User login
Delayed Bleeding: The Silent Risk for Seniors
This discussion was recorded on August 2, 2024. This transcript has been edited for clarity.
Robert D. Glatter, MD: Today, we’ll be discussing the results of a new study published in The Journal of Emergency Medicine, looking at the incidence of delayed intracranial hemorrhage among older patients taking preinjury anticoagulants who present to the emergency department (ED) with blunt head trauma.
Joining me today is the lead author of the study, Dr. Richard Shih, professor of emergency medicine at Florida Atlantic University. Also joining me is Dr. Christina Shenvi, associate professor of emergency medicine at the University of North Carolina (UNC) Chapel Hill, with fellowship training in geriatric emergency medicine.
Welcome to both of you.
Richard D. Shih, MD: Thanks, Rob.
Christina L. Shenvi, MD, PhD, MBA: Thanks. Pleasure to be here.
ICH Study Methodology
Dr. Glatter: It’s a pleasure to have you. Rich, this is a great study and targeted toward a population we see daily in the emergency department. I want you to describe your methodology, patient selection, and how you went about organizing your study to look at this important finding of delayed intracranial hemorrhage, especially in those on anticoagulants.
Dr. Shih: This all started for our research team when we first read the 2012 Annals of Emergency Medicine paper. The first author was Vincenzo Menditto, and he looked at a group of patients that had minor head injury, were anticoagulated, and had negative initial head CTs.
There were about 100 patients, of which about 10 of them did not consent, but they hospitalized all these patients. These were anticoagulated, negative-first head CTs. They hospitalized the patients and then did a routine second CT at about 24 hours. They also followed them for a week, and it turned out a little over 7% of them had delayed head CT.
We were wondering how many delayed intracranial hemorrhages we had missed because current practice for us was that, if patients had a good physical exam, their head CT was normal, and everything looked good, we would send them home.
Because of that, a number of people across the country wanted to verify those findings from the Menditto study. We tried to design a good study to answer that question. We happen to have a very large geriatric population in Florida, and our ED census is very high for age over 65, at nearly 60%.
There are two Level I trauma centers in Palm Beach County. We included a second multicenter hospital, and we prospectively enrolled patients. We know the current state of practice is not to routinely do second CTs, so we followed these patients over time and followed their medical records to try to identify delayed bleeding. That’s how we set up our methodology.
Is It Safe to Discharge Patients With Trauma After 24 Hours?
Dr. Glatter: For the bulk of these patients with negative head CTs, it’s been my practice that when they’re stable and they look fine and there’s no other apparent, distracting painful trauma, injuries and so forth, they’re safe to discharge.
The secondary outcome in your study is interesting: the need for neurosurgical intervention in terms of those with delayed intracranial hemorrhage.
Dr. Shih: I do believe that it’s certainly not the problem that Menditto described, which is 7%. There are two other prospective studies that have looked at this issue with delayed bleeding on anticoagulants. Both of these also showed a relatively low rate of delayed bleeding, which is between like 0.2% and 1.0%. In our study, it was 0.4%.
The difference in the studies is that Menditto and colleagues routinely did 24-hour head CTs. They admitted everybody. For these other studies, routine head CT was not part of it. My bet is that there is a rate of delayed bleeding somewhere in between that seen in the Menditto study and that in all the other studies.
However, talking about significant intracranial hemorrhage, ones that perhaps need neurosurgery, I believe most of them are not significant. There’s some number that do occur, but the vast majority of those probably don’t need neurosurgery. We had 14 delayed bleeds out of 6000 patients with head trauma. One of them ended up requiring neurosurgery, so the answer is not zero, but I don’t think it’s 7% either.
Dr. Glatter: Dr. Shenvi, I want to bring you into the conversation to talk about your experience at UNC, and how you run things in terms of older patients with blunt head trauma on preinjury anticoagulants.
Dr. Shenvi: Thanks, Rob. I remember when this paper came out showing this 7% rate of delayed bleeding and the question was, “Should we be admitting all these people?” Partly just from an overwhelming need for capacity that that would bring, it just wasn’t practical to say, “We’re going to admit every patient with a negative head CT to the hospital and rescan them.” That would be hundreds or thousands of patients each year in any given facility.
The other thing is that delayed bleeds don’t always happen just in the first 24 hours. It’s not even a matter of bringing patients into observation for 24 hours, watching them, and rescanning them if they have symptoms. It can occur several days out. That never, in almost any institution that I know of, became standard practice.
The way that it did change my care was to give good return precautions to patients, to make sure they have somebody with them to say, “Hey, sometimes you can have bleeding several days out after a fall, even though your CT scan here today looks perfect,” and to alert them that if they start having severe headaches, vomiting, or other symptoms of intracranial hemorrhage, that they should come back.
I don’t think it ever became standard practice, and for good reason, because that was one study. The subsequent studies that Richard mentioned, pretty quickly on the heels of that initial one, showed a much lower rate of delayed ICH with the caveats that the methodology was different.
Shift in Anticoagulants
Dr. Shenvi: One other big change from that original study, and now to Richard’s study, is the shift in anticoagulants. Back in the initial study you mentioned, it was all warfarin. We know from other studies looking at warfarin vs the direct oral anticoagulants (DOACs) that DOACs have lower rates of ICH after a head injury, lower rates of need for neurosurgical intervention, and lower rates of discharge to a skilled nursing facility after an intracranial hemorrhage.
Across the board, we know that the DOACs tend to do better. It’s difficult to compare newer studies because it’s a different medication. It did inform my practice to have an awareness of delayed intracranial hemorrhage so that I warn patients more proactively.
Dr. Glatter: I haven’t seen a patient on warfarin in years. I don’t know if either of you have, but it’s all DOACs now unless there’s some other reason. That shift is quite apparent.
Dr. Shih: The problem with looking at delayed bleeding for DOACs vs warfarin is the numbers were so low. I think we had 13 people, and seven were in the no-anticoagulant group. The numbers are even lower, so it’s hard to say.
I just wanted to comment on something that Dr. Shenvi said, and I pretty much agree with everything that she said. Anticoagulants and warfarin, and that Menditto study, have a carryover effect. People group DOACs with warfarin similarly. When a patient is brought in, the first thing they talk about with head trauma is, “Oh, they’re on an anticoagulant” or “They’re not on an anticoagulant.” It’s so ingrained.
I believe that, in emergency medicine, we’re pressed for space and time and we’re not as affected by that 24-hour observation. Maybe many of our surgeons will automatically admit those patients.
I haven’t seen a guideline from the United States, but there are two international guidelines. One is from Austria from 2019, and one is from Scandinavia. Both recommended 24-hour observation if you’re on an anticoagulant.
There is a bit of controversy left over with that. Hopefully, as more and more of information, like in our study, comes out, people will be a little bit more clear about it. I don’t think there’s a need to routinely admit them.
I do want to mention that the Menditto study had such a massive impact on everybody. They pointed out one subgroup (and it’s such a small number of patients). They had seven cases of delayed bleeding; four or five of them were within that 24 hours, and a couple were diagnosed later over the next couple days.
Of those seven people, four of them had international normalized ratios (INRs) greater than 3. Of those four patients, I’ve heard people talk about this and recommend, “Okay, that’s the subgroup I would admit.” There’s a toss-up with what to do with DOAC because it’s very hard to tell whether there’s an issue, whether there are problems with their dosing, and whatever.
We actually recently looked at that. We have a much larger sample than four: close to 300 patients who were on warfarin. We looked at patients who had INRs below 3 and above 3, and we didn’t show a difference. We still don’t believe that warfarin is a big issue with delayed bleeding.
Should We Be Asking: ‘Are They on Blood Thinners?’
Dr. Shenvi: One of the interesting trends related to warfarin and the DOACs vs no anticoagulant is that as you mentioned, Dr Shih, the first question out of people’s mouths or the first piece of information emergency medical services gives you when they come in with a patient who’s had a head injury is, “Are they on blood thinners or not?”
Yet, the paradigm is shifting to say it’s not actually the blood thinners themselves that are giving older patients the higher risk for bleeding; it’s age and other comorbidities.
Certainly, if you’re on an anticoagulant and you start to bleed, your prognosis is much worse because the bleeding doesn’t stop. In terms of who has a bleeding event, there’s much less impact of anticoagulation than we used to think. That, in part, may be due to the change from warfarin to other medications.
Some of the experts I’ve talked to who have done the research on this have said, “Well, actually, warfarin was more of a marker for being much older and more frail, because it was primarily prescribed to older patients who have significant heart disease, atrial fibrillation, and so on.” It was more a marker for somebody who is at risk for an intracranial hemorrhage. There are many changes that have happened in the past 10 years with medications and also our understanding.
Challenges in Patient Follow-up
Dr. Glatter: That’s a great point. One thing, Rich, I want to ask you about is in terms of your proxy outcome assessment. When you use that at 14 and 60 days with telephone follow-up and then chart review at 60 and 90 days (because, obviously, everyone can’t get another head CT or it’s difficult to follow patients up), did you find that worked out well in your prospective cohort study, in terms of using that as a proxy, so to speak?
Dr. Shih: I would say to a certain extent. Unfortunately, we don’t have access to the patients to come back to follow up all of them, and there was obviously a large number of patients in our study.
The next best thing was that we had dedicated research assistants calling all of the patients at 14 days and 60 days. I’ve certainly read research studies where, when they call them, they get 80%-90% follow-up, but we did not achieve that.
I don’t know if people are more inundated with spam phone calls now, or the older people are just afraid of picking up their phone sometimes with all the scams and so forth. I totally understand, but in all honesty, we only had about a 30%-35% follow-up using that follow-up pathway.
Then the proxy pathway was to look at their charts at 60 and 90 days. Also, we looked at the Florida death registry, which is pretty good, and then finally, we had both Level I trauma centers in the county that we were in participating. It’s standard practice that if you have an intracranial hemorrhage at a non–Level I trauma center, you would be transferred to a Level I trauma center. That’s the protocol. I know that’s not followed 100% of the time, but that’s part of the proxy follow-up. You could criticize the study for not having closer to 90% actual contact, but that’s the best we could do.
Dr. Glatter: I think that’s admirable. Using that paradigm of what you described certainly allows the reader to understand the difficulty in assessing patients that don’t get follow-up head CT, and hardly anyone does that, as we know.
To your point of having both Level I trauma centers in the county, that makes it pretty secure. If we’re going to do a study encompassing a similar type of regional aspect, it would be similar.
Dr. Shenvi: I think your proxies, to your credit, were as good as you can get. You can never get a 100% follow-up, but you really looked at all the different avenues by which patients might present, either in the death registry or a Level I center. Well done on that aspect.
Determining When to Admit Patients for Observation
Dr. Glatter: In terms of admissions: You admit a patient, then you hear back that this patient should not have been admitted because they had a negative head CT, but you put them in anyway in the sense of delayed bleeding happening or not happening.
It’s interesting. Maybe the insurers will start looking at this in some capacity, based on your study, that because it’s so infrequent that you see delayed bleeding, that admitting someone for any reason whatsoever would be declined. Do you see that being an issue? In other words, [do you see] this leading to a pattern in terms of the payers?
Dr. Shih: Certainly, you could interpret it that way, and that would be unfortunate. The [incidence of] delayed bleeding is definitely not zero. That’s the first thing.
The second thing is that when you’re dealing with an older population, having some sense that they’re not doing well is an important contributor to trying to fully assess what’s going on — whether or not they have a bleed or whether they’re at risk for falling again and then hitting their head and causing a second bleed, and making sure they can do the activities of daily life. There really should be some room for a physician to say, “They just got here, and we don’t know him that well. There’s something that bothers me about this person” and have the ability to watch them for at least another 24 hours. That’s how I feel.
Dr. Shenvi: In my location, it would be difficult to try to admit somebody purely for observation for delayed bleeding. I think we would get a lot of pushback on that. The reasons I might admit a patient after a fall with a negative head CT, though, are all the things that, Rob, you alluded to earlier — which are, what made them fall in the first place and were they unable to get up?
I had this happen just this week. A patient who fell couldn’t get off the ground for 12 hours, and so now she’s dehydrated and delirious with slight rhabdomyolysis. Then you’re admitting them either for the sequelae of the fall that are not related to the intracranial hemorrhage, or the fact that they are so debilitated and deconditioned that they cannot take care of themselves. They need physical therapy. Often, we will have physical and occupational therapists come see them in the ED during business hours and help make an assessment of whether they are safe to go home or whether they fall again. That can give more evidence for the need for admission.
Dr. Glatter: To bring artificial intelligence into this discussion, algorithms that are out there that say, “Push a button and the patient’s safe for discharge.” Well, this argues for a clinical gestalt and a human being to make an assessment because you can use these predictive models, which are coming and they’re going to be here soon, and they already are in some sense. Again, we have to use clinical human judgment.
Dr. Shih: I agree.
Advice for Primary Care Physicians
Dr. Glatter: What return precautions do you discuss with patients who’ve had blunt head trauma that maybe had a head CT, or even didn’t? What are the main things we’re looking for?
Dr. Shenvi: What I usually tell people is if you start to have a worse headache, nausea or vomiting, any weakness in one area of your body, or vision changes, and if there’s a family member or friend there, I’ll say, “If you notice that they’re acting differently or seem confused, come back.”
Dr. Shih: I agree with what she said, and I’m also going to add one thing. The most important part is they are trying to prevent a subsequent fall. We know that when they’ve fallen and they present to the ED, they’re at even higher risk for falling and reinjuring themselves, and that’s a population that’s already at risk.
One of the secondary studies that we published out of this project was looking at follow-up with their primary care physicians, and there were two things that we wanted to address. The first was, how often did they do it? Then, when they did do it, did their primary care physicians try to address and prevent subsequent falls?
Both the answers are actually bad. Amazingly, just over like 60% followed up.
In some of our subsequent research, because we’re in the midst of a randomized, controlled trial where we do a home visit, when we initially see these individuals that have fallen, they’ll schedule a home visit for us. Then a week or two later, when we schedule the home visit, many of them cancel because they think, Oh, that was a one-off and it’s not going to happen again. Part of the problem is the patients, because many of them believe that they just slipped and fell and it’s not going to happen again, or they’re not prone to it.
The second issue was when patients did go to a primary care physician, we have found that some primary care physicians believe that falling and injuring themselves is just part of the normal aging process. A percentage of them don’t go over assessment for fall risk or even initiate fall prevention treatments or programs.
I try to take that time to tell them that this is very common in their age group, and believe it or not, a fall from standing is the way people really injure themselves, and there may be ways to prevent subsequent falls and injuries.
Dr. Glatter: Absolutely. Do you find that their medications are a contributor in some sense? Say they’re antihypertensive, have issues of orthostasis, or a new medication was added in the last week.
Dr. Shenvi: It’s all of the above. Sometimes it’s one thing, like they just started tamsulosin for their kidney stone, they stood up, they felt lightheaded, and they fell. Usually, it’s multifactorial with some changes in their gait, vision, balance, reflex time, and strength, plus the medications or the need for assistive devices. Maybe they can’t take care of their home as well as they used to and there are things on the floor. It’s really all of the above.
‘Harder to Unlearn Something Than to Learn It’
Dr. Glatter: Would either of you like to add any additional points to the discussion or add a few pearls?
Dr. Shenvi: This just highlights the challenge of how it’s harder to unlearn something than to learn it, where one study that maybe wasn’t quite looking at what we needed to, or practice and prescribing patterns have changed, so it’s no longer really relevant.
The things that we learned from that, or the fears that we instilled in our minds of, Uh oh, they could go home and have delayed bleeding, are much harder to unlearn, and it takes more studies to unlearn that idea than it did to actually put it into place.
I’m glad that your team has done this much larger, prospective study and hopefully will reduce the concern about this entity.
Dr. Shih: I appreciate that segue. It is amazing that, for paramedics and medical students, the first thing out of their mouth is, “Are they on an anticoagulant?”
In terms of the risk of developing an intracranial hemorrhage, I think it’s much less than the weight we’ve put on it before. However, I believe if they have a bleed, the bleeds are worse. It’s kind of a double-edged sword. It’s still an important factor, but it doesn’t come with the Oh my gosh, they’re on an anticoagulant that everybody thinks about.
No. 1 Cause of Traumatic Injury Is a Fall from Standing
Dr. Glatter: These are obviously ground-level falls in most patients and not motor vehicle crashes. That’s an important part in the population that you looked at that should be mentioned clearly.
Dr. Shih: It’s astonishing. I’ve been a program director for over 20 years, and geriatrics is not well taught in the curriculum. It’s astonishing for many of our trainees and emergency physicians in general that the number-one cause for traumatic injury is a fall from standing.
Certainly, we get patients coming in the trauma center like a 95-year-old person who’s on a ladder putting up his Christmas lights. I’m like, oh my God.
For the vast majority, it’s closer to 90%, but in our study, for the patients we looked at, it was 80% that fall from standing. That’s the mechanism that causes these bleeds and these major injuries.
Dr. Shenvi: That’s reflective of what we see, so it’s good that that’s what you looked at also.
Dr. Glatter: Absolutely. Well, thank you both. This has been a very informative discussion. I appreciate your time, and our readers will certainly benefit from your knowledge and expertise. Thank you again.
Dr. Glatter, assistant professor of emergency medicine at Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, is a medical adviser for this news organization. He disclosed having no relevant financial conflicts. Dr. Shih is professor of emergency medicine at the Charles E. Schmidt College of Medicine at Florida Atlantic University, Boca Raton. His current grant funding and area of research interest involves geriatric emergency department patients with head injury and fall-related injury. He disclosed receiving a research grant from The Florida Medical Malpractice Joint Underwriting Association Grant for Safety of Health Care Services). Dr. Shenvi, associate professor of emergency medicine at the University of North Carolina at Chapel Hill, disclosed ties with the American College of Emergency Physicians, Institute for Healthcare Improvement, AstraZeneca, and CurvaFix.
A version of this article appeared on Medscape.com.
This discussion was recorded on August 2, 2024. This transcript has been edited for clarity.
Robert D. Glatter, MD: Today, we’ll be discussing the results of a new study published in The Journal of Emergency Medicine, looking at the incidence of delayed intracranial hemorrhage among older patients taking preinjury anticoagulants who present to the emergency department (ED) with blunt head trauma.
Joining me today is the lead author of the study, Dr. Richard Shih, professor of emergency medicine at Florida Atlantic University. Also joining me is Dr. Christina Shenvi, associate professor of emergency medicine at the University of North Carolina (UNC) Chapel Hill, with fellowship training in geriatric emergency medicine.
Welcome to both of you.
Richard D. Shih, MD: Thanks, Rob.
Christina L. Shenvi, MD, PhD, MBA: Thanks. Pleasure to be here.
ICH Study Methodology
Dr. Glatter: It’s a pleasure to have you. Rich, this is a great study and targeted toward a population we see daily in the emergency department. I want you to describe your methodology, patient selection, and how you went about organizing your study to look at this important finding of delayed intracranial hemorrhage, especially in those on anticoagulants.
Dr. Shih: This all started for our research team when we first read the 2012 Annals of Emergency Medicine paper. The first author was Vincenzo Menditto, and he looked at a group of patients that had minor head injury, were anticoagulated, and had negative initial head CTs.
There were about 100 patients, of which about 10 of them did not consent, but they hospitalized all these patients. These were anticoagulated, negative-first head CTs. They hospitalized the patients and then did a routine second CT at about 24 hours. They also followed them for a week, and it turned out a little over 7% of them had delayed head CT.
We were wondering how many delayed intracranial hemorrhages we had missed because current practice for us was that, if patients had a good physical exam, their head CT was normal, and everything looked good, we would send them home.
Because of that, a number of people across the country wanted to verify those findings from the Menditto study. We tried to design a good study to answer that question. We happen to have a very large geriatric population in Florida, and our ED census is very high for age over 65, at nearly 60%.
There are two Level I trauma centers in Palm Beach County. We included a second multicenter hospital, and we prospectively enrolled patients. We know the current state of practice is not to routinely do second CTs, so we followed these patients over time and followed their medical records to try to identify delayed bleeding. That’s how we set up our methodology.
Is It Safe to Discharge Patients With Trauma After 24 Hours?
Dr. Glatter: For the bulk of these patients with negative head CTs, it’s been my practice that when they’re stable and they look fine and there’s no other apparent, distracting painful trauma, injuries and so forth, they’re safe to discharge.
The secondary outcome in your study is interesting: the need for neurosurgical intervention in terms of those with delayed intracranial hemorrhage.
Dr. Shih: I do believe that it’s certainly not the problem that Menditto described, which is 7%. There are two other prospective studies that have looked at this issue with delayed bleeding on anticoagulants. Both of these also showed a relatively low rate of delayed bleeding, which is between like 0.2% and 1.0%. In our study, it was 0.4%.
The difference in the studies is that Menditto and colleagues routinely did 24-hour head CTs. They admitted everybody. For these other studies, routine head CT was not part of it. My bet is that there is a rate of delayed bleeding somewhere in between that seen in the Menditto study and that in all the other studies.
However, talking about significant intracranial hemorrhage, ones that perhaps need neurosurgery, I believe most of them are not significant. There’s some number that do occur, but the vast majority of those probably don’t need neurosurgery. We had 14 delayed bleeds out of 6000 patients with head trauma. One of them ended up requiring neurosurgery, so the answer is not zero, but I don’t think it’s 7% either.
Dr. Glatter: Dr. Shenvi, I want to bring you into the conversation to talk about your experience at UNC, and how you run things in terms of older patients with blunt head trauma on preinjury anticoagulants.
Dr. Shenvi: Thanks, Rob. I remember when this paper came out showing this 7% rate of delayed bleeding and the question was, “Should we be admitting all these people?” Partly just from an overwhelming need for capacity that that would bring, it just wasn’t practical to say, “We’re going to admit every patient with a negative head CT to the hospital and rescan them.” That would be hundreds or thousands of patients each year in any given facility.
The other thing is that delayed bleeds don’t always happen just in the first 24 hours. It’s not even a matter of bringing patients into observation for 24 hours, watching them, and rescanning them if they have symptoms. It can occur several days out. That never, in almost any institution that I know of, became standard practice.
The way that it did change my care was to give good return precautions to patients, to make sure they have somebody with them to say, “Hey, sometimes you can have bleeding several days out after a fall, even though your CT scan here today looks perfect,” and to alert them that if they start having severe headaches, vomiting, or other symptoms of intracranial hemorrhage, that they should come back.
I don’t think it ever became standard practice, and for good reason, because that was one study. The subsequent studies that Richard mentioned, pretty quickly on the heels of that initial one, showed a much lower rate of delayed ICH with the caveats that the methodology was different.
Shift in Anticoagulants
Dr. Shenvi: One other big change from that original study, and now to Richard’s study, is the shift in anticoagulants. Back in the initial study you mentioned, it was all warfarin. We know from other studies looking at warfarin vs the direct oral anticoagulants (DOACs) that DOACs have lower rates of ICH after a head injury, lower rates of need for neurosurgical intervention, and lower rates of discharge to a skilled nursing facility after an intracranial hemorrhage.
Across the board, we know that the DOACs tend to do better. It’s difficult to compare newer studies because it’s a different medication. It did inform my practice to have an awareness of delayed intracranial hemorrhage so that I warn patients more proactively.
Dr. Glatter: I haven’t seen a patient on warfarin in years. I don’t know if either of you have, but it’s all DOACs now unless there’s some other reason. That shift is quite apparent.
Dr. Shih: The problem with looking at delayed bleeding for DOACs vs warfarin is the numbers were so low. I think we had 13 people, and seven were in the no-anticoagulant group. The numbers are even lower, so it’s hard to say.
I just wanted to comment on something that Dr. Shenvi said, and I pretty much agree with everything that she said. Anticoagulants and warfarin, and that Menditto study, have a carryover effect. People group DOACs with warfarin similarly. When a patient is brought in, the first thing they talk about with head trauma is, “Oh, they’re on an anticoagulant” or “They’re not on an anticoagulant.” It’s so ingrained.
I believe that, in emergency medicine, we’re pressed for space and time and we’re not as affected by that 24-hour observation. Maybe many of our surgeons will automatically admit those patients.
I haven’t seen a guideline from the United States, but there are two international guidelines. One is from Austria from 2019, and one is from Scandinavia. Both recommended 24-hour observation if you’re on an anticoagulant.
There is a bit of controversy left over with that. Hopefully, as more and more of information, like in our study, comes out, people will be a little bit more clear about it. I don’t think there’s a need to routinely admit them.
I do want to mention that the Menditto study had such a massive impact on everybody. They pointed out one subgroup (and it’s such a small number of patients). They had seven cases of delayed bleeding; four or five of them were within that 24 hours, and a couple were diagnosed later over the next couple days.
Of those seven people, four of them had international normalized ratios (INRs) greater than 3. Of those four patients, I’ve heard people talk about this and recommend, “Okay, that’s the subgroup I would admit.” There’s a toss-up with what to do with DOAC because it’s very hard to tell whether there’s an issue, whether there are problems with their dosing, and whatever.
We actually recently looked at that. We have a much larger sample than four: close to 300 patients who were on warfarin. We looked at patients who had INRs below 3 and above 3, and we didn’t show a difference. We still don’t believe that warfarin is a big issue with delayed bleeding.
Should We Be Asking: ‘Are They on Blood Thinners?’
Dr. Shenvi: One of the interesting trends related to warfarin and the DOACs vs no anticoagulant is that as you mentioned, Dr Shih, the first question out of people’s mouths or the first piece of information emergency medical services gives you when they come in with a patient who’s had a head injury is, “Are they on blood thinners or not?”
Yet, the paradigm is shifting to say it’s not actually the blood thinners themselves that are giving older patients the higher risk for bleeding; it’s age and other comorbidities.
Certainly, if you’re on an anticoagulant and you start to bleed, your prognosis is much worse because the bleeding doesn’t stop. In terms of who has a bleeding event, there’s much less impact of anticoagulation than we used to think. That, in part, may be due to the change from warfarin to other medications.
Some of the experts I’ve talked to who have done the research on this have said, “Well, actually, warfarin was more of a marker for being much older and more frail, because it was primarily prescribed to older patients who have significant heart disease, atrial fibrillation, and so on.” It was more a marker for somebody who is at risk for an intracranial hemorrhage. There are many changes that have happened in the past 10 years with medications and also our understanding.
Challenges in Patient Follow-up
Dr. Glatter: That’s a great point. One thing, Rich, I want to ask you about is in terms of your proxy outcome assessment. When you use that at 14 and 60 days with telephone follow-up and then chart review at 60 and 90 days (because, obviously, everyone can’t get another head CT or it’s difficult to follow patients up), did you find that worked out well in your prospective cohort study, in terms of using that as a proxy, so to speak?
Dr. Shih: I would say to a certain extent. Unfortunately, we don’t have access to the patients to come back to follow up all of them, and there was obviously a large number of patients in our study.
The next best thing was that we had dedicated research assistants calling all of the patients at 14 days and 60 days. I’ve certainly read research studies where, when they call them, they get 80%-90% follow-up, but we did not achieve that.
I don’t know if people are more inundated with spam phone calls now, or the older people are just afraid of picking up their phone sometimes with all the scams and so forth. I totally understand, but in all honesty, we only had about a 30%-35% follow-up using that follow-up pathway.
Then the proxy pathway was to look at their charts at 60 and 90 days. Also, we looked at the Florida death registry, which is pretty good, and then finally, we had both Level I trauma centers in the county that we were in participating. It’s standard practice that if you have an intracranial hemorrhage at a non–Level I trauma center, you would be transferred to a Level I trauma center. That’s the protocol. I know that’s not followed 100% of the time, but that’s part of the proxy follow-up. You could criticize the study for not having closer to 90% actual contact, but that’s the best we could do.
Dr. Glatter: I think that’s admirable. Using that paradigm of what you described certainly allows the reader to understand the difficulty in assessing patients that don’t get follow-up head CT, and hardly anyone does that, as we know.
To your point of having both Level I trauma centers in the county, that makes it pretty secure. If we’re going to do a study encompassing a similar type of regional aspect, it would be similar.
Dr. Shenvi: I think your proxies, to your credit, were as good as you can get. You can never get a 100% follow-up, but you really looked at all the different avenues by which patients might present, either in the death registry or a Level I center. Well done on that aspect.
Determining When to Admit Patients for Observation
Dr. Glatter: In terms of admissions: You admit a patient, then you hear back that this patient should not have been admitted because they had a negative head CT, but you put them in anyway in the sense of delayed bleeding happening or not happening.
It’s interesting. Maybe the insurers will start looking at this in some capacity, based on your study, that because it’s so infrequent that you see delayed bleeding, that admitting someone for any reason whatsoever would be declined. Do you see that being an issue? In other words, [do you see] this leading to a pattern in terms of the payers?
Dr. Shih: Certainly, you could interpret it that way, and that would be unfortunate. The [incidence of] delayed bleeding is definitely not zero. That’s the first thing.
The second thing is that when you’re dealing with an older population, having some sense that they’re not doing well is an important contributor to trying to fully assess what’s going on — whether or not they have a bleed or whether they’re at risk for falling again and then hitting their head and causing a second bleed, and making sure they can do the activities of daily life. There really should be some room for a physician to say, “They just got here, and we don’t know him that well. There’s something that bothers me about this person” and have the ability to watch them for at least another 24 hours. That’s how I feel.
Dr. Shenvi: In my location, it would be difficult to try to admit somebody purely for observation for delayed bleeding. I think we would get a lot of pushback on that. The reasons I might admit a patient after a fall with a negative head CT, though, are all the things that, Rob, you alluded to earlier — which are, what made them fall in the first place and were they unable to get up?
I had this happen just this week. A patient who fell couldn’t get off the ground for 12 hours, and so now she’s dehydrated and delirious with slight rhabdomyolysis. Then you’re admitting them either for the sequelae of the fall that are not related to the intracranial hemorrhage, or the fact that they are so debilitated and deconditioned that they cannot take care of themselves. They need physical therapy. Often, we will have physical and occupational therapists come see them in the ED during business hours and help make an assessment of whether they are safe to go home or whether they fall again. That can give more evidence for the need for admission.
Dr. Glatter: To bring artificial intelligence into this discussion, algorithms that are out there that say, “Push a button and the patient’s safe for discharge.” Well, this argues for a clinical gestalt and a human being to make an assessment because you can use these predictive models, which are coming and they’re going to be here soon, and they already are in some sense. Again, we have to use clinical human judgment.
Dr. Shih: I agree.
Advice for Primary Care Physicians
Dr. Glatter: What return precautions do you discuss with patients who’ve had blunt head trauma that maybe had a head CT, or even didn’t? What are the main things we’re looking for?
Dr. Shenvi: What I usually tell people is if you start to have a worse headache, nausea or vomiting, any weakness in one area of your body, or vision changes, and if there’s a family member or friend there, I’ll say, “If you notice that they’re acting differently or seem confused, come back.”
Dr. Shih: I agree with what she said, and I’m also going to add one thing. The most important part is they are trying to prevent a subsequent fall. We know that when they’ve fallen and they present to the ED, they’re at even higher risk for falling and reinjuring themselves, and that’s a population that’s already at risk.
One of the secondary studies that we published out of this project was looking at follow-up with their primary care physicians, and there were two things that we wanted to address. The first was, how often did they do it? Then, when they did do it, did their primary care physicians try to address and prevent subsequent falls?
Both the answers are actually bad. Amazingly, just over like 60% followed up.
In some of our subsequent research, because we’re in the midst of a randomized, controlled trial where we do a home visit, when we initially see these individuals that have fallen, they’ll schedule a home visit for us. Then a week or two later, when we schedule the home visit, many of them cancel because they think, Oh, that was a one-off and it’s not going to happen again. Part of the problem is the patients, because many of them believe that they just slipped and fell and it’s not going to happen again, or they’re not prone to it.
The second issue was when patients did go to a primary care physician, we have found that some primary care physicians believe that falling and injuring themselves is just part of the normal aging process. A percentage of them don’t go over assessment for fall risk or even initiate fall prevention treatments or programs.
I try to take that time to tell them that this is very common in their age group, and believe it or not, a fall from standing is the way people really injure themselves, and there may be ways to prevent subsequent falls and injuries.
Dr. Glatter: Absolutely. Do you find that their medications are a contributor in some sense? Say they’re antihypertensive, have issues of orthostasis, or a new medication was added in the last week.
Dr. Shenvi: It’s all of the above. Sometimes it’s one thing, like they just started tamsulosin for their kidney stone, they stood up, they felt lightheaded, and they fell. Usually, it’s multifactorial with some changes in their gait, vision, balance, reflex time, and strength, plus the medications or the need for assistive devices. Maybe they can’t take care of their home as well as they used to and there are things on the floor. It’s really all of the above.
‘Harder to Unlearn Something Than to Learn It’
Dr. Glatter: Would either of you like to add any additional points to the discussion or add a few pearls?
Dr. Shenvi: This just highlights the challenge of how it’s harder to unlearn something than to learn it, where one study that maybe wasn’t quite looking at what we needed to, or practice and prescribing patterns have changed, so it’s no longer really relevant.
The things that we learned from that, or the fears that we instilled in our minds of, Uh oh, they could go home and have delayed bleeding, are much harder to unlearn, and it takes more studies to unlearn that idea than it did to actually put it into place.
I’m glad that your team has done this much larger, prospective study and hopefully will reduce the concern about this entity.
Dr. Shih: I appreciate that segue. It is amazing that, for paramedics and medical students, the first thing out of their mouth is, “Are they on an anticoagulant?”
In terms of the risk of developing an intracranial hemorrhage, I think it’s much less than the weight we’ve put on it before. However, I believe if they have a bleed, the bleeds are worse. It’s kind of a double-edged sword. It’s still an important factor, but it doesn’t come with the Oh my gosh, they’re on an anticoagulant that everybody thinks about.
No. 1 Cause of Traumatic Injury Is a Fall from Standing
Dr. Glatter: These are obviously ground-level falls in most patients and not motor vehicle crashes. That’s an important part in the population that you looked at that should be mentioned clearly.
Dr. Shih: It’s astonishing. I’ve been a program director for over 20 years, and geriatrics is not well taught in the curriculum. It’s astonishing for many of our trainees and emergency physicians in general that the number-one cause for traumatic injury is a fall from standing.
Certainly, we get patients coming in the trauma center like a 95-year-old person who’s on a ladder putting up his Christmas lights. I’m like, oh my God.
For the vast majority, it’s closer to 90%, but in our study, for the patients we looked at, it was 80% that fall from standing. That’s the mechanism that causes these bleeds and these major injuries.
Dr. Shenvi: That’s reflective of what we see, so it’s good that that’s what you looked at also.
Dr. Glatter: Absolutely. Well, thank you both. This has been a very informative discussion. I appreciate your time, and our readers will certainly benefit from your knowledge and expertise. Thank you again.
Dr. Glatter, assistant professor of emergency medicine at Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, is a medical adviser for this news organization. He disclosed having no relevant financial conflicts. Dr. Shih is professor of emergency medicine at the Charles E. Schmidt College of Medicine at Florida Atlantic University, Boca Raton. His current grant funding and area of research interest involves geriatric emergency department patients with head injury and fall-related injury. He disclosed receiving a research grant from The Florida Medical Malpractice Joint Underwriting Association Grant for Safety of Health Care Services). Dr. Shenvi, associate professor of emergency medicine at the University of North Carolina at Chapel Hill, disclosed ties with the American College of Emergency Physicians, Institute for Healthcare Improvement, AstraZeneca, and CurvaFix.
A version of this article appeared on Medscape.com.
This discussion was recorded on August 2, 2024. This transcript has been edited for clarity.
Robert D. Glatter, MD: Today, we’ll be discussing the results of a new study published in The Journal of Emergency Medicine, looking at the incidence of delayed intracranial hemorrhage among older patients taking preinjury anticoagulants who present to the emergency department (ED) with blunt head trauma.
Joining me today is the lead author of the study, Dr. Richard Shih, professor of emergency medicine at Florida Atlantic University. Also joining me is Dr. Christina Shenvi, associate professor of emergency medicine at the University of North Carolina (UNC) Chapel Hill, with fellowship training in geriatric emergency medicine.
Welcome to both of you.
Richard D. Shih, MD: Thanks, Rob.
Christina L. Shenvi, MD, PhD, MBA: Thanks. Pleasure to be here.
ICH Study Methodology
Dr. Glatter: It’s a pleasure to have you. Rich, this is a great study and targeted toward a population we see daily in the emergency department. I want you to describe your methodology, patient selection, and how you went about organizing your study to look at this important finding of delayed intracranial hemorrhage, especially in those on anticoagulants.
Dr. Shih: This all started for our research team when we first read the 2012 Annals of Emergency Medicine paper. The first author was Vincenzo Menditto, and he looked at a group of patients that had minor head injury, were anticoagulated, and had negative initial head CTs.
There were about 100 patients, of which about 10 of them did not consent, but they hospitalized all these patients. These were anticoagulated, negative-first head CTs. They hospitalized the patients and then did a routine second CT at about 24 hours. They also followed them for a week, and it turned out a little over 7% of them had delayed head CT.
We were wondering how many delayed intracranial hemorrhages we had missed because current practice for us was that, if patients had a good physical exam, their head CT was normal, and everything looked good, we would send them home.
Because of that, a number of people across the country wanted to verify those findings from the Menditto study. We tried to design a good study to answer that question. We happen to have a very large geriatric population in Florida, and our ED census is very high for age over 65, at nearly 60%.
There are two Level I trauma centers in Palm Beach County. We included a second multicenter hospital, and we prospectively enrolled patients. We know the current state of practice is not to routinely do second CTs, so we followed these patients over time and followed their medical records to try to identify delayed bleeding. That’s how we set up our methodology.
Is It Safe to Discharge Patients With Trauma After 24 Hours?
Dr. Glatter: For the bulk of these patients with negative head CTs, it’s been my practice that when they’re stable and they look fine and there’s no other apparent, distracting painful trauma, injuries and so forth, they’re safe to discharge.
The secondary outcome in your study is interesting: the need for neurosurgical intervention in terms of those with delayed intracranial hemorrhage.
Dr. Shih: I do believe that it’s certainly not the problem that Menditto described, which is 7%. There are two other prospective studies that have looked at this issue with delayed bleeding on anticoagulants. Both of these also showed a relatively low rate of delayed bleeding, which is between like 0.2% and 1.0%. In our study, it was 0.4%.
The difference in the studies is that Menditto and colleagues routinely did 24-hour head CTs. They admitted everybody. For these other studies, routine head CT was not part of it. My bet is that there is a rate of delayed bleeding somewhere in between that seen in the Menditto study and that in all the other studies.
However, talking about significant intracranial hemorrhage, ones that perhaps need neurosurgery, I believe most of them are not significant. There’s some number that do occur, but the vast majority of those probably don’t need neurosurgery. We had 14 delayed bleeds out of 6000 patients with head trauma. One of them ended up requiring neurosurgery, so the answer is not zero, but I don’t think it’s 7% either.
Dr. Glatter: Dr. Shenvi, I want to bring you into the conversation to talk about your experience at UNC, and how you run things in terms of older patients with blunt head trauma on preinjury anticoagulants.
Dr. Shenvi: Thanks, Rob. I remember when this paper came out showing this 7% rate of delayed bleeding and the question was, “Should we be admitting all these people?” Partly just from an overwhelming need for capacity that that would bring, it just wasn’t practical to say, “We’re going to admit every patient with a negative head CT to the hospital and rescan them.” That would be hundreds or thousands of patients each year in any given facility.
The other thing is that delayed bleeds don’t always happen just in the first 24 hours. It’s not even a matter of bringing patients into observation for 24 hours, watching them, and rescanning them if they have symptoms. It can occur several days out. That never, in almost any institution that I know of, became standard practice.
The way that it did change my care was to give good return precautions to patients, to make sure they have somebody with them to say, “Hey, sometimes you can have bleeding several days out after a fall, even though your CT scan here today looks perfect,” and to alert them that if they start having severe headaches, vomiting, or other symptoms of intracranial hemorrhage, that they should come back.
I don’t think it ever became standard practice, and for good reason, because that was one study. The subsequent studies that Richard mentioned, pretty quickly on the heels of that initial one, showed a much lower rate of delayed ICH with the caveats that the methodology was different.
Shift in Anticoagulants
Dr. Shenvi: One other big change from that original study, and now to Richard’s study, is the shift in anticoagulants. Back in the initial study you mentioned, it was all warfarin. We know from other studies looking at warfarin vs the direct oral anticoagulants (DOACs) that DOACs have lower rates of ICH after a head injury, lower rates of need for neurosurgical intervention, and lower rates of discharge to a skilled nursing facility after an intracranial hemorrhage.
Across the board, we know that the DOACs tend to do better. It’s difficult to compare newer studies because it’s a different medication. It did inform my practice to have an awareness of delayed intracranial hemorrhage so that I warn patients more proactively.
Dr. Glatter: I haven’t seen a patient on warfarin in years. I don’t know if either of you have, but it’s all DOACs now unless there’s some other reason. That shift is quite apparent.
Dr. Shih: The problem with looking at delayed bleeding for DOACs vs warfarin is the numbers were so low. I think we had 13 people, and seven were in the no-anticoagulant group. The numbers are even lower, so it’s hard to say.
I just wanted to comment on something that Dr. Shenvi said, and I pretty much agree with everything that she said. Anticoagulants and warfarin, and that Menditto study, have a carryover effect. People group DOACs with warfarin similarly. When a patient is brought in, the first thing they talk about with head trauma is, “Oh, they’re on an anticoagulant” or “They’re not on an anticoagulant.” It’s so ingrained.
I believe that, in emergency medicine, we’re pressed for space and time and we’re not as affected by that 24-hour observation. Maybe many of our surgeons will automatically admit those patients.
I haven’t seen a guideline from the United States, but there are two international guidelines. One is from Austria from 2019, and one is from Scandinavia. Both recommended 24-hour observation if you’re on an anticoagulant.
There is a bit of controversy left over with that. Hopefully, as more and more of information, like in our study, comes out, people will be a little bit more clear about it. I don’t think there’s a need to routinely admit them.
I do want to mention that the Menditto study had such a massive impact on everybody. They pointed out one subgroup (and it’s such a small number of patients). They had seven cases of delayed bleeding; four or five of them were within that 24 hours, and a couple were diagnosed later over the next couple days.
Of those seven people, four of them had international normalized ratios (INRs) greater than 3. Of those four patients, I’ve heard people talk about this and recommend, “Okay, that’s the subgroup I would admit.” There’s a toss-up with what to do with DOAC because it’s very hard to tell whether there’s an issue, whether there are problems with their dosing, and whatever.
We actually recently looked at that. We have a much larger sample than four: close to 300 patients who were on warfarin. We looked at patients who had INRs below 3 and above 3, and we didn’t show a difference. We still don’t believe that warfarin is a big issue with delayed bleeding.
Should We Be Asking: ‘Are They on Blood Thinners?’
Dr. Shenvi: One of the interesting trends related to warfarin and the DOACs vs no anticoagulant is that as you mentioned, Dr Shih, the first question out of people’s mouths or the first piece of information emergency medical services gives you when they come in with a patient who’s had a head injury is, “Are they on blood thinners or not?”
Yet, the paradigm is shifting to say it’s not actually the blood thinners themselves that are giving older patients the higher risk for bleeding; it’s age and other comorbidities.
Certainly, if you’re on an anticoagulant and you start to bleed, your prognosis is much worse because the bleeding doesn’t stop. In terms of who has a bleeding event, there’s much less impact of anticoagulation than we used to think. That, in part, may be due to the change from warfarin to other medications.
Some of the experts I’ve talked to who have done the research on this have said, “Well, actually, warfarin was more of a marker for being much older and more frail, because it was primarily prescribed to older patients who have significant heart disease, atrial fibrillation, and so on.” It was more a marker for somebody who is at risk for an intracranial hemorrhage. There are many changes that have happened in the past 10 years with medications and also our understanding.
Challenges in Patient Follow-up
Dr. Glatter: That’s a great point. One thing, Rich, I want to ask you about is in terms of your proxy outcome assessment. When you use that at 14 and 60 days with telephone follow-up and then chart review at 60 and 90 days (because, obviously, everyone can’t get another head CT or it’s difficult to follow patients up), did you find that worked out well in your prospective cohort study, in terms of using that as a proxy, so to speak?
Dr. Shih: I would say to a certain extent. Unfortunately, we don’t have access to the patients to come back to follow up all of them, and there was obviously a large number of patients in our study.
The next best thing was that we had dedicated research assistants calling all of the patients at 14 days and 60 days. I’ve certainly read research studies where, when they call them, they get 80%-90% follow-up, but we did not achieve that.
I don’t know if people are more inundated with spam phone calls now, or the older people are just afraid of picking up their phone sometimes with all the scams and so forth. I totally understand, but in all honesty, we only had about a 30%-35% follow-up using that follow-up pathway.
Then the proxy pathway was to look at their charts at 60 and 90 days. Also, we looked at the Florida death registry, which is pretty good, and then finally, we had both Level I trauma centers in the county that we were in participating. It’s standard practice that if you have an intracranial hemorrhage at a non–Level I trauma center, you would be transferred to a Level I trauma center. That’s the protocol. I know that’s not followed 100% of the time, but that’s part of the proxy follow-up. You could criticize the study for not having closer to 90% actual contact, but that’s the best we could do.
Dr. Glatter: I think that’s admirable. Using that paradigm of what you described certainly allows the reader to understand the difficulty in assessing patients that don’t get follow-up head CT, and hardly anyone does that, as we know.
To your point of having both Level I trauma centers in the county, that makes it pretty secure. If we’re going to do a study encompassing a similar type of regional aspect, it would be similar.
Dr. Shenvi: I think your proxies, to your credit, were as good as you can get. You can never get a 100% follow-up, but you really looked at all the different avenues by which patients might present, either in the death registry or a Level I center. Well done on that aspect.
Determining When to Admit Patients for Observation
Dr. Glatter: In terms of admissions: You admit a patient, then you hear back that this patient should not have been admitted because they had a negative head CT, but you put them in anyway in the sense of delayed bleeding happening or not happening.
It’s interesting. Maybe the insurers will start looking at this in some capacity, based on your study, that because it’s so infrequent that you see delayed bleeding, that admitting someone for any reason whatsoever would be declined. Do you see that being an issue? In other words, [do you see] this leading to a pattern in terms of the payers?
Dr. Shih: Certainly, you could interpret it that way, and that would be unfortunate. The [incidence of] delayed bleeding is definitely not zero. That’s the first thing.
The second thing is that when you’re dealing with an older population, having some sense that they’re not doing well is an important contributor to trying to fully assess what’s going on — whether or not they have a bleed or whether they’re at risk for falling again and then hitting their head and causing a second bleed, and making sure they can do the activities of daily life. There really should be some room for a physician to say, “They just got here, and we don’t know him that well. There’s something that bothers me about this person” and have the ability to watch them for at least another 24 hours. That’s how I feel.
Dr. Shenvi: In my location, it would be difficult to try to admit somebody purely for observation for delayed bleeding. I think we would get a lot of pushback on that. The reasons I might admit a patient after a fall with a negative head CT, though, are all the things that, Rob, you alluded to earlier — which are, what made them fall in the first place and were they unable to get up?
I had this happen just this week. A patient who fell couldn’t get off the ground for 12 hours, and so now she’s dehydrated and delirious with slight rhabdomyolysis. Then you’re admitting them either for the sequelae of the fall that are not related to the intracranial hemorrhage, or the fact that they are so debilitated and deconditioned that they cannot take care of themselves. They need physical therapy. Often, we will have physical and occupational therapists come see them in the ED during business hours and help make an assessment of whether they are safe to go home or whether they fall again. That can give more evidence for the need for admission.
Dr. Glatter: To bring artificial intelligence into this discussion, algorithms that are out there that say, “Push a button and the patient’s safe for discharge.” Well, this argues for a clinical gestalt and a human being to make an assessment because you can use these predictive models, which are coming and they’re going to be here soon, and they already are in some sense. Again, we have to use clinical human judgment.
Dr. Shih: I agree.
Advice for Primary Care Physicians
Dr. Glatter: What return precautions do you discuss with patients who’ve had blunt head trauma that maybe had a head CT, or even didn’t? What are the main things we’re looking for?
Dr. Shenvi: What I usually tell people is if you start to have a worse headache, nausea or vomiting, any weakness in one area of your body, or vision changes, and if there’s a family member or friend there, I’ll say, “If you notice that they’re acting differently or seem confused, come back.”
Dr. Shih: I agree with what she said, and I’m also going to add one thing. The most important part is they are trying to prevent a subsequent fall. We know that when they’ve fallen and they present to the ED, they’re at even higher risk for falling and reinjuring themselves, and that’s a population that’s already at risk.
One of the secondary studies that we published out of this project was looking at follow-up with their primary care physicians, and there were two things that we wanted to address. The first was, how often did they do it? Then, when they did do it, did their primary care physicians try to address and prevent subsequent falls?
Both the answers are actually bad. Amazingly, just over like 60% followed up.
In some of our subsequent research, because we’re in the midst of a randomized, controlled trial where we do a home visit, when we initially see these individuals that have fallen, they’ll schedule a home visit for us. Then a week or two later, when we schedule the home visit, many of them cancel because they think, Oh, that was a one-off and it’s not going to happen again. Part of the problem is the patients, because many of them believe that they just slipped and fell and it’s not going to happen again, or they’re not prone to it.
The second issue was when patients did go to a primary care physician, we have found that some primary care physicians believe that falling and injuring themselves is just part of the normal aging process. A percentage of them don’t go over assessment for fall risk or even initiate fall prevention treatments or programs.
I try to take that time to tell them that this is very common in their age group, and believe it or not, a fall from standing is the way people really injure themselves, and there may be ways to prevent subsequent falls and injuries.
Dr. Glatter: Absolutely. Do you find that their medications are a contributor in some sense? Say they’re antihypertensive, have issues of orthostasis, or a new medication was added in the last week.
Dr. Shenvi: It’s all of the above. Sometimes it’s one thing, like they just started tamsulosin for their kidney stone, they stood up, they felt lightheaded, and they fell. Usually, it’s multifactorial with some changes in their gait, vision, balance, reflex time, and strength, plus the medications or the need for assistive devices. Maybe they can’t take care of their home as well as they used to and there are things on the floor. It’s really all of the above.
‘Harder to Unlearn Something Than to Learn It’
Dr. Glatter: Would either of you like to add any additional points to the discussion or add a few pearls?
Dr. Shenvi: This just highlights the challenge of how it’s harder to unlearn something than to learn it, where one study that maybe wasn’t quite looking at what we needed to, or practice and prescribing patterns have changed, so it’s no longer really relevant.
The things that we learned from that, or the fears that we instilled in our minds of, Uh oh, they could go home and have delayed bleeding, are much harder to unlearn, and it takes more studies to unlearn that idea than it did to actually put it into place.
I’m glad that your team has done this much larger, prospective study and hopefully will reduce the concern about this entity.
Dr. Shih: I appreciate that segue. It is amazing that, for paramedics and medical students, the first thing out of their mouth is, “Are they on an anticoagulant?”
In terms of the risk of developing an intracranial hemorrhage, I think it’s much less than the weight we’ve put on it before. However, I believe if they have a bleed, the bleeds are worse. It’s kind of a double-edged sword. It’s still an important factor, but it doesn’t come with the Oh my gosh, they’re on an anticoagulant that everybody thinks about.
No. 1 Cause of Traumatic Injury Is a Fall from Standing
Dr. Glatter: These are obviously ground-level falls in most patients and not motor vehicle crashes. That’s an important part in the population that you looked at that should be mentioned clearly.
Dr. Shih: It’s astonishing. I’ve been a program director for over 20 years, and geriatrics is not well taught in the curriculum. It’s astonishing for many of our trainees and emergency physicians in general that the number-one cause for traumatic injury is a fall from standing.
Certainly, we get patients coming in the trauma center like a 95-year-old person who’s on a ladder putting up his Christmas lights. I’m like, oh my God.
For the vast majority, it’s closer to 90%, but in our study, for the patients we looked at, it was 80% that fall from standing. That’s the mechanism that causes these bleeds and these major injuries.
Dr. Shenvi: That’s reflective of what we see, so it’s good that that’s what you looked at also.
Dr. Glatter: Absolutely. Well, thank you both. This has been a very informative discussion. I appreciate your time, and our readers will certainly benefit from your knowledge and expertise. Thank you again.
Dr. Glatter, assistant professor of emergency medicine at Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York, is a medical adviser for this news organization. He disclosed having no relevant financial conflicts. Dr. Shih is professor of emergency medicine at the Charles E. Schmidt College of Medicine at Florida Atlantic University, Boca Raton. His current grant funding and area of research interest involves geriatric emergency department patients with head injury and fall-related injury. He disclosed receiving a research grant from The Florida Medical Malpractice Joint Underwriting Association Grant for Safety of Health Care Services). Dr. Shenvi, associate professor of emergency medicine at the University of North Carolina at Chapel Hill, disclosed ties with the American College of Emergency Physicians, Institute for Healthcare Improvement, AstraZeneca, and CurvaFix.
A version of this article appeared on Medscape.com.
Primary Care Physicians Track an Average of 57 Quality Measures for Value-Based Care Pay
A new analysis suggests one reason doctors are wary of value-based care arrangements: Overkill.
Researchers found that primary care physicians in one large integrated health system were required to track an average of 57 different quality measures across multiple insurers that linked outcomes to payments under value-based contracts.
Medicare contracts were the most likely to pile quality measures on physicians with an average of 13.42 measures vs 10.07 for commercial insurer contracts and 5.37 for Medicaid contracts, reported Claire Boone, PhD, of the University of Chicago in Illinois and Providence Research Network, Portland, Oregon, and colleagues in JAMA Health Forum. The analysis, which may be the first of its kind, tracked 890 primary care physicians from 2020 to 2022.
The average of 57 quality measures per physician was unexpectedly high, Dr. Boone said in an interview.
“The magnitude of that number surprised us,” Dr. Boone said. “Primary care physicians and their practices have a lot on their plate. Now we know that one of those things is a very large number of different quality metrics to pay attention to, measure, report on, and implement.
Value-based care programs use quality measures to evaluate how well clinicians are doing their jobs and adjust reimbursement accordingly. A payer, for example, may raise reimbursements if a clinician has higher numbers of patients who meet quality measure standards for depression screening or blood pressure.
Dr. Boone said her research group is studying the impact of quality measures and was surprised that data showed individual primary care physicians had to deal with a high number of value-based contracts.
The researchers tracked value-based contracts for 890 physicians (58.3% women, 41.7% men) in an unidentified West Coast Health system. (Several study authors work for the Providence Health System, which serves several Western States and Texas.) The average number of patients per physician was 1309.
The physicians were part of an average of 11.18 value-based contracts (commercial insurers, 49.50%; Medicaid, 21.49%; and Medicare, 29.01%). This number grew from 9.39 in 2020 to 12.26 in 2022. Quality measure data weren’t available for 29% of contracts.
Quality measures were considered unique if they referenced different conditions.
For example, colorectal cancer screening is unique from depression screening. The researchers also considered measures for the same condition unique if the target value differed — for example, blood pressure control defined as < 140/90 vs blood pressure control defined as < 130/80, Dr. Boone said.
Dr. Boone said she expected payers to coordinate quality measures.
“The fact that they largely are not is really the main finding of this paper. Without coordination, the use of value-based contracts and quality measures at scale leads to many unique measures being used. This may reflect the fact that there are so many important tasks to do in primary care, and there’s no consensus on which ones should be included in quality-based contracts.”
Ronald N. Adler, MD, an associate professor in the Department of Family Medicine and Community Health at UMass Chan Medical School, Worcester, Massachusetts, who’s familiar with the findings but didn’t take part in the research, said the study offers something new — the quantification of quality measures.
He said in an interview that physicians deal with quality measures in different ways. Some clinicians “don’t really care,” and have an attitude of “this is not why I got into medicine.” But others “are very competitive around this, and it leads to a lot of a lot of stress. Trying to address 50-plus measures is impossible and demoralizing.”
The metrics may measure things like mammogram screening that are out of the physician’s control, Dr. Adler said. “I can recommend a mammogram, and my patient can choose not to do it. Or maybe my patient is homeless; she doesn’t have transportation, and it’s not a priority for her, even though she wants to do it.”
Patients may not take medication as prescribed, or they may be unable to afford it, he said. “Can they afford to eat healthy foods? Or is ramen all they can afford, and their sugars are through the roof? There are a lot of factors at play here that are independent of the quality of care provided by the doctor.”
As for his own approach, Dr. Adler said he worries about some measures more than others. “I’m very proactive about screening my patients for colon cancer and maybe a little less so about mammography.”
For colon cancer screening, “there are a lot of benefits and not that many harms as opposed to mammography, which has harms such as false positives and overdiagnosis of breast cancer.”
Dr. Adler is a member of the Quality Measure Alignment Taskforce in Massachusetts, which is trying to establish consensus on appropriate quality measures. But payer participation is voluntary. “Our health systems are too siloed ... so there is no readily available mechanism for enforcing such recommendations.”
Wayne Altman, MD, chair of Family Medicine at Tufts University School of Medicine, Boston, Massachusetts, is also familiar with the study findings but didn’t take part in the research. He said in an interview that clinicians shouldn’t have to deal with more than 5-10 quality measures in total.
He pointed out that many measures don’t make sense in certain populations. Titrating blood pressure to < 140/90 isn’t ideal for elderly patients because aggressive control can send their blood pressure dangerously low. “They’re going to fall down, break a hip, and likely die within a year. You have to have the right population and be aware of unintended consequences.”
Still, Dr. Adler noted, there’s an important role for quality measures in healthcare.
“We need data to inform our quality improvement activities, but they need to be the right measures. People can’t respond reasonably to improve on 50-plus measures,” he said. “They need to be consolidated and prioritized. It would be really helpful if we could have a much lower number of measures that are meaningful, safe, and connect to things that matter.”
No funding has been reported. Dr. Boone disclosed a grant from the National Institute on Aging. Dr. Adler and Dr. Altman had no disclosures.
A version of this article first appeared on Medscape.com.
A new analysis suggests one reason doctors are wary of value-based care arrangements: Overkill.
Researchers found that primary care physicians in one large integrated health system were required to track an average of 57 different quality measures across multiple insurers that linked outcomes to payments under value-based contracts.
Medicare contracts were the most likely to pile quality measures on physicians with an average of 13.42 measures vs 10.07 for commercial insurer contracts and 5.37 for Medicaid contracts, reported Claire Boone, PhD, of the University of Chicago in Illinois and Providence Research Network, Portland, Oregon, and colleagues in JAMA Health Forum. The analysis, which may be the first of its kind, tracked 890 primary care physicians from 2020 to 2022.
The average of 57 quality measures per physician was unexpectedly high, Dr. Boone said in an interview.
“The magnitude of that number surprised us,” Dr. Boone said. “Primary care physicians and their practices have a lot on their plate. Now we know that one of those things is a very large number of different quality metrics to pay attention to, measure, report on, and implement.
Value-based care programs use quality measures to evaluate how well clinicians are doing their jobs and adjust reimbursement accordingly. A payer, for example, may raise reimbursements if a clinician has higher numbers of patients who meet quality measure standards for depression screening or blood pressure.
Dr. Boone said her research group is studying the impact of quality measures and was surprised that data showed individual primary care physicians had to deal with a high number of value-based contracts.
The researchers tracked value-based contracts for 890 physicians (58.3% women, 41.7% men) in an unidentified West Coast Health system. (Several study authors work for the Providence Health System, which serves several Western States and Texas.) The average number of patients per physician was 1309.
The physicians were part of an average of 11.18 value-based contracts (commercial insurers, 49.50%; Medicaid, 21.49%; and Medicare, 29.01%). This number grew from 9.39 in 2020 to 12.26 in 2022. Quality measure data weren’t available for 29% of contracts.
Quality measures were considered unique if they referenced different conditions.
For example, colorectal cancer screening is unique from depression screening. The researchers also considered measures for the same condition unique if the target value differed — for example, blood pressure control defined as < 140/90 vs blood pressure control defined as < 130/80, Dr. Boone said.
Dr. Boone said she expected payers to coordinate quality measures.
“The fact that they largely are not is really the main finding of this paper. Without coordination, the use of value-based contracts and quality measures at scale leads to many unique measures being used. This may reflect the fact that there are so many important tasks to do in primary care, and there’s no consensus on which ones should be included in quality-based contracts.”
Ronald N. Adler, MD, an associate professor in the Department of Family Medicine and Community Health at UMass Chan Medical School, Worcester, Massachusetts, who’s familiar with the findings but didn’t take part in the research, said the study offers something new — the quantification of quality measures.
He said in an interview that physicians deal with quality measures in different ways. Some clinicians “don’t really care,” and have an attitude of “this is not why I got into medicine.” But others “are very competitive around this, and it leads to a lot of a lot of stress. Trying to address 50-plus measures is impossible and demoralizing.”
The metrics may measure things like mammogram screening that are out of the physician’s control, Dr. Adler said. “I can recommend a mammogram, and my patient can choose not to do it. Or maybe my patient is homeless; she doesn’t have transportation, and it’s not a priority for her, even though she wants to do it.”
Patients may not take medication as prescribed, or they may be unable to afford it, he said. “Can they afford to eat healthy foods? Or is ramen all they can afford, and their sugars are through the roof? There are a lot of factors at play here that are independent of the quality of care provided by the doctor.”
As for his own approach, Dr. Adler said he worries about some measures more than others. “I’m very proactive about screening my patients for colon cancer and maybe a little less so about mammography.”
For colon cancer screening, “there are a lot of benefits and not that many harms as opposed to mammography, which has harms such as false positives and overdiagnosis of breast cancer.”
Dr. Adler is a member of the Quality Measure Alignment Taskforce in Massachusetts, which is trying to establish consensus on appropriate quality measures. But payer participation is voluntary. “Our health systems are too siloed ... so there is no readily available mechanism for enforcing such recommendations.”
Wayne Altman, MD, chair of Family Medicine at Tufts University School of Medicine, Boston, Massachusetts, is also familiar with the study findings but didn’t take part in the research. He said in an interview that clinicians shouldn’t have to deal with more than 5-10 quality measures in total.
He pointed out that many measures don’t make sense in certain populations. Titrating blood pressure to < 140/90 isn’t ideal for elderly patients because aggressive control can send their blood pressure dangerously low. “They’re going to fall down, break a hip, and likely die within a year. You have to have the right population and be aware of unintended consequences.”
Still, Dr. Adler noted, there’s an important role for quality measures in healthcare.
“We need data to inform our quality improvement activities, but they need to be the right measures. People can’t respond reasonably to improve on 50-plus measures,” he said. “They need to be consolidated and prioritized. It would be really helpful if we could have a much lower number of measures that are meaningful, safe, and connect to things that matter.”
No funding has been reported. Dr. Boone disclosed a grant from the National Institute on Aging. Dr. Adler and Dr. Altman had no disclosures.
A version of this article first appeared on Medscape.com.
A new analysis suggests one reason doctors are wary of value-based care arrangements: Overkill.
Researchers found that primary care physicians in one large integrated health system were required to track an average of 57 different quality measures across multiple insurers that linked outcomes to payments under value-based contracts.
Medicare contracts were the most likely to pile quality measures on physicians with an average of 13.42 measures vs 10.07 for commercial insurer contracts and 5.37 for Medicaid contracts, reported Claire Boone, PhD, of the University of Chicago in Illinois and Providence Research Network, Portland, Oregon, and colleagues in JAMA Health Forum. The analysis, which may be the first of its kind, tracked 890 primary care physicians from 2020 to 2022.
The average of 57 quality measures per physician was unexpectedly high, Dr. Boone said in an interview.
“The magnitude of that number surprised us,” Dr. Boone said. “Primary care physicians and their practices have a lot on their plate. Now we know that one of those things is a very large number of different quality metrics to pay attention to, measure, report on, and implement.
Value-based care programs use quality measures to evaluate how well clinicians are doing their jobs and adjust reimbursement accordingly. A payer, for example, may raise reimbursements if a clinician has higher numbers of patients who meet quality measure standards for depression screening or blood pressure.
Dr. Boone said her research group is studying the impact of quality measures and was surprised that data showed individual primary care physicians had to deal with a high number of value-based contracts.
The researchers tracked value-based contracts for 890 physicians (58.3% women, 41.7% men) in an unidentified West Coast Health system. (Several study authors work for the Providence Health System, which serves several Western States and Texas.) The average number of patients per physician was 1309.
The physicians were part of an average of 11.18 value-based contracts (commercial insurers, 49.50%; Medicaid, 21.49%; and Medicare, 29.01%). This number grew from 9.39 in 2020 to 12.26 in 2022. Quality measure data weren’t available for 29% of contracts.
Quality measures were considered unique if they referenced different conditions.
For example, colorectal cancer screening is unique from depression screening. The researchers also considered measures for the same condition unique if the target value differed — for example, blood pressure control defined as < 140/90 vs blood pressure control defined as < 130/80, Dr. Boone said.
Dr. Boone said she expected payers to coordinate quality measures.
“The fact that they largely are not is really the main finding of this paper. Without coordination, the use of value-based contracts and quality measures at scale leads to many unique measures being used. This may reflect the fact that there are so many important tasks to do in primary care, and there’s no consensus on which ones should be included in quality-based contracts.”
Ronald N. Adler, MD, an associate professor in the Department of Family Medicine and Community Health at UMass Chan Medical School, Worcester, Massachusetts, who’s familiar with the findings but didn’t take part in the research, said the study offers something new — the quantification of quality measures.
He said in an interview that physicians deal with quality measures in different ways. Some clinicians “don’t really care,” and have an attitude of “this is not why I got into medicine.” But others “are very competitive around this, and it leads to a lot of a lot of stress. Trying to address 50-plus measures is impossible and demoralizing.”
The metrics may measure things like mammogram screening that are out of the physician’s control, Dr. Adler said. “I can recommend a mammogram, and my patient can choose not to do it. Or maybe my patient is homeless; she doesn’t have transportation, and it’s not a priority for her, even though she wants to do it.”
Patients may not take medication as prescribed, or they may be unable to afford it, he said. “Can they afford to eat healthy foods? Or is ramen all they can afford, and their sugars are through the roof? There are a lot of factors at play here that are independent of the quality of care provided by the doctor.”
As for his own approach, Dr. Adler said he worries about some measures more than others. “I’m very proactive about screening my patients for colon cancer and maybe a little less so about mammography.”
For colon cancer screening, “there are a lot of benefits and not that many harms as opposed to mammography, which has harms such as false positives and overdiagnosis of breast cancer.”
Dr. Adler is a member of the Quality Measure Alignment Taskforce in Massachusetts, which is trying to establish consensus on appropriate quality measures. But payer participation is voluntary. “Our health systems are too siloed ... so there is no readily available mechanism for enforcing such recommendations.”
Wayne Altman, MD, chair of Family Medicine at Tufts University School of Medicine, Boston, Massachusetts, is also familiar with the study findings but didn’t take part in the research. He said in an interview that clinicians shouldn’t have to deal with more than 5-10 quality measures in total.
He pointed out that many measures don’t make sense in certain populations. Titrating blood pressure to < 140/90 isn’t ideal for elderly patients because aggressive control can send their blood pressure dangerously low. “They’re going to fall down, break a hip, and likely die within a year. You have to have the right population and be aware of unintended consequences.”
Still, Dr. Adler noted, there’s an important role for quality measures in healthcare.
“We need data to inform our quality improvement activities, but they need to be the right measures. People can’t respond reasonably to improve on 50-plus measures,” he said. “They need to be consolidated and prioritized. It would be really helpful if we could have a much lower number of measures that are meaningful, safe, and connect to things that matter.”
No funding has been reported. Dr. Boone disclosed a grant from the National Institute on Aging. Dr. Adler and Dr. Altman had no disclosures.
A version of this article first appeared on Medscape.com.
FROM JAMA HEALTH FORUM
Involuntary flashbacks
The correct diagnosis is posttraumatic stress disorder (PTSD). The patient's anxiety, irritability, sleep difficulties, and other symptoms are directly related to the recent traumatic event (car crash), and he has no significant physical injuries or neurologic abnormalities.
Generalized anxiety disorder is incorrect because it involves chronic worry about various life aspects for at least 6 months, unrelated to a specific trauma.
Postconcussion syndrome is not applicable because of the lack of concussion evidence and other symptoms, such as headaches or dizziness.
Acute stress disorder is similar to PTSD but is diagnosed when symptoms occur within 3 days to 1 month after a trauma. Because this patient's symptoms have persisted beyond 1 month, PTSD is the most likely diagnosis.
Patients with PTSD exhibit pronounced cognitive, affective, or behavioral responses to trauma reminders; these responses may include severe anxiety, dissociative episodes, flashbacks, and hyperreactive behaviors. The intensity of these symptoms and the resulting psychosocial impairment are more severe in individuals with PTSD compared with people who experience trauma without developing the disorder. To manage such heightened arousal, individuals with PTSD often engage in avoidance behaviors, leading to emotional numbing; reduced interest in daily activities; and, in severe cases, detachment from others.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals older than 6 years. These criteria include: (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the traumatic event; (C) persistent avoidance of stimuli associated with the trauma; (D) negative alterations in cognitions and mood related to the trauma; and (E) marked alterations in arousal and reactivity, evidenced by two or more specific symptoms.
Early intervention is key in the treatment of PTSD to prevent the condition from becoming chronic. Although more empirical data are needed, especially regarding pharmacotherapy, early supportive interventions such as psychoeducation and case management have shown promise in acutely traumatized individuals.
Trauma-focused psychotherapy is recommended as the first-line treatment for most adults with PTSD. This approach, which includes exposure-based therapies, is generally preferred over other therapies or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions (eg, depression, psychosis) that impair their ability to engage in trauma-focused therapy, initial pharmacologic management is advised until symptoms stabilize, after which psychotherapy can be introduced.
Clinical trials and meta-analyses have demonstrated the efficacy of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. The treatment choice should be collaborative, based on patient presentation, preference, and therapist expertise.
For individuals with PTSD experiencing significant sleep disturbances, particularly nightmares, prazosin is suggested. Clinical studies demonstrate that prazosin effectively reduces overall PTSD symptoms, nightmares, and sleep disturbances in approximately half of the patients treated.
Medication regimens effective for PTSD should be continued for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials in patients with PTSD who completed acute treatment with SSRIs have demonstrated that those who continued with SSRIs were less likely to have relapse compared with those receiving placebo.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is posttraumatic stress disorder (PTSD). The patient's anxiety, irritability, sleep difficulties, and other symptoms are directly related to the recent traumatic event (car crash), and he has no significant physical injuries or neurologic abnormalities.
Generalized anxiety disorder is incorrect because it involves chronic worry about various life aspects for at least 6 months, unrelated to a specific trauma.
Postconcussion syndrome is not applicable because of the lack of concussion evidence and other symptoms, such as headaches or dizziness.
Acute stress disorder is similar to PTSD but is diagnosed when symptoms occur within 3 days to 1 month after a trauma. Because this patient's symptoms have persisted beyond 1 month, PTSD is the most likely diagnosis.
Patients with PTSD exhibit pronounced cognitive, affective, or behavioral responses to trauma reminders; these responses may include severe anxiety, dissociative episodes, flashbacks, and hyperreactive behaviors. The intensity of these symptoms and the resulting psychosocial impairment are more severe in individuals with PTSD compared with people who experience trauma without developing the disorder. To manage such heightened arousal, individuals with PTSD often engage in avoidance behaviors, leading to emotional numbing; reduced interest in daily activities; and, in severe cases, detachment from others.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals older than 6 years. These criteria include: (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the traumatic event; (C) persistent avoidance of stimuli associated with the trauma; (D) negative alterations in cognitions and mood related to the trauma; and (E) marked alterations in arousal and reactivity, evidenced by two or more specific symptoms.
Early intervention is key in the treatment of PTSD to prevent the condition from becoming chronic. Although more empirical data are needed, especially regarding pharmacotherapy, early supportive interventions such as psychoeducation and case management have shown promise in acutely traumatized individuals.
Trauma-focused psychotherapy is recommended as the first-line treatment for most adults with PTSD. This approach, which includes exposure-based therapies, is generally preferred over other therapies or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions (eg, depression, psychosis) that impair their ability to engage in trauma-focused therapy, initial pharmacologic management is advised until symptoms stabilize, after which psychotherapy can be introduced.
Clinical trials and meta-analyses have demonstrated the efficacy of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. The treatment choice should be collaborative, based on patient presentation, preference, and therapist expertise.
For individuals with PTSD experiencing significant sleep disturbances, particularly nightmares, prazosin is suggested. Clinical studies demonstrate that prazosin effectively reduces overall PTSD symptoms, nightmares, and sleep disturbances in approximately half of the patients treated.
Medication regimens effective for PTSD should be continued for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials in patients with PTSD who completed acute treatment with SSRIs have demonstrated that those who continued with SSRIs were less likely to have relapse compared with those receiving placebo.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is posttraumatic stress disorder (PTSD). The patient's anxiety, irritability, sleep difficulties, and other symptoms are directly related to the recent traumatic event (car crash), and he has no significant physical injuries or neurologic abnormalities.
Generalized anxiety disorder is incorrect because it involves chronic worry about various life aspects for at least 6 months, unrelated to a specific trauma.
Postconcussion syndrome is not applicable because of the lack of concussion evidence and other symptoms, such as headaches or dizziness.
Acute stress disorder is similar to PTSD but is diagnosed when symptoms occur within 3 days to 1 month after a trauma. Because this patient's symptoms have persisted beyond 1 month, PTSD is the most likely diagnosis.
Patients with PTSD exhibit pronounced cognitive, affective, or behavioral responses to trauma reminders; these responses may include severe anxiety, dissociative episodes, flashbacks, and hyperreactive behaviors. The intensity of these symptoms and the resulting psychosocial impairment are more severe in individuals with PTSD compared with people who experience trauma without developing the disorder. To manage such heightened arousal, individuals with PTSD often engage in avoidance behaviors, leading to emotional numbing; reduced interest in daily activities; and, in severe cases, detachment from others.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals older than 6 years. These criteria include: (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the traumatic event; (C) persistent avoidance of stimuli associated with the trauma; (D) negative alterations in cognitions and mood related to the trauma; and (E) marked alterations in arousal and reactivity, evidenced by two or more specific symptoms.
Early intervention is key in the treatment of PTSD to prevent the condition from becoming chronic. Although more empirical data are needed, especially regarding pharmacotherapy, early supportive interventions such as psychoeducation and case management have shown promise in acutely traumatized individuals.
Trauma-focused psychotherapy is recommended as the first-line treatment for most adults with PTSD. This approach, which includes exposure-based therapies, is generally preferred over other therapies or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions (eg, depression, psychosis) that impair their ability to engage in trauma-focused therapy, initial pharmacologic management is advised until symptoms stabilize, after which psychotherapy can be introduced.
Clinical trials and meta-analyses have demonstrated the efficacy of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. The treatment choice should be collaborative, based on patient presentation, preference, and therapist expertise.
For individuals with PTSD experiencing significant sleep disturbances, particularly nightmares, prazosin is suggested. Clinical studies demonstrate that prazosin effectively reduces overall PTSD symptoms, nightmares, and sleep disturbances in approximately half of the patients treated.
Medication regimens effective for PTSD should be continued for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials in patients with PTSD who completed acute treatment with SSRIs have demonstrated that those who continued with SSRIs were less likely to have relapse compared with those receiving placebo.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
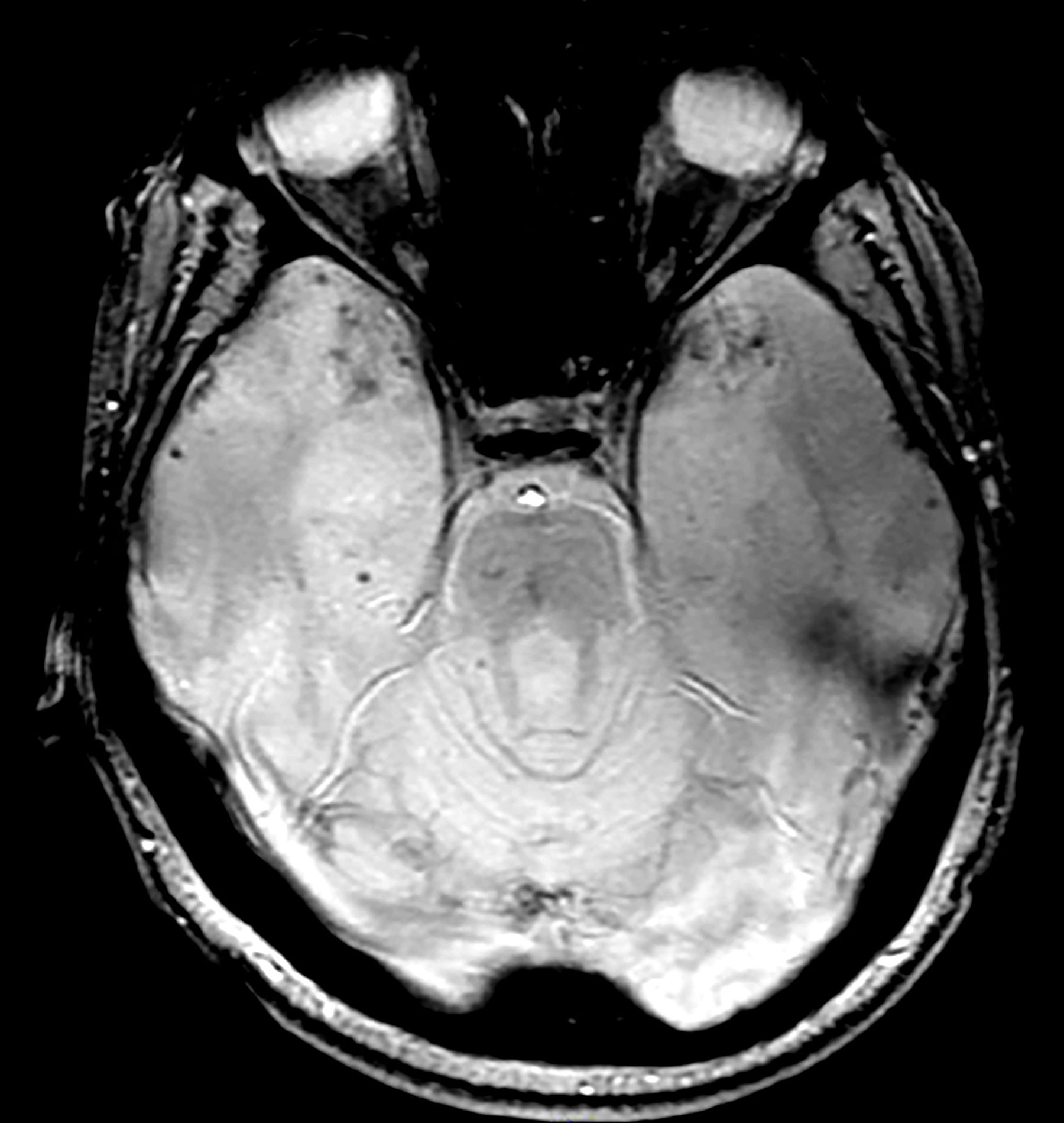
A 28-year-old man presented to the emergency department following a high-speed motor vehicle accident 2 months ago. He sustained no major physical injuries but had minor lacerations and bruising. The patient reported feeling unusually irritable and having difficulty sleeping since the accident, citing frequent flashbacks to the accident and occasional nightmares. He has started to feel more anxious and withdrawn, losing interest in hobbies such as swimming and biking that he previously enjoyed.
The patient's medical history is unremarkable, with no previous psychiatric or neurologic conditions. His neurologic examination was normal. An initial axial T2-weighted brain MRI demonstrated multiple small areas of hemorrhage, indicative of a diffuse axonal injury or shear-type injury. Despite the lack of significant physical injuries, the patient expressed ongoing distress related to the traumatic event.
Technoference
You see it all the time. It’s the family at the table next to you in the restaurant where the two teenage children are texting away on their phones. Or the playground, where a 3-year-old is playing with his toy truck and bulldozer in the sand and his father, immersed in his laptop, hasn’t said a word to his child.
It may trouble you when you witness social situations like that in which an electronic device is preventing or certainly interfering with interpersonal interactions. Or at least I hope it troubles you. Maybe it is so ubiquitous that you have come to accept it as the norm. It’s likely you may even be a participant. But, do you have a name for it?
It’s called “technoference,” a word coined by a doctoral student in human development and family studies at Penn State a decade ago “to describe the everyday intrusions and interruptions in couple interactions that take place due to technology devices and their always-on, ever-present nature.” Although, the original research that triggered the coinage was about couples, obviously the phenomenon occurs whenever people of any age are together in social situations.
While the word may not have crept into common parlance, we all know it when we see it. Technoference may not appear in the paper’s title, but it is a subject being investigated across a broad array of disciplines. One phone tracking study found that parents of young infants spend more than 5 hours each day on their smartphones. More than a quarter of that time the infant is engaged with the parent’s digital device. Technoference has been associated with decreased parent-child interaction during early childhood. It has been associated with more negative responses to children’s behavior, as well as an increased risk of child injury.
There are numerous studies suggesting an association between parental technoference and mental health difficulties in children. I have recently reviewed one of these studies that looks at the relationship of perceived parental technoference and the mental health of children entering adolescents. The authors collected longitudinal data of more than 1300 emerging adolescents, hoping to determine if the relationship between parental distraction and mental health was bidirectional. In other words, could a child’s mental health be contributing to his parents’ perceived distraction? Or was it primarily the parents’ technoference that was playing a role in the child’s mental health problems?
What investigators found was that higher levels of parental distraction were associated with higher levels of inattention and hyperactivity in the emerging adolescents, but not vice versa. On the other hand, higher levels of adolescent anxiety was associated with higher levels of perceived parental technoference, but not vice versa.
I know this sounds a bit confusing and a bit chicken-egg-chicken-eggish. The study was not designed to determine causation in these associations. However, the authors offer some possible scenarios that may provide a bit of clarity. It could be that parents who are concerned about their anxious child respond by retreating into the cyberspace to avoid tense situations or for support or information.
On the other hand, This explanation meshes with other studies demonstrating an association between parental distraction and aggression and attention problems in early childhood.
While one could spend more time imagining other factors that could be driving these bidirectional relationships, I’m not sure that it makes a heckuva lot of difference. Whether the child’s mental illness is the primary driver or the parent’s device-associated distraction is the dominant force isn’t the point. These are bidirectional relationships. If we are interested in pointing fingers, the common denominator is the device and our failure as a society to keep it in proper perspective. We all know that smartphones, tablets, and computers create an unhealthy distraction in personal relationships. The parents know and most of the children know. It’s time for us all to demonstrate some self-discipline. And that can begin for us as health care providers as we sit behind our computers spending more time looking at the screen than we do engaging the patient with our eyes.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
You see it all the time. It’s the family at the table next to you in the restaurant where the two teenage children are texting away on their phones. Or the playground, where a 3-year-old is playing with his toy truck and bulldozer in the sand and his father, immersed in his laptop, hasn’t said a word to his child.
It may trouble you when you witness social situations like that in which an electronic device is preventing or certainly interfering with interpersonal interactions. Or at least I hope it troubles you. Maybe it is so ubiquitous that you have come to accept it as the norm. It’s likely you may even be a participant. But, do you have a name for it?
It’s called “technoference,” a word coined by a doctoral student in human development and family studies at Penn State a decade ago “to describe the everyday intrusions and interruptions in couple interactions that take place due to technology devices and their always-on, ever-present nature.” Although, the original research that triggered the coinage was about couples, obviously the phenomenon occurs whenever people of any age are together in social situations.
While the word may not have crept into common parlance, we all know it when we see it. Technoference may not appear in the paper’s title, but it is a subject being investigated across a broad array of disciplines. One phone tracking study found that parents of young infants spend more than 5 hours each day on their smartphones. More than a quarter of that time the infant is engaged with the parent’s digital device. Technoference has been associated with decreased parent-child interaction during early childhood. It has been associated with more negative responses to children’s behavior, as well as an increased risk of child injury.
There are numerous studies suggesting an association between parental technoference and mental health difficulties in children. I have recently reviewed one of these studies that looks at the relationship of perceived parental technoference and the mental health of children entering adolescents. The authors collected longitudinal data of more than 1300 emerging adolescents, hoping to determine if the relationship between parental distraction and mental health was bidirectional. In other words, could a child’s mental health be contributing to his parents’ perceived distraction? Or was it primarily the parents’ technoference that was playing a role in the child’s mental health problems?
What investigators found was that higher levels of parental distraction were associated with higher levels of inattention and hyperactivity in the emerging adolescents, but not vice versa. On the other hand, higher levels of adolescent anxiety was associated with higher levels of perceived parental technoference, but not vice versa.
I know this sounds a bit confusing and a bit chicken-egg-chicken-eggish. The study was not designed to determine causation in these associations. However, the authors offer some possible scenarios that may provide a bit of clarity. It could be that parents who are concerned about their anxious child respond by retreating into the cyberspace to avoid tense situations or for support or information.
On the other hand, This explanation meshes with other studies demonstrating an association between parental distraction and aggression and attention problems in early childhood.
While one could spend more time imagining other factors that could be driving these bidirectional relationships, I’m not sure that it makes a heckuva lot of difference. Whether the child’s mental illness is the primary driver or the parent’s device-associated distraction is the dominant force isn’t the point. These are bidirectional relationships. If we are interested in pointing fingers, the common denominator is the device and our failure as a society to keep it in proper perspective. We all know that smartphones, tablets, and computers create an unhealthy distraction in personal relationships. The parents know and most of the children know. It’s time for us all to demonstrate some self-discipline. And that can begin for us as health care providers as we sit behind our computers spending more time looking at the screen than we do engaging the patient with our eyes.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
You see it all the time. It’s the family at the table next to you in the restaurant where the two teenage children are texting away on their phones. Or the playground, where a 3-year-old is playing with his toy truck and bulldozer in the sand and his father, immersed in his laptop, hasn’t said a word to his child.
It may trouble you when you witness social situations like that in which an electronic device is preventing or certainly interfering with interpersonal interactions. Or at least I hope it troubles you. Maybe it is so ubiquitous that you have come to accept it as the norm. It’s likely you may even be a participant. But, do you have a name for it?
It’s called “technoference,” a word coined by a doctoral student in human development and family studies at Penn State a decade ago “to describe the everyday intrusions and interruptions in couple interactions that take place due to technology devices and their always-on, ever-present nature.” Although, the original research that triggered the coinage was about couples, obviously the phenomenon occurs whenever people of any age are together in social situations.
While the word may not have crept into common parlance, we all know it when we see it. Technoference may not appear in the paper’s title, but it is a subject being investigated across a broad array of disciplines. One phone tracking study found that parents of young infants spend more than 5 hours each day on their smartphones. More than a quarter of that time the infant is engaged with the parent’s digital device. Technoference has been associated with decreased parent-child interaction during early childhood. It has been associated with more negative responses to children’s behavior, as well as an increased risk of child injury.
There are numerous studies suggesting an association between parental technoference and mental health difficulties in children. I have recently reviewed one of these studies that looks at the relationship of perceived parental technoference and the mental health of children entering adolescents. The authors collected longitudinal data of more than 1300 emerging adolescents, hoping to determine if the relationship between parental distraction and mental health was bidirectional. In other words, could a child’s mental health be contributing to his parents’ perceived distraction? Or was it primarily the parents’ technoference that was playing a role in the child’s mental health problems?
What investigators found was that higher levels of parental distraction were associated with higher levels of inattention and hyperactivity in the emerging adolescents, but not vice versa. On the other hand, higher levels of adolescent anxiety was associated with higher levels of perceived parental technoference, but not vice versa.
I know this sounds a bit confusing and a bit chicken-egg-chicken-eggish. The study was not designed to determine causation in these associations. However, the authors offer some possible scenarios that may provide a bit of clarity. It could be that parents who are concerned about their anxious child respond by retreating into the cyberspace to avoid tense situations or for support or information.
On the other hand, This explanation meshes with other studies demonstrating an association between parental distraction and aggression and attention problems in early childhood.
While one could spend more time imagining other factors that could be driving these bidirectional relationships, I’m not sure that it makes a heckuva lot of difference. Whether the child’s mental illness is the primary driver or the parent’s device-associated distraction is the dominant force isn’t the point. These are bidirectional relationships. If we are interested in pointing fingers, the common denominator is the device and our failure as a society to keep it in proper perspective. We all know that smartphones, tablets, and computers create an unhealthy distraction in personal relationships. The parents know and most of the children know. It’s time for us all to demonstrate some self-discipline. And that can begin for us as health care providers as we sit behind our computers spending more time looking at the screen than we do engaging the patient with our eyes.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Closing the GAP in Idiopathic Pulmonary Fibrosis
5 things you should know about IPF. American Lung Association. April 12, 2023. Accessed June 21, 2024. https://www.lung.org/blog/idiopathic-pulmonary-fibrosis-things-to-know
Raghu G, Chen SY, Yeh WS, et al. Idiopathic pulmonary fibrosis in US Medicare beneficiaries aged 65 years and older: incidence, prevalence, and survival, 2001-11. Lancet Respir Med. 2014;2(7):566-572. doi:10.1016/S2213-2600(14)70101-8
Morrow T. Improving outcomes and managing costs in idiopathic pulmonary fibrosis. Am J Manag Care. 2019;25(11 suppl):S204-S209. PMID: 31419090
Man RK, Gogikar A, Nanda A, et al. A comparison of the effectiveness of nintedanib and pirfenidone in treating idiopathic pulmonary fibrosis: a systematic review. Cureus. 2024;16(2):e54268. doi:10.7759/cureus.54268
Ley B, Ryerson CJ, Vittinghoff E, et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Intern Med. 2012;156(10):684-691. doi:10.7326/0003-4819-156-10-201205150-00004
Raghu G, Remy-Jardin M, Myers JL, et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198(5):e44-e68. doi:10.1164/rccm.201807-1255ST
Collard HR, Ryerson CJ, Corte TJ, et al. Acute exacerbation of idiopathic pulmonary fibrosis. An International Working Group report. Am J Respir Crit Care Med. 2016;194(3):265-275. doi:10.1164/rccm.201604-0801CI
Abuserewa ST, Duff R, Becker G. Treatment of idiopathic pulmonary fibrosis. Cureus. 2021;13(5):e15360. doi:10.7759/cureus.15360
Lee JH, Jang JH, Jang HJ, et al. New prognostic scoring system for mortality in idiopathic pulmonary fibrosis by modifying the gender, age, and physiology model with desaturation during the six-minute walk test. Front Med (Lausanne). 2023;10:1052129. doi:10.3389/fmed.2023.1052129
Chandel A, Pastre J, Valery S, King CS, Nathan SD. Derivation and validation of a simple multidimensional index incorporating exercise capacity parameters for survival prediction in idiopathic pulmonary fibrosis. Thorax. 2023;78(4):368-375. doi:10.1136/thoraxjnl-2021-218440
Chandel A, King CS, Ignacio RV, et al. External validation and longitudinal application of the DO-GAP index to individualise survival prediction in idiopathic pulmonary fibrosis. ERJ Open Res. 2023;9(3):00124-2023. doi:10.1183/23120541.00124-2023
Suzuki Y, Mori K, Aono Y, et al. Combined assessment of the GAP index and body mass index at antifibrotic therapy initiation for prognosis of idiopathic pulmonary fibrosis. Sci Rep. 2021;11(1):18579. doi:10.1038/s41598-021-98161-y
Lacedonia D, De Pace CC, Rea G, et al. Machine learning and BMI improve the prognostic value of GAP index in treated IPF patients. Bioengineering (Basel). 2023;10(2):251. doi:10.3390/bioengineering10020251
Fujii H, Hara Y, Saigusa Y, et al. ILD-GAP combined with the Charlson Comorbidity Index score (ILD-GAPC) as a prognostic prediction model in patients with interstitial lung disease. Can Respir J. 2023;2023:5088207. doi:10.1155/2023/5088207
Ley B, Bradford WZ, Weycker D, Vittinghoff E, du Bois RM, Collard HR. Unified baseline and longitudinal mortality prediction in idiopathic pulmonary fibrosis. Eur Respir J. 2015;45(5):1374-1381. doi:10.1183/09031936.00146314
Kreuter M, Lee JS, Tzouvelekis A, et al. Monocyte count as a prognostic biomarker in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2021;204(1):74-81. doi:10.1164/rccm.202003-0669OC
Kreuter M, Lee JS, Tzouvelekis A, et al. A modified blood cell GAP (cGAP) to prognosticate outcomes in IPF. Poster presented at: European Respiratory Society International Congress; September 4-6, 2022. https://medically.gene.com/global/en/unrestricted/respiratory/ERS-2022/ers-2022-poster-kreuter-a-modified-blood-cell-gap.html
Nishikiori H, Chiba H, Lee SH, et al. A modified GAP model for East-Asian populations with idiopathic pulmonary fibrosis. Respir Investig. 2020;58(5):395-402. doi:10.1016/j.resinv.2020.04.001
5 things you should know about IPF. American Lung Association. April 12, 2023. Accessed June 21, 2024. https://www.lung.org/blog/idiopathic-pulmonary-fibrosis-things-to-know
Raghu G, Chen SY, Yeh WS, et al. Idiopathic pulmonary fibrosis in US Medicare beneficiaries aged 65 years and older: incidence, prevalence, and survival, 2001-11. Lancet Respir Med. 2014;2(7):566-572. doi:10.1016/S2213-2600(14)70101-8
Morrow T. Improving outcomes and managing costs in idiopathic pulmonary fibrosis. Am J Manag Care. 2019;25(11 suppl):S204-S209. PMID: 31419090
Man RK, Gogikar A, Nanda A, et al. A comparison of the effectiveness of nintedanib and pirfenidone in treating idiopathic pulmonary fibrosis: a systematic review. Cureus. 2024;16(2):e54268. doi:10.7759/cureus.54268
Ley B, Ryerson CJ, Vittinghoff E, et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Intern Med. 2012;156(10):684-691. doi:10.7326/0003-4819-156-10-201205150-00004
Raghu G, Remy-Jardin M, Myers JL, et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198(5):e44-e68. doi:10.1164/rccm.201807-1255ST
Collard HR, Ryerson CJ, Corte TJ, et al. Acute exacerbation of idiopathic pulmonary fibrosis. An International Working Group report. Am J Respir Crit Care Med. 2016;194(3):265-275. doi:10.1164/rccm.201604-0801CI
Abuserewa ST, Duff R, Becker G. Treatment of idiopathic pulmonary fibrosis. Cureus. 2021;13(5):e15360. doi:10.7759/cureus.15360
Lee JH, Jang JH, Jang HJ, et al. New prognostic scoring system for mortality in idiopathic pulmonary fibrosis by modifying the gender, age, and physiology model with desaturation during the six-minute walk test. Front Med (Lausanne). 2023;10:1052129. doi:10.3389/fmed.2023.1052129
Chandel A, Pastre J, Valery S, King CS, Nathan SD. Derivation and validation of a simple multidimensional index incorporating exercise capacity parameters for survival prediction in idiopathic pulmonary fibrosis. Thorax. 2023;78(4):368-375. doi:10.1136/thoraxjnl-2021-218440
Chandel A, King CS, Ignacio RV, et al. External validation and longitudinal application of the DO-GAP index to individualise survival prediction in idiopathic pulmonary fibrosis. ERJ Open Res. 2023;9(3):00124-2023. doi:10.1183/23120541.00124-2023
Suzuki Y, Mori K, Aono Y, et al. Combined assessment of the GAP index and body mass index at antifibrotic therapy initiation for prognosis of idiopathic pulmonary fibrosis. Sci Rep. 2021;11(1):18579. doi:10.1038/s41598-021-98161-y
Lacedonia D, De Pace CC, Rea G, et al. Machine learning and BMI improve the prognostic value of GAP index in treated IPF patients. Bioengineering (Basel). 2023;10(2):251. doi:10.3390/bioengineering10020251
Fujii H, Hara Y, Saigusa Y, et al. ILD-GAP combined with the Charlson Comorbidity Index score (ILD-GAPC) as a prognostic prediction model in patients with interstitial lung disease. Can Respir J. 2023;2023:5088207. doi:10.1155/2023/5088207
Ley B, Bradford WZ, Weycker D, Vittinghoff E, du Bois RM, Collard HR. Unified baseline and longitudinal mortality prediction in idiopathic pulmonary fibrosis. Eur Respir J. 2015;45(5):1374-1381. doi:10.1183/09031936.00146314
Kreuter M, Lee JS, Tzouvelekis A, et al. Monocyte count as a prognostic biomarker in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2021;204(1):74-81. doi:10.1164/rccm.202003-0669OC
Kreuter M, Lee JS, Tzouvelekis A, et al. A modified blood cell GAP (cGAP) to prognosticate outcomes in IPF. Poster presented at: European Respiratory Society International Congress; September 4-6, 2022. https://medically.gene.com/global/en/unrestricted/respiratory/ERS-2022/ers-2022-poster-kreuter-a-modified-blood-cell-gap.html
Nishikiori H, Chiba H, Lee SH, et al. A modified GAP model for East-Asian populations with idiopathic pulmonary fibrosis. Respir Investig. 2020;58(5):395-402. doi:10.1016/j.resinv.2020.04.001
5 things you should know about IPF. American Lung Association. April 12, 2023. Accessed June 21, 2024. https://www.lung.org/blog/idiopathic-pulmonary-fibrosis-things-to-know
Raghu G, Chen SY, Yeh WS, et al. Idiopathic pulmonary fibrosis in US Medicare beneficiaries aged 65 years and older: incidence, prevalence, and survival, 2001-11. Lancet Respir Med. 2014;2(7):566-572. doi:10.1016/S2213-2600(14)70101-8
Morrow T. Improving outcomes and managing costs in idiopathic pulmonary fibrosis. Am J Manag Care. 2019;25(11 suppl):S204-S209. PMID: 31419090
Man RK, Gogikar A, Nanda A, et al. A comparison of the effectiveness of nintedanib and pirfenidone in treating idiopathic pulmonary fibrosis: a systematic review. Cureus. 2024;16(2):e54268. doi:10.7759/cureus.54268
Ley B, Ryerson CJ, Vittinghoff E, et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Intern Med. 2012;156(10):684-691. doi:10.7326/0003-4819-156-10-201205150-00004
Raghu G, Remy-Jardin M, Myers JL, et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198(5):e44-e68. doi:10.1164/rccm.201807-1255ST
Collard HR, Ryerson CJ, Corte TJ, et al. Acute exacerbation of idiopathic pulmonary fibrosis. An International Working Group report. Am J Respir Crit Care Med. 2016;194(3):265-275. doi:10.1164/rccm.201604-0801CI
Abuserewa ST, Duff R, Becker G. Treatment of idiopathic pulmonary fibrosis. Cureus. 2021;13(5):e15360. doi:10.7759/cureus.15360
Lee JH, Jang JH, Jang HJ, et al. New prognostic scoring system for mortality in idiopathic pulmonary fibrosis by modifying the gender, age, and physiology model with desaturation during the six-minute walk test. Front Med (Lausanne). 2023;10:1052129. doi:10.3389/fmed.2023.1052129
Chandel A, Pastre J, Valery S, King CS, Nathan SD. Derivation and validation of a simple multidimensional index incorporating exercise capacity parameters for survival prediction in idiopathic pulmonary fibrosis. Thorax. 2023;78(4):368-375. doi:10.1136/thoraxjnl-2021-218440
Chandel A, King CS, Ignacio RV, et al. External validation and longitudinal application of the DO-GAP index to individualise survival prediction in idiopathic pulmonary fibrosis. ERJ Open Res. 2023;9(3):00124-2023. doi:10.1183/23120541.00124-2023
Suzuki Y, Mori K, Aono Y, et al. Combined assessment of the GAP index and body mass index at antifibrotic therapy initiation for prognosis of idiopathic pulmonary fibrosis. Sci Rep. 2021;11(1):18579. doi:10.1038/s41598-021-98161-y
Lacedonia D, De Pace CC, Rea G, et al. Machine learning and BMI improve the prognostic value of GAP index in treated IPF patients. Bioengineering (Basel). 2023;10(2):251. doi:10.3390/bioengineering10020251
Fujii H, Hara Y, Saigusa Y, et al. ILD-GAP combined with the Charlson Comorbidity Index score (ILD-GAPC) as a prognostic prediction model in patients with interstitial lung disease. Can Respir J. 2023;2023:5088207. doi:10.1155/2023/5088207
Ley B, Bradford WZ, Weycker D, Vittinghoff E, du Bois RM, Collard HR. Unified baseline and longitudinal mortality prediction in idiopathic pulmonary fibrosis. Eur Respir J. 2015;45(5):1374-1381. doi:10.1183/09031936.00146314
Kreuter M, Lee JS, Tzouvelekis A, et al. Monocyte count as a prognostic biomarker in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2021;204(1):74-81. doi:10.1164/rccm.202003-0669OC
Kreuter M, Lee JS, Tzouvelekis A, et al. A modified blood cell GAP (cGAP) to prognosticate outcomes in IPF. Poster presented at: European Respiratory Society International Congress; September 4-6, 2022. https://medically.gene.com/global/en/unrestricted/respiratory/ERS-2022/ers-2022-poster-kreuter-a-modified-blood-cell-gap.html
Nishikiori H, Chiba H, Lee SH, et al. A modified GAP model for East-Asian populations with idiopathic pulmonary fibrosis. Respir Investig. 2020;58(5):395-402. doi:10.1016/j.resinv.2020.04.001
Pulmonology Data Trends 2024
Pulmonology Data Trends 2024 is a supplement to CHEST Physician highlighting the latest breakthroughs in pulmonology research and treatments through a series of infographics.
Read more:
Artificial Intelligence in Sleep Apnea
Ritwick Agrawal, MD, MS, FCCP
RSV Updates: Prophylaxis Approval and Hospitalization for Severe RSV
Riddhi Upadhyay, MD
Biologics in Asthma: Changing the Severe Asthma Paradigm
Shyam Subramanian, MD, FCCP
Updates in COPD Guidelines and Treatment
Dharani K. Narendra, MD, FCCP
Targeted Therapies and Surgical Resection for Lung Cancer: Evolving Treatment Options
Saadia A. Faiz, MD, FCCP
Closing the GAP in Idiopathic Pulmonary Fibrosis
Humayun Anjum, MD, FCCP
Severe Community-Acquired Pneumonia: Diagnostic Criteria, Treatment, and COVID-19
Sujith V. Cherian, MD, FCCP
Pulmonary Hypertension: Comorbidities and Novel Therapies
Mary Jo S. Farmer, MD, PhD, FCCP
The Genetic Side of Interstitial Lung Disease
Priya Balakrishnan, MD, MS, FCCP
Noninvasive Ventilation in Neuromuscular Disease
Sreelatha Naik, MD, FCCP, and Kelly Lobrutto, CRNP
Pulmonology Data Trends 2024 is a supplement to CHEST Physician highlighting the latest breakthroughs in pulmonology research and treatments through a series of infographics.
Read more:
Artificial Intelligence in Sleep Apnea
Ritwick Agrawal, MD, MS, FCCP
RSV Updates: Prophylaxis Approval and Hospitalization for Severe RSV
Riddhi Upadhyay, MD
Biologics in Asthma: Changing the Severe Asthma Paradigm
Shyam Subramanian, MD, FCCP
Updates in COPD Guidelines and Treatment
Dharani K. Narendra, MD, FCCP
Targeted Therapies and Surgical Resection for Lung Cancer: Evolving Treatment Options
Saadia A. Faiz, MD, FCCP
Closing the GAP in Idiopathic Pulmonary Fibrosis
Humayun Anjum, MD, FCCP
Severe Community-Acquired Pneumonia: Diagnostic Criteria, Treatment, and COVID-19
Sujith V. Cherian, MD, FCCP
Pulmonary Hypertension: Comorbidities and Novel Therapies
Mary Jo S. Farmer, MD, PhD, FCCP
The Genetic Side of Interstitial Lung Disease
Priya Balakrishnan, MD, MS, FCCP
Noninvasive Ventilation in Neuromuscular Disease
Sreelatha Naik, MD, FCCP, and Kelly Lobrutto, CRNP
Pulmonology Data Trends 2024 is a supplement to CHEST Physician highlighting the latest breakthroughs in pulmonology research and treatments through a series of infographics.
Read more:
Artificial Intelligence in Sleep Apnea
Ritwick Agrawal, MD, MS, FCCP
RSV Updates: Prophylaxis Approval and Hospitalization for Severe RSV
Riddhi Upadhyay, MD
Biologics in Asthma: Changing the Severe Asthma Paradigm
Shyam Subramanian, MD, FCCP
Updates in COPD Guidelines and Treatment
Dharani K. Narendra, MD, FCCP
Targeted Therapies and Surgical Resection for Lung Cancer: Evolving Treatment Options
Saadia A. Faiz, MD, FCCP
Closing the GAP in Idiopathic Pulmonary Fibrosis
Humayun Anjum, MD, FCCP
Severe Community-Acquired Pneumonia: Diagnostic Criteria, Treatment, and COVID-19
Sujith V. Cherian, MD, FCCP
Pulmonary Hypertension: Comorbidities and Novel Therapies
Mary Jo S. Farmer, MD, PhD, FCCP
The Genetic Side of Interstitial Lung Disease
Priya Balakrishnan, MD, MS, FCCP
Noninvasive Ventilation in Neuromuscular Disease
Sreelatha Naik, MD, FCCP, and Kelly Lobrutto, CRNP
UCSF Favors Pricey Doctoral Program for Nurse-Midwives Amid Maternal Care Crisis
One of California’s two programs for training nurse-midwives has stopped admitting students while it revamps its curriculum to offer only doctoral degrees, a move that’s drawn howls of protest from alumni, health policy experts, and faculty who accuse the University of California of putting profits above public health needs.
The University of California San Francisco’s (UCSF) renowned nursing school will graduate its final class of certified nurse-midwives in the spring of 2025. Then the university will cancel its 2-year master’s program in nurse-midwifery, along with other nursing disciplines, in favor of a 3-year doctor of nursing practice, or DNP, degree. The change will pause UCSF’s nearly 5 decades–long training of nurse-midwives until at least 2025 and will more than double the cost to students.
State Assembly member Mia Bonta, who chairs the health committee, said she was “disheartened” to learn that UCSF was eliminating its master’s nurse-midwifery program and feared the additional time and costs to get a doctorate would deter potential applicants. “Instead of adding hurdles, we need to be building and expanding a pipeline of culturally and racially concordant providers to support improved birth outcomes, especially for Black and Latina birthing people,” she said in an email.
The switch to doctoral education is part of a national movement to require all advanced-practice registered nurses, including nurse-midwives and nurse practitioners, to earn doctoral degrees, Kristen Bole, a UCSF spokesperson, said in response to written questions. The doctoral training will feature additional classes in leadership and quality improvement.
But the movement, which dates to 2004, has not caught on the way the American Association of Colleges of Nursing envisioned when it called for doctorate-level education to be required for entry-level advanced nursing practice by 2015. That deadline came and went. Now, an acute need for maternal health practitioners has some universities moving in the other direction.
This year, Rutgers University reinstated the nurse-midwifery master’s training it had eliminated in 2016. The University of Alabama at Birmingham also restarted its master’s in nurse-midwifery program in 2022 after a 25-year hiatus. In addition, George Washington University in Washington, DC, Loyola University in New Orleans, and the University of Nevada in Las Vagas added master’s training in nurse-midwifery.
UCSF estimates tuition and fees will cost $152,000 for a 3-year doctoral degree in midwifery, compared with $65,000 for a 2-year master’s. Studies show that 71% of nursing master’s students and 74% of nursing doctoral students rely on student loans, and nurses with doctorates earn negligibly or no more than nurses with master’s degrees.
Kim Q. Dau, who ran UCSF’s nurse-midwifery program for a decade, resigned in June because she was uncomfortable with the elimination of the master’s in favor of a doctoral requirement, she said, which is at odds with the state’s workforce needs and unnecessary for clinical practice.
“They’ll be equally prepared clinically but at more expense to the student and with a greater time investment,” she said.
Nurse-midwives are registered nurses with graduate degrees in nurse-midwifery. Licensed in all 50 states, they work mostly in hospitals and can perform abortions and prescribe medications, though they are also trained in managing labor pain with showers, massage, and other natural means. Certified midwives, by contrast, study midwifery at the graduate level outside of nursing schools and are licensed only in some states. Certified professional midwives attend births outside of hospitals.
The California Nurse-Midwives Association also criticized UCSF’s program change, which comes amid a national maternal mortality crisis, a serious shortage of obstetric providers, and a growing reliance on midwives. According to the 2022 “White House Blueprint for Addressing the Maternal Health Crisis” report, the United States has the highest maternal mortality rate of any developed nation and needs thousands more midwives and other women’s health providers to bridge the swelling gap.
Ginger Breedlove, founder and CEO of Grow Midwives, a national consulting firm, likened UCSF’s switch from master’s to doctoral training to “an earthquake.”
“Why are we delaying the entry of essential care providers by making them go to an additional year of school, which adds nothing to their clinical preparedness or safety to serve the community?” asked Ms. Breedlove, a past president of the American College of Nurse-Midwives. “Why they have chosen this during one of the worst workforce shortages combined with the worst maternal health crisis we have had in 50 years is beyond my imagination.”
A 2020 report published in Nursing Outlook failed to find that advanced-practice registered nurses with doctorates were more clinically proficient than those with master’s degrees. “Unfortunately, to date, the data are sparse,” it concluded.
The American College of Nurse-Midwives also denounced the doctoral requirement, as have trade associations for neonatal nurse practitioners and neonatal nurses, citing “the lack of scientific evidence that ... doctoral-level education is beneficial to patients, practitioners, or society.”
There is no evidence that doctoral-level nurse-midwives will provide better care, Ms. Breedlove said.
“This is profit over purpose,” she added.
Ms. Bole disputed Ms. Breedlove’s accusation of a profit motive. Asked for reasons for the change, she offered broad statements: “The decision to upgrade our program was made to ensure that our graduates are prepared for the challenges they will face in the evolving health care landscape.”
Like Ms. Breedlove, Liz Donnelly, vice chair of the health policy committee for the California Nurse-Midwives Association, worries that UCSF’s switch to a doctoral degree will exacerbate the twin crises of maternal mortality and a shrinking obstetrics workforce across California and the nation.
On average, 10-12 nurse-midwives graduated from the UCSF master’s program each year over the past decade, Ms. Bole said. California’s remaining master’s program in nurse-midwifery is at California State University in Fullerton, south of Los Angeles, and it graduated 8 nurse-midwives in 2023 and 11 in 2024.
More than half of rural counties in the United States lacked obstetric care in 2018, according to a Government Accountability Office report.
In some parts of California, expectant mothers must drive 2 hours for care, said Bethany Sasaki, who runs Midtown Nurse Midwives, a Sacramento birth center. It has had to stop accepting new clients because it cannot find midwives.
Ms. Donnelly predicted the closure of UCSF’s midwifery program will significantly reduce the number of nurse-midwives entering the workforce and will inhibit people with fewer resources from attending the program. “Specifically, I think it’s going to reduce folks of color, people from rural communities, people from poor communities,” she said.
UCSF’s change will also likely undercut efforts to train providers from diverse backgrounds.
Natasha, a 37-year-old Afro-Puerto Rican mother of two, has spent a decade preparing to train as a nurse-midwife so she could help women like herself through pregnancy and childbirth. She asked to be identified only by her first name out of fear of reducing her chances of graduate school admission.
The UCSF program’s pause, plus the added time and expense to get a doctoral degree, has muddied her career path.
“The master’s was just the perfect program,” said Natasha, who lives in the Bay Area and cannot travel to the other end of the state to attend California State University-Fullerton. “I’m frustrated, and I feel deflated. I now have to find another career path.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
One of California’s two programs for training nurse-midwives has stopped admitting students while it revamps its curriculum to offer only doctoral degrees, a move that’s drawn howls of protest from alumni, health policy experts, and faculty who accuse the University of California of putting profits above public health needs.
The University of California San Francisco’s (UCSF) renowned nursing school will graduate its final class of certified nurse-midwives in the spring of 2025. Then the university will cancel its 2-year master’s program in nurse-midwifery, along with other nursing disciplines, in favor of a 3-year doctor of nursing practice, or DNP, degree. The change will pause UCSF’s nearly 5 decades–long training of nurse-midwives until at least 2025 and will more than double the cost to students.
State Assembly member Mia Bonta, who chairs the health committee, said she was “disheartened” to learn that UCSF was eliminating its master’s nurse-midwifery program and feared the additional time and costs to get a doctorate would deter potential applicants. “Instead of adding hurdles, we need to be building and expanding a pipeline of culturally and racially concordant providers to support improved birth outcomes, especially for Black and Latina birthing people,” she said in an email.
The switch to doctoral education is part of a national movement to require all advanced-practice registered nurses, including nurse-midwives and nurse practitioners, to earn doctoral degrees, Kristen Bole, a UCSF spokesperson, said in response to written questions. The doctoral training will feature additional classes in leadership and quality improvement.
But the movement, which dates to 2004, has not caught on the way the American Association of Colleges of Nursing envisioned when it called for doctorate-level education to be required for entry-level advanced nursing practice by 2015. That deadline came and went. Now, an acute need for maternal health practitioners has some universities moving in the other direction.
This year, Rutgers University reinstated the nurse-midwifery master’s training it had eliminated in 2016. The University of Alabama at Birmingham also restarted its master’s in nurse-midwifery program in 2022 after a 25-year hiatus. In addition, George Washington University in Washington, DC, Loyola University in New Orleans, and the University of Nevada in Las Vagas added master’s training in nurse-midwifery.
UCSF estimates tuition and fees will cost $152,000 for a 3-year doctoral degree in midwifery, compared with $65,000 for a 2-year master’s. Studies show that 71% of nursing master’s students and 74% of nursing doctoral students rely on student loans, and nurses with doctorates earn negligibly or no more than nurses with master’s degrees.
Kim Q. Dau, who ran UCSF’s nurse-midwifery program for a decade, resigned in June because she was uncomfortable with the elimination of the master’s in favor of a doctoral requirement, she said, which is at odds with the state’s workforce needs and unnecessary for clinical practice.
“They’ll be equally prepared clinically but at more expense to the student and with a greater time investment,” she said.
Nurse-midwives are registered nurses with graduate degrees in nurse-midwifery. Licensed in all 50 states, they work mostly in hospitals and can perform abortions and prescribe medications, though they are also trained in managing labor pain with showers, massage, and other natural means. Certified midwives, by contrast, study midwifery at the graduate level outside of nursing schools and are licensed only in some states. Certified professional midwives attend births outside of hospitals.
The California Nurse-Midwives Association also criticized UCSF’s program change, which comes amid a national maternal mortality crisis, a serious shortage of obstetric providers, and a growing reliance on midwives. According to the 2022 “White House Blueprint for Addressing the Maternal Health Crisis” report, the United States has the highest maternal mortality rate of any developed nation and needs thousands more midwives and other women’s health providers to bridge the swelling gap.
Ginger Breedlove, founder and CEO of Grow Midwives, a national consulting firm, likened UCSF’s switch from master’s to doctoral training to “an earthquake.”
“Why are we delaying the entry of essential care providers by making them go to an additional year of school, which adds nothing to their clinical preparedness or safety to serve the community?” asked Ms. Breedlove, a past president of the American College of Nurse-Midwives. “Why they have chosen this during one of the worst workforce shortages combined with the worst maternal health crisis we have had in 50 years is beyond my imagination.”
A 2020 report published in Nursing Outlook failed to find that advanced-practice registered nurses with doctorates were more clinically proficient than those with master’s degrees. “Unfortunately, to date, the data are sparse,” it concluded.
The American College of Nurse-Midwives also denounced the doctoral requirement, as have trade associations for neonatal nurse practitioners and neonatal nurses, citing “the lack of scientific evidence that ... doctoral-level education is beneficial to patients, practitioners, or society.”
There is no evidence that doctoral-level nurse-midwives will provide better care, Ms. Breedlove said.
“This is profit over purpose,” she added.
Ms. Bole disputed Ms. Breedlove’s accusation of a profit motive. Asked for reasons for the change, she offered broad statements: “The decision to upgrade our program was made to ensure that our graduates are prepared for the challenges they will face in the evolving health care landscape.”
Like Ms. Breedlove, Liz Donnelly, vice chair of the health policy committee for the California Nurse-Midwives Association, worries that UCSF’s switch to a doctoral degree will exacerbate the twin crises of maternal mortality and a shrinking obstetrics workforce across California and the nation.
On average, 10-12 nurse-midwives graduated from the UCSF master’s program each year over the past decade, Ms. Bole said. California’s remaining master’s program in nurse-midwifery is at California State University in Fullerton, south of Los Angeles, and it graduated 8 nurse-midwives in 2023 and 11 in 2024.
More than half of rural counties in the United States lacked obstetric care in 2018, according to a Government Accountability Office report.
In some parts of California, expectant mothers must drive 2 hours for care, said Bethany Sasaki, who runs Midtown Nurse Midwives, a Sacramento birth center. It has had to stop accepting new clients because it cannot find midwives.
Ms. Donnelly predicted the closure of UCSF’s midwifery program will significantly reduce the number of nurse-midwives entering the workforce and will inhibit people with fewer resources from attending the program. “Specifically, I think it’s going to reduce folks of color, people from rural communities, people from poor communities,” she said.
UCSF’s change will also likely undercut efforts to train providers from diverse backgrounds.
Natasha, a 37-year-old Afro-Puerto Rican mother of two, has spent a decade preparing to train as a nurse-midwife so she could help women like herself through pregnancy and childbirth. She asked to be identified only by her first name out of fear of reducing her chances of graduate school admission.
The UCSF program’s pause, plus the added time and expense to get a doctoral degree, has muddied her career path.
“The master’s was just the perfect program,” said Natasha, who lives in the Bay Area and cannot travel to the other end of the state to attend California State University-Fullerton. “I’m frustrated, and I feel deflated. I now have to find another career path.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
One of California’s two programs for training nurse-midwives has stopped admitting students while it revamps its curriculum to offer only doctoral degrees, a move that’s drawn howls of protest from alumni, health policy experts, and faculty who accuse the University of California of putting profits above public health needs.
The University of California San Francisco’s (UCSF) renowned nursing school will graduate its final class of certified nurse-midwives in the spring of 2025. Then the university will cancel its 2-year master’s program in nurse-midwifery, along with other nursing disciplines, in favor of a 3-year doctor of nursing practice, or DNP, degree. The change will pause UCSF’s nearly 5 decades–long training of nurse-midwives until at least 2025 and will more than double the cost to students.
State Assembly member Mia Bonta, who chairs the health committee, said she was “disheartened” to learn that UCSF was eliminating its master’s nurse-midwifery program and feared the additional time and costs to get a doctorate would deter potential applicants. “Instead of adding hurdles, we need to be building and expanding a pipeline of culturally and racially concordant providers to support improved birth outcomes, especially for Black and Latina birthing people,” she said in an email.
The switch to doctoral education is part of a national movement to require all advanced-practice registered nurses, including nurse-midwives and nurse practitioners, to earn doctoral degrees, Kristen Bole, a UCSF spokesperson, said in response to written questions. The doctoral training will feature additional classes in leadership and quality improvement.
But the movement, which dates to 2004, has not caught on the way the American Association of Colleges of Nursing envisioned when it called for doctorate-level education to be required for entry-level advanced nursing practice by 2015. That deadline came and went. Now, an acute need for maternal health practitioners has some universities moving in the other direction.
This year, Rutgers University reinstated the nurse-midwifery master’s training it had eliminated in 2016. The University of Alabama at Birmingham also restarted its master’s in nurse-midwifery program in 2022 after a 25-year hiatus. In addition, George Washington University in Washington, DC, Loyola University in New Orleans, and the University of Nevada in Las Vagas added master’s training in nurse-midwifery.
UCSF estimates tuition and fees will cost $152,000 for a 3-year doctoral degree in midwifery, compared with $65,000 for a 2-year master’s. Studies show that 71% of nursing master’s students and 74% of nursing doctoral students rely on student loans, and nurses with doctorates earn negligibly or no more than nurses with master’s degrees.
Kim Q. Dau, who ran UCSF’s nurse-midwifery program for a decade, resigned in June because she was uncomfortable with the elimination of the master’s in favor of a doctoral requirement, she said, which is at odds with the state’s workforce needs and unnecessary for clinical practice.
“They’ll be equally prepared clinically but at more expense to the student and with a greater time investment,” she said.
Nurse-midwives are registered nurses with graduate degrees in nurse-midwifery. Licensed in all 50 states, they work mostly in hospitals and can perform abortions and prescribe medications, though they are also trained in managing labor pain with showers, massage, and other natural means. Certified midwives, by contrast, study midwifery at the graduate level outside of nursing schools and are licensed only in some states. Certified professional midwives attend births outside of hospitals.
The California Nurse-Midwives Association also criticized UCSF’s program change, which comes amid a national maternal mortality crisis, a serious shortage of obstetric providers, and a growing reliance on midwives. According to the 2022 “White House Blueprint for Addressing the Maternal Health Crisis” report, the United States has the highest maternal mortality rate of any developed nation and needs thousands more midwives and other women’s health providers to bridge the swelling gap.
Ginger Breedlove, founder and CEO of Grow Midwives, a national consulting firm, likened UCSF’s switch from master’s to doctoral training to “an earthquake.”
“Why are we delaying the entry of essential care providers by making them go to an additional year of school, which adds nothing to their clinical preparedness or safety to serve the community?” asked Ms. Breedlove, a past president of the American College of Nurse-Midwives. “Why they have chosen this during one of the worst workforce shortages combined with the worst maternal health crisis we have had in 50 years is beyond my imagination.”
A 2020 report published in Nursing Outlook failed to find that advanced-practice registered nurses with doctorates were more clinically proficient than those with master’s degrees. “Unfortunately, to date, the data are sparse,” it concluded.
The American College of Nurse-Midwives also denounced the doctoral requirement, as have trade associations for neonatal nurse practitioners and neonatal nurses, citing “the lack of scientific evidence that ... doctoral-level education is beneficial to patients, practitioners, or society.”
There is no evidence that doctoral-level nurse-midwives will provide better care, Ms. Breedlove said.
“This is profit over purpose,” she added.
Ms. Bole disputed Ms. Breedlove’s accusation of a profit motive. Asked for reasons for the change, she offered broad statements: “The decision to upgrade our program was made to ensure that our graduates are prepared for the challenges they will face in the evolving health care landscape.”
Like Ms. Breedlove, Liz Donnelly, vice chair of the health policy committee for the California Nurse-Midwives Association, worries that UCSF’s switch to a doctoral degree will exacerbate the twin crises of maternal mortality and a shrinking obstetrics workforce across California and the nation.
On average, 10-12 nurse-midwives graduated from the UCSF master’s program each year over the past decade, Ms. Bole said. California’s remaining master’s program in nurse-midwifery is at California State University in Fullerton, south of Los Angeles, and it graduated 8 nurse-midwives in 2023 and 11 in 2024.
More than half of rural counties in the United States lacked obstetric care in 2018, according to a Government Accountability Office report.
In some parts of California, expectant mothers must drive 2 hours for care, said Bethany Sasaki, who runs Midtown Nurse Midwives, a Sacramento birth center. It has had to stop accepting new clients because it cannot find midwives.
Ms. Donnelly predicted the closure of UCSF’s midwifery program will significantly reduce the number of nurse-midwives entering the workforce and will inhibit people with fewer resources from attending the program. “Specifically, I think it’s going to reduce folks of color, people from rural communities, people from poor communities,” she said.
UCSF’s change will also likely undercut efforts to train providers from diverse backgrounds.
Natasha, a 37-year-old Afro-Puerto Rican mother of two, has spent a decade preparing to train as a nurse-midwife so she could help women like herself through pregnancy and childbirth. She asked to be identified only by her first name out of fear of reducing her chances of graduate school admission.
The UCSF program’s pause, plus the added time and expense to get a doctoral degree, has muddied her career path.
“The master’s was just the perfect program,” said Natasha, who lives in the Bay Area and cannot travel to the other end of the state to attend California State University-Fullerton. “I’m frustrated, and I feel deflated. I now have to find another career path.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation. KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Updates in COPD Guidelines and Treatment
Al Wachami N, Guennouni M, Iderdar Y, et al. Estimating the global prevalence of chronic obstructive pulmonary disease (COPD): a systematic review and meta-analysis. BMC Public Health. 2024;24(1):297. doi:10.1186/s12889-024-17686-9
COPD trends brief. American Lung Association. Accessed July 11, 2024. https://www.lung.org/research/trends-in-lung-disease/copd-trends-brief
Chronic obstructive pulmonary disease (COPD). World Health Organization. March 16, 2023. Accessed July 11, 2024. https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
Shalabi MS, Aqdi SW, Alfort OA, et al. Effectiveness and safety of bronchodilators and inhaled corticosteroids in the management of chronic obstructive pulmonary disease. Int J Commun Med Public Health. 2023;10(8):2955-2959. doi:10.18203/2394-6040.ijcmph20232392
McCormick B. FDA approves ensifentrine for maintenance treatment of adult patients with COPD. AJMC. June 26, 2024. Accessed July 11, 2024. https://www.ajmc.com/view/fda-approves-ensifentrine-for-maintenance-treatment-of-adult-patients-with-copd
Kersul AL, Cosio BG. Biologics in COPD. Open Resp Arch. 2024;6(2):100306. doi:10.1016/j.opresp.2024.100306
2023 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease. Accessed July 11, 2024. https://goldcopd.org/2023-gold-report-2
2024 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease. Accessed July 11, 2024. https://goldcopd.org/2024-gold-report/
Regeneron Pharmaceuticals Inc. Dupixent® (dupilumab) late-breaking data from NOTUS confirmatory phase 3 COPD trial presented at ATS and published in the New England Journal of Medicine [press release]. May 20, 2024. Accessed July 11, 2024. https://investor.regeneron.com/news-releases/news-release-details/dupixentr-dupilumab-late-breaking-data-notus-confirmatory-phase
Pavord ID, Chapman KR, Bafadhel M, et al. Mepolizumab for eosinophil-associated COPD: analysis of METREX and METREO. Int J Chron Obstruct Pulmon Dis. 2021;16:1755-1770. doi:10.2147/COPD.S294333
Mepolizumab as add-on treatment in participants with COPD characterized by frequent exacerbations and eosinophil level (MATINEE). Clinicaltrials.gov. Updated August 28, 2023. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT04133909
Singh D, Criner GJ, Agustí A, et al. Benralizumab prevents recurrent exacerbations in patients with chronic obstructive pulmonary disease: a post hoc analysis. Int J Chron Obstruct Pulmon Dis. 2023;18:1595-1599. doi:10.2147/COPD.S418944
Efficacy and safety of benralizumab in moderate to very severe chronic obstructive pulmonary disease (COPD) with a history of frequent exacerbations (RESOLUTE). Clinicaltrials.gov. Updated May 8, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT04053634
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (TITANIA). Clinicaltrials.gov. Updated June 27, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05158387
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (OBERON). Clinicaltrials.gov. Updated June 21, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05166889
Long-term efficacy and safety of tozorakimab in participants with chronic obstructive pulmonary disease with a history of exacerbations (PROSPERO). Clinicaltrials.gov. Updated June 20, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05742802
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (MIRANDA). Clinicaltrials.gov. Updated June 4, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT06040086
Study to assess the efficacy, safety, and tolerability of SAR440340/REGN3500/itepekimab in chronic obstructive pulmonary disease (COPD) (AERIFY-1). ClinicalTrials.gov. Updated June 21, 2024. Accessed July 11, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04701983
Study to assess the efficacy, safety, and tolerability of SAR440340/REGN3500/itepekimab in chronic obstructive pulmonary disease (COPD) (AERIFY-2). ClinicalTrials.gov. Updated May 9, 2024. Accessed July 11, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04751487
ALIENTO and ARNASA: study designs of two randomised, double-blind, placebo-controlled trials of astegolimab in patients with COPD. Medically. 2023. Accessed July 11, 2024. https://medically.gene.com/global/en/unrestricted/respiratory/ERS-2023/ers-2023-poster-brightling-aliento-and-arnasa-study-des.html
Anzueto A, Barjaktarevic IZ, Siler TM, et al. Ensifentrine, a novel phosphodiesterase 3 and 4 inhibitor for the treatment of chronic obstructive pulmonary disease: randomized, double-blind, placebo-controlled, multicenter phase III trials (the ENHANCE trials). Am J Respir Crit Care Med. 2023;208(4):406-416. doi:10.1164/rccm.202306-0944OC
US Preventive Services Taskforce. Lung cancer: screening. March 9, 2021. Accessed July 11, 2024. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
Al Wachami N, Guennouni M, Iderdar Y, et al. Estimating the global prevalence of chronic obstructive pulmonary disease (COPD): a systematic review and meta-analysis. BMC Public Health. 2024;24(1):297. doi:10.1186/s12889-024-17686-9
COPD trends brief. American Lung Association. Accessed July 11, 2024. https://www.lung.org/research/trends-in-lung-disease/copd-trends-brief
Chronic obstructive pulmonary disease (COPD). World Health Organization. March 16, 2023. Accessed July 11, 2024. https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
Shalabi MS, Aqdi SW, Alfort OA, et al. Effectiveness and safety of bronchodilators and inhaled corticosteroids in the management of chronic obstructive pulmonary disease. Int J Commun Med Public Health. 2023;10(8):2955-2959. doi:10.18203/2394-6040.ijcmph20232392
McCormick B. FDA approves ensifentrine for maintenance treatment of adult patients with COPD. AJMC. June 26, 2024. Accessed July 11, 2024. https://www.ajmc.com/view/fda-approves-ensifentrine-for-maintenance-treatment-of-adult-patients-with-copd
Kersul AL, Cosio BG. Biologics in COPD. Open Resp Arch. 2024;6(2):100306. doi:10.1016/j.opresp.2024.100306
2023 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease. Accessed July 11, 2024. https://goldcopd.org/2023-gold-report-2
2024 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease. Accessed July 11, 2024. https://goldcopd.org/2024-gold-report/
Regeneron Pharmaceuticals Inc. Dupixent® (dupilumab) late-breaking data from NOTUS confirmatory phase 3 COPD trial presented at ATS and published in the New England Journal of Medicine [press release]. May 20, 2024. Accessed July 11, 2024. https://investor.regeneron.com/news-releases/news-release-details/dupixentr-dupilumab-late-breaking-data-notus-confirmatory-phase
Pavord ID, Chapman KR, Bafadhel M, et al. Mepolizumab for eosinophil-associated COPD: analysis of METREX and METREO. Int J Chron Obstruct Pulmon Dis. 2021;16:1755-1770. doi:10.2147/COPD.S294333
Mepolizumab as add-on treatment in participants with COPD characterized by frequent exacerbations and eosinophil level (MATINEE). Clinicaltrials.gov. Updated August 28, 2023. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT04133909
Singh D, Criner GJ, Agustí A, et al. Benralizumab prevents recurrent exacerbations in patients with chronic obstructive pulmonary disease: a post hoc analysis. Int J Chron Obstruct Pulmon Dis. 2023;18:1595-1599. doi:10.2147/COPD.S418944
Efficacy and safety of benralizumab in moderate to very severe chronic obstructive pulmonary disease (COPD) with a history of frequent exacerbations (RESOLUTE). Clinicaltrials.gov. Updated May 8, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT04053634
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (TITANIA). Clinicaltrials.gov. Updated June 27, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05158387
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (OBERON). Clinicaltrials.gov. Updated June 21, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05166889
Long-term efficacy and safety of tozorakimab in participants with chronic obstructive pulmonary disease with a history of exacerbations (PROSPERO). Clinicaltrials.gov. Updated June 20, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05742802
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (MIRANDA). Clinicaltrials.gov. Updated June 4, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT06040086
Study to assess the efficacy, safety, and tolerability of SAR440340/REGN3500/itepekimab in chronic obstructive pulmonary disease (COPD) (AERIFY-1). ClinicalTrials.gov. Updated June 21, 2024. Accessed July 11, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04701983
Study to assess the efficacy, safety, and tolerability of SAR440340/REGN3500/itepekimab in chronic obstructive pulmonary disease (COPD) (AERIFY-2). ClinicalTrials.gov. Updated May 9, 2024. Accessed July 11, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04751487
ALIENTO and ARNASA: study designs of two randomised, double-blind, placebo-controlled trials of astegolimab in patients with COPD. Medically. 2023. Accessed July 11, 2024. https://medically.gene.com/global/en/unrestricted/respiratory/ERS-2023/ers-2023-poster-brightling-aliento-and-arnasa-study-des.html
Anzueto A, Barjaktarevic IZ, Siler TM, et al. Ensifentrine, a novel phosphodiesterase 3 and 4 inhibitor for the treatment of chronic obstructive pulmonary disease: randomized, double-blind, placebo-controlled, multicenter phase III trials (the ENHANCE trials). Am J Respir Crit Care Med. 2023;208(4):406-416. doi:10.1164/rccm.202306-0944OC
US Preventive Services Taskforce. Lung cancer: screening. March 9, 2021. Accessed July 11, 2024. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
Al Wachami N, Guennouni M, Iderdar Y, et al. Estimating the global prevalence of chronic obstructive pulmonary disease (COPD): a systematic review and meta-analysis. BMC Public Health. 2024;24(1):297. doi:10.1186/s12889-024-17686-9
COPD trends brief. American Lung Association. Accessed July 11, 2024. https://www.lung.org/research/trends-in-lung-disease/copd-trends-brief
Chronic obstructive pulmonary disease (COPD). World Health Organization. March 16, 2023. Accessed July 11, 2024. https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
Shalabi MS, Aqdi SW, Alfort OA, et al. Effectiveness and safety of bronchodilators and inhaled corticosteroids in the management of chronic obstructive pulmonary disease. Int J Commun Med Public Health. 2023;10(8):2955-2959. doi:10.18203/2394-6040.ijcmph20232392
McCormick B. FDA approves ensifentrine for maintenance treatment of adult patients with COPD. AJMC. June 26, 2024. Accessed July 11, 2024. https://www.ajmc.com/view/fda-approves-ensifentrine-for-maintenance-treatment-of-adult-patients-with-copd
Kersul AL, Cosio BG. Biologics in COPD. Open Resp Arch. 2024;6(2):100306. doi:10.1016/j.opresp.2024.100306
2023 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease. Accessed July 11, 2024. https://goldcopd.org/2023-gold-report-2
2024 GOLD Report. Global Initiative for Chronic Obstructive Lung Disease. Accessed July 11, 2024. https://goldcopd.org/2024-gold-report/
Regeneron Pharmaceuticals Inc. Dupixent® (dupilumab) late-breaking data from NOTUS confirmatory phase 3 COPD trial presented at ATS and published in the New England Journal of Medicine [press release]. May 20, 2024. Accessed July 11, 2024. https://investor.regeneron.com/news-releases/news-release-details/dupixentr-dupilumab-late-breaking-data-notus-confirmatory-phase
Pavord ID, Chapman KR, Bafadhel M, et al. Mepolizumab for eosinophil-associated COPD: analysis of METREX and METREO. Int J Chron Obstruct Pulmon Dis. 2021;16:1755-1770. doi:10.2147/COPD.S294333
Mepolizumab as add-on treatment in participants with COPD characterized by frequent exacerbations and eosinophil level (MATINEE). Clinicaltrials.gov. Updated August 28, 2023. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT04133909
Singh D, Criner GJ, Agustí A, et al. Benralizumab prevents recurrent exacerbations in patients with chronic obstructive pulmonary disease: a post hoc analysis. Int J Chron Obstruct Pulmon Dis. 2023;18:1595-1599. doi:10.2147/COPD.S418944
Efficacy and safety of benralizumab in moderate to very severe chronic obstructive pulmonary disease (COPD) with a history of frequent exacerbations (RESOLUTE). Clinicaltrials.gov. Updated May 8, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT04053634
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (TITANIA). Clinicaltrials.gov. Updated June 27, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05158387
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (OBERON). Clinicaltrials.gov. Updated June 21, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05166889
Long-term efficacy and safety of tozorakimab in participants with chronic obstructive pulmonary disease with a history of exacerbations (PROSPERO). Clinicaltrials.gov. Updated June 20, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT05742802
Efficacy and safety of tozorakimab in symptomatic chronic obstructive pulmonary disease with a history of exacerbations (MIRANDA). Clinicaltrials.gov. Updated June 4, 2024. Accessed July 11, 2024. https://clinicaltrials.gov/study/NCT06040086
Study to assess the efficacy, safety, and tolerability of SAR440340/REGN3500/itepekimab in chronic obstructive pulmonary disease (COPD) (AERIFY-1). ClinicalTrials.gov. Updated June 21, 2024. Accessed July 11, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04701983
Study to assess the efficacy, safety, and tolerability of SAR440340/REGN3500/itepekimab in chronic obstructive pulmonary disease (COPD) (AERIFY-2). ClinicalTrials.gov. Updated May 9, 2024. Accessed July 11, 2024. https://classic.clinicaltrials.gov/ct2/show/NCT04751487
ALIENTO and ARNASA: study designs of two randomised, double-blind, placebo-controlled trials of astegolimab in patients with COPD. Medically. 2023. Accessed July 11, 2024. https://medically.gene.com/global/en/unrestricted/respiratory/ERS-2023/ers-2023-poster-brightling-aliento-and-arnasa-study-des.html
Anzueto A, Barjaktarevic IZ, Siler TM, et al. Ensifentrine, a novel phosphodiesterase 3 and 4 inhibitor for the treatment of chronic obstructive pulmonary disease: randomized, double-blind, placebo-controlled, multicenter phase III trials (the ENHANCE trials). Am J Respir Crit Care Med. 2023;208(4):406-416. doi:10.1164/rccm.202306-0944OC
US Preventive Services Taskforce. Lung cancer: screening. March 9, 2021. Accessed July 11, 2024. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening
Gram Stain Doesn’t Improve UTI Diagnosis in the ED
TOPLINE:
Compared with other urine analysis methods, urine Gram stain has a moderate predictive value for detecting gram-negative bacteria in urine culture but does not significantly improve urinary tract infection (UTI) diagnosis in the emergency department (ED).
METHODOLOGY:
- Researchers conducted an observational cohort study at the University Medical Center Groningen in the Netherlands, encompassing 1358 episodes across 1136 patients suspected of having a UTI.
- The study included the following predefined subgroups: patients using urinary catheters and patients with leukopenia (< 4.0×10⁹ leucocytes/L). Urine dipstick nitrite, automated urinalysis, Gram stain, and urine cultures were performed on urine samples collected from patients presenting at the ED.
- The sensitivity and specificity of Gram stain for “many” bacteria (quantified as > 15/high power field) were compared with those of urine dipstick nitrite and automated bacterial counting in urinalysis.
TAKEAWAY:
- The sensitivity and specificity of Gram stain for “many” bacteria were 51.3% and 91.0%, respectively, with an accuracy of 76.8%.
- Gram stain showed a positive predictive value (PPV) of 84.7% for gram-negative rods in urine culture; however, the PPV was only 38.4% for gram-positive cocci.
- In the catheter subgroup, the presence of monomorphic bacteria quantified as “many” had a higher PPV for diagnosing a UTI than the presence of polymorphic bacteria with the same quantification.
- The overall performance of Gram stain in diagnosing a UTI in the ED was comparable to that of automated bacterial counting in urinalysis but better than that of urine dipstick nitrite.
IN PRACTICE:
“With the exception of a moderate prediction of gram-negative bacteria in the UC [urine culture], urine GS [Gram stain] does not improve UTI diagnosis at the ED compared to other urine parameters,” the authors wrote.
SOURCE:
The study was led by Stephanie J.M. Middelkoop, University of Groningen, University Medical Center Groningen, the Netherlands. It was published online on August 16, 2024, in Infectious Diseases.
LIMITATIONS:
The study’s limitations included a small sample size within the leukopenia subgroup, which may have affected the generalizability of the findings. Additionally, the potential influence of refrigeration of urine samples on bacterial growth could have affected the results. In this study, indwelling catheters were not replaced before urine sample collection, which may have affected the accuracy of UTI diagnosis in patients using catheters.
DISCLOSURES:
No conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Compared with other urine analysis methods, urine Gram stain has a moderate predictive value for detecting gram-negative bacteria in urine culture but does not significantly improve urinary tract infection (UTI) diagnosis in the emergency department (ED).
METHODOLOGY:
- Researchers conducted an observational cohort study at the University Medical Center Groningen in the Netherlands, encompassing 1358 episodes across 1136 patients suspected of having a UTI.
- The study included the following predefined subgroups: patients using urinary catheters and patients with leukopenia (< 4.0×10⁹ leucocytes/L). Urine dipstick nitrite, automated urinalysis, Gram stain, and urine cultures were performed on urine samples collected from patients presenting at the ED.
- The sensitivity and specificity of Gram stain for “many” bacteria (quantified as > 15/high power field) were compared with those of urine dipstick nitrite and automated bacterial counting in urinalysis.
TAKEAWAY:
- The sensitivity and specificity of Gram stain for “many” bacteria were 51.3% and 91.0%, respectively, with an accuracy of 76.8%.
- Gram stain showed a positive predictive value (PPV) of 84.7% for gram-negative rods in urine culture; however, the PPV was only 38.4% for gram-positive cocci.
- In the catheter subgroup, the presence of monomorphic bacteria quantified as “many” had a higher PPV for diagnosing a UTI than the presence of polymorphic bacteria with the same quantification.
- The overall performance of Gram stain in diagnosing a UTI in the ED was comparable to that of automated bacterial counting in urinalysis but better than that of urine dipstick nitrite.
IN PRACTICE:
“With the exception of a moderate prediction of gram-negative bacteria in the UC [urine culture], urine GS [Gram stain] does not improve UTI diagnosis at the ED compared to other urine parameters,” the authors wrote.
SOURCE:
The study was led by Stephanie J.M. Middelkoop, University of Groningen, University Medical Center Groningen, the Netherlands. It was published online on August 16, 2024, in Infectious Diseases.
LIMITATIONS:
The study’s limitations included a small sample size within the leukopenia subgroup, which may have affected the generalizability of the findings. Additionally, the potential influence of refrigeration of urine samples on bacterial growth could have affected the results. In this study, indwelling catheters were not replaced before urine sample collection, which may have affected the accuracy of UTI diagnosis in patients using catheters.
DISCLOSURES:
No conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Compared with other urine analysis methods, urine Gram stain has a moderate predictive value for detecting gram-negative bacteria in urine culture but does not significantly improve urinary tract infection (UTI) diagnosis in the emergency department (ED).
METHODOLOGY:
- Researchers conducted an observational cohort study at the University Medical Center Groningen in the Netherlands, encompassing 1358 episodes across 1136 patients suspected of having a UTI.
- The study included the following predefined subgroups: patients using urinary catheters and patients with leukopenia (< 4.0×10⁹ leucocytes/L). Urine dipstick nitrite, automated urinalysis, Gram stain, and urine cultures were performed on urine samples collected from patients presenting at the ED.
- The sensitivity and specificity of Gram stain for “many” bacteria (quantified as > 15/high power field) were compared with those of urine dipstick nitrite and automated bacterial counting in urinalysis.
TAKEAWAY:
- The sensitivity and specificity of Gram stain for “many” bacteria were 51.3% and 91.0%, respectively, with an accuracy of 76.8%.
- Gram stain showed a positive predictive value (PPV) of 84.7% for gram-negative rods in urine culture; however, the PPV was only 38.4% for gram-positive cocci.
- In the catheter subgroup, the presence of monomorphic bacteria quantified as “many” had a higher PPV for diagnosing a UTI than the presence of polymorphic bacteria with the same quantification.
- The overall performance of Gram stain in diagnosing a UTI in the ED was comparable to that of automated bacterial counting in urinalysis but better than that of urine dipstick nitrite.
IN PRACTICE:
“With the exception of a moderate prediction of gram-negative bacteria in the UC [urine culture], urine GS [Gram stain] does not improve UTI diagnosis at the ED compared to other urine parameters,” the authors wrote.
SOURCE:
The study was led by Stephanie J.M. Middelkoop, University of Groningen, University Medical Center Groningen, the Netherlands. It was published online on August 16, 2024, in Infectious Diseases.
LIMITATIONS:
The study’s limitations included a small sample size within the leukopenia subgroup, which may have affected the generalizability of the findings. Additionally, the potential influence of refrigeration of urine samples on bacterial growth could have affected the results. In this study, indwelling catheters were not replaced before urine sample collection, which may have affected the accuracy of UTI diagnosis in patients using catheters.
DISCLOSURES:
No conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
In Colorectal Cancer, Donating Half a Liver Could Save Lives
This transcript has been edited for clarity.
Benjamin L. Schlechter, MD: Dr. Dib is the director of the Hepatobiliary Surgery and Living Donor Program at Beth Israel Deaconess Medical Center here in Boston, and a Harvard Medical School faculty member.
He was previously at the Pontificia Universidad Católica de Chile, a leading international institution investigating the role of liver transplant in colorectal cancer, among other diseases. Dr. Dib, before we move to our discussion, I’d like to hear a bit about your pathway to becoming a transplant surgeon. How did you end up working on colorectal cancer and liver transplants in this field?
Martin J. Dib, MD: Thank you so much, Dr. Schlechter. I am originally from Chile. I had an opportunity to come to Beth Israel Deaconess Medical Center after medical school and I did liver regeneration research at the transplant center. After that, I was lucky enough to match as a general surgery resident at Beth Israel Deaconess.
This is my alma mater and I was able to graduate as a surgeon here. You and I had some paths together. After graduating from Harvard as a surgeon, I was trained in liver transplant, abdominal transplant, surgical oncology, and hepatobiliary surgery at the University of Toronto.
I have been developing this passion for being able to transplant cancer patients and use organ transplant techniques to be able to do complex resections for cancer.
Dr. Schlechter: Let’s talk about the topic for today, which is liver transplant and colorectal cancer. I’ll be honest — this is not a very familiar topic for a lot of oncologists. There are a lot of details that I think are new to us as oncologists. We need to expand this conversation to get access to patients for this.
First and foremost, can you talk about some of the parameters for a resectable liver metastasis vs unresectable disease that would be an indication for a liver transplant?
Dr. Dib: I think this is a very interesting topic because liver transplantation for cancer is not new. Liver transplantation started in the 1960s when people started doing liver transplants for advanced liver tumors. The problem is that they were selecting patients who had very advanced — and poor tumor biology — tumors. The outcomes were not good.
It was only in 1996 when the Milan criteria started. Mazzaferro and colleagues, using strict patient selection, were able to do liver transplant for selected hepatocellular carcinoma patients. Having those excellent outcomes in selecting patients opened the field for what we now call transplant oncology, which is using selection criteria and using other methods to be able to select which patients will do well after transplantation, even with immunosuppression.
Liver transplantation for colorectal metastasis was used at the very beginning of the era of liver transplantation, but with very poor outcomes. It was abandoned because of the outcomes. It is exciting to see that after 20 years of not doing it, there was a group in Norway that started again. They are doing liver transplants for colorectal metastases (mets), but with very selected patients.
In Norway, they had a very unusual setting where they had more liver donors than patients on the list waiting for liver transplant. So they can’t share these livers and we’re all jealous, right? Every single country in the West struggles because we don’t have enough livers for the rest of the list. And they had a lot of livers to be able to transplant people.
They decided to transplant some selected patients with colorectal mets that were unresectable. And the surprise was that they found that they were able to get a 60% survival at 5 years. And so that was new. After that, in Norway, they started showing this data to other centers in the world. It wasn’t until this year that we could see not only the long-term data and long-term outcomes of using liver transplantation for unresectable colorectal mets, but also we’re now having data from a prospective clinical trial from France.
It was three countries in the prospective clinical trial: France, Belgium, and Italy. We now see that we have a little stronger data to support the use of liver transplants for unresectable colorectal mets.
Dr. Schlechter: That’s the TRANSMET study you’re referencing that was presented at ASCO in the late-breaking abstract session in 2024, and then more recently in The Lancet’s eClinicalMedicine. Both of those papers were led by René Adam. That was a cool presentation to sit through. I was in the room, and I was taking a ton of notes and there was a lot of info that came out of that.
First of all, it showed that patients who had received chemotherapy and were responding could then go on to liver transplant in that population. Impressively, 81% of the patients who were randomized to transplant received it. Frankly, that’s a big number, especially compared with the West, as you said, and in particular the US and here in New England where livers are a very precious commodity.
And even accounting for that, if you look at the intention-to-treat analysis, the 5-year overall survival in that population was 57% compared with 13% with chemotherapy. And that feels like a real number for chemotherapy. If you look at the per-protocol analysis, frankly, the numbers are higher.
It’s always a challenging assessment. What was also interesting to me was the pattern of recurrence, which in general was that recurrences were extrahepatic. So not only were patients rendered disease-free, but in general, the liver remained disease-free and only 3% of patients had liver-only recurrence and 11% had widespread metastatic disease.
The biggest group was lung metastases, at about 40%. Ultimately, they reported a progression-free survival of 17. 4 months for transplant compared with 6. 4 months with chemotherapy. On every parameter, it looks like liver transplant wins for these people. Help me out. Who are these people? How do we find these people?
What are the inclusions and exclusions for this population?
Dr. Dib: I think that’s very important. This is not a therapy that will be for every patient. These are selected patients who have liver-only unresectable colorectal mets. These are patients that don’t have any extrahepatic disease and that either the primary has been taken out already or that they have the primary present, but the plan is to take the primary and then do a liver transplantation after 3 months, hopefully after 6 months, of removing the primary.
These are patients who meet all the criteria that we have seen in terms of the best outcomes — patients that have Oslo scores of less than three. The Oslo trial, which included the SECA (Secondary Cancer)-I and SECA-II trials, basically showed that patients with a maximal tumor diameter of less than 5.5 with a pretransplant CEA (carcinoembryonic antigen) of less than 80 that do not have progression on chemotherapy, among other variables, do better. But the concept is that this is a therapy that will apply only to selected patients. That way we can continue to have adequate overall survival post-transplant that would be comparable to other diseases that we do liver transplants for.
Dr. Schlechter: Were there other biomarkers, any mutations that were included or excluded?
Dr. Dib: Yes. If you look at SECA-I, SECA-II trial outcomes, and also TRANSMET, they all say patients with BRAF mutations shouldn’t be transplanted. There are other parameters, including, for example, the site of the primary tumor. Patients with a left-sided colon primary tumor do much better than patients who have a right-sided primary tumor.
That’s not a complete contraindication, but if you look at the most updated inclusion criteria of programs, like the ones that the one that we have here at Beth Israel Deaconess and many others, the inclusion criteria protocols include patients who have only hepatic disease.
So, if there are no extrahepatic mets, the resection of the primary has been done or will be done after a multidisciplinary discussion. We want to make sure they have the absence of BRAF mutation, and that they don’t have disease progression while on chemotherapy. So hopefully we have data from enough months to be able to make sure that there’s no intrahepatic or extrahepatic progression while on chemotherapy.
And that’s including CEA and also looking at the imaging.
Dr. Schlechter: When you’re seeing a patient, how much chemo do you think they should have? What’s a good run chemotherapy-wise for these patients? Let’s say, before I refer a patient to you, how much chemo should they have? And then what should I do? Do I get a PET scan? Do I get MRI? What’s the right scanning I should do to prove there’s no extrahepatic disease before sending a patient in for consideration?
Dr. Dib: First, we need to confirm unresectability. Referring patients early is always a good measure to make sure that we’re all in agreement that it’s an unresectable patient. Having a PET scan from the very beginning is helpful because it shows the disease before doing chemotherapy.
In terms of the lines of chemotherapy, ideally in the TRANSMET trial, for example, the idea was to show tumor control for at least 3 months, with less than three lines of chemotherapy. Some patients will do that with FOLFIRI. It depends on the case.
I think some of those evaluations will need a multidisciplinary discussion. In our case, we are connected to the Norway team. We frequently talk with the Oslo team and an international community of transplant centers to get opinions on particular cases.
But I think referring patients early is a good measure. If we don’t think that they qualify, we will let the team know. We’re strictly looking at patients who have unresectable liver mets that don’t have extrahepatic disease. The idea is to do a primary tumor resection, and then get to transplantation, hopefully after 6 months. In some cases that have some concerns in terms of tumor biology, we may even extend the time from diagnosis to transplant to over 1.5 years.
Dr. Schlechter: Excellent. And what’s the experience like for these patients? In training as a resident many years ago, I saw patients with cirrhosis who went on to have a liver transplant, and that was sort of trading one disease for another. What is the posttransplant, or the remission, experience of a liver transplant for colorectal cancer like for the patient?
Dr. Dib: That’s a very important point. I think that transplantation has gotten better and better, as has chemotherapy systemic therapy. The liver transplantation experience from 20 years ago has improved dramatically. I think the quality of life of liver transplant patients after transplantation has increased quite a bit.
At Beth Israel Deaconess, we have a liver transplant program that is doing over a 100 livers a year. And when you have a high-volume center, usually the experience gets better. The time in the hospital post-transplant decreases.
In general, when we’re doing liver transplants, patients are getting extubated in the OR 30% of the time. The vast majority of patients are going home within 1 or 2 weeks. They need to have immunosuppression for the rest of their lives. We have a very good program of transplant coordinators that will help the family and the patient to live with immunosuppression and live with a transplanted organ.
But I would say that we have many, many patients, especially these patients who are not patients with cirrhosis. Their health is not as deteriorated as patients who have low MELD (model for end-stage liver disease) scores. They don’t have liver disease. They have cancer. So usually patients like that, many of them can go back to work and live a quality of life that is fairly reasonable.
Dr. Schlechter: That’s good to hear. When we hear statements like liver transplant for colon cancer, a lot of us have this picture of a much sicker population, but it’s interesting and true that the colorectal cancer population as a candidate for liver transplant is a much healthier population than the population with cirrhosis.
Let’s talk about organs and donors. Largely in the TRANSMET study, for example, that was cadaveric donors. Those were not living donors and you’ve done a lot of work on living donors. If the answer in the United States, because of limited access to organs, is going to be living donors, who are those donors?
What is that like? How do you identify them?
Dr. Dib: There’s a lot of advantages to using living donors for these patients. In any type of patient that needs a liver transplant, cadaveric donors or deceased donors is the same concept. There are two types of deceased donors: the brain-dead donors and donors after cardiac death. Those are hard to come by.
We still have 15%-20% mortality on the waiting list in the United States. We’re already still struggling to get enough donors to transplant the patients that are on the list. Now, if you add a new indication, which is unresectable colorectal mets, we need to make sure that the outcomes are equivalent to the patients who are going to be transplanted for other reasons.
Right now, for example, the 5-year overall survival of a patient with cirrhosis, or a patient with hepatocellular carcinoma, is over 80% 5-year survival. In the SECA trials and TRANSMET trial, if we do a good selection, I think we can get to 70% 5-year survival. But until we have more data, I think it’s a cautious measure to, as a field, try to use living donors and not compete with the rest of the list of patients who are already dying on the list for liver transplants.
Once we get more data, it’s going to be something that, in the transplant community, we may be able to use deceased donors. Especially deceased donors with maybe extended criteria that are not going to be used for other patients. We can do living-unrelated or living-related donations. Family members or also friends or neighbors or part of the community, even altruistic donors, can donate to a potential recipient. And that enables us to not only time the transplant in an adequate manner, because we’re able to transplant the patient early, but also time it so we can give the number of chemotherapy cycles that we want to give.
That’s a huge advantage. You don’t compete for a liver with the cadaveric waiting list of patients that are waiting for other reasons, and you can select the tumor biology very well because you know exactly when the surgery is going to be. For instance, we can say, okay, this patient has KRAS mutation, left-sided colon cancer, and has been having good tumor biology with no progression. We will wait 6 months from the primary tumor to the transplant, which is going to be 1 year from diagnosis to transplant. And we can see during that time whether they continue to have good tumor biology.
But if you have a deceased donor liver transplant, sometimes you can’t time that well and schedule it. It becomes a bit more tricky in terms of patient selection and making sure that we do this for the people who are going to benefit.
Dr. Schlechter: And how does donor matching work? Is it HLA (human leukocyte antigen) matched or ABO-matched? Who can donate when you say a living-related? For example, when we think about bone marrow transplantation, which we’re all familiar with in the oncology population, it’s an incredibly complex match process. Is this the same challenge?
Dr. Dib: No, it’s a little bit simpler. Living donors for liver transplants need to be between the ages of 18 and 60. They need to be relatively healthy, relatively fit, with a BMI hopefully less than 30, definitely less than 35. The compatibility is ABO compatibility. So, if they’re ABO-compatible, relatively young, relatively healthy, they would be a potential donor and we will go ahead and do a CT scan.
If the CT scan shows that they have a good, adequate anatomy, more than 90% of those will be good donors. I would say that out of 100 people who want to be donors, 25 of them will be adequate. One out of four people who want to save their family member and want to have this operation are able to donate half of their liver to their family member or loved one.
Dr. Schlechter: Excellent. And it’s helpful to know that the matching process is simpler. During his discussion, René Adam unequivocally stated that liver transplants are a new standard of care for colorectal cancer. And I guess my question is, do you agree with this statement? How do we balance the demand for living donors and the demand for deceased donors? Especially in a time of increasing fatty liver disease and obesity, other indications for liver transplant, causes of cirrhosis, and also in an era of young-onset colorectal cancer. Patients are younger. Is this a new standard of care? Do you agree with that statement?
Dr. Dib: I do agree with that statement. I think it’s important to understand that not all patients with colorectal mets are the same. Of the number of patients in the United States who have colorectal cancer, let’s say 50% of them will have liver metastasis. Only 15%-20% of them will have liver-only metastasis.
This is only for patients who have liver-only metastasis without extrahepatic disease. And only maybe 15%-20% of them will meet all the criteria to be able to undergo liver transplantation. I think it’s for a very selective subset of patients who have very good tumor biology, generally young patients who don’t have any other alternative to having even a complex liver resection and are not able to get R0 resection. That is when we could think about doing liver transplantation.
It’s one more of the skills that we can have. It doesn’t mean that it will be the only skill, or the best skill, for all of the patients.
Dr. Schlechter: When a patient volunteers to be a living donor for a loved one or a family member, and they go through all the screening and they’re found to be a candidate, what is the surgical experience for that patient?
How long are they in the hospital? What sort of operation is that?
Dr. Dib: Living donors are very special patients. These are patients who do not need an operation. And the only reason they’re doing this is to save the life of their loved one. Donor safety is our priority number one, two, three, and four. The donor operation needs to be perfect.
And so we take good care of, first of all, selecting the living donors, making sure that they’re young and they don’t have any big contraindications. We also ensure that they are well informed of the process. The living donor surgery that we’re now doing is laparoscopic and minimally invasive. Here at Beth Israel Deaconess, we have done it laparoscopically with very good results.
I think that experience before and after the surgery gets so much better because of the better recovery. They’re able to go home, in general, within 4 or 5 days, and they get on with their normal life within 6-8 weeks. I think it’s important for them to know all the processes and the actual risks and benefits for the recipient.
Among those risks, I think it’s important for them to understand that this is a complex operation. Even if we do it laparoscopically or robotically, so that the scar is less, inside we’re still taking out half of the liver. That is a surgery that needs to be undertaken very meticulously, with a focus on minimizing any bleeding.
It’s a surgery that takes a long time. It takes about 6 hours. We do our best to try to minimize any risks.
Dr. Schlechter: Excellent. Thanks for that. Today we had Dr. Martin Dib joining us to discuss liver transplant for metastatic colorectal cancer. We discussed the various important criteria. We discussed that early referral to multidisciplinary centers that manage these is important to help get patients set up.
We discussed the fact that there are certain inclusion and exclusion criteria to consider. Obviously, unresectable disease is a critical determination that should be made by a liver surgeon. The absence of extrahepatic disease is important in staging with PET or other imaging. We discussed certain other biological exclusions.
There’s a relative contraindication of right-sided vs left-sided cancers, but right-sided cancers can be transplanted. We discussed that an elevated CEA greater than 80 is a contraindication, as are mutations in BRAF. We reviewed data from both the TRANSMET trial recently published in The Lancet and presented at ASCO in 2024, as well as the older Oslo criteria and Oslo trials and SECA trials.
And finally, we heard that donors can now come as living donors, a laparoscopic robotic surgery with a better safety profile, and greater access to organs that are ABO matched and not HLA matched because of the nature of the biology. Thank you again for joining us.
Benjamin L. Schlechter, MD, is senior physician, Gastrointestinal Cancer Center, Dana-Farber Cancer Institute, Boston, Massachusetts. He has disclosed no relevant financial relationships. Martin J. Dib, MD, is member of the faculty, Department of Surgery, Harvard Medical School; director of Hepatobiliary Surgery, Division of Transplantation, Beth Israel Deaconess Medical Center, Boston. He has disclosed no relevant financial relationships.
A version of this transcript appeared on Medscape.com.
This transcript has been edited for clarity.
Benjamin L. Schlechter, MD: Dr. Dib is the director of the Hepatobiliary Surgery and Living Donor Program at Beth Israel Deaconess Medical Center here in Boston, and a Harvard Medical School faculty member.
He was previously at the Pontificia Universidad Católica de Chile, a leading international institution investigating the role of liver transplant in colorectal cancer, among other diseases. Dr. Dib, before we move to our discussion, I’d like to hear a bit about your pathway to becoming a transplant surgeon. How did you end up working on colorectal cancer and liver transplants in this field?
Martin J. Dib, MD: Thank you so much, Dr. Schlechter. I am originally from Chile. I had an opportunity to come to Beth Israel Deaconess Medical Center after medical school and I did liver regeneration research at the transplant center. After that, I was lucky enough to match as a general surgery resident at Beth Israel Deaconess.
This is my alma mater and I was able to graduate as a surgeon here. You and I had some paths together. After graduating from Harvard as a surgeon, I was trained in liver transplant, abdominal transplant, surgical oncology, and hepatobiliary surgery at the University of Toronto.
I have been developing this passion for being able to transplant cancer patients and use organ transplant techniques to be able to do complex resections for cancer.
Dr. Schlechter: Let’s talk about the topic for today, which is liver transplant and colorectal cancer. I’ll be honest — this is not a very familiar topic for a lot of oncologists. There are a lot of details that I think are new to us as oncologists. We need to expand this conversation to get access to patients for this.
First and foremost, can you talk about some of the parameters for a resectable liver metastasis vs unresectable disease that would be an indication for a liver transplant?
Dr. Dib: I think this is a very interesting topic because liver transplantation for cancer is not new. Liver transplantation started in the 1960s when people started doing liver transplants for advanced liver tumors. The problem is that they were selecting patients who had very advanced — and poor tumor biology — tumors. The outcomes were not good.
It was only in 1996 when the Milan criteria started. Mazzaferro and colleagues, using strict patient selection, were able to do liver transplant for selected hepatocellular carcinoma patients. Having those excellent outcomes in selecting patients opened the field for what we now call transplant oncology, which is using selection criteria and using other methods to be able to select which patients will do well after transplantation, even with immunosuppression.
Liver transplantation for colorectal metastasis was used at the very beginning of the era of liver transplantation, but with very poor outcomes. It was abandoned because of the outcomes. It is exciting to see that after 20 years of not doing it, there was a group in Norway that started again. They are doing liver transplants for colorectal metastases (mets), but with very selected patients.
In Norway, they had a very unusual setting where they had more liver donors than patients on the list waiting for liver transplant. So they can’t share these livers and we’re all jealous, right? Every single country in the West struggles because we don’t have enough livers for the rest of the list. And they had a lot of livers to be able to transplant people.
They decided to transplant some selected patients with colorectal mets that were unresectable. And the surprise was that they found that they were able to get a 60% survival at 5 years. And so that was new. After that, in Norway, they started showing this data to other centers in the world. It wasn’t until this year that we could see not only the long-term data and long-term outcomes of using liver transplantation for unresectable colorectal mets, but also we’re now having data from a prospective clinical trial from France.
It was three countries in the prospective clinical trial: France, Belgium, and Italy. We now see that we have a little stronger data to support the use of liver transplants for unresectable colorectal mets.
Dr. Schlechter: That’s the TRANSMET study you’re referencing that was presented at ASCO in the late-breaking abstract session in 2024, and then more recently in The Lancet’s eClinicalMedicine. Both of those papers were led by René Adam. That was a cool presentation to sit through. I was in the room, and I was taking a ton of notes and there was a lot of info that came out of that.
First of all, it showed that patients who had received chemotherapy and were responding could then go on to liver transplant in that population. Impressively, 81% of the patients who were randomized to transplant received it. Frankly, that’s a big number, especially compared with the West, as you said, and in particular the US and here in New England where livers are a very precious commodity.
And even accounting for that, if you look at the intention-to-treat analysis, the 5-year overall survival in that population was 57% compared with 13% with chemotherapy. And that feels like a real number for chemotherapy. If you look at the per-protocol analysis, frankly, the numbers are higher.
It’s always a challenging assessment. What was also interesting to me was the pattern of recurrence, which in general was that recurrences were extrahepatic. So not only were patients rendered disease-free, but in general, the liver remained disease-free and only 3% of patients had liver-only recurrence and 11% had widespread metastatic disease.
The biggest group was lung metastases, at about 40%. Ultimately, they reported a progression-free survival of 17. 4 months for transplant compared with 6. 4 months with chemotherapy. On every parameter, it looks like liver transplant wins for these people. Help me out. Who are these people? How do we find these people?
What are the inclusions and exclusions for this population?
Dr. Dib: I think that’s very important. This is not a therapy that will be for every patient. These are selected patients who have liver-only unresectable colorectal mets. These are patients that don’t have any extrahepatic disease and that either the primary has been taken out already or that they have the primary present, but the plan is to take the primary and then do a liver transplantation after 3 months, hopefully after 6 months, of removing the primary.
These are patients who meet all the criteria that we have seen in terms of the best outcomes — patients that have Oslo scores of less than three. The Oslo trial, which included the SECA (Secondary Cancer)-I and SECA-II trials, basically showed that patients with a maximal tumor diameter of less than 5.5 with a pretransplant CEA (carcinoembryonic antigen) of less than 80 that do not have progression on chemotherapy, among other variables, do better. But the concept is that this is a therapy that will apply only to selected patients. That way we can continue to have adequate overall survival post-transplant that would be comparable to other diseases that we do liver transplants for.
Dr. Schlechter: Were there other biomarkers, any mutations that were included or excluded?
Dr. Dib: Yes. If you look at SECA-I, SECA-II trial outcomes, and also TRANSMET, they all say patients with BRAF mutations shouldn’t be transplanted. There are other parameters, including, for example, the site of the primary tumor. Patients with a left-sided colon primary tumor do much better than patients who have a right-sided primary tumor.
That’s not a complete contraindication, but if you look at the most updated inclusion criteria of programs, like the ones that the one that we have here at Beth Israel Deaconess and many others, the inclusion criteria protocols include patients who have only hepatic disease.
So, if there are no extrahepatic mets, the resection of the primary has been done or will be done after a multidisciplinary discussion. We want to make sure they have the absence of BRAF mutation, and that they don’t have disease progression while on chemotherapy. So hopefully we have data from enough months to be able to make sure that there’s no intrahepatic or extrahepatic progression while on chemotherapy.
And that’s including CEA and also looking at the imaging.
Dr. Schlechter: When you’re seeing a patient, how much chemo do you think they should have? What’s a good run chemotherapy-wise for these patients? Let’s say, before I refer a patient to you, how much chemo should they have? And then what should I do? Do I get a PET scan? Do I get MRI? What’s the right scanning I should do to prove there’s no extrahepatic disease before sending a patient in for consideration?
Dr. Dib: First, we need to confirm unresectability. Referring patients early is always a good measure to make sure that we’re all in agreement that it’s an unresectable patient. Having a PET scan from the very beginning is helpful because it shows the disease before doing chemotherapy.
In terms of the lines of chemotherapy, ideally in the TRANSMET trial, for example, the idea was to show tumor control for at least 3 months, with less than three lines of chemotherapy. Some patients will do that with FOLFIRI. It depends on the case.
I think some of those evaluations will need a multidisciplinary discussion. In our case, we are connected to the Norway team. We frequently talk with the Oslo team and an international community of transplant centers to get opinions on particular cases.
But I think referring patients early is a good measure. If we don’t think that they qualify, we will let the team know. We’re strictly looking at patients who have unresectable liver mets that don’t have extrahepatic disease. The idea is to do a primary tumor resection, and then get to transplantation, hopefully after 6 months. In some cases that have some concerns in terms of tumor biology, we may even extend the time from diagnosis to transplant to over 1.5 years.
Dr. Schlechter: Excellent. And what’s the experience like for these patients? In training as a resident many years ago, I saw patients with cirrhosis who went on to have a liver transplant, and that was sort of trading one disease for another. What is the posttransplant, or the remission, experience of a liver transplant for colorectal cancer like for the patient?
Dr. Dib: That’s a very important point. I think that transplantation has gotten better and better, as has chemotherapy systemic therapy. The liver transplantation experience from 20 years ago has improved dramatically. I think the quality of life of liver transplant patients after transplantation has increased quite a bit.
At Beth Israel Deaconess, we have a liver transplant program that is doing over a 100 livers a year. And when you have a high-volume center, usually the experience gets better. The time in the hospital post-transplant decreases.
In general, when we’re doing liver transplants, patients are getting extubated in the OR 30% of the time. The vast majority of patients are going home within 1 or 2 weeks. They need to have immunosuppression for the rest of their lives. We have a very good program of transplant coordinators that will help the family and the patient to live with immunosuppression and live with a transplanted organ.
But I would say that we have many, many patients, especially these patients who are not patients with cirrhosis. Their health is not as deteriorated as patients who have low MELD (model for end-stage liver disease) scores. They don’t have liver disease. They have cancer. So usually patients like that, many of them can go back to work and live a quality of life that is fairly reasonable.
Dr. Schlechter: That’s good to hear. When we hear statements like liver transplant for colon cancer, a lot of us have this picture of a much sicker population, but it’s interesting and true that the colorectal cancer population as a candidate for liver transplant is a much healthier population than the population with cirrhosis.
Let’s talk about organs and donors. Largely in the TRANSMET study, for example, that was cadaveric donors. Those were not living donors and you’ve done a lot of work on living donors. If the answer in the United States, because of limited access to organs, is going to be living donors, who are those donors?
What is that like? How do you identify them?
Dr. Dib: There’s a lot of advantages to using living donors for these patients. In any type of patient that needs a liver transplant, cadaveric donors or deceased donors is the same concept. There are two types of deceased donors: the brain-dead donors and donors after cardiac death. Those are hard to come by.
We still have 15%-20% mortality on the waiting list in the United States. We’re already still struggling to get enough donors to transplant the patients that are on the list. Now, if you add a new indication, which is unresectable colorectal mets, we need to make sure that the outcomes are equivalent to the patients who are going to be transplanted for other reasons.
Right now, for example, the 5-year overall survival of a patient with cirrhosis, or a patient with hepatocellular carcinoma, is over 80% 5-year survival. In the SECA trials and TRANSMET trial, if we do a good selection, I think we can get to 70% 5-year survival. But until we have more data, I think it’s a cautious measure to, as a field, try to use living donors and not compete with the rest of the list of patients who are already dying on the list for liver transplants.
Once we get more data, it’s going to be something that, in the transplant community, we may be able to use deceased donors. Especially deceased donors with maybe extended criteria that are not going to be used for other patients. We can do living-unrelated or living-related donations. Family members or also friends or neighbors or part of the community, even altruistic donors, can donate to a potential recipient. And that enables us to not only time the transplant in an adequate manner, because we’re able to transplant the patient early, but also time it so we can give the number of chemotherapy cycles that we want to give.
That’s a huge advantage. You don’t compete for a liver with the cadaveric waiting list of patients that are waiting for other reasons, and you can select the tumor biology very well because you know exactly when the surgery is going to be. For instance, we can say, okay, this patient has KRAS mutation, left-sided colon cancer, and has been having good tumor biology with no progression. We will wait 6 months from the primary tumor to the transplant, which is going to be 1 year from diagnosis to transplant. And we can see during that time whether they continue to have good tumor biology.
But if you have a deceased donor liver transplant, sometimes you can’t time that well and schedule it. It becomes a bit more tricky in terms of patient selection and making sure that we do this for the people who are going to benefit.
Dr. Schlechter: And how does donor matching work? Is it HLA (human leukocyte antigen) matched or ABO-matched? Who can donate when you say a living-related? For example, when we think about bone marrow transplantation, which we’re all familiar with in the oncology population, it’s an incredibly complex match process. Is this the same challenge?
Dr. Dib: No, it’s a little bit simpler. Living donors for liver transplants need to be between the ages of 18 and 60. They need to be relatively healthy, relatively fit, with a BMI hopefully less than 30, definitely less than 35. The compatibility is ABO compatibility. So, if they’re ABO-compatible, relatively young, relatively healthy, they would be a potential donor and we will go ahead and do a CT scan.
If the CT scan shows that they have a good, adequate anatomy, more than 90% of those will be good donors. I would say that out of 100 people who want to be donors, 25 of them will be adequate. One out of four people who want to save their family member and want to have this operation are able to donate half of their liver to their family member or loved one.
Dr. Schlechter: Excellent. And it’s helpful to know that the matching process is simpler. During his discussion, René Adam unequivocally stated that liver transplants are a new standard of care for colorectal cancer. And I guess my question is, do you agree with this statement? How do we balance the demand for living donors and the demand for deceased donors? Especially in a time of increasing fatty liver disease and obesity, other indications for liver transplant, causes of cirrhosis, and also in an era of young-onset colorectal cancer. Patients are younger. Is this a new standard of care? Do you agree with that statement?
Dr. Dib: I do agree with that statement. I think it’s important to understand that not all patients with colorectal mets are the same. Of the number of patients in the United States who have colorectal cancer, let’s say 50% of them will have liver metastasis. Only 15%-20% of them will have liver-only metastasis.
This is only for patients who have liver-only metastasis without extrahepatic disease. And only maybe 15%-20% of them will meet all the criteria to be able to undergo liver transplantation. I think it’s for a very selective subset of patients who have very good tumor biology, generally young patients who don’t have any other alternative to having even a complex liver resection and are not able to get R0 resection. That is when we could think about doing liver transplantation.
It’s one more of the skills that we can have. It doesn’t mean that it will be the only skill, or the best skill, for all of the patients.
Dr. Schlechter: When a patient volunteers to be a living donor for a loved one or a family member, and they go through all the screening and they’re found to be a candidate, what is the surgical experience for that patient?
How long are they in the hospital? What sort of operation is that?
Dr. Dib: Living donors are very special patients. These are patients who do not need an operation. And the only reason they’re doing this is to save the life of their loved one. Donor safety is our priority number one, two, three, and four. The donor operation needs to be perfect.
And so we take good care of, first of all, selecting the living donors, making sure that they’re young and they don’t have any big contraindications. We also ensure that they are well informed of the process. The living donor surgery that we’re now doing is laparoscopic and minimally invasive. Here at Beth Israel Deaconess, we have done it laparoscopically with very good results.
I think that experience before and after the surgery gets so much better because of the better recovery. They’re able to go home, in general, within 4 or 5 days, and they get on with their normal life within 6-8 weeks. I think it’s important for them to know all the processes and the actual risks and benefits for the recipient.
Among those risks, I think it’s important for them to understand that this is a complex operation. Even if we do it laparoscopically or robotically, so that the scar is less, inside we’re still taking out half of the liver. That is a surgery that needs to be undertaken very meticulously, with a focus on minimizing any bleeding.
It’s a surgery that takes a long time. It takes about 6 hours. We do our best to try to minimize any risks.
Dr. Schlechter: Excellent. Thanks for that. Today we had Dr. Martin Dib joining us to discuss liver transplant for metastatic colorectal cancer. We discussed the various important criteria. We discussed that early referral to multidisciplinary centers that manage these is important to help get patients set up.
We discussed the fact that there are certain inclusion and exclusion criteria to consider. Obviously, unresectable disease is a critical determination that should be made by a liver surgeon. The absence of extrahepatic disease is important in staging with PET or other imaging. We discussed certain other biological exclusions.
There’s a relative contraindication of right-sided vs left-sided cancers, but right-sided cancers can be transplanted. We discussed that an elevated CEA greater than 80 is a contraindication, as are mutations in BRAF. We reviewed data from both the TRANSMET trial recently published in The Lancet and presented at ASCO in 2024, as well as the older Oslo criteria and Oslo trials and SECA trials.
And finally, we heard that donors can now come as living donors, a laparoscopic robotic surgery with a better safety profile, and greater access to organs that are ABO matched and not HLA matched because of the nature of the biology. Thank you again for joining us.
Benjamin L. Schlechter, MD, is senior physician, Gastrointestinal Cancer Center, Dana-Farber Cancer Institute, Boston, Massachusetts. He has disclosed no relevant financial relationships. Martin J. Dib, MD, is member of the faculty, Department of Surgery, Harvard Medical School; director of Hepatobiliary Surgery, Division of Transplantation, Beth Israel Deaconess Medical Center, Boston. He has disclosed no relevant financial relationships.
A version of this transcript appeared on Medscape.com.
This transcript has been edited for clarity.
Benjamin L. Schlechter, MD: Dr. Dib is the director of the Hepatobiliary Surgery and Living Donor Program at Beth Israel Deaconess Medical Center here in Boston, and a Harvard Medical School faculty member.
He was previously at the Pontificia Universidad Católica de Chile, a leading international institution investigating the role of liver transplant in colorectal cancer, among other diseases. Dr. Dib, before we move to our discussion, I’d like to hear a bit about your pathway to becoming a transplant surgeon. How did you end up working on colorectal cancer and liver transplants in this field?
Martin J. Dib, MD: Thank you so much, Dr. Schlechter. I am originally from Chile. I had an opportunity to come to Beth Israel Deaconess Medical Center after medical school and I did liver regeneration research at the transplant center. After that, I was lucky enough to match as a general surgery resident at Beth Israel Deaconess.
This is my alma mater and I was able to graduate as a surgeon here. You and I had some paths together. After graduating from Harvard as a surgeon, I was trained in liver transplant, abdominal transplant, surgical oncology, and hepatobiliary surgery at the University of Toronto.
I have been developing this passion for being able to transplant cancer patients and use organ transplant techniques to be able to do complex resections for cancer.
Dr. Schlechter: Let’s talk about the topic for today, which is liver transplant and colorectal cancer. I’ll be honest — this is not a very familiar topic for a lot of oncologists. There are a lot of details that I think are new to us as oncologists. We need to expand this conversation to get access to patients for this.
First and foremost, can you talk about some of the parameters for a resectable liver metastasis vs unresectable disease that would be an indication for a liver transplant?
Dr. Dib: I think this is a very interesting topic because liver transplantation for cancer is not new. Liver transplantation started in the 1960s when people started doing liver transplants for advanced liver tumors. The problem is that they were selecting patients who had very advanced — and poor tumor biology — tumors. The outcomes were not good.
It was only in 1996 when the Milan criteria started. Mazzaferro and colleagues, using strict patient selection, were able to do liver transplant for selected hepatocellular carcinoma patients. Having those excellent outcomes in selecting patients opened the field for what we now call transplant oncology, which is using selection criteria and using other methods to be able to select which patients will do well after transplantation, even with immunosuppression.
Liver transplantation for colorectal metastasis was used at the very beginning of the era of liver transplantation, but with very poor outcomes. It was abandoned because of the outcomes. It is exciting to see that after 20 years of not doing it, there was a group in Norway that started again. They are doing liver transplants for colorectal metastases (mets), but with very selected patients.
In Norway, they had a very unusual setting where they had more liver donors than patients on the list waiting for liver transplant. So they can’t share these livers and we’re all jealous, right? Every single country in the West struggles because we don’t have enough livers for the rest of the list. And they had a lot of livers to be able to transplant people.
They decided to transplant some selected patients with colorectal mets that were unresectable. And the surprise was that they found that they were able to get a 60% survival at 5 years. And so that was new. After that, in Norway, they started showing this data to other centers in the world. It wasn’t until this year that we could see not only the long-term data and long-term outcomes of using liver transplantation for unresectable colorectal mets, but also we’re now having data from a prospective clinical trial from France.
It was three countries in the prospective clinical trial: France, Belgium, and Italy. We now see that we have a little stronger data to support the use of liver transplants for unresectable colorectal mets.
Dr. Schlechter: That’s the TRANSMET study you’re referencing that was presented at ASCO in the late-breaking abstract session in 2024, and then more recently in The Lancet’s eClinicalMedicine. Both of those papers were led by René Adam. That was a cool presentation to sit through. I was in the room, and I was taking a ton of notes and there was a lot of info that came out of that.
First of all, it showed that patients who had received chemotherapy and were responding could then go on to liver transplant in that population. Impressively, 81% of the patients who were randomized to transplant received it. Frankly, that’s a big number, especially compared with the West, as you said, and in particular the US and here in New England where livers are a very precious commodity.
And even accounting for that, if you look at the intention-to-treat analysis, the 5-year overall survival in that population was 57% compared with 13% with chemotherapy. And that feels like a real number for chemotherapy. If you look at the per-protocol analysis, frankly, the numbers are higher.
It’s always a challenging assessment. What was also interesting to me was the pattern of recurrence, which in general was that recurrences were extrahepatic. So not only were patients rendered disease-free, but in general, the liver remained disease-free and only 3% of patients had liver-only recurrence and 11% had widespread metastatic disease.
The biggest group was lung metastases, at about 40%. Ultimately, they reported a progression-free survival of 17. 4 months for transplant compared with 6. 4 months with chemotherapy. On every parameter, it looks like liver transplant wins for these people. Help me out. Who are these people? How do we find these people?
What are the inclusions and exclusions for this population?
Dr. Dib: I think that’s very important. This is not a therapy that will be for every patient. These are selected patients who have liver-only unresectable colorectal mets. These are patients that don’t have any extrahepatic disease and that either the primary has been taken out already or that they have the primary present, but the plan is to take the primary and then do a liver transplantation after 3 months, hopefully after 6 months, of removing the primary.
These are patients who meet all the criteria that we have seen in terms of the best outcomes — patients that have Oslo scores of less than three. The Oslo trial, which included the SECA (Secondary Cancer)-I and SECA-II trials, basically showed that patients with a maximal tumor diameter of less than 5.5 with a pretransplant CEA (carcinoembryonic antigen) of less than 80 that do not have progression on chemotherapy, among other variables, do better. But the concept is that this is a therapy that will apply only to selected patients. That way we can continue to have adequate overall survival post-transplant that would be comparable to other diseases that we do liver transplants for.
Dr. Schlechter: Were there other biomarkers, any mutations that were included or excluded?
Dr. Dib: Yes. If you look at SECA-I, SECA-II trial outcomes, and also TRANSMET, they all say patients with BRAF mutations shouldn’t be transplanted. There are other parameters, including, for example, the site of the primary tumor. Patients with a left-sided colon primary tumor do much better than patients who have a right-sided primary tumor.
That’s not a complete contraindication, but if you look at the most updated inclusion criteria of programs, like the ones that the one that we have here at Beth Israel Deaconess and many others, the inclusion criteria protocols include patients who have only hepatic disease.
So, if there are no extrahepatic mets, the resection of the primary has been done or will be done after a multidisciplinary discussion. We want to make sure they have the absence of BRAF mutation, and that they don’t have disease progression while on chemotherapy. So hopefully we have data from enough months to be able to make sure that there’s no intrahepatic or extrahepatic progression while on chemotherapy.
And that’s including CEA and also looking at the imaging.
Dr. Schlechter: When you’re seeing a patient, how much chemo do you think they should have? What’s a good run chemotherapy-wise for these patients? Let’s say, before I refer a patient to you, how much chemo should they have? And then what should I do? Do I get a PET scan? Do I get MRI? What’s the right scanning I should do to prove there’s no extrahepatic disease before sending a patient in for consideration?
Dr. Dib: First, we need to confirm unresectability. Referring patients early is always a good measure to make sure that we’re all in agreement that it’s an unresectable patient. Having a PET scan from the very beginning is helpful because it shows the disease before doing chemotherapy.
In terms of the lines of chemotherapy, ideally in the TRANSMET trial, for example, the idea was to show tumor control for at least 3 months, with less than three lines of chemotherapy. Some patients will do that with FOLFIRI. It depends on the case.
I think some of those evaluations will need a multidisciplinary discussion. In our case, we are connected to the Norway team. We frequently talk with the Oslo team and an international community of transplant centers to get opinions on particular cases.
But I think referring patients early is a good measure. If we don’t think that they qualify, we will let the team know. We’re strictly looking at patients who have unresectable liver mets that don’t have extrahepatic disease. The idea is to do a primary tumor resection, and then get to transplantation, hopefully after 6 months. In some cases that have some concerns in terms of tumor biology, we may even extend the time from diagnosis to transplant to over 1.5 years.
Dr. Schlechter: Excellent. And what’s the experience like for these patients? In training as a resident many years ago, I saw patients with cirrhosis who went on to have a liver transplant, and that was sort of trading one disease for another. What is the posttransplant, or the remission, experience of a liver transplant for colorectal cancer like for the patient?
Dr. Dib: That’s a very important point. I think that transplantation has gotten better and better, as has chemotherapy systemic therapy. The liver transplantation experience from 20 years ago has improved dramatically. I think the quality of life of liver transplant patients after transplantation has increased quite a bit.
At Beth Israel Deaconess, we have a liver transplant program that is doing over a 100 livers a year. And when you have a high-volume center, usually the experience gets better. The time in the hospital post-transplant decreases.
In general, when we’re doing liver transplants, patients are getting extubated in the OR 30% of the time. The vast majority of patients are going home within 1 or 2 weeks. They need to have immunosuppression for the rest of their lives. We have a very good program of transplant coordinators that will help the family and the patient to live with immunosuppression and live with a transplanted organ.
But I would say that we have many, many patients, especially these patients who are not patients with cirrhosis. Their health is not as deteriorated as patients who have low MELD (model for end-stage liver disease) scores. They don’t have liver disease. They have cancer. So usually patients like that, many of them can go back to work and live a quality of life that is fairly reasonable.
Dr. Schlechter: That’s good to hear. When we hear statements like liver transplant for colon cancer, a lot of us have this picture of a much sicker population, but it’s interesting and true that the colorectal cancer population as a candidate for liver transplant is a much healthier population than the population with cirrhosis.
Let’s talk about organs and donors. Largely in the TRANSMET study, for example, that was cadaveric donors. Those were not living donors and you’ve done a lot of work on living donors. If the answer in the United States, because of limited access to organs, is going to be living donors, who are those donors?
What is that like? How do you identify them?
Dr. Dib: There’s a lot of advantages to using living donors for these patients. In any type of patient that needs a liver transplant, cadaveric donors or deceased donors is the same concept. There are two types of deceased donors: the brain-dead donors and donors after cardiac death. Those are hard to come by.
We still have 15%-20% mortality on the waiting list in the United States. We’re already still struggling to get enough donors to transplant the patients that are on the list. Now, if you add a new indication, which is unresectable colorectal mets, we need to make sure that the outcomes are equivalent to the patients who are going to be transplanted for other reasons.
Right now, for example, the 5-year overall survival of a patient with cirrhosis, or a patient with hepatocellular carcinoma, is over 80% 5-year survival. In the SECA trials and TRANSMET trial, if we do a good selection, I think we can get to 70% 5-year survival. But until we have more data, I think it’s a cautious measure to, as a field, try to use living donors and not compete with the rest of the list of patients who are already dying on the list for liver transplants.
Once we get more data, it’s going to be something that, in the transplant community, we may be able to use deceased donors. Especially deceased donors with maybe extended criteria that are not going to be used for other patients. We can do living-unrelated or living-related donations. Family members or also friends or neighbors or part of the community, even altruistic donors, can donate to a potential recipient. And that enables us to not only time the transplant in an adequate manner, because we’re able to transplant the patient early, but also time it so we can give the number of chemotherapy cycles that we want to give.
That’s a huge advantage. You don’t compete for a liver with the cadaveric waiting list of patients that are waiting for other reasons, and you can select the tumor biology very well because you know exactly when the surgery is going to be. For instance, we can say, okay, this patient has KRAS mutation, left-sided colon cancer, and has been having good tumor biology with no progression. We will wait 6 months from the primary tumor to the transplant, which is going to be 1 year from diagnosis to transplant. And we can see during that time whether they continue to have good tumor biology.
But if you have a deceased donor liver transplant, sometimes you can’t time that well and schedule it. It becomes a bit more tricky in terms of patient selection and making sure that we do this for the people who are going to benefit.
Dr. Schlechter: And how does donor matching work? Is it HLA (human leukocyte antigen) matched or ABO-matched? Who can donate when you say a living-related? For example, when we think about bone marrow transplantation, which we’re all familiar with in the oncology population, it’s an incredibly complex match process. Is this the same challenge?
Dr. Dib: No, it’s a little bit simpler. Living donors for liver transplants need to be between the ages of 18 and 60. They need to be relatively healthy, relatively fit, with a BMI hopefully less than 30, definitely less than 35. The compatibility is ABO compatibility. So, if they’re ABO-compatible, relatively young, relatively healthy, they would be a potential donor and we will go ahead and do a CT scan.
If the CT scan shows that they have a good, adequate anatomy, more than 90% of those will be good donors. I would say that out of 100 people who want to be donors, 25 of them will be adequate. One out of four people who want to save their family member and want to have this operation are able to donate half of their liver to their family member or loved one.
Dr. Schlechter: Excellent. And it’s helpful to know that the matching process is simpler. During his discussion, René Adam unequivocally stated that liver transplants are a new standard of care for colorectal cancer. And I guess my question is, do you agree with this statement? How do we balance the demand for living donors and the demand for deceased donors? Especially in a time of increasing fatty liver disease and obesity, other indications for liver transplant, causes of cirrhosis, and also in an era of young-onset colorectal cancer. Patients are younger. Is this a new standard of care? Do you agree with that statement?
Dr. Dib: I do agree with that statement. I think it’s important to understand that not all patients with colorectal mets are the same. Of the number of patients in the United States who have colorectal cancer, let’s say 50% of them will have liver metastasis. Only 15%-20% of them will have liver-only metastasis.
This is only for patients who have liver-only metastasis without extrahepatic disease. And only maybe 15%-20% of them will meet all the criteria to be able to undergo liver transplantation. I think it’s for a very selective subset of patients who have very good tumor biology, generally young patients who don’t have any other alternative to having even a complex liver resection and are not able to get R0 resection. That is when we could think about doing liver transplantation.
It’s one more of the skills that we can have. It doesn’t mean that it will be the only skill, or the best skill, for all of the patients.
Dr. Schlechter: When a patient volunteers to be a living donor for a loved one or a family member, and they go through all the screening and they’re found to be a candidate, what is the surgical experience for that patient?
How long are they in the hospital? What sort of operation is that?
Dr. Dib: Living donors are very special patients. These are patients who do not need an operation. And the only reason they’re doing this is to save the life of their loved one. Donor safety is our priority number one, two, three, and four. The donor operation needs to be perfect.
And so we take good care of, first of all, selecting the living donors, making sure that they’re young and they don’t have any big contraindications. We also ensure that they are well informed of the process. The living donor surgery that we’re now doing is laparoscopic and minimally invasive. Here at Beth Israel Deaconess, we have done it laparoscopically with very good results.
I think that experience before and after the surgery gets so much better because of the better recovery. They’re able to go home, in general, within 4 or 5 days, and they get on with their normal life within 6-8 weeks. I think it’s important for them to know all the processes and the actual risks and benefits for the recipient.
Among those risks, I think it’s important for them to understand that this is a complex operation. Even if we do it laparoscopically or robotically, so that the scar is less, inside we’re still taking out half of the liver. That is a surgery that needs to be undertaken very meticulously, with a focus on minimizing any bleeding.
It’s a surgery that takes a long time. It takes about 6 hours. We do our best to try to minimize any risks.
Dr. Schlechter: Excellent. Thanks for that. Today we had Dr. Martin Dib joining us to discuss liver transplant for metastatic colorectal cancer. We discussed the various important criteria. We discussed that early referral to multidisciplinary centers that manage these is important to help get patients set up.
We discussed the fact that there are certain inclusion and exclusion criteria to consider. Obviously, unresectable disease is a critical determination that should be made by a liver surgeon. The absence of extrahepatic disease is important in staging with PET or other imaging. We discussed certain other biological exclusions.
There’s a relative contraindication of right-sided vs left-sided cancers, but right-sided cancers can be transplanted. We discussed that an elevated CEA greater than 80 is a contraindication, as are mutations in BRAF. We reviewed data from both the TRANSMET trial recently published in The Lancet and presented at ASCO in 2024, as well as the older Oslo criteria and Oslo trials and SECA trials.
And finally, we heard that donors can now come as living donors, a laparoscopic robotic surgery with a better safety profile, and greater access to organs that are ABO matched and not HLA matched because of the nature of the biology. Thank you again for joining us.
Benjamin L. Schlechter, MD, is senior physician, Gastrointestinal Cancer Center, Dana-Farber Cancer Institute, Boston, Massachusetts. He has disclosed no relevant financial relationships. Martin J. Dib, MD, is member of the faculty, Department of Surgery, Harvard Medical School; director of Hepatobiliary Surgery, Division of Transplantation, Beth Israel Deaconess Medical Center, Boston. He has disclosed no relevant financial relationships.
A version of this transcript appeared on Medscape.com.