User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


ACE inhibitors and severe COVID-19: Protective in older patients?
.
In addition, a new meta-analysis of all the available data on the use of ACE inhibitors and angiotensin-receptor blockers (ARBs) in COVID-19–infected patients has concluded that these drugs are not associated with more severe disease and do not increase susceptibility to infection.
The observational study, which was published on the MedRxiv preprint server on May 19 and has not yet been peer reviewed, was conducted by the health insurance company United Heath Group and by Yale University, New Haven, Conn.
The investigators analyzed data from 10,000 patients from across the United States who had tested positive for COVID-19, who were enrolled in Medicare Advantage insurance plans or were commercially insured, and who had received a prescription for one or more antihypertensive medications.
Results showed that the use of ACE inhibitors was associated with an almost 40% lower risk for COVID-19 hospitalization for older people enrolled in Medicare Advantage plans. No such benefit was seen in the younger commercially insured patients or in either group with ARBs.
At a telephone media briefing on the study, senior investigator Harlan M. Krumholz, MD, said: “We don’t believe this is enough info to change practice, but we do think this is an interesting and intriguing result.
“These findings merit a clinical trial to formally test whether ACE inhibitors – which are cheap, widely available, and well-tolerated drugs – can reduce hospitalization of patients infected with COVID-19,” added Dr. Krumholz, professor of medicine at Yale and director of the Yale New Haven Hospital Center for Outcomes Research.
A pragmatic clinical trial is now being planned. In this trial, 10,000 older people who test positive for COVID-19 will be randomly assigned to receive either a low dose of an ACE inhibitor or placebo. It is hoped that recruitment for the trial will begin in June of 2020. It is open to all eligible Americans who are older than 50 years, who test negative for COVID-19, and who are not taking medications for hypertension. Prospective patients can sign up at a dedicated website.
The randomized trial, also conducted by United Health Group and Yale, is said to be “one of the first virtual COVID-19 clinical trials to be launched at scale.”
For the observational study, the researchers identified 2,263 people who were receiving medication for hypertension and who tested positive for COVID-19. Of these, approximately two-thirds were older, Medicare Advantage enrollees; one-third were younger, commercially insured individuals.
In a propensity score–matched analysis, the investigators matched 441 patients who were taking ACE inhibitors to 441 patients who were taking other antihypertensive agents; and 412 patients who were receiving an ARB to 412 patients who were receiving other antihypertensive agents.
Results showed that during a median of 30 days after testing positive, 12.7% of the cohort were hospitalized for COVID-19. In propensity score–matched analyses, neither ACE inhibitors (hazard ratio [HR], 0.77; P = .18) nor ARBs (HR, 0.88; P =.48) were significantly associated with risk for hospitalization.
However, in analyses stratified by the insurance group, ACE inhibitors (but not ARBs) were associated with a significant lower risk for hospitalization among the Medicare group (HR, 0.61; P = .02) but not among the commercially insured group (HR, 2.14; P = .12).
A second study examined outcomes of 7,933 individuals with hypertension who were hospitalized with COVID-19 (92% of these patients were Medicare Advantage enrollees). Of these, 14.2% died, 59.5% survived to discharge, and 26.3% underwent ongoing hospitalization. In propensity score–matched analyses, use of neither an ACE inhibitor (HR, 0.97; P = .74) nor an ARB (HR, 1.15; P = .15) was associated with risk of in-hospital mortality.
The researchers said their findings are consistent with prior evidence from randomized clinical trials suggesting a reduced risk for pneumonia with ACE inhibitors that is not observed with ARBs.
They also cited some preclinical evidence that they said suggests a possible protective role for ACE inhibitors in COVID-19: that ACE inhibitors, but not ARBs, are associated with the upregulation of ACE2 receptors, which modulate the local interactions of the renin-angiotensin-aldosterone system in the lung tissue.
“The presence of ACE2 receptors, therefore, exerts a protective effect against the development of acute lung injury in infections with SARS coronaviruses, which lead to dysregulation of these mechanisms and endothelial damage,” they added. “Further, our observations do not support theoretical concerns of adverse outcomes due to enhanced virulence of SARS coronaviruses due to overexpression of ACE2 receptors in cell cultures – an indirect binding site for these viruses.”
The authors also noted that their findings have “important implications” for four ongoing randomized trials of ACE inhibitors/ARBs in COVID-19, “as none of them align with the observations of our study.”
They pointed out that of the four ongoing trials, three are testing the use of ACE inhibitors or ARBs in the treatment of hospitalized COVID-19 patients, and one is testing the use of a 10-day course of ARBs after a positive SARS-CoV-2 test to prevent hospitalization.
Experts cautious
However, two cardiovascular experts who were asked to comment on this latest study were not overly optimistic about the data.
Michael A. Weber, MD, professor of medicine at the State University of New York, Brooklyn, said: “This report adds to the growing number of observational studies that show varying effects of ACE inhibitors and ARBs in increasing or decreasing hospitalizations for COVID-19 and the likelihood of in-hospital mortality. Overall, this new report differs from others in the remarkable effects of insurance coverage: In particular, for ACE inhibitors, there was a 40% reduction in fatal events in Medicare patients but a twofold increase in patients using commercial insurance – albeit the test for heterogeneity when comparing the two groups did not quite reach statistical significance.
“In essence, these authors are saying that ACE inhibitors are highly protective in patients aged 65 or older but bordering on harmful in patients aged below 65. I agree that it’s worthwhile to check this finding in a prospective trial ... but this hypothesis does seem to be a reach.”
Dr. Weber noted that both ACE inhibitors and ARBs increase the level of the ACE2 enzyme to which the COVID-19 virus binds in the lungs.
“The ACE inhibitors do so by inhibiting the enzyme’s action and thus stimulate further enzyme production; the ARBs block the effects of angiotensin II, which results in high angiotensin II levels that also upregulate ACE2 production,” he said. “Perhaps the ACE inhibitors, by binding to the ACE enzyme, can in some way interfere with the enzyme’s uptake of the COVID virus and thus provide some measure of clinical protection. This is possible, but why would this effect be apparent only in older people?”
John McMurray, MD, professor of medical cardiology at the University of Glasgow, Scotland, added: “This looks like a subgroup of a subgroup type analysis based on small numbers of events – I think there were only 77 hospitalizations among the 722 patients treated with an ACE inhibitor, and the Medicare Advantage subgroup was only 581 of those 722 patients.
“The hazard ratio had wide 95% CI [confidence interval] and a modest P value,” Dr. McMurray added. “So yes, interesting and hypothesis-generating, but not definitive.”
New meta-analysis
The new meta-analysis of all data so far available on ACE inhibitor and ARB use for patients with COVID-19 was published online in Annals of Internal Medicine on May 15.
The analysis is a living, systematic review with ongoing literature surveillance and critical appraisal, which will be updated as new data become available. It included 14 observational studies.
The authors, led by Katherine M. Mackey, MD, VA Portland Health Care System, Oregon, concluded: “High-certainty evidence suggests that ACE-inhibitor or ARB use is not associated with more severe COVID-19 disease, and moderate certainty evidence suggested no association between use of these medications and positive SARS-CoV-2 test results among symptomatic patients. Whether these medications increase the risk for mild or asymptomatic disease or are beneficial in COVID-19 treatment remains uncertain.”
In an accompanying editorial, William G. Kussmaul III, MD, Drexel University, Philadelphia, said that initial fears that these drugs may be harmful for patients with COVID-19 now seem to have been unfounded.
“We now have reasonable reassurance that drugs that alter the renin-angiotensin system do not pose substantial threats as either COVID-19 risk factors or severity multipliers,” he wrote.
A version of this article originally appeared on Medscape.com.
.
In addition, a new meta-analysis of all the available data on the use of ACE inhibitors and angiotensin-receptor blockers (ARBs) in COVID-19–infected patients has concluded that these drugs are not associated with more severe disease and do not increase susceptibility to infection.
The observational study, which was published on the MedRxiv preprint server on May 19 and has not yet been peer reviewed, was conducted by the health insurance company United Heath Group and by Yale University, New Haven, Conn.
The investigators analyzed data from 10,000 patients from across the United States who had tested positive for COVID-19, who were enrolled in Medicare Advantage insurance plans or were commercially insured, and who had received a prescription for one or more antihypertensive medications.
Results showed that the use of ACE inhibitors was associated with an almost 40% lower risk for COVID-19 hospitalization for older people enrolled in Medicare Advantage plans. No such benefit was seen in the younger commercially insured patients or in either group with ARBs.
At a telephone media briefing on the study, senior investigator Harlan M. Krumholz, MD, said: “We don’t believe this is enough info to change practice, but we do think this is an interesting and intriguing result.
“These findings merit a clinical trial to formally test whether ACE inhibitors – which are cheap, widely available, and well-tolerated drugs – can reduce hospitalization of patients infected with COVID-19,” added Dr. Krumholz, professor of medicine at Yale and director of the Yale New Haven Hospital Center for Outcomes Research.
A pragmatic clinical trial is now being planned. In this trial, 10,000 older people who test positive for COVID-19 will be randomly assigned to receive either a low dose of an ACE inhibitor or placebo. It is hoped that recruitment for the trial will begin in June of 2020. It is open to all eligible Americans who are older than 50 years, who test negative for COVID-19, and who are not taking medications for hypertension. Prospective patients can sign up at a dedicated website.
The randomized trial, also conducted by United Health Group and Yale, is said to be “one of the first virtual COVID-19 clinical trials to be launched at scale.”
For the observational study, the researchers identified 2,263 people who were receiving medication for hypertension and who tested positive for COVID-19. Of these, approximately two-thirds were older, Medicare Advantage enrollees; one-third were younger, commercially insured individuals.
In a propensity score–matched analysis, the investigators matched 441 patients who were taking ACE inhibitors to 441 patients who were taking other antihypertensive agents; and 412 patients who were receiving an ARB to 412 patients who were receiving other antihypertensive agents.
Results showed that during a median of 30 days after testing positive, 12.7% of the cohort were hospitalized for COVID-19. In propensity score–matched analyses, neither ACE inhibitors (hazard ratio [HR], 0.77; P = .18) nor ARBs (HR, 0.88; P =.48) were significantly associated with risk for hospitalization.
However, in analyses stratified by the insurance group, ACE inhibitors (but not ARBs) were associated with a significant lower risk for hospitalization among the Medicare group (HR, 0.61; P = .02) but not among the commercially insured group (HR, 2.14; P = .12).
A second study examined outcomes of 7,933 individuals with hypertension who were hospitalized with COVID-19 (92% of these patients were Medicare Advantage enrollees). Of these, 14.2% died, 59.5% survived to discharge, and 26.3% underwent ongoing hospitalization. In propensity score–matched analyses, use of neither an ACE inhibitor (HR, 0.97; P = .74) nor an ARB (HR, 1.15; P = .15) was associated with risk of in-hospital mortality.
The researchers said their findings are consistent with prior evidence from randomized clinical trials suggesting a reduced risk for pneumonia with ACE inhibitors that is not observed with ARBs.
They also cited some preclinical evidence that they said suggests a possible protective role for ACE inhibitors in COVID-19: that ACE inhibitors, but not ARBs, are associated with the upregulation of ACE2 receptors, which modulate the local interactions of the renin-angiotensin-aldosterone system in the lung tissue.
“The presence of ACE2 receptors, therefore, exerts a protective effect against the development of acute lung injury in infections with SARS coronaviruses, which lead to dysregulation of these mechanisms and endothelial damage,” they added. “Further, our observations do not support theoretical concerns of adverse outcomes due to enhanced virulence of SARS coronaviruses due to overexpression of ACE2 receptors in cell cultures – an indirect binding site for these viruses.”
The authors also noted that their findings have “important implications” for four ongoing randomized trials of ACE inhibitors/ARBs in COVID-19, “as none of them align with the observations of our study.”
They pointed out that of the four ongoing trials, three are testing the use of ACE inhibitors or ARBs in the treatment of hospitalized COVID-19 patients, and one is testing the use of a 10-day course of ARBs after a positive SARS-CoV-2 test to prevent hospitalization.
Experts cautious
However, two cardiovascular experts who were asked to comment on this latest study were not overly optimistic about the data.
Michael A. Weber, MD, professor of medicine at the State University of New York, Brooklyn, said: “This report adds to the growing number of observational studies that show varying effects of ACE inhibitors and ARBs in increasing or decreasing hospitalizations for COVID-19 and the likelihood of in-hospital mortality. Overall, this new report differs from others in the remarkable effects of insurance coverage: In particular, for ACE inhibitors, there was a 40% reduction in fatal events in Medicare patients but a twofold increase in patients using commercial insurance – albeit the test for heterogeneity when comparing the two groups did not quite reach statistical significance.
“In essence, these authors are saying that ACE inhibitors are highly protective in patients aged 65 or older but bordering on harmful in patients aged below 65. I agree that it’s worthwhile to check this finding in a prospective trial ... but this hypothesis does seem to be a reach.”
Dr. Weber noted that both ACE inhibitors and ARBs increase the level of the ACE2 enzyme to which the COVID-19 virus binds in the lungs.
“The ACE inhibitors do so by inhibiting the enzyme’s action and thus stimulate further enzyme production; the ARBs block the effects of angiotensin II, which results in high angiotensin II levels that also upregulate ACE2 production,” he said. “Perhaps the ACE inhibitors, by binding to the ACE enzyme, can in some way interfere with the enzyme’s uptake of the COVID virus and thus provide some measure of clinical protection. This is possible, but why would this effect be apparent only in older people?”
John McMurray, MD, professor of medical cardiology at the University of Glasgow, Scotland, added: “This looks like a subgroup of a subgroup type analysis based on small numbers of events – I think there were only 77 hospitalizations among the 722 patients treated with an ACE inhibitor, and the Medicare Advantage subgroup was only 581 of those 722 patients.
“The hazard ratio had wide 95% CI [confidence interval] and a modest P value,” Dr. McMurray added. “So yes, interesting and hypothesis-generating, but not definitive.”
New meta-analysis
The new meta-analysis of all data so far available on ACE inhibitor and ARB use for patients with COVID-19 was published online in Annals of Internal Medicine on May 15.
The analysis is a living, systematic review with ongoing literature surveillance and critical appraisal, which will be updated as new data become available. It included 14 observational studies.
The authors, led by Katherine M. Mackey, MD, VA Portland Health Care System, Oregon, concluded: “High-certainty evidence suggests that ACE-inhibitor or ARB use is not associated with more severe COVID-19 disease, and moderate certainty evidence suggested no association between use of these medications and positive SARS-CoV-2 test results among symptomatic patients. Whether these medications increase the risk for mild or asymptomatic disease or are beneficial in COVID-19 treatment remains uncertain.”
In an accompanying editorial, William G. Kussmaul III, MD, Drexel University, Philadelphia, said that initial fears that these drugs may be harmful for patients with COVID-19 now seem to have been unfounded.
“We now have reasonable reassurance that drugs that alter the renin-angiotensin system do not pose substantial threats as either COVID-19 risk factors or severity multipliers,” he wrote.
A version of this article originally appeared on Medscape.com.
.
In addition, a new meta-analysis of all the available data on the use of ACE inhibitors and angiotensin-receptor blockers (ARBs) in COVID-19–infected patients has concluded that these drugs are not associated with more severe disease and do not increase susceptibility to infection.
The observational study, which was published on the MedRxiv preprint server on May 19 and has not yet been peer reviewed, was conducted by the health insurance company United Heath Group and by Yale University, New Haven, Conn.
The investigators analyzed data from 10,000 patients from across the United States who had tested positive for COVID-19, who were enrolled in Medicare Advantage insurance plans or were commercially insured, and who had received a prescription for one or more antihypertensive medications.
Results showed that the use of ACE inhibitors was associated with an almost 40% lower risk for COVID-19 hospitalization for older people enrolled in Medicare Advantage plans. No such benefit was seen in the younger commercially insured patients or in either group with ARBs.
At a telephone media briefing on the study, senior investigator Harlan M. Krumholz, MD, said: “We don’t believe this is enough info to change practice, but we do think this is an interesting and intriguing result.
“These findings merit a clinical trial to formally test whether ACE inhibitors – which are cheap, widely available, and well-tolerated drugs – can reduce hospitalization of patients infected with COVID-19,” added Dr. Krumholz, professor of medicine at Yale and director of the Yale New Haven Hospital Center for Outcomes Research.
A pragmatic clinical trial is now being planned. In this trial, 10,000 older people who test positive for COVID-19 will be randomly assigned to receive either a low dose of an ACE inhibitor or placebo. It is hoped that recruitment for the trial will begin in June of 2020. It is open to all eligible Americans who are older than 50 years, who test negative for COVID-19, and who are not taking medications for hypertension. Prospective patients can sign up at a dedicated website.
The randomized trial, also conducted by United Health Group and Yale, is said to be “one of the first virtual COVID-19 clinical trials to be launched at scale.”
For the observational study, the researchers identified 2,263 people who were receiving medication for hypertension and who tested positive for COVID-19. Of these, approximately two-thirds were older, Medicare Advantage enrollees; one-third were younger, commercially insured individuals.
In a propensity score–matched analysis, the investigators matched 441 patients who were taking ACE inhibitors to 441 patients who were taking other antihypertensive agents; and 412 patients who were receiving an ARB to 412 patients who were receiving other antihypertensive agents.
Results showed that during a median of 30 days after testing positive, 12.7% of the cohort were hospitalized for COVID-19. In propensity score–matched analyses, neither ACE inhibitors (hazard ratio [HR], 0.77; P = .18) nor ARBs (HR, 0.88; P =.48) were significantly associated with risk for hospitalization.
However, in analyses stratified by the insurance group, ACE inhibitors (but not ARBs) were associated with a significant lower risk for hospitalization among the Medicare group (HR, 0.61; P = .02) but not among the commercially insured group (HR, 2.14; P = .12).
A second study examined outcomes of 7,933 individuals with hypertension who were hospitalized with COVID-19 (92% of these patients were Medicare Advantage enrollees). Of these, 14.2% died, 59.5% survived to discharge, and 26.3% underwent ongoing hospitalization. In propensity score–matched analyses, use of neither an ACE inhibitor (HR, 0.97; P = .74) nor an ARB (HR, 1.15; P = .15) was associated with risk of in-hospital mortality.
The researchers said their findings are consistent with prior evidence from randomized clinical trials suggesting a reduced risk for pneumonia with ACE inhibitors that is not observed with ARBs.
They also cited some preclinical evidence that they said suggests a possible protective role for ACE inhibitors in COVID-19: that ACE inhibitors, but not ARBs, are associated with the upregulation of ACE2 receptors, which modulate the local interactions of the renin-angiotensin-aldosterone system in the lung tissue.
“The presence of ACE2 receptors, therefore, exerts a protective effect against the development of acute lung injury in infections with SARS coronaviruses, which lead to dysregulation of these mechanisms and endothelial damage,” they added. “Further, our observations do not support theoretical concerns of adverse outcomes due to enhanced virulence of SARS coronaviruses due to overexpression of ACE2 receptors in cell cultures – an indirect binding site for these viruses.”
The authors also noted that their findings have “important implications” for four ongoing randomized trials of ACE inhibitors/ARBs in COVID-19, “as none of them align with the observations of our study.”
They pointed out that of the four ongoing trials, three are testing the use of ACE inhibitors or ARBs in the treatment of hospitalized COVID-19 patients, and one is testing the use of a 10-day course of ARBs after a positive SARS-CoV-2 test to prevent hospitalization.
Experts cautious
However, two cardiovascular experts who were asked to comment on this latest study were not overly optimistic about the data.
Michael A. Weber, MD, professor of medicine at the State University of New York, Brooklyn, said: “This report adds to the growing number of observational studies that show varying effects of ACE inhibitors and ARBs in increasing or decreasing hospitalizations for COVID-19 and the likelihood of in-hospital mortality. Overall, this new report differs from others in the remarkable effects of insurance coverage: In particular, for ACE inhibitors, there was a 40% reduction in fatal events in Medicare patients but a twofold increase in patients using commercial insurance – albeit the test for heterogeneity when comparing the two groups did not quite reach statistical significance.
“In essence, these authors are saying that ACE inhibitors are highly protective in patients aged 65 or older but bordering on harmful in patients aged below 65. I agree that it’s worthwhile to check this finding in a prospective trial ... but this hypothesis does seem to be a reach.”
Dr. Weber noted that both ACE inhibitors and ARBs increase the level of the ACE2 enzyme to which the COVID-19 virus binds in the lungs.
“The ACE inhibitors do so by inhibiting the enzyme’s action and thus stimulate further enzyme production; the ARBs block the effects of angiotensin II, which results in high angiotensin II levels that also upregulate ACE2 production,” he said. “Perhaps the ACE inhibitors, by binding to the ACE enzyme, can in some way interfere with the enzyme’s uptake of the COVID virus and thus provide some measure of clinical protection. This is possible, but why would this effect be apparent only in older people?”
John McMurray, MD, professor of medical cardiology at the University of Glasgow, Scotland, added: “This looks like a subgroup of a subgroup type analysis based on small numbers of events – I think there were only 77 hospitalizations among the 722 patients treated with an ACE inhibitor, and the Medicare Advantage subgroup was only 581 of those 722 patients.
“The hazard ratio had wide 95% CI [confidence interval] and a modest P value,” Dr. McMurray added. “So yes, interesting and hypothesis-generating, but not definitive.”
New meta-analysis
The new meta-analysis of all data so far available on ACE inhibitor and ARB use for patients with COVID-19 was published online in Annals of Internal Medicine on May 15.
The analysis is a living, systematic review with ongoing literature surveillance and critical appraisal, which will be updated as new data become available. It included 14 observational studies.
The authors, led by Katherine M. Mackey, MD, VA Portland Health Care System, Oregon, concluded: “High-certainty evidence suggests that ACE-inhibitor or ARB use is not associated with more severe COVID-19 disease, and moderate certainty evidence suggested no association between use of these medications and positive SARS-CoV-2 test results among symptomatic patients. Whether these medications increase the risk for mild or asymptomatic disease or are beneficial in COVID-19 treatment remains uncertain.”
In an accompanying editorial, William G. Kussmaul III, MD, Drexel University, Philadelphia, said that initial fears that these drugs may be harmful for patients with COVID-19 now seem to have been unfounded.
“We now have reasonable reassurance that drugs that alter the renin-angiotensin system do not pose substantial threats as either COVID-19 risk factors or severity multipliers,” he wrote.
A version of this article originally appeared on Medscape.com.
As visits for AMI drop during pandemic, deaths rise
The drastic drop in admissions for acute myocardial infarctions (AMI) during the COVID-19 pandemic in Italy has seen a parallel rise in MI fatality rates in those who do present to hospitals, according to a new report. This gives credence to suggestions that people have avoided hospitals during the pandemic despite life-threatening emergencies.
Salvatore De Rosa, MD, PhD, and colleagues reported their results in the European Heart Journal.
“These data return a frightening picture of about half of AMI patients not reaching out to the hospital at all, which will probably significantly increase mortality for AMI and bring with it a number of patients with post-MI heart failure, despite the fact that acute coronary syndrome management protocols were promptly implemented,” Dr. De Rosa, of Magna Graecia University in Catanzaro, Italy, and associates wrote.
Hospitalizations down
The study counted AMIs at 54 hospital coronary care units nationwide for the week of March 12-19, 2020, at the height of the coronavirus outbreak in northern Italy, and compared that with an equivalent week in 2019. The researchers reported 319 AMIs during the week in 2020, compared with 618 in the equivalent 2019 week, a 48% reduction (P < .001). Although the outbreak was worst in northern Italy, the decline in admissions occurred throughout the country.
An analysis of subtype determined the decline in the incidence of ST-segment elevation MI lagged significantly behind that of non-STEMI. STEMI declined from 268 in 2019 to 197 in 2020, a 27% reduction, while hospitalizations for non-STEMI went from 350 to 122, a 65% reduction.
The researchers also found substantial reductions in hospitalizations for heart failure, by 47%, and atrial fibrillation, by 53%. Incidentally, the mean age of atrial fibrillation patients was considerably younger in 2020: 64.6 vs. 70 years.
Death, complications up
AMI patients who managed to get to the hospital during the pandemic also had worse outcomes. Mortality for STEMI cases more than tripled, to 14% during the outbreak, compared with 4% in 2019 (P < .001) and complication rates increased by 80% to 19% (P = .025). Twenty-one STEMI patients were positive for COVID-19 and more than a quarter (29%) died, which was more than two and a half times the 12% death rate in non–COVID-19 STEMI patients.
Analysis of the STEMI group also found that the care gap for women with heart disease worsened significantly during the pandemic, as they comprised 20.3% of cases this year, compared with 25.4% before the pandemic. Also, the reduction in admissions for STEMI during the pandemic was statistically significant at 41% for women, but not for men at 18%.
Non-STEMI patients fared better overall than STEMI patients, but their outcomes also worsened during the pandemic. Non-STEMI patients were significantly less likely to have percutaneous coronary intervention during the pandemic than previously; the rate declined by 13%, from 77% to 66%. The non-STEMI mortality rate nearly doubled, although not statistically significantly, from 1.7% to 3.3%, whereas complication rates actually more than doubled, from 5.1% to 10.7%, a significant difference. Twelve (9.8%) of the non-STEMI patients were COVID-19 positive, but none died.
Trend extends beyond borders
Dr. De Rosa and colleagues noted that their findings are in line with studies that reported similar declines for STEMI interventions in the United States and Spain during the pandemic (J Am Coll Cardiol. 2020. doi: 10.1016/j.jacc.2020.04.011; REC Interv Cardiol. 2020. doi: 10.24875/RECIC.M20000120).
Additionally, a group at Kaiser Permanente in Northern California also reported a 50% decline in the incidence of AMI hospitalizations during the pandemic (N Engl J Med. 2020 May 19. doi: 10.1056/NEJMc2015630). Likewise, a study of aortic dissections in New York reported a sharp decline in procedures during the pandemic in the city, from 13 to 3 a month (J Am Coll Cardiol. 2020 May 15. doi: 10.1016/j.jacc.2020.05.022)
The researchers in Italy didn’t aim to determine the reasons for the decline in AMI hospitalizations, but Dr. De Rosa and colleagues speculated on the following explanations: Fear of contagion in response to media reports, concentration of resources to address COVID-19 may have engendered a sense to defer less urgent care among patients and health care systems, and a true reduction in acute cardiovascular disease because people under stay-at-home orders had low physical stress.
“The concern is fewer MIs most likely means people are dying at home or presenting later as this study suggests,” said Martha Gulati, MD, chief of cardiology at the University of Arizona, Phoenix, in interpreting the results of the Italian study.
That could be a result of a mixed message from the media about accessing health care during the pandemic. “What it suggests to a lot of us is that the media has transmitted this notion that hospitals are busy taking care of COVID-19 patients, but we never said don’t come to hospital if you’re having a heart attack,” Dr. Gulati said. “I think we created some sort of fear that patients if they didn’t have COVID-19 they didn’t want to bother physicians.”
Dr. Gulati, whose practice focuses on women with CVD, said the study’s findings that interventions in women dropped more precipitously than men were concerning. “We know already that women don’t do as well after a heart attack, compared to men, and now we see it worsen it even further when women aren’t presenting,” she said. “We’re worried that this is going to increase the gap.”
Dr. DeRosa and colleagues have no relevant financial relationships to disclose.
SOURCE: De Rosa S et al. Euro Heart J. 2020 May 15. doi: 10.1093/eurheartj/ehaa409.
The drastic drop in admissions for acute myocardial infarctions (AMI) during the COVID-19 pandemic in Italy has seen a parallel rise in MI fatality rates in those who do present to hospitals, according to a new report. This gives credence to suggestions that people have avoided hospitals during the pandemic despite life-threatening emergencies.
Salvatore De Rosa, MD, PhD, and colleagues reported their results in the European Heart Journal.
“These data return a frightening picture of about half of AMI patients not reaching out to the hospital at all, which will probably significantly increase mortality for AMI and bring with it a number of patients with post-MI heart failure, despite the fact that acute coronary syndrome management protocols were promptly implemented,” Dr. De Rosa, of Magna Graecia University in Catanzaro, Italy, and associates wrote.
Hospitalizations down
The study counted AMIs at 54 hospital coronary care units nationwide for the week of March 12-19, 2020, at the height of the coronavirus outbreak in northern Italy, and compared that with an equivalent week in 2019. The researchers reported 319 AMIs during the week in 2020, compared with 618 in the equivalent 2019 week, a 48% reduction (P < .001). Although the outbreak was worst in northern Italy, the decline in admissions occurred throughout the country.
An analysis of subtype determined the decline in the incidence of ST-segment elevation MI lagged significantly behind that of non-STEMI. STEMI declined from 268 in 2019 to 197 in 2020, a 27% reduction, while hospitalizations for non-STEMI went from 350 to 122, a 65% reduction.
The researchers also found substantial reductions in hospitalizations for heart failure, by 47%, and atrial fibrillation, by 53%. Incidentally, the mean age of atrial fibrillation patients was considerably younger in 2020: 64.6 vs. 70 years.
Death, complications up
AMI patients who managed to get to the hospital during the pandemic also had worse outcomes. Mortality for STEMI cases more than tripled, to 14% during the outbreak, compared with 4% in 2019 (P < .001) and complication rates increased by 80% to 19% (P = .025). Twenty-one STEMI patients were positive for COVID-19 and more than a quarter (29%) died, which was more than two and a half times the 12% death rate in non–COVID-19 STEMI patients.
Analysis of the STEMI group also found that the care gap for women with heart disease worsened significantly during the pandemic, as they comprised 20.3% of cases this year, compared with 25.4% before the pandemic. Also, the reduction in admissions for STEMI during the pandemic was statistically significant at 41% for women, but not for men at 18%.
Non-STEMI patients fared better overall than STEMI patients, but their outcomes also worsened during the pandemic. Non-STEMI patients were significantly less likely to have percutaneous coronary intervention during the pandemic than previously; the rate declined by 13%, from 77% to 66%. The non-STEMI mortality rate nearly doubled, although not statistically significantly, from 1.7% to 3.3%, whereas complication rates actually more than doubled, from 5.1% to 10.7%, a significant difference. Twelve (9.8%) of the non-STEMI patients were COVID-19 positive, but none died.
Trend extends beyond borders
Dr. De Rosa and colleagues noted that their findings are in line with studies that reported similar declines for STEMI interventions in the United States and Spain during the pandemic (J Am Coll Cardiol. 2020. doi: 10.1016/j.jacc.2020.04.011; REC Interv Cardiol. 2020. doi: 10.24875/RECIC.M20000120).
Additionally, a group at Kaiser Permanente in Northern California also reported a 50% decline in the incidence of AMI hospitalizations during the pandemic (N Engl J Med. 2020 May 19. doi: 10.1056/NEJMc2015630). Likewise, a study of aortic dissections in New York reported a sharp decline in procedures during the pandemic in the city, from 13 to 3 a month (J Am Coll Cardiol. 2020 May 15. doi: 10.1016/j.jacc.2020.05.022)
The researchers in Italy didn’t aim to determine the reasons for the decline in AMI hospitalizations, but Dr. De Rosa and colleagues speculated on the following explanations: Fear of contagion in response to media reports, concentration of resources to address COVID-19 may have engendered a sense to defer less urgent care among patients and health care systems, and a true reduction in acute cardiovascular disease because people under stay-at-home orders had low physical stress.
“The concern is fewer MIs most likely means people are dying at home or presenting later as this study suggests,” said Martha Gulati, MD, chief of cardiology at the University of Arizona, Phoenix, in interpreting the results of the Italian study.
That could be a result of a mixed message from the media about accessing health care during the pandemic. “What it suggests to a lot of us is that the media has transmitted this notion that hospitals are busy taking care of COVID-19 patients, but we never said don’t come to hospital if you’re having a heart attack,” Dr. Gulati said. “I think we created some sort of fear that patients if they didn’t have COVID-19 they didn’t want to bother physicians.”
Dr. Gulati, whose practice focuses on women with CVD, said the study’s findings that interventions in women dropped more precipitously than men were concerning. “We know already that women don’t do as well after a heart attack, compared to men, and now we see it worsen it even further when women aren’t presenting,” she said. “We’re worried that this is going to increase the gap.”
Dr. DeRosa and colleagues have no relevant financial relationships to disclose.
SOURCE: De Rosa S et al. Euro Heart J. 2020 May 15. doi: 10.1093/eurheartj/ehaa409.
The drastic drop in admissions for acute myocardial infarctions (AMI) during the COVID-19 pandemic in Italy has seen a parallel rise in MI fatality rates in those who do present to hospitals, according to a new report. This gives credence to suggestions that people have avoided hospitals during the pandemic despite life-threatening emergencies.
Salvatore De Rosa, MD, PhD, and colleagues reported their results in the European Heart Journal.
“These data return a frightening picture of about half of AMI patients not reaching out to the hospital at all, which will probably significantly increase mortality for AMI and bring with it a number of patients with post-MI heart failure, despite the fact that acute coronary syndrome management protocols were promptly implemented,” Dr. De Rosa, of Magna Graecia University in Catanzaro, Italy, and associates wrote.
Hospitalizations down
The study counted AMIs at 54 hospital coronary care units nationwide for the week of March 12-19, 2020, at the height of the coronavirus outbreak in northern Italy, and compared that with an equivalent week in 2019. The researchers reported 319 AMIs during the week in 2020, compared with 618 in the equivalent 2019 week, a 48% reduction (P < .001). Although the outbreak was worst in northern Italy, the decline in admissions occurred throughout the country.
An analysis of subtype determined the decline in the incidence of ST-segment elevation MI lagged significantly behind that of non-STEMI. STEMI declined from 268 in 2019 to 197 in 2020, a 27% reduction, while hospitalizations for non-STEMI went from 350 to 122, a 65% reduction.
The researchers also found substantial reductions in hospitalizations for heart failure, by 47%, and atrial fibrillation, by 53%. Incidentally, the mean age of atrial fibrillation patients was considerably younger in 2020: 64.6 vs. 70 years.
Death, complications up
AMI patients who managed to get to the hospital during the pandemic also had worse outcomes. Mortality for STEMI cases more than tripled, to 14% during the outbreak, compared with 4% in 2019 (P < .001) and complication rates increased by 80% to 19% (P = .025). Twenty-one STEMI patients were positive for COVID-19 and more than a quarter (29%) died, which was more than two and a half times the 12% death rate in non–COVID-19 STEMI patients.
Analysis of the STEMI group also found that the care gap for women with heart disease worsened significantly during the pandemic, as they comprised 20.3% of cases this year, compared with 25.4% before the pandemic. Also, the reduction in admissions for STEMI during the pandemic was statistically significant at 41% for women, but not for men at 18%.
Non-STEMI patients fared better overall than STEMI patients, but their outcomes also worsened during the pandemic. Non-STEMI patients were significantly less likely to have percutaneous coronary intervention during the pandemic than previously; the rate declined by 13%, from 77% to 66%. The non-STEMI mortality rate nearly doubled, although not statistically significantly, from 1.7% to 3.3%, whereas complication rates actually more than doubled, from 5.1% to 10.7%, a significant difference. Twelve (9.8%) of the non-STEMI patients were COVID-19 positive, but none died.
Trend extends beyond borders
Dr. De Rosa and colleagues noted that their findings are in line with studies that reported similar declines for STEMI interventions in the United States and Spain during the pandemic (J Am Coll Cardiol. 2020. doi: 10.1016/j.jacc.2020.04.011; REC Interv Cardiol. 2020. doi: 10.24875/RECIC.M20000120).
Additionally, a group at Kaiser Permanente in Northern California also reported a 50% decline in the incidence of AMI hospitalizations during the pandemic (N Engl J Med. 2020 May 19. doi: 10.1056/NEJMc2015630). Likewise, a study of aortic dissections in New York reported a sharp decline in procedures during the pandemic in the city, from 13 to 3 a month (J Am Coll Cardiol. 2020 May 15. doi: 10.1016/j.jacc.2020.05.022)
The researchers in Italy didn’t aim to determine the reasons for the decline in AMI hospitalizations, but Dr. De Rosa and colleagues speculated on the following explanations: Fear of contagion in response to media reports, concentration of resources to address COVID-19 may have engendered a sense to defer less urgent care among patients and health care systems, and a true reduction in acute cardiovascular disease because people under stay-at-home orders had low physical stress.
“The concern is fewer MIs most likely means people are dying at home or presenting later as this study suggests,” said Martha Gulati, MD, chief of cardiology at the University of Arizona, Phoenix, in interpreting the results of the Italian study.
That could be a result of a mixed message from the media about accessing health care during the pandemic. “What it suggests to a lot of us is that the media has transmitted this notion that hospitals are busy taking care of COVID-19 patients, but we never said don’t come to hospital if you’re having a heart attack,” Dr. Gulati said. “I think we created some sort of fear that patients if they didn’t have COVID-19 they didn’t want to bother physicians.”
Dr. Gulati, whose practice focuses on women with CVD, said the study’s findings that interventions in women dropped more precipitously than men were concerning. “We know already that women don’t do as well after a heart attack, compared to men, and now we see it worsen it even further when women aren’t presenting,” she said. “We’re worried that this is going to increase the gap.”
Dr. DeRosa and colleagues have no relevant financial relationships to disclose.
SOURCE: De Rosa S et al. Euro Heart J. 2020 May 15. doi: 10.1093/eurheartj/ehaa409.
FROM THE EUROPEAN HEART JOURNAL
COVID-19 may cause subacute thyroiditis
Coronavirus disease of 2019 (COVID-19) may lead to subacute thyroiditis in some patients, which is suspected to have viral or postviral origin, especially with upper respiratory tract infections, according to a case study in the Journal of Clinical Endocrinology & Metabolism.
Alessandro Brancatella, a PhD student at the University Hospital Pisa (Italy), and colleagues described the case of an 18-year-old woman who was tested Feb. 21 for SARS-CoV-2 infection after her father was hospitalized because of COVID-19. Her results were positive for the virus, and not long after, she developed mild symptoms. By March 13 and again on March 14, test swabs for SARS-CoV-2 were both negative.
On March 17, she presented with fever, fatigue, palpitations, and neck pain that radiated to her jaw. Testing and physical examination pointed to subacute thyroiditis, and she was soon diagnosed and treated with prednisone. Her neck pain and fever disappeared within 2 days, and the remaining symptoms went away within a week.
The authors noted that the woman’s thyroid had been evaluated before she tested positive for SARS-CoV-2, and at that time, thyroid disease was ruled out. They also pointed out that, although the exact etiology for subacute thyroiditis is unknown, “it is common opinion that the disease is due to a viral infection or to a post-viral inflammatory reaction in genetically predisposed subjects.” They cited examples of viruses with suspected causal associations, including mumps, Epstein-Barr virus, and HIV, and they suggested that, based on the timing of the woman’s subacute thyroiditis and the normal results of her thyroid evaluation before developing COVID-19, SARS-CoV-2 be added to that list.
“To our knowledge, this is the first case of [subacute thyroiditis] related to SARS-CoV-2,” they concluded. “We therefore believe that physicians should be alerted about the possibility of this additional clinical manifestation related to SARS-CoV-2 infection.”
One author reported funding from the University of Pisa.
SOURCE: Brancatella A et al. J Clin Endocrinol Metab. 2020 May 21. doi: 10.1210/clinem/dgaa276.
Coronavirus disease of 2019 (COVID-19) may lead to subacute thyroiditis in some patients, which is suspected to have viral or postviral origin, especially with upper respiratory tract infections, according to a case study in the Journal of Clinical Endocrinology & Metabolism.
Alessandro Brancatella, a PhD student at the University Hospital Pisa (Italy), and colleagues described the case of an 18-year-old woman who was tested Feb. 21 for SARS-CoV-2 infection after her father was hospitalized because of COVID-19. Her results were positive for the virus, and not long after, she developed mild symptoms. By March 13 and again on March 14, test swabs for SARS-CoV-2 were both negative.
On March 17, she presented with fever, fatigue, palpitations, and neck pain that radiated to her jaw. Testing and physical examination pointed to subacute thyroiditis, and she was soon diagnosed and treated with prednisone. Her neck pain and fever disappeared within 2 days, and the remaining symptoms went away within a week.
The authors noted that the woman’s thyroid had been evaluated before she tested positive for SARS-CoV-2, and at that time, thyroid disease was ruled out. They also pointed out that, although the exact etiology for subacute thyroiditis is unknown, “it is common opinion that the disease is due to a viral infection or to a post-viral inflammatory reaction in genetically predisposed subjects.” They cited examples of viruses with suspected causal associations, including mumps, Epstein-Barr virus, and HIV, and they suggested that, based on the timing of the woman’s subacute thyroiditis and the normal results of her thyroid evaluation before developing COVID-19, SARS-CoV-2 be added to that list.
“To our knowledge, this is the first case of [subacute thyroiditis] related to SARS-CoV-2,” they concluded. “We therefore believe that physicians should be alerted about the possibility of this additional clinical manifestation related to SARS-CoV-2 infection.”
One author reported funding from the University of Pisa.
SOURCE: Brancatella A et al. J Clin Endocrinol Metab. 2020 May 21. doi: 10.1210/clinem/dgaa276.
Coronavirus disease of 2019 (COVID-19) may lead to subacute thyroiditis in some patients, which is suspected to have viral or postviral origin, especially with upper respiratory tract infections, according to a case study in the Journal of Clinical Endocrinology & Metabolism.
Alessandro Brancatella, a PhD student at the University Hospital Pisa (Italy), and colleagues described the case of an 18-year-old woman who was tested Feb. 21 for SARS-CoV-2 infection after her father was hospitalized because of COVID-19. Her results were positive for the virus, and not long after, she developed mild symptoms. By March 13 and again on March 14, test swabs for SARS-CoV-2 were both negative.
On March 17, she presented with fever, fatigue, palpitations, and neck pain that radiated to her jaw. Testing and physical examination pointed to subacute thyroiditis, and she was soon diagnosed and treated with prednisone. Her neck pain and fever disappeared within 2 days, and the remaining symptoms went away within a week.
The authors noted that the woman’s thyroid had been evaluated before she tested positive for SARS-CoV-2, and at that time, thyroid disease was ruled out. They also pointed out that, although the exact etiology for subacute thyroiditis is unknown, “it is common opinion that the disease is due to a viral infection or to a post-viral inflammatory reaction in genetically predisposed subjects.” They cited examples of viruses with suspected causal associations, including mumps, Epstein-Barr virus, and HIV, and they suggested that, based on the timing of the woman’s subacute thyroiditis and the normal results of her thyroid evaluation before developing COVID-19, SARS-CoV-2 be added to that list.
“To our knowledge, this is the first case of [subacute thyroiditis] related to SARS-CoV-2,” they concluded. “We therefore believe that physicians should be alerted about the possibility of this additional clinical manifestation related to SARS-CoV-2 infection.”
One author reported funding from the University of Pisa.
SOURCE: Brancatella A et al. J Clin Endocrinol Metab. 2020 May 21. doi: 10.1210/clinem/dgaa276.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
COVID-19 vaccine won’t be a slam dunk
A successful vaccine for prevention of SARS-CoV-2 infection will probably need to incorporate T-cell epitopes to induce a long-term memory T-cell immune response to the virus, Mehrdad Matloubian, MD, PhD, predicted at the virtual edition of the American College of Rheumatology’s 2020 State-of-the-Art Clinical Symposium.
Vaccine-induced neutralizing antibodies may not be sufficient to reliably provide sustained protection against infection. In mouse studies, T-cell immunity has protected against reinfection with the novel coronaviruses. And in some but not all studies of patients infected with the SARS virus, which shares 80% genetic overlap with the SARS-CoV-2 virus responsible for the COVID-19 pandemic, neutralizing antibodies have waned over time.
“In one study, 20 of 26 patients with SARS had lost their antibody response by 6 years post infection. And they had no B-cell immunity against the SARS antigens. The good news is they did have T-cell memory against SARS virus, and people with more severe disease tended to have more T-cell memory against SARS. All of this has really important implications for vaccine development,” observed Dr. Matloubian, a rheumatologist at the University of California, San Francisco.
Dr. Matloubian is among those who are convinced that the ongoing massive global accelerated effort to develop a safe and effective vaccine affords the best opportunity to gain the upper hand in the COVID-19 pandemic. A large array of vaccines are in development.
A key safety concern to watch for in the coming months is whether a vaccine candidate is able to sidestep the issue of antibody-dependent enhancement, whereby prior infection with a non-SARS coronavirus, such as those that cause the common cold, might result in creation of rogue subneutralizing coronavirus antibodies in response to vaccination. There is concern that these nonneutralizing antibodies could facilitate entry of the virus into monocytes and other cells lacking the ACE2 receptor, its usual portal of entry. This in turn could trigger expanded viral replication, a hyperinflammatory response, and viral spread to sites beyond the lung, such as the heart or kidneys.
Little optimism about antivirals’ impact
Dr. Matloubian predicted that antiviral medications, including the much-ballyhooed remdesivir, are unlikely to be a game changer in the COVID-19 pandemic. That’s because most patients who become symptomatic don’t do so until at least 2 days post infection. By that point, their viral load has already peaked and is waning and the B- and T-cell immune responses are starting to gear up.
“Timing seems to be everything when it comes to treatment with antivirals,” he observed. “The virus titer is usually declining by the time people present with severe COVID-19, suggesting that at this time antiviral therapy might be of little use to change the course of the disease, especially if it’s mainly immune-mediated by then. Even with influenza virus, there’s a really short window where Tamiflu [oseltamivir] is effective. It’s going to be the same case for antivirals used for treatment of COVID-19.”
He noted that in a placebo-controlled, randomized trial of remdesivir in 236 Chinese patients with severe COVID-19, intravenous remdesivir wasn’t associated with a significantly shorter time to clinical improvement, although there was a trend in that direction in the subgroup with symptom duration of 10 days or less at initiation of treatment.
A National Institutes of Health press release announcing that remdesivir had a positive impact on duration of hospitalization in a separate randomized trial drew enormous attention from a public desperate for good news. However, the full study has yet to be published, and it’s unclear when during the disease course the antiviral agent was started.
“We need a blockbuster antiviral that’s oral, highly effective, and doesn’t have any side effects to be used in prophylaxis of health care workers and for people who are exposed by family members being infected. And so far there is no such thing, even on the horizon,” according to the rheumatologist.
Fellow panelist Jinoos Yazdany, MD, concurred.
“As we talk to experts around the country, it seems like there isn’t very much optimism about such a blockbuster drug. Most people are actually putting their hope in a vaccine,” said Dr. Yazdany, professor of medicine at the University of California, San Francisco, and chief of rheumatology at San Francisco General Hospital.
Another research priority is identification of biomarkers in blood or bronchoalveolar lavage fluid to identify early on the subgroup of infected patients who are likely to crash and develop severe disease. That would permit a targeted approach to inhibition of the inflammatory pathways contributing to development of acute respiratory distress syndrome before this full-blown cytokine storm-like syndrome can occur. There is great interest in trying to achieve this by repurposing many biologic agents widely used by rheumatologists, including the interleukin-1 blocker anakinra (Kineret) and the IL-6 blocker tocilizumab (Actemra).
Dr. Matloubian reported having no financial conflicts of interest regarding his presentation.
A successful vaccine for prevention of SARS-CoV-2 infection will probably need to incorporate T-cell epitopes to induce a long-term memory T-cell immune response to the virus, Mehrdad Matloubian, MD, PhD, predicted at the virtual edition of the American College of Rheumatology’s 2020 State-of-the-Art Clinical Symposium.
Vaccine-induced neutralizing antibodies may not be sufficient to reliably provide sustained protection against infection. In mouse studies, T-cell immunity has protected against reinfection with the novel coronaviruses. And in some but not all studies of patients infected with the SARS virus, which shares 80% genetic overlap with the SARS-CoV-2 virus responsible for the COVID-19 pandemic, neutralizing antibodies have waned over time.
“In one study, 20 of 26 patients with SARS had lost their antibody response by 6 years post infection. And they had no B-cell immunity against the SARS antigens. The good news is they did have T-cell memory against SARS virus, and people with more severe disease tended to have more T-cell memory against SARS. All of this has really important implications for vaccine development,” observed Dr. Matloubian, a rheumatologist at the University of California, San Francisco.
Dr. Matloubian is among those who are convinced that the ongoing massive global accelerated effort to develop a safe and effective vaccine affords the best opportunity to gain the upper hand in the COVID-19 pandemic. A large array of vaccines are in development.
A key safety concern to watch for in the coming months is whether a vaccine candidate is able to sidestep the issue of antibody-dependent enhancement, whereby prior infection with a non-SARS coronavirus, such as those that cause the common cold, might result in creation of rogue subneutralizing coronavirus antibodies in response to vaccination. There is concern that these nonneutralizing antibodies could facilitate entry of the virus into monocytes and other cells lacking the ACE2 receptor, its usual portal of entry. This in turn could trigger expanded viral replication, a hyperinflammatory response, and viral spread to sites beyond the lung, such as the heart or kidneys.
Little optimism about antivirals’ impact
Dr. Matloubian predicted that antiviral medications, including the much-ballyhooed remdesivir, are unlikely to be a game changer in the COVID-19 pandemic. That’s because most patients who become symptomatic don’t do so until at least 2 days post infection. By that point, their viral load has already peaked and is waning and the B- and T-cell immune responses are starting to gear up.
“Timing seems to be everything when it comes to treatment with antivirals,” he observed. “The virus titer is usually declining by the time people present with severe COVID-19, suggesting that at this time antiviral therapy might be of little use to change the course of the disease, especially if it’s mainly immune-mediated by then. Even with influenza virus, there’s a really short window where Tamiflu [oseltamivir] is effective. It’s going to be the same case for antivirals used for treatment of COVID-19.”
He noted that in a placebo-controlled, randomized trial of remdesivir in 236 Chinese patients with severe COVID-19, intravenous remdesivir wasn’t associated with a significantly shorter time to clinical improvement, although there was a trend in that direction in the subgroup with symptom duration of 10 days or less at initiation of treatment.
A National Institutes of Health press release announcing that remdesivir had a positive impact on duration of hospitalization in a separate randomized trial drew enormous attention from a public desperate for good news. However, the full study has yet to be published, and it’s unclear when during the disease course the antiviral agent was started.
“We need a blockbuster antiviral that’s oral, highly effective, and doesn’t have any side effects to be used in prophylaxis of health care workers and for people who are exposed by family members being infected. And so far there is no such thing, even on the horizon,” according to the rheumatologist.
Fellow panelist Jinoos Yazdany, MD, concurred.
“As we talk to experts around the country, it seems like there isn’t very much optimism about such a blockbuster drug. Most people are actually putting their hope in a vaccine,” said Dr. Yazdany, professor of medicine at the University of California, San Francisco, and chief of rheumatology at San Francisco General Hospital.
Another research priority is identification of biomarkers in blood or bronchoalveolar lavage fluid to identify early on the subgroup of infected patients who are likely to crash and develop severe disease. That would permit a targeted approach to inhibition of the inflammatory pathways contributing to development of acute respiratory distress syndrome before this full-blown cytokine storm-like syndrome can occur. There is great interest in trying to achieve this by repurposing many biologic agents widely used by rheumatologists, including the interleukin-1 blocker anakinra (Kineret) and the IL-6 blocker tocilizumab (Actemra).
Dr. Matloubian reported having no financial conflicts of interest regarding his presentation.
A successful vaccine for prevention of SARS-CoV-2 infection will probably need to incorporate T-cell epitopes to induce a long-term memory T-cell immune response to the virus, Mehrdad Matloubian, MD, PhD, predicted at the virtual edition of the American College of Rheumatology’s 2020 State-of-the-Art Clinical Symposium.
Vaccine-induced neutralizing antibodies may not be sufficient to reliably provide sustained protection against infection. In mouse studies, T-cell immunity has protected against reinfection with the novel coronaviruses. And in some but not all studies of patients infected with the SARS virus, which shares 80% genetic overlap with the SARS-CoV-2 virus responsible for the COVID-19 pandemic, neutralizing antibodies have waned over time.
“In one study, 20 of 26 patients with SARS had lost their antibody response by 6 years post infection. And they had no B-cell immunity against the SARS antigens. The good news is they did have T-cell memory against SARS virus, and people with more severe disease tended to have more T-cell memory against SARS. All of this has really important implications for vaccine development,” observed Dr. Matloubian, a rheumatologist at the University of California, San Francisco.
Dr. Matloubian is among those who are convinced that the ongoing massive global accelerated effort to develop a safe and effective vaccine affords the best opportunity to gain the upper hand in the COVID-19 pandemic. A large array of vaccines are in development.
A key safety concern to watch for in the coming months is whether a vaccine candidate is able to sidestep the issue of antibody-dependent enhancement, whereby prior infection with a non-SARS coronavirus, such as those that cause the common cold, might result in creation of rogue subneutralizing coronavirus antibodies in response to vaccination. There is concern that these nonneutralizing antibodies could facilitate entry of the virus into monocytes and other cells lacking the ACE2 receptor, its usual portal of entry. This in turn could trigger expanded viral replication, a hyperinflammatory response, and viral spread to sites beyond the lung, such as the heart or kidneys.
Little optimism about antivirals’ impact
Dr. Matloubian predicted that antiviral medications, including the much-ballyhooed remdesivir, are unlikely to be a game changer in the COVID-19 pandemic. That’s because most patients who become symptomatic don’t do so until at least 2 days post infection. By that point, their viral load has already peaked and is waning and the B- and T-cell immune responses are starting to gear up.
“Timing seems to be everything when it comes to treatment with antivirals,” he observed. “The virus titer is usually declining by the time people present with severe COVID-19, suggesting that at this time antiviral therapy might be of little use to change the course of the disease, especially if it’s mainly immune-mediated by then. Even with influenza virus, there’s a really short window where Tamiflu [oseltamivir] is effective. It’s going to be the same case for antivirals used for treatment of COVID-19.”
He noted that in a placebo-controlled, randomized trial of remdesivir in 236 Chinese patients with severe COVID-19, intravenous remdesivir wasn’t associated with a significantly shorter time to clinical improvement, although there was a trend in that direction in the subgroup with symptom duration of 10 days or less at initiation of treatment.
A National Institutes of Health press release announcing that remdesivir had a positive impact on duration of hospitalization in a separate randomized trial drew enormous attention from a public desperate for good news. However, the full study has yet to be published, and it’s unclear when during the disease course the antiviral agent was started.
“We need a blockbuster antiviral that’s oral, highly effective, and doesn’t have any side effects to be used in prophylaxis of health care workers and for people who are exposed by family members being infected. And so far there is no such thing, even on the horizon,” according to the rheumatologist.
Fellow panelist Jinoos Yazdany, MD, concurred.
“As we talk to experts around the country, it seems like there isn’t very much optimism about such a blockbuster drug. Most people are actually putting their hope in a vaccine,” said Dr. Yazdany, professor of medicine at the University of California, San Francisco, and chief of rheumatology at San Francisco General Hospital.
Another research priority is identification of biomarkers in blood or bronchoalveolar lavage fluid to identify early on the subgroup of infected patients who are likely to crash and develop severe disease. That would permit a targeted approach to inhibition of the inflammatory pathways contributing to development of acute respiratory distress syndrome before this full-blown cytokine storm-like syndrome can occur. There is great interest in trying to achieve this by repurposing many biologic agents widely used by rheumatologists, including the interleukin-1 blocker anakinra (Kineret) and the IL-6 blocker tocilizumab (Actemra).
Dr. Matloubian reported having no financial conflicts of interest regarding his presentation.
FROM SOTA 2020
AHA offers advice on prehospital acute stroke triage amid COVID-19
A key goal is to ensure timely transfer of patients while minimizing the risk of infectious exposure for EMS personnel, coworkers, and other patients, the writing group says.
“Acute ischemic stroke is still a highly devastating disease and the Time Is Brain paradigm remains true during the COVID-19 pandemic as well,” said writing group chair Mayank Goyal, MD, of the University of Calgary (Alta.)
“We have highly effective and proven treatments available. As such, treatment delays due to additional screening requirements and personal protection equipment (PPE) should be kept at a minimum,” Dr. Goyal said.
“Practicing COVID-19 stroke work flows, through simulation training, can help to reduce treatment delays, minimize the risk of infectious exposure for patients and staff, and help alleviate stress,” he added.
A new layer of complexity
The guidance statement, Prehospital Triage of Acute Stroke Patients During the COVID-19 Pandemic, was published online May 13 in the journal Stroke.
“The need to limit infectious spread during the COVID-19 pandemic has added a new layer of complexity to prehospital stroke triage and transfer,” the writing group noted. “Timely and enhanced” communication between EMS, hospitals, and local coordinating authorities are critical, especially ambulance-and facility-based telestroke networks, they wrote.
The main factors to guide the triage decision are the likelihood of a large vessel occlusion; the magnitude of additional delays because of interhospital transfer and work flow efficiency at the primary stroke center or acute stroke ready hospital; the need for advanced critical care resources; and the available bed, staff, and PPE resources at the hospitals.
The group said it “seems reasonable” to lower the threshold to bypass hospitals that can’t provide acute stroke treatment in favor of transporting to a hospital that is “stroke ready,” particularly in patients likely to require advanced care. They cautioned, however, that taking all acute stroke patients to a comprehensive stroke center could overwhelm these centers and lead to clustering of COVID-19 patients.
They said it is equally important to ensure “necessary transfers” of stroke patients who would benefit from endovascular therapy or neurocritical care and avoid unnecessary patient transfers. “Doing so will likely require local hospital boards and health care authorities to collaborate and establish local guidelines and protocols,” the writing group said.
“During the COVID-19 pandemic, it is more important than ever to ensure that stroke patients are taken to the right hospital that can meet their urgent needs at the outset,” Dr. Goyal commented in an AHA news release.
The writing group emphasized that the principles put forth in the document are intended as suggestions rather than strict rules and will be adapted and updated to meet the evolving needs during the COVID-19 crisis and future pandemics.
“The process of improving stroke work flow and getting the correct patient to the correct hospital fast is dependent on training, protocols, simulation, technology, and – probably most importantly – teamwork. These principles are extremely important during the current pandemic but will be useful in improving stroke care afterwards as well,” Dr. Goyal said.
This research had no commercial funding. Members of the writing committee are on several AHA/ASA Council Science Subcommittees, including the Emergency Neurovascular Care, the Telestroke, and the Neurovascular Intervention committees. Goyal is a consultant for Medtronic, Stryker, Microvention, GE Healthcare, and Mentice. A complete list of author disclosures is available with the original article.
This article first appeared on Medscape.com.
A key goal is to ensure timely transfer of patients while minimizing the risk of infectious exposure for EMS personnel, coworkers, and other patients, the writing group says.
“Acute ischemic stroke is still a highly devastating disease and the Time Is Brain paradigm remains true during the COVID-19 pandemic as well,” said writing group chair Mayank Goyal, MD, of the University of Calgary (Alta.)
“We have highly effective and proven treatments available. As such, treatment delays due to additional screening requirements and personal protection equipment (PPE) should be kept at a minimum,” Dr. Goyal said.
“Practicing COVID-19 stroke work flows, through simulation training, can help to reduce treatment delays, minimize the risk of infectious exposure for patients and staff, and help alleviate stress,” he added.
A new layer of complexity
The guidance statement, Prehospital Triage of Acute Stroke Patients During the COVID-19 Pandemic, was published online May 13 in the journal Stroke.
“The need to limit infectious spread during the COVID-19 pandemic has added a new layer of complexity to prehospital stroke triage and transfer,” the writing group noted. “Timely and enhanced” communication between EMS, hospitals, and local coordinating authorities are critical, especially ambulance-and facility-based telestroke networks, they wrote.
The main factors to guide the triage decision are the likelihood of a large vessel occlusion; the magnitude of additional delays because of interhospital transfer and work flow efficiency at the primary stroke center or acute stroke ready hospital; the need for advanced critical care resources; and the available bed, staff, and PPE resources at the hospitals.
The group said it “seems reasonable” to lower the threshold to bypass hospitals that can’t provide acute stroke treatment in favor of transporting to a hospital that is “stroke ready,” particularly in patients likely to require advanced care. They cautioned, however, that taking all acute stroke patients to a comprehensive stroke center could overwhelm these centers and lead to clustering of COVID-19 patients.
They said it is equally important to ensure “necessary transfers” of stroke patients who would benefit from endovascular therapy or neurocritical care and avoid unnecessary patient transfers. “Doing so will likely require local hospital boards and health care authorities to collaborate and establish local guidelines and protocols,” the writing group said.
“During the COVID-19 pandemic, it is more important than ever to ensure that stroke patients are taken to the right hospital that can meet their urgent needs at the outset,” Dr. Goyal commented in an AHA news release.
The writing group emphasized that the principles put forth in the document are intended as suggestions rather than strict rules and will be adapted and updated to meet the evolving needs during the COVID-19 crisis and future pandemics.
“The process of improving stroke work flow and getting the correct patient to the correct hospital fast is dependent on training, protocols, simulation, technology, and – probably most importantly – teamwork. These principles are extremely important during the current pandemic but will be useful in improving stroke care afterwards as well,” Dr. Goyal said.
This research had no commercial funding. Members of the writing committee are on several AHA/ASA Council Science Subcommittees, including the Emergency Neurovascular Care, the Telestroke, and the Neurovascular Intervention committees. Goyal is a consultant for Medtronic, Stryker, Microvention, GE Healthcare, and Mentice. A complete list of author disclosures is available with the original article.
This article first appeared on Medscape.com.
A key goal is to ensure timely transfer of patients while minimizing the risk of infectious exposure for EMS personnel, coworkers, and other patients, the writing group says.
“Acute ischemic stroke is still a highly devastating disease and the Time Is Brain paradigm remains true during the COVID-19 pandemic as well,” said writing group chair Mayank Goyal, MD, of the University of Calgary (Alta.)
“We have highly effective and proven treatments available. As such, treatment delays due to additional screening requirements and personal protection equipment (PPE) should be kept at a minimum,” Dr. Goyal said.
“Practicing COVID-19 stroke work flows, through simulation training, can help to reduce treatment delays, minimize the risk of infectious exposure for patients and staff, and help alleviate stress,” he added.
A new layer of complexity
The guidance statement, Prehospital Triage of Acute Stroke Patients During the COVID-19 Pandemic, was published online May 13 in the journal Stroke.
“The need to limit infectious spread during the COVID-19 pandemic has added a new layer of complexity to prehospital stroke triage and transfer,” the writing group noted. “Timely and enhanced” communication between EMS, hospitals, and local coordinating authorities are critical, especially ambulance-and facility-based telestroke networks, they wrote.
The main factors to guide the triage decision are the likelihood of a large vessel occlusion; the magnitude of additional delays because of interhospital transfer and work flow efficiency at the primary stroke center or acute stroke ready hospital; the need for advanced critical care resources; and the available bed, staff, and PPE resources at the hospitals.
The group said it “seems reasonable” to lower the threshold to bypass hospitals that can’t provide acute stroke treatment in favor of transporting to a hospital that is “stroke ready,” particularly in patients likely to require advanced care. They cautioned, however, that taking all acute stroke patients to a comprehensive stroke center could overwhelm these centers and lead to clustering of COVID-19 patients.
They said it is equally important to ensure “necessary transfers” of stroke patients who would benefit from endovascular therapy or neurocritical care and avoid unnecessary patient transfers. “Doing so will likely require local hospital boards and health care authorities to collaborate and establish local guidelines and protocols,” the writing group said.
“During the COVID-19 pandemic, it is more important than ever to ensure that stroke patients are taken to the right hospital that can meet their urgent needs at the outset,” Dr. Goyal commented in an AHA news release.
The writing group emphasized that the principles put forth in the document are intended as suggestions rather than strict rules and will be adapted and updated to meet the evolving needs during the COVID-19 crisis and future pandemics.
“The process of improving stroke work flow and getting the correct patient to the correct hospital fast is dependent on training, protocols, simulation, technology, and – probably most importantly – teamwork. These principles are extremely important during the current pandemic but will be useful in improving stroke care afterwards as well,” Dr. Goyal said.
This research had no commercial funding. Members of the writing committee are on several AHA/ASA Council Science Subcommittees, including the Emergency Neurovascular Care, the Telestroke, and the Neurovascular Intervention committees. Goyal is a consultant for Medtronic, Stryker, Microvention, GE Healthcare, and Mentice. A complete list of author disclosures is available with the original article.
This article first appeared on Medscape.com.
COVID-19: Delirium first, depression, anxiety, insomnia later?
Severe COVID-19 may cause delirium in the acute stage of illness, followed by the possibility of depression, anxiety, fatigue, insomnia, and posttraumatic stress disorder (PTSD) over the longer term, new research suggests.
Results from “the first systematic review and meta-analysis of the psychiatric consequences of coronavirus infection” showed that previous coronavirus epidemics were associated with a significant psychiatric burden in both the acute and post-illness stages.
“Most people with COVID-19 will not develop any mental health problems, even among those with severe cases requiring hospitalization, but given the huge numbers of people getting sick, the global impact on mental health could be considerable,” co–lead investigator Jonathan Rogers, MRCPsych, Department of Psychiatry, University College London, United Kingdom, said in a news release.
The study was published online May 18 in Lancet Psychiatry.
Need for Monitoring, Support
The researchers analyzed 65 peer-reviewed studies and seven preprint articles with data on acute and post-illness psychiatric and neuropsychiatric features of patients who had been hospitalized with COVID-19, as well as two other diseases caused by coronaviruses – severe acute respiratory syndrome (SARS), in 2002–2004, and Middle East respiratory syndrome (MERS), in 2012.
“Our main findings are that signs suggestive of delirium are common in the acute stage of SARS, MERS, and COVID-19; there is evidence of depression, anxiety, fatigue, and post-traumatic stress disorder in the post-illness stage of previous coronavirus epidemics, but there are few data yet on COVID-19,” the investigators write.
The data show that among patients acutely ill with SARS and MERS, 28% experienced confusion, 33% had depressed mood, 36% had anxiety, 34% suffered from impaired memory, and 42% had insomnia.
After recovery from SARS and MERS, sleep disorder, frequent recall of traumatic memories, emotional lability, impaired concentration, fatigue, and impaired memory were reported in more than 15% of patients during a follow-up period that ranged from 6 weeks to 39 months.
In a meta-analysis, the point prevalence in the post-illness stage was 32% for PTSD and about 15% for depression and anxiety.
In patients acutely ill with severe COVID-19, available data suggest that 65% experience delirium, 69% have agitation after withdrawal of sedation, and 21% have altered consciousness.
In one study, 33% of patients had a dysexecutive syndrome at discharge, characterized by symptoms such as inattention, disorientation, or poorly organized movements in response to command. Currently, data are very limited regarding patients who have recovered from COVID-19, the investigators caution.
“, and monitored after they recover to ensure they do not develop mental illnesses, and are able to access treatment if needed,” senior author Anthony David, FMedSci, from UCL Institute of Mental Health, said in a news release.
“While most people with COVID-19 will recover without experiencing mental illness, we need to research which factors may contribute to enduring mental health problems, and develop interventions to prevent and treat them,” he added.
Be Prepared
The coauthors of a linked commentary say it makes sense, from a biological perspective, to merge data on these three coronavirus diseases, given the degree to which they resemble each other.
They caution, however, that treatment of COVID-19 seems to be different from treatment of SARS and MERS. In addition, the social and economic situation of COVID-19 survivors’ return is completely different from that of SARS and MERS survivors.
Findings from previous coronavirus outbreaks are “useful, but might not be exact predictors of prevalences of psychiatric complications for patients with COVID-19,” write Iris Sommer, MD, PhD, from University Medical Center Groningen, the Netherlands, and P. Roberto Bakker, MD, PhD, from Maastricht University Medical Center, the Netherlands.
“The warning from [this study] that we should prepare to treat large numbers of patients with COVID-19 who go on to develop delirium, post-traumatic stress disorder, anxiety, and depression is an important message for the psychiatric community,” they add.
Sommer and Bakker also say the reported estimates of prevalence in this study should be interpreted with caution, “as true numbers of both acute and long-term psychiatric disorders for patients with COVID-19 might be considerably higher.”
Funding for the study was provided by the Wellcome Trust, the UK National Institute for Health Research (NIHR), the UK Medical Research Council, the NIHR Biomedical Research Center at the University College London Hospitals NHS Foundation Trust, and the University College London. The authors of the study and the commentary have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Severe COVID-19 may cause delirium in the acute stage of illness, followed by the possibility of depression, anxiety, fatigue, insomnia, and posttraumatic stress disorder (PTSD) over the longer term, new research suggests.
Results from “the first systematic review and meta-analysis of the psychiatric consequences of coronavirus infection” showed that previous coronavirus epidemics were associated with a significant psychiatric burden in both the acute and post-illness stages.
“Most people with COVID-19 will not develop any mental health problems, even among those with severe cases requiring hospitalization, but given the huge numbers of people getting sick, the global impact on mental health could be considerable,” co–lead investigator Jonathan Rogers, MRCPsych, Department of Psychiatry, University College London, United Kingdom, said in a news release.
The study was published online May 18 in Lancet Psychiatry.
Need for Monitoring, Support
The researchers analyzed 65 peer-reviewed studies and seven preprint articles with data on acute and post-illness psychiatric and neuropsychiatric features of patients who had been hospitalized with COVID-19, as well as two other diseases caused by coronaviruses – severe acute respiratory syndrome (SARS), in 2002–2004, and Middle East respiratory syndrome (MERS), in 2012.
“Our main findings are that signs suggestive of delirium are common in the acute stage of SARS, MERS, and COVID-19; there is evidence of depression, anxiety, fatigue, and post-traumatic stress disorder in the post-illness stage of previous coronavirus epidemics, but there are few data yet on COVID-19,” the investigators write.
The data show that among patients acutely ill with SARS and MERS, 28% experienced confusion, 33% had depressed mood, 36% had anxiety, 34% suffered from impaired memory, and 42% had insomnia.
After recovery from SARS and MERS, sleep disorder, frequent recall of traumatic memories, emotional lability, impaired concentration, fatigue, and impaired memory were reported in more than 15% of patients during a follow-up period that ranged from 6 weeks to 39 months.
In a meta-analysis, the point prevalence in the post-illness stage was 32% for PTSD and about 15% for depression and anxiety.
In patients acutely ill with severe COVID-19, available data suggest that 65% experience delirium, 69% have agitation after withdrawal of sedation, and 21% have altered consciousness.
In one study, 33% of patients had a dysexecutive syndrome at discharge, characterized by symptoms such as inattention, disorientation, or poorly organized movements in response to command. Currently, data are very limited regarding patients who have recovered from COVID-19, the investigators caution.
“, and monitored after they recover to ensure they do not develop mental illnesses, and are able to access treatment if needed,” senior author Anthony David, FMedSci, from UCL Institute of Mental Health, said in a news release.
“While most people with COVID-19 will recover without experiencing mental illness, we need to research which factors may contribute to enduring mental health problems, and develop interventions to prevent and treat them,” he added.
Be Prepared
The coauthors of a linked commentary say it makes sense, from a biological perspective, to merge data on these three coronavirus diseases, given the degree to which they resemble each other.
They caution, however, that treatment of COVID-19 seems to be different from treatment of SARS and MERS. In addition, the social and economic situation of COVID-19 survivors’ return is completely different from that of SARS and MERS survivors.
Findings from previous coronavirus outbreaks are “useful, but might not be exact predictors of prevalences of psychiatric complications for patients with COVID-19,” write Iris Sommer, MD, PhD, from University Medical Center Groningen, the Netherlands, and P. Roberto Bakker, MD, PhD, from Maastricht University Medical Center, the Netherlands.
“The warning from [this study] that we should prepare to treat large numbers of patients with COVID-19 who go on to develop delirium, post-traumatic stress disorder, anxiety, and depression is an important message for the psychiatric community,” they add.
Sommer and Bakker also say the reported estimates of prevalence in this study should be interpreted with caution, “as true numbers of both acute and long-term psychiatric disorders for patients with COVID-19 might be considerably higher.”
Funding for the study was provided by the Wellcome Trust, the UK National Institute for Health Research (NIHR), the UK Medical Research Council, the NIHR Biomedical Research Center at the University College London Hospitals NHS Foundation Trust, and the University College London. The authors of the study and the commentary have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Severe COVID-19 may cause delirium in the acute stage of illness, followed by the possibility of depression, anxiety, fatigue, insomnia, and posttraumatic stress disorder (PTSD) over the longer term, new research suggests.
Results from “the first systematic review and meta-analysis of the psychiatric consequences of coronavirus infection” showed that previous coronavirus epidemics were associated with a significant psychiatric burden in both the acute and post-illness stages.
“Most people with COVID-19 will not develop any mental health problems, even among those with severe cases requiring hospitalization, but given the huge numbers of people getting sick, the global impact on mental health could be considerable,” co–lead investigator Jonathan Rogers, MRCPsych, Department of Psychiatry, University College London, United Kingdom, said in a news release.
The study was published online May 18 in Lancet Psychiatry.
Need for Monitoring, Support
The researchers analyzed 65 peer-reviewed studies and seven preprint articles with data on acute and post-illness psychiatric and neuropsychiatric features of patients who had been hospitalized with COVID-19, as well as two other diseases caused by coronaviruses – severe acute respiratory syndrome (SARS), in 2002–2004, and Middle East respiratory syndrome (MERS), in 2012.
“Our main findings are that signs suggestive of delirium are common in the acute stage of SARS, MERS, and COVID-19; there is evidence of depression, anxiety, fatigue, and post-traumatic stress disorder in the post-illness stage of previous coronavirus epidemics, but there are few data yet on COVID-19,” the investigators write.
The data show that among patients acutely ill with SARS and MERS, 28% experienced confusion, 33% had depressed mood, 36% had anxiety, 34% suffered from impaired memory, and 42% had insomnia.
After recovery from SARS and MERS, sleep disorder, frequent recall of traumatic memories, emotional lability, impaired concentration, fatigue, and impaired memory were reported in more than 15% of patients during a follow-up period that ranged from 6 weeks to 39 months.
In a meta-analysis, the point prevalence in the post-illness stage was 32% for PTSD and about 15% for depression and anxiety.
In patients acutely ill with severe COVID-19, available data suggest that 65% experience delirium, 69% have agitation after withdrawal of sedation, and 21% have altered consciousness.
In one study, 33% of patients had a dysexecutive syndrome at discharge, characterized by symptoms such as inattention, disorientation, or poorly organized movements in response to command. Currently, data are very limited regarding patients who have recovered from COVID-19, the investigators caution.
“, and monitored after they recover to ensure they do not develop mental illnesses, and are able to access treatment if needed,” senior author Anthony David, FMedSci, from UCL Institute of Mental Health, said in a news release.
“While most people with COVID-19 will recover without experiencing mental illness, we need to research which factors may contribute to enduring mental health problems, and develop interventions to prevent and treat them,” he added.
Be Prepared
The coauthors of a linked commentary say it makes sense, from a biological perspective, to merge data on these three coronavirus diseases, given the degree to which they resemble each other.
They caution, however, that treatment of COVID-19 seems to be different from treatment of SARS and MERS. In addition, the social and economic situation of COVID-19 survivors’ return is completely different from that of SARS and MERS survivors.
Findings from previous coronavirus outbreaks are “useful, but might not be exact predictors of prevalences of psychiatric complications for patients with COVID-19,” write Iris Sommer, MD, PhD, from University Medical Center Groningen, the Netherlands, and P. Roberto Bakker, MD, PhD, from Maastricht University Medical Center, the Netherlands.
“The warning from [this study] that we should prepare to treat large numbers of patients with COVID-19 who go on to develop delirium, post-traumatic stress disorder, anxiety, and depression is an important message for the psychiatric community,” they add.
Sommer and Bakker also say the reported estimates of prevalence in this study should be interpreted with caution, “as true numbers of both acute and long-term psychiatric disorders for patients with COVID-19 might be considerably higher.”
Funding for the study was provided by the Wellcome Trust, the UK National Institute for Health Research (NIHR), the UK Medical Research Council, the NIHR Biomedical Research Center at the University College London Hospitals NHS Foundation Trust, and the University College London. The authors of the study and the commentary have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Chilblain-like lesions reported in children thought to have COVID-19
Two and elsewhere.
These symptoms should be considered a sign of infection with the virus, but the symptoms themselves typically don’t require treatment, according to the authors of the two new reports, from hospitals in Milan and Madrid, published in Pediatric Dermatology.
In the first study, Cristiana Colonna, MD, and colleagues at Hospital Maggiore Polyclinic in Milan described four cases of chilblain-like lesions in children ages 5-11 years with mild COVID-19 symptoms.
In the second, David Andina, MD, and colleagues in the ED and the departments of dermatology and pathology at the Child Jesus University Children’s Hospital in Madrid published a retrospective study of 22 cases in children and adolescents ages 6-17 years who reported to the hospital ED from April 6 to 17, the peak of the pandemic in Madrid.
In all four of the Milan cases, the skin lesions appeared several days after the onset of COVID-19 symptoms, although all four patients initially tested negative for COVID-19. However, Dr. Colonna and colleagues wrote that, “given the fact that the sensitivity and specificity of both nasopharyngeal swabs and antibody tests for COVID-19 (when available) are not 100% reliable, the question of the origin of these strange chilblain-like lesions is still elusive.” Until further studies are available, they emphasized that clinicians should be “alert to the presentation of chilblain-like findings” in children with mild symptoms “as a possible sign of COVID-19 infection.”
All the patients had lesions on their feet or toes, and a 5-year-old boy also had lesions on the right hand. One patient, an 11-year-old girl, had a biopsy that revealed dense lymphocytic perivascular cuffing and periadnexal infiltration.
“The finding of an elevated d-dimer in one of our patients, along with the clinical features suggestive of a vasoocclusive phenomenon, supports consideration of laboratory evaluation for coagulation defects in asymptomatic or mildly symptomatic children with acrovasculitis-like findings,” Dr. Colonna and colleagues wrote. None of the four cases in Milan required treatment, with three cases resolving within 5 days.
Like the Milan cases, all 22 patients in the Madrid series had foot or toe lesions and three had lesions on the fingers. This larger series also reported more detailed symptoms about the lesions: pruritus in nine patients (41%) and mild pain in seven (32%). A total of 10 patients had systemic symptoms of COVID-19, predominantly cough and rhinorrhea in 9 patients (41%), but 2 (9%) had abdominal pain and diarrhea. These symptoms, the authors said, appeared a median of 14 days (range, 1-28 days) before they developed chilblains.
A total of 19 patients were tested for COVID-19, but only 1 was positive.
This retrospective study also included contact information, with one patient having household contact with a single confirmed case of COVID-19; 12 patients recalled household contact who were considered probable cases of COVID-19, with respiratory symptoms.
Skin biopsies were obtained from the acral lesions in six patients, all showing similar results, although with varying degrees of intensity. All biopsies showed features of lymphocytic vasculopathy. Some cases showed mild dermal and perieccrine mucinosis, lymphocytic eccrine hidradenitis, vascular ectasia, red cell extravasation and focal thrombosis described as “mostly confined to scattered papillary dermal capillaries, but also in vessels of the reticular dermis.”
The only treatments Dr. Andina and colleagues reported were oral analgesics for pain and oral antihistamines for pruritus when needed. One patient was given topical corticosteroids and another a short course of oral steroids, both for erythema multiforme.
Dr. Andina and colleagues wrote that the skin lesions in these patients “were unequivocally categorized as chilblains, both clinically and histopathologically,” and, after 7-10 days, began to fade. None of the patients had complications, and had an “excellent outcome,” they noted.
Dr. Colonna and colleagues had no conflicts of interest to declare. Dr. Andina and colleagues provided no disclosure statement.
SOURCES: Colonna C et al. Ped Derm. 2020 May 6. doi: 10.1111/pde.14210; Andina D et al. Ped Derm. 2020 May 9. doi: 10.1111/pde.14215.
Two and elsewhere.
These symptoms should be considered a sign of infection with the virus, but the symptoms themselves typically don’t require treatment, according to the authors of the two new reports, from hospitals in Milan and Madrid, published in Pediatric Dermatology.
In the first study, Cristiana Colonna, MD, and colleagues at Hospital Maggiore Polyclinic in Milan described four cases of chilblain-like lesions in children ages 5-11 years with mild COVID-19 symptoms.
In the second, David Andina, MD, and colleagues in the ED and the departments of dermatology and pathology at the Child Jesus University Children’s Hospital in Madrid published a retrospective study of 22 cases in children and adolescents ages 6-17 years who reported to the hospital ED from April 6 to 17, the peak of the pandemic in Madrid.
In all four of the Milan cases, the skin lesions appeared several days after the onset of COVID-19 symptoms, although all four patients initially tested negative for COVID-19. However, Dr. Colonna and colleagues wrote that, “given the fact that the sensitivity and specificity of both nasopharyngeal swabs and antibody tests for COVID-19 (when available) are not 100% reliable, the question of the origin of these strange chilblain-like lesions is still elusive.” Until further studies are available, they emphasized that clinicians should be “alert to the presentation of chilblain-like findings” in children with mild symptoms “as a possible sign of COVID-19 infection.”
All the patients had lesions on their feet or toes, and a 5-year-old boy also had lesions on the right hand. One patient, an 11-year-old girl, had a biopsy that revealed dense lymphocytic perivascular cuffing and periadnexal infiltration.
“The finding of an elevated d-dimer in one of our patients, along with the clinical features suggestive of a vasoocclusive phenomenon, supports consideration of laboratory evaluation for coagulation defects in asymptomatic or mildly symptomatic children with acrovasculitis-like findings,” Dr. Colonna and colleagues wrote. None of the four cases in Milan required treatment, with three cases resolving within 5 days.
Like the Milan cases, all 22 patients in the Madrid series had foot or toe lesions and three had lesions on the fingers. This larger series also reported more detailed symptoms about the lesions: pruritus in nine patients (41%) and mild pain in seven (32%). A total of 10 patients had systemic symptoms of COVID-19, predominantly cough and rhinorrhea in 9 patients (41%), but 2 (9%) had abdominal pain and diarrhea. These symptoms, the authors said, appeared a median of 14 days (range, 1-28 days) before they developed chilblains.
A total of 19 patients were tested for COVID-19, but only 1 was positive.
This retrospective study also included contact information, with one patient having household contact with a single confirmed case of COVID-19; 12 patients recalled household contact who were considered probable cases of COVID-19, with respiratory symptoms.
Skin biopsies were obtained from the acral lesions in six patients, all showing similar results, although with varying degrees of intensity. All biopsies showed features of lymphocytic vasculopathy. Some cases showed mild dermal and perieccrine mucinosis, lymphocytic eccrine hidradenitis, vascular ectasia, red cell extravasation and focal thrombosis described as “mostly confined to scattered papillary dermal capillaries, but also in vessels of the reticular dermis.”
The only treatments Dr. Andina and colleagues reported were oral analgesics for pain and oral antihistamines for pruritus when needed. One patient was given topical corticosteroids and another a short course of oral steroids, both for erythema multiforme.
Dr. Andina and colleagues wrote that the skin lesions in these patients “were unequivocally categorized as chilblains, both clinically and histopathologically,” and, after 7-10 days, began to fade. None of the patients had complications, and had an “excellent outcome,” they noted.
Dr. Colonna and colleagues had no conflicts of interest to declare. Dr. Andina and colleagues provided no disclosure statement.
SOURCES: Colonna C et al. Ped Derm. 2020 May 6. doi: 10.1111/pde.14210; Andina D et al. Ped Derm. 2020 May 9. doi: 10.1111/pde.14215.
Two and elsewhere.
These symptoms should be considered a sign of infection with the virus, but the symptoms themselves typically don’t require treatment, according to the authors of the two new reports, from hospitals in Milan and Madrid, published in Pediatric Dermatology.
In the first study, Cristiana Colonna, MD, and colleagues at Hospital Maggiore Polyclinic in Milan described four cases of chilblain-like lesions in children ages 5-11 years with mild COVID-19 symptoms.
In the second, David Andina, MD, and colleagues in the ED and the departments of dermatology and pathology at the Child Jesus University Children’s Hospital in Madrid published a retrospective study of 22 cases in children and adolescents ages 6-17 years who reported to the hospital ED from April 6 to 17, the peak of the pandemic in Madrid.
In all four of the Milan cases, the skin lesions appeared several days after the onset of COVID-19 symptoms, although all four patients initially tested negative for COVID-19. However, Dr. Colonna and colleagues wrote that, “given the fact that the sensitivity and specificity of both nasopharyngeal swabs and antibody tests for COVID-19 (when available) are not 100% reliable, the question of the origin of these strange chilblain-like lesions is still elusive.” Until further studies are available, they emphasized that clinicians should be “alert to the presentation of chilblain-like findings” in children with mild symptoms “as a possible sign of COVID-19 infection.”
All the patients had lesions on their feet or toes, and a 5-year-old boy also had lesions on the right hand. One patient, an 11-year-old girl, had a biopsy that revealed dense lymphocytic perivascular cuffing and periadnexal infiltration.
“The finding of an elevated d-dimer in one of our patients, along with the clinical features suggestive of a vasoocclusive phenomenon, supports consideration of laboratory evaluation for coagulation defects in asymptomatic or mildly symptomatic children with acrovasculitis-like findings,” Dr. Colonna and colleagues wrote. None of the four cases in Milan required treatment, with three cases resolving within 5 days.
Like the Milan cases, all 22 patients in the Madrid series had foot or toe lesions and three had lesions on the fingers. This larger series also reported more detailed symptoms about the lesions: pruritus in nine patients (41%) and mild pain in seven (32%). A total of 10 patients had systemic symptoms of COVID-19, predominantly cough and rhinorrhea in 9 patients (41%), but 2 (9%) had abdominal pain and diarrhea. These symptoms, the authors said, appeared a median of 14 days (range, 1-28 days) before they developed chilblains.
A total of 19 patients were tested for COVID-19, but only 1 was positive.
This retrospective study also included contact information, with one patient having household contact with a single confirmed case of COVID-19; 12 patients recalled household contact who were considered probable cases of COVID-19, with respiratory symptoms.
Skin biopsies were obtained from the acral lesions in six patients, all showing similar results, although with varying degrees of intensity. All biopsies showed features of lymphocytic vasculopathy. Some cases showed mild dermal and perieccrine mucinosis, lymphocytic eccrine hidradenitis, vascular ectasia, red cell extravasation and focal thrombosis described as “mostly confined to scattered papillary dermal capillaries, but also in vessels of the reticular dermis.”
The only treatments Dr. Andina and colleagues reported were oral analgesics for pain and oral antihistamines for pruritus when needed. One patient was given topical corticosteroids and another a short course of oral steroids, both for erythema multiforme.
Dr. Andina and colleagues wrote that the skin lesions in these patients “were unequivocally categorized as chilblains, both clinically and histopathologically,” and, after 7-10 days, began to fade. None of the patients had complications, and had an “excellent outcome,” they noted.
Dr. Colonna and colleagues had no conflicts of interest to declare. Dr. Andina and colleagues provided no disclosure statement.
SOURCES: Colonna C et al. Ped Derm. 2020 May 6. doi: 10.1111/pde.14210; Andina D et al. Ped Derm. 2020 May 9. doi: 10.1111/pde.14215.
FROM PEDIATRIC DERMATOLOGY
The SHM 2019 Chapter Excellence Awards
The Society of Hospital Medicine is proud to recognize its chapters for their hard work and dedication in 2019 through Chapter Excellence Awards. Each year, chapters strive to demonstrate growth, sustenance, and innovation within their chapter activities, which are then applauded for their successes throughout the subsequent year. In 2019, a new Bronze category was established, for a total of four Status Awards that chapters can earn.
Please join SHM in congratulating the following chapters on their year of success in 2019!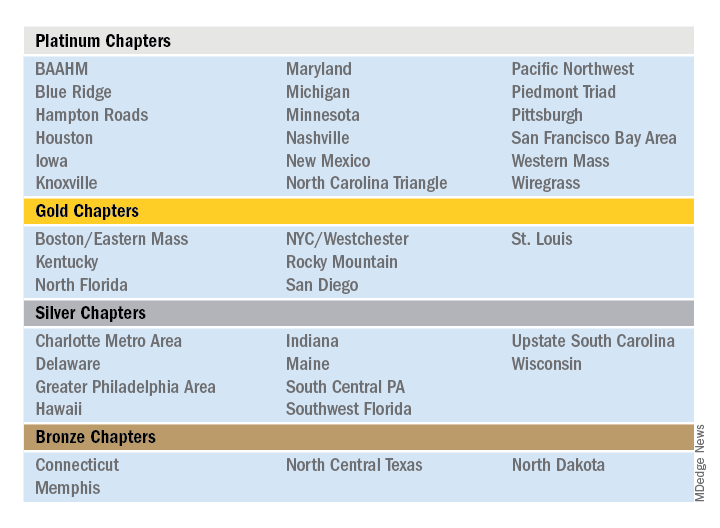
Outstanding Chapter of the Year
The Outstanding Chapter of the Year Award goes to one chapter who exemplifies high performance, going above and beyond the basic chapter requirements. The recipient of the Outstanding Chapter of the Year Award for 2019 is the Wiregrass Chapter of SHM. The chapter has a strong and engaged leadership which includes representation at all levels of the hospital medicine team, including physician hospitalists, advanced care provider hospitalists, practice administrators, nurses, residents, and medical students.
In the last year, the Wiregrass leadership team has organized programs and events to cater to and engage all the chapter’s members. This includes a variety of innovative ideas that catered toward medical education, health care provider well-being, engagement, mentorship, and community involvement.
The SHM Wiregrass Chapter’s biggest accomplishment in 2019 was the creation of an exchange program for physician and advanced practice provider hospitalists between the SHM New Mexico Chapter and the SHM Wiregrass Chapter. This idea first arose at HM19, where the chapter leaders had met during a networking event and debated the role of clinician wellbeing, quality of medical education, and faculty development to individual hospital medicine group (HMG) practice styles.
Clinician well-being is the prerequisite to the triple aim of improving the health of populations, enhancing the patient experience, and reducing the cost of care. Each HMG faces similar challenges but approaches to solving them vary. Professional challenges can affect the well-being of the individual clinicians. Having interinstitutional exchange programs provides a platform to exchange ideas and establish mentors. Also, the quality of medical education is directly linked to the quality of faculty development. Improving the quality of medical education requires a multifaceted approach by highly developed faculty. The complex factors affecting medical education and faculty development are further complicated by geographic location, patient characteristics, and professional growth opportunities. Overcoming these obstacles requires an innovative and collaborative approach. Although faculty exchanges are common in academic medicine, they are not commonly attempted with HMGs.
Hospitalists are responsible for a significant part of inpatient training for residents, medical students, and nurse practitioners/physician assistants (NPs/PAs), but their faculty training can vary based on location. Being a young specialty, only 2 decades old, hospital medicine is still evolving and incorporating NP/PA and physician hospitalists in varied practice models. Each HMG addresses common obstacles differently based on their culture and practice styles. The chapter leaders determined an exchange program would afford the opportunity for visiting faculty members to experience these differences. This emphasized the role and importance of exchanging ideas and contemplated a solution to benefit more practicing hospitalists.
The chapter leaders researched the characteristics of individual academic HMGs and structured a tailored faculty exchange involving physicians and NPs/PAs. During the exchange program planning, the visiting faculty itinerary was tailored to a well-planned agenda for 1 week, with separate tracks for physicians and NPs/PAs giving increased access to their individual peer practice styles. Additionally, the visiting faculty had meetings and discussions with HMG and hospital leadership, to specifically address each visiting faculty institution’s challenges. The overall goal of this exchange program was to promote cross-institutional collaboration, increase engagement, improve medical education through faculty development, and improve the quality of care. The focus of the exchange program was to share ideas and innovation and learn the approaches to unique challenges at each institution. Out of this also came collaboration and mentoring opportunities.
The evaluation process of the exchange involved interviews, a survey, and the establishment of shared QI projects in mutual areas of challenge. The survey provided feedback, lessons learned from the exchange, and areas to be improved. Collaborative QI projects currently underway as a result of the exchange include paging etiquette, quality of sleep for hospitalized patients, and onboarding of NPs/PAs in HMGs.
This innovation addressed faculty development and medical education via clinician well-being. The physician and NP/PA Faculty Exchange was an essential and meaningful innovation that resulted in increased SHM member engagement, cross-institutional collaboration, networking, and mentorship.
Additional projects that the SHM Wiregrass Chapter successfully implemented in 2019 include a “Women in Medicine” event that recognized women physician and advanced practice provider hospitalist leaders, a poster competition that expanded its research, clinical vignettes, and quality categories to include a fourth category of innovation, featuring 75 posters. Additionally, the chapter held a policy meeting with six Alabama state legislators, creating new channels of collaboration between the legislators and the chapter. Lastly, the chapter held a successful community event and launched a mentor program targeting medical students and residents.
Rising Star Chapter
The Rising Star Chapter Award goes to one chapter who has been active for 2 years or less, who in the past 12 months have made improvements to their leadership, stability and growth, and membership. The recipient of the Rising Star Chapter Award for 2019 is the Blue Ridge Chapter of SHM, which has made significant strides to develop since its launch in the fall of 2018. The chapter represents counties in northwest Tennessee, southwest Virginia, and western North Carolina.
The chapter held three meetings in 2019 which were well attended by hospitalists, residents/fellows, administrators, advanced practice providers, and nurses. On average, attendees from five to six different hospitalist groups are represented. The chapter hosted both Dr. Chris Frost, immediate past president of the SHM board of directors, and Dr. Ron Greeno, a past president of the SHM board of directors.
The SHM Blue Ridge Chapter has collaborated with both the ACP Tennessee Chapter and the Healthcare MBA program at Haslam College of Business at the University of Tennessee.
The chapter leadership regularly attends local medical residency programs at noon conferences to attract and recruit young physicians into chapter activities. Overall, the chapter has seen a growth in membership in 2019. The Blue Ridge Chapter is an active, enthusiastic chapter that is rapidly growing and thriving.
Outstanding Membership Recruitment and Retention
The Outstanding Membership Recruitment and Retention Award is a new exemplary award for 2019 that goes to one chapter who has gone above and beyond to implement initiatives to recruit and retain SHM members in their chapter. The recipient of the Outstanding Membership Recruitment and Retention Award for 2019 is the Western Massachusetts Chapter of SHM, which has done outstanding work to recruit and retain the membership. In 2019, the SHM membership in the chapter grew by 24%. The chapter utilized Chapter Development Funds to launch new initiatives to conduct outreach to nonmember hospitalists in the community and invite them to meetings to obtain the SHM experience. Additionally, the chapter encouraged residents to join and get involved by hosting a poster competition.
The Western Massachusetts Chapter focused on being innovative, inclusive, and creative to retain their existing meetings. For example, the chapter hosted a new “Jeopardy Session” event that featured a nontraditional jeopardy game that attracted a large attendance including local residents. Additionally, the chapter insured that all clinical and nonclinical members of the hospital medicine team were included and encouraged to participate in all chapter meetings. Lastly, the chapter launched a local awards program to recognize senior hospitalist and early career hospitalist who contributed to chapter development.
Most Engaged Chapter Leader
The Most Engaged Chapter Leader Award is a new exemplary award for 2019 that goes to one chapter leader or district chair who is either nominated or self-nominated and has demonstrated how they or their nominee has gone above and beyond in the past year to grow and sustain their chapter and/or district and continues to carry out the SHM mission. The recipient of the Most Engaged Chapter Leader Award for 2019 goes to Thérèse Franco, MD, SFHM, president of the Pacific Northwest Chapter.
Dr. Franco has served as the chapter’s president for 2 years and has served on the SHM Chapter Support Committee for 3 years. She has previously participated as a mentor in the glycemic control mentored implementation program, and as chair and cochair of the RIV contest. She continues to review abstracts, volunteer as a judge and offer local education on glycemic control through the Washington State Hospital Association, promoting SHM’s work there. One of Dr. Franco’s core strengths has been effective collaboration with past leaders (such as Rachel Thompson, MD, and Kimberly Bell, MD), future leaders, and other organizations (such as the Washington State Medical Association and the King County Medical Association). Dr. Franco has recruited an outstanding leadership team and new advisory committee for the Pacific Northwest Chapter, resulting a fantastic year of growth, innovation, and development.
The Society of Hospital Medicine is proud to recognize its chapters for their hard work and dedication in 2019 through Chapter Excellence Awards. Each year, chapters strive to demonstrate growth, sustenance, and innovation within their chapter activities, which are then applauded for their successes throughout the subsequent year. In 2019, a new Bronze category was established, for a total of four Status Awards that chapters can earn.
Please join SHM in congratulating the following chapters on their year of success in 2019!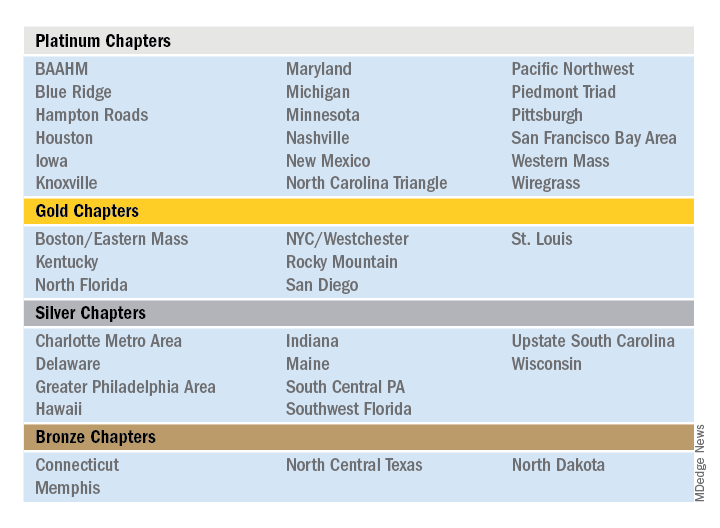
Outstanding Chapter of the Year
The Outstanding Chapter of the Year Award goes to one chapter who exemplifies high performance, going above and beyond the basic chapter requirements. The recipient of the Outstanding Chapter of the Year Award for 2019 is the Wiregrass Chapter of SHM. The chapter has a strong and engaged leadership which includes representation at all levels of the hospital medicine team, including physician hospitalists, advanced care provider hospitalists, practice administrators, nurses, residents, and medical students.
In the last year, the Wiregrass leadership team has organized programs and events to cater to and engage all the chapter’s members. This includes a variety of innovative ideas that catered toward medical education, health care provider well-being, engagement, mentorship, and community involvement.
The SHM Wiregrass Chapter’s biggest accomplishment in 2019 was the creation of an exchange program for physician and advanced practice provider hospitalists between the SHM New Mexico Chapter and the SHM Wiregrass Chapter. This idea first arose at HM19, where the chapter leaders had met during a networking event and debated the role of clinician wellbeing, quality of medical education, and faculty development to individual hospital medicine group (HMG) practice styles.
Clinician well-being is the prerequisite to the triple aim of improving the health of populations, enhancing the patient experience, and reducing the cost of care. Each HMG faces similar challenges but approaches to solving them vary. Professional challenges can affect the well-being of the individual clinicians. Having interinstitutional exchange programs provides a platform to exchange ideas and establish mentors. Also, the quality of medical education is directly linked to the quality of faculty development. Improving the quality of medical education requires a multifaceted approach by highly developed faculty. The complex factors affecting medical education and faculty development are further complicated by geographic location, patient characteristics, and professional growth opportunities. Overcoming these obstacles requires an innovative and collaborative approach. Although faculty exchanges are common in academic medicine, they are not commonly attempted with HMGs.
Hospitalists are responsible for a significant part of inpatient training for residents, medical students, and nurse practitioners/physician assistants (NPs/PAs), but their faculty training can vary based on location. Being a young specialty, only 2 decades old, hospital medicine is still evolving and incorporating NP/PA and physician hospitalists in varied practice models. Each HMG addresses common obstacles differently based on their culture and practice styles. The chapter leaders determined an exchange program would afford the opportunity for visiting faculty members to experience these differences. This emphasized the role and importance of exchanging ideas and contemplated a solution to benefit more practicing hospitalists.
The chapter leaders researched the characteristics of individual academic HMGs and structured a tailored faculty exchange involving physicians and NPs/PAs. During the exchange program planning, the visiting faculty itinerary was tailored to a well-planned agenda for 1 week, with separate tracks for physicians and NPs/PAs giving increased access to their individual peer practice styles. Additionally, the visiting faculty had meetings and discussions with HMG and hospital leadership, to specifically address each visiting faculty institution’s challenges. The overall goal of this exchange program was to promote cross-institutional collaboration, increase engagement, improve medical education through faculty development, and improve the quality of care. The focus of the exchange program was to share ideas and innovation and learn the approaches to unique challenges at each institution. Out of this also came collaboration and mentoring opportunities.
The evaluation process of the exchange involved interviews, a survey, and the establishment of shared QI projects in mutual areas of challenge. The survey provided feedback, lessons learned from the exchange, and areas to be improved. Collaborative QI projects currently underway as a result of the exchange include paging etiquette, quality of sleep for hospitalized patients, and onboarding of NPs/PAs in HMGs.
This innovation addressed faculty development and medical education via clinician well-being. The physician and NP/PA Faculty Exchange was an essential and meaningful innovation that resulted in increased SHM member engagement, cross-institutional collaboration, networking, and mentorship.
Additional projects that the SHM Wiregrass Chapter successfully implemented in 2019 include a “Women in Medicine” event that recognized women physician and advanced practice provider hospitalist leaders, a poster competition that expanded its research, clinical vignettes, and quality categories to include a fourth category of innovation, featuring 75 posters. Additionally, the chapter held a policy meeting with six Alabama state legislators, creating new channels of collaboration between the legislators and the chapter. Lastly, the chapter held a successful community event and launched a mentor program targeting medical students and residents.
Rising Star Chapter
The Rising Star Chapter Award goes to one chapter who has been active for 2 years or less, who in the past 12 months have made improvements to their leadership, stability and growth, and membership. The recipient of the Rising Star Chapter Award for 2019 is the Blue Ridge Chapter of SHM, which has made significant strides to develop since its launch in the fall of 2018. The chapter represents counties in northwest Tennessee, southwest Virginia, and western North Carolina.
The chapter held three meetings in 2019 which were well attended by hospitalists, residents/fellows, administrators, advanced practice providers, and nurses. On average, attendees from five to six different hospitalist groups are represented. The chapter hosted both Dr. Chris Frost, immediate past president of the SHM board of directors, and Dr. Ron Greeno, a past president of the SHM board of directors.
The SHM Blue Ridge Chapter has collaborated with both the ACP Tennessee Chapter and the Healthcare MBA program at Haslam College of Business at the University of Tennessee.
The chapter leadership regularly attends local medical residency programs at noon conferences to attract and recruit young physicians into chapter activities. Overall, the chapter has seen a growth in membership in 2019. The Blue Ridge Chapter is an active, enthusiastic chapter that is rapidly growing and thriving.
Outstanding Membership Recruitment and Retention
The Outstanding Membership Recruitment and Retention Award is a new exemplary award for 2019 that goes to one chapter who has gone above and beyond to implement initiatives to recruit and retain SHM members in their chapter. The recipient of the Outstanding Membership Recruitment and Retention Award for 2019 is the Western Massachusetts Chapter of SHM, which has done outstanding work to recruit and retain the membership. In 2019, the SHM membership in the chapter grew by 24%. The chapter utilized Chapter Development Funds to launch new initiatives to conduct outreach to nonmember hospitalists in the community and invite them to meetings to obtain the SHM experience. Additionally, the chapter encouraged residents to join and get involved by hosting a poster competition.
The Western Massachusetts Chapter focused on being innovative, inclusive, and creative to retain their existing meetings. For example, the chapter hosted a new “Jeopardy Session” event that featured a nontraditional jeopardy game that attracted a large attendance including local residents. Additionally, the chapter insured that all clinical and nonclinical members of the hospital medicine team were included and encouraged to participate in all chapter meetings. Lastly, the chapter launched a local awards program to recognize senior hospitalist and early career hospitalist who contributed to chapter development.
Most Engaged Chapter Leader
The Most Engaged Chapter Leader Award is a new exemplary award for 2019 that goes to one chapter leader or district chair who is either nominated or self-nominated and has demonstrated how they or their nominee has gone above and beyond in the past year to grow and sustain their chapter and/or district and continues to carry out the SHM mission. The recipient of the Most Engaged Chapter Leader Award for 2019 goes to Thérèse Franco, MD, SFHM, president of the Pacific Northwest Chapter.
Dr. Franco has served as the chapter’s president for 2 years and has served on the SHM Chapter Support Committee for 3 years. She has previously participated as a mentor in the glycemic control mentored implementation program, and as chair and cochair of the RIV contest. She continues to review abstracts, volunteer as a judge and offer local education on glycemic control through the Washington State Hospital Association, promoting SHM’s work there. One of Dr. Franco’s core strengths has been effective collaboration with past leaders (such as Rachel Thompson, MD, and Kimberly Bell, MD), future leaders, and other organizations (such as the Washington State Medical Association and the King County Medical Association). Dr. Franco has recruited an outstanding leadership team and new advisory committee for the Pacific Northwest Chapter, resulting a fantastic year of growth, innovation, and development.
The Society of Hospital Medicine is proud to recognize its chapters for their hard work and dedication in 2019 through Chapter Excellence Awards. Each year, chapters strive to demonstrate growth, sustenance, and innovation within their chapter activities, which are then applauded for their successes throughout the subsequent year. In 2019, a new Bronze category was established, for a total of four Status Awards that chapters can earn.
Please join SHM in congratulating the following chapters on their year of success in 2019!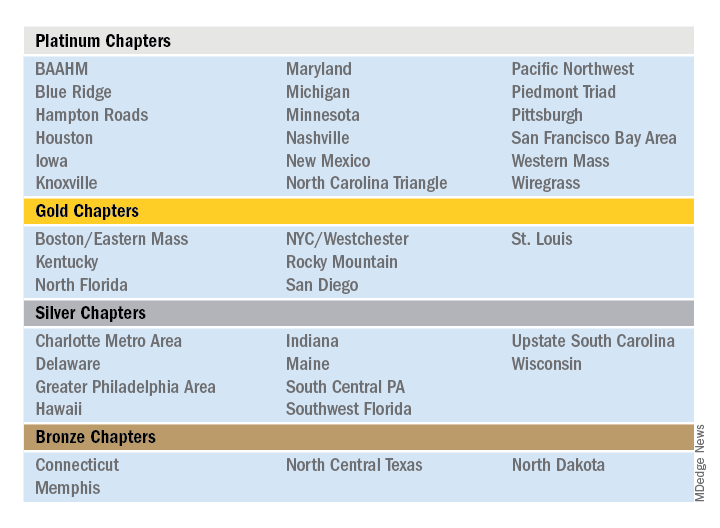
Outstanding Chapter of the Year
The Outstanding Chapter of the Year Award goes to one chapter who exemplifies high performance, going above and beyond the basic chapter requirements. The recipient of the Outstanding Chapter of the Year Award for 2019 is the Wiregrass Chapter of SHM. The chapter has a strong and engaged leadership which includes representation at all levels of the hospital medicine team, including physician hospitalists, advanced care provider hospitalists, practice administrators, nurses, residents, and medical students.
In the last year, the Wiregrass leadership team has organized programs and events to cater to and engage all the chapter’s members. This includes a variety of innovative ideas that catered toward medical education, health care provider well-being, engagement, mentorship, and community involvement.
The SHM Wiregrass Chapter’s biggest accomplishment in 2019 was the creation of an exchange program for physician and advanced practice provider hospitalists between the SHM New Mexico Chapter and the SHM Wiregrass Chapter. This idea first arose at HM19, where the chapter leaders had met during a networking event and debated the role of clinician wellbeing, quality of medical education, and faculty development to individual hospital medicine group (HMG) practice styles.
Clinician well-being is the prerequisite to the triple aim of improving the health of populations, enhancing the patient experience, and reducing the cost of care. Each HMG faces similar challenges but approaches to solving them vary. Professional challenges can affect the well-being of the individual clinicians. Having interinstitutional exchange programs provides a platform to exchange ideas and establish mentors. Also, the quality of medical education is directly linked to the quality of faculty development. Improving the quality of medical education requires a multifaceted approach by highly developed faculty. The complex factors affecting medical education and faculty development are further complicated by geographic location, patient characteristics, and professional growth opportunities. Overcoming these obstacles requires an innovative and collaborative approach. Although faculty exchanges are common in academic medicine, they are not commonly attempted with HMGs.
Hospitalists are responsible for a significant part of inpatient training for residents, medical students, and nurse practitioners/physician assistants (NPs/PAs), but their faculty training can vary based on location. Being a young specialty, only 2 decades old, hospital medicine is still evolving and incorporating NP/PA and physician hospitalists in varied practice models. Each HMG addresses common obstacles differently based on their culture and practice styles. The chapter leaders determined an exchange program would afford the opportunity for visiting faculty members to experience these differences. This emphasized the role and importance of exchanging ideas and contemplated a solution to benefit more practicing hospitalists.
The chapter leaders researched the characteristics of individual academic HMGs and structured a tailored faculty exchange involving physicians and NPs/PAs. During the exchange program planning, the visiting faculty itinerary was tailored to a well-planned agenda for 1 week, with separate tracks for physicians and NPs/PAs giving increased access to their individual peer practice styles. Additionally, the visiting faculty had meetings and discussions with HMG and hospital leadership, to specifically address each visiting faculty institution’s challenges. The overall goal of this exchange program was to promote cross-institutional collaboration, increase engagement, improve medical education through faculty development, and improve the quality of care. The focus of the exchange program was to share ideas and innovation and learn the approaches to unique challenges at each institution. Out of this also came collaboration and mentoring opportunities.
The evaluation process of the exchange involved interviews, a survey, and the establishment of shared QI projects in mutual areas of challenge. The survey provided feedback, lessons learned from the exchange, and areas to be improved. Collaborative QI projects currently underway as a result of the exchange include paging etiquette, quality of sleep for hospitalized patients, and onboarding of NPs/PAs in HMGs.
This innovation addressed faculty development and medical education via clinician well-being. The physician and NP/PA Faculty Exchange was an essential and meaningful innovation that resulted in increased SHM member engagement, cross-institutional collaboration, networking, and mentorship.
Additional projects that the SHM Wiregrass Chapter successfully implemented in 2019 include a “Women in Medicine” event that recognized women physician and advanced practice provider hospitalist leaders, a poster competition that expanded its research, clinical vignettes, and quality categories to include a fourth category of innovation, featuring 75 posters. Additionally, the chapter held a policy meeting with six Alabama state legislators, creating new channels of collaboration between the legislators and the chapter. Lastly, the chapter held a successful community event and launched a mentor program targeting medical students and residents.
Rising Star Chapter
The Rising Star Chapter Award goes to one chapter who has been active for 2 years or less, who in the past 12 months have made improvements to their leadership, stability and growth, and membership. The recipient of the Rising Star Chapter Award for 2019 is the Blue Ridge Chapter of SHM, which has made significant strides to develop since its launch in the fall of 2018. The chapter represents counties in northwest Tennessee, southwest Virginia, and western North Carolina.
The chapter held three meetings in 2019 which were well attended by hospitalists, residents/fellows, administrators, advanced practice providers, and nurses. On average, attendees from five to six different hospitalist groups are represented. The chapter hosted both Dr. Chris Frost, immediate past president of the SHM board of directors, and Dr. Ron Greeno, a past president of the SHM board of directors.
The SHM Blue Ridge Chapter has collaborated with both the ACP Tennessee Chapter and the Healthcare MBA program at Haslam College of Business at the University of Tennessee.
The chapter leadership regularly attends local medical residency programs at noon conferences to attract and recruit young physicians into chapter activities. Overall, the chapter has seen a growth in membership in 2019. The Blue Ridge Chapter is an active, enthusiastic chapter that is rapidly growing and thriving.
Outstanding Membership Recruitment and Retention
The Outstanding Membership Recruitment and Retention Award is a new exemplary award for 2019 that goes to one chapter who has gone above and beyond to implement initiatives to recruit and retain SHM members in their chapter. The recipient of the Outstanding Membership Recruitment and Retention Award for 2019 is the Western Massachusetts Chapter of SHM, which has done outstanding work to recruit and retain the membership. In 2019, the SHM membership in the chapter grew by 24%. The chapter utilized Chapter Development Funds to launch new initiatives to conduct outreach to nonmember hospitalists in the community and invite them to meetings to obtain the SHM experience. Additionally, the chapter encouraged residents to join and get involved by hosting a poster competition.
The Western Massachusetts Chapter focused on being innovative, inclusive, and creative to retain their existing meetings. For example, the chapter hosted a new “Jeopardy Session” event that featured a nontraditional jeopardy game that attracted a large attendance including local residents. Additionally, the chapter insured that all clinical and nonclinical members of the hospital medicine team were included and encouraged to participate in all chapter meetings. Lastly, the chapter launched a local awards program to recognize senior hospitalist and early career hospitalist who contributed to chapter development.
Most Engaged Chapter Leader
The Most Engaged Chapter Leader Award is a new exemplary award for 2019 that goes to one chapter leader or district chair who is either nominated or self-nominated and has demonstrated how they or their nominee has gone above and beyond in the past year to grow and sustain their chapter and/or district and continues to carry out the SHM mission. The recipient of the Most Engaged Chapter Leader Award for 2019 goes to Thérèse Franco, MD, SFHM, president of the Pacific Northwest Chapter.
Dr. Franco has served as the chapter’s president for 2 years and has served on the SHM Chapter Support Committee for 3 years. She has previously participated as a mentor in the glycemic control mentored implementation program, and as chair and cochair of the RIV contest. She continues to review abstracts, volunteer as a judge and offer local education on glycemic control through the Washington State Hospital Association, promoting SHM’s work there. One of Dr. Franco’s core strengths has been effective collaboration with past leaders (such as Rachel Thompson, MD, and Kimberly Bell, MD), future leaders, and other organizations (such as the Washington State Medical Association and the King County Medical Association). Dr. Franco has recruited an outstanding leadership team and new advisory committee for the Pacific Northwest Chapter, resulting a fantastic year of growth, innovation, and development.
Large COVID-19 dataset: Kidney injury in >35% of those in hospital
As a new report shows that over a third of U.S. patients hospitalized with COVID-19 developed acute kidney injury (AKI), and nearly 15% of these patients needed dialysis, experts in the field are calling for more robust research into multiple aspects of this increasingly important issue.
Among 5,449 patients admitted to 13 Northwell Health New York–based hospitals between March and April 2020, 36.6% (1,993) developed AKI.
– the rate of kidney injury was 89.7% among ventilated patients, compared with 21.7% among other patients.
AKI in COVID-19 was also linked to a poor prognosis: 35% of those who developed AKI had died at the time of publication.
The study includes the largest defined cohort of hospitalized COVID-19 patients to date with a focus on AKI, says Jamie S. Hirsch, MD, of Northwell Health in Great Neck, N.Y., and colleagues in their article published online in Kidney International.
The findings track with those of a study of New York hospitals published online in The Lancet. In that dataset, just under a third (31%) of critically ill patients developed severe kidney damage and needed dialysis.
Both of these studies help solidify the experiences of clinicians on the ground, with many U.S. hospitals in the early phases of the pandemic underestimating the problem of AKI and having to scramble to find enough dialysis machines and dialysate solution to treat the most severely affected patients.
“We hope to learn more about the COVID-19–related AKI in the coming weeks, and that by sharing what we have learned from our patients, other doctors and their patients can benefit,” said senior author of the new study, Kenar D. Jhaveri, MD, associated chief of nephrology at Hofstra/Northwell.
The new report also comes as scientists from the National Institute of Diabetes and Digestive and Kidney Diseases highlighted the importance of AKI as a sequela of COVID-19 in an editorial published in Diabetes Care.
They, too, said that it is vitally important to better understand what is happening, as more and more hospitals will face COVID-19 patients with this complication.
“The natural history and heterogeneity of the kidney disease caused by COVID-19 need to be unraveled,” one of the authors, Robert A. Star, MD, director of the division of kidney, urologic, and hematologic diseases at NIDDK, said in an interview.
Such research is key because “low kidney function is an exclusion criterion in current studies” examining antiviral medications in COVID-19, he said. “Clinical trials are needed to test therapeutic interventions to prevent or treat COVID-19–induced AKI.”
Extremely ill patients develop AKI as their condition deteriorates
Identifying risk factors for the development of AKI in COVID-19 will be critical in helping shed more light on diagnostic and predictive biomarkers, Dr. Star said.
Dr. Hirsch and colleagues said that extremely ill patients often develop kidney failure as their condition deteriorates, and this happens quickly. Indeed, the clearest risk factors for the development of AKI were “the need for ventilator support or vasopressor drug treatment.”
Other independent predictors of AKI were older age, black race, diabetes, hypertension, and cardiovascular disease.
Of those on mechanical ventilation overall in the more than 5,000-patient study, almost a quarter (23.2%) developed AKI and needed renal replacement therapy, which consisted of either intermittent or continuous hemodialysis.
Dr. Star and associates wrote that these numbers are important because of the knock-on effects.
“Hemodialysis in critically ill infected patients is associated with significant clotting complications and mortality as well as increased infection risk to staff,” they pointed out.
Dr. Star said that “the incidence rate of AKI reported in this study is higher than what had been previously reported by others in the United States and China and may reflect differences in population demographics, severity of illness, prevalence of comorbidities, socioeconomic factors, patient volume overwhelming hospital capacity, or other factors not yet determined.
“It may be caused by dehydration (volume depletion), heart failure, the inflammatory response to the virus (cytokine storm), respiratory failure, clotting of blood vessels (hypercoagulation), muscle tissue breakdown (rhabdomyolysis), and/or a direct viral infection of the kidney,” he said.
Renal biopsies from patients with AKI may help shed some light
The editorialists went on to say that findings from kidney biopsies of COVID-19 patients with AKI may help shed some light on this condition.
“While difficult to perform, kidney biopsies from patients with early AKI could help us understand the underlying pathophysiologies at the cellular and molecular level and begin to target specific treatments to specific subgroups of patients,” they wrote.
The authors noted that, as part of funding opportunities provided by the National Institutes of Health for COVID-19 research, the NIDDK has published a Notice of Special Interest outlining the most urgent areas in need of research, with one of the focuses being on the kidney.
“As the research community emerges from the crisis situation, there should be renewed efforts for multidisciplinary research to conduct integrated basic, translational, and clinical studies aimed at greatly increasing the knowledge base to understand how both the current COVID-19 threat and future health threats affect both healthy people and people with chronic diseases and conditions,” the editorials noted.
The authors of the Diabetes Care editorial have reported no relevant financial relationships. Dr. Jhaveri has reported being a consultant for Astex Pharmaceuticals.
A version of this article originally appeared on Medscape.com.
As a new report shows that over a third of U.S. patients hospitalized with COVID-19 developed acute kidney injury (AKI), and nearly 15% of these patients needed dialysis, experts in the field are calling for more robust research into multiple aspects of this increasingly important issue.
Among 5,449 patients admitted to 13 Northwell Health New York–based hospitals between March and April 2020, 36.6% (1,993) developed AKI.
– the rate of kidney injury was 89.7% among ventilated patients, compared with 21.7% among other patients.
AKI in COVID-19 was also linked to a poor prognosis: 35% of those who developed AKI had died at the time of publication.
The study includes the largest defined cohort of hospitalized COVID-19 patients to date with a focus on AKI, says Jamie S. Hirsch, MD, of Northwell Health in Great Neck, N.Y., and colleagues in their article published online in Kidney International.
The findings track with those of a study of New York hospitals published online in The Lancet. In that dataset, just under a third (31%) of critically ill patients developed severe kidney damage and needed dialysis.
Both of these studies help solidify the experiences of clinicians on the ground, with many U.S. hospitals in the early phases of the pandemic underestimating the problem of AKI and having to scramble to find enough dialysis machines and dialysate solution to treat the most severely affected patients.
“We hope to learn more about the COVID-19–related AKI in the coming weeks, and that by sharing what we have learned from our patients, other doctors and their patients can benefit,” said senior author of the new study, Kenar D. Jhaveri, MD, associated chief of nephrology at Hofstra/Northwell.
The new report also comes as scientists from the National Institute of Diabetes and Digestive and Kidney Diseases highlighted the importance of AKI as a sequela of COVID-19 in an editorial published in Diabetes Care.
They, too, said that it is vitally important to better understand what is happening, as more and more hospitals will face COVID-19 patients with this complication.
“The natural history and heterogeneity of the kidney disease caused by COVID-19 need to be unraveled,” one of the authors, Robert A. Star, MD, director of the division of kidney, urologic, and hematologic diseases at NIDDK, said in an interview.
Such research is key because “low kidney function is an exclusion criterion in current studies” examining antiviral medications in COVID-19, he said. “Clinical trials are needed to test therapeutic interventions to prevent or treat COVID-19–induced AKI.”
Extremely ill patients develop AKI as their condition deteriorates
Identifying risk factors for the development of AKI in COVID-19 will be critical in helping shed more light on diagnostic and predictive biomarkers, Dr. Star said.
Dr. Hirsch and colleagues said that extremely ill patients often develop kidney failure as their condition deteriorates, and this happens quickly. Indeed, the clearest risk factors for the development of AKI were “the need for ventilator support or vasopressor drug treatment.”
Other independent predictors of AKI were older age, black race, diabetes, hypertension, and cardiovascular disease.
Of those on mechanical ventilation overall in the more than 5,000-patient study, almost a quarter (23.2%) developed AKI and needed renal replacement therapy, which consisted of either intermittent or continuous hemodialysis.
Dr. Star and associates wrote that these numbers are important because of the knock-on effects.
“Hemodialysis in critically ill infected patients is associated with significant clotting complications and mortality as well as increased infection risk to staff,” they pointed out.
Dr. Star said that “the incidence rate of AKI reported in this study is higher than what had been previously reported by others in the United States and China and may reflect differences in population demographics, severity of illness, prevalence of comorbidities, socioeconomic factors, patient volume overwhelming hospital capacity, or other factors not yet determined.
“It may be caused by dehydration (volume depletion), heart failure, the inflammatory response to the virus (cytokine storm), respiratory failure, clotting of blood vessels (hypercoagulation), muscle tissue breakdown (rhabdomyolysis), and/or a direct viral infection of the kidney,” he said.
Renal biopsies from patients with AKI may help shed some light
The editorialists went on to say that findings from kidney biopsies of COVID-19 patients with AKI may help shed some light on this condition.
“While difficult to perform, kidney biopsies from patients with early AKI could help us understand the underlying pathophysiologies at the cellular and molecular level and begin to target specific treatments to specific subgroups of patients,” they wrote.
The authors noted that, as part of funding opportunities provided by the National Institutes of Health for COVID-19 research, the NIDDK has published a Notice of Special Interest outlining the most urgent areas in need of research, with one of the focuses being on the kidney.
“As the research community emerges from the crisis situation, there should be renewed efforts for multidisciplinary research to conduct integrated basic, translational, and clinical studies aimed at greatly increasing the knowledge base to understand how both the current COVID-19 threat and future health threats affect both healthy people and people with chronic diseases and conditions,” the editorials noted.
The authors of the Diabetes Care editorial have reported no relevant financial relationships. Dr. Jhaveri has reported being a consultant for Astex Pharmaceuticals.
A version of this article originally appeared on Medscape.com.
As a new report shows that over a third of U.S. patients hospitalized with COVID-19 developed acute kidney injury (AKI), and nearly 15% of these patients needed dialysis, experts in the field are calling for more robust research into multiple aspects of this increasingly important issue.
Among 5,449 patients admitted to 13 Northwell Health New York–based hospitals between March and April 2020, 36.6% (1,993) developed AKI.
– the rate of kidney injury was 89.7% among ventilated patients, compared with 21.7% among other patients.
AKI in COVID-19 was also linked to a poor prognosis: 35% of those who developed AKI had died at the time of publication.
The study includes the largest defined cohort of hospitalized COVID-19 patients to date with a focus on AKI, says Jamie S. Hirsch, MD, of Northwell Health in Great Neck, N.Y., and colleagues in their article published online in Kidney International.
The findings track with those of a study of New York hospitals published online in The Lancet. In that dataset, just under a third (31%) of critically ill patients developed severe kidney damage and needed dialysis.
Both of these studies help solidify the experiences of clinicians on the ground, with many U.S. hospitals in the early phases of the pandemic underestimating the problem of AKI and having to scramble to find enough dialysis machines and dialysate solution to treat the most severely affected patients.
“We hope to learn more about the COVID-19–related AKI in the coming weeks, and that by sharing what we have learned from our patients, other doctors and their patients can benefit,” said senior author of the new study, Kenar D. Jhaveri, MD, associated chief of nephrology at Hofstra/Northwell.
The new report also comes as scientists from the National Institute of Diabetes and Digestive and Kidney Diseases highlighted the importance of AKI as a sequela of COVID-19 in an editorial published in Diabetes Care.
They, too, said that it is vitally important to better understand what is happening, as more and more hospitals will face COVID-19 patients with this complication.
“The natural history and heterogeneity of the kidney disease caused by COVID-19 need to be unraveled,” one of the authors, Robert A. Star, MD, director of the division of kidney, urologic, and hematologic diseases at NIDDK, said in an interview.
Such research is key because “low kidney function is an exclusion criterion in current studies” examining antiviral medications in COVID-19, he said. “Clinical trials are needed to test therapeutic interventions to prevent or treat COVID-19–induced AKI.”
Extremely ill patients develop AKI as their condition deteriorates
Identifying risk factors for the development of AKI in COVID-19 will be critical in helping shed more light on diagnostic and predictive biomarkers, Dr. Star said.
Dr. Hirsch and colleagues said that extremely ill patients often develop kidney failure as their condition deteriorates, and this happens quickly. Indeed, the clearest risk factors for the development of AKI were “the need for ventilator support or vasopressor drug treatment.”
Other independent predictors of AKI were older age, black race, diabetes, hypertension, and cardiovascular disease.
Of those on mechanical ventilation overall in the more than 5,000-patient study, almost a quarter (23.2%) developed AKI and needed renal replacement therapy, which consisted of either intermittent or continuous hemodialysis.
Dr. Star and associates wrote that these numbers are important because of the knock-on effects.
“Hemodialysis in critically ill infected patients is associated with significant clotting complications and mortality as well as increased infection risk to staff,” they pointed out.
Dr. Star said that “the incidence rate of AKI reported in this study is higher than what had been previously reported by others in the United States and China and may reflect differences in population demographics, severity of illness, prevalence of comorbidities, socioeconomic factors, patient volume overwhelming hospital capacity, or other factors not yet determined.
“It may be caused by dehydration (volume depletion), heart failure, the inflammatory response to the virus (cytokine storm), respiratory failure, clotting of blood vessels (hypercoagulation), muscle tissue breakdown (rhabdomyolysis), and/or a direct viral infection of the kidney,” he said.
Renal biopsies from patients with AKI may help shed some light
The editorialists went on to say that findings from kidney biopsies of COVID-19 patients with AKI may help shed some light on this condition.
“While difficult to perform, kidney biopsies from patients with early AKI could help us understand the underlying pathophysiologies at the cellular and molecular level and begin to target specific treatments to specific subgroups of patients,” they wrote.
The authors noted that, as part of funding opportunities provided by the National Institutes of Health for COVID-19 research, the NIDDK has published a Notice of Special Interest outlining the most urgent areas in need of research, with one of the focuses being on the kidney.
“As the research community emerges from the crisis situation, there should be renewed efforts for multidisciplinary research to conduct integrated basic, translational, and clinical studies aimed at greatly increasing the knowledge base to understand how both the current COVID-19 threat and future health threats affect both healthy people and people with chronic diseases and conditions,” the editorials noted.
The authors of the Diabetes Care editorial have reported no relevant financial relationships. Dr. Jhaveri has reported being a consultant for Astex Pharmaceuticals.
A version of this article originally appeared on Medscape.com.
AAN publishes ethical guidance on patient care during the pandemic
The document, which was published online May 15 in Neurology, reviews adaptations to the inpatient and outpatient settings and addresses the need to develop protocols for the allocation of scarce medical resources. The guidance is the product of a joint committee of the AAN, the American Neurological Association, the Child Neurology Society, and the Neurocritical Care Society Ethics Committee.
“Now is one of the most challenging times of our careers as neurologists,” said James C. Stevens, MD, president of the AAN, in a press release. “Clinics and hospitals are adapting to caring for the most ill, managing scarce resources, and trying to protect people without the disease. As neurologists, we must continue to adapt our daily practice, continue to care for our most ill neurology patients, and help contribute to the care of those afflicted with COVID-19.”
The role of telehealth
The authors recommended that ordinary appointments be held using telehealth, which, they say, already has become part of patient care. Telehealth enables neurologists to continue providing care while reducing the risk of exposure to and spread of SARS-CoV-2. The disadvantages of telehealth are that it limits physical examinations and behavioral health examinations, the authors acknowledged. “Each clinician should decide, in concert with his or her patient, if an in-person evaluation warrants the risk of an encounter,” according to the guidance.
Neurologists also should advise their patients that their neurologic condition could affect their relative risk of hospitalization and death resulting from COVID-19. Patients with multiple sclerosis or myasthenia gravis, for example, may be receiving corticosteroids or immunomodulatory therapies that make them more vulnerable to COVID-19 infection. “Even if desired services are available, neurologists and their patients ought to consider whether their care plans can safely be delayed in order to mitigate risk,” wrote the authors. Neurologists must try to maintain the customary standard of care, however, for patients with neurologic disease severe enough to warrant hospitalization, such as stroke or epilepsy.
The potential need for triage
Resources such as ventilators and ICU beds are limited, and health care facilities have had to triage them during the pandemic. Patients with a neurologic disease that decreases their likelihood of survival from a respiratory illness may not be offered these resources. Neurologists should discuss with patients and decision makers the ways in which reduced resources might affect patient care. Neurologists must “be aware of the burden of disease in their local community and how healthcare leaders plan on coping with a surge,” according to the guidance.
Advance directives, which should be a standard part of clinical care, take on increased importance during the pandemic. Patients who have not completed advance care planning documents should be encouraged to do so, according to the authors. These documents include patients’ preferences for “do not attempt resuscitation” status. Nevertheless, “we must assure patients with chronic illness that diminished resources in this healthcare crisis will not restrict their access to comfort and palliative care,” the document states.
Scarce resource allocation protocols
In the event that a surge in patients overwhelms a hospital’s contingencies and forces it to operate in crisis mode, it should have a scarce resource allocation protocol in place.
“This will surely be the most challenging aspect of patient care during this pandemic public health emergency,” wrote the authors. To ensure transparency and to mitigate the emotional effect of these decisions on patients and clinicians, scarce resource allocation protocols should be developed by teams that include intensivists, clinical ethicists, and nursing representatives who are not directly involved in the care of the critically ill patients. The goal of these protocols is to maximize the number of lives saved. They generally include an initial patient assessment followed by regular reevaluations to determine whether patients using scarce resources are benefiting less than other patients who need the same resources. The protocols should consider not only patients with COVID-19 infection, but also patients with stroke, traumatic injury, influenza, and heart failure who may need the same resources. Race, gender, ethnicity, socioeconomics, and perceived social worth should not influence care decisions, according to the guidance. Validated mortality prediction scales, such as the Glasgow Outcome Scale, can contribute to care decisions. Obtaining community input into these protocols will ensure trust in the health care system.
“If the situation necessitates hard decisions, we need to be fair, objective, transparent, and adamantly preserve our professional integrity,” wrote the authors. “Through it all, we owe it to our patients and families, as well as ourselves, to maintain our own health and wellness.”
The guidance was developed without funding, and the authors reported no relevant disclosures.
SOURCE: Rubin MA et al. Neurology. 2020 May 15. doi: 10.1212/WNL.0000000000009744.
The document, which was published online May 15 in Neurology, reviews adaptations to the inpatient and outpatient settings and addresses the need to develop protocols for the allocation of scarce medical resources. The guidance is the product of a joint committee of the AAN, the American Neurological Association, the Child Neurology Society, and the Neurocritical Care Society Ethics Committee.
“Now is one of the most challenging times of our careers as neurologists,” said James C. Stevens, MD, president of the AAN, in a press release. “Clinics and hospitals are adapting to caring for the most ill, managing scarce resources, and trying to protect people without the disease. As neurologists, we must continue to adapt our daily practice, continue to care for our most ill neurology patients, and help contribute to the care of those afflicted with COVID-19.”
The role of telehealth
The authors recommended that ordinary appointments be held using telehealth, which, they say, already has become part of patient care. Telehealth enables neurologists to continue providing care while reducing the risk of exposure to and spread of SARS-CoV-2. The disadvantages of telehealth are that it limits physical examinations and behavioral health examinations, the authors acknowledged. “Each clinician should decide, in concert with his or her patient, if an in-person evaluation warrants the risk of an encounter,” according to the guidance.
Neurologists also should advise their patients that their neurologic condition could affect their relative risk of hospitalization and death resulting from COVID-19. Patients with multiple sclerosis or myasthenia gravis, for example, may be receiving corticosteroids or immunomodulatory therapies that make them more vulnerable to COVID-19 infection. “Even if desired services are available, neurologists and their patients ought to consider whether their care plans can safely be delayed in order to mitigate risk,” wrote the authors. Neurologists must try to maintain the customary standard of care, however, for patients with neurologic disease severe enough to warrant hospitalization, such as stroke or epilepsy.
The potential need for triage
Resources such as ventilators and ICU beds are limited, and health care facilities have had to triage them during the pandemic. Patients with a neurologic disease that decreases their likelihood of survival from a respiratory illness may not be offered these resources. Neurologists should discuss with patients and decision makers the ways in which reduced resources might affect patient care. Neurologists must “be aware of the burden of disease in their local community and how healthcare leaders plan on coping with a surge,” according to the guidance.
Advance directives, which should be a standard part of clinical care, take on increased importance during the pandemic. Patients who have not completed advance care planning documents should be encouraged to do so, according to the authors. These documents include patients’ preferences for “do not attempt resuscitation” status. Nevertheless, “we must assure patients with chronic illness that diminished resources in this healthcare crisis will not restrict their access to comfort and palliative care,” the document states.
Scarce resource allocation protocols
In the event that a surge in patients overwhelms a hospital’s contingencies and forces it to operate in crisis mode, it should have a scarce resource allocation protocol in place.
“This will surely be the most challenging aspect of patient care during this pandemic public health emergency,” wrote the authors. To ensure transparency and to mitigate the emotional effect of these decisions on patients and clinicians, scarce resource allocation protocols should be developed by teams that include intensivists, clinical ethicists, and nursing representatives who are not directly involved in the care of the critically ill patients. The goal of these protocols is to maximize the number of lives saved. They generally include an initial patient assessment followed by regular reevaluations to determine whether patients using scarce resources are benefiting less than other patients who need the same resources. The protocols should consider not only patients with COVID-19 infection, but also patients with stroke, traumatic injury, influenza, and heart failure who may need the same resources. Race, gender, ethnicity, socioeconomics, and perceived social worth should not influence care decisions, according to the guidance. Validated mortality prediction scales, such as the Glasgow Outcome Scale, can contribute to care decisions. Obtaining community input into these protocols will ensure trust in the health care system.
“If the situation necessitates hard decisions, we need to be fair, objective, transparent, and adamantly preserve our professional integrity,” wrote the authors. “Through it all, we owe it to our patients and families, as well as ourselves, to maintain our own health and wellness.”
The guidance was developed without funding, and the authors reported no relevant disclosures.
SOURCE: Rubin MA et al. Neurology. 2020 May 15. doi: 10.1212/WNL.0000000000009744.
The document, which was published online May 15 in Neurology, reviews adaptations to the inpatient and outpatient settings and addresses the need to develop protocols for the allocation of scarce medical resources. The guidance is the product of a joint committee of the AAN, the American Neurological Association, the Child Neurology Society, and the Neurocritical Care Society Ethics Committee.
“Now is one of the most challenging times of our careers as neurologists,” said James C. Stevens, MD, president of the AAN, in a press release. “Clinics and hospitals are adapting to caring for the most ill, managing scarce resources, and trying to protect people without the disease. As neurologists, we must continue to adapt our daily practice, continue to care for our most ill neurology patients, and help contribute to the care of those afflicted with COVID-19.”
The role of telehealth
The authors recommended that ordinary appointments be held using telehealth, which, they say, already has become part of patient care. Telehealth enables neurologists to continue providing care while reducing the risk of exposure to and spread of SARS-CoV-2. The disadvantages of telehealth are that it limits physical examinations and behavioral health examinations, the authors acknowledged. “Each clinician should decide, in concert with his or her patient, if an in-person evaluation warrants the risk of an encounter,” according to the guidance.
Neurologists also should advise their patients that their neurologic condition could affect their relative risk of hospitalization and death resulting from COVID-19. Patients with multiple sclerosis or myasthenia gravis, for example, may be receiving corticosteroids or immunomodulatory therapies that make them more vulnerable to COVID-19 infection. “Even if desired services are available, neurologists and their patients ought to consider whether their care plans can safely be delayed in order to mitigate risk,” wrote the authors. Neurologists must try to maintain the customary standard of care, however, for patients with neurologic disease severe enough to warrant hospitalization, such as stroke or epilepsy.
The potential need for triage
Resources such as ventilators and ICU beds are limited, and health care facilities have had to triage them during the pandemic. Patients with a neurologic disease that decreases their likelihood of survival from a respiratory illness may not be offered these resources. Neurologists should discuss with patients and decision makers the ways in which reduced resources might affect patient care. Neurologists must “be aware of the burden of disease in their local community and how healthcare leaders plan on coping with a surge,” according to the guidance.
Advance directives, which should be a standard part of clinical care, take on increased importance during the pandemic. Patients who have not completed advance care planning documents should be encouraged to do so, according to the authors. These documents include patients’ preferences for “do not attempt resuscitation” status. Nevertheless, “we must assure patients with chronic illness that diminished resources in this healthcare crisis will not restrict their access to comfort and palliative care,” the document states.
Scarce resource allocation protocols
In the event that a surge in patients overwhelms a hospital’s contingencies and forces it to operate in crisis mode, it should have a scarce resource allocation protocol in place.
“This will surely be the most challenging aspect of patient care during this pandemic public health emergency,” wrote the authors. To ensure transparency and to mitigate the emotional effect of these decisions on patients and clinicians, scarce resource allocation protocols should be developed by teams that include intensivists, clinical ethicists, and nursing representatives who are not directly involved in the care of the critically ill patients. The goal of these protocols is to maximize the number of lives saved. They generally include an initial patient assessment followed by regular reevaluations to determine whether patients using scarce resources are benefiting less than other patients who need the same resources. The protocols should consider not only patients with COVID-19 infection, but also patients with stroke, traumatic injury, influenza, and heart failure who may need the same resources. Race, gender, ethnicity, socioeconomics, and perceived social worth should not influence care decisions, according to the guidance. Validated mortality prediction scales, such as the Glasgow Outcome Scale, can contribute to care decisions. Obtaining community input into these protocols will ensure trust in the health care system.
“If the situation necessitates hard decisions, we need to be fair, objective, transparent, and adamantly preserve our professional integrity,” wrote the authors. “Through it all, we owe it to our patients and families, as well as ourselves, to maintain our own health and wellness.”
The guidance was developed without funding, and the authors reported no relevant disclosures.
SOURCE: Rubin MA et al. Neurology. 2020 May 15. doi: 10.1212/WNL.0000000000009744.
FROM NEUROLOGY