User login
Standing up to ‘injustice in health’: The Association of Black Gastroenterologists and Hepatologists
“Of all the forms of inequality, injustice in health is the most shocking and inhuman.” – Martin Luther King Jr., March 25, 1966. 1
This single disparity – health care injustice – too often results in needless mental anguish, physical suffering, or death. In the spring of 2020, at the peak of the COVID-19 pandemic, the convergence of injustices in health care and policing led to the disproportionate preventable physical deaths of Black men and women. This became the watershed moment for 11 gastroenterologists and hepatologists who collectively grieved but heeded the call of social responsibility to form the Association of Black Gastroenterologists and Hepatologists.
The mission of ABGH is laser focused. It is to promote health equity in Black communities, advance science, and develop the careers of Black gastroenterologists, hepatologists, and scientists. The vision is to improve gastrointestinal health outcomes in Black communities; to develop the pipeline of Black gastroenterologists and hepatologists given that currently only 4% in the United States identify as Black; to foster networking, mentoring, and sponsorship among Black students, clinical trainees, gastroenterologists, and hepatologists; and to promote the scholarship of Black gastroenterologists and hepatologists.
Through community engagement, ABGH stands to empower the Black community with knowledge and choices, which inherently strengthens the physician-patient relationship. ABGH also exists to implement positive change in long term outcome statistics in Black communities. Black Americans are 20% more likely to be diagnosed with colorectal cancer and 40% more likely to die from the disease. In addition to colorectal cancer, rates of esophageal squamous cancer, as well as cancer of the small bowel and pancreas, are highest in Black people.2 Through scientific research and clinical care, we aim to eradicate digestive health disparities.
Yet in this space, we know first-hand that, in the United States, the wellness of a community is not measured by the medical fitness of its members alone but also by the availability of equitable opportunities for fulfillment of nonmedical but health-impacting social needs. These needs, also known as social determinants of health, are made inaccessible to vulnerable populations because of systemic racism. Importantly, we recognize that dismantling racist systems is not a singular effort, nor are we pioneers in this work, but we look forward to executing health equity goals collaboratively with our fellow gastrointestinal national societies and other leading community and grassroots organizations.
The founders of ABGH are a distinctive group of practicing gastroenterologists and hepatologists from across the United States with a strong track record in DEI work through their community, clinical, and research activities. The board of directors reflects only the depth of talent shared throughout the ABGH membership. The strength of the organization lies in its diverse and energetic constituents who all exemplify outstanding training and the readiness to redefine the standard of health care delivery to the Black community. From medical students to senior level gastroenterologists, we collectively embody a considerable momentum for formation of this organization at this point in our history.
ABGH fulfills a professional career development need for budding gastroenterologists not so readily available from other organizations. The compelling impact of representing the embodiment of what many of us were told we could not become is limitless. The personal and professional growth enabled by our networking and learning from each other is both motivating and empowering since, even after overcoming the obstacles needed to become a medical provider, Black professionals are often not afforded the bandwidth, range of emotion, and protection to reveal their specific needs. For this author personally, the ABGH provides a psychological safety that allows authentic self-identity without code-switching.3 Through this authenticity has arisen formidable strength, creativity, and productivity. The leadership and innovation cultivated in ABGH stands to benefit many generations to come, both within and outside the organization.
Reflections from a junior member of ABGH: Dr. Kafayat Busari
My desire to pursue gastroenterology was bolstered by determination, curiosity, and passion, yet ironically was often met with skepticism by many in position to help advance this goal. Although projections of incertitude on members of a community that are often made to feel inadequate can diminish even the brightest of lights, conversely it can fuel the creation of an organization emboldened to specifically address GI-related health disparities. When I was a second-year internal medicine resident, I encountered a GI physician who told me GI “wasn’t something I wanted to do”—despite me expressing my interest.
Confused by the statement, I reached out to Renee L. Williams, MD, of NYU Langone Health, who I had met during my medical school training. She suggested I join a conference call later that week. On that call and the many that took place thereafter, I was introduced to Black gastroenterologists who are luminal disease experts, chair members, journal editors, transplant hepatologists, interventional endoscopists, researchers, and professors (in other words, GI professional leaders). My time on the initial call lasted perhaps less than 20 minutes, but the impact has been immeasurable.
I was provided the emotional reassurance that GI was indeed for me and told “there’s always a seat, and if it feels like there’s not, we just need to get more chairs.” Little did I know, but those metaphorical chairs were being gathered so that I and other aspiring gastroenterologists will be able to sit comfortably at these tables one day. I was witnessing these GI professional leaders set in motion the beginning of what will undoubtedly be a pivotal component in the way I approach my career as a gastroenterologist. The experience reignited my mental determination to one day attain the level of success represented by the ABGH board members and to persevere in my quest to help redefine how Black medical students and residents serve their communities as physicians.
The creation of the ABGH could not have come at a better time in my training. In the wake of recent public protests for equity of African Americans within every institution (academia, housing, banks, policing, health care, and beyond), which were fundamentally built on racism, being a junior member of ABGH has not only given me a platform to speak my truth but has also provided me with tools to help others do so as well. As someone very passionate about research, primarily in colorectal cancer, I have been given an opportunity to connect with a dream team of mentors who have taken research ideas to new levels and have challenged me to dig deeper and expand my curiosity to investigate what still needs to be uncovered. It has created opportunity after opportunity for actively building relationships, leading to meaningful collaborations and the sharing of innovative ideas and discoveries.
It is important to emphasize that ABGH is not an organization wanting to exclude themselves on the basis of ethnicity. ABGH is an example of how shared health goals within a medical discipline can be achieved when inclusion and equity is at the helm. ABGH led and represented events that raise awareness of diseases affecting all patients and aim to make the GI community more culturally competent. ABGH is future-oriented and embraces all members who align with the mission regardless of ethnicity, gender, orientation, or disability. The institution that is and will be the ABGH impresses upon me a feeling of excitement, gratitude, and humility. I look forward to continuing the mission created by the founding members and being to others what ABGH is to me.
For more information on this organization, please visit blackingastro.org.
Dr. Busari is a resident physician at Florida State University-SMH and a junior member of ABGH. Dr. Guillaume director of the Gastrointestinal Motility Center at Stony Brook (New York) University Hospital and an assistant professor of medicine at the Renaissance School of Medicine at Stony Brook University. They have no disclosures.
References
1. Galarneau C. J Health Care Poor Underserved. 2018;29(1):5-8.
2. Ashktorab H et al. Gastroenterology. 2017 Oct;153(4):910-923.
3. Blanchard AK. N Engl J Med. 2021 Jun 10;384(23):e87.
“Of all the forms of inequality, injustice in health is the most shocking and inhuman.” – Martin Luther King Jr., March 25, 1966. 1
This single disparity – health care injustice – too often results in needless mental anguish, physical suffering, or death. In the spring of 2020, at the peak of the COVID-19 pandemic, the convergence of injustices in health care and policing led to the disproportionate preventable physical deaths of Black men and women. This became the watershed moment for 11 gastroenterologists and hepatologists who collectively grieved but heeded the call of social responsibility to form the Association of Black Gastroenterologists and Hepatologists.
The mission of ABGH is laser focused. It is to promote health equity in Black communities, advance science, and develop the careers of Black gastroenterologists, hepatologists, and scientists. The vision is to improve gastrointestinal health outcomes in Black communities; to develop the pipeline of Black gastroenterologists and hepatologists given that currently only 4% in the United States identify as Black; to foster networking, mentoring, and sponsorship among Black students, clinical trainees, gastroenterologists, and hepatologists; and to promote the scholarship of Black gastroenterologists and hepatologists.
Through community engagement, ABGH stands to empower the Black community with knowledge and choices, which inherently strengthens the physician-patient relationship. ABGH also exists to implement positive change in long term outcome statistics in Black communities. Black Americans are 20% more likely to be diagnosed with colorectal cancer and 40% more likely to die from the disease. In addition to colorectal cancer, rates of esophageal squamous cancer, as well as cancer of the small bowel and pancreas, are highest in Black people.2 Through scientific research and clinical care, we aim to eradicate digestive health disparities.
Yet in this space, we know first-hand that, in the United States, the wellness of a community is not measured by the medical fitness of its members alone but also by the availability of equitable opportunities for fulfillment of nonmedical but health-impacting social needs. These needs, also known as social determinants of health, are made inaccessible to vulnerable populations because of systemic racism. Importantly, we recognize that dismantling racist systems is not a singular effort, nor are we pioneers in this work, but we look forward to executing health equity goals collaboratively with our fellow gastrointestinal national societies and other leading community and grassroots organizations.
The founders of ABGH are a distinctive group of practicing gastroenterologists and hepatologists from across the United States with a strong track record in DEI work through their community, clinical, and research activities. The board of directors reflects only the depth of talent shared throughout the ABGH membership. The strength of the organization lies in its diverse and energetic constituents who all exemplify outstanding training and the readiness to redefine the standard of health care delivery to the Black community. From medical students to senior level gastroenterologists, we collectively embody a considerable momentum for formation of this organization at this point in our history.
ABGH fulfills a professional career development need for budding gastroenterologists not so readily available from other organizations. The compelling impact of representing the embodiment of what many of us were told we could not become is limitless. The personal and professional growth enabled by our networking and learning from each other is both motivating and empowering since, even after overcoming the obstacles needed to become a medical provider, Black professionals are often not afforded the bandwidth, range of emotion, and protection to reveal their specific needs. For this author personally, the ABGH provides a psychological safety that allows authentic self-identity without code-switching.3 Through this authenticity has arisen formidable strength, creativity, and productivity. The leadership and innovation cultivated in ABGH stands to benefit many generations to come, both within and outside the organization.
Reflections from a junior member of ABGH: Dr. Kafayat Busari
My desire to pursue gastroenterology was bolstered by determination, curiosity, and passion, yet ironically was often met with skepticism by many in position to help advance this goal. Although projections of incertitude on members of a community that are often made to feel inadequate can diminish even the brightest of lights, conversely it can fuel the creation of an organization emboldened to specifically address GI-related health disparities. When I was a second-year internal medicine resident, I encountered a GI physician who told me GI “wasn’t something I wanted to do”—despite me expressing my interest.
Confused by the statement, I reached out to Renee L. Williams, MD, of NYU Langone Health, who I had met during my medical school training. She suggested I join a conference call later that week. On that call and the many that took place thereafter, I was introduced to Black gastroenterologists who are luminal disease experts, chair members, journal editors, transplant hepatologists, interventional endoscopists, researchers, and professors (in other words, GI professional leaders). My time on the initial call lasted perhaps less than 20 minutes, but the impact has been immeasurable.
I was provided the emotional reassurance that GI was indeed for me and told “there’s always a seat, and if it feels like there’s not, we just need to get more chairs.” Little did I know, but those metaphorical chairs were being gathered so that I and other aspiring gastroenterologists will be able to sit comfortably at these tables one day. I was witnessing these GI professional leaders set in motion the beginning of what will undoubtedly be a pivotal component in the way I approach my career as a gastroenterologist. The experience reignited my mental determination to one day attain the level of success represented by the ABGH board members and to persevere in my quest to help redefine how Black medical students and residents serve their communities as physicians.
The creation of the ABGH could not have come at a better time in my training. In the wake of recent public protests for equity of African Americans within every institution (academia, housing, banks, policing, health care, and beyond), which were fundamentally built on racism, being a junior member of ABGH has not only given me a platform to speak my truth but has also provided me with tools to help others do so as well. As someone very passionate about research, primarily in colorectal cancer, I have been given an opportunity to connect with a dream team of mentors who have taken research ideas to new levels and have challenged me to dig deeper and expand my curiosity to investigate what still needs to be uncovered. It has created opportunity after opportunity for actively building relationships, leading to meaningful collaborations and the sharing of innovative ideas and discoveries.
It is important to emphasize that ABGH is not an organization wanting to exclude themselves on the basis of ethnicity. ABGH is an example of how shared health goals within a medical discipline can be achieved when inclusion and equity is at the helm. ABGH led and represented events that raise awareness of diseases affecting all patients and aim to make the GI community more culturally competent. ABGH is future-oriented and embraces all members who align with the mission regardless of ethnicity, gender, orientation, or disability. The institution that is and will be the ABGH impresses upon me a feeling of excitement, gratitude, and humility. I look forward to continuing the mission created by the founding members and being to others what ABGH is to me.
For more information on this organization, please visit blackingastro.org.
Dr. Busari is a resident physician at Florida State University-SMH and a junior member of ABGH. Dr. Guillaume director of the Gastrointestinal Motility Center at Stony Brook (New York) University Hospital and an assistant professor of medicine at the Renaissance School of Medicine at Stony Brook University. They have no disclosures.
References
1. Galarneau C. J Health Care Poor Underserved. 2018;29(1):5-8.
2. Ashktorab H et al. Gastroenterology. 2017 Oct;153(4):910-923.
3. Blanchard AK. N Engl J Med. 2021 Jun 10;384(23):e87.
“Of all the forms of inequality, injustice in health is the most shocking and inhuman.” – Martin Luther King Jr., March 25, 1966. 1
This single disparity – health care injustice – too often results in needless mental anguish, physical suffering, or death. In the spring of 2020, at the peak of the COVID-19 pandemic, the convergence of injustices in health care and policing led to the disproportionate preventable physical deaths of Black men and women. This became the watershed moment for 11 gastroenterologists and hepatologists who collectively grieved but heeded the call of social responsibility to form the Association of Black Gastroenterologists and Hepatologists.
The mission of ABGH is laser focused. It is to promote health equity in Black communities, advance science, and develop the careers of Black gastroenterologists, hepatologists, and scientists. The vision is to improve gastrointestinal health outcomes in Black communities; to develop the pipeline of Black gastroenterologists and hepatologists given that currently only 4% in the United States identify as Black; to foster networking, mentoring, and sponsorship among Black students, clinical trainees, gastroenterologists, and hepatologists; and to promote the scholarship of Black gastroenterologists and hepatologists.
Through community engagement, ABGH stands to empower the Black community with knowledge and choices, which inherently strengthens the physician-patient relationship. ABGH also exists to implement positive change in long term outcome statistics in Black communities. Black Americans are 20% more likely to be diagnosed with colorectal cancer and 40% more likely to die from the disease. In addition to colorectal cancer, rates of esophageal squamous cancer, as well as cancer of the small bowel and pancreas, are highest in Black people.2 Through scientific research and clinical care, we aim to eradicate digestive health disparities.
Yet in this space, we know first-hand that, in the United States, the wellness of a community is not measured by the medical fitness of its members alone but also by the availability of equitable opportunities for fulfillment of nonmedical but health-impacting social needs. These needs, also known as social determinants of health, are made inaccessible to vulnerable populations because of systemic racism. Importantly, we recognize that dismantling racist systems is not a singular effort, nor are we pioneers in this work, but we look forward to executing health equity goals collaboratively with our fellow gastrointestinal national societies and other leading community and grassroots organizations.
The founders of ABGH are a distinctive group of practicing gastroenterologists and hepatologists from across the United States with a strong track record in DEI work through their community, clinical, and research activities. The board of directors reflects only the depth of talent shared throughout the ABGH membership. The strength of the organization lies in its diverse and energetic constituents who all exemplify outstanding training and the readiness to redefine the standard of health care delivery to the Black community. From medical students to senior level gastroenterologists, we collectively embody a considerable momentum for formation of this organization at this point in our history.
ABGH fulfills a professional career development need for budding gastroenterologists not so readily available from other organizations. The compelling impact of representing the embodiment of what many of us were told we could not become is limitless. The personal and professional growth enabled by our networking and learning from each other is both motivating and empowering since, even after overcoming the obstacles needed to become a medical provider, Black professionals are often not afforded the bandwidth, range of emotion, and protection to reveal their specific needs. For this author personally, the ABGH provides a psychological safety that allows authentic self-identity without code-switching.3 Through this authenticity has arisen formidable strength, creativity, and productivity. The leadership and innovation cultivated in ABGH stands to benefit many generations to come, both within and outside the organization.
Reflections from a junior member of ABGH: Dr. Kafayat Busari
My desire to pursue gastroenterology was bolstered by determination, curiosity, and passion, yet ironically was often met with skepticism by many in position to help advance this goal. Although projections of incertitude on members of a community that are often made to feel inadequate can diminish even the brightest of lights, conversely it can fuel the creation of an organization emboldened to specifically address GI-related health disparities. When I was a second-year internal medicine resident, I encountered a GI physician who told me GI “wasn’t something I wanted to do”—despite me expressing my interest.
Confused by the statement, I reached out to Renee L. Williams, MD, of NYU Langone Health, who I had met during my medical school training. She suggested I join a conference call later that week. On that call and the many that took place thereafter, I was introduced to Black gastroenterologists who are luminal disease experts, chair members, journal editors, transplant hepatologists, interventional endoscopists, researchers, and professors (in other words, GI professional leaders). My time on the initial call lasted perhaps less than 20 minutes, but the impact has been immeasurable.
I was provided the emotional reassurance that GI was indeed for me and told “there’s always a seat, and if it feels like there’s not, we just need to get more chairs.” Little did I know, but those metaphorical chairs were being gathered so that I and other aspiring gastroenterologists will be able to sit comfortably at these tables one day. I was witnessing these GI professional leaders set in motion the beginning of what will undoubtedly be a pivotal component in the way I approach my career as a gastroenterologist. The experience reignited my mental determination to one day attain the level of success represented by the ABGH board members and to persevere in my quest to help redefine how Black medical students and residents serve their communities as physicians.
The creation of the ABGH could not have come at a better time in my training. In the wake of recent public protests for equity of African Americans within every institution (academia, housing, banks, policing, health care, and beyond), which were fundamentally built on racism, being a junior member of ABGH has not only given me a platform to speak my truth but has also provided me with tools to help others do so as well. As someone very passionate about research, primarily in colorectal cancer, I have been given an opportunity to connect with a dream team of mentors who have taken research ideas to new levels and have challenged me to dig deeper and expand my curiosity to investigate what still needs to be uncovered. It has created opportunity after opportunity for actively building relationships, leading to meaningful collaborations and the sharing of innovative ideas and discoveries.
It is important to emphasize that ABGH is not an organization wanting to exclude themselves on the basis of ethnicity. ABGH is an example of how shared health goals within a medical discipline can be achieved when inclusion and equity is at the helm. ABGH led and represented events that raise awareness of diseases affecting all patients and aim to make the GI community more culturally competent. ABGH is future-oriented and embraces all members who align with the mission regardless of ethnicity, gender, orientation, or disability. The institution that is and will be the ABGH impresses upon me a feeling of excitement, gratitude, and humility. I look forward to continuing the mission created by the founding members and being to others what ABGH is to me.
For more information on this organization, please visit blackingastro.org.
Dr. Busari is a resident physician at Florida State University-SMH and a junior member of ABGH. Dr. Guillaume director of the Gastrointestinal Motility Center at Stony Brook (New York) University Hospital and an assistant professor of medicine at the Renaissance School of Medicine at Stony Brook University. They have no disclosures.
References
1. Galarneau C. J Health Care Poor Underserved. 2018;29(1):5-8.
2. Ashktorab H et al. Gastroenterology. 2017 Oct;153(4):910-923.
3. Blanchard AK. N Engl J Med. 2021 Jun 10;384(23):e87.
Long COVID appears to ‘impair’ survival in cancer patients
More than one in six cancer patients experience long-term sequelae following SARS-CoV-2 infection, placing them at increased risk of discontinuing their cancer treatment or dying, according to European registry data.
Given the “high lethality” of COVID-19 in cancer patients and the risk for long-term complications following infection in the general population, Alessio Cortellini, MD, a consultant medical oncologist at Hammersmith Hospital and Imperial College London, and colleagues wanted to explore the “prevalence and clinical significance of COVID-19 sequelae in cancer patients and their oncological continuity of care.”
Dr. Cortellini presented the OnCovid registry research on Sept. 21 at the 2021 European Society for Medical Oncology Congress. He reported that overall, the data suggest that post–COVID-19 complications may “impair” patients’ cancer survival as well as their cancer care.
The OnCovid registry data showed that the 15% of cancer patients who had long-term COVID-19 complications were 76% more likely to die than those without sequelae. Cancer patients with COVID-19 sequelae were significantly more likely to permanently stop taking their systemic anticancer therapy, and they were more than 3.5 times more likely to die than those who continued their treatment as planned. In terms of long-term complications, almost half of patients experienced dyspnea, and two-fifths reported chronic fatigue.
“This data confirms the need to continue to prioritize cancer patients,” Antonio Passaro, MD, PhD, division of thoracic oncology, European Institute of Oncology IRCCS, Milan, commented in a press release. “In the fight against the pandemic, it is of the utmost importance that we do not neglect to study and understand the curves of cancer incidence and mortality.”
Invited to discuss the results, Anne-Marie C. Dingemans, MD, PhD, a pulmonologist and professor of thoracic oncology at Erasmus Medical Center, Rotterdam, the Netherlands, said COVID-19 remains a “very important” issue for cancer patients.
Interestingly, Dr. Dingemans noted that COVID-19 sequelae in patients with cancer appear to occur slightly less frequently, compared with estimates in the general population – which range from 13% to 60% – though patients with cancer tend to have more respiratory problems.
However, Dr. Dingemans added, the difficulty with comparing sequelae rates between cancer patients and the general population is that cancer patients “probably already have a lot of symptoms” associated with long COVID, such as dyspnea and fatigue, and may not be aware that they are experiencing COVID sequelae.
The registry results
To investigate the long-term impact of COVID-19 on survival and continuity of care, the team examined data from the OnCovid registry, which was established at the beginning of the pandemic to study consecutive patients aged 18 years and older with confirmed SARS-CoV-2 infection and a history of solid or hematologic malignancies.
At the data cutoff on March 1, 2021, the registry included 35 institutions in six European countries. The institutions collected information on patient demographics and comorbidities, cancer history, anticancer therapy, COVID-19 investigations, and COVID-19–specific therapies.
For the current analysis, the team included 1,557 of 2,634 patients who had undergone a clinical reassessment after recovering from COVID-19. Information sufficient to conduct multivariate analysis was available for 840 of these patients.
About half of the patients were younger than 60 years, and just over half were women. The most common cancer diagnoses were breast cancer (23.4%), gastrointestinal tumors (16.5%), gynecologic/genitourinary tumors (19.3%), and hematologic cancers (14.1%), with even distribution between local/locoregional and advanced disease.
The median interval between COVID-19 recovery and reassessment was 44 days, and the mean post–COVID-19 follow-up period was 128 days.
About 15% of patients experienced at least one long-term sequela from COVID-19. The most common were dyspnea/shortness of breath (49.6%), fatigue (41.0%), chronic cough (33.8%), and other respiratory complications (10.7%).
Dr. Cortellini noted that cancer patients who experienced sequelae were more likely to be male, aged 65 years or older, to have at least two comorbidities, and to have a history of smoking. In addition, cancer patients who experienced long-term complications were significantly more likely to have had COVID-19 complications, to have required COVID-19 therapy, and to have been hospitalized for the disease.
Factoring in gender, age, comorbidity burden, primary tumor, stage, receipt of anticancer and anti–COVID-19 therapy, COVID-19 complications, and hospitalization, the team found that COVID-19 sequelae were independently associated with an increased risk for death (hazard ratio, 1.76).
Further analysis of patterns of systemic anticancer therapy in 471 patients revealed that 14.8% of COVID-19 survivors permanently discontinued therapy and that a dose or regimen adjustment occurred for 37.8%.
Patients who permanently discontinued anticancer therapy were more likely to be former or current smokers, to have had COVID-19 complications or been hospitalized for COVID-19, and to have had COVID-19 sequelae at reassessment. The investigators found no association between permanent discontinuation of therapy and cancer disease stage.
Dr. Cortellini and colleagues reported that permanent cessation of systemic anticancer therapy was associated with an increased risk for death. A change in dose or regimen did not affect survival.
The most common reason for stopping therapy permanently was deterioration of the patient’s performance status (61.3%), followed by disease progression (29.0%). Dose or regimen adjustments typically occurred to avoid immune suppression (50.0%), hospitalization (25.8%), and intravenous drug administration (19.1%).
Dr. Cortellini concluded his presentation by highlighting the importance of increasing awareness of long COVID in patients with cancer as well as early treatment of COVID-19 sequelae to improve patient outcomes.
The study was funded by the Imperial College Biomedical Research Center. Dr. Cortellini has relationships with MSD, Bristol-Myers Squibb, Roche, Novartis, AstraZeneca, Astellas, and Sun Pharma. Dr. Dingemans has relationships with Roche, Eli Lilly, Boehringer Ingelheim, AstraZeneca, Jansen, Chiesi, Amgen, Pfizer, Bayer, Takeda, Pharmamar, and Sanofi.
A version of this article first appeared on Medscape.com.
More than one in six cancer patients experience long-term sequelae following SARS-CoV-2 infection, placing them at increased risk of discontinuing their cancer treatment or dying, according to European registry data.
Given the “high lethality” of COVID-19 in cancer patients and the risk for long-term complications following infection in the general population, Alessio Cortellini, MD, a consultant medical oncologist at Hammersmith Hospital and Imperial College London, and colleagues wanted to explore the “prevalence and clinical significance of COVID-19 sequelae in cancer patients and their oncological continuity of care.”
Dr. Cortellini presented the OnCovid registry research on Sept. 21 at the 2021 European Society for Medical Oncology Congress. He reported that overall, the data suggest that post–COVID-19 complications may “impair” patients’ cancer survival as well as their cancer care.
The OnCovid registry data showed that the 15% of cancer patients who had long-term COVID-19 complications were 76% more likely to die than those without sequelae. Cancer patients with COVID-19 sequelae were significantly more likely to permanently stop taking their systemic anticancer therapy, and they were more than 3.5 times more likely to die than those who continued their treatment as planned. In terms of long-term complications, almost half of patients experienced dyspnea, and two-fifths reported chronic fatigue.
“This data confirms the need to continue to prioritize cancer patients,” Antonio Passaro, MD, PhD, division of thoracic oncology, European Institute of Oncology IRCCS, Milan, commented in a press release. “In the fight against the pandemic, it is of the utmost importance that we do not neglect to study and understand the curves of cancer incidence and mortality.”
Invited to discuss the results, Anne-Marie C. Dingemans, MD, PhD, a pulmonologist and professor of thoracic oncology at Erasmus Medical Center, Rotterdam, the Netherlands, said COVID-19 remains a “very important” issue for cancer patients.
Interestingly, Dr. Dingemans noted that COVID-19 sequelae in patients with cancer appear to occur slightly less frequently, compared with estimates in the general population – which range from 13% to 60% – though patients with cancer tend to have more respiratory problems.
However, Dr. Dingemans added, the difficulty with comparing sequelae rates between cancer patients and the general population is that cancer patients “probably already have a lot of symptoms” associated with long COVID, such as dyspnea and fatigue, and may not be aware that they are experiencing COVID sequelae.
The registry results
To investigate the long-term impact of COVID-19 on survival and continuity of care, the team examined data from the OnCovid registry, which was established at the beginning of the pandemic to study consecutive patients aged 18 years and older with confirmed SARS-CoV-2 infection and a history of solid or hematologic malignancies.
At the data cutoff on March 1, 2021, the registry included 35 institutions in six European countries. The institutions collected information on patient demographics and comorbidities, cancer history, anticancer therapy, COVID-19 investigations, and COVID-19–specific therapies.
For the current analysis, the team included 1,557 of 2,634 patients who had undergone a clinical reassessment after recovering from COVID-19. Information sufficient to conduct multivariate analysis was available for 840 of these patients.
About half of the patients were younger than 60 years, and just over half were women. The most common cancer diagnoses were breast cancer (23.4%), gastrointestinal tumors (16.5%), gynecologic/genitourinary tumors (19.3%), and hematologic cancers (14.1%), with even distribution between local/locoregional and advanced disease.
The median interval between COVID-19 recovery and reassessment was 44 days, and the mean post–COVID-19 follow-up period was 128 days.
About 15% of patients experienced at least one long-term sequela from COVID-19. The most common were dyspnea/shortness of breath (49.6%), fatigue (41.0%), chronic cough (33.8%), and other respiratory complications (10.7%).
Dr. Cortellini noted that cancer patients who experienced sequelae were more likely to be male, aged 65 years or older, to have at least two comorbidities, and to have a history of smoking. In addition, cancer patients who experienced long-term complications were significantly more likely to have had COVID-19 complications, to have required COVID-19 therapy, and to have been hospitalized for the disease.
Factoring in gender, age, comorbidity burden, primary tumor, stage, receipt of anticancer and anti–COVID-19 therapy, COVID-19 complications, and hospitalization, the team found that COVID-19 sequelae were independently associated with an increased risk for death (hazard ratio, 1.76).
Further analysis of patterns of systemic anticancer therapy in 471 patients revealed that 14.8% of COVID-19 survivors permanently discontinued therapy and that a dose or regimen adjustment occurred for 37.8%.
Patients who permanently discontinued anticancer therapy were more likely to be former or current smokers, to have had COVID-19 complications or been hospitalized for COVID-19, and to have had COVID-19 sequelae at reassessment. The investigators found no association between permanent discontinuation of therapy and cancer disease stage.
Dr. Cortellini and colleagues reported that permanent cessation of systemic anticancer therapy was associated with an increased risk for death. A change in dose or regimen did not affect survival.
The most common reason for stopping therapy permanently was deterioration of the patient’s performance status (61.3%), followed by disease progression (29.0%). Dose or regimen adjustments typically occurred to avoid immune suppression (50.0%), hospitalization (25.8%), and intravenous drug administration (19.1%).
Dr. Cortellini concluded his presentation by highlighting the importance of increasing awareness of long COVID in patients with cancer as well as early treatment of COVID-19 sequelae to improve patient outcomes.
The study was funded by the Imperial College Biomedical Research Center. Dr. Cortellini has relationships with MSD, Bristol-Myers Squibb, Roche, Novartis, AstraZeneca, Astellas, and Sun Pharma. Dr. Dingemans has relationships with Roche, Eli Lilly, Boehringer Ingelheim, AstraZeneca, Jansen, Chiesi, Amgen, Pfizer, Bayer, Takeda, Pharmamar, and Sanofi.
A version of this article first appeared on Medscape.com.
More than one in six cancer patients experience long-term sequelae following SARS-CoV-2 infection, placing them at increased risk of discontinuing their cancer treatment or dying, according to European registry data.
Given the “high lethality” of COVID-19 in cancer patients and the risk for long-term complications following infection in the general population, Alessio Cortellini, MD, a consultant medical oncologist at Hammersmith Hospital and Imperial College London, and colleagues wanted to explore the “prevalence and clinical significance of COVID-19 sequelae in cancer patients and their oncological continuity of care.”
Dr. Cortellini presented the OnCovid registry research on Sept. 21 at the 2021 European Society for Medical Oncology Congress. He reported that overall, the data suggest that post–COVID-19 complications may “impair” patients’ cancer survival as well as their cancer care.
The OnCovid registry data showed that the 15% of cancer patients who had long-term COVID-19 complications were 76% more likely to die than those without sequelae. Cancer patients with COVID-19 sequelae were significantly more likely to permanently stop taking their systemic anticancer therapy, and they were more than 3.5 times more likely to die than those who continued their treatment as planned. In terms of long-term complications, almost half of patients experienced dyspnea, and two-fifths reported chronic fatigue.
“This data confirms the need to continue to prioritize cancer patients,” Antonio Passaro, MD, PhD, division of thoracic oncology, European Institute of Oncology IRCCS, Milan, commented in a press release. “In the fight against the pandemic, it is of the utmost importance that we do not neglect to study and understand the curves of cancer incidence and mortality.”
Invited to discuss the results, Anne-Marie C. Dingemans, MD, PhD, a pulmonologist and professor of thoracic oncology at Erasmus Medical Center, Rotterdam, the Netherlands, said COVID-19 remains a “very important” issue for cancer patients.
Interestingly, Dr. Dingemans noted that COVID-19 sequelae in patients with cancer appear to occur slightly less frequently, compared with estimates in the general population – which range from 13% to 60% – though patients with cancer tend to have more respiratory problems.
However, Dr. Dingemans added, the difficulty with comparing sequelae rates between cancer patients and the general population is that cancer patients “probably already have a lot of symptoms” associated with long COVID, such as dyspnea and fatigue, and may not be aware that they are experiencing COVID sequelae.
The registry results
To investigate the long-term impact of COVID-19 on survival and continuity of care, the team examined data from the OnCovid registry, which was established at the beginning of the pandemic to study consecutive patients aged 18 years and older with confirmed SARS-CoV-2 infection and a history of solid or hematologic malignancies.
At the data cutoff on March 1, 2021, the registry included 35 institutions in six European countries. The institutions collected information on patient demographics and comorbidities, cancer history, anticancer therapy, COVID-19 investigations, and COVID-19–specific therapies.
For the current analysis, the team included 1,557 of 2,634 patients who had undergone a clinical reassessment after recovering from COVID-19. Information sufficient to conduct multivariate analysis was available for 840 of these patients.
About half of the patients were younger than 60 years, and just over half were women. The most common cancer diagnoses were breast cancer (23.4%), gastrointestinal tumors (16.5%), gynecologic/genitourinary tumors (19.3%), and hematologic cancers (14.1%), with even distribution between local/locoregional and advanced disease.
The median interval between COVID-19 recovery and reassessment was 44 days, and the mean post–COVID-19 follow-up period was 128 days.
About 15% of patients experienced at least one long-term sequela from COVID-19. The most common were dyspnea/shortness of breath (49.6%), fatigue (41.0%), chronic cough (33.8%), and other respiratory complications (10.7%).
Dr. Cortellini noted that cancer patients who experienced sequelae were more likely to be male, aged 65 years or older, to have at least two comorbidities, and to have a history of smoking. In addition, cancer patients who experienced long-term complications were significantly more likely to have had COVID-19 complications, to have required COVID-19 therapy, and to have been hospitalized for the disease.
Factoring in gender, age, comorbidity burden, primary tumor, stage, receipt of anticancer and anti–COVID-19 therapy, COVID-19 complications, and hospitalization, the team found that COVID-19 sequelae were independently associated with an increased risk for death (hazard ratio, 1.76).
Further analysis of patterns of systemic anticancer therapy in 471 patients revealed that 14.8% of COVID-19 survivors permanently discontinued therapy and that a dose or regimen adjustment occurred for 37.8%.
Patients who permanently discontinued anticancer therapy were more likely to be former or current smokers, to have had COVID-19 complications or been hospitalized for COVID-19, and to have had COVID-19 sequelae at reassessment. The investigators found no association between permanent discontinuation of therapy and cancer disease stage.
Dr. Cortellini and colleagues reported that permanent cessation of systemic anticancer therapy was associated with an increased risk for death. A change in dose or regimen did not affect survival.
The most common reason for stopping therapy permanently was deterioration of the patient’s performance status (61.3%), followed by disease progression (29.0%). Dose or regimen adjustments typically occurred to avoid immune suppression (50.0%), hospitalization (25.8%), and intravenous drug administration (19.1%).
Dr. Cortellini concluded his presentation by highlighting the importance of increasing awareness of long COVID in patients with cancer as well as early treatment of COVID-19 sequelae to improve patient outcomes.
The study was funded by the Imperial College Biomedical Research Center. Dr. Cortellini has relationships with MSD, Bristol-Myers Squibb, Roche, Novartis, AstraZeneca, Astellas, and Sun Pharma. Dr. Dingemans has relationships with Roche, Eli Lilly, Boehringer Ingelheim, AstraZeneca, Jansen, Chiesi, Amgen, Pfizer, Bayer, Takeda, Pharmamar, and Sanofi.
A version of this article first appeared on Medscape.com.
Management of advanced endometrial cancer
Endometrial cancer is most commonly diagnosed at an early stage. Unfortunately, there is a trend toward the diagnosis of more advanced disease, for which cure is rare, and this is an important contributing factor toward the overall increasing mortality trend for endometrial cancer.
Histology is a major risk factor for advanced disease. For example, serous carcinoma, which accounts for approximately only 10% of all endometrial cancer diagnoses, comprises 25% of cases of advanced cases. Similarly, carcinosarcoma, a cell type known to be particularly aggressive, is relatively overrepresented among cases of advanced disease.
Advanced endometrial cancer includes cases of stage III (involvement of lymph nodes, ovaries, and vagina) and stage IV disease (with direct extension into pelvic viscera and distant metastases). In most cases of stage III disease, extrauterine metastases are microscopic and are detected only at the time of surgical staging. Bulky nodal disease within the pelvic and para-aortic nodal basins is less common but associated with worse prognosis than for patients with microscopic nodal metastases. Stage IV disease usually presents with peritoneal spread of disease including carcinomatosis, omental disease, and involvement of the small and large intestine.
Once advanced, endometrial cancer requires more than surgery alone, relying heavily on adjuvant therapies to achieve responses, particularly systemic therapy with platinum and taxane chemotherapy. In some cases, molecularly targeted therapy (such as trastuzumab for serous carcinomas that demonstrate overexpression of HER2) has been shown to be superior in efficacy.1 Surgery may involve either radical nodal dissections to the infrarenal aortic basin, and/or peritoneal debulking procedures similar to that required for ovarian cancer. Perhaps because of patterns of disease distribution so similar to ovarian cancer, historically, sequencing of therapy focused on radical primary debulking surgery (PDS) followed by chemotherapy.
In 2000, a retrospective series from Johns Hopkins University documented the outcomes of 65 patients with advanced endometrial cancer who had undergone primary debulking surgery followed by chemotherapy.2 They noted that survival was directly associated with degree of cytoreduction, with the best outcomes seen for those patients whose surgery resulted in no gross residual disease. Following these data, PDS with complete resection of all disease became the goal of primary therapy.
However, unlike ovarian cancer (which shares a similar disease distribution with advanced endometrial cancer) patients with endometrial cancer are more obese, older, and typically have more comorbidities. Therefore, radical primary debulking surgeries may be associated with poor patient perioperative outcomes, and feasibility of complete cytoreduction, particularly in very obese patients, can be limited. For this reason, neoadjuvant chemotherapy (NACT) has been explored as an option. The potential virtue of NACT is that it allows for tumor deposits to decrease in size, or be eliminated, prior to surgery, resulting in a less morbid procedure for the patient.
Observed outcomes for NACT relative to PDS are mixed. When small series have compared the two for the treatment of advanced serous endometrial cancer, NACT was associated with decreased perioperative morbidity, with similar overall survival observed.3,4
However, in larger series exploring patients within the National Cancer Database (a collection of over 1,500 hospitals accredited by the Commission on Cancer) outcomes appear different for the two approaches.5,6 While PDS was initially associated with worse survival, at approximately 5-6 months from diagnosis, this changed and survival was observed to be consistently superior for this group. These data suggest that patients undergoing primary surgical cytoreduction may experience an early mortality risk, possibly secondary to the impact of surgery, but that if they are to survive beyond this point, they experience better outcomes. While the researchers attempted to control for risk factors of poor outcomes that might have systematically differed between the two groups, this specific database is limited in its ability to account for all fundamental differences between them. Only approximately 15% of women with advanced endometrial cancer were offered NACT during those time periods. This observation alone suggests that this likely represents a group specially selected for their poor candidacy for upfront debulking surgery, and inherently increased risk for death from all causes.
The question remains, is NACT appropriate for all patients or just those who are considered poor surgical candidates? Could all patients benefit from the decreased morbidity associated with surgery after NACT without compromising survival? Randomized controlled trials are necessary to answer this question as they are the only way to ensure that risk factors for poor outcomes (such as histology, disease distribution, medical comorbidities) are equally distributed among both groups.
In the meantime, gynecologic oncologists should take a cautious approach to decision making regarding sequencing of surgery and chemotherapy in the setting of a new diagnosis of advanced endometrial cancer. Arguably more important than surgical interventions, access to molecularly targeted systemic therapy is likely to bring the best outcomes for advanced endometrial cancer. Carboplatin and paclitaxel are the current gold standard of care for frontline systemic therapy; however, response rates with this regimen are less favorable for endometrial cancer than for ovarian cancer. Work is being done to test novel therapies against actionable targets to use as alternatives or as adjuncts to traditional chemotherapy regimens. In doing so, clinicians are learning to distinguish endometrial cancers by more than simply their histologic features, but also by their molecular profiles.
Advanced endometrial cancer is a serious disease with high lethality. Future research should focus on ways to ensure toxicities of therapy, including surgery, are minimized while improving upon existing poor clinical outcomes.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no financial disclosures.
References
1. Fader AN et al. J Clin Oncol 2018;36(20):2044-51.
2. Bristow RE et al. Gynecol Oncol 2000;78(2):85-91.
3. Bogani G et al. Tumori 2019;105(1):92-97.
4. Wilkinson-Ryan I et al. Int J Gynecol Cancer. 2015;25(1):63-8.
5. Tobias CJ et al. JAMA Netw Open 2020;3(12):e2028612.
6. Chambers LM et al. Gynecol Oncol 2021;160(2):405-12.
Endometrial cancer is most commonly diagnosed at an early stage. Unfortunately, there is a trend toward the diagnosis of more advanced disease, for which cure is rare, and this is an important contributing factor toward the overall increasing mortality trend for endometrial cancer.
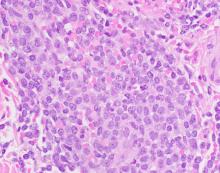
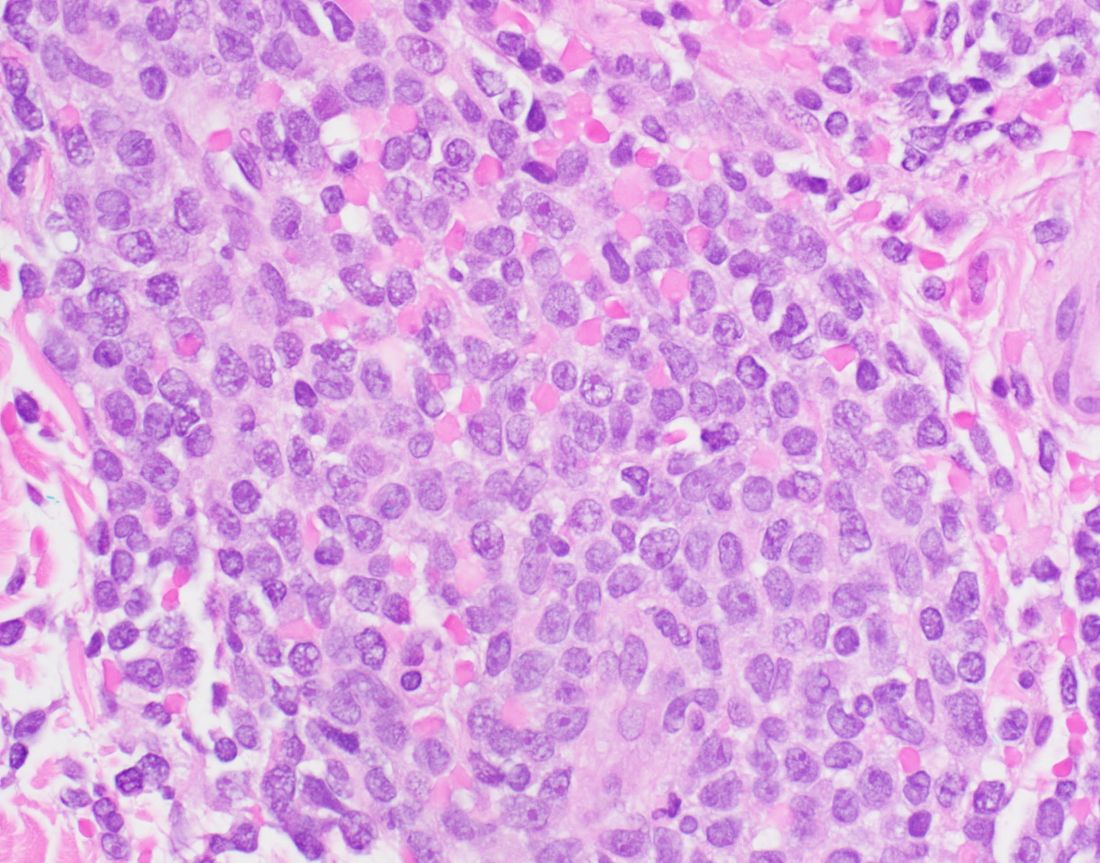
Histology is a major risk factor for advanced disease. For example, serous carcinoma, which accounts for approximately only 10% of all endometrial cancer diagnoses, comprises 25% of cases of advanced cases. Similarly, carcinosarcoma, a cell type known to be particularly aggressive, is relatively overrepresented among cases of advanced disease.
Advanced endometrial cancer includes cases of stage III (involvement of lymph nodes, ovaries, and vagina) and stage IV disease (with direct extension into pelvic viscera and distant metastases). In most cases of stage III disease, extrauterine metastases are microscopic and are detected only at the time of surgical staging. Bulky nodal disease within the pelvic and para-aortic nodal basins is less common but associated with worse prognosis than for patients with microscopic nodal metastases. Stage IV disease usually presents with peritoneal spread of disease including carcinomatosis, omental disease, and involvement of the small and large intestine.
Once advanced, endometrial cancer requires more than surgery alone, relying heavily on adjuvant therapies to achieve responses, particularly systemic therapy with platinum and taxane chemotherapy. In some cases, molecularly targeted therapy (such as trastuzumab for serous carcinomas that demonstrate overexpression of HER2) has been shown to be superior in efficacy.1 Surgery may involve either radical nodal dissections to the infrarenal aortic basin, and/or peritoneal debulking procedures similar to that required for ovarian cancer. Perhaps because of patterns of disease distribution so similar to ovarian cancer, historically, sequencing of therapy focused on radical primary debulking surgery (PDS) followed by chemotherapy.
In 2000, a retrospective series from Johns Hopkins University documented the outcomes of 65 patients with advanced endometrial cancer who had undergone primary debulking surgery followed by chemotherapy.2 They noted that survival was directly associated with degree of cytoreduction, with the best outcomes seen for those patients whose surgery resulted in no gross residual disease. Following these data, PDS with complete resection of all disease became the goal of primary therapy.
However, unlike ovarian cancer (which shares a similar disease distribution with advanced endometrial cancer) patients with endometrial cancer are more obese, older, and typically have more comorbidities. Therefore, radical primary debulking surgeries may be associated with poor patient perioperative outcomes, and feasibility of complete cytoreduction, particularly in very obese patients, can be limited. For this reason, neoadjuvant chemotherapy (NACT) has been explored as an option. The potential virtue of NACT is that it allows for tumor deposits to decrease in size, or be eliminated, prior to surgery, resulting in a less morbid procedure for the patient.
Observed outcomes for NACT relative to PDS are mixed. When small series have compared the two for the treatment of advanced serous endometrial cancer, NACT was associated with decreased perioperative morbidity, with similar overall survival observed.3,4
However, in larger series exploring patients within the National Cancer Database (a collection of over 1,500 hospitals accredited by the Commission on Cancer) outcomes appear different for the two approaches.5,6 While PDS was initially associated with worse survival, at approximately 5-6 months from diagnosis, this changed and survival was observed to be consistently superior for this group. These data suggest that patients undergoing primary surgical cytoreduction may experience an early mortality risk, possibly secondary to the impact of surgery, but that if they are to survive beyond this point, they experience better outcomes. While the researchers attempted to control for risk factors of poor outcomes that might have systematically differed between the two groups, this specific database is limited in its ability to account for all fundamental differences between them. Only approximately 15% of women with advanced endometrial cancer were offered NACT during those time periods. This observation alone suggests that this likely represents a group specially selected for their poor candidacy for upfront debulking surgery, and inherently increased risk for death from all causes.
The question remains, is NACT appropriate for all patients or just those who are considered poor surgical candidates? Could all patients benefit from the decreased morbidity associated with surgery after NACT without compromising survival? Randomized controlled trials are necessary to answer this question as they are the only way to ensure that risk factors for poor outcomes (such as histology, disease distribution, medical comorbidities) are equally distributed among both groups.
In the meantime, gynecologic oncologists should take a cautious approach to decision making regarding sequencing of surgery and chemotherapy in the setting of a new diagnosis of advanced endometrial cancer. Arguably more important than surgical interventions, access to molecularly targeted systemic therapy is likely to bring the best outcomes for advanced endometrial cancer. Carboplatin and paclitaxel are the current gold standard of care for frontline systemic therapy; however, response rates with this regimen are less favorable for endometrial cancer than for ovarian cancer. Work is being done to test novel therapies against actionable targets to use as alternatives or as adjuncts to traditional chemotherapy regimens. In doing so, clinicians are learning to distinguish endometrial cancers by more than simply their histologic features, but also by their molecular profiles.
Advanced endometrial cancer is a serious disease with high lethality. Future research should focus on ways to ensure toxicities of therapy, including surgery, are minimized while improving upon existing poor clinical outcomes.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no financial disclosures.
References
1. Fader AN et al. J Clin Oncol 2018;36(20):2044-51.
2. Bristow RE et al. Gynecol Oncol 2000;78(2):85-91.
3. Bogani G et al. Tumori 2019;105(1):92-97.
4. Wilkinson-Ryan I et al. Int J Gynecol Cancer. 2015;25(1):63-8.
5. Tobias CJ et al. JAMA Netw Open 2020;3(12):e2028612.
6. Chambers LM et al. Gynecol Oncol 2021;160(2):405-12.
Endometrial cancer is most commonly diagnosed at an early stage. Unfortunately, there is a trend toward the diagnosis of more advanced disease, for which cure is rare, and this is an important contributing factor toward the overall increasing mortality trend for endometrial cancer.
Histology is a major risk factor for advanced disease. For example, serous carcinoma, which accounts for approximately only 10% of all endometrial cancer diagnoses, comprises 25% of cases of advanced cases. Similarly, carcinosarcoma, a cell type known to be particularly aggressive, is relatively overrepresented among cases of advanced disease.
Advanced endometrial cancer includes cases of stage III (involvement of lymph nodes, ovaries, and vagina) and stage IV disease (with direct extension into pelvic viscera and distant metastases). In most cases of stage III disease, extrauterine metastases are microscopic and are detected only at the time of surgical staging. Bulky nodal disease within the pelvic and para-aortic nodal basins is less common but associated with worse prognosis than for patients with microscopic nodal metastases. Stage IV disease usually presents with peritoneal spread of disease including carcinomatosis, omental disease, and involvement of the small and large intestine.
Once advanced, endometrial cancer requires more than surgery alone, relying heavily on adjuvant therapies to achieve responses, particularly systemic therapy with platinum and taxane chemotherapy. In some cases, molecularly targeted therapy (such as trastuzumab for serous carcinomas that demonstrate overexpression of HER2) has been shown to be superior in efficacy.1 Surgery may involve either radical nodal dissections to the infrarenal aortic basin, and/or peritoneal debulking procedures similar to that required for ovarian cancer. Perhaps because of patterns of disease distribution so similar to ovarian cancer, historically, sequencing of therapy focused on radical primary debulking surgery (PDS) followed by chemotherapy.
In 2000, a retrospective series from Johns Hopkins University documented the outcomes of 65 patients with advanced endometrial cancer who had undergone primary debulking surgery followed by chemotherapy.2 They noted that survival was directly associated with degree of cytoreduction, with the best outcomes seen for those patients whose surgery resulted in no gross residual disease. Following these data, PDS with complete resection of all disease became the goal of primary therapy.
However, unlike ovarian cancer (which shares a similar disease distribution with advanced endometrial cancer) patients with endometrial cancer are more obese, older, and typically have more comorbidities. Therefore, radical primary debulking surgeries may be associated with poor patient perioperative outcomes, and feasibility of complete cytoreduction, particularly in very obese patients, can be limited. For this reason, neoadjuvant chemotherapy (NACT) has been explored as an option. The potential virtue of NACT is that it allows for tumor deposits to decrease in size, or be eliminated, prior to surgery, resulting in a less morbid procedure for the patient.
Observed outcomes for NACT relative to PDS are mixed. When small series have compared the two for the treatment of advanced serous endometrial cancer, NACT was associated with decreased perioperative morbidity, with similar overall survival observed.3,4
However, in larger series exploring patients within the National Cancer Database (a collection of over 1,500 hospitals accredited by the Commission on Cancer) outcomes appear different for the two approaches.5,6 While PDS was initially associated with worse survival, at approximately 5-6 months from diagnosis, this changed and survival was observed to be consistently superior for this group. These data suggest that patients undergoing primary surgical cytoreduction may experience an early mortality risk, possibly secondary to the impact of surgery, but that if they are to survive beyond this point, they experience better outcomes. While the researchers attempted to control for risk factors of poor outcomes that might have systematically differed between the two groups, this specific database is limited in its ability to account for all fundamental differences between them. Only approximately 15% of women with advanced endometrial cancer were offered NACT during those time periods. This observation alone suggests that this likely represents a group specially selected for their poor candidacy for upfront debulking surgery, and inherently increased risk for death from all causes.
The question remains, is NACT appropriate for all patients or just those who are considered poor surgical candidates? Could all patients benefit from the decreased morbidity associated with surgery after NACT without compromising survival? Randomized controlled trials are necessary to answer this question as they are the only way to ensure that risk factors for poor outcomes (such as histology, disease distribution, medical comorbidities) are equally distributed among both groups.
In the meantime, gynecologic oncologists should take a cautious approach to decision making regarding sequencing of surgery and chemotherapy in the setting of a new diagnosis of advanced endometrial cancer. Arguably more important than surgical interventions, access to molecularly targeted systemic therapy is likely to bring the best outcomes for advanced endometrial cancer. Carboplatin and paclitaxel are the current gold standard of care for frontline systemic therapy; however, response rates with this regimen are less favorable for endometrial cancer than for ovarian cancer. Work is being done to test novel therapies against actionable targets to use as alternatives or as adjuncts to traditional chemotherapy regimens. In doing so, clinicians are learning to distinguish endometrial cancers by more than simply their histologic features, but also by their molecular profiles.
Advanced endometrial cancer is a serious disease with high lethality. Future research should focus on ways to ensure toxicities of therapy, including surgery, are minimized while improving upon existing poor clinical outcomes.
Dr. Rossi is assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. She has no financial disclosures.
References
1. Fader AN et al. J Clin Oncol 2018;36(20):2044-51.
2. Bristow RE et al. Gynecol Oncol 2000;78(2):85-91.
3. Bogani G et al. Tumori 2019;105(1):92-97.
4. Wilkinson-Ryan I et al. Int J Gynecol Cancer. 2015;25(1):63-8.
5. Tobias CJ et al. JAMA Netw Open 2020;3(12):e2028612.
6. Chambers LM et al. Gynecol Oncol 2021;160(2):405-12.
An appeal for equitable access to care for early pregnancy loss
Remarkable advances in care for early pregnancy loss (EPL) have occurred over the past several years. Misoprostol with mifepristone pretreatment is now the gold standard for medical management after recent research showed that this regimen improves both the efficacy and cost-effectiveness of medical management.1 Manual vacuum aspiration (MVA)’s portability, effectiveness, and safety ensure that providers can offer procedural EPL management in almost any clinical setting. Medication management and in-office uterine aspiration are two evidence-based options for EPL management that may increase access for the 25% of pregnant women who experience EPL. Unfortunately, many women do not have access to either option. Equitable access to early pregnancy loss management can be achieved by expanding access to mifepristone and office-based MVA.
However, access to mifepristone and initiating office-based MVA is challenging. Mifepristone is one of several medications regulated under the Food and Drug Administration’s Risk Evaluation and Management Strategies (REMS) program.2
The REMS guidelines restrict clinicians in prescribing and dispensing mifepristone, including the key provision that mifepristone may be dispensed only in clinics, medical offices, and hospitals. Clinicians cannot write a prescription for mifepristone for a patient to pick up at the pharmacy. Efforts are underway to roll back the REMS. Barriers to office-based MVA include time, culture shift among staff, gathering equipment, and creating protocols. Clinicians can improve access to EPL management in a variety of ways:
- MVA training: Ob.gyns. who lack training in MVA use can take advantage of several programs designed to teach the skill to clinicians, including programs such as Training, Education, and Advocacy in Miscarriage Management (TEAMM).3,4 MVA is easy to learn for ob.gyns. and procedural complications are uncommon. In the office setting, complications requiring transfer to a higher level of care are rare.5 With adequate training, whether during residency or afterward, ob.gyns. can learn to safely and effectively use MVA for procedural EPL management in the office and in the emergency department.
- Partnerships with pharmacists to reduce barriers to mifepristone: Ob.gyns. working in a variety of clinical settings, including independent clinics, critical access hospitals, community hospitals, and academic medical centers, have worked closely with on-site pharmacists to place mifepristone on their practice sites’ formularies.6 These ob.gyn.–pharmacist collaborations often require explanations to institutional Pharmacy and Therapeutics (P&T) committees of the benefits of mifepristone to patients, detailed indications for mifepristone’s use, and methods to secure mifepristone on site.
- Partnerships with emergency department and outpatient nursing and administration to promote MVA: Provision of MVA is ideal for safe, effective, and cost-efficient procedural EPL management in both the emergency department and outpatient setting. However, access to MVA in emergency rooms and outpatient clinical settings is suboptimal. Some clinicians push back against MVA use in the emergency department, citing fears that performing the procedure in the emergency department unnecessarily uses staff and resources reserved for patients with more critical illnesses. Ob.gyns. should also work with emergency medicine physicians and emergency department nursing staff and hospital administrators in explaining that MVA in the emergency room is patient centered and cost effective.
Interdisciplinary collaboration and training are two strategies that can increase access to mifepristone and MVA for EPL management. Use of mifepristone/misoprostol and office/emergency department MVA for treatment of EPL is patient centered, evidence based, feasible, highly effective, and timely. These two health care interventions are practical in almost any setting, including rural and other low-resource settings. By using these strategies to overcome the logistical and institutional challenges, ob.gyns. can help countless women with EPL gain access to the best EPL care.
Dr. Espey is chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque. Dr. Jackson is an obstetrician/gynecologist at Michigan State University in Flint. They have no disclosures to report.
References
1. Schreiber CA et al. N Engl J Med. 2018 Jun 7;378(23):2161-70.
2. Food and Drug Administration. Mifeprex (mifepristone) information.
3. The TEAMM (Training, Education, and Advocacy in Miscarriage Management) Project. Training interprofessional teams to manage miscarriage. Accessed March 15, 2021.
4. Quinley KE et al. Ann Emerg Med. 2019 Jul;72(1):86-92.
5. Milingos DS et al. BJOG. 2009 Aug;116(9):1268-71.
6. Calloway D et al. Contraception. 2021 Jul;104(1):24-8.
Remarkable advances in care for early pregnancy loss (EPL) have occurred over the past several years. Misoprostol with mifepristone pretreatment is now the gold standard for medical management after recent research showed that this regimen improves both the efficacy and cost-effectiveness of medical management.1 Manual vacuum aspiration (MVA)’s portability, effectiveness, and safety ensure that providers can offer procedural EPL management in almost any clinical setting. Medication management and in-office uterine aspiration are two evidence-based options for EPL management that may increase access for the 25% of pregnant women who experience EPL. Unfortunately, many women do not have access to either option. Equitable access to early pregnancy loss management can be achieved by expanding access to mifepristone and office-based MVA.
However, access to mifepristone and initiating office-based MVA is challenging. Mifepristone is one of several medications regulated under the Food and Drug Administration’s Risk Evaluation and Management Strategies (REMS) program.2
The REMS guidelines restrict clinicians in prescribing and dispensing mifepristone, including the key provision that mifepristone may be dispensed only in clinics, medical offices, and hospitals. Clinicians cannot write a prescription for mifepristone for a patient to pick up at the pharmacy. Efforts are underway to roll back the REMS. Barriers to office-based MVA include time, culture shift among staff, gathering equipment, and creating protocols. Clinicians can improve access to EPL management in a variety of ways:
- MVA training: Ob.gyns. who lack training in MVA use can take advantage of several programs designed to teach the skill to clinicians, including programs such as Training, Education, and Advocacy in Miscarriage Management (TEAMM).3,4 MVA is easy to learn for ob.gyns. and procedural complications are uncommon. In the office setting, complications requiring transfer to a higher level of care are rare.5 With adequate training, whether during residency or afterward, ob.gyns. can learn to safely and effectively use MVA for procedural EPL management in the office and in the emergency department.
- Partnerships with pharmacists to reduce barriers to mifepristone: Ob.gyns. working in a variety of clinical settings, including independent clinics, critical access hospitals, community hospitals, and academic medical centers, have worked closely with on-site pharmacists to place mifepristone on their practice sites’ formularies.6 These ob.gyn.–pharmacist collaborations often require explanations to institutional Pharmacy and Therapeutics (P&T) committees of the benefits of mifepristone to patients, detailed indications for mifepristone’s use, and methods to secure mifepristone on site.
- Partnerships with emergency department and outpatient nursing and administration to promote MVA: Provision of MVA is ideal for safe, effective, and cost-efficient procedural EPL management in both the emergency department and outpatient setting. However, access to MVA in emergency rooms and outpatient clinical settings is suboptimal. Some clinicians push back against MVA use in the emergency department, citing fears that performing the procedure in the emergency department unnecessarily uses staff and resources reserved for patients with more critical illnesses. Ob.gyns. should also work with emergency medicine physicians and emergency department nursing staff and hospital administrators in explaining that MVA in the emergency room is patient centered and cost effective.
Interdisciplinary collaboration and training are two strategies that can increase access to mifepristone and MVA for EPL management. Use of mifepristone/misoprostol and office/emergency department MVA for treatment of EPL is patient centered, evidence based, feasible, highly effective, and timely. These two health care interventions are practical in almost any setting, including rural and other low-resource settings. By using these strategies to overcome the logistical and institutional challenges, ob.gyns. can help countless women with EPL gain access to the best EPL care.
Dr. Espey is chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque. Dr. Jackson is an obstetrician/gynecologist at Michigan State University in Flint. They have no disclosures to report.
References
1. Schreiber CA et al. N Engl J Med. 2018 Jun 7;378(23):2161-70.
2. Food and Drug Administration. Mifeprex (mifepristone) information.
3. The TEAMM (Training, Education, and Advocacy in Miscarriage Management) Project. Training interprofessional teams to manage miscarriage. Accessed March 15, 2021.
4. Quinley KE et al. Ann Emerg Med. 2019 Jul;72(1):86-92.
5. Milingos DS et al. BJOG. 2009 Aug;116(9):1268-71.
6. Calloway D et al. Contraception. 2021 Jul;104(1):24-8.
Remarkable advances in care for early pregnancy loss (EPL) have occurred over the past several years. Misoprostol with mifepristone pretreatment is now the gold standard for medical management after recent research showed that this regimen improves both the efficacy and cost-effectiveness of medical management.1 Manual vacuum aspiration (MVA)’s portability, effectiveness, and safety ensure that providers can offer procedural EPL management in almost any clinical setting. Medication management and in-office uterine aspiration are two evidence-based options for EPL management that may increase access for the 25% of pregnant women who experience EPL. Unfortunately, many women do not have access to either option. Equitable access to early pregnancy loss management can be achieved by expanding access to mifepristone and office-based MVA.
However, access to mifepristone and initiating office-based MVA is challenging. Mifepristone is one of several medications regulated under the Food and Drug Administration’s Risk Evaluation and Management Strategies (REMS) program.2
The REMS guidelines restrict clinicians in prescribing and dispensing mifepristone, including the key provision that mifepristone may be dispensed only in clinics, medical offices, and hospitals. Clinicians cannot write a prescription for mifepristone for a patient to pick up at the pharmacy. Efforts are underway to roll back the REMS. Barriers to office-based MVA include time, culture shift among staff, gathering equipment, and creating protocols. Clinicians can improve access to EPL management in a variety of ways:
- MVA training: Ob.gyns. who lack training in MVA use can take advantage of several programs designed to teach the skill to clinicians, including programs such as Training, Education, and Advocacy in Miscarriage Management (TEAMM).3,4 MVA is easy to learn for ob.gyns. and procedural complications are uncommon. In the office setting, complications requiring transfer to a higher level of care are rare.5 With adequate training, whether during residency or afterward, ob.gyns. can learn to safely and effectively use MVA for procedural EPL management in the office and in the emergency department.
- Partnerships with pharmacists to reduce barriers to mifepristone: Ob.gyns. working in a variety of clinical settings, including independent clinics, critical access hospitals, community hospitals, and academic medical centers, have worked closely with on-site pharmacists to place mifepristone on their practice sites’ formularies.6 These ob.gyn.–pharmacist collaborations often require explanations to institutional Pharmacy and Therapeutics (P&T) committees of the benefits of mifepristone to patients, detailed indications for mifepristone’s use, and methods to secure mifepristone on site.
- Partnerships with emergency department and outpatient nursing and administration to promote MVA: Provision of MVA is ideal for safe, effective, and cost-efficient procedural EPL management in both the emergency department and outpatient setting. However, access to MVA in emergency rooms and outpatient clinical settings is suboptimal. Some clinicians push back against MVA use in the emergency department, citing fears that performing the procedure in the emergency department unnecessarily uses staff and resources reserved for patients with more critical illnesses. Ob.gyns. should also work with emergency medicine physicians and emergency department nursing staff and hospital administrators in explaining that MVA in the emergency room is patient centered and cost effective.
Interdisciplinary collaboration and training are two strategies that can increase access to mifepristone and MVA for EPL management. Use of mifepristone/misoprostol and office/emergency department MVA for treatment of EPL is patient centered, evidence based, feasible, highly effective, and timely. These two health care interventions are practical in almost any setting, including rural and other low-resource settings. By using these strategies to overcome the logistical and institutional challenges, ob.gyns. can help countless women with EPL gain access to the best EPL care.
Dr. Espey is chair of the department of obstetrics and gynecology at the University of New Mexico, Albuquerque. Dr. Jackson is an obstetrician/gynecologist at Michigan State University in Flint. They have no disclosures to report.
References
1. Schreiber CA et al. N Engl J Med. 2018 Jun 7;378(23):2161-70.
2. Food and Drug Administration. Mifeprex (mifepristone) information.
3. The TEAMM (Training, Education, and Advocacy in Miscarriage Management) Project. Training interprofessional teams to manage miscarriage. Accessed March 15, 2021.
4. Quinley KE et al. Ann Emerg Med. 2019 Jul;72(1):86-92.
5. Milingos DS et al. BJOG. 2009 Aug;116(9):1268-71.
6. Calloway D et al. Contraception. 2021 Jul;104(1):24-8.
Remdesivir sharply cuts COVID hospitalization risk, Gilead says
Remdesivir (Veklury, Gilead) was found to reduce some COVID-19 patients’ risk of hospitalization by 87% in a phase 3 trial, the drug’s manufacturer announced Sept. 22 in a press release.
The randomized, double-blind, placebo-controlled trial evaluated the efficacy and safety of a 3-day course of intravenous remdesivir in an analysis of 562 nonhospitalized patients at high risk for disease progression.
Remdesivir demonstrated a statistically significant 87% reduction in risk for COVID-19–related hospitalization or all-cause death by Day 28 (0.7% [2/279]) compared with placebo (5.3% [15/283]) P = .008. Participants were assigned 1:1 to remdesivir or the placebo group.
Researchers also found an 81% reduction in risk for the composite secondary endpoint – medical visits due to COVID-19 or all-cause death by Day 28. Only 1.6% had COVID-19 medical visits ([4/246]) compared with those in the placebo group (8.3% [21/252]) P = .002. No deaths were observed in either arm by Day 28.
“These latest data show remdesivir’s potential to help high-risk patients recover before they get sicker and stay out of the hospital altogether,” coauthor Robert L. Gottlieb, MD, PhD, from Baylor University Medical Center, Houston, said in the press release.
Remdesivir is the only drug approved by the U.S. Food and Drug Administration for hospitalized COVID-19 patients at least 12 years old. Its treatment of nonhospitalized patients with 3 days of dosing is investigational, and the safety and efficacy for this use and dosing duration have not been established or approved by any regulatory agency, the Gilead press release notes.
The patients in this study were considered high-risk for disease progression based on comorbidities – commonly obesity, hypertension, and diabetes – and age, but had not recently been hospitalized due to COVID-19.
A third of the participants were at least 60 years old. Participants in the study must have received a positive diagnosis within 4 days of starting treatment and experienced symptoms for 7 days or less.
Use of remdesivir controversial
Results from the Adaptive COVID-19 Treatment Trial (ACTT-1) showed remdesivir was superior to placebo in shortening time to recovery in adults hospitalized with COVID-19 with evidence of lower respiratory tract infection.
However, a large trial of more than 11,000 people in 30 countries, sponsored by the World Health Organization, did not show any benefit for the drug in reducing COVID deaths.
The WHO has conditionally recommended against using remdesivir in hospitalized patients, regardless of disease severity, “as there is currently no evidence that remdesivir improves survival and other outcomes in these patients.”
The drug also is given intravenously, and this study tested three infusions over 3 days, a difficult treatment for nonhospitalized patients.
The study results were released ahead of IDWeek, where the late-breaking abstract will be presented at the virtual conference in full at the end of next week.
A version of this article first appeared on Medscape.com.
Remdesivir (Veklury, Gilead) was found to reduce some COVID-19 patients’ risk of hospitalization by 87% in a phase 3 trial, the drug’s manufacturer announced Sept. 22 in a press release.
The randomized, double-blind, placebo-controlled trial evaluated the efficacy and safety of a 3-day course of intravenous remdesivir in an analysis of 562 nonhospitalized patients at high risk for disease progression.
Remdesivir demonstrated a statistically significant 87% reduction in risk for COVID-19–related hospitalization or all-cause death by Day 28 (0.7% [2/279]) compared with placebo (5.3% [15/283]) P = .008. Participants were assigned 1:1 to remdesivir or the placebo group.
Researchers also found an 81% reduction in risk for the composite secondary endpoint – medical visits due to COVID-19 or all-cause death by Day 28. Only 1.6% had COVID-19 medical visits ([4/246]) compared with those in the placebo group (8.3% [21/252]) P = .002. No deaths were observed in either arm by Day 28.
“These latest data show remdesivir’s potential to help high-risk patients recover before they get sicker and stay out of the hospital altogether,” coauthor Robert L. Gottlieb, MD, PhD, from Baylor University Medical Center, Houston, said in the press release.
Remdesivir is the only drug approved by the U.S. Food and Drug Administration for hospitalized COVID-19 patients at least 12 years old. Its treatment of nonhospitalized patients with 3 days of dosing is investigational, and the safety and efficacy for this use and dosing duration have not been established or approved by any regulatory agency, the Gilead press release notes.
The patients in this study were considered high-risk for disease progression based on comorbidities – commonly obesity, hypertension, and diabetes – and age, but had not recently been hospitalized due to COVID-19.
A third of the participants were at least 60 years old. Participants in the study must have received a positive diagnosis within 4 days of starting treatment and experienced symptoms for 7 days or less.
Use of remdesivir controversial
Results from the Adaptive COVID-19 Treatment Trial (ACTT-1) showed remdesivir was superior to placebo in shortening time to recovery in adults hospitalized with COVID-19 with evidence of lower respiratory tract infection.
However, a large trial of more than 11,000 people in 30 countries, sponsored by the World Health Organization, did not show any benefit for the drug in reducing COVID deaths.
The WHO has conditionally recommended against using remdesivir in hospitalized patients, regardless of disease severity, “as there is currently no evidence that remdesivir improves survival and other outcomes in these patients.”
The drug also is given intravenously, and this study tested three infusions over 3 days, a difficult treatment for nonhospitalized patients.
The study results were released ahead of IDWeek, where the late-breaking abstract will be presented at the virtual conference in full at the end of next week.
A version of this article first appeared on Medscape.com.
Remdesivir (Veklury, Gilead) was found to reduce some COVID-19 patients’ risk of hospitalization by 87% in a phase 3 trial, the drug’s manufacturer announced Sept. 22 in a press release.
The randomized, double-blind, placebo-controlled trial evaluated the efficacy and safety of a 3-day course of intravenous remdesivir in an analysis of 562 nonhospitalized patients at high risk for disease progression.
Remdesivir demonstrated a statistically significant 87% reduction in risk for COVID-19–related hospitalization or all-cause death by Day 28 (0.7% [2/279]) compared with placebo (5.3% [15/283]) P = .008. Participants were assigned 1:1 to remdesivir or the placebo group.
Researchers also found an 81% reduction in risk for the composite secondary endpoint – medical visits due to COVID-19 or all-cause death by Day 28. Only 1.6% had COVID-19 medical visits ([4/246]) compared with those in the placebo group (8.3% [21/252]) P = .002. No deaths were observed in either arm by Day 28.
“These latest data show remdesivir’s potential to help high-risk patients recover before they get sicker and stay out of the hospital altogether,” coauthor Robert L. Gottlieb, MD, PhD, from Baylor University Medical Center, Houston, said in the press release.
Remdesivir is the only drug approved by the U.S. Food and Drug Administration for hospitalized COVID-19 patients at least 12 years old. Its treatment of nonhospitalized patients with 3 days of dosing is investigational, and the safety and efficacy for this use and dosing duration have not been established or approved by any regulatory agency, the Gilead press release notes.
The patients in this study were considered high-risk for disease progression based on comorbidities – commonly obesity, hypertension, and diabetes – and age, but had not recently been hospitalized due to COVID-19.
A third of the participants were at least 60 years old. Participants in the study must have received a positive diagnosis within 4 days of starting treatment and experienced symptoms for 7 days or less.
Use of remdesivir controversial
Results from the Adaptive COVID-19 Treatment Trial (ACTT-1) showed remdesivir was superior to placebo in shortening time to recovery in adults hospitalized with COVID-19 with evidence of lower respiratory tract infection.
However, a large trial of more than 11,000 people in 30 countries, sponsored by the World Health Organization, did not show any benefit for the drug in reducing COVID deaths.
The WHO has conditionally recommended against using remdesivir in hospitalized patients, regardless of disease severity, “as there is currently no evidence that remdesivir improves survival and other outcomes in these patients.”
The drug also is given intravenously, and this study tested three infusions over 3 days, a difficult treatment for nonhospitalized patients.
The study results were released ahead of IDWeek, where the late-breaking abstract will be presented at the virtual conference in full at the end of next week.
A version of this article first appeared on Medscape.com.
Rare hematologic malignancy may first present to a dermatologist
in about 80% of cases.
“You won’t see blastic plasmacytoid dendritic cell neoplasm listed on our primary cutaneous lymphoma classifications because it’s not technically a primary cutaneous disease,” Brittney K. DeClerck, MD, said during the annual meeting of the Pacific Dermatologic Association. “It’s a systemic disease that has secondary cutaneous manifestations. That’s a very important distinction to make, in terms of not missing the underlying disease associated with what might be commonly first seen on the skin.”
BPDCN is a malignancy of plasmacytoid dendritic cells, which capture, process, and present antigen, and allow the remainder of the immune system to be activated. “They are mainly derived from the myeloid cell lineage, and possibly from the lymphoid line in a subset of cases,” said Dr. DeClerck, associate professor of clinical pathology and dermatology at the University of Southern California, Los Angeles. “They secrete high levels of type I interferons, which is important for antiviral immunity, but they can also be implicated in severe systemic inflammatory diseases, such as systemic lupus erythematosus and systemic sclerosis.”
BPDCN involves the skin in about 80% of cases, she added, “but invariably at some point it involves the bone marrow and has an acute leukemic presentation, whether or not it happens concurrently with what we see on the skin as dermatologists. We also see variable involvement of the peripheral blood, lymph nodes, and the central nervous system.”
The classification of BPDCN has changed over time based on evolving immunohistochemical markers and technologies. For example, in 1995 it was called agranular CD4+ NK cell leukemia, in 2001 it was called blastic NK-cell lymphoma, in 2005 it was called CD4+/CD56+ hematodermic neoplasm, and in 2008 it was called BPDCN (AML subset). In 2016 it became classified as its own entity: BPDCN.
Because of changing nomenclature, the true incidence of the disease is unknown, but according to the best available literature, 75% of cases occur in men and the median age is between 60 and 70 years, “but all ages can be affected,” Dr. DeClerck said. “Cases seem to come in clusters. Our most recent cluster has been in our pediatric population. At Children’s Hospital Los Angeles, we’ve had three cases in the last couple of years. To me, that was a bit unusual.”
She added that 10%-20% of patients will have either a history of, or will develop another, hematologic malignancy, such as myelodysplastic syndrome (MDS), chronic myelogenous leukemia (CML), or acute myelogenous leukemia (AML).
The general prognosis of BPDCN is poor, and the mean time from onset of lesions to an actual diagnosis is about 6.2 months, which underscores the importance of early diagnosis, Dr. DeClerck said. “There can be some nondescript solitary lesions that patients can present with, so don’t hesitate to biopsy.” The median overall survival is less than 20 months, but patients under 60 years of age have a slightly better prognosis.
Clinical presentation
Clinically, the malignancy presents with variable involvement of the skin, bone marrow, lymph nodes, peripheral blood, and central nervous system. “Patients may have one or all of these,” she said. Because 80% of patients have skin lesions, “dermatologists should be aware of this entity in order to communicate with our pathologists to understand that maybe one biopsy isn’t enough. Several biopsies may be required.”
The most common dermatologic presentation of BPDCN is erythematous to deeply violaceous nodules. Other patients may present with infiltrated ecchymotic plaques or petechial to hyperpigmented macules, patches, and plaques. Biopsy reveals a diffusely infiltrated dermis of markedly atypical large cells, but occasionally can be more subtle. “Early lesions may only be perivascular in nature, so going on high power on anything that looks atypical on low power is important in these cases,” Dr. DeClerck said.
The recommended histochemical stains for suspected BPDCN include CD123, CD4, and CD56. “We need to have other stains to rule out other things, such as negative stains that are going to exclude other T cell and B cell processes, and Merkel cell carcinoma, which can express CD56. We also want to have another confirmatory stain because other things can express CD123, CD4, and CD56. Commonly we use TCL1 or TCF4.”
The differential diagnosis of cutaneous findings includes leukemia cutis, mycosis fungoides, NK/T-cell lymphoma, and cutaneous gamma-delta T-cell lymphoma, while the differential diagnosis of biopsy findings includes AML, acute lymphoblastic leukemia, and NK/T-cell lymphoma.
Treatment of BPDCN
Historically, BPDCN was treated with multiagent high-dose chemotherapy. “Patients would frequently respond early but would relapse quickly, progress, and have a poor outcome,” Dr. DeClerck said. Now, first-line therapy is tagraxofusp-erzs (Elzonris) or multiagent chemotherapy based on where the patient is in the course of disease. Tagraxofusp-erzs is an IL-3 conjugated diphtheria toxic fusion protein which binds to CD123, which was approved by the Food and Drug Administration in 2018 for treating BPDCN. After that initial therapy, it is determined whether the patient has a complete response or failed response, she said. “If they have a complete response, they frequently go on to bone marrow transplantation, which is the only curative therapy at this point for these patients.”
According to Dr. DeClerck, an anti-BCL-2 therapy, venetoclax, can be used for patients with BPDCN as well. National Comprehensive Cancer Network (NCCN) guidelines for the treatment of BPDCN can be found on the NCCN website.
Dr. DeClerck emphasized the importance of reviewing biopsy results with a hematopathologist, “because there are complex leukemias that are beyond what dermatopathologists have been trained in.” Once a patient is diagnosed with BPDCN, she recommends rapid referral to a large center for treatment and possible bone marrow transplantation.
Dr. DeClerck disclosed that she is an adviser for tagraxofusp-erzs manufacturer Stemline Therapeutics.
in about 80% of cases.
“You won’t see blastic plasmacytoid dendritic cell neoplasm listed on our primary cutaneous lymphoma classifications because it’s not technically a primary cutaneous disease,” Brittney K. DeClerck, MD, said during the annual meeting of the Pacific Dermatologic Association. “It’s a systemic disease that has secondary cutaneous manifestations. That’s a very important distinction to make, in terms of not missing the underlying disease associated with what might be commonly first seen on the skin.”
BPDCN is a malignancy of plasmacytoid dendritic cells, which capture, process, and present antigen, and allow the remainder of the immune system to be activated. “They are mainly derived from the myeloid cell lineage, and possibly from the lymphoid line in a subset of cases,” said Dr. DeClerck, associate professor of clinical pathology and dermatology at the University of Southern California, Los Angeles. “They secrete high levels of type I interferons, which is important for antiviral immunity, but they can also be implicated in severe systemic inflammatory diseases, such as systemic lupus erythematosus and systemic sclerosis.”
BPDCN involves the skin in about 80% of cases, she added, “but invariably at some point it involves the bone marrow and has an acute leukemic presentation, whether or not it happens concurrently with what we see on the skin as dermatologists. We also see variable involvement of the peripheral blood, lymph nodes, and the central nervous system.”
The classification of BPDCN has changed over time based on evolving immunohistochemical markers and technologies. For example, in 1995 it was called agranular CD4+ NK cell leukemia, in 2001 it was called blastic NK-cell lymphoma, in 2005 it was called CD4+/CD56+ hematodermic neoplasm, and in 2008 it was called BPDCN (AML subset). In 2016 it became classified as its own entity: BPDCN.
Because of changing nomenclature, the true incidence of the disease is unknown, but according to the best available literature, 75% of cases occur in men and the median age is between 60 and 70 years, “but all ages can be affected,” Dr. DeClerck said. “Cases seem to come in clusters. Our most recent cluster has been in our pediatric population. At Children’s Hospital Los Angeles, we’ve had three cases in the last couple of years. To me, that was a bit unusual.”
She added that 10%-20% of patients will have either a history of, or will develop another, hematologic malignancy, such as myelodysplastic syndrome (MDS), chronic myelogenous leukemia (CML), or acute myelogenous leukemia (AML).
The general prognosis of BPDCN is poor, and the mean time from onset of lesions to an actual diagnosis is about 6.2 months, which underscores the importance of early diagnosis, Dr. DeClerck said. “There can be some nondescript solitary lesions that patients can present with, so don’t hesitate to biopsy.” The median overall survival is less than 20 months, but patients under 60 years of age have a slightly better prognosis.
Clinical presentation
Clinically, the malignancy presents with variable involvement of the skin, bone marrow, lymph nodes, peripheral blood, and central nervous system. “Patients may have one or all of these,” she said. Because 80% of patients have skin lesions, “dermatologists should be aware of this entity in order to communicate with our pathologists to understand that maybe one biopsy isn’t enough. Several biopsies may be required.”
The most common dermatologic presentation of BPDCN is erythematous to deeply violaceous nodules. Other patients may present with infiltrated ecchymotic plaques or petechial to hyperpigmented macules, patches, and plaques. Biopsy reveals a diffusely infiltrated dermis of markedly atypical large cells, but occasionally can be more subtle. “Early lesions may only be perivascular in nature, so going on high power on anything that looks atypical on low power is important in these cases,” Dr. DeClerck said.
The recommended histochemical stains for suspected BPDCN include CD123, CD4, and CD56. “We need to have other stains to rule out other things, such as negative stains that are going to exclude other T cell and B cell processes, and Merkel cell carcinoma, which can express CD56. We also want to have another confirmatory stain because other things can express CD123, CD4, and CD56. Commonly we use TCL1 or TCF4.”
The differential diagnosis of cutaneous findings includes leukemia cutis, mycosis fungoides, NK/T-cell lymphoma, and cutaneous gamma-delta T-cell lymphoma, while the differential diagnosis of biopsy findings includes AML, acute lymphoblastic leukemia, and NK/T-cell lymphoma.
Treatment of BPDCN
Historically, BPDCN was treated with multiagent high-dose chemotherapy. “Patients would frequently respond early but would relapse quickly, progress, and have a poor outcome,” Dr. DeClerck said. Now, first-line therapy is tagraxofusp-erzs (Elzonris) or multiagent chemotherapy based on where the patient is in the course of disease. Tagraxofusp-erzs is an IL-3 conjugated diphtheria toxic fusion protein which binds to CD123, which was approved by the Food and Drug Administration in 2018 for treating BPDCN. After that initial therapy, it is determined whether the patient has a complete response or failed response, she said. “If they have a complete response, they frequently go on to bone marrow transplantation, which is the only curative therapy at this point for these patients.”
According to Dr. DeClerck, an anti-BCL-2 therapy, venetoclax, can be used for patients with BPDCN as well. National Comprehensive Cancer Network (NCCN) guidelines for the treatment of BPDCN can be found on the NCCN website.
Dr. DeClerck emphasized the importance of reviewing biopsy results with a hematopathologist, “because there are complex leukemias that are beyond what dermatopathologists have been trained in.” Once a patient is diagnosed with BPDCN, she recommends rapid referral to a large center for treatment and possible bone marrow transplantation.
Dr. DeClerck disclosed that she is an adviser for tagraxofusp-erzs manufacturer Stemline Therapeutics.
in about 80% of cases.
“You won’t see blastic plasmacytoid dendritic cell neoplasm listed on our primary cutaneous lymphoma classifications because it’s not technically a primary cutaneous disease,” Brittney K. DeClerck, MD, said during the annual meeting of the Pacific Dermatologic Association. “It’s a systemic disease that has secondary cutaneous manifestations. That’s a very important distinction to make, in terms of not missing the underlying disease associated with what might be commonly first seen on the skin.”
BPDCN is a malignancy of plasmacytoid dendritic cells, which capture, process, and present antigen, and allow the remainder of the immune system to be activated. “They are mainly derived from the myeloid cell lineage, and possibly from the lymphoid line in a subset of cases,” said Dr. DeClerck, associate professor of clinical pathology and dermatology at the University of Southern California, Los Angeles. “They secrete high levels of type I interferons, which is important for antiviral immunity, but they can also be implicated in severe systemic inflammatory diseases, such as systemic lupus erythematosus and systemic sclerosis.”
BPDCN involves the skin in about 80% of cases, she added, “but invariably at some point it involves the bone marrow and has an acute leukemic presentation, whether or not it happens concurrently with what we see on the skin as dermatologists. We also see variable involvement of the peripheral blood, lymph nodes, and the central nervous system.”
The classification of BPDCN has changed over time based on evolving immunohistochemical markers and technologies. For example, in 1995 it was called agranular CD4+ NK cell leukemia, in 2001 it was called blastic NK-cell lymphoma, in 2005 it was called CD4+/CD56+ hematodermic neoplasm, and in 2008 it was called BPDCN (AML subset). In 2016 it became classified as its own entity: BPDCN.
Because of changing nomenclature, the true incidence of the disease is unknown, but according to the best available literature, 75% of cases occur in men and the median age is between 60 and 70 years, “but all ages can be affected,” Dr. DeClerck said. “Cases seem to come in clusters. Our most recent cluster has been in our pediatric population. At Children’s Hospital Los Angeles, we’ve had three cases in the last couple of years. To me, that was a bit unusual.”
She added that 10%-20% of patients will have either a history of, or will develop another, hematologic malignancy, such as myelodysplastic syndrome (MDS), chronic myelogenous leukemia (CML), or acute myelogenous leukemia (AML).
The general prognosis of BPDCN is poor, and the mean time from onset of lesions to an actual diagnosis is about 6.2 months, which underscores the importance of early diagnosis, Dr. DeClerck said. “There can be some nondescript solitary lesions that patients can present with, so don’t hesitate to biopsy.” The median overall survival is less than 20 months, but patients under 60 years of age have a slightly better prognosis.
Clinical presentation
Clinically, the malignancy presents with variable involvement of the skin, bone marrow, lymph nodes, peripheral blood, and central nervous system. “Patients may have one or all of these,” she said. Because 80% of patients have skin lesions, “dermatologists should be aware of this entity in order to communicate with our pathologists to understand that maybe one biopsy isn’t enough. Several biopsies may be required.”
The most common dermatologic presentation of BPDCN is erythematous to deeply violaceous nodules. Other patients may present with infiltrated ecchymotic plaques or petechial to hyperpigmented macules, patches, and plaques. Biopsy reveals a diffusely infiltrated dermis of markedly atypical large cells, but occasionally can be more subtle. “Early lesions may only be perivascular in nature, so going on high power on anything that looks atypical on low power is important in these cases,” Dr. DeClerck said.
The recommended histochemical stains for suspected BPDCN include CD123, CD4, and CD56. “We need to have other stains to rule out other things, such as negative stains that are going to exclude other T cell and B cell processes, and Merkel cell carcinoma, which can express CD56. We also want to have another confirmatory stain because other things can express CD123, CD4, and CD56. Commonly we use TCL1 or TCF4.”
The differential diagnosis of cutaneous findings includes leukemia cutis, mycosis fungoides, NK/T-cell lymphoma, and cutaneous gamma-delta T-cell lymphoma, while the differential diagnosis of biopsy findings includes AML, acute lymphoblastic leukemia, and NK/T-cell lymphoma.
Treatment of BPDCN
Historically, BPDCN was treated with multiagent high-dose chemotherapy. “Patients would frequently respond early but would relapse quickly, progress, and have a poor outcome,” Dr. DeClerck said. Now, first-line therapy is tagraxofusp-erzs (Elzonris) or multiagent chemotherapy based on where the patient is in the course of disease. Tagraxofusp-erzs is an IL-3 conjugated diphtheria toxic fusion protein which binds to CD123, which was approved by the Food and Drug Administration in 2018 for treating BPDCN. After that initial therapy, it is determined whether the patient has a complete response or failed response, she said. “If they have a complete response, they frequently go on to bone marrow transplantation, which is the only curative therapy at this point for these patients.”
According to Dr. DeClerck, an anti-BCL-2 therapy, venetoclax, can be used for patients with BPDCN as well. National Comprehensive Cancer Network (NCCN) guidelines for the treatment of BPDCN can be found on the NCCN website.
Dr. DeClerck emphasized the importance of reviewing biopsy results with a hematopathologist, “because there are complex leukemias that are beyond what dermatopathologists have been trained in.” Once a patient is diagnosed with BPDCN, she recommends rapid referral to a large center for treatment and possible bone marrow transplantation.
Dr. DeClerck disclosed that she is an adviser for tagraxofusp-erzs manufacturer Stemline Therapeutics.
FROM PDA 2021
Dopamine and reward: The story of social media
How often do you find yourself on social media? The first thing I do when I wake up is check my email and text messages, as well as my Facebook, Snapchat, and Instagram notifications.
Some 150,000 messages are shared on Facebook each minute; 293 million daily active users worldwide were recorded on Snapchat during the second quarter of 2021; 127.2 million monthly active users in the United States are projected to be on Instagram by 2023.
Social media has gained the hearts and wonder of many around the world. It’s absolutely incredible how ingrained it has become in our lives as a medium for creativity, outlet for communication, and platform for information. In fact, these online network tools have now become essential during COVID-19 to ensure productive workflow, keep in touch with our loved ones, and, overall, maintain social capital. Social media has truly emerged as a powerful form of living beyond our physical selves.
Yet, increased (and addictive) social media use is associated with negative health outcomes, especially among adolescents. For example, in a study reporting parent and adolescent accounts of social media use, it was reported that social media use was associated with hyperactivity/impulsivity, depression, anxiety, loneliness, and a fear of missing out. Furthermore, a meta-analysis investigating the relationship between social media use and depressive symptoms among adolescents found a small but significant and positive relationship between the two. However, additional research is required to elucidate this association.
Notwithstanding, the addictive nature of social media has previously been called out as analogous to the addictive nature of gambling. Let’s think about it. Whether you’re on Instagram, TikTok, or a similar platform, you can’t help but scroll from one video to the next. It’s one 5- to 10-second video after the next, and before you know it, you’ve spent the past hour going through random videos – but you can’t stop. Why is that so?
Social media actually “rewires” our brain such that we expect instant gratification. In other words, when we get a notification, message, like, or share, we expect fast and short-term pleasure/reward because the brain will produce a “hit of dopamine.” However, it is important to note that the reward system is not delimited to the dopaminergic pathway and, in fact, should be understood as a complex network system (i.e., governed by changes in brain morphology through addiction and excessive behavior). Given the quick pace of the social media world, the reward pathways in our brain change and there’s an increasing demand for attention, perpetuating an addictive mindset.
When we refresh our page, we expect instant gratification. But what happens when we don’t get a like, or a message, or some sort of “reward”? Recounts of social media use by adolescents have likened online attention to popularity. Accordingly, a lack of constant attention on social media has created a vicious cycle of anxiety, loneliness, and depression because of a failure to receive “virtual” reward. Taken together, social media may be harmful because it distorts our self-image, and while social media platforms help connect us, they can also ironically make us feel isolated, lower our self-confidence, and diminish our overall sense of well-being.
As the platforms for communication and information have evolved so rapidly over the past decade, there is a need to establish boundaries between what is beneficial and what is potentially detrimental to our mental health. While social media companies should play a role in mitigating addictive social network behavior, it would also seem counterintuitive to the general business model. In that case, who takes charge? This multifaceted problem requires a multidisciplinary approach.
Leanna M.W. Lui is an MSc candidate at the University of Toronto.
A version of this article first appeared on Medscape.com.
How often do you find yourself on social media? The first thing I do when I wake up is check my email and text messages, as well as my Facebook, Snapchat, and Instagram notifications.
Some 150,000 messages are shared on Facebook each minute; 293 million daily active users worldwide were recorded on Snapchat during the second quarter of 2021; 127.2 million monthly active users in the United States are projected to be on Instagram by 2023.
Social media has gained the hearts and wonder of many around the world. It’s absolutely incredible how ingrained it has become in our lives as a medium for creativity, outlet for communication, and platform for information. In fact, these online network tools have now become essential during COVID-19 to ensure productive workflow, keep in touch with our loved ones, and, overall, maintain social capital. Social media has truly emerged as a powerful form of living beyond our physical selves.
Yet, increased (and addictive) social media use is associated with negative health outcomes, especially among adolescents. For example, in a study reporting parent and adolescent accounts of social media use, it was reported that social media use was associated with hyperactivity/impulsivity, depression, anxiety, loneliness, and a fear of missing out. Furthermore, a meta-analysis investigating the relationship between social media use and depressive symptoms among adolescents found a small but significant and positive relationship between the two. However, additional research is required to elucidate this association.
Notwithstanding, the addictive nature of social media has previously been called out as analogous to the addictive nature of gambling. Let’s think about it. Whether you’re on Instagram, TikTok, or a similar platform, you can’t help but scroll from one video to the next. It’s one 5- to 10-second video after the next, and before you know it, you’ve spent the past hour going through random videos – but you can’t stop. Why is that so?
Social media actually “rewires” our brain such that we expect instant gratification. In other words, when we get a notification, message, like, or share, we expect fast and short-term pleasure/reward because the brain will produce a “hit of dopamine.” However, it is important to note that the reward system is not delimited to the dopaminergic pathway and, in fact, should be understood as a complex network system (i.e., governed by changes in brain morphology through addiction and excessive behavior). Given the quick pace of the social media world, the reward pathways in our brain change and there’s an increasing demand for attention, perpetuating an addictive mindset.
When we refresh our page, we expect instant gratification. But what happens when we don’t get a like, or a message, or some sort of “reward”? Recounts of social media use by adolescents have likened online attention to popularity. Accordingly, a lack of constant attention on social media has created a vicious cycle of anxiety, loneliness, and depression because of a failure to receive “virtual” reward. Taken together, social media may be harmful because it distorts our self-image, and while social media platforms help connect us, they can also ironically make us feel isolated, lower our self-confidence, and diminish our overall sense of well-being.
As the platforms for communication and information have evolved so rapidly over the past decade, there is a need to establish boundaries between what is beneficial and what is potentially detrimental to our mental health. While social media companies should play a role in mitigating addictive social network behavior, it would also seem counterintuitive to the general business model. In that case, who takes charge? This multifaceted problem requires a multidisciplinary approach.
Leanna M.W. Lui is an MSc candidate at the University of Toronto.
A version of this article first appeared on Medscape.com.
How often do you find yourself on social media? The first thing I do when I wake up is check my email and text messages, as well as my Facebook, Snapchat, and Instagram notifications.
Some 150,000 messages are shared on Facebook each minute; 293 million daily active users worldwide were recorded on Snapchat during the second quarter of 2021; 127.2 million monthly active users in the United States are projected to be on Instagram by 2023.
Social media has gained the hearts and wonder of many around the world. It’s absolutely incredible how ingrained it has become in our lives as a medium for creativity, outlet for communication, and platform for information. In fact, these online network tools have now become essential during COVID-19 to ensure productive workflow, keep in touch with our loved ones, and, overall, maintain social capital. Social media has truly emerged as a powerful form of living beyond our physical selves.
Yet, increased (and addictive) social media use is associated with negative health outcomes, especially among adolescents. For example, in a study reporting parent and adolescent accounts of social media use, it was reported that social media use was associated with hyperactivity/impulsivity, depression, anxiety, loneliness, and a fear of missing out. Furthermore, a meta-analysis investigating the relationship between social media use and depressive symptoms among adolescents found a small but significant and positive relationship between the two. However, additional research is required to elucidate this association.
Notwithstanding, the addictive nature of social media has previously been called out as analogous to the addictive nature of gambling. Let’s think about it. Whether you’re on Instagram, TikTok, or a similar platform, you can’t help but scroll from one video to the next. It’s one 5- to 10-second video after the next, and before you know it, you’ve spent the past hour going through random videos – but you can’t stop. Why is that so?
Social media actually “rewires” our brain such that we expect instant gratification. In other words, when we get a notification, message, like, or share, we expect fast and short-term pleasure/reward because the brain will produce a “hit of dopamine.” However, it is important to note that the reward system is not delimited to the dopaminergic pathway and, in fact, should be understood as a complex network system (i.e., governed by changes in brain morphology through addiction and excessive behavior). Given the quick pace of the social media world, the reward pathways in our brain change and there’s an increasing demand for attention, perpetuating an addictive mindset.
When we refresh our page, we expect instant gratification. But what happens when we don’t get a like, or a message, or some sort of “reward”? Recounts of social media use by adolescents have likened online attention to popularity. Accordingly, a lack of constant attention on social media has created a vicious cycle of anxiety, loneliness, and depression because of a failure to receive “virtual” reward. Taken together, social media may be harmful because it distorts our self-image, and while social media platforms help connect us, they can also ironically make us feel isolated, lower our self-confidence, and diminish our overall sense of well-being.
As the platforms for communication and information have evolved so rapidly over the past decade, there is a need to establish boundaries between what is beneficial and what is potentially detrimental to our mental health. While social media companies should play a role in mitigating addictive social network behavior, it would also seem counterintuitive to the general business model. In that case, who takes charge? This multifaceted problem requires a multidisciplinary approach.
Leanna M.W. Lui is an MSc candidate at the University of Toronto.
A version of this article first appeared on Medscape.com.
Authors’ response
My co-authors and I appreciate the excellent comments regarding our Photo Rounds column, “Foot rash and joint pain,” and would like to provide some additional detail.
After our patient’s 27-day hospital stay, he was admitted to a rehabilitation center for continued inpatient physical therapy for 14 days due to weakness and deconditioning. Following his discharge from the rehabilitation center, the patient was still confined to a wheelchair. He was prescribed an oral prednisone taper (as mentioned in our article) and celecoxib 200 mg bid and referred for outpatient physical therapy. At a follow-up appointment with the rheumatologist, he received adalimumab 80 mg followed by 40 mg every other week, which led to improvement in his range of motion and pain. Two months after outpatient physical therapy, the patient was lost to follow-up.
We agree with Dr. Hahn et al that many of these patients with chlamydia-associated ReA become “long-haulers.” In medicine—especially when rare diseases are considered—we must often make decisions without perfect science. The studies referenced by Dr. Hahn et al suggest that combinations of doxycycline and rifampin or azithromycin and rifampin may treat not only chlamydial infection, but ReA and associated cutaneous disease, as well.1,2 While these studies are small in size, larger studies may never be funded. We agree that combination therapy should be considered in this population of patients.
Hannah R. Badon, MD
Ross L. Pearlman, MD
Robert T. Brodell, MD
Jackson, MS
1. Carter JD, Valeriano J, Vasey FB. Doxycycline versus doxycycline and rifampin in undifferentiated spondyloarthropathy, with special reference to chlamydia-induced arthritis. A prospective, randomized 9-month comparison. J Rheumatol. 2004;31:1973-1980.
2. Carter JD, Espinoza LR, Inman RD, et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis: a double-blind, placebo-controlled, prospective trial. Arthritis Rheum. 2010;62:1298-1307. doi: 10.1002/art.27394
My co-authors and I appreciate the excellent comments regarding our Photo Rounds column, “Foot rash and joint pain,” and would like to provide some additional detail.
After our patient’s 27-day hospital stay, he was admitted to a rehabilitation center for continued inpatient physical therapy for 14 days due to weakness and deconditioning. Following his discharge from the rehabilitation center, the patient was still confined to a wheelchair. He was prescribed an oral prednisone taper (as mentioned in our article) and celecoxib 200 mg bid and referred for outpatient physical therapy. At a follow-up appointment with the rheumatologist, he received adalimumab 80 mg followed by 40 mg every other week, which led to improvement in his range of motion and pain. Two months after outpatient physical therapy, the patient was lost to follow-up.
We agree with Dr. Hahn et al that many of these patients with chlamydia-associated ReA become “long-haulers.” In medicine—especially when rare diseases are considered—we must often make decisions without perfect science. The studies referenced by Dr. Hahn et al suggest that combinations of doxycycline and rifampin or azithromycin and rifampin may treat not only chlamydial infection, but ReA and associated cutaneous disease, as well.1,2 While these studies are small in size, larger studies may never be funded. We agree that combination therapy should be considered in this population of patients.
Hannah R. Badon, MD
Ross L. Pearlman, MD
Robert T. Brodell, MD
Jackson, MS
My co-authors and I appreciate the excellent comments regarding our Photo Rounds column, “Foot rash and joint pain,” and would like to provide some additional detail.
After our patient’s 27-day hospital stay, he was admitted to a rehabilitation center for continued inpatient physical therapy for 14 days due to weakness and deconditioning. Following his discharge from the rehabilitation center, the patient was still confined to a wheelchair. He was prescribed an oral prednisone taper (as mentioned in our article) and celecoxib 200 mg bid and referred for outpatient physical therapy. At a follow-up appointment with the rheumatologist, he received adalimumab 80 mg followed by 40 mg every other week, which led to improvement in his range of motion and pain. Two months after outpatient physical therapy, the patient was lost to follow-up.
We agree with Dr. Hahn et al that many of these patients with chlamydia-associated ReA become “long-haulers.” In medicine—especially when rare diseases are considered—we must often make decisions without perfect science. The studies referenced by Dr. Hahn et al suggest that combinations of doxycycline and rifampin or azithromycin and rifampin may treat not only chlamydial infection, but ReA and associated cutaneous disease, as well.1,2 While these studies are small in size, larger studies may never be funded. We agree that combination therapy should be considered in this population of patients.
Hannah R. Badon, MD
Ross L. Pearlman, MD
Robert T. Brodell, MD
Jackson, MS
1. Carter JD, Valeriano J, Vasey FB. Doxycycline versus doxycycline and rifampin in undifferentiated spondyloarthropathy, with special reference to chlamydia-induced arthritis. A prospective, randomized 9-month comparison. J Rheumatol. 2004;31:1973-1980.
2. Carter JD, Espinoza LR, Inman RD, et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis: a double-blind, placebo-controlled, prospective trial. Arthritis Rheum. 2010;62:1298-1307. doi: 10.1002/art.27394
1. Carter JD, Valeriano J, Vasey FB. Doxycycline versus doxycycline and rifampin in undifferentiated spondyloarthropathy, with special reference to chlamydia-induced arthritis. A prospective, randomized 9-month comparison. J Rheumatol. 2004;31:1973-1980.
2. Carter JD, Espinoza LR, Inman RD, et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis: a double-blind, placebo-controlled, prospective trial. Arthritis Rheum. 2010;62:1298-1307. doi: 10.1002/art.27394
How best to treat “long-haulers” with reactive arthritis?
In the June Photo Rounds column, “Foot rash and joint pain” (J Fam Pract. 2021;70:249-251), Badon et al presented a case of chlamydia-associated reactive arthritis (ReA), formerly called Reiter syndrome, in a 21-year-old man following Chlamydia trachomatis urethritis. We would like to point out that, contrary to the conventional definition of ReA, in which the causative pathogen can’t be cultured from the affected joints,1 chlamydia-associated ReA is associated with evidence of chronic joint infection that, while not cultivable, can be confirmed by real-time polymerase chain reaction testing of metabolically active pathogens in synovial tissue and/or fluid.2
C trachomatis and C pneumoniae are the most frequent causative pathogens to elicit ReA.3 Short-course antibiotics and anti-inflammatory treatments can palliate ReA, but these treatments often do not provide a cure.3 Two controlled clinical trials demonstrated that chlamydia-associated ReA can be treated successfully with longer-term combination antibiotic therapy.4,5 ReA is usually diagnosed in the acute stage (first 6 months) and can become chronic in 30% of cases.6 It would be interesting to know the long-term treatment and outcome data for the case patient.
David L. Hahn, MD, MS
Alan P. Hudson, PhD
Charles Stratton, MD
Wilmore Webley, PhD
Judith Whittum-Hudson, PhD
1. Yu D, van Tubergenm A. Reactive arthritis. UpToDate. Updated 2021. Accessed August 10, 2021. www.uptodate.com/contents/reactive-arthritis
2. Gérard HC, Carter JD, Hudson AP. Chlamydia trachomatis is present and metabolically active during the remitting phase in synovial tissues from patients with chronic chlamydia-induced reactive arthritis. Am J Med Sci. 2013;346:22-25. doi: 10.1097/MAJ.0b013e3182648740
3. Zeidler H, Hudson AP. New insights into chlamydia and arthritis. Promise of a cure? Ann Rheum Dis. 2014;73:637-644. doi: 10.1136/annrheumdis-2013-204110
4. Carter JD, Valeriano J, Vasey FB. Doxycycline versus doxycycline and rifampin in undifferentiated spondyloarthropathy, with special reference to chlamydia-induced arthritis. A prospective, randomized 9-month comparison. J Rheumatol. 2004;31:1973-1980.
5. Carter JD, Espinoza LR, Inman RD, et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis: a double-blind, placebo-controlled, prospective trial. Arthritis Rheum. 2010;62:1298-1307. doi: 10.1002/art.27394
6. Carter JD, Inman RD, Whittum-Hudson J, et al. Chlamydia and chronic arthritis. Ann Med. 2012;44:784-792. doi: 10.3109/07853890.2011.606830
In the June Photo Rounds column, “Foot rash and joint pain” (J Fam Pract. 2021;70:249-251), Badon et al presented a case of chlamydia-associated reactive arthritis (ReA), formerly called Reiter syndrome, in a 21-year-old man following Chlamydia trachomatis urethritis. We would like to point out that, contrary to the conventional definition of ReA, in which the causative pathogen can’t be cultured from the affected joints,1 chlamydia-associated ReA is associated with evidence of chronic joint infection that, while not cultivable, can be confirmed by real-time polymerase chain reaction testing of metabolically active pathogens in synovial tissue and/or fluid.2
C trachomatis and C pneumoniae are the most frequent causative pathogens to elicit ReA.3 Short-course antibiotics and anti-inflammatory treatments can palliate ReA, but these treatments often do not provide a cure.3 Two controlled clinical trials demonstrated that chlamydia-associated ReA can be treated successfully with longer-term combination antibiotic therapy.4,5 ReA is usually diagnosed in the acute stage (first 6 months) and can become chronic in 30% of cases.6 It would be interesting to know the long-term treatment and outcome data for the case patient.
David L. Hahn, MD, MS
Alan P. Hudson, PhD
Charles Stratton, MD
Wilmore Webley, PhD
Judith Whittum-Hudson, PhD
In the June Photo Rounds column, “Foot rash and joint pain” (J Fam Pract. 2021;70:249-251), Badon et al presented a case of chlamydia-associated reactive arthritis (ReA), formerly called Reiter syndrome, in a 21-year-old man following Chlamydia trachomatis urethritis. We would like to point out that, contrary to the conventional definition of ReA, in which the causative pathogen can’t be cultured from the affected joints,1 chlamydia-associated ReA is associated with evidence of chronic joint infection that, while not cultivable, can be confirmed by real-time polymerase chain reaction testing of metabolically active pathogens in synovial tissue and/or fluid.2
C trachomatis and C pneumoniae are the most frequent causative pathogens to elicit ReA.3 Short-course antibiotics and anti-inflammatory treatments can palliate ReA, but these treatments often do not provide a cure.3 Two controlled clinical trials demonstrated that chlamydia-associated ReA can be treated successfully with longer-term combination antibiotic therapy.4,5 ReA is usually diagnosed in the acute stage (first 6 months) and can become chronic in 30% of cases.6 It would be interesting to know the long-term treatment and outcome data for the case patient.
David L. Hahn, MD, MS
Alan P. Hudson, PhD
Charles Stratton, MD
Wilmore Webley, PhD
Judith Whittum-Hudson, PhD
1. Yu D, van Tubergenm A. Reactive arthritis. UpToDate. Updated 2021. Accessed August 10, 2021. www.uptodate.com/contents/reactive-arthritis
2. Gérard HC, Carter JD, Hudson AP. Chlamydia trachomatis is present and metabolically active during the remitting phase in synovial tissues from patients with chronic chlamydia-induced reactive arthritis. Am J Med Sci. 2013;346:22-25. doi: 10.1097/MAJ.0b013e3182648740
3. Zeidler H, Hudson AP. New insights into chlamydia and arthritis. Promise of a cure? Ann Rheum Dis. 2014;73:637-644. doi: 10.1136/annrheumdis-2013-204110
4. Carter JD, Valeriano J, Vasey FB. Doxycycline versus doxycycline and rifampin in undifferentiated spondyloarthropathy, with special reference to chlamydia-induced arthritis. A prospective, randomized 9-month comparison. J Rheumatol. 2004;31:1973-1980.
5. Carter JD, Espinoza LR, Inman RD, et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis: a double-blind, placebo-controlled, prospective trial. Arthritis Rheum. 2010;62:1298-1307. doi: 10.1002/art.27394
6. Carter JD, Inman RD, Whittum-Hudson J, et al. Chlamydia and chronic arthritis. Ann Med. 2012;44:784-792. doi: 10.3109/07853890.2011.606830
1. Yu D, van Tubergenm A. Reactive arthritis. UpToDate. Updated 2021. Accessed August 10, 2021. www.uptodate.com/contents/reactive-arthritis
2. Gérard HC, Carter JD, Hudson AP. Chlamydia trachomatis is present and metabolically active during the remitting phase in synovial tissues from patients with chronic chlamydia-induced reactive arthritis. Am J Med Sci. 2013;346:22-25. doi: 10.1097/MAJ.0b013e3182648740
3. Zeidler H, Hudson AP. New insights into chlamydia and arthritis. Promise of a cure? Ann Rheum Dis. 2014;73:637-644. doi: 10.1136/annrheumdis-2013-204110
4. Carter JD, Valeriano J, Vasey FB. Doxycycline versus doxycycline and rifampin in undifferentiated spondyloarthropathy, with special reference to chlamydia-induced arthritis. A prospective, randomized 9-month comparison. J Rheumatol. 2004;31:1973-1980.
5. Carter JD, Espinoza LR, Inman RD, et al. Combination antibiotics as a treatment for chronic Chlamydia-induced reactive arthritis: a double-blind, placebo-controlled, prospective trial. Arthritis Rheum. 2010;62:1298-1307. doi: 10.1002/art.27394
6. Carter JD, Inman RD, Whittum-Hudson J, et al. Chlamydia and chronic arthritis. Ann Med. 2012;44:784-792. doi: 10.3109/07853890.2011.606830
Study identifies pandemic-related stressor in Parkinson’s disease
a team of researchers in the Netherlands reported, but they also identified meaningful targets for intervention.
Lisanne Dommershuijsen, MSc, a PhD candidate and researcher in epidemiology at the Erasmus University Medical Center in Rotterdam, the Netherlands, reported on a cross-sectional study of 833 participants with Parkinson’s disease in the PRIME-NL study at the International Congress of Parkinson’s Disease and Movement Disorders. The average age of participants was 70.2 and 38% were women.
“We studied targeted hypothetical interventions on COVID-19 stressors in people with Parkinson’s disease,” Ms. Dommershuijsen said. “This disruption in normal life caused considerable psychological stress in community-dwelling individuals. People with Parkinson’s disease might be especially vulnerable to this stress.
“For instance, because reduced levels of physical activity have worsened symptoms or because people with Parkinson’s often have difficulty with flexible [adaptations] to drastic and rapid changes in daily routines, such as those introduced by the COVID-19 pandemic, previous studies found that COVID-19 worsened depression and anxiety symptoms and reduced quality of life (QOL) in people with Parkinson’s disease,” Ms. Dommershuijsen said.
Hence, the goal of the study was to identify the most vulnerable subgroups in the Parkinson’s population and to suggest potential interventions to ameliorate these impacts, she said.
The study focused on eight different stressors that emerged in the pandemic: access to care, medicine and nursing services; loss of social contact; canceled social events; tension or conflict in the home; inability to perform physical activity or relax; and COVID-19 symptoms. The outcomes of interest were depression, as measured with the Beck Depression Inventory (BDI); anxiety, as measured with the Spielberger State-Trait Anxiety Inventory (STAI); and QOL, with the Parkinson’s Disease Quality of Life Questionnaire. The aggregate resulted in a scale of 0-40, with the mean stressor score in the study being 9.6, Ms. Dommershuijsen said.
The BDI and STAI scores for social stressors – loss of social contacts, social events canceled and tension or conflict at home – exceeded those for the so-called care stressors – problems accessing care, medication or nursing – she said, although all eight stressors yielded higher BDI and STAI scores across the board.
Vulnerable subgroups
“When we looked at vulnerable subgroups of people with Parkinson’s disease, we found more pronounced associations between the COVID-19 stress and mental health in women, in highly educated participants, and in participants with advanced Parkinson’s disease,” Ms. Dommershuijsen said. The impact on women and people with advanced disease is explainable, Ms. Dommershuijsen added in an interview; the former because depressive symptoms are more common in women, and the latter because loss of access to care impacts mental wellness.
“The finding that social stressors were more related to anxiety in highly educated people was surprising to us, given that depression in general is more common in people with a lower education,” she said in an interview. “One previous study of the general population suggested this might be related to expectations about available resources, but this findings and the possible explanation warrants further investigation.”
When the study stratified for coping strategies, the COVID-19 stressors had a smaller effect on depressive and anxiety symptoms in Parkinson’s disease patients prone to confrontive coping and planful problem solving, she said. “Whereas, we observed a larger effect of these stressors in people who are prone to using distancing or seeking social support as coping mechanisms,” Ms. Dommershuijsen said.
The researchers also created a model of a hypothetical 50% reduction in COVID-19 stressors among all study participants, but the effect wasn’t clinically relevant, Ms. Dommershuijsen said. However, in people with advanced Parkinson’s disease – that is, with an Movement Disorder Society–Unified Parkinson Disease Rating Scale score above median – the effect was clinically relevant in all outcomes.
The potential interventions the study identified were telemedicine via virtual consultations to alleviate care stressors, and virtual support groups and online classes to address social stressors. “However, a more personalized approach is needed to target tension or conflict at home, which was the most important social stressor influencing depression and anxiety symptoms in our study,” she said. “Social work can play an important role here.”
Asked to comment on the study, Roy Alcalay, MD, professor of neurology at Columbia University Irving Medical Center in New York, said in an interview that the findings align with his research on the impact of COVID-19 and related restrictions on people with Parkinson’s disease.
“The pandemic has affected people in different ways,” he said. “Initially very acutely, people just didn’t have access to doctors. There was also the acute question in movement disorders, but also in other diseases where the people with Parkinson’s disease are going to have the worse outcome when they have COVID-19.” Dr. Alcalay authored two recent papers on the impact of COVID-19 in people with Parkinson’s disease.
“Then we see that, in addition to that question, there’s the question of even if they don’t have COVID-19, just the social distancing and the lack of access to health care, and specifically to physical and occupational therapy and other services, can be quite damaging,” he said.
What’s commendable about the study, he said, was that it just doesn’t highlight the problem. “They’re also highlighting potential solutions, that planful problem solving and coping strategies can be helpful to people.”
Neither Ms. Dommershuijsen nor Dr. Alcalay have any relevant relationships to disclose.
a team of researchers in the Netherlands reported, but they also identified meaningful targets for intervention.
Lisanne Dommershuijsen, MSc, a PhD candidate and researcher in epidemiology at the Erasmus University Medical Center in Rotterdam, the Netherlands, reported on a cross-sectional study of 833 participants with Parkinson’s disease in the PRIME-NL study at the International Congress of Parkinson’s Disease and Movement Disorders. The average age of participants was 70.2 and 38% were women.
“We studied targeted hypothetical interventions on COVID-19 stressors in people with Parkinson’s disease,” Ms. Dommershuijsen said. “This disruption in normal life caused considerable psychological stress in community-dwelling individuals. People with Parkinson’s disease might be especially vulnerable to this stress.
“For instance, because reduced levels of physical activity have worsened symptoms or because people with Parkinson’s often have difficulty with flexible [adaptations] to drastic and rapid changes in daily routines, such as those introduced by the COVID-19 pandemic, previous studies found that COVID-19 worsened depression and anxiety symptoms and reduced quality of life (QOL) in people with Parkinson’s disease,” Ms. Dommershuijsen said.
Hence, the goal of the study was to identify the most vulnerable subgroups in the Parkinson’s population and to suggest potential interventions to ameliorate these impacts, she said.
The study focused on eight different stressors that emerged in the pandemic: access to care, medicine and nursing services; loss of social contact; canceled social events; tension or conflict in the home; inability to perform physical activity or relax; and COVID-19 symptoms. The outcomes of interest were depression, as measured with the Beck Depression Inventory (BDI); anxiety, as measured with the Spielberger State-Trait Anxiety Inventory (STAI); and QOL, with the Parkinson’s Disease Quality of Life Questionnaire. The aggregate resulted in a scale of 0-40, with the mean stressor score in the study being 9.6, Ms. Dommershuijsen said.
The BDI and STAI scores for social stressors – loss of social contacts, social events canceled and tension or conflict at home – exceeded those for the so-called care stressors – problems accessing care, medication or nursing – she said, although all eight stressors yielded higher BDI and STAI scores across the board.
Vulnerable subgroups
“When we looked at vulnerable subgroups of people with Parkinson’s disease, we found more pronounced associations between the COVID-19 stress and mental health in women, in highly educated participants, and in participants with advanced Parkinson’s disease,” Ms. Dommershuijsen said. The impact on women and people with advanced disease is explainable, Ms. Dommershuijsen added in an interview; the former because depressive symptoms are more common in women, and the latter because loss of access to care impacts mental wellness.
“The finding that social stressors were more related to anxiety in highly educated people was surprising to us, given that depression in general is more common in people with a lower education,” she said in an interview. “One previous study of the general population suggested this might be related to expectations about available resources, but this findings and the possible explanation warrants further investigation.”
When the study stratified for coping strategies, the COVID-19 stressors had a smaller effect on depressive and anxiety symptoms in Parkinson’s disease patients prone to confrontive coping and planful problem solving, she said. “Whereas, we observed a larger effect of these stressors in people who are prone to using distancing or seeking social support as coping mechanisms,” Ms. Dommershuijsen said.
The researchers also created a model of a hypothetical 50% reduction in COVID-19 stressors among all study participants, but the effect wasn’t clinically relevant, Ms. Dommershuijsen said. However, in people with advanced Parkinson’s disease – that is, with an Movement Disorder Society–Unified Parkinson Disease Rating Scale score above median – the effect was clinically relevant in all outcomes.
The potential interventions the study identified were telemedicine via virtual consultations to alleviate care stressors, and virtual support groups and online classes to address social stressors. “However, a more personalized approach is needed to target tension or conflict at home, which was the most important social stressor influencing depression and anxiety symptoms in our study,” she said. “Social work can play an important role here.”
Asked to comment on the study, Roy Alcalay, MD, professor of neurology at Columbia University Irving Medical Center in New York, said in an interview that the findings align with his research on the impact of COVID-19 and related restrictions on people with Parkinson’s disease.
“The pandemic has affected people in different ways,” he said. “Initially very acutely, people just didn’t have access to doctors. There was also the acute question in movement disorders, but also in other diseases where the people with Parkinson’s disease are going to have the worse outcome when they have COVID-19.” Dr. Alcalay authored two recent papers on the impact of COVID-19 in people with Parkinson’s disease.
“Then we see that, in addition to that question, there’s the question of even if they don’t have COVID-19, just the social distancing and the lack of access to health care, and specifically to physical and occupational therapy and other services, can be quite damaging,” he said.
What’s commendable about the study, he said, was that it just doesn’t highlight the problem. “They’re also highlighting potential solutions, that planful problem solving and coping strategies can be helpful to people.”
Neither Ms. Dommershuijsen nor Dr. Alcalay have any relevant relationships to disclose.
a team of researchers in the Netherlands reported, but they also identified meaningful targets for intervention.
Lisanne Dommershuijsen, MSc, a PhD candidate and researcher in epidemiology at the Erasmus University Medical Center in Rotterdam, the Netherlands, reported on a cross-sectional study of 833 participants with Parkinson’s disease in the PRIME-NL study at the International Congress of Parkinson’s Disease and Movement Disorders. The average age of participants was 70.2 and 38% were women.
“We studied targeted hypothetical interventions on COVID-19 stressors in people with Parkinson’s disease,” Ms. Dommershuijsen said. “This disruption in normal life caused considerable psychological stress in community-dwelling individuals. People with Parkinson’s disease might be especially vulnerable to this stress.
“For instance, because reduced levels of physical activity have worsened symptoms or because people with Parkinson’s often have difficulty with flexible [adaptations] to drastic and rapid changes in daily routines, such as those introduced by the COVID-19 pandemic, previous studies found that COVID-19 worsened depression and anxiety symptoms and reduced quality of life (QOL) in people with Parkinson’s disease,” Ms. Dommershuijsen said.
Hence, the goal of the study was to identify the most vulnerable subgroups in the Parkinson’s population and to suggest potential interventions to ameliorate these impacts, she said.
The study focused on eight different stressors that emerged in the pandemic: access to care, medicine and nursing services; loss of social contact; canceled social events; tension or conflict in the home; inability to perform physical activity or relax; and COVID-19 symptoms. The outcomes of interest were depression, as measured with the Beck Depression Inventory (BDI); anxiety, as measured with the Spielberger State-Trait Anxiety Inventory (STAI); and QOL, with the Parkinson’s Disease Quality of Life Questionnaire. The aggregate resulted in a scale of 0-40, with the mean stressor score in the study being 9.6, Ms. Dommershuijsen said.
The BDI and STAI scores for social stressors – loss of social contacts, social events canceled and tension or conflict at home – exceeded those for the so-called care stressors – problems accessing care, medication or nursing – she said, although all eight stressors yielded higher BDI and STAI scores across the board.
Vulnerable subgroups
“When we looked at vulnerable subgroups of people with Parkinson’s disease, we found more pronounced associations between the COVID-19 stress and mental health in women, in highly educated participants, and in participants with advanced Parkinson’s disease,” Ms. Dommershuijsen said. The impact on women and people with advanced disease is explainable, Ms. Dommershuijsen added in an interview; the former because depressive symptoms are more common in women, and the latter because loss of access to care impacts mental wellness.
“The finding that social stressors were more related to anxiety in highly educated people was surprising to us, given that depression in general is more common in people with a lower education,” she said in an interview. “One previous study of the general population suggested this might be related to expectations about available resources, but this findings and the possible explanation warrants further investigation.”
When the study stratified for coping strategies, the COVID-19 stressors had a smaller effect on depressive and anxiety symptoms in Parkinson’s disease patients prone to confrontive coping and planful problem solving, she said. “Whereas, we observed a larger effect of these stressors in people who are prone to using distancing or seeking social support as coping mechanisms,” Ms. Dommershuijsen said.
The researchers also created a model of a hypothetical 50% reduction in COVID-19 stressors among all study participants, but the effect wasn’t clinically relevant, Ms. Dommershuijsen said. However, in people with advanced Parkinson’s disease – that is, with an Movement Disorder Society–Unified Parkinson Disease Rating Scale score above median – the effect was clinically relevant in all outcomes.
The potential interventions the study identified were telemedicine via virtual consultations to alleviate care stressors, and virtual support groups and online classes to address social stressors. “However, a more personalized approach is needed to target tension or conflict at home, which was the most important social stressor influencing depression and anxiety symptoms in our study,” she said. “Social work can play an important role here.”
Asked to comment on the study, Roy Alcalay, MD, professor of neurology at Columbia University Irving Medical Center in New York, said in an interview that the findings align with his research on the impact of COVID-19 and related restrictions on people with Parkinson’s disease.
“The pandemic has affected people in different ways,” he said. “Initially very acutely, people just didn’t have access to doctors. There was also the acute question in movement disorders, but also in other diseases where the people with Parkinson’s disease are going to have the worse outcome when they have COVID-19.” Dr. Alcalay authored two recent papers on the impact of COVID-19 in people with Parkinson’s disease.
“Then we see that, in addition to that question, there’s the question of even if they don’t have COVID-19, just the social distancing and the lack of access to health care, and specifically to physical and occupational therapy and other services, can be quite damaging,” he said.
What’s commendable about the study, he said, was that it just doesn’t highlight the problem. “They’re also highlighting potential solutions, that planful problem solving and coping strategies can be helpful to people.”
Neither Ms. Dommershuijsen nor Dr. Alcalay have any relevant relationships to disclose.
FROM MDS VIRTUAL CONGRESS 2021