User login
A healthy White male presented with a rash consisting of erythematous to purpuric macules
Vasculitis is a process in which blood vessels become inflamed and necrotic. Classic small vessel vasculitis reveals a leukocytoclastic vasculitis and most commonly presents as palpable purpura. .” A form of EIV has been described in the literature as “Disney dermatitis.” It is often seen in healthy adults after a long day of walking at the parks. Other forms of exercise, such as jogging, hiking, or swimming, may also cause the condition.
Clinically, EIV affects the lower legs and presents as purpuric macules. Edema may be present. Lesions may be asymptomatic or may present with pruritus or burning. Diagnosis is often made clinically. Skin biopsies for H&E and DIF (direct immunofluorescence) can help distinguish the type of vasculitis that is present. Laboratory tests may be needed to exclude other causes of vasculitis. Episodes may be recurrent.
Henoch-Schönlein purpura (HSP), also called anaphylactoid purpura, is a subtype of small-vessel vasculitis where IgA immunoglobulin is deposited in the vessel walls. It is the most common form of vasculitis is children (usually ages 4-8). In addition to skin, organs such as joints, kidneys, and intestines can be involved. Schamberg’s disease, or capillaritis, is also called pigmented purpura. In this benign condition, leakage from capillaries results in erythematous to brown patches on the lower extremities. A true vasculitis is not seen. The brown discoloration is due to hemosiderin deposition. Cryoglobulinemia is a rare condition in which abnormal immunoglobulin complexes deposit in tissues and vessels. Leukocytoclastic vasculitis is present in small vessels. Palpable purpura and livedo may be seen clinically, and systemic symptoms may be present.
Treatment of EIV is largely supportive as lesions will resolve on their own over 3-4 weeks. Postinflammatory hyperpigmentation may result. Temporary cessation of exercise and compression stockings can help speed up the resolution of lesions. Systemic medications used in the treatment of severe vasculitis, such as systemic steroids, dapsone, and colchicine, are not needed in EIV.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
Vasculitis is a process in which blood vessels become inflamed and necrotic. Classic small vessel vasculitis reveals a leukocytoclastic vasculitis and most commonly presents as palpable purpura. .” A form of EIV has been described in the literature as “Disney dermatitis.” It is often seen in healthy adults after a long day of walking at the parks. Other forms of exercise, such as jogging, hiking, or swimming, may also cause the condition.
Clinically, EIV affects the lower legs and presents as purpuric macules. Edema may be present. Lesions may be asymptomatic or may present with pruritus or burning. Diagnosis is often made clinically. Skin biopsies for H&E and DIF (direct immunofluorescence) can help distinguish the type of vasculitis that is present. Laboratory tests may be needed to exclude other causes of vasculitis. Episodes may be recurrent.
Henoch-Schönlein purpura (HSP), also called anaphylactoid purpura, is a subtype of small-vessel vasculitis where IgA immunoglobulin is deposited in the vessel walls. It is the most common form of vasculitis is children (usually ages 4-8). In addition to skin, organs such as joints, kidneys, and intestines can be involved. Schamberg’s disease, or capillaritis, is also called pigmented purpura. In this benign condition, leakage from capillaries results in erythematous to brown patches on the lower extremities. A true vasculitis is not seen. The brown discoloration is due to hemosiderin deposition. Cryoglobulinemia is a rare condition in which abnormal immunoglobulin complexes deposit in tissues and vessels. Leukocytoclastic vasculitis is present in small vessels. Palpable purpura and livedo may be seen clinically, and systemic symptoms may be present.
Treatment of EIV is largely supportive as lesions will resolve on their own over 3-4 weeks. Postinflammatory hyperpigmentation may result. Temporary cessation of exercise and compression stockings can help speed up the resolution of lesions. Systemic medications used in the treatment of severe vasculitis, such as systemic steroids, dapsone, and colchicine, are not needed in EIV.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
Vasculitis is a process in which blood vessels become inflamed and necrotic. Classic small vessel vasculitis reveals a leukocytoclastic vasculitis and most commonly presents as palpable purpura. .” A form of EIV has been described in the literature as “Disney dermatitis.” It is often seen in healthy adults after a long day of walking at the parks. Other forms of exercise, such as jogging, hiking, or swimming, may also cause the condition.
Clinically, EIV affects the lower legs and presents as purpuric macules. Edema may be present. Lesions may be asymptomatic or may present with pruritus or burning. Diagnosis is often made clinically. Skin biopsies for H&E and DIF (direct immunofluorescence) can help distinguish the type of vasculitis that is present. Laboratory tests may be needed to exclude other causes of vasculitis. Episodes may be recurrent.
Henoch-Schönlein purpura (HSP), also called anaphylactoid purpura, is a subtype of small-vessel vasculitis where IgA immunoglobulin is deposited in the vessel walls. It is the most common form of vasculitis is children (usually ages 4-8). In addition to skin, organs such as joints, kidneys, and intestines can be involved. Schamberg’s disease, or capillaritis, is also called pigmented purpura. In this benign condition, leakage from capillaries results in erythematous to brown patches on the lower extremities. A true vasculitis is not seen. The brown discoloration is due to hemosiderin deposition. Cryoglobulinemia is a rare condition in which abnormal immunoglobulin complexes deposit in tissues and vessels. Leukocytoclastic vasculitis is present in small vessels. Palpable purpura and livedo may be seen clinically, and systemic symptoms may be present.
Treatment of EIV is largely supportive as lesions will resolve on their own over 3-4 weeks. Postinflammatory hyperpigmentation may result. Temporary cessation of exercise and compression stockings can help speed up the resolution of lesions. Systemic medications used in the treatment of severe vasculitis, such as systemic steroids, dapsone, and colchicine, are not needed in EIV.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
Violent patient throws scalding oil on MD; other patient dangers
Ralph Newman, MD, got a taste of how dangerous medicine could be at age 10, when he witnessed a physician being shot by a patient.
“I was visiting a friend whose father was a psychiatrist,” Dr. Newman recalled. “We were playing in the living room when the doorbell rang. My friend went to the door and opened it. Then I heard a shot. I ran to the front hall and saw my friend’s father slumped at the bottom of the stairs. He had come down the stairs to see who was there. It was a patient armed with a shotgun.”
As a result of the shooting, a large portion of the psychiatrist’s intestines was removed. In spite of this traumatic incident, Dr. Newman went on to become a psychiatrist – who treated many violent prisoners. “I knew it was dangerous,” he said, “but I rationalized that I wouldn’t be attacked because I would be nicer.”
That attitude seemed to work until 2002, when a prisoner threw boiling oil on him. Dr. Newman was working at the Federal Medical Center Butner, a facility for prisoners in North Carolina. “A prisoner I had been treating was denied parole, based on my recommendation,” he said. “From then on, he was looking for a way to exact revenge.”
“One day I was sitting in the nursing station, typing up notes,” Dr. Newman said. “Two new nurses, who were also there, had forgotten to lock the door, and the prisoner noticed that. He heated up some baby oil in a microwave, which was available to prisoners at the time. Then he walked into the office, threw the oil on my back, and came at me with a sharp pencil.”
Dr. Newman said the nurses fled to an adjoining office, locked the door, and wouldn’t let him in. He went into another office and collapsed in exhaustion. He was saved by an inmate who came on the scene, fended off the attacker, and called for help.
“I was taken to the burn unit,” Dr. Newman recalled. “I had second- and third-degree burns on 9% of my body. It was extremely painful. It took me 45 days to recover enough to get back to work.” The two nurses were fired.
Doctors take threats by patients more seriously now
When orthopedic surgeon Preston Phillips, MD, was killed by a patient in Tulsa, Okla., on June 1, Jennifer M. Weiss, MD, recognized the potential danger to physicians.
“The news left me feeling very shaken,” said Dr. Weiss, a pediatric orthopedic surgeon at Southern California Permanente Medical Group, Los Angeles. “Every orthopedic surgeon I talked to about it felt shaken.”
Dr. Weiss said the impact of that event prompted her to take a patient’s abuse more seriously than she might have previously. “Before the killing, my colleagues and I might have swept the incident under the rug, but we reported it to the authorities,” she said.
“What happened was I told a parent of a school-aged child that the child wasn’t ready to go back to sports,” Dr. Weiss says. “This parent was incredibly triggered – screaming and making verbal threats. The parent was standing between me and the door, so I couldn’t get out.”
Coworkers down the hall heard the yelling and helped Dr. Weiss get out of the room. “The parent was escorted out of the building, and the incident was reported to our risk management team,” she said.
Shooters/killers vs. agitated patients
Patients who shoot to kill are very different from agitated patients seen by many doctors on a regular basis – particularly in emergency departments (EDs), psychiatric units, and pain clinics, said Scott Zeller, MD, a psychiatrist who is vice president of Acute Psychiatric Medicine at Vituity, a multistate physician partnership based in Emeryville, California.
“Agitated patients have trouble communicating their needs and can become physically and verbally aggressive,” Dr. Zeller said. He reports that there are 1.7 million such incidents a year in this country, but most of the incidents of verbal aggression can be kept from exploding into physical violence.
Shooters, however, are very hard to stop because they usually plan the action in advance, Dr. Zeller said. He recalled the 2017 murder of Todd Graham, MD, a friend from medical school. Dr. Graham, an orthopedic surgeon in South Bend, Ind., was gunned down by the husband of one of his patients after Dr. Graham declined to prescribe opioids for her.
Playing down the risk of violence
Doctors may play down the risk of violence, even after they have experienced it personally. “Patients can get angry and may make threatening comments,” Dr. Weiss said. “A lot of doctors just brush it off.”
Simple remarks can set off violence-prone patients, as happened to James P. Phillips, MD, director of disaster and operational medicine at George Washington University, Washington. He recalled asking a prisoner who was visiting his hospital to “lower the volume,” and the man exploded. “Even though he was handcuffed to the bed, he heaved an oxygen tank into a window,” Dr. Phillips said. “He said he would be coming back to kill me.”
Sometimes threats or other types of verbal abuse can be as destructive as physical violence. Diann Krywko, MD, an emergency physician at the Medical University of South Carolina (MUSC) Health, Charleston, has had some tough assignments. She worked in EDs in Detroit and Flint, Mich., for a decade before coming to MUSC, where she serves as director of wellness, health, and resilience. One of the incidents that has bothered her the most involved a threat.
It happened when Dr. Krywko denied a patient’s request for narcotics. “She was very angry and said she’d come to my home and cut my children’s heads off,” Dr. Krywko said. “To this day, what she said horrifies me. I still see her smile as she said that.”
Dr. Krywko considered filing for a restraining order against the patient but didn’t because the patient could have learned her address. Dr. Phillips said fear of retaliation is one reason many doctors don’t report threats from patients. “The patient you report knows where you work and may come there to take revenge,” he said. “Also, you may have to continue caring for the person who punched you.”
Online threats also may cause a great deal of angst. Dr. Phillips said he received many online threats when was a medical analyst for CNN in 2020. “Someone sent my address to his Twitter followers, and they shared it with others, so now the whole world knows where I live,” he said. “I had to upgrade security at my home.”
How to deal with volatile patients
Being nice may not always work, but in many cases, it can keep a volatile situation from exploding, according to Dr. Krywko.
“When patients begin to show signs of agitation or are already there, we always try to verbally deescalate the situation, which involves listening,” Dr. Krywko said. “They want someone to hear them out.”
Doctors speak to patients from a position of authority, but Dr. Krywko advises that they should not be too blunt. “Don’t tell patients they’re wrong,” she said. “Even if they may be incorrect, they feel their viewpoint is valid. Encourage a dialogue with words like, ‘Tell me more,’ ” Dr. Krywko said.
Defending yourself
Doctors may have little warning of an impending attack because a patient’s mood can change quickly. This happened several years ago to Jennifer Casaletto, MD, an emergency physician in Charlotte, N.C.
“A man was brought into my ED by ambulance,” she said. “He seemed very calm for a long while, but then he became completely unhinged. A male nurse placed himself between the patient and others and was attacked. He got hurt but was able to continue working.”
Dr. Zeller said health care teams sometimes overreact when patients lash out. “The old-fashioned way to deal with an agitated patient is to call in the cavalry – everyone does a group takedown,” he said. “The patient is put in restraints and heavily sedated. This is not good for anybody. Not only is it likely to injure and traumatize the patient, it can also injure the care team.”
Many hospital EDs have security guards. “I feel safer when a hospital has armed security guards, but they need to be well trained,” Dr. Casaletto said. “Many small hospitals and freestanding EDs do not have security officers at all, or the guards are undertrained or told not to touch anybody.”
In many electronic health record systems, doctors can flag violent patients so future caregivers can be forewarned. However, Dr. Zeller advises against writing about patients’ violence or rudeness in the medical record, because patients can have access to it and might take revenge.
Rising violence from patients
“It feels like it has become much more dangerous to work in the ED,” said Hasan Gokal, MD, an emergency physician working in EDs at the Texas Medical Center. “Just last week, a woman pulled out a gun and fired it in an ED near Houston.”
The statistics back up Dr. Gokal’s assessment. Injuries caused by violent attacks against medical professionals grew by 67% from 2011 to 2018, according to the U.S. Bureau of Labor Statistics. Those levels rose even more during the COVID-19 pandemic – the assault rate in hospitals rose 23% just in 2020.
Dr. Krywko said she had “a patient who said she wanted to hurt the next person who irritated her, and that happened to me. She jumped out of her bed swinging and punching, and I wasn’t ready for it. I yelled for help and the care team came.”
“The rise in violence has to do with a decline in respect for authority,” Dr. Phillips said. “Some people now believe doctors are lying to them about the need for COVID precautions because they are taking money from the vaccine companies. The pandemic has exacerbated violence in every way.”
Dr. Phillips said that a growing lack of resources had led to more anger among patients. “There are fewer nurses and reduced physician coverage,” he said. “That means longer wait times for patients, which increases patients’ frustrations.”
Dr. Weiss said patients have higher expectations. “In sports medicine, the expectations are incredible,” she said. “Parents want their kids to get back to playing as soon as possible.”
“Hospitals in particular are soft targets for violence,” Dr. Phillips said. “People know you can’t assault a flight attendant, because it’s a federal offense, but there is no such federal offense for violence against health care personnel.”
A version of this article first appeared on Medscape.com.
Ralph Newman, MD, got a taste of how dangerous medicine could be at age 10, when he witnessed a physician being shot by a patient.
“I was visiting a friend whose father was a psychiatrist,” Dr. Newman recalled. “We were playing in the living room when the doorbell rang. My friend went to the door and opened it. Then I heard a shot. I ran to the front hall and saw my friend’s father slumped at the bottom of the stairs. He had come down the stairs to see who was there. It was a patient armed with a shotgun.”
As a result of the shooting, a large portion of the psychiatrist’s intestines was removed. In spite of this traumatic incident, Dr. Newman went on to become a psychiatrist – who treated many violent prisoners. “I knew it was dangerous,” he said, “but I rationalized that I wouldn’t be attacked because I would be nicer.”
That attitude seemed to work until 2002, when a prisoner threw boiling oil on him. Dr. Newman was working at the Federal Medical Center Butner, a facility for prisoners in North Carolina. “A prisoner I had been treating was denied parole, based on my recommendation,” he said. “From then on, he was looking for a way to exact revenge.”
“One day I was sitting in the nursing station, typing up notes,” Dr. Newman said. “Two new nurses, who were also there, had forgotten to lock the door, and the prisoner noticed that. He heated up some baby oil in a microwave, which was available to prisoners at the time. Then he walked into the office, threw the oil on my back, and came at me with a sharp pencil.”
Dr. Newman said the nurses fled to an adjoining office, locked the door, and wouldn’t let him in. He went into another office and collapsed in exhaustion. He was saved by an inmate who came on the scene, fended off the attacker, and called for help.
“I was taken to the burn unit,” Dr. Newman recalled. “I had second- and third-degree burns on 9% of my body. It was extremely painful. It took me 45 days to recover enough to get back to work.” The two nurses were fired.
Doctors take threats by patients more seriously now
When orthopedic surgeon Preston Phillips, MD, was killed by a patient in Tulsa, Okla., on June 1, Jennifer M. Weiss, MD, recognized the potential danger to physicians.
“The news left me feeling very shaken,” said Dr. Weiss, a pediatric orthopedic surgeon at Southern California Permanente Medical Group, Los Angeles. “Every orthopedic surgeon I talked to about it felt shaken.”
Dr. Weiss said the impact of that event prompted her to take a patient’s abuse more seriously than she might have previously. “Before the killing, my colleagues and I might have swept the incident under the rug, but we reported it to the authorities,” she said.
“What happened was I told a parent of a school-aged child that the child wasn’t ready to go back to sports,” Dr. Weiss says. “This parent was incredibly triggered – screaming and making verbal threats. The parent was standing between me and the door, so I couldn’t get out.”
Coworkers down the hall heard the yelling and helped Dr. Weiss get out of the room. “The parent was escorted out of the building, and the incident was reported to our risk management team,” she said.
Shooters/killers vs. agitated patients
Patients who shoot to kill are very different from agitated patients seen by many doctors on a regular basis – particularly in emergency departments (EDs), psychiatric units, and pain clinics, said Scott Zeller, MD, a psychiatrist who is vice president of Acute Psychiatric Medicine at Vituity, a multistate physician partnership based in Emeryville, California.
“Agitated patients have trouble communicating their needs and can become physically and verbally aggressive,” Dr. Zeller said. He reports that there are 1.7 million such incidents a year in this country, but most of the incidents of verbal aggression can be kept from exploding into physical violence.
Shooters, however, are very hard to stop because they usually plan the action in advance, Dr. Zeller said. He recalled the 2017 murder of Todd Graham, MD, a friend from medical school. Dr. Graham, an orthopedic surgeon in South Bend, Ind., was gunned down by the husband of one of his patients after Dr. Graham declined to prescribe opioids for her.
Playing down the risk of violence
Doctors may play down the risk of violence, even after they have experienced it personally. “Patients can get angry and may make threatening comments,” Dr. Weiss said. “A lot of doctors just brush it off.”
Simple remarks can set off violence-prone patients, as happened to James P. Phillips, MD, director of disaster and operational medicine at George Washington University, Washington. He recalled asking a prisoner who was visiting his hospital to “lower the volume,” and the man exploded. “Even though he was handcuffed to the bed, he heaved an oxygen tank into a window,” Dr. Phillips said. “He said he would be coming back to kill me.”
Sometimes threats or other types of verbal abuse can be as destructive as physical violence. Diann Krywko, MD, an emergency physician at the Medical University of South Carolina (MUSC) Health, Charleston, has had some tough assignments. She worked in EDs in Detroit and Flint, Mich., for a decade before coming to MUSC, where she serves as director of wellness, health, and resilience. One of the incidents that has bothered her the most involved a threat.
It happened when Dr. Krywko denied a patient’s request for narcotics. “She was very angry and said she’d come to my home and cut my children’s heads off,” Dr. Krywko said. “To this day, what she said horrifies me. I still see her smile as she said that.”
Dr. Krywko considered filing for a restraining order against the patient but didn’t because the patient could have learned her address. Dr. Phillips said fear of retaliation is one reason many doctors don’t report threats from patients. “The patient you report knows where you work and may come there to take revenge,” he said. “Also, you may have to continue caring for the person who punched you.”
Online threats also may cause a great deal of angst. Dr. Phillips said he received many online threats when was a medical analyst for CNN in 2020. “Someone sent my address to his Twitter followers, and they shared it with others, so now the whole world knows where I live,” he said. “I had to upgrade security at my home.”
How to deal with volatile patients
Being nice may not always work, but in many cases, it can keep a volatile situation from exploding, according to Dr. Krywko.
“When patients begin to show signs of agitation or are already there, we always try to verbally deescalate the situation, which involves listening,” Dr. Krywko said. “They want someone to hear them out.”
Doctors speak to patients from a position of authority, but Dr. Krywko advises that they should not be too blunt. “Don’t tell patients they’re wrong,” she said. “Even if they may be incorrect, they feel their viewpoint is valid. Encourage a dialogue with words like, ‘Tell me more,’ ” Dr. Krywko said.
Defending yourself
Doctors may have little warning of an impending attack because a patient’s mood can change quickly. This happened several years ago to Jennifer Casaletto, MD, an emergency physician in Charlotte, N.C.
“A man was brought into my ED by ambulance,” she said. “He seemed very calm for a long while, but then he became completely unhinged. A male nurse placed himself between the patient and others and was attacked. He got hurt but was able to continue working.”
Dr. Zeller said health care teams sometimes overreact when patients lash out. “The old-fashioned way to deal with an agitated patient is to call in the cavalry – everyone does a group takedown,” he said. “The patient is put in restraints and heavily sedated. This is not good for anybody. Not only is it likely to injure and traumatize the patient, it can also injure the care team.”
Many hospital EDs have security guards. “I feel safer when a hospital has armed security guards, but they need to be well trained,” Dr. Casaletto said. “Many small hospitals and freestanding EDs do not have security officers at all, or the guards are undertrained or told not to touch anybody.”
In many electronic health record systems, doctors can flag violent patients so future caregivers can be forewarned. However, Dr. Zeller advises against writing about patients’ violence or rudeness in the medical record, because patients can have access to it and might take revenge.
Rising violence from patients
“It feels like it has become much more dangerous to work in the ED,” said Hasan Gokal, MD, an emergency physician working in EDs at the Texas Medical Center. “Just last week, a woman pulled out a gun and fired it in an ED near Houston.”
The statistics back up Dr. Gokal’s assessment. Injuries caused by violent attacks against medical professionals grew by 67% from 2011 to 2018, according to the U.S. Bureau of Labor Statistics. Those levels rose even more during the COVID-19 pandemic – the assault rate in hospitals rose 23% just in 2020.
Dr. Krywko said she had “a patient who said she wanted to hurt the next person who irritated her, and that happened to me. She jumped out of her bed swinging and punching, and I wasn’t ready for it. I yelled for help and the care team came.”
“The rise in violence has to do with a decline in respect for authority,” Dr. Phillips said. “Some people now believe doctors are lying to them about the need for COVID precautions because they are taking money from the vaccine companies. The pandemic has exacerbated violence in every way.”
Dr. Phillips said that a growing lack of resources had led to more anger among patients. “There are fewer nurses and reduced physician coverage,” he said. “That means longer wait times for patients, which increases patients’ frustrations.”
Dr. Weiss said patients have higher expectations. “In sports medicine, the expectations are incredible,” she said. “Parents want their kids to get back to playing as soon as possible.”
“Hospitals in particular are soft targets for violence,” Dr. Phillips said. “People know you can’t assault a flight attendant, because it’s a federal offense, but there is no such federal offense for violence against health care personnel.”
A version of this article first appeared on Medscape.com.
Ralph Newman, MD, got a taste of how dangerous medicine could be at age 10, when he witnessed a physician being shot by a patient.
“I was visiting a friend whose father was a psychiatrist,” Dr. Newman recalled. “We were playing in the living room when the doorbell rang. My friend went to the door and opened it. Then I heard a shot. I ran to the front hall and saw my friend’s father slumped at the bottom of the stairs. He had come down the stairs to see who was there. It was a patient armed with a shotgun.”
As a result of the shooting, a large portion of the psychiatrist’s intestines was removed. In spite of this traumatic incident, Dr. Newman went on to become a psychiatrist – who treated many violent prisoners. “I knew it was dangerous,” he said, “but I rationalized that I wouldn’t be attacked because I would be nicer.”
That attitude seemed to work until 2002, when a prisoner threw boiling oil on him. Dr. Newman was working at the Federal Medical Center Butner, a facility for prisoners in North Carolina. “A prisoner I had been treating was denied parole, based on my recommendation,” he said. “From then on, he was looking for a way to exact revenge.”
“One day I was sitting in the nursing station, typing up notes,” Dr. Newman said. “Two new nurses, who were also there, had forgotten to lock the door, and the prisoner noticed that. He heated up some baby oil in a microwave, which was available to prisoners at the time. Then he walked into the office, threw the oil on my back, and came at me with a sharp pencil.”
Dr. Newman said the nurses fled to an adjoining office, locked the door, and wouldn’t let him in. He went into another office and collapsed in exhaustion. He was saved by an inmate who came on the scene, fended off the attacker, and called for help.
“I was taken to the burn unit,” Dr. Newman recalled. “I had second- and third-degree burns on 9% of my body. It was extremely painful. It took me 45 days to recover enough to get back to work.” The two nurses were fired.
Doctors take threats by patients more seriously now
When orthopedic surgeon Preston Phillips, MD, was killed by a patient in Tulsa, Okla., on June 1, Jennifer M. Weiss, MD, recognized the potential danger to physicians.
“The news left me feeling very shaken,” said Dr. Weiss, a pediatric orthopedic surgeon at Southern California Permanente Medical Group, Los Angeles. “Every orthopedic surgeon I talked to about it felt shaken.”
Dr. Weiss said the impact of that event prompted her to take a patient’s abuse more seriously than she might have previously. “Before the killing, my colleagues and I might have swept the incident under the rug, but we reported it to the authorities,” she said.
“What happened was I told a parent of a school-aged child that the child wasn’t ready to go back to sports,” Dr. Weiss says. “This parent was incredibly triggered – screaming and making verbal threats. The parent was standing between me and the door, so I couldn’t get out.”
Coworkers down the hall heard the yelling and helped Dr. Weiss get out of the room. “The parent was escorted out of the building, and the incident was reported to our risk management team,” she said.
Shooters/killers vs. agitated patients
Patients who shoot to kill are very different from agitated patients seen by many doctors on a regular basis – particularly in emergency departments (EDs), psychiatric units, and pain clinics, said Scott Zeller, MD, a psychiatrist who is vice president of Acute Psychiatric Medicine at Vituity, a multistate physician partnership based in Emeryville, California.
“Agitated patients have trouble communicating their needs and can become physically and verbally aggressive,” Dr. Zeller said. He reports that there are 1.7 million such incidents a year in this country, but most of the incidents of verbal aggression can be kept from exploding into physical violence.
Shooters, however, are very hard to stop because they usually plan the action in advance, Dr. Zeller said. He recalled the 2017 murder of Todd Graham, MD, a friend from medical school. Dr. Graham, an orthopedic surgeon in South Bend, Ind., was gunned down by the husband of one of his patients after Dr. Graham declined to prescribe opioids for her.
Playing down the risk of violence
Doctors may play down the risk of violence, even after they have experienced it personally. “Patients can get angry and may make threatening comments,” Dr. Weiss said. “A lot of doctors just brush it off.”
Simple remarks can set off violence-prone patients, as happened to James P. Phillips, MD, director of disaster and operational medicine at George Washington University, Washington. He recalled asking a prisoner who was visiting his hospital to “lower the volume,” and the man exploded. “Even though he was handcuffed to the bed, he heaved an oxygen tank into a window,” Dr. Phillips said. “He said he would be coming back to kill me.”
Sometimes threats or other types of verbal abuse can be as destructive as physical violence. Diann Krywko, MD, an emergency physician at the Medical University of South Carolina (MUSC) Health, Charleston, has had some tough assignments. She worked in EDs in Detroit and Flint, Mich., for a decade before coming to MUSC, where she serves as director of wellness, health, and resilience. One of the incidents that has bothered her the most involved a threat.
It happened when Dr. Krywko denied a patient’s request for narcotics. “She was very angry and said she’d come to my home and cut my children’s heads off,” Dr. Krywko said. “To this day, what she said horrifies me. I still see her smile as she said that.”
Dr. Krywko considered filing for a restraining order against the patient but didn’t because the patient could have learned her address. Dr. Phillips said fear of retaliation is one reason many doctors don’t report threats from patients. “The patient you report knows where you work and may come there to take revenge,” he said. “Also, you may have to continue caring for the person who punched you.”
Online threats also may cause a great deal of angst. Dr. Phillips said he received many online threats when was a medical analyst for CNN in 2020. “Someone sent my address to his Twitter followers, and they shared it with others, so now the whole world knows where I live,” he said. “I had to upgrade security at my home.”
How to deal with volatile patients
Being nice may not always work, but in many cases, it can keep a volatile situation from exploding, according to Dr. Krywko.
“When patients begin to show signs of agitation or are already there, we always try to verbally deescalate the situation, which involves listening,” Dr. Krywko said. “They want someone to hear them out.”
Doctors speak to patients from a position of authority, but Dr. Krywko advises that they should not be too blunt. “Don’t tell patients they’re wrong,” she said. “Even if they may be incorrect, they feel their viewpoint is valid. Encourage a dialogue with words like, ‘Tell me more,’ ” Dr. Krywko said.
Defending yourself
Doctors may have little warning of an impending attack because a patient’s mood can change quickly. This happened several years ago to Jennifer Casaletto, MD, an emergency physician in Charlotte, N.C.
“A man was brought into my ED by ambulance,” she said. “He seemed very calm for a long while, but then he became completely unhinged. A male nurse placed himself between the patient and others and was attacked. He got hurt but was able to continue working.”
Dr. Zeller said health care teams sometimes overreact when patients lash out. “The old-fashioned way to deal with an agitated patient is to call in the cavalry – everyone does a group takedown,” he said. “The patient is put in restraints and heavily sedated. This is not good for anybody. Not only is it likely to injure and traumatize the patient, it can also injure the care team.”
Many hospital EDs have security guards. “I feel safer when a hospital has armed security guards, but they need to be well trained,” Dr. Casaletto said. “Many small hospitals and freestanding EDs do not have security officers at all, or the guards are undertrained or told not to touch anybody.”
In many electronic health record systems, doctors can flag violent patients so future caregivers can be forewarned. However, Dr. Zeller advises against writing about patients’ violence or rudeness in the medical record, because patients can have access to it and might take revenge.
Rising violence from patients
“It feels like it has become much more dangerous to work in the ED,” said Hasan Gokal, MD, an emergency physician working in EDs at the Texas Medical Center. “Just last week, a woman pulled out a gun and fired it in an ED near Houston.”
The statistics back up Dr. Gokal’s assessment. Injuries caused by violent attacks against medical professionals grew by 67% from 2011 to 2018, according to the U.S. Bureau of Labor Statistics. Those levels rose even more during the COVID-19 pandemic – the assault rate in hospitals rose 23% just in 2020.
Dr. Krywko said she had “a patient who said she wanted to hurt the next person who irritated her, and that happened to me. She jumped out of her bed swinging and punching, and I wasn’t ready for it. I yelled for help and the care team came.”
“The rise in violence has to do with a decline in respect for authority,” Dr. Phillips said. “Some people now believe doctors are lying to them about the need for COVID precautions because they are taking money from the vaccine companies. The pandemic has exacerbated violence in every way.”
Dr. Phillips said that a growing lack of resources had led to more anger among patients. “There are fewer nurses and reduced physician coverage,” he said. “That means longer wait times for patients, which increases patients’ frustrations.”
Dr. Weiss said patients have higher expectations. “In sports medicine, the expectations are incredible,” she said. “Parents want their kids to get back to playing as soon as possible.”
“Hospitals in particular are soft targets for violence,” Dr. Phillips said. “People know you can’t assault a flight attendant, because it’s a federal offense, but there is no such federal offense for violence against health care personnel.”
A version of this article first appeared on Medscape.com.
Marital status plays modest role in gastric cancer overall survival
, according to research published in the Journal of Investigative Medicine.
Tumor size remained the largest contributor to overall survival, but marital status was among several other significant factors, such as age, race, gender, treatment style, and pathologic stage, that can provide insight into a patient’s likelihood of overall survival, as it does with several other cancers.
“Married patients had the best prognosis, followed by single patients, and the prognosis of separated patients was the worst,” write Lixiang Zhang and colleagues at the First Affiliated Hospital of Anhui Medical University, Hefei, China. “We speculate that this might be due to the fact that married patients had better financial conditions and emotional encouragement, while separated patients might be more likely to experience financial difficulties [and] emotional loss.”
The results were not necessarily surprising to Richard M. Peek, Jr., MD, director of the division of gastroenterology and a professor of medicine at Vanderbilt University Medical Center, who was not involved in the research.
“Marital status is a reflection of support systems, and a strong support system is a prognosticator for increased compliance with medical appointments and medical therapies,” Dr. Peek told this news organization. “It is something to consider when somebody is being treated for gastric cancer, because if they don’t have a strong support system – and marital status can be a proxy for that – then they may need more intensive follow-up and surveillance, for example, than somebody who does not have that support system.”
Exploring the marital status–cancer survival connection
Gastric cancer is the third leading cause of cancer deaths across the world, causing 780,000 deaths in 2018, the authors note. Yet it’s difficult to accurately predict the prognosis in patients who undergo treatment for early stage gastric cancer. Previous research has found marital status to be associated with survival in prostate, cervical, and rectal cancers.
Mark A. Lewis, MD, director of gastrointestinal oncology at Intermountain Healthcare Cancer Center, Utah, told this news organization that the connection between marital status and cancer outcomes has been described previously, including in an even larger analysis using the U.S. Surveillance, Epidemiology, and End Results (SEER) database from 2013. That study found that “unmarried patients are at significantly higher risk of presentation with metastatic cancer, undertreatment, and death resulting from their cancer.”
In this study, the researchers compared marital status and survival rates among 3,647 patients with early-stage gastric cancer, using data from the SEER database. The study only included patients with tumors in the lamina propria, mucosa, and submucosa and excluded those with distant metastasis or distant lymph node metastases, a second cancer, no data on chemotherapy received, or unknown survival time.
Because they were using a nomogram and building a new predictive nomogram that would include marital status, the researchers divided the patient population into a training set of 2,719 patients and a testing set of 928 patients. Using overall survival as the primary endpoint, the analysis included the variables of “age at diagnosis, race, gender, tumor location, histology, grade, stage_T and stage_N, surgery in the primary site, lymph node dissection, chemotherapy, radiation, tumor size, insurance, and marital status,” the authors report.
Among the study population, 53.7% were married, 17.3% were widowed, 14% were single and never married, 7.5% were divorced, 1.1% were separated, and the status of 6.4% was unknown. Age at diagnosis, race, gender, histology, tumor grade, stage T, stage N, surgery type, tumor size, and insurance status were all significantly different between the marital status subgroups.
Married patients had the best prognosis, with an average overall survival of 72 months, compared with an average 60 months in widowed persons, the group with the poorest overall survival. Overall survival was higher in married women (76 months) than in married men (69 months). The same pattern held for women (62 months) and men (52 months) who had been widowed.
“It is worthy to note that survival was significantly better in divorced female patients than in divorced male patients,” the authors report. “Survival was better in female patients than in male patients” across all marital groups.
What long-term relationships reveal
These findings do not mean that simply getting married changes one’s likelihood of survival, however. Rather, a long-term relationship is revealing about other aspects in a person’s life.
“I think it represents more stability in the supportive relationship that you need to really deal with a serious disease like cancer,” Dr. Peek said.
If a patient does not have a long-term partner, their care team can ask other questions to get a sense of what their support network is like, Dr. Peek added. “We want to know, does anybody else live in the house with them? Do they have adequate transportation? Can they make medical appointments? Do they have somebody who can help with the medical issues that are going to come up? Do they have family in the area?”
Cancer treatment requires a multidisciplinary approach, and having someone other than just the patient around to help bring together the different aspects of care from different care teams can make a difference in how the patient fares, Dr. Peek explained. Patients without a strong support system may need closer follow-up and other accommodations, he said.
Providers “may schedule their clinical appointments closer together if they don’t have a support system, or they may be able to reach out and offer transportation assistance and those kinds of things that somebody living alone may need,” Dr. Peek said. Outside resources may be a higher priority for those who lack a support system at home, he added.
Dr. Peek also noted other factors that may play a role in a patient’s survival that these researchers did not have the data to address, such as socioeconomic status, employment, alcohol use, smoking, and infection with Helicobacter pylori, the strongest known risk factor for gastric cancer.
A potentially relevant limitation of the study is that it probably has some selection bias, because the patients who were included probably had the means to have received an earlier diagnosis, said Dr. Lewis, who was not involved in the research.
“Furthermore, just in terms of the group sizes, the baseline characteristics section makes it clear that the preponderance of patients were married, lending that group more statistical weight,” Dr. Lewis said.
“Of the seven attributes in the nomogram, the impact of the marital status seems comparatively meager relative to conventional clinicopathology risk factors like T stage,” he added.
“All in all, I think this study reinforces our awareness that socioeconomic status and social determinants of health play a huge role in cancer outcomes, but it’s not entirely clear that’s modifiable just by getting married,” Dr. Lewis said. “There is a saying in oncology that ‘expensive liquor causes less cancer than cheap liquor,’ which is not negating the carcinogenicity of alcohol but rather identifying different outcomes by socioeconomic status.”
The research was funded by the Natural Science Foundation of Anhui Province. The authors report no relevant financial relationships. Dr. Peek reports no relevant financial relationships. Dr. Lewis reports receiving speaking fees for AstraZeneca/Daiichi Sankyo and having done educational videos for Astellas.
A version of this article first appeared on Medscape.com.
, according to research published in the Journal of Investigative Medicine.
Tumor size remained the largest contributor to overall survival, but marital status was among several other significant factors, such as age, race, gender, treatment style, and pathologic stage, that can provide insight into a patient’s likelihood of overall survival, as it does with several other cancers.
“Married patients had the best prognosis, followed by single patients, and the prognosis of separated patients was the worst,” write Lixiang Zhang and colleagues at the First Affiliated Hospital of Anhui Medical University, Hefei, China. “We speculate that this might be due to the fact that married patients had better financial conditions and emotional encouragement, while separated patients might be more likely to experience financial difficulties [and] emotional loss.”
The results were not necessarily surprising to Richard M. Peek, Jr., MD, director of the division of gastroenterology and a professor of medicine at Vanderbilt University Medical Center, who was not involved in the research.
“Marital status is a reflection of support systems, and a strong support system is a prognosticator for increased compliance with medical appointments and medical therapies,” Dr. Peek told this news organization. “It is something to consider when somebody is being treated for gastric cancer, because if they don’t have a strong support system – and marital status can be a proxy for that – then they may need more intensive follow-up and surveillance, for example, than somebody who does not have that support system.”
Exploring the marital status–cancer survival connection
Gastric cancer is the third leading cause of cancer deaths across the world, causing 780,000 deaths in 2018, the authors note. Yet it’s difficult to accurately predict the prognosis in patients who undergo treatment for early stage gastric cancer. Previous research has found marital status to be associated with survival in prostate, cervical, and rectal cancers.
Mark A. Lewis, MD, director of gastrointestinal oncology at Intermountain Healthcare Cancer Center, Utah, told this news organization that the connection between marital status and cancer outcomes has been described previously, including in an even larger analysis using the U.S. Surveillance, Epidemiology, and End Results (SEER) database from 2013. That study found that “unmarried patients are at significantly higher risk of presentation with metastatic cancer, undertreatment, and death resulting from their cancer.”
In this study, the researchers compared marital status and survival rates among 3,647 patients with early-stage gastric cancer, using data from the SEER database. The study only included patients with tumors in the lamina propria, mucosa, and submucosa and excluded those with distant metastasis or distant lymph node metastases, a second cancer, no data on chemotherapy received, or unknown survival time.
Because they were using a nomogram and building a new predictive nomogram that would include marital status, the researchers divided the patient population into a training set of 2,719 patients and a testing set of 928 patients. Using overall survival as the primary endpoint, the analysis included the variables of “age at diagnosis, race, gender, tumor location, histology, grade, stage_T and stage_N, surgery in the primary site, lymph node dissection, chemotherapy, radiation, tumor size, insurance, and marital status,” the authors report.
Among the study population, 53.7% were married, 17.3% were widowed, 14% were single and never married, 7.5% were divorced, 1.1% were separated, and the status of 6.4% was unknown. Age at diagnosis, race, gender, histology, tumor grade, stage T, stage N, surgery type, tumor size, and insurance status were all significantly different between the marital status subgroups.
Married patients had the best prognosis, with an average overall survival of 72 months, compared with an average 60 months in widowed persons, the group with the poorest overall survival. Overall survival was higher in married women (76 months) than in married men (69 months). The same pattern held for women (62 months) and men (52 months) who had been widowed.
“It is worthy to note that survival was significantly better in divorced female patients than in divorced male patients,” the authors report. “Survival was better in female patients than in male patients” across all marital groups.
What long-term relationships reveal
These findings do not mean that simply getting married changes one’s likelihood of survival, however. Rather, a long-term relationship is revealing about other aspects in a person’s life.
“I think it represents more stability in the supportive relationship that you need to really deal with a serious disease like cancer,” Dr. Peek said.
If a patient does not have a long-term partner, their care team can ask other questions to get a sense of what their support network is like, Dr. Peek added. “We want to know, does anybody else live in the house with them? Do they have adequate transportation? Can they make medical appointments? Do they have somebody who can help with the medical issues that are going to come up? Do they have family in the area?”
Cancer treatment requires a multidisciplinary approach, and having someone other than just the patient around to help bring together the different aspects of care from different care teams can make a difference in how the patient fares, Dr. Peek explained. Patients without a strong support system may need closer follow-up and other accommodations, he said.
Providers “may schedule their clinical appointments closer together if they don’t have a support system, or they may be able to reach out and offer transportation assistance and those kinds of things that somebody living alone may need,” Dr. Peek said. Outside resources may be a higher priority for those who lack a support system at home, he added.
Dr. Peek also noted other factors that may play a role in a patient’s survival that these researchers did not have the data to address, such as socioeconomic status, employment, alcohol use, smoking, and infection with Helicobacter pylori, the strongest known risk factor for gastric cancer.
A potentially relevant limitation of the study is that it probably has some selection bias, because the patients who were included probably had the means to have received an earlier diagnosis, said Dr. Lewis, who was not involved in the research.
“Furthermore, just in terms of the group sizes, the baseline characteristics section makes it clear that the preponderance of patients were married, lending that group more statistical weight,” Dr. Lewis said.
“Of the seven attributes in the nomogram, the impact of the marital status seems comparatively meager relative to conventional clinicopathology risk factors like T stage,” he added.
“All in all, I think this study reinforces our awareness that socioeconomic status and social determinants of health play a huge role in cancer outcomes, but it’s not entirely clear that’s modifiable just by getting married,” Dr. Lewis said. “There is a saying in oncology that ‘expensive liquor causes less cancer than cheap liquor,’ which is not negating the carcinogenicity of alcohol but rather identifying different outcomes by socioeconomic status.”
The research was funded by the Natural Science Foundation of Anhui Province. The authors report no relevant financial relationships. Dr. Peek reports no relevant financial relationships. Dr. Lewis reports receiving speaking fees for AstraZeneca/Daiichi Sankyo and having done educational videos for Astellas.
A version of this article first appeared on Medscape.com.
, according to research published in the Journal of Investigative Medicine.
Tumor size remained the largest contributor to overall survival, but marital status was among several other significant factors, such as age, race, gender, treatment style, and pathologic stage, that can provide insight into a patient’s likelihood of overall survival, as it does with several other cancers.
“Married patients had the best prognosis, followed by single patients, and the prognosis of separated patients was the worst,” write Lixiang Zhang and colleagues at the First Affiliated Hospital of Anhui Medical University, Hefei, China. “We speculate that this might be due to the fact that married patients had better financial conditions and emotional encouragement, while separated patients might be more likely to experience financial difficulties [and] emotional loss.”
The results were not necessarily surprising to Richard M. Peek, Jr., MD, director of the division of gastroenterology and a professor of medicine at Vanderbilt University Medical Center, who was not involved in the research.
“Marital status is a reflection of support systems, and a strong support system is a prognosticator for increased compliance with medical appointments and medical therapies,” Dr. Peek told this news organization. “It is something to consider when somebody is being treated for gastric cancer, because if they don’t have a strong support system – and marital status can be a proxy for that – then they may need more intensive follow-up and surveillance, for example, than somebody who does not have that support system.”
Exploring the marital status–cancer survival connection
Gastric cancer is the third leading cause of cancer deaths across the world, causing 780,000 deaths in 2018, the authors note. Yet it’s difficult to accurately predict the prognosis in patients who undergo treatment for early stage gastric cancer. Previous research has found marital status to be associated with survival in prostate, cervical, and rectal cancers.
Mark A. Lewis, MD, director of gastrointestinal oncology at Intermountain Healthcare Cancer Center, Utah, told this news organization that the connection between marital status and cancer outcomes has been described previously, including in an even larger analysis using the U.S. Surveillance, Epidemiology, and End Results (SEER) database from 2013. That study found that “unmarried patients are at significantly higher risk of presentation with metastatic cancer, undertreatment, and death resulting from their cancer.”
In this study, the researchers compared marital status and survival rates among 3,647 patients with early-stage gastric cancer, using data from the SEER database. The study only included patients with tumors in the lamina propria, mucosa, and submucosa and excluded those with distant metastasis or distant lymph node metastases, a second cancer, no data on chemotherapy received, or unknown survival time.
Because they were using a nomogram and building a new predictive nomogram that would include marital status, the researchers divided the patient population into a training set of 2,719 patients and a testing set of 928 patients. Using overall survival as the primary endpoint, the analysis included the variables of “age at diagnosis, race, gender, tumor location, histology, grade, stage_T and stage_N, surgery in the primary site, lymph node dissection, chemotherapy, radiation, tumor size, insurance, and marital status,” the authors report.
Among the study population, 53.7% were married, 17.3% were widowed, 14% were single and never married, 7.5% were divorced, 1.1% were separated, and the status of 6.4% was unknown. Age at diagnosis, race, gender, histology, tumor grade, stage T, stage N, surgery type, tumor size, and insurance status were all significantly different between the marital status subgroups.
Married patients had the best prognosis, with an average overall survival of 72 months, compared with an average 60 months in widowed persons, the group with the poorest overall survival. Overall survival was higher in married women (76 months) than in married men (69 months). The same pattern held for women (62 months) and men (52 months) who had been widowed.
“It is worthy to note that survival was significantly better in divorced female patients than in divorced male patients,” the authors report. “Survival was better in female patients than in male patients” across all marital groups.
What long-term relationships reveal
These findings do not mean that simply getting married changes one’s likelihood of survival, however. Rather, a long-term relationship is revealing about other aspects in a person’s life.
“I think it represents more stability in the supportive relationship that you need to really deal with a serious disease like cancer,” Dr. Peek said.
If a patient does not have a long-term partner, their care team can ask other questions to get a sense of what their support network is like, Dr. Peek added. “We want to know, does anybody else live in the house with them? Do they have adequate transportation? Can they make medical appointments? Do they have somebody who can help with the medical issues that are going to come up? Do they have family in the area?”
Cancer treatment requires a multidisciplinary approach, and having someone other than just the patient around to help bring together the different aspects of care from different care teams can make a difference in how the patient fares, Dr. Peek explained. Patients without a strong support system may need closer follow-up and other accommodations, he said.
Providers “may schedule their clinical appointments closer together if they don’t have a support system, or they may be able to reach out and offer transportation assistance and those kinds of things that somebody living alone may need,” Dr. Peek said. Outside resources may be a higher priority for those who lack a support system at home, he added.
Dr. Peek also noted other factors that may play a role in a patient’s survival that these researchers did not have the data to address, such as socioeconomic status, employment, alcohol use, smoking, and infection with Helicobacter pylori, the strongest known risk factor for gastric cancer.
A potentially relevant limitation of the study is that it probably has some selection bias, because the patients who were included probably had the means to have received an earlier diagnosis, said Dr. Lewis, who was not involved in the research.
“Furthermore, just in terms of the group sizes, the baseline characteristics section makes it clear that the preponderance of patients were married, lending that group more statistical weight,” Dr. Lewis said.
“Of the seven attributes in the nomogram, the impact of the marital status seems comparatively meager relative to conventional clinicopathology risk factors like T stage,” he added.
“All in all, I think this study reinforces our awareness that socioeconomic status and social determinants of health play a huge role in cancer outcomes, but it’s not entirely clear that’s modifiable just by getting married,” Dr. Lewis said. “There is a saying in oncology that ‘expensive liquor causes less cancer than cheap liquor,’ which is not negating the carcinogenicity of alcohol but rather identifying different outcomes by socioeconomic status.”
The research was funded by the Natural Science Foundation of Anhui Province. The authors report no relevant financial relationships. Dr. Peek reports no relevant financial relationships. Dr. Lewis reports receiving speaking fees for AstraZeneca/Daiichi Sankyo and having done educational videos for Astellas.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF INVESTIGATIVE MEDICINE
Ten steps for clinicians to avoid being racist: The Francis commitment
As a Black man who grew up in this country, I can tell you first-hand what it does to you. The scars never go away, and your status is always in question, no matter your title or uniforms of respect. Eventually it wears you down.
I was born into poverty and the segregation of southwest Louisiana. I experienced the dehumanization intended for me: separate drinking fountains and poor foundational education. I was lucky to attend a historically Black college or university (Southern University, Baton Rouge, La.), that gave me my bearings. I then went to some of the very best, predominantly White institutions.
When I looked for a job after training, there were few integrated medical groups, so I started my own. It included practitioners who were White, Black, Jewish, Asian, Middle Eastern, Muslim, Christian, etc. We cross covered and treated patients from every corner of the globe.
In medicine, we treat human beings with disease. The disease should be the only difference that sets us apart. There is absolutely no place for racism.
It is difficult to be called a racist, and I have met only a handful of people in health care whom I would label as such. But racism is structural and institutionalized so that it is often hidden.
One way to overcome this is to make every effort possible to get to know people as individuals. Only then can we see that there are few real differences between us. I would often seek out a colleague from a different culture or race to have lunch with so I could learn more about them.
We all strive for the same things – validation, happiness, love, family, and a future. We all grieve over the same things.
What some caregivers may not realize is that, just as clinicians have been trained to recognize subtle signs and symptoms of disease, minorities can recognize racism immediately during a medical encounter. Our past experiences make us skilled at picking up a lack of eye contact or body language and tone of voice that are dismissive and disrespectful.
A patient who has felt racism may still return for care because of insurance coverage limitations, location, or a lack of alternatives. But trust and loyalty will never develop on the part of this patient, and empathy will be absent on the part of their caregiver.
To counter this in my own practice, I developed the Francis Commitment to avoid any hint of racism or bias toward my patients.
I commit to the following:
1. I see you.
2. I hear you.
3. I accept who you are.
4. I will try to understand how you must feel (empathy).
5. Treating you is very important to me.
6. I would like to gain your trust that I will do my very best to make you better.
7. I value you as a human being and will treat you as if you are family.
8. I care about what happens to you.
9. I want us to work together to fight this disease.
10. I am grateful that you chose me as your caregiver.
The INOVA health care system where I work has undertaken an initiative called What Matters Most to better understand the needs of every patient. We are currently working on a strategy of patient personalization to not only learn about their medical needs but also to discover who they are as a person. We incorporate Social Determinants of Health in our dealings with patients. We also have participated in a program called “A Long Talk”, where we learned that those of us who remain silent when we see or hear racism are responsible for its persistence and growth.
But we must do more. Racism will propagate if we live in silos surrounded by people whose ideas reflect our own. As long as we have nondiversified board rooms, departments, and staff, the problem will persist.
A lot of the biases that we unconsciously carry in our heads and hearts have no basis in reality and were placed there without our permission by parents, society, and friends. But we can replace these divisive thoughts and impulses.
What’s in your heart can only be known and controlled by you. How tolerant we are of racism is up to us: Do you call out racism; do you challenge any inkling of racism from friends or acquaintances; do you put pressure on institutions where you work to diversify in recruiting and hiring?
Think of all the advances in medicine that were achieved by people from different cultures and races. Racism has no place in what we have all devoted our lives to do – take care of our fellow humans.
A version of this article first appeared on Medscape.com.
As a Black man who grew up in this country, I can tell you first-hand what it does to you. The scars never go away, and your status is always in question, no matter your title or uniforms of respect. Eventually it wears you down.
I was born into poverty and the segregation of southwest Louisiana. I experienced the dehumanization intended for me: separate drinking fountains and poor foundational education. I was lucky to attend a historically Black college or university (Southern University, Baton Rouge, La.), that gave me my bearings. I then went to some of the very best, predominantly White institutions.
When I looked for a job after training, there were few integrated medical groups, so I started my own. It included practitioners who were White, Black, Jewish, Asian, Middle Eastern, Muslim, Christian, etc. We cross covered and treated patients from every corner of the globe.
In medicine, we treat human beings with disease. The disease should be the only difference that sets us apart. There is absolutely no place for racism.
It is difficult to be called a racist, and I have met only a handful of people in health care whom I would label as such. But racism is structural and institutionalized so that it is often hidden.
One way to overcome this is to make every effort possible to get to know people as individuals. Only then can we see that there are few real differences between us. I would often seek out a colleague from a different culture or race to have lunch with so I could learn more about them.
We all strive for the same things – validation, happiness, love, family, and a future. We all grieve over the same things.
What some caregivers may not realize is that, just as clinicians have been trained to recognize subtle signs and symptoms of disease, minorities can recognize racism immediately during a medical encounter. Our past experiences make us skilled at picking up a lack of eye contact or body language and tone of voice that are dismissive and disrespectful.
A patient who has felt racism may still return for care because of insurance coverage limitations, location, or a lack of alternatives. But trust and loyalty will never develop on the part of this patient, and empathy will be absent on the part of their caregiver.
To counter this in my own practice, I developed the Francis Commitment to avoid any hint of racism or bias toward my patients.
I commit to the following:
1. I see you.
2. I hear you.
3. I accept who you are.
4. I will try to understand how you must feel (empathy).
5. Treating you is very important to me.
6. I would like to gain your trust that I will do my very best to make you better.
7. I value you as a human being and will treat you as if you are family.
8. I care about what happens to you.
9. I want us to work together to fight this disease.
10. I am grateful that you chose me as your caregiver.
The INOVA health care system where I work has undertaken an initiative called What Matters Most to better understand the needs of every patient. We are currently working on a strategy of patient personalization to not only learn about their medical needs but also to discover who they are as a person. We incorporate Social Determinants of Health in our dealings with patients. We also have participated in a program called “A Long Talk”, where we learned that those of us who remain silent when we see or hear racism are responsible for its persistence and growth.
But we must do more. Racism will propagate if we live in silos surrounded by people whose ideas reflect our own. As long as we have nondiversified board rooms, departments, and staff, the problem will persist.
A lot of the biases that we unconsciously carry in our heads and hearts have no basis in reality and were placed there without our permission by parents, society, and friends. But we can replace these divisive thoughts and impulses.
What’s in your heart can only be known and controlled by you. How tolerant we are of racism is up to us: Do you call out racism; do you challenge any inkling of racism from friends or acquaintances; do you put pressure on institutions where you work to diversify in recruiting and hiring?
Think of all the advances in medicine that were achieved by people from different cultures and races. Racism has no place in what we have all devoted our lives to do – take care of our fellow humans.
A version of this article first appeared on Medscape.com.
As a Black man who grew up in this country, I can tell you first-hand what it does to you. The scars never go away, and your status is always in question, no matter your title or uniforms of respect. Eventually it wears you down.
I was born into poverty and the segregation of southwest Louisiana. I experienced the dehumanization intended for me: separate drinking fountains and poor foundational education. I was lucky to attend a historically Black college or university (Southern University, Baton Rouge, La.), that gave me my bearings. I then went to some of the very best, predominantly White institutions.
When I looked for a job after training, there were few integrated medical groups, so I started my own. It included practitioners who were White, Black, Jewish, Asian, Middle Eastern, Muslim, Christian, etc. We cross covered and treated patients from every corner of the globe.
In medicine, we treat human beings with disease. The disease should be the only difference that sets us apart. There is absolutely no place for racism.
It is difficult to be called a racist, and I have met only a handful of people in health care whom I would label as such. But racism is structural and institutionalized so that it is often hidden.
One way to overcome this is to make every effort possible to get to know people as individuals. Only then can we see that there are few real differences between us. I would often seek out a colleague from a different culture or race to have lunch with so I could learn more about them.
We all strive for the same things – validation, happiness, love, family, and a future. We all grieve over the same things.
What some caregivers may not realize is that, just as clinicians have been trained to recognize subtle signs and symptoms of disease, minorities can recognize racism immediately during a medical encounter. Our past experiences make us skilled at picking up a lack of eye contact or body language and tone of voice that are dismissive and disrespectful.
A patient who has felt racism may still return for care because of insurance coverage limitations, location, or a lack of alternatives. But trust and loyalty will never develop on the part of this patient, and empathy will be absent on the part of their caregiver.
To counter this in my own practice, I developed the Francis Commitment to avoid any hint of racism or bias toward my patients.
I commit to the following:
1. I see you.
2. I hear you.
3. I accept who you are.
4. I will try to understand how you must feel (empathy).
5. Treating you is very important to me.
6. I would like to gain your trust that I will do my very best to make you better.
7. I value you as a human being and will treat you as if you are family.
8. I care about what happens to you.
9. I want us to work together to fight this disease.
10. I am grateful that you chose me as your caregiver.
The INOVA health care system where I work has undertaken an initiative called What Matters Most to better understand the needs of every patient. We are currently working on a strategy of patient personalization to not only learn about their medical needs but also to discover who they are as a person. We incorporate Social Determinants of Health in our dealings with patients. We also have participated in a program called “A Long Talk”, where we learned that those of us who remain silent when we see or hear racism are responsible for its persistence and growth.
But we must do more. Racism will propagate if we live in silos surrounded by people whose ideas reflect our own. As long as we have nondiversified board rooms, departments, and staff, the problem will persist.
A lot of the biases that we unconsciously carry in our heads and hearts have no basis in reality and were placed there without our permission by parents, society, and friends. But we can replace these divisive thoughts and impulses.
What’s in your heart can only be known and controlled by you. How tolerant we are of racism is up to us: Do you call out racism; do you challenge any inkling of racism from friends or acquaintances; do you put pressure on institutions where you work to diversify in recruiting and hiring?
Think of all the advances in medicine that were achieved by people from different cultures and races. Racism has no place in what we have all devoted our lives to do – take care of our fellow humans.
A version of this article first appeared on Medscape.com.
New algorithm for initial PsA treatment choice is driven by T-cell behavior
T-cell behavior
Biologic selection is cytokine based
NEW YORK – An algorithm in development for psoriatic arthritis (PsA) is showing promise for directing patients to the biologic with the greatest likelihood of producing disease control, according to a proof-of-concept study presented at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“Our technique involves a more precise functional assay showing exact T-cell behavior, compared to the previous assessments that only analyzed cellular phenotypes,” reported Gizem Ayan, MD, a fellow in rheumatology at Hacettepe University Faculty of Medicine, Ankara, Turkey.
The concept of precision medicine in PsA as well as other autoimmune diseases is not new. Phenotypes and biomarkers have already shown potential for guiding treatment, according to Dr. Ayan, but she said none are yet guideline recommended or proven to improve patient outcomes.
The principle of the new algorithm that she and her coinvestigators are pursing is based on immunophenotype analysis conducted with a flow-cytometric cytokine secretion assay (FCCSA). In the protocol, monocytes obtained from peripheral blood undergo activation before an FCCSA to distinguish patients by their T-cell behavior.
The treatment decision tree is based on median ratios of tumor necrosis factor (TNF)-alpha, interleukin (IL)–22, IL-17, and interferon-gamma expression among CD4+ and CD8+ cells. Based on a yes-or-no response to specific immune patterns, the patient is funneled to a biologic that inhibits a dominant cytokine.
The proof-of-concept study, which enrolled 8 patients with PsA who were naive to conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) and 11 patients with PsA who were naive to biologic DMARDs (bDMARDs), was designed to demonstrate feasibility. It did not test clinical benefit, but it did show that immunophenotyping with this methodology can be performed efficiently.
“From the time a blood sample is obtained, the method provided results within 24 hours,” according to Dr. Ayan, who is now planning a randomized trial to test the ability of the algorithm to improve clinical outcomes.
In the decision tree, there are five yes-no pathways to a treatment choice. The first step of the algorithm is to test the ratio of TNF-alpha to interferon-gamma CD4+ T cells. A “yes’ response is produced if the ratio is greater than or equal to 2. These patients are then evaluated for the ratio of TNF-alpha to interferon-gamma CD8+ T cells. A yes response is produced if the ratio is greater than or equal to 0.5. If yes, they are candidates for a TNF-alpha inhibitor. If no, they are directed to an IL-12/23 inhibitor.
If the answer at the first decision point in the algorithm is a “no,” meaning they do not have a TNF-alpha to interferon-gamma CD4+ ratio of 2 or higher, they are evaluated for percentage of CD4+ T cells expressing IL-22 or IL-17. Is it greater than or equal to 2%? If the answer is “no,” they are candidates for an IL-12/23 inhibitor.
If “yes,” they are evaluated for percentage of IL-22 to IL-17 CD4+. If the IL-22 CD4+ percentage is lower than the IL-17 CD4+ percentage, meaning a “yes” to this decision point, they are directed to an IL-17 inhibitor. If the answer at this decision point is “no,” they are directed to an IL-12/23 inhibitor.
Prior to enrollment in this proof-of-concept study, 10 of the bDMARD patients were scheduled to receive an anti-TNF drug and 1 was scheduled to receive an IL-12/23 inhibitor. On the basis of this algorithm, only 5 patients were directed to an anti-TNF drug. Of the remaining, 5 were directed to an IL-17 inhibitor, and 1 was directed to an IL-12/23 inhibitor.
All 19 participants in the proof-of-concept study had peripheral arthritis; their median age was 45 years. Approximately 90% had skin lesions. Axial involvement was present in only one patient. Based on these and other characteristics and the median ratios of the cytokines measured, Dr. Ayan called this a representative population.
Based on the feasibility of this method for subtyping patients by T-cell behavior to guide drug selection, Dr. Ayan anticipates pursuing the additional steps that would show the algorithm makes a difference to patient care, including such adjunctive benefits as more cost-effective treatment selection.
“We aim to develop a treatment decision algorithm that can be implemented in daily practice,” Dr. Ayan said.
Is peripheral blood sampling adequate?
In addition to saying that the algorithm will need to prove that it alters outcomes, Samuel Tzen-yue Hwang, MD, PhD, professor and chair of the department of dermatology at the University of California, Davis, Sacramento, pointed out some potential practical issues.
“Flow cytometry is not typically available as a rapid throughput, and the cost is high,” he said. Moreover, he remains skeptical about performing this algorithm on the basis of peripheral blood samples.
“It is debatable that looking at peripheral cells would provide adequate information about what is taking place at sites of inflammation,” he said. Although it would “be fantastic” to develop an algorithm that required only a peripheral blood sample, he pointed out that “only a fraction of these cells is relevant” to disease activity.
Aspirating fluid from an involved joint “might be more useful,” but it is more work, he added. Yet, Dr. Hwang acknowledged that this approach is intriguing. He agreed that there is considerable heterogeneity among patients with PsA in their response to specific biologics, and a method to better direct patients to the treatment most likely to elicit a response is needed.
Dr. Ayan and Dr. Hwang reported no potential conflicts of interest.
Biologic selection is cytokine based
Biologic selection is cytokine based
NEW YORK – An algorithm in development for psoriatic arthritis (PsA) is showing promise for directing patients to the biologic with the greatest likelihood of producing disease control, according to a proof-of-concept study presented at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“Our technique involves a more precise functional assay showing exact T-cell behavior, compared to the previous assessments that only analyzed cellular phenotypes,” reported Gizem Ayan, MD, a fellow in rheumatology at Hacettepe University Faculty of Medicine, Ankara, Turkey.
The concept of precision medicine in PsA as well as other autoimmune diseases is not new. Phenotypes and biomarkers have already shown potential for guiding treatment, according to Dr. Ayan, but she said none are yet guideline recommended or proven to improve patient outcomes.
The principle of the new algorithm that she and her coinvestigators are pursing is based on immunophenotype analysis conducted with a flow-cytometric cytokine secretion assay (FCCSA). In the protocol, monocytes obtained from peripheral blood undergo activation before an FCCSA to distinguish patients by their T-cell behavior.
The treatment decision tree is based on median ratios of tumor necrosis factor (TNF)-alpha, interleukin (IL)–22, IL-17, and interferon-gamma expression among CD4+ and CD8+ cells. Based on a yes-or-no response to specific immune patterns, the patient is funneled to a biologic that inhibits a dominant cytokine.
The proof-of-concept study, which enrolled 8 patients with PsA who were naive to conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) and 11 patients with PsA who were naive to biologic DMARDs (bDMARDs), was designed to demonstrate feasibility. It did not test clinical benefit, but it did show that immunophenotyping with this methodology can be performed efficiently.
“From the time a blood sample is obtained, the method provided results within 24 hours,” according to Dr. Ayan, who is now planning a randomized trial to test the ability of the algorithm to improve clinical outcomes.
In the decision tree, there are five yes-no pathways to a treatment choice. The first step of the algorithm is to test the ratio of TNF-alpha to interferon-gamma CD4+ T cells. A “yes’ response is produced if the ratio is greater than or equal to 2. These patients are then evaluated for the ratio of TNF-alpha to interferon-gamma CD8+ T cells. A yes response is produced if the ratio is greater than or equal to 0.5. If yes, they are candidates for a TNF-alpha inhibitor. If no, they are directed to an IL-12/23 inhibitor.
If the answer at the first decision point in the algorithm is a “no,” meaning they do not have a TNF-alpha to interferon-gamma CD4+ ratio of 2 or higher, they are evaluated for percentage of CD4+ T cells expressing IL-22 or IL-17. Is it greater than or equal to 2%? If the answer is “no,” they are candidates for an IL-12/23 inhibitor.
If “yes,” they are evaluated for percentage of IL-22 to IL-17 CD4+. If the IL-22 CD4+ percentage is lower than the IL-17 CD4+ percentage, meaning a “yes” to this decision point, they are directed to an IL-17 inhibitor. If the answer at this decision point is “no,” they are directed to an IL-12/23 inhibitor.
Prior to enrollment in this proof-of-concept study, 10 of the bDMARD patients were scheduled to receive an anti-TNF drug and 1 was scheduled to receive an IL-12/23 inhibitor. On the basis of this algorithm, only 5 patients were directed to an anti-TNF drug. Of the remaining, 5 were directed to an IL-17 inhibitor, and 1 was directed to an IL-12/23 inhibitor.
All 19 participants in the proof-of-concept study had peripheral arthritis; their median age was 45 years. Approximately 90% had skin lesions. Axial involvement was present in only one patient. Based on these and other characteristics and the median ratios of the cytokines measured, Dr. Ayan called this a representative population.
Based on the feasibility of this method for subtyping patients by T-cell behavior to guide drug selection, Dr. Ayan anticipates pursuing the additional steps that would show the algorithm makes a difference to patient care, including such adjunctive benefits as more cost-effective treatment selection.
“We aim to develop a treatment decision algorithm that can be implemented in daily practice,” Dr. Ayan said.
Is peripheral blood sampling adequate?
In addition to saying that the algorithm will need to prove that it alters outcomes, Samuel Tzen-yue Hwang, MD, PhD, professor and chair of the department of dermatology at the University of California, Davis, Sacramento, pointed out some potential practical issues.
“Flow cytometry is not typically available as a rapid throughput, and the cost is high,” he said. Moreover, he remains skeptical about performing this algorithm on the basis of peripheral blood samples.
“It is debatable that looking at peripheral cells would provide adequate information about what is taking place at sites of inflammation,” he said. Although it would “be fantastic” to develop an algorithm that required only a peripheral blood sample, he pointed out that “only a fraction of these cells is relevant” to disease activity.
Aspirating fluid from an involved joint “might be more useful,” but it is more work, he added. Yet, Dr. Hwang acknowledged that this approach is intriguing. He agreed that there is considerable heterogeneity among patients with PsA in their response to specific biologics, and a method to better direct patients to the treatment most likely to elicit a response is needed.
Dr. Ayan and Dr. Hwang reported no potential conflicts of interest.
NEW YORK – An algorithm in development for psoriatic arthritis (PsA) is showing promise for directing patients to the biologic with the greatest likelihood of producing disease control, according to a proof-of-concept study presented at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“Our technique involves a more precise functional assay showing exact T-cell behavior, compared to the previous assessments that only analyzed cellular phenotypes,” reported Gizem Ayan, MD, a fellow in rheumatology at Hacettepe University Faculty of Medicine, Ankara, Turkey.
The concept of precision medicine in PsA as well as other autoimmune diseases is not new. Phenotypes and biomarkers have already shown potential for guiding treatment, according to Dr. Ayan, but she said none are yet guideline recommended or proven to improve patient outcomes.
The principle of the new algorithm that she and her coinvestigators are pursing is based on immunophenotype analysis conducted with a flow-cytometric cytokine secretion assay (FCCSA). In the protocol, monocytes obtained from peripheral blood undergo activation before an FCCSA to distinguish patients by their T-cell behavior.
The treatment decision tree is based on median ratios of tumor necrosis factor (TNF)-alpha, interleukin (IL)–22, IL-17, and interferon-gamma expression among CD4+ and CD8+ cells. Based on a yes-or-no response to specific immune patterns, the patient is funneled to a biologic that inhibits a dominant cytokine.
The proof-of-concept study, which enrolled 8 patients with PsA who were naive to conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) and 11 patients with PsA who were naive to biologic DMARDs (bDMARDs), was designed to demonstrate feasibility. It did not test clinical benefit, but it did show that immunophenotyping with this methodology can be performed efficiently.
“From the time a blood sample is obtained, the method provided results within 24 hours,” according to Dr. Ayan, who is now planning a randomized trial to test the ability of the algorithm to improve clinical outcomes.
In the decision tree, there are five yes-no pathways to a treatment choice. The first step of the algorithm is to test the ratio of TNF-alpha to interferon-gamma CD4+ T cells. A “yes’ response is produced if the ratio is greater than or equal to 2. These patients are then evaluated for the ratio of TNF-alpha to interferon-gamma CD8+ T cells. A yes response is produced if the ratio is greater than or equal to 0.5. If yes, they are candidates for a TNF-alpha inhibitor. If no, they are directed to an IL-12/23 inhibitor.
If the answer at the first decision point in the algorithm is a “no,” meaning they do not have a TNF-alpha to interferon-gamma CD4+ ratio of 2 or higher, they are evaluated for percentage of CD4+ T cells expressing IL-22 or IL-17. Is it greater than or equal to 2%? If the answer is “no,” they are candidates for an IL-12/23 inhibitor.
If “yes,” they are evaluated for percentage of IL-22 to IL-17 CD4+. If the IL-22 CD4+ percentage is lower than the IL-17 CD4+ percentage, meaning a “yes” to this decision point, they are directed to an IL-17 inhibitor. If the answer at this decision point is “no,” they are directed to an IL-12/23 inhibitor.
Prior to enrollment in this proof-of-concept study, 10 of the bDMARD patients were scheduled to receive an anti-TNF drug and 1 was scheduled to receive an IL-12/23 inhibitor. On the basis of this algorithm, only 5 patients were directed to an anti-TNF drug. Of the remaining, 5 were directed to an IL-17 inhibitor, and 1 was directed to an IL-12/23 inhibitor.
All 19 participants in the proof-of-concept study had peripheral arthritis; their median age was 45 years. Approximately 90% had skin lesions. Axial involvement was present in only one patient. Based on these and other characteristics and the median ratios of the cytokines measured, Dr. Ayan called this a representative population.
Based on the feasibility of this method for subtyping patients by T-cell behavior to guide drug selection, Dr. Ayan anticipates pursuing the additional steps that would show the algorithm makes a difference to patient care, including such adjunctive benefits as more cost-effective treatment selection.
“We aim to develop a treatment decision algorithm that can be implemented in daily practice,” Dr. Ayan said.
Is peripheral blood sampling adequate?
In addition to saying that the algorithm will need to prove that it alters outcomes, Samuel Tzen-yue Hwang, MD, PhD, professor and chair of the department of dermatology at the University of California, Davis, Sacramento, pointed out some potential practical issues.
“Flow cytometry is not typically available as a rapid throughput, and the cost is high,” he said. Moreover, he remains skeptical about performing this algorithm on the basis of peripheral blood samples.
“It is debatable that looking at peripheral cells would provide adequate information about what is taking place at sites of inflammation,” he said. Although it would “be fantastic” to develop an algorithm that required only a peripheral blood sample, he pointed out that “only a fraction of these cells is relevant” to disease activity.
Aspirating fluid from an involved joint “might be more useful,” but it is more work, he added. Yet, Dr. Hwang acknowledged that this approach is intriguing. He agreed that there is considerable heterogeneity among patients with PsA in their response to specific biologics, and a method to better direct patients to the treatment most likely to elicit a response is needed.
Dr. Ayan and Dr. Hwang reported no potential conflicts of interest.
T-cell behavior
T-cell behavior
AT GRAPPA 2022
Type 2 Diabetes Treatment
Migraine Treatment Guidelines
Diffuse annular lesions
A 24-YEAR-OLD WOMAN with a history of guttate psoriasis, for which she was taking adalimumab, presented with a 2-week history of diffuse papules and plaques on her neck, back, torso, and upper and lower extremities (FIGURE 1). She said that the lesions were pruritic and seemed similar to those that erupted during past outbreaks of psoriasis—although they were more numerous and progressive. So, the patient (a nurse) decided to take her biweekly dose (40 mg) of adalimumab 1 week early. After administration, the rash significantly worsened, spreading to the rest of her trunk and extremities.

Physical exam was notable for multiple erythematous papules and plaques with central clearing and light peripheral scaling on both arms and legs, as well as her chest and back. The patient also indicated she’d adopted a stray cat 2 weeks prior. Given the patient’s pet exposure and the annular nature of the lesions, a potassium hydroxide (KOH) preparation was done.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Tinea corporis
The KOH preparation was positive for hyphae in 4 separate sites (trunk, left arm, left leg, and left neck), confirming the diagnosis of severe extensive tinea corporis (FIGURE 2).
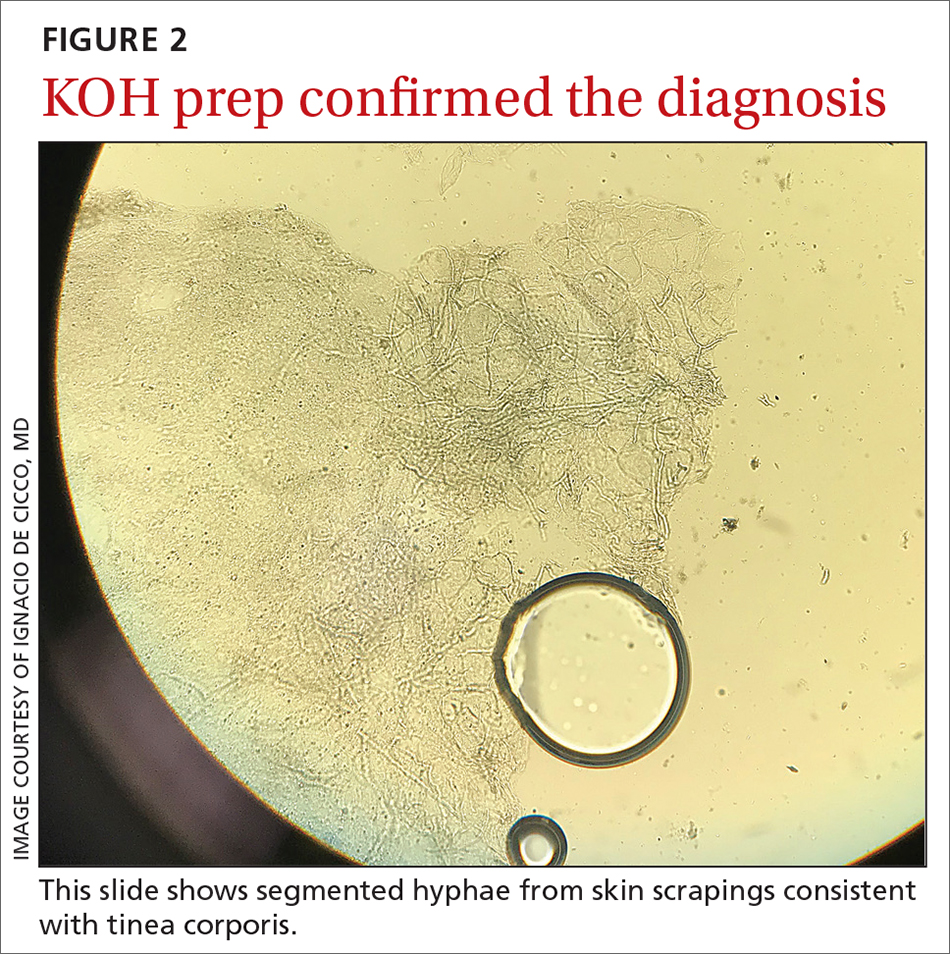
Dermatophyte (tinea) infections are caused by fungi that invade and reproduce in the skin, hair, and nails. Dermatophytes, which include the genera Trichophyton, Microsporum, and Epidermophyton, are the most common cause of superficial mycotic infections. As of 2016, the worldwide prevalence of superficial mycotic infections was 20% to 25%.1 Tinea corporis can result from contact with people, animals, or soil. Infections resulting from animal-to-human contact are often transmitted by domestic animals. In this case, the patient’s exposure was from her new cat.
Tinea corporis classically manifests as pruritic, erythematous patches or plaques with central clearing, giving it an annular appearance. The response to a tinea infection depends on the immune system of the host and can range in severity from superficial to severe.2 There are 2 forms of severe dermatophytosis: invasive, which involves localized perifollicular sites or deep dermatophytosis, and extensive, which is confined to the stratum corneum but results in numerous lesions.3
The diagnosis of tinea corporis is commonly confirmed using direct microscopic examination with 10% to 20% KOH preparation, which will show branching and septate hyphal filaments.4
Several conditions with annular lesions comprise the differential
The findings of pruritic annular erythematous lesions on the patient’s neck, chest, trunk, and bilateral extremities led the patient to suspect this was a worsening case of her guttate psoriasis. Other possible diagnoses included pityriasis rosea, subacute cutaneous lupus erythematosus (SCLE), and secondary syphilis.
Continue to: Guttate psoriasis
Guttate psoriasis would not typically progress during treatment with adalimumab, although tumor necrosis factor (TNF) inhibitors have been associated with worsening psoriasis. Guttate psoriasis manifests with small, pink to red, scaly raindrop-shaped patches over the trunk and extremities.
Pityriasis rosea, a rash that resembles branches of a Christmas tree, was strongly considered given the appearance of the lesions on the patient’s back. It commonly manifests as round to oval lesions with a subtle advancing border and central fine scaling, similar in shape and color to the lesions seen in tinea corporis.
SCLE has been associated with use of TNF inhibitors, but our patient had no other lupus-like symptoms, such as fatigue, fever, headaches, or joint pain. SCLE lesions are often annular with raised pink to red borders similar in appearance to tinea corporis.
Secondary syphilis was ruled out in this patient because she had a negative rapid plasma reagin test. Secondary syphilis most commonly manifests with diffuse, nonpruritic pink to red-brown lesions on the palms and soles of patients. Patients often have prodromal symptoms that include fever, weight loss, myalgias, headache, and sore throat.
Terbinafine, Yes, but for how long?
Historically, terbinafine has been prescribed at 250 mg once daily for 2 weeks for extensive tinea corporis. However, recent studies in India suggest that terbinafine should be dosed at 250 mg twice daily, with longer durations of treatment, due to resistance.5 In the United States, it is reasonable to prescribe oral terbinafine 250 mg once daily for 4 weeks and then re-evaluate the patient in a case of extensive tinea corporis.
Other oral antifungals that can effectively treat extensive tinea corporis include itraconazole, fluconazole, and griseofulvin.1 Itraconazole and terbinafine are equally effective and safe in the treatment of tinea corporis, although itraconazole is significantly more expensive.6 Furthermore, a recent study found that combination therapy with oral terbinafine and itraconazole is as safe as monotherapy and is an option when terbinafine resistance is suspected.7
Our patient was initially started on oral terbinafine 250 mg/d. After the first dose, the patient requested a change in medication because there was no improvement in the rash. The patient was then prescribed oral fluconazole 300 mg daily and the tinea cleared after 2 months of daily therapy. (We surmise the treatment course may have been prolonged due to the possible immunosuppressant effects of adalimumab.) At the completion of treatment for the tinea corporis, the patient was restarted on adalimumab 40 mg biweekly for her psoriasis.
1. Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: a comprehensive review. Indian Dermatol Online J. 2016;7:77-86. doi: 10.4103/2229-5178.178099
2. Weitzman I, Summerbell RC. The dermatophytes. Clin Microbial Rev. 1995:8:240-259. doi: 10.1128/CMR.8.2.240
3. Rouzaud C, Hay R, Chosidow O, et al. Severe dermatophytosis and acquired or innate immunodeficiency: a review. J Fungi (Basel). 2015;2:4. doi: 10.3390/jof2010004
4. Kurade SM, Amladi SA, Miskeen AK. Skin scraping and a potassium hydroxide mount. Indian J Dermatol Venereol Leprol. 2006;72:238-41. doi: 10.4103/0378-6323.25794
5. Khurana A, Sardana K, Chowdhary A. Antifungal resistance in dermatophytes: recent trends and therapeutic implications. Fungal Genet Biol. 2019;132:103255. doi: 10.1016/j.fgb.2019.103255
6. Bhatia A, Kanish B, Badyal DK, et al. Efficacy of oral terbinafine versus itraconazole in treatment of dermatophytic infection of skin - a prospective, randomized comparative study. Indian J Pharmacol. 2019;51:116-119.
7. Sharma P, Bhalla M, Thami GP, et al. Evaluation of efficacy and safety of oral terbinafine and itraconazole combination therapy in the management of dermatophytosis. J Dermatolog Treat. 2020;31:749-753. doi: 10.1080/09546634.2019.1612835
A 24-YEAR-OLD WOMAN with a history of guttate psoriasis, for which she was taking adalimumab, presented with a 2-week history of diffuse papules and plaques on her neck, back, torso, and upper and lower extremities (FIGURE 1). She said that the lesions were pruritic and seemed similar to those that erupted during past outbreaks of psoriasis—although they were more numerous and progressive. So, the patient (a nurse) decided to take her biweekly dose (40 mg) of adalimumab 1 week early. After administration, the rash significantly worsened, spreading to the rest of her trunk and extremities.

Physical exam was notable for multiple erythematous papules and plaques with central clearing and light peripheral scaling on both arms and legs, as well as her chest and back. The patient also indicated she’d adopted a stray cat 2 weeks prior. Given the patient’s pet exposure and the annular nature of the lesions, a potassium hydroxide (KOH) preparation was done.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Tinea corporis
The KOH preparation was positive for hyphae in 4 separate sites (trunk, left arm, left leg, and left neck), confirming the diagnosis of severe extensive tinea corporis (FIGURE 2).
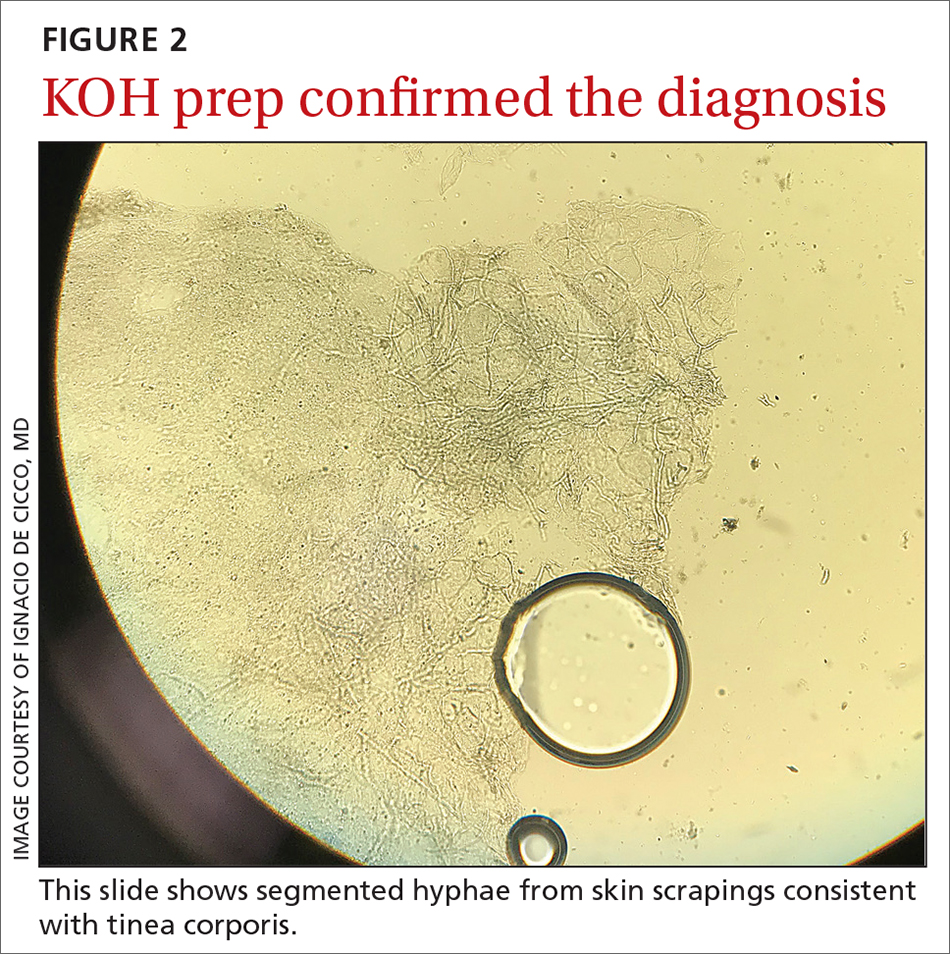
Dermatophyte (tinea) infections are caused by fungi that invade and reproduce in the skin, hair, and nails. Dermatophytes, which include the genera Trichophyton, Microsporum, and Epidermophyton, are the most common cause of superficial mycotic infections. As of 2016, the worldwide prevalence of superficial mycotic infections was 20% to 25%.1 Tinea corporis can result from contact with people, animals, or soil. Infections resulting from animal-to-human contact are often transmitted by domestic animals. In this case, the patient’s exposure was from her new cat.
Tinea corporis classically manifests as pruritic, erythematous patches or plaques with central clearing, giving it an annular appearance. The response to a tinea infection depends on the immune system of the host and can range in severity from superficial to severe.2 There are 2 forms of severe dermatophytosis: invasive, which involves localized perifollicular sites or deep dermatophytosis, and extensive, which is confined to the stratum corneum but results in numerous lesions.3
The diagnosis of tinea corporis is commonly confirmed using direct microscopic examination with 10% to 20% KOH preparation, which will show branching and septate hyphal filaments.4
Several conditions with annular lesions comprise the differential
The findings of pruritic annular erythematous lesions on the patient’s neck, chest, trunk, and bilateral extremities led the patient to suspect this was a worsening case of her guttate psoriasis. Other possible diagnoses included pityriasis rosea, subacute cutaneous lupus erythematosus (SCLE), and secondary syphilis.
Continue to: Guttate psoriasis
Guttate psoriasis would not typically progress during treatment with adalimumab, although tumor necrosis factor (TNF) inhibitors have been associated with worsening psoriasis. Guttate psoriasis manifests with small, pink to red, scaly raindrop-shaped patches over the trunk and extremities.
Pityriasis rosea, a rash that resembles branches of a Christmas tree, was strongly considered given the appearance of the lesions on the patient’s back. It commonly manifests as round to oval lesions with a subtle advancing border and central fine scaling, similar in shape and color to the lesions seen in tinea corporis.
SCLE has been associated with use of TNF inhibitors, but our patient had no other lupus-like symptoms, such as fatigue, fever, headaches, or joint pain. SCLE lesions are often annular with raised pink to red borders similar in appearance to tinea corporis.
Secondary syphilis was ruled out in this patient because she had a negative rapid plasma reagin test. Secondary syphilis most commonly manifests with diffuse, nonpruritic pink to red-brown lesions on the palms and soles of patients. Patients often have prodromal symptoms that include fever, weight loss, myalgias, headache, and sore throat.
Terbinafine, Yes, but for how long?
Historically, terbinafine has been prescribed at 250 mg once daily for 2 weeks for extensive tinea corporis. However, recent studies in India suggest that terbinafine should be dosed at 250 mg twice daily, with longer durations of treatment, due to resistance.5 In the United States, it is reasonable to prescribe oral terbinafine 250 mg once daily for 4 weeks and then re-evaluate the patient in a case of extensive tinea corporis.
Other oral antifungals that can effectively treat extensive tinea corporis include itraconazole, fluconazole, and griseofulvin.1 Itraconazole and terbinafine are equally effective and safe in the treatment of tinea corporis, although itraconazole is significantly more expensive.6 Furthermore, a recent study found that combination therapy with oral terbinafine and itraconazole is as safe as monotherapy and is an option when terbinafine resistance is suspected.7
Our patient was initially started on oral terbinafine 250 mg/d. After the first dose, the patient requested a change in medication because there was no improvement in the rash. The patient was then prescribed oral fluconazole 300 mg daily and the tinea cleared after 2 months of daily therapy. (We surmise the treatment course may have been prolonged due to the possible immunosuppressant effects of adalimumab.) At the completion of treatment for the tinea corporis, the patient was restarted on adalimumab 40 mg biweekly for her psoriasis.
A 24-YEAR-OLD WOMAN with a history of guttate psoriasis, for which she was taking adalimumab, presented with a 2-week history of diffuse papules and plaques on her neck, back, torso, and upper and lower extremities (FIGURE 1). She said that the lesions were pruritic and seemed similar to those that erupted during past outbreaks of psoriasis—although they were more numerous and progressive. So, the patient (a nurse) decided to take her biweekly dose (40 mg) of adalimumab 1 week early. After administration, the rash significantly worsened, spreading to the rest of her trunk and extremities.

Physical exam was notable for multiple erythematous papules and plaques with central clearing and light peripheral scaling on both arms and legs, as well as her chest and back. The patient also indicated she’d adopted a stray cat 2 weeks prior. Given the patient’s pet exposure and the annular nature of the lesions, a potassium hydroxide (KOH) preparation was done.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Tinea corporis
The KOH preparation was positive for hyphae in 4 separate sites (trunk, left arm, left leg, and left neck), confirming the diagnosis of severe extensive tinea corporis (FIGURE 2).
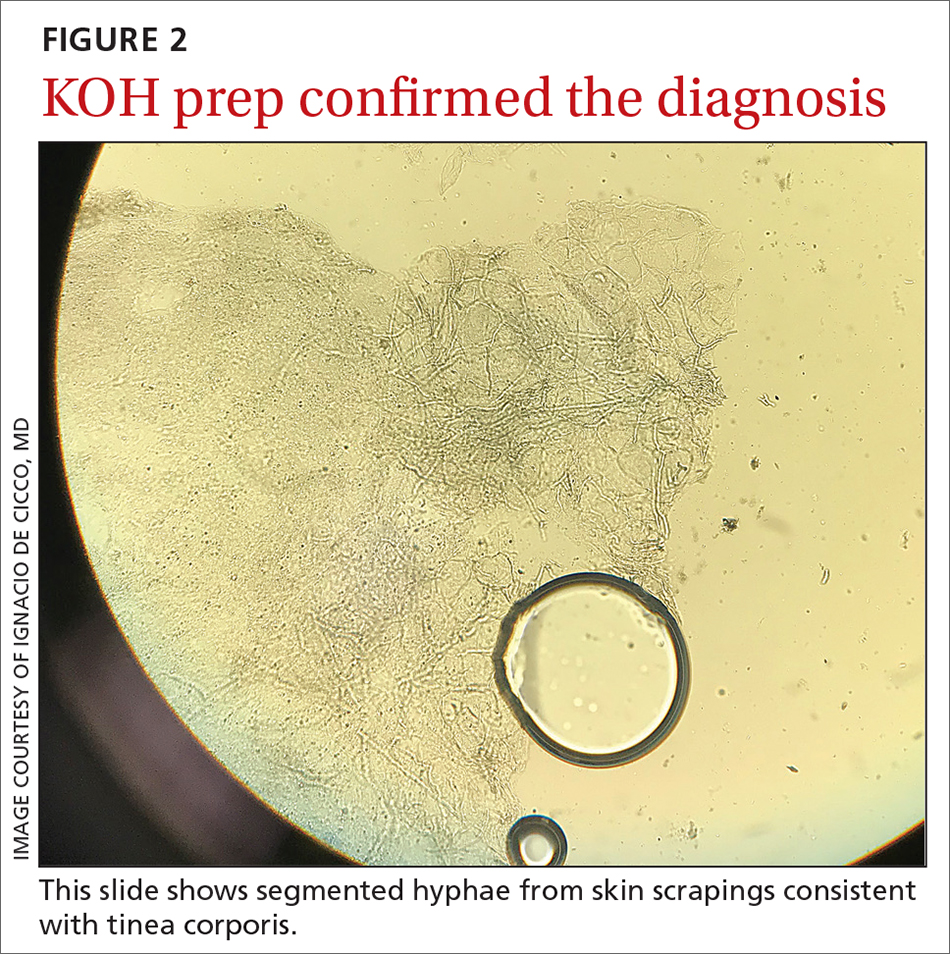
Dermatophyte (tinea) infections are caused by fungi that invade and reproduce in the skin, hair, and nails. Dermatophytes, which include the genera Trichophyton, Microsporum, and Epidermophyton, are the most common cause of superficial mycotic infections. As of 2016, the worldwide prevalence of superficial mycotic infections was 20% to 25%.1 Tinea corporis can result from contact with people, animals, or soil. Infections resulting from animal-to-human contact are often transmitted by domestic animals. In this case, the patient’s exposure was from her new cat.
Tinea corporis classically manifests as pruritic, erythematous patches or plaques with central clearing, giving it an annular appearance. The response to a tinea infection depends on the immune system of the host and can range in severity from superficial to severe.2 There are 2 forms of severe dermatophytosis: invasive, which involves localized perifollicular sites or deep dermatophytosis, and extensive, which is confined to the stratum corneum but results in numerous lesions.3
The diagnosis of tinea corporis is commonly confirmed using direct microscopic examination with 10% to 20% KOH preparation, which will show branching and septate hyphal filaments.4
Several conditions with annular lesions comprise the differential
The findings of pruritic annular erythematous lesions on the patient’s neck, chest, trunk, and bilateral extremities led the patient to suspect this was a worsening case of her guttate psoriasis. Other possible diagnoses included pityriasis rosea, subacute cutaneous lupus erythematosus (SCLE), and secondary syphilis.
Continue to: Guttate psoriasis
Guttate psoriasis would not typically progress during treatment with adalimumab, although tumor necrosis factor (TNF) inhibitors have been associated with worsening psoriasis. Guttate psoriasis manifests with small, pink to red, scaly raindrop-shaped patches over the trunk and extremities.
Pityriasis rosea, a rash that resembles branches of a Christmas tree, was strongly considered given the appearance of the lesions on the patient’s back. It commonly manifests as round to oval lesions with a subtle advancing border and central fine scaling, similar in shape and color to the lesions seen in tinea corporis.
SCLE has been associated with use of TNF inhibitors, but our patient had no other lupus-like symptoms, such as fatigue, fever, headaches, or joint pain. SCLE lesions are often annular with raised pink to red borders similar in appearance to tinea corporis.
Secondary syphilis was ruled out in this patient because she had a negative rapid plasma reagin test. Secondary syphilis most commonly manifests with diffuse, nonpruritic pink to red-brown lesions on the palms and soles of patients. Patients often have prodromal symptoms that include fever, weight loss, myalgias, headache, and sore throat.
Terbinafine, Yes, but for how long?
Historically, terbinafine has been prescribed at 250 mg once daily for 2 weeks for extensive tinea corporis. However, recent studies in India suggest that terbinafine should be dosed at 250 mg twice daily, with longer durations of treatment, due to resistance.5 In the United States, it is reasonable to prescribe oral terbinafine 250 mg once daily for 4 weeks and then re-evaluate the patient in a case of extensive tinea corporis.
Other oral antifungals that can effectively treat extensive tinea corporis include itraconazole, fluconazole, and griseofulvin.1 Itraconazole and terbinafine are equally effective and safe in the treatment of tinea corporis, although itraconazole is significantly more expensive.6 Furthermore, a recent study found that combination therapy with oral terbinafine and itraconazole is as safe as monotherapy and is an option when terbinafine resistance is suspected.7
Our patient was initially started on oral terbinafine 250 mg/d. After the first dose, the patient requested a change in medication because there was no improvement in the rash. The patient was then prescribed oral fluconazole 300 mg daily and the tinea cleared after 2 months of daily therapy. (We surmise the treatment course may have been prolonged due to the possible immunosuppressant effects of adalimumab.) At the completion of treatment for the tinea corporis, the patient was restarted on adalimumab 40 mg biweekly for her psoriasis.
1. Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: a comprehensive review. Indian Dermatol Online J. 2016;7:77-86. doi: 10.4103/2229-5178.178099
2. Weitzman I, Summerbell RC. The dermatophytes. Clin Microbial Rev. 1995:8:240-259. doi: 10.1128/CMR.8.2.240
3. Rouzaud C, Hay R, Chosidow O, et al. Severe dermatophytosis and acquired or innate immunodeficiency: a review. J Fungi (Basel). 2015;2:4. doi: 10.3390/jof2010004
4. Kurade SM, Amladi SA, Miskeen AK. Skin scraping and a potassium hydroxide mount. Indian J Dermatol Venereol Leprol. 2006;72:238-41. doi: 10.4103/0378-6323.25794
5. Khurana A, Sardana K, Chowdhary A. Antifungal resistance in dermatophytes: recent trends and therapeutic implications. Fungal Genet Biol. 2019;132:103255. doi: 10.1016/j.fgb.2019.103255
6. Bhatia A, Kanish B, Badyal DK, et al. Efficacy of oral terbinafine versus itraconazole in treatment of dermatophytic infection of skin - a prospective, randomized comparative study. Indian J Pharmacol. 2019;51:116-119.
7. Sharma P, Bhalla M, Thami GP, et al. Evaluation of efficacy and safety of oral terbinafine and itraconazole combination therapy in the management of dermatophytosis. J Dermatolog Treat. 2020;31:749-753. doi: 10.1080/09546634.2019.1612835
1. Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: a comprehensive review. Indian Dermatol Online J. 2016;7:77-86. doi: 10.4103/2229-5178.178099
2. Weitzman I, Summerbell RC. The dermatophytes. Clin Microbial Rev. 1995:8:240-259. doi: 10.1128/CMR.8.2.240
3. Rouzaud C, Hay R, Chosidow O, et al. Severe dermatophytosis and acquired or innate immunodeficiency: a review. J Fungi (Basel). 2015;2:4. doi: 10.3390/jof2010004
4. Kurade SM, Amladi SA, Miskeen AK. Skin scraping and a potassium hydroxide mount. Indian J Dermatol Venereol Leprol. 2006;72:238-41. doi: 10.4103/0378-6323.25794
5. Khurana A, Sardana K, Chowdhary A. Antifungal resistance in dermatophytes: recent trends and therapeutic implications. Fungal Genet Biol. 2019;132:103255. doi: 10.1016/j.fgb.2019.103255
6. Bhatia A, Kanish B, Badyal DK, et al. Efficacy of oral terbinafine versus itraconazole in treatment of dermatophytic infection of skin - a prospective, randomized comparative study. Indian J Pharmacol. 2019;51:116-119.
7. Sharma P, Bhalla M, Thami GP, et al. Evaluation of efficacy and safety of oral terbinafine and itraconazole combination therapy in the management of dermatophytosis. J Dermatolog Treat. 2020;31:749-753. doi: 10.1080/09546634.2019.1612835
52-year-old man • erectile dysfunction • insomnia • migraine headaches • disclosure of infidelity
THE CASE
A 52-year-old man requested medicine to help him with erectile dysfunction. After obtaining a medical history and performing a physical exam, the family physician (FP) asked for more details about the patient’s situation. He reported that his wife, who had recently seen the same FP for counseling related to her frustrations with her husband, was uninterested in sex. He then added that he was having an affair with a 32-year-old female co-worker and wanted to improve his sexual function.
He admitted to feeling guilty about this situation and was conflicted about whether to end the affair. He also stated that since the affair, his insomnia had worsened, he was drinking more alcohol, and he was having migraine headaches. As the FP for both patients, and with the knowledge that the wife was worried about possible infidelity, the physician felt some level of conflict about the situation. The following is a discussion of the issues that this patient encounter raised.
DISCUSSION
Issues related to infidelity are common to both men and women. They are also common in same-sex relationships; in general, however, lesbian couples have fewer outside partners, whereas gay men are more likely to seek variety by having multiple partners.1
It is widely understood that successfully committed couples spend quality time together, emphasize each other’s strengths, show respect, accept influence, and nurture their friendship. However, many couples experience infidelity at some time in the course of their marriage. It is difficult to put an exact estimate on rates of infidelity due to problems with research methodology, inaccurate reporting, and a lack of agreement on a definition for infidelity.2 General categories of infidelity include emotional only, sexual only, and combined sexual and emotional infidelity.3,4 In terms of sexual infidelity, one study found that 25% of married men and 15% of married women admitted to having had extramarital sex at least once during their relationship.5 However, other studies suggest that women are closing the “sexual infidelity” gap and engaging in sexual affairs at a similar rate to men.6 There are websites that, in fact, have made it easier for married individuals to engage in affairs.
Reasons for infidelity. Men and women often have different motives in engaging in infidelity. In general, men’s motivations are more often related to sexual dissatisfaction and women’s to emotional dissatisfaction.7,8 However, infidelity may not always be the result of marital unhappiness.
Some studies suggest that the presence of opportunity may override the positive aspects of a relationship.9 Opportunity is heightened in the work environment, as reflected by the finding that 50% of infidelity occurs in the office.10 Research suggests that all relationships may be vulnerable to infidelity if the right opportunities present themselves.11
In general, health care providers are encouraged to use caution in generalizing about infidelity, as the subject is extremely complex, nuanced, and difficult to measure with exactitude.12
Continue to: The impact of infidelity
The impact of infidelity on couples varies due to factors such as the pre-morbid health of the marriage,13 the depth of involvement with the affair partner,14 and pre-existing attitudes about infidelity.13
Infidelity is a common cause of divorce in America. However, in a sample, Schneider et al15 found that despite initial threats to leave the marriage after infidelity, less than one-quarter of partners divorced. Other studies have found that disclosure of the infidelity and a commitment to work on the marriage may be an essential component of healing.16
Emotionally focused couples therapy, with its emphasis on attachment and bonding, may hold promise for helping couples successfully work through the trauma brought on by extramarital relationships.17 Psychologist and infidelity researcher Shirley Glass found that of the two-thirds of couples who chose to stay together after an affair, 80% of them reported a better marriage after treatment.11
Initial steps to take, and questions to ask
Both male and female patients need to feel comfortable surfacing sexual concerns with their clinicians. In this case, the concerns of the husband are interwoven with broader marital issues, which are the source of emotional and psychosomatic distress. His decision regarding his affair carried with it potentially life-altering consequences for his wife, 3 children, and affair partner and her family. It also raised ethical issues for the FP, who was providing care to both the husband and the wife. Appropriate care requires that a physician in this situation
- demonstrate a nonjudgmental approach
- clarify personal ethics in response to patient behaviors
- maintain confidentiality
- apply an ethical framework to resolve value dilemmas
- avoid actions that would be harmful to patients.
Interviewing can help to elicit information that may be clarifying not only to the physician but also to the patient. When interviewing a patient such as the one in this case, it would be wise to ask:
- How long has the affair been going on?
- Why is the patient engaging in the affair?
- Is abuse (emotional or physical) a factor in the marriage?
- Does the patient still have feelings for their spouse? Does the patient want to work on the marriage?
- Has the patient talked to a friend or therapist about the situation?
- Would the patient be willing to talk to a therapist?
Continue to: Ethical and legal considerations
Ethical and legal considerations
Some therapists espouse the view that being “neutral” in the presence of an affair is as much a value judgment as taking one side or the other. In the presence of emotional or physical abuse, it might indeed be best to support a marital separation. However, in other situations when there are young children involved and the patient is undecided about what to do, the FP can discuss the pros and cons of working on a marriage that suffers from more treatable types of disrepair (ie, stress, disconnection, repetitive arguments).
Provision of care. If the patient is unwilling to end the affair, the physician needs to decide whether they feel ethically at ease with prescribing sexually enhancing performance medication, given that the patient’s wife is also a patient. A physician in this situation might feel that they are betraying the wife by providing such medications to the husband. In such cases, it might be appropriate to refer the husband to a colleague.
In all cases of infidelity, however, it is wise to discuss safe-sex practices in order to limit the risk of transmitting a sexually transmitted infection (STI) to the spouse (or affair partner) and offer testing for STIs.
Confidentiality. Despite feelings the physician might have about betraying the wife’s trust by providing the performance-enhancing medicine to the husband, there is very little justification for revealing the affair to the wife. In general, confidentiality can only be broken if there is a high level of imminent danger associated with nondisclosure. The physician needs to realize the serious legal implications of breaking confidentiality in this situation, as such disclosure may prompt the initiation of divorce proceedings.
Real-world recommendations
Check your own biases. Infidelity can trigger a whole host of emotional reactions in physicians based on their own personal and professional history. It is important to be aware of such emotions and if sufficiently triggered, discuss the case with a colleague.
Continue to: Encourage bibliotherapy and marriage therapy
Encourage bibliotherapy and marriage therapy. The conversation might go something like this:
“I would recommend you do some reading about infidelity. If you are interested in working on your marriage, you might want to consider a couples counselor who can help you. Research shows that while such counseling can help couples work through infidelity, disclosure needs to occur as part of that process. Research also indicates that about two-thirds of marriages stay together after the revelation of an affair and that such couples can experience healing if they commit to a therapeutic process. If you are unsure how you want to proceed, it might be helpful for you to explore your situation with an individual therapist. What would you like to do next?”
There are also written resources that the patient might find helpful; see “3 bibliotherapy resources for infidelity” for recommendations.
SIDEBAR
3 bibliotherapy resources for infidelity
Not ‘Just Friends’: Protect Your Relationship from Infidelity and Heal the Trauma of Betrayal (Shirley Glass)
After the Affair: Healing the Pain and Rebuilding Trust When a Partner Has Betrayed You (Janice Abrams-Spring)
How Can I Forgive You: The Courage to Forgive, the Freedom Not To (Janice Abrams-Spring)
Referral to an individual or marriage counselor is warranted if the patient wants to work through the issues alone or with their partner. Disclosure of infidelity may not always be necessary for successful reconciliation if the affair has ended. A marriage therapist to whom you refer needs to be competent in working with infidelity.
Our patient. At the completion of the initial consultation—and after a discussion focused on the issues described, including encouragement to seek counseling—the FP acceded to the patient’s request for sexual performance-enhancing medication.
Continue to: The patient returned a few months...
The patient returned a few months later. His wife had found texts between him and his affair partner and told the patient that they had to enter into couples therapy or she was going to file for divorce. The patient told his physician that he had ended the extramarital relationship and was working on his marriage with a qualified marriage therapist; however, he felt lingering feelings of loss, discomfort in the workplace, and confusion about his choices. The physician was supportive and encouraged him to share these feelings, if possible, with an individual therapist or to find a friend who could listen while being supportive of his marriage. The physician also offered his services as a sounding board.
A year later, the patient had found another job and was still working on his marriage.
THE TAKEAWAY
This case underscores the importance of some basic health care tenets. It reminds us that maintaining patient confidentiality is paramount, and that nonjudgmental interviewing can help us to help our patients navigate challenging situations. The particulars of this case also highlight the importance of referring patients out for individual or marriage counseling and making a referral to a colleague when a situation makes us feel as if we are betraying a patient’s trust.
CORRESPONDENCE
David C. Slawson, MD, 2001 Vail Avenue, Suite 400B, Mercy Medical Plaza, Charlotte, NC 28207; [email protected]
1. Blumstein P, Schwartz P. American Couples: Money, Work, Sex. William Morrow; 1983.
2. Blow A, Hartnett K. Infidelity in committed relationships I: a methodological review. J Marital Fam Ther. 2005;31:183-216. doi: 10.1111/j.1752-0606.2005.tb01555.x
3. Glass S, Wright TL. Sex differences in type of extramarital involvement and marital dissatisfaction. Sex Roles. 1985;12:1101-1120.
4. Thompson AP. Emotional and sexual components of extramarital relations. J Marriage Fam. 1984;46:35-42. doi: 10.2307/351861
5. Laumann EO, Gagnon JH, Michael RT, et al. The Social Organization of Sexuality: Sexual Practices in the United States. University of Chicago Press; 1994.
6. Oliver MB, Hyde JS. Gender differences in sexuality: a meta-analysis. Psychol Bull. 1993;114:29-51. doi: 10.1037/0033-2909.114.1.29
7. Glass SP, Wright TL. Justifications for extramarital relationships: the association between attitudes, behaviors, and gender. J Sex Res. 1992;29:361-387. doi: 10.1080/00224499209551654
8. Spanier GB, Margolis RL. Marital separation and extramarital sexual behavior. J Sex Res. 1983;19:23-48.
9. Atkins DC, Baucom DH, Jacobson NS. Understanding infidelity: correlates in a national random sample. J Fam Psychol. 2001;15:735-749. doi: 10.1037//0893-3200.15.4.735
10. Treas J, Giesen D. Sexual infidelity among married and cohabitating Americans. J Marriage Fam. 2000;62:48-60. doi: 10.1111/j.1741-3737.2000.00048.x
11. Glass SP. Not ‘Just Friends’: Protect Your Relationship From Infidelity and Heal the Trauma of Betrayal. Free Press; 2002.
12. Blow A, Hartnet K. Infidelity in committed relationships II: a substantive review. J Marital Fam Ther. 2005;31:2. doi: 10.1111/j.1752-0606.2005.tb01556.x
13. Buunk B. Conditions that promote breakups as a consequence of extradyadic involvements. J Soc Clin Psychol. 1987;5:271-284. doi: 10.1521/jscp.1987.5.3.271
14. Charn IW, Parnass S. The impact of extramarital relationships on the continuation of marriages. J Sex Marital Therapy. 1995;21:100-115. doi: 10.1080/00926239508404389
15. Schneider JP, Irons RR, Corley MD. Disclosure of extramarital sexual activities by sexually exploitative professionals and other persons with addictive or compulsive sexual disorders. J Sex Edu Therapy. 1999;24:277-287. doi: 10.1080/01614576.1999.11074316
16. Atkins DC, Eldridge KA, Baucom DH, et al. Infidelity and behavioral couple therapy: optimism in the face of betrayal. J Consult Clin Psychol. 2005;73:144-150. doi: 10.1037/0022-006X.73.1.144
17. Johnson SM, Makinen J, Millikin J. Attachment injuries in couple relationships: a new perspective on impasses in emotionally focused marital therapy. J Marital Fam Therapy. 2001;27:145-155. doi: 10.1111/j.1752-0606.2001.tb01152.x
THE CASE
A 52-year-old man requested medicine to help him with erectile dysfunction. After obtaining a medical history and performing a physical exam, the family physician (FP) asked for more details about the patient’s situation. He reported that his wife, who had recently seen the same FP for counseling related to her frustrations with her husband, was uninterested in sex. He then added that he was having an affair with a 32-year-old female co-worker and wanted to improve his sexual function.
He admitted to feeling guilty about this situation and was conflicted about whether to end the affair. He also stated that since the affair, his insomnia had worsened, he was drinking more alcohol, and he was having migraine headaches. As the FP for both patients, and with the knowledge that the wife was worried about possible infidelity, the physician felt some level of conflict about the situation. The following is a discussion of the issues that this patient encounter raised.
DISCUSSION
Issues related to infidelity are common to both men and women. They are also common in same-sex relationships; in general, however, lesbian couples have fewer outside partners, whereas gay men are more likely to seek variety by having multiple partners.1
It is widely understood that successfully committed couples spend quality time together, emphasize each other’s strengths, show respect, accept influence, and nurture their friendship. However, many couples experience infidelity at some time in the course of their marriage. It is difficult to put an exact estimate on rates of infidelity due to problems with research methodology, inaccurate reporting, and a lack of agreement on a definition for infidelity.2 General categories of infidelity include emotional only, sexual only, and combined sexual and emotional infidelity.3,4 In terms of sexual infidelity, one study found that 25% of married men and 15% of married women admitted to having had extramarital sex at least once during their relationship.5 However, other studies suggest that women are closing the “sexual infidelity” gap and engaging in sexual affairs at a similar rate to men.6 There are websites that, in fact, have made it easier for married individuals to engage in affairs.
Reasons for infidelity. Men and women often have different motives in engaging in infidelity. In general, men’s motivations are more often related to sexual dissatisfaction and women’s to emotional dissatisfaction.7,8 However, infidelity may not always be the result of marital unhappiness.
Some studies suggest that the presence of opportunity may override the positive aspects of a relationship.9 Opportunity is heightened in the work environment, as reflected by the finding that 50% of infidelity occurs in the office.10 Research suggests that all relationships may be vulnerable to infidelity if the right opportunities present themselves.11
In general, health care providers are encouraged to use caution in generalizing about infidelity, as the subject is extremely complex, nuanced, and difficult to measure with exactitude.12
Continue to: The impact of infidelity
The impact of infidelity on couples varies due to factors such as the pre-morbid health of the marriage,13 the depth of involvement with the affair partner,14 and pre-existing attitudes about infidelity.13
Infidelity is a common cause of divorce in America. However, in a sample, Schneider et al15 found that despite initial threats to leave the marriage after infidelity, less than one-quarter of partners divorced. Other studies have found that disclosure of the infidelity and a commitment to work on the marriage may be an essential component of healing.16
Emotionally focused couples therapy, with its emphasis on attachment and bonding, may hold promise for helping couples successfully work through the trauma brought on by extramarital relationships.17 Psychologist and infidelity researcher Shirley Glass found that of the two-thirds of couples who chose to stay together after an affair, 80% of them reported a better marriage after treatment.11
Initial steps to take, and questions to ask
Both male and female patients need to feel comfortable surfacing sexual concerns with their clinicians. In this case, the concerns of the husband are interwoven with broader marital issues, which are the source of emotional and psychosomatic distress. His decision regarding his affair carried with it potentially life-altering consequences for his wife, 3 children, and affair partner and her family. It also raised ethical issues for the FP, who was providing care to both the husband and the wife. Appropriate care requires that a physician in this situation
- demonstrate a nonjudgmental approach
- clarify personal ethics in response to patient behaviors
- maintain confidentiality
- apply an ethical framework to resolve value dilemmas
- avoid actions that would be harmful to patients.
Interviewing can help to elicit information that may be clarifying not only to the physician but also to the patient. When interviewing a patient such as the one in this case, it would be wise to ask:
- How long has the affair been going on?
- Why is the patient engaging in the affair?
- Is abuse (emotional or physical) a factor in the marriage?
- Does the patient still have feelings for their spouse? Does the patient want to work on the marriage?
- Has the patient talked to a friend or therapist about the situation?
- Would the patient be willing to talk to a therapist?
Continue to: Ethical and legal considerations
Ethical and legal considerations
Some therapists espouse the view that being “neutral” in the presence of an affair is as much a value judgment as taking one side or the other. In the presence of emotional or physical abuse, it might indeed be best to support a marital separation. However, in other situations when there are young children involved and the patient is undecided about what to do, the FP can discuss the pros and cons of working on a marriage that suffers from more treatable types of disrepair (ie, stress, disconnection, repetitive arguments).
Provision of care. If the patient is unwilling to end the affair, the physician needs to decide whether they feel ethically at ease with prescribing sexually enhancing performance medication, given that the patient’s wife is also a patient. A physician in this situation might feel that they are betraying the wife by providing such medications to the husband. In such cases, it might be appropriate to refer the husband to a colleague.
In all cases of infidelity, however, it is wise to discuss safe-sex practices in order to limit the risk of transmitting a sexually transmitted infection (STI) to the spouse (or affair partner) and offer testing for STIs.
Confidentiality. Despite feelings the physician might have about betraying the wife’s trust by providing the performance-enhancing medicine to the husband, there is very little justification for revealing the affair to the wife. In general, confidentiality can only be broken if there is a high level of imminent danger associated with nondisclosure. The physician needs to realize the serious legal implications of breaking confidentiality in this situation, as such disclosure may prompt the initiation of divorce proceedings.
Real-world recommendations
Check your own biases. Infidelity can trigger a whole host of emotional reactions in physicians based on their own personal and professional history. It is important to be aware of such emotions and if sufficiently triggered, discuss the case with a colleague.
Continue to: Encourage bibliotherapy and marriage therapy
Encourage bibliotherapy and marriage therapy. The conversation might go something like this:
“I would recommend you do some reading about infidelity. If you are interested in working on your marriage, you might want to consider a couples counselor who can help you. Research shows that while such counseling can help couples work through infidelity, disclosure needs to occur as part of that process. Research also indicates that about two-thirds of marriages stay together after the revelation of an affair and that such couples can experience healing if they commit to a therapeutic process. If you are unsure how you want to proceed, it might be helpful for you to explore your situation with an individual therapist. What would you like to do next?”
There are also written resources that the patient might find helpful; see “3 bibliotherapy resources for infidelity” for recommendations.
SIDEBAR
3 bibliotherapy resources for infidelity
Not ‘Just Friends’: Protect Your Relationship from Infidelity and Heal the Trauma of Betrayal (Shirley Glass)
After the Affair: Healing the Pain and Rebuilding Trust When a Partner Has Betrayed You (Janice Abrams-Spring)
How Can I Forgive You: The Courage to Forgive, the Freedom Not To (Janice Abrams-Spring)
Referral to an individual or marriage counselor is warranted if the patient wants to work through the issues alone or with their partner. Disclosure of infidelity may not always be necessary for successful reconciliation if the affair has ended. A marriage therapist to whom you refer needs to be competent in working with infidelity.
Our patient. At the completion of the initial consultation—and after a discussion focused on the issues described, including encouragement to seek counseling—the FP acceded to the patient’s request for sexual performance-enhancing medication.
Continue to: The patient returned a few months...
The patient returned a few months later. His wife had found texts between him and his affair partner and told the patient that they had to enter into couples therapy or she was going to file for divorce. The patient told his physician that he had ended the extramarital relationship and was working on his marriage with a qualified marriage therapist; however, he felt lingering feelings of loss, discomfort in the workplace, and confusion about his choices. The physician was supportive and encouraged him to share these feelings, if possible, with an individual therapist or to find a friend who could listen while being supportive of his marriage. The physician also offered his services as a sounding board.
A year later, the patient had found another job and was still working on his marriage.
THE TAKEAWAY
This case underscores the importance of some basic health care tenets. It reminds us that maintaining patient confidentiality is paramount, and that nonjudgmental interviewing can help us to help our patients navigate challenging situations. The particulars of this case also highlight the importance of referring patients out for individual or marriage counseling and making a referral to a colleague when a situation makes us feel as if we are betraying a patient’s trust.
CORRESPONDENCE
David C. Slawson, MD, 2001 Vail Avenue, Suite 400B, Mercy Medical Plaza, Charlotte, NC 28207; [email protected]
THE CASE
A 52-year-old man requested medicine to help him with erectile dysfunction. After obtaining a medical history and performing a physical exam, the family physician (FP) asked for more details about the patient’s situation. He reported that his wife, who had recently seen the same FP for counseling related to her frustrations with her husband, was uninterested in sex. He then added that he was having an affair with a 32-year-old female co-worker and wanted to improve his sexual function.
He admitted to feeling guilty about this situation and was conflicted about whether to end the affair. He also stated that since the affair, his insomnia had worsened, he was drinking more alcohol, and he was having migraine headaches. As the FP for both patients, and with the knowledge that the wife was worried about possible infidelity, the physician felt some level of conflict about the situation. The following is a discussion of the issues that this patient encounter raised.
DISCUSSION
Issues related to infidelity are common to both men and women. They are also common in same-sex relationships; in general, however, lesbian couples have fewer outside partners, whereas gay men are more likely to seek variety by having multiple partners.1
It is widely understood that successfully committed couples spend quality time together, emphasize each other’s strengths, show respect, accept influence, and nurture their friendship. However, many couples experience infidelity at some time in the course of their marriage. It is difficult to put an exact estimate on rates of infidelity due to problems with research methodology, inaccurate reporting, and a lack of agreement on a definition for infidelity.2 General categories of infidelity include emotional only, sexual only, and combined sexual and emotional infidelity.3,4 In terms of sexual infidelity, one study found that 25% of married men and 15% of married women admitted to having had extramarital sex at least once during their relationship.5 However, other studies suggest that women are closing the “sexual infidelity” gap and engaging in sexual affairs at a similar rate to men.6 There are websites that, in fact, have made it easier for married individuals to engage in affairs.
Reasons for infidelity. Men and women often have different motives in engaging in infidelity. In general, men’s motivations are more often related to sexual dissatisfaction and women’s to emotional dissatisfaction.7,8 However, infidelity may not always be the result of marital unhappiness.
Some studies suggest that the presence of opportunity may override the positive aspects of a relationship.9 Opportunity is heightened in the work environment, as reflected by the finding that 50% of infidelity occurs in the office.10 Research suggests that all relationships may be vulnerable to infidelity if the right opportunities present themselves.11
In general, health care providers are encouraged to use caution in generalizing about infidelity, as the subject is extremely complex, nuanced, and difficult to measure with exactitude.12
Continue to: The impact of infidelity
The impact of infidelity on couples varies due to factors such as the pre-morbid health of the marriage,13 the depth of involvement with the affair partner,14 and pre-existing attitudes about infidelity.13
Infidelity is a common cause of divorce in America. However, in a sample, Schneider et al15 found that despite initial threats to leave the marriage after infidelity, less than one-quarter of partners divorced. Other studies have found that disclosure of the infidelity and a commitment to work on the marriage may be an essential component of healing.16
Emotionally focused couples therapy, with its emphasis on attachment and bonding, may hold promise for helping couples successfully work through the trauma brought on by extramarital relationships.17 Psychologist and infidelity researcher Shirley Glass found that of the two-thirds of couples who chose to stay together after an affair, 80% of them reported a better marriage after treatment.11
Initial steps to take, and questions to ask
Both male and female patients need to feel comfortable surfacing sexual concerns with their clinicians. In this case, the concerns of the husband are interwoven with broader marital issues, which are the source of emotional and psychosomatic distress. His decision regarding his affair carried with it potentially life-altering consequences for his wife, 3 children, and affair partner and her family. It also raised ethical issues for the FP, who was providing care to both the husband and the wife. Appropriate care requires that a physician in this situation
- demonstrate a nonjudgmental approach
- clarify personal ethics in response to patient behaviors
- maintain confidentiality
- apply an ethical framework to resolve value dilemmas
- avoid actions that would be harmful to patients.
Interviewing can help to elicit information that may be clarifying not only to the physician but also to the patient. When interviewing a patient such as the one in this case, it would be wise to ask:
- How long has the affair been going on?
- Why is the patient engaging in the affair?
- Is abuse (emotional or physical) a factor in the marriage?
- Does the patient still have feelings for their spouse? Does the patient want to work on the marriage?
- Has the patient talked to a friend or therapist about the situation?
- Would the patient be willing to talk to a therapist?
Continue to: Ethical and legal considerations
Ethical and legal considerations
Some therapists espouse the view that being “neutral” in the presence of an affair is as much a value judgment as taking one side or the other. In the presence of emotional or physical abuse, it might indeed be best to support a marital separation. However, in other situations when there are young children involved and the patient is undecided about what to do, the FP can discuss the pros and cons of working on a marriage that suffers from more treatable types of disrepair (ie, stress, disconnection, repetitive arguments).
Provision of care. If the patient is unwilling to end the affair, the physician needs to decide whether they feel ethically at ease with prescribing sexually enhancing performance medication, given that the patient’s wife is also a patient. A physician in this situation might feel that they are betraying the wife by providing such medications to the husband. In such cases, it might be appropriate to refer the husband to a colleague.
In all cases of infidelity, however, it is wise to discuss safe-sex practices in order to limit the risk of transmitting a sexually transmitted infection (STI) to the spouse (or affair partner) and offer testing for STIs.
Confidentiality. Despite feelings the physician might have about betraying the wife’s trust by providing the performance-enhancing medicine to the husband, there is very little justification for revealing the affair to the wife. In general, confidentiality can only be broken if there is a high level of imminent danger associated with nondisclosure. The physician needs to realize the serious legal implications of breaking confidentiality in this situation, as such disclosure may prompt the initiation of divorce proceedings.
Real-world recommendations
Check your own biases. Infidelity can trigger a whole host of emotional reactions in physicians based on their own personal and professional history. It is important to be aware of such emotions and if sufficiently triggered, discuss the case with a colleague.
Continue to: Encourage bibliotherapy and marriage therapy
Encourage bibliotherapy and marriage therapy. The conversation might go something like this:
“I would recommend you do some reading about infidelity. If you are interested in working on your marriage, you might want to consider a couples counselor who can help you. Research shows that while such counseling can help couples work through infidelity, disclosure needs to occur as part of that process. Research also indicates that about two-thirds of marriages stay together after the revelation of an affair and that such couples can experience healing if they commit to a therapeutic process. If you are unsure how you want to proceed, it might be helpful for you to explore your situation with an individual therapist. What would you like to do next?”
There are also written resources that the patient might find helpful; see “3 bibliotherapy resources for infidelity” for recommendations.
SIDEBAR
3 bibliotherapy resources for infidelity
Not ‘Just Friends’: Protect Your Relationship from Infidelity and Heal the Trauma of Betrayal (Shirley Glass)
After the Affair: Healing the Pain and Rebuilding Trust When a Partner Has Betrayed You (Janice Abrams-Spring)
How Can I Forgive You: The Courage to Forgive, the Freedom Not To (Janice Abrams-Spring)
Referral to an individual or marriage counselor is warranted if the patient wants to work through the issues alone or with their partner. Disclosure of infidelity may not always be necessary for successful reconciliation if the affair has ended. A marriage therapist to whom you refer needs to be competent in working with infidelity.
Our patient. At the completion of the initial consultation—and after a discussion focused on the issues described, including encouragement to seek counseling—the FP acceded to the patient’s request for sexual performance-enhancing medication.
Continue to: The patient returned a few months...
The patient returned a few months later. His wife had found texts between him and his affair partner and told the patient that they had to enter into couples therapy or she was going to file for divorce. The patient told his physician that he had ended the extramarital relationship and was working on his marriage with a qualified marriage therapist; however, he felt lingering feelings of loss, discomfort in the workplace, and confusion about his choices. The physician was supportive and encouraged him to share these feelings, if possible, with an individual therapist or to find a friend who could listen while being supportive of his marriage. The physician also offered his services as a sounding board.
A year later, the patient had found another job and was still working on his marriage.
THE TAKEAWAY
This case underscores the importance of some basic health care tenets. It reminds us that maintaining patient confidentiality is paramount, and that nonjudgmental interviewing can help us to help our patients navigate challenging situations. The particulars of this case also highlight the importance of referring patients out for individual or marriage counseling and making a referral to a colleague when a situation makes us feel as if we are betraying a patient’s trust.
CORRESPONDENCE
David C. Slawson, MD, 2001 Vail Avenue, Suite 400B, Mercy Medical Plaza, Charlotte, NC 28207; [email protected]
1. Blumstein P, Schwartz P. American Couples: Money, Work, Sex. William Morrow; 1983.
2. Blow A, Hartnett K. Infidelity in committed relationships I: a methodological review. J Marital Fam Ther. 2005;31:183-216. doi: 10.1111/j.1752-0606.2005.tb01555.x
3. Glass S, Wright TL. Sex differences in type of extramarital involvement and marital dissatisfaction. Sex Roles. 1985;12:1101-1120.
4. Thompson AP. Emotional and sexual components of extramarital relations. J Marriage Fam. 1984;46:35-42. doi: 10.2307/351861
5. Laumann EO, Gagnon JH, Michael RT, et al. The Social Organization of Sexuality: Sexual Practices in the United States. University of Chicago Press; 1994.
6. Oliver MB, Hyde JS. Gender differences in sexuality: a meta-analysis. Psychol Bull. 1993;114:29-51. doi: 10.1037/0033-2909.114.1.29
7. Glass SP, Wright TL. Justifications for extramarital relationships: the association between attitudes, behaviors, and gender. J Sex Res. 1992;29:361-387. doi: 10.1080/00224499209551654
8. Spanier GB, Margolis RL. Marital separation and extramarital sexual behavior. J Sex Res. 1983;19:23-48.
9. Atkins DC, Baucom DH, Jacobson NS. Understanding infidelity: correlates in a national random sample. J Fam Psychol. 2001;15:735-749. doi: 10.1037//0893-3200.15.4.735
10. Treas J, Giesen D. Sexual infidelity among married and cohabitating Americans. J Marriage Fam. 2000;62:48-60. doi: 10.1111/j.1741-3737.2000.00048.x
11. Glass SP. Not ‘Just Friends’: Protect Your Relationship From Infidelity and Heal the Trauma of Betrayal. Free Press; 2002.
12. Blow A, Hartnet K. Infidelity in committed relationships II: a substantive review. J Marital Fam Ther. 2005;31:2. doi: 10.1111/j.1752-0606.2005.tb01556.x
13. Buunk B. Conditions that promote breakups as a consequence of extradyadic involvements. J Soc Clin Psychol. 1987;5:271-284. doi: 10.1521/jscp.1987.5.3.271
14. Charn IW, Parnass S. The impact of extramarital relationships on the continuation of marriages. J Sex Marital Therapy. 1995;21:100-115. doi: 10.1080/00926239508404389
15. Schneider JP, Irons RR, Corley MD. Disclosure of extramarital sexual activities by sexually exploitative professionals and other persons with addictive or compulsive sexual disorders. J Sex Edu Therapy. 1999;24:277-287. doi: 10.1080/01614576.1999.11074316
16. Atkins DC, Eldridge KA, Baucom DH, et al. Infidelity and behavioral couple therapy: optimism in the face of betrayal. J Consult Clin Psychol. 2005;73:144-150. doi: 10.1037/0022-006X.73.1.144
17. Johnson SM, Makinen J, Millikin J. Attachment injuries in couple relationships: a new perspective on impasses in emotionally focused marital therapy. J Marital Fam Therapy. 2001;27:145-155. doi: 10.1111/j.1752-0606.2001.tb01152.x
1. Blumstein P, Schwartz P. American Couples: Money, Work, Sex. William Morrow; 1983.
2. Blow A, Hartnett K. Infidelity in committed relationships I: a methodological review. J Marital Fam Ther. 2005;31:183-216. doi: 10.1111/j.1752-0606.2005.tb01555.x
3. Glass S, Wright TL. Sex differences in type of extramarital involvement and marital dissatisfaction. Sex Roles. 1985;12:1101-1120.
4. Thompson AP. Emotional and sexual components of extramarital relations. J Marriage Fam. 1984;46:35-42. doi: 10.2307/351861
5. Laumann EO, Gagnon JH, Michael RT, et al. The Social Organization of Sexuality: Sexual Practices in the United States. University of Chicago Press; 1994.
6. Oliver MB, Hyde JS. Gender differences in sexuality: a meta-analysis. Psychol Bull. 1993;114:29-51. doi: 10.1037/0033-2909.114.1.29
7. Glass SP, Wright TL. Justifications for extramarital relationships: the association between attitudes, behaviors, and gender. J Sex Res. 1992;29:361-387. doi: 10.1080/00224499209551654
8. Spanier GB, Margolis RL. Marital separation and extramarital sexual behavior. J Sex Res. 1983;19:23-48.
9. Atkins DC, Baucom DH, Jacobson NS. Understanding infidelity: correlates in a national random sample. J Fam Psychol. 2001;15:735-749. doi: 10.1037//0893-3200.15.4.735
10. Treas J, Giesen D. Sexual infidelity among married and cohabitating Americans. J Marriage Fam. 2000;62:48-60. doi: 10.1111/j.1741-3737.2000.00048.x
11. Glass SP. Not ‘Just Friends’: Protect Your Relationship From Infidelity and Heal the Trauma of Betrayal. Free Press; 2002.
12. Blow A, Hartnet K. Infidelity in committed relationships II: a substantive review. J Marital Fam Ther. 2005;31:2. doi: 10.1111/j.1752-0606.2005.tb01556.x
13. Buunk B. Conditions that promote breakups as a consequence of extradyadic involvements. J Soc Clin Psychol. 1987;5:271-284. doi: 10.1521/jscp.1987.5.3.271
14. Charn IW, Parnass S. The impact of extramarital relationships on the continuation of marriages. J Sex Marital Therapy. 1995;21:100-115. doi: 10.1080/00926239508404389
15. Schneider JP, Irons RR, Corley MD. Disclosure of extramarital sexual activities by sexually exploitative professionals and other persons with addictive or compulsive sexual disorders. J Sex Edu Therapy. 1999;24:277-287. doi: 10.1080/01614576.1999.11074316
16. Atkins DC, Eldridge KA, Baucom DH, et al. Infidelity and behavioral couple therapy: optimism in the face of betrayal. J Consult Clin Psychol. 2005;73:144-150. doi: 10.1037/0022-006X.73.1.144
17. Johnson SM, Makinen J, Millikin J. Attachment injuries in couple relationships: a new perspective on impasses in emotionally focused marital therapy. J Marital Fam Therapy. 2001;27:145-155. doi: 10.1111/j.1752-0606.2001.tb01152.x
Drug shortages plague hematology, but preparedness helps
Just before he took a call from a reporter asking about the impact of drug shortages in hematology, Bill Greene, PharmD, chief pharmaceutical officer at St. Jude Children’s Research Hospital, had spent an hour on the phone overseeing his institution’s response to a hematology drug shortage. The chemotherapy drug fludarabine, used to treat chronic lymphocytic leukemia, was in short supply.
“There are 5 different manufacturers, but none of them have had drug available over the past 2 weeks,” Dr. Greene said. “We’re trying to chase some emergency supplies to be able to continue treatment for patients who’ve had their treatments initiated and planned.”
Over the past several years, this predicament has become common at hematology clinics across the country. In fact, management of scarce medication resources has become a significant part of Dr. Greene’s workload these days, as critical drugs fail to show up on time or manufacturer supplies run low at his hospital in Memphis.
This shortage of hematology drugs got a new dose of national attention, thanks to a recent episode of CBS News’ “60 Minutes.” Through interviews with physicians and parents of children who suddenly could not get vital medications, the report highlighted the recent shortage of another leukemia drug, vincristine.
“As a cancer mom, we shouldn’t be fighting for our children to get a drug that is needed,” Cyndi Valenta was quoted as saying. She recalled that when the shortage began in 2019, her 13-year-old son, a leukemia patient at Loma Linda (Calif.) University Hospital, felt frightened. Ms. Valenta said she felt a “gut-wrenching feeling of just fear and anger.” They were finally able to get doses of the drug after launching a social media campaign.
Such drug shortages are especially widespread in oncology and hematology, according to a survey of oncology pharmacists at 68 organizations nationwide. Published in the May 2022 issue of Oncology Practice, the study showed that 63% of institutions reported one or more drug shortages every month, with a 34% increase in 2019, compared with 2018. Treatment delays, reduced doses, or alternative regimens were reported by 75% of respondents, the authors wrote.
The pharmacists surveyed between May 2019 and July 2020 were asked about the three most hard-to-get chemotherapy and supportive care agents. Vincristine topped the list, followed by vinblastine, IVIG, leucovorin, and BCG, as well as difficult-to-obtain ropine, erwinia asparaginase, etoposide, and leuprolide. Several of these drugs are used to treat conditions such as lymphoma and leukemia.
Eighty-two percent of respondents reported shortages of decitabine (IV), often used as part of a cocktail with vinblastine and other drugs to treat Hodgkin lymphoma.
The reasons for drug shortages are varied. The CBS News report declared that “pharmaceutical companies have stopped producing many life-saving generic drugs because they make too little profit,” and it suggested that the federal government isn’t doing enough.
But government action actually might be making a difference. According to the FDA, the number of new drug shortages has fallen dramatically from 250 in 2011 to 41 in 2021, and the number of prevented drug shortages rose from nearly 200 to more than 300 over that same period. Still, the number of ongoing drug shortages has risen from around 40 in 2017 to about 80 in 2021.
Reasons for the paucity of certain drugs are often unclear. In a June 12, 2022 post, for example, the American Society of Health-System Pharmacists’ drug shortage database noted that the chemotherapy drug fludarabine was in short supply and provided details about when some of the 5 manufacturers expected to have it available. (This is the shortage that Dr. Greene was trying to manage.) But 4 of the 5 manufacturers “did not provide a reason,” and the fifth blamed manufacturing delays.
“There’s a lot of closely held trade secrets that hinder the ability to share good information,” said Dr. Greene. To make things more complicated, shipping times are often unreliable. “The product doesn’t show up today, we place another order. Sometimes it will show up tomorrow, sometimes it doesn’t,” he said. “If you’re not tracking it carefully, you deplete your own supply.”
Patients’ families have grown used to dealing with drug shortages, and “they’re less quick to blame personnel at our institution.”
How can hematologists cope with this issue? “The best thing in the immediate term is to advocate for their hospital to have a pharmacist dedicated to shortage monitoring and taking proactive steps to obviate shortages,” hematologist/oncologist Andrew Hantel, MD, an instructor at Dana-Farber Cancer Institute, Harvard Medical School, Boston, said in an interview.
“We have ongoing communications with other large cancer centers and the FDA to recognize shortages early and develop plans to make sure we stay ahead of them,” Dr. Hantel said. “Most often this involves assessing supply, use rates, alternative manufacturers, and additional measures the Food and Drug Administration can take (for example, importation), and occasionally working with clinical teams to see if other medications are feasible alternatives.”
If a drug is unavailable, it can also be helpful to discuss alternative approaches. “We did not have any frank shortages of vincristine,” Dr. Hantel said, “but we did focus on conservation measures and considered different ethically appropriate ways to distribute vincristine if there was a point at which we did not have enough for everyone who needed it.”
If a drug is in short supply, options can include delaying treatment, giving an alternative, or providing the rest of the regimen without the scarce drug, he said. In a 2021 report in The Lancet Hematology, Dr. Hantel and his colleagues offered “model solutions for ethical allocation during cancer medicine shortages.”
The authors of the May 2022 drug-shortage report highlighted an alternative regimen in hematology. They noted that manufacturing delays have limited the supply of dacarbazine, used for Hodgkin lymphoma. Due to the current shortages, they wrote, clinicians are considering the use of escalated bleomycin, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone, replacing dacarbazine with procarbazine and using the doxorubicin, bleomycin, vinblastine, procarbazine, and prednisone regimen, or replacing dacarbazine with cyclophosphamide.
Dr. Greene emphasized the importance of tracking the news and the drug shortage websites run by the FDA and the American Society of Health-System Pharmacists.
It’s also crucial to have a good relationship with your wholesaler, he added, and to communicate about these problems within your facility. At his hospital, the pharmaceutical staff holds a multi-disciplinary meeting at least weekly to discuss the supply of medications. As he put it, “it’s a challenging environment.”
Dr. Greene and Dr. Hantel reported no relevant disclosures.
Just before he took a call from a reporter asking about the impact of drug shortages in hematology, Bill Greene, PharmD, chief pharmaceutical officer at St. Jude Children’s Research Hospital, had spent an hour on the phone overseeing his institution’s response to a hematology drug shortage. The chemotherapy drug fludarabine, used to treat chronic lymphocytic leukemia, was in short supply.
“There are 5 different manufacturers, but none of them have had drug available over the past 2 weeks,” Dr. Greene said. “We’re trying to chase some emergency supplies to be able to continue treatment for patients who’ve had their treatments initiated and planned.”
Over the past several years, this predicament has become common at hematology clinics across the country. In fact, management of scarce medication resources has become a significant part of Dr. Greene’s workload these days, as critical drugs fail to show up on time or manufacturer supplies run low at his hospital in Memphis.
This shortage of hematology drugs got a new dose of national attention, thanks to a recent episode of CBS News’ “60 Minutes.” Through interviews with physicians and parents of children who suddenly could not get vital medications, the report highlighted the recent shortage of another leukemia drug, vincristine.
“As a cancer mom, we shouldn’t be fighting for our children to get a drug that is needed,” Cyndi Valenta was quoted as saying. She recalled that when the shortage began in 2019, her 13-year-old son, a leukemia patient at Loma Linda (Calif.) University Hospital, felt frightened. Ms. Valenta said she felt a “gut-wrenching feeling of just fear and anger.” They were finally able to get doses of the drug after launching a social media campaign.
Such drug shortages are especially widespread in oncology and hematology, according to a survey of oncology pharmacists at 68 organizations nationwide. Published in the May 2022 issue of Oncology Practice, the study showed that 63% of institutions reported one or more drug shortages every month, with a 34% increase in 2019, compared with 2018. Treatment delays, reduced doses, or alternative regimens were reported by 75% of respondents, the authors wrote.
The pharmacists surveyed between May 2019 and July 2020 were asked about the three most hard-to-get chemotherapy and supportive care agents. Vincristine topped the list, followed by vinblastine, IVIG, leucovorin, and BCG, as well as difficult-to-obtain ropine, erwinia asparaginase, etoposide, and leuprolide. Several of these drugs are used to treat conditions such as lymphoma and leukemia.
Eighty-two percent of respondents reported shortages of decitabine (IV), often used as part of a cocktail with vinblastine and other drugs to treat Hodgkin lymphoma.
The reasons for drug shortages are varied. The CBS News report declared that “pharmaceutical companies have stopped producing many life-saving generic drugs because they make too little profit,” and it suggested that the federal government isn’t doing enough.
But government action actually might be making a difference. According to the FDA, the number of new drug shortages has fallen dramatically from 250 in 2011 to 41 in 2021, and the number of prevented drug shortages rose from nearly 200 to more than 300 over that same period. Still, the number of ongoing drug shortages has risen from around 40 in 2017 to about 80 in 2021.
Reasons for the paucity of certain drugs are often unclear. In a June 12, 2022 post, for example, the American Society of Health-System Pharmacists’ drug shortage database noted that the chemotherapy drug fludarabine was in short supply and provided details about when some of the 5 manufacturers expected to have it available. (This is the shortage that Dr. Greene was trying to manage.) But 4 of the 5 manufacturers “did not provide a reason,” and the fifth blamed manufacturing delays.
“There’s a lot of closely held trade secrets that hinder the ability to share good information,” said Dr. Greene. To make things more complicated, shipping times are often unreliable. “The product doesn’t show up today, we place another order. Sometimes it will show up tomorrow, sometimes it doesn’t,” he said. “If you’re not tracking it carefully, you deplete your own supply.”
Patients’ families have grown used to dealing with drug shortages, and “they’re less quick to blame personnel at our institution.”
How can hematologists cope with this issue? “The best thing in the immediate term is to advocate for their hospital to have a pharmacist dedicated to shortage monitoring and taking proactive steps to obviate shortages,” hematologist/oncologist Andrew Hantel, MD, an instructor at Dana-Farber Cancer Institute, Harvard Medical School, Boston, said in an interview.
“We have ongoing communications with other large cancer centers and the FDA to recognize shortages early and develop plans to make sure we stay ahead of them,” Dr. Hantel said. “Most often this involves assessing supply, use rates, alternative manufacturers, and additional measures the Food and Drug Administration can take (for example, importation), and occasionally working with clinical teams to see if other medications are feasible alternatives.”
If a drug is unavailable, it can also be helpful to discuss alternative approaches. “We did not have any frank shortages of vincristine,” Dr. Hantel said, “but we did focus on conservation measures and considered different ethically appropriate ways to distribute vincristine if there was a point at which we did not have enough for everyone who needed it.”
If a drug is in short supply, options can include delaying treatment, giving an alternative, or providing the rest of the regimen without the scarce drug, he said. In a 2021 report in The Lancet Hematology, Dr. Hantel and his colleagues offered “model solutions for ethical allocation during cancer medicine shortages.”
The authors of the May 2022 drug-shortage report highlighted an alternative regimen in hematology. They noted that manufacturing delays have limited the supply of dacarbazine, used for Hodgkin lymphoma. Due to the current shortages, they wrote, clinicians are considering the use of escalated bleomycin, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone, replacing dacarbazine with procarbazine and using the doxorubicin, bleomycin, vinblastine, procarbazine, and prednisone regimen, or replacing dacarbazine with cyclophosphamide.
Dr. Greene emphasized the importance of tracking the news and the drug shortage websites run by the FDA and the American Society of Health-System Pharmacists.
It’s also crucial to have a good relationship with your wholesaler, he added, and to communicate about these problems within your facility. At his hospital, the pharmaceutical staff holds a multi-disciplinary meeting at least weekly to discuss the supply of medications. As he put it, “it’s a challenging environment.”
Dr. Greene and Dr. Hantel reported no relevant disclosures.
Just before he took a call from a reporter asking about the impact of drug shortages in hematology, Bill Greene, PharmD, chief pharmaceutical officer at St. Jude Children’s Research Hospital, had spent an hour on the phone overseeing his institution’s response to a hematology drug shortage. The chemotherapy drug fludarabine, used to treat chronic lymphocytic leukemia, was in short supply.
“There are 5 different manufacturers, but none of them have had drug available over the past 2 weeks,” Dr. Greene said. “We’re trying to chase some emergency supplies to be able to continue treatment for patients who’ve had their treatments initiated and planned.”
Over the past several years, this predicament has become common at hematology clinics across the country. In fact, management of scarce medication resources has become a significant part of Dr. Greene’s workload these days, as critical drugs fail to show up on time or manufacturer supplies run low at his hospital in Memphis.
This shortage of hematology drugs got a new dose of national attention, thanks to a recent episode of CBS News’ “60 Minutes.” Through interviews with physicians and parents of children who suddenly could not get vital medications, the report highlighted the recent shortage of another leukemia drug, vincristine.
“As a cancer mom, we shouldn’t be fighting for our children to get a drug that is needed,” Cyndi Valenta was quoted as saying. She recalled that when the shortage began in 2019, her 13-year-old son, a leukemia patient at Loma Linda (Calif.) University Hospital, felt frightened. Ms. Valenta said she felt a “gut-wrenching feeling of just fear and anger.” They were finally able to get doses of the drug after launching a social media campaign.
Such drug shortages are especially widespread in oncology and hematology, according to a survey of oncology pharmacists at 68 organizations nationwide. Published in the May 2022 issue of Oncology Practice, the study showed that 63% of institutions reported one or more drug shortages every month, with a 34% increase in 2019, compared with 2018. Treatment delays, reduced doses, or alternative regimens were reported by 75% of respondents, the authors wrote.
The pharmacists surveyed between May 2019 and July 2020 were asked about the three most hard-to-get chemotherapy and supportive care agents. Vincristine topped the list, followed by vinblastine, IVIG, leucovorin, and BCG, as well as difficult-to-obtain ropine, erwinia asparaginase, etoposide, and leuprolide. Several of these drugs are used to treat conditions such as lymphoma and leukemia.
Eighty-two percent of respondents reported shortages of decitabine (IV), often used as part of a cocktail with vinblastine and other drugs to treat Hodgkin lymphoma.
The reasons for drug shortages are varied. The CBS News report declared that “pharmaceutical companies have stopped producing many life-saving generic drugs because they make too little profit,” and it suggested that the federal government isn’t doing enough.
But government action actually might be making a difference. According to the FDA, the number of new drug shortages has fallen dramatically from 250 in 2011 to 41 in 2021, and the number of prevented drug shortages rose from nearly 200 to more than 300 over that same period. Still, the number of ongoing drug shortages has risen from around 40 in 2017 to about 80 in 2021.
Reasons for the paucity of certain drugs are often unclear. In a June 12, 2022 post, for example, the American Society of Health-System Pharmacists’ drug shortage database noted that the chemotherapy drug fludarabine was in short supply and provided details about when some of the 5 manufacturers expected to have it available. (This is the shortage that Dr. Greene was trying to manage.) But 4 of the 5 manufacturers “did not provide a reason,” and the fifth blamed manufacturing delays.
“There’s a lot of closely held trade secrets that hinder the ability to share good information,” said Dr. Greene. To make things more complicated, shipping times are often unreliable. “The product doesn’t show up today, we place another order. Sometimes it will show up tomorrow, sometimes it doesn’t,” he said. “If you’re not tracking it carefully, you deplete your own supply.”
Patients’ families have grown used to dealing with drug shortages, and “they’re less quick to blame personnel at our institution.”
How can hematologists cope with this issue? “The best thing in the immediate term is to advocate for their hospital to have a pharmacist dedicated to shortage monitoring and taking proactive steps to obviate shortages,” hematologist/oncologist Andrew Hantel, MD, an instructor at Dana-Farber Cancer Institute, Harvard Medical School, Boston, said in an interview.
“We have ongoing communications with other large cancer centers and the FDA to recognize shortages early and develop plans to make sure we stay ahead of them,” Dr. Hantel said. “Most often this involves assessing supply, use rates, alternative manufacturers, and additional measures the Food and Drug Administration can take (for example, importation), and occasionally working with clinical teams to see if other medications are feasible alternatives.”
If a drug is unavailable, it can also be helpful to discuss alternative approaches. “We did not have any frank shortages of vincristine,” Dr. Hantel said, “but we did focus on conservation measures and considered different ethically appropriate ways to distribute vincristine if there was a point at which we did not have enough for everyone who needed it.”
If a drug is in short supply, options can include delaying treatment, giving an alternative, or providing the rest of the regimen without the scarce drug, he said. In a 2021 report in The Lancet Hematology, Dr. Hantel and his colleagues offered “model solutions for ethical allocation during cancer medicine shortages.”
The authors of the May 2022 drug-shortage report highlighted an alternative regimen in hematology. They noted that manufacturing delays have limited the supply of dacarbazine, used for Hodgkin lymphoma. Due to the current shortages, they wrote, clinicians are considering the use of escalated bleomycin, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone, replacing dacarbazine with procarbazine and using the doxorubicin, bleomycin, vinblastine, procarbazine, and prednisone regimen, or replacing dacarbazine with cyclophosphamide.
Dr. Greene emphasized the importance of tracking the news and the drug shortage websites run by the FDA and the American Society of Health-System Pharmacists.
It’s also crucial to have a good relationship with your wholesaler, he added, and to communicate about these problems within your facility. At his hospital, the pharmaceutical staff holds a multi-disciplinary meeting at least weekly to discuss the supply of medications. As he put it, “it’s a challenging environment.”
Dr. Greene and Dr. Hantel reported no relevant disclosures.