User login
ASCO updates NSCLC guidelines for adjuvant therapy
Adjuvant cisplatin-based chemotherapy is recommended for routine use in non–small cell lung cancer patients with stage IIA, IIB, or IIIA disease who have undergone complete surgical resections, according to updated guidelines from the American Society of Clinical Oncology.
In patients with stage IA disease, the guidelines recommend against cisplatin-based chemotherapy. The new guidelines are based on a systematic review current to January 2016 and an American Society for Radiation Oncology guideline and systematic review, which ASCO had already endorsed, which formed the basis for recommendations on adjuvant radiation therapy, Mark G. Kris, MD, and panel authors said (J Clin Oncol. 2017 April 26. doi: 10.1200/JCO.2017.72.4401).
The guidelines, available online, also recommend against routine cisplatin-based chemotherapy in patients with stage IB disease, but they suggest an evaluation of these patients to explore the pros and cons of adjuvant chemotherapy.
With respect to radiation, the authors recommend against it for patients with resected stage I or stage II disease, and they recommend against it for routine use in patients with stage IIIA. However, in patients with IIIA N2 disease, patients should be evaluated postoperatively, in consultation with a medical oncologist, for the potential risks and benefits of adjuvant radiation.
The authors also provide some recommendations for communicating with patients regarding treatment decisions. There are few studies examining this question, so the recommendations are based on low-quality evidence.
Non–small cell lung cancer patients may have complex social, psychological, and medical issues, and discussions should be carried out with this in mind. Pain, impaired breathing, and fatigue are common after surgery, and smoking cessation can lead to short-term stress as a result of nicotine withdrawal. Older patients may have a range of comorbidities.
Studies show that patients are most satisfied if they feel that physicians allow them to share in the decision making, and if they are given sufficient time to choose. To that end, the authors recommend a session dedicated to discussion of adjuvant therapy.
Communicating risk of death is challenging for many reasons. Patients should be asked how they would like to hear about their risks: some prefer general terms, while others may opt for numbers, charts, or graphs. The guidelines include a risk chart that can help patients understand the potential benefits and risks of chemotherapy.
The study authors report financial relationships with numerous pharmaceutical companies.
Adjuvant cisplatin-based chemotherapy is recommended for routine use in non–small cell lung cancer patients with stage IIA, IIB, or IIIA disease who have undergone complete surgical resections, according to updated guidelines from the American Society of Clinical Oncology.
In patients with stage IA disease, the guidelines recommend against cisplatin-based chemotherapy. The new guidelines are based on a systematic review current to January 2016 and an American Society for Radiation Oncology guideline and systematic review, which ASCO had already endorsed, which formed the basis for recommendations on adjuvant radiation therapy, Mark G. Kris, MD, and panel authors said (J Clin Oncol. 2017 April 26. doi: 10.1200/JCO.2017.72.4401).
The guidelines, available online, also recommend against routine cisplatin-based chemotherapy in patients with stage IB disease, but they suggest an evaluation of these patients to explore the pros and cons of adjuvant chemotherapy.
With respect to radiation, the authors recommend against it for patients with resected stage I or stage II disease, and they recommend against it for routine use in patients with stage IIIA. However, in patients with IIIA N2 disease, patients should be evaluated postoperatively, in consultation with a medical oncologist, for the potential risks and benefits of adjuvant radiation.
The authors also provide some recommendations for communicating with patients regarding treatment decisions. There are few studies examining this question, so the recommendations are based on low-quality evidence.
Non–small cell lung cancer patients may have complex social, psychological, and medical issues, and discussions should be carried out with this in mind. Pain, impaired breathing, and fatigue are common after surgery, and smoking cessation can lead to short-term stress as a result of nicotine withdrawal. Older patients may have a range of comorbidities.
Studies show that patients are most satisfied if they feel that physicians allow them to share in the decision making, and if they are given sufficient time to choose. To that end, the authors recommend a session dedicated to discussion of adjuvant therapy.
Communicating risk of death is challenging for many reasons. Patients should be asked how they would like to hear about their risks: some prefer general terms, while others may opt for numbers, charts, or graphs. The guidelines include a risk chart that can help patients understand the potential benefits and risks of chemotherapy.
The study authors report financial relationships with numerous pharmaceutical companies.
Adjuvant cisplatin-based chemotherapy is recommended for routine use in non–small cell lung cancer patients with stage IIA, IIB, or IIIA disease who have undergone complete surgical resections, according to updated guidelines from the American Society of Clinical Oncology.
In patients with stage IA disease, the guidelines recommend against cisplatin-based chemotherapy. The new guidelines are based on a systematic review current to January 2016 and an American Society for Radiation Oncology guideline and systematic review, which ASCO had already endorsed, which formed the basis for recommendations on adjuvant radiation therapy, Mark G. Kris, MD, and panel authors said (J Clin Oncol. 2017 April 26. doi: 10.1200/JCO.2017.72.4401).
The guidelines, available online, also recommend against routine cisplatin-based chemotherapy in patients with stage IB disease, but they suggest an evaluation of these patients to explore the pros and cons of adjuvant chemotherapy.
With respect to radiation, the authors recommend against it for patients with resected stage I or stage II disease, and they recommend against it for routine use in patients with stage IIIA. However, in patients with IIIA N2 disease, patients should be evaluated postoperatively, in consultation with a medical oncologist, for the potential risks and benefits of adjuvant radiation.
The authors also provide some recommendations for communicating with patients regarding treatment decisions. There are few studies examining this question, so the recommendations are based on low-quality evidence.
Non–small cell lung cancer patients may have complex social, psychological, and medical issues, and discussions should be carried out with this in mind. Pain, impaired breathing, and fatigue are common after surgery, and smoking cessation can lead to short-term stress as a result of nicotine withdrawal. Older patients may have a range of comorbidities.
Studies show that patients are most satisfied if they feel that physicians allow them to share in the decision making, and if they are given sufficient time to choose. To that end, the authors recommend a session dedicated to discussion of adjuvant therapy.
Communicating risk of death is challenging for many reasons. Patients should be asked how they would like to hear about their risks: some prefer general terms, while others may opt for numbers, charts, or graphs. The guidelines include a risk chart that can help patients understand the potential benefits and risks of chemotherapy.
The study authors report financial relationships with numerous pharmaceutical companies.
TNFSF13B variant linked to MS and SLE
A variant in the TNFSF13B gene has been linked to susceptibility to both multiple sclerosis and systemic lupus erythematosus, according to a report published online April 26 in the New England Journal of Medicine.
This gene encodes the cytokine B-cell activating factor (BAFF), which is essential for B-cell activation, differentiation, and survival. BAFF is targeted by agents such as belimumab that are used in the treatment of autoimmune disorders, and is primarily produced by monocytes and neutrophils, said Maristella Steri, PhD, of Istituto di Ricerca Genetica e Biomedica, Consiglio Nazionale delle Ricerche Monserrato (Italy), and her associates.
The researchers have named this TNFSF13B variation “BAFF-var.”
Previous genome-wide association studies have identified more than 110 independent signals for MS and 43 for SLE but have not yet delineated the effector mechanisms for most of these associations. To explore these mechanisms in greater detail, Dr. Steri and her associates studied the population in Sardinia, Italy, which has the highest prevalences of MS and SLE in the world.
They performed genome-wide association studies and other genetic investigations in case-control sets of 2,934 patients with MS, 411 with SLE, and 3,392 control subjects, analyzing roughly 12.2 million single-nucleotide polymorphisms (SNPs). They ruled out rs1287404 as a likely variant driving the association and identified BAFF-var as the variant most strongly associated with MS (odds ratio, 1.27).
The investigators then replicated their findings in a series of genetic studies in case-control sets from mainland Italy (2,292 patients with MS, 503 with SLE, and 2,563 controls), Sweden (4,548 patients with MS and 3,481 controls), the United Kingdom (3,176 patients with MS and 2,958 controls), and the Iberian peninsula (1,120 patients with SLE and 1,300 controls). BAFF-var was most common across Sardinia, with a frequency of 26.5%, and became progressively less common moving northward (5.7% in Italy, 4.9% in Spain, 1.8% in the United Kingdom and Sweden).
Taken together, “these findings pinpoint BAFF-var as the variant in TNFSF13B that is most strongly associated with MS,” wrote Dr. Steri and her associates (N Engl J Med. 2017 Apr 27. doi: 10.1056/NEJMoa1610528).
BAFF-var also proved to be associated with SLE in case-control sets from Sardinia (OR, 1.38), mainland Italy (OR, 1.49), and the Iberian peninsula (OR, 1.55). This indicates that “the effect of BAFF-var is not restricted to MS alone,” they noted.
Further analyses showed that BAFF-var “dramatically” increased levels of soluble BAFF and circulating B cells, especially CD24+CD27+ cells, as well as total IgG, IgA, IgM, and monocytes. In one notable analysis, preclinical blood samples taken from Sardinians participating in a longitudinal study showed elevated levels of soluble BAFF in people who did not go on to develop MS until years later.
“We infer [from this] that BAFF-var is the causal variant driving an increase in soluble BAFF and a cascade of immune effects leading to increased autoimmunity risk,” Dr. Steri and her associates said.
Further study suggested that positive selection specifically favoring BAFF-var, not random genetic drift, accounted for the high frequency of this mutation in Sardinia and its progressively lower frequency moving northward. The most likely possibility is that BAFF-var was positively selected because it provided resistance to malaria, which was “strikingly prevalent” in Sardinia until it was eradicated in the 1950s. In mouse models, BAFF overexpression confers protection against lethal malaria.
“In addition, as shown here, BAFF-var increases antibody production, and classic findings showed that antibody transfer from adults with immunity to malaria to acutely infected children reduced blood-stage parasitemia and disease severity,” the investigators said.
“The evolutionary scenario we propose is that BAFF-var was selected as an adaptive response to malaria infection, resulting in an increased present-day risk of autoimmunity,” they said.
The Italian Foundation for Multiple Sclerosis, the National Institute on Aging, the Italian Ministry of Economy and Finance, the European Union, the National Human Genome Research Institute, and other organizations supported the study. Dr. Steri reported having no relevant disclosures; some of her associates reported ties to numerous industry sources.
Perhaps the next challenge is the clinical application of the findings from Steri et al. is to determine whether BAFF-var status can be used to stratify patients for a specific therapy.
These data clearly point in that direction, but the discriminatory power of this single variant may not be sufficient for clinical decision making.
In contrast, it does seem reasonable to examine whether stratifying patients according to their BAFF-var status would be useful in clinical trials assessing B-cell–directed therapies.
Thomas Korn, MD, of the Technical University of Munich and the Munich Cluster for Systems Neurology, reported ties to Biogen, Novartis, Merck Serono, and Bayer. Mohamed Oukka, PhD, of the University of Washington, Seattle, and the Center for Immunity and Immunotherapies at Seattle Children’s Research Institute, reported having no relevant disclosures. They made these remarks in an editorial accompanying Dr. Steri’s report (N Engl J Med. 2017 Apr 27. doi: 10.1056/NEJMe1700720).
Perhaps the next challenge is the clinical application of the findings from Steri et al. is to determine whether BAFF-var status can be used to stratify patients for a specific therapy.
These data clearly point in that direction, but the discriminatory power of this single variant may not be sufficient for clinical decision making.
In contrast, it does seem reasonable to examine whether stratifying patients according to their BAFF-var status would be useful in clinical trials assessing B-cell–directed therapies.
Thomas Korn, MD, of the Technical University of Munich and the Munich Cluster for Systems Neurology, reported ties to Biogen, Novartis, Merck Serono, and Bayer. Mohamed Oukka, PhD, of the University of Washington, Seattle, and the Center for Immunity and Immunotherapies at Seattle Children’s Research Institute, reported having no relevant disclosures. They made these remarks in an editorial accompanying Dr. Steri’s report (N Engl J Med. 2017 Apr 27. doi: 10.1056/NEJMe1700720).
Perhaps the next challenge is the clinical application of the findings from Steri et al. is to determine whether BAFF-var status can be used to stratify patients for a specific therapy.
These data clearly point in that direction, but the discriminatory power of this single variant may not be sufficient for clinical decision making.
In contrast, it does seem reasonable to examine whether stratifying patients according to their BAFF-var status would be useful in clinical trials assessing B-cell–directed therapies.
Thomas Korn, MD, of the Technical University of Munich and the Munich Cluster for Systems Neurology, reported ties to Biogen, Novartis, Merck Serono, and Bayer. Mohamed Oukka, PhD, of the University of Washington, Seattle, and the Center for Immunity and Immunotherapies at Seattle Children’s Research Institute, reported having no relevant disclosures. They made these remarks in an editorial accompanying Dr. Steri’s report (N Engl J Med. 2017 Apr 27. doi: 10.1056/NEJMe1700720).
A variant in the TNFSF13B gene has been linked to susceptibility to both multiple sclerosis and systemic lupus erythematosus, according to a report published online April 26 in the New England Journal of Medicine.
This gene encodes the cytokine B-cell activating factor (BAFF), which is essential for B-cell activation, differentiation, and survival. BAFF is targeted by agents such as belimumab that are used in the treatment of autoimmune disorders, and is primarily produced by monocytes and neutrophils, said Maristella Steri, PhD, of Istituto di Ricerca Genetica e Biomedica, Consiglio Nazionale delle Ricerche Monserrato (Italy), and her associates.
The researchers have named this TNFSF13B variation “BAFF-var.”
Previous genome-wide association studies have identified more than 110 independent signals for MS and 43 for SLE but have not yet delineated the effector mechanisms for most of these associations. To explore these mechanisms in greater detail, Dr. Steri and her associates studied the population in Sardinia, Italy, which has the highest prevalences of MS and SLE in the world.
They performed genome-wide association studies and other genetic investigations in case-control sets of 2,934 patients with MS, 411 with SLE, and 3,392 control subjects, analyzing roughly 12.2 million single-nucleotide polymorphisms (SNPs). They ruled out rs1287404 as a likely variant driving the association and identified BAFF-var as the variant most strongly associated with MS (odds ratio, 1.27).
The investigators then replicated their findings in a series of genetic studies in case-control sets from mainland Italy (2,292 patients with MS, 503 with SLE, and 2,563 controls), Sweden (4,548 patients with MS and 3,481 controls), the United Kingdom (3,176 patients with MS and 2,958 controls), and the Iberian peninsula (1,120 patients with SLE and 1,300 controls). BAFF-var was most common across Sardinia, with a frequency of 26.5%, and became progressively less common moving northward (5.7% in Italy, 4.9% in Spain, 1.8% in the United Kingdom and Sweden).
Taken together, “these findings pinpoint BAFF-var as the variant in TNFSF13B that is most strongly associated with MS,” wrote Dr. Steri and her associates (N Engl J Med. 2017 Apr 27. doi: 10.1056/NEJMoa1610528).
BAFF-var also proved to be associated with SLE in case-control sets from Sardinia (OR, 1.38), mainland Italy (OR, 1.49), and the Iberian peninsula (OR, 1.55). This indicates that “the effect of BAFF-var is not restricted to MS alone,” they noted.
Further analyses showed that BAFF-var “dramatically” increased levels of soluble BAFF and circulating B cells, especially CD24+CD27+ cells, as well as total IgG, IgA, IgM, and monocytes. In one notable analysis, preclinical blood samples taken from Sardinians participating in a longitudinal study showed elevated levels of soluble BAFF in people who did not go on to develop MS until years later.
“We infer [from this] that BAFF-var is the causal variant driving an increase in soluble BAFF and a cascade of immune effects leading to increased autoimmunity risk,” Dr. Steri and her associates said.
Further study suggested that positive selection specifically favoring BAFF-var, not random genetic drift, accounted for the high frequency of this mutation in Sardinia and its progressively lower frequency moving northward. The most likely possibility is that BAFF-var was positively selected because it provided resistance to malaria, which was “strikingly prevalent” in Sardinia until it was eradicated in the 1950s. In mouse models, BAFF overexpression confers protection against lethal malaria.
“In addition, as shown here, BAFF-var increases antibody production, and classic findings showed that antibody transfer from adults with immunity to malaria to acutely infected children reduced blood-stage parasitemia and disease severity,” the investigators said.
“The evolutionary scenario we propose is that BAFF-var was selected as an adaptive response to malaria infection, resulting in an increased present-day risk of autoimmunity,” they said.
The Italian Foundation for Multiple Sclerosis, the National Institute on Aging, the Italian Ministry of Economy and Finance, the European Union, the National Human Genome Research Institute, and other organizations supported the study. Dr. Steri reported having no relevant disclosures; some of her associates reported ties to numerous industry sources.
A variant in the TNFSF13B gene has been linked to susceptibility to both multiple sclerosis and systemic lupus erythematosus, according to a report published online April 26 in the New England Journal of Medicine.
This gene encodes the cytokine B-cell activating factor (BAFF), which is essential for B-cell activation, differentiation, and survival. BAFF is targeted by agents such as belimumab that are used in the treatment of autoimmune disorders, and is primarily produced by monocytes and neutrophils, said Maristella Steri, PhD, of Istituto di Ricerca Genetica e Biomedica, Consiglio Nazionale delle Ricerche Monserrato (Italy), and her associates.
The researchers have named this TNFSF13B variation “BAFF-var.”
Previous genome-wide association studies have identified more than 110 independent signals for MS and 43 for SLE but have not yet delineated the effector mechanisms for most of these associations. To explore these mechanisms in greater detail, Dr. Steri and her associates studied the population in Sardinia, Italy, which has the highest prevalences of MS and SLE in the world.
They performed genome-wide association studies and other genetic investigations in case-control sets of 2,934 patients with MS, 411 with SLE, and 3,392 control subjects, analyzing roughly 12.2 million single-nucleotide polymorphisms (SNPs). They ruled out rs1287404 as a likely variant driving the association and identified BAFF-var as the variant most strongly associated with MS (odds ratio, 1.27).
The investigators then replicated their findings in a series of genetic studies in case-control sets from mainland Italy (2,292 patients with MS, 503 with SLE, and 2,563 controls), Sweden (4,548 patients with MS and 3,481 controls), the United Kingdom (3,176 patients with MS and 2,958 controls), and the Iberian peninsula (1,120 patients with SLE and 1,300 controls). BAFF-var was most common across Sardinia, with a frequency of 26.5%, and became progressively less common moving northward (5.7% in Italy, 4.9% in Spain, 1.8% in the United Kingdom and Sweden).
Taken together, “these findings pinpoint BAFF-var as the variant in TNFSF13B that is most strongly associated with MS,” wrote Dr. Steri and her associates (N Engl J Med. 2017 Apr 27. doi: 10.1056/NEJMoa1610528).
BAFF-var also proved to be associated with SLE in case-control sets from Sardinia (OR, 1.38), mainland Italy (OR, 1.49), and the Iberian peninsula (OR, 1.55). This indicates that “the effect of BAFF-var is not restricted to MS alone,” they noted.
Further analyses showed that BAFF-var “dramatically” increased levels of soluble BAFF and circulating B cells, especially CD24+CD27+ cells, as well as total IgG, IgA, IgM, and monocytes. In one notable analysis, preclinical blood samples taken from Sardinians participating in a longitudinal study showed elevated levels of soluble BAFF in people who did not go on to develop MS until years later.
“We infer [from this] that BAFF-var is the causal variant driving an increase in soluble BAFF and a cascade of immune effects leading to increased autoimmunity risk,” Dr. Steri and her associates said.
Further study suggested that positive selection specifically favoring BAFF-var, not random genetic drift, accounted for the high frequency of this mutation in Sardinia and its progressively lower frequency moving northward. The most likely possibility is that BAFF-var was positively selected because it provided resistance to malaria, which was “strikingly prevalent” in Sardinia until it was eradicated in the 1950s. In mouse models, BAFF overexpression confers protection against lethal malaria.
“In addition, as shown here, BAFF-var increases antibody production, and classic findings showed that antibody transfer from adults with immunity to malaria to acutely infected children reduced blood-stage parasitemia and disease severity,” the investigators said.
“The evolutionary scenario we propose is that BAFF-var was selected as an adaptive response to malaria infection, resulting in an increased present-day risk of autoimmunity,” they said.
The Italian Foundation for Multiple Sclerosis, the National Institute on Aging, the Italian Ministry of Economy and Finance, the European Union, the National Human Genome Research Institute, and other organizations supported the study. Dr. Steri reported having no relevant disclosures; some of her associates reported ties to numerous industry sources.
Key clinical point: A variant in the TNFSF13B gene has been linked to susceptibility to both multiple sclerosis and systemic lupus erythematosus.
Major finding: BAFF-var was the TNFSF13B variant most strongly associated with MS in Sardinia (OR, 1.27), and was also associated with SLE in Sardinia (OR, 1.38), mainland Italy (OR, 1.49), and the Iberian peninsula (OR, 1.55).
Data source: A series of genome-wide association studies and other genetic studies involving thousands of patients with MS or SLE in Sardinia and confirmed in thousands of patients across Italy, Spain, Sweden, and the United Kingdom.
Disclosures: The Italian Foundation for Multiple Sclerosis, the National Institute on Aging, the Italian Ministry of Economy and Finance, the European Union, the National Human Genome Research Institute, and other organizations supported the study. Dr. Steri reported having no relevant disclosures; some of her associates reported ties to numerous industry sources.
For girls with Turner syndrome, experimental fertility preservation may offer the hope of a baby of their own
ORLANDO – Fertility preservation techniques pioneered in young cancer patients may someday allow some women with Turner syndrome to give birth to their own children, without relying on donated eggs.
Spontaneous conception and live birth are exceedingly rare among women with the genetic disorder. Until very recently, adoption was the only practical way for most to grow a family. In the last decade, however, fertility specialists in Europe and the United States have had good success with in vitro fertilization using donated eggs. Now, those clinicians are aiming for a higher goal: babies born from a patient’s own eggs, cryopreserved either individually or within whole ovarian tissue.
These are not pipe dreams, according to experts interviewed for this story. Autologous oocyte freezing is well established in healthy women and is now coming of age in cancer patients, with recent reports of live births. Ovarian tissue freezing and reimplantation is a much newer technique, also pioneered in cancer patients. To date, more than 70 live births have occurred from ovarian cortical tissue conservation and later transplantation in adults. Last December brought the first report of a live birth to a childhood cancer survivor who had prepubertal ovarian tissue frozen before chemotherapy. And a 2015 report detailed the case of a girl with primary ovarian failure secondary to sickle cell anemia treatment. At 25, she gave birth to a healthy child conceived from ovarian tissue removed when she was 14 years old.
Not all clinicians so enthusiastically embrace this future, however. A new set of consensus guidelines for the management of girls and women with Turner syndrome is in the works and will recommend a more conservative clinical approach, according to Nelly Mauras, MD, chief of endocrinology, diabetes, and metabolism at the Nemours Children’s Health System in Jacksonville, Fla.
A group of academic and patient advocacy stakeholders is cooperatively honing the document based on a meeting last summer in Cincinnati. These groups include the European Society of Endocrinology, the Endocrine Society, the U.S. Pediatric Endocrine Society, the European Society for Pediatric Endocrinology, Cardiology, and Reproductive Endocrinology, as well as Turner syndrome patient advocacy groups.
Dr. Mauras said the guideline will be “less discouraging” than the existing one issued in 2012 by the American Society of Reproductive Medicine. In its 2012 guidelines, the society identified Turner syndrome as a relative contraindication to pregnancy and an absolute contraindication in those with documented cardiac anomalies. However, greater experience has since been accrued in reproductive techniques of oocyte donation in Turner, with better outcomes.
The upcoming guidelines, however, will still recommend strongly against ovarian stimulation for fertility preservation for girls younger than 12, Dr. Mauras said, and will not recommend ovarian tissue conservation. “We just do not have the safety data and pregnancy outcomes that we need to give strong recommendations for these treatments,” she said. “These are still considered experimental treatments for girls with Turner syndrome.”
Turner syndrome, caused by a deletion of one X chromosome, throws a unique curve into the game – very early ovarian failure. Those with a complete deletion (45,X) begin losing their primordial ovarian follicles even before birth. Most will never experience spontaneous puberty; even if they do, their egg reserve is virtually gone soon after. Ovarian reserve may not be completely lost in girls with mosaicism, however, who have the X deletion in only a portion of their cells (46,XX/45,X). Some will enter puberty, and about 5% may even conceive spontaneously in younger years. But of the majority of Turner girls eventually experience complete ovarian failure.
This means that fertility preservation can’t be a wait-and-see issue, according to Kutluk Oktay, MD, PhD, a fertility specialist on the leading edge of this issue in the United States.
“We have to be proactive,” said Dr. Oktay, professor of obstetrics and gynecology at New York Medical College, Valhalla. “If we wait until girls are 12 or 13 to address this, a majority will have totally depleted their ovarian reserve by then. They will have no option other than an egg donor or adoption. We are suggesting that they should be screened as soon as they are diagnosed, and if they and their parents wish it, something should be done before it’s too late.”
Dr. Oktay is also the founder of fertilitypreservation.org, which specializes in advanced fertility treatments for cancer patients. He is one of a handful of physicians in the United States who advocate early oocyte harvesting in peripubertal girls and ovarian tissue harvesting in prepubertal girls with Turner syndrome. Last year, in conjunction with the Turner Syndrome Foundation, he and his colleagues published a set of guidelines for preserving fertility in these patients.
The paper recommends fertility assessment pathways for pre- and postpubertal girls. For both groups, Dr. Oktay employs serial assessments of ovarian reserve by monitoring several hormones, including follicle-stimulating hormone, luteinizing hormone, and antimüllerian hormone (AMH). Produced by primordial follicles, AMH declines as egg reserve declines over a lifetime, and is considered an accurate marker of ovarian reserve. When a girl experiences two consecutive AMH declines, egg depletion is probably accelerating. “This is the time to consider fertility preservation,” he said.
If a girl is peri- or postpubertal, the choice would probably be ovarian stimulation with the goal of retrieving mature oocytes. For prepubertal girls, the best choice is probably ovarian tissue cryopreservation. But because the egg reserve may already be spotty inside the ovary, he recommended freezing it en bloc, rather than preserving just cortical sections.
Because these techniques are only beginning to be used in young Turner patients, neither has been tested yet to see if it would result in a pregnancy. However, Dr. Oktay said, more than 80 babies have been born to women with other disorders who had ovaries frozen as adults. And European women with Turner syndrome have been successfully bearing children with donated oocytes for years.
“I don’t differentiate Europe from the U.S.,” he said. “We have no reason to believe Turner syndrome girls would be any different here than they are there.”
Pregnancy rates by egg donation in Turner syndrome patients are about half that typically seen in an otherwise healthy infertile woman, according to numerous sources; with a take-home baby rate of about 18%. There are numerous reasons for this. The miscarriage rate in Turner patients is about 44%. Women with Turner tend to have smaller uteri, with thinner endometrium, mostly because of the lack of estrogen.
But with careful management, those who do conceive can safely deliver a healthy baby, said Outi Hovatta, MD, a Finnish fertility specialist who has done extensive work in the area. “In Europe, we have been doing this quite liberally for years, and haven’t had a bad experience,” she said in an interview.
A 2013 review summarized both the success and the risks of these pregnancies. It examined obstetric and neonatal outcomes among 106 women with Turner syndrome who gave birth via egg donation from 1992 to 2011 in Sweden, Finland, and Denmark.
Most (70%) had a single embryo transferred, as virtually all guidelines recommend. Women with Turner are prone to cardiac and aortic defects that can worsen under the strain of pregnancy, or even present for the first time during gestation. Aortic dissection is a real threat; up to a third of patients with Turner experience it during adulthood, and it’s a major cause of death among them. In the Nordic series, 10 women (9%) had a known cardiac anomaly.
The multiple birth rate was 7%. More than a third (35%) developed a hypertensive disorder, including preeclampsia (20%). Four women had potentially life-threatening complications, including one with aortic dissection, one who developed mild regurgitation of the tricuspid and mitral valve, one with a mechanical heart valve who developed HELLP syndrome (hemolysis, elevated liver enzymes, low platelets), and one who underwent a postpartum hysterectomy because of severe hemorrhaging.
The infants, nevertheless, did well. The preterm birth rate was 8%, with 9% of the singleton infants having a low birth weight. About 4% had a major birth defect. Of the 131 born, three died (2.3%), including a set of extremely preterm twins.
Close follow-up and cross-specialty cooperation are what make these positive outcomes possible, said Dr. Hovatta, who is now a professor emeritus at the Karolinska Institute, Sweden.
“We do everything we can to exclude things that could cause bad outcomes.” That includes extremely rigorous cardiac testing before pregnancy and continuous monitoring during it. “If a woman has any sign of cardiac anomaly, she is advised not to become pregnant. If she shows any signs of aortic dilation, we follow her extremely carefully with experienced cardiologists.”
Like Dr. Oktay, Dr. Hovatta and her European colleagues make fertility preservation an early topic of conversation. Unlike in the United States, where many girls aren’t diagnosed with the disorder until they fail to enter puberty, almost all Turner girls in Europe are identified very early in childhood. They receive early growth hormone treatment, and there is frequent consultation with interdisciplinary specialists. Fertility is spoken of early and often.
Early oocyte retrieval is common, Dr. Hovatta said. “Yes, it’s possible to wait until puberty, but for so many girls, most of the eggs have disappeared by then, so we typically don’t wait. We start looking at that option around 11 years, which is the same time we think about cryopreserving ovarian tissue.”
However, she added, as in the United States, the outcomes of these procedures are still unknown. But the existing data in other populations, the ability to carefully shepherd women through a successful pregnancy, and the willingness of families to provide the option all support further exploring them. Dr. Hovatta was at the Cincinnati gathering last summer and said she did not agree with the conservative tone she heard. Dr. Oktay also does not agree.
“This evidence we have so far is good evidence,” he said. “Look, where we are right now with Turner girls is where we were 15 years ago with cancer patients. People thought, ‘They have cancer. They should just be worrying about surviving cancer, not about their fertility.’ Now fertility counseling is a very important part of cancer care. We have all these tools available to us for cancer patients who don’t want to lose their fertility. This accumulated experience that has already been applied in other medical conditions … why not use that for Turner syndrome? This is my point: With all the data out there about the potential benefits and the ways to manage the risks, we shouldn’t have to tell girls, ‘Well, you have to become menopausal, and maybe you can adopt someday.’ That doesn’t sit well with parents any more. We want these girls to thrive. Not just to survive, but to have as close to a normal quality of life as possible.”
ORLANDO – Fertility preservation techniques pioneered in young cancer patients may someday allow some women with Turner syndrome to give birth to their own children, without relying on donated eggs.
Spontaneous conception and live birth are exceedingly rare among women with the genetic disorder. Until very recently, adoption was the only practical way for most to grow a family. In the last decade, however, fertility specialists in Europe and the United States have had good success with in vitro fertilization using donated eggs. Now, those clinicians are aiming for a higher goal: babies born from a patient’s own eggs, cryopreserved either individually or within whole ovarian tissue.
These are not pipe dreams, according to experts interviewed for this story. Autologous oocyte freezing is well established in healthy women and is now coming of age in cancer patients, with recent reports of live births. Ovarian tissue freezing and reimplantation is a much newer technique, also pioneered in cancer patients. To date, more than 70 live births have occurred from ovarian cortical tissue conservation and later transplantation in adults. Last December brought the first report of a live birth to a childhood cancer survivor who had prepubertal ovarian tissue frozen before chemotherapy. And a 2015 report detailed the case of a girl with primary ovarian failure secondary to sickle cell anemia treatment. At 25, she gave birth to a healthy child conceived from ovarian tissue removed when she was 14 years old.
Not all clinicians so enthusiastically embrace this future, however. A new set of consensus guidelines for the management of girls and women with Turner syndrome is in the works and will recommend a more conservative clinical approach, according to Nelly Mauras, MD, chief of endocrinology, diabetes, and metabolism at the Nemours Children’s Health System in Jacksonville, Fla.
A group of academic and patient advocacy stakeholders is cooperatively honing the document based on a meeting last summer in Cincinnati. These groups include the European Society of Endocrinology, the Endocrine Society, the U.S. Pediatric Endocrine Society, the European Society for Pediatric Endocrinology, Cardiology, and Reproductive Endocrinology, as well as Turner syndrome patient advocacy groups.
Dr. Mauras said the guideline will be “less discouraging” than the existing one issued in 2012 by the American Society of Reproductive Medicine. In its 2012 guidelines, the society identified Turner syndrome as a relative contraindication to pregnancy and an absolute contraindication in those with documented cardiac anomalies. However, greater experience has since been accrued in reproductive techniques of oocyte donation in Turner, with better outcomes.
The upcoming guidelines, however, will still recommend strongly against ovarian stimulation for fertility preservation for girls younger than 12, Dr. Mauras said, and will not recommend ovarian tissue conservation. “We just do not have the safety data and pregnancy outcomes that we need to give strong recommendations for these treatments,” she said. “These are still considered experimental treatments for girls with Turner syndrome.”
Turner syndrome, caused by a deletion of one X chromosome, throws a unique curve into the game – very early ovarian failure. Those with a complete deletion (45,X) begin losing their primordial ovarian follicles even before birth. Most will never experience spontaneous puberty; even if they do, their egg reserve is virtually gone soon after. Ovarian reserve may not be completely lost in girls with mosaicism, however, who have the X deletion in only a portion of their cells (46,XX/45,X). Some will enter puberty, and about 5% may even conceive spontaneously in younger years. But of the majority of Turner girls eventually experience complete ovarian failure.
This means that fertility preservation can’t be a wait-and-see issue, according to Kutluk Oktay, MD, PhD, a fertility specialist on the leading edge of this issue in the United States.
“We have to be proactive,” said Dr. Oktay, professor of obstetrics and gynecology at New York Medical College, Valhalla. “If we wait until girls are 12 or 13 to address this, a majority will have totally depleted their ovarian reserve by then. They will have no option other than an egg donor or adoption. We are suggesting that they should be screened as soon as they are diagnosed, and if they and their parents wish it, something should be done before it’s too late.”
Dr. Oktay is also the founder of fertilitypreservation.org, which specializes in advanced fertility treatments for cancer patients. He is one of a handful of physicians in the United States who advocate early oocyte harvesting in peripubertal girls and ovarian tissue harvesting in prepubertal girls with Turner syndrome. Last year, in conjunction with the Turner Syndrome Foundation, he and his colleagues published a set of guidelines for preserving fertility in these patients.
The paper recommends fertility assessment pathways for pre- and postpubertal girls. For both groups, Dr. Oktay employs serial assessments of ovarian reserve by monitoring several hormones, including follicle-stimulating hormone, luteinizing hormone, and antimüllerian hormone (AMH). Produced by primordial follicles, AMH declines as egg reserve declines over a lifetime, and is considered an accurate marker of ovarian reserve. When a girl experiences two consecutive AMH declines, egg depletion is probably accelerating. “This is the time to consider fertility preservation,” he said.
If a girl is peri- or postpubertal, the choice would probably be ovarian stimulation with the goal of retrieving mature oocytes. For prepubertal girls, the best choice is probably ovarian tissue cryopreservation. But because the egg reserve may already be spotty inside the ovary, he recommended freezing it en bloc, rather than preserving just cortical sections.
Because these techniques are only beginning to be used in young Turner patients, neither has been tested yet to see if it would result in a pregnancy. However, Dr. Oktay said, more than 80 babies have been born to women with other disorders who had ovaries frozen as adults. And European women with Turner syndrome have been successfully bearing children with donated oocytes for years.
“I don’t differentiate Europe from the U.S.,” he said. “We have no reason to believe Turner syndrome girls would be any different here than they are there.”
Pregnancy rates by egg donation in Turner syndrome patients are about half that typically seen in an otherwise healthy infertile woman, according to numerous sources; with a take-home baby rate of about 18%. There are numerous reasons for this. The miscarriage rate in Turner patients is about 44%. Women with Turner tend to have smaller uteri, with thinner endometrium, mostly because of the lack of estrogen.
But with careful management, those who do conceive can safely deliver a healthy baby, said Outi Hovatta, MD, a Finnish fertility specialist who has done extensive work in the area. “In Europe, we have been doing this quite liberally for years, and haven’t had a bad experience,” she said in an interview.
A 2013 review summarized both the success and the risks of these pregnancies. It examined obstetric and neonatal outcomes among 106 women with Turner syndrome who gave birth via egg donation from 1992 to 2011 in Sweden, Finland, and Denmark.
Most (70%) had a single embryo transferred, as virtually all guidelines recommend. Women with Turner are prone to cardiac and aortic defects that can worsen under the strain of pregnancy, or even present for the first time during gestation. Aortic dissection is a real threat; up to a third of patients with Turner experience it during adulthood, and it’s a major cause of death among them. In the Nordic series, 10 women (9%) had a known cardiac anomaly.
The multiple birth rate was 7%. More than a third (35%) developed a hypertensive disorder, including preeclampsia (20%). Four women had potentially life-threatening complications, including one with aortic dissection, one who developed mild regurgitation of the tricuspid and mitral valve, one with a mechanical heart valve who developed HELLP syndrome (hemolysis, elevated liver enzymes, low platelets), and one who underwent a postpartum hysterectomy because of severe hemorrhaging.
The infants, nevertheless, did well. The preterm birth rate was 8%, with 9% of the singleton infants having a low birth weight. About 4% had a major birth defect. Of the 131 born, three died (2.3%), including a set of extremely preterm twins.
Close follow-up and cross-specialty cooperation are what make these positive outcomes possible, said Dr. Hovatta, who is now a professor emeritus at the Karolinska Institute, Sweden.
“We do everything we can to exclude things that could cause bad outcomes.” That includes extremely rigorous cardiac testing before pregnancy and continuous monitoring during it. “If a woman has any sign of cardiac anomaly, she is advised not to become pregnant. If she shows any signs of aortic dilation, we follow her extremely carefully with experienced cardiologists.”
Like Dr. Oktay, Dr. Hovatta and her European colleagues make fertility preservation an early topic of conversation. Unlike in the United States, where many girls aren’t diagnosed with the disorder until they fail to enter puberty, almost all Turner girls in Europe are identified very early in childhood. They receive early growth hormone treatment, and there is frequent consultation with interdisciplinary specialists. Fertility is spoken of early and often.
Early oocyte retrieval is common, Dr. Hovatta said. “Yes, it’s possible to wait until puberty, but for so many girls, most of the eggs have disappeared by then, so we typically don’t wait. We start looking at that option around 11 years, which is the same time we think about cryopreserving ovarian tissue.”
However, she added, as in the United States, the outcomes of these procedures are still unknown. But the existing data in other populations, the ability to carefully shepherd women through a successful pregnancy, and the willingness of families to provide the option all support further exploring them. Dr. Hovatta was at the Cincinnati gathering last summer and said she did not agree with the conservative tone she heard. Dr. Oktay also does not agree.
“This evidence we have so far is good evidence,” he said. “Look, where we are right now with Turner girls is where we were 15 years ago with cancer patients. People thought, ‘They have cancer. They should just be worrying about surviving cancer, not about their fertility.’ Now fertility counseling is a very important part of cancer care. We have all these tools available to us for cancer patients who don’t want to lose their fertility. This accumulated experience that has already been applied in other medical conditions … why not use that for Turner syndrome? This is my point: With all the data out there about the potential benefits and the ways to manage the risks, we shouldn’t have to tell girls, ‘Well, you have to become menopausal, and maybe you can adopt someday.’ That doesn’t sit well with parents any more. We want these girls to thrive. Not just to survive, but to have as close to a normal quality of life as possible.”
ORLANDO – Fertility preservation techniques pioneered in young cancer patients may someday allow some women with Turner syndrome to give birth to their own children, without relying on donated eggs.
Spontaneous conception and live birth are exceedingly rare among women with the genetic disorder. Until very recently, adoption was the only practical way for most to grow a family. In the last decade, however, fertility specialists in Europe and the United States have had good success with in vitro fertilization using donated eggs. Now, those clinicians are aiming for a higher goal: babies born from a patient’s own eggs, cryopreserved either individually or within whole ovarian tissue.
These are not pipe dreams, according to experts interviewed for this story. Autologous oocyte freezing is well established in healthy women and is now coming of age in cancer patients, with recent reports of live births. Ovarian tissue freezing and reimplantation is a much newer technique, also pioneered in cancer patients. To date, more than 70 live births have occurred from ovarian cortical tissue conservation and later transplantation in adults. Last December brought the first report of a live birth to a childhood cancer survivor who had prepubertal ovarian tissue frozen before chemotherapy. And a 2015 report detailed the case of a girl with primary ovarian failure secondary to sickle cell anemia treatment. At 25, she gave birth to a healthy child conceived from ovarian tissue removed when she was 14 years old.
Not all clinicians so enthusiastically embrace this future, however. A new set of consensus guidelines for the management of girls and women with Turner syndrome is in the works and will recommend a more conservative clinical approach, according to Nelly Mauras, MD, chief of endocrinology, diabetes, and metabolism at the Nemours Children’s Health System in Jacksonville, Fla.
A group of academic and patient advocacy stakeholders is cooperatively honing the document based on a meeting last summer in Cincinnati. These groups include the European Society of Endocrinology, the Endocrine Society, the U.S. Pediatric Endocrine Society, the European Society for Pediatric Endocrinology, Cardiology, and Reproductive Endocrinology, as well as Turner syndrome patient advocacy groups.
Dr. Mauras said the guideline will be “less discouraging” than the existing one issued in 2012 by the American Society of Reproductive Medicine. In its 2012 guidelines, the society identified Turner syndrome as a relative contraindication to pregnancy and an absolute contraindication in those with documented cardiac anomalies. However, greater experience has since been accrued in reproductive techniques of oocyte donation in Turner, with better outcomes.
The upcoming guidelines, however, will still recommend strongly against ovarian stimulation for fertility preservation for girls younger than 12, Dr. Mauras said, and will not recommend ovarian tissue conservation. “We just do not have the safety data and pregnancy outcomes that we need to give strong recommendations for these treatments,” she said. “These are still considered experimental treatments for girls with Turner syndrome.”
Turner syndrome, caused by a deletion of one X chromosome, throws a unique curve into the game – very early ovarian failure. Those with a complete deletion (45,X) begin losing their primordial ovarian follicles even before birth. Most will never experience spontaneous puberty; even if they do, their egg reserve is virtually gone soon after. Ovarian reserve may not be completely lost in girls with mosaicism, however, who have the X deletion in only a portion of their cells (46,XX/45,X). Some will enter puberty, and about 5% may even conceive spontaneously in younger years. But of the majority of Turner girls eventually experience complete ovarian failure.
This means that fertility preservation can’t be a wait-and-see issue, according to Kutluk Oktay, MD, PhD, a fertility specialist on the leading edge of this issue in the United States.
“We have to be proactive,” said Dr. Oktay, professor of obstetrics and gynecology at New York Medical College, Valhalla. “If we wait until girls are 12 or 13 to address this, a majority will have totally depleted their ovarian reserve by then. They will have no option other than an egg donor or adoption. We are suggesting that they should be screened as soon as they are diagnosed, and if they and their parents wish it, something should be done before it’s too late.”
Dr. Oktay is also the founder of fertilitypreservation.org, which specializes in advanced fertility treatments for cancer patients. He is one of a handful of physicians in the United States who advocate early oocyte harvesting in peripubertal girls and ovarian tissue harvesting in prepubertal girls with Turner syndrome. Last year, in conjunction with the Turner Syndrome Foundation, he and his colleagues published a set of guidelines for preserving fertility in these patients.
The paper recommends fertility assessment pathways for pre- and postpubertal girls. For both groups, Dr. Oktay employs serial assessments of ovarian reserve by monitoring several hormones, including follicle-stimulating hormone, luteinizing hormone, and antimüllerian hormone (AMH). Produced by primordial follicles, AMH declines as egg reserve declines over a lifetime, and is considered an accurate marker of ovarian reserve. When a girl experiences two consecutive AMH declines, egg depletion is probably accelerating. “This is the time to consider fertility preservation,” he said.
If a girl is peri- or postpubertal, the choice would probably be ovarian stimulation with the goal of retrieving mature oocytes. For prepubertal girls, the best choice is probably ovarian tissue cryopreservation. But because the egg reserve may already be spotty inside the ovary, he recommended freezing it en bloc, rather than preserving just cortical sections.
Because these techniques are only beginning to be used in young Turner patients, neither has been tested yet to see if it would result in a pregnancy. However, Dr. Oktay said, more than 80 babies have been born to women with other disorders who had ovaries frozen as adults. And European women with Turner syndrome have been successfully bearing children with donated oocytes for years.
“I don’t differentiate Europe from the U.S.,” he said. “We have no reason to believe Turner syndrome girls would be any different here than they are there.”
Pregnancy rates by egg donation in Turner syndrome patients are about half that typically seen in an otherwise healthy infertile woman, according to numerous sources; with a take-home baby rate of about 18%. There are numerous reasons for this. The miscarriage rate in Turner patients is about 44%. Women with Turner tend to have smaller uteri, with thinner endometrium, mostly because of the lack of estrogen.
But with careful management, those who do conceive can safely deliver a healthy baby, said Outi Hovatta, MD, a Finnish fertility specialist who has done extensive work in the area. “In Europe, we have been doing this quite liberally for years, and haven’t had a bad experience,” she said in an interview.
A 2013 review summarized both the success and the risks of these pregnancies. It examined obstetric and neonatal outcomes among 106 women with Turner syndrome who gave birth via egg donation from 1992 to 2011 in Sweden, Finland, and Denmark.
Most (70%) had a single embryo transferred, as virtually all guidelines recommend. Women with Turner are prone to cardiac and aortic defects that can worsen under the strain of pregnancy, or even present for the first time during gestation. Aortic dissection is a real threat; up to a third of patients with Turner experience it during adulthood, and it’s a major cause of death among them. In the Nordic series, 10 women (9%) had a known cardiac anomaly.
The multiple birth rate was 7%. More than a third (35%) developed a hypertensive disorder, including preeclampsia (20%). Four women had potentially life-threatening complications, including one with aortic dissection, one who developed mild regurgitation of the tricuspid and mitral valve, one with a mechanical heart valve who developed HELLP syndrome (hemolysis, elevated liver enzymes, low platelets), and one who underwent a postpartum hysterectomy because of severe hemorrhaging.
The infants, nevertheless, did well. The preterm birth rate was 8%, with 9% of the singleton infants having a low birth weight. About 4% had a major birth defect. Of the 131 born, three died (2.3%), including a set of extremely preterm twins.
Close follow-up and cross-specialty cooperation are what make these positive outcomes possible, said Dr. Hovatta, who is now a professor emeritus at the Karolinska Institute, Sweden.
“We do everything we can to exclude things that could cause bad outcomes.” That includes extremely rigorous cardiac testing before pregnancy and continuous monitoring during it. “If a woman has any sign of cardiac anomaly, she is advised not to become pregnant. If she shows any signs of aortic dilation, we follow her extremely carefully with experienced cardiologists.”
Like Dr. Oktay, Dr. Hovatta and her European colleagues make fertility preservation an early topic of conversation. Unlike in the United States, where many girls aren’t diagnosed with the disorder until they fail to enter puberty, almost all Turner girls in Europe are identified very early in childhood. They receive early growth hormone treatment, and there is frequent consultation with interdisciplinary specialists. Fertility is spoken of early and often.
Early oocyte retrieval is common, Dr. Hovatta said. “Yes, it’s possible to wait until puberty, but for so many girls, most of the eggs have disappeared by then, so we typically don’t wait. We start looking at that option around 11 years, which is the same time we think about cryopreserving ovarian tissue.”
However, she added, as in the United States, the outcomes of these procedures are still unknown. But the existing data in other populations, the ability to carefully shepherd women through a successful pregnancy, and the willingness of families to provide the option all support further exploring them. Dr. Hovatta was at the Cincinnati gathering last summer and said she did not agree with the conservative tone she heard. Dr. Oktay also does not agree.
“This evidence we have so far is good evidence,” he said. “Look, where we are right now with Turner girls is where we were 15 years ago with cancer patients. People thought, ‘They have cancer. They should just be worrying about surviving cancer, not about their fertility.’ Now fertility counseling is a very important part of cancer care. We have all these tools available to us for cancer patients who don’t want to lose their fertility. This accumulated experience that has already been applied in other medical conditions … why not use that for Turner syndrome? This is my point: With all the data out there about the potential benefits and the ways to manage the risks, we shouldn’t have to tell girls, ‘Well, you have to become menopausal, and maybe you can adopt someday.’ That doesn’t sit well with parents any more. We want these girls to thrive. Not just to survive, but to have as close to a normal quality of life as possible.”
Failed expectations: When cultural similarities do not favor a therapeutic bond
The importance of establishing a bond with a patient early in treatment is instilled in psychiatry trainees during their first year of residency. It is well-known that a strong therapeutic connection is correlated with successful treatment and favorable outcomes.
We present a case in which sharing my cultural background with a patient was detrimental to the therapeutic relationship and forced me to look beyond superficial similarities to forge a meaningful connection.
A shared language, a shared connection?
When I, a psychiatry intern who emigrated from Honduras 11 years ago, met Ms. M, a middle-age, Spanish-speaking Honduran immigrant with schizoaffective disorder, I was curious to hear the story of how her immigration intermingled with her mental illness. As a budding psychiatrist, I was certain our common culture would intensify our interactions. It did, although in ways I did not expect.
Despite my enthusiasm and best intentions, our first meeting was less than ideal. Ms. M believed she not only was God’s wife and my attending physician’s wife, but that I was her rival for my attending’s affections. “I heard you are from Honduras. I am from Honduras, too. What part are you from?” I asked her. She became angry. “I am not from there. I am from Israel,” she said. For many days, we had the same hostile and disappointing conversations, during which I would try to tease out the basis for her delusions and understand our lack of connection. I felt hurt and puzzled. If I could not connect with someone with whom I shared a common background, then to whom could I connect with? I had to re-evaluate my approach. Should I alter my attire to seem less feminine? Should I tell her I am happily married? Should I not speak Spanish? Would these changes make our interactions feel less threatening to her?
“You are focused too much on you and not enough on her,” my attending retorted. I came to realize that, in my crusade to have Ms. M perceive me a certain way, I had lost sight of who she was and what lay at the core of her delusions. I stepped back and considered Ms. M: a patient, yes, but also a woman who was unable to communicate freely with others because she did not speak English. Because of her perpetual paranoia and psychosis, she was emotionally isolated, lacked necessary social support from her family, and had no sense of community. However, in her delusions she was a prophet, a herald for God’s news, with a vital role in His plans. In her mind, she was a mother and had the support of a life-long partner.
As I considered her struggles, I thought about myself. When I first came to the United States, it was difficult to develop relationships with my peers because I worried about my accent and idioms. In Honduras, my friends and family knew me as a gregarious, quick-witted individual. In acculturating to my new home, I became reclusive and insecure. It took years to regain a semblance of identity.
In my attending’s office, I found that it was not our shared heritage that was the path to engaging Ms. M, but rather our shared isolation, which I had not been validating. This helped me reframe the way I viewed the therapeutic relationship and changed the focus of my attempts to engage her. I stopped taking her rejection personally and focused on providing her support and solace. By tapping into her isolation, she opened up and eventually agreed to medication changes, which slowly reduced—but did not eliminate—her delusions, hallucinations, and hostility toward others. Because of her intractable psychotic symptoms, she required a long-term structured care setting and was transferred to the state hospital.
Culture is only ‘skin deep’
I assumed our shared background would have effortlessly led to a trustworthy relationship, but her resistance challenged that notion. My own desires to have a deep connection with a fellow immigrant contributed to my internalization of her rejection. Our physical and cultural similarities acted as a hindrance because she subconsciously projected her idealized image of a woman onto me. Nevertheless, she helped me recognize the importance of unexamined projective identification and countertransference, evidenced by wanting to change my appearance and behavior and my increased willingness for self-disclosure.
As I start my second year of residency and reflect on my experiences as an intern, Ms. M always comes to mind. She taught me that culture may be only “skin deep” and similarities between therapist and patient do not guarantee a successful bond. Searching for deeper, fundamental connections and validating these bonds can open the doors to connecting with those from all walks of life, from whichever road they come.
1. Krupnick JL, Sotsky SM, Simmens S, et al. The role of the therapeutic alliance in psychotherapy and pharmacotherapy outcome: findings in the National Institute of Mental Health Treatment of Depression Collaborative Research Program. J Consult Clin Psychol. 1996;64(3):532-539.
The importance of establishing a bond with a patient early in treatment is instilled in psychiatry trainees during their first year of residency. It is well-known that a strong therapeutic connection is correlated with successful treatment and favorable outcomes.
We present a case in which sharing my cultural background with a patient was detrimental to the therapeutic relationship and forced me to look beyond superficial similarities to forge a meaningful connection.
A shared language, a shared connection?
When I, a psychiatry intern who emigrated from Honduras 11 years ago, met Ms. M, a middle-age, Spanish-speaking Honduran immigrant with schizoaffective disorder, I was curious to hear the story of how her immigration intermingled with her mental illness. As a budding psychiatrist, I was certain our common culture would intensify our interactions. It did, although in ways I did not expect.
Despite my enthusiasm and best intentions, our first meeting was less than ideal. Ms. M believed she not only was God’s wife and my attending physician’s wife, but that I was her rival for my attending’s affections. “I heard you are from Honduras. I am from Honduras, too. What part are you from?” I asked her. She became angry. “I am not from there. I am from Israel,” she said. For many days, we had the same hostile and disappointing conversations, during which I would try to tease out the basis for her delusions and understand our lack of connection. I felt hurt and puzzled. If I could not connect with someone with whom I shared a common background, then to whom could I connect with? I had to re-evaluate my approach. Should I alter my attire to seem less feminine? Should I tell her I am happily married? Should I not speak Spanish? Would these changes make our interactions feel less threatening to her?
“You are focused too much on you and not enough on her,” my attending retorted. I came to realize that, in my crusade to have Ms. M perceive me a certain way, I had lost sight of who she was and what lay at the core of her delusions. I stepped back and considered Ms. M: a patient, yes, but also a woman who was unable to communicate freely with others because she did not speak English. Because of her perpetual paranoia and psychosis, she was emotionally isolated, lacked necessary social support from her family, and had no sense of community. However, in her delusions she was a prophet, a herald for God’s news, with a vital role in His plans. In her mind, she was a mother and had the support of a life-long partner.
As I considered her struggles, I thought about myself. When I first came to the United States, it was difficult to develop relationships with my peers because I worried about my accent and idioms. In Honduras, my friends and family knew me as a gregarious, quick-witted individual. In acculturating to my new home, I became reclusive and insecure. It took years to regain a semblance of identity.
In my attending’s office, I found that it was not our shared heritage that was the path to engaging Ms. M, but rather our shared isolation, which I had not been validating. This helped me reframe the way I viewed the therapeutic relationship and changed the focus of my attempts to engage her. I stopped taking her rejection personally and focused on providing her support and solace. By tapping into her isolation, she opened up and eventually agreed to medication changes, which slowly reduced—but did not eliminate—her delusions, hallucinations, and hostility toward others. Because of her intractable psychotic symptoms, she required a long-term structured care setting and was transferred to the state hospital.
Culture is only ‘skin deep’
I assumed our shared background would have effortlessly led to a trustworthy relationship, but her resistance challenged that notion. My own desires to have a deep connection with a fellow immigrant contributed to my internalization of her rejection. Our physical and cultural similarities acted as a hindrance because she subconsciously projected her idealized image of a woman onto me. Nevertheless, she helped me recognize the importance of unexamined projective identification and countertransference, evidenced by wanting to change my appearance and behavior and my increased willingness for self-disclosure.
As I start my second year of residency and reflect on my experiences as an intern, Ms. M always comes to mind. She taught me that culture may be only “skin deep” and similarities between therapist and patient do not guarantee a successful bond. Searching for deeper, fundamental connections and validating these bonds can open the doors to connecting with those from all walks of life, from whichever road they come.
The importance of establishing a bond with a patient early in treatment is instilled in psychiatry trainees during their first year of residency. It is well-known that a strong therapeutic connection is correlated with successful treatment and favorable outcomes.
We present a case in which sharing my cultural background with a patient was detrimental to the therapeutic relationship and forced me to look beyond superficial similarities to forge a meaningful connection.
A shared language, a shared connection?
When I, a psychiatry intern who emigrated from Honduras 11 years ago, met Ms. M, a middle-age, Spanish-speaking Honduran immigrant with schizoaffective disorder, I was curious to hear the story of how her immigration intermingled with her mental illness. As a budding psychiatrist, I was certain our common culture would intensify our interactions. It did, although in ways I did not expect.
Despite my enthusiasm and best intentions, our first meeting was less than ideal. Ms. M believed she not only was God’s wife and my attending physician’s wife, but that I was her rival for my attending’s affections. “I heard you are from Honduras. I am from Honduras, too. What part are you from?” I asked her. She became angry. “I am not from there. I am from Israel,” she said. For many days, we had the same hostile and disappointing conversations, during which I would try to tease out the basis for her delusions and understand our lack of connection. I felt hurt and puzzled. If I could not connect with someone with whom I shared a common background, then to whom could I connect with? I had to re-evaluate my approach. Should I alter my attire to seem less feminine? Should I tell her I am happily married? Should I not speak Spanish? Would these changes make our interactions feel less threatening to her?
“You are focused too much on you and not enough on her,” my attending retorted. I came to realize that, in my crusade to have Ms. M perceive me a certain way, I had lost sight of who she was and what lay at the core of her delusions. I stepped back and considered Ms. M: a patient, yes, but also a woman who was unable to communicate freely with others because she did not speak English. Because of her perpetual paranoia and psychosis, she was emotionally isolated, lacked necessary social support from her family, and had no sense of community. However, in her delusions she was a prophet, a herald for God’s news, with a vital role in His plans. In her mind, she was a mother and had the support of a life-long partner.
As I considered her struggles, I thought about myself. When I first came to the United States, it was difficult to develop relationships with my peers because I worried about my accent and idioms. In Honduras, my friends and family knew me as a gregarious, quick-witted individual. In acculturating to my new home, I became reclusive and insecure. It took years to regain a semblance of identity.
In my attending’s office, I found that it was not our shared heritage that was the path to engaging Ms. M, but rather our shared isolation, which I had not been validating. This helped me reframe the way I viewed the therapeutic relationship and changed the focus of my attempts to engage her. I stopped taking her rejection personally and focused on providing her support and solace. By tapping into her isolation, she opened up and eventually agreed to medication changes, which slowly reduced—but did not eliminate—her delusions, hallucinations, and hostility toward others. Because of her intractable psychotic symptoms, she required a long-term structured care setting and was transferred to the state hospital.
Culture is only ‘skin deep’
I assumed our shared background would have effortlessly led to a trustworthy relationship, but her resistance challenged that notion. My own desires to have a deep connection with a fellow immigrant contributed to my internalization of her rejection. Our physical and cultural similarities acted as a hindrance because she subconsciously projected her idealized image of a woman onto me. Nevertheless, she helped me recognize the importance of unexamined projective identification and countertransference, evidenced by wanting to change my appearance and behavior and my increased willingness for self-disclosure.
As I start my second year of residency and reflect on my experiences as an intern, Ms. M always comes to mind. She taught me that culture may be only “skin deep” and similarities between therapist and patient do not guarantee a successful bond. Searching for deeper, fundamental connections and validating these bonds can open the doors to connecting with those from all walks of life, from whichever road they come.
1. Krupnick JL, Sotsky SM, Simmens S, et al. The role of the therapeutic alliance in psychotherapy and pharmacotherapy outcome: findings in the National Institute of Mental Health Treatment of Depression Collaborative Research Program. J Consult Clin Psychol. 1996;64(3):532-539.
1. Krupnick JL, Sotsky SM, Simmens S, et al. The role of the therapeutic alliance in psychotherapy and pharmacotherapy outcome: findings in the National Institute of Mental Health Treatment of Depression Collaborative Research Program. J Consult Clin Psychol. 1996;64(3):532-539.
Truncal vagotomy might help delay Parkinson’s disease
Patients who were followed for more than 5 years after truncal vagotomy had about a 40% lower risk of being diagnosed with Parkinson’s disease, compared with matched population controls, according to the results of a cohort registry study.
Selective vagotomy did not decrease the risk of Parkinson’s disease (PD), however, reported Bojing Liu of Karolinska Institutet, Stockholm, and her associates. The findings, which reflect those from a prior Danish study, “provide preliminary and indirect support” for the idea that Lewy pathology in PD begins in peripheral nerves and spreads to the central nervous system through “prion-like mechanisms,” they added.
The findings reflect a prior registry study that found a 15% decrease in the risk of PD compared with the general population more than 5 years after truncal vagotomy (Ann Neurol. 2015 Oct. 78[4];522-9). “This Danish study, however, did not differentiate truncal from selective vagotomy and thus might have underestimated the association of truncal vagotomy with PD,” the researchers said.
Another study found that truncal vagotomy exhibited a nonsignificant protective effect overall and an insignificantly increased risk of PD more than 20 years after surgery (Neurology Today 2015 Dec 3;15[23]:27-30). Likewise, the current study yielded “stronger evidence for PD risk reduction more than 5 or 10 years after truncal vagotomy,” and the protective effect appeared to weaken with longer follow-up, the investigators noted. If PD started at multiple sites within the peripheral nervous system, “even truncal vagotomy may delay, rather than eliminate, the risk for PD,” they emphasized. “Indeed, abnormal alpha-synuclein accumulation has been found throughout the digestive tract of patients with PD with descending pattern of density, and even in the submandibular gland in patients with preclinical PD.”
The study was funded by the Swedish Research Council for Health, Working Life and Welfare, the Parkinson Research Foundation in Sweden, the Karolinska Institutet, the Swedish Society for Medical Research, the Stockholm County Council, and Karolinska Institutet–NIH Doctoral Partnership Program in Neuroscience. The investigators had no relevant disclosures.
The current study provides an independent dataset suggesting that truncal vagotomy may be protective in Parkinson’s disease. Therefore, the time has come to seriously consider the implications of these findings.
Could it be true that alpha-synuclein misfolding in PD may originate in the autonomic nerve terminals of the gastrointestinal tract? For the moment, more research is needed. One may consider studying the effects of vagotomy in patients with mutations in the leucine-rich repeat kinase-2 gene (LRRK2), which dramatically increases the risk of developing neurodegenerative parkinsonism. Some of these mutations have a penetrance of up to 80% in the very elderly. However, it is largely unknown whether alpha-synuclein aggregates are present in gastrointestinal nerve endings of these patients. At this stage, we have insufficient knowledge to propose vagotomy as a putative treatment for PD. Although vagotomy will likely never become a widespread treatment for PD, strategies to prevent alpha-synuclein misfolding in the gastrointestinal tract may be proposed, because nerve terminals are reachable by oral therapeutic interventions.
Per Borghammer, MD, PhD, is in the department of nuclear medicine and PET Centre, Aarhus University Hospital, Denmark. Clement Hamani, MD, PhD, is at the division of neurosurgery, Toronto Western Hospital, University of Toronto, and the department of neuroimaging, Centre for Addiction and Mental Health, Campbell Family Mental Health Research Institute, Toronto. They reported no conflicts of interest. These comments are excerpted from their editorial (Neurology. 2017 Apr 26. doi: 10.1212/WNL.0000000000003969).
The current study provides an independent dataset suggesting that truncal vagotomy may be protective in Parkinson’s disease. Therefore, the time has come to seriously consider the implications of these findings.
Could it be true that alpha-synuclein misfolding in PD may originate in the autonomic nerve terminals of the gastrointestinal tract? For the moment, more research is needed. One may consider studying the effects of vagotomy in patients with mutations in the leucine-rich repeat kinase-2 gene (LRRK2), which dramatically increases the risk of developing neurodegenerative parkinsonism. Some of these mutations have a penetrance of up to 80% in the very elderly. However, it is largely unknown whether alpha-synuclein aggregates are present in gastrointestinal nerve endings of these patients. At this stage, we have insufficient knowledge to propose vagotomy as a putative treatment for PD. Although vagotomy will likely never become a widespread treatment for PD, strategies to prevent alpha-synuclein misfolding in the gastrointestinal tract may be proposed, because nerve terminals are reachable by oral therapeutic interventions.
Per Borghammer, MD, PhD, is in the department of nuclear medicine and PET Centre, Aarhus University Hospital, Denmark. Clement Hamani, MD, PhD, is at the division of neurosurgery, Toronto Western Hospital, University of Toronto, and the department of neuroimaging, Centre for Addiction and Mental Health, Campbell Family Mental Health Research Institute, Toronto. They reported no conflicts of interest. These comments are excerpted from their editorial (Neurology. 2017 Apr 26. doi: 10.1212/WNL.0000000000003969).
The current study provides an independent dataset suggesting that truncal vagotomy may be protective in Parkinson’s disease. Therefore, the time has come to seriously consider the implications of these findings.
Could it be true that alpha-synuclein misfolding in PD may originate in the autonomic nerve terminals of the gastrointestinal tract? For the moment, more research is needed. One may consider studying the effects of vagotomy in patients with mutations in the leucine-rich repeat kinase-2 gene (LRRK2), which dramatically increases the risk of developing neurodegenerative parkinsonism. Some of these mutations have a penetrance of up to 80% in the very elderly. However, it is largely unknown whether alpha-synuclein aggregates are present in gastrointestinal nerve endings of these patients. At this stage, we have insufficient knowledge to propose vagotomy as a putative treatment for PD. Although vagotomy will likely never become a widespread treatment for PD, strategies to prevent alpha-synuclein misfolding in the gastrointestinal tract may be proposed, because nerve terminals are reachable by oral therapeutic interventions.
Per Borghammer, MD, PhD, is in the department of nuclear medicine and PET Centre, Aarhus University Hospital, Denmark. Clement Hamani, MD, PhD, is at the division of neurosurgery, Toronto Western Hospital, University of Toronto, and the department of neuroimaging, Centre for Addiction and Mental Health, Campbell Family Mental Health Research Institute, Toronto. They reported no conflicts of interest. These comments are excerpted from their editorial (Neurology. 2017 Apr 26. doi: 10.1212/WNL.0000000000003969).
Patients who were followed for more than 5 years after truncal vagotomy had about a 40% lower risk of being diagnosed with Parkinson’s disease, compared with matched population controls, according to the results of a cohort registry study.
Selective vagotomy did not decrease the risk of Parkinson’s disease (PD), however, reported Bojing Liu of Karolinska Institutet, Stockholm, and her associates. The findings, which reflect those from a prior Danish study, “provide preliminary and indirect support” for the idea that Lewy pathology in PD begins in peripheral nerves and spreads to the central nervous system through “prion-like mechanisms,” they added.
The findings reflect a prior registry study that found a 15% decrease in the risk of PD compared with the general population more than 5 years after truncal vagotomy (Ann Neurol. 2015 Oct. 78[4];522-9). “This Danish study, however, did not differentiate truncal from selective vagotomy and thus might have underestimated the association of truncal vagotomy with PD,” the researchers said.
Another study found that truncal vagotomy exhibited a nonsignificant protective effect overall and an insignificantly increased risk of PD more than 20 years after surgery (Neurology Today 2015 Dec 3;15[23]:27-30). Likewise, the current study yielded “stronger evidence for PD risk reduction more than 5 or 10 years after truncal vagotomy,” and the protective effect appeared to weaken with longer follow-up, the investigators noted. If PD started at multiple sites within the peripheral nervous system, “even truncal vagotomy may delay, rather than eliminate, the risk for PD,” they emphasized. “Indeed, abnormal alpha-synuclein accumulation has been found throughout the digestive tract of patients with PD with descending pattern of density, and even in the submandibular gland in patients with preclinical PD.”
The study was funded by the Swedish Research Council for Health, Working Life and Welfare, the Parkinson Research Foundation in Sweden, the Karolinska Institutet, the Swedish Society for Medical Research, the Stockholm County Council, and Karolinska Institutet–NIH Doctoral Partnership Program in Neuroscience. The investigators had no relevant disclosures.
Patients who were followed for more than 5 years after truncal vagotomy had about a 40% lower risk of being diagnosed with Parkinson’s disease, compared with matched population controls, according to the results of a cohort registry study.
Selective vagotomy did not decrease the risk of Parkinson’s disease (PD), however, reported Bojing Liu of Karolinska Institutet, Stockholm, and her associates. The findings, which reflect those from a prior Danish study, “provide preliminary and indirect support” for the idea that Lewy pathology in PD begins in peripheral nerves and spreads to the central nervous system through “prion-like mechanisms,” they added.
The findings reflect a prior registry study that found a 15% decrease in the risk of PD compared with the general population more than 5 years after truncal vagotomy (Ann Neurol. 2015 Oct. 78[4];522-9). “This Danish study, however, did not differentiate truncal from selective vagotomy and thus might have underestimated the association of truncal vagotomy with PD,” the researchers said.
Another study found that truncal vagotomy exhibited a nonsignificant protective effect overall and an insignificantly increased risk of PD more than 20 years after surgery (Neurology Today 2015 Dec 3;15[23]:27-30). Likewise, the current study yielded “stronger evidence for PD risk reduction more than 5 or 10 years after truncal vagotomy,” and the protective effect appeared to weaken with longer follow-up, the investigators noted. If PD started at multiple sites within the peripheral nervous system, “even truncal vagotomy may delay, rather than eliminate, the risk for PD,” they emphasized. “Indeed, abnormal alpha-synuclein accumulation has been found throughout the digestive tract of patients with PD with descending pattern of density, and even in the submandibular gland in patients with preclinical PD.”
The study was funded by the Swedish Research Council for Health, Working Life and Welfare, the Parkinson Research Foundation in Sweden, the Karolinska Institutet, the Swedish Society for Medical Research, the Stockholm County Council, and Karolinska Institutet–NIH Doctoral Partnership Program in Neuroscience. The investigators had no relevant disclosures.
Key clinical point:
Major finding: Compared with controls, patients who underwent truncal vagotomy were at decreased risk of Parkinson’s disease after more than 5 years (hazard ratio, 0.59, 95% confidence interval, 0.37-0.93). Selective vagotomy did not show this association.
Data source: A matched cohort study of 9,430 vagotomized patients (3,445 truncal, 5,978 selective, 7 unknown) between 1970 and 2010, and 377,200 population controls matched by age and sex.
Disclosures: The Swedish Research Council for Health, Working Life and Welfare, the Parkinson Research Foundation in Sweden, the Karolinska Institutet, the Swedish Society for Medical Research, the Stockholm County Council, and Karolinska Institutet–NIH Doctoral Partnership Program in Neuroscience funded the study. The investigators had no relevant disclosures.
RIV poster contest a meeting highlight
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
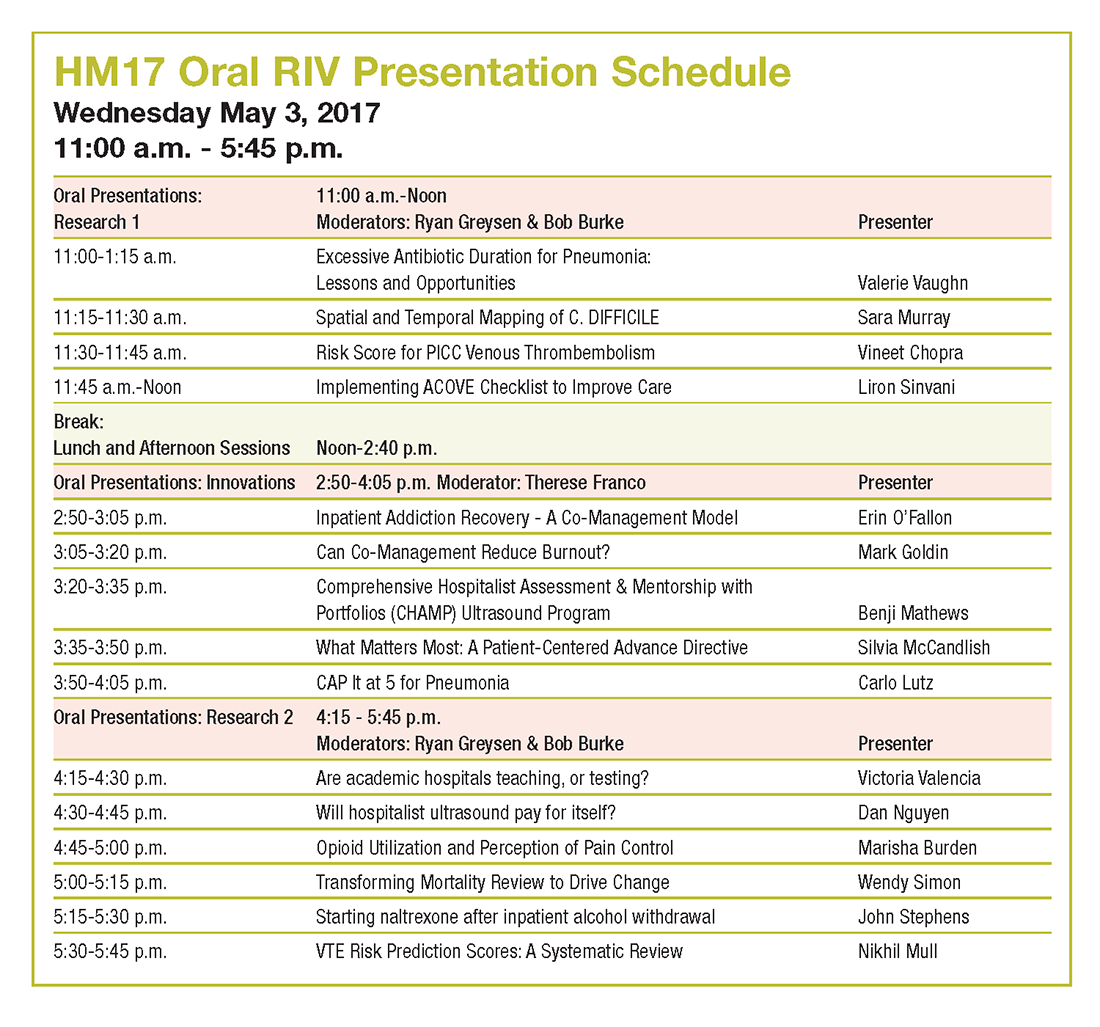
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
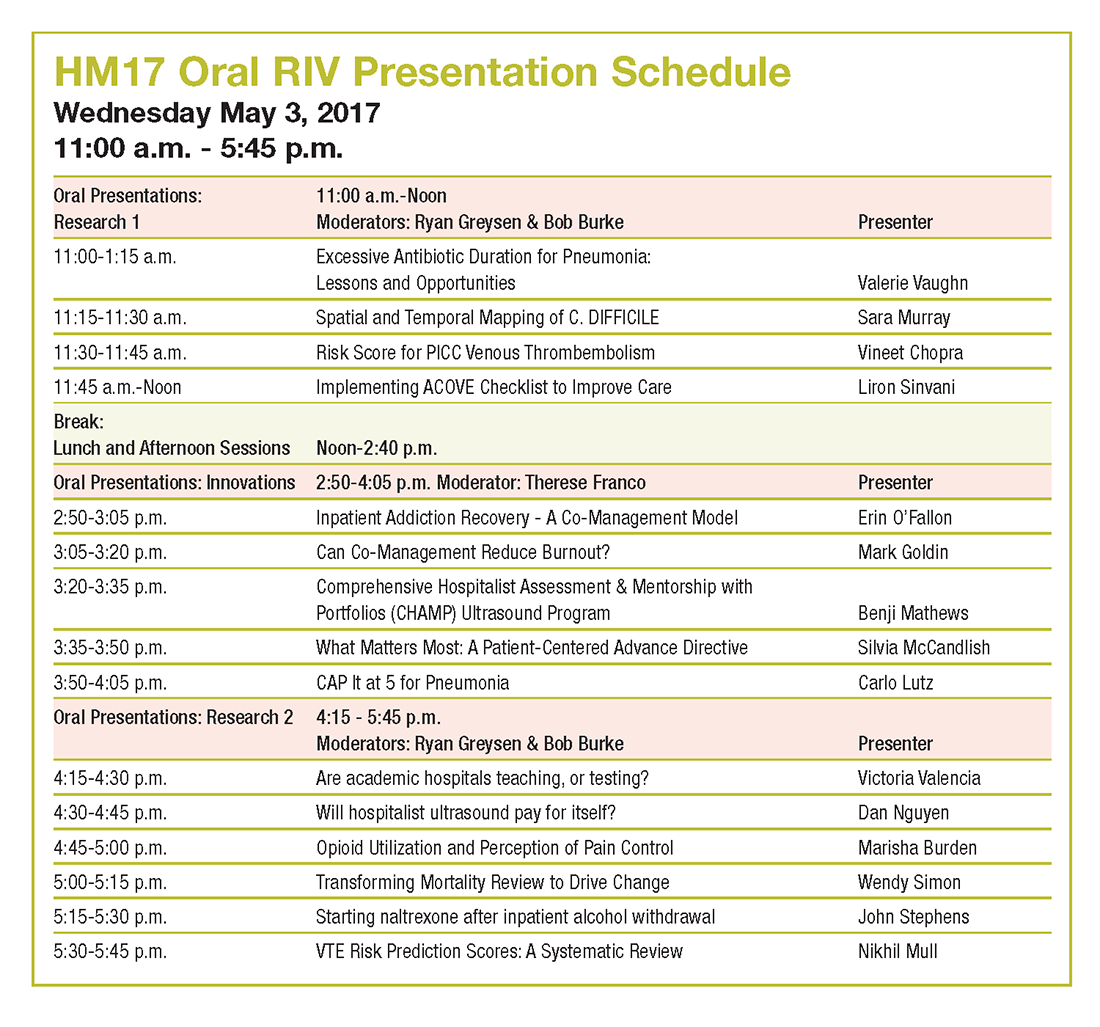
Look back at the history of SHM’s annual Research, Innovations and Clinical Vignettes poster competition – better known as the RIV – and it may seem inevitable that it’s grown into one of the main highlights of the conference. The RIV has become so popular that the number of submissions has nearly tripled from 634 in 2010 to 1,712 this year.
“Certainly, there is some natural evolution,” said Dr. Fang, a hospitalist, researcher, and anticoagulation clinic director at the University of California San Francisco. “But not all specialty societies embrace research or encourage its growth, so I would give a lot of credit to the Society of Hospital Medicine for being very deliberate in trying to strengthen its research program, highlight the research that hospitalists do, and make research a core pillar of what SHM stands for.”
The efforts have clearly worked, as RIV is a major driver for annual meeting attendance. The poster competition draws massive crowds that snake their way through the accepted posters.
For those interested in a deeper dive, SHM chooses a dozen or so top abstracts for oral presentations that are, in Dr. Fang’s words, “the creme de la creme of all the research and innovations for the given year.”
The growth of the abstracts competition comes, of course, as the specialty itself has seen its ranks skyrocket. Hospitalists now number an estimated 52,000 nationally, and in addition to providing direct clinical care, have taken ownership of key health care drivers like patient safety, quality improvement, and systems change.
“We do what we do for the good of health care and, ultimately, for the good of our patients,” Dr. Fang said. “Sometimes that’s rounding and taking care of patients in a clinical fashion, and sometimes it’s contributing to the medical literature. It could have been really easy for a specialty to say, ‘Not our problem,’ or ‘No, we’re just rounding.’ ”
HM17 course director Lenny Feldman, MD, FACP, FAAP, SFHM, believes that the commitment of SHM’s founding generation to do research for the past decade has created a group of mentors that push younger hospitalists to do more of the same.
“If we didn’t have the research engine part of hospital medicine, if we didn’t have the folks who are getting into administration and other important leadership areas, we wouldn’t see the maturation of this specialty and we would, in many ways, be stuck at the point at which we started,” Dr. Feldman said. “The only way for us to move forward is to do the research, to be in position to make sure that hospital medicine continues to grow in a direction that is good for our patients, for us, and for the entire system.”
That perspective is what motivates hospitalists to make the RIV bigger each year, said Dr. Fang.
“Having your abstract accepted as a poster or an oral presentation showcases all the work that you’ve put into it,” Dr. Fang said. “There’s a huge amount of pride in showing what you’ve been able to achieve. The driving force is the desire to see what other people are doing, and network to share ideas. That’s the really wonderful part of the RIV competition.”
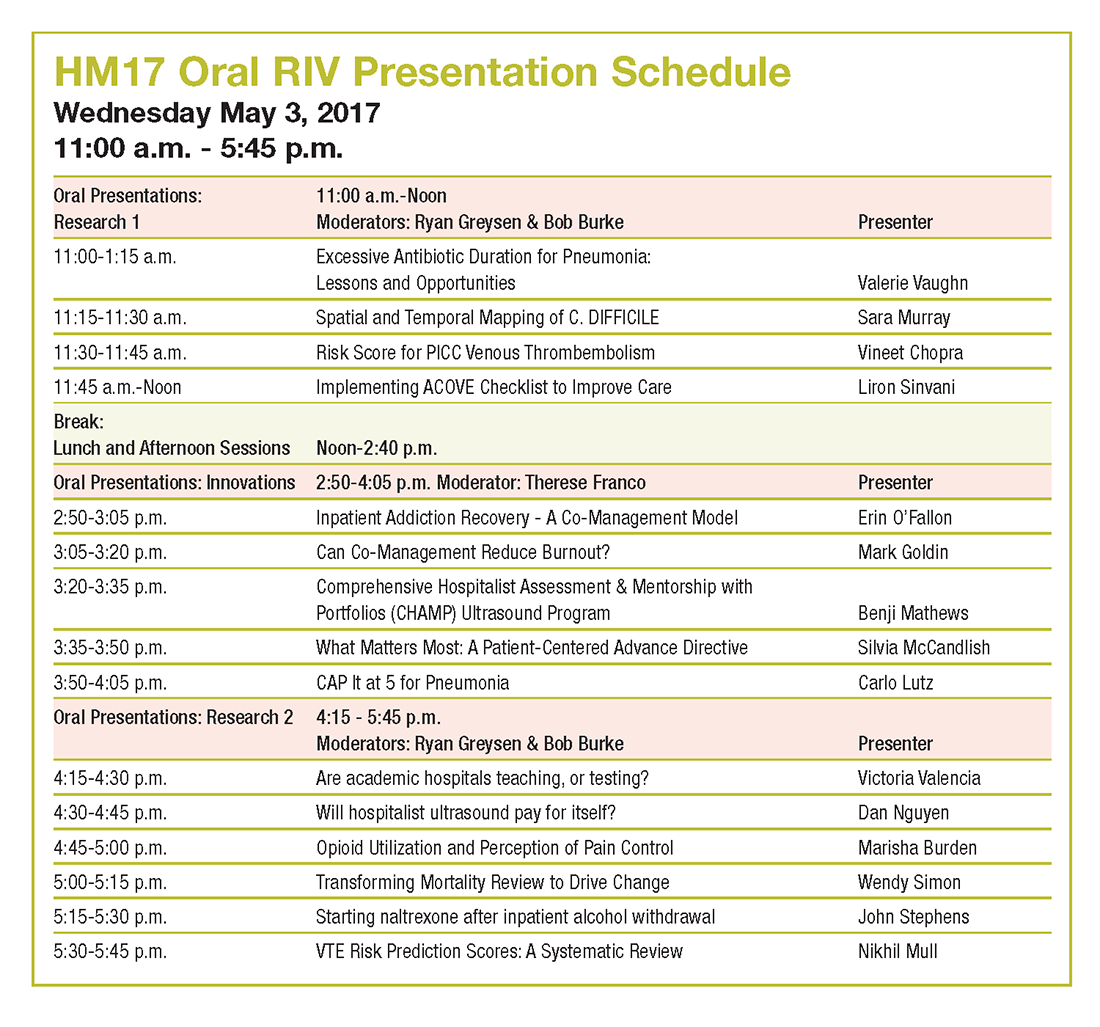
Postmenopausal hot flashes cut by 93% with novel nonhormonal treatment
AT ENDO 2017
ORLANDO –
After 12 weeks of treatment with the oral small molecule, women had a 93% reduction in moderate to severe hot flashes, compared with a 23% reduction for those taking placebo (P less than .0001). The effects of fezolinetant were seen earlier as well, with an 88% reduction in hot flashes at 4 weeks into the trial, compared with a 12% reduction for the placebo group (P less than .001).
The eight-site study enrolled 87 patients in a double-blind, randomized, placebo-controlled trial that assessed hot flash frequency and severity at study weeks 4 and 12. Postmenopausal women had to have frequent, moderate to severe hot flashes to qualify for enrollment, and they had to be otherwise healthy.
To capture data for a secondary endpoint, participants also completed a quality of life questionnaire. Dr. Fraser and his coinvestigators tracked safety and pharmacokinetic data by measuring levels of luteinizing hormone, follicle-stimulating hormone, estradiol, and sex hormone–binding globulin at baseline and 12 weeks, as well.
Evenly divided between study arms, 80 patients completed the trial. Two patients withdrew because of adverse events, one patient violated inclusion criteria, and the others withdrew for a variety of reasons. Mean age was similar between the two groups, at 53.7 years for those on placebo and 53.3 years for the fezolinetant group. Other anthropometric characteristics were similar, as well.
At baseline, patients taking placebo experienced a mean 10.3 moderate to severe hot flashes daily, compared with the fezolinetant group at a mean of 11.5. By study week 4, 14 of the 40 patients in the active arm had zero hot flashes, compared with 2 of 40 in the in the placebo arm, when the intention-to-treat population was examined. Hot flash severity dropped by 70% (P less than .0001).
Quality of life was assessed with the Hot Flash Related Daily Interference Scale (HFRDIS). When the two groups were compared, a significant (P less than .001) reduction in HFRDIS score was seen by week 4 and continued through to week 12 in the group on active treatment. Lower HFRDIS scores mean improved hot flash–related quality of life.
Using the Leeds Sleep Evaluation Questionnaire allowed Dr. Fraser and his colleagues to ask about how long it took patients to get to sleep while they were participating in the study, compared with their normal sleep latency. Patients taking fezolinetant reported getting to sleep significantly more quickly (P less than .01) than the placebo group. They also reported better quality of sleep (P less than .001) and a better awakening experience (P less than .05). However, they did not report feeling better after awakening (P = .08).
Women taking fezolinetant also showed significant improvement, compared with the placebo group, on other quality of life questionnaires, the Greene Climacteric Scale and the Sheehan Disability Scale. By week 8, a significant (P less than .001) improvement was seen on both scales and specifically at week 4 on the Sheehan Disability Scale.
Among the hormone biomarkers that were followed in the study, only plasma luteinizing-hormone levels dropped, compared with patients’ baseline levels. These were reduced 20% 12 hours after one of the two daily 60-mg oral doses, and 50% at 3 hours post dose, a point at which maximum serum fezolinetant concentration would be seen. These were all statistically significant reductions and expected effects of the drug’s mechanism of action.
Further pharmacokinetic analysis, said Dr. Fraser, “supports testing of once-daily dosing for vasomotor symptoms,” given that, when the drug was tested in premenopausal women in phase I clinical trials, there was no difference in peak and trough drug concentration.
The safety profile was good overall, said Dr. Fraser. No patients in the fezolinetant group reported serious treatment-emergent adverse events. “More patients reported treatment-emergent adverse events in the placebo group than in the fezolinetant group,” he said.
The NK3R antagonist is also under investigation for use in the treatment of polycystic ovary syndrome and uterine fibroids.
The study was funded by Ogeda, which employs Dr. Fraser. Another author reported serving as a clinical adviser for Ogeda.
[email protected]
On Twitter @karioakes
AT ENDO 2017
ORLANDO –
After 12 weeks of treatment with the oral small molecule, women had a 93% reduction in moderate to severe hot flashes, compared with a 23% reduction for those taking placebo (P less than .0001). The effects of fezolinetant were seen earlier as well, with an 88% reduction in hot flashes at 4 weeks into the trial, compared with a 12% reduction for the placebo group (P less than .001).
The eight-site study enrolled 87 patients in a double-blind, randomized, placebo-controlled trial that assessed hot flash frequency and severity at study weeks 4 and 12. Postmenopausal women had to have frequent, moderate to severe hot flashes to qualify for enrollment, and they had to be otherwise healthy.
To capture data for a secondary endpoint, participants also completed a quality of life questionnaire. Dr. Fraser and his coinvestigators tracked safety and pharmacokinetic data by measuring levels of luteinizing hormone, follicle-stimulating hormone, estradiol, and sex hormone–binding globulin at baseline and 12 weeks, as well.
Evenly divided between study arms, 80 patients completed the trial. Two patients withdrew because of adverse events, one patient violated inclusion criteria, and the others withdrew for a variety of reasons. Mean age was similar between the two groups, at 53.7 years for those on placebo and 53.3 years for the fezolinetant group. Other anthropometric characteristics were similar, as well.
At baseline, patients taking placebo experienced a mean 10.3 moderate to severe hot flashes daily, compared with the fezolinetant group at a mean of 11.5. By study week 4, 14 of the 40 patients in the active arm had zero hot flashes, compared with 2 of 40 in the in the placebo arm, when the intention-to-treat population was examined. Hot flash severity dropped by 70% (P less than .0001).
Quality of life was assessed with the Hot Flash Related Daily Interference Scale (HFRDIS). When the two groups were compared, a significant (P less than .001) reduction in HFRDIS score was seen by week 4 and continued through to week 12 in the group on active treatment. Lower HFRDIS scores mean improved hot flash–related quality of life.
Using the Leeds Sleep Evaluation Questionnaire allowed Dr. Fraser and his colleagues to ask about how long it took patients to get to sleep while they were participating in the study, compared with their normal sleep latency. Patients taking fezolinetant reported getting to sleep significantly more quickly (P less than .01) than the placebo group. They also reported better quality of sleep (P less than .001) and a better awakening experience (P less than .05). However, they did not report feeling better after awakening (P = .08).
Women taking fezolinetant also showed significant improvement, compared with the placebo group, on other quality of life questionnaires, the Greene Climacteric Scale and the Sheehan Disability Scale. By week 8, a significant (P less than .001) improvement was seen on both scales and specifically at week 4 on the Sheehan Disability Scale.
Among the hormone biomarkers that were followed in the study, only plasma luteinizing-hormone levels dropped, compared with patients’ baseline levels. These were reduced 20% 12 hours after one of the two daily 60-mg oral doses, and 50% at 3 hours post dose, a point at which maximum serum fezolinetant concentration would be seen. These were all statistically significant reductions and expected effects of the drug’s mechanism of action.
Further pharmacokinetic analysis, said Dr. Fraser, “supports testing of once-daily dosing for vasomotor symptoms,” given that, when the drug was tested in premenopausal women in phase I clinical trials, there was no difference in peak and trough drug concentration.
The safety profile was good overall, said Dr. Fraser. No patients in the fezolinetant group reported serious treatment-emergent adverse events. “More patients reported treatment-emergent adverse events in the placebo group than in the fezolinetant group,” he said.
The NK3R antagonist is also under investigation for use in the treatment of polycystic ovary syndrome and uterine fibroids.
The study was funded by Ogeda, which employs Dr. Fraser. Another author reported serving as a clinical adviser for Ogeda.
[email protected]
On Twitter @karioakes
AT ENDO 2017
ORLANDO –
After 12 weeks of treatment with the oral small molecule, women had a 93% reduction in moderate to severe hot flashes, compared with a 23% reduction for those taking placebo (P less than .0001). The effects of fezolinetant were seen earlier as well, with an 88% reduction in hot flashes at 4 weeks into the trial, compared with a 12% reduction for the placebo group (P less than .001).
The eight-site study enrolled 87 patients in a double-blind, randomized, placebo-controlled trial that assessed hot flash frequency and severity at study weeks 4 and 12. Postmenopausal women had to have frequent, moderate to severe hot flashes to qualify for enrollment, and they had to be otherwise healthy.
To capture data for a secondary endpoint, participants also completed a quality of life questionnaire. Dr. Fraser and his coinvestigators tracked safety and pharmacokinetic data by measuring levels of luteinizing hormone, follicle-stimulating hormone, estradiol, and sex hormone–binding globulin at baseline and 12 weeks, as well.
Evenly divided between study arms, 80 patients completed the trial. Two patients withdrew because of adverse events, one patient violated inclusion criteria, and the others withdrew for a variety of reasons. Mean age was similar between the two groups, at 53.7 years for those on placebo and 53.3 years for the fezolinetant group. Other anthropometric characteristics were similar, as well.
At baseline, patients taking placebo experienced a mean 10.3 moderate to severe hot flashes daily, compared with the fezolinetant group at a mean of 11.5. By study week 4, 14 of the 40 patients in the active arm had zero hot flashes, compared with 2 of 40 in the in the placebo arm, when the intention-to-treat population was examined. Hot flash severity dropped by 70% (P less than .0001).
Quality of life was assessed with the Hot Flash Related Daily Interference Scale (HFRDIS). When the two groups were compared, a significant (P less than .001) reduction in HFRDIS score was seen by week 4 and continued through to week 12 in the group on active treatment. Lower HFRDIS scores mean improved hot flash–related quality of life.
Using the Leeds Sleep Evaluation Questionnaire allowed Dr. Fraser and his colleagues to ask about how long it took patients to get to sleep while they were participating in the study, compared with their normal sleep latency. Patients taking fezolinetant reported getting to sleep significantly more quickly (P less than .01) than the placebo group. They also reported better quality of sleep (P less than .001) and a better awakening experience (P less than .05). However, they did not report feeling better after awakening (P = .08).
Women taking fezolinetant also showed significant improvement, compared with the placebo group, on other quality of life questionnaires, the Greene Climacteric Scale and the Sheehan Disability Scale. By week 8, a significant (P less than .001) improvement was seen on both scales and specifically at week 4 on the Sheehan Disability Scale.
Among the hormone biomarkers that were followed in the study, only plasma luteinizing-hormone levels dropped, compared with patients’ baseline levels. These were reduced 20% 12 hours after one of the two daily 60-mg oral doses, and 50% at 3 hours post dose, a point at which maximum serum fezolinetant concentration would be seen. These were all statistically significant reductions and expected effects of the drug’s mechanism of action.
Further pharmacokinetic analysis, said Dr. Fraser, “supports testing of once-daily dosing for vasomotor symptoms,” given that, when the drug was tested in premenopausal women in phase I clinical trials, there was no difference in peak and trough drug concentration.
The safety profile was good overall, said Dr. Fraser. No patients in the fezolinetant group reported serious treatment-emergent adverse events. “More patients reported treatment-emergent adverse events in the placebo group than in the fezolinetant group,” he said.
The NK3R antagonist is also under investigation for use in the treatment of polycystic ovary syndrome and uterine fibroids.
The study was funded by Ogeda, which employs Dr. Fraser. Another author reported serving as a clinical adviser for Ogeda.
[email protected]
On Twitter @karioakes
Key clinical point: .
Major finding: Women on fezolinetant had a 93% drop in hot flash frequency, compared with a 23% reduction for those on placebo (P less than .0001).
Data source: A phase II randomized, double-blind, placebo-controlled clinical trial of 87 postmenopausal women with moderate to severe hot flashes.
Disclosures: The study was funded by Ogeda, which employs Dr. Fraser. Another author reported serving as a clinical adviser for Ogeda.
Multiple miscarriages in a 29-year-old woman
A) Didelphys uterus INCORRECT
A didelphys uterus occurs as a result of complete nonfusion of the Müllerian duct, resulting in duplicated uterine horns, duplicated cervices, and occasionally the proximal vagina, which is often associated with a transverse or longitudinal vaginal septum.1,2 Fusion anomalies (didelphys and bicornuate) can be differentiated from resorption anomalies (septate and arcuate) on ultrasonography (US) by a deep fundal cleft (>1 cm).1 3D US is highly accurate in identifying Müllerian duct anomalies (MDAs), it correlates well with magnetic resonance imaging (MRI), and it is more cost effective and accessible.3 For the didelphys uterus, 3D US obtained coronal to the uterine fundus often demonstrates widely divergent uterine horns separated by a deep serosal fundal cleft (>1 cm) and noncommunicating endometrial cavities with 2 cervices.1 Identifying a duplicated vaginal canal can help differentiate a didelphys uterus from a bicornuate bicollis uterus.1

B) Unicornuate uterus INCORRECT
A unicornuate uterus results from arrested development of one Müllerian duct and normal development of the other. There are 4 different subtypes: no rudimentary horn, rudimentary horn without endometrial cavity, rudimentary horn with communicating endometrial cavity, and rudimentary horn with noncommunicating uterine cavity.1 Renal anomalies, especially renal agenesis when present, are usually ipsilateral to the rudimentary horn.1 On US, unicornuate uterus appears as a lobular oblong (banana-shaped) structure away from the midline. The rudimentary horn is often difficult to identify and, when seen, the presence or absence of endometrium is an important finding.1
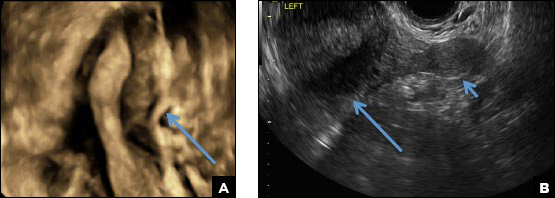
C) Partial septate uterus CORRECT
A septate uterus is a result of a resorption anomaly. The septum may be partial (subseptate) or complete secondary to failure of resorption of the uterovaginal septum. A complete septum extends to the external cervical os and occasionally to the vagina.1 US demonstrates interruption of the myometrium by a hypoechoic fibrous septum and/or a muscular septum which is isoechoic to the myometrium and arises midline from the fundus.1 3D US often clearly delineates the septum and improves visualization of the external fundal contour.2 The external fundal contour in septate uterus is convex (little or no serosal fundal cleft) and the apex is greater than 5 mm above the interostial line compared with a bicornuate or didelphys uterus, where the apex is less than 5 mm from the interostial line.1,2 Additionally, the intercornual distance is less than 4 cm.4 A septate uterus with duplicated cervix can appear similar to a bicornuate bicollis uterus and can be correctly diagnosed by evaluating the external fundal contour.1
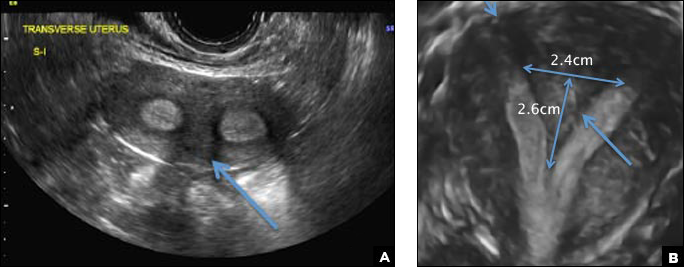
D) Arcuate uterus INCORRECT
The arcuate uterus also represents a resorption anomaly as a sequela of near-complete resorption of the uterovaginal septum.1 On 3D US, the fundal indentation in an arcuate uterus is well delineated and appears broad based with an obtuse angle at the most central point, which can help differentiate it from a septate uterus that has an acute angle.2,3 Both an arcuate and a septate uterus have a normal external (serosal) fundal contour.2,3 With an arcuate uterus, the length of the vertical measurement from the tubal ostia line, which is drawn horizontally between the tubal ostia to the fundal midline component of the endometrial cavity, is 1 cm or less. With a septate uterus, this vertical distance is greater than 1 cm.
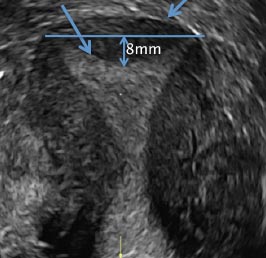
- CambriaBehr SC, Courtier JL, Qayyum A. Imaging of MMS PGothicüCambriallerian duct anomalies. RadioGraphics. 2012;32(6):e23.
- Bermejo C, Martinez Ten P, Diaz D, et al. Three-dimensional ultrasound in the diagnosis of MMS PGothicüCambriallerian duct anomaly and concordance with MRI. Ultrasound Obstet Gynecol.Cambria 2010;35(5):593–601.
- Deutch TD, Abuhamed AZ. The role of 3-dimensional ultrasonography and magnetic resonance imaging in the diagnosis of MMS PGothicüCambriallerian duct anomalies. J Ultrasound Med. 2008;27(3):413–423.
- CambriaChandler TM, Machan LS, Cooperberg PL, Harris AC, Chang SD. MMS PGothicüCambriallerian duct anomalies: from diagnosis to intervention.Cambria Br J Radiol. 2009;82(984):1034–1042.
A) Didelphys uterus INCORRECT
A didelphys uterus occurs as a result of complete nonfusion of the Müllerian duct, resulting in duplicated uterine horns, duplicated cervices, and occasionally the proximal vagina, which is often associated with a transverse or longitudinal vaginal septum.1,2 Fusion anomalies (didelphys and bicornuate) can be differentiated from resorption anomalies (septate and arcuate) on ultrasonography (US) by a deep fundal cleft (>1 cm).1 3D US is highly accurate in identifying Müllerian duct anomalies (MDAs), it correlates well with magnetic resonance imaging (MRI), and it is more cost effective and accessible.3 For the didelphys uterus, 3D US obtained coronal to the uterine fundus often demonstrates widely divergent uterine horns separated by a deep serosal fundal cleft (>1 cm) and noncommunicating endometrial cavities with 2 cervices.1 Identifying a duplicated vaginal canal can help differentiate a didelphys uterus from a bicornuate bicollis uterus.1

B) Unicornuate uterus INCORRECT
A unicornuate uterus results from arrested development of one Müllerian duct and normal development of the other. There are 4 different subtypes: no rudimentary horn, rudimentary horn without endometrial cavity, rudimentary horn with communicating endometrial cavity, and rudimentary horn with noncommunicating uterine cavity.1 Renal anomalies, especially renal agenesis when present, are usually ipsilateral to the rudimentary horn.1 On US, unicornuate uterus appears as a lobular oblong (banana-shaped) structure away from the midline. The rudimentary horn is often difficult to identify and, when seen, the presence or absence of endometrium is an important finding.1
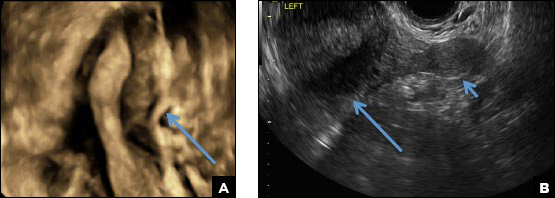
C) Partial septate uterus CORRECT
A septate uterus is a result of a resorption anomaly. The septum may be partial (subseptate) or complete secondary to failure of resorption of the uterovaginal septum. A complete septum extends to the external cervical os and occasionally to the vagina.1 US demonstrates interruption of the myometrium by a hypoechoic fibrous septum and/or a muscular septum which is isoechoic to the myometrium and arises midline from the fundus.1 3D US often clearly delineates the septum and improves visualization of the external fundal contour.2 The external fundal contour in septate uterus is convex (little or no serosal fundal cleft) and the apex is greater than 5 mm above the interostial line compared with a bicornuate or didelphys uterus, where the apex is less than 5 mm from the interostial line.1,2 Additionally, the intercornual distance is less than 4 cm.4 A septate uterus with duplicated cervix can appear similar to a bicornuate bicollis uterus and can be correctly diagnosed by evaluating the external fundal contour.1
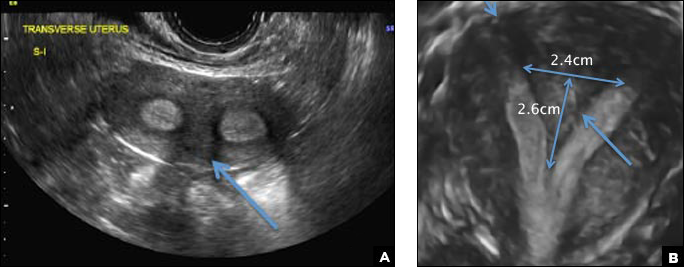
D) Arcuate uterus INCORRECT
The arcuate uterus also represents a resorption anomaly as a sequela of near-complete resorption of the uterovaginal septum.1 On 3D US, the fundal indentation in an arcuate uterus is well delineated and appears broad based with an obtuse angle at the most central point, which can help differentiate it from a septate uterus that has an acute angle.2,3 Both an arcuate and a septate uterus have a normal external (serosal) fundal contour.2,3 With an arcuate uterus, the length of the vertical measurement from the tubal ostia line, which is drawn horizontally between the tubal ostia to the fundal midline component of the endometrial cavity, is 1 cm or less. With a septate uterus, this vertical distance is greater than 1 cm.
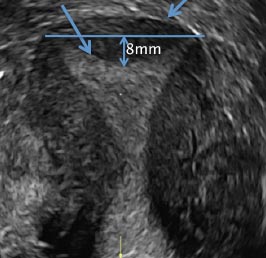
A) Didelphys uterus INCORRECT
A didelphys uterus occurs as a result of complete nonfusion of the Müllerian duct, resulting in duplicated uterine horns, duplicated cervices, and occasionally the proximal vagina, which is often associated with a transverse or longitudinal vaginal septum.1,2 Fusion anomalies (didelphys and bicornuate) can be differentiated from resorption anomalies (septate and arcuate) on ultrasonography (US) by a deep fundal cleft (>1 cm).1 3D US is highly accurate in identifying Müllerian duct anomalies (MDAs), it correlates well with magnetic resonance imaging (MRI), and it is more cost effective and accessible.3 For the didelphys uterus, 3D US obtained coronal to the uterine fundus often demonstrates widely divergent uterine horns separated by a deep serosal fundal cleft (>1 cm) and noncommunicating endometrial cavities with 2 cervices.1 Identifying a duplicated vaginal canal can help differentiate a didelphys uterus from a bicornuate bicollis uterus.1

B) Unicornuate uterus INCORRECT
A unicornuate uterus results from arrested development of one Müllerian duct and normal development of the other. There are 4 different subtypes: no rudimentary horn, rudimentary horn without endometrial cavity, rudimentary horn with communicating endometrial cavity, and rudimentary horn with noncommunicating uterine cavity.1 Renal anomalies, especially renal agenesis when present, are usually ipsilateral to the rudimentary horn.1 On US, unicornuate uterus appears as a lobular oblong (banana-shaped) structure away from the midline. The rudimentary horn is often difficult to identify and, when seen, the presence or absence of endometrium is an important finding.1
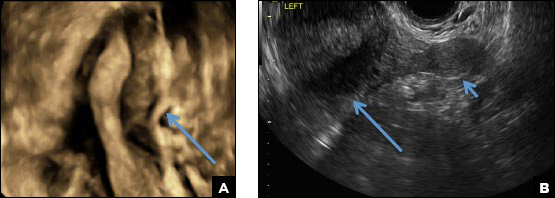
C) Partial septate uterus CORRECT
A septate uterus is a result of a resorption anomaly. The septum may be partial (subseptate) or complete secondary to failure of resorption of the uterovaginal septum. A complete septum extends to the external cervical os and occasionally to the vagina.1 US demonstrates interruption of the myometrium by a hypoechoic fibrous septum and/or a muscular septum which is isoechoic to the myometrium and arises midline from the fundus.1 3D US often clearly delineates the septum and improves visualization of the external fundal contour.2 The external fundal contour in septate uterus is convex (little or no serosal fundal cleft) and the apex is greater than 5 mm above the interostial line compared with a bicornuate or didelphys uterus, where the apex is less than 5 mm from the interostial line.1,2 Additionally, the intercornual distance is less than 4 cm.4 A septate uterus with duplicated cervix can appear similar to a bicornuate bicollis uterus and can be correctly diagnosed by evaluating the external fundal contour.1
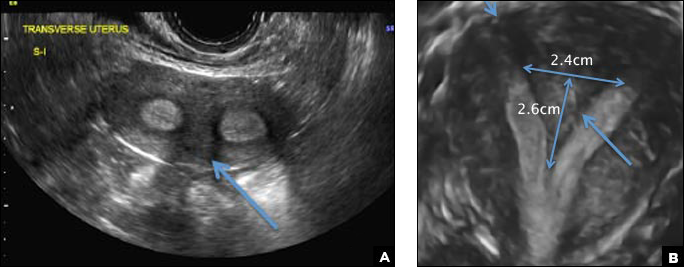
D) Arcuate uterus INCORRECT
The arcuate uterus also represents a resorption anomaly as a sequela of near-complete resorption of the uterovaginal septum.1 On 3D US, the fundal indentation in an arcuate uterus is well delineated and appears broad based with an obtuse angle at the most central point, which can help differentiate it from a septate uterus that has an acute angle.2,3 Both an arcuate and a septate uterus have a normal external (serosal) fundal contour.2,3 With an arcuate uterus, the length of the vertical measurement from the tubal ostia line, which is drawn horizontally between the tubal ostia to the fundal midline component of the endometrial cavity, is 1 cm or less. With a septate uterus, this vertical distance is greater than 1 cm.
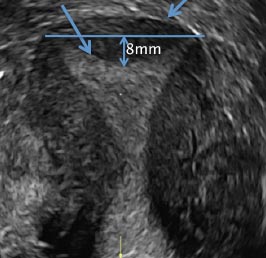
- CambriaBehr SC, Courtier JL, Qayyum A. Imaging of MMS PGothicüCambriallerian duct anomalies. RadioGraphics. 2012;32(6):e23.
- Bermejo C, Martinez Ten P, Diaz D, et al. Three-dimensional ultrasound in the diagnosis of MMS PGothicüCambriallerian duct anomaly and concordance with MRI. Ultrasound Obstet Gynecol.Cambria 2010;35(5):593–601.
- Deutch TD, Abuhamed AZ. The role of 3-dimensional ultrasonography and magnetic resonance imaging in the diagnosis of MMS PGothicüCambriallerian duct anomalies. J Ultrasound Med. 2008;27(3):413–423.
- CambriaChandler TM, Machan LS, Cooperberg PL, Harris AC, Chang SD. MMS PGothicüCambriallerian duct anomalies: from diagnosis to intervention.Cambria Br J Radiol. 2009;82(984):1034–1042.
- CambriaBehr SC, Courtier JL, Qayyum A. Imaging of MMS PGothicüCambriallerian duct anomalies. RadioGraphics. 2012;32(6):e23.
- Bermejo C, Martinez Ten P, Diaz D, et al. Three-dimensional ultrasound in the diagnosis of MMS PGothicüCambriallerian duct anomaly and concordance with MRI. Ultrasound Obstet Gynecol.Cambria 2010;35(5):593–601.
- Deutch TD, Abuhamed AZ. The role of 3-dimensional ultrasonography and magnetic resonance imaging in the diagnosis of MMS PGothicüCambriallerian duct anomalies. J Ultrasound Med. 2008;27(3):413–423.
- CambriaChandler TM, Machan LS, Cooperberg PL, Harris AC, Chang SD. MMS PGothicüCambriallerian duct anomalies: from diagnosis to intervention.Cambria Br J Radiol. 2009;82(984):1034–1042.
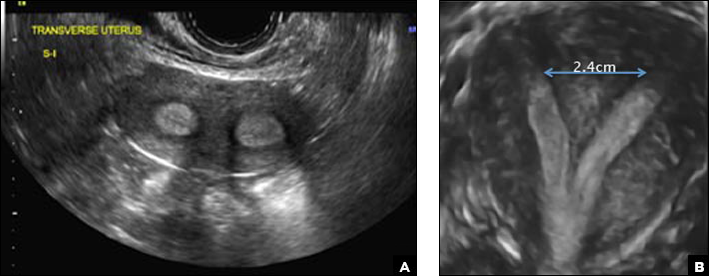
A 29-year-old woman presents to her ObGyn’s office with a history of multiple miscarriages. Transverse pelvic 2D ultrasonography of the uterus (A) and coronal 3D imaging (B) are performed.
GOP health reform: Essential health benefits, community rating under fire
Republicans are targeting two key consumer protections in their latest attempt to gain enough votes to pass the American Health Care Act, phase 1 of their Affordable Care Act repeal and replace plan.
On the chopping block are the essential health care benefits package and so-called community rating provisions – which prevent insurers from charging significantly more for older patients and those with preexisting conditions.
“Obamacare is already in a race to the bottom in terms of quality coverage for the sick and that’s because of the law’s community rating provisions, which penalize high-quality coverage for the sick,” Michael F. Cannon, director of health policy studies at the Cato Institute, said in an interview. “The [AHCA] would arguably accelerate that race to the bottom. The waiver provision in this amendment definitely would and it would because the bill would allow states to waive the community rating provisions, but only for people who were not previously insured.”
The waiver provisions would “increase premiums for the previously uninsured and discourage them from enrolling,” Mr. Cannon predicted.
David Anderson, research associate at the Margolis Center for Health Policy at Duke University, Durham, N.C., said that, if a state elects to take a waiver, so-called high-cost patients “such as individuals with cancer, individuals with cystic fibrosis, individuals with coagulation disorders, [would be] shrugged to the side into a high-cost risk pool or some kind of risk sharing ... with their own premium pool.” This could lower premium costs for healthy patients, he added.
This could be enhanced by narrowing the essential health benefits. For example, Mr. Anderson said that a state could keep the drug benefit, but apply for a waiver to narrow its coverage for all generics plus a limited list of brand names.
“Someone with cystic fibrosis with a $300,000-a-year medication will not have that covered and will be put in the high-cost risk pool,” Mr. Anderson said. “What it does is that it makes insurance cheaper for individuals who are highly unlikely to be high cost, and it makes it much more expensive for any individuals with known high-cost conditions.”
The draft amendment also would make it easier a whole lot easier to get such waivers approved: If enacted, the legislation would give default approval of such waivers and allow just 60 days for the Department of Health & Human Services to deny waiver request.
States would be able to apply for a waiver from the essential health benefits requirements for the 2020 plan year and a waiver to charge higher premiums to certain individuals for the 2019 plan year.
Waivers to change the essential health benefits package would need to meet one or more of the following conditions:
- Reduce average premiums.
- Increase enrollment.
- Stabilize the health insurance market.
- Stabilize premiums for individuals with preexisting conditions.
- Increase consumer choice.
For a state to change community rating provisions, its waiver also would need to create a mechanism, such as high-risk pools, to help those patients. Funding for these pools is provided for in the AHCA, but has been criticized as being inadequate on a national level.
Mr. Cannon of the Cato Institute predicted that such waivers ultimately would lead to more adverse selections for people needing comprehensive coverage and could force more people to lose coverage than to gain access to affordable, high-quality plans.
“If you waive essential health benefits in a community-rated market, you get even more adverse selection against comprehensive plans that sick people want, so those plans disappear,” Mr. Cannon said. “They either disappear because the insurers stop offering them or they disappear because insurers try to make the coverage worse, because Obamacare penalizes them if they don’t make coverage worse.”
He said these waivers provide little incentive for health insurers to stay in the individual markets and they could, as they are already, flee the individual markets.
The AHCA is phase 1 of the GOP repeal and replace plan. Congressional Republicans want to use the budget reconciliation process for the AHCA, so that they need only a simple majority to change revenue-generating provisions of the ACA. Phase 2 is a comprehensive review of all federal health care regulations and phase 3 is slated to be new legislation to replace the ACA with a new health care reform plan, which will require a two-thirds majority in the Senate to pass.
Republicans are targeting two key consumer protections in their latest attempt to gain enough votes to pass the American Health Care Act, phase 1 of their Affordable Care Act repeal and replace plan.
On the chopping block are the essential health care benefits package and so-called community rating provisions – which prevent insurers from charging significantly more for older patients and those with preexisting conditions.
“Obamacare is already in a race to the bottom in terms of quality coverage for the sick and that’s because of the law’s community rating provisions, which penalize high-quality coverage for the sick,” Michael F. Cannon, director of health policy studies at the Cato Institute, said in an interview. “The [AHCA] would arguably accelerate that race to the bottom. The waiver provision in this amendment definitely would and it would because the bill would allow states to waive the community rating provisions, but only for people who were not previously insured.”
The waiver provisions would “increase premiums for the previously uninsured and discourage them from enrolling,” Mr. Cannon predicted.
David Anderson, research associate at the Margolis Center for Health Policy at Duke University, Durham, N.C., said that, if a state elects to take a waiver, so-called high-cost patients “such as individuals with cancer, individuals with cystic fibrosis, individuals with coagulation disorders, [would be] shrugged to the side into a high-cost risk pool or some kind of risk sharing ... with their own premium pool.” This could lower premium costs for healthy patients, he added.
This could be enhanced by narrowing the essential health benefits. For example, Mr. Anderson said that a state could keep the drug benefit, but apply for a waiver to narrow its coverage for all generics plus a limited list of brand names.
“Someone with cystic fibrosis with a $300,000-a-year medication will not have that covered and will be put in the high-cost risk pool,” Mr. Anderson said. “What it does is that it makes insurance cheaper for individuals who are highly unlikely to be high cost, and it makes it much more expensive for any individuals with known high-cost conditions.”
The draft amendment also would make it easier a whole lot easier to get such waivers approved: If enacted, the legislation would give default approval of such waivers and allow just 60 days for the Department of Health & Human Services to deny waiver request.
States would be able to apply for a waiver from the essential health benefits requirements for the 2020 plan year and a waiver to charge higher premiums to certain individuals for the 2019 plan year.
Waivers to change the essential health benefits package would need to meet one or more of the following conditions:
- Reduce average premiums.
- Increase enrollment.
- Stabilize the health insurance market.
- Stabilize premiums for individuals with preexisting conditions.
- Increase consumer choice.
For a state to change community rating provisions, its waiver also would need to create a mechanism, such as high-risk pools, to help those patients. Funding for these pools is provided for in the AHCA, but has been criticized as being inadequate on a national level.
Mr. Cannon of the Cato Institute predicted that such waivers ultimately would lead to more adverse selections for people needing comprehensive coverage and could force more people to lose coverage than to gain access to affordable, high-quality plans.
“If you waive essential health benefits in a community-rated market, you get even more adverse selection against comprehensive plans that sick people want, so those plans disappear,” Mr. Cannon said. “They either disappear because the insurers stop offering them or they disappear because insurers try to make the coverage worse, because Obamacare penalizes them if they don’t make coverage worse.”
He said these waivers provide little incentive for health insurers to stay in the individual markets and they could, as they are already, flee the individual markets.
The AHCA is phase 1 of the GOP repeal and replace plan. Congressional Republicans want to use the budget reconciliation process for the AHCA, so that they need only a simple majority to change revenue-generating provisions of the ACA. Phase 2 is a comprehensive review of all federal health care regulations and phase 3 is slated to be new legislation to replace the ACA with a new health care reform plan, which will require a two-thirds majority in the Senate to pass.
Republicans are targeting two key consumer protections in their latest attempt to gain enough votes to pass the American Health Care Act, phase 1 of their Affordable Care Act repeal and replace plan.
On the chopping block are the essential health care benefits package and so-called community rating provisions – which prevent insurers from charging significantly more for older patients and those with preexisting conditions.
“Obamacare is already in a race to the bottom in terms of quality coverage for the sick and that’s because of the law’s community rating provisions, which penalize high-quality coverage for the sick,” Michael F. Cannon, director of health policy studies at the Cato Institute, said in an interview. “The [AHCA] would arguably accelerate that race to the bottom. The waiver provision in this amendment definitely would and it would because the bill would allow states to waive the community rating provisions, but only for people who were not previously insured.”
The waiver provisions would “increase premiums for the previously uninsured and discourage them from enrolling,” Mr. Cannon predicted.
David Anderson, research associate at the Margolis Center for Health Policy at Duke University, Durham, N.C., said that, if a state elects to take a waiver, so-called high-cost patients “such as individuals with cancer, individuals with cystic fibrosis, individuals with coagulation disorders, [would be] shrugged to the side into a high-cost risk pool or some kind of risk sharing ... with their own premium pool.” This could lower premium costs for healthy patients, he added.
This could be enhanced by narrowing the essential health benefits. For example, Mr. Anderson said that a state could keep the drug benefit, but apply for a waiver to narrow its coverage for all generics plus a limited list of brand names.
“Someone with cystic fibrosis with a $300,000-a-year medication will not have that covered and will be put in the high-cost risk pool,” Mr. Anderson said. “What it does is that it makes insurance cheaper for individuals who are highly unlikely to be high cost, and it makes it much more expensive for any individuals with known high-cost conditions.”
The draft amendment also would make it easier a whole lot easier to get such waivers approved: If enacted, the legislation would give default approval of such waivers and allow just 60 days for the Department of Health & Human Services to deny waiver request.
States would be able to apply for a waiver from the essential health benefits requirements for the 2020 plan year and a waiver to charge higher premiums to certain individuals for the 2019 plan year.
Waivers to change the essential health benefits package would need to meet one or more of the following conditions:
- Reduce average premiums.
- Increase enrollment.
- Stabilize the health insurance market.
- Stabilize premiums for individuals with preexisting conditions.
- Increase consumer choice.
For a state to change community rating provisions, its waiver also would need to create a mechanism, such as high-risk pools, to help those patients. Funding for these pools is provided for in the AHCA, but has been criticized as being inadequate on a national level.
Mr. Cannon of the Cato Institute predicted that such waivers ultimately would lead to more adverse selections for people needing comprehensive coverage and could force more people to lose coverage than to gain access to affordable, high-quality plans.
“If you waive essential health benefits in a community-rated market, you get even more adverse selection against comprehensive plans that sick people want, so those plans disappear,” Mr. Cannon said. “They either disappear because the insurers stop offering them or they disappear because insurers try to make the coverage worse, because Obamacare penalizes them if they don’t make coverage worse.”
He said these waivers provide little incentive for health insurers to stay in the individual markets and they could, as they are already, flee the individual markets.
The AHCA is phase 1 of the GOP repeal and replace plan. Congressional Republicans want to use the budget reconciliation process for the AHCA, so that they need only a simple majority to change revenue-generating provisions of the ACA. Phase 2 is a comprehensive review of all federal health care regulations and phase 3 is slated to be new legislation to replace the ACA with a new health care reform plan, which will require a two-thirds majority in the Senate to pass.
VIDEO: Cannabidiol reduces convulsive seizures in Dravet syndrome
BOSTON – Adjunctive treatment with cannabidiol significantly reduced convulsive seizure frequency in Dravet syndrome patients in a randomized, double-blind, placebo-controlled trial.
Over a 14-week treatment period, including 2 weeks of titration and 12 weeks of maintenance, convulsive seizure frequency in 61 treated children and adolescents decreased from a median of 12.4 to 5.9 per month (median reduction of 39%), compared with a decrease from a median of 14.9 to 14.1 per month (median reduction of 13%) in 59 patients who received placebo, J. Helen Cross, MD, reported at the annual meeting of the American Academy of Neurology.
The proportion of patients with at least a 50% reduction in convulsive seizures was 42.6% with cannabidiol vs. 27.1% with placebo (odds ratio, 2.0), but this difference did not reach statistical significance, said Dr. Cross of the University College London Great Ormond Street Institute of Child Health and the Great Ormond Street Hospital for Children NHS Trust, London.
In a video interview, Dr. Cross discussed the findings and the importance of improving seizure control in patients with Dravet syndrome, a rare infantile-onset developmental and epileptic encephalopathy with very poor prognosis for long-term seizure control and neurodevelopmental outcomes.
Participants in the study (GWPCARE1) had a mean age of 10 years, but nearly a third were younger than 6 years. All had Dravet syndrome and drug-resistant seizures; the median number of antiepilepsy drugs previously tried was four, and the median number being used was three. Those randomized to the treatment group received cannabidiol oral solution up to 20 mg/kg per day.
Adverse events were common, occurring in 93.4% and 74.6% of treatment group and placebo group patients, respectively. But adverse events reported in the treatment group were mild or moderate in 84% of patients, and treatment was generally well tolerated.
“These are very complex patients with a high seizure burden... and therefore, to have another medication that looks as if it can be of benefit is really very exciting for this population,” Dr. Cross said, noting that cannabidiol was also shown in other studies presented at the AAN meeting (GWPCARE3 and GWPCARE4) to reduce seizure frequency in patients with Lennox-Gastaut syndrome.
GW Research sponsored the study. Dr. Cross is a member of the advisory boards for Eisai, GW Pharmaceuticals, Shire, and Zogenix.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Adjunctive treatment with cannabidiol significantly reduced convulsive seizure frequency in Dravet syndrome patients in a randomized, double-blind, placebo-controlled trial.
Over a 14-week treatment period, including 2 weeks of titration and 12 weeks of maintenance, convulsive seizure frequency in 61 treated children and adolescents decreased from a median of 12.4 to 5.9 per month (median reduction of 39%), compared with a decrease from a median of 14.9 to 14.1 per month (median reduction of 13%) in 59 patients who received placebo, J. Helen Cross, MD, reported at the annual meeting of the American Academy of Neurology.
The proportion of patients with at least a 50% reduction in convulsive seizures was 42.6% with cannabidiol vs. 27.1% with placebo (odds ratio, 2.0), but this difference did not reach statistical significance, said Dr. Cross of the University College London Great Ormond Street Institute of Child Health and the Great Ormond Street Hospital for Children NHS Trust, London.
In a video interview, Dr. Cross discussed the findings and the importance of improving seizure control in patients with Dravet syndrome, a rare infantile-onset developmental and epileptic encephalopathy with very poor prognosis for long-term seizure control and neurodevelopmental outcomes.
Participants in the study (GWPCARE1) had a mean age of 10 years, but nearly a third were younger than 6 years. All had Dravet syndrome and drug-resistant seizures; the median number of antiepilepsy drugs previously tried was four, and the median number being used was three. Those randomized to the treatment group received cannabidiol oral solution up to 20 mg/kg per day.
Adverse events were common, occurring in 93.4% and 74.6% of treatment group and placebo group patients, respectively. But adverse events reported in the treatment group were mild or moderate in 84% of patients, and treatment was generally well tolerated.
“These are very complex patients with a high seizure burden... and therefore, to have another medication that looks as if it can be of benefit is really very exciting for this population,” Dr. Cross said, noting that cannabidiol was also shown in other studies presented at the AAN meeting (GWPCARE3 and GWPCARE4) to reduce seizure frequency in patients with Lennox-Gastaut syndrome.
GW Research sponsored the study. Dr. Cross is a member of the advisory boards for Eisai, GW Pharmaceuticals, Shire, and Zogenix.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BOSTON – Adjunctive treatment with cannabidiol significantly reduced convulsive seizure frequency in Dravet syndrome patients in a randomized, double-blind, placebo-controlled trial.
Over a 14-week treatment period, including 2 weeks of titration and 12 weeks of maintenance, convulsive seizure frequency in 61 treated children and adolescents decreased from a median of 12.4 to 5.9 per month (median reduction of 39%), compared with a decrease from a median of 14.9 to 14.1 per month (median reduction of 13%) in 59 patients who received placebo, J. Helen Cross, MD, reported at the annual meeting of the American Academy of Neurology.
The proportion of patients with at least a 50% reduction in convulsive seizures was 42.6% with cannabidiol vs. 27.1% with placebo (odds ratio, 2.0), but this difference did not reach statistical significance, said Dr. Cross of the University College London Great Ormond Street Institute of Child Health and the Great Ormond Street Hospital for Children NHS Trust, London.
In a video interview, Dr. Cross discussed the findings and the importance of improving seizure control in patients with Dravet syndrome, a rare infantile-onset developmental and epileptic encephalopathy with very poor prognosis for long-term seizure control and neurodevelopmental outcomes.
Participants in the study (GWPCARE1) had a mean age of 10 years, but nearly a third were younger than 6 years. All had Dravet syndrome and drug-resistant seizures; the median number of antiepilepsy drugs previously tried was four, and the median number being used was three. Those randomized to the treatment group received cannabidiol oral solution up to 20 mg/kg per day.
Adverse events were common, occurring in 93.4% and 74.6% of treatment group and placebo group patients, respectively. But adverse events reported in the treatment group were mild or moderate in 84% of patients, and treatment was generally well tolerated.
“These are very complex patients with a high seizure burden... and therefore, to have another medication that looks as if it can be of benefit is really very exciting for this population,” Dr. Cross said, noting that cannabidiol was also shown in other studies presented at the AAN meeting (GWPCARE3 and GWPCARE4) to reduce seizure frequency in patients with Lennox-Gastaut syndrome.
GW Research sponsored the study. Dr. Cross is a member of the advisory boards for Eisai, GW Pharmaceuticals, Shire, and Zogenix.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
At ANN 2017
Key clinical point:
Major finding: Children and adolescents treated with cannabidiol had a decline in convulsive seizure frequency, from a median of 12.4 to 5.9 per month (median reduction of 39%), compared with a decrease from a median of 14.9 to 14.1 per month with placebo (median reduction of 13%).
Data source: A randomized, double-blind, placebo-controlled trial of adjunctive treatment with cannabidiol in 120 children and adolescents with Dravet syndrome.
Disclosures: GW Research sponsored the study. Dr. Cross is a member of the advisory boards for Eisai, GW Pharmaceuticals, Shire, and Zogenix.