User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
COVID-19 a rare trigger for Guillain-Barré syndrome
Although Guillain-Barré syndrome may rarely follow a recent infection with SARS-CoV-2, a strong relationship of GBS with the novel coronavirus is unlikely, say researchers with the International GBS Outcome Study (IGOS) consortium.
“Our study shows that COVID-19 may precede Guillain-Barré syndrome in rare cases, but the existence of a true association or causal relation still needs to be established,” Bart Jacobs, MD, PhD, department of neurology and immunology, Erasmus Medical Center and University Medical Center, both in Rotterdam, the Netherlands, said in a statement.
The study was published online in the journal Brain.
No uptick in pandemic cases
Since the beginning of the pandemic, there are reports of more than 90 GBS diagnoses following a possible COVID-19 infection. However, it remains unclear whether COVID-19 is another potential infectious trigger or whether the reported cases are coincidental.
To investigate further, Dr. Jacobs and the IGOS consortium reviewed 49 patients (median age, 56 years) with GBS who were added to their ongoing prospective observational cohort study between Jan. 30 and May 30, 2020.
The patients came from China, Denmark, France, Greece, Italy, Japan, the Netherlands, Spain, Switzerland, and the United Kingdom.
Of the 49 GBS patients, 8 (16%) had a confirmed and 3 (6%) had a probable SARS-CoV-2 infection; 15 had possible SARS-CoV-2 infection, 21 had no suspicion of SARS-CoV-2 infection, and 2 were “unclassifiable.”
Of the 11 patients with confirmed/probable SARS-CoV-2 infection, 9 had no serological evidence of any other recent preceding infection known to be associated with GBS.
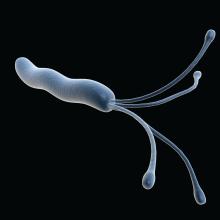
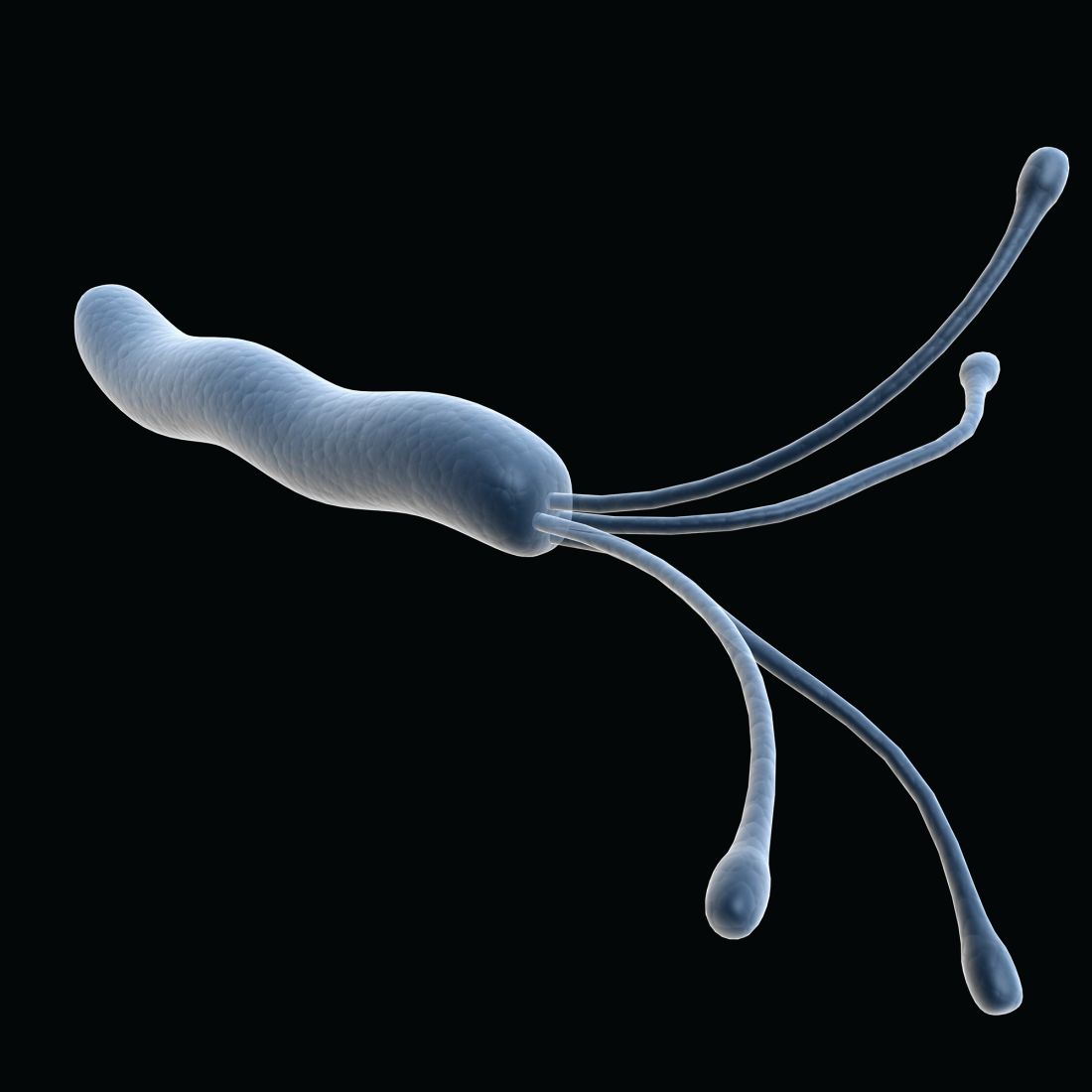
The other two had serological evidence of a recent Campylobacter jejuni infection, which could have played a role in GBS onset, the researchers noted.
Most patients with a confirmed/probable SARS-CoV-2 infection had a sensorimotor GBS variant (73%), although Miller Fisher syndrome–GBS overlap (18%) and an ataxic variant (9%) were also found.
All patients with a confirmed/probable SARS-CoV-2 infection had a severe form of GBS. Common early neurologic features were facial weakness (64%), sensory deficits (82%), and autonomic dysfunction (64%), although not significantly different, compared with the other patients.
All eight patients who underwent nerve conduction study had a demyelinating subtype, which was more frequent than in the other GBS patients (47%; P = .012) as well as historical region and age-matched controls included in the IGOS cohort before the pandemic (52%, P = .016).
The median time from the onset of SARS-CoV-2 infection to neurologic symptoms was 16 days and ranged from 12 to 22 days.
More research needed
The researchers noted that the 22% frequency of a preceding SARS-CoV-2 infection in this study population was “higher than estimates of the contemporaneous background prevalence of SARS-CoV-2, which may be a result of recruitment bias during the pandemic, but could also indicate that GBS may rarely follow a recent SARS-CoV-2 infection.”
Importantly, however, they did not find more patients diagnosed with GBS during the first 4 months of the pandemic, compared with previous years, “suggesting that a strong association between SARS-CoV-2 and GBS is unlikely.”
“Should SARS-CoV-2 indeed be able to trigger GBS, our data are consistent with a postinfectious disease mechanism rather than direct viral invasion,” they noted, adding that the study was not designed to quantify a causative link between GBS and SARS-CoV-2.
“An unbiased multicenter, international, case-control study is needed to determine whether there is an association or not,” they wrote.
The IGOS is financially supported by the GBS-CIDP Foundation International, Gain, Erasmus MC University Medical Center Rotterdam, Glasgow University, CSL Behring, Grifols, Annexon and Hansa Biopharma. Dr. Jacobs received grants from Grifols, CSL-Behring, Annexon, Prinses Beatrix Spierfonds, Hansa Biopharma, and GBS-CIDP Foundation International and is on the global medical advisory board of the GBS CIDP Foundation International.
A version of this article first appeared on Medscape.com.
Although Guillain-Barré syndrome may rarely follow a recent infection with SARS-CoV-2, a strong relationship of GBS with the novel coronavirus is unlikely, say researchers with the International GBS Outcome Study (IGOS) consortium.
“Our study shows that COVID-19 may precede Guillain-Barré syndrome in rare cases, but the existence of a true association or causal relation still needs to be established,” Bart Jacobs, MD, PhD, department of neurology and immunology, Erasmus Medical Center and University Medical Center, both in Rotterdam, the Netherlands, said in a statement.
The study was published online in the journal Brain.
No uptick in pandemic cases
Since the beginning of the pandemic, there are reports of more than 90 GBS diagnoses following a possible COVID-19 infection. However, it remains unclear whether COVID-19 is another potential infectious trigger or whether the reported cases are coincidental.
To investigate further, Dr. Jacobs and the IGOS consortium reviewed 49 patients (median age, 56 years) with GBS who were added to their ongoing prospective observational cohort study between Jan. 30 and May 30, 2020.
The patients came from China, Denmark, France, Greece, Italy, Japan, the Netherlands, Spain, Switzerland, and the United Kingdom.
Of the 49 GBS patients, 8 (16%) had a confirmed and 3 (6%) had a probable SARS-CoV-2 infection; 15 had possible SARS-CoV-2 infection, 21 had no suspicion of SARS-CoV-2 infection, and 2 were “unclassifiable.”
Of the 11 patients with confirmed/probable SARS-CoV-2 infection, 9 had no serological evidence of any other recent preceding infection known to be associated with GBS.
The other two had serological evidence of a recent Campylobacter jejuni infection, which could have played a role in GBS onset, the researchers noted.
Most patients with a confirmed/probable SARS-CoV-2 infection had a sensorimotor GBS variant (73%), although Miller Fisher syndrome–GBS overlap (18%) and an ataxic variant (9%) were also found.
All patients with a confirmed/probable SARS-CoV-2 infection had a severe form of GBS. Common early neurologic features were facial weakness (64%), sensory deficits (82%), and autonomic dysfunction (64%), although not significantly different, compared with the other patients.
All eight patients who underwent nerve conduction study had a demyelinating subtype, which was more frequent than in the other GBS patients (47%; P = .012) as well as historical region and age-matched controls included in the IGOS cohort before the pandemic (52%, P = .016).
The median time from the onset of SARS-CoV-2 infection to neurologic symptoms was 16 days and ranged from 12 to 22 days.
More research needed
The researchers noted that the 22% frequency of a preceding SARS-CoV-2 infection in this study population was “higher than estimates of the contemporaneous background prevalence of SARS-CoV-2, which may be a result of recruitment bias during the pandemic, but could also indicate that GBS may rarely follow a recent SARS-CoV-2 infection.”
Importantly, however, they did not find more patients diagnosed with GBS during the first 4 months of the pandemic, compared with previous years, “suggesting that a strong association between SARS-CoV-2 and GBS is unlikely.”
“Should SARS-CoV-2 indeed be able to trigger GBS, our data are consistent with a postinfectious disease mechanism rather than direct viral invasion,” they noted, adding that the study was not designed to quantify a causative link between GBS and SARS-CoV-2.
“An unbiased multicenter, international, case-control study is needed to determine whether there is an association or not,” they wrote.
The IGOS is financially supported by the GBS-CIDP Foundation International, Gain, Erasmus MC University Medical Center Rotterdam, Glasgow University, CSL Behring, Grifols, Annexon and Hansa Biopharma. Dr. Jacobs received grants from Grifols, CSL-Behring, Annexon, Prinses Beatrix Spierfonds, Hansa Biopharma, and GBS-CIDP Foundation International and is on the global medical advisory board of the GBS CIDP Foundation International.
A version of this article first appeared on Medscape.com.
Although Guillain-Barré syndrome may rarely follow a recent infection with SARS-CoV-2, a strong relationship of GBS with the novel coronavirus is unlikely, say researchers with the International GBS Outcome Study (IGOS) consortium.
“Our study shows that COVID-19 may precede Guillain-Barré syndrome in rare cases, but the existence of a true association or causal relation still needs to be established,” Bart Jacobs, MD, PhD, department of neurology and immunology, Erasmus Medical Center and University Medical Center, both in Rotterdam, the Netherlands, said in a statement.
The study was published online in the journal Brain.
No uptick in pandemic cases
Since the beginning of the pandemic, there are reports of more than 90 GBS diagnoses following a possible COVID-19 infection. However, it remains unclear whether COVID-19 is another potential infectious trigger or whether the reported cases are coincidental.
To investigate further, Dr. Jacobs and the IGOS consortium reviewed 49 patients (median age, 56 years) with GBS who were added to their ongoing prospective observational cohort study between Jan. 30 and May 30, 2020.
The patients came from China, Denmark, France, Greece, Italy, Japan, the Netherlands, Spain, Switzerland, and the United Kingdom.
Of the 49 GBS patients, 8 (16%) had a confirmed and 3 (6%) had a probable SARS-CoV-2 infection; 15 had possible SARS-CoV-2 infection, 21 had no suspicion of SARS-CoV-2 infection, and 2 were “unclassifiable.”
Of the 11 patients with confirmed/probable SARS-CoV-2 infection, 9 had no serological evidence of any other recent preceding infection known to be associated with GBS.
The other two had serological evidence of a recent Campylobacter jejuni infection, which could have played a role in GBS onset, the researchers noted.
Most patients with a confirmed/probable SARS-CoV-2 infection had a sensorimotor GBS variant (73%), although Miller Fisher syndrome–GBS overlap (18%) and an ataxic variant (9%) were also found.
All patients with a confirmed/probable SARS-CoV-2 infection had a severe form of GBS. Common early neurologic features were facial weakness (64%), sensory deficits (82%), and autonomic dysfunction (64%), although not significantly different, compared with the other patients.
All eight patients who underwent nerve conduction study had a demyelinating subtype, which was more frequent than in the other GBS patients (47%; P = .012) as well as historical region and age-matched controls included in the IGOS cohort before the pandemic (52%, P = .016).
The median time from the onset of SARS-CoV-2 infection to neurologic symptoms was 16 days and ranged from 12 to 22 days.
More research needed
The researchers noted that the 22% frequency of a preceding SARS-CoV-2 infection in this study population was “higher than estimates of the contemporaneous background prevalence of SARS-CoV-2, which may be a result of recruitment bias during the pandemic, but could also indicate that GBS may rarely follow a recent SARS-CoV-2 infection.”
Importantly, however, they did not find more patients diagnosed with GBS during the first 4 months of the pandemic, compared with previous years, “suggesting that a strong association between SARS-CoV-2 and GBS is unlikely.”
“Should SARS-CoV-2 indeed be able to trigger GBS, our data are consistent with a postinfectious disease mechanism rather than direct viral invasion,” they noted, adding that the study was not designed to quantify a causative link between GBS and SARS-CoV-2.
“An unbiased multicenter, international, case-control study is needed to determine whether there is an association or not,” they wrote.
The IGOS is financially supported by the GBS-CIDP Foundation International, Gain, Erasmus MC University Medical Center Rotterdam, Glasgow University, CSL Behring, Grifols, Annexon and Hansa Biopharma. Dr. Jacobs received grants from Grifols, CSL-Behring, Annexon, Prinses Beatrix Spierfonds, Hansa Biopharma, and GBS-CIDP Foundation International and is on the global medical advisory board of the GBS CIDP Foundation International.
A version of this article first appeared on Medscape.com.
CDC chief overrules panel, OKs boosters for health care workers
The CDC’s Advisory Committee on Immunization Practices earlier Thursday voted to allow several groups of Americans to get a booster shot, but voted not to recommend it for adults age 18 to 64 who live or work in a place where the risk of COVID-19 is high. That would have included health care workers and other frontline employees.
But CDC Director Rochelle Walensky, MD, decided to reverse that recommendation and include the 18-to-64-year-olds in her final decision.
“As CDC Director, it is my job to recognize where our actions can have the greatest impact,” Dr. Walensky said in a statement late Thursday night, according to published reports. “At CDC, we are tasked with analyzing complex, often imperfect data to make concrete recommendations that optimize health. In a pandemic, even with uncertainty, we must take actions that we anticipate will do the greatest good.”
Dr. Walensky agreed with the rest of the advisory committee's decisions, which included recommendations that the following groups also be eligible for a booster shot:
- Adults ages 65 and up and residents of long-term care facilities
- Adults ages 50 to 64 who have an underlying medical condition that may increase their risk from a COVID infection
- Adults ages 18 to 49 who may be at increased risk from a COVID-19 infection because of an underlying medical condition, if a person feels like they need one based on a consideration of their individual benefit and risks.
About 26 million Americans are at least 6 months past the last dose of the Pfizer vaccines, making them eligible to receive a third dose. About 13.6 million of them are over the age of 65. Another 5.3 million are ages 50 to 64.
In making the recommendations, the committee left out healthcare workers. This was a departure from the Food and Drug Administration’s authorization which included boosters for those 65 and over, and for people 18 through 64 years of age who are at high risk for severe illness from the coronavirus, including essential workers – such as those in healthcare -- whose jobs increase their risk for infection.
This is the group Dr. Walensky added to the eligible list on her own.
Committee members “did not buy the need in occupational or institutional settings,” said William Schaffner, MD, an infectious disease specialist at Vanderbilt University in Nashville. Dr. Schaffner sits on the ACIP workgroup that considered the evidence behind boosters. He said that he would have voted yes to offer boosters to healthcare and other essential workers.
“There was a real split in the committee,” he said.
The vote on boosters for healthcare and other high-risk workers was rejected 9 to 6.
“I think that there is ample evidence that people such as healthcare workers do not have repeated exposure in the workplace,” said Beth Bell, MD, a clinical professor at the University of Washington. “They’re using PPE as they should and they’re following the other policies within the healthcare setting. There’s lots of evidence that suggest that health care workers who become infected become infected because of exposures in the community.”
She was not alone in feeling cautious.
“I think this is an extremely slippery slope,” said Sarah Long, MD, a pediatric infectious disease specialist at Drexel University in Philadelphia, before her vote to reject boosters for healthcare and other high-risk workers.
“We might as well just say, ‘Give it to everybody 18 and over.’ We have an extremely effective vaccine. It’s like saying it’s not working, and it is working.”
The committee saw data showing that all of the vaccines remain highly protective against hospitalization and death for all age groups, though protection against getting sick with COVID has waned slightly over time and with the dominance of the more contagious Delta variant. Those at highest risk for a severe breakthrough infection — those that cause hospitalization or death — are older adults.
How much will the U.S. benefit from boosters?
Some felt squeamish about broadly recommending boosters at all.
“We have too much hope on the line with these boosters,” said James Loehr, MD, who is a family physician in Ithaca, N.Y. Dr. Loehr said he felt the goal of giving boosters in the United States should be to decrease hospitalizations, and he felt they would, but that the impact would likely be smaller than appreciated.
Based on his calculations of the benefits of boosters for each age group, Dr. Loehr said if boosters were given to all 13 million seniors previously vaccinated with the Pfizer vaccine, we might prevent 200 hospitalizations a day, “which would be a lot,” he noted. But, he said, “considering that we have 10,000 hospitalizations a day now, it’s probably not that much.”
Others agreed.
“I really think this is a solution looking for a problem,” said Jason Goldman, MD, an associate professor at Florida Atlantic University who was representing the American College of Physicians. “You know, I don’t think it’s going to address the issue of the pandemic. I really think it’s just going to create more confusion on the provider from the position of implementation, and I really think it’s going really far afield of the data.”
ACIP Chair Grace Lee, MD, a pediatric infectious disease specialist at Stanford, said she had cared for children who had died of COVID.
“I can tell you that their family members really wished they had extra protection for their kids, because they weren’t symptomatic. Nobody else was sick at home,” she said.
Dr. Lee said for her, access was paramount, and she was in favor of expanding access to boosters for as many people as possible.
Next steps
People who were initially vaccinated with either Moderna or Johnson & Johnson vaccines are excluded from booster recommendations, something many on the committee were uncomfortable with.
The FDA is still considering Moderna’s application to market booster doses. Johnson & Johnson hasn’t yet applied to the FDA for permission to offer second doses in the United States.
While the ACIP’s recommendations are important, in this case, they may not have a huge practical effect, said Schaffner. The CDC has already approved third shots for people who are immunocompromised, and no proof of a medical condition is required to get one.
More than 2 million people have already gotten a third dose, he noted, and not all of them are immunocompromised.
“They have heard the president say that, you know, everybody should get a booster, and they’ve taken that at face value,” he said.
A version of this article first appeared on WebMD.com.
The CDC’s Advisory Committee on Immunization Practices earlier Thursday voted to allow several groups of Americans to get a booster shot, but voted not to recommend it for adults age 18 to 64 who live or work in a place where the risk of COVID-19 is high. That would have included health care workers and other frontline employees.
But CDC Director Rochelle Walensky, MD, decided to reverse that recommendation and include the 18-to-64-year-olds in her final decision.
“As CDC Director, it is my job to recognize where our actions can have the greatest impact,” Dr. Walensky said in a statement late Thursday night, according to published reports. “At CDC, we are tasked with analyzing complex, often imperfect data to make concrete recommendations that optimize health. In a pandemic, even with uncertainty, we must take actions that we anticipate will do the greatest good.”
Dr. Walensky agreed with the rest of the advisory committee's decisions, which included recommendations that the following groups also be eligible for a booster shot:
- Adults ages 65 and up and residents of long-term care facilities
- Adults ages 50 to 64 who have an underlying medical condition that may increase their risk from a COVID infection
- Adults ages 18 to 49 who may be at increased risk from a COVID-19 infection because of an underlying medical condition, if a person feels like they need one based on a consideration of their individual benefit and risks.
About 26 million Americans are at least 6 months past the last dose of the Pfizer vaccines, making them eligible to receive a third dose. About 13.6 million of them are over the age of 65. Another 5.3 million are ages 50 to 64.
In making the recommendations, the committee left out healthcare workers. This was a departure from the Food and Drug Administration’s authorization which included boosters for those 65 and over, and for people 18 through 64 years of age who are at high risk for severe illness from the coronavirus, including essential workers – such as those in healthcare -- whose jobs increase their risk for infection.
This is the group Dr. Walensky added to the eligible list on her own.
Committee members “did not buy the need in occupational or institutional settings,” said William Schaffner, MD, an infectious disease specialist at Vanderbilt University in Nashville. Dr. Schaffner sits on the ACIP workgroup that considered the evidence behind boosters. He said that he would have voted yes to offer boosters to healthcare and other essential workers.
“There was a real split in the committee,” he said.
The vote on boosters for healthcare and other high-risk workers was rejected 9 to 6.
“I think that there is ample evidence that people such as healthcare workers do not have repeated exposure in the workplace,” said Beth Bell, MD, a clinical professor at the University of Washington. “They’re using PPE as they should and they’re following the other policies within the healthcare setting. There’s lots of evidence that suggest that health care workers who become infected become infected because of exposures in the community.”
She was not alone in feeling cautious.
“I think this is an extremely slippery slope,” said Sarah Long, MD, a pediatric infectious disease specialist at Drexel University in Philadelphia, before her vote to reject boosters for healthcare and other high-risk workers.
“We might as well just say, ‘Give it to everybody 18 and over.’ We have an extremely effective vaccine. It’s like saying it’s not working, and it is working.”
The committee saw data showing that all of the vaccines remain highly protective against hospitalization and death for all age groups, though protection against getting sick with COVID has waned slightly over time and with the dominance of the more contagious Delta variant. Those at highest risk for a severe breakthrough infection — those that cause hospitalization or death — are older adults.
How much will the U.S. benefit from boosters?
Some felt squeamish about broadly recommending boosters at all.
“We have too much hope on the line with these boosters,” said James Loehr, MD, who is a family physician in Ithaca, N.Y. Dr. Loehr said he felt the goal of giving boosters in the United States should be to decrease hospitalizations, and he felt they would, but that the impact would likely be smaller than appreciated.
Based on his calculations of the benefits of boosters for each age group, Dr. Loehr said if boosters were given to all 13 million seniors previously vaccinated with the Pfizer vaccine, we might prevent 200 hospitalizations a day, “which would be a lot,” he noted. But, he said, “considering that we have 10,000 hospitalizations a day now, it’s probably not that much.”
Others agreed.
“I really think this is a solution looking for a problem,” said Jason Goldman, MD, an associate professor at Florida Atlantic University who was representing the American College of Physicians. “You know, I don’t think it’s going to address the issue of the pandemic. I really think it’s just going to create more confusion on the provider from the position of implementation, and I really think it’s going really far afield of the data.”
ACIP Chair Grace Lee, MD, a pediatric infectious disease specialist at Stanford, said she had cared for children who had died of COVID.
“I can tell you that their family members really wished they had extra protection for their kids, because they weren’t symptomatic. Nobody else was sick at home,” she said.
Dr. Lee said for her, access was paramount, and she was in favor of expanding access to boosters for as many people as possible.
Next steps
People who were initially vaccinated with either Moderna or Johnson & Johnson vaccines are excluded from booster recommendations, something many on the committee were uncomfortable with.
The FDA is still considering Moderna’s application to market booster doses. Johnson & Johnson hasn’t yet applied to the FDA for permission to offer second doses in the United States.
While the ACIP’s recommendations are important, in this case, they may not have a huge practical effect, said Schaffner. The CDC has already approved third shots for people who are immunocompromised, and no proof of a medical condition is required to get one.
More than 2 million people have already gotten a third dose, he noted, and not all of them are immunocompromised.
“They have heard the president say that, you know, everybody should get a booster, and they’ve taken that at face value,” he said.
A version of this article first appeared on WebMD.com.
The CDC’s Advisory Committee on Immunization Practices earlier Thursday voted to allow several groups of Americans to get a booster shot, but voted not to recommend it for adults age 18 to 64 who live or work in a place where the risk of COVID-19 is high. That would have included health care workers and other frontline employees.
But CDC Director Rochelle Walensky, MD, decided to reverse that recommendation and include the 18-to-64-year-olds in her final decision.
“As CDC Director, it is my job to recognize where our actions can have the greatest impact,” Dr. Walensky said in a statement late Thursday night, according to published reports. “At CDC, we are tasked with analyzing complex, often imperfect data to make concrete recommendations that optimize health. In a pandemic, even with uncertainty, we must take actions that we anticipate will do the greatest good.”
Dr. Walensky agreed with the rest of the advisory committee's decisions, which included recommendations that the following groups also be eligible for a booster shot:
- Adults ages 65 and up and residents of long-term care facilities
- Adults ages 50 to 64 who have an underlying medical condition that may increase their risk from a COVID infection
- Adults ages 18 to 49 who may be at increased risk from a COVID-19 infection because of an underlying medical condition, if a person feels like they need one based on a consideration of their individual benefit and risks.
About 26 million Americans are at least 6 months past the last dose of the Pfizer vaccines, making them eligible to receive a third dose. About 13.6 million of them are over the age of 65. Another 5.3 million are ages 50 to 64.
In making the recommendations, the committee left out healthcare workers. This was a departure from the Food and Drug Administration’s authorization which included boosters for those 65 and over, and for people 18 through 64 years of age who are at high risk for severe illness from the coronavirus, including essential workers – such as those in healthcare -- whose jobs increase their risk for infection.
This is the group Dr. Walensky added to the eligible list on her own.
Committee members “did not buy the need in occupational or institutional settings,” said William Schaffner, MD, an infectious disease specialist at Vanderbilt University in Nashville. Dr. Schaffner sits on the ACIP workgroup that considered the evidence behind boosters. He said that he would have voted yes to offer boosters to healthcare and other essential workers.
“There was a real split in the committee,” he said.
The vote on boosters for healthcare and other high-risk workers was rejected 9 to 6.
“I think that there is ample evidence that people such as healthcare workers do not have repeated exposure in the workplace,” said Beth Bell, MD, a clinical professor at the University of Washington. “They’re using PPE as they should and they’re following the other policies within the healthcare setting. There’s lots of evidence that suggest that health care workers who become infected become infected because of exposures in the community.”
She was not alone in feeling cautious.
“I think this is an extremely slippery slope,” said Sarah Long, MD, a pediatric infectious disease specialist at Drexel University in Philadelphia, before her vote to reject boosters for healthcare and other high-risk workers.
“We might as well just say, ‘Give it to everybody 18 and over.’ We have an extremely effective vaccine. It’s like saying it’s not working, and it is working.”
The committee saw data showing that all of the vaccines remain highly protective against hospitalization and death for all age groups, though protection against getting sick with COVID has waned slightly over time and with the dominance of the more contagious Delta variant. Those at highest risk for a severe breakthrough infection — those that cause hospitalization or death — are older adults.
How much will the U.S. benefit from boosters?
Some felt squeamish about broadly recommending boosters at all.
“We have too much hope on the line with these boosters,” said James Loehr, MD, who is a family physician in Ithaca, N.Y. Dr. Loehr said he felt the goal of giving boosters in the United States should be to decrease hospitalizations, and he felt they would, but that the impact would likely be smaller than appreciated.
Based on his calculations of the benefits of boosters for each age group, Dr. Loehr said if boosters were given to all 13 million seniors previously vaccinated with the Pfizer vaccine, we might prevent 200 hospitalizations a day, “which would be a lot,” he noted. But, he said, “considering that we have 10,000 hospitalizations a day now, it’s probably not that much.”
Others agreed.
“I really think this is a solution looking for a problem,” said Jason Goldman, MD, an associate professor at Florida Atlantic University who was representing the American College of Physicians. “You know, I don’t think it’s going to address the issue of the pandemic. I really think it’s just going to create more confusion on the provider from the position of implementation, and I really think it’s going really far afield of the data.”
ACIP Chair Grace Lee, MD, a pediatric infectious disease specialist at Stanford, said she had cared for children who had died of COVID.
“I can tell you that their family members really wished they had extra protection for their kids, because they weren’t symptomatic. Nobody else was sick at home,” she said.
Dr. Lee said for her, access was paramount, and she was in favor of expanding access to boosters for as many people as possible.
Next steps
People who were initially vaccinated with either Moderna or Johnson & Johnson vaccines are excluded from booster recommendations, something many on the committee were uncomfortable with.
The FDA is still considering Moderna’s application to market booster doses. Johnson & Johnson hasn’t yet applied to the FDA for permission to offer second doses in the United States.
While the ACIP’s recommendations are important, in this case, they may not have a huge practical effect, said Schaffner. The CDC has already approved third shots for people who are immunocompromised, and no proof of a medical condition is required to get one.
More than 2 million people have already gotten a third dose, he noted, and not all of them are immunocompromised.
“They have heard the president say that, you know, everybody should get a booster, and they’ve taken that at face value,” he said.
A version of this article first appeared on WebMD.com.
Long COVID appears to ‘impair’ survival in cancer patients
More than one in six cancer patients experience long-term sequelae following SARS-CoV-2 infection, placing them at increased risk of discontinuing their cancer treatment or dying, according to European registry data.
Given the “high lethality” of COVID-19 in cancer patients and the risk for long-term complications following infection in the general population, Alessio Cortellini, MD, a consultant medical oncologist at Hammersmith Hospital and Imperial College London, and colleagues wanted to explore the “prevalence and clinical significance of COVID-19 sequelae in cancer patients and their oncological continuity of care.”
Dr. Cortellini presented the OnCovid registry research on Sept. 21 at the 2021 European Society for Medical Oncology Congress. He reported that overall, the data suggest that post–COVID-19 complications may “impair” patients’ cancer survival as well as their cancer care.
The OnCovid registry data showed that the 15% of cancer patients who had long-term COVID-19 complications were 76% more likely to die than those without sequelae. Cancer patients with COVID-19 sequelae were significantly more likely to permanently stop taking their systemic anticancer therapy, and they were more than 3.5 times more likely to die than those who continued their treatment as planned. In terms of long-term complications, almost half of patients experienced dyspnea, and two-fifths reported chronic fatigue.
“This data confirms the need to continue to prioritize cancer patients,” Antonio Passaro, MD, PhD, division of thoracic oncology, European Institute of Oncology IRCCS, Milan, commented in a press release. “In the fight against the pandemic, it is of the utmost importance that we do not neglect to study and understand the curves of cancer incidence and mortality.”
Invited to discuss the results, Anne-Marie C. Dingemans, MD, PhD, a pulmonologist and professor of thoracic oncology at Erasmus Medical Center, Rotterdam, the Netherlands, said COVID-19 remains a “very important” issue for cancer patients.
Interestingly, Dr. Dingemans noted that COVID-19 sequelae in patients with cancer appear to occur slightly less frequently, compared with estimates in the general population – which range from 13% to 60% – though patients with cancer tend to have more respiratory problems.
However, Dr. Dingemans added, the difficulty with comparing sequelae rates between cancer patients and the general population is that cancer patients “probably already have a lot of symptoms” associated with long COVID, such as dyspnea and fatigue, and may not be aware that they are experiencing COVID sequelae.
The registry results
To investigate the long-term impact of COVID-19 on survival and continuity of care, the team examined data from the OnCovid registry, which was established at the beginning of the pandemic to study consecutive patients aged 18 years and older with confirmed SARS-CoV-2 infection and a history of solid or hematologic malignancies.
At the data cutoff on March 1, 2021, the registry included 35 institutions in six European countries. The institutions collected information on patient demographics and comorbidities, cancer history, anticancer therapy, COVID-19 investigations, and COVID-19–specific therapies.
For the current analysis, the team included 1,557 of 2,634 patients who had undergone a clinical reassessment after recovering from COVID-19. Information sufficient to conduct multivariate analysis was available for 840 of these patients.
About half of the patients were younger than 60 years, and just over half were women. The most common cancer diagnoses were breast cancer (23.4%), gastrointestinal tumors (16.5%), gynecologic/genitourinary tumors (19.3%), and hematologic cancers (14.1%), with even distribution between local/locoregional and advanced disease.
The median interval between COVID-19 recovery and reassessment was 44 days, and the mean post–COVID-19 follow-up period was 128 days.
About 15% of patients experienced at least one long-term sequela from COVID-19. The most common were dyspnea/shortness of breath (49.6%), fatigue (41.0%), chronic cough (33.8%), and other respiratory complications (10.7%).
Dr. Cortellini noted that cancer patients who experienced sequelae were more likely to be male, aged 65 years or older, to have at least two comorbidities, and to have a history of smoking. In addition, cancer patients who experienced long-term complications were significantly more likely to have had COVID-19 complications, to have required COVID-19 therapy, and to have been hospitalized for the disease.
Factoring in gender, age, comorbidity burden, primary tumor, stage, receipt of anticancer and anti–COVID-19 therapy, COVID-19 complications, and hospitalization, the team found that COVID-19 sequelae were independently associated with an increased risk for death (hazard ratio, 1.76).
Further analysis of patterns of systemic anticancer therapy in 471 patients revealed that 14.8% of COVID-19 survivors permanently discontinued therapy and that a dose or regimen adjustment occurred for 37.8%.
Patients who permanently discontinued anticancer therapy were more likely to be former or current smokers, to have had COVID-19 complications or been hospitalized for COVID-19, and to have had COVID-19 sequelae at reassessment. The investigators found no association between permanent discontinuation of therapy and cancer disease stage.
Dr. Cortellini and colleagues reported that permanent cessation of systemic anticancer therapy was associated with an increased risk for death. A change in dose or regimen did not affect survival.
The most common reason for stopping therapy permanently was deterioration of the patient’s performance status (61.3%), followed by disease progression (29.0%). Dose or regimen adjustments typically occurred to avoid immune suppression (50.0%), hospitalization (25.8%), and intravenous drug administration (19.1%).
Dr. Cortellini concluded his presentation by highlighting the importance of increasing awareness of long COVID in patients with cancer as well as early treatment of COVID-19 sequelae to improve patient outcomes.
The study was funded by the Imperial College Biomedical Research Center. Dr. Cortellini has relationships with MSD, Bristol-Myers Squibb, Roche, Novartis, AstraZeneca, Astellas, and Sun Pharma. Dr. Dingemans has relationships with Roche, Eli Lilly, Boehringer Ingelheim, AstraZeneca, Jansen, Chiesi, Amgen, Pfizer, Bayer, Takeda, Pharmamar, and Sanofi.
A version of this article first appeared on Medscape.com.
More than one in six cancer patients experience long-term sequelae following SARS-CoV-2 infection, placing them at increased risk of discontinuing their cancer treatment or dying, according to European registry data.
Given the “high lethality” of COVID-19 in cancer patients and the risk for long-term complications following infection in the general population, Alessio Cortellini, MD, a consultant medical oncologist at Hammersmith Hospital and Imperial College London, and colleagues wanted to explore the “prevalence and clinical significance of COVID-19 sequelae in cancer patients and their oncological continuity of care.”
Dr. Cortellini presented the OnCovid registry research on Sept. 21 at the 2021 European Society for Medical Oncology Congress. He reported that overall, the data suggest that post–COVID-19 complications may “impair” patients’ cancer survival as well as their cancer care.
The OnCovid registry data showed that the 15% of cancer patients who had long-term COVID-19 complications were 76% more likely to die than those without sequelae. Cancer patients with COVID-19 sequelae were significantly more likely to permanently stop taking their systemic anticancer therapy, and they were more than 3.5 times more likely to die than those who continued their treatment as planned. In terms of long-term complications, almost half of patients experienced dyspnea, and two-fifths reported chronic fatigue.
“This data confirms the need to continue to prioritize cancer patients,” Antonio Passaro, MD, PhD, division of thoracic oncology, European Institute of Oncology IRCCS, Milan, commented in a press release. “In the fight against the pandemic, it is of the utmost importance that we do not neglect to study and understand the curves of cancer incidence and mortality.”
Invited to discuss the results, Anne-Marie C. Dingemans, MD, PhD, a pulmonologist and professor of thoracic oncology at Erasmus Medical Center, Rotterdam, the Netherlands, said COVID-19 remains a “very important” issue for cancer patients.
Interestingly, Dr. Dingemans noted that COVID-19 sequelae in patients with cancer appear to occur slightly less frequently, compared with estimates in the general population – which range from 13% to 60% – though patients with cancer tend to have more respiratory problems.
However, Dr. Dingemans added, the difficulty with comparing sequelae rates between cancer patients and the general population is that cancer patients “probably already have a lot of symptoms” associated with long COVID, such as dyspnea and fatigue, and may not be aware that they are experiencing COVID sequelae.
The registry results
To investigate the long-term impact of COVID-19 on survival and continuity of care, the team examined data from the OnCovid registry, which was established at the beginning of the pandemic to study consecutive patients aged 18 years and older with confirmed SARS-CoV-2 infection and a history of solid or hematologic malignancies.
At the data cutoff on March 1, 2021, the registry included 35 institutions in six European countries. The institutions collected information on patient demographics and comorbidities, cancer history, anticancer therapy, COVID-19 investigations, and COVID-19–specific therapies.
For the current analysis, the team included 1,557 of 2,634 patients who had undergone a clinical reassessment after recovering from COVID-19. Information sufficient to conduct multivariate analysis was available for 840 of these patients.
About half of the patients were younger than 60 years, and just over half were women. The most common cancer diagnoses were breast cancer (23.4%), gastrointestinal tumors (16.5%), gynecologic/genitourinary tumors (19.3%), and hematologic cancers (14.1%), with even distribution between local/locoregional and advanced disease.
The median interval between COVID-19 recovery and reassessment was 44 days, and the mean post–COVID-19 follow-up period was 128 days.
About 15% of patients experienced at least one long-term sequela from COVID-19. The most common were dyspnea/shortness of breath (49.6%), fatigue (41.0%), chronic cough (33.8%), and other respiratory complications (10.7%).
Dr. Cortellini noted that cancer patients who experienced sequelae were more likely to be male, aged 65 years or older, to have at least two comorbidities, and to have a history of smoking. In addition, cancer patients who experienced long-term complications were significantly more likely to have had COVID-19 complications, to have required COVID-19 therapy, and to have been hospitalized for the disease.
Factoring in gender, age, comorbidity burden, primary tumor, stage, receipt of anticancer and anti–COVID-19 therapy, COVID-19 complications, and hospitalization, the team found that COVID-19 sequelae were independently associated with an increased risk for death (hazard ratio, 1.76).
Further analysis of patterns of systemic anticancer therapy in 471 patients revealed that 14.8% of COVID-19 survivors permanently discontinued therapy and that a dose or regimen adjustment occurred for 37.8%.
Patients who permanently discontinued anticancer therapy were more likely to be former or current smokers, to have had COVID-19 complications or been hospitalized for COVID-19, and to have had COVID-19 sequelae at reassessment. The investigators found no association between permanent discontinuation of therapy and cancer disease stage.
Dr. Cortellini and colleagues reported that permanent cessation of systemic anticancer therapy was associated with an increased risk for death. A change in dose or regimen did not affect survival.
The most common reason for stopping therapy permanently was deterioration of the patient’s performance status (61.3%), followed by disease progression (29.0%). Dose or regimen adjustments typically occurred to avoid immune suppression (50.0%), hospitalization (25.8%), and intravenous drug administration (19.1%).
Dr. Cortellini concluded his presentation by highlighting the importance of increasing awareness of long COVID in patients with cancer as well as early treatment of COVID-19 sequelae to improve patient outcomes.
The study was funded by the Imperial College Biomedical Research Center. Dr. Cortellini has relationships with MSD, Bristol-Myers Squibb, Roche, Novartis, AstraZeneca, Astellas, and Sun Pharma. Dr. Dingemans has relationships with Roche, Eli Lilly, Boehringer Ingelheim, AstraZeneca, Jansen, Chiesi, Amgen, Pfizer, Bayer, Takeda, Pharmamar, and Sanofi.
A version of this article first appeared on Medscape.com.
More than one in six cancer patients experience long-term sequelae following SARS-CoV-2 infection, placing them at increased risk of discontinuing their cancer treatment or dying, according to European registry data.
Given the “high lethality” of COVID-19 in cancer patients and the risk for long-term complications following infection in the general population, Alessio Cortellini, MD, a consultant medical oncologist at Hammersmith Hospital and Imperial College London, and colleagues wanted to explore the “prevalence and clinical significance of COVID-19 sequelae in cancer patients and their oncological continuity of care.”
Dr. Cortellini presented the OnCovid registry research on Sept. 21 at the 2021 European Society for Medical Oncology Congress. He reported that overall, the data suggest that post–COVID-19 complications may “impair” patients’ cancer survival as well as their cancer care.
The OnCovid registry data showed that the 15% of cancer patients who had long-term COVID-19 complications were 76% more likely to die than those without sequelae. Cancer patients with COVID-19 sequelae were significantly more likely to permanently stop taking their systemic anticancer therapy, and they were more than 3.5 times more likely to die than those who continued their treatment as planned. In terms of long-term complications, almost half of patients experienced dyspnea, and two-fifths reported chronic fatigue.
“This data confirms the need to continue to prioritize cancer patients,” Antonio Passaro, MD, PhD, division of thoracic oncology, European Institute of Oncology IRCCS, Milan, commented in a press release. “In the fight against the pandemic, it is of the utmost importance that we do not neglect to study and understand the curves of cancer incidence and mortality.”
Invited to discuss the results, Anne-Marie C. Dingemans, MD, PhD, a pulmonologist and professor of thoracic oncology at Erasmus Medical Center, Rotterdam, the Netherlands, said COVID-19 remains a “very important” issue for cancer patients.
Interestingly, Dr. Dingemans noted that COVID-19 sequelae in patients with cancer appear to occur slightly less frequently, compared with estimates in the general population – which range from 13% to 60% – though patients with cancer tend to have more respiratory problems.
However, Dr. Dingemans added, the difficulty with comparing sequelae rates between cancer patients and the general population is that cancer patients “probably already have a lot of symptoms” associated with long COVID, such as dyspnea and fatigue, and may not be aware that they are experiencing COVID sequelae.
The registry results
To investigate the long-term impact of COVID-19 on survival and continuity of care, the team examined data from the OnCovid registry, which was established at the beginning of the pandemic to study consecutive patients aged 18 years and older with confirmed SARS-CoV-2 infection and a history of solid or hematologic malignancies.
At the data cutoff on March 1, 2021, the registry included 35 institutions in six European countries. The institutions collected information on patient demographics and comorbidities, cancer history, anticancer therapy, COVID-19 investigations, and COVID-19–specific therapies.
For the current analysis, the team included 1,557 of 2,634 patients who had undergone a clinical reassessment after recovering from COVID-19. Information sufficient to conduct multivariate analysis was available for 840 of these patients.
About half of the patients were younger than 60 years, and just over half were women. The most common cancer diagnoses were breast cancer (23.4%), gastrointestinal tumors (16.5%), gynecologic/genitourinary tumors (19.3%), and hematologic cancers (14.1%), with even distribution between local/locoregional and advanced disease.
The median interval between COVID-19 recovery and reassessment was 44 days, and the mean post–COVID-19 follow-up period was 128 days.
About 15% of patients experienced at least one long-term sequela from COVID-19. The most common were dyspnea/shortness of breath (49.6%), fatigue (41.0%), chronic cough (33.8%), and other respiratory complications (10.7%).
Dr. Cortellini noted that cancer patients who experienced sequelae were more likely to be male, aged 65 years or older, to have at least two comorbidities, and to have a history of smoking. In addition, cancer patients who experienced long-term complications were significantly more likely to have had COVID-19 complications, to have required COVID-19 therapy, and to have been hospitalized for the disease.
Factoring in gender, age, comorbidity burden, primary tumor, stage, receipt of anticancer and anti–COVID-19 therapy, COVID-19 complications, and hospitalization, the team found that COVID-19 sequelae were independently associated with an increased risk for death (hazard ratio, 1.76).
Further analysis of patterns of systemic anticancer therapy in 471 patients revealed that 14.8% of COVID-19 survivors permanently discontinued therapy and that a dose or regimen adjustment occurred for 37.8%.
Patients who permanently discontinued anticancer therapy were more likely to be former or current smokers, to have had COVID-19 complications or been hospitalized for COVID-19, and to have had COVID-19 sequelae at reassessment. The investigators found no association between permanent discontinuation of therapy and cancer disease stage.
Dr. Cortellini and colleagues reported that permanent cessation of systemic anticancer therapy was associated with an increased risk for death. A change in dose or regimen did not affect survival.
The most common reason for stopping therapy permanently was deterioration of the patient’s performance status (61.3%), followed by disease progression (29.0%). Dose or regimen adjustments typically occurred to avoid immune suppression (50.0%), hospitalization (25.8%), and intravenous drug administration (19.1%).
Dr. Cortellini concluded his presentation by highlighting the importance of increasing awareness of long COVID in patients with cancer as well as early treatment of COVID-19 sequelae to improve patient outcomes.
The study was funded by the Imperial College Biomedical Research Center. Dr. Cortellini has relationships with MSD, Bristol-Myers Squibb, Roche, Novartis, AstraZeneca, Astellas, and Sun Pharma. Dr. Dingemans has relationships with Roche, Eli Lilly, Boehringer Ingelheim, AstraZeneca, Jansen, Chiesi, Amgen, Pfizer, Bayer, Takeda, Pharmamar, and Sanofi.
A version of this article first appeared on Medscape.com.
An appeal for equitable access to care for early pregnancy loss
Remarkable advances in care for early pregnancy loss (EPL) have occurred over the past several years. Misoprostol with mifepristone pretreatment is now the gold standard for medical management after recent research showed that this regimen improves both the efficacy and cost-effectiveness of medical management.1 Manual vacuum aspiration (MVA)’s portability, effectiveness, and safety ensure that providers can offer procedural EPL management in almost any clinical setting. Medication management and in-office uterine aspiration are two evidence-based options for EPL management that may increase access for the 25% of pregnant women who experience EPL. Unfortunately, many women do not have access to either option. Equitable access to early pregnancy loss management can be achieved by expanding access to mifepristone and office-based MVA.
However, access to mifepristone and initiating office-based MVA is challenging. Mifepristone is one of several medications regulated under the Food and Drug Administration’s Risk Evaluation and Management Strategies (REMS) program.2
The REMS guidelines restrict clinicians in prescribing and dispensing mifepristone, including the key provision that mifepristone may be dispensed only in clinics, medical offices, and hospitals. Clinicians cannot write a prescription for mifepristone for a patient to pick up at the pharmacy. Efforts are underway to roll back the REMS. Barriers to office-based MVA include time, culture shift among staff, gathering equipment, and creating protocols. Clinicians can improve access to EPL management in a variety of ways:
- MVA training: Ob.gyns. who lack training in MVA use can take advantage of several programs designed to teach the skill to clinicians, including programs such as Training, Education, and Advocacy in Miscarriage Management (TEAMM).3,4 MVA is easy to learn for ob.gyns. and procedural complications are uncommon. In the office setting, complications requiring transfer to a higher level of care are rare.5 With adequate training, whether during residency or afterward, ob.gyns. can learn to safely and effectively use MVA for procedural EPL management in the office and in the emergency department.
- Partnerships with pharmacists to reduce barriers to mifepristone: Ob.gyns. working in a variety of clinical settings, including independent clinics, critical access hospitals, community hospitals, and academic medical centers, have worked closely with on-site pharmacists to place mifepristone on their practice sites’ formularies.6 These ob.gyn.–pharmacist collaborations often require explanations to institutional Pharmacy and Therapeutics (P&T) committees of the benefits of mifepristone to patients, detailed indications for mifepristone’s use, and methods to secure mifepristone on site.
- Partnerships with emergency department and outpatient nursing and administration to promote MVA: Provision of MVA is ideal for safe, effective, and cost-efficient procedural EPL management in both the emergency department and outpatient setting. However, access to MVA in emergency rooms and outpatient clinical settings is suboptimal. Some clinicians push back against MVA use in the emergency department, citing fears that performing the procedure in the emergency department unnecessarily uses staff and resources reserved for patients with more critical illnesses. Ob.gyns. should also work with emergency medicine physicians and emergency department nursing staff and hospital administrators in explaining that MVA in the emergency room is patient centered and cost effective.
Interdisciplinary collaboration and training are two strategies that can increase access to mifepristone and MVA for EPL management. Use of mifepristone/misoprostol and office/emergency department MVA for treatment of EPL is patient centered, evidence based, feasible, highly effective, and timely. These two health care interventions are practical in almost any setting, including rural and other low-resource settings. By using these strategies to overcome the logistical and institutional challenges, ob.gyns. can help countless women with EPL gain access to the best EPL care.
Dr. Espey is chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque. Dr. Jackson is an obstetrician/gynecologist at Michigan State University in Flint. They have no disclosures to report.
References
1. Schreiber CA et al. N Engl J Med. 2018 Jun 7;378(23):2161-70.
2. Food and Drug Administration. Mifeprex (mifepristone) information.
3. The TEAMM (Training, Education, and Advocacy in Miscarriage Management) Project. Training interprofessional teams to manage miscarriage. Accessed March 15, 2021.
4. Quinley KE et al. Ann Emerg Med. 2019 Jul;72(1):86-92.
5. Milingos DS et al. BJOG. 2009 Aug;116(9):1268-71.
6. Calloway D et al. Contraception. 2021 Jul;104(1):24-8.
Remarkable advances in care for early pregnancy loss (EPL) have occurred over the past several years. Misoprostol with mifepristone pretreatment is now the gold standard for medical management after recent research showed that this regimen improves both the efficacy and cost-effectiveness of medical management.1 Manual vacuum aspiration (MVA)’s portability, effectiveness, and safety ensure that providers can offer procedural EPL management in almost any clinical setting. Medication management and in-office uterine aspiration are two evidence-based options for EPL management that may increase access for the 25% of pregnant women who experience EPL. Unfortunately, many women do not have access to either option. Equitable access to early pregnancy loss management can be achieved by expanding access to mifepristone and office-based MVA.
However, access to mifepristone and initiating office-based MVA is challenging. Mifepristone is one of several medications regulated under the Food and Drug Administration’s Risk Evaluation and Management Strategies (REMS) program.2
The REMS guidelines restrict clinicians in prescribing and dispensing mifepristone, including the key provision that mifepristone may be dispensed only in clinics, medical offices, and hospitals. Clinicians cannot write a prescription for mifepristone for a patient to pick up at the pharmacy. Efforts are underway to roll back the REMS. Barriers to office-based MVA include time, culture shift among staff, gathering equipment, and creating protocols. Clinicians can improve access to EPL management in a variety of ways:
- MVA training: Ob.gyns. who lack training in MVA use can take advantage of several programs designed to teach the skill to clinicians, including programs such as Training, Education, and Advocacy in Miscarriage Management (TEAMM).3,4 MVA is easy to learn for ob.gyns. and procedural complications are uncommon. In the office setting, complications requiring transfer to a higher level of care are rare.5 With adequate training, whether during residency or afterward, ob.gyns. can learn to safely and effectively use MVA for procedural EPL management in the office and in the emergency department.
- Partnerships with pharmacists to reduce barriers to mifepristone: Ob.gyns. working in a variety of clinical settings, including independent clinics, critical access hospitals, community hospitals, and academic medical centers, have worked closely with on-site pharmacists to place mifepristone on their practice sites’ formularies.6 These ob.gyn.–pharmacist collaborations often require explanations to institutional Pharmacy and Therapeutics (P&T) committees of the benefits of mifepristone to patients, detailed indications for mifepristone’s use, and methods to secure mifepristone on site.
- Partnerships with emergency department and outpatient nursing and administration to promote MVA: Provision of MVA is ideal for safe, effective, and cost-efficient procedural EPL management in both the emergency department and outpatient setting. However, access to MVA in emergency rooms and outpatient clinical settings is suboptimal. Some clinicians push back against MVA use in the emergency department, citing fears that performing the procedure in the emergency department unnecessarily uses staff and resources reserved for patients with more critical illnesses. Ob.gyns. should also work with emergency medicine physicians and emergency department nursing staff and hospital administrators in explaining that MVA in the emergency room is patient centered and cost effective.
Interdisciplinary collaboration and training are two strategies that can increase access to mifepristone and MVA for EPL management. Use of mifepristone/misoprostol and office/emergency department MVA for treatment of EPL is patient centered, evidence based, feasible, highly effective, and timely. These two health care interventions are practical in almost any setting, including rural and other low-resource settings. By using these strategies to overcome the logistical and institutional challenges, ob.gyns. can help countless women with EPL gain access to the best EPL care.
Dr. Espey is chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque. Dr. Jackson is an obstetrician/gynecologist at Michigan State University in Flint. They have no disclosures to report.
References
1. Schreiber CA et al. N Engl J Med. 2018 Jun 7;378(23):2161-70.
2. Food and Drug Administration. Mifeprex (mifepristone) information.
3. The TEAMM (Training, Education, and Advocacy in Miscarriage Management) Project. Training interprofessional teams to manage miscarriage. Accessed March 15, 2021.
4. Quinley KE et al. Ann Emerg Med. 2019 Jul;72(1):86-92.
5. Milingos DS et al. BJOG. 2009 Aug;116(9):1268-71.
6. Calloway D et al. Contraception. 2021 Jul;104(1):24-8.
Remarkable advances in care for early pregnancy loss (EPL) have occurred over the past several years. Misoprostol with mifepristone pretreatment is now the gold standard for medical management after recent research showed that this regimen improves both the efficacy and cost-effectiveness of medical management.1 Manual vacuum aspiration (MVA)’s portability, effectiveness, and safety ensure that providers can offer procedural EPL management in almost any clinical setting. Medication management and in-office uterine aspiration are two evidence-based options for EPL management that may increase access for the 25% of pregnant women who experience EPL. Unfortunately, many women do not have access to either option. Equitable access to early pregnancy loss management can be achieved by expanding access to mifepristone and office-based MVA.
However, access to mifepristone and initiating office-based MVA is challenging. Mifepristone is one of several medications regulated under the Food and Drug Administration’s Risk Evaluation and Management Strategies (REMS) program.2
The REMS guidelines restrict clinicians in prescribing and dispensing mifepristone, including the key provision that mifepristone may be dispensed only in clinics, medical offices, and hospitals. Clinicians cannot write a prescription for mifepristone for a patient to pick up at the pharmacy. Efforts are underway to roll back the REMS. Barriers to office-based MVA include time, culture shift among staff, gathering equipment, and creating protocols. Clinicians can improve access to EPL management in a variety of ways:
- MVA training: Ob.gyns. who lack training in MVA use can take advantage of several programs designed to teach the skill to clinicians, including programs such as Training, Education, and Advocacy in Miscarriage Management (TEAMM).3,4 MVA is easy to learn for ob.gyns. and procedural complications are uncommon. In the office setting, complications requiring transfer to a higher level of care are rare.5 With adequate training, whether during residency or afterward, ob.gyns. can learn to safely and effectively use MVA for procedural EPL management in the office and in the emergency department.
- Partnerships with pharmacists to reduce barriers to mifepristone: Ob.gyns. working in a variety of clinical settings, including independent clinics, critical access hospitals, community hospitals, and academic medical centers, have worked closely with on-site pharmacists to place mifepristone on their practice sites’ formularies.6 These ob.gyn.–pharmacist collaborations often require explanations to institutional Pharmacy and Therapeutics (P&T) committees of the benefits of mifepristone to patients, detailed indications for mifepristone’s use, and methods to secure mifepristone on site.
- Partnerships with emergency department and outpatient nursing and administration to promote MVA: Provision of MVA is ideal for safe, effective, and cost-efficient procedural EPL management in both the emergency department and outpatient setting. However, access to MVA in emergency rooms and outpatient clinical settings is suboptimal. Some clinicians push back against MVA use in the emergency department, citing fears that performing the procedure in the emergency department unnecessarily uses staff and resources reserved for patients with more critical illnesses. Ob.gyns. should also work with emergency medicine physicians and emergency department nursing staff and hospital administrators in explaining that MVA in the emergency room is patient centered and cost effective.
Interdisciplinary collaboration and training are two strategies that can increase access to mifepristone and MVA for EPL management. Use of mifepristone/misoprostol and office/emergency department MVA for treatment of EPL is patient centered, evidence based, feasible, highly effective, and timely. These two health care interventions are practical in almost any setting, including rural and other low-resource settings. By using these strategies to overcome the logistical and institutional challenges, ob.gyns. can help countless women with EPL gain access to the best EPL care.
Dr. Espey is chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque. Dr. Jackson is an obstetrician/gynecologist at Michigan State University in Flint. They have no disclosures to report.
References
1. Schreiber CA et al. N Engl J Med. 2018 Jun 7;378(23):2161-70.
2. Food and Drug Administration. Mifeprex (mifepristone) information.
3. The TEAMM (Training, Education, and Advocacy in Miscarriage Management) Project. Training interprofessional teams to manage miscarriage. Accessed March 15, 2021.
4. Quinley KE et al. Ann Emerg Med. 2019 Jul;72(1):86-92.
5. Milingos DS et al. BJOG. 2009 Aug;116(9):1268-71.
6. Calloway D et al. Contraception. 2021 Jul;104(1):24-8.
Remdesivir sharply cuts COVID hospitalization risk, Gilead says
Remdesivir (Veklury, Gilead) was found to reduce some COVID-19 patients’ risk of hospitalization by 87% in a phase 3 trial, the drug’s manufacturer announced Sept. 22 in a press release.
The randomized, double-blind, placebo-controlled trial evaluated the efficacy and safety of a 3-day course of intravenous remdesivir in an analysis of 562 nonhospitalized patients at high risk for disease progression.
Remdesivir demonstrated a statistically significant 87% reduction in risk for COVID-19–related hospitalization or all-cause death by Day 28 (0.7% [2/279]) compared with placebo (5.3% [15/283]) P = .008. Participants were assigned 1:1 to remdesivir or the placebo group.
Researchers also found an 81% reduction in risk for the composite secondary endpoint – medical visits due to COVID-19 or all-cause death by Day 28. Only 1.6% had COVID-19 medical visits ([4/246]) compared with those in the placebo group (8.3% [21/252]) P = .002. No deaths were observed in either arm by Day 28.
“These latest data show remdesivir’s potential to help high-risk patients recover before they get sicker and stay out of the hospital altogether,” coauthor Robert L. Gottlieb, MD, PhD, from Baylor University Medical Center, Houston, said in the press release.
Remdesivir is the only drug approved by the U.S. Food and Drug Administration for hospitalized COVID-19 patients at least 12 years old. Its treatment of nonhospitalized patients with 3 days of dosing is investigational, and the safety and efficacy for this use and dosing duration have not been established or approved by any regulatory agency, the Gilead press release notes.
The patients in this study were considered high-risk for disease progression based on comorbidities – commonly obesity, hypertension, and diabetes – and age, but had not recently been hospitalized due to COVID-19.
A third of the participants were at least 60 years old. Participants in the study must have received a positive diagnosis within 4 days of starting treatment and experienced symptoms for 7 days or less.
Use of remdesivir controversial
Results from the Adaptive COVID-19 Treatment Trial (ACTT-1) showed remdesivir was superior to placebo in shortening time to recovery in adults hospitalized with COVID-19 with evidence of lower respiratory tract infection.
However, a large trial of more than 11,000 people in 30 countries, sponsored by the World Health Organization, did not show any benefit for the drug in reducing COVID deaths.
The WHO has conditionally recommended against using remdesivir in hospitalized patients, regardless of disease severity, “as there is currently no evidence that remdesivir improves survival and other outcomes in these patients.”
The drug also is given intravenously, and this study tested three infusions over 3 days, a difficult treatment for nonhospitalized patients.
The study results were released ahead of IDWeek, where the late-breaking abstract will be presented at the virtual conference in full at the end of next week.
A version of this article first appeared on Medscape.com.
Remdesivir (Veklury, Gilead) was found to reduce some COVID-19 patients’ risk of hospitalization by 87% in a phase 3 trial, the drug’s manufacturer announced Sept. 22 in a press release.
The randomized, double-blind, placebo-controlled trial evaluated the efficacy and safety of a 3-day course of intravenous remdesivir in an analysis of 562 nonhospitalized patients at high risk for disease progression.
Remdesivir demonstrated a statistically significant 87% reduction in risk for COVID-19–related hospitalization or all-cause death by Day 28 (0.7% [2/279]) compared with placebo (5.3% [15/283]) P = .008. Participants were assigned 1:1 to remdesivir or the placebo group.
Researchers also found an 81% reduction in risk for the composite secondary endpoint – medical visits due to COVID-19 or all-cause death by Day 28. Only 1.6% had COVID-19 medical visits ([4/246]) compared with those in the placebo group (8.3% [21/252]) P = .002. No deaths were observed in either arm by Day 28.
“These latest data show remdesivir’s potential to help high-risk patients recover before they get sicker and stay out of the hospital altogether,” coauthor Robert L. Gottlieb, MD, PhD, from Baylor University Medical Center, Houston, said in the press release.
Remdesivir is the only drug approved by the U.S. Food and Drug Administration for hospitalized COVID-19 patients at least 12 years old. Its treatment of nonhospitalized patients with 3 days of dosing is investigational, and the safety and efficacy for this use and dosing duration have not been established or approved by any regulatory agency, the Gilead press release notes.
The patients in this study were considered high-risk for disease progression based on comorbidities – commonly obesity, hypertension, and diabetes – and age, but had not recently been hospitalized due to COVID-19.
A third of the participants were at least 60 years old. Participants in the study must have received a positive diagnosis within 4 days of starting treatment and experienced symptoms for 7 days or less.
Use of remdesivir controversial
Results from the Adaptive COVID-19 Treatment Trial (ACTT-1) showed remdesivir was superior to placebo in shortening time to recovery in adults hospitalized with COVID-19 with evidence of lower respiratory tract infection.
However, a large trial of more than 11,000 people in 30 countries, sponsored by the World Health Organization, did not show any benefit for the drug in reducing COVID deaths.
The WHO has conditionally recommended against using remdesivir in hospitalized patients, regardless of disease severity, “as there is currently no evidence that remdesivir improves survival and other outcomes in these patients.”
The drug also is given intravenously, and this study tested three infusions over 3 days, a difficult treatment for nonhospitalized patients.
The study results were released ahead of IDWeek, where the late-breaking abstract will be presented at the virtual conference in full at the end of next week.
A version of this article first appeared on Medscape.com.
Remdesivir (Veklury, Gilead) was found to reduce some COVID-19 patients’ risk of hospitalization by 87% in a phase 3 trial, the drug’s manufacturer announced Sept. 22 in a press release.
The randomized, double-blind, placebo-controlled trial evaluated the efficacy and safety of a 3-day course of intravenous remdesivir in an analysis of 562 nonhospitalized patients at high risk for disease progression.
Remdesivir demonstrated a statistically significant 87% reduction in risk for COVID-19–related hospitalization or all-cause death by Day 28 (0.7% [2/279]) compared with placebo (5.3% [15/283]) P = .008. Participants were assigned 1:1 to remdesivir or the placebo group.
Researchers also found an 81% reduction in risk for the composite secondary endpoint – medical visits due to COVID-19 or all-cause death by Day 28. Only 1.6% had COVID-19 medical visits ([4/246]) compared with those in the placebo group (8.3% [21/252]) P = .002. No deaths were observed in either arm by Day 28.
“These latest data show remdesivir’s potential to help high-risk patients recover before they get sicker and stay out of the hospital altogether,” coauthor Robert L. Gottlieb, MD, PhD, from Baylor University Medical Center, Houston, said in the press release.
Remdesivir is the only drug approved by the U.S. Food and Drug Administration for hospitalized COVID-19 patients at least 12 years old. Its treatment of nonhospitalized patients with 3 days of dosing is investigational, and the safety and efficacy for this use and dosing duration have not been established or approved by any regulatory agency, the Gilead press release notes.
The patients in this study were considered high-risk for disease progression based on comorbidities – commonly obesity, hypertension, and diabetes – and age, but had not recently been hospitalized due to COVID-19.
A third of the participants were at least 60 years old. Participants in the study must have received a positive diagnosis within 4 days of starting treatment and experienced symptoms for 7 days or less.
Use of remdesivir controversial
Results from the Adaptive COVID-19 Treatment Trial (ACTT-1) showed remdesivir was superior to placebo in shortening time to recovery in adults hospitalized with COVID-19 with evidence of lower respiratory tract infection.
However, a large trial of more than 11,000 people in 30 countries, sponsored by the World Health Organization, did not show any benefit for the drug in reducing COVID deaths.
The WHO has conditionally recommended against using remdesivir in hospitalized patients, regardless of disease severity, “as there is currently no evidence that remdesivir improves survival and other outcomes in these patients.”
The drug also is given intravenously, and this study tested three infusions over 3 days, a difficult treatment for nonhospitalized patients.
The study results were released ahead of IDWeek, where the late-breaking abstract will be presented at the virtual conference in full at the end of next week.
A version of this article first appeared on Medscape.com.
Study identifies pandemic-related stressor in Parkinson’s disease
a team of researchers in the Netherlands reported, but they also identified meaningful targets for intervention.
Lisanne Dommershuijsen, MSc, a PhD candidate and researcher in epidemiology at the Erasmus University Medical Center in Rotterdam, the Netherlands, reported on a cross-sectional study of 833 participants with Parkinson’s disease in the PRIME-NL study at the International Congress of Parkinson’s Disease and Movement Disorders. The average age of participants was 70.2 and 38% were women.
“We studied targeted hypothetical interventions on COVID-19 stressors in people with Parkinson’s disease,” Ms. Dommershuijsen said. “This disruption in normal life caused considerable psychological stress in community-dwelling individuals. People with Parkinson’s disease might be especially vulnerable to this stress.
“For instance, because reduced levels of physical activity have worsened symptoms or because people with Parkinson’s often have difficulty with flexible [adaptations] to drastic and rapid changes in daily routines, such as those introduced by the COVID-19 pandemic, previous studies found that COVID-19 worsened depression and anxiety symptoms and reduced quality of life (QOL) in people with Parkinson’s disease,” Ms. Dommershuijsen said.
Hence, the goal of the study was to identify the most vulnerable subgroups in the Parkinson’s population and to suggest potential interventions to ameliorate these impacts, she said.
The study focused on eight different stressors that emerged in the pandemic: access to care, medicine and nursing services; loss of social contact; canceled social events; tension or conflict in the home; inability to perform physical activity or relax; and COVID-19 symptoms. The outcomes of interest were depression, as measured with the Beck Depression Inventory (BDI); anxiety, as measured with the Spielberger State-Trait Anxiety Inventory (STAI); and QOL, with the Parkinson’s Disease Quality of Life Questionnaire. The aggregate resulted in a scale of 0-40, with the mean stressor score in the study being 9.6, Ms. Dommershuijsen said.
The BDI and STAI scores for social stressors – loss of social contacts, social events canceled and tension or conflict at home – exceeded those for the so-called care stressors – problems accessing care, medication or nursing – she said, although all eight stressors yielded higher BDI and STAI scores across the board.
Vulnerable subgroups
“When we looked at vulnerable subgroups of people with Parkinson’s disease, we found more pronounced associations between the COVID-19 stress and mental health in women, in highly educated participants, and in participants with advanced Parkinson’s disease,” Ms. Dommershuijsen said. The impact on women and people with advanced disease is explainable, Ms. Dommershuijsen added in an interview; the former because depressive symptoms are more common in women, and the latter because loss of access to care impacts mental wellness.
“The finding that social stressors were more related to anxiety in highly educated people was surprising to us, given that depression in general is more common in people with a lower education,” she said in an interview. “One previous study of the general population suggested this might be related to expectations about available resources, but this findings and the possible explanation warrants further investigation.”
When the study stratified for coping strategies, the COVID-19 stressors had a smaller effect on depressive and anxiety symptoms in Parkinson’s disease patients prone to confrontive coping and planful problem solving, she said. “Whereas, we observed a larger effect of these stressors in people who are prone to using distancing or seeking social support as coping mechanisms,” Ms. Dommershuijsen said.
The researchers also created a model of a hypothetical 50% reduction in COVID-19 stressors among all study participants, but the effect wasn’t clinically relevant, Ms. Dommershuijsen said. However, in people with advanced Parkinson’s disease – that is, with an Movement Disorder Society–Unified Parkinson Disease Rating Scale score above median – the effect was clinically relevant in all outcomes.
The potential interventions the study identified were telemedicine via virtual consultations to alleviate care stressors, and virtual support groups and online classes to address social stressors. “However, a more personalized approach is needed to target tension or conflict at home, which was the most important social stressor influencing depression and anxiety symptoms in our study,” she said. “Social work can play an important role here.”
Asked to comment on the study, Roy Alcalay, MD, professor of neurology at Columbia University Irving Medical Center in New York, said in an interview that the findings align with his research on the impact of COVID-19 and related restrictions on people with Parkinson’s disease.
“The pandemic has affected people in different ways,” he said. “Initially very acutely, people just didn’t have access to doctors. There was also the acute question in movement disorders, but also in other diseases where the people with Parkinson’s disease are going to have the worse outcome when they have COVID-19.” Dr. Alcalay authored two recent papers on the impact of COVID-19 in people with Parkinson’s disease.
“Then we see that, in addition to that question, there’s the question of even if they don’t have COVID-19, just the social distancing and the lack of access to health care, and specifically to physical and occupational therapy and other services, can be quite damaging,” he said.
What’s commendable about the study, he said, was that it just doesn’t highlight the problem. “They’re also highlighting potential solutions, that planful problem solving and coping strategies can be helpful to people.”
Neither Ms. Dommershuijsen nor Dr. Alcalay have any relevant relationships to disclose.
a team of researchers in the Netherlands reported, but they also identified meaningful targets for intervention.
Lisanne Dommershuijsen, MSc, a PhD candidate and researcher in epidemiology at the Erasmus University Medical Center in Rotterdam, the Netherlands, reported on a cross-sectional study of 833 participants with Parkinson’s disease in the PRIME-NL study at the International Congress of Parkinson’s Disease and Movement Disorders. The average age of participants was 70.2 and 38% were women.
“We studied targeted hypothetical interventions on COVID-19 stressors in people with Parkinson’s disease,” Ms. Dommershuijsen said. “This disruption in normal life caused considerable psychological stress in community-dwelling individuals. People with Parkinson’s disease might be especially vulnerable to this stress.
“For instance, because reduced levels of physical activity have worsened symptoms or because people with Parkinson’s often have difficulty with flexible [adaptations] to drastic and rapid changes in daily routines, such as those introduced by the COVID-19 pandemic, previous studies found that COVID-19 worsened depression and anxiety symptoms and reduced quality of life (QOL) in people with Parkinson’s disease,” Ms. Dommershuijsen said.
Hence, the goal of the study was to identify the most vulnerable subgroups in the Parkinson’s population and to suggest potential interventions to ameliorate these impacts, she said.
The study focused on eight different stressors that emerged in the pandemic: access to care, medicine and nursing services; loss of social contact; canceled social events; tension or conflict in the home; inability to perform physical activity or relax; and COVID-19 symptoms. The outcomes of interest were depression, as measured with the Beck Depression Inventory (BDI); anxiety, as measured with the Spielberger State-Trait Anxiety Inventory (STAI); and QOL, with the Parkinson’s Disease Quality of Life Questionnaire. The aggregate resulted in a scale of 0-40, with the mean stressor score in the study being 9.6, Ms. Dommershuijsen said.
The BDI and STAI scores for social stressors – loss of social contacts, social events canceled and tension or conflict at home – exceeded those for the so-called care stressors – problems accessing care, medication or nursing – she said, although all eight stressors yielded higher BDI and STAI scores across the board.
Vulnerable subgroups
“When we looked at vulnerable subgroups of people with Parkinson’s disease, we found more pronounced associations between the COVID-19 stress and mental health in women, in highly educated participants, and in participants with advanced Parkinson’s disease,” Ms. Dommershuijsen said. The impact on women and people with advanced disease is explainable, Ms. Dommershuijsen added in an interview; the former because depressive symptoms are more common in women, and the latter because loss of access to care impacts mental wellness.
“The finding that social stressors were more related to anxiety in highly educated people was surprising to us, given that depression in general is more common in people with a lower education,” she said in an interview. “One previous study of the general population suggested this might be related to expectations about available resources, but this findings and the possible explanation warrants further investigation.”
When the study stratified for coping strategies, the COVID-19 stressors had a smaller effect on depressive and anxiety symptoms in Parkinson’s disease patients prone to confrontive coping and planful problem solving, she said. “Whereas, we observed a larger effect of these stressors in people who are prone to using distancing or seeking social support as coping mechanisms,” Ms. Dommershuijsen said.
The researchers also created a model of a hypothetical 50% reduction in COVID-19 stressors among all study participants, but the effect wasn’t clinically relevant, Ms. Dommershuijsen said. However, in people with advanced Parkinson’s disease – that is, with an Movement Disorder Society–Unified Parkinson Disease Rating Scale score above median – the effect was clinically relevant in all outcomes.
The potential interventions the study identified were telemedicine via virtual consultations to alleviate care stressors, and virtual support groups and online classes to address social stressors. “However, a more personalized approach is needed to target tension or conflict at home, which was the most important social stressor influencing depression and anxiety symptoms in our study,” she said. “Social work can play an important role here.”
Asked to comment on the study, Roy Alcalay, MD, professor of neurology at Columbia University Irving Medical Center in New York, said in an interview that the findings align with his research on the impact of COVID-19 and related restrictions on people with Parkinson’s disease.
“The pandemic has affected people in different ways,” he said. “Initially very acutely, people just didn’t have access to doctors. There was also the acute question in movement disorders, but also in other diseases where the people with Parkinson’s disease are going to have the worse outcome when they have COVID-19.” Dr. Alcalay authored two recent papers on the impact of COVID-19 in people with Parkinson’s disease.
“Then we see that, in addition to that question, there’s the question of even if they don’t have COVID-19, just the social distancing and the lack of access to health care, and specifically to physical and occupational therapy and other services, can be quite damaging,” he said.
What’s commendable about the study, he said, was that it just doesn’t highlight the problem. “They’re also highlighting potential solutions, that planful problem solving and coping strategies can be helpful to people.”
Neither Ms. Dommershuijsen nor Dr. Alcalay have any relevant relationships to disclose.
a team of researchers in the Netherlands reported, but they also identified meaningful targets for intervention.
Lisanne Dommershuijsen, MSc, a PhD candidate and researcher in epidemiology at the Erasmus University Medical Center in Rotterdam, the Netherlands, reported on a cross-sectional study of 833 participants with Parkinson’s disease in the PRIME-NL study at the International Congress of Parkinson’s Disease and Movement Disorders. The average age of participants was 70.2 and 38% were women.
“We studied targeted hypothetical interventions on COVID-19 stressors in people with Parkinson’s disease,” Ms. Dommershuijsen said. “This disruption in normal life caused considerable psychological stress in community-dwelling individuals. People with Parkinson’s disease might be especially vulnerable to this stress.
“For instance, because reduced levels of physical activity have worsened symptoms or because people with Parkinson’s often have difficulty with flexible [adaptations] to drastic and rapid changes in daily routines, such as those introduced by the COVID-19 pandemic, previous studies found that COVID-19 worsened depression and anxiety symptoms and reduced quality of life (QOL) in people with Parkinson’s disease,” Ms. Dommershuijsen said.
Hence, the goal of the study was to identify the most vulnerable subgroups in the Parkinson’s population and to suggest potential interventions to ameliorate these impacts, she said.
The study focused on eight different stressors that emerged in the pandemic: access to care, medicine and nursing services; loss of social contact; canceled social events; tension or conflict in the home; inability to perform physical activity or relax; and COVID-19 symptoms. The outcomes of interest were depression, as measured with the Beck Depression Inventory (BDI); anxiety, as measured with the Spielberger State-Trait Anxiety Inventory (STAI); and QOL, with the Parkinson’s Disease Quality of Life Questionnaire. The aggregate resulted in a scale of 0-40, with the mean stressor score in the study being 9.6, Ms. Dommershuijsen said.
The BDI and STAI scores for social stressors – loss of social contacts, social events canceled and tension or conflict at home – exceeded those for the so-called care stressors – problems accessing care, medication or nursing – she said, although all eight stressors yielded higher BDI and STAI scores across the board.
Vulnerable subgroups
“When we looked at vulnerable subgroups of people with Parkinson’s disease, we found more pronounced associations between the COVID-19 stress and mental health in women, in highly educated participants, and in participants with advanced Parkinson’s disease,” Ms. Dommershuijsen said. The impact on women and people with advanced disease is explainable, Ms. Dommershuijsen added in an interview; the former because depressive symptoms are more common in women, and the latter because loss of access to care impacts mental wellness.
“The finding that social stressors were more related to anxiety in highly educated people was surprising to us, given that depression in general is more common in people with a lower education,” she said in an interview. “One previous study of the general population suggested this might be related to expectations about available resources, but this findings and the possible explanation warrants further investigation.”
When the study stratified for coping strategies, the COVID-19 stressors had a smaller effect on depressive and anxiety symptoms in Parkinson’s disease patients prone to confrontive coping and planful problem solving, she said. “Whereas, we observed a larger effect of these stressors in people who are prone to using distancing or seeking social support as coping mechanisms,” Ms. Dommershuijsen said.
The researchers also created a model of a hypothetical 50% reduction in COVID-19 stressors among all study participants, but the effect wasn’t clinically relevant, Ms. Dommershuijsen said. However, in people with advanced Parkinson’s disease – that is, with an Movement Disorder Society–Unified Parkinson Disease Rating Scale score above median – the effect was clinically relevant in all outcomes.
The potential interventions the study identified were telemedicine via virtual consultations to alleviate care stressors, and virtual support groups and online classes to address social stressors. “However, a more personalized approach is needed to target tension or conflict at home, which was the most important social stressor influencing depression and anxiety symptoms in our study,” she said. “Social work can play an important role here.”
Asked to comment on the study, Roy Alcalay, MD, professor of neurology at Columbia University Irving Medical Center in New York, said in an interview that the findings align with his research on the impact of COVID-19 and related restrictions on people with Parkinson’s disease.
“The pandemic has affected people in different ways,” he said. “Initially very acutely, people just didn’t have access to doctors. There was also the acute question in movement disorders, but also in other diseases where the people with Parkinson’s disease are going to have the worse outcome when they have COVID-19.” Dr. Alcalay authored two recent papers on the impact of COVID-19 in people with Parkinson’s disease.
“Then we see that, in addition to that question, there’s the question of even if they don’t have COVID-19, just the social distancing and the lack of access to health care, and specifically to physical and occupational therapy and other services, can be quite damaging,” he said.
What’s commendable about the study, he said, was that it just doesn’t highlight the problem. “They’re also highlighting potential solutions, that planful problem solving and coping strategies can be helpful to people.”
Neither Ms. Dommershuijsen nor Dr. Alcalay have any relevant relationships to disclose.
FROM MDS VIRTUAL CONGRESS 2021
Gastric cancer: Family history–based H. pylori strategy would be cost effective
Testing for and treating Helicobacter pylori infection among individuals with a family history of gastric cancer could be a cost-effective strategy in the United States, according to a new model published in the journal Gastroenterology.
As many as 10% of gastric cancers aggregate within families, though just why this happens is unclear, according to Sheila D. Rustgi, MD, and colleagues. Shared environmental or genetic factors, or combinations of both, may be responsible. First-degree family history and H. pylori infection each raise gastric cancer risk by roughly 2.5-fold.
In the United States, universal screening for H. pylori infection is not currently recommended, but some studies have suggested a possible benefit in some high-risk populations. American Gastroenterological Association clinical practice guidelines suggest that a patient’s family history should be a factor when considering surveillance strategies for intestinal metaplasia.
Furthermore, a study by Il Ju Choi, MD, and colleagues in 2020 showed that H. pylori treatment with bismuth-based quadruple therapy reduced the risk of gastric cancer by 73% among individuals with a first-degree relative who had gastric cancer. The combination included a proton pump inhibitor, bismuth, metronidazole, and tetracycline for 10 days.
“We hypothesize that, given the dramatic reduction in GC demonstrated by Choi et al., that the screening strategy can be a cost-effective intervention,” Dr. Rustgi and colleagues wrote.
In the new study, the researchers used a Markov state-transition mode, employing a hypothetical cohort of 40-year-old U.S. men and women with a first-degree relative with gastric cancer. It simulated a follow-up period of 60 years or until death. The model assumed a 7-day treatment with triple therapy (proton pump inhibitor, clarithromycin, and amoxicillin) followed by a 14-day treatment period with quadruple therapy if needed. Although the model was analyzed from the U.S. perspective, the trial that informed the risk reduction was performed in a South Korean population.
No screening had a cost of $2,694.09 and resulted in 21.95 quality-adjusted life years (QALYs). 13C-Urea Breath Test screening had a cost of $2,105.28 and led to 22.37 QALYs. Stool antigen testing had a cost of $2,126.00 and yielded 22.30 QALYs.
In the no-screening group, an estimated 2.04% of patients would develop gastric cancer, and 1.82% would die of it. With screening, the frequency of gastric cancer dropped to 1.59%-1.65%, with a gastric cancer mortality rate of 1.41%-1.46%. Overall, screening was modeled to lead to a 19.1%-22.0% risk reduction.
The researchers validated their model by an assumption of an H. pylori infection rate of 100% and then compared the results of the model to the outcome of the study by Dr. Choi and colleagues. In the trial, there was a 55% reduction in gastric cancer among treated patients at a median of 9 years of follow-up. Those who had successful eradication of H. pylori had a 73% reduction. The new model estimated reductions from a testing and treatment strategy of 53.3%-64.5%.
The findings aren’t surprising, according to Joseph Jennings, MD, of the department of medicine at Georgetown University, Washington, and director of the Center for GI Bleeding at MedStar Georgetown University Hospital, who was not involved with the study. “Even eliminating one person getting gastric cancer, where they will then need major surgery, chemotherapy, all these very expensive interventions [is important],” said Dr. Jennings. “We have very efficient ways to test for these things that don’t involve endoscopy.”
One potential caveat to identifying and treating H. pylori infection is whether elimination of H. pylori may lead to some adverse effects. Some patients can experience increased acid reflux as a result, while others suffer no ill effects. “But when you’re dealing with the alternative, which is stomach cancer, those negatives would have to stack up really, really high to outweigh the positives of preventing a cancer that’s really hard to treat,” said Dr. Jennings.
Dr. Jennings pointed out that the model also projected testing and an intervention conducted in a South Korean population, and extrapolated it to a U.S. population, where the incidence of gastric cancer is lower. “There definitely are some questions about how well it would translate if applied to the general United States population,” said Dr. Jennings.
That question could prompt researchers to conduct a U.S.-based study modeled after the test and treat study in South Korea to see if the regimen produced similar results. The model should add weight to that argument, said Dr. Jennings: “This is raising the point that, at least from an intellectual level, it might be worth now designing the study to see if it works in our population,” said Dr. Jennings.
The authors and Dr. Jennings have no relevant financial disclosures.
Testing for and treating Helicobacter pylori infection among individuals with a family history of gastric cancer could be a cost-effective strategy in the United States, according to a new model published in the journal Gastroenterology.
As many as 10% of gastric cancers aggregate within families, though just why this happens is unclear, according to Sheila D. Rustgi, MD, and colleagues. Shared environmental or genetic factors, or combinations of both, may be responsible. First-degree family history and H. pylori infection each raise gastric cancer risk by roughly 2.5-fold.
In the United States, universal screening for H. pylori infection is not currently recommended, but some studies have suggested a possible benefit in some high-risk populations. American Gastroenterological Association clinical practice guidelines suggest that a patient’s family history should be a factor when considering surveillance strategies for intestinal metaplasia.
Furthermore, a study by Il Ju Choi, MD, and colleagues in 2020 showed that H. pylori treatment with bismuth-based quadruple therapy reduced the risk of gastric cancer by 73% among individuals with a first-degree relative who had gastric cancer. The combination included a proton pump inhibitor, bismuth, metronidazole, and tetracycline for 10 days.
“We hypothesize that, given the dramatic reduction in GC demonstrated by Choi et al., that the screening strategy can be a cost-effective intervention,” Dr. Rustgi and colleagues wrote.
In the new study, the researchers used a Markov state-transition mode, employing a hypothetical cohort of 40-year-old U.S. men and women with a first-degree relative with gastric cancer. It simulated a follow-up period of 60 years or until death. The model assumed a 7-day treatment with triple therapy (proton pump inhibitor, clarithromycin, and amoxicillin) followed by a 14-day treatment period with quadruple therapy if needed. Although the model was analyzed from the U.S. perspective, the trial that informed the risk reduction was performed in a South Korean population.
No screening had a cost of $2,694.09 and resulted in 21.95 quality-adjusted life years (QALYs). 13C-Urea Breath Test screening had a cost of $2,105.28 and led to 22.37 QALYs. Stool antigen testing had a cost of $2,126.00 and yielded 22.30 QALYs.
In the no-screening group, an estimated 2.04% of patients would develop gastric cancer, and 1.82% would die of it. With screening, the frequency of gastric cancer dropped to 1.59%-1.65%, with a gastric cancer mortality rate of 1.41%-1.46%. Overall, screening was modeled to lead to a 19.1%-22.0% risk reduction.
The researchers validated their model by an assumption of an H. pylori infection rate of 100% and then compared the results of the model to the outcome of the study by Dr. Choi and colleagues. In the trial, there was a 55% reduction in gastric cancer among treated patients at a median of 9 years of follow-up. Those who had successful eradication of H. pylori had a 73% reduction. The new model estimated reductions from a testing and treatment strategy of 53.3%-64.5%.
The findings aren’t surprising, according to Joseph Jennings, MD, of the department of medicine at Georgetown University, Washington, and director of the Center for GI Bleeding at MedStar Georgetown University Hospital, who was not involved with the study. “Even eliminating one person getting gastric cancer, where they will then need major surgery, chemotherapy, all these very expensive interventions [is important],” said Dr. Jennings. “We have very efficient ways to test for these things that don’t involve endoscopy.”
One potential caveat to identifying and treating H. pylori infection is whether elimination of H. pylori may lead to some adverse effects. Some patients can experience increased acid reflux as a result, while others suffer no ill effects. “But when you’re dealing with the alternative, which is stomach cancer, those negatives would have to stack up really, really high to outweigh the positives of preventing a cancer that’s really hard to treat,” said Dr. Jennings.
Dr. Jennings pointed out that the model also projected testing and an intervention conducted in a South Korean population, and extrapolated it to a U.S. population, where the incidence of gastric cancer is lower. “There definitely are some questions about how well it would translate if applied to the general United States population,” said Dr. Jennings.
That question could prompt researchers to conduct a U.S.-based study modeled after the test and treat study in South Korea to see if the regimen produced similar results. The model should add weight to that argument, said Dr. Jennings: “This is raising the point that, at least from an intellectual level, it might be worth now designing the study to see if it works in our population,” said Dr. Jennings.
The authors and Dr. Jennings have no relevant financial disclosures.
Testing for and treating Helicobacter pylori infection among individuals with a family history of gastric cancer could be a cost-effective strategy in the United States, according to a new model published in the journal Gastroenterology.
As many as 10% of gastric cancers aggregate within families, though just why this happens is unclear, according to Sheila D. Rustgi, MD, and colleagues. Shared environmental or genetic factors, or combinations of both, may be responsible. First-degree family history and H. pylori infection each raise gastric cancer risk by roughly 2.5-fold.
In the United States, universal screening for H. pylori infection is not currently recommended, but some studies have suggested a possible benefit in some high-risk populations. American Gastroenterological Association clinical practice guidelines suggest that a patient’s family history should be a factor when considering surveillance strategies for intestinal metaplasia.
Furthermore, a study by Il Ju Choi, MD, and colleagues in 2020 showed that H. pylori treatment with bismuth-based quadruple therapy reduced the risk of gastric cancer by 73% among individuals with a first-degree relative who had gastric cancer. The combination included a proton pump inhibitor, bismuth, metronidazole, and tetracycline for 10 days.
“We hypothesize that, given the dramatic reduction in GC demonstrated by Choi et al., that the screening strategy can be a cost-effective intervention,” Dr. Rustgi and colleagues wrote.
In the new study, the researchers used a Markov state-transition mode, employing a hypothetical cohort of 40-year-old U.S. men and women with a first-degree relative with gastric cancer. It simulated a follow-up period of 60 years or until death. The model assumed a 7-day treatment with triple therapy (proton pump inhibitor, clarithromycin, and amoxicillin) followed by a 14-day treatment period with quadruple therapy if needed. Although the model was analyzed from the U.S. perspective, the trial that informed the risk reduction was performed in a South Korean population.
No screening had a cost of $2,694.09 and resulted in 21.95 quality-adjusted life years (QALYs). 13C-Urea Breath Test screening had a cost of $2,105.28 and led to 22.37 QALYs. Stool antigen testing had a cost of $2,126.00 and yielded 22.30 QALYs.
In the no-screening group, an estimated 2.04% of patients would develop gastric cancer, and 1.82% would die of it. With screening, the frequency of gastric cancer dropped to 1.59%-1.65%, with a gastric cancer mortality rate of 1.41%-1.46%. Overall, screening was modeled to lead to a 19.1%-22.0% risk reduction.
The researchers validated their model by an assumption of an H. pylori infection rate of 100% and then compared the results of the model to the outcome of the study by Dr. Choi and colleagues. In the trial, there was a 55% reduction in gastric cancer among treated patients at a median of 9 years of follow-up. Those who had successful eradication of H. pylori had a 73% reduction. The new model estimated reductions from a testing and treatment strategy of 53.3%-64.5%.
The findings aren’t surprising, according to Joseph Jennings, MD, of the department of medicine at Georgetown University, Washington, and director of the Center for GI Bleeding at MedStar Georgetown University Hospital, who was not involved with the study. “Even eliminating one person getting gastric cancer, where they will then need major surgery, chemotherapy, all these very expensive interventions [is important],” said Dr. Jennings. “We have very efficient ways to test for these things that don’t involve endoscopy.”
One potential caveat to identifying and treating H. pylori infection is whether elimination of H. pylori may lead to some adverse effects. Some patients can experience increased acid reflux as a result, while others suffer no ill effects. “But when you’re dealing with the alternative, which is stomach cancer, those negatives would have to stack up really, really high to outweigh the positives of preventing a cancer that’s really hard to treat,” said Dr. Jennings.
Dr. Jennings pointed out that the model also projected testing and an intervention conducted in a South Korean population, and extrapolated it to a U.S. population, where the incidence of gastric cancer is lower. “There definitely are some questions about how well it would translate if applied to the general United States population,” said Dr. Jennings.
That question could prompt researchers to conduct a U.S.-based study modeled after the test and treat study in South Korea to see if the regimen produced similar results. The model should add weight to that argument, said Dr. Jennings: “This is raising the point that, at least from an intellectual level, it might be worth now designing the study to see if it works in our population,” said Dr. Jennings.
The authors and Dr. Jennings have no relevant financial disclosures.
FROM GASTROENTEROLOGY
New COVID-19 strain has reached the U.S.
Deadline, citing a Centers for Disease Control and Prevention report, said 26 residents and 20 workers tested positive for COVID-19 at a skilled care nursing home. The facility has 83 residents and 116 employees.
On March 1, 28 specimens that had been subjected to whole genome sequencing were found to have “mutations aligning with the R.1 lineage,” Deadline said.
About 90% of the facility’s residents and 52% of the staff had received two COVID vaccine doses, the CDC said. Because of the high vaccination rate, the finding raises concerns about “reduced protective immunity” in relation to the R.1 variant, the CDC said.
However, the nursing home case appears to show that the vaccine keeps most people from getting extremely sick, the CDC said. The vaccine was 86.5% protective against symptomatic illness among residents and 87.1% protective for employees.
“Compared with unvaccinated persons, vaccinated persons had reduced risk for SARS-CoV-2 infection and symptomatic COVID-19,” the CDC said. The vaccination of nursing home residents and health care workers “is essential to reduce the risk for symptomatic COVID-19, as is continued focus on infection prevention and control practices,” the CDC said.
Since being reported in Kentucky, R.1 has been detected more than 10,000 times in the United States, Forbes reported, basing that number on entries in the GISAID SARS-CoV-2 database.
Overall, more than 42 million cases of COVID have been reported since the start of the pandemic.
Deadline reported that the R.1 strain was first detected in Japan in January among three members of one family. The family members had no history of traveling abroad, Deadline said, citing an National Institutes of Health report.
The CDC has not classified R.1 as a variant of concern yet but noted it has “several mutations of importance” and “demonstrates evidence of increasing virus transmissibility.”
A version of this article first appeared on WebMD.com.
Deadline, citing a Centers for Disease Control and Prevention report, said 26 residents and 20 workers tested positive for COVID-19 at a skilled care nursing home. The facility has 83 residents and 116 employees.
On March 1, 28 specimens that had been subjected to whole genome sequencing were found to have “mutations aligning with the R.1 lineage,” Deadline said.
About 90% of the facility’s residents and 52% of the staff had received two COVID vaccine doses, the CDC said. Because of the high vaccination rate, the finding raises concerns about “reduced protective immunity” in relation to the R.1 variant, the CDC said.
However, the nursing home case appears to show that the vaccine keeps most people from getting extremely sick, the CDC said. The vaccine was 86.5% protective against symptomatic illness among residents and 87.1% protective for employees.
“Compared with unvaccinated persons, vaccinated persons had reduced risk for SARS-CoV-2 infection and symptomatic COVID-19,” the CDC said. The vaccination of nursing home residents and health care workers “is essential to reduce the risk for symptomatic COVID-19, as is continued focus on infection prevention and control practices,” the CDC said.
Since being reported in Kentucky, R.1 has been detected more than 10,000 times in the United States, Forbes reported, basing that number on entries in the GISAID SARS-CoV-2 database.
Overall, more than 42 million cases of COVID have been reported since the start of the pandemic.
Deadline reported that the R.1 strain was first detected in Japan in January among three members of one family. The family members had no history of traveling abroad, Deadline said, citing an National Institutes of Health report.
The CDC has not classified R.1 as a variant of concern yet but noted it has “several mutations of importance” and “demonstrates evidence of increasing virus transmissibility.”
A version of this article first appeared on WebMD.com.
Deadline, citing a Centers for Disease Control and Prevention report, said 26 residents and 20 workers tested positive for COVID-19 at a skilled care nursing home. The facility has 83 residents and 116 employees.
On March 1, 28 specimens that had been subjected to whole genome sequencing were found to have “mutations aligning with the R.1 lineage,” Deadline said.
About 90% of the facility’s residents and 52% of the staff had received two COVID vaccine doses, the CDC said. Because of the high vaccination rate, the finding raises concerns about “reduced protective immunity” in relation to the R.1 variant, the CDC said.
However, the nursing home case appears to show that the vaccine keeps most people from getting extremely sick, the CDC said. The vaccine was 86.5% protective against symptomatic illness among residents and 87.1% protective for employees.
“Compared with unvaccinated persons, vaccinated persons had reduced risk for SARS-CoV-2 infection and symptomatic COVID-19,” the CDC said. The vaccination of nursing home residents and health care workers “is essential to reduce the risk for symptomatic COVID-19, as is continued focus on infection prevention and control practices,” the CDC said.
Since being reported in Kentucky, R.1 has been detected more than 10,000 times in the United States, Forbes reported, basing that number on entries in the GISAID SARS-CoV-2 database.
Overall, more than 42 million cases of COVID have been reported since the start of the pandemic.
Deadline reported that the R.1 strain was first detected in Japan in January among three members of one family. The family members had no history of traveling abroad, Deadline said, citing an National Institutes of Health report.
The CDC has not classified R.1 as a variant of concern yet but noted it has “several mutations of importance” and “demonstrates evidence of increasing virus transmissibility.”
A version of this article first appeared on WebMD.com.
Sexual assault in women tied to increased stroke, dementia risk
Traumatic experiences, especially sexual assault, may put women at greater risk for poor brain health.
In the Ms Brain study, middle-aged women with trauma exposure had a greater volume of white matter hyperintensities (WMHs) than those without trauma. In addition, the differences persisted even after adjusting for depressive or post-traumatic stress symptoms.
WMHs are “an important indicator of small vessel disease in the brain and have been linked to future stroke risk, dementia risk, and mortality,” lead investigator Rebecca Thurston, PhD, from the University of Pittsburgh, told this news organization.
“What I take from this is, really, that sexual assault has implications for women’s health, far beyond exclusively mental health outcomes, but also for their cardiovascular health, as we have shown in other work and for their stroke and dementia risk as we are seeing in the present work,” Dr. Thurston added.
The study was presented at the North American Menopause Society (NAMS) Annual Meeting in Washington, D.C., and has been accepted for publication in the journal Brain Imaging and Behavior.
Beyond the usual suspects
As part of the study, 145 women (mean age, 59 years) free of clinical cardiovascular disease, stroke, or dementia provided their medical history, including history of traumatic experiences, depression, and post-traumatic stress disorder and underwent magnetic resonance brain imaging for WMHs.
More than two-thirds (68%) of the women reported at least one trauma, most commonly sexual assault (23%).
In multivariate analysis, women with trauma exposure had greater WMH volume than women without trauma (P = .01), with sexual assault most strongly associated with greater WMH volume (P = .02).
The associations persisted after adjusting for depressive or post-traumatic stress symptoms.
“A history of sexual assault was particularly related to white matter hyperintensities in the parietal lobe, and these kinds of white matter hyperintensities have been linked to Alzheimer’s disease in a fairly pronounced way,” Dr. Thurston said.
“When we think about risk factors for stroke, dementia, we need to think beyond exclusively our usual suspects and also think about women [who experienced] psychological trauma and experienced sexual assault in particular. So ask about it and consider it part of your screening regimen,” she added.
‘Burgeoning’ literature
Commenting on the findings, Charles Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, and director of its Institute for Early Life Adversity Research, said the research adds to the “burgeoning literature on the long term neurobiological consequences of trauma and more specifically, sexual abuse, on brain imaging measures.”
“Our group and others reported several years ago that patients with mood disorders, more specifically bipolar disorder and major depression, had higher rates of WMH than matched controls. Those older studies did not control for a history of early life adversity such as childhood maltreatment,” Dr. Nemeroff said.
“In addition to this finding of increased WMH in subjects exposed to trauma is a very large literature documenting other central nervous system (CNS) changes in this population, including cortical thinning in certain brain areas and clearly an emerging finding that different forms of childhood maltreatment are associated with quite distinct structural brain alterations in adulthood,” he noted.
The study was supported by grants from the National Institutes of Health. Dr. Thurston and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Traumatic experiences, especially sexual assault, may put women at greater risk for poor brain health.
In the Ms Brain study, middle-aged women with trauma exposure had a greater volume of white matter hyperintensities (WMHs) than those without trauma. In addition, the differences persisted even after adjusting for depressive or post-traumatic stress symptoms.
WMHs are “an important indicator of small vessel disease in the brain and have been linked to future stroke risk, dementia risk, and mortality,” lead investigator Rebecca Thurston, PhD, from the University of Pittsburgh, told this news organization.
“What I take from this is, really, that sexual assault has implications for women’s health, far beyond exclusively mental health outcomes, but also for their cardiovascular health, as we have shown in other work and for their stroke and dementia risk as we are seeing in the present work,” Dr. Thurston added.
The study was presented at the North American Menopause Society (NAMS) Annual Meeting in Washington, D.C., and has been accepted for publication in the journal Brain Imaging and Behavior.
Beyond the usual suspects
As part of the study, 145 women (mean age, 59 years) free of clinical cardiovascular disease, stroke, or dementia provided their medical history, including history of traumatic experiences, depression, and post-traumatic stress disorder and underwent magnetic resonance brain imaging for WMHs.
More than two-thirds (68%) of the women reported at least one trauma, most commonly sexual assault (23%).
In multivariate analysis, women with trauma exposure had greater WMH volume than women without trauma (P = .01), with sexual assault most strongly associated with greater WMH volume (P = .02).
The associations persisted after adjusting for depressive or post-traumatic stress symptoms.
“A history of sexual assault was particularly related to white matter hyperintensities in the parietal lobe, and these kinds of white matter hyperintensities have been linked to Alzheimer’s disease in a fairly pronounced way,” Dr. Thurston said.
“When we think about risk factors for stroke, dementia, we need to think beyond exclusively our usual suspects and also think about women [who experienced] psychological trauma and experienced sexual assault in particular. So ask about it and consider it part of your screening regimen,” she added.
‘Burgeoning’ literature
Commenting on the findings, Charles Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, and director of its Institute for Early Life Adversity Research, said the research adds to the “burgeoning literature on the long term neurobiological consequences of trauma and more specifically, sexual abuse, on brain imaging measures.”
“Our group and others reported several years ago that patients with mood disorders, more specifically bipolar disorder and major depression, had higher rates of WMH than matched controls. Those older studies did not control for a history of early life adversity such as childhood maltreatment,” Dr. Nemeroff said.
“In addition to this finding of increased WMH in subjects exposed to trauma is a very large literature documenting other central nervous system (CNS) changes in this population, including cortical thinning in certain brain areas and clearly an emerging finding that different forms of childhood maltreatment are associated with quite distinct structural brain alterations in adulthood,” he noted.
The study was supported by grants from the National Institutes of Health. Dr. Thurston and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Traumatic experiences, especially sexual assault, may put women at greater risk for poor brain health.
In the Ms Brain study, middle-aged women with trauma exposure had a greater volume of white matter hyperintensities (WMHs) than those without trauma. In addition, the differences persisted even after adjusting for depressive or post-traumatic stress symptoms.
WMHs are “an important indicator of small vessel disease in the brain and have been linked to future stroke risk, dementia risk, and mortality,” lead investigator Rebecca Thurston, PhD, from the University of Pittsburgh, told this news organization.
“What I take from this is, really, that sexual assault has implications for women’s health, far beyond exclusively mental health outcomes, but also for their cardiovascular health, as we have shown in other work and for their stroke and dementia risk as we are seeing in the present work,” Dr. Thurston added.
The study was presented at the North American Menopause Society (NAMS) Annual Meeting in Washington, D.C., and has been accepted for publication in the journal Brain Imaging and Behavior.
Beyond the usual suspects
As part of the study, 145 women (mean age, 59 years) free of clinical cardiovascular disease, stroke, or dementia provided their medical history, including history of traumatic experiences, depression, and post-traumatic stress disorder and underwent magnetic resonance brain imaging for WMHs.
More than two-thirds (68%) of the women reported at least one trauma, most commonly sexual assault (23%).
In multivariate analysis, women with trauma exposure had greater WMH volume than women without trauma (P = .01), with sexual assault most strongly associated with greater WMH volume (P = .02).
The associations persisted after adjusting for depressive or post-traumatic stress symptoms.
“A history of sexual assault was particularly related to white matter hyperintensities in the parietal lobe, and these kinds of white matter hyperintensities have been linked to Alzheimer’s disease in a fairly pronounced way,” Dr. Thurston said.
“When we think about risk factors for stroke, dementia, we need to think beyond exclusively our usual suspects and also think about women [who experienced] psychological trauma and experienced sexual assault in particular. So ask about it and consider it part of your screening regimen,” she added.
‘Burgeoning’ literature
Commenting on the findings, Charles Nemeroff, MD, PhD, professor and chair, department of psychiatry and behavioral sciences, Dell Medical School, University of Texas at Austin, and director of its Institute for Early Life Adversity Research, said the research adds to the “burgeoning literature on the long term neurobiological consequences of trauma and more specifically, sexual abuse, on brain imaging measures.”
“Our group and others reported several years ago that patients with mood disorders, more specifically bipolar disorder and major depression, had higher rates of WMH than matched controls. Those older studies did not control for a history of early life adversity such as childhood maltreatment,” Dr. Nemeroff said.
“In addition to this finding of increased WMH in subjects exposed to trauma is a very large literature documenting other central nervous system (CNS) changes in this population, including cortical thinning in certain brain areas and clearly an emerging finding that different forms of childhood maltreatment are associated with quite distinct structural brain alterations in adulthood,” he noted.
The study was supported by grants from the National Institutes of Health. Dr. Thurston and Dr. Nemeroff have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Smart watch glucose monitoring on the horizon
Earlier this year, technology news sites reported that the Apple Watch Series 7 and the Samsung Galaxy Watch 4 were going to have integrated optical sensors for checking interstitial fluid glucose levels with no blood sampling needed. By the summer, new articles indicated that the glucose sensing watches would not be released this year for either Apple or Samsung.
For now, the newest technology available for monitoring glucose is continuous glucose monitoring (CGM), which involves a tiny sensor being inserted under the skin. The sensor tests glucose every few minutes, and a transmitter wirelessly sends the information to a monitor, which may be part of an insulin pump or a separate device. Some CGMs send information directly to a smartphone or tablet, according to the National Institutes of Health.
In 1999 the Food and Drug Administration approved the first CGM, which was only approved for downloading 3 days of data at a doctor’s office. Interestingly, the first real-time CGM device for patients to use on their own was a watch, the Glucowatch Biographer. Because of irritation and other issues, that watch never caught on. In 2006 and 2008, Dexcom and then Abbott released the first real-time CGMs that allowed patients to frequently check their own blood sugars.1,2
How CGM has advanced diabetes management
The advent of CGM has advanced the field of diabetes management in many ways.
It has allowed patients to get real time feedback on how their behavior affects their blood sugar. The use of CGM along with the ensuing behavioral changes actually leads to a decrease in hemoglobin A1c, along with a lower risk of hypoglycemia. CGM has also resulted in patients having a better understanding of several aspects of glucose control, including glucose variability and nocturnal hypoglycemia.
Affordable, readily accessible CGM monitors that allow patients to intermittently use CGM have become available over the last 3 years.
In the United States alone, 34.2 million people have diabetes – nearly 1 in every 10 people. Many do not do self-monitoring of blood glucose and most do not use CGM. The current alternative to CGM – self monitoring of blood glucose – is cumbersome, and, since it requires regular finger sticks, is painful. Also, there is significant cost to each test strip that is used to self-monitor, and most insurance limits the number of times a day a patient can check their blood sugar. CGM used to be reserved only for patients who use multiple doses of insulin daily, and only began being approved for use for patients on basal insulin alone in June 2021.3
Most primary care doctors are just beginning to learn how to interpret CGM data.
Smart watch glucose monitoring predictions
When smart watch glucose monitoring arrives, it will suddenly change the playing field for patients with diabetes and their doctors alike.
We expect it to bring down the price of CGM and make it readily available to any patient who owns a smart watch with that function.
For doctors, the new technology will result in them suddenly being asked to advise their patients on how to use the data generated by watch-based CGM.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece. Dr. Persampiere is a second-year resident in the family medicine residency program at Abington Jefferson Health. You can contact them at [email protected].
References
1. Hirsh I. Introduction: History of Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association. 2018.
2. Peters A. The Evidence Base for Continuous Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association 2018.
3. “Medicare Loosening Restrictions for Continuous Glucose Monitor (CGM) Coverage,” Healthline. 2021 Jul 13.
Earlier this year, technology news sites reported that the Apple Watch Series 7 and the Samsung Galaxy Watch 4 were going to have integrated optical sensors for checking interstitial fluid glucose levels with no blood sampling needed. By the summer, new articles indicated that the glucose sensing watches would not be released this year for either Apple or Samsung.
For now, the newest technology available for monitoring glucose is continuous glucose monitoring (CGM), which involves a tiny sensor being inserted under the skin. The sensor tests glucose every few minutes, and a transmitter wirelessly sends the information to a monitor, which may be part of an insulin pump or a separate device. Some CGMs send information directly to a smartphone or tablet, according to the National Institutes of Health.
In 1999 the Food and Drug Administration approved the first CGM, which was only approved for downloading 3 days of data at a doctor’s office. Interestingly, the first real-time CGM device for patients to use on their own was a watch, the Glucowatch Biographer. Because of irritation and other issues, that watch never caught on. In 2006 and 2008, Dexcom and then Abbott released the first real-time CGMs that allowed patients to frequently check their own blood sugars.1,2
How CGM has advanced diabetes management
The advent of CGM has advanced the field of diabetes management in many ways.
It has allowed patients to get real time feedback on how their behavior affects their blood sugar. The use of CGM along with the ensuing behavioral changes actually leads to a decrease in hemoglobin A1c, along with a lower risk of hypoglycemia. CGM has also resulted in patients having a better understanding of several aspects of glucose control, including glucose variability and nocturnal hypoglycemia.
Affordable, readily accessible CGM monitors that allow patients to intermittently use CGM have become available over the last 3 years.
In the United States alone, 34.2 million people have diabetes – nearly 1 in every 10 people. Many do not do self-monitoring of blood glucose and most do not use CGM. The current alternative to CGM – self monitoring of blood glucose – is cumbersome, and, since it requires regular finger sticks, is painful. Also, there is significant cost to each test strip that is used to self-monitor, and most insurance limits the number of times a day a patient can check their blood sugar. CGM used to be reserved only for patients who use multiple doses of insulin daily, and only began being approved for use for patients on basal insulin alone in June 2021.3
Most primary care doctors are just beginning to learn how to interpret CGM data.
Smart watch glucose monitoring predictions
When smart watch glucose monitoring arrives, it will suddenly change the playing field for patients with diabetes and their doctors alike.
We expect it to bring down the price of CGM and make it readily available to any patient who owns a smart watch with that function.
For doctors, the new technology will result in them suddenly being asked to advise their patients on how to use the data generated by watch-based CGM.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece. Dr. Persampiere is a second-year resident in the family medicine residency program at Abington Jefferson Health. You can contact them at [email protected].
References
1. Hirsh I. Introduction: History of Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association. 2018.
2. Peters A. The Evidence Base for Continuous Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association 2018.
3. “Medicare Loosening Restrictions for Continuous Glucose Monitor (CGM) Coverage,” Healthline. 2021 Jul 13.
Earlier this year, technology news sites reported that the Apple Watch Series 7 and the Samsung Galaxy Watch 4 were going to have integrated optical sensors for checking interstitial fluid glucose levels with no blood sampling needed. By the summer, new articles indicated that the glucose sensing watches would not be released this year for either Apple or Samsung.
For now, the newest technology available for monitoring glucose is continuous glucose monitoring (CGM), which involves a tiny sensor being inserted under the skin. The sensor tests glucose every few minutes, and a transmitter wirelessly sends the information to a monitor, which may be part of an insulin pump or a separate device. Some CGMs send information directly to a smartphone or tablet, according to the National Institutes of Health.
In 1999 the Food and Drug Administration approved the first CGM, which was only approved for downloading 3 days of data at a doctor’s office. Interestingly, the first real-time CGM device for patients to use on their own was a watch, the Glucowatch Biographer. Because of irritation and other issues, that watch never caught on. In 2006 and 2008, Dexcom and then Abbott released the first real-time CGMs that allowed patients to frequently check their own blood sugars.1,2
How CGM has advanced diabetes management
The advent of CGM has advanced the field of diabetes management in many ways.
It has allowed patients to get real time feedback on how their behavior affects their blood sugar. The use of CGM along with the ensuing behavioral changes actually leads to a decrease in hemoglobin A1c, along with a lower risk of hypoglycemia. CGM has also resulted in patients having a better understanding of several aspects of glucose control, including glucose variability and nocturnal hypoglycemia.
Affordable, readily accessible CGM monitors that allow patients to intermittently use CGM have become available over the last 3 years.
In the United States alone, 34.2 million people have diabetes – nearly 1 in every 10 people. Many do not do self-monitoring of blood glucose and most do not use CGM. The current alternative to CGM – self monitoring of blood glucose – is cumbersome, and, since it requires regular finger sticks, is painful. Also, there is significant cost to each test strip that is used to self-monitor, and most insurance limits the number of times a day a patient can check their blood sugar. CGM used to be reserved only for patients who use multiple doses of insulin daily, and only began being approved for use for patients on basal insulin alone in June 2021.3
Most primary care doctors are just beginning to learn how to interpret CGM data.
Smart watch glucose monitoring predictions
When smart watch glucose monitoring arrives, it will suddenly change the playing field for patients with diabetes and their doctors alike.
We expect it to bring down the price of CGM and make it readily available to any patient who owns a smart watch with that function.
For doctors, the new technology will result in them suddenly being asked to advise their patients on how to use the data generated by watch-based CGM.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Hospital–Jefferson Health. They have no conflicts related to the content of this piece. Dr. Persampiere is a second-year resident in the family medicine residency program at Abington Jefferson Health. You can contact them at [email protected].
References
1. Hirsh I. Introduction: History of Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association. 2018.
2. Peters A. The Evidence Base for Continuous Glucose Monitoring, in “Role of Continuous Glucose Monitoring in Diabetes Treatment.” American Diabetes Association 2018.
3. “Medicare Loosening Restrictions for Continuous Glucose Monitor (CGM) Coverage,” Healthline. 2021 Jul 13.