User login
Cerebral protection in TAVI cuts ischemic lesions
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
As there was no significant difference in clinical neurological outcomes related to use of a filter device, although there was significantly fewer and smaller brain lesions in the stroke group, one is left to conclude that the majority of MRI findings after TAVI are not clinically relevant. Is the added cost of a cerebral protection device cost effective given the equivalent neurological outcomes in the both groups?
As there was no significant difference in clinical neurological outcomes related to use of a filter device, although there was significantly fewer and smaller brain lesions in the stroke group, one is left to conclude that the majority of MRI findings after TAVI are not clinically relevant. Is the added cost of a cerebral protection device cost effective given the equivalent neurological outcomes in the both groups?
As there was no significant difference in clinical neurological outcomes related to use of a filter device, although there was significantly fewer and smaller brain lesions in the stroke group, one is left to conclude that the majority of MRI findings after TAVI are not clinically relevant. Is the added cost of a cerebral protection device cost effective given the equivalent neurological outcomes in the both groups?
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
In patients undergoing transcatheter aortic valve implantation, use of a cerebral protection device to entrap and remove embolic debris reduced both the number and the size of ischemic brain lesions, according to a report published in JAMA.
The frequency and severity of postprocedure stroke symptoms were similar with and without the filter; however, the researchers noted that the study included only 100 patients and was not powered to assess differences in stroke rates.
Various cerebral protection devices were invented in response to the finding of a threefold increase in periprocedural stroke mortality following TAVI. Yet “clear evidence of the efficacy of any embolic protection device in TAVI is still missing,” said Stephan Haussig, MD, of the University of Leipzig (Germany) Heart Center, and his associates.
They performed a prospective randomized clinical trial at their center to assess the efficacy of the only cerebral protection device that was available when their study was designed. For the study, 100 patients with severe, symptomatic aortic stenosis were randomly assigned to undergo TAVI either with (50 patients) or without (50 patients) the use of a protective filter to capture embolic debris. The filter device was estimated to fully protect 74% of the brain and partially protect 24%, leaving only 2% unprotected.
The primary endpoint of the study was the number of ischemic brain lesions detected on diffusion-weighted MRI in the filter group, compared with the control group. This imaging was performed at baseline, 2 days after the procedure, and 7 days after the procedure.
In protected brain regions, the median number of new ischemic brain lesions was markedly lower in the filter group than in the control group (4 vs. 10) at 2 days, as well as at 7 days (3 vs. 7, respectively). In addition, the volume of new lesions in protected brain regions also was markedly lower in the filter group at 2 days (242 mm vs. 527 mm) and at 7 days (101 mm vs. 292 mm).
Similar protective effects were evident when the entire brain was evaluated. The median number of new lesions was markedly lower in the filter group than in the control group (8 vs. 16) at 2 days and at 7 days (5 vs. 10, respectively). The median lesion volume also was markedly lower in the filter group at 2 days (466 mm vs. 800 mm) and at 7 days (205 mm vs. 720 mm).
However, this protective effect didn’t translate into a substantive difference in neurologic outcomes between the two study groups, as assessed by the National Institutes of Health Stroke Scale and the modified Rankin scale. Five patients in each group developed symptoms of stroke, and all symptoms were deemed minor and nondisabling, the investigators said (JAMA 2016;316[6]:592-601).
It is important to note that this study wasn’t powered to assess differences in stroke rates. Larger studies will be needed to assess the impact of protective devices on neurological and functional outcomes, Dr. Haussig and his associates wrote.
The two study groups also did not differ with regard to complications. Thirty-day mortality was 0% in the filter group and 2% in the control group, a nonsignificant difference.
The investigators pointed out that protective filter devices can protect the brain only while they are in place during TAVI, “which usually takes less than 1 hour and represents only 2% of the first 48 hours after which the first MRI was performed in this study. Based on the analyzed material captured and removed by the filters – e.g., old and fresh thrombus, endothelium, atheromatous plaque, valve tissue, and calcium – it becomes evident that causes of cerebral injury are multifactorial and that the embolic risk does not resolve immediately at the end of the TAVI procedure,” they said.
Perhaps the study’s most surprising finding was that nearly every patient had new cerebral lesions consistent with infarcts, but most of these were very small and not associated with any neurocognitive or functional impairments.
This study was limited in that it involved a single cardiac team assessing only one brand of filter device at a single hospital, so the results are not necessarily generalizable to a broader patient population or to the many other devices that have since been developed, Dr. Haussig and his associates added.
This study was funded by a grant from Claret Medical and Medtronic. Dr. Haussig reported having no relevant financial disclosures; his associates reported ties to numerous industry sources.
‘Stepping’ up robotic lobectomy instruction
Teaching minimally invasive robotic surgery to residents can be difficult in a health care environment obsessed with quality outcome measures and under scrutiny by hospital administrators and payers, but researchers at the University of Alabama at Birmingham may have devised a method to instruct residents in robotic lobectomy without compromising patient outcomes, according to a study published in the October issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:991-7).
Robert J. Cerfolio, MD, MBA, FCCP, and his coauthors divided the procedure into 19 sequential, teachable steps and allowed residents to perform selected steps during operations that Dr. Cerfolio directed.
“We then applied simulation training, coaching techniques, and video review of each step to help improve the steps that residents could not complete,” Dr. Cerfolio and his coauthors said.
Surgeons in academic centers face the challenge of teaching “the art and science of surgery,” Dr. Cerfolio and his colleagues said, while maintaining quality outcomes. “Teaching minimally invasive surgery, especially robotic surgery, is challenging given the risks and the limited availability of the robot.”
The researchers acknowledged that other groups have taken a similar approach to training, but this is the first study that included video review, coaching, and instruction tied to time constraints, they said.
“A major concern is that while teaching robotic surgery, patients can be injured, care is worse, and metrics that are increasingly used as surrogates for quality outcomes suffer,” they noted.
They allotted each step in the procedure a set amount of time in which the resident had to complete it, totaling 80 minutes for all 19 steps and ranging from 1 minute to inspect the pleura after placing ports (9 minutes) to 20 minutes to close the five incisions. If the resident completed the task in the allotted time, it was recorded as “performed.”
Between February 2010 and December 2010 Dr. Cerfolio performed 520 robotic lobectomies, and over time the percentage of successful steps per resident improved.
For example, in the first year, 50% of thoracic surgery residents completed the first five steps (mark and place ports, inspect pleura, resect the inferior pulmonary ligament, and remove three lymph nodes), but by the last year of the study 90% of them successfully completed the five steps.
Dr. Cerfolio and coauthors acknowledged “many flaws” in their study, but the study also had strengths: It involved only one operation and corroborated the database with each resident’s own surgical logs.
“Operations such as robotic lobectomy can be successfully taught by dividing them into a series of surgical maneuvers or steps,” the researchers noted. Recording what residents can and can’t do, reviewing video, and coaching contribute to the process to improve their skills. “Further studies that scientifically measure ‘ways to teach’ and ways to coach and mentor are needed,” they said.
Dr. Cerfolio disclosed relationships with Intuitive Surgical, Ethicon, Community Health Services, KCL, Bovie and C-SATS. Coauthor Douglas Minnich, MD, is a consultant to Medtronic. The other co-authors had no financial relationships to disclose.
This in an interesting and clinically relevant study given the emphasis many institutions have placed on becoming “robotic” centers of excellence. The overall cost effectiveness of robotic surgery from a public policy standpoint remains a matter of intense study given the scarcity of resources in many health-care settings.
This in an interesting and clinically relevant study given the emphasis many institutions have placed on becoming “robotic” centers of excellence. The overall cost effectiveness of robotic surgery from a public policy standpoint remains a matter of intense study given the scarcity of resources in many health-care settings.
This in an interesting and clinically relevant study given the emphasis many institutions have placed on becoming “robotic” centers of excellence. The overall cost effectiveness of robotic surgery from a public policy standpoint remains a matter of intense study given the scarcity of resources in many health-care settings.
Teaching minimally invasive robotic surgery to residents can be difficult in a health care environment obsessed with quality outcome measures and under scrutiny by hospital administrators and payers, but researchers at the University of Alabama at Birmingham may have devised a method to instruct residents in robotic lobectomy without compromising patient outcomes, according to a study published in the October issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:991-7).
Robert J. Cerfolio, MD, MBA, FCCP, and his coauthors divided the procedure into 19 sequential, teachable steps and allowed residents to perform selected steps during operations that Dr. Cerfolio directed.
“We then applied simulation training, coaching techniques, and video review of each step to help improve the steps that residents could not complete,” Dr. Cerfolio and his coauthors said.
Surgeons in academic centers face the challenge of teaching “the art and science of surgery,” Dr. Cerfolio and his colleagues said, while maintaining quality outcomes. “Teaching minimally invasive surgery, especially robotic surgery, is challenging given the risks and the limited availability of the robot.”
The researchers acknowledged that other groups have taken a similar approach to training, but this is the first study that included video review, coaching, and instruction tied to time constraints, they said.
“A major concern is that while teaching robotic surgery, patients can be injured, care is worse, and metrics that are increasingly used as surrogates for quality outcomes suffer,” they noted.
They allotted each step in the procedure a set amount of time in which the resident had to complete it, totaling 80 minutes for all 19 steps and ranging from 1 minute to inspect the pleura after placing ports (9 minutes) to 20 minutes to close the five incisions. If the resident completed the task in the allotted time, it was recorded as “performed.”
Between February 2010 and December 2010 Dr. Cerfolio performed 520 robotic lobectomies, and over time the percentage of successful steps per resident improved.
For example, in the first year, 50% of thoracic surgery residents completed the first five steps (mark and place ports, inspect pleura, resect the inferior pulmonary ligament, and remove three lymph nodes), but by the last year of the study 90% of them successfully completed the five steps.
Dr. Cerfolio and coauthors acknowledged “many flaws” in their study, but the study also had strengths: It involved only one operation and corroborated the database with each resident’s own surgical logs.
“Operations such as robotic lobectomy can be successfully taught by dividing them into a series of surgical maneuvers or steps,” the researchers noted. Recording what residents can and can’t do, reviewing video, and coaching contribute to the process to improve their skills. “Further studies that scientifically measure ‘ways to teach’ and ways to coach and mentor are needed,” they said.
Dr. Cerfolio disclosed relationships with Intuitive Surgical, Ethicon, Community Health Services, KCL, Bovie and C-SATS. Coauthor Douglas Minnich, MD, is a consultant to Medtronic. The other co-authors had no financial relationships to disclose.
Teaching minimally invasive robotic surgery to residents can be difficult in a health care environment obsessed with quality outcome measures and under scrutiny by hospital administrators and payers, but researchers at the University of Alabama at Birmingham may have devised a method to instruct residents in robotic lobectomy without compromising patient outcomes, according to a study published in the October issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:991-7).
Robert J. Cerfolio, MD, MBA, FCCP, and his coauthors divided the procedure into 19 sequential, teachable steps and allowed residents to perform selected steps during operations that Dr. Cerfolio directed.
“We then applied simulation training, coaching techniques, and video review of each step to help improve the steps that residents could not complete,” Dr. Cerfolio and his coauthors said.
Surgeons in academic centers face the challenge of teaching “the art and science of surgery,” Dr. Cerfolio and his colleagues said, while maintaining quality outcomes. “Teaching minimally invasive surgery, especially robotic surgery, is challenging given the risks and the limited availability of the robot.”
The researchers acknowledged that other groups have taken a similar approach to training, but this is the first study that included video review, coaching, and instruction tied to time constraints, they said.
“A major concern is that while teaching robotic surgery, patients can be injured, care is worse, and metrics that are increasingly used as surrogates for quality outcomes suffer,” they noted.
They allotted each step in the procedure a set amount of time in which the resident had to complete it, totaling 80 minutes for all 19 steps and ranging from 1 minute to inspect the pleura after placing ports (9 minutes) to 20 minutes to close the five incisions. If the resident completed the task in the allotted time, it was recorded as “performed.”
Between February 2010 and December 2010 Dr. Cerfolio performed 520 robotic lobectomies, and over time the percentage of successful steps per resident improved.
For example, in the first year, 50% of thoracic surgery residents completed the first five steps (mark and place ports, inspect pleura, resect the inferior pulmonary ligament, and remove three lymph nodes), but by the last year of the study 90% of them successfully completed the five steps.
Dr. Cerfolio and coauthors acknowledged “many flaws” in their study, but the study also had strengths: It involved only one operation and corroborated the database with each resident’s own surgical logs.
“Operations such as robotic lobectomy can be successfully taught by dividing them into a series of surgical maneuvers or steps,” the researchers noted. Recording what residents can and can’t do, reviewing video, and coaching contribute to the process to improve their skills. “Further studies that scientifically measure ‘ways to teach’ and ways to coach and mentor are needed,” they said.
Dr. Cerfolio disclosed relationships with Intuitive Surgical, Ethicon, Community Health Services, KCL, Bovie and C-SATS. Coauthor Douglas Minnich, MD, is a consultant to Medtronic. The other co-authors had no financial relationships to disclose.
Staying open versus closed at the end of the year
To the horror of many colleagues, I close my office for the last 2 weeks of each year. I went back to work on Jan. 3.
For several years, I didn’t close for that long. My staff and I would try to work out who needed what days off for family holiday stuff, and try to be open at least 3 days each week in late December. With Hanukkah spanning 8 nights it was always easy to get around, working some days and not others since at least one weekend would be in there. But Christmas and New Year’s Day aren’t so easy. They can be any day of the week. Usually people want the day before off, and some people prefer the day after.
So in 2013, I decided that from then on we would be closed over the holidays.
Of course, being a doctor never quite stops. There are always test results, refills, and patient calls coming in, but I can handle them from my desk at home as well as the one at my office.
My kids are off from school. So we can take them to shows, light displays, movies, and other local bonding activities. Or drive 90 minutes north to spend time in the snow.
There is, of course, the financial drawback. If I’m out of the office for 2 weeks, then it means I’ll hit a shortfall 2-4 weeks later. So I have to plan ahead because I’ll likely need to skip a paycheck or two until cash flow is back up and running.
I’ll miss 10 days of December billing. But if you think about it, it’s closer to 6 days when you take away the holidays we’d be closed. And if you’re not packed full it comes down to 3-4 days ... So why bother?
I can’t do it as often as I’d like, but when they’re out of school I’ll gladly trade money for family time.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
To the horror of many colleagues, I close my office for the last 2 weeks of each year. I went back to work on Jan. 3.
For several years, I didn’t close for that long. My staff and I would try to work out who needed what days off for family holiday stuff, and try to be open at least 3 days each week in late December. With Hanukkah spanning 8 nights it was always easy to get around, working some days and not others since at least one weekend would be in there. But Christmas and New Year’s Day aren’t so easy. They can be any day of the week. Usually people want the day before off, and some people prefer the day after.
So in 2013, I decided that from then on we would be closed over the holidays.
Of course, being a doctor never quite stops. There are always test results, refills, and patient calls coming in, but I can handle them from my desk at home as well as the one at my office.
My kids are off from school. So we can take them to shows, light displays, movies, and other local bonding activities. Or drive 90 minutes north to spend time in the snow.
There is, of course, the financial drawback. If I’m out of the office for 2 weeks, then it means I’ll hit a shortfall 2-4 weeks later. So I have to plan ahead because I’ll likely need to skip a paycheck or two until cash flow is back up and running.
I’ll miss 10 days of December billing. But if you think about it, it’s closer to 6 days when you take away the holidays we’d be closed. And if you’re not packed full it comes down to 3-4 days ... So why bother?
I can’t do it as often as I’d like, but when they’re out of school I’ll gladly trade money for family time.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
To the horror of many colleagues, I close my office for the last 2 weeks of each year. I went back to work on Jan. 3.
For several years, I didn’t close for that long. My staff and I would try to work out who needed what days off for family holiday stuff, and try to be open at least 3 days each week in late December. With Hanukkah spanning 8 nights it was always easy to get around, working some days and not others since at least one weekend would be in there. But Christmas and New Year’s Day aren’t so easy. They can be any day of the week. Usually people want the day before off, and some people prefer the day after.
So in 2013, I decided that from then on we would be closed over the holidays.
Of course, being a doctor never quite stops. There are always test results, refills, and patient calls coming in, but I can handle them from my desk at home as well as the one at my office.
My kids are off from school. So we can take them to shows, light displays, movies, and other local bonding activities. Or drive 90 minutes north to spend time in the snow.
There is, of course, the financial drawback. If I’m out of the office for 2 weeks, then it means I’ll hit a shortfall 2-4 weeks later. So I have to plan ahead because I’ll likely need to skip a paycheck or two until cash flow is back up and running.
I’ll miss 10 days of December billing. But if you think about it, it’s closer to 6 days when you take away the holidays we’d be closed. And if you’re not packed full it comes down to 3-4 days ... So why bother?
I can’t do it as often as I’d like, but when they’re out of school I’ll gladly trade money for family time.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Understand form and function to make the most of fillers
LAS VEGAS – Combining the right products and anatomical knowledge translates patient concerns into better outcomes when using fillers, according to Burt Steffes, MD, a dermatologist in Fond du Lac, Wisc.
“If you understand differences in products, you’ll get better results and minimize complications” for different areas, Dr. Steffes said in a presentation at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
The physical properties of different fillers impact the results, he pointed out. For example, G prime, a measure of elasticity, varies among fillers; a filler with a higher G prime is more contour stable and is designed to lift tissue, while a product with a lower G prime is designed to spread through tissues and move more naturally with the face.
However, “lift capacity using G prime is only useful across products in the entire family and make up,” Dr. Steffes noted. A recent Allergan-sponsored study emphasized that “product performance is a complex interaction of various properties and tissue interactions not just G prime,” he said (Dermatol Surg, 2015;41:S373-81).
Determining the most effective filler to use depends on the location and area to be corrected.
• Tear troughs: Dr. Steffes recommends avoiding hydrophilic products; he prefers Belotero, Restylane, or Restylane Silk.
• Lips: More flexible products such as Juvederm, Restylane, or Belotero can provide patients with the desired result, he noted.
• Nasolabial fold: Juvederm, Restylane, or Radiesse are appropriate choices likely to produce favorable outcomes, Dr. Steffes said.
• Lateral and midface atrophy: For greater lift and cohesivity in these patients, Dr. Steffes considers Perlane, Voluma, Radiesse, or Sculptra as options.
“Fillers are a great way to help people look and feel better,” but complications occur, so be prepared, he said. “You have to know how to recognize and manage complications.”
Proper management starts with staff education. Provide instruction and training to staff (including reception) on how to recognize impending problems. “Have a written protocol available, and keep nitroglycerin paste, hyaluronidase, and aspirin on hand,” he advised.
Cases of swelling may require hyaluronidase to correct, as may lumps and bumps, Dr. Steffes said. Bruising may be managed with ice packs after the fact, but can often be avoided or minimized by using blunt tip cannulas, slow injections, small aliquots, and small-gauge needles, he added.
In cases of extreme complications such as vascular occlusion, start by massaging the area with nitroglycerin paste, and administer hyaluronidase if necessary, he said. However, be sure to proceed carefully if using hyaluronidase in patients with an allergy to bee stings; use it only in an emergency in these patients and treat anaphylaxis if necessary, he added.
Dr. Steffes had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Combining the right products and anatomical knowledge translates patient concerns into better outcomes when using fillers, according to Burt Steffes, MD, a dermatologist in Fond du Lac, Wisc.
“If you understand differences in products, you’ll get better results and minimize complications” for different areas, Dr. Steffes said in a presentation at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
The physical properties of different fillers impact the results, he pointed out. For example, G prime, a measure of elasticity, varies among fillers; a filler with a higher G prime is more contour stable and is designed to lift tissue, while a product with a lower G prime is designed to spread through tissues and move more naturally with the face.
However, “lift capacity using G prime is only useful across products in the entire family and make up,” Dr. Steffes noted. A recent Allergan-sponsored study emphasized that “product performance is a complex interaction of various properties and tissue interactions not just G prime,” he said (Dermatol Surg, 2015;41:S373-81).
Determining the most effective filler to use depends on the location and area to be corrected.
• Tear troughs: Dr. Steffes recommends avoiding hydrophilic products; he prefers Belotero, Restylane, or Restylane Silk.
• Lips: More flexible products such as Juvederm, Restylane, or Belotero can provide patients with the desired result, he noted.
• Nasolabial fold: Juvederm, Restylane, or Radiesse are appropriate choices likely to produce favorable outcomes, Dr. Steffes said.
• Lateral and midface atrophy: For greater lift and cohesivity in these patients, Dr. Steffes considers Perlane, Voluma, Radiesse, or Sculptra as options.
“Fillers are a great way to help people look and feel better,” but complications occur, so be prepared, he said. “You have to know how to recognize and manage complications.”
Proper management starts with staff education. Provide instruction and training to staff (including reception) on how to recognize impending problems. “Have a written protocol available, and keep nitroglycerin paste, hyaluronidase, and aspirin on hand,” he advised.
Cases of swelling may require hyaluronidase to correct, as may lumps and bumps, Dr. Steffes said. Bruising may be managed with ice packs after the fact, but can often be avoided or minimized by using blunt tip cannulas, slow injections, small aliquots, and small-gauge needles, he added.
In cases of extreme complications such as vascular occlusion, start by massaging the area with nitroglycerin paste, and administer hyaluronidase if necessary, he said. However, be sure to proceed carefully if using hyaluronidase in patients with an allergy to bee stings; use it only in an emergency in these patients and treat anaphylaxis if necessary, he added.
Dr. Steffes had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Combining the right products and anatomical knowledge translates patient concerns into better outcomes when using fillers, according to Burt Steffes, MD, a dermatologist in Fond du Lac, Wisc.
“If you understand differences in products, you’ll get better results and minimize complications” for different areas, Dr. Steffes said in a presentation at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
The physical properties of different fillers impact the results, he pointed out. For example, G prime, a measure of elasticity, varies among fillers; a filler with a higher G prime is more contour stable and is designed to lift tissue, while a product with a lower G prime is designed to spread through tissues and move more naturally with the face.
However, “lift capacity using G prime is only useful across products in the entire family and make up,” Dr. Steffes noted. A recent Allergan-sponsored study emphasized that “product performance is a complex interaction of various properties and tissue interactions not just G prime,” he said (Dermatol Surg, 2015;41:S373-81).
Determining the most effective filler to use depends on the location and area to be corrected.
• Tear troughs: Dr. Steffes recommends avoiding hydrophilic products; he prefers Belotero, Restylane, or Restylane Silk.
• Lips: More flexible products such as Juvederm, Restylane, or Belotero can provide patients with the desired result, he noted.
• Nasolabial fold: Juvederm, Restylane, or Radiesse are appropriate choices likely to produce favorable outcomes, Dr. Steffes said.
• Lateral and midface atrophy: For greater lift and cohesivity in these patients, Dr. Steffes considers Perlane, Voluma, Radiesse, or Sculptra as options.
“Fillers are a great way to help people look and feel better,” but complications occur, so be prepared, he said. “You have to know how to recognize and manage complications.”
Proper management starts with staff education. Provide instruction and training to staff (including reception) on how to recognize impending problems. “Have a written protocol available, and keep nitroglycerin paste, hyaluronidase, and aspirin on hand,” he advised.
Cases of swelling may require hyaluronidase to correct, as may lumps and bumps, Dr. Steffes said. Bruising may be managed with ice packs after the fact, but can often be avoided or minimized by using blunt tip cannulas, slow injections, small aliquots, and small-gauge needles, he added.
In cases of extreme complications such as vascular occlusion, start by massaging the area with nitroglycerin paste, and administer hyaluronidase if necessary, he said. However, be sure to proceed carefully if using hyaluronidase in patients with an allergy to bee stings; use it only in an emergency in these patients and treat anaphylaxis if necessary, he added.
Dr. Steffes had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Simple tips optimize toxin treatments
LAS VEGAS – Listening to patients is the “first and most important step” toward using neuromodulators successfully, according to Burt Steffes, MD.
Clinicians armed with a thorough knowledge of anatomy and the available products can use neuromodulators successfully for a range of aging concerns including the glabellar complex, crow’s feet, marionette lines, smoker’s lines, a dimpled chin, and platysmal bands, Dr. Steffes, a dermatologist in Fond du Lac, Wisc., said in a presentation at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
When diluting toxins, be consistent for best results, he advised. “Pick a concentration you like and stick with it,” he said. Establishing realistic expectations and taking preprocedure photos are essential for optimizing results, he added.
Dr. Steffes shared the following tips for successful toxin treatments:
• Horizontal forehead rhytids. Check the brow position and stay approximately 2 cm above the eyebrows. Be conservative with the amount of product used to avoid the frozen look. In cases of upper eyelid ptosis, “improvement can be achieved with apraclonidine 0.5% drops,” he said.
• Glabellar complex. Dr. Steffes said he usually uses 10-30 units. Avoid blood vessels to avoid bruising, he said, “and ask patients to scowl” to identify the exact location for injections.
• Crow’s feet. Treatment of crow’s feet means managing an area “of great variability,” Dr. Steffes said. He advised using superficial injections to minimize bruising, while staying 2 cm from the orbital rim and adjusting to match the patient’s rhytid pattern. He recommends 1-2 units placed 1 cm below the lower eyelid margin at the mid-pupillary line to decrease the bunching of the lower eyelid.
• Platysmal bands. Managing volume is the key to successful treatment of platysmal bands, said Dr. Steffes. “Injecting too much product into the neck can lead to asymmetry” he cautioned. Pinch the platysmal band between the fingers and inject intramuscularly, using 2 units per injection. “Use conservative amounts and adjust in two weeks if needed,” he said.
Be sure that all patients make follow-up appointments before they leave the office after a procedure, and schedule new patients for follow-up in 2 weeks, said Dr. Steffes. Instruct all patients to contact your office immediately for any concerns including bruising that may be managed within the first 24-48 hours with a low-fluence 595-nm, 532-nm, or 1,064-nm laser, he added.
Dr. Steffes had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Listening to patients is the “first and most important step” toward using neuromodulators successfully, according to Burt Steffes, MD.
Clinicians armed with a thorough knowledge of anatomy and the available products can use neuromodulators successfully for a range of aging concerns including the glabellar complex, crow’s feet, marionette lines, smoker’s lines, a dimpled chin, and platysmal bands, Dr. Steffes, a dermatologist in Fond du Lac, Wisc., said in a presentation at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
When diluting toxins, be consistent for best results, he advised. “Pick a concentration you like and stick with it,” he said. Establishing realistic expectations and taking preprocedure photos are essential for optimizing results, he added.
Dr. Steffes shared the following tips for successful toxin treatments:
• Horizontal forehead rhytids. Check the brow position and stay approximately 2 cm above the eyebrows. Be conservative with the amount of product used to avoid the frozen look. In cases of upper eyelid ptosis, “improvement can be achieved with apraclonidine 0.5% drops,” he said.
• Glabellar complex. Dr. Steffes said he usually uses 10-30 units. Avoid blood vessels to avoid bruising, he said, “and ask patients to scowl” to identify the exact location for injections.
• Crow’s feet. Treatment of crow’s feet means managing an area “of great variability,” Dr. Steffes said. He advised using superficial injections to minimize bruising, while staying 2 cm from the orbital rim and adjusting to match the patient’s rhytid pattern. He recommends 1-2 units placed 1 cm below the lower eyelid margin at the mid-pupillary line to decrease the bunching of the lower eyelid.
• Platysmal bands. Managing volume is the key to successful treatment of platysmal bands, said Dr. Steffes. “Injecting too much product into the neck can lead to asymmetry” he cautioned. Pinch the platysmal band between the fingers and inject intramuscularly, using 2 units per injection. “Use conservative amounts and adjust in two weeks if needed,” he said.
Be sure that all patients make follow-up appointments before they leave the office after a procedure, and schedule new patients for follow-up in 2 weeks, said Dr. Steffes. Instruct all patients to contact your office immediately for any concerns including bruising that may be managed within the first 24-48 hours with a low-fluence 595-nm, 532-nm, or 1,064-nm laser, he added.
Dr. Steffes had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
LAS VEGAS – Listening to patients is the “first and most important step” toward using neuromodulators successfully, according to Burt Steffes, MD.
Clinicians armed with a thorough knowledge of anatomy and the available products can use neuromodulators successfully for a range of aging concerns including the glabellar complex, crow’s feet, marionette lines, smoker’s lines, a dimpled chin, and platysmal bands, Dr. Steffes, a dermatologist in Fond du Lac, Wisc., said in a presentation at Skin Disease Education Foundation’s annual Las Vegas dermatology seminar.
When diluting toxins, be consistent for best results, he advised. “Pick a concentration you like and stick with it,” he said. Establishing realistic expectations and taking preprocedure photos are essential for optimizing results, he added.
Dr. Steffes shared the following tips for successful toxin treatments:
• Horizontal forehead rhytids. Check the brow position and stay approximately 2 cm above the eyebrows. Be conservative with the amount of product used to avoid the frozen look. In cases of upper eyelid ptosis, “improvement can be achieved with apraclonidine 0.5% drops,” he said.
• Glabellar complex. Dr. Steffes said he usually uses 10-30 units. Avoid blood vessels to avoid bruising, he said, “and ask patients to scowl” to identify the exact location for injections.
• Crow’s feet. Treatment of crow’s feet means managing an area “of great variability,” Dr. Steffes said. He advised using superficial injections to minimize bruising, while staying 2 cm from the orbital rim and adjusting to match the patient’s rhytid pattern. He recommends 1-2 units placed 1 cm below the lower eyelid margin at the mid-pupillary line to decrease the bunching of the lower eyelid.
• Platysmal bands. Managing volume is the key to successful treatment of platysmal bands, said Dr. Steffes. “Injecting too much product into the neck can lead to asymmetry” he cautioned. Pinch the platysmal band between the fingers and inject intramuscularly, using 2 units per injection. “Use conservative amounts and adjust in two weeks if needed,” he said.
Be sure that all patients make follow-up appointments before they leave the office after a procedure, and schedule new patients for follow-up in 2 weeks, said Dr. Steffes. Instruct all patients to contact your office immediately for any concerns including bruising that may be managed within the first 24-48 hours with a low-fluence 595-nm, 532-nm, or 1,064-nm laser, he added.
Dr. Steffes had no relevant financial conflicts to disclose.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF LAS VEGAS DERMATOLOGY SEMINAR
Depressive symptoms plague ‘significant number’ of active airline pilots
The number of active airline pilots managing depressive symptoms might be severely underreported because of pilots’ fear of facing workplace stigma, a cross-sectional study of pilots from across the globe suggests.
“This study fills an important gap of knowledge by providing a current glimpse of mental health among commercial airline pilots, which to date had not been available,” wrote the authors, who added that such data are even more important in the wake of the March 2015 Germanwings flight 9525 crash.
In the study, Alexander C. Wu, MPH, and his coinvestigators conducted a descriptive, cross-sectional study by distributing an anonymous online survey through airline unions, companies, and airports. The survey, administered between April and December 2015, was received by 3,485 airline pilots. Among that number, 1,866 completed half the survey and 1,837 completed the entire survey. Symptoms of depression were evaluated based on the Patient Health Questionnaire (PHQ-9) depression module, with questions taken from the National Health and Nutrition Examination Survey – created by the Centers for Disease Control and Prevention’s National Center for Health Statistics – and the standardized Job Content Questionnaire (JCQ) (Environ Health. 2016 Dec 15. doi: 10.1186/s12940-016-0200-6).
The median age of those who responded was 42 years for females and 50 for males, and the average career length was 16 years across both genders, reported Mr. Wu, a doctoral candidate at the Harvard School of Public Health in Boston, and his coinvestigators. Nearly half of the respondents (45.5%) were from the United States, which was one of more than 50 countries represented, including Canada, Australia, Spain, the United Kingdom, Germany, the United Arab Emirates, Hong Kong, and Thailand.
More than 60% of the respondents had either a 4-year college/university degree or graduate education, and 80% of respondents had flown at least one “major trip” in the 30 days prior to completing the survey. Most of the respondents did not smoke, were married, and were white. Depression threshold was defined as a score of at least 10 on the PHQ-9, which was reported by 233 of the 1,848 responding airline pilots (12.6%), and 193 (13.5%) of the 1,430 pilots who reported flying in the 7 days prior to completing the survey. Furthermore, 75 (4.1%) of the 1,829 who answered the relevant question reported having suicidal thoughts at some point in the prior 2 weeks.
“We found a significant trend in proportions of depression at higher levels of use of sleep-aid medication (P less than .001) and among those experiencing sexual harassment (P = .001) or verbal harassment (P less than .001),” the investigators noted. In addition, 75 of the pilots “reported having thoughts of being better off dead or self-harm within the past 2 weeks,” the investigators wrote. “To our knowledge, this is the most current measure of the prevalence of suicidal thoughts among airline pilots.”
When asked about the study, Mark S. Gold, MD, said in an interview that workplace stigmas and the fear of facing criticism from their colleagues may be the prevailing factor in preventing pilots from openly discussing these issues among themselves. “Being a pilot, like a physician, is a drug-free occupation, [but] substance use disorders and depression are so commonly found together that the question is often ‘chicken or egg,’ ” said Dr. Gold, adjunct professor of psychiatry at Washington University in St. Louis, and former Donald R. Dizney Eminent Scholar and chairman of the psychiatry department at the University of Florida, Gainesville. “Add shame, guilt, and denial, and suicide ideation, [and] attempts and completions become all the more common.”
The solution, Dr. Gold said, is early detection, along with “multidisciplinary evaluation and diagnosis, prompt treatment and long-term follow-up by a physician’s health program or [an employee assistance program that] is associated with sustained remissions.” Mr. Wu and his coinvestigators said they would neither rate nor recommend a specific treatment. “However, [Internet-based cognitive-behavioral therapy] is one example of a possible intervention found in the literature,” they wrote.
The investigators cited several limitations. They conceded, for example, that there is “potential underestimation of frequencies of adverse mental health outcomes due to less participation among participants with more severe depression compared to those with less severe or without depression,” as well as the fact that the age of those who completed the survey were, on average, older, and they had flown more recently than had noncompleters. The age discrepancy might have skewed the results.
Harvard T.H. Chan School of Public Health funded the study. Mr. Wu and his coinvestigators reported no relevant financial disclosures.
The number of active airline pilots managing depressive symptoms might be severely underreported because of pilots’ fear of facing workplace stigma, a cross-sectional study of pilots from across the globe suggests.
“This study fills an important gap of knowledge by providing a current glimpse of mental health among commercial airline pilots, which to date had not been available,” wrote the authors, who added that such data are even more important in the wake of the March 2015 Germanwings flight 9525 crash.
In the study, Alexander C. Wu, MPH, and his coinvestigators conducted a descriptive, cross-sectional study by distributing an anonymous online survey through airline unions, companies, and airports. The survey, administered between April and December 2015, was received by 3,485 airline pilots. Among that number, 1,866 completed half the survey and 1,837 completed the entire survey. Symptoms of depression were evaluated based on the Patient Health Questionnaire (PHQ-9) depression module, with questions taken from the National Health and Nutrition Examination Survey – created by the Centers for Disease Control and Prevention’s National Center for Health Statistics – and the standardized Job Content Questionnaire (JCQ) (Environ Health. 2016 Dec 15. doi: 10.1186/s12940-016-0200-6).
The median age of those who responded was 42 years for females and 50 for males, and the average career length was 16 years across both genders, reported Mr. Wu, a doctoral candidate at the Harvard School of Public Health in Boston, and his coinvestigators. Nearly half of the respondents (45.5%) were from the United States, which was one of more than 50 countries represented, including Canada, Australia, Spain, the United Kingdom, Germany, the United Arab Emirates, Hong Kong, and Thailand.
More than 60% of the respondents had either a 4-year college/university degree or graduate education, and 80% of respondents had flown at least one “major trip” in the 30 days prior to completing the survey. Most of the respondents did not smoke, were married, and were white. Depression threshold was defined as a score of at least 10 on the PHQ-9, which was reported by 233 of the 1,848 responding airline pilots (12.6%), and 193 (13.5%) of the 1,430 pilots who reported flying in the 7 days prior to completing the survey. Furthermore, 75 (4.1%) of the 1,829 who answered the relevant question reported having suicidal thoughts at some point in the prior 2 weeks.
“We found a significant trend in proportions of depression at higher levels of use of sleep-aid medication (P less than .001) and among those experiencing sexual harassment (P = .001) or verbal harassment (P less than .001),” the investigators noted. In addition, 75 of the pilots “reported having thoughts of being better off dead or self-harm within the past 2 weeks,” the investigators wrote. “To our knowledge, this is the most current measure of the prevalence of suicidal thoughts among airline pilots.”
When asked about the study, Mark S. Gold, MD, said in an interview that workplace stigmas and the fear of facing criticism from their colleagues may be the prevailing factor in preventing pilots from openly discussing these issues among themselves. “Being a pilot, like a physician, is a drug-free occupation, [but] substance use disorders and depression are so commonly found together that the question is often ‘chicken or egg,’ ” said Dr. Gold, adjunct professor of psychiatry at Washington University in St. Louis, and former Donald R. Dizney Eminent Scholar and chairman of the psychiatry department at the University of Florida, Gainesville. “Add shame, guilt, and denial, and suicide ideation, [and] attempts and completions become all the more common.”
The solution, Dr. Gold said, is early detection, along with “multidisciplinary evaluation and diagnosis, prompt treatment and long-term follow-up by a physician’s health program or [an employee assistance program that] is associated with sustained remissions.” Mr. Wu and his coinvestigators said they would neither rate nor recommend a specific treatment. “However, [Internet-based cognitive-behavioral therapy] is one example of a possible intervention found in the literature,” they wrote.
The investigators cited several limitations. They conceded, for example, that there is “potential underestimation of frequencies of adverse mental health outcomes due to less participation among participants with more severe depression compared to those with less severe or without depression,” as well as the fact that the age of those who completed the survey were, on average, older, and they had flown more recently than had noncompleters. The age discrepancy might have skewed the results.
Harvard T.H. Chan School of Public Health funded the study. Mr. Wu and his coinvestigators reported no relevant financial disclosures.
The number of active airline pilots managing depressive symptoms might be severely underreported because of pilots’ fear of facing workplace stigma, a cross-sectional study of pilots from across the globe suggests.
“This study fills an important gap of knowledge by providing a current glimpse of mental health among commercial airline pilots, which to date had not been available,” wrote the authors, who added that such data are even more important in the wake of the March 2015 Germanwings flight 9525 crash.
In the study, Alexander C. Wu, MPH, and his coinvestigators conducted a descriptive, cross-sectional study by distributing an anonymous online survey through airline unions, companies, and airports. The survey, administered between April and December 2015, was received by 3,485 airline pilots. Among that number, 1,866 completed half the survey and 1,837 completed the entire survey. Symptoms of depression were evaluated based on the Patient Health Questionnaire (PHQ-9) depression module, with questions taken from the National Health and Nutrition Examination Survey – created by the Centers for Disease Control and Prevention’s National Center for Health Statistics – and the standardized Job Content Questionnaire (JCQ) (Environ Health. 2016 Dec 15. doi: 10.1186/s12940-016-0200-6).
The median age of those who responded was 42 years for females and 50 for males, and the average career length was 16 years across both genders, reported Mr. Wu, a doctoral candidate at the Harvard School of Public Health in Boston, and his coinvestigators. Nearly half of the respondents (45.5%) were from the United States, which was one of more than 50 countries represented, including Canada, Australia, Spain, the United Kingdom, Germany, the United Arab Emirates, Hong Kong, and Thailand.
More than 60% of the respondents had either a 4-year college/university degree or graduate education, and 80% of respondents had flown at least one “major trip” in the 30 days prior to completing the survey. Most of the respondents did not smoke, were married, and were white. Depression threshold was defined as a score of at least 10 on the PHQ-9, which was reported by 233 of the 1,848 responding airline pilots (12.6%), and 193 (13.5%) of the 1,430 pilots who reported flying in the 7 days prior to completing the survey. Furthermore, 75 (4.1%) of the 1,829 who answered the relevant question reported having suicidal thoughts at some point in the prior 2 weeks.
“We found a significant trend in proportions of depression at higher levels of use of sleep-aid medication (P less than .001) and among those experiencing sexual harassment (P = .001) or verbal harassment (P less than .001),” the investigators noted. In addition, 75 of the pilots “reported having thoughts of being better off dead or self-harm within the past 2 weeks,” the investigators wrote. “To our knowledge, this is the most current measure of the prevalence of suicidal thoughts among airline pilots.”
When asked about the study, Mark S. Gold, MD, said in an interview that workplace stigmas and the fear of facing criticism from their colleagues may be the prevailing factor in preventing pilots from openly discussing these issues among themselves. “Being a pilot, like a physician, is a drug-free occupation, [but] substance use disorders and depression are so commonly found together that the question is often ‘chicken or egg,’ ” said Dr. Gold, adjunct professor of psychiatry at Washington University in St. Louis, and former Donald R. Dizney Eminent Scholar and chairman of the psychiatry department at the University of Florida, Gainesville. “Add shame, guilt, and denial, and suicide ideation, [and] attempts and completions become all the more common.”
The solution, Dr. Gold said, is early detection, along with “multidisciplinary evaluation and diagnosis, prompt treatment and long-term follow-up by a physician’s health program or [an employee assistance program that] is associated with sustained remissions.” Mr. Wu and his coinvestigators said they would neither rate nor recommend a specific treatment. “However, [Internet-based cognitive-behavioral therapy] is one example of a possible intervention found in the literature,” they wrote.
The investigators cited several limitations. They conceded, for example, that there is “potential underestimation of frequencies of adverse mental health outcomes due to less participation among participants with more severe depression compared to those with less severe or without depression,” as well as the fact that the age of those who completed the survey were, on average, older, and they had flown more recently than had noncompleters. The age discrepancy might have skewed the results.
Harvard T.H. Chan School of Public Health funded the study. Mr. Wu and his coinvestigators reported no relevant financial disclosures.
FROM ENVIRONMENTAL HEALTH
Key clinical point:
Major finding: Among airline pilots, 12.6% meet standards for depression, while 4.1% reported experiencing thoughts of committing suicide.
Data source: Descriptive cross-sectional study of 3,485 surveyed pilots from April through December 2015.
Disclosures: Harvard T.H. Chan School of Public Health funded the study. Mr. Wu and his coinvestigators reported no relevant financial disclosures.
Acetaminophen use in pregnancy: What is the evidence?
Among pregnant women, acetaminophen is the most commonly used pain reliever, and likely the most commonly used of any medication. Estimates suggest that anywhere from 40% to greater than 65% of pregnant women use an acetaminophen-containing product at some time in pregnancy. Recently, concerns have been raised in several studies about potential increased risks for a variety of neurobehavioral outcomes including attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorders (ASD), cognitive deficits, and other behavior problems.
A 2013 study conducted in the Norwegian Mother and Child Cohort Study (pregnant women enrolled 1999-2008) evaluated 2,919 same-sex siblings at 3 years of age whose mothers were enrolled in the cohort during pregnancy. Prenatal exposure to acetaminophen was collected from maternal interview data during and shortly after pregnancy. Behavioral performance in the children was measured using validated maternal questionnaires. After adjustment for maternal febrile illness, infection, and comorbidities, use of acetaminophen for 28 days or more in pregnancy was associated with poorer gross motor and communication performance, more externalizing and internalizing behaviors, and higher activity levels in the offspring. Exposure for less than 28 days was associated with poor gross motor skills only. There were no associations found between ibuprofen use in pregnancy and any of the neurobehavioral outcomes.1
Four additional studies on this topic were published in 2016. One study from the Avon Longitudinal Study of Parents and Children followed 7,796 pregnant women enrolled in Bristol, England, in 1991-1992. This study’s findings were similar to the Danish cohort, with increased risks for conduct problems and hyperactivity symptoms as assessed in the Strengths and Difficulties Questionnaire at 7 years of age. In contrast, there was no association found with postnatal maternal acetaminophen use or paternal use.3
Two additional studies published in 2016 were from the Danish cohort described above. The first assessed long term follow-up for an average of 12.7 years linked to incidence of ASD or infantile autism in the Danish Psychiatric and Hospital Registries. An increased risk for ASD was found only when the diagnosis was accompanied by hyperkinetic symptoms (RR,1.51; 95% CI, 1.19-1.92), and this risk was most pronounced when acetaminophen was used in the last half of pregnancy.5
The second study examined a smaller subset of 1,491 children who were tested at 5 years of age by trained psychologists using the Wechsler Preschool and Primary Scale of Intelligence – a measure of IQ. Maternal fever and acetaminophen use in pregnancy were associated with small but significant deficits. For example, children of mothers who used acetaminophen but reported no fever had on average a 3.4 point deficit in performance IQ, compared with children of mothers who reported neither. However, mothers who reported both acetaminophen use and fever showed no differences.6
The authors of the studies described above, as well as other experts in the field, have discussed the biological plausibility of such associations being causal. The endocrine disruptive effects of acetaminophen and/or an impact on oxidative stress have been suggested as possible mechanisms, although no convincing data have supported these theories to date. Several of the studies have been criticized for reliance on maternal report of the outcomes, and all studies relied on maternal report of the exposure, which raises possibilities for bias and misclassification. However, some studies included assessments by trained psychologists or linkage to diagnoses recorded in national health registries. Control for confounding is always problematic in observational studies, especially with long-term outcomes. The sibling-pair study conducted in Norway attempted to control for genetic and environmental confounding using this design. Confounding by indication is also a concern. Adjustment for maternal fever, infections, or other comorbidities may have addressed some of this concern; however, as with acetaminophen, vague and perhaps inaccurate maternal report of these events may be problematic. Findings for another pain reliever, ibuprofen, showed no association in one study, which provides some reassurance.
At the present time, the impacts on behavior including hyperactivity and perhaps ASD are most prominent in the published reports stemming from four countries with large cohort studies. There is conflicting evidence of any impact on cognitive performance. All associations reported are quite modest with relative risks in the 1.5 or lower range. Nevertheless, acetaminophen is a medication taken by most women in pregnancy, so the broad impact, if these associations are causal, is not trivial. Clinically, an urgent concern would be that women or clinicians might ignore the current advice to take acetaminophen to reduce maternal fever. In that regard, it is reassuring that the Danish Cohort study found no impact on IQ when acetaminophen was used to treat a fever, while fever itself was associated with increased risks.
In studies which examined frequency of use, longer duration was often associated with higher risks. However, no study reported on dose. Future studies should capture dose, as well as better information on the underlying conditions being treated. The findings from these epidemiologic studies also call for additional experimental work to better understand possible mechanisms. In the meantime, as with any over-the-counter medication, judicious and appropriate use of acetaminophen should be advised.
References
1. Int J Epidemiol. 2013 Dec;42(6):1702-13.
2. JAMA Pediatr. 2014 Apr;168(4):313-20.
3. JAMA Pediatr. 2016 Oct 1;170(10):964-970.
4. Int. J. Epidemiol. 2016 June 28. doi: 10.1093/ije/dyw115.
5. Autism Res. 2016 Sep;9(9):951-8.
6. Epidemiology. 2016 Nov;27(6):912-8.
Dr. Chambers is a professor of pediatrics and director of clinical research at Rady Children’s Hospital, and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no relevant financial disclosures. To comment, e-mail her at [email protected].
Among pregnant women, acetaminophen is the most commonly used pain reliever, and likely the most commonly used of any medication. Estimates suggest that anywhere from 40% to greater than 65% of pregnant women use an acetaminophen-containing product at some time in pregnancy. Recently, concerns have been raised in several studies about potential increased risks for a variety of neurobehavioral outcomes including attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorders (ASD), cognitive deficits, and other behavior problems.
A 2013 study conducted in the Norwegian Mother and Child Cohort Study (pregnant women enrolled 1999-2008) evaluated 2,919 same-sex siblings at 3 years of age whose mothers were enrolled in the cohort during pregnancy. Prenatal exposure to acetaminophen was collected from maternal interview data during and shortly after pregnancy. Behavioral performance in the children was measured using validated maternal questionnaires. After adjustment for maternal febrile illness, infection, and comorbidities, use of acetaminophen for 28 days or more in pregnancy was associated with poorer gross motor and communication performance, more externalizing and internalizing behaviors, and higher activity levels in the offspring. Exposure for less than 28 days was associated with poor gross motor skills only. There were no associations found between ibuprofen use in pregnancy and any of the neurobehavioral outcomes.1
Four additional studies on this topic were published in 2016. One study from the Avon Longitudinal Study of Parents and Children followed 7,796 pregnant women enrolled in Bristol, England, in 1991-1992. This study’s findings were similar to the Danish cohort, with increased risks for conduct problems and hyperactivity symptoms as assessed in the Strengths and Difficulties Questionnaire at 7 years of age. In contrast, there was no association found with postnatal maternal acetaminophen use or paternal use.3
Two additional studies published in 2016 were from the Danish cohort described above. The first assessed long term follow-up for an average of 12.7 years linked to incidence of ASD or infantile autism in the Danish Psychiatric and Hospital Registries. An increased risk for ASD was found only when the diagnosis was accompanied by hyperkinetic symptoms (RR,1.51; 95% CI, 1.19-1.92), and this risk was most pronounced when acetaminophen was used in the last half of pregnancy.5
The second study examined a smaller subset of 1,491 children who were tested at 5 years of age by trained psychologists using the Wechsler Preschool and Primary Scale of Intelligence – a measure of IQ. Maternal fever and acetaminophen use in pregnancy were associated with small but significant deficits. For example, children of mothers who used acetaminophen but reported no fever had on average a 3.4 point deficit in performance IQ, compared with children of mothers who reported neither. However, mothers who reported both acetaminophen use and fever showed no differences.6
The authors of the studies described above, as well as other experts in the field, have discussed the biological plausibility of such associations being causal. The endocrine disruptive effects of acetaminophen and/or an impact on oxidative stress have been suggested as possible mechanisms, although no convincing data have supported these theories to date. Several of the studies have been criticized for reliance on maternal report of the outcomes, and all studies relied on maternal report of the exposure, which raises possibilities for bias and misclassification. However, some studies included assessments by trained psychologists or linkage to diagnoses recorded in national health registries. Control for confounding is always problematic in observational studies, especially with long-term outcomes. The sibling-pair study conducted in Norway attempted to control for genetic and environmental confounding using this design. Confounding by indication is also a concern. Adjustment for maternal fever, infections, or other comorbidities may have addressed some of this concern; however, as with acetaminophen, vague and perhaps inaccurate maternal report of these events may be problematic. Findings for another pain reliever, ibuprofen, showed no association in one study, which provides some reassurance.
At the present time, the impacts on behavior including hyperactivity and perhaps ASD are most prominent in the published reports stemming from four countries with large cohort studies. There is conflicting evidence of any impact on cognitive performance. All associations reported are quite modest with relative risks in the 1.5 or lower range. Nevertheless, acetaminophen is a medication taken by most women in pregnancy, so the broad impact, if these associations are causal, is not trivial. Clinically, an urgent concern would be that women or clinicians might ignore the current advice to take acetaminophen to reduce maternal fever. In that regard, it is reassuring that the Danish Cohort study found no impact on IQ when acetaminophen was used to treat a fever, while fever itself was associated with increased risks.
In studies which examined frequency of use, longer duration was often associated with higher risks. However, no study reported on dose. Future studies should capture dose, as well as better information on the underlying conditions being treated. The findings from these epidemiologic studies also call for additional experimental work to better understand possible mechanisms. In the meantime, as with any over-the-counter medication, judicious and appropriate use of acetaminophen should be advised.
References
1. Int J Epidemiol. 2013 Dec;42(6):1702-13.
2. JAMA Pediatr. 2014 Apr;168(4):313-20.
3. JAMA Pediatr. 2016 Oct 1;170(10):964-970.
4. Int. J. Epidemiol. 2016 June 28. doi: 10.1093/ije/dyw115.
5. Autism Res. 2016 Sep;9(9):951-8.
6. Epidemiology. 2016 Nov;27(6):912-8.
Dr. Chambers is a professor of pediatrics and director of clinical research at Rady Children’s Hospital, and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no relevant financial disclosures. To comment, e-mail her at [email protected].
Among pregnant women, acetaminophen is the most commonly used pain reliever, and likely the most commonly used of any medication. Estimates suggest that anywhere from 40% to greater than 65% of pregnant women use an acetaminophen-containing product at some time in pregnancy. Recently, concerns have been raised in several studies about potential increased risks for a variety of neurobehavioral outcomes including attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorders (ASD), cognitive deficits, and other behavior problems.
A 2013 study conducted in the Norwegian Mother and Child Cohort Study (pregnant women enrolled 1999-2008) evaluated 2,919 same-sex siblings at 3 years of age whose mothers were enrolled in the cohort during pregnancy. Prenatal exposure to acetaminophen was collected from maternal interview data during and shortly after pregnancy. Behavioral performance in the children was measured using validated maternal questionnaires. After adjustment for maternal febrile illness, infection, and comorbidities, use of acetaminophen for 28 days or more in pregnancy was associated with poorer gross motor and communication performance, more externalizing and internalizing behaviors, and higher activity levels in the offspring. Exposure for less than 28 days was associated with poor gross motor skills only. There were no associations found between ibuprofen use in pregnancy and any of the neurobehavioral outcomes.1
Four additional studies on this topic were published in 2016. One study from the Avon Longitudinal Study of Parents and Children followed 7,796 pregnant women enrolled in Bristol, England, in 1991-1992. This study’s findings were similar to the Danish cohort, with increased risks for conduct problems and hyperactivity symptoms as assessed in the Strengths and Difficulties Questionnaire at 7 years of age. In contrast, there was no association found with postnatal maternal acetaminophen use or paternal use.3
Two additional studies published in 2016 were from the Danish cohort described above. The first assessed long term follow-up for an average of 12.7 years linked to incidence of ASD or infantile autism in the Danish Psychiatric and Hospital Registries. An increased risk for ASD was found only when the diagnosis was accompanied by hyperkinetic symptoms (RR,1.51; 95% CI, 1.19-1.92), and this risk was most pronounced when acetaminophen was used in the last half of pregnancy.5
The second study examined a smaller subset of 1,491 children who were tested at 5 years of age by trained psychologists using the Wechsler Preschool and Primary Scale of Intelligence – a measure of IQ. Maternal fever and acetaminophen use in pregnancy were associated with small but significant deficits. For example, children of mothers who used acetaminophen but reported no fever had on average a 3.4 point deficit in performance IQ, compared with children of mothers who reported neither. However, mothers who reported both acetaminophen use and fever showed no differences.6
The authors of the studies described above, as well as other experts in the field, have discussed the biological plausibility of such associations being causal. The endocrine disruptive effects of acetaminophen and/or an impact on oxidative stress have been suggested as possible mechanisms, although no convincing data have supported these theories to date. Several of the studies have been criticized for reliance on maternal report of the outcomes, and all studies relied on maternal report of the exposure, which raises possibilities for bias and misclassification. However, some studies included assessments by trained psychologists or linkage to diagnoses recorded in national health registries. Control for confounding is always problematic in observational studies, especially with long-term outcomes. The sibling-pair study conducted in Norway attempted to control for genetic and environmental confounding using this design. Confounding by indication is also a concern. Adjustment for maternal fever, infections, or other comorbidities may have addressed some of this concern; however, as with acetaminophen, vague and perhaps inaccurate maternal report of these events may be problematic. Findings for another pain reliever, ibuprofen, showed no association in one study, which provides some reassurance.
At the present time, the impacts on behavior including hyperactivity and perhaps ASD are most prominent in the published reports stemming from four countries with large cohort studies. There is conflicting evidence of any impact on cognitive performance. All associations reported are quite modest with relative risks in the 1.5 or lower range. Nevertheless, acetaminophen is a medication taken by most women in pregnancy, so the broad impact, if these associations are causal, is not trivial. Clinically, an urgent concern would be that women or clinicians might ignore the current advice to take acetaminophen to reduce maternal fever. In that regard, it is reassuring that the Danish Cohort study found no impact on IQ when acetaminophen was used to treat a fever, while fever itself was associated with increased risks.
In studies which examined frequency of use, longer duration was often associated with higher risks. However, no study reported on dose. Future studies should capture dose, as well as better information on the underlying conditions being treated. The findings from these epidemiologic studies also call for additional experimental work to better understand possible mechanisms. In the meantime, as with any over-the-counter medication, judicious and appropriate use of acetaminophen should be advised.
References
1. Int J Epidemiol. 2013 Dec;42(6):1702-13.
2. JAMA Pediatr. 2014 Apr;168(4):313-20.
3. JAMA Pediatr. 2016 Oct 1;170(10):964-970.
4. Int. J. Epidemiol. 2016 June 28. doi: 10.1093/ije/dyw115.
5. Autism Res. 2016 Sep;9(9):951-8.
6. Epidemiology. 2016 Nov;27(6):912-8.
Dr. Chambers is a professor of pediatrics and director of clinical research at Rady Children’s Hospital, and associate director of the Clinical and Translational Research Institute at the University of California, San Diego. She is director of MotherToBaby California, a past president of the Organization of Teratology Information Specialists, and past president of the Teratology Society. She has no relevant financial disclosures. To comment, e-mail her at [email protected].
Obesity-associated protein linked to AML
Photo courtesy of
University of Cincinnati
Preclinical research indicates that a protein associated with obesity is also involved in the development of acute myeloid leukemia (AML) and may affect AML patients’ response to treatment.
Researchers found evidence to suggest that the fat mass- and obesity-associated protein (FTO) regulates the expression of a set of genes through a mechanism involving RNA modification, thereby increasing the reproduction of leukemia cells and prohibiting drug response.
Jianjun Chen, PhD, of the University of Cincinnati in Ohio, and his colleagues conducted this research and reported the findings in Cancer Cell.
The team noted that N6-methyladenosine (m6A) RNA methylation is the most prevalent internal modification in messenger RNAs (mRNAs) in genes. And they found that FTO, an m6A demethylase, plays a critical oncogenic role in AML.
The researchers made this discovery by analyzing 2 microarray datasets of samples from AML as well as samples from control subjects.
The team found that FTO was highly expressed in AMLs with t(11q23)/MLL rearrangements, t(15;17)/PML-RARA, FLT3-ITD, and/or NPM1 mutations.
The high level of FTO expression contributed to leukemia cells multiplying and surviving and also promoted the development of AML in animal models and the non-response of AML cells to therapeutic agents.
Additionally, the researchers found that genes like ASB2 and RARA, which were reported to inhibit leukemia cell growth and/or mediate the response of leukemia cells to therapeutic agents, were suppressed in the AML samples with higher FTO expression.
The suppression of these genes was attributed to FTO-controlled decreased stability of their mRNA and was connected to FTO’s m6A demethylase activity.
“Our study shows, for the first time, the functional importance of the m6A modification machinery in leukemia,” Dr Chen said. “In addition, given the functional importance of FTO in the formation of leukemia and drug response, targeting FTO signaling may present a new therapeutic strategy to treat leukemia.”
“As FTO may also play a cancer-promoting role in various types of solid tumors, besides leukemia, our discoveries may have a broad impact in cancer biology and cancer therapy. Further studies are needed to advance our understanding of the critical role of FTO in various types of cancers and to develop more effective novel therapeutic strategies based on such understanding to treat cancers.” ![]()
Photo courtesy of
University of Cincinnati
Preclinical research indicates that a protein associated with obesity is also involved in the development of acute myeloid leukemia (AML) and may affect AML patients’ response to treatment.
Researchers found evidence to suggest that the fat mass- and obesity-associated protein (FTO) regulates the expression of a set of genes through a mechanism involving RNA modification, thereby increasing the reproduction of leukemia cells and prohibiting drug response.
Jianjun Chen, PhD, of the University of Cincinnati in Ohio, and his colleagues conducted this research and reported the findings in Cancer Cell.
The team noted that N6-methyladenosine (m6A) RNA methylation is the most prevalent internal modification in messenger RNAs (mRNAs) in genes. And they found that FTO, an m6A demethylase, plays a critical oncogenic role in AML.
The researchers made this discovery by analyzing 2 microarray datasets of samples from AML as well as samples from control subjects.
The team found that FTO was highly expressed in AMLs with t(11q23)/MLL rearrangements, t(15;17)/PML-RARA, FLT3-ITD, and/or NPM1 mutations.
The high level of FTO expression contributed to leukemia cells multiplying and surviving and also promoted the development of AML in animal models and the non-response of AML cells to therapeutic agents.
Additionally, the researchers found that genes like ASB2 and RARA, which were reported to inhibit leukemia cell growth and/or mediate the response of leukemia cells to therapeutic agents, were suppressed in the AML samples with higher FTO expression.
The suppression of these genes was attributed to FTO-controlled decreased stability of their mRNA and was connected to FTO’s m6A demethylase activity.
“Our study shows, for the first time, the functional importance of the m6A modification machinery in leukemia,” Dr Chen said. “In addition, given the functional importance of FTO in the formation of leukemia and drug response, targeting FTO signaling may present a new therapeutic strategy to treat leukemia.”
“As FTO may also play a cancer-promoting role in various types of solid tumors, besides leukemia, our discoveries may have a broad impact in cancer biology and cancer therapy. Further studies are needed to advance our understanding of the critical role of FTO in various types of cancers and to develop more effective novel therapeutic strategies based on such understanding to treat cancers.” ![]()
Photo courtesy of
University of Cincinnati
Preclinical research indicates that a protein associated with obesity is also involved in the development of acute myeloid leukemia (AML) and may affect AML patients’ response to treatment.
Researchers found evidence to suggest that the fat mass- and obesity-associated protein (FTO) regulates the expression of a set of genes through a mechanism involving RNA modification, thereby increasing the reproduction of leukemia cells and prohibiting drug response.
Jianjun Chen, PhD, of the University of Cincinnati in Ohio, and his colleagues conducted this research and reported the findings in Cancer Cell.
The team noted that N6-methyladenosine (m6A) RNA methylation is the most prevalent internal modification in messenger RNAs (mRNAs) in genes. And they found that FTO, an m6A demethylase, plays a critical oncogenic role in AML.
The researchers made this discovery by analyzing 2 microarray datasets of samples from AML as well as samples from control subjects.
The team found that FTO was highly expressed in AMLs with t(11q23)/MLL rearrangements, t(15;17)/PML-RARA, FLT3-ITD, and/or NPM1 mutations.
The high level of FTO expression contributed to leukemia cells multiplying and surviving and also promoted the development of AML in animal models and the non-response of AML cells to therapeutic agents.
Additionally, the researchers found that genes like ASB2 and RARA, which were reported to inhibit leukemia cell growth and/or mediate the response of leukemia cells to therapeutic agents, were suppressed in the AML samples with higher FTO expression.
The suppression of these genes was attributed to FTO-controlled decreased stability of their mRNA and was connected to FTO’s m6A demethylase activity.
“Our study shows, for the first time, the functional importance of the m6A modification machinery in leukemia,” Dr Chen said. “In addition, given the functional importance of FTO in the formation of leukemia and drug response, targeting FTO signaling may present a new therapeutic strategy to treat leukemia.”
“As FTO may also play a cancer-promoting role in various types of solid tumors, besides leukemia, our discoveries may have a broad impact in cancer biology and cancer therapy. Further studies are needed to advance our understanding of the critical role of FTO in various types of cancers and to develop more effective novel therapeutic strategies based on such understanding to treat cancers.” ![]()
Syringes recalled due to infection risk
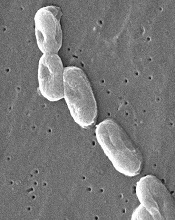
Image courtesy of
CDC/Janice Carr
The US Food and Drug Administration (FDA) has announced a Class I, nationwide recall of Nurse Assist Inc.’s normal saline flush syringes due to incidents of Burkholderia cepacia contamination.
Nurse Assist reported that patients developed B cepacia bloodstream infections while receiving intravenous care using the company’s prepackaged saline flush syringes, so the company voluntarily recalled all unexpired lots of the product.
This recall was first announced last October, but, yesterday, the FDA classified it as a Class I recall and said use of these syringes may cause serious injuries or death.
Nurse Assist said it is investigating the link between the syringes and the infections with the FDA, the US Centers for Disease Control, and various state health departments.
Until the investigation can be completed, all healthcare facilities with affected product should discontinue use and return the product to the supplier.
The normal saline flush is a plastic syringe filled with 0.9% sodium chloride (a 12 mL IV flush syringe with a 3 mL, 5 mL, or 10 mL fill volume). It is used to clear out medical devices that deliver medicine directly into the veins of a patient through a needle or catheter.
All unexpired lots of this product are covered by the recall. Product Numbers 1203, 1205, and 1210 are packaged 30 syringes to an inner carton and 6 inner cartons in a case (180 syringes).
For product number 1210-BP, 100 syringes are packaged in an inner carton with 4 inner cartons in a case (400 syringes). Lot code information can be found on the outer case panel, the back panel of the inner carton, and on each syringe label.
The lots being recalled were distributed to customers and distributors between February 16, 2016, and September 30, 2016. Product can be identified by the labeling on the packaging and device.
Customers with questions can contact Nurse Assist Inc. at 1-800-649-6800 ext. 10, Monday through Friday, between the hours of 8 am and 5 pm, Central Time, or via email at [email protected].
Healthcare professionals and consumers can report adverse reactions or quality problems they experienced using these devices to MedWatch: The FDA Safety Information and Adverse Event Reporting Program. ![]()
Image courtesy of
CDC/Janice Carr
The US Food and Drug Administration (FDA) has announced a Class I, nationwide recall of Nurse Assist Inc.’s normal saline flush syringes due to incidents of Burkholderia cepacia contamination.
Nurse Assist reported that patients developed B cepacia bloodstream infections while receiving intravenous care using the company’s prepackaged saline flush syringes, so the company voluntarily recalled all unexpired lots of the product.
This recall was first announced last October, but, yesterday, the FDA classified it as a Class I recall and said use of these syringes may cause serious injuries or death.
Nurse Assist said it is investigating the link between the syringes and the infections with the FDA, the US Centers for Disease Control, and various state health departments.
Until the investigation can be completed, all healthcare facilities with affected product should discontinue use and return the product to the supplier.
The normal saline flush is a plastic syringe filled with 0.9% sodium chloride (a 12 mL IV flush syringe with a 3 mL, 5 mL, or 10 mL fill volume). It is used to clear out medical devices that deliver medicine directly into the veins of a patient through a needle or catheter.
All unexpired lots of this product are covered by the recall. Product Numbers 1203, 1205, and 1210 are packaged 30 syringes to an inner carton and 6 inner cartons in a case (180 syringes).
For product number 1210-BP, 100 syringes are packaged in an inner carton with 4 inner cartons in a case (400 syringes). Lot code information can be found on the outer case panel, the back panel of the inner carton, and on each syringe label.
The lots being recalled were distributed to customers and distributors between February 16, 2016, and September 30, 2016. Product can be identified by the labeling on the packaging and device.
Customers with questions can contact Nurse Assist Inc. at 1-800-649-6800 ext. 10, Monday through Friday, between the hours of 8 am and 5 pm, Central Time, or via email at [email protected].
Healthcare professionals and consumers can report adverse reactions or quality problems they experienced using these devices to MedWatch: The FDA Safety Information and Adverse Event Reporting Program. ![]()
Image courtesy of
CDC/Janice Carr
The US Food and Drug Administration (FDA) has announced a Class I, nationwide recall of Nurse Assist Inc.’s normal saline flush syringes due to incidents of Burkholderia cepacia contamination.
Nurse Assist reported that patients developed B cepacia bloodstream infections while receiving intravenous care using the company’s prepackaged saline flush syringes, so the company voluntarily recalled all unexpired lots of the product.
This recall was first announced last October, but, yesterday, the FDA classified it as a Class I recall and said use of these syringes may cause serious injuries or death.
Nurse Assist said it is investigating the link between the syringes and the infections with the FDA, the US Centers for Disease Control, and various state health departments.
Until the investigation can be completed, all healthcare facilities with affected product should discontinue use and return the product to the supplier.
The normal saline flush is a plastic syringe filled with 0.9% sodium chloride (a 12 mL IV flush syringe with a 3 mL, 5 mL, or 10 mL fill volume). It is used to clear out medical devices that deliver medicine directly into the veins of a patient through a needle or catheter.
All unexpired lots of this product are covered by the recall. Product Numbers 1203, 1205, and 1210 are packaged 30 syringes to an inner carton and 6 inner cartons in a case (180 syringes).
For product number 1210-BP, 100 syringes are packaged in an inner carton with 4 inner cartons in a case (400 syringes). Lot code information can be found on the outer case panel, the back panel of the inner carton, and on each syringe label.
The lots being recalled were distributed to customers and distributors between February 16, 2016, and September 30, 2016. Product can be identified by the labeling on the packaging and device.
Customers with questions can contact Nurse Assist Inc. at 1-800-649-6800 ext. 10, Monday through Friday, between the hours of 8 am and 5 pm, Central Time, or via email at [email protected].
Healthcare professionals and consumers can report adverse reactions or quality problems they experienced using these devices to MedWatch: The FDA Safety Information and Adverse Event Reporting Program. ![]()
Antiplatelet agent may pose lower risk of bleeding

Photo by Sakurai Midori
Researchers say they have developed an antiplatelet agent that has demonstrated considerable
antithrombotic activity and low bleeding liability in monkeys.
The agent, known as BMS-986120, is a PAR4 antagonist.
Experiments in cynomolgus monkeys indicated that BMS-986120 can effectively fight thrombosis but poses a lower risk of bleeding than clopidogrel.
The researchers described these experiments in Science Translational Medicine.
The research was supported by Bristol-Myers Squibb but also benefited from funding from the “Fonds pour un Québec Innovant et en Santé” from the Ministry of Economy, Science and Innovation of Québec.
To investigate the effects of PAR4 inhibition, the researchers developed PAR4-targeted antibodies and tested them in guinea pigs. The antibodies exhibited antithrombotic activity in the animals, while posing a low risk of bleeding.
Because of these positive results, the researchers performed a high-throughput screen of more than 1 million molecules to find a PAR4 inhibitor. They identified BMS-986120 as a “highly potent, selective, and reversible” inhibitor of PAR4 in human platelets.
The researchers wanted to test BMS-986120 in cynomolgus monkey models of occlusive arterial thrombosis and provoked bleeding time (BT). But the team first had to validate the translatability of the models (for clinical prediction of efficacy and bleeding liability) by studying clopidogrel in the animals.
When compared to vehicle control, clopidogrel slowed vascular occlusion and reduced thrombus weight in the monkeys in a dose-dependent manner. But clopidogrel also had “strong effects” on hemostasis.
When the researchers tested BMS-986120 (vs vehicle control) in these models, they observed a wider therapeutic window with BMS-986120 than with clopidogrel.
The researchers said BMS-986120 was “highly effective” in preserving vascular patency during the induction of occlusive thrombosis. When given at 1 mg/kg, BMS-986120 prevented vascular occlusion in all monkeys.
BMS-986120 also decreased thrombus weight in a dose-dependent manner. When given at 1 mg/kg, BMS-986120 reduced thrombus formation by 82%.
BMS-986120 had a limited, though still statistically significant, impact on hemostasis. BMS-986120 at 1 mg/kg significantly increased kidney and mesenteric BT when compared to vehicle control (P<0.0001 for both).
The researchers plotted the relative antithrombotic (thrombus weight reduction) and BT effects of clopidogrel and BMS-986120 as a function of the dose of each drug.
They found that, at doses resulting in about 50% to 80% antithrombotic activity, clopidogrel produced about 8- to 9-fold increases in kidney and mesenteric BT. BMS-986120, on the other hand, produced increases of about 2-fold or less in kidney and mesenteric BT.
The researchers said these preclinical findings suggest that targeting PAR4 is an attractive antiplatelet strategy, and BMS-986120 has potential as an antiplatelet agent. The drug is currently being evaluated in clinical trials. ![]()

Photo by Sakurai Midori
Researchers say they have developed an antiplatelet agent that has demonstrated considerable
antithrombotic activity and low bleeding liability in monkeys.
The agent, known as BMS-986120, is a PAR4 antagonist.
Experiments in cynomolgus monkeys indicated that BMS-986120 can effectively fight thrombosis but poses a lower risk of bleeding than clopidogrel.
The researchers described these experiments in Science Translational Medicine.
The research was supported by Bristol-Myers Squibb but also benefited from funding from the “Fonds pour un Québec Innovant et en Santé” from the Ministry of Economy, Science and Innovation of Québec.
To investigate the effects of PAR4 inhibition, the researchers developed PAR4-targeted antibodies and tested them in guinea pigs. The antibodies exhibited antithrombotic activity in the animals, while posing a low risk of bleeding.
Because of these positive results, the researchers performed a high-throughput screen of more than 1 million molecules to find a PAR4 inhibitor. They identified BMS-986120 as a “highly potent, selective, and reversible” inhibitor of PAR4 in human platelets.
The researchers wanted to test BMS-986120 in cynomolgus monkey models of occlusive arterial thrombosis and provoked bleeding time (BT). But the team first had to validate the translatability of the models (for clinical prediction of efficacy and bleeding liability) by studying clopidogrel in the animals.
When compared to vehicle control, clopidogrel slowed vascular occlusion and reduced thrombus weight in the monkeys in a dose-dependent manner. But clopidogrel also had “strong effects” on hemostasis.
When the researchers tested BMS-986120 (vs vehicle control) in these models, they observed a wider therapeutic window with BMS-986120 than with clopidogrel.
The researchers said BMS-986120 was “highly effective” in preserving vascular patency during the induction of occlusive thrombosis. When given at 1 mg/kg, BMS-986120 prevented vascular occlusion in all monkeys.
BMS-986120 also decreased thrombus weight in a dose-dependent manner. When given at 1 mg/kg, BMS-986120 reduced thrombus formation by 82%.
BMS-986120 had a limited, though still statistically significant, impact on hemostasis. BMS-986120 at 1 mg/kg significantly increased kidney and mesenteric BT when compared to vehicle control (P<0.0001 for both).
The researchers plotted the relative antithrombotic (thrombus weight reduction) and BT effects of clopidogrel and BMS-986120 as a function of the dose of each drug.
They found that, at doses resulting in about 50% to 80% antithrombotic activity, clopidogrel produced about 8- to 9-fold increases in kidney and mesenteric BT. BMS-986120, on the other hand, produced increases of about 2-fold or less in kidney and mesenteric BT.
The researchers said these preclinical findings suggest that targeting PAR4 is an attractive antiplatelet strategy, and BMS-986120 has potential as an antiplatelet agent. The drug is currently being evaluated in clinical trials. ![]()

Photo by Sakurai Midori
Researchers say they have developed an antiplatelet agent that has demonstrated considerable
antithrombotic activity and low bleeding liability in monkeys.
The agent, known as BMS-986120, is a PAR4 antagonist.
Experiments in cynomolgus monkeys indicated that BMS-986120 can effectively fight thrombosis but poses a lower risk of bleeding than clopidogrel.
The researchers described these experiments in Science Translational Medicine.
The research was supported by Bristol-Myers Squibb but also benefited from funding from the “Fonds pour un Québec Innovant et en Santé” from the Ministry of Economy, Science and Innovation of Québec.
To investigate the effects of PAR4 inhibition, the researchers developed PAR4-targeted antibodies and tested them in guinea pigs. The antibodies exhibited antithrombotic activity in the animals, while posing a low risk of bleeding.
Because of these positive results, the researchers performed a high-throughput screen of more than 1 million molecules to find a PAR4 inhibitor. They identified BMS-986120 as a “highly potent, selective, and reversible” inhibitor of PAR4 in human platelets.
The researchers wanted to test BMS-986120 in cynomolgus monkey models of occlusive arterial thrombosis and provoked bleeding time (BT). But the team first had to validate the translatability of the models (for clinical prediction of efficacy and bleeding liability) by studying clopidogrel in the animals.
When compared to vehicle control, clopidogrel slowed vascular occlusion and reduced thrombus weight in the monkeys in a dose-dependent manner. But clopidogrel also had “strong effects” on hemostasis.
When the researchers tested BMS-986120 (vs vehicle control) in these models, they observed a wider therapeutic window with BMS-986120 than with clopidogrel.
The researchers said BMS-986120 was “highly effective” in preserving vascular patency during the induction of occlusive thrombosis. When given at 1 mg/kg, BMS-986120 prevented vascular occlusion in all monkeys.
BMS-986120 also decreased thrombus weight in a dose-dependent manner. When given at 1 mg/kg, BMS-986120 reduced thrombus formation by 82%.
BMS-986120 had a limited, though still statistically significant, impact on hemostasis. BMS-986120 at 1 mg/kg significantly increased kidney and mesenteric BT when compared to vehicle control (P<0.0001 for both).
The researchers plotted the relative antithrombotic (thrombus weight reduction) and BT effects of clopidogrel and BMS-986120 as a function of the dose of each drug.
They found that, at doses resulting in about 50% to 80% antithrombotic activity, clopidogrel produced about 8- to 9-fold increases in kidney and mesenteric BT. BMS-986120, on the other hand, produced increases of about 2-fold or less in kidney and mesenteric BT.
The researchers said these preclinical findings suggest that targeting PAR4 is an attractive antiplatelet strategy, and BMS-986120 has potential as an antiplatelet agent. The drug is currently being evaluated in clinical trials. ![]()






