User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Medicare hospital deaths decline, hospice usage increases
Since 2000, Medicare beneficiaries have become less likely to die in hospitals, and more likely to die in their homes or in community health care facilities.
A review of Medicare records also determined that there was a decline in health care transitions in the final 3 days of life for these patients, Joan M. Teno, MD, and her colleagues wrote in JAMA.
It is not possible to identify a specific reason for the shift, wrote Dr. Teno, professor of medicine at the Oregon Health & Science University, Portland. Between the study years of 2000 and 2015, there were several large efforts to improve care at the end of life.
“Since 2009, programs ranging from ensuring informed patient decision making to enhanced care coordination have had the goal of improving care at the end of life. Specific interventions have included promoting conversations about the goals of care, continued growth of hospice services and palliative care, and the debate and passage of the Affordable Care Act … It is difficult to disentangle efforts such as public education, promotion of advance directives through the Patient Self- Determination Act, increased access to hospice and palliative care services, financial incentives of payment policies, and other secular changes.”
The study mined data from the Centers for Medicare & Medicaid Services, and examined end-of-life outcomes among two Medicare groups: Medicare fee-for-service recipients (1,361,870) during 2009-2015, and Medicare Advantage recipients (871,845), comparing 2011 and 2015. The mean age of both cohorts was 82 years.
Outcomes included site of death and “potentially burdensome transitions,” during the last days of life. These were defined as three or more hospitalizations in the previous 3 months, or two or more hospitalizations for pneumonia, urinary tract infection, dehydration, or sepsis during the last 120 days of life. Prolonged mechanical ventilation also was deemed potentially burdensome.
Among fee-for-service recipients, deaths in acute care hospitals declined from 32.6% to19.8%. Deaths in nursing homes remained steady, at 27.2% and 24.9%. Many of these deaths (42.9%) were preceded by a stay in an ICU. There was a transient increase in end-of-life ICU use, around 2009, but by 2015, the percentage was down to 29%, compared with 65.2% in 2000.
Transitions between a nursing home and hospital in the last 90 days of life were 0.49/person in 2000 and 0.33/person in 2015. Hospitalizations for infection or dehydration fell from 14.6% to12.2%. Hospitalization with prolonged ventilation fell from 3.1% to 2.5%.
Dying in hospice care increased from 21.6% to 50.4%, and people were taking advantage of hospice services longer: the proportion using short-term services (3 days or less) fell from 9.8% to 7.7%.
Among Medicare Advantage recipients, the numbers were somewhat different. More than 50% of recipients entered hospice care in both 2011 and 2015; in both years, 8% had services for more than 3 days. About 27% had ICU care in the last days of life, in both years. Compared to fee-for-service recipients, fewer Medicare Advantage patients were in nursing homes at the time of death, and that number declined from 2011 to 2015 (37.7% to 33.2%).
In each year, about 10% of these patients had a hospitalization for dehydration or infection, and 3% had a stay requiring prolonged mechanical ventilation in each year. The mean number of health care transitions remained steady, at 0.23 and 0.21 per person each year.
Dr. Teno had no financial disclosures.
SOURCE: Teno JM et al. JAMA. 2018 Jun 25. doi: 10.1001/jama.2018.8981.
Since 2000, Medicare beneficiaries have become less likely to die in hospitals, and more likely to die in their homes or in community health care facilities.
A review of Medicare records also determined that there was a decline in health care transitions in the final 3 days of life for these patients, Joan M. Teno, MD, and her colleagues wrote in JAMA.
It is not possible to identify a specific reason for the shift, wrote Dr. Teno, professor of medicine at the Oregon Health & Science University, Portland. Between the study years of 2000 and 2015, there were several large efforts to improve care at the end of life.
“Since 2009, programs ranging from ensuring informed patient decision making to enhanced care coordination have had the goal of improving care at the end of life. Specific interventions have included promoting conversations about the goals of care, continued growth of hospice services and palliative care, and the debate and passage of the Affordable Care Act … It is difficult to disentangle efforts such as public education, promotion of advance directives through the Patient Self- Determination Act, increased access to hospice and palliative care services, financial incentives of payment policies, and other secular changes.”
The study mined data from the Centers for Medicare & Medicaid Services, and examined end-of-life outcomes among two Medicare groups: Medicare fee-for-service recipients (1,361,870) during 2009-2015, and Medicare Advantage recipients (871,845), comparing 2011 and 2015. The mean age of both cohorts was 82 years.
Outcomes included site of death and “potentially burdensome transitions,” during the last days of life. These were defined as three or more hospitalizations in the previous 3 months, or two or more hospitalizations for pneumonia, urinary tract infection, dehydration, or sepsis during the last 120 days of life. Prolonged mechanical ventilation also was deemed potentially burdensome.
Among fee-for-service recipients, deaths in acute care hospitals declined from 32.6% to19.8%. Deaths in nursing homes remained steady, at 27.2% and 24.9%. Many of these deaths (42.9%) were preceded by a stay in an ICU. There was a transient increase in end-of-life ICU use, around 2009, but by 2015, the percentage was down to 29%, compared with 65.2% in 2000.
Transitions between a nursing home and hospital in the last 90 days of life were 0.49/person in 2000 and 0.33/person in 2015. Hospitalizations for infection or dehydration fell from 14.6% to12.2%. Hospitalization with prolonged ventilation fell from 3.1% to 2.5%.
Dying in hospice care increased from 21.6% to 50.4%, and people were taking advantage of hospice services longer: the proportion using short-term services (3 days or less) fell from 9.8% to 7.7%.
Among Medicare Advantage recipients, the numbers were somewhat different. More than 50% of recipients entered hospice care in both 2011 and 2015; in both years, 8% had services for more than 3 days. About 27% had ICU care in the last days of life, in both years. Compared to fee-for-service recipients, fewer Medicare Advantage patients were in nursing homes at the time of death, and that number declined from 2011 to 2015 (37.7% to 33.2%).
In each year, about 10% of these patients had a hospitalization for dehydration or infection, and 3% had a stay requiring prolonged mechanical ventilation in each year. The mean number of health care transitions remained steady, at 0.23 and 0.21 per person each year.
Dr. Teno had no financial disclosures.
SOURCE: Teno JM et al. JAMA. 2018 Jun 25. doi: 10.1001/jama.2018.8981.
Since 2000, Medicare beneficiaries have become less likely to die in hospitals, and more likely to die in their homes or in community health care facilities.
A review of Medicare records also determined that there was a decline in health care transitions in the final 3 days of life for these patients, Joan M. Teno, MD, and her colleagues wrote in JAMA.
It is not possible to identify a specific reason for the shift, wrote Dr. Teno, professor of medicine at the Oregon Health & Science University, Portland. Between the study years of 2000 and 2015, there were several large efforts to improve care at the end of life.
“Since 2009, programs ranging from ensuring informed patient decision making to enhanced care coordination have had the goal of improving care at the end of life. Specific interventions have included promoting conversations about the goals of care, continued growth of hospice services and palliative care, and the debate and passage of the Affordable Care Act … It is difficult to disentangle efforts such as public education, promotion of advance directives through the Patient Self- Determination Act, increased access to hospice and palliative care services, financial incentives of payment policies, and other secular changes.”
The study mined data from the Centers for Medicare & Medicaid Services, and examined end-of-life outcomes among two Medicare groups: Medicare fee-for-service recipients (1,361,870) during 2009-2015, and Medicare Advantage recipients (871,845), comparing 2011 and 2015. The mean age of both cohorts was 82 years.
Outcomes included site of death and “potentially burdensome transitions,” during the last days of life. These were defined as three or more hospitalizations in the previous 3 months, or two or more hospitalizations for pneumonia, urinary tract infection, dehydration, or sepsis during the last 120 days of life. Prolonged mechanical ventilation also was deemed potentially burdensome.
Among fee-for-service recipients, deaths in acute care hospitals declined from 32.6% to19.8%. Deaths in nursing homes remained steady, at 27.2% and 24.9%. Many of these deaths (42.9%) were preceded by a stay in an ICU. There was a transient increase in end-of-life ICU use, around 2009, but by 2015, the percentage was down to 29%, compared with 65.2% in 2000.
Transitions between a nursing home and hospital in the last 90 days of life were 0.49/person in 2000 and 0.33/person in 2015. Hospitalizations for infection or dehydration fell from 14.6% to12.2%. Hospitalization with prolonged ventilation fell from 3.1% to 2.5%.
Dying in hospice care increased from 21.6% to 50.4%, and people were taking advantage of hospice services longer: the proportion using short-term services (3 days or less) fell from 9.8% to 7.7%.
Among Medicare Advantage recipients, the numbers were somewhat different. More than 50% of recipients entered hospice care in both 2011 and 2015; in both years, 8% had services for more than 3 days. About 27% had ICU care in the last days of life, in both years. Compared to fee-for-service recipients, fewer Medicare Advantage patients were in nursing homes at the time of death, and that number declined from 2011 to 2015 (37.7% to 33.2%).
In each year, about 10% of these patients had a hospitalization for dehydration or infection, and 3% had a stay requiring prolonged mechanical ventilation in each year. The mean number of health care transitions remained steady, at 0.23 and 0.21 per person each year.
Dr. Teno had no financial disclosures.
SOURCE: Teno JM et al. JAMA. 2018 Jun 25. doi: 10.1001/jama.2018.8981.
FROM JAMA
Key clinical point: During 2000-2015, Medicare recipients became less likely to die in hospitals.
Major finding:
Study details: The retrospective study comprised more than 2.3 million Medicare recipients.
Disclosures: Dr. Teno had no financial disclosures.
Source: Teno JM et al. JAMA. 2018 Jun 25. doi: 10.1001/jama.2018.8981.
Pediatric special interest group to open new era of opportunity
More visible, systemic pediatric presence within SHM
Editor’s note: Each month, the Society of Hospital Medicine puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help improve the care of hospitalized patients.
Why did you become a member of SHM?
After being in a general pediatrics practice for a few years, I saw a lot of value in and got a lot of support from working with other outpatient pediatricians and the American Academy of Pediatrics. When I left that outpatient practice to focus on hospital pediatrics 13 years ago, I needed to find people who knew a lot more than I did about inpatient work and an organization that could support my growth and development in this new role. Of course, SHM was the answer.
I knew there was a ton I could learn from the internists who had been doing this work a lot longer and senior pediatric hospitalists who could share their experiences. I found all of that, and more, and was honored to join the Pediatrics Committee in 2012 to help serve the community that’s helped me so much.
During your time on the Pediatrics Committee, what goals were accomplished?
Over the years, this great committee has been very active at the direction of some fantastic leaders. We have had the privilege and responsibility to advise the SHM Board on pediatric issues and concerns, and we’ve developed some interesting pediatric-specific educational content in areas such as quality and safe handoffs. We’ve worked on the Choosing Wisely campaign and are now in the process of updating the Pediatric Hospital Medicine Core Competencies.
Each year we develop the content for the Pediatric Track of the SHM annual conference, and for several years, I was also on the Annual Conference Committee, which was a fantastic opportunity to bring the pediatric world to the broader work of SHM.
The Pediatrics Committee is transitioning from a committee to a Pediatric Special Interest Group. What can members look forward to in this transition?
I was asked to lead the subcommittee that is working on the SIG transition, and I must say, I am excited! You know, as great as the Pediatrics Committee is, it’s still only 15-20 people. And there are opportunities for pediatric hospitalists to join other SHM committees, but even at that, the footprint of active, engaged pediatric hospitalists within SHM is fairly small. The transition to a much more open-ended pediatric hospitalist SIG will allow many more hospitalists who take care of children to become involved. That’s more people, from more places, with more perspectives and ideas. It’s more energy, more collaboration, and hopefully, in the long run, a more visible and systemic pediatric presence within SHM.
Sure, there are questions and a few concerns, and I’m not sure all the details have been quite worked out, but in the big picture, I think it’s good for pediatric hospital medicine and good for SHM. Stay tuned as the process develops, but I think SHM members are going to see the new opportunity to get involved directly in SIG projects and goals, collaborate with more pediatric hospitalists, and see some real dynamic and forward-thinking leadership in the SIG executive council ... and opportunities to be on that Executive Council in a transparent, collegial way.
What were your main takeaways from Pediatric Hospital Medicine 2017? What can attendees expect at PHM 2018?
The annual Pediatric Hospital Medicine (PHM) meeting is always a bit of a whirlwind and our meeting in Nashville in 2017, hosted by SHM and our very own board member, Kris Rehm, MD, SFHM, was no different. There is always so much to experience and a diversity of offerings, which is really representative of how broad and rapidly growing our field is.
Of course, the “Top Articles in PHM” review is always popular and well received, and the poster and platform research sessions really show how far PHM has come and how much incredibly detailed and diligent work is being done to advance it further. There were some particularly thought-provoking plenary sessions last year on evidence-based health policy challenges and how some things we take as PHM dogma might not even be true! Left us all scratching our heads a bit. The final plenary on magic and pediatrics was inspiring and hilarious.
As far as PHM 2018, I suppose for full disclosure I should mention that I’m on the planning committee, so of course it’s going to be awesome! We really are putting together a fantastic experience. We had so many high-quality submissions for workshops, clinical sessions, research – truly spanning the whole range of PHM work. Whatever you’re coming to learn about, you’ll find it. We have some tremendously gifted plenary speakers lined up; some are sure to inspire, some will make you smile with pride about being a hospitalist, and at least one will almost certainly crack you up. We’ve shortened the length of many of the workshops to allow attendees to have more experiences while making sure the content is still meaningful. There will be several opportunities to mentor and be mentored in a comfortable, casual setting. I could go on and on, but if you take care of kids, come to Atlanta and see for yourself in July!
Do you have any advice for early-stage pediatric hospitalists looking to advance their careers?
This is an exciting time to be a pediatric hospitalist. Like it or hate it, subspecialty designation in PHM is around the corner, the new SHM pediatric SIG is going to open up a new era of opportunities, research in the field is gathering tremendous momentum, and fellowship training is only going to fuel that.
But PHM is still so far from becoming a single, one-size-fits-all path. There is still a huge range of practice locations, settings, responsibilities, and challenges. I tell my junior folks: “Put yourself out there. Try some things. Try a lot of things. If you have opportunities to practice in a few different settings, try it. If there are learners, teach. Join a research or quality improvement group. Go to some big meetings; talk to 50 new people. If you hear someone give a great talk that gets you fired up about something you have a passion for, stick around, go talk with them; they get it, they were you once, and probably not even that long ago. Throw your hat in a ring and help out with a project. It might turn out to not be your ‘thing,’ but it might lead you to your ‘thing.’ Or not, but you’ll come away with some experience and two new friends.”
That’s what makes this journey fun. There is no goal, no endgame. It’s all about the journey and the joy you find in the ride.
Ms. Steele is a marketing communications specialist at the Society of Hospital Medicine.
More visible, systemic pediatric presence within SHM
More visible, systemic pediatric presence within SHM
Editor’s note: Each month, the Society of Hospital Medicine puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help improve the care of hospitalized patients.
Why did you become a member of SHM?
After being in a general pediatrics practice for a few years, I saw a lot of value in and got a lot of support from working with other outpatient pediatricians and the American Academy of Pediatrics. When I left that outpatient practice to focus on hospital pediatrics 13 years ago, I needed to find people who knew a lot more than I did about inpatient work and an organization that could support my growth and development in this new role. Of course, SHM was the answer.
I knew there was a ton I could learn from the internists who had been doing this work a lot longer and senior pediatric hospitalists who could share their experiences. I found all of that, and more, and was honored to join the Pediatrics Committee in 2012 to help serve the community that’s helped me so much.
During your time on the Pediatrics Committee, what goals were accomplished?
Over the years, this great committee has been very active at the direction of some fantastic leaders. We have had the privilege and responsibility to advise the SHM Board on pediatric issues and concerns, and we’ve developed some interesting pediatric-specific educational content in areas such as quality and safe handoffs. We’ve worked on the Choosing Wisely campaign and are now in the process of updating the Pediatric Hospital Medicine Core Competencies.
Each year we develop the content for the Pediatric Track of the SHM annual conference, and for several years, I was also on the Annual Conference Committee, which was a fantastic opportunity to bring the pediatric world to the broader work of SHM.
The Pediatrics Committee is transitioning from a committee to a Pediatric Special Interest Group. What can members look forward to in this transition?
I was asked to lead the subcommittee that is working on the SIG transition, and I must say, I am excited! You know, as great as the Pediatrics Committee is, it’s still only 15-20 people. And there are opportunities for pediatric hospitalists to join other SHM committees, but even at that, the footprint of active, engaged pediatric hospitalists within SHM is fairly small. The transition to a much more open-ended pediatric hospitalist SIG will allow many more hospitalists who take care of children to become involved. That’s more people, from more places, with more perspectives and ideas. It’s more energy, more collaboration, and hopefully, in the long run, a more visible and systemic pediatric presence within SHM.
Sure, there are questions and a few concerns, and I’m not sure all the details have been quite worked out, but in the big picture, I think it’s good for pediatric hospital medicine and good for SHM. Stay tuned as the process develops, but I think SHM members are going to see the new opportunity to get involved directly in SIG projects and goals, collaborate with more pediatric hospitalists, and see some real dynamic and forward-thinking leadership in the SIG executive council ... and opportunities to be on that Executive Council in a transparent, collegial way.
What were your main takeaways from Pediatric Hospital Medicine 2017? What can attendees expect at PHM 2018?
The annual Pediatric Hospital Medicine (PHM) meeting is always a bit of a whirlwind and our meeting in Nashville in 2017, hosted by SHM and our very own board member, Kris Rehm, MD, SFHM, was no different. There is always so much to experience and a diversity of offerings, which is really representative of how broad and rapidly growing our field is.
Of course, the “Top Articles in PHM” review is always popular and well received, and the poster and platform research sessions really show how far PHM has come and how much incredibly detailed and diligent work is being done to advance it further. There were some particularly thought-provoking plenary sessions last year on evidence-based health policy challenges and how some things we take as PHM dogma might not even be true! Left us all scratching our heads a bit. The final plenary on magic and pediatrics was inspiring and hilarious.
As far as PHM 2018, I suppose for full disclosure I should mention that I’m on the planning committee, so of course it’s going to be awesome! We really are putting together a fantastic experience. We had so many high-quality submissions for workshops, clinical sessions, research – truly spanning the whole range of PHM work. Whatever you’re coming to learn about, you’ll find it. We have some tremendously gifted plenary speakers lined up; some are sure to inspire, some will make you smile with pride about being a hospitalist, and at least one will almost certainly crack you up. We’ve shortened the length of many of the workshops to allow attendees to have more experiences while making sure the content is still meaningful. There will be several opportunities to mentor and be mentored in a comfortable, casual setting. I could go on and on, but if you take care of kids, come to Atlanta and see for yourself in July!
Do you have any advice for early-stage pediatric hospitalists looking to advance their careers?
This is an exciting time to be a pediatric hospitalist. Like it or hate it, subspecialty designation in PHM is around the corner, the new SHM pediatric SIG is going to open up a new era of opportunities, research in the field is gathering tremendous momentum, and fellowship training is only going to fuel that.
But PHM is still so far from becoming a single, one-size-fits-all path. There is still a huge range of practice locations, settings, responsibilities, and challenges. I tell my junior folks: “Put yourself out there. Try some things. Try a lot of things. If you have opportunities to practice in a few different settings, try it. If there are learners, teach. Join a research or quality improvement group. Go to some big meetings; talk to 50 new people. If you hear someone give a great talk that gets you fired up about something you have a passion for, stick around, go talk with them; they get it, they were you once, and probably not even that long ago. Throw your hat in a ring and help out with a project. It might turn out to not be your ‘thing,’ but it might lead you to your ‘thing.’ Or not, but you’ll come away with some experience and two new friends.”
That’s what makes this journey fun. There is no goal, no endgame. It’s all about the journey and the joy you find in the ride.
Ms. Steele is a marketing communications specialist at the Society of Hospital Medicine.
Editor’s note: Each month, the Society of Hospital Medicine puts the spotlight on some of our most active members who are making substantial contributions to hospital medicine. Visit www.hospitalmedicine.org for more information on how you can lend your expertise to help improve the care of hospitalized patients.
Why did you become a member of SHM?
After being in a general pediatrics practice for a few years, I saw a lot of value in and got a lot of support from working with other outpatient pediatricians and the American Academy of Pediatrics. When I left that outpatient practice to focus on hospital pediatrics 13 years ago, I needed to find people who knew a lot more than I did about inpatient work and an organization that could support my growth and development in this new role. Of course, SHM was the answer.
I knew there was a ton I could learn from the internists who had been doing this work a lot longer and senior pediatric hospitalists who could share their experiences. I found all of that, and more, and was honored to join the Pediatrics Committee in 2012 to help serve the community that’s helped me so much.
During your time on the Pediatrics Committee, what goals were accomplished?
Over the years, this great committee has been very active at the direction of some fantastic leaders. We have had the privilege and responsibility to advise the SHM Board on pediatric issues and concerns, and we’ve developed some interesting pediatric-specific educational content in areas such as quality and safe handoffs. We’ve worked on the Choosing Wisely campaign and are now in the process of updating the Pediatric Hospital Medicine Core Competencies.
Each year we develop the content for the Pediatric Track of the SHM annual conference, and for several years, I was also on the Annual Conference Committee, which was a fantastic opportunity to bring the pediatric world to the broader work of SHM.
The Pediatrics Committee is transitioning from a committee to a Pediatric Special Interest Group. What can members look forward to in this transition?
I was asked to lead the subcommittee that is working on the SIG transition, and I must say, I am excited! You know, as great as the Pediatrics Committee is, it’s still only 15-20 people. And there are opportunities for pediatric hospitalists to join other SHM committees, but even at that, the footprint of active, engaged pediatric hospitalists within SHM is fairly small. The transition to a much more open-ended pediatric hospitalist SIG will allow many more hospitalists who take care of children to become involved. That’s more people, from more places, with more perspectives and ideas. It’s more energy, more collaboration, and hopefully, in the long run, a more visible and systemic pediatric presence within SHM.
Sure, there are questions and a few concerns, and I’m not sure all the details have been quite worked out, but in the big picture, I think it’s good for pediatric hospital medicine and good for SHM. Stay tuned as the process develops, but I think SHM members are going to see the new opportunity to get involved directly in SIG projects and goals, collaborate with more pediatric hospitalists, and see some real dynamic and forward-thinking leadership in the SIG executive council ... and opportunities to be on that Executive Council in a transparent, collegial way.
What were your main takeaways from Pediatric Hospital Medicine 2017? What can attendees expect at PHM 2018?
The annual Pediatric Hospital Medicine (PHM) meeting is always a bit of a whirlwind and our meeting in Nashville in 2017, hosted by SHM and our very own board member, Kris Rehm, MD, SFHM, was no different. There is always so much to experience and a diversity of offerings, which is really representative of how broad and rapidly growing our field is.
Of course, the “Top Articles in PHM” review is always popular and well received, and the poster and platform research sessions really show how far PHM has come and how much incredibly detailed and diligent work is being done to advance it further. There were some particularly thought-provoking plenary sessions last year on evidence-based health policy challenges and how some things we take as PHM dogma might not even be true! Left us all scratching our heads a bit. The final plenary on magic and pediatrics was inspiring and hilarious.
As far as PHM 2018, I suppose for full disclosure I should mention that I’m on the planning committee, so of course it’s going to be awesome! We really are putting together a fantastic experience. We had so many high-quality submissions for workshops, clinical sessions, research – truly spanning the whole range of PHM work. Whatever you’re coming to learn about, you’ll find it. We have some tremendously gifted plenary speakers lined up; some are sure to inspire, some will make you smile with pride about being a hospitalist, and at least one will almost certainly crack you up. We’ve shortened the length of many of the workshops to allow attendees to have more experiences while making sure the content is still meaningful. There will be several opportunities to mentor and be mentored in a comfortable, casual setting. I could go on and on, but if you take care of kids, come to Atlanta and see for yourself in July!
Do you have any advice for early-stage pediatric hospitalists looking to advance their careers?
This is an exciting time to be a pediatric hospitalist. Like it or hate it, subspecialty designation in PHM is around the corner, the new SHM pediatric SIG is going to open up a new era of opportunities, research in the field is gathering tremendous momentum, and fellowship training is only going to fuel that.
But PHM is still so far from becoming a single, one-size-fits-all path. There is still a huge range of practice locations, settings, responsibilities, and challenges. I tell my junior folks: “Put yourself out there. Try some things. Try a lot of things. If you have opportunities to practice in a few different settings, try it. If there are learners, teach. Join a research or quality improvement group. Go to some big meetings; talk to 50 new people. If you hear someone give a great talk that gets you fired up about something you have a passion for, stick around, go talk with them; they get it, they were you once, and probably not even that long ago. Throw your hat in a ring and help out with a project. It might turn out to not be your ‘thing,’ but it might lead you to your ‘thing.’ Or not, but you’ll come away with some experience and two new friends.”
That’s what makes this journey fun. There is no goal, no endgame. It’s all about the journey and the joy you find in the ride.
Ms. Steele is a marketing communications specialist at the Society of Hospital Medicine.
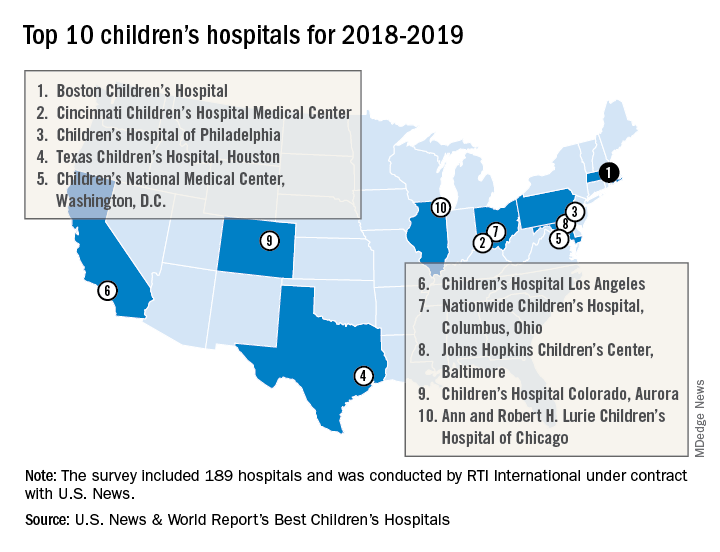
Boston Children’s Hospital named nation’s best
For the fourth consecutive year, Boston Children’s Hospital has been named the top children’s hospital by U.S. News & World Report.
The hospital finished among the top five in all 10 pediatric specialties included in the rankings: cancer (third), cardiology and heart surgery (second), diabetes and endocrinology (second), gastroenterology and GI surgery (second), neonatology (third), nephrology (first), neurology and neurosurgery (first), orthopedics (first), pulmonology (fourth), and urology (third), according to the 2018-2019 Best Children’s Hospitals rankings.
Of the 189 facilities that qualified for inclusion this year, 118 submitted sufficient data to be considered in at least 1 of the 10 specialties and 86 were ranked among the top 50 in at least 1 specialty. In addition, a survey of individuals conducted to establish the hospitals’ reputations – generally worth about 15% of a hospital’s score in each specialty – was completed by 4,165 physicians.
RTI International, a research and consulting firm, conducted the physician survey and produced the methodology and national rankings under contract with U.S. News.
For the fourth consecutive year, Boston Children’s Hospital has been named the top children’s hospital by U.S. News & World Report.
The hospital finished among the top five in all 10 pediatric specialties included in the rankings: cancer (third), cardiology and heart surgery (second), diabetes and endocrinology (second), gastroenterology and GI surgery (second), neonatology (third), nephrology (first), neurology and neurosurgery (first), orthopedics (first), pulmonology (fourth), and urology (third), according to the 2018-2019 Best Children’s Hospitals rankings.
Of the 189 facilities that qualified for inclusion this year, 118 submitted sufficient data to be considered in at least 1 of the 10 specialties and 86 were ranked among the top 50 in at least 1 specialty. In addition, a survey of individuals conducted to establish the hospitals’ reputations – generally worth about 15% of a hospital’s score in each specialty – was completed by 4,165 physicians.
RTI International, a research and consulting firm, conducted the physician survey and produced the methodology and national rankings under contract with U.S. News.
For the fourth consecutive year, Boston Children’s Hospital has been named the top children’s hospital by U.S. News & World Report.
The hospital finished among the top five in all 10 pediatric specialties included in the rankings: cancer (third), cardiology and heart surgery (second), diabetes and endocrinology (second), gastroenterology and GI surgery (second), neonatology (third), nephrology (first), neurology and neurosurgery (first), orthopedics (first), pulmonology (fourth), and urology (third), according to the 2018-2019 Best Children’s Hospitals rankings.
Of the 189 facilities that qualified for inclusion this year, 118 submitted sufficient data to be considered in at least 1 of the 10 specialties and 86 were ranked among the top 50 in at least 1 specialty. In addition, a survey of individuals conducted to establish the hospitals’ reputations – generally worth about 15% of a hospital’s score in each specialty – was completed by 4,165 physicians.
RTI International, a research and consulting firm, conducted the physician survey and produced the methodology and national rankings under contract with U.S. News.
Data suggest harm outweighs benefit of opioids for musculoskeletal pain
AMSTERDAM – Opioids cannot be justified for the routine treatment for musculoskeletal pain because risks outweigh benefits, according to a detailed review of published studies presented at the European Congress of Rheumatology.
“There is very little evidence of benefit for the long-term management of nonmalignant pain, but very good evidence for harm,” reported Blair Smith, MD, head of the population health sciences division, University of Dundee (Scotland).
In the treatment of musculoskeletal pain, the goals are increased function and quality of life, rather than complete relief of pain, according to Dr. Smith. On this basis, opioids are not an appropriate routine therapy. He reported that pain relief is not well documented, while side effects such as sedation, dizziness, and constipation, are likely to be counterproductive to improved outcomes.
There is no absolute contraindication for opioids in the control of chronic musculoskeletal pain, but Dr. Smith’s summary of the data led him to conclude that they should be used judiciously and “only for carefully selected patients.”
Of the many studies he reviewed to draw this conclusion, one of the most recent was identified as the most persuasive. Published earlier this year, the SPACE study is “the first good-quality study of long-term opioid use” in patients with musculoskeletal complaints. It was negative.
“The pain intensity at the end of 12 months of treatment was slightly but significantly worse among those randomized to opioids,” reported Dr. Smith. “There was no difference in patient function, but there was an increased risk of adverse events.”
In the SPACE study, 240 patients with moderate to severe chronic back pain or hip or knee osteoarthritis were randomized to opioid or nonopioid pain management. In the nonopioid group, the first therapeutic step was acetaminophen, but medications could be changed, added, or adjusted within both groups to improve patient response.
At the end of 12 months, a lack of benefit on both pain control and functional improvement from opioids relative to nonopioid treatment was accompanied by a higher rate of adverse effects. This led the authors to conclude that opioids are not supported for musculoskeletal pain.
Not all the evidence argues against opioids for noncancer pain management, according to Dr. Smith, but he emphasized that those who support use of opioids do so for pain control only. They do not confirm an advantage for function and quality of life, which he suggested are the key endpoints. For example, a 2010 Cochrane review concluded from a systematic literature review that there is “weak evidence” for pain relief but inconclusive evidence of an improvement in functioning and quality of life.
Other investigators have drawn the same conclusion, according to Dr. Smith. He cited a statement from the International Association for Study of Pain that advises, “Caution should be used for prescribing opioids for chronic pain.” Although this statement was not specific to musculoskeletal pain, the IASP does specify that pain medications should be employed “to promote increased function and improved quality of life rather than complete relief of pain,” according to Dr. Smith.
Opioid prescriptions for chronic pain have been increasing in Europe as they have in the United States, but Dr. Smith indicated that opioids, if used at all, should be prescribed for very short periods and for very specific goals, particularly improvement in function.
“Probably most important for my [primary care] colleagues, patients prescribed opioids should be evaluated early and frequently to gauge benefit,” Dr. Smith said. Although he believes pain control is an important and worthwhile goal, it must be approached within the context of improved well-being rather than as an isolated endpoint.
SOURCE: Smith B et al. EULAR 2018, Abstract No. SP0073.
AMSTERDAM – Opioids cannot be justified for the routine treatment for musculoskeletal pain because risks outweigh benefits, according to a detailed review of published studies presented at the European Congress of Rheumatology.
“There is very little evidence of benefit for the long-term management of nonmalignant pain, but very good evidence for harm,” reported Blair Smith, MD, head of the population health sciences division, University of Dundee (Scotland).
In the treatment of musculoskeletal pain, the goals are increased function and quality of life, rather than complete relief of pain, according to Dr. Smith. On this basis, opioids are not an appropriate routine therapy. He reported that pain relief is not well documented, while side effects such as sedation, dizziness, and constipation, are likely to be counterproductive to improved outcomes.
There is no absolute contraindication for opioids in the control of chronic musculoskeletal pain, but Dr. Smith’s summary of the data led him to conclude that they should be used judiciously and “only for carefully selected patients.”
Of the many studies he reviewed to draw this conclusion, one of the most recent was identified as the most persuasive. Published earlier this year, the SPACE study is “the first good-quality study of long-term opioid use” in patients with musculoskeletal complaints. It was negative.
“The pain intensity at the end of 12 months of treatment was slightly but significantly worse among those randomized to opioids,” reported Dr. Smith. “There was no difference in patient function, but there was an increased risk of adverse events.”
In the SPACE study, 240 patients with moderate to severe chronic back pain or hip or knee osteoarthritis were randomized to opioid or nonopioid pain management. In the nonopioid group, the first therapeutic step was acetaminophen, but medications could be changed, added, or adjusted within both groups to improve patient response.
At the end of 12 months, a lack of benefit on both pain control and functional improvement from opioids relative to nonopioid treatment was accompanied by a higher rate of adverse effects. This led the authors to conclude that opioids are not supported for musculoskeletal pain.
Not all the evidence argues against opioids for noncancer pain management, according to Dr. Smith, but he emphasized that those who support use of opioids do so for pain control only. They do not confirm an advantage for function and quality of life, which he suggested are the key endpoints. For example, a 2010 Cochrane review concluded from a systematic literature review that there is “weak evidence” for pain relief but inconclusive evidence of an improvement in functioning and quality of life.
Other investigators have drawn the same conclusion, according to Dr. Smith. He cited a statement from the International Association for Study of Pain that advises, “Caution should be used for prescribing opioids for chronic pain.” Although this statement was not specific to musculoskeletal pain, the IASP does specify that pain medications should be employed “to promote increased function and improved quality of life rather than complete relief of pain,” according to Dr. Smith.
Opioid prescriptions for chronic pain have been increasing in Europe as they have in the United States, but Dr. Smith indicated that opioids, if used at all, should be prescribed for very short periods and for very specific goals, particularly improvement in function.
“Probably most important for my [primary care] colleagues, patients prescribed opioids should be evaluated early and frequently to gauge benefit,” Dr. Smith said. Although he believes pain control is an important and worthwhile goal, it must be approached within the context of improved well-being rather than as an isolated endpoint.
SOURCE: Smith B et al. EULAR 2018, Abstract No. SP0073.
AMSTERDAM – Opioids cannot be justified for the routine treatment for musculoskeletal pain because risks outweigh benefits, according to a detailed review of published studies presented at the European Congress of Rheumatology.
“There is very little evidence of benefit for the long-term management of nonmalignant pain, but very good evidence for harm,” reported Blair Smith, MD, head of the population health sciences division, University of Dundee (Scotland).
In the treatment of musculoskeletal pain, the goals are increased function and quality of life, rather than complete relief of pain, according to Dr. Smith. On this basis, opioids are not an appropriate routine therapy. He reported that pain relief is not well documented, while side effects such as sedation, dizziness, and constipation, are likely to be counterproductive to improved outcomes.
There is no absolute contraindication for opioids in the control of chronic musculoskeletal pain, but Dr. Smith’s summary of the data led him to conclude that they should be used judiciously and “only for carefully selected patients.”
Of the many studies he reviewed to draw this conclusion, one of the most recent was identified as the most persuasive. Published earlier this year, the SPACE study is “the first good-quality study of long-term opioid use” in patients with musculoskeletal complaints. It was negative.
“The pain intensity at the end of 12 months of treatment was slightly but significantly worse among those randomized to opioids,” reported Dr. Smith. “There was no difference in patient function, but there was an increased risk of adverse events.”
In the SPACE study, 240 patients with moderate to severe chronic back pain or hip or knee osteoarthritis were randomized to opioid or nonopioid pain management. In the nonopioid group, the first therapeutic step was acetaminophen, but medications could be changed, added, or adjusted within both groups to improve patient response.
At the end of 12 months, a lack of benefit on both pain control and functional improvement from opioids relative to nonopioid treatment was accompanied by a higher rate of adverse effects. This led the authors to conclude that opioids are not supported for musculoskeletal pain.
Not all the evidence argues against opioids for noncancer pain management, according to Dr. Smith, but he emphasized that those who support use of opioids do so for pain control only. They do not confirm an advantage for function and quality of life, which he suggested are the key endpoints. For example, a 2010 Cochrane review concluded from a systematic literature review that there is “weak evidence” for pain relief but inconclusive evidence of an improvement in functioning and quality of life.
Other investigators have drawn the same conclusion, according to Dr. Smith. He cited a statement from the International Association for Study of Pain that advises, “Caution should be used for prescribing opioids for chronic pain.” Although this statement was not specific to musculoskeletal pain, the IASP does specify that pain medications should be employed “to promote increased function and improved quality of life rather than complete relief of pain,” according to Dr. Smith.
Opioid prescriptions for chronic pain have been increasing in Europe as they have in the United States, but Dr. Smith indicated that opioids, if used at all, should be prescribed for very short periods and for very specific goals, particularly improvement in function.
“Probably most important for my [primary care] colleagues, patients prescribed opioids should be evaluated early and frequently to gauge benefit,” Dr. Smith said. Although he believes pain control is an important and worthwhile goal, it must be approached within the context of improved well-being rather than as an isolated endpoint.
SOURCE: Smith B et al. EULAR 2018, Abstract No. SP0073.
REPORTING FROM THE EULAR 2018 CONGRESS
Health care, technology, and the future
Major forces combining to reshape care delivery
What will be the role of humans in the future health system?
At first blush, this is a peculiar question. Health care is all about humans. How could one doubt their presence or role? It is working with and for people that attracted many to this profession.
On the cusp of a significant health system reformulation, it is the very question that hospitalists now must ponder. Just as ATMs replaced bank cashiers, online shopping replaced retail stores, and autonomous cars will soon replace drivers, the human landscape of health care is about to change. What pressures will force the changes?
On one hand, there is increasing demand. The Affordable Care Act opened the insurance door for people previously uncovered. Aging is delivering the baby boomer bubble into their sicker years. Hospitalists witness this phenomenon every day in the ballooning parade of patients they serve. At times, those pressures can overwhelm.
On the other hand, the political will to provide government subsidized health coverage is waning. Washington is tripping over itself to dismantle Obamacare with glancing concern for how it will inflate the ranks of the uninsured. Employers are eager to free themselves from the burden of providing increasingly expensive health coverage benefits. By removing the mandate to buy health care insurance, the current political health system architects are liberating the healthy paying population from their contributions to the overall insurance pool. Simply put, there is and will be less money and less of all that it buys.
Combine building demand with decreasing budget into a system that does not follow general market forces: You get that earthquake. A consumer can forgo that new phone in hard times but not that cardiac procedure. People will be caught in the fissures of the system. Waits, quality, burnout, morale problems, and financial losses will all trend in the wrong directions. The process will evolve in slow motion. Some might argue that we have already arrived.
Enter entrepreneurs, technologic advances, and a growing savvy and willingness to engage tech solutions to everyday problems. If Alexa can turn on your toaster, could it take your blood pressure? If a robot can vacuum your rug, could a different robot provide personal care services? And, if an algorithm can drive your car, could it similarly diagnose what ails you?
On Jan. 30, 2018, one of the greatest disrupters of all time, Amazon, announced that it is joining forces with Berkshire Hathaway and JPMorgan Chase to leap into health care. While they are initially experimenting with health care changes for their corporate employees, the ultimate marketwide goal is to apply technology to both reduce costs and improve patient care. Warren Buffet, Berkshire Hathaway’s founder, said in a statement, “The ballooning costs of health care act as a hungry tapeworm on the American economy.” (And yes, I imagine that many hospitalists would take umbrage with that characterization.) In addition to the Amazon alliance, CVS Health and Aetna also recently agreed to join forces.
The rising health care interest by Amazon begs the imagination. Technology already is far along in automating routine procedures, elevating patient safety protocols, and recalculating patient flows and information. This added corporate interest and investment will further expand new ideas and innovative technologies. And, for sure, it will challenge long held beliefs and practices that shape the health system we have today.
Hospitalist insight needed
What is the role of hospitalist leaders in this shifting equation? Hospitalists already can claim significant credit for introducing major changes in the landscape of hospital care in this country, with all the concomitant improvements in the efficiencies and quality of more integrated service delivery. Can you also guide the system in strategically selecting where and how technology can best be applied to automate and reconfigure service delivery?
The most important questions are: What is it that humans in health care uniquely do that cannot otherwise be accomplished? Are we able to hold onto the humane sides of health care, even as we seek to introduce cost-saving efficiencies?
Top of mind come the most personal sides of health service delivery: touch, empathy, understanding, and care itself. Next come human analysis, understanding, and translation. And beyond that, leadership, direction, and the vision to craft a health care system that meets our societal expectations – not just for the wealthy who cannot afford it – but for everyone.
It would be easy to dismiss this conversation. Society never decided whether those bank tellers, travel agents, or journalists were critical to our functioning. Along these same lines, you and your patients are more than mere algorithms.
As I often share in my leadership seminars, one key function of leaders is to identify and ask the right questions and to be at the decision-making table. What are those questions?
As a hospitalist leader, which part of your work and your activities could be eased by automation? Where might technology ease pressures and enhance your interactions with patients? How do we improve the efficiencies and effectiveness of health service delivery while we preserve the very human qualities that are fundamental to its values? No patient wants to speak to a physician who stares at a computer screen without eye contact, reassurance, or genuine interest. We can do better than that.
Business stakeholders in the system – and clearly, they are positioning and are powerful – will hold great sway on the contours of our future health care system. They could see humans – with all their costs, imperfections, and distractions – as replaceable.
Know that as you lead and pose your questions, there are people interested in listening. Certainly, the tech industry is looking for opportunities to generate broad market appeal. Similarly, health system decision makers looking to enhance how the system functions likewise seek guidance on what could – and could not – work. And who knows: Those decision makers could very well be you.
This is a conversation the country deserves. There is nothing more intimate, more personally important, and more professionally satisfying than the genuine person-to-person quality of what we do in health care. What we arrive at in the end should be achieved by intent, not by accident.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration,” 2nd ed. (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Major forces combining to reshape care delivery
Major forces combining to reshape care delivery
What will be the role of humans in the future health system?
At first blush, this is a peculiar question. Health care is all about humans. How could one doubt their presence or role? It is working with and for people that attracted many to this profession.
On the cusp of a significant health system reformulation, it is the very question that hospitalists now must ponder. Just as ATMs replaced bank cashiers, online shopping replaced retail stores, and autonomous cars will soon replace drivers, the human landscape of health care is about to change. What pressures will force the changes?
On one hand, there is increasing demand. The Affordable Care Act opened the insurance door for people previously uncovered. Aging is delivering the baby boomer bubble into their sicker years. Hospitalists witness this phenomenon every day in the ballooning parade of patients they serve. At times, those pressures can overwhelm.
On the other hand, the political will to provide government subsidized health coverage is waning. Washington is tripping over itself to dismantle Obamacare with glancing concern for how it will inflate the ranks of the uninsured. Employers are eager to free themselves from the burden of providing increasingly expensive health coverage benefits. By removing the mandate to buy health care insurance, the current political health system architects are liberating the healthy paying population from their contributions to the overall insurance pool. Simply put, there is and will be less money and less of all that it buys.
Combine building demand with decreasing budget into a system that does not follow general market forces: You get that earthquake. A consumer can forgo that new phone in hard times but not that cardiac procedure. People will be caught in the fissures of the system. Waits, quality, burnout, morale problems, and financial losses will all trend in the wrong directions. The process will evolve in slow motion. Some might argue that we have already arrived.
Enter entrepreneurs, technologic advances, and a growing savvy and willingness to engage tech solutions to everyday problems. If Alexa can turn on your toaster, could it take your blood pressure? If a robot can vacuum your rug, could a different robot provide personal care services? And, if an algorithm can drive your car, could it similarly diagnose what ails you?
On Jan. 30, 2018, one of the greatest disrupters of all time, Amazon, announced that it is joining forces with Berkshire Hathaway and JPMorgan Chase to leap into health care. While they are initially experimenting with health care changes for their corporate employees, the ultimate marketwide goal is to apply technology to both reduce costs and improve patient care. Warren Buffet, Berkshire Hathaway’s founder, said in a statement, “The ballooning costs of health care act as a hungry tapeworm on the American economy.” (And yes, I imagine that many hospitalists would take umbrage with that characterization.) In addition to the Amazon alliance, CVS Health and Aetna also recently agreed to join forces.
The rising health care interest by Amazon begs the imagination. Technology already is far along in automating routine procedures, elevating patient safety protocols, and recalculating patient flows and information. This added corporate interest and investment will further expand new ideas and innovative technologies. And, for sure, it will challenge long held beliefs and practices that shape the health system we have today.
Hospitalist insight needed
What is the role of hospitalist leaders in this shifting equation? Hospitalists already can claim significant credit for introducing major changes in the landscape of hospital care in this country, with all the concomitant improvements in the efficiencies and quality of more integrated service delivery. Can you also guide the system in strategically selecting where and how technology can best be applied to automate and reconfigure service delivery?
The most important questions are: What is it that humans in health care uniquely do that cannot otherwise be accomplished? Are we able to hold onto the humane sides of health care, even as we seek to introduce cost-saving efficiencies?
Top of mind come the most personal sides of health service delivery: touch, empathy, understanding, and care itself. Next come human analysis, understanding, and translation. And beyond that, leadership, direction, and the vision to craft a health care system that meets our societal expectations – not just for the wealthy who cannot afford it – but for everyone.
It would be easy to dismiss this conversation. Society never decided whether those bank tellers, travel agents, or journalists were critical to our functioning. Along these same lines, you and your patients are more than mere algorithms.
As I often share in my leadership seminars, one key function of leaders is to identify and ask the right questions and to be at the decision-making table. What are those questions?
As a hospitalist leader, which part of your work and your activities could be eased by automation? Where might technology ease pressures and enhance your interactions with patients? How do we improve the efficiencies and effectiveness of health service delivery while we preserve the very human qualities that are fundamental to its values? No patient wants to speak to a physician who stares at a computer screen without eye contact, reassurance, or genuine interest. We can do better than that.
Business stakeholders in the system – and clearly, they are positioning and are powerful – will hold great sway on the contours of our future health care system. They could see humans – with all their costs, imperfections, and distractions – as replaceable.
Know that as you lead and pose your questions, there are people interested in listening. Certainly, the tech industry is looking for opportunities to generate broad market appeal. Similarly, health system decision makers looking to enhance how the system functions likewise seek guidance on what could – and could not – work. And who knows: Those decision makers could very well be you.
This is a conversation the country deserves. There is nothing more intimate, more personally important, and more professionally satisfying than the genuine person-to-person quality of what we do in health care. What we arrive at in the end should be achieved by intent, not by accident.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration,” 2nd ed. (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
What will be the role of humans in the future health system?
At first blush, this is a peculiar question. Health care is all about humans. How could one doubt their presence or role? It is working with and for people that attracted many to this profession.
On the cusp of a significant health system reformulation, it is the very question that hospitalists now must ponder. Just as ATMs replaced bank cashiers, online shopping replaced retail stores, and autonomous cars will soon replace drivers, the human landscape of health care is about to change. What pressures will force the changes?
On one hand, there is increasing demand. The Affordable Care Act opened the insurance door for people previously uncovered. Aging is delivering the baby boomer bubble into their sicker years. Hospitalists witness this phenomenon every day in the ballooning parade of patients they serve. At times, those pressures can overwhelm.
On the other hand, the political will to provide government subsidized health coverage is waning. Washington is tripping over itself to dismantle Obamacare with glancing concern for how it will inflate the ranks of the uninsured. Employers are eager to free themselves from the burden of providing increasingly expensive health coverage benefits. By removing the mandate to buy health care insurance, the current political health system architects are liberating the healthy paying population from their contributions to the overall insurance pool. Simply put, there is and will be less money and less of all that it buys.
Combine building demand with decreasing budget into a system that does not follow general market forces: You get that earthquake. A consumer can forgo that new phone in hard times but not that cardiac procedure. People will be caught in the fissures of the system. Waits, quality, burnout, morale problems, and financial losses will all trend in the wrong directions. The process will evolve in slow motion. Some might argue that we have already arrived.
Enter entrepreneurs, technologic advances, and a growing savvy and willingness to engage tech solutions to everyday problems. If Alexa can turn on your toaster, could it take your blood pressure? If a robot can vacuum your rug, could a different robot provide personal care services? And, if an algorithm can drive your car, could it similarly diagnose what ails you?
On Jan. 30, 2018, one of the greatest disrupters of all time, Amazon, announced that it is joining forces with Berkshire Hathaway and JPMorgan Chase to leap into health care. While they are initially experimenting with health care changes for their corporate employees, the ultimate marketwide goal is to apply technology to both reduce costs and improve patient care. Warren Buffet, Berkshire Hathaway’s founder, said in a statement, “The ballooning costs of health care act as a hungry tapeworm on the American economy.” (And yes, I imagine that many hospitalists would take umbrage with that characterization.) In addition to the Amazon alliance, CVS Health and Aetna also recently agreed to join forces.
The rising health care interest by Amazon begs the imagination. Technology already is far along in automating routine procedures, elevating patient safety protocols, and recalculating patient flows and information. This added corporate interest and investment will further expand new ideas and innovative technologies. And, for sure, it will challenge long held beliefs and practices that shape the health system we have today.
Hospitalist insight needed
What is the role of hospitalist leaders in this shifting equation? Hospitalists already can claim significant credit for introducing major changes in the landscape of hospital care in this country, with all the concomitant improvements in the efficiencies and quality of more integrated service delivery. Can you also guide the system in strategically selecting where and how technology can best be applied to automate and reconfigure service delivery?
The most important questions are: What is it that humans in health care uniquely do that cannot otherwise be accomplished? Are we able to hold onto the humane sides of health care, even as we seek to introduce cost-saving efficiencies?
Top of mind come the most personal sides of health service delivery: touch, empathy, understanding, and care itself. Next come human analysis, understanding, and translation. And beyond that, leadership, direction, and the vision to craft a health care system that meets our societal expectations – not just for the wealthy who cannot afford it – but for everyone.
It would be easy to dismiss this conversation. Society never decided whether those bank tellers, travel agents, or journalists were critical to our functioning. Along these same lines, you and your patients are more than mere algorithms.
As I often share in my leadership seminars, one key function of leaders is to identify and ask the right questions and to be at the decision-making table. What are those questions?
As a hospitalist leader, which part of your work and your activities could be eased by automation? Where might technology ease pressures and enhance your interactions with patients? How do we improve the efficiencies and effectiveness of health service delivery while we preserve the very human qualities that are fundamental to its values? No patient wants to speak to a physician who stares at a computer screen without eye contact, reassurance, or genuine interest. We can do better than that.
Business stakeholders in the system – and clearly, they are positioning and are powerful – will hold great sway on the contours of our future health care system. They could see humans – with all their costs, imperfections, and distractions – as replaceable.
Know that as you lead and pose your questions, there are people interested in listening. Certainly, the tech industry is looking for opportunities to generate broad market appeal. Similarly, health system decision makers looking to enhance how the system functions likewise seek guidance on what could – and could not – work. And who knows: Those decision makers could very well be you.
This is a conversation the country deserves. There is nothing more intimate, more personally important, and more professionally satisfying than the genuine person-to-person quality of what we do in health care. What we arrive at in the end should be achieved by intent, not by accident.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration,” 2nd ed. (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution, Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Buprenorphine endangers lives and health of children
Eleven children died from exposure to buprenorphine – a drug used to treat opioid exposure – from 2007 to 2016, mostly very young children who accidentally ingested the drug.
Four deaths, however, were teens who took buprenorphine recreationally or used it in a suicide attempt, according to a new database review by Sara Post, MS, of the Research Institute at Nationwide Children’s Hospital, Columbus, Ohio, and her associates.
“In 2016, the American Academy of Pediatrics issued a statement advocating for increased access to buprenorphine for opioid-addicted adolescents in primary care settings,” the authors noted. “This recommendation is warranted because of the high and increasing prevalence of opioid dependence among adolescents. However, caution should be used, because increased prescriptions among adolescents could lead to increased diversion and abuse and increased access to younger children in the home. Therefore, patient education for adolescents should include information about the dangers of misusing and/or abusing prescription drugs and the proper storage of medications.”
The deaths comprise a small fraction of the 11,275 children aged 19 years and younger whose buprenorphine ingestions were reported to a poison control center during that time, the investigators said. Nevertheless, almost half (45%) of the exposed children were admitted to a health care facility – with 22% needing treatment in a critical care unit.
The rate of exposures was highest during the years when only tablet formulations were available and fell after film was introduced, wrote Ms. Post, a medical student at the Northeast Ohio Medical University in Rootstown, and her colleagues. But after 2013, the rate held steady, at about 38 exposures per 1 million children per year.
Childproof packaging for all buprenorphine formulations could help protect younger children, and education could help protect older ones, she and her coinvestigators said. Manufacturers should use unit-dose packaging for all buprenorphine products to help prevent unintentional exposure among young children. Health care providers should inform caregivers of young children about the dangers of buprenorphine exposure and provide instructions on proper storage and disposal of medications. Adolescents should receive information regarding the risks of substance abuse and misuse.”
Ms. Post and her colleagues analyzed calls to poison control centers affiliated with the National Poison Data System from 2007 to 2016. During that time, the centers received 11,275 calls about buprenorphine exposure among children and adolescents 19 years and younger.
The mean age of exposure in children was about 4 years; children younger than 6 years comprised 86% of the exposures (9,709).
The investigators noted temporal trends in exposure rates in this group. From 2007 to 2013, the rate increased by 215%, peaking at 20 per 1 million in 2010. A decline followed, with exposure dropping to 12 per 1 million in 2013, before rising again to 13 in 2016.
The increase “was likely attributable to the increasing number of buprenorphine prescriptions dispensed since the Food and Drug Administration approved its use as a treatment of opioid dependence in 2002,” Ms. Post and her colleagues wrote.
The transient decrease may have been related to a shift in adult prescribing patterns, as the drug was prescribed less often to those in their 20s and gradually given more often to people aged 40-59 years.
The decrease also was probably related to the packaging shift from tablet to film. “In 2013, the leading brand-name tablets were voluntarily withdrawn from the U.S. market because of potential risk of unintentional pediatric exposures,” the team wrote. Unfortunately, the film packaging didn’t completely deter some children; from 2013 to 2016, there was a 30% increase in the frequency of exposures to buprenorphine film.
The bulk of exposures were unintentional (98%) and involved ingestion of a single buprenorphine product. However, the authors noted, even a single adult therapeutic dose can be extremely dangerous to a small child.
“Therapeutic doses of buprenorphine-naloxone for pediatric patients are 2 to 6 mcg/kg, so ingestion of a single 2-mg sublingual tablet in a 10-kg child can result in more than a 30-fold overdose. This is particularly dangerous, because children exposed to buprenorphine do not display the ‘ceiling effect’ reported in adults, in which escalating doses do not lead to additional increases in respiratory depression,” Ms. Post and her coauthors said.
This was reflected in the serious clinical effects experienced: respiratory depression, bradycardia, coma, cyanosis, respiratory arrest, seizure, and cardiac arrest. These youngest children experienced the most serious outcomes, with half requiring a hospital admittance and 21% experiencing a serious medical outcome. Seven died, six of whom were 2 years or younger.
There were 315 (3%) exposures in children aged 6-12 years; most of these (83%) were either unintentional or therapeutic errors (18%). About 30% of the group required hospital admission and about 12% experienced a serious medical outcome. There were no fatalities among this group, the investigators noted.
Among adolescents aged 13-19 years, there were 1,251 (11%) exposures and four deaths. The bulk of these (77%) was intentional, with suspected suicide accounting for 12%, and 30% involving more than one substance. The exposure rate followed the same general trends, rising to a peak of about 6 per 1 million in 2010 and the falling and leveling off at about 3 per 1 million in 2016, they said.
About 22% of teen exposures required hospital admission, with 11% needing treatment in a critical care unit. The four deaths, one of which was a suicide, all involved multiple substances (benzodiazepines, alcohol, and marijuana).
Ms. Post received a research stipend from the National Student Injury Research Training Program while she worked on the study. The coauthors had no relevant financial disclosures.
SOURCE: Post et al. Pediatrics. 2018;142:e20173652.
Eleven children died from exposure to buprenorphine – a drug used to treat opioid exposure – from 2007 to 2016, mostly very young children who accidentally ingested the drug.
Four deaths, however, were teens who took buprenorphine recreationally or used it in a suicide attempt, according to a new database review by Sara Post, MS, of the Research Institute at Nationwide Children’s Hospital, Columbus, Ohio, and her associates.
“In 2016, the American Academy of Pediatrics issued a statement advocating for increased access to buprenorphine for opioid-addicted adolescents in primary care settings,” the authors noted. “This recommendation is warranted because of the high and increasing prevalence of opioid dependence among adolescents. However, caution should be used, because increased prescriptions among adolescents could lead to increased diversion and abuse and increased access to younger children in the home. Therefore, patient education for adolescents should include information about the dangers of misusing and/or abusing prescription drugs and the proper storage of medications.”
The deaths comprise a small fraction of the 11,275 children aged 19 years and younger whose buprenorphine ingestions were reported to a poison control center during that time, the investigators said. Nevertheless, almost half (45%) of the exposed children were admitted to a health care facility – with 22% needing treatment in a critical care unit.
The rate of exposures was highest during the years when only tablet formulations were available and fell after film was introduced, wrote Ms. Post, a medical student at the Northeast Ohio Medical University in Rootstown, and her colleagues. But after 2013, the rate held steady, at about 38 exposures per 1 million children per year.
Childproof packaging for all buprenorphine formulations could help protect younger children, and education could help protect older ones, she and her coinvestigators said. Manufacturers should use unit-dose packaging for all buprenorphine products to help prevent unintentional exposure among young children. Health care providers should inform caregivers of young children about the dangers of buprenorphine exposure and provide instructions on proper storage and disposal of medications. Adolescents should receive information regarding the risks of substance abuse and misuse.”
Ms. Post and her colleagues analyzed calls to poison control centers affiliated with the National Poison Data System from 2007 to 2016. During that time, the centers received 11,275 calls about buprenorphine exposure among children and adolescents 19 years and younger.
The mean age of exposure in children was about 4 years; children younger than 6 years comprised 86% of the exposures (9,709).
The investigators noted temporal trends in exposure rates in this group. From 2007 to 2013, the rate increased by 215%, peaking at 20 per 1 million in 2010. A decline followed, with exposure dropping to 12 per 1 million in 2013, before rising again to 13 in 2016.
The increase “was likely attributable to the increasing number of buprenorphine prescriptions dispensed since the Food and Drug Administration approved its use as a treatment of opioid dependence in 2002,” Ms. Post and her colleagues wrote.
The transient decrease may have been related to a shift in adult prescribing patterns, as the drug was prescribed less often to those in their 20s and gradually given more often to people aged 40-59 years.
The decrease also was probably related to the packaging shift from tablet to film. “In 2013, the leading brand-name tablets were voluntarily withdrawn from the U.S. market because of potential risk of unintentional pediatric exposures,” the team wrote. Unfortunately, the film packaging didn’t completely deter some children; from 2013 to 2016, there was a 30% increase in the frequency of exposures to buprenorphine film.
The bulk of exposures were unintentional (98%) and involved ingestion of a single buprenorphine product. However, the authors noted, even a single adult therapeutic dose can be extremely dangerous to a small child.
“Therapeutic doses of buprenorphine-naloxone for pediatric patients are 2 to 6 mcg/kg, so ingestion of a single 2-mg sublingual tablet in a 10-kg child can result in more than a 30-fold overdose. This is particularly dangerous, because children exposed to buprenorphine do not display the ‘ceiling effect’ reported in adults, in which escalating doses do not lead to additional increases in respiratory depression,” Ms. Post and her coauthors said.
This was reflected in the serious clinical effects experienced: respiratory depression, bradycardia, coma, cyanosis, respiratory arrest, seizure, and cardiac arrest. These youngest children experienced the most serious outcomes, with half requiring a hospital admittance and 21% experiencing a serious medical outcome. Seven died, six of whom were 2 years or younger.
There were 315 (3%) exposures in children aged 6-12 years; most of these (83%) were either unintentional or therapeutic errors (18%). About 30% of the group required hospital admission and about 12% experienced a serious medical outcome. There were no fatalities among this group, the investigators noted.
Among adolescents aged 13-19 years, there were 1,251 (11%) exposures and four deaths. The bulk of these (77%) was intentional, with suspected suicide accounting for 12%, and 30% involving more than one substance. The exposure rate followed the same general trends, rising to a peak of about 6 per 1 million in 2010 and the falling and leveling off at about 3 per 1 million in 2016, they said.
About 22% of teen exposures required hospital admission, with 11% needing treatment in a critical care unit. The four deaths, one of which was a suicide, all involved multiple substances (benzodiazepines, alcohol, and marijuana).
Ms. Post received a research stipend from the National Student Injury Research Training Program while she worked on the study. The coauthors had no relevant financial disclosures.
SOURCE: Post et al. Pediatrics. 2018;142:e20173652.
Eleven children died from exposure to buprenorphine – a drug used to treat opioid exposure – from 2007 to 2016, mostly very young children who accidentally ingested the drug.
Four deaths, however, were teens who took buprenorphine recreationally or used it in a suicide attempt, according to a new database review by Sara Post, MS, of the Research Institute at Nationwide Children’s Hospital, Columbus, Ohio, and her associates.
“In 2016, the American Academy of Pediatrics issued a statement advocating for increased access to buprenorphine for opioid-addicted adolescents in primary care settings,” the authors noted. “This recommendation is warranted because of the high and increasing prevalence of opioid dependence among adolescents. However, caution should be used, because increased prescriptions among adolescents could lead to increased diversion and abuse and increased access to younger children in the home. Therefore, patient education for adolescents should include information about the dangers of misusing and/or abusing prescription drugs and the proper storage of medications.”
The deaths comprise a small fraction of the 11,275 children aged 19 years and younger whose buprenorphine ingestions were reported to a poison control center during that time, the investigators said. Nevertheless, almost half (45%) of the exposed children were admitted to a health care facility – with 22% needing treatment in a critical care unit.
The rate of exposures was highest during the years when only tablet formulations were available and fell after film was introduced, wrote Ms. Post, a medical student at the Northeast Ohio Medical University in Rootstown, and her colleagues. But after 2013, the rate held steady, at about 38 exposures per 1 million children per year.
Childproof packaging for all buprenorphine formulations could help protect younger children, and education could help protect older ones, she and her coinvestigators said. Manufacturers should use unit-dose packaging for all buprenorphine products to help prevent unintentional exposure among young children. Health care providers should inform caregivers of young children about the dangers of buprenorphine exposure and provide instructions on proper storage and disposal of medications. Adolescents should receive information regarding the risks of substance abuse and misuse.”
Ms. Post and her colleagues analyzed calls to poison control centers affiliated with the National Poison Data System from 2007 to 2016. During that time, the centers received 11,275 calls about buprenorphine exposure among children and adolescents 19 years and younger.
The mean age of exposure in children was about 4 years; children younger than 6 years comprised 86% of the exposures (9,709).
The investigators noted temporal trends in exposure rates in this group. From 2007 to 2013, the rate increased by 215%, peaking at 20 per 1 million in 2010. A decline followed, with exposure dropping to 12 per 1 million in 2013, before rising again to 13 in 2016.
The increase “was likely attributable to the increasing number of buprenorphine prescriptions dispensed since the Food and Drug Administration approved its use as a treatment of opioid dependence in 2002,” Ms. Post and her colleagues wrote.
The transient decrease may have been related to a shift in adult prescribing patterns, as the drug was prescribed less often to those in their 20s and gradually given more often to people aged 40-59 years.
The decrease also was probably related to the packaging shift from tablet to film. “In 2013, the leading brand-name tablets were voluntarily withdrawn from the U.S. market because of potential risk of unintentional pediatric exposures,” the team wrote. Unfortunately, the film packaging didn’t completely deter some children; from 2013 to 2016, there was a 30% increase in the frequency of exposures to buprenorphine film.
The bulk of exposures were unintentional (98%) and involved ingestion of a single buprenorphine product. However, the authors noted, even a single adult therapeutic dose can be extremely dangerous to a small child.
“Therapeutic doses of buprenorphine-naloxone for pediatric patients are 2 to 6 mcg/kg, so ingestion of a single 2-mg sublingual tablet in a 10-kg child can result in more than a 30-fold overdose. This is particularly dangerous, because children exposed to buprenorphine do not display the ‘ceiling effect’ reported in adults, in which escalating doses do not lead to additional increases in respiratory depression,” Ms. Post and her coauthors said.
This was reflected in the serious clinical effects experienced: respiratory depression, bradycardia, coma, cyanosis, respiratory arrest, seizure, and cardiac arrest. These youngest children experienced the most serious outcomes, with half requiring a hospital admittance and 21% experiencing a serious medical outcome. Seven died, six of whom were 2 years or younger.
There were 315 (3%) exposures in children aged 6-12 years; most of these (83%) were either unintentional or therapeutic errors (18%). About 30% of the group required hospital admission and about 12% experienced a serious medical outcome. There were no fatalities among this group, the investigators noted.
Among adolescents aged 13-19 years, there were 1,251 (11%) exposures and four deaths. The bulk of these (77%) was intentional, with suspected suicide accounting for 12%, and 30% involving more than one substance. The exposure rate followed the same general trends, rising to a peak of about 6 per 1 million in 2010 and the falling and leveling off at about 3 per 1 million in 2016, they said.
About 22% of teen exposures required hospital admission, with 11% needing treatment in a critical care unit. The four deaths, one of which was a suicide, all involved multiple substances (benzodiazepines, alcohol, and marijuana).
Ms. Post received a research stipend from the National Student Injury Research Training Program while she worked on the study. The coauthors had no relevant financial disclosures.
SOURCE: Post et al. Pediatrics. 2018;142:e20173652.
FROM PEDIATRICS
Key clinical point: Buprenorphine ingestion remains a threat to children, especially those younger than 6 years.
Major finding: From 2007 to 2016, 11,275 exposures were reported; 11 children died.
Study details: The database review looked at records from the National Poison Data System.
Disclosures: Ms. Post received a research stipend from the National Student Injury Research Training Program while she worked on the study. The coauthors had no relevant financial disclosures.
Source: Post et al. Pediatrics. 2018;142:e20173652.
Addressing malnutrition and improving performance
Stakeholders develop a malnutrition Toolkit
Hospitalists are key players in improving hospital performance, but they may be overlooking a leading cause of morbidity and mortality, especially among older adults.
Research suggests that at the time of hospital admission, some 20%-50% of all patients are at risk for malnutrition or are malnourished, but only 7% of those patients are diagnosed during their stay, according to research cited in an abstract presented at HM17.1
“Because individuals who are malnourished lack sufficient nutrients to promote healing and rehabilitation, and are at increased risk of medical complications, it can have a serious impact on patient safety indicators, such as rates of pressure ulcers, wound healing, and risk of falls,” said lead author Eleanor Fitall of Avalere Health. “Early identification and subsequent treatment of these patients is the best way to prevent this risk.”
To address the issue, Avalere Health and the Academy of Nutrition and Dietetics established the Malnutrition Quality Improvement Initiative (MQii), a multi-stakeholder effort to identify tools to support hospital-based care teams in improving malnutrition care quality. They developed a malnutrition Toolkit, which was piloted in 2016 and was shown to effectively improve malnutrition care.
“Since the poster presentation in May, we have successfully implemented the Toolkit at 50 hospitals via a multi-hospital Learning Collaborative,” Ms. Fitall said. They are now recruiting hospitals and health systems to participate in an expanded Learning Collaborative. Interested sites should contact the MQii team at [email protected].
“By supporting efforts to improve malnutrition care in the inpatient setting, hospitalists can help reduce the incidence of these problems as well as decrease rates of readmissions and reduce patient lengths of stay,” Ms. Fitall said. “Hospitalists are critical to addressing malnutrition care gaps in the hospital. Dietitians that have undertaken malnutrition quality improvement projects using the MQii Toolkit have found that they are most successful when hospitalists are actively engaged in the team, particularly when looking to improve the rate of malnutrition diagnosis. Hospitalists are ideally positioned to champion these efforts.”
Support for MQii was provided by Abbott, she said.
Reference
1. Fitall E, Bruno M, Jones K, Lynch J, Silver H, Godamunne K, Valladares A, Mitchell K. Malnutrition Care: “Low Hanging Fruit” for Hospitalist Clinical Performance Improvement [abstract]. J Hosp Med. 2017;12(suppl 2).
Stakeholders develop a malnutrition Toolkit
Stakeholders develop a malnutrition Toolkit
Hospitalists are key players in improving hospital performance, but they may be overlooking a leading cause of morbidity and mortality, especially among older adults.
Research suggests that at the time of hospital admission, some 20%-50% of all patients are at risk for malnutrition or are malnourished, but only 7% of those patients are diagnosed during their stay, according to research cited in an abstract presented at HM17.1
“Because individuals who are malnourished lack sufficient nutrients to promote healing and rehabilitation, and are at increased risk of medical complications, it can have a serious impact on patient safety indicators, such as rates of pressure ulcers, wound healing, and risk of falls,” said lead author Eleanor Fitall of Avalere Health. “Early identification and subsequent treatment of these patients is the best way to prevent this risk.”
To address the issue, Avalere Health and the Academy of Nutrition and Dietetics established the Malnutrition Quality Improvement Initiative (MQii), a multi-stakeholder effort to identify tools to support hospital-based care teams in improving malnutrition care quality. They developed a malnutrition Toolkit, which was piloted in 2016 and was shown to effectively improve malnutrition care.
“Since the poster presentation in May, we have successfully implemented the Toolkit at 50 hospitals via a multi-hospital Learning Collaborative,” Ms. Fitall said. They are now recruiting hospitals and health systems to participate in an expanded Learning Collaborative. Interested sites should contact the MQii team at [email protected].
“By supporting efforts to improve malnutrition care in the inpatient setting, hospitalists can help reduce the incidence of these problems as well as decrease rates of readmissions and reduce patient lengths of stay,” Ms. Fitall said. “Hospitalists are critical to addressing malnutrition care gaps in the hospital. Dietitians that have undertaken malnutrition quality improvement projects using the MQii Toolkit have found that they are most successful when hospitalists are actively engaged in the team, particularly when looking to improve the rate of malnutrition diagnosis. Hospitalists are ideally positioned to champion these efforts.”
Support for MQii was provided by Abbott, she said.
Reference
1. Fitall E, Bruno M, Jones K, Lynch J, Silver H, Godamunne K, Valladares A, Mitchell K. Malnutrition Care: “Low Hanging Fruit” for Hospitalist Clinical Performance Improvement [abstract]. J Hosp Med. 2017;12(suppl 2).
Hospitalists are key players in improving hospital performance, but they may be overlooking a leading cause of morbidity and mortality, especially among older adults.
Research suggests that at the time of hospital admission, some 20%-50% of all patients are at risk for malnutrition or are malnourished, but only 7% of those patients are diagnosed during their stay, according to research cited in an abstract presented at HM17.1
“Because individuals who are malnourished lack sufficient nutrients to promote healing and rehabilitation, and are at increased risk of medical complications, it can have a serious impact on patient safety indicators, such as rates of pressure ulcers, wound healing, and risk of falls,” said lead author Eleanor Fitall of Avalere Health. “Early identification and subsequent treatment of these patients is the best way to prevent this risk.”
To address the issue, Avalere Health and the Academy of Nutrition and Dietetics established the Malnutrition Quality Improvement Initiative (MQii), a multi-stakeholder effort to identify tools to support hospital-based care teams in improving malnutrition care quality. They developed a malnutrition Toolkit, which was piloted in 2016 and was shown to effectively improve malnutrition care.
“Since the poster presentation in May, we have successfully implemented the Toolkit at 50 hospitals via a multi-hospital Learning Collaborative,” Ms. Fitall said. They are now recruiting hospitals and health systems to participate in an expanded Learning Collaborative. Interested sites should contact the MQii team at [email protected].
“By supporting efforts to improve malnutrition care in the inpatient setting, hospitalists can help reduce the incidence of these problems as well as decrease rates of readmissions and reduce patient lengths of stay,” Ms. Fitall said. “Hospitalists are critical to addressing malnutrition care gaps in the hospital. Dietitians that have undertaken malnutrition quality improvement projects using the MQii Toolkit have found that they are most successful when hospitalists are actively engaged in the team, particularly when looking to improve the rate of malnutrition diagnosis. Hospitalists are ideally positioned to champion these efforts.”
Support for MQii was provided by Abbott, she said.
Reference
1. Fitall E, Bruno M, Jones K, Lynch J, Silver H, Godamunne K, Valladares A, Mitchell K. Malnutrition Care: “Low Hanging Fruit” for Hospitalist Clinical Performance Improvement [abstract]. J Hosp Med. 2017;12(suppl 2).
Quick Byte: PrEP advances
There are recent advances in preexposure prophylaxis, or PrEP, as a promising prevention option for HIV, according to a recent study.1
Reference
1. Desai M, Field N, Grant R, McCormack S. “Recent advances in pre-exposure prophylaxis for HIV.” BMJ. 2017;359:j5011.
There are recent advances in preexposure prophylaxis, or PrEP, as a promising prevention option for HIV, according to a recent study.1
Reference
1. Desai M, Field N, Grant R, McCormack S. “Recent advances in pre-exposure prophylaxis for HIV.” BMJ. 2017;359:j5011.
There are recent advances in preexposure prophylaxis, or PrEP, as a promising prevention option for HIV, according to a recent study.1
Reference
1. Desai M, Field N, Grant R, McCormack S. “Recent advances in pre-exposure prophylaxis for HIV.” BMJ. 2017;359:j5011.
Biomarker duo rapidly identifies serious bacterial infections
MALMO, SWEDEN – The combination of serum procalcitonin and C-reactive protein levels upon admission to a pediatric ICU displayed high utility for early diagnosis of serious bacterial infection in critically ill children in a large prospective observational study presented at the annual meeting of the European Society for Paediatric Infectious Diseases.
This winning combination significantly outperformed neutrophil gelatinase-associated lipocalin, activated partial thromboplastin time, and resistin, both individually and in various combinations, for the vital task of making a rapid distinction between infectious and noninfectious causes of pediatric systemic inflammatory response syndrome, reported Enitan D. Carrol, MD, professor of pediatric infection at the University of Liverpool (England).
“One of the clinical dilemmas we face in intensive care is being able to differentiate between infectious and noninfectious causes of systemic inflammatory response syndrome. This is important because we need to identify which children have life-threatening infections so that we can promptly initiate antimicrobial therapy,” she explained.
One in four deaths in pediatric ICUs are infection related, Dr. Carrol noted.
“There is an urgent need for infection markers which, firstly, change early in the course of bacterial infection, secondly, correlate with real-time clinical progression, and thirdly, have a rapid turn-around time to allow effective clinical decision making,” she observed.
The combination of procalcitonin and C-reactive protein (CRP) levels measured at admission fits the bill, Dr. Carrol continued. Of the five biomarkers evaluated in her study – all backed by some supporting evidence of efficacy in earlier studies – the top two individual performers in terms of negative predictive value (NPV) were a CRP less than 4.2 mg/dL with a negative NPV of 99%, and a procalcitonin less than 1.52 ng/mL with an NPV of 96%. The positive predictive value of each of the biomarkers was 37%. The sensitivity and specificity of procalcitonin for diagnosis of serious bacterial infection were 78% and 80%, respectively. For CRP, the figures were 93% and 76%.
The combination of procalcitonin and CRP outperformed a multitude of other two-, three-, and four-biomarker combinations tested, with an area under the curve of 93% for combined sensitivity and specificity.
The study included 657 children admitted to the pediatric ICU at Alder Hey Children’s Hospital in Liverpool with systemic inflammatory response syndrome. All had blood samples measured for the five biomarkers on days 1-7. Clinicians were blinded as to the biomarker results. Ninety-two (14%) patients were ultimately found to have a serious bacterial infection – essentially, bacterial meningitis or septic shock – and 565 (86%) had a nonbacterial etiology.
The 28-day mortality rate was 9% in the group with serious bacterial infection, significantly higher than the 2% rate in the group with other causes of their systemic inflammatory response syndrome.
Longitudinal trends in procalcitonin and CRP as evidenced in the study can be used in clinical decision making, according to Dr. Carrol. Mean values of procalcitonin plummeted by 80% from day 1 to day 5 in response to antimicrobial therapy in the group with serious bacterial infections. In contrast, CRP levels rose sharply from day 1 to a peak on day 2, then fell, although the 50% drop from day 2 to day 5 in response to antimicrobial therapy wasn’t as pronounced as the change in procalcitonin.
“There is an additive benefit for both biomarkers compared with CRP alone. The problem with CRP on admission, as I’ve demonstrated in this study, is it often hasn’t risen yet early after admission. So although it gave the best area under the curve of any of the biomarkers, I think that combined with procalcitonin you get a much better descriminator,” Dr. Carrol said.
The median duration of ICU stay in the patients with serious bacterial infection at admission was 5 days, compared with 3 days when the cause of systemic inflammatory response syndrome lay elsewhere. Their median duration of ventilation was significantly longer, too: 4 days versus 2 in children without a serious bacterial infection.
Stepwise logistic regression analysis pinpointed several clinical variables as being associated with prolonged ICU stay.
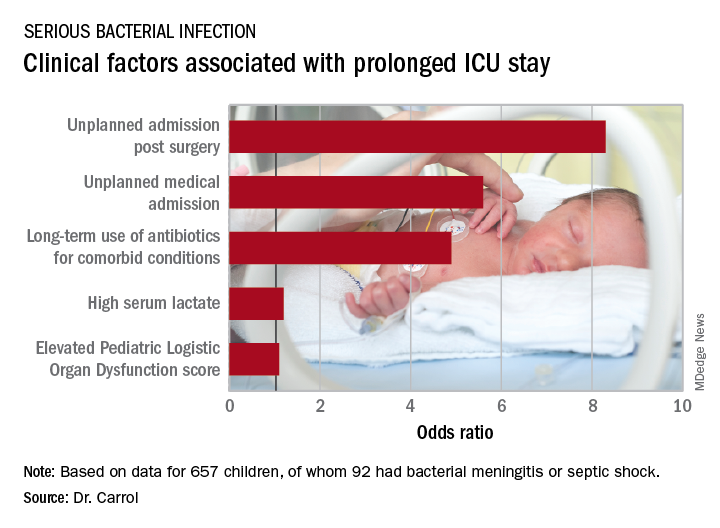
In addition, initiation of antibiotic therapy prior to admission to the pediatric ICU was associated with a 50% reduction in the likelihood of a prolonged ICU stay. “This reflects the fact that early antibiotics give you a better prognosis if you have sepsis,” according to Dr. Carrol.
She and her coinvestigators now have embarked on a multicenter U.K. study looking at the impact of procalcitonin to guide duration of antimicrobial therapy in critically ill children.
The Alder Hey study was funded by the U.K. National Institute for Health Research. Dr. Carrol reported having no financial conflicts. Although she serves as a consultant to several health care companies, all remuneration goes directly to the University of Liverpool.
MALMO, SWEDEN – The combination of serum procalcitonin and C-reactive protein levels upon admission to a pediatric ICU displayed high utility for early diagnosis of serious bacterial infection in critically ill children in a large prospective observational study presented at the annual meeting of the European Society for Paediatric Infectious Diseases.
This winning combination significantly outperformed neutrophil gelatinase-associated lipocalin, activated partial thromboplastin time, and resistin, both individually and in various combinations, for the vital task of making a rapid distinction between infectious and noninfectious causes of pediatric systemic inflammatory response syndrome, reported Enitan D. Carrol, MD, professor of pediatric infection at the University of Liverpool (England).
“One of the clinical dilemmas we face in intensive care is being able to differentiate between infectious and noninfectious causes of systemic inflammatory response syndrome. This is important because we need to identify which children have life-threatening infections so that we can promptly initiate antimicrobial therapy,” she explained.
One in four deaths in pediatric ICUs are infection related, Dr. Carrol noted.
“There is an urgent need for infection markers which, firstly, change early in the course of bacterial infection, secondly, correlate with real-time clinical progression, and thirdly, have a rapid turn-around time to allow effective clinical decision making,” she observed.
The combination of procalcitonin and C-reactive protein (CRP) levels measured at admission fits the bill, Dr. Carrol continued. Of the five biomarkers evaluated in her study – all backed by some supporting evidence of efficacy in earlier studies – the top two individual performers in terms of negative predictive value (NPV) were a CRP less than 4.2 mg/dL with a negative NPV of 99%, and a procalcitonin less than 1.52 ng/mL with an NPV of 96%. The positive predictive value of each of the biomarkers was 37%. The sensitivity and specificity of procalcitonin for diagnosis of serious bacterial infection were 78% and 80%, respectively. For CRP, the figures were 93% and 76%.
The combination of procalcitonin and CRP outperformed a multitude of other two-, three-, and four-biomarker combinations tested, with an area under the curve of 93% for combined sensitivity and specificity.
The study included 657 children admitted to the pediatric ICU at Alder Hey Children’s Hospital in Liverpool with systemic inflammatory response syndrome. All had blood samples measured for the five biomarkers on days 1-7. Clinicians were blinded as to the biomarker results. Ninety-two (14%) patients were ultimately found to have a serious bacterial infection – essentially, bacterial meningitis or septic shock – and 565 (86%) had a nonbacterial etiology.
The 28-day mortality rate was 9% in the group with serious bacterial infection, significantly higher than the 2% rate in the group with other causes of their systemic inflammatory response syndrome.
Longitudinal trends in procalcitonin and CRP as evidenced in the study can be used in clinical decision making, according to Dr. Carrol. Mean values of procalcitonin plummeted by 80% from day 1 to day 5 in response to antimicrobial therapy in the group with serious bacterial infections. In contrast, CRP levels rose sharply from day 1 to a peak on day 2, then fell, although the 50% drop from day 2 to day 5 in response to antimicrobial therapy wasn’t as pronounced as the change in procalcitonin.
“There is an additive benefit for both biomarkers compared with CRP alone. The problem with CRP on admission, as I’ve demonstrated in this study, is it often hasn’t risen yet early after admission. So although it gave the best area under the curve of any of the biomarkers, I think that combined with procalcitonin you get a much better descriminator,” Dr. Carrol said.
The median duration of ICU stay in the patients with serious bacterial infection at admission was 5 days, compared with 3 days when the cause of systemic inflammatory response syndrome lay elsewhere. Their median duration of ventilation was significantly longer, too: 4 days versus 2 in children without a serious bacterial infection.
Stepwise logistic regression analysis pinpointed several clinical variables as being associated with prolonged ICU stay.
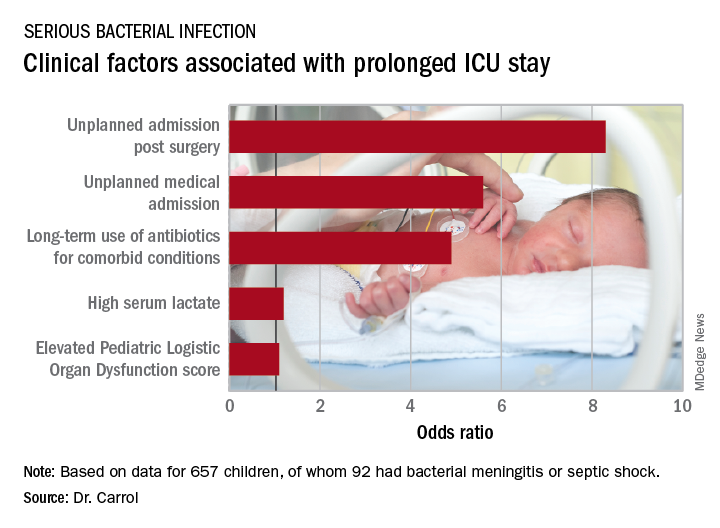
In addition, initiation of antibiotic therapy prior to admission to the pediatric ICU was associated with a 50% reduction in the likelihood of a prolonged ICU stay. “This reflects the fact that early antibiotics give you a better prognosis if you have sepsis,” according to Dr. Carrol.
She and her coinvestigators now have embarked on a multicenter U.K. study looking at the impact of procalcitonin to guide duration of antimicrobial therapy in critically ill children.
The Alder Hey study was funded by the U.K. National Institute for Health Research. Dr. Carrol reported having no financial conflicts. Although she serves as a consultant to several health care companies, all remuneration goes directly to the University of Liverpool.
MALMO, SWEDEN – The combination of serum procalcitonin and C-reactive protein levels upon admission to a pediatric ICU displayed high utility for early diagnosis of serious bacterial infection in critically ill children in a large prospective observational study presented at the annual meeting of the European Society for Paediatric Infectious Diseases.
This winning combination significantly outperformed neutrophil gelatinase-associated lipocalin, activated partial thromboplastin time, and resistin, both individually and in various combinations, for the vital task of making a rapid distinction between infectious and noninfectious causes of pediatric systemic inflammatory response syndrome, reported Enitan D. Carrol, MD, professor of pediatric infection at the University of Liverpool (England).
“One of the clinical dilemmas we face in intensive care is being able to differentiate between infectious and noninfectious causes of systemic inflammatory response syndrome. This is important because we need to identify which children have life-threatening infections so that we can promptly initiate antimicrobial therapy,” she explained.
One in four deaths in pediatric ICUs are infection related, Dr. Carrol noted.
“There is an urgent need for infection markers which, firstly, change early in the course of bacterial infection, secondly, correlate with real-time clinical progression, and thirdly, have a rapid turn-around time to allow effective clinical decision making,” she observed.
The combination of procalcitonin and C-reactive protein (CRP) levels measured at admission fits the bill, Dr. Carrol continued. Of the five biomarkers evaluated in her study – all backed by some supporting evidence of efficacy in earlier studies – the top two individual performers in terms of negative predictive value (NPV) were a CRP less than 4.2 mg/dL with a negative NPV of 99%, and a procalcitonin less than 1.52 ng/mL with an NPV of 96%. The positive predictive value of each of the biomarkers was 37%. The sensitivity and specificity of procalcitonin for diagnosis of serious bacterial infection were 78% and 80%, respectively. For CRP, the figures were 93% and 76%.
The combination of procalcitonin and CRP outperformed a multitude of other two-, three-, and four-biomarker combinations tested, with an area under the curve of 93% for combined sensitivity and specificity.
The study included 657 children admitted to the pediatric ICU at Alder Hey Children’s Hospital in Liverpool with systemic inflammatory response syndrome. All had blood samples measured for the five biomarkers on days 1-7. Clinicians were blinded as to the biomarker results. Ninety-two (14%) patients were ultimately found to have a serious bacterial infection – essentially, bacterial meningitis or septic shock – and 565 (86%) had a nonbacterial etiology.
The 28-day mortality rate was 9% in the group with serious bacterial infection, significantly higher than the 2% rate in the group with other causes of their systemic inflammatory response syndrome.
Longitudinal trends in procalcitonin and CRP as evidenced in the study can be used in clinical decision making, according to Dr. Carrol. Mean values of procalcitonin plummeted by 80% from day 1 to day 5 in response to antimicrobial therapy in the group with serious bacterial infections. In contrast, CRP levels rose sharply from day 1 to a peak on day 2, then fell, although the 50% drop from day 2 to day 5 in response to antimicrobial therapy wasn’t as pronounced as the change in procalcitonin.
“There is an additive benefit for both biomarkers compared with CRP alone. The problem with CRP on admission, as I’ve demonstrated in this study, is it often hasn’t risen yet early after admission. So although it gave the best area under the curve of any of the biomarkers, I think that combined with procalcitonin you get a much better descriminator,” Dr. Carrol said.
The median duration of ICU stay in the patients with serious bacterial infection at admission was 5 days, compared with 3 days when the cause of systemic inflammatory response syndrome lay elsewhere. Their median duration of ventilation was significantly longer, too: 4 days versus 2 in children without a serious bacterial infection.
Stepwise logistic regression analysis pinpointed several clinical variables as being associated with prolonged ICU stay.
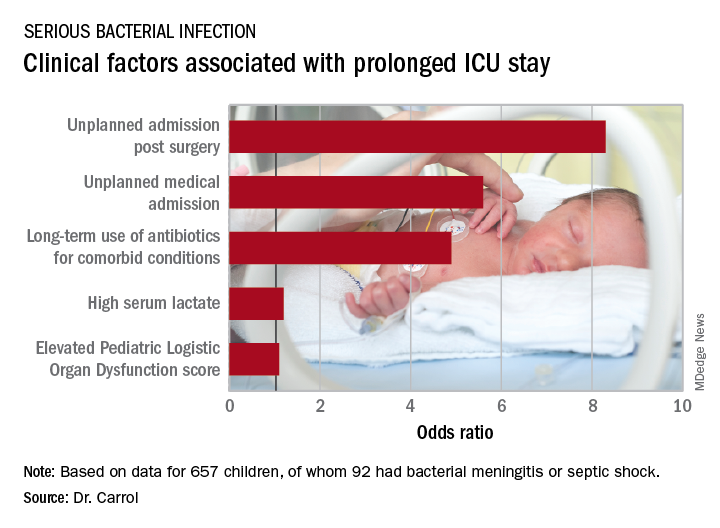
In addition, initiation of antibiotic therapy prior to admission to the pediatric ICU was associated with a 50% reduction in the likelihood of a prolonged ICU stay. “This reflects the fact that early antibiotics give you a better prognosis if you have sepsis,” according to Dr. Carrol.
She and her coinvestigators now have embarked on a multicenter U.K. study looking at the impact of procalcitonin to guide duration of antimicrobial therapy in critically ill children.
The Alder Hey study was funded by the U.K. National Institute for Health Research. Dr. Carrol reported having no financial conflicts. Although she serves as a consultant to several health care companies, all remuneration goes directly to the University of Liverpool.
REPORTING FROM ESPID 2018
Key clinical point:
Major finding: The area under the curve combining sensitivity and specificity was 93%.
Study details: This was a prospective, observational, single-center, clinician-blinded study of 657 patients admitted to a pediatric ICU with symptoms of systemic inflammatory response syndrome.
Disclosures: The study was funded by the U.K. National Institute for Health Research. The presenter reported having no relevant financial conflicts. Although she serves as a consultant to several health care companies, all remuneration goes directly to the University of Liverpool.
MI risk prediction after noncardiac surgery simplified
ORLANDO – The risk of perioperative MI or death associated with noncardiac surgery is vanishingly low in patients free of diabetes, hypertension, and smoking, Tanya Wilcox, MD, reported at the annual meeting of the American College of Cardiology.
How small is the risk? A mere 1 in 1,000, according to her analysis of more than 3.8 million major noncardiac surgeries in the American College of Surgeons National Surgical Quality Improvement Program database for 2009-2015, according to Dr. Wilcox of New York University.
Physicians are frequently asked by surgeons to clear patients for noncardiac surgery in terms of cardiovascular risk. Because current risk scores are complex, aren’t amenable to rapid bedside calculations, and may entail cardiac stress testing, Dr. Wilcox decided it was worth assessing the impact of three straightforward cardiovascular risk factors – current smoking and treatment for hypertension or diabetes – on 30-day postoperative MI-free survival. For this purpose she turned to the National Surgical Quality Improvement Program database, a validated, risk-adjusted, outcomes-based program to measure and improve the quality of surgical care utilizing data from 250 U.S. surgical centers.
Of the 3,817,113 patients who underwent major noncardiac surgery, 1,586,020 (42%) of them had none of the three cardiovascular risk factors of interest, 1,541,846 (40%) had one, 643,424 (17%) had two, and 45,823, or 1.2%, had all three. The patients’ mean age was 57, 75% were white, and 57% were women. About half of all patients underwent various operations within the realm of general surgery; next most frequent were orthopedic procedures, accounting for 18% of total noncardiac surgery. Of note, only 23% of patients with zero risk factors were American Society of Anesthesiologists Class 3-5, compared with 51% of those with one cardiovascular risk factor, 76% with two, and 71% with all three.
The incidence of acute MI or death within 30 days of noncardiac surgery climbed in stepwise fashion according to a patient’s risk factor burden. In a multivariate analysis adjusted for age, race, and gender, patients with any one of the cardiovascular risk factors had a 30-day risk of acute MI or death that was 1.52 times greater than those with no risk factors, patients with two risk factors were at 2.4-fold increased risk, and those with all three were at 3.63-fold greater risk than those with none. The degree of increased risk associated with any single risk factor ranged from 1.47-fold for hypertension to 1.94-fold for smoking.
“Further study is needed to determine whether aggressive risk factor modifications in the form of blood pressure control, glycemic control, and smoking cessation could reduce the incidence of postoperative MI,” Dr. Wilcox observed.
She reported having no financial conflicts regarding her study.
ORLANDO – The risk of perioperative MI or death associated with noncardiac surgery is vanishingly low in patients free of diabetes, hypertension, and smoking, Tanya Wilcox, MD, reported at the annual meeting of the American College of Cardiology.
How small is the risk? A mere 1 in 1,000, according to her analysis of more than 3.8 million major noncardiac surgeries in the American College of Surgeons National Surgical Quality Improvement Program database for 2009-2015, according to Dr. Wilcox of New York University.
Physicians are frequently asked by surgeons to clear patients for noncardiac surgery in terms of cardiovascular risk. Because current risk scores are complex, aren’t amenable to rapid bedside calculations, and may entail cardiac stress testing, Dr. Wilcox decided it was worth assessing the impact of three straightforward cardiovascular risk factors – current smoking and treatment for hypertension or diabetes – on 30-day postoperative MI-free survival. For this purpose she turned to the National Surgical Quality Improvement Program database, a validated, risk-adjusted, outcomes-based program to measure and improve the quality of surgical care utilizing data from 250 U.S. surgical centers.
Of the 3,817,113 patients who underwent major noncardiac surgery, 1,586,020 (42%) of them had none of the three cardiovascular risk factors of interest, 1,541,846 (40%) had one, 643,424 (17%) had two, and 45,823, or 1.2%, had all three. The patients’ mean age was 57, 75% were white, and 57% were women. About half of all patients underwent various operations within the realm of general surgery; next most frequent were orthopedic procedures, accounting for 18% of total noncardiac surgery. Of note, only 23% of patients with zero risk factors were American Society of Anesthesiologists Class 3-5, compared with 51% of those with one cardiovascular risk factor, 76% with two, and 71% with all three.
The incidence of acute MI or death within 30 days of noncardiac surgery climbed in stepwise fashion according to a patient’s risk factor burden. In a multivariate analysis adjusted for age, race, and gender, patients with any one of the cardiovascular risk factors had a 30-day risk of acute MI or death that was 1.52 times greater than those with no risk factors, patients with two risk factors were at 2.4-fold increased risk, and those with all three were at 3.63-fold greater risk than those with none. The degree of increased risk associated with any single risk factor ranged from 1.47-fold for hypertension to 1.94-fold for smoking.
“Further study is needed to determine whether aggressive risk factor modifications in the form of blood pressure control, glycemic control, and smoking cessation could reduce the incidence of postoperative MI,” Dr. Wilcox observed.
She reported having no financial conflicts regarding her study.
ORLANDO – The risk of perioperative MI or death associated with noncardiac surgery is vanishingly low in patients free of diabetes, hypertension, and smoking, Tanya Wilcox, MD, reported at the annual meeting of the American College of Cardiology.
How small is the risk? A mere 1 in 1,000, according to her analysis of more than 3.8 million major noncardiac surgeries in the American College of Surgeons National Surgical Quality Improvement Program database for 2009-2015, according to Dr. Wilcox of New York University.
Physicians are frequently asked by surgeons to clear patients for noncardiac surgery in terms of cardiovascular risk. Because current risk scores are complex, aren’t amenable to rapid bedside calculations, and may entail cardiac stress testing, Dr. Wilcox decided it was worth assessing the impact of three straightforward cardiovascular risk factors – current smoking and treatment for hypertension or diabetes – on 30-day postoperative MI-free survival. For this purpose she turned to the National Surgical Quality Improvement Program database, a validated, risk-adjusted, outcomes-based program to measure and improve the quality of surgical care utilizing data from 250 U.S. surgical centers.
Of the 3,817,113 patients who underwent major noncardiac surgery, 1,586,020 (42%) of them had none of the three cardiovascular risk factors of interest, 1,541,846 (40%) had one, 643,424 (17%) had two, and 45,823, or 1.2%, had all three. The patients’ mean age was 57, 75% were white, and 57% were women. About half of all patients underwent various operations within the realm of general surgery; next most frequent were orthopedic procedures, accounting for 18% of total noncardiac surgery. Of note, only 23% of patients with zero risk factors were American Society of Anesthesiologists Class 3-5, compared with 51% of those with one cardiovascular risk factor, 76% with two, and 71% with all three.
The incidence of acute MI or death within 30 days of noncardiac surgery climbed in stepwise fashion according to a patient’s risk factor burden. In a multivariate analysis adjusted for age, race, and gender, patients with any one of the cardiovascular risk factors had a 30-day risk of acute MI or death that was 1.52 times greater than those with no risk factors, patients with two risk factors were at 2.4-fold increased risk, and those with all three were at 3.63-fold greater risk than those with none. The degree of increased risk associated with any single risk factor ranged from 1.47-fold for hypertension to 1.94-fold for smoking.
“Further study is needed to determine whether aggressive risk factor modifications in the form of blood pressure control, glycemic control, and smoking cessation could reduce the incidence of postoperative MI,” Dr. Wilcox observed.
She reported having no financial conflicts regarding her study.
REPORTING FROM ACC 2018
Key clinical point: Noncardiac surgery patients can breathe easier regarding perioperative cardiovascular risk provided they don’t smoke and aren’t hypertensive or diabetic.
Major finding: .
Study details: This was a retrospective analysis of more than 3.8 million noncardiac surgeries contained in the American College of Surgeons National Surgical Quality Improvement Program database for 2009-2015.
Disclosures: The study presenter reported having no financial conflicts.