User login
Building a cancer genetics and prevention program
Gastroenterologists offer more than just high-quality colonoscopy for colon cancer prevention. We often are the specialists who first recognize a genetic cancer syndrome during our endoscopy or clinic sessions. The patient who piqued my interest in colon cancer genetics was a 24-year-old woman who was referred for postoperative nausea after a hysterectomy for early stage uterine cancer (that alone should have raised alarm bells). Endoscopy revealed (by happenstance) a stomach coated with polyps. This led to a colonoscopy and diagnosis of familial adenomatous polyposis (uterine cancer within FAP is unusual but reported, for those of you studying for boards). In 1991, no coordinated genetics program existed within my practice so I arranged referrals to genetic counselors, surgeons, and pathologists. This led to the discovery of FAP and early stage (and curable) cancers in her two brothers and her father, in addition to extended pedigree analysis that established multi-organ cancer risks in other relatives. Years later, she brought her two adopted children to meet me and told me of lighting candles in my honor during an American Cancer Society walk. This is why we become doctors.
In this column, Dr. Xavier Llor describes the cancer genetics program he and others have built at Yale. It provides practical steps that can be taken by health system or community-based gastroenterologists to recognize and manage these complex syndromes. We are the specialists on the front lines and Dr. Llor helps us provide the coordinated care our patients expect from us.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Among all common cancers, breast and colon have the highest percentage of cases that are due to hereditary syndromes. Many of the responsible genes have been identified, and the last few years have seen an increase in uptake of genetic testing supported by the refinement of the clinical criteria suggestive of these syndromes as well as the clear improvement in outcomes as a result of the adoption of cancer preventive measures in mutation carriers.1 In spite of this, genetic testing for colorectal cancer (CRC) syndromes is not ordered as often as it should be according to the prevalence of these syndromes.2 In contrast, testing for hereditary breast cancer has become more generalized, and the threshold for ordering genetic testing in the latter is often lower than for CRC. The are several reasons for this: 1) much greater awareness, by both providers and the general public, of hereditary breast cancer conditions; 2) fewer providers with expertise in CRC genetics; 3) lack of a systematic approach to identify patients with potential CRC syndromes; and 4) absence of a clear premorbid phenotype for the most common of all CRC syndromes, Lynch syndrome.3
The recent recommendation in practice guidelines to screen all CRC tumors for Lynch syndrome either with immunohistochemistry to evaluate mismatch repair (MMR) protein expression or through tandem repeat analysis to test for microsatellite instability4 has highlighted that about 10% of all CRCs (a percentage consistently seen in different ethnic groups5) need further cancer genetic evaluation, and many will require sequencing of germline DNA. Although data on cost-effectiveness of this approach are somewhat conflicting,6,7 it is sensible because it is systematic, and studies have shown an increase in diagnostic yield through universal tumor screening.8 Unfortunately, in practice, often suspicious tumor testing results are not followed up by cancer genetics referrals, and many patients with CRC syndrome remain undiagnosed.
Patients with oligopolyposis (fewer than 100 polyps over time) also present diagnostic challenges. Some have attenuated familial adenomatous polyposis because of an APC mutation or MUTYH-associated polyposis. Recent findings have revealed other less commonly mutated genes that also result in oligopolyposis and a significant CRC risk: polymerases POLE and POLD1, GREM1, MCM9, or NTHL1. Because of the relatively low number of polyps in many of these syndromes and the lack of a systematic strategy to add up all polyps diagnosed over time, we not uncommonly fail to suspect some polyposis syndromes. Furthermore, the mixed pattern of polyps that is often associated with some of the mentioned mutated genes adds an extra challenge to diagnosing these cases.
Once individuals with CRC syndromes are identified, the challenge is to provide them with the care that they need, because many gastroenterologists, oncologists, and other health care providers are not extremely familiar with the current options for these patients.
In summary, there is a need to find systematic ways to triage and appropriately refer patients with a potential CRC syndrome to cancer genetics specialists so patients and their families can benefit from proper diagnosis and cancer preventive measures.
Building a comprehensive cancer genetics program
Although implementing systematic approaches is key to selecting individuals at risk, the complexity of caring for these patients demands a service that can stand up to the multiple challenges. For instance, most CRC syndromes are in fact multi-cancer syndromes with an increased risk of cancer and other pathologies in different organs beside the colon. Furthermore, the psychological implications of having a heritable cancer condition often take an important toll on affected families, with common feelings of guilt for having passed the mutated genes to the offspring.
Thus, to provide the best care to affected families, there is a tremendous need for well-organized and comprehensive cancer genetics services that are capable of responding to the multiple needs of these families so state-of-the-art cancer preventive measures can be carried out and multilevel support can be provided. The mentioned considerations were the guiding force in the creation of the Smilow Cancer Genetics and Prevention Program (SCGPP) at Yale. Thus, we established a comprehensive program that brings together health professionals specializing in different aspects of these patients’ care that ensures their proper attention in a longitudinal fashion, making the program their home for health care. We integrated in the program, among others, physician leaders in gastrointestinal (GI), breast, gynecological, endocrine, and genitourinary high-risk malignancies; genetic counselors; an advanced practice registered nurse specializing in cancer prevention and risk reduction; and a scientific director who leads the Clinical Laboratory Improvement Amendments–certified laboratory at Yale that offers in-house genetic testing, including full exome sequencing. The SCGPP was started in July 2015, and it currently provides more than 250 new consultations per month.
The following are several key elements that I consider important for a cancer genetics program and how they have been addressed at the SCGPP.
Identification through risk stratification
Because the identification of all individuals who can benefit from cancer genetics consultation is complex yet essential, a comprehensive approach with different strategies is often necessary.9 Universal tumor testing is an effective tool, but other complementary approaches such as the use of questionnaires can also contribute to identifying patients in need for cancer genetics assessment. In our program, the pathology department tests for MMR protein expression in all bowel and endometrial tumors. The ones that have loss of expression of an MMR protein are reported to the SCGPP, which contacts the patient’s providers to request a referral. In a relatively short implementation time, this has already resulted in a significant increase in the number of patients referred for cancer genetics consultation and new Lynch syndrome diagnosis. On the other hand, two brief and simplified questionnaires have been developed and distributed in clinics, one for health providers and one administered directly to patients. The questionnaires contain questions related to the patient’s own cancer history, polyp history, cancer screening tests, and family history. The first one assists health care providers in identifying individuals. The second one is completed by patients, collected, and reviewed by a genetic counselor. Suitable patients are invited to a cancer genetics consultation through their primary health care providers. A third questionnaire directed to endoscopy services will be rolled out soon. This collects information on completed endoscopy procedures, polyps and cancers found, and family history.
The program is currently working with information technology to develop a system to pull from the electronic medical record (EMR) relevant information on the patient’s own medical history, family history, and endoscopy findings. A set of criteria has been established so relevant information will generate an alert for prompt referral for the SCGPP.
Because education of health care providers about these conditions is essential to foster collaboration and to help them better understand about cancer risk assessment, genetics, and what the SCGPP can offer to some of their patients, sessions are routinely held with some of them to discuss different aspects on cancer genetics.
In summary, a comprehensive and coordinated approach is key to substantially expand the number of individuals identified and referred for cancer genetics assessment.
Genetic testing
During the last few years we have witnessed changes at different levels around genetic testing that are having a tremendous impact. Some of these changes pose significant new challenges that require rapid adaptation on the providers’ side. Thus, we are quickly moving from single gene testing to panels of genes tested at once. This has resulted in unexpected findings such as mutated genes not initially suspected or variants of unknown significance that often should be interpreted in the context of the personal and family history of cancer because of the lack of definite information on their potential pathogenicity.10 Adding to that, genome-scale tumor sequencing is becoming more common as it increasingly informs on the types of anti-tumor therapies to be selected for a specific patient (precision medicine). This approach is revealing some unexpected information because in some cases it has helped identify significant mutations in the germline.11
Finally, the increasing number of commercial laboratories offering genetic testing has resulted in more competition and lower prices, in some cases to a point that direct-to-consumer charges may be even lower than insurance copayments. This is contributing to a rapid increase in individuals being tested including patients who otherwise would unlikely have been tested in the past because of lack of fulfillment of insurance criteria. The challenge for us is to be ready to help navigate the increasing amount of information obtained as a result of all these changes.
Integration of electronic platforms
In an era of full implementation of EMRs, a cancer genetics program should not simply adapt to the new environment but fully embrace it and explore the possibilities that come with it. Thus, from its inception, the SCGPP has been embracing the electronic platforms to the maximum extent so the clinical operation is streamlined and documentation is well-displayed and accessible in the EMR. The Yale health care system uses EPIC (Epic Systems, Verona, WI) as its EMR, and the SCGPP uses Progeny (Progeny Genetics LLC, Delray Beach, FL) to collect data, construct family pedigrees, and build the research registry of the Program. A joint effort by the developers of both systems has resulted in integration at different levels. Thus, after a referral is received, patients are called, registered, and asked several questions including their own cancer and polyp history as well as their family history of cancer. This assists in triaging patients to the most appropriate SCGPP provider: a genetic counselor, a disease physician leader, or a combined visit according to the established internal protocol. In all cases, for new patients with GI cancer syndromes, a combined appointment of a genetic counselor and the GI physician leader is scheduled. At the same time, patients are sent an email with a link to the Progeny online questionnaire that includes personal and family history of cancer as well as extensive clinical information. Once the questionnaire is completed, the program generates a preliminary pedigree that patients can print, and the SCGPP gets a message communicating that the patient has completed this questionnaire. Therefore, when patients are seen on consultation, providers already have the provisional data and pedigree. During the visit, information is verified and edited as needed, and the finalized pedigree goes live through a hyperlink in the EMR. Every revision results in an updated pedigree visible through the mentioned hyperlink. This process saves a considerable amount of time to the providers and increases clinic efficiency.
Informed consent for the research registry is also fully electronic, with signatures recorded in tablets that transmit the signed document to a secure server.
The necessary team approach
Another essential component of a cancer genetics program like this is the integrated and comprehensive approach to patients. Thus, in our Program, the combined appointments for GI patients with the genetic counselor and the physician leader cover all different aspects of care, and a complete plan is suggested and discussed. Once the initial assessment is finalized and genetic testing results (if ordered) are completed, patients are followed prospectively to ensure that prophylactic and cancer prevention measures are undertaken according to the updated standards of care. Complex cases are discussed with the entire team in the weekly case conference that is always followed by a scientific conference with alternating topics such as journal club, practice improvement, ongoing research projects, and extensive case reviews.
Network integration
Although the needs for cancer genetics can be found in any corner of the map, it is not realistic to believe that services like this can be provided in a consistent fashion without being part of a bigger program umbrella. In our case, Yale’s Smilow Cancer Center charged the SCGPP with the duty to provide high quality and consistent cancer genetics services to the entire network that currently includes a total of 5 affiliated hospitals and 10 care centers. To do so, all cases seen outside the main campus are brought up for discussion in the weekly case conference. Furthermore, counselors distributed throughout the network routinely also see patients in the main office, and when away, they participate in case conference and scientific conference via teleconference or videoconference. All this is considered critical to facilitate a cohesive and state-of-the-art program that extends beyond the main campus. Recently, telemedicine is used to provide consultations directly to patients so the program’s services are brought to the most remote locations. A senior genetic counselor is in charge of the network operations to facilitate all these services and help engage providers in the corresponding facilities. She regularly attends tumor board meetings in the local hospitals to help disseminate knowledge in cancer genetics as well as to assist in the identification of patients who can benefit from referral to the SCGPP.
Surveillance and recall program
Key to the success of a cancer genetics program is successfully coordinating care so preventive tests and measures are performed to decrease cancer risk. The SCGPP aims to be the home for familial and hereditary cancer patients. For these patients, this implies a strong commitment to their needs, with a special emphasis on the appropriate prophylactic and cancer surveillance measures. The registry database provides an extremely useful tool to track scheduled tests and procedures and to generate reminders. The advanced practice registered nurse meticulously follows them and ensures proper completion and review. She follows up on the scheduling of the specific tests, reviews results once these tests are completed, and brings them back to discussion with the physician leader. She also follows up on incomplete tests and helps to bring down potential barriers in the performance of these tests. Another key aspect of her job consists of facilitating the assistance of psychological support or risk reduction through lifestyle changes, such as smoking cessation or weight reduction, to patients in need of such services.
Cancer genetics research
Key to an academic program in cancer genetics like this one is to facilitate the study of familial and syndromic cancers, including aspects such as phenotype characterization or the efficacy of chemopreventive approaches. To accomplish this, a patient registry is essential. Registries are extremely useful tools that facilitate data accrual and analysis. The SCGPP registry is based on the Progeny suite that incorporates not only clinical and pedigree building components but also the genotype and sample management systems (LAB and LIMS). Thus, a fully searchable and robust database and biological sample repository have been created, and all patients are approached about participating in this institutional review board–approved registry.
Cancer prevention in nonfamilial, nonsyndromic cases
Some nongenetic factors such as diet, physical activity, or toxic exposure seem to underlie the important differences seen in CRC incidence around the world.12 Thus, interventions at this level can potentially have a very high impact for cancer prevention in all individuals. In fact, even individuals with genetic mutations that carry a high risk for developing malignancies can see their risk modified by addressing lifestyle/environmental factors.13 Thus, the SCGPP has created tools for assessment and risk stratification that take the mentioned factors into account and create a roadmap for primary prevention. The tools include questionnaires on all environmental exposures, lifestyle factors, and medications the patient is exposed to and that can influence cancer risk. The information is reviewed in a special clinic session, and all services to help modify risk factors are offered to the patient.
Conclusions
There is a clear need for GI cancer genetics services to reach all patients who can benefit from them, and at the same time the field is rapidly growing in complexity. More than ever, these services demand a multidisciplinary approach, with experts leading the care of these patients in a coordinated fashion with the rest of the health care community. However, payers have not fully recognized these complexities, and some critical aspects such as genetic counseling services are not always properly reimbursed. As we shape up the present and future of health care that should be fully personalized and patient-centered, embracing new ways of delivering it, we need to engage all the players and help them understand what this takes and the rewards in the form of better outcomes that will come with it.
References
1. Kastrinos F., Stoffel E.M. History, genetics, and strategies for cancer prevention in Lynch syndrome. Clin Gastroenterol Hepatol. 2014;12:715-27 (quiz e41-e43).
2. Karlitz J.J., Hsieh M.C., Liu Y., et al. Population-based Lynch syndrome screening by microsatellite instability in patients </=50: prevalence, testing determinants, and result availability prior to colon surgery. Am J Gastroenterol. 2015;110:948-55.
3. Llor X. When should we suspect hereditary colorectal cancer syndrome? Clin Gastroenterol Hepatol. 2012;10:363-7.
4. Giardiello F.M., Allen J.I., Axilbund J.E., et al. Guidelines on genetic evaluation and management of Lynch syndrome: a consensus statement by the US Multi-society Task Force on colorectal cancer. Am J Gastroenterol. 2014;109:1159-79.
5. Berera S., Koru-Sengul T., Miao F., et al. Colorectal tumors from different racial and ethnic minorities have similar rates of mismatch repair deficiency. Clin Gastroenterol Hepatol. 2016;14:1163-71.
6. Mvundura M., Grosse S.D., Hampel H., et al. The cost-effectiveness of genetic testing strategies for Lynch syndrome among newly diagnosed patients with colorectal cancer. Genet Med. 2010;12:93-104.
7. Barzi A., Sadeghi S., Kattan M.W., et al. Comparative effectiveness of screening strategies for Lynch syndrome. J Natl Cancer Inst. 2015;107:1-9.
8. Moreira L., Balaguer F., Lindor N., et al. Identification of Lynch syndrome among patients with colorectal cancer. JAMA. 2012;308:1555-65.
9. Stoffel E.M., Kastrinos F. Familial colorectal cancer, beyond Lynch syndrome. Clin Gastroenterol Hepatol. 2014;12:1059-68.
10. Desmond A., Kurian A.W., Gabree M., et al. Clinical actionability of multigene panel testing for hereditary breast and ovarian cancer risk assessment. JAMA Oncol. 2015;1:943-51.
11. Parsons D.W., Roy A., Yang Y., et al. Diagnostic yield of clinical tumor and germline whole-exome sequencing for children with solid tumors. JAMA Oncol. 2016;([Epub ahead of print])
12. Aleksandrova K., Pischon T., Jenab M., et al. Combined impact of healthy lifestyle factors on colorectal cancer: a large European cohort study. BMC Med. 2014;12:168.
13. Movahedi M., Bishop D.T., Macrae F., et al. Obesity, aspirin, and risk of colorectal cancer in carriers of hereditary colorectal cancer: a prospective investigation in the CAPP2 study. J Clin Oncol. 2015;33:3591-7.
Dr. Llor is in the department of medicine and cancer center, Yale University, New Haven, Conn. He discloses no conflicts of interest.
Gastroenterologists offer more than just high-quality colonoscopy for colon cancer prevention. We often are the specialists who first recognize a genetic cancer syndrome during our endoscopy or clinic sessions. The patient who piqued my interest in colon cancer genetics was a 24-year-old woman who was referred for postoperative nausea after a hysterectomy for early stage uterine cancer (that alone should have raised alarm bells). Endoscopy revealed (by happenstance) a stomach coated with polyps. This led to a colonoscopy and diagnosis of familial adenomatous polyposis (uterine cancer within FAP is unusual but reported, for those of you studying for boards). In 1991, no coordinated genetics program existed within my practice so I arranged referrals to genetic counselors, surgeons, and pathologists. This led to the discovery of FAP and early stage (and curable) cancers in her two brothers and her father, in addition to extended pedigree analysis that established multi-organ cancer risks in other relatives. Years later, she brought her two adopted children to meet me and told me of lighting candles in my honor during an American Cancer Society walk. This is why we become doctors.
In this column, Dr. Xavier Llor describes the cancer genetics program he and others have built at Yale. It provides practical steps that can be taken by health system or community-based gastroenterologists to recognize and manage these complex syndromes. We are the specialists on the front lines and Dr. Llor helps us provide the coordinated care our patients expect from us.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Among all common cancers, breast and colon have the highest percentage of cases that are due to hereditary syndromes. Many of the responsible genes have been identified, and the last few years have seen an increase in uptake of genetic testing supported by the refinement of the clinical criteria suggestive of these syndromes as well as the clear improvement in outcomes as a result of the adoption of cancer preventive measures in mutation carriers.1 In spite of this, genetic testing for colorectal cancer (CRC) syndromes is not ordered as often as it should be according to the prevalence of these syndromes.2 In contrast, testing for hereditary breast cancer has become more generalized, and the threshold for ordering genetic testing in the latter is often lower than for CRC. The are several reasons for this: 1) much greater awareness, by both providers and the general public, of hereditary breast cancer conditions; 2) fewer providers with expertise in CRC genetics; 3) lack of a systematic approach to identify patients with potential CRC syndromes; and 4) absence of a clear premorbid phenotype for the most common of all CRC syndromes, Lynch syndrome.3
The recent recommendation in practice guidelines to screen all CRC tumors for Lynch syndrome either with immunohistochemistry to evaluate mismatch repair (MMR) protein expression or through tandem repeat analysis to test for microsatellite instability4 has highlighted that about 10% of all CRCs (a percentage consistently seen in different ethnic groups5) need further cancer genetic evaluation, and many will require sequencing of germline DNA. Although data on cost-effectiveness of this approach are somewhat conflicting,6,7 it is sensible because it is systematic, and studies have shown an increase in diagnostic yield through universal tumor screening.8 Unfortunately, in practice, often suspicious tumor testing results are not followed up by cancer genetics referrals, and many patients with CRC syndrome remain undiagnosed.
Patients with oligopolyposis (fewer than 100 polyps over time) also present diagnostic challenges. Some have attenuated familial adenomatous polyposis because of an APC mutation or MUTYH-associated polyposis. Recent findings have revealed other less commonly mutated genes that also result in oligopolyposis and a significant CRC risk: polymerases POLE and POLD1, GREM1, MCM9, or NTHL1. Because of the relatively low number of polyps in many of these syndromes and the lack of a systematic strategy to add up all polyps diagnosed over time, we not uncommonly fail to suspect some polyposis syndromes. Furthermore, the mixed pattern of polyps that is often associated with some of the mentioned mutated genes adds an extra challenge to diagnosing these cases.
Once individuals with CRC syndromes are identified, the challenge is to provide them with the care that they need, because many gastroenterologists, oncologists, and other health care providers are not extremely familiar with the current options for these patients.
In summary, there is a need to find systematic ways to triage and appropriately refer patients with a potential CRC syndrome to cancer genetics specialists so patients and their families can benefit from proper diagnosis and cancer preventive measures.
Building a comprehensive cancer genetics program
Although implementing systematic approaches is key to selecting individuals at risk, the complexity of caring for these patients demands a service that can stand up to the multiple challenges. For instance, most CRC syndromes are in fact multi-cancer syndromes with an increased risk of cancer and other pathologies in different organs beside the colon. Furthermore, the psychological implications of having a heritable cancer condition often take an important toll on affected families, with common feelings of guilt for having passed the mutated genes to the offspring.
Thus, to provide the best care to affected families, there is a tremendous need for well-organized and comprehensive cancer genetics services that are capable of responding to the multiple needs of these families so state-of-the-art cancer preventive measures can be carried out and multilevel support can be provided. The mentioned considerations were the guiding force in the creation of the Smilow Cancer Genetics and Prevention Program (SCGPP) at Yale. Thus, we established a comprehensive program that brings together health professionals specializing in different aspects of these patients’ care that ensures their proper attention in a longitudinal fashion, making the program their home for health care. We integrated in the program, among others, physician leaders in gastrointestinal (GI), breast, gynecological, endocrine, and genitourinary high-risk malignancies; genetic counselors; an advanced practice registered nurse specializing in cancer prevention and risk reduction; and a scientific director who leads the Clinical Laboratory Improvement Amendments–certified laboratory at Yale that offers in-house genetic testing, including full exome sequencing. The SCGPP was started in July 2015, and it currently provides more than 250 new consultations per month.
The following are several key elements that I consider important for a cancer genetics program and how they have been addressed at the SCGPP.
Identification through risk stratification
Because the identification of all individuals who can benefit from cancer genetics consultation is complex yet essential, a comprehensive approach with different strategies is often necessary.9 Universal tumor testing is an effective tool, but other complementary approaches such as the use of questionnaires can also contribute to identifying patients in need for cancer genetics assessment. In our program, the pathology department tests for MMR protein expression in all bowel and endometrial tumors. The ones that have loss of expression of an MMR protein are reported to the SCGPP, which contacts the patient’s providers to request a referral. In a relatively short implementation time, this has already resulted in a significant increase in the number of patients referred for cancer genetics consultation and new Lynch syndrome diagnosis. On the other hand, two brief and simplified questionnaires have been developed and distributed in clinics, one for health providers and one administered directly to patients. The questionnaires contain questions related to the patient’s own cancer history, polyp history, cancer screening tests, and family history. The first one assists health care providers in identifying individuals. The second one is completed by patients, collected, and reviewed by a genetic counselor. Suitable patients are invited to a cancer genetics consultation through their primary health care providers. A third questionnaire directed to endoscopy services will be rolled out soon. This collects information on completed endoscopy procedures, polyps and cancers found, and family history.
The program is currently working with information technology to develop a system to pull from the electronic medical record (EMR) relevant information on the patient’s own medical history, family history, and endoscopy findings. A set of criteria has been established so relevant information will generate an alert for prompt referral for the SCGPP.
Because education of health care providers about these conditions is essential to foster collaboration and to help them better understand about cancer risk assessment, genetics, and what the SCGPP can offer to some of their patients, sessions are routinely held with some of them to discuss different aspects on cancer genetics.
In summary, a comprehensive and coordinated approach is key to substantially expand the number of individuals identified and referred for cancer genetics assessment.
Genetic testing
During the last few years we have witnessed changes at different levels around genetic testing that are having a tremendous impact. Some of these changes pose significant new challenges that require rapid adaptation on the providers’ side. Thus, we are quickly moving from single gene testing to panels of genes tested at once. This has resulted in unexpected findings such as mutated genes not initially suspected or variants of unknown significance that often should be interpreted in the context of the personal and family history of cancer because of the lack of definite information on their potential pathogenicity.10 Adding to that, genome-scale tumor sequencing is becoming more common as it increasingly informs on the types of anti-tumor therapies to be selected for a specific patient (precision medicine). This approach is revealing some unexpected information because in some cases it has helped identify significant mutations in the germline.11
Finally, the increasing number of commercial laboratories offering genetic testing has resulted in more competition and lower prices, in some cases to a point that direct-to-consumer charges may be even lower than insurance copayments. This is contributing to a rapid increase in individuals being tested including patients who otherwise would unlikely have been tested in the past because of lack of fulfillment of insurance criteria. The challenge for us is to be ready to help navigate the increasing amount of information obtained as a result of all these changes.
Integration of electronic platforms
In an era of full implementation of EMRs, a cancer genetics program should not simply adapt to the new environment but fully embrace it and explore the possibilities that come with it. Thus, from its inception, the SCGPP has been embracing the electronic platforms to the maximum extent so the clinical operation is streamlined and documentation is well-displayed and accessible in the EMR. The Yale health care system uses EPIC (Epic Systems, Verona, WI) as its EMR, and the SCGPP uses Progeny (Progeny Genetics LLC, Delray Beach, FL) to collect data, construct family pedigrees, and build the research registry of the Program. A joint effort by the developers of both systems has resulted in integration at different levels. Thus, after a referral is received, patients are called, registered, and asked several questions including their own cancer and polyp history as well as their family history of cancer. This assists in triaging patients to the most appropriate SCGPP provider: a genetic counselor, a disease physician leader, or a combined visit according to the established internal protocol. In all cases, for new patients with GI cancer syndromes, a combined appointment of a genetic counselor and the GI physician leader is scheduled. At the same time, patients are sent an email with a link to the Progeny online questionnaire that includes personal and family history of cancer as well as extensive clinical information. Once the questionnaire is completed, the program generates a preliminary pedigree that patients can print, and the SCGPP gets a message communicating that the patient has completed this questionnaire. Therefore, when patients are seen on consultation, providers already have the provisional data and pedigree. During the visit, information is verified and edited as needed, and the finalized pedigree goes live through a hyperlink in the EMR. Every revision results in an updated pedigree visible through the mentioned hyperlink. This process saves a considerable amount of time to the providers and increases clinic efficiency.
Informed consent for the research registry is also fully electronic, with signatures recorded in tablets that transmit the signed document to a secure server.
The necessary team approach
Another essential component of a cancer genetics program like this is the integrated and comprehensive approach to patients. Thus, in our Program, the combined appointments for GI patients with the genetic counselor and the physician leader cover all different aspects of care, and a complete plan is suggested and discussed. Once the initial assessment is finalized and genetic testing results (if ordered) are completed, patients are followed prospectively to ensure that prophylactic and cancer prevention measures are undertaken according to the updated standards of care. Complex cases are discussed with the entire team in the weekly case conference that is always followed by a scientific conference with alternating topics such as journal club, practice improvement, ongoing research projects, and extensive case reviews.
Network integration
Although the needs for cancer genetics can be found in any corner of the map, it is not realistic to believe that services like this can be provided in a consistent fashion without being part of a bigger program umbrella. In our case, Yale’s Smilow Cancer Center charged the SCGPP with the duty to provide high quality and consistent cancer genetics services to the entire network that currently includes a total of 5 affiliated hospitals and 10 care centers. To do so, all cases seen outside the main campus are brought up for discussion in the weekly case conference. Furthermore, counselors distributed throughout the network routinely also see patients in the main office, and when away, they participate in case conference and scientific conference via teleconference or videoconference. All this is considered critical to facilitate a cohesive and state-of-the-art program that extends beyond the main campus. Recently, telemedicine is used to provide consultations directly to patients so the program’s services are brought to the most remote locations. A senior genetic counselor is in charge of the network operations to facilitate all these services and help engage providers in the corresponding facilities. She regularly attends tumor board meetings in the local hospitals to help disseminate knowledge in cancer genetics as well as to assist in the identification of patients who can benefit from referral to the SCGPP.
Surveillance and recall program
Key to the success of a cancer genetics program is successfully coordinating care so preventive tests and measures are performed to decrease cancer risk. The SCGPP aims to be the home for familial and hereditary cancer patients. For these patients, this implies a strong commitment to their needs, with a special emphasis on the appropriate prophylactic and cancer surveillance measures. The registry database provides an extremely useful tool to track scheduled tests and procedures and to generate reminders. The advanced practice registered nurse meticulously follows them and ensures proper completion and review. She follows up on the scheduling of the specific tests, reviews results once these tests are completed, and brings them back to discussion with the physician leader. She also follows up on incomplete tests and helps to bring down potential barriers in the performance of these tests. Another key aspect of her job consists of facilitating the assistance of psychological support or risk reduction through lifestyle changes, such as smoking cessation or weight reduction, to patients in need of such services.
Cancer genetics research
Key to an academic program in cancer genetics like this one is to facilitate the study of familial and syndromic cancers, including aspects such as phenotype characterization or the efficacy of chemopreventive approaches. To accomplish this, a patient registry is essential. Registries are extremely useful tools that facilitate data accrual and analysis. The SCGPP registry is based on the Progeny suite that incorporates not only clinical and pedigree building components but also the genotype and sample management systems (LAB and LIMS). Thus, a fully searchable and robust database and biological sample repository have been created, and all patients are approached about participating in this institutional review board–approved registry.
Cancer prevention in nonfamilial, nonsyndromic cases
Some nongenetic factors such as diet, physical activity, or toxic exposure seem to underlie the important differences seen in CRC incidence around the world.12 Thus, interventions at this level can potentially have a very high impact for cancer prevention in all individuals. In fact, even individuals with genetic mutations that carry a high risk for developing malignancies can see their risk modified by addressing lifestyle/environmental factors.13 Thus, the SCGPP has created tools for assessment and risk stratification that take the mentioned factors into account and create a roadmap for primary prevention. The tools include questionnaires on all environmental exposures, lifestyle factors, and medications the patient is exposed to and that can influence cancer risk. The information is reviewed in a special clinic session, and all services to help modify risk factors are offered to the patient.
Conclusions
There is a clear need for GI cancer genetics services to reach all patients who can benefit from them, and at the same time the field is rapidly growing in complexity. More than ever, these services demand a multidisciplinary approach, with experts leading the care of these patients in a coordinated fashion with the rest of the health care community. However, payers have not fully recognized these complexities, and some critical aspects such as genetic counseling services are not always properly reimbursed. As we shape up the present and future of health care that should be fully personalized and patient-centered, embracing new ways of delivering it, we need to engage all the players and help them understand what this takes and the rewards in the form of better outcomes that will come with it.
References
1. Kastrinos F., Stoffel E.M. History, genetics, and strategies for cancer prevention in Lynch syndrome. Clin Gastroenterol Hepatol. 2014;12:715-27 (quiz e41-e43).
2. Karlitz J.J., Hsieh M.C., Liu Y., et al. Population-based Lynch syndrome screening by microsatellite instability in patients </=50: prevalence, testing determinants, and result availability prior to colon surgery. Am J Gastroenterol. 2015;110:948-55.
3. Llor X. When should we suspect hereditary colorectal cancer syndrome? Clin Gastroenterol Hepatol. 2012;10:363-7.
4. Giardiello F.M., Allen J.I., Axilbund J.E., et al. Guidelines on genetic evaluation and management of Lynch syndrome: a consensus statement by the US Multi-society Task Force on colorectal cancer. Am J Gastroenterol. 2014;109:1159-79.
5. Berera S., Koru-Sengul T., Miao F., et al. Colorectal tumors from different racial and ethnic minorities have similar rates of mismatch repair deficiency. Clin Gastroenterol Hepatol. 2016;14:1163-71.
6. Mvundura M., Grosse S.D., Hampel H., et al. The cost-effectiveness of genetic testing strategies for Lynch syndrome among newly diagnosed patients with colorectal cancer. Genet Med. 2010;12:93-104.
7. Barzi A., Sadeghi S., Kattan M.W., et al. Comparative effectiveness of screening strategies for Lynch syndrome. J Natl Cancer Inst. 2015;107:1-9.
8. Moreira L., Balaguer F., Lindor N., et al. Identification of Lynch syndrome among patients with colorectal cancer. JAMA. 2012;308:1555-65.
9. Stoffel E.M., Kastrinos F. Familial colorectal cancer, beyond Lynch syndrome. Clin Gastroenterol Hepatol. 2014;12:1059-68.
10. Desmond A., Kurian A.W., Gabree M., et al. Clinical actionability of multigene panel testing for hereditary breast and ovarian cancer risk assessment. JAMA Oncol. 2015;1:943-51.
11. Parsons D.W., Roy A., Yang Y., et al. Diagnostic yield of clinical tumor and germline whole-exome sequencing for children with solid tumors. JAMA Oncol. 2016;([Epub ahead of print])
12. Aleksandrova K., Pischon T., Jenab M., et al. Combined impact of healthy lifestyle factors on colorectal cancer: a large European cohort study. BMC Med. 2014;12:168.
13. Movahedi M., Bishop D.T., Macrae F., et al. Obesity, aspirin, and risk of colorectal cancer in carriers of hereditary colorectal cancer: a prospective investigation in the CAPP2 study. J Clin Oncol. 2015;33:3591-7.
Dr. Llor is in the department of medicine and cancer center, Yale University, New Haven, Conn. He discloses no conflicts of interest.
Gastroenterologists offer more than just high-quality colonoscopy for colon cancer prevention. We often are the specialists who first recognize a genetic cancer syndrome during our endoscopy or clinic sessions. The patient who piqued my interest in colon cancer genetics was a 24-year-old woman who was referred for postoperative nausea after a hysterectomy for early stage uterine cancer (that alone should have raised alarm bells). Endoscopy revealed (by happenstance) a stomach coated with polyps. This led to a colonoscopy and diagnosis of familial adenomatous polyposis (uterine cancer within FAP is unusual but reported, for those of you studying for boards). In 1991, no coordinated genetics program existed within my practice so I arranged referrals to genetic counselors, surgeons, and pathologists. This led to the discovery of FAP and early stage (and curable) cancers in her two brothers and her father, in addition to extended pedigree analysis that established multi-organ cancer risks in other relatives. Years later, she brought her two adopted children to meet me and told me of lighting candles in my honor during an American Cancer Society walk. This is why we become doctors.
In this column, Dr. Xavier Llor describes the cancer genetics program he and others have built at Yale. It provides practical steps that can be taken by health system or community-based gastroenterologists to recognize and manage these complex syndromes. We are the specialists on the front lines and Dr. Llor helps us provide the coordinated care our patients expect from us.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Among all common cancers, breast and colon have the highest percentage of cases that are due to hereditary syndromes. Many of the responsible genes have been identified, and the last few years have seen an increase in uptake of genetic testing supported by the refinement of the clinical criteria suggestive of these syndromes as well as the clear improvement in outcomes as a result of the adoption of cancer preventive measures in mutation carriers.1 In spite of this, genetic testing for colorectal cancer (CRC) syndromes is not ordered as often as it should be according to the prevalence of these syndromes.2 In contrast, testing for hereditary breast cancer has become more generalized, and the threshold for ordering genetic testing in the latter is often lower than for CRC. The are several reasons for this: 1) much greater awareness, by both providers and the general public, of hereditary breast cancer conditions; 2) fewer providers with expertise in CRC genetics; 3) lack of a systematic approach to identify patients with potential CRC syndromes; and 4) absence of a clear premorbid phenotype for the most common of all CRC syndromes, Lynch syndrome.3
The recent recommendation in practice guidelines to screen all CRC tumors for Lynch syndrome either with immunohistochemistry to evaluate mismatch repair (MMR) protein expression or through tandem repeat analysis to test for microsatellite instability4 has highlighted that about 10% of all CRCs (a percentage consistently seen in different ethnic groups5) need further cancer genetic evaluation, and many will require sequencing of germline DNA. Although data on cost-effectiveness of this approach are somewhat conflicting,6,7 it is sensible because it is systematic, and studies have shown an increase in diagnostic yield through universal tumor screening.8 Unfortunately, in practice, often suspicious tumor testing results are not followed up by cancer genetics referrals, and many patients with CRC syndrome remain undiagnosed.
Patients with oligopolyposis (fewer than 100 polyps over time) also present diagnostic challenges. Some have attenuated familial adenomatous polyposis because of an APC mutation or MUTYH-associated polyposis. Recent findings have revealed other less commonly mutated genes that also result in oligopolyposis and a significant CRC risk: polymerases POLE and POLD1, GREM1, MCM9, or NTHL1. Because of the relatively low number of polyps in many of these syndromes and the lack of a systematic strategy to add up all polyps diagnosed over time, we not uncommonly fail to suspect some polyposis syndromes. Furthermore, the mixed pattern of polyps that is often associated with some of the mentioned mutated genes adds an extra challenge to diagnosing these cases.
Once individuals with CRC syndromes are identified, the challenge is to provide them with the care that they need, because many gastroenterologists, oncologists, and other health care providers are not extremely familiar with the current options for these patients.
In summary, there is a need to find systematic ways to triage and appropriately refer patients with a potential CRC syndrome to cancer genetics specialists so patients and their families can benefit from proper diagnosis and cancer preventive measures.
Building a comprehensive cancer genetics program
Although implementing systematic approaches is key to selecting individuals at risk, the complexity of caring for these patients demands a service that can stand up to the multiple challenges. For instance, most CRC syndromes are in fact multi-cancer syndromes with an increased risk of cancer and other pathologies in different organs beside the colon. Furthermore, the psychological implications of having a heritable cancer condition often take an important toll on affected families, with common feelings of guilt for having passed the mutated genes to the offspring.
Thus, to provide the best care to affected families, there is a tremendous need for well-organized and comprehensive cancer genetics services that are capable of responding to the multiple needs of these families so state-of-the-art cancer preventive measures can be carried out and multilevel support can be provided. The mentioned considerations were the guiding force in the creation of the Smilow Cancer Genetics and Prevention Program (SCGPP) at Yale. Thus, we established a comprehensive program that brings together health professionals specializing in different aspects of these patients’ care that ensures their proper attention in a longitudinal fashion, making the program their home for health care. We integrated in the program, among others, physician leaders in gastrointestinal (GI), breast, gynecological, endocrine, and genitourinary high-risk malignancies; genetic counselors; an advanced practice registered nurse specializing in cancer prevention and risk reduction; and a scientific director who leads the Clinical Laboratory Improvement Amendments–certified laboratory at Yale that offers in-house genetic testing, including full exome sequencing. The SCGPP was started in July 2015, and it currently provides more than 250 new consultations per month.
The following are several key elements that I consider important for a cancer genetics program and how they have been addressed at the SCGPP.
Identification through risk stratification
Because the identification of all individuals who can benefit from cancer genetics consultation is complex yet essential, a comprehensive approach with different strategies is often necessary.9 Universal tumor testing is an effective tool, but other complementary approaches such as the use of questionnaires can also contribute to identifying patients in need for cancer genetics assessment. In our program, the pathology department tests for MMR protein expression in all bowel and endometrial tumors. The ones that have loss of expression of an MMR protein are reported to the SCGPP, which contacts the patient’s providers to request a referral. In a relatively short implementation time, this has already resulted in a significant increase in the number of patients referred for cancer genetics consultation and new Lynch syndrome diagnosis. On the other hand, two brief and simplified questionnaires have been developed and distributed in clinics, one for health providers and one administered directly to patients. The questionnaires contain questions related to the patient’s own cancer history, polyp history, cancer screening tests, and family history. The first one assists health care providers in identifying individuals. The second one is completed by patients, collected, and reviewed by a genetic counselor. Suitable patients are invited to a cancer genetics consultation through their primary health care providers. A third questionnaire directed to endoscopy services will be rolled out soon. This collects information on completed endoscopy procedures, polyps and cancers found, and family history.
The program is currently working with information technology to develop a system to pull from the electronic medical record (EMR) relevant information on the patient’s own medical history, family history, and endoscopy findings. A set of criteria has been established so relevant information will generate an alert for prompt referral for the SCGPP.
Because education of health care providers about these conditions is essential to foster collaboration and to help them better understand about cancer risk assessment, genetics, and what the SCGPP can offer to some of their patients, sessions are routinely held with some of them to discuss different aspects on cancer genetics.
In summary, a comprehensive and coordinated approach is key to substantially expand the number of individuals identified and referred for cancer genetics assessment.
Genetic testing
During the last few years we have witnessed changes at different levels around genetic testing that are having a tremendous impact. Some of these changes pose significant new challenges that require rapid adaptation on the providers’ side. Thus, we are quickly moving from single gene testing to panels of genes tested at once. This has resulted in unexpected findings such as mutated genes not initially suspected or variants of unknown significance that often should be interpreted in the context of the personal and family history of cancer because of the lack of definite information on their potential pathogenicity.10 Adding to that, genome-scale tumor sequencing is becoming more common as it increasingly informs on the types of anti-tumor therapies to be selected for a specific patient (precision medicine). This approach is revealing some unexpected information because in some cases it has helped identify significant mutations in the germline.11
Finally, the increasing number of commercial laboratories offering genetic testing has resulted in more competition and lower prices, in some cases to a point that direct-to-consumer charges may be even lower than insurance copayments. This is contributing to a rapid increase in individuals being tested including patients who otherwise would unlikely have been tested in the past because of lack of fulfillment of insurance criteria. The challenge for us is to be ready to help navigate the increasing amount of information obtained as a result of all these changes.
Integration of electronic platforms
In an era of full implementation of EMRs, a cancer genetics program should not simply adapt to the new environment but fully embrace it and explore the possibilities that come with it. Thus, from its inception, the SCGPP has been embracing the electronic platforms to the maximum extent so the clinical operation is streamlined and documentation is well-displayed and accessible in the EMR. The Yale health care system uses EPIC (Epic Systems, Verona, WI) as its EMR, and the SCGPP uses Progeny (Progeny Genetics LLC, Delray Beach, FL) to collect data, construct family pedigrees, and build the research registry of the Program. A joint effort by the developers of both systems has resulted in integration at different levels. Thus, after a referral is received, patients are called, registered, and asked several questions including their own cancer and polyp history as well as their family history of cancer. This assists in triaging patients to the most appropriate SCGPP provider: a genetic counselor, a disease physician leader, or a combined visit according to the established internal protocol. In all cases, for new patients with GI cancer syndromes, a combined appointment of a genetic counselor and the GI physician leader is scheduled. At the same time, patients are sent an email with a link to the Progeny online questionnaire that includes personal and family history of cancer as well as extensive clinical information. Once the questionnaire is completed, the program generates a preliminary pedigree that patients can print, and the SCGPP gets a message communicating that the patient has completed this questionnaire. Therefore, when patients are seen on consultation, providers already have the provisional data and pedigree. During the visit, information is verified and edited as needed, and the finalized pedigree goes live through a hyperlink in the EMR. Every revision results in an updated pedigree visible through the mentioned hyperlink. This process saves a considerable amount of time to the providers and increases clinic efficiency.
Informed consent for the research registry is also fully electronic, with signatures recorded in tablets that transmit the signed document to a secure server.
The necessary team approach
Another essential component of a cancer genetics program like this is the integrated and comprehensive approach to patients. Thus, in our Program, the combined appointments for GI patients with the genetic counselor and the physician leader cover all different aspects of care, and a complete plan is suggested and discussed. Once the initial assessment is finalized and genetic testing results (if ordered) are completed, patients are followed prospectively to ensure that prophylactic and cancer prevention measures are undertaken according to the updated standards of care. Complex cases are discussed with the entire team in the weekly case conference that is always followed by a scientific conference with alternating topics such as journal club, practice improvement, ongoing research projects, and extensive case reviews.
Network integration
Although the needs for cancer genetics can be found in any corner of the map, it is not realistic to believe that services like this can be provided in a consistent fashion without being part of a bigger program umbrella. In our case, Yale’s Smilow Cancer Center charged the SCGPP with the duty to provide high quality and consistent cancer genetics services to the entire network that currently includes a total of 5 affiliated hospitals and 10 care centers. To do so, all cases seen outside the main campus are brought up for discussion in the weekly case conference. Furthermore, counselors distributed throughout the network routinely also see patients in the main office, and when away, they participate in case conference and scientific conference via teleconference or videoconference. All this is considered critical to facilitate a cohesive and state-of-the-art program that extends beyond the main campus. Recently, telemedicine is used to provide consultations directly to patients so the program’s services are brought to the most remote locations. A senior genetic counselor is in charge of the network operations to facilitate all these services and help engage providers in the corresponding facilities. She regularly attends tumor board meetings in the local hospitals to help disseminate knowledge in cancer genetics as well as to assist in the identification of patients who can benefit from referral to the SCGPP.
Surveillance and recall program
Key to the success of a cancer genetics program is successfully coordinating care so preventive tests and measures are performed to decrease cancer risk. The SCGPP aims to be the home for familial and hereditary cancer patients. For these patients, this implies a strong commitment to their needs, with a special emphasis on the appropriate prophylactic and cancer surveillance measures. The registry database provides an extremely useful tool to track scheduled tests and procedures and to generate reminders. The advanced practice registered nurse meticulously follows them and ensures proper completion and review. She follows up on the scheduling of the specific tests, reviews results once these tests are completed, and brings them back to discussion with the physician leader. She also follows up on incomplete tests and helps to bring down potential barriers in the performance of these tests. Another key aspect of her job consists of facilitating the assistance of psychological support or risk reduction through lifestyle changes, such as smoking cessation or weight reduction, to patients in need of such services.
Cancer genetics research
Key to an academic program in cancer genetics like this one is to facilitate the study of familial and syndromic cancers, including aspects such as phenotype characterization or the efficacy of chemopreventive approaches. To accomplish this, a patient registry is essential. Registries are extremely useful tools that facilitate data accrual and analysis. The SCGPP registry is based on the Progeny suite that incorporates not only clinical and pedigree building components but also the genotype and sample management systems (LAB and LIMS). Thus, a fully searchable and robust database and biological sample repository have been created, and all patients are approached about participating in this institutional review board–approved registry.
Cancer prevention in nonfamilial, nonsyndromic cases
Some nongenetic factors such as diet, physical activity, or toxic exposure seem to underlie the important differences seen in CRC incidence around the world.12 Thus, interventions at this level can potentially have a very high impact for cancer prevention in all individuals. In fact, even individuals with genetic mutations that carry a high risk for developing malignancies can see their risk modified by addressing lifestyle/environmental factors.13 Thus, the SCGPP has created tools for assessment and risk stratification that take the mentioned factors into account and create a roadmap for primary prevention. The tools include questionnaires on all environmental exposures, lifestyle factors, and medications the patient is exposed to and that can influence cancer risk. The information is reviewed in a special clinic session, and all services to help modify risk factors are offered to the patient.
Conclusions
There is a clear need for GI cancer genetics services to reach all patients who can benefit from them, and at the same time the field is rapidly growing in complexity. More than ever, these services demand a multidisciplinary approach, with experts leading the care of these patients in a coordinated fashion with the rest of the health care community. However, payers have not fully recognized these complexities, and some critical aspects such as genetic counseling services are not always properly reimbursed. As we shape up the present and future of health care that should be fully personalized and patient-centered, embracing new ways of delivering it, we need to engage all the players and help them understand what this takes and the rewards in the form of better outcomes that will come with it.
References
1. Kastrinos F., Stoffel E.M. History, genetics, and strategies for cancer prevention in Lynch syndrome. Clin Gastroenterol Hepatol. 2014;12:715-27 (quiz e41-e43).
2. Karlitz J.J., Hsieh M.C., Liu Y., et al. Population-based Lynch syndrome screening by microsatellite instability in patients </=50: prevalence, testing determinants, and result availability prior to colon surgery. Am J Gastroenterol. 2015;110:948-55.
3. Llor X. When should we suspect hereditary colorectal cancer syndrome? Clin Gastroenterol Hepatol. 2012;10:363-7.
4. Giardiello F.M., Allen J.I., Axilbund J.E., et al. Guidelines on genetic evaluation and management of Lynch syndrome: a consensus statement by the US Multi-society Task Force on colorectal cancer. Am J Gastroenterol. 2014;109:1159-79.
5. Berera S., Koru-Sengul T., Miao F., et al. Colorectal tumors from different racial and ethnic minorities have similar rates of mismatch repair deficiency. Clin Gastroenterol Hepatol. 2016;14:1163-71.
6. Mvundura M., Grosse S.D., Hampel H., et al. The cost-effectiveness of genetic testing strategies for Lynch syndrome among newly diagnosed patients with colorectal cancer. Genet Med. 2010;12:93-104.
7. Barzi A., Sadeghi S., Kattan M.W., et al. Comparative effectiveness of screening strategies for Lynch syndrome. J Natl Cancer Inst. 2015;107:1-9.
8. Moreira L., Balaguer F., Lindor N., et al. Identification of Lynch syndrome among patients with colorectal cancer. JAMA. 2012;308:1555-65.
9. Stoffel E.M., Kastrinos F. Familial colorectal cancer, beyond Lynch syndrome. Clin Gastroenterol Hepatol. 2014;12:1059-68.
10. Desmond A., Kurian A.W., Gabree M., et al. Clinical actionability of multigene panel testing for hereditary breast and ovarian cancer risk assessment. JAMA Oncol. 2015;1:943-51.
11. Parsons D.W., Roy A., Yang Y., et al. Diagnostic yield of clinical tumor and germline whole-exome sequencing for children with solid tumors. JAMA Oncol. 2016;([Epub ahead of print])
12. Aleksandrova K., Pischon T., Jenab M., et al. Combined impact of healthy lifestyle factors on colorectal cancer: a large European cohort study. BMC Med. 2014;12:168.
13. Movahedi M., Bishop D.T., Macrae F., et al. Obesity, aspirin, and risk of colorectal cancer in carriers of hereditary colorectal cancer: a prospective investigation in the CAPP2 study. J Clin Oncol. 2015;33:3591-7.
Dr. Llor is in the department of medicine and cancer center, Yale University, New Haven, Conn. He discloses no conflicts of interest.
Mortality may be reduced when surgical ablation for AF is done with mitral operations
HOUSTON – At the time of mitral valve repair or replacement operations, the addition of surgical ablation to treat atrial fibrillation (AF) can be performed without increased risk of mortality, results from a large cohort study has demonstrated.
“Surgical ablation for atrial fibrillation performed concomitant to mitral valve repair or replacement is accepted to reduce long-term AF rates and improve quality of life, and has recently attained a class I, level of evidence A recommendation in the recent Society of Thoracic Surgeons Guidelines,” Vinay Badhwar, MD, said in an interview. Dr. Badhwar is the lead author of the STS Guidelines and senior author of the current study on mortality following surgical ablation of AF. “Nevertheless, the direct impact of surgical ablation on operative mortality has not been studied on a large scale using robust registry data.”
In an effort to examine the impact of performing or not performing surgical ablation (SA) on mortality of contemporary mitral valve repair or replacement (MVRR) operations, Dr. Badhwar, Gordon F. Murray Professor and Chair, department of cardiovascular and thoracic surgery at West Virginia University, Morgantown, W.Va., and his associates at eight other leading centers nationwide evaluated the medical records of 88,765 MVRR patients in the STS Adult Cardiac Surgery Database between July 2011 and June 2014.
The research, presented as the Richard E. Clark award winning paper in adult cardiac surgery by study leader J. Scott Rankin, MD, professor of surgery in the department of cardiovascular and thoracic surgery at West Virginia University, included cases of tricuspid repair and coronary artery bypass grafting and assessed all STS comorbid risk variables and mitral etiology for predictors of mortality. After performing multivariable logistic regression, the researchers compared risk-adjusted odds ratios for mortality by AF type at operation and SA performance: group 1 (no AF plus no SA), group 2 (no AF plus SA), group 3 (AF plus no SA), group 4 (AF plus SA), group 5 (persistent AF plus no SA), and group 6 (persistent AF plus SA).
The median age of patients ranged from 63 to 72 years. Compared with their counterparts in other groups, patients in groups 3 and 5 were older (median age of 71 and 72 years, respectively), had worse symptoms (50% in each group had NYHA class III or IV disease), had more reoperations (30% vs. 32%), and had higher unadjusted mortalities (6.7% vs. 6.6%).
Following multivariable risk adjustment, groups 2-6 with AF history plus or minus SA were referenced to group 1 patients without AF or SA. Groups 2-4 represented the overall population, and groups 5 and 6 were patients with persistent AF. Patients with AF at the time of operation not receiving SA (groups 3 and 5) had odds ratios of 1.16 and 1.17, respectively, or an increase of 16% and 17% in relative risk of mortality (P = .004 and P = .01, respectively). In groups 4 and 6, concomitant SA reduced the AF-related mortality to a level that was statistically comparable to reference baseline group 1 without a history of AF (P = .13 and P = .21, respectively).
“The present study appears to clearly illustrate the adverse effects of AF on operative mortality following MVRR,” Dr. Badhwar said. “After thorough risk adjustment, we were impressed to learn that the relative mortality risk of mitral procedures increased by nearly 15% for either paroxysmal or persistent AF, and results were similar for the two AF types. A remote history of AF with preoperative sinus rhythm immediately prior to surgery had little effect on prognosis, and these patients appeared to have outcomes more like those without AF. In patients with active AF at the time of mitral operation, SA reduced the AF-related mortality and decreased operative mortality to levels not statistically different from patients without AF.” He added that the findings of this study support the recent STS Guidelines on Surgical Ablation published in the January 2017 edition of Annals of Thoracic Surgery (Ann Thorac Surg. 2017 Jan;103[1]:329-41). “However, the ultimate decision on whether or not to add surgical ablation must always remain between the surgeon and the patient,” he said.
Dr. Badhwar acknowledged that the study is limited by the information available in version 2.73 of the STS Adult Cardiac Surgery Database. “This does highlight the ongoing need for participants in the database to provide as much complete information as possible for all patients undergoing cardiac operations, especially those involving surgical ablation,” he said.
Dr. Badhwar reported having no financial disclosures. Dr. Rankin disclosed ties with Admedus, AtriCure, and BioStable Science and Engineering.
HOUSTON – At the time of mitral valve repair or replacement operations, the addition of surgical ablation to treat atrial fibrillation (AF) can be performed without increased risk of mortality, results from a large cohort study has demonstrated.
“Surgical ablation for atrial fibrillation performed concomitant to mitral valve repair or replacement is accepted to reduce long-term AF rates and improve quality of life, and has recently attained a class I, level of evidence A recommendation in the recent Society of Thoracic Surgeons Guidelines,” Vinay Badhwar, MD, said in an interview. Dr. Badhwar is the lead author of the STS Guidelines and senior author of the current study on mortality following surgical ablation of AF. “Nevertheless, the direct impact of surgical ablation on operative mortality has not been studied on a large scale using robust registry data.”
In an effort to examine the impact of performing or not performing surgical ablation (SA) on mortality of contemporary mitral valve repair or replacement (MVRR) operations, Dr. Badhwar, Gordon F. Murray Professor and Chair, department of cardiovascular and thoracic surgery at West Virginia University, Morgantown, W.Va., and his associates at eight other leading centers nationwide evaluated the medical records of 88,765 MVRR patients in the STS Adult Cardiac Surgery Database between July 2011 and June 2014.
The research, presented as the Richard E. Clark award winning paper in adult cardiac surgery by study leader J. Scott Rankin, MD, professor of surgery in the department of cardiovascular and thoracic surgery at West Virginia University, included cases of tricuspid repair and coronary artery bypass grafting and assessed all STS comorbid risk variables and mitral etiology for predictors of mortality. After performing multivariable logistic regression, the researchers compared risk-adjusted odds ratios for mortality by AF type at operation and SA performance: group 1 (no AF plus no SA), group 2 (no AF plus SA), group 3 (AF plus no SA), group 4 (AF plus SA), group 5 (persistent AF plus no SA), and group 6 (persistent AF plus SA).
The median age of patients ranged from 63 to 72 years. Compared with their counterparts in other groups, patients in groups 3 and 5 were older (median age of 71 and 72 years, respectively), had worse symptoms (50% in each group had NYHA class III or IV disease), had more reoperations (30% vs. 32%), and had higher unadjusted mortalities (6.7% vs. 6.6%).
Following multivariable risk adjustment, groups 2-6 with AF history plus or minus SA were referenced to group 1 patients without AF or SA. Groups 2-4 represented the overall population, and groups 5 and 6 were patients with persistent AF. Patients with AF at the time of operation not receiving SA (groups 3 and 5) had odds ratios of 1.16 and 1.17, respectively, or an increase of 16% and 17% in relative risk of mortality (P = .004 and P = .01, respectively). In groups 4 and 6, concomitant SA reduced the AF-related mortality to a level that was statistically comparable to reference baseline group 1 without a history of AF (P = .13 and P = .21, respectively).
“The present study appears to clearly illustrate the adverse effects of AF on operative mortality following MVRR,” Dr. Badhwar said. “After thorough risk adjustment, we were impressed to learn that the relative mortality risk of mitral procedures increased by nearly 15% for either paroxysmal or persistent AF, and results were similar for the two AF types. A remote history of AF with preoperative sinus rhythm immediately prior to surgery had little effect on prognosis, and these patients appeared to have outcomes more like those without AF. In patients with active AF at the time of mitral operation, SA reduced the AF-related mortality and decreased operative mortality to levels not statistically different from patients without AF.” He added that the findings of this study support the recent STS Guidelines on Surgical Ablation published in the January 2017 edition of Annals of Thoracic Surgery (Ann Thorac Surg. 2017 Jan;103[1]:329-41). “However, the ultimate decision on whether or not to add surgical ablation must always remain between the surgeon and the patient,” he said.
Dr. Badhwar acknowledged that the study is limited by the information available in version 2.73 of the STS Adult Cardiac Surgery Database. “This does highlight the ongoing need for participants in the database to provide as much complete information as possible for all patients undergoing cardiac operations, especially those involving surgical ablation,” he said.
Dr. Badhwar reported having no financial disclosures. Dr. Rankin disclosed ties with Admedus, AtriCure, and BioStable Science and Engineering.
HOUSTON – At the time of mitral valve repair or replacement operations, the addition of surgical ablation to treat atrial fibrillation (AF) can be performed without increased risk of mortality, results from a large cohort study has demonstrated.
“Surgical ablation for atrial fibrillation performed concomitant to mitral valve repair or replacement is accepted to reduce long-term AF rates and improve quality of life, and has recently attained a class I, level of evidence A recommendation in the recent Society of Thoracic Surgeons Guidelines,” Vinay Badhwar, MD, said in an interview. Dr. Badhwar is the lead author of the STS Guidelines and senior author of the current study on mortality following surgical ablation of AF. “Nevertheless, the direct impact of surgical ablation on operative mortality has not been studied on a large scale using robust registry data.”
In an effort to examine the impact of performing or not performing surgical ablation (SA) on mortality of contemporary mitral valve repair or replacement (MVRR) operations, Dr. Badhwar, Gordon F. Murray Professor and Chair, department of cardiovascular and thoracic surgery at West Virginia University, Morgantown, W.Va., and his associates at eight other leading centers nationwide evaluated the medical records of 88,765 MVRR patients in the STS Adult Cardiac Surgery Database between July 2011 and June 2014.
The research, presented as the Richard E. Clark award winning paper in adult cardiac surgery by study leader J. Scott Rankin, MD, professor of surgery in the department of cardiovascular and thoracic surgery at West Virginia University, included cases of tricuspid repair and coronary artery bypass grafting and assessed all STS comorbid risk variables and mitral etiology for predictors of mortality. After performing multivariable logistic regression, the researchers compared risk-adjusted odds ratios for mortality by AF type at operation and SA performance: group 1 (no AF plus no SA), group 2 (no AF plus SA), group 3 (AF plus no SA), group 4 (AF plus SA), group 5 (persistent AF plus no SA), and group 6 (persistent AF plus SA).
The median age of patients ranged from 63 to 72 years. Compared with their counterparts in other groups, patients in groups 3 and 5 were older (median age of 71 and 72 years, respectively), had worse symptoms (50% in each group had NYHA class III or IV disease), had more reoperations (30% vs. 32%), and had higher unadjusted mortalities (6.7% vs. 6.6%).
Following multivariable risk adjustment, groups 2-6 with AF history plus or minus SA were referenced to group 1 patients without AF or SA. Groups 2-4 represented the overall population, and groups 5 and 6 were patients with persistent AF. Patients with AF at the time of operation not receiving SA (groups 3 and 5) had odds ratios of 1.16 and 1.17, respectively, or an increase of 16% and 17% in relative risk of mortality (P = .004 and P = .01, respectively). In groups 4 and 6, concomitant SA reduced the AF-related mortality to a level that was statistically comparable to reference baseline group 1 without a history of AF (P = .13 and P = .21, respectively).
“The present study appears to clearly illustrate the adverse effects of AF on operative mortality following MVRR,” Dr. Badhwar said. “After thorough risk adjustment, we were impressed to learn that the relative mortality risk of mitral procedures increased by nearly 15% for either paroxysmal or persistent AF, and results were similar for the two AF types. A remote history of AF with preoperative sinus rhythm immediately prior to surgery had little effect on prognosis, and these patients appeared to have outcomes more like those without AF. In patients with active AF at the time of mitral operation, SA reduced the AF-related mortality and decreased operative mortality to levels not statistically different from patients without AF.” He added that the findings of this study support the recent STS Guidelines on Surgical Ablation published in the January 2017 edition of Annals of Thoracic Surgery (Ann Thorac Surg. 2017 Jan;103[1]:329-41). “However, the ultimate decision on whether or not to add surgical ablation must always remain between the surgeon and the patient,” he said.
Dr. Badhwar acknowledged that the study is limited by the information available in version 2.73 of the STS Adult Cardiac Surgery Database. “This does highlight the ongoing need for participants in the database to provide as much complete information as possible for all patients undergoing cardiac operations, especially those involving surgical ablation,” he said.
Dr. Badhwar reported having no financial disclosures. Dr. Rankin disclosed ties with Admedus, AtriCure, and BioStable Science and Engineering.
AT THE STS ANNUAL MEETING
Key clinical point:
Major finding: Adding surgical ablation to treat AF at the time of MVRR reduced the AF-related mortality to a rate that was comparable to a reference baseline group that had no history of AF.
Data source: An analysis of medical records from 88,765 MVRR patients in the STS Adult Cardiac Surgery Database between July 2011 and June 2014.
Disclosures: Dr. Badhwar reported having no financial disclosures. Dr. Rankin disclosed ties with Admedus, AtriCure, and BioStable Science and Engineering.
Early, in-hospital shunt failure common among infants
HOUSTON – Among neonates and infants who underwent shunt construction as a source of pulmonary blood flow, early, in-hospital shunt failure occurred in 7.3% of cases, results from a large retrospective study showed.
“Approximately one in seven patients who experiences cardiac surgery in the first year of life undergoes construction of a systemic to pulmonary artery shunt of some type,” one of the study investigators, Marshall L. Jacobs, MD, said in an interview. The study was presented at the annual meeting of the Society of Thoracic Surgeons.
“Early failure of such shunts is an incompletely understood phenomenon which accounts for important morbidity and mortality among infants and neonates. Much of what is known about shunt failure is based on experiences reported from individual institutions. The few multicenter studies to date have been clinical trials that focused primarily on pharmacologic strategies intended to reduce the risk of shunt failure due to thrombosis. Their utility for guiding clinical decision making has been limited. Some have been underpowered; some have had limited risk adjustment of subjects.”
Dr. Do, who presented the findings at the meeting and is currently a Congenital Heart Surgery Fellow at the Children’s Hospital of Philadelphia, and a team of 11 other investigators utilized the STS Congenital Heart Surgery Database to identify 9,172 neonates and infants who underwent shunt construction as a source of pulmonary blood flow at 118 institutions from 2010 to 2015. Criteria for shunt failure included a documented diagnosis of in-hospital shunt failure, shunt revision, or catheter-based shunt intervention. The investigators used multivariable logistic regression to evaluate risk factors for in-hospital shunt failure.
Of the 9,172 at-risk neonates and infants, 674 (7.3%) experienced early, in-hospital shunt failure. “The observed rate of early shunt failure varied across the many specific types of shunts, and was lower with systemic ventricle to pulmonary artery shunts (as in the Sano modification of the Norwood procedure) than with the systemic artery to pulmonary artery shunts,” said Dr. Jacobs, who is a cardiothoracic surgeon at Johns Hopkins University, Baltimore.
In multivariable analysis, risk factors for in-hospital shunt failure included lower weight at operation for both neonates and infants, preoperative hypercoagulable state, and the collective presence of any other STS Congenital Heart Surgery Database preoperative risk factors. Neither cardiopulmonary bypass nor single ventricle diagnosis were risk factors for shunt failure. The investigators also observed that patients with in-hospital shunt failure had significantly higher rates of operative mortality (31.9% vs. 11.1%) and major morbidity (84.4% vs. 29.4%), and longer postoperative length of stay among survivors (a median of 45 vs. 22 days).
“Understanding the characteristics of the patient groups found to be at highest risk for early shunt failure is helpful in identifying individual patients that may warrant expectant surveillance, enhanced pharmacologic management, or other strategies to reduce the risk of shunt failure,” Dr. Jacobs concluded.
“But perhaps more importantly it provides key information that may be helpful in the design and development of future clinical trials and/or collaborative quality improvement initiatives designed to reduce the cost in lives and resources that is associated with early shunt dysfunction.”
He acknowledged certain limitations of the study, including its retrospective observational design and the voluntary nature of the STS Congenital Heart Surgery Database. “In addition, some potentially important variables, such as detailed data concerning preoperative test results of coagulation assays are not collected in the STS Congenital Heart Surgery Database,” he said.
The research was supported by the STS Access & Publications Research program. The investigators reported having no financial disclosures.
HOUSTON – Among neonates and infants who underwent shunt construction as a source of pulmonary blood flow, early, in-hospital shunt failure occurred in 7.3% of cases, results from a large retrospective study showed.
“Approximately one in seven patients who experiences cardiac surgery in the first year of life undergoes construction of a systemic to pulmonary artery shunt of some type,” one of the study investigators, Marshall L. Jacobs, MD, said in an interview. The study was presented at the annual meeting of the Society of Thoracic Surgeons.
“Early failure of such shunts is an incompletely understood phenomenon which accounts for important morbidity and mortality among infants and neonates. Much of what is known about shunt failure is based on experiences reported from individual institutions. The few multicenter studies to date have been clinical trials that focused primarily on pharmacologic strategies intended to reduce the risk of shunt failure due to thrombosis. Their utility for guiding clinical decision making has been limited. Some have been underpowered; some have had limited risk adjustment of subjects.”
Dr. Do, who presented the findings at the meeting and is currently a Congenital Heart Surgery Fellow at the Children’s Hospital of Philadelphia, and a team of 11 other investigators utilized the STS Congenital Heart Surgery Database to identify 9,172 neonates and infants who underwent shunt construction as a source of pulmonary blood flow at 118 institutions from 2010 to 2015. Criteria for shunt failure included a documented diagnosis of in-hospital shunt failure, shunt revision, or catheter-based shunt intervention. The investigators used multivariable logistic regression to evaluate risk factors for in-hospital shunt failure.
Of the 9,172 at-risk neonates and infants, 674 (7.3%) experienced early, in-hospital shunt failure. “The observed rate of early shunt failure varied across the many specific types of shunts, and was lower with systemic ventricle to pulmonary artery shunts (as in the Sano modification of the Norwood procedure) than with the systemic artery to pulmonary artery shunts,” said Dr. Jacobs, who is a cardiothoracic surgeon at Johns Hopkins University, Baltimore.
In multivariable analysis, risk factors for in-hospital shunt failure included lower weight at operation for both neonates and infants, preoperative hypercoagulable state, and the collective presence of any other STS Congenital Heart Surgery Database preoperative risk factors. Neither cardiopulmonary bypass nor single ventricle diagnosis were risk factors for shunt failure. The investigators also observed that patients with in-hospital shunt failure had significantly higher rates of operative mortality (31.9% vs. 11.1%) and major morbidity (84.4% vs. 29.4%), and longer postoperative length of stay among survivors (a median of 45 vs. 22 days).
“Understanding the characteristics of the patient groups found to be at highest risk for early shunt failure is helpful in identifying individual patients that may warrant expectant surveillance, enhanced pharmacologic management, or other strategies to reduce the risk of shunt failure,” Dr. Jacobs concluded.
“But perhaps more importantly it provides key information that may be helpful in the design and development of future clinical trials and/or collaborative quality improvement initiatives designed to reduce the cost in lives and resources that is associated with early shunt dysfunction.”
He acknowledged certain limitations of the study, including its retrospective observational design and the voluntary nature of the STS Congenital Heart Surgery Database. “In addition, some potentially important variables, such as detailed data concerning preoperative test results of coagulation assays are not collected in the STS Congenital Heart Surgery Database,” he said.
The research was supported by the STS Access & Publications Research program. The investigators reported having no financial disclosures.
HOUSTON – Among neonates and infants who underwent shunt construction as a source of pulmonary blood flow, early, in-hospital shunt failure occurred in 7.3% of cases, results from a large retrospective study showed.
“Approximately one in seven patients who experiences cardiac surgery in the first year of life undergoes construction of a systemic to pulmonary artery shunt of some type,” one of the study investigators, Marshall L. Jacobs, MD, said in an interview. The study was presented at the annual meeting of the Society of Thoracic Surgeons.
“Early failure of such shunts is an incompletely understood phenomenon which accounts for important morbidity and mortality among infants and neonates. Much of what is known about shunt failure is based on experiences reported from individual institutions. The few multicenter studies to date have been clinical trials that focused primarily on pharmacologic strategies intended to reduce the risk of shunt failure due to thrombosis. Their utility for guiding clinical decision making has been limited. Some have been underpowered; some have had limited risk adjustment of subjects.”
Dr. Do, who presented the findings at the meeting and is currently a Congenital Heart Surgery Fellow at the Children’s Hospital of Philadelphia, and a team of 11 other investigators utilized the STS Congenital Heart Surgery Database to identify 9,172 neonates and infants who underwent shunt construction as a source of pulmonary blood flow at 118 institutions from 2010 to 2015. Criteria for shunt failure included a documented diagnosis of in-hospital shunt failure, shunt revision, or catheter-based shunt intervention. The investigators used multivariable logistic regression to evaluate risk factors for in-hospital shunt failure.
Of the 9,172 at-risk neonates and infants, 674 (7.3%) experienced early, in-hospital shunt failure. “The observed rate of early shunt failure varied across the many specific types of shunts, and was lower with systemic ventricle to pulmonary artery shunts (as in the Sano modification of the Norwood procedure) than with the systemic artery to pulmonary artery shunts,” said Dr. Jacobs, who is a cardiothoracic surgeon at Johns Hopkins University, Baltimore.
In multivariable analysis, risk factors for in-hospital shunt failure included lower weight at operation for both neonates and infants, preoperative hypercoagulable state, and the collective presence of any other STS Congenital Heart Surgery Database preoperative risk factors. Neither cardiopulmonary bypass nor single ventricle diagnosis were risk factors for shunt failure. The investigators also observed that patients with in-hospital shunt failure had significantly higher rates of operative mortality (31.9% vs. 11.1%) and major morbidity (84.4% vs. 29.4%), and longer postoperative length of stay among survivors (a median of 45 vs. 22 days).
“Understanding the characteristics of the patient groups found to be at highest risk for early shunt failure is helpful in identifying individual patients that may warrant expectant surveillance, enhanced pharmacologic management, or other strategies to reduce the risk of shunt failure,” Dr. Jacobs concluded.
“But perhaps more importantly it provides key information that may be helpful in the design and development of future clinical trials and/or collaborative quality improvement initiatives designed to reduce the cost in lives and resources that is associated with early shunt dysfunction.”
He acknowledged certain limitations of the study, including its retrospective observational design and the voluntary nature of the STS Congenital Heart Surgery Database. “In addition, some potentially important variables, such as detailed data concerning preoperative test results of coagulation assays are not collected in the STS Congenital Heart Surgery Database,” he said.
The research was supported by the STS Access & Publications Research program. The investigators reported having no financial disclosures.
AT THE STS ANNUAL MEETING
Key clinical point:
Major finding: Among neonates and infants who underwent shunt operations, 7.3% experienced early, in-hospital shunt failure.
Data source: A retrospective analysis of 9,172 neonates and infants who underwent shunt construction as a source of pulmonary blood flow at 118 institutions from 2010 to 2015.
Disclosures: The research was supported by the STS Access & Publications Research program. The investigators reported having no financial disclosures.
Flashback to April 2008
The April 2008 issue of GI & Hepatology News (GIHN) featured an article by Roy M. Soetikno, MD, MS, FASGE and his colleagues from the Palo Alto VA Medical Center in California. They drew our attention to nonpolypoid (flat) colonic lesions in an article from JAMA (2008;299:1027-35).
Coincidentally, the week before this article appeared, I was sitting with Roy in Kyoto, Japan, at a conference of international experts focused on flat colonic lesions. The Japanese definitions of flat and depressed lesions were markedly different from those used by Western physicians. We now know that most flat lesions seen by U.S.-based endoscopists are sessile serrated adenomas (SSAs). SSAs at that time also were a new and controversial classification. SSAs were first described by Torlakovic and Snover in 1996 (Gastroenterology 1996;110:748-55).
Dale Snover, MD, was my golfing partner and read pathology slides for our practice in Minneapolis, so we were the first gastroenterologists in the country to grapple with the clinical implications of SSAs. Roy’s article was accompanied by an excellent commentary by Jerome D. Waye, MD, FASGE, who emphasized the importance of a slow withdrawal time and meticulous visual technique during colonoscopy.
Key points in the JAMA article were a) prevalence of flat lesions was about 9% in a screening population, b) small flat polyps can harbor advanced histologic changes including cancers, and c) many physicians who perform colonoscopy missed these lesions putting patients at risk for interval colon cancers.
The GIHN piece, referencing Soetikno’s article, helped inform us about an important (and confusing) problem in our colon cancer prevention efforts. As numerous authors subsequently highlighted (see Gastroenterology 2016;151:870-8) most cancers, missed at initial colonoscopy, are proximal and frequently develop from SSAs. We continue to work to reduce missed cancers and thanks to this seminal article, we have better insights about how to achieve this goal.
John I. Allen, MD, MBA, AGAF, is professor of medicine in the division of gastroenterology and hepatology at the University of Michigan, Ann Arbor, and the Editor in Chief of GI & Hepatology News.
The April 2008 issue of GI & Hepatology News (GIHN) featured an article by Roy M. Soetikno, MD, MS, FASGE and his colleagues from the Palo Alto VA Medical Center in California. They drew our attention to nonpolypoid (flat) colonic lesions in an article from JAMA (2008;299:1027-35).
Coincidentally, the week before this article appeared, I was sitting with Roy in Kyoto, Japan, at a conference of international experts focused on flat colonic lesions. The Japanese definitions of flat and depressed lesions were markedly different from those used by Western physicians. We now know that most flat lesions seen by U.S.-based endoscopists are sessile serrated adenomas (SSAs). SSAs at that time also were a new and controversial classification. SSAs were first described by Torlakovic and Snover in 1996 (Gastroenterology 1996;110:748-55).
Dale Snover, MD, was my golfing partner and read pathology slides for our practice in Minneapolis, so we were the first gastroenterologists in the country to grapple with the clinical implications of SSAs. Roy’s article was accompanied by an excellent commentary by Jerome D. Waye, MD, FASGE, who emphasized the importance of a slow withdrawal time and meticulous visual technique during colonoscopy.
Key points in the JAMA article were a) prevalence of flat lesions was about 9% in a screening population, b) small flat polyps can harbor advanced histologic changes including cancers, and c) many physicians who perform colonoscopy missed these lesions putting patients at risk for interval colon cancers.
The GIHN piece, referencing Soetikno’s article, helped inform us about an important (and confusing) problem in our colon cancer prevention efforts. As numerous authors subsequently highlighted (see Gastroenterology 2016;151:870-8) most cancers, missed at initial colonoscopy, are proximal and frequently develop from SSAs. We continue to work to reduce missed cancers and thanks to this seminal article, we have better insights about how to achieve this goal.
John I. Allen, MD, MBA, AGAF, is professor of medicine in the division of gastroenterology and hepatology at the University of Michigan, Ann Arbor, and the Editor in Chief of GI & Hepatology News.
The April 2008 issue of GI & Hepatology News (GIHN) featured an article by Roy M. Soetikno, MD, MS, FASGE and his colleagues from the Palo Alto VA Medical Center in California. They drew our attention to nonpolypoid (flat) colonic lesions in an article from JAMA (2008;299:1027-35).
Coincidentally, the week before this article appeared, I was sitting with Roy in Kyoto, Japan, at a conference of international experts focused on flat colonic lesions. The Japanese definitions of flat and depressed lesions were markedly different from those used by Western physicians. We now know that most flat lesions seen by U.S.-based endoscopists are sessile serrated adenomas (SSAs). SSAs at that time also were a new and controversial classification. SSAs were first described by Torlakovic and Snover in 1996 (Gastroenterology 1996;110:748-55).
Dale Snover, MD, was my golfing partner and read pathology slides for our practice in Minneapolis, so we were the first gastroenterologists in the country to grapple with the clinical implications of SSAs. Roy’s article was accompanied by an excellent commentary by Jerome D. Waye, MD, FASGE, who emphasized the importance of a slow withdrawal time and meticulous visual technique during colonoscopy.
Key points in the JAMA article were a) prevalence of flat lesions was about 9% in a screening population, b) small flat polyps can harbor advanced histologic changes including cancers, and c) many physicians who perform colonoscopy missed these lesions putting patients at risk for interval colon cancers.
The GIHN piece, referencing Soetikno’s article, helped inform us about an important (and confusing) problem in our colon cancer prevention efforts. As numerous authors subsequently highlighted (see Gastroenterology 2016;151:870-8) most cancers, missed at initial colonoscopy, are proximal and frequently develop from SSAs. We continue to work to reduce missed cancers and thanks to this seminal article, we have better insights about how to achieve this goal.
John I. Allen, MD, MBA, AGAF, is professor of medicine in the division of gastroenterology and hepatology at the University of Michigan, Ann Arbor, and the Editor in Chief of GI & Hepatology News.
Multivessel PCI in STEMI gains traction
SNOWMASS, COLO. – The tide appears to have turned regarding the merits of percutaneous coronary intervention in non-infarct-related arteries in conjunction with primary PCI for ST-elevation MI in patients with multivessel disease, Douglas E. Drachman, MD, said at the Annual Cardiovascular Conference at Snowmass.
Previously, multivessel PCI in STEMI patients who are hemodynamically stable was believed harmful and was given a Class IIIb recommendation – meaning don’t do it – in the 2013 American College of Cardiology/American Heart Association STEMI guidelines. Just 2 years later, however, new evidence in the form of three randomized trials prompted a focused update of the joint guidelines in which the practice was upgraded to Class IIb status, meaning it could be considered and may be beneficial.
Roughly 50% of STEMI patients have significant lesions in non-infarct-related arteries (non-IRA). The question of how best to treat such patients is an important one because multivessel coronary disease in STEMI is associated with increased risks of both reinfarction and mortality, noted Dr. Drachman, an interventional cardiologist at Massachusetts General Hospital in Boston.
He offered several reasons why the findings of the three influential randomized trials differed from earlier negative retrospective observational studies: “I would argue there’s been significant improvement in our technique in doing PCI. We’re primarily doing transradial interventions now for our patients, so the risk associated with multiple accesses is reduced. Our ability to use more potent antithrombotic strategies is enhanced by our concern about bleeding risk. And the stent platforms that we use in our interventional strategies have improved to the point that we are tackling ever more challenging lesions with greater aplomb and less concern that we may cause harm. I think all these factors have enhanced the ability of the interventionalist to select and treat non-IRAs in a staged fashion and be less parsimonious at the point of care.”
The remaining questions are which non-IRA lesions should be treated, in whom, when relative to primary PCI, and what are the cost implications? These issues are being tackled in at least eight active randomized controlled trials. Depending upon the answers to come, multivessel PCI in STEMI patients could receive a further upgrade in the guidelines.
Since release of the 2015 focused guideline update, several large studies have provided further backing for multivessel PCI in STEMI patients with significant multivessel disease, although these weren’t randomized prospective studies and hence must be considered hypothesis-generating.
One of these major pieces of evidence was a meta-analysis of observational studies led by Eric R. Bates, MD, professor of internal medicine at the University of Michigan in Ann Arbor. He and his coinvestigators analyzed studies comparing culprit vessel-only primary PCI for STEMI patients with multivessel disease versus staged PCI in which primary PCI was done first, followed by PCI of a non-infarct-related vessel later during the same hospitalization or soon after. Staged PCI was the clear winner, with a 2.2-fold greater likelihood of freedom from mortality (J Am Coll Cardiol. 2016 Sep 6;68(10):1066-81).
When the investigators compared studies of staged PCI versus multivessel PCI in the same session as primary PCI, staged PCI was again the clear winner, with a 4-fold greater freedom from mortality.
Among the possible risks of performing PCI of a non-IRA in the same session as primary PCI are increased risks of thrombosis, contrast-induced nephropathy, stent undersizing due to vasospasm, and unintended jeopardy of distant viable myocardium due to microembolization or side branch occlusion, Dr. Drachman said.
“Maybe in certain circumstances it’s best to let the dust settle after the urgent vessel intervention. Wait a couple of days and then make your plan,” the cardiologist advised.
Another informative recent piece of evidence was provided by a Canadian retrospective observational study which compared revascularization strategies in 6,503 consecutive STEMI patients with multivessel disease. Staged multivessel PCI during the index hospitalization was performed in 658 patients, multivessel PCI during the primary PCI session in 1,325, and PCI limited to the infarct-related artery in 4,520. The study endpoints were 2-year all-cause mortality and repeat revascularization.
Staged multivessel PCI had the lowest mortality and repeat revascularization rates. The 2-year mortality rate associated with this strategy was 45% less than with multivessel intervention at the time of primary PCI and 35% lower than for culprit vessel-only PCI, which unsurprisingly had the highest repeat revascularization rate (JACC Cardiovasc Interv. 2017 Jan 9;10(1):11-23).
The first of the three randomized trials that led to a change in the guidelines was the UK PRAMI study (Preventive Angioplasty in Acute Myocardial Infarction). It showed at a mean 23-months followup that STEMI patients with multivessel disease had a 65% reduction in the relative risk of a composite endoint of cardiovascular death, MI, or refractory angina if they received non-IRA PCI at the same time as primary PCI compared with PCI limited to the IRA (N Engl J Med. 2013 Sep 19;369(12):1115-23).
Next came another UK trial: CvLPRIT (Complete vs. Culprit-Lesion Only Primary PCI) demonstrated a 65% reduction in the composite 12-month outcome of all-cause mortality, MI, heart failure, or ischemia-driven PCI with staged PCI during the index hospitalization compared with culprit vessel-only PCI (J Am Coll Cardiol. 2015 Mar 17;65(10):963-72).
Finally, DANAMI-3-PRIMULTI (the Third Danish Study of Optimal Acute Treatment of Patients with STEMI: Primary PCI in Multivessel Disease) showed a dramatic reduction in the risk of ischemia-driven PCI during a median 27 months of followup in patients who underwent staged multivessel PCI guided by the findings of fractional flow reserve measurement compared with primary PCI limited to the IRA (Lancet. 2015 Aug 15;386(9994):665-71). However, fractional flow reserve-guided multivessel PCI didn’t decrease the risk of death or nonfatal recurrent MI, leaving its role unsettled pending the results of ongoing clinical trials.
Dr. Drachman said it’s clear certain STEMI patients should not undergo non-IRA PCI. These include anyone in whom the procedure would be lengthy due to vessel tortuosity or chronic total occlusion, as well as patients with stable saphenous vein graft disease or heavily calcified lesions requiring atherectomy, since multivessel PCI in those settings would pose a high risk for additional left ventricular dysfunction.
“Be thoughtful about patients who have renal dysfunction,” he added.
Dr. Drachman reported having no financial conflicts of interest.
SNOWMASS, COLO. – The tide appears to have turned regarding the merits of percutaneous coronary intervention in non-infarct-related arteries in conjunction with primary PCI for ST-elevation MI in patients with multivessel disease, Douglas E. Drachman, MD, said at the Annual Cardiovascular Conference at Snowmass.
Previously, multivessel PCI in STEMI patients who are hemodynamically stable was believed harmful and was given a Class IIIb recommendation – meaning don’t do it – in the 2013 American College of Cardiology/American Heart Association STEMI guidelines. Just 2 years later, however, new evidence in the form of three randomized trials prompted a focused update of the joint guidelines in which the practice was upgraded to Class IIb status, meaning it could be considered and may be beneficial.
Roughly 50% of STEMI patients have significant lesions in non-infarct-related arteries (non-IRA). The question of how best to treat such patients is an important one because multivessel coronary disease in STEMI is associated with increased risks of both reinfarction and mortality, noted Dr. Drachman, an interventional cardiologist at Massachusetts General Hospital in Boston.
He offered several reasons why the findings of the three influential randomized trials differed from earlier negative retrospective observational studies: “I would argue there’s been significant improvement in our technique in doing PCI. We’re primarily doing transradial interventions now for our patients, so the risk associated with multiple accesses is reduced. Our ability to use more potent antithrombotic strategies is enhanced by our concern about bleeding risk. And the stent platforms that we use in our interventional strategies have improved to the point that we are tackling ever more challenging lesions with greater aplomb and less concern that we may cause harm. I think all these factors have enhanced the ability of the interventionalist to select and treat non-IRAs in a staged fashion and be less parsimonious at the point of care.”
The remaining questions are which non-IRA lesions should be treated, in whom, when relative to primary PCI, and what are the cost implications? These issues are being tackled in at least eight active randomized controlled trials. Depending upon the answers to come, multivessel PCI in STEMI patients could receive a further upgrade in the guidelines.
Since release of the 2015 focused guideline update, several large studies have provided further backing for multivessel PCI in STEMI patients with significant multivessel disease, although these weren’t randomized prospective studies and hence must be considered hypothesis-generating.
One of these major pieces of evidence was a meta-analysis of observational studies led by Eric R. Bates, MD, professor of internal medicine at the University of Michigan in Ann Arbor. He and his coinvestigators analyzed studies comparing culprit vessel-only primary PCI for STEMI patients with multivessel disease versus staged PCI in which primary PCI was done first, followed by PCI of a non-infarct-related vessel later during the same hospitalization or soon after. Staged PCI was the clear winner, with a 2.2-fold greater likelihood of freedom from mortality (J Am Coll Cardiol. 2016 Sep 6;68(10):1066-81).
When the investigators compared studies of staged PCI versus multivessel PCI in the same session as primary PCI, staged PCI was again the clear winner, with a 4-fold greater freedom from mortality.
Among the possible risks of performing PCI of a non-IRA in the same session as primary PCI are increased risks of thrombosis, contrast-induced nephropathy, stent undersizing due to vasospasm, and unintended jeopardy of distant viable myocardium due to microembolization or side branch occlusion, Dr. Drachman said.
“Maybe in certain circumstances it’s best to let the dust settle after the urgent vessel intervention. Wait a couple of days and then make your plan,” the cardiologist advised.
Another informative recent piece of evidence was provided by a Canadian retrospective observational study which compared revascularization strategies in 6,503 consecutive STEMI patients with multivessel disease. Staged multivessel PCI during the index hospitalization was performed in 658 patients, multivessel PCI during the primary PCI session in 1,325, and PCI limited to the infarct-related artery in 4,520. The study endpoints were 2-year all-cause mortality and repeat revascularization.
Staged multivessel PCI had the lowest mortality and repeat revascularization rates. The 2-year mortality rate associated with this strategy was 45% less than with multivessel intervention at the time of primary PCI and 35% lower than for culprit vessel-only PCI, which unsurprisingly had the highest repeat revascularization rate (JACC Cardiovasc Interv. 2017 Jan 9;10(1):11-23).
The first of the three randomized trials that led to a change in the guidelines was the UK PRAMI study (Preventive Angioplasty in Acute Myocardial Infarction). It showed at a mean 23-months followup that STEMI patients with multivessel disease had a 65% reduction in the relative risk of a composite endoint of cardiovascular death, MI, or refractory angina if they received non-IRA PCI at the same time as primary PCI compared with PCI limited to the IRA (N Engl J Med. 2013 Sep 19;369(12):1115-23).
Next came another UK trial: CvLPRIT (Complete vs. Culprit-Lesion Only Primary PCI) demonstrated a 65% reduction in the composite 12-month outcome of all-cause mortality, MI, heart failure, or ischemia-driven PCI with staged PCI during the index hospitalization compared with culprit vessel-only PCI (J Am Coll Cardiol. 2015 Mar 17;65(10):963-72).
Finally, DANAMI-3-PRIMULTI (the Third Danish Study of Optimal Acute Treatment of Patients with STEMI: Primary PCI in Multivessel Disease) showed a dramatic reduction in the risk of ischemia-driven PCI during a median 27 months of followup in patients who underwent staged multivessel PCI guided by the findings of fractional flow reserve measurement compared with primary PCI limited to the IRA (Lancet. 2015 Aug 15;386(9994):665-71). However, fractional flow reserve-guided multivessel PCI didn’t decrease the risk of death or nonfatal recurrent MI, leaving its role unsettled pending the results of ongoing clinical trials.
Dr. Drachman said it’s clear certain STEMI patients should not undergo non-IRA PCI. These include anyone in whom the procedure would be lengthy due to vessel tortuosity or chronic total occlusion, as well as patients with stable saphenous vein graft disease or heavily calcified lesions requiring atherectomy, since multivessel PCI in those settings would pose a high risk for additional left ventricular dysfunction.
“Be thoughtful about patients who have renal dysfunction,” he added.
Dr. Drachman reported having no financial conflicts of interest.
SNOWMASS, COLO. – The tide appears to have turned regarding the merits of percutaneous coronary intervention in non-infarct-related arteries in conjunction with primary PCI for ST-elevation MI in patients with multivessel disease, Douglas E. Drachman, MD, said at the Annual Cardiovascular Conference at Snowmass.
Previously, multivessel PCI in STEMI patients who are hemodynamically stable was believed harmful and was given a Class IIIb recommendation – meaning don’t do it – in the 2013 American College of Cardiology/American Heart Association STEMI guidelines. Just 2 years later, however, new evidence in the form of three randomized trials prompted a focused update of the joint guidelines in which the practice was upgraded to Class IIb status, meaning it could be considered and may be beneficial.
Roughly 50% of STEMI patients have significant lesions in non-infarct-related arteries (non-IRA). The question of how best to treat such patients is an important one because multivessel coronary disease in STEMI is associated with increased risks of both reinfarction and mortality, noted Dr. Drachman, an interventional cardiologist at Massachusetts General Hospital in Boston.
He offered several reasons why the findings of the three influential randomized trials differed from earlier negative retrospective observational studies: “I would argue there’s been significant improvement in our technique in doing PCI. We’re primarily doing transradial interventions now for our patients, so the risk associated with multiple accesses is reduced. Our ability to use more potent antithrombotic strategies is enhanced by our concern about bleeding risk. And the stent platforms that we use in our interventional strategies have improved to the point that we are tackling ever more challenging lesions with greater aplomb and less concern that we may cause harm. I think all these factors have enhanced the ability of the interventionalist to select and treat non-IRAs in a staged fashion and be less parsimonious at the point of care.”
The remaining questions are which non-IRA lesions should be treated, in whom, when relative to primary PCI, and what are the cost implications? These issues are being tackled in at least eight active randomized controlled trials. Depending upon the answers to come, multivessel PCI in STEMI patients could receive a further upgrade in the guidelines.
Since release of the 2015 focused guideline update, several large studies have provided further backing for multivessel PCI in STEMI patients with significant multivessel disease, although these weren’t randomized prospective studies and hence must be considered hypothesis-generating.
One of these major pieces of evidence was a meta-analysis of observational studies led by Eric R. Bates, MD, professor of internal medicine at the University of Michigan in Ann Arbor. He and his coinvestigators analyzed studies comparing culprit vessel-only primary PCI for STEMI patients with multivessel disease versus staged PCI in which primary PCI was done first, followed by PCI of a non-infarct-related vessel later during the same hospitalization or soon after. Staged PCI was the clear winner, with a 2.2-fold greater likelihood of freedom from mortality (J Am Coll Cardiol. 2016 Sep 6;68(10):1066-81).
When the investigators compared studies of staged PCI versus multivessel PCI in the same session as primary PCI, staged PCI was again the clear winner, with a 4-fold greater freedom from mortality.
Among the possible risks of performing PCI of a non-IRA in the same session as primary PCI are increased risks of thrombosis, contrast-induced nephropathy, stent undersizing due to vasospasm, and unintended jeopardy of distant viable myocardium due to microembolization or side branch occlusion, Dr. Drachman said.
“Maybe in certain circumstances it’s best to let the dust settle after the urgent vessel intervention. Wait a couple of days and then make your plan,” the cardiologist advised.
Another informative recent piece of evidence was provided by a Canadian retrospective observational study which compared revascularization strategies in 6,503 consecutive STEMI patients with multivessel disease. Staged multivessel PCI during the index hospitalization was performed in 658 patients, multivessel PCI during the primary PCI session in 1,325, and PCI limited to the infarct-related artery in 4,520. The study endpoints were 2-year all-cause mortality and repeat revascularization.
Staged multivessel PCI had the lowest mortality and repeat revascularization rates. The 2-year mortality rate associated with this strategy was 45% less than with multivessel intervention at the time of primary PCI and 35% lower than for culprit vessel-only PCI, which unsurprisingly had the highest repeat revascularization rate (JACC Cardiovasc Interv. 2017 Jan 9;10(1):11-23).
The first of the three randomized trials that led to a change in the guidelines was the UK PRAMI study (Preventive Angioplasty in Acute Myocardial Infarction). It showed at a mean 23-months followup that STEMI patients with multivessel disease had a 65% reduction in the relative risk of a composite endoint of cardiovascular death, MI, or refractory angina if they received non-IRA PCI at the same time as primary PCI compared with PCI limited to the IRA (N Engl J Med. 2013 Sep 19;369(12):1115-23).
Next came another UK trial: CvLPRIT (Complete vs. Culprit-Lesion Only Primary PCI) demonstrated a 65% reduction in the composite 12-month outcome of all-cause mortality, MI, heart failure, or ischemia-driven PCI with staged PCI during the index hospitalization compared with culprit vessel-only PCI (J Am Coll Cardiol. 2015 Mar 17;65(10):963-72).
Finally, DANAMI-3-PRIMULTI (the Third Danish Study of Optimal Acute Treatment of Patients with STEMI: Primary PCI in Multivessel Disease) showed a dramatic reduction in the risk of ischemia-driven PCI during a median 27 months of followup in patients who underwent staged multivessel PCI guided by the findings of fractional flow reserve measurement compared with primary PCI limited to the IRA (Lancet. 2015 Aug 15;386(9994):665-71). However, fractional flow reserve-guided multivessel PCI didn’t decrease the risk of death or nonfatal recurrent MI, leaving its role unsettled pending the results of ongoing clinical trials.
Dr. Drachman said it’s clear certain STEMI patients should not undergo non-IRA PCI. These include anyone in whom the procedure would be lengthy due to vessel tortuosity or chronic total occlusion, as well as patients with stable saphenous vein graft disease or heavily calcified lesions requiring atherectomy, since multivessel PCI in those settings would pose a high risk for additional left ventricular dysfunction.
“Be thoughtful about patients who have renal dysfunction,” he added.
Dr. Drachman reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Flu activity up slightly, but still down from seasonal peak
After rising to a high point for the season in the last week of 2016, influenza activity dropped a bit in the first week of the new year but then rose again in the second week, according to the Centers for Disease Control and Prevention.
As measured by outpatient visits for influenza-like illness (ILI), activity slipped from 3.4% at the end of 2016 to 3.2% for the week ending Jan. 7 but then ticked up to 3.3% for the week ending Jan. 14, the CDC reported. The national baseline level of outpatient visits is 2.2% for ILI, which is defined as fever (temperature of 100° F or greater) and cough and/or sore throat.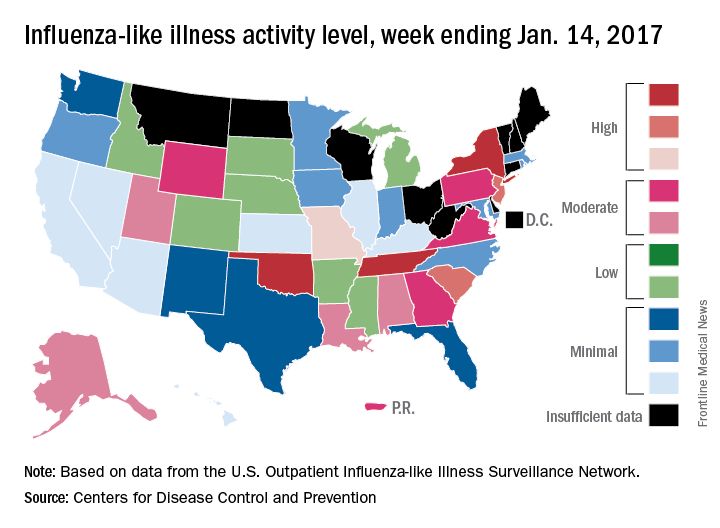
Two influenza-related pediatric deaths were reported for the week ending Jan. 14, although both occurred in earlier weeks: one during the week ending Dec. 10 and one during the week ending Jan. 7. So far for the 2016-2017 season, a total of five flu-related pediatric deaths have been reported, according to the CDC.
After rising to a high point for the season in the last week of 2016, influenza activity dropped a bit in the first week of the new year but then rose again in the second week, according to the Centers for Disease Control and Prevention.
As measured by outpatient visits for influenza-like illness (ILI), activity slipped from 3.4% at the end of 2016 to 3.2% for the week ending Jan. 7 but then ticked up to 3.3% for the week ending Jan. 14, the CDC reported. The national baseline level of outpatient visits is 2.2% for ILI, which is defined as fever (temperature of 100° F or greater) and cough and/or sore throat.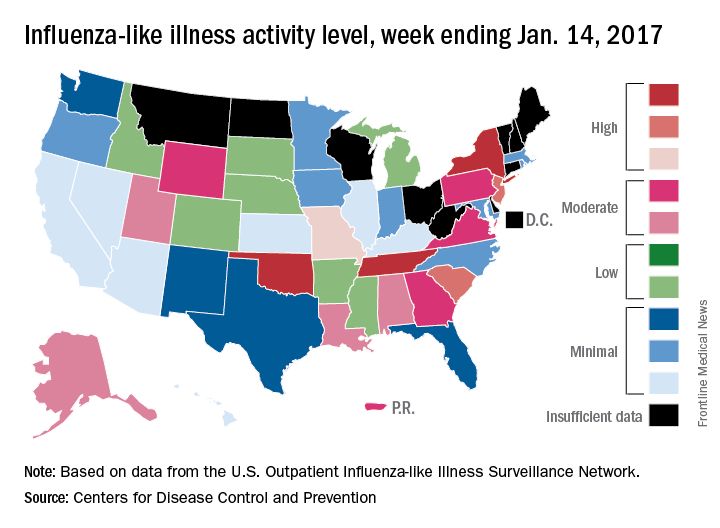
Two influenza-related pediatric deaths were reported for the week ending Jan. 14, although both occurred in earlier weeks: one during the week ending Dec. 10 and one during the week ending Jan. 7. So far for the 2016-2017 season, a total of five flu-related pediatric deaths have been reported, according to the CDC.
After rising to a high point for the season in the last week of 2016, influenza activity dropped a bit in the first week of the new year but then rose again in the second week, according to the Centers for Disease Control and Prevention.
As measured by outpatient visits for influenza-like illness (ILI), activity slipped from 3.4% at the end of 2016 to 3.2% for the week ending Jan. 7 but then ticked up to 3.3% for the week ending Jan. 14, the CDC reported. The national baseline level of outpatient visits is 2.2% for ILI, which is defined as fever (temperature of 100° F or greater) and cough and/or sore throat.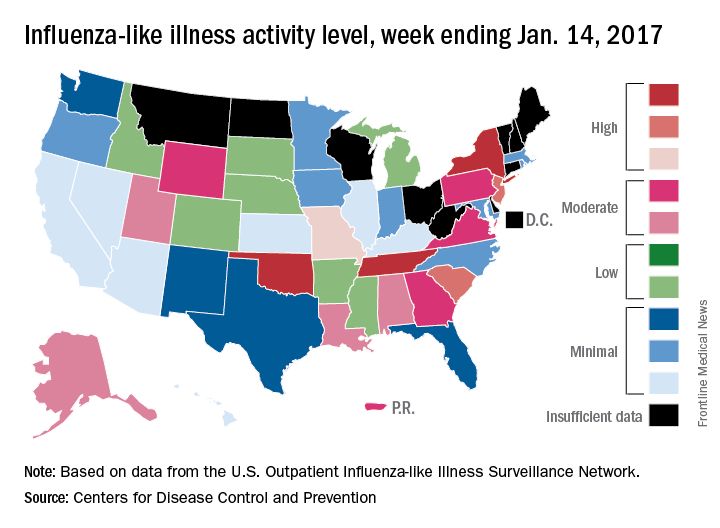
Two influenza-related pediatric deaths were reported for the week ending Jan. 14, although both occurred in earlier weeks: one during the week ending Dec. 10 and one during the week ending Jan. 7. So far for the 2016-2017 season, a total of five flu-related pediatric deaths have been reported, according to the CDC.
Resective epilepsy surgery found OK in septuagenarians
HOUSTON – With careful selection, patients in their 70s with refractory epilepsy may be offered resective epilepsy surgery, results from a small single-center study demonstrated.
The findings “were a surprise to us,” lead study author Ahmed Abdelkader, MD, said in an interview at the annual meeting of the American Epilepsy Society. “We expected that complications would be higher because this is a vulnerable age group with multiple comorbidities.”
Dr. Abdelkader and his associates searched the database of the Cleveland Clinic Epilepsy Center to identify patients aged 70 years and older who underwent respective epilepsy surgery between Jan. 1, 2000, and Sept. 30, 2015. They limited the analysis to seven patients who had at least one year of post-surgical follow-up. The mean age of the patients at surgery was 73 and the age of epilepsy onset ranged from 24-71 years, with a monthly frequency of 4.2 seizures. Their mean Charlson Combined Comorbidity Index score was 4, which translated into a 10-year mean survival probability of 53%. Four of the patients (57%) had a history of significant injuries due to seizures, while all but one had a positive MRI. Three of the patients had hippocampal sclerosis, “which is unique because most cases of hippocampal sclerosis are in younger age groups,” said Dr. Abdelkader, who is currently a research fellow at University Hospitals Case Medical Center, Cleveland.
All patients underwent anterior temporal lobectomy, four on the left side. None had a surgical complication. Six of the seven patients had a good surgical outcome, defined as a Class I or II on the Engel Epilepsy Surgery Outcome Scale, with four being completed free of seizures at one year of follow-up. One of the patients underwent two respective epilepsy surgeries: the first at age 72 and the second at age 75. He died of natural causes, 11 years after his first surgery, and was the only patient to pass away during the follow-up period.
In their abstract, the researchers called for future multi-center collaborative studies “to prospectively study factors influencing respective epilepsy surgery recommendation and its outcome in this rapidly growing population.”
Dr. Abdelkader reported having no financial disclosures.
HOUSTON – With careful selection, patients in their 70s with refractory epilepsy may be offered resective epilepsy surgery, results from a small single-center study demonstrated.
The findings “were a surprise to us,” lead study author Ahmed Abdelkader, MD, said in an interview at the annual meeting of the American Epilepsy Society. “We expected that complications would be higher because this is a vulnerable age group with multiple comorbidities.”
Dr. Abdelkader and his associates searched the database of the Cleveland Clinic Epilepsy Center to identify patients aged 70 years and older who underwent respective epilepsy surgery between Jan. 1, 2000, and Sept. 30, 2015. They limited the analysis to seven patients who had at least one year of post-surgical follow-up. The mean age of the patients at surgery was 73 and the age of epilepsy onset ranged from 24-71 years, with a monthly frequency of 4.2 seizures. Their mean Charlson Combined Comorbidity Index score was 4, which translated into a 10-year mean survival probability of 53%. Four of the patients (57%) had a history of significant injuries due to seizures, while all but one had a positive MRI. Three of the patients had hippocampal sclerosis, “which is unique because most cases of hippocampal sclerosis are in younger age groups,” said Dr. Abdelkader, who is currently a research fellow at University Hospitals Case Medical Center, Cleveland.
All patients underwent anterior temporal lobectomy, four on the left side. None had a surgical complication. Six of the seven patients had a good surgical outcome, defined as a Class I or II on the Engel Epilepsy Surgery Outcome Scale, with four being completed free of seizures at one year of follow-up. One of the patients underwent two respective epilepsy surgeries: the first at age 72 and the second at age 75. He died of natural causes, 11 years after his first surgery, and was the only patient to pass away during the follow-up period.
In their abstract, the researchers called for future multi-center collaborative studies “to prospectively study factors influencing respective epilepsy surgery recommendation and its outcome in this rapidly growing population.”
Dr. Abdelkader reported having no financial disclosures.
HOUSTON – With careful selection, patients in their 70s with refractory epilepsy may be offered resective epilepsy surgery, results from a small single-center study demonstrated.
The findings “were a surprise to us,” lead study author Ahmed Abdelkader, MD, said in an interview at the annual meeting of the American Epilepsy Society. “We expected that complications would be higher because this is a vulnerable age group with multiple comorbidities.”
Dr. Abdelkader and his associates searched the database of the Cleveland Clinic Epilepsy Center to identify patients aged 70 years and older who underwent respective epilepsy surgery between Jan. 1, 2000, and Sept. 30, 2015. They limited the analysis to seven patients who had at least one year of post-surgical follow-up. The mean age of the patients at surgery was 73 and the age of epilepsy onset ranged from 24-71 years, with a monthly frequency of 4.2 seizures. Their mean Charlson Combined Comorbidity Index score was 4, which translated into a 10-year mean survival probability of 53%. Four of the patients (57%) had a history of significant injuries due to seizures, while all but one had a positive MRI. Three of the patients had hippocampal sclerosis, “which is unique because most cases of hippocampal sclerosis are in younger age groups,” said Dr. Abdelkader, who is currently a research fellow at University Hospitals Case Medical Center, Cleveland.
All patients underwent anterior temporal lobectomy, four on the left side. None had a surgical complication. Six of the seven patients had a good surgical outcome, defined as a Class I or II on the Engel Epilepsy Surgery Outcome Scale, with four being completed free of seizures at one year of follow-up. One of the patients underwent two respective epilepsy surgeries: the first at age 72 and the second at age 75. He died of natural causes, 11 years after his first surgery, and was the only patient to pass away during the follow-up period.
In their abstract, the researchers called for future multi-center collaborative studies “to prospectively study factors influencing respective epilepsy surgery recommendation and its outcome in this rapidly growing population.”
Dr. Abdelkader reported having no financial disclosures.
AT AES 2016
Key clinical point:
Major finding: Six of the seven patients achieved good surgical outcome, with four being completed free of seizures at one year of follow-up.
Data source: A retrospective review of seven patients who underwent resective epilepsy surgery in their 70s.
Disclosures: Dr. Abdelkader reported having no financial disclosures.
Age and disease stage predict long-term survival in elderly lung cancer patients
AT THE STS ANNUAL MEETING
HOUSTON – Although certain medical factors predict long-term survival in patients over age 65 years with lung cancer, advanced age and disease stage are especially strong predictors, results from a large analysis of national data demonstrated.
The findings, which were presented by Mark Onaitis, MD, at the annual meeting of the Society of Thoracic Surgeons, come from a novel effort to pair Medicare data with files from the STS General Thoracic Surgery Database (GTSD).
For the current study, he and his associates linked GTSD data to Medicare data on 29,899 patients who underwent lung cancer resection from 2002 to 2013. They used Cox proportional hazards modeling to create a long-term survival model and used statistically significant univariate factors and known clinical predictors of outcome to perform variable selection.
Dr. Onaitis reported that the median age of patients was 73 years and that 52% were female. Of the 29,899 patients, 805 had a missing pathologic stage. Of the 29,094 patients not missing a pathologic stage, 69% were stage I, 18% stage II, 11% stage III, and 2% stage IV. Two-thirds of patients (66%) underwent lobectomy, followed by wedge resection (17%), segmentectomy (7%), bilobectomy (3%), pneumonectomy (3%), and sleeve lobectomy (1%). A thoracoscopic approach was performed in nearly half of resections (47%).
Cox analysis revealed the following strong negative predictors of long-term survival: having stage III or IV-V disease (hazard ratio, 1.23 and 1.37, respectively), being age 70-74 (HR, 1.19), 75-80 (HR, 1.40), or 80 and older (HR, 1.90).
After controlling for disease stage, the following procedures were associated with increased hazard of death, compared with lobectomy: wedge resection (HR, 1.22), segmentectomy (HR, 1.10), bilobectomy (HR, 1.30), and pneumonectomy (HR, 1.58). In addition, video-assisted thoracoscopic surgery was associated with improved long-term survival, compared with thoracotomy (HR, 0.86).
“Given the large number of patients and the excellent quality of the data, it was not surprising that age and stage and known medical conditions affect long-term survival,” Dr. Onaitis commented. “The deleterious effects of sublobar operations and open [as opposed to thoracoscopic or VATS] approach were more pronounced than expected.”
Other modifiable predictive factors include being a past or current smoker (HR, 1.35 and HR, 1.54, respectively) and having a body mass index below 18.5 kg/m2 (HR, 1.58).
Dr. Onaitis acknowledged certain limitations of the study, including its retrospective design. “Because the study involves linkage of STS data to Medicare data, the findings may not be applicable to patients less than 65 years of age,” he added. He reported having no financial disclosures.
AT THE STS ANNUAL MEETING
HOUSTON – Although certain medical factors predict long-term survival in patients over age 65 years with lung cancer, advanced age and disease stage are especially strong predictors, results from a large analysis of national data demonstrated.
The findings, which were presented by Mark Onaitis, MD, at the annual meeting of the Society of Thoracic Surgeons, come from a novel effort to pair Medicare data with files from the STS General Thoracic Surgery Database (GTSD).
For the current study, he and his associates linked GTSD data to Medicare data on 29,899 patients who underwent lung cancer resection from 2002 to 2013. They used Cox proportional hazards modeling to create a long-term survival model and used statistically significant univariate factors and known clinical predictors of outcome to perform variable selection.
Dr. Onaitis reported that the median age of patients was 73 years and that 52% were female. Of the 29,899 patients, 805 had a missing pathologic stage. Of the 29,094 patients not missing a pathologic stage, 69% were stage I, 18% stage II, 11% stage III, and 2% stage IV. Two-thirds of patients (66%) underwent lobectomy, followed by wedge resection (17%), segmentectomy (7%), bilobectomy (3%), pneumonectomy (3%), and sleeve lobectomy (1%). A thoracoscopic approach was performed in nearly half of resections (47%).
Cox analysis revealed the following strong negative predictors of long-term survival: having stage III or IV-V disease (hazard ratio, 1.23 and 1.37, respectively), being age 70-74 (HR, 1.19), 75-80 (HR, 1.40), or 80 and older (HR, 1.90).
After controlling for disease stage, the following procedures were associated with increased hazard of death, compared with lobectomy: wedge resection (HR, 1.22), segmentectomy (HR, 1.10), bilobectomy (HR, 1.30), and pneumonectomy (HR, 1.58). In addition, video-assisted thoracoscopic surgery was associated with improved long-term survival, compared with thoracotomy (HR, 0.86).
“Given the large number of patients and the excellent quality of the data, it was not surprising that age and stage and known medical conditions affect long-term survival,” Dr. Onaitis commented. “The deleterious effects of sublobar operations and open [as opposed to thoracoscopic or VATS] approach were more pronounced than expected.”
Other modifiable predictive factors include being a past or current smoker (HR, 1.35 and HR, 1.54, respectively) and having a body mass index below 18.5 kg/m2 (HR, 1.58).
Dr. Onaitis acknowledged certain limitations of the study, including its retrospective design. “Because the study involves linkage of STS data to Medicare data, the findings may not be applicable to patients less than 65 years of age,” he added. He reported having no financial disclosures.
AT THE STS ANNUAL MEETING
HOUSTON – Although certain medical factors predict long-term survival in patients over age 65 years with lung cancer, advanced age and disease stage are especially strong predictors, results from a large analysis of national data demonstrated.
The findings, which were presented by Mark Onaitis, MD, at the annual meeting of the Society of Thoracic Surgeons, come from a novel effort to pair Medicare data with files from the STS General Thoracic Surgery Database (GTSD).
For the current study, he and his associates linked GTSD data to Medicare data on 29,899 patients who underwent lung cancer resection from 2002 to 2013. They used Cox proportional hazards modeling to create a long-term survival model and used statistically significant univariate factors and known clinical predictors of outcome to perform variable selection.
Dr. Onaitis reported that the median age of patients was 73 years and that 52% were female. Of the 29,899 patients, 805 had a missing pathologic stage. Of the 29,094 patients not missing a pathologic stage, 69% were stage I, 18% stage II, 11% stage III, and 2% stage IV. Two-thirds of patients (66%) underwent lobectomy, followed by wedge resection (17%), segmentectomy (7%), bilobectomy (3%), pneumonectomy (3%), and sleeve lobectomy (1%). A thoracoscopic approach was performed in nearly half of resections (47%).
Cox analysis revealed the following strong negative predictors of long-term survival: having stage III or IV-V disease (hazard ratio, 1.23 and 1.37, respectively), being age 70-74 (HR, 1.19), 75-80 (HR, 1.40), or 80 and older (HR, 1.90).
After controlling for disease stage, the following procedures were associated with increased hazard of death, compared with lobectomy: wedge resection (HR, 1.22), segmentectomy (HR, 1.10), bilobectomy (HR, 1.30), and pneumonectomy (HR, 1.58). In addition, video-assisted thoracoscopic surgery was associated with improved long-term survival, compared with thoracotomy (HR, 0.86).
“Given the large number of patients and the excellent quality of the data, it was not surprising that age and stage and known medical conditions affect long-term survival,” Dr. Onaitis commented. “The deleterious effects of sublobar operations and open [as opposed to thoracoscopic or VATS] approach were more pronounced than expected.”
Other modifiable predictive factors include being a past or current smoker (HR, 1.35 and HR, 1.54, respectively) and having a body mass index below 18.5 kg/m2 (HR, 1.58).
Dr. Onaitis acknowledged certain limitations of the study, including its retrospective design. “Because the study involves linkage of STS data to Medicare data, the findings may not be applicable to patients less than 65 years of age,” he added. He reported having no financial disclosures.
Key clinical point:
Major finding: Strong negative predictors of long-term survival included having stage III or IV-V disease (HR, 1.23 and 1.37, respectively), being age 70-74 (HR, 1.19), 75-80 (HR, 1.40), or 80 and older (HR, 1.90).
Data source: A retrospective analysis of 29,899 patients over age 65 who underwent lung cancer resection from 2002 to 2013.
Disclosures: Dr. Onaitis reported having no financial disclosures.
Study IDs risk factors for ideal timing of stage 2 palliation following Norwood
HOUSTON – The optimal timing of stage 2 palliation after the Norwood operation depends on certain patient-specific risk factors, but in most cases should be done around 3-4 months of age, results from a multi-center study show.
While previous studies have investigated whether early stage-2 palliation (S2P) can be performed without increased post-S2P mortality, the effect of the timing of S2P on post-Norwood mortality remains unknown, Robert “Jake” Jaquiss, MD, said in an interview in advance of the annual meeting of the Society of Thoracic Surgeons.
“There has been a lot of dispute about how early is too early for S2P,” said Dr. Jaquiss, the study’s senior author, who is professor and division chief of pediatric cardiothoracic surgery at the University of Texas Southwestern Medical Center. “That is one of the few things that is in the control of the doctor. Most of the rest of the decisions are based entirely on the condition of the patient and the patient’s specific anatomy. So the timing of S2P is something that we can truly define most always. What we want to find out is, what is the ideal timing? How early is too early? Is there such a thing as too late?”
In an effort to determine the optimal timing of S2P that both minimizes pre-S2P attrition and maximizes long-term post-S2P survival, Dr. Jaquiss and his associates at 19 other institutions evaluated data from 534 neonates diagnosed with left ventricular outflow tract obstruction that precluded adequate systemic cardiac output through the aortic valve who initially underwent a Norwood operation from 2005 to 2016.
S2P was performed in 377 patients (71%) at a mean age of 5.4 months, while 115 (22%) died after Norwood, and the rest underwent biventricular repair or heart transplantation. After S2P, 38 (10%) died, 248 (66%) underwent Fontan, and the rest were alive awaiting Fontan or underwent heart transplantation.
Risk factors for death after Norwood included requiring pre-Norwood extracorporeal membrane oxygenation (P less than .0001), birth weight of less than 2.5 kg (P less than .0001), modified Blalock-Taussig shunt vs. a right ventricle to pulmonary artery conduit (P = .0003), larger baseline right pulmonary artery diameter (P = .0002), smaller baseline mitral valve diameter (P = .0002), smaller baseline tricuspid valve diameter (P = .0001), and nonwhite race (P = .03).
Risk factors for death after S2P included lower oxygen saturation at pre-S2P clinic visit (P = .02), having moderate or severe pre-S2P right ventricular dysfunction (P = .007), younger age at S2P (P = .03), and longer post-Norwood hospital length of stay (P = .03).
The risk-adjusted, 4-year, post-Norwood survival was 72%, with a confidence interval of 67%-75%. When plotted vs. the age at S2P, risk-adjusted, 4-year, post-Norwood survival for the 534 patients was maximized by S2P at 3-6 months of age. At the same time, risk-adjusted, 4-year survival in low-risk infants was compromised only by undergoing S2P earlier than 3 months of age. In high-risk infants, survival was severely compromised, especially when undergoing S2P earlier than 6 months of age.
“The results reinforced intuitions or expectations that most of the investigators already had,” Dr. Jaquiss said. “But we are in an era where evidence-based medicine is much preferable to intuition-based medicine. I’m very confident in the findings we have. I feel more confident in suggesting that we should be planning these surgeries around 3-4 months of age in usual-risk children and also more confident in suggesting that we need to consider transplantation earlier in children who are perceived to be at high risk. There is some hope [by clinicians in] some centers that you can convert a high-risk prognosis to a lower or intermediate risk prognosis by doing the S2P earlier or at some alternative time. Our data suggests that would not be helpful.”
Dr. Jaquiss and Dr. Meza reported having no financial disclosures.
HOUSTON – The optimal timing of stage 2 palliation after the Norwood operation depends on certain patient-specific risk factors, but in most cases should be done around 3-4 months of age, results from a multi-center study show.
While previous studies have investigated whether early stage-2 palliation (S2P) can be performed without increased post-S2P mortality, the effect of the timing of S2P on post-Norwood mortality remains unknown, Robert “Jake” Jaquiss, MD, said in an interview in advance of the annual meeting of the Society of Thoracic Surgeons.
“There has been a lot of dispute about how early is too early for S2P,” said Dr. Jaquiss, the study’s senior author, who is professor and division chief of pediatric cardiothoracic surgery at the University of Texas Southwestern Medical Center. “That is one of the few things that is in the control of the doctor. Most of the rest of the decisions are based entirely on the condition of the patient and the patient’s specific anatomy. So the timing of S2P is something that we can truly define most always. What we want to find out is, what is the ideal timing? How early is too early? Is there such a thing as too late?”
In an effort to determine the optimal timing of S2P that both minimizes pre-S2P attrition and maximizes long-term post-S2P survival, Dr. Jaquiss and his associates at 19 other institutions evaluated data from 534 neonates diagnosed with left ventricular outflow tract obstruction that precluded adequate systemic cardiac output through the aortic valve who initially underwent a Norwood operation from 2005 to 2016.
S2P was performed in 377 patients (71%) at a mean age of 5.4 months, while 115 (22%) died after Norwood, and the rest underwent biventricular repair or heart transplantation. After S2P, 38 (10%) died, 248 (66%) underwent Fontan, and the rest were alive awaiting Fontan or underwent heart transplantation.
Risk factors for death after Norwood included requiring pre-Norwood extracorporeal membrane oxygenation (P less than .0001), birth weight of less than 2.5 kg (P less than .0001), modified Blalock-Taussig shunt vs. a right ventricle to pulmonary artery conduit (P = .0003), larger baseline right pulmonary artery diameter (P = .0002), smaller baseline mitral valve diameter (P = .0002), smaller baseline tricuspid valve diameter (P = .0001), and nonwhite race (P = .03).
Risk factors for death after S2P included lower oxygen saturation at pre-S2P clinic visit (P = .02), having moderate or severe pre-S2P right ventricular dysfunction (P = .007), younger age at S2P (P = .03), and longer post-Norwood hospital length of stay (P = .03).
The risk-adjusted, 4-year, post-Norwood survival was 72%, with a confidence interval of 67%-75%. When plotted vs. the age at S2P, risk-adjusted, 4-year, post-Norwood survival for the 534 patients was maximized by S2P at 3-6 months of age. At the same time, risk-adjusted, 4-year survival in low-risk infants was compromised only by undergoing S2P earlier than 3 months of age. In high-risk infants, survival was severely compromised, especially when undergoing S2P earlier than 6 months of age.
“The results reinforced intuitions or expectations that most of the investigators already had,” Dr. Jaquiss said. “But we are in an era where evidence-based medicine is much preferable to intuition-based medicine. I’m very confident in the findings we have. I feel more confident in suggesting that we should be planning these surgeries around 3-4 months of age in usual-risk children and also more confident in suggesting that we need to consider transplantation earlier in children who are perceived to be at high risk. There is some hope [by clinicians in] some centers that you can convert a high-risk prognosis to a lower or intermediate risk prognosis by doing the S2P earlier or at some alternative time. Our data suggests that would not be helpful.”
Dr. Jaquiss and Dr. Meza reported having no financial disclosures.
HOUSTON – The optimal timing of stage 2 palliation after the Norwood operation depends on certain patient-specific risk factors, but in most cases should be done around 3-4 months of age, results from a multi-center study show.
While previous studies have investigated whether early stage-2 palliation (S2P) can be performed without increased post-S2P mortality, the effect of the timing of S2P on post-Norwood mortality remains unknown, Robert “Jake” Jaquiss, MD, said in an interview in advance of the annual meeting of the Society of Thoracic Surgeons.
“There has been a lot of dispute about how early is too early for S2P,” said Dr. Jaquiss, the study’s senior author, who is professor and division chief of pediatric cardiothoracic surgery at the University of Texas Southwestern Medical Center. “That is one of the few things that is in the control of the doctor. Most of the rest of the decisions are based entirely on the condition of the patient and the patient’s specific anatomy. So the timing of S2P is something that we can truly define most always. What we want to find out is, what is the ideal timing? How early is too early? Is there such a thing as too late?”
In an effort to determine the optimal timing of S2P that both minimizes pre-S2P attrition and maximizes long-term post-S2P survival, Dr. Jaquiss and his associates at 19 other institutions evaluated data from 534 neonates diagnosed with left ventricular outflow tract obstruction that precluded adequate systemic cardiac output through the aortic valve who initially underwent a Norwood operation from 2005 to 2016.
S2P was performed in 377 patients (71%) at a mean age of 5.4 months, while 115 (22%) died after Norwood, and the rest underwent biventricular repair or heart transplantation. After S2P, 38 (10%) died, 248 (66%) underwent Fontan, and the rest were alive awaiting Fontan or underwent heart transplantation.
Risk factors for death after Norwood included requiring pre-Norwood extracorporeal membrane oxygenation (P less than .0001), birth weight of less than 2.5 kg (P less than .0001), modified Blalock-Taussig shunt vs. a right ventricle to pulmonary artery conduit (P = .0003), larger baseline right pulmonary artery diameter (P = .0002), smaller baseline mitral valve diameter (P = .0002), smaller baseline tricuspid valve diameter (P = .0001), and nonwhite race (P = .03).
Risk factors for death after S2P included lower oxygen saturation at pre-S2P clinic visit (P = .02), having moderate or severe pre-S2P right ventricular dysfunction (P = .007), younger age at S2P (P = .03), and longer post-Norwood hospital length of stay (P = .03).
The risk-adjusted, 4-year, post-Norwood survival was 72%, with a confidence interval of 67%-75%. When plotted vs. the age at S2P, risk-adjusted, 4-year, post-Norwood survival for the 534 patients was maximized by S2P at 3-6 months of age. At the same time, risk-adjusted, 4-year survival in low-risk infants was compromised only by undergoing S2P earlier than 3 months of age. In high-risk infants, survival was severely compromised, especially when undergoing S2P earlier than 6 months of age.
“The results reinforced intuitions or expectations that most of the investigators already had,” Dr. Jaquiss said. “But we are in an era where evidence-based medicine is much preferable to intuition-based medicine. I’m very confident in the findings we have. I feel more confident in suggesting that we should be planning these surgeries around 3-4 months of age in usual-risk children and also more confident in suggesting that we need to consider transplantation earlier in children who are perceived to be at high risk. There is some hope [by clinicians in] some centers that you can convert a high-risk prognosis to a lower or intermediate risk prognosis by doing the S2P earlier or at some alternative time. Our data suggests that would not be helpful.”
Dr. Jaquiss and Dr. Meza reported having no financial disclosures.
Key clinical point:
Major finding: When plotted vs. the age at stage 2 palliation, risk-adjusted, 4-year, post-Norwood survival for the 534 patients was maximized by S2P at 3-6 months of age.
Data source: A multi-institutional analysis of 534 neonates diagnosed with left ventricular outflow tract obstruction that precluded adequate systemic cardiac output through the aortic valve who initially underwent a Norwood operation from 2005 to 2016.
Disclosures: Dr. Jaquiss and Dr. Meza reported having no financial disclosures.
New thinking on septal myectomy vs. alcohol ablation for obstructive cardiomyopathy
SNOWMASS, COLO. – The first-ever national study of the impact of hospital volume on outcomes of septal myectomy versus alcohol septal ablation for treatment of obstructive hypertrophic cardiomyopathy deserves to be practice-changing, Rick A. Nishimura, MD, said at the Annual Cardiovascular Conference at Snowmass.
Prior to release of these eye-opening data, conventional thinking held that referral for percutaneous septal ablation was the preferred option for elderly, sedentary patients with lots of comorbid conditions and a limited remaining lifespan, while surgical septal myectomy was the best fix for young, active, relatively healthy patients because of its impressive durability of benefit.
Similarly, 80% of alcohol ablations took place at centers doing less than 20 cases over 9 years. But the success of the percutaneous procedure was less dependent upon large institutional volumes. Only at the lowest-volume centers, where a total of fewer than 10 of the procedures were done over 9 years, was procedural mortality significantly higher – indeed, three- to fourfold higher – than at mid- or high-volume institutions or centers of excellence, all of which had similar mortality rates. The same was true for rates of postoperative complete heart block requiring a permanent pacemaker: significantly higher only at the lowest-volume institutions, according to the investigators from Weill Cornell Medical College in New York (JAMA Cardiol. 2016 Jun 1;1[3]:324-32).
“I think the bottom line is this: for the patient who is severely symptomatic with obstruction on optimal medical therapy, septal myectomy probably offers the best chance of excellent long-term symptomatic improvement, but the mortality depends on the center and the surgical expertise there, and complications do, too. This is something good to know that we never had data on before, that if you can’t get to a center with an experienced surgeon doing myectomies, it’s reasonable to go to a center doing ablations as long as there is some experience with the procedure there,” said Dr. Nishimura, professor of cardiovascular diseases and hypertension at the Mayo Clinic in Rochester, Minn.
Of the 11,248 patients treated for obstructive hypertrophic cardiomyopathy identified by the Cornell investigators using the Agency for Healthcare Research and Quality National Inpatient Sample database, 57% got myectomy and 43% underwent ablation. During the study years ablation increased in popularity by about 50%, rising from an annual rate of 1.6 to 2.5 procedures per million per year, while myectomy declined from 2.0 to 1.5 cases per million population per year. But that’s not what’s happened at the Mayo Clinic and other hypertrophic cardiomyopathy centers of excellence.
At the Mayo Clinic, for example, the volume of septal myectomies climbed from roughly 50 procedures per year in 2000 to close to 250 in 2015. Meanwhile the rate of alcohol septal ablation procedures remained steady at fewer than 20 per year.
“With shared decision making at Mayo, surgery has gone way up,” said Dr. Nishimura. “In an experienced surgeon’s hands, operative mortality is 0.8%, the gradient improves to 3%, and 94% of patients are postoperative New York Heart Association class I or II. This lasts for decades. We have 20-, 30-, and 40-year follow-up data now showing that over 90% of patients will have an excellent symptomatic benefit and be able to return to a normal lifestyle. The septum doesn’t come back. They’re good for life. So it’s a wonderful operation.”
In contrast, catheter-based septal ablation has a 4-year rate of survival free of death, NYHA class III or IV, or myectomy of 76%.
“One in four treated patients will not benefit,” the cardiologist emphasized.
The percutaneous procedure entails instilling alcohol into the septal perforator artery supplying the area of obstruction in order to cause a localized MI. Over a period of several weeks this causes the septum to shrink, thereby relieving the outflow tract obstruction.
When the procedure fails to bring about improvement, it’s often because the patient had a very long septal perforator artery and instilling the alcohol caused a large MI, making things worse. Or the patient didn’t have a septal perforator artery, or had one with so many branches that the cardiologist couldn’t identify the right one to treat to target the septum.
Dr. Nishimura reported having no financial conflicts.
SNOWMASS, COLO. – The first-ever national study of the impact of hospital volume on outcomes of septal myectomy versus alcohol septal ablation for treatment of obstructive hypertrophic cardiomyopathy deserves to be practice-changing, Rick A. Nishimura, MD, said at the Annual Cardiovascular Conference at Snowmass.
Prior to release of these eye-opening data, conventional thinking held that referral for percutaneous septal ablation was the preferred option for elderly, sedentary patients with lots of comorbid conditions and a limited remaining lifespan, while surgical septal myectomy was the best fix for young, active, relatively healthy patients because of its impressive durability of benefit.
Similarly, 80% of alcohol ablations took place at centers doing less than 20 cases over 9 years. But the success of the percutaneous procedure was less dependent upon large institutional volumes. Only at the lowest-volume centers, where a total of fewer than 10 of the procedures were done over 9 years, was procedural mortality significantly higher – indeed, three- to fourfold higher – than at mid- or high-volume institutions or centers of excellence, all of which had similar mortality rates. The same was true for rates of postoperative complete heart block requiring a permanent pacemaker: significantly higher only at the lowest-volume institutions, according to the investigators from Weill Cornell Medical College in New York (JAMA Cardiol. 2016 Jun 1;1[3]:324-32).
“I think the bottom line is this: for the patient who is severely symptomatic with obstruction on optimal medical therapy, septal myectomy probably offers the best chance of excellent long-term symptomatic improvement, but the mortality depends on the center and the surgical expertise there, and complications do, too. This is something good to know that we never had data on before, that if you can’t get to a center with an experienced surgeon doing myectomies, it’s reasonable to go to a center doing ablations as long as there is some experience with the procedure there,” said Dr. Nishimura, professor of cardiovascular diseases and hypertension at the Mayo Clinic in Rochester, Minn.
Of the 11,248 patients treated for obstructive hypertrophic cardiomyopathy identified by the Cornell investigators using the Agency for Healthcare Research and Quality National Inpatient Sample database, 57% got myectomy and 43% underwent ablation. During the study years ablation increased in popularity by about 50%, rising from an annual rate of 1.6 to 2.5 procedures per million per year, while myectomy declined from 2.0 to 1.5 cases per million population per year. But that’s not what’s happened at the Mayo Clinic and other hypertrophic cardiomyopathy centers of excellence.
At the Mayo Clinic, for example, the volume of septal myectomies climbed from roughly 50 procedures per year in 2000 to close to 250 in 2015. Meanwhile the rate of alcohol septal ablation procedures remained steady at fewer than 20 per year.
“With shared decision making at Mayo, surgery has gone way up,” said Dr. Nishimura. “In an experienced surgeon’s hands, operative mortality is 0.8%, the gradient improves to 3%, and 94% of patients are postoperative New York Heart Association class I or II. This lasts for decades. We have 20-, 30-, and 40-year follow-up data now showing that over 90% of patients will have an excellent symptomatic benefit and be able to return to a normal lifestyle. The septum doesn’t come back. They’re good for life. So it’s a wonderful operation.”
In contrast, catheter-based septal ablation has a 4-year rate of survival free of death, NYHA class III or IV, or myectomy of 76%.
“One in four treated patients will not benefit,” the cardiologist emphasized.
The percutaneous procedure entails instilling alcohol into the septal perforator artery supplying the area of obstruction in order to cause a localized MI. Over a period of several weeks this causes the septum to shrink, thereby relieving the outflow tract obstruction.
When the procedure fails to bring about improvement, it’s often because the patient had a very long septal perforator artery and instilling the alcohol caused a large MI, making things worse. Or the patient didn’t have a septal perforator artery, or had one with so many branches that the cardiologist couldn’t identify the right one to treat to target the septum.
Dr. Nishimura reported having no financial conflicts.
SNOWMASS, COLO. – The first-ever national study of the impact of hospital volume on outcomes of septal myectomy versus alcohol septal ablation for treatment of obstructive hypertrophic cardiomyopathy deserves to be practice-changing, Rick A. Nishimura, MD, said at the Annual Cardiovascular Conference at Snowmass.
Prior to release of these eye-opening data, conventional thinking held that referral for percutaneous septal ablation was the preferred option for elderly, sedentary patients with lots of comorbid conditions and a limited remaining lifespan, while surgical septal myectomy was the best fix for young, active, relatively healthy patients because of its impressive durability of benefit.
Similarly, 80% of alcohol ablations took place at centers doing less than 20 cases over 9 years. But the success of the percutaneous procedure was less dependent upon large institutional volumes. Only at the lowest-volume centers, where a total of fewer than 10 of the procedures were done over 9 years, was procedural mortality significantly higher – indeed, three- to fourfold higher – than at mid- or high-volume institutions or centers of excellence, all of which had similar mortality rates. The same was true for rates of postoperative complete heart block requiring a permanent pacemaker: significantly higher only at the lowest-volume institutions, according to the investigators from Weill Cornell Medical College in New York (JAMA Cardiol. 2016 Jun 1;1[3]:324-32).
“I think the bottom line is this: for the patient who is severely symptomatic with obstruction on optimal medical therapy, septal myectomy probably offers the best chance of excellent long-term symptomatic improvement, but the mortality depends on the center and the surgical expertise there, and complications do, too. This is something good to know that we never had data on before, that if you can’t get to a center with an experienced surgeon doing myectomies, it’s reasonable to go to a center doing ablations as long as there is some experience with the procedure there,” said Dr. Nishimura, professor of cardiovascular diseases and hypertension at the Mayo Clinic in Rochester, Minn.
Of the 11,248 patients treated for obstructive hypertrophic cardiomyopathy identified by the Cornell investigators using the Agency for Healthcare Research and Quality National Inpatient Sample database, 57% got myectomy and 43% underwent ablation. During the study years ablation increased in popularity by about 50%, rising from an annual rate of 1.6 to 2.5 procedures per million per year, while myectomy declined from 2.0 to 1.5 cases per million population per year. But that’s not what’s happened at the Mayo Clinic and other hypertrophic cardiomyopathy centers of excellence.
At the Mayo Clinic, for example, the volume of septal myectomies climbed from roughly 50 procedures per year in 2000 to close to 250 in 2015. Meanwhile the rate of alcohol septal ablation procedures remained steady at fewer than 20 per year.
“With shared decision making at Mayo, surgery has gone way up,” said Dr. Nishimura. “In an experienced surgeon’s hands, operative mortality is 0.8%, the gradient improves to 3%, and 94% of patients are postoperative New York Heart Association class I or II. This lasts for decades. We have 20-, 30-, and 40-year follow-up data now showing that over 90% of patients will have an excellent symptomatic benefit and be able to return to a normal lifestyle. The septum doesn’t come back. They’re good for life. So it’s a wonderful operation.”
In contrast, catheter-based septal ablation has a 4-year rate of survival free of death, NYHA class III or IV, or myectomy of 76%.
“One in four treated patients will not benefit,” the cardiologist emphasized.
The percutaneous procedure entails instilling alcohol into the septal perforator artery supplying the area of obstruction in order to cause a localized MI. Over a period of several weeks this causes the septum to shrink, thereby relieving the outflow tract obstruction.
When the procedure fails to bring about improvement, it’s often because the patient had a very long septal perforator artery and instilling the alcohol caused a large MI, making things worse. Or the patient didn’t have a septal perforator artery, or had one with so many branches that the cardiologist couldn’t identify the right one to treat to target the septum.
Dr. Nishimura reported having no financial conflicts.