User login
Exercise boosts anticancer effects of doxorubicin

Credit: Aaron Logan
Exercising during doxorubicin treatment can amplify the drug’s cancer-fighting ability, according to preclinical research.
Previous studies showed that adopting an exercise regimen before receiving doxorubicin could protect against the cardiac side effects associated with the drug.
Now, researchers have reported that exercising during doxorubicin treatment does not protect the heart, but it does help shrink tumors in mice.
Joseph Libonati, PhD, of the University of Pennsylvania in Philadelphia, and his colleagues reported these findings in the American Journal of Physiology—Regulatory, Integrative and Comparative Physiology.
The researchers conducted experiments with 4 groups of mice, all of which received an injection of melanoma cells.
During the next 2 weeks, 2 of the groups received doxorubicin in 2 doses, while the other 2 groups received placebo injections.
A treated group and a placebo group were put on exercise regimens, walking for 45 minutes 5 days a week on mouse-sized treadmills, while the rest of the mice remained sedentary.
After the 2-week trial, the researchers examined the animals’ hearts using echocardiogram and tissue analysis.
As expected, doxorubicin reduced the heart’s function and size and increased fibrosis. Mice that exercised were not protected from this damage.
“We looked, and the exercise didn’t do anything to the heart; it didn’t worsen it, it didn’t help it,” Dr Libonati said. “But the tumor data—I find them actually amazing.”
The mice that received doxorubicin and exercised had significantly smaller tumors after 2 weeks than mice that only received doxorubicin (P<0.05).
Further studies will investigate exactly how exercise enhances the effect of doxorubicin, but the researchers believe it could be, in part, because exercise increases blood flow to the tumor, bringing with it more of the drug in the bloodstream.
“If exercise helps in this way, you could potentially use a smaller dose of the drug and get fewer side effects,” Dr Libonati said.
Gaining a clearer understanding of the many ways that exercise affects various systems of the body could also pave the way for developing drugs that mimic the effects of exercise.
“People don’t take a drug and then sit down all day,” Dr Libonati said. “Something as simple as moving affects how drugs are metabolized. We’re only just beginning to understand the complexities.” ![]()

Credit: Aaron Logan
Exercising during doxorubicin treatment can amplify the drug’s cancer-fighting ability, according to preclinical research.
Previous studies showed that adopting an exercise regimen before receiving doxorubicin could protect against the cardiac side effects associated with the drug.
Now, researchers have reported that exercising during doxorubicin treatment does not protect the heart, but it does help shrink tumors in mice.
Joseph Libonati, PhD, of the University of Pennsylvania in Philadelphia, and his colleagues reported these findings in the American Journal of Physiology—Regulatory, Integrative and Comparative Physiology.
The researchers conducted experiments with 4 groups of mice, all of which received an injection of melanoma cells.
During the next 2 weeks, 2 of the groups received doxorubicin in 2 doses, while the other 2 groups received placebo injections.
A treated group and a placebo group were put on exercise regimens, walking for 45 minutes 5 days a week on mouse-sized treadmills, while the rest of the mice remained sedentary.
After the 2-week trial, the researchers examined the animals’ hearts using echocardiogram and tissue analysis.
As expected, doxorubicin reduced the heart’s function and size and increased fibrosis. Mice that exercised were not protected from this damage.
“We looked, and the exercise didn’t do anything to the heart; it didn’t worsen it, it didn’t help it,” Dr Libonati said. “But the tumor data—I find them actually amazing.”
The mice that received doxorubicin and exercised had significantly smaller tumors after 2 weeks than mice that only received doxorubicin (P<0.05).
Further studies will investigate exactly how exercise enhances the effect of doxorubicin, but the researchers believe it could be, in part, because exercise increases blood flow to the tumor, bringing with it more of the drug in the bloodstream.
“If exercise helps in this way, you could potentially use a smaller dose of the drug and get fewer side effects,” Dr Libonati said.
Gaining a clearer understanding of the many ways that exercise affects various systems of the body could also pave the way for developing drugs that mimic the effects of exercise.
“People don’t take a drug and then sit down all day,” Dr Libonati said. “Something as simple as moving affects how drugs are metabolized. We’re only just beginning to understand the complexities.” ![]()

Credit: Aaron Logan
Exercising during doxorubicin treatment can amplify the drug’s cancer-fighting ability, according to preclinical research.
Previous studies showed that adopting an exercise regimen before receiving doxorubicin could protect against the cardiac side effects associated with the drug.
Now, researchers have reported that exercising during doxorubicin treatment does not protect the heart, but it does help shrink tumors in mice.
Joseph Libonati, PhD, of the University of Pennsylvania in Philadelphia, and his colleagues reported these findings in the American Journal of Physiology—Regulatory, Integrative and Comparative Physiology.
The researchers conducted experiments with 4 groups of mice, all of which received an injection of melanoma cells.
During the next 2 weeks, 2 of the groups received doxorubicin in 2 doses, while the other 2 groups received placebo injections.
A treated group and a placebo group were put on exercise regimens, walking for 45 minutes 5 days a week on mouse-sized treadmills, while the rest of the mice remained sedentary.
After the 2-week trial, the researchers examined the animals’ hearts using echocardiogram and tissue analysis.
As expected, doxorubicin reduced the heart’s function and size and increased fibrosis. Mice that exercised were not protected from this damage.
“We looked, and the exercise didn’t do anything to the heart; it didn’t worsen it, it didn’t help it,” Dr Libonati said. “But the tumor data—I find them actually amazing.”
The mice that received doxorubicin and exercised had significantly smaller tumors after 2 weeks than mice that only received doxorubicin (P<0.05).
Further studies will investigate exactly how exercise enhances the effect of doxorubicin, but the researchers believe it could be, in part, because exercise increases blood flow to the tumor, bringing with it more of the drug in the bloodstream.
“If exercise helps in this way, you could potentially use a smaller dose of the drug and get fewer side effects,” Dr Libonati said.
Gaining a clearer understanding of the many ways that exercise affects various systems of the body could also pave the way for developing drugs that mimic the effects of exercise.
“People don’t take a drug and then sit down all day,” Dr Libonati said. “Something as simple as moving affects how drugs are metabolized. We’re only just beginning to understand the complexities.” ![]()
FDA approves 30-day pack of anticoagulant

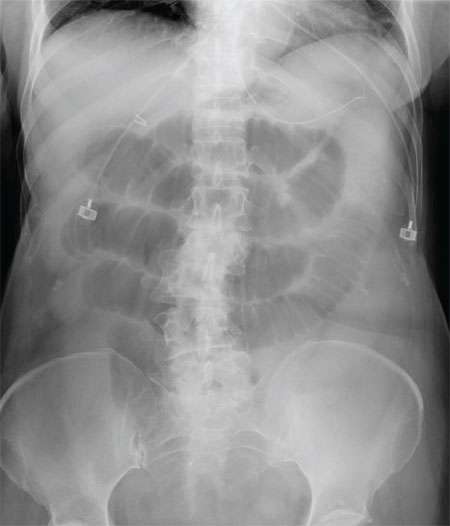
Credit: NHS
The US Food and Drug Administration (FDA) has approved the Xarelto Starter Pack™ for the treatment of deep vein thrombosis (DVT) and/or pulmonary embolism (PE).
The pack provides a 30-day supply of Xarelto (rivaroxaban), which gives patients time to follow up with their primary care physician after leaving the hospital, without missing treatment.
Patients have the greatest risk of recurrence in the first 30 days after a DVT or PE.
“The starter pack will make a difference for patients impacted by blood clots by offering a 30-day supply of the drug in a new, convenient package, which may help support patients as they transition from the hospital to outpatient care,” said Paul Burton, MD, PhD, Vice President of Medical Affairs at Janssen, the company developing Xarelto.
The Xarelto Starter Pack™ will be available at pharmacies in October.
Xarelto is a factor Xa inhibitor that is FDA-approved to treat and prevent the recurrence of DVT/PE, as thromboprophylaxis in patients who have undergone knee or hip replacement surgery, and to reduce the risk of stroke in patients with non-valvular atrial fibrillation.
For DVT/PE patients, Xarelto is given twice daily at 15 mg with food for the first 21 days. On day 22, patients transition to a once-daily dose of 20 mg with food for the remainder of treatment.
Xarelto has a boxed warning stating that premature discontinuation of the drug increases the risk of thrombotic events, and epidural or spinal hematomas have occurred in Xarelto-treated patients who are receiving neuraxial anesthesia or undergoing spinal puncture.
For more details on Xarelto, see the full prescribing information. ![]()

Credit: NHS
The US Food and Drug Administration (FDA) has approved the Xarelto Starter Pack™ for the treatment of deep vein thrombosis (DVT) and/or pulmonary embolism (PE).
The pack provides a 30-day supply of Xarelto (rivaroxaban), which gives patients time to follow up with their primary care physician after leaving the hospital, without missing treatment.
Patients have the greatest risk of recurrence in the first 30 days after a DVT or PE.
“The starter pack will make a difference for patients impacted by blood clots by offering a 30-day supply of the drug in a new, convenient package, which may help support patients as they transition from the hospital to outpatient care,” said Paul Burton, MD, PhD, Vice President of Medical Affairs at Janssen, the company developing Xarelto.
The Xarelto Starter Pack™ will be available at pharmacies in October.
Xarelto is a factor Xa inhibitor that is FDA-approved to treat and prevent the recurrence of DVT/PE, as thromboprophylaxis in patients who have undergone knee or hip replacement surgery, and to reduce the risk of stroke in patients with non-valvular atrial fibrillation.
For DVT/PE patients, Xarelto is given twice daily at 15 mg with food for the first 21 days. On day 22, patients transition to a once-daily dose of 20 mg with food for the remainder of treatment.
Xarelto has a boxed warning stating that premature discontinuation of the drug increases the risk of thrombotic events, and epidural or spinal hematomas have occurred in Xarelto-treated patients who are receiving neuraxial anesthesia or undergoing spinal puncture.
For more details on Xarelto, see the full prescribing information. ![]()

Credit: NHS
The US Food and Drug Administration (FDA) has approved the Xarelto Starter Pack™ for the treatment of deep vein thrombosis (DVT) and/or pulmonary embolism (PE).
The pack provides a 30-day supply of Xarelto (rivaroxaban), which gives patients time to follow up with their primary care physician after leaving the hospital, without missing treatment.
Patients have the greatest risk of recurrence in the first 30 days after a DVT or PE.
“The starter pack will make a difference for patients impacted by blood clots by offering a 30-day supply of the drug in a new, convenient package, which may help support patients as they transition from the hospital to outpatient care,” said Paul Burton, MD, PhD, Vice President of Medical Affairs at Janssen, the company developing Xarelto.
The Xarelto Starter Pack™ will be available at pharmacies in October.
Xarelto is a factor Xa inhibitor that is FDA-approved to treat and prevent the recurrence of DVT/PE, as thromboprophylaxis in patients who have undergone knee or hip replacement surgery, and to reduce the risk of stroke in patients with non-valvular atrial fibrillation.
For DVT/PE patients, Xarelto is given twice daily at 15 mg with food for the first 21 days. On day 22, patients transition to a once-daily dose of 20 mg with food for the remainder of treatment.
Xarelto has a boxed warning stating that premature discontinuation of the drug increases the risk of thrombotic events, and epidural or spinal hematomas have occurred in Xarelto-treated patients who are receiving neuraxial anesthesia or undergoing spinal puncture.
For more details on Xarelto, see the full prescribing information. ![]()
License to slip up?
The Food and Drug Administration recently approved another weight-loss drug (Contrave), a combination of naltrexone (indicated for opioid dependence) and bupropion (indicated for depression). This is the third weight-loss drug approved in the past 2 years. The FDA previously approved lorcaserin (Belviq) and topiramate/phentermine (Qsymia). This approval activity signals pharmaceutical interest in a multibillion dollar weight loss industry and perhaps, maybe less so, the FDA’s recognition of our public health crisis.
For patients who meet criteria for the use of these medications, they should be offered if they can be afforded. However, these medications may make patients behave differently.
It’s called “license.”
License is the psychological phenomenon in which people who feel they have made progress toward a goal feel liberated to make an incongruent choice. Think of a patient interested in losing weight who now takes a weight-loss pill. Despite not having lost any weight yet and perhaps just after taking the first pill, the patient then makes a choice to consume a high-calorie dessert.
Here are some data that support that this could be happening.
One team of investigators randomized subjects to being informed they were taking a placebo or a weight-loss supplement (which was actually the same placebo tablet as in the other study arm). After receiving the supplement, participants were allowed access to a reward buffet lunch at which their food consumption was recorded. Compared with controls, participants receiving a purported weight-loss supplement ate more food at the reward buffet. This effect seemed to occur through a perceived sense that they were making progress toward their weight-loss goal by taking the pill (Nutrition 2014;30:1007-14).
This is critical for us to think about and incorporate into our clinical teaching when prescribing these medications. Psychological liberation threatens any health gains we can make at a population level with any weight-loss approach. We need to help our patients understand that these medications should be used in combination with sustainable lifestyle changes or they may as well be taking a placebo.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician.
The Food and Drug Administration recently approved another weight-loss drug (Contrave), a combination of naltrexone (indicated for opioid dependence) and bupropion (indicated for depression). This is the third weight-loss drug approved in the past 2 years. The FDA previously approved lorcaserin (Belviq) and topiramate/phentermine (Qsymia). This approval activity signals pharmaceutical interest in a multibillion dollar weight loss industry and perhaps, maybe less so, the FDA’s recognition of our public health crisis.
For patients who meet criteria for the use of these medications, they should be offered if they can be afforded. However, these medications may make patients behave differently.
It’s called “license.”
License is the psychological phenomenon in which people who feel they have made progress toward a goal feel liberated to make an incongruent choice. Think of a patient interested in losing weight who now takes a weight-loss pill. Despite not having lost any weight yet and perhaps just after taking the first pill, the patient then makes a choice to consume a high-calorie dessert.
Here are some data that support that this could be happening.
One team of investigators randomized subjects to being informed they were taking a placebo or a weight-loss supplement (which was actually the same placebo tablet as in the other study arm). After receiving the supplement, participants were allowed access to a reward buffet lunch at which their food consumption was recorded. Compared with controls, participants receiving a purported weight-loss supplement ate more food at the reward buffet. This effect seemed to occur through a perceived sense that they were making progress toward their weight-loss goal by taking the pill (Nutrition 2014;30:1007-14).
This is critical for us to think about and incorporate into our clinical teaching when prescribing these medications. Psychological liberation threatens any health gains we can make at a population level with any weight-loss approach. We need to help our patients understand that these medications should be used in combination with sustainable lifestyle changes or they may as well be taking a placebo.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician.
The Food and Drug Administration recently approved another weight-loss drug (Contrave), a combination of naltrexone (indicated for opioid dependence) and bupropion (indicated for depression). This is the third weight-loss drug approved in the past 2 years. The FDA previously approved lorcaserin (Belviq) and topiramate/phentermine (Qsymia). This approval activity signals pharmaceutical interest in a multibillion dollar weight loss industry and perhaps, maybe less so, the FDA’s recognition of our public health crisis.
For patients who meet criteria for the use of these medications, they should be offered if they can be afforded. However, these medications may make patients behave differently.
It’s called “license.”
License is the psychological phenomenon in which people who feel they have made progress toward a goal feel liberated to make an incongruent choice. Think of a patient interested in losing weight who now takes a weight-loss pill. Despite not having lost any weight yet and perhaps just after taking the first pill, the patient then makes a choice to consume a high-calorie dessert.
Here are some data that support that this could be happening.
One team of investigators randomized subjects to being informed they were taking a placebo or a weight-loss supplement (which was actually the same placebo tablet as in the other study arm). After receiving the supplement, participants were allowed access to a reward buffet lunch at which their food consumption was recorded. Compared with controls, participants receiving a purported weight-loss supplement ate more food at the reward buffet. This effect seemed to occur through a perceived sense that they were making progress toward their weight-loss goal by taking the pill (Nutrition 2014;30:1007-14).
This is critical for us to think about and incorporate into our clinical teaching when prescribing these medications. Psychological liberation threatens any health gains we can make at a population level with any weight-loss approach. We need to help our patients understand that these medications should be used in combination with sustainable lifestyle changes or they may as well be taking a placebo.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician.
Combo improves PFS in multiple myeloma

Credit: NIH
Adding panobinostat to treatment with bortezomib and dexamethasone can improve progression-free survival (PFS) in previously treated patients with multiple myeloma, results of the PANORAMA-1 trial suggest.
The combination conferred a 4-month improvement in median PFS when compared to bortezomib and dexamethasone plus placebo.
There was no significant difference in overall survival between the treatment groups, but researchers said these data are not mature.
“The PANORAMA-1 study is the first phase 3 trial to show the superiority of [panobinostat] plus bortezomib and dexamethasone over one of the standard 2-drug regimens for patients with relapsing and/or refractory multiple myeloma,” said lead study investigator Jesus San-Miguel, MD, of Clínica Universidad de Navarra in Pamplona, Spain.
Dr San-Miguel and his colleagues reported the results of PANORAMA-1 in The Lancet Oncology. The trial was sponsored by Novartis Pharmaceuticals, the company developing panobinostat.
The trial included 768 patients with relapsed or relapsed and refractory multiple myeloma who had failed at least 1 prior treatment.
Three-hundred and eighty-seven patients were randomized to treatment with panobinostat, bortezomib, and dexamethasone. And 381 patients were randomized to receive placebo, bortezomib, and dexamethasone.
The median follow up was 6.47 months in the panobinostat arm 5.59 months in the placebo arm.
The study’s primary endpoint was PFS. And the median PFS was significantly longer in the panobinostat arm than the placebo arm—11.99 months and 8.08 months, respectively (P<0.0001).
The median overall survival, on the other hand, was similar between the treatment arms. It was 33.64 months in the panobinostat arm and 30.39 months in the placebo arm (P=0.26).
Likewise, the overall response rate was similar between the treatment arms—60.7% with panobinostat and 54.6% with placebo (P=0.09). But the rate of complete or near-complete response was higher with panobinostat—27.6% and 15.7%, respectively (P=0.00006).
The rate of serious adverse events was 60% in the panobinostat arm and 42% in the placebo arm.
The most common grade 3/4 adverse events were thrombocytopenia (67% and 31%, respectively), lymphopenia (53% and 40%, respectively), neutropenia (35% and 11%, respectively), diarrhea (26% and 8%, respectively), and neuropathy (18% and 15%, respectively).
Based on these data, panobinostat was granted priority review by the US Food and Drug Administration in May. Priority review is given to therapies that may offer major advances in treatment. ![]()

Credit: NIH
Adding panobinostat to treatment with bortezomib and dexamethasone can improve progression-free survival (PFS) in previously treated patients with multiple myeloma, results of the PANORAMA-1 trial suggest.
The combination conferred a 4-month improvement in median PFS when compared to bortezomib and dexamethasone plus placebo.
There was no significant difference in overall survival between the treatment groups, but researchers said these data are not mature.
“The PANORAMA-1 study is the first phase 3 trial to show the superiority of [panobinostat] plus bortezomib and dexamethasone over one of the standard 2-drug regimens for patients with relapsing and/or refractory multiple myeloma,” said lead study investigator Jesus San-Miguel, MD, of Clínica Universidad de Navarra in Pamplona, Spain.
Dr San-Miguel and his colleagues reported the results of PANORAMA-1 in The Lancet Oncology. The trial was sponsored by Novartis Pharmaceuticals, the company developing panobinostat.
The trial included 768 patients with relapsed or relapsed and refractory multiple myeloma who had failed at least 1 prior treatment.
Three-hundred and eighty-seven patients were randomized to treatment with panobinostat, bortezomib, and dexamethasone. And 381 patients were randomized to receive placebo, bortezomib, and dexamethasone.
The median follow up was 6.47 months in the panobinostat arm 5.59 months in the placebo arm.
The study’s primary endpoint was PFS. And the median PFS was significantly longer in the panobinostat arm than the placebo arm—11.99 months and 8.08 months, respectively (P<0.0001).
The median overall survival, on the other hand, was similar between the treatment arms. It was 33.64 months in the panobinostat arm and 30.39 months in the placebo arm (P=0.26).
Likewise, the overall response rate was similar between the treatment arms—60.7% with panobinostat and 54.6% with placebo (P=0.09). But the rate of complete or near-complete response was higher with panobinostat—27.6% and 15.7%, respectively (P=0.00006).
The rate of serious adverse events was 60% in the panobinostat arm and 42% in the placebo arm.
The most common grade 3/4 adverse events were thrombocytopenia (67% and 31%, respectively), lymphopenia (53% and 40%, respectively), neutropenia (35% and 11%, respectively), diarrhea (26% and 8%, respectively), and neuropathy (18% and 15%, respectively).
Based on these data, panobinostat was granted priority review by the US Food and Drug Administration in May. Priority review is given to therapies that may offer major advances in treatment. ![]()

Credit: NIH
Adding panobinostat to treatment with bortezomib and dexamethasone can improve progression-free survival (PFS) in previously treated patients with multiple myeloma, results of the PANORAMA-1 trial suggest.
The combination conferred a 4-month improvement in median PFS when compared to bortezomib and dexamethasone plus placebo.
There was no significant difference in overall survival between the treatment groups, but researchers said these data are not mature.
“The PANORAMA-1 study is the first phase 3 trial to show the superiority of [panobinostat] plus bortezomib and dexamethasone over one of the standard 2-drug regimens for patients with relapsing and/or refractory multiple myeloma,” said lead study investigator Jesus San-Miguel, MD, of Clínica Universidad de Navarra in Pamplona, Spain.
Dr San-Miguel and his colleagues reported the results of PANORAMA-1 in The Lancet Oncology. The trial was sponsored by Novartis Pharmaceuticals, the company developing panobinostat.
The trial included 768 patients with relapsed or relapsed and refractory multiple myeloma who had failed at least 1 prior treatment.
Three-hundred and eighty-seven patients were randomized to treatment with panobinostat, bortezomib, and dexamethasone. And 381 patients were randomized to receive placebo, bortezomib, and dexamethasone.
The median follow up was 6.47 months in the panobinostat arm 5.59 months in the placebo arm.
The study’s primary endpoint was PFS. And the median PFS was significantly longer in the panobinostat arm than the placebo arm—11.99 months and 8.08 months, respectively (P<0.0001).
The median overall survival, on the other hand, was similar between the treatment arms. It was 33.64 months in the panobinostat arm and 30.39 months in the placebo arm (P=0.26).
Likewise, the overall response rate was similar between the treatment arms—60.7% with panobinostat and 54.6% with placebo (P=0.09). But the rate of complete or near-complete response was higher with panobinostat—27.6% and 15.7%, respectively (P=0.00006).
The rate of serious adverse events was 60% in the panobinostat arm and 42% in the placebo arm.
The most common grade 3/4 adverse events were thrombocytopenia (67% and 31%, respectively), lymphopenia (53% and 40%, respectively), neutropenia (35% and 11%, respectively), diarrhea (26% and 8%, respectively), and neuropathy (18% and 15%, respectively).
Based on these data, panobinostat was granted priority review by the US Food and Drug Administration in May. Priority review is given to therapies that may offer major advances in treatment. ![]()
Studies explain gene’s role in thrombosis, hemostasis

Credit: Kevin MacKenzie
Two preclinical studies provide new insight into the activity of STXBP5, a gene that has been linked to changes in von Willebrand factor (VWF).
One research group found evidence suggesting that STXBP5 regulates endothelial exocytosis and thrombosis.
Another group’s work indicated that STXBP5 is required for normal arterial hemostasis, as it contributes to platelet packaging and secretion.
Both studies appear in The Journal of Clinical Investigation.
Charles Lowenstein, MD, of the University of Rochester in New York, and his colleagues began their research with the theory that STXBP5 inhibits endothelial cell exocytosis.
The group found that STXBP5 is expressed in human endothelial cells, and reducing STXBP5 increases exocytosis of VWF and P-selectin.
STXBP5-knockout mice had higher levels of VWF in their plasma, increased P-selectin translocation, and more platelet-endothelial interactions. This suggests that defective STXBP5 is a risk factor for thrombosis.
However, STXBP5-knockout mice also exhibited prolonged bleeding and impaired thrombosis. They had defects in platelet secretion and activation as well.
Sidney (Wally) Whiteheart, PhD, of the University of Kentucky in Lexington, and his colleagues helped to explain these findings with their research.
The group showed that platelets lacking SXTBP5 failed to function correctly, and SXTBP5 was required for platelets to assist in normal clot formation. This suggests STXBP5 plays different roles in endothelial cells and platelets.
Specifically, the researchers found that STXBP5 interacts with core secretion machinery complexes and the platelet cytoskeleton.
And platelets from STXBP5-knockout mice exhibited defects in granule secretion. These platelets had altered granule cargo levels, despite having normal morphology and granule numbers.
Like Dr Lowenstein’s group, Dr Whiteheart and his colleagues observed dramatic bleeding and defective hemostasis in STXBP5-knockout mice. Transplant experiments suggested these defects were due to a loss of STXBP5 in bone marrow-derived cells. ![]()

Credit: Kevin MacKenzie
Two preclinical studies provide new insight into the activity of STXBP5, a gene that has been linked to changes in von Willebrand factor (VWF).
One research group found evidence suggesting that STXBP5 regulates endothelial exocytosis and thrombosis.
Another group’s work indicated that STXBP5 is required for normal arterial hemostasis, as it contributes to platelet packaging and secretion.
Both studies appear in The Journal of Clinical Investigation.
Charles Lowenstein, MD, of the University of Rochester in New York, and his colleagues began their research with the theory that STXBP5 inhibits endothelial cell exocytosis.
The group found that STXBP5 is expressed in human endothelial cells, and reducing STXBP5 increases exocytosis of VWF and P-selectin.
STXBP5-knockout mice had higher levels of VWF in their plasma, increased P-selectin translocation, and more platelet-endothelial interactions. This suggests that defective STXBP5 is a risk factor for thrombosis.
However, STXBP5-knockout mice also exhibited prolonged bleeding and impaired thrombosis. They had defects in platelet secretion and activation as well.
Sidney (Wally) Whiteheart, PhD, of the University of Kentucky in Lexington, and his colleagues helped to explain these findings with their research.
The group showed that platelets lacking SXTBP5 failed to function correctly, and SXTBP5 was required for platelets to assist in normal clot formation. This suggests STXBP5 plays different roles in endothelial cells and platelets.
Specifically, the researchers found that STXBP5 interacts with core secretion machinery complexes and the platelet cytoskeleton.
And platelets from STXBP5-knockout mice exhibited defects in granule secretion. These platelets had altered granule cargo levels, despite having normal morphology and granule numbers.
Like Dr Lowenstein’s group, Dr Whiteheart and his colleagues observed dramatic bleeding and defective hemostasis in STXBP5-knockout mice. Transplant experiments suggested these defects were due to a loss of STXBP5 in bone marrow-derived cells. ![]()

Credit: Kevin MacKenzie
Two preclinical studies provide new insight into the activity of STXBP5, a gene that has been linked to changes in von Willebrand factor (VWF).
One research group found evidence suggesting that STXBP5 regulates endothelial exocytosis and thrombosis.
Another group’s work indicated that STXBP5 is required for normal arterial hemostasis, as it contributes to platelet packaging and secretion.
Both studies appear in The Journal of Clinical Investigation.
Charles Lowenstein, MD, of the University of Rochester in New York, and his colleagues began their research with the theory that STXBP5 inhibits endothelial cell exocytosis.
The group found that STXBP5 is expressed in human endothelial cells, and reducing STXBP5 increases exocytosis of VWF and P-selectin.
STXBP5-knockout mice had higher levels of VWF in their plasma, increased P-selectin translocation, and more platelet-endothelial interactions. This suggests that defective STXBP5 is a risk factor for thrombosis.
However, STXBP5-knockout mice also exhibited prolonged bleeding and impaired thrombosis. They had defects in platelet secretion and activation as well.
Sidney (Wally) Whiteheart, PhD, of the University of Kentucky in Lexington, and his colleagues helped to explain these findings with their research.
The group showed that platelets lacking SXTBP5 failed to function correctly, and SXTBP5 was required for platelets to assist in normal clot formation. This suggests STXBP5 plays different roles in endothelial cells and platelets.
Specifically, the researchers found that STXBP5 interacts with core secretion machinery complexes and the platelet cytoskeleton.
And platelets from STXBP5-knockout mice exhibited defects in granule secretion. These platelets had altered granule cargo levels, despite having normal morphology and granule numbers.
Like Dr Lowenstein’s group, Dr Whiteheart and his colleagues observed dramatic bleeding and defective hemostasis in STXBP5-knockout mice. Transplant experiments suggested these defects were due to a loss of STXBP5 in bone marrow-derived cells. ![]()
Dr. Robert L. Barbieri’s Editor’s Picks September 2014
Editor in Chief Robert L. Barbieri, MD, provides an overview of three articles appearing in OBG Management’s September 2014 issue. Listen to his take on why these articles are of particular importance to women’s health professionals.
Access all of the articles in the September 2014 issue here.
Editor in Chief Robert L. Barbieri, MD, provides an overview of three articles appearing in OBG Management’s September 2014 issue. Listen to his take on why these articles are of particular importance to women’s health professionals.
Access all of the articles in the September 2014 issue here.
Editor in Chief Robert L. Barbieri, MD, provides an overview of three articles appearing in OBG Management’s September 2014 issue. Listen to his take on why these articles are of particular importance to women’s health professionals.
Access all of the articles in the September 2014 issue here.
Library can help cut cost of syringe pumps

Credit: Darren Baker
Researchers have published an open-source library of designs that could allow scientists to cut the cost of syringe pumps.
These syringe-pump designs can be made on a RepRap 3D printer for the cost of the plastic filament, and the designs are customizable.
“Not only have we designed a single syringe pump, we’ve designed all future syringe pumps,” said Joshua Pearce, PhD, of Michigan Technological University in Houghton.
“Scientists can customize the design of a pump for exactly what they are doing, just by changing a couple of numbers in the software.”
Dr Pearce and his colleagues described their work creating the library of designs in PLOS ONE. The hardware plans, designs, and source code for the pumps are available on Appropedia.
The library includes recipes for most parts of a syringe pump. Scientists will have to buy the small electric stepper motor that drives the liquid, some simple hardware, and the syringe itself.
The researchers also incorporated a low-cost, credit card-sized Raspberry Pi computer as a wireless controller.
“That way, you can link the syringe pump to the network, sit on a beach in Hawaii, and control your lab,” Dr Pearce said. “Plenty of people can have access, and you can run multiple experiments at the same time. Our entire single-pump system costs only $50 and can replace pumps that run between $250 and $2500.”
It costs more to make a double-pump system, about $120, but it replaces a commercial system that costs $5000.
And Dr Pearce believes someone will find a way to make the pumps even better.
“I’m sure someone will improve our designs and share their results with us and the rest of the community,” he said. “That’s the beauty and power of open source.” ![]()

Credit: Darren Baker
Researchers have published an open-source library of designs that could allow scientists to cut the cost of syringe pumps.
These syringe-pump designs can be made on a RepRap 3D printer for the cost of the plastic filament, and the designs are customizable.
“Not only have we designed a single syringe pump, we’ve designed all future syringe pumps,” said Joshua Pearce, PhD, of Michigan Technological University in Houghton.
“Scientists can customize the design of a pump for exactly what they are doing, just by changing a couple of numbers in the software.”
Dr Pearce and his colleagues described their work creating the library of designs in PLOS ONE. The hardware plans, designs, and source code for the pumps are available on Appropedia.
The library includes recipes for most parts of a syringe pump. Scientists will have to buy the small electric stepper motor that drives the liquid, some simple hardware, and the syringe itself.
The researchers also incorporated a low-cost, credit card-sized Raspberry Pi computer as a wireless controller.
“That way, you can link the syringe pump to the network, sit on a beach in Hawaii, and control your lab,” Dr Pearce said. “Plenty of people can have access, and you can run multiple experiments at the same time. Our entire single-pump system costs only $50 and can replace pumps that run between $250 and $2500.”
It costs more to make a double-pump system, about $120, but it replaces a commercial system that costs $5000.
And Dr Pearce believes someone will find a way to make the pumps even better.
“I’m sure someone will improve our designs and share their results with us and the rest of the community,” he said. “That’s the beauty and power of open source.” ![]()

Credit: Darren Baker
Researchers have published an open-source library of designs that could allow scientists to cut the cost of syringe pumps.
These syringe-pump designs can be made on a RepRap 3D printer for the cost of the plastic filament, and the designs are customizable.
“Not only have we designed a single syringe pump, we’ve designed all future syringe pumps,” said Joshua Pearce, PhD, of Michigan Technological University in Houghton.
“Scientists can customize the design of a pump for exactly what they are doing, just by changing a couple of numbers in the software.”
Dr Pearce and his colleagues described their work creating the library of designs in PLOS ONE. The hardware plans, designs, and source code for the pumps are available on Appropedia.
The library includes recipes for most parts of a syringe pump. Scientists will have to buy the small electric stepper motor that drives the liquid, some simple hardware, and the syringe itself.
The researchers also incorporated a low-cost, credit card-sized Raspberry Pi computer as a wireless controller.
“That way, you can link the syringe pump to the network, sit on a beach in Hawaii, and control your lab,” Dr Pearce said. “Plenty of people can have access, and you can run multiple experiments at the same time. Our entire single-pump system costs only $50 and can replace pumps that run between $250 and $2500.”
It costs more to make a double-pump system, about $120, but it replaces a commercial system that costs $5000.
And Dr Pearce believes someone will find a way to make the pumps even better.
“I’m sure someone will improve our designs and share their results with us and the rest of the community,” he said. “That’s the beauty and power of open source.” ![]()
Idelalisib approved to treat CLL, FL in EU

The European Commission has granted marketing authorization for the PI3K delta inhibitor idelalisib (Zydelig) to treat chronic lymphocytic leukemia (CLL) and follicular lymphoma (FL) in the European Union.
The drug is now approved for use in combination with rituximab for CLL patients who have received at least 1 prior therapy or as first-line treatment in CLL patients who have 17p deletion or TP53 mutation and are not eligible for chemo-immunotherapy.
Idelalisib is also approved as monotherapy for FL patients who were refractory to 2 prior lines of treatment.
These approvals are based on data from 2 clinical trials—Study 116 and Study 101-09.
Study 116: Idelalisib in CLL
This phase 3 trial was stopped early because idelalisib had a significant impact on progression-free survival.
The study included 220 CLL patients who could not receive chemotherapy. Half were randomized to receive idelalisib plus rituximab, and the other half were randomized to rituximab plus placebo.
Patients in the rituximab-idelalisib arm had a much higher overall response rate than patients in the rituximab-placebo arm—81% and 13%, respectively (P<0.001). There were no complete responses.
At 24 weeks, the rate of progression-free survival was 93% in the rituximab-idelalisib arm and 46% in the rituximab-placebo arm (P<0.001). The median progression-free survival was 5.5 months in the rituximab-placebo arm and not reached in the rituximab-idelalisib arm (P<0.001).
At 12 months, the overall survival rate was 92% in the rituximab-idelalisib arm and 80% in the rituximab-placebo arm (P=0.02).
Most adverse events, in either treatment arm, were grade 2 or lower. The most common events in the rituximab-idelalisib arm were pyrexia, fatigue, nausea, chills, and diarrhea. In the rituximab-placebo arm, the most common events were infusion-related reactions, fatigue, cough, nausea, and dyspnea.
There were more serious adverse events in the rituximab-idelalisib arm than in the rituximab-placebo arm—40% and 35%, respectively. The most frequent serious events were pneumonia, pyrexia, and febrile neutropenia (in both treatment arms).
Study 101-09: Idelalisib in FL
This phase 2 trial enrolled 125 patients with indolent non-Hodgkin lymphoma who were refractory to rituximab and chemotherapy containing an alkylating agent. Patients received idelalisib monotherapy.
Of the 72 subjects with FL, 54% achieved a response, and 8% had a complete response. The median duration of response was not reached (range, 0-14.8 months).
Improvements in survival or disease-related symptoms have not been established.
In all patients, the most common grade 3 or higher adverse events were neutropenia (27%), elevations in aminotransferase levels (13%), diarrhea (13%), and pneumonia (7%).
Idelalisib is under development by Gilead Sciences. The drug is already approved in the US for the aforementioned indications, as well as to treat small lymphocytic lymphoma. ![]()

The European Commission has granted marketing authorization for the PI3K delta inhibitor idelalisib (Zydelig) to treat chronic lymphocytic leukemia (CLL) and follicular lymphoma (FL) in the European Union.
The drug is now approved for use in combination with rituximab for CLL patients who have received at least 1 prior therapy or as first-line treatment in CLL patients who have 17p deletion or TP53 mutation and are not eligible for chemo-immunotherapy.
Idelalisib is also approved as monotherapy for FL patients who were refractory to 2 prior lines of treatment.
These approvals are based on data from 2 clinical trials—Study 116 and Study 101-09.
Study 116: Idelalisib in CLL
This phase 3 trial was stopped early because idelalisib had a significant impact on progression-free survival.
The study included 220 CLL patients who could not receive chemotherapy. Half were randomized to receive idelalisib plus rituximab, and the other half were randomized to rituximab plus placebo.
Patients in the rituximab-idelalisib arm had a much higher overall response rate than patients in the rituximab-placebo arm—81% and 13%, respectively (P<0.001). There were no complete responses.
At 24 weeks, the rate of progression-free survival was 93% in the rituximab-idelalisib arm and 46% in the rituximab-placebo arm (P<0.001). The median progression-free survival was 5.5 months in the rituximab-placebo arm and not reached in the rituximab-idelalisib arm (P<0.001).
At 12 months, the overall survival rate was 92% in the rituximab-idelalisib arm and 80% in the rituximab-placebo arm (P=0.02).
Most adverse events, in either treatment arm, were grade 2 or lower. The most common events in the rituximab-idelalisib arm were pyrexia, fatigue, nausea, chills, and diarrhea. In the rituximab-placebo arm, the most common events were infusion-related reactions, fatigue, cough, nausea, and dyspnea.
There were more serious adverse events in the rituximab-idelalisib arm than in the rituximab-placebo arm—40% and 35%, respectively. The most frequent serious events were pneumonia, pyrexia, and febrile neutropenia (in both treatment arms).
Study 101-09: Idelalisib in FL
This phase 2 trial enrolled 125 patients with indolent non-Hodgkin lymphoma who were refractory to rituximab and chemotherapy containing an alkylating agent. Patients received idelalisib monotherapy.
Of the 72 subjects with FL, 54% achieved a response, and 8% had a complete response. The median duration of response was not reached (range, 0-14.8 months).
Improvements in survival or disease-related symptoms have not been established.
In all patients, the most common grade 3 or higher adverse events were neutropenia (27%), elevations in aminotransferase levels (13%), diarrhea (13%), and pneumonia (7%).
Idelalisib is under development by Gilead Sciences. The drug is already approved in the US for the aforementioned indications, as well as to treat small lymphocytic lymphoma. ![]()

The European Commission has granted marketing authorization for the PI3K delta inhibitor idelalisib (Zydelig) to treat chronic lymphocytic leukemia (CLL) and follicular lymphoma (FL) in the European Union.
The drug is now approved for use in combination with rituximab for CLL patients who have received at least 1 prior therapy or as first-line treatment in CLL patients who have 17p deletion or TP53 mutation and are not eligible for chemo-immunotherapy.
Idelalisib is also approved as monotherapy for FL patients who were refractory to 2 prior lines of treatment.
These approvals are based on data from 2 clinical trials—Study 116 and Study 101-09.
Study 116: Idelalisib in CLL
This phase 3 trial was stopped early because idelalisib had a significant impact on progression-free survival.
The study included 220 CLL patients who could not receive chemotherapy. Half were randomized to receive idelalisib plus rituximab, and the other half were randomized to rituximab plus placebo.
Patients in the rituximab-idelalisib arm had a much higher overall response rate than patients in the rituximab-placebo arm—81% and 13%, respectively (P<0.001). There were no complete responses.
At 24 weeks, the rate of progression-free survival was 93% in the rituximab-idelalisib arm and 46% in the rituximab-placebo arm (P<0.001). The median progression-free survival was 5.5 months in the rituximab-placebo arm and not reached in the rituximab-idelalisib arm (P<0.001).
At 12 months, the overall survival rate was 92% in the rituximab-idelalisib arm and 80% in the rituximab-placebo arm (P=0.02).
Most adverse events, in either treatment arm, were grade 2 or lower. The most common events in the rituximab-idelalisib arm were pyrexia, fatigue, nausea, chills, and diarrhea. In the rituximab-placebo arm, the most common events were infusion-related reactions, fatigue, cough, nausea, and dyspnea.
There were more serious adverse events in the rituximab-idelalisib arm than in the rituximab-placebo arm—40% and 35%, respectively. The most frequent serious events were pneumonia, pyrexia, and febrile neutropenia (in both treatment arms).
Study 101-09: Idelalisib in FL
This phase 2 trial enrolled 125 patients with indolent non-Hodgkin lymphoma who were refractory to rituximab and chemotherapy containing an alkylating agent. Patients received idelalisib monotherapy.
Of the 72 subjects with FL, 54% achieved a response, and 8% had a complete response. The median duration of response was not reached (range, 0-14.8 months).
Improvements in survival or disease-related symptoms have not been established.
In all patients, the most common grade 3 or higher adverse events were neutropenia (27%), elevations in aminotransferase levels (13%), diarrhea (13%), and pneumonia (7%).
Idelalisib is under development by Gilead Sciences. The drug is already approved in the US for the aforementioned indications, as well as to treat small lymphocytic lymphoma. ![]()
Targeting the Kidneys to Improve Glycemic Control
A 37-year-old woman with a history of papillary carcinoma (status post total thyroidectomy 12 years ago, with negative recurrence) presents for a check-up. She also has polycystic ovarian syndrome (PCOS) with obesity and is taking metformin XR (one 500-mg tablet bid). Her visit is uneventful, and she leaves the office with an order for labwork.
Results indicate normal thyroid function and negative thyroglobulin. However, her serum glucose level is 350 mg/dL, so the patient is called and informed of the result. She denies polyphagia, polydipsia, and polyuria. Repeat blood work confirms overt hyperglycemia (320 mg/dL) with an A1C of 13%, undetectable C-peptide, and negative glutamic acid decarboxylase 65 (GAD65) and islet cell antibodies.
She is advised to increase her metformin dose (to two 500-mg tablets bid) and is started on insulin detemir (20 U every evening), with instructions to increase the latter by three units every two to three days until a target fasting glucose level of 100 to 140 mg/dL is achieved. She is also advised to follow a low-carbohydrate diet and increase her exercise.
The patient returns in two weeks for follow-up. She remains asymptomatic and has now increased her insulin detemir to 34 U bid (she started splitting the dosage after it reached 50 U/d). However, her glucose is still in the low 200s in the morning and the high 200s during the day (after lunch and dinner).
Her overt hyperglycemia is most likely a result of her longstanding insulin resistance, essential lack of b-cell function, and PCOS-associated obesity. Once diabetes from autoimmunity is ruled out by laboratory findings (negative antibodies) and clinical assessment (classic metabolic syndrome features), we focus on her glycemic control.
Even with nearly 70 U/d of insulin, the patient’s glycemic improvement is disappointing, suggesting significant insulin resistance and glucose toxicity. Living in an era with numerous classes of antidiabetic medications, we have lengthy discussions on treatment options. Canagliflozin, recently (at the time) approved, is included. The patient is interested in this new medication, and it is a reasonable choice to get her out of the glucotoxic phase.
After a discussion of benefits and potential adverse effects, she is placed on canagliflozin 100 mg/d. Her glucose log in one week shows fasting glucose values in the range of 140 to 160 mg/dL and postprandial glucose values in the 180s. As a result, she lowers her insulin to 25 U bid. Her renal panel shows a potassium level of 4.3 mEq/L (reference range, 3.5 to 5.3) and a glomerular filtration rate (GFR) of 103 mL/min/1.73 m2. She is advised to further increase her canagliflozin to 300 mg and slowly titrate her insulin down as needed, with a target fasting glucose level of 80 to 110 mg/dL and a postprandial target of 100 to 140 mg/dL.
What are SGLT2 inhibitors, and how do they work?
What are SGLT2 inhibitors, and how do they work?
Sodium-GLucose co-Transporter 2 (SGLT2) inhibitors are a new class of antihyperglycemic agent. The first, canagliflozin, was approved by the FDA in March 2013, followed by dapagliflozin (January 2014) and empagliflozin (August 2014).
As glucose is filtered through the nephrons of the kidney, about 90% is reabsorbed via SGLT2 in the proximal tubule (SGLT1 is responsible for the remaining 10%) so that glucose calories are not eliminated through urine.1 In a healthy person, the renal glucose threshold is about 180 mg/dL.1 When blood glucose exceeds this level, glucose is excreted into the urine. However, in diabetic patients, this threshold is higher due to the up-regulation of SGLT2s (and other glucose transporters), which worsens hyperglycemia.1 SGLT2 inhibitors will reset the threshold, which in turn will increase glucosuria and thereby lower serum glucose.1
SGLT2 inhibitors lower A1C by about 0.7% to 0.8%.2 Independent of other mechanisms such as the degree of b-cell function or insulin resistance, these agents can be used regardless of the duration of diabetes3 if the GFR is intact (≥ 45 mL/min/1.73 m2 for canagliflozin and empagliflozin, ≥ 60 mL/min/ 1.73 m2 for dapagliflozin).4,5
What are the risks and benefits associated with these agents?
What are the risks and benefits associated with these agents?
Modest weight loss is seen with the use of SGLT2 inhibitors. Initial weight loss is believed to be related to volume loss, but more sustained weight loss is thought to be from loss of fat mass.6 This is not surprising, as excreting glucose means excreting calories through urine.
Risk for hypoglycemia is extremely low, which makes this therapeutic class an attractive option. However, caution should be exercised when SGLT2 inhibitors are combined with other agents known to cause hypoglycemia (sulfonylureas and insulin).6
The most common adverse effect is genital mycotic infection. Women with a history of recurrent genital mycotic infection and uncircumcised men are at the greatest risk.6
Due to increased glycosuria, which results in an osmotic diuresis, modest blood pressure improvement has been seen (3 to 4 mm Hg systolic and 1 to 2 mm Hg diastolic7,8) in patients taking SGLT2 inhibitors, which is an additional benefit for hypertensive diabetic patients.6 On the other hand, use of SGLT2 inhibitors can also cause dehydration and volume depletion and can raise serum creatinine in patients who are already taking diuretics (particularly loop diuretics).6 Drug tolerance and adherence can be improved by advising patients to expect transient increased urination (approximately 135 to 350 mL/d increase from baseline5,9) and emphasizing the importance of good hydration and maintaining good genital hygiene.
A slight increase in LDL cholesterol was seen in clinical trials of the SGLT2 inhibitors, although this phenomenon is poorly understood. However, HDL cholesterol increased as well, maintaining the LDL:HDL ratio.6 No long-term cardiovascular outcome data are available at this time; as with any new antidiabetic medication, postmarketing studies, as required by the FDA, are currently ongoing.6
What are the options in this therapeutic category, and how are they distinct?
What are the options in this therapeutic category, and how are they distinct?
As mentioned previously, there are currently three SGLT2 inhibitors on the market: canagliflozin, dapagliflozin, and empagliflozin. There are subtle clinical differences among these three agents, which might direct the clinician’s choice.
First, canagliflozin is available in dosages of 100 and 300 mg. The starting dosage is 100 mg, which can be titrated to 300 mg in patients with a GFR ≥ 60 mL/min/1.73 m2 who require a greater glucose-lowering effect. Those with a GFR < 60 mL/min/1.73 m2 but ≥ 45 mL/min/1.73 m2 are limited to the 100-mg dosage. Dapagliflozin is available in 5-mg and 10-mg dosages, the former being the starting dosage. But dapagliflozin is not recommended in patients whose GFR is < 60 mL/min/1.73 m2.4
Empagliflozin is available in dosages of 10 and 25 mg. The starting dosage of 10 mg can be increased to 25 mg if the patient has not achieved his/her target glucose level. Either can be used in patients with a GFR ≥ 45 mL/min/1.73 m2.5
Second, hyperkalemia was seen in patients taking canagliflozin but not in those taking dapagliflozin or empagliflozin. Therefore, serum potassium should be monitored and caution used, especially when patients are being treated with potassium-sparing diuretics and/or ACE inhibitors or angiotensin II receptor blockers.6
Third, dapagliflozin carries a warning for bladder cancer, as higher rates of newly diagnosed bladder cancer were seen with this drug compared with placebo or comparator drugs (0.17% vs 0.03%, respectively).4 However, this finding may have resulted from a randomization imbalance of patients in the study, and further research is needed to clarify this risk.6 It is not recommended that dapagliflozin be used in patients with active or a history of bladder cancer at this time.
With these agents, there is a paradoxical rise in glucagon that increases endogenous glucose production from the liver.10 The mechanism is poorly understood, but it might be due to the body’s compensatory (survival) mechanism to “make up” the loss of glucose through urine by increasing hepatic gluconeogenesis.
Using an incretin agent, such as dipeptidyl peptidase 4 (DPP-4) inhibitors or glucagon-like peptide 1 (GLP-1) receptor agonists, in conjunction with an SGLT2 inhibitor, has been suggested as a way to potentiate the glucose-lowering effect, as it may attenuate the paradoxical rise in glucagon.10 Since the incretin class is weight neutral (DPP-4 inhibitors) or associated with weight loss (GLP-1 agonists), using incretins with SGLT2 inhibitors might produce more significant weight loss, which has numerous additional benefits for diabetic patients.
SGLT2 inhibitors are currently approved as an adjunct to diet and exercise for patients with type 2 diabetes. They are not approved for those with type 1 diabetes, although the mechanism of action of these drugs (which is independent of the b-cell function) might make them effective in this population. Active pilot studies of this patient population are in progress.11
Conclusion
In summary, SGLT2 inhibitors are an exciting new class of antidiabetic medication that offers a unique mechanism to lower serum glucose. It is the only medication that will actually remove glucose from the body; by contrast, all other existing antidiabetic medications move glucose within the body (to liver, fat, muscle, etc).
There is no curative medication for diabetes. But with an increasing diabetic population and an emphasis on individualizing antihyperglycemic regimens, we always welcome medications with novel mechanisms of action. Due to SLGT2 inhibitors’ recent approval, however, short-term and long-term adverse effects are unknown, and ongoing postmarketing surveillance should be closely followed.
References
1. Abdul-Ghani MA, DeFronzo RA. Inhibition of renal glucose reabsorption: a novel strategy for achieving glucose control in type 2 diabetes mellitus. Endocr Pract. 2008;14:782-790.
2. Berhan A, Barker A. Sodium glucose co-transport 2 inhibitors in the treatment of type 2 diabetes mellitus: a meta-analysis of randomized double-blind controlled trials. BMC Endocr Disord. 2013;13(1):58.
3. Wilding JP, Norwood P, T’joen C, et al. A study of dapagliflozin in patients with type 2 diabetes receiving high doses of insulin plus insulin sensitizers. Diabetes Care. 2009;32:1656-1662.
4. Taylor JR. Dapagliflozin offers differences from other SGLT2 inhibitors. Endocrine Today. May 2014.
5. Jardiance [package insert]. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals, Inc; 2014.
6. Bakris G, Fonseca VA, Peters AL, Wysham CH. Clinical perspectives on the role of the kidney in the pathophysiology of T2DM: emerging options for treatment [video series]. 2013. www.thedoctorschannel.com/view/the-kid ney-in-t2dm-cme-part-1/. Accessed September 12, 2014.
7. Vercruysse F. Efficacy and safety of canagliflozin in subjects with type 2 diabetes mellitus inadequately controlled with metformin plus sulphonylurea over 52 weeks [abstract 934]. Presented at the 49th European Association for the Study of Diabetes Annual Meeting: Barcelona; September 24, 2013.
8. Hach T. Empagliflozin improves glycaemic parameters and cardiovascular risk factors in patients with type 2 diabetes: pooled data from four pivotal phase III trials [abstract 943]. Presented at the 49th European Association for the Study of Diabetes Annual Meeting: Barcelona; September 24, 2013.
9. List JF, Woo V, Morales E, et al. Sodium-glucose co-transport inhibition with dapagliflozin in type 2 diabetes mellitus. Diabetes Care. 2009;32(4):650-657.
10. Merovci A, Solis-Herrera C, Daniele G, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014;124(5):2287.
11. Perkins BA, Cherney DZ, Partridge H, et al. Sodium-glucose cotransporter 2 inhibition and glycemic control in type 1 diabetes: results of an 8-week open-label proof-of-concept trial. Diabetes Care. 2014;37(5):1480-1483.
A 37-year-old woman with a history of papillary carcinoma (status post total thyroidectomy 12 years ago, with negative recurrence) presents for a check-up. She also has polycystic ovarian syndrome (PCOS) with obesity and is taking metformin XR (one 500-mg tablet bid). Her visit is uneventful, and she leaves the office with an order for labwork.
Results indicate normal thyroid function and negative thyroglobulin. However, her serum glucose level is 350 mg/dL, so the patient is called and informed of the result. She denies polyphagia, polydipsia, and polyuria. Repeat blood work confirms overt hyperglycemia (320 mg/dL) with an A1C of 13%, undetectable C-peptide, and negative glutamic acid decarboxylase 65 (GAD65) and islet cell antibodies.
She is advised to increase her metformin dose (to two 500-mg tablets bid) and is started on insulin detemir (20 U every evening), with instructions to increase the latter by three units every two to three days until a target fasting glucose level of 100 to 140 mg/dL is achieved. She is also advised to follow a low-carbohydrate diet and increase her exercise.
The patient returns in two weeks for follow-up. She remains asymptomatic and has now increased her insulin detemir to 34 U bid (she started splitting the dosage after it reached 50 U/d). However, her glucose is still in the low 200s in the morning and the high 200s during the day (after lunch and dinner).
Her overt hyperglycemia is most likely a result of her longstanding insulin resistance, essential lack of b-cell function, and PCOS-associated obesity. Once diabetes from autoimmunity is ruled out by laboratory findings (negative antibodies) and clinical assessment (classic metabolic syndrome features), we focus on her glycemic control.
Even with nearly 70 U/d of insulin, the patient’s glycemic improvement is disappointing, suggesting significant insulin resistance and glucose toxicity. Living in an era with numerous classes of antidiabetic medications, we have lengthy discussions on treatment options. Canagliflozin, recently (at the time) approved, is included. The patient is interested in this new medication, and it is a reasonable choice to get her out of the glucotoxic phase.
After a discussion of benefits and potential adverse effects, she is placed on canagliflozin 100 mg/d. Her glucose log in one week shows fasting glucose values in the range of 140 to 160 mg/dL and postprandial glucose values in the 180s. As a result, she lowers her insulin to 25 U bid. Her renal panel shows a potassium level of 4.3 mEq/L (reference range, 3.5 to 5.3) and a glomerular filtration rate (GFR) of 103 mL/min/1.73 m2. She is advised to further increase her canagliflozin to 300 mg and slowly titrate her insulin down as needed, with a target fasting glucose level of 80 to 110 mg/dL and a postprandial target of 100 to 140 mg/dL.
What are SGLT2 inhibitors, and how do they work?
What are SGLT2 inhibitors, and how do they work?
Sodium-GLucose co-Transporter 2 (SGLT2) inhibitors are a new class of antihyperglycemic agent. The first, canagliflozin, was approved by the FDA in March 2013, followed by dapagliflozin (January 2014) and empagliflozin (August 2014).
As glucose is filtered through the nephrons of the kidney, about 90% is reabsorbed via SGLT2 in the proximal tubule (SGLT1 is responsible for the remaining 10%) so that glucose calories are not eliminated through urine.1 In a healthy person, the renal glucose threshold is about 180 mg/dL.1 When blood glucose exceeds this level, glucose is excreted into the urine. However, in diabetic patients, this threshold is higher due to the up-regulation of SGLT2s (and other glucose transporters), which worsens hyperglycemia.1 SGLT2 inhibitors will reset the threshold, which in turn will increase glucosuria and thereby lower serum glucose.1
SGLT2 inhibitors lower A1C by about 0.7% to 0.8%.2 Independent of other mechanisms such as the degree of b-cell function or insulin resistance, these agents can be used regardless of the duration of diabetes3 if the GFR is intact (≥ 45 mL/min/1.73 m2 for canagliflozin and empagliflozin, ≥ 60 mL/min/ 1.73 m2 for dapagliflozin).4,5
What are the risks and benefits associated with these agents?
What are the risks and benefits associated with these agents?
Modest weight loss is seen with the use of SGLT2 inhibitors. Initial weight loss is believed to be related to volume loss, but more sustained weight loss is thought to be from loss of fat mass.6 This is not surprising, as excreting glucose means excreting calories through urine.
Risk for hypoglycemia is extremely low, which makes this therapeutic class an attractive option. However, caution should be exercised when SGLT2 inhibitors are combined with other agents known to cause hypoglycemia (sulfonylureas and insulin).6
The most common adverse effect is genital mycotic infection. Women with a history of recurrent genital mycotic infection and uncircumcised men are at the greatest risk.6
Due to increased glycosuria, which results in an osmotic diuresis, modest blood pressure improvement has been seen (3 to 4 mm Hg systolic and 1 to 2 mm Hg diastolic7,8) in patients taking SGLT2 inhibitors, which is an additional benefit for hypertensive diabetic patients.6 On the other hand, use of SGLT2 inhibitors can also cause dehydration and volume depletion and can raise serum creatinine in patients who are already taking diuretics (particularly loop diuretics).6 Drug tolerance and adherence can be improved by advising patients to expect transient increased urination (approximately 135 to 350 mL/d increase from baseline5,9) and emphasizing the importance of good hydration and maintaining good genital hygiene.
A slight increase in LDL cholesterol was seen in clinical trials of the SGLT2 inhibitors, although this phenomenon is poorly understood. However, HDL cholesterol increased as well, maintaining the LDL:HDL ratio.6 No long-term cardiovascular outcome data are available at this time; as with any new antidiabetic medication, postmarketing studies, as required by the FDA, are currently ongoing.6
What are the options in this therapeutic category, and how are they distinct?
What are the options in this therapeutic category, and how are they distinct?
As mentioned previously, there are currently three SGLT2 inhibitors on the market: canagliflozin, dapagliflozin, and empagliflozin. There are subtle clinical differences among these three agents, which might direct the clinician’s choice.
First, canagliflozin is available in dosages of 100 and 300 mg. The starting dosage is 100 mg, which can be titrated to 300 mg in patients with a GFR ≥ 60 mL/min/1.73 m2 who require a greater glucose-lowering effect. Those with a GFR < 60 mL/min/1.73 m2 but ≥ 45 mL/min/1.73 m2 are limited to the 100-mg dosage. Dapagliflozin is available in 5-mg and 10-mg dosages, the former being the starting dosage. But dapagliflozin is not recommended in patients whose GFR is < 60 mL/min/1.73 m2.4
Empagliflozin is available in dosages of 10 and 25 mg. The starting dosage of 10 mg can be increased to 25 mg if the patient has not achieved his/her target glucose level. Either can be used in patients with a GFR ≥ 45 mL/min/1.73 m2.5
Second, hyperkalemia was seen in patients taking canagliflozin but not in those taking dapagliflozin or empagliflozin. Therefore, serum potassium should be monitored and caution used, especially when patients are being treated with potassium-sparing diuretics and/or ACE inhibitors or angiotensin II receptor blockers.6
Third, dapagliflozin carries a warning for bladder cancer, as higher rates of newly diagnosed bladder cancer were seen with this drug compared with placebo or comparator drugs (0.17% vs 0.03%, respectively).4 However, this finding may have resulted from a randomization imbalance of patients in the study, and further research is needed to clarify this risk.6 It is not recommended that dapagliflozin be used in patients with active or a history of bladder cancer at this time.
With these agents, there is a paradoxical rise in glucagon that increases endogenous glucose production from the liver.10 The mechanism is poorly understood, but it might be due to the body’s compensatory (survival) mechanism to “make up” the loss of glucose through urine by increasing hepatic gluconeogenesis.
Using an incretin agent, such as dipeptidyl peptidase 4 (DPP-4) inhibitors or glucagon-like peptide 1 (GLP-1) receptor agonists, in conjunction with an SGLT2 inhibitor, has been suggested as a way to potentiate the glucose-lowering effect, as it may attenuate the paradoxical rise in glucagon.10 Since the incretin class is weight neutral (DPP-4 inhibitors) or associated with weight loss (GLP-1 agonists), using incretins with SGLT2 inhibitors might produce more significant weight loss, which has numerous additional benefits for diabetic patients.
SGLT2 inhibitors are currently approved as an adjunct to diet and exercise for patients with type 2 diabetes. They are not approved for those with type 1 diabetes, although the mechanism of action of these drugs (which is independent of the b-cell function) might make them effective in this population. Active pilot studies of this patient population are in progress.11
Conclusion
In summary, SGLT2 inhibitors are an exciting new class of antidiabetic medication that offers a unique mechanism to lower serum glucose. It is the only medication that will actually remove glucose from the body; by contrast, all other existing antidiabetic medications move glucose within the body (to liver, fat, muscle, etc).
There is no curative medication for diabetes. But with an increasing diabetic population and an emphasis on individualizing antihyperglycemic regimens, we always welcome medications with novel mechanisms of action. Due to SLGT2 inhibitors’ recent approval, however, short-term and long-term adverse effects are unknown, and ongoing postmarketing surveillance should be closely followed.
References
1. Abdul-Ghani MA, DeFronzo RA. Inhibition of renal glucose reabsorption: a novel strategy for achieving glucose control in type 2 diabetes mellitus. Endocr Pract. 2008;14:782-790.
2. Berhan A, Barker A. Sodium glucose co-transport 2 inhibitors in the treatment of type 2 diabetes mellitus: a meta-analysis of randomized double-blind controlled trials. BMC Endocr Disord. 2013;13(1):58.
3. Wilding JP, Norwood P, T’joen C, et al. A study of dapagliflozin in patients with type 2 diabetes receiving high doses of insulin plus insulin sensitizers. Diabetes Care. 2009;32:1656-1662.
4. Taylor JR. Dapagliflozin offers differences from other SGLT2 inhibitors. Endocrine Today. May 2014.
5. Jardiance [package insert]. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals, Inc; 2014.
6. Bakris G, Fonseca VA, Peters AL, Wysham CH. Clinical perspectives on the role of the kidney in the pathophysiology of T2DM: emerging options for treatment [video series]. 2013. www.thedoctorschannel.com/view/the-kid ney-in-t2dm-cme-part-1/. Accessed September 12, 2014.
7. Vercruysse F. Efficacy and safety of canagliflozin in subjects with type 2 diabetes mellitus inadequately controlled with metformin plus sulphonylurea over 52 weeks [abstract 934]. Presented at the 49th European Association for the Study of Diabetes Annual Meeting: Barcelona; September 24, 2013.
8. Hach T. Empagliflozin improves glycaemic parameters and cardiovascular risk factors in patients with type 2 diabetes: pooled data from four pivotal phase III trials [abstract 943]. Presented at the 49th European Association for the Study of Diabetes Annual Meeting: Barcelona; September 24, 2013.
9. List JF, Woo V, Morales E, et al. Sodium-glucose co-transport inhibition with dapagliflozin in type 2 diabetes mellitus. Diabetes Care. 2009;32(4):650-657.
10. Merovci A, Solis-Herrera C, Daniele G, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014;124(5):2287.
11. Perkins BA, Cherney DZ, Partridge H, et al. Sodium-glucose cotransporter 2 inhibition and glycemic control in type 1 diabetes: results of an 8-week open-label proof-of-concept trial. Diabetes Care. 2014;37(5):1480-1483.
A 37-year-old woman with a history of papillary carcinoma (status post total thyroidectomy 12 years ago, with negative recurrence) presents for a check-up. She also has polycystic ovarian syndrome (PCOS) with obesity and is taking metformin XR (one 500-mg tablet bid). Her visit is uneventful, and she leaves the office with an order for labwork.
Results indicate normal thyroid function and negative thyroglobulin. However, her serum glucose level is 350 mg/dL, so the patient is called and informed of the result. She denies polyphagia, polydipsia, and polyuria. Repeat blood work confirms overt hyperglycemia (320 mg/dL) with an A1C of 13%, undetectable C-peptide, and negative glutamic acid decarboxylase 65 (GAD65) and islet cell antibodies.
She is advised to increase her metformin dose (to two 500-mg tablets bid) and is started on insulin detemir (20 U every evening), with instructions to increase the latter by three units every two to three days until a target fasting glucose level of 100 to 140 mg/dL is achieved. She is also advised to follow a low-carbohydrate diet and increase her exercise.
The patient returns in two weeks for follow-up. She remains asymptomatic and has now increased her insulin detemir to 34 U bid (she started splitting the dosage after it reached 50 U/d). However, her glucose is still in the low 200s in the morning and the high 200s during the day (after lunch and dinner).
Her overt hyperglycemia is most likely a result of her longstanding insulin resistance, essential lack of b-cell function, and PCOS-associated obesity. Once diabetes from autoimmunity is ruled out by laboratory findings (negative antibodies) and clinical assessment (classic metabolic syndrome features), we focus on her glycemic control.
Even with nearly 70 U/d of insulin, the patient’s glycemic improvement is disappointing, suggesting significant insulin resistance and glucose toxicity. Living in an era with numerous classes of antidiabetic medications, we have lengthy discussions on treatment options. Canagliflozin, recently (at the time) approved, is included. The patient is interested in this new medication, and it is a reasonable choice to get her out of the glucotoxic phase.
After a discussion of benefits and potential adverse effects, she is placed on canagliflozin 100 mg/d. Her glucose log in one week shows fasting glucose values in the range of 140 to 160 mg/dL and postprandial glucose values in the 180s. As a result, she lowers her insulin to 25 U bid. Her renal panel shows a potassium level of 4.3 mEq/L (reference range, 3.5 to 5.3) and a glomerular filtration rate (GFR) of 103 mL/min/1.73 m2. She is advised to further increase her canagliflozin to 300 mg and slowly titrate her insulin down as needed, with a target fasting glucose level of 80 to 110 mg/dL and a postprandial target of 100 to 140 mg/dL.
What are SGLT2 inhibitors, and how do they work?
What are SGLT2 inhibitors, and how do they work?
Sodium-GLucose co-Transporter 2 (SGLT2) inhibitors are a new class of antihyperglycemic agent. The first, canagliflozin, was approved by the FDA in March 2013, followed by dapagliflozin (January 2014) and empagliflozin (August 2014).
As glucose is filtered through the nephrons of the kidney, about 90% is reabsorbed via SGLT2 in the proximal tubule (SGLT1 is responsible for the remaining 10%) so that glucose calories are not eliminated through urine.1 In a healthy person, the renal glucose threshold is about 180 mg/dL.1 When blood glucose exceeds this level, glucose is excreted into the urine. However, in diabetic patients, this threshold is higher due to the up-regulation of SGLT2s (and other glucose transporters), which worsens hyperglycemia.1 SGLT2 inhibitors will reset the threshold, which in turn will increase glucosuria and thereby lower serum glucose.1
SGLT2 inhibitors lower A1C by about 0.7% to 0.8%.2 Independent of other mechanisms such as the degree of b-cell function or insulin resistance, these agents can be used regardless of the duration of diabetes3 if the GFR is intact (≥ 45 mL/min/1.73 m2 for canagliflozin and empagliflozin, ≥ 60 mL/min/ 1.73 m2 for dapagliflozin).4,5
What are the risks and benefits associated with these agents?
What are the risks and benefits associated with these agents?
Modest weight loss is seen with the use of SGLT2 inhibitors. Initial weight loss is believed to be related to volume loss, but more sustained weight loss is thought to be from loss of fat mass.6 This is not surprising, as excreting glucose means excreting calories through urine.
Risk for hypoglycemia is extremely low, which makes this therapeutic class an attractive option. However, caution should be exercised when SGLT2 inhibitors are combined with other agents known to cause hypoglycemia (sulfonylureas and insulin).6
The most common adverse effect is genital mycotic infection. Women with a history of recurrent genital mycotic infection and uncircumcised men are at the greatest risk.6
Due to increased glycosuria, which results in an osmotic diuresis, modest blood pressure improvement has been seen (3 to 4 mm Hg systolic and 1 to 2 mm Hg diastolic7,8) in patients taking SGLT2 inhibitors, which is an additional benefit for hypertensive diabetic patients.6 On the other hand, use of SGLT2 inhibitors can also cause dehydration and volume depletion and can raise serum creatinine in patients who are already taking diuretics (particularly loop diuretics).6 Drug tolerance and adherence can be improved by advising patients to expect transient increased urination (approximately 135 to 350 mL/d increase from baseline5,9) and emphasizing the importance of good hydration and maintaining good genital hygiene.
A slight increase in LDL cholesterol was seen in clinical trials of the SGLT2 inhibitors, although this phenomenon is poorly understood. However, HDL cholesterol increased as well, maintaining the LDL:HDL ratio.6 No long-term cardiovascular outcome data are available at this time; as with any new antidiabetic medication, postmarketing studies, as required by the FDA, are currently ongoing.6
What are the options in this therapeutic category, and how are they distinct?
What are the options in this therapeutic category, and how are they distinct?
As mentioned previously, there are currently three SGLT2 inhibitors on the market: canagliflozin, dapagliflozin, and empagliflozin. There are subtle clinical differences among these three agents, which might direct the clinician’s choice.
First, canagliflozin is available in dosages of 100 and 300 mg. The starting dosage is 100 mg, which can be titrated to 300 mg in patients with a GFR ≥ 60 mL/min/1.73 m2 who require a greater glucose-lowering effect. Those with a GFR < 60 mL/min/1.73 m2 but ≥ 45 mL/min/1.73 m2 are limited to the 100-mg dosage. Dapagliflozin is available in 5-mg and 10-mg dosages, the former being the starting dosage. But dapagliflozin is not recommended in patients whose GFR is < 60 mL/min/1.73 m2.4
Empagliflozin is available in dosages of 10 and 25 mg. The starting dosage of 10 mg can be increased to 25 mg if the patient has not achieved his/her target glucose level. Either can be used in patients with a GFR ≥ 45 mL/min/1.73 m2.5
Second, hyperkalemia was seen in patients taking canagliflozin but not in those taking dapagliflozin or empagliflozin. Therefore, serum potassium should be monitored and caution used, especially when patients are being treated with potassium-sparing diuretics and/or ACE inhibitors or angiotensin II receptor blockers.6
Third, dapagliflozin carries a warning for bladder cancer, as higher rates of newly diagnosed bladder cancer were seen with this drug compared with placebo or comparator drugs (0.17% vs 0.03%, respectively).4 However, this finding may have resulted from a randomization imbalance of patients in the study, and further research is needed to clarify this risk.6 It is not recommended that dapagliflozin be used in patients with active or a history of bladder cancer at this time.
With these agents, there is a paradoxical rise in glucagon that increases endogenous glucose production from the liver.10 The mechanism is poorly understood, but it might be due to the body’s compensatory (survival) mechanism to “make up” the loss of glucose through urine by increasing hepatic gluconeogenesis.
Using an incretin agent, such as dipeptidyl peptidase 4 (DPP-4) inhibitors or glucagon-like peptide 1 (GLP-1) receptor agonists, in conjunction with an SGLT2 inhibitor, has been suggested as a way to potentiate the glucose-lowering effect, as it may attenuate the paradoxical rise in glucagon.10 Since the incretin class is weight neutral (DPP-4 inhibitors) or associated with weight loss (GLP-1 agonists), using incretins with SGLT2 inhibitors might produce more significant weight loss, which has numerous additional benefits for diabetic patients.
SGLT2 inhibitors are currently approved as an adjunct to diet and exercise for patients with type 2 diabetes. They are not approved for those with type 1 diabetes, although the mechanism of action of these drugs (which is independent of the b-cell function) might make them effective in this population. Active pilot studies of this patient population are in progress.11
Conclusion
In summary, SGLT2 inhibitors are an exciting new class of antidiabetic medication that offers a unique mechanism to lower serum glucose. It is the only medication that will actually remove glucose from the body; by contrast, all other existing antidiabetic medications move glucose within the body (to liver, fat, muscle, etc).
There is no curative medication for diabetes. But with an increasing diabetic population and an emphasis on individualizing antihyperglycemic regimens, we always welcome medications with novel mechanisms of action. Due to SLGT2 inhibitors’ recent approval, however, short-term and long-term adverse effects are unknown, and ongoing postmarketing surveillance should be closely followed.
References
1. Abdul-Ghani MA, DeFronzo RA. Inhibition of renal glucose reabsorption: a novel strategy for achieving glucose control in type 2 diabetes mellitus. Endocr Pract. 2008;14:782-790.
2. Berhan A, Barker A. Sodium glucose co-transport 2 inhibitors in the treatment of type 2 diabetes mellitus: a meta-analysis of randomized double-blind controlled trials. BMC Endocr Disord. 2013;13(1):58.
3. Wilding JP, Norwood P, T’joen C, et al. A study of dapagliflozin in patients with type 2 diabetes receiving high doses of insulin plus insulin sensitizers. Diabetes Care. 2009;32:1656-1662.
4. Taylor JR. Dapagliflozin offers differences from other SGLT2 inhibitors. Endocrine Today. May 2014.
5. Jardiance [package insert]. Ridgefield, CT: Boehringer Ingelheim Pharmaceuticals, Inc; 2014.
6. Bakris G, Fonseca VA, Peters AL, Wysham CH. Clinical perspectives on the role of the kidney in the pathophysiology of T2DM: emerging options for treatment [video series]. 2013. www.thedoctorschannel.com/view/the-kid ney-in-t2dm-cme-part-1/. Accessed September 12, 2014.
7. Vercruysse F. Efficacy and safety of canagliflozin in subjects with type 2 diabetes mellitus inadequately controlled with metformin plus sulphonylurea over 52 weeks [abstract 934]. Presented at the 49th European Association for the Study of Diabetes Annual Meeting: Barcelona; September 24, 2013.
8. Hach T. Empagliflozin improves glycaemic parameters and cardiovascular risk factors in patients with type 2 diabetes: pooled data from four pivotal phase III trials [abstract 943]. Presented at the 49th European Association for the Study of Diabetes Annual Meeting: Barcelona; September 24, 2013.
9. List JF, Woo V, Morales E, et al. Sodium-glucose co-transport inhibition with dapagliflozin in type 2 diabetes mellitus. Diabetes Care. 2009;32(4):650-657.
10. Merovci A, Solis-Herrera C, Daniele G, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014;124(5):2287.
11. Perkins BA, Cherney DZ, Partridge H, et al. Sodium-glucose cotransporter 2 inhibition and glycemic control in type 1 diabetes: results of an 8-week open-label proof-of-concept trial. Diabetes Care. 2014;37(5):1480-1483.
Nausea, Vomiting, and Worsening Pain
ANSWER
The radiograph shows multiple stacked dilated loops of small bowel. The colon does not appear distended. (A nasogastric tube is also present, and there are degenerative changes in the spine.) Such a finding is typically associated with at least a partial small bowel obstruction, since no definite air fluid levels are noted.
The patient was admitted and made npo. Nasogastric decompression was started, and general surgery consultation was obtained.
ANSWER
The radiograph shows multiple stacked dilated loops of small bowel. The colon does not appear distended. (A nasogastric tube is also present, and there are degenerative changes in the spine.) Such a finding is typically associated with at least a partial small bowel obstruction, since no definite air fluid levels are noted.
The patient was admitted and made npo. Nasogastric decompression was started, and general surgery consultation was obtained.
ANSWER
The radiograph shows multiple stacked dilated loops of small bowel. The colon does not appear distended. (A nasogastric tube is also present, and there are degenerative changes in the spine.) Such a finding is typically associated with at least a partial small bowel obstruction, since no definite air fluid levels are noted.
The patient was admitted and made npo. Nasogastric decompression was started, and general surgery consultation was obtained.

A 75-year-old woman presents to the emergency department with a three-day history of abdominal pain. She does not recall eating anything unusual. She reports having nausea and vomiting and states that her pain is progressively worsening. Her medical history is significant for hypertension. Surgical history is significant for previous cholecystectomy and total abdominal hysterectomy. She is afebrile, and her vital signs are within normal limits. Her abdomen is soft and diffusely tender, with slightly decreased bowel sounds. No rebound or guarding is present. The rest of her physical examination overall is within normal limits. During the exam, she experiences a couple episodes of bilious vomiting. You order some laboratory studies as well as an abdominal radiograph (shown). What is your impression?