User login
Midlife fitness tied to lower later-life CVD mortality, depression risk
Higher cardiorespiratory fitness at midlife appears linked to a lower risk of depression in later life. In addition, higher midlife fitness is associated with a lower risk of cardiovascular mortality when depression preceded CVD death, according to a retrospective study published in JAMA Psychiatry.
“These findings ... should encourage physicians to consider fitness and physical activity in promoting healthy aging,” wrote Benjamin L. Willis, MD, MPH, of the Cooper Institute in Dallas, and his associates.
The study included 17,989 participants from the Cooper Center Longitudinal Study and linked data from those participants with a depression diagnosis based on Medicare claims and cardiovascular disease (CVD) mortality rates based on the National Death Index.
The participants were mostly men (80.2%), and their mean age at midlife assessment was 50 years. The participants’ treadmill time at midlife was used to categorize them into age- and sex-specific quintiles, with quintile 1 representing low fitness, quintiles 2 and 3 representing moderate fitness, and quintiles 4 and 5 representing high fitness.
After 117,218 person-years of follow-up, the investigators observed 2,701 depression diagnoses, 610 deaths tied to cardiovascular disease without prior depression, and 231 deaths associated with CVD after depression.
In addition, Dr. Willis and his associates found that (hazard ratio, 0.84; 95% confidence interval, 0.74-0.95), compared with participants with a low level of fitness. Participants with a high level of fitness also had a 61% lower risk of death from CVD without depression (HR, 0.39; 95% CI, 0.31-0.48), compared with those who had low fitness levels. Participants with a high fitness level who received a depression diagnosis had a 56% lower risk of death from CVD (HR, 0.44; 95% CI, 0.31-0.64), compared with those who had a low level of fitness.
The researchers pointed out that cardiovascular disease mortality is higher following depression but that cardiorespiratory fitness at midlife is a modifiable risk factor for both depression and CVD mortality.
Dr. Willis and his associates cited several limitations. Among them was the unavailability of information about participants’ use of medication that could influence either the presence or absence of a depression diagnosis.
Nevertheless, they said, the results provide lessons for clinicians and patients.
“This study shows that being fit at midlife is associated with a lower risk of later-life depression and subsequent CVD mortality, even in the presence of depression,” they wrote. “These findings suggest the importance of fitness in primary prevention of heart disease and associated CVD mortality in older aging adults.”
The investigators reported no conflicts of interest.
SOURCE: Willis BL et al. JAMA Psychiatry. 2018 Jun 27. doi: 10.1001/jamapsychiatry.2018.1467.
Higher cardiorespiratory fitness at midlife appears linked to a lower risk of depression in later life. In addition, higher midlife fitness is associated with a lower risk of cardiovascular mortality when depression preceded CVD death, according to a retrospective study published in JAMA Psychiatry.
“These findings ... should encourage physicians to consider fitness and physical activity in promoting healthy aging,” wrote Benjamin L. Willis, MD, MPH, of the Cooper Institute in Dallas, and his associates.
The study included 17,989 participants from the Cooper Center Longitudinal Study and linked data from those participants with a depression diagnosis based on Medicare claims and cardiovascular disease (CVD) mortality rates based on the National Death Index.
The participants were mostly men (80.2%), and their mean age at midlife assessment was 50 years. The participants’ treadmill time at midlife was used to categorize them into age- and sex-specific quintiles, with quintile 1 representing low fitness, quintiles 2 and 3 representing moderate fitness, and quintiles 4 and 5 representing high fitness.
After 117,218 person-years of follow-up, the investigators observed 2,701 depression diagnoses, 610 deaths tied to cardiovascular disease without prior depression, and 231 deaths associated with CVD after depression.
In addition, Dr. Willis and his associates found that (hazard ratio, 0.84; 95% confidence interval, 0.74-0.95), compared with participants with a low level of fitness. Participants with a high level of fitness also had a 61% lower risk of death from CVD without depression (HR, 0.39; 95% CI, 0.31-0.48), compared with those who had low fitness levels. Participants with a high fitness level who received a depression diagnosis had a 56% lower risk of death from CVD (HR, 0.44; 95% CI, 0.31-0.64), compared with those who had a low level of fitness.
The researchers pointed out that cardiovascular disease mortality is higher following depression but that cardiorespiratory fitness at midlife is a modifiable risk factor for both depression and CVD mortality.
Dr. Willis and his associates cited several limitations. Among them was the unavailability of information about participants’ use of medication that could influence either the presence or absence of a depression diagnosis.
Nevertheless, they said, the results provide lessons for clinicians and patients.
“This study shows that being fit at midlife is associated with a lower risk of later-life depression and subsequent CVD mortality, even in the presence of depression,” they wrote. “These findings suggest the importance of fitness in primary prevention of heart disease and associated CVD mortality in older aging adults.”
The investigators reported no conflicts of interest.
SOURCE: Willis BL et al. JAMA Psychiatry. 2018 Jun 27. doi: 10.1001/jamapsychiatry.2018.1467.
Higher cardiorespiratory fitness at midlife appears linked to a lower risk of depression in later life. In addition, higher midlife fitness is associated with a lower risk of cardiovascular mortality when depression preceded CVD death, according to a retrospective study published in JAMA Psychiatry.
“These findings ... should encourage physicians to consider fitness and physical activity in promoting healthy aging,” wrote Benjamin L. Willis, MD, MPH, of the Cooper Institute in Dallas, and his associates.
The study included 17,989 participants from the Cooper Center Longitudinal Study and linked data from those participants with a depression diagnosis based on Medicare claims and cardiovascular disease (CVD) mortality rates based on the National Death Index.
The participants were mostly men (80.2%), and their mean age at midlife assessment was 50 years. The participants’ treadmill time at midlife was used to categorize them into age- and sex-specific quintiles, with quintile 1 representing low fitness, quintiles 2 and 3 representing moderate fitness, and quintiles 4 and 5 representing high fitness.
After 117,218 person-years of follow-up, the investigators observed 2,701 depression diagnoses, 610 deaths tied to cardiovascular disease without prior depression, and 231 deaths associated with CVD after depression.
In addition, Dr. Willis and his associates found that (hazard ratio, 0.84; 95% confidence interval, 0.74-0.95), compared with participants with a low level of fitness. Participants with a high level of fitness also had a 61% lower risk of death from CVD without depression (HR, 0.39; 95% CI, 0.31-0.48), compared with those who had low fitness levels. Participants with a high fitness level who received a depression diagnosis had a 56% lower risk of death from CVD (HR, 0.44; 95% CI, 0.31-0.64), compared with those who had a low level of fitness.
The researchers pointed out that cardiovascular disease mortality is higher following depression but that cardiorespiratory fitness at midlife is a modifiable risk factor for both depression and CVD mortality.
Dr. Willis and his associates cited several limitations. Among them was the unavailability of information about participants’ use of medication that could influence either the presence or absence of a depression diagnosis.
Nevertheless, they said, the results provide lessons for clinicians and patients.
“This study shows that being fit at midlife is associated with a lower risk of later-life depression and subsequent CVD mortality, even in the presence of depression,” they wrote. “These findings suggest the importance of fitness in primary prevention of heart disease and associated CVD mortality in older aging adults.”
The investigators reported no conflicts of interest.
SOURCE: Willis BL et al. JAMA Psychiatry. 2018 Jun 27. doi: 10.1001/jamapsychiatry.2018.1467.
REPORTING FROM JAMA PSYCHIATRY
IMAGINE-RA: No need for MRI with treat-to-target strategy
AMSTERDAM – Results of the
“Despite patients achieving a target of clinical remission, we still see erosive progression in about 20%-30%,” study investigator Signe Møller-Bisgaard, MD, PhD, said at the European Congress of Rheumatology. That’s regardless of the definition of remission that you use, she added.
Dr. Møller-Bisgaard, a resident in rheumatology and postdoctoral researcher who works at Rigshospitalet and Frederiksberg Hospital in Copenhagen, observed that both synovial inflammation and bone marrow edema seen on MRI had been shown to predict progression in patients with rheumatoid arthritis.
What was not known, however, was whether there was any value in specifically targeting MRI remission in patients who had already achieved clinical remission. This is what the IMAGINE-RA study set out to address. It was a 2-year trial of 200 patients with rheumatoid arthritis in clinical remission who were recruited and randomized to either an MRI or conventional treat-to-target strategy. The study involved nine rheumatology and eight radiological departments, Dr. Møller-Bisgaard said.
The protocol for the study (Trials. 2015;16:178) defined clinical remission as a DAS28-CRP of 3.2 or lower and no swollen joints. Patients had to have erosions on x-ray, be anti–cyclic citrullinated peptide positive, and be treated only with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) at the time of entry.
During the study patients were assessed every 4 months via the DAS28 or DAS28 plus MRI of the dominant hand and wrist, with radiographs of the hands and feet performed annually in both groups and MRI also performed yearly in the conventional treat-to-target group.
“Treatment was intensified in both arms if the DAS28-CRP was above 3.2, and there was at least one clinical swollen joint,” Dr. Møller-Bisgaard explained. Treatment was also intensified in the MRI group if bone marrow edema was observed. Treatment intensification involved maximal doses of csDMARDs alone or in combinations, and then addition of biologic treatments, such as a tumor necrosis factor inhibitor.
“Targeting absence of MRI bone marrow edema in addition to a conventional treat-to-target strategy in RA patients in clinical remission had no effect on the probability of achieving DAS28-CRP remission or halting radiographic progression,” she said.
However, there were some positive effects on several predefined secondary endpoints. For instance, more patients in the MRI group than in the conventional treat-to-target group achieved American College of Rheumatology/EULAR remission (49% vs. 32%; P = .017). There was a significant improvement in the number of swollen joints and a patient and physician global assessment. “There was also more improvement in HAQ [Health Assessment Questionnaire], with a difference between the groups of .14 [P less than .001], Dr. Møller-Bisgaard reported.
The IMAGINE-RA study is funded by grants from the Danish Rheumatism Association and the Research Fund of Region Zealand. Funding is also provided by AbbVie via a nonrestricted grant, and adalimumab is provided free of charge. Dr. Møller-Bisgaard and coauthors had no personal conflicts of interest to declare.
SOURCE: Møller-Bisgaard S et al. EULAR 2018 Congress. Abstract OP0018.
AMSTERDAM – Results of the
“Despite patients achieving a target of clinical remission, we still see erosive progression in about 20%-30%,” study investigator Signe Møller-Bisgaard, MD, PhD, said at the European Congress of Rheumatology. That’s regardless of the definition of remission that you use, she added.
Dr. Møller-Bisgaard, a resident in rheumatology and postdoctoral researcher who works at Rigshospitalet and Frederiksberg Hospital in Copenhagen, observed that both synovial inflammation and bone marrow edema seen on MRI had been shown to predict progression in patients with rheumatoid arthritis.
What was not known, however, was whether there was any value in specifically targeting MRI remission in patients who had already achieved clinical remission. This is what the IMAGINE-RA study set out to address. It was a 2-year trial of 200 patients with rheumatoid arthritis in clinical remission who were recruited and randomized to either an MRI or conventional treat-to-target strategy. The study involved nine rheumatology and eight radiological departments, Dr. Møller-Bisgaard said.
The protocol for the study (Trials. 2015;16:178) defined clinical remission as a DAS28-CRP of 3.2 or lower and no swollen joints. Patients had to have erosions on x-ray, be anti–cyclic citrullinated peptide positive, and be treated only with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) at the time of entry.
During the study patients were assessed every 4 months via the DAS28 or DAS28 plus MRI of the dominant hand and wrist, with radiographs of the hands and feet performed annually in both groups and MRI also performed yearly in the conventional treat-to-target group.
“Treatment was intensified in both arms if the DAS28-CRP was above 3.2, and there was at least one clinical swollen joint,” Dr. Møller-Bisgaard explained. Treatment was also intensified in the MRI group if bone marrow edema was observed. Treatment intensification involved maximal doses of csDMARDs alone or in combinations, and then addition of biologic treatments, such as a tumor necrosis factor inhibitor.
“Targeting absence of MRI bone marrow edema in addition to a conventional treat-to-target strategy in RA patients in clinical remission had no effect on the probability of achieving DAS28-CRP remission or halting radiographic progression,” she said.
However, there were some positive effects on several predefined secondary endpoints. For instance, more patients in the MRI group than in the conventional treat-to-target group achieved American College of Rheumatology/EULAR remission (49% vs. 32%; P = .017). There was a significant improvement in the number of swollen joints and a patient and physician global assessment. “There was also more improvement in HAQ [Health Assessment Questionnaire], with a difference between the groups of .14 [P less than .001], Dr. Møller-Bisgaard reported.
The IMAGINE-RA study is funded by grants from the Danish Rheumatism Association and the Research Fund of Region Zealand. Funding is also provided by AbbVie via a nonrestricted grant, and adalimumab is provided free of charge. Dr. Møller-Bisgaard and coauthors had no personal conflicts of interest to declare.
SOURCE: Møller-Bisgaard S et al. EULAR 2018 Congress. Abstract OP0018.
AMSTERDAM – Results of the
“Despite patients achieving a target of clinical remission, we still see erosive progression in about 20%-30%,” study investigator Signe Møller-Bisgaard, MD, PhD, said at the European Congress of Rheumatology. That’s regardless of the definition of remission that you use, she added.
Dr. Møller-Bisgaard, a resident in rheumatology and postdoctoral researcher who works at Rigshospitalet and Frederiksberg Hospital in Copenhagen, observed that both synovial inflammation and bone marrow edema seen on MRI had been shown to predict progression in patients with rheumatoid arthritis.
What was not known, however, was whether there was any value in specifically targeting MRI remission in patients who had already achieved clinical remission. This is what the IMAGINE-RA study set out to address. It was a 2-year trial of 200 patients with rheumatoid arthritis in clinical remission who were recruited and randomized to either an MRI or conventional treat-to-target strategy. The study involved nine rheumatology and eight radiological departments, Dr. Møller-Bisgaard said.
The protocol for the study (Trials. 2015;16:178) defined clinical remission as a DAS28-CRP of 3.2 or lower and no swollen joints. Patients had to have erosions on x-ray, be anti–cyclic citrullinated peptide positive, and be treated only with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) at the time of entry.
During the study patients were assessed every 4 months via the DAS28 or DAS28 plus MRI of the dominant hand and wrist, with radiographs of the hands and feet performed annually in both groups and MRI also performed yearly in the conventional treat-to-target group.
“Treatment was intensified in both arms if the DAS28-CRP was above 3.2, and there was at least one clinical swollen joint,” Dr. Møller-Bisgaard explained. Treatment was also intensified in the MRI group if bone marrow edema was observed. Treatment intensification involved maximal doses of csDMARDs alone or in combinations, and then addition of biologic treatments, such as a tumor necrosis factor inhibitor.
“Targeting absence of MRI bone marrow edema in addition to a conventional treat-to-target strategy in RA patients in clinical remission had no effect on the probability of achieving DAS28-CRP remission or halting radiographic progression,” she said.
However, there were some positive effects on several predefined secondary endpoints. For instance, more patients in the MRI group than in the conventional treat-to-target group achieved American College of Rheumatology/EULAR remission (49% vs. 32%; P = .017). There was a significant improvement in the number of swollen joints and a patient and physician global assessment. “There was also more improvement in HAQ [Health Assessment Questionnaire], with a difference between the groups of .14 [P less than .001], Dr. Møller-Bisgaard reported.
The IMAGINE-RA study is funded by grants from the Danish Rheumatism Association and the Research Fund of Region Zealand. Funding is also provided by AbbVie via a nonrestricted grant, and adalimumab is provided free of charge. Dr. Møller-Bisgaard and coauthors had no personal conflicts of interest to declare.
SOURCE: Møller-Bisgaard S et al. EULAR 2018 Congress. Abstract OP0018.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: When a treat-to-target approach is used there is no added benefit of using magnetic resonance imaging.
Major finding: At 2 years, a similar percentage of patients achieved a DAS28-CRP of less than 2.6 and had no radiographic progression with an MRI-guided and conventional treat-to-target strategy.
Study details: The IMAGINE-RA study, a 2-year, prospective, randomized, multicenter trial of 200 patients with rheumatoid arthritis in clinical remission treated at 10 Danish hospitals.
Disclosures: The IMAGINE-RA study is funded by grants from the Danish Rheumatism Association and the Research Fund of Region Zealand. Funding is also provided by AbbVie via a nonrestricted grant and adalimumab is provided free of charge. Dr. Møller-Bisgaard and her coauthors had no personal conflicts of interest to declare.
Source: Møller-Bisgaard S et al. EULAR 2018 Congress. Abstract OP0018.
Many veterans with comorbid pain and OUD not receiving MAT
SAN DIEGO – Less than 30% of veterans on medication-assisted treatment for opioids had a diagnosis of opioid use disorder, and only 7% of veterans with an opioid use disorder initiated medication-assisted treatment.
Those are key findings from a large study that set out to assess factors associated with initiating medication-assisted treatment (MAT) among veterans seeking pain care and to characterize the cohort of veterans seeking specialty pain care who initiated MAT.
“ but it was really low,” lead study author Lisham Ashrafioun, PhD, said in an interview at the annual meeting of the College on Problems of Drug Dependence. “These findings are preliminary, but I think we need to understand a lot more about how to treat people with opioid use disorders who are receiving pain care as well.”
Dr. Ashrafioun, a research investigator at the Veteran Affairs Center of Excellence for Suicide Prevention at the Canandaigua VA Medical Center, N.Y., and his associates drew from national VA electronic medical record data to identify 219,443 veterans who initiated specialty pain services during fiscal year 2012-2014. They used procedure and billing codes to identify veterans who started using MAT for opioids within the year following initiation of pain services, and extracted data on demographics, psychiatric and medical diagnoses, and pain intensity scores.
Of the 219,443 veterans, only 2,406 had received MAT in the year following the index visit (1.1%). In addition, only 26.4% of those on MAT had an opioid use disorder and just 6.6% of those with an opioid use disorder initiated MAT.
In adjusted analyses, opioid use disorders (adjusted odds ratio, 5.71) and opioid prescriptions (aOR, 2.33) were significantly associated with greater odds of receiving MAT. Moreover, having a diagnosis of depression was associated with a greater odds of receiving MAT (aOR, 1.26), while having a diagnosis of PTSD was associated with a greater odds of not receiving it (aOR, 0.90). The researchers also found that having a diagnosis of alcohol use disorder was associated with a greater odds of not receiving MAT (aOR, 0.85), while having a diagnosis of drug use disorder was associated with a greater odds of receiving it (aOR, 1.32).
Dr. Ashrafioun, who also holds a faculty position in the department of psychiatry at the University of Rochester (N.Y.), acknowledged certain limitations of the study. For example, the sample was restricted to only those receiving specialty pain care, provider and facility variation was not accounted for, and study participants might have initiated MAT outside of the VA.
He reported having no financial disclosures.
[email protected]
SAN DIEGO – Less than 30% of veterans on medication-assisted treatment for opioids had a diagnosis of opioid use disorder, and only 7% of veterans with an opioid use disorder initiated medication-assisted treatment.
Those are key findings from a large study that set out to assess factors associated with initiating medication-assisted treatment (MAT) among veterans seeking pain care and to characterize the cohort of veterans seeking specialty pain care who initiated MAT.
“ but it was really low,” lead study author Lisham Ashrafioun, PhD, said in an interview at the annual meeting of the College on Problems of Drug Dependence. “These findings are preliminary, but I think we need to understand a lot more about how to treat people with opioid use disorders who are receiving pain care as well.”
Dr. Ashrafioun, a research investigator at the Veteran Affairs Center of Excellence for Suicide Prevention at the Canandaigua VA Medical Center, N.Y., and his associates drew from national VA electronic medical record data to identify 219,443 veterans who initiated specialty pain services during fiscal year 2012-2014. They used procedure and billing codes to identify veterans who started using MAT for opioids within the year following initiation of pain services, and extracted data on demographics, psychiatric and medical diagnoses, and pain intensity scores.
Of the 219,443 veterans, only 2,406 had received MAT in the year following the index visit (1.1%). In addition, only 26.4% of those on MAT had an opioid use disorder and just 6.6% of those with an opioid use disorder initiated MAT.
In adjusted analyses, opioid use disorders (adjusted odds ratio, 5.71) and opioid prescriptions (aOR, 2.33) were significantly associated with greater odds of receiving MAT. Moreover, having a diagnosis of depression was associated with a greater odds of receiving MAT (aOR, 1.26), while having a diagnosis of PTSD was associated with a greater odds of not receiving it (aOR, 0.90). The researchers also found that having a diagnosis of alcohol use disorder was associated with a greater odds of not receiving MAT (aOR, 0.85), while having a diagnosis of drug use disorder was associated with a greater odds of receiving it (aOR, 1.32).
Dr. Ashrafioun, who also holds a faculty position in the department of psychiatry at the University of Rochester (N.Y.), acknowledged certain limitations of the study. For example, the sample was restricted to only those receiving specialty pain care, provider and facility variation was not accounted for, and study participants might have initiated MAT outside of the VA.
He reported having no financial disclosures.
[email protected]
SAN DIEGO – Less than 30% of veterans on medication-assisted treatment for opioids had a diagnosis of opioid use disorder, and only 7% of veterans with an opioid use disorder initiated medication-assisted treatment.
Those are key findings from a large study that set out to assess factors associated with initiating medication-assisted treatment (MAT) among veterans seeking pain care and to characterize the cohort of veterans seeking specialty pain care who initiated MAT.
“ but it was really low,” lead study author Lisham Ashrafioun, PhD, said in an interview at the annual meeting of the College on Problems of Drug Dependence. “These findings are preliminary, but I think we need to understand a lot more about how to treat people with opioid use disorders who are receiving pain care as well.”
Dr. Ashrafioun, a research investigator at the Veteran Affairs Center of Excellence for Suicide Prevention at the Canandaigua VA Medical Center, N.Y., and his associates drew from national VA electronic medical record data to identify 219,443 veterans who initiated specialty pain services during fiscal year 2012-2014. They used procedure and billing codes to identify veterans who started using MAT for opioids within the year following initiation of pain services, and extracted data on demographics, psychiatric and medical diagnoses, and pain intensity scores.
Of the 219,443 veterans, only 2,406 had received MAT in the year following the index visit (1.1%). In addition, only 26.4% of those on MAT had an opioid use disorder and just 6.6% of those with an opioid use disorder initiated MAT.
In adjusted analyses, opioid use disorders (adjusted odds ratio, 5.71) and opioid prescriptions (aOR, 2.33) were significantly associated with greater odds of receiving MAT. Moreover, having a diagnosis of depression was associated with a greater odds of receiving MAT (aOR, 1.26), while having a diagnosis of PTSD was associated with a greater odds of not receiving it (aOR, 0.90). The researchers also found that having a diagnosis of alcohol use disorder was associated with a greater odds of not receiving MAT (aOR, 0.85), while having a diagnosis of drug use disorder was associated with a greater odds of receiving it (aOR, 1.32).
Dr. Ashrafioun, who also holds a faculty position in the department of psychiatry at the University of Rochester (N.Y.), acknowledged certain limitations of the study. For example, the sample was restricted to only those receiving specialty pain care, provider and facility variation was not accounted for, and study participants might have initiated MAT outside of the VA.
He reported having no financial disclosures.
[email protected]
REPORTING FROM CPDD 2018
Key clinical point: Several clinical features differentiate veterans seeking specialty pain care who receive medication-assisted treatment (MAT) from those who do not.
Major finding: Only 26.5% of veterans on MAT had an opioid use disorder.
Study details: An analysis of 219,443 veterans who initiated specialty pain services during fiscal year 2012-2014.
Disclosures: Dr. Ashrafioun reported having no financial disclosures.
Cocaine use declining among young adults
SAN DIEGO – Use of cocaine by young adults in the United States has declined significantly since the early 2000s, but it remains relatively common. In fact, results from an analysis of national data suggest that about 5% of 18- to 22-year-olds have used cocaine in the past 12 months.
“We don’t typically think of cocaine use amongst young people, but it is of a nontrivial prevalence,” lead study author Kristin E. Schneider said in an interview at the annual meeting of the College on Problems of Drug Dependence. “If someone has risky alcohol use they might also have risky substance use. We need to be screening for those things as well, while most interventions these days focus on problem drinking.”
Ms. Schneider, a graduate student in the department of mental health at Johns Hopkins University, Baltimore, and her associates drew from the 2002-2014 waves of the National Survey on Drug Use and Health to describe trends in cocaine use among young adults by race/ethnicity, sex, and college enrollment. They assessed for lifetime use, any past 12-month cocaine use, past 30-day use, and any past 12-month use disorder. They also tested for linear and quadratic trends over time.
When the researchers averaged across all years, they found that 12.1% of young adults had ever used cocaine, 5.9% had used it in the past 12 months, 1.8% had used in the past 30 days, and 1% had a use disorder in the past 12 months. They also observed significant linear declines in cocaine use across the entire study period. For example, between 2002 and 2014, the prevalence of lifetime cocaine use declined from 13.7% to 8.6%, past 12-month use declined from 6.3% to 4.1%, and past 30-day use declined from 1.8% to 1.4%.
Nonstudents had higher lifetime rates of cocaine use, compared with students (14.8% vs. 7.8%, respectively), but differences between the two groups were small for other indicators. “Perhaps being an emerging environment with other [young] adults who are also making risky health behavior decisions compensates for this baseline difference of risk between people who go to college and those who do not,” Ms. Schneider said. At the same time, the lowest rates of past 12-month cocaine use was observed in black males (1.6%), Asian females (0.8%), and black females (0.8%).
The National Institute on Drug Abuse supported the study. Ms. Schneider reported having no financial disclosures.
SAN DIEGO – Use of cocaine by young adults in the United States has declined significantly since the early 2000s, but it remains relatively common. In fact, results from an analysis of national data suggest that about 5% of 18- to 22-year-olds have used cocaine in the past 12 months.
“We don’t typically think of cocaine use amongst young people, but it is of a nontrivial prevalence,” lead study author Kristin E. Schneider said in an interview at the annual meeting of the College on Problems of Drug Dependence. “If someone has risky alcohol use they might also have risky substance use. We need to be screening for those things as well, while most interventions these days focus on problem drinking.”
Ms. Schneider, a graduate student in the department of mental health at Johns Hopkins University, Baltimore, and her associates drew from the 2002-2014 waves of the National Survey on Drug Use and Health to describe trends in cocaine use among young adults by race/ethnicity, sex, and college enrollment. They assessed for lifetime use, any past 12-month cocaine use, past 30-day use, and any past 12-month use disorder. They also tested for linear and quadratic trends over time.
When the researchers averaged across all years, they found that 12.1% of young adults had ever used cocaine, 5.9% had used it in the past 12 months, 1.8% had used in the past 30 days, and 1% had a use disorder in the past 12 months. They also observed significant linear declines in cocaine use across the entire study period. For example, between 2002 and 2014, the prevalence of lifetime cocaine use declined from 13.7% to 8.6%, past 12-month use declined from 6.3% to 4.1%, and past 30-day use declined from 1.8% to 1.4%.
Nonstudents had higher lifetime rates of cocaine use, compared with students (14.8% vs. 7.8%, respectively), but differences between the two groups were small for other indicators. “Perhaps being an emerging environment with other [young] adults who are also making risky health behavior decisions compensates for this baseline difference of risk between people who go to college and those who do not,” Ms. Schneider said. At the same time, the lowest rates of past 12-month cocaine use was observed in black males (1.6%), Asian females (0.8%), and black females (0.8%).
The National Institute on Drug Abuse supported the study. Ms. Schneider reported having no financial disclosures.
SAN DIEGO – Use of cocaine by young adults in the United States has declined significantly since the early 2000s, but it remains relatively common. In fact, results from an analysis of national data suggest that about 5% of 18- to 22-year-olds have used cocaine in the past 12 months.
“We don’t typically think of cocaine use amongst young people, but it is of a nontrivial prevalence,” lead study author Kristin E. Schneider said in an interview at the annual meeting of the College on Problems of Drug Dependence. “If someone has risky alcohol use they might also have risky substance use. We need to be screening for those things as well, while most interventions these days focus on problem drinking.”
Ms. Schneider, a graduate student in the department of mental health at Johns Hopkins University, Baltimore, and her associates drew from the 2002-2014 waves of the National Survey on Drug Use and Health to describe trends in cocaine use among young adults by race/ethnicity, sex, and college enrollment. They assessed for lifetime use, any past 12-month cocaine use, past 30-day use, and any past 12-month use disorder. They also tested for linear and quadratic trends over time.
When the researchers averaged across all years, they found that 12.1% of young adults had ever used cocaine, 5.9% had used it in the past 12 months, 1.8% had used in the past 30 days, and 1% had a use disorder in the past 12 months. They also observed significant linear declines in cocaine use across the entire study period. For example, between 2002 and 2014, the prevalence of lifetime cocaine use declined from 13.7% to 8.6%, past 12-month use declined from 6.3% to 4.1%, and past 30-day use declined from 1.8% to 1.4%.
Nonstudents had higher lifetime rates of cocaine use, compared with students (14.8% vs. 7.8%, respectively), but differences between the two groups were small for other indicators. “Perhaps being an emerging environment with other [young] adults who are also making risky health behavior decisions compensates for this baseline difference of risk between people who go to college and those who do not,” Ms. Schneider said. At the same time, the lowest rates of past 12-month cocaine use was observed in black males (1.6%), Asian females (0.8%), and black females (0.8%).
The National Institute on Drug Abuse supported the study. Ms. Schneider reported having no financial disclosures.
AT CPDD 2018
Key clinical point: Cocaine use has declined among young adults in the United States.
Major finding: Between 2002 and 2014, the prevalence of lifetime cocaine use declined from 13.7% to 8.6%.
Study details: An analysis drawn from the 2002-2014 waves of the National Survey on Drug Use and Health.
Disclosures: The National Institute on Drug Abuse supported the study. Ms. Schneider reported having no financial disclosures.
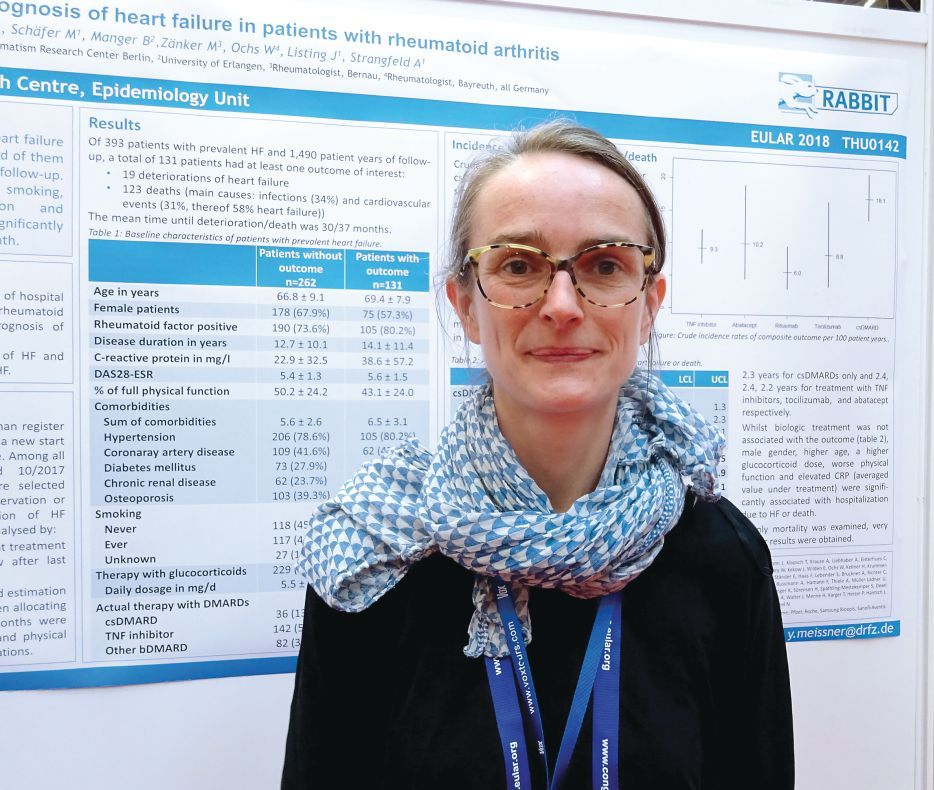
Heart failure confers poor prognosis in rheumatoid arthritis
AMSTERDAM – The combination of heart failure and rheumatoid arthritis carries a poor prognosis, according to data from the German biologics register.
Of 393 patients enrolled in RABBIT (Rheumatoide Arthritis: Beobachtung der Biologika-Therapie) who had heart failure in addition to their rheumatoid arthritis, 131 (33%) needed hospital treatment or died over a 10-year period. The mean time to hospitalization or death was 2.5-3.0 years.
“We include patients at the start of their DMARD [disease modifying antirheumatic drug] treatment and follow them up for at least 5 years,” said Dr. Meissner, explaining how the German biologics register works. “For this analysis, we selected all the patients with prevalent heart failure and followed them up until either the database was closed, they dropped out, or had an event.” In this case, an event was defined as a composite of deterioration in heart failure that required hospitalization or death from any cause.
Dr. Meissner, of the German Rheumatism Research Center in Berlin, noted that 19 (14.5%) patients experienced a deterioration in their heart failure and 123 deaths were recorded during the study period that started in May 2001 and ended in October 2017. Around one-third of deaths were attributable to infections (34%), and one-third were attributable to cardiovascular causes (31%). Of the CV deaths, more than half (58%) were attributed to patients’ heart failure.
“What impressed us the most is the number of comorbidities at baseline,” Dr. Meissner said. Not including heart failure or rheumatoid arthritis, patients who experienced an event had an average of 6.5 comorbidities versus 5.6 for those who did not have an event. These additional comorbidities included hypertension, coronary artery disease, diabetes mellitus, chronic renal disease, and osteoporosis.
Crude incidence rates (IRs) for heart failure deterioration or death were calculated according to the rheumatoid arthritis treatment being used and found to be highest in those treated with conventional DMARDs, at 18.1/100 patient-years. IRs with biologic treatments were lower, at 10.2/100 patient-years for abatacept, 9.3 for TNF inhibitors, 8.8 for tocilizumab, and 6.0 for rituximab. What this suggests it that better control of inflammation results in a lower risk for hospitalization and death, Dr. Meissner and her associates reported in their poster presentation.
“If patients are not effectively treated for rheumatoid arthritis, there might be other consequences like the deterioration of heart failure or death,” Dr. Meissner said.
She noted that investigators also looked at identifying risk factors for hospitalization or death and found that there was a greater adjusted relative risk if patients were male (RR = 2.4), older (RR = 1.3 per 5-year increase in age), or if they smoked (RR = 1.7). Using higher doses of glucocorticoids also was a risk factor, with a RR of 1.4 for every 5 mg/day increase in dose.
Better physical function was associated with a lower risk of an event (RR = 0.9) and, along with smoking and adjustment of the steroid dose, is a risk factor that could potentially be influenced, Dr. Meissner proposed.
No data on how the heart failure was being managed are available for this cohort and more research is needed.
“There is still not enough known about this topic, and we need the research to determine how to best manage these patients,” Dr. Meissner said. “The time to an event was only 3 years from the time of inclusion in the register, so we need better management of those patients with heart failure as a comorbidity.”
RABBIT is supported by a joint, unconditional grant from AbbVie, Bristol-Myers Squibb, Celltrion, Hexal AG, Lilly, MSD Sharp & Dohme, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Meissner disclosed being on a speakers bureau for Pfizer.
SOURCE: Meissner Y et al. EULAR 2018 Congress. Abstract THU0142 .
AMSTERDAM – The combination of heart failure and rheumatoid arthritis carries a poor prognosis, according to data from the German biologics register.
Of 393 patients enrolled in RABBIT (Rheumatoide Arthritis: Beobachtung der Biologika-Therapie) who had heart failure in addition to their rheumatoid arthritis, 131 (33%) needed hospital treatment or died over a 10-year period. The mean time to hospitalization or death was 2.5-3.0 years.
“We include patients at the start of their DMARD [disease modifying antirheumatic drug] treatment and follow them up for at least 5 years,” said Dr. Meissner, explaining how the German biologics register works. “For this analysis, we selected all the patients with prevalent heart failure and followed them up until either the database was closed, they dropped out, or had an event.” In this case, an event was defined as a composite of deterioration in heart failure that required hospitalization or death from any cause.
Dr. Meissner, of the German Rheumatism Research Center in Berlin, noted that 19 (14.5%) patients experienced a deterioration in their heart failure and 123 deaths were recorded during the study period that started in May 2001 and ended in October 2017. Around one-third of deaths were attributable to infections (34%), and one-third were attributable to cardiovascular causes (31%). Of the CV deaths, more than half (58%) were attributed to patients’ heart failure.
“What impressed us the most is the number of comorbidities at baseline,” Dr. Meissner said. Not including heart failure or rheumatoid arthritis, patients who experienced an event had an average of 6.5 comorbidities versus 5.6 for those who did not have an event. These additional comorbidities included hypertension, coronary artery disease, diabetes mellitus, chronic renal disease, and osteoporosis.
Crude incidence rates (IRs) for heart failure deterioration or death were calculated according to the rheumatoid arthritis treatment being used and found to be highest in those treated with conventional DMARDs, at 18.1/100 patient-years. IRs with biologic treatments were lower, at 10.2/100 patient-years for abatacept, 9.3 for TNF inhibitors, 8.8 for tocilizumab, and 6.0 for rituximab. What this suggests it that better control of inflammation results in a lower risk for hospitalization and death, Dr. Meissner and her associates reported in their poster presentation.
“If patients are not effectively treated for rheumatoid arthritis, there might be other consequences like the deterioration of heart failure or death,” Dr. Meissner said.
She noted that investigators also looked at identifying risk factors for hospitalization or death and found that there was a greater adjusted relative risk if patients were male (RR = 2.4), older (RR = 1.3 per 5-year increase in age), or if they smoked (RR = 1.7). Using higher doses of glucocorticoids also was a risk factor, with a RR of 1.4 for every 5 mg/day increase in dose.
Better physical function was associated with a lower risk of an event (RR = 0.9) and, along with smoking and adjustment of the steroid dose, is a risk factor that could potentially be influenced, Dr. Meissner proposed.
No data on how the heart failure was being managed are available for this cohort and more research is needed.
“There is still not enough known about this topic, and we need the research to determine how to best manage these patients,” Dr. Meissner said. “The time to an event was only 3 years from the time of inclusion in the register, so we need better management of those patients with heart failure as a comorbidity.”
RABBIT is supported by a joint, unconditional grant from AbbVie, Bristol-Myers Squibb, Celltrion, Hexal AG, Lilly, MSD Sharp & Dohme, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Meissner disclosed being on a speakers bureau for Pfizer.
SOURCE: Meissner Y et al. EULAR 2018 Congress. Abstract THU0142 .
AMSTERDAM – The combination of heart failure and rheumatoid arthritis carries a poor prognosis, according to data from the German biologics register.
Of 393 patients enrolled in RABBIT (Rheumatoide Arthritis: Beobachtung der Biologika-Therapie) who had heart failure in addition to their rheumatoid arthritis, 131 (33%) needed hospital treatment or died over a 10-year period. The mean time to hospitalization or death was 2.5-3.0 years.
“We include patients at the start of their DMARD [disease modifying antirheumatic drug] treatment and follow them up for at least 5 years,” said Dr. Meissner, explaining how the German biologics register works. “For this analysis, we selected all the patients with prevalent heart failure and followed them up until either the database was closed, they dropped out, or had an event.” In this case, an event was defined as a composite of deterioration in heart failure that required hospitalization or death from any cause.
Dr. Meissner, of the German Rheumatism Research Center in Berlin, noted that 19 (14.5%) patients experienced a deterioration in their heart failure and 123 deaths were recorded during the study period that started in May 2001 and ended in October 2017. Around one-third of deaths were attributable to infections (34%), and one-third were attributable to cardiovascular causes (31%). Of the CV deaths, more than half (58%) were attributed to patients’ heart failure.
“What impressed us the most is the number of comorbidities at baseline,” Dr. Meissner said. Not including heart failure or rheumatoid arthritis, patients who experienced an event had an average of 6.5 comorbidities versus 5.6 for those who did not have an event. These additional comorbidities included hypertension, coronary artery disease, diabetes mellitus, chronic renal disease, and osteoporosis.
Crude incidence rates (IRs) for heart failure deterioration or death were calculated according to the rheumatoid arthritis treatment being used and found to be highest in those treated with conventional DMARDs, at 18.1/100 patient-years. IRs with biologic treatments were lower, at 10.2/100 patient-years for abatacept, 9.3 for TNF inhibitors, 8.8 for tocilizumab, and 6.0 for rituximab. What this suggests it that better control of inflammation results in a lower risk for hospitalization and death, Dr. Meissner and her associates reported in their poster presentation.
“If patients are not effectively treated for rheumatoid arthritis, there might be other consequences like the deterioration of heart failure or death,” Dr. Meissner said.
She noted that investigators also looked at identifying risk factors for hospitalization or death and found that there was a greater adjusted relative risk if patients were male (RR = 2.4), older (RR = 1.3 per 5-year increase in age), or if they smoked (RR = 1.7). Using higher doses of glucocorticoids also was a risk factor, with a RR of 1.4 for every 5 mg/day increase in dose.
Better physical function was associated with a lower risk of an event (RR = 0.9) and, along with smoking and adjustment of the steroid dose, is a risk factor that could potentially be influenced, Dr. Meissner proposed.
No data on how the heart failure was being managed are available for this cohort and more research is needed.
“There is still not enough known about this topic, and we need the research to determine how to best manage these patients,” Dr. Meissner said. “The time to an event was only 3 years from the time of inclusion in the register, so we need better management of those patients with heart failure as a comorbidity.”
RABBIT is supported by a joint, unconditional grant from AbbVie, Bristol-Myers Squibb, Celltrion, Hexal AG, Lilly, MSD Sharp & Dohme, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Meissner disclosed being on a speakers bureau for Pfizer.
SOURCE: Meissner Y et al. EULAR 2018 Congress. Abstract THU0142 .
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: Comorbid heart failure and rheumatoid arthritis carry an unfavorable prognosis, but risk factors have been identified.
Major finding: One-third of patients were hospitalized or died, with a mean time to deterioration or death of 2.5-3 years.
Study details: 393 patients with both heart failure and rheumatoid arthritis enrolled in the German biologics register RABBIT.
Disclosures: RABBIT is supported by a joint, unconditional grant from AbbVie, Bristol-Myers Squibb, Celltrion, Hexal AG, Lilly, MSD Sharp & Dohme, Pfizer, Roche, Samsung Bioepis, Sanofi-Aventis, and UCB. Dr. Meissner disclosed being part of a speakers bureau for Pfizer.
Source: Meissner Y et al. EULAR 2018 Congress, Abstract THU0142.
Extramammary Paget Disease: Making the Correct Diagnosis
Resident debt burden may cloud professional future
Surgical trainees have a large, potentially unmanageable debt burden and are in need of long-term financial education to help better navigate the growing cost of medical education, according to new research.
“Surgical residents are highly leveraged financially and have minimal financial training,” Sarah E. Tevis, MD, of the University of Texas MD Anderson Cancer Center, Houston, and her colleagues wrote in a study in the Journal of the American College of Surgeons. “This places residents in a volatile financial situation as they complete their training and start accumulating debt liabilities, such as mortgages and child care, in the face of tremendous amounts of educational and other debt liabilities.”
Studies of resident debt load typically account for medical education debt, but not for other debts such as undergraduate loans, consumer debt, and mortgages. Residents’ actual debt burden may be considerably higher than has been reported.
The researchers sent surveys to all surgical residents at the University of Wisconsin, Madison, in 2015, with 105 responding (an 80% response rate). Of those responding, 38% reported having more than $200,000 in educational debt, and 82% had a moderate- or high-risk debt-to-asset ratio.
“We found that surgical residents are dangerously overleveraged, with 70% of residents found to have high debt-to-asset ratios,” Dr. Tevis and her colleagues wrote, with the addition of mortgages and vehicle debt on top of educational debt being the key factors of moving residents into the high-risk debt-to-asset category.
The debt-to-asset ratio was calculated as the sum of student loan debt + nonstudent loan debt + credit card balance + mortgage debt + vehicle debt divided by the value of home and other real estate + value of household vehicles + amount in savings + value of retirement investment. A debt-to-asset ratio of 0.5 to 0.9 was considered moderate risk, with a ratio greater than or equal to 0.9 considered high risk.
The debt-to-income ratio was calculated as the sum of student loan debt + nonstudent loan debt + credit card balance + mortgage debt + vehicle debt divided by total household income. A high-risk ratio defined as being greater than 0.4, the line at which surgical trainees might be restricted from obtaining a traditional mortgage.
Total household income included personal income, domestic partner income, military income, and any income from moonlighting, rental properties, and other sources of revenue. Assets included home and second home purchase prices when applicable, value of vehicles, amount in savings, value of retirement accounts, and value of investments. Contributors to debt included student loan, nonstudent loan, mortgage, vehicle financing, and credit card balances.
Salary data for U.S. residents, which strictly tracked U.S. inflation, was calculated over a 15-year period (2000-2015) using data from the Association of American Medical Colleges for comparison.
In examining debt-to-income, researchers found that “83% of residents have a high-risk debt-to-income ratio [greater than 0.4],” the authors wrote. “We found that the majority of residents were classified in the high financial risk exposure cohort when comprehensive total debt liabilities were considered. In this group of highly leveraged residents, over 80% of residents were dangerously unable to manage regular monthly liabilities with their current level of income.”
No statistically significant association between sex, residency year, residency program, or who manages finances and risk debt-to-asset ratios were found in this study.
The authors noted that, although this study did not look at the psychological impact of significant debt load and lack of training on how to manage finances, these factors have been shown in other studies to correlate with resident burnout and psychological stress.
Bruce A. Harms, MD, FACS, coauthor of the study said in an interview, “We are in an evolving era in surgery and in health care in general and financial resources are being stretched. We don’t know for sure that the rising educational debt and overall debt burden as residents enter their prime years will drive the next generation of physicians to certain career choices. It may even perhaps drive a given fully trained young surgeon away from a practice that is more exposed to an underserved population. Excessive financial debt induced stress may influence a resident’s decision on what they do with their skill set but to what degree is largely unknown.”
Dr. Harms added that residents may assume that when they eventually enter practice, they will have a pathway and the means to deal with educational debt. “They would be correct in that starting salaries are keeping pace with inflation. However, in many instances, they are also entering a time in their lives when they will be taking on additional debt in the form of home mortgage, family, and child care costs. I believe, in most instances, residents are focused almost totally on their residency training and many other financial considerations take a back seat and ‘we’ll deal with our debt problem in the future’ attitude. Residents for the most part don’t have the financial means and resources to deal with debt anyway during the course of their lengthy residency training. The exception would be having a secondary income from a spouse or partner that would allow for a more robust debt-attrition strategy. Also, residents are likely not focused on or considering a strategy for the best return on investment of their time, additional expense, and career delay from their prolonged pathway to becoming a fully trained surgeon.”
The bottom line is that basic financial educational is not included in core surgical training even though most surgical residents would like some degree of financial education. That is the basic problem and shortcoming of existing residency training programs, Dr. Tevis and her colleagues wrote.
Given the financial burdens that education and other factors are placing on surgical residents, Dr. Tevis and her colleagues proposed “that formal training in the business of medicine and personal finance for surgical residents be strongly considered at the training program level or in partnership with other organizations, such as the American College of Surgeons, in an effort to improve the financial status of residents and prepare them for their careers, both personally and professionally.”
Dr. Harms noted, “It is probable that in most cases, educational loan debt principal is not being paid down to any significant degree given the current residency salary structure. We can only hope that residents are given some degree of good information on strategies for managing educational loan debt, which may include federally sponsored loan repayment programs such as [those offered] through NIH-sponsored research or federal loan forgiveness programs that residents may qualify for. In most cases, federal loan forgiveness programs require a minimum monthly payment that is calculated based upon current income. As an absolute minimum, interest payments should be made as additional interest debt will add significantly to the overall debt burden as interest will continue to accrue.”
Getting that financial training early could have significant benefits on the back end. The study authors noted that salary data from the Association of American Medical Colleges showed assistant professor salaries mirrored inflation metrics, but even better, surgeon salaries continued to exceed inflation-indexed targets and continued upward trends even through recession periods.
“Therefore, the financial pathway, built on increases in surgeon starting salaries exceeding annual inflation, presently still exists for deleveraging of critical debt exposure if personal finances are optimally managed,” the authors stated.
The study did have its limitations. It did not include certain variable expenses such as utilities, food, and other shopping habits, although that may have been captured as the survey asked respondents to list other “major” sources of income and debt. It also was limited to surgical residents at a single institution and may not be applicable to other specialties or geographic locations. It did not assess whether residents with mortgage payments were able to make educational loan payments beyond the minimum.
The investigators reported no conflicts.
SOURCE: Tevis SE et al. J Am Coll Surg. 2018 May 31. doi: 10.1016/j.jamcollsurg.2018.05.002.
Surgical trainees have a large, potentially unmanageable debt burden and are in need of long-term financial education to help better navigate the growing cost of medical education, according to new research.
“Surgical residents are highly leveraged financially and have minimal financial training,” Sarah E. Tevis, MD, of the University of Texas MD Anderson Cancer Center, Houston, and her colleagues wrote in a study in the Journal of the American College of Surgeons. “This places residents in a volatile financial situation as they complete their training and start accumulating debt liabilities, such as mortgages and child care, in the face of tremendous amounts of educational and other debt liabilities.”
Studies of resident debt load typically account for medical education debt, but not for other debts such as undergraduate loans, consumer debt, and mortgages. Residents’ actual debt burden may be considerably higher than has been reported.
The researchers sent surveys to all surgical residents at the University of Wisconsin, Madison, in 2015, with 105 responding (an 80% response rate). Of those responding, 38% reported having more than $200,000 in educational debt, and 82% had a moderate- or high-risk debt-to-asset ratio.
“We found that surgical residents are dangerously overleveraged, with 70% of residents found to have high debt-to-asset ratios,” Dr. Tevis and her colleagues wrote, with the addition of mortgages and vehicle debt on top of educational debt being the key factors of moving residents into the high-risk debt-to-asset category.
The debt-to-asset ratio was calculated as the sum of student loan debt + nonstudent loan debt + credit card balance + mortgage debt + vehicle debt divided by the value of home and other real estate + value of household vehicles + amount in savings + value of retirement investment. A debt-to-asset ratio of 0.5 to 0.9 was considered moderate risk, with a ratio greater than or equal to 0.9 considered high risk.
The debt-to-income ratio was calculated as the sum of student loan debt + nonstudent loan debt + credit card balance + mortgage debt + vehicle debt divided by total household income. A high-risk ratio defined as being greater than 0.4, the line at which surgical trainees might be restricted from obtaining a traditional mortgage.
Total household income included personal income, domestic partner income, military income, and any income from moonlighting, rental properties, and other sources of revenue. Assets included home and second home purchase prices when applicable, value of vehicles, amount in savings, value of retirement accounts, and value of investments. Contributors to debt included student loan, nonstudent loan, mortgage, vehicle financing, and credit card balances.
Salary data for U.S. residents, which strictly tracked U.S. inflation, was calculated over a 15-year period (2000-2015) using data from the Association of American Medical Colleges for comparison.
In examining debt-to-income, researchers found that “83% of residents have a high-risk debt-to-income ratio [greater than 0.4],” the authors wrote. “We found that the majority of residents were classified in the high financial risk exposure cohort when comprehensive total debt liabilities were considered. In this group of highly leveraged residents, over 80% of residents were dangerously unable to manage regular monthly liabilities with their current level of income.”
No statistically significant association between sex, residency year, residency program, or who manages finances and risk debt-to-asset ratios were found in this study.
The authors noted that, although this study did not look at the psychological impact of significant debt load and lack of training on how to manage finances, these factors have been shown in other studies to correlate with resident burnout and psychological stress.
Bruce A. Harms, MD, FACS, coauthor of the study said in an interview, “We are in an evolving era in surgery and in health care in general and financial resources are being stretched. We don’t know for sure that the rising educational debt and overall debt burden as residents enter their prime years will drive the next generation of physicians to certain career choices. It may even perhaps drive a given fully trained young surgeon away from a practice that is more exposed to an underserved population. Excessive financial debt induced stress may influence a resident’s decision on what they do with their skill set but to what degree is largely unknown.”
Dr. Harms added that residents may assume that when they eventually enter practice, they will have a pathway and the means to deal with educational debt. “They would be correct in that starting salaries are keeping pace with inflation. However, in many instances, they are also entering a time in their lives when they will be taking on additional debt in the form of home mortgage, family, and child care costs. I believe, in most instances, residents are focused almost totally on their residency training and many other financial considerations take a back seat and ‘we’ll deal with our debt problem in the future’ attitude. Residents for the most part don’t have the financial means and resources to deal with debt anyway during the course of their lengthy residency training. The exception would be having a secondary income from a spouse or partner that would allow for a more robust debt-attrition strategy. Also, residents are likely not focused on or considering a strategy for the best return on investment of their time, additional expense, and career delay from their prolonged pathway to becoming a fully trained surgeon.”
The bottom line is that basic financial educational is not included in core surgical training even though most surgical residents would like some degree of financial education. That is the basic problem and shortcoming of existing residency training programs, Dr. Tevis and her colleagues wrote.
Given the financial burdens that education and other factors are placing on surgical residents, Dr. Tevis and her colleagues proposed “that formal training in the business of medicine and personal finance for surgical residents be strongly considered at the training program level or in partnership with other organizations, such as the American College of Surgeons, in an effort to improve the financial status of residents and prepare them for their careers, both personally and professionally.”
Dr. Harms noted, “It is probable that in most cases, educational loan debt principal is not being paid down to any significant degree given the current residency salary structure. We can only hope that residents are given some degree of good information on strategies for managing educational loan debt, which may include federally sponsored loan repayment programs such as [those offered] through NIH-sponsored research or federal loan forgiveness programs that residents may qualify for. In most cases, federal loan forgiveness programs require a minimum monthly payment that is calculated based upon current income. As an absolute minimum, interest payments should be made as additional interest debt will add significantly to the overall debt burden as interest will continue to accrue.”
Getting that financial training early could have significant benefits on the back end. The study authors noted that salary data from the Association of American Medical Colleges showed assistant professor salaries mirrored inflation metrics, but even better, surgeon salaries continued to exceed inflation-indexed targets and continued upward trends even through recession periods.
“Therefore, the financial pathway, built on increases in surgeon starting salaries exceeding annual inflation, presently still exists for deleveraging of critical debt exposure if personal finances are optimally managed,” the authors stated.
The study did have its limitations. It did not include certain variable expenses such as utilities, food, and other shopping habits, although that may have been captured as the survey asked respondents to list other “major” sources of income and debt. It also was limited to surgical residents at a single institution and may not be applicable to other specialties or geographic locations. It did not assess whether residents with mortgage payments were able to make educational loan payments beyond the minimum.
The investigators reported no conflicts.
SOURCE: Tevis SE et al. J Am Coll Surg. 2018 May 31. doi: 10.1016/j.jamcollsurg.2018.05.002.
Surgical trainees have a large, potentially unmanageable debt burden and are in need of long-term financial education to help better navigate the growing cost of medical education, according to new research.
“Surgical residents are highly leveraged financially and have minimal financial training,” Sarah E. Tevis, MD, of the University of Texas MD Anderson Cancer Center, Houston, and her colleagues wrote in a study in the Journal of the American College of Surgeons. “This places residents in a volatile financial situation as they complete their training and start accumulating debt liabilities, such as mortgages and child care, in the face of tremendous amounts of educational and other debt liabilities.”
Studies of resident debt load typically account for medical education debt, but not for other debts such as undergraduate loans, consumer debt, and mortgages. Residents’ actual debt burden may be considerably higher than has been reported.
The researchers sent surveys to all surgical residents at the University of Wisconsin, Madison, in 2015, with 105 responding (an 80% response rate). Of those responding, 38% reported having more than $200,000 in educational debt, and 82% had a moderate- or high-risk debt-to-asset ratio.
“We found that surgical residents are dangerously overleveraged, with 70% of residents found to have high debt-to-asset ratios,” Dr. Tevis and her colleagues wrote, with the addition of mortgages and vehicle debt on top of educational debt being the key factors of moving residents into the high-risk debt-to-asset category.
The debt-to-asset ratio was calculated as the sum of student loan debt + nonstudent loan debt + credit card balance + mortgage debt + vehicle debt divided by the value of home and other real estate + value of household vehicles + amount in savings + value of retirement investment. A debt-to-asset ratio of 0.5 to 0.9 was considered moderate risk, with a ratio greater than or equal to 0.9 considered high risk.
The debt-to-income ratio was calculated as the sum of student loan debt + nonstudent loan debt + credit card balance + mortgage debt + vehicle debt divided by total household income. A high-risk ratio defined as being greater than 0.4, the line at which surgical trainees might be restricted from obtaining a traditional mortgage.
Total household income included personal income, domestic partner income, military income, and any income from moonlighting, rental properties, and other sources of revenue. Assets included home and second home purchase prices when applicable, value of vehicles, amount in savings, value of retirement accounts, and value of investments. Contributors to debt included student loan, nonstudent loan, mortgage, vehicle financing, and credit card balances.
Salary data for U.S. residents, which strictly tracked U.S. inflation, was calculated over a 15-year period (2000-2015) using data from the Association of American Medical Colleges for comparison.
In examining debt-to-income, researchers found that “83% of residents have a high-risk debt-to-income ratio [greater than 0.4],” the authors wrote. “We found that the majority of residents were classified in the high financial risk exposure cohort when comprehensive total debt liabilities were considered. In this group of highly leveraged residents, over 80% of residents were dangerously unable to manage regular monthly liabilities with their current level of income.”
No statistically significant association between sex, residency year, residency program, or who manages finances and risk debt-to-asset ratios were found in this study.
The authors noted that, although this study did not look at the psychological impact of significant debt load and lack of training on how to manage finances, these factors have been shown in other studies to correlate with resident burnout and psychological stress.
Bruce A. Harms, MD, FACS, coauthor of the study said in an interview, “We are in an evolving era in surgery and in health care in general and financial resources are being stretched. We don’t know for sure that the rising educational debt and overall debt burden as residents enter their prime years will drive the next generation of physicians to certain career choices. It may even perhaps drive a given fully trained young surgeon away from a practice that is more exposed to an underserved population. Excessive financial debt induced stress may influence a resident’s decision on what they do with their skill set but to what degree is largely unknown.”
Dr. Harms added that residents may assume that when they eventually enter practice, they will have a pathway and the means to deal with educational debt. “They would be correct in that starting salaries are keeping pace with inflation. However, in many instances, they are also entering a time in their lives when they will be taking on additional debt in the form of home mortgage, family, and child care costs. I believe, in most instances, residents are focused almost totally on their residency training and many other financial considerations take a back seat and ‘we’ll deal with our debt problem in the future’ attitude. Residents for the most part don’t have the financial means and resources to deal with debt anyway during the course of their lengthy residency training. The exception would be having a secondary income from a spouse or partner that would allow for a more robust debt-attrition strategy. Also, residents are likely not focused on or considering a strategy for the best return on investment of their time, additional expense, and career delay from their prolonged pathway to becoming a fully trained surgeon.”
The bottom line is that basic financial educational is not included in core surgical training even though most surgical residents would like some degree of financial education. That is the basic problem and shortcoming of existing residency training programs, Dr. Tevis and her colleagues wrote.
Given the financial burdens that education and other factors are placing on surgical residents, Dr. Tevis and her colleagues proposed “that formal training in the business of medicine and personal finance for surgical residents be strongly considered at the training program level or in partnership with other organizations, such as the American College of Surgeons, in an effort to improve the financial status of residents and prepare them for their careers, both personally and professionally.”
Dr. Harms noted, “It is probable that in most cases, educational loan debt principal is not being paid down to any significant degree given the current residency salary structure. We can only hope that residents are given some degree of good information on strategies for managing educational loan debt, which may include federally sponsored loan repayment programs such as [those offered] through NIH-sponsored research or federal loan forgiveness programs that residents may qualify for. In most cases, federal loan forgiveness programs require a minimum monthly payment that is calculated based upon current income. As an absolute minimum, interest payments should be made as additional interest debt will add significantly to the overall debt burden as interest will continue to accrue.”
Getting that financial training early could have significant benefits on the back end. The study authors noted that salary data from the Association of American Medical Colleges showed assistant professor salaries mirrored inflation metrics, but even better, surgeon salaries continued to exceed inflation-indexed targets and continued upward trends even through recession periods.
“Therefore, the financial pathway, built on increases in surgeon starting salaries exceeding annual inflation, presently still exists for deleveraging of critical debt exposure if personal finances are optimally managed,” the authors stated.
The study did have its limitations. It did not include certain variable expenses such as utilities, food, and other shopping habits, although that may have been captured as the survey asked respondents to list other “major” sources of income and debt. It also was limited to surgical residents at a single institution and may not be applicable to other specialties or geographic locations. It did not assess whether residents with mortgage payments were able to make educational loan payments beyond the minimum.
The investigators reported no conflicts.
SOURCE: Tevis SE et al. J Am Coll Surg. 2018 May 31. doi: 10.1016/j.jamcollsurg.2018.05.002.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Residents’ actual debt may be considerably higher than has been reported.
Major finding: More than one-third of surgical residents responding to a survey reported more than $200,000 in educational debt.
Study details: An analysis of responses to a survey from 105 surgical residents at the University of Wisconsin.
Disclosures: The study authors reported no disclosures.
Source: Tevis SE et al. J Am Coll Surg. 2018 May 31. doi: 10.1016/j.jamcollsurg.2018.05.002.
Resilience, part 3
Major PHS Cuts Proposed in Reorg Plan
The Trump administration seeks to reorganize several federal agencies as part of a sweeping reform proposal, issued June 21. Although the plans hits many parts of federal health care, the most dramatic change is a proposed reduction of the Public Health Service (PHS) Commissioned Corps from more than 6,000 officers to no more than 4,500.
“Government in the 21st century is fundamentally a services business, and modern information technology should be at the heart of the U.S. government service delivery model,” according to the administration’s reform proposal. “And yet, today’s Executive branch is still aligned to the stove-piped organizational constructs of the 20th century, which in many cases have grown inefficient and out of date. Consequently, the public and our workforce are frustrated with government’s ability to deliver its mission in an effective, efficient, and secure way.”
If implemented, changes to the Commissioned Corp would be dramatic. The plan directs the Department of Health and Human Services (HHS) to “civilianize officers who do not provide critical public health services” and to ensure that the Corps is deployed at least once every 3 years to positions that either are difficult to fill or respond to a public health emergency. Instead the Commissioned Corps would be replaced with a Reserve Corps. Similar to the armed forces reserves, this group “would consist of Government employees and private citizens who agree to be deployed and serve in times of national need.” In addition, the plan would change the way federal agencies pay for the retirement benefits of Commissioned Corps members, potentially eliminating one of the fiscal benefits that agencies receive for hiring Commissioned Corps members.
In addition, under the proposal, nutrition assistance programs currently run out of the U.S. Department of Agriculture (USDA) including the Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) would move to the Department of Health and Human Services, which would be rebranded the Department of Health and Public Welfare.
Moving these programs “would allow for better and easier coordination across programs that serve similar populations, ensuring consistent policies and a single point of administration for the major public assistance programs,” according to the proposal. “This single point of administration would lead to reduced duplication in state reporting requirements and other administrative burdens, and a more streamlined process for issuing guidance, writing regulations, and approving waivers.”
Food oversight functions would move from the Food and Drug Administration to the USDA; FDA would be rebranded the Federal Drug Administration and focus on drugs, devices, biologics, tobacco, dietary supplements, and cosmetics.
The administration also proposed to create a Council on Public Assistance comprised of “all federal agencies that administer public benefits, with a statutory authority to set cross-cutting program policies, including uniform work requirements.”
Other functions of the council would include approving service plans and waivers by states under Welfare-to-Work projects; resolving disputes when multiple agencies disagree on a particular policy; and recommending policy changes to eliminate barriers at the federal, state, and local level to getting welfare beneficiaries to work.
The proposal also calls for a restructuring of the National Institutes of Health “to ensure operations are effective and efficient,” with no detail provided. It would also place the Agency for Healthcare Research and Quality under the auspices of NIH.
The Strategic National Stockpile would be managed by the Assistant Secretary for Preparedness and Response “to consolidate strategic decision making around the development and procurement of medical countermeasures, and streamline operational decisions during responses to public health and other emergencies to improve responsiveness.”
Senator Patty Murray (D-WA), the ranking member of the Senate Health, Education, Labor, and Pensions (HELP) Committee, was quick to dismiss the plan, labeling it as “futile” and an “attempt to make government work worse for the people it serves.”
This article originally appeared at Internal Medicine News. It has been edited for Federal Practitioner and includes additional reporting by Reid Paul.
The Trump administration seeks to reorganize several federal agencies as part of a sweeping reform proposal, issued June 21. Although the plans hits many parts of federal health care, the most dramatic change is a proposed reduction of the Public Health Service (PHS) Commissioned Corps from more than 6,000 officers to no more than 4,500.
“Government in the 21st century is fundamentally a services business, and modern information technology should be at the heart of the U.S. government service delivery model,” according to the administration’s reform proposal. “And yet, today’s Executive branch is still aligned to the stove-piped organizational constructs of the 20th century, which in many cases have grown inefficient and out of date. Consequently, the public and our workforce are frustrated with government’s ability to deliver its mission in an effective, efficient, and secure way.”
If implemented, changes to the Commissioned Corp would be dramatic. The plan directs the Department of Health and Human Services (HHS) to “civilianize officers who do not provide critical public health services” and to ensure that the Corps is deployed at least once every 3 years to positions that either are difficult to fill or respond to a public health emergency. Instead the Commissioned Corps would be replaced with a Reserve Corps. Similar to the armed forces reserves, this group “would consist of Government employees and private citizens who agree to be deployed and serve in times of national need.” In addition, the plan would change the way federal agencies pay for the retirement benefits of Commissioned Corps members, potentially eliminating one of the fiscal benefits that agencies receive for hiring Commissioned Corps members.
In addition, under the proposal, nutrition assistance programs currently run out of the U.S. Department of Agriculture (USDA) including the Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) would move to the Department of Health and Human Services, which would be rebranded the Department of Health and Public Welfare.
Moving these programs “would allow for better and easier coordination across programs that serve similar populations, ensuring consistent policies and a single point of administration for the major public assistance programs,” according to the proposal. “This single point of administration would lead to reduced duplication in state reporting requirements and other administrative burdens, and a more streamlined process for issuing guidance, writing regulations, and approving waivers.”
Food oversight functions would move from the Food and Drug Administration to the USDA; FDA would be rebranded the Federal Drug Administration and focus on drugs, devices, biologics, tobacco, dietary supplements, and cosmetics.
The administration also proposed to create a Council on Public Assistance comprised of “all federal agencies that administer public benefits, with a statutory authority to set cross-cutting program policies, including uniform work requirements.”
Other functions of the council would include approving service plans and waivers by states under Welfare-to-Work projects; resolving disputes when multiple agencies disagree on a particular policy; and recommending policy changes to eliminate barriers at the federal, state, and local level to getting welfare beneficiaries to work.
The proposal also calls for a restructuring of the National Institutes of Health “to ensure operations are effective and efficient,” with no detail provided. It would also place the Agency for Healthcare Research and Quality under the auspices of NIH.
The Strategic National Stockpile would be managed by the Assistant Secretary for Preparedness and Response “to consolidate strategic decision making around the development and procurement of medical countermeasures, and streamline operational decisions during responses to public health and other emergencies to improve responsiveness.”
Senator Patty Murray (D-WA), the ranking member of the Senate Health, Education, Labor, and Pensions (HELP) Committee, was quick to dismiss the plan, labeling it as “futile” and an “attempt to make government work worse for the people it serves.”
This article originally appeared at Internal Medicine News. It has been edited for Federal Practitioner and includes additional reporting by Reid Paul.
The Trump administration seeks to reorganize several federal agencies as part of a sweeping reform proposal, issued June 21. Although the plans hits many parts of federal health care, the most dramatic change is a proposed reduction of the Public Health Service (PHS) Commissioned Corps from more than 6,000 officers to no more than 4,500.
“Government in the 21st century is fundamentally a services business, and modern information technology should be at the heart of the U.S. government service delivery model,” according to the administration’s reform proposal. “And yet, today’s Executive branch is still aligned to the stove-piped organizational constructs of the 20th century, which in many cases have grown inefficient and out of date. Consequently, the public and our workforce are frustrated with government’s ability to deliver its mission in an effective, efficient, and secure way.”
If implemented, changes to the Commissioned Corp would be dramatic. The plan directs the Department of Health and Human Services (HHS) to “civilianize officers who do not provide critical public health services” and to ensure that the Corps is deployed at least once every 3 years to positions that either are difficult to fill or respond to a public health emergency. Instead the Commissioned Corps would be replaced with a Reserve Corps. Similar to the armed forces reserves, this group “would consist of Government employees and private citizens who agree to be deployed and serve in times of national need.” In addition, the plan would change the way federal agencies pay for the retirement benefits of Commissioned Corps members, potentially eliminating one of the fiscal benefits that agencies receive for hiring Commissioned Corps members.
In addition, under the proposal, nutrition assistance programs currently run out of the U.S. Department of Agriculture (USDA) including the Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) would move to the Department of Health and Human Services, which would be rebranded the Department of Health and Public Welfare.
Moving these programs “would allow for better and easier coordination across programs that serve similar populations, ensuring consistent policies and a single point of administration for the major public assistance programs,” according to the proposal. “This single point of administration would lead to reduced duplication in state reporting requirements and other administrative burdens, and a more streamlined process for issuing guidance, writing regulations, and approving waivers.”
Food oversight functions would move from the Food and Drug Administration to the USDA; FDA would be rebranded the Federal Drug Administration and focus on drugs, devices, biologics, tobacco, dietary supplements, and cosmetics.
The administration also proposed to create a Council on Public Assistance comprised of “all federal agencies that administer public benefits, with a statutory authority to set cross-cutting program policies, including uniform work requirements.”
Other functions of the council would include approving service plans and waivers by states under Welfare-to-Work projects; resolving disputes when multiple agencies disagree on a particular policy; and recommending policy changes to eliminate barriers at the federal, state, and local level to getting welfare beneficiaries to work.
The proposal also calls for a restructuring of the National Institutes of Health “to ensure operations are effective and efficient,” with no detail provided. It would also place the Agency for Healthcare Research and Quality under the auspices of NIH.
The Strategic National Stockpile would be managed by the Assistant Secretary for Preparedness and Response “to consolidate strategic decision making around the development and procurement of medical countermeasures, and streamline operational decisions during responses to public health and other emergencies to improve responsiveness.”
Senator Patty Murray (D-WA), the ranking member of the Senate Health, Education, Labor, and Pensions (HELP) Committee, was quick to dismiss the plan, labeling it as “futile” and an “attempt to make government work worse for the people it serves.”
This article originally appeared at Internal Medicine News. It has been edited for Federal Practitioner and includes additional reporting by Reid Paul.
FDA Boxed Warning Updates: June 2018
The FDA’s MedWatch program safety labeling changes for boxed warnings are compiled quarterly for drugs and therapeutic biologics where important changes have been made to the safety information. These and other label changes are searchable in the Drug Safety Labeling Changes (SLC) database, where data are available to the public in downloadable and searchable formats. Boxed warnings are ordinarily used to highlight either adverse reactions so serious in proportion to the potential benefi t from the drug that it is essential that it be considered in assessing the risks and benefi ts of using the drug; or serious adverse reactions that can be prevented/reduced in frequency or severity by appropriate use of the drug; or FDA approved the drug with restrictions to ensure safe use because FDA concluded that the drug can be safely used only if distribution or use is restricted. For complete FDA Drug Safety Labeling changes, please visit http://www.accessdata.fda.gov/scripts/cder/safetylabelingchanges.
VIDEX AND VIDEX EC (DIDANOSINE):
- Edited boxed warning, January 2018
WARNING: PANCREATITIS, LACTIC ACIDOSIS and HEPATOMEGALY with STEATOSIS
Coadministration of VIDEX or VIDEX EC and stavudine is contraindicated because of increased risk of serious and/or life-threatening events. Suspend treatment if clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity occurs.
ZYDELIG (IDELALISIB):
- Edited boxed warning, January 2018
WARNING: FATAL AND SERIOUS TOXICITIES: HEPATIC, SEVERE DIARRHEA, COLITIS, PNEUMONITIS, INFECTIONS, and INTESTINAL PERFORATION
Fatal and/or serious hepatotoxicity occurred in 16% to 18% of Zydelig-treated patients…
Fatal and/or serious and severe diarrhea or colitis occurred in 14% to 20% of Zydelig-treated patients…
Fatal and/or serious infections occurred in 21% to 48% of Zydelig-treated patients…
AQUAMEPHYTON (PHYTONADIONE):
- Edited boxed warning, March 2018
WARNING: HYPERSENSITIVITY REACTIONS WITH INTRAVENOUS AND INTRAMUSCULAR USE
Fatal hypersensitivity reactions, including anaphylaxis, have occurred during and immediately after INTRAVENOUS and INTRAMUSCULAR injection of Aqua-MEPHYTON. Reactions have occurred despite dilution to avoid rapid infusion and upon first dose. Avoid the intravenous and intramuscular routes of administration unless the subcutaneous route is not feasible and the serious risk is justified.
FERAHEME (FERUMOXYTOL):
- Edited boxed warning, February 2018
WARNING: RISK FOR SERIOUS HYPERSENSITIVITY/ANAPHYLAXIS REACTIONS
Fatal and serious hypersensitivity reactions including anaphylaxis have occurred in patients receiving feraheme. Initial symptoms may
include hypotension, syncope, unresponsiveness, cardiac/cardiorespiratory arrest.
Only administer feraheme as an intravenous infusion over at least 15 minutes and only when personnel and therapies are immediately available for the treatment of anaphylaxis and other hypersensitivity reactions.
METHADONE HYDROCHLORIDE, METHADOSE (METHADONE HYDROCHLORIDE):
- Edited boxed warning, February 2018
RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
Concomitant use with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, is a risk factor for respiratory depression and death.
Reserve concomitant prescribing of benzodiazepines or other CNS depressants for use in patients for whom alternatives to benzodiazepines or other CNS depressants are inadequate.
Follow patients for signs and symptoms of respiratory depression and sedation. If the patient is visibly sedated, evaluate the cause of sedation, and consider delaying or omitting daily methadone dosing.
DOLOPHINE HYDROCHLORIDE (METHADONE HYDROCHLORIDE):
- Edited boxed warning, February 2018
RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death.
Reserve concomitant prescribing of DOLOPHINE Tablets and benzodiazepines or other CNS depressants for use in patients for whom alternatives to benzodiazepines or other CNS depressants are inadequate.
Limit dosages and durations to the minimum required for patients being treated for pain.
Follow patients for signs and symptoms of respiratory depression and sedation. If the patient is visibly sedated, evaluate the cause of sedation, and consider delaying or omitting the daily methadone dose.
PARNATE (TRANYLCYPROMINE SULFATE):
- Edited boxed warning, January 2018
WARNING: SUICIDAL THOUGHTS AND BEHAVIORS AND HYPERTENSIVE CRISIS WITH SIGNIFICANT TYRAMINE USE
SUICIDAL THOUGHTS AND BEHAVIORS
Antidepressants increased the risk of suicidal thoughts and behaviors in pediatric and young adult patients in short-term studies. Closely monitor all antidepressant-treated patients for clinical worsening, and for emergence of suicidal thoughts and behaviors. PARNATE is not approved for use in pediatric patients.
HYPERTENSIVE CRISIS WITH SIGNIFICANT TYRAMINE USE
Excessive consumption of foods or beverages with significant tyramine content or the use of certain drugs with PARNATE or after PARNATE discontinuation can precipitate hypertensive crisis. Monitor blood pressure and allow for medication-free intervals between administration of PARNATE and interacting drugs. Instruct patients to avoid ingestion of foods and beverages with high tyramine content.
OCALIVA (OBETICHOLIC ACID):
- New boxed warning/Newly added section, February 2018
WARNING: HEPATIC DECOMPENSATION AND FAILURE IN INCORRECTLY DOSED PBC PATIENTS WITH CHILD-PUGH CLASS B OR C OR DECOMPENSATED CIRRHOSIS
In postmarketing reports, hepatic decompensation and failure, in some cases fatal, have been reported in patients with primary biliary cholangitis (PBC) with decompensated cirrhosis or Child-Pugh Class B or C hepatic impairment when OCALIVA was dosed more frequently than recommended.
The recommended starting dosage of OCALIVA is 5 mg once weekly for patients with Child-Pugh Class B or C hepatic impairment or a prior decompensation event.
The FDA’s MedWatch program safety labeling changes for boxed warnings are compiled quarterly for drugs and therapeutic biologics where important changes have been made to the safety information. These and other label changes are searchable in the Drug Safety Labeling Changes (SLC) database, where data are available to the public in downloadable and searchable formats. Boxed warnings are ordinarily used to highlight either adverse reactions so serious in proportion to the potential benefi t from the drug that it is essential that it be considered in assessing the risks and benefi ts of using the drug; or serious adverse reactions that can be prevented/reduced in frequency or severity by appropriate use of the drug; or FDA approved the drug with restrictions to ensure safe use because FDA concluded that the drug can be safely used only if distribution or use is restricted. For complete FDA Drug Safety Labeling changes, please visit http://www.accessdata.fda.gov/scripts/cder/safetylabelingchanges.
VIDEX AND VIDEX EC (DIDANOSINE):
- Edited boxed warning, January 2018
WARNING: PANCREATITIS, LACTIC ACIDOSIS and HEPATOMEGALY with STEATOSIS
Coadministration of VIDEX or VIDEX EC and stavudine is contraindicated because of increased risk of serious and/or life-threatening events. Suspend treatment if clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity occurs.
ZYDELIG (IDELALISIB):
- Edited boxed warning, January 2018
WARNING: FATAL AND SERIOUS TOXICITIES: HEPATIC, SEVERE DIARRHEA, COLITIS, PNEUMONITIS, INFECTIONS, and INTESTINAL PERFORATION
Fatal and/or serious hepatotoxicity occurred in 16% to 18% of Zydelig-treated patients…
Fatal and/or serious and severe diarrhea or colitis occurred in 14% to 20% of Zydelig-treated patients…
Fatal and/or serious infections occurred in 21% to 48% of Zydelig-treated patients…
AQUAMEPHYTON (PHYTONADIONE):
- Edited boxed warning, March 2018
WARNING: HYPERSENSITIVITY REACTIONS WITH INTRAVENOUS AND INTRAMUSCULAR USE
Fatal hypersensitivity reactions, including anaphylaxis, have occurred during and immediately after INTRAVENOUS and INTRAMUSCULAR injection of Aqua-MEPHYTON. Reactions have occurred despite dilution to avoid rapid infusion and upon first dose. Avoid the intravenous and intramuscular routes of administration unless the subcutaneous route is not feasible and the serious risk is justified.
FERAHEME (FERUMOXYTOL):
- Edited boxed warning, February 2018
WARNING: RISK FOR SERIOUS HYPERSENSITIVITY/ANAPHYLAXIS REACTIONS
Fatal and serious hypersensitivity reactions including anaphylaxis have occurred in patients receiving feraheme. Initial symptoms may
include hypotension, syncope, unresponsiveness, cardiac/cardiorespiratory arrest.
Only administer feraheme as an intravenous infusion over at least 15 minutes and only when personnel and therapies are immediately available for the treatment of anaphylaxis and other hypersensitivity reactions.
METHADONE HYDROCHLORIDE, METHADOSE (METHADONE HYDROCHLORIDE):
- Edited boxed warning, February 2018
RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
Concomitant use with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, is a risk factor for respiratory depression and death.
Reserve concomitant prescribing of benzodiazepines or other CNS depressants for use in patients for whom alternatives to benzodiazepines or other CNS depressants are inadequate.
Follow patients for signs and symptoms of respiratory depression and sedation. If the patient is visibly sedated, evaluate the cause of sedation, and consider delaying or omitting daily methadone dosing.
DOLOPHINE HYDROCHLORIDE (METHADONE HYDROCHLORIDE):
- Edited boxed warning, February 2018
RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death.
Reserve concomitant prescribing of DOLOPHINE Tablets and benzodiazepines or other CNS depressants for use in patients for whom alternatives to benzodiazepines or other CNS depressants are inadequate.
Limit dosages and durations to the minimum required for patients being treated for pain.
Follow patients for signs and symptoms of respiratory depression and sedation. If the patient is visibly sedated, evaluate the cause of sedation, and consider delaying or omitting the daily methadone dose.
PARNATE (TRANYLCYPROMINE SULFATE):
- Edited boxed warning, January 2018
WARNING: SUICIDAL THOUGHTS AND BEHAVIORS AND HYPERTENSIVE CRISIS WITH SIGNIFICANT TYRAMINE USE
SUICIDAL THOUGHTS AND BEHAVIORS
Antidepressants increased the risk of suicidal thoughts and behaviors in pediatric and young adult patients in short-term studies. Closely monitor all antidepressant-treated patients for clinical worsening, and for emergence of suicidal thoughts and behaviors. PARNATE is not approved for use in pediatric patients.
HYPERTENSIVE CRISIS WITH SIGNIFICANT TYRAMINE USE
Excessive consumption of foods or beverages with significant tyramine content or the use of certain drugs with PARNATE or after PARNATE discontinuation can precipitate hypertensive crisis. Monitor blood pressure and allow for medication-free intervals between administration of PARNATE and interacting drugs. Instruct patients to avoid ingestion of foods and beverages with high tyramine content.
OCALIVA (OBETICHOLIC ACID):
- New boxed warning/Newly added section, February 2018
WARNING: HEPATIC DECOMPENSATION AND FAILURE IN INCORRECTLY DOSED PBC PATIENTS WITH CHILD-PUGH CLASS B OR C OR DECOMPENSATED CIRRHOSIS
In postmarketing reports, hepatic decompensation and failure, in some cases fatal, have been reported in patients with primary biliary cholangitis (PBC) with decompensated cirrhosis or Child-Pugh Class B or C hepatic impairment when OCALIVA was dosed more frequently than recommended.
The recommended starting dosage of OCALIVA is 5 mg once weekly for patients with Child-Pugh Class B or C hepatic impairment or a prior decompensation event.
The FDA’s MedWatch program safety labeling changes for boxed warnings are compiled quarterly for drugs and therapeutic biologics where important changes have been made to the safety information. These and other label changes are searchable in the Drug Safety Labeling Changes (SLC) database, where data are available to the public in downloadable and searchable formats. Boxed warnings are ordinarily used to highlight either adverse reactions so serious in proportion to the potential benefi t from the drug that it is essential that it be considered in assessing the risks and benefi ts of using the drug; or serious adverse reactions that can be prevented/reduced in frequency or severity by appropriate use of the drug; or FDA approved the drug with restrictions to ensure safe use because FDA concluded that the drug can be safely used only if distribution or use is restricted. For complete FDA Drug Safety Labeling changes, please visit http://www.accessdata.fda.gov/scripts/cder/safetylabelingchanges.
VIDEX AND VIDEX EC (DIDANOSINE):
- Edited boxed warning, January 2018
WARNING: PANCREATITIS, LACTIC ACIDOSIS and HEPATOMEGALY with STEATOSIS
Coadministration of VIDEX or VIDEX EC and stavudine is contraindicated because of increased risk of serious and/or life-threatening events. Suspend treatment if clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity occurs.
ZYDELIG (IDELALISIB):
- Edited boxed warning, January 2018
WARNING: FATAL AND SERIOUS TOXICITIES: HEPATIC, SEVERE DIARRHEA, COLITIS, PNEUMONITIS, INFECTIONS, and INTESTINAL PERFORATION
Fatal and/or serious hepatotoxicity occurred in 16% to 18% of Zydelig-treated patients…
Fatal and/or serious and severe diarrhea or colitis occurred in 14% to 20% of Zydelig-treated patients…
Fatal and/or serious infections occurred in 21% to 48% of Zydelig-treated patients…
AQUAMEPHYTON (PHYTONADIONE):
- Edited boxed warning, March 2018
WARNING: HYPERSENSITIVITY REACTIONS WITH INTRAVENOUS AND INTRAMUSCULAR USE
Fatal hypersensitivity reactions, including anaphylaxis, have occurred during and immediately after INTRAVENOUS and INTRAMUSCULAR injection of Aqua-MEPHYTON. Reactions have occurred despite dilution to avoid rapid infusion and upon first dose. Avoid the intravenous and intramuscular routes of administration unless the subcutaneous route is not feasible and the serious risk is justified.
FERAHEME (FERUMOXYTOL):
- Edited boxed warning, February 2018
WARNING: RISK FOR SERIOUS HYPERSENSITIVITY/ANAPHYLAXIS REACTIONS
Fatal and serious hypersensitivity reactions including anaphylaxis have occurred in patients receiving feraheme. Initial symptoms may
include hypotension, syncope, unresponsiveness, cardiac/cardiorespiratory arrest.
Only administer feraheme as an intravenous infusion over at least 15 minutes and only when personnel and therapies are immediately available for the treatment of anaphylaxis and other hypersensitivity reactions.
METHADONE HYDROCHLORIDE, METHADOSE (METHADONE HYDROCHLORIDE):
- Edited boxed warning, February 2018
RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
Concomitant use with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, is a risk factor for respiratory depression and death.
Reserve concomitant prescribing of benzodiazepines or other CNS depressants for use in patients for whom alternatives to benzodiazepines or other CNS depressants are inadequate.
Follow patients for signs and symptoms of respiratory depression and sedation. If the patient is visibly sedated, evaluate the cause of sedation, and consider delaying or omitting daily methadone dosing.
DOLOPHINE HYDROCHLORIDE (METHADONE HYDROCHLORIDE):
- Edited boxed warning, February 2018
RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death.
Reserve concomitant prescribing of DOLOPHINE Tablets and benzodiazepines or other CNS depressants for use in patients for whom alternatives to benzodiazepines or other CNS depressants are inadequate.
Limit dosages and durations to the minimum required for patients being treated for pain.
Follow patients for signs and symptoms of respiratory depression and sedation. If the patient is visibly sedated, evaluate the cause of sedation, and consider delaying or omitting the daily methadone dose.
PARNATE (TRANYLCYPROMINE SULFATE):
- Edited boxed warning, January 2018
WARNING: SUICIDAL THOUGHTS AND BEHAVIORS AND HYPERTENSIVE CRISIS WITH SIGNIFICANT TYRAMINE USE
SUICIDAL THOUGHTS AND BEHAVIORS
Antidepressants increased the risk of suicidal thoughts and behaviors in pediatric and young adult patients in short-term studies. Closely monitor all antidepressant-treated patients for clinical worsening, and for emergence of suicidal thoughts and behaviors. PARNATE is not approved for use in pediatric patients.
HYPERTENSIVE CRISIS WITH SIGNIFICANT TYRAMINE USE
Excessive consumption of foods or beverages with significant tyramine content or the use of certain drugs with PARNATE or after PARNATE discontinuation can precipitate hypertensive crisis. Monitor blood pressure and allow for medication-free intervals between administration of PARNATE and interacting drugs. Instruct patients to avoid ingestion of foods and beverages with high tyramine content.
OCALIVA (OBETICHOLIC ACID):
- New boxed warning/Newly added section, February 2018
WARNING: HEPATIC DECOMPENSATION AND FAILURE IN INCORRECTLY DOSED PBC PATIENTS WITH CHILD-PUGH CLASS B OR C OR DECOMPENSATED CIRRHOSIS
In postmarketing reports, hepatic decompensation and failure, in some cases fatal, have been reported in patients with primary biliary cholangitis (PBC) with decompensated cirrhosis or Child-Pugh Class B or C hepatic impairment when OCALIVA was dosed more frequently than recommended.
The recommended starting dosage of OCALIVA is 5 mg once weekly for patients with Child-Pugh Class B or C hepatic impairment or a prior decompensation event.