User login
HIV PrEP safe for breastfeeding women, infants
Pre-exposure prophylaxis (PrEP) therapy is safe for HIV-uninfected women breastfeeding their infants, according to a study in PLOS Medicine.
As PrEP becomes more widely used in heterosexual populations, an important consideration is its safety in infants who are breastfed by women taking the drugs, reported Kenneth Mugwanya, MBChB, PhD, of the University of Washington, Seattle, and his associates (PLOS Med. 2016 Sep 27. doi: 10.1371/journal.pmed.1002132).
The purpose of this small, prospective short-term trialwas to quantify drug levels in maternal blood samples, breast milk, and infant blood samples to begin to understand if PrEP is safe for use in pregnant or breastfeeding women at high risk for contracting HIV.
Antiretroviral PrEP with 300 mg tenofovir disoproxil fumarate and 200 mg emtricitabine was administered to 50 HIV-uninfected breastfeeding mothers through daily directly observed therapy for 10 consecutive days and then discontinued thereafter. All mothers were African and resided in Kenya or Uganda. Median maternal age was 25 years; 48% of infants were younger than 12 weeks and 52% were between 13 and 24 weeks of age. Across the study cohort, the median daily frequency of breastfeeding was 15 times.
Maternal blood and breast milk samples were collected and analyzed for drug concentrations at days 7 and 10 of the study. Peak concentration samples, collected 1-2 hours after PrEP administration, and trough concentration levels, collected 23-24 hours after PrEP dose, were collected on day 7 and day 10. Infant blood samples were collected only once, on day 7.
In maternal blood samples, tenofovir was detected at concentrations consistent with steady-state use (median peak concentration, 152.0 ng/mL). In breast milk, tenofovir was present in significantly lower concentrations (3.2 ng/mL). Emtricitabine was also detected at concentrations consistent with steady-state use in maternal blood samples (median peak concentration, 267.5 ng/mL); however, unlike tenofovir, emtricitabine concentration in breast milk was similar to peak plasma concentrations (212.5 ng/mL). Tenofovir was undetectable in 46 of 49 (94%) infant plasma samples. For the three infants with detectable tenofovir, the plasma concentrations were 0.9, 0.9, and 17.4 ng/mL, corresponding body weights were 6.4, 5.8, and 6.2 kg, and their maternal milk tenofovir concentrations were “modestly greater” than the median at 6.57, 3.64, and 4.05 ng/mL, respectively.
Emtricitabine, on the other hand, was detectable in 47 of 49 (96%) infant plasma samples with a median concentration of 13.2 ng/mL.
“The estimated daily tenofovir and emtricitabine doses ingested by the infant through breastfeeding were 12,500-fold and 200-fold, respectively, lower than the proposed daily pediatric dose for prophylaxis against vertical HIV acquisition. Thus, infants had low exposures to tenofovir and emtricitabine, which would not be expected to pose substantial safety risk to infants of mothers who use PrEP during breastfeeding,” Dr. Mugwanya and his associates wrote.
“These data provide evidence suggesting that this PrEP regimen can be safely used during breastfeeding, which is informative for clinical guidelines for women who are at substantial risk of HIV during pregnancy and the postpartum period,” the researchers concluded.
This study was funded by the Bill and Melinda Gates Foundation and the National Institutes of Health. The authors did not report disclosures.
On Twitter @jessnicolecraig
The research article by Dr. Mugwanya and his colleagues in PLOS Medicine significantly contributes to the accumulating safety data for PrEP in breastfeeding women. This documents a prospective study of daily tenofovir disoproxil fumarate (TDF)/emtricitabine (FTC) in 50 HIV-uninfected breastfeeding women between 1-24 weeks postpartum; the drug combination was provided to women for 10 consecutive days and then discontinued. In infant plasma, tenofovir was below the limit of detection in 46 (94%) of 49 samples; 47 of 49 (96%) infant samples had detectable FTC. Based on breast milk concentrations, breastfeeding infants would have exposures to TDF 12,500-fold lower and to FTC 200-fold lower than those achieved with pediatric therapeutic dosing (less than 0.01% and 0.5% of therapeutic dose, respectively).
These data confirm and extend other studies that have reported very-low concentrations of tenofovir detectable in breast milk and strongly suggest that TDF and TDF/FTC can safely be given to breastfeeding women without putting their infants at risk of adverse effects.
Although the World Health Organization calls for further research, current WHO guidelines are permissive of the use of PrEP during pregnancy and breastfeeding, noting growing evidence for safety from maternal HIV and hepatitis B virus studies. WHO is currently reviewing data on safety of PrEP in pregnancy and lactation and will provide more detailed guidance in the near future. Although it will be important to collect additional safety data, the weight of the existing evidence does not support further delay in implementing TDF PrEP for pregnant and breastfeeding women at high risk of HIV acquisition. Those women on PrEP who become pregnant or are lactating should not have to stop an effective HIV prevention intervention.
Lynne M. Mofenson, MD, is a senior HIV technical adviser at the Elizabeth Glaser Pediatric AIDS Foundation. Dr. Mofenson had no relevant disclosures to report. These comments are adapted from her perspective accompanying the study (PLOS Med. 2016 Sep 27. doi: 10.1371/journal.pmed.1002133).
The research article by Dr. Mugwanya and his colleagues in PLOS Medicine significantly contributes to the accumulating safety data for PrEP in breastfeeding women. This documents a prospective study of daily tenofovir disoproxil fumarate (TDF)/emtricitabine (FTC) in 50 HIV-uninfected breastfeeding women between 1-24 weeks postpartum; the drug combination was provided to women for 10 consecutive days and then discontinued. In infant plasma, tenofovir was below the limit of detection in 46 (94%) of 49 samples; 47 of 49 (96%) infant samples had detectable FTC. Based on breast milk concentrations, breastfeeding infants would have exposures to TDF 12,500-fold lower and to FTC 200-fold lower than those achieved with pediatric therapeutic dosing (less than 0.01% and 0.5% of therapeutic dose, respectively).
These data confirm and extend other studies that have reported very-low concentrations of tenofovir detectable in breast milk and strongly suggest that TDF and TDF/FTC can safely be given to breastfeeding women without putting their infants at risk of adverse effects.
Although the World Health Organization calls for further research, current WHO guidelines are permissive of the use of PrEP during pregnancy and breastfeeding, noting growing evidence for safety from maternal HIV and hepatitis B virus studies. WHO is currently reviewing data on safety of PrEP in pregnancy and lactation and will provide more detailed guidance in the near future. Although it will be important to collect additional safety data, the weight of the existing evidence does not support further delay in implementing TDF PrEP for pregnant and breastfeeding women at high risk of HIV acquisition. Those women on PrEP who become pregnant or are lactating should not have to stop an effective HIV prevention intervention.
Lynne M. Mofenson, MD, is a senior HIV technical adviser at the Elizabeth Glaser Pediatric AIDS Foundation. Dr. Mofenson had no relevant disclosures to report. These comments are adapted from her perspective accompanying the study (PLOS Med. 2016 Sep 27. doi: 10.1371/journal.pmed.1002133).
The research article by Dr. Mugwanya and his colleagues in PLOS Medicine significantly contributes to the accumulating safety data for PrEP in breastfeeding women. This documents a prospective study of daily tenofovir disoproxil fumarate (TDF)/emtricitabine (FTC) in 50 HIV-uninfected breastfeeding women between 1-24 weeks postpartum; the drug combination was provided to women for 10 consecutive days and then discontinued. In infant plasma, tenofovir was below the limit of detection in 46 (94%) of 49 samples; 47 of 49 (96%) infant samples had detectable FTC. Based on breast milk concentrations, breastfeeding infants would have exposures to TDF 12,500-fold lower and to FTC 200-fold lower than those achieved with pediatric therapeutic dosing (less than 0.01% and 0.5% of therapeutic dose, respectively).
These data confirm and extend other studies that have reported very-low concentrations of tenofovir detectable in breast milk and strongly suggest that TDF and TDF/FTC can safely be given to breastfeeding women without putting their infants at risk of adverse effects.
Although the World Health Organization calls for further research, current WHO guidelines are permissive of the use of PrEP during pregnancy and breastfeeding, noting growing evidence for safety from maternal HIV and hepatitis B virus studies. WHO is currently reviewing data on safety of PrEP in pregnancy and lactation and will provide more detailed guidance in the near future. Although it will be important to collect additional safety data, the weight of the existing evidence does not support further delay in implementing TDF PrEP for pregnant and breastfeeding women at high risk of HIV acquisition. Those women on PrEP who become pregnant or are lactating should not have to stop an effective HIV prevention intervention.
Lynne M. Mofenson, MD, is a senior HIV technical adviser at the Elizabeth Glaser Pediatric AIDS Foundation. Dr. Mofenson had no relevant disclosures to report. These comments are adapted from her perspective accompanying the study (PLOS Med. 2016 Sep 27. doi: 10.1371/journal.pmed.1002133).
Pre-exposure prophylaxis (PrEP) therapy is safe for HIV-uninfected women breastfeeding their infants, according to a study in PLOS Medicine.
As PrEP becomes more widely used in heterosexual populations, an important consideration is its safety in infants who are breastfed by women taking the drugs, reported Kenneth Mugwanya, MBChB, PhD, of the University of Washington, Seattle, and his associates (PLOS Med. 2016 Sep 27. doi: 10.1371/journal.pmed.1002132).
The purpose of this small, prospective short-term trialwas to quantify drug levels in maternal blood samples, breast milk, and infant blood samples to begin to understand if PrEP is safe for use in pregnant or breastfeeding women at high risk for contracting HIV.
Antiretroviral PrEP with 300 mg tenofovir disoproxil fumarate and 200 mg emtricitabine was administered to 50 HIV-uninfected breastfeeding mothers through daily directly observed therapy for 10 consecutive days and then discontinued thereafter. All mothers were African and resided in Kenya or Uganda. Median maternal age was 25 years; 48% of infants were younger than 12 weeks and 52% were between 13 and 24 weeks of age. Across the study cohort, the median daily frequency of breastfeeding was 15 times.
Maternal blood and breast milk samples were collected and analyzed for drug concentrations at days 7 and 10 of the study. Peak concentration samples, collected 1-2 hours after PrEP administration, and trough concentration levels, collected 23-24 hours after PrEP dose, were collected on day 7 and day 10. Infant blood samples were collected only once, on day 7.
In maternal blood samples, tenofovir was detected at concentrations consistent with steady-state use (median peak concentration, 152.0 ng/mL). In breast milk, tenofovir was present in significantly lower concentrations (3.2 ng/mL). Emtricitabine was also detected at concentrations consistent with steady-state use in maternal blood samples (median peak concentration, 267.5 ng/mL); however, unlike tenofovir, emtricitabine concentration in breast milk was similar to peak plasma concentrations (212.5 ng/mL). Tenofovir was undetectable in 46 of 49 (94%) infant plasma samples. For the three infants with detectable tenofovir, the plasma concentrations were 0.9, 0.9, and 17.4 ng/mL, corresponding body weights were 6.4, 5.8, and 6.2 kg, and their maternal milk tenofovir concentrations were “modestly greater” than the median at 6.57, 3.64, and 4.05 ng/mL, respectively.
Emtricitabine, on the other hand, was detectable in 47 of 49 (96%) infant plasma samples with a median concentration of 13.2 ng/mL.
“The estimated daily tenofovir and emtricitabine doses ingested by the infant through breastfeeding were 12,500-fold and 200-fold, respectively, lower than the proposed daily pediatric dose for prophylaxis against vertical HIV acquisition. Thus, infants had low exposures to tenofovir and emtricitabine, which would not be expected to pose substantial safety risk to infants of mothers who use PrEP during breastfeeding,” Dr. Mugwanya and his associates wrote.
“These data provide evidence suggesting that this PrEP regimen can be safely used during breastfeeding, which is informative for clinical guidelines for women who are at substantial risk of HIV during pregnancy and the postpartum period,” the researchers concluded.
This study was funded by the Bill and Melinda Gates Foundation and the National Institutes of Health. The authors did not report disclosures.
On Twitter @jessnicolecraig
Pre-exposure prophylaxis (PrEP) therapy is safe for HIV-uninfected women breastfeeding their infants, according to a study in PLOS Medicine.
As PrEP becomes more widely used in heterosexual populations, an important consideration is its safety in infants who are breastfed by women taking the drugs, reported Kenneth Mugwanya, MBChB, PhD, of the University of Washington, Seattle, and his associates (PLOS Med. 2016 Sep 27. doi: 10.1371/journal.pmed.1002132).
The purpose of this small, prospective short-term trialwas to quantify drug levels in maternal blood samples, breast milk, and infant blood samples to begin to understand if PrEP is safe for use in pregnant or breastfeeding women at high risk for contracting HIV.
Antiretroviral PrEP with 300 mg tenofovir disoproxil fumarate and 200 mg emtricitabine was administered to 50 HIV-uninfected breastfeeding mothers through daily directly observed therapy for 10 consecutive days and then discontinued thereafter. All mothers were African and resided in Kenya or Uganda. Median maternal age was 25 years; 48% of infants were younger than 12 weeks and 52% were between 13 and 24 weeks of age. Across the study cohort, the median daily frequency of breastfeeding was 15 times.
Maternal blood and breast milk samples were collected and analyzed for drug concentrations at days 7 and 10 of the study. Peak concentration samples, collected 1-2 hours after PrEP administration, and trough concentration levels, collected 23-24 hours after PrEP dose, were collected on day 7 and day 10. Infant blood samples were collected only once, on day 7.
In maternal blood samples, tenofovir was detected at concentrations consistent with steady-state use (median peak concentration, 152.0 ng/mL). In breast milk, tenofovir was present in significantly lower concentrations (3.2 ng/mL). Emtricitabine was also detected at concentrations consistent with steady-state use in maternal blood samples (median peak concentration, 267.5 ng/mL); however, unlike tenofovir, emtricitabine concentration in breast milk was similar to peak plasma concentrations (212.5 ng/mL). Tenofovir was undetectable in 46 of 49 (94%) infant plasma samples. For the three infants with detectable tenofovir, the plasma concentrations were 0.9, 0.9, and 17.4 ng/mL, corresponding body weights were 6.4, 5.8, and 6.2 kg, and their maternal milk tenofovir concentrations were “modestly greater” than the median at 6.57, 3.64, and 4.05 ng/mL, respectively.
Emtricitabine, on the other hand, was detectable in 47 of 49 (96%) infant plasma samples with a median concentration of 13.2 ng/mL.
“The estimated daily tenofovir and emtricitabine doses ingested by the infant through breastfeeding were 12,500-fold and 200-fold, respectively, lower than the proposed daily pediatric dose for prophylaxis against vertical HIV acquisition. Thus, infants had low exposures to tenofovir and emtricitabine, which would not be expected to pose substantial safety risk to infants of mothers who use PrEP during breastfeeding,” Dr. Mugwanya and his associates wrote.
“These data provide evidence suggesting that this PrEP regimen can be safely used during breastfeeding, which is informative for clinical guidelines for women who are at substantial risk of HIV during pregnancy and the postpartum period,” the researchers concluded.
This study was funded by the Bill and Melinda Gates Foundation and the National Institutes of Health. The authors did not report disclosures.
On Twitter @jessnicolecraig
FROM PLOS MEDICINE
Key clinical point: PrEP can be used safely in HIV-uninfected women who are breastfeeding.
Major finding: Tenofovir was undetectable in 46 of 49 (94%) infant plasma samples. While emtricitabine was detectable in 47 of 49 (96%) infant plasma samples, median concentration was low (13.2 ng/mL).
Data source: A prospective short-term study of 50 mother-infant pairs in Kenya and Uganda.
Disclosures: This study was funded by the Bill and Melinda Gates Foundation and the National Institutes of Health. The authors did not report disclosures.
Planning, education smooth transition to longer-acting clotting factors
ORLANDO – Transitioning patients with hemophilia from standard clotting factor concentrates to newer extended half-life products takes planning, education, and a little patience, but the payoff can be better hemostasis, a hemophilia treatment specialist said.
“Real-world experience shows us that you can maintain effective protection with less infusion with these new products, but we also know that each person should be evaluated individually when determining what their specific optimal treatment is,” said Jennifer Maahs, a hemophilia nurse practitioner at the Indiana Hemophilia and Thrombosis Center in Indianapolis.
Staff and patient education about the proper use of newer extended half-life (EHL) products is the key to success, she added in an oral session at the World Federation of Hemophilia World Congress.
The new EHL products allow for longer intervals between doses, especially with EHL recombinant factor IX used to treat hemophilia B. Prophylaxis with standard factor IX concentrates requires doses of 25-40 IU/kg twice weekly; in contrasts, EHL products can be given in various doses based on patient responses of either 50 IU/kg every 7 days, 100 IU/kg every 10 days, 25-40 IU/kg every 7 days, or 50-75 IU/kg every 14 days.
In general, the longer intervals between dosing occur in adults; young children tend to require more frequent dosing and have lower levels of factor recovery, she noted.
Extended Experience
Her center currently has more than 100 patients maintained on prolonged half-life factor VIII and factor IX products.
“We have really learned a lot of lessons along the way, and we have had to modify our approach based on these lessons,” she said. “Each patient situation is unique, and everything needs to be individualized.”
Staff review the published literature to educate themselves on the EHL products and prepare answers to expected questions from patients. Ms. Maahs suggested identifying key staff who are best equipped to answer specific questions.
“From a patient standpoint, we’ve developed a patient notification letter, so for any new product that comes out – for example a new factor VIII product – the notification gets sent out factor VIII patients, and we do that for every new product that comes out,” she said.
PK OK
Pharmacokinetic (PK) analyses may also be helpful in transitioning patients to EHL products.
To test patient responses to new products, her center tests patients for recovery from 15 minutes to 1 hour post-infusion, which will provide information about how the patient may respond to the product during a bleeding episode.
If the patient is on prophylaxis they will evaluate trough effectiveness to determine that patient’s responsiveness at the lowest level prior to the next infusion. Testing at other time points may be required based on the patient’s individual clinical history.
Center staff talk with each patient to discuss his needs and capabilities. If the patient is currently being managed with on-demand therapy, the talk may center on obstacles to utilization of prophylaxis and the patient’s desired infusion interval.
For patients currently on prophylaxis, they discuss the current regimen frequency and dose and assess how well it’s working. Staff members also provide information about alternative approaches to therapy, and ask patients specifically about their activity levels and dates of activity, compared with currently scheduled infusion days.
Patients are also educated about the reconstitution requirements for the new product, and are told to use up any remaining concentrates before switching over to the new product.
“As we move forward, within 2 to 4 weeks of starting a new therapy, we like to obtain a trough to see how their prophylaxis is working. At that time we ask how have you been doing on the new product, are you having any breakthrough bleeding, and how are you feeling about it,” Ms. Maahs said.
Weekly phone calls to the patient during the first month are also very helpful for reinforcing information about dosing regimens for bleeding episodes, reminding patients to call in if they experience a lead, and encouraging them to keep a treatment log. The phone call can also be helpful in identifying potential product-related reactions or other issues, she said.
‘Big impact’
“What’s the impact that we’ve seen? With factor IX, it has been really big. Previous on-demand patients have agreed that, ‘gosh, I’m infusing a couple of times a month anyway,’ so starting an every 14-day prophylactic regimen seems pretty reasonable,” she said.
“We’ve had infusion schedules in children change from twice weekly to once weekly and that has really decreased the burden of disease,” she added.
A few adults, however, have gone back to standard half-life products because of concerns that they would not be able to infuse when they thought they needed treatment, she noted.
The impact of the EHL factor VIII products has been smaller, although it has allowed slight increases in the dosing intervals (from every other day to every third day in children, for example), and has overall decreased the average number of monthly infusions from about 15 to about 10.
Some adolescents and young adults, who often have been on prophylaxis for all of their lives, have experienced absent or only minimal joint disease, and some have been able to extend their dosing intervals from every 4 to every 5 to 7 days, she said.
Ms. Maahs disclosed serving on advisory committees to Baxalta, Novo Nordisk, Biogen, Genentech, and CSL, and receiving honoraria related to those activities.
ORLANDO – Transitioning patients with hemophilia from standard clotting factor concentrates to newer extended half-life products takes planning, education, and a little patience, but the payoff can be better hemostasis, a hemophilia treatment specialist said.
“Real-world experience shows us that you can maintain effective protection with less infusion with these new products, but we also know that each person should be evaluated individually when determining what their specific optimal treatment is,” said Jennifer Maahs, a hemophilia nurse practitioner at the Indiana Hemophilia and Thrombosis Center in Indianapolis.
Staff and patient education about the proper use of newer extended half-life (EHL) products is the key to success, she added in an oral session at the World Federation of Hemophilia World Congress.
The new EHL products allow for longer intervals between doses, especially with EHL recombinant factor IX used to treat hemophilia B. Prophylaxis with standard factor IX concentrates requires doses of 25-40 IU/kg twice weekly; in contrasts, EHL products can be given in various doses based on patient responses of either 50 IU/kg every 7 days, 100 IU/kg every 10 days, 25-40 IU/kg every 7 days, or 50-75 IU/kg every 14 days.
In general, the longer intervals between dosing occur in adults; young children tend to require more frequent dosing and have lower levels of factor recovery, she noted.
Extended Experience
Her center currently has more than 100 patients maintained on prolonged half-life factor VIII and factor IX products.
“We have really learned a lot of lessons along the way, and we have had to modify our approach based on these lessons,” she said. “Each patient situation is unique, and everything needs to be individualized.”
Staff review the published literature to educate themselves on the EHL products and prepare answers to expected questions from patients. Ms. Maahs suggested identifying key staff who are best equipped to answer specific questions.
“From a patient standpoint, we’ve developed a patient notification letter, so for any new product that comes out – for example a new factor VIII product – the notification gets sent out factor VIII patients, and we do that for every new product that comes out,” she said.
PK OK
Pharmacokinetic (PK) analyses may also be helpful in transitioning patients to EHL products.
To test patient responses to new products, her center tests patients for recovery from 15 minutes to 1 hour post-infusion, which will provide information about how the patient may respond to the product during a bleeding episode.
If the patient is on prophylaxis they will evaluate trough effectiveness to determine that patient’s responsiveness at the lowest level prior to the next infusion. Testing at other time points may be required based on the patient’s individual clinical history.
Center staff talk with each patient to discuss his needs and capabilities. If the patient is currently being managed with on-demand therapy, the talk may center on obstacles to utilization of prophylaxis and the patient’s desired infusion interval.
For patients currently on prophylaxis, they discuss the current regimen frequency and dose and assess how well it’s working. Staff members also provide information about alternative approaches to therapy, and ask patients specifically about their activity levels and dates of activity, compared with currently scheduled infusion days.
Patients are also educated about the reconstitution requirements for the new product, and are told to use up any remaining concentrates before switching over to the new product.
“As we move forward, within 2 to 4 weeks of starting a new therapy, we like to obtain a trough to see how their prophylaxis is working. At that time we ask how have you been doing on the new product, are you having any breakthrough bleeding, and how are you feeling about it,” Ms. Maahs said.
Weekly phone calls to the patient during the first month are also very helpful for reinforcing information about dosing regimens for bleeding episodes, reminding patients to call in if they experience a lead, and encouraging them to keep a treatment log. The phone call can also be helpful in identifying potential product-related reactions or other issues, she said.
‘Big impact’
“What’s the impact that we’ve seen? With factor IX, it has been really big. Previous on-demand patients have agreed that, ‘gosh, I’m infusing a couple of times a month anyway,’ so starting an every 14-day prophylactic regimen seems pretty reasonable,” she said.
“We’ve had infusion schedules in children change from twice weekly to once weekly and that has really decreased the burden of disease,” she added.
A few adults, however, have gone back to standard half-life products because of concerns that they would not be able to infuse when they thought they needed treatment, she noted.
The impact of the EHL factor VIII products has been smaller, although it has allowed slight increases in the dosing intervals (from every other day to every third day in children, for example), and has overall decreased the average number of monthly infusions from about 15 to about 10.
Some adolescents and young adults, who often have been on prophylaxis for all of their lives, have experienced absent or only minimal joint disease, and some have been able to extend their dosing intervals from every 4 to every 5 to 7 days, she said.
Ms. Maahs disclosed serving on advisory committees to Baxalta, Novo Nordisk, Biogen, Genentech, and CSL, and receiving honoraria related to those activities.
ORLANDO – Transitioning patients with hemophilia from standard clotting factor concentrates to newer extended half-life products takes planning, education, and a little patience, but the payoff can be better hemostasis, a hemophilia treatment specialist said.
“Real-world experience shows us that you can maintain effective protection with less infusion with these new products, but we also know that each person should be evaluated individually when determining what their specific optimal treatment is,” said Jennifer Maahs, a hemophilia nurse practitioner at the Indiana Hemophilia and Thrombosis Center in Indianapolis.
Staff and patient education about the proper use of newer extended half-life (EHL) products is the key to success, she added in an oral session at the World Federation of Hemophilia World Congress.
The new EHL products allow for longer intervals between doses, especially with EHL recombinant factor IX used to treat hemophilia B. Prophylaxis with standard factor IX concentrates requires doses of 25-40 IU/kg twice weekly; in contrasts, EHL products can be given in various doses based on patient responses of either 50 IU/kg every 7 days, 100 IU/kg every 10 days, 25-40 IU/kg every 7 days, or 50-75 IU/kg every 14 days.
In general, the longer intervals between dosing occur in adults; young children tend to require more frequent dosing and have lower levels of factor recovery, she noted.
Extended Experience
Her center currently has more than 100 patients maintained on prolonged half-life factor VIII and factor IX products.
“We have really learned a lot of lessons along the way, and we have had to modify our approach based on these lessons,” she said. “Each patient situation is unique, and everything needs to be individualized.”
Staff review the published literature to educate themselves on the EHL products and prepare answers to expected questions from patients. Ms. Maahs suggested identifying key staff who are best equipped to answer specific questions.
“From a patient standpoint, we’ve developed a patient notification letter, so for any new product that comes out – for example a new factor VIII product – the notification gets sent out factor VIII patients, and we do that for every new product that comes out,” she said.
PK OK
Pharmacokinetic (PK) analyses may also be helpful in transitioning patients to EHL products.
To test patient responses to new products, her center tests patients for recovery from 15 minutes to 1 hour post-infusion, which will provide information about how the patient may respond to the product during a bleeding episode.
If the patient is on prophylaxis they will evaluate trough effectiveness to determine that patient’s responsiveness at the lowest level prior to the next infusion. Testing at other time points may be required based on the patient’s individual clinical history.
Center staff talk with each patient to discuss his needs and capabilities. If the patient is currently being managed with on-demand therapy, the talk may center on obstacles to utilization of prophylaxis and the patient’s desired infusion interval.
For patients currently on prophylaxis, they discuss the current regimen frequency and dose and assess how well it’s working. Staff members also provide information about alternative approaches to therapy, and ask patients specifically about their activity levels and dates of activity, compared with currently scheduled infusion days.
Patients are also educated about the reconstitution requirements for the new product, and are told to use up any remaining concentrates before switching over to the new product.
“As we move forward, within 2 to 4 weeks of starting a new therapy, we like to obtain a trough to see how their prophylaxis is working. At that time we ask how have you been doing on the new product, are you having any breakthrough bleeding, and how are you feeling about it,” Ms. Maahs said.
Weekly phone calls to the patient during the first month are also very helpful for reinforcing information about dosing regimens for bleeding episodes, reminding patients to call in if they experience a lead, and encouraging them to keep a treatment log. The phone call can also be helpful in identifying potential product-related reactions or other issues, she said.
‘Big impact’
“What’s the impact that we’ve seen? With factor IX, it has been really big. Previous on-demand patients have agreed that, ‘gosh, I’m infusing a couple of times a month anyway,’ so starting an every 14-day prophylactic regimen seems pretty reasonable,” she said.
“We’ve had infusion schedules in children change from twice weekly to once weekly and that has really decreased the burden of disease,” she added.
A few adults, however, have gone back to standard half-life products because of concerns that they would not be able to infuse when they thought they needed treatment, she noted.
The impact of the EHL factor VIII products has been smaller, although it has allowed slight increases in the dosing intervals (from every other day to every third day in children, for example), and has overall decreased the average number of monthly infusions from about 15 to about 10.
Some adolescents and young adults, who often have been on prophylaxis for all of their lives, have experienced absent or only minimal joint disease, and some have been able to extend their dosing intervals from every 4 to every 5 to 7 days, she said.
Ms. Maahs disclosed serving on advisory committees to Baxalta, Novo Nordisk, Biogen, Genentech, and CSL, and receiving honoraria related to those activities.
EXPERT ANALYSIS AT WFH 2016 WORLD CONGRESS
Key clinical point: Transitioning patients to extended half-life clotting factor concentrates requires tailoring treatment to individual patients.
Major finding: Many patients can transition from on-demand dosing with factor IX to prophylaxis infusions once every 2 weeks.
Data source: Review of a hemophilia treatment center experience transitioning patients to extended half-life products.
Disclosures: Jennifer Maahs, RN-BC, disclosed serving on advisory committees to Baxalta, Novo Nordisk, Biogen, Genentech, and CSL, and receiving honoraria related to those activities.
New Board of Editors for GI & Hepatology News
Editor in Chief:
John I. Allen, MD, MBA, AGAF
In 1980, Dr. Allen completed training at the University of Minnesota, Minneapolis, and then spent 10 years on their faculty. In 1991, he joined a private gastroenterology practice in Minneapolis and helped build this single-specialty GI practice into Minnesota Gastroenterology, one of the largest GI practices in the country. In 2013, he left practice to become clinical chief of digestive diseases and professor of medicine at Yale University School of Medicine. In September, 2016, he joined the faculty at the University of Michigan Medical Center, Ann Arbor. He currently remains on the Board of Directors of Allina Health, a large integrated health system in Minnesota.
Dr. Allen has served the American Gastroenterological Association (AGA) in multiple roles. He chaired the Clinical Practice Committee and led development of most quality measures currently in Medicare’s value-based payment system. Dr. Allen serves on the GI Specialty Board of the American Board of Internal Medicine and from May 2014 until May 2015, was president of the AGA Institute.
Associate Editors:
Megan A. Adams, MD, JD, MSc
Dr. Adams is a general gastroenterologist at the Ann Arbor VA and investigator in the VA Ann Arbor Center for Clinical Management Research, with an academic appointment as a clinical lecturer in the division of gastroenterology at the University of Michigan. As a gastroenterologist, attorney, and health services/policy researcher, her primary area of interest lies in improving GI health care delivery. Her current work focuses on improving our understanding of the drivers of inappropriate use of endoscopic resources in order to devise mechanisms to deliver higher-value care. She also has expertise in medicolegal issues in gastroenterology, as well as patient safety and quality improvement. She has served various roles in the AGA over the past 4 years, including as a previous member of the Trainee and Young GI Committee and Future Leaders Program Advisory Board. She currently serves as chair-elect of the AGA Quality Measures Committee.
Ziad F. Gellad, MD, MPH
Dr. Gellad is an associate professor of medicine in the division of gastroenterology at Duke University Medical Center, Durham, N.C., and a faculty member of the Duke Clinical Research Institute. He is also a VA Career Development Awardee and holds an appointment in the Health Services Research and Development Center of Innovation at the Durham VA Medical Center. Dr. Gellad received his MD and MPH degrees from Johns Hopkins University. He completed a residency in internal medicine and a fellowship in gastroenterology at Duke University Medical Center. Dr. Gellad’s research is focused on the implementation of systems engineering methods, including discrete event simulation, to improve the value of health care delivery. He is the director of quality for the division of gastroenterology and director of clinical improvement for the department of medicine at Duke University Medical Center. He also serves as chair of the AGA Quality Measures Committee.
Kim L. Isaacs, MD, PhD, AGAF
Dr. Isaacs is professor of medicine in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. She is codirector of the UNC Center for Inflammatory Bowel Disease and associate program director of the gastroenterology fellowship program at the university. She received her MD and PhD at the State University of New York at Stony Brook and completed her internship, residency, and fellowship in gastroenterology at the University of North Carolina at Chapel Hill. She is active in the clinical care of patients with inflammatory bowel disease and is an investigator in numerous clinical studies in the management and treatment of gastrointestinal disorders including ulcerative colitis, pouchitis, and Crohn’s disease. She has served on the AGA’s constitution and bylaws committee and the Education and Training Committee.
Gyanprakash A. Ketwaroo MD, MSc
Dr. Ketwaroo is an assistant professor in the division of gastroenterology and hepatology at Baylor College of Medicine, Houston, and an advanced endoscopist at the Michael E. Debakey VA Medical Center in Houston. After graduating with a degree in chemical physics from Brown University, he studied at Oxford University on a Rhodes Scholarship. He attended Harvard Medical School and completed an internal medicine residency at the Massachusetts General Hospital. This was followed by gastroenterology and advanced endoscopy fellowship training at the Beth Israel Deaconess Medical Center. He is chair of the AGA Trainee and Young GI Committee. His research interests include Barrett’s esophagus, chronic pancreatitis, and advanced imaging of gastrointestinal disease.
Lawrence R. Kosinski, MD, MBA, AGAF, FACG
Dr. Kosinski has been in the practice of gastroenterology since 1984. He received his MD from Loyola University Chicago Stritch School of Medicine in 1978 and earned his MBA from Northwestern University Kellogg School of Management in 1998. He is currently one of the managing partners of the Illinois Gastroenterology Group (IGG), the largest gastroenterology practice in Illinois.
In addition to his medical practice, Dr. Kosinski is the Clinical Private Practice Councilor for the American Gastroenterological Association and serves on its Governing Board. Locally, he is a member of the Advocate Sherman Hospital Board of Directors, Elgin, Ill.
In January 2014, Dr. Kosinski started SonarMD, a technology company formed to bring the success of Project Sonar to a national presence. He serves as its president and chief medical officer.
Sonia S. Kupfer, MD
Dr. Kupfer is an adult gastroenterologist with clinical and research interests in the genetics of gastrointestinal diseases. She is an assistant professor in the section of gastroenterology and serves as director of the Gastrointestinal Cancer Risk and Prevention Clinic at the University of Chicago. She is also a member of the University of Chicago Celiac Disease Center. She graduated from Yale University and completed her medical training including chief residency and gastroenterology fellowship at the University of Chicago. She received an F32 individual training grant and an NCI K08 career development award to study colorectal cancer genetics in African Americans. She is site primary investigator on a number of National Institutes of Health–sponsored clinical trials in colorectal cancer chemoprevention and screening. She served as codirector of two national clinical cancer genetics conferences and is a core faculty member in the City of Hope cancer genetics educational program. Dr. Kupfer is active on several AGA committees and is president-elect of the Collaborative Group of the Americas on Inherited Colorectal Cancer. She has mentored numerous medical students, residents, and fellows and teaches in the medical school.
Wajahat Mehal, MD, DPhil
Dr. Mehal is a hepatologist and director of the Yale Weight Loss Program at Yale University, New Haven, Conn. He obtained his medical training and DPhil at the University of Oxford, and completed his residency, chief residency, and Howard Hughes postdoctoral fellowship at Yale University. He has an active research group working in the area of sterile liver inflammation which covers alcoholic and nonalcoholic steatohepatitis. His clinical training is in transplant hepatology, obesity medicine, and endobariatrics. His laboratory training is in immunobiology and liver fibrosis. He has published widely in areas of inflammation and liver disease.
Editor in Chief:
John I. Allen, MD, MBA, AGAF
In 1980, Dr. Allen completed training at the University of Minnesota, Minneapolis, and then spent 10 years on their faculty. In 1991, he joined a private gastroenterology practice in Minneapolis and helped build this single-specialty GI practice into Minnesota Gastroenterology, one of the largest GI practices in the country. In 2013, he left practice to become clinical chief of digestive diseases and professor of medicine at Yale University School of Medicine. In September, 2016, he joined the faculty at the University of Michigan Medical Center, Ann Arbor. He currently remains on the Board of Directors of Allina Health, a large integrated health system in Minnesota.
Dr. Allen has served the American Gastroenterological Association (AGA) in multiple roles. He chaired the Clinical Practice Committee and led development of most quality measures currently in Medicare’s value-based payment system. Dr. Allen serves on the GI Specialty Board of the American Board of Internal Medicine and from May 2014 until May 2015, was president of the AGA Institute.
Associate Editors:
Megan A. Adams, MD, JD, MSc
Dr. Adams is a general gastroenterologist at the Ann Arbor VA and investigator in the VA Ann Arbor Center for Clinical Management Research, with an academic appointment as a clinical lecturer in the division of gastroenterology at the University of Michigan. As a gastroenterologist, attorney, and health services/policy researcher, her primary area of interest lies in improving GI health care delivery. Her current work focuses on improving our understanding of the drivers of inappropriate use of endoscopic resources in order to devise mechanisms to deliver higher-value care. She also has expertise in medicolegal issues in gastroenterology, as well as patient safety and quality improvement. She has served various roles in the AGA over the past 4 years, including as a previous member of the Trainee and Young GI Committee and Future Leaders Program Advisory Board. She currently serves as chair-elect of the AGA Quality Measures Committee.
Ziad F. Gellad, MD, MPH
Dr. Gellad is an associate professor of medicine in the division of gastroenterology at Duke University Medical Center, Durham, N.C., and a faculty member of the Duke Clinical Research Institute. He is also a VA Career Development Awardee and holds an appointment in the Health Services Research and Development Center of Innovation at the Durham VA Medical Center. Dr. Gellad received his MD and MPH degrees from Johns Hopkins University. He completed a residency in internal medicine and a fellowship in gastroenterology at Duke University Medical Center. Dr. Gellad’s research is focused on the implementation of systems engineering methods, including discrete event simulation, to improve the value of health care delivery. He is the director of quality for the division of gastroenterology and director of clinical improvement for the department of medicine at Duke University Medical Center. He also serves as chair of the AGA Quality Measures Committee.
Kim L. Isaacs, MD, PhD, AGAF
Dr. Isaacs is professor of medicine in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. She is codirector of the UNC Center for Inflammatory Bowel Disease and associate program director of the gastroenterology fellowship program at the university. She received her MD and PhD at the State University of New York at Stony Brook and completed her internship, residency, and fellowship in gastroenterology at the University of North Carolina at Chapel Hill. She is active in the clinical care of patients with inflammatory bowel disease and is an investigator in numerous clinical studies in the management and treatment of gastrointestinal disorders including ulcerative colitis, pouchitis, and Crohn’s disease. She has served on the AGA’s constitution and bylaws committee and the Education and Training Committee.
Gyanprakash A. Ketwaroo MD, MSc
Dr. Ketwaroo is an assistant professor in the division of gastroenterology and hepatology at Baylor College of Medicine, Houston, and an advanced endoscopist at the Michael E. Debakey VA Medical Center in Houston. After graduating with a degree in chemical physics from Brown University, he studied at Oxford University on a Rhodes Scholarship. He attended Harvard Medical School and completed an internal medicine residency at the Massachusetts General Hospital. This was followed by gastroenterology and advanced endoscopy fellowship training at the Beth Israel Deaconess Medical Center. He is chair of the AGA Trainee and Young GI Committee. His research interests include Barrett’s esophagus, chronic pancreatitis, and advanced imaging of gastrointestinal disease.
Lawrence R. Kosinski, MD, MBA, AGAF, FACG
Dr. Kosinski has been in the practice of gastroenterology since 1984. He received his MD from Loyola University Chicago Stritch School of Medicine in 1978 and earned his MBA from Northwestern University Kellogg School of Management in 1998. He is currently one of the managing partners of the Illinois Gastroenterology Group (IGG), the largest gastroenterology practice in Illinois.
In addition to his medical practice, Dr. Kosinski is the Clinical Private Practice Councilor for the American Gastroenterological Association and serves on its Governing Board. Locally, he is a member of the Advocate Sherman Hospital Board of Directors, Elgin, Ill.
In January 2014, Dr. Kosinski started SonarMD, a technology company formed to bring the success of Project Sonar to a national presence. He serves as its president and chief medical officer.
Sonia S. Kupfer, MD
Dr. Kupfer is an adult gastroenterologist with clinical and research interests in the genetics of gastrointestinal diseases. She is an assistant professor in the section of gastroenterology and serves as director of the Gastrointestinal Cancer Risk and Prevention Clinic at the University of Chicago. She is also a member of the University of Chicago Celiac Disease Center. She graduated from Yale University and completed her medical training including chief residency and gastroenterology fellowship at the University of Chicago. She received an F32 individual training grant and an NCI K08 career development award to study colorectal cancer genetics in African Americans. She is site primary investigator on a number of National Institutes of Health–sponsored clinical trials in colorectal cancer chemoprevention and screening. She served as codirector of two national clinical cancer genetics conferences and is a core faculty member in the City of Hope cancer genetics educational program. Dr. Kupfer is active on several AGA committees and is president-elect of the Collaborative Group of the Americas on Inherited Colorectal Cancer. She has mentored numerous medical students, residents, and fellows and teaches in the medical school.
Wajahat Mehal, MD, DPhil
Dr. Mehal is a hepatologist and director of the Yale Weight Loss Program at Yale University, New Haven, Conn. He obtained his medical training and DPhil at the University of Oxford, and completed his residency, chief residency, and Howard Hughes postdoctoral fellowship at Yale University. He has an active research group working in the area of sterile liver inflammation which covers alcoholic and nonalcoholic steatohepatitis. His clinical training is in transplant hepatology, obesity medicine, and endobariatrics. His laboratory training is in immunobiology and liver fibrosis. He has published widely in areas of inflammation and liver disease.
Editor in Chief:
John I. Allen, MD, MBA, AGAF
In 1980, Dr. Allen completed training at the University of Minnesota, Minneapolis, and then spent 10 years on their faculty. In 1991, he joined a private gastroenterology practice in Minneapolis and helped build this single-specialty GI practice into Minnesota Gastroenterology, one of the largest GI practices in the country. In 2013, he left practice to become clinical chief of digestive diseases and professor of medicine at Yale University School of Medicine. In September, 2016, he joined the faculty at the University of Michigan Medical Center, Ann Arbor. He currently remains on the Board of Directors of Allina Health, a large integrated health system in Minnesota.
Dr. Allen has served the American Gastroenterological Association (AGA) in multiple roles. He chaired the Clinical Practice Committee and led development of most quality measures currently in Medicare’s value-based payment system. Dr. Allen serves on the GI Specialty Board of the American Board of Internal Medicine and from May 2014 until May 2015, was president of the AGA Institute.
Associate Editors:
Megan A. Adams, MD, JD, MSc
Dr. Adams is a general gastroenterologist at the Ann Arbor VA and investigator in the VA Ann Arbor Center for Clinical Management Research, with an academic appointment as a clinical lecturer in the division of gastroenterology at the University of Michigan. As a gastroenterologist, attorney, and health services/policy researcher, her primary area of interest lies in improving GI health care delivery. Her current work focuses on improving our understanding of the drivers of inappropriate use of endoscopic resources in order to devise mechanisms to deliver higher-value care. She also has expertise in medicolegal issues in gastroenterology, as well as patient safety and quality improvement. She has served various roles in the AGA over the past 4 years, including as a previous member of the Trainee and Young GI Committee and Future Leaders Program Advisory Board. She currently serves as chair-elect of the AGA Quality Measures Committee.
Ziad F. Gellad, MD, MPH
Dr. Gellad is an associate professor of medicine in the division of gastroenterology at Duke University Medical Center, Durham, N.C., and a faculty member of the Duke Clinical Research Institute. He is also a VA Career Development Awardee and holds an appointment in the Health Services Research and Development Center of Innovation at the Durham VA Medical Center. Dr. Gellad received his MD and MPH degrees from Johns Hopkins University. He completed a residency in internal medicine and a fellowship in gastroenterology at Duke University Medical Center. Dr. Gellad’s research is focused on the implementation of systems engineering methods, including discrete event simulation, to improve the value of health care delivery. He is the director of quality for the division of gastroenterology and director of clinical improvement for the department of medicine at Duke University Medical Center. He also serves as chair of the AGA Quality Measures Committee.
Kim L. Isaacs, MD, PhD, AGAF
Dr. Isaacs is professor of medicine in the division of gastroenterology and hepatology at the University of North Carolina at Chapel Hill. She is codirector of the UNC Center for Inflammatory Bowel Disease and associate program director of the gastroenterology fellowship program at the university. She received her MD and PhD at the State University of New York at Stony Brook and completed her internship, residency, and fellowship in gastroenterology at the University of North Carolina at Chapel Hill. She is active in the clinical care of patients with inflammatory bowel disease and is an investigator in numerous clinical studies in the management and treatment of gastrointestinal disorders including ulcerative colitis, pouchitis, and Crohn’s disease. She has served on the AGA’s constitution and bylaws committee and the Education and Training Committee.
Gyanprakash A. Ketwaroo MD, MSc
Dr. Ketwaroo is an assistant professor in the division of gastroenterology and hepatology at Baylor College of Medicine, Houston, and an advanced endoscopist at the Michael E. Debakey VA Medical Center in Houston. After graduating with a degree in chemical physics from Brown University, he studied at Oxford University on a Rhodes Scholarship. He attended Harvard Medical School and completed an internal medicine residency at the Massachusetts General Hospital. This was followed by gastroenterology and advanced endoscopy fellowship training at the Beth Israel Deaconess Medical Center. He is chair of the AGA Trainee and Young GI Committee. His research interests include Barrett’s esophagus, chronic pancreatitis, and advanced imaging of gastrointestinal disease.
Lawrence R. Kosinski, MD, MBA, AGAF, FACG
Dr. Kosinski has been in the practice of gastroenterology since 1984. He received his MD from Loyola University Chicago Stritch School of Medicine in 1978 and earned his MBA from Northwestern University Kellogg School of Management in 1998. He is currently one of the managing partners of the Illinois Gastroenterology Group (IGG), the largest gastroenterology practice in Illinois.
In addition to his medical practice, Dr. Kosinski is the Clinical Private Practice Councilor for the American Gastroenterological Association and serves on its Governing Board. Locally, he is a member of the Advocate Sherman Hospital Board of Directors, Elgin, Ill.
In January 2014, Dr. Kosinski started SonarMD, a technology company formed to bring the success of Project Sonar to a national presence. He serves as its president and chief medical officer.
Sonia S. Kupfer, MD
Dr. Kupfer is an adult gastroenterologist with clinical and research interests in the genetics of gastrointestinal diseases. She is an assistant professor in the section of gastroenterology and serves as director of the Gastrointestinal Cancer Risk and Prevention Clinic at the University of Chicago. She is also a member of the University of Chicago Celiac Disease Center. She graduated from Yale University and completed her medical training including chief residency and gastroenterology fellowship at the University of Chicago. She received an F32 individual training grant and an NCI K08 career development award to study colorectal cancer genetics in African Americans. She is site primary investigator on a number of National Institutes of Health–sponsored clinical trials in colorectal cancer chemoprevention and screening. She served as codirector of two national clinical cancer genetics conferences and is a core faculty member in the City of Hope cancer genetics educational program. Dr. Kupfer is active on several AGA committees and is president-elect of the Collaborative Group of the Americas on Inherited Colorectal Cancer. She has mentored numerous medical students, residents, and fellows and teaches in the medical school.
Wajahat Mehal, MD, DPhil
Dr. Mehal is a hepatologist and director of the Yale Weight Loss Program at Yale University, New Haven, Conn. He obtained his medical training and DPhil at the University of Oxford, and completed his residency, chief residency, and Howard Hughes postdoctoral fellowship at Yale University. He has an active research group working in the area of sterile liver inflammation which covers alcoholic and nonalcoholic steatohepatitis. His clinical training is in transplant hepatology, obesity medicine, and endobariatrics. His laboratory training is in immunobiology and liver fibrosis. He has published widely in areas of inflammation and liver disease.
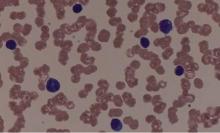
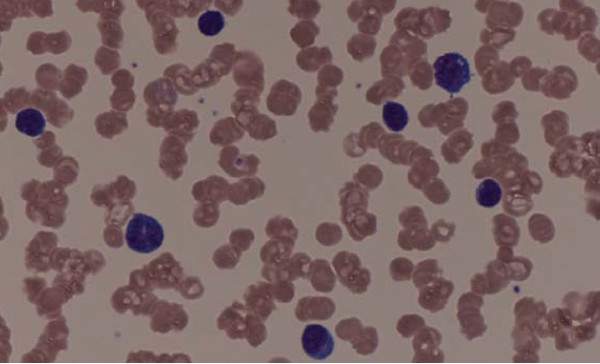
Expert panel offers treatment recommendations in Waldenström macroglobulinemia
Treatment recommendations for Waldenström macroglobulinemia have been updated based on the advice of a task force convened at the Eighth International Workshop on Waldenström Macroglobulinemia; the guidelines have been published in Blood.
The task force was impaneled to review recently published and ongoing clinical trial data as well as the impact of the newly recognized mutations MYD88 and CXCR4 on treatment decisions, indications for B-cell receptor and proteasome inhibitors, and future clinical trial initiatives.
The panel reiterated that the criteria for initiating therapy include immunoglobulin M (IgM)-related complications and/or symptoms that are related to direct involvement of the bone marrow by tumor cells, constitutional symptoms, and bulky extramedullary disease. Patients presenting with symptoms that include symptomatic hyperviscosity, moderate to severe hemolytic anemia, and symptomatic cryoglobulinemia need immediate treatment.
Close observation is recommended for the subgroup of patients who do not really fulfill the criteria for a diagnosis of Waldenström macroglobulinemia (WM), and whose laboratory findings may be the only indicator of the presence of a progressive disease.
Treatment recommendations
For symptomatic patients in the first-line setting, “anti-CD20 monoclonal antibody therapy alone or in combination with chemotherapy is an important standard of care for most patients with WM,” the authors, led by Veronique Leblond, MD, of Pitié-Salpêtrière Hôpital, Paris, wrote.
Rituximab is frequently used in WM, either as monotherapy or in combination with chemotherapeutic agents. The panel cautions that rituximab as monotherapy should be avoided in patients with high IgM levels, because of a lower chance of response and the risk of an IgM flare.
In patients with high IgM levels (typically around 4,000 mg/dL), plasmapheresis can be initiated before rituximab therapy, and plasmapheresis should always and immediately be used when symptomatic hyperviscosity is present. However, plasmapheresis alone is not an effective treatment for WM and must be followed by a rapidly acting cytoreductive regimen.
Several rituximab combinations are recommended by the panel. These include:
• Dexamethasone-rituximab-cyclophosphamide, which is an active and safe option, has a manageable toxicity, and can be considered for frail patients who need combination therapy.
• Bendamustine-rituximab is effective for front-line treatment and is well tolerated even in elderly patients who experience limited episodes of myelosuppression and infections.
Other therapeutic regimens include bortezomib-based therapy, which is recommended for patients with high IgM levels, symptomatic hyperviscosity, cryoglobulinemia or cold agglutinemia, amyloidosis, and renal impairment or in young patients who prefer to avoid alkylator or nucleoside analogue therapy.
Another option is carfilzomib-based therapy, which is an emerging “neuropathy-sparing” regimen for proteasome-inhibitor–based therapy, although it may not be the best choice for elderly patients with preexisting cardiac conditions due to potential cardiac toxicity.
Ibrutinib has been approved as a primary therapy for patients who are not candidates for chemoimmunotherapy, but the authors point out that the optimal use of this agent is still being investigated.
“The aim of the first-line treatments is to reach a high response rate with a prolonged progression-free survival,” write the authors. “The panel agrees that there is need to perform clinical trials with chemotherapy-free combinations with new compounds alone or in combination with anti-CD20 antibodies.”
For symptomatic previously treated patients
The panel also offered recommendations for previously treated symptomatic patients who have relapsed or are refractory to treatment.
Any of the interventions recommended for symptomatic, untreated patients can be considered for those who have already gone through first line therapy. Retreatment can be considered with a specific intervention if a response was achieved for 2 or more years with that therapy, although they caution that patients who have progressed on first-line ibrutinib should not use it again.
Ofatumumab is a potential option for patients who are unable to tolerate rituximab, and nucleoside analogues can be considered in fit patients who have not responded to less-toxic treatments.
Another option in this setting is everolimus, although since it is associated with considerable toxicities, the best candidates for this drug are those who have not responded to or have progressed after multiple lines of other better-tolerated regimens.
Immunomodulatory agents can also be considered, but in the context of a clinical trial only, because of their potential adverse events.
Finally, the panel also agreed that stem cell transplantation should be discussed with select patients, and while it is a feasible and effective treatment option for high-risk WM patients, it should be ideally offered at early relapse.
Investigating B-cell receptor (BCR) pathway inhibitors along with existing and novel compounds in patients in the relapsed/refractory setting should be a priority, according to the panel.
“BCR inhibitors, combined with proteasome inhibitors, would be of interest for overcoming resistance by interfering with the two key pathways that are affected by MYD88,” wrote Dr. Leblond and coauthors.
Treatment recommendations for Waldenström macroglobulinemia have been updated based on the advice of a task force convened at the Eighth International Workshop on Waldenström Macroglobulinemia; the guidelines have been published in Blood.
The task force was impaneled to review recently published and ongoing clinical trial data as well as the impact of the newly recognized mutations MYD88 and CXCR4 on treatment decisions, indications for B-cell receptor and proteasome inhibitors, and future clinical trial initiatives.
The panel reiterated that the criteria for initiating therapy include immunoglobulin M (IgM)-related complications and/or symptoms that are related to direct involvement of the bone marrow by tumor cells, constitutional symptoms, and bulky extramedullary disease. Patients presenting with symptoms that include symptomatic hyperviscosity, moderate to severe hemolytic anemia, and symptomatic cryoglobulinemia need immediate treatment.
Close observation is recommended for the subgroup of patients who do not really fulfill the criteria for a diagnosis of Waldenström macroglobulinemia (WM), and whose laboratory findings may be the only indicator of the presence of a progressive disease.
Treatment recommendations
For symptomatic patients in the first-line setting, “anti-CD20 monoclonal antibody therapy alone or in combination with chemotherapy is an important standard of care for most patients with WM,” the authors, led by Veronique Leblond, MD, of Pitié-Salpêtrière Hôpital, Paris, wrote.
Rituximab is frequently used in WM, either as monotherapy or in combination with chemotherapeutic agents. The panel cautions that rituximab as monotherapy should be avoided in patients with high IgM levels, because of a lower chance of response and the risk of an IgM flare.
In patients with high IgM levels (typically around 4,000 mg/dL), plasmapheresis can be initiated before rituximab therapy, and plasmapheresis should always and immediately be used when symptomatic hyperviscosity is present. However, plasmapheresis alone is not an effective treatment for WM and must be followed by a rapidly acting cytoreductive regimen.
Several rituximab combinations are recommended by the panel. These include:
• Dexamethasone-rituximab-cyclophosphamide, which is an active and safe option, has a manageable toxicity, and can be considered for frail patients who need combination therapy.
• Bendamustine-rituximab is effective for front-line treatment and is well tolerated even in elderly patients who experience limited episodes of myelosuppression and infections.
Other therapeutic regimens include bortezomib-based therapy, which is recommended for patients with high IgM levels, symptomatic hyperviscosity, cryoglobulinemia or cold agglutinemia, amyloidosis, and renal impairment or in young patients who prefer to avoid alkylator or nucleoside analogue therapy.
Another option is carfilzomib-based therapy, which is an emerging “neuropathy-sparing” regimen for proteasome-inhibitor–based therapy, although it may not be the best choice for elderly patients with preexisting cardiac conditions due to potential cardiac toxicity.
Ibrutinib has been approved as a primary therapy for patients who are not candidates for chemoimmunotherapy, but the authors point out that the optimal use of this agent is still being investigated.
“The aim of the first-line treatments is to reach a high response rate with a prolonged progression-free survival,” write the authors. “The panel agrees that there is need to perform clinical trials with chemotherapy-free combinations with new compounds alone or in combination with anti-CD20 antibodies.”
For symptomatic previously treated patients
The panel also offered recommendations for previously treated symptomatic patients who have relapsed or are refractory to treatment.
Any of the interventions recommended for symptomatic, untreated patients can be considered for those who have already gone through first line therapy. Retreatment can be considered with a specific intervention if a response was achieved for 2 or more years with that therapy, although they caution that patients who have progressed on first-line ibrutinib should not use it again.
Ofatumumab is a potential option for patients who are unable to tolerate rituximab, and nucleoside analogues can be considered in fit patients who have not responded to less-toxic treatments.
Another option in this setting is everolimus, although since it is associated with considerable toxicities, the best candidates for this drug are those who have not responded to or have progressed after multiple lines of other better-tolerated regimens.
Immunomodulatory agents can also be considered, but in the context of a clinical trial only, because of their potential adverse events.
Finally, the panel also agreed that stem cell transplantation should be discussed with select patients, and while it is a feasible and effective treatment option for high-risk WM patients, it should be ideally offered at early relapse.
Investigating B-cell receptor (BCR) pathway inhibitors along with existing and novel compounds in patients in the relapsed/refractory setting should be a priority, according to the panel.
“BCR inhibitors, combined with proteasome inhibitors, would be of interest for overcoming resistance by interfering with the two key pathways that are affected by MYD88,” wrote Dr. Leblond and coauthors.
Treatment recommendations for Waldenström macroglobulinemia have been updated based on the advice of a task force convened at the Eighth International Workshop on Waldenström Macroglobulinemia; the guidelines have been published in Blood.
The task force was impaneled to review recently published and ongoing clinical trial data as well as the impact of the newly recognized mutations MYD88 and CXCR4 on treatment decisions, indications for B-cell receptor and proteasome inhibitors, and future clinical trial initiatives.
The panel reiterated that the criteria for initiating therapy include immunoglobulin M (IgM)-related complications and/or symptoms that are related to direct involvement of the bone marrow by tumor cells, constitutional symptoms, and bulky extramedullary disease. Patients presenting with symptoms that include symptomatic hyperviscosity, moderate to severe hemolytic anemia, and symptomatic cryoglobulinemia need immediate treatment.
Close observation is recommended for the subgroup of patients who do not really fulfill the criteria for a diagnosis of Waldenström macroglobulinemia (WM), and whose laboratory findings may be the only indicator of the presence of a progressive disease.
Treatment recommendations
For symptomatic patients in the first-line setting, “anti-CD20 monoclonal antibody therapy alone or in combination with chemotherapy is an important standard of care for most patients with WM,” the authors, led by Veronique Leblond, MD, of Pitié-Salpêtrière Hôpital, Paris, wrote.
Rituximab is frequently used in WM, either as monotherapy or in combination with chemotherapeutic agents. The panel cautions that rituximab as monotherapy should be avoided in patients with high IgM levels, because of a lower chance of response and the risk of an IgM flare.
In patients with high IgM levels (typically around 4,000 mg/dL), plasmapheresis can be initiated before rituximab therapy, and plasmapheresis should always and immediately be used when symptomatic hyperviscosity is present. However, plasmapheresis alone is not an effective treatment for WM and must be followed by a rapidly acting cytoreductive regimen.
Several rituximab combinations are recommended by the panel. These include:
• Dexamethasone-rituximab-cyclophosphamide, which is an active and safe option, has a manageable toxicity, and can be considered for frail patients who need combination therapy.
• Bendamustine-rituximab is effective for front-line treatment and is well tolerated even in elderly patients who experience limited episodes of myelosuppression and infections.
Other therapeutic regimens include bortezomib-based therapy, which is recommended for patients with high IgM levels, symptomatic hyperviscosity, cryoglobulinemia or cold agglutinemia, amyloidosis, and renal impairment or in young patients who prefer to avoid alkylator or nucleoside analogue therapy.
Another option is carfilzomib-based therapy, which is an emerging “neuropathy-sparing” regimen for proteasome-inhibitor–based therapy, although it may not be the best choice for elderly patients with preexisting cardiac conditions due to potential cardiac toxicity.
Ibrutinib has been approved as a primary therapy for patients who are not candidates for chemoimmunotherapy, but the authors point out that the optimal use of this agent is still being investigated.
“The aim of the first-line treatments is to reach a high response rate with a prolonged progression-free survival,” write the authors. “The panel agrees that there is need to perform clinical trials with chemotherapy-free combinations with new compounds alone or in combination with anti-CD20 antibodies.”
For symptomatic previously treated patients
The panel also offered recommendations for previously treated symptomatic patients who have relapsed or are refractory to treatment.
Any of the interventions recommended for symptomatic, untreated patients can be considered for those who have already gone through first line therapy. Retreatment can be considered with a specific intervention if a response was achieved for 2 or more years with that therapy, although they caution that patients who have progressed on first-line ibrutinib should not use it again.
Ofatumumab is a potential option for patients who are unable to tolerate rituximab, and nucleoside analogues can be considered in fit patients who have not responded to less-toxic treatments.
Another option in this setting is everolimus, although since it is associated with considerable toxicities, the best candidates for this drug are those who have not responded to or have progressed after multiple lines of other better-tolerated regimens.
Immunomodulatory agents can also be considered, but in the context of a clinical trial only, because of their potential adverse events.
Finally, the panel also agreed that stem cell transplantation should be discussed with select patients, and while it is a feasible and effective treatment option for high-risk WM patients, it should be ideally offered at early relapse.
Investigating B-cell receptor (BCR) pathway inhibitors along with existing and novel compounds in patients in the relapsed/refractory setting should be a priority, according to the panel.
“BCR inhibitors, combined with proteasome inhibitors, would be of interest for overcoming resistance by interfering with the two key pathways that are affected by MYD88,” wrote Dr. Leblond and coauthors.
FROM BLOOD
FDA provides clearance for new colonoscope system
The U.S Food and Drug Administration provided 510(k) clearance for the new Aer-O-Scope colonoscope system, according to GI View of Ramat Gan, Israel.
The Aer-O-Scope is a self-propelled, disposable colonoscope with a 360-degree view of the colon that is controlled with a joystick.
The new system, which is an improvement on the earlier Aer-O-Scope colonoscope, also FDA approved, will have two working channels in order to provide therapeutic access for standard tools to take biopsies or perform polypectomies. It uses a soft multilumen tube designed to significantly reduce pressure on the colon wall, which may increase patient safety. It is also hydrophilic and reduces the friction between bowel and scope by more than 90%. The system has a self-propelled intubation process, created with balloons and low pressure CO2 gas. And, like all colonoscopes, the Aer-O-Scope provides insufflation, irrigation, and suction.
“The new Aer-O-Scope system with therapeutic access has many significant clinical benefits including enabling physicians to more easily, effectively, and efficiently identify and remove polyps and prevent colon cancer,” said GI View CEO Tal Simchony, PhD, in a press release. “We are now working on U.S. market introduction of the Aer-O-Scope. Postmarket studies are also in the plans.”
Colorectal cancer is one of the biggest causes of cancer death worldwide. It can be prevented by early detection and removal of polyps. Read more about Aer-O-Scope on GI View’s website.
The U.S Food and Drug Administration provided 510(k) clearance for the new Aer-O-Scope colonoscope system, according to GI View of Ramat Gan, Israel.
The Aer-O-Scope is a self-propelled, disposable colonoscope with a 360-degree view of the colon that is controlled with a joystick.
The new system, which is an improvement on the earlier Aer-O-Scope colonoscope, also FDA approved, will have two working channels in order to provide therapeutic access for standard tools to take biopsies or perform polypectomies. It uses a soft multilumen tube designed to significantly reduce pressure on the colon wall, which may increase patient safety. It is also hydrophilic and reduces the friction between bowel and scope by more than 90%. The system has a self-propelled intubation process, created with balloons and low pressure CO2 gas. And, like all colonoscopes, the Aer-O-Scope provides insufflation, irrigation, and suction.
“The new Aer-O-Scope system with therapeutic access has many significant clinical benefits including enabling physicians to more easily, effectively, and efficiently identify and remove polyps and prevent colon cancer,” said GI View CEO Tal Simchony, PhD, in a press release. “We are now working on U.S. market introduction of the Aer-O-Scope. Postmarket studies are also in the plans.”
Colorectal cancer is one of the biggest causes of cancer death worldwide. It can be prevented by early detection and removal of polyps. Read more about Aer-O-Scope on GI View’s website.
The U.S Food and Drug Administration provided 510(k) clearance for the new Aer-O-Scope colonoscope system, according to GI View of Ramat Gan, Israel.
The Aer-O-Scope is a self-propelled, disposable colonoscope with a 360-degree view of the colon that is controlled with a joystick.
The new system, which is an improvement on the earlier Aer-O-Scope colonoscope, also FDA approved, will have two working channels in order to provide therapeutic access for standard tools to take biopsies or perform polypectomies. It uses a soft multilumen tube designed to significantly reduce pressure on the colon wall, which may increase patient safety. It is also hydrophilic and reduces the friction between bowel and scope by more than 90%. The system has a self-propelled intubation process, created with balloons and low pressure CO2 gas. And, like all colonoscopes, the Aer-O-Scope provides insufflation, irrigation, and suction.
“The new Aer-O-Scope system with therapeutic access has many significant clinical benefits including enabling physicians to more easily, effectively, and efficiently identify and remove polyps and prevent colon cancer,” said GI View CEO Tal Simchony, PhD, in a press release. “We are now working on U.S. market introduction of the Aer-O-Scope. Postmarket studies are also in the plans.”
Colorectal cancer is one of the biggest causes of cancer death worldwide. It can be prevented by early detection and removal of polyps. Read more about Aer-O-Scope on GI View’s website.
DNA methylation rises sharply at progression of Ph+ CML
A large uptick in DNA methylation occurs at the time of progression in patients with Philadelphia chromosome–positive chronic myeloid leukemia (CML), according to results from a comparative cohort study. The observation raises the possibility of new therapeutic targets for advanced disease.
Researchers led by Gerwin Heller, PhD, of the Medical University of Vienna’s Clinical Division of Oncology and Comprehensive Cancer Center, Austria, collected peripheral blood mononuclear cells from 23 patients with CML during various disease phases (chronic phase in 17, acute phase in 5, and blast crisis in 9) and from 5 healthy controls.
They isolated DNA and analyzed it with a novel next-generation sequencing approach, known as reduced representation bisulfite sequencing, to identify the presence and extent of methylation.
Compared with the healthy controls, patients in chronic-phase CML had 666 differentially methylated CpG (cytosine-phosphate-guanine) sites, whereas those in blast crisis had 6,912 differentially methylated CpG sites (Leukemia. 2016;30:1861-8). Some 44% of the former but 88% of the latter affected CpG sites showed increased methylation.
Among patients with chronic-phase CML who experienced progression to the accelerated phase or blast crisis, analyses identified between 344 and 897 genes that were methylated at the time of progression but had not been at the time of diagnosis.
RNA sequencing determined that many of these newly methylated genes showed downregulated expression in the samples collected during blast crisis, compared with those collected during chronic phase disease. These genes included some tumor suppressor genes (EPB41L3, PRDX2), regulators of cell proliferation (BCL11B, NDRG2, PID1), and regulators of drug metabolism (CYP1B1), among others.
Treatment of CML cells with the epigenetically active drugs azacitidine (a DNA methyltransferase inhibitor) and trichostatin A (a histone deacetylase inhibitor) led to re-expression of the CYP1B1 gene.
“Together, our results demonstrate that CpG site methylation clearly increases during CML progression and that it may provide a useful basis for revealing new targets of therapy in advanced CML,” wrote Dr. Heller and colleagues, who disclosed that one of them has received research grants from Novartis and Ariad.
“Our findings suggest that investigating the efficacy of [DNA methyltransferase inhibitors] in patients with progressed CML should be considered,” they said.
A large uptick in DNA methylation occurs at the time of progression in patients with Philadelphia chromosome–positive chronic myeloid leukemia (CML), according to results from a comparative cohort study. The observation raises the possibility of new therapeutic targets for advanced disease.
Researchers led by Gerwin Heller, PhD, of the Medical University of Vienna’s Clinical Division of Oncology and Comprehensive Cancer Center, Austria, collected peripheral blood mononuclear cells from 23 patients with CML during various disease phases (chronic phase in 17, acute phase in 5, and blast crisis in 9) and from 5 healthy controls.
They isolated DNA and analyzed it with a novel next-generation sequencing approach, known as reduced representation bisulfite sequencing, to identify the presence and extent of methylation.
Compared with the healthy controls, patients in chronic-phase CML had 666 differentially methylated CpG (cytosine-phosphate-guanine) sites, whereas those in blast crisis had 6,912 differentially methylated CpG sites (Leukemia. 2016;30:1861-8). Some 44% of the former but 88% of the latter affected CpG sites showed increased methylation.
Among patients with chronic-phase CML who experienced progression to the accelerated phase or blast crisis, analyses identified between 344 and 897 genes that were methylated at the time of progression but had not been at the time of diagnosis.
RNA sequencing determined that many of these newly methylated genes showed downregulated expression in the samples collected during blast crisis, compared with those collected during chronic phase disease. These genes included some tumor suppressor genes (EPB41L3, PRDX2), regulators of cell proliferation (BCL11B, NDRG2, PID1), and regulators of drug metabolism (CYP1B1), among others.
Treatment of CML cells with the epigenetically active drugs azacitidine (a DNA methyltransferase inhibitor) and trichostatin A (a histone deacetylase inhibitor) led to re-expression of the CYP1B1 gene.
“Together, our results demonstrate that CpG site methylation clearly increases during CML progression and that it may provide a useful basis for revealing new targets of therapy in advanced CML,” wrote Dr. Heller and colleagues, who disclosed that one of them has received research grants from Novartis and Ariad.
“Our findings suggest that investigating the efficacy of [DNA methyltransferase inhibitors] in patients with progressed CML should be considered,” they said.
A large uptick in DNA methylation occurs at the time of progression in patients with Philadelphia chromosome–positive chronic myeloid leukemia (CML), according to results from a comparative cohort study. The observation raises the possibility of new therapeutic targets for advanced disease.
Researchers led by Gerwin Heller, PhD, of the Medical University of Vienna’s Clinical Division of Oncology and Comprehensive Cancer Center, Austria, collected peripheral blood mononuclear cells from 23 patients with CML during various disease phases (chronic phase in 17, acute phase in 5, and blast crisis in 9) and from 5 healthy controls.
They isolated DNA and analyzed it with a novel next-generation sequencing approach, known as reduced representation bisulfite sequencing, to identify the presence and extent of methylation.
Compared with the healthy controls, patients in chronic-phase CML had 666 differentially methylated CpG (cytosine-phosphate-guanine) sites, whereas those in blast crisis had 6,912 differentially methylated CpG sites (Leukemia. 2016;30:1861-8). Some 44% of the former but 88% of the latter affected CpG sites showed increased methylation.
Among patients with chronic-phase CML who experienced progression to the accelerated phase or blast crisis, analyses identified between 344 and 897 genes that were methylated at the time of progression but had not been at the time of diagnosis.
RNA sequencing determined that many of these newly methylated genes showed downregulated expression in the samples collected during blast crisis, compared with those collected during chronic phase disease. These genes included some tumor suppressor genes (EPB41L3, PRDX2), regulators of cell proliferation (BCL11B, NDRG2, PID1), and regulators of drug metabolism (CYP1B1), among others.
Treatment of CML cells with the epigenetically active drugs azacitidine (a DNA methyltransferase inhibitor) and trichostatin A (a histone deacetylase inhibitor) led to re-expression of the CYP1B1 gene.
“Together, our results demonstrate that CpG site methylation clearly increases during CML progression and that it may provide a useful basis for revealing new targets of therapy in advanced CML,” wrote Dr. Heller and colleagues, who disclosed that one of them has received research grants from Novartis and Ariad.
“Our findings suggest that investigating the efficacy of [DNA methyltransferase inhibitors] in patients with progressed CML should be considered,” they said.
FROM LEUKEMIA
Key clinical point: Increases in DNA methylation occur at progression of Ph+ CML; this realization may enable new therapeutic targets.
Major finding: Patients who progressed from chronic phase to accelerated phase or blast crisis had up to 897 genes that were newly methylated since diagnosis, including some tumor-suppressor genes and regulators of cell proliferation and drug metabolism.
Data source: A cohort study of 23 patients with CML and 5 healthy controls.
Disclosures: The investigators disclosed that one of the authors has received research grants from Novartis and Ariad.
Suicide Rate for People With Epilepsy Exceeds Level in the General Population
The annual suicide mortality rate among those with epilepsy is 22% higher than that in the general population, according to a report in the August issue of Epilepsy and Behavior. Researchers estimated that the annual suicide mortality rate in those with epilepsy during the period from 2003 through 2011 was 16.89 per 100,000 persons.
Researchers at Columbia University’s Mailman School of Public Health in New York and the Centers for Disease Control and Prevention in Atlanta studied the prevalence of suicide among people with epilepsy, compared with that in the population overall. This is the first study to estimate suicide rates among people with epilepsy in a large US general population. The researchers also investigated epilepsy-specific suicide risk factors.
The study, coauthored by Dale Hesdorffer, PhD, Professor of Epidemiology at the Mailman School of Public Health, was based on data from the US National Violent Death Reporting System, a multistate, population-based surveillance system that collects information on violent deaths, including suicide. From 2003 through 2011, the researchers identified, among people age 10 and older, 972 suicide cases with epilepsy and 81,529 suicide cases without epilepsy in 17 states. The investigators estimated suicide rates, evaluated suicide risk among people with epilepsy, and investigated suicide risk factors specific to epilepsy by comparing people with and without epilepsy. In 16 of the 17 states providing continual data from 2005 through 2011, they also compared suicide trends in people with and without epilepsy.
Compared with the non-epilepsy population, those with epilepsy were more likely to have died from suicide in houses, apartments, or residential institutions (81% vs 76%) and were more than twice as likely to poison themselves (38% vs 17%). More people with epilepsy ages 40 to 49 died from suicide than persons without epilepsy in the same age group (29% vs 22%). The proportion of suicides among those with epilepsy increased steadily from 2005 through 2010.
“Of particular significance is what we learned about those 40 to 49 years old,” said Dr. Hesdorffer. “Efforts for suicide prevention should target people with epilepsy in this age category specifically. Additional preventive efforts should include reducing the availability or exposure to poisons, especially at home, and supporting other evidence-based programs to reduce mental illness comorbidity associated with suicide.”
Suggested Reading
Tian N, Cui W, Zack M, et al. Suicide among people with epilepsy: a population-based analysis of data from the U.S. National Violent Death Reporting System, 17 states, 2003-2011. Epilepsy Behav. 2016;61:210-217.
Mula M, McGonigal A, Micoulaud-Franchi JA, et al. Validation of rapid suicidality screening in epilepsy using the NDDIE. Epilepsia. 2016;57(6):949-955.
The annual suicide mortality rate among those with epilepsy is 22% higher than that in the general population, according to a report in the August issue of Epilepsy and Behavior. Researchers estimated that the annual suicide mortality rate in those with epilepsy during the period from 2003 through 2011 was 16.89 per 100,000 persons.
Researchers at Columbia University’s Mailman School of Public Health in New York and the Centers for Disease Control and Prevention in Atlanta studied the prevalence of suicide among people with epilepsy, compared with that in the population overall. This is the first study to estimate suicide rates among people with epilepsy in a large US general population. The researchers also investigated epilepsy-specific suicide risk factors.
The study, coauthored by Dale Hesdorffer, PhD, Professor of Epidemiology at the Mailman School of Public Health, was based on data from the US National Violent Death Reporting System, a multistate, population-based surveillance system that collects information on violent deaths, including suicide. From 2003 through 2011, the researchers identified, among people age 10 and older, 972 suicide cases with epilepsy and 81,529 suicide cases without epilepsy in 17 states. The investigators estimated suicide rates, evaluated suicide risk among people with epilepsy, and investigated suicide risk factors specific to epilepsy by comparing people with and without epilepsy. In 16 of the 17 states providing continual data from 2005 through 2011, they also compared suicide trends in people with and without epilepsy.
Compared with the non-epilepsy population, those with epilepsy were more likely to have died from suicide in houses, apartments, or residential institutions (81% vs 76%) and were more than twice as likely to poison themselves (38% vs 17%). More people with epilepsy ages 40 to 49 died from suicide than persons without epilepsy in the same age group (29% vs 22%). The proportion of suicides among those with epilepsy increased steadily from 2005 through 2010.
“Of particular significance is what we learned about those 40 to 49 years old,” said Dr. Hesdorffer. “Efforts for suicide prevention should target people with epilepsy in this age category specifically. Additional preventive efforts should include reducing the availability or exposure to poisons, especially at home, and supporting other evidence-based programs to reduce mental illness comorbidity associated with suicide.”
Suggested Reading
Tian N, Cui W, Zack M, et al. Suicide among people with epilepsy: a population-based analysis of data from the U.S. National Violent Death Reporting System, 17 states, 2003-2011. Epilepsy Behav. 2016;61:210-217.
Mula M, McGonigal A, Micoulaud-Franchi JA, et al. Validation of rapid suicidality screening in epilepsy using the NDDIE. Epilepsia. 2016;57(6):949-955.
The annual suicide mortality rate among those with epilepsy is 22% higher than that in the general population, according to a report in the August issue of Epilepsy and Behavior. Researchers estimated that the annual suicide mortality rate in those with epilepsy during the period from 2003 through 2011 was 16.89 per 100,000 persons.
Researchers at Columbia University’s Mailman School of Public Health in New York and the Centers for Disease Control and Prevention in Atlanta studied the prevalence of suicide among people with epilepsy, compared with that in the population overall. This is the first study to estimate suicide rates among people with epilepsy in a large US general population. The researchers also investigated epilepsy-specific suicide risk factors.
The study, coauthored by Dale Hesdorffer, PhD, Professor of Epidemiology at the Mailman School of Public Health, was based on data from the US National Violent Death Reporting System, a multistate, population-based surveillance system that collects information on violent deaths, including suicide. From 2003 through 2011, the researchers identified, among people age 10 and older, 972 suicide cases with epilepsy and 81,529 suicide cases without epilepsy in 17 states. The investigators estimated suicide rates, evaluated suicide risk among people with epilepsy, and investigated suicide risk factors specific to epilepsy by comparing people with and without epilepsy. In 16 of the 17 states providing continual data from 2005 through 2011, they also compared suicide trends in people with and without epilepsy.
Compared with the non-epilepsy population, those with epilepsy were more likely to have died from suicide in houses, apartments, or residential institutions (81% vs 76%) and were more than twice as likely to poison themselves (38% vs 17%). More people with epilepsy ages 40 to 49 died from suicide than persons without epilepsy in the same age group (29% vs 22%). The proportion of suicides among those with epilepsy increased steadily from 2005 through 2010.
“Of particular significance is what we learned about those 40 to 49 years old,” said Dr. Hesdorffer. “Efforts for suicide prevention should target people with epilepsy in this age category specifically. Additional preventive efforts should include reducing the availability or exposure to poisons, especially at home, and supporting other evidence-based programs to reduce mental illness comorbidity associated with suicide.”
Suggested Reading
Tian N, Cui W, Zack M, et al. Suicide among people with epilepsy: a population-based analysis of data from the U.S. National Violent Death Reporting System, 17 states, 2003-2011. Epilepsy Behav. 2016;61:210-217.
Mula M, McGonigal A, Micoulaud-Franchi JA, et al. Validation of rapid suicidality screening in epilepsy using the NDDIE. Epilepsia. 2016;57(6):949-955.
Miscellany
Many interesting things happen in a medical office, most of which don’t merit a full column. Here are some from my own past few months:
Endocrine Knee? I was hard put to explain the calluses on both my patient’s knees. As I tried to formulate a question, he rescued me by saying, “I’m an endocrinologist. I spend a lot of my time on my knees, trimming the toenails of elderly diabetics.”
Who knew? At least bending the knee to insurers and regulators doesn’t require keratolytics ...
You can get anything online. My patient was about to graduate with a degree in psychoanalysis. “I have to set up my office,” she said, “drapes, analyst couch, and so forth.”
“Where do you buy an analyst couch?” I asked.
“Analyticcouch.com,” she explained. “Available in a variety of colors.”
What a country!
No I’m not, Officer! Many patients consider removing facial red spots that make them self-conscious, but Harriet’s reason was unique. “I got pulled over by a cop for an illegal change of lanes,” she said. “When he saw the red spot under my eye, he assumed I was a drunk. ‘Get over there, punk,’ he said.”
The other bathroom is upstairs. Stan listed his occupation as “muralist.” Picturing him sneaking up to blank walls on street corners in the middle of the night with a can of Benjamin Moore to ply his trade, I asked where he draws his murals.
“Most of my work is residential,” he said. “For instance, last year I did a bathroom in Framingham. The motif they wanted was ancient Egypt. I had to do a lot of research on the 18th dynasty, to get the details exactly right.”
That made sense. You wouldn’t want a dangling hieroglyphic participle in your downstairs lavatory. I asked him how it worked out.
“The client was delighted,” he said, “only there was one problem. Whenever guests came over for a dinner party, there was always a long line, because whoever was in the bathroom wouldn’t come out.”
There are always alternatives. By now I am used to hearing patients extol the virtues of exotic treatments: Vicks VapoRub for toenail tinea, tea tree oil for most anything. Apple cider vinegar for everything else.
Then the other day Marcy surprised me with this:
“I stopped the minocycline,” she said, “Instead I started using celery, which I ground up and boiled and then froze and then applied to the face.”
A little bit of a production, perhaps – grinding, boiling, freezing. As long as it works ...
You need a different kind of doctor. “I see I won’t be able to shower for 3 days,” said the new patient.
My jaw dropped, but no words came out.
“It’s that sign you put up,” he said, “right on the exam room door.”
As I don’t usually read my own signs, I turned to look. The sign read:
“If you have no-showed without notice three times, we reserve the right to reschedule you at our convenience.”
“It says, ‘No-Showed,” I said. Not ‘No Showers.”
I resisted the urge to refer him to an optometrist.
This reminded me of another episode some time ago, when a patient listed his Chief Complaint as, “I want Lasik Surgery.”
“Forgive me,” I said, “but why would you ask a dermatologist for Lasik surgery?”
“Doesn’t the sign on your door say, “Boston Ophthalmology?” he asked.
“Upstairs,” I said. “Seventh floor.”
Negotiating with Father Time. We suspected porphyria, and ordered a 24-hour urine collection. “I’m a busy executive,” said the patient. “I haven’t got time to collect it for that long.”
“But it has to be a whole day ...”
“Fifteen hours,” he said. “I’ll give you 15 hours.”
“But we need ...”
“Eighteen hours. OK?”
“Well, not really. You see, the test has to be a whole day ...”
“All right, 21 hours. That’s my best offer.”
Maybe if I could get him to spend the day in that Egyptian bathroom ...
Dr. Rockoff practices dermatology in Brookline, Mass, and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His new book, “Act Like a Doctor, Think Like a Patient,” is now available on amazon.com and barnesandnoble.com. This is his second book. Write to him at [email protected].
Many interesting things happen in a medical office, most of which don’t merit a full column. Here are some from my own past few months:
Endocrine Knee? I was hard put to explain the calluses on both my patient’s knees. As I tried to formulate a question, he rescued me by saying, “I’m an endocrinologist. I spend a lot of my time on my knees, trimming the toenails of elderly diabetics.”
Who knew? At least bending the knee to insurers and regulators doesn’t require keratolytics ...
You can get anything online. My patient was about to graduate with a degree in psychoanalysis. “I have to set up my office,” she said, “drapes, analyst couch, and so forth.”
“Where do you buy an analyst couch?” I asked.
“Analyticcouch.com,” she explained. “Available in a variety of colors.”
What a country!
No I’m not, Officer! Many patients consider removing facial red spots that make them self-conscious, but Harriet’s reason was unique. “I got pulled over by a cop for an illegal change of lanes,” she said. “When he saw the red spot under my eye, he assumed I was a drunk. ‘Get over there, punk,’ he said.”
The other bathroom is upstairs. Stan listed his occupation as “muralist.” Picturing him sneaking up to blank walls on street corners in the middle of the night with a can of Benjamin Moore to ply his trade, I asked where he draws his murals.
“Most of my work is residential,” he said. “For instance, last year I did a bathroom in Framingham. The motif they wanted was ancient Egypt. I had to do a lot of research on the 18th dynasty, to get the details exactly right.”
That made sense. You wouldn’t want a dangling hieroglyphic participle in your downstairs lavatory. I asked him how it worked out.
“The client was delighted,” he said, “only there was one problem. Whenever guests came over for a dinner party, there was always a long line, because whoever was in the bathroom wouldn’t come out.”
There are always alternatives. By now I am used to hearing patients extol the virtues of exotic treatments: Vicks VapoRub for toenail tinea, tea tree oil for most anything. Apple cider vinegar for everything else.
Then the other day Marcy surprised me with this:
“I stopped the minocycline,” she said, “Instead I started using celery, which I ground up and boiled and then froze and then applied to the face.”
A little bit of a production, perhaps – grinding, boiling, freezing. As long as it works ...
You need a different kind of doctor. “I see I won’t be able to shower for 3 days,” said the new patient.
My jaw dropped, but no words came out.
“It’s that sign you put up,” he said, “right on the exam room door.”
As I don’t usually read my own signs, I turned to look. The sign read:
“If you have no-showed without notice three times, we reserve the right to reschedule you at our convenience.”
“It says, ‘No-Showed,” I said. Not ‘No Showers.”
I resisted the urge to refer him to an optometrist.
This reminded me of another episode some time ago, when a patient listed his Chief Complaint as, “I want Lasik Surgery.”
“Forgive me,” I said, “but why would you ask a dermatologist for Lasik surgery?”
“Doesn’t the sign on your door say, “Boston Ophthalmology?” he asked.
“Upstairs,” I said. “Seventh floor.”
Negotiating with Father Time. We suspected porphyria, and ordered a 24-hour urine collection. “I’m a busy executive,” said the patient. “I haven’t got time to collect it for that long.”
“But it has to be a whole day ...”
“Fifteen hours,” he said. “I’ll give you 15 hours.”
“But we need ...”
“Eighteen hours. OK?”
“Well, not really. You see, the test has to be a whole day ...”
“All right, 21 hours. That’s my best offer.”
Maybe if I could get him to spend the day in that Egyptian bathroom ...
Dr. Rockoff practices dermatology in Brookline, Mass, and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His new book, “Act Like a Doctor, Think Like a Patient,” is now available on amazon.com and barnesandnoble.com. This is his second book. Write to him at [email protected].
Many interesting things happen in a medical office, most of which don’t merit a full column. Here are some from my own past few months:
Endocrine Knee? I was hard put to explain the calluses on both my patient’s knees. As I tried to formulate a question, he rescued me by saying, “I’m an endocrinologist. I spend a lot of my time on my knees, trimming the toenails of elderly diabetics.”
Who knew? At least bending the knee to insurers and regulators doesn’t require keratolytics ...
You can get anything online. My patient was about to graduate with a degree in psychoanalysis. “I have to set up my office,” she said, “drapes, analyst couch, and so forth.”
“Where do you buy an analyst couch?” I asked.
“Analyticcouch.com,” she explained. “Available in a variety of colors.”
What a country!
No I’m not, Officer! Many patients consider removing facial red spots that make them self-conscious, but Harriet’s reason was unique. “I got pulled over by a cop for an illegal change of lanes,” she said. “When he saw the red spot under my eye, he assumed I was a drunk. ‘Get over there, punk,’ he said.”
The other bathroom is upstairs. Stan listed his occupation as “muralist.” Picturing him sneaking up to blank walls on street corners in the middle of the night with a can of Benjamin Moore to ply his trade, I asked where he draws his murals.
“Most of my work is residential,” he said. “For instance, last year I did a bathroom in Framingham. The motif they wanted was ancient Egypt. I had to do a lot of research on the 18th dynasty, to get the details exactly right.”
That made sense. You wouldn’t want a dangling hieroglyphic participle in your downstairs lavatory. I asked him how it worked out.
“The client was delighted,” he said, “only there was one problem. Whenever guests came over for a dinner party, there was always a long line, because whoever was in the bathroom wouldn’t come out.”
There are always alternatives. By now I am used to hearing patients extol the virtues of exotic treatments: Vicks VapoRub for toenail tinea, tea tree oil for most anything. Apple cider vinegar for everything else.
Then the other day Marcy surprised me with this:
“I stopped the minocycline,” she said, “Instead I started using celery, which I ground up and boiled and then froze and then applied to the face.”
A little bit of a production, perhaps – grinding, boiling, freezing. As long as it works ...
You need a different kind of doctor. “I see I won’t be able to shower for 3 days,” said the new patient.
My jaw dropped, but no words came out.
“It’s that sign you put up,” he said, “right on the exam room door.”
As I don’t usually read my own signs, I turned to look. The sign read:
“If you have no-showed without notice three times, we reserve the right to reschedule you at our convenience.”
“It says, ‘No-Showed,” I said. Not ‘No Showers.”
I resisted the urge to refer him to an optometrist.
This reminded me of another episode some time ago, when a patient listed his Chief Complaint as, “I want Lasik Surgery.”
“Forgive me,” I said, “but why would you ask a dermatologist for Lasik surgery?”
“Doesn’t the sign on your door say, “Boston Ophthalmology?” he asked.
“Upstairs,” I said. “Seventh floor.”
Negotiating with Father Time. We suspected porphyria, and ordered a 24-hour urine collection. “I’m a busy executive,” said the patient. “I haven’t got time to collect it for that long.”
“But it has to be a whole day ...”
“Fifteen hours,” he said. “I’ll give you 15 hours.”
“But we need ...”
“Eighteen hours. OK?”
“Well, not really. You see, the test has to be a whole day ...”
“All right, 21 hours. That’s my best offer.”
Maybe if I could get him to spend the day in that Egyptian bathroom ...
Dr. Rockoff practices dermatology in Brookline, Mass, and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His new book, “Act Like a Doctor, Think Like a Patient,” is now available on amazon.com and barnesandnoble.com. This is his second book. Write to him at [email protected].
FDA to streamline development of antimicrobials, susceptibility test devices
The Food and Drug Administration has released a draft guidance document intended to help drug sponsors and device manufacturers coordinate the development of new antimicrobial drugs and antimicrobial susceptibility test devices (ASTs).
The FDA said it wants the guidance document, entitled “Coordinated Development of Antimicrobial Drugs and Antimicrobial Susceptibility Test Devices,” to help harmonize “development of these products such that the AST device could be cleared either at the time of new drug approval or shortly thereafter.” The agency acknowledged in the guidance document that development of antimicrobial drugs and ASTs – which test for in vitro susceptibility of bacterial pathogens isolated from clinical specimens to antimicrobials – has traditionally occurred independently, with AST device development “often initiated following drug approval.” A coordinated approach to developing new antimicrobial drugs with AST devices ideally would minimize the time between the approval of a new antimicrobial drug and clearance of an AST device.
The FDA highlighted three key goals of the guidance document:
• Describe interactions between antimicrobial drug sponsors and AST device manufacturers to help improve coordinated development of a new antimicrobial drug and an AST device to streamline the clearance process.
• Explain the considerations for submitting separate applications to the Center for Drug Evaluation and Research and the Center for Devices and Radiological Health when seeking to facilitate clearance of an AST device as close in time as possible to antimicrobial drug approval.
• Emphasize that the review of the new antimicrobial drug product and AST device(s) will remain independent, and that coordinated development does not influence the review timelines for either product.
The FDA will accept comments and suggestions on the draft guidance document within 60 days of publication in the Federal Register.
On Twitter @richpizzi
The Food and Drug Administration has released a draft guidance document intended to help drug sponsors and device manufacturers coordinate the development of new antimicrobial drugs and antimicrobial susceptibility test devices (ASTs).
The FDA said it wants the guidance document, entitled “Coordinated Development of Antimicrobial Drugs and Antimicrobial Susceptibility Test Devices,” to help harmonize “development of these products such that the AST device could be cleared either at the time of new drug approval or shortly thereafter.” The agency acknowledged in the guidance document that development of antimicrobial drugs and ASTs – which test for in vitro susceptibility of bacterial pathogens isolated from clinical specimens to antimicrobials – has traditionally occurred independently, with AST device development “often initiated following drug approval.” A coordinated approach to developing new antimicrobial drugs with AST devices ideally would minimize the time between the approval of a new antimicrobial drug and clearance of an AST device.
The FDA highlighted three key goals of the guidance document:
• Describe interactions between antimicrobial drug sponsors and AST device manufacturers to help improve coordinated development of a new antimicrobial drug and an AST device to streamline the clearance process.
• Explain the considerations for submitting separate applications to the Center for Drug Evaluation and Research and the Center for Devices and Radiological Health when seeking to facilitate clearance of an AST device as close in time as possible to antimicrobial drug approval.
• Emphasize that the review of the new antimicrobial drug product and AST device(s) will remain independent, and that coordinated development does not influence the review timelines for either product.
The FDA will accept comments and suggestions on the draft guidance document within 60 days of publication in the Federal Register.
On Twitter @richpizzi
The Food and Drug Administration has released a draft guidance document intended to help drug sponsors and device manufacturers coordinate the development of new antimicrobial drugs and antimicrobial susceptibility test devices (ASTs).
The FDA said it wants the guidance document, entitled “Coordinated Development of Antimicrobial Drugs and Antimicrobial Susceptibility Test Devices,” to help harmonize “development of these products such that the AST device could be cleared either at the time of new drug approval or shortly thereafter.” The agency acknowledged in the guidance document that development of antimicrobial drugs and ASTs – which test for in vitro susceptibility of bacterial pathogens isolated from clinical specimens to antimicrobials – has traditionally occurred independently, with AST device development “often initiated following drug approval.” A coordinated approach to developing new antimicrobial drugs with AST devices ideally would minimize the time between the approval of a new antimicrobial drug and clearance of an AST device.
The FDA highlighted three key goals of the guidance document:
• Describe interactions between antimicrobial drug sponsors and AST device manufacturers to help improve coordinated development of a new antimicrobial drug and an AST device to streamline the clearance process.
• Explain the considerations for submitting separate applications to the Center for Drug Evaluation and Research and the Center for Devices and Radiological Health when seeking to facilitate clearance of an AST device as close in time as possible to antimicrobial drug approval.
• Emphasize that the review of the new antimicrobial drug product and AST device(s) will remain independent, and that coordinated development does not influence the review timelines for either product.
The FDA will accept comments and suggestions on the draft guidance document within 60 days of publication in the Federal Register.
On Twitter @richpizzi
Do as I say, not as I do! A futile plea
I am constantly amazed when parents come in complaining about their child’s nail biting or irritable attitude “no matter how many times I tell her” as they do these same things in front of me!
We have not evolved that far from our nonverbal ancestors to expect that words will speak louder than actions. Looking closely, you can see even very young infants gazing closely at their parents, then mirroring their facial expressions a few minutes later (because of slower processing). Mirroring is probably the correct word for this as the mirror neuron system of the brain has as its primary and crucial function allowing humans to copy what they see in others.
Children look to model, especially those who are slightly older and more adept than they are. Older siblings bask in this adoration at times and squeal in frustration at other times that their younger sister is “mocking” them by copying their speech and actions. When children are picking up serious negative behaviors from siblings or peers, particularly in adolescence, we need to coach parents to take action.
But watching parents is the most powerful or “salient” stimulus for learning. Some theorize that the long period of childhood evolved to allow children to learn the incredible amount of information necessary to live independently in our complex culture. This learning begins very early and requires close contact and careful observation of the minute details of how the parent survives every day.
Eating is a great primitive example of why children must model their parents. How do animals know which plants are poisonous? By watching others eat and spit, choke, or vomit. Entire families have nonpreferred foods passed on by modeling refusal as well as lack of exposure on the table. Conversely, picky eaters need to observe others, preferably admired peers and parents, eating those vegetables. (Tasting is also necessary, but that’s a topic for another day!) It is worth asking about family meals, without the distraction of a TV, as they are key moments to model nutritious eating for their lifetime.
In “underdeveloped” countries, infants are naturally carried everywhere and observing constantly. In our “developed” country, many infants spend hours each day at day care, modeling their caregivers or watching media examples of people interacting, which may not be the models parents would consciously choose. Parents often ask us about childcare, anxious about the extremely rare threat of abduction, when we should instead be advising them about what models they want for their children during this critical learning period.
Emotion cueing is a crucial component of modeling and an untaught constant of typical parent-child interaction. Crawling infants placed on a clear surface over a “visual cliff” that appeared to be a sudden precipice look to the parent’s affect to decide how to act. The mother was instructed to show fear or joy when her baby reached the apparent danger and looked up for a warning. When fear was shown, the infants backed off and cried. When joy was shown, the baby crawled gaily across the “cliff.” For parents who do not come by signaling confidence naturally but want to model this for their children, I advise they “fake it until you make it!”
Parents are instructing their progeny in how to feel and act in every situation, whether they know it or not. Confident parents model bravery; kind parents model compassion; flexible parents model resilience; patient parents model tolerance; anxious parents model caution; angry parents model aggression. Ignoring parents (think: on their cellphone, distracted, depressed, inebriated, or high) leave their children to feel confused and insecure. An adaptive child of an ignoring parent may demand information by crying, clinging, fighting with siblings, or hitting the parent. They are desperate for the parental attention to teach them and keep them safe. A more passive child may become increasingly inhibited in their exploration of the world. We need to consider possible modeling failures when such child reaction patterns are the complaint, and remember that the adverse model may not be in the room, requiring us to ask, “What other adult models does he see?”
Studies have shown that infants learn resilience when experiencing “mistakes” in parent-infant interaction; learning how to tolerate and repair an interaction that is not perfect. This is really good news for parents who feel that they must be perfect models for their children! For parents of anxious or obsessive children, I sometimes prescribe making mistakes and saying “Oh well,” as well as rewarding the child when they can say “Oh well” themselves. No child is too old to benefit from observing a parent apologize sincerely for a mistake.
Language is modeled, right down to accent. But when parents complain about their child cussing, raising their voice in anger, having an “attitude,” or “talking back,” it is worth asking (parent and child) “Where do you think they/you have heard talk like that?” It may be childcare providers, peers, TV, video games or online media (all of which may warrant a change), but it also may reflect interactions at home.
Children make stronger memories when emotions are high as these may signal danger, making recall more salient to survival. This salience helps explain the lasting detriments to learning and health of growing up with psychological abuse, marital discord, partner violence, mental illness, or criminal behavior (among the Adverse Childhood Experiences). Such experiences cause stress and a sense of the world as a dangerous place, but also become models for the child’s own later relationships as adults. While unavoidable, they can be buffered by parents’ explaining them and providing alternative positive modeling.
Watching the parent conduct their craft, a key component of apprenticeship and family businesses in the past, has been replaced by YouTube and avatars for learning physical skills. But “modeling the process” of pride in craftsmanship, persistence in a task, and recovering and starting over when things go awry are omitted from training videos. These are good reasons to assure that parents do chores, crafts, cooking, or camping with their children as some things will surely go wrong, giving parents the chance to model resilience and problem solving!
Although teens may protest conversations and activities, they are watching their parents for how to be a spouse, a neighbor, a friend, a leader, a citizen. Parents, who may be cutting their teens loose, need to continue to expect/require participation in family meals and outings. Those are opportunities to model adult-level interactions with each other and with the community as well as to talk about their activities at work, in volunteering, in charity, and in religious practice. The moral development of the adolescent is shaped by what they see to the degree that when parents state one moral code but violate it themselves (for example, cheating on taxes, running red lights), the teen is less likely to follow the principles long term that the parents have verbalized.
Parents often relate to us as though we were their own parents. While this “projection” can interfere with disclosure on touchy subjects, it is also an opportunity for us to model ways of relating and reacting from sympathizing with the 4-year-old screaming about vaccines to asking an 8-year-old why he thinks his parents are getting a divorce.
Parenting (and being a pediatrician) is an opportunity to enjoy reliving your youth or to get a “do over” of parts you would like to have different for your child. Playfulness and silliness model joy for the child that can last a lifetime.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University School of Medicine, Baltimore, and creator of CHADIS (www.CHADIS.com). She has no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. Email her at [email protected].
I am constantly amazed when parents come in complaining about their child’s nail biting or irritable attitude “no matter how many times I tell her” as they do these same things in front of me!
We have not evolved that far from our nonverbal ancestors to expect that words will speak louder than actions. Looking closely, you can see even very young infants gazing closely at their parents, then mirroring their facial expressions a few minutes later (because of slower processing). Mirroring is probably the correct word for this as the mirror neuron system of the brain has as its primary and crucial function allowing humans to copy what they see in others.
Children look to model, especially those who are slightly older and more adept than they are. Older siblings bask in this adoration at times and squeal in frustration at other times that their younger sister is “mocking” them by copying their speech and actions. When children are picking up serious negative behaviors from siblings or peers, particularly in adolescence, we need to coach parents to take action.
But watching parents is the most powerful or “salient” stimulus for learning. Some theorize that the long period of childhood evolved to allow children to learn the incredible amount of information necessary to live independently in our complex culture. This learning begins very early and requires close contact and careful observation of the minute details of how the parent survives every day.
Eating is a great primitive example of why children must model their parents. How do animals know which plants are poisonous? By watching others eat and spit, choke, or vomit. Entire families have nonpreferred foods passed on by modeling refusal as well as lack of exposure on the table. Conversely, picky eaters need to observe others, preferably admired peers and parents, eating those vegetables. (Tasting is also necessary, but that’s a topic for another day!) It is worth asking about family meals, without the distraction of a TV, as they are key moments to model nutritious eating for their lifetime.
In “underdeveloped” countries, infants are naturally carried everywhere and observing constantly. In our “developed” country, many infants spend hours each day at day care, modeling their caregivers or watching media examples of people interacting, which may not be the models parents would consciously choose. Parents often ask us about childcare, anxious about the extremely rare threat of abduction, when we should instead be advising them about what models they want for their children during this critical learning period.
Emotion cueing is a crucial component of modeling and an untaught constant of typical parent-child interaction. Crawling infants placed on a clear surface over a “visual cliff” that appeared to be a sudden precipice look to the parent’s affect to decide how to act. The mother was instructed to show fear or joy when her baby reached the apparent danger and looked up for a warning. When fear was shown, the infants backed off and cried. When joy was shown, the baby crawled gaily across the “cliff.” For parents who do not come by signaling confidence naturally but want to model this for their children, I advise they “fake it until you make it!”
Parents are instructing their progeny in how to feel and act in every situation, whether they know it or not. Confident parents model bravery; kind parents model compassion; flexible parents model resilience; patient parents model tolerance; anxious parents model caution; angry parents model aggression. Ignoring parents (think: on their cellphone, distracted, depressed, inebriated, or high) leave their children to feel confused and insecure. An adaptive child of an ignoring parent may demand information by crying, clinging, fighting with siblings, or hitting the parent. They are desperate for the parental attention to teach them and keep them safe. A more passive child may become increasingly inhibited in their exploration of the world. We need to consider possible modeling failures when such child reaction patterns are the complaint, and remember that the adverse model may not be in the room, requiring us to ask, “What other adult models does he see?”
Studies have shown that infants learn resilience when experiencing “mistakes” in parent-infant interaction; learning how to tolerate and repair an interaction that is not perfect. This is really good news for parents who feel that they must be perfect models for their children! For parents of anxious or obsessive children, I sometimes prescribe making mistakes and saying “Oh well,” as well as rewarding the child when they can say “Oh well” themselves. No child is too old to benefit from observing a parent apologize sincerely for a mistake.
Language is modeled, right down to accent. But when parents complain about their child cussing, raising their voice in anger, having an “attitude,” or “talking back,” it is worth asking (parent and child) “Where do you think they/you have heard talk like that?” It may be childcare providers, peers, TV, video games or online media (all of which may warrant a change), but it also may reflect interactions at home.
Children make stronger memories when emotions are high as these may signal danger, making recall more salient to survival. This salience helps explain the lasting detriments to learning and health of growing up with psychological abuse, marital discord, partner violence, mental illness, or criminal behavior (among the Adverse Childhood Experiences). Such experiences cause stress and a sense of the world as a dangerous place, but also become models for the child’s own later relationships as adults. While unavoidable, they can be buffered by parents’ explaining them and providing alternative positive modeling.
Watching the parent conduct their craft, a key component of apprenticeship and family businesses in the past, has been replaced by YouTube and avatars for learning physical skills. But “modeling the process” of pride in craftsmanship, persistence in a task, and recovering and starting over when things go awry are omitted from training videos. These are good reasons to assure that parents do chores, crafts, cooking, or camping with their children as some things will surely go wrong, giving parents the chance to model resilience and problem solving!
Although teens may protest conversations and activities, they are watching their parents for how to be a spouse, a neighbor, a friend, a leader, a citizen. Parents, who may be cutting their teens loose, need to continue to expect/require participation in family meals and outings. Those are opportunities to model adult-level interactions with each other and with the community as well as to talk about their activities at work, in volunteering, in charity, and in religious practice. The moral development of the adolescent is shaped by what they see to the degree that when parents state one moral code but violate it themselves (for example, cheating on taxes, running red lights), the teen is less likely to follow the principles long term that the parents have verbalized.
Parents often relate to us as though we were their own parents. While this “projection” can interfere with disclosure on touchy subjects, it is also an opportunity for us to model ways of relating and reacting from sympathizing with the 4-year-old screaming about vaccines to asking an 8-year-old why he thinks his parents are getting a divorce.
Parenting (and being a pediatrician) is an opportunity to enjoy reliving your youth or to get a “do over” of parts you would like to have different for your child. Playfulness and silliness model joy for the child that can last a lifetime.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University School of Medicine, Baltimore, and creator of CHADIS (www.CHADIS.com). She has no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. Email her at [email protected].
I am constantly amazed when parents come in complaining about their child’s nail biting or irritable attitude “no matter how many times I tell her” as they do these same things in front of me!
We have not evolved that far from our nonverbal ancestors to expect that words will speak louder than actions. Looking closely, you can see even very young infants gazing closely at their parents, then mirroring their facial expressions a few minutes later (because of slower processing). Mirroring is probably the correct word for this as the mirror neuron system of the brain has as its primary and crucial function allowing humans to copy what they see in others.
Children look to model, especially those who are slightly older and more adept than they are. Older siblings bask in this adoration at times and squeal in frustration at other times that their younger sister is “mocking” them by copying their speech and actions. When children are picking up serious negative behaviors from siblings or peers, particularly in adolescence, we need to coach parents to take action.
But watching parents is the most powerful or “salient” stimulus for learning. Some theorize that the long period of childhood evolved to allow children to learn the incredible amount of information necessary to live independently in our complex culture. This learning begins very early and requires close contact and careful observation of the minute details of how the parent survives every day.
Eating is a great primitive example of why children must model their parents. How do animals know which plants are poisonous? By watching others eat and spit, choke, or vomit. Entire families have nonpreferred foods passed on by modeling refusal as well as lack of exposure on the table. Conversely, picky eaters need to observe others, preferably admired peers and parents, eating those vegetables. (Tasting is also necessary, but that’s a topic for another day!) It is worth asking about family meals, without the distraction of a TV, as they are key moments to model nutritious eating for their lifetime.
In “underdeveloped” countries, infants are naturally carried everywhere and observing constantly. In our “developed” country, many infants spend hours each day at day care, modeling their caregivers or watching media examples of people interacting, which may not be the models parents would consciously choose. Parents often ask us about childcare, anxious about the extremely rare threat of abduction, when we should instead be advising them about what models they want for their children during this critical learning period.
Emotion cueing is a crucial component of modeling and an untaught constant of typical parent-child interaction. Crawling infants placed on a clear surface over a “visual cliff” that appeared to be a sudden precipice look to the parent’s affect to decide how to act. The mother was instructed to show fear or joy when her baby reached the apparent danger and looked up for a warning. When fear was shown, the infants backed off and cried. When joy was shown, the baby crawled gaily across the “cliff.” For parents who do not come by signaling confidence naturally but want to model this for their children, I advise they “fake it until you make it!”
Parents are instructing their progeny in how to feel and act in every situation, whether they know it or not. Confident parents model bravery; kind parents model compassion; flexible parents model resilience; patient parents model tolerance; anxious parents model caution; angry parents model aggression. Ignoring parents (think: on their cellphone, distracted, depressed, inebriated, or high) leave their children to feel confused and insecure. An adaptive child of an ignoring parent may demand information by crying, clinging, fighting with siblings, or hitting the parent. They are desperate for the parental attention to teach them and keep them safe. A more passive child may become increasingly inhibited in their exploration of the world. We need to consider possible modeling failures when such child reaction patterns are the complaint, and remember that the adverse model may not be in the room, requiring us to ask, “What other adult models does he see?”
Studies have shown that infants learn resilience when experiencing “mistakes” in parent-infant interaction; learning how to tolerate and repair an interaction that is not perfect. This is really good news for parents who feel that they must be perfect models for their children! For parents of anxious or obsessive children, I sometimes prescribe making mistakes and saying “Oh well,” as well as rewarding the child when they can say “Oh well” themselves. No child is too old to benefit from observing a parent apologize sincerely for a mistake.
Language is modeled, right down to accent. But when parents complain about their child cussing, raising their voice in anger, having an “attitude,” or “talking back,” it is worth asking (parent and child) “Where do you think they/you have heard talk like that?” It may be childcare providers, peers, TV, video games or online media (all of which may warrant a change), but it also may reflect interactions at home.
Children make stronger memories when emotions are high as these may signal danger, making recall more salient to survival. This salience helps explain the lasting detriments to learning and health of growing up with psychological abuse, marital discord, partner violence, mental illness, or criminal behavior (among the Adverse Childhood Experiences). Such experiences cause stress and a sense of the world as a dangerous place, but also become models for the child’s own later relationships as adults. While unavoidable, they can be buffered by parents’ explaining them and providing alternative positive modeling.
Watching the parent conduct their craft, a key component of apprenticeship and family businesses in the past, has been replaced by YouTube and avatars for learning physical skills. But “modeling the process” of pride in craftsmanship, persistence in a task, and recovering and starting over when things go awry are omitted from training videos. These are good reasons to assure that parents do chores, crafts, cooking, or camping with their children as some things will surely go wrong, giving parents the chance to model resilience and problem solving!
Although teens may protest conversations and activities, they are watching their parents for how to be a spouse, a neighbor, a friend, a leader, a citizen. Parents, who may be cutting their teens loose, need to continue to expect/require participation in family meals and outings. Those are opportunities to model adult-level interactions with each other and with the community as well as to talk about their activities at work, in volunteering, in charity, and in religious practice. The moral development of the adolescent is shaped by what they see to the degree that when parents state one moral code but violate it themselves (for example, cheating on taxes, running red lights), the teen is less likely to follow the principles long term that the parents have verbalized.
Parents often relate to us as though we were their own parents. While this “projection” can interfere with disclosure on touchy subjects, it is also an opportunity for us to model ways of relating and reacting from sympathizing with the 4-year-old screaming about vaccines to asking an 8-year-old why he thinks his parents are getting a divorce.
Parenting (and being a pediatrician) is an opportunity to enjoy reliving your youth or to get a “do over” of parts you would like to have different for your child. Playfulness and silliness model joy for the child that can last a lifetime.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University School of Medicine, Baltimore, and creator of CHADIS (www.CHADIS.com). She has no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to Frontline Medical News. Email her at [email protected].