User login
Four of five health care providers get flu shot
Influenza vaccine coverage among U.S. health care personnel increased very slightly during the 2015-2016 flu season, with 79% reporting that they received the shot, compared with 77% in 2014-2015.
Hospital personnel were most likely to be covered (91%) and long-term care personnel least likely to be covered (69%), Carla L. Black, PhD, wrote in the Sept. 30 issue of Morbidity and Mortality Weekly Report (2016;65:1026-31). Coverage among health care personnel working in long-term care settings did increase, however, from 64% in the 2014-2015 seasons to 69% in the 2015-2016 season, Dr. Black and colleagues noted.
“Although low, this is the only setting with an appreciable increase in coverage, compared with last season. Influenza vaccination among health care personnel in long-term care settings is especially important because influenza vaccine effectiveness is generally lowest in the elderly,” according to Dr Black, an epidemiologist with the Centers for Disease Control and Prevention.
CDC conducted the Internet survey of 2,258 health care workers from March to April, 2016.
Physicians had the highest level of coverage (95.6%), while health care assistants and aides had the lowest (64.5%). Employers also exerted an influence on coverage. Most respondents (73%) were vaccinated at work. Coverage was highest (96.5%) at facilities where vaccination was required and lowest (45%) where vaccination was not required, promoted, or offered on site.
“Employer vaccination requirements likely contributed to the observed gradual increase in vaccination among health care personnel working in settings with the lowest coverage,” the investigators noted. “In the absence of vaccination requirements, expanding the number of health care locations offering vaccination on site, over multiple days, and at no cost might help sustain and improve influenza vaccination coverage among health care personnel, including in long-term care settings.”
As a CDC employee, Dr. Black has no financial conflicts.
Influenza vaccine coverage among U.S. health care personnel increased very slightly during the 2015-2016 flu season, with 79% reporting that they received the shot, compared with 77% in 2014-2015.
Hospital personnel were most likely to be covered (91%) and long-term care personnel least likely to be covered (69%), Carla L. Black, PhD, wrote in the Sept. 30 issue of Morbidity and Mortality Weekly Report (2016;65:1026-31). Coverage among health care personnel working in long-term care settings did increase, however, from 64% in the 2014-2015 seasons to 69% in the 2015-2016 season, Dr. Black and colleagues noted.
“Although low, this is the only setting with an appreciable increase in coverage, compared with last season. Influenza vaccination among health care personnel in long-term care settings is especially important because influenza vaccine effectiveness is generally lowest in the elderly,” according to Dr Black, an epidemiologist with the Centers for Disease Control and Prevention.
CDC conducted the Internet survey of 2,258 health care workers from March to April, 2016.
Physicians had the highest level of coverage (95.6%), while health care assistants and aides had the lowest (64.5%). Employers also exerted an influence on coverage. Most respondents (73%) were vaccinated at work. Coverage was highest (96.5%) at facilities where vaccination was required and lowest (45%) where vaccination was not required, promoted, or offered on site.
“Employer vaccination requirements likely contributed to the observed gradual increase in vaccination among health care personnel working in settings with the lowest coverage,” the investigators noted. “In the absence of vaccination requirements, expanding the number of health care locations offering vaccination on site, over multiple days, and at no cost might help sustain and improve influenza vaccination coverage among health care personnel, including in long-term care settings.”
As a CDC employee, Dr. Black has no financial conflicts.
Influenza vaccine coverage among U.S. health care personnel increased very slightly during the 2015-2016 flu season, with 79% reporting that they received the shot, compared with 77% in 2014-2015.
Hospital personnel were most likely to be covered (91%) and long-term care personnel least likely to be covered (69%), Carla L. Black, PhD, wrote in the Sept. 30 issue of Morbidity and Mortality Weekly Report (2016;65:1026-31). Coverage among health care personnel working in long-term care settings did increase, however, from 64% in the 2014-2015 seasons to 69% in the 2015-2016 season, Dr. Black and colleagues noted.
“Although low, this is the only setting with an appreciable increase in coverage, compared with last season. Influenza vaccination among health care personnel in long-term care settings is especially important because influenza vaccine effectiveness is generally lowest in the elderly,” according to Dr Black, an epidemiologist with the Centers for Disease Control and Prevention.
CDC conducted the Internet survey of 2,258 health care workers from March to April, 2016.
Physicians had the highest level of coverage (95.6%), while health care assistants and aides had the lowest (64.5%). Employers also exerted an influence on coverage. Most respondents (73%) were vaccinated at work. Coverage was highest (96.5%) at facilities where vaccination was required and lowest (45%) where vaccination was not required, promoted, or offered on site.
“Employer vaccination requirements likely contributed to the observed gradual increase in vaccination among health care personnel working in settings with the lowest coverage,” the investigators noted. “In the absence of vaccination requirements, expanding the number of health care locations offering vaccination on site, over multiple days, and at no cost might help sustain and improve influenza vaccination coverage among health care personnel, including in long-term care settings.”
As a CDC employee, Dr. Black has no financial conflicts.
Key clinical point:
Major finding: The flu vaccination rate was 79% among health care workers.
Data source: An Internet survey contained data on 2,258 people.
Disclosures: As a CDC employee, Dr. Black has no financial disclosures.
Many overweight Parkinson’s patients have insulin resistance
PORTLAND, ORE. – More than half of overweight, nondiabetic people with Parkinson’s disease were insulin resistant even though most had normal fasting glucose and insulin levels in a prospective, observational study, raising concerns about the potential role of insulin resistance in accelerating the progression of neurodegenerative diseases, including certain features of Parkinson’s disease.
Researchers at Cedars-Sinai Medical Center in Los Angeles tested 93 patients with Parkinson’s disease to determine the prevalence of undiagnosed insulin resistance (IR). They used the homeostatic model assessment of insulin resistance (HOMA-IR) formula, with a HOMA-IR index of 2.0 as a cut-off for abnormal insulin sensitivity. The index is a measure of how much insulin is needed to control blood sugar and uses just blood fasting insulin and glucose levels for the calculation.
Of the 93 patients (71 men), with an average age of 66 years, 9 were diabetic. Of the 84 nondiabetic patients, 49 (58%) had an abnormal HOMA-IR index, ranging from 2.01 to 9.92, which is consistent with IR. Of the 84, 63 were overweight (body mass index [BMI] greater than 25 kg/m2), and 60.3% had IR. Among the 27 nondiabetic, obese patients (BMI greater than 30 kg/m2), 96% had IR. Only 19% of patients with normal BMI had IR. All the nondiabetic subjects with abnormal HOMA-IR who had values available (n = 22) had normal fasting glucose and glycated hemoglobin levels.
The vast majority of subjects with IR had normal fasting glucose and insulin levels. “They’re using too much insulin to control the amount of glucose that they have even though their glucose itself is not abnormal,” Dr. Hogg said. “The relevance of this could be that this may promote some of the degenerative processes that are inherent to Parkinson’s and, more importantly, could potentially offer a reversible target, because if you can identify patients who are insulin resistant, you could, through diet and exercise and lifestyle changes or medications, potentially reverse this and potentially change their path from heading to Parkinson’s or worsening Parkinson’s to something else. That would be the ultimate hope for this research.”
Although overweight is a well known risk factor for insulin resistance, it may be particularly relevant in Parkinson’s disease “because it seems to promote aspects of the disease that could impact not just the motor features of Parkinson’s but also the nonmotor features. We’re most concerned about cognition. ... one of the most feared complications of Parkinson’s and something that we have very little to offer for right now,” Dr. Hogg explained.
He said he plans to look at brain glucose metabolism in Parkinson’s patients without insulin resistance and compare it to similar patients with insulin resistance using PET scanning to see if “these brains are potentially starved of energy.” He cited a British study that showed that exenatide, a glucagonlike peptide-1 (GLP-1) agonist used in diabetes, improved cognition in a treated group. He plans to test liraglutide, another GLP-1 agonist, to see if it will improve or at least stabilize motor or nonmotor symptoms of Parkinson’s disease in insulin-resistant patients.
He suggested that physicians may want to look at insulin and not just measures of blood glucose in appropriate patients.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center in New York, commented that the study indicates that there may be a cohort of patients who are seen routinely but have an undiagnosed risk factor. “Potentially, if we could address it and get their insulin resistance under control, perhaps with weight loss, then we might be able to potentially affect the progression of the Parkinson’s disease,” she said.
As for a mechanism of the effect, she said it is known that there is a “huge role of oxidative stress and apoptosis in the progression of Parkinson’s disease,” and insulin resistance may contribute to it.
She said she would like to see the study replicated in a much larger cohort before routinely adopting insulin measures in clinical practice. If the findings are sufficiently validated, “this is something that seems fairly easy and innocuous to test for.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, speculated that insulin may also have functions in the brain aside from its metabolic effects, specifically, promoting or maintaining neurons through neurotropic effects mediated through the insulinlike growth factor-1 receptors. Still, he cautioned that he would be “hesitant to look at insulin resistance peripherally and make some sort of comment about its relationship to Parkinson’s disease.”
The study was investigator initiated and had no commercial support. Dr. Hogg, Dr. Fleisher, and Dr. Smeyne reported having no financial disclosures.
PORTLAND, ORE. – More than half of overweight, nondiabetic people with Parkinson’s disease were insulin resistant even though most had normal fasting glucose and insulin levels in a prospective, observational study, raising concerns about the potential role of insulin resistance in accelerating the progression of neurodegenerative diseases, including certain features of Parkinson’s disease.
Researchers at Cedars-Sinai Medical Center in Los Angeles tested 93 patients with Parkinson’s disease to determine the prevalence of undiagnosed insulin resistance (IR). They used the homeostatic model assessment of insulin resistance (HOMA-IR) formula, with a HOMA-IR index of 2.0 as a cut-off for abnormal insulin sensitivity. The index is a measure of how much insulin is needed to control blood sugar and uses just blood fasting insulin and glucose levels for the calculation.
Of the 93 patients (71 men), with an average age of 66 years, 9 were diabetic. Of the 84 nondiabetic patients, 49 (58%) had an abnormal HOMA-IR index, ranging from 2.01 to 9.92, which is consistent with IR. Of the 84, 63 were overweight (body mass index [BMI] greater than 25 kg/m2), and 60.3% had IR. Among the 27 nondiabetic, obese patients (BMI greater than 30 kg/m2), 96% had IR. Only 19% of patients with normal BMI had IR. All the nondiabetic subjects with abnormal HOMA-IR who had values available (n = 22) had normal fasting glucose and glycated hemoglobin levels.
The vast majority of subjects with IR had normal fasting glucose and insulin levels. “They’re using too much insulin to control the amount of glucose that they have even though their glucose itself is not abnormal,” Dr. Hogg said. “The relevance of this could be that this may promote some of the degenerative processes that are inherent to Parkinson’s and, more importantly, could potentially offer a reversible target, because if you can identify patients who are insulin resistant, you could, through diet and exercise and lifestyle changes or medications, potentially reverse this and potentially change their path from heading to Parkinson’s or worsening Parkinson’s to something else. That would be the ultimate hope for this research.”
Although overweight is a well known risk factor for insulin resistance, it may be particularly relevant in Parkinson’s disease “because it seems to promote aspects of the disease that could impact not just the motor features of Parkinson’s but also the nonmotor features. We’re most concerned about cognition. ... one of the most feared complications of Parkinson’s and something that we have very little to offer for right now,” Dr. Hogg explained.
He said he plans to look at brain glucose metabolism in Parkinson’s patients without insulin resistance and compare it to similar patients with insulin resistance using PET scanning to see if “these brains are potentially starved of energy.” He cited a British study that showed that exenatide, a glucagonlike peptide-1 (GLP-1) agonist used in diabetes, improved cognition in a treated group. He plans to test liraglutide, another GLP-1 agonist, to see if it will improve or at least stabilize motor or nonmotor symptoms of Parkinson’s disease in insulin-resistant patients.
He suggested that physicians may want to look at insulin and not just measures of blood glucose in appropriate patients.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center in New York, commented that the study indicates that there may be a cohort of patients who are seen routinely but have an undiagnosed risk factor. “Potentially, if we could address it and get their insulin resistance under control, perhaps with weight loss, then we might be able to potentially affect the progression of the Parkinson’s disease,” she said.
As for a mechanism of the effect, she said it is known that there is a “huge role of oxidative stress and apoptosis in the progression of Parkinson’s disease,” and insulin resistance may contribute to it.
She said she would like to see the study replicated in a much larger cohort before routinely adopting insulin measures in clinical practice. If the findings are sufficiently validated, “this is something that seems fairly easy and innocuous to test for.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, speculated that insulin may also have functions in the brain aside from its metabolic effects, specifically, promoting or maintaining neurons through neurotropic effects mediated through the insulinlike growth factor-1 receptors. Still, he cautioned that he would be “hesitant to look at insulin resistance peripherally and make some sort of comment about its relationship to Parkinson’s disease.”
The study was investigator initiated and had no commercial support. Dr. Hogg, Dr. Fleisher, and Dr. Smeyne reported having no financial disclosures.
PORTLAND, ORE. – More than half of overweight, nondiabetic people with Parkinson’s disease were insulin resistant even though most had normal fasting glucose and insulin levels in a prospective, observational study, raising concerns about the potential role of insulin resistance in accelerating the progression of neurodegenerative diseases, including certain features of Parkinson’s disease.
Researchers at Cedars-Sinai Medical Center in Los Angeles tested 93 patients with Parkinson’s disease to determine the prevalence of undiagnosed insulin resistance (IR). They used the homeostatic model assessment of insulin resistance (HOMA-IR) formula, with a HOMA-IR index of 2.0 as a cut-off for abnormal insulin sensitivity. The index is a measure of how much insulin is needed to control blood sugar and uses just blood fasting insulin and glucose levels for the calculation.
Of the 93 patients (71 men), with an average age of 66 years, 9 were diabetic. Of the 84 nondiabetic patients, 49 (58%) had an abnormal HOMA-IR index, ranging from 2.01 to 9.92, which is consistent with IR. Of the 84, 63 were overweight (body mass index [BMI] greater than 25 kg/m2), and 60.3% had IR. Among the 27 nondiabetic, obese patients (BMI greater than 30 kg/m2), 96% had IR. Only 19% of patients with normal BMI had IR. All the nondiabetic subjects with abnormal HOMA-IR who had values available (n = 22) had normal fasting glucose and glycated hemoglobin levels.
The vast majority of subjects with IR had normal fasting glucose and insulin levels. “They’re using too much insulin to control the amount of glucose that they have even though their glucose itself is not abnormal,” Dr. Hogg said. “The relevance of this could be that this may promote some of the degenerative processes that are inherent to Parkinson’s and, more importantly, could potentially offer a reversible target, because if you can identify patients who are insulin resistant, you could, through diet and exercise and lifestyle changes or medications, potentially reverse this and potentially change their path from heading to Parkinson’s or worsening Parkinson’s to something else. That would be the ultimate hope for this research.”
Although overweight is a well known risk factor for insulin resistance, it may be particularly relevant in Parkinson’s disease “because it seems to promote aspects of the disease that could impact not just the motor features of Parkinson’s but also the nonmotor features. We’re most concerned about cognition. ... one of the most feared complications of Parkinson’s and something that we have very little to offer for right now,” Dr. Hogg explained.
He said he plans to look at brain glucose metabolism in Parkinson’s patients without insulin resistance and compare it to similar patients with insulin resistance using PET scanning to see if “these brains are potentially starved of energy.” He cited a British study that showed that exenatide, a glucagonlike peptide-1 (GLP-1) agonist used in diabetes, improved cognition in a treated group. He plans to test liraglutide, another GLP-1 agonist, to see if it will improve or at least stabilize motor or nonmotor symptoms of Parkinson’s disease in insulin-resistant patients.
He suggested that physicians may want to look at insulin and not just measures of blood glucose in appropriate patients.
Jori Fleisher, MD, a movement disorders neurologist at New York University Langone Medical Center in New York, commented that the study indicates that there may be a cohort of patients who are seen routinely but have an undiagnosed risk factor. “Potentially, if we could address it and get their insulin resistance under control, perhaps with weight loss, then we might be able to potentially affect the progression of the Parkinson’s disease,” she said.
As for a mechanism of the effect, she said it is known that there is a “huge role of oxidative stress and apoptosis in the progression of Parkinson’s disease,” and insulin resistance may contribute to it.
She said she would like to see the study replicated in a much larger cohort before routinely adopting insulin measures in clinical practice. If the findings are sufficiently validated, “this is something that seems fairly easy and innocuous to test for.”
Richard Smeyne, PhD, director of the Jefferson Comprehensive Parkinson’s Center at Thomas Jefferson University in Philadelphia, speculated that insulin may also have functions in the brain aside from its metabolic effects, specifically, promoting or maintaining neurons through neurotropic effects mediated through the insulinlike growth factor-1 receptors. Still, he cautioned that he would be “hesitant to look at insulin resistance peripherally and make some sort of comment about its relationship to Parkinson’s disease.”
The study was investigator initiated and had no commercial support. Dr. Hogg, Dr. Fleisher, and Dr. Smeyne reported having no financial disclosures.
AT WPC 2016
Key clinical point:
Major finding: Among 84 nondiabetic, Parkinson’s patients, 58% had insulin resistance, although their blood glucose and insulin levels were not abnormal.
Data source: Prospective, observational study of a total of 93 Parkinson’s patients.
Disclosures: The study was investigator initiated and had no commercial support. Dr. Hogg, Dr. Fleisher, and Dr. Smeyne reported having no financial disclosures.
Paulo Fontoura, MD, PhD
Biomarkers predict Parkinson’s among high-risk individuals
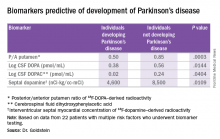
PORTLAND, ORE. – The presence of at least three out of four chemical biomarkers can predict the development of Parkinson’s disease at 3 years of follow-up in people with multiple risk factors for the disease, according to David Goldstein, MD.
These biomarkers, found in the cerebrospinal fluid and in the heart, represent catecholaminergic neurodegeneration.
The PDRisk study of the National Institute of Neurological Disorders and Stroke (NINDS) is investigating whether individuals with at least three out of four statistical risk factors for Parkinson’s disease (PD) develop the disease, based on chemical biomarkers of neurodegeneration. The risk factors are family history of the disease, olfactory dysfunction, dream enactment behavior, and orthostatic hypotension. The biomarkers are PET neuroimaging or cerebrospinal fluid (CSF) neurochemical indicators of catecholamine deficiency in the brain or heart. All the biomarkers are related to dopamine, its precursor, or its metabolites.
Four individuals out of the 22 reached the primary endpoint, which was a diagnosis of PD by a neurologist unaware of the biomarker data. Two of the four individuals with PD also had Lewy body dementia.
“All of the people who went on to convert [to PD], all of them, had at least three of those biomarkers positive. And among the 18 who so far haven’t developed Parkinson’s, none of them had three or more biomarkers. Most of them had none,” said Dr. Goldstein, director of the clinical neurocardiology section at the NINDS. He presented this first look at the PDRisk Study outcome data at the World Parkinson Congress.
Among 10 healthy control subjects without any risk factors for PD, 1 had two positive biomarkers, and the rest had none. Individuals who converted to PD could be distinguished from those who did not by low values for the posterior/anterior ratio of putamen 18F-DOPA–derived radioactivity, CSF DOPA, CSF 3,4-dihydroxyphenylacetic acid (DOPAC, a metabolite of dopamine), and septal myocardial 18F-dopamine-derived radioactivity. Almost 20 years ago, Dr. Goldstein found that there is a substantial loss of sympathetic noradrenergic nerves in the heart in PD.
He has weighted all the biomarkers as if they had equal contributions, which “is not fair,” he said. All four biomarkers were predictive on their own, but some were more potent than others, notably the ratio of DOPA in the anterior to posterior putamen and low values for DOPA in the CSF. He noted that this finding is the first time CSF DOPA has been documented as a biomarker for the development of PD.
The question remains about what to do with these predictors of PD if they are validated. Dr. Goldstein said they could be used to track the efficacy of any intervention to slow the decline to PD.
The study was run by the NINDS and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.
PORTLAND, ORE. – The presence of at least three out of four chemical biomarkers can predict the development of Parkinson’s disease at 3 years of follow-up in people with multiple risk factors for the disease, according to David Goldstein, MD.
These biomarkers, found in the cerebrospinal fluid and in the heart, represent catecholaminergic neurodegeneration.
The PDRisk study of the National Institute of Neurological Disorders and Stroke (NINDS) is investigating whether individuals with at least three out of four statistical risk factors for Parkinson’s disease (PD) develop the disease, based on chemical biomarkers of neurodegeneration. The risk factors are family history of the disease, olfactory dysfunction, dream enactment behavior, and orthostatic hypotension. The biomarkers are PET neuroimaging or cerebrospinal fluid (CSF) neurochemical indicators of catecholamine deficiency in the brain or heart. All the biomarkers are related to dopamine, its precursor, or its metabolites.
Four individuals out of the 22 reached the primary endpoint, which was a diagnosis of PD by a neurologist unaware of the biomarker data. Two of the four individuals with PD also had Lewy body dementia.
“All of the people who went on to convert [to PD], all of them, had at least three of those biomarkers positive. And among the 18 who so far haven’t developed Parkinson’s, none of them had three or more biomarkers. Most of them had none,” said Dr. Goldstein, director of the clinical neurocardiology section at the NINDS. He presented this first look at the PDRisk Study outcome data at the World Parkinson Congress.
Among 10 healthy control subjects without any risk factors for PD, 1 had two positive biomarkers, and the rest had none. Individuals who converted to PD could be distinguished from those who did not by low values for the posterior/anterior ratio of putamen 18F-DOPA–derived radioactivity, CSF DOPA, CSF 3,4-dihydroxyphenylacetic acid (DOPAC, a metabolite of dopamine), and septal myocardial 18F-dopamine-derived radioactivity. Almost 20 years ago, Dr. Goldstein found that there is a substantial loss of sympathetic noradrenergic nerves in the heart in PD.
He has weighted all the biomarkers as if they had equal contributions, which “is not fair,” he said. All four biomarkers were predictive on their own, but some were more potent than others, notably the ratio of DOPA in the anterior to posterior putamen and low values for DOPA in the CSF. He noted that this finding is the first time CSF DOPA has been documented as a biomarker for the development of PD.
The question remains about what to do with these predictors of PD if they are validated. Dr. Goldstein said they could be used to track the efficacy of any intervention to slow the decline to PD.
The study was run by the NINDS and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.
PORTLAND, ORE. – The presence of at least three out of four chemical biomarkers can predict the development of Parkinson’s disease at 3 years of follow-up in people with multiple risk factors for the disease, according to David Goldstein, MD.
These biomarkers, found in the cerebrospinal fluid and in the heart, represent catecholaminergic neurodegeneration.
The PDRisk study of the National Institute of Neurological Disorders and Stroke (NINDS) is investigating whether individuals with at least three out of four statistical risk factors for Parkinson’s disease (PD) develop the disease, based on chemical biomarkers of neurodegeneration. The risk factors are family history of the disease, olfactory dysfunction, dream enactment behavior, and orthostatic hypotension. The biomarkers are PET neuroimaging or cerebrospinal fluid (CSF) neurochemical indicators of catecholamine deficiency in the brain or heart. All the biomarkers are related to dopamine, its precursor, or its metabolites.
Four individuals out of the 22 reached the primary endpoint, which was a diagnosis of PD by a neurologist unaware of the biomarker data. Two of the four individuals with PD also had Lewy body dementia.
“All of the people who went on to convert [to PD], all of them, had at least three of those biomarkers positive. And among the 18 who so far haven’t developed Parkinson’s, none of them had three or more biomarkers. Most of them had none,” said Dr. Goldstein, director of the clinical neurocardiology section at the NINDS. He presented this first look at the PDRisk Study outcome data at the World Parkinson Congress.
Among 10 healthy control subjects without any risk factors for PD, 1 had two positive biomarkers, and the rest had none. Individuals who converted to PD could be distinguished from those who did not by low values for the posterior/anterior ratio of putamen 18F-DOPA–derived radioactivity, CSF DOPA, CSF 3,4-dihydroxyphenylacetic acid (DOPAC, a metabolite of dopamine), and septal myocardial 18F-dopamine-derived radioactivity. Almost 20 years ago, Dr. Goldstein found that there is a substantial loss of sympathetic noradrenergic nerves in the heart in PD.
He has weighted all the biomarkers as if they had equal contributions, which “is not fair,” he said. All four biomarkers were predictive on their own, but some were more potent than others, notably the ratio of DOPA in the anterior to posterior putamen and low values for DOPA in the CSF. He noted that this finding is the first time CSF DOPA has been documented as a biomarker for the development of PD.
The question remains about what to do with these predictors of PD if they are validated. Dr. Goldstein said they could be used to track the efficacy of any intervention to slow the decline to PD.
The study was run by the NINDS and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.
AT WPC 2016
Key clinical point:
Major finding: Among 22 individuals followed for at least 3 years, biomarkers were 100% positively or negatively predictive of developing Parkinson’s disease.
Data source: A prospective cohort study of 3,176 individuals supplying risk factor data, of whom 31 had three or more risk factors and biomarkers testing, and of whom 22 were followed for at least 3 years.
Disclosures: The study was run by the National Institute of Neurological Disorders and Stroke and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.
Steroids could reduce death rate for TB patients with acute respiratory failure
Tuberculosis patients admitted to intensive care units with acute respiratory failure had significantly better survival at 90 days after treatment with corticosteroids and anti-TB drugs, compared with patients not treated with the steroids, according to a retrospective study.
An adjusted inverse probability of treatment weighted analysis using propensity scores revealed corticosteroid use to be independently associated with a significantly reduced 90-day mortality rate (OR = 0.47; 95% CI, 0.22-0.98). This statistical approach was used because it reduces selection bias and other potential confounding factors in a way that a multivariate analysis cannot, wrote Ji Young Yang, MD, of Busan (South Korea) Paik Hospital and Inje University College of Medicine in Busan.
Mortality rates were similar between the steroid-treated and non–steroid-treated groups (48.6% and 50%, respectively), and unadjusted 90-day mortality risk was not affected by steroid administration (odds ratio, 0.94; 95% CI, 0.46-1.92; P = .875), reported Dr. Yang and colleagues (Clin Infect Dis. 2016 Sep 8. doi: 10.1093/cid/ciw616).
The study involved the examination of records of 124 patients (mean age 62, 64% men) admitted to a single center over a 25-year period ending in 2014. Of these, 56.5% received corticosteroids, and 49.2% of the cohort died within 90 days.
The investigators acknowledged that their study was limited by various factors, including its small size, its use of data from a single center, and its lack of a standardized approach to steroid treatment.
“Further prospective randomized controlled trials will therefore be necessary to clarify the role of steroids in the management of these patients,” they wrote in their analysis. However, Dr. Yang and colleagues argued, in acute respiratory failure – a rare but dangerous complication in TB – “corticosteroids represent an attractive option because they can suppress cytokine expression and are effective in managing the inflammatory complications of extrapulmonary tuberculosis. Moreover, corticosteroids have been recently been shown to reduce mortality or treatment failure in patients with tuberculosis or severe pneumonia.”
Robert C. Hyzy, MD, director of the critical care medicine unit at the University of Michigan, Ann Arbor, said the findings “should be considered hypothesis generating.
“Clinicians should wait for prospective validation of this observation before considering the use of corticosteroids in hospitalized patients with tuberculosis,” he added.
Dr. Yang and colleagues disclosed no conflicts of interest or outside funding for their study.
Tuberculosis patients admitted to intensive care units with acute respiratory failure had significantly better survival at 90 days after treatment with corticosteroids and anti-TB drugs, compared with patients not treated with the steroids, according to a retrospective study.
An adjusted inverse probability of treatment weighted analysis using propensity scores revealed corticosteroid use to be independently associated with a significantly reduced 90-day mortality rate (OR = 0.47; 95% CI, 0.22-0.98). This statistical approach was used because it reduces selection bias and other potential confounding factors in a way that a multivariate analysis cannot, wrote Ji Young Yang, MD, of Busan (South Korea) Paik Hospital and Inje University College of Medicine in Busan.
Mortality rates were similar between the steroid-treated and non–steroid-treated groups (48.6% and 50%, respectively), and unadjusted 90-day mortality risk was not affected by steroid administration (odds ratio, 0.94; 95% CI, 0.46-1.92; P = .875), reported Dr. Yang and colleagues (Clin Infect Dis. 2016 Sep 8. doi: 10.1093/cid/ciw616).
The study involved the examination of records of 124 patients (mean age 62, 64% men) admitted to a single center over a 25-year period ending in 2014. Of these, 56.5% received corticosteroids, and 49.2% of the cohort died within 90 days.
The investigators acknowledged that their study was limited by various factors, including its small size, its use of data from a single center, and its lack of a standardized approach to steroid treatment.
“Further prospective randomized controlled trials will therefore be necessary to clarify the role of steroids in the management of these patients,” they wrote in their analysis. However, Dr. Yang and colleagues argued, in acute respiratory failure – a rare but dangerous complication in TB – “corticosteroids represent an attractive option because they can suppress cytokine expression and are effective in managing the inflammatory complications of extrapulmonary tuberculosis. Moreover, corticosteroids have been recently been shown to reduce mortality or treatment failure in patients with tuberculosis or severe pneumonia.”
Robert C. Hyzy, MD, director of the critical care medicine unit at the University of Michigan, Ann Arbor, said the findings “should be considered hypothesis generating.
“Clinicians should wait for prospective validation of this observation before considering the use of corticosteroids in hospitalized patients with tuberculosis,” he added.
Dr. Yang and colleagues disclosed no conflicts of interest or outside funding for their study.
Tuberculosis patients admitted to intensive care units with acute respiratory failure had significantly better survival at 90 days after treatment with corticosteroids and anti-TB drugs, compared with patients not treated with the steroids, according to a retrospective study.
An adjusted inverse probability of treatment weighted analysis using propensity scores revealed corticosteroid use to be independently associated with a significantly reduced 90-day mortality rate (OR = 0.47; 95% CI, 0.22-0.98). This statistical approach was used because it reduces selection bias and other potential confounding factors in a way that a multivariate analysis cannot, wrote Ji Young Yang, MD, of Busan (South Korea) Paik Hospital and Inje University College of Medicine in Busan.
Mortality rates were similar between the steroid-treated and non–steroid-treated groups (48.6% and 50%, respectively), and unadjusted 90-day mortality risk was not affected by steroid administration (odds ratio, 0.94; 95% CI, 0.46-1.92; P = .875), reported Dr. Yang and colleagues (Clin Infect Dis. 2016 Sep 8. doi: 10.1093/cid/ciw616).
The study involved the examination of records of 124 patients (mean age 62, 64% men) admitted to a single center over a 25-year period ending in 2014. Of these, 56.5% received corticosteroids, and 49.2% of the cohort died within 90 days.
The investigators acknowledged that their study was limited by various factors, including its small size, its use of data from a single center, and its lack of a standardized approach to steroid treatment.
“Further prospective randomized controlled trials will therefore be necessary to clarify the role of steroids in the management of these patients,” they wrote in their analysis. However, Dr. Yang and colleagues argued, in acute respiratory failure – a rare but dangerous complication in TB – “corticosteroids represent an attractive option because they can suppress cytokine expression and are effective in managing the inflammatory complications of extrapulmonary tuberculosis. Moreover, corticosteroids have been recently been shown to reduce mortality or treatment failure in patients with tuberculosis or severe pneumonia.”
Robert C. Hyzy, MD, director of the critical care medicine unit at the University of Michigan, Ann Arbor, said the findings “should be considered hypothesis generating.
“Clinicians should wait for prospective validation of this observation before considering the use of corticosteroids in hospitalized patients with tuberculosis,” he added.
Dr. Yang and colleagues disclosed no conflicts of interest or outside funding for their study.
Key clinical point: Corticosteroids used in combination with anti-TB treatment appeared to lower 90-day mortality in TB patients with ARF.
Major finding: Reduced 90-day mortality was associated with corticosteroid use (odds ratio, 0.47; 95% CI, 0.22-0.98; P = .049).
Data source: A retrospective cohort study of 124 patients admitted to intensive care units with TB and ARF in a single Korean center from 1989 to 2014.
Disclosures: The investigators reported no outside funding or conflicts of interest.
Midterm results of thoracic stenting for acute type B dissection promising
LAS VEGAS – Patients with acute, complicated type B aortic dissections are reported to have a greater than 50% likelihood of dying from their condition. Three-year results of the Valiant thoracic stent graft in the treatment of these dissections showed freedom from all-cause mortality of 79.4%, and a freedom from dissection-related mortality of 90%, according to Ali Azizzadeh, MD.
Dr. Azizzadeh presented the midterm results of the Medtronic Dissection US IDE trial of endovascular treatment with the Valiant Captivia thoracic stent graft (Medtronic) in acute, complicated type B aortic dissection patients at the 2016 Vascular Interventional Advances meeting.
One-year outcomes of the trial were reported last year in the Annals of Thoracic Surgery (2015 Sep;100:802-9).
Dr. Azizzadeh is a vascular surgeon at the Memorial Hermann Heart and Vascular Institute, Houston.
Between June 2010 and May 2012, 50 patients with acute, complicated type B aortic dissection were enrolled at 16 clinical sites in the United States in this multicenter, prospective, nonrandomized trial with a planned 5-year follow-up.
The primary safety endpoint was all-cause mortality within 30 days from the index procedure.
A total of 28 patients completed their 3-year follow-up. Through 3 years, there were no postindex ruptures or conversions to open surgical repair reported in the trial.
At 3 years, true lumen diameter over the stented region (or endograft segment) remained stable or increased in 92.3% of patients, according to Dr. Azizzadeh. False lumen diameter remained stable or decreased in 69.3% of patients, and the false lumen was partially or completely thrombosed in 75% of patients.
One death (from sepsis) occurred between years 2 and 3; and was adjudicated by the clinical events committee as unrelated to the device, the procedure, or the dissection.
Although these midterm results are encouraging, said Dr. Azizzadeh, longer-term outcomes are needed to assess the durability of the stent graft in this indication.
The trial was sponsored by Medtronic. Dr. Azizzadeh has consulted for and received research/trial funding from W.L. Gore & Associates and Medtronic.
LAS VEGAS – Patients with acute, complicated type B aortic dissections are reported to have a greater than 50% likelihood of dying from their condition. Three-year results of the Valiant thoracic stent graft in the treatment of these dissections showed freedom from all-cause mortality of 79.4%, and a freedom from dissection-related mortality of 90%, according to Ali Azizzadeh, MD.
Dr. Azizzadeh presented the midterm results of the Medtronic Dissection US IDE trial of endovascular treatment with the Valiant Captivia thoracic stent graft (Medtronic) in acute, complicated type B aortic dissection patients at the 2016 Vascular Interventional Advances meeting.
One-year outcomes of the trial were reported last year in the Annals of Thoracic Surgery (2015 Sep;100:802-9).
Dr. Azizzadeh is a vascular surgeon at the Memorial Hermann Heart and Vascular Institute, Houston.
Between June 2010 and May 2012, 50 patients with acute, complicated type B aortic dissection were enrolled at 16 clinical sites in the United States in this multicenter, prospective, nonrandomized trial with a planned 5-year follow-up.
The primary safety endpoint was all-cause mortality within 30 days from the index procedure.
A total of 28 patients completed their 3-year follow-up. Through 3 years, there were no postindex ruptures or conversions to open surgical repair reported in the trial.
At 3 years, true lumen diameter over the stented region (or endograft segment) remained stable or increased in 92.3% of patients, according to Dr. Azizzadeh. False lumen diameter remained stable or decreased in 69.3% of patients, and the false lumen was partially or completely thrombosed in 75% of patients.
One death (from sepsis) occurred between years 2 and 3; and was adjudicated by the clinical events committee as unrelated to the device, the procedure, or the dissection.
Although these midterm results are encouraging, said Dr. Azizzadeh, longer-term outcomes are needed to assess the durability of the stent graft in this indication.
The trial was sponsored by Medtronic. Dr. Azizzadeh has consulted for and received research/trial funding from W.L. Gore & Associates and Medtronic.
LAS VEGAS – Patients with acute, complicated type B aortic dissections are reported to have a greater than 50% likelihood of dying from their condition. Three-year results of the Valiant thoracic stent graft in the treatment of these dissections showed freedom from all-cause mortality of 79.4%, and a freedom from dissection-related mortality of 90%, according to Ali Azizzadeh, MD.
Dr. Azizzadeh presented the midterm results of the Medtronic Dissection US IDE trial of endovascular treatment with the Valiant Captivia thoracic stent graft (Medtronic) in acute, complicated type B aortic dissection patients at the 2016 Vascular Interventional Advances meeting.
One-year outcomes of the trial were reported last year in the Annals of Thoracic Surgery (2015 Sep;100:802-9).
Dr. Azizzadeh is a vascular surgeon at the Memorial Hermann Heart and Vascular Institute, Houston.
Between June 2010 and May 2012, 50 patients with acute, complicated type B aortic dissection were enrolled at 16 clinical sites in the United States in this multicenter, prospective, nonrandomized trial with a planned 5-year follow-up.
The primary safety endpoint was all-cause mortality within 30 days from the index procedure.
A total of 28 patients completed their 3-year follow-up. Through 3 years, there were no postindex ruptures or conversions to open surgical repair reported in the trial.
At 3 years, true lumen diameter over the stented region (or endograft segment) remained stable or increased in 92.3% of patients, according to Dr. Azizzadeh. False lumen diameter remained stable or decreased in 69.3% of patients, and the false lumen was partially or completely thrombosed in 75% of patients.
One death (from sepsis) occurred between years 2 and 3; and was adjudicated by the clinical events committee as unrelated to the device, the procedure, or the dissection.
Although these midterm results are encouraging, said Dr. Azizzadeh, longer-term outcomes are needed to assess the durability of the stent graft in this indication.
The trial was sponsored by Medtronic. Dr. Azizzadeh has consulted for and received research/trial funding from W.L. Gore & Associates and Medtronic.
AT VIVA16 LAS VEGAS
Key clinical point:
Major finding: Three-year results of the Valiant thoracic stent graft in the treatment of acute type B dissections showed freedom from all-cause mortality of 79.4%, and a freedom from dissection-related mortality of 90%.
Data source: Midterm results were presented from the multicenter, prospective, nonrandomized Medtronic Dissection US IDE trial.
Disclosures: The trial was sponsored by Medtronic. Dr. Azizzadeh has consulted for and received research/trial funding from W.L. Gore & Associates and Medtronic.
VIDEO: Is your patient clinically depressed, or is there something else?
Is your 42-year-old patient with well-controlled hypertension and type 2 diabetes dealing with a mood disorder that should be regarded as a psychiatric illness – or is she experiencing demoralization and grief?
In this installment of Mental Health Consult, the patient screens positive for depression but is ambivalent about taking antidepressants. In addition, the patient believes she has a number of coping resources that she can utilize. Finding out whether there is a need for an evidence-based psychotherapy, medication, or if other interventions are appropriate requires four key questions when taking a history.
Our expert panel from George Washington University, Washington, includes James L. Griffith, MD, chair of psychiatry and behavioral sciences; April Barbour, MD, MPH, director of the division of general internal medicine; and Lorenzo Norris, MD, medical director of psychiatric and behavioral services.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @whitneymcknight
Is your 42-year-old patient with well-controlled hypertension and type 2 diabetes dealing with a mood disorder that should be regarded as a psychiatric illness – or is she experiencing demoralization and grief?
In this installment of Mental Health Consult, the patient screens positive for depression but is ambivalent about taking antidepressants. In addition, the patient believes she has a number of coping resources that she can utilize. Finding out whether there is a need for an evidence-based psychotherapy, medication, or if other interventions are appropriate requires four key questions when taking a history.
Our expert panel from George Washington University, Washington, includes James L. Griffith, MD, chair of psychiatry and behavioral sciences; April Barbour, MD, MPH, director of the division of general internal medicine; and Lorenzo Norris, MD, medical director of psychiatric and behavioral services.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @whitneymcknight
Is your 42-year-old patient with well-controlled hypertension and type 2 diabetes dealing with a mood disorder that should be regarded as a psychiatric illness – or is she experiencing demoralization and grief?
In this installment of Mental Health Consult, the patient screens positive for depression but is ambivalent about taking antidepressants. In addition, the patient believes she has a number of coping resources that she can utilize. Finding out whether there is a need for an evidence-based psychotherapy, medication, or if other interventions are appropriate requires four key questions when taking a history.
Our expert panel from George Washington University, Washington, includes James L. Griffith, MD, chair of psychiatry and behavioral sciences; April Barbour, MD, MPH, director of the division of general internal medicine; and Lorenzo Norris, MD, medical director of psychiatric and behavioral services.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @whitneymcknight
Intake of Vitamins and Minerals Is Inadequate for Most Americans: What Should We Advise Patients About Supplements?
Endovascular construction of arteriovenous fistulas shows promise
LAS VEGAS – Patients who had an arteriovenous fistula (AVF) created endovascularly using a new magnetic catheter system required fewer interventions and had fewer health care costs than patients whose AVF was created surgically, according to a late-breaking trial presented by Charmaine E. Lok, MD, at the 2016 Vascular Interventional Advances meeting.
The study compared AVF postcreation interventions between patients undergoing surgical (sAVF) creation and those whose fistula was created using a new endovascular AVF (endoAVF) system.
Medicare Standard Analytical Files were used to determine patient demographic and clinical characteristics and to identify and determine rates of sAVF postcreation interventions in patients with sAVF created from 2011 to 2013, according to Dr. Lok, a professor of medicine at the University of Toronto and senior scientist at the Toronto General Research Institute.
The rates of postcreation interventions per patient-year were determined based on patients’ outpatient and physician claims. Demographics and clinical information for patients with endoAVF were obtained from the single-arm Novel Endovascular Access Trial (NEAT) performed in Canada, Australia, and New Zealand.
The researchers determined the rates of postcreation interventions per patient-year from the trial based on patients’ outpatient and physician claims during specified follow-up.
Propensity score matching based on clinical and demographic factors was successful for comparing 60 Medicare patients who had surgical AVFs to NEAT patients. The matched surgical cohort had a significantly higher number of interventions than the endovascular cohort (3.4 vs. 0.6 per patient-year, respectively; P less than .0001). The associated average annual costs were $11,240 less for the endovascular patients, compared with the surgical patients.
In a breakdown of procedures, the endovascular cohort had lower event rates for angioplasty (0.04 vs. 0.93),respectively; thrombectomy (0.04 vs. 0.20); embolization/ligation of vein (0.13 vs. 0.1); revision (0.04 vs. 0.17); new AVF or transposition (0.11 vs. 0.30); catheter placement (0.11 vs. 0.43); vascular access–related infection (0.02 vs. 1.23), and arteriovenous graft placement (0.02 vs. 0.07), according to Dr. Lok.
The NEAT study assessed the FLEX system, which percutaneously creates a fistula in chronic kidney disease patients who require hemodialysis vascular access.
The FLEX system uses two catheters delivered percutaneously to an artery and a vein in proximity to each other in the arm. The catheters use magnets for alignment and a radio frequency system as an energy source. The catheters are magnetically aligned and an RF pulse creates an arteriovenous fistula endovascularly between the artery and vein and the catheters are then removed.
The technology used is not commercially available in the United States and is pending Food and Drug Administration review, according to Dr. Lok
The study was sponsored by TVA Medical. Dr. Lok has received honoraria from Maquet and W.L. Gore, and is a consultant for TVA Medical and W. L. Gore, and has received research funding from Maquet, Proteon, and TVA Medical.
LAS VEGAS – Patients who had an arteriovenous fistula (AVF) created endovascularly using a new magnetic catheter system required fewer interventions and had fewer health care costs than patients whose AVF was created surgically, according to a late-breaking trial presented by Charmaine E. Lok, MD, at the 2016 Vascular Interventional Advances meeting.
The study compared AVF postcreation interventions between patients undergoing surgical (sAVF) creation and those whose fistula was created using a new endovascular AVF (endoAVF) system.
Medicare Standard Analytical Files were used to determine patient demographic and clinical characteristics and to identify and determine rates of sAVF postcreation interventions in patients with sAVF created from 2011 to 2013, according to Dr. Lok, a professor of medicine at the University of Toronto and senior scientist at the Toronto General Research Institute.
The rates of postcreation interventions per patient-year were determined based on patients’ outpatient and physician claims. Demographics and clinical information for patients with endoAVF were obtained from the single-arm Novel Endovascular Access Trial (NEAT) performed in Canada, Australia, and New Zealand.
The researchers determined the rates of postcreation interventions per patient-year from the trial based on patients’ outpatient and physician claims during specified follow-up.
Propensity score matching based on clinical and demographic factors was successful for comparing 60 Medicare patients who had surgical AVFs to NEAT patients. The matched surgical cohort had a significantly higher number of interventions than the endovascular cohort (3.4 vs. 0.6 per patient-year, respectively; P less than .0001). The associated average annual costs were $11,240 less for the endovascular patients, compared with the surgical patients.
In a breakdown of procedures, the endovascular cohort had lower event rates for angioplasty (0.04 vs. 0.93),respectively; thrombectomy (0.04 vs. 0.20); embolization/ligation of vein (0.13 vs. 0.1); revision (0.04 vs. 0.17); new AVF or transposition (0.11 vs. 0.30); catheter placement (0.11 vs. 0.43); vascular access–related infection (0.02 vs. 1.23), and arteriovenous graft placement (0.02 vs. 0.07), according to Dr. Lok.
The NEAT study assessed the FLEX system, which percutaneously creates a fistula in chronic kidney disease patients who require hemodialysis vascular access.
The FLEX system uses two catheters delivered percutaneously to an artery and a vein in proximity to each other in the arm. The catheters use magnets for alignment and a radio frequency system as an energy source. The catheters are magnetically aligned and an RF pulse creates an arteriovenous fistula endovascularly between the artery and vein and the catheters are then removed.
The technology used is not commercially available in the United States and is pending Food and Drug Administration review, according to Dr. Lok
The study was sponsored by TVA Medical. Dr. Lok has received honoraria from Maquet and W.L. Gore, and is a consultant for TVA Medical and W. L. Gore, and has received research funding from Maquet, Proteon, and TVA Medical.
LAS VEGAS – Patients who had an arteriovenous fistula (AVF) created endovascularly using a new magnetic catheter system required fewer interventions and had fewer health care costs than patients whose AVF was created surgically, according to a late-breaking trial presented by Charmaine E. Lok, MD, at the 2016 Vascular Interventional Advances meeting.
The study compared AVF postcreation interventions between patients undergoing surgical (sAVF) creation and those whose fistula was created using a new endovascular AVF (endoAVF) system.
Medicare Standard Analytical Files were used to determine patient demographic and clinical characteristics and to identify and determine rates of sAVF postcreation interventions in patients with sAVF created from 2011 to 2013, according to Dr. Lok, a professor of medicine at the University of Toronto and senior scientist at the Toronto General Research Institute.
The rates of postcreation interventions per patient-year were determined based on patients’ outpatient and physician claims. Demographics and clinical information for patients with endoAVF were obtained from the single-arm Novel Endovascular Access Trial (NEAT) performed in Canada, Australia, and New Zealand.
The researchers determined the rates of postcreation interventions per patient-year from the trial based on patients’ outpatient and physician claims during specified follow-up.
Propensity score matching based on clinical and demographic factors was successful for comparing 60 Medicare patients who had surgical AVFs to NEAT patients. The matched surgical cohort had a significantly higher number of interventions than the endovascular cohort (3.4 vs. 0.6 per patient-year, respectively; P less than .0001). The associated average annual costs were $11,240 less for the endovascular patients, compared with the surgical patients.
In a breakdown of procedures, the endovascular cohort had lower event rates for angioplasty (0.04 vs. 0.93),respectively; thrombectomy (0.04 vs. 0.20); embolization/ligation of vein (0.13 vs. 0.1); revision (0.04 vs. 0.17); new AVF or transposition (0.11 vs. 0.30); catheter placement (0.11 vs. 0.43); vascular access–related infection (0.02 vs. 1.23), and arteriovenous graft placement (0.02 vs. 0.07), according to Dr. Lok.
The NEAT study assessed the FLEX system, which percutaneously creates a fistula in chronic kidney disease patients who require hemodialysis vascular access.
The FLEX system uses two catheters delivered percutaneously to an artery and a vein in proximity to each other in the arm. The catheters use magnets for alignment and a radio frequency system as an energy source. The catheters are magnetically aligned and an RF pulse creates an arteriovenous fistula endovascularly between the artery and vein and the catheters are then removed.
The technology used is not commercially available in the United States and is pending Food and Drug Administration review, according to Dr. Lok
The study was sponsored by TVA Medical. Dr. Lok has received honoraria from Maquet and W.L. Gore, and is a consultant for TVA Medical and W. L. Gore, and has received research funding from Maquet, Proteon, and TVA Medical.
Key clinical point: than patients whose AVF was created surgically
Major finding: A matched surgical cohort of patients with surgically constructed AVFs had a significantly higher number of interventions than an endovascular AVF cohort (3.4 vs. 0.6 per patient-year).
Data source: Researchers performed a propensity-matching analysis of Medicare patients to those patient who received an endovascularly created AVF in the NEAT trial.
Disclosures: The study was sponsored by TVA Medical. Dr. Lok has received honoraria from Maquet and W.L. Gore, and is a consultant for TVA Medical and W. L. Gore, and has received research funding from Maquet, Proteon, and TVA Medical.
Extended half-life clotting factors are safe, effective, and pricey
ORLANDO – Early experience with extended half-life clotting factor concentrates suggests these products are generally safe and effective, at least in the short term, according to hemophilia experts.
“In adolescent and adult patients, the extended half-life clotting factor concentrates demonstrate efficacy and safety in a variety of clinical settings, including prophylaxis, treatment of bleeds, and perisurgical hemostasis,” said Johnny Mahlangu, MD, director of the Haemophilia Comprehensive Care Centre in Johannesburg, South Africa.
Barriers to prophylaxis include “the need to inject the clotting factor concentrate at least two or three times a week, poor venous access, and, of course, poor adherence and compliance from our patients. Essentially, the extended half-life products were developed to mitigate these limitations,” he said.
Dr. Mahlangu and Guy Young, MD, a pediatric hematologist at Children’s Hospital Los Angeles, discussed results from published clinical trials of EHL products in children and adults.
The X factor
Extended half-life products currently available or in development include those created through fusion technology, including factor VIII products for treatment of hemophilia A, factor IX for treating hemophilia B, and factor VII products for treating factor VII deficiency (Alexander’s Disease).
More recent products created through pegylation technology include recombinant FVIII products.
Factor IX EHL CFCs
The three recombinant factor IX (rFIX) products that have completed phase III clinical trials are: nonacog beta pegol (N9-GP), rFIXFc (Alprolix), and rFIX-FP (Idelvion). The latter two are approved by the U.S. Food and Drug Administration; the former is waiting European and U.S. approval.
In clinical trials in adolescents and adults, these agents were associated with low median annualized bleeding rates, as follows:
• rFIXFc: 3.0 for a 50 IU/kg dose given every 7 days, and 1.4 for a 100 IU/kg dose given every 10 days
• rFIX-FP: 0.0 for a 40 IU/kg dose given every 7 days, and 1.08 for a 75 IU/kg dose given every 14 days
• Nonacog beta pegol: 2.93 for a 10 IU/kg dose and 1.0 for a 40 IU/kg dose, each given every 7 days.
All of these agents effectively treated bleeding episodes after one or two doses, Dr. Mahlangu said. The respective overall hemostatic efficacy rates were 97.2%, 96.7%, and 97.1%.
Safety analyses from published studies showed that no patients exposed to any of these agents developed inhibiting antibodies, although three patients treated with rFIXFc and nonacog beta pegol each developed noninhibitory antibodies.
There were no deaths from thromboembolic episodes and no drug-related serious adverse events.
Data are more limited for children treated with rFIX products, Dr. Young noted. In studies thus far, no children developed inhibitors, although this population had been heavily pretreated, he noted. Median annualized bleeding rates ranged from 1 to 3 and did not differ significantly between the products.
Factor VIII EHL CFCs
Four factor VIII EHL products are available or in development: rFVIIIFc (Eloctate); antihemophilic factor, pegylated (Adynovate); turoctocog alfa pegol (N8-GP); and BAY 94-9027. The former two agents are approved in the United States.
In adults and adolescents, these products have half-lives comparatively shorter than those seen with Factor IX products, the researchers noted.
Annualized bleeding rates for patients on prophylaxis with these agents were less than 4 bleeds per year, ranging from 1.3 to 3.6. In all, 96% of bleeds that did occur could be resolved with one or two injections of the extended half-life rFVIII products.
All patients had at least 50 exposures to these products, and none have developed inhibitors to date.
Only one study has been published to date of factor VIII products in children, comparing a standard half-life product with rFVIIIFc, Dr. Young said.
In this study, the patients were treated with a twice weekly, split-dose regimen. No patients developed inhibitors, and the mean annualized bleeding rate was a low 1.96.
Dr. Mahlangu disclosed research grants from Bayer, Biogen, CSL Behring, Novo Nordisk, and Roche, and speakers bureau participation for Amgen, Biotest, Biogen, CSL Behring, Novo Nordisk, and Sobi. Dr. Young disclosed honoraria and consulting fees from Baxalta, Bayer, Biogen, CSL Behring, and Novo Nordisk. Ellis J. Neufeld, MD, PhD, the invited discussant of the presentation, disclosed institutional grants from Baxalta, Novo Nordisk, and Octapharma, consulting/advising for those companies and for CSL Behring, Genentech, Hema Biologics, and Pfizer.
Improvements in half-life are incremental with the factor VIII products, but ground breaking with the factor IX products, allowing treatment intervals to be substantially prolonged. Pivotal trials of the several longer-acting products have been positive and generally convincing.
However, the pricing of these extended half-life products seems to reflect the so called “value proposition,” a concept from Big Pharma that puts a premium on convenience or novelty when determining the marketing price for a new drug. But the price may not always be commensurate with the clinical benefits patients derive from these newer agents.
How trials translate into treatment recommendations is complicated, and as Dr. Young and Dr. Mahlangu both made very clear, you need to consider that factor VIII and factor IX prolongation is entirely separate, even when the same technology is used, because the consequences are very different.
Ellis J. Neufeld, MD, PhD, is the associate chief of hematology/oncology at Boston Children’s Hospital, and was the invited discussant of the presentation.
Improvements in half-life are incremental with the factor VIII products, but ground breaking with the factor IX products, allowing treatment intervals to be substantially prolonged. Pivotal trials of the several longer-acting products have been positive and generally convincing.
However, the pricing of these extended half-life products seems to reflect the so called “value proposition,” a concept from Big Pharma that puts a premium on convenience or novelty when determining the marketing price for a new drug. But the price may not always be commensurate with the clinical benefits patients derive from these newer agents.
How trials translate into treatment recommendations is complicated, and as Dr. Young and Dr. Mahlangu both made very clear, you need to consider that factor VIII and factor IX prolongation is entirely separate, even when the same technology is used, because the consequences are very different.
Ellis J. Neufeld, MD, PhD, is the associate chief of hematology/oncology at Boston Children’s Hospital, and was the invited discussant of the presentation.
Improvements in half-life are incremental with the factor VIII products, but ground breaking with the factor IX products, allowing treatment intervals to be substantially prolonged. Pivotal trials of the several longer-acting products have been positive and generally convincing.
However, the pricing of these extended half-life products seems to reflect the so called “value proposition,” a concept from Big Pharma that puts a premium on convenience or novelty when determining the marketing price for a new drug. But the price may not always be commensurate with the clinical benefits patients derive from these newer agents.
How trials translate into treatment recommendations is complicated, and as Dr. Young and Dr. Mahlangu both made very clear, you need to consider that factor VIII and factor IX prolongation is entirely separate, even when the same technology is used, because the consequences are very different.
Ellis J. Neufeld, MD, PhD, is the associate chief of hematology/oncology at Boston Children’s Hospital, and was the invited discussant of the presentation.
ORLANDO – Early experience with extended half-life clotting factor concentrates suggests these products are generally safe and effective, at least in the short term, according to hemophilia experts.
“In adolescent and adult patients, the extended half-life clotting factor concentrates demonstrate efficacy and safety in a variety of clinical settings, including prophylaxis, treatment of bleeds, and perisurgical hemostasis,” said Johnny Mahlangu, MD, director of the Haemophilia Comprehensive Care Centre in Johannesburg, South Africa.
Barriers to prophylaxis include “the need to inject the clotting factor concentrate at least two or three times a week, poor venous access, and, of course, poor adherence and compliance from our patients. Essentially, the extended half-life products were developed to mitigate these limitations,” he said.
Dr. Mahlangu and Guy Young, MD, a pediatric hematologist at Children’s Hospital Los Angeles, discussed results from published clinical trials of EHL products in children and adults.
The X factor
Extended half-life products currently available or in development include those created through fusion technology, including factor VIII products for treatment of hemophilia A, factor IX for treating hemophilia B, and factor VII products for treating factor VII deficiency (Alexander’s Disease).
More recent products created through pegylation technology include recombinant FVIII products.
Factor IX EHL CFCs
The three recombinant factor IX (rFIX) products that have completed phase III clinical trials are: nonacog beta pegol (N9-GP), rFIXFc (Alprolix), and rFIX-FP (Idelvion). The latter two are approved by the U.S. Food and Drug Administration; the former is waiting European and U.S. approval.
In clinical trials in adolescents and adults, these agents were associated with low median annualized bleeding rates, as follows:
• rFIXFc: 3.0 for a 50 IU/kg dose given every 7 days, and 1.4 for a 100 IU/kg dose given every 10 days
• rFIX-FP: 0.0 for a 40 IU/kg dose given every 7 days, and 1.08 for a 75 IU/kg dose given every 14 days
• Nonacog beta pegol: 2.93 for a 10 IU/kg dose and 1.0 for a 40 IU/kg dose, each given every 7 days.
All of these agents effectively treated bleeding episodes after one or two doses, Dr. Mahlangu said. The respective overall hemostatic efficacy rates were 97.2%, 96.7%, and 97.1%.
Safety analyses from published studies showed that no patients exposed to any of these agents developed inhibiting antibodies, although three patients treated with rFIXFc and nonacog beta pegol each developed noninhibitory antibodies.
There were no deaths from thromboembolic episodes and no drug-related serious adverse events.
Data are more limited for children treated with rFIX products, Dr. Young noted. In studies thus far, no children developed inhibitors, although this population had been heavily pretreated, he noted. Median annualized bleeding rates ranged from 1 to 3 and did not differ significantly between the products.
Factor VIII EHL CFCs
Four factor VIII EHL products are available or in development: rFVIIIFc (Eloctate); antihemophilic factor, pegylated (Adynovate); turoctocog alfa pegol (N8-GP); and BAY 94-9027. The former two agents are approved in the United States.
In adults and adolescents, these products have half-lives comparatively shorter than those seen with Factor IX products, the researchers noted.
Annualized bleeding rates for patients on prophylaxis with these agents were less than 4 bleeds per year, ranging from 1.3 to 3.6. In all, 96% of bleeds that did occur could be resolved with one or two injections of the extended half-life rFVIII products.
All patients had at least 50 exposures to these products, and none have developed inhibitors to date.
Only one study has been published to date of factor VIII products in children, comparing a standard half-life product with rFVIIIFc, Dr. Young said.
In this study, the patients were treated with a twice weekly, split-dose regimen. No patients developed inhibitors, and the mean annualized bleeding rate was a low 1.96.
Dr. Mahlangu disclosed research grants from Bayer, Biogen, CSL Behring, Novo Nordisk, and Roche, and speakers bureau participation for Amgen, Biotest, Biogen, CSL Behring, Novo Nordisk, and Sobi. Dr. Young disclosed honoraria and consulting fees from Baxalta, Bayer, Biogen, CSL Behring, and Novo Nordisk. Ellis J. Neufeld, MD, PhD, the invited discussant of the presentation, disclosed institutional grants from Baxalta, Novo Nordisk, and Octapharma, consulting/advising for those companies and for CSL Behring, Genentech, Hema Biologics, and Pfizer.
ORLANDO – Early experience with extended half-life clotting factor concentrates suggests these products are generally safe and effective, at least in the short term, according to hemophilia experts.
“In adolescent and adult patients, the extended half-life clotting factor concentrates demonstrate efficacy and safety in a variety of clinical settings, including prophylaxis, treatment of bleeds, and perisurgical hemostasis,” said Johnny Mahlangu, MD, director of the Haemophilia Comprehensive Care Centre in Johannesburg, South Africa.
Barriers to prophylaxis include “the need to inject the clotting factor concentrate at least two or three times a week, poor venous access, and, of course, poor adherence and compliance from our patients. Essentially, the extended half-life products were developed to mitigate these limitations,” he said.
Dr. Mahlangu and Guy Young, MD, a pediatric hematologist at Children’s Hospital Los Angeles, discussed results from published clinical trials of EHL products in children and adults.
The X factor
Extended half-life products currently available or in development include those created through fusion technology, including factor VIII products for treatment of hemophilia A, factor IX for treating hemophilia B, and factor VII products for treating factor VII deficiency (Alexander’s Disease).
More recent products created through pegylation technology include recombinant FVIII products.
Factor IX EHL CFCs
The three recombinant factor IX (rFIX) products that have completed phase III clinical trials are: nonacog beta pegol (N9-GP), rFIXFc (Alprolix), and rFIX-FP (Idelvion). The latter two are approved by the U.S. Food and Drug Administration; the former is waiting European and U.S. approval.
In clinical trials in adolescents and adults, these agents were associated with low median annualized bleeding rates, as follows:
• rFIXFc: 3.0 for a 50 IU/kg dose given every 7 days, and 1.4 for a 100 IU/kg dose given every 10 days
• rFIX-FP: 0.0 for a 40 IU/kg dose given every 7 days, and 1.08 for a 75 IU/kg dose given every 14 days
• Nonacog beta pegol: 2.93 for a 10 IU/kg dose and 1.0 for a 40 IU/kg dose, each given every 7 days.
All of these agents effectively treated bleeding episodes after one or two doses, Dr. Mahlangu said. The respective overall hemostatic efficacy rates were 97.2%, 96.7%, and 97.1%.
Safety analyses from published studies showed that no patients exposed to any of these agents developed inhibiting antibodies, although three patients treated with rFIXFc and nonacog beta pegol each developed noninhibitory antibodies.
There were no deaths from thromboembolic episodes and no drug-related serious adverse events.
Data are more limited for children treated with rFIX products, Dr. Young noted. In studies thus far, no children developed inhibitors, although this population had been heavily pretreated, he noted. Median annualized bleeding rates ranged from 1 to 3 and did not differ significantly between the products.
Factor VIII EHL CFCs
Four factor VIII EHL products are available or in development: rFVIIIFc (Eloctate); antihemophilic factor, pegylated (Adynovate); turoctocog alfa pegol (N8-GP); and BAY 94-9027. The former two agents are approved in the United States.
In adults and adolescents, these products have half-lives comparatively shorter than those seen with Factor IX products, the researchers noted.
Annualized bleeding rates for patients on prophylaxis with these agents were less than 4 bleeds per year, ranging from 1.3 to 3.6. In all, 96% of bleeds that did occur could be resolved with one or two injections of the extended half-life rFVIII products.
All patients had at least 50 exposures to these products, and none have developed inhibitors to date.
Only one study has been published to date of factor VIII products in children, comparing a standard half-life product with rFVIIIFc, Dr. Young said.
In this study, the patients were treated with a twice weekly, split-dose regimen. No patients developed inhibitors, and the mean annualized bleeding rate was a low 1.96.
Dr. Mahlangu disclosed research grants from Bayer, Biogen, CSL Behring, Novo Nordisk, and Roche, and speakers bureau participation for Amgen, Biotest, Biogen, CSL Behring, Novo Nordisk, and Sobi. Dr. Young disclosed honoraria and consulting fees from Baxalta, Bayer, Biogen, CSL Behring, and Novo Nordisk. Ellis J. Neufeld, MD, PhD, the invited discussant of the presentation, disclosed institutional grants from Baxalta, Novo Nordisk, and Octapharma, consulting/advising for those companies and for CSL Behring, Genentech, Hema Biologics, and Pfizer.
AT WFH 2016 WORLD CONGRESS