User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Stroke thrombectomy alone fails noninferiority to bridging tPA
In the prospective, multicenter trial, the rate of good functional outcome was 57% for patients who underwent direct thrombectomy and 65% among patients who received IV thrombolysis before undergoing thrombectomy. This result failed to demonstrate noninferiority of direct mechanical thrombectomy compared to combination therapy, the researchers conclude.
“Good outcome was high in both treatment arms, with the point estimate in favor of the bridging cohort,” said lead investigator Urs Fischer, MD, co-chair of the stroke center at Inselspital, Bern University Hospital, Switzerland, during his presentation. “Postinterventional reperfusion was very high in both treatment arms and higher in patients with bridging thrombolysis, compared to direct mechanical thrombectomy.”
The findings were presented at the 13th World Stroke Congress (WSC) 2021.
Two views of thrombolysis
The value of bridging thrombolysis for patients who undergo mechanical thrombectomy is a matter of debate. One argument is that, for patients with large-vessel occlusion, IV thrombolysis may improve reperfusion before and after thrombectomy and yield better clinical outcomes. The opposing argument is that bridging thrombolysis may increase the risk for distal emboli, delay mechanical thrombectomy, and increase the rate of hemorrhage.
The researchers conducted the SWIFT DIRECT trial to investigate this question. They enrolled patients with acute ischemic stroke due to occlusion of the internal carotid artery or the M1 segment of the middle cerebral artery.
The trial was conducted at 48 sites in seven European countries and Canada. The investigators randomly assigned patients to receive IV alteplase (0.9 mg/kg) plus mechanical thrombectomy with the Solitaire device or to receive direct mechanical thrombectomy with the same device. Treatment was open label, but the assessment of endpoints was blinded.
Investigators assigned 423 patients to treatment, and 408 were included in the full analysis set. Of this group, 201 participants received direct mechanical thrombectomy, and 207 received IV thrombolysis plus thrombectomy. There were three crossovers in each treatment arm.
The primary outcome was functional independence, defined as a Modified Rankin Scale (mRS) score of 0-2, at 90 days. Secondary outcomes included mortality at 90 days, mRS shift, change in National Institutes of Health Stroke Scale (NIHSS) score at 24 hours, successful reperfusion, and symptomatic and asymptomatic intracranial hemorrhage (ICH).
Noninferiority not demonstrated
At baseline, patient characteristics were well balanced between the treatment groups. The median age of the patients was 72 years, and about 50% of participants were women. The median NIHSS score was 17 in both arms.
Approximately 57% of patients who underwent direct thrombectomy and 65% of those who received IV thrombolysis plus thrombectomy were functionally independent at 90 days, the primary outcome.
In addition, the researchers found no difference in mRS shift, mortality at 90 days, or change in NIHSS score at 24 hours. Postinterventional reperfusion was very high in both arms and was higher in patients who received IV tissue plasminogen activator, compared with those who received direct mechanical thrombectomy, said Dr. Fischer.
The rate of successful postinterventional reperfusion, however, was higher among patients who received thrombolysis than among those who underwent direct thrombectomy. The rate of symptomatic ICH was 1.5% in the direct thrombectomy group and 4.9% in the thrombolysis-plus-thrombectomy group.
New endpoints needed?
The investigators used noninferiority margins of 12%. “This question about the noninferiority margins, that’s a very tricky and difficult one in randomized clinical trials,” said Dr. Fischer. The investigators defined their margin using the 2015 HERMES data because no trials had yet compared direct mechanical thrombectomy and bridging thrombolysis at the time.
The researchers are performing a pooled analysis of all the trials that compared bridging thrombolysis with direct mechanical thrombectomy. “We are therefore looking at several margins, and I think this is the way we should look at these noninferiority margins,” said Dr. Fischer. “There’s not a clear-cut level which you can define.”
Enrollment in the trial was well balanced with respect to gender, which is not always the case in stroke studies, said Kevin Sheth, MD, professor of neurology and neurosurgery at Yale School of Medicine, New Haven, Conn., who commented on the study for this news organization.
The findings indicate that the likelihood of there being a difference between groups on this question is low, said Dr. Sheth. Both groups had large-vessel occlusion, both received thrombectomy, and both achieved reperfusion. But the higher rate of successful reperfusion in the bridging cohort was not reflected in any of the clinical endpoints that the investigators examined.
Observing a difference in this context will require very large trials or different endpoints that are more responsive to the intervention, said Dr. Sheth. “This is going to be a challenge for not just this but for any neuroprotection trial in the future,” he said.
The study was supported by Medtronic. Dr. Fischer has served as a consultant for Medtronic, Stryker, and CSL Behring. Dr. Sheth has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In the prospective, multicenter trial, the rate of good functional outcome was 57% for patients who underwent direct thrombectomy and 65% among patients who received IV thrombolysis before undergoing thrombectomy. This result failed to demonstrate noninferiority of direct mechanical thrombectomy compared to combination therapy, the researchers conclude.
“Good outcome was high in both treatment arms, with the point estimate in favor of the bridging cohort,” said lead investigator Urs Fischer, MD, co-chair of the stroke center at Inselspital, Bern University Hospital, Switzerland, during his presentation. “Postinterventional reperfusion was very high in both treatment arms and higher in patients with bridging thrombolysis, compared to direct mechanical thrombectomy.”
The findings were presented at the 13th World Stroke Congress (WSC) 2021.
Two views of thrombolysis
The value of bridging thrombolysis for patients who undergo mechanical thrombectomy is a matter of debate. One argument is that, for patients with large-vessel occlusion, IV thrombolysis may improve reperfusion before and after thrombectomy and yield better clinical outcomes. The opposing argument is that bridging thrombolysis may increase the risk for distal emboli, delay mechanical thrombectomy, and increase the rate of hemorrhage.
The researchers conducted the SWIFT DIRECT trial to investigate this question. They enrolled patients with acute ischemic stroke due to occlusion of the internal carotid artery or the M1 segment of the middle cerebral artery.
The trial was conducted at 48 sites in seven European countries and Canada. The investigators randomly assigned patients to receive IV alteplase (0.9 mg/kg) plus mechanical thrombectomy with the Solitaire device or to receive direct mechanical thrombectomy with the same device. Treatment was open label, but the assessment of endpoints was blinded.
Investigators assigned 423 patients to treatment, and 408 were included in the full analysis set. Of this group, 201 participants received direct mechanical thrombectomy, and 207 received IV thrombolysis plus thrombectomy. There were three crossovers in each treatment arm.
The primary outcome was functional independence, defined as a Modified Rankin Scale (mRS) score of 0-2, at 90 days. Secondary outcomes included mortality at 90 days, mRS shift, change in National Institutes of Health Stroke Scale (NIHSS) score at 24 hours, successful reperfusion, and symptomatic and asymptomatic intracranial hemorrhage (ICH).
Noninferiority not demonstrated
At baseline, patient characteristics were well balanced between the treatment groups. The median age of the patients was 72 years, and about 50% of participants were women. The median NIHSS score was 17 in both arms.
Approximately 57% of patients who underwent direct thrombectomy and 65% of those who received IV thrombolysis plus thrombectomy were functionally independent at 90 days, the primary outcome.
In addition, the researchers found no difference in mRS shift, mortality at 90 days, or change in NIHSS score at 24 hours. Postinterventional reperfusion was very high in both arms and was higher in patients who received IV tissue plasminogen activator, compared with those who received direct mechanical thrombectomy, said Dr. Fischer.
The rate of successful postinterventional reperfusion, however, was higher among patients who received thrombolysis than among those who underwent direct thrombectomy. The rate of symptomatic ICH was 1.5% in the direct thrombectomy group and 4.9% in the thrombolysis-plus-thrombectomy group.
New endpoints needed?
The investigators used noninferiority margins of 12%. “This question about the noninferiority margins, that’s a very tricky and difficult one in randomized clinical trials,” said Dr. Fischer. The investigators defined their margin using the 2015 HERMES data because no trials had yet compared direct mechanical thrombectomy and bridging thrombolysis at the time.
The researchers are performing a pooled analysis of all the trials that compared bridging thrombolysis with direct mechanical thrombectomy. “We are therefore looking at several margins, and I think this is the way we should look at these noninferiority margins,” said Dr. Fischer. “There’s not a clear-cut level which you can define.”
Enrollment in the trial was well balanced with respect to gender, which is not always the case in stroke studies, said Kevin Sheth, MD, professor of neurology and neurosurgery at Yale School of Medicine, New Haven, Conn., who commented on the study for this news organization.
The findings indicate that the likelihood of there being a difference between groups on this question is low, said Dr. Sheth. Both groups had large-vessel occlusion, both received thrombectomy, and both achieved reperfusion. But the higher rate of successful reperfusion in the bridging cohort was not reflected in any of the clinical endpoints that the investigators examined.
Observing a difference in this context will require very large trials or different endpoints that are more responsive to the intervention, said Dr. Sheth. “This is going to be a challenge for not just this but for any neuroprotection trial in the future,” he said.
The study was supported by Medtronic. Dr. Fischer has served as a consultant for Medtronic, Stryker, and CSL Behring. Dr. Sheth has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In the prospective, multicenter trial, the rate of good functional outcome was 57% for patients who underwent direct thrombectomy and 65% among patients who received IV thrombolysis before undergoing thrombectomy. This result failed to demonstrate noninferiority of direct mechanical thrombectomy compared to combination therapy, the researchers conclude.
“Good outcome was high in both treatment arms, with the point estimate in favor of the bridging cohort,” said lead investigator Urs Fischer, MD, co-chair of the stroke center at Inselspital, Bern University Hospital, Switzerland, during his presentation. “Postinterventional reperfusion was very high in both treatment arms and higher in patients with bridging thrombolysis, compared to direct mechanical thrombectomy.”
The findings were presented at the 13th World Stroke Congress (WSC) 2021.
Two views of thrombolysis
The value of bridging thrombolysis for patients who undergo mechanical thrombectomy is a matter of debate. One argument is that, for patients with large-vessel occlusion, IV thrombolysis may improve reperfusion before and after thrombectomy and yield better clinical outcomes. The opposing argument is that bridging thrombolysis may increase the risk for distal emboli, delay mechanical thrombectomy, and increase the rate of hemorrhage.
The researchers conducted the SWIFT DIRECT trial to investigate this question. They enrolled patients with acute ischemic stroke due to occlusion of the internal carotid artery or the M1 segment of the middle cerebral artery.
The trial was conducted at 48 sites in seven European countries and Canada. The investigators randomly assigned patients to receive IV alteplase (0.9 mg/kg) plus mechanical thrombectomy with the Solitaire device or to receive direct mechanical thrombectomy with the same device. Treatment was open label, but the assessment of endpoints was blinded.
Investigators assigned 423 patients to treatment, and 408 were included in the full analysis set. Of this group, 201 participants received direct mechanical thrombectomy, and 207 received IV thrombolysis plus thrombectomy. There were three crossovers in each treatment arm.
The primary outcome was functional independence, defined as a Modified Rankin Scale (mRS) score of 0-2, at 90 days. Secondary outcomes included mortality at 90 days, mRS shift, change in National Institutes of Health Stroke Scale (NIHSS) score at 24 hours, successful reperfusion, and symptomatic and asymptomatic intracranial hemorrhage (ICH).
Noninferiority not demonstrated
At baseline, patient characteristics were well balanced between the treatment groups. The median age of the patients was 72 years, and about 50% of participants were women. The median NIHSS score was 17 in both arms.
Approximately 57% of patients who underwent direct thrombectomy and 65% of those who received IV thrombolysis plus thrombectomy were functionally independent at 90 days, the primary outcome.
In addition, the researchers found no difference in mRS shift, mortality at 90 days, or change in NIHSS score at 24 hours. Postinterventional reperfusion was very high in both arms and was higher in patients who received IV tissue plasminogen activator, compared with those who received direct mechanical thrombectomy, said Dr. Fischer.
The rate of successful postinterventional reperfusion, however, was higher among patients who received thrombolysis than among those who underwent direct thrombectomy. The rate of symptomatic ICH was 1.5% in the direct thrombectomy group and 4.9% in the thrombolysis-plus-thrombectomy group.
New endpoints needed?
The investigators used noninferiority margins of 12%. “This question about the noninferiority margins, that’s a very tricky and difficult one in randomized clinical trials,” said Dr. Fischer. The investigators defined their margin using the 2015 HERMES data because no trials had yet compared direct mechanical thrombectomy and bridging thrombolysis at the time.
The researchers are performing a pooled analysis of all the trials that compared bridging thrombolysis with direct mechanical thrombectomy. “We are therefore looking at several margins, and I think this is the way we should look at these noninferiority margins,” said Dr. Fischer. “There’s not a clear-cut level which you can define.”
Enrollment in the trial was well balanced with respect to gender, which is not always the case in stroke studies, said Kevin Sheth, MD, professor of neurology and neurosurgery at Yale School of Medicine, New Haven, Conn., who commented on the study for this news organization.
The findings indicate that the likelihood of there being a difference between groups on this question is low, said Dr. Sheth. Both groups had large-vessel occlusion, both received thrombectomy, and both achieved reperfusion. But the higher rate of successful reperfusion in the bridging cohort was not reflected in any of the clinical endpoints that the investigators examined.
Observing a difference in this context will require very large trials or different endpoints that are more responsive to the intervention, said Dr. Sheth. “This is going to be a challenge for not just this but for any neuroprotection trial in the future,” he said.
The study was supported by Medtronic. Dr. Fischer has served as a consultant for Medtronic, Stryker, and CSL Behring. Dr. Sheth has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM WSC 2021
Pandemic stresses harder on physician moms than physician dads: Study
COVID-19 has been difficult for parents trying to balance careers, home life, and keeping their loved ones safe. A new study indicates that, not only are physicians not immune to these stressors, but the long-term effects could be devastating for health care overall.
In a study published Nov. 11, 2021, in JAMA Network Open , researchers found that stresses to work/life balance and family life caused by the pandemic have differed among men and women physicians.
Physicians and other health care workers have been at the front lines of the COVID-19 pandemic, and their work lives have been the focus of a lot of attention in the media and by researchers. Their family lives, not so much. But physicians have families, and the pandemic has upended almost everything about their lives, particularly where work life and home life intersect. School and day care closures, working from home, working extra hours, or working less – all of these changes have consequences on family life and the mental health of parents who are also physicians.
Findings from a Medscape survey published in early 2021 indicate that more female physicians than male physicians were either “conflicted” or “very conflicted” as parents because of work demands (42% vs. 23%) nearly 6 months into the pandemic.
In the current study, researchers from the University of Michigan, Harvard University, and the Medical University of South Carolina teamed up to investigate gender differences in how work/family factors affected the mental health of early-career physician parents in the United States during the first year of the COVID-19 pandemic. The results suggest that the pandemic has increased gender disparity and added disproportionately to the burden of female physicians.
Managing the household falls mostly on moms
Participants were physicians enrolled in the Intern Health Study, a longitudinal study that regularly surveys medical interns in the United States to assess stress and mood. When researchers compared survey results from before the onset of the pandemic (2018) with later results (2020), they found a striking gender difference in how the pandemic has changed family and work duties for physicians.
The authors of the study pointed out that previous research had found that female physicians take on a greater share of household and childcare duties than male physicians. The current study found that their share had increased with the pandemic. Physician moms are now 30 times more likely to be in charge of these tasks than physician dads.
In families in which both parents were physicians, none of the men said they took the primary role in managing the extra demands caused by the pandemic. In addition, women were twice as likely as men to work primarily from home and to work reduced hours.
The extra stress seems to be taking a toll on women physicians. In the 2020 survey, physician mothers had higher scores for anxiety and depression symptoms, compared with men. Notably, the 2018 survey did not show a significant difference in depression scores between men and women. Nor were there significant differences in depression and anxiety scores between women and men who were not parents or in reports of work/family conflict before and after the pandemic.
In general, the results indicate that the pandemic has only widened the gender gap between women and men physicians when it comes to managing family life and dealing with the stresses of maintaining a suitable work-life balance.
‘Long-term repercussions’ for gender equity in medicine
Although these are serious problems for women physicians and their families, the effects go beyond the home and beyond individuals. Even before the pandemic, women in medicine struggled for parity in career advancement and opportunities as well as in pay, and this new setback could make those challenges even greater.
“Even short-term adjustments can have serious long-term repercussions as they may lead to lower earnings and negatively impact opportunities for promotion, further exacerbating gender inequalities in compensation and advancement,” the study’s authors wrote.
The potential damage extends to the entire profession and the health care system itself. The profession is already struggling to retain young female physicians, and this situation is likely to make that problem worse and have long-term consequences. Citing data showing that female physicians spend more time with patients and that their patients may have better outcomes, the authors wrote that the consequences of losing more early-career female physicians “could be devastating to the U.S. health care system, particularly in the context of a global pandemic and an impending physician shortage.”
The sample size was small (276 U.S. physicians), and the study relied on self-reported data. The findings suggest that more research on this topic is needed, especially research that includes other demographic factors, such as sexual orientation and ethnicity. The authors recommend that institutional and public policymakers take into account the effects of the pandemic on physician mothers to ensure that recent gains in gender equity for women physicians do not fall victim to COVID-19.
A version of this article first appeared on Medscape.com.
COVID-19 has been difficult for parents trying to balance careers, home life, and keeping their loved ones safe. A new study indicates that, not only are physicians not immune to these stressors, but the long-term effects could be devastating for health care overall.
In a study published Nov. 11, 2021, in JAMA Network Open , researchers found that stresses to work/life balance and family life caused by the pandemic have differed among men and women physicians.
Physicians and other health care workers have been at the front lines of the COVID-19 pandemic, and their work lives have been the focus of a lot of attention in the media and by researchers. Their family lives, not so much. But physicians have families, and the pandemic has upended almost everything about their lives, particularly where work life and home life intersect. School and day care closures, working from home, working extra hours, or working less – all of these changes have consequences on family life and the mental health of parents who are also physicians.
Findings from a Medscape survey published in early 2021 indicate that more female physicians than male physicians were either “conflicted” or “very conflicted” as parents because of work demands (42% vs. 23%) nearly 6 months into the pandemic.
In the current study, researchers from the University of Michigan, Harvard University, and the Medical University of South Carolina teamed up to investigate gender differences in how work/family factors affected the mental health of early-career physician parents in the United States during the first year of the COVID-19 pandemic. The results suggest that the pandemic has increased gender disparity and added disproportionately to the burden of female physicians.
Managing the household falls mostly on moms
Participants were physicians enrolled in the Intern Health Study, a longitudinal study that regularly surveys medical interns in the United States to assess stress and mood. When researchers compared survey results from before the onset of the pandemic (2018) with later results (2020), they found a striking gender difference in how the pandemic has changed family and work duties for physicians.
The authors of the study pointed out that previous research had found that female physicians take on a greater share of household and childcare duties than male physicians. The current study found that their share had increased with the pandemic. Physician moms are now 30 times more likely to be in charge of these tasks than physician dads.
In families in which both parents were physicians, none of the men said they took the primary role in managing the extra demands caused by the pandemic. In addition, women were twice as likely as men to work primarily from home and to work reduced hours.
The extra stress seems to be taking a toll on women physicians. In the 2020 survey, physician mothers had higher scores for anxiety and depression symptoms, compared with men. Notably, the 2018 survey did not show a significant difference in depression scores between men and women. Nor were there significant differences in depression and anxiety scores between women and men who were not parents or in reports of work/family conflict before and after the pandemic.
In general, the results indicate that the pandemic has only widened the gender gap between women and men physicians when it comes to managing family life and dealing with the stresses of maintaining a suitable work-life balance.
‘Long-term repercussions’ for gender equity in medicine
Although these are serious problems for women physicians and their families, the effects go beyond the home and beyond individuals. Even before the pandemic, women in medicine struggled for parity in career advancement and opportunities as well as in pay, and this new setback could make those challenges even greater.
“Even short-term adjustments can have serious long-term repercussions as they may lead to lower earnings and negatively impact opportunities for promotion, further exacerbating gender inequalities in compensation and advancement,” the study’s authors wrote.
The potential damage extends to the entire profession and the health care system itself. The profession is already struggling to retain young female physicians, and this situation is likely to make that problem worse and have long-term consequences. Citing data showing that female physicians spend more time with patients and that their patients may have better outcomes, the authors wrote that the consequences of losing more early-career female physicians “could be devastating to the U.S. health care system, particularly in the context of a global pandemic and an impending physician shortage.”
The sample size was small (276 U.S. physicians), and the study relied on self-reported data. The findings suggest that more research on this topic is needed, especially research that includes other demographic factors, such as sexual orientation and ethnicity. The authors recommend that institutional and public policymakers take into account the effects of the pandemic on physician mothers to ensure that recent gains in gender equity for women physicians do not fall victim to COVID-19.
A version of this article first appeared on Medscape.com.
COVID-19 has been difficult for parents trying to balance careers, home life, and keeping their loved ones safe. A new study indicates that, not only are physicians not immune to these stressors, but the long-term effects could be devastating for health care overall.
In a study published Nov. 11, 2021, in JAMA Network Open , researchers found that stresses to work/life balance and family life caused by the pandemic have differed among men and women physicians.
Physicians and other health care workers have been at the front lines of the COVID-19 pandemic, and their work lives have been the focus of a lot of attention in the media and by researchers. Their family lives, not so much. But physicians have families, and the pandemic has upended almost everything about their lives, particularly where work life and home life intersect. School and day care closures, working from home, working extra hours, or working less – all of these changes have consequences on family life and the mental health of parents who are also physicians.
Findings from a Medscape survey published in early 2021 indicate that more female physicians than male physicians were either “conflicted” or “very conflicted” as parents because of work demands (42% vs. 23%) nearly 6 months into the pandemic.
In the current study, researchers from the University of Michigan, Harvard University, and the Medical University of South Carolina teamed up to investigate gender differences in how work/family factors affected the mental health of early-career physician parents in the United States during the first year of the COVID-19 pandemic. The results suggest that the pandemic has increased gender disparity and added disproportionately to the burden of female physicians.
Managing the household falls mostly on moms
Participants were physicians enrolled in the Intern Health Study, a longitudinal study that regularly surveys medical interns in the United States to assess stress and mood. When researchers compared survey results from before the onset of the pandemic (2018) with later results (2020), they found a striking gender difference in how the pandemic has changed family and work duties for physicians.
The authors of the study pointed out that previous research had found that female physicians take on a greater share of household and childcare duties than male physicians. The current study found that their share had increased with the pandemic. Physician moms are now 30 times more likely to be in charge of these tasks than physician dads.
In families in which both parents were physicians, none of the men said they took the primary role in managing the extra demands caused by the pandemic. In addition, women were twice as likely as men to work primarily from home and to work reduced hours.
The extra stress seems to be taking a toll on women physicians. In the 2020 survey, physician mothers had higher scores for anxiety and depression symptoms, compared with men. Notably, the 2018 survey did not show a significant difference in depression scores between men and women. Nor were there significant differences in depression and anxiety scores between women and men who were not parents or in reports of work/family conflict before and after the pandemic.
In general, the results indicate that the pandemic has only widened the gender gap between women and men physicians when it comes to managing family life and dealing with the stresses of maintaining a suitable work-life balance.
‘Long-term repercussions’ for gender equity in medicine
Although these are serious problems for women physicians and their families, the effects go beyond the home and beyond individuals. Even before the pandemic, women in medicine struggled for parity in career advancement and opportunities as well as in pay, and this new setback could make those challenges even greater.
“Even short-term adjustments can have serious long-term repercussions as they may lead to lower earnings and negatively impact opportunities for promotion, further exacerbating gender inequalities in compensation and advancement,” the study’s authors wrote.
The potential damage extends to the entire profession and the health care system itself. The profession is already struggling to retain young female physicians, and this situation is likely to make that problem worse and have long-term consequences. Citing data showing that female physicians spend more time with patients and that their patients may have better outcomes, the authors wrote that the consequences of losing more early-career female physicians “could be devastating to the U.S. health care system, particularly in the context of a global pandemic and an impending physician shortage.”
The sample size was small (276 U.S. physicians), and the study relied on self-reported data. The findings suggest that more research on this topic is needed, especially research that includes other demographic factors, such as sexual orientation and ethnicity. The authors recommend that institutional and public policymakers take into account the effects of the pandemic on physician mothers to ensure that recent gains in gender equity for women physicians do not fall victim to COVID-19.
A version of this article first appeared on Medscape.com.
Substantial declines in mortality for most cancers
according to a new analysis.
Researchers found that rates for all cancers combined declined by 27% overall between 1971 and 2019 and decreased significantly for 12 of the 15 top cancer sites analyzed.
The data revealed even greater mortality declines for certain cancers in particular years. For example, mortality from lung cancer was 44% lower in 2019, compared with its peak rate in 1993, whereas it was only 13% lower, compared with morality rates in 1971.
“The cancer mortality rate has reduced considerably since 1971 overall and for most cancer sites because of improvements in prevention, early detection, and treatment,” lead author Ahmedin Jemal, DVM, PhD, American Cancer Society, Kennesaw, Ga., and colleagues wrote.
Advances in surgery, radiotherapy, chemotherapy, precision medicine, and combinations therapies over the past 5 decades have contributed to these significant declines in mortality, Dr. Jemal and colleagues explained. The researchers also credit the “expanded investment” in the National Cancer Institute’s annual budget following the 1971 National Cancer Act, which increased the budget 25-fold from $227 million in 1971 to $6 billion in 2019.
The report, published online Nov. 11, 2021, in JAMA Oncology, analyzed mortality rates for all cancers as well as the top 15 sites using the National Center for Health Statistics.
The researchers found that, overall, deaths declined significantly for all cancers over the study period. Some of the biggest headway since 1971 occurred for stomach and cervical cancers – with 72% and 69% lower mortality rates, respectively – as well as colorectal cancer (56%), oral cavity and pharynx cancer (43%), and ovarian cancer (41%). Mortality rates of female breast cancer and prostate cancer also dropped considerably – both by 39%.
“The decline in mortality for female breast, cervical, colorectal, and prostate cancer in part reflects increased detection (and removal) of premalignant lesions and early-stage cancers,” Dr. Jemal and colleagues noted.
Data suggest that screening likely explains about half of the observed decline in mortality from colorectal cancer between 1975 and 2002. A 2018 study also found that the use of adjuvant chemotherapy was responsible for 63% of the decline in mortality from female breast cancer between 2000 and 2012.
In addition, the authors noted, “the decline in lung, oral cavity and bladder cancers largely reflects reductions in smoking because of enhanced public awareness of the health consequences, implementation of increased cigarette excise taxes, and comprehensive smoke-free laws.”
However, mortality did increase in a few categories. For instance, the mortality rate from pancreatic cancer increased by 3% between 1971 and 2019, and by 8% for both esophageal and brain cancers. Mortality rates from cancer were also greater for 29% of the U.S. counties included in the analysis, mostly those in the South.
The increase in mortality from pancreatic cancer likely reflects the growing rates of obesity in the United States, along with no real advances in pancreatic cancer prevention, early detection, or treatment, the authors suggested. In addition, lack of progress in regions of the south may be related to unequal access to improvements in treatment compared with other parts of the country.
“Improving equity through investment in the social determinants of health and implementation research is critical to furthering the national cancer-control agenda,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new analysis.
Researchers found that rates for all cancers combined declined by 27% overall between 1971 and 2019 and decreased significantly for 12 of the 15 top cancer sites analyzed.
The data revealed even greater mortality declines for certain cancers in particular years. For example, mortality from lung cancer was 44% lower in 2019, compared with its peak rate in 1993, whereas it was only 13% lower, compared with morality rates in 1971.
“The cancer mortality rate has reduced considerably since 1971 overall and for most cancer sites because of improvements in prevention, early detection, and treatment,” lead author Ahmedin Jemal, DVM, PhD, American Cancer Society, Kennesaw, Ga., and colleagues wrote.
Advances in surgery, radiotherapy, chemotherapy, precision medicine, and combinations therapies over the past 5 decades have contributed to these significant declines in mortality, Dr. Jemal and colleagues explained. The researchers also credit the “expanded investment” in the National Cancer Institute’s annual budget following the 1971 National Cancer Act, which increased the budget 25-fold from $227 million in 1971 to $6 billion in 2019.
The report, published online Nov. 11, 2021, in JAMA Oncology, analyzed mortality rates for all cancers as well as the top 15 sites using the National Center for Health Statistics.
The researchers found that, overall, deaths declined significantly for all cancers over the study period. Some of the biggest headway since 1971 occurred for stomach and cervical cancers – with 72% and 69% lower mortality rates, respectively – as well as colorectal cancer (56%), oral cavity and pharynx cancer (43%), and ovarian cancer (41%). Mortality rates of female breast cancer and prostate cancer also dropped considerably – both by 39%.
“The decline in mortality for female breast, cervical, colorectal, and prostate cancer in part reflects increased detection (and removal) of premalignant lesions and early-stage cancers,” Dr. Jemal and colleagues noted.
Data suggest that screening likely explains about half of the observed decline in mortality from colorectal cancer between 1975 and 2002. A 2018 study also found that the use of adjuvant chemotherapy was responsible for 63% of the decline in mortality from female breast cancer between 2000 and 2012.
In addition, the authors noted, “the decline in lung, oral cavity and bladder cancers largely reflects reductions in smoking because of enhanced public awareness of the health consequences, implementation of increased cigarette excise taxes, and comprehensive smoke-free laws.”
However, mortality did increase in a few categories. For instance, the mortality rate from pancreatic cancer increased by 3% between 1971 and 2019, and by 8% for both esophageal and brain cancers. Mortality rates from cancer were also greater for 29% of the U.S. counties included in the analysis, mostly those in the South.
The increase in mortality from pancreatic cancer likely reflects the growing rates of obesity in the United States, along with no real advances in pancreatic cancer prevention, early detection, or treatment, the authors suggested. In addition, lack of progress in regions of the south may be related to unequal access to improvements in treatment compared with other parts of the country.
“Improving equity through investment in the social determinants of health and implementation research is critical to furthering the national cancer-control agenda,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new analysis.
Researchers found that rates for all cancers combined declined by 27% overall between 1971 and 2019 and decreased significantly for 12 of the 15 top cancer sites analyzed.
The data revealed even greater mortality declines for certain cancers in particular years. For example, mortality from lung cancer was 44% lower in 2019, compared with its peak rate in 1993, whereas it was only 13% lower, compared with morality rates in 1971.
“The cancer mortality rate has reduced considerably since 1971 overall and for most cancer sites because of improvements in prevention, early detection, and treatment,” lead author Ahmedin Jemal, DVM, PhD, American Cancer Society, Kennesaw, Ga., and colleagues wrote.
Advances in surgery, radiotherapy, chemotherapy, precision medicine, and combinations therapies over the past 5 decades have contributed to these significant declines in mortality, Dr. Jemal and colleagues explained. The researchers also credit the “expanded investment” in the National Cancer Institute’s annual budget following the 1971 National Cancer Act, which increased the budget 25-fold from $227 million in 1971 to $6 billion in 2019.
The report, published online Nov. 11, 2021, in JAMA Oncology, analyzed mortality rates for all cancers as well as the top 15 sites using the National Center for Health Statistics.
The researchers found that, overall, deaths declined significantly for all cancers over the study period. Some of the biggest headway since 1971 occurred for stomach and cervical cancers – with 72% and 69% lower mortality rates, respectively – as well as colorectal cancer (56%), oral cavity and pharynx cancer (43%), and ovarian cancer (41%). Mortality rates of female breast cancer and prostate cancer also dropped considerably – both by 39%.
“The decline in mortality for female breast, cervical, colorectal, and prostate cancer in part reflects increased detection (and removal) of premalignant lesions and early-stage cancers,” Dr. Jemal and colleagues noted.
Data suggest that screening likely explains about half of the observed decline in mortality from colorectal cancer between 1975 and 2002. A 2018 study also found that the use of adjuvant chemotherapy was responsible for 63% of the decline in mortality from female breast cancer between 2000 and 2012.
In addition, the authors noted, “the decline in lung, oral cavity and bladder cancers largely reflects reductions in smoking because of enhanced public awareness of the health consequences, implementation of increased cigarette excise taxes, and comprehensive smoke-free laws.”
However, mortality did increase in a few categories. For instance, the mortality rate from pancreatic cancer increased by 3% between 1971 and 2019, and by 8% for both esophageal and brain cancers. Mortality rates from cancer were also greater for 29% of the U.S. counties included in the analysis, mostly those in the South.
The increase in mortality from pancreatic cancer likely reflects the growing rates of obesity in the United States, along with no real advances in pancreatic cancer prevention, early detection, or treatment, the authors suggested. In addition, lack of progress in regions of the south may be related to unequal access to improvements in treatment compared with other parts of the country.
“Improving equity through investment in the social determinants of health and implementation research is critical to furthering the national cancer-control agenda,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA ONCOLOGY
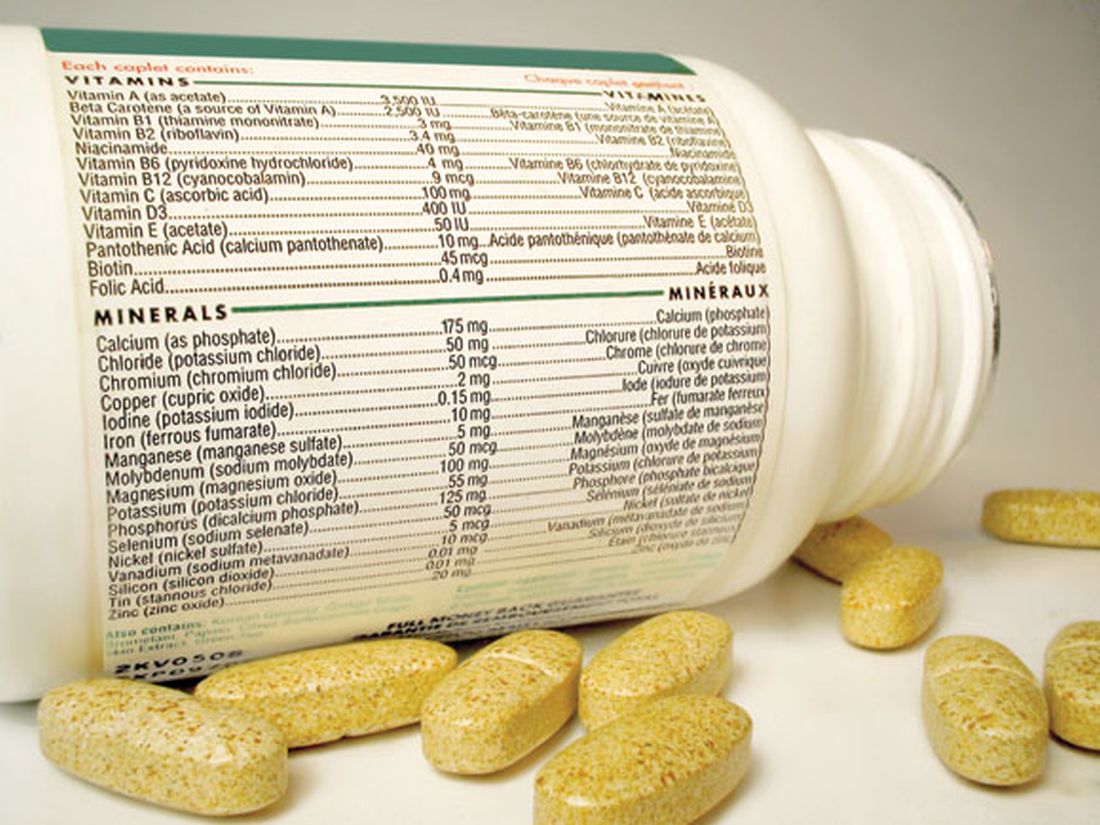
Multivitamins, but not cocoa, tied to slowed brain aging
, with the effects especially pronounced in patients with cardiovascular (CVD) disease, new research suggests.
In addition to testing the effect of a daily multivitamin on cognition, the COSMOS-Mind study examined the effect of cocoa flavanols, but showed no beneficial effect.
The findings “may have important public health implications, particularly for brain health, given the accessibility of multivitamins and minerals, and their low cost and safety,” said study investigator Laura D. Baker, PhD, professor, gerontology and geriatric medicine, Wake Forest University, Winston-Salem, N.C.
The findings were presented at the 14th Clinical Trials on Alzheimer’s Disease (CTAD) conference.
Placebo-controlled study
The study is a substudy of a large parent trial that compared the effects of cocoa extract (500 mg/day cocoa flavanols) and a standard multivitamin-mineral (MVM) to placebo on cardiovascular and cancer outcomes in more than 21,000 older participants.
COSMOS-Mind included 2,262 adults aged 65 and over without dementia who underwent cognitive testing at baseline and annually for 3 years. The mean age at baseline was 73 years, and 40.4% were men. Most participants (88.7%) were non-Hispanic White and almost half (49.2%) had some post-college education.
All study groups were balanced with respect to demographics, CVD history, diabetes, depression, smoking status, alcohol intake, chocolate intake, and prior multivitamin use. Baseline cognitive scores were similar between study groups. Researchers had complete data on 77% of study participants.
The primary endpoint was the effect of cocoa extract (CE) vs. placebo on Global Cognitive Function composite score. The secondary outcome was the effect of MVM vs. placebo on global cognitive function.
Additional outcomes included the impact of supplements on executive function and memory and the treatment effects for prespecified subgroups, including subjects with a history of CVD.
Using a graph of change over time, Dr. Baker showed there was no effect of cocoa on global cognitive function (effect: 0.03; 95% confidence interval, –0.02 to 0.08; P = .28). “We see the to-be-expected practice effects, but there’s no separation between the active and placebo groups,” she said.
It was a different story for MVM. Here, there was the same practice effect, but the graph showed the lines separated for global cognitive function composite score (effect: 0.07; 95% CI, 0.02-0.12; P = .007).
“We see a positive effect of multivitamins for the active group relative to placebo, peaking at 2 years and then remaining stable over time,” said Dr. Baker.
There were similar findings with MVM for the memory composite score, and the executive function composite score. “We have significance in all three, where the two lines do separate over and above the practice effects,” said Dr. Baker.
New evidence
Investigators found a baseline history of CVD, including transient ischemic attack, heart failure, coronary artery bypass graft, percutaneous transluminal coronary angioplasty, and stent, but not myocardial infarction or stroke as these were excluded in the parent trial because they affected the response to multivitamins.
As expected, those with CVD had lower cognitive scores at baseline. “But after an initial bump due to practice effect, at year 1, the cardiovascular disease history folks continue to benefit from multivitamins, whereas those who got placebo multivitamins continue to decline over time,” said Dr. Baker.
Based on information from a baseline scatter plot of cognitive function scores by age, the study’s modeling estimated the multivitamin treatment effect had a positive benefit of .028 standard deviations (SD) per year.
“Daily multivitamin-mineral supplementation appears to slow cognitive aging by 60% or by 1.8 years,” Dr. Baker added.
To date, the effect of MVM supplementation on cognition has been tested in only one large randomized clinical trial – the Physicians Health Study II. That study did not show an effect, but included only older male physicians – and cognitive testing began 2.5 years after randomization, said Dr. Baker.
“Our study provides new evidence that daily multivitamin supplementation may benefit cognitive function in older women and men, and the multivitamin effects may be more pronounced in participants with cardiovascular disease,” she noted.
For effects of multivitamins on Alzheimer’s disease prevalence and progression, “stay tuned,” Dr. Baker concluded.
Following the presentation, session cochair Suzanne Schindler, MD, PhD, instructor in the department of neurology at Washington University, St. Louis, said she and her colleagues “always check vitamin B12 levels” in patients with memory and cognitive difficulties and wondered if study subjects with a low level or deficiency of vitamin B12 benefited from the intervention.
“We are asking ourselves that as well,” said Dr. Baker.
“Some of this is a work in progress,” Dr. Baker added. “We still need to look at that more in-depth to understand whether it might be a mechanism for improvement. I think the results are still out on that topic.”
The study received support from the National Institute on Aging. Pfizer Consumer Healthcare (now GSK Consumer Healthcare) provided study pills and packaging. Dr. Baker has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, with the effects especially pronounced in patients with cardiovascular (CVD) disease, new research suggests.
In addition to testing the effect of a daily multivitamin on cognition, the COSMOS-Mind study examined the effect of cocoa flavanols, but showed no beneficial effect.
The findings “may have important public health implications, particularly for brain health, given the accessibility of multivitamins and minerals, and their low cost and safety,” said study investigator Laura D. Baker, PhD, professor, gerontology and geriatric medicine, Wake Forest University, Winston-Salem, N.C.
The findings were presented at the 14th Clinical Trials on Alzheimer’s Disease (CTAD) conference.
Placebo-controlled study
The study is a substudy of a large parent trial that compared the effects of cocoa extract (500 mg/day cocoa flavanols) and a standard multivitamin-mineral (MVM) to placebo on cardiovascular and cancer outcomes in more than 21,000 older participants.
COSMOS-Mind included 2,262 adults aged 65 and over without dementia who underwent cognitive testing at baseline and annually for 3 years. The mean age at baseline was 73 years, and 40.4% were men. Most participants (88.7%) were non-Hispanic White and almost half (49.2%) had some post-college education.
All study groups were balanced with respect to demographics, CVD history, diabetes, depression, smoking status, alcohol intake, chocolate intake, and prior multivitamin use. Baseline cognitive scores were similar between study groups. Researchers had complete data on 77% of study participants.
The primary endpoint was the effect of cocoa extract (CE) vs. placebo on Global Cognitive Function composite score. The secondary outcome was the effect of MVM vs. placebo on global cognitive function.
Additional outcomes included the impact of supplements on executive function and memory and the treatment effects for prespecified subgroups, including subjects with a history of CVD.
Using a graph of change over time, Dr. Baker showed there was no effect of cocoa on global cognitive function (effect: 0.03; 95% confidence interval, –0.02 to 0.08; P = .28). “We see the to-be-expected practice effects, but there’s no separation between the active and placebo groups,” she said.
It was a different story for MVM. Here, there was the same practice effect, but the graph showed the lines separated for global cognitive function composite score (effect: 0.07; 95% CI, 0.02-0.12; P = .007).
“We see a positive effect of multivitamins for the active group relative to placebo, peaking at 2 years and then remaining stable over time,” said Dr. Baker.
There were similar findings with MVM for the memory composite score, and the executive function composite score. “We have significance in all three, where the two lines do separate over and above the practice effects,” said Dr. Baker.
New evidence
Investigators found a baseline history of CVD, including transient ischemic attack, heart failure, coronary artery bypass graft, percutaneous transluminal coronary angioplasty, and stent, but not myocardial infarction or stroke as these were excluded in the parent trial because they affected the response to multivitamins.
As expected, those with CVD had lower cognitive scores at baseline. “But after an initial bump due to practice effect, at year 1, the cardiovascular disease history folks continue to benefit from multivitamins, whereas those who got placebo multivitamins continue to decline over time,” said Dr. Baker.
Based on information from a baseline scatter plot of cognitive function scores by age, the study’s modeling estimated the multivitamin treatment effect had a positive benefit of .028 standard deviations (SD) per year.
“Daily multivitamin-mineral supplementation appears to slow cognitive aging by 60% or by 1.8 years,” Dr. Baker added.
To date, the effect of MVM supplementation on cognition has been tested in only one large randomized clinical trial – the Physicians Health Study II. That study did not show an effect, but included only older male physicians – and cognitive testing began 2.5 years after randomization, said Dr. Baker.
“Our study provides new evidence that daily multivitamin supplementation may benefit cognitive function in older women and men, and the multivitamin effects may be more pronounced in participants with cardiovascular disease,” she noted.
For effects of multivitamins on Alzheimer’s disease prevalence and progression, “stay tuned,” Dr. Baker concluded.
Following the presentation, session cochair Suzanne Schindler, MD, PhD, instructor in the department of neurology at Washington University, St. Louis, said she and her colleagues “always check vitamin B12 levels” in patients with memory and cognitive difficulties and wondered if study subjects with a low level or deficiency of vitamin B12 benefited from the intervention.
“We are asking ourselves that as well,” said Dr. Baker.
“Some of this is a work in progress,” Dr. Baker added. “We still need to look at that more in-depth to understand whether it might be a mechanism for improvement. I think the results are still out on that topic.”
The study received support from the National Institute on Aging. Pfizer Consumer Healthcare (now GSK Consumer Healthcare) provided study pills and packaging. Dr. Baker has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, with the effects especially pronounced in patients with cardiovascular (CVD) disease, new research suggests.
In addition to testing the effect of a daily multivitamin on cognition, the COSMOS-Mind study examined the effect of cocoa flavanols, but showed no beneficial effect.
The findings “may have important public health implications, particularly for brain health, given the accessibility of multivitamins and minerals, and their low cost and safety,” said study investigator Laura D. Baker, PhD, professor, gerontology and geriatric medicine, Wake Forest University, Winston-Salem, N.C.
The findings were presented at the 14th Clinical Trials on Alzheimer’s Disease (CTAD) conference.
Placebo-controlled study
The study is a substudy of a large parent trial that compared the effects of cocoa extract (500 mg/day cocoa flavanols) and a standard multivitamin-mineral (MVM) to placebo on cardiovascular and cancer outcomes in more than 21,000 older participants.
COSMOS-Mind included 2,262 adults aged 65 and over without dementia who underwent cognitive testing at baseline and annually for 3 years. The mean age at baseline was 73 years, and 40.4% were men. Most participants (88.7%) were non-Hispanic White and almost half (49.2%) had some post-college education.
All study groups were balanced with respect to demographics, CVD history, diabetes, depression, smoking status, alcohol intake, chocolate intake, and prior multivitamin use. Baseline cognitive scores were similar between study groups. Researchers had complete data on 77% of study participants.
The primary endpoint was the effect of cocoa extract (CE) vs. placebo on Global Cognitive Function composite score. The secondary outcome was the effect of MVM vs. placebo on global cognitive function.
Additional outcomes included the impact of supplements on executive function and memory and the treatment effects for prespecified subgroups, including subjects with a history of CVD.
Using a graph of change over time, Dr. Baker showed there was no effect of cocoa on global cognitive function (effect: 0.03; 95% confidence interval, –0.02 to 0.08; P = .28). “We see the to-be-expected practice effects, but there’s no separation between the active and placebo groups,” she said.
It was a different story for MVM. Here, there was the same practice effect, but the graph showed the lines separated for global cognitive function composite score (effect: 0.07; 95% CI, 0.02-0.12; P = .007).
“We see a positive effect of multivitamins for the active group relative to placebo, peaking at 2 years and then remaining stable over time,” said Dr. Baker.
There were similar findings with MVM for the memory composite score, and the executive function composite score. “We have significance in all three, where the two lines do separate over and above the practice effects,” said Dr. Baker.
New evidence
Investigators found a baseline history of CVD, including transient ischemic attack, heart failure, coronary artery bypass graft, percutaneous transluminal coronary angioplasty, and stent, but not myocardial infarction or stroke as these were excluded in the parent trial because they affected the response to multivitamins.
As expected, those with CVD had lower cognitive scores at baseline. “But after an initial bump due to practice effect, at year 1, the cardiovascular disease history folks continue to benefit from multivitamins, whereas those who got placebo multivitamins continue to decline over time,” said Dr. Baker.
Based on information from a baseline scatter plot of cognitive function scores by age, the study’s modeling estimated the multivitamin treatment effect had a positive benefit of .028 standard deviations (SD) per year.
“Daily multivitamin-mineral supplementation appears to slow cognitive aging by 60% or by 1.8 years,” Dr. Baker added.
To date, the effect of MVM supplementation on cognition has been tested in only one large randomized clinical trial – the Physicians Health Study II. That study did not show an effect, but included only older male physicians – and cognitive testing began 2.5 years after randomization, said Dr. Baker.
“Our study provides new evidence that daily multivitamin supplementation may benefit cognitive function in older women and men, and the multivitamin effects may be more pronounced in participants with cardiovascular disease,” she noted.
For effects of multivitamins on Alzheimer’s disease prevalence and progression, “stay tuned,” Dr. Baker concluded.
Following the presentation, session cochair Suzanne Schindler, MD, PhD, instructor in the department of neurology at Washington University, St. Louis, said she and her colleagues “always check vitamin B12 levels” in patients with memory and cognitive difficulties and wondered if study subjects with a low level or deficiency of vitamin B12 benefited from the intervention.
“We are asking ourselves that as well,” said Dr. Baker.
“Some of this is a work in progress,” Dr. Baker added. “We still need to look at that more in-depth to understand whether it might be a mechanism for improvement. I think the results are still out on that topic.”
The study received support from the National Institute on Aging. Pfizer Consumer Healthcare (now GSK Consumer Healthcare) provided study pills and packaging. Dr. Baker has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
B-cell repletion is common with MS drug, but no symptom worsening
. However, there are no corresponding worsening of symptoms or signs of a “wearing off” effect, new research shows.
“Most people expect that since this is a B-cell depleting drug, that if you are not depleting B cells, then that should be reflected clinically and there should be some breakthrough activity,” said study investigator Joshua D. Katz, MD, codirector of the Elliot Lewis Center for Multiple Sclerosis Care in Wellesley, Massachusetts.
“So [these results] were a surprise, but I would not conclude from our data that B-cell repletion does not put someone at risk. We can only say that we didn’t observe anybody having a breakthrough,” he added.
The research was presented at the 2021 Annual Meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
Real-world study
Preapproval clinical trials of ocrelizumab suggest about 5% of patients experience a repletion of B cells. However, the timing and association with breakthrough symptoms were unclear.
To investigate, Dr. Katz and colleagues conducted two studies. The first is a substudy of the prospective ACAPELLA trial to assess ocrelizumab-associated adverse events in a real-world population. The study included 294 patients with relapsing and progressive forms of MS treated with at least two cycles of ocrelizumab, given as infusion once every 6 months.
The results showed that overall, 91 (31%) of the 294 patients had some degree of repletion at one or more timepoints.
In categorizing patients according to their highest CD19 measure after two cycles, 108 patients (64.7%) had no significant repletion of B-cells after infusion, defined as an increase of less than 10 cells/μL, while 45 (26.9%) were considered mild repleters, defined as having increases of 10-49 cells/μL.
Seven patients (4.2%) were moderate repleters, with an increase of 50-79 cells/μL, and 7 (4.2%) were categorized as marked repleters, with increases of 80 or more cells/μL.
Eight patients in the study fully repleted, with values from 114-319 cells/μL, occurring between 23 and 34 weeks of the last infusion.
However, there was no relationship between repletion of the B-cells and clinical or MRI evidence of relapse.
Of note, the proportion of patients who did not have B-cell repletion increased with greater numbers of infusions. Whereas 64.7% were non-repleters at cycle 2, that number increased to 88.8% by cycle 6, with a slight drop to 85.6% being non-repleters by cycle 7 (36 months).
“Mild B-cell repletion was fairly common after two cycles of ocrelizumab, but with repeated dosing, a greater proportion of patients were non-repleters, suggesting that cumulative exposure to ocrelizumab results in greater depletion,” the researchers noted.
However, “while the number of moderate or marked repleters in our study was small, they had a tendency to remain repleters over time with subsequent infusions,” they added.
In looking at patient characteristics, moderate and marketed repleters had higher mean BMI (34.1 and 32.6, respectively) compared with the non- and mild repleters (27.0 and 29.4, respectively; P < .0001).
Dr. Katz noted that the increased risk of B-cell repletion with higher BMI was not a surprise. This association, he said, “makes sense” because patients’ relative exposure to ocrelizumab decreases with higher BMI. Similar patterns with BMI were observed in the clinical trial for ocrelizumab approval, in which patients with lower BMI tended to have greater improvement.
No symptom worsening
In the second study, the investigators further examined changes in symptom burden related to the amount of time from ocrelizumab infusion. They evaluated 110 patients, aged 18-80 (mean age 44.8) who had Expanded Disability Status Scale (EDSS) scores between 0-7. Study participants were either initiating ocrelizumab or had been on the drug for at least 1 year.
Symptom burden was evaluated with the Neurological Disorders (Neuro-Qol) questionnaire and SymptoMScreen patient-reported outcomes at the beginning of the study at week 4, and near the end of the ocrelizumab infusion cycle, at week 22.
The researchers found that among 69 participants who completed the questionnaires, there were no significant differences at week 22 versus week 4 across a wide range of symptoms, including walking, spasticity, pain, fatigue, cognitive function, dizziness, and depression between the two timepoints.
The only change on the Neuro-QoL score was in the sleep disturbance domain, which improved marginally at the end of the cycle (P = .052). This study did not evaluate changes in B-cells.
Dr. Katz noted that the inclusion of patients over age of 55 in the study offered important insights.
“Our hypothesis was that we were going to start seeing a higher rate of complications, especially infections, in people who are older and may be at a higher risk of infection and disability,” Dr. Katz noted. “But so far, we haven’t seen any higher risk in older patients or those with more disability than anyone else, which is good news.”
Amplification of baseline symptoms not uncommon
Commenting on the research, Scott D. Newsome, DO, current president of the CMSC, noted that although no association was observed between the B-cell repletion and symptoms, amplification of flare-up symptoms that are linked to B-cell depleting therapy infusion timing are not uncommon.
“The ‘wearing-off’ phenomenon is not unique to the B-cell therapies,” said Dr. Newsome, who is also director of Johns Hopkins University’s Neurosciences Consultation and Infusion Center and an associate professor of neurology at the JHU med school. “With natalizumab (Tysabri), patients can have an amplification of baseline symptoms as they come closer to their next infusion, and it has been speculated that maybe it was something biologically happening, such as inflammatory cytokines ramping back up or some other mechanisms.”
“Now that we have the B-cell depleting therapies, we tend see the same kind of pattern, where a few weeks leading up to the next infusion, people will develop these amplified symptoms,” he said.
The possibility of a cumulative effect, appearing to address the B-cell repletion associated with early infusions, could have implications over time, Dr. Newsome noted.
“This is important because if people are going on these therapies long-term, the question we may need to ask is whether they actually need to continue to get an infusion every 6 months,” he said.
As these questions around the safety of long-term immunosuppressant drug use continue, different dosing regimens may need to be considered in order to mitigate potential infection risk, he added.
Dr. Katz reports consulting and/or speakers’ bureau relationships with Alexion, Biogen, EMD Serono, Genentech, Novartis, and Sanofi. Dr. Newsome reports relationships with Autobahn, BioIncept, Biogen, Genentech, Novartis, Bristol Myers Squibb, EMD Serono, Greenwich Biosciences, and MedDay Pharmaceuticals.
A version of this article first appeared on Medscape.com.
. However, there are no corresponding worsening of symptoms or signs of a “wearing off” effect, new research shows.
“Most people expect that since this is a B-cell depleting drug, that if you are not depleting B cells, then that should be reflected clinically and there should be some breakthrough activity,” said study investigator Joshua D. Katz, MD, codirector of the Elliot Lewis Center for Multiple Sclerosis Care in Wellesley, Massachusetts.
“So [these results] were a surprise, but I would not conclude from our data that B-cell repletion does not put someone at risk. We can only say that we didn’t observe anybody having a breakthrough,” he added.
The research was presented at the 2021 Annual Meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
Real-world study
Preapproval clinical trials of ocrelizumab suggest about 5% of patients experience a repletion of B cells. However, the timing and association with breakthrough symptoms were unclear.
To investigate, Dr. Katz and colleagues conducted two studies. The first is a substudy of the prospective ACAPELLA trial to assess ocrelizumab-associated adverse events in a real-world population. The study included 294 patients with relapsing and progressive forms of MS treated with at least two cycles of ocrelizumab, given as infusion once every 6 months.
The results showed that overall, 91 (31%) of the 294 patients had some degree of repletion at one or more timepoints.
In categorizing patients according to their highest CD19 measure after two cycles, 108 patients (64.7%) had no significant repletion of B-cells after infusion, defined as an increase of less than 10 cells/μL, while 45 (26.9%) were considered mild repleters, defined as having increases of 10-49 cells/μL.
Seven patients (4.2%) were moderate repleters, with an increase of 50-79 cells/μL, and 7 (4.2%) were categorized as marked repleters, with increases of 80 or more cells/μL.
Eight patients in the study fully repleted, with values from 114-319 cells/μL, occurring between 23 and 34 weeks of the last infusion.
However, there was no relationship between repletion of the B-cells and clinical or MRI evidence of relapse.
Of note, the proportion of patients who did not have B-cell repletion increased with greater numbers of infusions. Whereas 64.7% were non-repleters at cycle 2, that number increased to 88.8% by cycle 6, with a slight drop to 85.6% being non-repleters by cycle 7 (36 months).
“Mild B-cell repletion was fairly common after two cycles of ocrelizumab, but with repeated dosing, a greater proportion of patients were non-repleters, suggesting that cumulative exposure to ocrelizumab results in greater depletion,” the researchers noted.
However, “while the number of moderate or marked repleters in our study was small, they had a tendency to remain repleters over time with subsequent infusions,” they added.
In looking at patient characteristics, moderate and marketed repleters had higher mean BMI (34.1 and 32.6, respectively) compared with the non- and mild repleters (27.0 and 29.4, respectively; P < .0001).
Dr. Katz noted that the increased risk of B-cell repletion with higher BMI was not a surprise. This association, he said, “makes sense” because patients’ relative exposure to ocrelizumab decreases with higher BMI. Similar patterns with BMI were observed in the clinical trial for ocrelizumab approval, in which patients with lower BMI tended to have greater improvement.
No symptom worsening
In the second study, the investigators further examined changes in symptom burden related to the amount of time from ocrelizumab infusion. They evaluated 110 patients, aged 18-80 (mean age 44.8) who had Expanded Disability Status Scale (EDSS) scores between 0-7. Study participants were either initiating ocrelizumab or had been on the drug for at least 1 year.
Symptom burden was evaluated with the Neurological Disorders (Neuro-Qol) questionnaire and SymptoMScreen patient-reported outcomes at the beginning of the study at week 4, and near the end of the ocrelizumab infusion cycle, at week 22.
The researchers found that among 69 participants who completed the questionnaires, there were no significant differences at week 22 versus week 4 across a wide range of symptoms, including walking, spasticity, pain, fatigue, cognitive function, dizziness, and depression between the two timepoints.
The only change on the Neuro-QoL score was in the sleep disturbance domain, which improved marginally at the end of the cycle (P = .052). This study did not evaluate changes in B-cells.
Dr. Katz noted that the inclusion of patients over age of 55 in the study offered important insights.
“Our hypothesis was that we were going to start seeing a higher rate of complications, especially infections, in people who are older and may be at a higher risk of infection and disability,” Dr. Katz noted. “But so far, we haven’t seen any higher risk in older patients or those with more disability than anyone else, which is good news.”
Amplification of baseline symptoms not uncommon
Commenting on the research, Scott D. Newsome, DO, current president of the CMSC, noted that although no association was observed between the B-cell repletion and symptoms, amplification of flare-up symptoms that are linked to B-cell depleting therapy infusion timing are not uncommon.
“The ‘wearing-off’ phenomenon is not unique to the B-cell therapies,” said Dr. Newsome, who is also director of Johns Hopkins University’s Neurosciences Consultation and Infusion Center and an associate professor of neurology at the JHU med school. “With natalizumab (Tysabri), patients can have an amplification of baseline symptoms as they come closer to their next infusion, and it has been speculated that maybe it was something biologically happening, such as inflammatory cytokines ramping back up or some other mechanisms.”
“Now that we have the B-cell depleting therapies, we tend see the same kind of pattern, where a few weeks leading up to the next infusion, people will develop these amplified symptoms,” he said.
The possibility of a cumulative effect, appearing to address the B-cell repletion associated with early infusions, could have implications over time, Dr. Newsome noted.
“This is important because if people are going on these therapies long-term, the question we may need to ask is whether they actually need to continue to get an infusion every 6 months,” he said.
As these questions around the safety of long-term immunosuppressant drug use continue, different dosing regimens may need to be considered in order to mitigate potential infection risk, he added.
Dr. Katz reports consulting and/or speakers’ bureau relationships with Alexion, Biogen, EMD Serono, Genentech, Novartis, and Sanofi. Dr. Newsome reports relationships with Autobahn, BioIncept, Biogen, Genentech, Novartis, Bristol Myers Squibb, EMD Serono, Greenwich Biosciences, and MedDay Pharmaceuticals.
A version of this article first appeared on Medscape.com.
. However, there are no corresponding worsening of symptoms or signs of a “wearing off” effect, new research shows.
“Most people expect that since this is a B-cell depleting drug, that if you are not depleting B cells, then that should be reflected clinically and there should be some breakthrough activity,” said study investigator Joshua D. Katz, MD, codirector of the Elliot Lewis Center for Multiple Sclerosis Care in Wellesley, Massachusetts.
“So [these results] were a surprise, but I would not conclude from our data that B-cell repletion does not put someone at risk. We can only say that we didn’t observe anybody having a breakthrough,” he added.
The research was presented at the 2021 Annual Meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
Real-world study
Preapproval clinical trials of ocrelizumab suggest about 5% of patients experience a repletion of B cells. However, the timing and association with breakthrough symptoms were unclear.
To investigate, Dr. Katz and colleagues conducted two studies. The first is a substudy of the prospective ACAPELLA trial to assess ocrelizumab-associated adverse events in a real-world population. The study included 294 patients with relapsing and progressive forms of MS treated with at least two cycles of ocrelizumab, given as infusion once every 6 months.
The results showed that overall, 91 (31%) of the 294 patients had some degree of repletion at one or more timepoints.
In categorizing patients according to their highest CD19 measure after two cycles, 108 patients (64.7%) had no significant repletion of B-cells after infusion, defined as an increase of less than 10 cells/μL, while 45 (26.9%) were considered mild repleters, defined as having increases of 10-49 cells/μL.
Seven patients (4.2%) were moderate repleters, with an increase of 50-79 cells/μL, and 7 (4.2%) were categorized as marked repleters, with increases of 80 or more cells/μL.
Eight patients in the study fully repleted, with values from 114-319 cells/μL, occurring between 23 and 34 weeks of the last infusion.
However, there was no relationship between repletion of the B-cells and clinical or MRI evidence of relapse.
Of note, the proportion of patients who did not have B-cell repletion increased with greater numbers of infusions. Whereas 64.7% were non-repleters at cycle 2, that number increased to 88.8% by cycle 6, with a slight drop to 85.6% being non-repleters by cycle 7 (36 months).
“Mild B-cell repletion was fairly common after two cycles of ocrelizumab, but with repeated dosing, a greater proportion of patients were non-repleters, suggesting that cumulative exposure to ocrelizumab results in greater depletion,” the researchers noted.
However, “while the number of moderate or marked repleters in our study was small, they had a tendency to remain repleters over time with subsequent infusions,” they added.
In looking at patient characteristics, moderate and marketed repleters had higher mean BMI (34.1 and 32.6, respectively) compared with the non- and mild repleters (27.0 and 29.4, respectively; P < .0001).
Dr. Katz noted that the increased risk of B-cell repletion with higher BMI was not a surprise. This association, he said, “makes sense” because patients’ relative exposure to ocrelizumab decreases with higher BMI. Similar patterns with BMI were observed in the clinical trial for ocrelizumab approval, in which patients with lower BMI tended to have greater improvement.
No symptom worsening
In the second study, the investigators further examined changes in symptom burden related to the amount of time from ocrelizumab infusion. They evaluated 110 patients, aged 18-80 (mean age 44.8) who had Expanded Disability Status Scale (EDSS) scores between 0-7. Study participants were either initiating ocrelizumab or had been on the drug for at least 1 year.
Symptom burden was evaluated with the Neurological Disorders (Neuro-Qol) questionnaire and SymptoMScreen patient-reported outcomes at the beginning of the study at week 4, and near the end of the ocrelizumab infusion cycle, at week 22.
The researchers found that among 69 participants who completed the questionnaires, there were no significant differences at week 22 versus week 4 across a wide range of symptoms, including walking, spasticity, pain, fatigue, cognitive function, dizziness, and depression between the two timepoints.
The only change on the Neuro-QoL score was in the sleep disturbance domain, which improved marginally at the end of the cycle (P = .052). This study did not evaluate changes in B-cells.
Dr. Katz noted that the inclusion of patients over age of 55 in the study offered important insights.
“Our hypothesis was that we were going to start seeing a higher rate of complications, especially infections, in people who are older and may be at a higher risk of infection and disability,” Dr. Katz noted. “But so far, we haven’t seen any higher risk in older patients or those with more disability than anyone else, which is good news.”
Amplification of baseline symptoms not uncommon
Commenting on the research, Scott D. Newsome, DO, current president of the CMSC, noted that although no association was observed between the B-cell repletion and symptoms, amplification of flare-up symptoms that are linked to B-cell depleting therapy infusion timing are not uncommon.
“The ‘wearing-off’ phenomenon is not unique to the B-cell therapies,” said Dr. Newsome, who is also director of Johns Hopkins University’s Neurosciences Consultation and Infusion Center and an associate professor of neurology at the JHU med school. “With natalizumab (Tysabri), patients can have an amplification of baseline symptoms as they come closer to their next infusion, and it has been speculated that maybe it was something biologically happening, such as inflammatory cytokines ramping back up or some other mechanisms.”
“Now that we have the B-cell depleting therapies, we tend see the same kind of pattern, where a few weeks leading up to the next infusion, people will develop these amplified symptoms,” he said.
The possibility of a cumulative effect, appearing to address the B-cell repletion associated with early infusions, could have implications over time, Dr. Newsome noted.
“This is important because if people are going on these therapies long-term, the question we may need to ask is whether they actually need to continue to get an infusion every 6 months,” he said.
As these questions around the safety of long-term immunosuppressant drug use continue, different dosing regimens may need to be considered in order to mitigate potential infection risk, he added.
Dr. Katz reports consulting and/or speakers’ bureau relationships with Alexion, Biogen, EMD Serono, Genentech, Novartis, and Sanofi. Dr. Newsome reports relationships with Autobahn, BioIncept, Biogen, Genentech, Novartis, Bristol Myers Squibb, EMD Serono, Greenwich Biosciences, and MedDay Pharmaceuticals.
A version of this article first appeared on Medscape.com.
FROM CMSC 2021
Parkinson’s death rate rising, reasons unclear
, according to what investigators say is the most comprehensive study in the nation of temporal trends in Parkinson’s disease mortality.
“The reason behind the rising death rates from Parkinson’s disease is not clear at present and warrants further investigation,” Wei Bao, MD, PhD, associate professor in the department of epidemiology at the University of Iowa College of Public Health, in Iowa City, said in an interview. “We know that people are living longer and the general population is getting older, but that doesn’t fully explain the increase we saw in the death rate in people with Parkinson’s disease,” Dr. Bao added in a statement.
“Understanding why more people are dying from this disease is critical if we are going to reverse the trend,” Dr. Bao said.
The study was published online Oct. 27 in Neurology.
Long-term data
The researchers used data from the National Vital Statistics System to determine national trends in Parkinson’s disease mortality overall and in several key subgroups. The analyses included 479,059 people who died of Parkinson’s disease between 1999 and 2019.
Over the 21-year period, the age-adjusted mortality from Parkinson’s disease rose from 5.4 per 100,000 in 1999 to 8.8 per 100,000 in 2019. The average annual percent change (APC) was 2.4% for the entire period.
During the study period, the number of deaths from Parkinson’s disease more than doubled, from 14,593 to 35,311.
The death rate from Parkinson’s disease increased significantly across all age groups. The average APC was 5.0% among adults younger than 65 years, 1.9% among those aged 65-74 years, 2.2% among those 75-84 years, and 2.7% among those 85 and older.
The death rate increased in both men and women, but age-adjusted Parkinson’s disease mortality was twice as high in men as in women. The researchers say one possible explanation for the sex difference is estrogen, which leads to higher dopamine levels in areas of the brain that control motor responses and may protect women from Parkinson’s disease.
The study also showed that White people are more likely to die from Parkinson’s disease than persons of other racial and ethnic groups. In 2019, the death rate per 100,000 was 9.7 for Whites, 6.5 for Hispanics, and 4.7 for non-Hispanic Blacks.
Previous studies have shown that compared with White people, Black and Hispanic people are less likely to see a neurologist, owing to socioeconomic barriers. This suggests that White people may be more likely to receive a Parkinson’s disease diagnosis, the researchers noted.
“It’s important to continue to evaluate long-term trends in Parkinson’s death rates,” Dr. Bao said.
“This can inform future research that may help pinpoint why more people are dying of the disease. Also, updating vital statistics about Parkinson’s death rates may be used for priority setting and financing of health care and policy,” Dr. Bao added.
1.2 million patients by 2030
Reached for comment, James Beck, PhD, chief scientific officer for the Parkinson’s Foundation, said these findings are not surprising. “They are aligned with the work the Parkinson’s Foundation has done to show that the number of people with Parkinson’s disease has increased over time. We are working on an improved estimate of Parkinson’s disease incidence and predict that Parkinson’s disease will continue to rise as the population ages, so an increase in mortality rates would be expected,” Dr. Beck said.
He noted that much of the public health statistics regarding Parkinson’s disease are outdated and that the Parkinson’s Foundation has been partnering with others to update them.
“For instance, to calculate an accurate estimate of the prevalence of Parkinson’s disease, the Parkinson’s Foundation Prevalence Project was formed. The findings from this group demonstrated that the number of people living with Parkinson’s disease will rise to nearly 1.2 million by 2030, a substantial increase from the estimate of 930,000 for 2020,” Dr. Beck said.
“The overarching message is that more people are being diagnosed with Parkinson’s disease, not that more people are dying from the disease,” he added.
“Over the last 20 years, our understanding of Parkinson’s disease has changed and developed, so clinicians are more aware and better able to properly diagnose Parkinson’s disease. This could mean that the cause is likely due to an increase in diagnosis rates and better recognition of Parkinson’s disease, which would lead to higher rates of identifying Parkinson’s disease as a cause of death,” said Dr. Beck.
The study had no targeted funding. Dr. Bao and Dr. Beck have indicated no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to what investigators say is the most comprehensive study in the nation of temporal trends in Parkinson’s disease mortality.
“The reason behind the rising death rates from Parkinson’s disease is not clear at present and warrants further investigation,” Wei Bao, MD, PhD, associate professor in the department of epidemiology at the University of Iowa College of Public Health, in Iowa City, said in an interview. “We know that people are living longer and the general population is getting older, but that doesn’t fully explain the increase we saw in the death rate in people with Parkinson’s disease,” Dr. Bao added in a statement.
“Understanding why more people are dying from this disease is critical if we are going to reverse the trend,” Dr. Bao said.
The study was published online Oct. 27 in Neurology.
Long-term data
The researchers used data from the National Vital Statistics System to determine national trends in Parkinson’s disease mortality overall and in several key subgroups. The analyses included 479,059 people who died of Parkinson’s disease between 1999 and 2019.
Over the 21-year period, the age-adjusted mortality from Parkinson’s disease rose from 5.4 per 100,000 in 1999 to 8.8 per 100,000 in 2019. The average annual percent change (APC) was 2.4% for the entire period.
During the study period, the number of deaths from Parkinson’s disease more than doubled, from 14,593 to 35,311.
The death rate from Parkinson’s disease increased significantly across all age groups. The average APC was 5.0% among adults younger than 65 years, 1.9% among those aged 65-74 years, 2.2% among those 75-84 years, and 2.7% among those 85 and older.
The death rate increased in both men and women, but age-adjusted Parkinson’s disease mortality was twice as high in men as in women. The researchers say one possible explanation for the sex difference is estrogen, which leads to higher dopamine levels in areas of the brain that control motor responses and may protect women from Parkinson’s disease.
The study also showed that White people are more likely to die from Parkinson’s disease than persons of other racial and ethnic groups. In 2019, the death rate per 100,000 was 9.7 for Whites, 6.5 for Hispanics, and 4.7 for non-Hispanic Blacks.
Previous studies have shown that compared with White people, Black and Hispanic people are less likely to see a neurologist, owing to socioeconomic barriers. This suggests that White people may be more likely to receive a Parkinson’s disease diagnosis, the researchers noted.
“It’s important to continue to evaluate long-term trends in Parkinson’s death rates,” Dr. Bao said.
“This can inform future research that may help pinpoint why more people are dying of the disease. Also, updating vital statistics about Parkinson’s death rates may be used for priority setting and financing of health care and policy,” Dr. Bao added.
1.2 million patients by 2030
Reached for comment, James Beck, PhD, chief scientific officer for the Parkinson’s Foundation, said these findings are not surprising. “They are aligned with the work the Parkinson’s Foundation has done to show that the number of people with Parkinson’s disease has increased over time. We are working on an improved estimate of Parkinson’s disease incidence and predict that Parkinson’s disease will continue to rise as the population ages, so an increase in mortality rates would be expected,” Dr. Beck said.
He noted that much of the public health statistics regarding Parkinson’s disease are outdated and that the Parkinson’s Foundation has been partnering with others to update them.
“For instance, to calculate an accurate estimate of the prevalence of Parkinson’s disease, the Parkinson’s Foundation Prevalence Project was formed. The findings from this group demonstrated that the number of people living with Parkinson’s disease will rise to nearly 1.2 million by 2030, a substantial increase from the estimate of 930,000 for 2020,” Dr. Beck said.
“The overarching message is that more people are being diagnosed with Parkinson’s disease, not that more people are dying from the disease,” he added.
“Over the last 20 years, our understanding of Parkinson’s disease has changed and developed, so clinicians are more aware and better able to properly diagnose Parkinson’s disease. This could mean that the cause is likely due to an increase in diagnosis rates and better recognition of Parkinson’s disease, which would lead to higher rates of identifying Parkinson’s disease as a cause of death,” said Dr. Beck.
The study had no targeted funding. Dr. Bao and Dr. Beck have indicated no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to what investigators say is the most comprehensive study in the nation of temporal trends in Parkinson’s disease mortality.
“The reason behind the rising death rates from Parkinson’s disease is not clear at present and warrants further investigation,” Wei Bao, MD, PhD, associate professor in the department of epidemiology at the University of Iowa College of Public Health, in Iowa City, said in an interview. “We know that people are living longer and the general population is getting older, but that doesn’t fully explain the increase we saw in the death rate in people with Parkinson’s disease,” Dr. Bao added in a statement.
“Understanding why more people are dying from this disease is critical if we are going to reverse the trend,” Dr. Bao said.
The study was published online Oct. 27 in Neurology.
Long-term data
The researchers used data from the National Vital Statistics System to determine national trends in Parkinson’s disease mortality overall and in several key subgroups. The analyses included 479,059 people who died of Parkinson’s disease between 1999 and 2019.
Over the 21-year period, the age-adjusted mortality from Parkinson’s disease rose from 5.4 per 100,000 in 1999 to 8.8 per 100,000 in 2019. The average annual percent change (APC) was 2.4% for the entire period.
During the study period, the number of deaths from Parkinson’s disease more than doubled, from 14,593 to 35,311.
The death rate from Parkinson’s disease increased significantly across all age groups. The average APC was 5.0% among adults younger than 65 years, 1.9% among those aged 65-74 years, 2.2% among those 75-84 years, and 2.7% among those 85 and older.
The death rate increased in both men and women, but age-adjusted Parkinson’s disease mortality was twice as high in men as in women. The researchers say one possible explanation for the sex difference is estrogen, which leads to higher dopamine levels in areas of the brain that control motor responses and may protect women from Parkinson’s disease.
The study also showed that White people are more likely to die from Parkinson’s disease than persons of other racial and ethnic groups. In 2019, the death rate per 100,000 was 9.7 for Whites, 6.5 for Hispanics, and 4.7 for non-Hispanic Blacks.
Previous studies have shown that compared with White people, Black and Hispanic people are less likely to see a neurologist, owing to socioeconomic barriers. This suggests that White people may be more likely to receive a Parkinson’s disease diagnosis, the researchers noted.
“It’s important to continue to evaluate long-term trends in Parkinson’s death rates,” Dr. Bao said.
“This can inform future research that may help pinpoint why more people are dying of the disease. Also, updating vital statistics about Parkinson’s death rates may be used for priority setting and financing of health care and policy,” Dr. Bao added.
1.2 million patients by 2030
Reached for comment, James Beck, PhD, chief scientific officer for the Parkinson’s Foundation, said these findings are not surprising. “They are aligned with the work the Parkinson’s Foundation has done to show that the number of people with Parkinson’s disease has increased over time. We are working on an improved estimate of Parkinson’s disease incidence and predict that Parkinson’s disease will continue to rise as the population ages, so an increase in mortality rates would be expected,” Dr. Beck said.
He noted that much of the public health statistics regarding Parkinson’s disease are outdated and that the Parkinson’s Foundation has been partnering with others to update them.
“For instance, to calculate an accurate estimate of the prevalence of Parkinson’s disease, the Parkinson’s Foundation Prevalence Project was formed. The findings from this group demonstrated that the number of people living with Parkinson’s disease will rise to nearly 1.2 million by 2030, a substantial increase from the estimate of 930,000 for 2020,” Dr. Beck said.
“The overarching message is that more people are being diagnosed with Parkinson’s disease, not that more people are dying from the disease,” he added.
“Over the last 20 years, our understanding of Parkinson’s disease has changed and developed, so clinicians are more aware and better able to properly diagnose Parkinson’s disease. This could mean that the cause is likely due to an increase in diagnosis rates and better recognition of Parkinson’s disease, which would lead to higher rates of identifying Parkinson’s disease as a cause of death,” said Dr. Beck.
The study had no targeted funding. Dr. Bao and Dr. Beck have indicated no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Do adolescents develop CNS autoimmunity after COVID-19?
Recent research suggests that some pediatric patients who develop neuropsychiatric symptoms from COVID-19 may have intrathecal antineural SARS-CoV-2 autoantibodies, which may hint at central nervous system (CNS) autoimmunity in these patients.
“Overall, these findings indicate that severe neuropsychiatric symptoms can occur in the setting of pediatric COVID-19, including patients who lack many of the cardinal systemic features,” Christopher M. Bartley, MD, PhD, of the Weill Institute for Neurosciences at the University of California, San Francisco, and colleagues wrote in their study. “These data highlight the possibility of SARS-CoV-2 neuroinvasion and/or CNS autoimmunity in pediatric patients with COVID-19 and neuropsychiatric symptoms.”
In a case series published Oct. 25 in JAMA Neurology (doi: 10.1001/jamaneurol.2021.3821), Dr. Bartley and colleagues examined three pediatric patients who were infected with SARS-CoV-2 and, over a period of 5 months in 2020, were admitted to the hospital – where they received a neurology consultation for “subacute, functionally impairing behavioral changes.”
Patient 1 had a history of unspecified anxiety and depression, and was admitted for erratic behavior, paranoia-like fears, social withdrawal, and insomnia. The patient did not respond to treatment with risperidone and gabapentin, and was readmitted soon after discharge, then treated with olanzapine followed by a transition to valproate and lorazepam. It was found the patient had cerebrospinal fluid (CSF) abnormalities in the form of elevated protein levels, and an elevated IgG index, and was given intravenous immunoglobulin followed by IV methylprednisolone. While symptoms such as paranoia improved and the patient was able to better organize thoughts after 5 days, other symptoms such as delusions and hyperreflexia persisted for at least 1 month before resolving, and some symptoms, such as lability, did not resolve before discharge.
Patient 2 had a history of motor tics and anxiety, but showed signs of insomnia, mood lability, impaired concentration, difficulty finding words, and problems completing homework following a SARS-CoV-2 infection. The patient’s father previously had been diagnosed with COVID-19 and the patient developed respiratory symptoms and fever; an IgG serology test later confirmed a SARS-CoV-2 infection. The patient went on to experience internal preoccupation, aggression, and suicidal ideation. The patients was treated with aripiprazole and risperidone, but did not respond, and was admitted to the hospital. As with patient 1, patient 2 had CSF abnormalities in the form of elevated protein levels, and responded to IV methylprednisolone, with working memory and bradyphrenia improving. However, the patient developed insomnia, extreme anxiety, suicidal ideation, aggression, and sadness after discharge, and was readmitted. The patient was treated with IV immunoglobulin, and discharged with quetiapine and lithium.
“Six months later, although improved from initial presentation, the patient required academic accommodations and continued to endorse forgetfulness and attention difficulties. The patient’s chronic tics and anxiety were unchanged,” Dr. Bartley and colleagues wrote.
Patient 3 had no psychiatric history but started to demonstrate “odd behavior, including repetitive behaviors, anorexia, and insomnia” following a SARS-CoV-2 infection. After being hospitalized, the patient showed signs of “ideomotor apraxia, abulia, disorganized behavior, agitation, and diffusely brisk reflexes” and had a high white blood cell count, creatine kinase level, and C-reactive protein level. CSF was also abnormal for this patient, with three unique oligoclonal bands identified. The patient was treated with lorazepam and olanzapine, did not receive immunotherapy, and was discharged without psychiatric medications after 4 days.
When the researchers performed testing on each of the three patients, they found intrathecal anti–SARS-CoV-2 IgG and immunostained mouse brain tissue, and “a diverse set of candidate autoantigens by human phage immunoprecipitation sequencing” in patient 1 and patient 2. In comparison, patient 3 “neither appreciably immunostained nor enriched candidates by human phage immunoprecipitation sequencing,” the researchers said.
“ and the potential for immunotherapy in some,” Dr. Bartley and colleagues concluded.
Potential of CNS autoimmunity
Evan J. Kyzar, MD, PhD, a resident physician in psychiatry at New York State Psychiatric Institute in New York Presbyterian–Columbia Campus, said in an interview that the results of the case series show some pediatric patients with neuropsychiatric symptoms can have anti-SARS-CoV-2 antibodies after viral clearance.
“Interestingly, some of the patients in this study also had antibodies in the CSF that targeted native proteins, demonstrating that COVID-19 may lead to autoimmunity directed at the brain,” he said. “This study increases our knowledge of how COVID-19 interacts with the nervous system and how autoimmune mechanisms might be contributing to at least a portion of patients with neuropsychiatric symptoms during acute infection, and possibly even after viral clearance.”
Dr. Kyzar noted that the immunological methods in the study were “cutting-edge” and the validation exploring the immune responses was detailed, but was limited because of the small sample size.
“[T]he researchers are using similar techniques to explore psychiatric disorders such as depression and schizophrenia to determine if some patients diagnosed with these conditions may have CNS-targeting autoantibodies that contribute to their symptoms and clinical presentation,” Dr. Kyzar said. “This work has the potential to discover novel neuroimmune mechanisms contributing to neuropsychiatric disease and offer possible pathways for the discovery of new treatments.”
The authors reported financial relationships with Allen & Company, the Chan Zuckerberg Initiative, National Institutes of Health, Novartis, Public Health Company, Roche/Genentech, Sandler Foundation, and Takeda in the form of grants and personal fees. They reported funding and/or support from the Brain Research Foundation, Hanna H. Gray Fellowship, Howard Hughes Medical Institute, John A. Watson Scholar Program, Latinx Center of Excellence, the National Institute of Mental Health, the National Institute of Neurological Disorders and Stroke, President’s Postdoctoral Fellowship Program, and Shared Instrumentation grant. Dr. Kyzar reported no relevant financial disclosures.
Recent research suggests that some pediatric patients who develop neuropsychiatric symptoms from COVID-19 may have intrathecal antineural SARS-CoV-2 autoantibodies, which may hint at central nervous system (CNS) autoimmunity in these patients.
“Overall, these findings indicate that severe neuropsychiatric symptoms can occur in the setting of pediatric COVID-19, including patients who lack many of the cardinal systemic features,” Christopher M. Bartley, MD, PhD, of the Weill Institute for Neurosciences at the University of California, San Francisco, and colleagues wrote in their study. “These data highlight the possibility of SARS-CoV-2 neuroinvasion and/or CNS autoimmunity in pediatric patients with COVID-19 and neuropsychiatric symptoms.”
In a case series published Oct. 25 in JAMA Neurology (doi: 10.1001/jamaneurol.2021.3821), Dr. Bartley and colleagues examined three pediatric patients who were infected with SARS-CoV-2 and, over a period of 5 months in 2020, were admitted to the hospital – where they received a neurology consultation for “subacute, functionally impairing behavioral changes.”
Patient 1 had a history of unspecified anxiety and depression, and was admitted for erratic behavior, paranoia-like fears, social withdrawal, and insomnia. The patient did not respond to treatment with risperidone and gabapentin, and was readmitted soon after discharge, then treated with olanzapine followed by a transition to valproate and lorazepam. It was found the patient had cerebrospinal fluid (CSF) abnormalities in the form of elevated protein levels, and an elevated IgG index, and was given intravenous immunoglobulin followed by IV methylprednisolone. While symptoms such as paranoia improved and the patient was able to better organize thoughts after 5 days, other symptoms such as delusions and hyperreflexia persisted for at least 1 month before resolving, and some symptoms, such as lability, did not resolve before discharge.
Patient 2 had a history of motor tics and anxiety, but showed signs of insomnia, mood lability, impaired concentration, difficulty finding words, and problems completing homework following a SARS-CoV-2 infection. The patient’s father previously had been diagnosed with COVID-19 and the patient developed respiratory symptoms and fever; an IgG serology test later confirmed a SARS-CoV-2 infection. The patient went on to experience internal preoccupation, aggression, and suicidal ideation. The patients was treated with aripiprazole and risperidone, but did not respond, and was admitted to the hospital. As with patient 1, patient 2 had CSF abnormalities in the form of elevated protein levels, and responded to IV methylprednisolone, with working memory and bradyphrenia improving. However, the patient developed insomnia, extreme anxiety, suicidal ideation, aggression, and sadness after discharge, and was readmitted. The patient was treated with IV immunoglobulin, and discharged with quetiapine and lithium.
“Six months later, although improved from initial presentation, the patient required academic accommodations and continued to endorse forgetfulness and attention difficulties. The patient’s chronic tics and anxiety were unchanged,” Dr. Bartley and colleagues wrote.
Patient 3 had no psychiatric history but started to demonstrate “odd behavior, including repetitive behaviors, anorexia, and insomnia” following a SARS-CoV-2 infection. After being hospitalized, the patient showed signs of “ideomotor apraxia, abulia, disorganized behavior, agitation, and diffusely brisk reflexes” and had a high white blood cell count, creatine kinase level, and C-reactive protein level. CSF was also abnormal for this patient, with three unique oligoclonal bands identified. The patient was treated with lorazepam and olanzapine, did not receive immunotherapy, and was discharged without psychiatric medications after 4 days.
When the researchers performed testing on each of the three patients, they found intrathecal anti–SARS-CoV-2 IgG and immunostained mouse brain tissue, and “a diverse set of candidate autoantigens by human phage immunoprecipitation sequencing” in patient 1 and patient 2. In comparison, patient 3 “neither appreciably immunostained nor enriched candidates by human phage immunoprecipitation sequencing,” the researchers said.
“ and the potential for immunotherapy in some,” Dr. Bartley and colleagues concluded.
Potential of CNS autoimmunity
Evan J. Kyzar, MD, PhD, a resident physician in psychiatry at New York State Psychiatric Institute in New York Presbyterian–Columbia Campus, said in an interview that the results of the case series show some pediatric patients with neuropsychiatric symptoms can have anti-SARS-CoV-2 antibodies after viral clearance.
“Interestingly, some of the patients in this study also had antibodies in the CSF that targeted native proteins, demonstrating that COVID-19 may lead to autoimmunity directed at the brain,” he said. “This study increases our knowledge of how COVID-19 interacts with the nervous system and how autoimmune mechanisms might be contributing to at least a portion of patients with neuropsychiatric symptoms during acute infection, and possibly even after viral clearance.”
Dr. Kyzar noted that the immunological methods in the study were “cutting-edge” and the validation exploring the immune responses was detailed, but was limited because of the small sample size.
“[T]he researchers are using similar techniques to explore psychiatric disorders such as depression and schizophrenia to determine if some patients diagnosed with these conditions may have CNS-targeting autoantibodies that contribute to their symptoms and clinical presentation,” Dr. Kyzar said. “This work has the potential to discover novel neuroimmune mechanisms contributing to neuropsychiatric disease and offer possible pathways for the discovery of new treatments.”
The authors reported financial relationships with Allen & Company, the Chan Zuckerberg Initiative, National Institutes of Health, Novartis, Public Health Company, Roche/Genentech, Sandler Foundation, and Takeda in the form of grants and personal fees. They reported funding and/or support from the Brain Research Foundation, Hanna H. Gray Fellowship, Howard Hughes Medical Institute, John A. Watson Scholar Program, Latinx Center of Excellence, the National Institute of Mental Health, the National Institute of Neurological Disorders and Stroke, President’s Postdoctoral Fellowship Program, and Shared Instrumentation grant. Dr. Kyzar reported no relevant financial disclosures.
Recent research suggests that some pediatric patients who develop neuropsychiatric symptoms from COVID-19 may have intrathecal antineural SARS-CoV-2 autoantibodies, which may hint at central nervous system (CNS) autoimmunity in these patients.
“Overall, these findings indicate that severe neuropsychiatric symptoms can occur in the setting of pediatric COVID-19, including patients who lack many of the cardinal systemic features,” Christopher M. Bartley, MD, PhD, of the Weill Institute for Neurosciences at the University of California, San Francisco, and colleagues wrote in their study. “These data highlight the possibility of SARS-CoV-2 neuroinvasion and/or CNS autoimmunity in pediatric patients with COVID-19 and neuropsychiatric symptoms.”
In a case series published Oct. 25 in JAMA Neurology (doi: 10.1001/jamaneurol.2021.3821), Dr. Bartley and colleagues examined three pediatric patients who were infected with SARS-CoV-2 and, over a period of 5 months in 2020, were admitted to the hospital – where they received a neurology consultation for “subacute, functionally impairing behavioral changes.”
Patient 1 had a history of unspecified anxiety and depression, and was admitted for erratic behavior, paranoia-like fears, social withdrawal, and insomnia. The patient did not respond to treatment with risperidone and gabapentin, and was readmitted soon after discharge, then treated with olanzapine followed by a transition to valproate and lorazepam. It was found the patient had cerebrospinal fluid (CSF) abnormalities in the form of elevated protein levels, and an elevated IgG index, and was given intravenous immunoglobulin followed by IV methylprednisolone. While symptoms such as paranoia improved and the patient was able to better organize thoughts after 5 days, other symptoms such as delusions and hyperreflexia persisted for at least 1 month before resolving, and some symptoms, such as lability, did not resolve before discharge.
Patient 2 had a history of motor tics and anxiety, but showed signs of insomnia, mood lability, impaired concentration, difficulty finding words, and problems completing homework following a SARS-CoV-2 infection. The patient’s father previously had been diagnosed with COVID-19 and the patient developed respiratory symptoms and fever; an IgG serology test later confirmed a SARS-CoV-2 infection. The patient went on to experience internal preoccupation, aggression, and suicidal ideation. The patients was treated with aripiprazole and risperidone, but did not respond, and was admitted to the hospital. As with patient 1, patient 2 had CSF abnormalities in the form of elevated protein levels, and responded to IV methylprednisolone, with working memory and bradyphrenia improving. However, the patient developed insomnia, extreme anxiety, suicidal ideation, aggression, and sadness after discharge, and was readmitted. The patient was treated with IV immunoglobulin, and discharged with quetiapine and lithium.
“Six months later, although improved from initial presentation, the patient required academic accommodations and continued to endorse forgetfulness and attention difficulties. The patient’s chronic tics and anxiety were unchanged,” Dr. Bartley and colleagues wrote.
Patient 3 had no psychiatric history but started to demonstrate “odd behavior, including repetitive behaviors, anorexia, and insomnia” following a SARS-CoV-2 infection. After being hospitalized, the patient showed signs of “ideomotor apraxia, abulia, disorganized behavior, agitation, and diffusely brisk reflexes” and had a high white blood cell count, creatine kinase level, and C-reactive protein level. CSF was also abnormal for this patient, with three unique oligoclonal bands identified. The patient was treated with lorazepam and olanzapine, did not receive immunotherapy, and was discharged without psychiatric medications after 4 days.
When the researchers performed testing on each of the three patients, they found intrathecal anti–SARS-CoV-2 IgG and immunostained mouse brain tissue, and “a diverse set of candidate autoantigens by human phage immunoprecipitation sequencing” in patient 1 and patient 2. In comparison, patient 3 “neither appreciably immunostained nor enriched candidates by human phage immunoprecipitation sequencing,” the researchers said.
“ and the potential for immunotherapy in some,” Dr. Bartley and colleagues concluded.
Potential of CNS autoimmunity
Evan J. Kyzar, MD, PhD, a resident physician in psychiatry at New York State Psychiatric Institute in New York Presbyterian–Columbia Campus, said in an interview that the results of the case series show some pediatric patients with neuropsychiatric symptoms can have anti-SARS-CoV-2 antibodies after viral clearance.
“Interestingly, some of the patients in this study also had antibodies in the CSF that targeted native proteins, demonstrating that COVID-19 may lead to autoimmunity directed at the brain,” he said. “This study increases our knowledge of how COVID-19 interacts with the nervous system and how autoimmune mechanisms might be contributing to at least a portion of patients with neuropsychiatric symptoms during acute infection, and possibly even after viral clearance.”
Dr. Kyzar noted that the immunological methods in the study were “cutting-edge” and the validation exploring the immune responses was detailed, but was limited because of the small sample size.
“[T]he researchers are using similar techniques to explore psychiatric disorders such as depression and schizophrenia to determine if some patients diagnosed with these conditions may have CNS-targeting autoantibodies that contribute to their symptoms and clinical presentation,” Dr. Kyzar said. “This work has the potential to discover novel neuroimmune mechanisms contributing to neuropsychiatric disease and offer possible pathways for the discovery of new treatments.”
The authors reported financial relationships with Allen & Company, the Chan Zuckerberg Initiative, National Institutes of Health, Novartis, Public Health Company, Roche/Genentech, Sandler Foundation, and Takeda in the form of grants and personal fees. They reported funding and/or support from the Brain Research Foundation, Hanna H. Gray Fellowship, Howard Hughes Medical Institute, John A. Watson Scholar Program, Latinx Center of Excellence, the National Institute of Mental Health, the National Institute of Neurological Disorders and Stroke, President’s Postdoctoral Fellowship Program, and Shared Instrumentation grant. Dr. Kyzar reported no relevant financial disclosures.
FROM JAMA NEUROLOGY
Step right up, folks, for a public dissection
The greatest autopsy on Earth?
The LOTME staff would like to apologize in advance. The following item contains historical facts.
P.T. Barnum is a rather controversial figure in American history. The greatest show on Earth was certainly popular in its day. However, Barnum got his start in 1835 by leasing a slave named Joyce Heth, an elderly Black woman who told vivid stories of caring for a young George Washington. He toured her around the country, advertising her as a 160-year-old woman who served as George Washington’s nanny. When Ms. Heth died the next year, Barnum sold tickets to the autopsy, charging the equivalent of $30 in today’s money.
When a doctor announced that Ms. Heth was actually 75-80 when she died, it caused great controversy in the press and ruined Barnum’s career. Wait, no, that’s not right. The opposite, actually. He weathered the storm, built his famous circus, and never again committed a hoax.
It’s difficult to quantify how wrong publicly dissecting a person and charging people to see said dissection is, but that was almost 200 years ago. At the very least, we can say that such terrible behavior is firmly in the distant past.
Oh wait.
David Saunders, a 98-year-old veteran of World War II and the Korean War, donated his body to science. His body, however, was purchased by DeathScience.org from a medical lab – with the buyer supposedly misleading the medical lab about its intentions, which was for use at the traveling Oddities and Curiosities Expo. Tickets went for up to $500 each to witness the public autopsy of Mr. Saunders’ body, which took place at a Marriott in Portland, Ore. It promised to be an exciting, all-day event from 9 a.m. to 4 p.m., with a break for lunch, of course. You can’t have an autopsy without a catered lunch.
Another public autopsy event was scheduled in Seattle but canceled after news of the first event broke. Oh, and for that extra little kick, Mr. Saunders died from COVID-19, meaning that all those paying customers were exposed.
P.T. Barnum is probably rolling over in his grave right now. His autopsy tickets were a bargain.
Go ahead, have that soda before math
We should all know by now that sugary drinks are bad, even artificially sweetened ones. It might not always stop us from drinking them, but we know the deal. But what if sugary drinks like soda could be helpful for girls in school?
You read that right. We said girls. A soda before class might have boys bouncing off the walls, but not girls. A recent study showed that not only was girls’ behavior unaffected by having a sugary drink, their math skills even improved.
Researchers analyzed the behavior of 4- to 6-year-old children before and after having a sugary drink. The sugar rush was actually calming for girls and helped them perform better with numerical skills, but the opposite was true for boys. “Our study is the first to provide large-scale experimental evidence on the impact of sugary drinks on preschool children. The results clearly indicate a causal impact of sugary drinks on children’s behavior and test scores,” Fritz Schiltz, PhD, said in a written statement.
This probably isn’t the green light to have as many sugary drinks as you want, but it might be interesting to see how your work is affected after a soda.
Chicken nuggets and the meat paradox
Two young children are fighting over the last chicken nugget when an adult comes in to see what’s going on.
Liam: Vegetable!
Olivia: Meat!
Liam: Chicken nuggets are vegetables!
Olivia: No, dorkface! They’re meat.
Caregiver: Good news, kids. You’re both right.
Olivia: How can we both be right?
At this point, a woman enters the room. She’s wearing a white lab coat, so she must be a scientist.
Dr. Scientist: You can’t both be right, Olivia. You are being fed a serving of the meat paradox. That’s why Liam here doesn’t know that chicken nuggets are made of chicken, which is a form of meat. Sadly, he’s not the only one.
In a recent study, scientists from Furman University in Greenville, S.C., found that 38% of 176 children aged 4-7 years thought that chicken nuggets were vegetables and more than 46% identified French fries as animal based.
Olivia: Did our caregiver lie to us, Dr. Scientist?
Dr. Scientist: Yes, Olivia. The researchers I mentioned explained that “many people experience unease while eating meat. Omnivores eat foods that entail animal suffering and death while at the same time endorsing the compassionate treatment of animals.” That’s the meat paradox.
Liam: What else did they say, Dr. Scientist?
Dr. Scientist: Over 70% of those children said that cows and pigs were not edible and 5% thought that cats and horses were. The investigators wrote “that children and youth should be viewed as agents of environmental change” in the future, but suggested that parents need to bring honesty to the table.
Caregiver: How did you get in here anyway? And how do you know their names?
Dr. Scientist: I’ve been rooting through your garbage for years. All in the name of science, of course.
Bedtimes aren’t just for children
There are multiple ways to prevent heart disease, but what if it could be as easy as switching your bedtime? A recent study in European Heart Journal–Digital Health suggests that there’s a sweet spot when it comes to sleep timing.
Through smartwatch-like devices, researchers measured the sleep-onset and wake-up times for 7 days in 88,026 participants aged 43-79 years. After 5.7 years of follow-up to see if anyone had a heart attack, stroke, or any other cardiovascular event, 3.6% developed some kind of cardiovascular disease.
Those who went to bed between 10 p.m. and 11 p.m. had a lower risk of developing heart disease. The risk was 25% higher for subjects who went to bed at midnight or later, 24% higher for bedtimes before 10 p.m., and 12% higher for bedtimes between 11 p.m. and midnight.
So, why can you go to bed before “The Tonight Show” and lower your cardiovascular risk but not before the nightly news? Well, it has something to do with your body’s natural clock.
“The optimum time to go to sleep is at a specific point in the body’s 24-hour cycle and deviations may be detrimental to health. The riskiest time was after midnight, potentially because it may reduce the likelihood of seeing morning light, which resets the body clock,” said study author Dr. David Plans of the University of Exeter, England.
Although a sleep schedule is preferred, it isn’t realistic all the time for those in certain occupations who might have to resort to other methods to keep their circadian clocks ticking optimally for their health. But if all it takes is prescribing a sleep time to reduce heart disease on a massive scale it would make a great “low-cost public health target.”
So bedtimes aren’t just for children.
The greatest autopsy on Earth?
The LOTME staff would like to apologize in advance. The following item contains historical facts.
P.T. Barnum is a rather controversial figure in American history. The greatest show on Earth was certainly popular in its day. However, Barnum got his start in 1835 by leasing a slave named Joyce Heth, an elderly Black woman who told vivid stories of caring for a young George Washington. He toured her around the country, advertising her as a 160-year-old woman who served as George Washington’s nanny. When Ms. Heth died the next year, Barnum sold tickets to the autopsy, charging the equivalent of $30 in today’s money.
When a doctor announced that Ms. Heth was actually 75-80 when she died, it caused great controversy in the press and ruined Barnum’s career. Wait, no, that’s not right. The opposite, actually. He weathered the storm, built his famous circus, and never again committed a hoax.
It’s difficult to quantify how wrong publicly dissecting a person and charging people to see said dissection is, but that was almost 200 years ago. At the very least, we can say that such terrible behavior is firmly in the distant past.
Oh wait.
David Saunders, a 98-year-old veteran of World War II and the Korean War, donated his body to science. His body, however, was purchased by DeathScience.org from a medical lab – with the buyer supposedly misleading the medical lab about its intentions, which was for use at the traveling Oddities and Curiosities Expo. Tickets went for up to $500 each to witness the public autopsy of Mr. Saunders’ body, which took place at a Marriott in Portland, Ore. It promised to be an exciting, all-day event from 9 a.m. to 4 p.m., with a break for lunch, of course. You can’t have an autopsy without a catered lunch.
Another public autopsy event was scheduled in Seattle but canceled after news of the first event broke. Oh, and for that extra little kick, Mr. Saunders died from COVID-19, meaning that all those paying customers were exposed.
P.T. Barnum is probably rolling over in his grave right now. His autopsy tickets were a bargain.
Go ahead, have that soda before math
We should all know by now that sugary drinks are bad, even artificially sweetened ones. It might not always stop us from drinking them, but we know the deal. But what if sugary drinks like soda could be helpful for girls in school?
You read that right. We said girls. A soda before class might have boys bouncing off the walls, but not girls. A recent study showed that not only was girls’ behavior unaffected by having a sugary drink, their math skills even improved.
Researchers analyzed the behavior of 4- to 6-year-old children before and after having a sugary drink. The sugar rush was actually calming for girls and helped them perform better with numerical skills, but the opposite was true for boys. “Our study is the first to provide large-scale experimental evidence on the impact of sugary drinks on preschool children. The results clearly indicate a causal impact of sugary drinks on children’s behavior and test scores,” Fritz Schiltz, PhD, said in a written statement.
This probably isn’t the green light to have as many sugary drinks as you want, but it might be interesting to see how your work is affected after a soda.
Chicken nuggets and the meat paradox
Two young children are fighting over the last chicken nugget when an adult comes in to see what’s going on.
Liam: Vegetable!
Olivia: Meat!
Liam: Chicken nuggets are vegetables!
Olivia: No, dorkface! They’re meat.
Caregiver: Good news, kids. You’re both right.
Olivia: How can we both be right?
At this point, a woman enters the room. She’s wearing a white lab coat, so she must be a scientist.
Dr. Scientist: You can’t both be right, Olivia. You are being fed a serving of the meat paradox. That’s why Liam here doesn’t know that chicken nuggets are made of chicken, which is a form of meat. Sadly, he’s not the only one.
In a recent study, scientists from Furman University in Greenville, S.C., found that 38% of 176 children aged 4-7 years thought that chicken nuggets were vegetables and more than 46% identified French fries as animal based.
Olivia: Did our caregiver lie to us, Dr. Scientist?
Dr. Scientist: Yes, Olivia. The researchers I mentioned explained that “many people experience unease while eating meat. Omnivores eat foods that entail animal suffering and death while at the same time endorsing the compassionate treatment of animals.” That’s the meat paradox.
Liam: What else did they say, Dr. Scientist?
Dr. Scientist: Over 70% of those children said that cows and pigs were not edible and 5% thought that cats and horses were. The investigators wrote “that children and youth should be viewed as agents of environmental change” in the future, but suggested that parents need to bring honesty to the table.
Caregiver: How did you get in here anyway? And how do you know their names?
Dr. Scientist: I’ve been rooting through your garbage for years. All in the name of science, of course.
Bedtimes aren’t just for children
There are multiple ways to prevent heart disease, but what if it could be as easy as switching your bedtime? A recent study in European Heart Journal–Digital Health suggests that there’s a sweet spot when it comes to sleep timing.
Through smartwatch-like devices, researchers measured the sleep-onset and wake-up times for 7 days in 88,026 participants aged 43-79 years. After 5.7 years of follow-up to see if anyone had a heart attack, stroke, or any other cardiovascular event, 3.6% developed some kind of cardiovascular disease.
Those who went to bed between 10 p.m. and 11 p.m. had a lower risk of developing heart disease. The risk was 25% higher for subjects who went to bed at midnight or later, 24% higher for bedtimes before 10 p.m., and 12% higher for bedtimes between 11 p.m. and midnight.
So, why can you go to bed before “The Tonight Show” and lower your cardiovascular risk but not before the nightly news? Well, it has something to do with your body’s natural clock.
“The optimum time to go to sleep is at a specific point in the body’s 24-hour cycle and deviations may be detrimental to health. The riskiest time was after midnight, potentially because it may reduce the likelihood of seeing morning light, which resets the body clock,” said study author Dr. David Plans of the University of Exeter, England.
Although a sleep schedule is preferred, it isn’t realistic all the time for those in certain occupations who might have to resort to other methods to keep their circadian clocks ticking optimally for their health. But if all it takes is prescribing a sleep time to reduce heart disease on a massive scale it would make a great “low-cost public health target.”
So bedtimes aren’t just for children.
The greatest autopsy on Earth?
The LOTME staff would like to apologize in advance. The following item contains historical facts.
P.T. Barnum is a rather controversial figure in American history. The greatest show on Earth was certainly popular in its day. However, Barnum got his start in 1835 by leasing a slave named Joyce Heth, an elderly Black woman who told vivid stories of caring for a young George Washington. He toured her around the country, advertising her as a 160-year-old woman who served as George Washington’s nanny. When Ms. Heth died the next year, Barnum sold tickets to the autopsy, charging the equivalent of $30 in today’s money.
When a doctor announced that Ms. Heth was actually 75-80 when she died, it caused great controversy in the press and ruined Barnum’s career. Wait, no, that’s not right. The opposite, actually. He weathered the storm, built his famous circus, and never again committed a hoax.
It’s difficult to quantify how wrong publicly dissecting a person and charging people to see said dissection is, but that was almost 200 years ago. At the very least, we can say that such terrible behavior is firmly in the distant past.
Oh wait.
David Saunders, a 98-year-old veteran of World War II and the Korean War, donated his body to science. His body, however, was purchased by DeathScience.org from a medical lab – with the buyer supposedly misleading the medical lab about its intentions, which was for use at the traveling Oddities and Curiosities Expo. Tickets went for up to $500 each to witness the public autopsy of Mr. Saunders’ body, which took place at a Marriott in Portland, Ore. It promised to be an exciting, all-day event from 9 a.m. to 4 p.m., with a break for lunch, of course. You can’t have an autopsy without a catered lunch.
Another public autopsy event was scheduled in Seattle but canceled after news of the first event broke. Oh, and for that extra little kick, Mr. Saunders died from COVID-19, meaning that all those paying customers were exposed.
P.T. Barnum is probably rolling over in his grave right now. His autopsy tickets were a bargain.
Go ahead, have that soda before math
We should all know by now that sugary drinks are bad, even artificially sweetened ones. It might not always stop us from drinking them, but we know the deal. But what if sugary drinks like soda could be helpful for girls in school?
You read that right. We said girls. A soda before class might have boys bouncing off the walls, but not girls. A recent study showed that not only was girls’ behavior unaffected by having a sugary drink, their math skills even improved.
Researchers analyzed the behavior of 4- to 6-year-old children before and after having a sugary drink. The sugar rush was actually calming for girls and helped them perform better with numerical skills, but the opposite was true for boys. “Our study is the first to provide large-scale experimental evidence on the impact of sugary drinks on preschool children. The results clearly indicate a causal impact of sugary drinks on children’s behavior and test scores,” Fritz Schiltz, PhD, said in a written statement.
This probably isn’t the green light to have as many sugary drinks as you want, but it might be interesting to see how your work is affected after a soda.
Chicken nuggets and the meat paradox
Two young children are fighting over the last chicken nugget when an adult comes in to see what’s going on.
Liam: Vegetable!
Olivia: Meat!
Liam: Chicken nuggets are vegetables!
Olivia: No, dorkface! They’re meat.
Caregiver: Good news, kids. You’re both right.
Olivia: How can we both be right?
At this point, a woman enters the room. She’s wearing a white lab coat, so she must be a scientist.
Dr. Scientist: You can’t both be right, Olivia. You are being fed a serving of the meat paradox. That’s why Liam here doesn’t know that chicken nuggets are made of chicken, which is a form of meat. Sadly, he’s not the only one.
In a recent study, scientists from Furman University in Greenville, S.C., found that 38% of 176 children aged 4-7 years thought that chicken nuggets were vegetables and more than 46% identified French fries as animal based.
Olivia: Did our caregiver lie to us, Dr. Scientist?
Dr. Scientist: Yes, Olivia. The researchers I mentioned explained that “many people experience unease while eating meat. Omnivores eat foods that entail animal suffering and death while at the same time endorsing the compassionate treatment of animals.” That’s the meat paradox.
Liam: What else did they say, Dr. Scientist?
Dr. Scientist: Over 70% of those children said that cows and pigs were not edible and 5% thought that cats and horses were. The investigators wrote “that children and youth should be viewed as agents of environmental change” in the future, but suggested that parents need to bring honesty to the table.
Caregiver: How did you get in here anyway? And how do you know their names?
Dr. Scientist: I’ve been rooting through your garbage for years. All in the name of science, of course.
Bedtimes aren’t just for children
There are multiple ways to prevent heart disease, but what if it could be as easy as switching your bedtime? A recent study in European Heart Journal–Digital Health suggests that there’s a sweet spot when it comes to sleep timing.
Through smartwatch-like devices, researchers measured the sleep-onset and wake-up times for 7 days in 88,026 participants aged 43-79 years. After 5.7 years of follow-up to see if anyone had a heart attack, stroke, or any other cardiovascular event, 3.6% developed some kind of cardiovascular disease.
Those who went to bed between 10 p.m. and 11 p.m. had a lower risk of developing heart disease. The risk was 25% higher for subjects who went to bed at midnight or later, 24% higher for bedtimes before 10 p.m., and 12% higher for bedtimes between 11 p.m. and midnight.
So, why can you go to bed before “The Tonight Show” and lower your cardiovascular risk but not before the nightly news? Well, it has something to do with your body’s natural clock.
“The optimum time to go to sleep is at a specific point in the body’s 24-hour cycle and deviations may be detrimental to health. The riskiest time was after midnight, potentially because it may reduce the likelihood of seeing morning light, which resets the body clock,” said study author Dr. David Plans of the University of Exeter, England.
Although a sleep schedule is preferred, it isn’t realistic all the time for those in certain occupations who might have to resort to other methods to keep their circadian clocks ticking optimally for their health. But if all it takes is prescribing a sleep time to reduce heart disease on a massive scale it would make a great “low-cost public health target.”
So bedtimes aren’t just for children.
Brief, automated cognitive test may offer key advantages in MS
(RRMS), new research shows.
“To our knowledge this is the first psychometric evaluation of the NIH Toolbox Cognition Battery in MS,” said study investigator Heena R. Manglani, MA, a clinical psychology fellow at Massachusetts General Hospital and Harvard Medical School, Boston.
“[The findings] suggest that the NIH Toolbox Cognition Battery may be used as an alternative to other gold-standard measures which may cover limited domains or require manual scoring,” added Ms. Manglani, who is working toward her PhD in clinical psychology.
The study was presented at the 2021 Annual Meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
An indicator of disease activity?
Cognitive deficits affecting a range of functions – including memory, attention and communication – are common in MS and affect 34% to 65% of patients with the disease, and the ability to detect and monitor such deficits has important implications.
Cognitive changes can provide a unique opportunity to identify acute disease activity in patients with MS that might be already occurring before physical manifestations become apparent, said Ms. Manglani. “If we can detect subtle changes in cognition that might foreshadow other symptoms of disease worsening, we can then allocate interventions that might stave off cognitive decline,” she explained.
While there is an array of well-established neuropsychological tests for the assessment of cognitive deficits, each has limitations, so a shorter, computerized, convenient, and reliable test could prove beneficial.
The NIHTB-CB has been validated in a large, nationally representative sample of individuals aged 8 to 85 and represents a potentially attractive option, yielding composite measures and scores corrected for age, gender, education, race, and ethnicity.
Comparative testing
To compare the test with other leading cognition tools used in MS, the investigators recruited 87 patients with RRMS (79% female, mean age 47.3 years). Participants were recruited to perform the full NIHTB-CB (about 30 minutes) and the full Minimal Assessment of Cognitive Function in Multiple Sclerosis (MACFIMS), which takes about 90 minutes, as well as some subsets from the Wechsler Adult Intelligence Scale-IV (WAIS-IV) covering processing speed and working memory. All patients had an EDSS of 5.0 or below and, on average, had been living with MS for about a decade.
The results showed the normative scores for NIHTB-CB had significant concordance with the other measures in terms of processing speed (concordance correlation coefficient [CCC] range = 0.28-0.48), working memory (CCC range = 0.27-0.37), and episodic memory (CCC range = 0.21-0.32). However, agreement was not shown for executive function (CCC range = 0.096-0.11).
Ms. Manglani noted executive function included various submeasures such as planning and inhibitory control. “Perhaps our gold standard measures tapped into a different facet of executive function than measured by the NIHTB,” she said.
The investigators found the proportion of participants classified as cognitively impaired was similar between the MACFIMS and the NIHTB tests.
Further assessment of fluid cognition on the NIHTB-CB – a composite of processing speed, working memory, episodic memory, and executive function that is automatically generated by the toolbox – showed the measure was negatively associated with disease severity, as measured by the EDSS (P = .006). However, the measure was not associated with a difference in depression (P = .39) or fatigue (P = .69).
Of note, a similar association with lower disease severity on the EDSS was not observed with MACFIMS.
“Interestingly, we found that only the NIHTB-CB fluid cognition was associated with disease severity, such that it was associated with nearly 11% of the variance in EDSS scores, and we were surprised that we didn’t see this with MACFIMS,” Ms. Manglani said.
Key advantages
The NIHTB-CB was developed as part of the NIH Blueprint for Neuroscience Research initiative and commissioned by 16 NIH Institutes to provide brief, efficient assessment measures of cognitive function.
The battery has been validated in healthy individuals and tested in other populations with neurologic disorders, including patients who have suffered stroke and traumatic brain injury.
Ms. Manglani noted that the NIHTB-CB had key advantages over other tests. “First, it is a 30-minute iPad-based battery, which is shorter than most cognitive batteries available, and one of the few that is completely computerized. In addition, it automatically scores performance and yields a report with both composite scores and scores for each subtest,” she said.
In addition, said Ms. Manglani, “the NIH toolbox has a large validation sample of individuals between 8-85 years of age and provides normative scores that account for age, gender, education, and race/ethnicity, which allows individuals’ performances to be compared with their peers.”
The findings underscore that with further validation, the battery could have an important role in MS, she added.
“The NIH Toolbox needs to be tested in all subtypes of MS, with a full range of disease severity, and in MS clinics to gauge the clinical feasibility. Larger samples and repeated assessments are also needed to assess the test-retest reliability,” she said.
The study had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(RRMS), new research shows.
“To our knowledge this is the first psychometric evaluation of the NIH Toolbox Cognition Battery in MS,” said study investigator Heena R. Manglani, MA, a clinical psychology fellow at Massachusetts General Hospital and Harvard Medical School, Boston.
“[The findings] suggest that the NIH Toolbox Cognition Battery may be used as an alternative to other gold-standard measures which may cover limited domains or require manual scoring,” added Ms. Manglani, who is working toward her PhD in clinical psychology.
The study was presented at the 2021 Annual Meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
An indicator of disease activity?
Cognitive deficits affecting a range of functions – including memory, attention and communication – are common in MS and affect 34% to 65% of patients with the disease, and the ability to detect and monitor such deficits has important implications.
Cognitive changes can provide a unique opportunity to identify acute disease activity in patients with MS that might be already occurring before physical manifestations become apparent, said Ms. Manglani. “If we can detect subtle changes in cognition that might foreshadow other symptoms of disease worsening, we can then allocate interventions that might stave off cognitive decline,” she explained.
While there is an array of well-established neuropsychological tests for the assessment of cognitive deficits, each has limitations, so a shorter, computerized, convenient, and reliable test could prove beneficial.
The NIHTB-CB has been validated in a large, nationally representative sample of individuals aged 8 to 85 and represents a potentially attractive option, yielding composite measures and scores corrected for age, gender, education, race, and ethnicity.
Comparative testing
To compare the test with other leading cognition tools used in MS, the investigators recruited 87 patients with RRMS (79% female, mean age 47.3 years). Participants were recruited to perform the full NIHTB-CB (about 30 minutes) and the full Minimal Assessment of Cognitive Function in Multiple Sclerosis (MACFIMS), which takes about 90 minutes, as well as some subsets from the Wechsler Adult Intelligence Scale-IV (WAIS-IV) covering processing speed and working memory. All patients had an EDSS of 5.0 or below and, on average, had been living with MS for about a decade.
The results showed the normative scores for NIHTB-CB had significant concordance with the other measures in terms of processing speed (concordance correlation coefficient [CCC] range = 0.28-0.48), working memory (CCC range = 0.27-0.37), and episodic memory (CCC range = 0.21-0.32). However, agreement was not shown for executive function (CCC range = 0.096-0.11).
Ms. Manglani noted executive function included various submeasures such as planning and inhibitory control. “Perhaps our gold standard measures tapped into a different facet of executive function than measured by the NIHTB,” she said.
The investigators found the proportion of participants classified as cognitively impaired was similar between the MACFIMS and the NIHTB tests.
Further assessment of fluid cognition on the NIHTB-CB – a composite of processing speed, working memory, episodic memory, and executive function that is automatically generated by the toolbox – showed the measure was negatively associated with disease severity, as measured by the EDSS (P = .006). However, the measure was not associated with a difference in depression (P = .39) or fatigue (P = .69).
Of note, a similar association with lower disease severity on the EDSS was not observed with MACFIMS.
“Interestingly, we found that only the NIHTB-CB fluid cognition was associated with disease severity, such that it was associated with nearly 11% of the variance in EDSS scores, and we were surprised that we didn’t see this with MACFIMS,” Ms. Manglani said.
Key advantages
The NIHTB-CB was developed as part of the NIH Blueprint for Neuroscience Research initiative and commissioned by 16 NIH Institutes to provide brief, efficient assessment measures of cognitive function.
The battery has been validated in healthy individuals and tested in other populations with neurologic disorders, including patients who have suffered stroke and traumatic brain injury.
Ms. Manglani noted that the NIHTB-CB had key advantages over other tests. “First, it is a 30-minute iPad-based battery, which is shorter than most cognitive batteries available, and one of the few that is completely computerized. In addition, it automatically scores performance and yields a report with both composite scores and scores for each subtest,” she said.
In addition, said Ms. Manglani, “the NIH toolbox has a large validation sample of individuals between 8-85 years of age and provides normative scores that account for age, gender, education, and race/ethnicity, which allows individuals’ performances to be compared with their peers.”
The findings underscore that with further validation, the battery could have an important role in MS, she added.
“The NIH Toolbox needs to be tested in all subtypes of MS, with a full range of disease severity, and in MS clinics to gauge the clinical feasibility. Larger samples and repeated assessments are also needed to assess the test-retest reliability,” she said.
The study had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(RRMS), new research shows.
“To our knowledge this is the first psychometric evaluation of the NIH Toolbox Cognition Battery in MS,” said study investigator Heena R. Manglani, MA, a clinical psychology fellow at Massachusetts General Hospital and Harvard Medical School, Boston.
“[The findings] suggest that the NIH Toolbox Cognition Battery may be used as an alternative to other gold-standard measures which may cover limited domains or require manual scoring,” added Ms. Manglani, who is working toward her PhD in clinical psychology.
The study was presented at the 2021 Annual Meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
An indicator of disease activity?
Cognitive deficits affecting a range of functions – including memory, attention and communication – are common in MS and affect 34% to 65% of patients with the disease, and the ability to detect and monitor such deficits has important implications.
Cognitive changes can provide a unique opportunity to identify acute disease activity in patients with MS that might be already occurring before physical manifestations become apparent, said Ms. Manglani. “If we can detect subtle changes in cognition that might foreshadow other symptoms of disease worsening, we can then allocate interventions that might stave off cognitive decline,” she explained.
While there is an array of well-established neuropsychological tests for the assessment of cognitive deficits, each has limitations, so a shorter, computerized, convenient, and reliable test could prove beneficial.
The NIHTB-CB has been validated in a large, nationally representative sample of individuals aged 8 to 85 and represents a potentially attractive option, yielding composite measures and scores corrected for age, gender, education, race, and ethnicity.
Comparative testing
To compare the test with other leading cognition tools used in MS, the investigators recruited 87 patients with RRMS (79% female, mean age 47.3 years). Participants were recruited to perform the full NIHTB-CB (about 30 minutes) and the full Minimal Assessment of Cognitive Function in Multiple Sclerosis (MACFIMS), which takes about 90 minutes, as well as some subsets from the Wechsler Adult Intelligence Scale-IV (WAIS-IV) covering processing speed and working memory. All patients had an EDSS of 5.0 or below and, on average, had been living with MS for about a decade.
The results showed the normative scores for NIHTB-CB had significant concordance with the other measures in terms of processing speed (concordance correlation coefficient [CCC] range = 0.28-0.48), working memory (CCC range = 0.27-0.37), and episodic memory (CCC range = 0.21-0.32). However, agreement was not shown for executive function (CCC range = 0.096-0.11).
Ms. Manglani noted executive function included various submeasures such as planning and inhibitory control. “Perhaps our gold standard measures tapped into a different facet of executive function than measured by the NIHTB,” she said.
The investigators found the proportion of participants classified as cognitively impaired was similar between the MACFIMS and the NIHTB tests.
Further assessment of fluid cognition on the NIHTB-CB – a composite of processing speed, working memory, episodic memory, and executive function that is automatically generated by the toolbox – showed the measure was negatively associated with disease severity, as measured by the EDSS (P = .006). However, the measure was not associated with a difference in depression (P = .39) or fatigue (P = .69).
Of note, a similar association with lower disease severity on the EDSS was not observed with MACFIMS.
“Interestingly, we found that only the NIHTB-CB fluid cognition was associated with disease severity, such that it was associated with nearly 11% of the variance in EDSS scores, and we were surprised that we didn’t see this with MACFIMS,” Ms. Manglani said.
Key advantages
The NIHTB-CB was developed as part of the NIH Blueprint for Neuroscience Research initiative and commissioned by 16 NIH Institutes to provide brief, efficient assessment measures of cognitive function.
The battery has been validated in healthy individuals and tested in other populations with neurologic disorders, including patients who have suffered stroke and traumatic brain injury.
Ms. Manglani noted that the NIHTB-CB had key advantages over other tests. “First, it is a 30-minute iPad-based battery, which is shorter than most cognitive batteries available, and one of the few that is completely computerized. In addition, it automatically scores performance and yields a report with both composite scores and scores for each subtest,” she said.
In addition, said Ms. Manglani, “the NIH toolbox has a large validation sample of individuals between 8-85 years of age and provides normative scores that account for age, gender, education, and race/ethnicity, which allows individuals’ performances to be compared with their peers.”
The findings underscore that with further validation, the battery could have an important role in MS, she added.
“The NIH Toolbox needs to be tested in all subtypes of MS, with a full range of disease severity, and in MS clinics to gauge the clinical feasibility. Larger samples and repeated assessments are also needed to assess the test-retest reliability,” she said.
The study had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CMSC 2021
Specialty pharmacists may speed time to MS treatment
, new data suggest.
“As DMT management and treatment options for MS symptoms become more complex, clinical pharmacists can be utilized for medication education and management,” Jenelle Hall Montgomery, PharmD, a clinical pharmacist practitioner at the Multiple Sclerosis and Neuroimmunology Division, department of neurology, Duke University Hospital, Durham, N.C., told delegates attending the 2021 Annual Meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
Since 2018, more than half a dozen DMTs have been approved for MS by the U.S. Food and Drug Administration. However, there is currently no established DMT selection algorithm, and because of this, there is a need for specialty pharmacists, she added.
“DMT approvals by the FDA have outpaced MS guideline recommendations. This can be overwhelming for patients, especially now that they have so many options to choose from,” she said.
Key services provided by specialty pharmacists include coordinating pretreatment requirements, as well as help with dosing, side effects, safety monitoring, and treatment adherence. In addition, pharmacists help with switching therapies, dispensing, and cost and authorization problems.
In reporting on improvements associated with specialty pharmacists, researchers from prominent MS centers around the country described specific outcomes.
Aids early intervention
A report on the Kaiser Permanente Washington (KPWA) MS Pharmacy Program detailed significant reductions in the time to address patients’ needs through the use of specialty pharmacists. In an assessment of 391 referrals to the program from 2019 to 2020, the average total time spent per patient per year dropped from 145 minutes in 2019 to 109 minutes in 2020.
Services included assessment of medication adherence, adverse drug reaction consultation, lab monitoring, patient counseling on initiation of a DMT, shared decision making, and follow-up visits.
“The KPWA MS Pharmacy Program plays an integral role in the care of patients with MS. The MS clinical pharmacists ensure patients are well informed about their DMT options and are fully educated about selected treatment,” the investigators noted.
A report on an outpatient MS clinic at Emory Healthcare, Atlanta, described how use of specialty pharmacist services resulted in a 49% reduction in time to treatment initiation with fingolimod. The time decreased from 83.9 days to 42.9 days following the introduction of specialty pharmacist services.
“Integration of a clinical pharmacy specialist in the therapeutic management of MS patients is crucial to early intervention with disease-modifying therapy,” the investigators noted.
A report on the specialty pharmacy services provided at Johns Hopkins MS Precision Medicine Center of Excellence, Baltimore, described an evaluation of 708 assessments between July 2019 and June 2020. Results showed that the vast majority (98%) of patients reported no missed days from work or school due to MS-related symptoms and that 99.3% reported no hospitalizations due to MS relapses, which are both key measures of MS treatment adherence.
High patient satisfaction
Patients reported high satisfaction with the in-house pharmacy on the National Association of Specialty Pharmacy’s patient satisfaction survey. In the survey, the average score was 82, compared with 79 for external specialty pharmacies.
“Moreover, patients were highly satisfied with the services provided at the pharmacy and were likely to continue receiving their comprehensive pharmacy care at our institution,” the researchers reported.
The study “highlights the value of pharmacists’ involvement in patient care and supports the need for continuation of integrated clinical services in health system specialty pharmacy,” the investigators noted.
CMSC President Scott D. Newsome, DO, director of the Neurosciences Consultation and Infusion Center at Green Spring Station, Lutherville, Maryland, and associate professor of neurology at Johns Hopkins University School of Medicine, said that as a clinician, he is highly satisfied with the specialty pharmacy services for MS at Johns Hopkins.
“Our pharmacists are fantastic in communicating with the prescriber if something comes up related to medication safety or they are concerned that the patient isn’t adhering to the medication,” Dr. Newsome said.
He noted that in addition to helping to alleviate the burden of a myriad of tasks associated with prescribing for patients with MS, specialty pharmacists may have an important impact on outcomes, although more data are needed.
“Having a specialty pharmacy involved in the care of our patients can help navigate the challenges associated with the process of obtaining approval for DMTs,” he said. “We know how important it is to expedite and shorten the time frame from writing the prescription to getting the person on their DMT.”
Telemedicine, other models
Although integrated specialty pharmacist services may seem out of reach for smaller MS clinics, the use of telemedicine and other models may help achieve similar results.
“A model I have seen is having pharmacists split their time between a specialty pharmacy and the MS clinic,” said Dr. Montgomery.
“A telemedicine model can also be utilized, in which a pharmacist can reach out to patients by telephone or through video visits. This would allow a pharmacist to be utilized for multiple clinics or as an MS specialist within a specialty pharmacy,” she added.
Whether provided in house or through telemedicine, a key benefit for clinicians is in freeing up valuable time, which has a domino effect in improving quality all around.
“In addition to improving safety outcomes, specialty pharmacists help with the allocation of clinic staff to other clinic responsibilities, and the utilization of services by patients results in more resources allocated for their care,” Dr. Montgomery said.
Dr. Montgomery is a nonpromotional speaker for Novartis and is on its advisory board.
A version of this article first appeared on Medscape.com.
, new data suggest.
“As DMT management and treatment options for MS symptoms become more complex, clinical pharmacists can be utilized for medication education and management,” Jenelle Hall Montgomery, PharmD, a clinical pharmacist practitioner at the Multiple Sclerosis and Neuroimmunology Division, department of neurology, Duke University Hospital, Durham, N.C., told delegates attending the 2021 Annual Meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
Since 2018, more than half a dozen DMTs have been approved for MS by the U.S. Food and Drug Administration. However, there is currently no established DMT selection algorithm, and because of this, there is a need for specialty pharmacists, she added.
“DMT approvals by the FDA have outpaced MS guideline recommendations. This can be overwhelming for patients, especially now that they have so many options to choose from,” she said.
Key services provided by specialty pharmacists include coordinating pretreatment requirements, as well as help with dosing, side effects, safety monitoring, and treatment adherence. In addition, pharmacists help with switching therapies, dispensing, and cost and authorization problems.
In reporting on improvements associated with specialty pharmacists, researchers from prominent MS centers around the country described specific outcomes.
Aids early intervention
A report on the Kaiser Permanente Washington (KPWA) MS Pharmacy Program detailed significant reductions in the time to address patients’ needs through the use of specialty pharmacists. In an assessment of 391 referrals to the program from 2019 to 2020, the average total time spent per patient per year dropped from 145 minutes in 2019 to 109 minutes in 2020.
Services included assessment of medication adherence, adverse drug reaction consultation, lab monitoring, patient counseling on initiation of a DMT, shared decision making, and follow-up visits.
“The KPWA MS Pharmacy Program plays an integral role in the care of patients with MS. The MS clinical pharmacists ensure patients are well informed about their DMT options and are fully educated about selected treatment,” the investigators noted.
A report on an outpatient MS clinic at Emory Healthcare, Atlanta, described how use of specialty pharmacist services resulted in a 49% reduction in time to treatment initiation with fingolimod. The time decreased from 83.9 days to 42.9 days following the introduction of specialty pharmacist services.
“Integration of a clinical pharmacy specialist in the therapeutic management of MS patients is crucial to early intervention with disease-modifying therapy,” the investigators noted.
A report on the specialty pharmacy services provided at Johns Hopkins MS Precision Medicine Center of Excellence, Baltimore, described an evaluation of 708 assessments between July 2019 and June 2020. Results showed that the vast majority (98%) of patients reported no missed days from work or school due to MS-related symptoms and that 99.3% reported no hospitalizations due to MS relapses, which are both key measures of MS treatment adherence.
High patient satisfaction
Patients reported high satisfaction with the in-house pharmacy on the National Association of Specialty Pharmacy’s patient satisfaction survey. In the survey, the average score was 82, compared with 79 for external specialty pharmacies.
“Moreover, patients were highly satisfied with the services provided at the pharmacy and were likely to continue receiving their comprehensive pharmacy care at our institution,” the researchers reported.
The study “highlights the value of pharmacists’ involvement in patient care and supports the need for continuation of integrated clinical services in health system specialty pharmacy,” the investigators noted.
CMSC President Scott D. Newsome, DO, director of the Neurosciences Consultation and Infusion Center at Green Spring Station, Lutherville, Maryland, and associate professor of neurology at Johns Hopkins University School of Medicine, said that as a clinician, he is highly satisfied with the specialty pharmacy services for MS at Johns Hopkins.
“Our pharmacists are fantastic in communicating with the prescriber if something comes up related to medication safety or they are concerned that the patient isn’t adhering to the medication,” Dr. Newsome said.
He noted that in addition to helping to alleviate the burden of a myriad of tasks associated with prescribing for patients with MS, specialty pharmacists may have an important impact on outcomes, although more data are needed.
“Having a specialty pharmacy involved in the care of our patients can help navigate the challenges associated with the process of obtaining approval for DMTs,” he said. “We know how important it is to expedite and shorten the time frame from writing the prescription to getting the person on their DMT.”
Telemedicine, other models
Although integrated specialty pharmacist services may seem out of reach for smaller MS clinics, the use of telemedicine and other models may help achieve similar results.
“A model I have seen is having pharmacists split their time between a specialty pharmacy and the MS clinic,” said Dr. Montgomery.
“A telemedicine model can also be utilized, in which a pharmacist can reach out to patients by telephone or through video visits. This would allow a pharmacist to be utilized for multiple clinics or as an MS specialist within a specialty pharmacy,” she added.
Whether provided in house or through telemedicine, a key benefit for clinicians is in freeing up valuable time, which has a domino effect in improving quality all around.
“In addition to improving safety outcomes, specialty pharmacists help with the allocation of clinic staff to other clinic responsibilities, and the utilization of services by patients results in more resources allocated for their care,” Dr. Montgomery said.
Dr. Montgomery is a nonpromotional speaker for Novartis and is on its advisory board.
A version of this article first appeared on Medscape.com.
, new data suggest.
“As DMT management and treatment options for MS symptoms become more complex, clinical pharmacists can be utilized for medication education and management,” Jenelle Hall Montgomery, PharmD, a clinical pharmacist practitioner at the Multiple Sclerosis and Neuroimmunology Division, department of neurology, Duke University Hospital, Durham, N.C., told delegates attending the 2021 Annual Meeting of the Consortium of Multiple Sclerosis Centers (CMSC).
Since 2018, more than half a dozen DMTs have been approved for MS by the U.S. Food and Drug Administration. However, there is currently no established DMT selection algorithm, and because of this, there is a need for specialty pharmacists, she added.
“DMT approvals by the FDA have outpaced MS guideline recommendations. This can be overwhelming for patients, especially now that they have so many options to choose from,” she said.
Key services provided by specialty pharmacists include coordinating pretreatment requirements, as well as help with dosing, side effects, safety monitoring, and treatment adherence. In addition, pharmacists help with switching therapies, dispensing, and cost and authorization problems.
In reporting on improvements associated with specialty pharmacists, researchers from prominent MS centers around the country described specific outcomes.
Aids early intervention
A report on the Kaiser Permanente Washington (KPWA) MS Pharmacy Program detailed significant reductions in the time to address patients’ needs through the use of specialty pharmacists. In an assessment of 391 referrals to the program from 2019 to 2020, the average total time spent per patient per year dropped from 145 minutes in 2019 to 109 minutes in 2020.
Services included assessment of medication adherence, adverse drug reaction consultation, lab monitoring, patient counseling on initiation of a DMT, shared decision making, and follow-up visits.
“The KPWA MS Pharmacy Program plays an integral role in the care of patients with MS. The MS clinical pharmacists ensure patients are well informed about their DMT options and are fully educated about selected treatment,” the investigators noted.
A report on an outpatient MS clinic at Emory Healthcare, Atlanta, described how use of specialty pharmacist services resulted in a 49% reduction in time to treatment initiation with fingolimod. The time decreased from 83.9 days to 42.9 days following the introduction of specialty pharmacist services.
“Integration of a clinical pharmacy specialist in the therapeutic management of MS patients is crucial to early intervention with disease-modifying therapy,” the investigators noted.
A report on the specialty pharmacy services provided at Johns Hopkins MS Precision Medicine Center of Excellence, Baltimore, described an evaluation of 708 assessments between July 2019 and June 2020. Results showed that the vast majority (98%) of patients reported no missed days from work or school due to MS-related symptoms and that 99.3% reported no hospitalizations due to MS relapses, which are both key measures of MS treatment adherence.
High patient satisfaction
Patients reported high satisfaction with the in-house pharmacy on the National Association of Specialty Pharmacy’s patient satisfaction survey. In the survey, the average score was 82, compared with 79 for external specialty pharmacies.
“Moreover, patients were highly satisfied with the services provided at the pharmacy and were likely to continue receiving their comprehensive pharmacy care at our institution,” the researchers reported.
The study “highlights the value of pharmacists’ involvement in patient care and supports the need for continuation of integrated clinical services in health system specialty pharmacy,” the investigators noted.
CMSC President Scott D. Newsome, DO, director of the Neurosciences Consultation and Infusion Center at Green Spring Station, Lutherville, Maryland, and associate professor of neurology at Johns Hopkins University School of Medicine, said that as a clinician, he is highly satisfied with the specialty pharmacy services for MS at Johns Hopkins.
“Our pharmacists are fantastic in communicating with the prescriber if something comes up related to medication safety or they are concerned that the patient isn’t adhering to the medication,” Dr. Newsome said.
He noted that in addition to helping to alleviate the burden of a myriad of tasks associated with prescribing for patients with MS, specialty pharmacists may have an important impact on outcomes, although more data are needed.
“Having a specialty pharmacy involved in the care of our patients can help navigate the challenges associated with the process of obtaining approval for DMTs,” he said. “We know how important it is to expedite and shorten the time frame from writing the prescription to getting the person on their DMT.”
Telemedicine, other models
Although integrated specialty pharmacist services may seem out of reach for smaller MS clinics, the use of telemedicine and other models may help achieve similar results.
“A model I have seen is having pharmacists split their time between a specialty pharmacy and the MS clinic,” said Dr. Montgomery.
“A telemedicine model can also be utilized, in which a pharmacist can reach out to patients by telephone or through video visits. This would allow a pharmacist to be utilized for multiple clinics or as an MS specialist within a specialty pharmacy,” she added.
Whether provided in house or through telemedicine, a key benefit for clinicians is in freeing up valuable time, which has a domino effect in improving quality all around.
“In addition to improving safety outcomes, specialty pharmacists help with the allocation of clinic staff to other clinic responsibilities, and the utilization of services by patients results in more resources allocated for their care,” Dr. Montgomery said.
Dr. Montgomery is a nonpromotional speaker for Novartis and is on its advisory board.
A version of this article first appeared on Medscape.com.
FROM CMSC 2021