User login
Antiplatelet therapy could treat Alzheimer’s disease

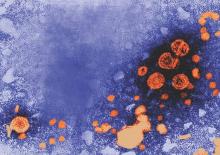
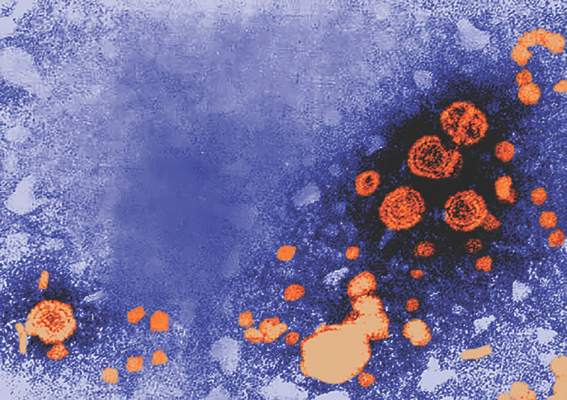
Image by Andre E.X. Brown
Antiplatelet drugs can significantly reduce amyloid plaques in cerebral vessels of transgenic mice with Alzheimer’s disease, according to new research.
The study revealed a mechanism for direct involvement of platelets in the progression of Alzheimer’s disease, and investigators believe this could be of great importance for the treatment of Alzheimer’s patients.
Alzheimer’s disease is characterized by the formation of amyloid aggregates and deposits of amyloid in the brain. The amyloid deposits damage the structure and function of nerve tissue in the brain and lead to the loss of neuronal cells and cognitive capability.
Amyloid deposits in Alzheimer’s disease occur not only in the brain parenchyma, but also in blood vessels in the brain. The current study, published in Science Signaling, deals with the vascular form of the disease.
Previous research demonstrated that platelets attach to amyloid deposits in the vessel wall, which leads to ongoing platelet activation in mice. The platelets then form a hemostatic plug, which occludes vessels in the brain and leads to insufficient perfusion of the surrounding tissue.
Investigators have now determined that the protein amyloid-ß binds to a specific integrin on the platelet surface that is important for the aggregation of platelets.
This binding induces the release of adenosine diphosphate and the chaperone protein clusterin and supports the formation of amyloid plaques.
In cell culture experiments, the investigators analyzed platelets from 5 patients with Glanzmann’s thrombasthenia, a hereditary defect of platelet activation, and found no amyloid plaques.
The team then treated Alzheimer’s transgenic mice with the antiplatelet agent clopidogrel. The mice exhibited reduced platelet activation and significantly reduced amyloid plaque formation, which improved the perfusion of the brain during the 3-month treatment with the drug.
The investigators suggest that antiplatelet therapy may alleviate fibril formation in cerebral vessels of Alzheimer’s disease patients. ![]()

Image by Andre E.X. Brown
Antiplatelet drugs can significantly reduce amyloid plaques in cerebral vessels of transgenic mice with Alzheimer’s disease, according to new research.
The study revealed a mechanism for direct involvement of platelets in the progression of Alzheimer’s disease, and investigators believe this could be of great importance for the treatment of Alzheimer’s patients.
Alzheimer’s disease is characterized by the formation of amyloid aggregates and deposits of amyloid in the brain. The amyloid deposits damage the structure and function of nerve tissue in the brain and lead to the loss of neuronal cells and cognitive capability.
Amyloid deposits in Alzheimer’s disease occur not only in the brain parenchyma, but also in blood vessels in the brain. The current study, published in Science Signaling, deals with the vascular form of the disease.
Previous research demonstrated that platelets attach to amyloid deposits in the vessel wall, which leads to ongoing platelet activation in mice. The platelets then form a hemostatic plug, which occludes vessels in the brain and leads to insufficient perfusion of the surrounding tissue.
Investigators have now determined that the protein amyloid-ß binds to a specific integrin on the platelet surface that is important for the aggregation of platelets.
This binding induces the release of adenosine diphosphate and the chaperone protein clusterin and supports the formation of amyloid plaques.
In cell culture experiments, the investigators analyzed platelets from 5 patients with Glanzmann’s thrombasthenia, a hereditary defect of platelet activation, and found no amyloid plaques.
The team then treated Alzheimer’s transgenic mice with the antiplatelet agent clopidogrel. The mice exhibited reduced platelet activation and significantly reduced amyloid plaque formation, which improved the perfusion of the brain during the 3-month treatment with the drug.
The investigators suggest that antiplatelet therapy may alleviate fibril formation in cerebral vessels of Alzheimer’s disease patients. ![]()

Image by Andre E.X. Brown
Antiplatelet drugs can significantly reduce amyloid plaques in cerebral vessels of transgenic mice with Alzheimer’s disease, according to new research.
The study revealed a mechanism for direct involvement of platelets in the progression of Alzheimer’s disease, and investigators believe this could be of great importance for the treatment of Alzheimer’s patients.
Alzheimer’s disease is characterized by the formation of amyloid aggregates and deposits of amyloid in the brain. The amyloid deposits damage the structure and function of nerve tissue in the brain and lead to the loss of neuronal cells and cognitive capability.
Amyloid deposits in Alzheimer’s disease occur not only in the brain parenchyma, but also in blood vessels in the brain. The current study, published in Science Signaling, deals with the vascular form of the disease.
Previous research demonstrated that platelets attach to amyloid deposits in the vessel wall, which leads to ongoing platelet activation in mice. The platelets then form a hemostatic plug, which occludes vessels in the brain and leads to insufficient perfusion of the surrounding tissue.
Investigators have now determined that the protein amyloid-ß binds to a specific integrin on the platelet surface that is important for the aggregation of platelets.
This binding induces the release of adenosine diphosphate and the chaperone protein clusterin and supports the formation of amyloid plaques.
In cell culture experiments, the investigators analyzed platelets from 5 patients with Glanzmann’s thrombasthenia, a hereditary defect of platelet activation, and found no amyloid plaques.
The team then treated Alzheimer’s transgenic mice with the antiplatelet agent clopidogrel. The mice exhibited reduced platelet activation and significantly reduced amyloid plaque formation, which improved the perfusion of the brain during the 3-month treatment with the drug.
The investigators suggest that antiplatelet therapy may alleviate fibril formation in cerebral vessels of Alzheimer’s disease patients. ![]()
EULAR-PReS guidelines aim to aid pediatric to adult care transition
LONDON – The first European guidelines developed to help the transition of young people from pediatric to adult rheumatology care within Europe were announced at the European Congress of Rheumatology.
The key aim of the guidelines, which have been jointly written by the European League Against Rheumatism (EULAR) and the Paediatric Rheumatology European Society (PReS), is to make the transition process more consistent across rheumatology practices throughout Europe, which in turn should help to ensure both the continuity and the quality of clinical care, explained Dr. Helen E. Fosterof Newcastle (England) University.
“There is evidence that there has been a long-standing problem of young people growing up with their condition moving to adult care and either falling between the services or being lost to follow-up, or there has not been continuity of care,” she said in an interview ahead of presenting the new EULAR/PReS guidelines at the congress.
“All in all, that’s translated into poorer health outcomes for young people,” said Dr. Foster, who was one of the main convenors of the EULAR/PReS Working Party for Transitional Care Management for Adolescents and Young People.
The premise is to try to provide practical recommendations that clinicians can use to help young people in their care from the age of 11 years and older as they get ready for the transfer to adult services. The latter process can occur anywhere from 16 to 19 years of age, Dr. Foster said, but it is important to try start the transition process early and get young people more involved and responsible for their own care.
“The idea is that young people are supported to be in control of their condition, that they can cope with being seen on their own in clinic, that they are getting on with their lives, and ultimately that they have a better outcome, which includes becoming healthy, getting a job, living independently, and having a family,” she said. The age at transfer is flexible and needs to fit with the young person’s home and school life. Ideally, it occurs at a time when their disease and medication are stable, they are attending routine appointments, and generally able to be independent and cope with their condition.
EULAR/PReS transition guidelines: 12 recommendations
• Access to high-quality coordinated transition care services should be available to all young people.
• Transition should ‘start early’ (11 years of age) or directly after diagnosis.
• Direct communication is needed between young people and their families and pediatric and adult care providers.
• Each young person should have an individualized transition plan.
• There should be a written transition policy within all relevant services; this should be regularly agreed and updated.
• The multidisciplinary team involved in transitional care should be clearly defined in a written document.
• Transition services should address the complexity of adolescent and young adult development.
• There must be an agreed upon and written transfer document.
• Health care teams should be given appropriate training in adolescent and young adult rheumatic diseases.
• Secure funding is needed for uninterrupted clinical care and transition into adult services.
• An open digital platform should host the recommendations and support tools and information.
• More evidence is needed to demonstrate the outcomes of the transition to adult services.
Developing the guidelines
Together with Dr. Kirsten Minden of the German Rheumatism Research Centre Berlin (DRFZ), Dr. Foster chaired the international, multidisciplinary EULAR/PReS Working Party to review existing national and international guidelines, consensus statements, and other supporting evidence on transitional care management in childhood-onset rheumatic illness.
The remit was to develop recommendations to facilitate optimal transitional care management in rheumatology across different European countries. As such, the recommendations cover both the ideal situation as well as the bare minimum requirements to hopefully allow widespread adoption. To this end, the working party performed a systematic literature review according to EULAR standard operating procedures. They developed a set of 12 recommendations based on the evidence they reviewed.
There are 47 different health systems within Europe, all running according to different health policies set by different governments, Dr. Minden observed. In fact, only a handful of countries have specific transition care policies or pathways, so the aim was to try to develop recommendations that would work across the board while giving some ideas on how to improve existing strategies further.
She noted that some examples of existing transition programs are “Growing up and moving on” in the United Kingdom (Pediatr Transplant. 2005;9:364-72), “On your own feet ahead” in the Netherlands (BMC Health Serv Res. 2014;14:47), and “Devices for Optimization of Transfer and Transition of Adolescents with Rheumatic Disorders (DON’T RETARD)” in Belgium (Rheumatology [Oxford]. 2016;55:133-42). Of these, two are specific to the transition of young people with juvenile idiopathic arthritis (JIA) and one is for rheumatologic conditions in general.
Core elements of these programs are the need to provide written information and have a transition care plan, the allocation of a dedicated transition coordinator, and an individualized transition plan for each patient, Dr. Minden said. These elements are also part of the EULAR/PReS transition guidelines.
One of the issues to be addressed, however, is whether these transition programs actually work in the long term. “Transitional care services in rheumatology are beginning to happen and their further development can surely be facilitated by the provision of tool kits and resources for health care providers and patients,” she noted. Some of the tools already exist, so the challenge now is to get these available to all so that there can be a wider dissemination of knowledge.
The North American perspective
Both the American Academy of Pediatrics and the Canadian Pediatric Society have issued general guidance on how to transition young people from pediatric to adult services, said Dr. Lori. B. Tucker, a pediatric specialist working at BC Children’s Hospital in Vancouver, which runs the ON TRAC (Transitioning Responsibly to Adult Care) program. This is a province-wide program aimed at supporting young people between the ages of 12 and 24 years with chronic health conditions and their families to transition from pediatric to adult health care services.
The ON TRAC program includes online and mobile-enabled checklists that can be used with young people and their families, although Dr. Tucker noted that the program had perhaps not been as successful as had been hoped. Another Canadian initiative specific to rheumatology practice is the RACER (Readiness for Adult Care in Rheumatology) questionnaire. This was developed to assess how ready young people with chronic ailments were to transition to adult service.
Dr. Tucker also highlighted the YARD (Young Adult Rheumatic Diseases) clinic at her institution, set up for those aged 18 years or older with a definite diagnosis of rheumatic disease. Parents are not allowed within the clinic so as to enable young adults to take responsibility for their overall care and collaborate with their health care providers. The clinic provides education, assistance with separation independence, and other issues pertinent to this young population of patients, and it also aims to encourage adherence to appointments and treatments.
“Collaboration between pediatric rheumatologists and adult colleagues is critical to improve the outcomes of young adults with rheumatic diseases,” Dr. Tucker said. She added, “Better articulated guidelines for transition care and use of new tools have great potential to improve the care of these patients ‘lost in-between.’ ”
Why the need for the EULAR/PReS recommendations?
Dr. Foster noted that, in many countries, there is a natural break between pediatric and adult care, with young people often moving from one center to another, perhaps in another part of the country. An important part of the transition process is therefore ensuring that there are appropriately trained staff members and good communication between centers to ensure that young people don’t get lost during the move.
“This is everyone’s business,” Dr. Foster said at the congress. “It is a shared responsibility to get it right.” That means adult and pediatric health care teams work together. Care needs to be “holistic,” she added, and cover medical, psychosocial, vocational issues, and be “developmentally appropriate throughout.” Young people also need to be involved from the start of the process, beginning early and continuing into young adulthood.
The recommendations aim to be flexible so that they can be widely implemented by health care teams throughout Europe. “It is not ‘one size fits all,” Dr. Foster acknowledged in the interview, noting the importance of being realistic and recognizing the differences between health systems, resources, and access across Europe.
Dr. Foster, who trained in adult rheumatology before turning to pediatric rheumatology, noted that there are existing resources that can be used and although funding will be an issue on some levels, there are things that can be done by using existing tools and resources.
“We don’t want to reinvent the wheel. We want to share best practice and resources,” she said. Indeed, one of the recommendations is that all the guidelines and all the resources used to develop them are made publicly available via an electronic platform so that anybody involved in the care of a young person with rheumatic disease, as well as the young person and their family, can access them.
“Transitional care is key to improving long-term outcomes for young people with rheumatic disease,” Dr. Foster concluded. The EULAR/PReS transition care management guidelines have been developed with the engagement of all relevant stakeholders, she said, so they should be widely applicable and “important levers for change” throughout Europe. “Implementation will require funding, but also our will and energy to make them actually work in practice.”
The EULAR/PReS transition guidelines are being finalized and will be published soon in Annals of the Rheumatic Diseases.
Dr. Foster, Dr. Minden, and Dr. Tucker had no disclosures relevant to the development of the recommendations.
LONDON – The first European guidelines developed to help the transition of young people from pediatric to adult rheumatology care within Europe were announced at the European Congress of Rheumatology.
The key aim of the guidelines, which have been jointly written by the European League Against Rheumatism (EULAR) and the Paediatric Rheumatology European Society (PReS), is to make the transition process more consistent across rheumatology practices throughout Europe, which in turn should help to ensure both the continuity and the quality of clinical care, explained Dr. Helen E. Fosterof Newcastle (England) University.
“There is evidence that there has been a long-standing problem of young people growing up with their condition moving to adult care and either falling between the services or being lost to follow-up, or there has not been continuity of care,” she said in an interview ahead of presenting the new EULAR/PReS guidelines at the congress.
“All in all, that’s translated into poorer health outcomes for young people,” said Dr. Foster, who was one of the main convenors of the EULAR/PReS Working Party for Transitional Care Management for Adolescents and Young People.
The premise is to try to provide practical recommendations that clinicians can use to help young people in their care from the age of 11 years and older as they get ready for the transfer to adult services. The latter process can occur anywhere from 16 to 19 years of age, Dr. Foster said, but it is important to try start the transition process early and get young people more involved and responsible for their own care.
“The idea is that young people are supported to be in control of their condition, that they can cope with being seen on their own in clinic, that they are getting on with their lives, and ultimately that they have a better outcome, which includes becoming healthy, getting a job, living independently, and having a family,” she said. The age at transfer is flexible and needs to fit with the young person’s home and school life. Ideally, it occurs at a time when their disease and medication are stable, they are attending routine appointments, and generally able to be independent and cope with their condition.
EULAR/PReS transition guidelines: 12 recommendations
• Access to high-quality coordinated transition care services should be available to all young people.
• Transition should ‘start early’ (11 years of age) or directly after diagnosis.
• Direct communication is needed between young people and their families and pediatric and adult care providers.
• Each young person should have an individualized transition plan.
• There should be a written transition policy within all relevant services; this should be regularly agreed and updated.
• The multidisciplinary team involved in transitional care should be clearly defined in a written document.
• Transition services should address the complexity of adolescent and young adult development.
• There must be an agreed upon and written transfer document.
• Health care teams should be given appropriate training in adolescent and young adult rheumatic diseases.
• Secure funding is needed for uninterrupted clinical care and transition into adult services.
• An open digital platform should host the recommendations and support tools and information.
• More evidence is needed to demonstrate the outcomes of the transition to adult services.
Developing the guidelines
Together with Dr. Kirsten Minden of the German Rheumatism Research Centre Berlin (DRFZ), Dr. Foster chaired the international, multidisciplinary EULAR/PReS Working Party to review existing national and international guidelines, consensus statements, and other supporting evidence on transitional care management in childhood-onset rheumatic illness.
The remit was to develop recommendations to facilitate optimal transitional care management in rheumatology across different European countries. As such, the recommendations cover both the ideal situation as well as the bare minimum requirements to hopefully allow widespread adoption. To this end, the working party performed a systematic literature review according to EULAR standard operating procedures. They developed a set of 12 recommendations based on the evidence they reviewed.
There are 47 different health systems within Europe, all running according to different health policies set by different governments, Dr. Minden observed. In fact, only a handful of countries have specific transition care policies or pathways, so the aim was to try to develop recommendations that would work across the board while giving some ideas on how to improve existing strategies further.
She noted that some examples of existing transition programs are “Growing up and moving on” in the United Kingdom (Pediatr Transplant. 2005;9:364-72), “On your own feet ahead” in the Netherlands (BMC Health Serv Res. 2014;14:47), and “Devices for Optimization of Transfer and Transition of Adolescents with Rheumatic Disorders (DON’T RETARD)” in Belgium (Rheumatology [Oxford]. 2016;55:133-42). Of these, two are specific to the transition of young people with juvenile idiopathic arthritis (JIA) and one is for rheumatologic conditions in general.
Core elements of these programs are the need to provide written information and have a transition care plan, the allocation of a dedicated transition coordinator, and an individualized transition plan for each patient, Dr. Minden said. These elements are also part of the EULAR/PReS transition guidelines.
One of the issues to be addressed, however, is whether these transition programs actually work in the long term. “Transitional care services in rheumatology are beginning to happen and their further development can surely be facilitated by the provision of tool kits and resources for health care providers and patients,” she noted. Some of the tools already exist, so the challenge now is to get these available to all so that there can be a wider dissemination of knowledge.
The North American perspective
Both the American Academy of Pediatrics and the Canadian Pediatric Society have issued general guidance on how to transition young people from pediatric to adult services, said Dr. Lori. B. Tucker, a pediatric specialist working at BC Children’s Hospital in Vancouver, which runs the ON TRAC (Transitioning Responsibly to Adult Care) program. This is a province-wide program aimed at supporting young people between the ages of 12 and 24 years with chronic health conditions and their families to transition from pediatric to adult health care services.
The ON TRAC program includes online and mobile-enabled checklists that can be used with young people and their families, although Dr. Tucker noted that the program had perhaps not been as successful as had been hoped. Another Canadian initiative specific to rheumatology practice is the RACER (Readiness for Adult Care in Rheumatology) questionnaire. This was developed to assess how ready young people with chronic ailments were to transition to adult service.
Dr. Tucker also highlighted the YARD (Young Adult Rheumatic Diseases) clinic at her institution, set up for those aged 18 years or older with a definite diagnosis of rheumatic disease. Parents are not allowed within the clinic so as to enable young adults to take responsibility for their overall care and collaborate with their health care providers. The clinic provides education, assistance with separation independence, and other issues pertinent to this young population of patients, and it also aims to encourage adherence to appointments and treatments.
“Collaboration between pediatric rheumatologists and adult colleagues is critical to improve the outcomes of young adults with rheumatic diseases,” Dr. Tucker said. She added, “Better articulated guidelines for transition care and use of new tools have great potential to improve the care of these patients ‘lost in-between.’ ”
Why the need for the EULAR/PReS recommendations?
Dr. Foster noted that, in many countries, there is a natural break between pediatric and adult care, with young people often moving from one center to another, perhaps in another part of the country. An important part of the transition process is therefore ensuring that there are appropriately trained staff members and good communication between centers to ensure that young people don’t get lost during the move.
“This is everyone’s business,” Dr. Foster said at the congress. “It is a shared responsibility to get it right.” That means adult and pediatric health care teams work together. Care needs to be “holistic,” she added, and cover medical, psychosocial, vocational issues, and be “developmentally appropriate throughout.” Young people also need to be involved from the start of the process, beginning early and continuing into young adulthood.
The recommendations aim to be flexible so that they can be widely implemented by health care teams throughout Europe. “It is not ‘one size fits all,” Dr. Foster acknowledged in the interview, noting the importance of being realistic and recognizing the differences between health systems, resources, and access across Europe.
Dr. Foster, who trained in adult rheumatology before turning to pediatric rheumatology, noted that there are existing resources that can be used and although funding will be an issue on some levels, there are things that can be done by using existing tools and resources.
“We don’t want to reinvent the wheel. We want to share best practice and resources,” she said. Indeed, one of the recommendations is that all the guidelines and all the resources used to develop them are made publicly available via an electronic platform so that anybody involved in the care of a young person with rheumatic disease, as well as the young person and their family, can access them.
“Transitional care is key to improving long-term outcomes for young people with rheumatic disease,” Dr. Foster concluded. The EULAR/PReS transition care management guidelines have been developed with the engagement of all relevant stakeholders, she said, so they should be widely applicable and “important levers for change” throughout Europe. “Implementation will require funding, but also our will and energy to make them actually work in practice.”
The EULAR/PReS transition guidelines are being finalized and will be published soon in Annals of the Rheumatic Diseases.
Dr. Foster, Dr. Minden, and Dr. Tucker had no disclosures relevant to the development of the recommendations.
LONDON – The first European guidelines developed to help the transition of young people from pediatric to adult rheumatology care within Europe were announced at the European Congress of Rheumatology.
The key aim of the guidelines, which have been jointly written by the European League Against Rheumatism (EULAR) and the Paediatric Rheumatology European Society (PReS), is to make the transition process more consistent across rheumatology practices throughout Europe, which in turn should help to ensure both the continuity and the quality of clinical care, explained Dr. Helen E. Fosterof Newcastle (England) University.
“There is evidence that there has been a long-standing problem of young people growing up with their condition moving to adult care and either falling between the services or being lost to follow-up, or there has not been continuity of care,” she said in an interview ahead of presenting the new EULAR/PReS guidelines at the congress.
“All in all, that’s translated into poorer health outcomes for young people,” said Dr. Foster, who was one of the main convenors of the EULAR/PReS Working Party for Transitional Care Management for Adolescents and Young People.
The premise is to try to provide practical recommendations that clinicians can use to help young people in their care from the age of 11 years and older as they get ready for the transfer to adult services. The latter process can occur anywhere from 16 to 19 years of age, Dr. Foster said, but it is important to try start the transition process early and get young people more involved and responsible for their own care.
“The idea is that young people are supported to be in control of their condition, that they can cope with being seen on their own in clinic, that they are getting on with their lives, and ultimately that they have a better outcome, which includes becoming healthy, getting a job, living independently, and having a family,” she said. The age at transfer is flexible and needs to fit with the young person’s home and school life. Ideally, it occurs at a time when their disease and medication are stable, they are attending routine appointments, and generally able to be independent and cope with their condition.
EULAR/PReS transition guidelines: 12 recommendations
• Access to high-quality coordinated transition care services should be available to all young people.
• Transition should ‘start early’ (11 years of age) or directly after diagnosis.
• Direct communication is needed between young people and their families and pediatric and adult care providers.
• Each young person should have an individualized transition plan.
• There should be a written transition policy within all relevant services; this should be regularly agreed and updated.
• The multidisciplinary team involved in transitional care should be clearly defined in a written document.
• Transition services should address the complexity of adolescent and young adult development.
• There must be an agreed upon and written transfer document.
• Health care teams should be given appropriate training in adolescent and young adult rheumatic diseases.
• Secure funding is needed for uninterrupted clinical care and transition into adult services.
• An open digital platform should host the recommendations and support tools and information.
• More evidence is needed to demonstrate the outcomes of the transition to adult services.
Developing the guidelines
Together with Dr. Kirsten Minden of the German Rheumatism Research Centre Berlin (DRFZ), Dr. Foster chaired the international, multidisciplinary EULAR/PReS Working Party to review existing national and international guidelines, consensus statements, and other supporting evidence on transitional care management in childhood-onset rheumatic illness.
The remit was to develop recommendations to facilitate optimal transitional care management in rheumatology across different European countries. As such, the recommendations cover both the ideal situation as well as the bare minimum requirements to hopefully allow widespread adoption. To this end, the working party performed a systematic literature review according to EULAR standard operating procedures. They developed a set of 12 recommendations based on the evidence they reviewed.
There are 47 different health systems within Europe, all running according to different health policies set by different governments, Dr. Minden observed. In fact, only a handful of countries have specific transition care policies or pathways, so the aim was to try to develop recommendations that would work across the board while giving some ideas on how to improve existing strategies further.
She noted that some examples of existing transition programs are “Growing up and moving on” in the United Kingdom (Pediatr Transplant. 2005;9:364-72), “On your own feet ahead” in the Netherlands (BMC Health Serv Res. 2014;14:47), and “Devices for Optimization of Transfer and Transition of Adolescents with Rheumatic Disorders (DON’T RETARD)” in Belgium (Rheumatology [Oxford]. 2016;55:133-42). Of these, two are specific to the transition of young people with juvenile idiopathic arthritis (JIA) and one is for rheumatologic conditions in general.
Core elements of these programs are the need to provide written information and have a transition care plan, the allocation of a dedicated transition coordinator, and an individualized transition plan for each patient, Dr. Minden said. These elements are also part of the EULAR/PReS transition guidelines.
One of the issues to be addressed, however, is whether these transition programs actually work in the long term. “Transitional care services in rheumatology are beginning to happen and their further development can surely be facilitated by the provision of tool kits and resources for health care providers and patients,” she noted. Some of the tools already exist, so the challenge now is to get these available to all so that there can be a wider dissemination of knowledge.
The North American perspective
Both the American Academy of Pediatrics and the Canadian Pediatric Society have issued general guidance on how to transition young people from pediatric to adult services, said Dr. Lori. B. Tucker, a pediatric specialist working at BC Children’s Hospital in Vancouver, which runs the ON TRAC (Transitioning Responsibly to Adult Care) program. This is a province-wide program aimed at supporting young people between the ages of 12 and 24 years with chronic health conditions and their families to transition from pediatric to adult health care services.
The ON TRAC program includes online and mobile-enabled checklists that can be used with young people and their families, although Dr. Tucker noted that the program had perhaps not been as successful as had been hoped. Another Canadian initiative specific to rheumatology practice is the RACER (Readiness for Adult Care in Rheumatology) questionnaire. This was developed to assess how ready young people with chronic ailments were to transition to adult service.
Dr. Tucker also highlighted the YARD (Young Adult Rheumatic Diseases) clinic at her institution, set up for those aged 18 years or older with a definite diagnosis of rheumatic disease. Parents are not allowed within the clinic so as to enable young adults to take responsibility for their overall care and collaborate with their health care providers. The clinic provides education, assistance with separation independence, and other issues pertinent to this young population of patients, and it also aims to encourage adherence to appointments and treatments.
“Collaboration between pediatric rheumatologists and adult colleagues is critical to improve the outcomes of young adults with rheumatic diseases,” Dr. Tucker said. She added, “Better articulated guidelines for transition care and use of new tools have great potential to improve the care of these patients ‘lost in-between.’ ”
Why the need for the EULAR/PReS recommendations?
Dr. Foster noted that, in many countries, there is a natural break between pediatric and adult care, with young people often moving from one center to another, perhaps in another part of the country. An important part of the transition process is therefore ensuring that there are appropriately trained staff members and good communication between centers to ensure that young people don’t get lost during the move.
“This is everyone’s business,” Dr. Foster said at the congress. “It is a shared responsibility to get it right.” That means adult and pediatric health care teams work together. Care needs to be “holistic,” she added, and cover medical, psychosocial, vocational issues, and be “developmentally appropriate throughout.” Young people also need to be involved from the start of the process, beginning early and continuing into young adulthood.
The recommendations aim to be flexible so that they can be widely implemented by health care teams throughout Europe. “It is not ‘one size fits all,” Dr. Foster acknowledged in the interview, noting the importance of being realistic and recognizing the differences between health systems, resources, and access across Europe.
Dr. Foster, who trained in adult rheumatology before turning to pediatric rheumatology, noted that there are existing resources that can be used and although funding will be an issue on some levels, there are things that can be done by using existing tools and resources.
“We don’t want to reinvent the wheel. We want to share best practice and resources,” she said. Indeed, one of the recommendations is that all the guidelines and all the resources used to develop them are made publicly available via an electronic platform so that anybody involved in the care of a young person with rheumatic disease, as well as the young person and their family, can access them.
“Transitional care is key to improving long-term outcomes for young people with rheumatic disease,” Dr. Foster concluded. The EULAR/PReS transition care management guidelines have been developed with the engagement of all relevant stakeholders, she said, so they should be widely applicable and “important levers for change” throughout Europe. “Implementation will require funding, but also our will and energy to make them actually work in practice.”
The EULAR/PReS transition guidelines are being finalized and will be published soon in Annals of the Rheumatic Diseases.
Dr. Foster, Dr. Minden, and Dr. Tucker had no disclosures relevant to the development of the recommendations.
AT THE EULAR 2016 CONGRESS
Aesthetic Dermatology: Synthetic second skin
Hot off the presses, a new so-called “second skin” is being redeveloped and rebranded for use in both cosmetic and medical dermatology. But what is this substance, and will it hold up to all the claims the manufacturer and research team suggest?
Recently described in Nature Materials, the liquid polymer developed by chemical engineers at MIT is a synthetic, adherent silicone-based film that lies perfectly invisibly on the skin – providing a pulling or temporary tightening of the skin. The product was initially marketed by the company Living Proof as “Neotensil” [an acronym for (Neo) new, (T) transforming, (E) elastic, (N) non-invasive, (S) supportive, (I) invisible, and immediate (L) layer solution]. When applied to the area under the eye, the product creates a so-called “Spanx” effect or tightening of periorbital skin.
The material – called XPL – is delivered in a two-step sequential process. First, a polysiloxane cream is applied to the skin, followed by a platinum catalyst that induces the polymer to harden and tighten the skin underneath. The product uses patented Strateris technology, which is described as creating invisible “shapewear” for the eye; a film that tightens, smooths, and lifts the appearance of skin for up to 24 hours. It was briefly on the market in 2014-2015, then taken off the market to be redeveloped.
Does it work? Yes. Although it takes about an hour to take effect, the clinical results are jaw dropping. However, it also has its drawbacks. The polymer – which hardens within 2 minutes – must be applied to clean skin, with no creams or makeup whatsoever. And makeup cannot be applied over the treated area either, as the area looks irregular and uneven with makeup. This is a very difficult obstacle to overcome for many female patients.
Additionally, to take off the product, the polymer must be dissolved with a special chemical remover that is packaged with the product. Without this key component, it is very difficult and very irritating to remove. Although none of the patients I have used this product on have developed allergic reactions, any synthetic polymer, particularly one with adherent properties, has the potential to be an irritant and/or an allergen. Long-term clinical trials are needed to both validate its efficacy and side-effect profile.
The potential for clinical uses is vast. The product has been shown to provide a synthetic skin barrier that minimizes transepidermal water loss, improving skin hydration. Its uses in burns, atopic dermatitis, bullous disease, and psoriasis could help those with altered skin-barrier function. The researchers are also hoping to use this product for targeted drug delivery and for UV protection.
After a decade of research, the MIT team has developed a skinlike material that is invisible and mimics both the mechanical and elastic properties of the skin. Future clinical studies are essential to evaluating its broad applicability in both dermatology and general medicine.
1. Nature Materials 2016. doi:10.1038/nmat4635.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Dr. Talakoub has no disclosures related to the product. Write to them at [email protected].
Hot off the presses, a new so-called “second skin” is being redeveloped and rebranded for use in both cosmetic and medical dermatology. But what is this substance, and will it hold up to all the claims the manufacturer and research team suggest?
Recently described in Nature Materials, the liquid polymer developed by chemical engineers at MIT is a synthetic, adherent silicone-based film that lies perfectly invisibly on the skin – providing a pulling or temporary tightening of the skin. The product was initially marketed by the company Living Proof as “Neotensil” [an acronym for (Neo) new, (T) transforming, (E) elastic, (N) non-invasive, (S) supportive, (I) invisible, and immediate (L) layer solution]. When applied to the area under the eye, the product creates a so-called “Spanx” effect or tightening of periorbital skin.
The material – called XPL – is delivered in a two-step sequential process. First, a polysiloxane cream is applied to the skin, followed by a platinum catalyst that induces the polymer to harden and tighten the skin underneath. The product uses patented Strateris technology, which is described as creating invisible “shapewear” for the eye; a film that tightens, smooths, and lifts the appearance of skin for up to 24 hours. It was briefly on the market in 2014-2015, then taken off the market to be redeveloped.
Does it work? Yes. Although it takes about an hour to take effect, the clinical results are jaw dropping. However, it also has its drawbacks. The polymer – which hardens within 2 minutes – must be applied to clean skin, with no creams or makeup whatsoever. And makeup cannot be applied over the treated area either, as the area looks irregular and uneven with makeup. This is a very difficult obstacle to overcome for many female patients.
Additionally, to take off the product, the polymer must be dissolved with a special chemical remover that is packaged with the product. Without this key component, it is very difficult and very irritating to remove. Although none of the patients I have used this product on have developed allergic reactions, any synthetic polymer, particularly one with adherent properties, has the potential to be an irritant and/or an allergen. Long-term clinical trials are needed to both validate its efficacy and side-effect profile.
The potential for clinical uses is vast. The product has been shown to provide a synthetic skin barrier that minimizes transepidermal water loss, improving skin hydration. Its uses in burns, atopic dermatitis, bullous disease, and psoriasis could help those with altered skin-barrier function. The researchers are also hoping to use this product for targeted drug delivery and for UV protection.
After a decade of research, the MIT team has developed a skinlike material that is invisible and mimics both the mechanical and elastic properties of the skin. Future clinical studies are essential to evaluating its broad applicability in both dermatology and general medicine.
1. Nature Materials 2016. doi:10.1038/nmat4635.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Dr. Talakoub has no disclosures related to the product. Write to them at [email protected].
Hot off the presses, a new so-called “second skin” is being redeveloped and rebranded for use in both cosmetic and medical dermatology. But what is this substance, and will it hold up to all the claims the manufacturer and research team suggest?
Recently described in Nature Materials, the liquid polymer developed by chemical engineers at MIT is a synthetic, adherent silicone-based film that lies perfectly invisibly on the skin – providing a pulling or temporary tightening of the skin. The product was initially marketed by the company Living Proof as “Neotensil” [an acronym for (Neo) new, (T) transforming, (E) elastic, (N) non-invasive, (S) supportive, (I) invisible, and immediate (L) layer solution]. When applied to the area under the eye, the product creates a so-called “Spanx” effect or tightening of periorbital skin.
The material – called XPL – is delivered in a two-step sequential process. First, a polysiloxane cream is applied to the skin, followed by a platinum catalyst that induces the polymer to harden and tighten the skin underneath. The product uses patented Strateris technology, which is described as creating invisible “shapewear” for the eye; a film that tightens, smooths, and lifts the appearance of skin for up to 24 hours. It was briefly on the market in 2014-2015, then taken off the market to be redeveloped.
Does it work? Yes. Although it takes about an hour to take effect, the clinical results are jaw dropping. However, it also has its drawbacks. The polymer – which hardens within 2 minutes – must be applied to clean skin, with no creams or makeup whatsoever. And makeup cannot be applied over the treated area either, as the area looks irregular and uneven with makeup. This is a very difficult obstacle to overcome for many female patients.
Additionally, to take off the product, the polymer must be dissolved with a special chemical remover that is packaged with the product. Without this key component, it is very difficult and very irritating to remove. Although none of the patients I have used this product on have developed allergic reactions, any synthetic polymer, particularly one with adherent properties, has the potential to be an irritant and/or an allergen. Long-term clinical trials are needed to both validate its efficacy and side-effect profile.
The potential for clinical uses is vast. The product has been shown to provide a synthetic skin barrier that minimizes transepidermal water loss, improving skin hydration. Its uses in burns, atopic dermatitis, bullous disease, and psoriasis could help those with altered skin-barrier function. The researchers are also hoping to use this product for targeted drug delivery and for UV protection.
After a decade of research, the MIT team has developed a skinlike material that is invisible and mimics both the mechanical and elastic properties of the skin. Future clinical studies are essential to evaluating its broad applicability in both dermatology and general medicine.
1. Nature Materials 2016. doi:10.1038/nmat4635.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Dr. Talakoub has no disclosures related to the product. Write to them at [email protected].
VIDEO: EULAR guidance on DMARD use in RA made ‘more concise’
LONDON – The European League Against Rheumatism guidelines on the use of disease-modifying antirheumatic drugs for the treatment of rheumatoid arthritis have been updated in line with current evidence and made more concise.
Dr. Josef S. Smolen of the department of rheumatology at the Medical University of Vienna who presented the 2016 guidelines at the European Congress of Rheumatology, noted that they now consist of 12 rather than the 14 recommendations that were included in the 2013 update (Ann Rheum Dis. 2014;73:492-509) and the 15 recommendations that were in the original 2010 version.
These 12 recommendations cover treatment targets and general approaches in the management of rheumatoid arthritis that incorporate disease-modifying antirheumatic drugs (DMARDs) and the use of glucocorticoids, and present treatment options as a hierarchy to help guide clinicians through appropriate procedures when initial and subsequent treatment fails. All DMARDs are considered in the recommendations, from the long-standing conventional synthetic (cs)DMARDs, such as methotrexate, sulfasalazine, and leflunomide, and the newer biologic DMARDs, such as the anti–tumor necrosis factor (TNF)–targeting drugs, to the newer biosimilar DMARDs, and targeted synthetic (ts)DMARDS, such as the Janus kinase (JAK) inhibitors tofacitinib and baricitinib.
The recommendations have been developed in accordance with EULAR’s standard operating procedure for the development of guidelines, Dr. Smolen observed, and involved three systematic literature reviews and expert opinion garnered from a task force of 50 experts and patients.
“This was the largest task force I have ever convened,” Dr. Smolen said, noting that rheumatologists from outside Europe had been invited to contribute their expertise and knowledge for the first time. Altogether 42 rheumatologists, three clinical fellows, two health professionals, and three patients were involved in revising the recommendations.
There are now four rather than three overarching principles, two of which are shared with early inflammatory arthritis recommendations that were also presented at the congress. The first two principles state that shared decision making is key to optimizing care and that rheumatologists should be the primary specialists looking after patients. The third principle recognizes the high burden that RA can have not only on an individual level but also on health care systems and society in general, which rheumatologists should be aware of. The fourth and final principle states that treatment decisions should be based on patients’ disease activity but that other factors, such as patients’ age, risk for progression, coexisting disease, and likely tolerance of treatment should also be kept in mind.
In an interview, Dr. Smolen highlighted that the EULAR recommendations cover three main phases of DMARD treatment: First is the DMARD-naive group of patients, who may be at an early or late stage of their disease. Second is the group in whom initial treatment has failed, and third is the group for whom subsequent treatment has not worked.
“In all these phases, we have some changes,” Dr. Smolen said. As an example, he noted that in the DMARD-naive setting, the use of csDMARDs has always been recommended but that the prior advice to consider combination csDMARD treatment has been edited out.
“We now say methotrexate should be part of the first treatment strategy, and the treatment strategy encompasses the use of additional, at least conventional synthetic, DMARDs.” Glucocorticoids are also more strongly recommended as part of the initial treatment strategy in combination with methotrexate, he said, although there is the proviso to use these for as short a time as possible.
In situations where patients do not respond to methotrexate plus glucocorticoids or they cannot tolerate methotrexate, then the recommendations advise stratifying patients into two groups. Those with poor prognostic factors might be switched to a biologic therapy, such as an anti-TNF agent or a tsDMARD. In regard to the latter, there is now more evidence behind the use of JAK inhibitors, notably tofacitinib, Dr. Smolen observed. Biologic DMARDs should be combined with csDMARDs, but if the latter is not tolerated then there is the option to use an IL-6 pathway inhibitor.
“There is now compelling evidence that all biologic DMARDs, including tocilizumab, convey better clinical, functional, and structural outcomes in combination with conventional synthetic DMARDs, especially methotrexate,” Dr. Smolen observed during his presentation of the recommendations. This may not be the case for the JAK inhibitors based on the current evidence.
When asked how the EULAR recommendations match up to those issued earlier this year by the American College of Rheumatology (Arthritis Care Res. 2016;68:1-25), Dr. Smolen observed that the two had become “much closer.” There remain differences in recommendations on glucocorticoid use, which are “somewhat clearer” in the European than in the American guidelines, and EULAR proposes combining biologic DMARDs with csDMARDs rather than using them as monotherapy. The EULAR recommendations also do not distinguish patients by disease duration but by treatment phase, and use prognostic factors for stratification.
The recommendations are currently in draft format and once finalized they will be published in Annals of the Rheumatic Diseases and also made freely available via the EULAR website, joining the organization’s many other recommendations for the management of rheumatic diseases. Dr. Smolen noted that these are intended as a template to provide national societies, health systems, and regulatory bodies a guide to the best evidence-based use of DMARDS in RA throughout Europe.
Dr. Smolen has received grant support and/or honoraria for consultations and/or for presentations from: AbbVie, Amgen, AstraZeneca, Astro-Pharma, Bristol-Myers Squibb, Celgene, GlaxoSmithKline, ILTOO Pharma, Janssen, Merck Serono, Merck Sharp & Dohme, Novartis-Sandoz, Pfizer, Roche-Chugai, Samsung, and UCB.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LONDON – The European League Against Rheumatism guidelines on the use of disease-modifying antirheumatic drugs for the treatment of rheumatoid arthritis have been updated in line with current evidence and made more concise.
Dr. Josef S. Smolen of the department of rheumatology at the Medical University of Vienna who presented the 2016 guidelines at the European Congress of Rheumatology, noted that they now consist of 12 rather than the 14 recommendations that were included in the 2013 update (Ann Rheum Dis. 2014;73:492-509) and the 15 recommendations that were in the original 2010 version.
These 12 recommendations cover treatment targets and general approaches in the management of rheumatoid arthritis that incorporate disease-modifying antirheumatic drugs (DMARDs) and the use of glucocorticoids, and present treatment options as a hierarchy to help guide clinicians through appropriate procedures when initial and subsequent treatment fails. All DMARDs are considered in the recommendations, from the long-standing conventional synthetic (cs)DMARDs, such as methotrexate, sulfasalazine, and leflunomide, and the newer biologic DMARDs, such as the anti–tumor necrosis factor (TNF)–targeting drugs, to the newer biosimilar DMARDs, and targeted synthetic (ts)DMARDS, such as the Janus kinase (JAK) inhibitors tofacitinib and baricitinib.
The recommendations have been developed in accordance with EULAR’s standard operating procedure for the development of guidelines, Dr. Smolen observed, and involved three systematic literature reviews and expert opinion garnered from a task force of 50 experts and patients.
“This was the largest task force I have ever convened,” Dr. Smolen said, noting that rheumatologists from outside Europe had been invited to contribute their expertise and knowledge for the first time. Altogether 42 rheumatologists, three clinical fellows, two health professionals, and three patients were involved in revising the recommendations.
There are now four rather than three overarching principles, two of which are shared with early inflammatory arthritis recommendations that were also presented at the congress. The first two principles state that shared decision making is key to optimizing care and that rheumatologists should be the primary specialists looking after patients. The third principle recognizes the high burden that RA can have not only on an individual level but also on health care systems and society in general, which rheumatologists should be aware of. The fourth and final principle states that treatment decisions should be based on patients’ disease activity but that other factors, such as patients’ age, risk for progression, coexisting disease, and likely tolerance of treatment should also be kept in mind.
In an interview, Dr. Smolen highlighted that the EULAR recommendations cover three main phases of DMARD treatment: First is the DMARD-naive group of patients, who may be at an early or late stage of their disease. Second is the group in whom initial treatment has failed, and third is the group for whom subsequent treatment has not worked.
“In all these phases, we have some changes,” Dr. Smolen said. As an example, he noted that in the DMARD-naive setting, the use of csDMARDs has always been recommended but that the prior advice to consider combination csDMARD treatment has been edited out.
“We now say methotrexate should be part of the first treatment strategy, and the treatment strategy encompasses the use of additional, at least conventional synthetic, DMARDs.” Glucocorticoids are also more strongly recommended as part of the initial treatment strategy in combination with methotrexate, he said, although there is the proviso to use these for as short a time as possible.
In situations where patients do not respond to methotrexate plus glucocorticoids or they cannot tolerate methotrexate, then the recommendations advise stratifying patients into two groups. Those with poor prognostic factors might be switched to a biologic therapy, such as an anti-TNF agent or a tsDMARD. In regard to the latter, there is now more evidence behind the use of JAK inhibitors, notably tofacitinib, Dr. Smolen observed. Biologic DMARDs should be combined with csDMARDs, but if the latter is not tolerated then there is the option to use an IL-6 pathway inhibitor.
“There is now compelling evidence that all biologic DMARDs, including tocilizumab, convey better clinical, functional, and structural outcomes in combination with conventional synthetic DMARDs, especially methotrexate,” Dr. Smolen observed during his presentation of the recommendations. This may not be the case for the JAK inhibitors based on the current evidence.
When asked how the EULAR recommendations match up to those issued earlier this year by the American College of Rheumatology (Arthritis Care Res. 2016;68:1-25), Dr. Smolen observed that the two had become “much closer.” There remain differences in recommendations on glucocorticoid use, which are “somewhat clearer” in the European than in the American guidelines, and EULAR proposes combining biologic DMARDs with csDMARDs rather than using them as monotherapy. The EULAR recommendations also do not distinguish patients by disease duration but by treatment phase, and use prognostic factors for stratification.
The recommendations are currently in draft format and once finalized they will be published in Annals of the Rheumatic Diseases and also made freely available via the EULAR website, joining the organization’s many other recommendations for the management of rheumatic diseases. Dr. Smolen noted that these are intended as a template to provide national societies, health systems, and regulatory bodies a guide to the best evidence-based use of DMARDS in RA throughout Europe.
Dr. Smolen has received grant support and/or honoraria for consultations and/or for presentations from: AbbVie, Amgen, AstraZeneca, Astro-Pharma, Bristol-Myers Squibb, Celgene, GlaxoSmithKline, ILTOO Pharma, Janssen, Merck Serono, Merck Sharp & Dohme, Novartis-Sandoz, Pfizer, Roche-Chugai, Samsung, and UCB.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
LONDON – The European League Against Rheumatism guidelines on the use of disease-modifying antirheumatic drugs for the treatment of rheumatoid arthritis have been updated in line with current evidence and made more concise.
Dr. Josef S. Smolen of the department of rheumatology at the Medical University of Vienna who presented the 2016 guidelines at the European Congress of Rheumatology, noted that they now consist of 12 rather than the 14 recommendations that were included in the 2013 update (Ann Rheum Dis. 2014;73:492-509) and the 15 recommendations that were in the original 2010 version.
These 12 recommendations cover treatment targets and general approaches in the management of rheumatoid arthritis that incorporate disease-modifying antirheumatic drugs (DMARDs) and the use of glucocorticoids, and present treatment options as a hierarchy to help guide clinicians through appropriate procedures when initial and subsequent treatment fails. All DMARDs are considered in the recommendations, from the long-standing conventional synthetic (cs)DMARDs, such as methotrexate, sulfasalazine, and leflunomide, and the newer biologic DMARDs, such as the anti–tumor necrosis factor (TNF)–targeting drugs, to the newer biosimilar DMARDs, and targeted synthetic (ts)DMARDS, such as the Janus kinase (JAK) inhibitors tofacitinib and baricitinib.
The recommendations have been developed in accordance with EULAR’s standard operating procedure for the development of guidelines, Dr. Smolen observed, and involved three systematic literature reviews and expert opinion garnered from a task force of 50 experts and patients.
“This was the largest task force I have ever convened,” Dr. Smolen said, noting that rheumatologists from outside Europe had been invited to contribute their expertise and knowledge for the first time. Altogether 42 rheumatologists, three clinical fellows, two health professionals, and three patients were involved in revising the recommendations.
There are now four rather than three overarching principles, two of which are shared with early inflammatory arthritis recommendations that were also presented at the congress. The first two principles state that shared decision making is key to optimizing care and that rheumatologists should be the primary specialists looking after patients. The third principle recognizes the high burden that RA can have not only on an individual level but also on health care systems and society in general, which rheumatologists should be aware of. The fourth and final principle states that treatment decisions should be based on patients’ disease activity but that other factors, such as patients’ age, risk for progression, coexisting disease, and likely tolerance of treatment should also be kept in mind.
In an interview, Dr. Smolen highlighted that the EULAR recommendations cover three main phases of DMARD treatment: First is the DMARD-naive group of patients, who may be at an early or late stage of their disease. Second is the group in whom initial treatment has failed, and third is the group for whom subsequent treatment has not worked.
“In all these phases, we have some changes,” Dr. Smolen said. As an example, he noted that in the DMARD-naive setting, the use of csDMARDs has always been recommended but that the prior advice to consider combination csDMARD treatment has been edited out.
“We now say methotrexate should be part of the first treatment strategy, and the treatment strategy encompasses the use of additional, at least conventional synthetic, DMARDs.” Glucocorticoids are also more strongly recommended as part of the initial treatment strategy in combination with methotrexate, he said, although there is the proviso to use these for as short a time as possible.
In situations where patients do not respond to methotrexate plus glucocorticoids or they cannot tolerate methotrexate, then the recommendations advise stratifying patients into two groups. Those with poor prognostic factors might be switched to a biologic therapy, such as an anti-TNF agent or a tsDMARD. In regard to the latter, there is now more evidence behind the use of JAK inhibitors, notably tofacitinib, Dr. Smolen observed. Biologic DMARDs should be combined with csDMARDs, but if the latter is not tolerated then there is the option to use an IL-6 pathway inhibitor.
“There is now compelling evidence that all biologic DMARDs, including tocilizumab, convey better clinical, functional, and structural outcomes in combination with conventional synthetic DMARDs, especially methotrexate,” Dr. Smolen observed during his presentation of the recommendations. This may not be the case for the JAK inhibitors based on the current evidence.
When asked how the EULAR recommendations match up to those issued earlier this year by the American College of Rheumatology (Arthritis Care Res. 2016;68:1-25), Dr. Smolen observed that the two had become “much closer.” There remain differences in recommendations on glucocorticoid use, which are “somewhat clearer” in the European than in the American guidelines, and EULAR proposes combining biologic DMARDs with csDMARDs rather than using them as monotherapy. The EULAR recommendations also do not distinguish patients by disease duration but by treatment phase, and use prognostic factors for stratification.
The recommendations are currently in draft format and once finalized they will be published in Annals of the Rheumatic Diseases and also made freely available via the EULAR website, joining the organization’s many other recommendations for the management of rheumatic diseases. Dr. Smolen noted that these are intended as a template to provide national societies, health systems, and regulatory bodies a guide to the best evidence-based use of DMARDS in RA throughout Europe.
Dr. Smolen has received grant support and/or honoraria for consultations and/or for presentations from: AbbVie, Amgen, AstraZeneca, Astro-Pharma, Bristol-Myers Squibb, Celgene, GlaxoSmithKline, ILTOO Pharma, Janssen, Merck Serono, Merck Sharp & Dohme, Novartis-Sandoz, Pfizer, Roche-Chugai, Samsung, and UCB.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE EULAR 2016 CONGRESS
Unanimous vote sends mental health reform to House floor
The much contested Helping Families in Mental Health Crisis Act is at last headed for the House floor. The bipartisan bill was passed 53-0 by members of the House Energy and Commerce Committee.
“The 53-0 vote marks another important milestone to delivering meaningful reforms to families in mental health crisis. Those suffering from mental illness need the attention of this Congress, and I hope the House will swiftly follow our lead,” Rep. Fred Upton (R-Mich.), chairman of the committee, said in a statement.
Much of the debate on H.R. 2646, introduced last year by Rep. Tim Murphy (R-Pa.), has centered on its call for relaxation of HIPAA rules, tougher assisted outpatient treatment requirements, and changes to the structure of the Substance Abuse and Mental Health Services Administration (SAMHSA).
The bill originally called for relaxing HIPAA somewhat so that parents and caregivers could receive patient care information, excluding psychotherapy notes. Instead, the bill as passed by the committee calls upon the Department of Health and Human Services to clarify the law and better educate medical personnel as to what is and isn’t appropriate to share, particularly when a patient is considered incapacitated.
Rep. Murphy, who is a clinical child psychologist, also wanted to more widely implement assisted outpatient treatment (AOT) for patients with serious mental illness. In the end, the committee approved a 2-year extension for AOT block grant funding into 2020, at a cost of an additional $5 million.
The bill as passed by the committee entrusts the administration of SAMHSA to a cabinet-level appointee and calls for that individual to be a physician or clinical psychologist. Various checks and balances have also been added to ensure that if the bill becomes law, SAMHSA will focus on evidence-based practices.
The bill (which greatly mirrors the U.S. Senate bill the Mental Health Reform Act of 2016, S. 2680) now heads to the House floor where Speaker Paul Ryan (R-Wis.) has pledged to give it priority this summer.
“Here and now this committee jointly proclaims that the diagnosis and treatment of mental illness must come out of the shadows. We declare a new dawn of hope for the care of those with mental illness and we pledge our unwavering commitment to continued work to bring help and hope in the future,” Rep. Murphy said in a statement.
On Twitter @whitneymcknight
The much contested Helping Families in Mental Health Crisis Act is at last headed for the House floor. The bipartisan bill was passed 53-0 by members of the House Energy and Commerce Committee.
“The 53-0 vote marks another important milestone to delivering meaningful reforms to families in mental health crisis. Those suffering from mental illness need the attention of this Congress, and I hope the House will swiftly follow our lead,” Rep. Fred Upton (R-Mich.), chairman of the committee, said in a statement.
Much of the debate on H.R. 2646, introduced last year by Rep. Tim Murphy (R-Pa.), has centered on its call for relaxation of HIPAA rules, tougher assisted outpatient treatment requirements, and changes to the structure of the Substance Abuse and Mental Health Services Administration (SAMHSA).
The bill originally called for relaxing HIPAA somewhat so that parents and caregivers could receive patient care information, excluding psychotherapy notes. Instead, the bill as passed by the committee calls upon the Department of Health and Human Services to clarify the law and better educate medical personnel as to what is and isn’t appropriate to share, particularly when a patient is considered incapacitated.
Rep. Murphy, who is a clinical child psychologist, also wanted to more widely implement assisted outpatient treatment (AOT) for patients with serious mental illness. In the end, the committee approved a 2-year extension for AOT block grant funding into 2020, at a cost of an additional $5 million.
The bill as passed by the committee entrusts the administration of SAMHSA to a cabinet-level appointee and calls for that individual to be a physician or clinical psychologist. Various checks and balances have also been added to ensure that if the bill becomes law, SAMHSA will focus on evidence-based practices.
The bill (which greatly mirrors the U.S. Senate bill the Mental Health Reform Act of 2016, S. 2680) now heads to the House floor where Speaker Paul Ryan (R-Wis.) has pledged to give it priority this summer.
“Here and now this committee jointly proclaims that the diagnosis and treatment of mental illness must come out of the shadows. We declare a new dawn of hope for the care of those with mental illness and we pledge our unwavering commitment to continued work to bring help and hope in the future,” Rep. Murphy said in a statement.
On Twitter @whitneymcknight
The much contested Helping Families in Mental Health Crisis Act is at last headed for the House floor. The bipartisan bill was passed 53-0 by members of the House Energy and Commerce Committee.
“The 53-0 vote marks another important milestone to delivering meaningful reforms to families in mental health crisis. Those suffering from mental illness need the attention of this Congress, and I hope the House will swiftly follow our lead,” Rep. Fred Upton (R-Mich.), chairman of the committee, said in a statement.
Much of the debate on H.R. 2646, introduced last year by Rep. Tim Murphy (R-Pa.), has centered on its call for relaxation of HIPAA rules, tougher assisted outpatient treatment requirements, and changes to the structure of the Substance Abuse and Mental Health Services Administration (SAMHSA).
The bill originally called for relaxing HIPAA somewhat so that parents and caregivers could receive patient care information, excluding psychotherapy notes. Instead, the bill as passed by the committee calls upon the Department of Health and Human Services to clarify the law and better educate medical personnel as to what is and isn’t appropriate to share, particularly when a patient is considered incapacitated.
Rep. Murphy, who is a clinical child psychologist, also wanted to more widely implement assisted outpatient treatment (AOT) for patients with serious mental illness. In the end, the committee approved a 2-year extension for AOT block grant funding into 2020, at a cost of an additional $5 million.
The bill as passed by the committee entrusts the administration of SAMHSA to a cabinet-level appointee and calls for that individual to be a physician or clinical psychologist. Various checks and balances have also been added to ensure that if the bill becomes law, SAMHSA will focus on evidence-based practices.
The bill (which greatly mirrors the U.S. Senate bill the Mental Health Reform Act of 2016, S. 2680) now heads to the House floor where Speaker Paul Ryan (R-Wis.) has pledged to give it priority this summer.
“Here and now this committee jointly proclaims that the diagnosis and treatment of mental illness must come out of the shadows. We declare a new dawn of hope for the care of those with mental illness and we pledge our unwavering commitment to continued work to bring help and hope in the future,” Rep. Murphy said in a statement.
On Twitter @whitneymcknight
Real-world MS relapse rate is low for dimethyl fumarate
NATIONAL HARBOR, MD. – A real-world comparison of relapse rates in multiple sclerosis (MS) patients for five disease-modifying therapies (DMTs) found the largest decrease for delayed-release dimethyl fumarate (DMF) followed by fingolimod. Patients were less likely to adhere to treatment involving teriflunomide, glatiramer acetate, or interferon-beta (IFN-beta).
Real-world outcome data have been limited, so these findings from nearly 6,400 patients presented as a poster at the annual meeting of the Consortium of Multiple Sclerosis Centers will likely be important in guiding decisions on therapy in the management of MS.
“We need real-world data to better understand the behavior of these drugs in our real-world patients. We learn a tremendous amount from phase II and III clinical trials. We attempt to look at clinical trial results and then extrapolate to our real-world patient. However, by virtue of their design, clinical trial populations represent an incomplete MS demographic,” said Dr. Aaron Boster of Riverside Methodist Hospital, Columbus, Ohio.
The retrospective study collected claims data from Truven Health MarketScan databases between January 2012 and September 2014 for adults with MS who commenced DMT with an oral or injectable drug. Annualized relapse rates (ARRs) and DMT adherence were compared for teriflunomide (n = 500), fingolimod (n = 579), IFN-beta (n = 884), glatiramer acetate (n = 1,057), and DMF (n = 3,352).
The primary outcome was ARR, which was determined before and after initiation of DMT, based on the number of MS-related relapses before and in the year following initiation of therapy. Adherence to therapy was measured using the proportion of days covered within the first year after therapy began.
The DMF cohort had the largest reduction in unadjusted ARR, from 0.425 prior to therapy to 0.296 after therapy began (–0.129; P less than .0001), followed by those treated with fingolimod, from 0.442 prior to therapy to 0.307 following therapy (–0.135; P less than .001).
After researchers adjusted for baseline demographics, clinical characteristics, and prior DMT exposure, DMF was associated with significantly lower ARR than was glatiramer acetate, IFN-beta, and teriflunomide. DMF remained better than fingolimod, but the difference was not significant.
Relative to the DMF cohort, the adjusted incidence rate ratio of ARR in the year after DMT began was 1.34 (95% confidence interval, 1.17-1.53) for glatiramer acetate, 1.27 (95% CI, 1.10-1.46) for IFN-beta, 1.23 (95% CI, 1.05-1.45) for teriflunomide, and 1.03 (95% CI, 0.88-1.21) for fingolimod.
“Despite differences in patient demographics and comorbidities between DMT clinical trial populations and these U.S. claims data, the real-world effectiveness reported here is consistent with previous mixed and indirect treatment comparisons based on clinical trial data,” Dr. Boster and his colleagues said.
The implied differences in the real-world comparative effectiveness of the various DMTs should be considered when making decisions about the best therapy to manage MS, according to the researchers.
Dr. Boster disclosed research funding from Genentech, Actelion, and Mallinckrodt, and has received consulting/speaking remuneration from Genzyme, Novartis, Teva, Biogen, and Medtronic. The other researchers have received compensation from or are employees of Biogen.
NATIONAL HARBOR, MD. – A real-world comparison of relapse rates in multiple sclerosis (MS) patients for five disease-modifying therapies (DMTs) found the largest decrease for delayed-release dimethyl fumarate (DMF) followed by fingolimod. Patients were less likely to adhere to treatment involving teriflunomide, glatiramer acetate, or interferon-beta (IFN-beta).
Real-world outcome data have been limited, so these findings from nearly 6,400 patients presented as a poster at the annual meeting of the Consortium of Multiple Sclerosis Centers will likely be important in guiding decisions on therapy in the management of MS.
“We need real-world data to better understand the behavior of these drugs in our real-world patients. We learn a tremendous amount from phase II and III clinical trials. We attempt to look at clinical trial results and then extrapolate to our real-world patient. However, by virtue of their design, clinical trial populations represent an incomplete MS demographic,” said Dr. Aaron Boster of Riverside Methodist Hospital, Columbus, Ohio.
The retrospective study collected claims data from Truven Health MarketScan databases between January 2012 and September 2014 for adults with MS who commenced DMT with an oral or injectable drug. Annualized relapse rates (ARRs) and DMT adherence were compared for teriflunomide (n = 500), fingolimod (n = 579), IFN-beta (n = 884), glatiramer acetate (n = 1,057), and DMF (n = 3,352).
The primary outcome was ARR, which was determined before and after initiation of DMT, based on the number of MS-related relapses before and in the year following initiation of therapy. Adherence to therapy was measured using the proportion of days covered within the first year after therapy began.
The DMF cohort had the largest reduction in unadjusted ARR, from 0.425 prior to therapy to 0.296 after therapy began (–0.129; P less than .0001), followed by those treated with fingolimod, from 0.442 prior to therapy to 0.307 following therapy (–0.135; P less than .001).
After researchers adjusted for baseline demographics, clinical characteristics, and prior DMT exposure, DMF was associated with significantly lower ARR than was glatiramer acetate, IFN-beta, and teriflunomide. DMF remained better than fingolimod, but the difference was not significant.
Relative to the DMF cohort, the adjusted incidence rate ratio of ARR in the year after DMT began was 1.34 (95% confidence interval, 1.17-1.53) for glatiramer acetate, 1.27 (95% CI, 1.10-1.46) for IFN-beta, 1.23 (95% CI, 1.05-1.45) for teriflunomide, and 1.03 (95% CI, 0.88-1.21) for fingolimod.
“Despite differences in patient demographics and comorbidities between DMT clinical trial populations and these U.S. claims data, the real-world effectiveness reported here is consistent with previous mixed and indirect treatment comparisons based on clinical trial data,” Dr. Boster and his colleagues said.
The implied differences in the real-world comparative effectiveness of the various DMTs should be considered when making decisions about the best therapy to manage MS, according to the researchers.
Dr. Boster disclosed research funding from Genentech, Actelion, and Mallinckrodt, and has received consulting/speaking remuneration from Genzyme, Novartis, Teva, Biogen, and Medtronic. The other researchers have received compensation from or are employees of Biogen.
NATIONAL HARBOR, MD. – A real-world comparison of relapse rates in multiple sclerosis (MS) patients for five disease-modifying therapies (DMTs) found the largest decrease for delayed-release dimethyl fumarate (DMF) followed by fingolimod. Patients were less likely to adhere to treatment involving teriflunomide, glatiramer acetate, or interferon-beta (IFN-beta).
Real-world outcome data have been limited, so these findings from nearly 6,400 patients presented as a poster at the annual meeting of the Consortium of Multiple Sclerosis Centers will likely be important in guiding decisions on therapy in the management of MS.
“We need real-world data to better understand the behavior of these drugs in our real-world patients. We learn a tremendous amount from phase II and III clinical trials. We attempt to look at clinical trial results and then extrapolate to our real-world patient. However, by virtue of their design, clinical trial populations represent an incomplete MS demographic,” said Dr. Aaron Boster of Riverside Methodist Hospital, Columbus, Ohio.
The retrospective study collected claims data from Truven Health MarketScan databases between January 2012 and September 2014 for adults with MS who commenced DMT with an oral or injectable drug. Annualized relapse rates (ARRs) and DMT adherence were compared for teriflunomide (n = 500), fingolimod (n = 579), IFN-beta (n = 884), glatiramer acetate (n = 1,057), and DMF (n = 3,352).
The primary outcome was ARR, which was determined before and after initiation of DMT, based on the number of MS-related relapses before and in the year following initiation of therapy. Adherence to therapy was measured using the proportion of days covered within the first year after therapy began.
The DMF cohort had the largest reduction in unadjusted ARR, from 0.425 prior to therapy to 0.296 after therapy began (–0.129; P less than .0001), followed by those treated with fingolimod, from 0.442 prior to therapy to 0.307 following therapy (–0.135; P less than .001).
After researchers adjusted for baseline demographics, clinical characteristics, and prior DMT exposure, DMF was associated with significantly lower ARR than was glatiramer acetate, IFN-beta, and teriflunomide. DMF remained better than fingolimod, but the difference was not significant.
Relative to the DMF cohort, the adjusted incidence rate ratio of ARR in the year after DMT began was 1.34 (95% confidence interval, 1.17-1.53) for glatiramer acetate, 1.27 (95% CI, 1.10-1.46) for IFN-beta, 1.23 (95% CI, 1.05-1.45) for teriflunomide, and 1.03 (95% CI, 0.88-1.21) for fingolimod.
“Despite differences in patient demographics and comorbidities between DMT clinical trial populations and these U.S. claims data, the real-world effectiveness reported here is consistent with previous mixed and indirect treatment comparisons based on clinical trial data,” Dr. Boster and his colleagues said.
The implied differences in the real-world comparative effectiveness of the various DMTs should be considered when making decisions about the best therapy to manage MS, according to the researchers.
Dr. Boster disclosed research funding from Genentech, Actelion, and Mallinckrodt, and has received consulting/speaking remuneration from Genzyme, Novartis, Teva, Biogen, and Medtronic. The other researchers have received compensation from or are employees of Biogen.
AT THE CMSC ANNUAL MEETING
Key clinical point: Comparison of five disease-modifying therapies for MS has revealed the lowest relapse rate for dimethyl fumarate, which should help guide management decisions.
Major finding: Dimethyl fumarate treatment was associated with an unadjusted annualized relapse rate of –0.129, with fingolimod also having a significantly decreased relapse rate.
Data source: Data from claims databases involving nearly 6,400 MS patients.
Disclosures: The study was funded by Biogen. Dr. Boster disclosed research funding from Genentech, Actelion, and Mallinckrodt, and has received consulting/speaking remuneration from Genzyme, Novartis, Teva, Biogen, and Medtronic.
Tenofovir may prevent mother-to-child transmission of hepatitis B
The antiviral drug tenofovir disoproxil fumarate (TDF) can be used by expectant mothers infected with the hepatitis B virus to decrease HBV DNA levels and, therefore, significantly decrease the risk of passing the virus onto their children, according to a new study.
“A small but growing body of evidence has suggested that antiviral treatment may reduce the risk of mother-to-child transmission among mothers with an HBV DNA level of more than 6 log10 copies per milliliter, although quality studies are lacking and the existing studies have shown conflicting results,” wrote Dr. Calvin Q. Pan of New York University and coauthors in a study published in the New England Journal of Medicine (2016;374[24]:2324-34. doi: 10.1056/NEJMoa1508660).
An international research team recruited pregnant women in China – all of whom were positive for hepatitis B e antigen and had a viral load of at least 200,000 IU/mL – from March 2012 through June 2013. A total of 200 women were selected for inclusion and randomized into either a control cohort, or a cohort taking TDF; 100 mothers with 88 infants ultimately completed the study in the control group, while 97 mothers with 92 children completed the study in the TDF cohort.
Women on TDF were given a 300-mg dose orally every day, beginning 30-32 weeks into their pregnancy and continuing through 4 weeks after giving birth. Follow-up examinations were conducted at 4, 12, 24, and 28 weeks post partum, and the primary outcome was determining transmission of HBV from mother to child, with transmission defined as an infant having an HBV DNA level higher than 20 IU/mL. Patients in the control group were given “usual care without antiviral therapy.”
Mothers on TDF had lower HBV DNA levels at delivery, with 68% (66/97) dropping to under 200,000 IU/mL levels versus just 2% (2/100) in the control group having levels under that threshold (P less than .001). At 28-week follow-up examinations, intent-to-treat analysis showed that 5% (5/97) of infants born to mothers on TDF were found to have HBV DNA levels higher than 20 IU/mL, compared with 18% of infants born to mothers in the control group (P = .007). In per-protocol analysis, none of the infants whose mothers were taking TDF had contracted the disease; on the other hand, 7% (6/88) of those in the control group had (P = .01). Rates of birth defects and HBV serologic outcomes were not significantly different between the two cohorts.
“TDF [may] be useful for preventing mother-to-child transmission, which is a critical step toward the global eradication of HBV and a reduction in the incidence of liver cancer,” Dr. Pan and his colleagues said, adding that “the postpartum cessation of TDF requires close monitoring” in order to further understand the drug’s longer-term effects.
The study was funded by Gilead Sciences. Dr. Pan reported grant support from Gilead Sciences during the conduct of the study; grant support from Merck, grant support and personal fees from Gilead Sciences and Bristol-Myers Squibb; and personal fees from Johnson and Johnson and AbbVie outside the submitted work.
The antiviral drug tenofovir disoproxil fumarate (TDF) can be used by expectant mothers infected with the hepatitis B virus to decrease HBV DNA levels and, therefore, significantly decrease the risk of passing the virus onto their children, according to a new study.
“A small but growing body of evidence has suggested that antiviral treatment may reduce the risk of mother-to-child transmission among mothers with an HBV DNA level of more than 6 log10 copies per milliliter, although quality studies are lacking and the existing studies have shown conflicting results,” wrote Dr. Calvin Q. Pan of New York University and coauthors in a study published in the New England Journal of Medicine (2016;374[24]:2324-34. doi: 10.1056/NEJMoa1508660).
An international research team recruited pregnant women in China – all of whom were positive for hepatitis B e antigen and had a viral load of at least 200,000 IU/mL – from March 2012 through June 2013. A total of 200 women were selected for inclusion and randomized into either a control cohort, or a cohort taking TDF; 100 mothers with 88 infants ultimately completed the study in the control group, while 97 mothers with 92 children completed the study in the TDF cohort.
Women on TDF were given a 300-mg dose orally every day, beginning 30-32 weeks into their pregnancy and continuing through 4 weeks after giving birth. Follow-up examinations were conducted at 4, 12, 24, and 28 weeks post partum, and the primary outcome was determining transmission of HBV from mother to child, with transmission defined as an infant having an HBV DNA level higher than 20 IU/mL. Patients in the control group were given “usual care without antiviral therapy.”
Mothers on TDF had lower HBV DNA levels at delivery, with 68% (66/97) dropping to under 200,000 IU/mL levels versus just 2% (2/100) in the control group having levels under that threshold (P less than .001). At 28-week follow-up examinations, intent-to-treat analysis showed that 5% (5/97) of infants born to mothers on TDF were found to have HBV DNA levels higher than 20 IU/mL, compared with 18% of infants born to mothers in the control group (P = .007). In per-protocol analysis, none of the infants whose mothers were taking TDF had contracted the disease; on the other hand, 7% (6/88) of those in the control group had (P = .01). Rates of birth defects and HBV serologic outcomes were not significantly different between the two cohorts.
“TDF [may] be useful for preventing mother-to-child transmission, which is a critical step toward the global eradication of HBV and a reduction in the incidence of liver cancer,” Dr. Pan and his colleagues said, adding that “the postpartum cessation of TDF requires close monitoring” in order to further understand the drug’s longer-term effects.
The study was funded by Gilead Sciences. Dr. Pan reported grant support from Gilead Sciences during the conduct of the study; grant support from Merck, grant support and personal fees from Gilead Sciences and Bristol-Myers Squibb; and personal fees from Johnson and Johnson and AbbVie outside the submitted work.
The antiviral drug tenofovir disoproxil fumarate (TDF) can be used by expectant mothers infected with the hepatitis B virus to decrease HBV DNA levels and, therefore, significantly decrease the risk of passing the virus onto their children, according to a new study.
“A small but growing body of evidence has suggested that antiviral treatment may reduce the risk of mother-to-child transmission among mothers with an HBV DNA level of more than 6 log10 copies per milliliter, although quality studies are lacking and the existing studies have shown conflicting results,” wrote Dr. Calvin Q. Pan of New York University and coauthors in a study published in the New England Journal of Medicine (2016;374[24]:2324-34. doi: 10.1056/NEJMoa1508660).
An international research team recruited pregnant women in China – all of whom were positive for hepatitis B e antigen and had a viral load of at least 200,000 IU/mL – from March 2012 through June 2013. A total of 200 women were selected for inclusion and randomized into either a control cohort, or a cohort taking TDF; 100 mothers with 88 infants ultimately completed the study in the control group, while 97 mothers with 92 children completed the study in the TDF cohort.
Women on TDF were given a 300-mg dose orally every day, beginning 30-32 weeks into their pregnancy and continuing through 4 weeks after giving birth. Follow-up examinations were conducted at 4, 12, 24, and 28 weeks post partum, and the primary outcome was determining transmission of HBV from mother to child, with transmission defined as an infant having an HBV DNA level higher than 20 IU/mL. Patients in the control group were given “usual care without antiviral therapy.”
Mothers on TDF had lower HBV DNA levels at delivery, with 68% (66/97) dropping to under 200,000 IU/mL levels versus just 2% (2/100) in the control group having levels under that threshold (P less than .001). At 28-week follow-up examinations, intent-to-treat analysis showed that 5% (5/97) of infants born to mothers on TDF were found to have HBV DNA levels higher than 20 IU/mL, compared with 18% of infants born to mothers in the control group (P = .007). In per-protocol analysis, none of the infants whose mothers were taking TDF had contracted the disease; on the other hand, 7% (6/88) of those in the control group had (P = .01). Rates of birth defects and HBV serologic outcomes were not significantly different between the two cohorts.
“TDF [may] be useful for preventing mother-to-child transmission, which is a critical step toward the global eradication of HBV and a reduction in the incidence of liver cancer,” Dr. Pan and his colleagues said, adding that “the postpartum cessation of TDF requires close monitoring” in order to further understand the drug’s longer-term effects.
The study was funded by Gilead Sciences. Dr. Pan reported grant support from Gilead Sciences during the conduct of the study; grant support from Merck, grant support and personal fees from Gilead Sciences and Bristol-Myers Squibb; and personal fees from Johnson and Johnson and AbbVie outside the submitted work.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: A 300-mg daily dose of tenofovir disoproxil fumarate significantly reduced the risk of pregnant mothers with HBV infection transmitting the disease to their children.
Major finding: In an intent-to-treat analysis, only 5% of children born to mothers taking TDF during pregnancy were found to have contracted the disease, versus 18% in the control group (P = .007); similarly, in the per-protocol analysis, 0% of children born to mothers taking TDF had HBV vs. 7% in the control group (P = .01).
Data source: A multicenter, open label, randomized, parallel-group study of 197 HBV-positive pregnant women from March 2012 through June 2013.
Disclosures: The study was funded by Gilead Sciences. Dr. Pan reported grant support from Gilead Sciences during the conduct of the study; grant support from Merck, grant support and personal fees from Gilead Sciences and Bristol-Myers Squibb; and personal fees from Johnson and Johnson and AbbVie outside the submitted work.
Insomnia linked to increased risk of pregnancy loss
DENVER – Women who experience difficulty staying asleep are at increased risk of having one or more pregnancies that don’t result in a live birth, a large epidemiologic study suggests.
In contrast, other expressions of insomnia – difficulty in falling asleep, early morning awakening, or nonrestorative sleep – were not significantly associated with pregnancy loss in this analysis of a nationally representative sample comprised of 5,554 women aged 18-45 years, Sara Nowakowski, Ph.D., reported at the annual meeting of the Associated Professional Sleep Societies.
The women were participants in the National Health and Nutrition Examination Survey for 2005-2008, which collected data on reproductive history as well as sleep patterns. Roughly 20% of the women self-reported experiencing insomnia. Eighty-three percent of the 18- to 45-year-old women had been pregnant at least once, and 1,870 (40%) of them had one or more prior pregnancies that didn’t result in a live birth.
In a multivariate logistic regression analysis adjusted for age, race, education level, and frequency of sleep apnea symptoms, such as snoring or snorting/gasping, frequent difficulty in maintaining sleep was independently associated with an 85% increased risk of having experienced a pregnancy that didn’t result in a live birth, according to Dr. Nowakowski, a clinical psychologist in the department of ob.gyn. at the University of Texas, Galveston.
In an interview, she was quick to note that these are correlational, hypothesis-generating data, and that an epidemiologic study such as this can’t establish causality.
Dr. Nowakowski and her coinvestigators hope to conduct a prospective randomized trial of cognitive behavioral therapy for insomnia – a well-established treatment – in a group of women with prior spontaneous abortion, miscarriage, or other infertility issues, to determine whether insomnia is a modifiable risk factor for adverse pregnancy outcomes.
One physician at the meeting remarked that if women with fertility problems and insomnia knew of Dr. Nowakowski’s work showing an association between insomnia and unsuccessful pregnancies, they would be pounding down the doors of sleep specialists. Dr. Nowakowski agreed.
“I surf the online networks set up for infertile women. They’re very distraught over their trouble conceiving. They’re doing yoga, de-stress programs, taking all sorts of supplements – including melatonin – to try to improve their chances of fertility,” she said. “If insomnia turns out to partially account for the risk of having pregnancies that don’t result in live birth, and treating the insomnia reduces that risk, there would be a huge amount of patient interest.”
The study was supported by the National Institutes of Health. Dr. Nowakowski reported having no financial conflicts.
DENVER – Women who experience difficulty staying asleep are at increased risk of having one or more pregnancies that don’t result in a live birth, a large epidemiologic study suggests.
In contrast, other expressions of insomnia – difficulty in falling asleep, early morning awakening, or nonrestorative sleep – were not significantly associated with pregnancy loss in this analysis of a nationally representative sample comprised of 5,554 women aged 18-45 years, Sara Nowakowski, Ph.D., reported at the annual meeting of the Associated Professional Sleep Societies.
The women were participants in the National Health and Nutrition Examination Survey for 2005-2008, which collected data on reproductive history as well as sleep patterns. Roughly 20% of the women self-reported experiencing insomnia. Eighty-three percent of the 18- to 45-year-old women had been pregnant at least once, and 1,870 (40%) of them had one or more prior pregnancies that didn’t result in a live birth.
In a multivariate logistic regression analysis adjusted for age, race, education level, and frequency of sleep apnea symptoms, such as snoring or snorting/gasping, frequent difficulty in maintaining sleep was independently associated with an 85% increased risk of having experienced a pregnancy that didn’t result in a live birth, according to Dr. Nowakowski, a clinical psychologist in the department of ob.gyn. at the University of Texas, Galveston.
In an interview, she was quick to note that these are correlational, hypothesis-generating data, and that an epidemiologic study such as this can’t establish causality.
Dr. Nowakowski and her coinvestigators hope to conduct a prospective randomized trial of cognitive behavioral therapy for insomnia – a well-established treatment – in a group of women with prior spontaneous abortion, miscarriage, or other infertility issues, to determine whether insomnia is a modifiable risk factor for adverse pregnancy outcomes.
One physician at the meeting remarked that if women with fertility problems and insomnia knew of Dr. Nowakowski’s work showing an association between insomnia and unsuccessful pregnancies, they would be pounding down the doors of sleep specialists. Dr. Nowakowski agreed.
“I surf the online networks set up for infertile women. They’re very distraught over their trouble conceiving. They’re doing yoga, de-stress programs, taking all sorts of supplements – including melatonin – to try to improve their chances of fertility,” she said. “If insomnia turns out to partially account for the risk of having pregnancies that don’t result in live birth, and treating the insomnia reduces that risk, there would be a huge amount of patient interest.”
The study was supported by the National Institutes of Health. Dr. Nowakowski reported having no financial conflicts.
DENVER – Women who experience difficulty staying asleep are at increased risk of having one or more pregnancies that don’t result in a live birth, a large epidemiologic study suggests.
In contrast, other expressions of insomnia – difficulty in falling asleep, early morning awakening, or nonrestorative sleep – were not significantly associated with pregnancy loss in this analysis of a nationally representative sample comprised of 5,554 women aged 18-45 years, Sara Nowakowski, Ph.D., reported at the annual meeting of the Associated Professional Sleep Societies.
The women were participants in the National Health and Nutrition Examination Survey for 2005-2008, which collected data on reproductive history as well as sleep patterns. Roughly 20% of the women self-reported experiencing insomnia. Eighty-three percent of the 18- to 45-year-old women had been pregnant at least once, and 1,870 (40%) of them had one or more prior pregnancies that didn’t result in a live birth.
In a multivariate logistic regression analysis adjusted for age, race, education level, and frequency of sleep apnea symptoms, such as snoring or snorting/gasping, frequent difficulty in maintaining sleep was independently associated with an 85% increased risk of having experienced a pregnancy that didn’t result in a live birth, according to Dr. Nowakowski, a clinical psychologist in the department of ob.gyn. at the University of Texas, Galveston.
In an interview, she was quick to note that these are correlational, hypothesis-generating data, and that an epidemiologic study such as this can’t establish causality.
Dr. Nowakowski and her coinvestigators hope to conduct a prospective randomized trial of cognitive behavioral therapy for insomnia – a well-established treatment – in a group of women with prior spontaneous abortion, miscarriage, or other infertility issues, to determine whether insomnia is a modifiable risk factor for adverse pregnancy outcomes.
One physician at the meeting remarked that if women with fertility problems and insomnia knew of Dr. Nowakowski’s work showing an association between insomnia and unsuccessful pregnancies, they would be pounding down the doors of sleep specialists. Dr. Nowakowski agreed.
“I surf the online networks set up for infertile women. They’re very distraught over their trouble conceiving. They’re doing yoga, de-stress programs, taking all sorts of supplements – including melatonin – to try to improve their chances of fertility,” she said. “If insomnia turns out to partially account for the risk of having pregnancies that don’t result in live birth, and treating the insomnia reduces that risk, there would be a huge amount of patient interest.”
The study was supported by the National Institutes of Health. Dr. Nowakowski reported having no financial conflicts.
AT SLEEP 2016
Key clinical point: Insomnia may be a factor in some cases of poor pregnancy outcomes.
Major finding: Reproductive-age women who experienced difficulty staying asleep had an 85% greater likelihood of having a pregnancy that didn’t result in a live birth.
Data source: This epidemiologic study included 5,554 women aged 18-45 who provided details of their reproductive history and sleep status in the National Health and Nutrition Examination Survey.
Disclosures: This study was supported by the National Institutes of Health. Dr. Nowakowski reported having no financial conflicts.
Acute myeloid leukemia genomic classification and prognosis
Acute myeloid leukemia (AML) consists of at least 11 disease classes that represent distinct paths in the evolution of AML and have prognostic implications, based on an analysis of somatic driver mutations in 1,540 patients.
In total, 5,234 driver mutations were identified in 76 genes or regions, with 96% of patients having at least one mutation and 86% having two or more mutations. However, nearly one-half of the cohort did not fall into one of the molecular groups defined by the World Health Organization in 2008.
“The characterization of many new leukemia genes, multiple driver mutations per patient, and complex co-mutation patterns prompted us to reevaluate genomic classification of AML from the beginning,” wrote Elli Papaemmanuil, Ph.D., a molecular geneticist at Memorial Sloan Kettering, New York, and of the Cancer Genome Project, Wellcome Trust Sanger Institute, and her colleagues (N Engl J Med. 2016 Jun 9; 374:2209-21).
The team developed a Bayesian statistical model to define 11 mutually exclusive subtypes based on patterns of co-mutations. The schema unambiguously classified 1,236 of 1,540 patients (80%) into a single subgroup and 56 (4%) into two or more groups. A subset of patients (166, 11%) remained unclassified, possibly due to mutations in genes not sequenced in the study.
NPM1-mutated AML was the largest class (27% of the cohort), followed by the chromatin-spliceosome group (18% of the cohort) that included mutations in genes regulating RNA splicing (SRSF2, SF3B1, U2AF1, and ZRSR2), chromatin (ASXL1, STAG2, BCOR, MLLPTD, EZH2, and PHF6), or transcription (RUNX1). Another subgroup consisted of mutations in TP53, as well as complex karyotype alterations, cytogenetically visible copy-number alterations (aneuploidies), or a combination. While broader than previous classifications, such as “monosomal karyotype AML” and “complex karyotype AML,” this group emerged from correlated chromosomal abnormalities and was mutually exclusive of other class-defining lesions. In general, patients in this group were older and had fewer RAS pathway mutations.
The groups had considerable differences in clinical presentation and overall survival, according to the report. The TP53-aneuploidy subgroup had poor outcomes, as previously described. Patients in the chromatin-spliceosome group had lower rates of response to induction chemotherapy, higher relapse rates, and poorer long-term outcomes, compared with other groups. Most of these patients (84%) would be classified as intermediate risk under current guidelines, but the characteristics were more similar to those of subgroups with adverse outcomes.
Overall survival was correlated with the number of driver mutations, and deleterious affects of mutations often were found to be additive. In some cases, complex gene interactions accounted for variation in outcomes, suggesting the clinical effect of some driver mutations may depend on the occurrence of co-mutations in a wider genomic context.
The study by Papaemmanuil and her colleagues offers practice-changing insights that redefine molecular classification of AML. The mutational analysis of more than 1,500 AML patients provides a deeper understanding of the specific paths from normal blood cell to leukemia.
Specific concurrent mutations were linked to clinical outcomes. For example, co-mutations in NPM1, FLT3ITD, and DNMT3A are associated with a poor clinical outcome, but NPM1 and DNMT3A mutations without FLT3ITD are associated with better outcomes. In addition, mutations in NPM1 and DNMT3A in the presence of NRASG12/13 are associated with a more favorable outcome. The evolution of DNMT3A-NPM1 mutated clones along separate paths appears to affect disease outcome and may be relevant to clinical trials in AML subgroups.
|
Dr. Aaron Viny |
Previous, smaller studies had suggested that somatic mutations in splicing factors and chromatin modifiers were specific for secondary AML that arises from myelodysplastic syndromes (MDS). Papaemmanuil and her colleagues provide extensive data to support that hypothesis. Patients with chromatin-spliceosome mutations, previously classified as intermediate-risk AML, are classed into the same molecular subgroup as patients with secondary AML arising from MDS.
These data may inform the design of mechanism-based clinical trials based on the presence of specific mutations and co-mutations.
Dr. Aaron Viny is a medical oncologist at Memorial Sloan Kettering Cancer Center, New York. Dr. Ross Levine is Director of the Memorial Sloan Kettering Center for Hematologic Malignancies. These remarks were part of an editorial accompanying a report in The New England Journal of Medicine (2016 Jun 9; 374:2282-4). Dr. Levine reports personal fees from Foundation Medicine outside the submitted work.
The study by Papaemmanuil and her colleagues offers practice-changing insights that redefine molecular classification of AML. The mutational analysis of more than 1,500 AML patients provides a deeper understanding of the specific paths from normal blood cell to leukemia.
Specific concurrent mutations were linked to clinical outcomes. For example, co-mutations in NPM1, FLT3ITD, and DNMT3A are associated with a poor clinical outcome, but NPM1 and DNMT3A mutations without FLT3ITD are associated with better outcomes. In addition, mutations in NPM1 and DNMT3A in the presence of NRASG12/13 are associated with a more favorable outcome. The evolution of DNMT3A-NPM1 mutated clones along separate paths appears to affect disease outcome and may be relevant to clinical trials in AML subgroups.
|
Dr. Aaron Viny |
Previous, smaller studies had suggested that somatic mutations in splicing factors and chromatin modifiers were specific for secondary AML that arises from myelodysplastic syndromes (MDS). Papaemmanuil and her colleagues provide extensive data to support that hypothesis. Patients with chromatin-spliceosome mutations, previously classified as intermediate-risk AML, are classed into the same molecular subgroup as patients with secondary AML arising from MDS.
These data may inform the design of mechanism-based clinical trials based on the presence of specific mutations and co-mutations.
Dr. Aaron Viny is a medical oncologist at Memorial Sloan Kettering Cancer Center, New York. Dr. Ross Levine is Director of the Memorial Sloan Kettering Center for Hematologic Malignancies. These remarks were part of an editorial accompanying a report in The New England Journal of Medicine (2016 Jun 9; 374:2282-4). Dr. Levine reports personal fees from Foundation Medicine outside the submitted work.
The study by Papaemmanuil and her colleagues offers practice-changing insights that redefine molecular classification of AML. The mutational analysis of more than 1,500 AML patients provides a deeper understanding of the specific paths from normal blood cell to leukemia.
Specific concurrent mutations were linked to clinical outcomes. For example, co-mutations in NPM1, FLT3ITD, and DNMT3A are associated with a poor clinical outcome, but NPM1 and DNMT3A mutations without FLT3ITD are associated with better outcomes. In addition, mutations in NPM1 and DNMT3A in the presence of NRASG12/13 are associated with a more favorable outcome. The evolution of DNMT3A-NPM1 mutated clones along separate paths appears to affect disease outcome and may be relevant to clinical trials in AML subgroups.
|
Dr. Aaron Viny |
Previous, smaller studies had suggested that somatic mutations in splicing factors and chromatin modifiers were specific for secondary AML that arises from myelodysplastic syndromes (MDS). Papaemmanuil and her colleagues provide extensive data to support that hypothesis. Patients with chromatin-spliceosome mutations, previously classified as intermediate-risk AML, are classed into the same molecular subgroup as patients with secondary AML arising from MDS.
These data may inform the design of mechanism-based clinical trials based on the presence of specific mutations and co-mutations.
Dr. Aaron Viny is a medical oncologist at Memorial Sloan Kettering Cancer Center, New York. Dr. Ross Levine is Director of the Memorial Sloan Kettering Center for Hematologic Malignancies. These remarks were part of an editorial accompanying a report in The New England Journal of Medicine (2016 Jun 9; 374:2282-4). Dr. Levine reports personal fees from Foundation Medicine outside the submitted work.
Acute myeloid leukemia (AML) consists of at least 11 disease classes that represent distinct paths in the evolution of AML and have prognostic implications, based on an analysis of somatic driver mutations in 1,540 patients.
In total, 5,234 driver mutations were identified in 76 genes or regions, with 96% of patients having at least one mutation and 86% having two or more mutations. However, nearly one-half of the cohort did not fall into one of the molecular groups defined by the World Health Organization in 2008.
“The characterization of many new leukemia genes, multiple driver mutations per patient, and complex co-mutation patterns prompted us to reevaluate genomic classification of AML from the beginning,” wrote Elli Papaemmanuil, Ph.D., a molecular geneticist at Memorial Sloan Kettering, New York, and of the Cancer Genome Project, Wellcome Trust Sanger Institute, and her colleagues (N Engl J Med. 2016 Jun 9; 374:2209-21).
The team developed a Bayesian statistical model to define 11 mutually exclusive subtypes based on patterns of co-mutations. The schema unambiguously classified 1,236 of 1,540 patients (80%) into a single subgroup and 56 (4%) into two or more groups. A subset of patients (166, 11%) remained unclassified, possibly due to mutations in genes not sequenced in the study.
NPM1-mutated AML was the largest class (27% of the cohort), followed by the chromatin-spliceosome group (18% of the cohort) that included mutations in genes regulating RNA splicing (SRSF2, SF3B1, U2AF1, and ZRSR2), chromatin (ASXL1, STAG2, BCOR, MLLPTD, EZH2, and PHF6), or transcription (RUNX1). Another subgroup consisted of mutations in TP53, as well as complex karyotype alterations, cytogenetically visible copy-number alterations (aneuploidies), or a combination. While broader than previous classifications, such as “monosomal karyotype AML” and “complex karyotype AML,” this group emerged from correlated chromosomal abnormalities and was mutually exclusive of other class-defining lesions. In general, patients in this group were older and had fewer RAS pathway mutations.
The groups had considerable differences in clinical presentation and overall survival, according to the report. The TP53-aneuploidy subgroup had poor outcomes, as previously described. Patients in the chromatin-spliceosome group had lower rates of response to induction chemotherapy, higher relapse rates, and poorer long-term outcomes, compared with other groups. Most of these patients (84%) would be classified as intermediate risk under current guidelines, but the characteristics were more similar to those of subgroups with adverse outcomes.
Overall survival was correlated with the number of driver mutations, and deleterious affects of mutations often were found to be additive. In some cases, complex gene interactions accounted for variation in outcomes, suggesting the clinical effect of some driver mutations may depend on the occurrence of co-mutations in a wider genomic context.
Acute myeloid leukemia (AML) consists of at least 11 disease classes that represent distinct paths in the evolution of AML and have prognostic implications, based on an analysis of somatic driver mutations in 1,540 patients.
In total, 5,234 driver mutations were identified in 76 genes or regions, with 96% of patients having at least one mutation and 86% having two or more mutations. However, nearly one-half of the cohort did not fall into one of the molecular groups defined by the World Health Organization in 2008.
“The characterization of many new leukemia genes, multiple driver mutations per patient, and complex co-mutation patterns prompted us to reevaluate genomic classification of AML from the beginning,” wrote Elli Papaemmanuil, Ph.D., a molecular geneticist at Memorial Sloan Kettering, New York, and of the Cancer Genome Project, Wellcome Trust Sanger Institute, and her colleagues (N Engl J Med. 2016 Jun 9; 374:2209-21).
The team developed a Bayesian statistical model to define 11 mutually exclusive subtypes based on patterns of co-mutations. The schema unambiguously classified 1,236 of 1,540 patients (80%) into a single subgroup and 56 (4%) into two or more groups. A subset of patients (166, 11%) remained unclassified, possibly due to mutations in genes not sequenced in the study.
NPM1-mutated AML was the largest class (27% of the cohort), followed by the chromatin-spliceosome group (18% of the cohort) that included mutations in genes regulating RNA splicing (SRSF2, SF3B1, U2AF1, and ZRSR2), chromatin (ASXL1, STAG2, BCOR, MLLPTD, EZH2, and PHF6), or transcription (RUNX1). Another subgroup consisted of mutations in TP53, as well as complex karyotype alterations, cytogenetically visible copy-number alterations (aneuploidies), or a combination. While broader than previous classifications, such as “monosomal karyotype AML” and “complex karyotype AML,” this group emerged from correlated chromosomal abnormalities and was mutually exclusive of other class-defining lesions. In general, patients in this group were older and had fewer RAS pathway mutations.
The groups had considerable differences in clinical presentation and overall survival, according to the report. The TP53-aneuploidy subgroup had poor outcomes, as previously described. Patients in the chromatin-spliceosome group had lower rates of response to induction chemotherapy, higher relapse rates, and poorer long-term outcomes, compared with other groups. Most of these patients (84%) would be classified as intermediate risk under current guidelines, but the characteristics were more similar to those of subgroups with adverse outcomes.
Overall survival was correlated with the number of driver mutations, and deleterious affects of mutations often were found to be additive. In some cases, complex gene interactions accounted for variation in outcomes, suggesting the clinical effect of some driver mutations may depend on the occurrence of co-mutations in a wider genomic context.
FROM NEJM
Key clinical point: Mutational analysis of 1,540 patients with acute myeloid leukemia (AML) identified 11 distinct classes with prognostic implications.
Major finding: In total, 5,234 driver mutations were identified involving 76 genes or regions; 96% of patients had at least one driver mutation, and 86% had two or more.
Data sources: Samples came from three prospective multicenter clinical trials of the German-Austrian AML Study Group: AMLHD98A, AML-HD98B, and AMLSG-07-04.
Disclosures: Dr. Papaemmanuil and most coauthors reported having no disclosures. Two coauthors reported financial ties to industry sources.
Hold that TKI – When it’s safe to stop in CML
COPENHAGEN – A year after stopping tyrosine kinase inhibitor therapy, more than half of patients with chronic myeloid leukemia (CML) in a large clinical trial remained in deep molecular remission.
Among 750 patients with CML in remission for at least 1 year before study entry, 62% retained a treatment response 6 months after stopping a tyrosine kinase inhibitor (TKI) such as imatinib (Gleevec) and 56% retained responses 1 year after being off their drugs, reported Dr. Johan Richter of Lund (Sweden) University at the annual congress of the European Hematology Association.
“About 6 years of therapy [with imatinib] would be optimal for therapy prior to a stop attempt,” he said at a briefing prior to the presentation of data at the congress.
Although in clinical practice patients with CML may remain on a TKI indefinitely, results from small clinical trials have suggested that in 40%-60% of patients with deep molecular responses (MR4.0 or better), TKIs can be safely stopped, Dr. Richter noted.
To get a better handle on when it might be safe to stop a TKI and under what conditions, EURO-SKI investigators enrolled 868 adults with CML in chronic phase from 11 countries, 750 of whom had complete data for the analysis.
In all, 94% of patients had received imatinib in the first line, 2% received dasatinib (Sprycel), and 4% had received nilotinib (Tasigna). Of this group, 115 had switched to a second-line agent due to intolerance of the first-line drug.
The median time from diagnosis was 7.7 years. The median duration of therapy was 7.6 years, and the median duration of MR4 before stopping was 4.7 years.
As noted, among 750 patients assessable for molecular relapse–free survival, 62% remained in remission at 6 months after stopping the TKI, as did 56% at 12 months, 52% at 24 months, and 49% at 36 months.
For patients who resumed therapy, the median time to restart was 4.1 months.
To see whether they could identify any factors prognostic for relapse after stopping a TKI, the investigators used data on 448 patients in the study who were treated with imatinib.
In univariate analysis there was no significant association between molecular relapse–free survival at 6 months and either age, gender, depth of molecular response, or any standard risk scores.
The only significant predictors of molecular remission status at 6 months were duration of imatinib therapy and duration of molecular response before stopping.
The odds ratio for treatment duration was 1.16, indicating that each additional year of imatinib treatment is associated with a 16% increase in the likelihood that a patient would remain in deep molecular remission 6 months after stopping.
The investigators used the minimal P value approach to determine the cutoff of approximately 6 years, based on a molecular relapse–free survival at 6 months of 65.5% for patients who remained on imatinib for more than 5.8 years, compared with 42.6% for those who were on it for 5.8 years or less.
Although the study is ongoing, to date more than 80% of patients who had a loss of deep molecular remission after stopping their TKI regained the remission after resuming therapy, Dr. Richter said.
Dr. Richter said in an interview that longer follow-up will be needed to confirm their findings, and that patients who were sensitive to TKIs prior to stopping therapy remained sensitive when restarting, suggesting that treatment interruption does not increase the likelihood of drug resistance.
Coprincipal investigator Dr. Francois-Xavier Mahon of Bordeaux University in France, noted that in the STIM (Stop Imatinib)–1 and –2 trials, the estimated annual savings to the French health care system were 20 million euros ($22.6 million).
COPENHAGEN – A year after stopping tyrosine kinase inhibitor therapy, more than half of patients with chronic myeloid leukemia (CML) in a large clinical trial remained in deep molecular remission.
Among 750 patients with CML in remission for at least 1 year before study entry, 62% retained a treatment response 6 months after stopping a tyrosine kinase inhibitor (TKI) such as imatinib (Gleevec) and 56% retained responses 1 year after being off their drugs, reported Dr. Johan Richter of Lund (Sweden) University at the annual congress of the European Hematology Association.
“About 6 years of therapy [with imatinib] would be optimal for therapy prior to a stop attempt,” he said at a briefing prior to the presentation of data at the congress.
Although in clinical practice patients with CML may remain on a TKI indefinitely, results from small clinical trials have suggested that in 40%-60% of patients with deep molecular responses (MR4.0 or better), TKIs can be safely stopped, Dr. Richter noted.
To get a better handle on when it might be safe to stop a TKI and under what conditions, EURO-SKI investigators enrolled 868 adults with CML in chronic phase from 11 countries, 750 of whom had complete data for the analysis.
In all, 94% of patients had received imatinib in the first line, 2% received dasatinib (Sprycel), and 4% had received nilotinib (Tasigna). Of this group, 115 had switched to a second-line agent due to intolerance of the first-line drug.
The median time from diagnosis was 7.7 years. The median duration of therapy was 7.6 years, and the median duration of MR4 before stopping was 4.7 years.
As noted, among 750 patients assessable for molecular relapse–free survival, 62% remained in remission at 6 months after stopping the TKI, as did 56% at 12 months, 52% at 24 months, and 49% at 36 months.
For patients who resumed therapy, the median time to restart was 4.1 months.
To see whether they could identify any factors prognostic for relapse after stopping a TKI, the investigators used data on 448 patients in the study who were treated with imatinib.
In univariate analysis there was no significant association between molecular relapse–free survival at 6 months and either age, gender, depth of molecular response, or any standard risk scores.
The only significant predictors of molecular remission status at 6 months were duration of imatinib therapy and duration of molecular response before stopping.
The odds ratio for treatment duration was 1.16, indicating that each additional year of imatinib treatment is associated with a 16% increase in the likelihood that a patient would remain in deep molecular remission 6 months after stopping.
The investigators used the minimal P value approach to determine the cutoff of approximately 6 years, based on a molecular relapse–free survival at 6 months of 65.5% for patients who remained on imatinib for more than 5.8 years, compared with 42.6% for those who were on it for 5.8 years or less.
Although the study is ongoing, to date more than 80% of patients who had a loss of deep molecular remission after stopping their TKI regained the remission after resuming therapy, Dr. Richter said.
Dr. Richter said in an interview that longer follow-up will be needed to confirm their findings, and that patients who were sensitive to TKIs prior to stopping therapy remained sensitive when restarting, suggesting that treatment interruption does not increase the likelihood of drug resistance.
Coprincipal investigator Dr. Francois-Xavier Mahon of Bordeaux University in France, noted that in the STIM (Stop Imatinib)–1 and –2 trials, the estimated annual savings to the French health care system were 20 million euros ($22.6 million).
COPENHAGEN – A year after stopping tyrosine kinase inhibitor therapy, more than half of patients with chronic myeloid leukemia (CML) in a large clinical trial remained in deep molecular remission.
Among 750 patients with CML in remission for at least 1 year before study entry, 62% retained a treatment response 6 months after stopping a tyrosine kinase inhibitor (TKI) such as imatinib (Gleevec) and 56% retained responses 1 year after being off their drugs, reported Dr. Johan Richter of Lund (Sweden) University at the annual congress of the European Hematology Association.
“About 6 years of therapy [with imatinib] would be optimal for therapy prior to a stop attempt,” he said at a briefing prior to the presentation of data at the congress.
Although in clinical practice patients with CML may remain on a TKI indefinitely, results from small clinical trials have suggested that in 40%-60% of patients with deep molecular responses (MR4.0 or better), TKIs can be safely stopped, Dr. Richter noted.
To get a better handle on when it might be safe to stop a TKI and under what conditions, EURO-SKI investigators enrolled 868 adults with CML in chronic phase from 11 countries, 750 of whom had complete data for the analysis.
In all, 94% of patients had received imatinib in the first line, 2% received dasatinib (Sprycel), and 4% had received nilotinib (Tasigna). Of this group, 115 had switched to a second-line agent due to intolerance of the first-line drug.
The median time from diagnosis was 7.7 years. The median duration of therapy was 7.6 years, and the median duration of MR4 before stopping was 4.7 years.
As noted, among 750 patients assessable for molecular relapse–free survival, 62% remained in remission at 6 months after stopping the TKI, as did 56% at 12 months, 52% at 24 months, and 49% at 36 months.
For patients who resumed therapy, the median time to restart was 4.1 months.
To see whether they could identify any factors prognostic for relapse after stopping a TKI, the investigators used data on 448 patients in the study who were treated with imatinib.
In univariate analysis there was no significant association between molecular relapse–free survival at 6 months and either age, gender, depth of molecular response, or any standard risk scores.
The only significant predictors of molecular remission status at 6 months were duration of imatinib therapy and duration of molecular response before stopping.
The odds ratio for treatment duration was 1.16, indicating that each additional year of imatinib treatment is associated with a 16% increase in the likelihood that a patient would remain in deep molecular remission 6 months after stopping.
The investigators used the minimal P value approach to determine the cutoff of approximately 6 years, based on a molecular relapse–free survival at 6 months of 65.5% for patients who remained on imatinib for more than 5.8 years, compared with 42.6% for those who were on it for 5.8 years or less.
Although the study is ongoing, to date more than 80% of patients who had a loss of deep molecular remission after stopping their TKI regained the remission after resuming therapy, Dr. Richter said.
Dr. Richter said in an interview that longer follow-up will be needed to confirm their findings, and that patients who were sensitive to TKIs prior to stopping therapy remained sensitive when restarting, suggesting that treatment interruption does not increase the likelihood of drug resistance.
Coprincipal investigator Dr. Francois-Xavier Mahon of Bordeaux University in France, noted that in the STIM (Stop Imatinib)–1 and –2 trials, the estimated annual savings to the French health care system were 20 million euros ($22.6 million).
AT THE EHA CONGRESS
Key clinical point:.Tyrosine kinase inhibitor therapy can be safely stopped and resumed in many patients with chronic-phase chronic myeloid leukemia (CML).
Major finding: After stopping a TKI, 62% of patients retained a treatment response at 6 months, and 56% retained a response at 1 year.
Data source: Study of therapeutic interruption in 750 adults in deep molecular remission for at least 1 year on TKI therapy.
Disclosures: The study was sponsored by the European LeukemiaNet. Dr. Richter has previously disclosed consultancy and equity ownership with Cantargia. Dr. Mahon has previously disclosed being on the scientific advisory board and receiving honoraria from Novartis Oncology and BMS, and serving as consultant to those companies and to Pfizer.