User login
The better mammogram: Experts explore sensitivity of new modalities
PHILADELPHIA – Is it time to think about “the better mammogram” as the new standard of care? Can nuclear medicine provide a cost-effective workaround for imaging of women with dense breasts? According to two leading breast imaging researchers,
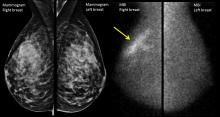
“Digital breast tomosynthesis is the new kid on the block for screening,” said Emily F. Conant, MD, professor of radiology and chief of breast imaging at the University of Pennsylvania, Philadelphia. “It’s becoming the new standard of care in mammography,” she said, speaking during a plenary session at the annual meeting of the North American Menopause Society.
Digital breast tomosynthesis (DBT) can involve simultaneous acquisition of a conventional 2D mammogram along with a series of images to create a 3D image. Another protocol, which delivers a lower radiation dose, produces a “synthetic” 2D reconstruction of 3D mammography.*
In addition to making visible tumors that otherwise might be obscured by the overlay of dense breast tissue, DBT can help reduce the recall rate, with the 3D images providing immediate clarification at the initial appointment. Studies show that the recall rate can go down by up to 31%, Dr. Conant said.
DBT has been shown to increase detection of invasive cancers, but it does not pick up more ductal carcinoma in situ, Dr. Conant said. This fact helps address the problem of overdiagnosis of small tumors that might regress. Overall, cancer detection is reported to increase by up to 53% with DBT, Dr. Conant said.
When primarily retrospective American studies are taken together with smaller prospective European studies, “the improvement in outcomes achieved with DBT directly addresses the major concerns regarding screening for breast cancer with mammography,” she said.
However, so far the studies have not offered DBT routinely to all comers. Since 2011, DBT has been offered to every woman screened at the University of Pennsylvania, at no additional cost. This created “a sort of natural experiment – there was no bias as to who got it.” Three consecutive years’ worth of outcomes have now been analyzed, Dr. Conant said.
Patient-level data from the University of Pennsylvania experience show statistically significant reductions in recall rate from diagnostic mammography alone. Also, researchers saw a steady increase in the rate of cancers detected per 1,000 patients, from 4.6 with digital mammography alone, to 6.1 by year three of DBT (JAMA Oncol. 2016 Jun 1;2[6]:737-43). This reflected the institutional learning curve with DBT, Dr. Conant said.
She said that the data also showed “a promising trend down in false negatives,” with an early reduction in cancers that were missed by DBT. Time is needed for mature cancer registry data to bear out these early trends, she added.
Other recent data show that DBT has promise to improve detection rates in a population of great interest – younger women, where there are often too many false positives and not enough cancers found, Dr. Conant said. If the risk-benefit ratio for DBT continues to play out as the data pile up, “I would strongly suggest that we should be doing screening in the 40s,” she said.
An important caveat, noted Dr. Conant, is that whether tomosynthesis is used or not, mammography captures anatomy, not physiology, and very dense breast tissue may still obscure a tumor, even when the tomographic slices are peeled back.
Though “DBT is ‘the better mammogram,’ additional outcome data are needed,” she said, including studies that compare modalities, include subgroup analyses, and better delineate the effect of cancer biology.
Molecular breast imaging
Another imaging modality uses nuclear medicine to capture the physiologic changes that accompany cancer. Molecular breast imaging (MBI), or scintimammography, can help “unveil the reservoir of hidden cancers in dense breasts,” said Deborah J. Rhodes, MD, professor of medicine at the Mayo Clinic, Rochester, Minn.
Dr. Rhodes – along with Michael O’Connor, PhD, Connie Hruska, PhD, Katie Hunt, MD, and Amy Conners, MD, her collaborators at the Mayo Clinic – uses a specialized array of gamma cameras to detect uptake of an injected radionuclide that’s preferentially avid for tumor tissue. This technique can unmask smaller tumors not seen on mammogram because it’s not impeded by having to “see” through dense breast tissue.
The radiation dose for an MBI study is a bit more than for DBT, but less than a coronary calcium score scan. The cost is about one-tenth that of breast magnetic resonance imaging (MRI), and interpretation is relatively straightforward, said Dr. Rhodes, who also presented data at the North American Menopause Society plenary.
“The traditional measure of mammography’s performance inflates its effectiveness,” especially in dense breast tissue, said Dr. Rhodes. “What is the sensitivity of mammography in the dense breast? It depends on what you measure it against.”
When cancers detected by MRI or MBI are added, the sensitivity of mammography drops from the 86.9% reported by the Breast Cancer Surveillance Consortium to 21%-31%, according to several published studies.
In one study, Dr. Rhodes and her Mayo colleagues found that the diagnostic yield per 1,000 patients with dense breasts by mammogram alone was 1.9 cancers. When MBI was added, that figure jumped to 8.8 cancers per 1,000 patients, an incremental gain of 363%.
“Tumor size matters profoundly,” she added. “If a tumor is detected above 2 cm, long-term survival drops below 50%.”
That contrasts with the better-than-80% long-term survival rate seen for those with sub-centimeter tumors, even in node-positive disease. “Only a third of tumors are detected when they are less than 1 cm” with regular screening mammography, Dr. Rhodes said.
However, in 2016 the U.S. Preventive Services Task Force concluded that the current evidence was insufficient to assess whether adjunctive screening for breast cancer using breast ultrasonography, MRI, DBT, or other methods should be used in women with dense breasts. The USPSTF noted that there weren’t studies that addressed the effect of supplemental screening on breast cancer morbidity or mortality.
The problem is that it can take 20 years or more to demonstrate mortality reduction, meaning that “no other imaging modality can compete” with mammography when this yardstick is used, Dr. Rhodes said. “This insistence on a mortality endpoint before we change practice” is impeding progress in screening, she said.
The American College of Obstetricians and Gynecologists “does not recommend adjunctive tests to screening mammography in women with dense breasts who are asymptomatic and have no additional risk factors.” However, the organization “strongly supports additional research to identify more effective screening methods” that will improve outcomes and minimize false positives in women with dense breasts.
Though DBT is becoming more widely available, MBI is still primarily used in research centers. Both Dr. Conant and Dr. Rhodes acknowledged that since these techniques are not required to be covered by insurance, payment – and patient access – may vary. Both physicians said their home institutions have worked hard to keep costs down for their studies.
Dr. Conant is consultant or advisory board member for Hologic. Dr. Rhodes reported having no conflicts of interest.
*Correction, 11/15/2017: An earlier version of this story misstated the synthetic mammography protocol.
[email protected]
On Twitter @karioakes
PHILADELPHIA – Is it time to think about “the better mammogram” as the new standard of care? Can nuclear medicine provide a cost-effective workaround for imaging of women with dense breasts? According to two leading breast imaging researchers,
“Digital breast tomosynthesis is the new kid on the block for screening,” said Emily F. Conant, MD, professor of radiology and chief of breast imaging at the University of Pennsylvania, Philadelphia. “It’s becoming the new standard of care in mammography,” she said, speaking during a plenary session at the annual meeting of the North American Menopause Society.
Digital breast tomosynthesis (DBT) can involve simultaneous acquisition of a conventional 2D mammogram along with a series of images to create a 3D image. Another protocol, which delivers a lower radiation dose, produces a “synthetic” 2D reconstruction of 3D mammography.*
In addition to making visible tumors that otherwise might be obscured by the overlay of dense breast tissue, DBT can help reduce the recall rate, with the 3D images providing immediate clarification at the initial appointment. Studies show that the recall rate can go down by up to 31%, Dr. Conant said.
DBT has been shown to increase detection of invasive cancers, but it does not pick up more ductal carcinoma in situ, Dr. Conant said. This fact helps address the problem of overdiagnosis of small tumors that might regress. Overall, cancer detection is reported to increase by up to 53% with DBT, Dr. Conant said.
When primarily retrospective American studies are taken together with smaller prospective European studies, “the improvement in outcomes achieved with DBT directly addresses the major concerns regarding screening for breast cancer with mammography,” she said.
However, so far the studies have not offered DBT routinely to all comers. Since 2011, DBT has been offered to every woman screened at the University of Pennsylvania, at no additional cost. This created “a sort of natural experiment – there was no bias as to who got it.” Three consecutive years’ worth of outcomes have now been analyzed, Dr. Conant said.
Patient-level data from the University of Pennsylvania experience show statistically significant reductions in recall rate from diagnostic mammography alone. Also, researchers saw a steady increase in the rate of cancers detected per 1,000 patients, from 4.6 with digital mammography alone, to 6.1 by year three of DBT (JAMA Oncol. 2016 Jun 1;2[6]:737-43). This reflected the institutional learning curve with DBT, Dr. Conant said.
She said that the data also showed “a promising trend down in false negatives,” with an early reduction in cancers that were missed by DBT. Time is needed for mature cancer registry data to bear out these early trends, she added.
Other recent data show that DBT has promise to improve detection rates in a population of great interest – younger women, where there are often too many false positives and not enough cancers found, Dr. Conant said. If the risk-benefit ratio for DBT continues to play out as the data pile up, “I would strongly suggest that we should be doing screening in the 40s,” she said.
An important caveat, noted Dr. Conant, is that whether tomosynthesis is used or not, mammography captures anatomy, not physiology, and very dense breast tissue may still obscure a tumor, even when the tomographic slices are peeled back.
Though “DBT is ‘the better mammogram,’ additional outcome data are needed,” she said, including studies that compare modalities, include subgroup analyses, and better delineate the effect of cancer biology.
Molecular breast imaging
Another imaging modality uses nuclear medicine to capture the physiologic changes that accompany cancer. Molecular breast imaging (MBI), or scintimammography, can help “unveil the reservoir of hidden cancers in dense breasts,” said Deborah J. Rhodes, MD, professor of medicine at the Mayo Clinic, Rochester, Minn.
Dr. Rhodes – along with Michael O’Connor, PhD, Connie Hruska, PhD, Katie Hunt, MD, and Amy Conners, MD, her collaborators at the Mayo Clinic – uses a specialized array of gamma cameras to detect uptake of an injected radionuclide that’s preferentially avid for tumor tissue. This technique can unmask smaller tumors not seen on mammogram because it’s not impeded by having to “see” through dense breast tissue.
The radiation dose for an MBI study is a bit more than for DBT, but less than a coronary calcium score scan. The cost is about one-tenth that of breast magnetic resonance imaging (MRI), and interpretation is relatively straightforward, said Dr. Rhodes, who also presented data at the North American Menopause Society plenary.
“The traditional measure of mammography’s performance inflates its effectiveness,” especially in dense breast tissue, said Dr. Rhodes. “What is the sensitivity of mammography in the dense breast? It depends on what you measure it against.”
When cancers detected by MRI or MBI are added, the sensitivity of mammography drops from the 86.9% reported by the Breast Cancer Surveillance Consortium to 21%-31%, according to several published studies.
In one study, Dr. Rhodes and her Mayo colleagues found that the diagnostic yield per 1,000 patients with dense breasts by mammogram alone was 1.9 cancers. When MBI was added, that figure jumped to 8.8 cancers per 1,000 patients, an incremental gain of 363%.
“Tumor size matters profoundly,” she added. “If a tumor is detected above 2 cm, long-term survival drops below 50%.”
That contrasts with the better-than-80% long-term survival rate seen for those with sub-centimeter tumors, even in node-positive disease. “Only a third of tumors are detected when they are less than 1 cm” with regular screening mammography, Dr. Rhodes said.
However, in 2016 the U.S. Preventive Services Task Force concluded that the current evidence was insufficient to assess whether adjunctive screening for breast cancer using breast ultrasonography, MRI, DBT, or other methods should be used in women with dense breasts. The USPSTF noted that there weren’t studies that addressed the effect of supplemental screening on breast cancer morbidity or mortality.
The problem is that it can take 20 years or more to demonstrate mortality reduction, meaning that “no other imaging modality can compete” with mammography when this yardstick is used, Dr. Rhodes said. “This insistence on a mortality endpoint before we change practice” is impeding progress in screening, she said.
The American College of Obstetricians and Gynecologists “does not recommend adjunctive tests to screening mammography in women with dense breasts who are asymptomatic and have no additional risk factors.” However, the organization “strongly supports additional research to identify more effective screening methods” that will improve outcomes and minimize false positives in women with dense breasts.
Though DBT is becoming more widely available, MBI is still primarily used in research centers. Both Dr. Conant and Dr. Rhodes acknowledged that since these techniques are not required to be covered by insurance, payment – and patient access – may vary. Both physicians said their home institutions have worked hard to keep costs down for their studies.
Dr. Conant is consultant or advisory board member for Hologic. Dr. Rhodes reported having no conflicts of interest.
*Correction, 11/15/2017: An earlier version of this story misstated the synthetic mammography protocol.
[email protected]
On Twitter @karioakes
PHILADELPHIA – Is it time to think about “the better mammogram” as the new standard of care? Can nuclear medicine provide a cost-effective workaround for imaging of women with dense breasts? According to two leading breast imaging researchers,
“Digital breast tomosynthesis is the new kid on the block for screening,” said Emily F. Conant, MD, professor of radiology and chief of breast imaging at the University of Pennsylvania, Philadelphia. “It’s becoming the new standard of care in mammography,” she said, speaking during a plenary session at the annual meeting of the North American Menopause Society.
Digital breast tomosynthesis (DBT) can involve simultaneous acquisition of a conventional 2D mammogram along with a series of images to create a 3D image. Another protocol, which delivers a lower radiation dose, produces a “synthetic” 2D reconstruction of 3D mammography.*
In addition to making visible tumors that otherwise might be obscured by the overlay of dense breast tissue, DBT can help reduce the recall rate, with the 3D images providing immediate clarification at the initial appointment. Studies show that the recall rate can go down by up to 31%, Dr. Conant said.
DBT has been shown to increase detection of invasive cancers, but it does not pick up more ductal carcinoma in situ, Dr. Conant said. This fact helps address the problem of overdiagnosis of small tumors that might regress. Overall, cancer detection is reported to increase by up to 53% with DBT, Dr. Conant said.
When primarily retrospective American studies are taken together with smaller prospective European studies, “the improvement in outcomes achieved with DBT directly addresses the major concerns regarding screening for breast cancer with mammography,” she said.
However, so far the studies have not offered DBT routinely to all comers. Since 2011, DBT has been offered to every woman screened at the University of Pennsylvania, at no additional cost. This created “a sort of natural experiment – there was no bias as to who got it.” Three consecutive years’ worth of outcomes have now been analyzed, Dr. Conant said.
Patient-level data from the University of Pennsylvania experience show statistically significant reductions in recall rate from diagnostic mammography alone. Also, researchers saw a steady increase in the rate of cancers detected per 1,000 patients, from 4.6 with digital mammography alone, to 6.1 by year three of DBT (JAMA Oncol. 2016 Jun 1;2[6]:737-43). This reflected the institutional learning curve with DBT, Dr. Conant said.
She said that the data also showed “a promising trend down in false negatives,” with an early reduction in cancers that were missed by DBT. Time is needed for mature cancer registry data to bear out these early trends, she added.
Other recent data show that DBT has promise to improve detection rates in a population of great interest – younger women, where there are often too many false positives and not enough cancers found, Dr. Conant said. If the risk-benefit ratio for DBT continues to play out as the data pile up, “I would strongly suggest that we should be doing screening in the 40s,” she said.
An important caveat, noted Dr. Conant, is that whether tomosynthesis is used or not, mammography captures anatomy, not physiology, and very dense breast tissue may still obscure a tumor, even when the tomographic slices are peeled back.
Though “DBT is ‘the better mammogram,’ additional outcome data are needed,” she said, including studies that compare modalities, include subgroup analyses, and better delineate the effect of cancer biology.
Molecular breast imaging
Another imaging modality uses nuclear medicine to capture the physiologic changes that accompany cancer. Molecular breast imaging (MBI), or scintimammography, can help “unveil the reservoir of hidden cancers in dense breasts,” said Deborah J. Rhodes, MD, professor of medicine at the Mayo Clinic, Rochester, Minn.
Dr. Rhodes – along with Michael O’Connor, PhD, Connie Hruska, PhD, Katie Hunt, MD, and Amy Conners, MD, her collaborators at the Mayo Clinic – uses a specialized array of gamma cameras to detect uptake of an injected radionuclide that’s preferentially avid for tumor tissue. This technique can unmask smaller tumors not seen on mammogram because it’s not impeded by having to “see” through dense breast tissue.
The radiation dose for an MBI study is a bit more than for DBT, but less than a coronary calcium score scan. The cost is about one-tenth that of breast magnetic resonance imaging (MRI), and interpretation is relatively straightforward, said Dr. Rhodes, who also presented data at the North American Menopause Society plenary.
“The traditional measure of mammography’s performance inflates its effectiveness,” especially in dense breast tissue, said Dr. Rhodes. “What is the sensitivity of mammography in the dense breast? It depends on what you measure it against.”
When cancers detected by MRI or MBI are added, the sensitivity of mammography drops from the 86.9% reported by the Breast Cancer Surveillance Consortium to 21%-31%, according to several published studies.
In one study, Dr. Rhodes and her Mayo colleagues found that the diagnostic yield per 1,000 patients with dense breasts by mammogram alone was 1.9 cancers. When MBI was added, that figure jumped to 8.8 cancers per 1,000 patients, an incremental gain of 363%.
“Tumor size matters profoundly,” she added. “If a tumor is detected above 2 cm, long-term survival drops below 50%.”
That contrasts with the better-than-80% long-term survival rate seen for those with sub-centimeter tumors, even in node-positive disease. “Only a third of tumors are detected when they are less than 1 cm” with regular screening mammography, Dr. Rhodes said.
However, in 2016 the U.S. Preventive Services Task Force concluded that the current evidence was insufficient to assess whether adjunctive screening for breast cancer using breast ultrasonography, MRI, DBT, or other methods should be used in women with dense breasts. The USPSTF noted that there weren’t studies that addressed the effect of supplemental screening on breast cancer morbidity or mortality.
The problem is that it can take 20 years or more to demonstrate mortality reduction, meaning that “no other imaging modality can compete” with mammography when this yardstick is used, Dr. Rhodes said. “This insistence on a mortality endpoint before we change practice” is impeding progress in screening, she said.
The American College of Obstetricians and Gynecologists “does not recommend adjunctive tests to screening mammography in women with dense breasts who are asymptomatic and have no additional risk factors.” However, the organization “strongly supports additional research to identify more effective screening methods” that will improve outcomes and minimize false positives in women with dense breasts.
Though DBT is becoming more widely available, MBI is still primarily used in research centers. Both Dr. Conant and Dr. Rhodes acknowledged that since these techniques are not required to be covered by insurance, payment – and patient access – may vary. Both physicians said their home institutions have worked hard to keep costs down for their studies.
Dr. Conant is consultant or advisory board member for Hologic. Dr. Rhodes reported having no conflicts of interest.
*Correction, 11/15/2017: An earlier version of this story misstated the synthetic mammography protocol.
[email protected]
On Twitter @karioakes
EXPERT ANALYSIS FROM NAMS 2017
Statin didn’t slow hepatic steatosis in HIV patients
SAN DIEGO – Statin therapy wasn’t effective against a rising rate of hepatic steatosis in HIV patients, and may increase nonalcoholic fatty liver disease (NAFLD) risk, according to a small study.
The findings are contrary to the limited data currently available, which suggest statins can have a beneficial effect on hepatic steatosis, according to the study’s investigators.
NAFLD is one of the leading causes of mortality and morbidity in people living with HIV, said Vanessa El Kamari, MD, of Case Western Reserve University, Cleveland, and rates are continuing to increase. With a lack of therapeutic interventions for NAFLD in patients with HIV, finding effective treatments is a major concern for providers.
Dr. El Kamari and her colleagues conducted a secondary analysis of the SATURN-HIV trial, a randomized, placebo-controlled trial of 147 patients with HIV who were on stable antiretroviral therapy (ART) with LDL cholesterol levels at or below 130 mg/dL. Patients were either treated with 10 mg rosuvastatin or placebo.
Patients in the treatment and placebo arms were an average age of 45 years, most patients were male (81% and 76%, respectively), and a majority was African American (69% and 67%, respectively). The two groups reported average CD4+ counts of 644 and 636, respectively.
Investigators used validated scores to determine hepatic steatosis in patients, although researchers acknowledged that liver biopsy is the gold standard for hepatic steatosis measurement.
“We understand liver fat score has its limitation,” said Dr. El Kamari in a question and answer session following the presentation at an annual scientific meeting on infectious diseases. “Further studies are needed in this area in order to detect, in noninvasive ways, hepatic steatosis.”
Liver fat scores (LFS) were measured on entry, at week 48, and week 96.
After 96 weeks, investigators saw significant increases in LFS in both the placebo and rosuvastatin groups (P = .01 and P less than .01, respectively). Progression from nonsteatosis at baseline to steatosis over 96 weeks was greater in patients given rosuvastatin than in those given placebo (odds ratio, 4.3; P = .03).
Studying predictors for LFS changes, a trend toward insignificance among the randomization group led investigators to the conclusion that statin may have negatively affected the liver fat score of patients over the 96-week time period.
The study researchers identified 92 patients who did not have hepatic steatosis at baseline to study how statins influenced the development of hepatic steatosis.
Of the 13 patients who developed steatosis during the trial period, 10 were part of the rosuvastatin group, while only 3 were from the placebo group.
Increases in LFS were associated with increases in insulin resistance, detected presence of HIV-1 RNA, and higher interferon-inducible proteins, according to Dr. El Kamari.
While increased homeostatic assessment of insulin resistance was associated with increased hepatic homeostasis, Dr. El Kamari was not able to determine if statins that are not associated with insulin resistance will have different outcomes.
The investigators cautioned that the findings may not be generalizable to the entire HIV population due to the overwhelming majority of African American patients with increased inflammation, as well as the study patients’ LDL cholesterol levels of less than or equal to 130 mg/dL.
The National Institutes of Health funded the study. Dr. El Kamari had no disclosures.
[email protected]
On Twitter @eaztweets
SAN DIEGO – Statin therapy wasn’t effective against a rising rate of hepatic steatosis in HIV patients, and may increase nonalcoholic fatty liver disease (NAFLD) risk, according to a small study.
The findings are contrary to the limited data currently available, which suggest statins can have a beneficial effect on hepatic steatosis, according to the study’s investigators.
NAFLD is one of the leading causes of mortality and morbidity in people living with HIV, said Vanessa El Kamari, MD, of Case Western Reserve University, Cleveland, and rates are continuing to increase. With a lack of therapeutic interventions for NAFLD in patients with HIV, finding effective treatments is a major concern for providers.
Dr. El Kamari and her colleagues conducted a secondary analysis of the SATURN-HIV trial, a randomized, placebo-controlled trial of 147 patients with HIV who were on stable antiretroviral therapy (ART) with LDL cholesterol levels at or below 130 mg/dL. Patients were either treated with 10 mg rosuvastatin or placebo.
Patients in the treatment and placebo arms were an average age of 45 years, most patients were male (81% and 76%, respectively), and a majority was African American (69% and 67%, respectively). The two groups reported average CD4+ counts of 644 and 636, respectively.
Investigators used validated scores to determine hepatic steatosis in patients, although researchers acknowledged that liver biopsy is the gold standard for hepatic steatosis measurement.
“We understand liver fat score has its limitation,” said Dr. El Kamari in a question and answer session following the presentation at an annual scientific meeting on infectious diseases. “Further studies are needed in this area in order to detect, in noninvasive ways, hepatic steatosis.”
Liver fat scores (LFS) were measured on entry, at week 48, and week 96.
After 96 weeks, investigators saw significant increases in LFS in both the placebo and rosuvastatin groups (P = .01 and P less than .01, respectively). Progression from nonsteatosis at baseline to steatosis over 96 weeks was greater in patients given rosuvastatin than in those given placebo (odds ratio, 4.3; P = .03).
Studying predictors for LFS changes, a trend toward insignificance among the randomization group led investigators to the conclusion that statin may have negatively affected the liver fat score of patients over the 96-week time period.
The study researchers identified 92 patients who did not have hepatic steatosis at baseline to study how statins influenced the development of hepatic steatosis.
Of the 13 patients who developed steatosis during the trial period, 10 were part of the rosuvastatin group, while only 3 were from the placebo group.
Increases in LFS were associated with increases in insulin resistance, detected presence of HIV-1 RNA, and higher interferon-inducible proteins, according to Dr. El Kamari.
While increased homeostatic assessment of insulin resistance was associated with increased hepatic homeostasis, Dr. El Kamari was not able to determine if statins that are not associated with insulin resistance will have different outcomes.
The investigators cautioned that the findings may not be generalizable to the entire HIV population due to the overwhelming majority of African American patients with increased inflammation, as well as the study patients’ LDL cholesterol levels of less than or equal to 130 mg/dL.
The National Institutes of Health funded the study. Dr. El Kamari had no disclosures.
[email protected]
On Twitter @eaztweets
SAN DIEGO – Statin therapy wasn’t effective against a rising rate of hepatic steatosis in HIV patients, and may increase nonalcoholic fatty liver disease (NAFLD) risk, according to a small study.
The findings are contrary to the limited data currently available, which suggest statins can have a beneficial effect on hepatic steatosis, according to the study’s investigators.
NAFLD is one of the leading causes of mortality and morbidity in people living with HIV, said Vanessa El Kamari, MD, of Case Western Reserve University, Cleveland, and rates are continuing to increase. With a lack of therapeutic interventions for NAFLD in patients with HIV, finding effective treatments is a major concern for providers.
Dr. El Kamari and her colleagues conducted a secondary analysis of the SATURN-HIV trial, a randomized, placebo-controlled trial of 147 patients with HIV who were on stable antiretroviral therapy (ART) with LDL cholesterol levels at or below 130 mg/dL. Patients were either treated with 10 mg rosuvastatin or placebo.
Patients in the treatment and placebo arms were an average age of 45 years, most patients were male (81% and 76%, respectively), and a majority was African American (69% and 67%, respectively). The two groups reported average CD4+ counts of 644 and 636, respectively.
Investigators used validated scores to determine hepatic steatosis in patients, although researchers acknowledged that liver biopsy is the gold standard for hepatic steatosis measurement.
“We understand liver fat score has its limitation,” said Dr. El Kamari in a question and answer session following the presentation at an annual scientific meeting on infectious diseases. “Further studies are needed in this area in order to detect, in noninvasive ways, hepatic steatosis.”
Liver fat scores (LFS) were measured on entry, at week 48, and week 96.
After 96 weeks, investigators saw significant increases in LFS in both the placebo and rosuvastatin groups (P = .01 and P less than .01, respectively). Progression from nonsteatosis at baseline to steatosis over 96 weeks was greater in patients given rosuvastatin than in those given placebo (odds ratio, 4.3; P = .03).
Studying predictors for LFS changes, a trend toward insignificance among the randomization group led investigators to the conclusion that statin may have negatively affected the liver fat score of patients over the 96-week time period.
The study researchers identified 92 patients who did not have hepatic steatosis at baseline to study how statins influenced the development of hepatic steatosis.
Of the 13 patients who developed steatosis during the trial period, 10 were part of the rosuvastatin group, while only 3 were from the placebo group.
Increases in LFS were associated with increases in insulin resistance, detected presence of HIV-1 RNA, and higher interferon-inducible proteins, according to Dr. El Kamari.
While increased homeostatic assessment of insulin resistance was associated with increased hepatic homeostasis, Dr. El Kamari was not able to determine if statins that are not associated with insulin resistance will have different outcomes.
The investigators cautioned that the findings may not be generalizable to the entire HIV population due to the overwhelming majority of African American patients with increased inflammation, as well as the study patients’ LDL cholesterol levels of less than or equal to 130 mg/dL.
The National Institutes of Health funded the study. Dr. El Kamari had no disclosures.
[email protected]
On Twitter @eaztweets
AT IDWEEK 2017
Key clinical point:
Major finding: Progression from nonsteatosis at baseline to steatosis over 96 weeks was greater in patients given rosuvastatin than in those given placebo (odds ratio, 4.3; P = .03).
Data source: A randomized, placebo-controlled study of 147 patients with HIV on stable ART.
Disclosures: The National Institutes of Health funded the study. Dr. El Kamari had no disclosures.
Large database analysis suggests safety of bariatric surgery in seniors
NATIONAL HARBOR, MD. – despite a slight increase in unadjusted mortality rates, according to an analysis of data from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP).
Based on data that was collected in 2015 and submitted to MBSAQIP, “bariatric surgery is safe in the elderly, even in those 70 years old and older,” reported Tallal Zeni, MD, director of the Michigan Bariatric Institute in Livonia.
There were 16,568 patients older than age 60 years entered into the MBSAQIP database in 2015. When those were compared with the 117,443 younger patients, the unadjusted rates of morbidity (6.5% vs. 6.0%) and mortality (0.3% vs. 0.1%) were higher for the older patients, but “they are close,” according to Dr. Zeni. Both rates reached significance by the conventional definition (P < .05), but he suggested that they are lower in this study than those in prior studies of MBSAQIP datasets and that they are acceptable relative to the anticipated health benefits.
Above the age of 60 years, no correlation could be made between increasing age and increasing risk of morbidity, mortality, or rate of reoperations, according to Dr. Zeni.
Why should bariatric surgery be considered in older patients? He cited data from a study that showed the life expectancy in a 70-year-old without functional limitations is 13 years. As a result, he added, “it behooves us to provide them with the best quality of life we can.”
Relative to prior MBSAQIP evaluations of bariatric surgery in the elderly, the proportion of patients undergoing sleeve gastrectomy relative to gastric bypass has been increasing, Dr. Zeni reported. In the analysis, approximately two-thirds of the bariatric procedures were performed with sleeve gastrectomy, which is higher relative to what previous MBSAQIP analyses have shown.
Based on rates of morbidity for those two surgical approaches in the analysis, that trend makes sense. While the higher 30-day mortality for gastric bypass, compared with sleeve gastrectomy, was not significant (0.38% vs. 0.26%; P = .221), all-cause morbidity was almost two times greater for those undergoing gastric bypass than it was for those undergoing sleeve gastrectomy (10.61% vs. 5.81%; P < .001), Dr. Zeni reported.
However, some of that difference may be explained by baseline disparities between the two groups. In the gastric bypass group, there were higher rates of preoperative diabetes (54% vs. 40%; P < .001), sleep apnea (57% vs. 50%; P < .001) and hyperlipidemia (59% vs. 54%; P < .001). Also, gastric bypass patients were more likely to have a history of a previous bariatric procedure (11% vs. 8.5%; P < .001) and to be in the American Society of Anesthesiologists Physical Status score of 3 (84% vs. 80%; P < .001), according to Dr. Zeni.
The specific complications more common in the gastric bypass group than the sleeve gastrectomy group included anastomotic leak (0.56% vs. 0.3%; P = .017), surgical site infection (1.74% vs. 0.61%; P < .001), pneumonia (0.87% vs. 0.32%; P < .001), and bleeding (1.14% vs. 0.5%; P = .024). Although the average operating time was 40 minutes longer in the bypass group, there were no significant differences in thromboembolic complications.
Overall, despite a modest increase in the risk of complications for bariatric surgery in elderly patients, that risk can be considered acceptable in relation to the potential health benefits, according to Dr. Zeni. He suggested that the data might encourage further growth in the rates of bariatric procedures among patients older than 60 years.
Dr. Zeni reports no relevant financial relationships.
NATIONAL HARBOR, MD. – despite a slight increase in unadjusted mortality rates, according to an analysis of data from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP).
Based on data that was collected in 2015 and submitted to MBSAQIP, “bariatric surgery is safe in the elderly, even in those 70 years old and older,” reported Tallal Zeni, MD, director of the Michigan Bariatric Institute in Livonia.
There were 16,568 patients older than age 60 years entered into the MBSAQIP database in 2015. When those were compared with the 117,443 younger patients, the unadjusted rates of morbidity (6.5% vs. 6.0%) and mortality (0.3% vs. 0.1%) were higher for the older patients, but “they are close,” according to Dr. Zeni. Both rates reached significance by the conventional definition (P < .05), but he suggested that they are lower in this study than those in prior studies of MBSAQIP datasets and that they are acceptable relative to the anticipated health benefits.
Above the age of 60 years, no correlation could be made between increasing age and increasing risk of morbidity, mortality, or rate of reoperations, according to Dr. Zeni.
Why should bariatric surgery be considered in older patients? He cited data from a study that showed the life expectancy in a 70-year-old without functional limitations is 13 years. As a result, he added, “it behooves us to provide them with the best quality of life we can.”
Relative to prior MBSAQIP evaluations of bariatric surgery in the elderly, the proportion of patients undergoing sleeve gastrectomy relative to gastric bypass has been increasing, Dr. Zeni reported. In the analysis, approximately two-thirds of the bariatric procedures were performed with sleeve gastrectomy, which is higher relative to what previous MBSAQIP analyses have shown.
Based on rates of morbidity for those two surgical approaches in the analysis, that trend makes sense. While the higher 30-day mortality for gastric bypass, compared with sleeve gastrectomy, was not significant (0.38% vs. 0.26%; P = .221), all-cause morbidity was almost two times greater for those undergoing gastric bypass than it was for those undergoing sleeve gastrectomy (10.61% vs. 5.81%; P < .001), Dr. Zeni reported.
However, some of that difference may be explained by baseline disparities between the two groups. In the gastric bypass group, there were higher rates of preoperative diabetes (54% vs. 40%; P < .001), sleep apnea (57% vs. 50%; P < .001) and hyperlipidemia (59% vs. 54%; P < .001). Also, gastric bypass patients were more likely to have a history of a previous bariatric procedure (11% vs. 8.5%; P < .001) and to be in the American Society of Anesthesiologists Physical Status score of 3 (84% vs. 80%; P < .001), according to Dr. Zeni.
The specific complications more common in the gastric bypass group than the sleeve gastrectomy group included anastomotic leak (0.56% vs. 0.3%; P = .017), surgical site infection (1.74% vs. 0.61%; P < .001), pneumonia (0.87% vs. 0.32%; P < .001), and bleeding (1.14% vs. 0.5%; P = .024). Although the average operating time was 40 minutes longer in the bypass group, there were no significant differences in thromboembolic complications.
Overall, despite a modest increase in the risk of complications for bariatric surgery in elderly patients, that risk can be considered acceptable in relation to the potential health benefits, according to Dr. Zeni. He suggested that the data might encourage further growth in the rates of bariatric procedures among patients older than 60 years.
Dr. Zeni reports no relevant financial relationships.
NATIONAL HARBOR, MD. – despite a slight increase in unadjusted mortality rates, according to an analysis of data from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP).
Based on data that was collected in 2015 and submitted to MBSAQIP, “bariatric surgery is safe in the elderly, even in those 70 years old and older,” reported Tallal Zeni, MD, director of the Michigan Bariatric Institute in Livonia.
There were 16,568 patients older than age 60 years entered into the MBSAQIP database in 2015. When those were compared with the 117,443 younger patients, the unadjusted rates of morbidity (6.5% vs. 6.0%) and mortality (0.3% vs. 0.1%) were higher for the older patients, but “they are close,” according to Dr. Zeni. Both rates reached significance by the conventional definition (P < .05), but he suggested that they are lower in this study than those in prior studies of MBSAQIP datasets and that they are acceptable relative to the anticipated health benefits.
Above the age of 60 years, no correlation could be made between increasing age and increasing risk of morbidity, mortality, or rate of reoperations, according to Dr. Zeni.
Why should bariatric surgery be considered in older patients? He cited data from a study that showed the life expectancy in a 70-year-old without functional limitations is 13 years. As a result, he added, “it behooves us to provide them with the best quality of life we can.”
Relative to prior MBSAQIP evaluations of bariatric surgery in the elderly, the proportion of patients undergoing sleeve gastrectomy relative to gastric bypass has been increasing, Dr. Zeni reported. In the analysis, approximately two-thirds of the bariatric procedures were performed with sleeve gastrectomy, which is higher relative to what previous MBSAQIP analyses have shown.
Based on rates of morbidity for those two surgical approaches in the analysis, that trend makes sense. While the higher 30-day mortality for gastric bypass, compared with sleeve gastrectomy, was not significant (0.38% vs. 0.26%; P = .221), all-cause morbidity was almost two times greater for those undergoing gastric bypass than it was for those undergoing sleeve gastrectomy (10.61% vs. 5.81%; P < .001), Dr. Zeni reported.
However, some of that difference may be explained by baseline disparities between the two groups. In the gastric bypass group, there were higher rates of preoperative diabetes (54% vs. 40%; P < .001), sleep apnea (57% vs. 50%; P < .001) and hyperlipidemia (59% vs. 54%; P < .001). Also, gastric bypass patients were more likely to have a history of a previous bariatric procedure (11% vs. 8.5%; P < .001) and to be in the American Society of Anesthesiologists Physical Status score of 3 (84% vs. 80%; P < .001), according to Dr. Zeni.
The specific complications more common in the gastric bypass group than the sleeve gastrectomy group included anastomotic leak (0.56% vs. 0.3%; P = .017), surgical site infection (1.74% vs. 0.61%; P < .001), pneumonia (0.87% vs. 0.32%; P < .001), and bleeding (1.14% vs. 0.5%; P = .024). Although the average operating time was 40 minutes longer in the bypass group, there were no significant differences in thromboembolic complications.
Overall, despite a modest increase in the risk of complications for bariatric surgery in elderly patients, that risk can be considered acceptable in relation to the potential health benefits, according to Dr. Zeni. He suggested that the data might encourage further growth in the rates of bariatric procedures among patients older than 60 years.
Dr. Zeni reports no relevant financial relationships.
AT OBESITY WEEK 2017
Key clinical point: Based on mortality and morbidity rates, bariatric surgery is acceptably safe in patients older than 60 years of age.
Major finding: Compared with patients younger than 60 years, older patients had only modestly increased rates of morbidity (6.5% vs. 6.0%) and mortality (0.3% vs. 0.1%).
Data source: A retrospective database analysis.
Disclosures: Dr. Zeni reports no relevant financial relationships.
Targeting PCSK9 inhibitors to reap most benefit
ANAHEIM, CALIF. – Patients with symptomatic peripheral artery disease or a high-risk history of MI got the biggest bang for the buck from aggressive LDL cholesterol lowering with evolocumab in two new prespecified subgroup analyses from the landmark FOURIER trial presented at the American Heart Association scientific sessions.
“At the end of the day, not all of our patients with ASCVD [atherosclerotic cardiovascular disease] can have these expensive medications. These subgroup analyses will help clinicians to target use of PCSK9 inhibitors to the patients who will benefit the most,” Lynne T. Braun, PhD, commented in her role as discussant of the two secondary analyses, presented back to back in a late-breaking science session. Dr. Braun is a professor in the department of internal medicine at Rush University, Chicago.
The FOURIER trial included 27,564 high-risk patients with prior MI, stroke, and/or symptomatic peripheral arterial disease (PAD) who had an LDL cholesterol level of 70 mg/dL or more on high- or moderate-intensity statin therapy. They were randomized in double-blind fashion to add-on subcutaneous evolocumab (Repatha) at either 140 mg every 2 weeks or 420 mg/month or to placebo, for a median of 2.5 years of follow-up. The evolocumab group experienced a 59% reduction in LDL cholesterol, compared with the controls on background statin therapy plus placebo, down to a mean LDL cholesterol level of just 30 mg/dL.
As previously reported, the risk of the primary composite endpoint – comprising cardiovascular death, MI, stroke, unstable angina, or coronary revascularization – was reduced by 15% in the evolocumab group at 3 years. The secondary endpoint of cardiovascular death, MI, or stroke was reduced by 20%, from 9.9% to 7.9% (N Engl J Med. 2017;376:1713-22).
Evolocumab tamed PAD
At the AHA scientific sessions, Marc P. Bonaca, MD, presented a secondary analysis restricted to the 3,642 FOURIER participants with symptomatic PAD. The goal was to answer two unresolved questions: Does LDL cholesterol lowering beyond what’s achievable with a statin further reduce PAD patients’ cardiovascular risk? And does it reduce their risk of major adverse leg events (MALE), defined as a composite of acute limb ischemia, major amputation, and urgent revascularization?
The rate of the composite endpoint comprising cardiovascular death, MI, or stroke was 13% over 3 years in PAD patients randomized to placebo, which was 81% greater than the 7.6% rate in placebo-treated participants with a baseline history of stroke or MI but no PAD, in an analysis adjusted for demographics, cardiovascular risk factors, kidney function, body mass index, and prior revascularization.
The event rate was even higher in patients with PAD plus a history of MI or stroke, at 14.9%. Evolocumab reduced that risk by 27%, compared with placebo in patients with PAD, for an absolute risk reduction of 3.5% and a number-needed-to-treat (NNT) of 29 for 2.5 years.
The benefit of evolocumab was even more pronounced in the subgroup of 1,505 patients with baseline PAD but no prior MI or stroke: a 43% relative risk reduction, from 10.3% to 5.5%, for an absolute risk reduction of 4.8% and a NNT of 21.
A linear relationship was seen between the MALE rate during follow-up and LDL cholesterol level after 1 month of therapy, down to an LDL cholesterol level of less than 10 mg/dL. The clinically relevant composite endpoint of MACE (major adverse cardiovascular events – a composite of cardiovascular death, MI, and stroke) or MALE in patients with baseline PAD but no history of MI or stroke occurred in 12.8% of controls and 6.5% of the evolocumab group. This translated to a 48% relative risk reduction, a 6.3% absolute risk reduction, and a NNT of 16. The event curves in the evolocumab and control arms separated quite early, within the first 90 days of treatment.
The take home message: “LDL reduction to very low levels should be considered in patients with PAD, regardless of their history of MI or stroke, to reduce the risk of MACE [major adverse cardiovascular event] and MALE,” declared Dr. Bonaca of Brigham and Women’s Hospital and Harvard Medical School, both in Boston.
Spotting the patients with a history of MI who’re at highest risk
Marc S. Sabatine, MD, presented the subanalysis involving the 22,351 FOURIER patients with a prior MI. He and his coinvestigators identified three high-risk features within this group: an MI within the past 2 years, a history of two or more MIs, and residual multivessel CAD. Each of these three features was individually associated with a 34%-90% increased risk of MACE during follow-up. All told, 63% of FOURIER participants with prior MI had one or more of the high-risk features.
The use of evolocumab in patients with at least one of the three high-risk features was associated with a 22% relative risk reduction and an absolute 2.5% risk reduction, compared with placebo. The event curves diverged at about 6 months, and the gap between them steadily widened during follow-up. Extrapolating from this pattern, it’s likely that evolocumab would achieve an absolute 5% risk reduction in MACE, compared with placebo over 5 years, with an NNT of 20, according to Dr. Sabatine, professor of medicine at Harvard Medical School and chairman of the Thrombolysis in Myocardial Infarction (TIMI) Study Group.
Lingering questions
Dr. Braun was particularly impressed that the absolute risk reduction in MACE was even larger in patients with baseline PAD but no history of stroke or MI than in PAD patients with such a history. She added that, while she recognizes the value of selecting objectively assessable hard clinical MACE as the primary endpoint in FOURIER, her own patients care even more about other outcomes.
“What my patients with PAD care most about is whether profound LDL lowering translates to less claudication, improved quality of life, and greater physical activity tolerance. These were prespecified secondary outcomes in FOURIER, and I look forward to future reports addressing those issues,” she said.
Another unanswered question involves the mechanism by which intensive LDL cholesterol lowering results in fewer MACE and MALE events in high-risk subgroups. The possibilities include the plaque regression that was documented in the GLAGOV trial, an anti-inflammatory plaque-stabilizing effect being exerted through PCSK9 inhibition, or perhaps the PCSK9 inhibitors’ ability to moderately lower lipoprotein(a) cholesterol levels.
Simultaneous with Dr. Bonaca’s presentation at the AHA, the FOURIER PAD analysis was published online in Circulation (2017 Nov 13; doi: 10.1161/CIRCULATIONAHA.117.032235).
The FOURIER trial was sponsored by Amgen. Dr. Bonaca and Dr. Sabatine reported receiving research grants from and serving as consultants to Amgen and other companies.
ANAHEIM, CALIF. – Patients with symptomatic peripheral artery disease or a high-risk history of MI got the biggest bang for the buck from aggressive LDL cholesterol lowering with evolocumab in two new prespecified subgroup analyses from the landmark FOURIER trial presented at the American Heart Association scientific sessions.
“At the end of the day, not all of our patients with ASCVD [atherosclerotic cardiovascular disease] can have these expensive medications. These subgroup analyses will help clinicians to target use of PCSK9 inhibitors to the patients who will benefit the most,” Lynne T. Braun, PhD, commented in her role as discussant of the two secondary analyses, presented back to back in a late-breaking science session. Dr. Braun is a professor in the department of internal medicine at Rush University, Chicago.
The FOURIER trial included 27,564 high-risk patients with prior MI, stroke, and/or symptomatic peripheral arterial disease (PAD) who had an LDL cholesterol level of 70 mg/dL or more on high- or moderate-intensity statin therapy. They were randomized in double-blind fashion to add-on subcutaneous evolocumab (Repatha) at either 140 mg every 2 weeks or 420 mg/month or to placebo, for a median of 2.5 years of follow-up. The evolocumab group experienced a 59% reduction in LDL cholesterol, compared with the controls on background statin therapy plus placebo, down to a mean LDL cholesterol level of just 30 mg/dL.
As previously reported, the risk of the primary composite endpoint – comprising cardiovascular death, MI, stroke, unstable angina, or coronary revascularization – was reduced by 15% in the evolocumab group at 3 years. The secondary endpoint of cardiovascular death, MI, or stroke was reduced by 20%, from 9.9% to 7.9% (N Engl J Med. 2017;376:1713-22).
Evolocumab tamed PAD
At the AHA scientific sessions, Marc P. Bonaca, MD, presented a secondary analysis restricted to the 3,642 FOURIER participants with symptomatic PAD. The goal was to answer two unresolved questions: Does LDL cholesterol lowering beyond what’s achievable with a statin further reduce PAD patients’ cardiovascular risk? And does it reduce their risk of major adverse leg events (MALE), defined as a composite of acute limb ischemia, major amputation, and urgent revascularization?
The rate of the composite endpoint comprising cardiovascular death, MI, or stroke was 13% over 3 years in PAD patients randomized to placebo, which was 81% greater than the 7.6% rate in placebo-treated participants with a baseline history of stroke or MI but no PAD, in an analysis adjusted for demographics, cardiovascular risk factors, kidney function, body mass index, and prior revascularization.
The event rate was even higher in patients with PAD plus a history of MI or stroke, at 14.9%. Evolocumab reduced that risk by 27%, compared with placebo in patients with PAD, for an absolute risk reduction of 3.5% and a number-needed-to-treat (NNT) of 29 for 2.5 years.
The benefit of evolocumab was even more pronounced in the subgroup of 1,505 patients with baseline PAD but no prior MI or stroke: a 43% relative risk reduction, from 10.3% to 5.5%, for an absolute risk reduction of 4.8% and a NNT of 21.
A linear relationship was seen between the MALE rate during follow-up and LDL cholesterol level after 1 month of therapy, down to an LDL cholesterol level of less than 10 mg/dL. The clinically relevant composite endpoint of MACE (major adverse cardiovascular events – a composite of cardiovascular death, MI, and stroke) or MALE in patients with baseline PAD but no history of MI or stroke occurred in 12.8% of controls and 6.5% of the evolocumab group. This translated to a 48% relative risk reduction, a 6.3% absolute risk reduction, and a NNT of 16. The event curves in the evolocumab and control arms separated quite early, within the first 90 days of treatment.
The take home message: “LDL reduction to very low levels should be considered in patients with PAD, regardless of their history of MI or stroke, to reduce the risk of MACE [major adverse cardiovascular event] and MALE,” declared Dr. Bonaca of Brigham and Women’s Hospital and Harvard Medical School, both in Boston.
Spotting the patients with a history of MI who’re at highest risk
Marc S. Sabatine, MD, presented the subanalysis involving the 22,351 FOURIER patients with a prior MI. He and his coinvestigators identified three high-risk features within this group: an MI within the past 2 years, a history of two or more MIs, and residual multivessel CAD. Each of these three features was individually associated with a 34%-90% increased risk of MACE during follow-up. All told, 63% of FOURIER participants with prior MI had one or more of the high-risk features.
The use of evolocumab in patients with at least one of the three high-risk features was associated with a 22% relative risk reduction and an absolute 2.5% risk reduction, compared with placebo. The event curves diverged at about 6 months, and the gap between them steadily widened during follow-up. Extrapolating from this pattern, it’s likely that evolocumab would achieve an absolute 5% risk reduction in MACE, compared with placebo over 5 years, with an NNT of 20, according to Dr. Sabatine, professor of medicine at Harvard Medical School and chairman of the Thrombolysis in Myocardial Infarction (TIMI) Study Group.
Lingering questions
Dr. Braun was particularly impressed that the absolute risk reduction in MACE was even larger in patients with baseline PAD but no history of stroke or MI than in PAD patients with such a history. She added that, while she recognizes the value of selecting objectively assessable hard clinical MACE as the primary endpoint in FOURIER, her own patients care even more about other outcomes.
“What my patients with PAD care most about is whether profound LDL lowering translates to less claudication, improved quality of life, and greater physical activity tolerance. These were prespecified secondary outcomes in FOURIER, and I look forward to future reports addressing those issues,” she said.
Another unanswered question involves the mechanism by which intensive LDL cholesterol lowering results in fewer MACE and MALE events in high-risk subgroups. The possibilities include the plaque regression that was documented in the GLAGOV trial, an anti-inflammatory plaque-stabilizing effect being exerted through PCSK9 inhibition, or perhaps the PCSK9 inhibitors’ ability to moderately lower lipoprotein(a) cholesterol levels.
Simultaneous with Dr. Bonaca’s presentation at the AHA, the FOURIER PAD analysis was published online in Circulation (2017 Nov 13; doi: 10.1161/CIRCULATIONAHA.117.032235).
The FOURIER trial was sponsored by Amgen. Dr. Bonaca and Dr. Sabatine reported receiving research grants from and serving as consultants to Amgen and other companies.
ANAHEIM, CALIF. – Patients with symptomatic peripheral artery disease or a high-risk history of MI got the biggest bang for the buck from aggressive LDL cholesterol lowering with evolocumab in two new prespecified subgroup analyses from the landmark FOURIER trial presented at the American Heart Association scientific sessions.
“At the end of the day, not all of our patients with ASCVD [atherosclerotic cardiovascular disease] can have these expensive medications. These subgroup analyses will help clinicians to target use of PCSK9 inhibitors to the patients who will benefit the most,” Lynne T. Braun, PhD, commented in her role as discussant of the two secondary analyses, presented back to back in a late-breaking science session. Dr. Braun is a professor in the department of internal medicine at Rush University, Chicago.
The FOURIER trial included 27,564 high-risk patients with prior MI, stroke, and/or symptomatic peripheral arterial disease (PAD) who had an LDL cholesterol level of 70 mg/dL or more on high- or moderate-intensity statin therapy. They were randomized in double-blind fashion to add-on subcutaneous evolocumab (Repatha) at either 140 mg every 2 weeks or 420 mg/month or to placebo, for a median of 2.5 years of follow-up. The evolocumab group experienced a 59% reduction in LDL cholesterol, compared with the controls on background statin therapy plus placebo, down to a mean LDL cholesterol level of just 30 mg/dL.
As previously reported, the risk of the primary composite endpoint – comprising cardiovascular death, MI, stroke, unstable angina, or coronary revascularization – was reduced by 15% in the evolocumab group at 3 years. The secondary endpoint of cardiovascular death, MI, or stroke was reduced by 20%, from 9.9% to 7.9% (N Engl J Med. 2017;376:1713-22).
Evolocumab tamed PAD
At the AHA scientific sessions, Marc P. Bonaca, MD, presented a secondary analysis restricted to the 3,642 FOURIER participants with symptomatic PAD. The goal was to answer two unresolved questions: Does LDL cholesterol lowering beyond what’s achievable with a statin further reduce PAD patients’ cardiovascular risk? And does it reduce their risk of major adverse leg events (MALE), defined as a composite of acute limb ischemia, major amputation, and urgent revascularization?
The rate of the composite endpoint comprising cardiovascular death, MI, or stroke was 13% over 3 years in PAD patients randomized to placebo, which was 81% greater than the 7.6% rate in placebo-treated participants with a baseline history of stroke or MI but no PAD, in an analysis adjusted for demographics, cardiovascular risk factors, kidney function, body mass index, and prior revascularization.
The event rate was even higher in patients with PAD plus a history of MI or stroke, at 14.9%. Evolocumab reduced that risk by 27%, compared with placebo in patients with PAD, for an absolute risk reduction of 3.5% and a number-needed-to-treat (NNT) of 29 for 2.5 years.
The benefit of evolocumab was even more pronounced in the subgroup of 1,505 patients with baseline PAD but no prior MI or stroke: a 43% relative risk reduction, from 10.3% to 5.5%, for an absolute risk reduction of 4.8% and a NNT of 21.
A linear relationship was seen between the MALE rate during follow-up and LDL cholesterol level after 1 month of therapy, down to an LDL cholesterol level of less than 10 mg/dL. The clinically relevant composite endpoint of MACE (major adverse cardiovascular events – a composite of cardiovascular death, MI, and stroke) or MALE in patients with baseline PAD but no history of MI or stroke occurred in 12.8% of controls and 6.5% of the evolocumab group. This translated to a 48% relative risk reduction, a 6.3% absolute risk reduction, and a NNT of 16. The event curves in the evolocumab and control arms separated quite early, within the first 90 days of treatment.
The take home message: “LDL reduction to very low levels should be considered in patients with PAD, regardless of their history of MI or stroke, to reduce the risk of MACE [major adverse cardiovascular event] and MALE,” declared Dr. Bonaca of Brigham and Women’s Hospital and Harvard Medical School, both in Boston.
Spotting the patients with a history of MI who’re at highest risk
Marc S. Sabatine, MD, presented the subanalysis involving the 22,351 FOURIER patients with a prior MI. He and his coinvestigators identified three high-risk features within this group: an MI within the past 2 years, a history of two or more MIs, and residual multivessel CAD. Each of these three features was individually associated with a 34%-90% increased risk of MACE during follow-up. All told, 63% of FOURIER participants with prior MI had one or more of the high-risk features.
The use of evolocumab in patients with at least one of the three high-risk features was associated with a 22% relative risk reduction and an absolute 2.5% risk reduction, compared with placebo. The event curves diverged at about 6 months, and the gap between them steadily widened during follow-up. Extrapolating from this pattern, it’s likely that evolocumab would achieve an absolute 5% risk reduction in MACE, compared with placebo over 5 years, with an NNT of 20, according to Dr. Sabatine, professor of medicine at Harvard Medical School and chairman of the Thrombolysis in Myocardial Infarction (TIMI) Study Group.
Lingering questions
Dr. Braun was particularly impressed that the absolute risk reduction in MACE was even larger in patients with baseline PAD but no history of stroke or MI than in PAD patients with such a history. She added that, while she recognizes the value of selecting objectively assessable hard clinical MACE as the primary endpoint in FOURIER, her own patients care even more about other outcomes.
“What my patients with PAD care most about is whether profound LDL lowering translates to less claudication, improved quality of life, and greater physical activity tolerance. These were prespecified secondary outcomes in FOURIER, and I look forward to future reports addressing those issues,” she said.
Another unanswered question involves the mechanism by which intensive LDL cholesterol lowering results in fewer MACE and MALE events in high-risk subgroups. The possibilities include the plaque regression that was documented in the GLAGOV trial, an anti-inflammatory plaque-stabilizing effect being exerted through PCSK9 inhibition, or perhaps the PCSK9 inhibitors’ ability to moderately lower lipoprotein(a) cholesterol levels.
Simultaneous with Dr. Bonaca’s presentation at the AHA, the FOURIER PAD analysis was published online in Circulation (2017 Nov 13; doi: 10.1161/CIRCULATIONAHA.117.032235).
The FOURIER trial was sponsored by Amgen. Dr. Bonaca and Dr. Sabatine reported receiving research grants from and serving as consultants to Amgen and other companies.
EXPERT ANALYSIS FROM THE AHA SCIENTIFIC SESSIONS
Adherence boon, or Big Brother loom?
The Food and Drug Administration has approved the first drug in the United States with a digital ingestion tracking system. Abilify MyCite (aripiprazole tablets with sensor) has an ingestible sensor embedded in the pill that records that the medication was taken. The product is approved for the treatment of schizophrenia, acute treatment of manic and mixed episodes associated with bipolar I disorder, and for use as an add-on treatment for depression in adults.
The system works by sending a message from the pill’s sensor to a wearable patch, according to a statement issued by the FDA. The patch transmits the information to a mobile application so that patients can track the ingestion of the medication on their smartphones. Patients can also permit their caregivers and physician to access the information through a web-based portal.
[polldaddy:9874958]
The Food and Drug Administration has approved the first drug in the United States with a digital ingestion tracking system. Abilify MyCite (aripiprazole tablets with sensor) has an ingestible sensor embedded in the pill that records that the medication was taken. The product is approved for the treatment of schizophrenia, acute treatment of manic and mixed episodes associated with bipolar I disorder, and for use as an add-on treatment for depression in adults.
The system works by sending a message from the pill’s sensor to a wearable patch, according to a statement issued by the FDA. The patch transmits the information to a mobile application so that patients can track the ingestion of the medication on their smartphones. Patients can also permit their caregivers and physician to access the information through a web-based portal.
[polldaddy:9874958]
The Food and Drug Administration has approved the first drug in the United States with a digital ingestion tracking system. Abilify MyCite (aripiprazole tablets with sensor) has an ingestible sensor embedded in the pill that records that the medication was taken. The product is approved for the treatment of schizophrenia, acute treatment of manic and mixed episodes associated with bipolar I disorder, and for use as an add-on treatment for depression in adults.
The system works by sending a message from the pill’s sensor to a wearable patch, according to a statement issued by the FDA. The patch transmits the information to a mobile application so that patients can track the ingestion of the medication on their smartphones. Patients can also permit their caregivers and physician to access the information through a web-based portal.
[polldaddy:9874958]
VIDEO: Beware of over-relying on MRI findings in axSpA
SAN DIEGO – Healthy individuals can show signs of spinal and pelvic inflammation on MRI, but these scans can be misleading if relied on to make a diagnosis of axial spondyloarthritis, according to findings from three separate studies at the annual meeting of the American College of Rheumatology.
“Don’t rely on MRI alone is our message,” said Robert Landewé, MD, PhD, of the University of Amsterdam, who was a coauthor of one of the three studies. “A positive MRI may occur in individuals that are completely healthy. We need to make sure that not too many patients with chronic lower back pain are diagnosed with a disease they don’t have.”
The axial form of spondyloarthritis (axSpA) affects the spinal and pelvic joints of an estimated 1.4% of the U.S. population, and the term encompasses the diagnosis of ankylosing spondylitis (0.5% of U.S. population) in which advanced sacroiliitis is seen on conventional radiography, according to the ACR. Axial SpA is particularly common in young people, especially males, in their teens and 20s.
Researchers believe that MRI scans can misleadingly suggest that patients have the condition. “We know that MRI is a sensitive method, but there’s a lack of data regarding its specificity,” Thomas Renson, MD, of Ghent (Belgium) University, said at a press conference during the meeting.
Dr. Landewé led a study that compared MRIs of sacroiliac joints in 47 healthy people, 47 axSpA patients matched for gender and age, 47 chronic back pain patients, 7 women with postpartum back pain, and 24 frequent runners. Positive MRIs were common in the axSpA patients (43 of 47), but they were also found in healthy people (11 of 47), chronic back pain patients (3 of 47), frequent runners (3 of 24), and women with postpartum back pain (4 of 7).
In another study, Dr. Renson and his colleagues sought to understand whether a sustained period of intense physical activity affected spinal findings in 22 healthy military recruits who did not have SpA.
However, there was a statistically significant increase of combined structural and inflammatory lesions (P = .038) from baseline to post training.
The findings underscore “the importance of interpretation of imaging in the right clinical context,” Dr. Renson said, since they point to the possibility of an incorrect diagnosis “even in a young, active population.”
Another study, led by Ulrich Weber, MD, of King Christian 10th Hospital for Rheumatic Diseases, Gråsten, Denmark, sought to understand levels of normal low-grade BME in 20 amateur runners (8 men) and 22 professional Danish hockey players (all men). On average, the researchers found signs of BME in 3.1 sacroiliac joint quadrants in the runners before and after they ran a race. Hockey players were scanned at the end of the competitive season and showed signs of BME in an average of 3.6 sacroiliac joint quadrants.
In an interview, Dr. Landewé said the studies point to how common positive MRIs are in healthy people. “It was far higher than we would have thought 10 years ago,” he said.
Are MRIs still useful then? Dr. Weber said MRI scans are still helpful in axSpA diagnoses even though they have major limitations. “The imaging method is the only one that’s halfway reliable,” he said. “These joints are deep in the body, so we have virtually no clinical ways to diagnose this.”
However, Dr. Landewé said, “you should do it only when you have sufficient suspicion of spondyloarthritis” – due to accompanying conditions such as positive family history, acute anterior uveitis, psoriasis, or peripheral arthritis – and not just when a patient has chronic back pain.
Dr. Renson reported having no relevant disclosures; two of his coauthors reported extensive disclosures. Dr. Weber and his coauthors reported having no relevant disclosures. Dr. Landewé reported having no relevant disclosures; several of his coauthors reported various disclosures. Funding for the studies was not reported.
SAN DIEGO – Healthy individuals can show signs of spinal and pelvic inflammation on MRI, but these scans can be misleading if relied on to make a diagnosis of axial spondyloarthritis, according to findings from three separate studies at the annual meeting of the American College of Rheumatology.
“Don’t rely on MRI alone is our message,” said Robert Landewé, MD, PhD, of the University of Amsterdam, who was a coauthor of one of the three studies. “A positive MRI may occur in individuals that are completely healthy. We need to make sure that not too many patients with chronic lower back pain are diagnosed with a disease they don’t have.”
The axial form of spondyloarthritis (axSpA) affects the spinal and pelvic joints of an estimated 1.4% of the U.S. population, and the term encompasses the diagnosis of ankylosing spondylitis (0.5% of U.S. population) in which advanced sacroiliitis is seen on conventional radiography, according to the ACR. Axial SpA is particularly common in young people, especially males, in their teens and 20s.
Researchers believe that MRI scans can misleadingly suggest that patients have the condition. “We know that MRI is a sensitive method, but there’s a lack of data regarding its specificity,” Thomas Renson, MD, of Ghent (Belgium) University, said at a press conference during the meeting.
Dr. Landewé led a study that compared MRIs of sacroiliac joints in 47 healthy people, 47 axSpA patients matched for gender and age, 47 chronic back pain patients, 7 women with postpartum back pain, and 24 frequent runners. Positive MRIs were common in the axSpA patients (43 of 47), but they were also found in healthy people (11 of 47), chronic back pain patients (3 of 47), frequent runners (3 of 24), and women with postpartum back pain (4 of 7).
In another study, Dr. Renson and his colleagues sought to understand whether a sustained period of intense physical activity affected spinal findings in 22 healthy military recruits who did not have SpA.
However, there was a statistically significant increase of combined structural and inflammatory lesions (P = .038) from baseline to post training.
The findings underscore “the importance of interpretation of imaging in the right clinical context,” Dr. Renson said, since they point to the possibility of an incorrect diagnosis “even in a young, active population.”
Another study, led by Ulrich Weber, MD, of King Christian 10th Hospital for Rheumatic Diseases, Gråsten, Denmark, sought to understand levels of normal low-grade BME in 20 amateur runners (8 men) and 22 professional Danish hockey players (all men). On average, the researchers found signs of BME in 3.1 sacroiliac joint quadrants in the runners before and after they ran a race. Hockey players were scanned at the end of the competitive season and showed signs of BME in an average of 3.6 sacroiliac joint quadrants.
In an interview, Dr. Landewé said the studies point to how common positive MRIs are in healthy people. “It was far higher than we would have thought 10 years ago,” he said.
Are MRIs still useful then? Dr. Weber said MRI scans are still helpful in axSpA diagnoses even though they have major limitations. “The imaging method is the only one that’s halfway reliable,” he said. “These joints are deep in the body, so we have virtually no clinical ways to diagnose this.”
However, Dr. Landewé said, “you should do it only when you have sufficient suspicion of spondyloarthritis” – due to accompanying conditions such as positive family history, acute anterior uveitis, psoriasis, or peripheral arthritis – and not just when a patient has chronic back pain.
Dr. Renson reported having no relevant disclosures; two of his coauthors reported extensive disclosures. Dr. Weber and his coauthors reported having no relevant disclosures. Dr. Landewé reported having no relevant disclosures; several of his coauthors reported various disclosures. Funding for the studies was not reported.
SAN DIEGO – Healthy individuals can show signs of spinal and pelvic inflammation on MRI, but these scans can be misleading if relied on to make a diagnosis of axial spondyloarthritis, according to findings from three separate studies at the annual meeting of the American College of Rheumatology.
“Don’t rely on MRI alone is our message,” said Robert Landewé, MD, PhD, of the University of Amsterdam, who was a coauthor of one of the three studies. “A positive MRI may occur in individuals that are completely healthy. We need to make sure that not too many patients with chronic lower back pain are diagnosed with a disease they don’t have.”
The axial form of spondyloarthritis (axSpA) affects the spinal and pelvic joints of an estimated 1.4% of the U.S. population, and the term encompasses the diagnosis of ankylosing spondylitis (0.5% of U.S. population) in which advanced sacroiliitis is seen on conventional radiography, according to the ACR. Axial SpA is particularly common in young people, especially males, in their teens and 20s.
Researchers believe that MRI scans can misleadingly suggest that patients have the condition. “We know that MRI is a sensitive method, but there’s a lack of data regarding its specificity,” Thomas Renson, MD, of Ghent (Belgium) University, said at a press conference during the meeting.
Dr. Landewé led a study that compared MRIs of sacroiliac joints in 47 healthy people, 47 axSpA patients matched for gender and age, 47 chronic back pain patients, 7 women with postpartum back pain, and 24 frequent runners. Positive MRIs were common in the axSpA patients (43 of 47), but they were also found in healthy people (11 of 47), chronic back pain patients (3 of 47), frequent runners (3 of 24), and women with postpartum back pain (4 of 7).
In another study, Dr. Renson and his colleagues sought to understand whether a sustained period of intense physical activity affected spinal findings in 22 healthy military recruits who did not have SpA.
However, there was a statistically significant increase of combined structural and inflammatory lesions (P = .038) from baseline to post training.
The findings underscore “the importance of interpretation of imaging in the right clinical context,” Dr. Renson said, since they point to the possibility of an incorrect diagnosis “even in a young, active population.”
Another study, led by Ulrich Weber, MD, of King Christian 10th Hospital for Rheumatic Diseases, Gråsten, Denmark, sought to understand levels of normal low-grade BME in 20 amateur runners (8 men) and 22 professional Danish hockey players (all men). On average, the researchers found signs of BME in 3.1 sacroiliac joint quadrants in the runners before and after they ran a race. Hockey players were scanned at the end of the competitive season and showed signs of BME in an average of 3.6 sacroiliac joint quadrants.
In an interview, Dr. Landewé said the studies point to how common positive MRIs are in healthy people. “It was far higher than we would have thought 10 years ago,” he said.
Are MRIs still useful then? Dr. Weber said MRI scans are still helpful in axSpA diagnoses even though they have major limitations. “The imaging method is the only one that’s halfway reliable,” he said. “These joints are deep in the body, so we have virtually no clinical ways to diagnose this.”
However, Dr. Landewé said, “you should do it only when you have sufficient suspicion of spondyloarthritis” – due to accompanying conditions such as positive family history, acute anterior uveitis, psoriasis, or peripheral arthritis – and not just when a patient has chronic back pain.
Dr. Renson reported having no relevant disclosures; two of his coauthors reported extensive disclosures. Dr. Weber and his coauthors reported having no relevant disclosures. Dr. Landewé reported having no relevant disclosures; several of his coauthors reported various disclosures. Funding for the studies was not reported.
AT ACR 2017
Fibroids associated with lower chance of unsuspected malignancy
NATIONAL HARBOR, MD. – Women undergoing hysterectomy or myomectomy for benign indications, who also had fibroids, were less likely to have a malignant diagnosis, according to a study presented at the AAGL Global Congress.
These findings could change the conversation when it comes to counseling patients about the risks associated with morcellation, a procedure that was strongly discouraged by the FDA in 2014 due to the concern that it might have the potential to spread malignancy.
“There’s a lot of things going on in the media about morcellation and risk of malignancy at the time of benign fibroid surgery, but this research actually makes apparent the higher risk of malignancy when fibroids are not present,” Farah Alvi, MD, a second-year fellow at Northwestern University, Chicago, said in an interview. Despite the concerns regarding morcellation and malignancy, this research suggests that patients who have fibroids at time of surgery may have a lower chance of malignancy, compared with patients who have other indications for surgery, she explained.
Dr. Alvi and her colleagues studied 2,987 hysterectomy or myomectomy patients with benign indications between January 2005 and December 2014.
Among patients studied, researchers found 33 confirmed malignant or borderline tumors, 16 of 1,790 (0.89%) in the leiomyoma group and 17 of 1,197 (1.42%) in the group with other indications (P = 0.04). The malignancies/borderline tumors included three leiomyosarcomas, two endometrial sarcomas, two endometrioid adenocarcinomas, one granulose cell tumor, three smooth muscle tumors of uncertain malignant potential, three atypical leiomyoma, and one serous papillary borderline ovarian tumor.
Of those with leiomyomata, 1 in 600 patients were diagnosed with leiomyosarcoma, compared with a risk of 1 in 350 for unanticipated malignancy in general.
Patients with surgical indications of symptomatic leiomyoma had an odds ratio of 0.63 (P = .18) for diagnosis of an unanticipated malignancy, compared with those without leiomyoma, according to Dr. Alvi. The odds of malignancy were also reduced in patients with uterine sizes of 15-20 weeks (OR, 0.65; P = .43) and those with specimen sizes of 250-500 grams (OR, 0.68; P = .64).
These findings will have implications for how physicians counsel women undergoing minimally invasive hysterectomy or myomectomy, Dr. Alvi said.
“In counseling patients about morcellation, we often have quoted them an estimated risk of 1 in 458 for leiomyosarcoma, based on the FDA morcellation warnings, and one thing we can learn is that risk is actually much lower than we think it is,” Dr. Alvi said.
The findings also suggest a shift in focus toward identifying the factors that put women at higher risk for malignancy. For example, older age is one of the most significant risk factors identified in the study, she added.
Dr. Alvi reported having no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
NATIONAL HARBOR, MD. – Women undergoing hysterectomy or myomectomy for benign indications, who also had fibroids, were less likely to have a malignant diagnosis, according to a study presented at the AAGL Global Congress.
These findings could change the conversation when it comes to counseling patients about the risks associated with morcellation, a procedure that was strongly discouraged by the FDA in 2014 due to the concern that it might have the potential to spread malignancy.
“There’s a lot of things going on in the media about morcellation and risk of malignancy at the time of benign fibroid surgery, but this research actually makes apparent the higher risk of malignancy when fibroids are not present,” Farah Alvi, MD, a second-year fellow at Northwestern University, Chicago, said in an interview. Despite the concerns regarding morcellation and malignancy, this research suggests that patients who have fibroids at time of surgery may have a lower chance of malignancy, compared with patients who have other indications for surgery, she explained.
Dr. Alvi and her colleagues studied 2,987 hysterectomy or myomectomy patients with benign indications between January 2005 and December 2014.
Among patients studied, researchers found 33 confirmed malignant or borderline tumors, 16 of 1,790 (0.89%) in the leiomyoma group and 17 of 1,197 (1.42%) in the group with other indications (P = 0.04). The malignancies/borderline tumors included three leiomyosarcomas, two endometrial sarcomas, two endometrioid adenocarcinomas, one granulose cell tumor, three smooth muscle tumors of uncertain malignant potential, three atypical leiomyoma, and one serous papillary borderline ovarian tumor.
Of those with leiomyomata, 1 in 600 patients were diagnosed with leiomyosarcoma, compared with a risk of 1 in 350 for unanticipated malignancy in general.
Patients with surgical indications of symptomatic leiomyoma had an odds ratio of 0.63 (P = .18) for diagnosis of an unanticipated malignancy, compared with those without leiomyoma, according to Dr. Alvi. The odds of malignancy were also reduced in patients with uterine sizes of 15-20 weeks (OR, 0.65; P = .43) and those with specimen sizes of 250-500 grams (OR, 0.68; P = .64).
These findings will have implications for how physicians counsel women undergoing minimally invasive hysterectomy or myomectomy, Dr. Alvi said.
“In counseling patients about morcellation, we often have quoted them an estimated risk of 1 in 458 for leiomyosarcoma, based on the FDA morcellation warnings, and one thing we can learn is that risk is actually much lower than we think it is,” Dr. Alvi said.
The findings also suggest a shift in focus toward identifying the factors that put women at higher risk for malignancy. For example, older age is one of the most significant risk factors identified in the study, she added.
Dr. Alvi reported having no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
NATIONAL HARBOR, MD. – Women undergoing hysterectomy or myomectomy for benign indications, who also had fibroids, were less likely to have a malignant diagnosis, according to a study presented at the AAGL Global Congress.
These findings could change the conversation when it comes to counseling patients about the risks associated with morcellation, a procedure that was strongly discouraged by the FDA in 2014 due to the concern that it might have the potential to spread malignancy.
“There’s a lot of things going on in the media about morcellation and risk of malignancy at the time of benign fibroid surgery, but this research actually makes apparent the higher risk of malignancy when fibroids are not present,” Farah Alvi, MD, a second-year fellow at Northwestern University, Chicago, said in an interview. Despite the concerns regarding morcellation and malignancy, this research suggests that patients who have fibroids at time of surgery may have a lower chance of malignancy, compared with patients who have other indications for surgery, she explained.
Dr. Alvi and her colleagues studied 2,987 hysterectomy or myomectomy patients with benign indications between January 2005 and December 2014.
Among patients studied, researchers found 33 confirmed malignant or borderline tumors, 16 of 1,790 (0.89%) in the leiomyoma group and 17 of 1,197 (1.42%) in the group with other indications (P = 0.04). The malignancies/borderline tumors included three leiomyosarcomas, two endometrial sarcomas, two endometrioid adenocarcinomas, one granulose cell tumor, three smooth muscle tumors of uncertain malignant potential, three atypical leiomyoma, and one serous papillary borderline ovarian tumor.
Of those with leiomyomata, 1 in 600 patients were diagnosed with leiomyosarcoma, compared with a risk of 1 in 350 for unanticipated malignancy in general.
Patients with surgical indications of symptomatic leiomyoma had an odds ratio of 0.63 (P = .18) for diagnosis of an unanticipated malignancy, compared with those without leiomyoma, according to Dr. Alvi. The odds of malignancy were also reduced in patients with uterine sizes of 15-20 weeks (OR, 0.65; P = .43) and those with specimen sizes of 250-500 grams (OR, 0.68; P = .64).
These findings will have implications for how physicians counsel women undergoing minimally invasive hysterectomy or myomectomy, Dr. Alvi said.
“In counseling patients about morcellation, we often have quoted them an estimated risk of 1 in 458 for leiomyosarcoma, based on the FDA morcellation warnings, and one thing we can learn is that risk is actually much lower than we think it is,” Dr. Alvi said.
The findings also suggest a shift in focus toward identifying the factors that put women at higher risk for malignancy. For example, older age is one of the most significant risk factors identified in the study, she added.
Dr. Alvi reported having no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
AT AAGL 2017
Key clinical point:
Major finding: Patients with preoperative indication of symptomatic leiomyoma had an odds ratio of 0.63 (P = .18) of having a diagnosis of malignancy.
Data source: Retrospective study of 2,987 hysterectomies or myomectomies between January 2005 and December 2014.
Disclosures: Dr. Alvi reported having no relevant financial disclosures.
Single-port laparoscopy has few complications but BMI matters
NATIONAL HARBOR, MD. – Single-port laparoscopy is both safe and feasible, and has the potential to decrease surgical complications and increase efficiency, according to findings presented at the AAGL Global Congress.
Ahmed N. Al-Niaimi, MD, of the University of Wisconsin–Madison, and his colleagues, conducted a retrospective cohort study analyzing 587 consecutive patients who underwent single-port laparoscopy from March 2012 to December 2016. Of the 587 patients, there were 27 clinically-relevant complications among 18 patients (3%). The complications included intensive care unit admission, reoperation, end organ damage, organ space surgical site infection, and readmission.
“Those factors leading to those complications are similar to the factors that cause complications in any other surgery,” Dr. Al-Niaimi said in an interview before the meeting.
Body mass index was found to be a primary contributor to surgical complications. Patients with a BMI of more than 30 kg/m2 experienced a 1% increase in the risk of surgical complications per unit value increase of BMI. This is significant because the median BMI of the patient population in the study was 33.9 kg/m2 and 57% of the study participants were considered obese or morbidly obese.
“The heavier the patient, the higher the complication rate,” Dr. Al-Niaimi said.
Surgeons who are learning single-port laparoscopy should choose patients with lower BMIs to gain efficiency in using the new technique, Dr. Al-Niaimi suggested. This will allow patients to decrease their risk of surgical complications while allowing surgeons to hone their abilities in a new surgical technique, he said.
The other prime contributor to surgical complications is the length of surgical time. The average time of surgery during the study was 156 minutes. Dr. Al-Niaimi and his colleagues found that for each 10-minute increase in surgical time, the risk of complications increased by 2%.
While the results of the study demonstrate safety in the single-port approach, Dr. Al-Niaimi said a randomized controlled trial is needed to validate the findings and determine whether single-port laparoscopy is more effective than multi-port laparoscopy.
Dr. Al-Niaimi reported having no financial disclosures.
NATIONAL HARBOR, MD. – Single-port laparoscopy is both safe and feasible, and has the potential to decrease surgical complications and increase efficiency, according to findings presented at the AAGL Global Congress.
Ahmed N. Al-Niaimi, MD, of the University of Wisconsin–Madison, and his colleagues, conducted a retrospective cohort study analyzing 587 consecutive patients who underwent single-port laparoscopy from March 2012 to December 2016. Of the 587 patients, there were 27 clinically-relevant complications among 18 patients (3%). The complications included intensive care unit admission, reoperation, end organ damage, organ space surgical site infection, and readmission.
“Those factors leading to those complications are similar to the factors that cause complications in any other surgery,” Dr. Al-Niaimi said in an interview before the meeting.
Body mass index was found to be a primary contributor to surgical complications. Patients with a BMI of more than 30 kg/m2 experienced a 1% increase in the risk of surgical complications per unit value increase of BMI. This is significant because the median BMI of the patient population in the study was 33.9 kg/m2 and 57% of the study participants were considered obese or morbidly obese.
“The heavier the patient, the higher the complication rate,” Dr. Al-Niaimi said.
Surgeons who are learning single-port laparoscopy should choose patients with lower BMIs to gain efficiency in using the new technique, Dr. Al-Niaimi suggested. This will allow patients to decrease their risk of surgical complications while allowing surgeons to hone their abilities in a new surgical technique, he said.
The other prime contributor to surgical complications is the length of surgical time. The average time of surgery during the study was 156 minutes. Dr. Al-Niaimi and his colleagues found that for each 10-minute increase in surgical time, the risk of complications increased by 2%.
While the results of the study demonstrate safety in the single-port approach, Dr. Al-Niaimi said a randomized controlled trial is needed to validate the findings and determine whether single-port laparoscopy is more effective than multi-port laparoscopy.
Dr. Al-Niaimi reported having no financial disclosures.
NATIONAL HARBOR, MD. – Single-port laparoscopy is both safe and feasible, and has the potential to decrease surgical complications and increase efficiency, according to findings presented at the AAGL Global Congress.
Ahmed N. Al-Niaimi, MD, of the University of Wisconsin–Madison, and his colleagues, conducted a retrospective cohort study analyzing 587 consecutive patients who underwent single-port laparoscopy from March 2012 to December 2016. Of the 587 patients, there were 27 clinically-relevant complications among 18 patients (3%). The complications included intensive care unit admission, reoperation, end organ damage, organ space surgical site infection, and readmission.
“Those factors leading to those complications are similar to the factors that cause complications in any other surgery,” Dr. Al-Niaimi said in an interview before the meeting.
Body mass index was found to be a primary contributor to surgical complications. Patients with a BMI of more than 30 kg/m2 experienced a 1% increase in the risk of surgical complications per unit value increase of BMI. This is significant because the median BMI of the patient population in the study was 33.9 kg/m2 and 57% of the study participants were considered obese or morbidly obese.
“The heavier the patient, the higher the complication rate,” Dr. Al-Niaimi said.
Surgeons who are learning single-port laparoscopy should choose patients with lower BMIs to gain efficiency in using the new technique, Dr. Al-Niaimi suggested. This will allow patients to decrease their risk of surgical complications while allowing surgeons to hone their abilities in a new surgical technique, he said.
The other prime contributor to surgical complications is the length of surgical time. The average time of surgery during the study was 156 minutes. Dr. Al-Niaimi and his colleagues found that for each 10-minute increase in surgical time, the risk of complications increased by 2%.
While the results of the study demonstrate safety in the single-port approach, Dr. Al-Niaimi said a randomized controlled trial is needed to validate the findings and determine whether single-port laparoscopy is more effective than multi-port laparoscopy.
Dr. Al-Niaimi reported having no financial disclosures.
AT AAGL 2017
Key clinical point:
Major finding: Obese patients experienced a 1% increase in risk of surgical complications per unit value increase of BMI.
Data source: Retrospective cohort study of 587 consecutive patients undergoing single-port laparoscopy at a single academic institution.
Disclosures: Dr. Al-Niaimi reported having no financial disclosures.
Direct oral anticoagulants okay during AF device placement
ANAHEIM, CALIF. – Whether direct oral anticoagulants are continued or interrupted for device placement in atrial fibrillation patients, the risk of device pocket hematoma or stroke is very low, based on results of the BRUISE CONTROL–2 trial in more than 600 subjects.
Either strategy is reasonable depending on the clinical scenario, coprincipal investigator David Birnie, MD, said in presenting the results at the American Heart Association scientific sessions.
When atrial fibrillation (AF) patients on direct oral anticoagulants (DOACs) present for device surgery, there’s concern that keeping them on the drugs will increase the bleeding risk, but that taking them off will increase the stroke risk. “We sought to resolve this dilemma,” said Dr. Birnie, an electrophysiologist and director of the arrhythmia service at the University of Ottawa Heart Institute.
The subjects were on dabigatran, rivaroxaban, or apixaban, about a third in each group; 328 were randomized to continue their daily dosing, including on the day of surgery. The other 334 were randomized to interrupted treatment. For rivaroxaban and apixaban, that meant taking their last dose 2 days before surgery. Dabigatran patients discontinued the drug 1-2 days beforehand, depending on glomerular filtration rate. Patients resumed treatment about 24 hours after surgery. CHA2DS2-VASc scores were a mean of 3.9 in both arms, and at least 2 in all participants.
The rate of clinically significant hematoma – the primary outcome in the study, defined as a hematoma requiring prolonged hospitalization, interrupted postoperative anticoagulation, or reoperation to evacuate – was identical in both arms, 2.1% (seven patients each). There were two ischemic strokes, one in each arm. There was one delayed cardiac tamponade in the continuation arm and one pericardial effusion in the interrupted arm. The three deaths in the trial were not related to device placement.
So, what to do depends on the clinical scenario, Dr. Birnie said in an interview. If someone needs urgent placement and there’s no time to wait for DOAC washout, “it’s quite reasonable to go ahead.” Also, “if somebody is at extremely high risk for stroke, then it’s very reasonable to continue the drug.”
On the other hand, “if someone has a much lower stroke risk, then the risk-benefit ratio is probably in the opposite direction, so temporarily discontinuing the drug is the right thing to do,” he said.
Dr. Birnie cautioned that although continued DOAC may reduce the risk of thromboembolism, “this study was not designed with power to answer this.”
“We are already putting these findings into practice” in Ottawa, he said. “Our protocol” – as in many places – “ was always to stop anticoagulation for 2 or 3 days, but now, for very high-risk patients – high-risk AF, unstable temporary pacing, that type of thing – we are very comfortable continuing it,” he said. The study follows up a previous randomized trial by Dr. Birnie and his colleagues that pitted continued warfarin against heparin bridging for AF device placement. There were far fewer device pocket hematomas with uninterrupted warfarin (N Engl J Med. 2013 May 30;368[22]:2084-93).
The team wanted to repeat the study using DOACs, since their use has grown substantially, with the majority of AF patients now on them.
The arms in BRUISE CONTROL–2 (Strategy of Continued Versus Interrupted Novel Oral Anticoagulant at Time of Device Surgery in Patients With Moderate to High Risk of Arterial Thromboembolic Events) were well matched, with a mean age of about 74 years; men made up more than 70% of the subjects in both arms. About 17% of the participants were on chronic aspirin therapy and about 4% were on clopidogrel, in each arm. The uninterrupted DOAC group went about 14 hours between their last preop and first postop DOAC dose. The interrupted group went about 72 hours.
BRUISE CONTROL–2 was funded by the Heart and Stroke Foundation of Canada, Boehringer Ingelheim, Bayer, Pfizer, and Bristol-Myers Squibb, among others. Dr. Birnie had no relevant financial disclosures.
ANAHEIM, CALIF. – Whether direct oral anticoagulants are continued or interrupted for device placement in atrial fibrillation patients, the risk of device pocket hematoma or stroke is very low, based on results of the BRUISE CONTROL–2 trial in more than 600 subjects.
Either strategy is reasonable depending on the clinical scenario, coprincipal investigator David Birnie, MD, said in presenting the results at the American Heart Association scientific sessions.
When atrial fibrillation (AF) patients on direct oral anticoagulants (DOACs) present for device surgery, there’s concern that keeping them on the drugs will increase the bleeding risk, but that taking them off will increase the stroke risk. “We sought to resolve this dilemma,” said Dr. Birnie, an electrophysiologist and director of the arrhythmia service at the University of Ottawa Heart Institute.
The subjects were on dabigatran, rivaroxaban, or apixaban, about a third in each group; 328 were randomized to continue their daily dosing, including on the day of surgery. The other 334 were randomized to interrupted treatment. For rivaroxaban and apixaban, that meant taking their last dose 2 days before surgery. Dabigatran patients discontinued the drug 1-2 days beforehand, depending on glomerular filtration rate. Patients resumed treatment about 24 hours after surgery. CHA2DS2-VASc scores were a mean of 3.9 in both arms, and at least 2 in all participants.
The rate of clinically significant hematoma – the primary outcome in the study, defined as a hematoma requiring prolonged hospitalization, interrupted postoperative anticoagulation, or reoperation to evacuate – was identical in both arms, 2.1% (seven patients each). There were two ischemic strokes, one in each arm. There was one delayed cardiac tamponade in the continuation arm and one pericardial effusion in the interrupted arm. The three deaths in the trial were not related to device placement.
So, what to do depends on the clinical scenario, Dr. Birnie said in an interview. If someone needs urgent placement and there’s no time to wait for DOAC washout, “it’s quite reasonable to go ahead.” Also, “if somebody is at extremely high risk for stroke, then it’s very reasonable to continue the drug.”
On the other hand, “if someone has a much lower stroke risk, then the risk-benefit ratio is probably in the opposite direction, so temporarily discontinuing the drug is the right thing to do,” he said.
Dr. Birnie cautioned that although continued DOAC may reduce the risk of thromboembolism, “this study was not designed with power to answer this.”
“We are already putting these findings into practice” in Ottawa, he said. “Our protocol” – as in many places – “ was always to stop anticoagulation for 2 or 3 days, but now, for very high-risk patients – high-risk AF, unstable temporary pacing, that type of thing – we are very comfortable continuing it,” he said. The study follows up a previous randomized trial by Dr. Birnie and his colleagues that pitted continued warfarin against heparin bridging for AF device placement. There were far fewer device pocket hematomas with uninterrupted warfarin (N Engl J Med. 2013 May 30;368[22]:2084-93).
The team wanted to repeat the study using DOACs, since their use has grown substantially, with the majority of AF patients now on them.
The arms in BRUISE CONTROL–2 (Strategy of Continued Versus Interrupted Novel Oral Anticoagulant at Time of Device Surgery in Patients With Moderate to High Risk of Arterial Thromboembolic Events) were well matched, with a mean age of about 74 years; men made up more than 70% of the subjects in both arms. About 17% of the participants were on chronic aspirin therapy and about 4% were on clopidogrel, in each arm. The uninterrupted DOAC group went about 14 hours between their last preop and first postop DOAC dose. The interrupted group went about 72 hours.
BRUISE CONTROL–2 was funded by the Heart and Stroke Foundation of Canada, Boehringer Ingelheim, Bayer, Pfizer, and Bristol-Myers Squibb, among others. Dr. Birnie had no relevant financial disclosures.
ANAHEIM, CALIF. – Whether direct oral anticoagulants are continued or interrupted for device placement in atrial fibrillation patients, the risk of device pocket hematoma or stroke is very low, based on results of the BRUISE CONTROL–2 trial in more than 600 subjects.
Either strategy is reasonable depending on the clinical scenario, coprincipal investigator David Birnie, MD, said in presenting the results at the American Heart Association scientific sessions.
When atrial fibrillation (AF) patients on direct oral anticoagulants (DOACs) present for device surgery, there’s concern that keeping them on the drugs will increase the bleeding risk, but that taking them off will increase the stroke risk. “We sought to resolve this dilemma,” said Dr. Birnie, an electrophysiologist and director of the arrhythmia service at the University of Ottawa Heart Institute.
The subjects were on dabigatran, rivaroxaban, or apixaban, about a third in each group; 328 were randomized to continue their daily dosing, including on the day of surgery. The other 334 were randomized to interrupted treatment. For rivaroxaban and apixaban, that meant taking their last dose 2 days before surgery. Dabigatran patients discontinued the drug 1-2 days beforehand, depending on glomerular filtration rate. Patients resumed treatment about 24 hours after surgery. CHA2DS2-VASc scores were a mean of 3.9 in both arms, and at least 2 in all participants.
The rate of clinically significant hematoma – the primary outcome in the study, defined as a hematoma requiring prolonged hospitalization, interrupted postoperative anticoagulation, or reoperation to evacuate – was identical in both arms, 2.1% (seven patients each). There were two ischemic strokes, one in each arm. There was one delayed cardiac tamponade in the continuation arm and one pericardial effusion in the interrupted arm. The three deaths in the trial were not related to device placement.
So, what to do depends on the clinical scenario, Dr. Birnie said in an interview. If someone needs urgent placement and there’s no time to wait for DOAC washout, “it’s quite reasonable to go ahead.” Also, “if somebody is at extremely high risk for stroke, then it’s very reasonable to continue the drug.”
On the other hand, “if someone has a much lower stroke risk, then the risk-benefit ratio is probably in the opposite direction, so temporarily discontinuing the drug is the right thing to do,” he said.
Dr. Birnie cautioned that although continued DOAC may reduce the risk of thromboembolism, “this study was not designed with power to answer this.”
“We are already putting these findings into practice” in Ottawa, he said. “Our protocol” – as in many places – “ was always to stop anticoagulation for 2 or 3 days, but now, for very high-risk patients – high-risk AF, unstable temporary pacing, that type of thing – we are very comfortable continuing it,” he said. The study follows up a previous randomized trial by Dr. Birnie and his colleagues that pitted continued warfarin against heparin bridging for AF device placement. There were far fewer device pocket hematomas with uninterrupted warfarin (N Engl J Med. 2013 May 30;368[22]:2084-93).
The team wanted to repeat the study using DOACs, since their use has grown substantially, with the majority of AF patients now on them.
The arms in BRUISE CONTROL–2 (Strategy of Continued Versus Interrupted Novel Oral Anticoagulant at Time of Device Surgery in Patients With Moderate to High Risk of Arterial Thromboembolic Events) were well matched, with a mean age of about 74 years; men made up more than 70% of the subjects in both arms. About 17% of the participants were on chronic aspirin therapy and about 4% were on clopidogrel, in each arm. The uninterrupted DOAC group went about 14 hours between their last preop and first postop DOAC dose. The interrupted group went about 72 hours.
BRUISE CONTROL–2 was funded by the Heart and Stroke Foundation of Canada, Boehringer Ingelheim, Bayer, Pfizer, and Bristol-Myers Squibb, among others. Dr. Birnie had no relevant financial disclosures.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: The rate of clinically significant hematoma was identical in both arms, at 2.1% (seven patients each).
Data source: BRUISE CONTROL-2, a randomized trial with more than 600 subjects.
Disclosures: The work was funded by the Heart and Stroke Foundation of Canada, Boehringer Ingelheim, Bayer, Pfizer, and Bristol-Myers Squibb, among others. The presenter had no relevant financial disclosures.
Pain is a risk factor for endometrial ablation failure
NATIONAL HARBOR, MD. – Second-generation endometrial ablations performed for an indication related to pain were significantly more likely to fail, according to findings presented at the AAGL Global Congress.
“We know that endometrial ablation carries a reasonable risk of failure – meaning a second ablation or hysterectomy procedure – and that rate can vary institutionally,” Matthew Hoffman, MD, chair of obstetrics and gynecology at Christiana Care Health Center, Newark, Del., said in an interview prior to the meeting. “Part of our goal is to examine patients who had pain as an indication for their procedure and to better understand if that served as an independent risk factor for women who would ultimately require additional surgical intervention.”
In a retrospective study, researchers identified 5,818 women who had undergone an ablation between October 2003 and March 2016 at a community hospital affiliated with the Christina Care Health System. Patients had either a radiofrequency ablation (3,706), hydrothermablation (1,786), or uterine balloon ablation (326).
The majority of the patients were white. Pain indications included pelvic pain, dysmenorrhea, dyspareunia, lower abdominal pain, endometriosis, and adenomyosis.
Investigators found a hysterectomy rate of 19.2% among the 437 patients who had pain as an indication for ablation, compared with 13.5% of patients with different indications (P = .001).
Secondary outcomes showed older women who underwent ablation for pain were still less likely to fail than were younger patients (odds ratio, 0.96, 95% confidence interval, .95-.97). “Older age, especially age 50 years or older, with the indication of pain, was actually protective against hysterectomy,” Meagan Cramer, MD, a resident physician at Christina Care Health System and one of the study researchers, said in an interview. “So even though pain itself was a risk factor, if you were in pain and older than 50 you were less likely to need a hysterectomy.”
The data used were collected at a single center, potentially limiting the generalizability of the findings.
Dr. Hoffman and Dr. Cramer suggested using hormonal IUDs as an alternative treatment when counseling patients who may be at risk for a failed ablation.
“This is a call for folks to look at a diverse number of risk factors and to look at this data to better counsel patients in how they choose and select procedures to get to the endpoints that you want,” Dr. Hoffman said.
The researchers reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
NATIONAL HARBOR, MD. – Second-generation endometrial ablations performed for an indication related to pain were significantly more likely to fail, according to findings presented at the AAGL Global Congress.
“We know that endometrial ablation carries a reasonable risk of failure – meaning a second ablation or hysterectomy procedure – and that rate can vary institutionally,” Matthew Hoffman, MD, chair of obstetrics and gynecology at Christiana Care Health Center, Newark, Del., said in an interview prior to the meeting. “Part of our goal is to examine patients who had pain as an indication for their procedure and to better understand if that served as an independent risk factor for women who would ultimately require additional surgical intervention.”
In a retrospective study, researchers identified 5,818 women who had undergone an ablation between October 2003 and March 2016 at a community hospital affiliated with the Christina Care Health System. Patients had either a radiofrequency ablation (3,706), hydrothermablation (1,786), or uterine balloon ablation (326).
The majority of the patients were white. Pain indications included pelvic pain, dysmenorrhea, dyspareunia, lower abdominal pain, endometriosis, and adenomyosis.
Investigators found a hysterectomy rate of 19.2% among the 437 patients who had pain as an indication for ablation, compared with 13.5% of patients with different indications (P = .001).
Secondary outcomes showed older women who underwent ablation for pain were still less likely to fail than were younger patients (odds ratio, 0.96, 95% confidence interval, .95-.97). “Older age, especially age 50 years or older, with the indication of pain, was actually protective against hysterectomy,” Meagan Cramer, MD, a resident physician at Christina Care Health System and one of the study researchers, said in an interview. “So even though pain itself was a risk factor, if you were in pain and older than 50 you were less likely to need a hysterectomy.”
The data used were collected at a single center, potentially limiting the generalizability of the findings.
Dr. Hoffman and Dr. Cramer suggested using hormonal IUDs as an alternative treatment when counseling patients who may be at risk for a failed ablation.
“This is a call for folks to look at a diverse number of risk factors and to look at this data to better counsel patients in how they choose and select procedures to get to the endpoints that you want,” Dr. Hoffman said.
The researchers reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
NATIONAL HARBOR, MD. – Second-generation endometrial ablations performed for an indication related to pain were significantly more likely to fail, according to findings presented at the AAGL Global Congress.
“We know that endometrial ablation carries a reasonable risk of failure – meaning a second ablation or hysterectomy procedure – and that rate can vary institutionally,” Matthew Hoffman, MD, chair of obstetrics and gynecology at Christiana Care Health Center, Newark, Del., said in an interview prior to the meeting. “Part of our goal is to examine patients who had pain as an indication for their procedure and to better understand if that served as an independent risk factor for women who would ultimately require additional surgical intervention.”
In a retrospective study, researchers identified 5,818 women who had undergone an ablation between October 2003 and March 2016 at a community hospital affiliated with the Christina Care Health System. Patients had either a radiofrequency ablation (3,706), hydrothermablation (1,786), or uterine balloon ablation (326).
The majority of the patients were white. Pain indications included pelvic pain, dysmenorrhea, dyspareunia, lower abdominal pain, endometriosis, and adenomyosis.
Investigators found a hysterectomy rate of 19.2% among the 437 patients who had pain as an indication for ablation, compared with 13.5% of patients with different indications (P = .001).
Secondary outcomes showed older women who underwent ablation for pain were still less likely to fail than were younger patients (odds ratio, 0.96, 95% confidence interval, .95-.97). “Older age, especially age 50 years or older, with the indication of pain, was actually protective against hysterectomy,” Meagan Cramer, MD, a resident physician at Christina Care Health System and one of the study researchers, said in an interview. “So even though pain itself was a risk factor, if you were in pain and older than 50 you were less likely to need a hysterectomy.”
The data used were collected at a single center, potentially limiting the generalizability of the findings.
Dr. Hoffman and Dr. Cramer suggested using hormonal IUDs as an alternative treatment when counseling patients who may be at risk for a failed ablation.
“This is a call for folks to look at a diverse number of risk factors and to look at this data to better counsel patients in how they choose and select procedures to get to the endpoints that you want,” Dr. Hoffman said.
The researchers reported no relevant financial disclosures.
[email protected]
On Twitter @eaztweets
AT AAGL 2017
Key clinical point:
Major finding: Ablation had a hysterectomy rate of 19.2% when pain was an indication, compared with 13.5% for other indications.
Data source: Retrospective study of 5,818 endometrial ablations conducted between October 2003 and March 2016 at a single institution.
Disclosures: The researchers reported no relevant financial disclosures.