User login
Predictors of County-Level Home Modification Use Across the US
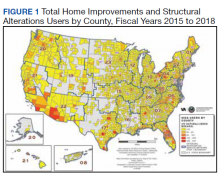
This article is part of a series of articles on the Home Improvements and Structural Alterations program (HISA), a home modification (HM) program within the Veterans Health Administration (VHA). HISA is a benefit awarded to veterans with disabilities (VWDs) and is instrumental in affording physical accessibility and structural alterations to veterans’ homes.1 The overarching goals of this project are to describe and understand HISA use by VWDs. Previous work has shown geographical variation in the number of HISA prescriptions across counties in the US (Figure 1).1 The current work seeks to describe and predict the county-level rates of HISA use. Information about what predicts HISA utilization at the county level is important because it enhances understanding of program utilization at a national level. The long-term goal of the series is to provide knowledge about HM services within VHA to improve community-based independent living of VWDs by increasing awareness and utilization of HM services.
Background
A health care professional (HCP) approves a HM support award by evaluating the practicality of the support to improve the built environment of a given veteran’s disability.1,2 Previously we detailed some of the preliminary research into the HISA program, including HISA user demographic and clinical characteristics, types of HMs received, user suggestions for improvement, and geospatial analysis of HISA prescriptions concentration.1-4
The geospatial analyses of HISA prescriptions revealed clusters of high numbers of HISA users (hot spots) and low numbers of HISA users (cold spots), indicating that HISA is either not prescribed or uniformly used across the US. The previous research prompted investigation into county-level variables that may impact HISA utilization rates. This inquiry focuses on county characteristics associated with HISA use rates, such as measures of clinical care and quality of care (eg, access to health services variables, lack of insurance, preventable hospital stays), physical environment, and sociodemographic characteristics. Clinical care and quality of care measures promote the interaction with HCPs. Moreover, access to health care is an important indicator of health outcomes.5,6 An individual’s capacity to access health services, such as a HM program, greatly impacts well-being, safety, independence, and health.2,4 Well-being, safety, independence, and health become compromised if individuals cannot access care, if needed care is lacking in their area, if HCPs are not available, or are unwilling to provide care due to lack of insurance coverage.7-12 In locations where health care services are minimal due to lack of specialists or health care facilities, the quality of (or access to) care may be compromised, resulting in preventable conditions becoming problematic.13,14 These conditions may result in unnecessary hospitalizations for conditions that could have been treated during routine care. Financial barriers to care particularly among low-income people and the uninsured have proven detrimental to health.15,16 On the other hand, preventable hospital stays are a quality of care measure (ie, a proxy for poor quality of care). HISA operates within a health care system; thus, it is imperative to include these measures impacting health.
In this study, we sought to identify county-level predictors—in particular, county-level proxies for access to care—that may be associated with county-level HISA use. We define HISA utilization rate as the percentage of a county’s VHA patients who have received a HISA award.
Methods
This study used data from the National Prosthetics Patient Database (NPPD), US Department of Veterans Affairs (VA) medical database inpatient and outpatient datasets, VHA Support Service Center (VSSC) data cubes, and the County Health Rankings database (CHRD). First, the study cohort was identified from NPPD users who have obtained a HISA award from fiscal years (FY) 2015 to 2018. Analysis started with FY 2015 following new regulations (38 CFR § 17) governing the operations of the HISA program.2 The study cohort was matched with records from NPPD and VA inpatient and outpatient datasets to obtain information about the veterans’ demographic characteristics and their HM characteristics and costs. The number of VHA end-of-year (EOY) patients per county was extracted from the VSSC Current Enrollment Cube, which was used in calculation of the county-level HISA utilization rate.17 Finally, zip code–based locational data were used to calculate approximate drive time and distance from the HISA user’s approximate location to the facility where they received their HM prescription. Drive times and drive distances were calculated with Esri ArcGIS Pro (v2.6.3) by placing zip code centroid and VHA facilities on a nationwide road network that contains both road speeds and distances.
Calculations
Patient-level data were aggregated up to county-level variables by calculating the sum, mean, or percent per county. HISA user sample characteristics, including sex, race, rurality (urban, rural), marital status, and Class 1 vs Class 2 disability-related eligibility groups, were aggregated to the county level by calculating percentages of HISA users of the given characteristics out of total HISA users in the county. Disability-related eligibility groups (Class 1 vs Class 2 HISA users) determines the maximum lifetime award dollar amount. Specifically, those with service-connected disabilities or those with a ≥ 50% disability rating (regardless of whether or not their disability is service connected) are classified as Class 1 HISA users and are eligible to receive a maximum lifetime award of $6800. Those with a recorded disability that is not connected to their military service, and who have a disability rating of < 50% are classified as Class 2 HISA users and are eligible to receive a lifetime maximum award of $2000.
The county-level number of HISA users was used as the numerator for calculation of county-level HISA utilization rate. Counties with zero HISA users were excluded. The number of EOY VHA patients per county in FY 2018 was divided by 1000 and used as the denominator in the calculation of county-level HISA utilization rate. Thus, the outcome variable is HISA utilization rate per 1000 VHA patients in FY 2018 (HISA utilization rate).
County-Level Variables
County-level variables were downloaded from the 2020 CHRD.5,6 An explanation of the CHRD model and the factors used in this study are shown in the eAppendix (available at doi: 10.12788/fp.0279).6 County-level aggregated HISA user data and the CHRD data were matched using county Federal Information Processing Standards codes. Access to care measures collected from CHRD included percentages uninsured and ratios of population to primary care physicians, dentists, mental health professionals, and other primary care professionals. Other CHRD measures included those for quality of care (rate of preventable hospital stay) and housing quality (percent of households with high housing costs, percent of households with overcrowding, percent of households with lack of kitchen or plumbing, percent of households with severe housing cost burden, percent of homeownership). Of secondary interest was county population rurality, as previous research findings showed the annual average of HISA users who are from rural areas ranged from 30 to 35%.
Analysis Methods
SAS (v9.4), R (v4.0.2), and RStudio (v1.3.1093) were used for data preparation and analysis.18 Multiple regression analysis was used to predict county-level utilization rate from county-level variables. Sociodemographic characteristics from CHRD and HISA data were included as important control predictors in the regression model, though our focus for this paper are the access to care and housing quality predictors.
Model diagnostics (examination of model residuals, Breusch-Godfrey test, Breusch-Pagan test) revealed significant heteroskedasticity of the model; thus, robust standard errors and associated P values were computed using the R estimatr package (v0.30.2).19 Some predictor variables of interest (eg, ratio of mental health professionals) were removed during the model building process either due to problems of multicollinearity or excessive missingness that would have resulted in listwise deletion.
Results
County-level HISA utilization rate per 1000 EOY VHA patients ranged from 0.09 to 59.7%, with a 6.6% mean and 5% median (Figure 2). The data were highly positively skewed. The final model included 33 total predictor variables (Table 1). The final regression model was a significantly better predictor of county-level HISA utilization rate than a null model (F[33-2184], 10.18; P < .001). The adjusted model R2 showed that the overall model accounted for approximately 23% of variance in county-level HISA utilization rate (Table 2).
Among the primary variables of interest, percent uninsured adults and rate of preventable hospital stays emerged as significant predictors of county-level HISA utilization rate. Specifically, county percentage of uninsured adults was negatively related to county-level HISA utilization rate (b = -8.99, P = .005), indicating that the higher the proportion of uninsured adults—with all other predictors held constant—the lower the HISA utilization rate. Percent uninsured adults ranged from 2.7 to 42.4% across counties, with a mean (SD) of 12.7% (5.8%) and 11.4% median.
County rate of preventable hospital stays, however, was significantly and positively related to county-level HISA utilization rate (b = .0004, P = .009), indicating that the higher the rate of preventable hospital stays—with all other predictors held constant—the higher the HISA utilization rate. The direction of this effect is the opposite of the direction of the effect of percent uninsured adults (positive rather than negative), even though both could be considered measures of access to care. The standardized β for these 2 predictors indicate that county rate of preventable hospital stays is a somewhat stronger predictor of county-level HISA utilization rate than is county percent of uninsured adults (β = .11 and β = -.09, respectively). Rate of preventable hospital stays ranged from 683 to 16,802 across counties included in this analysis, with a mean (SD) of 4,796.5 (1659.9) and a 4669 median.
Of secondary interest was county rurality. The county-level percentage of rural residents was significantly and positively related to county-level HISA utilization rate, indicating that the higher the proportion of individuals within county considered rural—all other predictors held constant—the higher the HISA utilization rate. The mean (SD) percentage of rural residents per county was 52.3% (30.2) and 52.7 % median.
Discussion
This study examined whether county-level characteristics, specifically variables for access to care, quality of care, and housing quality, were predictive of a county’s HISA utilization rate. Given that this series of work on the HISA program is (to our knowledge) the first of its kind, and given the exploratory nature of this analysis, we did not have specific predictions for the effects of any one given variable. Nevertheless, some of the results were surprising, and we believe they warrant additional study. In particular, the opposing direction of effects for access to care and quality of care variables were hard to reconcile.
The county percent of uninsured adults (an access to care variable, specifically, a proxy for poor access to care) was negatively associated with county-level HISA utilization rate, whereas the county rate of preventable hospital stays (a quality of care variable, but also potentially an access to care variable, and specifically, proxies for poor quality of care or poor access to care) was positively associated with county-level HISA utilization rate. To describe the relationships more generally, one coefficient in the regression model indicated that the poorer the access to care, the lower the HISA utilization rate (higher percent of uninsured adults predicts lower HISA utilization rate), while another coefficient in the regression model indicated the poorer the quality of and access to care, the higher the HISA utilization rate (higher rate of preventable hospital stays predicts higher HISA utilization rate). Future study is warranted to disentangle and reconcile the various community-level predictors of this service.
Housing quality measures (eg, percent of households with high housing costs, percent of households with overcrowding, percent of households with lack of kitchen or plumbing, percent of households with severe housing cost burden, and percent of homeownership) are important in the consideration of whether a HM will be performed or should be performed. For example, if a person is cost burdened by the amount of expenditure spent in housing there will be little discretionary funds to perform a HM. Individuals who do not own their home may experience complications in obtaining permission from landlords to perform a HM. County-level predictors of housing quality (percent of households with high housing costs, overcrowding, and lack of kitchen or plumbing) were not significantly associated with county-level HISA utilization rate but are also nevertheless relevant to the discussion of home modifications. Of particular interest is the percent of households with lack of kitchen or plumbing variable, which was positively related to county-level HISA utilization rate although not statistically significant. HM elements related to the kitchen (eg, heighten countertop) add to the accessibility of the home allowing for the performing of activities of daily living such as cooking. Between FY 2015 and FY 2018, we discovered 131 prescriptions for kitchen (n = 90) and plumbing (n = 41) HMs, which is a very small proportion of the 30,780 total HMs (there were 24,397 bathroom HMs). The nonsignificant coefficient for this variable may reflect the small number of veterans that obtained these HM.
Limitations
The potentially conflicting direction of effects for a significant access to care variable (percent uninsured adults) and a significant access to care and quality of care variable (preventable hospital stays) are interesting and warrant additional study, but the inability to interpret or explain this apparent inconsistency constitutes a limitation of the current data and analyses presented here. Another limitation is that this analysis uses county-level predictors for what is ultimately an individual-level outcome. It would have been ideal to have both individual- and county-level data to conduct a multilevel analysis; in particular, individual-level data within counties of individuals (both veterans and nonveterans) who did not receive a HISA award (including both those who applied and were denied, and who did not apply) would be highly valuable.
Conclusions
Our continuing research into veterans’ use of HM fills a gap in the literature about the characteristics of HISA users, the impact of county-level variables on the use of HISA, and the geographic distribution and use of HISA within the VHA. While it is important to examine the influence of broader systems on individual outcomes, there could be myriad other factors that are more proximal and more closely related to whether any one individual applies for, let alone receives, a HISA award. Indeed, a low overall adjusted model R2 indicates that there is considerable variability in county-level HISA utilization rate that was not accounted for by the current model; this further speaks to warranted additional study.
More research is needed to understand and account for geographical variation in HISA utilization rate across the US. However, this work serves as an exploratory first step at quantifying and predicting HISA utilization rate at a broad level, with the ultimate goal of increasing access to HMs for veterans with disabilities.
Acknowledgments
This research was supported by grant 15521 from the US Department of Veterans Affairs, Office of Rural Health. Furthermore, the research was supported in part by grant K12 HD055929 from the National Institutes of Health. We want to acknowledge Cheri E. Knecht, Project Coordinator, for her assistance throughout all aspects of our research study and for her thoughtful contributions during the writing of this manuscript.
1. Semeah LM, Ahrentzen S, Jia H, Cowper-Ripley DC, Levy CE, Mann WC. The home improvements and structural alterations benefits program: veterans with disabilities and home accessibility. J Disability Policy Studies. 2017;28(1):43-51. doi:10.1177/1044207317696275
2. Semeah LM, Wang X, Cowper Ripley DC, Lee MJ, Ahonle ZJ, Ganesh SP, et al. Improving health through a home modification service for veterans. In: Fiedler BA, ed. Three Facets of Public Health and Paths to Improvements. Academic Press; 2020:381-416.
3. Semeah LM, Ahrentzen S, Cowper-Ripley DC, Santos-Roman LM, Beamish JO, Farley K. Rental housing needs and barriers from the perspective of veterans with disabilities. Housing Policy Debate. 2019;29(4):542-558. doi:10.1080/10511482.2018.1543203
4. Semeah LM, Ganesh SP, Wang X, et al. Home modification and health services utilization by rural and urban veterans with disabilities. Housing Policy Debate. 2021;31(6):862-874.doi:10.1080/10511482.2020.1858923
5. University of Wisconsin Population Health Institute. County health rankings model. Accessed May 13, 2022. https://www.countyhealthrankings.org/about-us
6. Remington PL, Catlin BB, Gennuso KP. The County Health Rankings: rationale and methods. Popul Health Metr. 2015;13(11). doi:10.1186/s12963-015-0044-2
7. National Academies of Sciences, Engineering, and Medicine. Health-Care Utilization as a Proxy in Disability Determination. Washington, DC: The National Academies Press; 2018.
8. Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611-20. doi:10.1016/j.puhe.2015.04.001
9. Medicaid and Chip Payment and Access Commission (MACPAC). Medicaid access in brief: adults’ experiences in obtaining medical care. November 2016. Accessed May 13, 2022. https://www.macpac.gov/publication/access-in-brief-adults-experiences-in-obtaining-medical-care
10. Tolbert J, Orgera, K, Damico A. Key facts about the uninsured population. November 6, 2020. Accessed May 13, 2022. https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population
11. Meit M, Knudson A, Gilbert T, et al. The 2014 update of the rural-urban chartbook, 2014. October 2014. Accessed May 13, 2022. http://www.ruralhealthresearch.org
12. National Center for Health Statistics (US). Report No.: 2016-1232. Health, United States, 2015: with special feature on racial and ethnic health disparities. Hyattsville, MD: National Center for Health Statistics.
13. Broussard DL, Mason KE, Carruth AR, Carton TW. Assessing potentially preventable hospitalizations at the county level: a comparison of measures using Medicare data and state hospital discharge data. Popul Health Manag. 2018;21(6):438-445. doi:10.1089/pop.2017.0141
14. Pezzin LE, Bogner HR, Kurichi JE, et al. Preventable hospitalizations, barriers to care, and disability. Medicine (Baltimore). 2018;97:e0691 doi:10.1097/MD.0000000000010691
15. Davis K, Ballreich J. Equitable access to care: how the United States ranks internationally. N Engl J Med. 2014;371(17):1567-70. doi:10.1056/NEJMp1406707
16. Squires D, Anderson C. U.S. health care from a global perspective: spending, use of services, prices, and health in 13 countries. Issue Brief (Commonw Fund). 2015;15:1-15.
17. VHA Service Support Center. Current enrollment cube (vssc.med.va.gov). Retrieved August 06, 2019. [Data not verified.]
18. Bunn A, Korpela M. R: A language and environment for statistical computing: an introduction to dplR. January 29, 2021. Accessed May 13, 2022. http://r.meteo.uni.wroc.pl/web/packages/dplR/vignettes/intro-dplR.pdf
19. Sheppard BH, Hartwick J, Warshaw PR. The theory of reasoned action: a meta-analysis of past research with recommendations for modifications and future research. J Consumer Research. 1988;15(3):325-343. doi:10.1086/209170
This article is part of a series of articles on the Home Improvements and Structural Alterations program (HISA), a home modification (HM) program within the Veterans Health Administration (VHA). HISA is a benefit awarded to veterans with disabilities (VWDs) and is instrumental in affording physical accessibility and structural alterations to veterans’ homes.1 The overarching goals of this project are to describe and understand HISA use by VWDs. Previous work has shown geographical variation in the number of HISA prescriptions across counties in the US (Figure 1).1 The current work seeks to describe and predict the county-level rates of HISA use. Information about what predicts HISA utilization at the county level is important because it enhances understanding of program utilization at a national level. The long-term goal of the series is to provide knowledge about HM services within VHA to improve community-based independent living of VWDs by increasing awareness and utilization of HM services.
Background
A health care professional (HCP) approves a HM support award by evaluating the practicality of the support to improve the built environment of a given veteran’s disability.1,2 Previously we detailed some of the preliminary research into the HISA program, including HISA user demographic and clinical characteristics, types of HMs received, user suggestions for improvement, and geospatial analysis of HISA prescriptions concentration.1-4
The geospatial analyses of HISA prescriptions revealed clusters of high numbers of HISA users (hot spots) and low numbers of HISA users (cold spots), indicating that HISA is either not prescribed or uniformly used across the US. The previous research prompted investigation into county-level variables that may impact HISA utilization rates. This inquiry focuses on county characteristics associated with HISA use rates, such as measures of clinical care and quality of care (eg, access to health services variables, lack of insurance, preventable hospital stays), physical environment, and sociodemographic characteristics. Clinical care and quality of care measures promote the interaction with HCPs. Moreover, access to health care is an important indicator of health outcomes.5,6 An individual’s capacity to access health services, such as a HM program, greatly impacts well-being, safety, independence, and health.2,4 Well-being, safety, independence, and health become compromised if individuals cannot access care, if needed care is lacking in their area, if HCPs are not available, or are unwilling to provide care due to lack of insurance coverage.7-12 In locations where health care services are minimal due to lack of specialists or health care facilities, the quality of (or access to) care may be compromised, resulting in preventable conditions becoming problematic.13,14 These conditions may result in unnecessary hospitalizations for conditions that could have been treated during routine care. Financial barriers to care particularly among low-income people and the uninsured have proven detrimental to health.15,16 On the other hand, preventable hospital stays are a quality of care measure (ie, a proxy for poor quality of care). HISA operates within a health care system; thus, it is imperative to include these measures impacting health.
In this study, we sought to identify county-level predictors—in particular, county-level proxies for access to care—that may be associated with county-level HISA use. We define HISA utilization rate as the percentage of a county’s VHA patients who have received a HISA award.
Methods
This study used data from the National Prosthetics Patient Database (NPPD), US Department of Veterans Affairs (VA) medical database inpatient and outpatient datasets, VHA Support Service Center (VSSC) data cubes, and the County Health Rankings database (CHRD). First, the study cohort was identified from NPPD users who have obtained a HISA award from fiscal years (FY) 2015 to 2018. Analysis started with FY 2015 following new regulations (38 CFR § 17) governing the operations of the HISA program.2 The study cohort was matched with records from NPPD and VA inpatient and outpatient datasets to obtain information about the veterans’ demographic characteristics and their HM characteristics and costs. The number of VHA end-of-year (EOY) patients per county was extracted from the VSSC Current Enrollment Cube, which was used in calculation of the county-level HISA utilization rate.17 Finally, zip code–based locational data were used to calculate approximate drive time and distance from the HISA user’s approximate location to the facility where they received their HM prescription. Drive times and drive distances were calculated with Esri ArcGIS Pro (v2.6.3) by placing zip code centroid and VHA facilities on a nationwide road network that contains both road speeds and distances.
Calculations
Patient-level data were aggregated up to county-level variables by calculating the sum, mean, or percent per county. HISA user sample characteristics, including sex, race, rurality (urban, rural), marital status, and Class 1 vs Class 2 disability-related eligibility groups, were aggregated to the county level by calculating percentages of HISA users of the given characteristics out of total HISA users in the county. Disability-related eligibility groups (Class 1 vs Class 2 HISA users) determines the maximum lifetime award dollar amount. Specifically, those with service-connected disabilities or those with a ≥ 50% disability rating (regardless of whether or not their disability is service connected) are classified as Class 1 HISA users and are eligible to receive a maximum lifetime award of $6800. Those with a recorded disability that is not connected to their military service, and who have a disability rating of < 50% are classified as Class 2 HISA users and are eligible to receive a lifetime maximum award of $2000.
The county-level number of HISA users was used as the numerator for calculation of county-level HISA utilization rate. Counties with zero HISA users were excluded. The number of EOY VHA patients per county in FY 2018 was divided by 1000 and used as the denominator in the calculation of county-level HISA utilization rate. Thus, the outcome variable is HISA utilization rate per 1000 VHA patients in FY 2018 (HISA utilization rate).
County-Level Variables
County-level variables were downloaded from the 2020 CHRD.5,6 An explanation of the CHRD model and the factors used in this study are shown in the eAppendix (available at doi: 10.12788/fp.0279).6 County-level aggregated HISA user data and the CHRD data were matched using county Federal Information Processing Standards codes. Access to care measures collected from CHRD included percentages uninsured and ratios of population to primary care physicians, dentists, mental health professionals, and other primary care professionals. Other CHRD measures included those for quality of care (rate of preventable hospital stay) and housing quality (percent of households with high housing costs, percent of households with overcrowding, percent of households with lack of kitchen or plumbing, percent of households with severe housing cost burden, percent of homeownership). Of secondary interest was county population rurality, as previous research findings showed the annual average of HISA users who are from rural areas ranged from 30 to 35%.
Analysis Methods
SAS (v9.4), R (v4.0.2), and RStudio (v1.3.1093) were used for data preparation and analysis.18 Multiple regression analysis was used to predict county-level utilization rate from county-level variables. Sociodemographic characteristics from CHRD and HISA data were included as important control predictors in the regression model, though our focus for this paper are the access to care and housing quality predictors.
Model diagnostics (examination of model residuals, Breusch-Godfrey test, Breusch-Pagan test) revealed significant heteroskedasticity of the model; thus, robust standard errors and associated P values were computed using the R estimatr package (v0.30.2).19 Some predictor variables of interest (eg, ratio of mental health professionals) were removed during the model building process either due to problems of multicollinearity or excessive missingness that would have resulted in listwise deletion.
Results
County-level HISA utilization rate per 1000 EOY VHA patients ranged from 0.09 to 59.7%, with a 6.6% mean and 5% median (Figure 2). The data were highly positively skewed. The final model included 33 total predictor variables (Table 1). The final regression model was a significantly better predictor of county-level HISA utilization rate than a null model (F[33-2184], 10.18; P < .001). The adjusted model R2 showed that the overall model accounted for approximately 23% of variance in county-level HISA utilization rate (Table 2).
Among the primary variables of interest, percent uninsured adults and rate of preventable hospital stays emerged as significant predictors of county-level HISA utilization rate. Specifically, county percentage of uninsured adults was negatively related to county-level HISA utilization rate (b = -8.99, P = .005), indicating that the higher the proportion of uninsured adults—with all other predictors held constant—the lower the HISA utilization rate. Percent uninsured adults ranged from 2.7 to 42.4% across counties, with a mean (SD) of 12.7% (5.8%) and 11.4% median.
County rate of preventable hospital stays, however, was significantly and positively related to county-level HISA utilization rate (b = .0004, P = .009), indicating that the higher the rate of preventable hospital stays—with all other predictors held constant—the higher the HISA utilization rate. The direction of this effect is the opposite of the direction of the effect of percent uninsured adults (positive rather than negative), even though both could be considered measures of access to care. The standardized β for these 2 predictors indicate that county rate of preventable hospital stays is a somewhat stronger predictor of county-level HISA utilization rate than is county percent of uninsured adults (β = .11 and β = -.09, respectively). Rate of preventable hospital stays ranged from 683 to 16,802 across counties included in this analysis, with a mean (SD) of 4,796.5 (1659.9) and a 4669 median.
Of secondary interest was county rurality. The county-level percentage of rural residents was significantly and positively related to county-level HISA utilization rate, indicating that the higher the proportion of individuals within county considered rural—all other predictors held constant—the higher the HISA utilization rate. The mean (SD) percentage of rural residents per county was 52.3% (30.2) and 52.7 % median.
Discussion
This study examined whether county-level characteristics, specifically variables for access to care, quality of care, and housing quality, were predictive of a county’s HISA utilization rate. Given that this series of work on the HISA program is (to our knowledge) the first of its kind, and given the exploratory nature of this analysis, we did not have specific predictions for the effects of any one given variable. Nevertheless, some of the results were surprising, and we believe they warrant additional study. In particular, the opposing direction of effects for access to care and quality of care variables were hard to reconcile.
The county percent of uninsured adults (an access to care variable, specifically, a proxy for poor access to care) was negatively associated with county-level HISA utilization rate, whereas the county rate of preventable hospital stays (a quality of care variable, but also potentially an access to care variable, and specifically, proxies for poor quality of care or poor access to care) was positively associated with county-level HISA utilization rate. To describe the relationships more generally, one coefficient in the regression model indicated that the poorer the access to care, the lower the HISA utilization rate (higher percent of uninsured adults predicts lower HISA utilization rate), while another coefficient in the regression model indicated the poorer the quality of and access to care, the higher the HISA utilization rate (higher rate of preventable hospital stays predicts higher HISA utilization rate). Future study is warranted to disentangle and reconcile the various community-level predictors of this service.
Housing quality measures (eg, percent of households with high housing costs, percent of households with overcrowding, percent of households with lack of kitchen or plumbing, percent of households with severe housing cost burden, and percent of homeownership) are important in the consideration of whether a HM will be performed or should be performed. For example, if a person is cost burdened by the amount of expenditure spent in housing there will be little discretionary funds to perform a HM. Individuals who do not own their home may experience complications in obtaining permission from landlords to perform a HM. County-level predictors of housing quality (percent of households with high housing costs, overcrowding, and lack of kitchen or plumbing) were not significantly associated with county-level HISA utilization rate but are also nevertheless relevant to the discussion of home modifications. Of particular interest is the percent of households with lack of kitchen or plumbing variable, which was positively related to county-level HISA utilization rate although not statistically significant. HM elements related to the kitchen (eg, heighten countertop) add to the accessibility of the home allowing for the performing of activities of daily living such as cooking. Between FY 2015 and FY 2018, we discovered 131 prescriptions for kitchen (n = 90) and plumbing (n = 41) HMs, which is a very small proportion of the 30,780 total HMs (there were 24,397 bathroom HMs). The nonsignificant coefficient for this variable may reflect the small number of veterans that obtained these HM.
Limitations
The potentially conflicting direction of effects for a significant access to care variable (percent uninsured adults) and a significant access to care and quality of care variable (preventable hospital stays) are interesting and warrant additional study, but the inability to interpret or explain this apparent inconsistency constitutes a limitation of the current data and analyses presented here. Another limitation is that this analysis uses county-level predictors for what is ultimately an individual-level outcome. It would have been ideal to have both individual- and county-level data to conduct a multilevel analysis; in particular, individual-level data within counties of individuals (both veterans and nonveterans) who did not receive a HISA award (including both those who applied and were denied, and who did not apply) would be highly valuable.
Conclusions
Our continuing research into veterans’ use of HM fills a gap in the literature about the characteristics of HISA users, the impact of county-level variables on the use of HISA, and the geographic distribution and use of HISA within the VHA. While it is important to examine the influence of broader systems on individual outcomes, there could be myriad other factors that are more proximal and more closely related to whether any one individual applies for, let alone receives, a HISA award. Indeed, a low overall adjusted model R2 indicates that there is considerable variability in county-level HISA utilization rate that was not accounted for by the current model; this further speaks to warranted additional study.
More research is needed to understand and account for geographical variation in HISA utilization rate across the US. However, this work serves as an exploratory first step at quantifying and predicting HISA utilization rate at a broad level, with the ultimate goal of increasing access to HMs for veterans with disabilities.
Acknowledgments
This research was supported by grant 15521 from the US Department of Veterans Affairs, Office of Rural Health. Furthermore, the research was supported in part by grant K12 HD055929 from the National Institutes of Health. We want to acknowledge Cheri E. Knecht, Project Coordinator, for her assistance throughout all aspects of our research study and for her thoughtful contributions during the writing of this manuscript.
This article is part of a series of articles on the Home Improvements and Structural Alterations program (HISA), a home modification (HM) program within the Veterans Health Administration (VHA). HISA is a benefit awarded to veterans with disabilities (VWDs) and is instrumental in affording physical accessibility and structural alterations to veterans’ homes.1 The overarching goals of this project are to describe and understand HISA use by VWDs. Previous work has shown geographical variation in the number of HISA prescriptions across counties in the US (Figure 1).1 The current work seeks to describe and predict the county-level rates of HISA use. Information about what predicts HISA utilization at the county level is important because it enhances understanding of program utilization at a national level. The long-term goal of the series is to provide knowledge about HM services within VHA to improve community-based independent living of VWDs by increasing awareness and utilization of HM services.
Background
A health care professional (HCP) approves a HM support award by evaluating the practicality of the support to improve the built environment of a given veteran’s disability.1,2 Previously we detailed some of the preliminary research into the HISA program, including HISA user demographic and clinical characteristics, types of HMs received, user suggestions for improvement, and geospatial analysis of HISA prescriptions concentration.1-4
The geospatial analyses of HISA prescriptions revealed clusters of high numbers of HISA users (hot spots) and low numbers of HISA users (cold spots), indicating that HISA is either not prescribed or uniformly used across the US. The previous research prompted investigation into county-level variables that may impact HISA utilization rates. This inquiry focuses on county characteristics associated with HISA use rates, such as measures of clinical care and quality of care (eg, access to health services variables, lack of insurance, preventable hospital stays), physical environment, and sociodemographic characteristics. Clinical care and quality of care measures promote the interaction with HCPs. Moreover, access to health care is an important indicator of health outcomes.5,6 An individual’s capacity to access health services, such as a HM program, greatly impacts well-being, safety, independence, and health.2,4 Well-being, safety, independence, and health become compromised if individuals cannot access care, if needed care is lacking in their area, if HCPs are not available, or are unwilling to provide care due to lack of insurance coverage.7-12 In locations where health care services are minimal due to lack of specialists or health care facilities, the quality of (or access to) care may be compromised, resulting in preventable conditions becoming problematic.13,14 These conditions may result in unnecessary hospitalizations for conditions that could have been treated during routine care. Financial barriers to care particularly among low-income people and the uninsured have proven detrimental to health.15,16 On the other hand, preventable hospital stays are a quality of care measure (ie, a proxy for poor quality of care). HISA operates within a health care system; thus, it is imperative to include these measures impacting health.
In this study, we sought to identify county-level predictors—in particular, county-level proxies for access to care—that may be associated with county-level HISA use. We define HISA utilization rate as the percentage of a county’s VHA patients who have received a HISA award.
Methods
This study used data from the National Prosthetics Patient Database (NPPD), US Department of Veterans Affairs (VA) medical database inpatient and outpatient datasets, VHA Support Service Center (VSSC) data cubes, and the County Health Rankings database (CHRD). First, the study cohort was identified from NPPD users who have obtained a HISA award from fiscal years (FY) 2015 to 2018. Analysis started with FY 2015 following new regulations (38 CFR § 17) governing the operations of the HISA program.2 The study cohort was matched with records from NPPD and VA inpatient and outpatient datasets to obtain information about the veterans’ demographic characteristics and their HM characteristics and costs. The number of VHA end-of-year (EOY) patients per county was extracted from the VSSC Current Enrollment Cube, which was used in calculation of the county-level HISA utilization rate.17 Finally, zip code–based locational data were used to calculate approximate drive time and distance from the HISA user’s approximate location to the facility where they received their HM prescription. Drive times and drive distances were calculated with Esri ArcGIS Pro (v2.6.3) by placing zip code centroid and VHA facilities on a nationwide road network that contains both road speeds and distances.
Calculations
Patient-level data were aggregated up to county-level variables by calculating the sum, mean, or percent per county. HISA user sample characteristics, including sex, race, rurality (urban, rural), marital status, and Class 1 vs Class 2 disability-related eligibility groups, were aggregated to the county level by calculating percentages of HISA users of the given characteristics out of total HISA users in the county. Disability-related eligibility groups (Class 1 vs Class 2 HISA users) determines the maximum lifetime award dollar amount. Specifically, those with service-connected disabilities or those with a ≥ 50% disability rating (regardless of whether or not their disability is service connected) are classified as Class 1 HISA users and are eligible to receive a maximum lifetime award of $6800. Those with a recorded disability that is not connected to their military service, and who have a disability rating of < 50% are classified as Class 2 HISA users and are eligible to receive a lifetime maximum award of $2000.
The county-level number of HISA users was used as the numerator for calculation of county-level HISA utilization rate. Counties with zero HISA users were excluded. The number of EOY VHA patients per county in FY 2018 was divided by 1000 and used as the denominator in the calculation of county-level HISA utilization rate. Thus, the outcome variable is HISA utilization rate per 1000 VHA patients in FY 2018 (HISA utilization rate).
County-Level Variables
County-level variables were downloaded from the 2020 CHRD.5,6 An explanation of the CHRD model and the factors used in this study are shown in the eAppendix (available at doi: 10.12788/fp.0279).6 County-level aggregated HISA user data and the CHRD data were matched using county Federal Information Processing Standards codes. Access to care measures collected from CHRD included percentages uninsured and ratios of population to primary care physicians, dentists, mental health professionals, and other primary care professionals. Other CHRD measures included those for quality of care (rate of preventable hospital stay) and housing quality (percent of households with high housing costs, percent of households with overcrowding, percent of households with lack of kitchen or plumbing, percent of households with severe housing cost burden, percent of homeownership). Of secondary interest was county population rurality, as previous research findings showed the annual average of HISA users who are from rural areas ranged from 30 to 35%.
Analysis Methods
SAS (v9.4), R (v4.0.2), and RStudio (v1.3.1093) were used for data preparation and analysis.18 Multiple regression analysis was used to predict county-level utilization rate from county-level variables. Sociodemographic characteristics from CHRD and HISA data were included as important control predictors in the regression model, though our focus for this paper are the access to care and housing quality predictors.
Model diagnostics (examination of model residuals, Breusch-Godfrey test, Breusch-Pagan test) revealed significant heteroskedasticity of the model; thus, robust standard errors and associated P values were computed using the R estimatr package (v0.30.2).19 Some predictor variables of interest (eg, ratio of mental health professionals) were removed during the model building process either due to problems of multicollinearity or excessive missingness that would have resulted in listwise deletion.
Results
County-level HISA utilization rate per 1000 EOY VHA patients ranged from 0.09 to 59.7%, with a 6.6% mean and 5% median (Figure 2). The data were highly positively skewed. The final model included 33 total predictor variables (Table 1). The final regression model was a significantly better predictor of county-level HISA utilization rate than a null model (F[33-2184], 10.18; P < .001). The adjusted model R2 showed that the overall model accounted for approximately 23% of variance in county-level HISA utilization rate (Table 2).
Among the primary variables of interest, percent uninsured adults and rate of preventable hospital stays emerged as significant predictors of county-level HISA utilization rate. Specifically, county percentage of uninsured adults was negatively related to county-level HISA utilization rate (b = -8.99, P = .005), indicating that the higher the proportion of uninsured adults—with all other predictors held constant—the lower the HISA utilization rate. Percent uninsured adults ranged from 2.7 to 42.4% across counties, with a mean (SD) of 12.7% (5.8%) and 11.4% median.
County rate of preventable hospital stays, however, was significantly and positively related to county-level HISA utilization rate (b = .0004, P = .009), indicating that the higher the rate of preventable hospital stays—with all other predictors held constant—the higher the HISA utilization rate. The direction of this effect is the opposite of the direction of the effect of percent uninsured adults (positive rather than negative), even though both could be considered measures of access to care. The standardized β for these 2 predictors indicate that county rate of preventable hospital stays is a somewhat stronger predictor of county-level HISA utilization rate than is county percent of uninsured adults (β = .11 and β = -.09, respectively). Rate of preventable hospital stays ranged from 683 to 16,802 across counties included in this analysis, with a mean (SD) of 4,796.5 (1659.9) and a 4669 median.
Of secondary interest was county rurality. The county-level percentage of rural residents was significantly and positively related to county-level HISA utilization rate, indicating that the higher the proportion of individuals within county considered rural—all other predictors held constant—the higher the HISA utilization rate. The mean (SD) percentage of rural residents per county was 52.3% (30.2) and 52.7 % median.
Discussion
This study examined whether county-level characteristics, specifically variables for access to care, quality of care, and housing quality, were predictive of a county’s HISA utilization rate. Given that this series of work on the HISA program is (to our knowledge) the first of its kind, and given the exploratory nature of this analysis, we did not have specific predictions for the effects of any one given variable. Nevertheless, some of the results were surprising, and we believe they warrant additional study. In particular, the opposing direction of effects for access to care and quality of care variables were hard to reconcile.
The county percent of uninsured adults (an access to care variable, specifically, a proxy for poor access to care) was negatively associated with county-level HISA utilization rate, whereas the county rate of preventable hospital stays (a quality of care variable, but also potentially an access to care variable, and specifically, proxies for poor quality of care or poor access to care) was positively associated with county-level HISA utilization rate. To describe the relationships more generally, one coefficient in the regression model indicated that the poorer the access to care, the lower the HISA utilization rate (higher percent of uninsured adults predicts lower HISA utilization rate), while another coefficient in the regression model indicated the poorer the quality of and access to care, the higher the HISA utilization rate (higher rate of preventable hospital stays predicts higher HISA utilization rate). Future study is warranted to disentangle and reconcile the various community-level predictors of this service.
Housing quality measures (eg, percent of households with high housing costs, percent of households with overcrowding, percent of households with lack of kitchen or plumbing, percent of households with severe housing cost burden, and percent of homeownership) are important in the consideration of whether a HM will be performed or should be performed. For example, if a person is cost burdened by the amount of expenditure spent in housing there will be little discretionary funds to perform a HM. Individuals who do not own their home may experience complications in obtaining permission from landlords to perform a HM. County-level predictors of housing quality (percent of households with high housing costs, overcrowding, and lack of kitchen or plumbing) were not significantly associated with county-level HISA utilization rate but are also nevertheless relevant to the discussion of home modifications. Of particular interest is the percent of households with lack of kitchen or plumbing variable, which was positively related to county-level HISA utilization rate although not statistically significant. HM elements related to the kitchen (eg, heighten countertop) add to the accessibility of the home allowing for the performing of activities of daily living such as cooking. Between FY 2015 and FY 2018, we discovered 131 prescriptions for kitchen (n = 90) and plumbing (n = 41) HMs, which is a very small proportion of the 30,780 total HMs (there were 24,397 bathroom HMs). The nonsignificant coefficient for this variable may reflect the small number of veterans that obtained these HM.
Limitations
The potentially conflicting direction of effects for a significant access to care variable (percent uninsured adults) and a significant access to care and quality of care variable (preventable hospital stays) are interesting and warrant additional study, but the inability to interpret or explain this apparent inconsistency constitutes a limitation of the current data and analyses presented here. Another limitation is that this analysis uses county-level predictors for what is ultimately an individual-level outcome. It would have been ideal to have both individual- and county-level data to conduct a multilevel analysis; in particular, individual-level data within counties of individuals (both veterans and nonveterans) who did not receive a HISA award (including both those who applied and were denied, and who did not apply) would be highly valuable.
Conclusions
Our continuing research into veterans’ use of HM fills a gap in the literature about the characteristics of HISA users, the impact of county-level variables on the use of HISA, and the geographic distribution and use of HISA within the VHA. While it is important to examine the influence of broader systems on individual outcomes, there could be myriad other factors that are more proximal and more closely related to whether any one individual applies for, let alone receives, a HISA award. Indeed, a low overall adjusted model R2 indicates that there is considerable variability in county-level HISA utilization rate that was not accounted for by the current model; this further speaks to warranted additional study.
More research is needed to understand and account for geographical variation in HISA utilization rate across the US. However, this work serves as an exploratory first step at quantifying and predicting HISA utilization rate at a broad level, with the ultimate goal of increasing access to HMs for veterans with disabilities.
Acknowledgments
This research was supported by grant 15521 from the US Department of Veterans Affairs, Office of Rural Health. Furthermore, the research was supported in part by grant K12 HD055929 from the National Institutes of Health. We want to acknowledge Cheri E. Knecht, Project Coordinator, for her assistance throughout all aspects of our research study and for her thoughtful contributions during the writing of this manuscript.
1. Semeah LM, Ahrentzen S, Jia H, Cowper-Ripley DC, Levy CE, Mann WC. The home improvements and structural alterations benefits program: veterans with disabilities and home accessibility. J Disability Policy Studies. 2017;28(1):43-51. doi:10.1177/1044207317696275
2. Semeah LM, Wang X, Cowper Ripley DC, Lee MJ, Ahonle ZJ, Ganesh SP, et al. Improving health through a home modification service for veterans. In: Fiedler BA, ed. Three Facets of Public Health and Paths to Improvements. Academic Press; 2020:381-416.
3. Semeah LM, Ahrentzen S, Cowper-Ripley DC, Santos-Roman LM, Beamish JO, Farley K. Rental housing needs and barriers from the perspective of veterans with disabilities. Housing Policy Debate. 2019;29(4):542-558. doi:10.1080/10511482.2018.1543203
4. Semeah LM, Ganesh SP, Wang X, et al. Home modification and health services utilization by rural and urban veterans with disabilities. Housing Policy Debate. 2021;31(6):862-874.doi:10.1080/10511482.2020.1858923
5. University of Wisconsin Population Health Institute. County health rankings model. Accessed May 13, 2022. https://www.countyhealthrankings.org/about-us
6. Remington PL, Catlin BB, Gennuso KP. The County Health Rankings: rationale and methods. Popul Health Metr. 2015;13(11). doi:10.1186/s12963-015-0044-2
7. National Academies of Sciences, Engineering, and Medicine. Health-Care Utilization as a Proxy in Disability Determination. Washington, DC: The National Academies Press; 2018.
8. Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611-20. doi:10.1016/j.puhe.2015.04.001
9. Medicaid and Chip Payment and Access Commission (MACPAC). Medicaid access in brief: adults’ experiences in obtaining medical care. November 2016. Accessed May 13, 2022. https://www.macpac.gov/publication/access-in-brief-adults-experiences-in-obtaining-medical-care
10. Tolbert J, Orgera, K, Damico A. Key facts about the uninsured population. November 6, 2020. Accessed May 13, 2022. https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population
11. Meit M, Knudson A, Gilbert T, et al. The 2014 update of the rural-urban chartbook, 2014. October 2014. Accessed May 13, 2022. http://www.ruralhealthresearch.org
12. National Center for Health Statistics (US). Report No.: 2016-1232. Health, United States, 2015: with special feature on racial and ethnic health disparities. Hyattsville, MD: National Center for Health Statistics.
13. Broussard DL, Mason KE, Carruth AR, Carton TW. Assessing potentially preventable hospitalizations at the county level: a comparison of measures using Medicare data and state hospital discharge data. Popul Health Manag. 2018;21(6):438-445. doi:10.1089/pop.2017.0141
14. Pezzin LE, Bogner HR, Kurichi JE, et al. Preventable hospitalizations, barriers to care, and disability. Medicine (Baltimore). 2018;97:e0691 doi:10.1097/MD.0000000000010691
15. Davis K, Ballreich J. Equitable access to care: how the United States ranks internationally. N Engl J Med. 2014;371(17):1567-70. doi:10.1056/NEJMp1406707
16. Squires D, Anderson C. U.S. health care from a global perspective: spending, use of services, prices, and health in 13 countries. Issue Brief (Commonw Fund). 2015;15:1-15.
17. VHA Service Support Center. Current enrollment cube (vssc.med.va.gov). Retrieved August 06, 2019. [Data not verified.]
18. Bunn A, Korpela M. R: A language and environment for statistical computing: an introduction to dplR. January 29, 2021. Accessed May 13, 2022. http://r.meteo.uni.wroc.pl/web/packages/dplR/vignettes/intro-dplR.pdf
19. Sheppard BH, Hartwick J, Warshaw PR. The theory of reasoned action: a meta-analysis of past research with recommendations for modifications and future research. J Consumer Research. 1988;15(3):325-343. doi:10.1086/209170
1. Semeah LM, Ahrentzen S, Jia H, Cowper-Ripley DC, Levy CE, Mann WC. The home improvements and structural alterations benefits program: veterans with disabilities and home accessibility. J Disability Policy Studies. 2017;28(1):43-51. doi:10.1177/1044207317696275
2. Semeah LM, Wang X, Cowper Ripley DC, Lee MJ, Ahonle ZJ, Ganesh SP, et al. Improving health through a home modification service for veterans. In: Fiedler BA, ed. Three Facets of Public Health and Paths to Improvements. Academic Press; 2020:381-416.
3. Semeah LM, Ahrentzen S, Cowper-Ripley DC, Santos-Roman LM, Beamish JO, Farley K. Rental housing needs and barriers from the perspective of veterans with disabilities. Housing Policy Debate. 2019;29(4):542-558. doi:10.1080/10511482.2018.1543203
4. Semeah LM, Ganesh SP, Wang X, et al. Home modification and health services utilization by rural and urban veterans with disabilities. Housing Policy Debate. 2021;31(6):862-874.doi:10.1080/10511482.2020.1858923
5. University of Wisconsin Population Health Institute. County health rankings model. Accessed May 13, 2022. https://www.countyhealthrankings.org/about-us
6. Remington PL, Catlin BB, Gennuso KP. The County Health Rankings: rationale and methods. Popul Health Metr. 2015;13(11). doi:10.1186/s12963-015-0044-2
7. National Academies of Sciences, Engineering, and Medicine. Health-Care Utilization as a Proxy in Disability Determination. Washington, DC: The National Academies Press; 2018.
8. Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611-20. doi:10.1016/j.puhe.2015.04.001
9. Medicaid and Chip Payment and Access Commission (MACPAC). Medicaid access in brief: adults’ experiences in obtaining medical care. November 2016. Accessed May 13, 2022. https://www.macpac.gov/publication/access-in-brief-adults-experiences-in-obtaining-medical-care
10. Tolbert J, Orgera, K, Damico A. Key facts about the uninsured population. November 6, 2020. Accessed May 13, 2022. https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population
11. Meit M, Knudson A, Gilbert T, et al. The 2014 update of the rural-urban chartbook, 2014. October 2014. Accessed May 13, 2022. http://www.ruralhealthresearch.org
12. National Center for Health Statistics (US). Report No.: 2016-1232. Health, United States, 2015: with special feature on racial and ethnic health disparities. Hyattsville, MD: National Center for Health Statistics.
13. Broussard DL, Mason KE, Carruth AR, Carton TW. Assessing potentially preventable hospitalizations at the county level: a comparison of measures using Medicare data and state hospital discharge data. Popul Health Manag. 2018;21(6):438-445. doi:10.1089/pop.2017.0141
14. Pezzin LE, Bogner HR, Kurichi JE, et al. Preventable hospitalizations, barriers to care, and disability. Medicine (Baltimore). 2018;97:e0691 doi:10.1097/MD.0000000000010691
15. Davis K, Ballreich J. Equitable access to care: how the United States ranks internationally. N Engl J Med. 2014;371(17):1567-70. doi:10.1056/NEJMp1406707
16. Squires D, Anderson C. U.S. health care from a global perspective: spending, use of services, prices, and health in 13 countries. Issue Brief (Commonw Fund). 2015;15:1-15.
17. VHA Service Support Center. Current enrollment cube (vssc.med.va.gov). Retrieved August 06, 2019. [Data not verified.]
18. Bunn A, Korpela M. R: A language and environment for statistical computing: an introduction to dplR. January 29, 2021. Accessed May 13, 2022. http://r.meteo.uni.wroc.pl/web/packages/dplR/vignettes/intro-dplR.pdf
19. Sheppard BH, Hartwick J, Warshaw PR. The theory of reasoned action: a meta-analysis of past research with recommendations for modifications and future research. J Consumer Research. 1988;15(3):325-343. doi:10.1086/209170
Synthetic opioid use up almost 800% nationwide
The results of a national urine drug test (UDT) study come as the United States is reporting a record-high number of drug overdose deaths – more than 80% of which involved fentanyl or other synthetic opioids and prompting a push for better surveillance models.
Researchers found that UDTs can be used to accurately identify which drugs are circulating in a community, revealing in just a matter of days critically important drug use trends that current surveillance methods take a month or longer to report.
The faster turnaround could potentially allow clinicians and public health officials to be more proactive with targeted overdose prevention and harm-reduction strategies such as distribution of naloxone and fentanyl test strips.
“We’re talking about trying to come up with an early-warning system,” study author Steven Passik, PhD, vice president for scientific affairs for Millennium Health, San Diego, Calif., told this news organization. “We’re trying to find out if we can let people in the harm reduction and treatment space know about what might be coming weeks or a month or more in advance so that some interventions could be marshaled.”
The study was published online in JAMA Network Open.
Call for better surveillance
More than 100,000 people in the United States died of an unintended drug overdose in 2021, a record high and a 15% increase over 2020 figures, which also set a record.
Part of the federal government’s plan to address the crisis includes strengthening epidemiologic efforts by better collection and mining of public health surveillance data.
Sources currently used to detect drug use trends include mortality data, poison control centers, emergency departments, electronic health records, and crime laboratories. But analysis of these sources can take weeks or more.
“One of the real challenges in addressing and reducing overdose deaths has been the relative lack of accessible real-time data that can support agile responses to deployment of resources in a specific geographic region,” study coauthor Rebecca Jackson, MD, professor and associate dean for clinical and translational research at Ohio State University in Columbus, said in an interview.
Ohio State researchers partnered with scientists at Millennium Health, one of the largest urine test labs in the United States, on a cross-sectional study to find out if UDTs could be an accurate and speedier tool for drug surveillance.
They analyzed 500,000 unique urine samples from patients in substance use disorder (SUD) treatment facilities in all 50 states from 2013 to 2020, comparing levels of cocaine, heroin, methamphetamine, synthetic opioids, and other opioids found in the samples to levels of the same drugs from overdose mortality data at the national, state, and county level from the National Vital Statistics System.
On a national level, synthetic opioids and methamphetamine were highly correlated with overdose mortality data (Spearman’s rho = .96 for both). When synthetic opioids were coinvolved, methamphetamine (rho = .98), heroin (rho = .78), cocaine (rho = .94), and other opioids (rho = .83) were also highly correlated with overdose mortality data.
Similar correlations were found when examining state-level data from 24 states and at the county level upon analysis of 19 counties in Ohio.
A changing landscape
Researchers said the strong correlation between overdose deaths and UDT results for synthetic opioids and methamphetamine are likely explained by the drugs’ availability and lethality.
“The most important thing that we found was just the strength of the correlation, which goes right to the heart of why we considered correlation to be so critical,” lead author Penn Whitley, senior director of bioinformatics for Millennium Health, told this news organization. “We needed to demonstrate that there was a strong correlation of just the UDT positivity rates with mortality – in this case, fatal drug overdose rates – as a steppingstone to build out tools that could utilize UDT as a real-time data source.”
While the main goal of the study was to establish correlation between UDT results and national mortality data, the study also offers a view of a changing landscape in the opioid epidemic.
Overall, UDT positivity for total synthetic opioids increased from 2.1% in 2013 to 19.1% in 2020 (a 792.5% increase). Positivity rates for all included drug categories increased when synthetic opioids were present.
However, in the absence of synthetic opioids, UDT positivity decreased for almost all drug categories from 2013 to 2020 (from 7.7% to 4.7% for cocaine; 3.9% to 1.6% for heroin; 20.5% to 6.9% for other opioids).
Only methamphetamine positivity increased with or without involvement of synthetic opioids. With synthetic opioids, meth positivity rose from 0.1% in 2013 to 7.9% in 2020. Without them, meth positivity rates still rose, from 2.1% in 2013 to 13.1% in 2020.
The findings track with an earlier study showing methamphetamine-involved overdose deaths rose sharply between 2011 and 2018.
“The data from this manuscript support that the opioid epidemic is transitioning from an opioid epidemic to a polysubstance epidemic where illicit synthetic opioids, largely fentanyl, in combination with other substances are now responsible for upwards of 80% of OD deaths,” Dr. Jackson said.
In an accompanying editorial Jeffrey Brent, MD, PhD, clinical professor in internal medicine at the University of Colorado at Denver, Aurora, and Stephanie T. Weiss, MD, PhD, staff clinician in the Translational Addiction Medicine Branch at the National Institute on Drug Abuse, Baltimore, note that as new agents emerge, different harm-reduction strategies will be needed, adding that having a real-time tool to identify the trends will be key to preventing deaths.
“Surveillance systems are an integral component of reducing morbidity and mortality associated with illicit drug use. On local, regional, and national levels, information of this type is needed to most efficiently allocate limited resources to maximize benefit and save lives,” Dr. Brent and Dr. Weiss write.
The study was funded by Millennium Health and the National Center for Advancing Translational Sciences. Full disclosures are included in the original articles, but no sources reported conflicts related to the study.
A version of this article first appeared on Medscape.com.
The results of a national urine drug test (UDT) study come as the United States is reporting a record-high number of drug overdose deaths – more than 80% of which involved fentanyl or other synthetic opioids and prompting a push for better surveillance models.
Researchers found that UDTs can be used to accurately identify which drugs are circulating in a community, revealing in just a matter of days critically important drug use trends that current surveillance methods take a month or longer to report.
The faster turnaround could potentially allow clinicians and public health officials to be more proactive with targeted overdose prevention and harm-reduction strategies such as distribution of naloxone and fentanyl test strips.
“We’re talking about trying to come up with an early-warning system,” study author Steven Passik, PhD, vice president for scientific affairs for Millennium Health, San Diego, Calif., told this news organization. “We’re trying to find out if we can let people in the harm reduction and treatment space know about what might be coming weeks or a month or more in advance so that some interventions could be marshaled.”
The study was published online in JAMA Network Open.
Call for better surveillance
More than 100,000 people in the United States died of an unintended drug overdose in 2021, a record high and a 15% increase over 2020 figures, which also set a record.
Part of the federal government’s plan to address the crisis includes strengthening epidemiologic efforts by better collection and mining of public health surveillance data.
Sources currently used to detect drug use trends include mortality data, poison control centers, emergency departments, electronic health records, and crime laboratories. But analysis of these sources can take weeks or more.
“One of the real challenges in addressing and reducing overdose deaths has been the relative lack of accessible real-time data that can support agile responses to deployment of resources in a specific geographic region,” study coauthor Rebecca Jackson, MD, professor and associate dean for clinical and translational research at Ohio State University in Columbus, said in an interview.
Ohio State researchers partnered with scientists at Millennium Health, one of the largest urine test labs in the United States, on a cross-sectional study to find out if UDTs could be an accurate and speedier tool for drug surveillance.
They analyzed 500,000 unique urine samples from patients in substance use disorder (SUD) treatment facilities in all 50 states from 2013 to 2020, comparing levels of cocaine, heroin, methamphetamine, synthetic opioids, and other opioids found in the samples to levels of the same drugs from overdose mortality data at the national, state, and county level from the National Vital Statistics System.
On a national level, synthetic opioids and methamphetamine were highly correlated with overdose mortality data (Spearman’s rho = .96 for both). When synthetic opioids were coinvolved, methamphetamine (rho = .98), heroin (rho = .78), cocaine (rho = .94), and other opioids (rho = .83) were also highly correlated with overdose mortality data.
Similar correlations were found when examining state-level data from 24 states and at the county level upon analysis of 19 counties in Ohio.
A changing landscape
Researchers said the strong correlation between overdose deaths and UDT results for synthetic opioids and methamphetamine are likely explained by the drugs’ availability and lethality.
“The most important thing that we found was just the strength of the correlation, which goes right to the heart of why we considered correlation to be so critical,” lead author Penn Whitley, senior director of bioinformatics for Millennium Health, told this news organization. “We needed to demonstrate that there was a strong correlation of just the UDT positivity rates with mortality – in this case, fatal drug overdose rates – as a steppingstone to build out tools that could utilize UDT as a real-time data source.”
While the main goal of the study was to establish correlation between UDT results and national mortality data, the study also offers a view of a changing landscape in the opioid epidemic.
Overall, UDT positivity for total synthetic opioids increased from 2.1% in 2013 to 19.1% in 2020 (a 792.5% increase). Positivity rates for all included drug categories increased when synthetic opioids were present.
However, in the absence of synthetic opioids, UDT positivity decreased for almost all drug categories from 2013 to 2020 (from 7.7% to 4.7% for cocaine; 3.9% to 1.6% for heroin; 20.5% to 6.9% for other opioids).
Only methamphetamine positivity increased with or without involvement of synthetic opioids. With synthetic opioids, meth positivity rose from 0.1% in 2013 to 7.9% in 2020. Without them, meth positivity rates still rose, from 2.1% in 2013 to 13.1% in 2020.
The findings track with an earlier study showing methamphetamine-involved overdose deaths rose sharply between 2011 and 2018.
“The data from this manuscript support that the opioid epidemic is transitioning from an opioid epidemic to a polysubstance epidemic where illicit synthetic opioids, largely fentanyl, in combination with other substances are now responsible for upwards of 80% of OD deaths,” Dr. Jackson said.
In an accompanying editorial Jeffrey Brent, MD, PhD, clinical professor in internal medicine at the University of Colorado at Denver, Aurora, and Stephanie T. Weiss, MD, PhD, staff clinician in the Translational Addiction Medicine Branch at the National Institute on Drug Abuse, Baltimore, note that as new agents emerge, different harm-reduction strategies will be needed, adding that having a real-time tool to identify the trends will be key to preventing deaths.
“Surveillance systems are an integral component of reducing morbidity and mortality associated with illicit drug use. On local, regional, and national levels, information of this type is needed to most efficiently allocate limited resources to maximize benefit and save lives,” Dr. Brent and Dr. Weiss write.
The study was funded by Millennium Health and the National Center for Advancing Translational Sciences. Full disclosures are included in the original articles, but no sources reported conflicts related to the study.
A version of this article first appeared on Medscape.com.
The results of a national urine drug test (UDT) study come as the United States is reporting a record-high number of drug overdose deaths – more than 80% of which involved fentanyl or other synthetic opioids and prompting a push for better surveillance models.
Researchers found that UDTs can be used to accurately identify which drugs are circulating in a community, revealing in just a matter of days critically important drug use trends that current surveillance methods take a month or longer to report.
The faster turnaround could potentially allow clinicians and public health officials to be more proactive with targeted overdose prevention and harm-reduction strategies such as distribution of naloxone and fentanyl test strips.
“We’re talking about trying to come up with an early-warning system,” study author Steven Passik, PhD, vice president for scientific affairs for Millennium Health, San Diego, Calif., told this news organization. “We’re trying to find out if we can let people in the harm reduction and treatment space know about what might be coming weeks or a month or more in advance so that some interventions could be marshaled.”
The study was published online in JAMA Network Open.
Call for better surveillance
More than 100,000 people in the United States died of an unintended drug overdose in 2021, a record high and a 15% increase over 2020 figures, which also set a record.
Part of the federal government’s plan to address the crisis includes strengthening epidemiologic efforts by better collection and mining of public health surveillance data.
Sources currently used to detect drug use trends include mortality data, poison control centers, emergency departments, electronic health records, and crime laboratories. But analysis of these sources can take weeks or more.
“One of the real challenges in addressing and reducing overdose deaths has been the relative lack of accessible real-time data that can support agile responses to deployment of resources in a specific geographic region,” study coauthor Rebecca Jackson, MD, professor and associate dean for clinical and translational research at Ohio State University in Columbus, said in an interview.
Ohio State researchers partnered with scientists at Millennium Health, one of the largest urine test labs in the United States, on a cross-sectional study to find out if UDTs could be an accurate and speedier tool for drug surveillance.
They analyzed 500,000 unique urine samples from patients in substance use disorder (SUD) treatment facilities in all 50 states from 2013 to 2020, comparing levels of cocaine, heroin, methamphetamine, synthetic opioids, and other opioids found in the samples to levels of the same drugs from overdose mortality data at the national, state, and county level from the National Vital Statistics System.
On a national level, synthetic opioids and methamphetamine were highly correlated with overdose mortality data (Spearman’s rho = .96 for both). When synthetic opioids were coinvolved, methamphetamine (rho = .98), heroin (rho = .78), cocaine (rho = .94), and other opioids (rho = .83) were also highly correlated with overdose mortality data.
Similar correlations were found when examining state-level data from 24 states and at the county level upon analysis of 19 counties in Ohio.
A changing landscape
Researchers said the strong correlation between overdose deaths and UDT results for synthetic opioids and methamphetamine are likely explained by the drugs’ availability and lethality.
“The most important thing that we found was just the strength of the correlation, which goes right to the heart of why we considered correlation to be so critical,” lead author Penn Whitley, senior director of bioinformatics for Millennium Health, told this news organization. “We needed to demonstrate that there was a strong correlation of just the UDT positivity rates with mortality – in this case, fatal drug overdose rates – as a steppingstone to build out tools that could utilize UDT as a real-time data source.”
While the main goal of the study was to establish correlation between UDT results and national mortality data, the study also offers a view of a changing landscape in the opioid epidemic.
Overall, UDT positivity for total synthetic opioids increased from 2.1% in 2013 to 19.1% in 2020 (a 792.5% increase). Positivity rates for all included drug categories increased when synthetic opioids were present.
However, in the absence of synthetic opioids, UDT positivity decreased for almost all drug categories from 2013 to 2020 (from 7.7% to 4.7% for cocaine; 3.9% to 1.6% for heroin; 20.5% to 6.9% for other opioids).
Only methamphetamine positivity increased with or without involvement of synthetic opioids. With synthetic opioids, meth positivity rose from 0.1% in 2013 to 7.9% in 2020. Without them, meth positivity rates still rose, from 2.1% in 2013 to 13.1% in 2020.
The findings track with an earlier study showing methamphetamine-involved overdose deaths rose sharply between 2011 and 2018.
“The data from this manuscript support that the opioid epidemic is transitioning from an opioid epidemic to a polysubstance epidemic where illicit synthetic opioids, largely fentanyl, in combination with other substances are now responsible for upwards of 80% of OD deaths,” Dr. Jackson said.
In an accompanying editorial Jeffrey Brent, MD, PhD, clinical professor in internal medicine at the University of Colorado at Denver, Aurora, and Stephanie T. Weiss, MD, PhD, staff clinician in the Translational Addiction Medicine Branch at the National Institute on Drug Abuse, Baltimore, note that as new agents emerge, different harm-reduction strategies will be needed, adding that having a real-time tool to identify the trends will be key to preventing deaths.
“Surveillance systems are an integral component of reducing morbidity and mortality associated with illicit drug use. On local, regional, and national levels, information of this type is needed to most efficiently allocate limited resources to maximize benefit and save lives,” Dr. Brent and Dr. Weiss write.
The study was funded by Millennium Health and the National Center for Advancing Translational Sciences. Full disclosures are included in the original articles, but no sources reported conflicts related to the study.
A version of this article first appeared on Medscape.com.
Why do young men target schools for violent attacks? And what can we do about it?
Schools are intended to be a safe place to acquire knowledge, try out ideas, practice socializing, and build a foundation for adulthood. Many schools fulfill this mission for most children, but for children at both extremes of ability their school experience does not suffice.
When asked, “If you had the choice, would you rather stay home or go to school?” my patients almost universally prefer school. They all know that school is where they should be; they want to be normal, accepted by peers, getting ready for the world’s coming demands, and validation that they will make it as adults. Endorsement otherwise is a warning sign.
When such important tasks of childhood are thwarted children may despair, withdraw, give up, or a small number become furious. These may profoundly resent the children who are experiencing success when they could not. They may hate the teachers and the place where they experienced failure and humiliation. Lack of a positive connection to school characterizes children who are violent toward schools as well as those who drop out.
Schools may fail to support the basic needs of children for many reasons. Schools may avoid physical violence but fail to protect the children’s self-esteem. I have heard stories of teachers calling on children to perform who are clearly struggling or shy, insulting incorrect answers, calling names, putting names on the board, reading out failed grades, posting grades publicly, even allowing peers to mock students. Teachers may deny or disregard parent complaints, or even worsen treatment of the child. Although children may at times falsify complaints, children’s and parents’ reports must be taken seriously and remain anonymous. When we hear of such toxic situations for our patients, we can get details and contact school administrators without naming the child, as often the family feels they can’t. Repeated humiliation may require not only remediation, but consequences. We can advocate for a change in classroom or request a 504 Plan if emotional health is affected.
All children learn best and experience success and even joy when the tasks they face are at or slightly beyond their skill level. But with the wide range of abilities, especially for boys, education may need to be individualized. This is very difficult in larger classrooms with fewer resources, too few adult helpers, inexperienced teachers, or high levels of student misbehavior. Basing teacher promotion mainly on standardized test results makes individualizing instruction even less likely. Smaller class size is better; even the recommended (less than 20) or regulated (less than 30) class sizes are associated with suboptimal achievement, compared with smaller ones. Some ways to attain smaller class size include split days or alternate-day sessions, although these also have disadvantages.
While we can advocate for these changes, we can also encourage parents to promote academic skills by talking to and reading to their children of all ages, trying Reach Out and Read for young children, providing counting games, board games, and math songs! Besides screening for attention-deficit/hyperactivity disorder, we can use standard paragraphs and math problems (for example, WRAT, Einstein) to check skills when performance is low or behavior is a problem the school denies. When concerned, we can write letters for parents to sign requesting testing and an individualized education plan to determine need for tutoring or special education.
While Federal legislation requiring the “least restrictive environment” for education was intended to avoid sidelining differently able children, some can’t learn in a regular class. Conversely, if instruction in a special class is adjusted to the child with the lowest skills, minimal learning may occur for others. Although we can speak with the teacher about “this child’s abilities among those in his class” we can first suggest that the parent visit class to observe. Outside tutoring or home schooling may help a child move up to a regular class.
Sometimes a child’s learning is hampered by classrooms with numerous children misbehaving; this is also a reason for resentment. We can inform school administrators about methods such as The Good Behavior Game (paxis.org) that can improve behavior and connection for the whole class.
While a social “pecking order” is universal, it is unacceptable for children to be allowed to humiliate or hurt a peer, or damage their reputation. While this moral teaching should occur at home, it needs to continue at school where peers are forced into groups they did not choose. Screening for bullying at pediatric visits is now a universal recommendation as 30% report being bullied. We need to ask all children about “mean kids in school” or gang involvement for older children.
Parents can support their children experiencing cyberbullying and switch them to a “dumb phone” with no texting option, limited phone time, or no phone at all. Policies against bullying coming from school administrators are most effective but we can inform schools about the STOPit app for children to report bullying anonymously as well as education for students to stand together against a bully (stopbullying.gov). A Lunch Bunch for younger children or a buddy system for older ones can be requested to help them make friends.
With diverse child aptitudes, schools need to offer students alternative opportunities for self-expression and contribution. We can ask about a child’s strengths and suggest related extracurriculars activities in school or outside, including volunteering. Participation on teams or in clubs must not be blocked for those with poor grades. Perhaps tying participation to tutoring would satisfy the school’s desire to motivate instead. Parents can be encouraged to advocate for music, art, and drama classes – programs that are often victims of budget cuts – that can create the essential school connection.
Students in many areas lack access to classes in trades early enough in their education. The requirements for English or math may be out of reach and result in students dropping out before trade classes are an option. We may identify our patients who may do better with a trade education and advise families to request transfer to a high school offering this.
The best connection a child can have to a school is an adult who values them. The child may identify a preferred teacher to us so that we, or the parent, can call to ask them to provide special attention. Facilitating times for students to get to know teachers may require alteration in bus schedules, lunch times, study halls, or breaks, or keeping the school open longer outside class hours. While more mental health providers are clearly needed, sometimes it is the groundskeeper, the secretary, or the lunch helper who can make the best connection with a child.
As pediatricians, we must listen to struggling youth, acknowledge their pain, and model this empathy for their parents who may be obsessing over grades. Problem-solving about how to get accommodations, informal or formal, can inspire hope. We can coach parents and youth to meet respectfully with the school about issues to avoid labeling the child as a problem.
As pediatricians, our recommendations for school funding and policies may carry extra weight. We may share ideas through talks at PTA meetings, serve on school boards, or endorse leaders planning greater resources for schools to optimize each child’s experience and connection to school.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Schools are intended to be a safe place to acquire knowledge, try out ideas, practice socializing, and build a foundation for adulthood. Many schools fulfill this mission for most children, but for children at both extremes of ability their school experience does not suffice.
When asked, “If you had the choice, would you rather stay home or go to school?” my patients almost universally prefer school. They all know that school is where they should be; they want to be normal, accepted by peers, getting ready for the world’s coming demands, and validation that they will make it as adults. Endorsement otherwise is a warning sign.
When such important tasks of childhood are thwarted children may despair, withdraw, give up, or a small number become furious. These may profoundly resent the children who are experiencing success when they could not. They may hate the teachers and the place where they experienced failure and humiliation. Lack of a positive connection to school characterizes children who are violent toward schools as well as those who drop out.
Schools may fail to support the basic needs of children for many reasons. Schools may avoid physical violence but fail to protect the children’s self-esteem. I have heard stories of teachers calling on children to perform who are clearly struggling or shy, insulting incorrect answers, calling names, putting names on the board, reading out failed grades, posting grades publicly, even allowing peers to mock students. Teachers may deny or disregard parent complaints, or even worsen treatment of the child. Although children may at times falsify complaints, children’s and parents’ reports must be taken seriously and remain anonymous. When we hear of such toxic situations for our patients, we can get details and contact school administrators without naming the child, as often the family feels they can’t. Repeated humiliation may require not only remediation, but consequences. We can advocate for a change in classroom or request a 504 Plan if emotional health is affected.
All children learn best and experience success and even joy when the tasks they face are at or slightly beyond their skill level. But with the wide range of abilities, especially for boys, education may need to be individualized. This is very difficult in larger classrooms with fewer resources, too few adult helpers, inexperienced teachers, or high levels of student misbehavior. Basing teacher promotion mainly on standardized test results makes individualizing instruction even less likely. Smaller class size is better; even the recommended (less than 20) or regulated (less than 30) class sizes are associated with suboptimal achievement, compared with smaller ones. Some ways to attain smaller class size include split days or alternate-day sessions, although these also have disadvantages.
While we can advocate for these changes, we can also encourage parents to promote academic skills by talking to and reading to their children of all ages, trying Reach Out and Read for young children, providing counting games, board games, and math songs! Besides screening for attention-deficit/hyperactivity disorder, we can use standard paragraphs and math problems (for example, WRAT, Einstein) to check skills when performance is low or behavior is a problem the school denies. When concerned, we can write letters for parents to sign requesting testing and an individualized education plan to determine need for tutoring or special education.
While Federal legislation requiring the “least restrictive environment” for education was intended to avoid sidelining differently able children, some can’t learn in a regular class. Conversely, if instruction in a special class is adjusted to the child with the lowest skills, minimal learning may occur for others. Although we can speak with the teacher about “this child’s abilities among those in his class” we can first suggest that the parent visit class to observe. Outside tutoring or home schooling may help a child move up to a regular class.
Sometimes a child’s learning is hampered by classrooms with numerous children misbehaving; this is also a reason for resentment. We can inform school administrators about methods such as The Good Behavior Game (paxis.org) that can improve behavior and connection for the whole class.
While a social “pecking order” is universal, it is unacceptable for children to be allowed to humiliate or hurt a peer, or damage their reputation. While this moral teaching should occur at home, it needs to continue at school where peers are forced into groups they did not choose. Screening for bullying at pediatric visits is now a universal recommendation as 30% report being bullied. We need to ask all children about “mean kids in school” or gang involvement for older children.
Parents can support their children experiencing cyberbullying and switch them to a “dumb phone” with no texting option, limited phone time, or no phone at all. Policies against bullying coming from school administrators are most effective but we can inform schools about the STOPit app for children to report bullying anonymously as well as education for students to stand together against a bully (stopbullying.gov). A Lunch Bunch for younger children or a buddy system for older ones can be requested to help them make friends.
With diverse child aptitudes, schools need to offer students alternative opportunities for self-expression and contribution. We can ask about a child’s strengths and suggest related extracurriculars activities in school or outside, including volunteering. Participation on teams or in clubs must not be blocked for those with poor grades. Perhaps tying participation to tutoring would satisfy the school’s desire to motivate instead. Parents can be encouraged to advocate for music, art, and drama classes – programs that are often victims of budget cuts – that can create the essential school connection.
Students in many areas lack access to classes in trades early enough in their education. The requirements for English or math may be out of reach and result in students dropping out before trade classes are an option. We may identify our patients who may do better with a trade education and advise families to request transfer to a high school offering this.
The best connection a child can have to a school is an adult who values them. The child may identify a preferred teacher to us so that we, or the parent, can call to ask them to provide special attention. Facilitating times for students to get to know teachers may require alteration in bus schedules, lunch times, study halls, or breaks, or keeping the school open longer outside class hours. While more mental health providers are clearly needed, sometimes it is the groundskeeper, the secretary, or the lunch helper who can make the best connection with a child.
As pediatricians, we must listen to struggling youth, acknowledge their pain, and model this empathy for their parents who may be obsessing over grades. Problem-solving about how to get accommodations, informal or formal, can inspire hope. We can coach parents and youth to meet respectfully with the school about issues to avoid labeling the child as a problem.
As pediatricians, our recommendations for school funding and policies may carry extra weight. We may share ideas through talks at PTA meetings, serve on school boards, or endorse leaders planning greater resources for schools to optimize each child’s experience and connection to school.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Schools are intended to be a safe place to acquire knowledge, try out ideas, practice socializing, and build a foundation for adulthood. Many schools fulfill this mission for most children, but for children at both extremes of ability their school experience does not suffice.
When asked, “If you had the choice, would you rather stay home or go to school?” my patients almost universally prefer school. They all know that school is where they should be; they want to be normal, accepted by peers, getting ready for the world’s coming demands, and validation that they will make it as adults. Endorsement otherwise is a warning sign.
When such important tasks of childhood are thwarted children may despair, withdraw, give up, or a small number become furious. These may profoundly resent the children who are experiencing success when they could not. They may hate the teachers and the place where they experienced failure and humiliation. Lack of a positive connection to school characterizes children who are violent toward schools as well as those who drop out.
Schools may fail to support the basic needs of children for many reasons. Schools may avoid physical violence but fail to protect the children’s self-esteem. I have heard stories of teachers calling on children to perform who are clearly struggling or shy, insulting incorrect answers, calling names, putting names on the board, reading out failed grades, posting grades publicly, even allowing peers to mock students. Teachers may deny or disregard parent complaints, or even worsen treatment of the child. Although children may at times falsify complaints, children’s and parents’ reports must be taken seriously and remain anonymous. When we hear of such toxic situations for our patients, we can get details and contact school administrators without naming the child, as often the family feels they can’t. Repeated humiliation may require not only remediation, but consequences. We can advocate for a change in classroom or request a 504 Plan if emotional health is affected.
All children learn best and experience success and even joy when the tasks they face are at or slightly beyond their skill level. But with the wide range of abilities, especially for boys, education may need to be individualized. This is very difficult in larger classrooms with fewer resources, too few adult helpers, inexperienced teachers, or high levels of student misbehavior. Basing teacher promotion mainly on standardized test results makes individualizing instruction even less likely. Smaller class size is better; even the recommended (less than 20) or regulated (less than 30) class sizes are associated with suboptimal achievement, compared with smaller ones. Some ways to attain smaller class size include split days or alternate-day sessions, although these also have disadvantages.
While we can advocate for these changes, we can also encourage parents to promote academic skills by talking to and reading to their children of all ages, trying Reach Out and Read for young children, providing counting games, board games, and math songs! Besides screening for attention-deficit/hyperactivity disorder, we can use standard paragraphs and math problems (for example, WRAT, Einstein) to check skills when performance is low or behavior is a problem the school denies. When concerned, we can write letters for parents to sign requesting testing and an individualized education plan to determine need for tutoring or special education.
While Federal legislation requiring the “least restrictive environment” for education was intended to avoid sidelining differently able children, some can’t learn in a regular class. Conversely, if instruction in a special class is adjusted to the child with the lowest skills, minimal learning may occur for others. Although we can speak with the teacher about “this child’s abilities among those in his class” we can first suggest that the parent visit class to observe. Outside tutoring or home schooling may help a child move up to a regular class.
Sometimes a child’s learning is hampered by classrooms with numerous children misbehaving; this is also a reason for resentment. We can inform school administrators about methods such as The Good Behavior Game (paxis.org) that can improve behavior and connection for the whole class.
While a social “pecking order” is universal, it is unacceptable for children to be allowed to humiliate or hurt a peer, or damage their reputation. While this moral teaching should occur at home, it needs to continue at school where peers are forced into groups they did not choose. Screening for bullying at pediatric visits is now a universal recommendation as 30% report being bullied. We need to ask all children about “mean kids in school” or gang involvement for older children.
Parents can support their children experiencing cyberbullying and switch them to a “dumb phone” with no texting option, limited phone time, or no phone at all. Policies against bullying coming from school administrators are most effective but we can inform schools about the STOPit app for children to report bullying anonymously as well as education for students to stand together against a bully (stopbullying.gov). A Lunch Bunch for younger children or a buddy system for older ones can be requested to help them make friends.
With diverse child aptitudes, schools need to offer students alternative opportunities for self-expression and contribution. We can ask about a child’s strengths and suggest related extracurriculars activities in school or outside, including volunteering. Participation on teams or in clubs must not be blocked for those with poor grades. Perhaps tying participation to tutoring would satisfy the school’s desire to motivate instead. Parents can be encouraged to advocate for music, art, and drama classes – programs that are often victims of budget cuts – that can create the essential school connection.
Students in many areas lack access to classes in trades early enough in their education. The requirements for English or math may be out of reach and result in students dropping out before trade classes are an option. We may identify our patients who may do better with a trade education and advise families to request transfer to a high school offering this.
The best connection a child can have to a school is an adult who values them. The child may identify a preferred teacher to us so that we, or the parent, can call to ask them to provide special attention. Facilitating times for students to get to know teachers may require alteration in bus schedules, lunch times, study halls, or breaks, or keeping the school open longer outside class hours. While more mental health providers are clearly needed, sometimes it is the groundskeeper, the secretary, or the lunch helper who can make the best connection with a child.
As pediatricians, we must listen to struggling youth, acknowledge their pain, and model this empathy for their parents who may be obsessing over grades. Problem-solving about how to get accommodations, informal or formal, can inspire hope. We can coach parents and youth to meet respectfully with the school about issues to avoid labeling the child as a problem.
As pediatricians, our recommendations for school funding and policies may carry extra weight. We may share ideas through talks at PTA meetings, serve on school boards, or endorse leaders planning greater resources for schools to optimize each child’s experience and connection to school.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
‘DIY’ artificial pancreas systems found to be safe, effective: CREATE trial
NEW ORLEANS – Open-source automated insulin delivery systems appear to be both effective and safe in adults and children, new research finds.
Automated insulin delivery (AID) system, also known as closed-loop systems or an artificial pancreas, link an insulin pump and a continuous glucose monitor (CGM) with an algorithm that automatically adjusts insulin delivery to optimize glycemic control.
Prior to the availability of commercial AID systems, Dana Lewis, a patient with type 1 diabetes, and her partner codeveloped an algorithm that could link older versions of an insulin pump and CGM.
In 2015, they made the code and all related materials open-source, so that anyone who wanted to create their own AID system could do so. Today thousands of people worldwide with type 1 diabetes are using the systems, which are sometimes called “do-it-yourself (DIY)” AID systems although the approach has been community based.
AID systems are not approved by any regulatory body, and despite several nonrandomized studies demonstrating their effectiveness and safety, there is still concern among some health professionals about their safety. In 2019, the U.S. Food and Drug Administration warned against the use of any nonapproved devices or algorithms. (Now, though, at least one open-source AID system algorithm is under FDA review.)
Aimed at addressing those concerns, CREATE (Community Derived Automated Insulin Delivery) is the first randomized controlled clinical trial to compare an open-source AID system to insulin pump therapy and CGM (without any communication between the two) in patients with type 1 diabetes, most of whom were naive to AID systems.
Doctors uncomfortable with open source; study provides reassurance
The findings were presented at the American Diabetes Association scientific sessions by Martin I. de Bock, PhD, a pediatric endocrinologist and senior lecturer at the University of Otago, Christchurch, New Zealand.
The study compared the most commonly used open-source AID system (using the OpenAPS algorithm from a version of AndroidAPS implemented in a smartphone with the DANA-i insulin pump and Dexcom G6 CGM) to any insulin pump plus CGM as a comparator group.
The open-source AID system led to a significant reduction in hemoglobin A1c with no major safety issues.
“The acceptance [among clinicians] of open-source systems is diverse and complicated, [with varying] personal comfort levels of seeing someone using an AID system that has no regulatory approval,” Dr. de Bock told this news organization.
“This is one of the reasons that it was so important to conduct the CREATE trial for the many thousands of open-source AID users. Given that the trial demonstrated safety and efficacy using the most robust scientific methodology available – a long-term randomized controlled trial – it may go some way to provide assurance for providers when they are seeing people using an open-source automated system,” he said.
Asked for comment, session moderator Diana Isaacs, PharmD, CDCES, an endocrine clinical pharmacist at the Cleveland Clinic, told this news organization: “There has been concern that these systems aren’t safe, so showing the safety is important. I think people deserve choice. As long as they’re safe, patients should be able to use what they want to use, and we should support them.”
Dr. Isaacs pointed out that an advantage of open-source systems over current commercial AIDs for patients is the ability to customize glucose targets, but in CREATE, those targets were established in the protocol by the investigators.
“I think it’s nice having the data, although in the trial they had specific requirements. They had a target range and active insulin time that they were recommending. So it’s a little different than true DIY where you don’t really have those guidelines you have to follow. It is exciting, it’s very interesting, but I wouldn’t say it’s a true mirror of the real world.”
Open-source systems improved time-in-range, no safety issues
For the CREATE study, 100 participants were enrolled, including 50 children aged 7-15 years and 50 adults aged 16-70 years. All participants had been using insulin pumps for at least 6 months. Most of the children and about two-thirds of the adults were also using CGMs, but just 6% of the children and 18% of the adults had prior experience with AID systems.
Baseline A1c in children was 7.5% and in adults was 7.7%.
After a 4-week run-in, all patients were randomized to the open-source AID or insulin pump plus CGM for 6 months.
The final group analyzed consisted of 42 patients in the open-source AID group and 53 patients in the comparator group.
The primary outcome, the adjusted mean difference in percent time-in-range (glucose of 70-180 mg/dL) during the final 2 weeks of the 6-month trial, showed a significant difference of 14% (P < .001) with open-source AID compared with pump plus CGM only.
Time-in-range in the open-source AID group rose from 61.2% to 71.2%, while it actually dropped slightly in the comparator group, from 57.7% to 54.5%.
The proportion of patients achieving time-in-range greater than 70% with open-source AID was 60% versus just 15% with pump plus CGM.
Glycemic improvements with open-source AID were significant for adults and children and were greater for those with higher baseline A1c levels. The effect was immediate and sustained throughout the study period, “which is super-pleasing, because there was a worry that the technical burden of open source might be [leading to] dropout, but we didn’t see that. It was sustained right through to the end of the trial,” Dr. de Bock commented.
Hypoglycemic rates didn’t differ between groups, and there were no episodes of severe hypoglycemia or diabetic ketoacidosis.
No more waiting: What is the future of open-source AID?
When the open-source APS was first developed, users coined the motto: “We are not waiting.” But now that the “wait” is over and several commercial AIDs have been approved by regulatory bodies, with others still in the pipeline, will people still use open-source systems?
There are no current data on people moving from DIY to commercial systems. However, Dr. de Bock said, “For most who undertook an open-source option, the precision of the settings that they can use and enjoy would mean that most would likely stick to their open source.”
Dr. Isaacs agrees: “I actually don’t think it’s going to go away in the near future, because the FDA has very specific criteria for where these [formally approved] devices can be in terms of their target ranges and requirements versus with open source you can really customize. So I still think there’s going to be a subset of people who want that customization, who want the lower targets.”
Dana Lewis, the originator of the DIY system and a CREATE coauthor, told this news organization: “I don’t believe there has been a fall-off, and in fact, I think open-source AID has continued to have ongoing uptake as awareness increases about options and as more pumps and CGMs become interoperable with various open-source AID choices.”
“I think uptake increasing is also influenced by the fact that in places like Europe, Asia, and Australia there are in-warranty on-the-market pumps that are compatible and interoperable with open-source AID. I think awareness of AID overall increases uptake of commercial and open source alike,” she said.
“Clinicians, as emphasized in recent position statements, must maintain support of the person with diabetes, irrespective of the mode of treatment they are on. ... Health care providers should be encouraged to learn from the experiences of the people who have stuck with open-source AID or switched, so that they can inform themselves of the relative strengths and benefits of each system,” Dr. de Bock advised.
Ms. Lewis noted: “We are seeing increasing awareness and comfort in endocrinologists from the community perspective, and we do hope that this study helps increase conversation and awareness of the safety and efficacy of open-source AID systems as an option for people with diabetes.”
In fact, the team published an article specifically about clinicians’ experience in CREATE. “The learning curve is similar across AID technology,” she observed.
Findings of a 6-month continuation phase of CREATE, in which all participants used the open-source AID, are scheduled to be presented in September at the European Association for the Study of Diabetes annual meeting.
The study was funded by the Health Research Council of New Zealand, with hardware support from SOOIL Developments, South Korea; Dexcom; and Vodafone New Zealand. Dr. de Bock has reported receiving honoraria and/or research funding from Novo Nordisk, Sanofi, Pfizer, Medtronic, Lilly, Ypsomed, and Dexcom. Dr. Isaacs has reported serving as a consultant for LifeScan, Lilly, and Insulet, and as a speaker for Dexcom, Medtronic, Abbott, and Novo Nordisk. Ms. Lewis has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Open-source automated insulin delivery systems appear to be both effective and safe in adults and children, new research finds.
Automated insulin delivery (AID) system, also known as closed-loop systems or an artificial pancreas, link an insulin pump and a continuous glucose monitor (CGM) with an algorithm that automatically adjusts insulin delivery to optimize glycemic control.
Prior to the availability of commercial AID systems, Dana Lewis, a patient with type 1 diabetes, and her partner codeveloped an algorithm that could link older versions of an insulin pump and CGM.
In 2015, they made the code and all related materials open-source, so that anyone who wanted to create their own AID system could do so. Today thousands of people worldwide with type 1 diabetes are using the systems, which are sometimes called “do-it-yourself (DIY)” AID systems although the approach has been community based.
AID systems are not approved by any regulatory body, and despite several nonrandomized studies demonstrating their effectiveness and safety, there is still concern among some health professionals about their safety. In 2019, the U.S. Food and Drug Administration warned against the use of any nonapproved devices or algorithms. (Now, though, at least one open-source AID system algorithm is under FDA review.)
Aimed at addressing those concerns, CREATE (Community Derived Automated Insulin Delivery) is the first randomized controlled clinical trial to compare an open-source AID system to insulin pump therapy and CGM (without any communication between the two) in patients with type 1 diabetes, most of whom were naive to AID systems.
Doctors uncomfortable with open source; study provides reassurance
The findings were presented at the American Diabetes Association scientific sessions by Martin I. de Bock, PhD, a pediatric endocrinologist and senior lecturer at the University of Otago, Christchurch, New Zealand.
The study compared the most commonly used open-source AID system (using the OpenAPS algorithm from a version of AndroidAPS implemented in a smartphone with the DANA-i insulin pump and Dexcom G6 CGM) to any insulin pump plus CGM as a comparator group.
The open-source AID system led to a significant reduction in hemoglobin A1c with no major safety issues.
“The acceptance [among clinicians] of open-source systems is diverse and complicated, [with varying] personal comfort levels of seeing someone using an AID system that has no regulatory approval,” Dr. de Bock told this news organization.
“This is one of the reasons that it was so important to conduct the CREATE trial for the many thousands of open-source AID users. Given that the trial demonstrated safety and efficacy using the most robust scientific methodology available – a long-term randomized controlled trial – it may go some way to provide assurance for providers when they are seeing people using an open-source automated system,” he said.
Asked for comment, session moderator Diana Isaacs, PharmD, CDCES, an endocrine clinical pharmacist at the Cleveland Clinic, told this news organization: “There has been concern that these systems aren’t safe, so showing the safety is important. I think people deserve choice. As long as they’re safe, patients should be able to use what they want to use, and we should support them.”
Dr. Isaacs pointed out that an advantage of open-source systems over current commercial AIDs for patients is the ability to customize glucose targets, but in CREATE, those targets were established in the protocol by the investigators.
“I think it’s nice having the data, although in the trial they had specific requirements. They had a target range and active insulin time that they were recommending. So it’s a little different than true DIY where you don’t really have those guidelines you have to follow. It is exciting, it’s very interesting, but I wouldn’t say it’s a true mirror of the real world.”
Open-source systems improved time-in-range, no safety issues
For the CREATE study, 100 participants were enrolled, including 50 children aged 7-15 years and 50 adults aged 16-70 years. All participants had been using insulin pumps for at least 6 months. Most of the children and about two-thirds of the adults were also using CGMs, but just 6% of the children and 18% of the adults had prior experience with AID systems.
Baseline A1c in children was 7.5% and in adults was 7.7%.
After a 4-week run-in, all patients were randomized to the open-source AID or insulin pump plus CGM for 6 months.
The final group analyzed consisted of 42 patients in the open-source AID group and 53 patients in the comparator group.
The primary outcome, the adjusted mean difference in percent time-in-range (glucose of 70-180 mg/dL) during the final 2 weeks of the 6-month trial, showed a significant difference of 14% (P < .001) with open-source AID compared with pump plus CGM only.
Time-in-range in the open-source AID group rose from 61.2% to 71.2%, while it actually dropped slightly in the comparator group, from 57.7% to 54.5%.
The proportion of patients achieving time-in-range greater than 70% with open-source AID was 60% versus just 15% with pump plus CGM.
Glycemic improvements with open-source AID were significant for adults and children and were greater for those with higher baseline A1c levels. The effect was immediate and sustained throughout the study period, “which is super-pleasing, because there was a worry that the technical burden of open source might be [leading to] dropout, but we didn’t see that. It was sustained right through to the end of the trial,” Dr. de Bock commented.
Hypoglycemic rates didn’t differ between groups, and there were no episodes of severe hypoglycemia or diabetic ketoacidosis.
No more waiting: What is the future of open-source AID?
When the open-source APS was first developed, users coined the motto: “We are not waiting.” But now that the “wait” is over and several commercial AIDs have been approved by regulatory bodies, with others still in the pipeline, will people still use open-source systems?
There are no current data on people moving from DIY to commercial systems. However, Dr. de Bock said, “For most who undertook an open-source option, the precision of the settings that they can use and enjoy would mean that most would likely stick to their open source.”
Dr. Isaacs agrees: “I actually don’t think it’s going to go away in the near future, because the FDA has very specific criteria for where these [formally approved] devices can be in terms of their target ranges and requirements versus with open source you can really customize. So I still think there’s going to be a subset of people who want that customization, who want the lower targets.”
Dana Lewis, the originator of the DIY system and a CREATE coauthor, told this news organization: “I don’t believe there has been a fall-off, and in fact, I think open-source AID has continued to have ongoing uptake as awareness increases about options and as more pumps and CGMs become interoperable with various open-source AID choices.”
“I think uptake increasing is also influenced by the fact that in places like Europe, Asia, and Australia there are in-warranty on-the-market pumps that are compatible and interoperable with open-source AID. I think awareness of AID overall increases uptake of commercial and open source alike,” she said.
“Clinicians, as emphasized in recent position statements, must maintain support of the person with diabetes, irrespective of the mode of treatment they are on. ... Health care providers should be encouraged to learn from the experiences of the people who have stuck with open-source AID or switched, so that they can inform themselves of the relative strengths and benefits of each system,” Dr. de Bock advised.
Ms. Lewis noted: “We are seeing increasing awareness and comfort in endocrinologists from the community perspective, and we do hope that this study helps increase conversation and awareness of the safety and efficacy of open-source AID systems as an option for people with diabetes.”
In fact, the team published an article specifically about clinicians’ experience in CREATE. “The learning curve is similar across AID technology,” she observed.
Findings of a 6-month continuation phase of CREATE, in which all participants used the open-source AID, are scheduled to be presented in September at the European Association for the Study of Diabetes annual meeting.
The study was funded by the Health Research Council of New Zealand, with hardware support from SOOIL Developments, South Korea; Dexcom; and Vodafone New Zealand. Dr. de Bock has reported receiving honoraria and/or research funding from Novo Nordisk, Sanofi, Pfizer, Medtronic, Lilly, Ypsomed, and Dexcom. Dr. Isaacs has reported serving as a consultant for LifeScan, Lilly, and Insulet, and as a speaker for Dexcom, Medtronic, Abbott, and Novo Nordisk. Ms. Lewis has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Open-source automated insulin delivery systems appear to be both effective and safe in adults and children, new research finds.
Automated insulin delivery (AID) system, also known as closed-loop systems or an artificial pancreas, link an insulin pump and a continuous glucose monitor (CGM) with an algorithm that automatically adjusts insulin delivery to optimize glycemic control.
Prior to the availability of commercial AID systems, Dana Lewis, a patient with type 1 diabetes, and her partner codeveloped an algorithm that could link older versions of an insulin pump and CGM.
In 2015, they made the code and all related materials open-source, so that anyone who wanted to create their own AID system could do so. Today thousands of people worldwide with type 1 diabetes are using the systems, which are sometimes called “do-it-yourself (DIY)” AID systems although the approach has been community based.
AID systems are not approved by any regulatory body, and despite several nonrandomized studies demonstrating their effectiveness and safety, there is still concern among some health professionals about their safety. In 2019, the U.S. Food and Drug Administration warned against the use of any nonapproved devices or algorithms. (Now, though, at least one open-source AID system algorithm is under FDA review.)
Aimed at addressing those concerns, CREATE (Community Derived Automated Insulin Delivery) is the first randomized controlled clinical trial to compare an open-source AID system to insulin pump therapy and CGM (without any communication between the two) in patients with type 1 diabetes, most of whom were naive to AID systems.
Doctors uncomfortable with open source; study provides reassurance
The findings were presented at the American Diabetes Association scientific sessions by Martin I. de Bock, PhD, a pediatric endocrinologist and senior lecturer at the University of Otago, Christchurch, New Zealand.
The study compared the most commonly used open-source AID system (using the OpenAPS algorithm from a version of AndroidAPS implemented in a smartphone with the DANA-i insulin pump and Dexcom G6 CGM) to any insulin pump plus CGM as a comparator group.
The open-source AID system led to a significant reduction in hemoglobin A1c with no major safety issues.
“The acceptance [among clinicians] of open-source systems is diverse and complicated, [with varying] personal comfort levels of seeing someone using an AID system that has no regulatory approval,” Dr. de Bock told this news organization.
“This is one of the reasons that it was so important to conduct the CREATE trial for the many thousands of open-source AID users. Given that the trial demonstrated safety and efficacy using the most robust scientific methodology available – a long-term randomized controlled trial – it may go some way to provide assurance for providers when they are seeing people using an open-source automated system,” he said.
Asked for comment, session moderator Diana Isaacs, PharmD, CDCES, an endocrine clinical pharmacist at the Cleveland Clinic, told this news organization: “There has been concern that these systems aren’t safe, so showing the safety is important. I think people deserve choice. As long as they’re safe, patients should be able to use what they want to use, and we should support them.”
Dr. Isaacs pointed out that an advantage of open-source systems over current commercial AIDs for patients is the ability to customize glucose targets, but in CREATE, those targets were established in the protocol by the investigators.
“I think it’s nice having the data, although in the trial they had specific requirements. They had a target range and active insulin time that they were recommending. So it’s a little different than true DIY where you don’t really have those guidelines you have to follow. It is exciting, it’s very interesting, but I wouldn’t say it’s a true mirror of the real world.”
Open-source systems improved time-in-range, no safety issues
For the CREATE study, 100 participants were enrolled, including 50 children aged 7-15 years and 50 adults aged 16-70 years. All participants had been using insulin pumps for at least 6 months. Most of the children and about two-thirds of the adults were also using CGMs, but just 6% of the children and 18% of the adults had prior experience with AID systems.
Baseline A1c in children was 7.5% and in adults was 7.7%.
After a 4-week run-in, all patients were randomized to the open-source AID or insulin pump plus CGM for 6 months.
The final group analyzed consisted of 42 patients in the open-source AID group and 53 patients in the comparator group.
The primary outcome, the adjusted mean difference in percent time-in-range (glucose of 70-180 mg/dL) during the final 2 weeks of the 6-month trial, showed a significant difference of 14% (P < .001) with open-source AID compared with pump plus CGM only.
Time-in-range in the open-source AID group rose from 61.2% to 71.2%, while it actually dropped slightly in the comparator group, from 57.7% to 54.5%.
The proportion of patients achieving time-in-range greater than 70% with open-source AID was 60% versus just 15% with pump plus CGM.
Glycemic improvements with open-source AID were significant for adults and children and were greater for those with higher baseline A1c levels. The effect was immediate and sustained throughout the study period, “which is super-pleasing, because there was a worry that the technical burden of open source might be [leading to] dropout, but we didn’t see that. It was sustained right through to the end of the trial,” Dr. de Bock commented.
Hypoglycemic rates didn’t differ between groups, and there were no episodes of severe hypoglycemia or diabetic ketoacidosis.
No more waiting: What is the future of open-source AID?
When the open-source APS was first developed, users coined the motto: “We are not waiting.” But now that the “wait” is over and several commercial AIDs have been approved by regulatory bodies, with others still in the pipeline, will people still use open-source systems?
There are no current data on people moving from DIY to commercial systems. However, Dr. de Bock said, “For most who undertook an open-source option, the precision of the settings that they can use and enjoy would mean that most would likely stick to their open source.”
Dr. Isaacs agrees: “I actually don’t think it’s going to go away in the near future, because the FDA has very specific criteria for where these [formally approved] devices can be in terms of their target ranges and requirements versus with open source you can really customize. So I still think there’s going to be a subset of people who want that customization, who want the lower targets.”
Dana Lewis, the originator of the DIY system and a CREATE coauthor, told this news organization: “I don’t believe there has been a fall-off, and in fact, I think open-source AID has continued to have ongoing uptake as awareness increases about options and as more pumps and CGMs become interoperable with various open-source AID choices.”
“I think uptake increasing is also influenced by the fact that in places like Europe, Asia, and Australia there are in-warranty on-the-market pumps that are compatible and interoperable with open-source AID. I think awareness of AID overall increases uptake of commercial and open source alike,” she said.
“Clinicians, as emphasized in recent position statements, must maintain support of the person with diabetes, irrespective of the mode of treatment they are on. ... Health care providers should be encouraged to learn from the experiences of the people who have stuck with open-source AID or switched, so that they can inform themselves of the relative strengths and benefits of each system,” Dr. de Bock advised.
Ms. Lewis noted: “We are seeing increasing awareness and comfort in endocrinologists from the community perspective, and we do hope that this study helps increase conversation and awareness of the safety and efficacy of open-source AID systems as an option for people with diabetes.”
In fact, the team published an article specifically about clinicians’ experience in CREATE. “The learning curve is similar across AID technology,” she observed.
Findings of a 6-month continuation phase of CREATE, in which all participants used the open-source AID, are scheduled to be presented in September at the European Association for the Study of Diabetes annual meeting.
The study was funded by the Health Research Council of New Zealand, with hardware support from SOOIL Developments, South Korea; Dexcom; and Vodafone New Zealand. Dr. de Bock has reported receiving honoraria and/or research funding from Novo Nordisk, Sanofi, Pfizer, Medtronic, Lilly, Ypsomed, and Dexcom. Dr. Isaacs has reported serving as a consultant for LifeScan, Lilly, and Insulet, and as a speaker for Dexcom, Medtronic, Abbott, and Novo Nordisk. Ms. Lewis has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ADA 2022
Diagnostic axSpA MRI features differ in men and women
MRI criteria used to diagnose axial spondyloarthritis (axSpA) may require gender-specific revision, according to research conducted at Charité Universitätsmedizin Berlin.
Although established MRI markers were detected in both sexes, their prevalence was substantially different in some cases – ankylosis and fat metaplasia were more prevalent in male than female patients, for example, while sclerosis was far more common in females.
“There’s increasing evidence in the literature and awareness in clinical practice that there are some sex differences in the clinical presentation of axSpA,” said radiologist Sevtap Tugce Ulas, MD, at the annual European Congress of Rheumatology.
She presented the first results of a study examining the diagnostic performance of MRI findings for men and women. “Men have a high risk of structural damage, while women are more likely to be affected by peripheral manifestations with a higher risk for pain, stiffness, and fatigue.”
Joint biomechanics are different in men and women, she pointed out, which might explain some of the disparities. She observed that diagnostic delay – a known problem in axSpA – was “significantly longer” in female patients.
Dr. Ulas and colleagues conducted a post hoc analysis of participants in six prospective axSpA cohorts. From a total of more than 1,100 participants, the researchers identified 684 who had both a clinical diagnosis and complete imaging data available for evaluation. The study population included 379 men and women with and 305 men and women without axSpA.
The mean age overall in all groups was 37 years, with axSpA patients more likely than controls to have elevated C-reactive protein levels; levels were also higher in men with axSpA, compared with in women with axSpA.
Men with axSpA also were more likely than women to be HLA-B27 positive (91% vs. 79%), but there were similar mean Bath Ankylosing Spondylitis Disease Activity Index scores recorded (4.4 vs. 4.6) among the subjects with axSpA.
Two experienced radiologists, blinded to the clinical diagnosis, scored the MRI images independently of each other, looking for the presence of ankylosis; erosions; sclerosis; fat metaplasia; and bone marrow edema in the ventral, mid, and dorsal regions of the sacroiliac joints. Any disagreement between the two reviewers was assessed by a third, more experienced radiologist.
Clear differences in MRI markers
“If you look in detail, we found no major sex-specific differences for erosion and bone marrow edema,” Dr. Ulas reported.
The situation was quite different for other MRI parameters examined. Indeed, more men than women had evidence of ankylosis (24.3% vs. 7.4%) and fat metaplasia (58.8% vs. 42.6%). Conversely, women were more likely than men to have evidence of sclerosis (75.0% vs. 57.6%).
“To make the performance more easily comparable, we calculated a diagnostic odds ratio, which is simply positive likelihood ratio divided by negative likelihood ratio,” Dr. Ulas said.
Doing this showed that the presence of ankylosis had “an almost 10 times stronger performance in men,” with a DOR of 40.1 versus 4.7 for women.
“Interestingly, this was not only caused by low prevalence in females, but also by high rates of false positives,” she said.
DOR for the other parameters in men and women were 18.6 and 6.3 for fat metaplasia, 2.5 and 3.0 for sclerosis, 17.6 and 11.1 for joint erosion, and 2.5 and 3.7 for bone edema.
Overall, diagnostic accuracy was improved only when middle and dorsal lesions were considered.
‘Remarkably different’ results
“By definition, these patients have the same disease,” said Hendrik Schulze-Koops, MD, of Ludwig Maximilian University of Munich (Germany).
Yet these are “remarkably different” findings, Dr. Schulze-Koops said during a closing highlights session of the congress.
Current imaging practices don’t differentiate between the sexes but perhaps they might need to, he said, because these data suggest “female patients have a different MRI pattern from what we learn from the textbooks.
“[The investigators] say diagnostic performance of established imaging markers on MRI is significantly lower in female axSpA patients, and we should consider this when we are in the situation where we question the disease.”
Marta Mosca, MD, PhD, of the University of Pisa (Italy) and who cochaired the session in which Dr. Ulas had presented the findings commented: “I think is very interesting. We always talk about gender differences in treatment and in the assessment.”
However, Dr. Mosca asked if there were plans to study other patient cohorts, notably those not just referred by a rheumatologist, as that was “a big limitation.”
Dr. Ulas replied: “I think we need follow-up studies to investigate this problem, because we know that there are differences in the clinical presentation and also in the imaging, and this is an important point.”
Of course, there are other limitations, Dr. Ulas said, such as the sole use of conventional T1-weighted spin echo sequences. Although often routinely used in clinical practice, this imaging technique can lead to overestimation of structural damage. Moreover, “subtle differences might have been missed” in bone marrow edema because it wasn’t included in the semiquantitative scoring system used.
“Most importantly, the MRI images under investigation were also used in the diagnostic process, which carries the risk of circular reasoning,” Dr. Ulas said.
However, there are clearly some differences in imaging appearance between men and women, and “we show a significantly lower performance of many typical MRI findings in women,” Dr. Ulas said. “We hope that these findings might spark a critical discussion on the appropriateness of sex-blind classification criteria for axSpA, and hopefully, eventually lead to refined criteria for both sexes.”
Dr. Ulas had no conflicts of interest to disclose. Dr. Schulze-Koops and Dr. Mosca were not involved in the study and had no relevant disclosures.
MRI criteria used to diagnose axial spondyloarthritis (axSpA) may require gender-specific revision, according to research conducted at Charité Universitätsmedizin Berlin.
Although established MRI markers were detected in both sexes, their prevalence was substantially different in some cases – ankylosis and fat metaplasia were more prevalent in male than female patients, for example, while sclerosis was far more common in females.
“There’s increasing evidence in the literature and awareness in clinical practice that there are some sex differences in the clinical presentation of axSpA,” said radiologist Sevtap Tugce Ulas, MD, at the annual European Congress of Rheumatology.
She presented the first results of a study examining the diagnostic performance of MRI findings for men and women. “Men have a high risk of structural damage, while women are more likely to be affected by peripheral manifestations with a higher risk for pain, stiffness, and fatigue.”
Joint biomechanics are different in men and women, she pointed out, which might explain some of the disparities. She observed that diagnostic delay – a known problem in axSpA – was “significantly longer” in female patients.
Dr. Ulas and colleagues conducted a post hoc analysis of participants in six prospective axSpA cohorts. From a total of more than 1,100 participants, the researchers identified 684 who had both a clinical diagnosis and complete imaging data available for evaluation. The study population included 379 men and women with and 305 men and women without axSpA.
The mean age overall in all groups was 37 years, with axSpA patients more likely than controls to have elevated C-reactive protein levels; levels were also higher in men with axSpA, compared with in women with axSpA.
Men with axSpA also were more likely than women to be HLA-B27 positive (91% vs. 79%), but there were similar mean Bath Ankylosing Spondylitis Disease Activity Index scores recorded (4.4 vs. 4.6) among the subjects with axSpA.
Two experienced radiologists, blinded to the clinical diagnosis, scored the MRI images independently of each other, looking for the presence of ankylosis; erosions; sclerosis; fat metaplasia; and bone marrow edema in the ventral, mid, and dorsal regions of the sacroiliac joints. Any disagreement between the two reviewers was assessed by a third, more experienced radiologist.
Clear differences in MRI markers
“If you look in detail, we found no major sex-specific differences for erosion and bone marrow edema,” Dr. Ulas reported.
The situation was quite different for other MRI parameters examined. Indeed, more men than women had evidence of ankylosis (24.3% vs. 7.4%) and fat metaplasia (58.8% vs. 42.6%). Conversely, women were more likely than men to have evidence of sclerosis (75.0% vs. 57.6%).
“To make the performance more easily comparable, we calculated a diagnostic odds ratio, which is simply positive likelihood ratio divided by negative likelihood ratio,” Dr. Ulas said.
Doing this showed that the presence of ankylosis had “an almost 10 times stronger performance in men,” with a DOR of 40.1 versus 4.7 for women.
“Interestingly, this was not only caused by low prevalence in females, but also by high rates of false positives,” she said.
DOR for the other parameters in men and women were 18.6 and 6.3 for fat metaplasia, 2.5 and 3.0 for sclerosis, 17.6 and 11.1 for joint erosion, and 2.5 and 3.7 for bone edema.
Overall, diagnostic accuracy was improved only when middle and dorsal lesions were considered.
‘Remarkably different’ results
“By definition, these patients have the same disease,” said Hendrik Schulze-Koops, MD, of Ludwig Maximilian University of Munich (Germany).
Yet these are “remarkably different” findings, Dr. Schulze-Koops said during a closing highlights session of the congress.
Current imaging practices don’t differentiate between the sexes but perhaps they might need to, he said, because these data suggest “female patients have a different MRI pattern from what we learn from the textbooks.
“[The investigators] say diagnostic performance of established imaging markers on MRI is significantly lower in female axSpA patients, and we should consider this when we are in the situation where we question the disease.”
Marta Mosca, MD, PhD, of the University of Pisa (Italy) and who cochaired the session in which Dr. Ulas had presented the findings commented: “I think is very interesting. We always talk about gender differences in treatment and in the assessment.”
However, Dr. Mosca asked if there were plans to study other patient cohorts, notably those not just referred by a rheumatologist, as that was “a big limitation.”
Dr. Ulas replied: “I think we need follow-up studies to investigate this problem, because we know that there are differences in the clinical presentation and also in the imaging, and this is an important point.”
Of course, there are other limitations, Dr. Ulas said, such as the sole use of conventional T1-weighted spin echo sequences. Although often routinely used in clinical practice, this imaging technique can lead to overestimation of structural damage. Moreover, “subtle differences might have been missed” in bone marrow edema because it wasn’t included in the semiquantitative scoring system used.
“Most importantly, the MRI images under investigation were also used in the diagnostic process, which carries the risk of circular reasoning,” Dr. Ulas said.
However, there are clearly some differences in imaging appearance between men and women, and “we show a significantly lower performance of many typical MRI findings in women,” Dr. Ulas said. “We hope that these findings might spark a critical discussion on the appropriateness of sex-blind classification criteria for axSpA, and hopefully, eventually lead to refined criteria for both sexes.”
Dr. Ulas had no conflicts of interest to disclose. Dr. Schulze-Koops and Dr. Mosca were not involved in the study and had no relevant disclosures.
MRI criteria used to diagnose axial spondyloarthritis (axSpA) may require gender-specific revision, according to research conducted at Charité Universitätsmedizin Berlin.
Although established MRI markers were detected in both sexes, their prevalence was substantially different in some cases – ankylosis and fat metaplasia were more prevalent in male than female patients, for example, while sclerosis was far more common in females.
“There’s increasing evidence in the literature and awareness in clinical practice that there are some sex differences in the clinical presentation of axSpA,” said radiologist Sevtap Tugce Ulas, MD, at the annual European Congress of Rheumatology.
She presented the first results of a study examining the diagnostic performance of MRI findings for men and women. “Men have a high risk of structural damage, while women are more likely to be affected by peripheral manifestations with a higher risk for pain, stiffness, and fatigue.”
Joint biomechanics are different in men and women, she pointed out, which might explain some of the disparities. She observed that diagnostic delay – a known problem in axSpA – was “significantly longer” in female patients.
Dr. Ulas and colleagues conducted a post hoc analysis of participants in six prospective axSpA cohorts. From a total of more than 1,100 participants, the researchers identified 684 who had both a clinical diagnosis and complete imaging data available for evaluation. The study population included 379 men and women with and 305 men and women without axSpA.
The mean age overall in all groups was 37 years, with axSpA patients more likely than controls to have elevated C-reactive protein levels; levels were also higher in men with axSpA, compared with in women with axSpA.
Men with axSpA also were more likely than women to be HLA-B27 positive (91% vs. 79%), but there were similar mean Bath Ankylosing Spondylitis Disease Activity Index scores recorded (4.4 vs. 4.6) among the subjects with axSpA.
Two experienced radiologists, blinded to the clinical diagnosis, scored the MRI images independently of each other, looking for the presence of ankylosis; erosions; sclerosis; fat metaplasia; and bone marrow edema in the ventral, mid, and dorsal regions of the sacroiliac joints. Any disagreement between the two reviewers was assessed by a third, more experienced radiologist.
Clear differences in MRI markers
“If you look in detail, we found no major sex-specific differences for erosion and bone marrow edema,” Dr. Ulas reported.
The situation was quite different for other MRI parameters examined. Indeed, more men than women had evidence of ankylosis (24.3% vs. 7.4%) and fat metaplasia (58.8% vs. 42.6%). Conversely, women were more likely than men to have evidence of sclerosis (75.0% vs. 57.6%).
“To make the performance more easily comparable, we calculated a diagnostic odds ratio, which is simply positive likelihood ratio divided by negative likelihood ratio,” Dr. Ulas said.
Doing this showed that the presence of ankylosis had “an almost 10 times stronger performance in men,” with a DOR of 40.1 versus 4.7 for women.
“Interestingly, this was not only caused by low prevalence in females, but also by high rates of false positives,” she said.
DOR for the other parameters in men and women were 18.6 and 6.3 for fat metaplasia, 2.5 and 3.0 for sclerosis, 17.6 and 11.1 for joint erosion, and 2.5 and 3.7 for bone edema.
Overall, diagnostic accuracy was improved only when middle and dorsal lesions were considered.
‘Remarkably different’ results
“By definition, these patients have the same disease,” said Hendrik Schulze-Koops, MD, of Ludwig Maximilian University of Munich (Germany).
Yet these are “remarkably different” findings, Dr. Schulze-Koops said during a closing highlights session of the congress.
Current imaging practices don’t differentiate between the sexes but perhaps they might need to, he said, because these data suggest “female patients have a different MRI pattern from what we learn from the textbooks.
“[The investigators] say diagnostic performance of established imaging markers on MRI is significantly lower in female axSpA patients, and we should consider this when we are in the situation where we question the disease.”
Marta Mosca, MD, PhD, of the University of Pisa (Italy) and who cochaired the session in which Dr. Ulas had presented the findings commented: “I think is very interesting. We always talk about gender differences in treatment and in the assessment.”
However, Dr. Mosca asked if there were plans to study other patient cohorts, notably those not just referred by a rheumatologist, as that was “a big limitation.”
Dr. Ulas replied: “I think we need follow-up studies to investigate this problem, because we know that there are differences in the clinical presentation and also in the imaging, and this is an important point.”
Of course, there are other limitations, Dr. Ulas said, such as the sole use of conventional T1-weighted spin echo sequences. Although often routinely used in clinical practice, this imaging technique can lead to overestimation of structural damage. Moreover, “subtle differences might have been missed” in bone marrow edema because it wasn’t included in the semiquantitative scoring system used.
“Most importantly, the MRI images under investigation were also used in the diagnostic process, which carries the risk of circular reasoning,” Dr. Ulas said.
However, there are clearly some differences in imaging appearance between men and women, and “we show a significantly lower performance of many typical MRI findings in women,” Dr. Ulas said. “We hope that these findings might spark a critical discussion on the appropriateness of sex-blind classification criteria for axSpA, and hopefully, eventually lead to refined criteria for both sexes.”
Dr. Ulas had no conflicts of interest to disclose. Dr. Schulze-Koops and Dr. Mosca were not involved in the study and had no relevant disclosures.
FROM THE EULAR 2022 CONGRESS
Nonhealing Violaceous Plaque of the Hand Following a Splinter Injury
The Diagnosis: Chromoblastomycosis
This case highlights the importance of routine skin biopsy and tissue culture when clinical suspicion for mycotic infection is high. Despite nonspecific biopsy results (Figure), a diagnosis of chromoblastomycosis (CBM) was reached based on tissue culture. Surgical excision was not possible in our patient due to the size and location of the lesion. The patient was referred to infectious disease, with the plan to start long-term itraconazole for at least 6 to 12 months.
Cases of CBM were first documented in 1914 and distinguished by the appearance of spherical, brown, muriform cells on skin biopsy—features that now serve as the hallmark of CBM diagnoses.1,2 The implantation mycosis commonly is caused by agents such as Fonsecaea pedrosoi and Fonsecaea monophora of the bantiana-clade, as classified according to molecular phylogeny2; these agents have been isolated from soil, plants, and wood sources in tropical and subtropical regions and are strongly associated with agricultural activities.3
Chromoblastomycosis lesions tend to be asymptomatic with a variable amount of time between inoculation and lesion presentation, delaying medical care by months to years.3 The fungus causes a granulomatous reaction after skin damage, with noticeable pseudoepitheliomatous hyperplasia of the epidermis and granulomas formed by epithelioid and Langerhans cells in the dermis.4 Typically, CBM initially presents as an erythematous macular skin lesion, which then progresses to become more pink, papular, and sometimes pruritic.2 Muriform (sclerotic) bodies, which reflect fungal components, extrude transepidermally and appear as black dots on the lesion’s surface.4 Chromoblastomycosis is limited to the subcutaneous tissue and has been classified into 5 types of lesions: nodular, tumoral, verrucous, scarring, and plaque.2 Diagnosis is established using fungal tests such as potassium hydroxide direct microscopy, which exposes muriform bodies often in combination with dematiaceous hyphae, while fungal culture of F pedrosoi in Sabouraud agar produces velvety dark colonies.3 Although an immune response to CBM infection remains unclear, it has been demonstrated that the response differs based on the severity of the infection. The severe form of CBM produces high levels of IL-10, low levels of IFN-γ, and inefficient T-cell proliferation, while milder forms of CBM display low levels of IL-10, high levels of IFN-γ, and efficient T-cell proliferation.5 Complications of CBM include chronic lymphedema, ankylosis, and secondary bacterial infections, which largely are observed in advanced cases; malignant transformation to squamous cell carcinoma, though rare, also has been observed.6
Several therapeutic methods have been implemented in the treatment of CBM, but lesions often remain refractory, especially in advanced cases.6 Approaches to treatment can be divided into antifungal and physical methods. Commonly employed antifungal agents include itraconazole and terbinafine, which must be taken daily for a period ranging from 6 months to 1 year or longer; flucytosine with or without amphotericin also has been employed.4 Among the physical methods, surgical excision is not suggested due to possible dissemination of disease; other options include cryotherapy, thermotherapy, and laser vaporization.6 The prognosis has improved since the use of extended-spectrum triazoles, but high rates of refractory disease remain unchanged.2
The differential diagnosis includes other infections. Nocardiosis is a bacterial infection in which cutaneous disease can result in actinomycetoma, which presents with grains that are small, round, and stain blue on hematoxylin and eosin with eosinophilic rays at the periphery.7 Although the clinical features and pseudoepitheliomatous hyperplasia seen in CBM can mimic squamous cell carcinoma, the latter would show variable degrees of differentiation, keratinization, nuclear atypia, and architectural atypia with a negative tissue culture.8 Eumycetoma is a fungal infection that typically is not caused by F pedrosoi but rather most commonly Madurella mycetomatis.9 Leishmaniasis is a parasitic infection in which a biopsy of cutaneous lesions often displays parasite-filled histiocytes.10
- Rudolph M. Über die brasilianische “figueira” (vorläufige mitteilung). Arch Schiffs Trop Hyg. 1914;18:498-499.
- Queiroz-Telles F, de Hoog S, Santos DW, et al. Chromoblastomycosis. Clin Microbiol Rev. 2017;30:233-276. doi:10.1128/CMR.00032-16
- Brito AC, Bittencourt MJS. Chromoblastomycosis: an etiological, epidemiological, clinical, diagnostic, and treatment update. An Bras Dermatol. 2018;93:495-506. doi:10.1590/abd1806-4841.20187321
- Kurien G, Sugumar K, Chandran V. Chromoblastomycosis. StatPearls. StatPearls Publishing; 2021. Accessed June 4, 2022. https://www.ncbi.nlm.nih.gov/books/NBK470253/
- Mazo Fávero Gimenes V, Da Glória de Souza M, Ferreira KS, et al. Cytokines and lymphocyte proliferation in patients with different clinical forms of chromoblastomycosis. Microbes Infect. 2005;7:708-713. doi:10.1016/j.micinf.2005.01.006
- Krzys´ciak PM, Pindycka-Piaszczyn´ska M, Piaszczyn´ski M. Chromoblastomycosis. Postepy Dermatol Alergol. 2014;31:310-321. doi:10.5114/pdia.2014.40949
- Siddig EE, van de Sande WWJ, Fahal AH. Actinomycetoma laboratory-based diagnosis: a mini-review. Trans R Soc Trop Med Hyg. 2021;115:355-363.
- Parekh V, Seykora JT. Cutaneous squamous cell carcinoma. Clin Lab Med. 2017;37:503-525. doi:10.1016/j.cll .2017.06.003
- Nenoff P, van de Sande WWJ, Fahal AH, et al. Eumycetoma and actinomycetoma—an update on causative agents, epidemiology, pathogenesis, diagnostics and therapy. J Eur Acad Dermatol Venereol. 2015;29:1873-1883. doi:10.1111/jdv.13008
- Saliba M, Shalhoub A, Taraif S, et al. Cutaneous leishmaniasis: an evolving disease with ancient roots. Int J Dermatol. 2019;58:834-843. doi:10.1111/ijd.14451
The Diagnosis: Chromoblastomycosis
This case highlights the importance of routine skin biopsy and tissue culture when clinical suspicion for mycotic infection is high. Despite nonspecific biopsy results (Figure), a diagnosis of chromoblastomycosis (CBM) was reached based on tissue culture. Surgical excision was not possible in our patient due to the size and location of the lesion. The patient was referred to infectious disease, with the plan to start long-term itraconazole for at least 6 to 12 months.
Cases of CBM were first documented in 1914 and distinguished by the appearance of spherical, brown, muriform cells on skin biopsy—features that now serve as the hallmark of CBM diagnoses.1,2 The implantation mycosis commonly is caused by agents such as Fonsecaea pedrosoi and Fonsecaea monophora of the bantiana-clade, as classified according to molecular phylogeny2; these agents have been isolated from soil, plants, and wood sources in tropical and subtropical regions and are strongly associated with agricultural activities.3
Chromoblastomycosis lesions tend to be asymptomatic with a variable amount of time between inoculation and lesion presentation, delaying medical care by months to years.3 The fungus causes a granulomatous reaction after skin damage, with noticeable pseudoepitheliomatous hyperplasia of the epidermis and granulomas formed by epithelioid and Langerhans cells in the dermis.4 Typically, CBM initially presents as an erythematous macular skin lesion, which then progresses to become more pink, papular, and sometimes pruritic.2 Muriform (sclerotic) bodies, which reflect fungal components, extrude transepidermally and appear as black dots on the lesion’s surface.4 Chromoblastomycosis is limited to the subcutaneous tissue and has been classified into 5 types of lesions: nodular, tumoral, verrucous, scarring, and plaque.2 Diagnosis is established using fungal tests such as potassium hydroxide direct microscopy, which exposes muriform bodies often in combination with dematiaceous hyphae, while fungal culture of F pedrosoi in Sabouraud agar produces velvety dark colonies.3 Although an immune response to CBM infection remains unclear, it has been demonstrated that the response differs based on the severity of the infection. The severe form of CBM produces high levels of IL-10, low levels of IFN-γ, and inefficient T-cell proliferation, while milder forms of CBM display low levels of IL-10, high levels of IFN-γ, and efficient T-cell proliferation.5 Complications of CBM include chronic lymphedema, ankylosis, and secondary bacterial infections, which largely are observed in advanced cases; malignant transformation to squamous cell carcinoma, though rare, also has been observed.6
Several therapeutic methods have been implemented in the treatment of CBM, but lesions often remain refractory, especially in advanced cases.6 Approaches to treatment can be divided into antifungal and physical methods. Commonly employed antifungal agents include itraconazole and terbinafine, which must be taken daily for a period ranging from 6 months to 1 year or longer; flucytosine with or without amphotericin also has been employed.4 Among the physical methods, surgical excision is not suggested due to possible dissemination of disease; other options include cryotherapy, thermotherapy, and laser vaporization.6 The prognosis has improved since the use of extended-spectrum triazoles, but high rates of refractory disease remain unchanged.2
The differential diagnosis includes other infections. Nocardiosis is a bacterial infection in which cutaneous disease can result in actinomycetoma, which presents with grains that are small, round, and stain blue on hematoxylin and eosin with eosinophilic rays at the periphery.7 Although the clinical features and pseudoepitheliomatous hyperplasia seen in CBM can mimic squamous cell carcinoma, the latter would show variable degrees of differentiation, keratinization, nuclear atypia, and architectural atypia with a negative tissue culture.8 Eumycetoma is a fungal infection that typically is not caused by F pedrosoi but rather most commonly Madurella mycetomatis.9 Leishmaniasis is a parasitic infection in which a biopsy of cutaneous lesions often displays parasite-filled histiocytes.10
The Diagnosis: Chromoblastomycosis
This case highlights the importance of routine skin biopsy and tissue culture when clinical suspicion for mycotic infection is high. Despite nonspecific biopsy results (Figure), a diagnosis of chromoblastomycosis (CBM) was reached based on tissue culture. Surgical excision was not possible in our patient due to the size and location of the lesion. The patient was referred to infectious disease, with the plan to start long-term itraconazole for at least 6 to 12 months.
Cases of CBM were first documented in 1914 and distinguished by the appearance of spherical, brown, muriform cells on skin biopsy—features that now serve as the hallmark of CBM diagnoses.1,2 The implantation mycosis commonly is caused by agents such as Fonsecaea pedrosoi and Fonsecaea monophora of the bantiana-clade, as classified according to molecular phylogeny2; these agents have been isolated from soil, plants, and wood sources in tropical and subtropical regions and are strongly associated with agricultural activities.3
Chromoblastomycosis lesions tend to be asymptomatic with a variable amount of time between inoculation and lesion presentation, delaying medical care by months to years.3 The fungus causes a granulomatous reaction after skin damage, with noticeable pseudoepitheliomatous hyperplasia of the epidermis and granulomas formed by epithelioid and Langerhans cells in the dermis.4 Typically, CBM initially presents as an erythematous macular skin lesion, which then progresses to become more pink, papular, and sometimes pruritic.2 Muriform (sclerotic) bodies, which reflect fungal components, extrude transepidermally and appear as black dots on the lesion’s surface.4 Chromoblastomycosis is limited to the subcutaneous tissue and has been classified into 5 types of lesions: nodular, tumoral, verrucous, scarring, and plaque.2 Diagnosis is established using fungal tests such as potassium hydroxide direct microscopy, which exposes muriform bodies often in combination with dematiaceous hyphae, while fungal culture of F pedrosoi in Sabouraud agar produces velvety dark colonies.3 Although an immune response to CBM infection remains unclear, it has been demonstrated that the response differs based on the severity of the infection. The severe form of CBM produces high levels of IL-10, low levels of IFN-γ, and inefficient T-cell proliferation, while milder forms of CBM display low levels of IL-10, high levels of IFN-γ, and efficient T-cell proliferation.5 Complications of CBM include chronic lymphedema, ankylosis, and secondary bacterial infections, which largely are observed in advanced cases; malignant transformation to squamous cell carcinoma, though rare, also has been observed.6
Several therapeutic methods have been implemented in the treatment of CBM, but lesions often remain refractory, especially in advanced cases.6 Approaches to treatment can be divided into antifungal and physical methods. Commonly employed antifungal agents include itraconazole and terbinafine, which must be taken daily for a period ranging from 6 months to 1 year or longer; flucytosine with or without amphotericin also has been employed.4 Among the physical methods, surgical excision is not suggested due to possible dissemination of disease; other options include cryotherapy, thermotherapy, and laser vaporization.6 The prognosis has improved since the use of extended-spectrum triazoles, but high rates of refractory disease remain unchanged.2
The differential diagnosis includes other infections. Nocardiosis is a bacterial infection in which cutaneous disease can result in actinomycetoma, which presents with grains that are small, round, and stain blue on hematoxylin and eosin with eosinophilic rays at the periphery.7 Although the clinical features and pseudoepitheliomatous hyperplasia seen in CBM can mimic squamous cell carcinoma, the latter would show variable degrees of differentiation, keratinization, nuclear atypia, and architectural atypia with a negative tissue culture.8 Eumycetoma is a fungal infection that typically is not caused by F pedrosoi but rather most commonly Madurella mycetomatis.9 Leishmaniasis is a parasitic infection in which a biopsy of cutaneous lesions often displays parasite-filled histiocytes.10
- Rudolph M. Über die brasilianische “figueira” (vorläufige mitteilung). Arch Schiffs Trop Hyg. 1914;18:498-499.
- Queiroz-Telles F, de Hoog S, Santos DW, et al. Chromoblastomycosis. Clin Microbiol Rev. 2017;30:233-276. doi:10.1128/CMR.00032-16
- Brito AC, Bittencourt MJS. Chromoblastomycosis: an etiological, epidemiological, clinical, diagnostic, and treatment update. An Bras Dermatol. 2018;93:495-506. doi:10.1590/abd1806-4841.20187321
- Kurien G, Sugumar K, Chandran V. Chromoblastomycosis. StatPearls. StatPearls Publishing; 2021. Accessed June 4, 2022. https://www.ncbi.nlm.nih.gov/books/NBK470253/
- Mazo Fávero Gimenes V, Da Glória de Souza M, Ferreira KS, et al. Cytokines and lymphocyte proliferation in patients with different clinical forms of chromoblastomycosis. Microbes Infect. 2005;7:708-713. doi:10.1016/j.micinf.2005.01.006
- Krzys´ciak PM, Pindycka-Piaszczyn´ska M, Piaszczyn´ski M. Chromoblastomycosis. Postepy Dermatol Alergol. 2014;31:310-321. doi:10.5114/pdia.2014.40949
- Siddig EE, van de Sande WWJ, Fahal AH. Actinomycetoma laboratory-based diagnosis: a mini-review. Trans R Soc Trop Med Hyg. 2021;115:355-363.
- Parekh V, Seykora JT. Cutaneous squamous cell carcinoma. Clin Lab Med. 2017;37:503-525. doi:10.1016/j.cll .2017.06.003
- Nenoff P, van de Sande WWJ, Fahal AH, et al. Eumycetoma and actinomycetoma—an update on causative agents, epidemiology, pathogenesis, diagnostics and therapy. J Eur Acad Dermatol Venereol. 2015;29:1873-1883. doi:10.1111/jdv.13008
- Saliba M, Shalhoub A, Taraif S, et al. Cutaneous leishmaniasis: an evolving disease with ancient roots. Int J Dermatol. 2019;58:834-843. doi:10.1111/ijd.14451
- Rudolph M. Über die brasilianische “figueira” (vorläufige mitteilung). Arch Schiffs Trop Hyg. 1914;18:498-499.
- Queiroz-Telles F, de Hoog S, Santos DW, et al. Chromoblastomycosis. Clin Microbiol Rev. 2017;30:233-276. doi:10.1128/CMR.00032-16
- Brito AC, Bittencourt MJS. Chromoblastomycosis: an etiological, epidemiological, clinical, diagnostic, and treatment update. An Bras Dermatol. 2018;93:495-506. doi:10.1590/abd1806-4841.20187321
- Kurien G, Sugumar K, Chandran V. Chromoblastomycosis. StatPearls. StatPearls Publishing; 2021. Accessed June 4, 2022. https://www.ncbi.nlm.nih.gov/books/NBK470253/
- Mazo Fávero Gimenes V, Da Glória de Souza M, Ferreira KS, et al. Cytokines and lymphocyte proliferation in patients with different clinical forms of chromoblastomycosis. Microbes Infect. 2005;7:708-713. doi:10.1016/j.micinf.2005.01.006
- Krzys´ciak PM, Pindycka-Piaszczyn´ska M, Piaszczyn´ski M. Chromoblastomycosis. Postepy Dermatol Alergol. 2014;31:310-321. doi:10.5114/pdia.2014.40949
- Siddig EE, van de Sande WWJ, Fahal AH. Actinomycetoma laboratory-based diagnosis: a mini-review. Trans R Soc Trop Med Hyg. 2021;115:355-363.
- Parekh V, Seykora JT. Cutaneous squamous cell carcinoma. Clin Lab Med. 2017;37:503-525. doi:10.1016/j.cll .2017.06.003
- Nenoff P, van de Sande WWJ, Fahal AH, et al. Eumycetoma and actinomycetoma—an update on causative agents, epidemiology, pathogenesis, diagnostics and therapy. J Eur Acad Dermatol Venereol. 2015;29:1873-1883. doi:10.1111/jdv.13008
- Saliba M, Shalhoub A, Taraif S, et al. Cutaneous leishmaniasis: an evolving disease with ancient roots. Int J Dermatol. 2019;58:834-843. doi:10.1111/ijd.14451
A 70-year-old immunocompetent man presented to the dermatology department with a progressive asymptomatic hand wound of 2 years’ duration following a splinter injury in Belize. Prior treatment included oral antibiotics without improvement. Physical examination revealed a 5.1×3.0 cm, pink to violaceous, nonpurulent plaque with a cobblestonelike appearance on the dorsal aspect of the right hand. Both the initial and a repeat skin biopsy revealed nonspecific changes, including hyperkeratosis, hypergranulosis, acute and chronic inflammation, and vascular ectasia. Grocott-Gomori methenamine-silver staining was negative for fungal organisms. One month after the repeat biopsy, a tissue culture returned positive for the rare Fonsecaea pedrosoi.

Private Payer Engagement
Payer Advocacy in Dermatology
Frustrations with payers is a common source of annoyance among dermatologists. Payment rules can seem arbitrary, ever-changing, and not uniform among the various payers. Keeping track of payer requirements can be nearly impossible.
To assist members in handling these concerns, the American Academy of Dermatology Association (AADA) created the Patient Access and Payer Relations (PAPR) committee, which seeks to promote patient access to dermatologic care by addressing issues that may arise with private payers. The committee utilizes a multipronged approach to develop strategies to educate payers on the value of dermatology, addressing systematic payment issues as they arise over time, and building relationships with insurers and employers to promote coverage and payment policies allowing for the highest quality of dermatologic care. The committee is comprised of practicing dermatologists who meet regularly to help guide and implement the AADA’s payer advocacy initiatives.
Identifying payer contacts and forging working relationships is a cornerstone of payer advocacy. In addition to patient access to quality dermatologic services, fair reimbursement is always a primary concern.
Hot Topics in Payer Advocacy
How to Use Modifier −25 Appropriately—The AADA has been advocating for appropriate coverage and reimbursement for services billed by dermatologists; recent examples include assuring appropriate payment for services reported with modifier −25, which is used when a procedure such as a biopsy is performed on the same day as a separate and unrelated evaluation and management (E/M) service, such as psoriasis management. Some payers claim the concurrent nature of the services results in an overlap of office expenses such that these claims should be paid at a lesser amount; however, when procedure codes are frequently billed in association with an office visit, that overlap has already been accounted for as part of the code valuation process, negating the need for additional reduction.
The AADA PAPR committee has created numerous resources for our members to ensure they are using modifier −25 appropriately, particularly now that the US Department of Health and Human Services Office of the Inspector General (OIG) has announced a work plan to audit dermatologists claims reporting modifier −25.1 The AADA immediately formed a work group, including PAPR committee members, to develop and employ a strategy to educate key decision-makers on the correct use of modifier −25 and highlight appropriate resources to guide members. An introductory call was held with the OIG audit team to discuss the appropriate use of modifier −25 in dermatology as the OIG prepares to develop the parameters of its audit sometime in the future (AADA, unpublished data, 2021).
Working With Dermatology Societies on Payer Issues—The American Academy of Dermatology Association PAPR committee works collaboratively with members of the American Academy of Dermatology, state and local dermatology societies, and private payers to alleviate administrative burdens for dermatologists, maintain appropriate reimbursement for furnished services, and ensure patients can access covered quality care. Collaboration with state dermatology societies is essential to address payer issues that impact their members and provide guidance on effective engagement with their state payers. Recent examples include working with dermatology societies in Massachusetts, Rhode Island, and Florida on strategies to advocate against modifier −25 payment reductions by insurance carriers (AADA, unpublished data, 2021). Additionally, the AADA PAPR committee has been able to provide guidance and technical support as needed to state dermatology societies, such as to the Rhode Island Dermatology Society and the Pennsylvania Academy of Dermatology and Dermatologic Surgery to address payer quality metrics and access to laboratory services, respectively (AADA, unpublished data, 2021).
Patient Access to Affordable Treatments—American Academy of Dermatology Association payer advocacy is anchored to published position statements and clinical guidelines. To strengthen AADA advocacy on payer-mandated drug substitutions for nonmedical reasons and to preserve patient access to medications, the PAPR committee collaborated with the American Academy of Dermatology’s Drug Pricing and Transparency Task Force to update the AADA Position Statement on Patient Access to Affordable Treatments2 to address this issue. Essentially, patients who are stable on a medication should be allowed to keep using the same medication without payers changing their coverage for nonmedical reasons or by offering financial incentives to switch.
Relationships With Major Insurance Carriers—Integral to the PAPR committee’s private payer advocacy success are our proactive relationships with major insurance carriers. In 2021, the PAPR committee established quarterly dermatology-specific meetings with the major national carriers. In nurturing these relationships, the PAPR committee has been able to expand on opportunities to provide payer policy reviews as well as identify dermatologists as subject matter experts available to payers to assist with physician panels or policy reviews. These regular contacts also have proved beneficial in addressing issues raised by members; a few such examples include when one major payer reversed its denials on dermatologists’ claims for Current Procedural Terminology code 88304 (surgical pathology, gross and microscopic tissue exam) after it was brought to their attention by the AADA (AADA, unpublished data, 2021). This payer worked with its external vendor to correct the denials. When the AADA learned that another major payer was improperly denying payment for claims for 1 stage of Mohs micrographic surgery reported using Current Procedural Terminology code 17311, we worked with contacts at this payer to resolve the issue. They were receptive to our concerns and readily researched the issue. Leadership of the PAPR committee continued working with the AADA coding team and this payer to develop training guidance to prevent future denials, and the payer has reviewed prior denials and reprocessed claims for payment (AADA, unpublished data, 2021).
E/M Coding Issues
Another issue under consideration by several national insurers is E/M-level reassignment. Payers are reviewing claims from providers who are identified as coding at a higher E/M level as compared to their specialty peers. Some insurance carriers are using proprietary algorithms that attempt to link specific diagnoses to certain levels of E/M, triggering claim edits within their claim processing systems (AADA, unpublished data, 2021). The carrier will then either deny the claim or adjust reimbursement to a lower-level E/M service. In discussions with a national carrier on its E/M Leveling Program, the AADA has offered to work with them on appropriate E/M documentation and reporting (AADA, unpublished data, 2021). The AADA also has extensive member resources for guidance on E/M reporting as well as preparing for audits and appealing payer downcoding developed by the coding staff in conjunction with the Coding and Reimbursement Committee.
Recent Efforts From the AADA
Within the AADA, the PAPR committee works closely with the coding, practice management, and regulatory teams to address payer issues and develop resources for members. Recent examples include resources for dermatology practices on the No Surprises Act and what practices need to do to comply (AADA, unpublished data, 2021). The PAPR committee also works collaboratively with other AADA committees and task forces on payer issues as needed; for example, the PAPR committee has been working with the Dermatopathology Rapid Response committee to address member concerns regarding access to the pathology laboratory of their choice. Many payers are seeking to consolidate and save money by requiring the use of preferred laboratories, which impacts patient access to physician office laboratories and physician-recommended reference laboratories. The AADA, along with other medical specialties, has advocated for payers to not create a restrictive network of pathology laboratories within their provider networks and to support dermatologists’ laboratories of choice (AADA, unpublished data, 2021).
Within the payer space, the role of employers in impacting payment and coverage policies continues to rise. In 2021, the AADA leadership approved the employer outreach strategy to engage employers. The overall objectives are to advocate to employers on the value of dermatologic care and access to care provided by board-certified dermatologists. This is a long-term project that is just getting underway (AADA, unpublished data, 2021).
Payer Resource Center for AADA Members
To ensure that AADA members have the resources they need to advocate with payers as well as to keep the PAPR committee aware of emerging payer issues, the AADA created a new private payer resource center for members (https://www.aad.org/member/advocacy/priorities/payer-advocacy), which assists AADA members with common dermatologic concerns with insurers as well as contracting issues. The website also includes an email address for members to report payer issues ([email protected]). This information helps the PAPR committee identify and prioritize issues of concern.
Final Thoughts
Given the control that private insurance companies exert over the health care that dermatology patients can access, the AADA in general and the PAPR committee specifically play a valuable role in advocating access to care for dermatology patients.
- US Department of Health and Human Services Office of the Inspector General. Dermatologist claims for evaluation and management services on the same day as minor surgical procedures. Accessed May 16, 2022. https://www.oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000577.asp
- American Academy of Dermatology Association. Position Statement on Patient Access to Affordable Treatments. Updated November 4, 2017. Accessed May 24, 2022. https://server.aad.org/forms/policies/uploads/ps/ps%20-%20patient%20access%20to%20affordable%20treatments.pdf?)
Payer Advocacy in Dermatology
Frustrations with payers is a common source of annoyance among dermatologists. Payment rules can seem arbitrary, ever-changing, and not uniform among the various payers. Keeping track of payer requirements can be nearly impossible.
To assist members in handling these concerns, the American Academy of Dermatology Association (AADA) created the Patient Access and Payer Relations (PAPR) committee, which seeks to promote patient access to dermatologic care by addressing issues that may arise with private payers. The committee utilizes a multipronged approach to develop strategies to educate payers on the value of dermatology, addressing systematic payment issues as they arise over time, and building relationships with insurers and employers to promote coverage and payment policies allowing for the highest quality of dermatologic care. The committee is comprised of practicing dermatologists who meet regularly to help guide and implement the AADA’s payer advocacy initiatives.
Identifying payer contacts and forging working relationships is a cornerstone of payer advocacy. In addition to patient access to quality dermatologic services, fair reimbursement is always a primary concern.
Hot Topics in Payer Advocacy
How to Use Modifier −25 Appropriately—The AADA has been advocating for appropriate coverage and reimbursement for services billed by dermatologists; recent examples include assuring appropriate payment for services reported with modifier −25, which is used when a procedure such as a biopsy is performed on the same day as a separate and unrelated evaluation and management (E/M) service, such as psoriasis management. Some payers claim the concurrent nature of the services results in an overlap of office expenses such that these claims should be paid at a lesser amount; however, when procedure codes are frequently billed in association with an office visit, that overlap has already been accounted for as part of the code valuation process, negating the need for additional reduction.
The AADA PAPR committee has created numerous resources for our members to ensure they are using modifier −25 appropriately, particularly now that the US Department of Health and Human Services Office of the Inspector General (OIG) has announced a work plan to audit dermatologists claims reporting modifier −25.1 The AADA immediately formed a work group, including PAPR committee members, to develop and employ a strategy to educate key decision-makers on the correct use of modifier −25 and highlight appropriate resources to guide members. An introductory call was held with the OIG audit team to discuss the appropriate use of modifier −25 in dermatology as the OIG prepares to develop the parameters of its audit sometime in the future (AADA, unpublished data, 2021).
Working With Dermatology Societies on Payer Issues—The American Academy of Dermatology Association PAPR committee works collaboratively with members of the American Academy of Dermatology, state and local dermatology societies, and private payers to alleviate administrative burdens for dermatologists, maintain appropriate reimbursement for furnished services, and ensure patients can access covered quality care. Collaboration with state dermatology societies is essential to address payer issues that impact their members and provide guidance on effective engagement with their state payers. Recent examples include working with dermatology societies in Massachusetts, Rhode Island, and Florida on strategies to advocate against modifier −25 payment reductions by insurance carriers (AADA, unpublished data, 2021). Additionally, the AADA PAPR committee has been able to provide guidance and technical support as needed to state dermatology societies, such as to the Rhode Island Dermatology Society and the Pennsylvania Academy of Dermatology and Dermatologic Surgery to address payer quality metrics and access to laboratory services, respectively (AADA, unpublished data, 2021).
Patient Access to Affordable Treatments—American Academy of Dermatology Association payer advocacy is anchored to published position statements and clinical guidelines. To strengthen AADA advocacy on payer-mandated drug substitutions for nonmedical reasons and to preserve patient access to medications, the PAPR committee collaborated with the American Academy of Dermatology’s Drug Pricing and Transparency Task Force to update the AADA Position Statement on Patient Access to Affordable Treatments2 to address this issue. Essentially, patients who are stable on a medication should be allowed to keep using the same medication without payers changing their coverage for nonmedical reasons or by offering financial incentives to switch.
Relationships With Major Insurance Carriers—Integral to the PAPR committee’s private payer advocacy success are our proactive relationships with major insurance carriers. In 2021, the PAPR committee established quarterly dermatology-specific meetings with the major national carriers. In nurturing these relationships, the PAPR committee has been able to expand on opportunities to provide payer policy reviews as well as identify dermatologists as subject matter experts available to payers to assist with physician panels or policy reviews. These regular contacts also have proved beneficial in addressing issues raised by members; a few such examples include when one major payer reversed its denials on dermatologists’ claims for Current Procedural Terminology code 88304 (surgical pathology, gross and microscopic tissue exam) after it was brought to their attention by the AADA (AADA, unpublished data, 2021). This payer worked with its external vendor to correct the denials. When the AADA learned that another major payer was improperly denying payment for claims for 1 stage of Mohs micrographic surgery reported using Current Procedural Terminology code 17311, we worked with contacts at this payer to resolve the issue. They were receptive to our concerns and readily researched the issue. Leadership of the PAPR committee continued working with the AADA coding team and this payer to develop training guidance to prevent future denials, and the payer has reviewed prior denials and reprocessed claims for payment (AADA, unpublished data, 2021).
E/M Coding Issues
Another issue under consideration by several national insurers is E/M-level reassignment. Payers are reviewing claims from providers who are identified as coding at a higher E/M level as compared to their specialty peers. Some insurance carriers are using proprietary algorithms that attempt to link specific diagnoses to certain levels of E/M, triggering claim edits within their claim processing systems (AADA, unpublished data, 2021). The carrier will then either deny the claim or adjust reimbursement to a lower-level E/M service. In discussions with a national carrier on its E/M Leveling Program, the AADA has offered to work with them on appropriate E/M documentation and reporting (AADA, unpublished data, 2021). The AADA also has extensive member resources for guidance on E/M reporting as well as preparing for audits and appealing payer downcoding developed by the coding staff in conjunction with the Coding and Reimbursement Committee.
Recent Efforts From the AADA
Within the AADA, the PAPR committee works closely with the coding, practice management, and regulatory teams to address payer issues and develop resources for members. Recent examples include resources for dermatology practices on the No Surprises Act and what practices need to do to comply (AADA, unpublished data, 2021). The PAPR committee also works collaboratively with other AADA committees and task forces on payer issues as needed; for example, the PAPR committee has been working with the Dermatopathology Rapid Response committee to address member concerns regarding access to the pathology laboratory of their choice. Many payers are seeking to consolidate and save money by requiring the use of preferred laboratories, which impacts patient access to physician office laboratories and physician-recommended reference laboratories. The AADA, along with other medical specialties, has advocated for payers to not create a restrictive network of pathology laboratories within their provider networks and to support dermatologists’ laboratories of choice (AADA, unpublished data, 2021).
Within the payer space, the role of employers in impacting payment and coverage policies continues to rise. In 2021, the AADA leadership approved the employer outreach strategy to engage employers. The overall objectives are to advocate to employers on the value of dermatologic care and access to care provided by board-certified dermatologists. This is a long-term project that is just getting underway (AADA, unpublished data, 2021).
Payer Resource Center for AADA Members
To ensure that AADA members have the resources they need to advocate with payers as well as to keep the PAPR committee aware of emerging payer issues, the AADA created a new private payer resource center for members (https://www.aad.org/member/advocacy/priorities/payer-advocacy), which assists AADA members with common dermatologic concerns with insurers as well as contracting issues. The website also includes an email address for members to report payer issues ([email protected]). This information helps the PAPR committee identify and prioritize issues of concern.
Final Thoughts
Given the control that private insurance companies exert over the health care that dermatology patients can access, the AADA in general and the PAPR committee specifically play a valuable role in advocating access to care for dermatology patients.
Payer Advocacy in Dermatology
Frustrations with payers is a common source of annoyance among dermatologists. Payment rules can seem arbitrary, ever-changing, and not uniform among the various payers. Keeping track of payer requirements can be nearly impossible.
To assist members in handling these concerns, the American Academy of Dermatology Association (AADA) created the Patient Access and Payer Relations (PAPR) committee, which seeks to promote patient access to dermatologic care by addressing issues that may arise with private payers. The committee utilizes a multipronged approach to develop strategies to educate payers on the value of dermatology, addressing systematic payment issues as they arise over time, and building relationships with insurers and employers to promote coverage and payment policies allowing for the highest quality of dermatologic care. The committee is comprised of practicing dermatologists who meet regularly to help guide and implement the AADA’s payer advocacy initiatives.
Identifying payer contacts and forging working relationships is a cornerstone of payer advocacy. In addition to patient access to quality dermatologic services, fair reimbursement is always a primary concern.
Hot Topics in Payer Advocacy
How to Use Modifier −25 Appropriately—The AADA has been advocating for appropriate coverage and reimbursement for services billed by dermatologists; recent examples include assuring appropriate payment for services reported with modifier −25, which is used when a procedure such as a biopsy is performed on the same day as a separate and unrelated evaluation and management (E/M) service, such as psoriasis management. Some payers claim the concurrent nature of the services results in an overlap of office expenses such that these claims should be paid at a lesser amount; however, when procedure codes are frequently billed in association with an office visit, that overlap has already been accounted for as part of the code valuation process, negating the need for additional reduction.
The AADA PAPR committee has created numerous resources for our members to ensure they are using modifier −25 appropriately, particularly now that the US Department of Health and Human Services Office of the Inspector General (OIG) has announced a work plan to audit dermatologists claims reporting modifier −25.1 The AADA immediately formed a work group, including PAPR committee members, to develop and employ a strategy to educate key decision-makers on the correct use of modifier −25 and highlight appropriate resources to guide members. An introductory call was held with the OIG audit team to discuss the appropriate use of modifier −25 in dermatology as the OIG prepares to develop the parameters of its audit sometime in the future (AADA, unpublished data, 2021).
Working With Dermatology Societies on Payer Issues—The American Academy of Dermatology Association PAPR committee works collaboratively with members of the American Academy of Dermatology, state and local dermatology societies, and private payers to alleviate administrative burdens for dermatologists, maintain appropriate reimbursement for furnished services, and ensure patients can access covered quality care. Collaboration with state dermatology societies is essential to address payer issues that impact their members and provide guidance on effective engagement with their state payers. Recent examples include working with dermatology societies in Massachusetts, Rhode Island, and Florida on strategies to advocate against modifier −25 payment reductions by insurance carriers (AADA, unpublished data, 2021). Additionally, the AADA PAPR committee has been able to provide guidance and technical support as needed to state dermatology societies, such as to the Rhode Island Dermatology Society and the Pennsylvania Academy of Dermatology and Dermatologic Surgery to address payer quality metrics and access to laboratory services, respectively (AADA, unpublished data, 2021).
Patient Access to Affordable Treatments—American Academy of Dermatology Association payer advocacy is anchored to published position statements and clinical guidelines. To strengthen AADA advocacy on payer-mandated drug substitutions for nonmedical reasons and to preserve patient access to medications, the PAPR committee collaborated with the American Academy of Dermatology’s Drug Pricing and Transparency Task Force to update the AADA Position Statement on Patient Access to Affordable Treatments2 to address this issue. Essentially, patients who are stable on a medication should be allowed to keep using the same medication without payers changing their coverage for nonmedical reasons or by offering financial incentives to switch.
Relationships With Major Insurance Carriers—Integral to the PAPR committee’s private payer advocacy success are our proactive relationships with major insurance carriers. In 2021, the PAPR committee established quarterly dermatology-specific meetings with the major national carriers. In nurturing these relationships, the PAPR committee has been able to expand on opportunities to provide payer policy reviews as well as identify dermatologists as subject matter experts available to payers to assist with physician panels or policy reviews. These regular contacts also have proved beneficial in addressing issues raised by members; a few such examples include when one major payer reversed its denials on dermatologists’ claims for Current Procedural Terminology code 88304 (surgical pathology, gross and microscopic tissue exam) after it was brought to their attention by the AADA (AADA, unpublished data, 2021). This payer worked with its external vendor to correct the denials. When the AADA learned that another major payer was improperly denying payment for claims for 1 stage of Mohs micrographic surgery reported using Current Procedural Terminology code 17311, we worked with contacts at this payer to resolve the issue. They were receptive to our concerns and readily researched the issue. Leadership of the PAPR committee continued working with the AADA coding team and this payer to develop training guidance to prevent future denials, and the payer has reviewed prior denials and reprocessed claims for payment (AADA, unpublished data, 2021).
E/M Coding Issues
Another issue under consideration by several national insurers is E/M-level reassignment. Payers are reviewing claims from providers who are identified as coding at a higher E/M level as compared to their specialty peers. Some insurance carriers are using proprietary algorithms that attempt to link specific diagnoses to certain levels of E/M, triggering claim edits within their claim processing systems (AADA, unpublished data, 2021). The carrier will then either deny the claim or adjust reimbursement to a lower-level E/M service. In discussions with a national carrier on its E/M Leveling Program, the AADA has offered to work with them on appropriate E/M documentation and reporting (AADA, unpublished data, 2021). The AADA also has extensive member resources for guidance on E/M reporting as well as preparing for audits and appealing payer downcoding developed by the coding staff in conjunction with the Coding and Reimbursement Committee.
Recent Efforts From the AADA
Within the AADA, the PAPR committee works closely with the coding, practice management, and regulatory teams to address payer issues and develop resources for members. Recent examples include resources for dermatology practices on the No Surprises Act and what practices need to do to comply (AADA, unpublished data, 2021). The PAPR committee also works collaboratively with other AADA committees and task forces on payer issues as needed; for example, the PAPR committee has been working with the Dermatopathology Rapid Response committee to address member concerns regarding access to the pathology laboratory of their choice. Many payers are seeking to consolidate and save money by requiring the use of preferred laboratories, which impacts patient access to physician office laboratories and physician-recommended reference laboratories. The AADA, along with other medical specialties, has advocated for payers to not create a restrictive network of pathology laboratories within their provider networks and to support dermatologists’ laboratories of choice (AADA, unpublished data, 2021).
Within the payer space, the role of employers in impacting payment and coverage policies continues to rise. In 2021, the AADA leadership approved the employer outreach strategy to engage employers. The overall objectives are to advocate to employers on the value of dermatologic care and access to care provided by board-certified dermatologists. This is a long-term project that is just getting underway (AADA, unpublished data, 2021).
Payer Resource Center for AADA Members
To ensure that AADA members have the resources they need to advocate with payers as well as to keep the PAPR committee aware of emerging payer issues, the AADA created a new private payer resource center for members (https://www.aad.org/member/advocacy/priorities/payer-advocacy), which assists AADA members with common dermatologic concerns with insurers as well as contracting issues. The website also includes an email address for members to report payer issues ([email protected]). This information helps the PAPR committee identify and prioritize issues of concern.
Final Thoughts
Given the control that private insurance companies exert over the health care that dermatology patients can access, the AADA in general and the PAPR committee specifically play a valuable role in advocating access to care for dermatology patients.
- US Department of Health and Human Services Office of the Inspector General. Dermatologist claims for evaluation and management services on the same day as minor surgical procedures. Accessed May 16, 2022. https://www.oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000577.asp
- American Academy of Dermatology Association. Position Statement on Patient Access to Affordable Treatments. Updated November 4, 2017. Accessed May 24, 2022. https://server.aad.org/forms/policies/uploads/ps/ps%20-%20patient%20access%20to%20affordable%20treatments.pdf?)
- US Department of Health and Human Services Office of the Inspector General. Dermatologist claims for evaluation and management services on the same day as minor surgical procedures. Accessed May 16, 2022. https://www.oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000577.asp
- American Academy of Dermatology Association. Position Statement on Patient Access to Affordable Treatments. Updated November 4, 2017. Accessed May 24, 2022. https://server.aad.org/forms/policies/uploads/ps/ps%20-%20patient%20access%20to%20affordable%20treatments.pdf?)
Practice Points
- The American Academy of Dermatology Association routinely interacts with private medical payers on behalf of dermatologists and to insure access to dermatologic care for patients.
- Members of the American Academy of Dermatology are encouraged to work with the association when issues with payers arise.
Children and COVID: New cases hold steady in nonholiday week
The new-case count for the most recent reporting week – 87,644 for June 3-9 – did go up from the previous week, but by only 270 cases, the American Academy of Pediatrics and Children’s Hospital Association said in their weekly COVID report. That’s just 0.31% higher than a week ago and probably is affected by reduced testing and reporting because of Memorial Day, as the AAP and CHA noted earlier.
That hint of a continued decline accompanies the latest trend for new cases for all age groups: They have leveled out over the last month, with the moving 7-day daily average hovering around 100,000-110,000 since mid-May, data from the Centers for Disease Control and Prevention show.
The Food and Drug Administration, meanwhile, is in the news this week as two of its advisory panels take the next steps toward pediatric approvals of vaccines from Pfizer/BioNTtech and Moderna. The panels could advance the approvals of the Pfizer vaccine for children under the age of 5 years and the Moderna vaccine for children aged 6 months to 17 years.
Matthew Harris, MD, medical director of the COVID-19 vaccination program for Northwell Health in New Hyde Park, N.Y., emphasized the importance of vaccinations, as well as the continued challenge of convincing parents to get the shots for eligible children. “We still have a long way to go for primary vaccines and boosters for children 5 years and above,” he said in an interview.
The vaccination effort against COVID-19 has stalled somewhat as interest has waned since the Omicron surge. Weekly initial vaccinations for children aged 5-11 years, which topped 100,000 as recently as mid-March, have been about 43,000 a week for the last 3 weeks, while 12- to 17-year-olds had around 27,000 or 28,000 initial vaccinations per week over that span, the AAP said in a separate report.
The latest data available from the CDC show that overall vaccine coverage levels for the younger group are only about half those of the 12- to 17-year-olds, both in terms of initial doses and completions. The 5- to 11-year-olds are not eligible for boosters yet, but 26.5% of the older children had received one as of June 13, according to the CDC’s COVID Data Tracker.
The new-case count for the most recent reporting week – 87,644 for June 3-9 – did go up from the previous week, but by only 270 cases, the American Academy of Pediatrics and Children’s Hospital Association said in their weekly COVID report. That’s just 0.31% higher than a week ago and probably is affected by reduced testing and reporting because of Memorial Day, as the AAP and CHA noted earlier.
That hint of a continued decline accompanies the latest trend for new cases for all age groups: They have leveled out over the last month, with the moving 7-day daily average hovering around 100,000-110,000 since mid-May, data from the Centers for Disease Control and Prevention show.
The Food and Drug Administration, meanwhile, is in the news this week as two of its advisory panels take the next steps toward pediatric approvals of vaccines from Pfizer/BioNTtech and Moderna. The panels could advance the approvals of the Pfizer vaccine for children under the age of 5 years and the Moderna vaccine for children aged 6 months to 17 years.
Matthew Harris, MD, medical director of the COVID-19 vaccination program for Northwell Health in New Hyde Park, N.Y., emphasized the importance of vaccinations, as well as the continued challenge of convincing parents to get the shots for eligible children. “We still have a long way to go for primary vaccines and boosters for children 5 years and above,” he said in an interview.
The vaccination effort against COVID-19 has stalled somewhat as interest has waned since the Omicron surge. Weekly initial vaccinations for children aged 5-11 years, which topped 100,000 as recently as mid-March, have been about 43,000 a week for the last 3 weeks, while 12- to 17-year-olds had around 27,000 or 28,000 initial vaccinations per week over that span, the AAP said in a separate report.
The latest data available from the CDC show that overall vaccine coverage levels for the younger group are only about half those of the 12- to 17-year-olds, both in terms of initial doses and completions. The 5- to 11-year-olds are not eligible for boosters yet, but 26.5% of the older children had received one as of June 13, according to the CDC’s COVID Data Tracker.
The new-case count for the most recent reporting week – 87,644 for June 3-9 – did go up from the previous week, but by only 270 cases, the American Academy of Pediatrics and Children’s Hospital Association said in their weekly COVID report. That’s just 0.31% higher than a week ago and probably is affected by reduced testing and reporting because of Memorial Day, as the AAP and CHA noted earlier.
That hint of a continued decline accompanies the latest trend for new cases for all age groups: They have leveled out over the last month, with the moving 7-day daily average hovering around 100,000-110,000 since mid-May, data from the Centers for Disease Control and Prevention show.
The Food and Drug Administration, meanwhile, is in the news this week as two of its advisory panels take the next steps toward pediatric approvals of vaccines from Pfizer/BioNTtech and Moderna. The panels could advance the approvals of the Pfizer vaccine for children under the age of 5 years and the Moderna vaccine for children aged 6 months to 17 years.
Matthew Harris, MD, medical director of the COVID-19 vaccination program for Northwell Health in New Hyde Park, N.Y., emphasized the importance of vaccinations, as well as the continued challenge of convincing parents to get the shots for eligible children. “We still have a long way to go for primary vaccines and boosters for children 5 years and above,” he said in an interview.
The vaccination effort against COVID-19 has stalled somewhat as interest has waned since the Omicron surge. Weekly initial vaccinations for children aged 5-11 years, which topped 100,000 as recently as mid-March, have been about 43,000 a week for the last 3 weeks, while 12- to 17-year-olds had around 27,000 or 28,000 initial vaccinations per week over that span, the AAP said in a separate report.
The latest data available from the CDC show that overall vaccine coverage levels for the younger group are only about half those of the 12- to 17-year-olds, both in terms of initial doses and completions. The 5- to 11-year-olds are not eligible for boosters yet, but 26.5% of the older children had received one as of June 13, according to the CDC’s COVID Data Tracker.
Autoimmune disease linked to better late-stage breast cancer survival
CHICAGO – Comorbid autoimmune disease is associated with a greater chance of survival among women with stage IV breast cancer, according to a retrospective study presented at the annual meeting of the American Society of Clinical Oncology.
“It’s counterintuitive that, if you have two diseases instead of one, that you live longer, so then we had to scratch our heads a little bit and think about why these people are living longer,” said lead author Demitrios Dedousis, MD, University Hospitals, Case Medical Center, Cleveland.
Dr. Dedousis and colleagues conducted a retrospective analysis of patients from Surveillance, Epidemiology, and End Results–Medicare databases between 2007 and 2014 with breast cancer. The study included data from 137,324 patients diagnosed between 2007 and 2012, before the widespread use of immunotherapy. 27% of patients had an autoimmune disease, most commonly rheumatoid arthritis (23%), psoriasis (2.4%), and systemic lupus erythematosus (1.1%).
When all patients were included in the analysis, those with autoimmune disorders had slightly longer survival times, but these weren’t clinically significant. A subanalysis found a greater difference in survival.
The association appears more pronounced in metastatic cancer. Patients with stage 4 breast cancer and autoimmune disease had a longer mean overall survival (36 months vs. 30 months; hazard ratio, 1.46; P < .0001. Cancer-specific survival: HR, 1.39; P < .0001). Patients with autoimmune disease and stage 1-3 breast cancer had lower overall survival (P < .0001, P < 0.0001, and P = 0.026 respectively), compared with patients without autoimmune disease.
“What we thought was happening is that the lack of increased survival in stages 1 through 3 was hiding the increase in survival among the stage IV patients when looking at the overall cohort,” Dr. Dedousis said.
The retrospective nature of the study makes it impossible to draw any firm conclusions about causation. It could be that patients who have already been diagnosed with an autoimmune disease are more vigilant about going to health checkups. “There are other possible explanations, but the one that’s most interesting to us is that their immune system is involved in fighting the cancer. Our study certainly didn’t prove that, but it’s suggesting that’s a possibility,” Dr. Dedousis said.
He and his coauthors anticipate conducting similar studies in other cancers to see if there are similar relationships. Some preliminary work has already suggested something similar in lung cancer. “I think demonstrating this in a few kinds of cancer goes part of the way towards showing that this is a real biological phenomenon,” he said.
Another research avenue is to examine the immune systems and pathology specimens in patients with both an autoimmune disease and cancer to see if there is a greater immune response within the tumor. If so, that could suggest new immunotherapy strategies.
Another possibility is to look at the specific immune pathways within “protective” autoimmune conditions. “For the sake of argument, if we find a particular autoimmune condition is improving survival across multiple kinds of cancers, we could look at those pathways that are specifically involved in that autoimmune condition. It might help us identify a target for drug development,” Dr. Dedousis said.
Asked why a potential benefit might be more apparent in late-stage disease, he suggested that, in early-stage breast cancer, surgery and other treatments may be so effective that the immune system’s role only rarely makes a difference. It could play a larger role in late-stage disease when there are less effective therapies. It could also be that the immune system doesn’t recognize the cancer until it has spread beyond the regional lymph nodes on its way to metastasizing.
According to the National Cancer Institute, 10%-30% of people with cancer also have an autoimmune disease.
Dr. Dedousis has no relevant financial disclosures.
CHICAGO – Comorbid autoimmune disease is associated with a greater chance of survival among women with stage IV breast cancer, according to a retrospective study presented at the annual meeting of the American Society of Clinical Oncology.
“It’s counterintuitive that, if you have two diseases instead of one, that you live longer, so then we had to scratch our heads a little bit and think about why these people are living longer,” said lead author Demitrios Dedousis, MD, University Hospitals, Case Medical Center, Cleveland.
Dr. Dedousis and colleagues conducted a retrospective analysis of patients from Surveillance, Epidemiology, and End Results–Medicare databases between 2007 and 2014 with breast cancer. The study included data from 137,324 patients diagnosed between 2007 and 2012, before the widespread use of immunotherapy. 27% of patients had an autoimmune disease, most commonly rheumatoid arthritis (23%), psoriasis (2.4%), and systemic lupus erythematosus (1.1%).
When all patients were included in the analysis, those with autoimmune disorders had slightly longer survival times, but these weren’t clinically significant. A subanalysis found a greater difference in survival.
The association appears more pronounced in metastatic cancer. Patients with stage 4 breast cancer and autoimmune disease had a longer mean overall survival (36 months vs. 30 months; hazard ratio, 1.46; P < .0001. Cancer-specific survival: HR, 1.39; P < .0001). Patients with autoimmune disease and stage 1-3 breast cancer had lower overall survival (P < .0001, P < 0.0001, and P = 0.026 respectively), compared with patients without autoimmune disease.
“What we thought was happening is that the lack of increased survival in stages 1 through 3 was hiding the increase in survival among the stage IV patients when looking at the overall cohort,” Dr. Dedousis said.
The retrospective nature of the study makes it impossible to draw any firm conclusions about causation. It could be that patients who have already been diagnosed with an autoimmune disease are more vigilant about going to health checkups. “There are other possible explanations, but the one that’s most interesting to us is that their immune system is involved in fighting the cancer. Our study certainly didn’t prove that, but it’s suggesting that’s a possibility,” Dr. Dedousis said.
He and his coauthors anticipate conducting similar studies in other cancers to see if there are similar relationships. Some preliminary work has already suggested something similar in lung cancer. “I think demonstrating this in a few kinds of cancer goes part of the way towards showing that this is a real biological phenomenon,” he said.
Another research avenue is to examine the immune systems and pathology specimens in patients with both an autoimmune disease and cancer to see if there is a greater immune response within the tumor. If so, that could suggest new immunotherapy strategies.
Another possibility is to look at the specific immune pathways within “protective” autoimmune conditions. “For the sake of argument, if we find a particular autoimmune condition is improving survival across multiple kinds of cancers, we could look at those pathways that are specifically involved in that autoimmune condition. It might help us identify a target for drug development,” Dr. Dedousis said.
Asked why a potential benefit might be more apparent in late-stage disease, he suggested that, in early-stage breast cancer, surgery and other treatments may be so effective that the immune system’s role only rarely makes a difference. It could play a larger role in late-stage disease when there are less effective therapies. It could also be that the immune system doesn’t recognize the cancer until it has spread beyond the regional lymph nodes on its way to metastasizing.
According to the National Cancer Institute, 10%-30% of people with cancer also have an autoimmune disease.
Dr. Dedousis has no relevant financial disclosures.
CHICAGO – Comorbid autoimmune disease is associated with a greater chance of survival among women with stage IV breast cancer, according to a retrospective study presented at the annual meeting of the American Society of Clinical Oncology.
“It’s counterintuitive that, if you have two diseases instead of one, that you live longer, so then we had to scratch our heads a little bit and think about why these people are living longer,” said lead author Demitrios Dedousis, MD, University Hospitals, Case Medical Center, Cleveland.
Dr. Dedousis and colleagues conducted a retrospective analysis of patients from Surveillance, Epidemiology, and End Results–Medicare databases between 2007 and 2014 with breast cancer. The study included data from 137,324 patients diagnosed between 2007 and 2012, before the widespread use of immunotherapy. 27% of patients had an autoimmune disease, most commonly rheumatoid arthritis (23%), psoriasis (2.4%), and systemic lupus erythematosus (1.1%).
When all patients were included in the analysis, those with autoimmune disorders had slightly longer survival times, but these weren’t clinically significant. A subanalysis found a greater difference in survival.
The association appears more pronounced in metastatic cancer. Patients with stage 4 breast cancer and autoimmune disease had a longer mean overall survival (36 months vs. 30 months; hazard ratio, 1.46; P < .0001. Cancer-specific survival: HR, 1.39; P < .0001). Patients with autoimmune disease and stage 1-3 breast cancer had lower overall survival (P < .0001, P < 0.0001, and P = 0.026 respectively), compared with patients without autoimmune disease.
“What we thought was happening is that the lack of increased survival in stages 1 through 3 was hiding the increase in survival among the stage IV patients when looking at the overall cohort,” Dr. Dedousis said.
The retrospective nature of the study makes it impossible to draw any firm conclusions about causation. It could be that patients who have already been diagnosed with an autoimmune disease are more vigilant about going to health checkups. “There are other possible explanations, but the one that’s most interesting to us is that their immune system is involved in fighting the cancer. Our study certainly didn’t prove that, but it’s suggesting that’s a possibility,” Dr. Dedousis said.
He and his coauthors anticipate conducting similar studies in other cancers to see if there are similar relationships. Some preliminary work has already suggested something similar in lung cancer. “I think demonstrating this in a few kinds of cancer goes part of the way towards showing that this is a real biological phenomenon,” he said.
Another research avenue is to examine the immune systems and pathology specimens in patients with both an autoimmune disease and cancer to see if there is a greater immune response within the tumor. If so, that could suggest new immunotherapy strategies.
Another possibility is to look at the specific immune pathways within “protective” autoimmune conditions. “For the sake of argument, if we find a particular autoimmune condition is improving survival across multiple kinds of cancers, we could look at those pathways that are specifically involved in that autoimmune condition. It might help us identify a target for drug development,” Dr. Dedousis said.
Asked why a potential benefit might be more apparent in late-stage disease, he suggested that, in early-stage breast cancer, surgery and other treatments may be so effective that the immune system’s role only rarely makes a difference. It could play a larger role in late-stage disease when there are less effective therapies. It could also be that the immune system doesn’t recognize the cancer until it has spread beyond the regional lymph nodes on its way to metastasizing.
According to the National Cancer Institute, 10%-30% of people with cancer also have an autoimmune disease.
Dr. Dedousis has no relevant financial disclosures.
AT ASCO 2022
Breast cancer deaths take a big dip because of new medicines
CHICAGO – Progress in breast cancer treatment over the past 2 decades has reduced expected mortality from both early-stage and metastatic disease, according to a new model that looked at 10-year distant recurrence-free survival and survival time after metastatic diagnosis, among other factors.
“There has been an accelerating influx of new treatments for breast cancer starting around 1990. We wished to ask whether and to what extent decades of metastatic treatment advances may have affected population level breast cancer mortality,” said Jennifer Lee Caswell-Jin, MD, during a presentation of the study at the annual meeting of the American Society of Clinical Oncology.
“Our models find that metastatic treatments improved population-level survival in all breast cancer subtypes since 2000 with substantial variability by subtype," said Dr. Caswell-Jin, who is a medical oncologist with Stanford (Calif.) Medicine specializing in breast cancer.
The study is based on an analysis of four models from the Cancer Intervention and Surveillance Modeling Network (CISNET). The models simulated breast cancer mortality between 2000 and 2019 factoring in the use of mammography, efficacy and dissemination of estrogen receptor (ER) and HER2-specific treatments of early-stage (stages I-III) and metastatic (stage IV or distant recurrence) disease, but also non–cancer-related mortality. The models compared overall and ER/HER2-specific breast cancer mortality rates during this period with estimated rates with no screening or treatment, and then attributed mortality reductions to screening, early-stage, or metastatic treatment.
The results were compared with three clinical trials that tested therapies in different subtypes of metastatic disease. Dr. Caswell-Jin and colleagues adjusted the analysis to reflect expected differences between clinical trial populations and the broader population by sampling simulated patients who resembled the trial population.
The investigators found that, at 71%, the biggest drop in mortality rates were for women with ER+/HER2+ breast cancer, followed by 61% for women with ER-/HER2+ breast cancer and 59% for women with ER+/HER2– breast cancer. Triple-negative breast cancer – one of the most challenging breast cancers to treat – only saw a drop of 40% during this period. About 19% of the overall reduction in breast cancer mortality were caused by treatments after metastasis.
The median survival after a diagnosis of ER+/HER2– metastatic recurrence increased from 2 years in 2000 to 3.5 years in 2019. In triple-negative breast cancer, the increase was more modest, from 1.2 years in 2000 to 1.8 years in 2019. After a diagnosis of metastatic recurrence of ER+/HER2+ breast cancer, median survival increased from 2.3 years in 2000 to 4.8 years in 2019, and for ER–/HER2+ breast cancer, from 2.2 years in 2000 to 3.9 years in 2019.
“How much metastatic treatments contributed to the overall mortality reduction varied over time depending on what therapies were entering the metastatic setting at that time and what therapies were transitioning from the metastatic to early-stage setting,” Dr. Caswell-Jin said.
The study did not include sacituzumab govitecan for metastatic triple-negative breast cancer, or trastuzumab deruxtecan and tucatinib for HER2-positive disease, which were approved after 2020. “The numbers that we cite will be better today for triple-negative breast cancer because of those two drugs. And will be even better for HER2-positive breast cancer because of those two drugs,” she said.
During the Q&A portion of the presentation, Daniel Hayes, MD, the Stuart B. Padnos Professor of Breast Cancer Research at the University of Michigan Rogel Cancer Center, Ann Arbor, asked about the potential of CISNET as an in-practice diagnostic tool.
“We’ve traditionally told patients who have metastatic disease that they will not be cured. I told two patients that on Tuesday. Can CISNET modeling let us begin to see if there is indeed now, with the improved therapies we have, a group of patients who do appear to be cured, or is that not possible?” he asked.
Perhaps, Dr. Caswell-Jin said, in a very small population of older patients with HER2-positive breast cancer that did in fact occur, but to a very small degree.
CHICAGO – Progress in breast cancer treatment over the past 2 decades has reduced expected mortality from both early-stage and metastatic disease, according to a new model that looked at 10-year distant recurrence-free survival and survival time after metastatic diagnosis, among other factors.
“There has been an accelerating influx of new treatments for breast cancer starting around 1990. We wished to ask whether and to what extent decades of metastatic treatment advances may have affected population level breast cancer mortality,” said Jennifer Lee Caswell-Jin, MD, during a presentation of the study at the annual meeting of the American Society of Clinical Oncology.
“Our models find that metastatic treatments improved population-level survival in all breast cancer subtypes since 2000 with substantial variability by subtype," said Dr. Caswell-Jin, who is a medical oncologist with Stanford (Calif.) Medicine specializing in breast cancer.
The study is based on an analysis of four models from the Cancer Intervention and Surveillance Modeling Network (CISNET). The models simulated breast cancer mortality between 2000 and 2019 factoring in the use of mammography, efficacy and dissemination of estrogen receptor (ER) and HER2-specific treatments of early-stage (stages I-III) and metastatic (stage IV or distant recurrence) disease, but also non–cancer-related mortality. The models compared overall and ER/HER2-specific breast cancer mortality rates during this period with estimated rates with no screening or treatment, and then attributed mortality reductions to screening, early-stage, or metastatic treatment.
The results were compared with three clinical trials that tested therapies in different subtypes of metastatic disease. Dr. Caswell-Jin and colleagues adjusted the analysis to reflect expected differences between clinical trial populations and the broader population by sampling simulated patients who resembled the trial population.
The investigators found that, at 71%, the biggest drop in mortality rates were for women with ER+/HER2+ breast cancer, followed by 61% for women with ER-/HER2+ breast cancer and 59% for women with ER+/HER2– breast cancer. Triple-negative breast cancer – one of the most challenging breast cancers to treat – only saw a drop of 40% during this period. About 19% of the overall reduction in breast cancer mortality were caused by treatments after metastasis.
The median survival after a diagnosis of ER+/HER2– metastatic recurrence increased from 2 years in 2000 to 3.5 years in 2019. In triple-negative breast cancer, the increase was more modest, from 1.2 years in 2000 to 1.8 years in 2019. After a diagnosis of metastatic recurrence of ER+/HER2+ breast cancer, median survival increased from 2.3 years in 2000 to 4.8 years in 2019, and for ER–/HER2+ breast cancer, from 2.2 years in 2000 to 3.9 years in 2019.
“How much metastatic treatments contributed to the overall mortality reduction varied over time depending on what therapies were entering the metastatic setting at that time and what therapies were transitioning from the metastatic to early-stage setting,” Dr. Caswell-Jin said.
The study did not include sacituzumab govitecan for metastatic triple-negative breast cancer, or trastuzumab deruxtecan and tucatinib for HER2-positive disease, which were approved after 2020. “The numbers that we cite will be better today for triple-negative breast cancer because of those two drugs. And will be even better for HER2-positive breast cancer because of those two drugs,” she said.
During the Q&A portion of the presentation, Daniel Hayes, MD, the Stuart B. Padnos Professor of Breast Cancer Research at the University of Michigan Rogel Cancer Center, Ann Arbor, asked about the potential of CISNET as an in-practice diagnostic tool.
“We’ve traditionally told patients who have metastatic disease that they will not be cured. I told two patients that on Tuesday. Can CISNET modeling let us begin to see if there is indeed now, with the improved therapies we have, a group of patients who do appear to be cured, or is that not possible?” he asked.
Perhaps, Dr. Caswell-Jin said, in a very small population of older patients with HER2-positive breast cancer that did in fact occur, but to a very small degree.
CHICAGO – Progress in breast cancer treatment over the past 2 decades has reduced expected mortality from both early-stage and metastatic disease, according to a new model that looked at 10-year distant recurrence-free survival and survival time after metastatic diagnosis, among other factors.
“There has been an accelerating influx of new treatments for breast cancer starting around 1990. We wished to ask whether and to what extent decades of metastatic treatment advances may have affected population level breast cancer mortality,” said Jennifer Lee Caswell-Jin, MD, during a presentation of the study at the annual meeting of the American Society of Clinical Oncology.
“Our models find that metastatic treatments improved population-level survival in all breast cancer subtypes since 2000 with substantial variability by subtype," said Dr. Caswell-Jin, who is a medical oncologist with Stanford (Calif.) Medicine specializing in breast cancer.
The study is based on an analysis of four models from the Cancer Intervention and Surveillance Modeling Network (CISNET). The models simulated breast cancer mortality between 2000 and 2019 factoring in the use of mammography, efficacy and dissemination of estrogen receptor (ER) and HER2-specific treatments of early-stage (stages I-III) and metastatic (stage IV or distant recurrence) disease, but also non–cancer-related mortality. The models compared overall and ER/HER2-specific breast cancer mortality rates during this period with estimated rates with no screening or treatment, and then attributed mortality reductions to screening, early-stage, or metastatic treatment.
The results were compared with three clinical trials that tested therapies in different subtypes of metastatic disease. Dr. Caswell-Jin and colleagues adjusted the analysis to reflect expected differences between clinical trial populations and the broader population by sampling simulated patients who resembled the trial population.
The investigators found that, at 71%, the biggest drop in mortality rates were for women with ER+/HER2+ breast cancer, followed by 61% for women with ER-/HER2+ breast cancer and 59% for women with ER+/HER2– breast cancer. Triple-negative breast cancer – one of the most challenging breast cancers to treat – only saw a drop of 40% during this period. About 19% of the overall reduction in breast cancer mortality were caused by treatments after metastasis.
The median survival after a diagnosis of ER+/HER2– metastatic recurrence increased from 2 years in 2000 to 3.5 years in 2019. In triple-negative breast cancer, the increase was more modest, from 1.2 years in 2000 to 1.8 years in 2019. After a diagnosis of metastatic recurrence of ER+/HER2+ breast cancer, median survival increased from 2.3 years in 2000 to 4.8 years in 2019, and for ER–/HER2+ breast cancer, from 2.2 years in 2000 to 3.9 years in 2019.
“How much metastatic treatments contributed to the overall mortality reduction varied over time depending on what therapies were entering the metastatic setting at that time and what therapies were transitioning from the metastatic to early-stage setting,” Dr. Caswell-Jin said.
The study did not include sacituzumab govitecan for metastatic triple-negative breast cancer, or trastuzumab deruxtecan and tucatinib for HER2-positive disease, which were approved after 2020. “The numbers that we cite will be better today for triple-negative breast cancer because of those two drugs. And will be even better for HER2-positive breast cancer because of those two drugs,” she said.
During the Q&A portion of the presentation, Daniel Hayes, MD, the Stuart B. Padnos Professor of Breast Cancer Research at the University of Michigan Rogel Cancer Center, Ann Arbor, asked about the potential of CISNET as an in-practice diagnostic tool.
“We’ve traditionally told patients who have metastatic disease that they will not be cured. I told two patients that on Tuesday. Can CISNET modeling let us begin to see if there is indeed now, with the improved therapies we have, a group of patients who do appear to be cured, or is that not possible?” he asked.
Perhaps, Dr. Caswell-Jin said, in a very small population of older patients with HER2-positive breast cancer that did in fact occur, but to a very small degree.
AT ASCO 2022