User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Mycetomalike Skin Infection Due to Gordonia bronchialis in an Immunocompetent Patient
Mycetoma is a chronic subcutaneous infection due to fungal (eumycetoma) or aerobic actinomycetes (actinomycetoma) organisms. Clinical lesions develop from a granulomatous infiltrate organizing around the infectious organism. Patients can present with extensive subcutaneous nodularity and draining sinuses that can lead to deformation of the affected extremity. These infections are rare in developed countries, and the prevalence and incidence remain unknown. It has been reported that actinomycetes represent 60% of mycetoma cases worldwide, with the majority of cases in Central America from Nocardia (86%) and Actinomadura madurae (10%). 1Gordonia species are aerobic, partially acid-fast, gram-positive actinobacteria that may comprise a notable minority of actinomycete isolates. 2 The species Gordonia bronchialis is of particular interest as a human pathogen because of increasing reports of nosocomial infections. 3,4 We describe a case of a mycetomalike infection due to G bronchialis in an immunocompetent patient with complete resolution after 3 months of antibiotics.

Case Report
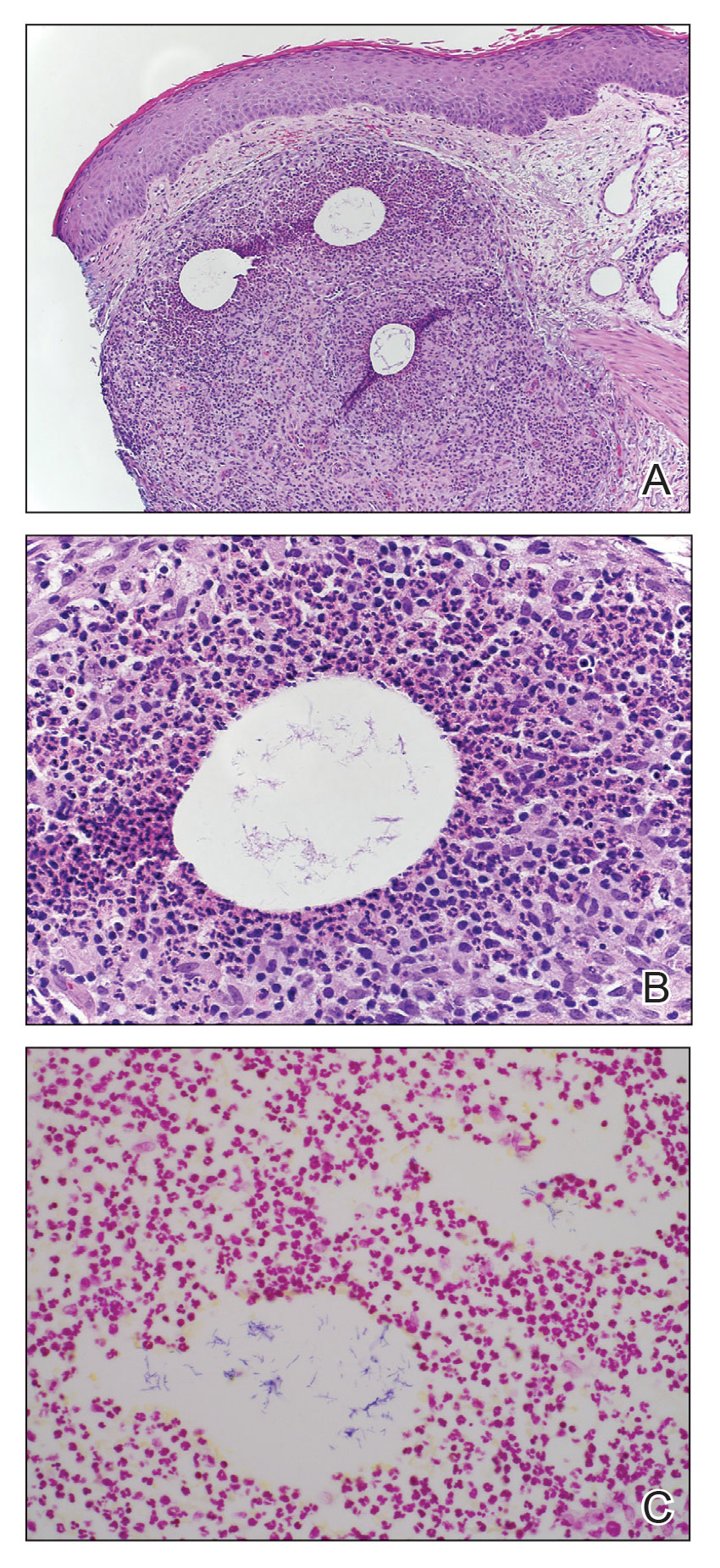
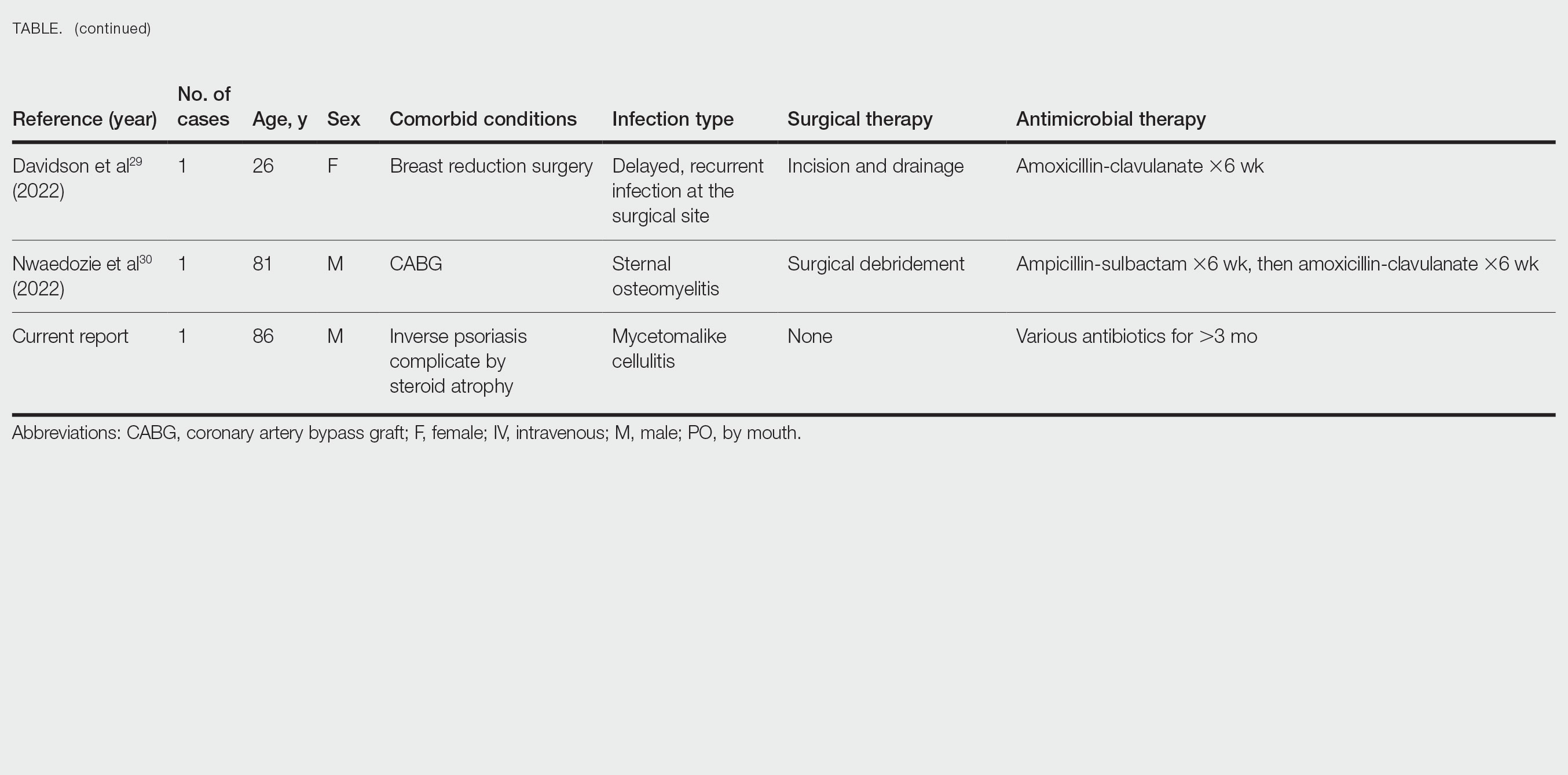
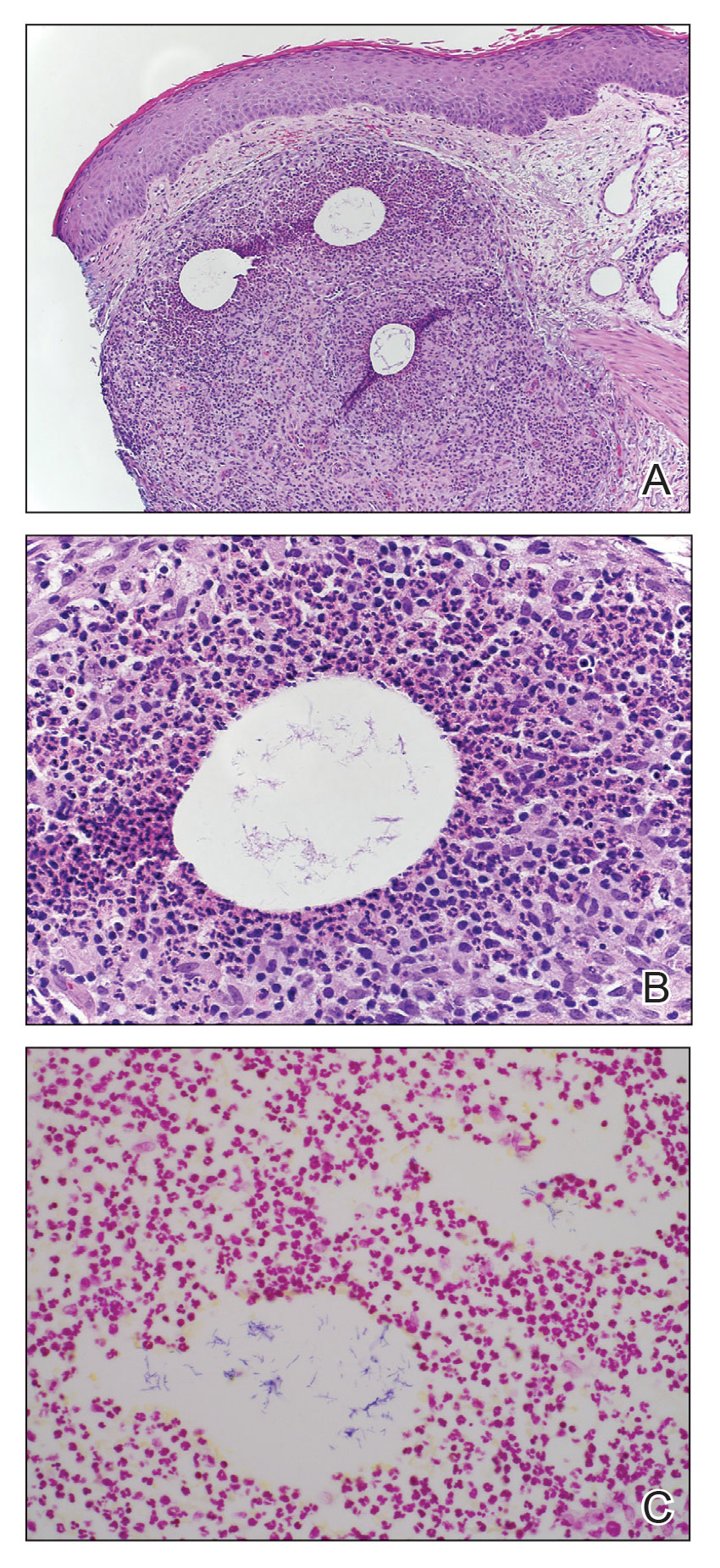
An 86-year-old man presented to the emergency department with a pruritic rash on the right forearm. He had a history of chronic kidney disease, hypertension, and inverse psoriasis complicated by steroid atrophy. He reported trauma to the right antecubital fossa approximately 1 to 2 months prior from a car door; he received wound care over several weeks at an outside hospital. The initial wound healed completely, but he subsequently noticed erythema spreading down the forearm. At the current presentation, he was empirically treated with mid-potency topical steroids and cefuroxime for 7 days. Initial laboratory results were notable for a white blood cell count of 5.7×103 cells/μL (reference range,3.7–8.4×103 cells/μL) and a creatinine level of 1.5 mg/dL (reference range, 0.57–1.25 mg/dL). The patient returned to the emergency department 2 weeks later with spreading of the initial rash and worsening pruritus. Dermatologic evaluation revealed the patient was afebrile and had violaceous papules and nodules that coalesced into plaques on the right arm, with the largest measuring approximately 15 cm. Areas of superficial erosion and crusting were noted (Figure 1A). The patient denied constitutional symptoms and had no axillary or cervical lymphadenopathy. The differential initially included an atypical infection vs a neoplasm. Two 5-mm punch biopsies were performed, which demonstrated a suppurative granulomatous infiltrate in the dermis with extension into the subcutis (Figure 2A). Focal vacuolations within the dermis demonstrated aggregates of gram-positive pseudofilamentous organisms (Figures 2B and 2C). Aerobic tissue cultures grew G bronchialis that was susceptible to all antibiotics tested and Staphylococcus epidermidis. Fungal and mycobacterial cultures were negative. The patient was placed on amoxicillin 875 mg–clavulanate 125 mg twice daily for 3 weeks. However, he demonstrated progression of the rash, with increased induration and confluence of plaques on the forearm (Figure 1B). A repeat excisional biopsy was performed, and a tissue sample was sent for 16S ribosomal RNA sequencing identification. However, neither conventional cultures nor sequencing demonstrated evidence of G bronchialis or any other pathogen. Additionally, bacterial, fungal, and mycobacterial blood cultures were negative. Amoxicillin-clavulanate was stopped, and he was placed on trimethoprim-sulfamethoxazole for 2 weeks, then changed to linezolid (600 mg twice daily) due to continued lack of improvement of the rash. After 2 weeks of linezolid, the rash was slightly improved, but the patient had notable side effects (eg, nausea, mucositis). Therefore, he was switched back to trimethoprim-sulfamethoxazole for another 6 weeks. Antibiotic therapy was discontinued after there was notable regression of indurated plaques (Figure 1C); he received more than 3 months of antibiotics in all. At 1 month after completion of antibiotic therapy, the patient had no evidence of recurrence.
Comment
Microbiology of Gordonia Species—Gordonia bronchialis originally was isolated in 1971 by Tsukamura et al5 from the sputum of patients with cavitary tuberculosis and bronchiectasis in Japan. Other Gordonia species (formerly Rhodococcus or Gordona) later were identified in soil, seawater, sediment, and wastewater. Gordonia bronchialis is a gram-positive aerobic actinomycete short rod that organizes in cordlike compact groups. It is weakly acid fast, nonmotile, and nonsporulating. Colonies exhibit pinkish-brown pigmentation. Our understanding of the clinical significance of this organism continues to evolve, and it is not always clearly pathogenic. Because Gordonia isolates may be dismissed as commensals or misidentified as Nocardia or Rhodococcus by routine biochemical tests, it is possible that infections may go undetected. Speciation requires gene sequencing; as our utilization of molecular methods has increased, the identification of clinically relevant aerobic actinomycetes, including Gordonia, has improved,6 and the following species have been recognized as pathogens: Gordonia araii, G bronchialis, Gordonia effusa, Gordonia otitidis, Gordonia polyisoprenivorans, Gordonia rubirpertincta, Gordonia sputi, and Gordonia terrae.7
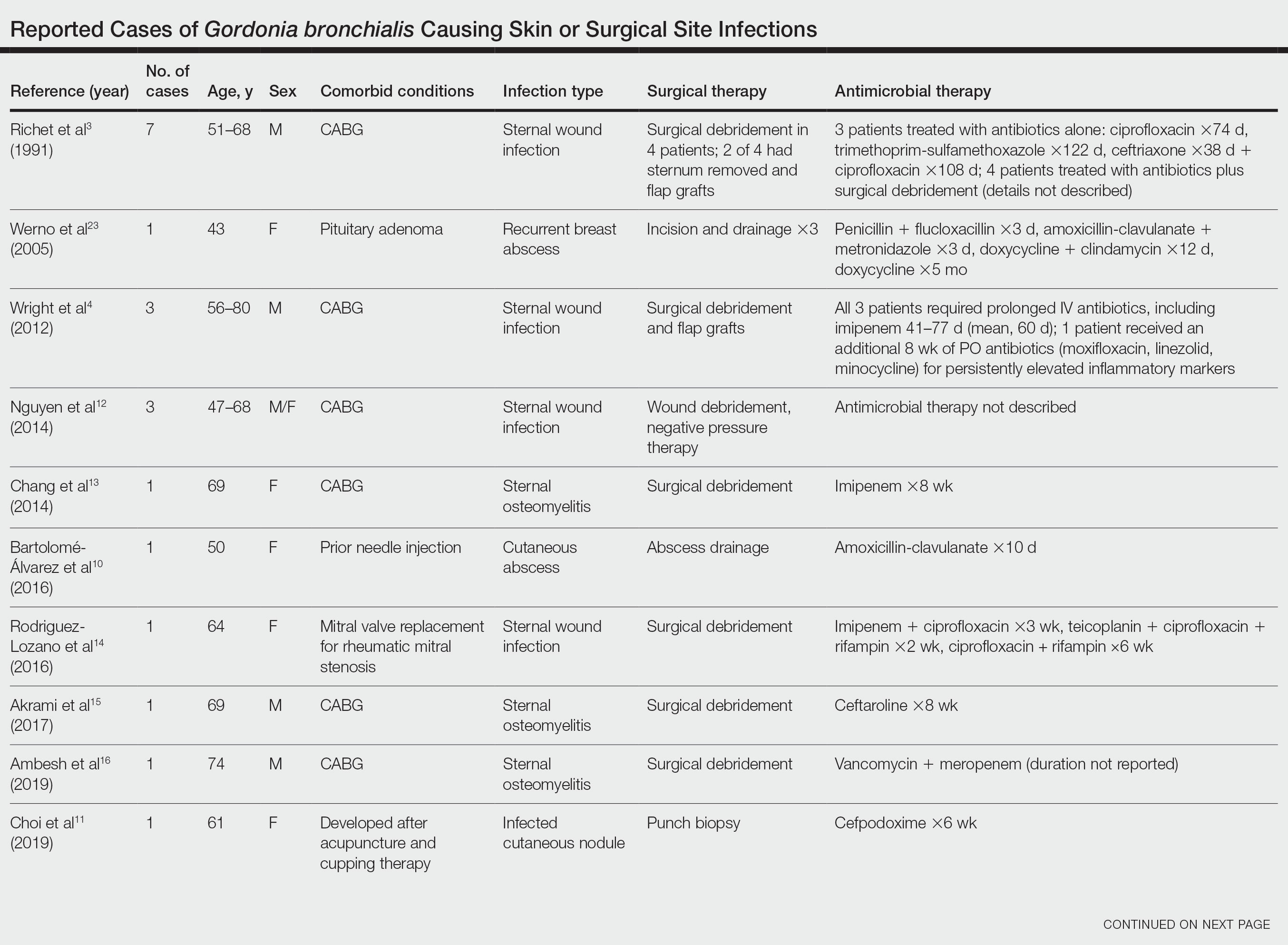
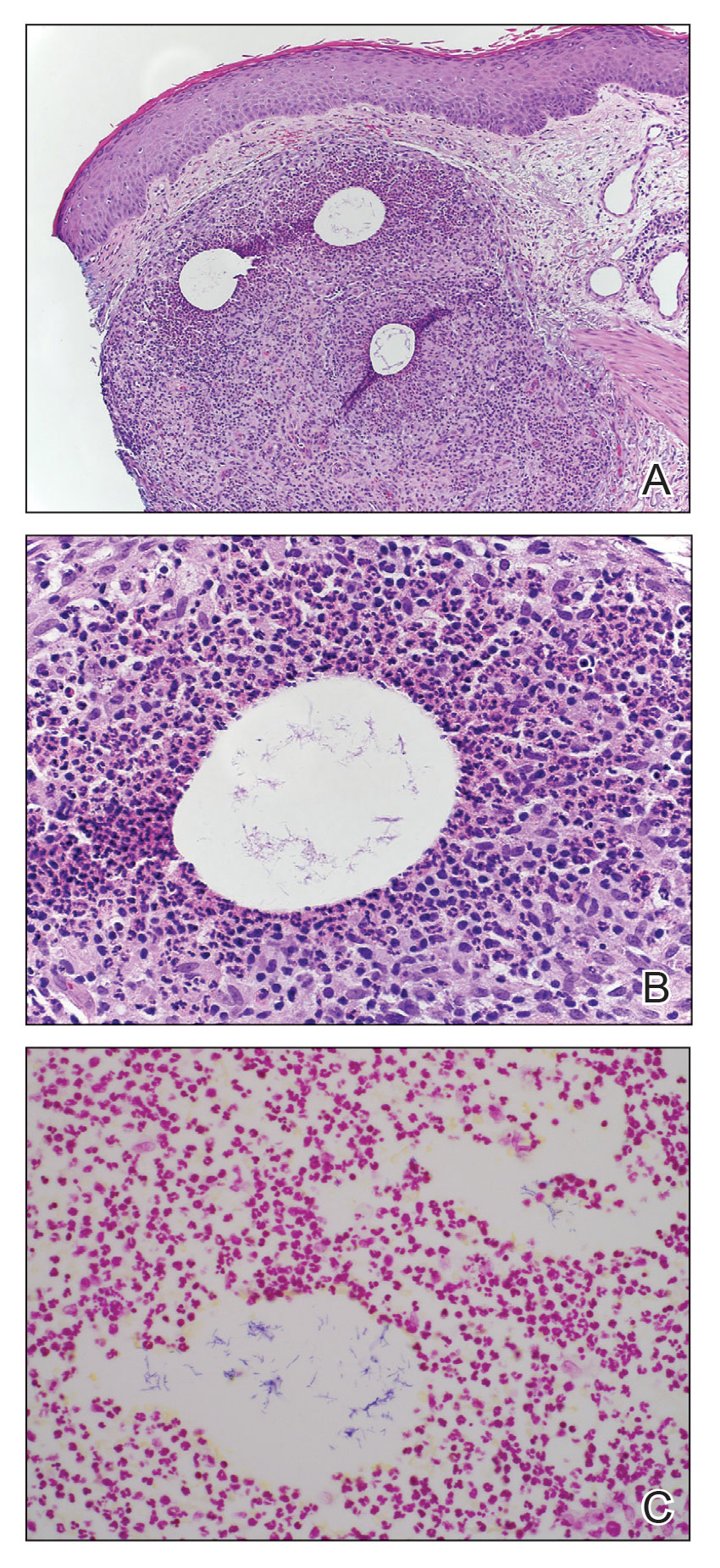
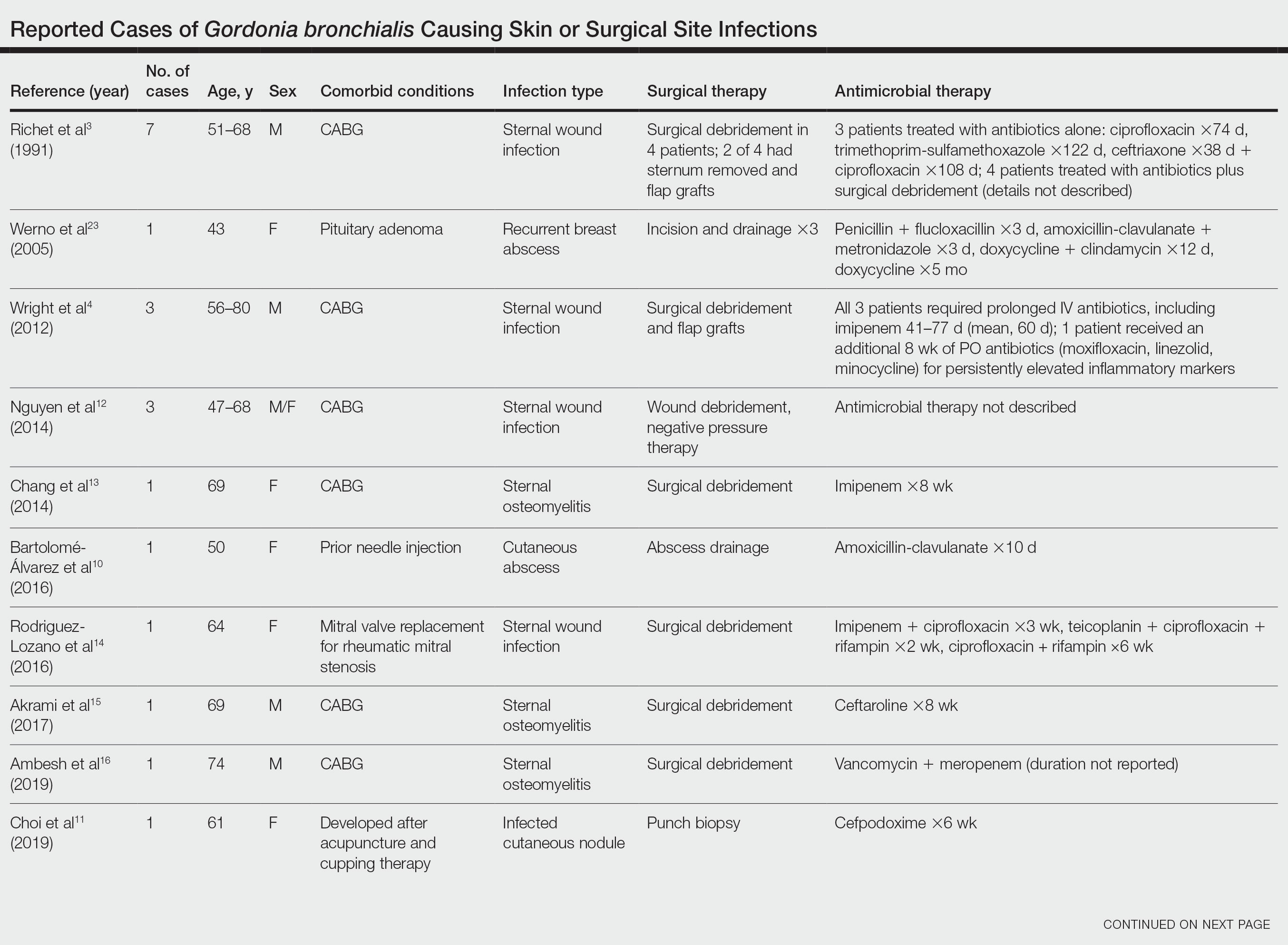
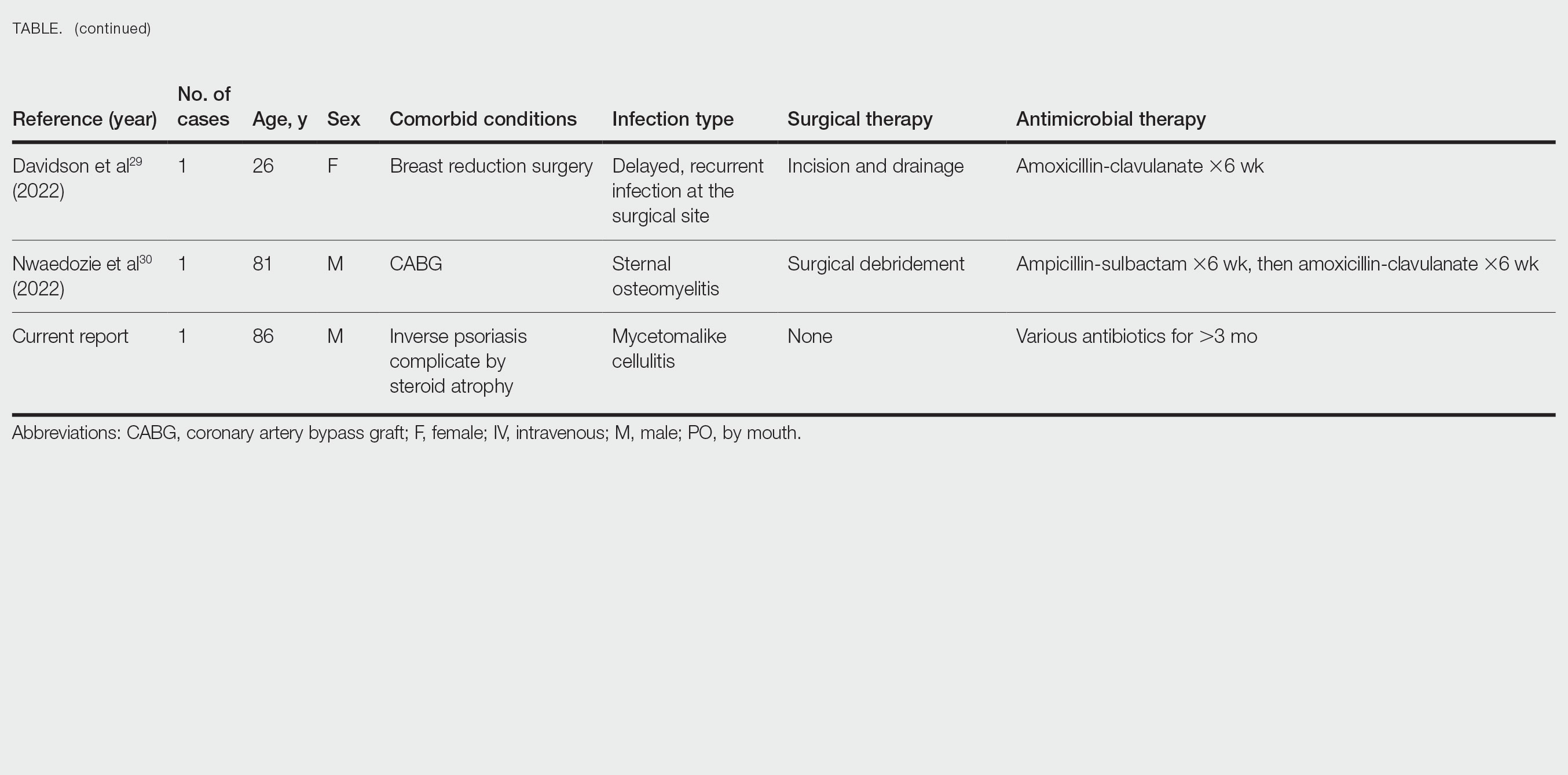
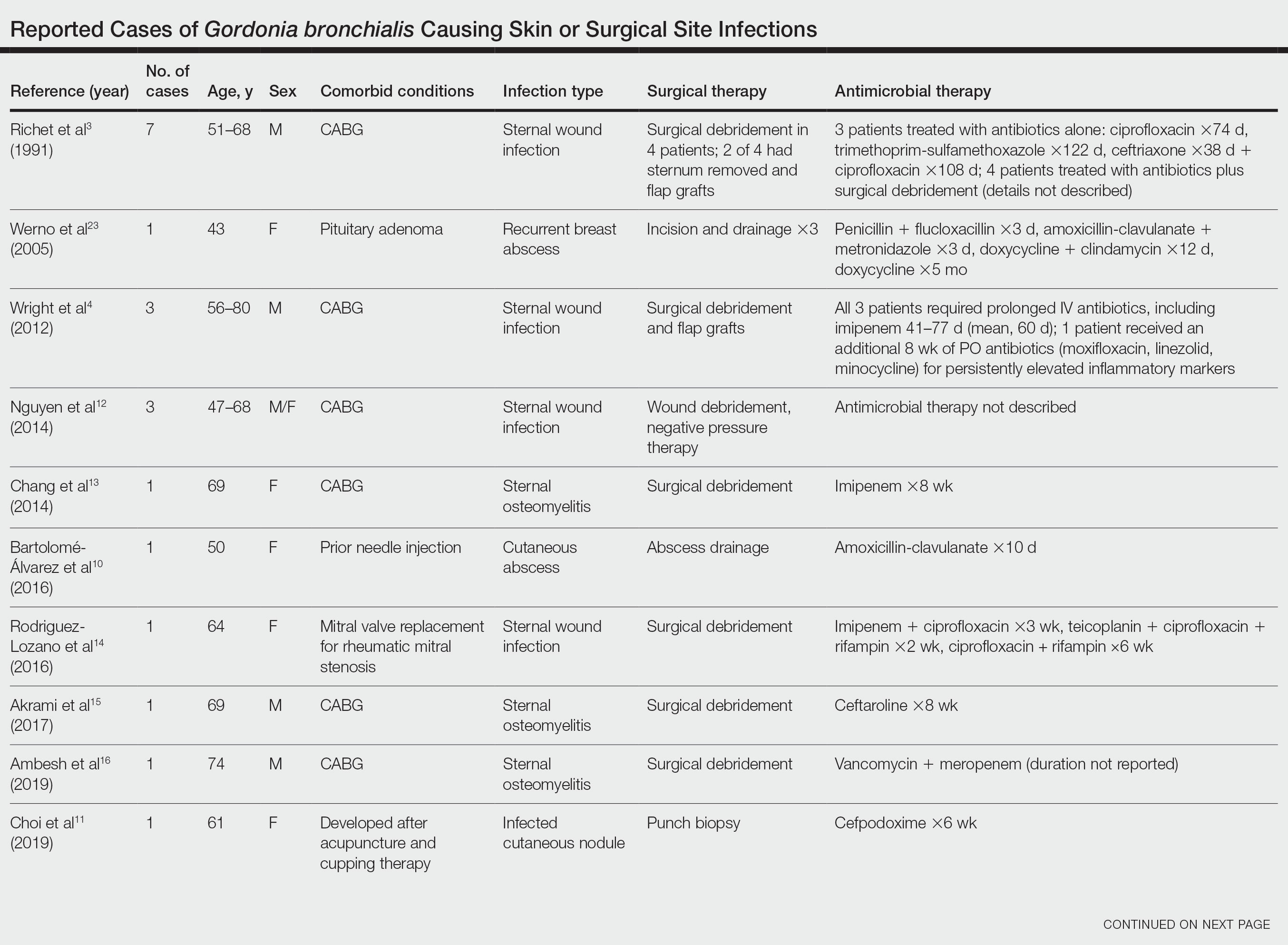
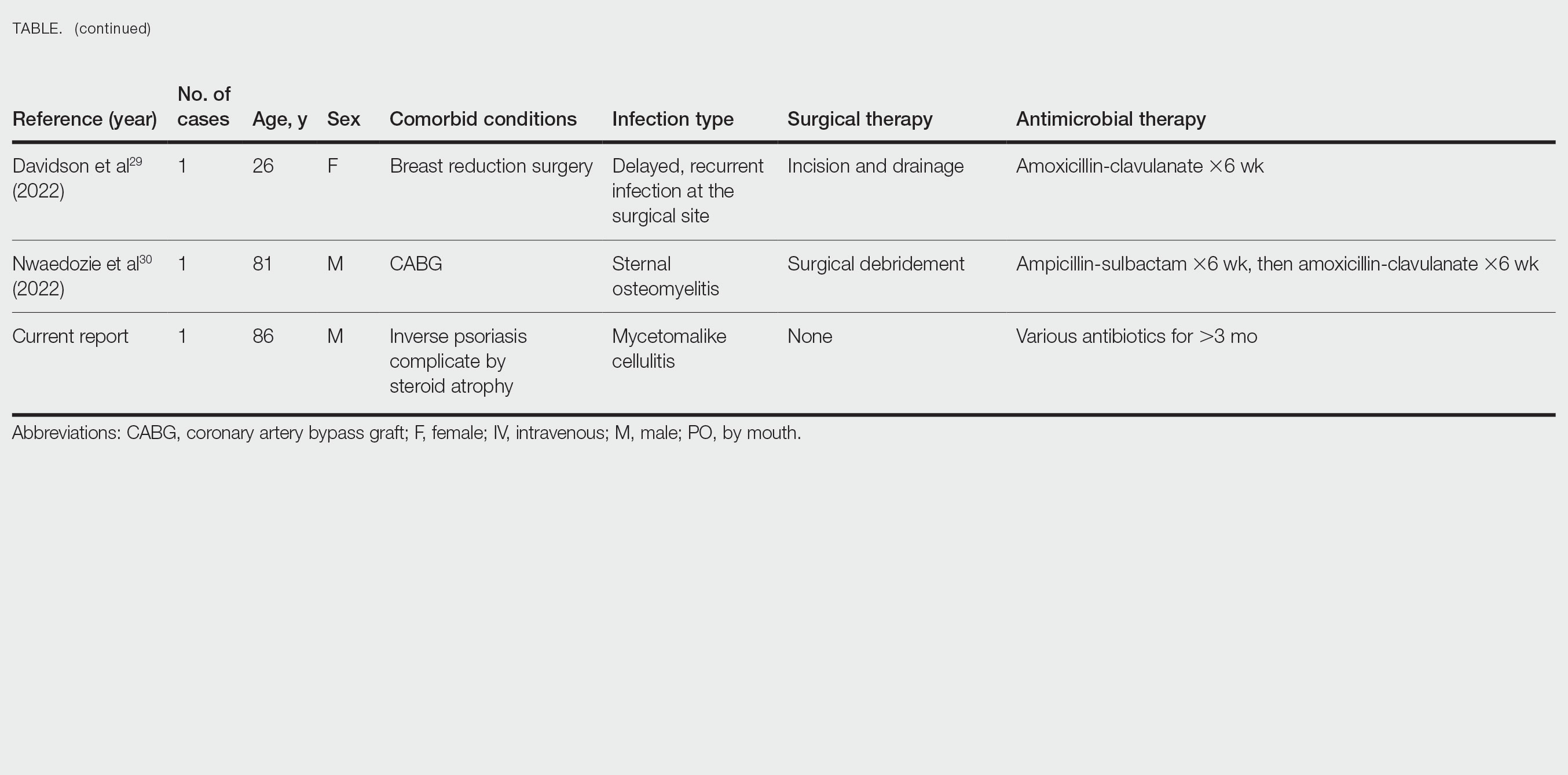
Cases Reported in the Literature—A PubMed search of articles indexed for MEDLINE using the term Gordonia bronchialis yielded 35 previously reported human cases of G bronchialis infection, most often associated with medical devices or procedures.8-31 Eighteen of these cases were sternal surgical site infections in patients with a history of cardiac surgery,3,4,12-16,30 including 2 outbreaks following coronary artery bypass grafting that were thought to be related to intraoperative transmission from a nurse.3,4 Of the remaining cases, 12 were linked to a procedure or an indwelling catheter: 4 cases of peritonitis in the setting of continuous ambulatory peritoneal dialysis17,18,26,27; 3 cases of skin and soft tissue infection (1 at the site of a prior needle injection,10 1 after acupuncture,11 and 1 after breast reduction surgery29); 1 case of ventriculitis in a premature neonate with an underlying intraventricular shunt19; 2 cases of pacemaker-induced endocarditis20,28; 1 case of tibial osteomyelitis related to a bioresorbable polymer screw21; and 1 case of chronic endophthalmitis with underlying intraocular lens implants.22 The Table lists all cases of G bronchialis skin or surgical site infections encountered in our literature search as well as the treatment provided in each case.
Only 4 of these 35 cases of G bronchialis infections were skin and soft tissue infections. All 4 occurred in immunocompetent hosts, and 3 were associated with needle punctures or surgery. The fourth case involved a recurrent breast abscess that occurred in a patient without known risk factors or recent procedures.23 Other Gordonia species have been associated with cutaneous infections, including Gordonia amicalis, G terrae, and recently Gordonia westfalica, with the latter 2 demonstrating actinomycetoma formation.32-34 Our case is remarkable in that it represents actinomycetoma due to G bronchialis. Of note, our patient was immunocompetent and did not have any radiation or chronic lymphedema involving the affected extremity. However, his history of steroid-induced skin atrophy may have predisposed him to this rare infection.
Clinical Presentation—Classic mycetoma demonstrate organismal granules within the dermis, surrounded by a neutrophilic infiltrate, which is in turn surrounded by histiocytes and multinucleated giant cells. Periodic acid–Schiff and silver stains can identify fungal organisms, while Gram stain helps to elucidate bacterial etiologies.1 In our patient, a biopsy revealed several dermal aggregates of pseudofilamentous gram-positive organisms surrounded by a neutrophilic and histiocytic infiltrate.8 Because this case presented over weeks to months rather than months to years, it progressed more rapidly than a classic mycetoma. However, the dermatologic and histologic features were consistent with mycetoma.
Management—General treatment of actinomycetoma requires identification of the causative organism and prolonged administration of antibiotics, typically in combination.35-37 Most G bronchialis infections associated with surgical intervention or implants in the literature required surgical debridement and removal of contaminated material for clinical cure, with the exception of 3 cases of sternal wound infection and 1 case of peritonitis that recovered with antimicrobial therapy alone.3,17 Combination therapy often was used, but monotherapy, particularly with a fluoroquinolone, has been reported. Susceptibility data are limited, but in general, Gordonia species appear susceptible to imipenem, ciprofloxacin, amikacin, gentamicin, and linezolid, with variable susceptibility to vancomycin (89% of isolates), third-generation cephalosporins (80%–90% of isolates), tetracyclines (≤85% of isolates), penicillin (≤70% of isolates), and trimethoprim-sulfamethoxazole (≤65% of isolates).7,10,19,38-40 Although there are no standardized recommendations for the treatment of these infections, the most commonly used drugs to treat Gordonia are carbapenems and fluoroquinolones, with or without an aminoglycoside, followed by third-generation cephalosporins and vancomycin, depending on susceptibilities. Additional antibiotics (alone or in combination) that have previously been used with favorable outcomes include amoxicillin or amoxicillin-clavulanate, piperacillin-tazobactam, rifampicin, trimethoprim-sulfamethoxazole, minocycline, doxycycline, and daptomycin.
Our patient received amoxicillin-clavulanate, trimethoprim-sulfamethoxazole, and linezolid. We considered combination therapy but decided against it due to concern for toxicity, given his age and poor renal function. The antibiotic that was most important to his recovery was unclear; the patient insisted that his body, not antibiotics, deserved most of the credit for healing his arm. Although cultures and polymerase chain reaction assays were negative after 3 weeks of amoxicillin-clavulanate, the patient did not show clinical improvement—reasons could be because the antibiotic reduced but did not eliminate the bacterial burden, sampling error of the biopsy, or it takes much longer for the body to heal than it takes to kill the bacteria. Most likely a combination of factors was at play.
Conclusion
Gordonia bronchialis is an emerging cause of human infections typically occurring after trauma, inoculation, or surgery. Most infections are localized; however, the present case highlights the ability of this species to form a massive cutaneous infection. Treatment should be tailored to susceptibility, with close follow-up to ensure improvement and resolution. For clinicians encountering a similar case, we encourage biopsy prior to empiric antibiotics, as antibiotic therapy can decrease the yield of subsequent testing. Treatment should be guided by the clinical course and may need to last weeks to months. Combination therapy for Gordonia infections should be considered in severe cases, in cases presenting as actinomycetoma, in those not responding to therapy, or when the susceptibility profile is unknown or unreliable.
Acknowledgments—The authors thank this veteran for allowing us to participate in his care and to learn from his experience. He gave his consent for us to share his story and the photographs of the arm.
- Arenas R, Fernandez Martinez RF, Torres-Guerrero E, et al. Actinomycetoma: an update on diagnosis and treatment. Cutis. 2017;99:E11-E15.
- Poonwan N, Mekha N, Yazawa K, et al. Characterization of clinical isolates of pathogenic Nocardia strains and related actinomycetes in Thailand from 1996 to 2003. Mycopathologia. 2005;159:361-368.
- Richet HM, Craven PC, Brown JM, et al. A cluster of Rhodococcus (Gordona) bronchialis sternal-wound infections after coronary-artery bypass surgery. N Engl J Med. 1991;324:104-109.
- Wright SN, Gerry JS, Busowski MT, et al. Gordonia bronchialis sternal wound infection in 3 patients following open heart surgery: intraoperative transmission from a healthcare worker. Infect Control Hosp Epidemiol. 2012;33:1238-1241.
- Tsukamura M. Proposal of a new genus, Gordona, for slightly acid-fast organisms occurring in sputa of patients with pulmonary disease and in soil. J Gen Microbiol. 1971;68:15-26.
- Wang T, Kong F, Chen S, et al. Improved identification of Gordonia, Rhodococcus and Tsukamurella species by 5′-end 16s rRNA gene sequencing. Pathology. 2011;43:58-63.
- Aoyama K, Kang Y, Yazawa K, et al. Characterization of clinical isolates of Gordonia species in Japanese clinical samples during 1998-2008. Mycopathologia. 2009;168:175-183.
- Ivanova N, Sikorski J, Jando M, et al. Complete genome sequence of Gordonia bronchialis type strain (3410 T). Stand Genomic Sci. 2010;2:19-28.
- Johnson JA, Onderdonk AB, Cosimi LA, et al. Gordonia bronchialis bacteremia and pleural infection: case report and review of the literature. J Clin Microbiol. 2011;49:1662-1666.
- Bartolomé-Álvarez J, Sáez-Nieto JA, Escudero-Jiménez A, et al. Cutaneous abscess due to Gordonia bronchialis: case report and literature review. Rev Esp Quimioter. 2016;29:170-173.
- Choi ME, Jung CJ, Won CH, et al. Case report of cutaneous nodule caused by Gordonia bronchialis in an immunocompetent patient after receiving acupuncture. J Dermatol. 2019;46:343-346.
- Nguyen DB, Gupta N, Abou-Daoud A, et al. A polymicrobial outbreak of surgical site infections following cardiac surgery at a community hospital in Florida, 2011-2012. Am J Infect Control. 2014;42:432-435.
- Chang JH, Ji M, Hong HL, et al. Sternal osteomyelitis caused byGordonia bronchialis after open-heart surgery. Infect Chemother. 2014;46:110-114.
- Rodriguez-Lozano J, Pérez-Llantada E, Agüero J, et al. Sternal wound infection caused by Gordonia bronchialis: identification by MALDI-TOF MS. JMM Case Rep. 2016;3:e005067.
- Akrami K, Coletta J, Mehta S, et al. Gordonia sternal wound infection treated with ceftaroline: case report and literature review. JMM Case Rep. 2017;4:e005113.
- Ambesh P, Kapoor A, Kazmi D, et al. Sternal osteomyelitis by Gordonia bronchialis in an immunocompetent patient after open heart surgery. Ann Card Anaesth. 2019;22:221-224.
- Ma TKW, Chow KM, Kwan BCH, et al. Peritoneal-dialysis related peritonitis caused by Gordonia species: report of four cases and literature review. Nephrology. 2014;19:379-383.
- Lam JYW, Wu AKL, Leung WS, et al. Gordonia species as emerging causes of continuous-ambulatory-peritoneal-dialysis-related peritonitis identified by 16S rRNA and secA1 gene sequencing and matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS). J Clin Microbiol. 2015;53:671-676.
- Blaschke AJ, Bender J, Byington CL, et al. Gordonia species: emerging pathogens in pediatric patients that are identified by 16S ribosomal RNA gene sequencing. Clin Infect Dis. 2007;45:483-486.
- Titécat M, Loïez C, Courcol RJ, et al. Difficulty with Gordonia bronchialis identification by Microflex mass spectrometer in a pacemaker‐induced endocarditis. JMM Case Rep. 2014;1:E003681.
- Siddiqui N, Toumeh A, Georgescu C. Tibial osteomyelitis caused by Gordonia bronchialis in an immunocompetent patient. J Clin Microbiol. 2012;50:3119-3121.
- Choi R, Strnad L, Flaxel CJ, et al. Gordonia bronchialis–associated endophthalmitis. Emerg Infect Dis. 2019;25:1017-1019.
- Werno AM, Anderson TP, Chambers ST, et al. Recurrent breast abscess caused by Gordonia bronchialis in an immunocompetent patient. J Clin Microbiol. 2005;43:3009-3010.
- Sng LH, Koh TH, Toney SR, et al. Bacteremia caused by Gordonia bronchialis in a patient with sequestrated lung. J Clin Microbiol. 2004;42:2870-2871.
- Ramanan P, Deziel PJ, Wengenack NL. Gordonia bacteremia. J Clin Microbiol. 2013;51:3443-3447.
- Sukackiene D, Rimsevicius L, Kiveryte S, et al. A case of successfully treated relapsing peritoneal dialysis-associated peritonitis caused by Gordonia bronchialis in a farmer. Nephrol Ther. 2018;14:109-111.
- Bruno V, Tjon J, Lin S, et al. Peritoneal dialysis-related peritonitis caused by Gordonia bronchialis: first pediatric report. Pediatr Nephrol. 2022;37:217-220. doi: 10.1007/s00467-021-05313-3
- Mormeneo Bayo S, Palacián Ruíz MP, Asin Samper U, et al. Pacemaker-induced endocarditis by Gordonia bronchialis. Enferm Infecc Microbiol Clin (Engl Ed). 2022;40:255-257.
- Davidson AL, Driscoll CR, Luther VP, et al. Recurrent skin and soft tissue infection following breast reduction surgery caused by Gordonia bronchialis: a case report. Plast Reconstr Surg Glob Open. 2022;10:E4395.
- Nwaedozie S, Mojarrab JN, Gopinath P, et al. Sternal osteomyelitis caused by Gordonia bronchialis in an immunocompetent patient following coronary artery bypass surgery. IDCases. 2022;29:E01548.
- Nakahama H, Hanada S, Takada K, et al. Obstructive pneumonia caused by Gordonia bronchialis with a bronchial foreign body. Int J Infect Dis. 2022;124:157-158. doi:10.1016/j.ijid.2022.09.028
- Lai CC, Hsieh JH, Tsai HY, et al. Cutaneous infection caused by Gordonia amicalis after a traumatic injury. J Clin Microbiol. 2012;50:1821-1822.
- Bakker XR, Spauwen PHM, Dolmans WMV. Mycetoma of the hand caused by Gordona terrae: a case report. J Hand Surg Am. 2004;29:188-190.
- Gueneau R, Blanchet D, Rodriguez-Nava V, et al. Actinomycetoma caused by Gordonia westfalica: first reported case of human infection. New Microbes New Infect. 2020;34:100658.
- Auwaerter PG, ed. The Johns Hopkins POC-IT ABX Guide. Johns Hopkins Medicine; 2021.
- Welsh O, Sauceda E, Gonzalez J, et al. Amikacin alone andin combination with trimethoprim-sulfamethoxazole in the treatment of actinomycotic mycetoma. J Am Acad Dermatol. 1987;17:443-448.
- Zijlstra EE, van de Sande WWJ, Welsh O, et al. Mycetoma: a unique neglected tropical disease. Lancet Infect Dis. 2016;16:100-112.
- Pham AS, Dé I, Rolston KV, et al. Catheter-related bacteremia caused by the nocardioform actinomycete Gordonia terrae. Clin Infect Dis. 2003;36:524-527.
- Renvoise A, Harle JR, Raoult D, et al. Gordonia sputi bacteremia. Emerg Infect Dis. 2009;15:1535-1537.
- Moser BD, Pellegrini GJ, Lasker BA, et al. Pattern of antimicrobial susceptibility obtained from blood isolates of a rare but emerging human pathogen, Gordonia polyisoprenivorans. Antimicrob Agents Chemother. 2012;56:4991-4993.
Mycetoma is a chronic subcutaneous infection due to fungal (eumycetoma) or aerobic actinomycetes (actinomycetoma) organisms. Clinical lesions develop from a granulomatous infiltrate organizing around the infectious organism. Patients can present with extensive subcutaneous nodularity and draining sinuses that can lead to deformation of the affected extremity. These infections are rare in developed countries, and the prevalence and incidence remain unknown. It has been reported that actinomycetes represent 60% of mycetoma cases worldwide, with the majority of cases in Central America from Nocardia (86%) and Actinomadura madurae (10%). 1Gordonia species are aerobic, partially acid-fast, gram-positive actinobacteria that may comprise a notable minority of actinomycete isolates. 2 The species Gordonia bronchialis is of particular interest as a human pathogen because of increasing reports of nosocomial infections. 3,4 We describe a case of a mycetomalike infection due to G bronchialis in an immunocompetent patient with complete resolution after 3 months of antibiotics.

Case Report
An 86-year-old man presented to the emergency department with a pruritic rash on the right forearm. He had a history of chronic kidney disease, hypertension, and inverse psoriasis complicated by steroid atrophy. He reported trauma to the right antecubital fossa approximately 1 to 2 months prior from a car door; he received wound care over several weeks at an outside hospital. The initial wound healed completely, but he subsequently noticed erythema spreading down the forearm. At the current presentation, he was empirically treated with mid-potency topical steroids and cefuroxime for 7 days. Initial laboratory results were notable for a white blood cell count of 5.7×103 cells/μL (reference range,3.7–8.4×103 cells/μL) and a creatinine level of 1.5 mg/dL (reference range, 0.57–1.25 mg/dL). The patient returned to the emergency department 2 weeks later with spreading of the initial rash and worsening pruritus. Dermatologic evaluation revealed the patient was afebrile and had violaceous papules and nodules that coalesced into plaques on the right arm, with the largest measuring approximately 15 cm. Areas of superficial erosion and crusting were noted (Figure 1A). The patient denied constitutional symptoms and had no axillary or cervical lymphadenopathy. The differential initially included an atypical infection vs a neoplasm. Two 5-mm punch biopsies were performed, which demonstrated a suppurative granulomatous infiltrate in the dermis with extension into the subcutis (Figure 2A). Focal vacuolations within the dermis demonstrated aggregates of gram-positive pseudofilamentous organisms (Figures 2B and 2C). Aerobic tissue cultures grew G bronchialis that was susceptible to all antibiotics tested and Staphylococcus epidermidis. Fungal and mycobacterial cultures were negative. The patient was placed on amoxicillin 875 mg–clavulanate 125 mg twice daily for 3 weeks. However, he demonstrated progression of the rash, with increased induration and confluence of plaques on the forearm (Figure 1B). A repeat excisional biopsy was performed, and a tissue sample was sent for 16S ribosomal RNA sequencing identification. However, neither conventional cultures nor sequencing demonstrated evidence of G bronchialis or any other pathogen. Additionally, bacterial, fungal, and mycobacterial blood cultures were negative. Amoxicillin-clavulanate was stopped, and he was placed on trimethoprim-sulfamethoxazole for 2 weeks, then changed to linezolid (600 mg twice daily) due to continued lack of improvement of the rash. After 2 weeks of linezolid, the rash was slightly improved, but the patient had notable side effects (eg, nausea, mucositis). Therefore, he was switched back to trimethoprim-sulfamethoxazole for another 6 weeks. Antibiotic therapy was discontinued after there was notable regression of indurated plaques (Figure 1C); he received more than 3 months of antibiotics in all. At 1 month after completion of antibiotic therapy, the patient had no evidence of recurrence.
Comment
Microbiology of Gordonia Species—Gordonia bronchialis originally was isolated in 1971 by Tsukamura et al5 from the sputum of patients with cavitary tuberculosis and bronchiectasis in Japan. Other Gordonia species (formerly Rhodococcus or Gordona) later were identified in soil, seawater, sediment, and wastewater. Gordonia bronchialis is a gram-positive aerobic actinomycete short rod that organizes in cordlike compact groups. It is weakly acid fast, nonmotile, and nonsporulating. Colonies exhibit pinkish-brown pigmentation. Our understanding of the clinical significance of this organism continues to evolve, and it is not always clearly pathogenic. Because Gordonia isolates may be dismissed as commensals or misidentified as Nocardia or Rhodococcus by routine biochemical tests, it is possible that infections may go undetected. Speciation requires gene sequencing; as our utilization of molecular methods has increased, the identification of clinically relevant aerobic actinomycetes, including Gordonia, has improved,6 and the following species have been recognized as pathogens: Gordonia araii, G bronchialis, Gordonia effusa, Gordonia otitidis, Gordonia polyisoprenivorans, Gordonia rubirpertincta, Gordonia sputi, and Gordonia terrae.7
Cases Reported in the Literature—A PubMed search of articles indexed for MEDLINE using the term Gordonia bronchialis yielded 35 previously reported human cases of G bronchialis infection, most often associated with medical devices or procedures.8-31 Eighteen of these cases were sternal surgical site infections in patients with a history of cardiac surgery,3,4,12-16,30 including 2 outbreaks following coronary artery bypass grafting that were thought to be related to intraoperative transmission from a nurse.3,4 Of the remaining cases, 12 were linked to a procedure or an indwelling catheter: 4 cases of peritonitis in the setting of continuous ambulatory peritoneal dialysis17,18,26,27; 3 cases of skin and soft tissue infection (1 at the site of a prior needle injection,10 1 after acupuncture,11 and 1 after breast reduction surgery29); 1 case of ventriculitis in a premature neonate with an underlying intraventricular shunt19; 2 cases of pacemaker-induced endocarditis20,28; 1 case of tibial osteomyelitis related to a bioresorbable polymer screw21; and 1 case of chronic endophthalmitis with underlying intraocular lens implants.22 The Table lists all cases of G bronchialis skin or surgical site infections encountered in our literature search as well as the treatment provided in each case.
Only 4 of these 35 cases of G bronchialis infections were skin and soft tissue infections. All 4 occurred in immunocompetent hosts, and 3 were associated with needle punctures or surgery. The fourth case involved a recurrent breast abscess that occurred in a patient without known risk factors or recent procedures.23 Other Gordonia species have been associated with cutaneous infections, including Gordonia amicalis, G terrae, and recently Gordonia westfalica, with the latter 2 demonstrating actinomycetoma formation.32-34 Our case is remarkable in that it represents actinomycetoma due to G bronchialis. Of note, our patient was immunocompetent and did not have any radiation or chronic lymphedema involving the affected extremity. However, his history of steroid-induced skin atrophy may have predisposed him to this rare infection.
Clinical Presentation—Classic mycetoma demonstrate organismal granules within the dermis, surrounded by a neutrophilic infiltrate, which is in turn surrounded by histiocytes and multinucleated giant cells. Periodic acid–Schiff and silver stains can identify fungal organisms, while Gram stain helps to elucidate bacterial etiologies.1 In our patient, a biopsy revealed several dermal aggregates of pseudofilamentous gram-positive organisms surrounded by a neutrophilic and histiocytic infiltrate.8 Because this case presented over weeks to months rather than months to years, it progressed more rapidly than a classic mycetoma. However, the dermatologic and histologic features were consistent with mycetoma.
Management—General treatment of actinomycetoma requires identification of the causative organism and prolonged administration of antibiotics, typically in combination.35-37 Most G bronchialis infections associated with surgical intervention or implants in the literature required surgical debridement and removal of contaminated material for clinical cure, with the exception of 3 cases of sternal wound infection and 1 case of peritonitis that recovered with antimicrobial therapy alone.3,17 Combination therapy often was used, but monotherapy, particularly with a fluoroquinolone, has been reported. Susceptibility data are limited, but in general, Gordonia species appear susceptible to imipenem, ciprofloxacin, amikacin, gentamicin, and linezolid, with variable susceptibility to vancomycin (89% of isolates), third-generation cephalosporins (80%–90% of isolates), tetracyclines (≤85% of isolates), penicillin (≤70% of isolates), and trimethoprim-sulfamethoxazole (≤65% of isolates).7,10,19,38-40 Although there are no standardized recommendations for the treatment of these infections, the most commonly used drugs to treat Gordonia are carbapenems and fluoroquinolones, with or without an aminoglycoside, followed by third-generation cephalosporins and vancomycin, depending on susceptibilities. Additional antibiotics (alone or in combination) that have previously been used with favorable outcomes include amoxicillin or amoxicillin-clavulanate, piperacillin-tazobactam, rifampicin, trimethoprim-sulfamethoxazole, minocycline, doxycycline, and daptomycin.
Our patient received amoxicillin-clavulanate, trimethoprim-sulfamethoxazole, and linezolid. We considered combination therapy but decided against it due to concern for toxicity, given his age and poor renal function. The antibiotic that was most important to his recovery was unclear; the patient insisted that his body, not antibiotics, deserved most of the credit for healing his arm. Although cultures and polymerase chain reaction assays were negative after 3 weeks of amoxicillin-clavulanate, the patient did not show clinical improvement—reasons could be because the antibiotic reduced but did not eliminate the bacterial burden, sampling error of the biopsy, or it takes much longer for the body to heal than it takes to kill the bacteria. Most likely a combination of factors was at play.
Conclusion
Gordonia bronchialis is an emerging cause of human infections typically occurring after trauma, inoculation, or surgery. Most infections are localized; however, the present case highlights the ability of this species to form a massive cutaneous infection. Treatment should be tailored to susceptibility, with close follow-up to ensure improvement and resolution. For clinicians encountering a similar case, we encourage biopsy prior to empiric antibiotics, as antibiotic therapy can decrease the yield of subsequent testing. Treatment should be guided by the clinical course and may need to last weeks to months. Combination therapy for Gordonia infections should be considered in severe cases, in cases presenting as actinomycetoma, in those not responding to therapy, or when the susceptibility profile is unknown or unreliable.
Acknowledgments—The authors thank this veteran for allowing us to participate in his care and to learn from his experience. He gave his consent for us to share his story and the photographs of the arm.
Mycetoma is a chronic subcutaneous infection due to fungal (eumycetoma) or aerobic actinomycetes (actinomycetoma) organisms. Clinical lesions develop from a granulomatous infiltrate organizing around the infectious organism. Patients can present with extensive subcutaneous nodularity and draining sinuses that can lead to deformation of the affected extremity. These infections are rare in developed countries, and the prevalence and incidence remain unknown. It has been reported that actinomycetes represent 60% of mycetoma cases worldwide, with the majority of cases in Central America from Nocardia (86%) and Actinomadura madurae (10%). 1Gordonia species are aerobic, partially acid-fast, gram-positive actinobacteria that may comprise a notable minority of actinomycete isolates. 2 The species Gordonia bronchialis is of particular interest as a human pathogen because of increasing reports of nosocomial infections. 3,4 We describe a case of a mycetomalike infection due to G bronchialis in an immunocompetent patient with complete resolution after 3 months of antibiotics.

Case Report
An 86-year-old man presented to the emergency department with a pruritic rash on the right forearm. He had a history of chronic kidney disease, hypertension, and inverse psoriasis complicated by steroid atrophy. He reported trauma to the right antecubital fossa approximately 1 to 2 months prior from a car door; he received wound care over several weeks at an outside hospital. The initial wound healed completely, but he subsequently noticed erythema spreading down the forearm. At the current presentation, he was empirically treated with mid-potency topical steroids and cefuroxime for 7 days. Initial laboratory results were notable for a white blood cell count of 5.7×103 cells/μL (reference range,3.7–8.4×103 cells/μL) and a creatinine level of 1.5 mg/dL (reference range, 0.57–1.25 mg/dL). The patient returned to the emergency department 2 weeks later with spreading of the initial rash and worsening pruritus. Dermatologic evaluation revealed the patient was afebrile and had violaceous papules and nodules that coalesced into plaques on the right arm, with the largest measuring approximately 15 cm. Areas of superficial erosion and crusting were noted (Figure 1A). The patient denied constitutional symptoms and had no axillary or cervical lymphadenopathy. The differential initially included an atypical infection vs a neoplasm. Two 5-mm punch biopsies were performed, which demonstrated a suppurative granulomatous infiltrate in the dermis with extension into the subcutis (Figure 2A). Focal vacuolations within the dermis demonstrated aggregates of gram-positive pseudofilamentous organisms (Figures 2B and 2C). Aerobic tissue cultures grew G bronchialis that was susceptible to all antibiotics tested and Staphylococcus epidermidis. Fungal and mycobacterial cultures were negative. The patient was placed on amoxicillin 875 mg–clavulanate 125 mg twice daily for 3 weeks. However, he demonstrated progression of the rash, with increased induration and confluence of plaques on the forearm (Figure 1B). A repeat excisional biopsy was performed, and a tissue sample was sent for 16S ribosomal RNA sequencing identification. However, neither conventional cultures nor sequencing demonstrated evidence of G bronchialis or any other pathogen. Additionally, bacterial, fungal, and mycobacterial blood cultures were negative. Amoxicillin-clavulanate was stopped, and he was placed on trimethoprim-sulfamethoxazole for 2 weeks, then changed to linezolid (600 mg twice daily) due to continued lack of improvement of the rash. After 2 weeks of linezolid, the rash was slightly improved, but the patient had notable side effects (eg, nausea, mucositis). Therefore, he was switched back to trimethoprim-sulfamethoxazole for another 6 weeks. Antibiotic therapy was discontinued after there was notable regression of indurated plaques (Figure 1C); he received more than 3 months of antibiotics in all. At 1 month after completion of antibiotic therapy, the patient had no evidence of recurrence.
Comment
Microbiology of Gordonia Species—Gordonia bronchialis originally was isolated in 1971 by Tsukamura et al5 from the sputum of patients with cavitary tuberculosis and bronchiectasis in Japan. Other Gordonia species (formerly Rhodococcus or Gordona) later were identified in soil, seawater, sediment, and wastewater. Gordonia bronchialis is a gram-positive aerobic actinomycete short rod that organizes in cordlike compact groups. It is weakly acid fast, nonmotile, and nonsporulating. Colonies exhibit pinkish-brown pigmentation. Our understanding of the clinical significance of this organism continues to evolve, and it is not always clearly pathogenic. Because Gordonia isolates may be dismissed as commensals or misidentified as Nocardia or Rhodococcus by routine biochemical tests, it is possible that infections may go undetected. Speciation requires gene sequencing; as our utilization of molecular methods has increased, the identification of clinically relevant aerobic actinomycetes, including Gordonia, has improved,6 and the following species have been recognized as pathogens: Gordonia araii, G bronchialis, Gordonia effusa, Gordonia otitidis, Gordonia polyisoprenivorans, Gordonia rubirpertincta, Gordonia sputi, and Gordonia terrae.7
Cases Reported in the Literature—A PubMed search of articles indexed for MEDLINE using the term Gordonia bronchialis yielded 35 previously reported human cases of G bronchialis infection, most often associated with medical devices or procedures.8-31 Eighteen of these cases were sternal surgical site infections in patients with a history of cardiac surgery,3,4,12-16,30 including 2 outbreaks following coronary artery bypass grafting that were thought to be related to intraoperative transmission from a nurse.3,4 Of the remaining cases, 12 were linked to a procedure or an indwelling catheter: 4 cases of peritonitis in the setting of continuous ambulatory peritoneal dialysis17,18,26,27; 3 cases of skin and soft tissue infection (1 at the site of a prior needle injection,10 1 after acupuncture,11 and 1 after breast reduction surgery29); 1 case of ventriculitis in a premature neonate with an underlying intraventricular shunt19; 2 cases of pacemaker-induced endocarditis20,28; 1 case of tibial osteomyelitis related to a bioresorbable polymer screw21; and 1 case of chronic endophthalmitis with underlying intraocular lens implants.22 The Table lists all cases of G bronchialis skin or surgical site infections encountered in our literature search as well as the treatment provided in each case.
Only 4 of these 35 cases of G bronchialis infections were skin and soft tissue infections. All 4 occurred in immunocompetent hosts, and 3 were associated with needle punctures or surgery. The fourth case involved a recurrent breast abscess that occurred in a patient without known risk factors or recent procedures.23 Other Gordonia species have been associated with cutaneous infections, including Gordonia amicalis, G terrae, and recently Gordonia westfalica, with the latter 2 demonstrating actinomycetoma formation.32-34 Our case is remarkable in that it represents actinomycetoma due to G bronchialis. Of note, our patient was immunocompetent and did not have any radiation or chronic lymphedema involving the affected extremity. However, his history of steroid-induced skin atrophy may have predisposed him to this rare infection.
Clinical Presentation—Classic mycetoma demonstrate organismal granules within the dermis, surrounded by a neutrophilic infiltrate, which is in turn surrounded by histiocytes and multinucleated giant cells. Periodic acid–Schiff and silver stains can identify fungal organisms, while Gram stain helps to elucidate bacterial etiologies.1 In our patient, a biopsy revealed several dermal aggregates of pseudofilamentous gram-positive organisms surrounded by a neutrophilic and histiocytic infiltrate.8 Because this case presented over weeks to months rather than months to years, it progressed more rapidly than a classic mycetoma. However, the dermatologic and histologic features were consistent with mycetoma.
Management—General treatment of actinomycetoma requires identification of the causative organism and prolonged administration of antibiotics, typically in combination.35-37 Most G bronchialis infections associated with surgical intervention or implants in the literature required surgical debridement and removal of contaminated material for clinical cure, with the exception of 3 cases of sternal wound infection and 1 case of peritonitis that recovered with antimicrobial therapy alone.3,17 Combination therapy often was used, but monotherapy, particularly with a fluoroquinolone, has been reported. Susceptibility data are limited, but in general, Gordonia species appear susceptible to imipenem, ciprofloxacin, amikacin, gentamicin, and linezolid, with variable susceptibility to vancomycin (89% of isolates), third-generation cephalosporins (80%–90% of isolates), tetracyclines (≤85% of isolates), penicillin (≤70% of isolates), and trimethoprim-sulfamethoxazole (≤65% of isolates).7,10,19,38-40 Although there are no standardized recommendations for the treatment of these infections, the most commonly used drugs to treat Gordonia are carbapenems and fluoroquinolones, with or without an aminoglycoside, followed by third-generation cephalosporins and vancomycin, depending on susceptibilities. Additional antibiotics (alone or in combination) that have previously been used with favorable outcomes include amoxicillin or amoxicillin-clavulanate, piperacillin-tazobactam, rifampicin, trimethoprim-sulfamethoxazole, minocycline, doxycycline, and daptomycin.
Our patient received amoxicillin-clavulanate, trimethoprim-sulfamethoxazole, and linezolid. We considered combination therapy but decided against it due to concern for toxicity, given his age and poor renal function. The antibiotic that was most important to his recovery was unclear; the patient insisted that his body, not antibiotics, deserved most of the credit for healing his arm. Although cultures and polymerase chain reaction assays were negative after 3 weeks of amoxicillin-clavulanate, the patient did not show clinical improvement—reasons could be because the antibiotic reduced but did not eliminate the bacterial burden, sampling error of the biopsy, or it takes much longer for the body to heal than it takes to kill the bacteria. Most likely a combination of factors was at play.
Conclusion
Gordonia bronchialis is an emerging cause of human infections typically occurring after trauma, inoculation, or surgery. Most infections are localized; however, the present case highlights the ability of this species to form a massive cutaneous infection. Treatment should be tailored to susceptibility, with close follow-up to ensure improvement and resolution. For clinicians encountering a similar case, we encourage biopsy prior to empiric antibiotics, as antibiotic therapy can decrease the yield of subsequent testing. Treatment should be guided by the clinical course and may need to last weeks to months. Combination therapy for Gordonia infections should be considered in severe cases, in cases presenting as actinomycetoma, in those not responding to therapy, or when the susceptibility profile is unknown or unreliable.
Acknowledgments—The authors thank this veteran for allowing us to participate in his care and to learn from his experience. He gave his consent for us to share his story and the photographs of the arm.
- Arenas R, Fernandez Martinez RF, Torres-Guerrero E, et al. Actinomycetoma: an update on diagnosis and treatment. Cutis. 2017;99:E11-E15.
- Poonwan N, Mekha N, Yazawa K, et al. Characterization of clinical isolates of pathogenic Nocardia strains and related actinomycetes in Thailand from 1996 to 2003. Mycopathologia. 2005;159:361-368.
- Richet HM, Craven PC, Brown JM, et al. A cluster of Rhodococcus (Gordona) bronchialis sternal-wound infections after coronary-artery bypass surgery. N Engl J Med. 1991;324:104-109.
- Wright SN, Gerry JS, Busowski MT, et al. Gordonia bronchialis sternal wound infection in 3 patients following open heart surgery: intraoperative transmission from a healthcare worker. Infect Control Hosp Epidemiol. 2012;33:1238-1241.
- Tsukamura M. Proposal of a new genus, Gordona, for slightly acid-fast organisms occurring in sputa of patients with pulmonary disease and in soil. J Gen Microbiol. 1971;68:15-26.
- Wang T, Kong F, Chen S, et al. Improved identification of Gordonia, Rhodococcus and Tsukamurella species by 5′-end 16s rRNA gene sequencing. Pathology. 2011;43:58-63.
- Aoyama K, Kang Y, Yazawa K, et al. Characterization of clinical isolates of Gordonia species in Japanese clinical samples during 1998-2008. Mycopathologia. 2009;168:175-183.
- Ivanova N, Sikorski J, Jando M, et al. Complete genome sequence of Gordonia bronchialis type strain (3410 T). Stand Genomic Sci. 2010;2:19-28.
- Johnson JA, Onderdonk AB, Cosimi LA, et al. Gordonia bronchialis bacteremia and pleural infection: case report and review of the literature. J Clin Microbiol. 2011;49:1662-1666.
- Bartolomé-Álvarez J, Sáez-Nieto JA, Escudero-Jiménez A, et al. Cutaneous abscess due to Gordonia bronchialis: case report and literature review. Rev Esp Quimioter. 2016;29:170-173.
- Choi ME, Jung CJ, Won CH, et al. Case report of cutaneous nodule caused by Gordonia bronchialis in an immunocompetent patient after receiving acupuncture. J Dermatol. 2019;46:343-346.
- Nguyen DB, Gupta N, Abou-Daoud A, et al. A polymicrobial outbreak of surgical site infections following cardiac surgery at a community hospital in Florida, 2011-2012. Am J Infect Control. 2014;42:432-435.
- Chang JH, Ji M, Hong HL, et al. Sternal osteomyelitis caused byGordonia bronchialis after open-heart surgery. Infect Chemother. 2014;46:110-114.
- Rodriguez-Lozano J, Pérez-Llantada E, Agüero J, et al. Sternal wound infection caused by Gordonia bronchialis: identification by MALDI-TOF MS. JMM Case Rep. 2016;3:e005067.
- Akrami K, Coletta J, Mehta S, et al. Gordonia sternal wound infection treated with ceftaroline: case report and literature review. JMM Case Rep. 2017;4:e005113.
- Ambesh P, Kapoor A, Kazmi D, et al. Sternal osteomyelitis by Gordonia bronchialis in an immunocompetent patient after open heart surgery. Ann Card Anaesth. 2019;22:221-224.
- Ma TKW, Chow KM, Kwan BCH, et al. Peritoneal-dialysis related peritonitis caused by Gordonia species: report of four cases and literature review. Nephrology. 2014;19:379-383.
- Lam JYW, Wu AKL, Leung WS, et al. Gordonia species as emerging causes of continuous-ambulatory-peritoneal-dialysis-related peritonitis identified by 16S rRNA and secA1 gene sequencing and matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS). J Clin Microbiol. 2015;53:671-676.
- Blaschke AJ, Bender J, Byington CL, et al. Gordonia species: emerging pathogens in pediatric patients that are identified by 16S ribosomal RNA gene sequencing. Clin Infect Dis. 2007;45:483-486.
- Titécat M, Loïez C, Courcol RJ, et al. Difficulty with Gordonia bronchialis identification by Microflex mass spectrometer in a pacemaker‐induced endocarditis. JMM Case Rep. 2014;1:E003681.
- Siddiqui N, Toumeh A, Georgescu C. Tibial osteomyelitis caused by Gordonia bronchialis in an immunocompetent patient. J Clin Microbiol. 2012;50:3119-3121.
- Choi R, Strnad L, Flaxel CJ, et al. Gordonia bronchialis–associated endophthalmitis. Emerg Infect Dis. 2019;25:1017-1019.
- Werno AM, Anderson TP, Chambers ST, et al. Recurrent breast abscess caused by Gordonia bronchialis in an immunocompetent patient. J Clin Microbiol. 2005;43:3009-3010.
- Sng LH, Koh TH, Toney SR, et al. Bacteremia caused by Gordonia bronchialis in a patient with sequestrated lung. J Clin Microbiol. 2004;42:2870-2871.
- Ramanan P, Deziel PJ, Wengenack NL. Gordonia bacteremia. J Clin Microbiol. 2013;51:3443-3447.
- Sukackiene D, Rimsevicius L, Kiveryte S, et al. A case of successfully treated relapsing peritoneal dialysis-associated peritonitis caused by Gordonia bronchialis in a farmer. Nephrol Ther. 2018;14:109-111.
- Bruno V, Tjon J, Lin S, et al. Peritoneal dialysis-related peritonitis caused by Gordonia bronchialis: first pediatric report. Pediatr Nephrol. 2022;37:217-220. doi: 10.1007/s00467-021-05313-3
- Mormeneo Bayo S, Palacián Ruíz MP, Asin Samper U, et al. Pacemaker-induced endocarditis by Gordonia bronchialis. Enferm Infecc Microbiol Clin (Engl Ed). 2022;40:255-257.
- Davidson AL, Driscoll CR, Luther VP, et al. Recurrent skin and soft tissue infection following breast reduction surgery caused by Gordonia bronchialis: a case report. Plast Reconstr Surg Glob Open. 2022;10:E4395.
- Nwaedozie S, Mojarrab JN, Gopinath P, et al. Sternal osteomyelitis caused by Gordonia bronchialis in an immunocompetent patient following coronary artery bypass surgery. IDCases. 2022;29:E01548.
- Nakahama H, Hanada S, Takada K, et al. Obstructive pneumonia caused by Gordonia bronchialis with a bronchial foreign body. Int J Infect Dis. 2022;124:157-158. doi:10.1016/j.ijid.2022.09.028
- Lai CC, Hsieh JH, Tsai HY, et al. Cutaneous infection caused by Gordonia amicalis after a traumatic injury. J Clin Microbiol. 2012;50:1821-1822.
- Bakker XR, Spauwen PHM, Dolmans WMV. Mycetoma of the hand caused by Gordona terrae: a case report. J Hand Surg Am. 2004;29:188-190.
- Gueneau R, Blanchet D, Rodriguez-Nava V, et al. Actinomycetoma caused by Gordonia westfalica: first reported case of human infection. New Microbes New Infect. 2020;34:100658.
- Auwaerter PG, ed. The Johns Hopkins POC-IT ABX Guide. Johns Hopkins Medicine; 2021.
- Welsh O, Sauceda E, Gonzalez J, et al. Amikacin alone andin combination with trimethoprim-sulfamethoxazole in the treatment of actinomycotic mycetoma. J Am Acad Dermatol. 1987;17:443-448.
- Zijlstra EE, van de Sande WWJ, Welsh O, et al. Mycetoma: a unique neglected tropical disease. Lancet Infect Dis. 2016;16:100-112.
- Pham AS, Dé I, Rolston KV, et al. Catheter-related bacteremia caused by the nocardioform actinomycete Gordonia terrae. Clin Infect Dis. 2003;36:524-527.
- Renvoise A, Harle JR, Raoult D, et al. Gordonia sputi bacteremia. Emerg Infect Dis. 2009;15:1535-1537.
- Moser BD, Pellegrini GJ, Lasker BA, et al. Pattern of antimicrobial susceptibility obtained from blood isolates of a rare but emerging human pathogen, Gordonia polyisoprenivorans. Antimicrob Agents Chemother. 2012;56:4991-4993.
- Arenas R, Fernandez Martinez RF, Torres-Guerrero E, et al. Actinomycetoma: an update on diagnosis and treatment. Cutis. 2017;99:E11-E15.
- Poonwan N, Mekha N, Yazawa K, et al. Characterization of clinical isolates of pathogenic Nocardia strains and related actinomycetes in Thailand from 1996 to 2003. Mycopathologia. 2005;159:361-368.
- Richet HM, Craven PC, Brown JM, et al. A cluster of Rhodococcus (Gordona) bronchialis sternal-wound infections after coronary-artery bypass surgery. N Engl J Med. 1991;324:104-109.
- Wright SN, Gerry JS, Busowski MT, et al. Gordonia bronchialis sternal wound infection in 3 patients following open heart surgery: intraoperative transmission from a healthcare worker. Infect Control Hosp Epidemiol. 2012;33:1238-1241.
- Tsukamura M. Proposal of a new genus, Gordona, for slightly acid-fast organisms occurring in sputa of patients with pulmonary disease and in soil. J Gen Microbiol. 1971;68:15-26.
- Wang T, Kong F, Chen S, et al. Improved identification of Gordonia, Rhodococcus and Tsukamurella species by 5′-end 16s rRNA gene sequencing. Pathology. 2011;43:58-63.
- Aoyama K, Kang Y, Yazawa K, et al. Characterization of clinical isolates of Gordonia species in Japanese clinical samples during 1998-2008. Mycopathologia. 2009;168:175-183.
- Ivanova N, Sikorski J, Jando M, et al. Complete genome sequence of Gordonia bronchialis type strain (3410 T). Stand Genomic Sci. 2010;2:19-28.
- Johnson JA, Onderdonk AB, Cosimi LA, et al. Gordonia bronchialis bacteremia and pleural infection: case report and review of the literature. J Clin Microbiol. 2011;49:1662-1666.
- Bartolomé-Álvarez J, Sáez-Nieto JA, Escudero-Jiménez A, et al. Cutaneous abscess due to Gordonia bronchialis: case report and literature review. Rev Esp Quimioter. 2016;29:170-173.
- Choi ME, Jung CJ, Won CH, et al. Case report of cutaneous nodule caused by Gordonia bronchialis in an immunocompetent patient after receiving acupuncture. J Dermatol. 2019;46:343-346.
- Nguyen DB, Gupta N, Abou-Daoud A, et al. A polymicrobial outbreak of surgical site infections following cardiac surgery at a community hospital in Florida, 2011-2012. Am J Infect Control. 2014;42:432-435.
- Chang JH, Ji M, Hong HL, et al. Sternal osteomyelitis caused byGordonia bronchialis after open-heart surgery. Infect Chemother. 2014;46:110-114.
- Rodriguez-Lozano J, Pérez-Llantada E, Agüero J, et al. Sternal wound infection caused by Gordonia bronchialis: identification by MALDI-TOF MS. JMM Case Rep. 2016;3:e005067.
- Akrami K, Coletta J, Mehta S, et al. Gordonia sternal wound infection treated with ceftaroline: case report and literature review. JMM Case Rep. 2017;4:e005113.
- Ambesh P, Kapoor A, Kazmi D, et al. Sternal osteomyelitis by Gordonia bronchialis in an immunocompetent patient after open heart surgery. Ann Card Anaesth. 2019;22:221-224.
- Ma TKW, Chow KM, Kwan BCH, et al. Peritoneal-dialysis related peritonitis caused by Gordonia species: report of four cases and literature review. Nephrology. 2014;19:379-383.
- Lam JYW, Wu AKL, Leung WS, et al. Gordonia species as emerging causes of continuous-ambulatory-peritoneal-dialysis-related peritonitis identified by 16S rRNA and secA1 gene sequencing and matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS). J Clin Microbiol. 2015;53:671-676.
- Blaschke AJ, Bender J, Byington CL, et al. Gordonia species: emerging pathogens in pediatric patients that are identified by 16S ribosomal RNA gene sequencing. Clin Infect Dis. 2007;45:483-486.
- Titécat M, Loïez C, Courcol RJ, et al. Difficulty with Gordonia bronchialis identification by Microflex mass spectrometer in a pacemaker‐induced endocarditis. JMM Case Rep. 2014;1:E003681.
- Siddiqui N, Toumeh A, Georgescu C. Tibial osteomyelitis caused by Gordonia bronchialis in an immunocompetent patient. J Clin Microbiol. 2012;50:3119-3121.
- Choi R, Strnad L, Flaxel CJ, et al. Gordonia bronchialis–associated endophthalmitis. Emerg Infect Dis. 2019;25:1017-1019.
- Werno AM, Anderson TP, Chambers ST, et al. Recurrent breast abscess caused by Gordonia bronchialis in an immunocompetent patient. J Clin Microbiol. 2005;43:3009-3010.
- Sng LH, Koh TH, Toney SR, et al. Bacteremia caused by Gordonia bronchialis in a patient with sequestrated lung. J Clin Microbiol. 2004;42:2870-2871.
- Ramanan P, Deziel PJ, Wengenack NL. Gordonia bacteremia. J Clin Microbiol. 2013;51:3443-3447.
- Sukackiene D, Rimsevicius L, Kiveryte S, et al. A case of successfully treated relapsing peritoneal dialysis-associated peritonitis caused by Gordonia bronchialis in a farmer. Nephrol Ther. 2018;14:109-111.
- Bruno V, Tjon J, Lin S, et al. Peritoneal dialysis-related peritonitis caused by Gordonia bronchialis: first pediatric report. Pediatr Nephrol. 2022;37:217-220. doi: 10.1007/s00467-021-05313-3
- Mormeneo Bayo S, Palacián Ruíz MP, Asin Samper U, et al. Pacemaker-induced endocarditis by Gordonia bronchialis. Enferm Infecc Microbiol Clin (Engl Ed). 2022;40:255-257.
- Davidson AL, Driscoll CR, Luther VP, et al. Recurrent skin and soft tissue infection following breast reduction surgery caused by Gordonia bronchialis: a case report. Plast Reconstr Surg Glob Open. 2022;10:E4395.
- Nwaedozie S, Mojarrab JN, Gopinath P, et al. Sternal osteomyelitis caused by Gordonia bronchialis in an immunocompetent patient following coronary artery bypass surgery. IDCases. 2022;29:E01548.
- Nakahama H, Hanada S, Takada K, et al. Obstructive pneumonia caused by Gordonia bronchialis with a bronchial foreign body. Int J Infect Dis. 2022;124:157-158. doi:10.1016/j.ijid.2022.09.028
- Lai CC, Hsieh JH, Tsai HY, et al. Cutaneous infection caused by Gordonia amicalis after a traumatic injury. J Clin Microbiol. 2012;50:1821-1822.
- Bakker XR, Spauwen PHM, Dolmans WMV. Mycetoma of the hand caused by Gordona terrae: a case report. J Hand Surg Am. 2004;29:188-190.
- Gueneau R, Blanchet D, Rodriguez-Nava V, et al. Actinomycetoma caused by Gordonia westfalica: first reported case of human infection. New Microbes New Infect. 2020;34:100658.
- Auwaerter PG, ed. The Johns Hopkins POC-IT ABX Guide. Johns Hopkins Medicine; 2021.
- Welsh O, Sauceda E, Gonzalez J, et al. Amikacin alone andin combination with trimethoprim-sulfamethoxazole in the treatment of actinomycotic mycetoma. J Am Acad Dermatol. 1987;17:443-448.
- Zijlstra EE, van de Sande WWJ, Welsh O, et al. Mycetoma: a unique neglected tropical disease. Lancet Infect Dis. 2016;16:100-112.
- Pham AS, Dé I, Rolston KV, et al. Catheter-related bacteremia caused by the nocardioform actinomycete Gordonia terrae. Clin Infect Dis. 2003;36:524-527.
- Renvoise A, Harle JR, Raoult D, et al. Gordonia sputi bacteremia. Emerg Infect Dis. 2009;15:1535-1537.
- Moser BD, Pellegrini GJ, Lasker BA, et al. Pattern of antimicrobial susceptibility obtained from blood isolates of a rare but emerging human pathogen, Gordonia polyisoprenivorans. Antimicrob Agents Chemother. 2012;56:4991-4993.
Practice Points
- Gordonia bronchialis is an emerging cause of human skin and soft tissue infection, typically occurring after trauma, inoculation, or surgery.
- Gordonia species can cause a mycetomalike skin infection.
- Increasing use of molecular methods to identify bacteria has improved identification of clinically relevant actinomycetes, such as Helvetica Neue LT StdGordonia, and increases the likelihood that clinicians will see these organisms on culture results.
Iron Screening in Alopecia Areata Patients May Catch Hereditary Hemochromatosis Early
The role of micronutrients in the hair follicle cycle is not fully understood; thus deficiency and/or excess of certain micronutrients may be a modifiable risk factor associated with the development and/or treatment of some types of hair loss and therefore may be included in the workup during an alopecia consultation.
Hereditary hemochromatosis (HHC) is the most common genetic disorder identified in White individuals, with a worldwide prevalence of 1 in 220 to 1 in 250 individuals for a homozygous mutation. It most commonly affects individuals of Northern European descent.1 Men usually present in the fourth to sixth decades of life, while women usually develop symptoms after menopause, as pregnancy and menstruation delay the onset of the disease.2 Early symptoms of HHC include fatigue, joint pain, abdominal pain, and weight loss. Men are more likely to develop complications; in fact, 1 in 10 men with HHC will develop severe liver disease.3 As the disease progresses, affected individuals can present with cardiomyopathy (restrictive and dilated), cirrhosis, hypogonadism (usually hypogonadotrophic), arthropathy, diabetes mellitus, hepatomegaly, hepatic cirrhosis, and primary liver cancer (eg, hepatocellular carcinoma, cholangiocarcinoma).2 Approximately 90% of patients with HHC present with hyperpigmentation at the time of diagnosis.4 Thinning or loss of hair is another finding in HHC, primarily reported in the axillae and pubic regions, and is ascribed to hepatotesticular insufficiency.5
Alopecia areata (AA) is the most common cause of autoimmune, inflammation-induced hair loss, with a calculated lifetime risk of 2%.6 This disease manifests as loss of hair in well-circumscribed patches of skin, most commonly on the scalp; AA also may affect other hair-bearing sites on the body. It is associated with an increased risk for other autoimmune disorders, such as psoriasis, thyroid disease, rheumatoid arthritis, systemic lupus erythematosus, and vitiligo.7
Alopecia areata is induced by an inflammatory infiltrate of CD4+ and CD8+ T lymphocytes around hair follicles in the anagen stage, the active growth phase.8 Although the diagnosis is clinical, some clinicians order laboratory thyroid studies to investigate conditions that may be associated with AA. Common treatments include topical, intralesional, and/or systemic corticosteroids; contact immunotherapy; topical and more recently oral minoxidil; phototherapy; and topical and systemic JAK inhibitors, including tofacitinib.4,9
We reviewed the medical records of 533 patients who were seen in The University of Texas Southwestern (Dallas, Texas) dermatology clinic from January 2015 through January 2020 and were diagnosed with AA. We examined their demographic data and medical history. We sought to determine any relationship between various types of alopecia and certain micronutrient levels through laboratory test results. Ferritin and iron saturation studies were evaluated. We report 4 cases of HHC concurrent with AA, of which 2 HHC diagnoses were uncovered through iron studies as part of the alopecia evaluation.
Case Reports
Patient 1—A 55-year-old White woman presented to the clinic for an alopecia consultation. She had a medical history of hypothyroidism and AA that was treated unsuccessfully with triamcinolone acetonide steroid injections; topical minoxidil; topical steroids; and systemic steroids, specifically oral prednisone. Following evaluation, she successfully transitioned to treatment with oral tofacitinib and continued to do well on tofacitinib.
The patient’s alopecia workup revealed a ferritin level of 245 ng/mL (reference range, 13–150 ng/mL) and iron saturation of 60% (reference range, 20%–50%). She was referred to the hematology department for further evaluation and was diagnosed with HHC. Genetic testing revealed a heterozygous H63D mutation; therapeutic phlebotomy was recommended. Her sister also was recently diagnosed with HHC.
Patient 2—A 55-year-old White man was referred for evaluation and treatment of alopecia universalis. He had a medical history of skin cancer and vitiligo. He attempted contact immunotherapy with diphenylcyclopropenone scalp treatment but stopped due to intolerable inflammation. Intervention with a topical steroid and topical minoxidil was unsuccessful, but use of triamcinolone acetonide steroid injection on the scalp and topical bimatoprost 0.03% on the eyebrows produced satisfactory results.
The patient’s alopecia workup revealed a ferritin level of 422 ng/mL (reference range, 30–400 ng/mL), which prompted a hematology consultation for further evaluation. Notably, the patient ate red meat several times a week, used iron skillets, and denied receiving blood transfusions. His social habits included 3 alcoholic beverages a night, 5 days a week. Ultrasonography of the liver was recommended to assess potential damage from iron overload and alcohol consumption; the results suggested chronic liver disease, not definitive for cirrhosis, and no evidence of hepatocellular carcinoma. Genetic analysis later revealed the heterozygous H63D variant; therapeutic phlebotomy was recommended.
Patient 3—A 22-year-old White man presented with AA involving his facial beard. He had a medical history of vitiligo and psoriasis and a family history of AA as well as other autoimmune diseases including Hashimoto thyroiditis, psoriasis, eczema, and autoimmune hepatitis. Diphenylcyclopropenone treatment was not successful.
Laboratory studies revealed mildly elevated transaminase and ferritin levels. The patient also presented to the gastroenterologist for evaluation of abdominal pain. Subsequent hematology evaluation confirmed the presence of compound heterozygous C282Y and H63D mutations in the HFE gene, and the patient’s mother was later determined to be homozygous for the C282Y mutation with no elevated ferritin level. The patient’s ferritin level at diagnosis was approximately 500 ng/mL (reference range, 22–322 ng/mL); he required a modest number of therapeutic phlebotomies to normalize his ferritin level.
Patient 4—A 62-year-old White woman presented for evaluation and treatment of patchy hair loss on the scalp of 7 months’ duration. She was subsequently diagnosed with AA. After unsuccessful treatment with a triamcinolone acetonide steroid injection, topical immunotherapy with diphenylcyclopropenone was recommended. The patient achieved full hair regrowth after 35 treatments administered at 3-week intervals.
The patient had a medical history of HHC, including homozygosity for the C282Y mutation, and a family history of HHC in 1 sister. Treatment was therapeutic phlebotomy.
Comment
HHC in the Setting of AA—We presented 4 White patients with both HHC and AA. A PubMed search of articles indexed for MEDLINE using the terms HHC and AA yielded only 1 other reported case of newly identified HHC in a 56-year-old man who presented with pigmented purpuric dermatitis and AA that affected the beard.10 Because HHC is the most common genetic disorder identified in White individuals and has a varied clinical presentation, the documentation of AA may be an important cutaneous clue to help clinicians diagnose HHC early.
Iron Overload in Patients With HHC—The genetic association between HHC and AA, if any, is unknown. What is known is that iron overload can catalyze reactive oxygen species, which can overwhelm cellular antioxidant capacities at particular levels and cause injury to its constituents.11 Data show that the levels of oxidative stress are elevated in the scalp of patients with AA compared to controls and increased 2-fold during the early phase of disease vs late-phase disease.12 Thus, it is possible that increased iron levels in HHC may contribute to AA in genetically susceptible individuals by direct toxicity that ultimately results in the AA hair disorder that is CD8+ T-cell mediated.
Data show that 78% (31/40) of men and 36% (14/39) of women identified with homozygous C282Y mutations determined from family genetic analyses exhibited iron overload.13 In general, a normal life expectancy is possible for patients promptly treated with appropriate therapeutic phlebotomies.14 Thus, early diagnosis and appropriate therapy can prevent consequences of iron overload, which include cirrhosis, diabetes mellitus, and cardiomyopathy.13Iron Screening in the Alopecia Workup—Our cases illustrate how iron screening tests as part of the alopecia workup identified a cohort of White patients with iron overload and subsequently led to an early diagnosis of HHC. The calculated 2% lifetime risk for developing AA highlights the importance of evaluating iron status as part of the AA workup, particularly for White men, and the potential health benefit from early diagnosis of HHC. Limitations of this case series included its retrospective nature and small patient number.
- Bacon BR, Adams PC, Kowdley KV, et al. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54:328-343.
- Barton JC, Edwards CQ. HFE hemochromatosis. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. GeneReviews® [Internet]. University of Washington, Seattle; 1993-2020.
- Centers for Disease Control and Prevention. Hereditary hemochromatosis. Accessed September 13, 2022. https://www.cdc.gov/genomics/disease/hemochromatosis.htm
- Ibrahim O, Bayart CB, Hogan S, et al. Treatment of alopecia areata with tofacitinib. JAMA Dermatol. 2017;153:600-602.
- Tweed MJ, Roland JM. Haemochromatosis as an endocrine cause of subfertility. BMJ. 1998;316:915-916. doi:10.1136/bmj.316.7135.915
- Gilhar A, Etzioni A, Paus R. Alopecia areata. N Engl J Med. 2012;366:1515-1525.
- Barahmani N, Schabath MB, Duvic M, et al. History of atopy or autoimmunity increases risk of alopecia areata. J Am Acad Dermatol. 2009;61:581-591.
- McElwee KJ, Freyschmidt-Paul P, Hoffmann R, et al. Transfer of CD8(+) cells induces localized hair loss whereas CD4(+)/CD25(−) cells promote systemic alopecia areata and CD4(+)/CD25(+) cells blockade disease onset in the C3H/HeJ mouse model. J Invest Dermatol. 2005;124:947-957.
- MacDonald Hull SP, Wood ML, Hutchinson PE, et al. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692-699.
- Sredoja Tišma V, Bulimbašic´ S, Jaganjac M, et al. Progressive pigmented purpuric dermatitis and alopecia areata as unusual skin manifestations in recognizing hereditary hemochromatosis. Acta Dermatovenerol Croat. 2012;20:181-186.
- Cabantchik ZI. Labile iron in cells and body fluids: physiology, pathology, and pharmacology. Front Pharmacol. 2014;5:45.
- Akar A, Arca E, Erbil H, et al. Antioxidant enzymes and lipid peroxidation in the scalp of patients with alopecia areata. J Dermatol Sci. 2002;29:85-90.
- Ryan E, Byrnes V, Coughlan B, et al. Underdiagnosis of hereditary haemochromatosis: lack of presentation or penetration? Gut. 2002;51:108-112.
- Niederau C, Strohmeyer G. Strategies for early diagnosis of haemochromatosis. Eur J Gastroenterol Hepatol. 2002;14:217-221.
The role of micronutrients in the hair follicle cycle is not fully understood; thus deficiency and/or excess of certain micronutrients may be a modifiable risk factor associated with the development and/or treatment of some types of hair loss and therefore may be included in the workup during an alopecia consultation.
Hereditary hemochromatosis (HHC) is the most common genetic disorder identified in White individuals, with a worldwide prevalence of 1 in 220 to 1 in 250 individuals for a homozygous mutation. It most commonly affects individuals of Northern European descent.1 Men usually present in the fourth to sixth decades of life, while women usually develop symptoms after menopause, as pregnancy and menstruation delay the onset of the disease.2 Early symptoms of HHC include fatigue, joint pain, abdominal pain, and weight loss. Men are more likely to develop complications; in fact, 1 in 10 men with HHC will develop severe liver disease.3 As the disease progresses, affected individuals can present with cardiomyopathy (restrictive and dilated), cirrhosis, hypogonadism (usually hypogonadotrophic), arthropathy, diabetes mellitus, hepatomegaly, hepatic cirrhosis, and primary liver cancer (eg, hepatocellular carcinoma, cholangiocarcinoma).2 Approximately 90% of patients with HHC present with hyperpigmentation at the time of diagnosis.4 Thinning or loss of hair is another finding in HHC, primarily reported in the axillae and pubic regions, and is ascribed to hepatotesticular insufficiency.5
Alopecia areata (AA) is the most common cause of autoimmune, inflammation-induced hair loss, with a calculated lifetime risk of 2%.6 This disease manifests as loss of hair in well-circumscribed patches of skin, most commonly on the scalp; AA also may affect other hair-bearing sites on the body. It is associated with an increased risk for other autoimmune disorders, such as psoriasis, thyroid disease, rheumatoid arthritis, systemic lupus erythematosus, and vitiligo.7
Alopecia areata is induced by an inflammatory infiltrate of CD4+ and CD8+ T lymphocytes around hair follicles in the anagen stage, the active growth phase.8 Although the diagnosis is clinical, some clinicians order laboratory thyroid studies to investigate conditions that may be associated with AA. Common treatments include topical, intralesional, and/or systemic corticosteroids; contact immunotherapy; topical and more recently oral minoxidil; phototherapy; and topical and systemic JAK inhibitors, including tofacitinib.4,9
We reviewed the medical records of 533 patients who were seen in The University of Texas Southwestern (Dallas, Texas) dermatology clinic from January 2015 through January 2020 and were diagnosed with AA. We examined their demographic data and medical history. We sought to determine any relationship between various types of alopecia and certain micronutrient levels through laboratory test results. Ferritin and iron saturation studies were evaluated. We report 4 cases of HHC concurrent with AA, of which 2 HHC diagnoses were uncovered through iron studies as part of the alopecia evaluation.
Case Reports
Patient 1—A 55-year-old White woman presented to the clinic for an alopecia consultation. She had a medical history of hypothyroidism and AA that was treated unsuccessfully with triamcinolone acetonide steroid injections; topical minoxidil; topical steroids; and systemic steroids, specifically oral prednisone. Following evaluation, she successfully transitioned to treatment with oral tofacitinib and continued to do well on tofacitinib.
The patient’s alopecia workup revealed a ferritin level of 245 ng/mL (reference range, 13–150 ng/mL) and iron saturation of 60% (reference range, 20%–50%). She was referred to the hematology department for further evaluation and was diagnosed with HHC. Genetic testing revealed a heterozygous H63D mutation; therapeutic phlebotomy was recommended. Her sister also was recently diagnosed with HHC.
Patient 2—A 55-year-old White man was referred for evaluation and treatment of alopecia universalis. He had a medical history of skin cancer and vitiligo. He attempted contact immunotherapy with diphenylcyclopropenone scalp treatment but stopped due to intolerable inflammation. Intervention with a topical steroid and topical minoxidil was unsuccessful, but use of triamcinolone acetonide steroid injection on the scalp and topical bimatoprost 0.03% on the eyebrows produced satisfactory results.
The patient’s alopecia workup revealed a ferritin level of 422 ng/mL (reference range, 30–400 ng/mL), which prompted a hematology consultation for further evaluation. Notably, the patient ate red meat several times a week, used iron skillets, and denied receiving blood transfusions. His social habits included 3 alcoholic beverages a night, 5 days a week. Ultrasonography of the liver was recommended to assess potential damage from iron overload and alcohol consumption; the results suggested chronic liver disease, not definitive for cirrhosis, and no evidence of hepatocellular carcinoma. Genetic analysis later revealed the heterozygous H63D variant; therapeutic phlebotomy was recommended.
Patient 3—A 22-year-old White man presented with AA involving his facial beard. He had a medical history of vitiligo and psoriasis and a family history of AA as well as other autoimmune diseases including Hashimoto thyroiditis, psoriasis, eczema, and autoimmune hepatitis. Diphenylcyclopropenone treatment was not successful.
Laboratory studies revealed mildly elevated transaminase and ferritin levels. The patient also presented to the gastroenterologist for evaluation of abdominal pain. Subsequent hematology evaluation confirmed the presence of compound heterozygous C282Y and H63D mutations in the HFE gene, and the patient’s mother was later determined to be homozygous for the C282Y mutation with no elevated ferritin level. The patient’s ferritin level at diagnosis was approximately 500 ng/mL (reference range, 22–322 ng/mL); he required a modest number of therapeutic phlebotomies to normalize his ferritin level.
Patient 4—A 62-year-old White woman presented for evaluation and treatment of patchy hair loss on the scalp of 7 months’ duration. She was subsequently diagnosed with AA. After unsuccessful treatment with a triamcinolone acetonide steroid injection, topical immunotherapy with diphenylcyclopropenone was recommended. The patient achieved full hair regrowth after 35 treatments administered at 3-week intervals.
The patient had a medical history of HHC, including homozygosity for the C282Y mutation, and a family history of HHC in 1 sister. Treatment was therapeutic phlebotomy.
Comment
HHC in the Setting of AA—We presented 4 White patients with both HHC and AA. A PubMed search of articles indexed for MEDLINE using the terms HHC and AA yielded only 1 other reported case of newly identified HHC in a 56-year-old man who presented with pigmented purpuric dermatitis and AA that affected the beard.10 Because HHC is the most common genetic disorder identified in White individuals and has a varied clinical presentation, the documentation of AA may be an important cutaneous clue to help clinicians diagnose HHC early.
Iron Overload in Patients With HHC—The genetic association between HHC and AA, if any, is unknown. What is known is that iron overload can catalyze reactive oxygen species, which can overwhelm cellular antioxidant capacities at particular levels and cause injury to its constituents.11 Data show that the levels of oxidative stress are elevated in the scalp of patients with AA compared to controls and increased 2-fold during the early phase of disease vs late-phase disease.12 Thus, it is possible that increased iron levels in HHC may contribute to AA in genetically susceptible individuals by direct toxicity that ultimately results in the AA hair disorder that is CD8+ T-cell mediated.
Data show that 78% (31/40) of men and 36% (14/39) of women identified with homozygous C282Y mutations determined from family genetic analyses exhibited iron overload.13 In general, a normal life expectancy is possible for patients promptly treated with appropriate therapeutic phlebotomies.14 Thus, early diagnosis and appropriate therapy can prevent consequences of iron overload, which include cirrhosis, diabetes mellitus, and cardiomyopathy.13Iron Screening in the Alopecia Workup—Our cases illustrate how iron screening tests as part of the alopecia workup identified a cohort of White patients with iron overload and subsequently led to an early diagnosis of HHC. The calculated 2% lifetime risk for developing AA highlights the importance of evaluating iron status as part of the AA workup, particularly for White men, and the potential health benefit from early diagnosis of HHC. Limitations of this case series included its retrospective nature and small patient number.
The role of micronutrients in the hair follicle cycle is not fully understood; thus deficiency and/or excess of certain micronutrients may be a modifiable risk factor associated with the development and/or treatment of some types of hair loss and therefore may be included in the workup during an alopecia consultation.
Hereditary hemochromatosis (HHC) is the most common genetic disorder identified in White individuals, with a worldwide prevalence of 1 in 220 to 1 in 250 individuals for a homozygous mutation. It most commonly affects individuals of Northern European descent.1 Men usually present in the fourth to sixth decades of life, while women usually develop symptoms after menopause, as pregnancy and menstruation delay the onset of the disease.2 Early symptoms of HHC include fatigue, joint pain, abdominal pain, and weight loss. Men are more likely to develop complications; in fact, 1 in 10 men with HHC will develop severe liver disease.3 As the disease progresses, affected individuals can present with cardiomyopathy (restrictive and dilated), cirrhosis, hypogonadism (usually hypogonadotrophic), arthropathy, diabetes mellitus, hepatomegaly, hepatic cirrhosis, and primary liver cancer (eg, hepatocellular carcinoma, cholangiocarcinoma).2 Approximately 90% of patients with HHC present with hyperpigmentation at the time of diagnosis.4 Thinning or loss of hair is another finding in HHC, primarily reported in the axillae and pubic regions, and is ascribed to hepatotesticular insufficiency.5
Alopecia areata (AA) is the most common cause of autoimmune, inflammation-induced hair loss, with a calculated lifetime risk of 2%.6 This disease manifests as loss of hair in well-circumscribed patches of skin, most commonly on the scalp; AA also may affect other hair-bearing sites on the body. It is associated with an increased risk for other autoimmune disorders, such as psoriasis, thyroid disease, rheumatoid arthritis, systemic lupus erythematosus, and vitiligo.7
Alopecia areata is induced by an inflammatory infiltrate of CD4+ and CD8+ T lymphocytes around hair follicles in the anagen stage, the active growth phase.8 Although the diagnosis is clinical, some clinicians order laboratory thyroid studies to investigate conditions that may be associated with AA. Common treatments include topical, intralesional, and/or systemic corticosteroids; contact immunotherapy; topical and more recently oral minoxidil; phototherapy; and topical and systemic JAK inhibitors, including tofacitinib.4,9
We reviewed the medical records of 533 patients who were seen in The University of Texas Southwestern (Dallas, Texas) dermatology clinic from January 2015 through January 2020 and were diagnosed with AA. We examined their demographic data and medical history. We sought to determine any relationship between various types of alopecia and certain micronutrient levels through laboratory test results. Ferritin and iron saturation studies were evaluated. We report 4 cases of HHC concurrent with AA, of which 2 HHC diagnoses were uncovered through iron studies as part of the alopecia evaluation.
Case Reports
Patient 1—A 55-year-old White woman presented to the clinic for an alopecia consultation. She had a medical history of hypothyroidism and AA that was treated unsuccessfully with triamcinolone acetonide steroid injections; topical minoxidil; topical steroids; and systemic steroids, specifically oral prednisone. Following evaluation, she successfully transitioned to treatment with oral tofacitinib and continued to do well on tofacitinib.
The patient’s alopecia workup revealed a ferritin level of 245 ng/mL (reference range, 13–150 ng/mL) and iron saturation of 60% (reference range, 20%–50%). She was referred to the hematology department for further evaluation and was diagnosed with HHC. Genetic testing revealed a heterozygous H63D mutation; therapeutic phlebotomy was recommended. Her sister also was recently diagnosed with HHC.
Patient 2—A 55-year-old White man was referred for evaluation and treatment of alopecia universalis. He had a medical history of skin cancer and vitiligo. He attempted contact immunotherapy with diphenylcyclopropenone scalp treatment but stopped due to intolerable inflammation. Intervention with a topical steroid and topical minoxidil was unsuccessful, but use of triamcinolone acetonide steroid injection on the scalp and topical bimatoprost 0.03% on the eyebrows produced satisfactory results.
The patient’s alopecia workup revealed a ferritin level of 422 ng/mL (reference range, 30–400 ng/mL), which prompted a hematology consultation for further evaluation. Notably, the patient ate red meat several times a week, used iron skillets, and denied receiving blood transfusions. His social habits included 3 alcoholic beverages a night, 5 days a week. Ultrasonography of the liver was recommended to assess potential damage from iron overload and alcohol consumption; the results suggested chronic liver disease, not definitive for cirrhosis, and no evidence of hepatocellular carcinoma. Genetic analysis later revealed the heterozygous H63D variant; therapeutic phlebotomy was recommended.
Patient 3—A 22-year-old White man presented with AA involving his facial beard. He had a medical history of vitiligo and psoriasis and a family history of AA as well as other autoimmune diseases including Hashimoto thyroiditis, psoriasis, eczema, and autoimmune hepatitis. Diphenylcyclopropenone treatment was not successful.
Laboratory studies revealed mildly elevated transaminase and ferritin levels. The patient also presented to the gastroenterologist for evaluation of abdominal pain. Subsequent hematology evaluation confirmed the presence of compound heterozygous C282Y and H63D mutations in the HFE gene, and the patient’s mother was later determined to be homozygous for the C282Y mutation with no elevated ferritin level. The patient’s ferritin level at diagnosis was approximately 500 ng/mL (reference range, 22–322 ng/mL); he required a modest number of therapeutic phlebotomies to normalize his ferritin level.
Patient 4—A 62-year-old White woman presented for evaluation and treatment of patchy hair loss on the scalp of 7 months’ duration. She was subsequently diagnosed with AA. After unsuccessful treatment with a triamcinolone acetonide steroid injection, topical immunotherapy with diphenylcyclopropenone was recommended. The patient achieved full hair regrowth after 35 treatments administered at 3-week intervals.
The patient had a medical history of HHC, including homozygosity for the C282Y mutation, and a family history of HHC in 1 sister. Treatment was therapeutic phlebotomy.
Comment
HHC in the Setting of AA—We presented 4 White patients with both HHC and AA. A PubMed search of articles indexed for MEDLINE using the terms HHC and AA yielded only 1 other reported case of newly identified HHC in a 56-year-old man who presented with pigmented purpuric dermatitis and AA that affected the beard.10 Because HHC is the most common genetic disorder identified in White individuals and has a varied clinical presentation, the documentation of AA may be an important cutaneous clue to help clinicians diagnose HHC early.
Iron Overload in Patients With HHC—The genetic association between HHC and AA, if any, is unknown. What is known is that iron overload can catalyze reactive oxygen species, which can overwhelm cellular antioxidant capacities at particular levels and cause injury to its constituents.11 Data show that the levels of oxidative stress are elevated in the scalp of patients with AA compared to controls and increased 2-fold during the early phase of disease vs late-phase disease.12 Thus, it is possible that increased iron levels in HHC may contribute to AA in genetically susceptible individuals by direct toxicity that ultimately results in the AA hair disorder that is CD8+ T-cell mediated.
Data show that 78% (31/40) of men and 36% (14/39) of women identified with homozygous C282Y mutations determined from family genetic analyses exhibited iron overload.13 In general, a normal life expectancy is possible for patients promptly treated with appropriate therapeutic phlebotomies.14 Thus, early diagnosis and appropriate therapy can prevent consequences of iron overload, which include cirrhosis, diabetes mellitus, and cardiomyopathy.13Iron Screening in the Alopecia Workup—Our cases illustrate how iron screening tests as part of the alopecia workup identified a cohort of White patients with iron overload and subsequently led to an early diagnosis of HHC. The calculated 2% lifetime risk for developing AA highlights the importance of evaluating iron status as part of the AA workup, particularly for White men, and the potential health benefit from early diagnosis of HHC. Limitations of this case series included its retrospective nature and small patient number.
- Bacon BR, Adams PC, Kowdley KV, et al. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54:328-343.
- Barton JC, Edwards CQ. HFE hemochromatosis. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. GeneReviews® [Internet]. University of Washington, Seattle; 1993-2020.
- Centers for Disease Control and Prevention. Hereditary hemochromatosis. Accessed September 13, 2022. https://www.cdc.gov/genomics/disease/hemochromatosis.htm
- Ibrahim O, Bayart CB, Hogan S, et al. Treatment of alopecia areata with tofacitinib. JAMA Dermatol. 2017;153:600-602.
- Tweed MJ, Roland JM. Haemochromatosis as an endocrine cause of subfertility. BMJ. 1998;316:915-916. doi:10.1136/bmj.316.7135.915
- Gilhar A, Etzioni A, Paus R. Alopecia areata. N Engl J Med. 2012;366:1515-1525.
- Barahmani N, Schabath MB, Duvic M, et al. History of atopy or autoimmunity increases risk of alopecia areata. J Am Acad Dermatol. 2009;61:581-591.
- McElwee KJ, Freyschmidt-Paul P, Hoffmann R, et al. Transfer of CD8(+) cells induces localized hair loss whereas CD4(+)/CD25(−) cells promote systemic alopecia areata and CD4(+)/CD25(+) cells blockade disease onset in the C3H/HeJ mouse model. J Invest Dermatol. 2005;124:947-957.
- MacDonald Hull SP, Wood ML, Hutchinson PE, et al. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692-699.
- Sredoja Tišma V, Bulimbašic´ S, Jaganjac M, et al. Progressive pigmented purpuric dermatitis and alopecia areata as unusual skin manifestations in recognizing hereditary hemochromatosis. Acta Dermatovenerol Croat. 2012;20:181-186.
- Cabantchik ZI. Labile iron in cells and body fluids: physiology, pathology, and pharmacology. Front Pharmacol. 2014;5:45.
- Akar A, Arca E, Erbil H, et al. Antioxidant enzymes and lipid peroxidation in the scalp of patients with alopecia areata. J Dermatol Sci. 2002;29:85-90.
- Ryan E, Byrnes V, Coughlan B, et al. Underdiagnosis of hereditary haemochromatosis: lack of presentation or penetration? Gut. 2002;51:108-112.
- Niederau C, Strohmeyer G. Strategies for early diagnosis of haemochromatosis. Eur J Gastroenterol Hepatol. 2002;14:217-221.
- Bacon BR, Adams PC, Kowdley KV, et al. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54:328-343.
- Barton JC, Edwards CQ. HFE hemochromatosis. In: Adam MP, Ardinger HH, Pagon RA, et al, eds. GeneReviews® [Internet]. University of Washington, Seattle; 1993-2020.
- Centers for Disease Control and Prevention. Hereditary hemochromatosis. Accessed September 13, 2022. https://www.cdc.gov/genomics/disease/hemochromatosis.htm
- Ibrahim O, Bayart CB, Hogan S, et al. Treatment of alopecia areata with tofacitinib. JAMA Dermatol. 2017;153:600-602.
- Tweed MJ, Roland JM. Haemochromatosis as an endocrine cause of subfertility. BMJ. 1998;316:915-916. doi:10.1136/bmj.316.7135.915
- Gilhar A, Etzioni A, Paus R. Alopecia areata. N Engl J Med. 2012;366:1515-1525.
- Barahmani N, Schabath MB, Duvic M, et al. History of atopy or autoimmunity increases risk of alopecia areata. J Am Acad Dermatol. 2009;61:581-591.
- McElwee KJ, Freyschmidt-Paul P, Hoffmann R, et al. Transfer of CD8(+) cells induces localized hair loss whereas CD4(+)/CD25(−) cells promote systemic alopecia areata and CD4(+)/CD25(+) cells blockade disease onset in the C3H/HeJ mouse model. J Invest Dermatol. 2005;124:947-957.
- MacDonald Hull SP, Wood ML, Hutchinson PE, et al. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692-699.
- Sredoja Tišma V, Bulimbašic´ S, Jaganjac M, et al. Progressive pigmented purpuric dermatitis and alopecia areata as unusual skin manifestations in recognizing hereditary hemochromatosis. Acta Dermatovenerol Croat. 2012;20:181-186.
- Cabantchik ZI. Labile iron in cells and body fluids: physiology, pathology, and pharmacology. Front Pharmacol. 2014;5:45.
- Akar A, Arca E, Erbil H, et al. Antioxidant enzymes and lipid peroxidation in the scalp of patients with alopecia areata. J Dermatol Sci. 2002;29:85-90.
- Ryan E, Byrnes V, Coughlan B, et al. Underdiagnosis of hereditary haemochromatosis: lack of presentation or penetration? Gut. 2002;51:108-112.
- Niederau C, Strohmeyer G. Strategies for early diagnosis of haemochromatosis. Eur J Gastroenterol Hepatol. 2002;14:217-221.
Practice Points
- Hereditary hemochromatosis (HHC) is a disorder of iron overload that presents with clinical phenotypic heterogeneity. Complications can be mitigated with early intervention.
- Alopecia areata (AA) may be a rare early cutaneous manifestation of HHC in individuals with a predisposition for autoimmunity; therefore, it is important to evaluate iron status as part of the AA workup.
Genital HSV shedding declines rapidly in first year post infection
Shedding of genital herpes simplex virus was frequent soon after first-time infection but declined significantly during the first year, based on data from 82 individuals.
Genital herpes simplex virus (HSV) infections remain common and incurable; consequently, the population with residual infection continues to rise, Christine Johnston, MD, of the University of Washington, Seattle, and colleagues wrote. However, data on the viral shedding trajectory of genital HSV-1 are limited, although HSV-1 accounts for an increasing number of infections.
In a study published in JAMA the researchers recruited 82 women with first-episode genital HSV-1 infections from sexual health and primary care clinics in Seattle, between 2013 and 2018. The participants supplied self-collected oral and genital swabs for daily HSV polymerase chain reaction testing for two 30-day periods at 2 months and 11 months after their initial symptoms. The study population was not pregnant and did not have HIV infection. The median age of the participants was 26 years, 54 were women, and 42 had primary HSV-1 infections. Primary HSV-1 infection was defined as the lack of HSV antibody at baseline or an evolving antibody profile, based on the University of Washington HSV Western Blot.
The primary outcome was the rates of genital and oral HSV shedding and lesions at 2 and 11 months and up to 2 years after an initial HSV-1 infection.
At 2 months, approximately two-thirds (64.6%) of the participants had HSV-1 in the genital tract and 29.3% had virus in the mouth. Genital shedding of HSV-1 was detected in 12.1% of 2,264 total testing days at 2 months, but this rate declined to 7.1% of 1,719 testing days at 11 months (relative risk, 0.52).
The researchers identified oral HSV-1 shedding on 3.9% of 2,247 testing days at 2 months, with a slight increase to 5.1% of 1,714 testing days at 11 months.
Both genital and oral lesions were rare, with reports of 2.6% and 0.4%, respectively, at 2 months and 3.8% and 0.5%, respectively, at 11 months.
The risk of genital shedding was significantly higher in individuals with primary HSV-1, compared with those with nonprimary infections (7.9% vs. 2.9%; RR, 2.75). The overall rate of genital shedding was 17.2% for those with primary HSV-1, of which 15.2% was asymptomatic. Oral shedding was similar for individuals with primary and nonprimary HSV in a multivariate analysis.
In addition, HSV-specific CD4+ and CD8+ T-cell responses were identified in all participants, and these remained stable during the study period. No association appeared between rates of genital and oral shedding and the proportion of cells that expressed two, three, or four cytokines.
The current study is the first known to comprehensively assess genital and oral HSV-1 viral shedding using polymerase chain reaction, the researchers wrote. “Characterizing shedding rates is clinically important because patients with genital herpes are often concerned about transmission to sexual partners, which usually occurs in the absence of lesions.”
The study findings were limited by several factors including the 22% loss of participants to follow-up by the end of the first year, and the use of data from a single location with a primarily White population, the researchers noted. Another limitation was reliance on self-reports and the potential underestimation of recurrences because of the possible use of antiviral medications between swabbing periods.
However, the results indicate the early frequency of HSV-1 shedding and suggest that suppressive therapy might benefit individuals with primary HSV-1 during their first year of infection, the researchers said.
Findings may improve HSV management
The current study helps fill a knowledge gap regarding the natural history of genital HSV-1 infections, Richard J. Whitley, MD, and Edward W. Hook III, MD, both of the University of Alabama at Birmingham, wrote in an accompanying editorial. Despite the small study population, the data represent the largest cohort to date of individuals with first-episode infection and up to 2 years’ follow-up.
Although HSV-2 shedding is greater and associated with more symptoms, seroprevalence of HSV-2 in the United States is declining, they noted. Therefore, the findings can inform patient counseling and recommendations for antiviral therapy that may extend to managing HSV-1 in pregnant women as well, although no pregnant women were included in the study.
“For clinicians, these data emphasize the importance of determining the HSV viral type in persons presenting with initial episodes of genital herpes to accurately counsel patients regarding risk of clinical recurrence, the likelihood of asymptomatic shedding of virus and hence transmission, and antiviral prophylaxis,” the editorialists emphasized. For investigators, the results should prompt additional studies of the host defense against HSV and improved serological testing.
Study supports need for attention to HSV-1
“Genital herpes is an extremely common sexually transmitted infection, and often only HSV-2 is measured,” Sarah W. Prager, MD, of the University of Washington, Seattle, said in an interview. “This study shows that HSV-1 also accounts for a significant amount of genital disease, and should also be considered when determining prevalence of genital herpes.
“I was not surprised to see that viral shedding decreased significantly over the first year after diagnosis, and similarly not surprised that lesions were rare after the initial infection,” said Dr. Prager, who was not involved in the study. “I was somewhat surprised to see that genital HSV-1 shedding was more common than oral shedding.”
Dr. Prager said that she would advise clinicians against serum HSV testing unless someone has an active genital lesion. “Testing after a lesion will often reveal HSV-1, and patients should be counseled that shedding will decrease over the first year. Subsequent genital lesions are uncommon, but certainly possible, and oral lesions and shedding are both rare.” ]
More research is needed in a more diverse population, Dr. Prager emphasized. Following patients for more than a year and learning more about the use of antiviral medications also would be useful.
The study was supported in part by the National Institutes of Health/National Institute of Allergy and Infectious Diseases through grants to several authors, including lead author Dr. Johnston. Dr. Johnston also disclosed personal fees from AbbVie, grants from Gilead, royalties from UpToDate, and personal fees from GlaxoSmithKline unrelated to the current study. Dr. Whitley disclosed personal fees from Virios Therapeutics as a board member and shareholder during the conduct of the study, royalties from Aettis unrelated to the submitted work, and serving on an advisory board for Visby Diagnostics. Dr. Hook disclosed serving on an advisory board for Visby Diagnostics unrelated to the submitted work. Dr. Prager had no conflicts to disclose and serves on the editorial advisory board of Ob.Gyn News.
Shedding of genital herpes simplex virus was frequent soon after first-time infection but declined significantly during the first year, based on data from 82 individuals.
Genital herpes simplex virus (HSV) infections remain common and incurable; consequently, the population with residual infection continues to rise, Christine Johnston, MD, of the University of Washington, Seattle, and colleagues wrote. However, data on the viral shedding trajectory of genital HSV-1 are limited, although HSV-1 accounts for an increasing number of infections.
In a study published in JAMA the researchers recruited 82 women with first-episode genital HSV-1 infections from sexual health and primary care clinics in Seattle, between 2013 and 2018. The participants supplied self-collected oral and genital swabs for daily HSV polymerase chain reaction testing for two 30-day periods at 2 months and 11 months after their initial symptoms. The study population was not pregnant and did not have HIV infection. The median age of the participants was 26 years, 54 were women, and 42 had primary HSV-1 infections. Primary HSV-1 infection was defined as the lack of HSV antibody at baseline or an evolving antibody profile, based on the University of Washington HSV Western Blot.
The primary outcome was the rates of genital and oral HSV shedding and lesions at 2 and 11 months and up to 2 years after an initial HSV-1 infection.
At 2 months, approximately two-thirds (64.6%) of the participants had HSV-1 in the genital tract and 29.3% had virus in the mouth. Genital shedding of HSV-1 was detected in 12.1% of 2,264 total testing days at 2 months, but this rate declined to 7.1% of 1,719 testing days at 11 months (relative risk, 0.52).
The researchers identified oral HSV-1 shedding on 3.9% of 2,247 testing days at 2 months, with a slight increase to 5.1% of 1,714 testing days at 11 months.
Both genital and oral lesions were rare, with reports of 2.6% and 0.4%, respectively, at 2 months and 3.8% and 0.5%, respectively, at 11 months.
The risk of genital shedding was significantly higher in individuals with primary HSV-1, compared with those with nonprimary infections (7.9% vs. 2.9%; RR, 2.75). The overall rate of genital shedding was 17.2% for those with primary HSV-1, of which 15.2% was asymptomatic. Oral shedding was similar for individuals with primary and nonprimary HSV in a multivariate analysis.
In addition, HSV-specific CD4+ and CD8+ T-cell responses were identified in all participants, and these remained stable during the study period. No association appeared between rates of genital and oral shedding and the proportion of cells that expressed two, three, or four cytokines.
The current study is the first known to comprehensively assess genital and oral HSV-1 viral shedding using polymerase chain reaction, the researchers wrote. “Characterizing shedding rates is clinically important because patients with genital herpes are often concerned about transmission to sexual partners, which usually occurs in the absence of lesions.”
The study findings were limited by several factors including the 22% loss of participants to follow-up by the end of the first year, and the use of data from a single location with a primarily White population, the researchers noted. Another limitation was reliance on self-reports and the potential underestimation of recurrences because of the possible use of antiviral medications between swabbing periods.
However, the results indicate the early frequency of HSV-1 shedding and suggest that suppressive therapy might benefit individuals with primary HSV-1 during their first year of infection, the researchers said.
Findings may improve HSV management
The current study helps fill a knowledge gap regarding the natural history of genital HSV-1 infections, Richard J. Whitley, MD, and Edward W. Hook III, MD, both of the University of Alabama at Birmingham, wrote in an accompanying editorial. Despite the small study population, the data represent the largest cohort to date of individuals with first-episode infection and up to 2 years’ follow-up.
Although HSV-2 shedding is greater and associated with more symptoms, seroprevalence of HSV-2 in the United States is declining, they noted. Therefore, the findings can inform patient counseling and recommendations for antiviral therapy that may extend to managing HSV-1 in pregnant women as well, although no pregnant women were included in the study.
“For clinicians, these data emphasize the importance of determining the HSV viral type in persons presenting with initial episodes of genital herpes to accurately counsel patients regarding risk of clinical recurrence, the likelihood of asymptomatic shedding of virus and hence transmission, and antiviral prophylaxis,” the editorialists emphasized. For investigators, the results should prompt additional studies of the host defense against HSV and improved serological testing.
Study supports need for attention to HSV-1
“Genital herpes is an extremely common sexually transmitted infection, and often only HSV-2 is measured,” Sarah W. Prager, MD, of the University of Washington, Seattle, said in an interview. “This study shows that HSV-1 also accounts for a significant amount of genital disease, and should also be considered when determining prevalence of genital herpes.
“I was not surprised to see that viral shedding decreased significantly over the first year after diagnosis, and similarly not surprised that lesions were rare after the initial infection,” said Dr. Prager, who was not involved in the study. “I was somewhat surprised to see that genital HSV-1 shedding was more common than oral shedding.”
Dr. Prager said that she would advise clinicians against serum HSV testing unless someone has an active genital lesion. “Testing after a lesion will often reveal HSV-1, and patients should be counseled that shedding will decrease over the first year. Subsequent genital lesions are uncommon, but certainly possible, and oral lesions and shedding are both rare.” ]
More research is needed in a more diverse population, Dr. Prager emphasized. Following patients for more than a year and learning more about the use of antiviral medications also would be useful.
The study was supported in part by the National Institutes of Health/National Institute of Allergy and Infectious Diseases through grants to several authors, including lead author Dr. Johnston. Dr. Johnston also disclosed personal fees from AbbVie, grants from Gilead, royalties from UpToDate, and personal fees from GlaxoSmithKline unrelated to the current study. Dr. Whitley disclosed personal fees from Virios Therapeutics as a board member and shareholder during the conduct of the study, royalties from Aettis unrelated to the submitted work, and serving on an advisory board for Visby Diagnostics. Dr. Hook disclosed serving on an advisory board for Visby Diagnostics unrelated to the submitted work. Dr. Prager had no conflicts to disclose and serves on the editorial advisory board of Ob.Gyn News.
Shedding of genital herpes simplex virus was frequent soon after first-time infection but declined significantly during the first year, based on data from 82 individuals.
Genital herpes simplex virus (HSV) infections remain common and incurable; consequently, the population with residual infection continues to rise, Christine Johnston, MD, of the University of Washington, Seattle, and colleagues wrote. However, data on the viral shedding trajectory of genital HSV-1 are limited, although HSV-1 accounts for an increasing number of infections.
In a study published in JAMA the researchers recruited 82 women with first-episode genital HSV-1 infections from sexual health and primary care clinics in Seattle, between 2013 and 2018. The participants supplied self-collected oral and genital swabs for daily HSV polymerase chain reaction testing for two 30-day periods at 2 months and 11 months after their initial symptoms. The study population was not pregnant and did not have HIV infection. The median age of the participants was 26 years, 54 were women, and 42 had primary HSV-1 infections. Primary HSV-1 infection was defined as the lack of HSV antibody at baseline or an evolving antibody profile, based on the University of Washington HSV Western Blot.
The primary outcome was the rates of genital and oral HSV shedding and lesions at 2 and 11 months and up to 2 years after an initial HSV-1 infection.
At 2 months, approximately two-thirds (64.6%) of the participants had HSV-1 in the genital tract and 29.3% had virus in the mouth. Genital shedding of HSV-1 was detected in 12.1% of 2,264 total testing days at 2 months, but this rate declined to 7.1% of 1,719 testing days at 11 months (relative risk, 0.52).
The researchers identified oral HSV-1 shedding on 3.9% of 2,247 testing days at 2 months, with a slight increase to 5.1% of 1,714 testing days at 11 months.
Both genital and oral lesions were rare, with reports of 2.6% and 0.4%, respectively, at 2 months and 3.8% and 0.5%, respectively, at 11 months.
The risk of genital shedding was significantly higher in individuals with primary HSV-1, compared with those with nonprimary infections (7.9% vs. 2.9%; RR, 2.75). The overall rate of genital shedding was 17.2% for those with primary HSV-1, of which 15.2% was asymptomatic. Oral shedding was similar for individuals with primary and nonprimary HSV in a multivariate analysis.
In addition, HSV-specific CD4+ and CD8+ T-cell responses were identified in all participants, and these remained stable during the study period. No association appeared between rates of genital and oral shedding and the proportion of cells that expressed two, three, or four cytokines.
The current study is the first known to comprehensively assess genital and oral HSV-1 viral shedding using polymerase chain reaction, the researchers wrote. “Characterizing shedding rates is clinically important because patients with genital herpes are often concerned about transmission to sexual partners, which usually occurs in the absence of lesions.”
The study findings were limited by several factors including the 22% loss of participants to follow-up by the end of the first year, and the use of data from a single location with a primarily White population, the researchers noted. Another limitation was reliance on self-reports and the potential underestimation of recurrences because of the possible use of antiviral medications between swabbing periods.
However, the results indicate the early frequency of HSV-1 shedding and suggest that suppressive therapy might benefit individuals with primary HSV-1 during their first year of infection, the researchers said.
Findings may improve HSV management
The current study helps fill a knowledge gap regarding the natural history of genital HSV-1 infections, Richard J. Whitley, MD, and Edward W. Hook III, MD, both of the University of Alabama at Birmingham, wrote in an accompanying editorial. Despite the small study population, the data represent the largest cohort to date of individuals with first-episode infection and up to 2 years’ follow-up.
Although HSV-2 shedding is greater and associated with more symptoms, seroprevalence of HSV-2 in the United States is declining, they noted. Therefore, the findings can inform patient counseling and recommendations for antiviral therapy that may extend to managing HSV-1 in pregnant women as well, although no pregnant women were included in the study.
“For clinicians, these data emphasize the importance of determining the HSV viral type in persons presenting with initial episodes of genital herpes to accurately counsel patients regarding risk of clinical recurrence, the likelihood of asymptomatic shedding of virus and hence transmission, and antiviral prophylaxis,” the editorialists emphasized. For investigators, the results should prompt additional studies of the host defense against HSV and improved serological testing.
Study supports need for attention to HSV-1
“Genital herpes is an extremely common sexually transmitted infection, and often only HSV-2 is measured,” Sarah W. Prager, MD, of the University of Washington, Seattle, said in an interview. “This study shows that HSV-1 also accounts for a significant amount of genital disease, and should also be considered when determining prevalence of genital herpes.
“I was not surprised to see that viral shedding decreased significantly over the first year after diagnosis, and similarly not surprised that lesions were rare after the initial infection,” said Dr. Prager, who was not involved in the study. “I was somewhat surprised to see that genital HSV-1 shedding was more common than oral shedding.”
Dr. Prager said that she would advise clinicians against serum HSV testing unless someone has an active genital lesion. “Testing after a lesion will often reveal HSV-1, and patients should be counseled that shedding will decrease over the first year. Subsequent genital lesions are uncommon, but certainly possible, and oral lesions and shedding are both rare.” ]
More research is needed in a more diverse population, Dr. Prager emphasized. Following patients for more than a year and learning more about the use of antiviral medications also would be useful.
The study was supported in part by the National Institutes of Health/National Institute of Allergy and Infectious Diseases through grants to several authors, including lead author Dr. Johnston. Dr. Johnston also disclosed personal fees from AbbVie, grants from Gilead, royalties from UpToDate, and personal fees from GlaxoSmithKline unrelated to the current study. Dr. Whitley disclosed personal fees from Virios Therapeutics as a board member and shareholder during the conduct of the study, royalties from Aettis unrelated to the submitted work, and serving on an advisory board for Visby Diagnostics. Dr. Hook disclosed serving on an advisory board for Visby Diagnostics unrelated to the submitted work. Dr. Prager had no conflicts to disclose and serves on the editorial advisory board of Ob.Gyn News.
FROM JAMA
Rapid action or sustained effect? Methotrexate vs. ciclosporin for pediatric AD
MONTREAL – in the TREAT study, investigators reported at the annual meeting of the International Society of Atopic Dermatitis.
The findings are important, since many regulatory bodies require patients to have tried such first-line conventional systemic therapies before moving on to novel therapeutics, explained Carsten Flohr, MD, PhD, research and development lead at St John’s Institute of Dermatology, Guy’s and St Thomas’ NHS Foundation Trust London.
“We don’t really have much pediatric trial data; very often the pediatric data that we have is buried in adult trials and when it comes to an adequately powered randomized controlled trial with conventional systemic medication in pediatric patients, we don’t have one – so we’re lacking that gold standard,” said Dr. Flohr, chair in dermatology and population health sciences at King’s College London.
In the TREAT trial, 103 patients with AD (mean age, 10 years) who had not responded to topical treatment, were randomly assigned to oral ciclosporin (4 mg/kg daily) or methotrexate (0.4 mg/kg weekly) for 36 weeks and then followed for another 24 weeks off therapy for the co-primary outcomes of change in objective Scoring Atopic Dermatitis (o-SCORAD) at 12 weeks, as well as time to first significant flare after treatment cessation, defined as returning to baseline o-SCORAD, or restarting a systemic treatment.
Secondary outcomes included disease severity and quality of life (QOL) measures, as well as safety. At baseline, the mean o-SCORAD was 46.81, with mean Eczema Area and Severity Index (EASI) and Patient Oriented Eczema Measure (POEM) scores of 28.05 and 20.62 respectively. The mean Children’s Dermatology Life Quality Index (CDLQI) score was 14.96.
Looking at change in eczema severity measured by o-SCORAD at 12 weeks, ciclosporin was superior to methotrexate, with a mean difference in o-SCORAD change of -5.69 (P =.01). For the co-primary endpoint of time to first significant flare during the 24 weeks after treatment cessation, “there was a trend toward more flare activity in the ciclosporin group, although with a hazard ratio of 1.55, this was statistically not significant,” Dr. Flohr said.
On a graph showing mean EASI scores from baseline through the 60-week study period, Dr. Flohr explained how the score first dropped more precipitously in patients treated with ciclosporin compared with those treated with methotrexate, reaching a statistically significant difference between the groups by 12 weeks (–3.13, P = .0145).
However, after that time, while the EASI score among those on methotrexate continued to drop, the ciclosporin score evened out, so that by 20 weeks, methotrexate EASI scores were better, and remained so until the end of treatment and further, out to 60 weeks (mean difference -6.36, P < .001). “The most interesting bit of this graph is [that] the curve is pointing downwards for methotrexate up to the 9-month point, suggesting these people had not reached their full therapeutic potential yet, whereas if you’re on ciclosporin you plateau and there’s not much additional improvement, if at all, and then people [on ciclosporin] start going up in their disease activity off therapy,” he said.
The same pattern was seen with all the other outcome measures, including o-SCORAD and POEM.
Quality of life significantly improved by about 8 points in both treatment groups, with no significant differences between groups, and this improvement was sustained through the 24 weeks following cessation of therapy. However, during this treatment-free phase, patients on methotrexate had fewer parent-reported flares compared with those on ciclosporin (mean 6.19 vs 5.40 flares, P =.0251), although there was no difference between groups in time to first flare.
Describing the treatment safety as “overall reassuring,” Dr. Flohr said there were slightly more nonserious adverse events in the methotrexate arm (407 vs. 369), with nausea occurring more often in this group (43.1% vs. 17.6%).
“I think we were seeing this clinically, but to see it in a clinical trial gives us more confidence in discussing with parents,” said session moderator Melinda Gooderham, MD, assistant professor at Queens University, Kingston, Ont., and medical director at the SKiN Centre for Dermatology in Peterborough.
What she also took away from the study was safety of these treatments. “The discontinuation rate was not different with either drug, so it’s not like ciclosporin works fast but all these people have problems and discontinue,” Dr. Gooderham told this news organization. “That’s also reassuring.”
Asked which treatment she prefers, Dr. Gooderham, a consultant physician at Peterborough Regional Health Centre, picked methotrexate “because of the lasting effect. But there are times when you may need more rapid control ... where I might choose ciclosporin first, but for me it’s maybe 90% methotrexate first, 10% ciclosporin.”
Dr. Flohr and Dr. Gooderham report no relevant financial relationships. The study was funded by the National Institute for Health and Care Research.
A version of this article first appeared on Medscape.com.
MONTREAL – in the TREAT study, investigators reported at the annual meeting of the International Society of Atopic Dermatitis.
The findings are important, since many regulatory bodies require patients to have tried such first-line conventional systemic therapies before moving on to novel therapeutics, explained Carsten Flohr, MD, PhD, research and development lead at St John’s Institute of Dermatology, Guy’s and St Thomas’ NHS Foundation Trust London.
“We don’t really have much pediatric trial data; very often the pediatric data that we have is buried in adult trials and when it comes to an adequately powered randomized controlled trial with conventional systemic medication in pediatric patients, we don’t have one – so we’re lacking that gold standard,” said Dr. Flohr, chair in dermatology and population health sciences at King’s College London.
In the TREAT trial, 103 patients with AD (mean age, 10 years) who had not responded to topical treatment, were randomly assigned to oral ciclosporin (4 mg/kg daily) or methotrexate (0.4 mg/kg weekly) for 36 weeks and then followed for another 24 weeks off therapy for the co-primary outcomes of change in objective Scoring Atopic Dermatitis (o-SCORAD) at 12 weeks, as well as time to first significant flare after treatment cessation, defined as returning to baseline o-SCORAD, or restarting a systemic treatment.
Secondary outcomes included disease severity and quality of life (QOL) measures, as well as safety. At baseline, the mean o-SCORAD was 46.81, with mean Eczema Area and Severity Index (EASI) and Patient Oriented Eczema Measure (POEM) scores of 28.05 and 20.62 respectively. The mean Children’s Dermatology Life Quality Index (CDLQI) score was 14.96.
Looking at change in eczema severity measured by o-SCORAD at 12 weeks, ciclosporin was superior to methotrexate, with a mean difference in o-SCORAD change of -5.69 (P =.01). For the co-primary endpoint of time to first significant flare during the 24 weeks after treatment cessation, “there was a trend toward more flare activity in the ciclosporin group, although with a hazard ratio of 1.55, this was statistically not significant,” Dr. Flohr said.
On a graph showing mean EASI scores from baseline through the 60-week study period, Dr. Flohr explained how the score first dropped more precipitously in patients treated with ciclosporin compared with those treated with methotrexate, reaching a statistically significant difference between the groups by 12 weeks (–3.13, P = .0145).
However, after that time, while the EASI score among those on methotrexate continued to drop, the ciclosporin score evened out, so that by 20 weeks, methotrexate EASI scores were better, and remained so until the end of treatment and further, out to 60 weeks (mean difference -6.36, P < .001). “The most interesting bit of this graph is [that] the curve is pointing downwards for methotrexate up to the 9-month point, suggesting these people had not reached their full therapeutic potential yet, whereas if you’re on ciclosporin you plateau and there’s not much additional improvement, if at all, and then people [on ciclosporin] start going up in their disease activity off therapy,” he said.
The same pattern was seen with all the other outcome measures, including o-SCORAD and POEM.
Quality of life significantly improved by about 8 points in both treatment groups, with no significant differences between groups, and this improvement was sustained through the 24 weeks following cessation of therapy. However, during this treatment-free phase, patients on methotrexate had fewer parent-reported flares compared with those on ciclosporin (mean 6.19 vs 5.40 flares, P =.0251), although there was no difference between groups in time to first flare.
Describing the treatment safety as “overall reassuring,” Dr. Flohr said there were slightly more nonserious adverse events in the methotrexate arm (407 vs. 369), with nausea occurring more often in this group (43.1% vs. 17.6%).
“I think we were seeing this clinically, but to see it in a clinical trial gives us more confidence in discussing with parents,” said session moderator Melinda Gooderham, MD, assistant professor at Queens University, Kingston, Ont., and medical director at the SKiN Centre for Dermatology in Peterborough.
What she also took away from the study was safety of these treatments. “The discontinuation rate was not different with either drug, so it’s not like ciclosporin works fast but all these people have problems and discontinue,” Dr. Gooderham told this news organization. “That’s also reassuring.”
Asked which treatment she prefers, Dr. Gooderham, a consultant physician at Peterborough Regional Health Centre, picked methotrexate “because of the lasting effect. But there are times when you may need more rapid control ... where I might choose ciclosporin first, but for me it’s maybe 90% methotrexate first, 10% ciclosporin.”
Dr. Flohr and Dr. Gooderham report no relevant financial relationships. The study was funded by the National Institute for Health and Care Research.
A version of this article first appeared on Medscape.com.
MONTREAL – in the TREAT study, investigators reported at the annual meeting of the International Society of Atopic Dermatitis.
The findings are important, since many regulatory bodies require patients to have tried such first-line conventional systemic therapies before moving on to novel therapeutics, explained Carsten Flohr, MD, PhD, research and development lead at St John’s Institute of Dermatology, Guy’s and St Thomas’ NHS Foundation Trust London.
“We don’t really have much pediatric trial data; very often the pediatric data that we have is buried in adult trials and when it comes to an adequately powered randomized controlled trial with conventional systemic medication in pediatric patients, we don’t have one – so we’re lacking that gold standard,” said Dr. Flohr, chair in dermatology and population health sciences at King’s College London.
In the TREAT trial, 103 patients with AD (mean age, 10 years) who had not responded to topical treatment, were randomly assigned to oral ciclosporin (4 mg/kg daily) or methotrexate (0.4 mg/kg weekly) for 36 weeks and then followed for another 24 weeks off therapy for the co-primary outcomes of change in objective Scoring Atopic Dermatitis (o-SCORAD) at 12 weeks, as well as time to first significant flare after treatment cessation, defined as returning to baseline o-SCORAD, or restarting a systemic treatment.
Secondary outcomes included disease severity and quality of life (QOL) measures, as well as safety. At baseline, the mean o-SCORAD was 46.81, with mean Eczema Area and Severity Index (EASI) and Patient Oriented Eczema Measure (POEM) scores of 28.05 and 20.62 respectively. The mean Children’s Dermatology Life Quality Index (CDLQI) score was 14.96.
Looking at change in eczema severity measured by o-SCORAD at 12 weeks, ciclosporin was superior to methotrexate, with a mean difference in o-SCORAD change of -5.69 (P =.01). For the co-primary endpoint of time to first significant flare during the 24 weeks after treatment cessation, “there was a trend toward more flare activity in the ciclosporin group, although with a hazard ratio of 1.55, this was statistically not significant,” Dr. Flohr said.
On a graph showing mean EASI scores from baseline through the 60-week study period, Dr. Flohr explained how the score first dropped more precipitously in patients treated with ciclosporin compared with those treated with methotrexate, reaching a statistically significant difference between the groups by 12 weeks (–3.13, P = .0145).
However, after that time, while the EASI score among those on methotrexate continued to drop, the ciclosporin score evened out, so that by 20 weeks, methotrexate EASI scores were better, and remained so until the end of treatment and further, out to 60 weeks (mean difference -6.36, P < .001). “The most interesting bit of this graph is [that] the curve is pointing downwards for methotrexate up to the 9-month point, suggesting these people had not reached their full therapeutic potential yet, whereas if you’re on ciclosporin you plateau and there’s not much additional improvement, if at all, and then people [on ciclosporin] start going up in their disease activity off therapy,” he said.
The same pattern was seen with all the other outcome measures, including o-SCORAD and POEM.
Quality of life significantly improved by about 8 points in both treatment groups, with no significant differences between groups, and this improvement was sustained through the 24 weeks following cessation of therapy. However, during this treatment-free phase, patients on methotrexate had fewer parent-reported flares compared with those on ciclosporin (mean 6.19 vs 5.40 flares, P =.0251), although there was no difference between groups in time to first flare.
Describing the treatment safety as “overall reassuring,” Dr. Flohr said there were slightly more nonserious adverse events in the methotrexate arm (407 vs. 369), with nausea occurring more often in this group (43.1% vs. 17.6%).
“I think we were seeing this clinically, but to see it in a clinical trial gives us more confidence in discussing with parents,” said session moderator Melinda Gooderham, MD, assistant professor at Queens University, Kingston, Ont., and medical director at the SKiN Centre for Dermatology in Peterborough.
What she also took away from the study was safety of these treatments. “The discontinuation rate was not different with either drug, so it’s not like ciclosporin works fast but all these people have problems and discontinue,” Dr. Gooderham told this news organization. “That’s also reassuring.”
Asked which treatment she prefers, Dr. Gooderham, a consultant physician at Peterborough Regional Health Centre, picked methotrexate “because of the lasting effect. But there are times when you may need more rapid control ... where I might choose ciclosporin first, but for me it’s maybe 90% methotrexate first, 10% ciclosporin.”
Dr. Flohr and Dr. Gooderham report no relevant financial relationships. The study was funded by the National Institute for Health and Care Research.
A version of this article first appeared on Medscape.com.
AT ISAD 2022
Online support tool improves AD self-management
MONTREAL – for up to 1 year, according to two randomized controlled trials presented at the annual meeting of the International Society of Atopic Dermatitis.
The intervention, directed either at parents of children with AD or young adults with AD, “is very low cost, evidence based, easily accessible, and free from possible commercial bias,” said investigator Kim Thomas, MD, professor of applied dermatology research and codirector of the Centre of Evidence Based Dermatology, faculty of medicine & health sciences, University of Nottingham (England).
The main focus of the intervention, along with general education, is “getting control” of the condition with flare-control creams and “keeping control” with regular emollient use.
Efficacy of the intervention, available free online, was compared with “usual eczema care” in 340 parents of children with AD up to age 12 and 337 young patients with AD aged 13-25. Participants were randomized to the intervention plus usual care or usual care alone. The primary outcome was the Patient-Oriented Eczema Measure(POEM) at 24 weeks, with a further measurement at 52 weeks.
In the parent group, about half were women and 83% were White, and the median age of their children was 4 years. About 50% of parents had a university degree, making them “possibly better educated than we might want our target audience for this type of intervention,” Dr. Thomas commented. Most of the children had moderate AD.
In the young patient group, the mean age was 19 years, more than three-quarters were female, 83% were White, and most had moderate AD.
At 24 weeks, both intervention groups had improved POEM scores, compared with controls, with a mean difference of 1.5 points in the parent group (P = .002) and 1.7 points in the young patient group (P = .04). “A small difference, but statistically significant and sustained,” Dr. Thomas said, adding that this difference was sustained up to 52 weeks.
In terms of mechanism of action, a secondary outcome looked at the concept of enablement, “which again, seemed to be improved in the intervention group, which suggests it’s something to do with being able to understand and cope with their disease better,” she said. The tool is targeted to “people who wouldn’t normally get to a dermatologist and certainly wouldn’t get access to group interventions.”
An additional aim of the intervention was “to provide a single, consistent message received from every point of contact that people might engage with ... [from] community doctors, pharmacists, dermatologists, and importantly, eczema charities all signposting [the intervention] and sharing a consistent message.”
While the intervention is free and available to patients anywhere, Dr. Thomas emphasized that it is tailored to the U.K. health care system. “If people would like to get in touch and help work with us to maybe adapt it slightly to make it more suitable for your own health care systems, that’s something we’d be very happy to look at with you.”
Asked for comment, Natalie Cunningham, MD, panel moderator, was lukewarm about the tool. “It can be a supplement, but you can never replace the one-on-one patient–health care provider interaction,” she told this news organization. “That could be provided by a nondermatologist and supplemented by an online component,” said Dr. Cunningham, from the Izaak Walton Killam Hospital for Children in Halifax, N.S.
“First-line treatment for eczema, no matter what kind of eczema, is topical steroids, and that is something that requires a lot of education – and something you want to do one on one in person because everyone comes to it with a different experience, baggage, or understanding,” she said. “We need to figure out what the barrier is so that you can do the right education.”
In addition, with systemic AD therapies currently approved for children, parents and young patients need to be able to advocate for specialist care to access these medications, she noted.
Dr. Thomas and Dr. Cunningham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – for up to 1 year, according to two randomized controlled trials presented at the annual meeting of the International Society of Atopic Dermatitis.
The intervention, directed either at parents of children with AD or young adults with AD, “is very low cost, evidence based, easily accessible, and free from possible commercial bias,” said investigator Kim Thomas, MD, professor of applied dermatology research and codirector of the Centre of Evidence Based Dermatology, faculty of medicine & health sciences, University of Nottingham (England).
The main focus of the intervention, along with general education, is “getting control” of the condition with flare-control creams and “keeping control” with regular emollient use.
Efficacy of the intervention, available free online, was compared with “usual eczema care” in 340 parents of children with AD up to age 12 and 337 young patients with AD aged 13-25. Participants were randomized to the intervention plus usual care or usual care alone. The primary outcome was the Patient-Oriented Eczema Measure(POEM) at 24 weeks, with a further measurement at 52 weeks.
In the parent group, about half were women and 83% were White, and the median age of their children was 4 years. About 50% of parents had a university degree, making them “possibly better educated than we might want our target audience for this type of intervention,” Dr. Thomas commented. Most of the children had moderate AD.
In the young patient group, the mean age was 19 years, more than three-quarters were female, 83% were White, and most had moderate AD.
At 24 weeks, both intervention groups had improved POEM scores, compared with controls, with a mean difference of 1.5 points in the parent group (P = .002) and 1.7 points in the young patient group (P = .04). “A small difference, but statistically significant and sustained,” Dr. Thomas said, adding that this difference was sustained up to 52 weeks.
In terms of mechanism of action, a secondary outcome looked at the concept of enablement, “which again, seemed to be improved in the intervention group, which suggests it’s something to do with being able to understand and cope with their disease better,” she said. The tool is targeted to “people who wouldn’t normally get to a dermatologist and certainly wouldn’t get access to group interventions.”
An additional aim of the intervention was “to provide a single, consistent message received from every point of contact that people might engage with ... [from] community doctors, pharmacists, dermatologists, and importantly, eczema charities all signposting [the intervention] and sharing a consistent message.”
While the intervention is free and available to patients anywhere, Dr. Thomas emphasized that it is tailored to the U.K. health care system. “If people would like to get in touch and help work with us to maybe adapt it slightly to make it more suitable for your own health care systems, that’s something we’d be very happy to look at with you.”
Asked for comment, Natalie Cunningham, MD, panel moderator, was lukewarm about the tool. “It can be a supplement, but you can never replace the one-on-one patient–health care provider interaction,” she told this news organization. “That could be provided by a nondermatologist and supplemented by an online component,” said Dr. Cunningham, from the Izaak Walton Killam Hospital for Children in Halifax, N.S.
“First-line treatment for eczema, no matter what kind of eczema, is topical steroids, and that is something that requires a lot of education – and something you want to do one on one in person because everyone comes to it with a different experience, baggage, or understanding,” she said. “We need to figure out what the barrier is so that you can do the right education.”
In addition, with systemic AD therapies currently approved for children, parents and young patients need to be able to advocate for specialist care to access these medications, she noted.
Dr. Thomas and Dr. Cunningham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
MONTREAL – for up to 1 year, according to two randomized controlled trials presented at the annual meeting of the International Society of Atopic Dermatitis.
The intervention, directed either at parents of children with AD or young adults with AD, “is very low cost, evidence based, easily accessible, and free from possible commercial bias,” said investigator Kim Thomas, MD, professor of applied dermatology research and codirector of the Centre of Evidence Based Dermatology, faculty of medicine & health sciences, University of Nottingham (England).
The main focus of the intervention, along with general education, is “getting control” of the condition with flare-control creams and “keeping control” with regular emollient use.
Efficacy of the intervention, available free online, was compared with “usual eczema care” in 340 parents of children with AD up to age 12 and 337 young patients with AD aged 13-25. Participants were randomized to the intervention plus usual care or usual care alone. The primary outcome was the Patient-Oriented Eczema Measure(POEM) at 24 weeks, with a further measurement at 52 weeks.
In the parent group, about half were women and 83% were White, and the median age of their children was 4 years. About 50% of parents had a university degree, making them “possibly better educated than we might want our target audience for this type of intervention,” Dr. Thomas commented. Most of the children had moderate AD.
In the young patient group, the mean age was 19 years, more than three-quarters were female, 83% were White, and most had moderate AD.
At 24 weeks, both intervention groups had improved POEM scores, compared with controls, with a mean difference of 1.5 points in the parent group (P = .002) and 1.7 points in the young patient group (P = .04). “A small difference, but statistically significant and sustained,” Dr. Thomas said, adding that this difference was sustained up to 52 weeks.
In terms of mechanism of action, a secondary outcome looked at the concept of enablement, “which again, seemed to be improved in the intervention group, which suggests it’s something to do with being able to understand and cope with their disease better,” she said. The tool is targeted to “people who wouldn’t normally get to a dermatologist and certainly wouldn’t get access to group interventions.”
An additional aim of the intervention was “to provide a single, consistent message received from every point of contact that people might engage with ... [from] community doctors, pharmacists, dermatologists, and importantly, eczema charities all signposting [the intervention] and sharing a consistent message.”
While the intervention is free and available to patients anywhere, Dr. Thomas emphasized that it is tailored to the U.K. health care system. “If people would like to get in touch and help work with us to maybe adapt it slightly to make it more suitable for your own health care systems, that’s something we’d be very happy to look at with you.”
Asked for comment, Natalie Cunningham, MD, panel moderator, was lukewarm about the tool. “It can be a supplement, but you can never replace the one-on-one patient–health care provider interaction,” she told this news organization. “That could be provided by a nondermatologist and supplemented by an online component,” said Dr. Cunningham, from the Izaak Walton Killam Hospital for Children in Halifax, N.S.
“First-line treatment for eczema, no matter what kind of eczema, is topical steroids, and that is something that requires a lot of education – and something you want to do one on one in person because everyone comes to it with a different experience, baggage, or understanding,” she said. “We need to figure out what the barrier is so that you can do the right education.”
In addition, with systemic AD therapies currently approved for children, parents and young patients need to be able to advocate for specialist care to access these medications, she noted.
Dr. Thomas and Dr. Cunningham reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ISAD 2022
Metabolites may distinguish severe subtypes of PAH
, based on data from approximately 1,500 individuals.
The overall prognosis and therapeutic response for patients with pulmonary arterial hypertension associated with systemic sclerosis (SSc-PAH) tends to be worse than for patients with other types of PAH, such as idiopathic pulmonary arterial hypertension (IPAH), but the impact of different metabolite profiles among subtypes of disease has not been explored, wrote Mona Alotaibi, MD, of the University of California, San Diego, and colleagues.
“Recently, metabolic dysregulation has been proposed as a key mechanism by which IPAH and SSc-PAH differ and could control such disparities,” they noted. Clarifying the molecular mechanisms of SSc-PAH could inform management and treatment, they added.
In a study published in the journal Chest, the researchers sought to identify a bioactive lipid signature unique to SSc-PAH. They identified 400 patients with SSc-PAH and 1,082 with IPAH. An additional 100 patients with scleroderma but no PH and 44 patients with scleroderma who had PH were included for external validation. The mean ages of the patients with IPAH and SSc-PAH in the discovery and validation cohorts ranged from approximately 51 to 65 years; more than 75% of patients across the groups were women.
The researchers tested more than 700 bioactive lipid metabolites using liquid chromatography/mass spectrometry. They found five metabolites that distinguished SSc-PAH and IPAH that were significantly associated with markers of disease severity: 17-beta estradiol, novel Eic, nervonic acid, fatty acid esters of hydroxy fatty acids, and prostaglandin F2 alpha (PGF 2 alpha).
The biomarkers were increased in SSc-PAH patients compared to patients with SSC alone, which suggests that the biomarkers are related to PAH and not to scleroderma alone, the researchers noted.
In particular, nervonic acid was associated with worse functional capacity, in SSc-PAH patients, as were higher levels of 17-beta estradiol and prostaglandin F2 alpha. Also, 17-beta estradiol was associated with lower cardiac impairment (CI) and stroke volume index (SVI) in SSc-PAH patients, but higher SVI in IPAH patients. PGF 2 alpha was associated with lower CI and SVI and higher pulmonary vascular resistance in SSc-PAH and IPAH combined.
The study findings were limited by several factors including the inability to adjust for all potential confounders between IPAH and SSc-PAH, and the fact that a clear causal relationship could not be determined, the researchers noted. Inadequate statistical power to analyze SSc-PAH data was another limitation, and studies with detailed scleroderma phenotypes are needed to validate the results, they said.
However, the current study provides insight on the metabolic differences in SSc-PAH and the potential impact on disease pathology that may inform diagnosis, prognosis, and treatment strategies for SSc-PAH patients, they concluded.
The study was supported by the National Institutes of Health. Several individual investigators received support from organizations including the American Heart Association and the Chest Foundation, and from companies including Livanova, Equillium, Corvus, Bayer, and Actelion, but the authors had no relevant financial conflicts to disclose.
, based on data from approximately 1,500 individuals.
The overall prognosis and therapeutic response for patients with pulmonary arterial hypertension associated with systemic sclerosis (SSc-PAH) tends to be worse than for patients with other types of PAH, such as idiopathic pulmonary arterial hypertension (IPAH), but the impact of different metabolite profiles among subtypes of disease has not been explored, wrote Mona Alotaibi, MD, of the University of California, San Diego, and colleagues.
“Recently, metabolic dysregulation has been proposed as a key mechanism by which IPAH and SSc-PAH differ and could control such disparities,” they noted. Clarifying the molecular mechanisms of SSc-PAH could inform management and treatment, they added.
In a study published in the journal Chest, the researchers sought to identify a bioactive lipid signature unique to SSc-PAH. They identified 400 patients with SSc-PAH and 1,082 with IPAH. An additional 100 patients with scleroderma but no PH and 44 patients with scleroderma who had PH were included for external validation. The mean ages of the patients with IPAH and SSc-PAH in the discovery and validation cohorts ranged from approximately 51 to 65 years; more than 75% of patients across the groups were women.
The researchers tested more than 700 bioactive lipid metabolites using liquid chromatography/mass spectrometry. They found five metabolites that distinguished SSc-PAH and IPAH that were significantly associated with markers of disease severity: 17-beta estradiol, novel Eic, nervonic acid, fatty acid esters of hydroxy fatty acids, and prostaglandin F2 alpha (PGF 2 alpha).
The biomarkers were increased in SSc-PAH patients compared to patients with SSC alone, which suggests that the biomarkers are related to PAH and not to scleroderma alone, the researchers noted.
In particular, nervonic acid was associated with worse functional capacity, in SSc-PAH patients, as were higher levels of 17-beta estradiol and prostaglandin F2 alpha. Also, 17-beta estradiol was associated with lower cardiac impairment (CI) and stroke volume index (SVI) in SSc-PAH patients, but higher SVI in IPAH patients. PGF 2 alpha was associated with lower CI and SVI and higher pulmonary vascular resistance in SSc-PAH and IPAH combined.
The study findings were limited by several factors including the inability to adjust for all potential confounders between IPAH and SSc-PAH, and the fact that a clear causal relationship could not be determined, the researchers noted. Inadequate statistical power to analyze SSc-PAH data was another limitation, and studies with detailed scleroderma phenotypes are needed to validate the results, they said.
However, the current study provides insight on the metabolic differences in SSc-PAH and the potential impact on disease pathology that may inform diagnosis, prognosis, and treatment strategies for SSc-PAH patients, they concluded.
The study was supported by the National Institutes of Health. Several individual investigators received support from organizations including the American Heart Association and the Chest Foundation, and from companies including Livanova, Equillium, Corvus, Bayer, and Actelion, but the authors had no relevant financial conflicts to disclose.
, based on data from approximately 1,500 individuals.
The overall prognosis and therapeutic response for patients with pulmonary arterial hypertension associated with systemic sclerosis (SSc-PAH) tends to be worse than for patients with other types of PAH, such as idiopathic pulmonary arterial hypertension (IPAH), but the impact of different metabolite profiles among subtypes of disease has not been explored, wrote Mona Alotaibi, MD, of the University of California, San Diego, and colleagues.
“Recently, metabolic dysregulation has been proposed as a key mechanism by which IPAH and SSc-PAH differ and could control such disparities,” they noted. Clarifying the molecular mechanisms of SSc-PAH could inform management and treatment, they added.
In a study published in the journal Chest, the researchers sought to identify a bioactive lipid signature unique to SSc-PAH. They identified 400 patients with SSc-PAH and 1,082 with IPAH. An additional 100 patients with scleroderma but no PH and 44 patients with scleroderma who had PH were included for external validation. The mean ages of the patients with IPAH and SSc-PAH in the discovery and validation cohorts ranged from approximately 51 to 65 years; more than 75% of patients across the groups were women.
The researchers tested more than 700 bioactive lipid metabolites using liquid chromatography/mass spectrometry. They found five metabolites that distinguished SSc-PAH and IPAH that were significantly associated with markers of disease severity: 17-beta estradiol, novel Eic, nervonic acid, fatty acid esters of hydroxy fatty acids, and prostaglandin F2 alpha (PGF 2 alpha).
The biomarkers were increased in SSc-PAH patients compared to patients with SSC alone, which suggests that the biomarkers are related to PAH and not to scleroderma alone, the researchers noted.
In particular, nervonic acid was associated with worse functional capacity, in SSc-PAH patients, as were higher levels of 17-beta estradiol and prostaglandin F2 alpha. Also, 17-beta estradiol was associated with lower cardiac impairment (CI) and stroke volume index (SVI) in SSc-PAH patients, but higher SVI in IPAH patients. PGF 2 alpha was associated with lower CI and SVI and higher pulmonary vascular resistance in SSc-PAH and IPAH combined.
The study findings were limited by several factors including the inability to adjust for all potential confounders between IPAH and SSc-PAH, and the fact that a clear causal relationship could not be determined, the researchers noted. Inadequate statistical power to analyze SSc-PAH data was another limitation, and studies with detailed scleroderma phenotypes are needed to validate the results, they said.
However, the current study provides insight on the metabolic differences in SSc-PAH and the potential impact on disease pathology that may inform diagnosis, prognosis, and treatment strategies for SSc-PAH patients, they concluded.
The study was supported by the National Institutes of Health. Several individual investigators received support from organizations including the American Heart Association and the Chest Foundation, and from companies including Livanova, Equillium, Corvus, Bayer, and Actelion, but the authors had no relevant financial conflicts to disclose.
FROM CHEST
Itchy Red-Brown Spots on a Child
The Diagnosis: Maculopapular Cutaneous Mastocytosis (Urticaria Pigmentosa)
A stroke test revealed urtication at the exact traumatized site (Figure). A skin biopsy performed 2 years prior by another physician in the same hospital had revealed mast cell infiltration of virtually the entire dermis. The diagnosis was then firmly established as maculopapular cutaneous mastocytosis (CM)(also known as urticaria pigmentosa) with both the pathology results and a confirmative stroke test, and no additional biopsy was attempted. Serum IgE and tryptase levels were within the reference range. General recommendations about the avoidance of trigger factors were given to the family, and a new-generation H1 blocker antihistaminic syrup was prescribed for flushing, itching, and urtication.

Mastocytosis is a canopy term for a heterogeneous group of disorders caused by clonal proliferation and accumulation of abnormal mast cells within the skin and visceral organs (ie, bone marrow, liver, spleen, lymph nodes, gastrointestinal tract). Cutaneous mastocytosis, the skin-restricted variant, is by far the most common form of childhood mastocytosis (90% of mastocytosis cases in children)1 and generally appears within the first 2 years of life.1-7 Pediatric CM usually is a benign and transient disease with an excellent prognosis and a negligible risk for systemic involvement.2,3,5
The pathogenesis of CM in children is obscure1; however, somatic or germline gain-of-function mutations of the c-KIT proto-oncogene, which encodes KIT (ie, a tyrosine kinase membrane receptor for stem cell factor), may account for most pediatric CM phenotypes.1,3,6 Activating c-KIT mutations leads to constitutive activation of the KIT receptor (expressed on the surface membrane of mast cells) and instigates autonomous (stem cell factor– independent) clonal proliferation, enhanced survival, and accumulation of mast cells.2
Maculopapular CM is the most common clinical form of CM.2,4,5 In children, maculopapular CM usually presents with polymorphous red-brown lesions of varying sizes and types—macule, papule, plaque, or nodule—on the torso and extremities.1-5 The distribution may be widespread and rarely is almost universal, as in our patient.2 Darier sign typically is positive, with a wheal and flare developing upon stroking or rubbing 1 or several lesions.1-6 The lesions gradually involute and often spontaneously regress at the time of puberty.1-3,5-7
The clinical signs and symptoms of mastocytosis are not only related to mast cell infiltration but also to mast cell activation within the tissues. The release of intracellular mediators from activated mast cells may have local and/or systemic consequences.4,7 Erythema, edema, flushing, pruritus, urticaria, blistering, and dermatographism are among the local cutaneous symptoms of mast cell activation.2-4,7 Systemic symptoms are rare in childhood CM and consist of wheezing, shortness of breath, nausea, vomiting, reflux, abdominal cramping, diarrhea, tachycardia, hypotension, syncope, anaphylaxis, and cyanotic spells.1-7 An elevated serum tryptase level is an indicator of both mast cell burden and risk for mast cell activation in the skin.4,7
Treatment of pediatric CM is conservative and symptomatic.3 Prevention of mediator release may be accomplished through avoidance of trigger factors.1 Alleviation of mediator-related symptoms might be attained using H1 and H2 histamine receptor blockers, oral cromolyn sodium, leukotriene antagonists, and epinephrine autoinjectors.1-3,5 Short-term topical or oral corticosteroids; calcineurin inhibitors (eg, pimecrolimus, tacrolimus); phototherapy; psoralen plus UVA; omalizumab; and innovative agents such as topical miltefosine, nemolizumab (an IL-31 antagonist), kinase inhibitors such as midostaurin, and tyrosine kinase inhibitors such as imatinib and masitinib may be tried in refractory or extensive pediatric CM.1,2,5,6
Although several disorders in childhood may present with red-brown macules and papules, Darier sign is unique to cutaneous mastocytosis. A biopsy also will be helpful in establishing the definitive diagnosis.
Histiocytosis X (also referred to as Langerhans cell histiocytosis) is the most common proliferative histiocytic disorder. Cutaneous lesions are polymorphic and consist of seborrheic involvement of the scalp with yellow, scaly or crusted papules; eroded patches; pustules; vesicles; petechiae; purpura; or red to purplish papules on the groin, abdomen, back, or chest.8
LEOPARD syndrome (also known as Noonan syndrome with multiple lentigines) is an acronym denoting lentigines (multiple), electrocardiographic conduction abnormalities, ocular hypertelorism, pulmonary stenosis, abnormalities of the genitalia, retarded growth, and deafness (sensorineural). The disorder is caused by a genetic mutation involving the PTPN11 gene and currently is categorized under the canopy of RASopathies. Cutaneous findings consist of lentiginous and café-au-lait macules and patches.9
Neurofibromatosis is a genetic disorder with a plethora of cutaneous and systemic manifestations. The type 1 variant that constitutes more than 95% of cases is caused by mutations in the neurofibromin gene. The main cutaneous findings include café-au-lait macules, freckling in axillary and inguinal locations (Crowe sign), and neurofibromas. These lesions may present as macules, patches, papules, or nodules.10
Xanthoma disseminatum is a rare sporadic proliferative histiocyte disorder involving the skin and mucosa. The disorder may be a harbinger of diabetes insipidus. Cutaneous lesions consist of asymptomatic, symmetrical, discrete, erythematous to yellow-brown papules and nodules.11
- Sandru F, Petca RC, Costescu M, et al. Cutaneous mastocytosis in childhood: update from the literature. J Clin Med. 2021;10:1474. doi:10.3390/jcm10071474
- Lange M, Hartmann K, Carter MC, et al. Molecular background, clinical features and management of pediatric mastocytosis: status 2021. Int J Mol Sci. 2021;22:2586. doi:10.3390/ijms22052586
- Castells M, Metcalfe DD, Escribano L. Diagnosis and treatment of cutaneous mastocytosis in children: practical recommendations. Am J Clin Dermatol. 2011;12:259-270. doi:10.2165/11588890-000000000-00000
- Nedoszytko B, Arock M, Lyons JJ, et al. Clinical impact of inherited and acquired genetic variants in mastocytosis. Int J Mol Sci. 2021;22:411. doi:10.3390/ijms22010411
- Nemat K, Abraham S. Cutaneous mastocytosis in childhood. Allergol Select. 2022;6:1-10. doi:10.5414/ALX02304E
- Giona F. Pediatric mastocytosis: an update. Mediterr J Hematol Infect Dis. 2021;13:E2021069. doi:10.4084/MJHID.2021.069
- Brockow K, Plata-Nazar K, Lange M, et al. Mediator-related symptoms and anaphylaxis in children with mastocytosis. Int J Mol Sci. 2021;22:2684. doi:10.3390/ijms22052684
- Grana N. Langerhans cell histiocytosis. Cancer Control. 2014;21: 328-334.
- García-Gil MF, Álvarez-Salafranca M, Valero-Torres A, et al. Melanoma in Noonan syndrome with multiple lentigines (LEOPARD syndrome): a new case. Actas Dermosifiliogr (Engl Ed). 2020;111:619-621.
- Ozarslan B, Russo T, Argenziano G, et al. Cutaneous findings in neurofibromatosis type 1. Cancers (Basel). 2021;13:463.
- Behra A, Sa DK, Naik R, et al. A rare case of persistent xanthoma disseminatum without any systemic involvement. Indian J Dermatol. 2020;65:239-241.
The Diagnosis: Maculopapular Cutaneous Mastocytosis (Urticaria Pigmentosa)
A stroke test revealed urtication at the exact traumatized site (Figure). A skin biopsy performed 2 years prior by another physician in the same hospital had revealed mast cell infiltration of virtually the entire dermis. The diagnosis was then firmly established as maculopapular cutaneous mastocytosis (CM)(also known as urticaria pigmentosa) with both the pathology results and a confirmative stroke test, and no additional biopsy was attempted. Serum IgE and tryptase levels were within the reference range. General recommendations about the avoidance of trigger factors were given to the family, and a new-generation H1 blocker antihistaminic syrup was prescribed for flushing, itching, and urtication.

Mastocytosis is a canopy term for a heterogeneous group of disorders caused by clonal proliferation and accumulation of abnormal mast cells within the skin and visceral organs (ie, bone marrow, liver, spleen, lymph nodes, gastrointestinal tract). Cutaneous mastocytosis, the skin-restricted variant, is by far the most common form of childhood mastocytosis (90% of mastocytosis cases in children)1 and generally appears within the first 2 years of life.1-7 Pediatric CM usually is a benign and transient disease with an excellent prognosis and a negligible risk for systemic involvement.2,3,5
The pathogenesis of CM in children is obscure1; however, somatic or germline gain-of-function mutations of the c-KIT proto-oncogene, which encodes KIT (ie, a tyrosine kinase membrane receptor for stem cell factor), may account for most pediatric CM phenotypes.1,3,6 Activating c-KIT mutations leads to constitutive activation of the KIT receptor (expressed on the surface membrane of mast cells) and instigates autonomous (stem cell factor– independent) clonal proliferation, enhanced survival, and accumulation of mast cells.2
Maculopapular CM is the most common clinical form of CM.2,4,5 In children, maculopapular CM usually presents with polymorphous red-brown lesions of varying sizes and types—macule, papule, plaque, or nodule—on the torso and extremities.1-5 The distribution may be widespread and rarely is almost universal, as in our patient.2 Darier sign typically is positive, with a wheal and flare developing upon stroking or rubbing 1 or several lesions.1-6 The lesions gradually involute and often spontaneously regress at the time of puberty.1-3,5-7
The clinical signs and symptoms of mastocytosis are not only related to mast cell infiltration but also to mast cell activation within the tissues. The release of intracellular mediators from activated mast cells may have local and/or systemic consequences.4,7 Erythema, edema, flushing, pruritus, urticaria, blistering, and dermatographism are among the local cutaneous symptoms of mast cell activation.2-4,7 Systemic symptoms are rare in childhood CM and consist of wheezing, shortness of breath, nausea, vomiting, reflux, abdominal cramping, diarrhea, tachycardia, hypotension, syncope, anaphylaxis, and cyanotic spells.1-7 An elevated serum tryptase level is an indicator of both mast cell burden and risk for mast cell activation in the skin.4,7
Treatment of pediatric CM is conservative and symptomatic.3 Prevention of mediator release may be accomplished through avoidance of trigger factors.1 Alleviation of mediator-related symptoms might be attained using H1 and H2 histamine receptor blockers, oral cromolyn sodium, leukotriene antagonists, and epinephrine autoinjectors.1-3,5 Short-term topical or oral corticosteroids; calcineurin inhibitors (eg, pimecrolimus, tacrolimus); phototherapy; psoralen plus UVA; omalizumab; and innovative agents such as topical miltefosine, nemolizumab (an IL-31 antagonist), kinase inhibitors such as midostaurin, and tyrosine kinase inhibitors such as imatinib and masitinib may be tried in refractory or extensive pediatric CM.1,2,5,6
Although several disorders in childhood may present with red-brown macules and papules, Darier sign is unique to cutaneous mastocytosis. A biopsy also will be helpful in establishing the definitive diagnosis.
Histiocytosis X (also referred to as Langerhans cell histiocytosis) is the most common proliferative histiocytic disorder. Cutaneous lesions are polymorphic and consist of seborrheic involvement of the scalp with yellow, scaly or crusted papules; eroded patches; pustules; vesicles; petechiae; purpura; or red to purplish papules on the groin, abdomen, back, or chest.8
LEOPARD syndrome (also known as Noonan syndrome with multiple lentigines) is an acronym denoting lentigines (multiple), electrocardiographic conduction abnormalities, ocular hypertelorism, pulmonary stenosis, abnormalities of the genitalia, retarded growth, and deafness (sensorineural). The disorder is caused by a genetic mutation involving the PTPN11 gene and currently is categorized under the canopy of RASopathies. Cutaneous findings consist of lentiginous and café-au-lait macules and patches.9
Neurofibromatosis is a genetic disorder with a plethora of cutaneous and systemic manifestations. The type 1 variant that constitutes more than 95% of cases is caused by mutations in the neurofibromin gene. The main cutaneous findings include café-au-lait macules, freckling in axillary and inguinal locations (Crowe sign), and neurofibromas. These lesions may present as macules, patches, papules, or nodules.10
Xanthoma disseminatum is a rare sporadic proliferative histiocyte disorder involving the skin and mucosa. The disorder may be a harbinger of diabetes insipidus. Cutaneous lesions consist of asymptomatic, symmetrical, discrete, erythematous to yellow-brown papules and nodules.11
The Diagnosis: Maculopapular Cutaneous Mastocytosis (Urticaria Pigmentosa)
A stroke test revealed urtication at the exact traumatized site (Figure). A skin biopsy performed 2 years prior by another physician in the same hospital had revealed mast cell infiltration of virtually the entire dermis. The diagnosis was then firmly established as maculopapular cutaneous mastocytosis (CM)(also known as urticaria pigmentosa) with both the pathology results and a confirmative stroke test, and no additional biopsy was attempted. Serum IgE and tryptase levels were within the reference range. General recommendations about the avoidance of trigger factors were given to the family, and a new-generation H1 blocker antihistaminic syrup was prescribed for flushing, itching, and urtication.

Mastocytosis is a canopy term for a heterogeneous group of disorders caused by clonal proliferation and accumulation of abnormal mast cells within the skin and visceral organs (ie, bone marrow, liver, spleen, lymph nodes, gastrointestinal tract). Cutaneous mastocytosis, the skin-restricted variant, is by far the most common form of childhood mastocytosis (90% of mastocytosis cases in children)1 and generally appears within the first 2 years of life.1-7 Pediatric CM usually is a benign and transient disease with an excellent prognosis and a negligible risk for systemic involvement.2,3,5
The pathogenesis of CM in children is obscure1; however, somatic or germline gain-of-function mutations of the c-KIT proto-oncogene, which encodes KIT (ie, a tyrosine kinase membrane receptor for stem cell factor), may account for most pediatric CM phenotypes.1,3,6 Activating c-KIT mutations leads to constitutive activation of the KIT receptor (expressed on the surface membrane of mast cells) and instigates autonomous (stem cell factor– independent) clonal proliferation, enhanced survival, and accumulation of mast cells.2
Maculopapular CM is the most common clinical form of CM.2,4,5 In children, maculopapular CM usually presents with polymorphous red-brown lesions of varying sizes and types—macule, papule, plaque, or nodule—on the torso and extremities.1-5 The distribution may be widespread and rarely is almost universal, as in our patient.2 Darier sign typically is positive, with a wheal and flare developing upon stroking or rubbing 1 or several lesions.1-6 The lesions gradually involute and often spontaneously regress at the time of puberty.1-3,5-7
The clinical signs and symptoms of mastocytosis are not only related to mast cell infiltration but also to mast cell activation within the tissues. The release of intracellular mediators from activated mast cells may have local and/or systemic consequences.4,7 Erythema, edema, flushing, pruritus, urticaria, blistering, and dermatographism are among the local cutaneous symptoms of mast cell activation.2-4,7 Systemic symptoms are rare in childhood CM and consist of wheezing, shortness of breath, nausea, vomiting, reflux, abdominal cramping, diarrhea, tachycardia, hypotension, syncope, anaphylaxis, and cyanotic spells.1-7 An elevated serum tryptase level is an indicator of both mast cell burden and risk for mast cell activation in the skin.4,7
Treatment of pediatric CM is conservative and symptomatic.3 Prevention of mediator release may be accomplished through avoidance of trigger factors.1 Alleviation of mediator-related symptoms might be attained using H1 and H2 histamine receptor blockers, oral cromolyn sodium, leukotriene antagonists, and epinephrine autoinjectors.1-3,5 Short-term topical or oral corticosteroids; calcineurin inhibitors (eg, pimecrolimus, tacrolimus); phototherapy; psoralen plus UVA; omalizumab; and innovative agents such as topical miltefosine, nemolizumab (an IL-31 antagonist), kinase inhibitors such as midostaurin, and tyrosine kinase inhibitors such as imatinib and masitinib may be tried in refractory or extensive pediatric CM.1,2,5,6
Although several disorders in childhood may present with red-brown macules and papules, Darier sign is unique to cutaneous mastocytosis. A biopsy also will be helpful in establishing the definitive diagnosis.
Histiocytosis X (also referred to as Langerhans cell histiocytosis) is the most common proliferative histiocytic disorder. Cutaneous lesions are polymorphic and consist of seborrheic involvement of the scalp with yellow, scaly or crusted papules; eroded patches; pustules; vesicles; petechiae; purpura; or red to purplish papules on the groin, abdomen, back, or chest.8
LEOPARD syndrome (also known as Noonan syndrome with multiple lentigines) is an acronym denoting lentigines (multiple), electrocardiographic conduction abnormalities, ocular hypertelorism, pulmonary stenosis, abnormalities of the genitalia, retarded growth, and deafness (sensorineural). The disorder is caused by a genetic mutation involving the PTPN11 gene and currently is categorized under the canopy of RASopathies. Cutaneous findings consist of lentiginous and café-au-lait macules and patches.9
Neurofibromatosis is a genetic disorder with a plethora of cutaneous and systemic manifestations. The type 1 variant that constitutes more than 95% of cases is caused by mutations in the neurofibromin gene. The main cutaneous findings include café-au-lait macules, freckling in axillary and inguinal locations (Crowe sign), and neurofibromas. These lesions may present as macules, patches, papules, or nodules.10
Xanthoma disseminatum is a rare sporadic proliferative histiocyte disorder involving the skin and mucosa. The disorder may be a harbinger of diabetes insipidus. Cutaneous lesions consist of asymptomatic, symmetrical, discrete, erythematous to yellow-brown papules and nodules.11
- Sandru F, Petca RC, Costescu M, et al. Cutaneous mastocytosis in childhood: update from the literature. J Clin Med. 2021;10:1474. doi:10.3390/jcm10071474
- Lange M, Hartmann K, Carter MC, et al. Molecular background, clinical features and management of pediatric mastocytosis: status 2021. Int J Mol Sci. 2021;22:2586. doi:10.3390/ijms22052586
- Castells M, Metcalfe DD, Escribano L. Diagnosis and treatment of cutaneous mastocytosis in children: practical recommendations. Am J Clin Dermatol. 2011;12:259-270. doi:10.2165/11588890-000000000-00000
- Nedoszytko B, Arock M, Lyons JJ, et al. Clinical impact of inherited and acquired genetic variants in mastocytosis. Int J Mol Sci. 2021;22:411. doi:10.3390/ijms22010411
- Nemat K, Abraham S. Cutaneous mastocytosis in childhood. Allergol Select. 2022;6:1-10. doi:10.5414/ALX02304E
- Giona F. Pediatric mastocytosis: an update. Mediterr J Hematol Infect Dis. 2021;13:E2021069. doi:10.4084/MJHID.2021.069
- Brockow K, Plata-Nazar K, Lange M, et al. Mediator-related symptoms and anaphylaxis in children with mastocytosis. Int J Mol Sci. 2021;22:2684. doi:10.3390/ijms22052684
- Grana N. Langerhans cell histiocytosis. Cancer Control. 2014;21: 328-334.
- García-Gil MF, Álvarez-Salafranca M, Valero-Torres A, et al. Melanoma in Noonan syndrome with multiple lentigines (LEOPARD syndrome): a new case. Actas Dermosifiliogr (Engl Ed). 2020;111:619-621.
- Ozarslan B, Russo T, Argenziano G, et al. Cutaneous findings in neurofibromatosis type 1. Cancers (Basel). 2021;13:463.
- Behra A, Sa DK, Naik R, et al. A rare case of persistent xanthoma disseminatum without any systemic involvement. Indian J Dermatol. 2020;65:239-241.
- Sandru F, Petca RC, Costescu M, et al. Cutaneous mastocytosis in childhood: update from the literature. J Clin Med. 2021;10:1474. doi:10.3390/jcm10071474
- Lange M, Hartmann K, Carter MC, et al. Molecular background, clinical features and management of pediatric mastocytosis: status 2021. Int J Mol Sci. 2021;22:2586. doi:10.3390/ijms22052586
- Castells M, Metcalfe DD, Escribano L. Diagnosis and treatment of cutaneous mastocytosis in children: practical recommendations. Am J Clin Dermatol. 2011;12:259-270. doi:10.2165/11588890-000000000-00000
- Nedoszytko B, Arock M, Lyons JJ, et al. Clinical impact of inherited and acquired genetic variants in mastocytosis. Int J Mol Sci. 2021;22:411. doi:10.3390/ijms22010411
- Nemat K, Abraham S. Cutaneous mastocytosis in childhood. Allergol Select. 2022;6:1-10. doi:10.5414/ALX02304E
- Giona F. Pediatric mastocytosis: an update. Mediterr J Hematol Infect Dis. 2021;13:E2021069. doi:10.4084/MJHID.2021.069
- Brockow K, Plata-Nazar K, Lange M, et al. Mediator-related symptoms and anaphylaxis in children with mastocytosis. Int J Mol Sci. 2021;22:2684. doi:10.3390/ijms22052684
- Grana N. Langerhans cell histiocytosis. Cancer Control. 2014;21: 328-334.
- García-Gil MF, Álvarez-Salafranca M, Valero-Torres A, et al. Melanoma in Noonan syndrome with multiple lentigines (LEOPARD syndrome): a new case. Actas Dermosifiliogr (Engl Ed). 2020;111:619-621.
- Ozarslan B, Russo T, Argenziano G, et al. Cutaneous findings in neurofibromatosis type 1. Cancers (Basel). 2021;13:463.
- Behra A, Sa DK, Naik R, et al. A rare case of persistent xanthoma disseminatum without any systemic involvement. Indian J Dermatol. 2020;65:239-241.
A 5-year-old boy presented with red-brown spots diffusely spread over the body that were present since birth. There were no subjective symptoms, except for rare instances of flushing, itching, and urtication following hot baths and abrasive scrubs. Dermatologic examination revealed widespread brown polymorphic macules and papules of varying sizes on the forehead, neck, torso, and extremities. Physical examination was otherwise normal.

How do patients perceive aesthetic providers on social media?
DENVER – However, in a recent survey, when asked if an aesthetic medical provider’s social media presence positively affects their desire to see that provider, 48% of patients were neutral or had no opinion, while 41% indicated yes.
Those are key findings from the survey, which aimed to evaluate the social media preferences and perceptions of patients who undergo aesthetic procedures.
“Aesthetic providers have firmly established a presence on social media,” Morgan Murphrey, MD, said at the annual meeting of the American Society for Dermatologic Surgery, where she presented the results. “According to the dermatology literature, somewhere between 25% and 50% of patients are looking up aesthetic providers on social media before they even see them in the clinic. This raises the question: How do patients perceive aesthetic providers that are on social media, and what do they want to see on their professional accounts?”
To find out, Dr. Murphrey, chief dermatology resident at the University of California, Davis, and Sabrina Fabi, MD, a San Diego–based cosmetic dermatologist, used Survey Monkey to randomly survey 2,063 individuals in the United States. They used descriptive statistics to analyze characteristics and responses of the study participants.
Of the 2,063 respondents, 651 (32%) indicated that they undergo medical aesthetic treatments including Botox injections, fillers, or laser procedures. More than half (56%) were women, 25% were 18-30 years old, 64% were 31-60 years old, and 11% were 61 years or older.
The three most common social media platforms they used were Facebook (70%), Instagram (65%), and YouTube (63%), followed by TikTok (45%) and Snapchat (29%). When the researchers stratified respondents by income level, individuals making $200,000 or more per year were statistically more likely to be on Instagram while those making less than $200,000 were more likely to be on Facebook and YouTube.
When asked if their aesthetic medical provider’s social media presence positively impacts their desire to see them as a patient, 48% of respondent were neutral or had no opinion, while 41% answered yes. “Only 2% felt strongly about this if the provider was on a specific social media platform, while 9% of respondents preferred that their provider not be on social media,” Dr. Murphrey added.
When asked if the number of social media followers influences their perception of an aesthetic provider as an expert, 43% of respondents answered no while 57% answered yes. “Once you get to about 20,000 followers, there seems to be somewhat of a law of diminishing returns in the number of followers,” she said. However, 55% indicated that they prefer to see a provider with a social media account that is verified with a blue check mark.
As for content published, 70% of respondents found it very important (36%) or important (34%) that a provider show before-and-after photos on their social media pages, while 67% said that they favor viewing personal content such as posts about the provider’s family and hobbies.
“This study summarizes to us that there is really low risk to creating a social media account; it’s something to think about,” Dr. Murphrey said. “Only 9% of respondents really didn’t want aesthetic providers to be on social media, but when we stratified our results, those individuals were less likely to be on social media themselves.”
Patricia Richey, MD, who practices Mohs surgery and cosmetic dermatology in Washington, D.C., and was asked to comment on the results, characterized the findings as important, “as the role of social media (especially visually based platforms like Instagram) will only continue to grow in our dermatologic and aesthetic practices.” Several studies have displayed a trend of plastic surgeons and other subspecialities outnumbering dermatologists within the aesthetic realm of social media, she noted. “As our patients increasingly seek out health care information and advice through these platforms, studies like Dr. Murphrey’s and Dr. Fabi’s are helpful in allowing us to better understand patient preferences and perspectives, in that we, as dermatologists, may be able to better aid their medical decisions in the future,” she added.
Neither the researchers nor Dr. Richey reported having relevant financial disclosures.
DENVER – However, in a recent survey, when asked if an aesthetic medical provider’s social media presence positively affects their desire to see that provider, 48% of patients were neutral or had no opinion, while 41% indicated yes.
Those are key findings from the survey, which aimed to evaluate the social media preferences and perceptions of patients who undergo aesthetic procedures.
“Aesthetic providers have firmly established a presence on social media,” Morgan Murphrey, MD, said at the annual meeting of the American Society for Dermatologic Surgery, where she presented the results. “According to the dermatology literature, somewhere between 25% and 50% of patients are looking up aesthetic providers on social media before they even see them in the clinic. This raises the question: How do patients perceive aesthetic providers that are on social media, and what do they want to see on their professional accounts?”
To find out, Dr. Murphrey, chief dermatology resident at the University of California, Davis, and Sabrina Fabi, MD, a San Diego–based cosmetic dermatologist, used Survey Monkey to randomly survey 2,063 individuals in the United States. They used descriptive statistics to analyze characteristics and responses of the study participants.
Of the 2,063 respondents, 651 (32%) indicated that they undergo medical aesthetic treatments including Botox injections, fillers, or laser procedures. More than half (56%) were women, 25% were 18-30 years old, 64% were 31-60 years old, and 11% were 61 years or older.
The three most common social media platforms they used were Facebook (70%), Instagram (65%), and YouTube (63%), followed by TikTok (45%) and Snapchat (29%). When the researchers stratified respondents by income level, individuals making $200,000 or more per year were statistically more likely to be on Instagram while those making less than $200,000 were more likely to be on Facebook and YouTube.
When asked if their aesthetic medical provider’s social media presence positively impacts their desire to see them as a patient, 48% of respondent were neutral or had no opinion, while 41% answered yes. “Only 2% felt strongly about this if the provider was on a specific social media platform, while 9% of respondents preferred that their provider not be on social media,” Dr. Murphrey added.
When asked if the number of social media followers influences their perception of an aesthetic provider as an expert, 43% of respondents answered no while 57% answered yes. “Once you get to about 20,000 followers, there seems to be somewhat of a law of diminishing returns in the number of followers,” she said. However, 55% indicated that they prefer to see a provider with a social media account that is verified with a blue check mark.
As for content published, 70% of respondents found it very important (36%) or important (34%) that a provider show before-and-after photos on their social media pages, while 67% said that they favor viewing personal content such as posts about the provider’s family and hobbies.
“This study summarizes to us that there is really low risk to creating a social media account; it’s something to think about,” Dr. Murphrey said. “Only 9% of respondents really didn’t want aesthetic providers to be on social media, but when we stratified our results, those individuals were less likely to be on social media themselves.”
Patricia Richey, MD, who practices Mohs surgery and cosmetic dermatology in Washington, D.C., and was asked to comment on the results, characterized the findings as important, “as the role of social media (especially visually based platforms like Instagram) will only continue to grow in our dermatologic and aesthetic practices.” Several studies have displayed a trend of plastic surgeons and other subspecialities outnumbering dermatologists within the aesthetic realm of social media, she noted. “As our patients increasingly seek out health care information and advice through these platforms, studies like Dr. Murphrey’s and Dr. Fabi’s are helpful in allowing us to better understand patient preferences and perspectives, in that we, as dermatologists, may be able to better aid their medical decisions in the future,” she added.
Neither the researchers nor Dr. Richey reported having relevant financial disclosures.
DENVER – However, in a recent survey, when asked if an aesthetic medical provider’s social media presence positively affects their desire to see that provider, 48% of patients were neutral or had no opinion, while 41% indicated yes.
Those are key findings from the survey, which aimed to evaluate the social media preferences and perceptions of patients who undergo aesthetic procedures.
“Aesthetic providers have firmly established a presence on social media,” Morgan Murphrey, MD, said at the annual meeting of the American Society for Dermatologic Surgery, where she presented the results. “According to the dermatology literature, somewhere between 25% and 50% of patients are looking up aesthetic providers on social media before they even see them in the clinic. This raises the question: How do patients perceive aesthetic providers that are on social media, and what do they want to see on their professional accounts?”
To find out, Dr. Murphrey, chief dermatology resident at the University of California, Davis, and Sabrina Fabi, MD, a San Diego–based cosmetic dermatologist, used Survey Monkey to randomly survey 2,063 individuals in the United States. They used descriptive statistics to analyze characteristics and responses of the study participants.
Of the 2,063 respondents, 651 (32%) indicated that they undergo medical aesthetic treatments including Botox injections, fillers, or laser procedures. More than half (56%) were women, 25% were 18-30 years old, 64% were 31-60 years old, and 11% were 61 years or older.
The three most common social media platforms they used were Facebook (70%), Instagram (65%), and YouTube (63%), followed by TikTok (45%) and Snapchat (29%). When the researchers stratified respondents by income level, individuals making $200,000 or more per year were statistically more likely to be on Instagram while those making less than $200,000 were more likely to be on Facebook and YouTube.
When asked if their aesthetic medical provider’s social media presence positively impacts their desire to see them as a patient, 48% of respondent were neutral or had no opinion, while 41% answered yes. “Only 2% felt strongly about this if the provider was on a specific social media platform, while 9% of respondents preferred that their provider not be on social media,” Dr. Murphrey added.
When asked if the number of social media followers influences their perception of an aesthetic provider as an expert, 43% of respondents answered no while 57% answered yes. “Once you get to about 20,000 followers, there seems to be somewhat of a law of diminishing returns in the number of followers,” she said. However, 55% indicated that they prefer to see a provider with a social media account that is verified with a blue check mark.
As for content published, 70% of respondents found it very important (36%) or important (34%) that a provider show before-and-after photos on their social media pages, while 67% said that they favor viewing personal content such as posts about the provider’s family and hobbies.
“This study summarizes to us that there is really low risk to creating a social media account; it’s something to think about,” Dr. Murphrey said. “Only 9% of respondents really didn’t want aesthetic providers to be on social media, but when we stratified our results, those individuals were less likely to be on social media themselves.”
Patricia Richey, MD, who practices Mohs surgery and cosmetic dermatology in Washington, D.C., and was asked to comment on the results, characterized the findings as important, “as the role of social media (especially visually based platforms like Instagram) will only continue to grow in our dermatologic and aesthetic practices.” Several studies have displayed a trend of plastic surgeons and other subspecialities outnumbering dermatologists within the aesthetic realm of social media, she noted. “As our patients increasingly seek out health care information and advice through these platforms, studies like Dr. Murphrey’s and Dr. Fabi’s are helpful in allowing us to better understand patient preferences and perspectives, in that we, as dermatologists, may be able to better aid their medical decisions in the future,” she added.
Neither the researchers nor Dr. Richey reported having relevant financial disclosures.
AT ASDS 2022
An integrative approach to atopic dermatitis features a long list of options
to probiotics and acupressure – that he encourages patients to try as they use the big guns, or as they attempt to wean off of them or avoid their use altogether.
During a presentation at the annual Integrative Dermatology Symposium, Dr. Lio said that he uses “5 pillars” to guide his integrative treatment plans: The skin barrier, the psyche, the microbiome, inflammation, and itch. “I try to flag approaches that predominantly address the categories that I think need the most help,” he said. “And I tell patients [which pillar or pillars] each treatment is addressing.”
Most commonly, the greatest challenge with AD – and the “single biggest weakness of conventional Western medicine” – lies not with getting patients clear in the first place, but in keeping them clear safely, he said. “I don’t think that using immunosuppressive [medications] is okay for the long-term unless there is no other choice,” said Dr. Lio, who cofounded the Chicago Integrative Eczema Center about 6 years ago and is clinical assistant professor of dermatology and pediatrics at Northwestern University, Chicago. Oftentimes, he said, complementary approaches, including dietary changes, can also serve as supportive adjunctive therapy to biologics and JAK inhibitors.
He has three main criteria, or “filters,” for evaluating these treatments before recommending them to patients: At least some clinical evidence for efficacy (preferably randomized trials but not necessarily), safety, and practicality. The “only way we’re going to move things forward [for AD and other conditions] is to try out less tested treatments ... to open up to them,” Dr. Lio said in an interview after the meeting. And in doing so, he said, dermatologists “can connect with a lot of patients whom naysayers can’t connect with.”
An integrative menu
Dr. Lio individualizes plans, suggesting treatments after “listening to patients’ stories” and considering their age, history, symptoms and skin presentation, and other factors. He said he “goes little by little,” telling a patient, for instance, “I’d love for us to try adding a little hemp oil to your diet.”
If patients aren’t pleased with or are tired of treatments, he said in the interview, “we move on and try something else.”
At the meeting, he described some of the treatments on his menu and the supporting evidence for those treatments:
Oral hempseed oil. A randomized crossover study of 20 adult patients with AD found that daily consumption of 2 tablespoons of hempseed oil decreased skin dryness, itchiness, and use of topical medications compared with consumption of olive oil. “It was statistically significant and seemed clinically meaningful,” likely resulting from the high concentration of polyunsaturated fatty acids in the oil, Dr. Lio said.
Topical vitamin B12. In a phase 3 randomized controlled trial of topical B12 applied twice a day for 8 weeks, patients experienced significant improvements in the extent and severity of AD compared with placebo. Another study in children with AD aged 6 months to 18 years found significant improvement in as early as 2 weeks of use. “It really does help, and is very gentle in babies,” Dr. Lio said.
Black tea compresses. “It’s absolutely my favorite kind of compress,” he said. “It was studied on the face and eyelids but I use it all over the body for adults and kids.” A German study of 22 patients with AD or contact facial dermatitis showed significant improvements in facial dermatitis within the first 3 days of treatment with application of black tea dressings plus an emollient cream, with significant reductions in four disease activity scores (the Facial Eczema Area and Severity Index, visual analog scale for pruritus, Investigator’s Global Assessment score, and Patient’s Self-Assessment Score) that continued through day 6.
Oolong tea. In a 2001 study, after 1 month of drinking oolong tea after each meal, 64% of patients with recalcitrant AD who continued with their regular treatment showed marked to moderate improvements in AD, with a beneficial effect first noticed after 1-2 weeks. At 6 months, 54% still had a good response to treatment. “It’s super cheap and accessible,” Dr. Lio said.
Coconut oil. One of the greatest benefits of coconut oil is on the microbiome and the dysbiosis that can result from a disrupted, or “leaky,” skin barrier – especially overgrowth of Staphylococcus aureus, which “drives AD,” Dr. Lio said. In a study of adults with AD from the Philippines, topically applied coconut oil decreased S. aureus colonization by 95% when applied twice daily for 4 weeks, compared with a 50% decrease in an olive oil control group. Other research has shown coconut oil to be superior to mineral oil as a moisturizer, he said at the meeting.
Acupressure. After a pilot study conducted by Dr. Lio and colleagues showed greater decreases in itch (per the visual analogue scale) in adults with AD who applied an acupressure bead at the LI11 point (near the elbow) for 3 minutes three times a week for 4 weeks, than among those who did not use the acupressure tool, Dr. Lio began trying it with some of his patients. “Now I use it broadly,” he added in the interview. “Kids over 10 can figure out how to use it and teenagers love it [to relief itch]. Some don’t use the beads anymore, they just use their fingertips.”
Advice on diet, vitamin D, and probiotics
AD severity is “powerfully” correlated with IgE food allergy, but Dr. Lio said at the meeting that he currently takes a cautious approach toward strict elimination diets.
There is a growing school of thought among allergists, he said, that positive IgE tests without evidence of acute reactions may not indicate true allergy, but rather sensitivity – and may not warrant food eliminations. And as has been shown with peanuts, there can be a serious downside to elimination, as food avoidance can lead to serious allergy later on, he said.
“More and more people are thinking that if you can tolerate [a food], continue it,” he added in the interview. In the absence of clear reactions, the only way to really know if a food is making eczema worse is to do a double-blind, placebo-controlled food challenge test, he noted.
Patients often come to see him believing that food is the “root cause” of their eczema and feeling frustrated, even anxious, about strict dietary restrictions they’ve implemented. But for many of these patients, the right question “would be to ask, why is my eczema causing my food allergy?” he said at the meeting, referring to the epithelial barrier hypothesis, which posits that skin barrier dysfunction can lead to asthma, allergic rhinitis, and food allergy.
Dr. Lio often recommends the Autoimmune Protocol (AIP) diet, a “close cousin” of the paleo diet for patients with AD, as general guidance to be followed “holistically” and often without the strict eliminations it prescribes. Minimizing processed foods and dairy and grains, which “can be inflammatory in some people,” and focusing on whole, nutrient-rich foods – all in keeping with the AIP principles – should have positive effects on the microbiome, overall health, and likely AD as well, he said.
Across the board, Dr. Lio recommends vitamin D (at nationally recommended dosages) and probiotics. Vitamin D has been shown to significantly help a small percentage of patients with eczema, he said, so he advises patients that it’s worth a trial. “I tell patients that I don’t know how to pick that small group out, so let’s try for a few months and see,” he said. “Inevitably, a percentage of patients come back and say it makes a huge difference.”
Dr. Lio’s understanding and use of probiotics has been “dynamic” over the years. “The “best, most reliable evidence” that probiotics can improve AD symptoms comes with the use of multiple probiotic strains together, he said. Based on limited but growing literature, he ensures that recommended formulations for babies include Lactobacillus rhamnosus, and that formulations for adults include Lactobacillus salivarius.
Dr. Lio works closely with dietitians, hypnotherapists, and psychologists – and will occasionally refer interested patients with AD to a Chinese medicine practitioner who personalizes the use of herbal formulations.
He reported no relevant disclosures.
to probiotics and acupressure – that he encourages patients to try as they use the big guns, or as they attempt to wean off of them or avoid their use altogether.
During a presentation at the annual Integrative Dermatology Symposium, Dr. Lio said that he uses “5 pillars” to guide his integrative treatment plans: The skin barrier, the psyche, the microbiome, inflammation, and itch. “I try to flag approaches that predominantly address the categories that I think need the most help,” he said. “And I tell patients [which pillar or pillars] each treatment is addressing.”
Most commonly, the greatest challenge with AD – and the “single biggest weakness of conventional Western medicine” – lies not with getting patients clear in the first place, but in keeping them clear safely, he said. “I don’t think that using immunosuppressive [medications] is okay for the long-term unless there is no other choice,” said Dr. Lio, who cofounded the Chicago Integrative Eczema Center about 6 years ago and is clinical assistant professor of dermatology and pediatrics at Northwestern University, Chicago. Oftentimes, he said, complementary approaches, including dietary changes, can also serve as supportive adjunctive therapy to biologics and JAK inhibitors.
He has three main criteria, or “filters,” for evaluating these treatments before recommending them to patients: At least some clinical evidence for efficacy (preferably randomized trials but not necessarily), safety, and practicality. The “only way we’re going to move things forward [for AD and other conditions] is to try out less tested treatments ... to open up to them,” Dr. Lio said in an interview after the meeting. And in doing so, he said, dermatologists “can connect with a lot of patients whom naysayers can’t connect with.”
An integrative menu
Dr. Lio individualizes plans, suggesting treatments after “listening to patients’ stories” and considering their age, history, symptoms and skin presentation, and other factors. He said he “goes little by little,” telling a patient, for instance, “I’d love for us to try adding a little hemp oil to your diet.”
If patients aren’t pleased with or are tired of treatments, he said in the interview, “we move on and try something else.”
At the meeting, he described some of the treatments on his menu and the supporting evidence for those treatments:
Oral hempseed oil. A randomized crossover study of 20 adult patients with AD found that daily consumption of 2 tablespoons of hempseed oil decreased skin dryness, itchiness, and use of topical medications compared with consumption of olive oil. “It was statistically significant and seemed clinically meaningful,” likely resulting from the high concentration of polyunsaturated fatty acids in the oil, Dr. Lio said.
Topical vitamin B12. In a phase 3 randomized controlled trial of topical B12 applied twice a day for 8 weeks, patients experienced significant improvements in the extent and severity of AD compared with placebo. Another study in children with AD aged 6 months to 18 years found significant improvement in as early as 2 weeks of use. “It really does help, and is very gentle in babies,” Dr. Lio said.
Black tea compresses. “It’s absolutely my favorite kind of compress,” he said. “It was studied on the face and eyelids but I use it all over the body for adults and kids.” A German study of 22 patients with AD or contact facial dermatitis showed significant improvements in facial dermatitis within the first 3 days of treatment with application of black tea dressings plus an emollient cream, with significant reductions in four disease activity scores (the Facial Eczema Area and Severity Index, visual analog scale for pruritus, Investigator’s Global Assessment score, and Patient’s Self-Assessment Score) that continued through day 6.
Oolong tea. In a 2001 study, after 1 month of drinking oolong tea after each meal, 64% of patients with recalcitrant AD who continued with their regular treatment showed marked to moderate improvements in AD, with a beneficial effect first noticed after 1-2 weeks. At 6 months, 54% still had a good response to treatment. “It’s super cheap and accessible,” Dr. Lio said.
Coconut oil. One of the greatest benefits of coconut oil is on the microbiome and the dysbiosis that can result from a disrupted, or “leaky,” skin barrier – especially overgrowth of Staphylococcus aureus, which “drives AD,” Dr. Lio said. In a study of adults with AD from the Philippines, topically applied coconut oil decreased S. aureus colonization by 95% when applied twice daily for 4 weeks, compared with a 50% decrease in an olive oil control group. Other research has shown coconut oil to be superior to mineral oil as a moisturizer, he said at the meeting.
Acupressure. After a pilot study conducted by Dr. Lio and colleagues showed greater decreases in itch (per the visual analogue scale) in adults with AD who applied an acupressure bead at the LI11 point (near the elbow) for 3 minutes three times a week for 4 weeks, than among those who did not use the acupressure tool, Dr. Lio began trying it with some of his patients. “Now I use it broadly,” he added in the interview. “Kids over 10 can figure out how to use it and teenagers love it [to relief itch]. Some don’t use the beads anymore, they just use their fingertips.”
Advice on diet, vitamin D, and probiotics
AD severity is “powerfully” correlated with IgE food allergy, but Dr. Lio said at the meeting that he currently takes a cautious approach toward strict elimination diets.
There is a growing school of thought among allergists, he said, that positive IgE tests without evidence of acute reactions may not indicate true allergy, but rather sensitivity – and may not warrant food eliminations. And as has been shown with peanuts, there can be a serious downside to elimination, as food avoidance can lead to serious allergy later on, he said.
“More and more people are thinking that if you can tolerate [a food], continue it,” he added in the interview. In the absence of clear reactions, the only way to really know if a food is making eczema worse is to do a double-blind, placebo-controlled food challenge test, he noted.
Patients often come to see him believing that food is the “root cause” of their eczema and feeling frustrated, even anxious, about strict dietary restrictions they’ve implemented. But for many of these patients, the right question “would be to ask, why is my eczema causing my food allergy?” he said at the meeting, referring to the epithelial barrier hypothesis, which posits that skin barrier dysfunction can lead to asthma, allergic rhinitis, and food allergy.
Dr. Lio often recommends the Autoimmune Protocol (AIP) diet, a “close cousin” of the paleo diet for patients with AD, as general guidance to be followed “holistically” and often without the strict eliminations it prescribes. Minimizing processed foods and dairy and grains, which “can be inflammatory in some people,” and focusing on whole, nutrient-rich foods – all in keeping with the AIP principles – should have positive effects on the microbiome, overall health, and likely AD as well, he said.
Across the board, Dr. Lio recommends vitamin D (at nationally recommended dosages) and probiotics. Vitamin D has been shown to significantly help a small percentage of patients with eczema, he said, so he advises patients that it’s worth a trial. “I tell patients that I don’t know how to pick that small group out, so let’s try for a few months and see,” he said. “Inevitably, a percentage of patients come back and say it makes a huge difference.”
Dr. Lio’s understanding and use of probiotics has been “dynamic” over the years. “The “best, most reliable evidence” that probiotics can improve AD symptoms comes with the use of multiple probiotic strains together, he said. Based on limited but growing literature, he ensures that recommended formulations for babies include Lactobacillus rhamnosus, and that formulations for adults include Lactobacillus salivarius.
Dr. Lio works closely with dietitians, hypnotherapists, and psychologists – and will occasionally refer interested patients with AD to a Chinese medicine practitioner who personalizes the use of herbal formulations.
He reported no relevant disclosures.
to probiotics and acupressure – that he encourages patients to try as they use the big guns, or as they attempt to wean off of them or avoid their use altogether.
During a presentation at the annual Integrative Dermatology Symposium, Dr. Lio said that he uses “5 pillars” to guide his integrative treatment plans: The skin barrier, the psyche, the microbiome, inflammation, and itch. “I try to flag approaches that predominantly address the categories that I think need the most help,” he said. “And I tell patients [which pillar or pillars] each treatment is addressing.”
Most commonly, the greatest challenge with AD – and the “single biggest weakness of conventional Western medicine” – lies not with getting patients clear in the first place, but in keeping them clear safely, he said. “I don’t think that using immunosuppressive [medications] is okay for the long-term unless there is no other choice,” said Dr. Lio, who cofounded the Chicago Integrative Eczema Center about 6 years ago and is clinical assistant professor of dermatology and pediatrics at Northwestern University, Chicago. Oftentimes, he said, complementary approaches, including dietary changes, can also serve as supportive adjunctive therapy to biologics and JAK inhibitors.
He has three main criteria, or “filters,” for evaluating these treatments before recommending them to patients: At least some clinical evidence for efficacy (preferably randomized trials but not necessarily), safety, and practicality. The “only way we’re going to move things forward [for AD and other conditions] is to try out less tested treatments ... to open up to them,” Dr. Lio said in an interview after the meeting. And in doing so, he said, dermatologists “can connect with a lot of patients whom naysayers can’t connect with.”
An integrative menu
Dr. Lio individualizes plans, suggesting treatments after “listening to patients’ stories” and considering their age, history, symptoms and skin presentation, and other factors. He said he “goes little by little,” telling a patient, for instance, “I’d love for us to try adding a little hemp oil to your diet.”
If patients aren’t pleased with or are tired of treatments, he said in the interview, “we move on and try something else.”
At the meeting, he described some of the treatments on his menu and the supporting evidence for those treatments:
Oral hempseed oil. A randomized crossover study of 20 adult patients with AD found that daily consumption of 2 tablespoons of hempseed oil decreased skin dryness, itchiness, and use of topical medications compared with consumption of olive oil. “It was statistically significant and seemed clinically meaningful,” likely resulting from the high concentration of polyunsaturated fatty acids in the oil, Dr. Lio said.
Topical vitamin B12. In a phase 3 randomized controlled trial of topical B12 applied twice a day for 8 weeks, patients experienced significant improvements in the extent and severity of AD compared with placebo. Another study in children with AD aged 6 months to 18 years found significant improvement in as early as 2 weeks of use. “It really does help, and is very gentle in babies,” Dr. Lio said.
Black tea compresses. “It’s absolutely my favorite kind of compress,” he said. “It was studied on the face and eyelids but I use it all over the body for adults and kids.” A German study of 22 patients with AD or contact facial dermatitis showed significant improvements in facial dermatitis within the first 3 days of treatment with application of black tea dressings plus an emollient cream, with significant reductions in four disease activity scores (the Facial Eczema Area and Severity Index, visual analog scale for pruritus, Investigator’s Global Assessment score, and Patient’s Self-Assessment Score) that continued through day 6.
Oolong tea. In a 2001 study, after 1 month of drinking oolong tea after each meal, 64% of patients with recalcitrant AD who continued with their regular treatment showed marked to moderate improvements in AD, with a beneficial effect first noticed after 1-2 weeks. At 6 months, 54% still had a good response to treatment. “It’s super cheap and accessible,” Dr. Lio said.
Coconut oil. One of the greatest benefits of coconut oil is on the microbiome and the dysbiosis that can result from a disrupted, or “leaky,” skin barrier – especially overgrowth of Staphylococcus aureus, which “drives AD,” Dr. Lio said. In a study of adults with AD from the Philippines, topically applied coconut oil decreased S. aureus colonization by 95% when applied twice daily for 4 weeks, compared with a 50% decrease in an olive oil control group. Other research has shown coconut oil to be superior to mineral oil as a moisturizer, he said at the meeting.
Acupressure. After a pilot study conducted by Dr. Lio and colleagues showed greater decreases in itch (per the visual analogue scale) in adults with AD who applied an acupressure bead at the LI11 point (near the elbow) for 3 minutes three times a week for 4 weeks, than among those who did not use the acupressure tool, Dr. Lio began trying it with some of his patients. “Now I use it broadly,” he added in the interview. “Kids over 10 can figure out how to use it and teenagers love it [to relief itch]. Some don’t use the beads anymore, they just use their fingertips.”
Advice on diet, vitamin D, and probiotics
AD severity is “powerfully” correlated with IgE food allergy, but Dr. Lio said at the meeting that he currently takes a cautious approach toward strict elimination diets.
There is a growing school of thought among allergists, he said, that positive IgE tests without evidence of acute reactions may not indicate true allergy, but rather sensitivity – and may not warrant food eliminations. And as has been shown with peanuts, there can be a serious downside to elimination, as food avoidance can lead to serious allergy later on, he said.
“More and more people are thinking that if you can tolerate [a food], continue it,” he added in the interview. In the absence of clear reactions, the only way to really know if a food is making eczema worse is to do a double-blind, placebo-controlled food challenge test, he noted.
Patients often come to see him believing that food is the “root cause” of their eczema and feeling frustrated, even anxious, about strict dietary restrictions they’ve implemented. But for many of these patients, the right question “would be to ask, why is my eczema causing my food allergy?” he said at the meeting, referring to the epithelial barrier hypothesis, which posits that skin barrier dysfunction can lead to asthma, allergic rhinitis, and food allergy.
Dr. Lio often recommends the Autoimmune Protocol (AIP) diet, a “close cousin” of the paleo diet for patients with AD, as general guidance to be followed “holistically” and often without the strict eliminations it prescribes. Minimizing processed foods and dairy and grains, which “can be inflammatory in some people,” and focusing on whole, nutrient-rich foods – all in keeping with the AIP principles – should have positive effects on the microbiome, overall health, and likely AD as well, he said.
Across the board, Dr. Lio recommends vitamin D (at nationally recommended dosages) and probiotics. Vitamin D has been shown to significantly help a small percentage of patients with eczema, he said, so he advises patients that it’s worth a trial. “I tell patients that I don’t know how to pick that small group out, so let’s try for a few months and see,” he said. “Inevitably, a percentage of patients come back and say it makes a huge difference.”
Dr. Lio’s understanding and use of probiotics has been “dynamic” over the years. “The “best, most reliable evidence” that probiotics can improve AD symptoms comes with the use of multiple probiotic strains together, he said. Based on limited but growing literature, he ensures that recommended formulations for babies include Lactobacillus rhamnosus, and that formulations for adults include Lactobacillus salivarius.
Dr. Lio works closely with dietitians, hypnotherapists, and psychologists – and will occasionally refer interested patients with AD to a Chinese medicine practitioner who personalizes the use of herbal formulations.
He reported no relevant disclosures.
FROM IDS 2022
Commentary: Complementary treatments for AD, November 2022
Still, some patients seek alternative or adjunctive treatment approaches, owing to a desire to identify the root cause of disease, their aversion toward Western medicine, or fear of adverse events. Yepes-Nuñez and colleagues performed a systematic review and meta-analysis including 23 studies of benefits and harms of allergen immunotherapy for AD. I had the privilege of participating in this study and can testify to the astronomical amount of work that went into comprehensively identifying all of the relevant studies and synthesizing the data. We found that adjunctive subcutaneous or sublingual allergen immunotherapy, particularly for house dust mites, led to modest but generally delayed improvements of AD severity, itch, and quality of life, and less definitive effects on sleep disturbance and AD flares. Overall, both were well tolerated, though subcutaneous immunotherapy was associated with more adverse events than sublingual immunotherapy. Allergen immunotherapy requires a significant investment of time by patients and was only modestly effective. Nevertheless, it may be a reasonable approach to consider in select patients with AD.
Benjamin Franklin famously stated that "an ounce of prevention is worth a pound of cure." Likewise, while successful treatment of AD is great, how can we advise patients and caregivers of children who are at high risk for AD? To answer this question, Voigt and Lele performed a systematic review and meta-analysis of 11 randomized controlled trials examining the efficacy of Lactobacillus rhamnosus at preventing AD in children when taken by mothers during pregnancy. They found that L. rhamnosus significantly reduced the risk of developing AD within 2 years, marginally significantly reduced risk at 4-5 years, and significantly reduced risk at 6-7 years, but no significant risk differences were observed at 10-11 years. The authors concluded that use of L. rhamnosus with or without other probiotics during pregnancy reduces the incidence of childhood AD at least up to age 7 years.
Wang and colleagues conducted an observational study of the relationship of home environment exposures with atopic disease, including AD, in 17,881 offspring from Iceland, Norway, Sweden, Denmark, and Estonia who had undergone two follow-up investigations every 10 years. They found that AD was associated with parent-reported visible mold and dampness/mold at home, living in an apartment, and living in newer buildings. Avoidance of these environmental exposures could possibly decrease the risk of developing AD, although future confirmatory studies are needed.
For each of these treatment/prevention approaches, the magnitude of benefit is not very large. Thus, these approaches do not replace our armamentarium of treatments and avoidance strategies for AD. Rather, they can be used complementarily as low-risk add-on interventions with a potential upside.
Still, some patients seek alternative or adjunctive treatment approaches, owing to a desire to identify the root cause of disease, their aversion toward Western medicine, or fear of adverse events. Yepes-Nuñez and colleagues performed a systematic review and meta-analysis including 23 studies of benefits and harms of allergen immunotherapy for AD. I had the privilege of participating in this study and can testify to the astronomical amount of work that went into comprehensively identifying all of the relevant studies and synthesizing the data. We found that adjunctive subcutaneous or sublingual allergen immunotherapy, particularly for house dust mites, led to modest but generally delayed improvements of AD severity, itch, and quality of life, and less definitive effects on sleep disturbance and AD flares. Overall, both were well tolerated, though subcutaneous immunotherapy was associated with more adverse events than sublingual immunotherapy. Allergen immunotherapy requires a significant investment of time by patients and was only modestly effective. Nevertheless, it may be a reasonable approach to consider in select patients with AD.
Benjamin Franklin famously stated that "an ounce of prevention is worth a pound of cure." Likewise, while successful treatment of AD is great, how can we advise patients and caregivers of children who are at high risk for AD? To answer this question, Voigt and Lele performed a systematic review and meta-analysis of 11 randomized controlled trials examining the efficacy of Lactobacillus rhamnosus at preventing AD in children when taken by mothers during pregnancy. They found that L. rhamnosus significantly reduced the risk of developing AD within 2 years, marginally significantly reduced risk at 4-5 years, and significantly reduced risk at 6-7 years, but no significant risk differences were observed at 10-11 years. The authors concluded that use of L. rhamnosus with or without other probiotics during pregnancy reduces the incidence of childhood AD at least up to age 7 years.
Wang and colleagues conducted an observational study of the relationship of home environment exposures with atopic disease, including AD, in 17,881 offspring from Iceland, Norway, Sweden, Denmark, and Estonia who had undergone two follow-up investigations every 10 years. They found that AD was associated with parent-reported visible mold and dampness/mold at home, living in an apartment, and living in newer buildings. Avoidance of these environmental exposures could possibly decrease the risk of developing AD, although future confirmatory studies are needed.
For each of these treatment/prevention approaches, the magnitude of benefit is not very large. Thus, these approaches do not replace our armamentarium of treatments and avoidance strategies for AD. Rather, they can be used complementarily as low-risk add-on interventions with a potential upside.
Still, some patients seek alternative or adjunctive treatment approaches, owing to a desire to identify the root cause of disease, their aversion toward Western medicine, or fear of adverse events. Yepes-Nuñez and colleagues performed a systematic review and meta-analysis including 23 studies of benefits and harms of allergen immunotherapy for AD. I had the privilege of participating in this study and can testify to the astronomical amount of work that went into comprehensively identifying all of the relevant studies and synthesizing the data. We found that adjunctive subcutaneous or sublingual allergen immunotherapy, particularly for house dust mites, led to modest but generally delayed improvements of AD severity, itch, and quality of life, and less definitive effects on sleep disturbance and AD flares. Overall, both were well tolerated, though subcutaneous immunotherapy was associated with more adverse events than sublingual immunotherapy. Allergen immunotherapy requires a significant investment of time by patients and was only modestly effective. Nevertheless, it may be a reasonable approach to consider in select patients with AD.
Benjamin Franklin famously stated that "an ounce of prevention is worth a pound of cure." Likewise, while successful treatment of AD is great, how can we advise patients and caregivers of children who are at high risk for AD? To answer this question, Voigt and Lele performed a systematic review and meta-analysis of 11 randomized controlled trials examining the efficacy of Lactobacillus rhamnosus at preventing AD in children when taken by mothers during pregnancy. They found that L. rhamnosus significantly reduced the risk of developing AD within 2 years, marginally significantly reduced risk at 4-5 years, and significantly reduced risk at 6-7 years, but no significant risk differences were observed at 10-11 years. The authors concluded that use of L. rhamnosus with or without other probiotics during pregnancy reduces the incidence of childhood AD at least up to age 7 years.
Wang and colleagues conducted an observational study of the relationship of home environment exposures with atopic disease, including AD, in 17,881 offspring from Iceland, Norway, Sweden, Denmark, and Estonia who had undergone two follow-up investigations every 10 years. They found that AD was associated with parent-reported visible mold and dampness/mold at home, living in an apartment, and living in newer buildings. Avoidance of these environmental exposures could possibly decrease the risk of developing AD, although future confirmatory studies are needed.
For each of these treatment/prevention approaches, the magnitude of benefit is not very large. Thus, these approaches do not replace our armamentarium of treatments and avoidance strategies for AD. Rather, they can be used complementarily as low-risk add-on interventions with a potential upside.









