User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Moderate alcohol intake may curb subsequent diabetes after gestational diabetes
Among women with a history of gestational diabetes, alcohol intake of half a drink to one drink daily was associated with a 55% lower risk for subsequent type 2 diabetes, based on data from approximately 4,700 women in the Nurses’ Health Study II cohort.
However, the findings must be considered in the context of other risks and benefits of alcohol consumption before making statements or clinical recommendations, wrote Stefanie N. Hinkle, PhD, of the National Institutes of Health, Bethesda, Md., and colleagues.
Women with a history of gestational diabetes remain at increased risk for developing type 2 diabetes, so modifiable diet and lifestyle factors deserve further study, the researchers noted. Previous research has shown an association between light to moderate alcohol consumption and reduced risk of type 2 diabetes among women in the general population, but data on a similar risk reduction for women with a history of gestational diabetes are lacking, they added.
In a study published in JAMA Network Open, the researchers reviewed data from 4,740 women enrolled in the Nurses’ Health Study II who reported a history of gestational diabetes. These women were followed from Jan. 1, 1991, to Dec. 31, 2017, as part of the Diabetes & Women’s Health Study; dietary intake, including alcohol intake, was assessed every 4 years via validated food frequency questionnaires.
The average age at baseline was 38 years, and the median follow-up time was 24 years, yielding a total of 78,328 person-years of follow-up. Alcohol consumption was divided into four categories: none; 0.1 g/day to 4.9 g/day; 5.0 to 14.9 g/day, and 15.0 g/day or higher.
A total of 897 incident cases of type 2 diabetes were reported during the study period. After adjustment for multiple dietary and lifestyle variables, including diet and physical activity, only alcohol consumption of 5.0-14.9 g/day (approximately half a drink to one drink) was associated with a significantly decreased risk for incident type 2 diabetes (hazard ratio, 0.45) compared with women who reported no alcohol consumption.
On further adjustment for body mass index, women who reported alcohol consumption in the 5.0-14.9 g/day range had a 41% lower risk for developing incident type 2 diabetes (HR, 0.59); alcohol consumption in the other ranges remained unassociated with type 2 diabetes risk, although the researchers noted that these estimates were attenuated.
The median daily intake for women who consumed alcohol was 2.3 g/day, approximately one drink per week. Beer was the most frequently consumed type of alcohol.
When the researchers analyzed the data by alcohol type, notably, “only beer consumption of 1 or more servings a week was associated with a lower risk for type 2 diabetes,” although previous studies have suggested a stronger association in diabetes risk reduction with wine consumption vs. beer, the researchers noted.
The study findings were the potential for confounding factors not included in the adjustment, potential underreporting of alcohol intake, and potential screening bias toward women who were more health conscious, the researchers noted. Other limitations were lack of generalizability given that most of the study participants were white women, and a lack of data on binge drinking and whether alcohol was consumed with meals, they added. The study strengths included the prospective design, large size, long-term follow-up, and use of validated questionnaires, they said.
The researchers cautioned that the results should not be interpreted without considering other health outcomes. “Consistent with the 2020 Dietary Guidelines for Americans, which recommend that adults who do not consume alcohol do not initiate drinking, it may not be prudent for those with a history of gestational diabetes who do not consume alcohol to initiate drinking alcohol solely to reduce their risk for type 2 diabetes,” they emphasized.
Risk/benefit ratio for alcohol includes many factors
“There is a relative paucity of data regarding women’s long-term health as it may relate to pregnancy and pregnancy outcomes,” Angela Bianco, MD, of Mount Sinai Hospital, New York, said in an interview.
Dr. Bianco said she was surprised by some of the study findings.
“Generally speaking, I consider alcohol to be of little to no nutritional value, and to have a high sugar content/glycemic index,” she said. “However, a reduced incidence of adult-onset diabetes has been observed among moderate drinkers in other large prospective studies as well,” she noted. “In contrast, some studies have shown an increased risk of diabetes among a proportion of subjects in the top alcohol consumption category, while other studies have found no association. Possible inconsistencies may be due to differences in drinking patterns and the types of beverages consumed,” Dr. Bianco explained.
A key point for clinicians to keep in mind is that “the study may be flawed based on the different criteria used to make a diagnosis of history of gestational diabetes, the fact that they excluded patients that did not return the questionnaires, and the fact that respondents may not have answered correctly due to recall bias” or other reasons, Dr. Bianco said. “Additionally, those who responded obviously had access to health care, which in and of itself is a confounder,” she noted.
Another key point is that “the effect of alcohol being consumed with or without a meal was not examined,” said Dr. Bianco. “Alcohol concentration is reduced if consumed with meals. Alcohol can lead to hypoglycemia (from reduced gluconeogenesis) during fasting states, but after meals (postprandial states) it can result in lower glucose disposal and higher blood glucose levels,” she said. “The available literature suggests that alcohol may improve insulin sensitivity and reduce resistance, but there is likely a U-shaped association between alcohol consumption and the risk of diabetes,” Dr. Bianco noted. “There is likely a delicate balance between benefits and risks of alcohol intake. The inherent benefit/risk ratio must take into account with other potential comorbidities including BMI, activity level, stress, and preexisting conditions,” she said.
“Additional long-term studies engaging patients with diverse ethnic and socioeconomic backgrounds with detailed information regarding the role of nutrition, alcohol intake, tobacco and drug use, environmental exposures, and medical comorbidities need to be performed,” Dr. Bianco concluded.
The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute of General Medical Sciences, and the National Institute of Diabetes and Digestive and Kidney Diseases; the Nurses’ Health Study II was supported by the National Institutes of Health. Lead author Dr. Hinkle and coauthor Cuilin Zhang, MD, are employees of the U.S. federal government. The researchers and Dr. Bianco had no financial conflicts to disclose.
Among women with a history of gestational diabetes, alcohol intake of half a drink to one drink daily was associated with a 55% lower risk for subsequent type 2 diabetes, based on data from approximately 4,700 women in the Nurses’ Health Study II cohort.
However, the findings must be considered in the context of other risks and benefits of alcohol consumption before making statements or clinical recommendations, wrote Stefanie N. Hinkle, PhD, of the National Institutes of Health, Bethesda, Md., and colleagues.
Women with a history of gestational diabetes remain at increased risk for developing type 2 diabetes, so modifiable diet and lifestyle factors deserve further study, the researchers noted. Previous research has shown an association between light to moderate alcohol consumption and reduced risk of type 2 diabetes among women in the general population, but data on a similar risk reduction for women with a history of gestational diabetes are lacking, they added.
In a study published in JAMA Network Open, the researchers reviewed data from 4,740 women enrolled in the Nurses’ Health Study II who reported a history of gestational diabetes. These women were followed from Jan. 1, 1991, to Dec. 31, 2017, as part of the Diabetes & Women’s Health Study; dietary intake, including alcohol intake, was assessed every 4 years via validated food frequency questionnaires.
The average age at baseline was 38 years, and the median follow-up time was 24 years, yielding a total of 78,328 person-years of follow-up. Alcohol consumption was divided into four categories: none; 0.1 g/day to 4.9 g/day; 5.0 to 14.9 g/day, and 15.0 g/day or higher.
A total of 897 incident cases of type 2 diabetes were reported during the study period. After adjustment for multiple dietary and lifestyle variables, including diet and physical activity, only alcohol consumption of 5.0-14.9 g/day (approximately half a drink to one drink) was associated with a significantly decreased risk for incident type 2 diabetes (hazard ratio, 0.45) compared with women who reported no alcohol consumption.
On further adjustment for body mass index, women who reported alcohol consumption in the 5.0-14.9 g/day range had a 41% lower risk for developing incident type 2 diabetes (HR, 0.59); alcohol consumption in the other ranges remained unassociated with type 2 diabetes risk, although the researchers noted that these estimates were attenuated.
The median daily intake for women who consumed alcohol was 2.3 g/day, approximately one drink per week. Beer was the most frequently consumed type of alcohol.
When the researchers analyzed the data by alcohol type, notably, “only beer consumption of 1 or more servings a week was associated with a lower risk for type 2 diabetes,” although previous studies have suggested a stronger association in diabetes risk reduction with wine consumption vs. beer, the researchers noted.
The study findings were the potential for confounding factors not included in the adjustment, potential underreporting of alcohol intake, and potential screening bias toward women who were more health conscious, the researchers noted. Other limitations were lack of generalizability given that most of the study participants were white women, and a lack of data on binge drinking and whether alcohol was consumed with meals, they added. The study strengths included the prospective design, large size, long-term follow-up, and use of validated questionnaires, they said.
The researchers cautioned that the results should not be interpreted without considering other health outcomes. “Consistent with the 2020 Dietary Guidelines for Americans, which recommend that adults who do not consume alcohol do not initiate drinking, it may not be prudent for those with a history of gestational diabetes who do not consume alcohol to initiate drinking alcohol solely to reduce their risk for type 2 diabetes,” they emphasized.
Risk/benefit ratio for alcohol includes many factors
“There is a relative paucity of data regarding women’s long-term health as it may relate to pregnancy and pregnancy outcomes,” Angela Bianco, MD, of Mount Sinai Hospital, New York, said in an interview.
Dr. Bianco said she was surprised by some of the study findings.
“Generally speaking, I consider alcohol to be of little to no nutritional value, and to have a high sugar content/glycemic index,” she said. “However, a reduced incidence of adult-onset diabetes has been observed among moderate drinkers in other large prospective studies as well,” she noted. “In contrast, some studies have shown an increased risk of diabetes among a proportion of subjects in the top alcohol consumption category, while other studies have found no association. Possible inconsistencies may be due to differences in drinking patterns and the types of beverages consumed,” Dr. Bianco explained.
A key point for clinicians to keep in mind is that “the study may be flawed based on the different criteria used to make a diagnosis of history of gestational diabetes, the fact that they excluded patients that did not return the questionnaires, and the fact that respondents may not have answered correctly due to recall bias” or other reasons, Dr. Bianco said. “Additionally, those who responded obviously had access to health care, which in and of itself is a confounder,” she noted.
Another key point is that “the effect of alcohol being consumed with or without a meal was not examined,” said Dr. Bianco. “Alcohol concentration is reduced if consumed with meals. Alcohol can lead to hypoglycemia (from reduced gluconeogenesis) during fasting states, but after meals (postprandial states) it can result in lower glucose disposal and higher blood glucose levels,” she said. “The available literature suggests that alcohol may improve insulin sensitivity and reduce resistance, but there is likely a U-shaped association between alcohol consumption and the risk of diabetes,” Dr. Bianco noted. “There is likely a delicate balance between benefits and risks of alcohol intake. The inherent benefit/risk ratio must take into account with other potential comorbidities including BMI, activity level, stress, and preexisting conditions,” she said.
“Additional long-term studies engaging patients with diverse ethnic and socioeconomic backgrounds with detailed information regarding the role of nutrition, alcohol intake, tobacco and drug use, environmental exposures, and medical comorbidities need to be performed,” Dr. Bianco concluded.
The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute of General Medical Sciences, and the National Institute of Diabetes and Digestive and Kidney Diseases; the Nurses’ Health Study II was supported by the National Institutes of Health. Lead author Dr. Hinkle and coauthor Cuilin Zhang, MD, are employees of the U.S. federal government. The researchers and Dr. Bianco had no financial conflicts to disclose.
Among women with a history of gestational diabetes, alcohol intake of half a drink to one drink daily was associated with a 55% lower risk for subsequent type 2 diabetes, based on data from approximately 4,700 women in the Nurses’ Health Study II cohort.
However, the findings must be considered in the context of other risks and benefits of alcohol consumption before making statements or clinical recommendations, wrote Stefanie N. Hinkle, PhD, of the National Institutes of Health, Bethesda, Md., and colleagues.
Women with a history of gestational diabetes remain at increased risk for developing type 2 diabetes, so modifiable diet and lifestyle factors deserve further study, the researchers noted. Previous research has shown an association between light to moderate alcohol consumption and reduced risk of type 2 diabetes among women in the general population, but data on a similar risk reduction for women with a history of gestational diabetes are lacking, they added.
In a study published in JAMA Network Open, the researchers reviewed data from 4,740 women enrolled in the Nurses’ Health Study II who reported a history of gestational diabetes. These women were followed from Jan. 1, 1991, to Dec. 31, 2017, as part of the Diabetes & Women’s Health Study; dietary intake, including alcohol intake, was assessed every 4 years via validated food frequency questionnaires.
The average age at baseline was 38 years, and the median follow-up time was 24 years, yielding a total of 78,328 person-years of follow-up. Alcohol consumption was divided into four categories: none; 0.1 g/day to 4.9 g/day; 5.0 to 14.9 g/day, and 15.0 g/day or higher.
A total of 897 incident cases of type 2 diabetes were reported during the study period. After adjustment for multiple dietary and lifestyle variables, including diet and physical activity, only alcohol consumption of 5.0-14.9 g/day (approximately half a drink to one drink) was associated with a significantly decreased risk for incident type 2 diabetes (hazard ratio, 0.45) compared with women who reported no alcohol consumption.
On further adjustment for body mass index, women who reported alcohol consumption in the 5.0-14.9 g/day range had a 41% lower risk for developing incident type 2 diabetes (HR, 0.59); alcohol consumption in the other ranges remained unassociated with type 2 diabetes risk, although the researchers noted that these estimates were attenuated.
The median daily intake for women who consumed alcohol was 2.3 g/day, approximately one drink per week. Beer was the most frequently consumed type of alcohol.
When the researchers analyzed the data by alcohol type, notably, “only beer consumption of 1 or more servings a week was associated with a lower risk for type 2 diabetes,” although previous studies have suggested a stronger association in diabetes risk reduction with wine consumption vs. beer, the researchers noted.
The study findings were the potential for confounding factors not included in the adjustment, potential underreporting of alcohol intake, and potential screening bias toward women who were more health conscious, the researchers noted. Other limitations were lack of generalizability given that most of the study participants were white women, and a lack of data on binge drinking and whether alcohol was consumed with meals, they added. The study strengths included the prospective design, large size, long-term follow-up, and use of validated questionnaires, they said.
The researchers cautioned that the results should not be interpreted without considering other health outcomes. “Consistent with the 2020 Dietary Guidelines for Americans, which recommend that adults who do not consume alcohol do not initiate drinking, it may not be prudent for those with a history of gestational diabetes who do not consume alcohol to initiate drinking alcohol solely to reduce their risk for type 2 diabetes,” they emphasized.
Risk/benefit ratio for alcohol includes many factors
“There is a relative paucity of data regarding women’s long-term health as it may relate to pregnancy and pregnancy outcomes,” Angela Bianco, MD, of Mount Sinai Hospital, New York, said in an interview.
Dr. Bianco said she was surprised by some of the study findings.
“Generally speaking, I consider alcohol to be of little to no nutritional value, and to have a high sugar content/glycemic index,” she said. “However, a reduced incidence of adult-onset diabetes has been observed among moderate drinkers in other large prospective studies as well,” she noted. “In contrast, some studies have shown an increased risk of diabetes among a proportion of subjects in the top alcohol consumption category, while other studies have found no association. Possible inconsistencies may be due to differences in drinking patterns and the types of beverages consumed,” Dr. Bianco explained.
A key point for clinicians to keep in mind is that “the study may be flawed based on the different criteria used to make a diagnosis of history of gestational diabetes, the fact that they excluded patients that did not return the questionnaires, and the fact that respondents may not have answered correctly due to recall bias” or other reasons, Dr. Bianco said. “Additionally, those who responded obviously had access to health care, which in and of itself is a confounder,” she noted.
Another key point is that “the effect of alcohol being consumed with or without a meal was not examined,” said Dr. Bianco. “Alcohol concentration is reduced if consumed with meals. Alcohol can lead to hypoglycemia (from reduced gluconeogenesis) during fasting states, but after meals (postprandial states) it can result in lower glucose disposal and higher blood glucose levels,” she said. “The available literature suggests that alcohol may improve insulin sensitivity and reduce resistance, but there is likely a U-shaped association between alcohol consumption and the risk of diabetes,” Dr. Bianco noted. “There is likely a delicate balance between benefits and risks of alcohol intake. The inherent benefit/risk ratio must take into account with other potential comorbidities including BMI, activity level, stress, and preexisting conditions,” she said.
“Additional long-term studies engaging patients with diverse ethnic and socioeconomic backgrounds with detailed information regarding the role of nutrition, alcohol intake, tobacco and drug use, environmental exposures, and medical comorbidities need to be performed,” Dr. Bianco concluded.
The study was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute of General Medical Sciences, and the National Institute of Diabetes and Digestive and Kidney Diseases; the Nurses’ Health Study II was supported by the National Institutes of Health. Lead author Dr. Hinkle and coauthor Cuilin Zhang, MD, are employees of the U.S. federal government. The researchers and Dr. Bianco had no financial conflicts to disclose.
FROM JAMA NETWORK OPEN
COVID-19 claims more than 675,000 U.S. lives, surpassing the 1918 flu
, according to data collected by Johns Hopkins University.
Although the raw numbers match, epidemiologists point out that 675,000 deaths in 1918 was a much greater proportion of the population. In 1918, the U.S. population was 105 million, less than one third of what it is today.
The AIDS pandemic of the 1980s remains the deadliest of the 20th Century, claiming the lives of 700,000 Americans. But at our current pace of 2,000 COVID deaths a day, we could quickly eclipse that death toll, too.
Even though the 1918 epidemic is often called the “Spanish Flu,” there is no universal consensus regarding where the virus originated, according to the Centers for Disease Control and Prevention.
Still, the almost incomprehensible loss harkens back to a time when medicine and technology were far less advanced than they are today.
In 1918, the United States didn’t have access to a vaccine, or near real-time tools to trace the spread and communicate the threat.
In some ways, the United States has failed to learn from the mistakes of the past.
There are many similarities between the two pandemics. In the spring of 1918, when the first wave of influenza hit, the United States and its allies were nearing victory in Europe in World War I. Just this summer the United States has ended its longest war, the conflict in Afghanistan, as COVID cases surge.
In both pandemics, hospitals and funeral homes were overrun and makeshift clinics were opened where space was available. Mask mandates were installed; schools, churches, and theaters closed; and social distancing was encouraged.
As is the case today, different jurisdictions took different steps to fight the pandemic and some were more successful than others.
According to History.com, in 1918, Philadelphia’s mayor said a popular annual parade could be held, and an estimated 200,000 people attended. In less than 2 weeks, more than 1,000 local residents were dead. But in St. Louis, public gatherings were banned, schools and theaters closed, and the death toll there was one eighth of Philadelphia’s.
Just as in 1918, America has at times continued to fan the flames of the epidemic by relaxing restrictions too quickly and relying on unproven treatments. Poor communication allowed younger people to feel that they wouldn’t necessarily face the worst consequences of the virus, contributing to a false sense of security in the age group that was fueling the spread.
“A lot of the mistakes that we definitely fell into in 1918, we hoped we wouldn’t fall into in 2020,” epidemiologist Stephen Kissler, PhD, of the Harvard T.H. Chan School of Public Health, told CNN. “We did.”
A version of this article first appeared on Medscape.com.
, according to data collected by Johns Hopkins University.
Although the raw numbers match, epidemiologists point out that 675,000 deaths in 1918 was a much greater proportion of the population. In 1918, the U.S. population was 105 million, less than one third of what it is today.
The AIDS pandemic of the 1980s remains the deadliest of the 20th Century, claiming the lives of 700,000 Americans. But at our current pace of 2,000 COVID deaths a day, we could quickly eclipse that death toll, too.
Even though the 1918 epidemic is often called the “Spanish Flu,” there is no universal consensus regarding where the virus originated, according to the Centers for Disease Control and Prevention.
Still, the almost incomprehensible loss harkens back to a time when medicine and technology were far less advanced than they are today.
In 1918, the United States didn’t have access to a vaccine, or near real-time tools to trace the spread and communicate the threat.
In some ways, the United States has failed to learn from the mistakes of the past.
There are many similarities between the two pandemics. In the spring of 1918, when the first wave of influenza hit, the United States and its allies were nearing victory in Europe in World War I. Just this summer the United States has ended its longest war, the conflict in Afghanistan, as COVID cases surge.
In both pandemics, hospitals and funeral homes were overrun and makeshift clinics were opened where space was available. Mask mandates were installed; schools, churches, and theaters closed; and social distancing was encouraged.
As is the case today, different jurisdictions took different steps to fight the pandemic and some were more successful than others.
According to History.com, in 1918, Philadelphia’s mayor said a popular annual parade could be held, and an estimated 200,000 people attended. In less than 2 weeks, more than 1,000 local residents were dead. But in St. Louis, public gatherings were banned, schools and theaters closed, and the death toll there was one eighth of Philadelphia’s.
Just as in 1918, America has at times continued to fan the flames of the epidemic by relaxing restrictions too quickly and relying on unproven treatments. Poor communication allowed younger people to feel that they wouldn’t necessarily face the worst consequences of the virus, contributing to a false sense of security in the age group that was fueling the spread.
“A lot of the mistakes that we definitely fell into in 1918, we hoped we wouldn’t fall into in 2020,” epidemiologist Stephen Kissler, PhD, of the Harvard T.H. Chan School of Public Health, told CNN. “We did.”
A version of this article first appeared on Medscape.com.
, according to data collected by Johns Hopkins University.
Although the raw numbers match, epidemiologists point out that 675,000 deaths in 1918 was a much greater proportion of the population. In 1918, the U.S. population was 105 million, less than one third of what it is today.
The AIDS pandemic of the 1980s remains the deadliest of the 20th Century, claiming the lives of 700,000 Americans. But at our current pace of 2,000 COVID deaths a day, we could quickly eclipse that death toll, too.
Even though the 1918 epidemic is often called the “Spanish Flu,” there is no universal consensus regarding where the virus originated, according to the Centers for Disease Control and Prevention.
Still, the almost incomprehensible loss harkens back to a time when medicine and technology were far less advanced than they are today.
In 1918, the United States didn’t have access to a vaccine, or near real-time tools to trace the spread and communicate the threat.
In some ways, the United States has failed to learn from the mistakes of the past.
There are many similarities between the two pandemics. In the spring of 1918, when the first wave of influenza hit, the United States and its allies were nearing victory in Europe in World War I. Just this summer the United States has ended its longest war, the conflict in Afghanistan, as COVID cases surge.
In both pandemics, hospitals and funeral homes were overrun and makeshift clinics were opened where space was available. Mask mandates were installed; schools, churches, and theaters closed; and social distancing was encouraged.
As is the case today, different jurisdictions took different steps to fight the pandemic and some were more successful than others.
According to History.com, in 1918, Philadelphia’s mayor said a popular annual parade could be held, and an estimated 200,000 people attended. In less than 2 weeks, more than 1,000 local residents were dead. But in St. Louis, public gatherings were banned, schools and theaters closed, and the death toll there was one eighth of Philadelphia’s.
Just as in 1918, America has at times continued to fan the flames of the epidemic by relaxing restrictions too quickly and relying on unproven treatments. Poor communication allowed younger people to feel that they wouldn’t necessarily face the worst consequences of the virus, contributing to a false sense of security in the age group that was fueling the spread.
“A lot of the mistakes that we definitely fell into in 1918, we hoped we wouldn’t fall into in 2020,” epidemiologist Stephen Kissler, PhD, of the Harvard T.H. Chan School of Public Health, told CNN. “We did.”
A version of this article first appeared on Medscape.com.
Adolescent immunizations and protecting our children from COVID-19
I began thinking of a topic for this column weeks ago determined to discuss anything except COVID-19. Yet, news reports from all sources blasted daily reminders of rising COVID-19 cases overall and specifically in children.
In August, school resumed for many of our patients and the battle over mandating masks for school attendance was in full swing. The fact that it is a Centers for Disease Control and Prevention recommendation supported by both the American Academy of Pediatrics and the Pediatric Infectious Disease Society fell on deaf ears. One day, I heard a report that over 25,000 students attending Texas public schools were diagnosed with COVID-19 between Aug. 23 and Aug. 29. This peak in activity occurred just 2 weeks after the start of school and led to the closure of 45 school districts. Texas does not have a monopoly on these rising cases. Delta, a more contagious variant, began circulating in June 2021 and by July it was the most predominant. Emergency department visits and hospitalizations have increased nationwide. During the latter 2 weeks of August 2021, COVID-19–related ED visits and hospitalizations for persons aged 0-17 years were 3.4 and 3.7 times higher in states with the lowest vaccination coverage, compared with states with high vaccination coverage (MMWR Morb Mortal Wkly Rep. 2021;70:1249-54). Specifically, the rates of hospitalization the week ending Aug. 14, 2021, were nearly 5 times the rates for the week ending June 26, 2021, for 0- to 17-year-olds and nearly 10 times the rates for children 0-4 years of age. Hospitalization rates were 10.1 times higher for unimmunized adolescents than for fully vaccinated ones (MMWR Morb Mortal Wkly Rep. 2021;70:1255-60).
Multiple elected state leaders have opposed interventions such as mandating masks in school, and our children are paying for it. These leaders have relinquished their responsibility to local school boards. Several have reinforced the no-mask mandate while others have had the courage and insight to ignore state government leaders and have established mask mandates.
How is this lack of enforcement of national recommendations affecting our patients? Let’s look at two neighboring school districts in Texas. School districts have COVID-19 dashboards that are updated daily and accessible to the general public. School District A requires masks for school entry. It serves 196,171 students and has 27,195 teachers and staff. Since school opened in August, 1,606 cumulative cases of COVID-19 in students (0.8%) and 282 in staff (1%) have been reported. Fifty-five percent of the student cases occurred in elementary schools. In contrast, School District B located in the adjacent county serves 64,517 students and has 3,906 teachers and staff with no mask mandate. Since August, there have been 4,506 cumulative COVID-19 cases in students (6.9%) and 578 (14.7%) in staff. Information regarding the specific school type was not provided; however, the dashboard indicates that 2,924 cases (64.8%) occurred in children younger than 11 years of age. County data indicate 62% of those older than 12 years of age were fully vaccinated in District A, compared with 54% of persons older than 12 years in District B. The county COVID-19 positivity rate in District A is 17.6% and in District B it is 20%. Both counties are experiencing increased COVID-19 activity yet have had strikingly different outcomes in the student/staff population. While supporting the case for wearing masks to prevent disease transmission, one can’t ignore the adolescents who were infected and vaccine eligible (District A: 706; District B: 1,582). Their vaccination status could not be determined.
As pediatricians we have played an integral part in the elimination of diseases through educating and administering vaccinations. Adolescents are relatively healthy, thus limiting the number of encounters with them. The majority complete the 11-year visit; however, many fail to return for the 16- to 18-year visit.
So how are we doing? CDC data from 10 U.S. jurisdictions demonstrated a substantial decrease in vaccine administration between March and May of 2020, compared with the same period in 2018 and 2019. A decline was anticipated because of the nationwide lockdown. Doses of HPV administered declined almost 64% and 71% for 9- to 12-year-olds and 13- to 17-year-olds, respectively. Tdap administration declined 66% and 61% for the same respective age groups. Although administered doses increased between June and September of 2020, it was not sufficient to achieve catch-up coverage. Compared to the same period in 2018-2019, administration of the HPV vaccine declined 12.8% and 28% (ages 9-12 and ages 13-17) and for Tdap it was 21% and 30% lower (ages 9-12 and ages 13-17) (MMWR Morb Mortal Wkly Rep. 2021;70:840-5).
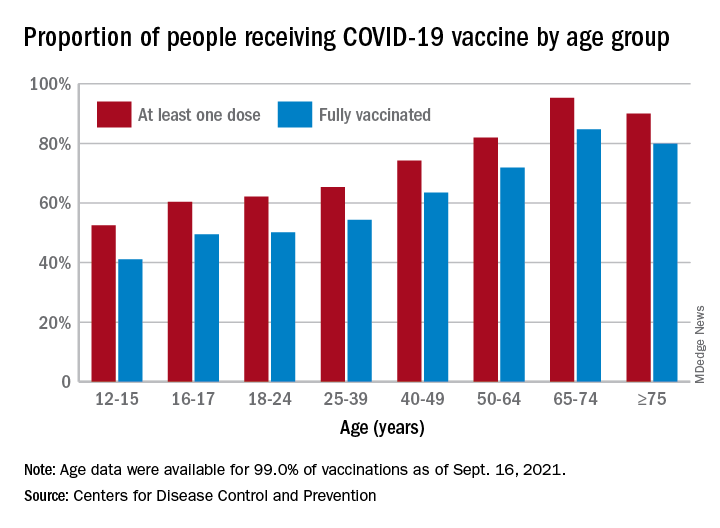
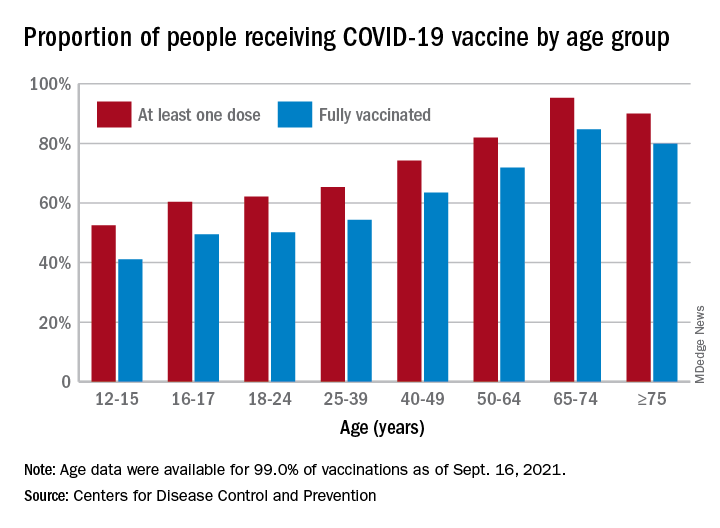
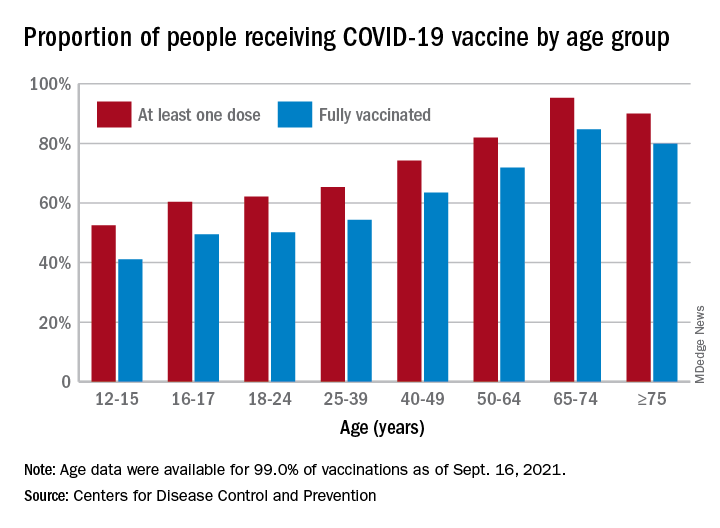
Now, we have another adolescent vaccine to discuss and encourage our patients to receive. We also need to address their concerns and/or to at least direct them to a reliable source to obtain accurate information. For the first time, a recommended vaccine may not be available at their medical home. Many don’t know where to go to receive it (http://www.vaccines.gov). Results of a Kaiser Family Foundation COVID-19 survey (August 2021) indicated that parents trusted their pediatricians most often (78%) for vaccine advice. The respondents voiced concern about trusting the location where the child would be immunized and long-term effects especially related to fertility. Parents who received communications regarding the benefits of vaccination were twice as likely to have their adolescents immunized. Finally, remember: Like parent, like child. An immunized parent is more likely to immunize the adolescent. (See Fig. 1.)
It is beyond the scope of this column to discuss the psychosocial aspects of this disease: children experiencing the death of teachers, classmates, family members, and those viewing the vitriol between pro- and antimask proponents often exhibited on school premises. And let’s not forget the child who wants to wear a mask but may be ostracized or bullied for doing so.
Our job is to do our very best to advocate for and to protect our patients by promoting mandatory masks at schools and encouraging vaccination of adolescents as we patiently wait for vaccines to become available for all of our children.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
I began thinking of a topic for this column weeks ago determined to discuss anything except COVID-19. Yet, news reports from all sources blasted daily reminders of rising COVID-19 cases overall and specifically in children.
In August, school resumed for many of our patients and the battle over mandating masks for school attendance was in full swing. The fact that it is a Centers for Disease Control and Prevention recommendation supported by both the American Academy of Pediatrics and the Pediatric Infectious Disease Society fell on deaf ears. One day, I heard a report that over 25,000 students attending Texas public schools were diagnosed with COVID-19 between Aug. 23 and Aug. 29. This peak in activity occurred just 2 weeks after the start of school and led to the closure of 45 school districts. Texas does not have a monopoly on these rising cases. Delta, a more contagious variant, began circulating in June 2021 and by July it was the most predominant. Emergency department visits and hospitalizations have increased nationwide. During the latter 2 weeks of August 2021, COVID-19–related ED visits and hospitalizations for persons aged 0-17 years were 3.4 and 3.7 times higher in states with the lowest vaccination coverage, compared with states with high vaccination coverage (MMWR Morb Mortal Wkly Rep. 2021;70:1249-54). Specifically, the rates of hospitalization the week ending Aug. 14, 2021, were nearly 5 times the rates for the week ending June 26, 2021, for 0- to 17-year-olds and nearly 10 times the rates for children 0-4 years of age. Hospitalization rates were 10.1 times higher for unimmunized adolescents than for fully vaccinated ones (MMWR Morb Mortal Wkly Rep. 2021;70:1255-60).
Multiple elected state leaders have opposed interventions such as mandating masks in school, and our children are paying for it. These leaders have relinquished their responsibility to local school boards. Several have reinforced the no-mask mandate while others have had the courage and insight to ignore state government leaders and have established mask mandates.
How is this lack of enforcement of national recommendations affecting our patients? Let’s look at two neighboring school districts in Texas. School districts have COVID-19 dashboards that are updated daily and accessible to the general public. School District A requires masks for school entry. It serves 196,171 students and has 27,195 teachers and staff. Since school opened in August, 1,606 cumulative cases of COVID-19 in students (0.8%) and 282 in staff (1%) have been reported. Fifty-five percent of the student cases occurred in elementary schools. In contrast, School District B located in the adjacent county serves 64,517 students and has 3,906 teachers and staff with no mask mandate. Since August, there have been 4,506 cumulative COVID-19 cases in students (6.9%) and 578 (14.7%) in staff. Information regarding the specific school type was not provided; however, the dashboard indicates that 2,924 cases (64.8%) occurred in children younger than 11 years of age. County data indicate 62% of those older than 12 years of age were fully vaccinated in District A, compared with 54% of persons older than 12 years in District B. The county COVID-19 positivity rate in District A is 17.6% and in District B it is 20%. Both counties are experiencing increased COVID-19 activity yet have had strikingly different outcomes in the student/staff population. While supporting the case for wearing masks to prevent disease transmission, one can’t ignore the adolescents who were infected and vaccine eligible (District A: 706; District B: 1,582). Their vaccination status could not be determined.
As pediatricians we have played an integral part in the elimination of diseases through educating and administering vaccinations. Adolescents are relatively healthy, thus limiting the number of encounters with them. The majority complete the 11-year visit; however, many fail to return for the 16- to 18-year visit.
So how are we doing? CDC data from 10 U.S. jurisdictions demonstrated a substantial decrease in vaccine administration between March and May of 2020, compared with the same period in 2018 and 2019. A decline was anticipated because of the nationwide lockdown. Doses of HPV administered declined almost 64% and 71% for 9- to 12-year-olds and 13- to 17-year-olds, respectively. Tdap administration declined 66% and 61% for the same respective age groups. Although administered doses increased between June and September of 2020, it was not sufficient to achieve catch-up coverage. Compared to the same period in 2018-2019, administration of the HPV vaccine declined 12.8% and 28% (ages 9-12 and ages 13-17) and for Tdap it was 21% and 30% lower (ages 9-12 and ages 13-17) (MMWR Morb Mortal Wkly Rep. 2021;70:840-5).
Now, we have another adolescent vaccine to discuss and encourage our patients to receive. We also need to address their concerns and/or to at least direct them to a reliable source to obtain accurate information. For the first time, a recommended vaccine may not be available at their medical home. Many don’t know where to go to receive it (http://www.vaccines.gov). Results of a Kaiser Family Foundation COVID-19 survey (August 2021) indicated that parents trusted their pediatricians most often (78%) for vaccine advice. The respondents voiced concern about trusting the location where the child would be immunized and long-term effects especially related to fertility. Parents who received communications regarding the benefits of vaccination were twice as likely to have their adolescents immunized. Finally, remember: Like parent, like child. An immunized parent is more likely to immunize the adolescent. (See Fig. 1.)
It is beyond the scope of this column to discuss the psychosocial aspects of this disease: children experiencing the death of teachers, classmates, family members, and those viewing the vitriol between pro- and antimask proponents often exhibited on school premises. And let’s not forget the child who wants to wear a mask but may be ostracized or bullied for doing so.
Our job is to do our very best to advocate for and to protect our patients by promoting mandatory masks at schools and encouraging vaccination of adolescents as we patiently wait for vaccines to become available for all of our children.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
I began thinking of a topic for this column weeks ago determined to discuss anything except COVID-19. Yet, news reports from all sources blasted daily reminders of rising COVID-19 cases overall and specifically in children.
In August, school resumed for many of our patients and the battle over mandating masks for school attendance was in full swing. The fact that it is a Centers for Disease Control and Prevention recommendation supported by both the American Academy of Pediatrics and the Pediatric Infectious Disease Society fell on deaf ears. One day, I heard a report that over 25,000 students attending Texas public schools were diagnosed with COVID-19 between Aug. 23 and Aug. 29. This peak in activity occurred just 2 weeks after the start of school and led to the closure of 45 school districts. Texas does not have a monopoly on these rising cases. Delta, a more contagious variant, began circulating in June 2021 and by July it was the most predominant. Emergency department visits and hospitalizations have increased nationwide. During the latter 2 weeks of August 2021, COVID-19–related ED visits and hospitalizations for persons aged 0-17 years were 3.4 and 3.7 times higher in states with the lowest vaccination coverage, compared with states with high vaccination coverage (MMWR Morb Mortal Wkly Rep. 2021;70:1249-54). Specifically, the rates of hospitalization the week ending Aug. 14, 2021, were nearly 5 times the rates for the week ending June 26, 2021, for 0- to 17-year-olds and nearly 10 times the rates for children 0-4 years of age. Hospitalization rates were 10.1 times higher for unimmunized adolescents than for fully vaccinated ones (MMWR Morb Mortal Wkly Rep. 2021;70:1255-60).
Multiple elected state leaders have opposed interventions such as mandating masks in school, and our children are paying for it. These leaders have relinquished their responsibility to local school boards. Several have reinforced the no-mask mandate while others have had the courage and insight to ignore state government leaders and have established mask mandates.
How is this lack of enforcement of national recommendations affecting our patients? Let’s look at two neighboring school districts in Texas. School districts have COVID-19 dashboards that are updated daily and accessible to the general public. School District A requires masks for school entry. It serves 196,171 students and has 27,195 teachers and staff. Since school opened in August, 1,606 cumulative cases of COVID-19 in students (0.8%) and 282 in staff (1%) have been reported. Fifty-five percent of the student cases occurred in elementary schools. In contrast, School District B located in the adjacent county serves 64,517 students and has 3,906 teachers and staff with no mask mandate. Since August, there have been 4,506 cumulative COVID-19 cases in students (6.9%) and 578 (14.7%) in staff. Information regarding the specific school type was not provided; however, the dashboard indicates that 2,924 cases (64.8%) occurred in children younger than 11 years of age. County data indicate 62% of those older than 12 years of age were fully vaccinated in District A, compared with 54% of persons older than 12 years in District B. The county COVID-19 positivity rate in District A is 17.6% and in District B it is 20%. Both counties are experiencing increased COVID-19 activity yet have had strikingly different outcomes in the student/staff population. While supporting the case for wearing masks to prevent disease transmission, one can’t ignore the adolescents who were infected and vaccine eligible (District A: 706; District B: 1,582). Their vaccination status could not be determined.
As pediatricians we have played an integral part in the elimination of diseases through educating and administering vaccinations. Adolescents are relatively healthy, thus limiting the number of encounters with them. The majority complete the 11-year visit; however, many fail to return for the 16- to 18-year visit.
So how are we doing? CDC data from 10 U.S. jurisdictions demonstrated a substantial decrease in vaccine administration between March and May of 2020, compared with the same period in 2018 and 2019. A decline was anticipated because of the nationwide lockdown. Doses of HPV administered declined almost 64% and 71% for 9- to 12-year-olds and 13- to 17-year-olds, respectively. Tdap administration declined 66% and 61% for the same respective age groups. Although administered doses increased between June and September of 2020, it was not sufficient to achieve catch-up coverage. Compared to the same period in 2018-2019, administration of the HPV vaccine declined 12.8% and 28% (ages 9-12 and ages 13-17) and for Tdap it was 21% and 30% lower (ages 9-12 and ages 13-17) (MMWR Morb Mortal Wkly Rep. 2021;70:840-5).
Now, we have another adolescent vaccine to discuss and encourage our patients to receive. We also need to address their concerns and/or to at least direct them to a reliable source to obtain accurate information. For the first time, a recommended vaccine may not be available at their medical home. Many don’t know where to go to receive it (http://www.vaccines.gov). Results of a Kaiser Family Foundation COVID-19 survey (August 2021) indicated that parents trusted their pediatricians most often (78%) for vaccine advice. The respondents voiced concern about trusting the location where the child would be immunized and long-term effects especially related to fertility. Parents who received communications regarding the benefits of vaccination were twice as likely to have their adolescents immunized. Finally, remember: Like parent, like child. An immunized parent is more likely to immunize the adolescent. (See Fig. 1.)
It is beyond the scope of this column to discuss the psychosocial aspects of this disease: children experiencing the death of teachers, classmates, family members, and those viewing the vitriol between pro- and antimask proponents often exhibited on school premises. And let’s not forget the child who wants to wear a mask but may be ostracized or bullied for doing so.
Our job is to do our very best to advocate for and to protect our patients by promoting mandatory masks at schools and encouraging vaccination of adolescents as we patiently wait for vaccines to become available for all of our children.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
EMPEROR-Preserved: Empagliflozin’s HFpEF efficacy catalyzes a heart failure redefinition
Groundbreaking results from the EMPEROR-Preserved trial did more than establish for the first time that a drug, empagliflozin, has clearly proven efficacy for treating patients with heart failure with preserved ejection fraction (HFpEF). The results also helped catalyze a paradigm shift in how heart failure thought leaders think about the role of ejection fraction for making important distinctions among patients with heart failure.
EMPEROR-Preserved may also be the final nail in the coffin for defining patients with heart failure as having HFpEF or heart failure with reduced ejection fraction (HFrEF).
This new consensus essentially throws out left ventricular ejection fraction (EF) as the key metric for matching patients to heart failure treatments. Experts have instead begun suggesting a more unified treatment approach for all heart failure patients regardless of their EF.
‘Forget about ejection fraction’
“We encourage you to forget about ejection fraction,” declared Milton Packer, MD, during discussion at a session of the annual scientific meeting of the Heart Failure Society of America. “We certainly encourage you to forget about an ejection fraction of less than 40%” as having special significance,” added Dr. Packer, a lead investigator for both the EMPEROR-Reduced and EMPEROR-Preserved trials (which researchers combined in a unified analysis with a total of 9,718 patients with heart failure called EMPEROR-Pooled), and a heart failure researcher at Baylor University Medical Center in Dallas.
“The 40% ejection fraction divide is artificial. It was created in 2003 as part of a trial design, but it has no physiological significance,” Dr. Packer explained. A much better way to distinguish systolic and diastolic heart failure is by strain assessment rather than by ejection fraction. “Strain is a measure of myocardial shortening, a measure of what the heart does. Ejection fraction is a measure of volume,” said Dr. Packer. “Sign me up to get rid of ejection fraction,” he added.
“Ejection fraction is not as valuable as we thought for distinguishing the therapeutic benefit” of heart failure drugs, agreed Marvin A. Konstam, MD, professor of medicine at Tufts University and chief physician executive of the CardioVascular Center of Tufts Medical Center, both in Boston, who spoke during a different session at the meeting.
“It would easier if we didn’t spend time parsing this number,” ejection fraction, commented Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern Medicine in Chicago. “Wouldn’t it be easier if we said that every patient with heart failure needs to receive one agent from each of the four [pillar] drug classes, and put them in a polypill” at reduced dosages, he proposed, envisioning one potential consequence of jettisoning ejection fraction.
The four pillar drug classes, recently identified as essential for patients with HFrEF but until now not endorsed for patients with HFpEF, are the sodium-glucose cotransporter 2 (SGLT2) inhibitors, such as empagliflozin (Jardiance); an angiotensin receptor blocker neprilysin inhibitor compound such as sacubitril/valsartan (Entresto); beta-blockers; and mineralocorticoid receptor antagonists such as spironolactone and eplerenone.
An opportunity for ‘simpler and easier’ treatments
“This is an opportunity to disrupt the way we’ve been doing things and think about something that is simpler and easier,” said Dr. Yancy, who chaired some of the panels serially formed by the American Heart Association and American College of Cardiology to write guidelines for treating heart failure. “An approach that would be easier to implement without worrying about staggering the start of each drug class and an incessant focus on titrating individual elements and taking 6 months to get to a certain place.”
Results from EMPEROR-Preserved and the combined EMPEROR-Pooled analysis triggered these paradigm-shifting sentiments by showing clear evidence that treatment with empagliflozin exerts consistent benefit – and is consistently safe – for patients with heart failure across a spectrum of EFs, from less than 25% to 64%, though its performance in patients with HFpEF and EFs of 65% or greater in the EMPEROR-Preserved trial remains unclear.
The consequence is that clinicians should feel comfortable prescribing empagliflozin to most patients with heart failure without regard to EF, even patients with EF values in the mid-60% range.
The EMPEROR-Preserved results showed a clear signal of attenuated benefit among patients with an EF of 65% or greater “on a population basis,” stressed Dr. Packer. “But on an individual basis, ejection fraction is not that reproducible, so measuring ejection fraction will not help you determine whom to treat or not treat. “
“There is significant variability” measuring EF using the most common modality, echocardiography, noted Javed Butler, MD, an EMPEROR coinvestigator who also spoke at the meeting session. A person with a measured EF of 65% could actually have a value that may be as low as 58% or as high as about 72%, noted Dr. Butler, who is professor and chair of medicine at the University of Mississippi, Jackson. The upshot is that any patient diagnosed with heart failure should receive an SGLT2 inhibitor “irrespective of their ejection fraction,” Dr. Butler advised.
“Ejection fraction is very crude, and probably not sufficient to identify a phenotype,” for treatment, said Dr. Yancy. “The real takeaway may be that we need to revisit what we call HFrEF, and then let that be the new standard for treatment.”
“Is [an EF of] 60% the new 40%?” asked Dr. Packer, implying that the answer was yes.
Results from several trials suggest redefining HFrEF
The idea that patients without traditionally defined HFrEF – an EF of 40% or less – could also benefit from other classes of heart failure drugs has been gestating for a while, and then rose to a new level with the August 2021 report of results from EMPEROR-Preserved. Two years ago, in September 2019, Dr. Butler, Dr. Packer, and a third colleague advanced the notion of redefining HFrEF by raising the ejection fraction ceiling in a published commentary.
They cited the experience with the angiotensin receptor blocker candesartan in a post hoc analysis of data collected in the CHARM-Preserved trial, which showed a strong signal of benefit in the subgroup of patients with EFs of 41%-49%, but not in those with an EF of 50% or higher. This finding prompted Dr. Konstam to express doubts about relying on EF to define heart failure subgroups in trials and guide management in a commentary published more than 3 years ago.
Another crack in the traditional EF framework came from analysis of results from the TOPCAT trial that tested spironolactone as a treatment for patients with HFpEF, according to the 2019 opinion published by Dr. Butler and Dr. Packer. Once again a post hoc analysis, this time using data from TOPCAT, suggested a benefit from the mineralocorticoid receptor antagonist spironolactone in patients with heart failure and an EF of 45%-49% (45% was the minimum EF for enrollment into the study).
Recently, data from a third trial that tested sacubitril/valsartan in patients with HFpEF, PARAGON-HF, showed benefit among patients with EFs below the study median of 57%. This finding led the Food and Drug Administration in February 2021 to amend its initial approval for sacubitril/valsartan by removing a specific EF ceiling from the drug’s indication and instead saying that patient’s receiving the drug should have a “below normal” EF.
Writing in a recent commentary, Dr. Yancy called the FDA’s action on sacubitril/valsartan “reasonable,” and that the subgroup assessment of data from the PARAGON-HF trial creates a “new, reasonably evidence-based therapy for HFpEF.” He also predicted that guideline-writing panels will “likely align with a permissive statement of indication” for sacubitril/valsartan in patients with HFpEF, especially those with EFs of less than 57%.
The idea of using an SGLT2 inhibitor like empagliflozin on all heart failure patients, and also adding agents like sacubitril/valsartan and spironolactone in patients with HFpEF and EFs in the mid-50% range or lower may take some time to catch on, but it already has one influential advocate.
“If a patient has HFpEF with an EF of less than 55%, use quadruple-class therapy,” summed up Dr. Butler during the HFSA session, while also suggesting prescribing an SGLT2 inhibitor to essentially all patients with heart failure regardless of their EF.
The EMPEROR-Preserved and EMPEROR-Reduced trials and the EMPEROR-Pooled analysis were sponsored by Boehringer Ingelheim and Lilly, the companies that jointly market empagliflozin (Jardiance). Dr. Packer has had financial relationships with BI and Lilly and numerous other companies. Dr. Konstam has served on data monitoring committees for trials funded by Boehringer Ingelheim and by Amgen, Luitpold, and Pfizer, and has been a consultant to Arena, LivaNova, Merck, SC Pharma, and Takeda. Dr. Yancy had no disclosures. Dr. Butler has had financial relationships with Boehringer Ingelheim and numerous other companies.
Groundbreaking results from the EMPEROR-Preserved trial did more than establish for the first time that a drug, empagliflozin, has clearly proven efficacy for treating patients with heart failure with preserved ejection fraction (HFpEF). The results also helped catalyze a paradigm shift in how heart failure thought leaders think about the role of ejection fraction for making important distinctions among patients with heart failure.
EMPEROR-Preserved may also be the final nail in the coffin for defining patients with heart failure as having HFpEF or heart failure with reduced ejection fraction (HFrEF).
This new consensus essentially throws out left ventricular ejection fraction (EF) as the key metric for matching patients to heart failure treatments. Experts have instead begun suggesting a more unified treatment approach for all heart failure patients regardless of their EF.
‘Forget about ejection fraction’
“We encourage you to forget about ejection fraction,” declared Milton Packer, MD, during discussion at a session of the annual scientific meeting of the Heart Failure Society of America. “We certainly encourage you to forget about an ejection fraction of less than 40%” as having special significance,” added Dr. Packer, a lead investigator for both the EMPEROR-Reduced and EMPEROR-Preserved trials (which researchers combined in a unified analysis with a total of 9,718 patients with heart failure called EMPEROR-Pooled), and a heart failure researcher at Baylor University Medical Center in Dallas.
“The 40% ejection fraction divide is artificial. It was created in 2003 as part of a trial design, but it has no physiological significance,” Dr. Packer explained. A much better way to distinguish systolic and diastolic heart failure is by strain assessment rather than by ejection fraction. “Strain is a measure of myocardial shortening, a measure of what the heart does. Ejection fraction is a measure of volume,” said Dr. Packer. “Sign me up to get rid of ejection fraction,” he added.
“Ejection fraction is not as valuable as we thought for distinguishing the therapeutic benefit” of heart failure drugs, agreed Marvin A. Konstam, MD, professor of medicine at Tufts University and chief physician executive of the CardioVascular Center of Tufts Medical Center, both in Boston, who spoke during a different session at the meeting.
“It would easier if we didn’t spend time parsing this number,” ejection fraction, commented Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern Medicine in Chicago. “Wouldn’t it be easier if we said that every patient with heart failure needs to receive one agent from each of the four [pillar] drug classes, and put them in a polypill” at reduced dosages, he proposed, envisioning one potential consequence of jettisoning ejection fraction.
The four pillar drug classes, recently identified as essential for patients with HFrEF but until now not endorsed for patients with HFpEF, are the sodium-glucose cotransporter 2 (SGLT2) inhibitors, such as empagliflozin (Jardiance); an angiotensin receptor blocker neprilysin inhibitor compound such as sacubitril/valsartan (Entresto); beta-blockers; and mineralocorticoid receptor antagonists such as spironolactone and eplerenone.
An opportunity for ‘simpler and easier’ treatments
“This is an opportunity to disrupt the way we’ve been doing things and think about something that is simpler and easier,” said Dr. Yancy, who chaired some of the panels serially formed by the American Heart Association and American College of Cardiology to write guidelines for treating heart failure. “An approach that would be easier to implement without worrying about staggering the start of each drug class and an incessant focus on titrating individual elements and taking 6 months to get to a certain place.”
Results from EMPEROR-Preserved and the combined EMPEROR-Pooled analysis triggered these paradigm-shifting sentiments by showing clear evidence that treatment with empagliflozin exerts consistent benefit – and is consistently safe – for patients with heart failure across a spectrum of EFs, from less than 25% to 64%, though its performance in patients with HFpEF and EFs of 65% or greater in the EMPEROR-Preserved trial remains unclear.
The consequence is that clinicians should feel comfortable prescribing empagliflozin to most patients with heart failure without regard to EF, even patients with EF values in the mid-60% range.
The EMPEROR-Preserved results showed a clear signal of attenuated benefit among patients with an EF of 65% or greater “on a population basis,” stressed Dr. Packer. “But on an individual basis, ejection fraction is not that reproducible, so measuring ejection fraction will not help you determine whom to treat or not treat. “
“There is significant variability” measuring EF using the most common modality, echocardiography, noted Javed Butler, MD, an EMPEROR coinvestigator who also spoke at the meeting session. A person with a measured EF of 65% could actually have a value that may be as low as 58% or as high as about 72%, noted Dr. Butler, who is professor and chair of medicine at the University of Mississippi, Jackson. The upshot is that any patient diagnosed with heart failure should receive an SGLT2 inhibitor “irrespective of their ejection fraction,” Dr. Butler advised.
“Ejection fraction is very crude, and probably not sufficient to identify a phenotype,” for treatment, said Dr. Yancy. “The real takeaway may be that we need to revisit what we call HFrEF, and then let that be the new standard for treatment.”
“Is [an EF of] 60% the new 40%?” asked Dr. Packer, implying that the answer was yes.
Results from several trials suggest redefining HFrEF
The idea that patients without traditionally defined HFrEF – an EF of 40% or less – could also benefit from other classes of heart failure drugs has been gestating for a while, and then rose to a new level with the August 2021 report of results from EMPEROR-Preserved. Two years ago, in September 2019, Dr. Butler, Dr. Packer, and a third colleague advanced the notion of redefining HFrEF by raising the ejection fraction ceiling in a published commentary.
They cited the experience with the angiotensin receptor blocker candesartan in a post hoc analysis of data collected in the CHARM-Preserved trial, which showed a strong signal of benefit in the subgroup of patients with EFs of 41%-49%, but not in those with an EF of 50% or higher. This finding prompted Dr. Konstam to express doubts about relying on EF to define heart failure subgroups in trials and guide management in a commentary published more than 3 years ago.
Another crack in the traditional EF framework came from analysis of results from the TOPCAT trial that tested spironolactone as a treatment for patients with HFpEF, according to the 2019 opinion published by Dr. Butler and Dr. Packer. Once again a post hoc analysis, this time using data from TOPCAT, suggested a benefit from the mineralocorticoid receptor antagonist spironolactone in patients with heart failure and an EF of 45%-49% (45% was the minimum EF for enrollment into the study).
Recently, data from a third trial that tested sacubitril/valsartan in patients with HFpEF, PARAGON-HF, showed benefit among patients with EFs below the study median of 57%. This finding led the Food and Drug Administration in February 2021 to amend its initial approval for sacubitril/valsartan by removing a specific EF ceiling from the drug’s indication and instead saying that patient’s receiving the drug should have a “below normal” EF.
Writing in a recent commentary, Dr. Yancy called the FDA’s action on sacubitril/valsartan “reasonable,” and that the subgroup assessment of data from the PARAGON-HF trial creates a “new, reasonably evidence-based therapy for HFpEF.” He also predicted that guideline-writing panels will “likely align with a permissive statement of indication” for sacubitril/valsartan in patients with HFpEF, especially those with EFs of less than 57%.
The idea of using an SGLT2 inhibitor like empagliflozin on all heart failure patients, and also adding agents like sacubitril/valsartan and spironolactone in patients with HFpEF and EFs in the mid-50% range or lower may take some time to catch on, but it already has one influential advocate.
“If a patient has HFpEF with an EF of less than 55%, use quadruple-class therapy,” summed up Dr. Butler during the HFSA session, while also suggesting prescribing an SGLT2 inhibitor to essentially all patients with heart failure regardless of their EF.
The EMPEROR-Preserved and EMPEROR-Reduced trials and the EMPEROR-Pooled analysis were sponsored by Boehringer Ingelheim and Lilly, the companies that jointly market empagliflozin (Jardiance). Dr. Packer has had financial relationships with BI and Lilly and numerous other companies. Dr. Konstam has served on data monitoring committees for trials funded by Boehringer Ingelheim and by Amgen, Luitpold, and Pfizer, and has been a consultant to Arena, LivaNova, Merck, SC Pharma, and Takeda. Dr. Yancy had no disclosures. Dr. Butler has had financial relationships with Boehringer Ingelheim and numerous other companies.
Groundbreaking results from the EMPEROR-Preserved trial did more than establish for the first time that a drug, empagliflozin, has clearly proven efficacy for treating patients with heart failure with preserved ejection fraction (HFpEF). The results also helped catalyze a paradigm shift in how heart failure thought leaders think about the role of ejection fraction for making important distinctions among patients with heart failure.
EMPEROR-Preserved may also be the final nail in the coffin for defining patients with heart failure as having HFpEF or heart failure with reduced ejection fraction (HFrEF).
This new consensus essentially throws out left ventricular ejection fraction (EF) as the key metric for matching patients to heart failure treatments. Experts have instead begun suggesting a more unified treatment approach for all heart failure patients regardless of their EF.
‘Forget about ejection fraction’
“We encourage you to forget about ejection fraction,” declared Milton Packer, MD, during discussion at a session of the annual scientific meeting of the Heart Failure Society of America. “We certainly encourage you to forget about an ejection fraction of less than 40%” as having special significance,” added Dr. Packer, a lead investigator for both the EMPEROR-Reduced and EMPEROR-Preserved trials (which researchers combined in a unified analysis with a total of 9,718 patients with heart failure called EMPEROR-Pooled), and a heart failure researcher at Baylor University Medical Center in Dallas.
“The 40% ejection fraction divide is artificial. It was created in 2003 as part of a trial design, but it has no physiological significance,” Dr. Packer explained. A much better way to distinguish systolic and diastolic heart failure is by strain assessment rather than by ejection fraction. “Strain is a measure of myocardial shortening, a measure of what the heart does. Ejection fraction is a measure of volume,” said Dr. Packer. “Sign me up to get rid of ejection fraction,” he added.
“Ejection fraction is not as valuable as we thought for distinguishing the therapeutic benefit” of heart failure drugs, agreed Marvin A. Konstam, MD, professor of medicine at Tufts University and chief physician executive of the CardioVascular Center of Tufts Medical Center, both in Boston, who spoke during a different session at the meeting.
“It would easier if we didn’t spend time parsing this number,” ejection fraction, commented Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern Medicine in Chicago. “Wouldn’t it be easier if we said that every patient with heart failure needs to receive one agent from each of the four [pillar] drug classes, and put them in a polypill” at reduced dosages, he proposed, envisioning one potential consequence of jettisoning ejection fraction.
The four pillar drug classes, recently identified as essential for patients with HFrEF but until now not endorsed for patients with HFpEF, are the sodium-glucose cotransporter 2 (SGLT2) inhibitors, such as empagliflozin (Jardiance); an angiotensin receptor blocker neprilysin inhibitor compound such as sacubitril/valsartan (Entresto); beta-blockers; and mineralocorticoid receptor antagonists such as spironolactone and eplerenone.
An opportunity for ‘simpler and easier’ treatments
“This is an opportunity to disrupt the way we’ve been doing things and think about something that is simpler and easier,” said Dr. Yancy, who chaired some of the panels serially formed by the American Heart Association and American College of Cardiology to write guidelines for treating heart failure. “An approach that would be easier to implement without worrying about staggering the start of each drug class and an incessant focus on titrating individual elements and taking 6 months to get to a certain place.”
Results from EMPEROR-Preserved and the combined EMPEROR-Pooled analysis triggered these paradigm-shifting sentiments by showing clear evidence that treatment with empagliflozin exerts consistent benefit – and is consistently safe – for patients with heart failure across a spectrum of EFs, from less than 25% to 64%, though its performance in patients with HFpEF and EFs of 65% or greater in the EMPEROR-Preserved trial remains unclear.
The consequence is that clinicians should feel comfortable prescribing empagliflozin to most patients with heart failure without regard to EF, even patients with EF values in the mid-60% range.
The EMPEROR-Preserved results showed a clear signal of attenuated benefit among patients with an EF of 65% or greater “on a population basis,” stressed Dr. Packer. “But on an individual basis, ejection fraction is not that reproducible, so measuring ejection fraction will not help you determine whom to treat or not treat. “
“There is significant variability” measuring EF using the most common modality, echocardiography, noted Javed Butler, MD, an EMPEROR coinvestigator who also spoke at the meeting session. A person with a measured EF of 65% could actually have a value that may be as low as 58% or as high as about 72%, noted Dr. Butler, who is professor and chair of medicine at the University of Mississippi, Jackson. The upshot is that any patient diagnosed with heart failure should receive an SGLT2 inhibitor “irrespective of their ejection fraction,” Dr. Butler advised.
“Ejection fraction is very crude, and probably not sufficient to identify a phenotype,” for treatment, said Dr. Yancy. “The real takeaway may be that we need to revisit what we call HFrEF, and then let that be the new standard for treatment.”
“Is [an EF of] 60% the new 40%?” asked Dr. Packer, implying that the answer was yes.
Results from several trials suggest redefining HFrEF
The idea that patients without traditionally defined HFrEF – an EF of 40% or less – could also benefit from other classes of heart failure drugs has been gestating for a while, and then rose to a new level with the August 2021 report of results from EMPEROR-Preserved. Two years ago, in September 2019, Dr. Butler, Dr. Packer, and a third colleague advanced the notion of redefining HFrEF by raising the ejection fraction ceiling in a published commentary.
They cited the experience with the angiotensin receptor blocker candesartan in a post hoc analysis of data collected in the CHARM-Preserved trial, which showed a strong signal of benefit in the subgroup of patients with EFs of 41%-49%, but not in those with an EF of 50% or higher. This finding prompted Dr. Konstam to express doubts about relying on EF to define heart failure subgroups in trials and guide management in a commentary published more than 3 years ago.
Another crack in the traditional EF framework came from analysis of results from the TOPCAT trial that tested spironolactone as a treatment for patients with HFpEF, according to the 2019 opinion published by Dr. Butler and Dr. Packer. Once again a post hoc analysis, this time using data from TOPCAT, suggested a benefit from the mineralocorticoid receptor antagonist spironolactone in patients with heart failure and an EF of 45%-49% (45% was the minimum EF for enrollment into the study).
Recently, data from a third trial that tested sacubitril/valsartan in patients with HFpEF, PARAGON-HF, showed benefit among patients with EFs below the study median of 57%. This finding led the Food and Drug Administration in February 2021 to amend its initial approval for sacubitril/valsartan by removing a specific EF ceiling from the drug’s indication and instead saying that patient’s receiving the drug should have a “below normal” EF.
Writing in a recent commentary, Dr. Yancy called the FDA’s action on sacubitril/valsartan “reasonable,” and that the subgroup assessment of data from the PARAGON-HF trial creates a “new, reasonably evidence-based therapy for HFpEF.” He also predicted that guideline-writing panels will “likely align with a permissive statement of indication” for sacubitril/valsartan in patients with HFpEF, especially those with EFs of less than 57%.
The idea of using an SGLT2 inhibitor like empagliflozin on all heart failure patients, and also adding agents like sacubitril/valsartan and spironolactone in patients with HFpEF and EFs in the mid-50% range or lower may take some time to catch on, but it already has one influential advocate.
“If a patient has HFpEF with an EF of less than 55%, use quadruple-class therapy,” summed up Dr. Butler during the HFSA session, while also suggesting prescribing an SGLT2 inhibitor to essentially all patients with heart failure regardless of their EF.
The EMPEROR-Preserved and EMPEROR-Reduced trials and the EMPEROR-Pooled analysis were sponsored by Boehringer Ingelheim and Lilly, the companies that jointly market empagliflozin (Jardiance). Dr. Packer has had financial relationships with BI and Lilly and numerous other companies. Dr. Konstam has served on data monitoring committees for trials funded by Boehringer Ingelheim and by Amgen, Luitpold, and Pfizer, and has been a consultant to Arena, LivaNova, Merck, SC Pharma, and Takeda. Dr. Yancy had no disclosures. Dr. Butler has had financial relationships with Boehringer Ingelheim and numerous other companies.
FROM HFSA 2021
A new weight loss threshold for T2d remission after bariatric surgery?
Patients with type 2 diabetes who underwent bariatric surgery commonly experienced remission, but there was little increase in rates of remission above a threshold of 20% total weight loss (TWL), according to a retrospective analysis of 5,928 patients with diabetes in an integrated health care system in Southern California.
The findings should reassure physicians and patients that surgery will be beneficial, according to lead author Karen Coleman, PhD, professor of health systems science at Kaiser Permanente Southern California.
Dr. Coleman has heard from many physicians saying they recommend against bariatric surgery because of concerns that patients gain weight back and therefore won’t get a long-term benefit, but this is not supported by the literature. “Hundreds of articles at this point show that this simply is not true. In addition, providers seem to think about bariatric surgery as an ‘all or none’ treatment. Gaining any weight back means that patients ‘fail.’ Weight regain is a normal part of massive weight loss; however, maintaining a certain amount of weight loss still provides benefits for patients, especially those with cardiovascular conditions like diabetes,” said Dr. Coleman.
Most patients lose 20%-30% of their body weight after bariatric surgery, but they don’t have to lose that much to see an improvement in type 2 diabetes (T2D). In addition, if patients lose that much or more, and then gain some weight back, it doesn’t eliminate benefit. “Although we did not measure weight regain, a corollary statement is that patients can regain some of the weight they lose, but if they stay around 20% of their total weight lost, then their diabetes still remits,” said Dr. Coleman.
In the past, some standards to treat severe weight loss and metabolic disease called for 50% or more TWL. More recent standards target a 30% threshold. “We want physicians to understand that they need to have more reasonable expectations of weight loss with surgery and that these reasonable expectations still result in profound improvements in cardiovascular risk, death, and quality of life. A 20% TWL threshold is easier for these patients to get to, and like other patients, they still get the benefit. So even if these patients may not have as much weight loss they can still benefit from the surgery for their diabetes,” Dr. Coleman added.
Physicians have long assumed that the effect of bariatric surgery on T2D remission is tied to weight loss, but this has been tested only recently. Previous studies found a link and suggested that 25% TWL may be the needed threshold, but more data are needed, especially for sleeve gastrectomy.
In the current study, published in Diabetes Care, 73% of patients were female. Mean age was 49.8 years, and mean body mass index was 43.8 kg/m2. Fifty-seven percent underwent Roux-en-Y gastric bypass (RYGB). Follow-up averaged 5.9 years. Overall, 71% of patients had an initial remission of their diabetes (72% RYGB, 70% sleeve). The average time to remission was 1.0 years. The researchers categorized participants by percentage TWL. Compared with the 0%-5% group, each 5% increase in TWL was linked with a greater likelihood of achieving remission: 5%-10%, hazard ratio 1.22 (P = .23); 10%-15%, HR 1.97 (95% confidence interval, 1.47-2.64); 15%-20%, HR 2.33 (95% CI, 1.74-3.11); 20%-25%, HR 2.81 (95% CI, 2.11-3.75); 25%-30%, HR 2.88 (95% CI, 2.16-3.83); >30%, HR, 2.92 (95% CI, 2.19-3.88). Categories above 25% TWL had remission rates similar to those of the 20%-25% group. Those in the over 20% TWL group who were taking insulin at the time of surgery had better odds of T2D remission than did those in the 0%-5% TWL group who were not taking insulin (HR, 2.18; 95% CI, 1.64-2.88).
The study is a useful addition to the literature on the topic, according to W. Timothy Garvey, MD, director of the diabetes research center at the University of Alabama at Birmingham. “This tends to quantify it a little bit more than people might have had before,” he said.
Dr. Garvey noted that there were wide error bars in the outcomes grouped by TWL, and suggested that individual results of surgery may vary widely. “There are plenty of individuals in each of those bins that will require more weight loss for remission or less weight loss. That’s just the average of people in that weight loss category. So if a clinician is going to use this information, they need to take it with a grain of salt and realize that, just because they reach that 20% weight loss threshold, it doesn’t mean that their patient is going to go into remission. As a loose guide, as something to shoot for, I think this is valuable,” he added.
Dr. Coleman recommended that physicians not wait too long to suggest bariatric surgery, since patients are likely to have better outcomes if they are healthier going in. “Bariatric surgery is by far the most effective long-term treatment we have for severe obesity and we should be treating it as a secondary prevention strategy, not a last resort to save people’s lives. Bariatric surgery cannot regrow the cells in the pancreas that make insulin. So if we wait until patients with type 2 diabetes are insulin dependent to offer bariatric surgery, we are compromising the great effect surgery can have for them,” said Dr. Coleman.
Patients with type 2 diabetes who underwent bariatric surgery commonly experienced remission, but there was little increase in rates of remission above a threshold of 20% total weight loss (TWL), according to a retrospective analysis of 5,928 patients with diabetes in an integrated health care system in Southern California.
The findings should reassure physicians and patients that surgery will be beneficial, according to lead author Karen Coleman, PhD, professor of health systems science at Kaiser Permanente Southern California.
Dr. Coleman has heard from many physicians saying they recommend against bariatric surgery because of concerns that patients gain weight back and therefore won’t get a long-term benefit, but this is not supported by the literature. “Hundreds of articles at this point show that this simply is not true. In addition, providers seem to think about bariatric surgery as an ‘all or none’ treatment. Gaining any weight back means that patients ‘fail.’ Weight regain is a normal part of massive weight loss; however, maintaining a certain amount of weight loss still provides benefits for patients, especially those with cardiovascular conditions like diabetes,” said Dr. Coleman.
Most patients lose 20%-30% of their body weight after bariatric surgery, but they don’t have to lose that much to see an improvement in type 2 diabetes (T2D). In addition, if patients lose that much or more, and then gain some weight back, it doesn’t eliminate benefit. “Although we did not measure weight regain, a corollary statement is that patients can regain some of the weight they lose, but if they stay around 20% of their total weight lost, then their diabetes still remits,” said Dr. Coleman.
In the past, some standards to treat severe weight loss and metabolic disease called for 50% or more TWL. More recent standards target a 30% threshold. “We want physicians to understand that they need to have more reasonable expectations of weight loss with surgery and that these reasonable expectations still result in profound improvements in cardiovascular risk, death, and quality of life. A 20% TWL threshold is easier for these patients to get to, and like other patients, they still get the benefit. So even if these patients may not have as much weight loss they can still benefit from the surgery for their diabetes,” Dr. Coleman added.
Physicians have long assumed that the effect of bariatric surgery on T2D remission is tied to weight loss, but this has been tested only recently. Previous studies found a link and suggested that 25% TWL may be the needed threshold, but more data are needed, especially for sleeve gastrectomy.
In the current study, published in Diabetes Care, 73% of patients were female. Mean age was 49.8 years, and mean body mass index was 43.8 kg/m2. Fifty-seven percent underwent Roux-en-Y gastric bypass (RYGB). Follow-up averaged 5.9 years. Overall, 71% of patients had an initial remission of their diabetes (72% RYGB, 70% sleeve). The average time to remission was 1.0 years. The researchers categorized participants by percentage TWL. Compared with the 0%-5% group, each 5% increase in TWL was linked with a greater likelihood of achieving remission: 5%-10%, hazard ratio 1.22 (P = .23); 10%-15%, HR 1.97 (95% confidence interval, 1.47-2.64); 15%-20%, HR 2.33 (95% CI, 1.74-3.11); 20%-25%, HR 2.81 (95% CI, 2.11-3.75); 25%-30%, HR 2.88 (95% CI, 2.16-3.83); >30%, HR, 2.92 (95% CI, 2.19-3.88). Categories above 25% TWL had remission rates similar to those of the 20%-25% group. Those in the over 20% TWL group who were taking insulin at the time of surgery had better odds of T2D remission than did those in the 0%-5% TWL group who were not taking insulin (HR, 2.18; 95% CI, 1.64-2.88).
The study is a useful addition to the literature on the topic, according to W. Timothy Garvey, MD, director of the diabetes research center at the University of Alabama at Birmingham. “This tends to quantify it a little bit more than people might have had before,” he said.
Dr. Garvey noted that there were wide error bars in the outcomes grouped by TWL, and suggested that individual results of surgery may vary widely. “There are plenty of individuals in each of those bins that will require more weight loss for remission or less weight loss. That’s just the average of people in that weight loss category. So if a clinician is going to use this information, they need to take it with a grain of salt and realize that, just because they reach that 20% weight loss threshold, it doesn’t mean that their patient is going to go into remission. As a loose guide, as something to shoot for, I think this is valuable,” he added.
Dr. Coleman recommended that physicians not wait too long to suggest bariatric surgery, since patients are likely to have better outcomes if they are healthier going in. “Bariatric surgery is by far the most effective long-term treatment we have for severe obesity and we should be treating it as a secondary prevention strategy, not a last resort to save people’s lives. Bariatric surgery cannot regrow the cells in the pancreas that make insulin. So if we wait until patients with type 2 diabetes are insulin dependent to offer bariatric surgery, we are compromising the great effect surgery can have for them,” said Dr. Coleman.
Patients with type 2 diabetes who underwent bariatric surgery commonly experienced remission, but there was little increase in rates of remission above a threshold of 20% total weight loss (TWL), according to a retrospective analysis of 5,928 patients with diabetes in an integrated health care system in Southern California.
The findings should reassure physicians and patients that surgery will be beneficial, according to lead author Karen Coleman, PhD, professor of health systems science at Kaiser Permanente Southern California.
Dr. Coleman has heard from many physicians saying they recommend against bariatric surgery because of concerns that patients gain weight back and therefore won’t get a long-term benefit, but this is not supported by the literature. “Hundreds of articles at this point show that this simply is not true. In addition, providers seem to think about bariatric surgery as an ‘all or none’ treatment. Gaining any weight back means that patients ‘fail.’ Weight regain is a normal part of massive weight loss; however, maintaining a certain amount of weight loss still provides benefits for patients, especially those with cardiovascular conditions like diabetes,” said Dr. Coleman.
Most patients lose 20%-30% of their body weight after bariatric surgery, but they don’t have to lose that much to see an improvement in type 2 diabetes (T2D). In addition, if patients lose that much or more, and then gain some weight back, it doesn’t eliminate benefit. “Although we did not measure weight regain, a corollary statement is that patients can regain some of the weight they lose, but if they stay around 20% of their total weight lost, then their diabetes still remits,” said Dr. Coleman.
In the past, some standards to treat severe weight loss and metabolic disease called for 50% or more TWL. More recent standards target a 30% threshold. “We want physicians to understand that they need to have more reasonable expectations of weight loss with surgery and that these reasonable expectations still result in profound improvements in cardiovascular risk, death, and quality of life. A 20% TWL threshold is easier for these patients to get to, and like other patients, they still get the benefit. So even if these patients may not have as much weight loss they can still benefit from the surgery for their diabetes,” Dr. Coleman added.
Physicians have long assumed that the effect of bariatric surgery on T2D remission is tied to weight loss, but this has been tested only recently. Previous studies found a link and suggested that 25% TWL may be the needed threshold, but more data are needed, especially for sleeve gastrectomy.
In the current study, published in Diabetes Care, 73% of patients were female. Mean age was 49.8 years, and mean body mass index was 43.8 kg/m2. Fifty-seven percent underwent Roux-en-Y gastric bypass (RYGB). Follow-up averaged 5.9 years. Overall, 71% of patients had an initial remission of their diabetes (72% RYGB, 70% sleeve). The average time to remission was 1.0 years. The researchers categorized participants by percentage TWL. Compared with the 0%-5% group, each 5% increase in TWL was linked with a greater likelihood of achieving remission: 5%-10%, hazard ratio 1.22 (P = .23); 10%-15%, HR 1.97 (95% confidence interval, 1.47-2.64); 15%-20%, HR 2.33 (95% CI, 1.74-3.11); 20%-25%, HR 2.81 (95% CI, 2.11-3.75); 25%-30%, HR 2.88 (95% CI, 2.16-3.83); >30%, HR, 2.92 (95% CI, 2.19-3.88). Categories above 25% TWL had remission rates similar to those of the 20%-25% group. Those in the over 20% TWL group who were taking insulin at the time of surgery had better odds of T2D remission than did those in the 0%-5% TWL group who were not taking insulin (HR, 2.18; 95% CI, 1.64-2.88).
The study is a useful addition to the literature on the topic, according to W. Timothy Garvey, MD, director of the diabetes research center at the University of Alabama at Birmingham. “This tends to quantify it a little bit more than people might have had before,” he said.
Dr. Garvey noted that there were wide error bars in the outcomes grouped by TWL, and suggested that individual results of surgery may vary widely. “There are plenty of individuals in each of those bins that will require more weight loss for remission or less weight loss. That’s just the average of people in that weight loss category. So if a clinician is going to use this information, they need to take it with a grain of salt and realize that, just because they reach that 20% weight loss threshold, it doesn’t mean that their patient is going to go into remission. As a loose guide, as something to shoot for, I think this is valuable,” he added.
Dr. Coleman recommended that physicians not wait too long to suggest bariatric surgery, since patients are likely to have better outcomes if they are healthier going in. “Bariatric surgery is by far the most effective long-term treatment we have for severe obesity and we should be treating it as a secondary prevention strategy, not a last resort to save people’s lives. Bariatric surgery cannot regrow the cells in the pancreas that make insulin. So if we wait until patients with type 2 diabetes are insulin dependent to offer bariatric surgery, we are compromising the great effect surgery can have for them,” said Dr. Coleman.
FROM DIABETES CARE
Moderna vaccine more effective than Pfizer and J&J
the Centers for Disease Control and Protection has said.
“Among U.S. adults without immunocompromising conditions, vaccine effectiveness against COVID-19 hospitalization during March 11–Aug. 15, 2021, was higher for the Moderna vaccine (93%) than the Pfizer-BioNTech vaccine (88%) and the Janssen vaccine (71%),” the agency’s Morbidity and Mortality Weekly Report said. Janssen refers to the Johnson & Johnson vaccine.
The CDC said the data could help people make informed decisions.
“Understanding differences in VE [vaccine effectiveness] by vaccine product can guide individual choices and policy recommendations regarding vaccine boosters. All Food and Drug Administration–approved or authorized COVID-19 vaccines provide substantial protection against COVID-19 hospitalization,” the report said.
The study also broke down effectiveness for longer periods. Moderna came out on top again.
After 120 days, the Moderna vaccine provided 92% effectiveness against hospitalization, whereas the Pfizer vaccine’s effectiveness dropped to 77%, the CDC said. There was no similar calculation for the Johnson & Johnson vaccine.
The CDC studied 3,689 adults at 21 hospitals in 18 states who got the two-shot Pfizer or Moderna vaccine or the one-shot Johnson & Johnson vaccine between March and August.
The agency noted some factors that could have come into play.
“Differences in vaccine effectiveness between the Moderna and Pfizer-BioNTech vaccine might be due to higher mRNA content in the Moderna vaccine, differences in timing between doses (3 weeks for Pfizer-BioNTech vs. 4 weeks for Moderna), or possible differences between groups that received each vaccine that were not accounted for in the analysis,” the report said.
The CDC noted limitations in the findings. Children, immunocompromised adults, and vaccine effectiveness against COVID-19 that did not result in hospitalization were not studied.
Other studies have shown all three U.S. vaccines provide a high rate of protection against coronavirus.
A version of this article first appeared on WebMD.com.
the Centers for Disease Control and Protection has said.
“Among U.S. adults without immunocompromising conditions, vaccine effectiveness against COVID-19 hospitalization during March 11–Aug. 15, 2021, was higher for the Moderna vaccine (93%) than the Pfizer-BioNTech vaccine (88%) and the Janssen vaccine (71%),” the agency’s Morbidity and Mortality Weekly Report said. Janssen refers to the Johnson & Johnson vaccine.
The CDC said the data could help people make informed decisions.
“Understanding differences in VE [vaccine effectiveness] by vaccine product can guide individual choices and policy recommendations regarding vaccine boosters. All Food and Drug Administration–approved or authorized COVID-19 vaccines provide substantial protection against COVID-19 hospitalization,” the report said.
The study also broke down effectiveness for longer periods. Moderna came out on top again.
After 120 days, the Moderna vaccine provided 92% effectiveness against hospitalization, whereas the Pfizer vaccine’s effectiveness dropped to 77%, the CDC said. There was no similar calculation for the Johnson & Johnson vaccine.
The CDC studied 3,689 adults at 21 hospitals in 18 states who got the two-shot Pfizer or Moderna vaccine or the one-shot Johnson & Johnson vaccine between March and August.
The agency noted some factors that could have come into play.
“Differences in vaccine effectiveness between the Moderna and Pfizer-BioNTech vaccine might be due to higher mRNA content in the Moderna vaccine, differences in timing between doses (3 weeks for Pfizer-BioNTech vs. 4 weeks for Moderna), or possible differences between groups that received each vaccine that were not accounted for in the analysis,” the report said.
The CDC noted limitations in the findings. Children, immunocompromised adults, and vaccine effectiveness against COVID-19 that did not result in hospitalization were not studied.
Other studies have shown all three U.S. vaccines provide a high rate of protection against coronavirus.
A version of this article first appeared on WebMD.com.
the Centers for Disease Control and Protection has said.
“Among U.S. adults without immunocompromising conditions, vaccine effectiveness against COVID-19 hospitalization during March 11–Aug. 15, 2021, was higher for the Moderna vaccine (93%) than the Pfizer-BioNTech vaccine (88%) and the Janssen vaccine (71%),” the agency’s Morbidity and Mortality Weekly Report said. Janssen refers to the Johnson & Johnson vaccine.
The CDC said the data could help people make informed decisions.
“Understanding differences in VE [vaccine effectiveness] by vaccine product can guide individual choices and policy recommendations regarding vaccine boosters. All Food and Drug Administration–approved or authorized COVID-19 vaccines provide substantial protection against COVID-19 hospitalization,” the report said.
The study also broke down effectiveness for longer periods. Moderna came out on top again.
After 120 days, the Moderna vaccine provided 92% effectiveness against hospitalization, whereas the Pfizer vaccine’s effectiveness dropped to 77%, the CDC said. There was no similar calculation for the Johnson & Johnson vaccine.
The CDC studied 3,689 adults at 21 hospitals in 18 states who got the two-shot Pfizer or Moderna vaccine or the one-shot Johnson & Johnson vaccine between March and August.
The agency noted some factors that could have come into play.
“Differences in vaccine effectiveness between the Moderna and Pfizer-BioNTech vaccine might be due to higher mRNA content in the Moderna vaccine, differences in timing between doses (3 weeks for Pfizer-BioNTech vs. 4 weeks for Moderna), or possible differences between groups that received each vaccine that were not accounted for in the analysis,” the report said.
The CDC noted limitations in the findings. Children, immunocompromised adults, and vaccine effectiveness against COVID-19 that did not result in hospitalization were not studied.
Other studies have shown all three U.S. vaccines provide a high rate of protection against coronavirus.
A version of this article first appeared on WebMD.com.
COVID vaccine is safe, effective for children aged 5-11, Pfizer says
With record numbers of COVID-19 cases being reported in kids, Pfizer and its partner BioNTech have announced that their mRNA vaccine for COVID-19 is safe and appears to generate a protective immune response in children as young as 5.
The companies have been testing a lower dose of the vaccine -- just 10 milligrams -- in children between the ages of 5 and 11. That’s one-third the dose given to adults.
In a clinical trial that included more than 2,200 children, Pfizer says two doses of the vaccines given 3 weeks apart generated a high level of neutralizing antibodies, comparable to the level seen in older children who get a higher dose of the vaccine.
On the advice of its vaccine advisory committee, the Food and Drug Administration asked vaccine makers to include more children in these studies earlier this year.
Rather than testing whether the vaccines are preventing COVID-19 illness in children, as they did in adults, the pharmaceutical companies that make the COVID-19 vaccines are looking at the antibody levels generated by the vaccines instead. The FDA has approved the approach in hopes of speeding vaccines to children, who are now back in school full time in most parts of the United States.
With that in mind, Evan Anderson, MD, a doctor with Children’s Healthcare of Atlanta who is an investigator for the trial — and is therefore kept in the dark about its results — said it’s important to keep in mind that the company didn’t share any efficacy data today.
“We don’t know whether there were cases of COVID-19 among children that were enrolled in the study and how those compared in those who received placebo versus those that received vaccine,” he said.
The company says side effects seen in the trial are comparable to those seen in older children. The company said there were no cases of heart inflammation called myocarditis observed. Pfizer says they plan to send their data to the FDA as soon as possible.
The company says side effects seen in the trial are comparable to those seen in older children. Pfizer says they plan to send their data to the FDA as soon as possible.
“We are pleased to be able to submit data to regulatory authorities for this group of school-aged children before the start of the winter season,” Ugur Sahin, MD, CEO and co-founder of BioNTech, said in a news release. “The safety profile and immunogenicity data in children aged 5 to 11 years vaccinated at a lower dose are consistent with those we have observed with our vaccine in other older populations at a higher dose.”
When asked how soon the FDA might act on Pfizer’s application, Anderson said others had speculated about timelines of 4 to 6 weeks, but he also noted that the FDA could still exercise its authority to ask the company for more information, which could slow the process down.
“As a parent myself, I would love to see that timeline occurring quickly. However, I do want the FDA to fully review the data and ask the necessary questions,” he said. “It’s a little speculative to get too definitive with timelines.”
A version of this article first appeared on WebMD.com.
With record numbers of COVID-19 cases being reported in kids, Pfizer and its partner BioNTech have announced that their mRNA vaccine for COVID-19 is safe and appears to generate a protective immune response in children as young as 5.
The companies have been testing a lower dose of the vaccine -- just 10 milligrams -- in children between the ages of 5 and 11. That’s one-third the dose given to adults.
In a clinical trial that included more than 2,200 children, Pfizer says two doses of the vaccines given 3 weeks apart generated a high level of neutralizing antibodies, comparable to the level seen in older children who get a higher dose of the vaccine.
On the advice of its vaccine advisory committee, the Food and Drug Administration asked vaccine makers to include more children in these studies earlier this year.
Rather than testing whether the vaccines are preventing COVID-19 illness in children, as they did in adults, the pharmaceutical companies that make the COVID-19 vaccines are looking at the antibody levels generated by the vaccines instead. The FDA has approved the approach in hopes of speeding vaccines to children, who are now back in school full time in most parts of the United States.
With that in mind, Evan Anderson, MD, a doctor with Children’s Healthcare of Atlanta who is an investigator for the trial — and is therefore kept in the dark about its results — said it’s important to keep in mind that the company didn’t share any efficacy data today.
“We don’t know whether there were cases of COVID-19 among children that were enrolled in the study and how those compared in those who received placebo versus those that received vaccine,” he said.
The company says side effects seen in the trial are comparable to those seen in older children. The company said there were no cases of heart inflammation called myocarditis observed. Pfizer says they plan to send their data to the FDA as soon as possible.
The company says side effects seen in the trial are comparable to those seen in older children. Pfizer says they plan to send their data to the FDA as soon as possible.
“We are pleased to be able to submit data to regulatory authorities for this group of school-aged children before the start of the winter season,” Ugur Sahin, MD, CEO and co-founder of BioNTech, said in a news release. “The safety profile and immunogenicity data in children aged 5 to 11 years vaccinated at a lower dose are consistent with those we have observed with our vaccine in other older populations at a higher dose.”
When asked how soon the FDA might act on Pfizer’s application, Anderson said others had speculated about timelines of 4 to 6 weeks, but he also noted that the FDA could still exercise its authority to ask the company for more information, which could slow the process down.
“As a parent myself, I would love to see that timeline occurring quickly. However, I do want the FDA to fully review the data and ask the necessary questions,” he said. “It’s a little speculative to get too definitive with timelines.”
A version of this article first appeared on WebMD.com.
With record numbers of COVID-19 cases being reported in kids, Pfizer and its partner BioNTech have announced that their mRNA vaccine for COVID-19 is safe and appears to generate a protective immune response in children as young as 5.
The companies have been testing a lower dose of the vaccine -- just 10 milligrams -- in children between the ages of 5 and 11. That’s one-third the dose given to adults.
In a clinical trial that included more than 2,200 children, Pfizer says two doses of the vaccines given 3 weeks apart generated a high level of neutralizing antibodies, comparable to the level seen in older children who get a higher dose of the vaccine.
On the advice of its vaccine advisory committee, the Food and Drug Administration asked vaccine makers to include more children in these studies earlier this year.
Rather than testing whether the vaccines are preventing COVID-19 illness in children, as they did in adults, the pharmaceutical companies that make the COVID-19 vaccines are looking at the antibody levels generated by the vaccines instead. The FDA has approved the approach in hopes of speeding vaccines to children, who are now back in school full time in most parts of the United States.
With that in mind, Evan Anderson, MD, a doctor with Children’s Healthcare of Atlanta who is an investigator for the trial — and is therefore kept in the dark about its results — said it’s important to keep in mind that the company didn’t share any efficacy data today.
“We don’t know whether there were cases of COVID-19 among children that were enrolled in the study and how those compared in those who received placebo versus those that received vaccine,” he said.
The company says side effects seen in the trial are comparable to those seen in older children. The company said there were no cases of heart inflammation called myocarditis observed. Pfizer says they plan to send their data to the FDA as soon as possible.
The company says side effects seen in the trial are comparable to those seen in older children. Pfizer says they plan to send their data to the FDA as soon as possible.
“We are pleased to be able to submit data to regulatory authorities for this group of school-aged children before the start of the winter season,” Ugur Sahin, MD, CEO and co-founder of BioNTech, said in a news release. “The safety profile and immunogenicity data in children aged 5 to 11 years vaccinated at a lower dose are consistent with those we have observed with our vaccine in other older populations at a higher dose.”
When asked how soon the FDA might act on Pfizer’s application, Anderson said others had speculated about timelines of 4 to 6 weeks, but he also noted that the FDA could still exercise its authority to ask the company for more information, which could slow the process down.
“As a parent myself, I would love to see that timeline occurring quickly. However, I do want the FDA to fully review the data and ask the necessary questions,” he said. “It’s a little speculative to get too definitive with timelines.”
A version of this article first appeared on WebMD.com.
U.S. seniors’ pandemic care worst among wealthy nations: Survey
Older adults in the United States – particularly among Black and Latino/Hispanic populations – experienced worse access to health care for chronic conditions during the pandemic than older adults in 10 other wealthy countries, according to findings from The Commonwealth Fund’s 2021 International Health Policy Survey of Older Adults released today.
David Blumenthal, MD, president of The Commonwealth Fund, said during a press briefing that surveying the senior population in the United States is particularly insightful because it is the only group with the universal coverage of Medicare, which offers a more direct comparison with other countries’ universal health care coverage.
More than one-third (37%) of older U.S. adults with multiple chronic conditions reported pandemic-related disruptions in their care – higher than rates in Canada, the Netherlands, and U.K. In Germany, only 11% had canceled or postponed appointments.
The survey was conducted between March and June 2021 and included responses from 18,477 adults age 65 and older in Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and U.K., and U.S. adults age 60 and older.
Among older adults who need help with daily activities, those in the United States, Canada, U.K., and Australia were the most likely to say they did not receive needed services from professionals or family members.
In the United States, 23% of people who said they needed help with activities such as housework, meal preparation, and medication management experienced a disruption in care because services were canceled or very limited during the pandemic. For comparison, only 8% of seniors in Germany and 11% of seniors in the Netherlands did not receive help with basic daily activities.
Many U.S. seniors used up savings
“Nearly one in five older adults report that they used up their savings or lost their main source of income because of the pandemic. We see much lower rates in other countries like Germany, Switzerland, the Netherlands, and Sweden,” Reginald D. Williams, vice president for international health policy and practice innovations at The Commonwealth Fund, said during a briefing.
Older U.S. adults reported economic difficulties related to the pandemic at a rate of up to six times that of other countries, he said.
The differences by race were stark. While 19% of U.S. seniors overall experienced financial hardships related to the pandemic, 32% of Black seniors and 39% of Latino/Hispanic seniors in the United States experienced hardships. Germany had the lowest rate, at 3% overall.
“As the COVID-19 pandemic in the United States continues to evolve,” Mr. Williams said, “finding ways to reduce care barriers – affordability and connecting adults to usual sources of primary care, enhancing access to economic supports and social services – can help narrow the gaps.”
Dr. Blumenthal said that even though “Medicare is a critical lifeline,” it has flaws.
“Medicare plans have significant gaps that leave beneficiaries vulnerable to sizable out-of-pocket expenses,” he said.
Placing caps on out-of-pocket costs and covering more health services, such as dental, vision, and hearing care, could help make the population less vulnerable, Dr. Blumenthal said. “The chronic lack of security facing U.S. seniors, especially those who are Black or Hispanic, is exacerbating the pandemic’s devastating toll,” he added.
Dr. Blumenthal and Mr. Williams have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults in the United States – particularly among Black and Latino/Hispanic populations – experienced worse access to health care for chronic conditions during the pandemic than older adults in 10 other wealthy countries, according to findings from The Commonwealth Fund’s 2021 International Health Policy Survey of Older Adults released today.
David Blumenthal, MD, president of The Commonwealth Fund, said during a press briefing that surveying the senior population in the United States is particularly insightful because it is the only group with the universal coverage of Medicare, which offers a more direct comparison with other countries’ universal health care coverage.
More than one-third (37%) of older U.S. adults with multiple chronic conditions reported pandemic-related disruptions in their care – higher than rates in Canada, the Netherlands, and U.K. In Germany, only 11% had canceled or postponed appointments.
The survey was conducted between March and June 2021 and included responses from 18,477 adults age 65 and older in Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and U.K., and U.S. adults age 60 and older.
Among older adults who need help with daily activities, those in the United States, Canada, U.K., and Australia were the most likely to say they did not receive needed services from professionals or family members.
In the United States, 23% of people who said they needed help with activities such as housework, meal preparation, and medication management experienced a disruption in care because services were canceled or very limited during the pandemic. For comparison, only 8% of seniors in Germany and 11% of seniors in the Netherlands did not receive help with basic daily activities.
Many U.S. seniors used up savings
“Nearly one in five older adults report that they used up their savings or lost their main source of income because of the pandemic. We see much lower rates in other countries like Germany, Switzerland, the Netherlands, and Sweden,” Reginald D. Williams, vice president for international health policy and practice innovations at The Commonwealth Fund, said during a briefing.
Older U.S. adults reported economic difficulties related to the pandemic at a rate of up to six times that of other countries, he said.
The differences by race were stark. While 19% of U.S. seniors overall experienced financial hardships related to the pandemic, 32% of Black seniors and 39% of Latino/Hispanic seniors in the United States experienced hardships. Germany had the lowest rate, at 3% overall.
“As the COVID-19 pandemic in the United States continues to evolve,” Mr. Williams said, “finding ways to reduce care barriers – affordability and connecting adults to usual sources of primary care, enhancing access to economic supports and social services – can help narrow the gaps.”
Dr. Blumenthal said that even though “Medicare is a critical lifeline,” it has flaws.
“Medicare plans have significant gaps that leave beneficiaries vulnerable to sizable out-of-pocket expenses,” he said.
Placing caps on out-of-pocket costs and covering more health services, such as dental, vision, and hearing care, could help make the population less vulnerable, Dr. Blumenthal said. “The chronic lack of security facing U.S. seniors, especially those who are Black or Hispanic, is exacerbating the pandemic’s devastating toll,” he added.
Dr. Blumenthal and Mr. Williams have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults in the United States – particularly among Black and Latino/Hispanic populations – experienced worse access to health care for chronic conditions during the pandemic than older adults in 10 other wealthy countries, according to findings from The Commonwealth Fund’s 2021 International Health Policy Survey of Older Adults released today.
David Blumenthal, MD, president of The Commonwealth Fund, said during a press briefing that surveying the senior population in the United States is particularly insightful because it is the only group with the universal coverage of Medicare, which offers a more direct comparison with other countries’ universal health care coverage.
More than one-third (37%) of older U.S. adults with multiple chronic conditions reported pandemic-related disruptions in their care – higher than rates in Canada, the Netherlands, and U.K. In Germany, only 11% had canceled or postponed appointments.
The survey was conducted between March and June 2021 and included responses from 18,477 adults age 65 and older in Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and U.K., and U.S. adults age 60 and older.
Among older adults who need help with daily activities, those in the United States, Canada, U.K., and Australia were the most likely to say they did not receive needed services from professionals or family members.
In the United States, 23% of people who said they needed help with activities such as housework, meal preparation, and medication management experienced a disruption in care because services were canceled or very limited during the pandemic. For comparison, only 8% of seniors in Germany and 11% of seniors in the Netherlands did not receive help with basic daily activities.
Many U.S. seniors used up savings
“Nearly one in five older adults report that they used up their savings or lost their main source of income because of the pandemic. We see much lower rates in other countries like Germany, Switzerland, the Netherlands, and Sweden,” Reginald D. Williams, vice president for international health policy and practice innovations at The Commonwealth Fund, said during a briefing.
Older U.S. adults reported economic difficulties related to the pandemic at a rate of up to six times that of other countries, he said.
The differences by race were stark. While 19% of U.S. seniors overall experienced financial hardships related to the pandemic, 32% of Black seniors and 39% of Latino/Hispanic seniors in the United States experienced hardships. Germany had the lowest rate, at 3% overall.
“As the COVID-19 pandemic in the United States continues to evolve,” Mr. Williams said, “finding ways to reduce care barriers – affordability and connecting adults to usual sources of primary care, enhancing access to economic supports and social services – can help narrow the gaps.”
Dr. Blumenthal said that even though “Medicare is a critical lifeline,” it has flaws.
“Medicare plans have significant gaps that leave beneficiaries vulnerable to sizable out-of-pocket expenses,” he said.
Placing caps on out-of-pocket costs and covering more health services, such as dental, vision, and hearing care, could help make the population less vulnerable, Dr. Blumenthal said. “The chronic lack of security facing U.S. seniors, especially those who are Black or Hispanic, is exacerbating the pandemic’s devastating toll,” he added.
Dr. Blumenthal and Mr. Williams have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA panel backs Pfizer's COVID booster for 65 and older, those at high risk
An expert panel that advises the Food and Drug Administration on its regulatory decisions voted Sept. 17 against recommending third doses of Pfizer’s COVID-19 vaccine for younger Americans.
But they didn’t kill the idea of booster shots completely.
In a dramatic, last-minute pivot, the 18 members of the FDA’s Vaccines and Related Biological Products Advisory Committee unanimously voted to recommend the FDA make boosters available for seniors and others at high risk of severe outcomes from COVID-19, including health care workers.
The 16-2 vote was a rebuttal to Pfizer’s initial request. The company had asked the FDA to allow it to offer third doses to all Americans over the age of 16 at least six months after their second shot.
The company requested an amendment to the full approval the FDA granted in August. That is the typical way boosters are authorized in the U.S., but it requires a higher bar of evidence and more regulatory scrutiny than the agency had been able to give since Pfizer filed for the change just days after its vaccine was granted full approval.
The committee’s actions were also a rebuff to the Biden administration, which announced before the FDA approved them that boosters would be rolled out to the general public Sept. 20. The announcement triggered the resignations of two of the agency’s top vaccine reviewers, who both participated in the Sept. 17 meeting.
After initially voting against Pfizer’s request to amend its license, the committee then worked on the fly with FDA officials to craft a strategy that would allow third doses to be offered under an emergency use authorization (EUA).
An EUA requires a lower standard of evidence and is more specific. It will restrict third doses to a more defined population than a change to the license would. It will also require Pfizer to continue to monitor the safety of third doses as they begin to be administered.
“This should demonstrate to the public that the members of this committee are independent of the FDA and that we do, in fact, bring our voices to the table when we are asked to serve on this committee,” said Archana Chattergee, MD, a pediatric infectious disease specialist who is dean of the Chicago Medical School at Rosalind Franklin University in Illinois.
The FDA doesn’t have to follow the committee’s recommendation, but almost certainly will, though regulators said they may still make some changes.
“We are not bound at FDA by your vote, we can tweak this,” said Peter Marks, MD, director of the Center for Biologics Evaluation and Research at the FDA. Dr. Marks participated in the meeting and helped to draft the revised proposal.
If the FDA issues the recommended EUA, a council of independent advisors to the CDC will make specific recommendations about how the third doses should be given. After the CDC director weighs in, boosters will begin rolling out to the public.
Moderna submitted data to the FDA on Sept. 1 in support of adding a booster dose to its regimen. The agency has not yet scheduled a public review of that data.
The Biden administration is prepared to administer shots as soon as they get the green light, Surgeon General Vivek Murthy, MD, said at a White House briefing earlier Sept. 17.
"This process is consistent with what we outlined in August where our goals were to stay ahead of the virus," Dr. Murthy said. "Our goal then and now is to protect the health and well-being of the public. As soon as the FDA and CDC complete their evaluations, we will be ready to move forward accordingly."
He added, "We've used this time since our August announcement to communicate and coordinate with pharmacy partners, nursing homes, states, and localities."
White House COVID-19 Response Coordinator Jeff Zients said vaccine supply is "in good shape for all Americans to get boosters as recommended."
Taking cues from Israel
In considering Pfizer’s original request, the committee overwhelmingly felt that they didn’t have enough information to say that the benefits of an additional dose of vaccine in 16- and 17-year-olds would outweigh its risk. Teens have the highest risk of rare heart inflammation after vaccination, a side effect known as myocarditis. It is not known how the vaccines are causing these cases of heart swelling. Most who have been diagnosed with the condition have recovered, though some have needed hospital care.
Pfizer didn’t include 16- and 17-year-olds in its studies of boosters, which included about 300 people between the ages of 18 and 55. The company acknowledged that gap in its data but pointed to FDA guidance that said evidence from adults could be extrapolated to teens.
“We don’t know that much about risks,” said committee member Eric Rubin, MD, who is editor-in-chief of the New England Journal of Medicine.
Much of the data on the potential benefits and harms of third Pfizer doses comes from Israel, which first began rolling out boosters to older adults in July.
In a highly anticipated presentation, Sharon Alroy-Preis, Israel’s director of public health services, joined the meeting to describe Israel’s experience with boosters.
Israel began to see a third surge of COVID-19 cases in December.
“This was after having two waves and two lockdowns,” Ms. Alroy-Preis said. By the third surge, she said, Israelis were tired.
“We decided on a lockdown, but the compliance of the public wasn’t as it was in the previous two waves,” she said.
Then the vaccine arrived. Israel started vaccinations as soon as the FDA approved it, and they quickly vaccinated a high percentage of their population, about 3 months faster than the rest of the world.
All vaccinations are reported and tracked by the Ministry of Health, so the country is able to keep close tabs on how well the shots are working.
As vaccines rolled out, cases fell dramatically. The pandemic seemed to be behind them. Delta arrived in March. By June, their cases were doubling every 10 days, despite about 80% of their most vulnerable adults being fully vaccinated, she said.
Most concerning was that about 60% of severe cases were breakthrough cases in fully vaccinated individuals.
“We had to stop and figure out, was this a Delta issue,” she said. “Or was this a waning immunity issue.”
“We had some clue that it might not be the Delta variant, at least not alone,” she said.
People who had originally been first in line for the vaccines, seniors and health care workers, were having the highest rates of breakthrough infections. People further away from their second dose were more likely to get a breakthrough infection.
Ms. Alroy-Preis said that if they had not started booster doses in July, their hospitals would have been overwhelmed. They had projected that they would have 2,000 cases in the hospital each day.
Boosters have helped to flatten the curve, though they are still seeing a significant number of infections.
Data from Israel presented at the meeting show boosters are largely safe and effective at reducing severe outcomes in seniors. Israeli experience also showed that third doses, which generate very high levels of neutralizing antibodies—the first and fastest line of the body’s immune defense - -may also slow transmission of the virus.
Key differences in the U.S.
The benefit of slowing down the explosive spread of a highly contagious virus was tantalizing, but many members noted that circumstances in Israel are very different than in the United States. Israel went into its current Delta surge already having high levels of vaccination in its population. They also relied on the Pfizer vaccine almost exclusively for their campaign.
The United States used a different mix of vaccines – Pfizer, Moderna, and Johnson & Johnson -- and doesn’t have the same high level of vaccination coverage of its population.
In the United States, transmission is mainly being driven by unvaccinated people, Dr. Rubin noted.
“That really means the primary benefit is going to be in reducing disease,” he said, “And we know the people who are going to benefit from that … and those are the kinds of people the FDA has already approved a third dose for,” he said, referring to those with underlying health conditions.
But Israel only began vaccinating younger people a few weeks ago. Most are still within a window where rare risks like myocarditis could appear, Rubin noted.
He and other members of the committee said they wished they had more information about the safety of third doses in younger adults.
“We don’t have that right now, and I don’t think I would be comfortable giving it to a 16-year-old,” he said.
At the same time, the primary benefit for third doses would be in preventing severe disease, and overall, data from the United States and other countries show that two doses of the vaccines remain highly effective at preventing hospitalization and death.
Asked why Israel began to see more severe cases in fully vaccinated people, the CDC’s Sara Oliver, MD, a disease detective with the CDC, said it was probably due to a mix of factors including the fact that Israel defines severe cases a little differently.
In the United States, a severe case is generally a person who has to be hospitalized or who has died from the infection. In Israel, a person with a severe case is someone who has an elevated respiratory rate and someone who has a blood oxygen level less than 94%. In the United States, that kind of patient wouldn’t necessarily be hospitalized.
In the end, one of the two committee members who wanted full approval for Pfizer’s third doses said he was satisfied with the outcome.
Mark Sawyer, MD, a professor of pediatrics and infectious disease at the University of California at San Diego, said he voted yes on the first question because he thought full approval was the best way to give doctors the flexibility to prescribe the shots to vulnerable individuals.
“I’m really glad we authorized a vaccine for a third dose, and I plan to go out and get my vaccine this afternoon,” Dr. Sawyer said, noting that he was at high risk as a health care provider.
This article was updated 9/19/21.
A version of this article first appeared on Medscape.com.
An expert panel that advises the Food and Drug Administration on its regulatory decisions voted Sept. 17 against recommending third doses of Pfizer’s COVID-19 vaccine for younger Americans.
But they didn’t kill the idea of booster shots completely.
In a dramatic, last-minute pivot, the 18 members of the FDA’s Vaccines and Related Biological Products Advisory Committee unanimously voted to recommend the FDA make boosters available for seniors and others at high risk of severe outcomes from COVID-19, including health care workers.
The 16-2 vote was a rebuttal to Pfizer’s initial request. The company had asked the FDA to allow it to offer third doses to all Americans over the age of 16 at least six months after their second shot.
The company requested an amendment to the full approval the FDA granted in August. That is the typical way boosters are authorized in the U.S., but it requires a higher bar of evidence and more regulatory scrutiny than the agency had been able to give since Pfizer filed for the change just days after its vaccine was granted full approval.
The committee’s actions were also a rebuff to the Biden administration, which announced before the FDA approved them that boosters would be rolled out to the general public Sept. 20. The announcement triggered the resignations of two of the agency’s top vaccine reviewers, who both participated in the Sept. 17 meeting.
After initially voting against Pfizer’s request to amend its license, the committee then worked on the fly with FDA officials to craft a strategy that would allow third doses to be offered under an emergency use authorization (EUA).
An EUA requires a lower standard of evidence and is more specific. It will restrict third doses to a more defined population than a change to the license would. It will also require Pfizer to continue to monitor the safety of third doses as they begin to be administered.
“This should demonstrate to the public that the members of this committee are independent of the FDA and that we do, in fact, bring our voices to the table when we are asked to serve on this committee,” said Archana Chattergee, MD, a pediatric infectious disease specialist who is dean of the Chicago Medical School at Rosalind Franklin University in Illinois.
The FDA doesn’t have to follow the committee’s recommendation, but almost certainly will, though regulators said they may still make some changes.
“We are not bound at FDA by your vote, we can tweak this,” said Peter Marks, MD, director of the Center for Biologics Evaluation and Research at the FDA. Dr. Marks participated in the meeting and helped to draft the revised proposal.
If the FDA issues the recommended EUA, a council of independent advisors to the CDC will make specific recommendations about how the third doses should be given. After the CDC director weighs in, boosters will begin rolling out to the public.
Moderna submitted data to the FDA on Sept. 1 in support of adding a booster dose to its regimen. The agency has not yet scheduled a public review of that data.
The Biden administration is prepared to administer shots as soon as they get the green light, Surgeon General Vivek Murthy, MD, said at a White House briefing earlier Sept. 17.
"This process is consistent with what we outlined in August where our goals were to stay ahead of the virus," Dr. Murthy said. "Our goal then and now is to protect the health and well-being of the public. As soon as the FDA and CDC complete their evaluations, we will be ready to move forward accordingly."
He added, "We've used this time since our August announcement to communicate and coordinate with pharmacy partners, nursing homes, states, and localities."
White House COVID-19 Response Coordinator Jeff Zients said vaccine supply is "in good shape for all Americans to get boosters as recommended."
Taking cues from Israel
In considering Pfizer’s original request, the committee overwhelmingly felt that they didn’t have enough information to say that the benefits of an additional dose of vaccine in 16- and 17-year-olds would outweigh its risk. Teens have the highest risk of rare heart inflammation after vaccination, a side effect known as myocarditis. It is not known how the vaccines are causing these cases of heart swelling. Most who have been diagnosed with the condition have recovered, though some have needed hospital care.
Pfizer didn’t include 16- and 17-year-olds in its studies of boosters, which included about 300 people between the ages of 18 and 55. The company acknowledged that gap in its data but pointed to FDA guidance that said evidence from adults could be extrapolated to teens.
“We don’t know that much about risks,” said committee member Eric Rubin, MD, who is editor-in-chief of the New England Journal of Medicine.
Much of the data on the potential benefits and harms of third Pfizer doses comes from Israel, which first began rolling out boosters to older adults in July.
In a highly anticipated presentation, Sharon Alroy-Preis, Israel’s director of public health services, joined the meeting to describe Israel’s experience with boosters.
Israel began to see a third surge of COVID-19 cases in December.
“This was after having two waves and two lockdowns,” Ms. Alroy-Preis said. By the third surge, she said, Israelis were tired.
“We decided on a lockdown, but the compliance of the public wasn’t as it was in the previous two waves,” she said.
Then the vaccine arrived. Israel started vaccinations as soon as the FDA approved it, and they quickly vaccinated a high percentage of their population, about 3 months faster than the rest of the world.
All vaccinations are reported and tracked by the Ministry of Health, so the country is able to keep close tabs on how well the shots are working.
As vaccines rolled out, cases fell dramatically. The pandemic seemed to be behind them. Delta arrived in March. By June, their cases were doubling every 10 days, despite about 80% of their most vulnerable adults being fully vaccinated, she said.
Most concerning was that about 60% of severe cases were breakthrough cases in fully vaccinated individuals.
“We had to stop and figure out, was this a Delta issue,” she said. “Or was this a waning immunity issue.”
“We had some clue that it might not be the Delta variant, at least not alone,” she said.
People who had originally been first in line for the vaccines, seniors and health care workers, were having the highest rates of breakthrough infections. People further away from their second dose were more likely to get a breakthrough infection.
Ms. Alroy-Preis said that if they had not started booster doses in July, their hospitals would have been overwhelmed. They had projected that they would have 2,000 cases in the hospital each day.
Boosters have helped to flatten the curve, though they are still seeing a significant number of infections.
Data from Israel presented at the meeting show boosters are largely safe and effective at reducing severe outcomes in seniors. Israeli experience also showed that third doses, which generate very high levels of neutralizing antibodies—the first and fastest line of the body’s immune defense - -may also slow transmission of the virus.
Key differences in the U.S.
The benefit of slowing down the explosive spread of a highly contagious virus was tantalizing, but many members noted that circumstances in Israel are very different than in the United States. Israel went into its current Delta surge already having high levels of vaccination in its population. They also relied on the Pfizer vaccine almost exclusively for their campaign.
The United States used a different mix of vaccines – Pfizer, Moderna, and Johnson & Johnson -- and doesn’t have the same high level of vaccination coverage of its population.
In the United States, transmission is mainly being driven by unvaccinated people, Dr. Rubin noted.
“That really means the primary benefit is going to be in reducing disease,” he said, “And we know the people who are going to benefit from that … and those are the kinds of people the FDA has already approved a third dose for,” he said, referring to those with underlying health conditions.
But Israel only began vaccinating younger people a few weeks ago. Most are still within a window where rare risks like myocarditis could appear, Rubin noted.
He and other members of the committee said they wished they had more information about the safety of third doses in younger adults.
“We don’t have that right now, and I don’t think I would be comfortable giving it to a 16-year-old,” he said.
At the same time, the primary benefit for third doses would be in preventing severe disease, and overall, data from the United States and other countries show that two doses of the vaccines remain highly effective at preventing hospitalization and death.
Asked why Israel began to see more severe cases in fully vaccinated people, the CDC’s Sara Oliver, MD, a disease detective with the CDC, said it was probably due to a mix of factors including the fact that Israel defines severe cases a little differently.
In the United States, a severe case is generally a person who has to be hospitalized or who has died from the infection. In Israel, a person with a severe case is someone who has an elevated respiratory rate and someone who has a blood oxygen level less than 94%. In the United States, that kind of patient wouldn’t necessarily be hospitalized.
In the end, one of the two committee members who wanted full approval for Pfizer’s third doses said he was satisfied with the outcome.
Mark Sawyer, MD, a professor of pediatrics and infectious disease at the University of California at San Diego, said he voted yes on the first question because he thought full approval was the best way to give doctors the flexibility to prescribe the shots to vulnerable individuals.
“I’m really glad we authorized a vaccine for a third dose, and I plan to go out and get my vaccine this afternoon,” Dr. Sawyer said, noting that he was at high risk as a health care provider.
This article was updated 9/19/21.
A version of this article first appeared on Medscape.com.
An expert panel that advises the Food and Drug Administration on its regulatory decisions voted Sept. 17 against recommending third doses of Pfizer’s COVID-19 vaccine for younger Americans.
But they didn’t kill the idea of booster shots completely.
In a dramatic, last-minute pivot, the 18 members of the FDA’s Vaccines and Related Biological Products Advisory Committee unanimously voted to recommend the FDA make boosters available for seniors and others at high risk of severe outcomes from COVID-19, including health care workers.
The 16-2 vote was a rebuttal to Pfizer’s initial request. The company had asked the FDA to allow it to offer third doses to all Americans over the age of 16 at least six months after their second shot.
The company requested an amendment to the full approval the FDA granted in August. That is the typical way boosters are authorized in the U.S., but it requires a higher bar of evidence and more regulatory scrutiny than the agency had been able to give since Pfizer filed for the change just days after its vaccine was granted full approval.
The committee’s actions were also a rebuff to the Biden administration, which announced before the FDA approved them that boosters would be rolled out to the general public Sept. 20. The announcement triggered the resignations of two of the agency’s top vaccine reviewers, who both participated in the Sept. 17 meeting.
After initially voting against Pfizer’s request to amend its license, the committee then worked on the fly with FDA officials to craft a strategy that would allow third doses to be offered under an emergency use authorization (EUA).
An EUA requires a lower standard of evidence and is more specific. It will restrict third doses to a more defined population than a change to the license would. It will also require Pfizer to continue to monitor the safety of third doses as they begin to be administered.
“This should demonstrate to the public that the members of this committee are independent of the FDA and that we do, in fact, bring our voices to the table when we are asked to serve on this committee,” said Archana Chattergee, MD, a pediatric infectious disease specialist who is dean of the Chicago Medical School at Rosalind Franklin University in Illinois.
The FDA doesn’t have to follow the committee’s recommendation, but almost certainly will, though regulators said they may still make some changes.
“We are not bound at FDA by your vote, we can tweak this,” said Peter Marks, MD, director of the Center for Biologics Evaluation and Research at the FDA. Dr. Marks participated in the meeting and helped to draft the revised proposal.
If the FDA issues the recommended EUA, a council of independent advisors to the CDC will make specific recommendations about how the third doses should be given. After the CDC director weighs in, boosters will begin rolling out to the public.
Moderna submitted data to the FDA on Sept. 1 in support of adding a booster dose to its regimen. The agency has not yet scheduled a public review of that data.
The Biden administration is prepared to administer shots as soon as they get the green light, Surgeon General Vivek Murthy, MD, said at a White House briefing earlier Sept. 17.
"This process is consistent with what we outlined in August where our goals were to stay ahead of the virus," Dr. Murthy said. "Our goal then and now is to protect the health and well-being of the public. As soon as the FDA and CDC complete their evaluations, we will be ready to move forward accordingly."
He added, "We've used this time since our August announcement to communicate and coordinate with pharmacy partners, nursing homes, states, and localities."
White House COVID-19 Response Coordinator Jeff Zients said vaccine supply is "in good shape for all Americans to get boosters as recommended."
Taking cues from Israel
In considering Pfizer’s original request, the committee overwhelmingly felt that they didn’t have enough information to say that the benefits of an additional dose of vaccine in 16- and 17-year-olds would outweigh its risk. Teens have the highest risk of rare heart inflammation after vaccination, a side effect known as myocarditis. It is not known how the vaccines are causing these cases of heart swelling. Most who have been diagnosed with the condition have recovered, though some have needed hospital care.
Pfizer didn’t include 16- and 17-year-olds in its studies of boosters, which included about 300 people between the ages of 18 and 55. The company acknowledged that gap in its data but pointed to FDA guidance that said evidence from adults could be extrapolated to teens.
“We don’t know that much about risks,” said committee member Eric Rubin, MD, who is editor-in-chief of the New England Journal of Medicine.
Much of the data on the potential benefits and harms of third Pfizer doses comes from Israel, which first began rolling out boosters to older adults in July.
In a highly anticipated presentation, Sharon Alroy-Preis, Israel’s director of public health services, joined the meeting to describe Israel’s experience with boosters.
Israel began to see a third surge of COVID-19 cases in December.
“This was after having two waves and two lockdowns,” Ms. Alroy-Preis said. By the third surge, she said, Israelis were tired.
“We decided on a lockdown, but the compliance of the public wasn’t as it was in the previous two waves,” she said.
Then the vaccine arrived. Israel started vaccinations as soon as the FDA approved it, and they quickly vaccinated a high percentage of their population, about 3 months faster than the rest of the world.
All vaccinations are reported and tracked by the Ministry of Health, so the country is able to keep close tabs on how well the shots are working.
As vaccines rolled out, cases fell dramatically. The pandemic seemed to be behind them. Delta arrived in March. By June, their cases were doubling every 10 days, despite about 80% of their most vulnerable adults being fully vaccinated, she said.
Most concerning was that about 60% of severe cases were breakthrough cases in fully vaccinated individuals.
“We had to stop and figure out, was this a Delta issue,” she said. “Or was this a waning immunity issue.”
“We had some clue that it might not be the Delta variant, at least not alone,” she said.
People who had originally been first in line for the vaccines, seniors and health care workers, were having the highest rates of breakthrough infections. People further away from their second dose were more likely to get a breakthrough infection.
Ms. Alroy-Preis said that if they had not started booster doses in July, their hospitals would have been overwhelmed. They had projected that they would have 2,000 cases in the hospital each day.
Boosters have helped to flatten the curve, though they are still seeing a significant number of infections.
Data from Israel presented at the meeting show boosters are largely safe and effective at reducing severe outcomes in seniors. Israeli experience also showed that third doses, which generate very high levels of neutralizing antibodies—the first and fastest line of the body’s immune defense - -may also slow transmission of the virus.
Key differences in the U.S.
The benefit of slowing down the explosive spread of a highly contagious virus was tantalizing, but many members noted that circumstances in Israel are very different than in the United States. Israel went into its current Delta surge already having high levels of vaccination in its population. They also relied on the Pfizer vaccine almost exclusively for their campaign.
The United States used a different mix of vaccines – Pfizer, Moderna, and Johnson & Johnson -- and doesn’t have the same high level of vaccination coverage of its population.
In the United States, transmission is mainly being driven by unvaccinated people, Dr. Rubin noted.
“That really means the primary benefit is going to be in reducing disease,” he said, “And we know the people who are going to benefit from that … and those are the kinds of people the FDA has already approved a third dose for,” he said, referring to those with underlying health conditions.
But Israel only began vaccinating younger people a few weeks ago. Most are still within a window where rare risks like myocarditis could appear, Rubin noted.
He and other members of the committee said they wished they had more information about the safety of third doses in younger adults.
“We don’t have that right now, and I don’t think I would be comfortable giving it to a 16-year-old,” he said.
At the same time, the primary benefit for third doses would be in preventing severe disease, and overall, data from the United States and other countries show that two doses of the vaccines remain highly effective at preventing hospitalization and death.
Asked why Israel began to see more severe cases in fully vaccinated people, the CDC’s Sara Oliver, MD, a disease detective with the CDC, said it was probably due to a mix of factors including the fact that Israel defines severe cases a little differently.
In the United States, a severe case is generally a person who has to be hospitalized or who has died from the infection. In Israel, a person with a severe case is someone who has an elevated respiratory rate and someone who has a blood oxygen level less than 94%. In the United States, that kind of patient wouldn’t necessarily be hospitalized.
In the end, one of the two committee members who wanted full approval for Pfizer’s third doses said he was satisfied with the outcome.
Mark Sawyer, MD, a professor of pediatrics and infectious disease at the University of California at San Diego, said he voted yes on the first question because he thought full approval was the best way to give doctors the flexibility to prescribe the shots to vulnerable individuals.
“I’m really glad we authorized a vaccine for a third dose, and I plan to go out and get my vaccine this afternoon,” Dr. Sawyer said, noting that he was at high risk as a health care provider.
This article was updated 9/19/21.
A version of this article first appeared on Medscape.com.
Step-wise medical therapy is cost effective for endometriosis
For patients with endometriosis-related dysmenorrhea, it is cost effective to use medical therapy before surgery, according to investigators.
A stepwise strategy involving two medications, then surgery, was associated with the lowest cost per quality-adjusted life-years (QALYs), reported lead author, Jacqueline A. Bohn, MD, of Oregon Health & Science University, Portland, and colleagues.
“In 2009, the medical costs associated with endometriosis in the United States were estimated at $69.4 billion annually,” the investigators wrote in Obstetrics and Gynecology. “Despite the recognized cost burden of this disease, cost-effectiveness data on the various treatment strategies is limited. Previous studies have investigated the direct and indirect costs regarding endometriosis; however, there are no prior studies that evaluate the cost-effectiveness of a stepwise regimen to guide management.”
To fill this knowledge gap, Dr. Bohn and colleagues created a cost-effectiveness model comparing four treatment strategies:
NSAIDs, then surgery
NSAIDs, then short-acting reversible contraceptives or long-acting reversible contraceptives (LARCs), then surgery
NSAIDs, then a short-acting reversible contraceptive or a LARC, then a LARC or gonadotropin-releasing hormone (GnRH) modulator, then surgery
Surgery alone
The analysis, which compared costs, QALYs, and incremental cost-effectiveness ratios, involved a theoretical cohort of 4,817,894 women aged 18-45 years, representing the estimated number of reproductive-age women in the United States with endometriosis-related dysmenorrhea. Costs were determined from published literature and inflated to 2019 dollars. Medical treatments were theoretically given for 6 months each, and the cost of laparoscopic surgery incorporated 12 months of postoperative care.
Of the four strategies, the two-medication approach was most cost effective, with a cost per QALY of $1,158. This was followed closely by the three-medication regimen, at $1,158, the single-medication regimen, at $2,108, and finally, surgery alone, at $4,338.
“We found that, although cost effective, requiring trial of a third medication offered little comparative advantage before proceeding directly to surgery after the second therapy fails,” the investigators wrote. “Yet, for the woman who is anxious about surgical intervention, or when a prolonged wait for a surgical specialist occurs, trial of a GnRH modulator may be worthwhile.”
Compared with surgery alone, each regimen starting with medical therapy remained below the standard willingness-to-pay threshold of $100,000 per QALY; however, the investigators recommend against trying more than three medications.
“Delaying surgical management in a woman with pain refractory to more than three medications may decrease quality of life and further increase cost,” they wrote.
To make surgery alone the most cost-effective option, surgery success would need to exceed 83%, Dr. Bohn and colleagues concluded.
According to Hugh Taylor, MD, of Yale University, New Haven, Conn., it’s unlikely that this surgery success threshold will be met, since surgery alone typically leads to recurrence.
“We know there’s a very high relapse rate after surgery,” Dr. Taylor said in an interview. “Even if the surgery may be initially successful, there’s roughly a 50% recurrence rate after about 2 years. So, finding the right medical therapy will give you more chance for long-term success.”
Dr. Taylor said it’s “really nice” that Dr. Bohn and colleagues conducted a sequential analysis because the findings support the most common approach in real-world practice.
“It confirms that starting with a medical therapy prior to surgery is an appropriate, successful treatment for endometriosis, which is something that many, many people in the community do, but we haven’t had a real trial to show that,” he said.
Dr. Taylor offered two areas of improvement for similar studies in the future: First, he suggested separating LARCs from oral contraceptives because LARCs may be less effective for some patients with endometriosis; and second, he suggested that limiting the third medication to a GnRH antagonist would be more applicable to real-world practice than using the broader category of GnRH modulators.
Although the three-medication approach involving a GnRH modulator was slightly more expensive than the two-medication approach, Dr. Taylor said the costs were so similar that a three-medication approach is “still reasonable,” particularly because it could spare patients from surgery.
Dr. Taylor also speculated that trying a GnRH antagonist could become more cost effective soon. Although only one GnRH antagonist is currently on the market, he noted that a second agent is poised for Food and Drug Administration approval, while a third is in the pipeline, and this competition may decrease drug prices.
The investigators disclosed support from the National Institutes of Health, Arnold Ventures, the World Health Organization, Merck, and others. Dr. Taylor reported that Yale University receives funding for endometriosis biomarker research from AbbVie.
For patients with endometriosis-related dysmenorrhea, it is cost effective to use medical therapy before surgery, according to investigators.
A stepwise strategy involving two medications, then surgery, was associated with the lowest cost per quality-adjusted life-years (QALYs), reported lead author, Jacqueline A. Bohn, MD, of Oregon Health & Science University, Portland, and colleagues.
“In 2009, the medical costs associated with endometriosis in the United States were estimated at $69.4 billion annually,” the investigators wrote in Obstetrics and Gynecology. “Despite the recognized cost burden of this disease, cost-effectiveness data on the various treatment strategies is limited. Previous studies have investigated the direct and indirect costs regarding endometriosis; however, there are no prior studies that evaluate the cost-effectiveness of a stepwise regimen to guide management.”
To fill this knowledge gap, Dr. Bohn and colleagues created a cost-effectiveness model comparing four treatment strategies:
NSAIDs, then surgery
NSAIDs, then short-acting reversible contraceptives or long-acting reversible contraceptives (LARCs), then surgery
NSAIDs, then a short-acting reversible contraceptive or a LARC, then a LARC or gonadotropin-releasing hormone (GnRH) modulator, then surgery
Surgery alone
The analysis, which compared costs, QALYs, and incremental cost-effectiveness ratios, involved a theoretical cohort of 4,817,894 women aged 18-45 years, representing the estimated number of reproductive-age women in the United States with endometriosis-related dysmenorrhea. Costs were determined from published literature and inflated to 2019 dollars. Medical treatments were theoretically given for 6 months each, and the cost of laparoscopic surgery incorporated 12 months of postoperative care.
Of the four strategies, the two-medication approach was most cost effective, with a cost per QALY of $1,158. This was followed closely by the three-medication regimen, at $1,158, the single-medication regimen, at $2,108, and finally, surgery alone, at $4,338.
“We found that, although cost effective, requiring trial of a third medication offered little comparative advantage before proceeding directly to surgery after the second therapy fails,” the investigators wrote. “Yet, for the woman who is anxious about surgical intervention, or when a prolonged wait for a surgical specialist occurs, trial of a GnRH modulator may be worthwhile.”
Compared with surgery alone, each regimen starting with medical therapy remained below the standard willingness-to-pay threshold of $100,000 per QALY; however, the investigators recommend against trying more than three medications.
“Delaying surgical management in a woman with pain refractory to more than three medications may decrease quality of life and further increase cost,” they wrote.
To make surgery alone the most cost-effective option, surgery success would need to exceed 83%, Dr. Bohn and colleagues concluded.
According to Hugh Taylor, MD, of Yale University, New Haven, Conn., it’s unlikely that this surgery success threshold will be met, since surgery alone typically leads to recurrence.
“We know there’s a very high relapse rate after surgery,” Dr. Taylor said in an interview. “Even if the surgery may be initially successful, there’s roughly a 50% recurrence rate after about 2 years. So, finding the right medical therapy will give you more chance for long-term success.”
Dr. Taylor said it’s “really nice” that Dr. Bohn and colleagues conducted a sequential analysis because the findings support the most common approach in real-world practice.
“It confirms that starting with a medical therapy prior to surgery is an appropriate, successful treatment for endometriosis, which is something that many, many people in the community do, but we haven’t had a real trial to show that,” he said.
Dr. Taylor offered two areas of improvement for similar studies in the future: First, he suggested separating LARCs from oral contraceptives because LARCs may be less effective for some patients with endometriosis; and second, he suggested that limiting the third medication to a GnRH antagonist would be more applicable to real-world practice than using the broader category of GnRH modulators.
Although the three-medication approach involving a GnRH modulator was slightly more expensive than the two-medication approach, Dr. Taylor said the costs were so similar that a three-medication approach is “still reasonable,” particularly because it could spare patients from surgery.
Dr. Taylor also speculated that trying a GnRH antagonist could become more cost effective soon. Although only one GnRH antagonist is currently on the market, he noted that a second agent is poised for Food and Drug Administration approval, while a third is in the pipeline, and this competition may decrease drug prices.
The investigators disclosed support from the National Institutes of Health, Arnold Ventures, the World Health Organization, Merck, and others. Dr. Taylor reported that Yale University receives funding for endometriosis biomarker research from AbbVie.
For patients with endometriosis-related dysmenorrhea, it is cost effective to use medical therapy before surgery, according to investigators.
A stepwise strategy involving two medications, then surgery, was associated with the lowest cost per quality-adjusted life-years (QALYs), reported lead author, Jacqueline A. Bohn, MD, of Oregon Health & Science University, Portland, and colleagues.
“In 2009, the medical costs associated with endometriosis in the United States were estimated at $69.4 billion annually,” the investigators wrote in Obstetrics and Gynecology. “Despite the recognized cost burden of this disease, cost-effectiveness data on the various treatment strategies is limited. Previous studies have investigated the direct and indirect costs regarding endometriosis; however, there are no prior studies that evaluate the cost-effectiveness of a stepwise regimen to guide management.”
To fill this knowledge gap, Dr. Bohn and colleagues created a cost-effectiveness model comparing four treatment strategies:
NSAIDs, then surgery
NSAIDs, then short-acting reversible contraceptives or long-acting reversible contraceptives (LARCs), then surgery
NSAIDs, then a short-acting reversible contraceptive or a LARC, then a LARC or gonadotropin-releasing hormone (GnRH) modulator, then surgery
Surgery alone
The analysis, which compared costs, QALYs, and incremental cost-effectiveness ratios, involved a theoretical cohort of 4,817,894 women aged 18-45 years, representing the estimated number of reproductive-age women in the United States with endometriosis-related dysmenorrhea. Costs were determined from published literature and inflated to 2019 dollars. Medical treatments were theoretically given for 6 months each, and the cost of laparoscopic surgery incorporated 12 months of postoperative care.
Of the four strategies, the two-medication approach was most cost effective, with a cost per QALY of $1,158. This was followed closely by the three-medication regimen, at $1,158, the single-medication regimen, at $2,108, and finally, surgery alone, at $4,338.
“We found that, although cost effective, requiring trial of a third medication offered little comparative advantage before proceeding directly to surgery after the second therapy fails,” the investigators wrote. “Yet, for the woman who is anxious about surgical intervention, or when a prolonged wait for a surgical specialist occurs, trial of a GnRH modulator may be worthwhile.”
Compared with surgery alone, each regimen starting with medical therapy remained below the standard willingness-to-pay threshold of $100,000 per QALY; however, the investigators recommend against trying more than three medications.
“Delaying surgical management in a woman with pain refractory to more than three medications may decrease quality of life and further increase cost,” they wrote.
To make surgery alone the most cost-effective option, surgery success would need to exceed 83%, Dr. Bohn and colleagues concluded.
According to Hugh Taylor, MD, of Yale University, New Haven, Conn., it’s unlikely that this surgery success threshold will be met, since surgery alone typically leads to recurrence.
“We know there’s a very high relapse rate after surgery,” Dr. Taylor said in an interview. “Even if the surgery may be initially successful, there’s roughly a 50% recurrence rate after about 2 years. So, finding the right medical therapy will give you more chance for long-term success.”
Dr. Taylor said it’s “really nice” that Dr. Bohn and colleagues conducted a sequential analysis because the findings support the most common approach in real-world practice.
“It confirms that starting with a medical therapy prior to surgery is an appropriate, successful treatment for endometriosis, which is something that many, many people in the community do, but we haven’t had a real trial to show that,” he said.
Dr. Taylor offered two areas of improvement for similar studies in the future: First, he suggested separating LARCs from oral contraceptives because LARCs may be less effective for some patients with endometriosis; and second, he suggested that limiting the third medication to a GnRH antagonist would be more applicable to real-world practice than using the broader category of GnRH modulators.
Although the three-medication approach involving a GnRH modulator was slightly more expensive than the two-medication approach, Dr. Taylor said the costs were so similar that a three-medication approach is “still reasonable,” particularly because it could spare patients from surgery.
Dr. Taylor also speculated that trying a GnRH antagonist could become more cost effective soon. Although only one GnRH antagonist is currently on the market, he noted that a second agent is poised for Food and Drug Administration approval, while a third is in the pipeline, and this competition may decrease drug prices.
The investigators disclosed support from the National Institutes of Health, Arnold Ventures, the World Health Organization, Merck, and others. Dr. Taylor reported that Yale University receives funding for endometriosis biomarker research from AbbVie.
FROM OBSTETRICS & GYNECOLOGY










