User login
FDA Black Box, VA Red Ink? A Successful Service-Connected Disability Claim for Chronic Neuropsychiatric Adverse Effects From Mefloquine
Mefloquine is a synthetic antimalarial drug structurally related to quinine. The drug was developed by the Walter Reed Army Institute of Research during a decades-long program that started during the Vietnam War in response to concerns of rising resistance to chloroquine.1
The prelicensing clinical testing of mefloquine, originally known as WR 142,490, was conducted in part among U.S. military service members.2,3 Soon after receiving FDA approval in 1989, under the brand name Lariam, it was recommended for use within the U.S. military.4 Over the following 2 decades, mefloquine was a common exposure during military deployments to malaria endemic areas.
Although the original U.S. mefloquine drug label noted that neuropsychiatric reactions could occur with use, changes to the drug label mandated by the FDA in July 2013, including a black box warning, described a potential for these to persist long after the drug has been discontinued.5,6 These changes have served to reinforce earlier U.S. military policy changes beginning in 2009 that deprioritized use of the drug in favor of safer and better-tolerated antimalarials. Consequently, more than a quarter century after its introduction, mefloquine now is only rarely prescribed to members of the U.S. military.7
In addition to limiting current use of the drug, the recent boxed warning may have important implications for service-connected disability claims adjudication by the VA for veterans previously exposed to the drug. This report presents a case of a nondeployed veteran exposed to mefloquine during an early military postmarketing study who developed chronic neuropsychiatric symptoms linked to the drug that were recently deemed service-connected. This report concludes with some comments on the likely implications of this case for future similar disability claims.
Case Presentation
In 2014, a 56-year-old nondeployed U.S. Marine Corps veteran submitted a claim to the VA for disabling conditions. The veteran alleged these conditions were due to his exposure to mefloquine while in military service more than 2 decades earlier. The veteran enlisted in 1975 and experienced a motor vehicle accident with prolonged loss of consciousness in 1978 but had no other significant medical history.
Thirteen years later, stationed in Hawaii in 1991, he was encouraged to volunteer for a double-blinded postmarketing study, evaluating the adverse effects (AEs) of chloroquine and mefloquine.8 As documentation following the trial revealed, he was randomly assigned to the mefloquine arm and received a loading dose of 250 mg daily for 3 days, followed by 250 mg per week for 11 weeks.
During the study he experienced insomnia, abnormal dreams, and nightmares. He also developed symptoms of anxiety, depression, cognitive dysfunction, and changes in personality—including anger and irritability—that were severe enough to be noted by his family members. The patient had not been advised of the significance of these symptoms and therefore did not report them during the clinical trial, nor did he report their intermittent presence after the study’s conclusion through his retirement in 1996, fearing adverse career consequences. Subsequent exacerbations of these chronic symptoms later contributed to the patient’s loss of civilian employment in 2010.
After becoming aware of the 2013 boxed warning that these chronic symptoms could be due to his earlier exposure to mefloquine, the veteran sought evaluation by a VA clinician. On evaluation, the clinician noted no history of deployment, and no history of posttraumatic stress disorder (PTSD) criteria A stressors, and posited that the veteran’s chronic neuropsychiatric symptoms were most likely a consequence of his earlier use of mefloquine. The VA subsequently awarded the veteran 50% disability for an anxiety disorder characterized by chronic sleep impairment and frequent panic attacks, attributing these to his service-connected use of the drug.
Discussion
Although the original 1989 FDA-approved mefloquine label had warned to discontinue the drug if specific prodromal symptoms of “anxiety, depression, restlessness or confusion” were noted,as illustrated by this case, this guidance was not always consistently communicated to service members.5 Indeed, few service members in the 1991 military postmarketing study discontinued the medication even after reporting such symptoms.8 Vivid dreams, often described as “terrifying nightmares with technicolor clarity” were reported by 7% of study participants. Similarly, concentration problems were reported in 5%; irritability in 4%; anger and moodiness each in 1%; and insomnia in 25%. Two study participants, after failing to discontinue mefloquine at the onset of severe insomnia, were later hospitalized for severe depression and suicidal thoughts, later deemed due to preexisting conditions. Despite these seemingly unfavorable results, mefloquine was nonetheless deemed well tolerated.8
Military Use of Mefloquine
Beginning in 1992, use of mefloquine for prophylaxis of malaria was then widely directed within the U.S. military during operations in Somalia. There, a majority of personnel received mefloquine under conditions of command-directed and directly observed administration of the drug.9,10 Again, drug label guidance describing the prodromal psychiatric symptoms that should have prompted discontinuation of mefloquine were either not consistently adhered to or not communicated. In one Somalia-era study, only 1 in 344 service members, or 0.3%, discontinued the drug.11
Throughout the remainder of the 1990s, mefloquine remained the antimalarial drug of choice for most U.S. military operations, and when combat began in Afghanistan in 2001, widespread use was also directed there.12,13 The following year, after national attention was directed to concerns of severe behavioral toxicity from the drug among personnel returning from Afghanistan, the manufacturer issued subtle changes to the mefloquine label warnings.5,14
These label changes adjusted the previously exclusive list of prodromal symptoms to an illustrative list, emphasizing that “if psychiatric symptoms such as [emphasis added] acute anxiety, depression, restlessness or confusion occur, these may be considered prodromal to a more serious event. In these cases, the drug must be discontinued and an alternative medication should be substituted.”5
In 2001 a randomized double-blinded trial demonstrated that symptoms of anxiety and depression occurred in at least 4% of mefloquine users, insomnia in 13%, and abnormal dreams in 14%. Nevertheless, an Army memorandum issued soon after the labeling change significantly understated the known risks of developing such psychiatric symptoms, erroneously claiming that these occurred from mefloquine only “at a rate of one per 2,000 to 13,000 persons.”15,16
Updated FDA Guidelines
In 2003, with widespread use of the drug being again directed during operations in Iraq, the FDA required that all mefloquine prescriptions be accompanied by a patient medication guide with warnings echoing those of the drug label that users seek medical attention should “possible signs of more serious mental problems” develop.5,17 However, surveys suggested that few U.S. service members received these warnings or even verbal instructions to that effect.17-19 During later congressional testimony, a service member who had experienced 3 weeks of nightmares prior to self-discontinuing the drug testified “every soldier I know has problems with it.”20
In response, a senior military medical leader—failing to recognize that the nightmares the soldier reported were in fact psychiatric symptoms and possible signs of more serious mental problems that required the drug’s discontinuation—may have undermined the FDA-directed warnings by dismissing the soldier’s testimony as “perception,” maintaining instead “that perceptions can become realities” should it become “held that this medication is widely problematic.”20
Given that certain preexisting conditions, including anxiety and depression, were known to confound recognition of incident psychiatric symptoms that required discontinuation of the drug, the original 1989 mefloquine label had noted that the drug should be used with caution in such patients. In subsequent years, this language was strengthened, and such patients were formally contraindicated the drug.21
Citing formal policy, senior military medical leaders provided assurance during congressional testimony that service members with these conditions would not be prescribed mefloquine.16,18,20 However, later analysis of a large group of deployed service members revealed that 1 in 7 with contraindications to mefloquine had been prescribed the drug contrary to drug label guidance.21
Black Box Warning
With growing recognition of the challenges in using mefloquine as directed by the drug label, a 2009 Army policy memorandum prioritized the use of safer and better-tolerated daily medications, such as doxycycline and atovaquone-proguanil, and stated that “[m]efloquine should only be used for personnel with contraindications to doxycycline.”22 This policy was extended throughout the other military services later that year.23 After concerns were raised that service members were still being prescribed the drug contrary to policy, further restrictions were formalized in early 2013 prior to the boxed warning, with mefloquine reserved for those only “with intolerance or contraindications” to the first-line drugs.24,25
In a later memorandum announcing the July 2013 boxed warning, the military revealed that the number of active-duty personnel prescribed mefloquine had steadily decreased in prior years from 17,361 in 2008 to only 2,040 in 2012.7 Although the military has not released precise figures on the number of U.S. military personnel exposed to mefloquine since the drug’s introduction, based on a variety of sources, the total is likely to far exceed 100,000.7,26
The major changes to the mefloquine label in 2013, including the boxed warning, clarified that neurologic and psychiatric effects from mefloquine could “persist after mefloquine has been discontinued.” The accompanying FDA Drug Safety Communication noted neurologic AEs from the drug, which include but are not limited to “dizziness, loss of balance, or ringing in the ears,” could “occur at any time during drug use, and can last for months to years after the drug is stopped or can be permanent.”6 Other neurologic symptoms listed in the drug label include vertigo, hearing impairment, headache, visual disturbances, sensory and motor neuropathies, including paresthesia, tremor, ataxia, convulsions, and encephalopathy.6
The updated drug label also made clear that psychiatric AEs from mefloquine, such as anxiety, paranoia, and depression to hallucinations and psychotic behavior, “have been reported to continue for months or years after mefloquine has been stopped.” Other psychiatric symptoms listed in the drug label include memory impairment, confusion, somnolence, insomnia, abnormal dreams, aggression, agitation, restlessness, mood swings, panic attacks, psychosis, and suicidal ideation.6
The 2013 boxed warning also served to reemphasize guidance first articulated in 2002 that any psychiatric symptom—presumably including abnormal dreams and insomnia—occurring during mefloquine use should be considered prodromal, prompting the drug’s immediate discontinuation.5 Specifically, the boxed warning explicitly cautioned that given the risk for serious psychiatric disturbances or neurologic AEs when used for malaria prophylaxis, “if psychiatric or neurologic symptoms occur, the drug should be discontinued and an alternative medication should be substituted.”6
Drug of Last Resort
By late 2013, partially on the basis of the boxed warning, the U.S. military declared mefloquine a “drug of last resort.”7,27 The U.S. Army Special Operations Command (USASOC) took the further step of prohibiting use of mefloquine altogether and, according to news reports, directed that medical and command staff assess whether certain personnel experiencing AEs from the drug may mistakenly have been thought to be malingering, have PTSD, or have other psychological problems.28
As the boxed warning and the USASOC order suggest, veterans exposed to mefloquine may have incurred a broad range of neurologic or psychiatric disorders or had others aggravated during military service as a result of their use of the drug. The effects of mefloquine may have confounded the diagnosis of neurologic or psychiatric disorders related to military service.26,29 As these AEs may be a direct result of mefloquine prescribed during military service, those with disabling diagnoses consistent with these effects may be entitled to claim disability compensation through the VA.
Of potential significant relevance to this adjudication process is a memorandum written in early 2012, in which the military conceded:
Some deploying Service members have been provided mefloquine for malaria prophylaxis without appropriate documentation in their medical records and without proper screening for contraindications. In addition, not all individuals have been provided the required mefloquine medication guide and wallet information card, as required by the Food and Drug Administration. 24
Veterans claiming a service-connected disability as a result of their use of mefloquine should therefore not always be expected to have documentation of prescribing in their military medical records. Although the VA could consider denying such claims for absence of proof of a nexus to military service, in light of this memorandum, the VA may need to consider other evidence of plausible exposure, including veteran testimony and deployment history.
It is also conceivable that the VA could consider denying such claims by arguing that the veteran directly contributed to the disability through willful misconduct by not adhering to mefloquine label guidance. However, as this memorandum establishes that mefloquine use was frequently directed without communication of the drug label precautions and warnings, the VA should consider that veterans claiming a service-connected disability frequently will not have known or otherwise been unable to discontinue the medication at the onset of prodromal symptoms.
It is also possible that the VA might deny claims on the basis that the claimed disabilities reflect preexisting conditions. However, as the memorandum establishes, use of mefloquine also was occasionally inappropriately directed to those with documented contraindications to the medication, who would have increased risk of AEs. As a result, veterans with preexisting neurologic or psychiatric conditions or disorders who nonetheless were prescribed mefloquine may reasonably claim these were aggravated during military service.
Conclusion
As this case suggests, in the coming years, as awareness of the chronic AEs of mefloquine increases among the veteran population, claims related to prior use of the drug are likely to increase and become of significant interest to the VA. Veterans with plausible exposure to mefloquine with neuropsychiatric disabilities who have yet to file a claim may be able to do so, and those veterans whose claims for service-connection were unfavorably adjudicated may be able to reopen their claims on the basis of the new material evidence in the 2012 military memorandum and the 2013 boxed warning.
This case report also suggests that service-connected disability claims arising from chronic neuropsychiatric AEs from mefloquine may prove to be of significant financial consequence. Further research to better define both the extent of prior mefloquine use among U.S. military personnel and the nature and prevalence of those chronic neurologic and psychiatric disorders caused by the drug would be helpful in informing improvements in the efficient and fair adjudication of such service-connected disability claims.
1. Tigertt WD. The army malaria research program. Ann Intern Med. 1969;70(1):150-153.
2. Trenholme CM, Williams RL, Desjardins RE, et al. Mefloquine (WR 142,490) in the treatment of human malaria. Science. 1975;190(4216):792-794.
3. Shanks GD, Karwacki J, Kanesa-thasan N, et al. Diseases transmitted primarily by arthropod vectors. In: Kelley PW, ed. Military Preventive Medicine: Mobilization and Deployment. Vol 2. Washington, DC: Borden Institute; 2005:803-935.
4. Armed Forces Epidemiological Board. Memorandum. Subject: Recommendations on Mefloquine Chemoprophylaxis for Military Personnel. Published October 3, 1989.
5. Nevin RL, Byrd AM. Neuropsychiatric adverse reactions to mefloquine: a systematic comparison of prescribing and patient safety guidance in the US, UK, Ireland, Australia, New Zealand, and Canada. Neurol Ther. 2016;5(1):69-83.
6. U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA approves label changes for antimalarial drug mefloquine hydrochloride due to risk of serious psychiatric and nerve side effects. http://www.fda.gov/Drugs/DrugSafety/ucm362227.htm. Published July 29, 2013. Accessed August 26, 2016.
7. Assistant Secretary of Defense for Health Affairs. Memorandum. Subject: Notification for Healthcare Providers of Mefloquine Boxed Warning. Published August 12, 2013.
8. Boudreau E, Schuster B, Sanchez J, et al. Tolerability of prophylactic Lariam regimens. Trop Med Parasitol. 1993;44(3):257-265.
9. Wallace MR, Sharp TW, Smoak B, et al. Malaria among United States troops in Somalia. Am J Med. 1996;100(1):49-55.
10. Smoak BL, Writer JV, Keep LW, Cowan J, Chantelois JL. The effects of inadvertent exposure of mefloquine chemoprophylaxis on pregnancy outcomes and infants of US Army servicewomen. J Infect Dis. 1997;176(3):831-833.
11. Sánchez JL, DeFraites RF, Sharp TW, Hanson RK. Mefloquine or doxycycline prophylaxis in US troops in Somalia. Lancet. 1993;341(8851):1021-1022.
12. Jones R, Kunsman G, Levine B, Smith M, Stahl C. Mefloquine distribution in postmortem cases. Forensic Sci Int. 1994;68(1):29-32.
13. Kotwal RS, Wenzel RB, Sterling RA, Porter WD, Jordan NN, Petruccelli BP. An outbreak of malaria in US Army Rangers returning from Afghanistan. JAMA. 2005;293(2):212-216.
14. Hess BP. Army fears rebellion on Lariam. United Press International. http://www.upi.com/Business_News/Security-Industry/2002/08/29/Analysis-Army-fears-rebellion-on-Lariam/UPI-39351030635930. Published August 29, 2002. Accessed August 29, 2016.
15. Overbosch D, Schilthuis H, Bienzle U, et al; Malarone International Study Team. Atovaquone-proguanil versus mefloquine for malaria prophylaxis in nonimmune travelers: results from a randomized, double-blind study. Clin Infect Dis. 2001;33(7):1015-1021.
16. U.S. Army Surgeon General. Memorandum. Subject: Updated Health Care Provider Information on Use of Mefloquine Hydrochloride for Malaria Prophylaxis. October 3, 2002.
17. Associated Press. Hallucinations linked to drug given to troops. http://www.nbcnews.com/id/6947472/ns/health-mental_health/t/hallucinations-linked-drug-given-troops. Published February 14, 2005. Accessed August 26, 2016.
18. Benjamin M. Army sent mentally ill troops to Iraq. United Press International. http://www.upi.com/Business_News/Security-Industry/2004/03/12/Army-sent-mentally-ill-troops-to-Iraq/UPI-97331079131967. Published March 12, 2004. Accessed August 26, 2016.
19. Fleet M, Mann J. Military’s use of malaria drug in question. http://edition.cnn.com/2004/HEALTH/05/20/lariam. Published May 21, 2004. Accessed August 26, 2016.
20. 108th Congress. Hearing on National Defense Authorization Act for Fiscal Year 2005 - H.R. 4200, February 25, 2004. http://commdocs.house.gov/committees/security/has056270.000/has056270_0f.htm. Accessed August 26, 2016.
21. Nevin RL. Mefloquine prescriptions in the presence of contraindications: prevalence among US military personnel deployed to Afghanistan, 2007. Pharmacoepidemiol Drug Saf. 2010;19(2):206-210.
22. U.S. Army Surgeon General. Memorandum. Subject: Updated Guidance on the Use of Mefloquine for Malaria Prophylaxis. February 2, 2009.
23. Assistant Secretary of Defense for Health Affairs. Memorandum. Subject: Policy Memorandum on the Use of Mefloquine (Lariam) in Malaria Prophylaxis. HA Policy 09-017. http://www.health.mil/~/media/MHS/Policy%20Files/Import/09-017.ashx. September 4, 2009. Accessed August 26, 2016.
24. Assistant Secretary of Defense for Health Affairs. Memorandum. Subject: Service Review of Mefloquine Prescribing Practices. January 17, 2012.
25. Assistant Secretary of Defense for Health Affairs. Memorandum. Subject: Guidance on Medications for Prophylaxis of Malaria. April 15, 2013.
26. Nevin RL. Mefloquine and posttraumatic stress disorder. In: Ritchie EC, ed. Forensic and Ethical Issues in Military Behavioral Health. Washington, DC: Borden Institute; 2014:275-296.
27. Pellerin C. DOD mefloquine policy mirrors FDA update on malaria drug. American Forces Press Service. http://archive.defense.gov/news/newsarticle.aspx?id=120857. Published September 26, 2013. Accessed August 26, 2016.
28. Jelinek P. Elite Army units to stop taking anti-malarial drug. Associated Press. http://www.military.com/daily-news/2013/09/19/elite-army-units-to-stop-taking-anti-malarial-drug.html. Published September 19, 2013. Accessed August 26, 2016.
29. Nevin RL, Ritchie EC. The Mefloquine intoxication syndrome: a significant potential confounder in the diagnosis and management of PTSD and other chronic deployment-related neuropsychiatric disorders. In: Ritchie EC, ed. Posttraumatic Stress Disorder and Related Disorders in Combat Veterans. Cham, Switzerland: Springer; 2015:257-278.
Mefloquine is a synthetic antimalarial drug structurally related to quinine. The drug was developed by the Walter Reed Army Institute of Research during a decades-long program that started during the Vietnam War in response to concerns of rising resistance to chloroquine.1
The prelicensing clinical testing of mefloquine, originally known as WR 142,490, was conducted in part among U.S. military service members.2,3 Soon after receiving FDA approval in 1989, under the brand name Lariam, it was recommended for use within the U.S. military.4 Over the following 2 decades, mefloquine was a common exposure during military deployments to malaria endemic areas.
Although the original U.S. mefloquine drug label noted that neuropsychiatric reactions could occur with use, changes to the drug label mandated by the FDA in July 2013, including a black box warning, described a potential for these to persist long after the drug has been discontinued.5,6 These changes have served to reinforce earlier U.S. military policy changes beginning in 2009 that deprioritized use of the drug in favor of safer and better-tolerated antimalarials. Consequently, more than a quarter century after its introduction, mefloquine now is only rarely prescribed to members of the U.S. military.7
In addition to limiting current use of the drug, the recent boxed warning may have important implications for service-connected disability claims adjudication by the VA for veterans previously exposed to the drug. This report presents a case of a nondeployed veteran exposed to mefloquine during an early military postmarketing study who developed chronic neuropsychiatric symptoms linked to the drug that were recently deemed service-connected. This report concludes with some comments on the likely implications of this case for future similar disability claims.
Case Presentation
In 2014, a 56-year-old nondeployed U.S. Marine Corps veteran submitted a claim to the VA for disabling conditions. The veteran alleged these conditions were due to his exposure to mefloquine while in military service more than 2 decades earlier. The veteran enlisted in 1975 and experienced a motor vehicle accident with prolonged loss of consciousness in 1978 but had no other significant medical history.
Thirteen years later, stationed in Hawaii in 1991, he was encouraged to volunteer for a double-blinded postmarketing study, evaluating the adverse effects (AEs) of chloroquine and mefloquine.8 As documentation following the trial revealed, he was randomly assigned to the mefloquine arm and received a loading dose of 250 mg daily for 3 days, followed by 250 mg per week for 11 weeks.
During the study he experienced insomnia, abnormal dreams, and nightmares. He also developed symptoms of anxiety, depression, cognitive dysfunction, and changes in personality—including anger and irritability—that were severe enough to be noted by his family members. The patient had not been advised of the significance of these symptoms and therefore did not report them during the clinical trial, nor did he report their intermittent presence after the study’s conclusion through his retirement in 1996, fearing adverse career consequences. Subsequent exacerbations of these chronic symptoms later contributed to the patient’s loss of civilian employment in 2010.
After becoming aware of the 2013 boxed warning that these chronic symptoms could be due to his earlier exposure to mefloquine, the veteran sought evaluation by a VA clinician. On evaluation, the clinician noted no history of deployment, and no history of posttraumatic stress disorder (PTSD) criteria A stressors, and posited that the veteran’s chronic neuropsychiatric symptoms were most likely a consequence of his earlier use of mefloquine. The VA subsequently awarded the veteran 50% disability for an anxiety disorder characterized by chronic sleep impairment and frequent panic attacks, attributing these to his service-connected use of the drug.
Discussion
Although the original 1989 FDA-approved mefloquine label had warned to discontinue the drug if specific prodromal symptoms of “anxiety, depression, restlessness or confusion” were noted,as illustrated by this case, this guidance was not always consistently communicated to service members.5 Indeed, few service members in the 1991 military postmarketing study discontinued the medication even after reporting such symptoms.8 Vivid dreams, often described as “terrifying nightmares with technicolor clarity” were reported by 7% of study participants. Similarly, concentration problems were reported in 5%; irritability in 4%; anger and moodiness each in 1%; and insomnia in 25%. Two study participants, after failing to discontinue mefloquine at the onset of severe insomnia, were later hospitalized for severe depression and suicidal thoughts, later deemed due to preexisting conditions. Despite these seemingly unfavorable results, mefloquine was nonetheless deemed well tolerated.8
Military Use of Mefloquine
Beginning in 1992, use of mefloquine for prophylaxis of malaria was then widely directed within the U.S. military during operations in Somalia. There, a majority of personnel received mefloquine under conditions of command-directed and directly observed administration of the drug.9,10 Again, drug label guidance describing the prodromal psychiatric symptoms that should have prompted discontinuation of mefloquine were either not consistently adhered to or not communicated. In one Somalia-era study, only 1 in 344 service members, or 0.3%, discontinued the drug.11
Throughout the remainder of the 1990s, mefloquine remained the antimalarial drug of choice for most U.S. military operations, and when combat began in Afghanistan in 2001, widespread use was also directed there.12,13 The following year, after national attention was directed to concerns of severe behavioral toxicity from the drug among personnel returning from Afghanistan, the manufacturer issued subtle changes to the mefloquine label warnings.5,14
These label changes adjusted the previously exclusive list of prodromal symptoms to an illustrative list, emphasizing that “if psychiatric symptoms such as [emphasis added] acute anxiety, depression, restlessness or confusion occur, these may be considered prodromal to a more serious event. In these cases, the drug must be discontinued and an alternative medication should be substituted.”5
In 2001 a randomized double-blinded trial demonstrated that symptoms of anxiety and depression occurred in at least 4% of mefloquine users, insomnia in 13%, and abnormal dreams in 14%. Nevertheless, an Army memorandum issued soon after the labeling change significantly understated the known risks of developing such psychiatric symptoms, erroneously claiming that these occurred from mefloquine only “at a rate of one per 2,000 to 13,000 persons.”15,16
Updated FDA Guidelines
In 2003, with widespread use of the drug being again directed during operations in Iraq, the FDA required that all mefloquine prescriptions be accompanied by a patient medication guide with warnings echoing those of the drug label that users seek medical attention should “possible signs of more serious mental problems” develop.5,17 However, surveys suggested that few U.S. service members received these warnings or even verbal instructions to that effect.17-19 During later congressional testimony, a service member who had experienced 3 weeks of nightmares prior to self-discontinuing the drug testified “every soldier I know has problems with it.”20
In response, a senior military medical leader—failing to recognize that the nightmares the soldier reported were in fact psychiatric symptoms and possible signs of more serious mental problems that required the drug’s discontinuation—may have undermined the FDA-directed warnings by dismissing the soldier’s testimony as “perception,” maintaining instead “that perceptions can become realities” should it become “held that this medication is widely problematic.”20
Given that certain preexisting conditions, including anxiety and depression, were known to confound recognition of incident psychiatric symptoms that required discontinuation of the drug, the original 1989 mefloquine label had noted that the drug should be used with caution in such patients. In subsequent years, this language was strengthened, and such patients were formally contraindicated the drug.21
Citing formal policy, senior military medical leaders provided assurance during congressional testimony that service members with these conditions would not be prescribed mefloquine.16,18,20 However, later analysis of a large group of deployed service members revealed that 1 in 7 with contraindications to mefloquine had been prescribed the drug contrary to drug label guidance.21
Black Box Warning
With growing recognition of the challenges in using mefloquine as directed by the drug label, a 2009 Army policy memorandum prioritized the use of safer and better-tolerated daily medications, such as doxycycline and atovaquone-proguanil, and stated that “[m]efloquine should only be used for personnel with contraindications to doxycycline.”22 This policy was extended throughout the other military services later that year.23 After concerns were raised that service members were still being prescribed the drug contrary to policy, further restrictions were formalized in early 2013 prior to the boxed warning, with mefloquine reserved for those only “with intolerance or contraindications” to the first-line drugs.24,25
In a later memorandum announcing the July 2013 boxed warning, the military revealed that the number of active-duty personnel prescribed mefloquine had steadily decreased in prior years from 17,361 in 2008 to only 2,040 in 2012.7 Although the military has not released precise figures on the number of U.S. military personnel exposed to mefloquine since the drug’s introduction, based on a variety of sources, the total is likely to far exceed 100,000.7,26
The major changes to the mefloquine label in 2013, including the boxed warning, clarified that neurologic and psychiatric effects from mefloquine could “persist after mefloquine has been discontinued.” The accompanying FDA Drug Safety Communication noted neurologic AEs from the drug, which include but are not limited to “dizziness, loss of balance, or ringing in the ears,” could “occur at any time during drug use, and can last for months to years after the drug is stopped or can be permanent.”6 Other neurologic symptoms listed in the drug label include vertigo, hearing impairment, headache, visual disturbances, sensory and motor neuropathies, including paresthesia, tremor, ataxia, convulsions, and encephalopathy.6
The updated drug label also made clear that psychiatric AEs from mefloquine, such as anxiety, paranoia, and depression to hallucinations and psychotic behavior, “have been reported to continue for months or years after mefloquine has been stopped.” Other psychiatric symptoms listed in the drug label include memory impairment, confusion, somnolence, insomnia, abnormal dreams, aggression, agitation, restlessness, mood swings, panic attacks, psychosis, and suicidal ideation.6
The 2013 boxed warning also served to reemphasize guidance first articulated in 2002 that any psychiatric symptom—presumably including abnormal dreams and insomnia—occurring during mefloquine use should be considered prodromal, prompting the drug’s immediate discontinuation.5 Specifically, the boxed warning explicitly cautioned that given the risk for serious psychiatric disturbances or neurologic AEs when used for malaria prophylaxis, “if psychiatric or neurologic symptoms occur, the drug should be discontinued and an alternative medication should be substituted.”6
Drug of Last Resort
By late 2013, partially on the basis of the boxed warning, the U.S. military declared mefloquine a “drug of last resort.”7,27 The U.S. Army Special Operations Command (USASOC) took the further step of prohibiting use of mefloquine altogether and, according to news reports, directed that medical and command staff assess whether certain personnel experiencing AEs from the drug may mistakenly have been thought to be malingering, have PTSD, or have other psychological problems.28
As the boxed warning and the USASOC order suggest, veterans exposed to mefloquine may have incurred a broad range of neurologic or psychiatric disorders or had others aggravated during military service as a result of their use of the drug. The effects of mefloquine may have confounded the diagnosis of neurologic or psychiatric disorders related to military service.26,29 As these AEs may be a direct result of mefloquine prescribed during military service, those with disabling diagnoses consistent with these effects may be entitled to claim disability compensation through the VA.
Of potential significant relevance to this adjudication process is a memorandum written in early 2012, in which the military conceded:
Some deploying Service members have been provided mefloquine for malaria prophylaxis without appropriate documentation in their medical records and without proper screening for contraindications. In addition, not all individuals have been provided the required mefloquine medication guide and wallet information card, as required by the Food and Drug Administration. 24
Veterans claiming a service-connected disability as a result of their use of mefloquine should therefore not always be expected to have documentation of prescribing in their military medical records. Although the VA could consider denying such claims for absence of proof of a nexus to military service, in light of this memorandum, the VA may need to consider other evidence of plausible exposure, including veteran testimony and deployment history.
It is also conceivable that the VA could consider denying such claims by arguing that the veteran directly contributed to the disability through willful misconduct by not adhering to mefloquine label guidance. However, as this memorandum establishes that mefloquine use was frequently directed without communication of the drug label precautions and warnings, the VA should consider that veterans claiming a service-connected disability frequently will not have known or otherwise been unable to discontinue the medication at the onset of prodromal symptoms.
It is also possible that the VA might deny claims on the basis that the claimed disabilities reflect preexisting conditions. However, as the memorandum establishes, use of mefloquine also was occasionally inappropriately directed to those with documented contraindications to the medication, who would have increased risk of AEs. As a result, veterans with preexisting neurologic or psychiatric conditions or disorders who nonetheless were prescribed mefloquine may reasonably claim these were aggravated during military service.
Conclusion
As this case suggests, in the coming years, as awareness of the chronic AEs of mefloquine increases among the veteran population, claims related to prior use of the drug are likely to increase and become of significant interest to the VA. Veterans with plausible exposure to mefloquine with neuropsychiatric disabilities who have yet to file a claim may be able to do so, and those veterans whose claims for service-connection were unfavorably adjudicated may be able to reopen their claims on the basis of the new material evidence in the 2012 military memorandum and the 2013 boxed warning.
This case report also suggests that service-connected disability claims arising from chronic neuropsychiatric AEs from mefloquine may prove to be of significant financial consequence. Further research to better define both the extent of prior mefloquine use among U.S. military personnel and the nature and prevalence of those chronic neurologic and psychiatric disorders caused by the drug would be helpful in informing improvements in the efficient and fair adjudication of such service-connected disability claims.
Mefloquine is a synthetic antimalarial drug structurally related to quinine. The drug was developed by the Walter Reed Army Institute of Research during a decades-long program that started during the Vietnam War in response to concerns of rising resistance to chloroquine.1
The prelicensing clinical testing of mefloquine, originally known as WR 142,490, was conducted in part among U.S. military service members.2,3 Soon after receiving FDA approval in 1989, under the brand name Lariam, it was recommended for use within the U.S. military.4 Over the following 2 decades, mefloquine was a common exposure during military deployments to malaria endemic areas.
Although the original U.S. mefloquine drug label noted that neuropsychiatric reactions could occur with use, changes to the drug label mandated by the FDA in July 2013, including a black box warning, described a potential for these to persist long after the drug has been discontinued.5,6 These changes have served to reinforce earlier U.S. military policy changes beginning in 2009 that deprioritized use of the drug in favor of safer and better-tolerated antimalarials. Consequently, more than a quarter century after its introduction, mefloquine now is only rarely prescribed to members of the U.S. military.7
In addition to limiting current use of the drug, the recent boxed warning may have important implications for service-connected disability claims adjudication by the VA for veterans previously exposed to the drug. This report presents a case of a nondeployed veteran exposed to mefloquine during an early military postmarketing study who developed chronic neuropsychiatric symptoms linked to the drug that were recently deemed service-connected. This report concludes with some comments on the likely implications of this case for future similar disability claims.
Case Presentation
In 2014, a 56-year-old nondeployed U.S. Marine Corps veteran submitted a claim to the VA for disabling conditions. The veteran alleged these conditions were due to his exposure to mefloquine while in military service more than 2 decades earlier. The veteran enlisted in 1975 and experienced a motor vehicle accident with prolonged loss of consciousness in 1978 but had no other significant medical history.
Thirteen years later, stationed in Hawaii in 1991, he was encouraged to volunteer for a double-blinded postmarketing study, evaluating the adverse effects (AEs) of chloroquine and mefloquine.8 As documentation following the trial revealed, he was randomly assigned to the mefloquine arm and received a loading dose of 250 mg daily for 3 days, followed by 250 mg per week for 11 weeks.
During the study he experienced insomnia, abnormal dreams, and nightmares. He also developed symptoms of anxiety, depression, cognitive dysfunction, and changes in personality—including anger and irritability—that were severe enough to be noted by his family members. The patient had not been advised of the significance of these symptoms and therefore did not report them during the clinical trial, nor did he report their intermittent presence after the study’s conclusion through his retirement in 1996, fearing adverse career consequences. Subsequent exacerbations of these chronic symptoms later contributed to the patient’s loss of civilian employment in 2010.
After becoming aware of the 2013 boxed warning that these chronic symptoms could be due to his earlier exposure to mefloquine, the veteran sought evaluation by a VA clinician. On evaluation, the clinician noted no history of deployment, and no history of posttraumatic stress disorder (PTSD) criteria A stressors, and posited that the veteran’s chronic neuropsychiatric symptoms were most likely a consequence of his earlier use of mefloquine. The VA subsequently awarded the veteran 50% disability for an anxiety disorder characterized by chronic sleep impairment and frequent panic attacks, attributing these to his service-connected use of the drug.
Discussion
Although the original 1989 FDA-approved mefloquine label had warned to discontinue the drug if specific prodromal symptoms of “anxiety, depression, restlessness or confusion” were noted,as illustrated by this case, this guidance was not always consistently communicated to service members.5 Indeed, few service members in the 1991 military postmarketing study discontinued the medication even after reporting such symptoms.8 Vivid dreams, often described as “terrifying nightmares with technicolor clarity” were reported by 7% of study participants. Similarly, concentration problems were reported in 5%; irritability in 4%; anger and moodiness each in 1%; and insomnia in 25%. Two study participants, after failing to discontinue mefloquine at the onset of severe insomnia, were later hospitalized for severe depression and suicidal thoughts, later deemed due to preexisting conditions. Despite these seemingly unfavorable results, mefloquine was nonetheless deemed well tolerated.8
Military Use of Mefloquine
Beginning in 1992, use of mefloquine for prophylaxis of malaria was then widely directed within the U.S. military during operations in Somalia. There, a majority of personnel received mefloquine under conditions of command-directed and directly observed administration of the drug.9,10 Again, drug label guidance describing the prodromal psychiatric symptoms that should have prompted discontinuation of mefloquine were either not consistently adhered to or not communicated. In one Somalia-era study, only 1 in 344 service members, or 0.3%, discontinued the drug.11
Throughout the remainder of the 1990s, mefloquine remained the antimalarial drug of choice for most U.S. military operations, and when combat began in Afghanistan in 2001, widespread use was also directed there.12,13 The following year, after national attention was directed to concerns of severe behavioral toxicity from the drug among personnel returning from Afghanistan, the manufacturer issued subtle changes to the mefloquine label warnings.5,14
These label changes adjusted the previously exclusive list of prodromal symptoms to an illustrative list, emphasizing that “if psychiatric symptoms such as [emphasis added] acute anxiety, depression, restlessness or confusion occur, these may be considered prodromal to a more serious event. In these cases, the drug must be discontinued and an alternative medication should be substituted.”5
In 2001 a randomized double-blinded trial demonstrated that symptoms of anxiety and depression occurred in at least 4% of mefloquine users, insomnia in 13%, and abnormal dreams in 14%. Nevertheless, an Army memorandum issued soon after the labeling change significantly understated the known risks of developing such psychiatric symptoms, erroneously claiming that these occurred from mefloquine only “at a rate of one per 2,000 to 13,000 persons.”15,16
Updated FDA Guidelines
In 2003, with widespread use of the drug being again directed during operations in Iraq, the FDA required that all mefloquine prescriptions be accompanied by a patient medication guide with warnings echoing those of the drug label that users seek medical attention should “possible signs of more serious mental problems” develop.5,17 However, surveys suggested that few U.S. service members received these warnings or even verbal instructions to that effect.17-19 During later congressional testimony, a service member who had experienced 3 weeks of nightmares prior to self-discontinuing the drug testified “every soldier I know has problems with it.”20
In response, a senior military medical leader—failing to recognize that the nightmares the soldier reported were in fact psychiatric symptoms and possible signs of more serious mental problems that required the drug’s discontinuation—may have undermined the FDA-directed warnings by dismissing the soldier’s testimony as “perception,” maintaining instead “that perceptions can become realities” should it become “held that this medication is widely problematic.”20
Given that certain preexisting conditions, including anxiety and depression, were known to confound recognition of incident psychiatric symptoms that required discontinuation of the drug, the original 1989 mefloquine label had noted that the drug should be used with caution in such patients. In subsequent years, this language was strengthened, and such patients were formally contraindicated the drug.21
Citing formal policy, senior military medical leaders provided assurance during congressional testimony that service members with these conditions would not be prescribed mefloquine.16,18,20 However, later analysis of a large group of deployed service members revealed that 1 in 7 with contraindications to mefloquine had been prescribed the drug contrary to drug label guidance.21
Black Box Warning
With growing recognition of the challenges in using mefloquine as directed by the drug label, a 2009 Army policy memorandum prioritized the use of safer and better-tolerated daily medications, such as doxycycline and atovaquone-proguanil, and stated that “[m]efloquine should only be used for personnel with contraindications to doxycycline.”22 This policy was extended throughout the other military services later that year.23 After concerns were raised that service members were still being prescribed the drug contrary to policy, further restrictions were formalized in early 2013 prior to the boxed warning, with mefloquine reserved for those only “with intolerance or contraindications” to the first-line drugs.24,25
In a later memorandum announcing the July 2013 boxed warning, the military revealed that the number of active-duty personnel prescribed mefloquine had steadily decreased in prior years from 17,361 in 2008 to only 2,040 in 2012.7 Although the military has not released precise figures on the number of U.S. military personnel exposed to mefloquine since the drug’s introduction, based on a variety of sources, the total is likely to far exceed 100,000.7,26
The major changes to the mefloquine label in 2013, including the boxed warning, clarified that neurologic and psychiatric effects from mefloquine could “persist after mefloquine has been discontinued.” The accompanying FDA Drug Safety Communication noted neurologic AEs from the drug, which include but are not limited to “dizziness, loss of balance, or ringing in the ears,” could “occur at any time during drug use, and can last for months to years after the drug is stopped or can be permanent.”6 Other neurologic symptoms listed in the drug label include vertigo, hearing impairment, headache, visual disturbances, sensory and motor neuropathies, including paresthesia, tremor, ataxia, convulsions, and encephalopathy.6
The updated drug label also made clear that psychiatric AEs from mefloquine, such as anxiety, paranoia, and depression to hallucinations and psychotic behavior, “have been reported to continue for months or years after mefloquine has been stopped.” Other psychiatric symptoms listed in the drug label include memory impairment, confusion, somnolence, insomnia, abnormal dreams, aggression, agitation, restlessness, mood swings, panic attacks, psychosis, and suicidal ideation.6
The 2013 boxed warning also served to reemphasize guidance first articulated in 2002 that any psychiatric symptom—presumably including abnormal dreams and insomnia—occurring during mefloquine use should be considered prodromal, prompting the drug’s immediate discontinuation.5 Specifically, the boxed warning explicitly cautioned that given the risk for serious psychiatric disturbances or neurologic AEs when used for malaria prophylaxis, “if psychiatric or neurologic symptoms occur, the drug should be discontinued and an alternative medication should be substituted.”6
Drug of Last Resort
By late 2013, partially on the basis of the boxed warning, the U.S. military declared mefloquine a “drug of last resort.”7,27 The U.S. Army Special Operations Command (USASOC) took the further step of prohibiting use of mefloquine altogether and, according to news reports, directed that medical and command staff assess whether certain personnel experiencing AEs from the drug may mistakenly have been thought to be malingering, have PTSD, or have other psychological problems.28
As the boxed warning and the USASOC order suggest, veterans exposed to mefloquine may have incurred a broad range of neurologic or psychiatric disorders or had others aggravated during military service as a result of their use of the drug. The effects of mefloquine may have confounded the diagnosis of neurologic or psychiatric disorders related to military service.26,29 As these AEs may be a direct result of mefloquine prescribed during military service, those with disabling diagnoses consistent with these effects may be entitled to claim disability compensation through the VA.
Of potential significant relevance to this adjudication process is a memorandum written in early 2012, in which the military conceded:
Some deploying Service members have been provided mefloquine for malaria prophylaxis without appropriate documentation in their medical records and without proper screening for contraindications. In addition, not all individuals have been provided the required mefloquine medication guide and wallet information card, as required by the Food and Drug Administration. 24
Veterans claiming a service-connected disability as a result of their use of mefloquine should therefore not always be expected to have documentation of prescribing in their military medical records. Although the VA could consider denying such claims for absence of proof of a nexus to military service, in light of this memorandum, the VA may need to consider other evidence of plausible exposure, including veteran testimony and deployment history.
It is also conceivable that the VA could consider denying such claims by arguing that the veteran directly contributed to the disability through willful misconduct by not adhering to mefloquine label guidance. However, as this memorandum establishes that mefloquine use was frequently directed without communication of the drug label precautions and warnings, the VA should consider that veterans claiming a service-connected disability frequently will not have known or otherwise been unable to discontinue the medication at the onset of prodromal symptoms.
It is also possible that the VA might deny claims on the basis that the claimed disabilities reflect preexisting conditions. However, as the memorandum establishes, use of mefloquine also was occasionally inappropriately directed to those with documented contraindications to the medication, who would have increased risk of AEs. As a result, veterans with preexisting neurologic or psychiatric conditions or disorders who nonetheless were prescribed mefloquine may reasonably claim these were aggravated during military service.
Conclusion
As this case suggests, in the coming years, as awareness of the chronic AEs of mefloquine increases among the veteran population, claims related to prior use of the drug are likely to increase and become of significant interest to the VA. Veterans with plausible exposure to mefloquine with neuropsychiatric disabilities who have yet to file a claim may be able to do so, and those veterans whose claims for service-connection were unfavorably adjudicated may be able to reopen their claims on the basis of the new material evidence in the 2012 military memorandum and the 2013 boxed warning.
This case report also suggests that service-connected disability claims arising from chronic neuropsychiatric AEs from mefloquine may prove to be of significant financial consequence. Further research to better define both the extent of prior mefloquine use among U.S. military personnel and the nature and prevalence of those chronic neurologic and psychiatric disorders caused by the drug would be helpful in informing improvements in the efficient and fair adjudication of such service-connected disability claims.
1. Tigertt WD. The army malaria research program. Ann Intern Med. 1969;70(1):150-153.
2. Trenholme CM, Williams RL, Desjardins RE, et al. Mefloquine (WR 142,490) in the treatment of human malaria. Science. 1975;190(4216):792-794.
3. Shanks GD, Karwacki J, Kanesa-thasan N, et al. Diseases transmitted primarily by arthropod vectors. In: Kelley PW, ed. Military Preventive Medicine: Mobilization and Deployment. Vol 2. Washington, DC: Borden Institute; 2005:803-935.
4. Armed Forces Epidemiological Board. Memorandum. Subject: Recommendations on Mefloquine Chemoprophylaxis for Military Personnel. Published October 3, 1989.
5. Nevin RL, Byrd AM. Neuropsychiatric adverse reactions to mefloquine: a systematic comparison of prescribing and patient safety guidance in the US, UK, Ireland, Australia, New Zealand, and Canada. Neurol Ther. 2016;5(1):69-83.
6. U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA approves label changes for antimalarial drug mefloquine hydrochloride due to risk of serious psychiatric and nerve side effects. http://www.fda.gov/Drugs/DrugSafety/ucm362227.htm. Published July 29, 2013. Accessed August 26, 2016.
7. Assistant Secretary of Defense for Health Affairs. Memorandum. Subject: Notification for Healthcare Providers of Mefloquine Boxed Warning. Published August 12, 2013.
8. Boudreau E, Schuster B, Sanchez J, et al. Tolerability of prophylactic Lariam regimens. Trop Med Parasitol. 1993;44(3):257-265.
9. Wallace MR, Sharp TW, Smoak B, et al. Malaria among United States troops in Somalia. Am J Med. 1996;100(1):49-55.
10. Smoak BL, Writer JV, Keep LW, Cowan J, Chantelois JL. The effects of inadvertent exposure of mefloquine chemoprophylaxis on pregnancy outcomes and infants of US Army servicewomen. J Infect Dis. 1997;176(3):831-833.
11. Sánchez JL, DeFraites RF, Sharp TW, Hanson RK. Mefloquine or doxycycline prophylaxis in US troops in Somalia. Lancet. 1993;341(8851):1021-1022.
12. Jones R, Kunsman G, Levine B, Smith M, Stahl C. Mefloquine distribution in postmortem cases. Forensic Sci Int. 1994;68(1):29-32.
13. Kotwal RS, Wenzel RB, Sterling RA, Porter WD, Jordan NN, Petruccelli BP. An outbreak of malaria in US Army Rangers returning from Afghanistan. JAMA. 2005;293(2):212-216.
14. Hess BP. Army fears rebellion on Lariam. United Press International. http://www.upi.com/Business_News/Security-Industry/2002/08/29/Analysis-Army-fears-rebellion-on-Lariam/UPI-39351030635930. Published August 29, 2002. Accessed August 29, 2016.
15. Overbosch D, Schilthuis H, Bienzle U, et al; Malarone International Study Team. Atovaquone-proguanil versus mefloquine for malaria prophylaxis in nonimmune travelers: results from a randomized, double-blind study. Clin Infect Dis. 2001;33(7):1015-1021.
16. U.S. Army Surgeon General. Memorandum. Subject: Updated Health Care Provider Information on Use of Mefloquine Hydrochloride for Malaria Prophylaxis. October 3, 2002.
17. Associated Press. Hallucinations linked to drug given to troops. http://www.nbcnews.com/id/6947472/ns/health-mental_health/t/hallucinations-linked-drug-given-troops. Published February 14, 2005. Accessed August 26, 2016.
18. Benjamin M. Army sent mentally ill troops to Iraq. United Press International. http://www.upi.com/Business_News/Security-Industry/2004/03/12/Army-sent-mentally-ill-troops-to-Iraq/UPI-97331079131967. Published March 12, 2004. Accessed August 26, 2016.
19. Fleet M, Mann J. Military’s use of malaria drug in question. http://edition.cnn.com/2004/HEALTH/05/20/lariam. Published May 21, 2004. Accessed August 26, 2016.
20. 108th Congress. Hearing on National Defense Authorization Act for Fiscal Year 2005 - H.R. 4200, February 25, 2004. http://commdocs.house.gov/committees/security/has056270.000/has056270_0f.htm. Accessed August 26, 2016.
21. Nevin RL. Mefloquine prescriptions in the presence of contraindications: prevalence among US military personnel deployed to Afghanistan, 2007. Pharmacoepidemiol Drug Saf. 2010;19(2):206-210.
22. U.S. Army Surgeon General. Memorandum. Subject: Updated Guidance on the Use of Mefloquine for Malaria Prophylaxis. February 2, 2009.
23. Assistant Secretary of Defense for Health Affairs. Memorandum. Subject: Policy Memorandum on the Use of Mefloquine (Lariam) in Malaria Prophylaxis. HA Policy 09-017. http://www.health.mil/~/media/MHS/Policy%20Files/Import/09-017.ashx. September 4, 2009. Accessed August 26, 2016.
24. Assistant Secretary of Defense for Health Affairs. Memorandum. Subject: Service Review of Mefloquine Prescribing Practices. January 17, 2012.
25. Assistant Secretary of Defense for Health Affairs. Memorandum. Subject: Guidance on Medications for Prophylaxis of Malaria. April 15, 2013.
26. Nevin RL. Mefloquine and posttraumatic stress disorder. In: Ritchie EC, ed. Forensic and Ethical Issues in Military Behavioral Health. Washington, DC: Borden Institute; 2014:275-296.
27. Pellerin C. DOD mefloquine policy mirrors FDA update on malaria drug. American Forces Press Service. http://archive.defense.gov/news/newsarticle.aspx?id=120857. Published September 26, 2013. Accessed August 26, 2016.
28. Jelinek P. Elite Army units to stop taking anti-malarial drug. Associated Press. http://www.military.com/daily-news/2013/09/19/elite-army-units-to-stop-taking-anti-malarial-drug.html. Published September 19, 2013. Accessed August 26, 2016.
29. Nevin RL, Ritchie EC. The Mefloquine intoxication syndrome: a significant potential confounder in the diagnosis and management of PTSD and other chronic deployment-related neuropsychiatric disorders. In: Ritchie EC, ed. Posttraumatic Stress Disorder and Related Disorders in Combat Veterans. Cham, Switzerland: Springer; 2015:257-278.
1. Tigertt WD. The army malaria research program. Ann Intern Med. 1969;70(1):150-153.
2. Trenholme CM, Williams RL, Desjardins RE, et al. Mefloquine (WR 142,490) in the treatment of human malaria. Science. 1975;190(4216):792-794.
3. Shanks GD, Karwacki J, Kanesa-thasan N, et al. Diseases transmitted primarily by arthropod vectors. In: Kelley PW, ed. Military Preventive Medicine: Mobilization and Deployment. Vol 2. Washington, DC: Borden Institute; 2005:803-935.
4. Armed Forces Epidemiological Board. Memorandum. Subject: Recommendations on Mefloquine Chemoprophylaxis for Military Personnel. Published October 3, 1989.
5. Nevin RL, Byrd AM. Neuropsychiatric adverse reactions to mefloquine: a systematic comparison of prescribing and patient safety guidance in the US, UK, Ireland, Australia, New Zealand, and Canada. Neurol Ther. 2016;5(1):69-83.
6. U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA approves label changes for antimalarial drug mefloquine hydrochloride due to risk of serious psychiatric and nerve side effects. http://www.fda.gov/Drugs/DrugSafety/ucm362227.htm. Published July 29, 2013. Accessed August 26, 2016.
7. Assistant Secretary of Defense for Health Affairs. Memorandum. Subject: Notification for Healthcare Providers of Mefloquine Boxed Warning. Published August 12, 2013.
8. Boudreau E, Schuster B, Sanchez J, et al. Tolerability of prophylactic Lariam regimens. Trop Med Parasitol. 1993;44(3):257-265.
9. Wallace MR, Sharp TW, Smoak B, et al. Malaria among United States troops in Somalia. Am J Med. 1996;100(1):49-55.
10. Smoak BL, Writer JV, Keep LW, Cowan J, Chantelois JL. The effects of inadvertent exposure of mefloquine chemoprophylaxis on pregnancy outcomes and infants of US Army servicewomen. J Infect Dis. 1997;176(3):831-833.
11. Sánchez JL, DeFraites RF, Sharp TW, Hanson RK. Mefloquine or doxycycline prophylaxis in US troops in Somalia. Lancet. 1993;341(8851):1021-1022.
12. Jones R, Kunsman G, Levine B, Smith M, Stahl C. Mefloquine distribution in postmortem cases. Forensic Sci Int. 1994;68(1):29-32.
13. Kotwal RS, Wenzel RB, Sterling RA, Porter WD, Jordan NN, Petruccelli BP. An outbreak of malaria in US Army Rangers returning from Afghanistan. JAMA. 2005;293(2):212-216.
14. Hess BP. Army fears rebellion on Lariam. United Press International. http://www.upi.com/Business_News/Security-Industry/2002/08/29/Analysis-Army-fears-rebellion-on-Lariam/UPI-39351030635930. Published August 29, 2002. Accessed August 29, 2016.
15. Overbosch D, Schilthuis H, Bienzle U, et al; Malarone International Study Team. Atovaquone-proguanil versus mefloquine for malaria prophylaxis in nonimmune travelers: results from a randomized, double-blind study. Clin Infect Dis. 2001;33(7):1015-1021.
16. U.S. Army Surgeon General. Memorandum. Subject: Updated Health Care Provider Information on Use of Mefloquine Hydrochloride for Malaria Prophylaxis. October 3, 2002.
17. Associated Press. Hallucinations linked to drug given to troops. http://www.nbcnews.com/id/6947472/ns/health-mental_health/t/hallucinations-linked-drug-given-troops. Published February 14, 2005. Accessed August 26, 2016.
18. Benjamin M. Army sent mentally ill troops to Iraq. United Press International. http://www.upi.com/Business_News/Security-Industry/2004/03/12/Army-sent-mentally-ill-troops-to-Iraq/UPI-97331079131967. Published March 12, 2004. Accessed August 26, 2016.
19. Fleet M, Mann J. Military’s use of malaria drug in question. http://edition.cnn.com/2004/HEALTH/05/20/lariam. Published May 21, 2004. Accessed August 26, 2016.
20. 108th Congress. Hearing on National Defense Authorization Act for Fiscal Year 2005 - H.R. 4200, February 25, 2004. http://commdocs.house.gov/committees/security/has056270.000/has056270_0f.htm. Accessed August 26, 2016.
21. Nevin RL. Mefloquine prescriptions in the presence of contraindications: prevalence among US military personnel deployed to Afghanistan, 2007. Pharmacoepidemiol Drug Saf. 2010;19(2):206-210.
22. U.S. Army Surgeon General. Memorandum. Subject: Updated Guidance on the Use of Mefloquine for Malaria Prophylaxis. February 2, 2009.
23. Assistant Secretary of Defense for Health Affairs. Memorandum. Subject: Policy Memorandum on the Use of Mefloquine (Lariam) in Malaria Prophylaxis. HA Policy 09-017. http://www.health.mil/~/media/MHS/Policy%20Files/Import/09-017.ashx. September 4, 2009. Accessed August 26, 2016.
24. Assistant Secretary of Defense for Health Affairs. Memorandum. Subject: Service Review of Mefloquine Prescribing Practices. January 17, 2012.
25. Assistant Secretary of Defense for Health Affairs. Memorandum. Subject: Guidance on Medications for Prophylaxis of Malaria. April 15, 2013.
26. Nevin RL. Mefloquine and posttraumatic stress disorder. In: Ritchie EC, ed. Forensic and Ethical Issues in Military Behavioral Health. Washington, DC: Borden Institute; 2014:275-296.
27. Pellerin C. DOD mefloquine policy mirrors FDA update on malaria drug. American Forces Press Service. http://archive.defense.gov/news/newsarticle.aspx?id=120857. Published September 26, 2013. Accessed August 26, 2016.
28. Jelinek P. Elite Army units to stop taking anti-malarial drug. Associated Press. http://www.military.com/daily-news/2013/09/19/elite-army-units-to-stop-taking-anti-malarial-drug.html. Published September 19, 2013. Accessed August 26, 2016.
29. Nevin RL, Ritchie EC. The Mefloquine intoxication syndrome: a significant potential confounder in the diagnosis and management of PTSD and other chronic deployment-related neuropsychiatric disorders. In: Ritchie EC, ed. Posttraumatic Stress Disorder and Related Disorders in Combat Veterans. Cham, Switzerland: Springer; 2015:257-278.
Combo could treat AML, other cancers

A novel combination has shown promise for treating acute myeloid leukemia (AML) and other cancers, according to preclinical research published in Cancer Cell.
Researchers found that combining a DNMT inhibitor and a PARP inhibitor greatly increases the drugs’ anti-tumor activity, and the combination could be effective in malignancies that are not responsive to PARP inhibitors or DNMT inhibitors alone.
Experiments showed that, when combined, the 2 types of inhibitors cause interactions that significantly disrupt cancer cells’ ability to survive DNA damage.
“Our preclinical data suggest that combining low doses of these inhibitors will enhance the clinical effects of both drugs as a potential treatment for patients with AML,” said study author Feyruz V. Rassool, PhD, of the University of Maryland School of Medicine in Baltimore.
“Moreover, our initial data suggest that subtypes of AML with a poor prognosis are likely to be sensitive to this new therapeutic approach.”
Dr Rassool and her colleagues assessed the activity of a DNMT inhibitor—decitabine or 5-azacytidine—in combination with a PARP inhibitor—veliparib or talazoparib—against AML and breast cancer.
In both AML and breast cancer cells, combination treatment increased cytotoxicity and decreased clonogenicity, compared to treatment with either type of inhibitor alone.
The combination of 5-azacytidine and talazoparib produced “very robust responses” in 2 mouse models of AML (MV411 and MOLM14), according to the researchers.
“[It was] somewhat of a surprise that leukemia cells were this sensitive to the combination treatment,” said study author Stephen B. Baylin, MD, of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins Medical Institutions in Baltimore.
“And if further research confirms our findings, it looks like it also could be useful for breast cancer and ovarian cancers for which PARP inhibitors have not been useful as yet.”
How the inhibitors work together
Dr Baylin noted that PARP helps repair naturally occurring breaks in strands of DNA, and some cancers rely more frequently on PARP than others.
“[PARP inhibitors] work according to how intensely and durably the PARP enzyme is trapped at certain DNA damage sites,” he explained. “If you can ramp up the duration and intensity of this trapping, you could potentially increase the efficacy of the drug[s].”
“We figured that if we pair 5-azacytidine and a PARP inhibitor like talazoparib, we may be able to increase PARP trapping at DNA damage sites.”
That’s because 5-azacytidine blocks proteins that attach gene-regulating methyl groups to DNA and traps those proteins on DNA. The proteins blocked by 5-azacytidine also interact with PARP enzymes at DNA damage sites.
In fact, the researchers did find that combining 5-azacytidine and talazoparib increased the time that PARP was trapped at sites of DNA damage in cancer cells. The time was extended from 30 minutes to 3-6 hours after treatment.
Next steps
Based on the results of this research, a clinical trial is planned to test whether low doses of decitabine and talazoparib can be safely combined and whether this therapy will be effective in AML patients.
The researchers are especially interested in testing the combination in patients who cannot receive intensive chemotherapy, whose leukemia is resistant to treatment, or who have relapsed after treatment.
“This is really a new paradigm mechanism that is being translated into a clinical trial,” Dr Rassool said. “It’s not just putting 2 drugs together.”
“We have shown in the laboratory that the proteins that these inhibitors target actually interact, so the effects of these inhibitors are enhanced through this interaction. Therein lies the novelty of this new approach.” ![]()

A novel combination has shown promise for treating acute myeloid leukemia (AML) and other cancers, according to preclinical research published in Cancer Cell.
Researchers found that combining a DNMT inhibitor and a PARP inhibitor greatly increases the drugs’ anti-tumor activity, and the combination could be effective in malignancies that are not responsive to PARP inhibitors or DNMT inhibitors alone.
Experiments showed that, when combined, the 2 types of inhibitors cause interactions that significantly disrupt cancer cells’ ability to survive DNA damage.
“Our preclinical data suggest that combining low doses of these inhibitors will enhance the clinical effects of both drugs as a potential treatment for patients with AML,” said study author Feyruz V. Rassool, PhD, of the University of Maryland School of Medicine in Baltimore.
“Moreover, our initial data suggest that subtypes of AML with a poor prognosis are likely to be sensitive to this new therapeutic approach.”
Dr Rassool and her colleagues assessed the activity of a DNMT inhibitor—decitabine or 5-azacytidine—in combination with a PARP inhibitor—veliparib or talazoparib—against AML and breast cancer.
In both AML and breast cancer cells, combination treatment increased cytotoxicity and decreased clonogenicity, compared to treatment with either type of inhibitor alone.
The combination of 5-azacytidine and talazoparib produced “very robust responses” in 2 mouse models of AML (MV411 and MOLM14), according to the researchers.
“[It was] somewhat of a surprise that leukemia cells were this sensitive to the combination treatment,” said study author Stephen B. Baylin, MD, of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins Medical Institutions in Baltimore.
“And if further research confirms our findings, it looks like it also could be useful for breast cancer and ovarian cancers for which PARP inhibitors have not been useful as yet.”
How the inhibitors work together
Dr Baylin noted that PARP helps repair naturally occurring breaks in strands of DNA, and some cancers rely more frequently on PARP than others.
“[PARP inhibitors] work according to how intensely and durably the PARP enzyme is trapped at certain DNA damage sites,” he explained. “If you can ramp up the duration and intensity of this trapping, you could potentially increase the efficacy of the drug[s].”
“We figured that if we pair 5-azacytidine and a PARP inhibitor like talazoparib, we may be able to increase PARP trapping at DNA damage sites.”
That’s because 5-azacytidine blocks proteins that attach gene-regulating methyl groups to DNA and traps those proteins on DNA. The proteins blocked by 5-azacytidine also interact with PARP enzymes at DNA damage sites.
In fact, the researchers did find that combining 5-azacytidine and talazoparib increased the time that PARP was trapped at sites of DNA damage in cancer cells. The time was extended from 30 minutes to 3-6 hours after treatment.
Next steps
Based on the results of this research, a clinical trial is planned to test whether low doses of decitabine and talazoparib can be safely combined and whether this therapy will be effective in AML patients.
The researchers are especially interested in testing the combination in patients who cannot receive intensive chemotherapy, whose leukemia is resistant to treatment, or who have relapsed after treatment.
“This is really a new paradigm mechanism that is being translated into a clinical trial,” Dr Rassool said. “It’s not just putting 2 drugs together.”
“We have shown in the laboratory that the proteins that these inhibitors target actually interact, so the effects of these inhibitors are enhanced through this interaction. Therein lies the novelty of this new approach.” ![]()

A novel combination has shown promise for treating acute myeloid leukemia (AML) and other cancers, according to preclinical research published in Cancer Cell.
Researchers found that combining a DNMT inhibitor and a PARP inhibitor greatly increases the drugs’ anti-tumor activity, and the combination could be effective in malignancies that are not responsive to PARP inhibitors or DNMT inhibitors alone.
Experiments showed that, when combined, the 2 types of inhibitors cause interactions that significantly disrupt cancer cells’ ability to survive DNA damage.
“Our preclinical data suggest that combining low doses of these inhibitors will enhance the clinical effects of both drugs as a potential treatment for patients with AML,” said study author Feyruz V. Rassool, PhD, of the University of Maryland School of Medicine in Baltimore.
“Moreover, our initial data suggest that subtypes of AML with a poor prognosis are likely to be sensitive to this new therapeutic approach.”
Dr Rassool and her colleagues assessed the activity of a DNMT inhibitor—decitabine or 5-azacytidine—in combination with a PARP inhibitor—veliparib or talazoparib—against AML and breast cancer.
In both AML and breast cancer cells, combination treatment increased cytotoxicity and decreased clonogenicity, compared to treatment with either type of inhibitor alone.
The combination of 5-azacytidine and talazoparib produced “very robust responses” in 2 mouse models of AML (MV411 and MOLM14), according to the researchers.
“[It was] somewhat of a surprise that leukemia cells were this sensitive to the combination treatment,” said study author Stephen B. Baylin, MD, of the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins Medical Institutions in Baltimore.
“And if further research confirms our findings, it looks like it also could be useful for breast cancer and ovarian cancers for which PARP inhibitors have not been useful as yet.”
How the inhibitors work together
Dr Baylin noted that PARP helps repair naturally occurring breaks in strands of DNA, and some cancers rely more frequently on PARP than others.
“[PARP inhibitors] work according to how intensely and durably the PARP enzyme is trapped at certain DNA damage sites,” he explained. “If you can ramp up the duration and intensity of this trapping, you could potentially increase the efficacy of the drug[s].”
“We figured that if we pair 5-azacytidine and a PARP inhibitor like talazoparib, we may be able to increase PARP trapping at DNA damage sites.”
That’s because 5-azacytidine blocks proteins that attach gene-regulating methyl groups to DNA and traps those proteins on DNA. The proteins blocked by 5-azacytidine also interact with PARP enzymes at DNA damage sites.
In fact, the researchers did find that combining 5-azacytidine and talazoparib increased the time that PARP was trapped at sites of DNA damage in cancer cells. The time was extended from 30 minutes to 3-6 hours after treatment.
Next steps
Based on the results of this research, a clinical trial is planned to test whether low doses of decitabine and talazoparib can be safely combined and whether this therapy will be effective in AML patients.
The researchers are especially interested in testing the combination in patients who cannot receive intensive chemotherapy, whose leukemia is resistant to treatment, or who have relapsed after treatment.
“This is really a new paradigm mechanism that is being translated into a clinical trial,” Dr Rassool said. “It’s not just putting 2 drugs together.”
“We have shown in the laboratory that the proteins that these inhibitors target actually interact, so the effects of these inhibitors are enhanced through this interaction. Therein lies the novelty of this new approach.” ![]()
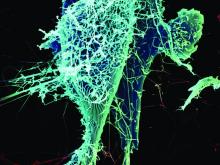
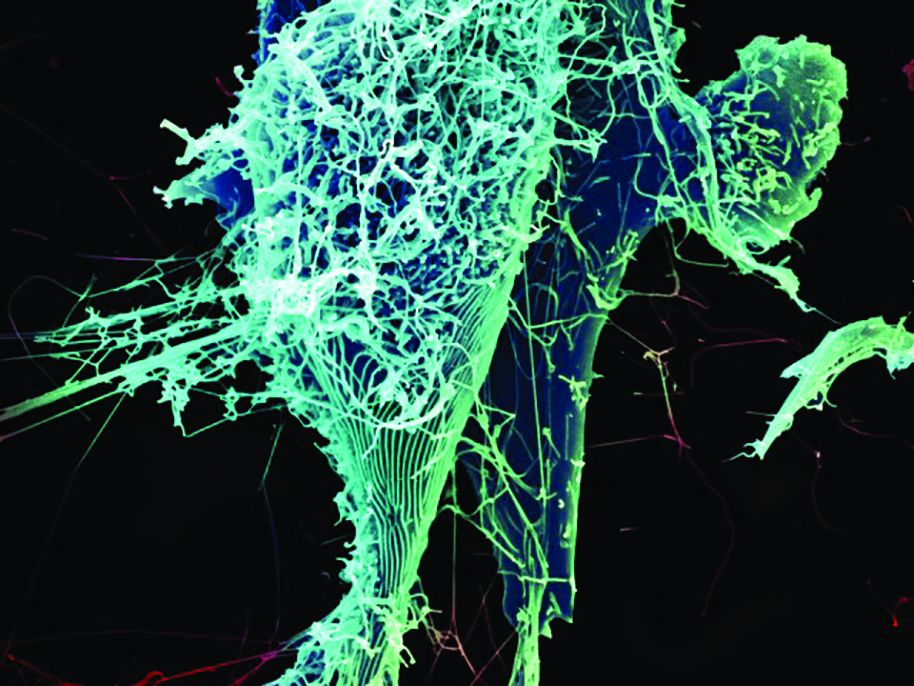
How a protein regulates blood cell fate

Image by Ian Johnston
Results of preclinical research explain the role endoglin plays in hematopoietic cell fate during embryogenesis.
Previous research showed that endoglin, a cell surface protein belonging to the TGF-beta receptor complex, is required for early hematopoietic lineage specification.
A new study shows that endoglin modulates the BMP and Wnt signaling pathways to encourage progenitor cells to develop into blood cells rather than cardiac cells.
This study was published in Nature Communications.
“During the early stages of development, cells have to make decisions very quickly,” said study author Rita Perlingeiro, PhD, of the University of Minnesota in Minneapolis.
“Fine-tuning of these early cell fate decisions can be easily disrupted by levels of key proteins within these cells. When one cell type is favored, this implies less of another. In this case, high levels of endoglin expression enhance the cell differentiation into blood cells, whereas cardiac cells are in deficit.”
Dr Perlingeiro and her colleagues made this discovery studying zebrafish and mouse models. The team wanted to pinpoint the mechanism underlying the dual function of endoglin in blood cell and cardiac cell fate.
The researchers found that endoglin is expressed in early mesoderm, and it marks both hematopoietic and cardiac progenitors.
Experiments showed that high levels of endoglin increase hematopoiesis while inhibiting cardiogenesis. And the levels of endoglin determine the activation of the BMP and Wnt signaling pathways.
With further investigation, the researchers identified JDP2, a member of the AP-1 transcription factor family, as an endoglin-dependent downstream target of Wnt signaling.
The team found that JDP2 expression is sufficient to establish blood cell fate when BMP and Wnt crosstalk is disturbed.
“The blood and heart systems are the first organs to develop in mammals, but the mechanisms regulating these earliest cell fate decisions are poorly understood,” Dr Perlingeiro said.
“By using multiple model systems, combined with specialized cell sorting technology and sequencing tools, our findings help uncover mechanisms previously unseen in the few cells engaged in these early development decisions.” ![]()

Image by Ian Johnston
Results of preclinical research explain the role endoglin plays in hematopoietic cell fate during embryogenesis.
Previous research showed that endoglin, a cell surface protein belonging to the TGF-beta receptor complex, is required for early hematopoietic lineage specification.
A new study shows that endoglin modulates the BMP and Wnt signaling pathways to encourage progenitor cells to develop into blood cells rather than cardiac cells.
This study was published in Nature Communications.
“During the early stages of development, cells have to make decisions very quickly,” said study author Rita Perlingeiro, PhD, of the University of Minnesota in Minneapolis.
“Fine-tuning of these early cell fate decisions can be easily disrupted by levels of key proteins within these cells. When one cell type is favored, this implies less of another. In this case, high levels of endoglin expression enhance the cell differentiation into blood cells, whereas cardiac cells are in deficit.”
Dr Perlingeiro and her colleagues made this discovery studying zebrafish and mouse models. The team wanted to pinpoint the mechanism underlying the dual function of endoglin in blood cell and cardiac cell fate.
The researchers found that endoglin is expressed in early mesoderm, and it marks both hematopoietic and cardiac progenitors.
Experiments showed that high levels of endoglin increase hematopoiesis while inhibiting cardiogenesis. And the levels of endoglin determine the activation of the BMP and Wnt signaling pathways.
With further investigation, the researchers identified JDP2, a member of the AP-1 transcription factor family, as an endoglin-dependent downstream target of Wnt signaling.
The team found that JDP2 expression is sufficient to establish blood cell fate when BMP and Wnt crosstalk is disturbed.
“The blood and heart systems are the first organs to develop in mammals, but the mechanisms regulating these earliest cell fate decisions are poorly understood,” Dr Perlingeiro said.
“By using multiple model systems, combined with specialized cell sorting technology and sequencing tools, our findings help uncover mechanisms previously unseen in the few cells engaged in these early development decisions.” ![]()

Image by Ian Johnston
Results of preclinical research explain the role endoglin plays in hematopoietic cell fate during embryogenesis.
Previous research showed that endoglin, a cell surface protein belonging to the TGF-beta receptor complex, is required for early hematopoietic lineage specification.
A new study shows that endoglin modulates the BMP and Wnt signaling pathways to encourage progenitor cells to develop into blood cells rather than cardiac cells.
This study was published in Nature Communications.
“During the early stages of development, cells have to make decisions very quickly,” said study author Rita Perlingeiro, PhD, of the University of Minnesota in Minneapolis.
“Fine-tuning of these early cell fate decisions can be easily disrupted by levels of key proteins within these cells. When one cell type is favored, this implies less of another. In this case, high levels of endoglin expression enhance the cell differentiation into blood cells, whereas cardiac cells are in deficit.”
Dr Perlingeiro and her colleagues made this discovery studying zebrafish and mouse models. The team wanted to pinpoint the mechanism underlying the dual function of endoglin in blood cell and cardiac cell fate.
The researchers found that endoglin is expressed in early mesoderm, and it marks both hematopoietic and cardiac progenitors.
Experiments showed that high levels of endoglin increase hematopoiesis while inhibiting cardiogenesis. And the levels of endoglin determine the activation of the BMP and Wnt signaling pathways.
With further investigation, the researchers identified JDP2, a member of the AP-1 transcription factor family, as an endoglin-dependent downstream target of Wnt signaling.
The team found that JDP2 expression is sufficient to establish blood cell fate when BMP and Wnt crosstalk is disturbed.
“The blood and heart systems are the first organs to develop in mammals, but the mechanisms regulating these earliest cell fate decisions are poorly understood,” Dr Perlingeiro said.
“By using multiple model systems, combined with specialized cell sorting technology and sequencing tools, our findings help uncover mechanisms previously unseen in the few cells engaged in these early development decisions.” ![]()
Beta-blockers reduce pain, opioid use in osteoarthritis
Beta-blockers were associated with less pain and lower opioid consumption in a case-control study of nearly 900 patients with osteoarthritis, Ana Valdes, PhD, and her colleagues reported in Arthritis Care & Research.
There is some mechanistic support for the association, which has been observed in other pain disorders, noted Dr. Valdes of the University of Nottingham (England) and her coauthors (Arthritis Care Res. 2016 Oct 1. doi: 10.1002/acr.23091).
The cohort was drawn from the Genetics of Osteoarthritis and Lifestyle (GOAL) study. Dr. Valdes and her associates examined the effect of beta-blocker use on pain as measured by the Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain score in 873 patients with knee and/or hip osteoarthritis. All were already taking at least one antihypertensive drug. The presence of “joint pain” was defined as a WOMAC score of less than 75. The multivariate analysis adjusted for age, gender, body mass index, knee or hip OA, history of other joint replacement, anxiety, and depression. Patients were a mean of about 69 years old; 347 were taking a beta-blocker.
After adjusting for the confounders, those taking the drugs were 32% less likely to report joint pain (odds ratio, 0.68). The effect seemed time bound: For every year on a beta-blocker, patients had a 4% decline in the risk of joint pain. The benefit was of similar magnitude regardless of whether patients had joint replacement. Beta-blockers also reduced the rate of opioid prescription by 27% (OR, 0.73), the authors noted.
They also found a similar benefit to the use of adrenergic blockers in general, but not with alpha-blockers. No other class of antihypertensive drugs showed any association with joint pain or with prescription of analgesics.
“These results might raise some future research questions for the treatment of hypertension in individuals with joint pain. Current guidance [in both the United Kingdom and United States] state that beta-blockers should no longer be preferred as an initial therapy for routine hypertension and should be used only when there is a compelling indication other than blood pressure control (for example, angina or chronic heart failure). If confirmed in randomized controlled trials, the data presented here could suggest that, in people with chronic joint pain beta-blockers may be considered as part of their antihypertensive regimen.”
The study was funded by the Arthritis Research UK Pain Centre, the European League Against Rheumatism, and AstraZeneca. Dr. Valdes had no financial disclosure, but one coauthor reported owning AstraZeneca stock.
Beta-blockers were associated with less pain and lower opioid consumption in a case-control study of nearly 900 patients with osteoarthritis, Ana Valdes, PhD, and her colleagues reported in Arthritis Care & Research.
There is some mechanistic support for the association, which has been observed in other pain disorders, noted Dr. Valdes of the University of Nottingham (England) and her coauthors (Arthritis Care Res. 2016 Oct 1. doi: 10.1002/acr.23091).
The cohort was drawn from the Genetics of Osteoarthritis and Lifestyle (GOAL) study. Dr. Valdes and her associates examined the effect of beta-blocker use on pain as measured by the Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain score in 873 patients with knee and/or hip osteoarthritis. All were already taking at least one antihypertensive drug. The presence of “joint pain” was defined as a WOMAC score of less than 75. The multivariate analysis adjusted for age, gender, body mass index, knee or hip OA, history of other joint replacement, anxiety, and depression. Patients were a mean of about 69 years old; 347 were taking a beta-blocker.
After adjusting for the confounders, those taking the drugs were 32% less likely to report joint pain (odds ratio, 0.68). The effect seemed time bound: For every year on a beta-blocker, patients had a 4% decline in the risk of joint pain. The benefit was of similar magnitude regardless of whether patients had joint replacement. Beta-blockers also reduced the rate of opioid prescription by 27% (OR, 0.73), the authors noted.
They also found a similar benefit to the use of adrenergic blockers in general, but not with alpha-blockers. No other class of antihypertensive drugs showed any association with joint pain or with prescription of analgesics.
“These results might raise some future research questions for the treatment of hypertension in individuals with joint pain. Current guidance [in both the United Kingdom and United States] state that beta-blockers should no longer be preferred as an initial therapy for routine hypertension and should be used only when there is a compelling indication other than blood pressure control (for example, angina or chronic heart failure). If confirmed in randomized controlled trials, the data presented here could suggest that, in people with chronic joint pain beta-blockers may be considered as part of their antihypertensive regimen.”
The study was funded by the Arthritis Research UK Pain Centre, the European League Against Rheumatism, and AstraZeneca. Dr. Valdes had no financial disclosure, but one coauthor reported owning AstraZeneca stock.
Beta-blockers were associated with less pain and lower opioid consumption in a case-control study of nearly 900 patients with osteoarthritis, Ana Valdes, PhD, and her colleagues reported in Arthritis Care & Research.
There is some mechanistic support for the association, which has been observed in other pain disorders, noted Dr. Valdes of the University of Nottingham (England) and her coauthors (Arthritis Care Res. 2016 Oct 1. doi: 10.1002/acr.23091).
The cohort was drawn from the Genetics of Osteoarthritis and Lifestyle (GOAL) study. Dr. Valdes and her associates examined the effect of beta-blocker use on pain as measured by the Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain score in 873 patients with knee and/or hip osteoarthritis. All were already taking at least one antihypertensive drug. The presence of “joint pain” was defined as a WOMAC score of less than 75. The multivariate analysis adjusted for age, gender, body mass index, knee or hip OA, history of other joint replacement, anxiety, and depression. Patients were a mean of about 69 years old; 347 were taking a beta-blocker.
After adjusting for the confounders, those taking the drugs were 32% less likely to report joint pain (odds ratio, 0.68). The effect seemed time bound: For every year on a beta-blocker, patients had a 4% decline in the risk of joint pain. The benefit was of similar magnitude regardless of whether patients had joint replacement. Beta-blockers also reduced the rate of opioid prescription by 27% (OR, 0.73), the authors noted.
They also found a similar benefit to the use of adrenergic blockers in general, but not with alpha-blockers. No other class of antihypertensive drugs showed any association with joint pain or with prescription of analgesics.
“These results might raise some future research questions for the treatment of hypertension in individuals with joint pain. Current guidance [in both the United Kingdom and United States] state that beta-blockers should no longer be preferred as an initial therapy for routine hypertension and should be used only when there is a compelling indication other than blood pressure control (for example, angina or chronic heart failure). If confirmed in randomized controlled trials, the data presented here could suggest that, in people with chronic joint pain beta-blockers may be considered as part of their antihypertensive regimen.”
The study was funded by the Arthritis Research UK Pain Centre, the European League Against Rheumatism, and AstraZeneca. Dr. Valdes had no financial disclosure, but one coauthor reported owning AstraZeneca stock.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point:
Major finding: The likelihood of joint pain was 32% and opioid use 27% lower in patients taking beta-blockers, compared with those not taking them.
Data source: The case-control study comprised 873 patients.
Disclosures: The study was funded by the Arthritis Research UK Pain Centre, the European League Against Rheumatism, and AstraZeneca. Dr. Valdes had no financial disclosure, but one coauthor reported owning AstraZeneca stock.
Risk model predicts chronic postop pain for VHR patients
Postoperative pain that lingers for months is a common outcome of ventral hernia repair surgery. A predictive model has been developed by investigators at the Carolina Medical Center in Charlotte, N.C., to determine which hernia patients are at risk for chronic postoperative pain.
Tiffany C. Cox, MD, and the research team used the International Hernia Mesh Registry to obtain a sample of 887 ventral hernia repair patients that had surgery between 2007 and 2014. Data on postoperative pain was based on the Carolinas Comfort Scale questionnaire administered at 1, 6 and 12 months after surgery. Logistic regression analyses were used to determine independent predictors of postoperative chronic pain and a risk model was developed (Am J Surg. 2016 Sep; 212[3]:501-10).
The investigators concluded that the statistically significant predictors of risk for developing chronic postoperative pain at 1 year were preoperative pain and pain at 1 month of 2 or greater on the Carolina Comfort Scale (odds ratio, 2.97 and 2.64, respectively), female sex (OR, 1.74), and repair of recurrent hernias (OR, 1.59).
The predictive model for chronic postoperative pain may be helpful to surgeons in counseling patients and in devising postoperative interventions.
The investigators had no disclosures.
Read the full study at goo.gl/MRjM66.
Postoperative pain that lingers for months is a common outcome of ventral hernia repair surgery. A predictive model has been developed by investigators at the Carolina Medical Center in Charlotte, N.C., to determine which hernia patients are at risk for chronic postoperative pain.
Tiffany C. Cox, MD, and the research team used the International Hernia Mesh Registry to obtain a sample of 887 ventral hernia repair patients that had surgery between 2007 and 2014. Data on postoperative pain was based on the Carolinas Comfort Scale questionnaire administered at 1, 6 and 12 months after surgery. Logistic regression analyses were used to determine independent predictors of postoperative chronic pain and a risk model was developed (Am J Surg. 2016 Sep; 212[3]:501-10).
The investigators concluded that the statistically significant predictors of risk for developing chronic postoperative pain at 1 year were preoperative pain and pain at 1 month of 2 or greater on the Carolina Comfort Scale (odds ratio, 2.97 and 2.64, respectively), female sex (OR, 1.74), and repair of recurrent hernias (OR, 1.59).
The predictive model for chronic postoperative pain may be helpful to surgeons in counseling patients and in devising postoperative interventions.
The investigators had no disclosures.
Read the full study at goo.gl/MRjM66.
Postoperative pain that lingers for months is a common outcome of ventral hernia repair surgery. A predictive model has been developed by investigators at the Carolina Medical Center in Charlotte, N.C., to determine which hernia patients are at risk for chronic postoperative pain.
Tiffany C. Cox, MD, and the research team used the International Hernia Mesh Registry to obtain a sample of 887 ventral hernia repair patients that had surgery between 2007 and 2014. Data on postoperative pain was based on the Carolinas Comfort Scale questionnaire administered at 1, 6 and 12 months after surgery. Logistic regression analyses were used to determine independent predictors of postoperative chronic pain and a risk model was developed (Am J Surg. 2016 Sep; 212[3]:501-10).
The investigators concluded that the statistically significant predictors of risk for developing chronic postoperative pain at 1 year were preoperative pain and pain at 1 month of 2 or greater on the Carolina Comfort Scale (odds ratio, 2.97 and 2.64, respectively), female sex (OR, 1.74), and repair of recurrent hernias (OR, 1.59).
The predictive model for chronic postoperative pain may be helpful to surgeons in counseling patients and in devising postoperative interventions.
The investigators had no disclosures.
Read the full study at goo.gl/MRjM66.
FROM THE AMERICAN JOURNAL OF SURGERY
Overdiagnosis more likely than early detection of threatening cancer with mammography screening
Following the introduction of mammography, women were considerably more likely to have tumors that were overdiagnosed than to have earlier detection of a tumor that was destined to become large, according to an analysis of trends from the Surveillance, Epidemiology, and End Results (SEER) database.
To assess the effectiveness of screening mammography in the real-world clinical and community setting, H. Gilbert Welch, MD, of the Dartmouth Institute for Health Policy and Clinical Practice and his associates examined trends in breast tumor size between the years of 1975 and 2012, a span of time that can be broken down into two distinct periods: a baseline period that predated the widespread use of screening mammography (1975-1979) and a period encompassing the most recent years for which 10 years of follow-up data were available (2000 through 2002).
Retrospective analysis of the SEER database revealed a shift in the size distribution of breast tumors: Large tumors, defined as invasive tumors measuring two centimeters or more, predominated in the period before widespread screening mammography, and small tumors, defined as in situ carcinomas or invasive tumors measuring less than two centimeters, predominated after.
This shift, the researchers noted, can, in part, be attributed to the use of screening mammography.
Overall, from 1975 to 2012, the proportion of breast tumors that were small increased from 36% to 68%. In that same time period, the proportion of large tumors decreased from 64% to 32%.
“This shift in size distribution was less the result of a substantial decrease in the incidence of large tumors and more the result of substantial increases in the detection of small tumors,” Dr. Welch and his associates wrote.
Put another way, the incidence of small tumors increased by 162 cases of cancer per 100,000 women, from 82 to 244 cases, while the incidence of large tumors decreased by 30 cases of cancer per 100,000 women, from 145 to 115 cases. “Assuming that the underlying burden of clinically meaningful breast cancer was unchanged, these data suggest that 30 cases of cancer per 100,000 women were destined to become large but were detected earlier, and the remaining 132 cases of cancer per 100,000 women were overdiagnosed,” the researchers wrote.
“The magnitude of the imbalance indicates that women were considerably more likely to have tumors that were overdiagnosed than to have earlier detection of a tumor that was destined to become large,” the researchers continued. “Our analysis of size-specific incidence highlights the fact that the introduction of screening mammography has produced a mixture of effects,” Dr. Welch and his associates added.
The Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth’s Geisel School of Medicine, and the National Cancer Institute supported this study. The investigators had no relevant disclosures.
Overdiagnosis of breast cancer has been suggested on the basis of multiple studies that used different designs and approaches and is acknowledged by national organizations such as the American Cancer Society and the U.S. Preventive Services Task Force. Although Dr. Welch and his associates present powerful data on a large number of women in a very clear fashion, they also rely on data with extensive missing values, make assumptions about underlying disease burden that cannot be verified, and acknowledge that their estimates are imprecise.
Rather than focusing on statistical issues and study design, we should move forward by agreeing that overdiagnosis does occur, even though the exact percentage of overdiagnosed cases remains unknown. Some consider overdiagnosis to be an intractable problem. No single approach will adequately address the issue. Instead, a multilevel approach ranging from research and education at the population level to intensified focus at the patient level is needed. One way to reduce overdiagnosis is targeted, precision screening of persons who have a higher risk of breast cancer rather than screening large populations in which the majority of persons are at a lower risk for harmful disease.
At the provider level, we need better tools to evaluate medical data and classify findings on the basis of clinical judgment. Previous research has documented extensive diagnostic variability among radiologists in their interpretation of mammograms and among pathologists in their interpretation of breast biopsy specimens. We are using archaic disease-classification systems with inadequate vetting and defective nosologic boundaries. Diagnostic thresholds for “abnormality” need to be revised because the middle and lower boundaries of these classification systems have expanded without a clear benefit to patients.
Rigorous analytic methods are required for the development of disease nosologies, and physicians need more sophisticated tools to improve diagnostic precision and accuracy. At the patient level, we need better methods of distinguishing biologically self-limited tumors from harmful tumors that progress. We must also improve communication regarding overdiagnosis at all levels, from dissemination of scientific findings at a population level to education of patients before they undergo screening.
Clinicians face time constraints and lack experience in communicating screening nuances. Better training may help. Building trust in science and medicine starts by taking ownership of all aspects of the screening cascade, including the collateral damage of our well-intentioned efforts.
Dr. Elmore is a professor of medicine and adjunct professor of epidemiology at the University of Washington. Dr. Elmore reported having no relevant disclosures related to this commentary but did report receiving financial compensation from UpToDate and Healthwise/Informed Medical Decisions Foundation. These comments are excerpted from an accompanying editorial (N Engl J Med. 2016 Oct 12;375[15]:1483-6).
Overdiagnosis of breast cancer has been suggested on the basis of multiple studies that used different designs and approaches and is acknowledged by national organizations such as the American Cancer Society and the U.S. Preventive Services Task Force. Although Dr. Welch and his associates present powerful data on a large number of women in a very clear fashion, they also rely on data with extensive missing values, make assumptions about underlying disease burden that cannot be verified, and acknowledge that their estimates are imprecise.
Rather than focusing on statistical issues and study design, we should move forward by agreeing that overdiagnosis does occur, even though the exact percentage of overdiagnosed cases remains unknown. Some consider overdiagnosis to be an intractable problem. No single approach will adequately address the issue. Instead, a multilevel approach ranging from research and education at the population level to intensified focus at the patient level is needed. One way to reduce overdiagnosis is targeted, precision screening of persons who have a higher risk of breast cancer rather than screening large populations in which the majority of persons are at a lower risk for harmful disease.
At the provider level, we need better tools to evaluate medical data and classify findings on the basis of clinical judgment. Previous research has documented extensive diagnostic variability among radiologists in their interpretation of mammograms and among pathologists in their interpretation of breast biopsy specimens. We are using archaic disease-classification systems with inadequate vetting and defective nosologic boundaries. Diagnostic thresholds for “abnormality” need to be revised because the middle and lower boundaries of these classification systems have expanded without a clear benefit to patients.
Rigorous analytic methods are required for the development of disease nosologies, and physicians need more sophisticated tools to improve diagnostic precision and accuracy. At the patient level, we need better methods of distinguishing biologically self-limited tumors from harmful tumors that progress. We must also improve communication regarding overdiagnosis at all levels, from dissemination of scientific findings at a population level to education of patients before they undergo screening.
Clinicians face time constraints and lack experience in communicating screening nuances. Better training may help. Building trust in science and medicine starts by taking ownership of all aspects of the screening cascade, including the collateral damage of our well-intentioned efforts.
Dr. Elmore is a professor of medicine and adjunct professor of epidemiology at the University of Washington. Dr. Elmore reported having no relevant disclosures related to this commentary but did report receiving financial compensation from UpToDate and Healthwise/Informed Medical Decisions Foundation. These comments are excerpted from an accompanying editorial (N Engl J Med. 2016 Oct 12;375[15]:1483-6).
Overdiagnosis of breast cancer has been suggested on the basis of multiple studies that used different designs and approaches and is acknowledged by national organizations such as the American Cancer Society and the U.S. Preventive Services Task Force. Although Dr. Welch and his associates present powerful data on a large number of women in a very clear fashion, they also rely on data with extensive missing values, make assumptions about underlying disease burden that cannot be verified, and acknowledge that their estimates are imprecise.
Rather than focusing on statistical issues and study design, we should move forward by agreeing that overdiagnosis does occur, even though the exact percentage of overdiagnosed cases remains unknown. Some consider overdiagnosis to be an intractable problem. No single approach will adequately address the issue. Instead, a multilevel approach ranging from research and education at the population level to intensified focus at the patient level is needed. One way to reduce overdiagnosis is targeted, precision screening of persons who have a higher risk of breast cancer rather than screening large populations in which the majority of persons are at a lower risk for harmful disease.
At the provider level, we need better tools to evaluate medical data and classify findings on the basis of clinical judgment. Previous research has documented extensive diagnostic variability among radiologists in their interpretation of mammograms and among pathologists in their interpretation of breast biopsy specimens. We are using archaic disease-classification systems with inadequate vetting and defective nosologic boundaries. Diagnostic thresholds for “abnormality” need to be revised because the middle and lower boundaries of these classification systems have expanded without a clear benefit to patients.
Rigorous analytic methods are required for the development of disease nosologies, and physicians need more sophisticated tools to improve diagnostic precision and accuracy. At the patient level, we need better methods of distinguishing biologically self-limited tumors from harmful tumors that progress. We must also improve communication regarding overdiagnosis at all levels, from dissemination of scientific findings at a population level to education of patients before they undergo screening.
Clinicians face time constraints and lack experience in communicating screening nuances. Better training may help. Building trust in science and medicine starts by taking ownership of all aspects of the screening cascade, including the collateral damage of our well-intentioned efforts.
Dr. Elmore is a professor of medicine and adjunct professor of epidemiology at the University of Washington. Dr. Elmore reported having no relevant disclosures related to this commentary but did report receiving financial compensation from UpToDate and Healthwise/Informed Medical Decisions Foundation. These comments are excerpted from an accompanying editorial (N Engl J Med. 2016 Oct 12;375[15]:1483-6).
Following the introduction of mammography, women were considerably more likely to have tumors that were overdiagnosed than to have earlier detection of a tumor that was destined to become large, according to an analysis of trends from the Surveillance, Epidemiology, and End Results (SEER) database.
To assess the effectiveness of screening mammography in the real-world clinical and community setting, H. Gilbert Welch, MD, of the Dartmouth Institute for Health Policy and Clinical Practice and his associates examined trends in breast tumor size between the years of 1975 and 2012, a span of time that can be broken down into two distinct periods: a baseline period that predated the widespread use of screening mammography (1975-1979) and a period encompassing the most recent years for which 10 years of follow-up data were available (2000 through 2002).
Retrospective analysis of the SEER database revealed a shift in the size distribution of breast tumors: Large tumors, defined as invasive tumors measuring two centimeters or more, predominated in the period before widespread screening mammography, and small tumors, defined as in situ carcinomas or invasive tumors measuring less than two centimeters, predominated after.
This shift, the researchers noted, can, in part, be attributed to the use of screening mammography.
Overall, from 1975 to 2012, the proportion of breast tumors that were small increased from 36% to 68%. In that same time period, the proportion of large tumors decreased from 64% to 32%.
“This shift in size distribution was less the result of a substantial decrease in the incidence of large tumors and more the result of substantial increases in the detection of small tumors,” Dr. Welch and his associates wrote.
Put another way, the incidence of small tumors increased by 162 cases of cancer per 100,000 women, from 82 to 244 cases, while the incidence of large tumors decreased by 30 cases of cancer per 100,000 women, from 145 to 115 cases. “Assuming that the underlying burden of clinically meaningful breast cancer was unchanged, these data suggest that 30 cases of cancer per 100,000 women were destined to become large but were detected earlier, and the remaining 132 cases of cancer per 100,000 women were overdiagnosed,” the researchers wrote.
“The magnitude of the imbalance indicates that women were considerably more likely to have tumors that were overdiagnosed than to have earlier detection of a tumor that was destined to become large,” the researchers continued. “Our analysis of size-specific incidence highlights the fact that the introduction of screening mammography has produced a mixture of effects,” Dr. Welch and his associates added.
The Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth’s Geisel School of Medicine, and the National Cancer Institute supported this study. The investigators had no relevant disclosures.
Following the introduction of mammography, women were considerably more likely to have tumors that were overdiagnosed than to have earlier detection of a tumor that was destined to become large, according to an analysis of trends from the Surveillance, Epidemiology, and End Results (SEER) database.
To assess the effectiveness of screening mammography in the real-world clinical and community setting, H. Gilbert Welch, MD, of the Dartmouth Institute for Health Policy and Clinical Practice and his associates examined trends in breast tumor size between the years of 1975 and 2012, a span of time that can be broken down into two distinct periods: a baseline period that predated the widespread use of screening mammography (1975-1979) and a period encompassing the most recent years for which 10 years of follow-up data were available (2000 through 2002).
Retrospective analysis of the SEER database revealed a shift in the size distribution of breast tumors: Large tumors, defined as invasive tumors measuring two centimeters or more, predominated in the period before widespread screening mammography, and small tumors, defined as in situ carcinomas or invasive tumors measuring less than two centimeters, predominated after.
This shift, the researchers noted, can, in part, be attributed to the use of screening mammography.
Overall, from 1975 to 2012, the proportion of breast tumors that were small increased from 36% to 68%. In that same time period, the proportion of large tumors decreased from 64% to 32%.
“This shift in size distribution was less the result of a substantial decrease in the incidence of large tumors and more the result of substantial increases in the detection of small tumors,” Dr. Welch and his associates wrote.
Put another way, the incidence of small tumors increased by 162 cases of cancer per 100,000 women, from 82 to 244 cases, while the incidence of large tumors decreased by 30 cases of cancer per 100,000 women, from 145 to 115 cases. “Assuming that the underlying burden of clinically meaningful breast cancer was unchanged, these data suggest that 30 cases of cancer per 100,000 women were destined to become large but were detected earlier, and the remaining 132 cases of cancer per 100,000 women were overdiagnosed,” the researchers wrote.
“The magnitude of the imbalance indicates that women were considerably more likely to have tumors that were overdiagnosed than to have earlier detection of a tumor that was destined to become large,” the researchers continued. “Our analysis of size-specific incidence highlights the fact that the introduction of screening mammography has produced a mixture of effects,” Dr. Welch and his associates added.
The Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth’s Geisel School of Medicine, and the National Cancer Institute supported this study. The investigators had no relevant disclosures.
Key clinical point:
Major finding: Of a population of 100,000 women, mammography detected 30 small tumors that were destined to become large but were detected earlier, while 132 cases of cancer were overdiagnosed.
Data source: Retrospective analysis of SEER data from 1975 to 2012.
Disclosures: The Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth’s Geisel School of Medicine, and the National Cancer Institute supported this study. The investigators had no relevant disclosures.
ZMapp shows promise for Ebola treatment, but misses efficacy goal
ZMapp, a potential monoclonal antibody treatment for Ebola virus disease, did not meet its efficacy goal in a clinical trial of patients in Liberia, Sierra Leone, and Guinea, according to a report in the New England Journal of Medicine.
ZMapp, developed by Mapp Biopharmaceutical, comprises three different laboratory-generated monoclonal antibodies. The drug targets the main surface protein of the Ebola virus. Earlier studies in nonhuman primates demonstrated that ZMapp had strong antiviral activity and prevented death when administered as late as 5 days after experimental infection with the Zaire Ebola virus strain.
The process of ZMapp infusion was generally safe, with only one serious adverse event – hypertension – attributed to the infusion itself. Of the 93 infusions attempted in the ZMapp group, 8 were stopped because of adverse events, and 9 were slowed down to accommodate for side effects.
While ZMapp did not meet its goal, the relative risk of death was 40% lower in the ZMapp group then in the control group. Treatment with ZMapp was delayed for a week after patients became symptomatic, exceeding the 5-day window where ZMapp has been shown to have at least 90% effectiveness. In addition, of the eight patients who died in the ZMapp group, seven died before the second of the three planned ZMapp infusions were delivered.
The abrupt end to the Ebola epidemic prevented the ZMapp trial from being adequately completed. A goal of 100 patients in both groups was desired but could not be reached.
“Despite the concerted efforts of many dedicated researchers domestically and internationally who participated in this and other trials, the outbreak appears to have ended with no incontrovertible evidence that any single treatment intervention, or combination of interventions, was unequivocally superior to the types of supportive medical care typically provided,” the investigators said.
Find the full study in the New England Journal of Medicine (doi: 10.1056/NEJMoa1604330).
ZMapp, a potential monoclonal antibody treatment for Ebola virus disease, did not meet its efficacy goal in a clinical trial of patients in Liberia, Sierra Leone, and Guinea, according to a report in the New England Journal of Medicine.
ZMapp, developed by Mapp Biopharmaceutical, comprises three different laboratory-generated monoclonal antibodies. The drug targets the main surface protein of the Ebola virus. Earlier studies in nonhuman primates demonstrated that ZMapp had strong antiviral activity and prevented death when administered as late as 5 days after experimental infection with the Zaire Ebola virus strain.
The process of ZMapp infusion was generally safe, with only one serious adverse event – hypertension – attributed to the infusion itself. Of the 93 infusions attempted in the ZMapp group, 8 were stopped because of adverse events, and 9 were slowed down to accommodate for side effects.
While ZMapp did not meet its goal, the relative risk of death was 40% lower in the ZMapp group then in the control group. Treatment with ZMapp was delayed for a week after patients became symptomatic, exceeding the 5-day window where ZMapp has been shown to have at least 90% effectiveness. In addition, of the eight patients who died in the ZMapp group, seven died before the second of the three planned ZMapp infusions were delivered.
The abrupt end to the Ebola epidemic prevented the ZMapp trial from being adequately completed. A goal of 100 patients in both groups was desired but could not be reached.
“Despite the concerted efforts of many dedicated researchers domestically and internationally who participated in this and other trials, the outbreak appears to have ended with no incontrovertible evidence that any single treatment intervention, or combination of interventions, was unequivocally superior to the types of supportive medical care typically provided,” the investigators said.
Find the full study in the New England Journal of Medicine (doi: 10.1056/NEJMoa1604330).
ZMapp, a potential monoclonal antibody treatment for Ebola virus disease, did not meet its efficacy goal in a clinical trial of patients in Liberia, Sierra Leone, and Guinea, according to a report in the New England Journal of Medicine.
ZMapp, developed by Mapp Biopharmaceutical, comprises three different laboratory-generated monoclonal antibodies. The drug targets the main surface protein of the Ebola virus. Earlier studies in nonhuman primates demonstrated that ZMapp had strong antiviral activity and prevented death when administered as late as 5 days after experimental infection with the Zaire Ebola virus strain.
The process of ZMapp infusion was generally safe, with only one serious adverse event – hypertension – attributed to the infusion itself. Of the 93 infusions attempted in the ZMapp group, 8 were stopped because of adverse events, and 9 were slowed down to accommodate for side effects.
While ZMapp did not meet its goal, the relative risk of death was 40% lower in the ZMapp group then in the control group. Treatment with ZMapp was delayed for a week after patients became symptomatic, exceeding the 5-day window where ZMapp has been shown to have at least 90% effectiveness. In addition, of the eight patients who died in the ZMapp group, seven died before the second of the three planned ZMapp infusions were delivered.
The abrupt end to the Ebola epidemic prevented the ZMapp trial from being adequately completed. A goal of 100 patients in both groups was desired but could not be reached.
“Despite the concerted efforts of many dedicated researchers domestically and internationally who participated in this and other trials, the outbreak appears to have ended with no incontrovertible evidence that any single treatment intervention, or combination of interventions, was unequivocally superior to the types of supportive medical care typically provided,” the investigators said.
Find the full study in the New England Journal of Medicine (doi: 10.1056/NEJMoa1604330).
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
VIDEO: The Business of Hospital Medicine
The business of hospital medicine is an important factor in individual clinicians' careers and for the specialty as a whole. Dr. Jasen Gundersen of TeamHealth and James Levy of Indigo Health Partners talk about the importance of recognizing the personal, and the system-wide, impacts and opportunities of the business side of HM.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The business of hospital medicine is an important factor in individual clinicians' careers and for the specialty as a whole. Dr. Jasen Gundersen of TeamHealth and James Levy of Indigo Health Partners talk about the importance of recognizing the personal, and the system-wide, impacts and opportunities of the business side of HM.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The business of hospital medicine is an important factor in individual clinicians' careers and for the specialty as a whole. Dr. Jasen Gundersen of TeamHealth and James Levy of Indigo Health Partners talk about the importance of recognizing the personal, and the system-wide, impacts and opportunities of the business side of HM.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Hepatitis Outlook: August 2016
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
A study in Hepatology has provided a preclinical risk assessment paradigm with which to better understand cardiovascular drug-drug interaction risk for hepatitis C–virus infected patients treated with sofosbuvir in combination with other direct acting antivirals and the antiarrhythmic drug amiodarone.
A Japanese study found that, although levels of Wisteria floribunda agglutinin-positive Mac-2-binding protein could be a useful indicator of liver fibrosis in patients with hepatitis B or C infection, WFA+-M2BP levels in the two groups significantly differed, even in the same degree of fibrosis.
Interferon-free, guideline-tailored therapy with direct-acting antivirals is highly effective and safe for hepatitis C virus–associated mixed cryoglobulinemia patients, according to a recent study.
Another recent study found that pegylated interferon (PegIFN) intensification in hepatitis B “e” antigen (HBeAg)-positive coinfected patients did not lead to increased clearance rates of HBeAg or hepatitis B surface antigen quantification (qHBsAg), despite faster declines of antigen levels while on PegIFN.
A study in HIV Medicine found that, under real-life conditions, treatment of patients infected with hepatitis C virus and of patients coinfected with HCV/HIV with all-oral direct-acting antiviral combinations led to high and similar rates of sustained virological response 12 weeks after the end of therapy.
Hepatitis B virus coinfection was the most important risk factor for liver fibrosis and cirrhosis in HIV-infected patients, and should be diagnosed early in HIV care to optimize treatment outcomes, a recent study showed.
Immunity persisted 24 months after a single dose of inactivated hepatitis A vaccine and live attenuated hepatitis A vaccine was administered to school-age children, according to a study published in Human Vaccines & Immunotherapeutics.
A hepatitis C treatment scale-up strategy in Rhode Island could reduce cirrhosis cases and liver-related deaths by 78.9% and 72.4%, respectively, by 2030, according to a study in Epidemiology and Infection.
Viral blipping is a frequent event during nucleoside analogue treatment of patients with chronic hepatitis B virus infection, a study found, although it did not lead to any clinically significant outcomes and thus may not require more frequent blood work and patient visits in clinical practice.
A study of liver and spleen stiffness in hepatitis C virus–infected patients – with advanced liver disease and sustained virologic response after interferon-free treatment – found that improvement of liver stiffness may be due to reduced necroinflammation, and to a lesser extent regression of cirrhosis. Improvement was more pronounced between therapy baseline and end of treatment than therapy baseline and 24 weeks after end of treatment.
From 2000 to 2011, 4,346 adults who died in New York City had a report of a hepatitis B virus infection (0.7%), according to a study in Epidemiology and Infection. Of the HBV-infected decedents, 1,074 (25%) were HIV coinfected. Fifty-five percent of HBV monoinfected and 95% of HBV/HIV coinfected decedents died prematurely, the researchers found.
Prison-based hepatitis C virus treatment achieves outcomes similar to those of community-based treatment, according to a study in the Journal of Viral Hepatitis, with those not released or transferred during treatment doing particularly well.
Treatment interventions to curb the hepatitis C virus epidemic among HIV-infected men who have sex with men are effective if high-risk behavior does not increase as it has during the last decade, according to a study in Hepatology.
The results of an international quality control study underline the urgent need to improve methods used to monitor hepatitis Delta virus viremia.
An investigation of a hepatitis E virus genotype 4 outbreak in Zhejiang Province, China, found that the outbreak was most likely caused by contaminated tap water rather than food.
A German study found that short treatment with 8 weeks of sofosbuvir and ledipasvir seems highly effective and safe in well-selected hepatitis C virus mono- and HIV/HCV-coinfected patients in a real-world setting.
A study of historical events fueling the cross-continental spread of hepatitis C virus epidemics said drivers for the epidemic were the advent of intravenous medical therapies and devices, growth in the heroin trade, and population mixing during armed conflicts.
AGA Resource
Through the AGA Roadmap to the Future of Practice, AGA offers a Hepatitis C Clinical Service line to support high-quality patient care, which is available at http://www.gastro.org/patient-care/conditions-diseases/hepatitis-c.
[email protected]
On Twitter @richpizzi
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
A study in Hepatology has provided a preclinical risk assessment paradigm with which to better understand cardiovascular drug-drug interaction risk for hepatitis C–virus infected patients treated with sofosbuvir in combination with other direct acting antivirals and the antiarrhythmic drug amiodarone.
A Japanese study found that, although levels of Wisteria floribunda agglutinin-positive Mac-2-binding protein could be a useful indicator of liver fibrosis in patients with hepatitis B or C infection, WFA+-M2BP levels in the two groups significantly differed, even in the same degree of fibrosis.
Interferon-free, guideline-tailored therapy with direct-acting antivirals is highly effective and safe for hepatitis C virus–associated mixed cryoglobulinemia patients, according to a recent study.
Another recent study found that pegylated interferon (PegIFN) intensification in hepatitis B “e” antigen (HBeAg)-positive coinfected patients did not lead to increased clearance rates of HBeAg or hepatitis B surface antigen quantification (qHBsAg), despite faster declines of antigen levels while on PegIFN.
A study in HIV Medicine found that, under real-life conditions, treatment of patients infected with hepatitis C virus and of patients coinfected with HCV/HIV with all-oral direct-acting antiviral combinations led to high and similar rates of sustained virological response 12 weeks after the end of therapy.
Hepatitis B virus coinfection was the most important risk factor for liver fibrosis and cirrhosis in HIV-infected patients, and should be diagnosed early in HIV care to optimize treatment outcomes, a recent study showed.
Immunity persisted 24 months after a single dose of inactivated hepatitis A vaccine and live attenuated hepatitis A vaccine was administered to school-age children, according to a study published in Human Vaccines & Immunotherapeutics.
A hepatitis C treatment scale-up strategy in Rhode Island could reduce cirrhosis cases and liver-related deaths by 78.9% and 72.4%, respectively, by 2030, according to a study in Epidemiology and Infection.
Viral blipping is a frequent event during nucleoside analogue treatment of patients with chronic hepatitis B virus infection, a study found, although it did not lead to any clinically significant outcomes and thus may not require more frequent blood work and patient visits in clinical practice.
A study of liver and spleen stiffness in hepatitis C virus–infected patients – with advanced liver disease and sustained virologic response after interferon-free treatment – found that improvement of liver stiffness may be due to reduced necroinflammation, and to a lesser extent regression of cirrhosis. Improvement was more pronounced between therapy baseline and end of treatment than therapy baseline and 24 weeks after end of treatment.
From 2000 to 2011, 4,346 adults who died in New York City had a report of a hepatitis B virus infection (0.7%), according to a study in Epidemiology and Infection. Of the HBV-infected decedents, 1,074 (25%) were HIV coinfected. Fifty-five percent of HBV monoinfected and 95% of HBV/HIV coinfected decedents died prematurely, the researchers found.
Prison-based hepatitis C virus treatment achieves outcomes similar to those of community-based treatment, according to a study in the Journal of Viral Hepatitis, with those not released or transferred during treatment doing particularly well.
Treatment interventions to curb the hepatitis C virus epidemic among HIV-infected men who have sex with men are effective if high-risk behavior does not increase as it has during the last decade, according to a study in Hepatology.
The results of an international quality control study underline the urgent need to improve methods used to monitor hepatitis Delta virus viremia.
An investigation of a hepatitis E virus genotype 4 outbreak in Zhejiang Province, China, found that the outbreak was most likely caused by contaminated tap water rather than food.
A German study found that short treatment with 8 weeks of sofosbuvir and ledipasvir seems highly effective and safe in well-selected hepatitis C virus mono- and HIV/HCV-coinfected patients in a real-world setting.
A study of historical events fueling the cross-continental spread of hepatitis C virus epidemics said drivers for the epidemic were the advent of intravenous medical therapies and devices, growth in the heroin trade, and population mixing during armed conflicts.
AGA Resource
Through the AGA Roadmap to the Future of Practice, AGA offers a Hepatitis C Clinical Service line to support high-quality patient care, which is available at http://www.gastro.org/patient-care/conditions-diseases/hepatitis-c.
[email protected]
On Twitter @richpizzi
If you work on the front lines of medical care treating patients with hepatitis, you may not have time to review all the hepatitis research that enters the medical literature every month. Here’s a quick look at some notable news items and journal articles published over the past month, covering a variety of the major hepatitis viruses.
A study in Hepatology has provided a preclinical risk assessment paradigm with which to better understand cardiovascular drug-drug interaction risk for hepatitis C–virus infected patients treated with sofosbuvir in combination with other direct acting antivirals and the antiarrhythmic drug amiodarone.
A Japanese study found that, although levels of Wisteria floribunda agglutinin-positive Mac-2-binding protein could be a useful indicator of liver fibrosis in patients with hepatitis B or C infection, WFA+-M2BP levels in the two groups significantly differed, even in the same degree of fibrosis.
Interferon-free, guideline-tailored therapy with direct-acting antivirals is highly effective and safe for hepatitis C virus–associated mixed cryoglobulinemia patients, according to a recent study.
Another recent study found that pegylated interferon (PegIFN) intensification in hepatitis B “e” antigen (HBeAg)-positive coinfected patients did not lead to increased clearance rates of HBeAg or hepatitis B surface antigen quantification (qHBsAg), despite faster declines of antigen levels while on PegIFN.
A study in HIV Medicine found that, under real-life conditions, treatment of patients infected with hepatitis C virus and of patients coinfected with HCV/HIV with all-oral direct-acting antiviral combinations led to high and similar rates of sustained virological response 12 weeks after the end of therapy.
Hepatitis B virus coinfection was the most important risk factor for liver fibrosis and cirrhosis in HIV-infected patients, and should be diagnosed early in HIV care to optimize treatment outcomes, a recent study showed.
Immunity persisted 24 months after a single dose of inactivated hepatitis A vaccine and live attenuated hepatitis A vaccine was administered to school-age children, according to a study published in Human Vaccines & Immunotherapeutics.
A hepatitis C treatment scale-up strategy in Rhode Island could reduce cirrhosis cases and liver-related deaths by 78.9% and 72.4%, respectively, by 2030, according to a study in Epidemiology and Infection.
Viral blipping is a frequent event during nucleoside analogue treatment of patients with chronic hepatitis B virus infection, a study found, although it did not lead to any clinically significant outcomes and thus may not require more frequent blood work and patient visits in clinical practice.
A study of liver and spleen stiffness in hepatitis C virus–infected patients – with advanced liver disease and sustained virologic response after interferon-free treatment – found that improvement of liver stiffness may be due to reduced necroinflammation, and to a lesser extent regression of cirrhosis. Improvement was more pronounced between therapy baseline and end of treatment than therapy baseline and 24 weeks after end of treatment.
From 2000 to 2011, 4,346 adults who died in New York City had a report of a hepatitis B virus infection (0.7%), according to a study in Epidemiology and Infection. Of the HBV-infected decedents, 1,074 (25%) were HIV coinfected. Fifty-five percent of HBV monoinfected and 95% of HBV/HIV coinfected decedents died prematurely, the researchers found.
Prison-based hepatitis C virus treatment achieves outcomes similar to those of community-based treatment, according to a study in the Journal of Viral Hepatitis, with those not released or transferred during treatment doing particularly well.
Treatment interventions to curb the hepatitis C virus epidemic among HIV-infected men who have sex with men are effective if high-risk behavior does not increase as it has during the last decade, according to a study in Hepatology.
The results of an international quality control study underline the urgent need to improve methods used to monitor hepatitis Delta virus viremia.
An investigation of a hepatitis E virus genotype 4 outbreak in Zhejiang Province, China, found that the outbreak was most likely caused by contaminated tap water rather than food.
A German study found that short treatment with 8 weeks of sofosbuvir and ledipasvir seems highly effective and safe in well-selected hepatitis C virus mono- and HIV/HCV-coinfected patients in a real-world setting.
A study of historical events fueling the cross-continental spread of hepatitis C virus epidemics said drivers for the epidemic were the advent of intravenous medical therapies and devices, growth in the heroin trade, and population mixing during armed conflicts.
AGA Resource
Through the AGA Roadmap to the Future of Practice, AGA offers a Hepatitis C Clinical Service line to support high-quality patient care, which is available at http://www.gastro.org/patient-care/conditions-diseases/hepatitis-c.
[email protected]
On Twitter @richpizzi
CDC: Improvement in breast cancer mortality slower among black women
Breast cancer mortality rates decreased for both white and black women from 2000 to 2014, but the decrease was slower for black women, according to a report by investigators with the Centers for Disease Control and Prevention.
The mortality rate decreased an average of 1.9% per year for white women, compared with an average decrease of 1.5% per year for black women, in an analysis of data from United States Cancer Statistics (USCS). Between 2010 and 2014, breast cancer mortality was 41% higher among black women (29.2 deaths per 100,000 people) than among white women (20.6 deaths per 100,000 population), reported Lisa C. Richardson, MD, and her associates at the CDC’s National Center for Chronic Disease Prevention and Health Promotion (MMWR. 2016 Oct 14;65[40]:1093-8).
Between 1999 and 2004, mortality rates decreased only for white woman older than 50 years.
USCS includes incidence data from the CDC’s National Program of Cancer Registries and the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program, and mortality data from the National Vital Statistics System.
“When combined with population-based approaches to increase knowledge of family history of cancer, increase physical activity, promote a healthy diet to maintain a healthy bodyweight, and increase screening for breast cancer, targeted treatment interventions could reduce racial disparities in breast cancer,” the investigators said. “A fuller understanding of [breast cancer’s] exact mechanisms might lead to more tailored interventions that could decrease mortality disparities.”
[email protected]
On Twitter @jessnicolecraig
Breast cancer mortality rates decreased for both white and black women from 2000 to 2014, but the decrease was slower for black women, according to a report by investigators with the Centers for Disease Control and Prevention.
The mortality rate decreased an average of 1.9% per year for white women, compared with an average decrease of 1.5% per year for black women, in an analysis of data from United States Cancer Statistics (USCS). Between 2010 and 2014, breast cancer mortality was 41% higher among black women (29.2 deaths per 100,000 people) than among white women (20.6 deaths per 100,000 population), reported Lisa C. Richardson, MD, and her associates at the CDC’s National Center for Chronic Disease Prevention and Health Promotion (MMWR. 2016 Oct 14;65[40]:1093-8).
Between 1999 and 2004, mortality rates decreased only for white woman older than 50 years.
USCS includes incidence data from the CDC’s National Program of Cancer Registries and the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program, and mortality data from the National Vital Statistics System.
“When combined with population-based approaches to increase knowledge of family history of cancer, increase physical activity, promote a healthy diet to maintain a healthy bodyweight, and increase screening for breast cancer, targeted treatment interventions could reduce racial disparities in breast cancer,” the investigators said. “A fuller understanding of [breast cancer’s] exact mechanisms might lead to more tailored interventions that could decrease mortality disparities.”
[email protected]
On Twitter @jessnicolecraig
Breast cancer mortality rates decreased for both white and black women from 2000 to 2014, but the decrease was slower for black women, according to a report by investigators with the Centers for Disease Control and Prevention.
The mortality rate decreased an average of 1.9% per year for white women, compared with an average decrease of 1.5% per year for black women, in an analysis of data from United States Cancer Statistics (USCS). Between 2010 and 2014, breast cancer mortality was 41% higher among black women (29.2 deaths per 100,000 people) than among white women (20.6 deaths per 100,000 population), reported Lisa C. Richardson, MD, and her associates at the CDC’s National Center for Chronic Disease Prevention and Health Promotion (MMWR. 2016 Oct 14;65[40]:1093-8).
Between 1999 and 2004, mortality rates decreased only for white woman older than 50 years.
USCS includes incidence data from the CDC’s National Program of Cancer Registries and the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program, and mortality data from the National Vital Statistics System.
“When combined with population-based approaches to increase knowledge of family history of cancer, increase physical activity, promote a healthy diet to maintain a healthy bodyweight, and increase screening for breast cancer, targeted treatment interventions could reduce racial disparities in breast cancer,” the investigators said. “A fuller understanding of [breast cancer’s] exact mechanisms might lead to more tailored interventions that could decrease mortality disparities.”
[email protected]
On Twitter @jessnicolecraig
Key clinical point:
Major finding: The mortality rate decreased an average of 1.9% per year for white women, compared with an average decrease of 1.5% per year for black women.
Data source: United States Cancer Statistics (USCS).
Disclosures: The CDC supported this study.