User login
Unusual antibiotic resistance found in more than 200 bacteria
The Centers for Disease Control and Prevention’s Antibiotic Resistance (AR) Lab Network has detected 221 instances of bacteria with especially rare resistance genes in the United States, according to a Vital Signs report published online and expanded upon in CDC’s MMWR Weekly.
The MMWR Weekly report, “Containment of Novel Multidrug-Resistant Organisms and Resistance Mechanisms,” which goes deeper into the science behind the issue, shows that in 9 months, in all states and Puerto Rico, health department workers in the AR lab network tested 5,776 samples of highly resistant bacteria, according to Anne Schuchat, MD, principal deputy director of the CDC. These bacteria were immediately tested for unusual resistance – “those genes that were highly resistant, or rare, with special resistance that could spread,” she said.
“Of the 5,776, about 1 in 4 of the bacteria had a gene that helped it spread its resistance. And there were 221 instances of an especially rare resistance gene,” she added. This prompted intense screening, revealing “that 1 in 10 tests were also positive. Meaning the unusual resistance may have spread to other patients. And could have continued spreading if left undetected.”
The report looked at carbapenem-resistant Enterobacteriaceae (CRE) and Enterobacteriaceae with extended-spectrum beta-lactamases (ESBL) infection data from the National Healthcare Safety Network from 2006-2015 to calculate changes in the year over year proportions of these infections and how an enhanced detection and control strategy curbs carbapenem resistance.
This strategy includes components such as timely implementation of appropriate infection control measures, conducting a health care and contact investigation with follow-up, and implementing a system to ensure adherence to infection control measures.
“With independent, or single facility approaches to control spread, a dangerous type of unusual resistance in Enterobacteriaceae [ESBL phenotype] decreased by about 2% per year [(risk ratio [RR] = 0.98, P less than .001)].” With a more aggressive approach, using guidance such as CDC’s CRE toolkit, released in 2009, another type of unusual resistance [CRE] in the same bacteria (Enterobacteriaceae) decreased by nearly 15% per year (RR = 0.85, P less than .01).
The difference may be due in part to the more directed response utilized to slow the spread of the “nightmare bacteria,” once it was identified, said Dr. Schuchat.
These results show massive promise even if only partially effective, specifically for CRE.
“CDC estimates show that if only 20% effective, the containment strategy can reduce the number of nightmare bacteria [CRE] cases by 76% over 3 years in one area.”
Due to the nature of antibiotic resistance and its ability to spread, this poses a significant public health threat. Antibiotics are not simply used to treat infections but are a safety net that is used in cancer treatment, surgery, and ICU care, Dr. Schuchat pointed out. The rise of antibiotic resistance is a threat to that safety net and accounts for nearly 2,000,000 antibiotic resistant infections and approximately 23,000 deaths per year.
But aggressive responses to these infections can control their spread. Dr. Schuchat used the analogy of controlling a fire to illustrate the concept.
“Much like a fire, finding and stopping unusual resistance early when it’s just a spark protects people.”
Dr. Schuchat reiterated that simply identifying the issue is only part of the equation.
“Detection is not enough on its own. When there is a fire, somebody needs to put it out. CDC supports more than 500 local staff across the country to combat antibiotic resistance wherever it emerges.”
While the report highlights the strides that have been made in combating antibiotic resistance, Paul Auwaerter, MD, president of the Infectious Diseases Society of America, released a statement highlighting the need to further fund these efforts.
“The report spells out the need to accelerate efforts to curb resistance or face an increasing burden including novel resistance mutations that threaten health,” stated Dr. Auwaerter. “The efforts detailed in the Vital Signs report were made possible through new congressional funding in 2016 to combat antibiotic resistance. We urge Congress to sustain and to grow that investment so that further progress will prepare us to meet the future challenges of antibiotic resistance from a position of strength,” he added.
A fact sheet with a brief summation of the vital signs report is available here.
The Centers for Disease Control and Prevention’s Antibiotic Resistance (AR) Lab Network has detected 221 instances of bacteria with especially rare resistance genes in the United States, according to a Vital Signs report published online and expanded upon in CDC’s MMWR Weekly.
The MMWR Weekly report, “Containment of Novel Multidrug-Resistant Organisms and Resistance Mechanisms,” which goes deeper into the science behind the issue, shows that in 9 months, in all states and Puerto Rico, health department workers in the AR lab network tested 5,776 samples of highly resistant bacteria, according to Anne Schuchat, MD, principal deputy director of the CDC. These bacteria were immediately tested for unusual resistance – “those genes that were highly resistant, or rare, with special resistance that could spread,” she said.
“Of the 5,776, about 1 in 4 of the bacteria had a gene that helped it spread its resistance. And there were 221 instances of an especially rare resistance gene,” she added. This prompted intense screening, revealing “that 1 in 10 tests were also positive. Meaning the unusual resistance may have spread to other patients. And could have continued spreading if left undetected.”
The report looked at carbapenem-resistant Enterobacteriaceae (CRE) and Enterobacteriaceae with extended-spectrum beta-lactamases (ESBL) infection data from the National Healthcare Safety Network from 2006-2015 to calculate changes in the year over year proportions of these infections and how an enhanced detection and control strategy curbs carbapenem resistance.
This strategy includes components such as timely implementation of appropriate infection control measures, conducting a health care and contact investigation with follow-up, and implementing a system to ensure adherence to infection control measures.
“With independent, or single facility approaches to control spread, a dangerous type of unusual resistance in Enterobacteriaceae [ESBL phenotype] decreased by about 2% per year [(risk ratio [RR] = 0.98, P less than .001)].” With a more aggressive approach, using guidance such as CDC’s CRE toolkit, released in 2009, another type of unusual resistance [CRE] in the same bacteria (Enterobacteriaceae) decreased by nearly 15% per year (RR = 0.85, P less than .01).
The difference may be due in part to the more directed response utilized to slow the spread of the “nightmare bacteria,” once it was identified, said Dr. Schuchat.
These results show massive promise even if only partially effective, specifically for CRE.
“CDC estimates show that if only 20% effective, the containment strategy can reduce the number of nightmare bacteria [CRE] cases by 76% over 3 years in one area.”
Due to the nature of antibiotic resistance and its ability to spread, this poses a significant public health threat. Antibiotics are not simply used to treat infections but are a safety net that is used in cancer treatment, surgery, and ICU care, Dr. Schuchat pointed out. The rise of antibiotic resistance is a threat to that safety net and accounts for nearly 2,000,000 antibiotic resistant infections and approximately 23,000 deaths per year.
But aggressive responses to these infections can control their spread. Dr. Schuchat used the analogy of controlling a fire to illustrate the concept.
“Much like a fire, finding and stopping unusual resistance early when it’s just a spark protects people.”
Dr. Schuchat reiterated that simply identifying the issue is only part of the equation.
“Detection is not enough on its own. When there is a fire, somebody needs to put it out. CDC supports more than 500 local staff across the country to combat antibiotic resistance wherever it emerges.”
While the report highlights the strides that have been made in combating antibiotic resistance, Paul Auwaerter, MD, president of the Infectious Diseases Society of America, released a statement highlighting the need to further fund these efforts.
“The report spells out the need to accelerate efforts to curb resistance or face an increasing burden including novel resistance mutations that threaten health,” stated Dr. Auwaerter. “The efforts detailed in the Vital Signs report were made possible through new congressional funding in 2016 to combat antibiotic resistance. We urge Congress to sustain and to grow that investment so that further progress will prepare us to meet the future challenges of antibiotic resistance from a position of strength,” he added.
A fact sheet with a brief summation of the vital signs report is available here.
The Centers for Disease Control and Prevention’s Antibiotic Resistance (AR) Lab Network has detected 221 instances of bacteria with especially rare resistance genes in the United States, according to a Vital Signs report published online and expanded upon in CDC’s MMWR Weekly.
The MMWR Weekly report, “Containment of Novel Multidrug-Resistant Organisms and Resistance Mechanisms,” which goes deeper into the science behind the issue, shows that in 9 months, in all states and Puerto Rico, health department workers in the AR lab network tested 5,776 samples of highly resistant bacteria, according to Anne Schuchat, MD, principal deputy director of the CDC. These bacteria were immediately tested for unusual resistance – “those genes that were highly resistant, or rare, with special resistance that could spread,” she said.
“Of the 5,776, about 1 in 4 of the bacteria had a gene that helped it spread its resistance. And there were 221 instances of an especially rare resistance gene,” she added. This prompted intense screening, revealing “that 1 in 10 tests were also positive. Meaning the unusual resistance may have spread to other patients. And could have continued spreading if left undetected.”
The report looked at carbapenem-resistant Enterobacteriaceae (CRE) and Enterobacteriaceae with extended-spectrum beta-lactamases (ESBL) infection data from the National Healthcare Safety Network from 2006-2015 to calculate changes in the year over year proportions of these infections and how an enhanced detection and control strategy curbs carbapenem resistance.
This strategy includes components such as timely implementation of appropriate infection control measures, conducting a health care and contact investigation with follow-up, and implementing a system to ensure adherence to infection control measures.
“With independent, or single facility approaches to control spread, a dangerous type of unusual resistance in Enterobacteriaceae [ESBL phenotype] decreased by about 2% per year [(risk ratio [RR] = 0.98, P less than .001)].” With a more aggressive approach, using guidance such as CDC’s CRE toolkit, released in 2009, another type of unusual resistance [CRE] in the same bacteria (Enterobacteriaceae) decreased by nearly 15% per year (RR = 0.85, P less than .01).
The difference may be due in part to the more directed response utilized to slow the spread of the “nightmare bacteria,” once it was identified, said Dr. Schuchat.
These results show massive promise even if only partially effective, specifically for CRE.
“CDC estimates show that if only 20% effective, the containment strategy can reduce the number of nightmare bacteria [CRE] cases by 76% over 3 years in one area.”
Due to the nature of antibiotic resistance and its ability to spread, this poses a significant public health threat. Antibiotics are not simply used to treat infections but are a safety net that is used in cancer treatment, surgery, and ICU care, Dr. Schuchat pointed out. The rise of antibiotic resistance is a threat to that safety net and accounts for nearly 2,000,000 antibiotic resistant infections and approximately 23,000 deaths per year.
But aggressive responses to these infections can control their spread. Dr. Schuchat used the analogy of controlling a fire to illustrate the concept.
“Much like a fire, finding and stopping unusual resistance early when it’s just a spark protects people.”
Dr. Schuchat reiterated that simply identifying the issue is only part of the equation.
“Detection is not enough on its own. When there is a fire, somebody needs to put it out. CDC supports more than 500 local staff across the country to combat antibiotic resistance wherever it emerges.”
While the report highlights the strides that have been made in combating antibiotic resistance, Paul Auwaerter, MD, president of the Infectious Diseases Society of America, released a statement highlighting the need to further fund these efforts.
“The report spells out the need to accelerate efforts to curb resistance or face an increasing burden including novel resistance mutations that threaten health,” stated Dr. Auwaerter. “The efforts detailed in the Vital Signs report were made possible through new congressional funding in 2016 to combat antibiotic resistance. We urge Congress to sustain and to grow that investment so that further progress will prepare us to meet the future challenges of antibiotic resistance from a position of strength,” he added.
A fact sheet with a brief summation of the vital signs report is available here.
FROM A CDC TELEBRIEFING
Late Thrombectomy Improves Ischemic Stroke Outcomes
LOS ANGELES—When performed between six and 16 hours after stroke onset, thrombectomy plus standard medical management yields better functional outcomes than medical management alone, according to research presented at the International Stroke Conference 2018. Adjunctive thrombectomy also reduces the rates of death and severe disability, compared with medical management alone.
In 2006, Gregory W. Albers, MD, Coyote Foundation Professor of Neurology and Neurological Sciences and Professor, by courtesy, of Neurosurgery at Stanford University Medical Center in California, and colleagues found that MRI could identify patients with stroke who would benefit from IV t-PA as late as six hours after onset. The investigators developed software called RAPID that could determine how much brain tissue was salvageable in a patient with stroke. In a subsequent study, the software allowed researchers to identify patients who would benefit from thrombectomy at a later point after stroke onset than had been considered possible.
The DEFUSE 3 Trial
Dr. Albers and colleagues conducted the DEFUSE 3 study to analyze whether patients could benefit from thrombectomy if administered between six and 16 hours after stroke onset. Eligible participants in the open-label trial had an occlusion in the middle cerebral artery or the internal carotid artery, an initial infarct size of less than 70 mL, and a ratio of ischemic tissue volume to infarct volume of 1.8 or more on perfusion imaging. The researchers used the RAPID software to determine how much salvageable tissue each patient had.
“We used fairly broad inclusion criteria,” said Dr. Albers. Patients as old as 90 were included, as were patients with moderate to severe strokes. Participants were required to be free of disability at stroke onset.
Patients were randomized to standard medical management alone or thrombectomy plus standard medical management. Medical management included standard stroke prevention therapies, management of blood pressure, and interventions to prevent complications for stroke such as deep venous thrombosis. The primary efficacy end point was modified Rankin scale score at 90 days. The secondary efficacy outcome was modified Rankin scale score of 0 to 2 at 90 days (ie, functional independence). The primary safety outcomes were death within 90 days and symptomatic intracranial hemorrhage within 36 hours.
Study Was Terminated Early
The patients in DEFUSE 3 were similar to those included in trials of thrombectomy administered within six hours, said Dr. Albers. Median age was about 70 in both study arms. About 50% of the study population was female, and median NIH Stroke Scale score was 16.
The researchers conducted an interim analysis when 182 patients had been enrolled at 38 sites, including 92 randomized to thrombectomy. The results of the analysis prompted them to end the study early because of treatment efficacy.
The unadjusted odds ratio (OR) of a favorable outcome on the modified Rankin scale at 90 days was 2.77 in the thrombectomy group, compared with the medical management group. After adjusting for between-group differences, the OR was 3.36. This result “is the largest odds ratio ever reported for a thrombectomy study,” said Dr. Albers. Approximately 45% of participants in the thrombectomy group achieved functional independence, compared with 17% in the medical management group.
The rate of mortality at 90 days was 14% in the thrombectomy arm and 26% in the medical management arm. The combined rate of death or severe disability was 22% in the thrombectomy group and 42% in the medical management group. The rate of symptomatic intracranial hemorrhage did not differ significantly between groups.
The benefit of thrombectomy on the primary and secondary end points was similar for patients with wake-up stroke and patients for whom stroke onset had been witnessed. “This [result] demonstrates that the DEFUSE 3 treatment benefit is not explained by a potentially shorter onset to treatment time in the wake-up group,” said Dr. Albers. The rate of good outcome was also similar in all three prespecified time periods that the investigators examined (ie, treatment at six to nine hours, nine to 12 hours, and 12 to 16 hours after onset).
Results Informed New Stroke Guidelines
The treatment benefits in this study are “even more significant” than when patients receive treatment within six hours of stroke onset, said Dr. Albers. Part of the reason for this difference is that the doctors who performed thrombectomy were successful at reperfusing the brain. About 80% of patients in the thrombectomy arm had excellent reperfusion, but spontaneous reperfusion occurred in less than 20% of the medical arm.
The updated guidelines from the American Heart Association and American Stroke Association for the management of acute ischemic stroke, which were published in the March issue of Stroke, recommend that neurologists use the DEFUSE 3 criteria to select patients for thrombectomy at six to 16 hours after stroke onset.
“Now that we know that we can successfully treat patients in later time windows, it is going to be important for primary stroke centers to be able to do the type of imaging that was done in the DEFUSE 3 and DAWN trials,” said Dr. Albers.
He added that it is still important to rush as quickly as possible to evaluate stroke patients. “Every minute still counts, and there are some unfortunate individuals whose minutes run dry even when they present during the golden hours after symptom onset. But more importantly, we now know that many stroke patients are considerably more fortunate; their hourglass is much kinder and affords medical providers with a golden opportunity to improve outcomes even in time frames that were once thought to be impossible.”
—Erik Greb
Suggested Reading
Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708-718.
Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110.
LOS ANGELES—When performed between six and 16 hours after stroke onset, thrombectomy plus standard medical management yields better functional outcomes than medical management alone, according to research presented at the International Stroke Conference 2018. Adjunctive thrombectomy also reduces the rates of death and severe disability, compared with medical management alone.
In 2006, Gregory W. Albers, MD, Coyote Foundation Professor of Neurology and Neurological Sciences and Professor, by courtesy, of Neurosurgery at Stanford University Medical Center in California, and colleagues found that MRI could identify patients with stroke who would benefit from IV t-PA as late as six hours after onset. The investigators developed software called RAPID that could determine how much brain tissue was salvageable in a patient with stroke. In a subsequent study, the software allowed researchers to identify patients who would benefit from thrombectomy at a later point after stroke onset than had been considered possible.
The DEFUSE 3 Trial
Dr. Albers and colleagues conducted the DEFUSE 3 study to analyze whether patients could benefit from thrombectomy if administered between six and 16 hours after stroke onset. Eligible participants in the open-label trial had an occlusion in the middle cerebral artery or the internal carotid artery, an initial infarct size of less than 70 mL, and a ratio of ischemic tissue volume to infarct volume of 1.8 or more on perfusion imaging. The researchers used the RAPID software to determine how much salvageable tissue each patient had.
“We used fairly broad inclusion criteria,” said Dr. Albers. Patients as old as 90 were included, as were patients with moderate to severe strokes. Participants were required to be free of disability at stroke onset.
Patients were randomized to standard medical management alone or thrombectomy plus standard medical management. Medical management included standard stroke prevention therapies, management of blood pressure, and interventions to prevent complications for stroke such as deep venous thrombosis. The primary efficacy end point was modified Rankin scale score at 90 days. The secondary efficacy outcome was modified Rankin scale score of 0 to 2 at 90 days (ie, functional independence). The primary safety outcomes were death within 90 days and symptomatic intracranial hemorrhage within 36 hours.
Study Was Terminated Early
The patients in DEFUSE 3 were similar to those included in trials of thrombectomy administered within six hours, said Dr. Albers. Median age was about 70 in both study arms. About 50% of the study population was female, and median NIH Stroke Scale score was 16.
The researchers conducted an interim analysis when 182 patients had been enrolled at 38 sites, including 92 randomized to thrombectomy. The results of the analysis prompted them to end the study early because of treatment efficacy.
The unadjusted odds ratio (OR) of a favorable outcome on the modified Rankin scale at 90 days was 2.77 in the thrombectomy group, compared with the medical management group. After adjusting for between-group differences, the OR was 3.36. This result “is the largest odds ratio ever reported for a thrombectomy study,” said Dr. Albers. Approximately 45% of participants in the thrombectomy group achieved functional independence, compared with 17% in the medical management group.
The rate of mortality at 90 days was 14% in the thrombectomy arm and 26% in the medical management arm. The combined rate of death or severe disability was 22% in the thrombectomy group and 42% in the medical management group. The rate of symptomatic intracranial hemorrhage did not differ significantly between groups.
The benefit of thrombectomy on the primary and secondary end points was similar for patients with wake-up stroke and patients for whom stroke onset had been witnessed. “This [result] demonstrates that the DEFUSE 3 treatment benefit is not explained by a potentially shorter onset to treatment time in the wake-up group,” said Dr. Albers. The rate of good outcome was also similar in all three prespecified time periods that the investigators examined (ie, treatment at six to nine hours, nine to 12 hours, and 12 to 16 hours after onset).
Results Informed New Stroke Guidelines
The treatment benefits in this study are “even more significant” than when patients receive treatment within six hours of stroke onset, said Dr. Albers. Part of the reason for this difference is that the doctors who performed thrombectomy were successful at reperfusing the brain. About 80% of patients in the thrombectomy arm had excellent reperfusion, but spontaneous reperfusion occurred in less than 20% of the medical arm.
The updated guidelines from the American Heart Association and American Stroke Association for the management of acute ischemic stroke, which were published in the March issue of Stroke, recommend that neurologists use the DEFUSE 3 criteria to select patients for thrombectomy at six to 16 hours after stroke onset.
“Now that we know that we can successfully treat patients in later time windows, it is going to be important for primary stroke centers to be able to do the type of imaging that was done in the DEFUSE 3 and DAWN trials,” said Dr. Albers.
He added that it is still important to rush as quickly as possible to evaluate stroke patients. “Every minute still counts, and there are some unfortunate individuals whose minutes run dry even when they present during the golden hours after symptom onset. But more importantly, we now know that many stroke patients are considerably more fortunate; their hourglass is much kinder and affords medical providers with a golden opportunity to improve outcomes even in time frames that were once thought to be impossible.”
—Erik Greb
Suggested Reading
Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708-718.
Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110.
LOS ANGELES—When performed between six and 16 hours after stroke onset, thrombectomy plus standard medical management yields better functional outcomes than medical management alone, according to research presented at the International Stroke Conference 2018. Adjunctive thrombectomy also reduces the rates of death and severe disability, compared with medical management alone.
In 2006, Gregory W. Albers, MD, Coyote Foundation Professor of Neurology and Neurological Sciences and Professor, by courtesy, of Neurosurgery at Stanford University Medical Center in California, and colleagues found that MRI could identify patients with stroke who would benefit from IV t-PA as late as six hours after onset. The investigators developed software called RAPID that could determine how much brain tissue was salvageable in a patient with stroke. In a subsequent study, the software allowed researchers to identify patients who would benefit from thrombectomy at a later point after stroke onset than had been considered possible.
The DEFUSE 3 Trial
Dr. Albers and colleagues conducted the DEFUSE 3 study to analyze whether patients could benefit from thrombectomy if administered between six and 16 hours after stroke onset. Eligible participants in the open-label trial had an occlusion in the middle cerebral artery or the internal carotid artery, an initial infarct size of less than 70 mL, and a ratio of ischemic tissue volume to infarct volume of 1.8 or more on perfusion imaging. The researchers used the RAPID software to determine how much salvageable tissue each patient had.
“We used fairly broad inclusion criteria,” said Dr. Albers. Patients as old as 90 were included, as were patients with moderate to severe strokes. Participants were required to be free of disability at stroke onset.
Patients were randomized to standard medical management alone or thrombectomy plus standard medical management. Medical management included standard stroke prevention therapies, management of blood pressure, and interventions to prevent complications for stroke such as deep venous thrombosis. The primary efficacy end point was modified Rankin scale score at 90 days. The secondary efficacy outcome was modified Rankin scale score of 0 to 2 at 90 days (ie, functional independence). The primary safety outcomes were death within 90 days and symptomatic intracranial hemorrhage within 36 hours.
Study Was Terminated Early
The patients in DEFUSE 3 were similar to those included in trials of thrombectomy administered within six hours, said Dr. Albers. Median age was about 70 in both study arms. About 50% of the study population was female, and median NIH Stroke Scale score was 16.
The researchers conducted an interim analysis when 182 patients had been enrolled at 38 sites, including 92 randomized to thrombectomy. The results of the analysis prompted them to end the study early because of treatment efficacy.
The unadjusted odds ratio (OR) of a favorable outcome on the modified Rankin scale at 90 days was 2.77 in the thrombectomy group, compared with the medical management group. After adjusting for between-group differences, the OR was 3.36. This result “is the largest odds ratio ever reported for a thrombectomy study,” said Dr. Albers. Approximately 45% of participants in the thrombectomy group achieved functional independence, compared with 17% in the medical management group.
The rate of mortality at 90 days was 14% in the thrombectomy arm and 26% in the medical management arm. The combined rate of death or severe disability was 22% in the thrombectomy group and 42% in the medical management group. The rate of symptomatic intracranial hemorrhage did not differ significantly between groups.
The benefit of thrombectomy on the primary and secondary end points was similar for patients with wake-up stroke and patients for whom stroke onset had been witnessed. “This [result] demonstrates that the DEFUSE 3 treatment benefit is not explained by a potentially shorter onset to treatment time in the wake-up group,” said Dr. Albers. The rate of good outcome was also similar in all three prespecified time periods that the investigators examined (ie, treatment at six to nine hours, nine to 12 hours, and 12 to 16 hours after onset).
Results Informed New Stroke Guidelines
The treatment benefits in this study are “even more significant” than when patients receive treatment within six hours of stroke onset, said Dr. Albers. Part of the reason for this difference is that the doctors who performed thrombectomy were successful at reperfusing the brain. About 80% of patients in the thrombectomy arm had excellent reperfusion, but spontaneous reperfusion occurred in less than 20% of the medical arm.
The updated guidelines from the American Heart Association and American Stroke Association for the management of acute ischemic stroke, which were published in the March issue of Stroke, recommend that neurologists use the DEFUSE 3 criteria to select patients for thrombectomy at six to 16 hours after stroke onset.
“Now that we know that we can successfully treat patients in later time windows, it is going to be important for primary stroke centers to be able to do the type of imaging that was done in the DEFUSE 3 and DAWN trials,” said Dr. Albers.
He added that it is still important to rush as quickly as possible to evaluate stroke patients. “Every minute still counts, and there are some unfortunate individuals whose minutes run dry even when they present during the golden hours after symptom onset. But more importantly, we now know that many stroke patients are considerably more fortunate; their hourglass is much kinder and affords medical providers with a golden opportunity to improve outcomes even in time frames that were once thought to be impossible.”
—Erik Greb
Suggested Reading
Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708-718.
Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46-e110.
Lower heart disease mortality brings increased disparity
The overall death rate from heart disease is down 68% since 1968 in the United States, but the disparity between blacks and whites has increased over that time, according to the Centers for Disease Control and Prevention.
Overall, heart disease mortality for adults aged 35 years and older went from 1,035 per 100,000 population in 1968 to 327 per 100,000 in 2015, a drop of 68%. For whites, the story was very similar: The death rate dropped from 1,032 to 326, or 68%. For blacks, who had a higher death rate to begin with, at 1,072 per 100,000, the drop was 63% to 396 per 100,000, Miriam Van Dyke, MPH, of Emory University, Atlanta, and her associates reported in MMWR Surveillance Summaries.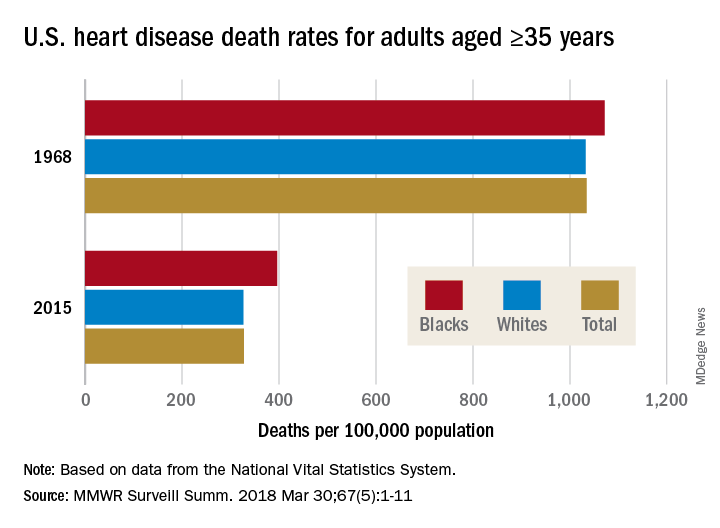
Disparities can be seen at the state level as well. For blacks aged 35 years and older, heart disease death rates ranged from 200 per 100,000 in Oregon to 516 per 100,000 in Arkansas in 2015. For whites in that age group, the death rate was lowest in the District of Columbia (198 per 100,000) and highest in Oklahoma (446 per 100,000), Ms. Van Dyke and her associates wrote.
To help them pinpoint differences by race within geographic areas, the investigators calculated ratios of black to white heart disease death rates. In 1968, the state with the highest ratio, or the largest excess of black mortality, was Rhode Island at 1.38, and the state with the lowest ratio, meaning the largest excess of white mortality, was Minnesota at 0.64. There were 27 states that year with a ratio over 1.0, 12 states with a ratio below 1.0, 1 state with a ratio of 1.0 (Wisconsin), and 11 states that did not have a black population large enough to make a reliable estimate, they said.
In 2015, the jurisdiction with the largest excess of black mortality was D.C., with a ratio of 2.42; the state with the lowest ratio was Rhode Island, at 0.69. That year, there were 34 states with a ratio over 1.0, 6 states with a ratio below 1.0, and 11 states – the same 11 as in 1968 – with black populations too small to reliably estimate death rates, the investigators noted.
“The elimination of racial disparities in heart disease death rates, along with continued decreases in heart disease death rates for all persons in the United States, is important for the overall state of health. The trends in black-white disparities in heart disease death rates … highlight the importance of continued surveillance of these trends at the national and state level,” the investigators wrote.
SOURCE: Van Dyke M et al. MMWR Surveill Summ. 2018 Mar 30;67(5):1-11.
The overall death rate from heart disease is down 68% since 1968 in the United States, but the disparity between blacks and whites has increased over that time, according to the Centers for Disease Control and Prevention.
Overall, heart disease mortality for adults aged 35 years and older went from 1,035 per 100,000 population in 1968 to 327 per 100,000 in 2015, a drop of 68%. For whites, the story was very similar: The death rate dropped from 1,032 to 326, or 68%. For blacks, who had a higher death rate to begin with, at 1,072 per 100,000, the drop was 63% to 396 per 100,000, Miriam Van Dyke, MPH, of Emory University, Atlanta, and her associates reported in MMWR Surveillance Summaries.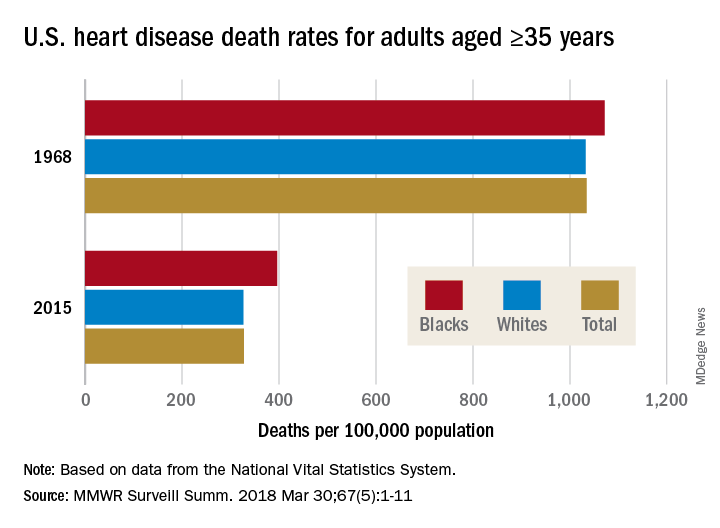
Disparities can be seen at the state level as well. For blacks aged 35 years and older, heart disease death rates ranged from 200 per 100,000 in Oregon to 516 per 100,000 in Arkansas in 2015. For whites in that age group, the death rate was lowest in the District of Columbia (198 per 100,000) and highest in Oklahoma (446 per 100,000), Ms. Van Dyke and her associates wrote.
To help them pinpoint differences by race within geographic areas, the investigators calculated ratios of black to white heart disease death rates. In 1968, the state with the highest ratio, or the largest excess of black mortality, was Rhode Island at 1.38, and the state with the lowest ratio, meaning the largest excess of white mortality, was Minnesota at 0.64. There were 27 states that year with a ratio over 1.0, 12 states with a ratio below 1.0, 1 state with a ratio of 1.0 (Wisconsin), and 11 states that did not have a black population large enough to make a reliable estimate, they said.
In 2015, the jurisdiction with the largest excess of black mortality was D.C., with a ratio of 2.42; the state with the lowest ratio was Rhode Island, at 0.69. That year, there were 34 states with a ratio over 1.0, 6 states with a ratio below 1.0, and 11 states – the same 11 as in 1968 – with black populations too small to reliably estimate death rates, the investigators noted.
“The elimination of racial disparities in heart disease death rates, along with continued decreases in heart disease death rates for all persons in the United States, is important for the overall state of health. The trends in black-white disparities in heart disease death rates … highlight the importance of continued surveillance of these trends at the national and state level,” the investigators wrote.
SOURCE: Van Dyke M et al. MMWR Surveill Summ. 2018 Mar 30;67(5):1-11.
The overall death rate from heart disease is down 68% since 1968 in the United States, but the disparity between blacks and whites has increased over that time, according to the Centers for Disease Control and Prevention.
Overall, heart disease mortality for adults aged 35 years and older went from 1,035 per 100,000 population in 1968 to 327 per 100,000 in 2015, a drop of 68%. For whites, the story was very similar: The death rate dropped from 1,032 to 326, or 68%. For blacks, who had a higher death rate to begin with, at 1,072 per 100,000, the drop was 63% to 396 per 100,000, Miriam Van Dyke, MPH, of Emory University, Atlanta, and her associates reported in MMWR Surveillance Summaries.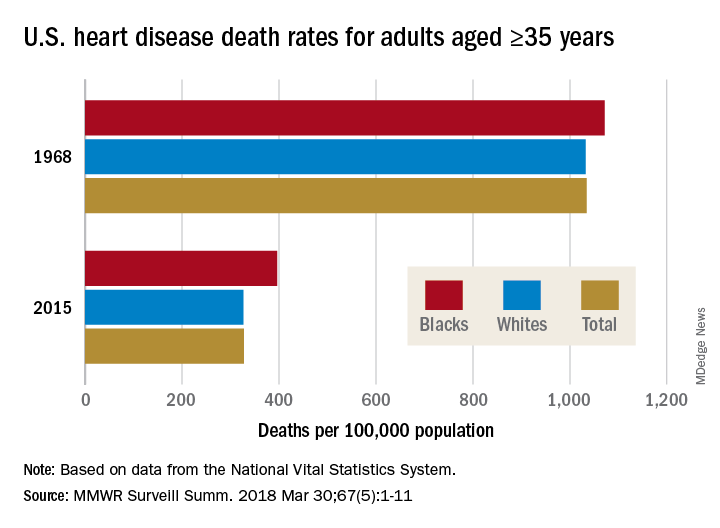
Disparities can be seen at the state level as well. For blacks aged 35 years and older, heart disease death rates ranged from 200 per 100,000 in Oregon to 516 per 100,000 in Arkansas in 2015. For whites in that age group, the death rate was lowest in the District of Columbia (198 per 100,000) and highest in Oklahoma (446 per 100,000), Ms. Van Dyke and her associates wrote.
To help them pinpoint differences by race within geographic areas, the investigators calculated ratios of black to white heart disease death rates. In 1968, the state with the highest ratio, or the largest excess of black mortality, was Rhode Island at 1.38, and the state with the lowest ratio, meaning the largest excess of white mortality, was Minnesota at 0.64. There were 27 states that year with a ratio over 1.0, 12 states with a ratio below 1.0, 1 state with a ratio of 1.0 (Wisconsin), and 11 states that did not have a black population large enough to make a reliable estimate, they said.
In 2015, the jurisdiction with the largest excess of black mortality was D.C., with a ratio of 2.42; the state with the lowest ratio was Rhode Island, at 0.69. That year, there were 34 states with a ratio over 1.0, 6 states with a ratio below 1.0, and 11 states – the same 11 as in 1968 – with black populations too small to reliably estimate death rates, the investigators noted.
“The elimination of racial disparities in heart disease death rates, along with continued decreases in heart disease death rates for all persons in the United States, is important for the overall state of health. The trends in black-white disparities in heart disease death rates … highlight the importance of continued surveillance of these trends at the national and state level,” the investigators wrote.
SOURCE: Van Dyke M et al. MMWR Surveill Summ. 2018 Mar 30;67(5):1-11.
FROM MMWR SURVEILLANCE SUMMARIES
Senators seek answers on Gleostine price hike
The drug, which is used to treat Hodgkin lymphoma and brain cancer, has seen its price increase by 1,400% ($50 to $786) since NextSource acquired it. Gleostine, which was approved by the Food and Drug Administration in 1976 and has long been off patent, has no generic competition.
“Recent reports of price increases for off-patent drugs have demonstrated the need for continued oversight by the United States Senate,” Sen. Susan Collins (R-Maine), Sen. Claire McCaskill (D-Mo.), and Sen. Catherine Cortez Masto (D-Nev.) wrote in a letter to Tri-Source Pharma CEO Robert DiCrisci. Tri-Source is the parent company of NextSource.
The senators requested information on the gross and net revenues of the drug; expenses related to the sale of the drug; annual profit data; internal and external communications related to current and future sales of the drug, including cost estimates, profit projections, and market share analysis; and a list of other drugs sold by the company along with relevant pricing information.
The manufacturer has previously defended its price increases, citing the increased cost of a key manufacturing component, the cost of providing discounted drugs to Medicaid and uninsured patients, and higher regulatory fees, as well as the maintenance of a year’s worth of “safety stock” to prevent shortages.
The drug, which is used to treat Hodgkin lymphoma and brain cancer, has seen its price increase by 1,400% ($50 to $786) since NextSource acquired it. Gleostine, which was approved by the Food and Drug Administration in 1976 and has long been off patent, has no generic competition.
“Recent reports of price increases for off-patent drugs have demonstrated the need for continued oversight by the United States Senate,” Sen. Susan Collins (R-Maine), Sen. Claire McCaskill (D-Mo.), and Sen. Catherine Cortez Masto (D-Nev.) wrote in a letter to Tri-Source Pharma CEO Robert DiCrisci. Tri-Source is the parent company of NextSource.
The senators requested information on the gross and net revenues of the drug; expenses related to the sale of the drug; annual profit data; internal and external communications related to current and future sales of the drug, including cost estimates, profit projections, and market share analysis; and a list of other drugs sold by the company along with relevant pricing information.
The manufacturer has previously defended its price increases, citing the increased cost of a key manufacturing component, the cost of providing discounted drugs to Medicaid and uninsured patients, and higher regulatory fees, as well as the maintenance of a year’s worth of “safety stock” to prevent shortages.
The drug, which is used to treat Hodgkin lymphoma and brain cancer, has seen its price increase by 1,400% ($50 to $786) since NextSource acquired it. Gleostine, which was approved by the Food and Drug Administration in 1976 and has long been off patent, has no generic competition.
“Recent reports of price increases for off-patent drugs have demonstrated the need for continued oversight by the United States Senate,” Sen. Susan Collins (R-Maine), Sen. Claire McCaskill (D-Mo.), and Sen. Catherine Cortez Masto (D-Nev.) wrote in a letter to Tri-Source Pharma CEO Robert DiCrisci. Tri-Source is the parent company of NextSource.
The senators requested information on the gross and net revenues of the drug; expenses related to the sale of the drug; annual profit data; internal and external communications related to current and future sales of the drug, including cost estimates, profit projections, and market share analysis; and a list of other drugs sold by the company along with relevant pricing information.
The manufacturer has previously defended its price increases, citing the increased cost of a key manufacturing component, the cost of providing discounted drugs to Medicaid and uninsured patients, and higher regulatory fees, as well as the maintenance of a year’s worth of “safety stock” to prevent shortages.
Medicare Part D plans get more flexibility to make midyear changes
Medicare Part D prescription drug plan sponsors will have flexibility to make maintenance changes to their formularies in 2019 as part of a broader effort to lower costs for Part D enrollees.
The ability to make so-called “maintenance changes” to a formulary can now be made prior to receiving approval from the Centers for Medicare & Medicaid Services after the agency finalized a proposal in a rule updating regulations governing Medicare Part D and Medicare Advantage.
The new rule allows plans to make formulary changes immediately upon generic approval assuming certain requirements are met, including generally advising Part D plan members beforehand that changes can occur without a specific advance notice and later providing information about any specific generic substitutions that occur.
The agency cited a Medicare Payment Advisory Commission June 2016 report to Congress as the source of the proposal. That report notes that while plan sponsors can notify beneficiaries of changes when they alert CMS, it can take up to 6 months to get formal notice of an approval, leaving some plan sponsors waiting.
CMS noted that the proposed changes drew concerns, particularly regarding changes that could be made without giving patients a chance to discuss them with their doctors about transitioning to a new medication and other concerns. However, the rule states that the policy “strikes the right balance between providing beneficiaries with access to needed drugs and Part D sponsors with flexibility to administer plans.”
Another area in the rule that CMS expects will generate savings is a new policy on biosimilars that affects beneficiaries receiving low-income subsidy benefits. Going forward, the agency will treat biosimilars and interchangeable biological products the same as generics in terms of determining copays for low-income subsidy enrollees.
Other changes in the rule eliminate requirements that sponsors eliminate plan offerings unless they “meaningfully differ” from one another, allowing plans to offer more choices to beneficiaries, and potentially more cost-saving options to meet their needs. It also clarifies rules regarding the “any willing provider” requirement to allow for more pharmacy options available to Part D enrollees and allow them to shop for best deals for their pharmaceuticals.
In combination with the final 2019 call letter that provides Medicare Advantage and Part D sponsors with the guidelines for submitting their plan designs for the coming coverage year, the rule also finalizes policies related to stemming the opioid crisis, including providing tools to help prevent opioid overprescribing and abuse. The rule implements provisions of the Comprehensive Addiction and Recovery Act of 2016 that require CMS to supply a framework that allows Part D sponsors to implement drug management programs to limit at-risk beneficiaries’ access to coverage for frequently abused drugs.
For example, plans will be allowed to limit at-risk beneficiaries to selected physicians and/or pharmacies to receive their prescriptions, although it will exempt patients who are being treated for cancer-related pain, are receiving palliative or end-of-life care, or are in hospice or long-term care from these drug management programs.
CMS also is limiting the availability of special enrollment periods for beneficiaries dually eligible for Medicare and Medicaid or eligible for the low-income subsidy who are identified as at-risk or potentially at-risk for prescription drug abuse.
Medicare Part D prescription drug plan sponsors will have flexibility to make maintenance changes to their formularies in 2019 as part of a broader effort to lower costs for Part D enrollees.
The ability to make so-called “maintenance changes” to a formulary can now be made prior to receiving approval from the Centers for Medicare & Medicaid Services after the agency finalized a proposal in a rule updating regulations governing Medicare Part D and Medicare Advantage.
The new rule allows plans to make formulary changes immediately upon generic approval assuming certain requirements are met, including generally advising Part D plan members beforehand that changes can occur without a specific advance notice and later providing information about any specific generic substitutions that occur.
The agency cited a Medicare Payment Advisory Commission June 2016 report to Congress as the source of the proposal. That report notes that while plan sponsors can notify beneficiaries of changes when they alert CMS, it can take up to 6 months to get formal notice of an approval, leaving some plan sponsors waiting.
CMS noted that the proposed changes drew concerns, particularly regarding changes that could be made without giving patients a chance to discuss them with their doctors about transitioning to a new medication and other concerns. However, the rule states that the policy “strikes the right balance between providing beneficiaries with access to needed drugs and Part D sponsors with flexibility to administer plans.”
Another area in the rule that CMS expects will generate savings is a new policy on biosimilars that affects beneficiaries receiving low-income subsidy benefits. Going forward, the agency will treat biosimilars and interchangeable biological products the same as generics in terms of determining copays for low-income subsidy enrollees.
Other changes in the rule eliminate requirements that sponsors eliminate plan offerings unless they “meaningfully differ” from one another, allowing plans to offer more choices to beneficiaries, and potentially more cost-saving options to meet their needs. It also clarifies rules regarding the “any willing provider” requirement to allow for more pharmacy options available to Part D enrollees and allow them to shop for best deals for their pharmaceuticals.
In combination with the final 2019 call letter that provides Medicare Advantage and Part D sponsors with the guidelines for submitting their plan designs for the coming coverage year, the rule also finalizes policies related to stemming the opioid crisis, including providing tools to help prevent opioid overprescribing and abuse. The rule implements provisions of the Comprehensive Addiction and Recovery Act of 2016 that require CMS to supply a framework that allows Part D sponsors to implement drug management programs to limit at-risk beneficiaries’ access to coverage for frequently abused drugs.
For example, plans will be allowed to limit at-risk beneficiaries to selected physicians and/or pharmacies to receive their prescriptions, although it will exempt patients who are being treated for cancer-related pain, are receiving palliative or end-of-life care, or are in hospice or long-term care from these drug management programs.
CMS also is limiting the availability of special enrollment periods for beneficiaries dually eligible for Medicare and Medicaid or eligible for the low-income subsidy who are identified as at-risk or potentially at-risk for prescription drug abuse.
Medicare Part D prescription drug plan sponsors will have flexibility to make maintenance changes to their formularies in 2019 as part of a broader effort to lower costs for Part D enrollees.
The ability to make so-called “maintenance changes” to a formulary can now be made prior to receiving approval from the Centers for Medicare & Medicaid Services after the agency finalized a proposal in a rule updating regulations governing Medicare Part D and Medicare Advantage.
The new rule allows plans to make formulary changes immediately upon generic approval assuming certain requirements are met, including generally advising Part D plan members beforehand that changes can occur without a specific advance notice and later providing information about any specific generic substitutions that occur.
The agency cited a Medicare Payment Advisory Commission June 2016 report to Congress as the source of the proposal. That report notes that while plan sponsors can notify beneficiaries of changes when they alert CMS, it can take up to 6 months to get formal notice of an approval, leaving some plan sponsors waiting.
CMS noted that the proposed changes drew concerns, particularly regarding changes that could be made without giving patients a chance to discuss them with their doctors about transitioning to a new medication and other concerns. However, the rule states that the policy “strikes the right balance between providing beneficiaries with access to needed drugs and Part D sponsors with flexibility to administer plans.”
Another area in the rule that CMS expects will generate savings is a new policy on biosimilars that affects beneficiaries receiving low-income subsidy benefits. Going forward, the agency will treat biosimilars and interchangeable biological products the same as generics in terms of determining copays for low-income subsidy enrollees.
Other changes in the rule eliminate requirements that sponsors eliminate plan offerings unless they “meaningfully differ” from one another, allowing plans to offer more choices to beneficiaries, and potentially more cost-saving options to meet their needs. It also clarifies rules regarding the “any willing provider” requirement to allow for more pharmacy options available to Part D enrollees and allow them to shop for best deals for their pharmaceuticals.
In combination with the final 2019 call letter that provides Medicare Advantage and Part D sponsors with the guidelines for submitting their plan designs for the coming coverage year, the rule also finalizes policies related to stemming the opioid crisis, including providing tools to help prevent opioid overprescribing and abuse. The rule implements provisions of the Comprehensive Addiction and Recovery Act of 2016 that require CMS to supply a framework that allows Part D sponsors to implement drug management programs to limit at-risk beneficiaries’ access to coverage for frequently abused drugs.
For example, plans will be allowed to limit at-risk beneficiaries to selected physicians and/or pharmacies to receive their prescriptions, although it will exempt patients who are being treated for cancer-related pain, are receiving palliative or end-of-life care, or are in hospice or long-term care from these drug management programs.
CMS also is limiting the availability of special enrollment periods for beneficiaries dually eligible for Medicare and Medicaid or eligible for the low-income subsidy who are identified as at-risk or potentially at-risk for prescription drug abuse.
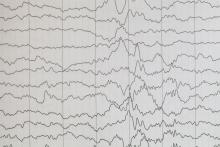
Sonified EEG could be useful triage tool
Medical students and nurses who listened to 15 seconds of single-channel sonified electroencephalograms detected seizures with 95%-98% sensitivity, outperforming neurologists who reviewed traditional visual EEG displays, according to the results of a single-center study.
“We confirm that individuals without EEG training can detect ongoing seizures or seizurelike rhythmic and periodic patterns by merely listening to short clips of sonified EEG,” wrote Josef Parvizi, MD, PhD, and his associates at Stanford (Calif.) University. “Ours is also the first study to test the capability of a sonification method to detect a range of significant abnormalities when it is used by clinical staff (e.g., physicians, nurses, and students).” The findings were published online March 20 in Epilepsia.
To test the method, 34 medical students and 30 nurses watched a 4-minute training video before listening to 84 sonified EEGs: seven seizures, 52 slowing or normal patterns, and 25 seizurelike abnormalities (generalized periodic discharges, lateralized periodic discharges, triphasic waves, or burst suppression). For each patient, listeners heard two sonified EEG clips, one from each hemisphere, and designated them as “seizure,” “nonseizure,” or “don’t know.” For comparison, 12 EEG-trained neurologists and 29 EEG-trained medical students reviewed traditional visual displays of the same EEGs.
Sonified EEGs identified seizures with a sensitivity of 95% (standard deviation, 14%) when heard by nurses and 98% (SD, 5%) when heard by medical students. In contrast, the sensitivity of visual displays was only 88% (SD, 11%) when reviewed by neurologists and 76% (SD, 19%) when reviewed by EEG-trained medical students. Specificity of sonified EEGs was 85% when heard by the medical students and 82% when heard by the nurses. Specificity of traditional review was 90% for neurologists and 65% for medical students.
The study was based on a representative sample, not a prospectively and consecutively recruited cohort, which constrains insights into how this technique might perform “at the bedside,” the researchers said. Additionally, the sonification method would not identify focal seizures occurring outside the individual channels selected (in this study, T3-T5 or T4-T6).
The study was funded by a Stanford University BioX Seed Grant. Dr. Parvizi and one coinvestigator invented the sonification method described and cofounded a startup that has licensed the technology from Stanford University. The other two investigators had no conflicts.
SOURCE: Parvizi J et al. Epilepsia. 2018 Mar 20. doi: 10.1111/epi.14043.
Medical students and nurses who listened to 15 seconds of single-channel sonified electroencephalograms detected seizures with 95%-98% sensitivity, outperforming neurologists who reviewed traditional visual EEG displays, according to the results of a single-center study.
“We confirm that individuals without EEG training can detect ongoing seizures or seizurelike rhythmic and periodic patterns by merely listening to short clips of sonified EEG,” wrote Josef Parvizi, MD, PhD, and his associates at Stanford (Calif.) University. “Ours is also the first study to test the capability of a sonification method to detect a range of significant abnormalities when it is used by clinical staff (e.g., physicians, nurses, and students).” The findings were published online March 20 in Epilepsia.
To test the method, 34 medical students and 30 nurses watched a 4-minute training video before listening to 84 sonified EEGs: seven seizures, 52 slowing or normal patterns, and 25 seizurelike abnormalities (generalized periodic discharges, lateralized periodic discharges, triphasic waves, or burst suppression). For each patient, listeners heard two sonified EEG clips, one from each hemisphere, and designated them as “seizure,” “nonseizure,” or “don’t know.” For comparison, 12 EEG-trained neurologists and 29 EEG-trained medical students reviewed traditional visual displays of the same EEGs.
Sonified EEGs identified seizures with a sensitivity of 95% (standard deviation, 14%) when heard by nurses and 98% (SD, 5%) when heard by medical students. In contrast, the sensitivity of visual displays was only 88% (SD, 11%) when reviewed by neurologists and 76% (SD, 19%) when reviewed by EEG-trained medical students. Specificity of sonified EEGs was 85% when heard by the medical students and 82% when heard by the nurses. Specificity of traditional review was 90% for neurologists and 65% for medical students.
The study was based on a representative sample, not a prospectively and consecutively recruited cohort, which constrains insights into how this technique might perform “at the bedside,” the researchers said. Additionally, the sonification method would not identify focal seizures occurring outside the individual channels selected (in this study, T3-T5 or T4-T6).
The study was funded by a Stanford University BioX Seed Grant. Dr. Parvizi and one coinvestigator invented the sonification method described and cofounded a startup that has licensed the technology from Stanford University. The other two investigators had no conflicts.
SOURCE: Parvizi J et al. Epilepsia. 2018 Mar 20. doi: 10.1111/epi.14043.
Medical students and nurses who listened to 15 seconds of single-channel sonified electroencephalograms detected seizures with 95%-98% sensitivity, outperforming neurologists who reviewed traditional visual EEG displays, according to the results of a single-center study.
“We confirm that individuals without EEG training can detect ongoing seizures or seizurelike rhythmic and periodic patterns by merely listening to short clips of sonified EEG,” wrote Josef Parvizi, MD, PhD, and his associates at Stanford (Calif.) University. “Ours is also the first study to test the capability of a sonification method to detect a range of significant abnormalities when it is used by clinical staff (e.g., physicians, nurses, and students).” The findings were published online March 20 in Epilepsia.
To test the method, 34 medical students and 30 nurses watched a 4-minute training video before listening to 84 sonified EEGs: seven seizures, 52 slowing or normal patterns, and 25 seizurelike abnormalities (generalized periodic discharges, lateralized periodic discharges, triphasic waves, or burst suppression). For each patient, listeners heard two sonified EEG clips, one from each hemisphere, and designated them as “seizure,” “nonseizure,” or “don’t know.” For comparison, 12 EEG-trained neurologists and 29 EEG-trained medical students reviewed traditional visual displays of the same EEGs.
Sonified EEGs identified seizures with a sensitivity of 95% (standard deviation, 14%) when heard by nurses and 98% (SD, 5%) when heard by medical students. In contrast, the sensitivity of visual displays was only 88% (SD, 11%) when reviewed by neurologists and 76% (SD, 19%) when reviewed by EEG-trained medical students. Specificity of sonified EEGs was 85% when heard by the medical students and 82% when heard by the nurses. Specificity of traditional review was 90% for neurologists and 65% for medical students.
The study was based on a representative sample, not a prospectively and consecutively recruited cohort, which constrains insights into how this technique might perform “at the bedside,” the researchers said. Additionally, the sonification method would not identify focal seizures occurring outside the individual channels selected (in this study, T3-T5 or T4-T6).
The study was funded by a Stanford University BioX Seed Grant. Dr. Parvizi and one coinvestigator invented the sonification method described and cofounded a startup that has licensed the technology from Stanford University. The other two investigators had no conflicts.
SOURCE: Parvizi J et al. Epilepsia. 2018 Mar 20. doi: 10.1111/epi.14043.
FROM EPILEPSIA
Key clinical point: Trained nonexperts reliably detected seizures by listening to short clips of sonified electroencephalograms.
Major finding: Sensitivity ranged from 95% (nurses) to 98% (medical students). Specificities were 82% and 85%, respectively.
Study details: Comparative reviews of 84 EEGs, including seven seizures, 25 seizurelike abnormalities, and 52 slowing or normal patterns.
Disclosures: The study was funded by a Stanford University BioX Seed Grant. Dr. Parvizi and one coinvestigator invented the sonification method described and cofounded a startup that has licensed the technology from Stanford University. The other two investigators had no conflicts.
Source: Parvizi J et al., Epilepsia. 2018 Mar 20. doi: 10.1111/epi.14043.
Debunking Atopic Dermatitis Myths: Do Most Children Outgrow Atopic Dermatitis?
Myth: Children eventually outgrow atopic dermatitis and therefore do not need treatment
The negative impact of atopic dermatitis (AD) on quality of life in the pediatric population often prompts parents/guardians to inquire about whether a child with AD will ever outgrow their disease. If remission is expected as the child gets older, many may question if it is necessary to pursue treatment or just let the disease run its course. Although AD often is reported to resolve soon after the first decade of life, symptoms can persist well into the second decade and beyond, suggesting that AD may be a lifelong disease with periods of waxing and waning symptoms that require persistent treatment throughout the patient’s life.
A 2014 study included 7157 children with AD (mean age of disease onset, 1.7 years) who were enrolled in the Pediatric Eczema Elective Registry (PEER) program between the ages of 2 and 17 years with measurement of disease activity at regular 6-month intervals for up to 5 years. The study results indicated that more than 80% of patients at every age (age range, 2–26 years) had symptoms of AD and/or were using medication to treat their disease, and the majority (64%) of patients had never reported a 6-month period during which they achieved clearance of symptoms without medication. At the age of 20 years, 50% of patients reported at least 1 lifetime 6-month period during which they were both symptom and treatment free. In another study of adolescents with AD who also had AD in childhood (N=82), 48% of patients remained in the same AD severity grades and 13% deteriorated from childhood to adolescence; only 39% of patients showed improvement in disease severity from childhood to adolescence. The findings of these reports are contradictory to conventional clinical teaching, which indicates that AD generally resolves by age 12 in 50% to 70% of children.
Even though some children with AD may experience periods of disease clearance, these findings often do not persist and should not be confused with a permanent remission. Most patients require continued treatment with medications to achieve relief of symptoms. Therefore, physicians should not assure parents/guardians that a child can outgrow AD; rather, they should educate pediatric patients and their caregivers about the potentially lifelong disease course and encourage early intervention to mitigate symptoms and manage comorbidities as the patient ages.
Hon KL, Tsang YCK, Poon TCW, et al. Predicating eczema severity beyond childhood. World J Pediatr. 2016;12:44-48.
Margolis JS, Abuabara K, Bilker W, et al. Persistence of mild to moderate atopic dermatitis [published online April 2, 2014]. JAMA Dermatol. 2014;150:593-600.
Myth: Children eventually outgrow atopic dermatitis and therefore do not need treatment
The negative impact of atopic dermatitis (AD) on quality of life in the pediatric population often prompts parents/guardians to inquire about whether a child with AD will ever outgrow their disease. If remission is expected as the child gets older, many may question if it is necessary to pursue treatment or just let the disease run its course. Although AD often is reported to resolve soon after the first decade of life, symptoms can persist well into the second decade and beyond, suggesting that AD may be a lifelong disease with periods of waxing and waning symptoms that require persistent treatment throughout the patient’s life.
A 2014 study included 7157 children with AD (mean age of disease onset, 1.7 years) who were enrolled in the Pediatric Eczema Elective Registry (PEER) program between the ages of 2 and 17 years with measurement of disease activity at regular 6-month intervals for up to 5 years. The study results indicated that more than 80% of patients at every age (age range, 2–26 years) had symptoms of AD and/or were using medication to treat their disease, and the majority (64%) of patients had never reported a 6-month period during which they achieved clearance of symptoms without medication. At the age of 20 years, 50% of patients reported at least 1 lifetime 6-month period during which they were both symptom and treatment free. In another study of adolescents with AD who also had AD in childhood (N=82), 48% of patients remained in the same AD severity grades and 13% deteriorated from childhood to adolescence; only 39% of patients showed improvement in disease severity from childhood to adolescence. The findings of these reports are contradictory to conventional clinical teaching, which indicates that AD generally resolves by age 12 in 50% to 70% of children.
Even though some children with AD may experience periods of disease clearance, these findings often do not persist and should not be confused with a permanent remission. Most patients require continued treatment with medications to achieve relief of symptoms. Therefore, physicians should not assure parents/guardians that a child can outgrow AD; rather, they should educate pediatric patients and their caregivers about the potentially lifelong disease course and encourage early intervention to mitigate symptoms and manage comorbidities as the patient ages.
Myth: Children eventually outgrow atopic dermatitis and therefore do not need treatment
The negative impact of atopic dermatitis (AD) on quality of life in the pediatric population often prompts parents/guardians to inquire about whether a child with AD will ever outgrow their disease. If remission is expected as the child gets older, many may question if it is necessary to pursue treatment or just let the disease run its course. Although AD often is reported to resolve soon after the first decade of life, symptoms can persist well into the second decade and beyond, suggesting that AD may be a lifelong disease with periods of waxing and waning symptoms that require persistent treatment throughout the patient’s life.
A 2014 study included 7157 children with AD (mean age of disease onset, 1.7 years) who were enrolled in the Pediatric Eczema Elective Registry (PEER) program between the ages of 2 and 17 years with measurement of disease activity at regular 6-month intervals for up to 5 years. The study results indicated that more than 80% of patients at every age (age range, 2–26 years) had symptoms of AD and/or were using medication to treat their disease, and the majority (64%) of patients had never reported a 6-month period during which they achieved clearance of symptoms without medication. At the age of 20 years, 50% of patients reported at least 1 lifetime 6-month period during which they were both symptom and treatment free. In another study of adolescents with AD who also had AD in childhood (N=82), 48% of patients remained in the same AD severity grades and 13% deteriorated from childhood to adolescence; only 39% of patients showed improvement in disease severity from childhood to adolescence. The findings of these reports are contradictory to conventional clinical teaching, which indicates that AD generally resolves by age 12 in 50% to 70% of children.
Even though some children with AD may experience periods of disease clearance, these findings often do not persist and should not be confused with a permanent remission. Most patients require continued treatment with medications to achieve relief of symptoms. Therefore, physicians should not assure parents/guardians that a child can outgrow AD; rather, they should educate pediatric patients and their caregivers about the potentially lifelong disease course and encourage early intervention to mitigate symptoms and manage comorbidities as the patient ages.
Hon KL, Tsang YCK, Poon TCW, et al. Predicating eczema severity beyond childhood. World J Pediatr. 2016;12:44-48.
Margolis JS, Abuabara K, Bilker W, et al. Persistence of mild to moderate atopic dermatitis [published online April 2, 2014]. JAMA Dermatol. 2014;150:593-600.
Hon KL, Tsang YCK, Poon TCW, et al. Predicating eczema severity beyond childhood. World J Pediatr. 2016;12:44-48.
Margolis JS, Abuabara K, Bilker W, et al. Persistence of mild to moderate atopic dermatitis [published online April 2, 2014]. JAMA Dermatol. 2014;150:593-600.
A refined strategy for confirming diagnosis in suspected NSTEMI
ORLANDO – A novel diagnostic strategy of performing CT angiography or cardiovascular MRI first in patients with suspected non-ST-elevation MI safely improved appropriate selection for invasive coronary angiography in the Dutch randomized CARMENTA trial.
The strategy of using noninvasive imaging first significantly cut down on the high proportion of diagnostic invasive angiography procedures that end up showing no significant obstructive coronary artery disease in the current era of high-sensitivity cardiac troponin assays, Martijn W. Smulders, MD, reported at the annual meeting of the American College of Cardiology.
CARMENTA (Cardiovascular Magnetic Resonance Imaging and Computed Tomography Angiography) was a single-center, prospective, randomized trial including 207 patients with suspected NSTEMI on the basis of acute chest pain, an elevated high-sensitivity cardiac troponin level, and an inconclusive ECG. They were randomized to one of three diagnostic strategies: a routine invasive strategy in which they were sent straight to the cardiac catheterization lab for invasive coronary angiography, or either CTA- or CMR-first as gatekeeper strategies in which referral for invasive angiography was reserved for only those patients whose noninvasive imaging demonstrated myocardial ischemia, infarction, or obstructive CAD with at least a 70% stenosis.
The impetus for the trial was the investigators’ concern that widespread embrace of high-sensitivity cardiac troponin assays has resulted in a serious clinical problem: Although these assays offer very high sensitivity for rapid detection of acute MI, their positive predictive value is only 56%, compared with 76% for the older troponin assays.
“That means almost one out of two patients with acute chest pain and an elevated high-sensitivity troponin level does not have a type 1 MI. We see a twofold higher incidence of elevated troponin levels with these assays, so there has been a significant increase in referrals for invasive angiography – and up to one-third of these patients with suspected NSTEMI don’t have an obstructive stenosis. We need a strategy to improve patient selection,” explained Dr. Smulders of Maastricht (the Netherlands) University.
The CARMENTA strategy worked. The primary outcome – the proportion of patients with suspected NSTEMI who underwent invasive coronary angiography during their initial hospitalization – was 65% in the CTA-first group and 77% in the CMR group, compared with 100% in the routine invasive-strategy control group. Moreover, fully 38% of patients in the control group turned out not to have obstructive CAD, compared with 15% who were sent for invasive angiography only after CTA and 31% who first had CMR.
Procedure-related complications, a secondary outcome, occurred in 12% of the CMR-first group, 13% of the CTA-first group, and 16% of patients in the routine invasive strategy control group. Major adverse cardiac events during 1 year of follow-up, which was the other secondary outcome, occurred in 9% of the CMR group, 6% of the CTA group, and 9% of the control group.
A limitation of the CARMENTA trial was that, even though it was scheduled to enroll 288 patients to achieve strong statistical power, the study’s data safety monitoring committee recommended on the basis of an interim analysis that the trial be halted early. The reasoning was that the experience of the first 200 enrollees made it clear that the noninvasive-imaging-first strategy would achieve the goal of reducing the volume of referrals to invasive angiography for suspected NSTEMI.
Session cochair Stefan D. Anker, MD, was irked by the trial’s early termination, which weakened the strength of the conclusions, especially with regard to the safety of the novel strategy.
“I agree that this imaging-first strategy reduces procedures, but the use of the word ‘safely’ is premature,” said Dr. Anker, professor of homeostasis and cachexia at Charite Medical School in Berlin.
“I totally agree with you,” Dr. Smulders replied. “We need a bigger trial to confirm our results – preferably a multicenter trial.”
“How can you do a bigger trial when your data safety monitoring board didn’t allow you to complete even this trial? They killed your trial. That’s the way I see it,” Dr. Anker said.
The CARMENTA trial was funded by the Dutch Heart Foundation. Dr. Smulders reported having no financial conflicts of interest.
SOURCE: Smulders M. ACC 18.
ORLANDO – A novel diagnostic strategy of performing CT angiography or cardiovascular MRI first in patients with suspected non-ST-elevation MI safely improved appropriate selection for invasive coronary angiography in the Dutch randomized CARMENTA trial.
The strategy of using noninvasive imaging first significantly cut down on the high proportion of diagnostic invasive angiography procedures that end up showing no significant obstructive coronary artery disease in the current era of high-sensitivity cardiac troponin assays, Martijn W. Smulders, MD, reported at the annual meeting of the American College of Cardiology.
CARMENTA (Cardiovascular Magnetic Resonance Imaging and Computed Tomography Angiography) was a single-center, prospective, randomized trial including 207 patients with suspected NSTEMI on the basis of acute chest pain, an elevated high-sensitivity cardiac troponin level, and an inconclusive ECG. They were randomized to one of three diagnostic strategies: a routine invasive strategy in which they were sent straight to the cardiac catheterization lab for invasive coronary angiography, or either CTA- or CMR-first as gatekeeper strategies in which referral for invasive angiography was reserved for only those patients whose noninvasive imaging demonstrated myocardial ischemia, infarction, or obstructive CAD with at least a 70% stenosis.
The impetus for the trial was the investigators’ concern that widespread embrace of high-sensitivity cardiac troponin assays has resulted in a serious clinical problem: Although these assays offer very high sensitivity for rapid detection of acute MI, their positive predictive value is only 56%, compared with 76% for the older troponin assays.
“That means almost one out of two patients with acute chest pain and an elevated high-sensitivity troponin level does not have a type 1 MI. We see a twofold higher incidence of elevated troponin levels with these assays, so there has been a significant increase in referrals for invasive angiography – and up to one-third of these patients with suspected NSTEMI don’t have an obstructive stenosis. We need a strategy to improve patient selection,” explained Dr. Smulders of Maastricht (the Netherlands) University.
The CARMENTA strategy worked. The primary outcome – the proportion of patients with suspected NSTEMI who underwent invasive coronary angiography during their initial hospitalization – was 65% in the CTA-first group and 77% in the CMR group, compared with 100% in the routine invasive-strategy control group. Moreover, fully 38% of patients in the control group turned out not to have obstructive CAD, compared with 15% who were sent for invasive angiography only after CTA and 31% who first had CMR.
Procedure-related complications, a secondary outcome, occurred in 12% of the CMR-first group, 13% of the CTA-first group, and 16% of patients in the routine invasive strategy control group. Major adverse cardiac events during 1 year of follow-up, which was the other secondary outcome, occurred in 9% of the CMR group, 6% of the CTA group, and 9% of the control group.
A limitation of the CARMENTA trial was that, even though it was scheduled to enroll 288 patients to achieve strong statistical power, the study’s data safety monitoring committee recommended on the basis of an interim analysis that the trial be halted early. The reasoning was that the experience of the first 200 enrollees made it clear that the noninvasive-imaging-first strategy would achieve the goal of reducing the volume of referrals to invasive angiography for suspected NSTEMI.
Session cochair Stefan D. Anker, MD, was irked by the trial’s early termination, which weakened the strength of the conclusions, especially with regard to the safety of the novel strategy.
“I agree that this imaging-first strategy reduces procedures, but the use of the word ‘safely’ is premature,” said Dr. Anker, professor of homeostasis and cachexia at Charite Medical School in Berlin.
“I totally agree with you,” Dr. Smulders replied. “We need a bigger trial to confirm our results – preferably a multicenter trial.”
“How can you do a bigger trial when your data safety monitoring board didn’t allow you to complete even this trial? They killed your trial. That’s the way I see it,” Dr. Anker said.
The CARMENTA trial was funded by the Dutch Heart Foundation. Dr. Smulders reported having no financial conflicts of interest.
SOURCE: Smulders M. ACC 18.
ORLANDO – A novel diagnostic strategy of performing CT angiography or cardiovascular MRI first in patients with suspected non-ST-elevation MI safely improved appropriate selection for invasive coronary angiography in the Dutch randomized CARMENTA trial.
The strategy of using noninvasive imaging first significantly cut down on the high proportion of diagnostic invasive angiography procedures that end up showing no significant obstructive coronary artery disease in the current era of high-sensitivity cardiac troponin assays, Martijn W. Smulders, MD, reported at the annual meeting of the American College of Cardiology.
CARMENTA (Cardiovascular Magnetic Resonance Imaging and Computed Tomography Angiography) was a single-center, prospective, randomized trial including 207 patients with suspected NSTEMI on the basis of acute chest pain, an elevated high-sensitivity cardiac troponin level, and an inconclusive ECG. They were randomized to one of three diagnostic strategies: a routine invasive strategy in which they were sent straight to the cardiac catheterization lab for invasive coronary angiography, or either CTA- or CMR-first as gatekeeper strategies in which referral for invasive angiography was reserved for only those patients whose noninvasive imaging demonstrated myocardial ischemia, infarction, or obstructive CAD with at least a 70% stenosis.
The impetus for the trial was the investigators’ concern that widespread embrace of high-sensitivity cardiac troponin assays has resulted in a serious clinical problem: Although these assays offer very high sensitivity for rapid detection of acute MI, their positive predictive value is only 56%, compared with 76% for the older troponin assays.
“That means almost one out of two patients with acute chest pain and an elevated high-sensitivity troponin level does not have a type 1 MI. We see a twofold higher incidence of elevated troponin levels with these assays, so there has been a significant increase in referrals for invasive angiography – and up to one-third of these patients with suspected NSTEMI don’t have an obstructive stenosis. We need a strategy to improve patient selection,” explained Dr. Smulders of Maastricht (the Netherlands) University.
The CARMENTA strategy worked. The primary outcome – the proportion of patients with suspected NSTEMI who underwent invasive coronary angiography during their initial hospitalization – was 65% in the CTA-first group and 77% in the CMR group, compared with 100% in the routine invasive-strategy control group. Moreover, fully 38% of patients in the control group turned out not to have obstructive CAD, compared with 15% who were sent for invasive angiography only after CTA and 31% who first had CMR.
Procedure-related complications, a secondary outcome, occurred in 12% of the CMR-first group, 13% of the CTA-first group, and 16% of patients in the routine invasive strategy control group. Major adverse cardiac events during 1 year of follow-up, which was the other secondary outcome, occurred in 9% of the CMR group, 6% of the CTA group, and 9% of the control group.
A limitation of the CARMENTA trial was that, even though it was scheduled to enroll 288 patients to achieve strong statistical power, the study’s data safety monitoring committee recommended on the basis of an interim analysis that the trial be halted early. The reasoning was that the experience of the first 200 enrollees made it clear that the noninvasive-imaging-first strategy would achieve the goal of reducing the volume of referrals to invasive angiography for suspected NSTEMI.
Session cochair Stefan D. Anker, MD, was irked by the trial’s early termination, which weakened the strength of the conclusions, especially with regard to the safety of the novel strategy.
“I agree that this imaging-first strategy reduces procedures, but the use of the word ‘safely’ is premature,” said Dr. Anker, professor of homeostasis and cachexia at Charite Medical School in Berlin.
“I totally agree with you,” Dr. Smulders replied. “We need a bigger trial to confirm our results – preferably a multicenter trial.”
“How can you do a bigger trial when your data safety monitoring board didn’t allow you to complete even this trial? They killed your trial. That’s the way I see it,” Dr. Anker said.
The CARMENTA trial was funded by the Dutch Heart Foundation. Dr. Smulders reported having no financial conflicts of interest.
SOURCE: Smulders M. ACC 18.
REPORTING FROM ACC 18
Key clinical point: Dutch cardiologists have come up with a novel way to reduce the high rate of negative diagnostic coronary angiography in patients with suspected NSTEMI.
Major finding: Reserving invasive coronary angiography for only those patients with suspected NSTEMI who first showed positive findings on noninvasive CT angiography reduced invasive angiography volume by 35%.
Study details: This single-center, randomized, prospective, three-arm clinical trial included 207 patients with suspected NSTEMI.
Disclosures: The CARMENTA trial was funded by the Dutch Heart Foundation. The presenter reported having no financial conflicts of interest.
Source: Smulders M. ACC 18.
Commentary—Could Prazosin Play a Role in Treating Chronic Posttraumatic Headache?
Headache is a common symptom after any severity traumatic brain injury in the civilian and military populations. Currently, there is no evidence-based treatment protocol for posttraumatic headache, and management largely is based on therapies used in the primary headache disorders.
There is a complex interaction between mood disorders, posttraumatic stress disorder (PTSD), sleep disorders, and headache. Depression and PTSD are frequently seen in civilian and military populations accompanying chronic posttraumatic headache. In civilians, about one-third of patients with posttraumatic headache meet criteria for depression and PTSD. A longitudinal study of Iraq and Afghanistan veterans followed over three years found that co-occurrence of depression, PTSD, or both would increase the risk of chronic posttraumatic headache more than TBI alone. Another meta-analysis of civilian and military TBI found that, though PTSD could affect intensity and severity of chronic posttraumatic headache, TBI was an independent risk factor for chronic posttraumatic headache. PTSD and depression can cause sleep disruption and intensify pain syndromes, including headache.
Though prazosin had been shown to be effective in decreasing nightmares, improving sleep, or decreasing daytime sleepiness in many prior studies, the PACT trial, a randomized, double-blind controlled trial of 304 participants at Veterans Affairs medical centers, did not meet its primary end points of less frequent and less intense trauma-related nightmares, greater improvement in sleep quality, and overall clinical status among veterans assigned to prazosin, compared with veterans assigned to placebo. While disappointing, and surprising given the results of the preceding studies, do these results predict a similar failure in the use of prazosin for treatment of posttraumatic headache?
In an observational study of 126 veterans with blast-related mild TBI during Operation Iraqi Freedom or Operation Enduring Freedom, 82% of participants had co-occurring conditions, including frequent, severe headache, neurologic exam abnormalities, or cognitive disorders. This pilot study found that treatment with prazosin and sleep hygiene counseling improved sleep, but also decreased headache pain and frequency, as well as improved cognitive function over nine weeks. Improvements were maintained for six months. Though difficult to determine the interplay of sleep, posttraumatic headache, and depression, could prazosin independently reduce the burden of headache? Currently, a double-blind, randomized, controlled trial in veterans is examining the effectiveness of prazosin as a preventive agent in treating combat-related posttraumatic headache. This study was scheduled to enroll its last patient at the end of 2017, and results may be out soon.
There may be specific pharmacologic properties that make prazosin a useful drug for headache treatment. Prazosin is a very potent, selective alpha 1-adrenergic antagonist that passes through the blood–brain barrier. It is highly protein bound (97%), so absolute amounts in the CNS are likely to be low. Its use in the treatment of hypertension is based on decreased peripheral vascular resistance as a result of arteriolar and venous receptor blockade. It also can act in the CNS to decrease sympathetic outflow. While an effect on headache could be central, peripheral, or both, other drugs with alpha-adrenergic blocking effects have been used in the treatment of migraine for decades. The ergots, for example, were the first alpha-adrenergic agents to be discovered acting as partial agonists or antagonists at adrenergic, tryptaminergic, and dopaminergic receptors. The hydrogenated ergot alkaloids are among the most potent alpha-adrenergic blocking agents, but adverse effects prevent doses that can cause more than minimal blockade. Chlorpromazine and other dopamine (D2) receptor antagonists, which are highly effective in acute treatment of migraine, particularly with parenteral delivery, also produce significant alpha-adrenergic receptor blockade, while trazodone, amitriptyline, and the atypical antipsychotics, with various levels of alpha-adrenergic antagonism, have found some success in migraine prevention.
Clinical experience has shown that there is wide response variability to acute and chronic medication for migraine. Genetic studies of patients with migraine, though at an early stage, have identified genes involved with vascular and neuronal function. It is likely that clinical observation will be borne out by individual responses to drug classes based on individual genetic profiles, so that subtypes of patients in clinical trial populations may show efficacy based on these profiles. It is likely that prazosin will be useful in certain patient subtypes for the treatment of headache. Posttraumatic headache, which may share some similar pathways of headache physiology with primary headache disorders, adds another layer of response complexity.
—Sylvia Lucas, MD, PhD
Clinical Professor of Neurology and Neurological Surgery
University of Washington
Seattle
Suggested Reading
Nampiaparampil DE. Prevalence of chronic pain after traumatic brain injury: a systematic review. JAMA. 2008;300(6):711-719.
Peterlin BL, Nijjar SS, Tietjen GE. Post-traumatic stress disorder and migraine: epidemiology, sex differences, and potential mechanisms. Headache. 2011;51(6):860-868.
Ruff RL, Riechers RG, Wang XF, et al. For veterans with mild traumatic brain injury, improved posttraumatic stress disorder severity and sleep correlated with symptomatic improvement. J Rehabil Res Dev. 2012;49(9):1305-1320.
Headache is a common symptom after any severity traumatic brain injury in the civilian and military populations. Currently, there is no evidence-based treatment protocol for posttraumatic headache, and management largely is based on therapies used in the primary headache disorders.
There is a complex interaction between mood disorders, posttraumatic stress disorder (PTSD), sleep disorders, and headache. Depression and PTSD are frequently seen in civilian and military populations accompanying chronic posttraumatic headache. In civilians, about one-third of patients with posttraumatic headache meet criteria for depression and PTSD. A longitudinal study of Iraq and Afghanistan veterans followed over three years found that co-occurrence of depression, PTSD, or both would increase the risk of chronic posttraumatic headache more than TBI alone. Another meta-analysis of civilian and military TBI found that, though PTSD could affect intensity and severity of chronic posttraumatic headache, TBI was an independent risk factor for chronic posttraumatic headache. PTSD and depression can cause sleep disruption and intensify pain syndromes, including headache.
Though prazosin had been shown to be effective in decreasing nightmares, improving sleep, or decreasing daytime sleepiness in many prior studies, the PACT trial, a randomized, double-blind controlled trial of 304 participants at Veterans Affairs medical centers, did not meet its primary end points of less frequent and less intense trauma-related nightmares, greater improvement in sleep quality, and overall clinical status among veterans assigned to prazosin, compared with veterans assigned to placebo. While disappointing, and surprising given the results of the preceding studies, do these results predict a similar failure in the use of prazosin for treatment of posttraumatic headache?
In an observational study of 126 veterans with blast-related mild TBI during Operation Iraqi Freedom or Operation Enduring Freedom, 82% of participants had co-occurring conditions, including frequent, severe headache, neurologic exam abnormalities, or cognitive disorders. This pilot study found that treatment with prazosin and sleep hygiene counseling improved sleep, but also decreased headache pain and frequency, as well as improved cognitive function over nine weeks. Improvements were maintained for six months. Though difficult to determine the interplay of sleep, posttraumatic headache, and depression, could prazosin independently reduce the burden of headache? Currently, a double-blind, randomized, controlled trial in veterans is examining the effectiveness of prazosin as a preventive agent in treating combat-related posttraumatic headache. This study was scheduled to enroll its last patient at the end of 2017, and results may be out soon.
There may be specific pharmacologic properties that make prazosin a useful drug for headache treatment. Prazosin is a very potent, selective alpha 1-adrenergic antagonist that passes through the blood–brain barrier. It is highly protein bound (97%), so absolute amounts in the CNS are likely to be low. Its use in the treatment of hypertension is based on decreased peripheral vascular resistance as a result of arteriolar and venous receptor blockade. It also can act in the CNS to decrease sympathetic outflow. While an effect on headache could be central, peripheral, or both, other drugs with alpha-adrenergic blocking effects have been used in the treatment of migraine for decades. The ergots, for example, were the first alpha-adrenergic agents to be discovered acting as partial agonists or antagonists at adrenergic, tryptaminergic, and dopaminergic receptors. The hydrogenated ergot alkaloids are among the most potent alpha-adrenergic blocking agents, but adverse effects prevent doses that can cause more than minimal blockade. Chlorpromazine and other dopamine (D2) receptor antagonists, which are highly effective in acute treatment of migraine, particularly with parenteral delivery, also produce significant alpha-adrenergic receptor blockade, while trazodone, amitriptyline, and the atypical antipsychotics, with various levels of alpha-adrenergic antagonism, have found some success in migraine prevention.
Clinical experience has shown that there is wide response variability to acute and chronic medication for migraine. Genetic studies of patients with migraine, though at an early stage, have identified genes involved with vascular and neuronal function. It is likely that clinical observation will be borne out by individual responses to drug classes based on individual genetic profiles, so that subtypes of patients in clinical trial populations may show efficacy based on these profiles. It is likely that prazosin will be useful in certain patient subtypes for the treatment of headache. Posttraumatic headache, which may share some similar pathways of headache physiology with primary headache disorders, adds another layer of response complexity.
—Sylvia Lucas, MD, PhD
Clinical Professor of Neurology and Neurological Surgery
University of Washington
Seattle
Suggested Reading
Nampiaparampil DE. Prevalence of chronic pain after traumatic brain injury: a systematic review. JAMA. 2008;300(6):711-719.
Peterlin BL, Nijjar SS, Tietjen GE. Post-traumatic stress disorder and migraine: epidemiology, sex differences, and potential mechanisms. Headache. 2011;51(6):860-868.
Ruff RL, Riechers RG, Wang XF, et al. For veterans with mild traumatic brain injury, improved posttraumatic stress disorder severity and sleep correlated with symptomatic improvement. J Rehabil Res Dev. 2012;49(9):1305-1320.
Headache is a common symptom after any severity traumatic brain injury in the civilian and military populations. Currently, there is no evidence-based treatment protocol for posttraumatic headache, and management largely is based on therapies used in the primary headache disorders.
There is a complex interaction between mood disorders, posttraumatic stress disorder (PTSD), sleep disorders, and headache. Depression and PTSD are frequently seen in civilian and military populations accompanying chronic posttraumatic headache. In civilians, about one-third of patients with posttraumatic headache meet criteria for depression and PTSD. A longitudinal study of Iraq and Afghanistan veterans followed over three years found that co-occurrence of depression, PTSD, or both would increase the risk of chronic posttraumatic headache more than TBI alone. Another meta-analysis of civilian and military TBI found that, though PTSD could affect intensity and severity of chronic posttraumatic headache, TBI was an independent risk factor for chronic posttraumatic headache. PTSD and depression can cause sleep disruption and intensify pain syndromes, including headache.
Though prazosin had been shown to be effective in decreasing nightmares, improving sleep, or decreasing daytime sleepiness in many prior studies, the PACT trial, a randomized, double-blind controlled trial of 304 participants at Veterans Affairs medical centers, did not meet its primary end points of less frequent and less intense trauma-related nightmares, greater improvement in sleep quality, and overall clinical status among veterans assigned to prazosin, compared with veterans assigned to placebo. While disappointing, and surprising given the results of the preceding studies, do these results predict a similar failure in the use of prazosin for treatment of posttraumatic headache?
In an observational study of 126 veterans with blast-related mild TBI during Operation Iraqi Freedom or Operation Enduring Freedom, 82% of participants had co-occurring conditions, including frequent, severe headache, neurologic exam abnormalities, or cognitive disorders. This pilot study found that treatment with prazosin and sleep hygiene counseling improved sleep, but also decreased headache pain and frequency, as well as improved cognitive function over nine weeks. Improvements were maintained for six months. Though difficult to determine the interplay of sleep, posttraumatic headache, and depression, could prazosin independently reduce the burden of headache? Currently, a double-blind, randomized, controlled trial in veterans is examining the effectiveness of prazosin as a preventive agent in treating combat-related posttraumatic headache. This study was scheduled to enroll its last patient at the end of 2017, and results may be out soon.
There may be specific pharmacologic properties that make prazosin a useful drug for headache treatment. Prazosin is a very potent, selective alpha 1-adrenergic antagonist that passes through the blood–brain barrier. It is highly protein bound (97%), so absolute amounts in the CNS are likely to be low. Its use in the treatment of hypertension is based on decreased peripheral vascular resistance as a result of arteriolar and venous receptor blockade. It also can act in the CNS to decrease sympathetic outflow. While an effect on headache could be central, peripheral, or both, other drugs with alpha-adrenergic blocking effects have been used in the treatment of migraine for decades. The ergots, for example, were the first alpha-adrenergic agents to be discovered acting as partial agonists or antagonists at adrenergic, tryptaminergic, and dopaminergic receptors. The hydrogenated ergot alkaloids are among the most potent alpha-adrenergic blocking agents, but adverse effects prevent doses that can cause more than minimal blockade. Chlorpromazine and other dopamine (D2) receptor antagonists, which are highly effective in acute treatment of migraine, particularly with parenteral delivery, also produce significant alpha-adrenergic receptor blockade, while trazodone, amitriptyline, and the atypical antipsychotics, with various levels of alpha-adrenergic antagonism, have found some success in migraine prevention.
Clinical experience has shown that there is wide response variability to acute and chronic medication for migraine. Genetic studies of patients with migraine, though at an early stage, have identified genes involved with vascular and neuronal function. It is likely that clinical observation will be borne out by individual responses to drug classes based on individual genetic profiles, so that subtypes of patients in clinical trial populations may show efficacy based on these profiles. It is likely that prazosin will be useful in certain patient subtypes for the treatment of headache. Posttraumatic headache, which may share some similar pathways of headache physiology with primary headache disorders, adds another layer of response complexity.
—Sylvia Lucas, MD, PhD
Clinical Professor of Neurology and Neurological Surgery
University of Washington
Seattle
Suggested Reading
Nampiaparampil DE. Prevalence of chronic pain after traumatic brain injury: a systematic review. JAMA. 2008;300(6):711-719.
Peterlin BL, Nijjar SS, Tietjen GE. Post-traumatic stress disorder and migraine: epidemiology, sex differences, and potential mechanisms. Headache. 2011;51(6):860-868.
Ruff RL, Riechers RG, Wang XF, et al. For veterans with mild traumatic brain injury, improved posttraumatic stress disorder severity and sleep correlated with symptomatic improvement. J Rehabil Res Dev. 2012;49(9):1305-1320.
Does Prazosin Benefit Patients With Posttraumatic Stress Disorder?
Among military veterans with chronic posttraumatic stress disorder (PTSD) and frequent nightmares, prazosin does not alleviate distressing dreams or improve sleep quality, according to trial results published in the February 8 issue of the New England Journal of Medicine.
Prior single-center trials found that prazosin, an alpha 1-adrenoreceptor antagonist, may alleviate nightmares associated with PTSD and improve overall clinical status. The present study’s eligibility criteria may have led to selection bias that contributed to its negative results, the researchers said.
The PACT Trial
To investigate the efficacy of prazosin in patients with chronic combat-related PTSD and frequent nightmares, Murray A. Raskind, MD, and colleagues conducted the Prazosin and Combat Trauma PTSD (PACT) trial. Dr. Raskind is the Director of the Veterans Affairs (VA) Northwest Network Mental Illness Research, Education, and Clinical Center and Professor and Vice Chair of Psychiatry and Behavioral Sciences at the University of Washington School of Medicine in Seattle.
The 26-week, double-blind, randomized, controlled trial included 304 veterans from 12 VA medical centers. Participants met DSM-IV criteria for PTSD; had a total score of at least 50 on the 17-item Clinician-Administered PTSD Scale (CAPS); had been exposed to one or more traumatic, life-threatening events in a war zone before the onset of recurrent nightmares; could recall combat-related nightmares; had a frequency score of at least 2 and a cumulative score of at least 5 on CAPS item B2 (ie, “recurrent distressing dreams”); and, for at least four weeks before randomization, were receiving a stable dose of nonexcluded medications or supportive psychotherapy. Exclusion criteria included unstable medical illness, a systolic blood pressure of less than 110 mm Hg in the supine position, active suicidal or homicidal ideation with plan or intent, and psychosocial instability.
Of 413 people screened, 304 underwent randomization (about 98% male; average age, 52); 152 patients were assigned to each treatment group. The two groups’ patient characteristics did not differ significantly at baseline. Researchers administered prazosin or placebo in escalating divided doses over five weeks to a daily maximum of 20 mg in men and 12 mg in women.
Primary Outcome Measures
The three primary outcome measures were change in score from baseline to 10 weeks on the CAPS item B2, change in score from baseline to 10 weeks on the Pittsburgh Sleep Quality Index, and the Clinical Global Impression of Change score at 10 weeks. None of the primary outcome measures significantly differed between the groups at 10 weeks. The groups’ outcome measures at 26 weeks and other secondary outcomes also were not significantly different.
The number of serious adverse events did not differ significantly by group. Of the adverse events, dizziness, lightheadedness, and urinary incontinence were significantly more common in the prazosin group, compared with the placebo group, whereas new or worsening suicidal ideation was significantly less common among participants who received prazosin, compared with patients who received placebo (8% vs 15%, respectively).
The investigators enrolled patients who were mainly in clinically stable condition, which may have led the trial to include patients whose distressing dreams were unlikely to respond to prazosin, Dr. Raskind and colleagues said.
Future Directions
“The failure of this new, large, multisite trial to replicate the previous studies is surprising and disappointing,” said Kerry J. Ressler, MD, PhD, Chief of the Division of Depression and Anxiety Disorders at McLean Hospital in Belmont, Massachusetts, and Professor of Psychiatry at Harvard Medical School in Boston, in an accompanying editorial. “PTSD remains a psychiatric malady that in some respects seems understandable and treatable on the basis of known neurobiologic pathways. Yet it is a complex syndrome with innumerable subtypes and variations…. There is a need to define clinical subtypes of PTSD on the basis of biologic markers.”
Studies of prazosin for the treatment of other conditions are under way. Investigators have initiated trials to examine whether prazosin reduces the frequency of chronic postconcussive headaches, compared with placebo.
—Jake Remaly
Suggested Reading
Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507-517.
Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003-1010.
Ressler KJ. Alpha-adrenergic receptors in PTSD - Failure or time for precision medicine? N Engl J Med. 2018; 378(6):575-576.
Among military veterans with chronic posttraumatic stress disorder (PTSD) and frequent nightmares, prazosin does not alleviate distressing dreams or improve sleep quality, according to trial results published in the February 8 issue of the New England Journal of Medicine.
Prior single-center trials found that prazosin, an alpha 1-adrenoreceptor antagonist, may alleviate nightmares associated with PTSD and improve overall clinical status. The present study’s eligibility criteria may have led to selection bias that contributed to its negative results, the researchers said.
The PACT Trial
To investigate the efficacy of prazosin in patients with chronic combat-related PTSD and frequent nightmares, Murray A. Raskind, MD, and colleagues conducted the Prazosin and Combat Trauma PTSD (PACT) trial. Dr. Raskind is the Director of the Veterans Affairs (VA) Northwest Network Mental Illness Research, Education, and Clinical Center and Professor and Vice Chair of Psychiatry and Behavioral Sciences at the University of Washington School of Medicine in Seattle.
The 26-week, double-blind, randomized, controlled trial included 304 veterans from 12 VA medical centers. Participants met DSM-IV criteria for PTSD; had a total score of at least 50 on the 17-item Clinician-Administered PTSD Scale (CAPS); had been exposed to one or more traumatic, life-threatening events in a war zone before the onset of recurrent nightmares; could recall combat-related nightmares; had a frequency score of at least 2 and a cumulative score of at least 5 on CAPS item B2 (ie, “recurrent distressing dreams”); and, for at least four weeks before randomization, were receiving a stable dose of nonexcluded medications or supportive psychotherapy. Exclusion criteria included unstable medical illness, a systolic blood pressure of less than 110 mm Hg in the supine position, active suicidal or homicidal ideation with plan or intent, and psychosocial instability.
Of 413 people screened, 304 underwent randomization (about 98% male; average age, 52); 152 patients were assigned to each treatment group. The two groups’ patient characteristics did not differ significantly at baseline. Researchers administered prazosin or placebo in escalating divided doses over five weeks to a daily maximum of 20 mg in men and 12 mg in women.
Primary Outcome Measures
The three primary outcome measures were change in score from baseline to 10 weeks on the CAPS item B2, change in score from baseline to 10 weeks on the Pittsburgh Sleep Quality Index, and the Clinical Global Impression of Change score at 10 weeks. None of the primary outcome measures significantly differed between the groups at 10 weeks. The groups’ outcome measures at 26 weeks and other secondary outcomes also were not significantly different.
The number of serious adverse events did not differ significantly by group. Of the adverse events, dizziness, lightheadedness, and urinary incontinence were significantly more common in the prazosin group, compared with the placebo group, whereas new or worsening suicidal ideation was significantly less common among participants who received prazosin, compared with patients who received placebo (8% vs 15%, respectively).
The investigators enrolled patients who were mainly in clinically stable condition, which may have led the trial to include patients whose distressing dreams were unlikely to respond to prazosin, Dr. Raskind and colleagues said.
Future Directions
“The failure of this new, large, multisite trial to replicate the previous studies is surprising and disappointing,” said Kerry J. Ressler, MD, PhD, Chief of the Division of Depression and Anxiety Disorders at McLean Hospital in Belmont, Massachusetts, and Professor of Psychiatry at Harvard Medical School in Boston, in an accompanying editorial. “PTSD remains a psychiatric malady that in some respects seems understandable and treatable on the basis of known neurobiologic pathways. Yet it is a complex syndrome with innumerable subtypes and variations…. There is a need to define clinical subtypes of PTSD on the basis of biologic markers.”
Studies of prazosin for the treatment of other conditions are under way. Investigators have initiated trials to examine whether prazosin reduces the frequency of chronic postconcussive headaches, compared with placebo.
—Jake Remaly
Suggested Reading
Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507-517.
Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003-1010.
Ressler KJ. Alpha-adrenergic receptors in PTSD - Failure or time for precision medicine? N Engl J Med. 2018; 378(6):575-576.
Among military veterans with chronic posttraumatic stress disorder (PTSD) and frequent nightmares, prazosin does not alleviate distressing dreams or improve sleep quality, according to trial results published in the February 8 issue of the New England Journal of Medicine.
Prior single-center trials found that prazosin, an alpha 1-adrenoreceptor antagonist, may alleviate nightmares associated with PTSD and improve overall clinical status. The present study’s eligibility criteria may have led to selection bias that contributed to its negative results, the researchers said.
The PACT Trial
To investigate the efficacy of prazosin in patients with chronic combat-related PTSD and frequent nightmares, Murray A. Raskind, MD, and colleagues conducted the Prazosin and Combat Trauma PTSD (PACT) trial. Dr. Raskind is the Director of the Veterans Affairs (VA) Northwest Network Mental Illness Research, Education, and Clinical Center and Professor and Vice Chair of Psychiatry and Behavioral Sciences at the University of Washington School of Medicine in Seattle.
The 26-week, double-blind, randomized, controlled trial included 304 veterans from 12 VA medical centers. Participants met DSM-IV criteria for PTSD; had a total score of at least 50 on the 17-item Clinician-Administered PTSD Scale (CAPS); had been exposed to one or more traumatic, life-threatening events in a war zone before the onset of recurrent nightmares; could recall combat-related nightmares; had a frequency score of at least 2 and a cumulative score of at least 5 on CAPS item B2 (ie, “recurrent distressing dreams”); and, for at least four weeks before randomization, were receiving a stable dose of nonexcluded medications or supportive psychotherapy. Exclusion criteria included unstable medical illness, a systolic blood pressure of less than 110 mm Hg in the supine position, active suicidal or homicidal ideation with plan or intent, and psychosocial instability.
Of 413 people screened, 304 underwent randomization (about 98% male; average age, 52); 152 patients were assigned to each treatment group. The two groups’ patient characteristics did not differ significantly at baseline. Researchers administered prazosin or placebo in escalating divided doses over five weeks to a daily maximum of 20 mg in men and 12 mg in women.
Primary Outcome Measures
The three primary outcome measures were change in score from baseline to 10 weeks on the CAPS item B2, change in score from baseline to 10 weeks on the Pittsburgh Sleep Quality Index, and the Clinical Global Impression of Change score at 10 weeks. None of the primary outcome measures significantly differed between the groups at 10 weeks. The groups’ outcome measures at 26 weeks and other secondary outcomes also were not significantly different.
The number of serious adverse events did not differ significantly by group. Of the adverse events, dizziness, lightheadedness, and urinary incontinence were significantly more common in the prazosin group, compared with the placebo group, whereas new or worsening suicidal ideation was significantly less common among participants who received prazosin, compared with patients who received placebo (8% vs 15%, respectively).
The investigators enrolled patients who were mainly in clinically stable condition, which may have led the trial to include patients whose distressing dreams were unlikely to respond to prazosin, Dr. Raskind and colleagues said.
Future Directions
“The failure of this new, large, multisite trial to replicate the previous studies is surprising and disappointing,” said Kerry J. Ressler, MD, PhD, Chief of the Division of Depression and Anxiety Disorders at McLean Hospital in Belmont, Massachusetts, and Professor of Psychiatry at Harvard Medical School in Boston, in an accompanying editorial. “PTSD remains a psychiatric malady that in some respects seems understandable and treatable on the basis of known neurobiologic pathways. Yet it is a complex syndrome with innumerable subtypes and variations…. There is a need to define clinical subtypes of PTSD on the basis of biologic markers.”
Studies of prazosin for the treatment of other conditions are under way. Investigators have initiated trials to examine whether prazosin reduces the frequency of chronic postconcussive headaches, compared with placebo.
—Jake Remaly
Suggested Reading
Raskind MA, Peskind ER, Chow B, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378(6):507-517.
Raskind MA, Peterson K, Williams T, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003-1010.
Ressler KJ. Alpha-adrenergic receptors in PTSD - Failure or time for precision medicine? N Engl J Med. 2018; 378(6):575-576.