User login
FDA approves two JAK-1 inhibitors for moderate to severe atopic dermatitis
The available for this indication in the United States.
“It’s big news because a few years ago we didn’t have any systemic treatments that are safer than the classical immunosuppressants like cyclosporine and methotrexate,” Emma Guttman-Yassky, MD, PhD, Waldman professor and system chair of dermatology at the Icahn School of Medicine at Mount Sinai in New York, told this news organization commenting on upadacitinib’s approval.
“The only oral approved drug for AD up to now was oral prednisone, which has terrible safety concerns. This is basically the first oral medication that we can provide our patients for long-term use.”
Upadacitinib
The approval of upadacitinib (Rinvoq), marketed by AbbVie, for moderate to severe AD in patients ages 12 and older, comes on the heels of findings from three pivotal phase 3 studies involving more than 2,500 adults and children 12 years of age and older with moderate to severe AD: Measure Up 1 and 2, led by Dr. Guttman-Yassky, which evaluated upadacitinib compared with placebo, and AD UP, which compared upadacitinib along with topical corticosteroids, compared with placebo.
Across the three studies, upadacitinib – both 15 mg and 30 mg once daily monotherapy – met all primary and secondary endpoints at week 16, with some patients achieving higher levels of skin clearance based on the Eczema Area and Severity Index 90 (EASI-90) and EASI-100.
“I always say that patients with AD need options,” Dr. Guttman-Yassky said. “We need biologics. We need oral medications. Not everybody likes an injectable. The plus of the class of JAK inhibitors in general is the quick onset of action.” Many patients in her clinic are maintained on upadacitinib more than two years later “and are super happy,” she said. “Many of them failed cyclosporine and other immunosuppressants such as methotrexate and prednisone.”
She predicted that health insurance companies will find coverage cost-effective “because it sets a new bar for efficacy, and because many patients have failed other treatments.”
Abrocitinib
Abrocitinib (Cibinqo), marketed by Pfizer, was approved for adults with moderate to severe AD. The approval was based on results of five clinical trials from a large-scale clinical trial program of more than 1,600 patients. The recommended doses are 100 mg and 200 mg, with the 200 mg dose recommended for patients who are not responding to the 100 mg dose.
The labeling of abrocitinib and upadacitinib include a boxed warning for JAK inhibitors, regarding the risk of serious infections, mortality, malignancy, major adverse cardiovascular events, and thrombosis.
Dr. Guttman-Yassky has served as a principal investigator for AbbVie and has received consulting fees from the company.
The available for this indication in the United States.
“It’s big news because a few years ago we didn’t have any systemic treatments that are safer than the classical immunosuppressants like cyclosporine and methotrexate,” Emma Guttman-Yassky, MD, PhD, Waldman professor and system chair of dermatology at the Icahn School of Medicine at Mount Sinai in New York, told this news organization commenting on upadacitinib’s approval.
“The only oral approved drug for AD up to now was oral prednisone, which has terrible safety concerns. This is basically the first oral medication that we can provide our patients for long-term use.”
Upadacitinib
The approval of upadacitinib (Rinvoq), marketed by AbbVie, for moderate to severe AD in patients ages 12 and older, comes on the heels of findings from three pivotal phase 3 studies involving more than 2,500 adults and children 12 years of age and older with moderate to severe AD: Measure Up 1 and 2, led by Dr. Guttman-Yassky, which evaluated upadacitinib compared with placebo, and AD UP, which compared upadacitinib along with topical corticosteroids, compared with placebo.
Across the three studies, upadacitinib – both 15 mg and 30 mg once daily monotherapy – met all primary and secondary endpoints at week 16, with some patients achieving higher levels of skin clearance based on the Eczema Area and Severity Index 90 (EASI-90) and EASI-100.
“I always say that patients with AD need options,” Dr. Guttman-Yassky said. “We need biologics. We need oral medications. Not everybody likes an injectable. The plus of the class of JAK inhibitors in general is the quick onset of action.” Many patients in her clinic are maintained on upadacitinib more than two years later “and are super happy,” she said. “Many of them failed cyclosporine and other immunosuppressants such as methotrexate and prednisone.”
She predicted that health insurance companies will find coverage cost-effective “because it sets a new bar for efficacy, and because many patients have failed other treatments.”
Abrocitinib
Abrocitinib (Cibinqo), marketed by Pfizer, was approved for adults with moderate to severe AD. The approval was based on results of five clinical trials from a large-scale clinical trial program of more than 1,600 patients. The recommended doses are 100 mg and 200 mg, with the 200 mg dose recommended for patients who are not responding to the 100 mg dose.
The labeling of abrocitinib and upadacitinib include a boxed warning for JAK inhibitors, regarding the risk of serious infections, mortality, malignancy, major adverse cardiovascular events, and thrombosis.
Dr. Guttman-Yassky has served as a principal investigator for AbbVie and has received consulting fees from the company.
The available for this indication in the United States.
“It’s big news because a few years ago we didn’t have any systemic treatments that are safer than the classical immunosuppressants like cyclosporine and methotrexate,” Emma Guttman-Yassky, MD, PhD, Waldman professor and system chair of dermatology at the Icahn School of Medicine at Mount Sinai in New York, told this news organization commenting on upadacitinib’s approval.
“The only oral approved drug for AD up to now was oral prednisone, which has terrible safety concerns. This is basically the first oral medication that we can provide our patients for long-term use.”
Upadacitinib
The approval of upadacitinib (Rinvoq), marketed by AbbVie, for moderate to severe AD in patients ages 12 and older, comes on the heels of findings from three pivotal phase 3 studies involving more than 2,500 adults and children 12 years of age and older with moderate to severe AD: Measure Up 1 and 2, led by Dr. Guttman-Yassky, which evaluated upadacitinib compared with placebo, and AD UP, which compared upadacitinib along with topical corticosteroids, compared with placebo.
Across the three studies, upadacitinib – both 15 mg and 30 mg once daily monotherapy – met all primary and secondary endpoints at week 16, with some patients achieving higher levels of skin clearance based on the Eczema Area and Severity Index 90 (EASI-90) and EASI-100.
“I always say that patients with AD need options,” Dr. Guttman-Yassky said. “We need biologics. We need oral medications. Not everybody likes an injectable. The plus of the class of JAK inhibitors in general is the quick onset of action.” Many patients in her clinic are maintained on upadacitinib more than two years later “and are super happy,” she said. “Many of them failed cyclosporine and other immunosuppressants such as methotrexate and prednisone.”
She predicted that health insurance companies will find coverage cost-effective “because it sets a new bar for efficacy, and because many patients have failed other treatments.”
Abrocitinib
Abrocitinib (Cibinqo), marketed by Pfizer, was approved for adults with moderate to severe AD. The approval was based on results of five clinical trials from a large-scale clinical trial program of more than 1,600 patients. The recommended doses are 100 mg and 200 mg, with the 200 mg dose recommended for patients who are not responding to the 100 mg dose.
The labeling of abrocitinib and upadacitinib include a boxed warning for JAK inhibitors, regarding the risk of serious infections, mortality, malignancy, major adverse cardiovascular events, and thrombosis.
Dr. Guttman-Yassky has served as a principal investigator for AbbVie and has received consulting fees from the company.
FDA updates status of iPLEDGE access problems
The, one month after a modified program was launched, the Food and Drug Administration announced on Jan. 14.
The IPMG has “created a new tool within the system to help resolve account access for some user groups without using the call center. This tool is intended to allow prescribers and designees to send login links directly to their patients’ desired email address through the Manage Patients page of the iPLEDGE REMS portal,” the FDA statement said.
“Prescribers can also send login links to their designees still having difficulty accessing their iPLEDGE account,” and users should check their emails for messages from iPLEDGE, including spam folders, the FDA advises. The iPLEDGE strategy is designed to prevent fetal exposure to isotretinoin, which is highly teratogenic.
Days after the new, gender-neutral approach to the isotretinoin risk mitigation program was launched on Dec. 13, the FDA convened an emergency meeting with representatives from the American Academy of Dermatology Association (AADA) to discuss the problematic rollout of the program, which was described as disastrous, chaotic, and a failure, with dermatologists on Twitter and elsewhere expressing anger and frustration over not being able to access the program or reach the call center.
A statement by the FDA on Dec. 23 followed, urging manufacturers to develop solutions for the website and to work with the AADA and pharmacy organizations to find solutions that would minimize treatment interruptions during the transition.
The modified REMS, launched on Dec. 13, is designed to make it more inclusive for transgender patients prescribed isotretinoin. Instead of three risk categories (females of reproductive potential, females not of reproductive potential, and males), patients who are prescribed isotretinoin for acne are assigned to one of two risk categories: those who can get pregnant and those who cannot get pregnant.
In the Jan. 14 statement, the FDA notes that the agency is continuing to work with the IPMG regarding the problems clinicians, pharmacists, and patients have had with accessing iPLEDGE over the last month.
“Although there has been progress, there is a significant amount of work still to be done,” the FDA acknowledged. “While we consider potential steps within the scope of FDA’s authorities, we will continue to meet with the IPMG for updates on the status of the problems with the iPLEDGE REMS and their progress towards having the system work as intended for all users.”
The, one month after a modified program was launched, the Food and Drug Administration announced on Jan. 14.
The IPMG has “created a new tool within the system to help resolve account access for some user groups without using the call center. This tool is intended to allow prescribers and designees to send login links directly to their patients’ desired email address through the Manage Patients page of the iPLEDGE REMS portal,” the FDA statement said.
“Prescribers can also send login links to their designees still having difficulty accessing their iPLEDGE account,” and users should check their emails for messages from iPLEDGE, including spam folders, the FDA advises. The iPLEDGE strategy is designed to prevent fetal exposure to isotretinoin, which is highly teratogenic.
Days after the new, gender-neutral approach to the isotretinoin risk mitigation program was launched on Dec. 13, the FDA convened an emergency meeting with representatives from the American Academy of Dermatology Association (AADA) to discuss the problematic rollout of the program, which was described as disastrous, chaotic, and a failure, with dermatologists on Twitter and elsewhere expressing anger and frustration over not being able to access the program or reach the call center.
A statement by the FDA on Dec. 23 followed, urging manufacturers to develop solutions for the website and to work with the AADA and pharmacy organizations to find solutions that would minimize treatment interruptions during the transition.
The modified REMS, launched on Dec. 13, is designed to make it more inclusive for transgender patients prescribed isotretinoin. Instead of three risk categories (females of reproductive potential, females not of reproductive potential, and males), patients who are prescribed isotretinoin for acne are assigned to one of two risk categories: those who can get pregnant and those who cannot get pregnant.
In the Jan. 14 statement, the FDA notes that the agency is continuing to work with the IPMG regarding the problems clinicians, pharmacists, and patients have had with accessing iPLEDGE over the last month.
“Although there has been progress, there is a significant amount of work still to be done,” the FDA acknowledged. “While we consider potential steps within the scope of FDA’s authorities, we will continue to meet with the IPMG for updates on the status of the problems with the iPLEDGE REMS and their progress towards having the system work as intended for all users.”
The, one month after a modified program was launched, the Food and Drug Administration announced on Jan. 14.
The IPMG has “created a new tool within the system to help resolve account access for some user groups without using the call center. This tool is intended to allow prescribers and designees to send login links directly to their patients’ desired email address through the Manage Patients page of the iPLEDGE REMS portal,” the FDA statement said.
“Prescribers can also send login links to their designees still having difficulty accessing their iPLEDGE account,” and users should check their emails for messages from iPLEDGE, including spam folders, the FDA advises. The iPLEDGE strategy is designed to prevent fetal exposure to isotretinoin, which is highly teratogenic.
Days after the new, gender-neutral approach to the isotretinoin risk mitigation program was launched on Dec. 13, the FDA convened an emergency meeting with representatives from the American Academy of Dermatology Association (AADA) to discuss the problematic rollout of the program, which was described as disastrous, chaotic, and a failure, with dermatologists on Twitter and elsewhere expressing anger and frustration over not being able to access the program or reach the call center.
A statement by the FDA on Dec. 23 followed, urging manufacturers to develop solutions for the website and to work with the AADA and pharmacy organizations to find solutions that would minimize treatment interruptions during the transition.
The modified REMS, launched on Dec. 13, is designed to make it more inclusive for transgender patients prescribed isotretinoin. Instead of three risk categories (females of reproductive potential, females not of reproductive potential, and males), patients who are prescribed isotretinoin for acne are assigned to one of two risk categories: those who can get pregnant and those who cannot get pregnant.
In the Jan. 14 statement, the FDA notes that the agency is continuing to work with the IPMG regarding the problems clinicians, pharmacists, and patients have had with accessing iPLEDGE over the last month.
“Although there has been progress, there is a significant amount of work still to be done,” the FDA acknowledged. “While we consider potential steps within the scope of FDA’s authorities, we will continue to meet with the IPMG for updates on the status of the problems with the iPLEDGE REMS and their progress towards having the system work as intended for all users.”
Atopic Dermatitis: A supplement to Dermatology News
- PATIENT SATISFACTION WITH TREATMENT
- REDUCING ITCH
- BURDEN OF DISEASE IN BLACK PATIENTS
- BATHING RECOMMENDATIONS
- PATIENT SATISFACTION WITH TREATMENT
- REDUCING ITCH
- BURDEN OF DISEASE IN BLACK PATIENTS
- BATHING RECOMMENDATIONS
- PATIENT SATISFACTION WITH TREATMENT
- REDUCING ITCH
- BURDEN OF DISEASE IN BLACK PATIENTS
- BATHING RECOMMENDATIONS
NPs, PAs say stop attacks and support health care colleagues
This commentary was submitted as a rebuttal to “PA name change bad for patients and the profession.”
To the Editor:
At a time when COVID-19 cases are climbing and health care workers are struggling to meet the needs of our nation’s healthcare system, the commentary by Rebekah Bernard, MD, divides health care providers and demeans the education, experience, and value of physician associates (PA) and nurse practitioners (NP) in our opinion.
The ill timing of this negative message is equally matched by her mischaracterization of the PA title change and PA efforts to eliminate outdated administrative barriers, as well as her baseless attack on NP education and clinical training.
Let us be clear about one thing: What patients really want and deserve is access to high-quality care delivered by the health care provider of their choice. Patients deserve health care providers who are committed to modern, integrated, and coordinated health care delivery, led by professionals who are dedicated to ensuring that everyone is practicing to the full extent of their education, clinical experience, and scope of practice. Patients deserve health care providers who respect each other and work together to embrace solutions that will improve health care for the future.
Decades of research confirm the high quality of PA- and NP-delivered health care. The evidence is in, and it is irrefutable: PA- and NP-delivered care is associated with improved access to care, lower health care costs, and fewer avoidable emergency room visits.
With regard to the PA title change, the fact is this: Changing the profession’s title does not change what PAs do or affect a PA’s scope of practice. The new title – physician associate – directly addresses the common misperception that PAs merely “assist” physicians. It is in the best interest of patients and the health care system for PAs to hold a professional title that ensures clarity about the work that PAs do.
For the sake of patients, we urge Bernard and her organization to stop continuously attacking other professions and focus on what really matters – providing access to safe, effective, equitable, high-quality care to all patients.
We are committed to patient-centered, coordinated health care, and we continue to work with like-minded physicians and other colleagues to make this a reality.
Ms. Orozco is president and chair of the board of directors for the American Academy of Physician Associates. Dr. Kapu is president of the American Association of Nurse Practitioners.
A version of this article first appeared on Medscape.com.
This commentary was submitted as a rebuttal to “PA name change bad for patients and the profession.”
To the Editor:
At a time when COVID-19 cases are climbing and health care workers are struggling to meet the needs of our nation’s healthcare system, the commentary by Rebekah Bernard, MD, divides health care providers and demeans the education, experience, and value of physician associates (PA) and nurse practitioners (NP) in our opinion.
The ill timing of this negative message is equally matched by her mischaracterization of the PA title change and PA efforts to eliminate outdated administrative barriers, as well as her baseless attack on NP education and clinical training.
Let us be clear about one thing: What patients really want and deserve is access to high-quality care delivered by the health care provider of their choice. Patients deserve health care providers who are committed to modern, integrated, and coordinated health care delivery, led by professionals who are dedicated to ensuring that everyone is practicing to the full extent of their education, clinical experience, and scope of practice. Patients deserve health care providers who respect each other and work together to embrace solutions that will improve health care for the future.
Decades of research confirm the high quality of PA- and NP-delivered health care. The evidence is in, and it is irrefutable: PA- and NP-delivered care is associated with improved access to care, lower health care costs, and fewer avoidable emergency room visits.
With regard to the PA title change, the fact is this: Changing the profession’s title does not change what PAs do or affect a PA’s scope of practice. The new title – physician associate – directly addresses the common misperception that PAs merely “assist” physicians. It is in the best interest of patients and the health care system for PAs to hold a professional title that ensures clarity about the work that PAs do.
For the sake of patients, we urge Bernard and her organization to stop continuously attacking other professions and focus on what really matters – providing access to safe, effective, equitable, high-quality care to all patients.
We are committed to patient-centered, coordinated health care, and we continue to work with like-minded physicians and other colleagues to make this a reality.
Ms. Orozco is president and chair of the board of directors for the American Academy of Physician Associates. Dr. Kapu is president of the American Association of Nurse Practitioners.
A version of this article first appeared on Medscape.com.
This commentary was submitted as a rebuttal to “PA name change bad for patients and the profession.”
To the Editor:
At a time when COVID-19 cases are climbing and health care workers are struggling to meet the needs of our nation’s healthcare system, the commentary by Rebekah Bernard, MD, divides health care providers and demeans the education, experience, and value of physician associates (PA) and nurse practitioners (NP) in our opinion.
The ill timing of this negative message is equally matched by her mischaracterization of the PA title change and PA efforts to eliminate outdated administrative barriers, as well as her baseless attack on NP education and clinical training.
Let us be clear about one thing: What patients really want and deserve is access to high-quality care delivered by the health care provider of their choice. Patients deserve health care providers who are committed to modern, integrated, and coordinated health care delivery, led by professionals who are dedicated to ensuring that everyone is practicing to the full extent of their education, clinical experience, and scope of practice. Patients deserve health care providers who respect each other and work together to embrace solutions that will improve health care for the future.
Decades of research confirm the high quality of PA- and NP-delivered health care. The evidence is in, and it is irrefutable: PA- and NP-delivered care is associated with improved access to care, lower health care costs, and fewer avoidable emergency room visits.
With regard to the PA title change, the fact is this: Changing the profession’s title does not change what PAs do or affect a PA’s scope of practice. The new title – physician associate – directly addresses the common misperception that PAs merely “assist” physicians. It is in the best interest of patients and the health care system for PAs to hold a professional title that ensures clarity about the work that PAs do.
For the sake of patients, we urge Bernard and her organization to stop continuously attacking other professions and focus on what really matters – providing access to safe, effective, equitable, high-quality care to all patients.
We are committed to patient-centered, coordinated health care, and we continue to work with like-minded physicians and other colleagues to make this a reality.
Ms. Orozco is president and chair of the board of directors for the American Academy of Physician Associates. Dr. Kapu is president of the American Association of Nurse Practitioners.
A version of this article first appeared on Medscape.com.
75-year-old White male presenting with progressive pruritus and a worsening rash
, although it can also be contracted through contaminated bedding and clothing. It can affect all races and ages.
Patients typically present with extremely pruritic, symmetric papules and excoriations. In nodular scabies, nodules and large papules are seen on exam. Thin lines in the skin called burrows may be present, especially in the webs between fingers. Female mites create burrows as they tunnel through the epidermis and lay eggs. The wrists, areola, waistline, and groin may all be involved, creating an imaginary circle between the areas described as the “circle of Hebra.” Penile and scrotal lesions are common in men.
Patients usually experience worse pruritus at night, which disturbs sleep. Crusted scabies is a severe form of scabies more often seen in those with immunocompromised immune systems. Clinically, thick crusted and scaly patches are present that are teeming with mites.
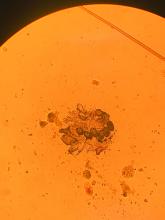
Diagnosis can be confirmed by performing a scabies prep, during which a burrow is scraped with a surgical blade. A drop of mineral oil is placed on the skin cells. The mite, ova, and feces can be visualized under the microscope. Wrists and hands usually have the highest yield for finding the parasites.
Topical treatments include permethrin 5% cream, lindane, benzyl benzoate, and crotamiton, and should be applied as two treatments a week apart. In the United States, permethrin is most commonly used. Ivermectin pills are used off label and are very effective and may be repeated for 1-2 weeks. All household contacts should be treated. Patients may still have pruritus for 2-4 weeks following treatment.
In this patient, a scabies prep was performed prior to performing repeat skin biopsies. Microscopic examination revealed ova, one mite, and feces. Treatment was initiated with ivermectin and permethrin.
Photos and case were submitted by Susannah Berke, MD, and Damon McClain, MD, Three Rivers Dermatology, Coraopolis, Pa.; and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
, although it can also be contracted through contaminated bedding and clothing. It can affect all races and ages.
Patients typically present with extremely pruritic, symmetric papules and excoriations. In nodular scabies, nodules and large papules are seen on exam. Thin lines in the skin called burrows may be present, especially in the webs between fingers. Female mites create burrows as they tunnel through the epidermis and lay eggs. The wrists, areola, waistline, and groin may all be involved, creating an imaginary circle between the areas described as the “circle of Hebra.” Penile and scrotal lesions are common in men.
Patients usually experience worse pruritus at night, which disturbs sleep. Crusted scabies is a severe form of scabies more often seen in those with immunocompromised immune systems. Clinically, thick crusted and scaly patches are present that are teeming with mites.
Diagnosis can be confirmed by performing a scabies prep, during which a burrow is scraped with a surgical blade. A drop of mineral oil is placed on the skin cells. The mite, ova, and feces can be visualized under the microscope. Wrists and hands usually have the highest yield for finding the parasites.
Topical treatments include permethrin 5% cream, lindane, benzyl benzoate, and crotamiton, and should be applied as two treatments a week apart. In the United States, permethrin is most commonly used. Ivermectin pills are used off label and are very effective and may be repeated for 1-2 weeks. All household contacts should be treated. Patients may still have pruritus for 2-4 weeks following treatment.
In this patient, a scabies prep was performed prior to performing repeat skin biopsies. Microscopic examination revealed ova, one mite, and feces. Treatment was initiated with ivermectin and permethrin.
Photos and case were submitted by Susannah Berke, MD, and Damon McClain, MD, Three Rivers Dermatology, Coraopolis, Pa.; and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
, although it can also be contracted through contaminated bedding and clothing. It can affect all races and ages.
Patients typically present with extremely pruritic, symmetric papules and excoriations. In nodular scabies, nodules and large papules are seen on exam. Thin lines in the skin called burrows may be present, especially in the webs between fingers. Female mites create burrows as they tunnel through the epidermis and lay eggs. The wrists, areola, waistline, and groin may all be involved, creating an imaginary circle between the areas described as the “circle of Hebra.” Penile and scrotal lesions are common in men.
Patients usually experience worse pruritus at night, which disturbs sleep. Crusted scabies is a severe form of scabies more often seen in those with immunocompromised immune systems. Clinically, thick crusted and scaly patches are present that are teeming with mites.
Diagnosis can be confirmed by performing a scabies prep, during which a burrow is scraped with a surgical blade. A drop of mineral oil is placed on the skin cells. The mite, ova, and feces can be visualized under the microscope. Wrists and hands usually have the highest yield for finding the parasites.
Topical treatments include permethrin 5% cream, lindane, benzyl benzoate, and crotamiton, and should be applied as two treatments a week apart. In the United States, permethrin is most commonly used. Ivermectin pills are used off label and are very effective and may be repeated for 1-2 weeks. All household contacts should be treated. Patients may still have pruritus for 2-4 weeks following treatment.
In this patient, a scabies prep was performed prior to performing repeat skin biopsies. Microscopic examination revealed ova, one mite, and feces. Treatment was initiated with ivermectin and permethrin.
Photos and case were submitted by Susannah Berke, MD, and Damon McClain, MD, Three Rivers Dermatology, Coraopolis, Pa.; and Dr. Bilu Martin.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
Parent group warns of social media/eating disorders link
A parents’ advocacy group with more than 2.5 million members nationwide sent an advisory to its members on Jan. 11, warning that social media’s January onslaught of messages for dieting and weight loss may be particularly harmful to kids struggling with weight and body image.
The guidance from ParentsTogether noted that such messages can trigger eating disorders and body dysmorphia. But some are particularly dangerous.
A Wall Street Journal investigation recently found that TikTok is distributing videos of rapid-weight-loss competitions and ways to purge food.
According to the ParentsTogether advisory, the Wall Street Journal also found TikTok has sent thousands of videos to teen accounts with messages such as “how to eat only 300 calories a day” or ”how to hide not eating from parents.” The group says similar messages appear on other social media platforms children use daily.
The seasonal January barrage of ads comes on top of a pandemic trend of worsening eating disorder patterns in young people worldwide.
Amanda Kloer, an organizer of the campaign behind the advisory and mother of two teenagers, said in an interview: “We know that January is a particularly sensitive month for this because of the amount of ad spending the wellness industry does.
“We wanted parents to be aware that while these risks exist year round, if they have a kid who is at risk, who is struggling a bit, they should pay particular attention to what they’re seeing on social media in January.”
Ms. Kloer sets up accounts on different platforms to test the messages a teen might receive and says the algorithms ramp up the frequency and the severity of the content as interest by the user grows.
“It sends kids down an extremely dangerous rabbit hole,” she said.
Debra Katzman, MD, with the division of adolescent medicine, department of pediatrics, University of Toronto, wrote in the Journal of Adolescent Health: “The COVID-19 pandemic has had a severe impact on individuals with eating disorders. Since the onset of the COVID-19 pandemic, eating disorder experts from across the globe have observed a substantial increase in the number and severity of new and preexisting young people suffering with eating disorders compared to prior years.”
Contributors beyond social media include lockdowns that bring steady access to food, distancing from peers, anxiety over school closures, and lack of a steady routine.
Eleanor Benner, PsyD, with Children’s Hospital of Philadelphia, said in an interview that awareness is growing regarding the increase in eating disorders correlated with social media use.
Researchers and experts have acknowledged that social media use has increased and changed during the pandemic. Awareness is heightened as parents have been home with kids and noticing what kids are seeing online.
Dr. Benner, a psychologist for the eating disorder assessment and treatment program at CHOP, said platforms have made attempts to limit eating disorder content, but “the reality is that content producers can find ways around this, and unfortunately, we don’t know for whom exactly that content poses greatest risk of contributing to the onset of an eating disorder.”
The most important change for physicians and families to watch for is weight loss, Dr. Benner said.
“Weight loss or lack of weight in children and teenagers is not okay,” she said. “Kids and adolescents should be continually growing and gaining weight through their early 20s.”
Signs of trouble may include diet changes, rejections of favorite foods, and abnormal changes in physical activity, mood, and personality.
Dr. Benner said parents should feel empowered to share these changes with their pediatrician and request that the doctor not discuss weight in front of their children.
Parents should initiate conversations around what kids are seeing to help encourage critical questioning of social media content, Dr. Benner said.
“Parents can also promote body neutrality, the idea that bodies are neither good nor bad, that we don’t have to love our bodies, but acknowledge what they do for us and go about our lives without getting stuck on what they look or feel like,” she said.
Neutrality also extends to categorizing food, and Dr. Benner advised calling foods what they are – ice cream or broccoli, not “junk” or “healthy,” she said. “Food should not be a moral issue. Moralizing and labeling foods perpetuates diet culture and can contribute to shame and guilt around eating.”
ParentsTogether also called on social media platforms to:
- Remove extreme content and stop sending weight-loss material to kids’ accounts: Social media platforms should remove the most extreme and dangerous content such as promoting skin lightening, the group said.
- Create parental account settings. That way, parents can see what their kids see and initiate conversations about bodies and health.
- Feature diverse content creators. The group urges platforms to promote creators with diverse personal appearances and backgrounds and those who support body acceptance and self-love.
ParentsTogether had collected more than 2,700 signatures by Jan. 13 on an online petition asking Instagram and TikTok to “Stop pushing extreme weight loss and dieting on kids.”
Pinterest became the first major platform to prohibit all weight loss ads, according to its announcement in July 2021.
The platform announced, “It’s an expansion of our ad policies that have long prohibited body shaming and dangerous weight loss products or claims. We encourage others in the industry to do the same and acknowledge, once and for all, that there’s no such thing as one size fits all.”
Ms. Kloer and Dr. Benner report no relevant financial relationships.
A parents’ advocacy group with more than 2.5 million members nationwide sent an advisory to its members on Jan. 11, warning that social media’s January onslaught of messages for dieting and weight loss may be particularly harmful to kids struggling with weight and body image.
The guidance from ParentsTogether noted that such messages can trigger eating disorders and body dysmorphia. But some are particularly dangerous.
A Wall Street Journal investigation recently found that TikTok is distributing videos of rapid-weight-loss competitions and ways to purge food.
According to the ParentsTogether advisory, the Wall Street Journal also found TikTok has sent thousands of videos to teen accounts with messages such as “how to eat only 300 calories a day” or ”how to hide not eating from parents.” The group says similar messages appear on other social media platforms children use daily.
The seasonal January barrage of ads comes on top of a pandemic trend of worsening eating disorder patterns in young people worldwide.
Amanda Kloer, an organizer of the campaign behind the advisory and mother of two teenagers, said in an interview: “We know that January is a particularly sensitive month for this because of the amount of ad spending the wellness industry does.
“We wanted parents to be aware that while these risks exist year round, if they have a kid who is at risk, who is struggling a bit, they should pay particular attention to what they’re seeing on social media in January.”
Ms. Kloer sets up accounts on different platforms to test the messages a teen might receive and says the algorithms ramp up the frequency and the severity of the content as interest by the user grows.
“It sends kids down an extremely dangerous rabbit hole,” she said.
Debra Katzman, MD, with the division of adolescent medicine, department of pediatrics, University of Toronto, wrote in the Journal of Adolescent Health: “The COVID-19 pandemic has had a severe impact on individuals with eating disorders. Since the onset of the COVID-19 pandemic, eating disorder experts from across the globe have observed a substantial increase in the number and severity of new and preexisting young people suffering with eating disorders compared to prior years.”
Contributors beyond social media include lockdowns that bring steady access to food, distancing from peers, anxiety over school closures, and lack of a steady routine.
Eleanor Benner, PsyD, with Children’s Hospital of Philadelphia, said in an interview that awareness is growing regarding the increase in eating disorders correlated with social media use.
Researchers and experts have acknowledged that social media use has increased and changed during the pandemic. Awareness is heightened as parents have been home with kids and noticing what kids are seeing online.
Dr. Benner, a psychologist for the eating disorder assessment and treatment program at CHOP, said platforms have made attempts to limit eating disorder content, but “the reality is that content producers can find ways around this, and unfortunately, we don’t know for whom exactly that content poses greatest risk of contributing to the onset of an eating disorder.”
The most important change for physicians and families to watch for is weight loss, Dr. Benner said.
“Weight loss or lack of weight in children and teenagers is not okay,” she said. “Kids and adolescents should be continually growing and gaining weight through their early 20s.”
Signs of trouble may include diet changes, rejections of favorite foods, and abnormal changes in physical activity, mood, and personality.
Dr. Benner said parents should feel empowered to share these changes with their pediatrician and request that the doctor not discuss weight in front of their children.
Parents should initiate conversations around what kids are seeing to help encourage critical questioning of social media content, Dr. Benner said.
“Parents can also promote body neutrality, the idea that bodies are neither good nor bad, that we don’t have to love our bodies, but acknowledge what they do for us and go about our lives without getting stuck on what they look or feel like,” she said.
Neutrality also extends to categorizing food, and Dr. Benner advised calling foods what they are – ice cream or broccoli, not “junk” or “healthy,” she said. “Food should not be a moral issue. Moralizing and labeling foods perpetuates diet culture and can contribute to shame and guilt around eating.”
ParentsTogether also called on social media platforms to:
- Remove extreme content and stop sending weight-loss material to kids’ accounts: Social media platforms should remove the most extreme and dangerous content such as promoting skin lightening, the group said.
- Create parental account settings. That way, parents can see what their kids see and initiate conversations about bodies and health.
- Feature diverse content creators. The group urges platforms to promote creators with diverse personal appearances and backgrounds and those who support body acceptance and self-love.
ParentsTogether had collected more than 2,700 signatures by Jan. 13 on an online petition asking Instagram and TikTok to “Stop pushing extreme weight loss and dieting on kids.”
Pinterest became the first major platform to prohibit all weight loss ads, according to its announcement in July 2021.
The platform announced, “It’s an expansion of our ad policies that have long prohibited body shaming and dangerous weight loss products or claims. We encourage others in the industry to do the same and acknowledge, once and for all, that there’s no such thing as one size fits all.”
Ms. Kloer and Dr. Benner report no relevant financial relationships.
A parents’ advocacy group with more than 2.5 million members nationwide sent an advisory to its members on Jan. 11, warning that social media’s January onslaught of messages for dieting and weight loss may be particularly harmful to kids struggling with weight and body image.
The guidance from ParentsTogether noted that such messages can trigger eating disorders and body dysmorphia. But some are particularly dangerous.
A Wall Street Journal investigation recently found that TikTok is distributing videos of rapid-weight-loss competitions and ways to purge food.
According to the ParentsTogether advisory, the Wall Street Journal also found TikTok has sent thousands of videos to teen accounts with messages such as “how to eat only 300 calories a day” or ”how to hide not eating from parents.” The group says similar messages appear on other social media platforms children use daily.
The seasonal January barrage of ads comes on top of a pandemic trend of worsening eating disorder patterns in young people worldwide.
Amanda Kloer, an organizer of the campaign behind the advisory and mother of two teenagers, said in an interview: “We know that January is a particularly sensitive month for this because of the amount of ad spending the wellness industry does.
“We wanted parents to be aware that while these risks exist year round, if they have a kid who is at risk, who is struggling a bit, they should pay particular attention to what they’re seeing on social media in January.”
Ms. Kloer sets up accounts on different platforms to test the messages a teen might receive and says the algorithms ramp up the frequency and the severity of the content as interest by the user grows.
“It sends kids down an extremely dangerous rabbit hole,” she said.
Debra Katzman, MD, with the division of adolescent medicine, department of pediatrics, University of Toronto, wrote in the Journal of Adolescent Health: “The COVID-19 pandemic has had a severe impact on individuals with eating disorders. Since the onset of the COVID-19 pandemic, eating disorder experts from across the globe have observed a substantial increase in the number and severity of new and preexisting young people suffering with eating disorders compared to prior years.”
Contributors beyond social media include lockdowns that bring steady access to food, distancing from peers, anxiety over school closures, and lack of a steady routine.
Eleanor Benner, PsyD, with Children’s Hospital of Philadelphia, said in an interview that awareness is growing regarding the increase in eating disorders correlated with social media use.
Researchers and experts have acknowledged that social media use has increased and changed during the pandemic. Awareness is heightened as parents have been home with kids and noticing what kids are seeing online.
Dr. Benner, a psychologist for the eating disorder assessment and treatment program at CHOP, said platforms have made attempts to limit eating disorder content, but “the reality is that content producers can find ways around this, and unfortunately, we don’t know for whom exactly that content poses greatest risk of contributing to the onset of an eating disorder.”
The most important change for physicians and families to watch for is weight loss, Dr. Benner said.
“Weight loss or lack of weight in children and teenagers is not okay,” she said. “Kids and adolescents should be continually growing and gaining weight through their early 20s.”
Signs of trouble may include diet changes, rejections of favorite foods, and abnormal changes in physical activity, mood, and personality.
Dr. Benner said parents should feel empowered to share these changes with their pediatrician and request that the doctor not discuss weight in front of their children.
Parents should initiate conversations around what kids are seeing to help encourage critical questioning of social media content, Dr. Benner said.
“Parents can also promote body neutrality, the idea that bodies are neither good nor bad, that we don’t have to love our bodies, but acknowledge what they do for us and go about our lives without getting stuck on what they look or feel like,” she said.
Neutrality also extends to categorizing food, and Dr. Benner advised calling foods what they are – ice cream or broccoli, not “junk” or “healthy,” she said. “Food should not be a moral issue. Moralizing and labeling foods perpetuates diet culture and can contribute to shame and guilt around eating.”
ParentsTogether also called on social media platforms to:
- Remove extreme content and stop sending weight-loss material to kids’ accounts: Social media platforms should remove the most extreme and dangerous content such as promoting skin lightening, the group said.
- Create parental account settings. That way, parents can see what their kids see and initiate conversations about bodies and health.
- Feature diverse content creators. The group urges platforms to promote creators with diverse personal appearances and backgrounds and those who support body acceptance and self-love.
ParentsTogether had collected more than 2,700 signatures by Jan. 13 on an online petition asking Instagram and TikTok to “Stop pushing extreme weight loss and dieting on kids.”
Pinterest became the first major platform to prohibit all weight loss ads, according to its announcement in July 2021.
The platform announced, “It’s an expansion of our ad policies that have long prohibited body shaming and dangerous weight loss products or claims. We encourage others in the industry to do the same and acknowledge, once and for all, that there’s no such thing as one size fits all.”
Ms. Kloer and Dr. Benner report no relevant financial relationships.
Stabilizing circadian rhythm tied to lower suicide risk in bipolar disorder
Social rhythm therapy (SRT), which uses behavioral strategies to support healthy sleep and other routines, is linked to improved mood and reduced suicide risk in young people with bipolar disorder (BD), early research suggests.
The small study also showed SRT is both feasible and acceptable in this patient population.
Results showed SRT, which was primarily delivered via telehealth sessions, began to show efficacy approximately 6 weeks into the 12-week therapeutic program, the researchers noted.
“Improving the regularity of daily rhythms like sleep, physical activity, and social activities can be really robust in improving mental health and even reducing suicide risk,” study investigator Hilary P. Blumberg, MD, the John and Hope Furth Professor of Psychiatric Neuroscience and director of the mood disorders research program at Yale University, New Haven, Conn., said in an interview.
The findings are published in the American Journal of Psychotherapy.
Trigger for depression, mania
Previous research shows unstable circadian rhythms may trigger depressive and manic symptoms – and are risk factors for suicidal thoughts and behaviors. Although interpersonal and social rhythm therapy has shown promise in patients with mood disorders, there is little research focusing only on the social rhythm aspect of the therapy.
The researchers only examined SRT, modified to create a therapeutic program aimed at adolescents and young adults.
The study included 13 participants (mean age, 20.5 years) with BD and a score of 15 or more on the 29-item Hamilton Depression Rating Scale (HDRS-29) and/or a score of 12 or more on the Young Mania Rating Scale (YMRS).
Participants were enrolled in the National Institute of Mental Health Brain Emotion Circuitry Targeted Self-Monitoring and Regulation Therapy (BE-SMART) program, which requires MRI sessions at three in-person visits to assess brain changes with the therapy. All but one participant was taking mood-stabilizing medications.
“We didn’t ask them to come off medications because we didn’t want to exacerbate things,” said Dr. Blumberg. She added the therapeutic approach “could be adjunctive to further improve symptoms and reduce risk.”
The majority occurred on a secure video platform. Three were conducted in person.
Working with a therapist, participants were taught how to follow a daily routine. Dr. Blumberg noted this is not just a matter of going to sleep and getting up at the same time every day, but thoroughly reviewing details of all daily activities and routines, including who participants eat with and when, their exercise schedule, and social engagements.
Each week, participants completed the five-item version of the Social Rhythm Metric. At the end of the intervention, they also completed the Client Satisfaction Questionnaire (CSQ). Scores on the CSQ range from 8 to 32, with scores of 26-32 indicating “excellent” satisfaction.
In addition, participants and therapists completed the Working Alliance Inventory, which assesses the client-therapist relationship by asking about such things as degree of comfort and respect.
Before and after the intervention, participants reported the regularity of their social rhythms using the Brief Social Rhythm Scale (BSRS) and risk for suicidal behavior using a subscale of the Concise Health Risk Tracking (CHRT) scale.
High retention, ‘excellent satisfaction’
Results showed 10 of the 13 participants (9 females) completed all study procedures, for a retention rate of 77%. Treatment satisfaction was excellent (mean CSQ, 29.4).
Both therapists and participants had high scores on all aspects of the Working Alliance Inventory scale.
“High treatment retention, excellent client satisfaction, and strong working alliance scores support the feasibility and acceptability of this intervention for adolescents and young adults with bipolar disorder,” the investigators wrote.
Participants showed significant improvement in social rhythm regularity and reductions in depression and manic symptoms as well as suicide propensity (P = .016 for BSRS; .024 for HDRS-29; .028 for YMRS; and .028 for CHRT suicide propensity). Effect sizes were in the moderate to high range.
By the midpoint of the therapy, there were significant improvements in social rhythm regularity and suicide propensity and trend-level reductions in depression, suggesting the potential for early benefits.
Dr. Blumberg noted it is difficult to find a therapy that helps with both depressive and mania symptoms. “An antidepressant may reduce depression, but sometimes can worsen manic symptoms.”
Impact on emotional brain circuitry?
The association between improved regularity of social rhythms and reduced suicide propensity persisted even after controlling for mood symptom changes.
“Suicide risk was reduced not just because subjects were less depressed. There’s something about regularizing rhythms that can reduce suicide risk,” said Dr. Blumberg.
The reviewers noted that SRT administered remotely improves accessibility; and this intervention “is well suited to the future of psychotherapy delivery, which will undoubtedly include remote treatment delivery.”
The absence of a comparator condition was cited as a study limitation. The investigators noted the small sample size means the findings should be interpreted cautiously and verified in an adequately powered randomized controlled trial.
The researchers now have early results from the brain scanning component of the study. “Preliminary findings suggest the intervention seems to benefit emotional brain circuitry,” Dr. Blumberg said.
The researchers are about to embark on a new study funded by a grant from the American Foundation of Suicide Prevention. It will investigate SRT in preventing suicide in adolescents and adults to age 29 years with depression or BD.
In addition, the researchers have secured support from the Klingenstein Third Generation Foundation to research prevention in youth at risk for BD – and from Women’s Health Access Matters to examine the therapy in women 50 and older with depression, a population possibly at increased risk for dementia.
‘Promising’ results
Commenting on the findings, Michael Thase, MD, professor of psychiatry, University of Pennsylvania, and research psychiatrist at the Corporal Michael J. Crescenz Veterans Affairs Medical Center, both in Philadelphia, praised the study.
“It’s a very, very promising initial study because even though there’s no control group, it does show that participants liked the program, most finished it, and on average, people got quite a bit better,” said Dr. Thase, who was not involved with the research.
The treatment may be especially beneficial for young patients with bipolar disorder who, just by their very age, experience lifestyle disruptions, Dr. Thase noted. Results from a previous study of the therapeutic approach in adults showed “probably half of the adults didn’t take to it.”
However, not everyone in this new study benefited either, as some dropped out, which Dr. Thase noted is not atypical.
“No form of intervention is suitable for everyone,” he said.
The study was supported by grants from the National Institute of Mental Health, AIM Youth Mental Health Foundation, Klingenstein Third Generation Foundation, American Foundation for Suicide Prevention, International Bipolar Foundation, MQ Brighter Futures Program, For the Love of Travis Foundation, and the John and Hope Furth Endowment. Dr. Blumberg and Dr. Thase reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Social rhythm therapy (SRT), which uses behavioral strategies to support healthy sleep and other routines, is linked to improved mood and reduced suicide risk in young people with bipolar disorder (BD), early research suggests.
The small study also showed SRT is both feasible and acceptable in this patient population.
Results showed SRT, which was primarily delivered via telehealth sessions, began to show efficacy approximately 6 weeks into the 12-week therapeutic program, the researchers noted.
“Improving the regularity of daily rhythms like sleep, physical activity, and social activities can be really robust in improving mental health and even reducing suicide risk,” study investigator Hilary P. Blumberg, MD, the John and Hope Furth Professor of Psychiatric Neuroscience and director of the mood disorders research program at Yale University, New Haven, Conn., said in an interview.
The findings are published in the American Journal of Psychotherapy.
Trigger for depression, mania
Previous research shows unstable circadian rhythms may trigger depressive and manic symptoms – and are risk factors for suicidal thoughts and behaviors. Although interpersonal and social rhythm therapy has shown promise in patients with mood disorders, there is little research focusing only on the social rhythm aspect of the therapy.
The researchers only examined SRT, modified to create a therapeutic program aimed at adolescents and young adults.
The study included 13 participants (mean age, 20.5 years) with BD and a score of 15 or more on the 29-item Hamilton Depression Rating Scale (HDRS-29) and/or a score of 12 or more on the Young Mania Rating Scale (YMRS).
Participants were enrolled in the National Institute of Mental Health Brain Emotion Circuitry Targeted Self-Monitoring and Regulation Therapy (BE-SMART) program, which requires MRI sessions at three in-person visits to assess brain changes with the therapy. All but one participant was taking mood-stabilizing medications.
“We didn’t ask them to come off medications because we didn’t want to exacerbate things,” said Dr. Blumberg. She added the therapeutic approach “could be adjunctive to further improve symptoms and reduce risk.”
The majority occurred on a secure video platform. Three were conducted in person.
Working with a therapist, participants were taught how to follow a daily routine. Dr. Blumberg noted this is not just a matter of going to sleep and getting up at the same time every day, but thoroughly reviewing details of all daily activities and routines, including who participants eat with and when, their exercise schedule, and social engagements.
Each week, participants completed the five-item version of the Social Rhythm Metric. At the end of the intervention, they also completed the Client Satisfaction Questionnaire (CSQ). Scores on the CSQ range from 8 to 32, with scores of 26-32 indicating “excellent” satisfaction.
In addition, participants and therapists completed the Working Alliance Inventory, which assesses the client-therapist relationship by asking about such things as degree of comfort and respect.
Before and after the intervention, participants reported the regularity of their social rhythms using the Brief Social Rhythm Scale (BSRS) and risk for suicidal behavior using a subscale of the Concise Health Risk Tracking (CHRT) scale.
High retention, ‘excellent satisfaction’
Results showed 10 of the 13 participants (9 females) completed all study procedures, for a retention rate of 77%. Treatment satisfaction was excellent (mean CSQ, 29.4).
Both therapists and participants had high scores on all aspects of the Working Alliance Inventory scale.
“High treatment retention, excellent client satisfaction, and strong working alliance scores support the feasibility and acceptability of this intervention for adolescents and young adults with bipolar disorder,” the investigators wrote.
Participants showed significant improvement in social rhythm regularity and reductions in depression and manic symptoms as well as suicide propensity (P = .016 for BSRS; .024 for HDRS-29; .028 for YMRS; and .028 for CHRT suicide propensity). Effect sizes were in the moderate to high range.
By the midpoint of the therapy, there were significant improvements in social rhythm regularity and suicide propensity and trend-level reductions in depression, suggesting the potential for early benefits.
Dr. Blumberg noted it is difficult to find a therapy that helps with both depressive and mania symptoms. “An antidepressant may reduce depression, but sometimes can worsen manic symptoms.”
Impact on emotional brain circuitry?
The association between improved regularity of social rhythms and reduced suicide propensity persisted even after controlling for mood symptom changes.
“Suicide risk was reduced not just because subjects were less depressed. There’s something about regularizing rhythms that can reduce suicide risk,” said Dr. Blumberg.
The reviewers noted that SRT administered remotely improves accessibility; and this intervention “is well suited to the future of psychotherapy delivery, which will undoubtedly include remote treatment delivery.”
The absence of a comparator condition was cited as a study limitation. The investigators noted the small sample size means the findings should be interpreted cautiously and verified in an adequately powered randomized controlled trial.
The researchers now have early results from the brain scanning component of the study. “Preliminary findings suggest the intervention seems to benefit emotional brain circuitry,” Dr. Blumberg said.
The researchers are about to embark on a new study funded by a grant from the American Foundation of Suicide Prevention. It will investigate SRT in preventing suicide in adolescents and adults to age 29 years with depression or BD.
In addition, the researchers have secured support from the Klingenstein Third Generation Foundation to research prevention in youth at risk for BD – and from Women’s Health Access Matters to examine the therapy in women 50 and older with depression, a population possibly at increased risk for dementia.
‘Promising’ results
Commenting on the findings, Michael Thase, MD, professor of psychiatry, University of Pennsylvania, and research psychiatrist at the Corporal Michael J. Crescenz Veterans Affairs Medical Center, both in Philadelphia, praised the study.
“It’s a very, very promising initial study because even though there’s no control group, it does show that participants liked the program, most finished it, and on average, people got quite a bit better,” said Dr. Thase, who was not involved with the research.
The treatment may be especially beneficial for young patients with bipolar disorder who, just by their very age, experience lifestyle disruptions, Dr. Thase noted. Results from a previous study of the therapeutic approach in adults showed “probably half of the adults didn’t take to it.”
However, not everyone in this new study benefited either, as some dropped out, which Dr. Thase noted is not atypical.
“No form of intervention is suitable for everyone,” he said.
The study was supported by grants from the National Institute of Mental Health, AIM Youth Mental Health Foundation, Klingenstein Third Generation Foundation, American Foundation for Suicide Prevention, International Bipolar Foundation, MQ Brighter Futures Program, For the Love of Travis Foundation, and the John and Hope Furth Endowment. Dr. Blumberg and Dr. Thase reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Social rhythm therapy (SRT), which uses behavioral strategies to support healthy sleep and other routines, is linked to improved mood and reduced suicide risk in young people with bipolar disorder (BD), early research suggests.
The small study also showed SRT is both feasible and acceptable in this patient population.
Results showed SRT, which was primarily delivered via telehealth sessions, began to show efficacy approximately 6 weeks into the 12-week therapeutic program, the researchers noted.
“Improving the regularity of daily rhythms like sleep, physical activity, and social activities can be really robust in improving mental health and even reducing suicide risk,” study investigator Hilary P. Blumberg, MD, the John and Hope Furth Professor of Psychiatric Neuroscience and director of the mood disorders research program at Yale University, New Haven, Conn., said in an interview.
The findings are published in the American Journal of Psychotherapy.
Trigger for depression, mania
Previous research shows unstable circadian rhythms may trigger depressive and manic symptoms – and are risk factors for suicidal thoughts and behaviors. Although interpersonal and social rhythm therapy has shown promise in patients with mood disorders, there is little research focusing only on the social rhythm aspect of the therapy.
The researchers only examined SRT, modified to create a therapeutic program aimed at adolescents and young adults.
The study included 13 participants (mean age, 20.5 years) with BD and a score of 15 or more on the 29-item Hamilton Depression Rating Scale (HDRS-29) and/or a score of 12 or more on the Young Mania Rating Scale (YMRS).
Participants were enrolled in the National Institute of Mental Health Brain Emotion Circuitry Targeted Self-Monitoring and Regulation Therapy (BE-SMART) program, which requires MRI sessions at three in-person visits to assess brain changes with the therapy. All but one participant was taking mood-stabilizing medications.
“We didn’t ask them to come off medications because we didn’t want to exacerbate things,” said Dr. Blumberg. She added the therapeutic approach “could be adjunctive to further improve symptoms and reduce risk.”
The majority occurred on a secure video platform. Three were conducted in person.
Working with a therapist, participants were taught how to follow a daily routine. Dr. Blumberg noted this is not just a matter of going to sleep and getting up at the same time every day, but thoroughly reviewing details of all daily activities and routines, including who participants eat with and when, their exercise schedule, and social engagements.
Each week, participants completed the five-item version of the Social Rhythm Metric. At the end of the intervention, they also completed the Client Satisfaction Questionnaire (CSQ). Scores on the CSQ range from 8 to 32, with scores of 26-32 indicating “excellent” satisfaction.
In addition, participants and therapists completed the Working Alliance Inventory, which assesses the client-therapist relationship by asking about such things as degree of comfort and respect.
Before and after the intervention, participants reported the regularity of their social rhythms using the Brief Social Rhythm Scale (BSRS) and risk for suicidal behavior using a subscale of the Concise Health Risk Tracking (CHRT) scale.
High retention, ‘excellent satisfaction’
Results showed 10 of the 13 participants (9 females) completed all study procedures, for a retention rate of 77%. Treatment satisfaction was excellent (mean CSQ, 29.4).
Both therapists and participants had high scores on all aspects of the Working Alliance Inventory scale.
“High treatment retention, excellent client satisfaction, and strong working alliance scores support the feasibility and acceptability of this intervention for adolescents and young adults with bipolar disorder,” the investigators wrote.
Participants showed significant improvement in social rhythm regularity and reductions in depression and manic symptoms as well as suicide propensity (P = .016 for BSRS; .024 for HDRS-29; .028 for YMRS; and .028 for CHRT suicide propensity). Effect sizes were in the moderate to high range.
By the midpoint of the therapy, there were significant improvements in social rhythm regularity and suicide propensity and trend-level reductions in depression, suggesting the potential for early benefits.
Dr. Blumberg noted it is difficult to find a therapy that helps with both depressive and mania symptoms. “An antidepressant may reduce depression, but sometimes can worsen manic symptoms.”
Impact on emotional brain circuitry?
The association between improved regularity of social rhythms and reduced suicide propensity persisted even after controlling for mood symptom changes.
“Suicide risk was reduced not just because subjects were less depressed. There’s something about regularizing rhythms that can reduce suicide risk,” said Dr. Blumberg.
The reviewers noted that SRT administered remotely improves accessibility; and this intervention “is well suited to the future of psychotherapy delivery, which will undoubtedly include remote treatment delivery.”
The absence of a comparator condition was cited as a study limitation. The investigators noted the small sample size means the findings should be interpreted cautiously and verified in an adequately powered randomized controlled trial.
The researchers now have early results from the brain scanning component of the study. “Preliminary findings suggest the intervention seems to benefit emotional brain circuitry,” Dr. Blumberg said.
The researchers are about to embark on a new study funded by a grant from the American Foundation of Suicide Prevention. It will investigate SRT in preventing suicide in adolescents and adults to age 29 years with depression or BD.
In addition, the researchers have secured support from the Klingenstein Third Generation Foundation to research prevention in youth at risk for BD – and from Women’s Health Access Matters to examine the therapy in women 50 and older with depression, a population possibly at increased risk for dementia.
‘Promising’ results
Commenting on the findings, Michael Thase, MD, professor of psychiatry, University of Pennsylvania, and research psychiatrist at the Corporal Michael J. Crescenz Veterans Affairs Medical Center, both in Philadelphia, praised the study.
“It’s a very, very promising initial study because even though there’s no control group, it does show that participants liked the program, most finished it, and on average, people got quite a bit better,” said Dr. Thase, who was not involved with the research.
The treatment may be especially beneficial for young patients with bipolar disorder who, just by their very age, experience lifestyle disruptions, Dr. Thase noted. Results from a previous study of the therapeutic approach in adults showed “probably half of the adults didn’t take to it.”
However, not everyone in this new study benefited either, as some dropped out, which Dr. Thase noted is not atypical.
“No form of intervention is suitable for everyone,” he said.
The study was supported by grants from the National Institute of Mental Health, AIM Youth Mental Health Foundation, Klingenstein Third Generation Foundation, American Foundation for Suicide Prevention, International Bipolar Foundation, MQ Brighter Futures Program, For the Love of Travis Foundation, and the John and Hope Furth Endowment. Dr. Blumberg and Dr. Thase reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF PSYCHOTHERAPY
Medicaid expansion curbs disparities, increases immigrant access, in postpartum care
Expanding Medicaid coverage has proved beneficial to postpartum women and may even help reduce disparities, say two new papers.
In the first study, expansion of Medicaid coverage under the Affordable Care Act was associated with higher rates of postpartum coverage and outpatient visits, according to results published in JAMA Health Forum.
Racial and ethnic disparities were also reduced in postpartum coverage, although these disparities remained between Black and White women for outpatient visits.
In the second study, published in JAMA Network Open, researchers found that when postpartum care is covered as part of Emergency Medicaid, women who have been denied access because of their citizenship status are able to use these services, which includes contraception.
Federal law currently prohibits undocumented and documented immigrants who have been in the United States for less than 5 years from receiving full-benefit Medicaid. Coverage is limited to Emergency Medicaid, which offers benefits only for life-threatening conditions, including hospital admission for childbirth. Coverage is not available for prenatal or postpartum care, including contraception.
For the first article, lead author Maria W. Steenland, SD, of Brown University, Providence, R.I., and colleagues point out that compared with other high-income countries, maternal mortality is higher in the United States and largely driven by persistent racial disparities. Compared with non-Hispanic White women, the rates of maternal death are more than twice as high among American Indian and Alaska Native women, and more than threefold greater in non-Hispanic Black women.
“To be clear, visits increased by around the same amount for Black and White individuals after Medicaid expansion, it is just that visits started off lower among Black women, and remained lower by a similar degree,” said Dr. Steenland.
One explanation is that Black women experience racial discrimination during pregnancy-related health care including childbirth hospitalizations and this may make them more reticent to seek postpartum care, she explained. “In addition, the ability to seek health care is determined by insurance as well as other social factors such as paid leave from work, childcare, and transportation, and these other factors may have remained a larger barrier for Black women after expansion.”
In this cohort study, they looked at the association of Medicaid expansion in Arkansas with continuous postpartum coverage, postpartum health care use, and change in racial disparities in the study outcomes. Using the Arkansas All-Payer Claims Database for persons with a childbirth between 2013 and 2015, the authors identified 60,990 childbirths. Of this group, 67% were White, 22% Black, and 7% Hispanic, and 72.3% were covered by Medicaid. The remaining 27.7% were paid for by a commercial payer.
Before Medicaid expansion, 50.6% of women with Medicaid had continuous coverage during the 6 months postpartum, and the share of women with Medicaid childbirth coverage who were continuously covered for 6 months postpartum increased to 69.3% in 2014 and 90.0% in 2015. Medicaid expansion was associated with a 27.8% increase in continuous coverage for 6-12 months postpartum, and 0.9 increase in visits or a relative increase of 75.0% in outpatient care compared with the visit rate of 1.2 visits within the first 6 months postpartum during the pre-expansion period.
A subgroup analysis was conducted to see if Medicaid expansion had any effect on the disparities between White and Black patients. In the 2-year period after expansion, the percentage of both Black and White women with continuous 6-month postpartum coverage increased to 87.9% and 85.9%, respectively. White individuals averaged 2 visits in the first 6 months postpartum versus 1.6 for Black individuals before expansion, and even though there was no difference in postpartum insurance coverage after expansion, racial disparities in the number of visits during the first 6 months postpartum remained after Medicaid expansion (2.5 vs. 2).
Commenting on the paper, Catherine Cansino, MD, MPH, associate clinical professor in the department of obstetrics and gynecology at the University of California, Davis, noted that she has seen the benefits of Medicaid expansion among obstetric population in California. “I’m glad to see similar expansion in other states,” she said. “But to address persistent health care inequities, I think concierge services or patient care navigation serve a role and can hopefully put a little dent in narrowing gaps.”
Dr. Cansino noted that there are many postpartum patients who need help arranging both pediatric and postpartum care, often prioritizing the newborn appointments. “They also need childcare help so they can focus on their own care as well as transportation,” she said, adding that “it would also be interesting to review racial/ethnic differences with regard to knowledge about contraceptive need immediately postpartum and also about the stigma related to postpartum mental health disorders. If patients don’t see the value of a postpartum visit, they would tend not to attend this visit especially given the many other challenges in the postpartum period.”
Access for immigrants
In the second study, the authors note that the decision to expand Emergency Medicaid options is largely up to individual states. Led by Maria I. Rodriguez, MD, MPH, of the department of obstetrics and gynecology, Oregon Health & Science University, Portland, and colleagues, they decided to compare two states – Oregon, which expanded Emergency Medicaid to include postpartum services and South Carolina, which kept only the federal minimum services – to see how it affected postpartum care among immigrant women.
Compared with South Carolina, there was a 40.6 percentage-point increase (95% confidence interval [CI] in postpartum care visits, P < .001) and postpartum contraception within 60 days grew by 33.2 percentage points (95% CI, P < .001), in Oregon after expansion went into effect.
“When postpartum care was covered for women who would have qualified for Medicaid, except for their citizenship status, their rates of attendance at a postpartum visit and use of postpartum contraception increased to levels observed in the traditional Medicaid population,” the authors wrote.
The calculations, drawn from Medicaid claims and birth certificate data from 2010 to 2019, assumed parallel trends, meaning the researchers made the assumption that use patterns would have remained the same in Oregon if the Emergency Medicaid expansion hadn’t happened and use in South Carolina would have remained consistent as well. A differential trend analysis showed significant increases in use of the services in Oregon relative to South Carolina.
“We included Oregon and South Carolina because both states have experienced similar growth in their immigrant population and have comparable immigrant populations, in terms of size and country of origin, residing in each state,” the authors noted.
Commenting on the study, Laura Mercer MD, MBA, MPH, associate professor in obstetrics and gynecology and director of the obstetrics and gynecology clerkship at the University of Arizona in Phoenix, said she was “excited and encouraged by the results” but not surprised, as it’s logical to assume that there would be more uptake of the services when they are provided free of charge or at low cost.
“Oftentimes, the mother of the family deprioritizes her own health and well-being in favor of diverting those resources to her children and her family,” said Dr. Mercer, who specializes in prenatal and postpartum care.
She added that the significant increase in contraception is a particularly representative sign of improvement as it is easier to quantify, compared to improvements in mental health or counseling.
But comprehensive postpartum care extends to physical, psychological, and social well-being. “Its components include counseling on the importance of birth spacing and providing the contraceptive method of their choice,” the authors wrote. “An absence of postpartum care has been associated with unintended pregnancy, short interpregnancy intervals, exacerbation of chronic diseases, and preterm birth.”
Dr. Mercer noted that closely spaced pregnancies, particularly less than 6 months but at least less than 18 months carry increased risk for mother and child. And for those who would say that immigrant women should be excluded from the Emergency Medicaid postpartum services, Dr. Mercer said she would encourage them to look at the data around the improved outcomes of comprehensive maternal care.
Being able to track health markers and intervene before a woman requires emergency care will reduce costs in the long run, she pointed out. But, regardless of the cost, policymakers have to ask themselves, “What do we value as a society? If we value families and healthy families and we want to promote the best possible outcomes, then I think this question becomes very easy to answer.”
The first study was funded by the National Institute for Health Care Management. Dr. Steenland was also supported by the Agency for Healthcare Research and Quality and the National Institutes of Health. Dr. Steenland reported grants from the Agency for Healthcare Research and Quality and from the National Institute for Child Health and Human Development during the conduct of the study. The second study was supported by the National Institute on Minority Health and Health Disparities. Dr. Rodriguez reports grants from Arnold Ventures and personal fees from the American College of Obstetricians and Gynecologists, Bayer, and Merck outside the submitted work. A coauthor reports grants from Merck/Organon and the Office of Population Affairs outside the submitted work, as well as membership on the board of directors of the Society of Family Planning and the ACOG Gynecology Clinical Practice Guideline committee. Dr. Mercer reported no relevant financial relationships.
Expanding Medicaid coverage has proved beneficial to postpartum women and may even help reduce disparities, say two new papers.
In the first study, expansion of Medicaid coverage under the Affordable Care Act was associated with higher rates of postpartum coverage and outpatient visits, according to results published in JAMA Health Forum.
Racial and ethnic disparities were also reduced in postpartum coverage, although these disparities remained between Black and White women for outpatient visits.
In the second study, published in JAMA Network Open, researchers found that when postpartum care is covered as part of Emergency Medicaid, women who have been denied access because of their citizenship status are able to use these services, which includes contraception.
Federal law currently prohibits undocumented and documented immigrants who have been in the United States for less than 5 years from receiving full-benefit Medicaid. Coverage is limited to Emergency Medicaid, which offers benefits only for life-threatening conditions, including hospital admission for childbirth. Coverage is not available for prenatal or postpartum care, including contraception.
For the first article, lead author Maria W. Steenland, SD, of Brown University, Providence, R.I., and colleagues point out that compared with other high-income countries, maternal mortality is higher in the United States and largely driven by persistent racial disparities. Compared with non-Hispanic White women, the rates of maternal death are more than twice as high among American Indian and Alaska Native women, and more than threefold greater in non-Hispanic Black women.
“To be clear, visits increased by around the same amount for Black and White individuals after Medicaid expansion, it is just that visits started off lower among Black women, and remained lower by a similar degree,” said Dr. Steenland.
One explanation is that Black women experience racial discrimination during pregnancy-related health care including childbirth hospitalizations and this may make them more reticent to seek postpartum care, she explained. “In addition, the ability to seek health care is determined by insurance as well as other social factors such as paid leave from work, childcare, and transportation, and these other factors may have remained a larger barrier for Black women after expansion.”
In this cohort study, they looked at the association of Medicaid expansion in Arkansas with continuous postpartum coverage, postpartum health care use, and change in racial disparities in the study outcomes. Using the Arkansas All-Payer Claims Database for persons with a childbirth between 2013 and 2015, the authors identified 60,990 childbirths. Of this group, 67% were White, 22% Black, and 7% Hispanic, and 72.3% were covered by Medicaid. The remaining 27.7% were paid for by a commercial payer.
Before Medicaid expansion, 50.6% of women with Medicaid had continuous coverage during the 6 months postpartum, and the share of women with Medicaid childbirth coverage who were continuously covered for 6 months postpartum increased to 69.3% in 2014 and 90.0% in 2015. Medicaid expansion was associated with a 27.8% increase in continuous coverage for 6-12 months postpartum, and 0.9 increase in visits or a relative increase of 75.0% in outpatient care compared with the visit rate of 1.2 visits within the first 6 months postpartum during the pre-expansion period.
A subgroup analysis was conducted to see if Medicaid expansion had any effect on the disparities between White and Black patients. In the 2-year period after expansion, the percentage of both Black and White women with continuous 6-month postpartum coverage increased to 87.9% and 85.9%, respectively. White individuals averaged 2 visits in the first 6 months postpartum versus 1.6 for Black individuals before expansion, and even though there was no difference in postpartum insurance coverage after expansion, racial disparities in the number of visits during the first 6 months postpartum remained after Medicaid expansion (2.5 vs. 2).
Commenting on the paper, Catherine Cansino, MD, MPH, associate clinical professor in the department of obstetrics and gynecology at the University of California, Davis, noted that she has seen the benefits of Medicaid expansion among obstetric population in California. “I’m glad to see similar expansion in other states,” she said. “But to address persistent health care inequities, I think concierge services or patient care navigation serve a role and can hopefully put a little dent in narrowing gaps.”
Dr. Cansino noted that there are many postpartum patients who need help arranging both pediatric and postpartum care, often prioritizing the newborn appointments. “They also need childcare help so they can focus on their own care as well as transportation,” she said, adding that “it would also be interesting to review racial/ethnic differences with regard to knowledge about contraceptive need immediately postpartum and also about the stigma related to postpartum mental health disorders. If patients don’t see the value of a postpartum visit, they would tend not to attend this visit especially given the many other challenges in the postpartum period.”
Access for immigrants
In the second study, the authors note that the decision to expand Emergency Medicaid options is largely up to individual states. Led by Maria I. Rodriguez, MD, MPH, of the department of obstetrics and gynecology, Oregon Health & Science University, Portland, and colleagues, they decided to compare two states – Oregon, which expanded Emergency Medicaid to include postpartum services and South Carolina, which kept only the federal minimum services – to see how it affected postpartum care among immigrant women.
Compared with South Carolina, there was a 40.6 percentage-point increase (95% confidence interval [CI] in postpartum care visits, P < .001) and postpartum contraception within 60 days grew by 33.2 percentage points (95% CI, P < .001), in Oregon after expansion went into effect.
“When postpartum care was covered for women who would have qualified for Medicaid, except for their citizenship status, their rates of attendance at a postpartum visit and use of postpartum contraception increased to levels observed in the traditional Medicaid population,” the authors wrote.
The calculations, drawn from Medicaid claims and birth certificate data from 2010 to 2019, assumed parallel trends, meaning the researchers made the assumption that use patterns would have remained the same in Oregon if the Emergency Medicaid expansion hadn’t happened and use in South Carolina would have remained consistent as well. A differential trend analysis showed significant increases in use of the services in Oregon relative to South Carolina.
“We included Oregon and South Carolina because both states have experienced similar growth in their immigrant population and have comparable immigrant populations, in terms of size and country of origin, residing in each state,” the authors noted.
Commenting on the study, Laura Mercer MD, MBA, MPH, associate professor in obstetrics and gynecology and director of the obstetrics and gynecology clerkship at the University of Arizona in Phoenix, said she was “excited and encouraged by the results” but not surprised, as it’s logical to assume that there would be more uptake of the services when they are provided free of charge or at low cost.
“Oftentimes, the mother of the family deprioritizes her own health and well-being in favor of diverting those resources to her children and her family,” said Dr. Mercer, who specializes in prenatal and postpartum care.
She added that the significant increase in contraception is a particularly representative sign of improvement as it is easier to quantify, compared to improvements in mental health or counseling.
But comprehensive postpartum care extends to physical, psychological, and social well-being. “Its components include counseling on the importance of birth spacing and providing the contraceptive method of their choice,” the authors wrote. “An absence of postpartum care has been associated with unintended pregnancy, short interpregnancy intervals, exacerbation of chronic diseases, and preterm birth.”
Dr. Mercer noted that closely spaced pregnancies, particularly less than 6 months but at least less than 18 months carry increased risk for mother and child. And for those who would say that immigrant women should be excluded from the Emergency Medicaid postpartum services, Dr. Mercer said she would encourage them to look at the data around the improved outcomes of comprehensive maternal care.
Being able to track health markers and intervene before a woman requires emergency care will reduce costs in the long run, she pointed out. But, regardless of the cost, policymakers have to ask themselves, “What do we value as a society? If we value families and healthy families and we want to promote the best possible outcomes, then I think this question becomes very easy to answer.”
The first study was funded by the National Institute for Health Care Management. Dr. Steenland was also supported by the Agency for Healthcare Research and Quality and the National Institutes of Health. Dr. Steenland reported grants from the Agency for Healthcare Research and Quality and from the National Institute for Child Health and Human Development during the conduct of the study. The second study was supported by the National Institute on Minority Health and Health Disparities. Dr. Rodriguez reports grants from Arnold Ventures and personal fees from the American College of Obstetricians and Gynecologists, Bayer, and Merck outside the submitted work. A coauthor reports grants from Merck/Organon and the Office of Population Affairs outside the submitted work, as well as membership on the board of directors of the Society of Family Planning and the ACOG Gynecology Clinical Practice Guideline committee. Dr. Mercer reported no relevant financial relationships.
Expanding Medicaid coverage has proved beneficial to postpartum women and may even help reduce disparities, say two new papers.
In the first study, expansion of Medicaid coverage under the Affordable Care Act was associated with higher rates of postpartum coverage and outpatient visits, according to results published in JAMA Health Forum.
Racial and ethnic disparities were also reduced in postpartum coverage, although these disparities remained between Black and White women for outpatient visits.
In the second study, published in JAMA Network Open, researchers found that when postpartum care is covered as part of Emergency Medicaid, women who have been denied access because of their citizenship status are able to use these services, which includes contraception.
Federal law currently prohibits undocumented and documented immigrants who have been in the United States for less than 5 years from receiving full-benefit Medicaid. Coverage is limited to Emergency Medicaid, which offers benefits only for life-threatening conditions, including hospital admission for childbirth. Coverage is not available for prenatal or postpartum care, including contraception.
For the first article, lead author Maria W. Steenland, SD, of Brown University, Providence, R.I., and colleagues point out that compared with other high-income countries, maternal mortality is higher in the United States and largely driven by persistent racial disparities. Compared with non-Hispanic White women, the rates of maternal death are more than twice as high among American Indian and Alaska Native women, and more than threefold greater in non-Hispanic Black women.
“To be clear, visits increased by around the same amount for Black and White individuals after Medicaid expansion, it is just that visits started off lower among Black women, and remained lower by a similar degree,” said Dr. Steenland.
One explanation is that Black women experience racial discrimination during pregnancy-related health care including childbirth hospitalizations and this may make them more reticent to seek postpartum care, she explained. “In addition, the ability to seek health care is determined by insurance as well as other social factors such as paid leave from work, childcare, and transportation, and these other factors may have remained a larger barrier for Black women after expansion.”
In this cohort study, they looked at the association of Medicaid expansion in Arkansas with continuous postpartum coverage, postpartum health care use, and change in racial disparities in the study outcomes. Using the Arkansas All-Payer Claims Database for persons with a childbirth between 2013 and 2015, the authors identified 60,990 childbirths. Of this group, 67% were White, 22% Black, and 7% Hispanic, and 72.3% were covered by Medicaid. The remaining 27.7% were paid for by a commercial payer.
Before Medicaid expansion, 50.6% of women with Medicaid had continuous coverage during the 6 months postpartum, and the share of women with Medicaid childbirth coverage who were continuously covered for 6 months postpartum increased to 69.3% in 2014 and 90.0% in 2015. Medicaid expansion was associated with a 27.8% increase in continuous coverage for 6-12 months postpartum, and 0.9 increase in visits or a relative increase of 75.0% in outpatient care compared with the visit rate of 1.2 visits within the first 6 months postpartum during the pre-expansion period.
A subgroup analysis was conducted to see if Medicaid expansion had any effect on the disparities between White and Black patients. In the 2-year period after expansion, the percentage of both Black and White women with continuous 6-month postpartum coverage increased to 87.9% and 85.9%, respectively. White individuals averaged 2 visits in the first 6 months postpartum versus 1.6 for Black individuals before expansion, and even though there was no difference in postpartum insurance coverage after expansion, racial disparities in the number of visits during the first 6 months postpartum remained after Medicaid expansion (2.5 vs. 2).
Commenting on the paper, Catherine Cansino, MD, MPH, associate clinical professor in the department of obstetrics and gynecology at the University of California, Davis, noted that she has seen the benefits of Medicaid expansion among obstetric population in California. “I’m glad to see similar expansion in other states,” she said. “But to address persistent health care inequities, I think concierge services or patient care navigation serve a role and can hopefully put a little dent in narrowing gaps.”
Dr. Cansino noted that there are many postpartum patients who need help arranging both pediatric and postpartum care, often prioritizing the newborn appointments. “They also need childcare help so they can focus on their own care as well as transportation,” she said, adding that “it would also be interesting to review racial/ethnic differences with regard to knowledge about contraceptive need immediately postpartum and also about the stigma related to postpartum mental health disorders. If patients don’t see the value of a postpartum visit, they would tend not to attend this visit especially given the many other challenges in the postpartum period.”
Access for immigrants
In the second study, the authors note that the decision to expand Emergency Medicaid options is largely up to individual states. Led by Maria I. Rodriguez, MD, MPH, of the department of obstetrics and gynecology, Oregon Health & Science University, Portland, and colleagues, they decided to compare two states – Oregon, which expanded Emergency Medicaid to include postpartum services and South Carolina, which kept only the federal minimum services – to see how it affected postpartum care among immigrant women.
Compared with South Carolina, there was a 40.6 percentage-point increase (95% confidence interval [CI] in postpartum care visits, P < .001) and postpartum contraception within 60 days grew by 33.2 percentage points (95% CI, P < .001), in Oregon after expansion went into effect.
“When postpartum care was covered for women who would have qualified for Medicaid, except for their citizenship status, their rates of attendance at a postpartum visit and use of postpartum contraception increased to levels observed in the traditional Medicaid population,” the authors wrote.
The calculations, drawn from Medicaid claims and birth certificate data from 2010 to 2019, assumed parallel trends, meaning the researchers made the assumption that use patterns would have remained the same in Oregon if the Emergency Medicaid expansion hadn’t happened and use in South Carolina would have remained consistent as well. A differential trend analysis showed significant increases in use of the services in Oregon relative to South Carolina.
“We included Oregon and South Carolina because both states have experienced similar growth in their immigrant population and have comparable immigrant populations, in terms of size and country of origin, residing in each state,” the authors noted.
Commenting on the study, Laura Mercer MD, MBA, MPH, associate professor in obstetrics and gynecology and director of the obstetrics and gynecology clerkship at the University of Arizona in Phoenix, said she was “excited and encouraged by the results” but not surprised, as it’s logical to assume that there would be more uptake of the services when they are provided free of charge or at low cost.
“Oftentimes, the mother of the family deprioritizes her own health and well-being in favor of diverting those resources to her children and her family,” said Dr. Mercer, who specializes in prenatal and postpartum care.
She added that the significant increase in contraception is a particularly representative sign of improvement as it is easier to quantify, compared to improvements in mental health or counseling.
But comprehensive postpartum care extends to physical, psychological, and social well-being. “Its components include counseling on the importance of birth spacing and providing the contraceptive method of their choice,” the authors wrote. “An absence of postpartum care has been associated with unintended pregnancy, short interpregnancy intervals, exacerbation of chronic diseases, and preterm birth.”
Dr. Mercer noted that closely spaced pregnancies, particularly less than 6 months but at least less than 18 months carry increased risk for mother and child. And for those who would say that immigrant women should be excluded from the Emergency Medicaid postpartum services, Dr. Mercer said she would encourage them to look at the data around the improved outcomes of comprehensive maternal care.
Being able to track health markers and intervene before a woman requires emergency care will reduce costs in the long run, she pointed out. But, regardless of the cost, policymakers have to ask themselves, “What do we value as a society? If we value families and healthy families and we want to promote the best possible outcomes, then I think this question becomes very easy to answer.”
The first study was funded by the National Institute for Health Care Management. Dr. Steenland was also supported by the Agency for Healthcare Research and Quality and the National Institutes of Health. Dr. Steenland reported grants from the Agency for Healthcare Research and Quality and from the National Institute for Child Health and Human Development during the conduct of the study. The second study was supported by the National Institute on Minority Health and Health Disparities. Dr. Rodriguez reports grants from Arnold Ventures and personal fees from the American College of Obstetricians and Gynecologists, Bayer, and Merck outside the submitted work. A coauthor reports grants from Merck/Organon and the Office of Population Affairs outside the submitted work, as well as membership on the board of directors of the Society of Family Planning and the ACOG Gynecology Clinical Practice Guideline committee. Dr. Mercer reported no relevant financial relationships.
FROM JAMA HEALTH FORUM AND JAMA NETWORK OPEN