User login
HIV drug may overcome proteasome-inhibitor resistance in multiple myeloma
The protease inhibitor nelfinavir was used successfully to resensitize patients with proteasome inhibitor–refractory multiple myeloma for proteasome-inhibitor treatment, Dr. Christoph Driessen of Kantonsspital St. Gallen (Switzerland) and colleagues reported in Haematologica.
The researchers had hypothesized that nelfinavir would induce the unfolded protein response and would overcome proteasome-inhibitor resistance. The researchers determined a nelfinavir dose of 2,500 mg twice daily based on a dose-finding study in 12 patients with advanced hematologic malignancies.
In an exploratory extension cohort trial that followed, six patients with relapsed, bortezomib-refractory, lenalidomide-resistant myeloma were treated with 2,500 mg of nelfinavir twice daily in combination with bortezomib; three reached a partial response, two had a minor response, and one had progressive disease. All began the investigational therapy less than 2 months after progressing under therapies with bortezomib/bendamustine/dexamethasone, bortezomib/bendamustine, or bortezomib monotherapy, respectively, the researchers said (Haematologica March 2016;101:346-55).
The study protocol did not allow dexamethasone co-administration until completion of cycle three, when patients who did not achieve a minor response were allowed to co-administer 8 mg dexamethasone with bortezomib. Higher doses were excluded because of potential interactions with nelfinavir through the Cyp3A4 system.
Future research should assess whether bortezomib may be replaced by next-generation drugs like carfilzomib to avoid drug interactions and improve activity and whether nelfinavir may likewise be used in combination with novel oral proteasome inhibitors to boost their low single agent activity. “This ultimately suggests exploring the addition of HIV protease inhibitors to established combinations of proteasome inhibitors with immunomodulatory drugs, for example, in the carfilzomib/lenalidomide/dexamethasone regimen, one of the most powerful and tolerable regimens available to date for advanced multiple myeloma,” they concluded.
On Twitter @maryjodales
The protease inhibitor nelfinavir was used successfully to resensitize patients with proteasome inhibitor–refractory multiple myeloma for proteasome-inhibitor treatment, Dr. Christoph Driessen of Kantonsspital St. Gallen (Switzerland) and colleagues reported in Haematologica.
The researchers had hypothesized that nelfinavir would induce the unfolded protein response and would overcome proteasome-inhibitor resistance. The researchers determined a nelfinavir dose of 2,500 mg twice daily based on a dose-finding study in 12 patients with advanced hematologic malignancies.
In an exploratory extension cohort trial that followed, six patients with relapsed, bortezomib-refractory, lenalidomide-resistant myeloma were treated with 2,500 mg of nelfinavir twice daily in combination with bortezomib; three reached a partial response, two had a minor response, and one had progressive disease. All began the investigational therapy less than 2 months after progressing under therapies with bortezomib/bendamustine/dexamethasone, bortezomib/bendamustine, or bortezomib monotherapy, respectively, the researchers said (Haematologica March 2016;101:346-55).
The study protocol did not allow dexamethasone co-administration until completion of cycle three, when patients who did not achieve a minor response were allowed to co-administer 8 mg dexamethasone with bortezomib. Higher doses were excluded because of potential interactions with nelfinavir through the Cyp3A4 system.
Future research should assess whether bortezomib may be replaced by next-generation drugs like carfilzomib to avoid drug interactions and improve activity and whether nelfinavir may likewise be used in combination with novel oral proteasome inhibitors to boost their low single agent activity. “This ultimately suggests exploring the addition of HIV protease inhibitors to established combinations of proteasome inhibitors with immunomodulatory drugs, for example, in the carfilzomib/lenalidomide/dexamethasone regimen, one of the most powerful and tolerable regimens available to date for advanced multiple myeloma,” they concluded.
On Twitter @maryjodales
The protease inhibitor nelfinavir was used successfully to resensitize patients with proteasome inhibitor–refractory multiple myeloma for proteasome-inhibitor treatment, Dr. Christoph Driessen of Kantonsspital St. Gallen (Switzerland) and colleagues reported in Haematologica.
The researchers had hypothesized that nelfinavir would induce the unfolded protein response and would overcome proteasome-inhibitor resistance. The researchers determined a nelfinavir dose of 2,500 mg twice daily based on a dose-finding study in 12 patients with advanced hematologic malignancies.
In an exploratory extension cohort trial that followed, six patients with relapsed, bortezomib-refractory, lenalidomide-resistant myeloma were treated with 2,500 mg of nelfinavir twice daily in combination with bortezomib; three reached a partial response, two had a minor response, and one had progressive disease. All began the investigational therapy less than 2 months after progressing under therapies with bortezomib/bendamustine/dexamethasone, bortezomib/bendamustine, or bortezomib monotherapy, respectively, the researchers said (Haematologica March 2016;101:346-55).
The study protocol did not allow dexamethasone co-administration until completion of cycle three, when patients who did not achieve a minor response were allowed to co-administer 8 mg dexamethasone with bortezomib. Higher doses were excluded because of potential interactions with nelfinavir through the Cyp3A4 system.
Future research should assess whether bortezomib may be replaced by next-generation drugs like carfilzomib to avoid drug interactions and improve activity and whether nelfinavir may likewise be used in combination with novel oral proteasome inhibitors to boost their low single agent activity. “This ultimately suggests exploring the addition of HIV protease inhibitors to established combinations of proteasome inhibitors with immunomodulatory drugs, for example, in the carfilzomib/lenalidomide/dexamethasone regimen, one of the most powerful and tolerable regimens available to date for advanced multiple myeloma,” they concluded.
On Twitter @maryjodales
FROM HAEMATOLOGIA
Key clinical point: Adding HIV protease inhibitors to established combinations of proteasome inhibitors may improve outcomes in patients with multiple myeloma.
Major finding: When six patients with relapsed, bortezomib-refractory, lenalidomide-resistant myeloma were treated with 2,500 mg of nelfinavir twice daily in combination with bortezomib, three reached a partial response, two had a minor response, and disease progressed in one.
Data source: A dose-finding study in 12 patients with advanced hematologic malignancies and an exploratory extension cohort trial that followed.
Disclosures: None of the authors had financial conflicts of interest in relation to the study.
Infection rates similar for in- and out-of-hospital pediatric cardiac arrest
ORLANDO – Infection rates didn’t differ between children who suffered cardiac arrest in or out of the hospital, and in both groups, few children’s infections were confirmed by culture, in a multicenter study.
The study explored infectious complications associated with pediatric cardiac arrest, Dr. Fasiha Saeed said at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.
She and her colleagues examined records of 491 pediatric patients who had return of spontaneous circulation after cardiac arrest (CA), 269 in hospital (IH) and 115 out of hospital (OH). Overall, more children who had in-hospital cardiac arrest were suspected of having an infection (242 [90%], compared with 83 [74%], in the OHCA group; P less than 0.0001).
However, cultures were actually sent for only about one in three patients with suspected infection in either group (34% IHCA and 35% OHCA). Definite infection was found in most patients who were cultured (82% and 86%, respectively).
Patients had “suspected infection” if they received cultures or antimicrobials, and were termed to have “definite infection” only if cultures were positive for infection.
“Infectious complications following out-of-hospital cardiac arrest have been reported in the adult literature, but the pediatric experience post–cardiac arrest is limited to case reports and small case series,” said Dr. Saeed, a pediatric critical care physician at Advocate Hospital, Park Ridge, Ill.
Data from PECARN (Pediatric Emergency Care Applied Research Network) had previously shown that in-hospital pediatric cardiac arrest patients were more likely to receive antimicrobials after return of spontaneous circulation. However, infectious etiologies and the early hospital course of these patients after their cardiac arrest was not known, said Dr. Saeed.
Dr. Saeed and her coinvestigators had hypothesized that “children with out-of-hospital cardiac arrest have a higher incidence of infections after return of spontaneous circulation and worse outcomes compared to children with in-hospital cardiac arrest,” she said. “We were surprised to see how infrequently cultures were sent,” said Dr. Saeed, in discussing the findings that were contrary to the study’s hypothesis.
Dr. Saeed and her colleagues conducted a retrospective analysis of the multi-institutional, deidentified PECARN database, examining 491 pediatric cardiac arrest patients who had required at least 1 minute of cardiopulmonary resuscitation. The patients were aged 24 hours to 18 years; the period of data collection was July 2003-December 2004.
Exclusion criteria included a diagnosis of septic shock, the use of therapeutic hypothermia, or patient death within 24 hours of the cardiac arrest.
Among other findings presented by Dr. Saeed, no association was seen between either suspected or definite infection and mortality. Antibiotic usage was also not associated with mortality. However, definite infection was positively associated with a respiratory etiology for cardiac arrest (odds ratio, 2.6). Post–cardiac arrest central venous pressure monitoring was also associated with definite infection (OR, 2.1).
Support for the study was provided by the Medical College of Wisconsin. The investigators disclosed no relevant conflicts of interest.
On Twitter @karioakes
ORLANDO – Infection rates didn’t differ between children who suffered cardiac arrest in or out of the hospital, and in both groups, few children’s infections were confirmed by culture, in a multicenter study.
The study explored infectious complications associated with pediatric cardiac arrest, Dr. Fasiha Saeed said at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.
She and her colleagues examined records of 491 pediatric patients who had return of spontaneous circulation after cardiac arrest (CA), 269 in hospital (IH) and 115 out of hospital (OH). Overall, more children who had in-hospital cardiac arrest were suspected of having an infection (242 [90%], compared with 83 [74%], in the OHCA group; P less than 0.0001).
However, cultures were actually sent for only about one in three patients with suspected infection in either group (34% IHCA and 35% OHCA). Definite infection was found in most patients who were cultured (82% and 86%, respectively).
Patients had “suspected infection” if they received cultures or antimicrobials, and were termed to have “definite infection” only if cultures were positive for infection.
“Infectious complications following out-of-hospital cardiac arrest have been reported in the adult literature, but the pediatric experience post–cardiac arrest is limited to case reports and small case series,” said Dr. Saeed, a pediatric critical care physician at Advocate Hospital, Park Ridge, Ill.
Data from PECARN (Pediatric Emergency Care Applied Research Network) had previously shown that in-hospital pediatric cardiac arrest patients were more likely to receive antimicrobials after return of spontaneous circulation. However, infectious etiologies and the early hospital course of these patients after their cardiac arrest was not known, said Dr. Saeed.
Dr. Saeed and her coinvestigators had hypothesized that “children with out-of-hospital cardiac arrest have a higher incidence of infections after return of spontaneous circulation and worse outcomes compared to children with in-hospital cardiac arrest,” she said. “We were surprised to see how infrequently cultures were sent,” said Dr. Saeed, in discussing the findings that were contrary to the study’s hypothesis.
Dr. Saeed and her colleagues conducted a retrospective analysis of the multi-institutional, deidentified PECARN database, examining 491 pediatric cardiac arrest patients who had required at least 1 minute of cardiopulmonary resuscitation. The patients were aged 24 hours to 18 years; the period of data collection was July 2003-December 2004.
Exclusion criteria included a diagnosis of septic shock, the use of therapeutic hypothermia, or patient death within 24 hours of the cardiac arrest.
Among other findings presented by Dr. Saeed, no association was seen between either suspected or definite infection and mortality. Antibiotic usage was also not associated with mortality. However, definite infection was positively associated with a respiratory etiology for cardiac arrest (odds ratio, 2.6). Post–cardiac arrest central venous pressure monitoring was also associated with definite infection (OR, 2.1).
Support for the study was provided by the Medical College of Wisconsin. The investigators disclosed no relevant conflicts of interest.
On Twitter @karioakes
ORLANDO – Infection rates didn’t differ between children who suffered cardiac arrest in or out of the hospital, and in both groups, few children’s infections were confirmed by culture, in a multicenter study.
The study explored infectious complications associated with pediatric cardiac arrest, Dr. Fasiha Saeed said at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.
She and her colleagues examined records of 491 pediatric patients who had return of spontaneous circulation after cardiac arrest (CA), 269 in hospital (IH) and 115 out of hospital (OH). Overall, more children who had in-hospital cardiac arrest were suspected of having an infection (242 [90%], compared with 83 [74%], in the OHCA group; P less than 0.0001).
However, cultures were actually sent for only about one in three patients with suspected infection in either group (34% IHCA and 35% OHCA). Definite infection was found in most patients who were cultured (82% and 86%, respectively).
Patients had “suspected infection” if they received cultures or antimicrobials, and were termed to have “definite infection” only if cultures were positive for infection.
“Infectious complications following out-of-hospital cardiac arrest have been reported in the adult literature, but the pediatric experience post–cardiac arrest is limited to case reports and small case series,” said Dr. Saeed, a pediatric critical care physician at Advocate Hospital, Park Ridge, Ill.
Data from PECARN (Pediatric Emergency Care Applied Research Network) had previously shown that in-hospital pediatric cardiac arrest patients were more likely to receive antimicrobials after return of spontaneous circulation. However, infectious etiologies and the early hospital course of these patients after their cardiac arrest was not known, said Dr. Saeed.
Dr. Saeed and her coinvestigators had hypothesized that “children with out-of-hospital cardiac arrest have a higher incidence of infections after return of spontaneous circulation and worse outcomes compared to children with in-hospital cardiac arrest,” she said. “We were surprised to see how infrequently cultures were sent,” said Dr. Saeed, in discussing the findings that were contrary to the study’s hypothesis.
Dr. Saeed and her colleagues conducted a retrospective analysis of the multi-institutional, deidentified PECARN database, examining 491 pediatric cardiac arrest patients who had required at least 1 minute of cardiopulmonary resuscitation. The patients were aged 24 hours to 18 years; the period of data collection was July 2003-December 2004.
Exclusion criteria included a diagnosis of septic shock, the use of therapeutic hypothermia, or patient death within 24 hours of the cardiac arrest.
Among other findings presented by Dr. Saeed, no association was seen between either suspected or definite infection and mortality. Antibiotic usage was also not associated with mortality. However, definite infection was positively associated with a respiratory etiology for cardiac arrest (odds ratio, 2.6). Post–cardiac arrest central venous pressure monitoring was also associated with definite infection (OR, 2.1).
Support for the study was provided by the Medical College of Wisconsin. The investigators disclosed no relevant conflicts of interest.
On Twitter @karioakes
AT THE CRITICAL CARE CONGRESS
Key clinical point: Postresuscitation infection rates were similar for in- and out-of-hospital pediatric cardiac arrest (IHCA and OHCA).
Major finding: More patients who had in-hospital arrest were suspected of having infection, Definite infection was found in most patients who were cultured (68/83 [82%] IHCA, and 25/29 [86%] OHCA).
Data source: Retrospective review of records of 491 pediatric patients who suffered cardiac arrest and had spontaneous return of circulation, drawn from the PECARN (Pediatric Emergency Care Applied Research Network) database.
Disclosures: Support for the study was provided by the Medical College of Wisconsin. The investigators disclosed no relevant conflicts of interest.
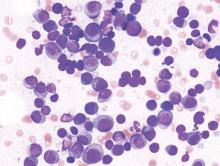
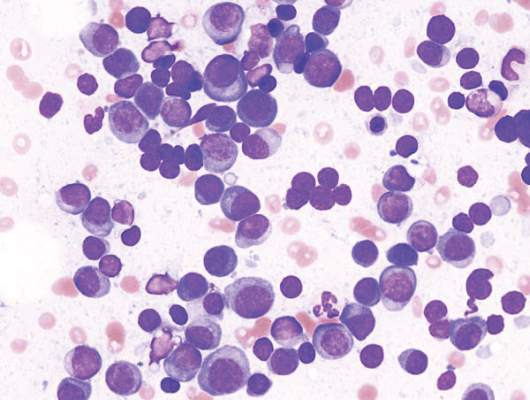
Allele associated with poor outcome in CLL

A form of the CYP3A7 gene is associated with poor outcomes in chronic lymphocytic leukemia (CLL) and other cancers, according to a study published in Cancer Research.
Among patients with CLL, breast cancer, or lung cancer, those with the CYP3A7*1C allele were more likely than those without it to experience disease progression or death.
Researchers believe this may be related to how patients metabolize treatment.
“The CYP3A7 gene encodes an enzyme that breaks down all sorts of naturally occurring substances—such as sex steroids like estrogen and testosterone—as well as a wide range of drugs that are used in the treatment of cancer,” said Olivia Fletcher, PhD, of The Institute of Cancer Research in London, UK.
“The CYP3A7 gene is normally turned on in an embryo and then turned off shortly after a baby is born, but individuals who have 1 or more copies of the CYP3A7*1C form of the gene turn on their CYP3A7 gene in adult life.”
“We found that individuals with breast cancer, lung cancer, or CLL who carry 1 or more copies of the CYP3A7*1C allele tend to have worse outcomes. One possibility is that these patients break down the drugs that they are given to treat their cancer too fast. However, further independent studies that replicate our findings in larger numbers of patients and rule out biases are needed before we could recommend any changes to the treatment that cancer patients with the CYP3A7*1C allele receive.”
To assess the impact of the CYP3A7*1C allele on patient outcomes, Dr Fletcher and her colleagues analyzed DNA samples from 1008 breast cancer patients, 1142 patients with lung cancer, and 356 patients with CLL.
The team looked for the presence of the single nucleotide polymorphism (SNP) rs45446698. Dr Fletcher explained that rs45446698 is 1 of 7 SNPs that cluster together to form the CYP3A7*1C allele.
The researchers found that, among CLL patients, rs45446698 (and, therefore, the CYP3A7*1C allele) was associated with a 62% increased risk of disease progression (P=0.03).
Among breast cancer patients, rs45446698 was associated with a 74% increased risk of breast cancer mortality (P=0.03). And among the lung cancer patients, the SNP was associated with a 43% increased risk of death from any cause (P=0.009).
The researchers also found borderline evidence of a statistical interaction between the CYP3A7*1C allele, treatment of patients with a cytotoxic agent that is a CYP3A substrate, and clinical outcome (P=0.06).
“Even though we did not see a statistically significant difference when stratifying patients by treatment with a CYP3A7 substrate, the fact that we see the same effect in 3 very different cancer types suggests to me that it is more likely to be something to do with treatment than the disease itself,” Dr Fletcher said.
“However, we are looking at ways of replicating these results in additional cohorts of patients and types of cancer, as well as overcoming the limitations of this study.”
Dr Fletcher explained that the main limitation of this study is that the researchers used samples and clinical information collected for other studies. So they did not have the same clinical information for each patient, and the samples were collected at different time points and for patients treated with various drugs.
She also noted that the researchers were not able to determine how quickly the patients broke down their treatments.
This study was supported by Sanofi-Aventis, Breast Cancer Now, Bloodwise, Cancer Research UK, the Medical Research Council, the Cridlan Trust, and the Helen Rollason Cancer Charity. The authors’ institutions received funding from the National Health Service of the United Kingdom. ![]()

A form of the CYP3A7 gene is associated with poor outcomes in chronic lymphocytic leukemia (CLL) and other cancers, according to a study published in Cancer Research.
Among patients with CLL, breast cancer, or lung cancer, those with the CYP3A7*1C allele were more likely than those without it to experience disease progression or death.
Researchers believe this may be related to how patients metabolize treatment.
“The CYP3A7 gene encodes an enzyme that breaks down all sorts of naturally occurring substances—such as sex steroids like estrogen and testosterone—as well as a wide range of drugs that are used in the treatment of cancer,” said Olivia Fletcher, PhD, of The Institute of Cancer Research in London, UK.
“The CYP3A7 gene is normally turned on in an embryo and then turned off shortly after a baby is born, but individuals who have 1 or more copies of the CYP3A7*1C form of the gene turn on their CYP3A7 gene in adult life.”
“We found that individuals with breast cancer, lung cancer, or CLL who carry 1 or more copies of the CYP3A7*1C allele tend to have worse outcomes. One possibility is that these patients break down the drugs that they are given to treat their cancer too fast. However, further independent studies that replicate our findings in larger numbers of patients and rule out biases are needed before we could recommend any changes to the treatment that cancer patients with the CYP3A7*1C allele receive.”
To assess the impact of the CYP3A7*1C allele on patient outcomes, Dr Fletcher and her colleagues analyzed DNA samples from 1008 breast cancer patients, 1142 patients with lung cancer, and 356 patients with CLL.
The team looked for the presence of the single nucleotide polymorphism (SNP) rs45446698. Dr Fletcher explained that rs45446698 is 1 of 7 SNPs that cluster together to form the CYP3A7*1C allele.
The researchers found that, among CLL patients, rs45446698 (and, therefore, the CYP3A7*1C allele) was associated with a 62% increased risk of disease progression (P=0.03).
Among breast cancer patients, rs45446698 was associated with a 74% increased risk of breast cancer mortality (P=0.03). And among the lung cancer patients, the SNP was associated with a 43% increased risk of death from any cause (P=0.009).
The researchers also found borderline evidence of a statistical interaction between the CYP3A7*1C allele, treatment of patients with a cytotoxic agent that is a CYP3A substrate, and clinical outcome (P=0.06).
“Even though we did not see a statistically significant difference when stratifying patients by treatment with a CYP3A7 substrate, the fact that we see the same effect in 3 very different cancer types suggests to me that it is more likely to be something to do with treatment than the disease itself,” Dr Fletcher said.
“However, we are looking at ways of replicating these results in additional cohorts of patients and types of cancer, as well as overcoming the limitations of this study.”
Dr Fletcher explained that the main limitation of this study is that the researchers used samples and clinical information collected for other studies. So they did not have the same clinical information for each patient, and the samples were collected at different time points and for patients treated with various drugs.
She also noted that the researchers were not able to determine how quickly the patients broke down their treatments.
This study was supported by Sanofi-Aventis, Breast Cancer Now, Bloodwise, Cancer Research UK, the Medical Research Council, the Cridlan Trust, and the Helen Rollason Cancer Charity. The authors’ institutions received funding from the National Health Service of the United Kingdom. ![]()

A form of the CYP3A7 gene is associated with poor outcomes in chronic lymphocytic leukemia (CLL) and other cancers, according to a study published in Cancer Research.
Among patients with CLL, breast cancer, or lung cancer, those with the CYP3A7*1C allele were more likely than those without it to experience disease progression or death.
Researchers believe this may be related to how patients metabolize treatment.
“The CYP3A7 gene encodes an enzyme that breaks down all sorts of naturally occurring substances—such as sex steroids like estrogen and testosterone—as well as a wide range of drugs that are used in the treatment of cancer,” said Olivia Fletcher, PhD, of The Institute of Cancer Research in London, UK.
“The CYP3A7 gene is normally turned on in an embryo and then turned off shortly after a baby is born, but individuals who have 1 or more copies of the CYP3A7*1C form of the gene turn on their CYP3A7 gene in adult life.”
“We found that individuals with breast cancer, lung cancer, or CLL who carry 1 or more copies of the CYP3A7*1C allele tend to have worse outcomes. One possibility is that these patients break down the drugs that they are given to treat their cancer too fast. However, further independent studies that replicate our findings in larger numbers of patients and rule out biases are needed before we could recommend any changes to the treatment that cancer patients with the CYP3A7*1C allele receive.”
To assess the impact of the CYP3A7*1C allele on patient outcomes, Dr Fletcher and her colleagues analyzed DNA samples from 1008 breast cancer patients, 1142 patients with lung cancer, and 356 patients with CLL.
The team looked for the presence of the single nucleotide polymorphism (SNP) rs45446698. Dr Fletcher explained that rs45446698 is 1 of 7 SNPs that cluster together to form the CYP3A7*1C allele.
The researchers found that, among CLL patients, rs45446698 (and, therefore, the CYP3A7*1C allele) was associated with a 62% increased risk of disease progression (P=0.03).
Among breast cancer patients, rs45446698 was associated with a 74% increased risk of breast cancer mortality (P=0.03). And among the lung cancer patients, the SNP was associated with a 43% increased risk of death from any cause (P=0.009).
The researchers also found borderline evidence of a statistical interaction between the CYP3A7*1C allele, treatment of patients with a cytotoxic agent that is a CYP3A substrate, and clinical outcome (P=0.06).
“Even though we did not see a statistically significant difference when stratifying patients by treatment with a CYP3A7 substrate, the fact that we see the same effect in 3 very different cancer types suggests to me that it is more likely to be something to do with treatment than the disease itself,” Dr Fletcher said.
“However, we are looking at ways of replicating these results in additional cohorts of patients and types of cancer, as well as overcoming the limitations of this study.”
Dr Fletcher explained that the main limitation of this study is that the researchers used samples and clinical information collected for other studies. So they did not have the same clinical information for each patient, and the samples were collected at different time points and for patients treated with various drugs.
She also noted that the researchers were not able to determine how quickly the patients broke down their treatments.
This study was supported by Sanofi-Aventis, Breast Cancer Now, Bloodwise, Cancer Research UK, the Medical Research Council, the Cridlan Trust, and the Helen Rollason Cancer Charity. The authors’ institutions received funding from the National Health Service of the United Kingdom. ![]()
A trip through the history of gynecologic oncology
The subspecialty of gynecologic oncology was formalized less than 50 years ago with the creation of the Society of Gynecologic Oncology and subspecialty training and board certification. The formation of the Gynecologic Oncology Group (GOG) – and the many clinical trials spearheaded by that group – has further advanced evidence-based treatments, resulting in improved survival outcomes, quality of life, and preventive strategies.
While it is not possible to provide a comprehensive and exhaustive review of all of the advances, we hope to highlight many of the notable advances in this article.Cervical cancer
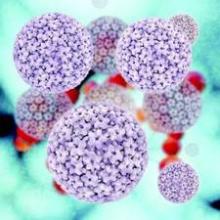
Cervical cancer is the fourth most common cancer in women worldwide with 528,000 new cases in 2012. The majority of cervical cancer cases are caused by infection with human papillomavirus (HPV). While the standard therapies for cervical cancer have been long established (radical hysterectomy for stage I and radiation therapy for locally advanced disease), one of the most significant advances in the past 50 years was the addition of radiation-sensitizing chemotherapy (cisplatin) administered concurrently with radiation therapy.
In randomized trials in both early and advanced cervical cancer, the risk of death was reduced by 30%-50%. These studies changed the paradigm for the treatment of cervical cancer (N Engl J Med. 1999 Apr 15;340[15]:1137-43; N Engl J Med. 1999 Apr 15;340[15]:1144-53; J Clin Oncol. 2000 Apr;18[8]:1606-13).
Future studies evaluating biologic adjuncts or additional chemotherapy are currently underway or awaiting data maturation.
The American Society of Clinical Oncology (ASCO) highlighted the “Top 5 advances in 50 years of Modern Oncology” in 2014, and second on the list was the approval of the HPV vaccine to prevent cervical cancer. Vaccines have been developed that can protect against types 2, 4 or 9 of HPV. In a 2014 study, depending on vaccination coverage, the relative number of cervical cancer cases avoided was 34% in Africa, 27% for America, 26% for Asia, 21% for Europe, and worldwide was estimated at 27% (Vaccine. 2014 Feb 3;32[6]:733-9).
While the benefit from HPV vaccination has been proven, in the United States, only about a third of eligible girls and women have been vaccinated. Efforts should focus on expanding vaccination penetration to eligible girls, boys, women, and men.
Endometrial cancer
Endometrial cancer is the most common gynecologic malignancy in the United States with an estimated 54,870 cases and 10,170 deaths annually. Notable advances in the management of women with endometrial cancer have arisen because of a better understanding that there are two types of endometrial cancer – type I and type II.
The type I endometrial cancers tend to be associated with lower stage of disease at the time of diagnosis and fewer recurrences, while type II endometrial cancer is associated with worse outcomes.
Tailoring the surgical approaches and adjuvant therapy for women with endometrial cancer has led to improved outcomes. The GOG conducted a large prospective randomized trial of laparotomy versus laparoscopic surgical staging for women with clinical early-stage endometrial cancer (LAP2). Laparoscopy was associated with improved perioperative outcomes and was found to be noninferior to laparotomy with regards to survival outcomes (J Clin Oncol. 2012 Mar 1;30[7]:695-700). Therefore, minimally invasive surgery has become widely accepted for the surgical staging of women with endometrial cancer.
Appropriate surgical staging allows for tailoring of postoperative adjuvant therapy. The current evidence suggests that vaginal brachytherapy should be the adjuvant treatment of choice over whole pelvic radiation in women with early-stage endometrial cancer (Lancet. 2010 Mar 6;375[9717]:816-23). Studies are underway to evaluate the role of both adjuvant radiation and chemotherapy in women with early-stage type II endometrial cancer who are felt to be at high risk for recurrent disease, as well as how to improve on the therapeutic options for women with advanced or recurrent disease.
Ovarian cancer
Epithelial ovarian cancer is the most deadly gynecologic malignancy in the United States with 21,290 cases and 14,180 deaths in 2015. The concept of ovarian tumor debulking was first described by Dr. Joe Meigs in 1934, but did not gain traction until the mid-1970s when Dr. C. Thomas Griffiths published his work (Natl Cancer Inst Monogr. 1975 Oct;42:101-4).
While there are no randomized trials proving that surgical cytoreduction improves overall survival, most retrospective studies support this concept. In 2009, Chi et al. showed improved median survival in women with ovarian cancer based on the increased percentage of women who underwent optimal cytoreduction (Gynecol Oncol. 2009 Jul;114[1]:26-31). This has led to modifications of surgical techniques and surgical goals with an effort to maximally cytoreduce all of the visible disease.
While initial surgical debulking is the goal, there are circumstances when a different approach may be indicated. Vergote et al. conducted a prospective randomized trial of 670 women with advanced ovarian cancer. In this study, neoadjuvant chemotherapy followed by interval debulking was not inferior to primary debulking followed by chemotherapy with regards to progression-free survival and overall survival. However, initial surgery was associated with increased surgical complications and perioperative mortality as compared with interval surgery. Therefore, in women who are not felt to be candidates for optimal cytoreduction, neoadjuvant chemotherapy followed by interval surgery may be an appropriate treatment strategy (N Engl J Med. 2010 Sep 2;363[10]:943-53.).
There have been several notable advances and a series of randomized trials – predominately conducted by the GOG – that have resulted in improved overall survival and progression-free interval in women with ovarian cancer. However, none are as significant as the discovery of paclitaxel and platinum-based chemotherapy (cisplatin and carboplatin).
In 1962, samples of the Pacific Yew’s bark were collected and, 2 years later, the extracts from this bark were found to have cytotoxic activity. There were initial difficulties suspending the drug in solution; however, ultimately a formulation in ethanol, cremophor, and saline was found to be effective. In 1984, the National Cancer Institute began clinical trials of paclitaxel and it was found to be highly effective in ovarian cancer. In 1992, it was approved for the treatment of ovarian cancer.
Cisplatin was approved in 1978. Carboplatin entered clinical trials in 1982 and was approved for women with recurrent ovarian cancer in 1989.
There were a series of trials beginning in the late 1980s that established the role of platinum agents and led us to GOG 111. This trial evaluated cisplatin with either cyclophosphamide or paclitaxel. The paclitaxel combination was superior and in 2003 two trials were published that solidified carboplatin and paclitaxel as the cornerstone in the treatment of women with ovarian cancer (J Clin Oncol. 2003 Sep 1;21[17]:3194-200; J Natl Cancer Inst. 2003 Sep 3;95[17]:1320-9).
What has most recently been debated is the route and schedule for both paclitaxel and the platinum agents. In January 2006, the National Cancer Institute released a Clinical Announcement regarding the role of intraperitoneal (IP) chemotherapy for the treatment of women with optimally debulked ovarian cancer. Of the six trials included in the announcement, four trials showed a benefit for progression-free survival and five studies showed an improvement in overall survival. Armstrong et al (GOG 172) showed a 16-month improvement in overall survival with intravenous (IV) paclitaxel, IP cisplatin, and IP paclitaxel. IP chemotherapy has not been universally embraced by physicians and patients in part because of its toxicity, treatment schedule, and the fact that no IP regimen has been compared with the current standard of IV carboplatin and paclitaxel (N Engl J Med. 2006 Jan 5;354[1]:34-43).
While there have been improvements in 5-year survival over time, most women with advanced ovarian cancer will undergo additional chemotherapy in order to achieve subsequent remissions or maintain stability of disease. Other drugs that have Food and Drug Administration approval in the setting of recurrent ovarian cancer include topotecan, liposomal doxorubicin, gemcitabine, bevacizumab, altretamine, carboplatin, cisplatin, cyclophosphamide, and melphalan. Olaparib was recently approved as monotherapy in women with a germline BRCA-mutation who had received three or more prior lines of chemotherapy.
Minimally invasive surgery
Over the last 30 years, minimally invasive surgery (MIS) in gynecologic oncology, particularly for endometrial cancer, has gone from a niche procedure to the standard of care. The introduction of laparoscopy into gynecologic oncology started in the early 1990s. In a series of 59 women undergoing laparoscopy for endometrial cancer, Childers et al. demonstrated feasibility of the technique and low laparotomy conversion rates (Gynecol Oncol. 1993 Oct;51[1]:33-8.). The GOG trial, LAP2, supported the equivalent oncologic outcomes of MIS versus laparotomy for the treatment of endometrial cancer. While many surgeons and centers offered laparoscopic surgery, there were issues with the learning curve that limited its widespread use.
In 2005, the FDA approval of the robotic platform for gynecologic surgery resulted in at least a doubling of the proportion of endometrial cancer patients treated with MIS (Int J Med Robot. 2009 Dec;5[4]:392-7.). In 2012, the Society of Gynecologic Oncology published a consensus statement regarding robotic-assisted surgery in gynecologic oncology (Gynecol Oncol. 2012 Feb;124[2]:180-4.). This review highlights the advantages of the robotics platform with regards to expanding MIS to women with cervical and ovarian cancer; the improvements in outcomes in the obese woman with endometrial cancer; and that the learning curve for robotic surgery is shorter than for traditional laparoscopy. Issues requiring further research include cost analysis as the cost of the new technology decreases, and opportunities for improvement in patient and physician quality of life.
Sentinel node mapping
The rationale for sentinel node mapping is that if one or more sentinel lymph nodes is/are negative for malignancy, then the other regional lymph nodes will also be negative. This would thereby avoid the need for a complete lymph node dissection and its resultant complications, including chronic lymphedema. Much of the work pioneering this strategy has been in breast cancer and melanoma, but data are rapidly emerging for these techniques in gynecologic malignancies.
Candidates for sentinel lymph node biopsy for vulvar cancer include those with a lesion more than 1mm in depth, a tumor less than 4 cm in size, and no obvious metastatic disease on exam or preoperative imaging. Additionally, recommendations have been made regarding case volume in order to achieve limited numbers of false-negative results and to maintain competency. In the study by Van der Zee et al. of 403 patients (623 groins) who underwent sentinel node procedures, the false-negative rate was 0-2%. The overall survival rate was 97% at 3 years (J Clin Oncol. 2008 Feb 20;26[6]:884-9). However, a more recent data from the Gynecologic Oncology Group (GOG 173) showed a slightly higher false-negative rate of 8% (J Clin Oncol. 2012 Nov 1;30[31]:3786-91). Overall survival data are pending from this study.
While sentinel lymph node mapping for endometrial cancer has been feasible for many years and has been well described, the questioned role of completed lymphadenectomy for early-stage endometrial cancer has led to a resurgence of interest in these techniques. While blue dye and radiolabeled tracer methods have historically been the most popular mapping solutions, the advent of endoscopic near-infrared imaging, with its higher sensitivity and good depth penetration, has added options. Indocyanine green fluorescence can be easily detected during robotic surgery and as experience with these techniques increase, successful mapping and sensitivity will increase.
Genetics
While hereditary cancer syndromes have been recognized for many years, detecting the genetic mutations that may increase an individual’s risk of developing a malignancy were not elucidated until the early 1990s. In gynecologic oncology, the most commonly encountered syndromes involve mutations in BRCA1 and BRCA2 and hereditary non–polyposis colorectal cancer, which causes mutations in DNA mismatch-repair genes and increase the risk of endometrial and ovarian cancer.
The SGO recently published a statement on risk assessment for inherited gynecologic cancer predispositions. In this statement “the evaluation for the presence of a hereditary cancer syndrome enables physicians to provide individualized and quantified assessment of cancer risk, as well as options for tailored screening and preventions strategies that may reduce morbidity associated with the development of malignancy” (Gynecol Oncol. 2015 Jan;136[1]:3-7). Beyond risk-reducing salpingo-oophorectomy, therapeutic strategies targeting patients with germline mutations have been developed (PARP inhibitors in BRCA-mutated women with ovarian cancer).
In August 2015, ASCO released an updated policy statement on genetic and genomic testing for cancer susceptibility and highlighted five key areas: germ-line implications of somatic mutation profiling; multigene panel testing for cancer susceptibility; quality assurance in genetic testing; education for oncology professionals; and access to cancer genetic services.
Antiemetics
Rounding out ASCO’s “Top 5 advances in 50 years of Modern Oncology” was the improvement in patients’ quality of life from supportive therapies, in particular antinausea medications.
Several of the agents commonly used in gynecologic oncology rate high (cisplatin) to moderate (carboplatin, cyclophosphamide, doxorubicin, ifosfamide) with regards to emetogenicity. The advent of 5-HT3 receptor antagonists (for example, ondansetron) has significantly improved the quality of life of patients undergoing cytotoxic chemotherapy. In addition to improving quality of life, the decrease in nausea and vomiting can also decrease life-threatening complications such as dehydration and electrolyte imbalance. Both ASCO and the National Comprehensive Cancer Network both have guidelines for the management of nausea and vomiting in patients undergoing chemotherapy.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina, Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology, and a professor in the division of gynecologic oncology at UNC. They reported having no relevant financial disclosures.
The subspecialty of gynecologic oncology was formalized less than 50 years ago with the creation of the Society of Gynecologic Oncology and subspecialty training and board certification. The formation of the Gynecologic Oncology Group (GOG) – and the many clinical trials spearheaded by that group – has further advanced evidence-based treatments, resulting in improved survival outcomes, quality of life, and preventive strategies.
While it is not possible to provide a comprehensive and exhaustive review of all of the advances, we hope to highlight many of the notable advances in this article.Cervical cancer
Cervical cancer is the fourth most common cancer in women worldwide with 528,000 new cases in 2012. The majority of cervical cancer cases are caused by infection with human papillomavirus (HPV). While the standard therapies for cervical cancer have been long established (radical hysterectomy for stage I and radiation therapy for locally advanced disease), one of the most significant advances in the past 50 years was the addition of radiation-sensitizing chemotherapy (cisplatin) administered concurrently with radiation therapy.
In randomized trials in both early and advanced cervical cancer, the risk of death was reduced by 30%-50%. These studies changed the paradigm for the treatment of cervical cancer (N Engl J Med. 1999 Apr 15;340[15]:1137-43; N Engl J Med. 1999 Apr 15;340[15]:1144-53; J Clin Oncol. 2000 Apr;18[8]:1606-13).
Future studies evaluating biologic adjuncts or additional chemotherapy are currently underway or awaiting data maturation.
The American Society of Clinical Oncology (ASCO) highlighted the “Top 5 advances in 50 years of Modern Oncology” in 2014, and second on the list was the approval of the HPV vaccine to prevent cervical cancer. Vaccines have been developed that can protect against types 2, 4 or 9 of HPV. In a 2014 study, depending on vaccination coverage, the relative number of cervical cancer cases avoided was 34% in Africa, 27% for America, 26% for Asia, 21% for Europe, and worldwide was estimated at 27% (Vaccine. 2014 Feb 3;32[6]:733-9).
While the benefit from HPV vaccination has been proven, in the United States, only about a third of eligible girls and women have been vaccinated. Efforts should focus on expanding vaccination penetration to eligible girls, boys, women, and men.
Endometrial cancer
Endometrial cancer is the most common gynecologic malignancy in the United States with an estimated 54,870 cases and 10,170 deaths annually. Notable advances in the management of women with endometrial cancer have arisen because of a better understanding that there are two types of endometrial cancer – type I and type II.
The type I endometrial cancers tend to be associated with lower stage of disease at the time of diagnosis and fewer recurrences, while type II endometrial cancer is associated with worse outcomes.
Tailoring the surgical approaches and adjuvant therapy for women with endometrial cancer has led to improved outcomes. The GOG conducted a large prospective randomized trial of laparotomy versus laparoscopic surgical staging for women with clinical early-stage endometrial cancer (LAP2). Laparoscopy was associated with improved perioperative outcomes and was found to be noninferior to laparotomy with regards to survival outcomes (J Clin Oncol. 2012 Mar 1;30[7]:695-700). Therefore, minimally invasive surgery has become widely accepted for the surgical staging of women with endometrial cancer.
Appropriate surgical staging allows for tailoring of postoperative adjuvant therapy. The current evidence suggests that vaginal brachytherapy should be the adjuvant treatment of choice over whole pelvic radiation in women with early-stage endometrial cancer (Lancet. 2010 Mar 6;375[9717]:816-23). Studies are underway to evaluate the role of both adjuvant radiation and chemotherapy in women with early-stage type II endometrial cancer who are felt to be at high risk for recurrent disease, as well as how to improve on the therapeutic options for women with advanced or recurrent disease.
Ovarian cancer
Epithelial ovarian cancer is the most deadly gynecologic malignancy in the United States with 21,290 cases and 14,180 deaths in 2015. The concept of ovarian tumor debulking was first described by Dr. Joe Meigs in 1934, but did not gain traction until the mid-1970s when Dr. C. Thomas Griffiths published his work (Natl Cancer Inst Monogr. 1975 Oct;42:101-4).
While there are no randomized trials proving that surgical cytoreduction improves overall survival, most retrospective studies support this concept. In 2009, Chi et al. showed improved median survival in women with ovarian cancer based on the increased percentage of women who underwent optimal cytoreduction (Gynecol Oncol. 2009 Jul;114[1]:26-31). This has led to modifications of surgical techniques and surgical goals with an effort to maximally cytoreduce all of the visible disease.
While initial surgical debulking is the goal, there are circumstances when a different approach may be indicated. Vergote et al. conducted a prospective randomized trial of 670 women with advanced ovarian cancer. In this study, neoadjuvant chemotherapy followed by interval debulking was not inferior to primary debulking followed by chemotherapy with regards to progression-free survival and overall survival. However, initial surgery was associated with increased surgical complications and perioperative mortality as compared with interval surgery. Therefore, in women who are not felt to be candidates for optimal cytoreduction, neoadjuvant chemotherapy followed by interval surgery may be an appropriate treatment strategy (N Engl J Med. 2010 Sep 2;363[10]:943-53.).
There have been several notable advances and a series of randomized trials – predominately conducted by the GOG – that have resulted in improved overall survival and progression-free interval in women with ovarian cancer. However, none are as significant as the discovery of paclitaxel and platinum-based chemotherapy (cisplatin and carboplatin).
In 1962, samples of the Pacific Yew’s bark were collected and, 2 years later, the extracts from this bark were found to have cytotoxic activity. There were initial difficulties suspending the drug in solution; however, ultimately a formulation in ethanol, cremophor, and saline was found to be effective. In 1984, the National Cancer Institute began clinical trials of paclitaxel and it was found to be highly effective in ovarian cancer. In 1992, it was approved for the treatment of ovarian cancer.
Cisplatin was approved in 1978. Carboplatin entered clinical trials in 1982 and was approved for women with recurrent ovarian cancer in 1989.
There were a series of trials beginning in the late 1980s that established the role of platinum agents and led us to GOG 111. This trial evaluated cisplatin with either cyclophosphamide or paclitaxel. The paclitaxel combination was superior and in 2003 two trials were published that solidified carboplatin and paclitaxel as the cornerstone in the treatment of women with ovarian cancer (J Clin Oncol. 2003 Sep 1;21[17]:3194-200; J Natl Cancer Inst. 2003 Sep 3;95[17]:1320-9).
What has most recently been debated is the route and schedule for both paclitaxel and the platinum agents. In January 2006, the National Cancer Institute released a Clinical Announcement regarding the role of intraperitoneal (IP) chemotherapy for the treatment of women with optimally debulked ovarian cancer. Of the six trials included in the announcement, four trials showed a benefit for progression-free survival and five studies showed an improvement in overall survival. Armstrong et al (GOG 172) showed a 16-month improvement in overall survival with intravenous (IV) paclitaxel, IP cisplatin, and IP paclitaxel. IP chemotherapy has not been universally embraced by physicians and patients in part because of its toxicity, treatment schedule, and the fact that no IP regimen has been compared with the current standard of IV carboplatin and paclitaxel (N Engl J Med. 2006 Jan 5;354[1]:34-43).
While there have been improvements in 5-year survival over time, most women with advanced ovarian cancer will undergo additional chemotherapy in order to achieve subsequent remissions or maintain stability of disease. Other drugs that have Food and Drug Administration approval in the setting of recurrent ovarian cancer include topotecan, liposomal doxorubicin, gemcitabine, bevacizumab, altretamine, carboplatin, cisplatin, cyclophosphamide, and melphalan. Olaparib was recently approved as monotherapy in women with a germline BRCA-mutation who had received three or more prior lines of chemotherapy.
Minimally invasive surgery
Over the last 30 years, minimally invasive surgery (MIS) in gynecologic oncology, particularly for endometrial cancer, has gone from a niche procedure to the standard of care. The introduction of laparoscopy into gynecologic oncology started in the early 1990s. In a series of 59 women undergoing laparoscopy for endometrial cancer, Childers et al. demonstrated feasibility of the technique and low laparotomy conversion rates (Gynecol Oncol. 1993 Oct;51[1]:33-8.). The GOG trial, LAP2, supported the equivalent oncologic outcomes of MIS versus laparotomy for the treatment of endometrial cancer. While many surgeons and centers offered laparoscopic surgery, there were issues with the learning curve that limited its widespread use.
In 2005, the FDA approval of the robotic platform for gynecologic surgery resulted in at least a doubling of the proportion of endometrial cancer patients treated with MIS (Int J Med Robot. 2009 Dec;5[4]:392-7.). In 2012, the Society of Gynecologic Oncology published a consensus statement regarding robotic-assisted surgery in gynecologic oncology (Gynecol Oncol. 2012 Feb;124[2]:180-4.). This review highlights the advantages of the robotics platform with regards to expanding MIS to women with cervical and ovarian cancer; the improvements in outcomes in the obese woman with endometrial cancer; and that the learning curve for robotic surgery is shorter than for traditional laparoscopy. Issues requiring further research include cost analysis as the cost of the new technology decreases, and opportunities for improvement in patient and physician quality of life.
Sentinel node mapping
The rationale for sentinel node mapping is that if one or more sentinel lymph nodes is/are negative for malignancy, then the other regional lymph nodes will also be negative. This would thereby avoid the need for a complete lymph node dissection and its resultant complications, including chronic lymphedema. Much of the work pioneering this strategy has been in breast cancer and melanoma, but data are rapidly emerging for these techniques in gynecologic malignancies.
Candidates for sentinel lymph node biopsy for vulvar cancer include those with a lesion more than 1mm in depth, a tumor less than 4 cm in size, and no obvious metastatic disease on exam or preoperative imaging. Additionally, recommendations have been made regarding case volume in order to achieve limited numbers of false-negative results and to maintain competency. In the study by Van der Zee et al. of 403 patients (623 groins) who underwent sentinel node procedures, the false-negative rate was 0-2%. The overall survival rate was 97% at 3 years (J Clin Oncol. 2008 Feb 20;26[6]:884-9). However, a more recent data from the Gynecologic Oncology Group (GOG 173) showed a slightly higher false-negative rate of 8% (J Clin Oncol. 2012 Nov 1;30[31]:3786-91). Overall survival data are pending from this study.
While sentinel lymph node mapping for endometrial cancer has been feasible for many years and has been well described, the questioned role of completed lymphadenectomy for early-stage endometrial cancer has led to a resurgence of interest in these techniques. While blue dye and radiolabeled tracer methods have historically been the most popular mapping solutions, the advent of endoscopic near-infrared imaging, with its higher sensitivity and good depth penetration, has added options. Indocyanine green fluorescence can be easily detected during robotic surgery and as experience with these techniques increase, successful mapping and sensitivity will increase.
Genetics
While hereditary cancer syndromes have been recognized for many years, detecting the genetic mutations that may increase an individual’s risk of developing a malignancy were not elucidated until the early 1990s. In gynecologic oncology, the most commonly encountered syndromes involve mutations in BRCA1 and BRCA2 and hereditary non–polyposis colorectal cancer, which causes mutations in DNA mismatch-repair genes and increase the risk of endometrial and ovarian cancer.
The SGO recently published a statement on risk assessment for inherited gynecologic cancer predispositions. In this statement “the evaluation for the presence of a hereditary cancer syndrome enables physicians to provide individualized and quantified assessment of cancer risk, as well as options for tailored screening and preventions strategies that may reduce morbidity associated with the development of malignancy” (Gynecol Oncol. 2015 Jan;136[1]:3-7). Beyond risk-reducing salpingo-oophorectomy, therapeutic strategies targeting patients with germline mutations have been developed (PARP inhibitors in BRCA-mutated women with ovarian cancer).
In August 2015, ASCO released an updated policy statement on genetic and genomic testing for cancer susceptibility and highlighted five key areas: germ-line implications of somatic mutation profiling; multigene panel testing for cancer susceptibility; quality assurance in genetic testing; education for oncology professionals; and access to cancer genetic services.
Antiemetics
Rounding out ASCO’s “Top 5 advances in 50 years of Modern Oncology” was the improvement in patients’ quality of life from supportive therapies, in particular antinausea medications.
Several of the agents commonly used in gynecologic oncology rate high (cisplatin) to moderate (carboplatin, cyclophosphamide, doxorubicin, ifosfamide) with regards to emetogenicity. The advent of 5-HT3 receptor antagonists (for example, ondansetron) has significantly improved the quality of life of patients undergoing cytotoxic chemotherapy. In addition to improving quality of life, the decrease in nausea and vomiting can also decrease life-threatening complications such as dehydration and electrolyte imbalance. Both ASCO and the National Comprehensive Cancer Network both have guidelines for the management of nausea and vomiting in patients undergoing chemotherapy.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina, Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology, and a professor in the division of gynecologic oncology at UNC. They reported having no relevant financial disclosures.
The subspecialty of gynecologic oncology was formalized less than 50 years ago with the creation of the Society of Gynecologic Oncology and subspecialty training and board certification. The formation of the Gynecologic Oncology Group (GOG) – and the many clinical trials spearheaded by that group – has further advanced evidence-based treatments, resulting in improved survival outcomes, quality of life, and preventive strategies.
While it is not possible to provide a comprehensive and exhaustive review of all of the advances, we hope to highlight many of the notable advances in this article.Cervical cancer
Cervical cancer is the fourth most common cancer in women worldwide with 528,000 new cases in 2012. The majority of cervical cancer cases are caused by infection with human papillomavirus (HPV). While the standard therapies for cervical cancer have been long established (radical hysterectomy for stage I and radiation therapy for locally advanced disease), one of the most significant advances in the past 50 years was the addition of radiation-sensitizing chemotherapy (cisplatin) administered concurrently with radiation therapy.
In randomized trials in both early and advanced cervical cancer, the risk of death was reduced by 30%-50%. These studies changed the paradigm for the treatment of cervical cancer (N Engl J Med. 1999 Apr 15;340[15]:1137-43; N Engl J Med. 1999 Apr 15;340[15]:1144-53; J Clin Oncol. 2000 Apr;18[8]:1606-13).
Future studies evaluating biologic adjuncts or additional chemotherapy are currently underway or awaiting data maturation.
The American Society of Clinical Oncology (ASCO) highlighted the “Top 5 advances in 50 years of Modern Oncology” in 2014, and second on the list was the approval of the HPV vaccine to prevent cervical cancer. Vaccines have been developed that can protect against types 2, 4 or 9 of HPV. In a 2014 study, depending on vaccination coverage, the relative number of cervical cancer cases avoided was 34% in Africa, 27% for America, 26% for Asia, 21% for Europe, and worldwide was estimated at 27% (Vaccine. 2014 Feb 3;32[6]:733-9).
While the benefit from HPV vaccination has been proven, in the United States, only about a third of eligible girls and women have been vaccinated. Efforts should focus on expanding vaccination penetration to eligible girls, boys, women, and men.
Endometrial cancer
Endometrial cancer is the most common gynecologic malignancy in the United States with an estimated 54,870 cases and 10,170 deaths annually. Notable advances in the management of women with endometrial cancer have arisen because of a better understanding that there are two types of endometrial cancer – type I and type II.
The type I endometrial cancers tend to be associated with lower stage of disease at the time of diagnosis and fewer recurrences, while type II endometrial cancer is associated with worse outcomes.
Tailoring the surgical approaches and adjuvant therapy for women with endometrial cancer has led to improved outcomes. The GOG conducted a large prospective randomized trial of laparotomy versus laparoscopic surgical staging for women with clinical early-stage endometrial cancer (LAP2). Laparoscopy was associated with improved perioperative outcomes and was found to be noninferior to laparotomy with regards to survival outcomes (J Clin Oncol. 2012 Mar 1;30[7]:695-700). Therefore, minimally invasive surgery has become widely accepted for the surgical staging of women with endometrial cancer.
Appropriate surgical staging allows for tailoring of postoperative adjuvant therapy. The current evidence suggests that vaginal brachytherapy should be the adjuvant treatment of choice over whole pelvic radiation in women with early-stage endometrial cancer (Lancet. 2010 Mar 6;375[9717]:816-23). Studies are underway to evaluate the role of both adjuvant radiation and chemotherapy in women with early-stage type II endometrial cancer who are felt to be at high risk for recurrent disease, as well as how to improve on the therapeutic options for women with advanced or recurrent disease.
Ovarian cancer
Epithelial ovarian cancer is the most deadly gynecologic malignancy in the United States with 21,290 cases and 14,180 deaths in 2015. The concept of ovarian tumor debulking was first described by Dr. Joe Meigs in 1934, but did not gain traction until the mid-1970s when Dr. C. Thomas Griffiths published his work (Natl Cancer Inst Monogr. 1975 Oct;42:101-4).
While there are no randomized trials proving that surgical cytoreduction improves overall survival, most retrospective studies support this concept. In 2009, Chi et al. showed improved median survival in women with ovarian cancer based on the increased percentage of women who underwent optimal cytoreduction (Gynecol Oncol. 2009 Jul;114[1]:26-31). This has led to modifications of surgical techniques and surgical goals with an effort to maximally cytoreduce all of the visible disease.
While initial surgical debulking is the goal, there are circumstances when a different approach may be indicated. Vergote et al. conducted a prospective randomized trial of 670 women with advanced ovarian cancer. In this study, neoadjuvant chemotherapy followed by interval debulking was not inferior to primary debulking followed by chemotherapy with regards to progression-free survival and overall survival. However, initial surgery was associated with increased surgical complications and perioperative mortality as compared with interval surgery. Therefore, in women who are not felt to be candidates for optimal cytoreduction, neoadjuvant chemotherapy followed by interval surgery may be an appropriate treatment strategy (N Engl J Med. 2010 Sep 2;363[10]:943-53.).
There have been several notable advances and a series of randomized trials – predominately conducted by the GOG – that have resulted in improved overall survival and progression-free interval in women with ovarian cancer. However, none are as significant as the discovery of paclitaxel and platinum-based chemotherapy (cisplatin and carboplatin).
In 1962, samples of the Pacific Yew’s bark were collected and, 2 years later, the extracts from this bark were found to have cytotoxic activity. There were initial difficulties suspending the drug in solution; however, ultimately a formulation in ethanol, cremophor, and saline was found to be effective. In 1984, the National Cancer Institute began clinical trials of paclitaxel and it was found to be highly effective in ovarian cancer. In 1992, it was approved for the treatment of ovarian cancer.
Cisplatin was approved in 1978. Carboplatin entered clinical trials in 1982 and was approved for women with recurrent ovarian cancer in 1989.
There were a series of trials beginning in the late 1980s that established the role of platinum agents and led us to GOG 111. This trial evaluated cisplatin with either cyclophosphamide or paclitaxel. The paclitaxel combination was superior and in 2003 two trials were published that solidified carboplatin and paclitaxel as the cornerstone in the treatment of women with ovarian cancer (J Clin Oncol. 2003 Sep 1;21[17]:3194-200; J Natl Cancer Inst. 2003 Sep 3;95[17]:1320-9).
What has most recently been debated is the route and schedule for both paclitaxel and the platinum agents. In January 2006, the National Cancer Institute released a Clinical Announcement regarding the role of intraperitoneal (IP) chemotherapy for the treatment of women with optimally debulked ovarian cancer. Of the six trials included in the announcement, four trials showed a benefit for progression-free survival and five studies showed an improvement in overall survival. Armstrong et al (GOG 172) showed a 16-month improvement in overall survival with intravenous (IV) paclitaxel, IP cisplatin, and IP paclitaxel. IP chemotherapy has not been universally embraced by physicians and patients in part because of its toxicity, treatment schedule, and the fact that no IP regimen has been compared with the current standard of IV carboplatin and paclitaxel (N Engl J Med. 2006 Jan 5;354[1]:34-43).
While there have been improvements in 5-year survival over time, most women with advanced ovarian cancer will undergo additional chemotherapy in order to achieve subsequent remissions or maintain stability of disease. Other drugs that have Food and Drug Administration approval in the setting of recurrent ovarian cancer include topotecan, liposomal doxorubicin, gemcitabine, bevacizumab, altretamine, carboplatin, cisplatin, cyclophosphamide, and melphalan. Olaparib was recently approved as monotherapy in women with a germline BRCA-mutation who had received three or more prior lines of chemotherapy.
Minimally invasive surgery
Over the last 30 years, minimally invasive surgery (MIS) in gynecologic oncology, particularly for endometrial cancer, has gone from a niche procedure to the standard of care. The introduction of laparoscopy into gynecologic oncology started in the early 1990s. In a series of 59 women undergoing laparoscopy for endometrial cancer, Childers et al. demonstrated feasibility of the technique and low laparotomy conversion rates (Gynecol Oncol. 1993 Oct;51[1]:33-8.). The GOG trial, LAP2, supported the equivalent oncologic outcomes of MIS versus laparotomy for the treatment of endometrial cancer. While many surgeons and centers offered laparoscopic surgery, there were issues with the learning curve that limited its widespread use.
In 2005, the FDA approval of the robotic platform for gynecologic surgery resulted in at least a doubling of the proportion of endometrial cancer patients treated with MIS (Int J Med Robot. 2009 Dec;5[4]:392-7.). In 2012, the Society of Gynecologic Oncology published a consensus statement regarding robotic-assisted surgery in gynecologic oncology (Gynecol Oncol. 2012 Feb;124[2]:180-4.). This review highlights the advantages of the robotics platform with regards to expanding MIS to women with cervical and ovarian cancer; the improvements in outcomes in the obese woman with endometrial cancer; and that the learning curve for robotic surgery is shorter than for traditional laparoscopy. Issues requiring further research include cost analysis as the cost of the new technology decreases, and opportunities for improvement in patient and physician quality of life.
Sentinel node mapping
The rationale for sentinel node mapping is that if one or more sentinel lymph nodes is/are negative for malignancy, then the other regional lymph nodes will also be negative. This would thereby avoid the need for a complete lymph node dissection and its resultant complications, including chronic lymphedema. Much of the work pioneering this strategy has been in breast cancer and melanoma, but data are rapidly emerging for these techniques in gynecologic malignancies.
Candidates for sentinel lymph node biopsy for vulvar cancer include those with a lesion more than 1mm in depth, a tumor less than 4 cm in size, and no obvious metastatic disease on exam or preoperative imaging. Additionally, recommendations have been made regarding case volume in order to achieve limited numbers of false-negative results and to maintain competency. In the study by Van der Zee et al. of 403 patients (623 groins) who underwent sentinel node procedures, the false-negative rate was 0-2%. The overall survival rate was 97% at 3 years (J Clin Oncol. 2008 Feb 20;26[6]:884-9). However, a more recent data from the Gynecologic Oncology Group (GOG 173) showed a slightly higher false-negative rate of 8% (J Clin Oncol. 2012 Nov 1;30[31]:3786-91). Overall survival data are pending from this study.
While sentinel lymph node mapping for endometrial cancer has been feasible for many years and has been well described, the questioned role of completed lymphadenectomy for early-stage endometrial cancer has led to a resurgence of interest in these techniques. While blue dye and radiolabeled tracer methods have historically been the most popular mapping solutions, the advent of endoscopic near-infrared imaging, with its higher sensitivity and good depth penetration, has added options. Indocyanine green fluorescence can be easily detected during robotic surgery and as experience with these techniques increase, successful mapping and sensitivity will increase.
Genetics
While hereditary cancer syndromes have been recognized for many years, detecting the genetic mutations that may increase an individual’s risk of developing a malignancy were not elucidated until the early 1990s. In gynecologic oncology, the most commonly encountered syndromes involve mutations in BRCA1 and BRCA2 and hereditary non–polyposis colorectal cancer, which causes mutations in DNA mismatch-repair genes and increase the risk of endometrial and ovarian cancer.
The SGO recently published a statement on risk assessment for inherited gynecologic cancer predispositions. In this statement “the evaluation for the presence of a hereditary cancer syndrome enables physicians to provide individualized and quantified assessment of cancer risk, as well as options for tailored screening and preventions strategies that may reduce morbidity associated with the development of malignancy” (Gynecol Oncol. 2015 Jan;136[1]:3-7). Beyond risk-reducing salpingo-oophorectomy, therapeutic strategies targeting patients with germline mutations have been developed (PARP inhibitors in BRCA-mutated women with ovarian cancer).
In August 2015, ASCO released an updated policy statement on genetic and genomic testing for cancer susceptibility and highlighted five key areas: germ-line implications of somatic mutation profiling; multigene panel testing for cancer susceptibility; quality assurance in genetic testing; education for oncology professionals; and access to cancer genetic services.
Antiemetics
Rounding out ASCO’s “Top 5 advances in 50 years of Modern Oncology” was the improvement in patients’ quality of life from supportive therapies, in particular antinausea medications.
Several of the agents commonly used in gynecologic oncology rate high (cisplatin) to moderate (carboplatin, cyclophosphamide, doxorubicin, ifosfamide) with regards to emetogenicity. The advent of 5-HT3 receptor antagonists (for example, ondansetron) has significantly improved the quality of life of patients undergoing cytotoxic chemotherapy. In addition to improving quality of life, the decrease in nausea and vomiting can also decrease life-threatening complications such as dehydration and electrolyte imbalance. Both ASCO and the National Comprehensive Cancer Network both have guidelines for the management of nausea and vomiting in patients undergoing chemotherapy.
Throughout 2016, Ob.Gyn. News will celebrate its 50th anniversary with exclusive articles looking at the evolution of the specialty, including the history of contraception, changes in gynecologic surgery, and the transformation of the well-woman visit. Look for these articles and more special features in the pages of Ob.Gyn. News and online at obgynnews.com.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina, Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology, and a professor in the division of gynecologic oncology at UNC. They reported having no relevant financial disclosures.
Product can reduce bleeding in hemophilia B

In a phase 3 study, prophylaxis with the recombinant factor IX product nonacog alfa (BeneFIX) reduced bleeding in patients with hemophilia B.
Once-weekly prophylaxis with nonacog alfa significantly reduced the annualized bleeding rate (ABR) when compared to on-demand treatment with the drug.
Nonacog alfa was generally well tolerated, and none of the patients who received it developed inhibitors or experienced thrombotic events.
These results were published in Haemophilia. The study was sponsored by Pfizer, the company developing nonacog alfa.
The study was a sequential-period trial with a 6-month period of on-demand treatment followed by a 12-month period of prophylaxis, with a mean total therapy duration of 550 days.
All 25 male participants had moderately severe or severe hemophilia B (factor IX activity of 2 IU/dL or less), and their mean age was 31.3.
Participants had experienced at least 12 bleeding events, 6 of them in joints, in the previous year. All participants received nonacog alfa, and no one discontinued treatment early.
The median ABR values were 2.0 (range, 0.0-13.8) for the prophylaxis period and 33.6 (range, 6.1-69.0) for the on-demand treatment period. The mean ABR values were 3.6 ± 4.6 and 32.9 ±17.4, respectively (P<0.0001).
Bleeding occurred in 16 patients (64%) during the prophylaxis period and all 25 patients (100%) during the on-demand treatment period.
During the prophylaxis period, 13 patients (52%) experienced spontaneous bleeding events, with a mean ABR of 2.6. Thirteen patients (52%) experienced traumatic bleeding events, with a mean ABR of 1.0.
During the on-demand treatment period, 21 patients (84%) experienced spontaneous bleeding events, with a mean ABR of 23.1. Eighteen patients (72.0%) experienced traumatic bleeding events, with a mean ABR of 9.9.
Most bleeds had “excellent” (53.5%) or “good” (34.9%) responses to the first infusion of nonacog alfa, 10.8% had “moderate” responses, and 0.6% had no response. All bleeds responded to follow-up infusions.
The incidence of treatment-emergent adverse events was 96% in all patients—96% during the prophylaxis period and 64% during the on-demand treatment period.
The most common adverse events, occurring in at least 10% of patients during either regimen, were arthralgia (24%), back pain (12%), headache (36%), joint swelling (20%), local swelling (12%), nasopharyngitis (12%), pharyngitis (20%), pyrexia (20%), toothache (24%), and upper respiratory tract infection (24%). ![]()

In a phase 3 study, prophylaxis with the recombinant factor IX product nonacog alfa (BeneFIX) reduced bleeding in patients with hemophilia B.
Once-weekly prophylaxis with nonacog alfa significantly reduced the annualized bleeding rate (ABR) when compared to on-demand treatment with the drug.
Nonacog alfa was generally well tolerated, and none of the patients who received it developed inhibitors or experienced thrombotic events.
These results were published in Haemophilia. The study was sponsored by Pfizer, the company developing nonacog alfa.
The study was a sequential-period trial with a 6-month period of on-demand treatment followed by a 12-month period of prophylaxis, with a mean total therapy duration of 550 days.
All 25 male participants had moderately severe or severe hemophilia B (factor IX activity of 2 IU/dL or less), and their mean age was 31.3.
Participants had experienced at least 12 bleeding events, 6 of them in joints, in the previous year. All participants received nonacog alfa, and no one discontinued treatment early.
The median ABR values were 2.0 (range, 0.0-13.8) for the prophylaxis period and 33.6 (range, 6.1-69.0) for the on-demand treatment period. The mean ABR values were 3.6 ± 4.6 and 32.9 ±17.4, respectively (P<0.0001).
Bleeding occurred in 16 patients (64%) during the prophylaxis period and all 25 patients (100%) during the on-demand treatment period.
During the prophylaxis period, 13 patients (52%) experienced spontaneous bleeding events, with a mean ABR of 2.6. Thirteen patients (52%) experienced traumatic bleeding events, with a mean ABR of 1.0.
During the on-demand treatment period, 21 patients (84%) experienced spontaneous bleeding events, with a mean ABR of 23.1. Eighteen patients (72.0%) experienced traumatic bleeding events, with a mean ABR of 9.9.
Most bleeds had “excellent” (53.5%) or “good” (34.9%) responses to the first infusion of nonacog alfa, 10.8% had “moderate” responses, and 0.6% had no response. All bleeds responded to follow-up infusions.
The incidence of treatment-emergent adverse events was 96% in all patients—96% during the prophylaxis period and 64% during the on-demand treatment period.
The most common adverse events, occurring in at least 10% of patients during either regimen, were arthralgia (24%), back pain (12%), headache (36%), joint swelling (20%), local swelling (12%), nasopharyngitis (12%), pharyngitis (20%), pyrexia (20%), toothache (24%), and upper respiratory tract infection (24%). ![]()

In a phase 3 study, prophylaxis with the recombinant factor IX product nonacog alfa (BeneFIX) reduced bleeding in patients with hemophilia B.
Once-weekly prophylaxis with nonacog alfa significantly reduced the annualized bleeding rate (ABR) when compared to on-demand treatment with the drug.
Nonacog alfa was generally well tolerated, and none of the patients who received it developed inhibitors or experienced thrombotic events.
These results were published in Haemophilia. The study was sponsored by Pfizer, the company developing nonacog alfa.
The study was a sequential-period trial with a 6-month period of on-demand treatment followed by a 12-month period of prophylaxis, with a mean total therapy duration of 550 days.
All 25 male participants had moderately severe or severe hemophilia B (factor IX activity of 2 IU/dL or less), and their mean age was 31.3.
Participants had experienced at least 12 bleeding events, 6 of them in joints, in the previous year. All participants received nonacog alfa, and no one discontinued treatment early.
The median ABR values were 2.0 (range, 0.0-13.8) for the prophylaxis period and 33.6 (range, 6.1-69.0) for the on-demand treatment period. The mean ABR values were 3.6 ± 4.6 and 32.9 ±17.4, respectively (P<0.0001).
Bleeding occurred in 16 patients (64%) during the prophylaxis period and all 25 patients (100%) during the on-demand treatment period.
During the prophylaxis period, 13 patients (52%) experienced spontaneous bleeding events, with a mean ABR of 2.6. Thirteen patients (52%) experienced traumatic bleeding events, with a mean ABR of 1.0.
During the on-demand treatment period, 21 patients (84%) experienced spontaneous bleeding events, with a mean ABR of 23.1. Eighteen patients (72.0%) experienced traumatic bleeding events, with a mean ABR of 9.9.
Most bleeds had “excellent” (53.5%) or “good” (34.9%) responses to the first infusion of nonacog alfa, 10.8% had “moderate” responses, and 0.6% had no response. All bleeds responded to follow-up infusions.
The incidence of treatment-emergent adverse events was 96% in all patients—96% during the prophylaxis period and 64% during the on-demand treatment period.
The most common adverse events, occurring in at least 10% of patients during either regimen, were arthralgia (24%), back pain (12%), headache (36%), joint swelling (20%), local swelling (12%), nasopharyngitis (12%), pharyngitis (20%), pyrexia (20%), toothache (24%), and upper respiratory tract infection (24%). ![]()
Preventing Patient Falls
Patient falls are a national issue, creating costs for every player in the healthcare system.
“Patient falls negatively impact patient outcomes, hospital costs, and costs for insurance and health systems,” says Jennifer Hefner, PhD, MPH, lead author of “A Falls Wheel in a Large Academic Medical Center: An Intervention to Reduce Patient Falls with Harm,” published in the Journal of Healthcare Quality.
“Patients are negatively impacted by falls in terms of outcomes like loss of confidence and readmission risks,” Dr. Hefner says. “Centers for Medicare & Medicaid Services in 2008 declared they wouldn’t reimburse hospitals for treatment of fall injuries if they occurred during a patient’s stay and they could be prevented by hospitals. In terms of the cost to society, the length of stay is longer if there’s been a fall with harm, and the total charges are 60% higher between those who fell and sustained an injury and those who didn’t.”
In the researchers’ yearlong study, a falls wheel—a tool that categorized each patient on two dimensions: risk of fall and risk of injury from fall—was placed on every patient’s door. During the year, the rate of falls with harm dropped by almost 50%.
The falls wheel was just one element—the main innovative element—of the hospital’s multifaceted approach to falls prevention. The hospital also enhanced staff education and focus on the issue, launched a resource website, and sent a daily email reporting the number of falls.
“The most important thing we learned is that falls are not a nurse-sensitive indicator,” says co-author Susan Moffatt-Bruce, MD, PhD. “Falls are a team-sensitive indicator. It’s only when you realize falls are not just a nurse’s responsibility but everybody’s responsibility can you actually impact them and reduce them.”
Focusing on the problem and developing specific, multifaceted interventions was the key, the authors say.
“I don’t think everybody needs to use a falls wheel, but you need some kind of system or program,” Dr. Moffatt-Bruce says. “Just putting a wristband on someone to say they’re at high risk is great, but so what? What are you going to do about it? What are the actual items you’re asking the team to do to prevent falls?”
Reference
- Hefner JL, McAlearney AS, Mansfield J, Knupp AM, Moffatt-Bruce SD. A falls wheel in a large academic medical center: an intervention to reduce patient falls with harm. J Healthc Qual. 2015;37(6):374-380.
Patient falls are a national issue, creating costs for every player in the healthcare system.
“Patient falls negatively impact patient outcomes, hospital costs, and costs for insurance and health systems,” says Jennifer Hefner, PhD, MPH, lead author of “A Falls Wheel in a Large Academic Medical Center: An Intervention to Reduce Patient Falls with Harm,” published in the Journal of Healthcare Quality.
“Patients are negatively impacted by falls in terms of outcomes like loss of confidence and readmission risks,” Dr. Hefner says. “Centers for Medicare & Medicaid Services in 2008 declared they wouldn’t reimburse hospitals for treatment of fall injuries if they occurred during a patient’s stay and they could be prevented by hospitals. In terms of the cost to society, the length of stay is longer if there’s been a fall with harm, and the total charges are 60% higher between those who fell and sustained an injury and those who didn’t.”
In the researchers’ yearlong study, a falls wheel—a tool that categorized each patient on two dimensions: risk of fall and risk of injury from fall—was placed on every patient’s door. During the year, the rate of falls with harm dropped by almost 50%.
The falls wheel was just one element—the main innovative element—of the hospital’s multifaceted approach to falls prevention. The hospital also enhanced staff education and focus on the issue, launched a resource website, and sent a daily email reporting the number of falls.
“The most important thing we learned is that falls are not a nurse-sensitive indicator,” says co-author Susan Moffatt-Bruce, MD, PhD. “Falls are a team-sensitive indicator. It’s only when you realize falls are not just a nurse’s responsibility but everybody’s responsibility can you actually impact them and reduce them.”
Focusing on the problem and developing specific, multifaceted interventions was the key, the authors say.
“I don’t think everybody needs to use a falls wheel, but you need some kind of system or program,” Dr. Moffatt-Bruce says. “Just putting a wristband on someone to say they’re at high risk is great, but so what? What are you going to do about it? What are the actual items you’re asking the team to do to prevent falls?”
Reference
- Hefner JL, McAlearney AS, Mansfield J, Knupp AM, Moffatt-Bruce SD. A falls wheel in a large academic medical center: an intervention to reduce patient falls with harm. J Healthc Qual. 2015;37(6):374-380.
Patient falls are a national issue, creating costs for every player in the healthcare system.
“Patient falls negatively impact patient outcomes, hospital costs, and costs for insurance and health systems,” says Jennifer Hefner, PhD, MPH, lead author of “A Falls Wheel in a Large Academic Medical Center: An Intervention to Reduce Patient Falls with Harm,” published in the Journal of Healthcare Quality.
“Patients are negatively impacted by falls in terms of outcomes like loss of confidence and readmission risks,” Dr. Hefner says. “Centers for Medicare & Medicaid Services in 2008 declared they wouldn’t reimburse hospitals for treatment of fall injuries if they occurred during a patient’s stay and they could be prevented by hospitals. In terms of the cost to society, the length of stay is longer if there’s been a fall with harm, and the total charges are 60% higher between those who fell and sustained an injury and those who didn’t.”
In the researchers’ yearlong study, a falls wheel—a tool that categorized each patient on two dimensions: risk of fall and risk of injury from fall—was placed on every patient’s door. During the year, the rate of falls with harm dropped by almost 50%.
The falls wheel was just one element—the main innovative element—of the hospital’s multifaceted approach to falls prevention. The hospital also enhanced staff education and focus on the issue, launched a resource website, and sent a daily email reporting the number of falls.
“The most important thing we learned is that falls are not a nurse-sensitive indicator,” says co-author Susan Moffatt-Bruce, MD, PhD. “Falls are a team-sensitive indicator. It’s only when you realize falls are not just a nurse’s responsibility but everybody’s responsibility can you actually impact them and reduce them.”
Focusing on the problem and developing specific, multifaceted interventions was the key, the authors say.
“I don’t think everybody needs to use a falls wheel, but you need some kind of system or program,” Dr. Moffatt-Bruce says. “Just putting a wristband on someone to say they’re at high risk is great, but so what? What are you going to do about it? What are the actual items you’re asking the team to do to prevent falls?”
Reference
- Hefner JL, McAlearney AS, Mansfield J, Knupp AM, Moffatt-Bruce SD. A falls wheel in a large academic medical center: an intervention to reduce patient falls with harm. J Healthc Qual. 2015;37(6):374-380.
Frontline Teams Needed for Rapidly Changing Healthcare
Healthcare is changing rapidly, shifting focus from volume to value, says Jeffrey Glasheen, MD, SFHM, lead author of the abstract “Developing Frontline Teams to Drive Health System Transformation.” To support this transformation, frontline clinical leaders need to be able to build and manage teams and care processes—skills not taught in traditional health professional training.
That’s why the University of Colorado Anschutz Medical Campus launched the Certificate Training Program (CTP). The CTP curriculum focuses on enhancing team performance, leadership development, and process improvement. Participants meet weekly and receive support from a coach, a process-improvement specialist, and a data analyst.
Following the yearlong program, participants showed significant improvements in self-perception of leadership (37% to 75% able to manage change), quality improvement (23% to 78% able to use QI tools), and efficiency (31% to 69% able to reduce operational waste) skills. The participants’ work resulted in measurable improvements for the hospital: multiday reductions in length of stays, more than $200,000 in antibiotic cost avoidance for hospitalized pediatric patients, and improvement in pain and symptom scores for palliative care patients. Overall cost avoidance and revenue benefit exceeded $5 million.\
“We aimed to demonstrate that the work that we all need to accomplish—improving the value equation—can best be accomplished through the creation, development, and resourcing of high-functioning teams,” says Dr. Glasheen, an SHM board member. “Most important, we showed that a comprehensive training and development program aimed at creating, resourcing, and supporting high-functioning clinical leadership teams can facilitate academic medical centers’ efforts to pursue high-value care and achieve measurable improvement.”
Reference
1. Glasheen J, Cumbler E, Kneeland P, et al. Developing frontline teams to drive health system transformation [abstract]. Journal of Hospital Medicine. 2015;10(suppl 2). Available at: http://www.shmabstracts.com/abstract/developing-frontline-teams-to-drive-health-system-transformation/. Accessed January 28, 2016.
Healthcare is changing rapidly, shifting focus from volume to value, says Jeffrey Glasheen, MD, SFHM, lead author of the abstract “Developing Frontline Teams to Drive Health System Transformation.” To support this transformation, frontline clinical leaders need to be able to build and manage teams and care processes—skills not taught in traditional health professional training.
That’s why the University of Colorado Anschutz Medical Campus launched the Certificate Training Program (CTP). The CTP curriculum focuses on enhancing team performance, leadership development, and process improvement. Participants meet weekly and receive support from a coach, a process-improvement specialist, and a data analyst.
Following the yearlong program, participants showed significant improvements in self-perception of leadership (37% to 75% able to manage change), quality improvement (23% to 78% able to use QI tools), and efficiency (31% to 69% able to reduce operational waste) skills. The participants’ work resulted in measurable improvements for the hospital: multiday reductions in length of stays, more than $200,000 in antibiotic cost avoidance for hospitalized pediatric patients, and improvement in pain and symptom scores for palliative care patients. Overall cost avoidance and revenue benefit exceeded $5 million.\
“We aimed to demonstrate that the work that we all need to accomplish—improving the value equation—can best be accomplished through the creation, development, and resourcing of high-functioning teams,” says Dr. Glasheen, an SHM board member. “Most important, we showed that a comprehensive training and development program aimed at creating, resourcing, and supporting high-functioning clinical leadership teams can facilitate academic medical centers’ efforts to pursue high-value care and achieve measurable improvement.”
Reference
1. Glasheen J, Cumbler E, Kneeland P, et al. Developing frontline teams to drive health system transformation [abstract]. Journal of Hospital Medicine. 2015;10(suppl 2). Available at: http://www.shmabstracts.com/abstract/developing-frontline-teams-to-drive-health-system-transformation/. Accessed January 28, 2016.
Healthcare is changing rapidly, shifting focus from volume to value, says Jeffrey Glasheen, MD, SFHM, lead author of the abstract “Developing Frontline Teams to Drive Health System Transformation.” To support this transformation, frontline clinical leaders need to be able to build and manage teams and care processes—skills not taught in traditional health professional training.
That’s why the University of Colorado Anschutz Medical Campus launched the Certificate Training Program (CTP). The CTP curriculum focuses on enhancing team performance, leadership development, and process improvement. Participants meet weekly and receive support from a coach, a process-improvement specialist, and a data analyst.
Following the yearlong program, participants showed significant improvements in self-perception of leadership (37% to 75% able to manage change), quality improvement (23% to 78% able to use QI tools), and efficiency (31% to 69% able to reduce operational waste) skills. The participants’ work resulted in measurable improvements for the hospital: multiday reductions in length of stays, more than $200,000 in antibiotic cost avoidance for hospitalized pediatric patients, and improvement in pain and symptom scores for palliative care patients. Overall cost avoidance and revenue benefit exceeded $5 million.\
“We aimed to demonstrate that the work that we all need to accomplish—improving the value equation—can best be accomplished through the creation, development, and resourcing of high-functioning teams,” says Dr. Glasheen, an SHM board member. “Most important, we showed that a comprehensive training and development program aimed at creating, resourcing, and supporting high-functioning clinical leadership teams can facilitate academic medical centers’ efforts to pursue high-value care and achieve measurable improvement.”
Reference
1. Glasheen J, Cumbler E, Kneeland P, et al. Developing frontline teams to drive health system transformation [abstract]. Journal of Hospital Medicine. 2015;10(suppl 2). Available at: http://www.shmabstracts.com/abstract/developing-frontline-teams-to-drive-health-system-transformation/. Accessed January 28, 2016.
The Cost of Oncology Drugs: A Pharmacy Perspective, Part I
Health care costs are the fastest growing financial segment of the U.S. economy. The Centers for Medicare and Medicaid Services (CMS) estimates health care spending in the U.S. will increase from $3.0 trillion in 2014 to $5.4 trillion by 2024.1 About 19.3% of the U.S. gross domestic product is consumed by health care, which is twice that of any other country in the world. It is often stated that the increasing cost of health care is the most significant financial threat to the U.S. economy. The cost of medications, including those for treating cancer, is the leading cause of increased health care spending.2
The cost of cancer care is the most rapidly increasing component of U.S. health care spending and will increase from $125 billion in 2010 to an estimated $158 billion in 2020, a 27% increase.3 Most experts agree that the current escalation of costs is unsustainable and, if left unchecked, will have a devastating effect on the quality of health care and an increasing negative financial impact on individuals, businesses, and government. However, that discussion is outside the scope of this article.
The affordability of health care has become a major concern for most Americans. During the recent U.S. financial crisis, most of the focus was on the bursting of the housing bubble, plummeting real estate prices, the loss of jobs, and the failure of large financial institutions. However, medical bills were still the leading cause of personal bankruptcies during this period. In 2007, 62% of personal bankruptcies in the U.S. were due to medical costs, and 78% of those bankruptcies involved patients who had health insurance at the beginning of their illness.4
The cost of prescription medications is causing financial difficulties for many patients, especially elderly.
Americans who have multiple chronic medical conditions and live on fixed incomes. A recently released survey by the nonpartisan Kaiser Family Foundation found that the high cost of prescription medications, especially those to treat serious medical conditions such as cancer, is the top health concern of 77% of those Americans polled.5 In this environment, oncology providers face many challenges in their obligation to treat cancer patients in a cost-effective manner.
This article will appear in 2 parts. Part 1 will focus on the emerging discussion of the financial impact of high-cost drugs in the U.S. The drivers of increasing oncology drug costs will also be reviewed. Part 2 will focus on the challenges of high cost medications in the VA and the role the VA Pharmacy Benefits Management (PBM) Service has in evaluating new oncology agents. Clinical guidance tools designed to aid the clinician in the cost-effective use of these agents and results of a nationwide survey of VA oncology pharmacists regarding the use of cost-containment strategies will also be presented.
Background
When discussing the value of targeted therapies, it is useful to define both targeted therapy and value. A targeted therapy is a type of treatment using drugs or other substances to identify and attack cancer cells with less harm to normal cells, according to the National Cancer Institute. 6 Some targeted therapies block the action of certain enzymes, proteins, or other molecules involved in the growth and spread of cancer cells (the molecular target). Other types of targeted therapies help the immune system kill cancer cells or deliver toxic substances directly to cancer cells and kill them.
Targeted therapy may have fewer adverse effects (AEs) than do other types of cancer treatment. Most targeted therapies are either small molecules or monoclonal antibodies. Although imatinib, released in 2001, is the drug that coined the phrase targeted therapy, many drugs released earlier, such as rituximab, can be considered targeted therapies due to their specific, or targeted, mechanism of action.
Value is the price an object will bring in an open and competitive, or free, market as determined by the consumer. To put the definition of value in simpler terms, Warren Buffet has been quoted as saying, “Cost is what you pay, value is what you get.” The oncology market is not entirely free and open. Market price is determined by the manufacturer, entry into the market is regulated by the FDA, purchasers (like the VA and the Centers for Medicare and Medicaid Services) have only limited ability to negotiate prices, and refusing to pay for life-saving or life-prolonging medications often is not an option. As costs for oncology drugs rapidly increase, the cost-benefit ratio, or value, is being increasingly debated. When comparing the clinical benefits these agents provide with cost, the perception of value is highly subjective and can change significantly based on who is paying the bill.
Questioning High-Cost Drugs
Charles Moertel and colleagues published a landmark trial 25 years ago, which reported that treatment with fluorouracil and levamisole for 1 year decreased the death rate of patients with stage C (stage III) colon cancer by 33% following curative surgery.7 Although this trial was clinically significant, there was as much discussion about the high cost of levamisole (Ergamisol) tablets as there
was about its clinical benefit for patients.
In a 1991 letter to the New England Journal of Medicine, Rossof and colleagues questioned the high cost of the levamisole in the treatment regimen.8 Rossof and colleagues were surprised at the drug’s price on approval, about $5 for each tablet, and detailed their concerns on how this price was determined. “On the basis of the cost to a veterinarian, the calculated cost of a hypothetical 50-mg tablet should be in the range of 3 to 6 cents,” they argued. The total cost to the patient of 1 year of treament was nearly $1,200. Their conclusion was that “…the price chosen for the new American consumer is far too high and requires justification by the manufacturer.”
A reply from Janssen Pharmaceutica, the drug’s manufacturer, offered many justifications for the price.8 According to the company, Ergamisol was supplied free to 5,000 research patients prior to FDA approval. It was also given for free to indigent patients. The company also insisted that its pricing compared favorably with its competitors, such as zidovudine, octreotide, newer generation nonsteroidal anti-inflammatories, and antihypertension drugs. “Drug pricing includes additional expensive research, physician education, compassionate use programs, and ensuring high-quality control. Janssen scientists studied immunomodulating effect of Ergamisol for 25 years with no financial return. Drug development is high-risk, so companies must be able to derive a reasonable return on sales.”8
The cost of levamisole was $1,200 per year in 1991, and after adjustment for inflation would cost about $1,988 in 2015, or $166 per month. If these prices caused outrage in 1990, it is easy to see how current prices of well over $10,000 per month for therapies, which often render small clinical benefits, can seem outrageous by comparison.
Public Debate Over Cancer Drug Prices
In the U.S., about 1.66 million patients will be diagnosed with cancer in 2015.9 Although about 30% to 40% of these patients will be effectively cured, only 3% to 4% will be cured using pharmacotherapy (usually traditional chemotherapy) as a sole modality. Therefore, the use of oncology drugs by the vast majority of cancer patients is not to cure but to control or palliate patients with advanced cancer. It is important to note that the cost of most curative regimens is cheap compared with many medications used for advanced disease. Until a few years ago, discussion of the high costs of cancer treatment was rarely made public due to the devastating nature of cancer. However, with the rapid price increases and relatively disappointing clinical benefits of the many new drugs entering the market, the question of value can no longer be ignored. Many authors havepresented commentaries and strategies addressing the issues
surrounding the high cost of cancer drugs.10-15
It was a groundbreaking 2012 letter to the New York Times that brought the issue to public attention.16 Dr. Peter Bach and his colleagues at Memorial Sloan Kettering Cancer Center announced they would not purchase a “phenomenally expensive new cancer drug” for their patients, calling their decision a no-brainer. The drug, ziv-afilbercept (Zaltrap), was twice the price of a similar drug, bevacizumab (Avastin), but was no more efficacious in the treatment of metastatic colorectal cancer. Bach and colleagues went on to say how high drug prices are having a potentially devastating financial impact on patients and that laws protect drug manufacturers to set drug prices at what they feel the market will bear.
Considering the value of cancer treatments is now actively encouraged. To that point, the American Society of Clinical Oncology (ASCO) has recently published a groundbreaking paper entitled “A Conceptual Framework to Assess the Value of Cancer Treatment Options.”17 This tool, which is still in development, will allow oncologists to quantify clinical benefit, toxicity, and out-of-pocket drug costs so patients can compare treatment options with cost as a consideration.
The financial burden put on patients has become the driving force for drug cost reform. In an attempt to control their costs, third-party payers have increased the cost burden for patients by demanding larger copays and other out-of-pocket expenses for medications. It is felt that requiring patients to have more “skin in the game” would force them to make treatment decisions based on cost. Unfortunately, this approach may lead to devastating financial consequences for patients.18-20 The overwhelming emotions patients experience following the diagnosis of cancer make it difficult to focus on the financial impact of treatment recommendations. In addition, many oncologists are not comfortable, or even capable, of discussing costs so patients can make financially informed treatment decisions.14 Unfortunately for patients, “shopping for health care” has very little in common with shopping for a car, television sets, or any other commodity.
The VA Health Care System
The VA is government-sponsored health care and is therefore unique in the U.S. health care environment. The VA might be considered a form of “socialized medicine” that operates under a different economic model than do private health care systems. The treatment of VA patients for common diseases is based on nationally accepted evidence-based guidelines, which allow the best care in a cost-effective manner. For the treatment of cancer, the use of expensive therapies must be made in the context of the finite resources allocated for the treatment of all veterans within the system.
The VA provides lifelong free or minimal cost health care to eligible veterans. For veterans receiving care within the VA, out-of-pocket expenses are considerably less than for non-VA patients. Current medication copays range from free to $9 per month for all medications, regardless of acquisition cost. This is in stark contrast to the private sector, where patients must often pay large, percentage- based copays for oncology medications, which can reach several thousand dollars per month. VA patients are not subject to percentage-based copays; therefore, they are not a financial stakeholder in the treatment
decision process.
Prior to 1995, the VA was a much criticized and poorly performing health care system that had experienced significant budget cuts, forcing many veterans to lose their benefits and seek care outside the VA. Beginning in 1995 with the creation of PBM, a remarkable transformation occurred that modernized and transformed the VA into a system that consistently outperforms the private sector in quality of care, patient safety, and patient satisfaction while maintaining low overall costs. The role of the VA PBM was to develop and maintain the National Drug Formulary, create clinical guidance documents, and manage drug costs and use.
Part 2 of this article will more closely examine the high cost of cancer drugs. It will also discuss the role of VA PBM and other VA efforts to control cost
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Click here for the digital edition.
1. Centers for Medicare and Medicaid. National health expenditure projections 2014-2024 Table 01. Centers for Medicare and Medicaid Website. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountsprojected.html. Updated July 30, 2015. Accessed January 11, 2016.
2. Bach PB. Limits of Medicare’s ability to control rising spending on cancer drugs. N Engl J Med. 2009;360(6):626-633.
3. Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128.
4. Himmelstein DU, Thorne D, Warren E, Woolhandler S. Medical bankruptcy in the United States, 2007: results of a national study. Am J Med. 2009;122(8):741-746.
5. The Henry J. Kaiser Family Foundation. Prescription drug costs remain atop the public’s national health care agenda, well ahead of Affordable Care Act revisions and repeal [press release]. Kaiser Family Foundation Website. http://kff.org/health-costs/press-release/prescription-drug-costs-remain-atop-the-publics-national-health-care-agenda-well-ahead-of-affordable-care-act-revisions-and-repeal. Published October 28, 2015. Accessed January 11, 2016.
6. National Cancer Institute (NCI). NCI dictionary of cancer terms: targeted therapy. National Cancer Institute Website. http://www.cancer.gov/publications/dictionaries/cancer-terms?cdrid=270742. Accessed January 11, 2016.
7. Moertel CG, Fleming TR, Macdonald JS, et al. Levamisole and fluorouracil for adjuvant therapy resected colon carcinoma. N Engl J Med. 1990;322(6):352-358.
8. Rossof AH, Philpot TR, Bunch RS, Letcher J. The high cost of levamisole for humans. N Engl J Med. 1991;324(10):701-702.
9. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5-29.
10. Nadler E, Eckert B, Neumann PJ. Do oncologists believe new cancer drugs offer good value? Oncologist. 2006;11(2):90-95.
11. Hillner BE, Smith TJ. Efficacy does not necessarily translate into cost effectiveness: a case study of the challenges associated with 21st century cancer drug pricing. J Clin Oncol. 2009;27(13):2111-2113.
12. Neumann PJ, Weinstein MC. Legislating against use of cost-effectiveness information. N Engl J Med. 2010;363(16):1495-1497.
13. Elkin EB, Bach PB. Cancer’s next frontier: addressing high and increasing costs. JAMA. 2010;303(11):1086-1087.
14. Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364(21):2060-2065.
15. Siddiqui M, Rajkumar SV. The high cost of cancer drugs and what we can do
about it. Mayo Clin Proc. 2012;87(10):935-943.
16. Bach PB, Saltz LB, Wittes RE. In cancer care, cost matters [op-ed]. New York Times. October 14, 2012.
17. Schnipper LE, Davidson NE, Wollins DS, et al; American Society of Clinical Oncology. American Society of Clinical Oncology statement: a conceptual framework to assess the value of cancer treatment options. J Clin Oncol. 2015;33(23): 2563-2577.
18. Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18(4):381-390.
19. Fenn KM, Evans SB, McCorkle R, et al. Impact of financial burden of cancer on
survivors’ quality of life. J Oncol Prac. 2014;10(5):332-338.
20. Zafar SY, McNeil RB, Thomas CM, Lathan CS, Ayanian JZ, Provenzale D. Population-based assessment of cancer survivors’ financial burden and quality of life: a prospective cohort study. J Oncol Pract. 2015;11(2):145-150.
Note: Page numbers differ between the print issue and digital edition.
Health care costs are the fastest growing financial segment of the U.S. economy. The Centers for Medicare and Medicaid Services (CMS) estimates health care spending in the U.S. will increase from $3.0 trillion in 2014 to $5.4 trillion by 2024.1 About 19.3% of the U.S. gross domestic product is consumed by health care, which is twice that of any other country in the world. It is often stated that the increasing cost of health care is the most significant financial threat to the U.S. economy. The cost of medications, including those for treating cancer, is the leading cause of increased health care spending.2
The cost of cancer care is the most rapidly increasing component of U.S. health care spending and will increase from $125 billion in 2010 to an estimated $158 billion in 2020, a 27% increase.3 Most experts agree that the current escalation of costs is unsustainable and, if left unchecked, will have a devastating effect on the quality of health care and an increasing negative financial impact on individuals, businesses, and government. However, that discussion is outside the scope of this article.
The affordability of health care has become a major concern for most Americans. During the recent U.S. financial crisis, most of the focus was on the bursting of the housing bubble, plummeting real estate prices, the loss of jobs, and the failure of large financial institutions. However, medical bills were still the leading cause of personal bankruptcies during this period. In 2007, 62% of personal bankruptcies in the U.S. were due to medical costs, and 78% of those bankruptcies involved patients who had health insurance at the beginning of their illness.4
The cost of prescription medications is causing financial difficulties for many patients, especially elderly.
Americans who have multiple chronic medical conditions and live on fixed incomes. A recently released survey by the nonpartisan Kaiser Family Foundation found that the high cost of prescription medications, especially those to treat serious medical conditions such as cancer, is the top health concern of 77% of those Americans polled.5 In this environment, oncology providers face many challenges in their obligation to treat cancer patients in a cost-effective manner.
This article will appear in 2 parts. Part 1 will focus on the emerging discussion of the financial impact of high-cost drugs in the U.S. The drivers of increasing oncology drug costs will also be reviewed. Part 2 will focus on the challenges of high cost medications in the VA and the role the VA Pharmacy Benefits Management (PBM) Service has in evaluating new oncology agents. Clinical guidance tools designed to aid the clinician in the cost-effective use of these agents and results of a nationwide survey of VA oncology pharmacists regarding the use of cost-containment strategies will also be presented.
Background
When discussing the value of targeted therapies, it is useful to define both targeted therapy and value. A targeted therapy is a type of treatment using drugs or other substances to identify and attack cancer cells with less harm to normal cells, according to the National Cancer Institute. 6 Some targeted therapies block the action of certain enzymes, proteins, or other molecules involved in the growth and spread of cancer cells (the molecular target). Other types of targeted therapies help the immune system kill cancer cells or deliver toxic substances directly to cancer cells and kill them.
Targeted therapy may have fewer adverse effects (AEs) than do other types of cancer treatment. Most targeted therapies are either small molecules or monoclonal antibodies. Although imatinib, released in 2001, is the drug that coined the phrase targeted therapy, many drugs released earlier, such as rituximab, can be considered targeted therapies due to their specific, or targeted, mechanism of action.
Value is the price an object will bring in an open and competitive, or free, market as determined by the consumer. To put the definition of value in simpler terms, Warren Buffet has been quoted as saying, “Cost is what you pay, value is what you get.” The oncology market is not entirely free and open. Market price is determined by the manufacturer, entry into the market is regulated by the FDA, purchasers (like the VA and the Centers for Medicare and Medicaid Services) have only limited ability to negotiate prices, and refusing to pay for life-saving or life-prolonging medications often is not an option. As costs for oncology drugs rapidly increase, the cost-benefit ratio, or value, is being increasingly debated. When comparing the clinical benefits these agents provide with cost, the perception of value is highly subjective and can change significantly based on who is paying the bill.
Questioning High-Cost Drugs
Charles Moertel and colleagues published a landmark trial 25 years ago, which reported that treatment with fluorouracil and levamisole for 1 year decreased the death rate of patients with stage C (stage III) colon cancer by 33% following curative surgery.7 Although this trial was clinically significant, there was as much discussion about the high cost of levamisole (Ergamisol) tablets as there
was about its clinical benefit for patients.
In a 1991 letter to the New England Journal of Medicine, Rossof and colleagues questioned the high cost of the levamisole in the treatment regimen.8 Rossof and colleagues were surprised at the drug’s price on approval, about $5 for each tablet, and detailed their concerns on how this price was determined. “On the basis of the cost to a veterinarian, the calculated cost of a hypothetical 50-mg tablet should be in the range of 3 to 6 cents,” they argued. The total cost to the patient of 1 year of treament was nearly $1,200. Their conclusion was that “…the price chosen for the new American consumer is far too high and requires justification by the manufacturer.”
A reply from Janssen Pharmaceutica, the drug’s manufacturer, offered many justifications for the price.8 According to the company, Ergamisol was supplied free to 5,000 research patients prior to FDA approval. It was also given for free to indigent patients. The company also insisted that its pricing compared favorably with its competitors, such as zidovudine, octreotide, newer generation nonsteroidal anti-inflammatories, and antihypertension drugs. “Drug pricing includes additional expensive research, physician education, compassionate use programs, and ensuring high-quality control. Janssen scientists studied immunomodulating effect of Ergamisol for 25 years with no financial return. Drug development is high-risk, so companies must be able to derive a reasonable return on sales.”8
The cost of levamisole was $1,200 per year in 1991, and after adjustment for inflation would cost about $1,988 in 2015, or $166 per month. If these prices caused outrage in 1990, it is easy to see how current prices of well over $10,000 per month for therapies, which often render small clinical benefits, can seem outrageous by comparison.
Public Debate Over Cancer Drug Prices
In the U.S., about 1.66 million patients will be diagnosed with cancer in 2015.9 Although about 30% to 40% of these patients will be effectively cured, only 3% to 4% will be cured using pharmacotherapy (usually traditional chemotherapy) as a sole modality. Therefore, the use of oncology drugs by the vast majority of cancer patients is not to cure but to control or palliate patients with advanced cancer. It is important to note that the cost of most curative regimens is cheap compared with many medications used for advanced disease. Until a few years ago, discussion of the high costs of cancer treatment was rarely made public due to the devastating nature of cancer. However, with the rapid price increases and relatively disappointing clinical benefits of the many new drugs entering the market, the question of value can no longer be ignored. Many authors havepresented commentaries and strategies addressing the issues
surrounding the high cost of cancer drugs.10-15
It was a groundbreaking 2012 letter to the New York Times that brought the issue to public attention.16 Dr. Peter Bach and his colleagues at Memorial Sloan Kettering Cancer Center announced they would not purchase a “phenomenally expensive new cancer drug” for their patients, calling their decision a no-brainer. The drug, ziv-afilbercept (Zaltrap), was twice the price of a similar drug, bevacizumab (Avastin), but was no more efficacious in the treatment of metastatic colorectal cancer. Bach and colleagues went on to say how high drug prices are having a potentially devastating financial impact on patients and that laws protect drug manufacturers to set drug prices at what they feel the market will bear.
Considering the value of cancer treatments is now actively encouraged. To that point, the American Society of Clinical Oncology (ASCO) has recently published a groundbreaking paper entitled “A Conceptual Framework to Assess the Value of Cancer Treatment Options.”17 This tool, which is still in development, will allow oncologists to quantify clinical benefit, toxicity, and out-of-pocket drug costs so patients can compare treatment options with cost as a consideration.
The financial burden put on patients has become the driving force for drug cost reform. In an attempt to control their costs, third-party payers have increased the cost burden for patients by demanding larger copays and other out-of-pocket expenses for medications. It is felt that requiring patients to have more “skin in the game” would force them to make treatment decisions based on cost. Unfortunately, this approach may lead to devastating financial consequences for patients.18-20 The overwhelming emotions patients experience following the diagnosis of cancer make it difficult to focus on the financial impact of treatment recommendations. In addition, many oncologists are not comfortable, or even capable, of discussing costs so patients can make financially informed treatment decisions.14 Unfortunately for patients, “shopping for health care” has very little in common with shopping for a car, television sets, or any other commodity.
The VA Health Care System
The VA is government-sponsored health care and is therefore unique in the U.S. health care environment. The VA might be considered a form of “socialized medicine” that operates under a different economic model than do private health care systems. The treatment of VA patients for common diseases is based on nationally accepted evidence-based guidelines, which allow the best care in a cost-effective manner. For the treatment of cancer, the use of expensive therapies must be made in the context of the finite resources allocated for the treatment of all veterans within the system.
The VA provides lifelong free or minimal cost health care to eligible veterans. For veterans receiving care within the VA, out-of-pocket expenses are considerably less than for non-VA patients. Current medication copays range from free to $9 per month for all medications, regardless of acquisition cost. This is in stark contrast to the private sector, where patients must often pay large, percentage- based copays for oncology medications, which can reach several thousand dollars per month. VA patients are not subject to percentage-based copays; therefore, they are not a financial stakeholder in the treatment
decision process.
Prior to 1995, the VA was a much criticized and poorly performing health care system that had experienced significant budget cuts, forcing many veterans to lose their benefits and seek care outside the VA. Beginning in 1995 with the creation of PBM, a remarkable transformation occurred that modernized and transformed the VA into a system that consistently outperforms the private sector in quality of care, patient safety, and patient satisfaction while maintaining low overall costs. The role of the VA PBM was to develop and maintain the National Drug Formulary, create clinical guidance documents, and manage drug costs and use.
Part 2 of this article will more closely examine the high cost of cancer drugs. It will also discuss the role of VA PBM and other VA efforts to control cost
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Click here for the digital edition.
Health care costs are the fastest growing financial segment of the U.S. economy. The Centers for Medicare and Medicaid Services (CMS) estimates health care spending in the U.S. will increase from $3.0 trillion in 2014 to $5.4 trillion by 2024.1 About 19.3% of the U.S. gross domestic product is consumed by health care, which is twice that of any other country in the world. It is often stated that the increasing cost of health care is the most significant financial threat to the U.S. economy. The cost of medications, including those for treating cancer, is the leading cause of increased health care spending.2
The cost of cancer care is the most rapidly increasing component of U.S. health care spending and will increase from $125 billion in 2010 to an estimated $158 billion in 2020, a 27% increase.3 Most experts agree that the current escalation of costs is unsustainable and, if left unchecked, will have a devastating effect on the quality of health care and an increasing negative financial impact on individuals, businesses, and government. However, that discussion is outside the scope of this article.
The affordability of health care has become a major concern for most Americans. During the recent U.S. financial crisis, most of the focus was on the bursting of the housing bubble, plummeting real estate prices, the loss of jobs, and the failure of large financial institutions. However, medical bills were still the leading cause of personal bankruptcies during this period. In 2007, 62% of personal bankruptcies in the U.S. were due to medical costs, and 78% of those bankruptcies involved patients who had health insurance at the beginning of their illness.4
The cost of prescription medications is causing financial difficulties for many patients, especially elderly.
Americans who have multiple chronic medical conditions and live on fixed incomes. A recently released survey by the nonpartisan Kaiser Family Foundation found that the high cost of prescription medications, especially those to treat serious medical conditions such as cancer, is the top health concern of 77% of those Americans polled.5 In this environment, oncology providers face many challenges in their obligation to treat cancer patients in a cost-effective manner.
This article will appear in 2 parts. Part 1 will focus on the emerging discussion of the financial impact of high-cost drugs in the U.S. The drivers of increasing oncology drug costs will also be reviewed. Part 2 will focus on the challenges of high cost medications in the VA and the role the VA Pharmacy Benefits Management (PBM) Service has in evaluating new oncology agents. Clinical guidance tools designed to aid the clinician in the cost-effective use of these agents and results of a nationwide survey of VA oncology pharmacists regarding the use of cost-containment strategies will also be presented.
Background
When discussing the value of targeted therapies, it is useful to define both targeted therapy and value. A targeted therapy is a type of treatment using drugs or other substances to identify and attack cancer cells with less harm to normal cells, according to the National Cancer Institute. 6 Some targeted therapies block the action of certain enzymes, proteins, or other molecules involved in the growth and spread of cancer cells (the molecular target). Other types of targeted therapies help the immune system kill cancer cells or deliver toxic substances directly to cancer cells and kill them.
Targeted therapy may have fewer adverse effects (AEs) than do other types of cancer treatment. Most targeted therapies are either small molecules or monoclonal antibodies. Although imatinib, released in 2001, is the drug that coined the phrase targeted therapy, many drugs released earlier, such as rituximab, can be considered targeted therapies due to their specific, or targeted, mechanism of action.
Value is the price an object will bring in an open and competitive, or free, market as determined by the consumer. To put the definition of value in simpler terms, Warren Buffet has been quoted as saying, “Cost is what you pay, value is what you get.” The oncology market is not entirely free and open. Market price is determined by the manufacturer, entry into the market is regulated by the FDA, purchasers (like the VA and the Centers for Medicare and Medicaid Services) have only limited ability to negotiate prices, and refusing to pay for life-saving or life-prolonging medications often is not an option. As costs for oncology drugs rapidly increase, the cost-benefit ratio, or value, is being increasingly debated. When comparing the clinical benefits these agents provide with cost, the perception of value is highly subjective and can change significantly based on who is paying the bill.
Questioning High-Cost Drugs
Charles Moertel and colleagues published a landmark trial 25 years ago, which reported that treatment with fluorouracil and levamisole for 1 year decreased the death rate of patients with stage C (stage III) colon cancer by 33% following curative surgery.7 Although this trial was clinically significant, there was as much discussion about the high cost of levamisole (Ergamisol) tablets as there
was about its clinical benefit for patients.
In a 1991 letter to the New England Journal of Medicine, Rossof and colleagues questioned the high cost of the levamisole in the treatment regimen.8 Rossof and colleagues were surprised at the drug’s price on approval, about $5 for each tablet, and detailed their concerns on how this price was determined. “On the basis of the cost to a veterinarian, the calculated cost of a hypothetical 50-mg tablet should be in the range of 3 to 6 cents,” they argued. The total cost to the patient of 1 year of treament was nearly $1,200. Their conclusion was that “…the price chosen for the new American consumer is far too high and requires justification by the manufacturer.”
A reply from Janssen Pharmaceutica, the drug’s manufacturer, offered many justifications for the price.8 According to the company, Ergamisol was supplied free to 5,000 research patients prior to FDA approval. It was also given for free to indigent patients. The company also insisted that its pricing compared favorably with its competitors, such as zidovudine, octreotide, newer generation nonsteroidal anti-inflammatories, and antihypertension drugs. “Drug pricing includes additional expensive research, physician education, compassionate use programs, and ensuring high-quality control. Janssen scientists studied immunomodulating effect of Ergamisol for 25 years with no financial return. Drug development is high-risk, so companies must be able to derive a reasonable return on sales.”8
The cost of levamisole was $1,200 per year in 1991, and after adjustment for inflation would cost about $1,988 in 2015, or $166 per month. If these prices caused outrage in 1990, it is easy to see how current prices of well over $10,000 per month for therapies, which often render small clinical benefits, can seem outrageous by comparison.
Public Debate Over Cancer Drug Prices
In the U.S., about 1.66 million patients will be diagnosed with cancer in 2015.9 Although about 30% to 40% of these patients will be effectively cured, only 3% to 4% will be cured using pharmacotherapy (usually traditional chemotherapy) as a sole modality. Therefore, the use of oncology drugs by the vast majority of cancer patients is not to cure but to control or palliate patients with advanced cancer. It is important to note that the cost of most curative regimens is cheap compared with many medications used for advanced disease. Until a few years ago, discussion of the high costs of cancer treatment was rarely made public due to the devastating nature of cancer. However, with the rapid price increases and relatively disappointing clinical benefits of the many new drugs entering the market, the question of value can no longer be ignored. Many authors havepresented commentaries and strategies addressing the issues
surrounding the high cost of cancer drugs.10-15
It was a groundbreaking 2012 letter to the New York Times that brought the issue to public attention.16 Dr. Peter Bach and his colleagues at Memorial Sloan Kettering Cancer Center announced they would not purchase a “phenomenally expensive new cancer drug” for their patients, calling their decision a no-brainer. The drug, ziv-afilbercept (Zaltrap), was twice the price of a similar drug, bevacizumab (Avastin), but was no more efficacious in the treatment of metastatic colorectal cancer. Bach and colleagues went on to say how high drug prices are having a potentially devastating financial impact on patients and that laws protect drug manufacturers to set drug prices at what they feel the market will bear.
Considering the value of cancer treatments is now actively encouraged. To that point, the American Society of Clinical Oncology (ASCO) has recently published a groundbreaking paper entitled “A Conceptual Framework to Assess the Value of Cancer Treatment Options.”17 This tool, which is still in development, will allow oncologists to quantify clinical benefit, toxicity, and out-of-pocket drug costs so patients can compare treatment options with cost as a consideration.
The financial burden put on patients has become the driving force for drug cost reform. In an attempt to control their costs, third-party payers have increased the cost burden for patients by demanding larger copays and other out-of-pocket expenses for medications. It is felt that requiring patients to have more “skin in the game” would force them to make treatment decisions based on cost. Unfortunately, this approach may lead to devastating financial consequences for patients.18-20 The overwhelming emotions patients experience following the diagnosis of cancer make it difficult to focus on the financial impact of treatment recommendations. In addition, many oncologists are not comfortable, or even capable, of discussing costs so patients can make financially informed treatment decisions.14 Unfortunately for patients, “shopping for health care” has very little in common with shopping for a car, television sets, or any other commodity.
The VA Health Care System
The VA is government-sponsored health care and is therefore unique in the U.S. health care environment. The VA might be considered a form of “socialized medicine” that operates under a different economic model than do private health care systems. The treatment of VA patients for common diseases is based on nationally accepted evidence-based guidelines, which allow the best care in a cost-effective manner. For the treatment of cancer, the use of expensive therapies must be made in the context of the finite resources allocated for the treatment of all veterans within the system.
The VA provides lifelong free or minimal cost health care to eligible veterans. For veterans receiving care within the VA, out-of-pocket expenses are considerably less than for non-VA patients. Current medication copays range from free to $9 per month for all medications, regardless of acquisition cost. This is in stark contrast to the private sector, where patients must often pay large, percentage- based copays for oncology medications, which can reach several thousand dollars per month. VA patients are not subject to percentage-based copays; therefore, they are not a financial stakeholder in the treatment
decision process.
Prior to 1995, the VA was a much criticized and poorly performing health care system that had experienced significant budget cuts, forcing many veterans to lose their benefits and seek care outside the VA. Beginning in 1995 with the creation of PBM, a remarkable transformation occurred that modernized and transformed the VA into a system that consistently outperforms the private sector in quality of care, patient safety, and patient satisfaction while maintaining low overall costs. The role of the VA PBM was to develop and maintain the National Drug Formulary, create clinical guidance documents, and manage drug costs and use.
Part 2 of this article will more closely examine the high cost of cancer drugs. It will also discuss the role of VA PBM and other VA efforts to control cost
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Click here for the digital edition.
1. Centers for Medicare and Medicaid. National health expenditure projections 2014-2024 Table 01. Centers for Medicare and Medicaid Website. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountsprojected.html. Updated July 30, 2015. Accessed January 11, 2016.
2. Bach PB. Limits of Medicare’s ability to control rising spending on cancer drugs. N Engl J Med. 2009;360(6):626-633.
3. Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128.
4. Himmelstein DU, Thorne D, Warren E, Woolhandler S. Medical bankruptcy in the United States, 2007: results of a national study. Am J Med. 2009;122(8):741-746.
5. The Henry J. Kaiser Family Foundation. Prescription drug costs remain atop the public’s national health care agenda, well ahead of Affordable Care Act revisions and repeal [press release]. Kaiser Family Foundation Website. http://kff.org/health-costs/press-release/prescription-drug-costs-remain-atop-the-publics-national-health-care-agenda-well-ahead-of-affordable-care-act-revisions-and-repeal. Published October 28, 2015. Accessed January 11, 2016.
6. National Cancer Institute (NCI). NCI dictionary of cancer terms: targeted therapy. National Cancer Institute Website. http://www.cancer.gov/publications/dictionaries/cancer-terms?cdrid=270742. Accessed January 11, 2016.
7. Moertel CG, Fleming TR, Macdonald JS, et al. Levamisole and fluorouracil for adjuvant therapy resected colon carcinoma. N Engl J Med. 1990;322(6):352-358.
8. Rossof AH, Philpot TR, Bunch RS, Letcher J. The high cost of levamisole for humans. N Engl J Med. 1991;324(10):701-702.
9. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5-29.
10. Nadler E, Eckert B, Neumann PJ. Do oncologists believe new cancer drugs offer good value? Oncologist. 2006;11(2):90-95.
11. Hillner BE, Smith TJ. Efficacy does not necessarily translate into cost effectiveness: a case study of the challenges associated with 21st century cancer drug pricing. J Clin Oncol. 2009;27(13):2111-2113.
12. Neumann PJ, Weinstein MC. Legislating against use of cost-effectiveness information. N Engl J Med. 2010;363(16):1495-1497.
13. Elkin EB, Bach PB. Cancer’s next frontier: addressing high and increasing costs. JAMA. 2010;303(11):1086-1087.
14. Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364(21):2060-2065.
15. Siddiqui M, Rajkumar SV. The high cost of cancer drugs and what we can do
about it. Mayo Clin Proc. 2012;87(10):935-943.
16. Bach PB, Saltz LB, Wittes RE. In cancer care, cost matters [op-ed]. New York Times. October 14, 2012.
17. Schnipper LE, Davidson NE, Wollins DS, et al; American Society of Clinical Oncology. American Society of Clinical Oncology statement: a conceptual framework to assess the value of cancer treatment options. J Clin Oncol. 2015;33(23): 2563-2577.
18. Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18(4):381-390.
19. Fenn KM, Evans SB, McCorkle R, et al. Impact of financial burden of cancer on
survivors’ quality of life. J Oncol Prac. 2014;10(5):332-338.
20. Zafar SY, McNeil RB, Thomas CM, Lathan CS, Ayanian JZ, Provenzale D. Population-based assessment of cancer survivors’ financial burden and quality of life: a prospective cohort study. J Oncol Pract. 2015;11(2):145-150.
Note: Page numbers differ between the print issue and digital edition.
1. Centers for Medicare and Medicaid. National health expenditure projections 2014-2024 Table 01. Centers for Medicare and Medicaid Website. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountsprojected.html. Updated July 30, 2015. Accessed January 11, 2016.
2. Bach PB. Limits of Medicare’s ability to control rising spending on cancer drugs. N Engl J Med. 2009;360(6):626-633.
3. Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):117-128.
4. Himmelstein DU, Thorne D, Warren E, Woolhandler S. Medical bankruptcy in the United States, 2007: results of a national study. Am J Med. 2009;122(8):741-746.
5. The Henry J. Kaiser Family Foundation. Prescription drug costs remain atop the public’s national health care agenda, well ahead of Affordable Care Act revisions and repeal [press release]. Kaiser Family Foundation Website. http://kff.org/health-costs/press-release/prescription-drug-costs-remain-atop-the-publics-national-health-care-agenda-well-ahead-of-affordable-care-act-revisions-and-repeal. Published October 28, 2015. Accessed January 11, 2016.
6. National Cancer Institute (NCI). NCI dictionary of cancer terms: targeted therapy. National Cancer Institute Website. http://www.cancer.gov/publications/dictionaries/cancer-terms?cdrid=270742. Accessed January 11, 2016.
7. Moertel CG, Fleming TR, Macdonald JS, et al. Levamisole and fluorouracil for adjuvant therapy resected colon carcinoma. N Engl J Med. 1990;322(6):352-358.
8. Rossof AH, Philpot TR, Bunch RS, Letcher J. The high cost of levamisole for humans. N Engl J Med. 1991;324(10):701-702.
9. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5-29.
10. Nadler E, Eckert B, Neumann PJ. Do oncologists believe new cancer drugs offer good value? Oncologist. 2006;11(2):90-95.
11. Hillner BE, Smith TJ. Efficacy does not necessarily translate into cost effectiveness: a case study of the challenges associated with 21st century cancer drug pricing. J Clin Oncol. 2009;27(13):2111-2113.
12. Neumann PJ, Weinstein MC. Legislating against use of cost-effectiveness information. N Engl J Med. 2010;363(16):1495-1497.
13. Elkin EB, Bach PB. Cancer’s next frontier: addressing high and increasing costs. JAMA. 2010;303(11):1086-1087.
14. Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364(21):2060-2065.
15. Siddiqui M, Rajkumar SV. The high cost of cancer drugs and what we can do
about it. Mayo Clin Proc. 2012;87(10):935-943.
16. Bach PB, Saltz LB, Wittes RE. In cancer care, cost matters [op-ed]. New York Times. October 14, 2012.
17. Schnipper LE, Davidson NE, Wollins DS, et al; American Society of Clinical Oncology. American Society of Clinical Oncology statement: a conceptual framework to assess the value of cancer treatment options. J Clin Oncol. 2015;33(23): 2563-2577.
18. Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18(4):381-390.
19. Fenn KM, Evans SB, McCorkle R, et al. Impact of financial burden of cancer on
survivors’ quality of life. J Oncol Prac. 2014;10(5):332-338.
20. Zafar SY, McNeil RB, Thomas CM, Lathan CS, Ayanian JZ, Provenzale D. Population-based assessment of cancer survivors’ financial burden and quality of life: a prospective cohort study. J Oncol Pract. 2015;11(2):145-150.
Note: Page numbers differ between the print issue and digital edition.
Caring for Patients With Prostate Cancer Who Are BRCA Positive
There are several risk assessment tools and clinical practice guidelines used in the management of localized prostate cancer (PCa). These include the D’Amico classification, the Cancer of the Prostate Risk Assessment (CAPRA) score, the National Comprehensive Cancer Network (NCCN) risk criteria, and the American Urological Association (AUA) clinical practice guidelines.1-4 None of these tools incorporate the BRCA1 and BRCA2 genes in the risk assessment or treatment recommendations for localized PCa.5 The BRCA mutations are most strongly associated with breast and ovarian cancer risk. However, BRCA mutations also increase susceptibility and disease progression in PCa.6 This article illustrates the current knowledge gap in PCa treatment algorithms for the BRCA2-positive patient population.
Traditional risk assessment tools use clinical and pathologic features of PCa, including prostate-specific antigen (PSA) level, Gleason score, tumor stage, and disease burden to measure cancer aggressiveness.1,7,8 These criteria are the basis of the AUA and NCCN guidelines for management of clinically localized PCa, which recognize 3 categories of clinically localized disease (low, intermediate, and high risk).3,4 The NCCN guidelines (version 1.2016) include a fourth category (very low risk or pathologically insignificant PCa) among some stage T1c patients, based on additional criteria, including PSA density. Both the AUA and NCCN recommend active surveillance as a treatment option for men with low-risk PCa. The NCCN recently revised its guidelines to state that intermediate-risk patients with PCa with favorable features (Gleason grade 3 and < 50% of positive biopsy cores) may also be considered for active surveillance.3
BRCA Mutations in Prostate Cancer
Estimates of the relative risk of PCa for men with BRCA1 and BRCA2 mutations have varied, but recent data suggest that it is 3.75-fold for BRCA1 mutations and 8.6-fold for BRCA2 by age 65 years.9-11 Moreover, PCas associated with BRCA1/2 mutations, particularly those in the BRCA2 gene, are often more aggressive and characterized by poor outcomes.12,13 The presence of a BRCA2 mutation is a negative prognostic factor in PCa, independent of tumor grade, stage, and PSA levels.14 Both PCa-specific survival and metastasis-free survival rates following surgical or radiation therapy are significantly lower in the BRCA mutation carriers than in noncarriers.15 Preliminary results of the IMPACT study demonstrate that targeted PCa screening in men with BRCA1 or BRCA2 mutations may result in identification of tumors more likely to require treatment.16
As a result of these increased risks, it is recommended that men with BRCA2 mutations begin PCa screening at age 40 years; however, there are no clear guidelines for clinical management of PCa in this group of patients.5 The lack of guidelines presents a challenge for clinical management of BRCA1/2 mutation carriers with localized PCa who otherwise qualify for active surveillance. A recent editorial by Bratt and Loman specifically
calls for aggressive therapy for patients who are BRCA positive, particularly BRCA2 carriers, suggesting the need to combine early radical local treatment with adjuvant systemic therapy.17 However, data on the effectiveness of aggressive therapies in patients with PCa who carry BRCA2 mutations are sparse.5
Genomic Test for Risk
There is growing recognition of the need to include molecular testing to improve risk assessment in PCa. Using traditional risk assessment tools, about 8% of low-risk patients are found to have progressive disease postoperatively.3 Current AUA guidelines from 2007 are silent on the issue of molecular testing. The 2015 and 2016 NCCN guidelines include molecular testing for better risk stratification of patients with PCa, specifically naming Oncotype DX Prostate Cancer Assay (Genomic Health, Redwood City, CA) and Prolaris (Myriad Genetics, Salt Lake City, UT).3 However, they do not address molecular BRCA mutation testing.
There are several genomic tests aimed at improving PCa risk assessment. These include Oncotype DX PCa Assay; Prolaris; Decipher Prostate Cancer Classifier (GenomeDx Biosciences, San Diego, CA); and ProMark (Metamark Laboratories, Cambridge, MA). These assays are tissuebased and measure gene expression on the RNA or protein level to identify low- or intermediate-risk patients who may be candidates for active surveillance, as well as patients at higher risk who may benefit from closer monitoring or additional therapy after their initial treatment. By 2015, the Centers for Medicare and Medicaid Services had issued positive coverage decisions for several tests.18
The Oncotype DX test is a quantitative real-time polymerase chain reaction assay that measures the expression of 17 genes (12 cancer-related genes and 5 reference genes) representing 4 biologic pathways, including from the androgen signaling, stromal response, cellular organization, and cellular proliferation (Table). Prolaris focuses on a larger number of genes in the cell-cycle progression (CCP) pathway (31 cell-cycle-related genes and 15 reference genes). There is no overlap between the 2 gene sets. Both tests integrate genomic data with clinical and histopathologic characteristics of the tumor to arrive at prognostic information. The Oncotype DX test yields a specific Genomic Prostate Score (GPS; scaled 0-100) that is integrated with the patient’s NCCN clinical risk group to quantify the likelihood of favorable pathology, which is defined as low-grade organ-confined disease.19 The Prolaris test uses the patient’s AUA risk category and then evaluates the patient’s risk based on the cell-cycle progression
gene panel compared with that risk category. It also provides an estimate of disease-specific mortality as validated by 2 independent cohorts that were managed conservatively initially with watchful waiting.
In this article, the authors present a case report of a BRCA2-positive veteran with newly diagnosed lowrisk PCa and a history of breast cancer. In addition to evaluating clinical criteria, Oncotype DX and Prolaris gene expression tests were ordered for this patient. The authors obtained veteran and institutional review board permission. To protect the identity of the patient, minor changes were made to patient demographics.
Case Presentation
A 68-year-old white man with a history of coronary artery disease, dyslipidemia, and hypertension, was recently diagnosed with PCa. He presented to Genomic Medicine Service to discuss how his BRCA2 mutation status might impact management decisions for PCa. Priorto the PCa diagnosis, the veteran had a history of breast and skin cancer. He was diagnosed with invasive ductal carcinoma of the right breast (ER+/PR+/Her2+) at age 62 years and treated with mastectomy and tamoxifen. He had testing at that time, which revealed a BRCA2 mutation: 3773delTT. Squamous cell carcinoma was detected on his right leg and removed at age 64 years. Basal cell carcinoma was removed from his left forehead first at age 65 years, and then residual basal cell carcinoma was removed from the forehead 2 months later.
The veteran was diagnosed with PCa at age 67 years at a non-VA clinic. The urology consult note reported a sudden increase of his PSA level to 5.9. A prostate needle biopsy was performed. The Gleason score was 3 + 3 = 6 in 2 of 12, with < 1% PCa involvement and focal highgrade prostatic intraepithelial neoplasia. The patient was asymptomatic, and his cancer was identified by needle biopsy due to elevated PSA. His clinical stage was T1c. According to AUA and NCCN guidelines, the patient was categorized as low risk, defined as Gleason Score ≤ 6, PSA < 10 ng/mL, and clinical stage up to T2a.3,4 Additionally, the veteran met 3 criteria for the NCCN very low-risk category (stage T1c, < 3 positive biopsy cores and ≤ 50% cancer in any core). However, because he was initially diagnosed at a non-VA clinic, his PSA density (the remaining criterion) was not available to the VA urologist. Therefore, the low-risk category was assumed for molecular test interpretation.
The non-VA urologist recommended active surveillance. The VA urologist agreed that active surveillance was an appropriate treatment recommendation at this time. However, the veteran and his family members remained concerned that his PCa might be more aggressive due to his BRCA2 mutation, and they worried that active surveillance would result in a worse outcome. Their concern was exacerbated by the veteran’s comorbidities, which could have potential implications on the timing of surgical options. The patient expressed these concerns to his VA primary care physician, who then referred him to the VA Genomic Medicine Services.
Genetic Consult
The genetic counselor scheduled a telegenetics consult and conducted an assessment of the veteran, which included a review of his medical history, mutation status, and relevant family history. The family history was consistent with hereditary breast/ovarian cancer. However, the primary reason the veteran underwent genetic testing was the diagnosis of breast cancer in a male. The genetic counselor provided the patient with information relevant to his mutation carrier status, including that men with BRCA2 mutations are at increased risk of developing more aggressive PCa, have higher rates of lymph node involvement, and greater mortality compared with men without BRCA2 mutations. The veteran was informed that there were no published guidelines that suggest PCa in BRCA2 carriers should be treated differently from sporadic PCa.
Tumor Testing Strategy
Although the veteran was comfortable with active surveillance at the time of consultation, he was concerned that, given his comorbidities, it would be better to pursue surgery sooner. The veteran asked the genetic counselor for more information about his prognosis given his BRCA2 status. The genetic counselor discussed possible use of tumor gene expression profiling and informed him about 2 active studies within the VA that are evaluating the clinical utility of gene expression tests for PCa risk stratification (Oncotype DX at Genomic Health and Prolaris at Myriad Genetic Laboratories). The veteran expressed an interest in having his biopsy tissue tested by both assays. Tumor biopsy tissue was obtained and sent to both Genomic Health and Myriad Genetics for testing. Neither test incorporated the veteran’s other health conditions or his BRCA mutation status into risk stratification results or the patient report.
Test Results
The Oncotype DX GPS result for this NCCN low-risk patient was 31 (Figure 1). This score corresponds to a likelihood of favorable pathology at radical prostatectomy of 71% (95% confidence interval [CI]: 63%-78%). Favorable pathology is defined as freedom from highgrade (Gleason score > 4+3) and/or nonorgan-confined (pT3) disease. This GPS result was consistent with the range of risk expected for NCCN low-risk patients based on the validation cohorts for the assay. The estimate of likelihood of favorable pathology would be modified if the PSA density result were available and if it placed the patient in the NCCN very low-risk category.
The Prolaris report demonstrated a score of 0.4 (Figure 2). This puts the veteran in the 94th percentile of contemporary U.S. men who are AUA low risk. The CCP score makes his cancer more aggressive than most AUA low-risk men, and the projected 10-year disease-specific mortality is 3%. In conjunction with the patient’s BRCA2 status, he may benefit from definitive intervention. If active surveillance is chosen, careful and regular follow-up for disease progression is mandated.
Interpretation of Genomic Testing in PCa
For both tests, the results are derived from 2-tiered calculations. For Oncotype DX, the gene expression measurement yields the GPS, which is then integrated with the patient’s clinical and pathologic information to yield the likelihood of favorable pathology. Although the Oncotype DX GPS is an independent measure of disease aggressiveness, on the patient report, the GPS is combined with the NCCN clinical risk group to provide a likelihood of favorable pathology. Therefore, 2 patients with the same GPS but different levels of clinical risk will have different likelihoods of favorable pathology.
The Prolaris test provides the Prolaris CCP score as well as the percentile group of patients with a lower score within the same risk category. Also, the Prolaris test yields a numerical 10-year PCa-specific mortality risk. The Prolaris score has been shown to impact therapeutic decisions in patients with newly diagnosed PCa.20
Recently, Myriad defined a threshold for active surveillance combining the CCP and CAPRA scores.21 Myriad validated this cutoff in 2 cohorts of men initially managed conservatively. Although the model predicts up to 3.2% disease-specific mortality, there were no observed deaths during a decade of follow-up. Myriad reports that by using this cutoff in contemporary patients tested commercially with Prolaris, a health care system could increase the percentage of men who would fit current criteria for active surveillance from 36% to 60% with no increase in risk of disease-specific mortality.
The results of these 2 tests are presented in 2 different formats and provide risk estimates for different clinical endpoints, making it challenging for a clinician to directly compare them. Moreover, each genomic test is based on a different set of genes and uses different clinical risk criteria (AUA vs NCCN), which may result in different test output. Finally, and most relevant to the case described here, there is no evidence-based consensus on how to interpret these test results in the context of a BRCA2 mutation.
Based on the published literature reporting that BRCA2 mutations are associated with more aggressive disease, one prediction would be that test scores from genomic assays such as Oncotype DX and Prolaris would tend to be higher in BRCA2 carriers than those of the overall population of PCa patients. This has, in fact, been reported for the Oncotype DX Breast Cancer Assay recurrence score in women who are BRCA carriers.22 Further research is required to ascertain whether this will be true for Oncotype DX GPS and Prolaris CCP score in PCa. The mechanism of action that predisposes BRCA2 mutation carriers to develop a more aggressive variant of PCa may not be detectable by the genomic markers included in the Oncotype DX PCa and Prolaris tests. The degree to which a mutated BRCA2 gene may interact with the genes comprising these assays and the reported tumor aggressiveness is not yet understood but deserving of future study.
Treatment Recommendation and Patient’s Decision
After considering his test results, the veteran chose active surveillance. The sum of clinical, pathologic, and molecular factors, combined with the patient’s preference, determined his course of treatment. Because prostatectomy was not performed, it has not been positively determined whether or not the patient harbors aggressive disease. As the molecular test results place the patient at the high end of the low-risk group, the VA urologist recommended close monitoring and suggested a follow-up biopsy with magnetic resonance-ultrasound fusion guidance.
Conclusions
Molecular testing found that the patient’s PCa stage and grade are consistent with NCCN low risk (Oncotype DX) and that the disease-specific mortality risk is slightly higher than predicted by clinical features alone (Prolaris). Previous studies have shown that molecular testing in men with PCa provides information that influences clinical decisions. The findings reported here suggest that molecular testing may also be a vital component in the medical management of patients with complex clinical phenotypes and common chronic conditions. Additional studies are necessary to evaluate whether the finding reported here is typical of individuals diagnosed with PCa who also have a BRCA2 mutation.
For any new genomic test to be clinically useful, its results must have clinical actionability. In this case, the clinical decision point was whether to recommend immediate definitive treatment or active surveillance. For this patient, the Oncotype DX assay provided a likelihood of favorable surgical pathology of 71% (or conversely a 29% risk of unfavorable pathology); by comparison, the Prolaris CCP score provided a 3% estimate of PCaspecific
mortality at 10 years. A key question is: How do clinicians perceive the actionability of risk estimates for these different endpoints?
The current case illustrates the challenges that rapidly developing genomic medicine pose for physicians trying to optimize care and communicate results to patients in a meaningful and consistent manner. For example, some urologists find the different 2-tiered calculations confusing. When laboratories use proprietary scalesbased on internally develop algorithms, differing interpretations are to be expected. The risk-assessment tests described here use different algorithms, and their interpretations are based on clinical categories from different sets of guidelines. This underscores the need for better standardization of PCa care.23
Oncology and urology professional associations should collaborate to develop consistent guidelines for use of new technologies in the management of PCa. A positive example is the evolution of testing recommendations in lung cancer, which initially varied between professional entities. In April 2013, the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology jointly issued a unified clinical practice guideline on molecular testing in patients with lung cancer.24 In October 2014, the American Society of Clinical Oncology issued an endorsement of the CAP/IASLC/AMP guideline.25 As the number of complex tests being used in PCa increases, it will be important for professional associations such as AUA and NCCN to collaborate in evaluating utility of innovations to make consistent recommendations
Author disclosures
Myriad Genetics and Genomic Health provided funding for research on their tests within the VA. Dr. Dash and Dr. Lynch are principal investigators of the Genomic Health study. Dr. Lowrance is the principal investigator of the Myriad Genetics study.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Click here to continue reading.
1. D’Amico AV, Whittington R, Malkowicz SB, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280(11):969-974.
2. Cooperberg MR, Pasta DJ, Elkin EP, et al. The University of California, San Francisco Cancer of the Prostate Risk Assessment score: a straightforward and reliable preoperative predictor of disease recurrence after radical prostatectomy. J Urol. 2005;173(6):1938-1942.
3. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: prostate cancer. National Comprehensive Cancer Network Website. http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. Updated November 10, 2015. Accessed December 8, 2016.
4. Thompson I, Thrasher JB, Aus G, et al; AUA Prostate Cancer Clinical Guideline Update Panel. Guideline for the management of clinically localized prostate cancer: 2007 update. J Urol. 2007;177(6):2106-2131.
5. Alanee SR, Glogowski EA, Schrader KA, Eastham JA, Offit K. Clinical features and management of BRCA1 and BRCA2-associated prostate cancer. Front Biosci (Elite Ed). 2014;6:15-30.
6. Castro E, Eeles R. The role of BRCA1 and BRCA2 in prostate cancer. Asian J Androl. 2012;14(3):409-414.
7. Boorjian SA, Karnes RJ, Rangel LJ, Bergstralh EJ, Blute ML. Mayo Clinic validation of the D’amico risk group classification for predicting survival following radical prostatectomy. J Urol. 2008;179(4):1354-1360.
8. Lowrance WT, Scardino PT. Predictive models for newly diagnosed prostate cancer patients. Rev Urol. 2009;11(3):117-126.
9. Levy-Lahad E, Friedman E. Cancer risks among BRCA1 and BRCA2 mutation carriers. Br J Cancer. 2007;96(1):11-15.
10. Leongamornlert D, Mahmud N, Tymrakiewicz M, et al; UKGPCS Collaborators. Germline BRCA1 mutations increase prostate cancer risk. Br J Cancer. 2012;106(10):1697-1701.
11. Kote-Jarai Z, Leongamornlert D, Saunders E, et al; UKGPCS Collaborators. BRCA2 is a moderate penetrance gene contributing to young-onset prostate cancer: implications for genetic testing in prostate cancer patients. Br J Cancer. 2011;105(8):1230-1234.
12. Tryggvadóttir L, Vidarsdóttir L, Thorgeirsson T, et al. Prostate cancer progression and survival in BRCA2 mutation carriers. J Natl Cancer Inst. 2007;99(12):929-935.
13. Gallagher DJ, Gaudet MM, Pal P, et al. Germline BRCA mutations denote a clinicopathologic subset of prostate cancer. Clin Cancer Res. 2010;16(7):2115-2121.
14. Castro E, Goh C, Olmos D, et al. Germline BRCA mutations are associated with higher risk of nodal involvement, distant metastasis, and poor survival outcomes in prostate cancer. J Clin Oncol. 2013;31(14):1748-1757.
15. Castro E, Goh C, Leongamornlert D, et al. Effect of BRCA mutations on metastatic relapse and cause-specific survival after radical treatment for localised prostate cancer. Eur Urol. 2015;68(2):186-193.
16. Bancroft EK, Page EC, Castro E, et al; IMPACT Collaborators. Targeted prostate cancer screening in BRCA1 and BRCA2 mutation carriers: results from the initial screening round of the IMPACT study. Eur Urol. 2014;66(3):489-499.
17. Bratt O, Loman N. Clinical management of prostate cancer in men with BRCA mutations. Eur Urol. 2015;68(2):194-195.
18. Centers for Medicare & Medicaid Services (CMS). MCD archive site. CMS Website. http://localcoverage.cms.gov/mcd_archive/overview.aspx. Accessed January 8, 2016.
19. Klein EA, Cooperberg MR, Magi-Galluzzi C, et al. A 17-gene assay to predict prostate cancer aggressiveness in the context of Gleason grade heterogeneity, tumor multifocality, and biopsy undersampling. Eur Urol. 2014;66(3):550-560.
20. Shore ND, Kella N, Moran B, et al. Impact of the cell cycle progression test on physician and patient treatment selection for localized prostate cancer. J Urol. 2015;pii:S0022-5347(15)04811-9 [epub ahead of print].
21. Stone S, Cuzick JM, Fisher G, et al. Validation of an active surveillance threshold for the CCP score in conservatively managed men with localized prostate cancer. J Clin Oncol. 2015;33(suppl 15):e16040.
22. Lewin R, Rizel S, Hendler D, et al. Oncotype-DX recurrence score distribution among breast cancer patients harboring a germline mutation in the BRCA1/2 genes. J Clin Oncol. 2015;33(suppl; abstr 564).
23. Dahm P, Yeung LL, Chang SS, Cookson MS. A critical review of clinical practice guidelines for the management of clinically localized prostate cancer. J Urol. 2008;180(2):451-459.
24. Lindeman NI, Cagle PT, Beasley MB, et al. Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J Thorac Oncol. 2013;8(7):823-859.
25. Leighl NB, Rekhtman N, Biermann WA, et al. Molecular testing for selection of patients with lung cancer for epidermal growth factor receptor and anaplastic lymphoma kinase tyrosine kinase inhibitors: American Society of Clinical Oncology endorsement of the College of American Pathologists/International Association for the Study of Lung Cancer/Association for Molecular Pathology guideline. J Clin Oncol. 2014;32(32):3673-3679.
Note: Page numbers differ between the print issue and digital edition.
There are several risk assessment tools and clinical practice guidelines used in the management of localized prostate cancer (PCa). These include the D’Amico classification, the Cancer of the Prostate Risk Assessment (CAPRA) score, the National Comprehensive Cancer Network (NCCN) risk criteria, and the American Urological Association (AUA) clinical practice guidelines.1-4 None of these tools incorporate the BRCA1 and BRCA2 genes in the risk assessment or treatment recommendations for localized PCa.5 The BRCA mutations are most strongly associated with breast and ovarian cancer risk. However, BRCA mutations also increase susceptibility and disease progression in PCa.6 This article illustrates the current knowledge gap in PCa treatment algorithms for the BRCA2-positive patient population.
Traditional risk assessment tools use clinical and pathologic features of PCa, including prostate-specific antigen (PSA) level, Gleason score, tumor stage, and disease burden to measure cancer aggressiveness.1,7,8 These criteria are the basis of the AUA and NCCN guidelines for management of clinically localized PCa, which recognize 3 categories of clinically localized disease (low, intermediate, and high risk).3,4 The NCCN guidelines (version 1.2016) include a fourth category (very low risk or pathologically insignificant PCa) among some stage T1c patients, based on additional criteria, including PSA density. Both the AUA and NCCN recommend active surveillance as a treatment option for men with low-risk PCa. The NCCN recently revised its guidelines to state that intermediate-risk patients with PCa with favorable features (Gleason grade 3 and < 50% of positive biopsy cores) may also be considered for active surveillance.3
BRCA Mutations in Prostate Cancer
Estimates of the relative risk of PCa for men with BRCA1 and BRCA2 mutations have varied, but recent data suggest that it is 3.75-fold for BRCA1 mutations and 8.6-fold for BRCA2 by age 65 years.9-11 Moreover, PCas associated with BRCA1/2 mutations, particularly those in the BRCA2 gene, are often more aggressive and characterized by poor outcomes.12,13 The presence of a BRCA2 mutation is a negative prognostic factor in PCa, independent of tumor grade, stage, and PSA levels.14 Both PCa-specific survival and metastasis-free survival rates following surgical or radiation therapy are significantly lower in the BRCA mutation carriers than in noncarriers.15 Preliminary results of the IMPACT study demonstrate that targeted PCa screening in men with BRCA1 or BRCA2 mutations may result in identification of tumors more likely to require treatment.16
As a result of these increased risks, it is recommended that men with BRCA2 mutations begin PCa screening at age 40 years; however, there are no clear guidelines for clinical management of PCa in this group of patients.5 The lack of guidelines presents a challenge for clinical management of BRCA1/2 mutation carriers with localized PCa who otherwise qualify for active surveillance. A recent editorial by Bratt and Loman specifically
calls for aggressive therapy for patients who are BRCA positive, particularly BRCA2 carriers, suggesting the need to combine early radical local treatment with adjuvant systemic therapy.17 However, data on the effectiveness of aggressive therapies in patients with PCa who carry BRCA2 mutations are sparse.5
Genomic Test for Risk
There is growing recognition of the need to include molecular testing to improve risk assessment in PCa. Using traditional risk assessment tools, about 8% of low-risk patients are found to have progressive disease postoperatively.3 Current AUA guidelines from 2007 are silent on the issue of molecular testing. The 2015 and 2016 NCCN guidelines include molecular testing for better risk stratification of patients with PCa, specifically naming Oncotype DX Prostate Cancer Assay (Genomic Health, Redwood City, CA) and Prolaris (Myriad Genetics, Salt Lake City, UT).3 However, they do not address molecular BRCA mutation testing.
There are several genomic tests aimed at improving PCa risk assessment. These include Oncotype DX PCa Assay; Prolaris; Decipher Prostate Cancer Classifier (GenomeDx Biosciences, San Diego, CA); and ProMark (Metamark Laboratories, Cambridge, MA). These assays are tissuebased and measure gene expression on the RNA or protein level to identify low- or intermediate-risk patients who may be candidates for active surveillance, as well as patients at higher risk who may benefit from closer monitoring or additional therapy after their initial treatment. By 2015, the Centers for Medicare and Medicaid Services had issued positive coverage decisions for several tests.18
The Oncotype DX test is a quantitative real-time polymerase chain reaction assay that measures the expression of 17 genes (12 cancer-related genes and 5 reference genes) representing 4 biologic pathways, including from the androgen signaling, stromal response, cellular organization, and cellular proliferation (Table). Prolaris focuses on a larger number of genes in the cell-cycle progression (CCP) pathway (31 cell-cycle-related genes and 15 reference genes). There is no overlap between the 2 gene sets. Both tests integrate genomic data with clinical and histopathologic characteristics of the tumor to arrive at prognostic information. The Oncotype DX test yields a specific Genomic Prostate Score (GPS; scaled 0-100) that is integrated with the patient’s NCCN clinical risk group to quantify the likelihood of favorable pathology, which is defined as low-grade organ-confined disease.19 The Prolaris test uses the patient’s AUA risk category and then evaluates the patient’s risk based on the cell-cycle progression
gene panel compared with that risk category. It also provides an estimate of disease-specific mortality as validated by 2 independent cohorts that were managed conservatively initially with watchful waiting.
In this article, the authors present a case report of a BRCA2-positive veteran with newly diagnosed lowrisk PCa and a history of breast cancer. In addition to evaluating clinical criteria, Oncotype DX and Prolaris gene expression tests were ordered for this patient. The authors obtained veteran and institutional review board permission. To protect the identity of the patient, minor changes were made to patient demographics.
Case Presentation
A 68-year-old white man with a history of coronary artery disease, dyslipidemia, and hypertension, was recently diagnosed with PCa. He presented to Genomic Medicine Service to discuss how his BRCA2 mutation status might impact management decisions for PCa. Priorto the PCa diagnosis, the veteran had a history of breast and skin cancer. He was diagnosed with invasive ductal carcinoma of the right breast (ER+/PR+/Her2+) at age 62 years and treated with mastectomy and tamoxifen. He had testing at that time, which revealed a BRCA2 mutation: 3773delTT. Squamous cell carcinoma was detected on his right leg and removed at age 64 years. Basal cell carcinoma was removed from his left forehead first at age 65 years, and then residual basal cell carcinoma was removed from the forehead 2 months later.
The veteran was diagnosed with PCa at age 67 years at a non-VA clinic. The urology consult note reported a sudden increase of his PSA level to 5.9. A prostate needle biopsy was performed. The Gleason score was 3 + 3 = 6 in 2 of 12, with < 1% PCa involvement and focal highgrade prostatic intraepithelial neoplasia. The patient was asymptomatic, and his cancer was identified by needle biopsy due to elevated PSA. His clinical stage was T1c. According to AUA and NCCN guidelines, the patient was categorized as low risk, defined as Gleason Score ≤ 6, PSA < 10 ng/mL, and clinical stage up to T2a.3,4 Additionally, the veteran met 3 criteria for the NCCN very low-risk category (stage T1c, < 3 positive biopsy cores and ≤ 50% cancer in any core). However, because he was initially diagnosed at a non-VA clinic, his PSA density (the remaining criterion) was not available to the VA urologist. Therefore, the low-risk category was assumed for molecular test interpretation.
The non-VA urologist recommended active surveillance. The VA urologist agreed that active surveillance was an appropriate treatment recommendation at this time. However, the veteran and his family members remained concerned that his PCa might be more aggressive due to his BRCA2 mutation, and they worried that active surveillance would result in a worse outcome. Their concern was exacerbated by the veteran’s comorbidities, which could have potential implications on the timing of surgical options. The patient expressed these concerns to his VA primary care physician, who then referred him to the VA Genomic Medicine Services.
Genetic Consult
The genetic counselor scheduled a telegenetics consult and conducted an assessment of the veteran, which included a review of his medical history, mutation status, and relevant family history. The family history was consistent with hereditary breast/ovarian cancer. However, the primary reason the veteran underwent genetic testing was the diagnosis of breast cancer in a male. The genetic counselor provided the patient with information relevant to his mutation carrier status, including that men with BRCA2 mutations are at increased risk of developing more aggressive PCa, have higher rates of lymph node involvement, and greater mortality compared with men without BRCA2 mutations. The veteran was informed that there were no published guidelines that suggest PCa in BRCA2 carriers should be treated differently from sporadic PCa.
Tumor Testing Strategy
Although the veteran was comfortable with active surveillance at the time of consultation, he was concerned that, given his comorbidities, it would be better to pursue surgery sooner. The veteran asked the genetic counselor for more information about his prognosis given his BRCA2 status. The genetic counselor discussed possible use of tumor gene expression profiling and informed him about 2 active studies within the VA that are evaluating the clinical utility of gene expression tests for PCa risk stratification (Oncotype DX at Genomic Health and Prolaris at Myriad Genetic Laboratories). The veteran expressed an interest in having his biopsy tissue tested by both assays. Tumor biopsy tissue was obtained and sent to both Genomic Health and Myriad Genetics for testing. Neither test incorporated the veteran’s other health conditions or his BRCA mutation status into risk stratification results or the patient report.
Test Results
The Oncotype DX GPS result for this NCCN low-risk patient was 31 (Figure 1). This score corresponds to a likelihood of favorable pathology at radical prostatectomy of 71% (95% confidence interval [CI]: 63%-78%). Favorable pathology is defined as freedom from highgrade (Gleason score > 4+3) and/or nonorgan-confined (pT3) disease. This GPS result was consistent with the range of risk expected for NCCN low-risk patients based on the validation cohorts for the assay. The estimate of likelihood of favorable pathology would be modified if the PSA density result were available and if it placed the patient in the NCCN very low-risk category.
The Prolaris report demonstrated a score of 0.4 (Figure 2). This puts the veteran in the 94th percentile of contemporary U.S. men who are AUA low risk. The CCP score makes his cancer more aggressive than most AUA low-risk men, and the projected 10-year disease-specific mortality is 3%. In conjunction with the patient’s BRCA2 status, he may benefit from definitive intervention. If active surveillance is chosen, careful and regular follow-up for disease progression is mandated.
Interpretation of Genomic Testing in PCa
For both tests, the results are derived from 2-tiered calculations. For Oncotype DX, the gene expression measurement yields the GPS, which is then integrated with the patient’s clinical and pathologic information to yield the likelihood of favorable pathology. Although the Oncotype DX GPS is an independent measure of disease aggressiveness, on the patient report, the GPS is combined with the NCCN clinical risk group to provide a likelihood of favorable pathology. Therefore, 2 patients with the same GPS but different levels of clinical risk will have different likelihoods of favorable pathology.
The Prolaris test provides the Prolaris CCP score as well as the percentile group of patients with a lower score within the same risk category. Also, the Prolaris test yields a numerical 10-year PCa-specific mortality risk. The Prolaris score has been shown to impact therapeutic decisions in patients with newly diagnosed PCa.20
Recently, Myriad defined a threshold for active surveillance combining the CCP and CAPRA scores.21 Myriad validated this cutoff in 2 cohorts of men initially managed conservatively. Although the model predicts up to 3.2% disease-specific mortality, there were no observed deaths during a decade of follow-up. Myriad reports that by using this cutoff in contemporary patients tested commercially with Prolaris, a health care system could increase the percentage of men who would fit current criteria for active surveillance from 36% to 60% with no increase in risk of disease-specific mortality.
The results of these 2 tests are presented in 2 different formats and provide risk estimates for different clinical endpoints, making it challenging for a clinician to directly compare them. Moreover, each genomic test is based on a different set of genes and uses different clinical risk criteria (AUA vs NCCN), which may result in different test output. Finally, and most relevant to the case described here, there is no evidence-based consensus on how to interpret these test results in the context of a BRCA2 mutation.
Based on the published literature reporting that BRCA2 mutations are associated with more aggressive disease, one prediction would be that test scores from genomic assays such as Oncotype DX and Prolaris would tend to be higher in BRCA2 carriers than those of the overall population of PCa patients. This has, in fact, been reported for the Oncotype DX Breast Cancer Assay recurrence score in women who are BRCA carriers.22 Further research is required to ascertain whether this will be true for Oncotype DX GPS and Prolaris CCP score in PCa. The mechanism of action that predisposes BRCA2 mutation carriers to develop a more aggressive variant of PCa may not be detectable by the genomic markers included in the Oncotype DX PCa and Prolaris tests. The degree to which a mutated BRCA2 gene may interact with the genes comprising these assays and the reported tumor aggressiveness is not yet understood but deserving of future study.
Treatment Recommendation and Patient’s Decision
After considering his test results, the veteran chose active surveillance. The sum of clinical, pathologic, and molecular factors, combined with the patient’s preference, determined his course of treatment. Because prostatectomy was not performed, it has not been positively determined whether or not the patient harbors aggressive disease. As the molecular test results place the patient at the high end of the low-risk group, the VA urologist recommended close monitoring and suggested a follow-up biopsy with magnetic resonance-ultrasound fusion guidance.
Conclusions
Molecular testing found that the patient’s PCa stage and grade are consistent with NCCN low risk (Oncotype DX) and that the disease-specific mortality risk is slightly higher than predicted by clinical features alone (Prolaris). Previous studies have shown that molecular testing in men with PCa provides information that influences clinical decisions. The findings reported here suggest that molecular testing may also be a vital component in the medical management of patients with complex clinical phenotypes and common chronic conditions. Additional studies are necessary to evaluate whether the finding reported here is typical of individuals diagnosed with PCa who also have a BRCA2 mutation.
For any new genomic test to be clinically useful, its results must have clinical actionability. In this case, the clinical decision point was whether to recommend immediate definitive treatment or active surveillance. For this patient, the Oncotype DX assay provided a likelihood of favorable surgical pathology of 71% (or conversely a 29% risk of unfavorable pathology); by comparison, the Prolaris CCP score provided a 3% estimate of PCaspecific
mortality at 10 years. A key question is: How do clinicians perceive the actionability of risk estimates for these different endpoints?
The current case illustrates the challenges that rapidly developing genomic medicine pose for physicians trying to optimize care and communicate results to patients in a meaningful and consistent manner. For example, some urologists find the different 2-tiered calculations confusing. When laboratories use proprietary scalesbased on internally develop algorithms, differing interpretations are to be expected. The risk-assessment tests described here use different algorithms, and their interpretations are based on clinical categories from different sets of guidelines. This underscores the need for better standardization of PCa care.23
Oncology and urology professional associations should collaborate to develop consistent guidelines for use of new technologies in the management of PCa. A positive example is the evolution of testing recommendations in lung cancer, which initially varied between professional entities. In April 2013, the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology jointly issued a unified clinical practice guideline on molecular testing in patients with lung cancer.24 In October 2014, the American Society of Clinical Oncology issued an endorsement of the CAP/IASLC/AMP guideline.25 As the number of complex tests being used in PCa increases, it will be important for professional associations such as AUA and NCCN to collaborate in evaluating utility of innovations to make consistent recommendations
Author disclosures
Myriad Genetics and Genomic Health provided funding for research on their tests within the VA. Dr. Dash and Dr. Lynch are principal investigators of the Genomic Health study. Dr. Lowrance is the principal investigator of the Myriad Genetics study.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Click here to continue reading.
There are several risk assessment tools and clinical practice guidelines used in the management of localized prostate cancer (PCa). These include the D’Amico classification, the Cancer of the Prostate Risk Assessment (CAPRA) score, the National Comprehensive Cancer Network (NCCN) risk criteria, and the American Urological Association (AUA) clinical practice guidelines.1-4 None of these tools incorporate the BRCA1 and BRCA2 genes in the risk assessment or treatment recommendations for localized PCa.5 The BRCA mutations are most strongly associated with breast and ovarian cancer risk. However, BRCA mutations also increase susceptibility and disease progression in PCa.6 This article illustrates the current knowledge gap in PCa treatment algorithms for the BRCA2-positive patient population.
Traditional risk assessment tools use clinical and pathologic features of PCa, including prostate-specific antigen (PSA) level, Gleason score, tumor stage, and disease burden to measure cancer aggressiveness.1,7,8 These criteria are the basis of the AUA and NCCN guidelines for management of clinically localized PCa, which recognize 3 categories of clinically localized disease (low, intermediate, and high risk).3,4 The NCCN guidelines (version 1.2016) include a fourth category (very low risk or pathologically insignificant PCa) among some stage T1c patients, based on additional criteria, including PSA density. Both the AUA and NCCN recommend active surveillance as a treatment option for men with low-risk PCa. The NCCN recently revised its guidelines to state that intermediate-risk patients with PCa with favorable features (Gleason grade 3 and < 50% of positive biopsy cores) may also be considered for active surveillance.3
BRCA Mutations in Prostate Cancer
Estimates of the relative risk of PCa for men with BRCA1 and BRCA2 mutations have varied, but recent data suggest that it is 3.75-fold for BRCA1 mutations and 8.6-fold for BRCA2 by age 65 years.9-11 Moreover, PCas associated with BRCA1/2 mutations, particularly those in the BRCA2 gene, are often more aggressive and characterized by poor outcomes.12,13 The presence of a BRCA2 mutation is a negative prognostic factor in PCa, independent of tumor grade, stage, and PSA levels.14 Both PCa-specific survival and metastasis-free survival rates following surgical or radiation therapy are significantly lower in the BRCA mutation carriers than in noncarriers.15 Preliminary results of the IMPACT study demonstrate that targeted PCa screening in men with BRCA1 or BRCA2 mutations may result in identification of tumors more likely to require treatment.16
As a result of these increased risks, it is recommended that men with BRCA2 mutations begin PCa screening at age 40 years; however, there are no clear guidelines for clinical management of PCa in this group of patients.5 The lack of guidelines presents a challenge for clinical management of BRCA1/2 mutation carriers with localized PCa who otherwise qualify for active surveillance. A recent editorial by Bratt and Loman specifically
calls for aggressive therapy for patients who are BRCA positive, particularly BRCA2 carriers, suggesting the need to combine early radical local treatment with adjuvant systemic therapy.17 However, data on the effectiveness of aggressive therapies in patients with PCa who carry BRCA2 mutations are sparse.5
Genomic Test for Risk
There is growing recognition of the need to include molecular testing to improve risk assessment in PCa. Using traditional risk assessment tools, about 8% of low-risk patients are found to have progressive disease postoperatively.3 Current AUA guidelines from 2007 are silent on the issue of molecular testing. The 2015 and 2016 NCCN guidelines include molecular testing for better risk stratification of patients with PCa, specifically naming Oncotype DX Prostate Cancer Assay (Genomic Health, Redwood City, CA) and Prolaris (Myriad Genetics, Salt Lake City, UT).3 However, they do not address molecular BRCA mutation testing.
There are several genomic tests aimed at improving PCa risk assessment. These include Oncotype DX PCa Assay; Prolaris; Decipher Prostate Cancer Classifier (GenomeDx Biosciences, San Diego, CA); and ProMark (Metamark Laboratories, Cambridge, MA). These assays are tissuebased and measure gene expression on the RNA or protein level to identify low- or intermediate-risk patients who may be candidates for active surveillance, as well as patients at higher risk who may benefit from closer monitoring or additional therapy after their initial treatment. By 2015, the Centers for Medicare and Medicaid Services had issued positive coverage decisions for several tests.18
The Oncotype DX test is a quantitative real-time polymerase chain reaction assay that measures the expression of 17 genes (12 cancer-related genes and 5 reference genes) representing 4 biologic pathways, including from the androgen signaling, stromal response, cellular organization, and cellular proliferation (Table). Prolaris focuses on a larger number of genes in the cell-cycle progression (CCP) pathway (31 cell-cycle-related genes and 15 reference genes). There is no overlap between the 2 gene sets. Both tests integrate genomic data with clinical and histopathologic characteristics of the tumor to arrive at prognostic information. The Oncotype DX test yields a specific Genomic Prostate Score (GPS; scaled 0-100) that is integrated with the patient’s NCCN clinical risk group to quantify the likelihood of favorable pathology, which is defined as low-grade organ-confined disease.19 The Prolaris test uses the patient’s AUA risk category and then evaluates the patient’s risk based on the cell-cycle progression
gene panel compared with that risk category. It also provides an estimate of disease-specific mortality as validated by 2 independent cohorts that were managed conservatively initially with watchful waiting.
In this article, the authors present a case report of a BRCA2-positive veteran with newly diagnosed lowrisk PCa and a history of breast cancer. In addition to evaluating clinical criteria, Oncotype DX and Prolaris gene expression tests were ordered for this patient. The authors obtained veteran and institutional review board permission. To protect the identity of the patient, minor changes were made to patient demographics.
Case Presentation
A 68-year-old white man with a history of coronary artery disease, dyslipidemia, and hypertension, was recently diagnosed with PCa. He presented to Genomic Medicine Service to discuss how his BRCA2 mutation status might impact management decisions for PCa. Priorto the PCa diagnosis, the veteran had a history of breast and skin cancer. He was diagnosed with invasive ductal carcinoma of the right breast (ER+/PR+/Her2+) at age 62 years and treated with mastectomy and tamoxifen. He had testing at that time, which revealed a BRCA2 mutation: 3773delTT. Squamous cell carcinoma was detected on his right leg and removed at age 64 years. Basal cell carcinoma was removed from his left forehead first at age 65 years, and then residual basal cell carcinoma was removed from the forehead 2 months later.
The veteran was diagnosed with PCa at age 67 years at a non-VA clinic. The urology consult note reported a sudden increase of his PSA level to 5.9. A prostate needle biopsy was performed. The Gleason score was 3 + 3 = 6 in 2 of 12, with < 1% PCa involvement and focal highgrade prostatic intraepithelial neoplasia. The patient was asymptomatic, and his cancer was identified by needle biopsy due to elevated PSA. His clinical stage was T1c. According to AUA and NCCN guidelines, the patient was categorized as low risk, defined as Gleason Score ≤ 6, PSA < 10 ng/mL, and clinical stage up to T2a.3,4 Additionally, the veteran met 3 criteria for the NCCN very low-risk category (stage T1c, < 3 positive biopsy cores and ≤ 50% cancer in any core). However, because he was initially diagnosed at a non-VA clinic, his PSA density (the remaining criterion) was not available to the VA urologist. Therefore, the low-risk category was assumed for molecular test interpretation.
The non-VA urologist recommended active surveillance. The VA urologist agreed that active surveillance was an appropriate treatment recommendation at this time. However, the veteran and his family members remained concerned that his PCa might be more aggressive due to his BRCA2 mutation, and they worried that active surveillance would result in a worse outcome. Their concern was exacerbated by the veteran’s comorbidities, which could have potential implications on the timing of surgical options. The patient expressed these concerns to his VA primary care physician, who then referred him to the VA Genomic Medicine Services.
Genetic Consult
The genetic counselor scheduled a telegenetics consult and conducted an assessment of the veteran, which included a review of his medical history, mutation status, and relevant family history. The family history was consistent with hereditary breast/ovarian cancer. However, the primary reason the veteran underwent genetic testing was the diagnosis of breast cancer in a male. The genetic counselor provided the patient with information relevant to his mutation carrier status, including that men with BRCA2 mutations are at increased risk of developing more aggressive PCa, have higher rates of lymph node involvement, and greater mortality compared with men without BRCA2 mutations. The veteran was informed that there were no published guidelines that suggest PCa in BRCA2 carriers should be treated differently from sporadic PCa.
Tumor Testing Strategy
Although the veteran was comfortable with active surveillance at the time of consultation, he was concerned that, given his comorbidities, it would be better to pursue surgery sooner. The veteran asked the genetic counselor for more information about his prognosis given his BRCA2 status. The genetic counselor discussed possible use of tumor gene expression profiling and informed him about 2 active studies within the VA that are evaluating the clinical utility of gene expression tests for PCa risk stratification (Oncotype DX at Genomic Health and Prolaris at Myriad Genetic Laboratories). The veteran expressed an interest in having his biopsy tissue tested by both assays. Tumor biopsy tissue was obtained and sent to both Genomic Health and Myriad Genetics for testing. Neither test incorporated the veteran’s other health conditions or his BRCA mutation status into risk stratification results or the patient report.
Test Results
The Oncotype DX GPS result for this NCCN low-risk patient was 31 (Figure 1). This score corresponds to a likelihood of favorable pathology at radical prostatectomy of 71% (95% confidence interval [CI]: 63%-78%). Favorable pathology is defined as freedom from highgrade (Gleason score > 4+3) and/or nonorgan-confined (pT3) disease. This GPS result was consistent with the range of risk expected for NCCN low-risk patients based on the validation cohorts for the assay. The estimate of likelihood of favorable pathology would be modified if the PSA density result were available and if it placed the patient in the NCCN very low-risk category.
The Prolaris report demonstrated a score of 0.4 (Figure 2). This puts the veteran in the 94th percentile of contemporary U.S. men who are AUA low risk. The CCP score makes his cancer more aggressive than most AUA low-risk men, and the projected 10-year disease-specific mortality is 3%. In conjunction with the patient’s BRCA2 status, he may benefit from definitive intervention. If active surveillance is chosen, careful and regular follow-up for disease progression is mandated.
Interpretation of Genomic Testing in PCa
For both tests, the results are derived from 2-tiered calculations. For Oncotype DX, the gene expression measurement yields the GPS, which is then integrated with the patient’s clinical and pathologic information to yield the likelihood of favorable pathology. Although the Oncotype DX GPS is an independent measure of disease aggressiveness, on the patient report, the GPS is combined with the NCCN clinical risk group to provide a likelihood of favorable pathology. Therefore, 2 patients with the same GPS but different levels of clinical risk will have different likelihoods of favorable pathology.
The Prolaris test provides the Prolaris CCP score as well as the percentile group of patients with a lower score within the same risk category. Also, the Prolaris test yields a numerical 10-year PCa-specific mortality risk. The Prolaris score has been shown to impact therapeutic decisions in patients with newly diagnosed PCa.20
Recently, Myriad defined a threshold for active surveillance combining the CCP and CAPRA scores.21 Myriad validated this cutoff in 2 cohorts of men initially managed conservatively. Although the model predicts up to 3.2% disease-specific mortality, there were no observed deaths during a decade of follow-up. Myriad reports that by using this cutoff in contemporary patients tested commercially with Prolaris, a health care system could increase the percentage of men who would fit current criteria for active surveillance from 36% to 60% with no increase in risk of disease-specific mortality.
The results of these 2 tests are presented in 2 different formats and provide risk estimates for different clinical endpoints, making it challenging for a clinician to directly compare them. Moreover, each genomic test is based on a different set of genes and uses different clinical risk criteria (AUA vs NCCN), which may result in different test output. Finally, and most relevant to the case described here, there is no evidence-based consensus on how to interpret these test results in the context of a BRCA2 mutation.
Based on the published literature reporting that BRCA2 mutations are associated with more aggressive disease, one prediction would be that test scores from genomic assays such as Oncotype DX and Prolaris would tend to be higher in BRCA2 carriers than those of the overall population of PCa patients. This has, in fact, been reported for the Oncotype DX Breast Cancer Assay recurrence score in women who are BRCA carriers.22 Further research is required to ascertain whether this will be true for Oncotype DX GPS and Prolaris CCP score in PCa. The mechanism of action that predisposes BRCA2 mutation carriers to develop a more aggressive variant of PCa may not be detectable by the genomic markers included in the Oncotype DX PCa and Prolaris tests. The degree to which a mutated BRCA2 gene may interact with the genes comprising these assays and the reported tumor aggressiveness is not yet understood but deserving of future study.
Treatment Recommendation and Patient’s Decision
After considering his test results, the veteran chose active surveillance. The sum of clinical, pathologic, and molecular factors, combined with the patient’s preference, determined his course of treatment. Because prostatectomy was not performed, it has not been positively determined whether or not the patient harbors aggressive disease. As the molecular test results place the patient at the high end of the low-risk group, the VA urologist recommended close monitoring and suggested a follow-up biopsy with magnetic resonance-ultrasound fusion guidance.
Conclusions
Molecular testing found that the patient’s PCa stage and grade are consistent with NCCN low risk (Oncotype DX) and that the disease-specific mortality risk is slightly higher than predicted by clinical features alone (Prolaris). Previous studies have shown that molecular testing in men with PCa provides information that influences clinical decisions. The findings reported here suggest that molecular testing may also be a vital component in the medical management of patients with complex clinical phenotypes and common chronic conditions. Additional studies are necessary to evaluate whether the finding reported here is typical of individuals diagnosed with PCa who also have a BRCA2 mutation.
For any new genomic test to be clinically useful, its results must have clinical actionability. In this case, the clinical decision point was whether to recommend immediate definitive treatment or active surveillance. For this patient, the Oncotype DX assay provided a likelihood of favorable surgical pathology of 71% (or conversely a 29% risk of unfavorable pathology); by comparison, the Prolaris CCP score provided a 3% estimate of PCaspecific
mortality at 10 years. A key question is: How do clinicians perceive the actionability of risk estimates for these different endpoints?
The current case illustrates the challenges that rapidly developing genomic medicine pose for physicians trying to optimize care and communicate results to patients in a meaningful and consistent manner. For example, some urologists find the different 2-tiered calculations confusing. When laboratories use proprietary scalesbased on internally develop algorithms, differing interpretations are to be expected. The risk-assessment tests described here use different algorithms, and their interpretations are based on clinical categories from different sets of guidelines. This underscores the need for better standardization of PCa care.23
Oncology and urology professional associations should collaborate to develop consistent guidelines for use of new technologies in the management of PCa. A positive example is the evolution of testing recommendations in lung cancer, which initially varied between professional entities. In April 2013, the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology jointly issued a unified clinical practice guideline on molecular testing in patients with lung cancer.24 In October 2014, the American Society of Clinical Oncology issued an endorsement of the CAP/IASLC/AMP guideline.25 As the number of complex tests being used in PCa increases, it will be important for professional associations such as AUA and NCCN to collaborate in evaluating utility of innovations to make consistent recommendations
Author disclosures
Myriad Genetics and Genomic Health provided funding for research on their tests within the VA. Dr. Dash and Dr. Lynch are principal investigators of the Genomic Health study. Dr. Lowrance is the principal investigator of the Myriad Genetics study.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Click here to continue reading.
1. D’Amico AV, Whittington R, Malkowicz SB, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280(11):969-974.
2. Cooperberg MR, Pasta DJ, Elkin EP, et al. The University of California, San Francisco Cancer of the Prostate Risk Assessment score: a straightforward and reliable preoperative predictor of disease recurrence after radical prostatectomy. J Urol. 2005;173(6):1938-1942.
3. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: prostate cancer. National Comprehensive Cancer Network Website. http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. Updated November 10, 2015. Accessed December 8, 2016.
4. Thompson I, Thrasher JB, Aus G, et al; AUA Prostate Cancer Clinical Guideline Update Panel. Guideline for the management of clinically localized prostate cancer: 2007 update. J Urol. 2007;177(6):2106-2131.
5. Alanee SR, Glogowski EA, Schrader KA, Eastham JA, Offit K. Clinical features and management of BRCA1 and BRCA2-associated prostate cancer. Front Biosci (Elite Ed). 2014;6:15-30.
6. Castro E, Eeles R. The role of BRCA1 and BRCA2 in prostate cancer. Asian J Androl. 2012;14(3):409-414.
7. Boorjian SA, Karnes RJ, Rangel LJ, Bergstralh EJ, Blute ML. Mayo Clinic validation of the D’amico risk group classification for predicting survival following radical prostatectomy. J Urol. 2008;179(4):1354-1360.
8. Lowrance WT, Scardino PT. Predictive models for newly diagnosed prostate cancer patients. Rev Urol. 2009;11(3):117-126.
9. Levy-Lahad E, Friedman E. Cancer risks among BRCA1 and BRCA2 mutation carriers. Br J Cancer. 2007;96(1):11-15.
10. Leongamornlert D, Mahmud N, Tymrakiewicz M, et al; UKGPCS Collaborators. Germline BRCA1 mutations increase prostate cancer risk. Br J Cancer. 2012;106(10):1697-1701.
11. Kote-Jarai Z, Leongamornlert D, Saunders E, et al; UKGPCS Collaborators. BRCA2 is a moderate penetrance gene contributing to young-onset prostate cancer: implications for genetic testing in prostate cancer patients. Br J Cancer. 2011;105(8):1230-1234.
12. Tryggvadóttir L, Vidarsdóttir L, Thorgeirsson T, et al. Prostate cancer progression and survival in BRCA2 mutation carriers. J Natl Cancer Inst. 2007;99(12):929-935.
13. Gallagher DJ, Gaudet MM, Pal P, et al. Germline BRCA mutations denote a clinicopathologic subset of prostate cancer. Clin Cancer Res. 2010;16(7):2115-2121.
14. Castro E, Goh C, Olmos D, et al. Germline BRCA mutations are associated with higher risk of nodal involvement, distant metastasis, and poor survival outcomes in prostate cancer. J Clin Oncol. 2013;31(14):1748-1757.
15. Castro E, Goh C, Leongamornlert D, et al. Effect of BRCA mutations on metastatic relapse and cause-specific survival after radical treatment for localised prostate cancer. Eur Urol. 2015;68(2):186-193.
16. Bancroft EK, Page EC, Castro E, et al; IMPACT Collaborators. Targeted prostate cancer screening in BRCA1 and BRCA2 mutation carriers: results from the initial screening round of the IMPACT study. Eur Urol. 2014;66(3):489-499.
17. Bratt O, Loman N. Clinical management of prostate cancer in men with BRCA mutations. Eur Urol. 2015;68(2):194-195.
18. Centers for Medicare & Medicaid Services (CMS). MCD archive site. CMS Website. http://localcoverage.cms.gov/mcd_archive/overview.aspx. Accessed January 8, 2016.
19. Klein EA, Cooperberg MR, Magi-Galluzzi C, et al. A 17-gene assay to predict prostate cancer aggressiveness in the context of Gleason grade heterogeneity, tumor multifocality, and biopsy undersampling. Eur Urol. 2014;66(3):550-560.
20. Shore ND, Kella N, Moran B, et al. Impact of the cell cycle progression test on physician and patient treatment selection for localized prostate cancer. J Urol. 2015;pii:S0022-5347(15)04811-9 [epub ahead of print].
21. Stone S, Cuzick JM, Fisher G, et al. Validation of an active surveillance threshold for the CCP score in conservatively managed men with localized prostate cancer. J Clin Oncol. 2015;33(suppl 15):e16040.
22. Lewin R, Rizel S, Hendler D, et al. Oncotype-DX recurrence score distribution among breast cancer patients harboring a germline mutation in the BRCA1/2 genes. J Clin Oncol. 2015;33(suppl; abstr 564).
23. Dahm P, Yeung LL, Chang SS, Cookson MS. A critical review of clinical practice guidelines for the management of clinically localized prostate cancer. J Urol. 2008;180(2):451-459.
24. Lindeman NI, Cagle PT, Beasley MB, et al. Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J Thorac Oncol. 2013;8(7):823-859.
25. Leighl NB, Rekhtman N, Biermann WA, et al. Molecular testing for selection of patients with lung cancer for epidermal growth factor receptor and anaplastic lymphoma kinase tyrosine kinase inhibitors: American Society of Clinical Oncology endorsement of the College of American Pathologists/International Association for the Study of Lung Cancer/Association for Molecular Pathology guideline. J Clin Oncol. 2014;32(32):3673-3679.
Note: Page numbers differ between the print issue and digital edition.
1. D’Amico AV, Whittington R, Malkowicz SB, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280(11):969-974.
2. Cooperberg MR, Pasta DJ, Elkin EP, et al. The University of California, San Francisco Cancer of the Prostate Risk Assessment score: a straightforward and reliable preoperative predictor of disease recurrence after radical prostatectomy. J Urol. 2005;173(6):1938-1942.
3. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: prostate cancer. National Comprehensive Cancer Network Website. http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. Updated November 10, 2015. Accessed December 8, 2016.
4. Thompson I, Thrasher JB, Aus G, et al; AUA Prostate Cancer Clinical Guideline Update Panel. Guideline for the management of clinically localized prostate cancer: 2007 update. J Urol. 2007;177(6):2106-2131.
5. Alanee SR, Glogowski EA, Schrader KA, Eastham JA, Offit K. Clinical features and management of BRCA1 and BRCA2-associated prostate cancer. Front Biosci (Elite Ed). 2014;6:15-30.
6. Castro E, Eeles R. The role of BRCA1 and BRCA2 in prostate cancer. Asian J Androl. 2012;14(3):409-414.
7. Boorjian SA, Karnes RJ, Rangel LJ, Bergstralh EJ, Blute ML. Mayo Clinic validation of the D’amico risk group classification for predicting survival following radical prostatectomy. J Urol. 2008;179(4):1354-1360.
8. Lowrance WT, Scardino PT. Predictive models for newly diagnosed prostate cancer patients. Rev Urol. 2009;11(3):117-126.
9. Levy-Lahad E, Friedman E. Cancer risks among BRCA1 and BRCA2 mutation carriers. Br J Cancer. 2007;96(1):11-15.
10. Leongamornlert D, Mahmud N, Tymrakiewicz M, et al; UKGPCS Collaborators. Germline BRCA1 mutations increase prostate cancer risk. Br J Cancer. 2012;106(10):1697-1701.
11. Kote-Jarai Z, Leongamornlert D, Saunders E, et al; UKGPCS Collaborators. BRCA2 is a moderate penetrance gene contributing to young-onset prostate cancer: implications for genetic testing in prostate cancer patients. Br J Cancer. 2011;105(8):1230-1234.
12. Tryggvadóttir L, Vidarsdóttir L, Thorgeirsson T, et al. Prostate cancer progression and survival in BRCA2 mutation carriers. J Natl Cancer Inst. 2007;99(12):929-935.
13. Gallagher DJ, Gaudet MM, Pal P, et al. Germline BRCA mutations denote a clinicopathologic subset of prostate cancer. Clin Cancer Res. 2010;16(7):2115-2121.
14. Castro E, Goh C, Olmos D, et al. Germline BRCA mutations are associated with higher risk of nodal involvement, distant metastasis, and poor survival outcomes in prostate cancer. J Clin Oncol. 2013;31(14):1748-1757.
15. Castro E, Goh C, Leongamornlert D, et al. Effect of BRCA mutations on metastatic relapse and cause-specific survival after radical treatment for localised prostate cancer. Eur Urol. 2015;68(2):186-193.
16. Bancroft EK, Page EC, Castro E, et al; IMPACT Collaborators. Targeted prostate cancer screening in BRCA1 and BRCA2 mutation carriers: results from the initial screening round of the IMPACT study. Eur Urol. 2014;66(3):489-499.
17. Bratt O, Loman N. Clinical management of prostate cancer in men with BRCA mutations. Eur Urol. 2015;68(2):194-195.
18. Centers for Medicare & Medicaid Services (CMS). MCD archive site. CMS Website. http://localcoverage.cms.gov/mcd_archive/overview.aspx. Accessed January 8, 2016.
19. Klein EA, Cooperberg MR, Magi-Galluzzi C, et al. A 17-gene assay to predict prostate cancer aggressiveness in the context of Gleason grade heterogeneity, tumor multifocality, and biopsy undersampling. Eur Urol. 2014;66(3):550-560.
20. Shore ND, Kella N, Moran B, et al. Impact of the cell cycle progression test on physician and patient treatment selection for localized prostate cancer. J Urol. 2015;pii:S0022-5347(15)04811-9 [epub ahead of print].
21. Stone S, Cuzick JM, Fisher G, et al. Validation of an active surveillance threshold for the CCP score in conservatively managed men with localized prostate cancer. J Clin Oncol. 2015;33(suppl 15):e16040.
22. Lewin R, Rizel S, Hendler D, et al. Oncotype-DX recurrence score distribution among breast cancer patients harboring a germline mutation in the BRCA1/2 genes. J Clin Oncol. 2015;33(suppl; abstr 564).
23. Dahm P, Yeung LL, Chang SS, Cookson MS. A critical review of clinical practice guidelines for the management of clinically localized prostate cancer. J Urol. 2008;180(2):451-459.
24. Lindeman NI, Cagle PT, Beasley MB, et al. Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J Thorac Oncol. 2013;8(7):823-859.
25. Leighl NB, Rekhtman N, Biermann WA, et al. Molecular testing for selection of patients with lung cancer for epidermal growth factor receptor and anaplastic lymphoma kinase tyrosine kinase inhibitors: American Society of Clinical Oncology endorsement of the College of American Pathologists/International Association for the Study of Lung Cancer/Association for Molecular Pathology guideline. J Clin Oncol. 2014;32(32):3673-3679.
Note: Page numbers differ between the print issue and digital edition.
Implementation of a Precision Oncology Program as an Exemplar of a Learning Health Care System in the VA
Traditional research methods, well suited for scientific discovery and drug development, fall short of providing health care systems with pragmatic information in 2 important ways: Current funding and institutions cannot support comparative effectiveness studies in sufficient numbers to answer the plethora of important clinical questions that confront health care providers (HCPs). The resultant knowledge gap manifests in treatment variability based on clinician impression rather than on direct evidence. A second equally important deficiency is the inability to make full use of the knowledge acquired in treating past patients to determine the best treatment option for the current patient.
Digitization of medical records, creation of health care system corporate data warehouses, and state-of-the-art analytical tools already allow for this revolutionary approach to patient care. Obstructing progress, however, is a lack of understanding by health care system managers and HCPs of the capability of the approach, and unfamiliarity with the requisite informatics by traditional medical researchers. Furthermore the regulatory approach is tilted against the reuse of medical record data for learning and toward strict adherence to patient confidentiality.
Note: Page numbers differ between the print issue and digital edition.
Traditional research methods, well suited for scientific discovery and drug development, fall short of providing health care systems with pragmatic information in 2 important ways: Current funding and institutions cannot support comparative effectiveness studies in sufficient numbers to answer the plethora of important clinical questions that confront health care providers (HCPs). The resultant knowledge gap manifests in treatment variability based on clinician impression rather than on direct evidence. A second equally important deficiency is the inability to make full use of the knowledge acquired in treating past patients to determine the best treatment option for the current patient.
Digitization of medical records, creation of health care system corporate data warehouses, and state-of-the-art analytical tools already allow for this revolutionary approach to patient care. Obstructing progress, however, is a lack of understanding by health care system managers and HCPs of the capability of the approach, and unfamiliarity with the requisite informatics by traditional medical researchers. Furthermore the regulatory approach is tilted against the reuse of medical record data for learning and toward strict adherence to patient confidentiality.
Traditional research methods, well suited for scientific discovery and drug development, fall short of providing health care systems with pragmatic information in 2 important ways: Current funding and institutions cannot support comparative effectiveness studies in sufficient numbers to answer the plethora of important clinical questions that confront health care providers (HCPs). The resultant knowledge gap manifests in treatment variability based on clinician impression rather than on direct evidence. A second equally important deficiency is the inability to make full use of the knowledge acquired in treating past patients to determine the best treatment option for the current patient.
Digitization of medical records, creation of health care system corporate data warehouses, and state-of-the-art analytical tools already allow for this revolutionary approach to patient care. Obstructing progress, however, is a lack of understanding by health care system managers and HCPs of the capability of the approach, and unfamiliarity with the requisite informatics by traditional medical researchers. Furthermore the regulatory approach is tilted against the reuse of medical record data for learning and toward strict adherence to patient confidentiality.
Note: Page numbers differ between the print issue and digital edition.
Note: Page numbers differ between the print issue and digital edition.