User login
Supraglottitis
Case
A 39-year-old woman, previously in good health, presented to the ED with a chief complaint of severe sore throat, which she said had begun approximately 4 hours prior and was rapidly worsening. She thought her voice sounded muffled, and said she was now having difficulty swallowing her saliva. The patient denied fever but did admit to chills. She experienced onset of shortness of breath 30 minutes prior to arrival to the ED.
The patient stated that she was a house painter and had been working in the home of someone who had several dogs. While not previously allergic to animals, the patient was concerned exposure to the dogs might have contributed to her symptoms. Regarding her social history, the patient admitted to daily consumption of beer, but denied smoking cigarettes. She had no known drug allergies.
On physical examination, the patient was afebrile. Her vital signs were: heart rate, 125 beats/min; blood pressure, 137/74 mm Hg; and respiratory rate, 18 breaths/min. Oxygen saturation was 99% on room air. Overall, the patient appeared anxious and exhibited mild inspiratory stridor. Examination of the eyes and ears were normal. There was no obvious inflammation or swelling of the posterior pharynx; the tongue was normal; there was no swelling of the floor of the mouth; and the uvula was midline and without swelling.
The patient was noted to having difficulty handling her secretions. She exhibited full range of motion of her neck. Her trachea was tender upon palpation but without jugular venous distension or lymphadenopathy. The cardiac examination was significant for tachycardia with a regular rhythm and without murmurs, rubs, or gallops; the pulmonary examination was normal except for transmitted upper airway sounds. The patient’s abdominal, dermatological, and neurological examinations were all normal.
Based on the examination findings, the differential diagnosis included allergic reaction, angioedema, epiglottitis, and retropharyngeal abscess. An intravenous (IV) line was placed and blood was drawn for laboratory evaluation, which included a complete blood count, basic metabolic panel (BMP), and a quantitative pregnancy test. Given the patient’s history, the emergency
A portable soft-tissue lateral radiograph of the neck was obtained. Radiology services interpreted the film as showing “prominent prevertebral soft tissues and epiglottis.
At this point, the patient appeared relatively stable and without progression of symptoms. Since there was the possibility of an infectious etiology, she was given piperacillin/tazobactam, 4.5 g IV.
Laboratory evaluation results were significant for an elevated white blood cell count (WBC) of 14.8 ×109/L, but without a left shift; BMP results were within normal limits, and the pregnancy test was negative.
Based on these findings, otolaryngology services were consulted. The consulting otolaryngologist sprayed oxymetazoline and tetracaine into both of the patient’s nostrils and performed a flexible fiberoptic nasopharyngolaryngoscopy. During the procedure, a significant amount of diffuse supraglottic edema was noted, but no posterior pharyngeal wall edema.
Based on the presence of stridor, difficulty managing secretions, and significant amount of supraglottic edema, the patient was taken to the surgical suite for urgent airway control. She was given dexamethasone, 10 mg IV, and after some difficulty, the anesthesiologist orally intubated the patient with a 7.0-mm endotracheal tube. Examination during the procedure noted diffuse supraglottic edema but no other abnormalities.
The patient was transferred to the intensive care unit (ICU) and treated with IV piperacillin/tazobactam and dexamethasone. While in the ICU, the patient became extremely agitated and combative. After further inquiry into the patient’s social history, the patient’s husband reported that his wife drank 12 to 13 beers nightly. The patient required treatment for alcohol withdrawal with IV benzodiazepines, sedation, and physical restraints. By hospital day 9, she was extubated and tolerated fluids by mouth. On hospital day 10, her mental status had returned to baseline, her WBC was within normal limits, and she no longer complained of difficulty swallowing. The patient was discharged home on hospital day 11 with a final diagnosis of supraglottitis and alcohol withdrawal, and she was given a prescription for amoxicillin/clavulanate. Unfortunately, she did not return for her follow-up appointments.
Discussion
While the incidence of pediatric epiglottitis has decreased since the introduction of the Haemophilus influenzae type b (Hib) vaccine in 1985, adult epiglottitis continues to represent a potentially life-threatening condition whose incidence has remained constant over the past several decades.1,2 The incidence of supraglottitis in adults is now 2.5 times greater than the incidence in children.3,4
Several important differences exist in the presentation and management of adults who present with inflammation of the epiglottis as compared to children. Children commonly present with an acute onset of symptoms, and due to their smaller and more pliant airway anatomy, they often experience stridor and respiratory distress.3,5 The inflammation in children is typically confined to the epiglottis and aryepiglottic folds, while in adults the inflammation can affect not only the epiglottis, but also supraglottic structures such as the pharynx, uvula, and aryepiglottic folds. For this reason, in adults the condition is often referred to as “supraglottitis.”2,6 Adults with supraglottitis most likely present in their 30s, 40s, and 50s, while children present between the ages of 2 and 5 years old.1,3,7 In adults, men more commonly present with supraglottitis than women.1,2 Cigarette smokers and patients with hypertension, diabetes mellitus (DM), chronic obstructive pulmonary disease, or human immunodeficiency virus/AIDS are at increased risk for supraglottitis.3,4 The mortality rate for adults with supraglottitis ranges from 1.2% to 7.1%.3
Etiology
Prior to the use of the Hib vaccine, Hib was the most common cause of epiglottitis, and remains so for children.1 Currently, the most common cause of supraglottitis in adults is Group A beta-hemolytic Streptococci.2 Other etiologies include other bacteria (Haemophilus influenzae, Streptococcus pneumoniae, Staphylococcus aureus, Pseudomonas species, Klebsiella pneumoniae, Pasteurella multocida, Neisseria species), viruses (herpes simplex, varicella, parainfluenza), trauma, and thermal injuries.1,4,5,8
Signs and Symptoms
Throat pain, dysphagia, odynophagia, and muffled voice are common complaints of adults presenting to the ED with supraglottitis.2,7 Fever is usually, but not always, present; the complaint of cough, however, is rare.2,3,4 Other less frequent complaints include hoarseness and drooling. Adults can also present with cervical lymphadenopathy, anterior neck tenderness, and cellulitis of the neck and chest.2,4 In general, the more severe cases will progress rapidly over a few hours. Due to the larger anatomy in adults, they are more likely than children to experience a gradual progression of symptoms, and supraglottitis will be missed on the initial presentation in up to 50% of adults.3,4 Stridor or respiratory compromise does occur in a minority of adult patients with supraglottitis. The need for artificial airway support (ie, endotracheal intubation, cricothyroidotomy) in adults ranges from 6.6% to 16%.9,10
Making the Diagnosis
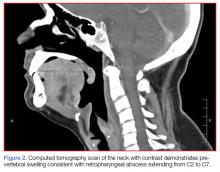
The gold standard for diagnosing supraglottitis is direct laryngoscopy.3,4 This point is emphasized in our case report, since the CT scan was concerning for a retropharyngeal abscess, and not supraglottitis. The examination of the oropharynx is generally safer and better tolerated in adults compared to pediatric patients, since airway compromise is much less likely. On occasion, inflammation, erythema, and edema of the epiglottis, aryepiglottic folds, or arytenoid cartilages can be observed.5 More commonly, the supraglottic structures are not visualized, and the posterior oropharynx appears relatively normal. This should serve as a clue for possible supraglottitis.
In suspected cases of adult supraglottitis without emergent airway compromise, lateral soft-tissue radiographs can be obtained to look for the “thumb sign,” indicating a swollen epiglottis. In adult supraglottitis, the width of the epiglottis is usually greater than 8 mm.11 Other abnormal radiographic findings include arytenoid and aryepiglottic fold enlargement, thinning of the airway, and an increase in size of the prevertebral space. Plain film sensitivity rates range from 38% to 98%.
Complete blood count and throat cultures are not particularly helpful in adult cases. Blood cultures, while only about 30% sensitive in adults, should be considered as supraglottitis can result in secondary infection in the central nervous system, lungs, and surrounding structures.3,5
If available, otolaryngology services should be consulted to evaluate the airway, and IV antibiotics, such as a third-generation cephalosporin (eg, ceftriaxone, cefotaxime), should be initiated to include coverage of Hib.3 If methicillin-resistant S aureus is a concern, vancomycin should be added. Clindamycin or metronidazole should also be given if anaerobes are suspected.4,7 The location for performing the nasopharyngeal laryngoscopy varies, depending on the patient’s age (ie, pediatric vs adult), severity of symptoms, presence of airway compromise, and local practice and custom.
Advanced imaging studies (CT scan or magnetic resonance imaging) can help identify the presence of an abscess and delineate the extent of the infection, but are not indicated in the early diagnosis and management of suspected adult supraglottitis.4 As our case demonstrates, CT is neither highly sensitive nor specific for the diagnosis of epiglottitis. The role of ultrasound in the evaluation of suspected epiglottitis is still being developed. One recent study compared 15 healthy volunteers with 15 patients diagnosed with epiglottitis by an otolaryngologist using laryngoscopy.12 A statistically significant difference was observed in the anteroposterior diameter of the epiglottis at the midpoint and both lateral edges between the study subjects and healthy volunteers.12 While there was overlap in the ranges for the midpoint, there was no overlap in both lateral edges between the two groups.12
Treatment
The vast majority of adult cases of supraglottitis are managed medically without airway intervention. Patients presenting with a rapid onset of symptoms and in respiratory distress or with stridor, drooling, or cyanosis, should be managed with early airway intervention. The use of corticosteroids is controversial, and has not been proven beneficial in any prospective trials.1-4,6,7,13
Admission to a critical care unit is indicated initially, even in patients who are not intubated, as they can experience delayed airway compromise with progression of the infection and edema.13
Complications
Abscess formation is a serious complication of supraglottitis, is present in up to 30% of cases, and is more likely to be seen in adults than in children.13 Since the adult larynx and surrounding tissues are larger than in children, often the infection is present longer, which allows for an abscess to develop. The risk of abscess formation is increased in patients with DM or those in whom a foreign body is present.
Numerous organisms have been isolated from supraglottic abscesses in adults, and in addition to incision and drainage, antibiotics covering both gram-positive organisms and anaerobes should be initiated.5 The presence of a supraglottic abscess increases the need for emergent intubation.13 In addition, a supraglottic abscess increases the mortality rate to 30%.3 Other complications from supraglottitis include mediastinitis, cervical adenitis, meningitis, and pneumonia.4,5
Conclusion
While the incidence of epiglottitis in the pediatric patient population has fallen, the incidence in adults remains relatively stable. Clinicians should consider supraglottitis in the differential diagnosis of adults presenting with severe sore throat, dysphagia, or stridor. While airway compromise in adults is uncommon, it does occur. Soft-tissue lateral neck radiographs can help make the diagnosis, but the gold standard remains laryngoscopy. All patients should be started on IV antibiotics and admitted to the ICU initially for airway watch.
1. Glynn F, Fenton JE. Diagnosis and management of supraglottitis (epiglottitis). Curr Infect Dis Rep. 2008;10(3):200-204.
2. Lichtor JL, Roche Rodriguez M, Aaronson NL, Spock T, Goodman TR, Baum ED. Epiglottitis: It hasn’t gone away. Anesthesiology. 2016;124(6):1404-1407. doi: 10.1097/ALN.0000000000001125.
3. Westerhuis B, Bietz MG, Lindemann J. Acute epiglottitis in adults: an under-recognized and life-threatening condition. S D Med. 2013;66(8):309-311, 313.
4. Al-Qudah M, Shetty S, Alomari M, Alqdah M. Acute adult supraglottitis: Current management and treatment. South Med J. 2010;103(8):800-804. doi: 10.1097/SMJ.0b013e3181e538d8.
5. Verbruggen K, Halewyck S, Deron P, Foulon I, Gordts F. Epiglottitis and related complications in adults. Case reports and review of the literature. B-ENT. 2012;8(2):143-148.
6. Mayo-Smith MF, Spinale JW, Donskey CJ, Yukawa M, Li RH, Schiffman FJ. Acute epiglottitis. An 18-year experience in Rhode Island. Chest. 1995;108(6):1640-1647.
7. Bizaki AJ, Numminen J, Vasama JP, Laranne J, Rautiainen M. Acute supraglottitis in adults in Finland: review and analysis of 308 cases. Laryngoscope. 2011;121(10):2107-2113. doi: 10.1002/lary.22147.
8. Charles R, Fadden M, Brook J. Acute epiglottitis. BMJ. 2013;347:f5235. doi: 10.1136/bmj.f5235.
9. Ng HL, Sin LM, Li MF, Que TL, Anandaciva S. Acute epiglottitis in adults: a retrospective review of 106 patients in Hong Kong. Emerg Med J. 2008;25(5):253-255. doi: 10.1136/emj.2007.050153.
10. Solomon P, Weisbrod M, Irish JC, Gullane PJ. Adult epiglottitis: the Toronto Hospital experience. J Otolaryngol. 1998;27(6):332-336.
11. Schumaker HM, Doris PE, Birnbaum G. Radiographic parameters in adult epiglottitis. Ann Emerg Med. 1984;13(8):588-590.
12. Ko DR, Chung YE, Park I, et al. Use of bedside sonography for diagnosing acute epiglottitis in the emergency department: a preliminary study. J Ultrasound Med. 2012;31(1):19-22.
13. Berger G, Landau T, Berger S, Finkelstein Y, Bernheim J, Ophir D. The rising incidence of adult acute epiglottitis and epiglottic abscess. Am J Otolaryngol. 2003;24(6):374-383.
Case
A 39-year-old woman, previously in good health, presented to the ED with a chief complaint of severe sore throat, which she said had begun approximately 4 hours prior and was rapidly worsening. She thought her voice sounded muffled, and said she was now having difficulty swallowing her saliva. The patient denied fever but did admit to chills. She experienced onset of shortness of breath 30 minutes prior to arrival to the ED.
The patient stated that she was a house painter and had been working in the home of someone who had several dogs. While not previously allergic to animals, the patient was concerned exposure to the dogs might have contributed to her symptoms. Regarding her social history, the patient admitted to daily consumption of beer, but denied smoking cigarettes. She had no known drug allergies.
On physical examination, the patient was afebrile. Her vital signs were: heart rate, 125 beats/min; blood pressure, 137/74 mm Hg; and respiratory rate, 18 breaths/min. Oxygen saturation was 99% on room air. Overall, the patient appeared anxious and exhibited mild inspiratory stridor. Examination of the eyes and ears were normal. There was no obvious inflammation or swelling of the posterior pharynx; the tongue was normal; there was no swelling of the floor of the mouth; and the uvula was midline and without swelling.
The patient was noted to having difficulty handling her secretions. She exhibited full range of motion of her neck. Her trachea was tender upon palpation but without jugular venous distension or lymphadenopathy. The cardiac examination was significant for tachycardia with a regular rhythm and without murmurs, rubs, or gallops; the pulmonary examination was normal except for transmitted upper airway sounds. The patient’s abdominal, dermatological, and neurological examinations were all normal.
Based on the examination findings, the differential diagnosis included allergic reaction, angioedema, epiglottitis, and retropharyngeal abscess. An intravenous (IV) line was placed and blood was drawn for laboratory evaluation, which included a complete blood count, basic metabolic panel (BMP), and a quantitative pregnancy test. Given the patient’s history, the emergency
A portable soft-tissue lateral radiograph of the neck was obtained. Radiology services interpreted the film as showing “prominent prevertebral soft tissues and epiglottis.
At this point, the patient appeared relatively stable and without progression of symptoms. Since there was the possibility of an infectious etiology, she was given piperacillin/tazobactam, 4.5 g IV.
Laboratory evaluation results were significant for an elevated white blood cell count (WBC) of 14.8 ×109/L, but without a left shift; BMP results were within normal limits, and the pregnancy test was negative.
Based on these findings, otolaryngology services were consulted. The consulting otolaryngologist sprayed oxymetazoline and tetracaine into both of the patient’s nostrils and performed a flexible fiberoptic nasopharyngolaryngoscopy. During the procedure, a significant amount of diffuse supraglottic edema was noted, but no posterior pharyngeal wall edema.
Based on the presence of stridor, difficulty managing secretions, and significant amount of supraglottic edema, the patient was taken to the surgical suite for urgent airway control. She was given dexamethasone, 10 mg IV, and after some difficulty, the anesthesiologist orally intubated the patient with a 7.0-mm endotracheal tube. Examination during the procedure noted diffuse supraglottic edema but no other abnormalities.
The patient was transferred to the intensive care unit (ICU) and treated with IV piperacillin/tazobactam and dexamethasone. While in the ICU, the patient became extremely agitated and combative. After further inquiry into the patient’s social history, the patient’s husband reported that his wife drank 12 to 13 beers nightly. The patient required treatment for alcohol withdrawal with IV benzodiazepines, sedation, and physical restraints. By hospital day 9, she was extubated and tolerated fluids by mouth. On hospital day 10, her mental status had returned to baseline, her WBC was within normal limits, and she no longer complained of difficulty swallowing. The patient was discharged home on hospital day 11 with a final diagnosis of supraglottitis and alcohol withdrawal, and she was given a prescription for amoxicillin/clavulanate. Unfortunately, she did not return for her follow-up appointments.
Discussion
While the incidence of pediatric epiglottitis has decreased since the introduction of the Haemophilus influenzae type b (Hib) vaccine in 1985, adult epiglottitis continues to represent a potentially life-threatening condition whose incidence has remained constant over the past several decades.1,2 The incidence of supraglottitis in adults is now 2.5 times greater than the incidence in children.3,4
Several important differences exist in the presentation and management of adults who present with inflammation of the epiglottis as compared to children. Children commonly present with an acute onset of symptoms, and due to their smaller and more pliant airway anatomy, they often experience stridor and respiratory distress.3,5 The inflammation in children is typically confined to the epiglottis and aryepiglottic folds, while in adults the inflammation can affect not only the epiglottis, but also supraglottic structures such as the pharynx, uvula, and aryepiglottic folds. For this reason, in adults the condition is often referred to as “supraglottitis.”2,6 Adults with supraglottitis most likely present in their 30s, 40s, and 50s, while children present between the ages of 2 and 5 years old.1,3,7 In adults, men more commonly present with supraglottitis than women.1,2 Cigarette smokers and patients with hypertension, diabetes mellitus (DM), chronic obstructive pulmonary disease, or human immunodeficiency virus/AIDS are at increased risk for supraglottitis.3,4 The mortality rate for adults with supraglottitis ranges from 1.2% to 7.1%.3
Etiology
Prior to the use of the Hib vaccine, Hib was the most common cause of epiglottitis, and remains so for children.1 Currently, the most common cause of supraglottitis in adults is Group A beta-hemolytic Streptococci.2 Other etiologies include other bacteria (Haemophilus influenzae, Streptococcus pneumoniae, Staphylococcus aureus, Pseudomonas species, Klebsiella pneumoniae, Pasteurella multocida, Neisseria species), viruses (herpes simplex, varicella, parainfluenza), trauma, and thermal injuries.1,4,5,8
Signs and Symptoms
Throat pain, dysphagia, odynophagia, and muffled voice are common complaints of adults presenting to the ED with supraglottitis.2,7 Fever is usually, but not always, present; the complaint of cough, however, is rare.2,3,4 Other less frequent complaints include hoarseness and drooling. Adults can also present with cervical lymphadenopathy, anterior neck tenderness, and cellulitis of the neck and chest.2,4 In general, the more severe cases will progress rapidly over a few hours. Due to the larger anatomy in adults, they are more likely than children to experience a gradual progression of symptoms, and supraglottitis will be missed on the initial presentation in up to 50% of adults.3,4 Stridor or respiratory compromise does occur in a minority of adult patients with supraglottitis. The need for artificial airway support (ie, endotracheal intubation, cricothyroidotomy) in adults ranges from 6.6% to 16%.9,10
Making the Diagnosis
The gold standard for diagnosing supraglottitis is direct laryngoscopy.3,4 This point is emphasized in our case report, since the CT scan was concerning for a retropharyngeal abscess, and not supraglottitis. The examination of the oropharynx is generally safer and better tolerated in adults compared to pediatric patients, since airway compromise is much less likely. On occasion, inflammation, erythema, and edema of the epiglottis, aryepiglottic folds, or arytenoid cartilages can be observed.5 More commonly, the supraglottic structures are not visualized, and the posterior oropharynx appears relatively normal. This should serve as a clue for possible supraglottitis.
In suspected cases of adult supraglottitis without emergent airway compromise, lateral soft-tissue radiographs can be obtained to look for the “thumb sign,” indicating a swollen epiglottis. In adult supraglottitis, the width of the epiglottis is usually greater than 8 mm.11 Other abnormal radiographic findings include arytenoid and aryepiglottic fold enlargement, thinning of the airway, and an increase in size of the prevertebral space. Plain film sensitivity rates range from 38% to 98%.
Complete blood count and throat cultures are not particularly helpful in adult cases. Blood cultures, while only about 30% sensitive in adults, should be considered as supraglottitis can result in secondary infection in the central nervous system, lungs, and surrounding structures.3,5
If available, otolaryngology services should be consulted to evaluate the airway, and IV antibiotics, such as a third-generation cephalosporin (eg, ceftriaxone, cefotaxime), should be initiated to include coverage of Hib.3 If methicillin-resistant S aureus is a concern, vancomycin should be added. Clindamycin or metronidazole should also be given if anaerobes are suspected.4,7 The location for performing the nasopharyngeal laryngoscopy varies, depending on the patient’s age (ie, pediatric vs adult), severity of symptoms, presence of airway compromise, and local practice and custom.
Advanced imaging studies (CT scan or magnetic resonance imaging) can help identify the presence of an abscess and delineate the extent of the infection, but are not indicated in the early diagnosis and management of suspected adult supraglottitis.4 As our case demonstrates, CT is neither highly sensitive nor specific for the diagnosis of epiglottitis. The role of ultrasound in the evaluation of suspected epiglottitis is still being developed. One recent study compared 15 healthy volunteers with 15 patients diagnosed with epiglottitis by an otolaryngologist using laryngoscopy.12 A statistically significant difference was observed in the anteroposterior diameter of the epiglottis at the midpoint and both lateral edges between the study subjects and healthy volunteers.12 While there was overlap in the ranges for the midpoint, there was no overlap in both lateral edges between the two groups.12
Treatment
The vast majority of adult cases of supraglottitis are managed medically without airway intervention. Patients presenting with a rapid onset of symptoms and in respiratory distress or with stridor, drooling, or cyanosis, should be managed with early airway intervention. The use of corticosteroids is controversial, and has not been proven beneficial in any prospective trials.1-4,6,7,13
Admission to a critical care unit is indicated initially, even in patients who are not intubated, as they can experience delayed airway compromise with progression of the infection and edema.13
Complications
Abscess formation is a serious complication of supraglottitis, is present in up to 30% of cases, and is more likely to be seen in adults than in children.13 Since the adult larynx and surrounding tissues are larger than in children, often the infection is present longer, which allows for an abscess to develop. The risk of abscess formation is increased in patients with DM or those in whom a foreign body is present.
Numerous organisms have been isolated from supraglottic abscesses in adults, and in addition to incision and drainage, antibiotics covering both gram-positive organisms and anaerobes should be initiated.5 The presence of a supraglottic abscess increases the need for emergent intubation.13 In addition, a supraglottic abscess increases the mortality rate to 30%.3 Other complications from supraglottitis include mediastinitis, cervical adenitis, meningitis, and pneumonia.4,5
Conclusion
While the incidence of epiglottitis in the pediatric patient population has fallen, the incidence in adults remains relatively stable. Clinicians should consider supraglottitis in the differential diagnosis of adults presenting with severe sore throat, dysphagia, or stridor. While airway compromise in adults is uncommon, it does occur. Soft-tissue lateral neck radiographs can help make the diagnosis, but the gold standard remains laryngoscopy. All patients should be started on IV antibiotics and admitted to the ICU initially for airway watch.
Case
A 39-year-old woman, previously in good health, presented to the ED with a chief complaint of severe sore throat, which she said had begun approximately 4 hours prior and was rapidly worsening. She thought her voice sounded muffled, and said she was now having difficulty swallowing her saliva. The patient denied fever but did admit to chills. She experienced onset of shortness of breath 30 minutes prior to arrival to the ED.
The patient stated that she was a house painter and had been working in the home of someone who had several dogs. While not previously allergic to animals, the patient was concerned exposure to the dogs might have contributed to her symptoms. Regarding her social history, the patient admitted to daily consumption of beer, but denied smoking cigarettes. She had no known drug allergies.
On physical examination, the patient was afebrile. Her vital signs were: heart rate, 125 beats/min; blood pressure, 137/74 mm Hg; and respiratory rate, 18 breaths/min. Oxygen saturation was 99% on room air. Overall, the patient appeared anxious and exhibited mild inspiratory stridor. Examination of the eyes and ears were normal. There was no obvious inflammation or swelling of the posterior pharynx; the tongue was normal; there was no swelling of the floor of the mouth; and the uvula was midline and without swelling.
The patient was noted to having difficulty handling her secretions. She exhibited full range of motion of her neck. Her trachea was tender upon palpation but without jugular venous distension or lymphadenopathy. The cardiac examination was significant for tachycardia with a regular rhythm and without murmurs, rubs, or gallops; the pulmonary examination was normal except for transmitted upper airway sounds. The patient’s abdominal, dermatological, and neurological examinations were all normal.
Based on the examination findings, the differential diagnosis included allergic reaction, angioedema, epiglottitis, and retropharyngeal abscess. An intravenous (IV) line was placed and blood was drawn for laboratory evaluation, which included a complete blood count, basic metabolic panel (BMP), and a quantitative pregnancy test. Given the patient’s history, the emergency
A portable soft-tissue lateral radiograph of the neck was obtained. Radiology services interpreted the film as showing “prominent prevertebral soft tissues and epiglottis.
At this point, the patient appeared relatively stable and without progression of symptoms. Since there was the possibility of an infectious etiology, she was given piperacillin/tazobactam, 4.5 g IV.
Laboratory evaluation results were significant for an elevated white blood cell count (WBC) of 14.8 ×109/L, but without a left shift; BMP results were within normal limits, and the pregnancy test was negative.
Based on these findings, otolaryngology services were consulted. The consulting otolaryngologist sprayed oxymetazoline and tetracaine into both of the patient’s nostrils and performed a flexible fiberoptic nasopharyngolaryngoscopy. During the procedure, a significant amount of diffuse supraglottic edema was noted, but no posterior pharyngeal wall edema.
Based on the presence of stridor, difficulty managing secretions, and significant amount of supraglottic edema, the patient was taken to the surgical suite for urgent airway control. She was given dexamethasone, 10 mg IV, and after some difficulty, the anesthesiologist orally intubated the patient with a 7.0-mm endotracheal tube. Examination during the procedure noted diffuse supraglottic edema but no other abnormalities.
The patient was transferred to the intensive care unit (ICU) and treated with IV piperacillin/tazobactam and dexamethasone. While in the ICU, the patient became extremely agitated and combative. After further inquiry into the patient’s social history, the patient’s husband reported that his wife drank 12 to 13 beers nightly. The patient required treatment for alcohol withdrawal with IV benzodiazepines, sedation, and physical restraints. By hospital day 9, she was extubated and tolerated fluids by mouth. On hospital day 10, her mental status had returned to baseline, her WBC was within normal limits, and she no longer complained of difficulty swallowing. The patient was discharged home on hospital day 11 with a final diagnosis of supraglottitis and alcohol withdrawal, and she was given a prescription for amoxicillin/clavulanate. Unfortunately, she did not return for her follow-up appointments.
Discussion
While the incidence of pediatric epiglottitis has decreased since the introduction of the Haemophilus influenzae type b (Hib) vaccine in 1985, adult epiglottitis continues to represent a potentially life-threatening condition whose incidence has remained constant over the past several decades.1,2 The incidence of supraglottitis in adults is now 2.5 times greater than the incidence in children.3,4
Several important differences exist in the presentation and management of adults who present with inflammation of the epiglottis as compared to children. Children commonly present with an acute onset of symptoms, and due to their smaller and more pliant airway anatomy, they often experience stridor and respiratory distress.3,5 The inflammation in children is typically confined to the epiglottis and aryepiglottic folds, while in adults the inflammation can affect not only the epiglottis, but also supraglottic structures such as the pharynx, uvula, and aryepiglottic folds. For this reason, in adults the condition is often referred to as “supraglottitis.”2,6 Adults with supraglottitis most likely present in their 30s, 40s, and 50s, while children present between the ages of 2 and 5 years old.1,3,7 In adults, men more commonly present with supraglottitis than women.1,2 Cigarette smokers and patients with hypertension, diabetes mellitus (DM), chronic obstructive pulmonary disease, or human immunodeficiency virus/AIDS are at increased risk for supraglottitis.3,4 The mortality rate for adults with supraglottitis ranges from 1.2% to 7.1%.3
Etiology
Prior to the use of the Hib vaccine, Hib was the most common cause of epiglottitis, and remains so for children.1 Currently, the most common cause of supraglottitis in adults is Group A beta-hemolytic Streptococci.2 Other etiologies include other bacteria (Haemophilus influenzae, Streptococcus pneumoniae, Staphylococcus aureus, Pseudomonas species, Klebsiella pneumoniae, Pasteurella multocida, Neisseria species), viruses (herpes simplex, varicella, parainfluenza), trauma, and thermal injuries.1,4,5,8
Signs and Symptoms
Throat pain, dysphagia, odynophagia, and muffled voice are common complaints of adults presenting to the ED with supraglottitis.2,7 Fever is usually, but not always, present; the complaint of cough, however, is rare.2,3,4 Other less frequent complaints include hoarseness and drooling. Adults can also present with cervical lymphadenopathy, anterior neck tenderness, and cellulitis of the neck and chest.2,4 In general, the more severe cases will progress rapidly over a few hours. Due to the larger anatomy in adults, they are more likely than children to experience a gradual progression of symptoms, and supraglottitis will be missed on the initial presentation in up to 50% of adults.3,4 Stridor or respiratory compromise does occur in a minority of adult patients with supraglottitis. The need for artificial airway support (ie, endotracheal intubation, cricothyroidotomy) in adults ranges from 6.6% to 16%.9,10
Making the Diagnosis
The gold standard for diagnosing supraglottitis is direct laryngoscopy.3,4 This point is emphasized in our case report, since the CT scan was concerning for a retropharyngeal abscess, and not supraglottitis. The examination of the oropharynx is generally safer and better tolerated in adults compared to pediatric patients, since airway compromise is much less likely. On occasion, inflammation, erythema, and edema of the epiglottis, aryepiglottic folds, or arytenoid cartilages can be observed.5 More commonly, the supraglottic structures are not visualized, and the posterior oropharynx appears relatively normal. This should serve as a clue for possible supraglottitis.
In suspected cases of adult supraglottitis without emergent airway compromise, lateral soft-tissue radiographs can be obtained to look for the “thumb sign,” indicating a swollen epiglottis. In adult supraglottitis, the width of the epiglottis is usually greater than 8 mm.11 Other abnormal radiographic findings include arytenoid and aryepiglottic fold enlargement, thinning of the airway, and an increase in size of the prevertebral space. Plain film sensitivity rates range from 38% to 98%.
Complete blood count and throat cultures are not particularly helpful in adult cases. Blood cultures, while only about 30% sensitive in adults, should be considered as supraglottitis can result in secondary infection in the central nervous system, lungs, and surrounding structures.3,5
If available, otolaryngology services should be consulted to evaluate the airway, and IV antibiotics, such as a third-generation cephalosporin (eg, ceftriaxone, cefotaxime), should be initiated to include coverage of Hib.3 If methicillin-resistant S aureus is a concern, vancomycin should be added. Clindamycin or metronidazole should also be given if anaerobes are suspected.4,7 The location for performing the nasopharyngeal laryngoscopy varies, depending on the patient’s age (ie, pediatric vs adult), severity of symptoms, presence of airway compromise, and local practice and custom.
Advanced imaging studies (CT scan or magnetic resonance imaging) can help identify the presence of an abscess and delineate the extent of the infection, but are not indicated in the early diagnosis and management of suspected adult supraglottitis.4 As our case demonstrates, CT is neither highly sensitive nor specific for the diagnosis of epiglottitis. The role of ultrasound in the evaluation of suspected epiglottitis is still being developed. One recent study compared 15 healthy volunteers with 15 patients diagnosed with epiglottitis by an otolaryngologist using laryngoscopy.12 A statistically significant difference was observed in the anteroposterior diameter of the epiglottis at the midpoint and both lateral edges between the study subjects and healthy volunteers.12 While there was overlap in the ranges for the midpoint, there was no overlap in both lateral edges between the two groups.12
Treatment
The vast majority of adult cases of supraglottitis are managed medically without airway intervention. Patients presenting with a rapid onset of symptoms and in respiratory distress or with stridor, drooling, or cyanosis, should be managed with early airway intervention. The use of corticosteroids is controversial, and has not been proven beneficial in any prospective trials.1-4,6,7,13
Admission to a critical care unit is indicated initially, even in patients who are not intubated, as they can experience delayed airway compromise with progression of the infection and edema.13
Complications
Abscess formation is a serious complication of supraglottitis, is present in up to 30% of cases, and is more likely to be seen in adults than in children.13 Since the adult larynx and surrounding tissues are larger than in children, often the infection is present longer, which allows for an abscess to develop. The risk of abscess formation is increased in patients with DM or those in whom a foreign body is present.
Numerous organisms have been isolated from supraglottic abscesses in adults, and in addition to incision and drainage, antibiotics covering both gram-positive organisms and anaerobes should be initiated.5 The presence of a supraglottic abscess increases the need for emergent intubation.13 In addition, a supraglottic abscess increases the mortality rate to 30%.3 Other complications from supraglottitis include mediastinitis, cervical adenitis, meningitis, and pneumonia.4,5
Conclusion
While the incidence of epiglottitis in the pediatric patient population has fallen, the incidence in adults remains relatively stable. Clinicians should consider supraglottitis in the differential diagnosis of adults presenting with severe sore throat, dysphagia, or stridor. While airway compromise in adults is uncommon, it does occur. Soft-tissue lateral neck radiographs can help make the diagnosis, but the gold standard remains laryngoscopy. All patients should be started on IV antibiotics and admitted to the ICU initially for airway watch.
1. Glynn F, Fenton JE. Diagnosis and management of supraglottitis (epiglottitis). Curr Infect Dis Rep. 2008;10(3):200-204.
2. Lichtor JL, Roche Rodriguez M, Aaronson NL, Spock T, Goodman TR, Baum ED. Epiglottitis: It hasn’t gone away. Anesthesiology. 2016;124(6):1404-1407. doi: 10.1097/ALN.0000000000001125.
3. Westerhuis B, Bietz MG, Lindemann J. Acute epiglottitis in adults: an under-recognized and life-threatening condition. S D Med. 2013;66(8):309-311, 313.
4. Al-Qudah M, Shetty S, Alomari M, Alqdah M. Acute adult supraglottitis: Current management and treatment. South Med J. 2010;103(8):800-804. doi: 10.1097/SMJ.0b013e3181e538d8.
5. Verbruggen K, Halewyck S, Deron P, Foulon I, Gordts F. Epiglottitis and related complications in adults. Case reports and review of the literature. B-ENT. 2012;8(2):143-148.
6. Mayo-Smith MF, Spinale JW, Donskey CJ, Yukawa M, Li RH, Schiffman FJ. Acute epiglottitis. An 18-year experience in Rhode Island. Chest. 1995;108(6):1640-1647.
7. Bizaki AJ, Numminen J, Vasama JP, Laranne J, Rautiainen M. Acute supraglottitis in adults in Finland: review and analysis of 308 cases. Laryngoscope. 2011;121(10):2107-2113. doi: 10.1002/lary.22147.
8. Charles R, Fadden M, Brook J. Acute epiglottitis. BMJ. 2013;347:f5235. doi: 10.1136/bmj.f5235.
9. Ng HL, Sin LM, Li MF, Que TL, Anandaciva S. Acute epiglottitis in adults: a retrospective review of 106 patients in Hong Kong. Emerg Med J. 2008;25(5):253-255. doi: 10.1136/emj.2007.050153.
10. Solomon P, Weisbrod M, Irish JC, Gullane PJ. Adult epiglottitis: the Toronto Hospital experience. J Otolaryngol. 1998;27(6):332-336.
11. Schumaker HM, Doris PE, Birnbaum G. Radiographic parameters in adult epiglottitis. Ann Emerg Med. 1984;13(8):588-590.
12. Ko DR, Chung YE, Park I, et al. Use of bedside sonography for diagnosing acute epiglottitis in the emergency department: a preliminary study. J Ultrasound Med. 2012;31(1):19-22.
13. Berger G, Landau T, Berger S, Finkelstein Y, Bernheim J, Ophir D. The rising incidence of adult acute epiglottitis and epiglottic abscess. Am J Otolaryngol. 2003;24(6):374-383.
1. Glynn F, Fenton JE. Diagnosis and management of supraglottitis (epiglottitis). Curr Infect Dis Rep. 2008;10(3):200-204.
2. Lichtor JL, Roche Rodriguez M, Aaronson NL, Spock T, Goodman TR, Baum ED. Epiglottitis: It hasn’t gone away. Anesthesiology. 2016;124(6):1404-1407. doi: 10.1097/ALN.0000000000001125.
3. Westerhuis B, Bietz MG, Lindemann J. Acute epiglottitis in adults: an under-recognized and life-threatening condition. S D Med. 2013;66(8):309-311, 313.
4. Al-Qudah M, Shetty S, Alomari M, Alqdah M. Acute adult supraglottitis: Current management and treatment. South Med J. 2010;103(8):800-804. doi: 10.1097/SMJ.0b013e3181e538d8.
5. Verbruggen K, Halewyck S, Deron P, Foulon I, Gordts F. Epiglottitis and related complications in adults. Case reports and review of the literature. B-ENT. 2012;8(2):143-148.
6. Mayo-Smith MF, Spinale JW, Donskey CJ, Yukawa M, Li RH, Schiffman FJ. Acute epiglottitis. An 18-year experience in Rhode Island. Chest. 1995;108(6):1640-1647.
7. Bizaki AJ, Numminen J, Vasama JP, Laranne J, Rautiainen M. Acute supraglottitis in adults in Finland: review and analysis of 308 cases. Laryngoscope. 2011;121(10):2107-2113. doi: 10.1002/lary.22147.
8. Charles R, Fadden M, Brook J. Acute epiglottitis. BMJ. 2013;347:f5235. doi: 10.1136/bmj.f5235.
9. Ng HL, Sin LM, Li MF, Que TL, Anandaciva S. Acute epiglottitis in adults: a retrospective review of 106 patients in Hong Kong. Emerg Med J. 2008;25(5):253-255. doi: 10.1136/emj.2007.050153.
10. Solomon P, Weisbrod M, Irish JC, Gullane PJ. Adult epiglottitis: the Toronto Hospital experience. J Otolaryngol. 1998;27(6):332-336.
11. Schumaker HM, Doris PE, Birnbaum G. Radiographic parameters in adult epiglottitis. Ann Emerg Med. 1984;13(8):588-590.
12. Ko DR, Chung YE, Park I, et al. Use of bedside sonography for diagnosing acute epiglottitis in the emergency department: a preliminary study. J Ultrasound Med. 2012;31(1):19-22.
13. Berger G, Landau T, Berger S, Finkelstein Y, Bernheim J, Ophir D. The rising incidence of adult acute epiglottitis and epiglottic abscess. Am J Otolaryngol. 2003;24(6):374-383.
Nontraumatic Splenic Rupture
Case
A 25-year-old college student presented to the ED following a near-syncopal episode. The patient stated he had felt lightheaded and had fallen to his knees immediately after taking a shower earlier that morning, but did not experience any loss of consciousness or injury. He denied a history of syncope or any recent trauma or fatigue. A review of the patient’s systems was negative. His medical history was remarkable for irritable bowel syndrome; he had no surgical history. Regarding his social history, he admitted to occasional alcohol use but denied any tobacco or illicit drug use. He was not on any current prescription or over-the-counter medications and denied any allergies.
The patient’s initial vital signs at presentation were: blood pressure, 112/58 mm Hg; heart rate, 86 beats/min; temperature, 97.9°F; and respiratory rate, 18 breaths/min. Oxygen saturation was 100% on room air. The patient reported pain in his left shoulder, epigastric region, and right flank. He rated his pain as a “4” on a 0-to-10 pain scale.
On physical examination, the patient was alert and oriented; he was thin and had mild pallor. His head, eyes, ears, nose, and throat; cardiac; pulmonary; and neurological examinations were normal. The abdominal examination revealed a soft, minimally tender epigastrium but with normal bowel sounds. Initial laboratory studies were remarkable for low hemoglobin (Hgb; 12.0 g/dL) and elevated aspartate transaminase (105 U/L), alanine aminotransferase (168 U/L), total bilirubin (1.6 mg/dL), and glucose (179 mg/dL) levels. The patient’s troponin I and lipase levels were within normal range. An electrocardiogram was unremarkable.
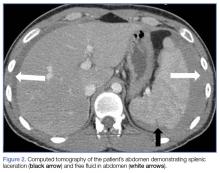
Given the patient’s elevated hepatic enzymes, right upper quadrant ultrasound was obtained, which demonstrated a normal gallbladder, a moderate amount of complicated free fluid (with hyper-echoic densities suggestive of coagulated blood) in all four quadrants, and splenomegaly measuring 13.7 cm (Figure 1a and 1b).
The patient’s status, including his vital signs, remained stable throughout his entire ED course. However, repeat laboratory studies taken 4 hours aft
Positive:
- Epstein-Barr virus (EBV)
- Viral capsid antigen (VCA) immunoglobulin G
- VCA immunoglobulin M
Negative:
- Mononuclear spot test
- Human immunodeficiency virus
- Hepatitis B and C
- Antinuclear antibodies
- Venereal disease research laboratory test
The rest of the patient’s recovery was uneventful, and he was discharged home in stable condition on hospital day 3.
Discussion
Although the spleen is the most common intra-abdominal organ that can rupture with blunt abdominal trauma, splenic rupture in the absence of trauma is very rare. Nontraumatic splenic rupture (NSR) has been associated with pathological and nonpathological spleens.1,2 A systemic review of NSRs showed that 7% of the 845 patients in the review had completely normal spleens; the remaining 93% had some form of splenic pathology.1
Etiology
The top three causes of splenic enlargement associated with NSR include hematologic malignancies, viral infections, and inflammation.1,2 Although viruses, such as EBV and cytomegalovirus, represent almost 15% of the pathological causes of NSR, it is not uncommon for a patient to have multiple pathological processes present.1 Our patient’s enlarged spleen was due to acute infectious mononucleosis.
Signs and Symptoms
Diagnosing NSR can be challenging and it is often missed or discovered incidentally during evaluation (as was initially the case with our patient).3 Several signs and symptoms present in our patient were red herrings that warranted closer analysis. The patient’s complaint of left shoulder pain suggested left hemidiaphragm irritation from the NSR. Furthermore, our patient’s near-syncopal episode was possibly due to acute vagal simulation from the initial contact of blood with the peritoneal cavity.4 The maximal vagal stimulus was likely transient, as our patient returned to baseline after a brief near-syncopal episode.
As illustrated in our case, though tachycardia is common in splenic rupture, not all patients present with this sign. The absence of tachycardia in our patient can be explained by the elevation of his baseline enteric vagal tone due to the continued presence of blood in the peritoneum.5 There are also other factors associated with the absence of tachycardia. For example, a well-conditioned athlete presenting with states of shock due to splenic rupture may not show signs of tachycardia.6
San Francisco Syncope Rule
The San Francisco Syncope Rule (SFSR) is a clinical decision-making risk-stratification tool used to determine outcomes and disposition of ED patients presenting with syncope.7 It is important to note that if we had used a straightforward application of the SFSR upon our patient’s initial presentation, the results would have been negative, suggesting he was not at risk for short-term serious outcomes.7
Imaging Studies
As demonstrated in our patient, a quick point-of-care (POC) bedside ultrasound scan can reveal the presence of free fluid in the abdomen to help with the diagnosis. On ultrasound, the presence of free fluid in the right upper quadrant is more commonly found in the hepatorenal recess, whereas in the left upper quadrant free fluid is seen sub-diaphragmatic/suprasplenic first before fluid is seen in the splenorenal recess. Bedside ultrasound can accurately detect as little as 100 mL of free fluid in the abdominal cavity, with a 90% sensitivity and 99% specificity.8
An ultrasound is highly sensitive as a preliminary screening tool to identify the presence of free intraperitoneal fluid and has some limited utility in identifying any disruption in the splenic echotexture that may suggest a laceration or hematoma. Ultrasound, however, has poor specificity in identifying solid organ injuries.9
Computed tomography scanning is the imaging modality of choice for assessing splenic injuries, and should be obtained to confirm the presence of a solid organ injury, as well as to grade the degree of injury and thereby determine the need for surgical intervention.10 It is worth noting that in a hemodynamically unstable patient, exploratory laparotomy may be embarked upon without a CT scan and positive free fluid on ultrasound.
Splenic Injury Scale
Splenic injury is classified on a scale of 1 (mild injury) to 5 (severe injury) (Table).11
Conclusion
This case illustrates an uncommon presentation of NSR and underscores the importance of considering NSR in the differential diagnoses of patients presenting with abdominal pain—a sign with such a broad differential that NSR could easily be missed during evaluation. Based on its high sensitivity and specificity in detecting the presence of free fluid in the abdominal cavity, POC ultrasound imaging should be used to evaluate patients presenting with abdominal pain and syncopal or near-syncopal symptoms. This case further demonstrates that the absence of tachycardia or signs of shock should not rule out NSR.
1. Renzulli P, Hostettler A, Schoepfer AM, Gloor B, Candinas D. Systematic review of atraumatic splenic rupture. Br J Surg. 2009;96(10):1114-1121. doi: 10.1002/bjs.6737.
2. Aubrey-Bassler FK, Sowers N. 613 cases of splenic rupture without risk factors or previously diagnosed disease: a systematic review. BMC Emerg Med. 2012;12:11. doi: 10.1186/1471-227X-12-11.
3. Schattner A, Meital A, Mavor E. Red-flag syncope: spontaneous splenic rupture. Am J Med. 2014;127(6):501-502. doi: 10.1016/j.amjmed.2014.02.024.
4. Moya A, Sutton R, Ammirati F, et al; Task Force for the Diagnosis and Management of Syncope; European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA); Heart Failure Association (HFA); Heart Rhythm Society (HRS). Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J. 2009;30(21):2631-2671. doi: 10.1093/eurheartj/ehp298.
5. Rana MS, Khalid U, Law S. Paradoxical bradycardia in a patient with haemorrhagic shock secondary to blunt abdominal trauma. BMJ Case Rep. 2010;2010. doi: 10.1136/bcr.04.2010.2872.
6. Kiss O, Sydó N, Vargha P, et al. Prevalence of physiological and pathological electrocardiographic findings in Hungarian athletes. Acta Physiol Hung. 2015;102(2):228-237. doi: 10.1556/036.102.2015.2.13.
7. Quinn JV, Stiell IG, McDermott DA, Sellers KL, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med. 2004;43(2):224-232.
8. Ma OJ, Mateer JR, Ogata M, Kefer MP, Wittmann D, Aprahamian C. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995;38(6):879-885.
9. Kendall JL, Faragher J, Hewitt GJ, Burcham G, Haukoos JS. Emergency Department Ultrasound Is not a Sensitive Detector of Solid Organ Injury. West J Emerg Med. 2009;10(1):1-5.
10. Hassan R, Abd Aziz A, Md Ralib AR, Saat A. Computed tomography of blunt spleen injury: a pictorial review. Malays J Med Sci. 2011;18(1):60-67.
11. Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision). J Trauma. 1995;38(3):323-324.
12. Cirocchi R, Boselli C, Corsi A, et al. Is non-operative management safe and effective for all splenic blunt trauma? A systematic review. Crit Care. 2013;17(5):R185. doi: 10.1186/cc12868.
Case
A 25-year-old college student presented to the ED following a near-syncopal episode. The patient stated he had felt lightheaded and had fallen to his knees immediately after taking a shower earlier that morning, but did not experience any loss of consciousness or injury. He denied a history of syncope or any recent trauma or fatigue. A review of the patient’s systems was negative. His medical history was remarkable for irritable bowel syndrome; he had no surgical history. Regarding his social history, he admitted to occasional alcohol use but denied any tobacco or illicit drug use. He was not on any current prescription or over-the-counter medications and denied any allergies.
The patient’s initial vital signs at presentation were: blood pressure, 112/58 mm Hg; heart rate, 86 beats/min; temperature, 97.9°F; and respiratory rate, 18 breaths/min. Oxygen saturation was 100% on room air. The patient reported pain in his left shoulder, epigastric region, and right flank. He rated his pain as a “4” on a 0-to-10 pain scale.
On physical examination, the patient was alert and oriented; he was thin and had mild pallor. His head, eyes, ears, nose, and throat; cardiac; pulmonary; and neurological examinations were normal. The abdominal examination revealed a soft, minimally tender epigastrium but with normal bowel sounds. Initial laboratory studies were remarkable for low hemoglobin (Hgb; 12.0 g/dL) and elevated aspartate transaminase (105 U/L), alanine aminotransferase (168 U/L), total bilirubin (1.6 mg/dL), and glucose (179 mg/dL) levels. The patient’s troponin I and lipase levels were within normal range. An electrocardiogram was unremarkable.
Given the patient’s elevated hepatic enzymes, right upper quadrant ultrasound was obtained, which demonstrated a normal gallbladder, a moderate amount of complicated free fluid (with hyper-echoic densities suggestive of coagulated blood) in all four quadrants, and splenomegaly measuring 13.7 cm (Figure 1a and 1b).
The patient’s status, including his vital signs, remained stable throughout his entire ED course. However, repeat laboratory studies taken 4 hours aft
Positive:
- Epstein-Barr virus (EBV)
- Viral capsid antigen (VCA) immunoglobulin G
- VCA immunoglobulin M
Negative:
- Mononuclear spot test
- Human immunodeficiency virus
- Hepatitis B and C
- Antinuclear antibodies
- Venereal disease research laboratory test
The rest of the patient’s recovery was uneventful, and he was discharged home in stable condition on hospital day 3.
Discussion
Although the spleen is the most common intra-abdominal organ that can rupture with blunt abdominal trauma, splenic rupture in the absence of trauma is very rare. Nontraumatic splenic rupture (NSR) has been associated with pathological and nonpathological spleens.1,2 A systemic review of NSRs showed that 7% of the 845 patients in the review had completely normal spleens; the remaining 93% had some form of splenic pathology.1
Etiology
The top three causes of splenic enlargement associated with NSR include hematologic malignancies, viral infections, and inflammation.1,2 Although viruses, such as EBV and cytomegalovirus, represent almost 15% of the pathological causes of NSR, it is not uncommon for a patient to have multiple pathological processes present.1 Our patient’s enlarged spleen was due to acute infectious mononucleosis.
Signs and Symptoms
Diagnosing NSR can be challenging and it is often missed or discovered incidentally during evaluation (as was initially the case with our patient).3 Several signs and symptoms present in our patient were red herrings that warranted closer analysis. The patient’s complaint of left shoulder pain suggested left hemidiaphragm irritation from the NSR. Furthermore, our patient’s near-syncopal episode was possibly due to acute vagal simulation from the initial contact of blood with the peritoneal cavity.4 The maximal vagal stimulus was likely transient, as our patient returned to baseline after a brief near-syncopal episode.
As illustrated in our case, though tachycardia is common in splenic rupture, not all patients present with this sign. The absence of tachycardia in our patient can be explained by the elevation of his baseline enteric vagal tone due to the continued presence of blood in the peritoneum.5 There are also other factors associated with the absence of tachycardia. For example, a well-conditioned athlete presenting with states of shock due to splenic rupture may not show signs of tachycardia.6
San Francisco Syncope Rule
The San Francisco Syncope Rule (SFSR) is a clinical decision-making risk-stratification tool used to determine outcomes and disposition of ED patients presenting with syncope.7 It is important to note that if we had used a straightforward application of the SFSR upon our patient’s initial presentation, the results would have been negative, suggesting he was not at risk for short-term serious outcomes.7
Imaging Studies
As demonstrated in our patient, a quick point-of-care (POC) bedside ultrasound scan can reveal the presence of free fluid in the abdomen to help with the diagnosis. On ultrasound, the presence of free fluid in the right upper quadrant is more commonly found in the hepatorenal recess, whereas in the left upper quadrant free fluid is seen sub-diaphragmatic/suprasplenic first before fluid is seen in the splenorenal recess. Bedside ultrasound can accurately detect as little as 100 mL of free fluid in the abdominal cavity, with a 90% sensitivity and 99% specificity.8
An ultrasound is highly sensitive as a preliminary screening tool to identify the presence of free intraperitoneal fluid and has some limited utility in identifying any disruption in the splenic echotexture that may suggest a laceration or hematoma. Ultrasound, however, has poor specificity in identifying solid organ injuries.9
Computed tomography scanning is the imaging modality of choice for assessing splenic injuries, and should be obtained to confirm the presence of a solid organ injury, as well as to grade the degree of injury and thereby determine the need for surgical intervention.10 It is worth noting that in a hemodynamically unstable patient, exploratory laparotomy may be embarked upon without a CT scan and positive free fluid on ultrasound.
Splenic Injury Scale
Splenic injury is classified on a scale of 1 (mild injury) to 5 (severe injury) (Table).11
Conclusion
This case illustrates an uncommon presentation of NSR and underscores the importance of considering NSR in the differential diagnoses of patients presenting with abdominal pain—a sign with such a broad differential that NSR could easily be missed during evaluation. Based on its high sensitivity and specificity in detecting the presence of free fluid in the abdominal cavity, POC ultrasound imaging should be used to evaluate patients presenting with abdominal pain and syncopal or near-syncopal symptoms. This case further demonstrates that the absence of tachycardia or signs of shock should not rule out NSR.
Case
A 25-year-old college student presented to the ED following a near-syncopal episode. The patient stated he had felt lightheaded and had fallen to his knees immediately after taking a shower earlier that morning, but did not experience any loss of consciousness or injury. He denied a history of syncope or any recent trauma or fatigue. A review of the patient’s systems was negative. His medical history was remarkable for irritable bowel syndrome; he had no surgical history. Regarding his social history, he admitted to occasional alcohol use but denied any tobacco or illicit drug use. He was not on any current prescription or over-the-counter medications and denied any allergies.
The patient’s initial vital signs at presentation were: blood pressure, 112/58 mm Hg; heart rate, 86 beats/min; temperature, 97.9°F; and respiratory rate, 18 breaths/min. Oxygen saturation was 100% on room air. The patient reported pain in his left shoulder, epigastric region, and right flank. He rated his pain as a “4” on a 0-to-10 pain scale.
On physical examination, the patient was alert and oriented; he was thin and had mild pallor. His head, eyes, ears, nose, and throat; cardiac; pulmonary; and neurological examinations were normal. The abdominal examination revealed a soft, minimally tender epigastrium but with normal bowel sounds. Initial laboratory studies were remarkable for low hemoglobin (Hgb; 12.0 g/dL) and elevated aspartate transaminase (105 U/L), alanine aminotransferase (168 U/L), total bilirubin (1.6 mg/dL), and glucose (179 mg/dL) levels. The patient’s troponin I and lipase levels were within normal range. An electrocardiogram was unremarkable.
Given the patient’s elevated hepatic enzymes, right upper quadrant ultrasound was obtained, which demonstrated a normal gallbladder, a moderate amount of complicated free fluid (with hyper-echoic densities suggestive of coagulated blood) in all four quadrants, and splenomegaly measuring 13.7 cm (Figure 1a and 1b).
The patient’s status, including his vital signs, remained stable throughout his entire ED course. However, repeat laboratory studies taken 4 hours aft
Positive:
- Epstein-Barr virus (EBV)
- Viral capsid antigen (VCA) immunoglobulin G
- VCA immunoglobulin M
Negative:
- Mononuclear spot test
- Human immunodeficiency virus
- Hepatitis B and C
- Antinuclear antibodies
- Venereal disease research laboratory test
The rest of the patient’s recovery was uneventful, and he was discharged home in stable condition on hospital day 3.
Discussion
Although the spleen is the most common intra-abdominal organ that can rupture with blunt abdominal trauma, splenic rupture in the absence of trauma is very rare. Nontraumatic splenic rupture (NSR) has been associated with pathological and nonpathological spleens.1,2 A systemic review of NSRs showed that 7% of the 845 patients in the review had completely normal spleens; the remaining 93% had some form of splenic pathology.1
Etiology
The top three causes of splenic enlargement associated with NSR include hematologic malignancies, viral infections, and inflammation.1,2 Although viruses, such as EBV and cytomegalovirus, represent almost 15% of the pathological causes of NSR, it is not uncommon for a patient to have multiple pathological processes present.1 Our patient’s enlarged spleen was due to acute infectious mononucleosis.
Signs and Symptoms
Diagnosing NSR can be challenging and it is often missed or discovered incidentally during evaluation (as was initially the case with our patient).3 Several signs and symptoms present in our patient were red herrings that warranted closer analysis. The patient’s complaint of left shoulder pain suggested left hemidiaphragm irritation from the NSR. Furthermore, our patient’s near-syncopal episode was possibly due to acute vagal simulation from the initial contact of blood with the peritoneal cavity.4 The maximal vagal stimulus was likely transient, as our patient returned to baseline after a brief near-syncopal episode.
As illustrated in our case, though tachycardia is common in splenic rupture, not all patients present with this sign. The absence of tachycardia in our patient can be explained by the elevation of his baseline enteric vagal tone due to the continued presence of blood in the peritoneum.5 There are also other factors associated with the absence of tachycardia. For example, a well-conditioned athlete presenting with states of shock due to splenic rupture may not show signs of tachycardia.6
San Francisco Syncope Rule
The San Francisco Syncope Rule (SFSR) is a clinical decision-making risk-stratification tool used to determine outcomes and disposition of ED patients presenting with syncope.7 It is important to note that if we had used a straightforward application of the SFSR upon our patient’s initial presentation, the results would have been negative, suggesting he was not at risk for short-term serious outcomes.7
Imaging Studies
As demonstrated in our patient, a quick point-of-care (POC) bedside ultrasound scan can reveal the presence of free fluid in the abdomen to help with the diagnosis. On ultrasound, the presence of free fluid in the right upper quadrant is more commonly found in the hepatorenal recess, whereas in the left upper quadrant free fluid is seen sub-diaphragmatic/suprasplenic first before fluid is seen in the splenorenal recess. Bedside ultrasound can accurately detect as little as 100 mL of free fluid in the abdominal cavity, with a 90% sensitivity and 99% specificity.8
An ultrasound is highly sensitive as a preliminary screening tool to identify the presence of free intraperitoneal fluid and has some limited utility in identifying any disruption in the splenic echotexture that may suggest a laceration or hematoma. Ultrasound, however, has poor specificity in identifying solid organ injuries.9
Computed tomography scanning is the imaging modality of choice for assessing splenic injuries, and should be obtained to confirm the presence of a solid organ injury, as well as to grade the degree of injury and thereby determine the need for surgical intervention.10 It is worth noting that in a hemodynamically unstable patient, exploratory laparotomy may be embarked upon without a CT scan and positive free fluid on ultrasound.
Splenic Injury Scale
Splenic injury is classified on a scale of 1 (mild injury) to 5 (severe injury) (Table).11
Conclusion
This case illustrates an uncommon presentation of NSR and underscores the importance of considering NSR in the differential diagnoses of patients presenting with abdominal pain—a sign with such a broad differential that NSR could easily be missed during evaluation. Based on its high sensitivity and specificity in detecting the presence of free fluid in the abdominal cavity, POC ultrasound imaging should be used to evaluate patients presenting with abdominal pain and syncopal or near-syncopal symptoms. This case further demonstrates that the absence of tachycardia or signs of shock should not rule out NSR.
1. Renzulli P, Hostettler A, Schoepfer AM, Gloor B, Candinas D. Systematic review of atraumatic splenic rupture. Br J Surg. 2009;96(10):1114-1121. doi: 10.1002/bjs.6737.
2. Aubrey-Bassler FK, Sowers N. 613 cases of splenic rupture without risk factors or previously diagnosed disease: a systematic review. BMC Emerg Med. 2012;12:11. doi: 10.1186/1471-227X-12-11.
3. Schattner A, Meital A, Mavor E. Red-flag syncope: spontaneous splenic rupture. Am J Med. 2014;127(6):501-502. doi: 10.1016/j.amjmed.2014.02.024.
4. Moya A, Sutton R, Ammirati F, et al; Task Force for the Diagnosis and Management of Syncope; European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA); Heart Failure Association (HFA); Heart Rhythm Society (HRS). Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J. 2009;30(21):2631-2671. doi: 10.1093/eurheartj/ehp298.
5. Rana MS, Khalid U, Law S. Paradoxical bradycardia in a patient with haemorrhagic shock secondary to blunt abdominal trauma. BMJ Case Rep. 2010;2010. doi: 10.1136/bcr.04.2010.2872.
6. Kiss O, Sydó N, Vargha P, et al. Prevalence of physiological and pathological electrocardiographic findings in Hungarian athletes. Acta Physiol Hung. 2015;102(2):228-237. doi: 10.1556/036.102.2015.2.13.
7. Quinn JV, Stiell IG, McDermott DA, Sellers KL, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med. 2004;43(2):224-232.
8. Ma OJ, Mateer JR, Ogata M, Kefer MP, Wittmann D, Aprahamian C. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995;38(6):879-885.
9. Kendall JL, Faragher J, Hewitt GJ, Burcham G, Haukoos JS. Emergency Department Ultrasound Is not a Sensitive Detector of Solid Organ Injury. West J Emerg Med. 2009;10(1):1-5.
10. Hassan R, Abd Aziz A, Md Ralib AR, Saat A. Computed tomography of blunt spleen injury: a pictorial review. Malays J Med Sci. 2011;18(1):60-67.
11. Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision). J Trauma. 1995;38(3):323-324.
12. Cirocchi R, Boselli C, Corsi A, et al. Is non-operative management safe and effective for all splenic blunt trauma? A systematic review. Crit Care. 2013;17(5):R185. doi: 10.1186/cc12868.
1. Renzulli P, Hostettler A, Schoepfer AM, Gloor B, Candinas D. Systematic review of atraumatic splenic rupture. Br J Surg. 2009;96(10):1114-1121. doi: 10.1002/bjs.6737.
2. Aubrey-Bassler FK, Sowers N. 613 cases of splenic rupture without risk factors or previously diagnosed disease: a systematic review. BMC Emerg Med. 2012;12:11. doi: 10.1186/1471-227X-12-11.
3. Schattner A, Meital A, Mavor E. Red-flag syncope: spontaneous splenic rupture. Am J Med. 2014;127(6):501-502. doi: 10.1016/j.amjmed.2014.02.024.
4. Moya A, Sutton R, Ammirati F, et al; Task Force for the Diagnosis and Management of Syncope; European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA); Heart Failure Association (HFA); Heart Rhythm Society (HRS). Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J. 2009;30(21):2631-2671. doi: 10.1093/eurheartj/ehp298.
5. Rana MS, Khalid U, Law S. Paradoxical bradycardia in a patient with haemorrhagic shock secondary to blunt abdominal trauma. BMJ Case Rep. 2010;2010. doi: 10.1136/bcr.04.2010.2872.
6. Kiss O, Sydó N, Vargha P, et al. Prevalence of physiological and pathological electrocardiographic findings in Hungarian athletes. Acta Physiol Hung. 2015;102(2):228-237. doi: 10.1556/036.102.2015.2.13.
7. Quinn JV, Stiell IG, McDermott DA, Sellers KL, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med. 2004;43(2):224-232.
8. Ma OJ, Mateer JR, Ogata M, Kefer MP, Wittmann D, Aprahamian C. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995;38(6):879-885.
9. Kendall JL, Faragher J, Hewitt GJ, Burcham G, Haukoos JS. Emergency Department Ultrasound Is not a Sensitive Detector of Solid Organ Injury. West J Emerg Med. 2009;10(1):1-5.
10. Hassan R, Abd Aziz A, Md Ralib AR, Saat A. Computed tomography of blunt spleen injury: a pictorial review. Malays J Med Sci. 2011;18(1):60-67.
11. Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision). J Trauma. 1995;38(3):323-324.
12. Cirocchi R, Boselli C, Corsi A, et al. Is non-operative management safe and effective for all splenic blunt trauma? A systematic review. Crit Care. 2013;17(5):R185. doi: 10.1186/cc12868.
Hypertension in the ED
Case Scenarios
Case 1
You had just started your shift, and your first patient presented with symptoms of headache and dizziness, and a blood pressure (BP) of 240/130 mm Hg, without any vomiting or visual symptoms. Physical examination revealed an alert, pleasant 65-year-old black man whose ocular, neurological, and cardiovascular (CV) examinations were normal. The patient reported a history of borderline hypertension, but had never taken any medications for it.
After placing some initial orders, including an electrocardiogram (ECG), basic metabolic panel (BMP), and head computed tomography (CT) scan, and ordering 10 mg intravenous (IV) prochlorperazine and 25 mg IV diphenhydramine to treat the patient’s headache, you are left asking yourself what steps you should take next.
Case 2
Your next patient was a 90-year-old white woman who had been referred to the ED by her primary care physician (PCP) for “hypertensive urgency.” She had no complaints to report. Similar to the first patient, this patient’s physical examination was also normal, with the exception of a persistently elevated BP of 220/140 mm Hg. Her history was significant for congestive heart failure (CHF), but she exhibited no current CV signs or symptoms. The patient had been taking furosemide but was not on any other antihypertensive medications.
Case 3
In the room next to your 90-year-old patient is a 32-year-old uninsured hypertensive white woman. During the history taking, the patient stated that she was trying to become pregnant and was not currently using any form of contraception. Similar to the second patient, she had no complaints to report. Regarding her reason for presentation, the patient stated that when she had her BP checked at a pharmacy earlier that day, the reading was “too high,” and the pharmacist had advised her to go to the ED. She seemed anxious but otherwise well. Her initial BP at presentation was 240/100 mm Hg, but her physical examination was otherwise normal.
Hypertensive Emergencies
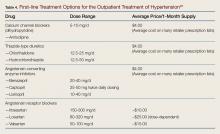
As emergency physicians (EPs), we see hypertensive patients every day. According to the US Centers for Disease Control and Prevention, 33% of American adults have hypertension, which is defined by a BP of ≥140/90 mm Hg (Table 1).
Almost 25% of total annual US adult ED visits are directly or indirectly related to hypertension, and about 1% of all ED visits are due solely to elevated BP.3 In an ambulatory care survey for 2007, moderate or severe hypertensive BP readings were found to be more common in patients presenting to the ED (43.5%) than to primary care clinics (27%).4 Patients presenting to the ED with hypertensive BP readings disproportionately represented patients who were older, male, non-Hispanic black, Medicare beneficiaries, or uninsured. Certainly, some patients presenting to the ED have hypertensive BP readings due to pain or anxiety, but multiple studies have suggested that 50% to 70% of ED patients who have hypertensive BP readings will be diagnosed with hypertension on office follow-up.5,6 While a minority of these patients present to the ED with hypertensive emergencies, the majority present either without symptoms of hypertension or with only mild headache. Given the disease burden of hypertension combined with the benefits of treatment, it is worthwhile for the practicing EP to review the most up-to-date guidelines on outpatient management of hypertension.
When a patient presents to the ED with a hypertensive BP reading, the initial priority of the EP is to exclude hypertensive emergency. Hypertensive emergencies are defined by the presence of hypertension (generally grade 3/severe hypertension with BP ≥180/110 mm Hg; see Table 1) in conjunction with evidence of target organ damage.
Target Organ Manifestations
The acuity and/or presence of target organ damage are not always clear on initial ED evaluation. For instance, when a patient who has no history of primary care presents to the ED with severe hypertension, laboratory evaluation may demonstrate protein and blood in his or her urine and an elevated serum creatinine level. In the absence of values from past laboratory studies, it is difficult to determine whether these test results represent normal laboratory parameters for this patient due to longstanding hypertensive kidney disease (ie, hypertensive nephrosclerosis) or if they represent a true hypertensive emergency, (ie, hypertensive emergency-related nephropathy).7 In patients with severe hypertension and possibly new acute kidney injury, it is probably safest to either assume hypertensive emergency-related nephropathy and to treat accordingly or consult with nephrology services. The picture of hypertensive emergency-related nephropathy often only becomes clear after renal biopsy results and improvement in renal parameters with BP control.
The ocular manifestations of hypertensive emergency require detailed fundoscopy, which at times can be challenging in the ED. In assessing for cardiac target organ damage, at our institution, we typically ask patients if they have experienced symptoms of dyspnea and chest pain or pressure. Generally, we also evaluate cardiac enzymes, B-type natriuretic peptide, and order ECG and chest X-ray studies when suggested by history or physical examination. Alarmingly, a study of 161 ED hypertensive (average BP of 183/109 mm Hg), asymptomatic, predominantly black patients found that 146 (90.7%) had subclinical hypertensive heart disease on point-of-care echocardiogram.8
Neurological/Hypertensive Encephalopathy
Hypertensive encephalopathy is a diagnosis of exclusion as alternate causes of confusion and headache, such as intracranial hemorrhage, are excluded and mental status improves with titrated BP control. Nonetheless, it is difficult to confidently state from the literature that patients who present with headache but have a normal mental status in the presence of severe hypertension are not on an early spectrum of hypertensive encephalopathy. Therefore, it is likely that the degree of symptoms should define whether target organ damage exists, though there is certainly a spectrum of hypertensive emergency—the strict definition of which is not always clear.
When a hypertensive emergency is diagnosed, management typically involves the use of antihypertensive IV medication in the intensive care unit. While such management is outside the scope of this paper, Adebayo and Rogers9 have published an excellent review of the care of hypertensive emergencies.
Asymptomatic Hypertension
The American College of Emergency Physicians (ACEP) has developed two clinical policies on the evaluation and management of asymptomatic hypertension in the ED. The original, published in 2006, advised that initially high BP readings of ED patients should be repeated: two separate high readings are adequate for screening, and those patients with hypertension should be referred for follow-up. Furthermore, ACEP policies note that initiating treatment in the ED is not necessary when patients are referred for follow-up. If treatment for hypertension is initiated in the ED, ACEP recommends that such management should attempt only to gradually lower BP, and not to normalize it during the initial ED visit.10
The 2013 update to ACEP’s clinical policy on managing asymptomatic hypertension expanded on the original policy. The updated policy advised against routine testing for target organ damage in patients who have asymptomatic severe hypertension. However, ACEP policy notes that evaluating serum creatinine in these patients with poor follow-up may influence patient disposition.11
The 2013 policy further stated that medical intervention is not required in ED patients who have asymptomatic severe hypertension, but may be considered in patients with poor follow-up. The policies emphasize that all asymptomatic hypertensive patients should be referred for follow-up. The literature cited for the recommendation that ED patients with asymptomatic severe hypertension do not require routine investigation stems from two observational studies. These studies found that screening asymptomatic ED patients who presented with severe hypertension revealed serum creatinine abnormalities in approximately 6%, which impacted patient disposition, though it was not clear from the study results whether admission correlated to meaningful patient outcomes.12,13
Patient Disposition
Since ACEP’s 2013 clinical policy, a study from the Cleveland Clinic has been published. This retrospective cohort study reviewed 6 years of data looking at all patients in its system with a BP of ≥180/110 mm Hg, and compared those office patients discharged to home to those referred to the ED or directly admitted to the inpatient hospital solely on the basis of severe hypertension.14 The study found that 0.5% of 387 patients referred to the ED by primary care clinics for asymptomatic severe hypertension had confirmed acute kidney injury on BMP.14 The Cleveland Clinic study also found that 2.1% of patients had evidence of target organ damage and 5.5% had any abnormal results.14 In addition, referral to the ED from the clinic for hypertension was associated with a slightly higher rate of major adverse CV events at 7 days (2 of 426 [0.5%] versus 61 of 58,109 [0.1%]; P = .02).14
The results of the Cleveland Clinic study confirm that in the absence of target organ damage, hypertension is probably best managed in the outpatient setting. The European Task Force hypertensive guidelines state “hospitalization for hypertension is regarded as inappropriate in most European countries.”15 However, from 2006 to 2012, 26% of US ED patients with primary diagnoses of hypertension were admitted to the hospital.3 In Canada’s most populous province of Ontario, from 2002 to 2011, approximately 8% of hypertensive patients were admitted.16 Part of this discrepancy may be due to the sometimes ambiguous nature of the presentation of patients with hypertension, making it unclear whether a true hypertensive emergency exists. Many patients perceive visual symptoms, headache, dizziness, and even chest pressure as the result of their elevated BP—without clear findings on fundoscopy, ECG, or cardiac marker testing. Perhaps more of these patients would be discharged if EPs felt comfortable initiating appropriate initial antihypertensive treatment.
Management
Initiating Antihypertensive Treatment
Some EPs may feel that an accurate diagnosis of hypertension requires repeat BP testing in the primary care office setting, and for this reason are reluctant to initiate antihypertensive treatment in the ED. The most recent guidelines by the Joint National Committee (JNC 8) do not address how many BP readings are necessary to diagnose hypertension, but JNC 7 suggested that diagnosis of hypertension requires two separate office visits.17 Evidence cited in ACEP’s first clinical policy states that two separate BP measurements in the ED are adequate for screening—but not necessarily for initiating treatment.10 However, European and British outpatient clinical recommendations advocate initiation of antihypertensive medication for a single visit in patients who have an elevated BP categorized as grade 3/severe hypertension (BP of ≥180/110 mm Hg).15,18 Furthermore, for patients with severe hypertension seen in the ED, as many as 97% are likely to have true hypertension at office follow-up.6 Those ED patients presenting with severe hypertension are very likely to have a true diagnosis of hypertension.
A recent retrospective analysis of a group of hypertensive ED patients by Brody et al19 found that patients prescribed BP medications by an EP were more likely to have improved BP control at follow-up 2 weeks later. In their study, the decision to prescribe antihypertensive medications were at the discretion of the EP. Seventy-six patients were given one or more prescriptions for antihypertensive therapy, compared to a control group of 141 patients who were not given a prescription. On follow-up at 2 weeks, there was an 11 mm Hg greater reduction of BP in the group who received prescriptions compared to the control group. None of the patients in either group on follow-up had experienced any new neurological deficits, ischemic events, life-threatening anaphylactic reactions, or clinically significant hypotension.
The Cleveland Clinic study14 also reported on those patents given who received new prescriptions from the ED. Similar to the study by Brody et al,19 none of the 82 patients discharged to home from the ED with a new antihypertensive prescription had any major adverse event at 30-day follow-up.14
Pharmacological Treatment Recommendations
When choosing to treat patients with new prescriptions for antihypertensives, it is important to follow the most current outpatient treatment recommendations. In 2014, JNC 8 released new guidelines for the outpatient management of adults with hypertension.20 The panel issued recommendations based on its systematic review of randomized controlled trials on antihypertensive treatments. The key recommendations are as follows:
- In patients aged 60 years or older, initiate pharmacological treatment at a BP of ≥150/90 mm Hg.
- In patients aged 18 to 59 years, initiate pharmacological treatment at a BP of ≥140/90 mm Hg.
- In the general nonblack population, initial antihypertensive treatment should include a thiazide-type diuretic, a calcium channel blocker (CCB), an angiotensin-converting enzyme inhibitor (ACE-I), or an angiotensin receptor blocker (ARB).
- In the general black population, initial treatment should include a thiazide-type diuretic or a CCB.
- In patients with chronic kidney disease (CKD) (including black patients), initial (or add-on) antihypertensive treatment should include an ACE-I or ARB to improve kidney outcomes—but not both.
- If goal BP is not reached within 1 month of initial treatment, increase the dose of the initial drug or add a second agent (eg, thiazide-type diuretic, CCB, ACE-I, or ARB). If goal is not reached with two drugs, use the third drug from that list if no contraindications exist, but do not use both an ACE-I and an ARB together in the same patient.
Of note, JNC 8, in departure from JNC 7, no longer recommends beta-blockers as first-line therapy for isolated hypertension (there may be compelling alternate indications, such as atrial fibrillation or postmyocardial infarction (MI), such that a beta-blocker would still be the first medication considered). The reason for this stems from a single randomized controlled trial of 9,193 patients that found that despite equivalent BP reduction, use of a beta-blocker in comparison to an ARB resulted in a higher rate of a composite outcome of death, MI, or stroke.21 The main difference was a 25% relative risk reduction for stroke with use of an ARB (losartan) in comparison to a beta-blocker (atenolol). The most recent European guidelines still include beta-blockers among its first-line recommended BP medications, but do acknowledge that they are not as effective in reducing stroke incidence as other alternative medications.15 The European guidelines otherwise include the same list of first-line agents. The British guidelines mirror JNC 8 in terms of first-line antihypertensive medication choices.18
Since the release of JNC 8, the Systolic Blood Pressure Intervention Trial (SPRINT) has been published, and will likely impact future national recommendations on BP management. The SPRINT study was a randomized controlled trial enrolling over 9,000 hypertensive nondiabetic patients older than age 50 years that treated individuals to a standard BP goal (systolic BP of 140 mm Hg) versus an intensive BP goal (systolic BP of 120 mm Hg) over a 3.5-year period. The trial was stopped early for safety as a 25% mortality reduction was observed in the intensive treatment group (1.65 vs 2.19 deaths/y).22 This was in contrast to previous trials that had mostly failed to show this sort of benefit, though previous trials were smaller in number or included only diabetic patients.23 While it is likely that this trial may influence lowering treatment thresholds from the office, it is not likely to impact care from the ED.
The recommendations of JNC 8 do not necessarily coincide with current US EP practice. In the study by Brody et al,19 of patients provided ED antihypertensive prescriptions, 54% received thiazide-type diuretics, 26% ACE-I, 10% CCBs, and 6% beta-blockers. This is noteworthy because 96% of those in the study were black patients who would benefit most from either a thiazide or a CCB. Another recent study of ED patients showed that of patients who were both treated in the ED and discharged with antihypertensive medications, 34% received a diuretic prescription, 32% clonidine, 15% a beta-blocker, 19% an ARB or ACE-I, 12% a CCB, and 2% hydrazine.24 These results are important because according to many published guidelines, including JNC 8, clonidine is only considered one of several fourth-line options for severe resistant hypertension.15,18,20 Since clonidine use can be complicated by rebound hypertension, it is not an ideal agent to be prescribed de novo to patients in the ED. This is particularly true if these patients are not already on maximum doses of the three most recommended agents previously noted, or if there are concerns over patient compliance.
Of the drug classes recommended by JNC 8, Table 3 lists the absolute and relative contraindications.
In clinical trials, amlodipine is among the most effective BP medications and is considered first-line therapy for all groups of patients with hypertension.15,18,20 A simplistic approach for most patients presenting with severe asymptomatic hypertension (BP of ≥180/110 mm Hg) not currently on treatment would be to recheck the BP and assure it remains elevated over the period of the ED visit.
Conclusion
Hypertension is among the most common medical conditions for which emergency patients seek care. The ACEP clinical policies provide guidance on the appropriate work-up and treatment of these patients. Given the occasional lack of clarity on whether a patient’s presentation is on the spectrum of more acute/serious, EPs may feel more comfortable in discharging patients with poor follow-up if they are able to safely prescribe antihypertensive treatment. Prior to prescribing treatment, EPs should refer to the JNC 8 guidelines to appropriately start antihypertensive treatment in select patient groups in the ED. The guidelines of JNC 8 are therefore worth referring to in order to appropriately start treatment in select patient groups from the ED.
Case Scenarios Continued
Case 1
[The 65-year-old black man who presented with headache and dizziness, and had an initial BP of 240/130 mm Hg.]
After treating the patient with prochlorperazine and diphenhydramine, his headache resolved. His BP improved but remained elevated at 190/120 mm Hg. On further questioning, the patient reported a history of similar headaches and wondered whether it was related to his BP. The head CT scan was negative for any acute hemorrhage, infarct, or mass; the ECG only showed evidence of left ventricular hypertrophy; and the BMP showed normal renal function.
After a long discussion with the patient, you agreed to start him on amlodipine 5 mg/d and referred him for follow-up with a local PCP.
Case 2
[The 90-year-old white woman with a history of CHF and an initial BP of 220/140 mm Hg at presentation.]
The BMP evaluation showed a baseline creatinine level of 1.3 mg/dL. Given this patient’s history of CHF, amlodipine would not be the ideal next agent to prescribe. After discussion with her PCP, you elected to start her on losartan at 25 mg/d, and instructed her to follow-up with her PCP within 1 week.
Case 3
[The 32-year-old white woman who presented at the advice of a pharmacist and had an initial BP of 240/100 mm Hg.]While reviewing the patient’s work-up and history, you noted her plans to become pregnant, and recalled a recent review on BP management, noting the contraindications associated with ARB or ACE-I in pregnancy. Based on the patient’s uninsured status and poor follow-up, you considered prescribing amlodipine. Prior to issuing the prescription, you performed a repeat BP check and noted that the patient’s BP had decreased to 130/85 mm Hg. Given the marked improvement in the patient’s BP during her ED course, you were not convinced that she truly had hypertension.
Instead of prescribing an antihypertensive agent, which may not ultimately benefit this patient, you advised her to seek follow-up care at an outpatient clinic to have her BP rechecked. The patient agreed, and you referred her to a local free clinic.
1. Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011-2012. NCHS Data Brief. 2013;(133):1-8.
2. Turnbull F; Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2013;362(9395):1527-1535.
3. McNaughton CD, Self WH, Zhu Y, Janke AT, Storrow AB, Levy P. Incidence of hypertension-related emergency department visits in the United States, 2006 to 2012. Am J Cardiol. 2015;116(11):1717-1723. doi: 10.1016/j.amjcard.2015.09.007.
4. Niska RW. Blood pressure measurements at emergency department visits by adults: United States, 2007-2008. NCHS Data Brief. 2011;(72):1-8.
5. Chernow SM, Iserson KV, Criss E. Use of the emergency department for hypertension screening: a prospective study. Ann Emerg Med. 1987;16(2):180-182.
6. Backer HD, Decker L, Ackerson L. Reproducibility of increased blood pressure during an emergency department or urgent care visit. Ann Emerg Med. 2003.41(4):507-512.
7. Nonaka K, Ubara Y, Sumida K, et al. Clinical and pathological evaluation of hypertensive emergency-related nephropathy. Intern Med. 2013;52(1):45-53.
8. Levy P, Ye H, Compton S, et al. Subclinical hypertensive heart disease in black patients with elevated blood pressure in an inner-city emergency department. Ann Emerg Med. 2012;60(4):467-474.e1. doi: 10.1016/j.annemergmed.2012.03.030.
9. Adebayo O, Rogers RL. Hypertensive emergencies in the emergency department. Emerg Med Clin North Am. 2015;33(3):539-551. doi: 10.1016/j.emc.2015.04.005.
10. Decker WW, Godwin SA, Hess EP, Lenamond CC, Jagoda AS; American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Asymptomatic Hypertension in the ED. Clinical policy: critical issues in the evaluation and management of adult patients with asymptomatic hypertension in the emergency department. Ann Emerg Med. 2006;47(3):237-234. doi: 10.1016/j.annemergmed.2005.10.003
11. Wolf SJ, Lo B, Shih RD, Smith MD, Fesmire FM; American College of Emergency Physicians Clinical Policies Committee. Clinical policy: critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med. 2013;62(1):59-68. doi: 10.1016/j.annemergmed.2013.05.012.
12. Karras DJ, Kruus LK, Cienki JJ, et al. Evaluation and treatment of patients with severely elevated blood pressure in academic emergency departments: a multicenter study. Ann Emerg Med. 2006;47(3):230-236.
13. Nishijima DK, Paladino L, Sinert R. Routine testing in patients with asymptomatic elevated blood pressure in the ED. Am J Emerg Med. 2010;28(2):235-242. doi: 10.1016/j.ajem.2008.11.015.
14. Patel KK, Young L, Howell EH, et al. Characteristics and outcomes of patients presenting with hypertensive urgency in the office setting. JAMA Intern Med. 2016;176(7):981-988. doi: 10.1001/jamainternmed.2016.1509.
15. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159-2219. doi: 10.1093/eurheartj/eht151.
16. Masood S, Austin PC, Atzema CL. A population-based analysis of outcomes in patients with a primary diagnosis of hypertension in the emergency department. Ann Emerg Med. 2016;68(3):258-267.e5. doi: 10.1016/j.annemergmed.2016.04.060.
17. Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560-2572. Erratum in: JAMA. 2003;290(2):197.
18. Krause T, Lovibond K, Caulfield M, McCormack T, Williams B; Guideline Development Group. Management of hypertension: summary of NICE guidance. BMJ. 2011;343:d4891. doi: 10.1136/bmj.d4891.
19. Brody A, Rahman T, Reed B, et al. Safety and efficacy of antihypertensive prescription at emergency department discharge. Acad Emerg Med. 2015;22(5):632-635. doi: 10.1111/acem.12660.
20. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520. doi: 10.1001/jama.2013.284427. Erratum in: JAMA. 2014;311(17):1809.
21. Dahlöf B, Devereux RB, Kjeldsen SE, et al; LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995-1003.
22. PRINT Research Group, Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103-2116. doi: 10.1056/NEJMoa1511939.
23. ACCORD Study Group, Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575-1585. doi: 10.1056/NEJMoa1001286.
24. Levy PD, Mahn JJ, Miller J, et al. Blood pressure treatment and outcomes in hypertensive patients without acute target organ damage: a retrospective cohort. Am J Emerg Med. 2015;33(9):1219-1224. doi: 10.1016/j.ajem.2015.05.036.
25. Leung AA, Wright A, Pazo V, Karson A, Bates DW. Risk of thiazide-induced hyponatremia in patients with hypertension. Am J Med. 2011;124(11):1064-1072. doi: 10.1016/j.amjmed.2011.06.031.
26. Mann JFE, Hilgers KF. Renin-angiotensin system inhibition in the treatment of hypertension. http://www.uptodate.com/contents/renin-angiotensin-system-inhibition-in-the-treatment-of-hypertension. Accessed September 21, 2016.
Case Scenarios
Case 1
You had just started your shift, and your first patient presented with symptoms of headache and dizziness, and a blood pressure (BP) of 240/130 mm Hg, without any vomiting or visual symptoms. Physical examination revealed an alert, pleasant 65-year-old black man whose ocular, neurological, and cardiovascular (CV) examinations were normal. The patient reported a history of borderline hypertension, but had never taken any medications for it.
After placing some initial orders, including an electrocardiogram (ECG), basic metabolic panel (BMP), and head computed tomography (CT) scan, and ordering 10 mg intravenous (IV) prochlorperazine and 25 mg IV diphenhydramine to treat the patient’s headache, you are left asking yourself what steps you should take next.
Case 2
Your next patient was a 90-year-old white woman who had been referred to the ED by her primary care physician (PCP) for “hypertensive urgency.” She had no complaints to report. Similar to the first patient, this patient’s physical examination was also normal, with the exception of a persistently elevated BP of 220/140 mm Hg. Her history was significant for congestive heart failure (CHF), but she exhibited no current CV signs or symptoms. The patient had been taking furosemide but was not on any other antihypertensive medications.
Case 3
In the room next to your 90-year-old patient is a 32-year-old uninsured hypertensive white woman. During the history taking, the patient stated that she was trying to become pregnant and was not currently using any form of contraception. Similar to the second patient, she had no complaints to report. Regarding her reason for presentation, the patient stated that when she had her BP checked at a pharmacy earlier that day, the reading was “too high,” and the pharmacist had advised her to go to the ED. She seemed anxious but otherwise well. Her initial BP at presentation was 240/100 mm Hg, but her physical examination was otherwise normal.
Hypertensive Emergencies
As emergency physicians (EPs), we see hypertensive patients every day. According to the US Centers for Disease Control and Prevention, 33% of American adults have hypertension, which is defined by a BP of ≥140/90 mm Hg (Table 1).
Almost 25% of total annual US adult ED visits are directly or indirectly related to hypertension, and about 1% of all ED visits are due solely to elevated BP.3 In an ambulatory care survey for 2007, moderate or severe hypertensive BP readings were found to be more common in patients presenting to the ED (43.5%) than to primary care clinics (27%).4 Patients presenting to the ED with hypertensive BP readings disproportionately represented patients who were older, male, non-Hispanic black, Medicare beneficiaries, or uninsured. Certainly, some patients presenting to the ED have hypertensive BP readings due to pain or anxiety, but multiple studies have suggested that 50% to 70% of ED patients who have hypertensive BP readings will be diagnosed with hypertension on office follow-up.5,6 While a minority of these patients present to the ED with hypertensive emergencies, the majority present either without symptoms of hypertension or with only mild headache. Given the disease burden of hypertension combined with the benefits of treatment, it is worthwhile for the practicing EP to review the most up-to-date guidelines on outpatient management of hypertension.
When a patient presents to the ED with a hypertensive BP reading, the initial priority of the EP is to exclude hypertensive emergency. Hypertensive emergencies are defined by the presence of hypertension (generally grade 3/severe hypertension with BP ≥180/110 mm Hg; see Table 1) in conjunction with evidence of target organ damage.
Target Organ Manifestations
The acuity and/or presence of target organ damage are not always clear on initial ED evaluation. For instance, when a patient who has no history of primary care presents to the ED with severe hypertension, laboratory evaluation may demonstrate protein and blood in his or her urine and an elevated serum creatinine level. In the absence of values from past laboratory studies, it is difficult to determine whether these test results represent normal laboratory parameters for this patient due to longstanding hypertensive kidney disease (ie, hypertensive nephrosclerosis) or if they represent a true hypertensive emergency, (ie, hypertensive emergency-related nephropathy).7 In patients with severe hypertension and possibly new acute kidney injury, it is probably safest to either assume hypertensive emergency-related nephropathy and to treat accordingly or consult with nephrology services. The picture of hypertensive emergency-related nephropathy often only becomes clear after renal biopsy results and improvement in renal parameters with BP control.
The ocular manifestations of hypertensive emergency require detailed fundoscopy, which at times can be challenging in the ED. In assessing for cardiac target organ damage, at our institution, we typically ask patients if they have experienced symptoms of dyspnea and chest pain or pressure. Generally, we also evaluate cardiac enzymes, B-type natriuretic peptide, and order ECG and chest X-ray studies when suggested by history or physical examination. Alarmingly, a study of 161 ED hypertensive (average BP of 183/109 mm Hg), asymptomatic, predominantly black patients found that 146 (90.7%) had subclinical hypertensive heart disease on point-of-care echocardiogram.8
Neurological/Hypertensive Encephalopathy
Hypertensive encephalopathy is a diagnosis of exclusion as alternate causes of confusion and headache, such as intracranial hemorrhage, are excluded and mental status improves with titrated BP control. Nonetheless, it is difficult to confidently state from the literature that patients who present with headache but have a normal mental status in the presence of severe hypertension are not on an early spectrum of hypertensive encephalopathy. Therefore, it is likely that the degree of symptoms should define whether target organ damage exists, though there is certainly a spectrum of hypertensive emergency—the strict definition of which is not always clear.
When a hypertensive emergency is diagnosed, management typically involves the use of antihypertensive IV medication in the intensive care unit. While such management is outside the scope of this paper, Adebayo and Rogers9 have published an excellent review of the care of hypertensive emergencies.
Asymptomatic Hypertension
The American College of Emergency Physicians (ACEP) has developed two clinical policies on the evaluation and management of asymptomatic hypertension in the ED. The original, published in 2006, advised that initially high BP readings of ED patients should be repeated: two separate high readings are adequate for screening, and those patients with hypertension should be referred for follow-up. Furthermore, ACEP policies note that initiating treatment in the ED is not necessary when patients are referred for follow-up. If treatment for hypertension is initiated in the ED, ACEP recommends that such management should attempt only to gradually lower BP, and not to normalize it during the initial ED visit.10
The 2013 update to ACEP’s clinical policy on managing asymptomatic hypertension expanded on the original policy. The updated policy advised against routine testing for target organ damage in patients who have asymptomatic severe hypertension. However, ACEP policy notes that evaluating serum creatinine in these patients with poor follow-up may influence patient disposition.11
The 2013 policy further stated that medical intervention is not required in ED patients who have asymptomatic severe hypertension, but may be considered in patients with poor follow-up. The policies emphasize that all asymptomatic hypertensive patients should be referred for follow-up. The literature cited for the recommendation that ED patients with asymptomatic severe hypertension do not require routine investigation stems from two observational studies. These studies found that screening asymptomatic ED patients who presented with severe hypertension revealed serum creatinine abnormalities in approximately 6%, which impacted patient disposition, though it was not clear from the study results whether admission correlated to meaningful patient outcomes.12,13
Patient Disposition
Since ACEP’s 2013 clinical policy, a study from the Cleveland Clinic has been published. This retrospective cohort study reviewed 6 years of data looking at all patients in its system with a BP of ≥180/110 mm Hg, and compared those office patients discharged to home to those referred to the ED or directly admitted to the inpatient hospital solely on the basis of severe hypertension.14 The study found that 0.5% of 387 patients referred to the ED by primary care clinics for asymptomatic severe hypertension had confirmed acute kidney injury on BMP.14 The Cleveland Clinic study also found that 2.1% of patients had evidence of target organ damage and 5.5% had any abnormal results.14 In addition, referral to the ED from the clinic for hypertension was associated with a slightly higher rate of major adverse CV events at 7 days (2 of 426 [0.5%] versus 61 of 58,109 [0.1%]; P = .02).14
The results of the Cleveland Clinic study confirm that in the absence of target organ damage, hypertension is probably best managed in the outpatient setting. The European Task Force hypertensive guidelines state “hospitalization for hypertension is regarded as inappropriate in most European countries.”15 However, from 2006 to 2012, 26% of US ED patients with primary diagnoses of hypertension were admitted to the hospital.3 In Canada’s most populous province of Ontario, from 2002 to 2011, approximately 8% of hypertensive patients were admitted.16 Part of this discrepancy may be due to the sometimes ambiguous nature of the presentation of patients with hypertension, making it unclear whether a true hypertensive emergency exists. Many patients perceive visual symptoms, headache, dizziness, and even chest pressure as the result of their elevated BP—without clear findings on fundoscopy, ECG, or cardiac marker testing. Perhaps more of these patients would be discharged if EPs felt comfortable initiating appropriate initial antihypertensive treatment.
Management
Initiating Antihypertensive Treatment
Some EPs may feel that an accurate diagnosis of hypertension requires repeat BP testing in the primary care office setting, and for this reason are reluctant to initiate antihypertensive treatment in the ED. The most recent guidelines by the Joint National Committee (JNC 8) do not address how many BP readings are necessary to diagnose hypertension, but JNC 7 suggested that diagnosis of hypertension requires two separate office visits.17 Evidence cited in ACEP’s first clinical policy states that two separate BP measurements in the ED are adequate for screening—but not necessarily for initiating treatment.10 However, European and British outpatient clinical recommendations advocate initiation of antihypertensive medication for a single visit in patients who have an elevated BP categorized as grade 3/severe hypertension (BP of ≥180/110 mm Hg).15,18 Furthermore, for patients with severe hypertension seen in the ED, as many as 97% are likely to have true hypertension at office follow-up.6 Those ED patients presenting with severe hypertension are very likely to have a true diagnosis of hypertension.
A recent retrospective analysis of a group of hypertensive ED patients by Brody et al19 found that patients prescribed BP medications by an EP were more likely to have improved BP control at follow-up 2 weeks later. In their study, the decision to prescribe antihypertensive medications were at the discretion of the EP. Seventy-six patients were given one or more prescriptions for antihypertensive therapy, compared to a control group of 141 patients who were not given a prescription. On follow-up at 2 weeks, there was an 11 mm Hg greater reduction of BP in the group who received prescriptions compared to the control group. None of the patients in either group on follow-up had experienced any new neurological deficits, ischemic events, life-threatening anaphylactic reactions, or clinically significant hypotension.
The Cleveland Clinic study14 also reported on those patents given who received new prescriptions from the ED. Similar to the study by Brody et al,19 none of the 82 patients discharged to home from the ED with a new antihypertensive prescription had any major adverse event at 30-day follow-up.14
Pharmacological Treatment Recommendations
When choosing to treat patients with new prescriptions for antihypertensives, it is important to follow the most current outpatient treatment recommendations. In 2014, JNC 8 released new guidelines for the outpatient management of adults with hypertension.20 The panel issued recommendations based on its systematic review of randomized controlled trials on antihypertensive treatments. The key recommendations are as follows:
- In patients aged 60 years or older, initiate pharmacological treatment at a BP of ≥150/90 mm Hg.
- In patients aged 18 to 59 years, initiate pharmacological treatment at a BP of ≥140/90 mm Hg.
- In the general nonblack population, initial antihypertensive treatment should include a thiazide-type diuretic, a calcium channel blocker (CCB), an angiotensin-converting enzyme inhibitor (ACE-I), or an angiotensin receptor blocker (ARB).
- In the general black population, initial treatment should include a thiazide-type diuretic or a CCB.
- In patients with chronic kidney disease (CKD) (including black patients), initial (or add-on) antihypertensive treatment should include an ACE-I or ARB to improve kidney outcomes—but not both.
- If goal BP is not reached within 1 month of initial treatment, increase the dose of the initial drug or add a second agent (eg, thiazide-type diuretic, CCB, ACE-I, or ARB). If goal is not reached with two drugs, use the third drug from that list if no contraindications exist, but do not use both an ACE-I and an ARB together in the same patient.
Of note, JNC 8, in departure from JNC 7, no longer recommends beta-blockers as first-line therapy for isolated hypertension (there may be compelling alternate indications, such as atrial fibrillation or postmyocardial infarction (MI), such that a beta-blocker would still be the first medication considered). The reason for this stems from a single randomized controlled trial of 9,193 patients that found that despite equivalent BP reduction, use of a beta-blocker in comparison to an ARB resulted in a higher rate of a composite outcome of death, MI, or stroke.21 The main difference was a 25% relative risk reduction for stroke with use of an ARB (losartan) in comparison to a beta-blocker (atenolol). The most recent European guidelines still include beta-blockers among its first-line recommended BP medications, but do acknowledge that they are not as effective in reducing stroke incidence as other alternative medications.15 The European guidelines otherwise include the same list of first-line agents. The British guidelines mirror JNC 8 in terms of first-line antihypertensive medication choices.18
Since the release of JNC 8, the Systolic Blood Pressure Intervention Trial (SPRINT) has been published, and will likely impact future national recommendations on BP management. The SPRINT study was a randomized controlled trial enrolling over 9,000 hypertensive nondiabetic patients older than age 50 years that treated individuals to a standard BP goal (systolic BP of 140 mm Hg) versus an intensive BP goal (systolic BP of 120 mm Hg) over a 3.5-year period. The trial was stopped early for safety as a 25% mortality reduction was observed in the intensive treatment group (1.65 vs 2.19 deaths/y).22 This was in contrast to previous trials that had mostly failed to show this sort of benefit, though previous trials were smaller in number or included only diabetic patients.23 While it is likely that this trial may influence lowering treatment thresholds from the office, it is not likely to impact care from the ED.
The recommendations of JNC 8 do not necessarily coincide with current US EP practice. In the study by Brody et al,19 of patients provided ED antihypertensive prescriptions, 54% received thiazide-type diuretics, 26% ACE-I, 10% CCBs, and 6% beta-blockers. This is noteworthy because 96% of those in the study were black patients who would benefit most from either a thiazide or a CCB. Another recent study of ED patients showed that of patients who were both treated in the ED and discharged with antihypertensive medications, 34% received a diuretic prescription, 32% clonidine, 15% a beta-blocker, 19% an ARB or ACE-I, 12% a CCB, and 2% hydrazine.24 These results are important because according to many published guidelines, including JNC 8, clonidine is only considered one of several fourth-line options for severe resistant hypertension.15,18,20 Since clonidine use can be complicated by rebound hypertension, it is not an ideal agent to be prescribed de novo to patients in the ED. This is particularly true if these patients are not already on maximum doses of the three most recommended agents previously noted, or if there are concerns over patient compliance.
Of the drug classes recommended by JNC 8, Table 3 lists the absolute and relative contraindications.
In clinical trials, amlodipine is among the most effective BP medications and is considered first-line therapy for all groups of patients with hypertension.15,18,20 A simplistic approach for most patients presenting with severe asymptomatic hypertension (BP of ≥180/110 mm Hg) not currently on treatment would be to recheck the BP and assure it remains elevated over the period of the ED visit.
Conclusion
Hypertension is among the most common medical conditions for which emergency patients seek care. The ACEP clinical policies provide guidance on the appropriate work-up and treatment of these patients. Given the occasional lack of clarity on whether a patient’s presentation is on the spectrum of more acute/serious, EPs may feel more comfortable in discharging patients with poor follow-up if they are able to safely prescribe antihypertensive treatment. Prior to prescribing treatment, EPs should refer to the JNC 8 guidelines to appropriately start antihypertensive treatment in select patient groups in the ED. The guidelines of JNC 8 are therefore worth referring to in order to appropriately start treatment in select patient groups from the ED.
Case Scenarios Continued
Case 1
[The 65-year-old black man who presented with headache and dizziness, and had an initial BP of 240/130 mm Hg.]
After treating the patient with prochlorperazine and diphenhydramine, his headache resolved. His BP improved but remained elevated at 190/120 mm Hg. On further questioning, the patient reported a history of similar headaches and wondered whether it was related to his BP. The head CT scan was negative for any acute hemorrhage, infarct, or mass; the ECG only showed evidence of left ventricular hypertrophy; and the BMP showed normal renal function.
After a long discussion with the patient, you agreed to start him on amlodipine 5 mg/d and referred him for follow-up with a local PCP.
Case 2
[The 90-year-old white woman with a history of CHF and an initial BP of 220/140 mm Hg at presentation.]
The BMP evaluation showed a baseline creatinine level of 1.3 mg/dL. Given this patient’s history of CHF, amlodipine would not be the ideal next agent to prescribe. After discussion with her PCP, you elected to start her on losartan at 25 mg/d, and instructed her to follow-up with her PCP within 1 week.
Case 3
[The 32-year-old white woman who presented at the advice of a pharmacist and had an initial BP of 240/100 mm Hg.]While reviewing the patient’s work-up and history, you noted her plans to become pregnant, and recalled a recent review on BP management, noting the contraindications associated with ARB or ACE-I in pregnancy. Based on the patient’s uninsured status and poor follow-up, you considered prescribing amlodipine. Prior to issuing the prescription, you performed a repeat BP check and noted that the patient’s BP had decreased to 130/85 mm Hg. Given the marked improvement in the patient’s BP during her ED course, you were not convinced that she truly had hypertension.
Instead of prescribing an antihypertensive agent, which may not ultimately benefit this patient, you advised her to seek follow-up care at an outpatient clinic to have her BP rechecked. The patient agreed, and you referred her to a local free clinic.
Case Scenarios
Case 1
You had just started your shift, and your first patient presented with symptoms of headache and dizziness, and a blood pressure (BP) of 240/130 mm Hg, without any vomiting or visual symptoms. Physical examination revealed an alert, pleasant 65-year-old black man whose ocular, neurological, and cardiovascular (CV) examinations were normal. The patient reported a history of borderline hypertension, but had never taken any medications for it.
After placing some initial orders, including an electrocardiogram (ECG), basic metabolic panel (BMP), and head computed tomography (CT) scan, and ordering 10 mg intravenous (IV) prochlorperazine and 25 mg IV diphenhydramine to treat the patient’s headache, you are left asking yourself what steps you should take next.
Case 2
Your next patient was a 90-year-old white woman who had been referred to the ED by her primary care physician (PCP) for “hypertensive urgency.” She had no complaints to report. Similar to the first patient, this patient’s physical examination was also normal, with the exception of a persistently elevated BP of 220/140 mm Hg. Her history was significant for congestive heart failure (CHF), but she exhibited no current CV signs or symptoms. The patient had been taking furosemide but was not on any other antihypertensive medications.
Case 3
In the room next to your 90-year-old patient is a 32-year-old uninsured hypertensive white woman. During the history taking, the patient stated that she was trying to become pregnant and was not currently using any form of contraception. Similar to the second patient, she had no complaints to report. Regarding her reason for presentation, the patient stated that when she had her BP checked at a pharmacy earlier that day, the reading was “too high,” and the pharmacist had advised her to go to the ED. She seemed anxious but otherwise well. Her initial BP at presentation was 240/100 mm Hg, but her physical examination was otherwise normal.
Hypertensive Emergencies
As emergency physicians (EPs), we see hypertensive patients every day. According to the US Centers for Disease Control and Prevention, 33% of American adults have hypertension, which is defined by a BP of ≥140/90 mm Hg (Table 1).
Almost 25% of total annual US adult ED visits are directly or indirectly related to hypertension, and about 1% of all ED visits are due solely to elevated BP.3 In an ambulatory care survey for 2007, moderate or severe hypertensive BP readings were found to be more common in patients presenting to the ED (43.5%) than to primary care clinics (27%).4 Patients presenting to the ED with hypertensive BP readings disproportionately represented patients who were older, male, non-Hispanic black, Medicare beneficiaries, or uninsured. Certainly, some patients presenting to the ED have hypertensive BP readings due to pain or anxiety, but multiple studies have suggested that 50% to 70% of ED patients who have hypertensive BP readings will be diagnosed with hypertension on office follow-up.5,6 While a minority of these patients present to the ED with hypertensive emergencies, the majority present either without symptoms of hypertension or with only mild headache. Given the disease burden of hypertension combined with the benefits of treatment, it is worthwhile for the practicing EP to review the most up-to-date guidelines on outpatient management of hypertension.
When a patient presents to the ED with a hypertensive BP reading, the initial priority of the EP is to exclude hypertensive emergency. Hypertensive emergencies are defined by the presence of hypertension (generally grade 3/severe hypertension with BP ≥180/110 mm Hg; see Table 1) in conjunction with evidence of target organ damage.
Target Organ Manifestations
The acuity and/or presence of target organ damage are not always clear on initial ED evaluation. For instance, when a patient who has no history of primary care presents to the ED with severe hypertension, laboratory evaluation may demonstrate protein and blood in his or her urine and an elevated serum creatinine level. In the absence of values from past laboratory studies, it is difficult to determine whether these test results represent normal laboratory parameters for this patient due to longstanding hypertensive kidney disease (ie, hypertensive nephrosclerosis) or if they represent a true hypertensive emergency, (ie, hypertensive emergency-related nephropathy).7 In patients with severe hypertension and possibly new acute kidney injury, it is probably safest to either assume hypertensive emergency-related nephropathy and to treat accordingly or consult with nephrology services. The picture of hypertensive emergency-related nephropathy often only becomes clear after renal biopsy results and improvement in renal parameters with BP control.
The ocular manifestations of hypertensive emergency require detailed fundoscopy, which at times can be challenging in the ED. In assessing for cardiac target organ damage, at our institution, we typically ask patients if they have experienced symptoms of dyspnea and chest pain or pressure. Generally, we also evaluate cardiac enzymes, B-type natriuretic peptide, and order ECG and chest X-ray studies when suggested by history or physical examination. Alarmingly, a study of 161 ED hypertensive (average BP of 183/109 mm Hg), asymptomatic, predominantly black patients found that 146 (90.7%) had subclinical hypertensive heart disease on point-of-care echocardiogram.8
Neurological/Hypertensive Encephalopathy
Hypertensive encephalopathy is a diagnosis of exclusion as alternate causes of confusion and headache, such as intracranial hemorrhage, are excluded and mental status improves with titrated BP control. Nonetheless, it is difficult to confidently state from the literature that patients who present with headache but have a normal mental status in the presence of severe hypertension are not on an early spectrum of hypertensive encephalopathy. Therefore, it is likely that the degree of symptoms should define whether target organ damage exists, though there is certainly a spectrum of hypertensive emergency—the strict definition of which is not always clear.
When a hypertensive emergency is diagnosed, management typically involves the use of antihypertensive IV medication in the intensive care unit. While such management is outside the scope of this paper, Adebayo and Rogers9 have published an excellent review of the care of hypertensive emergencies.
Asymptomatic Hypertension
The American College of Emergency Physicians (ACEP) has developed two clinical policies on the evaluation and management of asymptomatic hypertension in the ED. The original, published in 2006, advised that initially high BP readings of ED patients should be repeated: two separate high readings are adequate for screening, and those patients with hypertension should be referred for follow-up. Furthermore, ACEP policies note that initiating treatment in the ED is not necessary when patients are referred for follow-up. If treatment for hypertension is initiated in the ED, ACEP recommends that such management should attempt only to gradually lower BP, and not to normalize it during the initial ED visit.10
The 2013 update to ACEP’s clinical policy on managing asymptomatic hypertension expanded on the original policy. The updated policy advised against routine testing for target organ damage in patients who have asymptomatic severe hypertension. However, ACEP policy notes that evaluating serum creatinine in these patients with poor follow-up may influence patient disposition.11
The 2013 policy further stated that medical intervention is not required in ED patients who have asymptomatic severe hypertension, but may be considered in patients with poor follow-up. The policies emphasize that all asymptomatic hypertensive patients should be referred for follow-up. The literature cited for the recommendation that ED patients with asymptomatic severe hypertension do not require routine investigation stems from two observational studies. These studies found that screening asymptomatic ED patients who presented with severe hypertension revealed serum creatinine abnormalities in approximately 6%, which impacted patient disposition, though it was not clear from the study results whether admission correlated to meaningful patient outcomes.12,13
Patient Disposition
Since ACEP’s 2013 clinical policy, a study from the Cleveland Clinic has been published. This retrospective cohort study reviewed 6 years of data looking at all patients in its system with a BP of ≥180/110 mm Hg, and compared those office patients discharged to home to those referred to the ED or directly admitted to the inpatient hospital solely on the basis of severe hypertension.14 The study found that 0.5% of 387 patients referred to the ED by primary care clinics for asymptomatic severe hypertension had confirmed acute kidney injury on BMP.14 The Cleveland Clinic study also found that 2.1% of patients had evidence of target organ damage and 5.5% had any abnormal results.14 In addition, referral to the ED from the clinic for hypertension was associated with a slightly higher rate of major adverse CV events at 7 days (2 of 426 [0.5%] versus 61 of 58,109 [0.1%]; P = .02).14
The results of the Cleveland Clinic study confirm that in the absence of target organ damage, hypertension is probably best managed in the outpatient setting. The European Task Force hypertensive guidelines state “hospitalization for hypertension is regarded as inappropriate in most European countries.”15 However, from 2006 to 2012, 26% of US ED patients with primary diagnoses of hypertension were admitted to the hospital.3 In Canada’s most populous province of Ontario, from 2002 to 2011, approximately 8% of hypertensive patients were admitted.16 Part of this discrepancy may be due to the sometimes ambiguous nature of the presentation of patients with hypertension, making it unclear whether a true hypertensive emergency exists. Many patients perceive visual symptoms, headache, dizziness, and even chest pressure as the result of their elevated BP—without clear findings on fundoscopy, ECG, or cardiac marker testing. Perhaps more of these patients would be discharged if EPs felt comfortable initiating appropriate initial antihypertensive treatment.
Management
Initiating Antihypertensive Treatment
Some EPs may feel that an accurate diagnosis of hypertension requires repeat BP testing in the primary care office setting, and for this reason are reluctant to initiate antihypertensive treatment in the ED. The most recent guidelines by the Joint National Committee (JNC 8) do not address how many BP readings are necessary to diagnose hypertension, but JNC 7 suggested that diagnosis of hypertension requires two separate office visits.17 Evidence cited in ACEP’s first clinical policy states that two separate BP measurements in the ED are adequate for screening—but not necessarily for initiating treatment.10 However, European and British outpatient clinical recommendations advocate initiation of antihypertensive medication for a single visit in patients who have an elevated BP categorized as grade 3/severe hypertension (BP of ≥180/110 mm Hg).15,18 Furthermore, for patients with severe hypertension seen in the ED, as many as 97% are likely to have true hypertension at office follow-up.6 Those ED patients presenting with severe hypertension are very likely to have a true diagnosis of hypertension.
A recent retrospective analysis of a group of hypertensive ED patients by Brody et al19 found that patients prescribed BP medications by an EP were more likely to have improved BP control at follow-up 2 weeks later. In their study, the decision to prescribe antihypertensive medications were at the discretion of the EP. Seventy-six patients were given one or more prescriptions for antihypertensive therapy, compared to a control group of 141 patients who were not given a prescription. On follow-up at 2 weeks, there was an 11 mm Hg greater reduction of BP in the group who received prescriptions compared to the control group. None of the patients in either group on follow-up had experienced any new neurological deficits, ischemic events, life-threatening anaphylactic reactions, or clinically significant hypotension.
The Cleveland Clinic study14 also reported on those patents given who received new prescriptions from the ED. Similar to the study by Brody et al,19 none of the 82 patients discharged to home from the ED with a new antihypertensive prescription had any major adverse event at 30-day follow-up.14
Pharmacological Treatment Recommendations
When choosing to treat patients with new prescriptions for antihypertensives, it is important to follow the most current outpatient treatment recommendations. In 2014, JNC 8 released new guidelines for the outpatient management of adults with hypertension.20 The panel issued recommendations based on its systematic review of randomized controlled trials on antihypertensive treatments. The key recommendations are as follows:
- In patients aged 60 years or older, initiate pharmacological treatment at a BP of ≥150/90 mm Hg.
- In patients aged 18 to 59 years, initiate pharmacological treatment at a BP of ≥140/90 mm Hg.
- In the general nonblack population, initial antihypertensive treatment should include a thiazide-type diuretic, a calcium channel blocker (CCB), an angiotensin-converting enzyme inhibitor (ACE-I), or an angiotensin receptor blocker (ARB).
- In the general black population, initial treatment should include a thiazide-type diuretic or a CCB.
- In patients with chronic kidney disease (CKD) (including black patients), initial (or add-on) antihypertensive treatment should include an ACE-I or ARB to improve kidney outcomes—but not both.
- If goal BP is not reached within 1 month of initial treatment, increase the dose of the initial drug or add a second agent (eg, thiazide-type diuretic, CCB, ACE-I, or ARB). If goal is not reached with two drugs, use the third drug from that list if no contraindications exist, but do not use both an ACE-I and an ARB together in the same patient.
Of note, JNC 8, in departure from JNC 7, no longer recommends beta-blockers as first-line therapy for isolated hypertension (there may be compelling alternate indications, such as atrial fibrillation or postmyocardial infarction (MI), such that a beta-blocker would still be the first medication considered). The reason for this stems from a single randomized controlled trial of 9,193 patients that found that despite equivalent BP reduction, use of a beta-blocker in comparison to an ARB resulted in a higher rate of a composite outcome of death, MI, or stroke.21 The main difference was a 25% relative risk reduction for stroke with use of an ARB (losartan) in comparison to a beta-blocker (atenolol). The most recent European guidelines still include beta-blockers among its first-line recommended BP medications, but do acknowledge that they are not as effective in reducing stroke incidence as other alternative medications.15 The European guidelines otherwise include the same list of first-line agents. The British guidelines mirror JNC 8 in terms of first-line antihypertensive medication choices.18
Since the release of JNC 8, the Systolic Blood Pressure Intervention Trial (SPRINT) has been published, and will likely impact future national recommendations on BP management. The SPRINT study was a randomized controlled trial enrolling over 9,000 hypertensive nondiabetic patients older than age 50 years that treated individuals to a standard BP goal (systolic BP of 140 mm Hg) versus an intensive BP goal (systolic BP of 120 mm Hg) over a 3.5-year period. The trial was stopped early for safety as a 25% mortality reduction was observed in the intensive treatment group (1.65 vs 2.19 deaths/y).22 This was in contrast to previous trials that had mostly failed to show this sort of benefit, though previous trials were smaller in number or included only diabetic patients.23 While it is likely that this trial may influence lowering treatment thresholds from the office, it is not likely to impact care from the ED.
The recommendations of JNC 8 do not necessarily coincide with current US EP practice. In the study by Brody et al,19 of patients provided ED antihypertensive prescriptions, 54% received thiazide-type diuretics, 26% ACE-I, 10% CCBs, and 6% beta-blockers. This is noteworthy because 96% of those in the study were black patients who would benefit most from either a thiazide or a CCB. Another recent study of ED patients showed that of patients who were both treated in the ED and discharged with antihypertensive medications, 34% received a diuretic prescription, 32% clonidine, 15% a beta-blocker, 19% an ARB or ACE-I, 12% a CCB, and 2% hydrazine.24 These results are important because according to many published guidelines, including JNC 8, clonidine is only considered one of several fourth-line options for severe resistant hypertension.15,18,20 Since clonidine use can be complicated by rebound hypertension, it is not an ideal agent to be prescribed de novo to patients in the ED. This is particularly true if these patients are not already on maximum doses of the three most recommended agents previously noted, or if there are concerns over patient compliance.
Of the drug classes recommended by JNC 8, Table 3 lists the absolute and relative contraindications.
In clinical trials, amlodipine is among the most effective BP medications and is considered first-line therapy for all groups of patients with hypertension.15,18,20 A simplistic approach for most patients presenting with severe asymptomatic hypertension (BP of ≥180/110 mm Hg) not currently on treatment would be to recheck the BP and assure it remains elevated over the period of the ED visit.
Conclusion
Hypertension is among the most common medical conditions for which emergency patients seek care. The ACEP clinical policies provide guidance on the appropriate work-up and treatment of these patients. Given the occasional lack of clarity on whether a patient’s presentation is on the spectrum of more acute/serious, EPs may feel more comfortable in discharging patients with poor follow-up if they are able to safely prescribe antihypertensive treatment. Prior to prescribing treatment, EPs should refer to the JNC 8 guidelines to appropriately start antihypertensive treatment in select patient groups in the ED. The guidelines of JNC 8 are therefore worth referring to in order to appropriately start treatment in select patient groups from the ED.
Case Scenarios Continued
Case 1
[The 65-year-old black man who presented with headache and dizziness, and had an initial BP of 240/130 mm Hg.]
After treating the patient with prochlorperazine and diphenhydramine, his headache resolved. His BP improved but remained elevated at 190/120 mm Hg. On further questioning, the patient reported a history of similar headaches and wondered whether it was related to his BP. The head CT scan was negative for any acute hemorrhage, infarct, or mass; the ECG only showed evidence of left ventricular hypertrophy; and the BMP showed normal renal function.
After a long discussion with the patient, you agreed to start him on amlodipine 5 mg/d and referred him for follow-up with a local PCP.
Case 2
[The 90-year-old white woman with a history of CHF and an initial BP of 220/140 mm Hg at presentation.]
The BMP evaluation showed a baseline creatinine level of 1.3 mg/dL. Given this patient’s history of CHF, amlodipine would not be the ideal next agent to prescribe. After discussion with her PCP, you elected to start her on losartan at 25 mg/d, and instructed her to follow-up with her PCP within 1 week.
Case 3
[The 32-year-old white woman who presented at the advice of a pharmacist and had an initial BP of 240/100 mm Hg.]While reviewing the patient’s work-up and history, you noted her plans to become pregnant, and recalled a recent review on BP management, noting the contraindications associated with ARB or ACE-I in pregnancy. Based on the patient’s uninsured status and poor follow-up, you considered prescribing amlodipine. Prior to issuing the prescription, you performed a repeat BP check and noted that the patient’s BP had decreased to 130/85 mm Hg. Given the marked improvement in the patient’s BP during her ED course, you were not convinced that she truly had hypertension.
Instead of prescribing an antihypertensive agent, which may not ultimately benefit this patient, you advised her to seek follow-up care at an outpatient clinic to have her BP rechecked. The patient agreed, and you referred her to a local free clinic.
1. Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011-2012. NCHS Data Brief. 2013;(133):1-8.
2. Turnbull F; Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2013;362(9395):1527-1535.
3. McNaughton CD, Self WH, Zhu Y, Janke AT, Storrow AB, Levy P. Incidence of hypertension-related emergency department visits in the United States, 2006 to 2012. Am J Cardiol. 2015;116(11):1717-1723. doi: 10.1016/j.amjcard.2015.09.007.
4. Niska RW. Blood pressure measurements at emergency department visits by adults: United States, 2007-2008. NCHS Data Brief. 2011;(72):1-8.
5. Chernow SM, Iserson KV, Criss E. Use of the emergency department for hypertension screening: a prospective study. Ann Emerg Med. 1987;16(2):180-182.
6. Backer HD, Decker L, Ackerson L. Reproducibility of increased blood pressure during an emergency department or urgent care visit. Ann Emerg Med. 2003.41(4):507-512.
7. Nonaka K, Ubara Y, Sumida K, et al. Clinical and pathological evaluation of hypertensive emergency-related nephropathy. Intern Med. 2013;52(1):45-53.
8. Levy P, Ye H, Compton S, et al. Subclinical hypertensive heart disease in black patients with elevated blood pressure in an inner-city emergency department. Ann Emerg Med. 2012;60(4):467-474.e1. doi: 10.1016/j.annemergmed.2012.03.030.
9. Adebayo O, Rogers RL. Hypertensive emergencies in the emergency department. Emerg Med Clin North Am. 2015;33(3):539-551. doi: 10.1016/j.emc.2015.04.005.
10. Decker WW, Godwin SA, Hess EP, Lenamond CC, Jagoda AS; American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Asymptomatic Hypertension in the ED. Clinical policy: critical issues in the evaluation and management of adult patients with asymptomatic hypertension in the emergency department. Ann Emerg Med. 2006;47(3):237-234. doi: 10.1016/j.annemergmed.2005.10.003
11. Wolf SJ, Lo B, Shih RD, Smith MD, Fesmire FM; American College of Emergency Physicians Clinical Policies Committee. Clinical policy: critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med. 2013;62(1):59-68. doi: 10.1016/j.annemergmed.2013.05.012.
12. Karras DJ, Kruus LK, Cienki JJ, et al. Evaluation and treatment of patients with severely elevated blood pressure in academic emergency departments: a multicenter study. Ann Emerg Med. 2006;47(3):230-236.
13. Nishijima DK, Paladino L, Sinert R. Routine testing in patients with asymptomatic elevated blood pressure in the ED. Am J Emerg Med. 2010;28(2):235-242. doi: 10.1016/j.ajem.2008.11.015.
14. Patel KK, Young L, Howell EH, et al. Characteristics and outcomes of patients presenting with hypertensive urgency in the office setting. JAMA Intern Med. 2016;176(7):981-988. doi: 10.1001/jamainternmed.2016.1509.
15. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159-2219. doi: 10.1093/eurheartj/eht151.
16. Masood S, Austin PC, Atzema CL. A population-based analysis of outcomes in patients with a primary diagnosis of hypertension in the emergency department. Ann Emerg Med. 2016;68(3):258-267.e5. doi: 10.1016/j.annemergmed.2016.04.060.
17. Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560-2572. Erratum in: JAMA. 2003;290(2):197.
18. Krause T, Lovibond K, Caulfield M, McCormack T, Williams B; Guideline Development Group. Management of hypertension: summary of NICE guidance. BMJ. 2011;343:d4891. doi: 10.1136/bmj.d4891.
19. Brody A, Rahman T, Reed B, et al. Safety and efficacy of antihypertensive prescription at emergency department discharge. Acad Emerg Med. 2015;22(5):632-635. doi: 10.1111/acem.12660.
20. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520. doi: 10.1001/jama.2013.284427. Erratum in: JAMA. 2014;311(17):1809.
21. Dahlöf B, Devereux RB, Kjeldsen SE, et al; LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995-1003.
22. PRINT Research Group, Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103-2116. doi: 10.1056/NEJMoa1511939.
23. ACCORD Study Group, Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575-1585. doi: 10.1056/NEJMoa1001286.
24. Levy PD, Mahn JJ, Miller J, et al. Blood pressure treatment and outcomes in hypertensive patients without acute target organ damage: a retrospective cohort. Am J Emerg Med. 2015;33(9):1219-1224. doi: 10.1016/j.ajem.2015.05.036.
25. Leung AA, Wright A, Pazo V, Karson A, Bates DW. Risk of thiazide-induced hyponatremia in patients with hypertension. Am J Med. 2011;124(11):1064-1072. doi: 10.1016/j.amjmed.2011.06.031.
26. Mann JFE, Hilgers KF. Renin-angiotensin system inhibition in the treatment of hypertension. http://www.uptodate.com/contents/renin-angiotensin-system-inhibition-in-the-treatment-of-hypertension. Accessed September 21, 2016.
1. Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011-2012. NCHS Data Brief. 2013;(133):1-8.
2. Turnbull F; Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2013;362(9395):1527-1535.
3. McNaughton CD, Self WH, Zhu Y, Janke AT, Storrow AB, Levy P. Incidence of hypertension-related emergency department visits in the United States, 2006 to 2012. Am J Cardiol. 2015;116(11):1717-1723. doi: 10.1016/j.amjcard.2015.09.007.
4. Niska RW. Blood pressure measurements at emergency department visits by adults: United States, 2007-2008. NCHS Data Brief. 2011;(72):1-8.
5. Chernow SM, Iserson KV, Criss E. Use of the emergency department for hypertension screening: a prospective study. Ann Emerg Med. 1987;16(2):180-182.
6. Backer HD, Decker L, Ackerson L. Reproducibility of increased blood pressure during an emergency department or urgent care visit. Ann Emerg Med. 2003.41(4):507-512.
7. Nonaka K, Ubara Y, Sumida K, et al. Clinical and pathological evaluation of hypertensive emergency-related nephropathy. Intern Med. 2013;52(1):45-53.
8. Levy P, Ye H, Compton S, et al. Subclinical hypertensive heart disease in black patients with elevated blood pressure in an inner-city emergency department. Ann Emerg Med. 2012;60(4):467-474.e1. doi: 10.1016/j.annemergmed.2012.03.030.
9. Adebayo O, Rogers RL. Hypertensive emergencies in the emergency department. Emerg Med Clin North Am. 2015;33(3):539-551. doi: 10.1016/j.emc.2015.04.005.
10. Decker WW, Godwin SA, Hess EP, Lenamond CC, Jagoda AS; American College of Emergency Physicians Clinical Policies Subcommittee (Writing Committee) on Asymptomatic Hypertension in the ED. Clinical policy: critical issues in the evaluation and management of adult patients with asymptomatic hypertension in the emergency department. Ann Emerg Med. 2006;47(3):237-234. doi: 10.1016/j.annemergmed.2005.10.003
11. Wolf SJ, Lo B, Shih RD, Smith MD, Fesmire FM; American College of Emergency Physicians Clinical Policies Committee. Clinical policy: critical issues in the evaluation and management of adult patients in the emergency department with asymptomatic elevated blood pressure. Ann Emerg Med. 2013;62(1):59-68. doi: 10.1016/j.annemergmed.2013.05.012.
12. Karras DJ, Kruus LK, Cienki JJ, et al. Evaluation and treatment of patients with severely elevated blood pressure in academic emergency departments: a multicenter study. Ann Emerg Med. 2006;47(3):230-236.
13. Nishijima DK, Paladino L, Sinert R. Routine testing in patients with asymptomatic elevated blood pressure in the ED. Am J Emerg Med. 2010;28(2):235-242. doi: 10.1016/j.ajem.2008.11.015.
14. Patel KK, Young L, Howell EH, et al. Characteristics and outcomes of patients presenting with hypertensive urgency in the office setting. JAMA Intern Med. 2016;176(7):981-988. doi: 10.1001/jamainternmed.2016.1509.
15. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159-2219. doi: 10.1093/eurheartj/eht151.
16. Masood S, Austin PC, Atzema CL. A population-based analysis of outcomes in patients with a primary diagnosis of hypertension in the emergency department. Ann Emerg Med. 2016;68(3):258-267.e5. doi: 10.1016/j.annemergmed.2016.04.060.
17. Chobanian AV, Bakris GL, Black HR, et al; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560-2572. Erratum in: JAMA. 2003;290(2):197.
18. Krause T, Lovibond K, Caulfield M, McCormack T, Williams B; Guideline Development Group. Management of hypertension: summary of NICE guidance. BMJ. 2011;343:d4891. doi: 10.1136/bmj.d4891.
19. Brody A, Rahman T, Reed B, et al. Safety and efficacy of antihypertensive prescription at emergency department discharge. Acad Emerg Med. 2015;22(5):632-635. doi: 10.1111/acem.12660.
20. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520. doi: 10.1001/jama.2013.284427. Erratum in: JAMA. 2014;311(17):1809.
21. Dahlöf B, Devereux RB, Kjeldsen SE, et al; LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359(9311):995-1003.
22. PRINT Research Group, Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103-2116. doi: 10.1056/NEJMoa1511939.
23. ACCORD Study Group, Cushman WC, Evans GW, Byington RP, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575-1585. doi: 10.1056/NEJMoa1001286.
24. Levy PD, Mahn JJ, Miller J, et al. Blood pressure treatment and outcomes in hypertensive patients without acute target organ damage: a retrospective cohort. Am J Emerg Med. 2015;33(9):1219-1224. doi: 10.1016/j.ajem.2015.05.036.
25. Leung AA, Wright A, Pazo V, Karson A, Bates DW. Risk of thiazide-induced hyponatremia in patients with hypertension. Am J Med. 2011;124(11):1064-1072. doi: 10.1016/j.amjmed.2011.06.031.
26. Mann JFE, Hilgers KF. Renin-angiotensin system inhibition in the treatment of hypertension. http://www.uptodate.com/contents/renin-angiotensin-system-inhibition-in-the-treatment-of-hypertension. Accessed September 21, 2016.
Malpractice Counsel: Acute Pulmonary Embolism Masquerading as Acute Coronary Syndrome
Case
A 37-year-old woman presented to the ED with a 90-minute history of chest tightness and shortness of breath. She admitted to feeling anxious but denied nausea, vomiting, or diaphoresis. The patient was in good health overall and had no history of similar symptoms. The only medication she took on a regular basis was a combination oral contraceptive (OC). Regarding the patient’s social history, she admitted to smoking one-half of a pack of cigarettes per day and occasional alcohol use.
On physical examination, the patient’s vital signs were: heart rate (HR), 102 beats/min; blood pressure, 118/64 mm Hg; respiratory rate, 20 breaths/min; and temperature, 98.6˚F. Oxygen saturation was 95% on room air. The head, eyes, ears, nose, and throat examination was normal. The cardiopulmonary examination revealed slight tachycardia with a regular rhythm but no murmurs, rubs, or gallops; the lungs were clear to auscultation bilaterally. The abdominal examination revealed a soft, nontender abdomen, without mass, and no guarding or rebound was present. An examination of the lower extremities was not documented.
The emergency physician (EP) ordered laboratory studies, which included a complete blood count (CBC), basic metabolic profile (BMP), and troponin I level. A chest X-ray and electrocardiogram (ECG) were also ordered. The chest X-ray was interpreted as normal, and the ECG revealed mild sinus tachycardia with nonspecific ST-T segment changes in V1 through V3. The CBC and BMP were all within normal limits, but the troponin I level was slightly elevated.
Given the patient’s clinical presentation and slightly elevated troponin I level, the EP was concerned for an acute coronary syndrome (ACS) and admitted the patient to the care of the on-call cardiologist. Prior to transfer, the patient was given 325 mg of aspirin by mouth, but no anticoagulation therapy was ordered. The cardiologist, who evaluated the patient after she was admitted to the inpatient floor, was concerned the patient had a pulmonary embolism (PE), and ordered a stat computed tomography angiography (CTA) scan of the chest. While the patient was undergoing the chest CTA scan, she went into cardiac arrest. Despite aggressive resuscitative measures, the patient could not be revived and was pronounced dead. An autopsy revealed a PE as the cause of death.
Plaintiff’s Claim
The patient’s estate sued the EP for failure to properly diagnose the PE, stating the hospital was vicariously liable for the EP’s actions. The emergency medicine (EM) expert for the plaintiff opined that the decedent’s symptoms should have prompted the EP to suspect she was suffering from a PE, and he should have immediately ordered anticoagulation, a D-dimer test, or a chest CTA scan. The expert cardiologist for the plaintiff stated the EP should have immediately started the patient on anticoagulation prior to the chest CTA scan.
The Defense
The defense EM expert stated the defendant’s diagnosis of ACS was appropriate given the patient’s overall clinical presentation, and the defense expert cardiologist stated the standard of care did not require the EP to administer anticoagulation prior to her diagnosis of PE, since the bleeding risks outweighed the benefits.
Verdict
At trial, the jury returned a defense verdict.
Discussion
This is not the first (nor probably the last) malpractice case in this column to involve a missed PE. While there have been improvements to the tools we currently possess to evaluate patients for suspected PE, it remains a difficult condition to reliably and timely identify in the ED. Although the two predominating symptoms—shortness of breath and chest pain—are common presentations in the ED, each is associated with large differential diagnoses.
Acute Coronary Syndrome Versus Pulmonary Embolism
From what we know of the published details of this case, the patient had only one risk factor for ACS (cigarette smoking) and two risk factors for PE (cigarette smoking and estrogen-containing contraceptive use). The only abnormal physical finding (tachycardia) was slightly more suggestive of PE than ACS. This patient’s primary complaint was chest fullness and shortness of breath. According to the Prospective Investigation of Pulmonary Embolism Diagnosis II study, shortness of breath is the most common complaint in PE (73%), followed by pleuritic chest pain (44%).1
In ACS, which is more common in men versus women and in patients of both sexes over age 55 years, the clinical presentation most commonly involves chest pain that patients describe as a pressure or fullness (as demonstrated in this patient). Unfortunately, in certain patient populations (eg, women, elderly patients, patients with diabetes mellitus) the presenting complaint can be shortness of breath, weakness, or nausea and vomiting. In a study evaluating how frequently an acute PE can mimic ACS, Kukla et al2 found that one-third of patients with an acute PE can present with all of the manifestations suggestive of ACS (ie, chest pain, ECG changes, and elevated troponin).
It is probably safe to assume the elevated troponin I level played a factor in influencing the EP to diagnose ACS, rather than pursuing an alternative diagnosis such as PE. Unfortunately, since both serum troponin T and I can be markers of right ventricle dysfunction, they are elevated in 30% to 50% of patients with moderate-to-large PE.3 However, neither serum troponin T nor troponin I is specific for myocardial infarction or unstable angina.
Pretest Probability: Wells Criteria
Determining pretest probability for any disease process is important when evaluating complaints in the ED; this is especially true for PE. One of the most frequently used tools for determining the likelihood of PE in ED patients is the Wells criteria (Table 1).4
Based on the published information available, the patient in this case would have scored a 1.5, placing her in the unlikely or low-risk category for PE. Patients whose Wells score places them in the low-risk group can benefit from serum D-dimer testing to help diagnose PE. However, serum D-dimer testing should not be ordered for patients in the likely or high-risk categories; these patients should instead be sent directly for imaging studies such as a chest CTA scan.
Pulmonary Embolism Rule-Out Criteria
For patients whose Wells criteria score places them in the “unlikely group,” the PE rule-out criteria (PERC) can be used to determine the need for ordering a D-dimer. If all eight criteria are met, no further testing is necessary to exclude PE from the differential diagnosis (Table 2).5
Summary
Evaluating chest pain and shortness of breath in the ED is a humbling experience for even the most seasoned EP. Thoroughly reviewing the patient’s history and physical examination, and determining the pretest probability of disease entities high on the differential diagnoses list, go a long way in helping make the correct diagnosis—and in turn initiating possible life-saving interventions and treatment.
1. Stein PD, Beemath A, Matta F, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med. 2007;120(10):871-879.
2. Kukla P, Dlugopolski R, Krupa E, et al. How often pulmonary embolism mimics acute coronary syndrome? Kardiol Pol. 2011;69(3):235-240.
3. Meyer T, Binder L, Hruska N, Luthe H, Buchwald AB. Cardiac troponin I elevation in acute pulmonary embolism is associated with right ventricular dysfunction. J Am Coll Cardiol. 2000;36(5):1632-1636.
4. Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83(3):416-420.
5. Kline JA, Courtney DM, Kabrhel C, et al. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008;6(5):772-780. doi: 10.1111/j.1538-7836.2008.02944.x.
Case
A 37-year-old woman presented to the ED with a 90-minute history of chest tightness and shortness of breath. She admitted to feeling anxious but denied nausea, vomiting, or diaphoresis. The patient was in good health overall and had no history of similar symptoms. The only medication she took on a regular basis was a combination oral contraceptive (OC). Regarding the patient’s social history, she admitted to smoking one-half of a pack of cigarettes per day and occasional alcohol use.
On physical examination, the patient’s vital signs were: heart rate (HR), 102 beats/min; blood pressure, 118/64 mm Hg; respiratory rate, 20 breaths/min; and temperature, 98.6˚F. Oxygen saturation was 95% on room air. The head, eyes, ears, nose, and throat examination was normal. The cardiopulmonary examination revealed slight tachycardia with a regular rhythm but no murmurs, rubs, or gallops; the lungs were clear to auscultation bilaterally. The abdominal examination revealed a soft, nontender abdomen, without mass, and no guarding or rebound was present. An examination of the lower extremities was not documented.
The emergency physician (EP) ordered laboratory studies, which included a complete blood count (CBC), basic metabolic profile (BMP), and troponin I level. A chest X-ray and electrocardiogram (ECG) were also ordered. The chest X-ray was interpreted as normal, and the ECG revealed mild sinus tachycardia with nonspecific ST-T segment changes in V1 through V3. The CBC and BMP were all within normal limits, but the troponin I level was slightly elevated.
Given the patient’s clinical presentation and slightly elevated troponin I level, the EP was concerned for an acute coronary syndrome (ACS) and admitted the patient to the care of the on-call cardiologist. Prior to transfer, the patient was given 325 mg of aspirin by mouth, but no anticoagulation therapy was ordered. The cardiologist, who evaluated the patient after she was admitted to the inpatient floor, was concerned the patient had a pulmonary embolism (PE), and ordered a stat computed tomography angiography (CTA) scan of the chest. While the patient was undergoing the chest CTA scan, she went into cardiac arrest. Despite aggressive resuscitative measures, the patient could not be revived and was pronounced dead. An autopsy revealed a PE as the cause of death.
Plaintiff’s Claim
The patient’s estate sued the EP for failure to properly diagnose the PE, stating the hospital was vicariously liable for the EP’s actions. The emergency medicine (EM) expert for the plaintiff opined that the decedent’s symptoms should have prompted the EP to suspect she was suffering from a PE, and he should have immediately ordered anticoagulation, a D-dimer test, or a chest CTA scan. The expert cardiologist for the plaintiff stated the EP should have immediately started the patient on anticoagulation prior to the chest CTA scan.
The Defense
The defense EM expert stated the defendant’s diagnosis of ACS was appropriate given the patient’s overall clinical presentation, and the defense expert cardiologist stated the standard of care did not require the EP to administer anticoagulation prior to her diagnosis of PE, since the bleeding risks outweighed the benefits.
Verdict
At trial, the jury returned a defense verdict.
Discussion
This is not the first (nor probably the last) malpractice case in this column to involve a missed PE. While there have been improvements to the tools we currently possess to evaluate patients for suspected PE, it remains a difficult condition to reliably and timely identify in the ED. Although the two predominating symptoms—shortness of breath and chest pain—are common presentations in the ED, each is associated with large differential diagnoses.
Acute Coronary Syndrome Versus Pulmonary Embolism
From what we know of the published details of this case, the patient had only one risk factor for ACS (cigarette smoking) and two risk factors for PE (cigarette smoking and estrogen-containing contraceptive use). The only abnormal physical finding (tachycardia) was slightly more suggestive of PE than ACS. This patient’s primary complaint was chest fullness and shortness of breath. According to the Prospective Investigation of Pulmonary Embolism Diagnosis II study, shortness of breath is the most common complaint in PE (73%), followed by pleuritic chest pain (44%).1
In ACS, which is more common in men versus women and in patients of both sexes over age 55 years, the clinical presentation most commonly involves chest pain that patients describe as a pressure or fullness (as demonstrated in this patient). Unfortunately, in certain patient populations (eg, women, elderly patients, patients with diabetes mellitus) the presenting complaint can be shortness of breath, weakness, or nausea and vomiting. In a study evaluating how frequently an acute PE can mimic ACS, Kukla et al2 found that one-third of patients with an acute PE can present with all of the manifestations suggestive of ACS (ie, chest pain, ECG changes, and elevated troponin).
It is probably safe to assume the elevated troponin I level played a factor in influencing the EP to diagnose ACS, rather than pursuing an alternative diagnosis such as PE. Unfortunately, since both serum troponin T and I can be markers of right ventricle dysfunction, they are elevated in 30% to 50% of patients with moderate-to-large PE.3 However, neither serum troponin T nor troponin I is specific for myocardial infarction or unstable angina.
Pretest Probability: Wells Criteria
Determining pretest probability for any disease process is important when evaluating complaints in the ED; this is especially true for PE. One of the most frequently used tools for determining the likelihood of PE in ED patients is the Wells criteria (Table 1).4
Based on the published information available, the patient in this case would have scored a 1.5, placing her in the unlikely or low-risk category for PE. Patients whose Wells score places them in the low-risk group can benefit from serum D-dimer testing to help diagnose PE. However, serum D-dimer testing should not be ordered for patients in the likely or high-risk categories; these patients should instead be sent directly for imaging studies such as a chest CTA scan.
Pulmonary Embolism Rule-Out Criteria
For patients whose Wells criteria score places them in the “unlikely group,” the PE rule-out criteria (PERC) can be used to determine the need for ordering a D-dimer. If all eight criteria are met, no further testing is necessary to exclude PE from the differential diagnosis (Table 2).5
Summary
Evaluating chest pain and shortness of breath in the ED is a humbling experience for even the most seasoned EP. Thoroughly reviewing the patient’s history and physical examination, and determining the pretest probability of disease entities high on the differential diagnoses list, go a long way in helping make the correct diagnosis—and in turn initiating possible life-saving interventions and treatment.
Case
A 37-year-old woman presented to the ED with a 90-minute history of chest tightness and shortness of breath. She admitted to feeling anxious but denied nausea, vomiting, or diaphoresis. The patient was in good health overall and had no history of similar symptoms. The only medication she took on a regular basis was a combination oral contraceptive (OC). Regarding the patient’s social history, she admitted to smoking one-half of a pack of cigarettes per day and occasional alcohol use.
On physical examination, the patient’s vital signs were: heart rate (HR), 102 beats/min; blood pressure, 118/64 mm Hg; respiratory rate, 20 breaths/min; and temperature, 98.6˚F. Oxygen saturation was 95% on room air. The head, eyes, ears, nose, and throat examination was normal. The cardiopulmonary examination revealed slight tachycardia with a regular rhythm but no murmurs, rubs, or gallops; the lungs were clear to auscultation bilaterally. The abdominal examination revealed a soft, nontender abdomen, without mass, and no guarding or rebound was present. An examination of the lower extremities was not documented.
The emergency physician (EP) ordered laboratory studies, which included a complete blood count (CBC), basic metabolic profile (BMP), and troponin I level. A chest X-ray and electrocardiogram (ECG) were also ordered. The chest X-ray was interpreted as normal, and the ECG revealed mild sinus tachycardia with nonspecific ST-T segment changes in V1 through V3. The CBC and BMP were all within normal limits, but the troponin I level was slightly elevated.
Given the patient’s clinical presentation and slightly elevated troponin I level, the EP was concerned for an acute coronary syndrome (ACS) and admitted the patient to the care of the on-call cardiologist. Prior to transfer, the patient was given 325 mg of aspirin by mouth, but no anticoagulation therapy was ordered. The cardiologist, who evaluated the patient after she was admitted to the inpatient floor, was concerned the patient had a pulmonary embolism (PE), and ordered a stat computed tomography angiography (CTA) scan of the chest. While the patient was undergoing the chest CTA scan, she went into cardiac arrest. Despite aggressive resuscitative measures, the patient could not be revived and was pronounced dead. An autopsy revealed a PE as the cause of death.
Plaintiff’s Claim
The patient’s estate sued the EP for failure to properly diagnose the PE, stating the hospital was vicariously liable for the EP’s actions. The emergency medicine (EM) expert for the plaintiff opined that the decedent’s symptoms should have prompted the EP to suspect she was suffering from a PE, and he should have immediately ordered anticoagulation, a D-dimer test, or a chest CTA scan. The expert cardiologist for the plaintiff stated the EP should have immediately started the patient on anticoagulation prior to the chest CTA scan.
The Defense
The defense EM expert stated the defendant’s diagnosis of ACS was appropriate given the patient’s overall clinical presentation, and the defense expert cardiologist stated the standard of care did not require the EP to administer anticoagulation prior to her diagnosis of PE, since the bleeding risks outweighed the benefits.
Verdict
At trial, the jury returned a defense verdict.
Discussion
This is not the first (nor probably the last) malpractice case in this column to involve a missed PE. While there have been improvements to the tools we currently possess to evaluate patients for suspected PE, it remains a difficult condition to reliably and timely identify in the ED. Although the two predominating symptoms—shortness of breath and chest pain—are common presentations in the ED, each is associated with large differential diagnoses.
Acute Coronary Syndrome Versus Pulmonary Embolism
From what we know of the published details of this case, the patient had only one risk factor for ACS (cigarette smoking) and two risk factors for PE (cigarette smoking and estrogen-containing contraceptive use). The only abnormal physical finding (tachycardia) was slightly more suggestive of PE than ACS. This patient’s primary complaint was chest fullness and shortness of breath. According to the Prospective Investigation of Pulmonary Embolism Diagnosis II study, shortness of breath is the most common complaint in PE (73%), followed by pleuritic chest pain (44%).1
In ACS, which is more common in men versus women and in patients of both sexes over age 55 years, the clinical presentation most commonly involves chest pain that patients describe as a pressure or fullness (as demonstrated in this patient). Unfortunately, in certain patient populations (eg, women, elderly patients, patients with diabetes mellitus) the presenting complaint can be shortness of breath, weakness, or nausea and vomiting. In a study evaluating how frequently an acute PE can mimic ACS, Kukla et al2 found that one-third of patients with an acute PE can present with all of the manifestations suggestive of ACS (ie, chest pain, ECG changes, and elevated troponin).
It is probably safe to assume the elevated troponin I level played a factor in influencing the EP to diagnose ACS, rather than pursuing an alternative diagnosis such as PE. Unfortunately, since both serum troponin T and I can be markers of right ventricle dysfunction, they are elevated in 30% to 50% of patients with moderate-to-large PE.3 However, neither serum troponin T nor troponin I is specific for myocardial infarction or unstable angina.
Pretest Probability: Wells Criteria
Determining pretest probability for any disease process is important when evaluating complaints in the ED; this is especially true for PE. One of the most frequently used tools for determining the likelihood of PE in ED patients is the Wells criteria (Table 1).4
Based on the published information available, the patient in this case would have scored a 1.5, placing her in the unlikely or low-risk category for PE. Patients whose Wells score places them in the low-risk group can benefit from serum D-dimer testing to help diagnose PE. However, serum D-dimer testing should not be ordered for patients in the likely or high-risk categories; these patients should instead be sent directly for imaging studies such as a chest CTA scan.
Pulmonary Embolism Rule-Out Criteria
For patients whose Wells criteria score places them in the “unlikely group,” the PE rule-out criteria (PERC) can be used to determine the need for ordering a D-dimer. If all eight criteria are met, no further testing is necessary to exclude PE from the differential diagnosis (Table 2).5
Summary
Evaluating chest pain and shortness of breath in the ED is a humbling experience for even the most seasoned EP. Thoroughly reviewing the patient’s history and physical examination, and determining the pretest probability of disease entities high on the differential diagnoses list, go a long way in helping make the correct diagnosis—and in turn initiating possible life-saving interventions and treatment.
1. Stein PD, Beemath A, Matta F, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med. 2007;120(10):871-879.
2. Kukla P, Dlugopolski R, Krupa E, et al. How often pulmonary embolism mimics acute coronary syndrome? Kardiol Pol. 2011;69(3):235-240.
3. Meyer T, Binder L, Hruska N, Luthe H, Buchwald AB. Cardiac troponin I elevation in acute pulmonary embolism is associated with right ventricular dysfunction. J Am Coll Cardiol. 2000;36(5):1632-1636.
4. Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83(3):416-420.
5. Kline JA, Courtney DM, Kabrhel C, et al. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008;6(5):772-780. doi: 10.1111/j.1538-7836.2008.02944.x.
1. Stein PD, Beemath A, Matta F, et al. Clinical characteristics of patients with acute pulmonary embolism: data from PIOPED II. Am J Med. 2007;120(10):871-879.
2. Kukla P, Dlugopolski R, Krupa E, et al. How often pulmonary embolism mimics acute coronary syndrome? Kardiol Pol. 2011;69(3):235-240.
3. Meyer T, Binder L, Hruska N, Luthe H, Buchwald AB. Cardiac troponin I elevation in acute pulmonary embolism is associated with right ventricular dysfunction. J Am Coll Cardiol. 2000;36(5):1632-1636.
4. Wells PS, Anderson DR, Rodger M, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83(3):416-420.
5. Kline JA, Courtney DM, Kabrhel C, et al. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008;6(5):772-780. doi: 10.1111/j.1538-7836.2008.02944.x.
First EDition: Zika—Not the Only Mosquito-Borne Virus to Worry About
BY DOUG BRUNK
FRONTLINE MEDICAL NEWS
As the spread of the Zika virus continues to garner attention in the national spotlight, two other mosquito-borne viral infections pose a potential threat to the United States: dengue fever and chikungunya.
At the annual meeting of the Pacific Dermatologic Association, Iris Z. Ahronowitz, MD, shared tips on how to spot and diagnose patients with these viral infections.
“You really need to use all the data at your disposal, including a thorough symptom history, a thorough exposure history, and of course, our most important tool in all of this: our eyes,” said Dr Ahronowitz, a dermatologist at the University of Southern California, Los Angeles. Reaching a diagnosis involves asking about epidemiologic exposure, symptoms, morphology, and performing confirmatory testing by polymerase chain reaction (PCR) and/or enzyme-linked immunosorbent assay (ELISA). “Unfortunately we are not getting these results very quickly,” she said. “Sometimes the turnaround time can be 3 weeks or longer.”
She discussed the case of a 32-year-old woman who had returned from travel to Central Mexico. Two days later, the patient developed fever, fatigue, and retro-orbital headache, as well as flushing macular erythema over the chest. Three days later, she developed a generalized morbilliform eruption. Her white blood cell count was 1.5 x 109/L, platelet count was 37 x 109/L, aspartate aminotransferase (AST) was 124 U/L, and alanine aminotransferase (ALT) was 87 U/L.
The differential diagnosis for morbilliform eruption plus fever in a returning traveler is extensive, Dr Ahronowitz said. It includes measles, chikungunya, West Nile virus, O’nyong-nyong virus, Mayaro virus, Sindbis virus, Ross river disease, Ebola/Marburg, dengue, and Zika. Bacterial/rickettsial possibilities include typhoid fever, typhus, and leptospirosis.
The patient was ultimately diagnosed with dengue virus, a mosquito-borne flavivirus. Five serotypes have been identified, the most recent in 2013. According to Dr Ahronowitz, dengue ranks as the most common febrile illness in travelers returning from the Caribbean, South America, and Southeast Asia. “There are up to 100 million cases every year, 40% of the world population is at risk, and an estimated 80% of people are asymptomatic carriers, which is facilitating the spread of this disease,” she said. The most common vector is Aedes aegypti, a daytime biting mosquito that is endemic to the tropics and subtropics. But a new vector is emerging, Aedes albopictus, which is common in temperate areas. “Both types of mosquitoes are in the United States, and they’re spreading rapidly,” she said. “This is probably due to a combination of climate change and international travel.”
Dengue classically presents with sudden onset of fever, headache, retro-orbital pain, and severe myalgia; 50% to 82% of cases develop a distinctive rash. “While most viruses have nonspecific lab abnormalities, one that can be very helpful to you with suspected dengue is thrombocytopenia,” she said. “The incubation period ranges from 3 to 14 days.”
Rashes associated with dengue are classically biphasic and sequential. The initial rash occurs within 24 to 48 hours of symptom onset and is often mistaken for sunburn, with a flushing erythema of the face, neck, and chest. Three to 5 days later, a subsequent rash develops that starts out as a generalized morbilliform eruption but becomes confluent with petechiae and islands of sparing. “It’s been described as ‘white islands in a sea of red,’” Dr Ahronowitz said.
A more severe form of the disease, dengue hemorrhagic fever, is characterized by extensive purpura and bleeding from mucosa, gastrointestinal tract, and injection sites. “The patients who get this have prior immunity to a different serotype,” she said. “This is thought to be due to a phenomenon called antibody-dependent enhancement, whereby the presence of preexisting antibodies facilitates entry of the virus and produces a more robust inflammatory response. Most of these patients, even the ones with severe dengue, recover fully. The most common long-term sequela we’re seeing is chronic fatigue.”
The diagnosis is made with viral PCR from serum less than 7 days from onset of symptoms, or immunoglobulin M (IgM)ELISA more than 4 days from onset of symptoms. The treatment is supportive care with fluid resuscitation and analgesia; there is no specific treatment. “Do not give nonsteroidal anti-inflammatory drugs (NSAIDs) which can potentiate hemorrhage; give acetaminophen for pain and fevers,” she advised. “A tetravalent vaccine is now available for dengue. Prevention is so important because there is no treatment.”
Next, Dr Ahronowitz discussed the case of a 38-year-old man who returned from travel to Bangladesh. Two days after returning he developed fever to 104˚F, headache, and cervical lymphadenopathy. Three days after returning, he developed severe pain in the wrist, knees, and ankles, and a rash. “This rash was not specific; it was a morbilliform eruption primarily on the chest,” she said.
The patient was ultimately diagnosed with chikungunya, a single-strand RNA mosquito-borne virus with the same vectors as dengue. “This has been wreaking havoc across the Caribbean in the past few years,” Dr Ahronowitz said. “Chikungunya was first identified in the Americas in 2013, and there have been hundreds of thousands of cases in the Caribbean.” The first case acquired in the United States occurred in Florida in the summer of 2014. As of January 2016 there were 679 imported cases of the infection in the United States. “Fortunately, this most recent epidemic is slowing down a bit, but it’s important to be aware of,” she said.
Clinical presentation of chikungunya includes an incubation period of 3 to 7 days, acute onset of high fevers, chills, and myalgia. Nonspecific exanthem around 3 days occurs in 40% to 75% of cases, and symmetric polyarthralgias are common in the fingers, wrists, and ankles. Labs may reveal lymphopenia, acute kidney injury, and elevated AST and ALT levels. Acute symptoms resolve within 7 to 10 days.
Besides the rash, other cutaneous signs of the disease include aphthous-like ulcers and anogenital ulcers, particularly around the scrotum. Other patients may present with facial hyperpigmentation, also known as “brownie nose,” that appears with the rash. In babies, bullous lesions can occur. More than 20% of patients who acquire chikungunya still have severe joint pain 1 year after initial presentation. “This can be really debilitating,” she said. “A subset of patients will develop an inflammatory seronegative rheumatoid-like arthritis. It’s generally not a fatal condition except in the extremes of age and in people with a lot of comorbidities. Most people recover fully.”
As in dengue, clinicians can diagnose chikungunya by viral culture in the first 3 days of illness, and by reverse transcription PCR in the first 8 days of illness. On serology, IgM is positive by 5 days of symptom onset.
“If testing is not available locally, contact the Centers for Disease Control and Prevention,” Dr Ahronowitz said. “Treatment is supportive. Evaluate for and treat potential coinfections, including dengue, malaria, and bacterial infections. If dengue is in the differential diagnosis, avoid NSAIDs.” A new vaccine for chikungunya is currently in phase II trials.
BY DOUG BRUNK
FRONTLINE MEDICAL NEWS
As the spread of the Zika virus continues to garner attention in the national spotlight, two other mosquito-borne viral infections pose a potential threat to the United States: dengue fever and chikungunya.
At the annual meeting of the Pacific Dermatologic Association, Iris Z. Ahronowitz, MD, shared tips on how to spot and diagnose patients with these viral infections.
“You really need to use all the data at your disposal, including a thorough symptom history, a thorough exposure history, and of course, our most important tool in all of this: our eyes,” said Dr Ahronowitz, a dermatologist at the University of Southern California, Los Angeles. Reaching a diagnosis involves asking about epidemiologic exposure, symptoms, morphology, and performing confirmatory testing by polymerase chain reaction (PCR) and/or enzyme-linked immunosorbent assay (ELISA). “Unfortunately we are not getting these results very quickly,” she said. “Sometimes the turnaround time can be 3 weeks or longer.”
She discussed the case of a 32-year-old woman who had returned from travel to Central Mexico. Two days later, the patient developed fever, fatigue, and retro-orbital headache, as well as flushing macular erythema over the chest. Three days later, she developed a generalized morbilliform eruption. Her white blood cell count was 1.5 x 109/L, platelet count was 37 x 109/L, aspartate aminotransferase (AST) was 124 U/L, and alanine aminotransferase (ALT) was 87 U/L.
The differential diagnosis for morbilliform eruption plus fever in a returning traveler is extensive, Dr Ahronowitz said. It includes measles, chikungunya, West Nile virus, O’nyong-nyong virus, Mayaro virus, Sindbis virus, Ross river disease, Ebola/Marburg, dengue, and Zika. Bacterial/rickettsial possibilities include typhoid fever, typhus, and leptospirosis.
The patient was ultimately diagnosed with dengue virus, a mosquito-borne flavivirus. Five serotypes have been identified, the most recent in 2013. According to Dr Ahronowitz, dengue ranks as the most common febrile illness in travelers returning from the Caribbean, South America, and Southeast Asia. “There are up to 100 million cases every year, 40% of the world population is at risk, and an estimated 80% of people are asymptomatic carriers, which is facilitating the spread of this disease,” she said. The most common vector is Aedes aegypti, a daytime biting mosquito that is endemic to the tropics and subtropics. But a new vector is emerging, Aedes albopictus, which is common in temperate areas. “Both types of mosquitoes are in the United States, and they’re spreading rapidly,” she said. “This is probably due to a combination of climate change and international travel.”
Dengue classically presents with sudden onset of fever, headache, retro-orbital pain, and severe myalgia; 50% to 82% of cases develop a distinctive rash. “While most viruses have nonspecific lab abnormalities, one that can be very helpful to you with suspected dengue is thrombocytopenia,” she said. “The incubation period ranges from 3 to 14 days.”
Rashes associated with dengue are classically biphasic and sequential. The initial rash occurs within 24 to 48 hours of symptom onset and is often mistaken for sunburn, with a flushing erythema of the face, neck, and chest. Three to 5 days later, a subsequent rash develops that starts out as a generalized morbilliform eruption but becomes confluent with petechiae and islands of sparing. “It’s been described as ‘white islands in a sea of red,’” Dr Ahronowitz said.
A more severe form of the disease, dengue hemorrhagic fever, is characterized by extensive purpura and bleeding from mucosa, gastrointestinal tract, and injection sites. “The patients who get this have prior immunity to a different serotype,” she said. “This is thought to be due to a phenomenon called antibody-dependent enhancement, whereby the presence of preexisting antibodies facilitates entry of the virus and produces a more robust inflammatory response. Most of these patients, even the ones with severe dengue, recover fully. The most common long-term sequela we’re seeing is chronic fatigue.”
The diagnosis is made with viral PCR from serum less than 7 days from onset of symptoms, or immunoglobulin M (IgM)ELISA more than 4 days from onset of symptoms. The treatment is supportive care with fluid resuscitation and analgesia; there is no specific treatment. “Do not give nonsteroidal anti-inflammatory drugs (NSAIDs) which can potentiate hemorrhage; give acetaminophen for pain and fevers,” she advised. “A tetravalent vaccine is now available for dengue. Prevention is so important because there is no treatment.”
Next, Dr Ahronowitz discussed the case of a 38-year-old man who returned from travel to Bangladesh. Two days after returning he developed fever to 104˚F, headache, and cervical lymphadenopathy. Three days after returning, he developed severe pain in the wrist, knees, and ankles, and a rash. “This rash was not specific; it was a morbilliform eruption primarily on the chest,” she said.
The patient was ultimately diagnosed with chikungunya, a single-strand RNA mosquito-borne virus with the same vectors as dengue. “This has been wreaking havoc across the Caribbean in the past few years,” Dr Ahronowitz said. “Chikungunya was first identified in the Americas in 2013, and there have been hundreds of thousands of cases in the Caribbean.” The first case acquired in the United States occurred in Florida in the summer of 2014. As of January 2016 there were 679 imported cases of the infection in the United States. “Fortunately, this most recent epidemic is slowing down a bit, but it’s important to be aware of,” she said.
Clinical presentation of chikungunya includes an incubation period of 3 to 7 days, acute onset of high fevers, chills, and myalgia. Nonspecific exanthem around 3 days occurs in 40% to 75% of cases, and symmetric polyarthralgias are common in the fingers, wrists, and ankles. Labs may reveal lymphopenia, acute kidney injury, and elevated AST and ALT levels. Acute symptoms resolve within 7 to 10 days.
Besides the rash, other cutaneous signs of the disease include aphthous-like ulcers and anogenital ulcers, particularly around the scrotum. Other patients may present with facial hyperpigmentation, also known as “brownie nose,” that appears with the rash. In babies, bullous lesions can occur. More than 20% of patients who acquire chikungunya still have severe joint pain 1 year after initial presentation. “This can be really debilitating,” she said. “A subset of patients will develop an inflammatory seronegative rheumatoid-like arthritis. It’s generally not a fatal condition except in the extremes of age and in people with a lot of comorbidities. Most people recover fully.”
As in dengue, clinicians can diagnose chikungunya by viral culture in the first 3 days of illness, and by reverse transcription PCR in the first 8 days of illness. On serology, IgM is positive by 5 days of symptom onset.
“If testing is not available locally, contact the Centers for Disease Control and Prevention,” Dr Ahronowitz said. “Treatment is supportive. Evaluate for and treat potential coinfections, including dengue, malaria, and bacterial infections. If dengue is in the differential diagnosis, avoid NSAIDs.” A new vaccine for chikungunya is currently in phase II trials.
BY DOUG BRUNK
FRONTLINE MEDICAL NEWS
As the spread of the Zika virus continues to garner attention in the national spotlight, two other mosquito-borne viral infections pose a potential threat to the United States: dengue fever and chikungunya.
At the annual meeting of the Pacific Dermatologic Association, Iris Z. Ahronowitz, MD, shared tips on how to spot and diagnose patients with these viral infections.
“You really need to use all the data at your disposal, including a thorough symptom history, a thorough exposure history, and of course, our most important tool in all of this: our eyes,” said Dr Ahronowitz, a dermatologist at the University of Southern California, Los Angeles. Reaching a diagnosis involves asking about epidemiologic exposure, symptoms, morphology, and performing confirmatory testing by polymerase chain reaction (PCR) and/or enzyme-linked immunosorbent assay (ELISA). “Unfortunately we are not getting these results very quickly,” she said. “Sometimes the turnaround time can be 3 weeks or longer.”
She discussed the case of a 32-year-old woman who had returned from travel to Central Mexico. Two days later, the patient developed fever, fatigue, and retro-orbital headache, as well as flushing macular erythema over the chest. Three days later, she developed a generalized morbilliform eruption. Her white blood cell count was 1.5 x 109/L, platelet count was 37 x 109/L, aspartate aminotransferase (AST) was 124 U/L, and alanine aminotransferase (ALT) was 87 U/L.
The differential diagnosis for morbilliform eruption plus fever in a returning traveler is extensive, Dr Ahronowitz said. It includes measles, chikungunya, West Nile virus, O’nyong-nyong virus, Mayaro virus, Sindbis virus, Ross river disease, Ebola/Marburg, dengue, and Zika. Bacterial/rickettsial possibilities include typhoid fever, typhus, and leptospirosis.
The patient was ultimately diagnosed with dengue virus, a mosquito-borne flavivirus. Five serotypes have been identified, the most recent in 2013. According to Dr Ahronowitz, dengue ranks as the most common febrile illness in travelers returning from the Caribbean, South America, and Southeast Asia. “There are up to 100 million cases every year, 40% of the world population is at risk, and an estimated 80% of people are asymptomatic carriers, which is facilitating the spread of this disease,” she said. The most common vector is Aedes aegypti, a daytime biting mosquito that is endemic to the tropics and subtropics. But a new vector is emerging, Aedes albopictus, which is common in temperate areas. “Both types of mosquitoes are in the United States, and they’re spreading rapidly,” she said. “This is probably due to a combination of climate change and international travel.”
Dengue classically presents with sudden onset of fever, headache, retro-orbital pain, and severe myalgia; 50% to 82% of cases develop a distinctive rash. “While most viruses have nonspecific lab abnormalities, one that can be very helpful to you with suspected dengue is thrombocytopenia,” she said. “The incubation period ranges from 3 to 14 days.”
Rashes associated with dengue are classically biphasic and sequential. The initial rash occurs within 24 to 48 hours of symptom onset and is often mistaken for sunburn, with a flushing erythema of the face, neck, and chest. Three to 5 days later, a subsequent rash develops that starts out as a generalized morbilliform eruption but becomes confluent with petechiae and islands of sparing. “It’s been described as ‘white islands in a sea of red,’” Dr Ahronowitz said.
A more severe form of the disease, dengue hemorrhagic fever, is characterized by extensive purpura and bleeding from mucosa, gastrointestinal tract, and injection sites. “The patients who get this have prior immunity to a different serotype,” she said. “This is thought to be due to a phenomenon called antibody-dependent enhancement, whereby the presence of preexisting antibodies facilitates entry of the virus and produces a more robust inflammatory response. Most of these patients, even the ones with severe dengue, recover fully. The most common long-term sequela we’re seeing is chronic fatigue.”
The diagnosis is made with viral PCR from serum less than 7 days from onset of symptoms, or immunoglobulin M (IgM)ELISA more than 4 days from onset of symptoms. The treatment is supportive care with fluid resuscitation and analgesia; there is no specific treatment. “Do not give nonsteroidal anti-inflammatory drugs (NSAIDs) which can potentiate hemorrhage; give acetaminophen for pain and fevers,” she advised. “A tetravalent vaccine is now available for dengue. Prevention is so important because there is no treatment.”
Next, Dr Ahronowitz discussed the case of a 38-year-old man who returned from travel to Bangladesh. Two days after returning he developed fever to 104˚F, headache, and cervical lymphadenopathy. Three days after returning, he developed severe pain in the wrist, knees, and ankles, and a rash. “This rash was not specific; it was a morbilliform eruption primarily on the chest,” she said.
The patient was ultimately diagnosed with chikungunya, a single-strand RNA mosquito-borne virus with the same vectors as dengue. “This has been wreaking havoc across the Caribbean in the past few years,” Dr Ahronowitz said. “Chikungunya was first identified in the Americas in 2013, and there have been hundreds of thousands of cases in the Caribbean.” The first case acquired in the United States occurred in Florida in the summer of 2014. As of January 2016 there were 679 imported cases of the infection in the United States. “Fortunately, this most recent epidemic is slowing down a bit, but it’s important to be aware of,” she said.
Clinical presentation of chikungunya includes an incubation period of 3 to 7 days, acute onset of high fevers, chills, and myalgia. Nonspecific exanthem around 3 days occurs in 40% to 75% of cases, and symmetric polyarthralgias are common in the fingers, wrists, and ankles. Labs may reveal lymphopenia, acute kidney injury, and elevated AST and ALT levels. Acute symptoms resolve within 7 to 10 days.
Besides the rash, other cutaneous signs of the disease include aphthous-like ulcers and anogenital ulcers, particularly around the scrotum. Other patients may present with facial hyperpigmentation, also known as “brownie nose,” that appears with the rash. In babies, bullous lesions can occur. More than 20% of patients who acquire chikungunya still have severe joint pain 1 year after initial presentation. “This can be really debilitating,” she said. “A subset of patients will develop an inflammatory seronegative rheumatoid-like arthritis. It’s generally not a fatal condition except in the extremes of age and in people with a lot of comorbidities. Most people recover fully.”
As in dengue, clinicians can diagnose chikungunya by viral culture in the first 3 days of illness, and by reverse transcription PCR in the first 8 days of illness. On serology, IgM is positive by 5 days of symptom onset.
“If testing is not available locally, contact the Centers for Disease Control and Prevention,” Dr Ahronowitz said. “Treatment is supportive. Evaluate for and treat potential coinfections, including dengue, malaria, and bacterial infections. If dengue is in the differential diagnosis, avoid NSAIDs.” A new vaccine for chikungunya is currently in phase II trials.
The Long Hot Summer of 2016
Months of extremely high temperatures throughout the United States made the summer of 2016 one of the hottest summers on record. The summer may also be remembered for the excessive amounts of hot air generated in the run-up to the 2016 presidential election. But most oppressive of all has been the failure of Congress to appropriate funds for Zika virus research, prevention, and treatment before it recessed for vacation.
Emergency physicians (EPs) in the United States are already dealing with frightened, symptomatic patients who may have been exposed to the Zika, dengue, or chikungunya viruses, transmitted by the bite of the Aedes aegypti mosquito. In the First EDition section of this issue, dermatologist Iris Z. Ahronowitz, MD, describes some of the similarities in the acute clinical presentations of those infections (see page 438). But among this group of related viruses, only Zika has been positively linked to microcephaly and severely underdeveloped, damaged brains in babies born to women who are infected during pregnancy. An increasing number of newborn babies severely affected by Zika virus in utero began appearing in South America in late 2015. By summer’s end (September 21, 2016), the Centers for Disease Control and Prevention reports of Zika virus disease in the United States included over 3,300 travel-related cases, 43 locally acquired mosquito-borne cases, 28 sexually transmitted cases, and eight cases of Guillain-Barré syndrome (http://www.cdc.gov/zika/geo/united-states.html). Most importantly, as of September 15, 2016, there have been 20 live-born infants with birth defects and five pregnancy losses with birth defects—numbers that do not reflect the outcomes of ongoing pregnancies.
The life expectancy of babies severely affected by Zika virus and the nature and extent of disability in less physically affected babies are presently unknown. But according to The Washington Post (http://wapo.st/29Y5CnR), estimates of the cost of caring for a severely affected Zika baby through adulthood run as high as $10 million or more, and as high a total price as we will pay for the congressional intransigence this summer, such cost estimates do not even consider the terrible human suffering these babies will experience or the anguish their parents may have for the rest of their lives.
Emergency physicians are all too familiar with the emotional and behavioral problems that complicate our efforts to manage acute medical problems of children and adults born with autism or Down syndrome when they present to the ED. Most such congenital illnesses are not preventable, but when one potentially is, delaying needed resources because of partisan politics is unconscionable.
By summer’s end, as the last of leftover Ebola dollars were being spent on Zika-related programs, Democrats and Republicans finally appeared to be reaching a consensus to provide $1.1 billion of the $1.9 billion originally requested by the President long before the long hot summer began. This sudden agreement may be driven by the importance both parties place on winning the Florida vote in the upcoming election. But whatever the reason, Zika funding now will help prevent untold hardships and suffering in the years to come. In the meantime, EPs will continue to evaluate, diagnose, counsel, and, hopefully someday soon, be able to treat all who come to our EDs with Zika infection.
Months of extremely high temperatures throughout the United States made the summer of 2016 one of the hottest summers on record. The summer may also be remembered for the excessive amounts of hot air generated in the run-up to the 2016 presidential election. But most oppressive of all has been the failure of Congress to appropriate funds for Zika virus research, prevention, and treatment before it recessed for vacation.
Emergency physicians (EPs) in the United States are already dealing with frightened, symptomatic patients who may have been exposed to the Zika, dengue, or chikungunya viruses, transmitted by the bite of the Aedes aegypti mosquito. In the First EDition section of this issue, dermatologist Iris Z. Ahronowitz, MD, describes some of the similarities in the acute clinical presentations of those infections (see page 438). But among this group of related viruses, only Zika has been positively linked to microcephaly and severely underdeveloped, damaged brains in babies born to women who are infected during pregnancy. An increasing number of newborn babies severely affected by Zika virus in utero began appearing in South America in late 2015. By summer’s end (September 21, 2016), the Centers for Disease Control and Prevention reports of Zika virus disease in the United States included over 3,300 travel-related cases, 43 locally acquired mosquito-borne cases, 28 sexually transmitted cases, and eight cases of Guillain-Barré syndrome (http://www.cdc.gov/zika/geo/united-states.html). Most importantly, as of September 15, 2016, there have been 20 live-born infants with birth defects and five pregnancy losses with birth defects—numbers that do not reflect the outcomes of ongoing pregnancies.
The life expectancy of babies severely affected by Zika virus and the nature and extent of disability in less physically affected babies are presently unknown. But according to The Washington Post (http://wapo.st/29Y5CnR), estimates of the cost of caring for a severely affected Zika baby through adulthood run as high as $10 million or more, and as high a total price as we will pay for the congressional intransigence this summer, such cost estimates do not even consider the terrible human suffering these babies will experience or the anguish their parents may have for the rest of their lives.
Emergency physicians are all too familiar with the emotional and behavioral problems that complicate our efforts to manage acute medical problems of children and adults born with autism or Down syndrome when they present to the ED. Most such congenital illnesses are not preventable, but when one potentially is, delaying needed resources because of partisan politics is unconscionable.
By summer’s end, as the last of leftover Ebola dollars were being spent on Zika-related programs, Democrats and Republicans finally appeared to be reaching a consensus to provide $1.1 billion of the $1.9 billion originally requested by the President long before the long hot summer began. This sudden agreement may be driven by the importance both parties place on winning the Florida vote in the upcoming election. But whatever the reason, Zika funding now will help prevent untold hardships and suffering in the years to come. In the meantime, EPs will continue to evaluate, diagnose, counsel, and, hopefully someday soon, be able to treat all who come to our EDs with Zika infection.
Months of extremely high temperatures throughout the United States made the summer of 2016 one of the hottest summers on record. The summer may also be remembered for the excessive amounts of hot air generated in the run-up to the 2016 presidential election. But most oppressive of all has been the failure of Congress to appropriate funds for Zika virus research, prevention, and treatment before it recessed for vacation.
Emergency physicians (EPs) in the United States are already dealing with frightened, symptomatic patients who may have been exposed to the Zika, dengue, or chikungunya viruses, transmitted by the bite of the Aedes aegypti mosquito. In the First EDition section of this issue, dermatologist Iris Z. Ahronowitz, MD, describes some of the similarities in the acute clinical presentations of those infections (see page 438). But among this group of related viruses, only Zika has been positively linked to microcephaly and severely underdeveloped, damaged brains in babies born to women who are infected during pregnancy. An increasing number of newborn babies severely affected by Zika virus in utero began appearing in South America in late 2015. By summer’s end (September 21, 2016), the Centers for Disease Control and Prevention reports of Zika virus disease in the United States included over 3,300 travel-related cases, 43 locally acquired mosquito-borne cases, 28 sexually transmitted cases, and eight cases of Guillain-Barré syndrome (http://www.cdc.gov/zika/geo/united-states.html). Most importantly, as of September 15, 2016, there have been 20 live-born infants with birth defects and five pregnancy losses with birth defects—numbers that do not reflect the outcomes of ongoing pregnancies.
The life expectancy of babies severely affected by Zika virus and the nature and extent of disability in less physically affected babies are presently unknown. But according to The Washington Post (http://wapo.st/29Y5CnR), estimates of the cost of caring for a severely affected Zika baby through adulthood run as high as $10 million or more, and as high a total price as we will pay for the congressional intransigence this summer, such cost estimates do not even consider the terrible human suffering these babies will experience or the anguish their parents may have for the rest of their lives.
Emergency physicians are all too familiar with the emotional and behavioral problems that complicate our efforts to manage acute medical problems of children and adults born with autism or Down syndrome when they present to the ED. Most such congenital illnesses are not preventable, but when one potentially is, delaying needed resources because of partisan politics is unconscionable.
By summer’s end, as the last of leftover Ebola dollars were being spent on Zika-related programs, Democrats and Republicans finally appeared to be reaching a consensus to provide $1.1 billion of the $1.9 billion originally requested by the President long before the long hot summer began. This sudden agreement may be driven by the importance both parties place on winning the Florida vote in the upcoming election. But whatever the reason, Zika funding now will help prevent untold hardships and suffering in the years to come. In the meantime, EPs will continue to evaluate, diagnose, counsel, and, hopefully someday soon, be able to treat all who come to our EDs with Zika infection.
Direct Anterior Versus Posterior Simultaneous Bilateral Total Hip Arthroplasties: No Major Differences at 90 Days
End-stage osteoarthritis of the hip is a debilitating disease that is reliably treated with total hip arthroplasty (THA).1 Up to 35% of patients who undergo THA eventually require contralateral THA.2,3 In patients who present with advanced bilateral disease and undergo unilateral THA, the risk of ultimately requiring a contralateral procedure is as high as 97%.3-6 In patients with bilateral hip disease, function is not fully optimized until both hips have been replaced, particularly in the setting of fixed flexion contractures.7-9 Naturally, there has been some interest in simultaneous bilateral THAs for select patients.
The potential benefits of bilateral THAs over staged procedures include faster overall rehabilitation, exposure to a single anesthetic, reduced hospital length of stay (LOS), and cost savings.10-12 However, opinion on recommending bilateral THAs is mixed. Although bilateral procedures historically have been fraught with perioperative complications,13,14 advances in surgical and anesthetic techniques have led to improved outcomes.15 Whether surgical approach is a factor in these outcomes is unclear.
The popularity of the direct anterior (DA) approach for THA has increased in recent years.16 Although the relative advantages of various approaches remain in debate, one potential benefit of the DA approach is supine positioning, which allows simultaneous bilateral THAs to be performed without the need for repositioning before proceeding with the contralateral side. However, simultaneous bilateral THAs performed through the DA approach and those performed through other surgical approaches are lacking in comparative outcomes data.17In this study, we evaluated operative times, transfusion requirements, hospital discharge data, and 90-day complication rates in patients who had simultaneous bilateral THAs through either the DA approach or the posterior approach.
Methods
Study Design
This single-center study was conducted at the Mayo Clinic in Rochester, Minnesota. After obtaining approval from our Institutional Review Board, we performed a retrospective cohort analysis. We used our institution’s total joint registry to identify all patients who underwent simultaneous bilateral THAs through either the DA approach or the posterior approach. The first bilateral THAs to use the DA approach at our institution were performed in 2012. To ensure that the DA and posterior groups’ perioperative management would be similar, we included only cases performed between 2012 and 2014.
There were 19 patients in the DA group and 21 in the posterior group. The groups were similar in mean age (54 vs 54 years; P = .90), sex (73% vs 57% males; P = .33), body mass index (BMI; 25 vs 28 kg/m2; P = .38), preoperative hemoglobin level (14.3 vs 14.0 g/dL; P = .37), preoperative diagnosis (71.1% vs 78.6% degenerative joint disease; P = .75), and American Society of Anesthesiologists (ASA) score (1.9 vs 2.0; P = .63) (Table 1).
Patient Care
All cases were performed by 1 of 3 dedicated arthroplasty surgeons (Dr. Taunton, Dr. Sierra, Dr. Trousdale). Dr. Taunton exclusively uses the DA approach, and Dr. Sierra and Dr. Trousdale exclusively use the posterior approach. Patients in both groups received preoperative medical clearance and attended the same preoperative education class.
Patients in the DA group were positioned supine on an orthopedic table that allows hyperextension and adduction of the operative leg. Both hips were prepared and draped simultaneously. The most symptomatic hip was operated on first, with a sterile drape covering the contralateral hip. Between hips, fluoroscopy was moved to the other side of the operative suite, but no changes in positioning or preparation were necessary. A deep drain was placed on each side, and then was removed the morning of postoperative day 1. The same set of instruments was used on both sides.
Patients in the posterior group were positioned lateral on a regular operative table with hip rests. The most symptomatic hip was operated on first. After wound closure and dressing application, the patient was flipped to allow access to the contralateral hip and was prepared and draped again. The same instruments were used on each side. Drains were not used.
All patients received the same comprehensive multimodal pain management, which combined general and epidural anesthesia (remaining in place until postoperative day 2) and included an oral pain regimen of scheduled acetaminophen and as-needed tramadol and oxycodone. In all cases, intraoperative blood salvage and intravenous tranexamic acid (1 g at time of incision on first hip, 1 g at wound closure on second hip) were used. Preoperative autologous blood donation was not used. For deep vein thrombosis prophylaxis, patients were treated with bilateral sequential compression devices while hospitalized, but chemoprophylaxis was different between groups. Patients in the DA group received prophylactic low-molecular-weight heparin for 10 days, followed by twice-daily aspirin (325 mg) for 4 weeks. Patients in the posterior group received warfarin (goal international normalized ratio, 1.7-2.2) for 3 weeks, followed by twice-daily aspirin (325 mg) for 3 weeks. The decision to transfuse allogenic red blood cells was made by the treating surgeon, based on standardized hospital protocols, wherein patients are transfused for hemoglobin levels under 7.0 g/dL, or for hemoglobin levels less than 8.0 g/dL in the presence of persistent symptoms. All patients received care on an orthopedic specialty floor and were assisted by the same physical therapists. Discharge disposition was coordinated with the same group of social workers.
Two to 3 months after surgery, patients returned for routine examination and radiographs. All patients were followed up for at least 90 days.
Statistical Analysis
All outcomes were analyzed with appropriate summary statistics. Chi-square tests or logistic regression analyses (for categorical outcomes) were used to compare baseline covariates with perioperative outcomes, and 2-sample tests or Wilcoxon rank-sum tests were used to compare outcomes measured on a continuous scale. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated as appropriate. Operative time was calculated by adding time from incision to wound closure for both hips (room turnover time between hips was not included). Anesthesia time was defined as total time patients were in the operating room. All statistical tests were 2-sided, and the threshold for statistical significance was set at α = 0.05.
Results
Compared with patients who underwent simultaneous bilateral THAs through the posterior approach, patients who underwent simultaneous bilateral THAs through the DA approach had longer mean operative times (153 vs 106 min; P < .001) and anesthesia times (257 vs 221 min; P = .007). The 2 groups’ hospital stays were similar in length (3.1 vs 3.5 days; P = .31), but patients in the DA group were more likely to be discharged home (100.0% vs 71.4%; P = .02) (Table 2).
Patients in the DA group were more likely to have sufficient intraoperative blood salvage for autologous transfusion (89.5% vs 57.1%; OR, 6.4; 95% CI, 1.16-34.94; P = .03) (Table 3) and received more mean units of salvaged autologous blood (1.4 vs 0.5; P = .003) (Table 2). Allogenic blood was not given to any patients in the DA group, but 3 patients in the posterior group (14.3%) required allogenic blood transfusion (P = .23) (Table 2). Salvaged autologous and allogenic blood transfusion was not associated with sex, age 60 years or older, or hospital LOS of 4 days or more (Table 3). The groups’ mean hemoglobin levels, measured the morning of postoperative day 1, were similar: 10.6 g/dL (range, 8.5-12.4 g/dL) for the DA group and 10.3 g/dL (range 8.6-12.3 g/dL) for the posterior group (Table 2).
In-hospital complications were uncommon in both groups (5% vs 14%; P = .61) (Table 2). One patient in the posterior group sustained a unilateral dislocation the day of surgery, and closed reduction was required; other complications (1 ileus, 2 tachyarrhythmias) did not require intervention. Ninety-day complications were also rare; 1 patient in the posterior group developed a hematoma with wound drainage, and this was successfully managed conservatively. There were no reoperations or readmissions in either group (Table 2).
Discussion
Although bilateral procedures account for less than 1% of THAs in the United States,11 debate about their role in patients with severe bilateral hip disease continues. The potential benefits of a single episode of care must be weighed against the slightly increased risk for systemic complications.7,10-15 Recent innovations in perioperative management have been shown to minimize complications,15 but it is unclear whether surgical approach affects perioperative outcomes. Our goals in this study were to evaluate operative times, transfusion requirements, hospital discharge data, and 90-day complication rates in patients who underwent simultaneous bilateral THAs through either the DA approach or the posterior approach.
Patients in our DA group had longer operative and anesthesia times. Other studies have found longer operative times for the DA approach relative to the posterior approach in unilateral THAs.18 One potential benefit of the DA approach in the setting of simultaneous bilateral THAs is the ability to prepare and drape both sides before surgery and thereby keep the interruption between hips to a minimum. In the present study, however, time saved during turnover between hips was overshadowed by the time added for each THA.
Although it was uncommon for complications to occur within 90 days after surgery in this study, many patients are needed to fully investigate these rare occurrences. Because of inherent selection bias, these risks are difficult to directly compare in patients who undergo unilateral procedures. Although small studies have failed to clarify the issue,7,19,20 a recent review of the almost 20,000 bilateral THA cases in the US Nationwide Inpatient Sample database found that bilateral (vs unilateral) THAs were associated with increased risk of local and systemic complications.11 Therefore, bilateral THAs should be reserved for select cases, with attention given to excluding patients with preexisting cardiopulmonary disease and providing appropriate preoperative counseling.
Most studies have reported a higher transfusion rate in bilateral THAs relative to staged procedures.7,21-23 Allogenic blood transfusion leads to immune suppression, coagulopathy, and other systemic effects in general, and has been specifically associated with infection in patients who undergo total joint arthroplasty.24-29 Parvizi and colleagues17 reported reduced blood loss and fewer blood transfusions in patients who had simultaneous bilateral THAs through the DA approach, compared with the direct lateral approach. Patients in our DA group received more salvaged autologous blood, which we suppose was a function of longer operative times. However, postoperative hemoglobin levels and allogenic blood transfusion rates were statistically similar between the 2 groups. It is important to consider the increased risk of required allogenic blood transfusion associated with simultaneous bilateral THAs, but it is not fully clear if this risk is lower in THAs performed through the DA approach relative to other approaches. In our experience, the required transfusion risk is limited in DA and posterior approaches with use of contemporary perioperative blood management strategies.
Although hospital LOS is longer with simultaneous bilateral THAs than with unilateral THAs, historically it is shorter than the combined LOS of staged bilateral THAs.20 Patients in our study had a relatively short LOS after bilateral THAs, and there was no difference in LOS between groups. However, patients were more likely to be discharged home after bilateral THAs through the DA approach vs the posterior approach. Although discharge location was not affected by age, sex, ASA score, or LOS, unrecognized social factors unrelated to surgical approach likely influenced this finding.
This study should be interpreted in light of important limitations. Foremost, although data were prospectively collected, we examined them retrospectively. Thus, it is possible there may be unaccounted for differences between our DA and posterior THA groups. For example, the DA and posterior approaches were used by different surgeons with differing experience, technique, and preferences, all of which could have affected outcomes. Furthermore, our sample was relatively small (simultaneous bilateral THAs are performed relatively infrequently). Last, although anesthesia, pain management, blood conservation, and physical therapy were similar for the 2 groups, there was no standardized protocol for determining eligibility for simultaneous bilateral THAs.
In conclusion, we found that simultaneous bilateral THAs can be safely performed through either the DA approach or the posterior approach. Although the transition between hips is shorter with the DA approach, this time savings is overshadowed by the increased duration of each procedure. Transfusion rates are low in both groups, and in-hospital and 90-day complications are quite rare. Furthermore, patients can routinely be discharged home without elevating readmission rates. We will continue to perform simultaneous bilateral THAs through the DA approach or the posterior approach, according to surgeon preference.
Am J Orthop. 2016;45(6):E373-E378. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370(9597):1508-1519.
2. Sayeed SA, Johnson AJ, Jaffe DE, Mont MA. Incidence of contralateral THA after index THA for osteoarthritis. Clin Orthop Relat Res. 2012;470(2):535-540.
3. Sayeed SA, Trousdale RT, Barnes SA, Kaufman KR, Pagnano MW. Joint arthroplasty within 10 years after primary Charnley total hip arthroplasty. Am J Orthop. 2009;38(8):E141-E143.
4. Goker B, Doughan AM, Schnitzer TJ, Block JA. Quantification of progressive joint space narrowing in osteoarthritis of the hip: longitudinal analysis of the contralateral hip after total hip arthroplasty. Arthritis Rheum. 2000;43(5):988-994.
5. Husted H, Overgaard S, Laursen JO, et al. Need for bilateral arthroplasty for coxarthrosis. 1,477 replacements in 1,199 patients followed for 0-14 years. Acta Orthop Scand. 1996;67(5):421-423.
6. Ritter MA, Carr K, Herbst SA, et al. Outcome of the contralateral hip following total hip arthroplasty for osteoarthritis. J Arthroplasty. 1996;11(3):242-246.
7. Alfaro- Adrián J, Bayona F, Rech JA, Murray DW. One- or two-stage bilateral total hip replacement. J Arthroplasty. 1999;14(4):439-445.
8. Wykman A, Olsson E. Walking ability after total hip replacement. A comparison of gait analysis in unilateral and bilateral cases. J Bone Joint Surg Br. 1992;74(1):53-56.
9. Yoshii T, Jinno T, Morita S, et al. Postoperative hip motion and functional recovery after simultaneous bilateral total hip arthroplasty for bilateral osteoarthritis. J Orthop Sci. 2009;14(2):161-166.
10. Lorenze M, Huo MH, Zatorski LE, Keggi KJ. A comparison of the cost effectiveness of one-stage versus two-stage bilateral total hip replacement. Orthopedics. 1998;21(12):1249-1252.
11. Rasouli MR, Maltenfort MG, Ross D, Hozack WJ, Memtsoudis SG, Parvizi J. Perioperative morbidity and mortality following bilateral total hip arthroplasty. J Arthroplasty. 2014;29(1):142-148.
12. Reuben JD, Meyers SJ, Cox DD, Elliott M, Watson M, Shim SD. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty. 1998;13(2):172-179.
13. Bracy D, Wroblewski BM. Bilateral Charnley arthroplasty as a single procedure. A report on 400 patients. J Bone Joint Surg Br. 1981;63(3):354-356.
14. Ritter MA, Randolph JC. Bilateral total hip arthroplasty: a simultaneous procedure. Acta Orthop Scand. 1976;47(2):203-208.
15. Ritter MA, Stringer EA. Bilateral total hip arthroplasty: a single procedure. Clin Orthop Relat Res. 1980;(149):185-190.
16. Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;(441):115-124.
17. Parvizi J, Rasouli MR, Jaberi M, et al. Does the surgical approach in one stage bilateral total hip arthroplasty affect blood loss? Int Orthop. 2013;37(12):2357-2362.
18. Poehling-Monaghan KL, Kamath AF, Taunton MJ, Pagnano MW. Direct anterior versus miniposterior THA with the same advanced perioperative protocols: surprising early clinical results. Clin Orthop Relat Res. 2015;473(2):623-631.
19. Macaulay W, Salvati EA, Sculco TP, Pellicci PM. Single-stage bilateral total hip arthroplasty. J Am Acad Orthop Surg. 2002;10(3):217-221.
20. Romagnoli S, Zacchetti S, Perazzo P, Verde F, Banfi G, Viganò M. Simultaneous bilateral total hip arthroplasties do not lead to higher complication or allogeneic transfusion rates compared to unilateral procedures. Int Orthop. 2013;37(11):2125-2130.
21. Salvati EA, Hughes P, Lachiewicz P. Bilateral total hip-replacement arthroplasty in one stage. J Bone Joint Surg Am. 1978;60(5):640-644.
22. Parvizi J, Chaudhry S, Rasouli MR, et al. Who needs autologous blood donation in joint replacement? J Knee Surg. 2011;24(1):25-31.
23. Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am. 2007;89(1):27-32.
24. Blair SD, Janvrin SB, McCollum CN, Greenhalgh RM. Effect of early blood transfusion on gastrointestinal haemorrhage. Br J Surg. 1986;73(10):783-785.
25. Blumberg N, Heal JM. Immunomodulation by blood transfusion: an evolving scientific and clinical challenge. Am J Med. 1996;101(3):299-308.
26. Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340(6):409-417.
27. Iturbe T, Cornudella R, de Miguel R, et al. Hypercoagulability state in hip and knee surgery: influence of ABO antigenic system and allogenic transfusion. Transfus Sci. 1999;20(1):17-20.
28. Murphy P, Heal JM, Blumberg N. Infection or suspected infection after hip replacement surgery with autologous or homologous blood transfusions. Transfusion. 1991;31(3):212-217.
29. Watts CD, Pagnano MW. Minimising blood loss and transfusion in contemporary hip and knee arthroplasty. J Bone Joint Surg Br. 2012;94(11 suppl A):8-10.
End-stage osteoarthritis of the hip is a debilitating disease that is reliably treated with total hip arthroplasty (THA).1 Up to 35% of patients who undergo THA eventually require contralateral THA.2,3 In patients who present with advanced bilateral disease and undergo unilateral THA, the risk of ultimately requiring a contralateral procedure is as high as 97%.3-6 In patients with bilateral hip disease, function is not fully optimized until both hips have been replaced, particularly in the setting of fixed flexion contractures.7-9 Naturally, there has been some interest in simultaneous bilateral THAs for select patients.
The potential benefits of bilateral THAs over staged procedures include faster overall rehabilitation, exposure to a single anesthetic, reduced hospital length of stay (LOS), and cost savings.10-12 However, opinion on recommending bilateral THAs is mixed. Although bilateral procedures historically have been fraught with perioperative complications,13,14 advances in surgical and anesthetic techniques have led to improved outcomes.15 Whether surgical approach is a factor in these outcomes is unclear.
The popularity of the direct anterior (DA) approach for THA has increased in recent years.16 Although the relative advantages of various approaches remain in debate, one potential benefit of the DA approach is supine positioning, which allows simultaneous bilateral THAs to be performed without the need for repositioning before proceeding with the contralateral side. However, simultaneous bilateral THAs performed through the DA approach and those performed through other surgical approaches are lacking in comparative outcomes data.17In this study, we evaluated operative times, transfusion requirements, hospital discharge data, and 90-day complication rates in patients who had simultaneous bilateral THAs through either the DA approach or the posterior approach.
Methods
Study Design
This single-center study was conducted at the Mayo Clinic in Rochester, Minnesota. After obtaining approval from our Institutional Review Board, we performed a retrospective cohort analysis. We used our institution’s total joint registry to identify all patients who underwent simultaneous bilateral THAs through either the DA approach or the posterior approach. The first bilateral THAs to use the DA approach at our institution were performed in 2012. To ensure that the DA and posterior groups’ perioperative management would be similar, we included only cases performed between 2012 and 2014.
There were 19 patients in the DA group and 21 in the posterior group. The groups were similar in mean age (54 vs 54 years; P = .90), sex (73% vs 57% males; P = .33), body mass index (BMI; 25 vs 28 kg/m2; P = .38), preoperative hemoglobin level (14.3 vs 14.0 g/dL; P = .37), preoperative diagnosis (71.1% vs 78.6% degenerative joint disease; P = .75), and American Society of Anesthesiologists (ASA) score (1.9 vs 2.0; P = .63) (Table 1).
Patient Care
All cases were performed by 1 of 3 dedicated arthroplasty surgeons (Dr. Taunton, Dr. Sierra, Dr. Trousdale). Dr. Taunton exclusively uses the DA approach, and Dr. Sierra and Dr. Trousdale exclusively use the posterior approach. Patients in both groups received preoperative medical clearance and attended the same preoperative education class.
Patients in the DA group were positioned supine on an orthopedic table that allows hyperextension and adduction of the operative leg. Both hips were prepared and draped simultaneously. The most symptomatic hip was operated on first, with a sterile drape covering the contralateral hip. Between hips, fluoroscopy was moved to the other side of the operative suite, but no changes in positioning or preparation were necessary. A deep drain was placed on each side, and then was removed the morning of postoperative day 1. The same set of instruments was used on both sides.
Patients in the posterior group were positioned lateral on a regular operative table with hip rests. The most symptomatic hip was operated on first. After wound closure and dressing application, the patient was flipped to allow access to the contralateral hip and was prepared and draped again. The same instruments were used on each side. Drains were not used.
All patients received the same comprehensive multimodal pain management, which combined general and epidural anesthesia (remaining in place until postoperative day 2) and included an oral pain regimen of scheduled acetaminophen and as-needed tramadol and oxycodone. In all cases, intraoperative blood salvage and intravenous tranexamic acid (1 g at time of incision on first hip, 1 g at wound closure on second hip) were used. Preoperative autologous blood donation was not used. For deep vein thrombosis prophylaxis, patients were treated with bilateral sequential compression devices while hospitalized, but chemoprophylaxis was different between groups. Patients in the DA group received prophylactic low-molecular-weight heparin for 10 days, followed by twice-daily aspirin (325 mg) for 4 weeks. Patients in the posterior group received warfarin (goal international normalized ratio, 1.7-2.2) for 3 weeks, followed by twice-daily aspirin (325 mg) for 3 weeks. The decision to transfuse allogenic red blood cells was made by the treating surgeon, based on standardized hospital protocols, wherein patients are transfused for hemoglobin levels under 7.0 g/dL, or for hemoglobin levels less than 8.0 g/dL in the presence of persistent symptoms. All patients received care on an orthopedic specialty floor and were assisted by the same physical therapists. Discharge disposition was coordinated with the same group of social workers.
Two to 3 months after surgery, patients returned for routine examination and radiographs. All patients were followed up for at least 90 days.
Statistical Analysis
All outcomes were analyzed with appropriate summary statistics. Chi-square tests or logistic regression analyses (for categorical outcomes) were used to compare baseline covariates with perioperative outcomes, and 2-sample tests or Wilcoxon rank-sum tests were used to compare outcomes measured on a continuous scale. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated as appropriate. Operative time was calculated by adding time from incision to wound closure for both hips (room turnover time between hips was not included). Anesthesia time was defined as total time patients were in the operating room. All statistical tests were 2-sided, and the threshold for statistical significance was set at α = 0.05.
Results
Compared with patients who underwent simultaneous bilateral THAs through the posterior approach, patients who underwent simultaneous bilateral THAs through the DA approach had longer mean operative times (153 vs 106 min; P < .001) and anesthesia times (257 vs 221 min; P = .007). The 2 groups’ hospital stays were similar in length (3.1 vs 3.5 days; P = .31), but patients in the DA group were more likely to be discharged home (100.0% vs 71.4%; P = .02) (Table 2).
Patients in the DA group were more likely to have sufficient intraoperative blood salvage for autologous transfusion (89.5% vs 57.1%; OR, 6.4; 95% CI, 1.16-34.94; P = .03) (Table 3) and received more mean units of salvaged autologous blood (1.4 vs 0.5; P = .003) (Table 2). Allogenic blood was not given to any patients in the DA group, but 3 patients in the posterior group (14.3%) required allogenic blood transfusion (P = .23) (Table 2). Salvaged autologous and allogenic blood transfusion was not associated with sex, age 60 years or older, or hospital LOS of 4 days or more (Table 3). The groups’ mean hemoglobin levels, measured the morning of postoperative day 1, were similar: 10.6 g/dL (range, 8.5-12.4 g/dL) for the DA group and 10.3 g/dL (range 8.6-12.3 g/dL) for the posterior group (Table 2).
In-hospital complications were uncommon in both groups (5% vs 14%; P = .61) (Table 2). One patient in the posterior group sustained a unilateral dislocation the day of surgery, and closed reduction was required; other complications (1 ileus, 2 tachyarrhythmias) did not require intervention. Ninety-day complications were also rare; 1 patient in the posterior group developed a hematoma with wound drainage, and this was successfully managed conservatively. There were no reoperations or readmissions in either group (Table 2).
Discussion
Although bilateral procedures account for less than 1% of THAs in the United States,11 debate about their role in patients with severe bilateral hip disease continues. The potential benefits of a single episode of care must be weighed against the slightly increased risk for systemic complications.7,10-15 Recent innovations in perioperative management have been shown to minimize complications,15 but it is unclear whether surgical approach affects perioperative outcomes. Our goals in this study were to evaluate operative times, transfusion requirements, hospital discharge data, and 90-day complication rates in patients who underwent simultaneous bilateral THAs through either the DA approach or the posterior approach.
Patients in our DA group had longer operative and anesthesia times. Other studies have found longer operative times for the DA approach relative to the posterior approach in unilateral THAs.18 One potential benefit of the DA approach in the setting of simultaneous bilateral THAs is the ability to prepare and drape both sides before surgery and thereby keep the interruption between hips to a minimum. In the present study, however, time saved during turnover between hips was overshadowed by the time added for each THA.
Although it was uncommon for complications to occur within 90 days after surgery in this study, many patients are needed to fully investigate these rare occurrences. Because of inherent selection bias, these risks are difficult to directly compare in patients who undergo unilateral procedures. Although small studies have failed to clarify the issue,7,19,20 a recent review of the almost 20,000 bilateral THA cases in the US Nationwide Inpatient Sample database found that bilateral (vs unilateral) THAs were associated with increased risk of local and systemic complications.11 Therefore, bilateral THAs should be reserved for select cases, with attention given to excluding patients with preexisting cardiopulmonary disease and providing appropriate preoperative counseling.
Most studies have reported a higher transfusion rate in bilateral THAs relative to staged procedures.7,21-23 Allogenic blood transfusion leads to immune suppression, coagulopathy, and other systemic effects in general, and has been specifically associated with infection in patients who undergo total joint arthroplasty.24-29 Parvizi and colleagues17 reported reduced blood loss and fewer blood transfusions in patients who had simultaneous bilateral THAs through the DA approach, compared with the direct lateral approach. Patients in our DA group received more salvaged autologous blood, which we suppose was a function of longer operative times. However, postoperative hemoglobin levels and allogenic blood transfusion rates were statistically similar between the 2 groups. It is important to consider the increased risk of required allogenic blood transfusion associated with simultaneous bilateral THAs, but it is not fully clear if this risk is lower in THAs performed through the DA approach relative to other approaches. In our experience, the required transfusion risk is limited in DA and posterior approaches with use of contemporary perioperative blood management strategies.
Although hospital LOS is longer with simultaneous bilateral THAs than with unilateral THAs, historically it is shorter than the combined LOS of staged bilateral THAs.20 Patients in our study had a relatively short LOS after bilateral THAs, and there was no difference in LOS between groups. However, patients were more likely to be discharged home after bilateral THAs through the DA approach vs the posterior approach. Although discharge location was not affected by age, sex, ASA score, or LOS, unrecognized social factors unrelated to surgical approach likely influenced this finding.
This study should be interpreted in light of important limitations. Foremost, although data were prospectively collected, we examined them retrospectively. Thus, it is possible there may be unaccounted for differences between our DA and posterior THA groups. For example, the DA and posterior approaches were used by different surgeons with differing experience, technique, and preferences, all of which could have affected outcomes. Furthermore, our sample was relatively small (simultaneous bilateral THAs are performed relatively infrequently). Last, although anesthesia, pain management, blood conservation, and physical therapy were similar for the 2 groups, there was no standardized protocol for determining eligibility for simultaneous bilateral THAs.
In conclusion, we found that simultaneous bilateral THAs can be safely performed through either the DA approach or the posterior approach. Although the transition between hips is shorter with the DA approach, this time savings is overshadowed by the increased duration of each procedure. Transfusion rates are low in both groups, and in-hospital and 90-day complications are quite rare. Furthermore, patients can routinely be discharged home without elevating readmission rates. We will continue to perform simultaneous bilateral THAs through the DA approach or the posterior approach, according to surgeon preference.
Am J Orthop. 2016;45(6):E373-E378. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
End-stage osteoarthritis of the hip is a debilitating disease that is reliably treated with total hip arthroplasty (THA).1 Up to 35% of patients who undergo THA eventually require contralateral THA.2,3 In patients who present with advanced bilateral disease and undergo unilateral THA, the risk of ultimately requiring a contralateral procedure is as high as 97%.3-6 In patients with bilateral hip disease, function is not fully optimized until both hips have been replaced, particularly in the setting of fixed flexion contractures.7-9 Naturally, there has been some interest in simultaneous bilateral THAs for select patients.
The potential benefits of bilateral THAs over staged procedures include faster overall rehabilitation, exposure to a single anesthetic, reduced hospital length of stay (LOS), and cost savings.10-12 However, opinion on recommending bilateral THAs is mixed. Although bilateral procedures historically have been fraught with perioperative complications,13,14 advances in surgical and anesthetic techniques have led to improved outcomes.15 Whether surgical approach is a factor in these outcomes is unclear.
The popularity of the direct anterior (DA) approach for THA has increased in recent years.16 Although the relative advantages of various approaches remain in debate, one potential benefit of the DA approach is supine positioning, which allows simultaneous bilateral THAs to be performed without the need for repositioning before proceeding with the contralateral side. However, simultaneous bilateral THAs performed through the DA approach and those performed through other surgical approaches are lacking in comparative outcomes data.17In this study, we evaluated operative times, transfusion requirements, hospital discharge data, and 90-day complication rates in patients who had simultaneous bilateral THAs through either the DA approach or the posterior approach.
Methods
Study Design
This single-center study was conducted at the Mayo Clinic in Rochester, Minnesota. After obtaining approval from our Institutional Review Board, we performed a retrospective cohort analysis. We used our institution’s total joint registry to identify all patients who underwent simultaneous bilateral THAs through either the DA approach or the posterior approach. The first bilateral THAs to use the DA approach at our institution were performed in 2012. To ensure that the DA and posterior groups’ perioperative management would be similar, we included only cases performed between 2012 and 2014.
There were 19 patients in the DA group and 21 in the posterior group. The groups were similar in mean age (54 vs 54 years; P = .90), sex (73% vs 57% males; P = .33), body mass index (BMI; 25 vs 28 kg/m2; P = .38), preoperative hemoglobin level (14.3 vs 14.0 g/dL; P = .37), preoperative diagnosis (71.1% vs 78.6% degenerative joint disease; P = .75), and American Society of Anesthesiologists (ASA) score (1.9 vs 2.0; P = .63) (Table 1).
Patient Care
All cases were performed by 1 of 3 dedicated arthroplasty surgeons (Dr. Taunton, Dr. Sierra, Dr. Trousdale). Dr. Taunton exclusively uses the DA approach, and Dr. Sierra and Dr. Trousdale exclusively use the posterior approach. Patients in both groups received preoperative medical clearance and attended the same preoperative education class.
Patients in the DA group were positioned supine on an orthopedic table that allows hyperextension and adduction of the operative leg. Both hips were prepared and draped simultaneously. The most symptomatic hip was operated on first, with a sterile drape covering the contralateral hip. Between hips, fluoroscopy was moved to the other side of the operative suite, but no changes in positioning or preparation were necessary. A deep drain was placed on each side, and then was removed the morning of postoperative day 1. The same set of instruments was used on both sides.
Patients in the posterior group were positioned lateral on a regular operative table with hip rests. The most symptomatic hip was operated on first. After wound closure and dressing application, the patient was flipped to allow access to the contralateral hip and was prepared and draped again. The same instruments were used on each side. Drains were not used.
All patients received the same comprehensive multimodal pain management, which combined general and epidural anesthesia (remaining in place until postoperative day 2) and included an oral pain regimen of scheduled acetaminophen and as-needed tramadol and oxycodone. In all cases, intraoperative blood salvage and intravenous tranexamic acid (1 g at time of incision on first hip, 1 g at wound closure on second hip) were used. Preoperative autologous blood donation was not used. For deep vein thrombosis prophylaxis, patients were treated with bilateral sequential compression devices while hospitalized, but chemoprophylaxis was different between groups. Patients in the DA group received prophylactic low-molecular-weight heparin for 10 days, followed by twice-daily aspirin (325 mg) for 4 weeks. Patients in the posterior group received warfarin (goal international normalized ratio, 1.7-2.2) for 3 weeks, followed by twice-daily aspirin (325 mg) for 3 weeks. The decision to transfuse allogenic red blood cells was made by the treating surgeon, based on standardized hospital protocols, wherein patients are transfused for hemoglobin levels under 7.0 g/dL, or for hemoglobin levels less than 8.0 g/dL in the presence of persistent symptoms. All patients received care on an orthopedic specialty floor and were assisted by the same physical therapists. Discharge disposition was coordinated with the same group of social workers.
Two to 3 months after surgery, patients returned for routine examination and radiographs. All patients were followed up for at least 90 days.
Statistical Analysis
All outcomes were analyzed with appropriate summary statistics. Chi-square tests or logistic regression analyses (for categorical outcomes) were used to compare baseline covariates with perioperative outcomes, and 2-sample tests or Wilcoxon rank-sum tests were used to compare outcomes measured on a continuous scale. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated as appropriate. Operative time was calculated by adding time from incision to wound closure for both hips (room turnover time between hips was not included). Anesthesia time was defined as total time patients were in the operating room. All statistical tests were 2-sided, and the threshold for statistical significance was set at α = 0.05.
Results
Compared with patients who underwent simultaneous bilateral THAs through the posterior approach, patients who underwent simultaneous bilateral THAs through the DA approach had longer mean operative times (153 vs 106 min; P < .001) and anesthesia times (257 vs 221 min; P = .007). The 2 groups’ hospital stays were similar in length (3.1 vs 3.5 days; P = .31), but patients in the DA group were more likely to be discharged home (100.0% vs 71.4%; P = .02) (Table 2).
Patients in the DA group were more likely to have sufficient intraoperative blood salvage for autologous transfusion (89.5% vs 57.1%; OR, 6.4; 95% CI, 1.16-34.94; P = .03) (Table 3) and received more mean units of salvaged autologous blood (1.4 vs 0.5; P = .003) (Table 2). Allogenic blood was not given to any patients in the DA group, but 3 patients in the posterior group (14.3%) required allogenic blood transfusion (P = .23) (Table 2). Salvaged autologous and allogenic blood transfusion was not associated with sex, age 60 years or older, or hospital LOS of 4 days or more (Table 3). The groups’ mean hemoglobin levels, measured the morning of postoperative day 1, were similar: 10.6 g/dL (range, 8.5-12.4 g/dL) for the DA group and 10.3 g/dL (range 8.6-12.3 g/dL) for the posterior group (Table 2).
In-hospital complications were uncommon in both groups (5% vs 14%; P = .61) (Table 2). One patient in the posterior group sustained a unilateral dislocation the day of surgery, and closed reduction was required; other complications (1 ileus, 2 tachyarrhythmias) did not require intervention. Ninety-day complications were also rare; 1 patient in the posterior group developed a hematoma with wound drainage, and this was successfully managed conservatively. There were no reoperations or readmissions in either group (Table 2).
Discussion
Although bilateral procedures account for less than 1% of THAs in the United States,11 debate about their role in patients with severe bilateral hip disease continues. The potential benefits of a single episode of care must be weighed against the slightly increased risk for systemic complications.7,10-15 Recent innovations in perioperative management have been shown to minimize complications,15 but it is unclear whether surgical approach affects perioperative outcomes. Our goals in this study were to evaluate operative times, transfusion requirements, hospital discharge data, and 90-day complication rates in patients who underwent simultaneous bilateral THAs through either the DA approach or the posterior approach.
Patients in our DA group had longer operative and anesthesia times. Other studies have found longer operative times for the DA approach relative to the posterior approach in unilateral THAs.18 One potential benefit of the DA approach in the setting of simultaneous bilateral THAs is the ability to prepare and drape both sides before surgery and thereby keep the interruption between hips to a minimum. In the present study, however, time saved during turnover between hips was overshadowed by the time added for each THA.
Although it was uncommon for complications to occur within 90 days after surgery in this study, many patients are needed to fully investigate these rare occurrences. Because of inherent selection bias, these risks are difficult to directly compare in patients who undergo unilateral procedures. Although small studies have failed to clarify the issue,7,19,20 a recent review of the almost 20,000 bilateral THA cases in the US Nationwide Inpatient Sample database found that bilateral (vs unilateral) THAs were associated with increased risk of local and systemic complications.11 Therefore, bilateral THAs should be reserved for select cases, with attention given to excluding patients with preexisting cardiopulmonary disease and providing appropriate preoperative counseling.
Most studies have reported a higher transfusion rate in bilateral THAs relative to staged procedures.7,21-23 Allogenic blood transfusion leads to immune suppression, coagulopathy, and other systemic effects in general, and has been specifically associated with infection in patients who undergo total joint arthroplasty.24-29 Parvizi and colleagues17 reported reduced blood loss and fewer blood transfusions in patients who had simultaneous bilateral THAs through the DA approach, compared with the direct lateral approach. Patients in our DA group received more salvaged autologous blood, which we suppose was a function of longer operative times. However, postoperative hemoglobin levels and allogenic blood transfusion rates were statistically similar between the 2 groups. It is important to consider the increased risk of required allogenic blood transfusion associated with simultaneous bilateral THAs, but it is not fully clear if this risk is lower in THAs performed through the DA approach relative to other approaches. In our experience, the required transfusion risk is limited in DA and posterior approaches with use of contemporary perioperative blood management strategies.
Although hospital LOS is longer with simultaneous bilateral THAs than with unilateral THAs, historically it is shorter than the combined LOS of staged bilateral THAs.20 Patients in our study had a relatively short LOS after bilateral THAs, and there was no difference in LOS between groups. However, patients were more likely to be discharged home after bilateral THAs through the DA approach vs the posterior approach. Although discharge location was not affected by age, sex, ASA score, or LOS, unrecognized social factors unrelated to surgical approach likely influenced this finding.
This study should be interpreted in light of important limitations. Foremost, although data were prospectively collected, we examined them retrospectively. Thus, it is possible there may be unaccounted for differences between our DA and posterior THA groups. For example, the DA and posterior approaches were used by different surgeons with differing experience, technique, and preferences, all of which could have affected outcomes. Furthermore, our sample was relatively small (simultaneous bilateral THAs are performed relatively infrequently). Last, although anesthesia, pain management, blood conservation, and physical therapy were similar for the 2 groups, there was no standardized protocol for determining eligibility for simultaneous bilateral THAs.
In conclusion, we found that simultaneous bilateral THAs can be safely performed through either the DA approach or the posterior approach. Although the transition between hips is shorter with the DA approach, this time savings is overshadowed by the increased duration of each procedure. Transfusion rates are low in both groups, and in-hospital and 90-day complications are quite rare. Furthermore, patients can routinely be discharged home without elevating readmission rates. We will continue to perform simultaneous bilateral THAs through the DA approach or the posterior approach, according to surgeon preference.
Am J Orthop. 2016;45(6):E373-E378. Copyright Frontline Medical Communications Inc. 2016. All rights reserved.
1. Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370(9597):1508-1519.
2. Sayeed SA, Johnson AJ, Jaffe DE, Mont MA. Incidence of contralateral THA after index THA for osteoarthritis. Clin Orthop Relat Res. 2012;470(2):535-540.
3. Sayeed SA, Trousdale RT, Barnes SA, Kaufman KR, Pagnano MW. Joint arthroplasty within 10 years after primary Charnley total hip arthroplasty. Am J Orthop. 2009;38(8):E141-E143.
4. Goker B, Doughan AM, Schnitzer TJ, Block JA. Quantification of progressive joint space narrowing in osteoarthritis of the hip: longitudinal analysis of the contralateral hip after total hip arthroplasty. Arthritis Rheum. 2000;43(5):988-994.
5. Husted H, Overgaard S, Laursen JO, et al. Need for bilateral arthroplasty for coxarthrosis. 1,477 replacements in 1,199 patients followed for 0-14 years. Acta Orthop Scand. 1996;67(5):421-423.
6. Ritter MA, Carr K, Herbst SA, et al. Outcome of the contralateral hip following total hip arthroplasty for osteoarthritis. J Arthroplasty. 1996;11(3):242-246.
7. Alfaro- Adrián J, Bayona F, Rech JA, Murray DW. One- or two-stage bilateral total hip replacement. J Arthroplasty. 1999;14(4):439-445.
8. Wykman A, Olsson E. Walking ability after total hip replacement. A comparison of gait analysis in unilateral and bilateral cases. J Bone Joint Surg Br. 1992;74(1):53-56.
9. Yoshii T, Jinno T, Morita S, et al. Postoperative hip motion and functional recovery after simultaneous bilateral total hip arthroplasty for bilateral osteoarthritis. J Orthop Sci. 2009;14(2):161-166.
10. Lorenze M, Huo MH, Zatorski LE, Keggi KJ. A comparison of the cost effectiveness of one-stage versus two-stage bilateral total hip replacement. Orthopedics. 1998;21(12):1249-1252.
11. Rasouli MR, Maltenfort MG, Ross D, Hozack WJ, Memtsoudis SG, Parvizi J. Perioperative morbidity and mortality following bilateral total hip arthroplasty. J Arthroplasty. 2014;29(1):142-148.
12. Reuben JD, Meyers SJ, Cox DD, Elliott M, Watson M, Shim SD. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty. 1998;13(2):172-179.
13. Bracy D, Wroblewski BM. Bilateral Charnley arthroplasty as a single procedure. A report on 400 patients. J Bone Joint Surg Br. 1981;63(3):354-356.
14. Ritter MA, Randolph JC. Bilateral total hip arthroplasty: a simultaneous procedure. Acta Orthop Scand. 1976;47(2):203-208.
15. Ritter MA, Stringer EA. Bilateral total hip arthroplasty: a single procedure. Clin Orthop Relat Res. 1980;(149):185-190.
16. Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;(441):115-124.
17. Parvizi J, Rasouli MR, Jaberi M, et al. Does the surgical approach in one stage bilateral total hip arthroplasty affect blood loss? Int Orthop. 2013;37(12):2357-2362.
18. Poehling-Monaghan KL, Kamath AF, Taunton MJ, Pagnano MW. Direct anterior versus miniposterior THA with the same advanced perioperative protocols: surprising early clinical results. Clin Orthop Relat Res. 2015;473(2):623-631.
19. Macaulay W, Salvati EA, Sculco TP, Pellicci PM. Single-stage bilateral total hip arthroplasty. J Am Acad Orthop Surg. 2002;10(3):217-221.
20. Romagnoli S, Zacchetti S, Perazzo P, Verde F, Banfi G, Viganò M. Simultaneous bilateral total hip arthroplasties do not lead to higher complication or allogeneic transfusion rates compared to unilateral procedures. Int Orthop. 2013;37(11):2125-2130.
21. Salvati EA, Hughes P, Lachiewicz P. Bilateral total hip-replacement arthroplasty in one stage. J Bone Joint Surg Am. 1978;60(5):640-644.
22. Parvizi J, Chaudhry S, Rasouli MR, et al. Who needs autologous blood donation in joint replacement? J Knee Surg. 2011;24(1):25-31.
23. Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am. 2007;89(1):27-32.
24. Blair SD, Janvrin SB, McCollum CN, Greenhalgh RM. Effect of early blood transfusion on gastrointestinal haemorrhage. Br J Surg. 1986;73(10):783-785.
25. Blumberg N, Heal JM. Immunomodulation by blood transfusion: an evolving scientific and clinical challenge. Am J Med. 1996;101(3):299-308.
26. Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340(6):409-417.
27. Iturbe T, Cornudella R, de Miguel R, et al. Hypercoagulability state in hip and knee surgery: influence of ABO antigenic system and allogenic transfusion. Transfus Sci. 1999;20(1):17-20.
28. Murphy P, Heal JM, Blumberg N. Infection or suspected infection after hip replacement surgery with autologous or homologous blood transfusions. Transfusion. 1991;31(3):212-217.
29. Watts CD, Pagnano MW. Minimising blood loss and transfusion in contemporary hip and knee arthroplasty. J Bone Joint Surg Br. 2012;94(11 suppl A):8-10.
1. Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370(9597):1508-1519.
2. Sayeed SA, Johnson AJ, Jaffe DE, Mont MA. Incidence of contralateral THA after index THA for osteoarthritis. Clin Orthop Relat Res. 2012;470(2):535-540.
3. Sayeed SA, Trousdale RT, Barnes SA, Kaufman KR, Pagnano MW. Joint arthroplasty within 10 years after primary Charnley total hip arthroplasty. Am J Orthop. 2009;38(8):E141-E143.
4. Goker B, Doughan AM, Schnitzer TJ, Block JA. Quantification of progressive joint space narrowing in osteoarthritis of the hip: longitudinal analysis of the contralateral hip after total hip arthroplasty. Arthritis Rheum. 2000;43(5):988-994.
5. Husted H, Overgaard S, Laursen JO, et al. Need for bilateral arthroplasty for coxarthrosis. 1,477 replacements in 1,199 patients followed for 0-14 years. Acta Orthop Scand. 1996;67(5):421-423.
6. Ritter MA, Carr K, Herbst SA, et al. Outcome of the contralateral hip following total hip arthroplasty for osteoarthritis. J Arthroplasty. 1996;11(3):242-246.
7. Alfaro- Adrián J, Bayona F, Rech JA, Murray DW. One- or two-stage bilateral total hip replacement. J Arthroplasty. 1999;14(4):439-445.
8. Wykman A, Olsson E. Walking ability after total hip replacement. A comparison of gait analysis in unilateral and bilateral cases. J Bone Joint Surg Br. 1992;74(1):53-56.
9. Yoshii T, Jinno T, Morita S, et al. Postoperative hip motion and functional recovery after simultaneous bilateral total hip arthroplasty for bilateral osteoarthritis. J Orthop Sci. 2009;14(2):161-166.
10. Lorenze M, Huo MH, Zatorski LE, Keggi KJ. A comparison of the cost effectiveness of one-stage versus two-stage bilateral total hip replacement. Orthopedics. 1998;21(12):1249-1252.
11. Rasouli MR, Maltenfort MG, Ross D, Hozack WJ, Memtsoudis SG, Parvizi J. Perioperative morbidity and mortality following bilateral total hip arthroplasty. J Arthroplasty. 2014;29(1):142-148.
12. Reuben JD, Meyers SJ, Cox DD, Elliott M, Watson M, Shim SD. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty. 1998;13(2):172-179.
13. Bracy D, Wroblewski BM. Bilateral Charnley arthroplasty as a single procedure. A report on 400 patients. J Bone Joint Surg Br. 1981;63(3):354-356.
14. Ritter MA, Randolph JC. Bilateral total hip arthroplasty: a simultaneous procedure. Acta Orthop Scand. 1976;47(2):203-208.
15. Ritter MA, Stringer EA. Bilateral total hip arthroplasty: a single procedure. Clin Orthop Relat Res. 1980;(149):185-190.
16. Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;(441):115-124.
17. Parvizi J, Rasouli MR, Jaberi M, et al. Does the surgical approach in one stage bilateral total hip arthroplasty affect blood loss? Int Orthop. 2013;37(12):2357-2362.
18. Poehling-Monaghan KL, Kamath AF, Taunton MJ, Pagnano MW. Direct anterior versus miniposterior THA with the same advanced perioperative protocols: surprising early clinical results. Clin Orthop Relat Res. 2015;473(2):623-631.
19. Macaulay W, Salvati EA, Sculco TP, Pellicci PM. Single-stage bilateral total hip arthroplasty. J Am Acad Orthop Surg. 2002;10(3):217-221.
20. Romagnoli S, Zacchetti S, Perazzo P, Verde F, Banfi G, Viganò M. Simultaneous bilateral total hip arthroplasties do not lead to higher complication or allogeneic transfusion rates compared to unilateral procedures. Int Orthop. 2013;37(11):2125-2130.
21. Salvati EA, Hughes P, Lachiewicz P. Bilateral total hip-replacement arthroplasty in one stage. J Bone Joint Surg Am. 1978;60(5):640-644.
22. Parvizi J, Chaudhry S, Rasouli MR, et al. Who needs autologous blood donation in joint replacement? J Knee Surg. 2011;24(1):25-31.
23. Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am. 2007;89(1):27-32.
24. Blair SD, Janvrin SB, McCollum CN, Greenhalgh RM. Effect of early blood transfusion on gastrointestinal haemorrhage. Br J Surg. 1986;73(10):783-785.
25. Blumberg N, Heal JM. Immunomodulation by blood transfusion: an evolving scientific and clinical challenge. Am J Med. 1996;101(3):299-308.
26. Hébert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340(6):409-417.
27. Iturbe T, Cornudella R, de Miguel R, et al. Hypercoagulability state in hip and knee surgery: influence of ABO antigenic system and allogenic transfusion. Transfus Sci. 1999;20(1):17-20.
28. Murphy P, Heal JM, Blumberg N. Infection or suspected infection after hip replacement surgery with autologous or homologous blood transfusions. Transfusion. 1991;31(3):212-217.
29. Watts CD, Pagnano MW. Minimising blood loss and transfusion in contemporary hip and knee arthroplasty. J Bone Joint Surg Br. 2012;94(11 suppl A):8-10.
Biopsy scalp area for alopecia diagnosis
BOSTON – Getting a proper scalp biopsy and providing the dermatopathologist with a good supporting history are important elements in diagnosing a patient with hair loss, according to Eleanor Knopp, MD, a dermatologist and dermatopathologist with Group Health Permanente, Seattle.
The keys to a good scalp biopsy in a patient with alopecia are to take an adequate sample of scalp in both size and degree of involvement. With regard to where to biopsy, “it’s important ... to select an area of advanced thinning if you’re doing a biopsy of a nonscarring alopecia,” Dr. Knopp said at the American Academy of Dermatology summer meeting. She advised being “generous” with an anesthetic, preferably one containing epinephrine, to help keep the wound dry and to help with visualization during the procedure.
Evaluating for the presence or absence of follicular ostia with a dermatoscope helps distinguish scarring from nonscarring alopecia. Scarring alopecias typically show loss of follicular ostia, she noted.
While this method is effective at identifying nonscarring areas in white patients, it can be difficult to appreciate the disappearance of follicular ostia with a dermatoscope in patients of African descent or patients with darkly pigmented skin. In these patients, eccrine ostia appear as white pinpoint dots under a dermatoscope and mimic the appearance of follicular ostia, despite the presence of scarring alopecia, she noted.
In this situation, Dr. Knopp said the threshold for biopsying patients with darkly pigmented skin should be lower to rule out an early cicatricial alopecia.
For any specimen sent to the dermatopathologist, it is important to note patient characteristics, including age and race, duration of the condition, and clinical pattern. Not only is race helpful for interpreting what is seen in the specimen, but certain racial groups have higher predilections for certain diseases. There are also differences in normal hair densities depending on race although there can be a wide range even within a race, she added. Providing a photo of the involved area of the scalp is also a good idea, she added.
When biopsying a scarring alopecia, Dr. Knopp said that her preference is to find an area of relatively early thinning with visible erythema, and scale if it is present, “so that you know you have active inflammatory disease, but it’s not so advanced that you’re just seeing end-stage changes of scarring.”
It is worth having a discussion with the dermatopathologist about sectioning specimens, Dr. Knopp said. The consensus among most dermatopathologists is that horizontal sections are “absolutely the way to go for nonscarring alopecias,” but some dermatopathologists strongly prefer vertical sections, especially in cicatricial alopecias. Clinicians can always choose among the many reference laboratories to obtain the type of sections they prefer.
In cases of cicatricial alopecia, Dr. Knopp cautioned that clinicians may see “juicy pustules or fluctuant nodules” and consider these findings indicative of a highly active area of disease, but these changes may obscure early findings that are helpful to a pathologist. A better choice for a biopsy site is an area of early involvement that is not too inflamed and not so advanced that it is just scar, she noted.
Another potential pitfall is the temptation to biopsy a tuft of hairs. If there is polytrichia or compounding of follicles, it may be tempting to fit the punch tool over what are also sometimes called “doll’s hairs.” But those structures are nonspecific, end-stage features of many different cicatricial alopecias, including lichen planopilaris, central centrifugal cicatricial alopecia, and even lupus. Instead, Dr. Knopp recommended taking a specimen at the periphery where compounding is not present but where there is thinning and active inflammation.
Dr. Knopp, also with the University of Washington, Seattle, reported no financial relationships.
BOSTON – Getting a proper scalp biopsy and providing the dermatopathologist with a good supporting history are important elements in diagnosing a patient with hair loss, according to Eleanor Knopp, MD, a dermatologist and dermatopathologist with Group Health Permanente, Seattle.
The keys to a good scalp biopsy in a patient with alopecia are to take an adequate sample of scalp in both size and degree of involvement. With regard to where to biopsy, “it’s important ... to select an area of advanced thinning if you’re doing a biopsy of a nonscarring alopecia,” Dr. Knopp said at the American Academy of Dermatology summer meeting. She advised being “generous” with an anesthetic, preferably one containing epinephrine, to help keep the wound dry and to help with visualization during the procedure.
Evaluating for the presence or absence of follicular ostia with a dermatoscope helps distinguish scarring from nonscarring alopecia. Scarring alopecias typically show loss of follicular ostia, she noted.
While this method is effective at identifying nonscarring areas in white patients, it can be difficult to appreciate the disappearance of follicular ostia with a dermatoscope in patients of African descent or patients with darkly pigmented skin. In these patients, eccrine ostia appear as white pinpoint dots under a dermatoscope and mimic the appearance of follicular ostia, despite the presence of scarring alopecia, she noted.
In this situation, Dr. Knopp said the threshold for biopsying patients with darkly pigmented skin should be lower to rule out an early cicatricial alopecia.
For any specimen sent to the dermatopathologist, it is important to note patient characteristics, including age and race, duration of the condition, and clinical pattern. Not only is race helpful for interpreting what is seen in the specimen, but certain racial groups have higher predilections for certain diseases. There are also differences in normal hair densities depending on race although there can be a wide range even within a race, she added. Providing a photo of the involved area of the scalp is also a good idea, she added.
When biopsying a scarring alopecia, Dr. Knopp said that her preference is to find an area of relatively early thinning with visible erythema, and scale if it is present, “so that you know you have active inflammatory disease, but it’s not so advanced that you’re just seeing end-stage changes of scarring.”
It is worth having a discussion with the dermatopathologist about sectioning specimens, Dr. Knopp said. The consensus among most dermatopathologists is that horizontal sections are “absolutely the way to go for nonscarring alopecias,” but some dermatopathologists strongly prefer vertical sections, especially in cicatricial alopecias. Clinicians can always choose among the many reference laboratories to obtain the type of sections they prefer.
In cases of cicatricial alopecia, Dr. Knopp cautioned that clinicians may see “juicy pustules or fluctuant nodules” and consider these findings indicative of a highly active area of disease, but these changes may obscure early findings that are helpful to a pathologist. A better choice for a biopsy site is an area of early involvement that is not too inflamed and not so advanced that it is just scar, she noted.
Another potential pitfall is the temptation to biopsy a tuft of hairs. If there is polytrichia or compounding of follicles, it may be tempting to fit the punch tool over what are also sometimes called “doll’s hairs.” But those structures are nonspecific, end-stage features of many different cicatricial alopecias, including lichen planopilaris, central centrifugal cicatricial alopecia, and even lupus. Instead, Dr. Knopp recommended taking a specimen at the periphery where compounding is not present but where there is thinning and active inflammation.
Dr. Knopp, also with the University of Washington, Seattle, reported no financial relationships.
BOSTON – Getting a proper scalp biopsy and providing the dermatopathologist with a good supporting history are important elements in diagnosing a patient with hair loss, according to Eleanor Knopp, MD, a dermatologist and dermatopathologist with Group Health Permanente, Seattle.
The keys to a good scalp biopsy in a patient with alopecia are to take an adequate sample of scalp in both size and degree of involvement. With regard to where to biopsy, “it’s important ... to select an area of advanced thinning if you’re doing a biopsy of a nonscarring alopecia,” Dr. Knopp said at the American Academy of Dermatology summer meeting. She advised being “generous” with an anesthetic, preferably one containing epinephrine, to help keep the wound dry and to help with visualization during the procedure.
Evaluating for the presence or absence of follicular ostia with a dermatoscope helps distinguish scarring from nonscarring alopecia. Scarring alopecias typically show loss of follicular ostia, she noted.
While this method is effective at identifying nonscarring areas in white patients, it can be difficult to appreciate the disappearance of follicular ostia with a dermatoscope in patients of African descent or patients with darkly pigmented skin. In these patients, eccrine ostia appear as white pinpoint dots under a dermatoscope and mimic the appearance of follicular ostia, despite the presence of scarring alopecia, she noted.
In this situation, Dr. Knopp said the threshold for biopsying patients with darkly pigmented skin should be lower to rule out an early cicatricial alopecia.
For any specimen sent to the dermatopathologist, it is important to note patient characteristics, including age and race, duration of the condition, and clinical pattern. Not only is race helpful for interpreting what is seen in the specimen, but certain racial groups have higher predilections for certain diseases. There are also differences in normal hair densities depending on race although there can be a wide range even within a race, she added. Providing a photo of the involved area of the scalp is also a good idea, she added.
When biopsying a scarring alopecia, Dr. Knopp said that her preference is to find an area of relatively early thinning with visible erythema, and scale if it is present, “so that you know you have active inflammatory disease, but it’s not so advanced that you’re just seeing end-stage changes of scarring.”
It is worth having a discussion with the dermatopathologist about sectioning specimens, Dr. Knopp said. The consensus among most dermatopathologists is that horizontal sections are “absolutely the way to go for nonscarring alopecias,” but some dermatopathologists strongly prefer vertical sections, especially in cicatricial alopecias. Clinicians can always choose among the many reference laboratories to obtain the type of sections they prefer.
In cases of cicatricial alopecia, Dr. Knopp cautioned that clinicians may see “juicy pustules or fluctuant nodules” and consider these findings indicative of a highly active area of disease, but these changes may obscure early findings that are helpful to a pathologist. A better choice for a biopsy site is an area of early involvement that is not too inflamed and not so advanced that it is just scar, she noted.
Another potential pitfall is the temptation to biopsy a tuft of hairs. If there is polytrichia or compounding of follicles, it may be tempting to fit the punch tool over what are also sometimes called “doll’s hairs.” But those structures are nonspecific, end-stage features of many different cicatricial alopecias, including lichen planopilaris, central centrifugal cicatricial alopecia, and even lupus. Instead, Dr. Knopp recommended taking a specimen at the periphery where compounding is not present but where there is thinning and active inflammation.
Dr. Knopp, also with the University of Washington, Seattle, reported no financial relationships.
Further evidence links Zika, Guillain-Barré syndrome
Evidence of Zika virus found in Colombian patients with Guillain-Barré syndrome supports the theory that Zika virus infection and Guillain-Barré syndrome are related and could occur parainfectiously, according to a study published in the New England Journal of Medicine.
“Our study provides virologic evidence of [Zika virus] infection in patients with Guillain-Barré syndrome,” wrote Beatriz Parra, PhD, of the Hospital Universitario del Valle in Valle del Cauca, Colombia, and her coauthors (N Engl J Med. 2016 Oct 5. doi: 10.1056/NEJMoa1605564).
Results indicated that 66 (97%) of subjects had symptoms consistent with a Zika virus infection prior to the onset of Guillain-Barré syndrome. The median number of days between onset of Zika-like symptoms and the onset of Guillain-Barré syndrome was found to be 7 days (interquartile range, 3-10 days). Seventeen (40%) of the 42 patients who underwent laboratory testing tested positive for Zika virus RNA in their sample, with 16 of those 17 positive tests coming from urine samples. Additionally, 18 of the 42 laboratory-tested subjects had “clinical and immunologic findings [that] supported” a Zika virus infection.
“The onset of the Guillain-Barré syndrome can parallel the onset of systemic manifestations of [Zika virus] infection, indicating a so-called parainfectious onset, which suggests that factors different from the known postinfectious mechanisms may be present in [Zika virus]–related Guillain-Barré syndrome,” the authors explained, adding that 20 (48%) of the 42 laboratory-tested subjects had a parainfectious onset.
“RT-PCR testing of urine is a valuable diagnostic tool for the identification of [Zika virus] infection in patients with Guillain-Barré syndrome,” Dr. Parra and her coauthors concluded.
The study was funded by the Bart McLean Fund for Neuroimmunology Research, Johns Hopkins Project Restore, and the Universidad del Valle. Dr. Parra reported no relevant financial disclosures.
Dr. Parra and her colleagues report in the Journal the results of a prospective study of 68 Colombian patients who had a syndrome consistent with the Guillain-Barré syndrome, 66 of whom had previously had symptoms of Zika virus (ZIKV) infection. Major strengths of this study include the documentation of a temporal relationship between the Guillain-Barré syndrome and ZIKV infection (marked by a substantial increase in the incidence of the Guillain-Barré syndrome after the introduction of ZIKV, from 20 to 90 cases per month throughout Colombia), the criteria applied for the diagnosis of the Guillain-Barré syndrome, and the molecular and serologic flavivirus data from analyses of serum, cerebrospinal fluid, and urine.
The difficulties in diagnosing ZIKV infection are borne out in this study, as only 17 patients had definitive laboratory evidence of recent ZIKV infection. Of these 17 patients, only 14 had electrophysiologic data consistent with the Guillain-Barré syndrome and therefore could have met Brighton level 1 diagnostic criteria for the syndrome. Among the 25 ZIKV PCR–negative patients, dengue virus (DENV) IgG antibodies were present in the cerebrospinal fluid of 12 patients and in the serum of 10 patients, and serum DENV IgM test results were positive in 1. These data raise the possibility of primary DENV infection and false-positive ZIKV serologic test results from cross reactivity.
Overall, the study by Dr. Parra and her colleagues supports the association between ZIKV and the Guillain-Barré syndrome, although confirmation in another cohort would strengthen this assertion. Although high rates of seropositivity may prove protective against further waves of ZIKV-related Guillain-Barré syndrome in Central and South America, the ZIKV pandemic is just beginning in North America and Africa, and an increase in the incidence of the Guillain-Barré syndrome may follow.
Jennifer A. Frontera, MD, is with the Cerebrovascular Center at the Cleveland Clinic in Cleveland. Ivan R.F. da Silva. MD, is with the Federal Fluminense University in Niterói, Brazil. These comments were adapted from their editorial accompanying the study ( N Engl J Med. 2016 Oct 5. doi: 10.1056/NEJMe1611840 ).
Dr. Parra and her colleagues report in the Journal the results of a prospective study of 68 Colombian patients who had a syndrome consistent with the Guillain-Barré syndrome, 66 of whom had previously had symptoms of Zika virus (ZIKV) infection. Major strengths of this study include the documentation of a temporal relationship between the Guillain-Barré syndrome and ZIKV infection (marked by a substantial increase in the incidence of the Guillain-Barré syndrome after the introduction of ZIKV, from 20 to 90 cases per month throughout Colombia), the criteria applied for the diagnosis of the Guillain-Barré syndrome, and the molecular and serologic flavivirus data from analyses of serum, cerebrospinal fluid, and urine.
The difficulties in diagnosing ZIKV infection are borne out in this study, as only 17 patients had definitive laboratory evidence of recent ZIKV infection. Of these 17 patients, only 14 had electrophysiologic data consistent with the Guillain-Barré syndrome and therefore could have met Brighton level 1 diagnostic criteria for the syndrome. Among the 25 ZIKV PCR–negative patients, dengue virus (DENV) IgG antibodies were present in the cerebrospinal fluid of 12 patients and in the serum of 10 patients, and serum DENV IgM test results were positive in 1. These data raise the possibility of primary DENV infection and false-positive ZIKV serologic test results from cross reactivity.
Overall, the study by Dr. Parra and her colleagues supports the association between ZIKV and the Guillain-Barré syndrome, although confirmation in another cohort would strengthen this assertion. Although high rates of seropositivity may prove protective against further waves of ZIKV-related Guillain-Barré syndrome in Central and South America, the ZIKV pandemic is just beginning in North America and Africa, and an increase in the incidence of the Guillain-Barré syndrome may follow.
Jennifer A. Frontera, MD, is with the Cerebrovascular Center at the Cleveland Clinic in Cleveland. Ivan R.F. da Silva. MD, is with the Federal Fluminense University in Niterói, Brazil. These comments were adapted from their editorial accompanying the study ( N Engl J Med. 2016 Oct 5. doi: 10.1056/NEJMe1611840 ).
Dr. Parra and her colleagues report in the Journal the results of a prospective study of 68 Colombian patients who had a syndrome consistent with the Guillain-Barré syndrome, 66 of whom had previously had symptoms of Zika virus (ZIKV) infection. Major strengths of this study include the documentation of a temporal relationship between the Guillain-Barré syndrome and ZIKV infection (marked by a substantial increase in the incidence of the Guillain-Barré syndrome after the introduction of ZIKV, from 20 to 90 cases per month throughout Colombia), the criteria applied for the diagnosis of the Guillain-Barré syndrome, and the molecular and serologic flavivirus data from analyses of serum, cerebrospinal fluid, and urine.
The difficulties in diagnosing ZIKV infection are borne out in this study, as only 17 patients had definitive laboratory evidence of recent ZIKV infection. Of these 17 patients, only 14 had electrophysiologic data consistent with the Guillain-Barré syndrome and therefore could have met Brighton level 1 diagnostic criteria for the syndrome. Among the 25 ZIKV PCR–negative patients, dengue virus (DENV) IgG antibodies were present in the cerebrospinal fluid of 12 patients and in the serum of 10 patients, and serum DENV IgM test results were positive in 1. These data raise the possibility of primary DENV infection and false-positive ZIKV serologic test results from cross reactivity.
Overall, the study by Dr. Parra and her colleagues supports the association between ZIKV and the Guillain-Barré syndrome, although confirmation in another cohort would strengthen this assertion. Although high rates of seropositivity may prove protective against further waves of ZIKV-related Guillain-Barré syndrome in Central and South America, the ZIKV pandemic is just beginning in North America and Africa, and an increase in the incidence of the Guillain-Barré syndrome may follow.
Jennifer A. Frontera, MD, is with the Cerebrovascular Center at the Cleveland Clinic in Cleveland. Ivan R.F. da Silva. MD, is with the Federal Fluminense University in Niterói, Brazil. These comments were adapted from their editorial accompanying the study ( N Engl J Med. 2016 Oct 5. doi: 10.1056/NEJMe1611840 ).
Evidence of Zika virus found in Colombian patients with Guillain-Barré syndrome supports the theory that Zika virus infection and Guillain-Barré syndrome are related and could occur parainfectiously, according to a study published in the New England Journal of Medicine.
“Our study provides virologic evidence of [Zika virus] infection in patients with Guillain-Barré syndrome,” wrote Beatriz Parra, PhD, of the Hospital Universitario del Valle in Valle del Cauca, Colombia, and her coauthors (N Engl J Med. 2016 Oct 5. doi: 10.1056/NEJMoa1605564).
Results indicated that 66 (97%) of subjects had symptoms consistent with a Zika virus infection prior to the onset of Guillain-Barré syndrome. The median number of days between onset of Zika-like symptoms and the onset of Guillain-Barré syndrome was found to be 7 days (interquartile range, 3-10 days). Seventeen (40%) of the 42 patients who underwent laboratory testing tested positive for Zika virus RNA in their sample, with 16 of those 17 positive tests coming from urine samples. Additionally, 18 of the 42 laboratory-tested subjects had “clinical and immunologic findings [that] supported” a Zika virus infection.
“The onset of the Guillain-Barré syndrome can parallel the onset of systemic manifestations of [Zika virus] infection, indicating a so-called parainfectious onset, which suggests that factors different from the known postinfectious mechanisms may be present in [Zika virus]–related Guillain-Barré syndrome,” the authors explained, adding that 20 (48%) of the 42 laboratory-tested subjects had a parainfectious onset.
“RT-PCR testing of urine is a valuable diagnostic tool for the identification of [Zika virus] infection in patients with Guillain-Barré syndrome,” Dr. Parra and her coauthors concluded.
The study was funded by the Bart McLean Fund for Neuroimmunology Research, Johns Hopkins Project Restore, and the Universidad del Valle. Dr. Parra reported no relevant financial disclosures.
Evidence of Zika virus found in Colombian patients with Guillain-Barré syndrome supports the theory that Zika virus infection and Guillain-Barré syndrome are related and could occur parainfectiously, according to a study published in the New England Journal of Medicine.
“Our study provides virologic evidence of [Zika virus] infection in patients with Guillain-Barré syndrome,” wrote Beatriz Parra, PhD, of the Hospital Universitario del Valle in Valle del Cauca, Colombia, and her coauthors (N Engl J Med. 2016 Oct 5. doi: 10.1056/NEJMoa1605564).
Results indicated that 66 (97%) of subjects had symptoms consistent with a Zika virus infection prior to the onset of Guillain-Barré syndrome. The median number of days between onset of Zika-like symptoms and the onset of Guillain-Barré syndrome was found to be 7 days (interquartile range, 3-10 days). Seventeen (40%) of the 42 patients who underwent laboratory testing tested positive for Zika virus RNA in their sample, with 16 of those 17 positive tests coming from urine samples. Additionally, 18 of the 42 laboratory-tested subjects had “clinical and immunologic findings [that] supported” a Zika virus infection.
“The onset of the Guillain-Barré syndrome can parallel the onset of systemic manifestations of [Zika virus] infection, indicating a so-called parainfectious onset, which suggests that factors different from the known postinfectious mechanisms may be present in [Zika virus]–related Guillain-Barré syndrome,” the authors explained, adding that 20 (48%) of the 42 laboratory-tested subjects had a parainfectious onset.
“RT-PCR testing of urine is a valuable diagnostic tool for the identification of [Zika virus] infection in patients with Guillain-Barré syndrome,” Dr. Parra and her coauthors concluded.
The study was funded by the Bart McLean Fund for Neuroimmunology Research, Johns Hopkins Project Restore, and the Universidad del Valle. Dr. Parra reported no relevant financial disclosures.
Key clinical point:
Major finding: 97% of subjects had Zika-like symptoms prior to onset of GBS, and 40% of GBS patients who underwent RT-PCR testing were positive for Zika virus.
Data source: Study of 68 GBS patients from six hospitals in Colombia, with 42 patients undergoing RT-PCR analysis.
Disclosures: Funding provided by the Bart McLean Fund for Neuroimmunology Research, Johns Hopkins Project Restore, and the Universidad del Valle. Dr. Parra reported no relevant financial disclosures.
‘Practice-changing’ treatments emerging in AML

NEW YORK—We are “finally” making progress in the treatment of acute myeloid leukemia (AML), according to a speaker at the NCCN 11th Annual Congress: Hematologic Malignancies.
Jessica K. Altman, MD, said a number of developments have resulted in improved AML treatment, including a better understanding of biology and prognostic assessment, continued advances in transplant, and updating standard treatments and incorporating novel agents in both relapsed/refractory and newly diagnosed patients.
“There are a couple of practice-changing treatments in acute myeloid leukemia, 2 of which happened over the last decade: daunorubicin intensification and the use of FLT3 inhibitors,” said Dr Altman, an associate professor at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
Dr Altman went on to explain that novel therapies for AML can be divided into 2 basic categories. There are agents that don’t depend on mutation status (like daunorubicin) and those that are mutation-specific (like FLT3 inhibitors).
Therapies not dependent on mutational complexity
The therapies that are not dependent on mutational complexity include anti-CD33 antibodies, BCL‐2 inhibitors, a dose-intensified anthracycline regimen, and different formulations of 7+3, including CPX‐351.
Escalated daunorubicin
Randomized trials of escalated daunorubicin (90 vs 45 mg/m2) have demonstrated benefit in complete responses (CRs) and overall survival (OS) in intermediate-risk patients and patients with core-binding factor mutation. They have demonstrated benefit in OS in FLT3 ITD+ patients.
In patients up to 65 years of age, 60–90 mg/m2 of daunorubicin is now standard.
“It’s still not clear to me—and I don’t know if it ever will be—if 90 is equivalent to 60,” Dr Altman said.
CPX-351
CPX-351 is a liposomal formulation of cytarabine and daunorubicin. In a randomized, phase 3 study of older adults with secondary AML, the median OS was 9.56 months for patients treated with CPX-351 and 5.95 months for patients on the 7+3 regimen (P=0.005).
The median event-free survival was significantly better with CPX-351 (P=0.021), as was the rate of CR + CR with incomplete blood count recovery (CRi). The rate of CR + CRi was 47.7% with CPX-351 and 33.3% for 7+3 (P=0.016).
A similar number of patients went on to transplant in each arm. Grade 3-5 adverse events were similar in frequency and severity in both arms—92% with CPX-351 vs 91% with 7+3.
SGN-CD33A
CD33 is not a new target in myeloid leukemia, Dr Altman pointed out. Gemtuzumab ozogamicin has been studied, approved by the US Food and Drug Administration, and then withdrawn.
However, an increasing number of studies with gemtuzumab are underway, she said, and the agent may once again have a place in the AML armamentarium.
The newest CD33 construct is SGN-CD33A, a stable dipeptide linker that enables uniform drug loading of a pyrrolobenzodiazepine dimer that crosslinks DNA and leads to cell death.
“Single-agent data was quite promising,” Dr Altman noted, with a CR + CRi rate of 41% in previously treated patients and 58% in 12 treatment-naïve patients.
These results prompted a combination study of SGN-CD33A with hypomethylating agents.
“Results were higher than expected with a hypomethylating agent,” Dr Altman pointed out.
The CR + CRi + CR with incomplete platelet recovery was 58%. And the median relapse-free survival was 7.7 months.
A phase 3 randomized trial of SGN-CD33A is planned.
Venetoclax
BCL-2 inhibitors are the fourth type of agent not dependent on mutation complexity. Venetoclax (ABT‐199) is a small‐molecule BCL-2 inhibitor that leads to the initiation of apoptosis.
In a phase 1b trial of venetoclax in combination with a hypomethylating agent, the overall CR rate was 35%, and the CRi rate was 35%.
“Again, higher than what would be expected with a hypomethylating agent alone,” Dr Altman said.
In a phase 1b/2 trial of venetoclax in combination with low‐dose cytarabine, the CR + CRi rate was 54%. Patients responded even if they had prior exposure to hypomethylating agents.
Mutation-specific novel agents
The FLT3 inhibitor midostaurin and the IDH inhibitors AG-120 and AG-221 are among the most exciting mutation-specific agents and the ones most progressed, according to Dr Altman.
FLT3-ITD is mutated in about 30% of AML patients and carries an unfavorable prognosis, and the IDH mutation occurs in about 10% and confers a favorable prognosis.
Midostaurin
A phase 3, randomized, double-blind study of daunorubicin/cytarabine induction and high-dose cytarabine consolidation with midostaurin (PKC412) or placebo had a 59% CR rate by day 60 in the midostaurin arm, compared with 53% in the placebo arm.
“The CR rate was slightly higher in the midostaurin arm,” Dr Altman said, “but what’s the most remarkable about this study is the difference in overall survival.”
The median OS in the midostaurin arm was 74.7 months, compared with 25.6 months in the placebo arm (P=0.0074).
“The major take-home message from this clinical trial,” Dr Altman said, “is that midostaurin improved the overall survival when added to standard therapy and represents a new standard of care.”
AG-120 and AG-221
Two IDH inhibitors that have substantial data available are the IDH1 inhibitor AG-120 and the IDH2 inhibitor AG-221.
As of October 2015, 78 patients had been treated with AG-120 in a phase 1 trial, yielding an overall response rate of 35% and a CR rate of 15%.
As of September 2015, 209 patients had been treated with AG-221 in a phase 1/2 trial, and 66 are still on study. The overall response rate was 37% in 159 adults with relapsed/refractory AML, with a median duration of response of 6.9 months. The CR rate was 18%.
Investigators have initiated a phase 3 study of AG-221 compared to conventional care regimens. ![]()

NEW YORK—We are “finally” making progress in the treatment of acute myeloid leukemia (AML), according to a speaker at the NCCN 11th Annual Congress: Hematologic Malignancies.
Jessica K. Altman, MD, said a number of developments have resulted in improved AML treatment, including a better understanding of biology and prognostic assessment, continued advances in transplant, and updating standard treatments and incorporating novel agents in both relapsed/refractory and newly diagnosed patients.
“There are a couple of practice-changing treatments in acute myeloid leukemia, 2 of which happened over the last decade: daunorubicin intensification and the use of FLT3 inhibitors,” said Dr Altman, an associate professor at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
Dr Altman went on to explain that novel therapies for AML can be divided into 2 basic categories. There are agents that don’t depend on mutation status (like daunorubicin) and those that are mutation-specific (like FLT3 inhibitors).
Therapies not dependent on mutational complexity
The therapies that are not dependent on mutational complexity include anti-CD33 antibodies, BCL‐2 inhibitors, a dose-intensified anthracycline regimen, and different formulations of 7+3, including CPX‐351.
Escalated daunorubicin
Randomized trials of escalated daunorubicin (90 vs 45 mg/m2) have demonstrated benefit in complete responses (CRs) and overall survival (OS) in intermediate-risk patients and patients with core-binding factor mutation. They have demonstrated benefit in OS in FLT3 ITD+ patients.
In patients up to 65 years of age, 60–90 mg/m2 of daunorubicin is now standard.
“It’s still not clear to me—and I don’t know if it ever will be—if 90 is equivalent to 60,” Dr Altman said.
CPX-351
CPX-351 is a liposomal formulation of cytarabine and daunorubicin. In a randomized, phase 3 study of older adults with secondary AML, the median OS was 9.56 months for patients treated with CPX-351 and 5.95 months for patients on the 7+3 regimen (P=0.005).
The median event-free survival was significantly better with CPX-351 (P=0.021), as was the rate of CR + CR with incomplete blood count recovery (CRi). The rate of CR + CRi was 47.7% with CPX-351 and 33.3% for 7+3 (P=0.016).
A similar number of patients went on to transplant in each arm. Grade 3-5 adverse events were similar in frequency and severity in both arms—92% with CPX-351 vs 91% with 7+3.
SGN-CD33A
CD33 is not a new target in myeloid leukemia, Dr Altman pointed out. Gemtuzumab ozogamicin has been studied, approved by the US Food and Drug Administration, and then withdrawn.
However, an increasing number of studies with gemtuzumab are underway, she said, and the agent may once again have a place in the AML armamentarium.
The newest CD33 construct is SGN-CD33A, a stable dipeptide linker that enables uniform drug loading of a pyrrolobenzodiazepine dimer that crosslinks DNA and leads to cell death.
“Single-agent data was quite promising,” Dr Altman noted, with a CR + CRi rate of 41% in previously treated patients and 58% in 12 treatment-naïve patients.
These results prompted a combination study of SGN-CD33A with hypomethylating agents.
“Results were higher than expected with a hypomethylating agent,” Dr Altman pointed out.
The CR + CRi + CR with incomplete platelet recovery was 58%. And the median relapse-free survival was 7.7 months.
A phase 3 randomized trial of SGN-CD33A is planned.
Venetoclax
BCL-2 inhibitors are the fourth type of agent not dependent on mutation complexity. Venetoclax (ABT‐199) is a small‐molecule BCL-2 inhibitor that leads to the initiation of apoptosis.
In a phase 1b trial of venetoclax in combination with a hypomethylating agent, the overall CR rate was 35%, and the CRi rate was 35%.
“Again, higher than what would be expected with a hypomethylating agent alone,” Dr Altman said.
In a phase 1b/2 trial of venetoclax in combination with low‐dose cytarabine, the CR + CRi rate was 54%. Patients responded even if they had prior exposure to hypomethylating agents.
Mutation-specific novel agents
The FLT3 inhibitor midostaurin and the IDH inhibitors AG-120 and AG-221 are among the most exciting mutation-specific agents and the ones most progressed, according to Dr Altman.
FLT3-ITD is mutated in about 30% of AML patients and carries an unfavorable prognosis, and the IDH mutation occurs in about 10% and confers a favorable prognosis.
Midostaurin
A phase 3, randomized, double-blind study of daunorubicin/cytarabine induction and high-dose cytarabine consolidation with midostaurin (PKC412) or placebo had a 59% CR rate by day 60 in the midostaurin arm, compared with 53% in the placebo arm.
“The CR rate was slightly higher in the midostaurin arm,” Dr Altman said, “but what’s the most remarkable about this study is the difference in overall survival.”
The median OS in the midostaurin arm was 74.7 months, compared with 25.6 months in the placebo arm (P=0.0074).
“The major take-home message from this clinical trial,” Dr Altman said, “is that midostaurin improved the overall survival when added to standard therapy and represents a new standard of care.”
AG-120 and AG-221
Two IDH inhibitors that have substantial data available are the IDH1 inhibitor AG-120 and the IDH2 inhibitor AG-221.
As of October 2015, 78 patients had been treated with AG-120 in a phase 1 trial, yielding an overall response rate of 35% and a CR rate of 15%.
As of September 2015, 209 patients had been treated with AG-221 in a phase 1/2 trial, and 66 are still on study. The overall response rate was 37% in 159 adults with relapsed/refractory AML, with a median duration of response of 6.9 months. The CR rate was 18%.
Investigators have initiated a phase 3 study of AG-221 compared to conventional care regimens. ![]()

NEW YORK—We are “finally” making progress in the treatment of acute myeloid leukemia (AML), according to a speaker at the NCCN 11th Annual Congress: Hematologic Malignancies.
Jessica K. Altman, MD, said a number of developments have resulted in improved AML treatment, including a better understanding of biology and prognostic assessment, continued advances in transplant, and updating standard treatments and incorporating novel agents in both relapsed/refractory and newly diagnosed patients.
“There are a couple of practice-changing treatments in acute myeloid leukemia, 2 of which happened over the last decade: daunorubicin intensification and the use of FLT3 inhibitors,” said Dr Altman, an associate professor at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
Dr Altman went on to explain that novel therapies for AML can be divided into 2 basic categories. There are agents that don’t depend on mutation status (like daunorubicin) and those that are mutation-specific (like FLT3 inhibitors).
Therapies not dependent on mutational complexity
The therapies that are not dependent on mutational complexity include anti-CD33 antibodies, BCL‐2 inhibitors, a dose-intensified anthracycline regimen, and different formulations of 7+3, including CPX‐351.
Escalated daunorubicin
Randomized trials of escalated daunorubicin (90 vs 45 mg/m2) have demonstrated benefit in complete responses (CRs) and overall survival (OS) in intermediate-risk patients and patients with core-binding factor mutation. They have demonstrated benefit in OS in FLT3 ITD+ patients.
In patients up to 65 years of age, 60–90 mg/m2 of daunorubicin is now standard.
“It’s still not clear to me—and I don’t know if it ever will be—if 90 is equivalent to 60,” Dr Altman said.
CPX-351
CPX-351 is a liposomal formulation of cytarabine and daunorubicin. In a randomized, phase 3 study of older adults with secondary AML, the median OS was 9.56 months for patients treated with CPX-351 and 5.95 months for patients on the 7+3 regimen (P=0.005).
The median event-free survival was significantly better with CPX-351 (P=0.021), as was the rate of CR + CR with incomplete blood count recovery (CRi). The rate of CR + CRi was 47.7% with CPX-351 and 33.3% for 7+3 (P=0.016).
A similar number of patients went on to transplant in each arm. Grade 3-5 adverse events were similar in frequency and severity in both arms—92% with CPX-351 vs 91% with 7+3.
SGN-CD33A
CD33 is not a new target in myeloid leukemia, Dr Altman pointed out. Gemtuzumab ozogamicin has been studied, approved by the US Food and Drug Administration, and then withdrawn.
However, an increasing number of studies with gemtuzumab are underway, she said, and the agent may once again have a place in the AML armamentarium.
The newest CD33 construct is SGN-CD33A, a stable dipeptide linker that enables uniform drug loading of a pyrrolobenzodiazepine dimer that crosslinks DNA and leads to cell death.
“Single-agent data was quite promising,” Dr Altman noted, with a CR + CRi rate of 41% in previously treated patients and 58% in 12 treatment-naïve patients.
These results prompted a combination study of SGN-CD33A with hypomethylating agents.
“Results were higher than expected with a hypomethylating agent,” Dr Altman pointed out.
The CR + CRi + CR with incomplete platelet recovery was 58%. And the median relapse-free survival was 7.7 months.
A phase 3 randomized trial of SGN-CD33A is planned.
Venetoclax
BCL-2 inhibitors are the fourth type of agent not dependent on mutation complexity. Venetoclax (ABT‐199) is a small‐molecule BCL-2 inhibitor that leads to the initiation of apoptosis.
In a phase 1b trial of venetoclax in combination with a hypomethylating agent, the overall CR rate was 35%, and the CRi rate was 35%.
“Again, higher than what would be expected with a hypomethylating agent alone,” Dr Altman said.
In a phase 1b/2 trial of venetoclax in combination with low‐dose cytarabine, the CR + CRi rate was 54%. Patients responded even if they had prior exposure to hypomethylating agents.
Mutation-specific novel agents
The FLT3 inhibitor midostaurin and the IDH inhibitors AG-120 and AG-221 are among the most exciting mutation-specific agents and the ones most progressed, according to Dr Altman.
FLT3-ITD is mutated in about 30% of AML patients and carries an unfavorable prognosis, and the IDH mutation occurs in about 10% and confers a favorable prognosis.
Midostaurin
A phase 3, randomized, double-blind study of daunorubicin/cytarabine induction and high-dose cytarabine consolidation with midostaurin (PKC412) or placebo had a 59% CR rate by day 60 in the midostaurin arm, compared with 53% in the placebo arm.
“The CR rate was slightly higher in the midostaurin arm,” Dr Altman said, “but what’s the most remarkable about this study is the difference in overall survival.”
The median OS in the midostaurin arm was 74.7 months, compared with 25.6 months in the placebo arm (P=0.0074).
“The major take-home message from this clinical trial,” Dr Altman said, “is that midostaurin improved the overall survival when added to standard therapy and represents a new standard of care.”
AG-120 and AG-221
Two IDH inhibitors that have substantial data available are the IDH1 inhibitor AG-120 and the IDH2 inhibitor AG-221.
As of October 2015, 78 patients had been treated with AG-120 in a phase 1 trial, yielding an overall response rate of 35% and a CR rate of 15%.
As of September 2015, 209 patients had been treated with AG-221 in a phase 1/2 trial, and 66 are still on study. The overall response rate was 37% in 159 adults with relapsed/refractory AML, with a median duration of response of 6.9 months. The CR rate was 18%.
Investigators have initiated a phase 3 study of AG-221 compared to conventional care regimens. ![]()