User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
‘Encouraging’ new national data on chronic pain management
Most adults in the United States who have chronic pain favor a combination of nondrug and nonopioid approaches to control their pain, which is “encouraging,” new research shows.
A national survey reveals 55% of adults with chronic pain used pain management techniques that did not involve any opioids at all during the prior 3-month period.
However, few participants took advantage of cognitive-behavioral therapy (CBT), which is effective for easing chronic pain, Cornelius Groenewald, MB ChB, department of anesthesiology and pain medicine, University of Seattle, and colleagues write.
The results were published online in a research letter Feb. 7 in JAMA Network Open.
First time for pain questions
An estimated 50.2 million U.S. adults experience chronic pain, according to the 2019 National Health Interview Survey.
The 2019 version of the survey included questions on pain management techniques for the first time. Adults with chronic pain were asked to report on their use of 11 pain management techniques during the previous 3 months.
Among the 31,916 survey respondents, 64% were women; 69% were non-Hispanic White, 13% were Hispanic, and 11% were non-Hispanic Black; 71% were between 18 and 64 years of age, and 29% were 65 and older.
Among the key findings, an estimated 55% of adults with chronic pain used only nonopioid pain management techniques, 11% used both opioids and nonopioid techniques, and 4% used only opioids for chronic pain management; 30% did not report any pain management techniques during the previous 3 months.
Complementary therapies were the most commonly used nonopioid pain management technique (by 35% of adults with chronic pain), followed by physical, occupational, or rehabilitative therapies (19%).
Only about 4% of adults with chronic pain used CBT.
Other techniques used included self-management programs (5%) and chronic pain peer support groups (2%). In addition, 39% of adults with chronic pain reported using other pain approaches not specifically captured in the data set.
Benchmark data
Participants using complementary and psychological or psychotherapeutic interventions were more likely to be younger women with more education, the investigators report.
Adults using physical, occupational, or rehabilitative therapy were more likely to be highly educated older women with medical insurance.
Prescription opioid use for chronic pain was more common among older adults aged 45-64 years vs. those aged 18-44 years (19% vs. 8%).
It was also more common in women than men (17% vs. 13%), in adults with vs. without health insurance (16% vs. 6%), and in those with a high school education or lower, compared with those had more than a high school education (17% vs. 14%).
Prescription opioid use was less common among adults making $100,000 or more annually than in those making less than $35,000 a year (9% vs. 20%).
“While effective for some, opioids prescribed for chronic pain management remain an important determinant of the national opioid crisis,” the investigators write.
The study “provides baseline information on opioid and nonopioid pain management techniques used for chronic pain and serves as a benchmark for evaluating the outcome of health care policies aimed at reducing prescription opioid use,” they add.
The study had no specific funding. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Most adults in the United States who have chronic pain favor a combination of nondrug and nonopioid approaches to control their pain, which is “encouraging,” new research shows.
A national survey reveals 55% of adults with chronic pain used pain management techniques that did not involve any opioids at all during the prior 3-month period.
However, few participants took advantage of cognitive-behavioral therapy (CBT), which is effective for easing chronic pain, Cornelius Groenewald, MB ChB, department of anesthesiology and pain medicine, University of Seattle, and colleagues write.
The results were published online in a research letter Feb. 7 in JAMA Network Open.
First time for pain questions
An estimated 50.2 million U.S. adults experience chronic pain, according to the 2019 National Health Interview Survey.
The 2019 version of the survey included questions on pain management techniques for the first time. Adults with chronic pain were asked to report on their use of 11 pain management techniques during the previous 3 months.
Among the 31,916 survey respondents, 64% were women; 69% were non-Hispanic White, 13% were Hispanic, and 11% were non-Hispanic Black; 71% were between 18 and 64 years of age, and 29% were 65 and older.
Among the key findings, an estimated 55% of adults with chronic pain used only nonopioid pain management techniques, 11% used both opioids and nonopioid techniques, and 4% used only opioids for chronic pain management; 30% did not report any pain management techniques during the previous 3 months.
Complementary therapies were the most commonly used nonopioid pain management technique (by 35% of adults with chronic pain), followed by physical, occupational, or rehabilitative therapies (19%).
Only about 4% of adults with chronic pain used CBT.
Other techniques used included self-management programs (5%) and chronic pain peer support groups (2%). In addition, 39% of adults with chronic pain reported using other pain approaches not specifically captured in the data set.
Benchmark data
Participants using complementary and psychological or psychotherapeutic interventions were more likely to be younger women with more education, the investigators report.
Adults using physical, occupational, or rehabilitative therapy were more likely to be highly educated older women with medical insurance.
Prescription opioid use for chronic pain was more common among older adults aged 45-64 years vs. those aged 18-44 years (19% vs. 8%).
It was also more common in women than men (17% vs. 13%), in adults with vs. without health insurance (16% vs. 6%), and in those with a high school education or lower, compared with those had more than a high school education (17% vs. 14%).
Prescription opioid use was less common among adults making $100,000 or more annually than in those making less than $35,000 a year (9% vs. 20%).
“While effective for some, opioids prescribed for chronic pain management remain an important determinant of the national opioid crisis,” the investigators write.
The study “provides baseline information on opioid and nonopioid pain management techniques used for chronic pain and serves as a benchmark for evaluating the outcome of health care policies aimed at reducing prescription opioid use,” they add.
The study had no specific funding. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Most adults in the United States who have chronic pain favor a combination of nondrug and nonopioid approaches to control their pain, which is “encouraging,” new research shows.
A national survey reveals 55% of adults with chronic pain used pain management techniques that did not involve any opioids at all during the prior 3-month period.
However, few participants took advantage of cognitive-behavioral therapy (CBT), which is effective for easing chronic pain, Cornelius Groenewald, MB ChB, department of anesthesiology and pain medicine, University of Seattle, and colleagues write.
The results were published online in a research letter Feb. 7 in JAMA Network Open.
First time for pain questions
An estimated 50.2 million U.S. adults experience chronic pain, according to the 2019 National Health Interview Survey.
The 2019 version of the survey included questions on pain management techniques for the first time. Adults with chronic pain were asked to report on their use of 11 pain management techniques during the previous 3 months.
Among the 31,916 survey respondents, 64% were women; 69% were non-Hispanic White, 13% were Hispanic, and 11% were non-Hispanic Black; 71% were between 18 and 64 years of age, and 29% were 65 and older.
Among the key findings, an estimated 55% of adults with chronic pain used only nonopioid pain management techniques, 11% used both opioids and nonopioid techniques, and 4% used only opioids for chronic pain management; 30% did not report any pain management techniques during the previous 3 months.
Complementary therapies were the most commonly used nonopioid pain management technique (by 35% of adults with chronic pain), followed by physical, occupational, or rehabilitative therapies (19%).
Only about 4% of adults with chronic pain used CBT.
Other techniques used included self-management programs (5%) and chronic pain peer support groups (2%). In addition, 39% of adults with chronic pain reported using other pain approaches not specifically captured in the data set.
Benchmark data
Participants using complementary and psychological or psychotherapeutic interventions were more likely to be younger women with more education, the investigators report.
Adults using physical, occupational, or rehabilitative therapy were more likely to be highly educated older women with medical insurance.
Prescription opioid use for chronic pain was more common among older adults aged 45-64 years vs. those aged 18-44 years (19% vs. 8%).
It was also more common in women than men (17% vs. 13%), in adults with vs. without health insurance (16% vs. 6%), and in those with a high school education or lower, compared with those had more than a high school education (17% vs. 14%).
Prescription opioid use was less common among adults making $100,000 or more annually than in those making less than $35,000 a year (9% vs. 20%).
“While effective for some, opioids prescribed for chronic pain management remain an important determinant of the national opioid crisis,” the investigators write.
The study “provides baseline information on opioid and nonopioid pain management techniques used for chronic pain and serves as a benchmark for evaluating the outcome of health care policies aimed at reducing prescription opioid use,” they add.
The study had no specific funding. The investigators have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
‘Substantial’ CVD risks, burden up to a year after COVID-19
People who have had COVID-19 have an increased risk for, and 12-month burden of, cardiovascular disease (CVD) that is substantial and spans an array of cardiovascular disorders, a deep dive into federal data suggests.
“I went into this thinking that this is most likely happening in people to start with who have a higher risk of cardiovascular disorders, smokers, people with high BMI, diabetes, but what we found is something different,” Ziyad Al-Aly, MD, said in an interview. “It’s evident in people at high risk, but it was also as clear as the sun even in people who have no cardiovascular risk whatsoever.”
Rates were increased in younger adults, never smokers, White and Black people, and males and females, he said. “So the risk confirmed by the SARS-CoV-2 virus seems to spare almost no one.”
Although cardiovascular outcomes increased with the severity of the acute infection, the excess risks and burdens were also evident in those who never required hospitalization, a group that represents the majority of people with COVID-19, observed Dr. Al-Aly, who directs the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System.
“This study is very important because it underscores not just the acute cardiovascular risk associated with COVID but the increased risk of chronic cardiovascular outcomes as well,” cardiologist C. Michael Gibson, MD, professor of medicine, Harvard Medical School, Boston, said in an interview. “Given the number of patients in the U.S. who have been infected with COVID, this could represent a significant chronic burden on the health care system, particularly as health care professionals leave the profession.”
For the study, the investigators used national VA databases to build a cohort of 153,760 veterans who were alive 30 days after testing positive for COVID-19 between March 1, 2020, and January 2021. They were compared with a contemporary cohort of 5.6 million veterans with no evidence of SARS-CoV-2 infection and a historical cohort of 5.8 million veterans using the system in 2017 prior to the pandemic. Median follow-up was 347, 348, and 347 days, respectively.
As reported in Nature Medicine, the risk for a major adverse cardiovascular event, a composite of myocardial infarction, stroke, and all-cause mortality, was 4% higher in people who had been infected with COVID-19 than in those who had not.
“People say 4% is small, but actually it’s really, really big if you think about it in the context of the huge number of people who have had COVID-19 in the United States, and also globally,” Dr. Al-Aly said.
Compared with the contemporary control group, people who had COVID-19 had an increased risk (hazard ratio [HR]) and burden per 1,000 people at 1 year for the following cardiovascular outcomes:
- Stroke: HR, 1.52; burden, 4.03
- Transient ischemic attack: HR, 1.49; burden, 1.84
- Dysrhythmias: HR, 1.69; burden, 19.86
- Ischemic heart disease: HR, 1.66; burden, 7.28
- Heart failure: HR, 1.72; burden, 11.61
- Nonischemic cardiomyopathy: HR, 1.62; burden 3.56
- Pulmonary embolism: HR, 2.93; burden, 5.47
- Deep vein thrombosis: HR, 2.09; burden, 4.18
- Pericarditis: HR, 1.85, burden, 0.98
- Myocarditis: HR, 5.38; burden, 0.31
Recent reports have raised concerns about an association between COVID-19 vaccines and myocarditis and pericarditis, particularly in young males. Although very few of the participants were vaccinated prior to becoming infected, as vaccines were not yet widely available, the researchers performed two analyses censoring participants at the time of the first dose of any COVID-19 vaccine and adjusting for vaccination as a time-varying covariate.
The absolute numbers of myocarditis and pericarditis were still higher than the contemporary and historical cohorts. These numbers are much larger than those reported for myocarditis after vaccines, which are generally around 40 cases per 1 million people, observed Dr. Al-Aly.
The overall results were also consistent when compared with the historical control subjects.
“What we’re seeing in our report and others is that SARS-CoV-2 can leave a sort of scar or imprint on people, and some of these conditions are likely chronic conditions,” Dr. Al-Aly said. “So you’re going to have a generation of people who will bear the scar of COVID for their lifetime and I think that requires recognition and attention, so we’re aware of the magnitude of the problem and prepared to deal with it.”
With more than 76 million COVID-19 cases in the United States, that effort will likely have to be at the federal level, similar to President Joe Biden’s recent relaunch of the “Cancer Moonshot,” he added. “We need a greater and broader recognition at the federal level to try and recognize that when you have an earthquake, you don’t just deal with the earthquake when the earth is shaking, but you also need to deal with the aftermath.”
Dr. Gibson pointed out that this was a study of predominantly males and, thus, it’s unclear if the results can be extended to females. Nevertheless, he added, “long COVID may include outcomes beyond the central nervous system and we should educate patients about the risk of late cardiovascular outcomes.”
The authors noted the largely White, male cohort may limit generalizability of the findings. Other limitations include the possibility that some people may have had COVID-19 but were not tested, the datasets lacked information on cause of death, and possible residual confounding not accounted for in the adjusted analyses.
The research was funded by the U.S. Department of Veterans Affairs and two American Society of Nephrology and Kidney Cure fellowship awards. The authors declared no competing interests. Dr. Gibson reports having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
People who have had COVID-19 have an increased risk for, and 12-month burden of, cardiovascular disease (CVD) that is substantial and spans an array of cardiovascular disorders, a deep dive into federal data suggests.
“I went into this thinking that this is most likely happening in people to start with who have a higher risk of cardiovascular disorders, smokers, people with high BMI, diabetes, but what we found is something different,” Ziyad Al-Aly, MD, said in an interview. “It’s evident in people at high risk, but it was also as clear as the sun even in people who have no cardiovascular risk whatsoever.”
Rates were increased in younger adults, never smokers, White and Black people, and males and females, he said. “So the risk confirmed by the SARS-CoV-2 virus seems to spare almost no one.”
Although cardiovascular outcomes increased with the severity of the acute infection, the excess risks and burdens were also evident in those who never required hospitalization, a group that represents the majority of people with COVID-19, observed Dr. Al-Aly, who directs the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System.
“This study is very important because it underscores not just the acute cardiovascular risk associated with COVID but the increased risk of chronic cardiovascular outcomes as well,” cardiologist C. Michael Gibson, MD, professor of medicine, Harvard Medical School, Boston, said in an interview. “Given the number of patients in the U.S. who have been infected with COVID, this could represent a significant chronic burden on the health care system, particularly as health care professionals leave the profession.”
For the study, the investigators used national VA databases to build a cohort of 153,760 veterans who were alive 30 days after testing positive for COVID-19 between March 1, 2020, and January 2021. They were compared with a contemporary cohort of 5.6 million veterans with no evidence of SARS-CoV-2 infection and a historical cohort of 5.8 million veterans using the system in 2017 prior to the pandemic. Median follow-up was 347, 348, and 347 days, respectively.
As reported in Nature Medicine, the risk for a major adverse cardiovascular event, a composite of myocardial infarction, stroke, and all-cause mortality, was 4% higher in people who had been infected with COVID-19 than in those who had not.
“People say 4% is small, but actually it’s really, really big if you think about it in the context of the huge number of people who have had COVID-19 in the United States, and also globally,” Dr. Al-Aly said.
Compared with the contemporary control group, people who had COVID-19 had an increased risk (hazard ratio [HR]) and burden per 1,000 people at 1 year for the following cardiovascular outcomes:
- Stroke: HR, 1.52; burden, 4.03
- Transient ischemic attack: HR, 1.49; burden, 1.84
- Dysrhythmias: HR, 1.69; burden, 19.86
- Ischemic heart disease: HR, 1.66; burden, 7.28
- Heart failure: HR, 1.72; burden, 11.61
- Nonischemic cardiomyopathy: HR, 1.62; burden 3.56
- Pulmonary embolism: HR, 2.93; burden, 5.47
- Deep vein thrombosis: HR, 2.09; burden, 4.18
- Pericarditis: HR, 1.85, burden, 0.98
- Myocarditis: HR, 5.38; burden, 0.31
Recent reports have raised concerns about an association between COVID-19 vaccines and myocarditis and pericarditis, particularly in young males. Although very few of the participants were vaccinated prior to becoming infected, as vaccines were not yet widely available, the researchers performed two analyses censoring participants at the time of the first dose of any COVID-19 vaccine and adjusting for vaccination as a time-varying covariate.
The absolute numbers of myocarditis and pericarditis were still higher than the contemporary and historical cohorts. These numbers are much larger than those reported for myocarditis after vaccines, which are generally around 40 cases per 1 million people, observed Dr. Al-Aly.
The overall results were also consistent when compared with the historical control subjects.
“What we’re seeing in our report and others is that SARS-CoV-2 can leave a sort of scar or imprint on people, and some of these conditions are likely chronic conditions,” Dr. Al-Aly said. “So you’re going to have a generation of people who will bear the scar of COVID for their lifetime and I think that requires recognition and attention, so we’re aware of the magnitude of the problem and prepared to deal with it.”
With more than 76 million COVID-19 cases in the United States, that effort will likely have to be at the federal level, similar to President Joe Biden’s recent relaunch of the “Cancer Moonshot,” he added. “We need a greater and broader recognition at the federal level to try and recognize that when you have an earthquake, you don’t just deal with the earthquake when the earth is shaking, but you also need to deal with the aftermath.”
Dr. Gibson pointed out that this was a study of predominantly males and, thus, it’s unclear if the results can be extended to females. Nevertheless, he added, “long COVID may include outcomes beyond the central nervous system and we should educate patients about the risk of late cardiovascular outcomes.”
The authors noted the largely White, male cohort may limit generalizability of the findings. Other limitations include the possibility that some people may have had COVID-19 but were not tested, the datasets lacked information on cause of death, and possible residual confounding not accounted for in the adjusted analyses.
The research was funded by the U.S. Department of Veterans Affairs and two American Society of Nephrology and Kidney Cure fellowship awards. The authors declared no competing interests. Dr. Gibson reports having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
People who have had COVID-19 have an increased risk for, and 12-month burden of, cardiovascular disease (CVD) that is substantial and spans an array of cardiovascular disorders, a deep dive into federal data suggests.
“I went into this thinking that this is most likely happening in people to start with who have a higher risk of cardiovascular disorders, smokers, people with high BMI, diabetes, but what we found is something different,” Ziyad Al-Aly, MD, said in an interview. “It’s evident in people at high risk, but it was also as clear as the sun even in people who have no cardiovascular risk whatsoever.”
Rates were increased in younger adults, never smokers, White and Black people, and males and females, he said. “So the risk confirmed by the SARS-CoV-2 virus seems to spare almost no one.”
Although cardiovascular outcomes increased with the severity of the acute infection, the excess risks and burdens were also evident in those who never required hospitalization, a group that represents the majority of people with COVID-19, observed Dr. Al-Aly, who directs the Clinical Epidemiology Center at the Veterans Affairs St. Louis Health Care System.
“This study is very important because it underscores not just the acute cardiovascular risk associated with COVID but the increased risk of chronic cardiovascular outcomes as well,” cardiologist C. Michael Gibson, MD, professor of medicine, Harvard Medical School, Boston, said in an interview. “Given the number of patients in the U.S. who have been infected with COVID, this could represent a significant chronic burden on the health care system, particularly as health care professionals leave the profession.”
For the study, the investigators used national VA databases to build a cohort of 153,760 veterans who were alive 30 days after testing positive for COVID-19 between March 1, 2020, and January 2021. They were compared with a contemporary cohort of 5.6 million veterans with no evidence of SARS-CoV-2 infection and a historical cohort of 5.8 million veterans using the system in 2017 prior to the pandemic. Median follow-up was 347, 348, and 347 days, respectively.
As reported in Nature Medicine, the risk for a major adverse cardiovascular event, a composite of myocardial infarction, stroke, and all-cause mortality, was 4% higher in people who had been infected with COVID-19 than in those who had not.
“People say 4% is small, but actually it’s really, really big if you think about it in the context of the huge number of people who have had COVID-19 in the United States, and also globally,” Dr. Al-Aly said.
Compared with the contemporary control group, people who had COVID-19 had an increased risk (hazard ratio [HR]) and burden per 1,000 people at 1 year for the following cardiovascular outcomes:
- Stroke: HR, 1.52; burden, 4.03
- Transient ischemic attack: HR, 1.49; burden, 1.84
- Dysrhythmias: HR, 1.69; burden, 19.86
- Ischemic heart disease: HR, 1.66; burden, 7.28
- Heart failure: HR, 1.72; burden, 11.61
- Nonischemic cardiomyopathy: HR, 1.62; burden 3.56
- Pulmonary embolism: HR, 2.93; burden, 5.47
- Deep vein thrombosis: HR, 2.09; burden, 4.18
- Pericarditis: HR, 1.85, burden, 0.98
- Myocarditis: HR, 5.38; burden, 0.31
Recent reports have raised concerns about an association between COVID-19 vaccines and myocarditis and pericarditis, particularly in young males. Although very few of the participants were vaccinated prior to becoming infected, as vaccines were not yet widely available, the researchers performed two analyses censoring participants at the time of the first dose of any COVID-19 vaccine and adjusting for vaccination as a time-varying covariate.
The absolute numbers of myocarditis and pericarditis were still higher than the contemporary and historical cohorts. These numbers are much larger than those reported for myocarditis after vaccines, which are generally around 40 cases per 1 million people, observed Dr. Al-Aly.
The overall results were also consistent when compared with the historical control subjects.
“What we’re seeing in our report and others is that SARS-CoV-2 can leave a sort of scar or imprint on people, and some of these conditions are likely chronic conditions,” Dr. Al-Aly said. “So you’re going to have a generation of people who will bear the scar of COVID for their lifetime and I think that requires recognition and attention, so we’re aware of the magnitude of the problem and prepared to deal with it.”
With more than 76 million COVID-19 cases in the United States, that effort will likely have to be at the federal level, similar to President Joe Biden’s recent relaunch of the “Cancer Moonshot,” he added. “We need a greater and broader recognition at the federal level to try and recognize that when you have an earthquake, you don’t just deal with the earthquake when the earth is shaking, but you also need to deal with the aftermath.”
Dr. Gibson pointed out that this was a study of predominantly males and, thus, it’s unclear if the results can be extended to females. Nevertheless, he added, “long COVID may include outcomes beyond the central nervous system and we should educate patients about the risk of late cardiovascular outcomes.”
The authors noted the largely White, male cohort may limit generalizability of the findings. Other limitations include the possibility that some people may have had COVID-19 but were not tested, the datasets lacked information on cause of death, and possible residual confounding not accounted for in the adjusted analyses.
The research was funded by the U.S. Department of Veterans Affairs and two American Society of Nephrology and Kidney Cure fellowship awards. The authors declared no competing interests. Dr. Gibson reports having no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Dupilumab under FDA review for atopic dermatitis in children aged 6 months to 5 years
The and Sanofi.
If approved, dupilumab would be the first biologic approved for children in this age group in the United States, according to the statement. The proposed indication is as add-on therapy for children with moderate to severe AD not adequately controlled with topical prescription therapies or for whom topical therapies are not advised. The FDA granted breakthrough therapy designation for dupilumab for the treatment of severe AD in children aged 6 months to 11 years in 2016.
Approximately 85%-95% of atopic dermatitis patients develop symptoms before 5 years of age, and these symptoms often continue into adulthood, with an increased risk of skin infections and a significant impact on quality of life, according to the statement.
The sBLA is based on data from a phase 3 pivotal study of 162 children aged 6 months to 5 years in which dupilumab was added to standard-of-care topical corticosteroids, presented in December 2021. In the study, dupilumab plus standard of care significantly improved skin clearance and reduced overall disease severity and itch at 16 weeks compared with standard of care alone. Overall, 28% of the children randomized to dupilumab achieved the primary endpoint of clear or almost-clear skin, compared with 4% with those on standard of care alone (P < .0001), according to the manufacturers. Patients in the dupilumab group received either 200 mg (for children weighing ≥ 5 to < 15 kg) or 300 mg (for children weighing ≥ 15 to < 30 kg) every 4 weeks. Safety results were similar to those seen with dupilumab for children aged 6 years and older.
Conjunctivitis and herpes infections were among the most common adverse events associated with dupilumab in the study, according to the statement.
The target action date for the FDA decision on this application is June 9, 2022.
The and Sanofi.
If approved, dupilumab would be the first biologic approved for children in this age group in the United States, according to the statement. The proposed indication is as add-on therapy for children with moderate to severe AD not adequately controlled with topical prescription therapies or for whom topical therapies are not advised. The FDA granted breakthrough therapy designation for dupilumab for the treatment of severe AD in children aged 6 months to 11 years in 2016.
Approximately 85%-95% of atopic dermatitis patients develop symptoms before 5 years of age, and these symptoms often continue into adulthood, with an increased risk of skin infections and a significant impact on quality of life, according to the statement.
The sBLA is based on data from a phase 3 pivotal study of 162 children aged 6 months to 5 years in which dupilumab was added to standard-of-care topical corticosteroids, presented in December 2021. In the study, dupilumab plus standard of care significantly improved skin clearance and reduced overall disease severity and itch at 16 weeks compared with standard of care alone. Overall, 28% of the children randomized to dupilumab achieved the primary endpoint of clear or almost-clear skin, compared with 4% with those on standard of care alone (P < .0001), according to the manufacturers. Patients in the dupilumab group received either 200 mg (for children weighing ≥ 5 to < 15 kg) or 300 mg (for children weighing ≥ 15 to < 30 kg) every 4 weeks. Safety results were similar to those seen with dupilumab for children aged 6 years and older.
Conjunctivitis and herpes infections were among the most common adverse events associated with dupilumab in the study, according to the statement.
The target action date for the FDA decision on this application is June 9, 2022.
The and Sanofi.
If approved, dupilumab would be the first biologic approved for children in this age group in the United States, according to the statement. The proposed indication is as add-on therapy for children with moderate to severe AD not adequately controlled with topical prescription therapies or for whom topical therapies are not advised. The FDA granted breakthrough therapy designation for dupilumab for the treatment of severe AD in children aged 6 months to 11 years in 2016.
Approximately 85%-95% of atopic dermatitis patients develop symptoms before 5 years of age, and these symptoms often continue into adulthood, with an increased risk of skin infections and a significant impact on quality of life, according to the statement.
The sBLA is based on data from a phase 3 pivotal study of 162 children aged 6 months to 5 years in which dupilumab was added to standard-of-care topical corticosteroids, presented in December 2021. In the study, dupilumab plus standard of care significantly improved skin clearance and reduced overall disease severity and itch at 16 weeks compared with standard of care alone. Overall, 28% of the children randomized to dupilumab achieved the primary endpoint of clear or almost-clear skin, compared with 4% with those on standard of care alone (P < .0001), according to the manufacturers. Patients in the dupilumab group received either 200 mg (for children weighing ≥ 5 to < 15 kg) or 300 mg (for children weighing ≥ 15 to < 30 kg) every 4 weeks. Safety results were similar to those seen with dupilumab for children aged 6 years and older.
Conjunctivitis and herpes infections were among the most common adverse events associated with dupilumab in the study, according to the statement.
The target action date for the FDA decision on this application is June 9, 2022.
FROM THE FDA
Scientists see hope in new therapy for COVID-19 brain fog patients
People with long-COVID “brain fog” may be able to recover mental abilities that were dulled or stolen from them by the virus through an approach that has improved the effects of stroke, traumatic brain injury, and other post-viral disorders, doctors and scientists say.
For a lucky portion of the population, COVID-19 lasts a handful of days with minor symptoms. But for an estimated 37% who contract the virus, symptoms can linger for weeks, months, or even years. One of the most common symptoms of long COVID is brain fog: a life-altering condition characterized by slow thinking, confusion, difficulty remembering things, and poor concentration.
The approaches are based on the concept of neuroplasticity: The ability of neural networks in the brain to change, adapt, and strengthen, much like a muscle in the body that has been trained and exercised.
“The brain’s ability to bounce back from injury is what neuroplasticity is, and I’ve worked with people in our rehab clinic who have had brain tumors or suffer the effects of surgery or radiation on the brain, and people who have had West Nile virus, HIV, and meningitis,” said Tom Bergquist, PhD, clinical neuropsychologist at Mayo Clinic in Rochester, Minn. “There’s not a week that goes by that I don’t see someone recovering from COVID-19.”
One of the approaches used in the clinic is errorless learning, or having a patient with memory problems repeat information a certain number of times without error. The repetition helps rebuild those memory skills that were weakened during infection, Dr. Bergquist says.
People who have experienced brain fog after other viral infections have seen improvements with these approaches. Ben Ahrens, co-founder and CEO of re-origin – a company that offers neuroplasticity therapy – says he had long-term cognitive issues after a Lyme disease infection. Posttreatment Lyme disease syndrome, or chronic Lyme disease, occurs in about 1 in 10 people who are infected.
Mr. Ahrens says he was struck with Lyme 10 years ago and had brain fog, joint pain, and brain lesions detectable on scans for several years after infection.
According to Mr. Ahrens, neuroplasticity-based therapies help combat what researchers have found may be a lingering memory of past infections that lead to a heightened immune response, causing lingering symptoms.
“Essentially, what we believe is happening here, is the brain has learned that these symptoms are life-threatening – because, in fact, they can be,” Mr. Ahrens said. “The brain’s one job is to protect the body, and once it’s learned to associate these symptoms with that potentially very dangerous pathogen, even after it’s gone, things like a normal headache can trigger an immune cascade.”
Studies are underway at the University of Alabama at Birmingham to examine whether constraint-induced therapy – an approach rooted in neuroplasticity and historically used for loss of limb and speech function – is also effective for cognitive impairments like brain fog.
One technique they use is called shaping, which requires a person to repeatedly carry out their personal best function of impaired use – for example, remembering household tasks they have previously forgotten. That is done multiple times over several weeks in the clinic, and patients are given ways to transfer those skills to real-life use.
So far, the results are promising, said Edward Taub, PhD, researcher and professor of psychology at the University of Alabama at Birmingham.
When used in the past for physical impairments, researchers have noted not just clinical improvements, but structural changes. It led to an increase in the brain’s gray matter – which allows individuals to control movement, memory, and emotions – and improved white matter, which helps communication between gray matter areas.
Though results of the cognitive studies have not been published, Dr. Taub said patients with brain fog have shown improvement after just 35 hours of therapy and are nearly 100% improved after 6 months.
“The idea behind this is that the brain is responsive to use,” Dr. Taub said. “The amount of brain territory that’s dedicated to supporting or mediating a given behavioral function depends on the demands placed on the brain.”
A version of this article first appeared on WebMD.com.
People with long-COVID “brain fog” may be able to recover mental abilities that were dulled or stolen from them by the virus through an approach that has improved the effects of stroke, traumatic brain injury, and other post-viral disorders, doctors and scientists say.
For a lucky portion of the population, COVID-19 lasts a handful of days with minor symptoms. But for an estimated 37% who contract the virus, symptoms can linger for weeks, months, or even years. One of the most common symptoms of long COVID is brain fog: a life-altering condition characterized by slow thinking, confusion, difficulty remembering things, and poor concentration.
The approaches are based on the concept of neuroplasticity: The ability of neural networks in the brain to change, adapt, and strengthen, much like a muscle in the body that has been trained and exercised.
“The brain’s ability to bounce back from injury is what neuroplasticity is, and I’ve worked with people in our rehab clinic who have had brain tumors or suffer the effects of surgery or radiation on the brain, and people who have had West Nile virus, HIV, and meningitis,” said Tom Bergquist, PhD, clinical neuropsychologist at Mayo Clinic in Rochester, Minn. “There’s not a week that goes by that I don’t see someone recovering from COVID-19.”
One of the approaches used in the clinic is errorless learning, or having a patient with memory problems repeat information a certain number of times without error. The repetition helps rebuild those memory skills that were weakened during infection, Dr. Bergquist says.
People who have experienced brain fog after other viral infections have seen improvements with these approaches. Ben Ahrens, co-founder and CEO of re-origin – a company that offers neuroplasticity therapy – says he had long-term cognitive issues after a Lyme disease infection. Posttreatment Lyme disease syndrome, or chronic Lyme disease, occurs in about 1 in 10 people who are infected.
Mr. Ahrens says he was struck with Lyme 10 years ago and had brain fog, joint pain, and brain lesions detectable on scans for several years after infection.
According to Mr. Ahrens, neuroplasticity-based therapies help combat what researchers have found may be a lingering memory of past infections that lead to a heightened immune response, causing lingering symptoms.
“Essentially, what we believe is happening here, is the brain has learned that these symptoms are life-threatening – because, in fact, they can be,” Mr. Ahrens said. “The brain’s one job is to protect the body, and once it’s learned to associate these symptoms with that potentially very dangerous pathogen, even after it’s gone, things like a normal headache can trigger an immune cascade.”
Studies are underway at the University of Alabama at Birmingham to examine whether constraint-induced therapy – an approach rooted in neuroplasticity and historically used for loss of limb and speech function – is also effective for cognitive impairments like brain fog.
One technique they use is called shaping, which requires a person to repeatedly carry out their personal best function of impaired use – for example, remembering household tasks they have previously forgotten. That is done multiple times over several weeks in the clinic, and patients are given ways to transfer those skills to real-life use.
So far, the results are promising, said Edward Taub, PhD, researcher and professor of psychology at the University of Alabama at Birmingham.
When used in the past for physical impairments, researchers have noted not just clinical improvements, but structural changes. It led to an increase in the brain’s gray matter – which allows individuals to control movement, memory, and emotions – and improved white matter, which helps communication between gray matter areas.
Though results of the cognitive studies have not been published, Dr. Taub said patients with brain fog have shown improvement after just 35 hours of therapy and are nearly 100% improved after 6 months.
“The idea behind this is that the brain is responsive to use,” Dr. Taub said. “The amount of brain territory that’s dedicated to supporting or mediating a given behavioral function depends on the demands placed on the brain.”
A version of this article first appeared on WebMD.com.
People with long-COVID “brain fog” may be able to recover mental abilities that were dulled or stolen from them by the virus through an approach that has improved the effects of stroke, traumatic brain injury, and other post-viral disorders, doctors and scientists say.
For a lucky portion of the population, COVID-19 lasts a handful of days with minor symptoms. But for an estimated 37% who contract the virus, symptoms can linger for weeks, months, or even years. One of the most common symptoms of long COVID is brain fog: a life-altering condition characterized by slow thinking, confusion, difficulty remembering things, and poor concentration.
The approaches are based on the concept of neuroplasticity: The ability of neural networks in the brain to change, adapt, and strengthen, much like a muscle in the body that has been trained and exercised.
“The brain’s ability to bounce back from injury is what neuroplasticity is, and I’ve worked with people in our rehab clinic who have had brain tumors or suffer the effects of surgery or radiation on the brain, and people who have had West Nile virus, HIV, and meningitis,” said Tom Bergquist, PhD, clinical neuropsychologist at Mayo Clinic in Rochester, Minn. “There’s not a week that goes by that I don’t see someone recovering from COVID-19.”
One of the approaches used in the clinic is errorless learning, or having a patient with memory problems repeat information a certain number of times without error. The repetition helps rebuild those memory skills that were weakened during infection, Dr. Bergquist says.
People who have experienced brain fog after other viral infections have seen improvements with these approaches. Ben Ahrens, co-founder and CEO of re-origin – a company that offers neuroplasticity therapy – says he had long-term cognitive issues after a Lyme disease infection. Posttreatment Lyme disease syndrome, or chronic Lyme disease, occurs in about 1 in 10 people who are infected.
Mr. Ahrens says he was struck with Lyme 10 years ago and had brain fog, joint pain, and brain lesions detectable on scans for several years after infection.
According to Mr. Ahrens, neuroplasticity-based therapies help combat what researchers have found may be a lingering memory of past infections that lead to a heightened immune response, causing lingering symptoms.
“Essentially, what we believe is happening here, is the brain has learned that these symptoms are life-threatening – because, in fact, they can be,” Mr. Ahrens said. “The brain’s one job is to protect the body, and once it’s learned to associate these symptoms with that potentially very dangerous pathogen, even after it’s gone, things like a normal headache can trigger an immune cascade.”
Studies are underway at the University of Alabama at Birmingham to examine whether constraint-induced therapy – an approach rooted in neuroplasticity and historically used for loss of limb and speech function – is also effective for cognitive impairments like brain fog.
One technique they use is called shaping, which requires a person to repeatedly carry out their personal best function of impaired use – for example, remembering household tasks they have previously forgotten. That is done multiple times over several weeks in the clinic, and patients are given ways to transfer those skills to real-life use.
So far, the results are promising, said Edward Taub, PhD, researcher and professor of psychology at the University of Alabama at Birmingham.
When used in the past for physical impairments, researchers have noted not just clinical improvements, but structural changes. It led to an increase in the brain’s gray matter – which allows individuals to control movement, memory, and emotions – and improved white matter, which helps communication between gray matter areas.
Though results of the cognitive studies have not been published, Dr. Taub said patients with brain fog have shown improvement after just 35 hours of therapy and are nearly 100% improved after 6 months.
“The idea behind this is that the brain is responsive to use,” Dr. Taub said. “The amount of brain territory that’s dedicated to supporting or mediating a given behavioral function depends on the demands placed on the brain.”
A version of this article first appeared on WebMD.com.
Seniors face higher risk of other medical conditions after COVID-19
The findings of the observational study, which were published in the BMJ, show the risk of a new condition being triggered by COVID is more than twice as high in seniors, compared with younger patients. Plus, the researchers observed an even higher risk among those who were hospitalized, with nearly half (46%) of patients having developed new conditions after the acute COVID-19 infection period.
Respiratory failure with shortness of breath was the most common postacute sequela, but a wide range of heart, kidney, lung, liver, cognitive, mental health, and other conditions were diagnosed at least 3 weeks after initial infection and persisted beyond 30 days.
This is one of the first studies to specifically describe the incidence and severity of new conditions triggered by COVID-19 infection in a general sample of older adults, said study author Ken Cohen MD, FACP, executive director of translational research at Optum Labs and national senior medical director at Optum Care.
“Much of what has been published on the postacute sequelae of COVID-19 has been predominantly from a younger population, and many of the patients had been hospitalized,” Dr. Cohen noted. “This was the first study to focus on a large population of seniors, most of whom did not require hospitalization.”
Dr. Cohen and colleagues reviewed the health insurance records of more than 133,000 Medicare beneficiaries aged 65 or older who were diagnosed with COVID-19 before April 2020. They also matched individuals by age, race, sex, hospitalization status, and other factors to comparison groups without COVID-19 (one from 2020 and one from 2019), and to a group diagnosed with other lower respiratory tract viral infections before the pandemic.
Risk of developing new conditions was higher in hospitalized
After acute COVID-19 infection, 32% of seniors sought medical care for at least one new medical condition in 2020, compared with 21% of uninfected people in the same year.
The most commonly observed conditions included:
- Respiratory failure (7.55% higher risk).
- Fatigue (5.66% higher risk).
- High blood pressure (4.43% higher risk).
- Memory problems (2.63% higher risk).
- Kidney injury (2.59% higher risk).
- Mental health diagnoses (2.5% higher risk).
- Blood-clotting disorders (1.47 % higher risk).
- Heart rhythm disorders (2.9% higher risk).
The risk of developing new conditions was even higher among those 23,486 who were hospitalized in 2020. Those individuals showed a 23.6% higher risk for developing at least one new condition, compared with uninfected seniors in the same year. Also, patients older than 75 had a higher risk for neurological disorders, including dementia, encephalopathy, and memory problems. The researchers also found that respiratory failure and kidney injury were significantly more likely to affect men and Black patients.
When those who had COVID were compared with the group with other lower respiratory viral infections before the pandemic, only the risks of respiratory failure (2.39% higher), dementia (0.71% higher), and fatigue (0.18% higher) were higher.
Primary care providers can learn from these data to better evaluate and manage their geriatric patients with COVID-19 infection, said Amit Shah, MD, a geriatrician with the Mayo Clinic in Phoenix, in an interview.
“We must assess older patients who have had COVID-19 for more than just improvement from the respiratory symptoms of COVID-19 in post-COVID follow-up visits,” he said. “Older individuals with frailty have vulnerability to subsequent complications from severe illnesses and it is common to see post-illness diagnoses, such as new diagnosis of delirium; dementia; or renal, respiratory, or cardiac issues that is precipitated by the original illness. This study confirms that this is likely the case with COVID-19 as well.
“Primary care physicians should be vigilant for these complications, including attention to the rehabilitation needs of older patients with longer-term postviral fatigue from COVID-19,” Dr. Shah added.
Data predates ‘Omicron wave’
It remains uncertain whether sequelae will differ with the Omicron variant, but the findings remain applicable, Dr. Cohen said.
“We know that illness from the Omicron variant is on average less severe in those that have been vaccinated. However, throughout the Omicron wave, individuals who have not been vaccinated continue to have significant rates of serious illness and hospitalization,” he said.
“Our findings showed that serious illness with hospitalization was associated with a higher rate of sequelae. It can therefore be inferred that the rates of sequelae seen in our study would continue to occur in unvaccinated individuals who contract Omicron, but might occur less frequently in vaccinated individuals who contract Omicron and have less severe illness.”
Dr. Cohen serves as a consultant for Pfizer. Dr. Shah has disclosed no relevant financial relationships.
The findings of the observational study, which were published in the BMJ, show the risk of a new condition being triggered by COVID is more than twice as high in seniors, compared with younger patients. Plus, the researchers observed an even higher risk among those who were hospitalized, with nearly half (46%) of patients having developed new conditions after the acute COVID-19 infection period.
Respiratory failure with shortness of breath was the most common postacute sequela, but a wide range of heart, kidney, lung, liver, cognitive, mental health, and other conditions were diagnosed at least 3 weeks after initial infection and persisted beyond 30 days.
This is one of the first studies to specifically describe the incidence and severity of new conditions triggered by COVID-19 infection in a general sample of older adults, said study author Ken Cohen MD, FACP, executive director of translational research at Optum Labs and national senior medical director at Optum Care.
“Much of what has been published on the postacute sequelae of COVID-19 has been predominantly from a younger population, and many of the patients had been hospitalized,” Dr. Cohen noted. “This was the first study to focus on a large population of seniors, most of whom did not require hospitalization.”
Dr. Cohen and colleagues reviewed the health insurance records of more than 133,000 Medicare beneficiaries aged 65 or older who were diagnosed with COVID-19 before April 2020. They also matched individuals by age, race, sex, hospitalization status, and other factors to comparison groups without COVID-19 (one from 2020 and one from 2019), and to a group diagnosed with other lower respiratory tract viral infections before the pandemic.
Risk of developing new conditions was higher in hospitalized
After acute COVID-19 infection, 32% of seniors sought medical care for at least one new medical condition in 2020, compared with 21% of uninfected people in the same year.
The most commonly observed conditions included:
- Respiratory failure (7.55% higher risk).
- Fatigue (5.66% higher risk).
- High blood pressure (4.43% higher risk).
- Memory problems (2.63% higher risk).
- Kidney injury (2.59% higher risk).
- Mental health diagnoses (2.5% higher risk).
- Blood-clotting disorders (1.47 % higher risk).
- Heart rhythm disorders (2.9% higher risk).
The risk of developing new conditions was even higher among those 23,486 who were hospitalized in 2020. Those individuals showed a 23.6% higher risk for developing at least one new condition, compared with uninfected seniors in the same year. Also, patients older than 75 had a higher risk for neurological disorders, including dementia, encephalopathy, and memory problems. The researchers also found that respiratory failure and kidney injury were significantly more likely to affect men and Black patients.
When those who had COVID were compared with the group with other lower respiratory viral infections before the pandemic, only the risks of respiratory failure (2.39% higher), dementia (0.71% higher), and fatigue (0.18% higher) were higher.
Primary care providers can learn from these data to better evaluate and manage their geriatric patients with COVID-19 infection, said Amit Shah, MD, a geriatrician with the Mayo Clinic in Phoenix, in an interview.
“We must assess older patients who have had COVID-19 for more than just improvement from the respiratory symptoms of COVID-19 in post-COVID follow-up visits,” he said. “Older individuals with frailty have vulnerability to subsequent complications from severe illnesses and it is common to see post-illness diagnoses, such as new diagnosis of delirium; dementia; or renal, respiratory, or cardiac issues that is precipitated by the original illness. This study confirms that this is likely the case with COVID-19 as well.
“Primary care physicians should be vigilant for these complications, including attention to the rehabilitation needs of older patients with longer-term postviral fatigue from COVID-19,” Dr. Shah added.
Data predates ‘Omicron wave’
It remains uncertain whether sequelae will differ with the Omicron variant, but the findings remain applicable, Dr. Cohen said.
“We know that illness from the Omicron variant is on average less severe in those that have been vaccinated. However, throughout the Omicron wave, individuals who have not been vaccinated continue to have significant rates of serious illness and hospitalization,” he said.
“Our findings showed that serious illness with hospitalization was associated with a higher rate of sequelae. It can therefore be inferred that the rates of sequelae seen in our study would continue to occur in unvaccinated individuals who contract Omicron, but might occur less frequently in vaccinated individuals who contract Omicron and have less severe illness.”
Dr. Cohen serves as a consultant for Pfizer. Dr. Shah has disclosed no relevant financial relationships.
The findings of the observational study, which were published in the BMJ, show the risk of a new condition being triggered by COVID is more than twice as high in seniors, compared with younger patients. Plus, the researchers observed an even higher risk among those who were hospitalized, with nearly half (46%) of patients having developed new conditions after the acute COVID-19 infection period.
Respiratory failure with shortness of breath was the most common postacute sequela, but a wide range of heart, kidney, lung, liver, cognitive, mental health, and other conditions were diagnosed at least 3 weeks after initial infection and persisted beyond 30 days.
This is one of the first studies to specifically describe the incidence and severity of new conditions triggered by COVID-19 infection in a general sample of older adults, said study author Ken Cohen MD, FACP, executive director of translational research at Optum Labs and national senior medical director at Optum Care.
“Much of what has been published on the postacute sequelae of COVID-19 has been predominantly from a younger population, and many of the patients had been hospitalized,” Dr. Cohen noted. “This was the first study to focus on a large population of seniors, most of whom did not require hospitalization.”
Dr. Cohen and colleagues reviewed the health insurance records of more than 133,000 Medicare beneficiaries aged 65 or older who were diagnosed with COVID-19 before April 2020. They also matched individuals by age, race, sex, hospitalization status, and other factors to comparison groups without COVID-19 (one from 2020 and one from 2019), and to a group diagnosed with other lower respiratory tract viral infections before the pandemic.
Risk of developing new conditions was higher in hospitalized
After acute COVID-19 infection, 32% of seniors sought medical care for at least one new medical condition in 2020, compared with 21% of uninfected people in the same year.
The most commonly observed conditions included:
- Respiratory failure (7.55% higher risk).
- Fatigue (5.66% higher risk).
- High blood pressure (4.43% higher risk).
- Memory problems (2.63% higher risk).
- Kidney injury (2.59% higher risk).
- Mental health diagnoses (2.5% higher risk).
- Blood-clotting disorders (1.47 % higher risk).
- Heart rhythm disorders (2.9% higher risk).
The risk of developing new conditions was even higher among those 23,486 who were hospitalized in 2020. Those individuals showed a 23.6% higher risk for developing at least one new condition, compared with uninfected seniors in the same year. Also, patients older than 75 had a higher risk for neurological disorders, including dementia, encephalopathy, and memory problems. The researchers also found that respiratory failure and kidney injury were significantly more likely to affect men and Black patients.
When those who had COVID were compared with the group with other lower respiratory viral infections before the pandemic, only the risks of respiratory failure (2.39% higher), dementia (0.71% higher), and fatigue (0.18% higher) were higher.
Primary care providers can learn from these data to better evaluate and manage their geriatric patients with COVID-19 infection, said Amit Shah, MD, a geriatrician with the Mayo Clinic in Phoenix, in an interview.
“We must assess older patients who have had COVID-19 for more than just improvement from the respiratory symptoms of COVID-19 in post-COVID follow-up visits,” he said. “Older individuals with frailty have vulnerability to subsequent complications from severe illnesses and it is common to see post-illness diagnoses, such as new diagnosis of delirium; dementia; or renal, respiratory, or cardiac issues that is precipitated by the original illness. This study confirms that this is likely the case with COVID-19 as well.
“Primary care physicians should be vigilant for these complications, including attention to the rehabilitation needs of older patients with longer-term postviral fatigue from COVID-19,” Dr. Shah added.
Data predates ‘Omicron wave’
It remains uncertain whether sequelae will differ with the Omicron variant, but the findings remain applicable, Dr. Cohen said.
“We know that illness from the Omicron variant is on average less severe in those that have been vaccinated. However, throughout the Omicron wave, individuals who have not been vaccinated continue to have significant rates of serious illness and hospitalization,” he said.
“Our findings showed that serious illness with hospitalization was associated with a higher rate of sequelae. It can therefore be inferred that the rates of sequelae seen in our study would continue to occur in unvaccinated individuals who contract Omicron, but might occur less frequently in vaccinated individuals who contract Omicron and have less severe illness.”
Dr. Cohen serves as a consultant for Pfizer. Dr. Shah has disclosed no relevant financial relationships.
FROM BMJ
Growth in early life may predict early puberty
Faster gains in weight, length or height, or body mass index in the first 5 years of life were associated with an earlier onset of puberty in boys and girls, based on data from a cohort study of more than 7,000 children.
In recent decades, clinicians and parents have raised concerns about an earlier onset of puberty in children in the United States and other countries, Izzudin M. Aris, PhD, of Harvard Medical School, Boston, and colleagues wrote.
“Children with earlier pubertal onset not only may be at increased risk for long-term chronic diseases, but also may experience adverse consequences during adolescence, including psychosocial difficulties and dysmetabolism,” they said. However, the effect of growth in the first 5 years of life on pubertal onset has not been well studied.
In a study published in JAMA Network Open, the researchers identified 7,495 children from 36 cohorts participating in the Environmental Influences on Child Health Outcomes program from Jan. 1, 1986, to Dec. 31, 2015.
The study population included 3,772 girls and 3,723 boys; 60% reported as White, 23% as Black, 15% as Hispanic, 12% as one of the following: American Indian or Alaska Native, Native Hawaiian or Pacific Islander, multiple races, or other race. Most (84.1%) were born during or after the year 2000.
The primary outcome was the pubertal growth spurt, also known as age at peak height velocity (APHV). The researchers measured growth at 3 age periods in the first 5 years (early infancy, late infancy, and early childhood) and estimated rates of weight, length or height, and body mass index (BMI) gain. Secondary outcomes included self-reported pubic hair staging and scores on the Pubertal Development Scale.
Overall, weight and length or height gain velocities declined in the first 5 years of life, and boys had faster gains in early infancy, compared with girls.
APHV was negatively correlated with puberty scores and Tanner staging for pubic hair development in both boys and girls, while puberty score was positively correlated with Tanner staging for pubic hair in both sexes.
After controlling for maternal and child confounders including maternal age at delivery, maternal education level, and year of birth, faster gains in weight, length or height, or BMI at each of the three measurement periods in early life was associated with earlier APHV in boys. No effect was noted for race, maternal education level, or birth year.
In girls, faster gains in weight, length, or height, only at the latest measurement period (early childhood) were associated with younger APHV. No associations with APHV occurred for velocities of BMI gain at any age period in girls, the researchers noted. However, age at menarche was positively correlated with early APHV and negatively correlated with puberty score and Tanner staging for pubic hair.
The findings support previous studies of associations between child growth and pubertal onset, the researchers wrote. The mechanisms of action are many, and have not been explained, the researchers wrote in their discussion of the findings.
“We speculate that insulinlike growth factor 1 may be a factor in the associations observed in the present study, either directly or indirectly through sex steroid synthesis and secretion. Alternatively, in girls, androgens and adipokines may be factors in the observed associations for pubic hair staging and menarche, respectively,” they said. Genetics and other factors including social factors, environmental exposures, diet, and physical activity also affect growth in early life.
The study findings were limited by several factors including the use of child-reported measures of pubic hair staging and parent reports of pubertal scores, with the potential for error and misclassification, the researchers noted. Other limitations include a lack of data on maternal age at menarche and the use of weight-for-length rather than BMI for children younger than 2 years.
However, the results were strengthened by the large sample size, long-term follow-up, and especially the use of a nationally representative contemporary cohort that addresses gaps in the current literature from later time periods. The results support the associations of sex-specific early pubertal onset in children with faster growth early in life. “In the long term, results of the present study may inform future research that aims to develop and/or test preventive interventions to optimize nutrition, environmental exposures, physical activity, and other behaviors related to growth during these age periods,” they concluded.
Time and timing limit practical application of results
The current study addresses two issues that are ongoing concerns for clinicians, specifically, the rise in obesity in childhood and its potential link to an earlier age of entry into puberty, M. Susan Jay, MD, of the Medical College of Wisconsin, Milwaukee, said in an interview.
“Authors in prior studies have suggested that earlier puberty, and indeed earlier menarche, in females may be associated with the potential of long-term health issues,” Dr. Jay noted. “It has also been suggested that both early maturing females and males may be impacted psychosocially. Others have suggested that the pathways through puberty are key and environmental factors as well as nutrition can have an impact on adolescence as well as health consequences later in life.”
The current study is important because it focused on children born in the present era of the obesity epidemic, while earlier studies were conducted on a group in the 1960s-1980s. “This study suggests that there are sex-specific associations of faster growth and earlier entry into puberty,” Dr. Jay said.
“While it is exciting to consider closer monitoring of pubertal progression in pediatric settings, often patients and families do not present in a timely manner for assessment,” she said. “Also, the authors suggest that preventive support may be offered to children who are traversing puberty at earlier ages. However, given the current stress on practices with COVID as well as stress on providers offering clinical services, identifying supportive interventions may be a stretch at best for practitioners already burdened by clinical and administrative demands.
“Ongoing studies are needed to address the knowledge gaps that exist in the arena of pubertal onset and growth during childhood across life periods,” said Dr. Jay. “In the long term, the present study may help direct research that could focus on preventive interventions to optimize nutrition, physical activity, environmental exposures, and other factors that intersect growth during infancy through early childhood, which may hasten early pubertal development’s later sequelae in adulthood.”
The study was supported by various grants to the researchers from the Environmental Influences on Child Health Outcomes program, Office of the Director, National Institutes of Health, as well as the Colorado Clinical and Translational Sciences Institute, University of Colorado at Denver. Lead author Dr. Aris had no financial conflicts to disclose. Dr. Jay had no conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Faster gains in weight, length or height, or body mass index in the first 5 years of life were associated with an earlier onset of puberty in boys and girls, based on data from a cohort study of more than 7,000 children.
In recent decades, clinicians and parents have raised concerns about an earlier onset of puberty in children in the United States and other countries, Izzudin M. Aris, PhD, of Harvard Medical School, Boston, and colleagues wrote.
“Children with earlier pubertal onset not only may be at increased risk for long-term chronic diseases, but also may experience adverse consequences during adolescence, including psychosocial difficulties and dysmetabolism,” they said. However, the effect of growth in the first 5 years of life on pubertal onset has not been well studied.
In a study published in JAMA Network Open, the researchers identified 7,495 children from 36 cohorts participating in the Environmental Influences on Child Health Outcomes program from Jan. 1, 1986, to Dec. 31, 2015.
The study population included 3,772 girls and 3,723 boys; 60% reported as White, 23% as Black, 15% as Hispanic, 12% as one of the following: American Indian or Alaska Native, Native Hawaiian or Pacific Islander, multiple races, or other race. Most (84.1%) were born during or after the year 2000.
The primary outcome was the pubertal growth spurt, also known as age at peak height velocity (APHV). The researchers measured growth at 3 age periods in the first 5 years (early infancy, late infancy, and early childhood) and estimated rates of weight, length or height, and body mass index (BMI) gain. Secondary outcomes included self-reported pubic hair staging and scores on the Pubertal Development Scale.
Overall, weight and length or height gain velocities declined in the first 5 years of life, and boys had faster gains in early infancy, compared with girls.
APHV was negatively correlated with puberty scores and Tanner staging for pubic hair development in both boys and girls, while puberty score was positively correlated with Tanner staging for pubic hair in both sexes.
After controlling for maternal and child confounders including maternal age at delivery, maternal education level, and year of birth, faster gains in weight, length or height, or BMI at each of the three measurement periods in early life was associated with earlier APHV in boys. No effect was noted for race, maternal education level, or birth year.
In girls, faster gains in weight, length, or height, only at the latest measurement period (early childhood) were associated with younger APHV. No associations with APHV occurred for velocities of BMI gain at any age period in girls, the researchers noted. However, age at menarche was positively correlated with early APHV and negatively correlated with puberty score and Tanner staging for pubic hair.
The findings support previous studies of associations between child growth and pubertal onset, the researchers wrote. The mechanisms of action are many, and have not been explained, the researchers wrote in their discussion of the findings.
“We speculate that insulinlike growth factor 1 may be a factor in the associations observed in the present study, either directly or indirectly through sex steroid synthesis and secretion. Alternatively, in girls, androgens and adipokines may be factors in the observed associations for pubic hair staging and menarche, respectively,” they said. Genetics and other factors including social factors, environmental exposures, diet, and physical activity also affect growth in early life.
The study findings were limited by several factors including the use of child-reported measures of pubic hair staging and parent reports of pubertal scores, with the potential for error and misclassification, the researchers noted. Other limitations include a lack of data on maternal age at menarche and the use of weight-for-length rather than BMI for children younger than 2 years.
However, the results were strengthened by the large sample size, long-term follow-up, and especially the use of a nationally representative contemporary cohort that addresses gaps in the current literature from later time periods. The results support the associations of sex-specific early pubertal onset in children with faster growth early in life. “In the long term, results of the present study may inform future research that aims to develop and/or test preventive interventions to optimize nutrition, environmental exposures, physical activity, and other behaviors related to growth during these age periods,” they concluded.
Time and timing limit practical application of results
The current study addresses two issues that are ongoing concerns for clinicians, specifically, the rise in obesity in childhood and its potential link to an earlier age of entry into puberty, M. Susan Jay, MD, of the Medical College of Wisconsin, Milwaukee, said in an interview.
“Authors in prior studies have suggested that earlier puberty, and indeed earlier menarche, in females may be associated with the potential of long-term health issues,” Dr. Jay noted. “It has also been suggested that both early maturing females and males may be impacted psychosocially. Others have suggested that the pathways through puberty are key and environmental factors as well as nutrition can have an impact on adolescence as well as health consequences later in life.”
The current study is important because it focused on children born in the present era of the obesity epidemic, while earlier studies were conducted on a group in the 1960s-1980s. “This study suggests that there are sex-specific associations of faster growth and earlier entry into puberty,” Dr. Jay said.
“While it is exciting to consider closer monitoring of pubertal progression in pediatric settings, often patients and families do not present in a timely manner for assessment,” she said. “Also, the authors suggest that preventive support may be offered to children who are traversing puberty at earlier ages. However, given the current stress on practices with COVID as well as stress on providers offering clinical services, identifying supportive interventions may be a stretch at best for practitioners already burdened by clinical and administrative demands.
“Ongoing studies are needed to address the knowledge gaps that exist in the arena of pubertal onset and growth during childhood across life periods,” said Dr. Jay. “In the long term, the present study may help direct research that could focus on preventive interventions to optimize nutrition, physical activity, environmental exposures, and other factors that intersect growth during infancy through early childhood, which may hasten early pubertal development’s later sequelae in adulthood.”
The study was supported by various grants to the researchers from the Environmental Influences on Child Health Outcomes program, Office of the Director, National Institutes of Health, as well as the Colorado Clinical and Translational Sciences Institute, University of Colorado at Denver. Lead author Dr. Aris had no financial conflicts to disclose. Dr. Jay had no conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Faster gains in weight, length or height, or body mass index in the first 5 years of life were associated with an earlier onset of puberty in boys and girls, based on data from a cohort study of more than 7,000 children.
In recent decades, clinicians and parents have raised concerns about an earlier onset of puberty in children in the United States and other countries, Izzudin M. Aris, PhD, of Harvard Medical School, Boston, and colleagues wrote.
“Children with earlier pubertal onset not only may be at increased risk for long-term chronic diseases, but also may experience adverse consequences during adolescence, including psychosocial difficulties and dysmetabolism,” they said. However, the effect of growth in the first 5 years of life on pubertal onset has not been well studied.
In a study published in JAMA Network Open, the researchers identified 7,495 children from 36 cohorts participating in the Environmental Influences on Child Health Outcomes program from Jan. 1, 1986, to Dec. 31, 2015.
The study population included 3,772 girls and 3,723 boys; 60% reported as White, 23% as Black, 15% as Hispanic, 12% as one of the following: American Indian or Alaska Native, Native Hawaiian or Pacific Islander, multiple races, or other race. Most (84.1%) were born during or after the year 2000.
The primary outcome was the pubertal growth spurt, also known as age at peak height velocity (APHV). The researchers measured growth at 3 age periods in the first 5 years (early infancy, late infancy, and early childhood) and estimated rates of weight, length or height, and body mass index (BMI) gain. Secondary outcomes included self-reported pubic hair staging and scores on the Pubertal Development Scale.
Overall, weight and length or height gain velocities declined in the first 5 years of life, and boys had faster gains in early infancy, compared with girls.
APHV was negatively correlated with puberty scores and Tanner staging for pubic hair development in both boys and girls, while puberty score was positively correlated with Tanner staging for pubic hair in both sexes.
After controlling for maternal and child confounders including maternal age at delivery, maternal education level, and year of birth, faster gains in weight, length or height, or BMI at each of the three measurement periods in early life was associated with earlier APHV in boys. No effect was noted for race, maternal education level, or birth year.
In girls, faster gains in weight, length, or height, only at the latest measurement period (early childhood) were associated with younger APHV. No associations with APHV occurred for velocities of BMI gain at any age period in girls, the researchers noted. However, age at menarche was positively correlated with early APHV and negatively correlated with puberty score and Tanner staging for pubic hair.
The findings support previous studies of associations between child growth and pubertal onset, the researchers wrote. The mechanisms of action are many, and have not been explained, the researchers wrote in their discussion of the findings.
“We speculate that insulinlike growth factor 1 may be a factor in the associations observed in the present study, either directly or indirectly through sex steroid synthesis and secretion. Alternatively, in girls, androgens and adipokines may be factors in the observed associations for pubic hair staging and menarche, respectively,” they said. Genetics and other factors including social factors, environmental exposures, diet, and physical activity also affect growth in early life.
The study findings were limited by several factors including the use of child-reported measures of pubic hair staging and parent reports of pubertal scores, with the potential for error and misclassification, the researchers noted. Other limitations include a lack of data on maternal age at menarche and the use of weight-for-length rather than BMI for children younger than 2 years.
However, the results were strengthened by the large sample size, long-term follow-up, and especially the use of a nationally representative contemporary cohort that addresses gaps in the current literature from later time periods. The results support the associations of sex-specific early pubertal onset in children with faster growth early in life. “In the long term, results of the present study may inform future research that aims to develop and/or test preventive interventions to optimize nutrition, environmental exposures, physical activity, and other behaviors related to growth during these age periods,” they concluded.
Time and timing limit practical application of results
The current study addresses two issues that are ongoing concerns for clinicians, specifically, the rise in obesity in childhood and its potential link to an earlier age of entry into puberty, M. Susan Jay, MD, of the Medical College of Wisconsin, Milwaukee, said in an interview.
“Authors in prior studies have suggested that earlier puberty, and indeed earlier menarche, in females may be associated with the potential of long-term health issues,” Dr. Jay noted. “It has also been suggested that both early maturing females and males may be impacted psychosocially. Others have suggested that the pathways through puberty are key and environmental factors as well as nutrition can have an impact on adolescence as well as health consequences later in life.”
The current study is important because it focused on children born in the present era of the obesity epidemic, while earlier studies were conducted on a group in the 1960s-1980s. “This study suggests that there are sex-specific associations of faster growth and earlier entry into puberty,” Dr. Jay said.
“While it is exciting to consider closer monitoring of pubertal progression in pediatric settings, often patients and families do not present in a timely manner for assessment,” she said. “Also, the authors suggest that preventive support may be offered to children who are traversing puberty at earlier ages. However, given the current stress on practices with COVID as well as stress on providers offering clinical services, identifying supportive interventions may be a stretch at best for practitioners already burdened by clinical and administrative demands.
“Ongoing studies are needed to address the knowledge gaps that exist in the arena of pubertal onset and growth during childhood across life periods,” said Dr. Jay. “In the long term, the present study may help direct research that could focus on preventive interventions to optimize nutrition, physical activity, environmental exposures, and other factors that intersect growth during infancy through early childhood, which may hasten early pubertal development’s later sequelae in adulthood.”
The study was supported by various grants to the researchers from the Environmental Influences on Child Health Outcomes program, Office of the Director, National Institutes of Health, as well as the Colorado Clinical and Translational Sciences Institute, University of Colorado at Denver. Lead author Dr. Aris had no financial conflicts to disclose. Dr. Jay had no conflicts to disclose and serves on the editorial advisory board of Pediatric News.
FROM JAMA NETWORK OPEN
J&J pauses production of COVID vaccine
Johnson & Johnson stopped making its COVID-19 vaccine at a key facility in the Netherlands.
The Johnson & Johnson shot is seen as a critical vaccine for poorer countries. , people familiar with the decision told The New York Times.
The plant, located in Leiden, has been making an experimental but potentially more profitable vaccine instead. The experimental vaccine is for an unrelated virus -- respiratory syncytial virus, or RSV -- that will be used for a clinical trial.
The pause is said to be temporary. The Leiden plant is expected to restart production of the COVID-19 vaccine next month. The company has said that it has millions of COVID-19 doses in inventory, though it’s unclear whether the pause has affected vaccine supplies.
The interruption could reduce the supply of Johnson & Johnson’s COVID-19 vaccine by a few hundred million doses, one of the sources told the newspaper, since the doses made from renewed production won’t likely ship until May or June. Other facilities have been hired to produce the vaccine but aren’t running yet or haven’t received regulatory approval to ship doses for packaging.
Jake Sargent, a spokesman for Johnson & Johnson, told the Times that the company is “focused on ensuring our vaccine is available where people are in need” and that its global production network “is working day and night.” He said that the company has millions of doses in inventory and is continuing to deliver vaccine batches to facilities that package doses.
The pause has surprised officials at two main recipients of the Johnson & Johnson shots -- the African Union and Covax, the organization that coordinates COVID-19 vaccines for poorer countries. Leaders of the two organizations learned about the halt in production from reporters at the Times.
“This is not the time to be switching production lines of anything, when the lives of people across the developing world hang in the balance,” Ayoade Alakija, coleader of the African Union’s vaccine delivery program, told the newspaper.
Poorer countries rely on Johnson & Johnson’s vaccine because it doesn’t require ultracold refrigeration. The vaccine is also less expensive than others and easy to provide to hard-to-reach populations.
“In many low- and middle-income countries, our vaccine is the most important and sometimes only option,” Penny Heaton, MD, a Johnson & Johnson executive, said in December during a meeting with the CDC’s vaccine advisory committee.
“We have a global vaccine, and the world is depending on us,” she said.
A version of this article first appeared on WebMD.com.
Johnson & Johnson stopped making its COVID-19 vaccine at a key facility in the Netherlands.
The Johnson & Johnson shot is seen as a critical vaccine for poorer countries. , people familiar with the decision told The New York Times.
The plant, located in Leiden, has been making an experimental but potentially more profitable vaccine instead. The experimental vaccine is for an unrelated virus -- respiratory syncytial virus, or RSV -- that will be used for a clinical trial.
The pause is said to be temporary. The Leiden plant is expected to restart production of the COVID-19 vaccine next month. The company has said that it has millions of COVID-19 doses in inventory, though it’s unclear whether the pause has affected vaccine supplies.
The interruption could reduce the supply of Johnson & Johnson’s COVID-19 vaccine by a few hundred million doses, one of the sources told the newspaper, since the doses made from renewed production won’t likely ship until May or June. Other facilities have been hired to produce the vaccine but aren’t running yet or haven’t received regulatory approval to ship doses for packaging.
Jake Sargent, a spokesman for Johnson & Johnson, told the Times that the company is “focused on ensuring our vaccine is available where people are in need” and that its global production network “is working day and night.” He said that the company has millions of doses in inventory and is continuing to deliver vaccine batches to facilities that package doses.
The pause has surprised officials at two main recipients of the Johnson & Johnson shots -- the African Union and Covax, the organization that coordinates COVID-19 vaccines for poorer countries. Leaders of the two organizations learned about the halt in production from reporters at the Times.
“This is not the time to be switching production lines of anything, when the lives of people across the developing world hang in the balance,” Ayoade Alakija, coleader of the African Union’s vaccine delivery program, told the newspaper.
Poorer countries rely on Johnson & Johnson’s vaccine because it doesn’t require ultracold refrigeration. The vaccine is also less expensive than others and easy to provide to hard-to-reach populations.
“In many low- and middle-income countries, our vaccine is the most important and sometimes only option,” Penny Heaton, MD, a Johnson & Johnson executive, said in December during a meeting with the CDC’s vaccine advisory committee.
“We have a global vaccine, and the world is depending on us,” she said.
A version of this article first appeared on WebMD.com.
Johnson & Johnson stopped making its COVID-19 vaccine at a key facility in the Netherlands.
The Johnson & Johnson shot is seen as a critical vaccine for poorer countries. , people familiar with the decision told The New York Times.
The plant, located in Leiden, has been making an experimental but potentially more profitable vaccine instead. The experimental vaccine is for an unrelated virus -- respiratory syncytial virus, or RSV -- that will be used for a clinical trial.
The pause is said to be temporary. The Leiden plant is expected to restart production of the COVID-19 vaccine next month. The company has said that it has millions of COVID-19 doses in inventory, though it’s unclear whether the pause has affected vaccine supplies.
The interruption could reduce the supply of Johnson & Johnson’s COVID-19 vaccine by a few hundred million doses, one of the sources told the newspaper, since the doses made from renewed production won’t likely ship until May or June. Other facilities have been hired to produce the vaccine but aren’t running yet or haven’t received regulatory approval to ship doses for packaging.
Jake Sargent, a spokesman for Johnson & Johnson, told the Times that the company is “focused on ensuring our vaccine is available where people are in need” and that its global production network “is working day and night.” He said that the company has millions of doses in inventory and is continuing to deliver vaccine batches to facilities that package doses.
The pause has surprised officials at two main recipients of the Johnson & Johnson shots -- the African Union and Covax, the organization that coordinates COVID-19 vaccines for poorer countries. Leaders of the two organizations learned about the halt in production from reporters at the Times.
“This is not the time to be switching production lines of anything, when the lives of people across the developing world hang in the balance,” Ayoade Alakija, coleader of the African Union’s vaccine delivery program, told the newspaper.
Poorer countries rely on Johnson & Johnson’s vaccine because it doesn’t require ultracold refrigeration. The vaccine is also less expensive than others and easy to provide to hard-to-reach populations.
“In many low- and middle-income countries, our vaccine is the most important and sometimes only option,” Penny Heaton, MD, a Johnson & Johnson executive, said in December during a meeting with the CDC’s vaccine advisory committee.
“We have a global vaccine, and the world is depending on us,” she said.
A version of this article first appeared on WebMD.com.
Chronic truncal rash
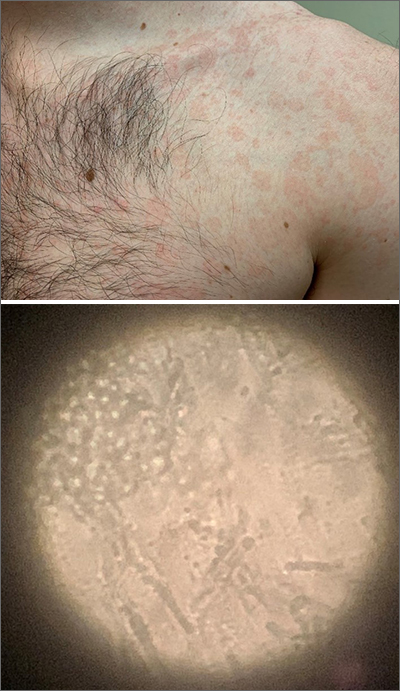
The patient was given a diagnosis of tinea versicolor (TV), also known as pityriasis versicolor, after a potassium hydroxide (KOH) prep test on a skin scraping confirmed the spaghetti and meatballs pattern of Malassezia Furfur (see image above). Note that in most cases, a KOH prep is not required for the diagnosis. Experienced clinicians will usually make the diagnosis based on the appearance of hyper- or hypopigmented macules or patches with fine scale on the trunk of adults. KOH prep is useful if the diagnosis is uncertain.
TV is a common fungal infection that’s seen more frequently in tropical climates and occurs equally in men and women.1 M. Furfur thrives on the lipids in the skin of sebum-rich areas, which explains its truncal distribution and rare occurrence in children (who have much lower sebum production).
Usually, topical antifungal medications are considered first-line treatment, but since large areas of skin are involved, adequate amounts need to be used. One of the most common and inexpensive treatments is to apply selenium sulfide shampoo (Selsun Blue) undiluted to the entire trunk, then allow to dry and remain in place overnight before showering. A repeat application should be done 1 week later. Topical terbinafine cream applied bid for 2 weeks is another option, as is oral itraconazole in a single 400 mg dose.
This patient declined the selenium sulfide topical treatment and requested systemic therapy, so he was prescribed itraconazole 400 mg orally as a single dose. He was advised that it might take a few weeks to clear up, and to use the selenium sulfide application if the itraconazole was not effective. Follow-up was not planned due to the high success rate of these therapies.
Image courtesy of Daniel Stulberg, MD. Text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Saunte DML, Gaitanis G, Hay RJ. Malassezia-associated skin diseases, the use of diagnostics and treatment. Front Cell Infect Microbiol. 2020;10:112. doi: 10.3389/fcimb.2020.00112
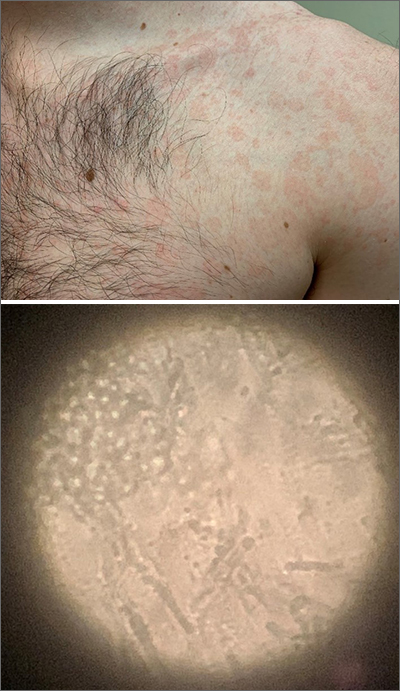
The patient was given a diagnosis of tinea versicolor (TV), also known as pityriasis versicolor, after a potassium hydroxide (KOH) prep test on a skin scraping confirmed the spaghetti and meatballs pattern of Malassezia Furfur (see image above). Note that in most cases, a KOH prep is not required for the diagnosis. Experienced clinicians will usually make the diagnosis based on the appearance of hyper- or hypopigmented macules or patches with fine scale on the trunk of adults. KOH prep is useful if the diagnosis is uncertain.
TV is a common fungal infection that’s seen more frequently in tropical climates and occurs equally in men and women.1 M. Furfur thrives on the lipids in the skin of sebum-rich areas, which explains its truncal distribution and rare occurrence in children (who have much lower sebum production).
Usually, topical antifungal medications are considered first-line treatment, but since large areas of skin are involved, adequate amounts need to be used. One of the most common and inexpensive treatments is to apply selenium sulfide shampoo (Selsun Blue) undiluted to the entire trunk, then allow to dry and remain in place overnight before showering. A repeat application should be done 1 week later. Topical terbinafine cream applied bid for 2 weeks is another option, as is oral itraconazole in a single 400 mg dose.
This patient declined the selenium sulfide topical treatment and requested systemic therapy, so he was prescribed itraconazole 400 mg orally as a single dose. He was advised that it might take a few weeks to clear up, and to use the selenium sulfide application if the itraconazole was not effective. Follow-up was not planned due to the high success rate of these therapies.
Image courtesy of Daniel Stulberg, MD. Text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
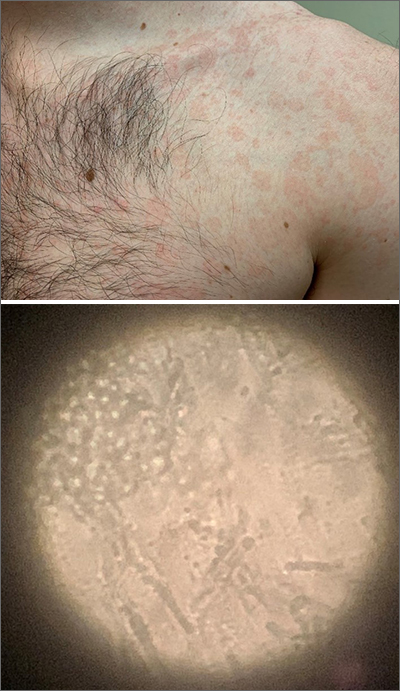
The patient was given a diagnosis of tinea versicolor (TV), also known as pityriasis versicolor, after a potassium hydroxide (KOH) prep test on a skin scraping confirmed the spaghetti and meatballs pattern of Malassezia Furfur (see image above). Note that in most cases, a KOH prep is not required for the diagnosis. Experienced clinicians will usually make the diagnosis based on the appearance of hyper- or hypopigmented macules or patches with fine scale on the trunk of adults. KOH prep is useful if the diagnosis is uncertain.
TV is a common fungal infection that’s seen more frequently in tropical climates and occurs equally in men and women.1 M. Furfur thrives on the lipids in the skin of sebum-rich areas, which explains its truncal distribution and rare occurrence in children (who have much lower sebum production).
Usually, topical antifungal medications are considered first-line treatment, but since large areas of skin are involved, adequate amounts need to be used. One of the most common and inexpensive treatments is to apply selenium sulfide shampoo (Selsun Blue) undiluted to the entire trunk, then allow to dry and remain in place overnight before showering. A repeat application should be done 1 week later. Topical terbinafine cream applied bid for 2 weeks is another option, as is oral itraconazole in a single 400 mg dose.
This patient declined the selenium sulfide topical treatment and requested systemic therapy, so he was prescribed itraconazole 400 mg orally as a single dose. He was advised that it might take a few weeks to clear up, and to use the selenium sulfide application if the itraconazole was not effective. Follow-up was not planned due to the high success rate of these therapies.
Image courtesy of Daniel Stulberg, MD. Text courtesy of Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, University of New Mexico School of Medicine, Albuquerque.
1. Saunte DML, Gaitanis G, Hay RJ. Malassezia-associated skin diseases, the use of diagnostics and treatment. Front Cell Infect Microbiol. 2020;10:112. doi: 10.3389/fcimb.2020.00112
1. Saunte DML, Gaitanis G, Hay RJ. Malassezia-associated skin diseases, the use of diagnostics and treatment. Front Cell Infect Microbiol. 2020;10:112. doi: 10.3389/fcimb.2020.00112
Expert shares workup pearls for children with severe atopic dermatitis
“Many patients who have failed topical steroids have never had adequate treatment,” Anna Yasmine Kirkorian, MD, chief of dermatology at National Children’s Hospital in Washington, said during the ODAC Dermatology, Aesthetic & Surgical Conference. “There is no lower age limit on the use of topical corticosteroids, and low potency corticosteroids are inadequate to treat severe eczema. The idea that only over-the-counter 2.5% hydrocortisone cream is necessary is not true,” she added.
“You also want to scrutinize the vehicle,” she said, noting that children are often prescribed cream formulations that hurt when applied, so parents stop applying them. “Ointments are generally the vehicles of choice in childhood,” she added.
It is generally not advised to use topical and oral antibiotics in children with AD, unless there are clear signs of infection. “If they’re just slightly oozy, don’t use them,” she continued. “Of course, every child or adult with eczema has Staph aureus on them, but most of the time, what you need to do is repair the barrier. We know that from data and common sense. When we repair their barrier, their rates of infection decrease.”
A focal area with pustules and pus should be cultured and treated, Dr. Kirkorian said. “Monotherapy with antibiotics is going to do nothing for you.” In cases of children with failure to thrive, she recommends referral to pediatric dermatology, allergy/immunology, GI, or genetics, as appropriate.
For children with severe AD, Dr. Kirkorian favors a rescue plan with a one-pound jar of triamcinolone ointment 0.1%. She recommends application of the ointment to all areas, including the face and scalp once nightly for 2 weeks, with a follow-up appointment at the end of that time. “If you just give people medicine and ask them to come back in 6 months, they are not able to comply with that and they don’t have faith that it’s going to work,” explained Dr. Kirkorian, associate professor of dermatology and pediatrics at George Washington University, Washington. At the end of 2 weeks, “the majority will have improved dramatically, and then you can implement maintenance therapy with topical calcineurin inhibitors, crisaborole, or possibly topical ruxolitinib.”
Some clinicians prescribe oral antihistamines for AD, but Dr. Kirkorian said that data supporting their use are limited and antihistamines are not approved for use in children younger than 6 months of age. Sedating antihistamines will induce sleep, “but do not provide durable night-long sleep,” and routine use may have an impact on learning and school performance. In addition, exposure to antihistamines in children under age 2 may be associated with development of ADHD at school age.
The interleukin-4 receptor alpha antagonist dupilumab (Dupixent) is approved by the Food and Drug Administration for moderate to severe AD in patients ages 6 and older. But obtaining it for patients can be tricky, she said, as this requires documented failure of corticosteroids, calcineurin inhibitors, crisaborole ointment, and phototherapy (if prescribed). Patients are often obligated to do step therapy with an off-label drug such as cyclosporine or methotrexate for 3 months, and they need to demonstrate responses with objective measures of severity such as the SCORAD (SCORing Atopic Dermatitis) and the validated Investigator Global Assessment.
“Most of my patients carry insurance that does not approve dupilumab without failure of a prior off-label systemic immunosuppressant medication,” Dr. Kirkorian said. Cyclosporine is her first choice for a systemic immunosuppressant “because it has a fast onset of action, it’s effective for treatment of atopic dermatitis, and safe for short-term use,” she said. “I don’t think that methotrexate works well for eczema. It can take weeks and weeks to work.”
She typically starts patients on a 5 mg/kg dose of cyclosporine. Baseline tests include CBC, CMP (comprehensive metabolic panel), lipids, and vitals. She repeats the labs at 1 month, and includes a blood pressure check. Potential adverse effects of cyclosporine include infections (including opportunistic infections), cytopenias, hypertension, nephrotoxicity, hepatotoxicity, neurotoxicity (including posterior reversible encephalopathy syndrome), electrolyte disturbance, lymphoma, and cutaneous malignancy.
“The good news is that we generally don’t see the adverse effects with short-term use,” Dr. Kirkorian said. “We will see some hypertrichosis and gingival hypertrophy, which resolves with cessation of therapy. There are serious side effects if you use it for long enough.”
As for methotrexate, “it is still a very important drug in pediatric dermatology, particularly in other conditions such as psoriasis,” she said. “The problem is that weekly dosing of methotrexate poses a greater risk of dosing errors. People aren’t really triggered to think of a once-weekly medication. If you do use it, give them a short supply to make sure that they come back, and that they don’t give it daily accidentally.”
Practical tips she offered for prescribing cyclosporine include supplying a patient handout with information on all adverse effects, dosing information, vaccination information, and pregnancy precautions, with contact information (a patient portal or on-call number) for the treating clinician in case a patient develops adverse effects. Administration of live vaccines while patients are on cyclosporine is not recommended.
When transitioning patients from cyclosporine or methotrexate to dupilumab, Dr. Kirkorian recommends tapering the immunosuppressant dose by half every 2 weeks to complete cessation by week 8 of treatment. For patients who experience a severe baseline flare once the immunosuppressant is tapered, despite the switch to dupilumab, she recommends restarting methotrexate at a full dose and then reducing the dose every 2 weeks until the lowest effective dose (2.5-5 mg weekly) is reached.
“Waning efficacy is real,” she said. “We can add methotrexate to recapture efficacy. Check for superimposed allergic contact dermatitis.”
With upadacitinib (Rinvoq), an oral Janus kinase (JAK) inhibitor recently approved for treating refractory, moderate to severe AD in patients 12 years of age and older, is the risk profile acceptable to parents and physicians? “I think the answer is yes,” Dr. Kirkorian said. “But we’re going to have to think through that very carefully. It’s going to be exciting to see how this drug changes management in our patients.”
Dr. Kirkorian disclosed that she is a member of the advisory board for Verrica Pharmaceuticals.
“Many patients who have failed topical steroids have never had adequate treatment,” Anna Yasmine Kirkorian, MD, chief of dermatology at National Children’s Hospital in Washington, said during the ODAC Dermatology, Aesthetic & Surgical Conference. “There is no lower age limit on the use of topical corticosteroids, and low potency corticosteroids are inadequate to treat severe eczema. The idea that only over-the-counter 2.5% hydrocortisone cream is necessary is not true,” she added.
“You also want to scrutinize the vehicle,” she said, noting that children are often prescribed cream formulations that hurt when applied, so parents stop applying them. “Ointments are generally the vehicles of choice in childhood,” she added.
It is generally not advised to use topical and oral antibiotics in children with AD, unless there are clear signs of infection. “If they’re just slightly oozy, don’t use them,” she continued. “Of course, every child or adult with eczema has Staph aureus on them, but most of the time, what you need to do is repair the barrier. We know that from data and common sense. When we repair their barrier, their rates of infection decrease.”
A focal area with pustules and pus should be cultured and treated, Dr. Kirkorian said. “Monotherapy with antibiotics is going to do nothing for you.” In cases of children with failure to thrive, she recommends referral to pediatric dermatology, allergy/immunology, GI, or genetics, as appropriate.
For children with severe AD, Dr. Kirkorian favors a rescue plan with a one-pound jar of triamcinolone ointment 0.1%. She recommends application of the ointment to all areas, including the face and scalp once nightly for 2 weeks, with a follow-up appointment at the end of that time. “If you just give people medicine and ask them to come back in 6 months, they are not able to comply with that and they don’t have faith that it’s going to work,” explained Dr. Kirkorian, associate professor of dermatology and pediatrics at George Washington University, Washington. At the end of 2 weeks, “the majority will have improved dramatically, and then you can implement maintenance therapy with topical calcineurin inhibitors, crisaborole, or possibly topical ruxolitinib.”
Some clinicians prescribe oral antihistamines for AD, but Dr. Kirkorian said that data supporting their use are limited and antihistamines are not approved for use in children younger than 6 months of age. Sedating antihistamines will induce sleep, “but do not provide durable night-long sleep,” and routine use may have an impact on learning and school performance. In addition, exposure to antihistamines in children under age 2 may be associated with development of ADHD at school age.
The interleukin-4 receptor alpha antagonist dupilumab (Dupixent) is approved by the Food and Drug Administration for moderate to severe AD in patients ages 6 and older. But obtaining it for patients can be tricky, she said, as this requires documented failure of corticosteroids, calcineurin inhibitors, crisaborole ointment, and phototherapy (if prescribed). Patients are often obligated to do step therapy with an off-label drug such as cyclosporine or methotrexate for 3 months, and they need to demonstrate responses with objective measures of severity such as the SCORAD (SCORing Atopic Dermatitis) and the validated Investigator Global Assessment.
“Most of my patients carry insurance that does not approve dupilumab without failure of a prior off-label systemic immunosuppressant medication,” Dr. Kirkorian said. Cyclosporine is her first choice for a systemic immunosuppressant “because it has a fast onset of action, it’s effective for treatment of atopic dermatitis, and safe for short-term use,” she said. “I don’t think that methotrexate works well for eczema. It can take weeks and weeks to work.”
She typically starts patients on a 5 mg/kg dose of cyclosporine. Baseline tests include CBC, CMP (comprehensive metabolic panel), lipids, and vitals. She repeats the labs at 1 month, and includes a blood pressure check. Potential adverse effects of cyclosporine include infections (including opportunistic infections), cytopenias, hypertension, nephrotoxicity, hepatotoxicity, neurotoxicity (including posterior reversible encephalopathy syndrome), electrolyte disturbance, lymphoma, and cutaneous malignancy.
“The good news is that we generally don’t see the adverse effects with short-term use,” Dr. Kirkorian said. “We will see some hypertrichosis and gingival hypertrophy, which resolves with cessation of therapy. There are serious side effects if you use it for long enough.”
As for methotrexate, “it is still a very important drug in pediatric dermatology, particularly in other conditions such as psoriasis,” she said. “The problem is that weekly dosing of methotrexate poses a greater risk of dosing errors. People aren’t really triggered to think of a once-weekly medication. If you do use it, give them a short supply to make sure that they come back, and that they don’t give it daily accidentally.”
Practical tips she offered for prescribing cyclosporine include supplying a patient handout with information on all adverse effects, dosing information, vaccination information, and pregnancy precautions, with contact information (a patient portal or on-call number) for the treating clinician in case a patient develops adverse effects. Administration of live vaccines while patients are on cyclosporine is not recommended.
When transitioning patients from cyclosporine or methotrexate to dupilumab, Dr. Kirkorian recommends tapering the immunosuppressant dose by half every 2 weeks to complete cessation by week 8 of treatment. For patients who experience a severe baseline flare once the immunosuppressant is tapered, despite the switch to dupilumab, she recommends restarting methotrexate at a full dose and then reducing the dose every 2 weeks until the lowest effective dose (2.5-5 mg weekly) is reached.
“Waning efficacy is real,” she said. “We can add methotrexate to recapture efficacy. Check for superimposed allergic contact dermatitis.”
With upadacitinib (Rinvoq), an oral Janus kinase (JAK) inhibitor recently approved for treating refractory, moderate to severe AD in patients 12 years of age and older, is the risk profile acceptable to parents and physicians? “I think the answer is yes,” Dr. Kirkorian said. “But we’re going to have to think through that very carefully. It’s going to be exciting to see how this drug changes management in our patients.”
Dr. Kirkorian disclosed that she is a member of the advisory board for Verrica Pharmaceuticals.
“Many patients who have failed topical steroids have never had adequate treatment,” Anna Yasmine Kirkorian, MD, chief of dermatology at National Children’s Hospital in Washington, said during the ODAC Dermatology, Aesthetic & Surgical Conference. “There is no lower age limit on the use of topical corticosteroids, and low potency corticosteroids are inadequate to treat severe eczema. The idea that only over-the-counter 2.5% hydrocortisone cream is necessary is not true,” she added.
“You also want to scrutinize the vehicle,” she said, noting that children are often prescribed cream formulations that hurt when applied, so parents stop applying them. “Ointments are generally the vehicles of choice in childhood,” she added.
It is generally not advised to use topical and oral antibiotics in children with AD, unless there are clear signs of infection. “If they’re just slightly oozy, don’t use them,” she continued. “Of course, every child or adult with eczema has Staph aureus on them, but most of the time, what you need to do is repair the barrier. We know that from data and common sense. When we repair their barrier, their rates of infection decrease.”
A focal area with pustules and pus should be cultured and treated, Dr. Kirkorian said. “Monotherapy with antibiotics is going to do nothing for you.” In cases of children with failure to thrive, she recommends referral to pediatric dermatology, allergy/immunology, GI, or genetics, as appropriate.
For children with severe AD, Dr. Kirkorian favors a rescue plan with a one-pound jar of triamcinolone ointment 0.1%. She recommends application of the ointment to all areas, including the face and scalp once nightly for 2 weeks, with a follow-up appointment at the end of that time. “If you just give people medicine and ask them to come back in 6 months, they are not able to comply with that and they don’t have faith that it’s going to work,” explained Dr. Kirkorian, associate professor of dermatology and pediatrics at George Washington University, Washington. At the end of 2 weeks, “the majority will have improved dramatically, and then you can implement maintenance therapy with topical calcineurin inhibitors, crisaborole, or possibly topical ruxolitinib.”
Some clinicians prescribe oral antihistamines for AD, but Dr. Kirkorian said that data supporting their use are limited and antihistamines are not approved for use in children younger than 6 months of age. Sedating antihistamines will induce sleep, “but do not provide durable night-long sleep,” and routine use may have an impact on learning and school performance. In addition, exposure to antihistamines in children under age 2 may be associated with development of ADHD at school age.
The interleukin-4 receptor alpha antagonist dupilumab (Dupixent) is approved by the Food and Drug Administration for moderate to severe AD in patients ages 6 and older. But obtaining it for patients can be tricky, she said, as this requires documented failure of corticosteroids, calcineurin inhibitors, crisaborole ointment, and phototherapy (if prescribed). Patients are often obligated to do step therapy with an off-label drug such as cyclosporine or methotrexate for 3 months, and they need to demonstrate responses with objective measures of severity such as the SCORAD (SCORing Atopic Dermatitis) and the validated Investigator Global Assessment.
“Most of my patients carry insurance that does not approve dupilumab without failure of a prior off-label systemic immunosuppressant medication,” Dr. Kirkorian said. Cyclosporine is her first choice for a systemic immunosuppressant “because it has a fast onset of action, it’s effective for treatment of atopic dermatitis, and safe for short-term use,” she said. “I don’t think that methotrexate works well for eczema. It can take weeks and weeks to work.”
She typically starts patients on a 5 mg/kg dose of cyclosporine. Baseline tests include CBC, CMP (comprehensive metabolic panel), lipids, and vitals. She repeats the labs at 1 month, and includes a blood pressure check. Potential adverse effects of cyclosporine include infections (including opportunistic infections), cytopenias, hypertension, nephrotoxicity, hepatotoxicity, neurotoxicity (including posterior reversible encephalopathy syndrome), electrolyte disturbance, lymphoma, and cutaneous malignancy.
“The good news is that we generally don’t see the adverse effects with short-term use,” Dr. Kirkorian said. “We will see some hypertrichosis and gingival hypertrophy, which resolves with cessation of therapy. There are serious side effects if you use it for long enough.”
As for methotrexate, “it is still a very important drug in pediatric dermatology, particularly in other conditions such as psoriasis,” she said. “The problem is that weekly dosing of methotrexate poses a greater risk of dosing errors. People aren’t really triggered to think of a once-weekly medication. If you do use it, give them a short supply to make sure that they come back, and that they don’t give it daily accidentally.”
Practical tips she offered for prescribing cyclosporine include supplying a patient handout with information on all adverse effects, dosing information, vaccination information, and pregnancy precautions, with contact information (a patient portal or on-call number) for the treating clinician in case a patient develops adverse effects. Administration of live vaccines while patients are on cyclosporine is not recommended.
When transitioning patients from cyclosporine or methotrexate to dupilumab, Dr. Kirkorian recommends tapering the immunosuppressant dose by half every 2 weeks to complete cessation by week 8 of treatment. For patients who experience a severe baseline flare once the immunosuppressant is tapered, despite the switch to dupilumab, she recommends restarting methotrexate at a full dose and then reducing the dose every 2 weeks until the lowest effective dose (2.5-5 mg weekly) is reached.
“Waning efficacy is real,” she said. “We can add methotrexate to recapture efficacy. Check for superimposed allergic contact dermatitis.”
With upadacitinib (Rinvoq), an oral Janus kinase (JAK) inhibitor recently approved for treating refractory, moderate to severe AD in patients 12 years of age and older, is the risk profile acceptable to parents and physicians? “I think the answer is yes,” Dr. Kirkorian said. “But we’re going to have to think through that very carefully. It’s going to be exciting to see how this drug changes management in our patients.”
Dr. Kirkorian disclosed that she is a member of the advisory board for Verrica Pharmaceuticals.
FROM ODAC 2022
Agreement reached for research definition of ‘long COVID’ in children and young people
Long COVID can affect adults, young people, and children, and now for the first time, in a landmark study accepted for publication in the Archives of Disease in Childhood, formal agreement has been made on a research definition for post–acute COVID-19, or “long COVID” as it is commonly known, in children and young people.
The researchers charged themselves with a single objective – to derive a research definition for long COVID (post–acute COVID-19) in children and young people to allow comparisons between research studies. Specifically, so studies on prevalence, course, and outcome of long COVID in this age group can be reliably compared, because to date there has been no consensus. In fact, the authors pointed out how the “slew of definitions” currently used all differ in number, type, and duration of symptoms, which hampers research efforts. In addition, the lack of definition consensus has contributed to very wide reported variations in the estimated prevalence of long COVID in children of 1%-51%, with the authors saying that a “consistently applied definition of long COVID will help reduce the variability of prevalence estimates.”
Statements sequentially whittled down
“Using robust consensus methodology,” the authors said, “we derived a research definition for long COVID in children and young people.”
To achieve the definition consensus, a three-phase online Delphi process was used, followed by a virtual consensus meeting. The 123 participants registered to take part in the study included 23 people (19%) in a lived experience panel, 50 (42%) in the researcher or researcher/service delivery combined panel and 47 (39%) in the service delivery panel. Of 120 registered participants, 105 (88%) completed phase 1, 86 eligible participants (82% of those completing phase 1) completed phase 2 and 77 eligible participants (90% of those completing phase 2) completed phase 3. Seventeen participants attended and voted at the consensus meeting – 4 (23%) from the service delivery panel, 11 (65%) from the researcher panel, and 2 (12%) from the lived experience panel.
Presented with 49 statements in each phase, participants scored these from 1-9 based on how important they were perceived to be with regards inclusion in the research definition of long COVID in children and young people. Having been sequentially whittled down in three phases, 10 statements were discussed at the consensus meeting, and a panel of eight 11- to 17-year-olds affected by long COVID also reviewed the statements to reach a final agreement.
Five of the statements were agreed to be included in the definition, which stated that long COVID in children and young people is a condition in which a child or young person has symptoms (at least one of which is a physical symptom) that have continued or developed after a diagnosis of COVID-19 (confirmed with one or more positive COVID tests); impact their physical, mental, or social well-being; are interfering with some aspect of daily living (for example, school, work, home, or relationships); and persist for a minimum duration of 12 weeks after initial testing for COVID-19 (even if symptoms have waxed and waned over that period).
David Strain, MBChB, MD, chair of the BMA board of science and clinical senior lecturer and honorary consultant, University of Exeter (England), told the Science Media Centre: “A Delphi study builds a consensus from the world’s experts by presenting a series of statements and continuing to refine them until there is agreement as to what the definition of pediatric long COVID should be.” He added: “This is vitally important in order to align the global research effort into long COVID.”
Reassuringly similar
From the agreed five statements, a further research definition was proposed to align with the World Health Organization definition for adults: “Post–COVID-19 condition occurs in young people with a history of confirmed SARS CoV-2 infection, with at least one persisting physical symptom for a minimum duration of 12 weeks after initial testing that cannot be explained by an alternative diagnosis. The symptoms have an impact on everyday functioning, may continue or develop after COVID-19 infection, and may fluctuate or relapse over time.”
The authors concluded: “This is the first research definition of long COVID (post–COVID-19 condition) in children and young people and complements the clinical case definition in adults proposed by WHO,” adding that the two definitions are “reassuringly similar.”
They reiterated how widespread adoption of this definition would allow comparisons between studies such that a core outcome set can be developed and the prevalence, course and outcome of long COVID in children and young people can be reliably evaluated, which “will substantially help strengthen the evidence base on this debilitating condition.”
In addition, the authors said that a consistently applied definition of long COVID will help to provide a “more accurate picture on the true impact of the condition.”
The researchers emphasized the need to differentiate between a clinical case definition and a research definition of long COVID and explained: “It is understandable that the patient groups representing people with long COVID are concerned about a definition that could restrict access to services that are needed.”
They went on to say that in their view the decision whether a child or young person can see a health care professional, access any support needed, or be referred, investigated, or treated for long COVID should be a “shared decision involving the young person, their carers, and clinicians.”
Dr. Strain reinforced that it was important that the definition was a research one and not a clinical one, pointing out that the 12-week period in the research definition “does not necessarily mean that a child or young person should need to wait 3 months before being offered help or assistance from their health care team, indeed a 3-month delay in offering support to a child or young person, at this vitally important period of their educational development, could have lasting long-term impacts.”
A version of this article first appeared on Medscape.co.uk.
Long COVID can affect adults, young people, and children, and now for the first time, in a landmark study accepted for publication in the Archives of Disease in Childhood, formal agreement has been made on a research definition for post–acute COVID-19, or “long COVID” as it is commonly known, in children and young people.
The researchers charged themselves with a single objective – to derive a research definition for long COVID (post–acute COVID-19) in children and young people to allow comparisons between research studies. Specifically, so studies on prevalence, course, and outcome of long COVID in this age group can be reliably compared, because to date there has been no consensus. In fact, the authors pointed out how the “slew of definitions” currently used all differ in number, type, and duration of symptoms, which hampers research efforts. In addition, the lack of definition consensus has contributed to very wide reported variations in the estimated prevalence of long COVID in children of 1%-51%, with the authors saying that a “consistently applied definition of long COVID will help reduce the variability of prevalence estimates.”
Statements sequentially whittled down
“Using robust consensus methodology,” the authors said, “we derived a research definition for long COVID in children and young people.”
To achieve the definition consensus, a three-phase online Delphi process was used, followed by a virtual consensus meeting. The 123 participants registered to take part in the study included 23 people (19%) in a lived experience panel, 50 (42%) in the researcher or researcher/service delivery combined panel and 47 (39%) in the service delivery panel. Of 120 registered participants, 105 (88%) completed phase 1, 86 eligible participants (82% of those completing phase 1) completed phase 2 and 77 eligible participants (90% of those completing phase 2) completed phase 3. Seventeen participants attended and voted at the consensus meeting – 4 (23%) from the service delivery panel, 11 (65%) from the researcher panel, and 2 (12%) from the lived experience panel.
Presented with 49 statements in each phase, participants scored these from 1-9 based on how important they were perceived to be with regards inclusion in the research definition of long COVID in children and young people. Having been sequentially whittled down in three phases, 10 statements were discussed at the consensus meeting, and a panel of eight 11- to 17-year-olds affected by long COVID also reviewed the statements to reach a final agreement.
Five of the statements were agreed to be included in the definition, which stated that long COVID in children and young people is a condition in which a child or young person has symptoms (at least one of which is a physical symptom) that have continued or developed after a diagnosis of COVID-19 (confirmed with one or more positive COVID tests); impact their physical, mental, or social well-being; are interfering with some aspect of daily living (for example, school, work, home, or relationships); and persist for a minimum duration of 12 weeks after initial testing for COVID-19 (even if symptoms have waxed and waned over that period).
David Strain, MBChB, MD, chair of the BMA board of science and clinical senior lecturer and honorary consultant, University of Exeter (England), told the Science Media Centre: “A Delphi study builds a consensus from the world’s experts by presenting a series of statements and continuing to refine them until there is agreement as to what the definition of pediatric long COVID should be.” He added: “This is vitally important in order to align the global research effort into long COVID.”
Reassuringly similar
From the agreed five statements, a further research definition was proposed to align with the World Health Organization definition for adults: “Post–COVID-19 condition occurs in young people with a history of confirmed SARS CoV-2 infection, with at least one persisting physical symptom for a minimum duration of 12 weeks after initial testing that cannot be explained by an alternative diagnosis. The symptoms have an impact on everyday functioning, may continue or develop after COVID-19 infection, and may fluctuate or relapse over time.”
The authors concluded: “This is the first research definition of long COVID (post–COVID-19 condition) in children and young people and complements the clinical case definition in adults proposed by WHO,” adding that the two definitions are “reassuringly similar.”
They reiterated how widespread adoption of this definition would allow comparisons between studies such that a core outcome set can be developed and the prevalence, course and outcome of long COVID in children and young people can be reliably evaluated, which “will substantially help strengthen the evidence base on this debilitating condition.”
In addition, the authors said that a consistently applied definition of long COVID will help to provide a “more accurate picture on the true impact of the condition.”
The researchers emphasized the need to differentiate between a clinical case definition and a research definition of long COVID and explained: “It is understandable that the patient groups representing people with long COVID are concerned about a definition that could restrict access to services that are needed.”
They went on to say that in their view the decision whether a child or young person can see a health care professional, access any support needed, or be referred, investigated, or treated for long COVID should be a “shared decision involving the young person, their carers, and clinicians.”
Dr. Strain reinforced that it was important that the definition was a research one and not a clinical one, pointing out that the 12-week period in the research definition “does not necessarily mean that a child or young person should need to wait 3 months before being offered help or assistance from their health care team, indeed a 3-month delay in offering support to a child or young person, at this vitally important period of their educational development, could have lasting long-term impacts.”
A version of this article first appeared on Medscape.co.uk.
Long COVID can affect adults, young people, and children, and now for the first time, in a landmark study accepted for publication in the Archives of Disease in Childhood, formal agreement has been made on a research definition for post–acute COVID-19, or “long COVID” as it is commonly known, in children and young people.
The researchers charged themselves with a single objective – to derive a research definition for long COVID (post–acute COVID-19) in children and young people to allow comparisons between research studies. Specifically, so studies on prevalence, course, and outcome of long COVID in this age group can be reliably compared, because to date there has been no consensus. In fact, the authors pointed out how the “slew of definitions” currently used all differ in number, type, and duration of symptoms, which hampers research efforts. In addition, the lack of definition consensus has contributed to very wide reported variations in the estimated prevalence of long COVID in children of 1%-51%, with the authors saying that a “consistently applied definition of long COVID will help reduce the variability of prevalence estimates.”
Statements sequentially whittled down
“Using robust consensus methodology,” the authors said, “we derived a research definition for long COVID in children and young people.”
To achieve the definition consensus, a three-phase online Delphi process was used, followed by a virtual consensus meeting. The 123 participants registered to take part in the study included 23 people (19%) in a lived experience panel, 50 (42%) in the researcher or researcher/service delivery combined panel and 47 (39%) in the service delivery panel. Of 120 registered participants, 105 (88%) completed phase 1, 86 eligible participants (82% of those completing phase 1) completed phase 2 and 77 eligible participants (90% of those completing phase 2) completed phase 3. Seventeen participants attended and voted at the consensus meeting – 4 (23%) from the service delivery panel, 11 (65%) from the researcher panel, and 2 (12%) from the lived experience panel.
Presented with 49 statements in each phase, participants scored these from 1-9 based on how important they were perceived to be with regards inclusion in the research definition of long COVID in children and young people. Having been sequentially whittled down in three phases, 10 statements were discussed at the consensus meeting, and a panel of eight 11- to 17-year-olds affected by long COVID also reviewed the statements to reach a final agreement.
Five of the statements were agreed to be included in the definition, which stated that long COVID in children and young people is a condition in which a child or young person has symptoms (at least one of which is a physical symptom) that have continued or developed after a diagnosis of COVID-19 (confirmed with one or more positive COVID tests); impact their physical, mental, or social well-being; are interfering with some aspect of daily living (for example, school, work, home, or relationships); and persist for a minimum duration of 12 weeks after initial testing for COVID-19 (even if symptoms have waxed and waned over that period).
David Strain, MBChB, MD, chair of the BMA board of science and clinical senior lecturer and honorary consultant, University of Exeter (England), told the Science Media Centre: “A Delphi study builds a consensus from the world’s experts by presenting a series of statements and continuing to refine them until there is agreement as to what the definition of pediatric long COVID should be.” He added: “This is vitally important in order to align the global research effort into long COVID.”
Reassuringly similar
From the agreed five statements, a further research definition was proposed to align with the World Health Organization definition for adults: “Post–COVID-19 condition occurs in young people with a history of confirmed SARS CoV-2 infection, with at least one persisting physical symptom for a minimum duration of 12 weeks after initial testing that cannot be explained by an alternative diagnosis. The symptoms have an impact on everyday functioning, may continue or develop after COVID-19 infection, and may fluctuate or relapse over time.”
The authors concluded: “This is the first research definition of long COVID (post–COVID-19 condition) in children and young people and complements the clinical case definition in adults proposed by WHO,” adding that the two definitions are “reassuringly similar.”
They reiterated how widespread adoption of this definition would allow comparisons between studies such that a core outcome set can be developed and the prevalence, course and outcome of long COVID in children and young people can be reliably evaluated, which “will substantially help strengthen the evidence base on this debilitating condition.”
In addition, the authors said that a consistently applied definition of long COVID will help to provide a “more accurate picture on the true impact of the condition.”
The researchers emphasized the need to differentiate between a clinical case definition and a research definition of long COVID and explained: “It is understandable that the patient groups representing people with long COVID are concerned about a definition that could restrict access to services that are needed.”
They went on to say that in their view the decision whether a child or young person can see a health care professional, access any support needed, or be referred, investigated, or treated for long COVID should be a “shared decision involving the young person, their carers, and clinicians.”
Dr. Strain reinforced that it was important that the definition was a research one and not a clinical one, pointing out that the 12-week period in the research definition “does not necessarily mean that a child or young person should need to wait 3 months before being offered help or assistance from their health care team, indeed a 3-month delay in offering support to a child or young person, at this vitally important period of their educational development, could have lasting long-term impacts.”
A version of this article first appeared on Medscape.co.uk.
FROM THE ARCHIVES OF DISEASE IN CHILDHOOD


