User login
FDA approves two new hemophilia therapies
The Food and Drug Administration has approved Idelvion, the first hemophilia B therapy with up to 14-day dosing intervals, and Kovaltry, an unmodified, full-length factor VIII compound for the treatment of hemophilia A.
Idelvion is a novel long-acting recombinant albumin fusion protein administered intravenously. In clinical trials from the PROLONG-9FP clinical development program – including phase I through III open-label, multicenter studies – the biotherapeutic agent maintained factor IX activity levels above 5% over 14 days at a dose of 75 IU/kg, resulting in a median annualized spontaneous bleeding rate of zero in patients, according to a statement by Idelvion’s manufacturer, CSL Behring. That “reduces the monthly number of units needed for prophylaxis therapy,” the company noted.
Idelvion is indicated in children and adults with hemophilia B for routine prophylaxis, as well as for on-demand control and prevention of bleeding episodes. It is also indicated for the perioperative management of bleeding. With on-demand treatment, 94% of bleeds were controlled with one infusion, and 99% were controlled with one or two infusions.
Appropriate patients 12 years and older can go up to 14 days between infusions, according to CSL Behring. The most common adverse reaction in the clinical trials was headache.
Idelvion is expected to be available later this month.
“The approval of this long-acting recombinant factor IX therapy for hemophilia B is vital, as physicians need more options to help their patients effectively and safely manage their bleeding disorder,” said Elena Santagostino, M.D., Ph.D., of the University of Milan/IRCCS Maggiore Hospital, and lead investigator of PROLONG-9FP, in a statement. “This provides them with greater freedom from frequent infusions.”
The FDA approved Kovaltry for children and adults with hemophilia A based on the results of the LEOPOLD (Long-Term Efficacy Open-Label Program in Severe Hemophilia A Disease) clinical trials. Kovaltry received approval in Europe and Canada earlier this year.
The LEOPOLD findings supported the approval for routine prophylaxis to reduce the frequency of bleeding episodes.
“In the LEOPOLD trials, Kovaltry reduced bleeding episodes in patients with hemophilia A when infused twice to three times per week with routine prophylaxis,” said Dr. Sanjay P. Ahuja, LEOPOLD investigator and director of the hemostasis and thrombosis center at University Hospitals Rainbow Babies & Children’s Hospital, Cleveland, in a statement by Kovaltry manufacturer Bayer. “Kovaltry may offer appropriate patients a twice-weekly prophylaxis dosing option.”
Dosing is 20-40 IU/kg of body weight 2-3 times per week in adolescents and adults, and 25-50 IU/kg of body weight 2-3 times per week or every other day in children aged 12 years or younger.
The most common adverse events associated with Kovaltry in the clinical trials were headache, fever, and pruritus.
The Food and Drug Administration has approved Idelvion, the first hemophilia B therapy with up to 14-day dosing intervals, and Kovaltry, an unmodified, full-length factor VIII compound for the treatment of hemophilia A.
Idelvion is a novel long-acting recombinant albumin fusion protein administered intravenously. In clinical trials from the PROLONG-9FP clinical development program – including phase I through III open-label, multicenter studies – the biotherapeutic agent maintained factor IX activity levels above 5% over 14 days at a dose of 75 IU/kg, resulting in a median annualized spontaneous bleeding rate of zero in patients, according to a statement by Idelvion’s manufacturer, CSL Behring. That “reduces the monthly number of units needed for prophylaxis therapy,” the company noted.
Idelvion is indicated in children and adults with hemophilia B for routine prophylaxis, as well as for on-demand control and prevention of bleeding episodes. It is also indicated for the perioperative management of bleeding. With on-demand treatment, 94% of bleeds were controlled with one infusion, and 99% were controlled with one or two infusions.
Appropriate patients 12 years and older can go up to 14 days between infusions, according to CSL Behring. The most common adverse reaction in the clinical trials was headache.
Idelvion is expected to be available later this month.
“The approval of this long-acting recombinant factor IX therapy for hemophilia B is vital, as physicians need more options to help their patients effectively and safely manage their bleeding disorder,” said Elena Santagostino, M.D., Ph.D., of the University of Milan/IRCCS Maggiore Hospital, and lead investigator of PROLONG-9FP, in a statement. “This provides them with greater freedom from frequent infusions.”
The FDA approved Kovaltry for children and adults with hemophilia A based on the results of the LEOPOLD (Long-Term Efficacy Open-Label Program in Severe Hemophilia A Disease) clinical trials. Kovaltry received approval in Europe and Canada earlier this year.
The LEOPOLD findings supported the approval for routine prophylaxis to reduce the frequency of bleeding episodes.
“In the LEOPOLD trials, Kovaltry reduced bleeding episodes in patients with hemophilia A when infused twice to three times per week with routine prophylaxis,” said Dr. Sanjay P. Ahuja, LEOPOLD investigator and director of the hemostasis and thrombosis center at University Hospitals Rainbow Babies & Children’s Hospital, Cleveland, in a statement by Kovaltry manufacturer Bayer. “Kovaltry may offer appropriate patients a twice-weekly prophylaxis dosing option.”
Dosing is 20-40 IU/kg of body weight 2-3 times per week in adolescents and adults, and 25-50 IU/kg of body weight 2-3 times per week or every other day in children aged 12 years or younger.
The most common adverse events associated with Kovaltry in the clinical trials were headache, fever, and pruritus.
The Food and Drug Administration has approved Idelvion, the first hemophilia B therapy with up to 14-day dosing intervals, and Kovaltry, an unmodified, full-length factor VIII compound for the treatment of hemophilia A.
Idelvion is a novel long-acting recombinant albumin fusion protein administered intravenously. In clinical trials from the PROLONG-9FP clinical development program – including phase I through III open-label, multicenter studies – the biotherapeutic agent maintained factor IX activity levels above 5% over 14 days at a dose of 75 IU/kg, resulting in a median annualized spontaneous bleeding rate of zero in patients, according to a statement by Idelvion’s manufacturer, CSL Behring. That “reduces the monthly number of units needed for prophylaxis therapy,” the company noted.
Idelvion is indicated in children and adults with hemophilia B for routine prophylaxis, as well as for on-demand control and prevention of bleeding episodes. It is also indicated for the perioperative management of bleeding. With on-demand treatment, 94% of bleeds were controlled with one infusion, and 99% were controlled with one or two infusions.
Appropriate patients 12 years and older can go up to 14 days between infusions, according to CSL Behring. The most common adverse reaction in the clinical trials was headache.
Idelvion is expected to be available later this month.
“The approval of this long-acting recombinant factor IX therapy for hemophilia B is vital, as physicians need more options to help their patients effectively and safely manage their bleeding disorder,” said Elena Santagostino, M.D., Ph.D., of the University of Milan/IRCCS Maggiore Hospital, and lead investigator of PROLONG-9FP, in a statement. “This provides them with greater freedom from frequent infusions.”
The FDA approved Kovaltry for children and adults with hemophilia A based on the results of the LEOPOLD (Long-Term Efficacy Open-Label Program in Severe Hemophilia A Disease) clinical trials. Kovaltry received approval in Europe and Canada earlier this year.
The LEOPOLD findings supported the approval for routine prophylaxis to reduce the frequency of bleeding episodes.
“In the LEOPOLD trials, Kovaltry reduced bleeding episodes in patients with hemophilia A when infused twice to three times per week with routine prophylaxis,” said Dr. Sanjay P. Ahuja, LEOPOLD investigator and director of the hemostasis and thrombosis center at University Hospitals Rainbow Babies & Children’s Hospital, Cleveland, in a statement by Kovaltry manufacturer Bayer. “Kovaltry may offer appropriate patients a twice-weekly prophylaxis dosing option.”
Dosing is 20-40 IU/kg of body weight 2-3 times per week in adolescents and adults, and 25-50 IU/kg of body weight 2-3 times per week or every other day in children aged 12 years or younger.
The most common adverse events associated with Kovaltry in the clinical trials were headache, fever, and pruritus.
Evaluation of Internet Information About Rotator Cuff Repair
Patients are learning about health and disease more independently than before, but such self-education may pose a unique challenge for practicing physicians. Although educated patients can assist in the critical appraisal of treatment options,1 misinformed patients may have preconceived treatment biases and unrealistic expectations. More than 66 million Americans use the Internet daily, and recent surveys have shown 86% have used the Internet for health-related information.2,3 With Internet use increasing, the number of patients turning to the web for medical information is increasing as well.4 For many patients, this information can be useful in making decisions about their health and health care.5
Although accessing medical information from the Internet has grown exponentially, analysis of information quality has grown considerably slower.6 With no regulatory body monitoring content, there is easy circumvention of the peer review process, an essential feature of academic publishing.7 With no external regulation, the information retrieved may be incorrect, outdated, or misleading. Many orthopedic studies have analyzed Internet content about numerous diagnoses.3-6,8-18 Most of these studies have found this information highly variable and of poor quality.
We conducted a study to evaluate and analyze rotator cuff repair information available to the general public through the Internet; to assess changes in the quality of information over time; to determine if sites sponsored by academic institutions offered higher-quality information; and to assess whether the readability of the material varied according to DISCERN scores.
Rotator cuff repairs are among the most common surgeries performed by orthopedic surgeons. To our knowledge, this is the first study to assess the quality of web information about rotator cuff repairs. We hypothesized that the quality of information would positively correlate with the reading level of the material presented, that academic institutions would present the highest-quality information, and that the type of information presented would change over time.
Materials and Methods
We used the search phrase rotator cuff repair on the 3 most popular search engines: Google, Yahoo!, and Bing. Google is the dominant engine, taking 83.06% of total market share, followed by Yahoo! (6.86%) and Bing (4.27%).5 The first 50 websites identified by each search engine were selected for evaluation, excluding duplicates or overlapping websites. Similarly, advertisements and strictly video results lacking text were excluded. After each engine was queried, a master list of 150 websites was created for individual evaluation and assessment. To assess changes in results over time, we performed 2 searches, on November 16, 2011, and May 18, 2014.
The content of each website was analyzed for authorship, ability to contact the author, discussion of disorder, surgical treatment, complications, surgical eligibility, rehabilitation, other treatment options, and use of peer-reviewed sources. Authorship was placed in 1 of 6 categories:
1. Academic—university-affiliated physician or research group.
2. Private—physician or group without stated affiliation to an academic organization.
3. Industry—manufacturing or marketing company advertising a product or service for profit.
4. News source—bulletin or article without affiliation to a hospital or an academic institution.
5. Public education—individual or organization with noncommercial website providing third-party information (eg, Wikipedia, About.com).
6. Blog—website publishing an individual’s personal experiences in diary or journal form.
Websites were also assessed for accuracy and validity based on presence or absence of Health On the Net code (HONcode) certification and DISCERN score. Designed by the Health On the Net Foundation in 1996, HONcode provides a framework for disseminating high-quality medical information over the web.19 Website owners can request that their sites be evaluated for HONcode certification; a site that qualifies can display the HONcode seal.20 The DISCERN project, initially funded by the National Health Service in the United Kingdom, judges the quality of written information available on health-related websites.21 It determines the quality of a publication on the basis of 16 questions: The first 8 address the publication’s reliability, the next 7 involve specific details of treatment choices, and the last is an overall rating of the website.
Website readability was assessed with the Flesch-Kincaid test. This test, designed under contract with the US Navy in 1975, has been used in other orthopedic studies.19 Regression analysis was performed to check for correlation between website readability and DISCERN score. Analysis of variance was used to analyze differences between scores.
Results
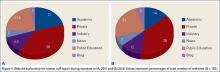
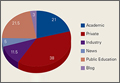
We performed a comprehensive analysis of the top 50 websites from each of the 3 search engines (N = 150 websites) (Figures 1–5, Table). Regarding authorship, our 2 searches demonstrated similar values (Figure 1). In 2011, 21% of websites were associated with an academic institution, 38% were authored by private physicians or hospital or physician groups not associated with an academic institution, 11.5% were industry-sponsored, 5% were news bulletins or media reports, 21.5% were public education websites, and 3% were personal blogs. Our 2014 search found a similar distribution of contributors. Between 2011 and 2014, the largest change was in academic authors, which decreased by 7%, from 21% to 14%. Percentage of websites authored by private physicians remained constant from the first to the second search: 38%.
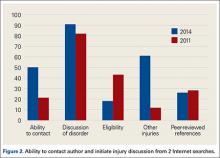
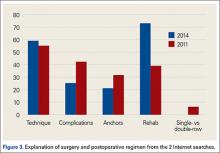
When the 2011 and 2014 website content was compared, several changes were noted. Percentage of websites providing an author contact method increased from 21% to 50% (Figure 2), percentage detailing rotator cuff repairs increased from 82% to 91%, and percentage introducing treatment options in addition to surgical management increased from 11.5% to 61%. Percentage discussing surgical eligibility, however, decreased from 43% to 18%. Percentage citing peer-reviewed sources remained relatively constant (28%, 26%), as did percentage discussing surgical technique for rotator cuff repair (55%, 59%) (Figure 3). A major decrease was found in percentage of websites discussing surgical complications, 42% in 2011 down to 25% in 2014, whereas a major increase was found in percentage discussing rehabilitation, from 39% in 2011 up to 73% in 2014. In 2014, no websites discussed double- versus single-row surgery—compared with 6% in 2011. False claims remained low between 2011 and 2014. In both searches, no website guaranteed a return to sport, and few made claims of painless or bloodless surgery.
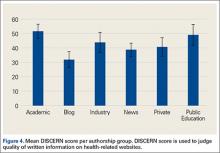
DISCERN scores for websites found during the 2014 search were averaged for each of the 6 authorship groups (Figure 4). The highest DISCERN scores were given to academic institution websites (51.6) and public education websites (49). For the academic websites, this difference was significant relative to news, blog, and private physician websites (Ps = .012, .001, .001) The lowest DISCERN scores were given to news organization websites and personal blogs. DISCERN scores were 43.8 for industry sources and 40.7 for private physician groups; the difference was not significant (P = .229). Overall mean DISCERN score for all websites was 44. Eleven percent of websites were HONcode-certified.
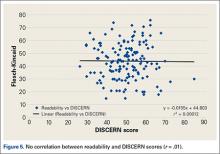
No correlation was found between website readability and DISCERN score; correlation coefficient r was .01 (Figure 5). For the websites in 2014, mean Flesch-Kincaid readability score was 50.17, and mean grade level was 10.98; coefficient of determination r2 was 0.00012.
The Table compares our data with data from other orthopedic studies that have analyzed the quality of Internet information about various orthopedic injuries, diseases, and procedures.3-6,8,9,11-18 With its mean DISCERN score of 44, the present rotator cuff tear study was ranked third of 6 studies that have used this scoring system to analyze website content. Of these 6 studies, those reviewing osteosarcoma and juvenile idiopathic arthritis were ranked highest (mean scores, 49.8 and 48.9, respectively), and the study reviewing scoliosis surgery was ranked lowest (38.9). Bruce-Brand and colleagues9 recently found a mean DISCERN score of 41 for anterior cruciate ligament (ACL) reconstruction. When considering HONcode-certified websites, our Internet search for rotator cuff tears found the third lowest percentage, 10.5%, compared with the other studies (Table); the highest percentage, 30%, was found for websites discussing concussions in athletes. When considering authorship, our rotator cuff study found the third highest percentage, 76%, authored by academic centers, physicians, and public education websites; the highest percentage was found in websites discussing ACL reconstruction. Websites discussing ACL reconstruction also had the highest percentage of websites authored by industry.9
Discussion
To our knowledge, this is the first study specifically analyzing the quality of Internet information about rotator cuff repairs. A similar study, conducted by Starman and colleagues15 in 2010, addressed the quality of web information about 10 common sports medicine diagnoses, one of which was rotator cuff tears. In that study, only 16 of the websites included discussed rotator cuff tears. In addition, the authors used a customized, HONcode-based grading system to analyze each website, making their data difficult to compare across studies.
Ideally, a high-quality medical website should be written by a credible source and should cover a disorder, treatment options, eligibility, rehabilitation, and complications. As there is no standard grading system for analyzing web content about rotator cuff repairs, we analyzed the websites for specific information we thought should be included in a high-quality website (Figures 2, 3). When considering authorship, we found academic centers, private physicians, and educational sources comprised 76% of the sources; industry sources made up only 12%. Similar findings were noted by investigators analyzing Internet information about other orthopedic topics, including ACL reconstruction, lumbar arthroplasty, osteosarcoma, and cervical spine surgery.5,11,22 Studies analyzing websites for information on ACL tears and distal radius fractures found have a higher percentage of industry-sponsored websites.9,10
DISCERN showed that the highest-quality information came from websites with academic affiliations, consistent with previous studies,3,9,17 and its mean score (51.6) was significantly higher than the scores for private physician websites, news sites, and blogs (Ps = .001, .016, .001); the least reliable information was from personal blogs and news outlets. Of note, mean DISCERN score was higher for the industry websites we found than for private physician websites (43.8 vs 40.7), though the difference was not significant (P = .229). Previous investigators considered number of industry-sponsored websites as a marker of poor quality of information relating to a given topic; however, given the DISCERN scores in our study, this might not necessarily be true.6 Based on the present study’s data, websites affiliated with academic institutions would be recommended for patients searching for high-quality information about rotator cuff tears.
Given DISCERN scores across studies, information about rotator cuff tears ranked below information about osteosarcoma and juvenile idiopathic arthritis but above information about scoliosis, cervical spine surgery, and ACL reconstruction (Table). DISCERN scores must be compared across studies, as there are no definitions for good and poor DISCERN scores.
Of the 4 studies that analyzed percentage of websites citing peer-reviewed sources, only our study and the study of cervical spine surgery18 analyzed that percentage as well as DISCERN score. Percentage citing peer-reviewed sources was 26% for rotator cuff tears and 24% for cervical spine surgery; the respective DISCERN scores were 44 and 43.6. As only these 2 studies could be compared, no real correlation between percentage of websites citing peer-reviewed sources and the quality of the content on a given topic can be assessed. More research into this relationship is needed. One already delineated association is the correlation between HONcode-certified sites and high DISCERN scores.21 For high-quality medical information, physicians can direct their patients both to academic institution websites and to HONcode-certified websites.
When we compared the present study with previous investigations, we found a large difference between search results for a given topic. In 2013, Duncan and colleagues6 and Bruce-Brand and colleagues9 used similar study designs (eg, search terms, search engines) for their investigations of quality of web information. Their results, however, were widely different. For example, percentages of industry authorship were 4.5% (Duncan and colleagues6) and 64% (Bruce-Brand and colleagues9). This inconsistency between studies conducted during similar periods might be related to what appears at the top of the results queue for a search. Duncan and colleagues6 analyzed 200 websites, Bruce-Brand and colleagues9 only 45. Industries may have made financial arrangements and used search engine optimization techniques to have their websites listed first in search results.
In our study, we also analyzed how web information has changed over time. On the Internet, information changes daily, and we hypothesized that the content found during our 2 searches (2011, 2014) would yield different results. Surprisingly, the data were similar, particularly concerning authorship (Figures 1, 2). In both searches, the largest authorship source was private physician or physician groups (38% in 2011 and 2014). Other authorship sources showed little change in percentage between searches. As for content, we found both increases and decreases in specific web information. Ability to contact authors increased from 21% (2011) to 50% (2014). We think it is important that websites offer a communication channel to people who read the medical information the sites provide. Percentage of websites discussing nonoperative treatment options increased from 11.5% to 61%. Therefore, patients in 2014 were being introduced to more options (in addition to surgery) for managing shoulder pain—an improvement in quality of information between the searches. Percentage of websites discussing surgical eligibility, however, decreased from 43% to 18%—a negative development in information quality. Another decrease, from 42% to 25%, was found for websites discussing surgical complications. Given the data as a whole, and our finding both negative and positive changes, it appears the quality of web content has not improved significantly. Interestingly, no websites discussed double- versus single-row surgery in 2014, but 6% did so in 2011.
Lost in the discussion of quality and reliability of information is whether patients comprehend what they are reading.23 Yi and colleagues19 recentlyassessed the readability level of arthroscopy information in articles published online by the American Academy of Orthopaedic Surgeons (AAOS) and the Arthroscopy Association of North America (AANA). The investigators used the Flesch-Kincaid readability test to determine readability level in terms of grade level. They found that the majority of the patient education articles on the AAOS and AANA sites had a readability level far above the national average; only 4 articles were written at or below the eighth-grade level, the current average reading level in the United States.24 Information that is not comprehensible is of no use to patients, and information that physicians and researchers consider high-quality might not be what patients consider high-quality. As we pursue higher-quality web content, we need to consider that its audience includes nonmedical readers, our patients. In the present study, we found that the readability of a website had no correlation with the site’s DISCERN score (Figure 5). Therefore, for information about rotator cuff repairs, higher-quality websites are no harder than lower-quality sites for patients to comprehend. The Flesch-Kincaid readability test is flawed in that it considers only total number of syllables per word and words per sentence, not nontextual elements of patient education materials, such as illustrations on a website. The 10.98 mean grade level found in our study is higher than the levels found for most studies reviewed by Yi and colleagues.19
This study had several limitations. During an Internet search, the number of websites a user visits drops precipitously after the first page of results. Studies have shown the top 20 sites in a given search receive 97% of the views, and the top 3 receive 58.4%. Whether patients visit websites far down in the list of 150 we found in our given search is unknown. Last, the Flesch-Kincaid readability test is flawed in several ways but nevertheless is used extensively in research. Grading is based on number of words and syllables used in a given sentence; it does not take into account the complexity or common usage of a given word or definition. Therefore, websites may receive low Flesch-Kincaid scores—indicating ease of reading—despite their use of complex medical terminology and jargon that complicate patients’ comprehension of the material.
Conclusion
Numerous authors have evaluated orthopedic patients’ accessing of medical information from the Internet. Although the Internet makes access easier, unreliable content can lead patients to develop certain notions about the direction of their care and certain expectations regarding their clinical outcomes. With there being no regulatory body monitoring content, the peer review process, an essential feature of academic publishing, can be easily circumvented.25
In this study, the highest-quality websites had academic affiliations. Quality of information about rotator cuff repairs was similar to what was found for other orthopedic topics in comparable studies. Surprisingly, there was little change in authorship and content of web information between our 2 search periods (2011, 2014). Although there has been a rapid increase in the number of medical websites, quality of content seems not to have changed significantly. Patients look to physicians for guidance but increasingly are accessing the Internet for additional information. It is essential that physicians understand the quality of information available on the Internet when counseling patients regarding surgery.
1. Brunnekreef JJ, Schreurs BW. Total hip arthroplasty: what information do we offer patients on websites of hospitals? BMC Health Serv Res. 2011;11:83.
2. Koh HS, In Y, Kong CG, Won HY, Kim KH, Lee JH. Factors affecting patients’ graft choice in anterior cruciate ligament reconstruction. Clin Orthop Surg. 2010;2(2):69-75.
3. Nason GJ, Baker JF, Byrne DP, Noel J, Moore D, Kiely PJ. Scoliosis-specific information on the Internet: has the “information highway” led to better information provision? Spine. 2012;37(21):E1364-E1369.
4. Groves ND, Humphreys HW, Williams AJ, Jones A. Effect of informational Internet web pages on patients’ decision making: randomised controlled trial regarding choice of spinal or general anaesthesia for orthopaedic surgery. Anaesthesia. 2010;65(3):277-282.
5. Purcell K, Brenner J, Rainie L. Search Engine Use 2012. Washington, DC: Pew Internet & American Life Project; 2012.
6. Duncan IC, Kane PW, Lawson KA, Cohen SB, Ciccotti MG, Dodson CC. Evaluation of information available on the Internet regarding anterior cruciate ligament reconstruction. Arthroscopy. 2013;29(6):1101-1107.
7. Lichtenfeld LJ. Can the beast be tamed? The woeful tale of accurate health information on the Internet. Ann Surg Oncol. 2012;19(3):701-702.
8. Ahmed OH, Sullivan SJ, Schneiders AG, McCrory PR. Concussion information online: evaluation of information quality, content and readability of concussion-related websites. Br J Sports Med. 2012;46(9):675-683.
9. Bruce-Brand RA, Baker JF, Byrne DP, Hogan NA, McCarthy T. Assessment of the quality and content of information on anterior cruciate ligament reconstruction on the Internet. Arthroscopy. 2013;29(6):1095-1100.
10. Dy JC, Taylor SA, Patel RM, Kitay A, Roberts TR, Daluiski A. The effect of search term on the quality and accuracy of online information regarding distal radius fractures. J Hand Surg Am. 2012;37(9):1881-1887.
11. Garcia RM, Messerschmitt PJ, Ahn NU. An evaluation of information on the Internet of a new device: the lumbar artificial disc replacement. J Spinal Disord Tech. 2009;22(1):52-57.
12. Gosselin MM, Mulcahey MK, Feller E, Hulstyn MJ. Examining Internet resources on gender differences in ACL injuries: what patients are reading. Knee. 2013;20(3):196-202.
13. Lam CG, Roter DL, Cohen KJ. Survey of quality, readability, and social reach of websites on osteosarcoma in adolescents. Patient Educ Couns. 2013;90(1):82-87.
14. Morr S, Shanti N, Carrer A, Kubeck J, Gerling MC. Quality of information concerning cervical disc herniation on the Internet. Spine J. 2010;10(4):350-354.
15. Starman JS, Gettys FK, Capo JA, Fleischli JE, Norton HJ, Karunakar MA. Quality and content of Internet-based information for ten common orthopaedic sports medicine diagnoses. J Bone Joint Surg Am. 2010;92(7):1612-1618.
16. Stinson JN, Tucker L, Huber A, et al. Surfing for juvenile idiopathic arthritis: perspectives on quality and content of information on the Internet. J Rheumatol. 2009;36(8):1755-1762.
17. Sullivan TB, Anderson JS, Ahn UM, Ahn NU. Can Internet information on vertebroplasty be a reliable means of patient self-education? Clin Orthop Relat Res. 2014;472(5):1597-1604.
18. Weil AG, Bojanowski MW, Jamart J, Gustin T, Lévêque M. Evaluation of the quality of information on the Internet available to patients undergoing cervical spine surgery. World Neurosurg. 2014;82(1-2):e31-e39.
19. Yi PH, Ganta A, Hussein KI, Frank RM, Jawa A. Readability of arthroscopy-related patient education materials from the American Academy of Orthopaedic Surgeons and Arthroscopy Association of North America web sites. Arthroscopy. 2013;29(6):1108-1112.
20. Boyer C, Selby M, Scherrer JR, Appel RD. The Health On the Net code of conduct for medical and health websites. Comput Biol Med. 1998;28(5):603-610.
21. Silberg WM, Lundberg GD, Musacchio RA. Assessing, controlling, and assuring the quality of medical information on the Internet: Caveant lector et viewor—Let the reader and viewer beware. JAMA. 1997;277(15):1244-1245.
22. Fabricant PD, Dy CJ, Patel RM, Blanco JS, Doyle SM. Internet search term affects the quality and accuracy of online information about developmental hip dysplasia. J Pediatr Orthop. 2013;33(4):361-365.
23. Aslam N, Bowyer D, Wainwright A, Theologis T, Benson M. Evaluation of Internet use by paediatric orthopaedic outpatients and the quality of information available. J Pediatr Orthop B. 2005;14(2):129-133.
24. Wetzler MJ. “I found it on the Internet”: how reliable and readable is patient information? Arthroscopy. 2013;29(6):967-968.
25. Qureshi SA, Koehler SM, Lin JD, Bird J, Garcia RM, Hecht AC. An evaluation of information on the Internet about a new device: the cervical artificial disc replacement. Spine. 2012;37(10):881-883.
Patients are learning about health and disease more independently than before, but such self-education may pose a unique challenge for practicing physicians. Although educated patients can assist in the critical appraisal of treatment options,1 misinformed patients may have preconceived treatment biases and unrealistic expectations. More than 66 million Americans use the Internet daily, and recent surveys have shown 86% have used the Internet for health-related information.2,3 With Internet use increasing, the number of patients turning to the web for medical information is increasing as well.4 For many patients, this information can be useful in making decisions about their health and health care.5
Although accessing medical information from the Internet has grown exponentially, analysis of information quality has grown considerably slower.6 With no regulatory body monitoring content, there is easy circumvention of the peer review process, an essential feature of academic publishing.7 With no external regulation, the information retrieved may be incorrect, outdated, or misleading. Many orthopedic studies have analyzed Internet content about numerous diagnoses.3-6,8-18 Most of these studies have found this information highly variable and of poor quality.
We conducted a study to evaluate and analyze rotator cuff repair information available to the general public through the Internet; to assess changes in the quality of information over time; to determine if sites sponsored by academic institutions offered higher-quality information; and to assess whether the readability of the material varied according to DISCERN scores.
Rotator cuff repairs are among the most common surgeries performed by orthopedic surgeons. To our knowledge, this is the first study to assess the quality of web information about rotator cuff repairs. We hypothesized that the quality of information would positively correlate with the reading level of the material presented, that academic institutions would present the highest-quality information, and that the type of information presented would change over time.
Materials and Methods
We used the search phrase rotator cuff repair on the 3 most popular search engines: Google, Yahoo!, and Bing. Google is the dominant engine, taking 83.06% of total market share, followed by Yahoo! (6.86%) and Bing (4.27%).5 The first 50 websites identified by each search engine were selected for evaluation, excluding duplicates or overlapping websites. Similarly, advertisements and strictly video results lacking text were excluded. After each engine was queried, a master list of 150 websites was created for individual evaluation and assessment. To assess changes in results over time, we performed 2 searches, on November 16, 2011, and May 18, 2014.
The content of each website was analyzed for authorship, ability to contact the author, discussion of disorder, surgical treatment, complications, surgical eligibility, rehabilitation, other treatment options, and use of peer-reviewed sources. Authorship was placed in 1 of 6 categories:
1. Academic—university-affiliated physician or research group.
2. Private—physician or group without stated affiliation to an academic organization.
3. Industry—manufacturing or marketing company advertising a product or service for profit.
4. News source—bulletin or article without affiliation to a hospital or an academic institution.
5. Public education—individual or organization with noncommercial website providing third-party information (eg, Wikipedia, About.com).
6. Blog—website publishing an individual’s personal experiences in diary or journal form.
Websites were also assessed for accuracy and validity based on presence or absence of Health On the Net code (HONcode) certification and DISCERN score. Designed by the Health On the Net Foundation in 1996, HONcode provides a framework for disseminating high-quality medical information over the web.19 Website owners can request that their sites be evaluated for HONcode certification; a site that qualifies can display the HONcode seal.20 The DISCERN project, initially funded by the National Health Service in the United Kingdom, judges the quality of written information available on health-related websites.21 It determines the quality of a publication on the basis of 16 questions: The first 8 address the publication’s reliability, the next 7 involve specific details of treatment choices, and the last is an overall rating of the website.
Website readability was assessed with the Flesch-Kincaid test. This test, designed under contract with the US Navy in 1975, has been used in other orthopedic studies.19 Regression analysis was performed to check for correlation between website readability and DISCERN score. Analysis of variance was used to analyze differences between scores.
Results
We performed a comprehensive analysis of the top 50 websites from each of the 3 search engines (N = 150 websites) (Figures 1–5, Table). Regarding authorship, our 2 searches demonstrated similar values (Figure 1). In 2011, 21% of websites were associated with an academic institution, 38% were authored by private physicians or hospital or physician groups not associated with an academic institution, 11.5% were industry-sponsored, 5% were news bulletins or media reports, 21.5% were public education websites, and 3% were personal blogs. Our 2014 search found a similar distribution of contributors. Between 2011 and 2014, the largest change was in academic authors, which decreased by 7%, from 21% to 14%. Percentage of websites authored by private physicians remained constant from the first to the second search: 38%.
When the 2011 and 2014 website content was compared, several changes were noted. Percentage of websites providing an author contact method increased from 21% to 50% (Figure 2), percentage detailing rotator cuff repairs increased from 82% to 91%, and percentage introducing treatment options in addition to surgical management increased from 11.5% to 61%. Percentage discussing surgical eligibility, however, decreased from 43% to 18%. Percentage citing peer-reviewed sources remained relatively constant (28%, 26%), as did percentage discussing surgical technique for rotator cuff repair (55%, 59%) (Figure 3). A major decrease was found in percentage of websites discussing surgical complications, 42% in 2011 down to 25% in 2014, whereas a major increase was found in percentage discussing rehabilitation, from 39% in 2011 up to 73% in 2014. In 2014, no websites discussed double- versus single-row surgery—compared with 6% in 2011. False claims remained low between 2011 and 2014. In both searches, no website guaranteed a return to sport, and few made claims of painless or bloodless surgery.
DISCERN scores for websites found during the 2014 search were averaged for each of the 6 authorship groups (Figure 4). The highest DISCERN scores were given to academic institution websites (51.6) and public education websites (49). For the academic websites, this difference was significant relative to news, blog, and private physician websites (Ps = .012, .001, .001) The lowest DISCERN scores were given to news organization websites and personal blogs. DISCERN scores were 43.8 for industry sources and 40.7 for private physician groups; the difference was not significant (P = .229). Overall mean DISCERN score for all websites was 44. Eleven percent of websites were HONcode-certified.
No correlation was found between website readability and DISCERN score; correlation coefficient r was .01 (Figure 5). For the websites in 2014, mean Flesch-Kincaid readability score was 50.17, and mean grade level was 10.98; coefficient of determination r2 was 0.00012.
The Table compares our data with data from other orthopedic studies that have analyzed the quality of Internet information about various orthopedic injuries, diseases, and procedures.3-6,8,9,11-18 With its mean DISCERN score of 44, the present rotator cuff tear study was ranked third of 6 studies that have used this scoring system to analyze website content. Of these 6 studies, those reviewing osteosarcoma and juvenile idiopathic arthritis were ranked highest (mean scores, 49.8 and 48.9, respectively), and the study reviewing scoliosis surgery was ranked lowest (38.9). Bruce-Brand and colleagues9 recently found a mean DISCERN score of 41 for anterior cruciate ligament (ACL) reconstruction. When considering HONcode-certified websites, our Internet search for rotator cuff tears found the third lowest percentage, 10.5%, compared with the other studies (Table); the highest percentage, 30%, was found for websites discussing concussions in athletes. When considering authorship, our rotator cuff study found the third highest percentage, 76%, authored by academic centers, physicians, and public education websites; the highest percentage was found in websites discussing ACL reconstruction. Websites discussing ACL reconstruction also had the highest percentage of websites authored by industry.9
Discussion
To our knowledge, this is the first study specifically analyzing the quality of Internet information about rotator cuff repairs. A similar study, conducted by Starman and colleagues15 in 2010, addressed the quality of web information about 10 common sports medicine diagnoses, one of which was rotator cuff tears. In that study, only 16 of the websites included discussed rotator cuff tears. In addition, the authors used a customized, HONcode-based grading system to analyze each website, making their data difficult to compare across studies.
Ideally, a high-quality medical website should be written by a credible source and should cover a disorder, treatment options, eligibility, rehabilitation, and complications. As there is no standard grading system for analyzing web content about rotator cuff repairs, we analyzed the websites for specific information we thought should be included in a high-quality website (Figures 2, 3). When considering authorship, we found academic centers, private physicians, and educational sources comprised 76% of the sources; industry sources made up only 12%. Similar findings were noted by investigators analyzing Internet information about other orthopedic topics, including ACL reconstruction, lumbar arthroplasty, osteosarcoma, and cervical spine surgery.5,11,22 Studies analyzing websites for information on ACL tears and distal radius fractures found have a higher percentage of industry-sponsored websites.9,10
DISCERN showed that the highest-quality information came from websites with academic affiliations, consistent with previous studies,3,9,17 and its mean score (51.6) was significantly higher than the scores for private physician websites, news sites, and blogs (Ps = .001, .016, .001); the least reliable information was from personal blogs and news outlets. Of note, mean DISCERN score was higher for the industry websites we found than for private physician websites (43.8 vs 40.7), though the difference was not significant (P = .229). Previous investigators considered number of industry-sponsored websites as a marker of poor quality of information relating to a given topic; however, given the DISCERN scores in our study, this might not necessarily be true.6 Based on the present study’s data, websites affiliated with academic institutions would be recommended for patients searching for high-quality information about rotator cuff tears.
Given DISCERN scores across studies, information about rotator cuff tears ranked below information about osteosarcoma and juvenile idiopathic arthritis but above information about scoliosis, cervical spine surgery, and ACL reconstruction (Table). DISCERN scores must be compared across studies, as there are no definitions for good and poor DISCERN scores.
Of the 4 studies that analyzed percentage of websites citing peer-reviewed sources, only our study and the study of cervical spine surgery18 analyzed that percentage as well as DISCERN score. Percentage citing peer-reviewed sources was 26% for rotator cuff tears and 24% for cervical spine surgery; the respective DISCERN scores were 44 and 43.6. As only these 2 studies could be compared, no real correlation between percentage of websites citing peer-reviewed sources and the quality of the content on a given topic can be assessed. More research into this relationship is needed. One already delineated association is the correlation between HONcode-certified sites and high DISCERN scores.21 For high-quality medical information, physicians can direct their patients both to academic institution websites and to HONcode-certified websites.
When we compared the present study with previous investigations, we found a large difference between search results for a given topic. In 2013, Duncan and colleagues6 and Bruce-Brand and colleagues9 used similar study designs (eg, search terms, search engines) for their investigations of quality of web information. Their results, however, were widely different. For example, percentages of industry authorship were 4.5% (Duncan and colleagues6) and 64% (Bruce-Brand and colleagues9). This inconsistency between studies conducted during similar periods might be related to what appears at the top of the results queue for a search. Duncan and colleagues6 analyzed 200 websites, Bruce-Brand and colleagues9 only 45. Industries may have made financial arrangements and used search engine optimization techniques to have their websites listed first in search results.
In our study, we also analyzed how web information has changed over time. On the Internet, information changes daily, and we hypothesized that the content found during our 2 searches (2011, 2014) would yield different results. Surprisingly, the data were similar, particularly concerning authorship (Figures 1, 2). In both searches, the largest authorship source was private physician or physician groups (38% in 2011 and 2014). Other authorship sources showed little change in percentage between searches. As for content, we found both increases and decreases in specific web information. Ability to contact authors increased from 21% (2011) to 50% (2014). We think it is important that websites offer a communication channel to people who read the medical information the sites provide. Percentage of websites discussing nonoperative treatment options increased from 11.5% to 61%. Therefore, patients in 2014 were being introduced to more options (in addition to surgery) for managing shoulder pain—an improvement in quality of information between the searches. Percentage of websites discussing surgical eligibility, however, decreased from 43% to 18%—a negative development in information quality. Another decrease, from 42% to 25%, was found for websites discussing surgical complications. Given the data as a whole, and our finding both negative and positive changes, it appears the quality of web content has not improved significantly. Interestingly, no websites discussed double- versus single-row surgery in 2014, but 6% did so in 2011.
Lost in the discussion of quality and reliability of information is whether patients comprehend what they are reading.23 Yi and colleagues19 recentlyassessed the readability level of arthroscopy information in articles published online by the American Academy of Orthopaedic Surgeons (AAOS) and the Arthroscopy Association of North America (AANA). The investigators used the Flesch-Kincaid readability test to determine readability level in terms of grade level. They found that the majority of the patient education articles on the AAOS and AANA sites had a readability level far above the national average; only 4 articles were written at or below the eighth-grade level, the current average reading level in the United States.24 Information that is not comprehensible is of no use to patients, and information that physicians and researchers consider high-quality might not be what patients consider high-quality. As we pursue higher-quality web content, we need to consider that its audience includes nonmedical readers, our patients. In the present study, we found that the readability of a website had no correlation with the site’s DISCERN score (Figure 5). Therefore, for information about rotator cuff repairs, higher-quality websites are no harder than lower-quality sites for patients to comprehend. The Flesch-Kincaid readability test is flawed in that it considers only total number of syllables per word and words per sentence, not nontextual elements of patient education materials, such as illustrations on a website. The 10.98 mean grade level found in our study is higher than the levels found for most studies reviewed by Yi and colleagues.19
This study had several limitations. During an Internet search, the number of websites a user visits drops precipitously after the first page of results. Studies have shown the top 20 sites in a given search receive 97% of the views, and the top 3 receive 58.4%. Whether patients visit websites far down in the list of 150 we found in our given search is unknown. Last, the Flesch-Kincaid readability test is flawed in several ways but nevertheless is used extensively in research. Grading is based on number of words and syllables used in a given sentence; it does not take into account the complexity or common usage of a given word or definition. Therefore, websites may receive low Flesch-Kincaid scores—indicating ease of reading—despite their use of complex medical terminology and jargon that complicate patients’ comprehension of the material.
Conclusion
Numerous authors have evaluated orthopedic patients’ accessing of medical information from the Internet. Although the Internet makes access easier, unreliable content can lead patients to develop certain notions about the direction of their care and certain expectations regarding their clinical outcomes. With there being no regulatory body monitoring content, the peer review process, an essential feature of academic publishing, can be easily circumvented.25
In this study, the highest-quality websites had academic affiliations. Quality of information about rotator cuff repairs was similar to what was found for other orthopedic topics in comparable studies. Surprisingly, there was little change in authorship and content of web information between our 2 search periods (2011, 2014). Although there has been a rapid increase in the number of medical websites, quality of content seems not to have changed significantly. Patients look to physicians for guidance but increasingly are accessing the Internet for additional information. It is essential that physicians understand the quality of information available on the Internet when counseling patients regarding surgery.
Patients are learning about health and disease more independently than before, but such self-education may pose a unique challenge for practicing physicians. Although educated patients can assist in the critical appraisal of treatment options,1 misinformed patients may have preconceived treatment biases and unrealistic expectations. More than 66 million Americans use the Internet daily, and recent surveys have shown 86% have used the Internet for health-related information.2,3 With Internet use increasing, the number of patients turning to the web for medical information is increasing as well.4 For many patients, this information can be useful in making decisions about their health and health care.5
Although accessing medical information from the Internet has grown exponentially, analysis of information quality has grown considerably slower.6 With no regulatory body monitoring content, there is easy circumvention of the peer review process, an essential feature of academic publishing.7 With no external regulation, the information retrieved may be incorrect, outdated, or misleading. Many orthopedic studies have analyzed Internet content about numerous diagnoses.3-6,8-18 Most of these studies have found this information highly variable and of poor quality.
We conducted a study to evaluate and analyze rotator cuff repair information available to the general public through the Internet; to assess changes in the quality of information over time; to determine if sites sponsored by academic institutions offered higher-quality information; and to assess whether the readability of the material varied according to DISCERN scores.
Rotator cuff repairs are among the most common surgeries performed by orthopedic surgeons. To our knowledge, this is the first study to assess the quality of web information about rotator cuff repairs. We hypothesized that the quality of information would positively correlate with the reading level of the material presented, that academic institutions would present the highest-quality information, and that the type of information presented would change over time.
Materials and Methods
We used the search phrase rotator cuff repair on the 3 most popular search engines: Google, Yahoo!, and Bing. Google is the dominant engine, taking 83.06% of total market share, followed by Yahoo! (6.86%) and Bing (4.27%).5 The first 50 websites identified by each search engine were selected for evaluation, excluding duplicates or overlapping websites. Similarly, advertisements and strictly video results lacking text were excluded. After each engine was queried, a master list of 150 websites was created for individual evaluation and assessment. To assess changes in results over time, we performed 2 searches, on November 16, 2011, and May 18, 2014.
The content of each website was analyzed for authorship, ability to contact the author, discussion of disorder, surgical treatment, complications, surgical eligibility, rehabilitation, other treatment options, and use of peer-reviewed sources. Authorship was placed in 1 of 6 categories:
1. Academic—university-affiliated physician or research group.
2. Private—physician or group without stated affiliation to an academic organization.
3. Industry—manufacturing or marketing company advertising a product or service for profit.
4. News source—bulletin or article without affiliation to a hospital or an academic institution.
5. Public education—individual or organization with noncommercial website providing third-party information (eg, Wikipedia, About.com).
6. Blog—website publishing an individual’s personal experiences in diary or journal form.
Websites were also assessed for accuracy and validity based on presence or absence of Health On the Net code (HONcode) certification and DISCERN score. Designed by the Health On the Net Foundation in 1996, HONcode provides a framework for disseminating high-quality medical information over the web.19 Website owners can request that their sites be evaluated for HONcode certification; a site that qualifies can display the HONcode seal.20 The DISCERN project, initially funded by the National Health Service in the United Kingdom, judges the quality of written information available on health-related websites.21 It determines the quality of a publication on the basis of 16 questions: The first 8 address the publication’s reliability, the next 7 involve specific details of treatment choices, and the last is an overall rating of the website.
Website readability was assessed with the Flesch-Kincaid test. This test, designed under contract with the US Navy in 1975, has been used in other orthopedic studies.19 Regression analysis was performed to check for correlation between website readability and DISCERN score. Analysis of variance was used to analyze differences between scores.
Results
We performed a comprehensive analysis of the top 50 websites from each of the 3 search engines (N = 150 websites) (Figures 1–5, Table). Regarding authorship, our 2 searches demonstrated similar values (Figure 1). In 2011, 21% of websites were associated with an academic institution, 38% were authored by private physicians or hospital or physician groups not associated with an academic institution, 11.5% were industry-sponsored, 5% were news bulletins or media reports, 21.5% were public education websites, and 3% were personal blogs. Our 2014 search found a similar distribution of contributors. Between 2011 and 2014, the largest change was in academic authors, which decreased by 7%, from 21% to 14%. Percentage of websites authored by private physicians remained constant from the first to the second search: 38%.
When the 2011 and 2014 website content was compared, several changes were noted. Percentage of websites providing an author contact method increased from 21% to 50% (Figure 2), percentage detailing rotator cuff repairs increased from 82% to 91%, and percentage introducing treatment options in addition to surgical management increased from 11.5% to 61%. Percentage discussing surgical eligibility, however, decreased from 43% to 18%. Percentage citing peer-reviewed sources remained relatively constant (28%, 26%), as did percentage discussing surgical technique for rotator cuff repair (55%, 59%) (Figure 3). A major decrease was found in percentage of websites discussing surgical complications, 42% in 2011 down to 25% in 2014, whereas a major increase was found in percentage discussing rehabilitation, from 39% in 2011 up to 73% in 2014. In 2014, no websites discussed double- versus single-row surgery—compared with 6% in 2011. False claims remained low between 2011 and 2014. In both searches, no website guaranteed a return to sport, and few made claims of painless or bloodless surgery.
DISCERN scores for websites found during the 2014 search were averaged for each of the 6 authorship groups (Figure 4). The highest DISCERN scores were given to academic institution websites (51.6) and public education websites (49). For the academic websites, this difference was significant relative to news, blog, and private physician websites (Ps = .012, .001, .001) The lowest DISCERN scores were given to news organization websites and personal blogs. DISCERN scores were 43.8 for industry sources and 40.7 for private physician groups; the difference was not significant (P = .229). Overall mean DISCERN score for all websites was 44. Eleven percent of websites were HONcode-certified.
No correlation was found between website readability and DISCERN score; correlation coefficient r was .01 (Figure 5). For the websites in 2014, mean Flesch-Kincaid readability score was 50.17, and mean grade level was 10.98; coefficient of determination r2 was 0.00012.
The Table compares our data with data from other orthopedic studies that have analyzed the quality of Internet information about various orthopedic injuries, diseases, and procedures.3-6,8,9,11-18 With its mean DISCERN score of 44, the present rotator cuff tear study was ranked third of 6 studies that have used this scoring system to analyze website content. Of these 6 studies, those reviewing osteosarcoma and juvenile idiopathic arthritis were ranked highest (mean scores, 49.8 and 48.9, respectively), and the study reviewing scoliosis surgery was ranked lowest (38.9). Bruce-Brand and colleagues9 recently found a mean DISCERN score of 41 for anterior cruciate ligament (ACL) reconstruction. When considering HONcode-certified websites, our Internet search for rotator cuff tears found the third lowest percentage, 10.5%, compared with the other studies (Table); the highest percentage, 30%, was found for websites discussing concussions in athletes. When considering authorship, our rotator cuff study found the third highest percentage, 76%, authored by academic centers, physicians, and public education websites; the highest percentage was found in websites discussing ACL reconstruction. Websites discussing ACL reconstruction also had the highest percentage of websites authored by industry.9
Discussion
To our knowledge, this is the first study specifically analyzing the quality of Internet information about rotator cuff repairs. A similar study, conducted by Starman and colleagues15 in 2010, addressed the quality of web information about 10 common sports medicine diagnoses, one of which was rotator cuff tears. In that study, only 16 of the websites included discussed rotator cuff tears. In addition, the authors used a customized, HONcode-based grading system to analyze each website, making their data difficult to compare across studies.
Ideally, a high-quality medical website should be written by a credible source and should cover a disorder, treatment options, eligibility, rehabilitation, and complications. As there is no standard grading system for analyzing web content about rotator cuff repairs, we analyzed the websites for specific information we thought should be included in a high-quality website (Figures 2, 3). When considering authorship, we found academic centers, private physicians, and educational sources comprised 76% of the sources; industry sources made up only 12%. Similar findings were noted by investigators analyzing Internet information about other orthopedic topics, including ACL reconstruction, lumbar arthroplasty, osteosarcoma, and cervical spine surgery.5,11,22 Studies analyzing websites for information on ACL tears and distal radius fractures found have a higher percentage of industry-sponsored websites.9,10
DISCERN showed that the highest-quality information came from websites with academic affiliations, consistent with previous studies,3,9,17 and its mean score (51.6) was significantly higher than the scores for private physician websites, news sites, and blogs (Ps = .001, .016, .001); the least reliable information was from personal blogs and news outlets. Of note, mean DISCERN score was higher for the industry websites we found than for private physician websites (43.8 vs 40.7), though the difference was not significant (P = .229). Previous investigators considered number of industry-sponsored websites as a marker of poor quality of information relating to a given topic; however, given the DISCERN scores in our study, this might not necessarily be true.6 Based on the present study’s data, websites affiliated with academic institutions would be recommended for patients searching for high-quality information about rotator cuff tears.
Given DISCERN scores across studies, information about rotator cuff tears ranked below information about osteosarcoma and juvenile idiopathic arthritis but above information about scoliosis, cervical spine surgery, and ACL reconstruction (Table). DISCERN scores must be compared across studies, as there are no definitions for good and poor DISCERN scores.
Of the 4 studies that analyzed percentage of websites citing peer-reviewed sources, only our study and the study of cervical spine surgery18 analyzed that percentage as well as DISCERN score. Percentage citing peer-reviewed sources was 26% for rotator cuff tears and 24% for cervical spine surgery; the respective DISCERN scores were 44 and 43.6. As only these 2 studies could be compared, no real correlation between percentage of websites citing peer-reviewed sources and the quality of the content on a given topic can be assessed. More research into this relationship is needed. One already delineated association is the correlation between HONcode-certified sites and high DISCERN scores.21 For high-quality medical information, physicians can direct their patients both to academic institution websites and to HONcode-certified websites.
When we compared the present study with previous investigations, we found a large difference between search results for a given topic. In 2013, Duncan and colleagues6 and Bruce-Brand and colleagues9 used similar study designs (eg, search terms, search engines) for their investigations of quality of web information. Their results, however, were widely different. For example, percentages of industry authorship were 4.5% (Duncan and colleagues6) and 64% (Bruce-Brand and colleagues9). This inconsistency between studies conducted during similar periods might be related to what appears at the top of the results queue for a search. Duncan and colleagues6 analyzed 200 websites, Bruce-Brand and colleagues9 only 45. Industries may have made financial arrangements and used search engine optimization techniques to have their websites listed first in search results.
In our study, we also analyzed how web information has changed over time. On the Internet, information changes daily, and we hypothesized that the content found during our 2 searches (2011, 2014) would yield different results. Surprisingly, the data were similar, particularly concerning authorship (Figures 1, 2). In both searches, the largest authorship source was private physician or physician groups (38% in 2011 and 2014). Other authorship sources showed little change in percentage between searches. As for content, we found both increases and decreases in specific web information. Ability to contact authors increased from 21% (2011) to 50% (2014). We think it is important that websites offer a communication channel to people who read the medical information the sites provide. Percentage of websites discussing nonoperative treatment options increased from 11.5% to 61%. Therefore, patients in 2014 were being introduced to more options (in addition to surgery) for managing shoulder pain—an improvement in quality of information between the searches. Percentage of websites discussing surgical eligibility, however, decreased from 43% to 18%—a negative development in information quality. Another decrease, from 42% to 25%, was found for websites discussing surgical complications. Given the data as a whole, and our finding both negative and positive changes, it appears the quality of web content has not improved significantly. Interestingly, no websites discussed double- versus single-row surgery in 2014, but 6% did so in 2011.
Lost in the discussion of quality and reliability of information is whether patients comprehend what they are reading.23 Yi and colleagues19 recentlyassessed the readability level of arthroscopy information in articles published online by the American Academy of Orthopaedic Surgeons (AAOS) and the Arthroscopy Association of North America (AANA). The investigators used the Flesch-Kincaid readability test to determine readability level in terms of grade level. They found that the majority of the patient education articles on the AAOS and AANA sites had a readability level far above the national average; only 4 articles were written at or below the eighth-grade level, the current average reading level in the United States.24 Information that is not comprehensible is of no use to patients, and information that physicians and researchers consider high-quality might not be what patients consider high-quality. As we pursue higher-quality web content, we need to consider that its audience includes nonmedical readers, our patients. In the present study, we found that the readability of a website had no correlation with the site’s DISCERN score (Figure 5). Therefore, for information about rotator cuff repairs, higher-quality websites are no harder than lower-quality sites for patients to comprehend. The Flesch-Kincaid readability test is flawed in that it considers only total number of syllables per word and words per sentence, not nontextual elements of patient education materials, such as illustrations on a website. The 10.98 mean grade level found in our study is higher than the levels found for most studies reviewed by Yi and colleagues.19
This study had several limitations. During an Internet search, the number of websites a user visits drops precipitously after the first page of results. Studies have shown the top 20 sites in a given search receive 97% of the views, and the top 3 receive 58.4%. Whether patients visit websites far down in the list of 150 we found in our given search is unknown. Last, the Flesch-Kincaid readability test is flawed in several ways but nevertheless is used extensively in research. Grading is based on number of words and syllables used in a given sentence; it does not take into account the complexity or common usage of a given word or definition. Therefore, websites may receive low Flesch-Kincaid scores—indicating ease of reading—despite their use of complex medical terminology and jargon that complicate patients’ comprehension of the material.
Conclusion
Numerous authors have evaluated orthopedic patients’ accessing of medical information from the Internet. Although the Internet makes access easier, unreliable content can lead patients to develop certain notions about the direction of their care and certain expectations regarding their clinical outcomes. With there being no regulatory body monitoring content, the peer review process, an essential feature of academic publishing, can be easily circumvented.25
In this study, the highest-quality websites had academic affiliations. Quality of information about rotator cuff repairs was similar to what was found for other orthopedic topics in comparable studies. Surprisingly, there was little change in authorship and content of web information between our 2 search periods (2011, 2014). Although there has been a rapid increase in the number of medical websites, quality of content seems not to have changed significantly. Patients look to physicians for guidance but increasingly are accessing the Internet for additional information. It is essential that physicians understand the quality of information available on the Internet when counseling patients regarding surgery.
1. Brunnekreef JJ, Schreurs BW. Total hip arthroplasty: what information do we offer patients on websites of hospitals? BMC Health Serv Res. 2011;11:83.
2. Koh HS, In Y, Kong CG, Won HY, Kim KH, Lee JH. Factors affecting patients’ graft choice in anterior cruciate ligament reconstruction. Clin Orthop Surg. 2010;2(2):69-75.
3. Nason GJ, Baker JF, Byrne DP, Noel J, Moore D, Kiely PJ. Scoliosis-specific information on the Internet: has the “information highway” led to better information provision? Spine. 2012;37(21):E1364-E1369.
4. Groves ND, Humphreys HW, Williams AJ, Jones A. Effect of informational Internet web pages on patients’ decision making: randomised controlled trial regarding choice of spinal or general anaesthesia for orthopaedic surgery. Anaesthesia. 2010;65(3):277-282.
5. Purcell K, Brenner J, Rainie L. Search Engine Use 2012. Washington, DC: Pew Internet & American Life Project; 2012.
6. Duncan IC, Kane PW, Lawson KA, Cohen SB, Ciccotti MG, Dodson CC. Evaluation of information available on the Internet regarding anterior cruciate ligament reconstruction. Arthroscopy. 2013;29(6):1101-1107.
7. Lichtenfeld LJ. Can the beast be tamed? The woeful tale of accurate health information on the Internet. Ann Surg Oncol. 2012;19(3):701-702.
8. Ahmed OH, Sullivan SJ, Schneiders AG, McCrory PR. Concussion information online: evaluation of information quality, content and readability of concussion-related websites. Br J Sports Med. 2012;46(9):675-683.
9. Bruce-Brand RA, Baker JF, Byrne DP, Hogan NA, McCarthy T. Assessment of the quality and content of information on anterior cruciate ligament reconstruction on the Internet. Arthroscopy. 2013;29(6):1095-1100.
10. Dy JC, Taylor SA, Patel RM, Kitay A, Roberts TR, Daluiski A. The effect of search term on the quality and accuracy of online information regarding distal radius fractures. J Hand Surg Am. 2012;37(9):1881-1887.
11. Garcia RM, Messerschmitt PJ, Ahn NU. An evaluation of information on the Internet of a new device: the lumbar artificial disc replacement. J Spinal Disord Tech. 2009;22(1):52-57.
12. Gosselin MM, Mulcahey MK, Feller E, Hulstyn MJ. Examining Internet resources on gender differences in ACL injuries: what patients are reading. Knee. 2013;20(3):196-202.
13. Lam CG, Roter DL, Cohen KJ. Survey of quality, readability, and social reach of websites on osteosarcoma in adolescents. Patient Educ Couns. 2013;90(1):82-87.
14. Morr S, Shanti N, Carrer A, Kubeck J, Gerling MC. Quality of information concerning cervical disc herniation on the Internet. Spine J. 2010;10(4):350-354.
15. Starman JS, Gettys FK, Capo JA, Fleischli JE, Norton HJ, Karunakar MA. Quality and content of Internet-based information for ten common orthopaedic sports medicine diagnoses. J Bone Joint Surg Am. 2010;92(7):1612-1618.
16. Stinson JN, Tucker L, Huber A, et al. Surfing for juvenile idiopathic arthritis: perspectives on quality and content of information on the Internet. J Rheumatol. 2009;36(8):1755-1762.
17. Sullivan TB, Anderson JS, Ahn UM, Ahn NU. Can Internet information on vertebroplasty be a reliable means of patient self-education? Clin Orthop Relat Res. 2014;472(5):1597-1604.
18. Weil AG, Bojanowski MW, Jamart J, Gustin T, Lévêque M. Evaluation of the quality of information on the Internet available to patients undergoing cervical spine surgery. World Neurosurg. 2014;82(1-2):e31-e39.
19. Yi PH, Ganta A, Hussein KI, Frank RM, Jawa A. Readability of arthroscopy-related patient education materials from the American Academy of Orthopaedic Surgeons and Arthroscopy Association of North America web sites. Arthroscopy. 2013;29(6):1108-1112.
20. Boyer C, Selby M, Scherrer JR, Appel RD. The Health On the Net code of conduct for medical and health websites. Comput Biol Med. 1998;28(5):603-610.
21. Silberg WM, Lundberg GD, Musacchio RA. Assessing, controlling, and assuring the quality of medical information on the Internet: Caveant lector et viewor—Let the reader and viewer beware. JAMA. 1997;277(15):1244-1245.
22. Fabricant PD, Dy CJ, Patel RM, Blanco JS, Doyle SM. Internet search term affects the quality and accuracy of online information about developmental hip dysplasia. J Pediatr Orthop. 2013;33(4):361-365.
23. Aslam N, Bowyer D, Wainwright A, Theologis T, Benson M. Evaluation of Internet use by paediatric orthopaedic outpatients and the quality of information available. J Pediatr Orthop B. 2005;14(2):129-133.
24. Wetzler MJ. “I found it on the Internet”: how reliable and readable is patient information? Arthroscopy. 2013;29(6):967-968.
25. Qureshi SA, Koehler SM, Lin JD, Bird J, Garcia RM, Hecht AC. An evaluation of information on the Internet about a new device: the cervical artificial disc replacement. Spine. 2012;37(10):881-883.
1. Brunnekreef JJ, Schreurs BW. Total hip arthroplasty: what information do we offer patients on websites of hospitals? BMC Health Serv Res. 2011;11:83.
2. Koh HS, In Y, Kong CG, Won HY, Kim KH, Lee JH. Factors affecting patients’ graft choice in anterior cruciate ligament reconstruction. Clin Orthop Surg. 2010;2(2):69-75.
3. Nason GJ, Baker JF, Byrne DP, Noel J, Moore D, Kiely PJ. Scoliosis-specific information on the Internet: has the “information highway” led to better information provision? Spine. 2012;37(21):E1364-E1369.
4. Groves ND, Humphreys HW, Williams AJ, Jones A. Effect of informational Internet web pages on patients’ decision making: randomised controlled trial regarding choice of spinal or general anaesthesia for orthopaedic surgery. Anaesthesia. 2010;65(3):277-282.
5. Purcell K, Brenner J, Rainie L. Search Engine Use 2012. Washington, DC: Pew Internet & American Life Project; 2012.
6. Duncan IC, Kane PW, Lawson KA, Cohen SB, Ciccotti MG, Dodson CC. Evaluation of information available on the Internet regarding anterior cruciate ligament reconstruction. Arthroscopy. 2013;29(6):1101-1107.
7. Lichtenfeld LJ. Can the beast be tamed? The woeful tale of accurate health information on the Internet. Ann Surg Oncol. 2012;19(3):701-702.
8. Ahmed OH, Sullivan SJ, Schneiders AG, McCrory PR. Concussion information online: evaluation of information quality, content and readability of concussion-related websites. Br J Sports Med. 2012;46(9):675-683.
9. Bruce-Brand RA, Baker JF, Byrne DP, Hogan NA, McCarthy T. Assessment of the quality and content of information on anterior cruciate ligament reconstruction on the Internet. Arthroscopy. 2013;29(6):1095-1100.
10. Dy JC, Taylor SA, Patel RM, Kitay A, Roberts TR, Daluiski A. The effect of search term on the quality and accuracy of online information regarding distal radius fractures. J Hand Surg Am. 2012;37(9):1881-1887.
11. Garcia RM, Messerschmitt PJ, Ahn NU. An evaluation of information on the Internet of a new device: the lumbar artificial disc replacement. J Spinal Disord Tech. 2009;22(1):52-57.
12. Gosselin MM, Mulcahey MK, Feller E, Hulstyn MJ. Examining Internet resources on gender differences in ACL injuries: what patients are reading. Knee. 2013;20(3):196-202.
13. Lam CG, Roter DL, Cohen KJ. Survey of quality, readability, and social reach of websites on osteosarcoma in adolescents. Patient Educ Couns. 2013;90(1):82-87.
14. Morr S, Shanti N, Carrer A, Kubeck J, Gerling MC. Quality of information concerning cervical disc herniation on the Internet. Spine J. 2010;10(4):350-354.
15. Starman JS, Gettys FK, Capo JA, Fleischli JE, Norton HJ, Karunakar MA. Quality and content of Internet-based information for ten common orthopaedic sports medicine diagnoses. J Bone Joint Surg Am. 2010;92(7):1612-1618.
16. Stinson JN, Tucker L, Huber A, et al. Surfing for juvenile idiopathic arthritis: perspectives on quality and content of information on the Internet. J Rheumatol. 2009;36(8):1755-1762.
17. Sullivan TB, Anderson JS, Ahn UM, Ahn NU. Can Internet information on vertebroplasty be a reliable means of patient self-education? Clin Orthop Relat Res. 2014;472(5):1597-1604.
18. Weil AG, Bojanowski MW, Jamart J, Gustin T, Lévêque M. Evaluation of the quality of information on the Internet available to patients undergoing cervical spine surgery. World Neurosurg. 2014;82(1-2):e31-e39.
19. Yi PH, Ganta A, Hussein KI, Frank RM, Jawa A. Readability of arthroscopy-related patient education materials from the American Academy of Orthopaedic Surgeons and Arthroscopy Association of North America web sites. Arthroscopy. 2013;29(6):1108-1112.
20. Boyer C, Selby M, Scherrer JR, Appel RD. The Health On the Net code of conduct for medical and health websites. Comput Biol Med. 1998;28(5):603-610.
21. Silberg WM, Lundberg GD, Musacchio RA. Assessing, controlling, and assuring the quality of medical information on the Internet: Caveant lector et viewor—Let the reader and viewer beware. JAMA. 1997;277(15):1244-1245.
22. Fabricant PD, Dy CJ, Patel RM, Blanco JS, Doyle SM. Internet search term affects the quality and accuracy of online information about developmental hip dysplasia. J Pediatr Orthop. 2013;33(4):361-365.
23. Aslam N, Bowyer D, Wainwright A, Theologis T, Benson M. Evaluation of Internet use by paediatric orthopaedic outpatients and the quality of information available. J Pediatr Orthop B. 2005;14(2):129-133.
24. Wetzler MJ. “I found it on the Internet”: how reliable and readable is patient information? Arthroscopy. 2013;29(6):967-968.
25. Qureshi SA, Koehler SM, Lin JD, Bird J, Garcia RM, Hecht AC. An evaluation of information on the Internet about a new device: the cervical artificial disc replacement. Spine. 2012;37(10):881-883.
Thyroid surgery access and acceptance varies along racial lines
BOSTON – Access to and acceptance of thyroid cancer surgery varies by race, with black patients in particular appearing to be disadvantaged, compared with whites, investigators reported.
A review of data on nearly 138,000 patients diagnosed with thyroid cancer showed that blacks were significantly less likely than were whites to be offered surgery – despite its generally excellent outcomes and low rates of morbidity and mortality, reported Dr. Herbert Castillo Valladares and his colleagues from the department of surgery at the Yale University in New Haven, Conn.
American Indians/Alaskan natives and Asian/Pacific Islanders were significantly more likely to refuse surgery than were whites, the investigators also reported in a poster session at the Society of Surgical Oncology annual cancer symposium.
“In this project, we wanted to focus on the provider-level factors that might be perpetuating these racial disparities, and it appears that we need to educate some providers about the recommendation of surgery or how to educate patients who refuse thyroid cancer surgery,” Dr. Valladares said in an interview.
The investigators noted that although incidence and prevalence rates of thyroid cancer are similar among various racial groups, survival differs by race, and they wanted to find out why. To do so, they polled the Surveillance, Epidemiology, and End Results (SEER) registry to identify 137,483 patients diagnosed with thyroid cancer during 1988-2012. Results were stratified by thyroid cancer type, either papillary, medullary, follicular, or anaplastic.
In all, 82% of the sample were white, 75% were female, 87% had a diagnosis of papillary thyroid cancer, and 95% underwent thyroid cancer surgery.
In logistic regression analysis that controlled for race, the investigators found that blacks, Asian/Pacific Islanders, and persons of unknown race were significantly less likely than whites were to have thyroid cancer surgery (odds ratios, 0.7, 0.82, and 0.34, respectively; P for each less than .0001).
Similarly, surgery was more frequently not recommended for blacks (OR, 1.34; P less than .0001), Asian/Pacific Islanders (OR, 1.2; P = .004) and those of unknown race (OR, 3.06; P less than .0001).
American Indians/Alaskan natives and Asian/Pacific Islanders were also significantly more likely than were whites to refuse surgery (OR, 4.45; P = .0001; OR, 2.96; P less than .0001, respectively).
Compared with whites, blacks – but not other races – had significantly worse 5-year survival (hazard ratio, 1.14; P = .0002).
In an analysis by cancer type, the investigators saw that race was not a predictor for surgery recommendation or refusal of surgery by patients with medullary or anaplastic cancer. However, among patients with papillary thyroid cancer, the most common type, surgery was recommended less often for blacks (OR, 1.2), Asian/Pacific Islanders (OR, 1.3), and patients of unknown race (OR, 3.1; all comparisons significant by 95% confidence interval).
Among patients with follicular histology, patients of unknown race were significantly less likely than were whites to have the surgery recommended (OR, 2.7; significant by 95% CI).
Dr. Valladares explained that the SEER data set does not include information about provider type, such as those in community based versus academic settings, so the next step will be to find a method for analyzing factors at both the patient level and the provider level that might influence recommendations for surgery or patient refusals to accept surgery.
The study was supported by the Paul H. Lavietes, M.D., Summer Research Fellowship of Yale University. The investigators reported no relevant conflicts of interest.
BOSTON – Access to and acceptance of thyroid cancer surgery varies by race, with black patients in particular appearing to be disadvantaged, compared with whites, investigators reported.
A review of data on nearly 138,000 patients diagnosed with thyroid cancer showed that blacks were significantly less likely than were whites to be offered surgery – despite its generally excellent outcomes and low rates of morbidity and mortality, reported Dr. Herbert Castillo Valladares and his colleagues from the department of surgery at the Yale University in New Haven, Conn.
American Indians/Alaskan natives and Asian/Pacific Islanders were significantly more likely to refuse surgery than were whites, the investigators also reported in a poster session at the Society of Surgical Oncology annual cancer symposium.
“In this project, we wanted to focus on the provider-level factors that might be perpetuating these racial disparities, and it appears that we need to educate some providers about the recommendation of surgery or how to educate patients who refuse thyroid cancer surgery,” Dr. Valladares said in an interview.
The investigators noted that although incidence and prevalence rates of thyroid cancer are similar among various racial groups, survival differs by race, and they wanted to find out why. To do so, they polled the Surveillance, Epidemiology, and End Results (SEER) registry to identify 137,483 patients diagnosed with thyroid cancer during 1988-2012. Results were stratified by thyroid cancer type, either papillary, medullary, follicular, or anaplastic.
In all, 82% of the sample were white, 75% were female, 87% had a diagnosis of papillary thyroid cancer, and 95% underwent thyroid cancer surgery.
In logistic regression analysis that controlled for race, the investigators found that blacks, Asian/Pacific Islanders, and persons of unknown race were significantly less likely than whites were to have thyroid cancer surgery (odds ratios, 0.7, 0.82, and 0.34, respectively; P for each less than .0001).
Similarly, surgery was more frequently not recommended for blacks (OR, 1.34; P less than .0001), Asian/Pacific Islanders (OR, 1.2; P = .004) and those of unknown race (OR, 3.06; P less than .0001).
American Indians/Alaskan natives and Asian/Pacific Islanders were also significantly more likely than were whites to refuse surgery (OR, 4.45; P = .0001; OR, 2.96; P less than .0001, respectively).
Compared with whites, blacks – but not other races – had significantly worse 5-year survival (hazard ratio, 1.14; P = .0002).
In an analysis by cancer type, the investigators saw that race was not a predictor for surgery recommendation or refusal of surgery by patients with medullary or anaplastic cancer. However, among patients with papillary thyroid cancer, the most common type, surgery was recommended less often for blacks (OR, 1.2), Asian/Pacific Islanders (OR, 1.3), and patients of unknown race (OR, 3.1; all comparisons significant by 95% confidence interval).
Among patients with follicular histology, patients of unknown race were significantly less likely than were whites to have the surgery recommended (OR, 2.7; significant by 95% CI).
Dr. Valladares explained that the SEER data set does not include information about provider type, such as those in community based versus academic settings, so the next step will be to find a method for analyzing factors at both the patient level and the provider level that might influence recommendations for surgery or patient refusals to accept surgery.
The study was supported by the Paul H. Lavietes, M.D., Summer Research Fellowship of Yale University. The investigators reported no relevant conflicts of interest.
BOSTON – Access to and acceptance of thyroid cancer surgery varies by race, with black patients in particular appearing to be disadvantaged, compared with whites, investigators reported.
A review of data on nearly 138,000 patients diagnosed with thyroid cancer showed that blacks were significantly less likely than were whites to be offered surgery – despite its generally excellent outcomes and low rates of morbidity and mortality, reported Dr. Herbert Castillo Valladares and his colleagues from the department of surgery at the Yale University in New Haven, Conn.
American Indians/Alaskan natives and Asian/Pacific Islanders were significantly more likely to refuse surgery than were whites, the investigators also reported in a poster session at the Society of Surgical Oncology annual cancer symposium.
“In this project, we wanted to focus on the provider-level factors that might be perpetuating these racial disparities, and it appears that we need to educate some providers about the recommendation of surgery or how to educate patients who refuse thyroid cancer surgery,” Dr. Valladares said in an interview.
The investigators noted that although incidence and prevalence rates of thyroid cancer are similar among various racial groups, survival differs by race, and they wanted to find out why. To do so, they polled the Surveillance, Epidemiology, and End Results (SEER) registry to identify 137,483 patients diagnosed with thyroid cancer during 1988-2012. Results were stratified by thyroid cancer type, either papillary, medullary, follicular, or anaplastic.
In all, 82% of the sample were white, 75% were female, 87% had a diagnosis of papillary thyroid cancer, and 95% underwent thyroid cancer surgery.
In logistic regression analysis that controlled for race, the investigators found that blacks, Asian/Pacific Islanders, and persons of unknown race were significantly less likely than whites were to have thyroid cancer surgery (odds ratios, 0.7, 0.82, and 0.34, respectively; P for each less than .0001).
Similarly, surgery was more frequently not recommended for blacks (OR, 1.34; P less than .0001), Asian/Pacific Islanders (OR, 1.2; P = .004) and those of unknown race (OR, 3.06; P less than .0001).
American Indians/Alaskan natives and Asian/Pacific Islanders were also significantly more likely than were whites to refuse surgery (OR, 4.45; P = .0001; OR, 2.96; P less than .0001, respectively).
Compared with whites, blacks – but not other races – had significantly worse 5-year survival (hazard ratio, 1.14; P = .0002).
In an analysis by cancer type, the investigators saw that race was not a predictor for surgery recommendation or refusal of surgery by patients with medullary or anaplastic cancer. However, among patients with papillary thyroid cancer, the most common type, surgery was recommended less often for blacks (OR, 1.2), Asian/Pacific Islanders (OR, 1.3), and patients of unknown race (OR, 3.1; all comparisons significant by 95% confidence interval).
Among patients with follicular histology, patients of unknown race were significantly less likely than were whites to have the surgery recommended (OR, 2.7; significant by 95% CI).
Dr. Valladares explained that the SEER data set does not include information about provider type, such as those in community based versus academic settings, so the next step will be to find a method for analyzing factors at both the patient level and the provider level that might influence recommendations for surgery or patient refusals to accept surgery.
The study was supported by the Paul H. Lavietes, M.D., Summer Research Fellowship of Yale University. The investigators reported no relevant conflicts of interest.
FROM SSO 2016
Key clinical point: Compared with whites, blacks, Asian/Pacific Islanders and persons of unknown race were significantly less likely than were whites to have thyroid cancer surgery.
Major finding: Asian/Pacific Islanders and persons of unknown race were significantly less likely than were whites to have thyroid cancer surgery (OR, 0.7, 0.82, and 0.34, respectively; P for each less than .0001).
Data source: SEER data on 137,483 patients with thyroid cancer during 1988-2012.
Disclosures: The study was supported by a Paul H. Lavietes, M.D., Summer Research Fellowship at Yale University. The investigators reported no relevant conflicts of interest.
Supreme Court to hear debate over contraception coverage mandate
The U.S. Supreme Court will hear oral arguments March 23 in a case that pits the federal government against religious employers who oppose contraceptive use.
Zubik v. Burwell centers on whether an accommodation under the Affordable Care Act’s contraceptive mandate is enough to protect the religious freedoms of nonprofit employers with strongly held religious beliefs.
The ruling in Zubik will have broad implications for contraception care nationwide and the way in which the Religious Freedom Restoration Act (RFRA) is applied going forward, said Laurie Sobel, a senior policy analyst for the Henry J. Kaiser Family Foundation.
“Ultimately, if the court were to rule in favor of Zubik, it would mean the workers and dependents of nonprofits are at risk of losing some or all contraceptive coverage,” Ms. Sobel said during a March 16 Kaiser press briefing. “The burden on women to pay out of pocket has [been] shown to really limit their choices and possibly limit [all] contraceptives for them.”
The ACA’s accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities, such as churches. The plaintiffs – part of seven consolidated cases that include a Catholic bishop and an order of nuns – argue that the opt-out process put in place by the government makes them complicit in offering contraception coverage indirectly.
The government contends that the exception does not impose a burden on the groups and that courts should not disregard the interest of employees who may not share their employers’ religious beliefs. The 8th U.S. Circuit Court of Appeals struck down the exception twice, ruling that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The 8th Circuit’s decisions are at odds with rulings by the 2nd and 5th Circuit courts.
The case comes down to whether the plaintiffs can prove the accommodation places a substantial burden on their religious conduct, and if so, whether the government can prove its provision is the least restrictive means of advancing a compelling interest, said Marci A. Hamilton, a law professor at the Benjamin N. Cardozo School of Law, Yeshiva University, New York.
“[If the court sides with Zubik], one possible precedent this could set is that religious objectors – the employers in these cases – will be able to limit independent third-party actions,” Ms. Hamilton said during the media conference. “It doesn’t matter the faith. You can have your decisions about birth control and the cost and reproductive care determined by the faith of your employer.”
A ruling for Zubik would also throw a monkey wrench in the country’s long tradition of legislative accommodations, Ms. Hamilton said, noting that there are many laws that include accommodations for certain populations.
“That means the legislative weighing of harm and safety is going to be pushed aside and essentially, we’re going to be talking about, how can every single law including the accommodations be fine-tuned for one set of believers?”
The recent death of Associate Justice Antonin Scalia, who was the court’s most outspoken conservative, could significantly impact the case’s outcome, analysts said. Justice Scalia was among majority in the 5-4 decision in Burwell v. Hobby Lobby, a 2014 opinion that protected religiously devout owners of closely held, for-profit businesses from having to offer birth control under the mandate. His absence could mean a 4-4 split in the Zubik case, which would allow the lower court rulings to stand, said Lyle Denniston, a Supreme Court analyst who writes for SCOTUSblog.
“My own sense is that the court is going to try very hard to find a way to resolve this case without a 4-4 split,” Mr. Denniston said during the Kaiser media conference. “If the Supreme Court issues a 4-4 decision, that leaves division in the lower courts, and it will vary from region to region in the country as to what the rights for women under the ACA are.”
More than 70 briefs have been issued to the high court in support of or opposition to the plaintiffs, including pleas by religious organizations, women’s advocacy groups, law professors, medical associations, and attorneys.
The American College of Obstetricians and Gynecologists and the American Academy of Family Physicians wrote in a joint brief that contraception coverage under the ACA ensures that patients have access to medically appropriate contraception without regard to their ability to pay. At the same time, the law respects an employer’s sincerely held religious objections to contraception through the accommodation, the brief said.
However, the Council for Christian Colleges & Universities argues the government’s decision to exempt some religious employers from providing contraceptive coverage while requiring others to comply with the mandate “demonstrates that the government’s approach is not the least restrictive means necessary to advance its interests.”
“Civil rights should not vary based on whether that institution is or is not affiliated with a church or other house of worship,” the council wrote in its brief to the Supreme Court. “Religious exercise is not tied to one’s affiliation but rather the source and sincerity of one’s belief and the desire to exercise it. That truth appears to be one the government has been unable to grasp or comprehend as it decides who is sufficiently ‘religious’ to have religious beliefs worthy of protection.”
On Twitter @legal_med
The U.S. Supreme Court will hear oral arguments March 23 in a case that pits the federal government against religious employers who oppose contraceptive use.
Zubik v. Burwell centers on whether an accommodation under the Affordable Care Act’s contraceptive mandate is enough to protect the religious freedoms of nonprofit employers with strongly held religious beliefs.
The ruling in Zubik will have broad implications for contraception care nationwide and the way in which the Religious Freedom Restoration Act (RFRA) is applied going forward, said Laurie Sobel, a senior policy analyst for the Henry J. Kaiser Family Foundation.
“Ultimately, if the court were to rule in favor of Zubik, it would mean the workers and dependents of nonprofits are at risk of losing some or all contraceptive coverage,” Ms. Sobel said during a March 16 Kaiser press briefing. “The burden on women to pay out of pocket has [been] shown to really limit their choices and possibly limit [all] contraceptives for them.”
The ACA’s accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities, such as churches. The plaintiffs – part of seven consolidated cases that include a Catholic bishop and an order of nuns – argue that the opt-out process put in place by the government makes them complicit in offering contraception coverage indirectly.
The government contends that the exception does not impose a burden on the groups and that courts should not disregard the interest of employees who may not share their employers’ religious beliefs. The 8th U.S. Circuit Court of Appeals struck down the exception twice, ruling that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The 8th Circuit’s decisions are at odds with rulings by the 2nd and 5th Circuit courts.
The case comes down to whether the plaintiffs can prove the accommodation places a substantial burden on their religious conduct, and if so, whether the government can prove its provision is the least restrictive means of advancing a compelling interest, said Marci A. Hamilton, a law professor at the Benjamin N. Cardozo School of Law, Yeshiva University, New York.
“[If the court sides with Zubik], one possible precedent this could set is that religious objectors – the employers in these cases – will be able to limit independent third-party actions,” Ms. Hamilton said during the media conference. “It doesn’t matter the faith. You can have your decisions about birth control and the cost and reproductive care determined by the faith of your employer.”
A ruling for Zubik would also throw a monkey wrench in the country’s long tradition of legislative accommodations, Ms. Hamilton said, noting that there are many laws that include accommodations for certain populations.
“That means the legislative weighing of harm and safety is going to be pushed aside and essentially, we’re going to be talking about, how can every single law including the accommodations be fine-tuned for one set of believers?”
The recent death of Associate Justice Antonin Scalia, who was the court’s most outspoken conservative, could significantly impact the case’s outcome, analysts said. Justice Scalia was among majority in the 5-4 decision in Burwell v. Hobby Lobby, a 2014 opinion that protected religiously devout owners of closely held, for-profit businesses from having to offer birth control under the mandate. His absence could mean a 4-4 split in the Zubik case, which would allow the lower court rulings to stand, said Lyle Denniston, a Supreme Court analyst who writes for SCOTUSblog.
“My own sense is that the court is going to try very hard to find a way to resolve this case without a 4-4 split,” Mr. Denniston said during the Kaiser media conference. “If the Supreme Court issues a 4-4 decision, that leaves division in the lower courts, and it will vary from region to region in the country as to what the rights for women under the ACA are.”
More than 70 briefs have been issued to the high court in support of or opposition to the plaintiffs, including pleas by religious organizations, women’s advocacy groups, law professors, medical associations, and attorneys.
The American College of Obstetricians and Gynecologists and the American Academy of Family Physicians wrote in a joint brief that contraception coverage under the ACA ensures that patients have access to medically appropriate contraception without regard to their ability to pay. At the same time, the law respects an employer’s sincerely held religious objections to contraception through the accommodation, the brief said.
However, the Council for Christian Colleges & Universities argues the government’s decision to exempt some religious employers from providing contraceptive coverage while requiring others to comply with the mandate “demonstrates that the government’s approach is not the least restrictive means necessary to advance its interests.”
“Civil rights should not vary based on whether that institution is or is not affiliated with a church or other house of worship,” the council wrote in its brief to the Supreme Court. “Religious exercise is not tied to one’s affiliation but rather the source and sincerity of one’s belief and the desire to exercise it. That truth appears to be one the government has been unable to grasp or comprehend as it decides who is sufficiently ‘religious’ to have religious beliefs worthy of protection.”
On Twitter @legal_med
The U.S. Supreme Court will hear oral arguments March 23 in a case that pits the federal government against religious employers who oppose contraceptive use.
Zubik v. Burwell centers on whether an accommodation under the Affordable Care Act’s contraceptive mandate is enough to protect the religious freedoms of nonprofit employers with strongly held religious beliefs.
The ruling in Zubik will have broad implications for contraception care nationwide and the way in which the Religious Freedom Restoration Act (RFRA) is applied going forward, said Laurie Sobel, a senior policy analyst for the Henry J. Kaiser Family Foundation.
“Ultimately, if the court were to rule in favor of Zubik, it would mean the workers and dependents of nonprofits are at risk of losing some or all contraceptive coverage,” Ms. Sobel said during a March 16 Kaiser press briefing. “The burden on women to pay out of pocket has [been] shown to really limit their choices and possibly limit [all] contraceptives for them.”
The ACA’s accommodation clause refers to an exception for organizations that oppose coverage for contraceptives but are not exempted entities, such as churches. The plaintiffs – part of seven consolidated cases that include a Catholic bishop and an order of nuns – argue that the opt-out process put in place by the government makes them complicit in offering contraception coverage indirectly.
The government contends that the exception does not impose a burden on the groups and that courts should not disregard the interest of employees who may not share their employers’ religious beliefs. The 8th U.S. Circuit Court of Appeals struck down the exception twice, ruling that forcing organizations to offer contraceptive coverage – even indirectly – violates their religious rights. The 8th Circuit’s decisions are at odds with rulings by the 2nd and 5th Circuit courts.
The case comes down to whether the plaintiffs can prove the accommodation places a substantial burden on their religious conduct, and if so, whether the government can prove its provision is the least restrictive means of advancing a compelling interest, said Marci A. Hamilton, a law professor at the Benjamin N. Cardozo School of Law, Yeshiva University, New York.
“[If the court sides with Zubik], one possible precedent this could set is that religious objectors – the employers in these cases – will be able to limit independent third-party actions,” Ms. Hamilton said during the media conference. “It doesn’t matter the faith. You can have your decisions about birth control and the cost and reproductive care determined by the faith of your employer.”
A ruling for Zubik would also throw a monkey wrench in the country’s long tradition of legislative accommodations, Ms. Hamilton said, noting that there are many laws that include accommodations for certain populations.
“That means the legislative weighing of harm and safety is going to be pushed aside and essentially, we’re going to be talking about, how can every single law including the accommodations be fine-tuned for one set of believers?”
The recent death of Associate Justice Antonin Scalia, who was the court’s most outspoken conservative, could significantly impact the case’s outcome, analysts said. Justice Scalia was among majority in the 5-4 decision in Burwell v. Hobby Lobby, a 2014 opinion that protected religiously devout owners of closely held, for-profit businesses from having to offer birth control under the mandate. His absence could mean a 4-4 split in the Zubik case, which would allow the lower court rulings to stand, said Lyle Denniston, a Supreme Court analyst who writes for SCOTUSblog.
“My own sense is that the court is going to try very hard to find a way to resolve this case without a 4-4 split,” Mr. Denniston said during the Kaiser media conference. “If the Supreme Court issues a 4-4 decision, that leaves division in the lower courts, and it will vary from region to region in the country as to what the rights for women under the ACA are.”
More than 70 briefs have been issued to the high court in support of or opposition to the plaintiffs, including pleas by religious organizations, women’s advocacy groups, law professors, medical associations, and attorneys.
The American College of Obstetricians and Gynecologists and the American Academy of Family Physicians wrote in a joint brief that contraception coverage under the ACA ensures that patients have access to medically appropriate contraception without regard to their ability to pay. At the same time, the law respects an employer’s sincerely held religious objections to contraception through the accommodation, the brief said.
However, the Council for Christian Colleges & Universities argues the government’s decision to exempt some religious employers from providing contraceptive coverage while requiring others to comply with the mandate “demonstrates that the government’s approach is not the least restrictive means necessary to advance its interests.”
“Civil rights should not vary based on whether that institution is or is not affiliated with a church or other house of worship,” the council wrote in its brief to the Supreme Court. “Religious exercise is not tied to one’s affiliation but rather the source and sincerity of one’s belief and the desire to exercise it. That truth appears to be one the government has been unable to grasp or comprehend as it decides who is sufficiently ‘religious’ to have religious beliefs worthy of protection.”
On Twitter @legal_med
Key differences found between patients with bipolar I, bipolar II
Second-generation antipsychotic use is associated with a previous incidence of psychiatric hospitalization in patients with bipolar disorder I but not in those with bipolar II, a study by Dr. Dong Yeon Park and associates shows.
The researchers found that the use of the second-generation agents (SGAs) was twice as common in the bipolar disorder I study group. Forty-four percent of 243 bipolar I patients used at least one of the antipsychotics, compared with 21.2% of 260 patients with bipolar disorder II.
Most bipolar I patients had a history of psychiatric hospitalization; however, hospitalization was significantly more common among patients in an SGA subgroup. In that group, more than 80% of those patients had a history of psychiatric hospitalization, compared with 58.1% of patients with bipolar I who were not taking SGAs. Comparatively, 12.7% of bipolar II patients taking SGAs had a history of psychiatric hospitalization, compared with 9.3% of bipolar II patients who were not taking SGAs.
Patients with bipolar I who were on SGAs also were more likely to be currently depressed, have current complex pharmacotherapy, and have a higher Clinical Global Impression for Bipolar Version Overall Severity score. Meanwhile, bipolar disorder II patients taking SGAs were more likely to be currently using mood stabilizers than were bipolar II patients who were not taking SGAs, reported Dr. Park, of the department of psychiatry at Seoul National Hospital, South Korea.
“More research is needed to assess differential demographic and clinical correlates of current SGA use in patients with bipolar II disorder compared to bipolar I disorder. Challenges related to the variable expense and side effects of SGAs highlight the importance of increasing knowledge of the strengths and limitations of use of these agents in patients with different types of bipolar disorders,” the investigators concluded.
Find the study in the Journal of Psychiatric Research (doi: 10.1016/j.jpsychires.2016.01.016).
Second-generation antipsychotic use is associated with a previous incidence of psychiatric hospitalization in patients with bipolar disorder I but not in those with bipolar II, a study by Dr. Dong Yeon Park and associates shows.
The researchers found that the use of the second-generation agents (SGAs) was twice as common in the bipolar disorder I study group. Forty-four percent of 243 bipolar I patients used at least one of the antipsychotics, compared with 21.2% of 260 patients with bipolar disorder II.
Most bipolar I patients had a history of psychiatric hospitalization; however, hospitalization was significantly more common among patients in an SGA subgroup. In that group, more than 80% of those patients had a history of psychiatric hospitalization, compared with 58.1% of patients with bipolar I who were not taking SGAs. Comparatively, 12.7% of bipolar II patients taking SGAs had a history of psychiatric hospitalization, compared with 9.3% of bipolar II patients who were not taking SGAs.
Patients with bipolar I who were on SGAs also were more likely to be currently depressed, have current complex pharmacotherapy, and have a higher Clinical Global Impression for Bipolar Version Overall Severity score. Meanwhile, bipolar disorder II patients taking SGAs were more likely to be currently using mood stabilizers than were bipolar II patients who were not taking SGAs, reported Dr. Park, of the department of psychiatry at Seoul National Hospital, South Korea.
“More research is needed to assess differential demographic and clinical correlates of current SGA use in patients with bipolar II disorder compared to bipolar I disorder. Challenges related to the variable expense and side effects of SGAs highlight the importance of increasing knowledge of the strengths and limitations of use of these agents in patients with different types of bipolar disorders,” the investigators concluded.
Find the study in the Journal of Psychiatric Research (doi: 10.1016/j.jpsychires.2016.01.016).
Second-generation antipsychotic use is associated with a previous incidence of psychiatric hospitalization in patients with bipolar disorder I but not in those with bipolar II, a study by Dr. Dong Yeon Park and associates shows.
The researchers found that the use of the second-generation agents (SGAs) was twice as common in the bipolar disorder I study group. Forty-four percent of 243 bipolar I patients used at least one of the antipsychotics, compared with 21.2% of 260 patients with bipolar disorder II.
Most bipolar I patients had a history of psychiatric hospitalization; however, hospitalization was significantly more common among patients in an SGA subgroup. In that group, more than 80% of those patients had a history of psychiatric hospitalization, compared with 58.1% of patients with bipolar I who were not taking SGAs. Comparatively, 12.7% of bipolar II patients taking SGAs had a history of psychiatric hospitalization, compared with 9.3% of bipolar II patients who were not taking SGAs.
Patients with bipolar I who were on SGAs also were more likely to be currently depressed, have current complex pharmacotherapy, and have a higher Clinical Global Impression for Bipolar Version Overall Severity score. Meanwhile, bipolar disorder II patients taking SGAs were more likely to be currently using mood stabilizers than were bipolar II patients who were not taking SGAs, reported Dr. Park, of the department of psychiatry at Seoul National Hospital, South Korea.
“More research is needed to assess differential demographic and clinical correlates of current SGA use in patients with bipolar II disorder compared to bipolar I disorder. Challenges related to the variable expense and side effects of SGAs highlight the importance of increasing knowledge of the strengths and limitations of use of these agents in patients with different types of bipolar disorders,” the investigators concluded.
Find the study in the Journal of Psychiatric Research (doi: 10.1016/j.jpsychires.2016.01.016).
FROM THE JOURNAL OF PSYCHIATRIC RESEARCH
FDA approves first generic form of oxiconazole nitrate cream
A generic formulation of oxiconazole nitrate cream, 1% has been approved by the Food and Drug Administration, for the treatment of tinea pedis, tinea cruris, tinea corporis due to Trichophyton rubrum, Trichophyton mentagrophytes, or Epidermophyton floccosum) and tinea (pityriasis) versicolor due to Malassezia furfur.
This is the first generic version of Oxistat to be approved, according to the FDA’s statement announcing the approval.
The label for the generic, manufactured by Taro Pharmaceuticals U.S.A. is available here.
A generic formulation of oxiconazole nitrate cream, 1% has been approved by the Food and Drug Administration, for the treatment of tinea pedis, tinea cruris, tinea corporis due to Trichophyton rubrum, Trichophyton mentagrophytes, or Epidermophyton floccosum) and tinea (pityriasis) versicolor due to Malassezia furfur.
This is the first generic version of Oxistat to be approved, according to the FDA’s statement announcing the approval.
The label for the generic, manufactured by Taro Pharmaceuticals U.S.A. is available here.
A generic formulation of oxiconazole nitrate cream, 1% has been approved by the Food and Drug Administration, for the treatment of tinea pedis, tinea cruris, tinea corporis due to Trichophyton rubrum, Trichophyton mentagrophytes, or Epidermophyton floccosum) and tinea (pityriasis) versicolor due to Malassezia furfur.
This is the first generic version of Oxistat to be approved, according to the FDA’s statement announcing the approval.
The label for the generic, manufactured by Taro Pharmaceuticals U.S.A. is available here.
Serious complications after cancer surgery linked to worse long-term survival
BOSTON – The operation was a success, but the patient died.
It’s an old chestnut for sure, but there is a painful kernel of truth in it, say investigators who found that patients who undergo complex cancer surgery and have serious complications are at significantly increased risk for death for at least 6 months after surgery, compared with patients who undergo the same procedure with few or no complications.
“Our work has important implications for quality assessment. I think in cancer surgery in particular we have to get away from the short-term metrics of survival, and we have to think about the implications of complications for long-term survival, even if at a very high-quality hospital we’re good at salvaging those patients who do experience those complications,” said Dr. Hari Nathan of the University of Michigan, Ann Arbor.
In a retrospective study, results of which were presented at the annual Society of Surgical Oncology Cancer Symposium, Dr. Nathan and colleagues showed that patients who underwent surgery for cancers of the esophagus and lung who had serious complications but survived at least 30 days after surgery had a more than twofold greater risk for death than did patients who had no complications, and patients with serious complications following surgery for cancer of the pancreas had a nearly twofold greater risk.
The effects of serious complications on survival persisted out to at least 180 days after surgery for each of the three procedures.
The findings suggest that just getting the patient through the operation and keeping him or her alive in the ICU is not sufficient cause for celebration by surgeons, Dr. Nathan said.
The investigators conducted the study to examine the incidence of complications following cancer surgery in older patients, the relationship between surgical complications and long-term survival, and whether the effects of complications would diminish or “wash out” over time. They reviewed Surveillance, Epidemiology and End Results–Medicare data on patients aged 65 years and older who underwent surgery with curative intent for esophageal cancer, non–small cell lung cancer, or pancreatic adenocarcinoma from 2005 through 2009.
They defined serious complications as “the appearance of a complication associated with a hospital length of stay greater than the 75th percentile for that procedure.”
The cohort included 965 patients who underwent esophageal surgery, 12,395 who had lung surgery, and 1,966 who underwent pancreatic resection. The proportion of patients over 80 years who underwent the procedures, respectively, were 12%, 18%, and 19%.
Serious complications occurred in 17% of patients with esophageal cancer, 10% of those with lung cancer, and 12% of those with cancer of the pancreas. The respective 30-day mortality rates were 6.%, 3.3%, and 3.9%.
Looking only at those patients with lung cancer who survived at least 30 days after surgery, the investigators found that median survival among those who had no complications was 79 months, compared with 60 months for those who had mild complications, and 33 months for patients who had serious complications (P less than .001)
“And indeed, when we performed adjusted survival analyses looking at all three disease sites, we saw a very consistent story: that those patients who had serious complications had decreased long-term survival for all three malignancies we looked at,” Dr. Nathan said.
Specifically, in survival analyses adjusted for sex, age, and procedure code, hazard ratios for patients with serious complications compared with those who had no complications were 2.55 for esophageal cancer patients, 2.13 for lung cancer patients, and 1.57 for pancreatic cancer patients (all comparisons significant as shown by 95% confidence intervals).
The investigators questioned whether the differences in mortality were due to the late effects of perioperative complications.
“In modern ICUs, we can keep virtually anybody alive for 30 days, and there has been a lot interest in longer-term metrics for perioperative mortality, for example, at 30 or 90 days, so we thought maybe that’s what we were seeing here,” he said. To test this idea, the investigators looked at the effects of complications on patient who survived lung cancer surgery for at least 90 days, and those who lived for at least 180 days after surgery, and they saw that the survival curves were similar to those seen with the 30-day survivors, showing significantly and persistently worse survival for patients with serious complications (P less than .001).
For each of the disease states, patients with serious complications were also significantly less likely than were those with no or mild complications to receive adjuvant chemotherapy, even after adjustment for patient age and cancer stage, two significant determinants of the likelihood of receiving chemotherapy.
And even when the effect of chemotherapy for those who did receive it was added into the survival models, patients with serious complications still had significantly worse overall survival, Dr. Nathan noted.
“Serious complications after these three cancer resections are common and they are associated with dramatically inferior long-term survival. Thirty, 60, 90, and even 180-day measures of mortality do not capture the full impact of complications on long-term survival,” he said.
Asked whether it may be possible to identify those patients at higher risk for serious complications due to comorbidities or other factors, and perhaps suggest withholding surgery from such patients, Dr. Nathan agreed, but added that “the best chance for survival for all of these patients is a high-quality surgical resection, so it’s hard to deny a patient that chance unless you think they have a really high risk of perioperative death.”
The study was internally funded. Dr. Nathan reported no significant disclosures.
BOSTON – The operation was a success, but the patient died.
It’s an old chestnut for sure, but there is a painful kernel of truth in it, say investigators who found that patients who undergo complex cancer surgery and have serious complications are at significantly increased risk for death for at least 6 months after surgery, compared with patients who undergo the same procedure with few or no complications.
“Our work has important implications for quality assessment. I think in cancer surgery in particular we have to get away from the short-term metrics of survival, and we have to think about the implications of complications for long-term survival, even if at a very high-quality hospital we’re good at salvaging those patients who do experience those complications,” said Dr. Hari Nathan of the University of Michigan, Ann Arbor.
In a retrospective study, results of which were presented at the annual Society of Surgical Oncology Cancer Symposium, Dr. Nathan and colleagues showed that patients who underwent surgery for cancers of the esophagus and lung who had serious complications but survived at least 30 days after surgery had a more than twofold greater risk for death than did patients who had no complications, and patients with serious complications following surgery for cancer of the pancreas had a nearly twofold greater risk.
The effects of serious complications on survival persisted out to at least 180 days after surgery for each of the three procedures.
The findings suggest that just getting the patient through the operation and keeping him or her alive in the ICU is not sufficient cause for celebration by surgeons, Dr. Nathan said.
The investigators conducted the study to examine the incidence of complications following cancer surgery in older patients, the relationship between surgical complications and long-term survival, and whether the effects of complications would diminish or “wash out” over time. They reviewed Surveillance, Epidemiology and End Results–Medicare data on patients aged 65 years and older who underwent surgery with curative intent for esophageal cancer, non–small cell lung cancer, or pancreatic adenocarcinoma from 2005 through 2009.
They defined serious complications as “the appearance of a complication associated with a hospital length of stay greater than the 75th percentile for that procedure.”
The cohort included 965 patients who underwent esophageal surgery, 12,395 who had lung surgery, and 1,966 who underwent pancreatic resection. The proportion of patients over 80 years who underwent the procedures, respectively, were 12%, 18%, and 19%.
Serious complications occurred in 17% of patients with esophageal cancer, 10% of those with lung cancer, and 12% of those with cancer of the pancreas. The respective 30-day mortality rates were 6.%, 3.3%, and 3.9%.
Looking only at those patients with lung cancer who survived at least 30 days after surgery, the investigators found that median survival among those who had no complications was 79 months, compared with 60 months for those who had mild complications, and 33 months for patients who had serious complications (P less than .001)
“And indeed, when we performed adjusted survival analyses looking at all three disease sites, we saw a very consistent story: that those patients who had serious complications had decreased long-term survival for all three malignancies we looked at,” Dr. Nathan said.
Specifically, in survival analyses adjusted for sex, age, and procedure code, hazard ratios for patients with serious complications compared with those who had no complications were 2.55 for esophageal cancer patients, 2.13 for lung cancer patients, and 1.57 for pancreatic cancer patients (all comparisons significant as shown by 95% confidence intervals).
The investigators questioned whether the differences in mortality were due to the late effects of perioperative complications.
“In modern ICUs, we can keep virtually anybody alive for 30 days, and there has been a lot interest in longer-term metrics for perioperative mortality, for example, at 30 or 90 days, so we thought maybe that’s what we were seeing here,” he said. To test this idea, the investigators looked at the effects of complications on patient who survived lung cancer surgery for at least 90 days, and those who lived for at least 180 days after surgery, and they saw that the survival curves were similar to those seen with the 30-day survivors, showing significantly and persistently worse survival for patients with serious complications (P less than .001).
For each of the disease states, patients with serious complications were also significantly less likely than were those with no or mild complications to receive adjuvant chemotherapy, even after adjustment for patient age and cancer stage, two significant determinants of the likelihood of receiving chemotherapy.
And even when the effect of chemotherapy for those who did receive it was added into the survival models, patients with serious complications still had significantly worse overall survival, Dr. Nathan noted.
“Serious complications after these three cancer resections are common and they are associated with dramatically inferior long-term survival. Thirty, 60, 90, and even 180-day measures of mortality do not capture the full impact of complications on long-term survival,” he said.
Asked whether it may be possible to identify those patients at higher risk for serious complications due to comorbidities or other factors, and perhaps suggest withholding surgery from such patients, Dr. Nathan agreed, but added that “the best chance for survival for all of these patients is a high-quality surgical resection, so it’s hard to deny a patient that chance unless you think they have a really high risk of perioperative death.”
The study was internally funded. Dr. Nathan reported no significant disclosures.
BOSTON – The operation was a success, but the patient died.
It’s an old chestnut for sure, but there is a painful kernel of truth in it, say investigators who found that patients who undergo complex cancer surgery and have serious complications are at significantly increased risk for death for at least 6 months after surgery, compared with patients who undergo the same procedure with few or no complications.
“Our work has important implications for quality assessment. I think in cancer surgery in particular we have to get away from the short-term metrics of survival, and we have to think about the implications of complications for long-term survival, even if at a very high-quality hospital we’re good at salvaging those patients who do experience those complications,” said Dr. Hari Nathan of the University of Michigan, Ann Arbor.
In a retrospective study, results of which were presented at the annual Society of Surgical Oncology Cancer Symposium, Dr. Nathan and colleagues showed that patients who underwent surgery for cancers of the esophagus and lung who had serious complications but survived at least 30 days after surgery had a more than twofold greater risk for death than did patients who had no complications, and patients with serious complications following surgery for cancer of the pancreas had a nearly twofold greater risk.
The effects of serious complications on survival persisted out to at least 180 days after surgery for each of the three procedures.
The findings suggest that just getting the patient through the operation and keeping him or her alive in the ICU is not sufficient cause for celebration by surgeons, Dr. Nathan said.
The investigators conducted the study to examine the incidence of complications following cancer surgery in older patients, the relationship between surgical complications and long-term survival, and whether the effects of complications would diminish or “wash out” over time. They reviewed Surveillance, Epidemiology and End Results–Medicare data on patients aged 65 years and older who underwent surgery with curative intent for esophageal cancer, non–small cell lung cancer, or pancreatic adenocarcinoma from 2005 through 2009.
They defined serious complications as “the appearance of a complication associated with a hospital length of stay greater than the 75th percentile for that procedure.”
The cohort included 965 patients who underwent esophageal surgery, 12,395 who had lung surgery, and 1,966 who underwent pancreatic resection. The proportion of patients over 80 years who underwent the procedures, respectively, were 12%, 18%, and 19%.
Serious complications occurred in 17% of patients with esophageal cancer, 10% of those with lung cancer, and 12% of those with cancer of the pancreas. The respective 30-day mortality rates were 6.%, 3.3%, and 3.9%.
Looking only at those patients with lung cancer who survived at least 30 days after surgery, the investigators found that median survival among those who had no complications was 79 months, compared with 60 months for those who had mild complications, and 33 months for patients who had serious complications (P less than .001)
“And indeed, when we performed adjusted survival analyses looking at all three disease sites, we saw a very consistent story: that those patients who had serious complications had decreased long-term survival for all three malignancies we looked at,” Dr. Nathan said.
Specifically, in survival analyses adjusted for sex, age, and procedure code, hazard ratios for patients with serious complications compared with those who had no complications were 2.55 for esophageal cancer patients, 2.13 for lung cancer patients, and 1.57 for pancreatic cancer patients (all comparisons significant as shown by 95% confidence intervals).
The investigators questioned whether the differences in mortality were due to the late effects of perioperative complications.
“In modern ICUs, we can keep virtually anybody alive for 30 days, and there has been a lot interest in longer-term metrics for perioperative mortality, for example, at 30 or 90 days, so we thought maybe that’s what we were seeing here,” he said. To test this idea, the investigators looked at the effects of complications on patient who survived lung cancer surgery for at least 90 days, and those who lived for at least 180 days after surgery, and they saw that the survival curves were similar to those seen with the 30-day survivors, showing significantly and persistently worse survival for patients with serious complications (P less than .001).
For each of the disease states, patients with serious complications were also significantly less likely than were those with no or mild complications to receive adjuvant chemotherapy, even after adjustment for patient age and cancer stage, two significant determinants of the likelihood of receiving chemotherapy.
And even when the effect of chemotherapy for those who did receive it was added into the survival models, patients with serious complications still had significantly worse overall survival, Dr. Nathan noted.
“Serious complications after these three cancer resections are common and they are associated with dramatically inferior long-term survival. Thirty, 60, 90, and even 180-day measures of mortality do not capture the full impact of complications on long-term survival,” he said.
Asked whether it may be possible to identify those patients at higher risk for serious complications due to comorbidities or other factors, and perhaps suggest withholding surgery from such patients, Dr. Nathan agreed, but added that “the best chance for survival for all of these patients is a high-quality surgical resection, so it’s hard to deny a patient that chance unless you think they have a really high risk of perioperative death.”
The study was internally funded. Dr. Nathan reported no significant disclosures.
AT SSO 2016
Key clinical point: Thirty-day postoperative survival may not be an adequate measure of success of complex cancer surgeries.
Major finding: Patients with serious complications from esophageal, lung, and pancreatic cancer operations had significantly worse survival out to 180 days ,compared with those with mild or no complications.
Data source: Retrospective review of SEER-Medicare data from 2005-2009.
Disclosures: The study was internally funded. Dr. Nathan reported no significant disclosures.
Those annoying EHR pop-up windows
In 1986, the United States and Canada mandated the adoption of a center brake light on all new cars. Studies had shown that this was better at getting attention than the two side lights alone, and reduced collisions.
Of course, as the years went by the safety benefit gradually faded. It never returned to the previous level, but clearly, as people got used to it, the new light faded into the background of their attention.
Today, we have electronic health record (EHR) systems that use all kinds of pop-up warnings to check INRs, to give flu shots, to consider COPD in the differential ... a million things. I’m sure the attorneys love them. (“Doctor, since the computer clearly warned you about this, why did you click ‘ignore’ and move on?”)
I don’t use one of those systems, but I talk to plenty of doctors who do. Initially, it was interesting and got their attention, then became annoying. Each pop-up window interrupted the chain of thought, distracting them from the task at hand: patient care. As time went on, they just began ignoring them. It’s easier to click “cancel” than it is have to think through something you’ve probably already considered.
So, like the center brake light, the well-intentioned pop-up window is ignored and pushed to the far side of your attention span.
Do these things improve quality of care? Probably no more than the center brake light reduces car accidents these days. They’re likely useful in training, to remind medical students and residents of things that are important, but beyond that would be a tough case to make.
I’m not saying attending physicians are infallible. We all make our share of mistakes in this world. But medicine is not a one-size-fits-all field. The EHRs, at least at present, can’t take into account as we do all the variables of each patient’s personality, social situation, compliance history, medication tolerance issues, and other factors.
Not only that, but the pop-up window saying, “Have you considered this?” is no less distracting than having to take a phone call during a visit. It’s intrusive, throws your train of thought temporarily onto another track, and requires a minute to refocus on the task at hand. In that time, you may have forgotten something equally, if not more important. Or missed some critical piece of information the patient mentioned.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In 1986, the United States and Canada mandated the adoption of a center brake light on all new cars. Studies had shown that this was better at getting attention than the two side lights alone, and reduced collisions.
Of course, as the years went by the safety benefit gradually faded. It never returned to the previous level, but clearly, as people got used to it, the new light faded into the background of their attention.
Today, we have electronic health record (EHR) systems that use all kinds of pop-up warnings to check INRs, to give flu shots, to consider COPD in the differential ... a million things. I’m sure the attorneys love them. (“Doctor, since the computer clearly warned you about this, why did you click ‘ignore’ and move on?”)
I don’t use one of those systems, but I talk to plenty of doctors who do. Initially, it was interesting and got their attention, then became annoying. Each pop-up window interrupted the chain of thought, distracting them from the task at hand: patient care. As time went on, they just began ignoring them. It’s easier to click “cancel” than it is have to think through something you’ve probably already considered.
So, like the center brake light, the well-intentioned pop-up window is ignored and pushed to the far side of your attention span.
Do these things improve quality of care? Probably no more than the center brake light reduces car accidents these days. They’re likely useful in training, to remind medical students and residents of things that are important, but beyond that would be a tough case to make.
I’m not saying attending physicians are infallible. We all make our share of mistakes in this world. But medicine is not a one-size-fits-all field. The EHRs, at least at present, can’t take into account as we do all the variables of each patient’s personality, social situation, compliance history, medication tolerance issues, and other factors.
Not only that, but the pop-up window saying, “Have you considered this?” is no less distracting than having to take a phone call during a visit. It’s intrusive, throws your train of thought temporarily onto another track, and requires a minute to refocus on the task at hand. In that time, you may have forgotten something equally, if not more important. Or missed some critical piece of information the patient mentioned.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
In 1986, the United States and Canada mandated the adoption of a center brake light on all new cars. Studies had shown that this was better at getting attention than the two side lights alone, and reduced collisions.
Of course, as the years went by the safety benefit gradually faded. It never returned to the previous level, but clearly, as people got used to it, the new light faded into the background of their attention.
Today, we have electronic health record (EHR) systems that use all kinds of pop-up warnings to check INRs, to give flu shots, to consider COPD in the differential ... a million things. I’m sure the attorneys love them. (“Doctor, since the computer clearly warned you about this, why did you click ‘ignore’ and move on?”)
I don’t use one of those systems, but I talk to plenty of doctors who do. Initially, it was interesting and got their attention, then became annoying. Each pop-up window interrupted the chain of thought, distracting them from the task at hand: patient care. As time went on, they just began ignoring them. It’s easier to click “cancel” than it is have to think through something you’ve probably already considered.
So, like the center brake light, the well-intentioned pop-up window is ignored and pushed to the far side of your attention span.
Do these things improve quality of care? Probably no more than the center brake light reduces car accidents these days. They’re likely useful in training, to remind medical students and residents of things that are important, but beyond that would be a tough case to make.
I’m not saying attending physicians are infallible. We all make our share of mistakes in this world. But medicine is not a one-size-fits-all field. The EHRs, at least at present, can’t take into account as we do all the variables of each patient’s personality, social situation, compliance history, medication tolerance issues, and other factors.
Not only that, but the pop-up window saying, “Have you considered this?” is no less distracting than having to take a phone call during a visit. It’s intrusive, throws your train of thought temporarily onto another track, and requires a minute to refocus on the task at hand. In that time, you may have forgotten something equally, if not more important. Or missed some critical piece of information the patient mentioned.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
ABMS approves new addiction medicine subspecialty
Many more physicians seeking to subspecialize in addiction medicine will now have the official blessing of the American Board of Medical Specialties.
ABMS announced March 14 its approval of an addiction medicine subspecialty that the American Board of Preventive Medicine (ABPM) will sponsor.
Physicians who are certified by any of the 24 ABMS member boards can apply for the addiction medicine certification. The American Board of Psychiatry and Neurology offers certification in addiction psychiatry, but only to psychiatrists.
ABPM hasn’t set a date for the addiction medicine subspecialty’s first board certification exam, which the board will develop. ABPM will post updates on its website, www.theabpm.org.
“Increasing the number of well-trained and certified specialists in addiction medicine will significantly increase access to care for those in need of intervention and treatment,” said ABPM’s board chair, Dr. Denece O. Kesler, in a statement.
One in seven Americans older than 12 years meets medical criteria for an addiction to nicotine, alcohol, or other drugs, according to statistics from the National Center on Addiction and Substance Abuse. But only 11% of those who need treatment are able to receive it, in part because of a lack of addiction medicine providers.
The American Board of Addiction Medicine (ABAM) hailed the new subspecialty. “This is a great day for addiction medicine,” Dr. Robert J. Sokol, president of ABAM and the Addiction Medicine Foundation (AMF), said in a statement. “This landmark event, more than any other, recognizes addiction as a preventable and treatable disease.”
ABAM has certified 3,902 physicians, according to the organization, which is not an ABMS member board. There are 40 AMF-sponsored fellowship training programs nationally, with a commitment to establish 125 more by 2025. AMF expects the ABMS recognition will lead to the fellowships gaining the imprimatur of the Accreditation Council on Graduate Medical Education.
“This is a positive development that has the potential to address a serious public health problem,” Dr. Daniel Lieberman, vice chairman of the psychiatry and behavioral health department at George Washington University, Washington, said in an interview. “This action will reassure doctors who are interested in addiction medicine that the time and effort they put into obtaining additional training will give them the status of a subspecialist with recognized expertise. It may also encourage young doctors to consider addiction medicine as a career path.”
Meanwhile, a package of mental health reforms moving in the U.S. Senate could improve patients’ access to addiction medicine providers. One of the bills, the TREAT Act, would increase the number of substance use detoxification patients that a qualified provider is legally allowed to treat annually, from 30 patients to 100 patients. The legislation also would allow those practitioners to request permission to annually treat unlimited numbers of patients thereafter.
On Twitter @whitneymcknight
Many more physicians seeking to subspecialize in addiction medicine will now have the official blessing of the American Board of Medical Specialties.
ABMS announced March 14 its approval of an addiction medicine subspecialty that the American Board of Preventive Medicine (ABPM) will sponsor.
Physicians who are certified by any of the 24 ABMS member boards can apply for the addiction medicine certification. The American Board of Psychiatry and Neurology offers certification in addiction psychiatry, but only to psychiatrists.
ABPM hasn’t set a date for the addiction medicine subspecialty’s first board certification exam, which the board will develop. ABPM will post updates on its website, www.theabpm.org.
“Increasing the number of well-trained and certified specialists in addiction medicine will significantly increase access to care for those in need of intervention and treatment,” said ABPM’s board chair, Dr. Denece O. Kesler, in a statement.
One in seven Americans older than 12 years meets medical criteria for an addiction to nicotine, alcohol, or other drugs, according to statistics from the National Center on Addiction and Substance Abuse. But only 11% of those who need treatment are able to receive it, in part because of a lack of addiction medicine providers.
The American Board of Addiction Medicine (ABAM) hailed the new subspecialty. “This is a great day for addiction medicine,” Dr. Robert J. Sokol, president of ABAM and the Addiction Medicine Foundation (AMF), said in a statement. “This landmark event, more than any other, recognizes addiction as a preventable and treatable disease.”
ABAM has certified 3,902 physicians, according to the organization, which is not an ABMS member board. There are 40 AMF-sponsored fellowship training programs nationally, with a commitment to establish 125 more by 2025. AMF expects the ABMS recognition will lead to the fellowships gaining the imprimatur of the Accreditation Council on Graduate Medical Education.
“This is a positive development that has the potential to address a serious public health problem,” Dr. Daniel Lieberman, vice chairman of the psychiatry and behavioral health department at George Washington University, Washington, said in an interview. “This action will reassure doctors who are interested in addiction medicine that the time and effort they put into obtaining additional training will give them the status of a subspecialist with recognized expertise. It may also encourage young doctors to consider addiction medicine as a career path.”
Meanwhile, a package of mental health reforms moving in the U.S. Senate could improve patients’ access to addiction medicine providers. One of the bills, the TREAT Act, would increase the number of substance use detoxification patients that a qualified provider is legally allowed to treat annually, from 30 patients to 100 patients. The legislation also would allow those practitioners to request permission to annually treat unlimited numbers of patients thereafter.
On Twitter @whitneymcknight
Many more physicians seeking to subspecialize in addiction medicine will now have the official blessing of the American Board of Medical Specialties.
ABMS announced March 14 its approval of an addiction medicine subspecialty that the American Board of Preventive Medicine (ABPM) will sponsor.
Physicians who are certified by any of the 24 ABMS member boards can apply for the addiction medicine certification. The American Board of Psychiatry and Neurology offers certification in addiction psychiatry, but only to psychiatrists.
ABPM hasn’t set a date for the addiction medicine subspecialty’s first board certification exam, which the board will develop. ABPM will post updates on its website, www.theabpm.org.
“Increasing the number of well-trained and certified specialists in addiction medicine will significantly increase access to care for those in need of intervention and treatment,” said ABPM’s board chair, Dr. Denece O. Kesler, in a statement.
One in seven Americans older than 12 years meets medical criteria for an addiction to nicotine, alcohol, or other drugs, according to statistics from the National Center on Addiction and Substance Abuse. But only 11% of those who need treatment are able to receive it, in part because of a lack of addiction medicine providers.
The American Board of Addiction Medicine (ABAM) hailed the new subspecialty. “This is a great day for addiction medicine,” Dr. Robert J. Sokol, president of ABAM and the Addiction Medicine Foundation (AMF), said in a statement. “This landmark event, more than any other, recognizes addiction as a preventable and treatable disease.”
ABAM has certified 3,902 physicians, according to the organization, which is not an ABMS member board. There are 40 AMF-sponsored fellowship training programs nationally, with a commitment to establish 125 more by 2025. AMF expects the ABMS recognition will lead to the fellowships gaining the imprimatur of the Accreditation Council on Graduate Medical Education.
“This is a positive development that has the potential to address a serious public health problem,” Dr. Daniel Lieberman, vice chairman of the psychiatry and behavioral health department at George Washington University, Washington, said in an interview. “This action will reassure doctors who are interested in addiction medicine that the time and effort they put into obtaining additional training will give them the status of a subspecialist with recognized expertise. It may also encourage young doctors to consider addiction medicine as a career path.”
Meanwhile, a package of mental health reforms moving in the U.S. Senate could improve patients’ access to addiction medicine providers. One of the bills, the TREAT Act, would increase the number of substance use detoxification patients that a qualified provider is legally allowed to treat annually, from 30 patients to 100 patients. The legislation also would allow those practitioners to request permission to annually treat unlimited numbers of patients thereafter.
On Twitter @whitneymcknight
The year in osteoarthritis
MAUI, HAWAII – One of the major happenings in the field of osteoarthritis in the past year was a disturbing report of dramatically increased risk of acute MI for at least 6 months after total knee replacement, panelists agreed at the 2016 Rheumatology Winter Clinical Symposium.
“What they found borders on frightening,” according to Dr. Martin J. Bergman of Drexel University, Philadelphia, and chief of rheumatology at Taylor Hospital in Ridley Park, Pa.
Dr. Bergman and copanelist Dr. Orrin M. Troum of the University of Southern California in Los Angeles highlighted key developments in osteoarthritis during the past year, including two major studies on total knee replacement, the Food and Drug Administration’s updated stronger warning on the cardiac and stroke risks of NSAIDs, a randomized trial which effectively takes hydroxychloroquine (Plaquenil) off the treatment menu for hand osteoarthritis, and a reassuring report on the safety of repeated intra-articular corticosteroid injections in patients with synovitic knee osteoarthritis.
Acute MI risk after total knee replacement
British investigators utilizing the U.K. National Health Service database retrospectively identified 13,849 patients who underwent total knee replacement (TKR) and an equal number of nonsurgical controls propensity-matched for cardiovascular risk factors. These two very large groups were followed for 5 years.
During the first month after TKR, the acute MI risk was 8.75-fold greater than in the matched controls. The elevated risk gradually declined thereafter, but it remained significantly higher than in controls until 1 year after surgery. At 3 months post surgery the TKR group was at fourfold increased risk of MI, compared with controls, and at 6 months their risk was still nearly double that of controls (Arthritis Rheumatol. 2015 Oct;67[10]:2771-9).
The British investigators also found a prolonged postsurgical elevated risk of MI in a large group of patients who underwent total hip replacement, although the magnitude of the increased risk, compared with matched controls, wasn’t as large as that seen after TKR.
Dr. Troum commented that the increased risk of MI during the first year after TKR identified in this study is something physicians now need to bring up in the risk/benefit discussion with patients considering TKR.
“Also, this study underscores that it may behoove us to make sure that these presurgical patients are really well worked up by a cardiologist or their primary care physician to mitigate that coronary risk as much as possible,” he added.
Another key finding in the U.K. study was that unlike the acute MI risk, the risk of venous thromboembolism following TKR remained elevated throughout the full 5 years of follow-up.
“Once you’ve had that surgery, you are at increased risk for venous thromboembolism. I think that’s something we have to keep in mind when a patient comes in with a history of total knee replacement and a complaint of calf pain or swelling – at that point, you have to think about deep venous thrombosis,” Dr. Bergman said.
TKR – Why wait?
In a Danish trial of 100 knee osteoarthritis patients deemed eligible for TKR, participants were randomized to prompt TKR followed by a 3-month regimen of exercise, dietary weight loss, physical therapy, and pain medication or to the nonsurgical regimen alone. At 12 months of follow-up, the prompt TKR group showed significantly greater improvement in a standardized score encompassing pain, symptoms, quality of life, and activities of daily living, even though one-quarter of patients in the nonsurgical treatment group bailed and underwent TKR before 12 months was up (N Engl J Med. 2015 Oct 22;373[17]:1597-606).
“My conclusion is that once you’ve determined that a patient needs and wants a total knee replacement, the patient should probably get it. Delaying – trying other modalities in an effort to lose weight and improve function – is really not going to buy you much in the way of time,” Dr. Bergman observed.
Hydroxychloroquine for hand osteoarthritis
At the 2015 European League Against Rheumatism (EULAR) meeting in Rome, Dutch investigators presented a randomized, double-blind trial in which 196 patients with symptomatic hand osteoarthritis received 6 months of hydroxychloroquine at 400 mg/day or placebo. Unlike in mild rheumatoid arthritis or lupus, hydroxychloroquine had no beneficial effect on hand osteoarthritis pain, disability, or quality of life measures.
“Plaquenil [Hydroxychloroquine] is not a good choice for patients with osteoarthritis of the hand. I think it’s a dead therapy,” Dr. Troum declared.
FDA expands warning on NSAIDs’ cardiovascular risk
On July 9, 2015, the FDA announced updated labels for NSAIDs. The new warning states that MI and stroke risk can increase as early as in the first week of NSAID use and appear to be dose- and duration-related. The agency also warned that patients who take an NSAID after a first MI are more likely to die within 1 year.
“This really brought a lot of folks to my office,” Dr. Troum recalled.
“Absolutely, this was big stuff,” Dr. Bergman agreed. “This became a nightmare for many of us because all of a sudden patients were scared to death about taking their NSAIDs.”
Intra-articular corticosteroids for knee osteoarthritis don’t accelerate cartilage deterioration
At last fall’s American College of Rheumatology meeting in San Francisco, Jeffrey B. Driban, Ph.D., of Tufts Medical Center, Boston, presented a double-blind, randomized trial of intra-articular injections of triamcinolone hexacetonide 40 mg versus saline quarterly for 2 years in 140 patients with symptomatic knee osteoarthritis with ultrasound evidence of synovitis. Participants underwent annual evaluation of periarticular bone and cartilage changes via MRI and dual-energy x-ray absorptiometry.
After 2 years, there was no difference between the two groups in terms of pain scores, walk time, or other functional measures. The injections – eight in total over 2 years – were safe, with new-onset hypertension and hyperglycemia rates of 3% in this obese population. And most important of all, there were no major differences between the two groups in terms of quantitative or semiquantitative structural endpoints; in other words, the injections didn’t increase the rate of structural disease progression. The intra-articular steroid group showed a modestly greater rate of loss of cartilage thickness, which the investigators deemed of uncertain clinical significance.
“The structural changes were minimal,” Dr. Troum noted. “This is only a 2-year study, but I can say that I now feel more comfortable giving these injections in patients who for whatever reason can’t get surgery.”
Dr. Bergman said that many orthopedic surgeons talk up the potential risk that intra-articular steroid injections will accelerate cartilage damage. They place an arbitrary limit on the number of injections a patient can receive.
“I think this study really helps us push back and say, ‘No, I think you’re fine in getting this procedure,’” the rheumatologist commented.
Dr. Bergman and Dr. Troum reported having no financial conflicts regarding their presentation.
MAUI, HAWAII – One of the major happenings in the field of osteoarthritis in the past year was a disturbing report of dramatically increased risk of acute MI for at least 6 months after total knee replacement, panelists agreed at the 2016 Rheumatology Winter Clinical Symposium.
“What they found borders on frightening,” according to Dr. Martin J. Bergman of Drexel University, Philadelphia, and chief of rheumatology at Taylor Hospital in Ridley Park, Pa.
Dr. Bergman and copanelist Dr. Orrin M. Troum of the University of Southern California in Los Angeles highlighted key developments in osteoarthritis during the past year, including two major studies on total knee replacement, the Food and Drug Administration’s updated stronger warning on the cardiac and stroke risks of NSAIDs, a randomized trial which effectively takes hydroxychloroquine (Plaquenil) off the treatment menu for hand osteoarthritis, and a reassuring report on the safety of repeated intra-articular corticosteroid injections in patients with synovitic knee osteoarthritis.
Acute MI risk after total knee replacement
British investigators utilizing the U.K. National Health Service database retrospectively identified 13,849 patients who underwent total knee replacement (TKR) and an equal number of nonsurgical controls propensity-matched for cardiovascular risk factors. These two very large groups were followed for 5 years.
During the first month after TKR, the acute MI risk was 8.75-fold greater than in the matched controls. The elevated risk gradually declined thereafter, but it remained significantly higher than in controls until 1 year after surgery. At 3 months post surgery the TKR group was at fourfold increased risk of MI, compared with controls, and at 6 months their risk was still nearly double that of controls (Arthritis Rheumatol. 2015 Oct;67[10]:2771-9).
The British investigators also found a prolonged postsurgical elevated risk of MI in a large group of patients who underwent total hip replacement, although the magnitude of the increased risk, compared with matched controls, wasn’t as large as that seen after TKR.
Dr. Troum commented that the increased risk of MI during the first year after TKR identified in this study is something physicians now need to bring up in the risk/benefit discussion with patients considering TKR.
“Also, this study underscores that it may behoove us to make sure that these presurgical patients are really well worked up by a cardiologist or their primary care physician to mitigate that coronary risk as much as possible,” he added.
Another key finding in the U.K. study was that unlike the acute MI risk, the risk of venous thromboembolism following TKR remained elevated throughout the full 5 years of follow-up.
“Once you’ve had that surgery, you are at increased risk for venous thromboembolism. I think that’s something we have to keep in mind when a patient comes in with a history of total knee replacement and a complaint of calf pain or swelling – at that point, you have to think about deep venous thrombosis,” Dr. Bergman said.
TKR – Why wait?
In a Danish trial of 100 knee osteoarthritis patients deemed eligible for TKR, participants were randomized to prompt TKR followed by a 3-month regimen of exercise, dietary weight loss, physical therapy, and pain medication or to the nonsurgical regimen alone. At 12 months of follow-up, the prompt TKR group showed significantly greater improvement in a standardized score encompassing pain, symptoms, quality of life, and activities of daily living, even though one-quarter of patients in the nonsurgical treatment group bailed and underwent TKR before 12 months was up (N Engl J Med. 2015 Oct 22;373[17]:1597-606).
“My conclusion is that once you’ve determined that a patient needs and wants a total knee replacement, the patient should probably get it. Delaying – trying other modalities in an effort to lose weight and improve function – is really not going to buy you much in the way of time,” Dr. Bergman observed.
Hydroxychloroquine for hand osteoarthritis
At the 2015 European League Against Rheumatism (EULAR) meeting in Rome, Dutch investigators presented a randomized, double-blind trial in which 196 patients with symptomatic hand osteoarthritis received 6 months of hydroxychloroquine at 400 mg/day or placebo. Unlike in mild rheumatoid arthritis or lupus, hydroxychloroquine had no beneficial effect on hand osteoarthritis pain, disability, or quality of life measures.
“Plaquenil [Hydroxychloroquine] is not a good choice for patients with osteoarthritis of the hand. I think it’s a dead therapy,” Dr. Troum declared.
FDA expands warning on NSAIDs’ cardiovascular risk
On July 9, 2015, the FDA announced updated labels for NSAIDs. The new warning states that MI and stroke risk can increase as early as in the first week of NSAID use and appear to be dose- and duration-related. The agency also warned that patients who take an NSAID after a first MI are more likely to die within 1 year.
“This really brought a lot of folks to my office,” Dr. Troum recalled.
“Absolutely, this was big stuff,” Dr. Bergman agreed. “This became a nightmare for many of us because all of a sudden patients were scared to death about taking their NSAIDs.”
Intra-articular corticosteroids for knee osteoarthritis don’t accelerate cartilage deterioration
At last fall’s American College of Rheumatology meeting in San Francisco, Jeffrey B. Driban, Ph.D., of Tufts Medical Center, Boston, presented a double-blind, randomized trial of intra-articular injections of triamcinolone hexacetonide 40 mg versus saline quarterly for 2 years in 140 patients with symptomatic knee osteoarthritis with ultrasound evidence of synovitis. Participants underwent annual evaluation of periarticular bone and cartilage changes via MRI and dual-energy x-ray absorptiometry.
After 2 years, there was no difference between the two groups in terms of pain scores, walk time, or other functional measures. The injections – eight in total over 2 years – were safe, with new-onset hypertension and hyperglycemia rates of 3% in this obese population. And most important of all, there were no major differences between the two groups in terms of quantitative or semiquantitative structural endpoints; in other words, the injections didn’t increase the rate of structural disease progression. The intra-articular steroid group showed a modestly greater rate of loss of cartilage thickness, which the investigators deemed of uncertain clinical significance.
“The structural changes were minimal,” Dr. Troum noted. “This is only a 2-year study, but I can say that I now feel more comfortable giving these injections in patients who for whatever reason can’t get surgery.”
Dr. Bergman said that many orthopedic surgeons talk up the potential risk that intra-articular steroid injections will accelerate cartilage damage. They place an arbitrary limit on the number of injections a patient can receive.
“I think this study really helps us push back and say, ‘No, I think you’re fine in getting this procedure,’” the rheumatologist commented.
Dr. Bergman and Dr. Troum reported having no financial conflicts regarding their presentation.
MAUI, HAWAII – One of the major happenings in the field of osteoarthritis in the past year was a disturbing report of dramatically increased risk of acute MI for at least 6 months after total knee replacement, panelists agreed at the 2016 Rheumatology Winter Clinical Symposium.
“What they found borders on frightening,” according to Dr. Martin J. Bergman of Drexel University, Philadelphia, and chief of rheumatology at Taylor Hospital in Ridley Park, Pa.
Dr. Bergman and copanelist Dr. Orrin M. Troum of the University of Southern California in Los Angeles highlighted key developments in osteoarthritis during the past year, including two major studies on total knee replacement, the Food and Drug Administration’s updated stronger warning on the cardiac and stroke risks of NSAIDs, a randomized trial which effectively takes hydroxychloroquine (Plaquenil) off the treatment menu for hand osteoarthritis, and a reassuring report on the safety of repeated intra-articular corticosteroid injections in patients with synovitic knee osteoarthritis.
Acute MI risk after total knee replacement
British investigators utilizing the U.K. National Health Service database retrospectively identified 13,849 patients who underwent total knee replacement (TKR) and an equal number of nonsurgical controls propensity-matched for cardiovascular risk factors. These two very large groups were followed for 5 years.
During the first month after TKR, the acute MI risk was 8.75-fold greater than in the matched controls. The elevated risk gradually declined thereafter, but it remained significantly higher than in controls until 1 year after surgery. At 3 months post surgery the TKR group was at fourfold increased risk of MI, compared with controls, and at 6 months their risk was still nearly double that of controls (Arthritis Rheumatol. 2015 Oct;67[10]:2771-9).
The British investigators also found a prolonged postsurgical elevated risk of MI in a large group of patients who underwent total hip replacement, although the magnitude of the increased risk, compared with matched controls, wasn’t as large as that seen after TKR.
Dr. Troum commented that the increased risk of MI during the first year after TKR identified in this study is something physicians now need to bring up in the risk/benefit discussion with patients considering TKR.
“Also, this study underscores that it may behoove us to make sure that these presurgical patients are really well worked up by a cardiologist or their primary care physician to mitigate that coronary risk as much as possible,” he added.
Another key finding in the U.K. study was that unlike the acute MI risk, the risk of venous thromboembolism following TKR remained elevated throughout the full 5 years of follow-up.
“Once you’ve had that surgery, you are at increased risk for venous thromboembolism. I think that’s something we have to keep in mind when a patient comes in with a history of total knee replacement and a complaint of calf pain or swelling – at that point, you have to think about deep venous thrombosis,” Dr. Bergman said.
TKR – Why wait?
In a Danish trial of 100 knee osteoarthritis patients deemed eligible for TKR, participants were randomized to prompt TKR followed by a 3-month regimen of exercise, dietary weight loss, physical therapy, and pain medication or to the nonsurgical regimen alone. At 12 months of follow-up, the prompt TKR group showed significantly greater improvement in a standardized score encompassing pain, symptoms, quality of life, and activities of daily living, even though one-quarter of patients in the nonsurgical treatment group bailed and underwent TKR before 12 months was up (N Engl J Med. 2015 Oct 22;373[17]:1597-606).
“My conclusion is that once you’ve determined that a patient needs and wants a total knee replacement, the patient should probably get it. Delaying – trying other modalities in an effort to lose weight and improve function – is really not going to buy you much in the way of time,” Dr. Bergman observed.
Hydroxychloroquine for hand osteoarthritis
At the 2015 European League Against Rheumatism (EULAR) meeting in Rome, Dutch investigators presented a randomized, double-blind trial in which 196 patients with symptomatic hand osteoarthritis received 6 months of hydroxychloroquine at 400 mg/day or placebo. Unlike in mild rheumatoid arthritis or lupus, hydroxychloroquine had no beneficial effect on hand osteoarthritis pain, disability, or quality of life measures.
“Plaquenil [Hydroxychloroquine] is not a good choice for patients with osteoarthritis of the hand. I think it’s a dead therapy,” Dr. Troum declared.
FDA expands warning on NSAIDs’ cardiovascular risk
On July 9, 2015, the FDA announced updated labels for NSAIDs. The new warning states that MI and stroke risk can increase as early as in the first week of NSAID use and appear to be dose- and duration-related. The agency also warned that patients who take an NSAID after a first MI are more likely to die within 1 year.
“This really brought a lot of folks to my office,” Dr. Troum recalled.
“Absolutely, this was big stuff,” Dr. Bergman agreed. “This became a nightmare for many of us because all of a sudden patients were scared to death about taking their NSAIDs.”
Intra-articular corticosteroids for knee osteoarthritis don’t accelerate cartilage deterioration
At last fall’s American College of Rheumatology meeting in San Francisco, Jeffrey B. Driban, Ph.D., of Tufts Medical Center, Boston, presented a double-blind, randomized trial of intra-articular injections of triamcinolone hexacetonide 40 mg versus saline quarterly for 2 years in 140 patients with symptomatic knee osteoarthritis with ultrasound evidence of synovitis. Participants underwent annual evaluation of periarticular bone and cartilage changes via MRI and dual-energy x-ray absorptiometry.
After 2 years, there was no difference between the two groups in terms of pain scores, walk time, or other functional measures. The injections – eight in total over 2 years – were safe, with new-onset hypertension and hyperglycemia rates of 3% in this obese population. And most important of all, there were no major differences between the two groups in terms of quantitative or semiquantitative structural endpoints; in other words, the injections didn’t increase the rate of structural disease progression. The intra-articular steroid group showed a modestly greater rate of loss of cartilage thickness, which the investigators deemed of uncertain clinical significance.
“The structural changes were minimal,” Dr. Troum noted. “This is only a 2-year study, but I can say that I now feel more comfortable giving these injections in patients who for whatever reason can’t get surgery.”
Dr. Bergman said that many orthopedic surgeons talk up the potential risk that intra-articular steroid injections will accelerate cartilage damage. They place an arbitrary limit on the number of injections a patient can receive.
“I think this study really helps us push back and say, ‘No, I think you’re fine in getting this procedure,’” the rheumatologist commented.
Dr. Bergman and Dr. Troum reported having no financial conflicts regarding their presentation.
EXPERT ANALYSIS FROM RWCS 2016