User login
FDA study suggests dabigatran’s pros outweigh cons

Credit: Darren Baker
After reviewing data from more than 134,000 patients, researchers at the US Food and Drug Administration (FDA) have concluded that dabigatran has a favorable risk-benefit profile.
Their research showed that, compared to warfarin, dabigatran decreased the risk of stroke, death, and intracranial hemorrhage in patients with atrial fibrillation.
On the other hand, dabigatran increased the risk of gastrointestinal bleeding, and the risk of myocardial infarction was similar for the 2 drugs.
This study was part of the FDA’s ongoing review of dabigatran. The agency has been investigating the safety of dabigatran since 2011, following reports of serious bleeding events associated with the drug.
A previous FDA study, announced in 2012, suggested dabigatran does not pose an increased risk of serious bleeding when compared to warfarin. But other studies have provided conflicting results, so the FDA decided to conduct additional research.
This study included information from more than 134,000 Medicare patients, aged 65 years or older. The researchers compared dabigatran and warfarin, evaluating the risk of ischemic stroke, intracranial hemorrhage, major gastrointestinal bleeding, myocardial infarction, and death.
The FDA said this study is based on a much larger and older patient population than those used in the agency’s earlier review of post-market data, and researchers employed a more sophisticated analytical method to capture and analyze the events of concern.
The data showed that, among new users of anticoagulants, dabigatran was associated with a lower risk of ischemic stroke, intracranial hemorrhage, and death, when compared to warfarin.
The incidence rate of ischemic stroke per 1000 person-years was 11.3 among dabigatran users and 13.9 among warfarin users (hazard ratio [HR]=0.80).
The incidence of intracranial hemorrhage was 3.3 and 9.6, respectively (HR=0.34). And the incidence of death was 32.6 and 37.8, respectively (HR=0.86).
The study also showed an increased risk of major gastrointestinal bleeding with the use of dabigatran compared to warfarin. The incidence rate per 1000 person-years was 34.2 and 26.5, respectively (HR=1.28).
The risk of myocardial infarction was similar for the 2 drugs. The incidence rate per 1000 person-years was 15.7 for dabigatran users and 16.9 for warfarin users (HR=0.92).
These results, except with regard to myocardial infarction, are consistent with the clinical trial results that provided the basis for dabigatran’s approval.
The FDA said these findings suggest dabigatran has a favorable risk-benefit profile, so the agency has made no changes to the drug’s current label or recommendations for use.
The FDA is planning to publish detailed data from this study. Until then, some information is available on the agency’s website.
The FDA said it will continue to investigate the reasons for differences in major gastrointestinal bleeding rates for dabigatran and warfarin. And it will continue reviewing anticoagulant use and the risk of bleeding. ![]()

Credit: Darren Baker
After reviewing data from more than 134,000 patients, researchers at the US Food and Drug Administration (FDA) have concluded that dabigatran has a favorable risk-benefit profile.
Their research showed that, compared to warfarin, dabigatran decreased the risk of stroke, death, and intracranial hemorrhage in patients with atrial fibrillation.
On the other hand, dabigatran increased the risk of gastrointestinal bleeding, and the risk of myocardial infarction was similar for the 2 drugs.
This study was part of the FDA’s ongoing review of dabigatran. The agency has been investigating the safety of dabigatran since 2011, following reports of serious bleeding events associated with the drug.
A previous FDA study, announced in 2012, suggested dabigatran does not pose an increased risk of serious bleeding when compared to warfarin. But other studies have provided conflicting results, so the FDA decided to conduct additional research.
This study included information from more than 134,000 Medicare patients, aged 65 years or older. The researchers compared dabigatran and warfarin, evaluating the risk of ischemic stroke, intracranial hemorrhage, major gastrointestinal bleeding, myocardial infarction, and death.
The FDA said this study is based on a much larger and older patient population than those used in the agency’s earlier review of post-market data, and researchers employed a more sophisticated analytical method to capture and analyze the events of concern.
The data showed that, among new users of anticoagulants, dabigatran was associated with a lower risk of ischemic stroke, intracranial hemorrhage, and death, when compared to warfarin.
The incidence rate of ischemic stroke per 1000 person-years was 11.3 among dabigatran users and 13.9 among warfarin users (hazard ratio [HR]=0.80).
The incidence of intracranial hemorrhage was 3.3 and 9.6, respectively (HR=0.34). And the incidence of death was 32.6 and 37.8, respectively (HR=0.86).
The study also showed an increased risk of major gastrointestinal bleeding with the use of dabigatran compared to warfarin. The incidence rate per 1000 person-years was 34.2 and 26.5, respectively (HR=1.28).
The risk of myocardial infarction was similar for the 2 drugs. The incidence rate per 1000 person-years was 15.7 for dabigatran users and 16.9 for warfarin users (HR=0.92).
These results, except with regard to myocardial infarction, are consistent with the clinical trial results that provided the basis for dabigatran’s approval.
The FDA said these findings suggest dabigatran has a favorable risk-benefit profile, so the agency has made no changes to the drug’s current label or recommendations for use.
The FDA is planning to publish detailed data from this study. Until then, some information is available on the agency’s website.
The FDA said it will continue to investigate the reasons for differences in major gastrointestinal bleeding rates for dabigatran and warfarin. And it will continue reviewing anticoagulant use and the risk of bleeding. ![]()

Credit: Darren Baker
After reviewing data from more than 134,000 patients, researchers at the US Food and Drug Administration (FDA) have concluded that dabigatran has a favorable risk-benefit profile.
Their research showed that, compared to warfarin, dabigatran decreased the risk of stroke, death, and intracranial hemorrhage in patients with atrial fibrillation.
On the other hand, dabigatran increased the risk of gastrointestinal bleeding, and the risk of myocardial infarction was similar for the 2 drugs.
This study was part of the FDA’s ongoing review of dabigatran. The agency has been investigating the safety of dabigatran since 2011, following reports of serious bleeding events associated with the drug.
A previous FDA study, announced in 2012, suggested dabigatran does not pose an increased risk of serious bleeding when compared to warfarin. But other studies have provided conflicting results, so the FDA decided to conduct additional research.
This study included information from more than 134,000 Medicare patients, aged 65 years or older. The researchers compared dabigatran and warfarin, evaluating the risk of ischemic stroke, intracranial hemorrhage, major gastrointestinal bleeding, myocardial infarction, and death.
The FDA said this study is based on a much larger and older patient population than those used in the agency’s earlier review of post-market data, and researchers employed a more sophisticated analytical method to capture and analyze the events of concern.
The data showed that, among new users of anticoagulants, dabigatran was associated with a lower risk of ischemic stroke, intracranial hemorrhage, and death, when compared to warfarin.
The incidence rate of ischemic stroke per 1000 person-years was 11.3 among dabigatran users and 13.9 among warfarin users (hazard ratio [HR]=0.80).
The incidence of intracranial hemorrhage was 3.3 and 9.6, respectively (HR=0.34). And the incidence of death was 32.6 and 37.8, respectively (HR=0.86).
The study also showed an increased risk of major gastrointestinal bleeding with the use of dabigatran compared to warfarin. The incidence rate per 1000 person-years was 34.2 and 26.5, respectively (HR=1.28).
The risk of myocardial infarction was similar for the 2 drugs. The incidence rate per 1000 person-years was 15.7 for dabigatran users and 16.9 for warfarin users (HR=0.92).
These results, except with regard to myocardial infarction, are consistent with the clinical trial results that provided the basis for dabigatran’s approval.
The FDA said these findings suggest dabigatran has a favorable risk-benefit profile, so the agency has made no changes to the drug’s current label or recommendations for use.
The FDA is planning to publish detailed data from this study. Until then, some information is available on the agency’s website.
The FDA said it will continue to investigate the reasons for differences in major gastrointestinal bleeding rates for dabigatran and warfarin. And it will continue reviewing anticoagulant use and the risk of bleeding. ![]()
Study links warfarin dosing and dementia

SAN FRANSICO—New research suggests bleeds and thrombosis are not the only adverse effects of improper warfarin dosing.
The study showed an increased risk of dementia among patients with atrial fibrillation whose warfarin doses were outside the therapeutic range for an extended period of time.
Jared Bunch, MD, of the Intermountain Medical Center Heart Institute in Murray, Utah, and his colleagues presented this finding at the 2014 Annual Heart Rhythm Society Scientific Session (PO05-169).
Previous research suggested that patients with atrial fibrillation had an increased risk of developing dementia. But the cause of that association
was unknown.
“[W]e now know that if warfarin doses are consistently too high or too low, one of the long-term consequences can be brain damage,” Dr Bunch said. “This points to the possibility that dementia in atrial fibrillation patients is partly due to small, repetitive clots and/or bleeds in the brain.”
To make this connection, the researchers analyzed data from 2693 atrial fibrillation patients receiving warfarin. The team evaluated the relationship between dementia and the percentage of time that patients’ warfarin doses were within the therapeutic range (international normalized ratio of 2 to 3).
In all, 4.1% of patients (n=111) were diagnosed with dementia. This included senile dementia (n=37, 1.4%), vascular dementia (n=8, 0.3%), and Alzheimer’s dementia (n=66, 2.4%).
The researchers’ analysis (adjusted for the risk of stroke and bleeding) revealed that the more time a patient’s warfarin dosages were outside the therapeutic range, the greater his risk of developing dementia.
Specifically, patients within the therapeutic range less than 25% of the time were 4.6 times more likely to develop dementia than patients within range more than 75% of the time.
Patients within the therapeutic range 25% to 50% of the time were 4.1 times more likely to develop dementia. And patients within the therapeutic range 51% to 75% of the time were 2.5 times more likely to develop dementia.
“Our results from the study tell us 2 things,” Dr Bunch said. “With careful use of anticoagulation medications, the dementia risk can be reduced.
Patients on warfarin need very close follow-up in specialized anticoagulation centers, if possible, to ensure their blood levels are within the recommended levels more often.”
“Second, these results also point to a potential new long-term consequence of dependency on long-term anticoagulation medications. In this regard, stroke prevention therapies do not require long-term anticoagulation medications, and reducing the use of these drugs will hopefully lower
dementia risk.” ![]()

SAN FRANSICO—New research suggests bleeds and thrombosis are not the only adverse effects of improper warfarin dosing.
The study showed an increased risk of dementia among patients with atrial fibrillation whose warfarin doses were outside the therapeutic range for an extended period of time.
Jared Bunch, MD, of the Intermountain Medical Center Heart Institute in Murray, Utah, and his colleagues presented this finding at the 2014 Annual Heart Rhythm Society Scientific Session (PO05-169).
Previous research suggested that patients with atrial fibrillation had an increased risk of developing dementia. But the cause of that association
was unknown.
“[W]e now know that if warfarin doses are consistently too high or too low, one of the long-term consequences can be brain damage,” Dr Bunch said. “This points to the possibility that dementia in atrial fibrillation patients is partly due to small, repetitive clots and/or bleeds in the brain.”
To make this connection, the researchers analyzed data from 2693 atrial fibrillation patients receiving warfarin. The team evaluated the relationship between dementia and the percentage of time that patients’ warfarin doses were within the therapeutic range (international normalized ratio of 2 to 3).
In all, 4.1% of patients (n=111) were diagnosed with dementia. This included senile dementia (n=37, 1.4%), vascular dementia (n=8, 0.3%), and Alzheimer’s dementia (n=66, 2.4%).
The researchers’ analysis (adjusted for the risk of stroke and bleeding) revealed that the more time a patient’s warfarin dosages were outside the therapeutic range, the greater his risk of developing dementia.
Specifically, patients within the therapeutic range less than 25% of the time were 4.6 times more likely to develop dementia than patients within range more than 75% of the time.
Patients within the therapeutic range 25% to 50% of the time were 4.1 times more likely to develop dementia. And patients within the therapeutic range 51% to 75% of the time were 2.5 times more likely to develop dementia.
“Our results from the study tell us 2 things,” Dr Bunch said. “With careful use of anticoagulation medications, the dementia risk can be reduced.
Patients on warfarin need very close follow-up in specialized anticoagulation centers, if possible, to ensure their blood levels are within the recommended levels more often.”
“Second, these results also point to a potential new long-term consequence of dependency on long-term anticoagulation medications. In this regard, stroke prevention therapies do not require long-term anticoagulation medications, and reducing the use of these drugs will hopefully lower
dementia risk.” ![]()

SAN FRANSICO—New research suggests bleeds and thrombosis are not the only adverse effects of improper warfarin dosing.
The study showed an increased risk of dementia among patients with atrial fibrillation whose warfarin doses were outside the therapeutic range for an extended period of time.
Jared Bunch, MD, of the Intermountain Medical Center Heart Institute in Murray, Utah, and his colleagues presented this finding at the 2014 Annual Heart Rhythm Society Scientific Session (PO05-169).
Previous research suggested that patients with atrial fibrillation had an increased risk of developing dementia. But the cause of that association
was unknown.
“[W]e now know that if warfarin doses are consistently too high or too low, one of the long-term consequences can be brain damage,” Dr Bunch said. “This points to the possibility that dementia in atrial fibrillation patients is partly due to small, repetitive clots and/or bleeds in the brain.”
To make this connection, the researchers analyzed data from 2693 atrial fibrillation patients receiving warfarin. The team evaluated the relationship between dementia and the percentage of time that patients’ warfarin doses were within the therapeutic range (international normalized ratio of 2 to 3).
In all, 4.1% of patients (n=111) were diagnosed with dementia. This included senile dementia (n=37, 1.4%), vascular dementia (n=8, 0.3%), and Alzheimer’s dementia (n=66, 2.4%).
The researchers’ analysis (adjusted for the risk of stroke and bleeding) revealed that the more time a patient’s warfarin dosages were outside the therapeutic range, the greater his risk of developing dementia.
Specifically, patients within the therapeutic range less than 25% of the time were 4.6 times more likely to develop dementia than patients within range more than 75% of the time.
Patients within the therapeutic range 25% to 50% of the time were 4.1 times more likely to develop dementia. And patients within the therapeutic range 51% to 75% of the time were 2.5 times more likely to develop dementia.
“Our results from the study tell us 2 things,” Dr Bunch said. “With careful use of anticoagulation medications, the dementia risk can be reduced.
Patients on warfarin need very close follow-up in specialized anticoagulation centers, if possible, to ensure their blood levels are within the recommended levels more often.”
“Second, these results also point to a potential new long-term consequence of dependency on long-term anticoagulation medications. In this regard, stroke prevention therapies do not require long-term anticoagulation medications, and reducing the use of these drugs will hopefully lower
dementia risk.” ![]()
Discharge Planning Tool in the EHR
According to the American Academy of Pediatrics clinical report on physicians' roles in coordinating care of hospitalized children, there are several important components of hospital discharge planning.[1] Foremost is that discharge planning should begin, and discharge criteria should be set, at the time of hospital admission. This allows for optimal engagement of parents and providers in the effort to adequately prepare patients for the transition to home.
As pediatric inpatients become increasingly complex,[2] adequately preparing families for the transition to home becomes more challenging.[3] There are a myriad of issues to address and the burden of this preparation effort falls on multiple individuals other than the bedside nurse and physician. Large multidisciplinary teams often play a significant role in the discharge of medically complex children.[4] Several challenges may hinder the team's ability to effectively navigate the discharge process such as financial or insurance‐related issues, language differences, or geographic barriers. Patient and family anxieties may also complicate the transition to home.[5]
The challenges of a multidisciplinary approach to discharge planning are further magnified by the limitations of the electronic health record (EHR). The EHR is well designed to record individual encounters, but poorly designed to coordinate longitudinal care across settings.[6] Although multidisciplinary providers may spend significant and well‐intentioned energy to facilitate hospital discharge, their efforts may go unseen or be duplicative.
We developed a discharge readiness report (DRR) for the EHR, an integrated summary of discharge‐related issues, organized into a highly visible and easily accessible report. The development of the discharge planning tool was the first step in a larger quality improvement (QI) initiative aimed at improving the efficiency, effectiveness, and safety of hospital discharge. Our team recognized that improving the flow and visibility of information between disciplines was the first step toward accomplishing this larger aim. Health information technology offers an important opportunity for the improvement of patient safety and care transitions7; therefore, we leveraged the EHR to create an integrated discharge report. We used QI methods to understand our hospital's discharge processes, examined potential pitfalls in interdisciplinary communication, determined relevant information to include in the report, and optimized ways to display the data. To our knowledge, this use of the EHR is novel. The objectives of this article were to describe our team's development and implementation strategies, as well as challenges encountered, in the design of this electronic discharge planning tool.
METHODS
Setting
Children's Hospital Colorado is a 413‐bed freestanding tertiary care teaching hospital with over 13,000 inpatient admissions annually and an average patient length of stay of 5.7 days. We were the first children's hospital to fully implement a single EHR (Epic Systems, Madison, WI) in 2006. This discharge improvement initiative emerged from our hospital's involvement in the Children's Hospital Association Discharge Collaborative between October 2011 and October 2012. We were 1 of 12 participating hospitals and developed several different projects within the framework of the initiative.
Improvement Team
Our multidisciplinary project team included hospitalist physicians, case managers, social workers, respiratory therapists, pharmacists, medical interpreters, process improvement specialists, clinical application specialists whose daily role is management of our hospital's EHR software, and resident liaisons whose daily role is working with residents to facilitate care coordination.
Ethics
The project was determined to be QI work by the Children's Hospital Colorado Organizational Research Risk and Quality Improvement Review Panel.
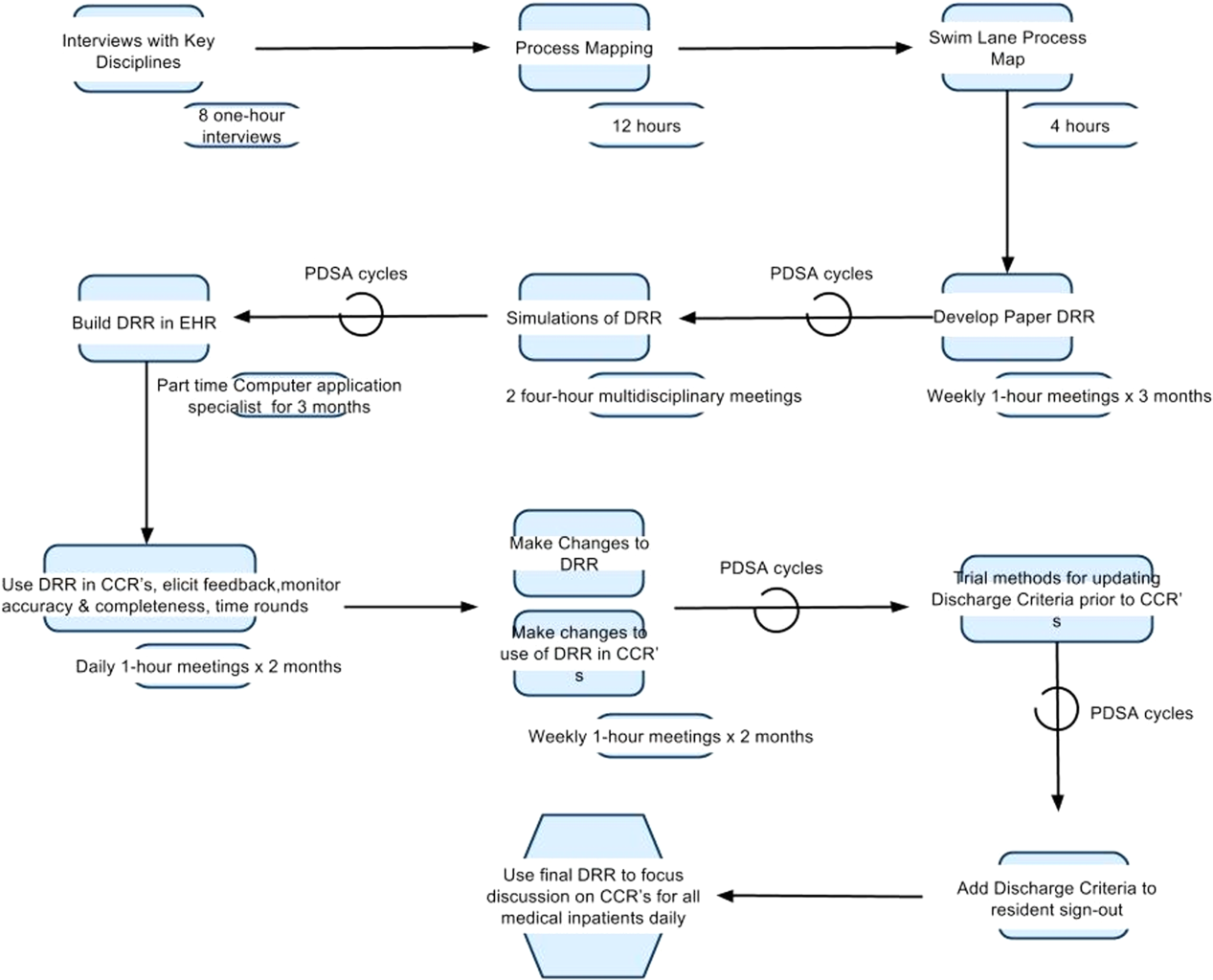
Understanding the Problem
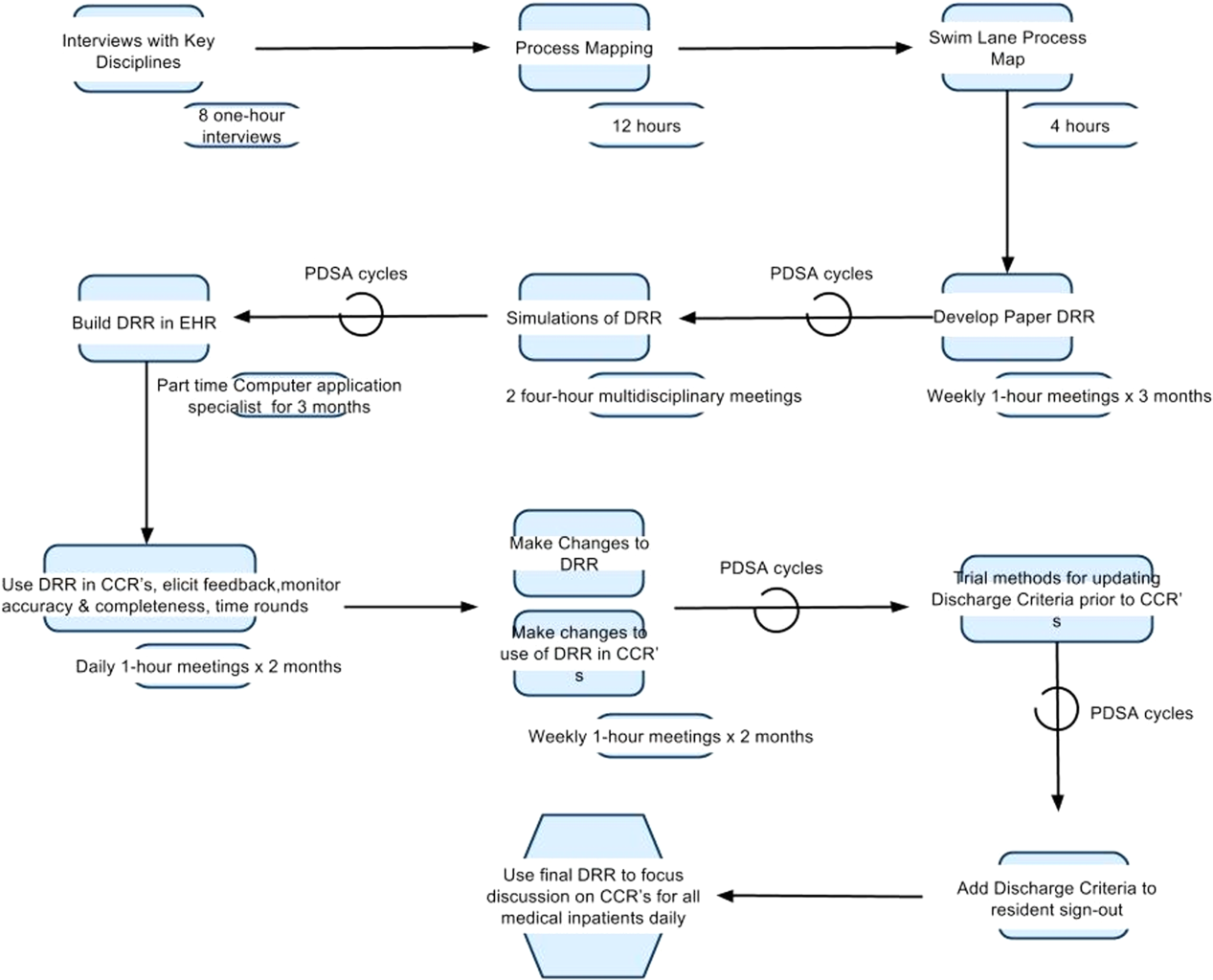
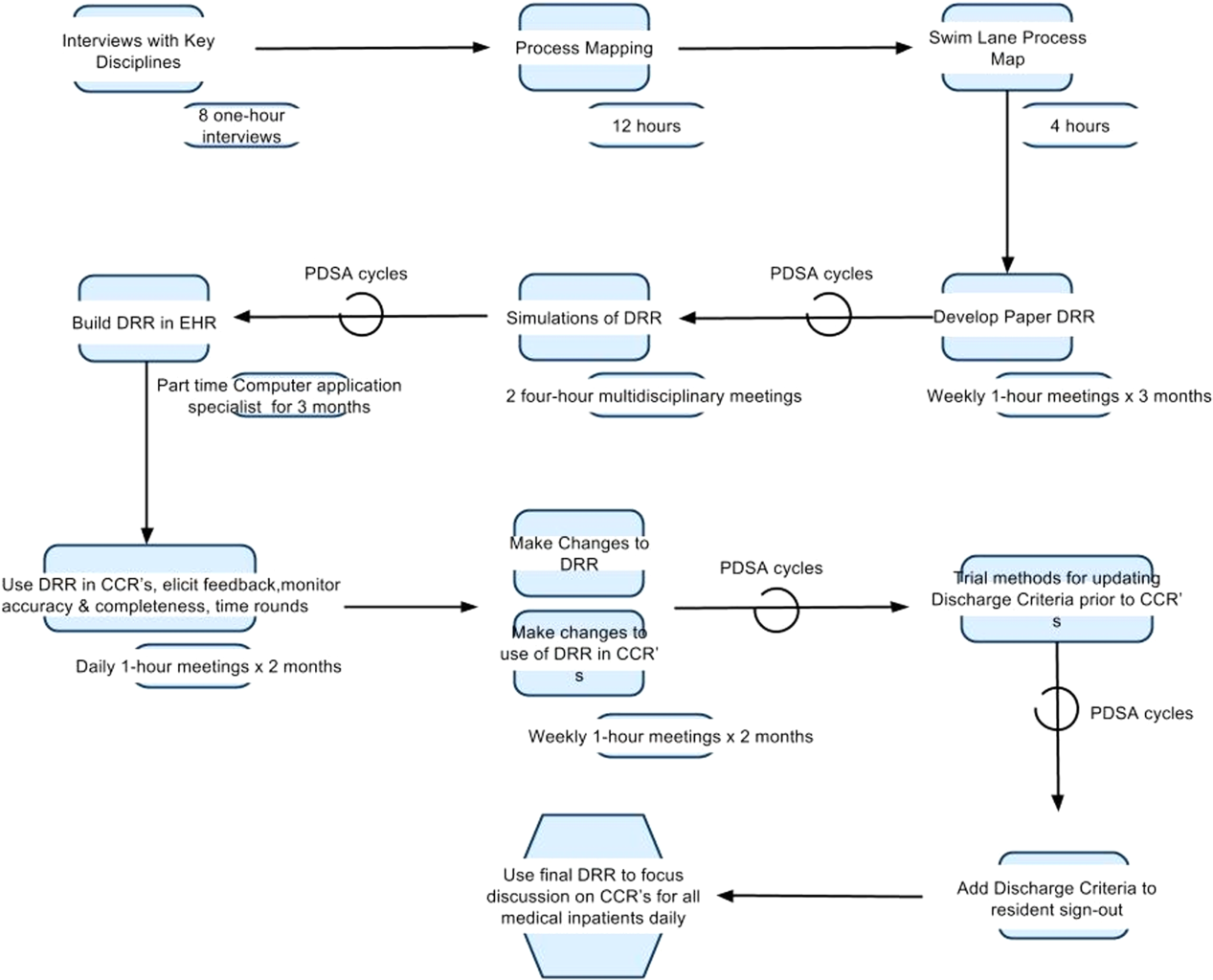
To understand the perspectives of each discipline involved in discharge planning, the lead hospitalist physician and a process improvement specialist interviewed key representatives from each group. Key informant interviews were conducted with hospitalist physicians, case managers, nurses, social workers, resident liaisons, respiratory therapists, pharmacists, medical interpreters, and residents. We inquired about their informational needs, their methods for obtaining relevant information, and whether the information was currently documented in the EHR. We then used process mapping to learn each disciplines' workflow related to discharge planning. Finally, we gathered key stakeholders together for a group session where discharge planning was mapped using the example of a patient admitted with asthma. From this session, we created a detailed multidisciplinary swim lane process map, a flowchart displaying the sequence of events in the overall discharge process grouped visually by placing the events in lanes. Each lane represented a discipline involved in patient discharge, and the arrows between lanes showed how information is passed between the various disciplines. Using this diagram, the team was able to fully understand provider interdependence in discharge planning and longitudinal timing of discharge‐related tasks during the patient's hospitalization.
We learned that: (1) discharge planning is complex, and there were often multiple provider types involved in the discharge of a single patient; (2) communication and coordination between the multitude of providers was often suboptimal; and (3) many of the tasks related to discharge were left to the last minute, resulting in unnecessary delays. Underlying these problems was a clear lack of organized and visible discharge planning information within the EHR.
There were many examples of obscure and siloed discharge processes. Physicians were aware of discharge criteria, but did not document these criteria for others to see. Case management assessments of home health needs were conveyed verbally to other team members, creating the potential for omissions, mistakes, or delays in appropriate home health planning. Social workers helped families to navigate financial hurdles (eg, assistance with payments for prescription medications). However, the presence of financial or insurance problems was not readily apparent to front‐line clinicians making discharge decisions. Other factors with potential significance for discharge planning, such as English‐language proficiency or a family's geographic distance from the hospital, were buried in disparate flow sheets or reports and not available or apparent to all health team members. There were also clear examples of discharge‐related tasks occurring at the end of hospitalization that could easily have been completed earlier in the admission such as identifying a primary care provider (PCP), scheduling follow‐up appointments, and completing work/subhool excuses because of lack of care team awareness that these items were needed.
Planning the Intervention
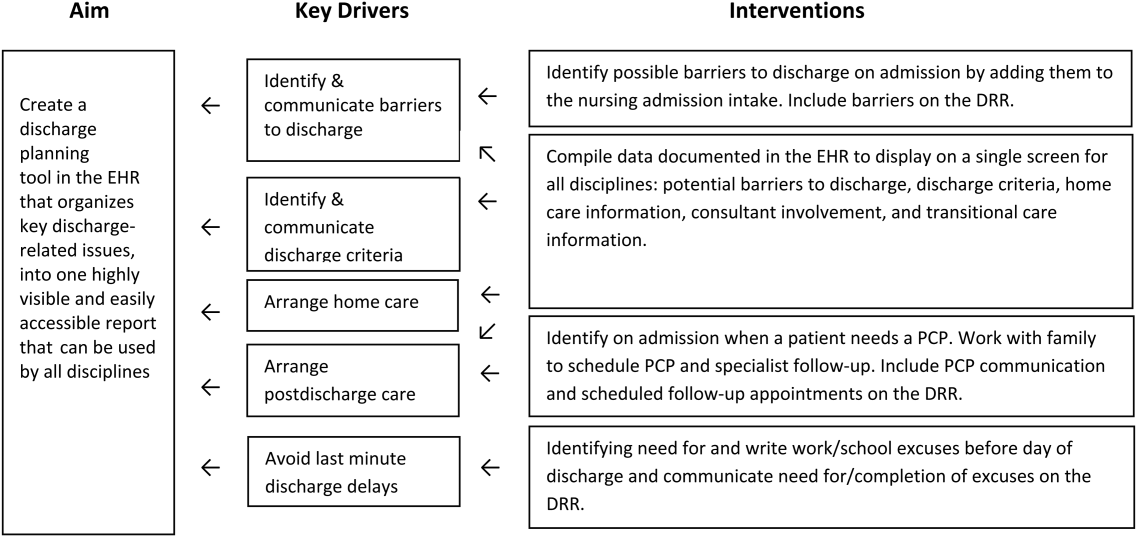
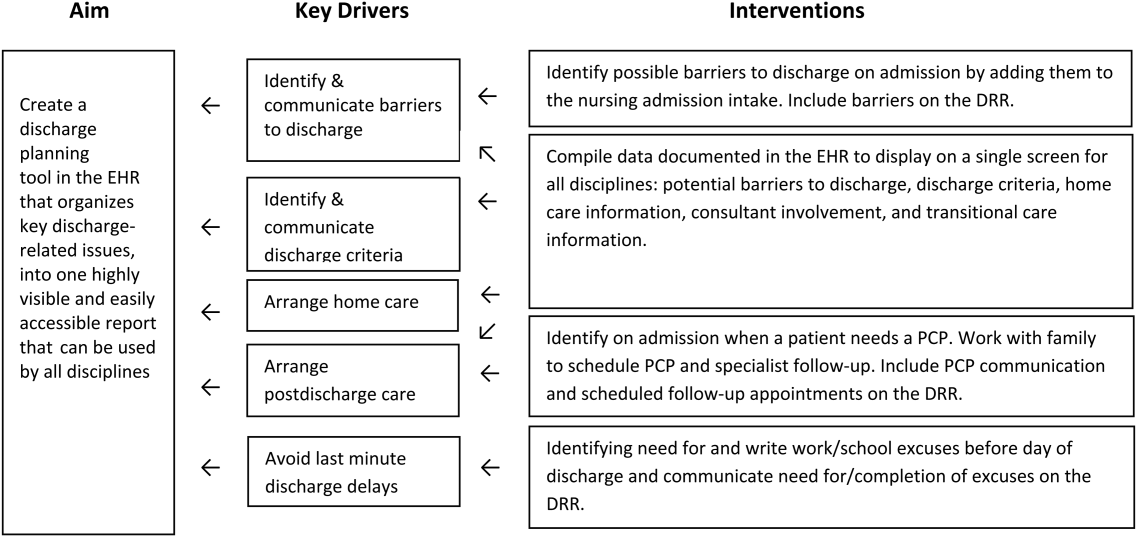
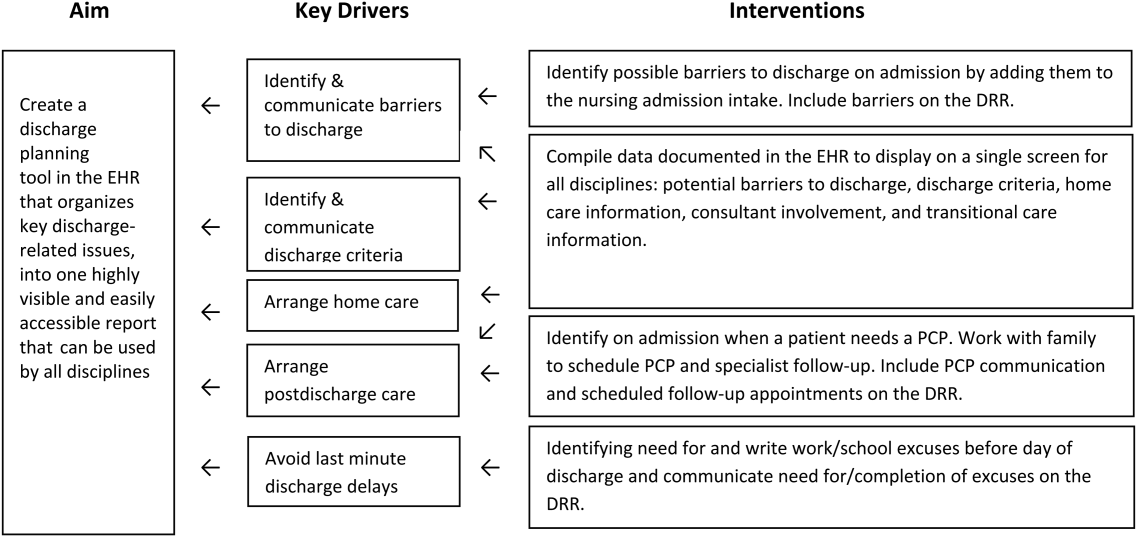
Based on our learning, we developed a key driver diagram (Figure 1). Our aim was to create a DRR that organized important discharge‐related information into 1 easily accessible report. Key drivers that were identified as relevant to the content of the DRR included: barriers to discharge, discharge criteria, home care, postdischarge care, and last minute delays. We also identified secondary drivers related to the design of the DRR. We hypothesized that addressing the secondary drivers would be essential to end user adoption of the tool. The secondary drivers included: accessibility, relevance, ease of updating, automation, and readability.
With the swim lane diagram as well as our primary and secondary drivers in mind, we created a mock DRR on paper. We conducted multiple patient discharge simulations with representatives from all disciplines, walking through each step of a patient hospitalization from registration to discharge. This allowed us to map out how preexisting, yet disparate, EHR data could be channeled into 1 report. A few changes were made to processes involving data collection and documentation to facilitate timely transfer of information to the report. For example, questions addressing potential barriers to discharge and whether a school/work excuse was needed were added to the admission nursing assessment.
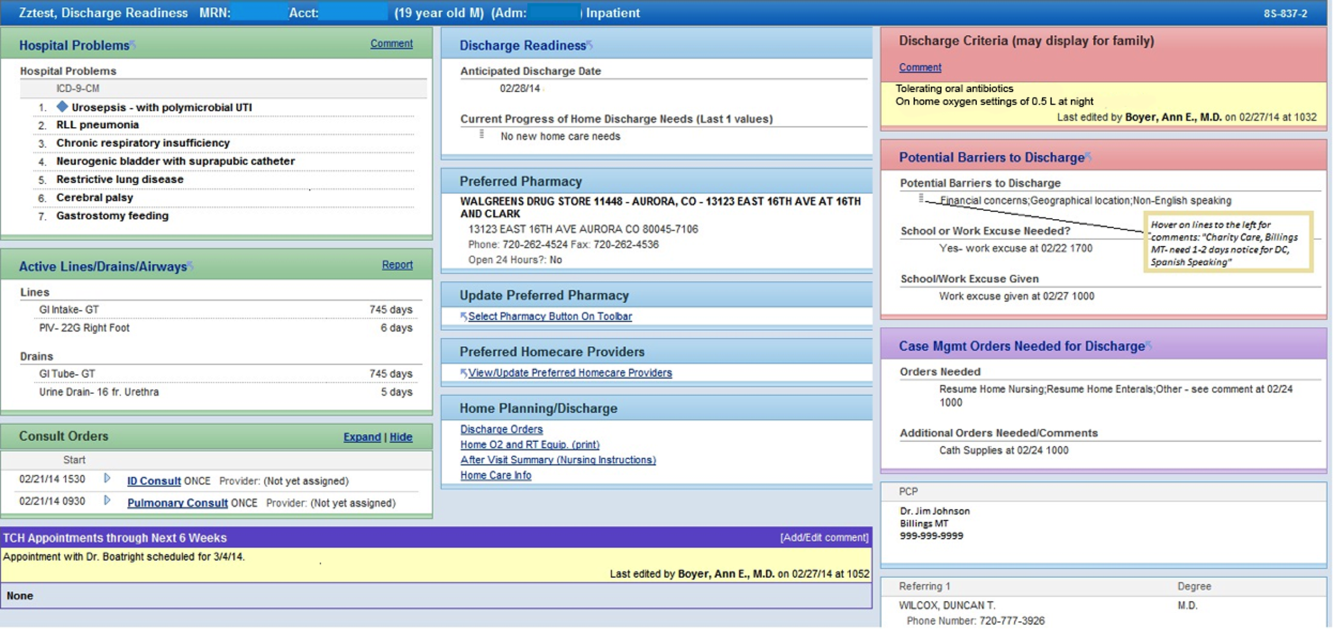
We then moved the paper DRR to the electronic environment. Data elements that were pulled automatically into the report included: potential barriers to discharge collected during nursing intake, case management information on home care needs, discharge criteria entered by resident and attending physicians, PCP, home pharmacy, follow‐up appointments, school/work excuse information gathered by resident liaisons, and active patient problems drawn from the problem list section. These data were organized into 4 distinct domains within the final DRR: potential barriers, transitional care, home care, and discharge criteria (Table 1).
| Discharge Readiness Report Domain | Example Content |
|---|---|
| |
| Potential barriers to discharge | Geographic location of the family, whether patient lives in more than 1 household, primary spoken language, financial or insurance concern, and need for work/subhool excuses |
| Transitional care | PCP and home pharmacy information, follow‐up ambulatory and imaging appointments, and care team communications with the PCP |
| Home care | Planned discharge date/time and home care needs assessments such as needs for special equipment or skilled home nursing |
| Discharge criteria | Clinical, social, or other care coordination conditions for discharge |
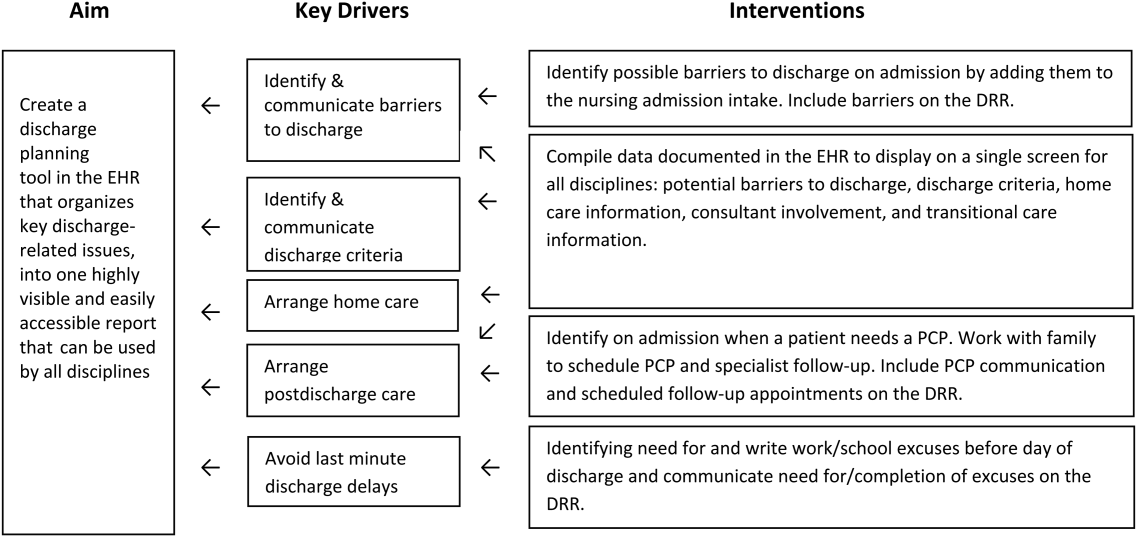
Additional features potentially important to discharge planning were also incorporated into the report based on end user feedback. These included hyperlinks to discharge orders, home oxygen prescriptions, and the after‐visit summary for families, and the patient's home care company (if present). To facilitate discharge and transitional care related communication between the primary team and subspecialty teams, consults involved during the hospitalization were included on the report. As home care arrangements often involve care for active lines and drains, they were added to the report (Figure 2).
Implementation
The report was activated within the EHR in June 2012. The team focused initial promotion and education efforts on medical floors. Education was widely disseminated via email and in‐person presentations.
The DRR was incorporated into daily CCRs for medical patients in July 2012. These multidisciplinary rounds occurred after medical‐team bedside rounds, focusing on care coordination and discharge planning. For each patient discussed, the DRR was projected onto a large screen, allowing all team members to view and discuss relevant discharge information. A process improvement (PI) specialist attended CCRs daily for several months, educating participants and monitoring use of the DRR. The PI specialist solicited feedback on ways to improve the DRR, and timed rounds to measure whether use of the DRR prolonged CCRs.
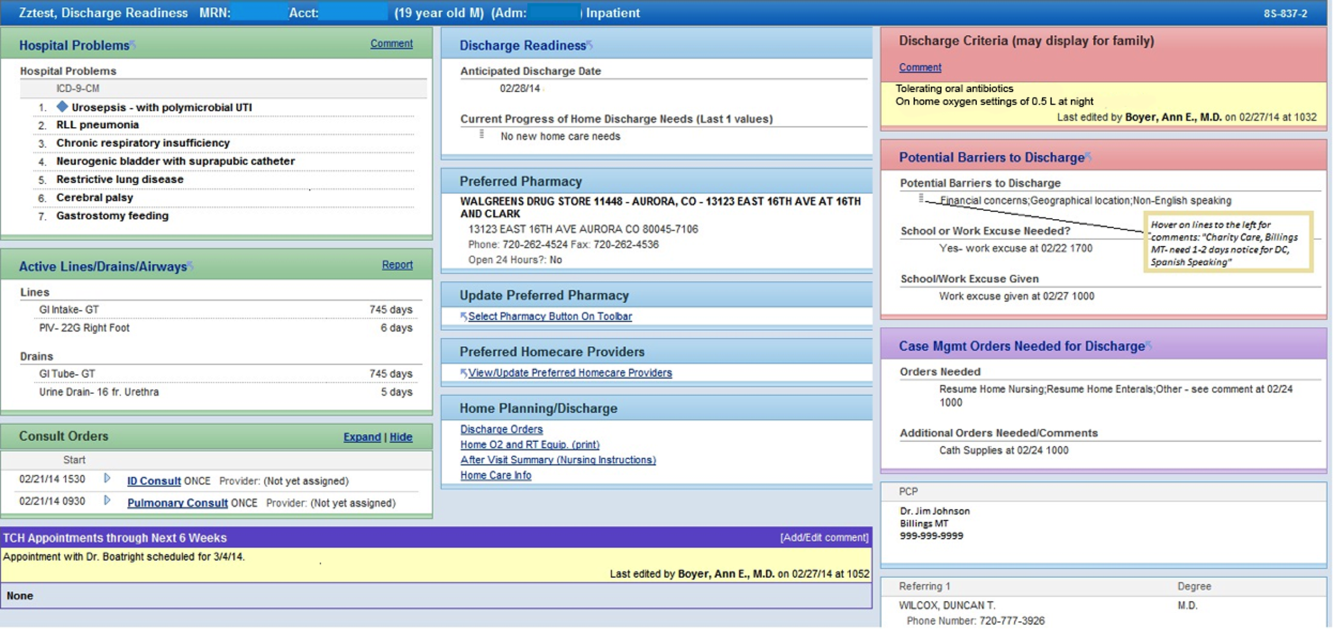
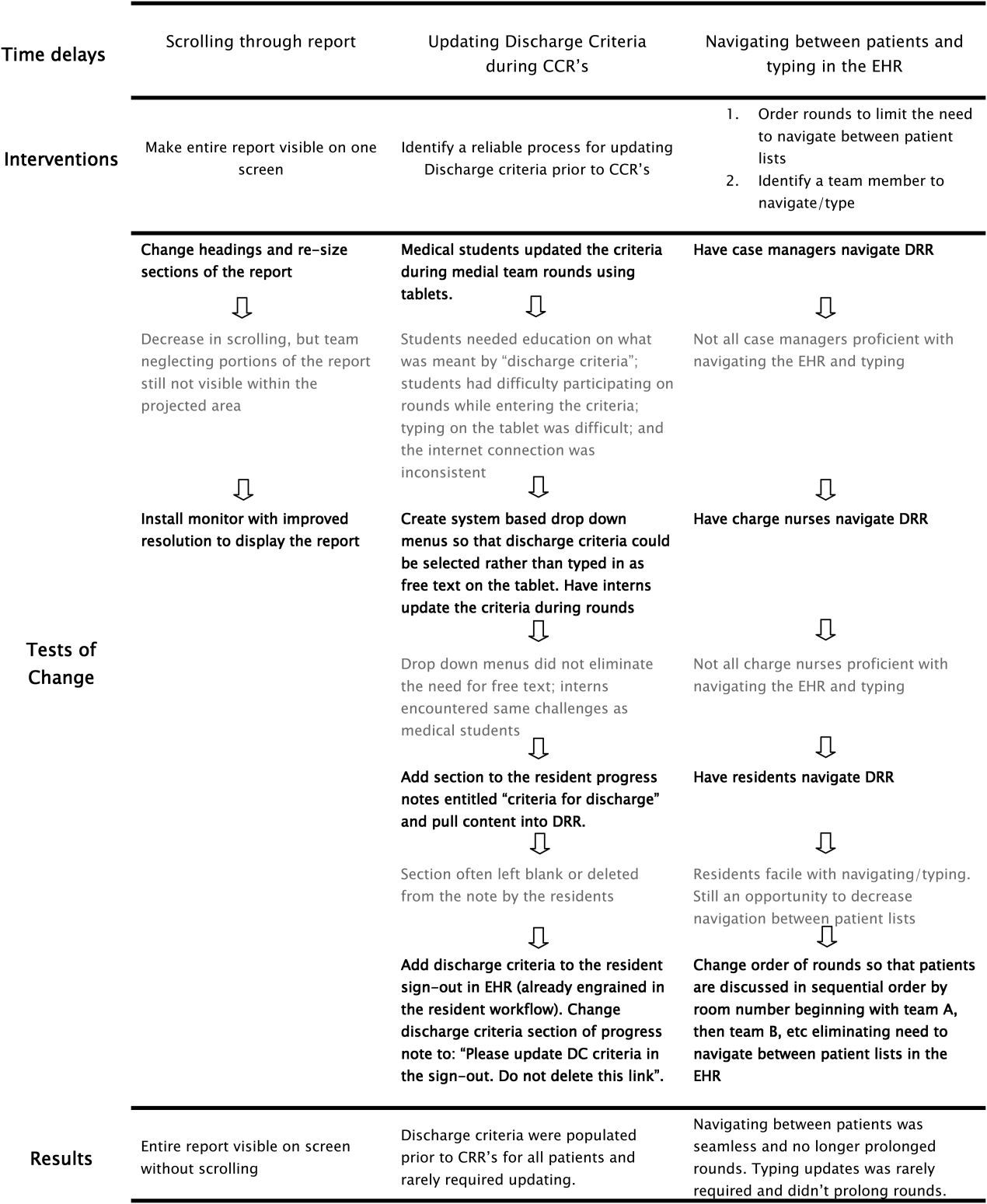
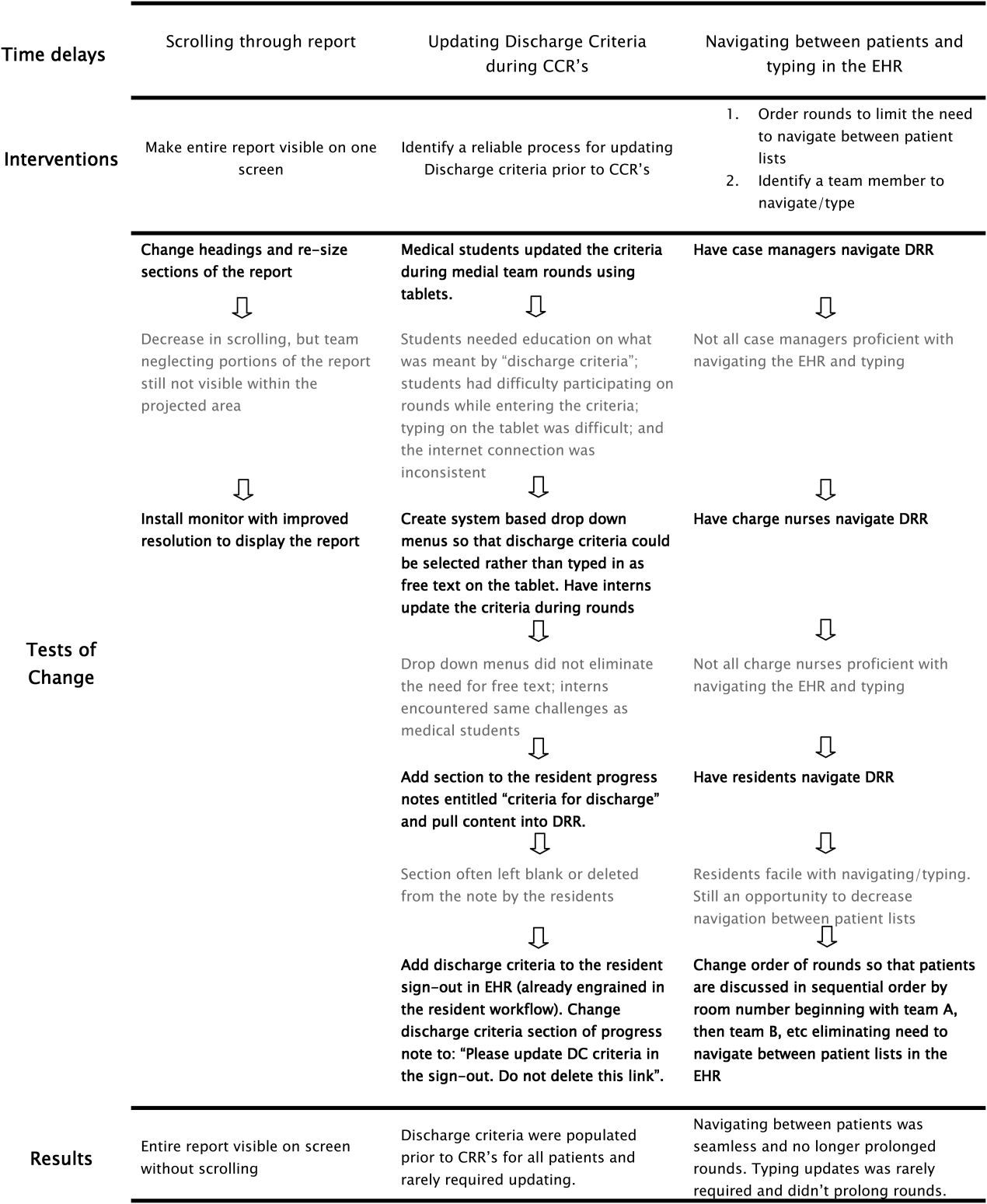
In the first weeks postimplementation, the use of the DRR prolonged rounds by as much as 1 minute per patient. Based on direct observation, the team focused interventions on barriers to the efficient use of the report during CCRs including: the need to scroll through the report, which was not visible on 1 screen; the need to navigate between patients; the need to quickly update the report based on discussion; and the need to update discharge criteria (Figure 3).
RESULTS
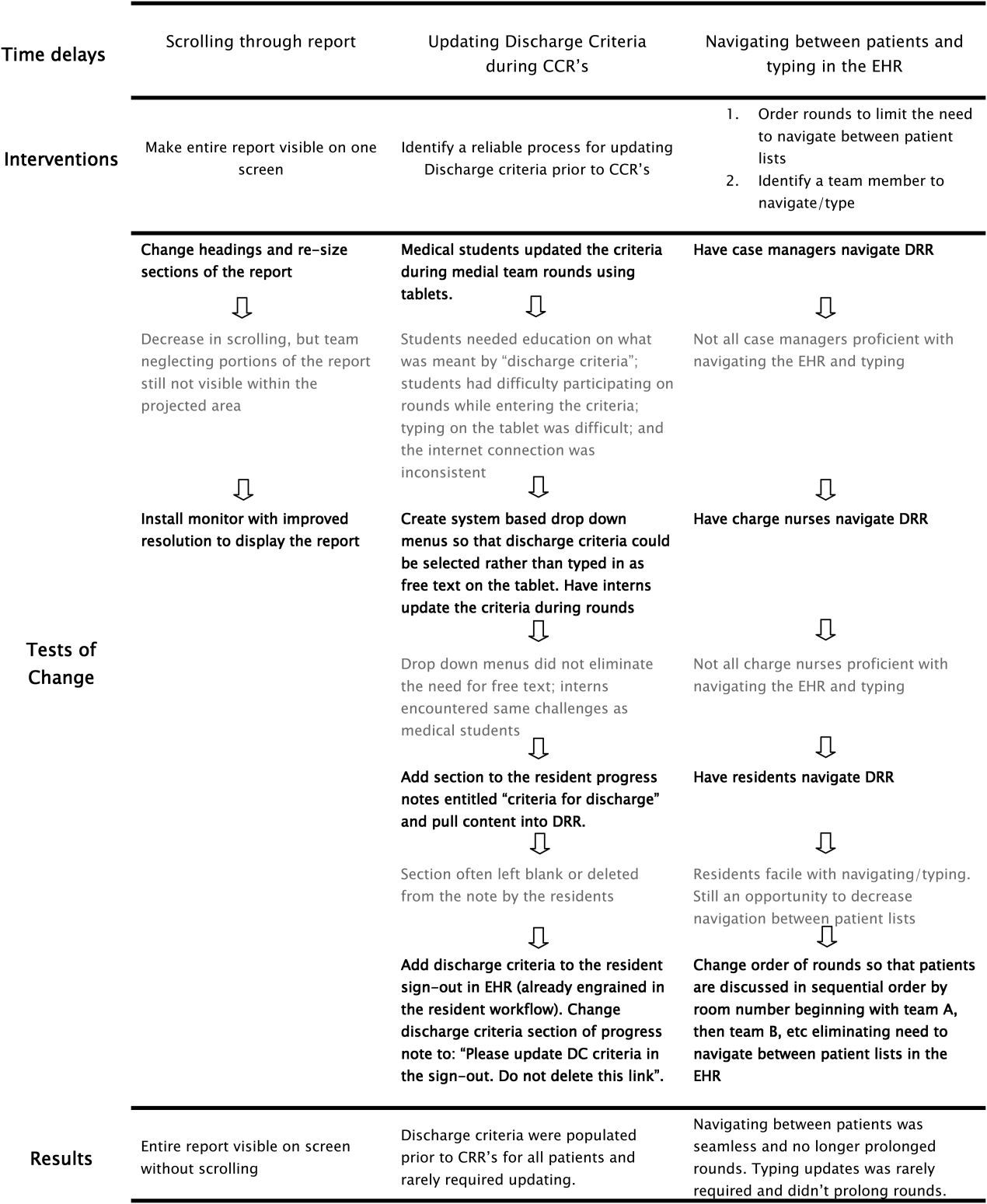
Creation of the final DRR required significant time and effort and was the culmination of a uniquely collaborative effort between clinicians, ancillary staff, and information technology specialists (Figure 4). The report is used consistently for all general medical and medical subspecialty patients during CCRs. After interventions were implemented to improve the efficiency of using the DRR during CCRs, the use of the DRR did not prolong CCRs. Members of the care team acknowledge that all sections of the report are populated and accurate. Though end users have commented on their use of the report outside of CCRs, we have not been able to formally measure this.
We have noticed a shift in the focus of discussion since implementation of the DRR. Prior to this initiative, care teams at our institution did not regularly discuss discharge criteria during bedside or CCRs. The phrase discharge criteria has now become part of our shared language.
Informally, the DRR appears to have reduced inefficiency and the potential for communication error. The practice of writing notes on printed patient lists to be used to sign‐out or communicate to other team members not in attendance at CCRs has largely disappeared.
The DRR has proven to be adaptable across patient units, and can be tailored to the specific transitional care needs of a given patient population. At discharge institution, the DRR has been modified for, and has taken on a prominent role in, the discharge planning of highly complex populations such as rehabilitation and ventilated patients.
DISCUSSION
Discharge planning is a multifaceted, multidisciplinary process that should begin at the time of hospital admission. Safe patient transition depends on efficient discharge processes and effective communication across settings.[8] Although not well studied in the inpatient setting, care process variability can result in inefficient patient flow and increased stress among staff.[9] Patients and families may experience confusion, coping difficulties, and increased readmission due to ineffective discharge planning.[10] These potential pitfalls highlight the need for healthcare providers to develop patient‐centered, systematic approaches to improving the discharge process.[11]
To our knowledge, this is the first description of a discharge planning tool for the EHR in the pediatric setting. Our discharge report is centralized, easily accessible by all members of the care team, and includes important patient‐specific discharge‐related information that be used to focus discussion and streamline multidisciplinary discharge planning rounds.
We anticipate that the report will allow the entire healthcare team to function more efficiently, decrease discharge‐related delays and failures based on communication roadblocks, and improve family and caregiver satisfaction with the discharge process. We are currently testing these hypotheses and evaluating several implementation strategies in an ongoing research study. Assuming positive impact, we plan to spread the use of the DRR to all inpatient care areas at our hospital, and potentially to other hospitals.
The limitations of this QI project are consistent with other initiatives to improve care. The challenges we encounter at our freestanding tertiary care teaching hospital with regard to effective discharge planning and multidisciplinary communication may not be generalizable to other nonteaching or community hospitals, and the DRR may not be useful in other settings. Though the report is now a part of our EHR, the most impactful implementation strategies remain to be determined. The report and related changes represent significant diversion from years of deeply ingrained workflows for some providers, and we encountered some resistance from staff during the early stages of implementation. The most important of which was that some team members are uncomfortable with technology and prefer to use paper. Most of this initial resistance was overcome by implementing changes to improve the ease of use of the report (Figure 3). Though input from end users and key stakeholders has been incorporated throughout this initiative, more work is needed to measure end user adoption and satisfaction with the report.
CONCLUSION
High‐quality hospital discharge planning requires an increasingly multidisciplinary approach. The EHR can be leveraged to improve transparency and interdisciplinary communication around the discharge process. An integrated summary of discharge‐related issues, organized into 1 highly visible and easily accessible report in the EHR has the potential to improve care transitions.
Disclosure
Nothing to report.
- . Clinical report—physicians' roles in coordinating care of hospitalized children. Pediatrics. 2010;126:829–832.
- , , , , , . Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126:638–646.
- , , . Hospitalist care of the medically complex child. Pediatr Clin North Am. 2005;52:1165–1187, x.
- , . Discharge planning and home care of the technology‐dependent infant. J Obstet Gynecol Neonatal Nurs. 1995;24:77–83.
- , , , . Pediatric discharge planning: complications, efficiency, and adequacy. Soc Work Health Care. 1995;22:1–18.
- , , , et al. The current capabilities of health information technology to support care transitions. AMIA Annu Symp Proc. 2013;2013:1231.
- , , , et al. Provider‐to‐provider electronic communication in the era of meaningful use: a review of the evidence. J Hosp Med. 2013;8:589–597.
- , , , . Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2:314–323.
- , , , , . A 5‐year time study analysis of emergency department patient care efficiency. Ann Emerg Med. 1999;34:326–335.
- , , , et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med. 2013;173(18):1715–1722.
- , . Addressing postdischarge adverse events: a neglected area. Jt Comm J Qual Patient Saf. 2008;34:85–97.
According to the American Academy of Pediatrics clinical report on physicians' roles in coordinating care of hospitalized children, there are several important components of hospital discharge planning.[1] Foremost is that discharge planning should begin, and discharge criteria should be set, at the time of hospital admission. This allows for optimal engagement of parents and providers in the effort to adequately prepare patients for the transition to home.
As pediatric inpatients become increasingly complex,[2] adequately preparing families for the transition to home becomes more challenging.[3] There are a myriad of issues to address and the burden of this preparation effort falls on multiple individuals other than the bedside nurse and physician. Large multidisciplinary teams often play a significant role in the discharge of medically complex children.[4] Several challenges may hinder the team's ability to effectively navigate the discharge process such as financial or insurance‐related issues, language differences, or geographic barriers. Patient and family anxieties may also complicate the transition to home.[5]
The challenges of a multidisciplinary approach to discharge planning are further magnified by the limitations of the electronic health record (EHR). The EHR is well designed to record individual encounters, but poorly designed to coordinate longitudinal care across settings.[6] Although multidisciplinary providers may spend significant and well‐intentioned energy to facilitate hospital discharge, their efforts may go unseen or be duplicative.
We developed a discharge readiness report (DRR) for the EHR, an integrated summary of discharge‐related issues, organized into a highly visible and easily accessible report. The development of the discharge planning tool was the first step in a larger quality improvement (QI) initiative aimed at improving the efficiency, effectiveness, and safety of hospital discharge. Our team recognized that improving the flow and visibility of information between disciplines was the first step toward accomplishing this larger aim. Health information technology offers an important opportunity for the improvement of patient safety and care transitions7; therefore, we leveraged the EHR to create an integrated discharge report. We used QI methods to understand our hospital's discharge processes, examined potential pitfalls in interdisciplinary communication, determined relevant information to include in the report, and optimized ways to display the data. To our knowledge, this use of the EHR is novel. The objectives of this article were to describe our team's development and implementation strategies, as well as challenges encountered, in the design of this electronic discharge planning tool.
METHODS
Setting
Children's Hospital Colorado is a 413‐bed freestanding tertiary care teaching hospital with over 13,000 inpatient admissions annually and an average patient length of stay of 5.7 days. We were the first children's hospital to fully implement a single EHR (Epic Systems, Madison, WI) in 2006. This discharge improvement initiative emerged from our hospital's involvement in the Children's Hospital Association Discharge Collaborative between October 2011 and October 2012. We were 1 of 12 participating hospitals and developed several different projects within the framework of the initiative.
Improvement Team
Our multidisciplinary project team included hospitalist physicians, case managers, social workers, respiratory therapists, pharmacists, medical interpreters, process improvement specialists, clinical application specialists whose daily role is management of our hospital's EHR software, and resident liaisons whose daily role is working with residents to facilitate care coordination.
Ethics
The project was determined to be QI work by the Children's Hospital Colorado Organizational Research Risk and Quality Improvement Review Panel.
Understanding the Problem
To understand the perspectives of each discipline involved in discharge planning, the lead hospitalist physician and a process improvement specialist interviewed key representatives from each group. Key informant interviews were conducted with hospitalist physicians, case managers, nurses, social workers, resident liaisons, respiratory therapists, pharmacists, medical interpreters, and residents. We inquired about their informational needs, their methods for obtaining relevant information, and whether the information was currently documented in the EHR. We then used process mapping to learn each disciplines' workflow related to discharge planning. Finally, we gathered key stakeholders together for a group session where discharge planning was mapped using the example of a patient admitted with asthma. From this session, we created a detailed multidisciplinary swim lane process map, a flowchart displaying the sequence of events in the overall discharge process grouped visually by placing the events in lanes. Each lane represented a discipline involved in patient discharge, and the arrows between lanes showed how information is passed between the various disciplines. Using this diagram, the team was able to fully understand provider interdependence in discharge planning and longitudinal timing of discharge‐related tasks during the patient's hospitalization.
We learned that: (1) discharge planning is complex, and there were often multiple provider types involved in the discharge of a single patient; (2) communication and coordination between the multitude of providers was often suboptimal; and (3) many of the tasks related to discharge were left to the last minute, resulting in unnecessary delays. Underlying these problems was a clear lack of organized and visible discharge planning information within the EHR.
There were many examples of obscure and siloed discharge processes. Physicians were aware of discharge criteria, but did not document these criteria for others to see. Case management assessments of home health needs were conveyed verbally to other team members, creating the potential for omissions, mistakes, or delays in appropriate home health planning. Social workers helped families to navigate financial hurdles (eg, assistance with payments for prescription medications). However, the presence of financial or insurance problems was not readily apparent to front‐line clinicians making discharge decisions. Other factors with potential significance for discharge planning, such as English‐language proficiency or a family's geographic distance from the hospital, were buried in disparate flow sheets or reports and not available or apparent to all health team members. There were also clear examples of discharge‐related tasks occurring at the end of hospitalization that could easily have been completed earlier in the admission such as identifying a primary care provider (PCP), scheduling follow‐up appointments, and completing work/subhool excuses because of lack of care team awareness that these items were needed.
Planning the Intervention
Based on our learning, we developed a key driver diagram (Figure 1). Our aim was to create a DRR that organized important discharge‐related information into 1 easily accessible report. Key drivers that were identified as relevant to the content of the DRR included: barriers to discharge, discharge criteria, home care, postdischarge care, and last minute delays. We also identified secondary drivers related to the design of the DRR. We hypothesized that addressing the secondary drivers would be essential to end user adoption of the tool. The secondary drivers included: accessibility, relevance, ease of updating, automation, and readability.
With the swim lane diagram as well as our primary and secondary drivers in mind, we created a mock DRR on paper. We conducted multiple patient discharge simulations with representatives from all disciplines, walking through each step of a patient hospitalization from registration to discharge. This allowed us to map out how preexisting, yet disparate, EHR data could be channeled into 1 report. A few changes were made to processes involving data collection and documentation to facilitate timely transfer of information to the report. For example, questions addressing potential barriers to discharge and whether a school/work excuse was needed were added to the admission nursing assessment.
We then moved the paper DRR to the electronic environment. Data elements that were pulled automatically into the report included: potential barriers to discharge collected during nursing intake, case management information on home care needs, discharge criteria entered by resident and attending physicians, PCP, home pharmacy, follow‐up appointments, school/work excuse information gathered by resident liaisons, and active patient problems drawn from the problem list section. These data were organized into 4 distinct domains within the final DRR: potential barriers, transitional care, home care, and discharge criteria (Table 1).
| Discharge Readiness Report Domain | Example Content |
|---|---|
| |
| Potential barriers to discharge | Geographic location of the family, whether patient lives in more than 1 household, primary spoken language, financial or insurance concern, and need for work/subhool excuses |
| Transitional care | PCP and home pharmacy information, follow‐up ambulatory and imaging appointments, and care team communications with the PCP |
| Home care | Planned discharge date/time and home care needs assessments such as needs for special equipment or skilled home nursing |
| Discharge criteria | Clinical, social, or other care coordination conditions for discharge |
Additional features potentially important to discharge planning were also incorporated into the report based on end user feedback. These included hyperlinks to discharge orders, home oxygen prescriptions, and the after‐visit summary for families, and the patient's home care company (if present). To facilitate discharge and transitional care related communication between the primary team and subspecialty teams, consults involved during the hospitalization were included on the report. As home care arrangements often involve care for active lines and drains, they were added to the report (Figure 2).
Implementation
The report was activated within the EHR in June 2012. The team focused initial promotion and education efforts on medical floors. Education was widely disseminated via email and in‐person presentations.
The DRR was incorporated into daily CCRs for medical patients in July 2012. These multidisciplinary rounds occurred after medical‐team bedside rounds, focusing on care coordination and discharge planning. For each patient discussed, the DRR was projected onto a large screen, allowing all team members to view and discuss relevant discharge information. A process improvement (PI) specialist attended CCRs daily for several months, educating participants and monitoring use of the DRR. The PI specialist solicited feedback on ways to improve the DRR, and timed rounds to measure whether use of the DRR prolonged CCRs.
In the first weeks postimplementation, the use of the DRR prolonged rounds by as much as 1 minute per patient. Based on direct observation, the team focused interventions on barriers to the efficient use of the report during CCRs including: the need to scroll through the report, which was not visible on 1 screen; the need to navigate between patients; the need to quickly update the report based on discussion; and the need to update discharge criteria (Figure 3).
RESULTS
Creation of the final DRR required significant time and effort and was the culmination of a uniquely collaborative effort between clinicians, ancillary staff, and information technology specialists (Figure 4). The report is used consistently for all general medical and medical subspecialty patients during CCRs. After interventions were implemented to improve the efficiency of using the DRR during CCRs, the use of the DRR did not prolong CCRs. Members of the care team acknowledge that all sections of the report are populated and accurate. Though end users have commented on their use of the report outside of CCRs, we have not been able to formally measure this.
We have noticed a shift in the focus of discussion since implementation of the DRR. Prior to this initiative, care teams at our institution did not regularly discuss discharge criteria during bedside or CCRs. The phrase discharge criteria has now become part of our shared language.
Informally, the DRR appears to have reduced inefficiency and the potential for communication error. The practice of writing notes on printed patient lists to be used to sign‐out or communicate to other team members not in attendance at CCRs has largely disappeared.
The DRR has proven to be adaptable across patient units, and can be tailored to the specific transitional care needs of a given patient population. At discharge institution, the DRR has been modified for, and has taken on a prominent role in, the discharge planning of highly complex populations such as rehabilitation and ventilated patients.
DISCUSSION
Discharge planning is a multifaceted, multidisciplinary process that should begin at the time of hospital admission. Safe patient transition depends on efficient discharge processes and effective communication across settings.[8] Although not well studied in the inpatient setting, care process variability can result in inefficient patient flow and increased stress among staff.[9] Patients and families may experience confusion, coping difficulties, and increased readmission due to ineffective discharge planning.[10] These potential pitfalls highlight the need for healthcare providers to develop patient‐centered, systematic approaches to improving the discharge process.[11]
To our knowledge, this is the first description of a discharge planning tool for the EHR in the pediatric setting. Our discharge report is centralized, easily accessible by all members of the care team, and includes important patient‐specific discharge‐related information that be used to focus discussion and streamline multidisciplinary discharge planning rounds.
We anticipate that the report will allow the entire healthcare team to function more efficiently, decrease discharge‐related delays and failures based on communication roadblocks, and improve family and caregiver satisfaction with the discharge process. We are currently testing these hypotheses and evaluating several implementation strategies in an ongoing research study. Assuming positive impact, we plan to spread the use of the DRR to all inpatient care areas at our hospital, and potentially to other hospitals.
The limitations of this QI project are consistent with other initiatives to improve care. The challenges we encounter at our freestanding tertiary care teaching hospital with regard to effective discharge planning and multidisciplinary communication may not be generalizable to other nonteaching or community hospitals, and the DRR may not be useful in other settings. Though the report is now a part of our EHR, the most impactful implementation strategies remain to be determined. The report and related changes represent significant diversion from years of deeply ingrained workflows for some providers, and we encountered some resistance from staff during the early stages of implementation. The most important of which was that some team members are uncomfortable with technology and prefer to use paper. Most of this initial resistance was overcome by implementing changes to improve the ease of use of the report (Figure 3). Though input from end users and key stakeholders has been incorporated throughout this initiative, more work is needed to measure end user adoption and satisfaction with the report.
CONCLUSION
High‐quality hospital discharge planning requires an increasingly multidisciplinary approach. The EHR can be leveraged to improve transparency and interdisciplinary communication around the discharge process. An integrated summary of discharge‐related issues, organized into 1 highly visible and easily accessible report in the EHR has the potential to improve care transitions.
Disclosure
Nothing to report.
According to the American Academy of Pediatrics clinical report on physicians' roles in coordinating care of hospitalized children, there are several important components of hospital discharge planning.[1] Foremost is that discharge planning should begin, and discharge criteria should be set, at the time of hospital admission. This allows for optimal engagement of parents and providers in the effort to adequately prepare patients for the transition to home.
As pediatric inpatients become increasingly complex,[2] adequately preparing families for the transition to home becomes more challenging.[3] There are a myriad of issues to address and the burden of this preparation effort falls on multiple individuals other than the bedside nurse and physician. Large multidisciplinary teams often play a significant role in the discharge of medically complex children.[4] Several challenges may hinder the team's ability to effectively navigate the discharge process such as financial or insurance‐related issues, language differences, or geographic barriers. Patient and family anxieties may also complicate the transition to home.[5]
The challenges of a multidisciplinary approach to discharge planning are further magnified by the limitations of the electronic health record (EHR). The EHR is well designed to record individual encounters, but poorly designed to coordinate longitudinal care across settings.[6] Although multidisciplinary providers may spend significant and well‐intentioned energy to facilitate hospital discharge, their efforts may go unseen or be duplicative.
We developed a discharge readiness report (DRR) for the EHR, an integrated summary of discharge‐related issues, organized into a highly visible and easily accessible report. The development of the discharge planning tool was the first step in a larger quality improvement (QI) initiative aimed at improving the efficiency, effectiveness, and safety of hospital discharge. Our team recognized that improving the flow and visibility of information between disciplines was the first step toward accomplishing this larger aim. Health information technology offers an important opportunity for the improvement of patient safety and care transitions7; therefore, we leveraged the EHR to create an integrated discharge report. We used QI methods to understand our hospital's discharge processes, examined potential pitfalls in interdisciplinary communication, determined relevant information to include in the report, and optimized ways to display the data. To our knowledge, this use of the EHR is novel. The objectives of this article were to describe our team's development and implementation strategies, as well as challenges encountered, in the design of this electronic discharge planning tool.
METHODS
Setting
Children's Hospital Colorado is a 413‐bed freestanding tertiary care teaching hospital with over 13,000 inpatient admissions annually and an average patient length of stay of 5.7 days. We were the first children's hospital to fully implement a single EHR (Epic Systems, Madison, WI) in 2006. This discharge improvement initiative emerged from our hospital's involvement in the Children's Hospital Association Discharge Collaborative between October 2011 and October 2012. We were 1 of 12 participating hospitals and developed several different projects within the framework of the initiative.
Improvement Team
Our multidisciplinary project team included hospitalist physicians, case managers, social workers, respiratory therapists, pharmacists, medical interpreters, process improvement specialists, clinical application specialists whose daily role is management of our hospital's EHR software, and resident liaisons whose daily role is working with residents to facilitate care coordination.
Ethics
The project was determined to be QI work by the Children's Hospital Colorado Organizational Research Risk and Quality Improvement Review Panel.
Understanding the Problem
To understand the perspectives of each discipline involved in discharge planning, the lead hospitalist physician and a process improvement specialist interviewed key representatives from each group. Key informant interviews were conducted with hospitalist physicians, case managers, nurses, social workers, resident liaisons, respiratory therapists, pharmacists, medical interpreters, and residents. We inquired about their informational needs, their methods for obtaining relevant information, and whether the information was currently documented in the EHR. We then used process mapping to learn each disciplines' workflow related to discharge planning. Finally, we gathered key stakeholders together for a group session where discharge planning was mapped using the example of a patient admitted with asthma. From this session, we created a detailed multidisciplinary swim lane process map, a flowchart displaying the sequence of events in the overall discharge process grouped visually by placing the events in lanes. Each lane represented a discipline involved in patient discharge, and the arrows between lanes showed how information is passed between the various disciplines. Using this diagram, the team was able to fully understand provider interdependence in discharge planning and longitudinal timing of discharge‐related tasks during the patient's hospitalization.
We learned that: (1) discharge planning is complex, and there were often multiple provider types involved in the discharge of a single patient; (2) communication and coordination between the multitude of providers was often suboptimal; and (3) many of the tasks related to discharge were left to the last minute, resulting in unnecessary delays. Underlying these problems was a clear lack of organized and visible discharge planning information within the EHR.
There were many examples of obscure and siloed discharge processes. Physicians were aware of discharge criteria, but did not document these criteria for others to see. Case management assessments of home health needs were conveyed verbally to other team members, creating the potential for omissions, mistakes, or delays in appropriate home health planning. Social workers helped families to navigate financial hurdles (eg, assistance with payments for prescription medications). However, the presence of financial or insurance problems was not readily apparent to front‐line clinicians making discharge decisions. Other factors with potential significance for discharge planning, such as English‐language proficiency or a family's geographic distance from the hospital, were buried in disparate flow sheets or reports and not available or apparent to all health team members. There were also clear examples of discharge‐related tasks occurring at the end of hospitalization that could easily have been completed earlier in the admission such as identifying a primary care provider (PCP), scheduling follow‐up appointments, and completing work/subhool excuses because of lack of care team awareness that these items were needed.
Planning the Intervention
Based on our learning, we developed a key driver diagram (Figure 1). Our aim was to create a DRR that organized important discharge‐related information into 1 easily accessible report. Key drivers that were identified as relevant to the content of the DRR included: barriers to discharge, discharge criteria, home care, postdischarge care, and last minute delays. We also identified secondary drivers related to the design of the DRR. We hypothesized that addressing the secondary drivers would be essential to end user adoption of the tool. The secondary drivers included: accessibility, relevance, ease of updating, automation, and readability.
With the swim lane diagram as well as our primary and secondary drivers in mind, we created a mock DRR on paper. We conducted multiple patient discharge simulations with representatives from all disciplines, walking through each step of a patient hospitalization from registration to discharge. This allowed us to map out how preexisting, yet disparate, EHR data could be channeled into 1 report. A few changes were made to processes involving data collection and documentation to facilitate timely transfer of information to the report. For example, questions addressing potential barriers to discharge and whether a school/work excuse was needed were added to the admission nursing assessment.
We then moved the paper DRR to the electronic environment. Data elements that were pulled automatically into the report included: potential barriers to discharge collected during nursing intake, case management information on home care needs, discharge criteria entered by resident and attending physicians, PCP, home pharmacy, follow‐up appointments, school/work excuse information gathered by resident liaisons, and active patient problems drawn from the problem list section. These data were organized into 4 distinct domains within the final DRR: potential barriers, transitional care, home care, and discharge criteria (Table 1).
| Discharge Readiness Report Domain | Example Content |
|---|---|
| |
| Potential barriers to discharge | Geographic location of the family, whether patient lives in more than 1 household, primary spoken language, financial or insurance concern, and need for work/subhool excuses |
| Transitional care | PCP and home pharmacy information, follow‐up ambulatory and imaging appointments, and care team communications with the PCP |
| Home care | Planned discharge date/time and home care needs assessments such as needs for special equipment or skilled home nursing |
| Discharge criteria | Clinical, social, or other care coordination conditions for discharge |
Additional features potentially important to discharge planning were also incorporated into the report based on end user feedback. These included hyperlinks to discharge orders, home oxygen prescriptions, and the after‐visit summary for families, and the patient's home care company (if present). To facilitate discharge and transitional care related communication between the primary team and subspecialty teams, consults involved during the hospitalization were included on the report. As home care arrangements often involve care for active lines and drains, they were added to the report (Figure 2).
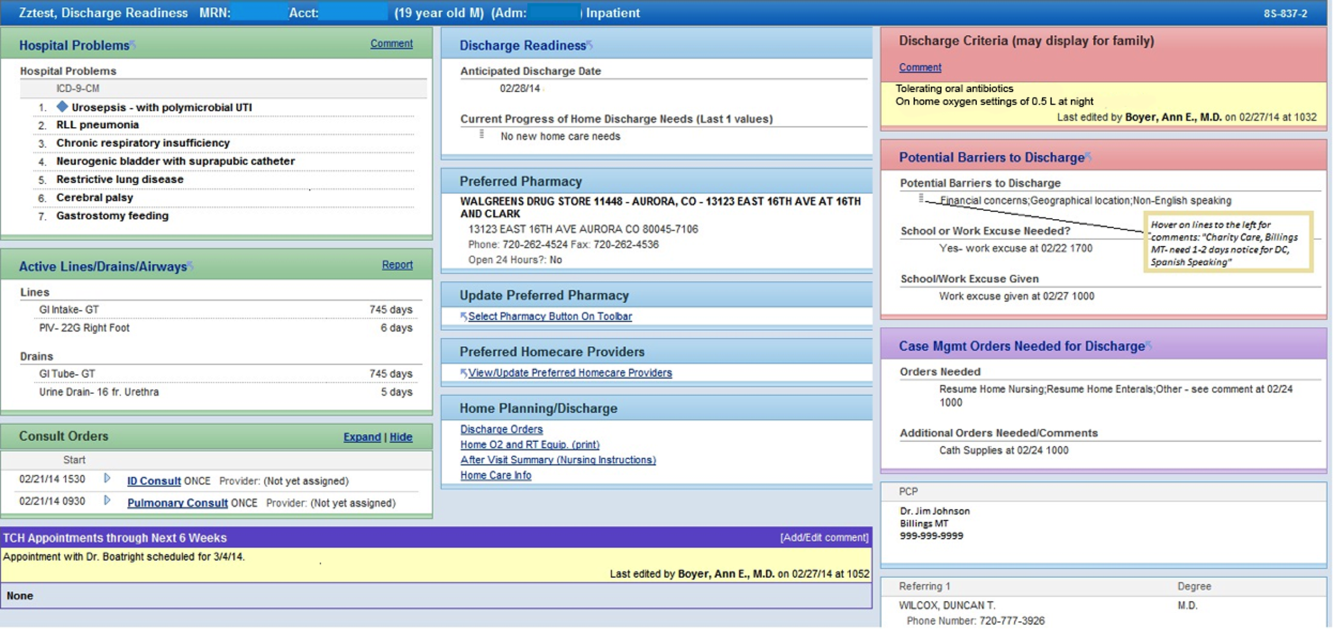
Implementation
The report was activated within the EHR in June 2012. The team focused initial promotion and education efforts on medical floors. Education was widely disseminated via email and in‐person presentations.
The DRR was incorporated into daily CCRs for medical patients in July 2012. These multidisciplinary rounds occurred after medical‐team bedside rounds, focusing on care coordination and discharge planning. For each patient discussed, the DRR was projected onto a large screen, allowing all team members to view and discuss relevant discharge information. A process improvement (PI) specialist attended CCRs daily for several months, educating participants and monitoring use of the DRR. The PI specialist solicited feedback on ways to improve the DRR, and timed rounds to measure whether use of the DRR prolonged CCRs.
In the first weeks postimplementation, the use of the DRR prolonged rounds by as much as 1 minute per patient. Based on direct observation, the team focused interventions on barriers to the efficient use of the report during CCRs including: the need to scroll through the report, which was not visible on 1 screen; the need to navigate between patients; the need to quickly update the report based on discussion; and the need to update discharge criteria (Figure 3).
RESULTS
Creation of the final DRR required significant time and effort and was the culmination of a uniquely collaborative effort between clinicians, ancillary staff, and information technology specialists (Figure 4). The report is used consistently for all general medical and medical subspecialty patients during CCRs. After interventions were implemented to improve the efficiency of using the DRR during CCRs, the use of the DRR did not prolong CCRs. Members of the care team acknowledge that all sections of the report are populated and accurate. Though end users have commented on their use of the report outside of CCRs, we have not been able to formally measure this.
We have noticed a shift in the focus of discussion since implementation of the DRR. Prior to this initiative, care teams at our institution did not regularly discuss discharge criteria during bedside or CCRs. The phrase discharge criteria has now become part of our shared language.
Informally, the DRR appears to have reduced inefficiency and the potential for communication error. The practice of writing notes on printed patient lists to be used to sign‐out or communicate to other team members not in attendance at CCRs has largely disappeared.
The DRR has proven to be adaptable across patient units, and can be tailored to the specific transitional care needs of a given patient population. At discharge institution, the DRR has been modified for, and has taken on a prominent role in, the discharge planning of highly complex populations such as rehabilitation and ventilated patients.
DISCUSSION
Discharge planning is a multifaceted, multidisciplinary process that should begin at the time of hospital admission. Safe patient transition depends on efficient discharge processes and effective communication across settings.[8] Although not well studied in the inpatient setting, care process variability can result in inefficient patient flow and increased stress among staff.[9] Patients and families may experience confusion, coping difficulties, and increased readmission due to ineffective discharge planning.[10] These potential pitfalls highlight the need for healthcare providers to develop patient‐centered, systematic approaches to improving the discharge process.[11]
To our knowledge, this is the first description of a discharge planning tool for the EHR in the pediatric setting. Our discharge report is centralized, easily accessible by all members of the care team, and includes important patient‐specific discharge‐related information that be used to focus discussion and streamline multidisciplinary discharge planning rounds.
We anticipate that the report will allow the entire healthcare team to function more efficiently, decrease discharge‐related delays and failures based on communication roadblocks, and improve family and caregiver satisfaction with the discharge process. We are currently testing these hypotheses and evaluating several implementation strategies in an ongoing research study. Assuming positive impact, we plan to spread the use of the DRR to all inpatient care areas at our hospital, and potentially to other hospitals.
The limitations of this QI project are consistent with other initiatives to improve care. The challenges we encounter at our freestanding tertiary care teaching hospital with regard to effective discharge planning and multidisciplinary communication may not be generalizable to other nonteaching or community hospitals, and the DRR may not be useful in other settings. Though the report is now a part of our EHR, the most impactful implementation strategies remain to be determined. The report and related changes represent significant diversion from years of deeply ingrained workflows for some providers, and we encountered some resistance from staff during the early stages of implementation. The most important of which was that some team members are uncomfortable with technology and prefer to use paper. Most of this initial resistance was overcome by implementing changes to improve the ease of use of the report (Figure 3). Though input from end users and key stakeholders has been incorporated throughout this initiative, more work is needed to measure end user adoption and satisfaction with the report.
CONCLUSION
High‐quality hospital discharge planning requires an increasingly multidisciplinary approach. The EHR can be leveraged to improve transparency and interdisciplinary communication around the discharge process. An integrated summary of discharge‐related issues, organized into 1 highly visible and easily accessible report in the EHR has the potential to improve care transitions.
Disclosure
Nothing to report.
- . Clinical report—physicians' roles in coordinating care of hospitalized children. Pediatrics. 2010;126:829–832.
- , , , , , . Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126:638–646.
- , , . Hospitalist care of the medically complex child. Pediatr Clin North Am. 2005;52:1165–1187, x.
- , . Discharge planning and home care of the technology‐dependent infant. J Obstet Gynecol Neonatal Nurs. 1995;24:77–83.
- , , , . Pediatric discharge planning: complications, efficiency, and adequacy. Soc Work Health Care. 1995;22:1–18.
- , , , et al. The current capabilities of health information technology to support care transitions. AMIA Annu Symp Proc. 2013;2013:1231.
- , , , et al. Provider‐to‐provider electronic communication in the era of meaningful use: a review of the evidence. J Hosp Med. 2013;8:589–597.
- , , , . Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2:314–323.
- , , , , . A 5‐year time study analysis of emergency department patient care efficiency. Ann Emerg Med. 1999;34:326–335.
- , , , et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med. 2013;173(18):1715–1722.
- , . Addressing postdischarge adverse events: a neglected area. Jt Comm J Qual Patient Saf. 2008;34:85–97.
- . Clinical report—physicians' roles in coordinating care of hospitalized children. Pediatrics. 2010;126:829–832.
- , , , , , . Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126:638–646.
- , , . Hospitalist care of the medically complex child. Pediatr Clin North Am. 2005;52:1165–1187, x.
- , . Discharge planning and home care of the technology‐dependent infant. J Obstet Gynecol Neonatal Nurs. 1995;24:77–83.
- , , , . Pediatric discharge planning: complications, efficiency, and adequacy. Soc Work Health Care. 1995;22:1–18.
- , , , et al. The current capabilities of health information technology to support care transitions. AMIA Annu Symp Proc. 2013;2013:1231.
- , , , et al. Provider‐to‐provider electronic communication in the era of meaningful use: a review of the evidence. J Hosp Med. 2013;8:589–597.
- , , , . Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2:314–323.
- , , , , . A 5‐year time study analysis of emergency department patient care efficiency. Ann Emerg Med. 1999;34:326–335.
- , , , et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med. 2013;173(18):1715–1722.
- , . Addressing postdischarge adverse events: a neglected area. Jt Comm J Qual Patient Saf. 2008;34:85–97.
Outcomes in CVC Occlusions
Long‐term central venous catheters (CVCs) facilitate care for patients with chronic illness by providing easy venous access for laboratory tests, administration of medication, and parenteral nutrition. However, several complications resulting from the use of CVCs, including sepsis, extravasation of infusions, and venous thrombosis, can increase associated morbidity and mortality. These complications can also interrupt and delay treatment for the underlying disease and thereby affect outcomes. One of the most common CVC complications is catheter occlusion.[1]
Catheter occlusion occurs in 14% to 36% of patients within 1 to 2 years of catheter placement.[2, 3, 4, 5, 6, 7, 8] A catheter occlusion can be partial or complete, and can occur secondary to a variety of mechanical problems, including an uncommon, but potentially life‐threatening, pinch‐off syndrome. Medication or parenteral nutrition can also cause occlusion, which can be acute or gradual, with increasingly sluggish flow through the catheter. Inappropriate concentrations or incompatible mixtures can cause medications to precipitate within the catheter lumen.
Occlusions are either thrombotic or nonthrombotic. One autopsy study of patients with a long‐term CVC found that a fibrin sheath encased the catheter tip in every case.[9] An occluded catheter may compromise patient care[9, 10]; it may cause cancellation or delay of procedures, it potentially interrupts administration of critical therapies including vesicants, it may result in risk of infection, and it potentially leads to catheter replacement. This can further complicate care, leading to increased length of stay (LOS) and hospital costs.
To better understand resource utilization, LOS, and cost implications of alteplase compared with catheter replacement, we conducted a preplanned, retrospective analysis of hospitalized patients captured between January 2006 and December 2011 in the database maintained by Premier. The Premier database is a large, US hospital‐based, service‐level, all‐payer, comparative database, with information collected primarily from nearly 600 geographically diverse, nonprofit, nongovernment community and teaching hospitals.
METHODS
Data Sources
The Premier database contains information on over 42 million hospital discharges (mean 5.5 million discharges/year)one‐fifth of all US hospitalizationsfrom the year 2000 to the present. The database contains data from standard hospital discharge files, including patient demographic information and disease state. Patients can be tracked, with a unique identifier, across the inpatient and hospital‐based outpatient settings, as well as across visits. In addition to the data elements available in most of the standard hospital discharge files, the Premier database also contains a date‐stamped log of billed items, including procedures, medications, and laboratory, diagnostic, and therapeutic services at the individual patient level. Drug utilization information is available by day of stay and includes quantity, dosing, strength used, and cost.
The Premier database has been used extensively to benchmark hospital clinical and financial performance as well as by the US Food and Drug Administration (FDA) for drug surveillance and by the Centers for Medicare and Medicaid Services to evaluate next‐generation payment models. Preliminary comparisons between patient and hospital characteristics for hospitals that submit data to Premier and those of the probability sample of hospitals and patients selected for the National Hospital Discharge Survey suggest that the patient populations are similar with regard to patient age, gender, LOS, mortality, primary discharge diagnosis, and primary procedure groups.
Patient Population
In this retrospective observational database analysis, inpatients of all ages were initially identified who were discharged from a hospital between January 1, 2006 and December 31, 2011 and whose records contained 1 or more International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9) procedural codes or Current Procedural Terminology (CPT‐4) codes signifying CVC placement. The catheter replacement group comprised patients having a catheter replacement during the hospitalization. The alteplase treatment group was identified through patient billing records and by computing the dose administered (2 mg) during the index hospitalization period. Healthcare Common Procedure Coding System J‐codes (J2996, alteplase recombinant injection 10 mg; J2997, alteplase recombinant 1 mg) were also evaluated during the analysis to supplement the search string identification. To account for and eliminate catheter replacement due to mechanical failure rather than occlusion, patients with ICD‐9 diagnosis code 996.1 for mechanical failure were excluded. Patients with an ICD‐9 diagnosis code for infection or who received antibiotics on the day of replacement were excluded as an additional way to narrow the study to patients with occlusion as the reason for catheter replacement. In addition, patients receiving kidney dialysis, a chronic condition prone to greater‐than‐usual risk of catheter occlusion, were excluded. When a patient had multiple hospital stays with CVC insertions or placement during the study period, the first hospitalization with insertions or placement was used in our analyses.
Of the CVC patient population (N=574,252), 36,680 patient discharges resulted in the need for CVC replacement, alteplase therapy, or both. Patients receiving both replacement and alteplase (N=144) were excluded from analysis, resulting in 33,551 patient discharges with alteplase and 1028 patient discharges with CVC replacement.
Outcome Measures
The main outcomes of interest were LOS and hospital costs after occlusion, and readmissions at 30 and 90 days. Secondary measures, as they were thought to play a role in influencing outcomes, included LOS and costs before occlusion, as well as departmental costs such as pharmacy, radiology, and days in the intensive care unit (ICU).
Statistical Analysis
Univariate descriptive statistics were used to characterize the patient population by patient, clinical, and hospital attributes. In addition, subgroup analyses were performed among patients with any cardiology diagnosis (using ICD‐9 diagnosis or procedure codes), heart failure, myocardial infarction, and cancer, which were potentially overlapping categories chosen prior to initiating the analyses. Data measured on a continuous scale were expressed as mean, standard deviation, range, and median. Categorical data were expressed as count/percentages in the categories. In addition, categorical costs were also examined before and after occlusion. Tables of results included P values comparing patients who received CVC replacement with those who received alteplase across all measures. The [2] tests were used to test for differences in categorical variables, and t tests were utilized for differences in continuous variables.
Multivariable regression modeling was conducted to better compare outcomes associated with catheter replacement versus alteplase treatment. Linear regression models were performed to evaluate hospital costs and LOS during the initial hospital discharge. Logistic regression models were performed to evaluate the odds of readmission at 30 and 90 days following discharge. All multivariable models controlled for factors found to be statistically significant in univariate analysis. The covariates varied by model, but generally included age, race, sex, cancer, 3M All Patient Refined Diagnosis Related Group risk of mortality and severity of illness, cerebrovascular disease, renal disease, payer, myocardial infarction, hemiplegia/paraplegia, chronic or acute diabetes, peripheral vascular disease, complication, admission source, admission type, congestive heart failure, dementia, metastatic solid tumor, rheumatic disease, peptic ulcer disease, chronic pulmonary disease, hospital teaching status, urban/rural location, US Census region, and number of hospital beds. Certain of these variables, such as 3M measures of severity and risk, as well as measures of LOS and costs before occlusion, were considered as ways to understand differences in risk of increased costs among patients. For each multivariable model, covariates eligible for inclusion in the models were selected using a backward selection method (logistic used stepwise) until all variables remaining in the model were significant at P0.2.
RESULTS
This study included 34,579 patients who first had a CVC insertion and then were treated for a CVC occlusion by receiving a replacement CVC (n=1028) or by receiving alteplase (2 mg) administration (n=33,551) during the same hospitalization (Table 1). Patients who received alteplase tended to be younger (6019 vs 6220 years old). More than 50% were at least 65 years of age. Twelve percent of alteplase patients were black, whereas 18.5% of catheter‐replacement patients were black.
| Catheter Replacement, n=1,028 | Alteplase Treatment, n=33,551 | |
|---|---|---|
| ||
| Age group, ya | ||
| Under 18 | 29 (2.8%) | 984 (2.9%) |
| 1834 | 84 (8.2%) | 2,479 (7.4%) |
| 3544 | 73 (7.1%) | 2,826 (8.4%) |
| 4554 | 116 (11.3%) | 5,217 (15.5%) |
| 5564 | 210 (20.4%) | 6,761 (20.1%) |
| 6574 | 203 (19.7%) | 6,741 (20.1%) |
| 75+ | 313 (30.4%) | 8,543 (25.5%) |
| Mean (SD) | 62 (20) | 60 (19) |
| Sex | ||
| Female | 565 (55.0%) | 18,172 (54.2%) |
| Male | 463 (45.0%) | 15,378 (45.8%) |
| Unknown | 0 (0%) | 1 (0%) |
| Race/ethnicitya | ||
| Black | 190 (18.5%) | 4,057 (12.1%) |
| Hispanic | 40 (3.9%) | 1,098 (3.3%) |
| Other | 126 (12.3%) | 6,250 (18.6%) |
| White | 672 (65.4%) | 22,146 (66.0%) |
| Comorbid conditions | ||
| Myocardial infarction | 96 (9.3%) | 3,746 (11.2%) |
| Congestive heart failure | 258 (25.1%) | 8,210 (24.5%) |
| Peripheral vascular disease | 104 (10.1%) | 3,451 (10.3%) |
| Cerebrovascular disease | 115 (11.2%) | 3,528 (10.5%) |
| Dementia | 33 (3.2%) | 838 (2.5%) |
| Chronic pulmonary diseasea | 264 (25.7%) | 10,495 (31.3%) |
| Rheumatic disease | 37 (3.6%) | 1,344 (4.0%) |
| Peptic ulcer disease | 41 (4.0%) | 1,068 (3.2%) |
| Mild liver diseasea | 94 (9.1%) | 2,392 (7.1%) |
| Moderate/severe liver diseasea | 29 (2.8%) | 531 (1.6%) |
| Acute diabetes | 255 (24.8%) | 9,185 (27.4%) |
| Chronic diabetesa | 44 (4.3%) | 2,327 (6.9%) |
| Hemiplegia paraplegia | 51 (5.0%) | 1,909 (5.7%) |
| Renal diseasea | 209 (20.3%) | 5,351 (16.0%) |
| Cancera | 207 (20.1%) | 5,685 (16.9%) |
| Metastatic solid tumora | 100 (9.7%) | 2,441 (7.3%) |
| AIDS/HIV | 4 (0.4%) | 244 (0.7%) |
| 3M APR‐DRG Severity of Illnessa | ||
| 1‐minor | 36 (3.5%) | 769 (2.3%) |
| 2‐moderate | 172 (16.7%) | 4,109 (12.2%) |
| 3‐major | 384 (37.3%) | 12,175 (36.3%) |
| 4‐extreme | 436 (42.4%) | 16,497 (49.2%) |
| Unknown | 0 (0%) | 1 (0%) |
| 3M APR‐DRG Risk of Mortalitya | ||
| 1‐minor | 159 (15.5%) | 4,716 (14.1%) |
| 2‐moderate | 253 (24.6%) | 6,746 (20.1%) |
| 3‐major | 313 (30.4%) | 10,569 (31.5%) |
| 4‐mxtreme | 303 (29.5%) | 11,519 (34.3%) |
| Unknown | 0 (0%) | 1 (0%) |
Alteplase patients were significantly more likely to have a diagnosis of chronic pulmonary disease, liver disease, renal disease, chronic diabetes (ie, diabetes with complications), and cancer. There was an equivalent number of urban and rural hospitals across the 2 groups of patients (Table 2); however, there were regional differences including a higher proportion of catheter‐replacement patients from the East North Central and Middle Atlantic areas and a lower proportion of catheter‐replacement patients from Mountain and Pacific states. Catheter‐replacement patients more frequently were treated in teaching hospitals and in hospitals of larger size.
| Catheter Replacement, n=1,028 | Alteplase Treatment, n=33,551 | |
|---|---|---|
| ||
| Provider regiona | ||
| New England | 28 (2.7%) | 976 (2.9%) |
| Middle Atlantic | 227 (22.1%) | 1,944 (5.8%) |
| South Atlantic | 247 (24.0%) | 8,047 (24.0%) |
| East North Central | 153 (14.9%) | 3,015 (9.0%) |
| East South Central | 14 (1.4%) | 1,345 (4.0%) |
| West North Central | 98 (9.5%) | 3,590 (10.7%) |
| West South Central | 112 (10.9%) | 5,096 (15.2%) |
| Mountain | 48 (4.7%) | 3,339 (9.9%) |
| Pacific | 94 (9.1%) | 6,083 (18.1%) |
| Unknown | 7 (0.7%) | 116 (0.3%) |
| Population served | ||
| Rural | 56 (5.4%) | 1,838 (5.5%) |
| Urban | 972 (94.6%) | 31,713 (94.5%) |
| Teaching statusa | ||
| Nonteaching | 431 (41.9%) | 18,598 (55.4%) |
| Teaching | 597 (58.1%) | 14,953 (4.6%) |
| Hospital size, no. of bedsa | ||
| <100 | 4 (0.4%) | 475 (1.4%) |
| 100199 | 56 (5.4%) | 1,725 (5.1%) |
| 200299 | 124 (12.1%) | 5,907 (17.6%) |
| 300499 | 432 (42.0%) | 13,790 (41.1%) |
| 500+ | 412 (40.1%) | 11,654 (34.7%) |
| Primary payora | ||
| Commercial | 50 (4.9%) | 1,779 (5.3%) |
| Managed care | 221 (21.5%) | 6,888 (20.5%) |
| Medicaid | 132 (12.8%) | 4,146 (12.4%) |
| Medicare | 572 (55.6%) | 17,226 (51.3%) |
| Other government programs | 9 (0.9%) | 439 (1.3%) |
| Any other payor | 44 (4.3%) | 3,073 (9.2%) |
| Admission sourcea | ||
| Emergency department | 424 (41.2%) | 12,741 (38.0%) |
| Physician referral | 390 (37.9%) | 14,502 (43.2%) |
| Transfer from another health facility | 154 (15.0%) | 4,109 (12.2%) |
| Unknown | 60 (5.8%) | 2,199 (6.5%) |
| Admission typea | ||
| Elective | 205 (19.9%) | 5,872 (17.5%) |
| Emergency | 613 (59.6%) | 19,660 (58.6%) |
| Newborn | 9 (0.9%) | 37 (0.1%) |
| Trauma center | 3 (0.3%) | 279 (0.8%) |
| Urgent | 192 (18.7%) | 7,573 (22.6%) |
| Unknown | 6 (0.6%) | 130 (0.4%) |
After covariate adjustment for baseline measurements significantly related to each outcome, average daily post occlusion costs were estimated to be $317 lower for alteplase recipients than for patients who received catheter replacement ($317; 95% confidence interval [CI]: $238‐$392; P<0.0001) (Table 3). Average adjusted total post occlusion costs were $1419 lower for alteplase recipients than for patients who received catheter replacement ($1418; 95% CI: $307‐$2458; P=0.012).
| CVC Replace Only, n=1,028 | Alteplase Only, n=33,551 | |
|---|---|---|
| ||
| 30‐day readmission | 24.6% | 23.7% |
| 90‐day readmission | 35.1% | 33.9% |
| Preocclusion | ||
| Mean (SD) length of stay, days | 3.8 (6.7) | 7.3 (6.9) |
| Mean (SD) total cost | $10,485 ($29,088) | $18,546 ($22,658) |
| Mean (SD) cost per day | $2,876 ($3,046) | $2,637 ($1,783) |
| Postocclusion | ||
| Mean (SD) length of stay, days | 8.8 (11.0) | 8.8 (10.0) |
| Mean (SD) total cost | $18,714 ($32,189) | $16,765 ($29,966) |
| Mean (SD) cost per day | $2,146 ($2,995) | $2,058 ($6,585) |
Contributing to the lower cost were certain revenue‐center specific costs (Table 4). Total room and board costs were different between the alteplase and catheter‐replacement groups in both the pre‐ and postocclusion periods; this was related to the difference between the 2 comparison groups in postocclusion LOS of about 0.3 days (Table 5). However, the differences favored alteplase use over catheter replacement. Cardiology/electrocardiography costs were lower for catheter replacement in the preocclusion period but lower for alteplase use in the postocclusion period. Emergency department costs were higher for catheter replacement in both periods, as were respiratory costs in the same manner. Additionally, costs for laboratory tests, nursing, operating room/surgery, pharmacy, radiology, supplies, and ICU room and board were lower in the preocclusion period but higher in the postocclusion period for catheter‐replacement patients. It was unclear why the pharmacy costs after catheter replacement would have increased for catheter‐replacement patients in contrast to the decrease for alteplase‐treated patients, but because this occurred at an average daily basis as well, it appeared that catheter‐replacement patients may have received additional medications. Average adjusted postocclusion LOS was similar for alteplase and catheter‐replacement recipients (P=0.24), suggesting that decreased total costs were due to reasons other than shorter LOS.
| Preocclusiona | Postocclusiona | |||
|---|---|---|---|---|
| CVC Replacement Only, n=1,028 | Alteplase Only, n=33,551 | CVC Replacement Only, n=1,028 | Alteplase Onlyn=33,551 | |
| ||||
| Total room and board cost | ||||
| Mean (SD) total cost | $4,380 ($9,545) | $8,535 ($10,175)b | $8,394 ($14,393) | $8,437 ($18,341)b |
| Mean (SD) cost per day | $693 ($734) | $1,097 ($724)b | $751 ($536) | $983 ($3,250) |
| Cardiology/ECG cost | ||||
| Mean (SD) total cost | $82 ($806) | $154 ($605)b | $124 ($540) | $107 ($735)b |
| Mean (SD) cost per day | $17 ($96) | $26 ($131)b | $17 ($93) | $19 ($217)b |
| Emergency department cost | ||||
| Mean (SD) total cost | $10 ($91) | $36 ($284)b | $10 ($67) | $12 ($195) |
| Mean (SD) cost per day | $4 ($32) | $8 ($65)b | $2 ($19) | $6 ($76) |
| Laboratory cost | ||||
| Mean (SD) total cost | $864 ($2,538) | $1,425 ($3,622)b | $1,471 ($5,614) | $1,175 ($3,961) |
| Mean (SD) cost per day | $140 ($314) | $180 ($269)b | $139 ($313) | $142 ($465)b |
| Nursing Cost | ||||
| Mean (SD) total cost | $218 ($1,497) | $224 ($2,364)b | $432 ($2,538) | $231 ($2,785) |
| Mean (SD) cost per day | $39 ($166) | $24 ($127)b | $35 ($140) | $21 ($112) |
| OR/surgery cost | ||||
| Mean (SD) total cost | $902 ($4,743) | $1,602 ($3,597)b | $1,437 ($3,029) | $847 ($2,701)b |
| Mean (SD) cost per day | $207 ($495) | $267 ($513)b | $302 ($646) | $130 ($827)b |
| Pharmacy cost | ||||
| Mean (SD) total cost | $2,085 ($20,338) | $3,014 ($6,408)b | $3,200 ($16,396) | $2,914 ($8,383)b |
| Mean (SD) cost per day | $263 ($1,509) | $368 ($583)b | $362 ($2,427) | $347 ($853)b |
| Radiology cost | ||||
| Mean (SD) total cost | $470 ($869) | $782 ($1,031)b | $731 ($1,160) | $505 ($1,550)b |
| Mean (SD) cost per day | $133 ($362) | $130 ($189)b | $144 ($293) | $83 ($469)b |
| Respiratory cost | ||||
| Mean (SD) total cost | $391 ($1,442) | $895 ($2,160)b | $673 ($2,209) | $783 ($2,297)b |
| Mean (SD) cost per day | $51 ($121) | $104 ($170)b | $61 ($115) | $81 ($280)b |
| Supply cost | ||||
| Mean (SD) total cost | $834 ($3,221) | $1,408 ($5,871)b | $1,636 ($7,250) | $1,117 ($4,477)b |
| Mean (SD) cost per day | $208 ($1,244) | $211 ($789)b | $264 ($871) | $165 ($1,529)b |
| Other therapy cost | ||||
| Mean (SD) total cost | $179 ($702) | $355 ($815)b | $436 ($837) | $509 ($1,263)b |
| Mean (SD) cost per day | $30 ($81) | $46 ($98)b | $51 ($106) | $66 ($481)b |
| Other departments cost | ||||
| Mean (SD) total cost | $26 ($710) | $1 ($36) | $74 ($1,127) | $3 ($144) b |
| Mean (SD) cost per day | $3 ($56) | $0 ($5) | $6 ($86) | $0 ($13)b |
| Fees cost | ||||
| Mean (SD) total cost | $38 ($370) | $82 ($969)b | $67 ($340) | $86 ($2,704) |
| Mean (SD) cost per day | $7 ($47) | $12 ($77)b | $12 ($120) | $12 ($843) |
| Healthcare services cost | ||||
| Mean (SD) total cost | $5 ($53) | $31 ($1,052)b | $29 ($515) | $35 ($1,162) |
| Mean (SD) cost per day | $1 ($10) | $3 ($65)b | $2 ($11) | $3 ($54) |
| ICU room and board cost | ||||
| Mean (SD) total cost | $2,085 ($7,700) | $4,333 ($8,826)b | $3,158 ($10,767) | $2,884 ($15,863) |
| Mean (SD) cost per day | $293 ($677) | $543 ($854)b | $222 ($512) | $323 ($2,330) |
| Model | Parameter Estimate | Summary Statistic | Estimate (95% CI) |
|---|---|---|---|
| |||
| 30‐day readmissiona | 0.0234 | Odds ratio | 1.048 (0.899 to 1.221) |
| 90‐day readmissionb | 0.0248 | Odds ratio | 1.051 (0.915 to 1.207) |
| Postocclusion total costsc | 0.0842 | Mean differenced | $1,418.69 ($2,458.12 to $307.27)f |
| Postocclusion total cost per daye | 0.1857 | Mean differenced | $317.20 ($392.24 to $238.22)f |
| Post occlusion length of stayg | 0.0313 | Mean differenced | 0.299 (0.196 to 0.820) |
Unadjusted 30‐ and 90‐day readmission rates were 24.6% and 35.1% for CVC replacement and slightly lower at 23.7% and 33.9% for alteplase (Table 3), respectively. Odds of readmission after adjusting for patient and hospital factors were not significantly different at 30 days (odds ratio [OR]: 1.048, 95% CI: 0.899‐1.221; P=0.55) or at 90 days (OR: 1.051, 95% CI: 0.915‐1.207; P=0.48) (Table 5). Subgroup analyses for patients with a diagnosis of heart failure, myocardial infarction, and cancer revealed similar results.
DISCUSSION
The cost of healthcare in the United States has risen at an outstanding rate compared with other countries. Our percentage of gross national product spent on healthcare is on the order of 16% to 18%, almost twice as much as the next most industrialized country in terms of healthcare expenditure.[11] In the current era, finding opportunities to reduce healthcare costs without negatively impacting quality of care is the name of the game. Professional societies have come together under the campaign of Choosing Wisely: An Initiative of the ABIM (American Board of Internal Medicine) Foundation to help educate clinicians and patients on cost‐containment strategies.[12] Research that demonstrates opportunities to reduce cost will help healthcare providers choose wisely among diagnostic and therapeutic options for patients. Our study demonstrated that the use of a drug such as alteplase in clearing CVC catheter obstruction was significantly less costly to the hospital than catheter replacement.
Cathflo Activase (alteplase: Genentech, South San Francisco, CA), the only FDA‐approved thrombolytic for the restoration of central venous catheter function, is the current standard treatment for catheter occlusions in the United States. A dose of 2 mg in 2 mL is instilled in patients weighing 30 kg or 110% of the internal lumen volume of the catheter not to exceed 2 mg in 2 mL for those patients weighing <30 kg. Haire et al. showed that a 2‐mg dose of alteplase was more effective than urokinase (5000 IU) for treating radiographically proven thrombotic occlusion of a CVC after a dwell time of 120 minutes.[13] In the Cardiovascular thrombolytic used to Open Occluded Lines (COOL) trial, one 2‐mg dose of alteplase cleared the catheter occlusion after 120 minutes in 74% of patients, compared with only 17% of patients who received a placebo. Studies have confirmed the safety and efficacy of alteplase administered at various time intervals in different long‐term catheters, including peripherally inserted central catheters, with major hemorrhage reported in 0.3% of patients.[14, 15, 16]
Adding to the knowledge of patient outcomes from clinical studies, many health outcomes studies have demonstrated benefit in cost containment through decreasing LOS, which one can argue is just shifting the cost to an earlier part of the stay. Even though this is highly beneficial, it does not address the core resource utilization within the hospital. Our study found its cost benefit not in the LOS, but in decreasing core resource utilization such as radiology, lab, nursing, and supplies. If patients are admitted for a noncardiovascular condition and have CVC occlusion, using alteplase to clear the CVC occlusion along with implementing strategies to manage the underlying disease to reduce the LOS becomes a powerful opportunity to impact cost. Among patients who may come to the hospital for just the CVC occlusion, the LOS should be short. There may be no significant opportunity to reduce the LOS in those cases, but opportunities to decrease core hospital resource utilization with alteplase make this approach beneficial if the patient can tolerate it.
Limitations of the study include the retrospective and administrative nature of the database used, which is unable to provide certain clinical measures as would be available at the patient's bedside when treatment choices are being made. Had they been available, we might have included them in our assessment of whether patients who underwent CVC replacement were significantly different from those who received alteplase. In addition, not all hospitals in the database had charge masters that facilitated identification of CVC replacements or reinsertions, requiring the use of CPT‐4 codes and evidence of new CVCs being placed or inserted. Certain patients were excluded if there was conflicting information about whether the CVC was new within the hospital stay or dwelling in the patient prior to admission. Also, dialysis patients were excluded because they were not part of any approved indication for alteplase 2 mg, and this group is particularly prone to catheter obstruction. As such, they represent more complicated cases than the norm; this exclusion may have limited the overall generalizability of the study. The study also relied on charge master (billing) data to identify the use of alteplase and other treatments, where there is the potential, albeit minimal, for inaccuracies in the data. Of greater importance, the study relied on ICD‐9 coding to identify comorbid conditions, and as in other studies using similar data sources, such methods are subject to coding errors and omissions. However, many of the listed limitations above were not thought to be different between the comparison groups or more problematic for this study than for other studies based on similar data sources.
CONCLUSION
Among patients treated for an occluded CVC, alteplase‐treated patients had lower daily postocclusion costs and lower total postocclusion costs than patients who received catheter replacement. Differences in costs did not appear to be driven by differences in postocclusion LOS. Readmissions at 30‐ and 90‐day periods were found to be similar between alteplase recipients and catheter‐replacement patients.
Acknowledgements
The authors thank W. Kenne Mountford for his editorial assistance with a prior version of the article and Dima Qato for assistance with the analyses. Additional editorial assistance was provided by Steve Melvin. This assistance was funded by Genentech, Inc.
Disclosures: This study was funded by Genentech, Inc. F. R. Ernst and C. Lipkin are employees of Premier, which was contracted by Genentech to conduct the study covered in this article. E. Chen is an employee of and holds stock in Genentech. D. Tayama is an employee of Genentech. A. N. Amin received research funding from Premier, which was contracted by Genentech to conduct the study covered in this article.
- , , , , et al. Management of occlusion and thrombosis associated with long‐term indwelling central venous catheters. Lancet. 2009;374:159–169.
- , , , , , ; Children's Oncology Group. Prophylactic urokinase in the management of long‐term venous access devices in children; a Children's Oncology Group study. J Clin Oncol. 2004;22:2718–2723.
- , , , et al. Central venous catheter‐related complications in children with oncological/hematological diseases: an observational study of 418 devices. Ann Oncol. 1985;16:648–654.
- , , , et al. A cross‐sectional study evaluating post‐thrombotic syndrome in children. Thromb Res. 2003;111:227–233.
- , , , . Complications and management of implanted venous access catheters. J Clin Oncol. 1985;3:710–717.
- . Local installation of small doses of streptokinase for treatment of thrombotic occlusions of long‐term access catheters. J Clin Oncol. 1983;1:572–573.
- , , . Are clinical signs accurate indicators of the cause of central venous catheter occlusion? J Parenter Enteral Nutr. 1995;19:75–79.
- , . Mechanism and management of persistent withdrawal occlusion. Am Surg. 1988;54:326–328.
- . Catheter‐related thrombosis in pediatrics. Pediatr Nurs. 2002;28:97–102, 105–106.
- . Reopen the pipeline. Nursing. 2005;35:54–61.
- , . Chemotherapy extravasation: a consequence of fibrin sheath formation around venous access devices. Oncol Nurs Forum. 1995;22:675–680.
- Organisation for Economic Co‐operation and Development (OECD). Statistics. OECD Health Data 2010, June 2010. http://www.oecd.org/unitedstates/Briefing‐Note‐USA‐2013.pdf. Accessed May 8, 2014.
- ABIM Foundation. Choosing Wisely: An Initiative of the ABIM Foundation. (2013). Available at: http://www.choosingwisely.org. Accessed April 6, 2013.
- , , , . Urokinase versus recombinant tissue plasminogen activator in thrombosed central venous catheters: a double‐blinded, randomized trial. Thromb Haemost. 1994;72:543–547.
- , , , et al. Recombinant tissue plasminogen activator (alteplase) for restoration of flow in occluded central venous access devices: a double‐blind placebo‐controlled trial—the Cardiovascular Thrombolytic to Open Occluded Lines (COOL) efficacy trial. J Vasc Interv Radiol. 2001;12:951–955.
- , , , et al. Safety and efficacy of alteplase for restoring function in occluded central venous catheters: results of the cardiovascular thrombolytic to open occluded lines trial. J Clin Oncol. 2002;20:317–324.
- , , , . Alteplase for treatment of occluded peripherally inserted central catheters: safety and efficacy in 240 patients. J Vasc Interv Radiol. 2004;15:45–49.
Long‐term central venous catheters (CVCs) facilitate care for patients with chronic illness by providing easy venous access for laboratory tests, administration of medication, and parenteral nutrition. However, several complications resulting from the use of CVCs, including sepsis, extravasation of infusions, and venous thrombosis, can increase associated morbidity and mortality. These complications can also interrupt and delay treatment for the underlying disease and thereby affect outcomes. One of the most common CVC complications is catheter occlusion.[1]
Catheter occlusion occurs in 14% to 36% of patients within 1 to 2 years of catheter placement.[2, 3, 4, 5, 6, 7, 8] A catheter occlusion can be partial or complete, and can occur secondary to a variety of mechanical problems, including an uncommon, but potentially life‐threatening, pinch‐off syndrome. Medication or parenteral nutrition can also cause occlusion, which can be acute or gradual, with increasingly sluggish flow through the catheter. Inappropriate concentrations or incompatible mixtures can cause medications to precipitate within the catheter lumen.
Occlusions are either thrombotic or nonthrombotic. One autopsy study of patients with a long‐term CVC found that a fibrin sheath encased the catheter tip in every case.[9] An occluded catheter may compromise patient care[9, 10]; it may cause cancellation or delay of procedures, it potentially interrupts administration of critical therapies including vesicants, it may result in risk of infection, and it potentially leads to catheter replacement. This can further complicate care, leading to increased length of stay (LOS) and hospital costs.
To better understand resource utilization, LOS, and cost implications of alteplase compared with catheter replacement, we conducted a preplanned, retrospective analysis of hospitalized patients captured between January 2006 and December 2011 in the database maintained by Premier. The Premier database is a large, US hospital‐based, service‐level, all‐payer, comparative database, with information collected primarily from nearly 600 geographically diverse, nonprofit, nongovernment community and teaching hospitals.
METHODS
Data Sources
The Premier database contains information on over 42 million hospital discharges (mean 5.5 million discharges/year)one‐fifth of all US hospitalizationsfrom the year 2000 to the present. The database contains data from standard hospital discharge files, including patient demographic information and disease state. Patients can be tracked, with a unique identifier, across the inpatient and hospital‐based outpatient settings, as well as across visits. In addition to the data elements available in most of the standard hospital discharge files, the Premier database also contains a date‐stamped log of billed items, including procedures, medications, and laboratory, diagnostic, and therapeutic services at the individual patient level. Drug utilization information is available by day of stay and includes quantity, dosing, strength used, and cost.
The Premier database has been used extensively to benchmark hospital clinical and financial performance as well as by the US Food and Drug Administration (FDA) for drug surveillance and by the Centers for Medicare and Medicaid Services to evaluate next‐generation payment models. Preliminary comparisons between patient and hospital characteristics for hospitals that submit data to Premier and those of the probability sample of hospitals and patients selected for the National Hospital Discharge Survey suggest that the patient populations are similar with regard to patient age, gender, LOS, mortality, primary discharge diagnosis, and primary procedure groups.
Patient Population
In this retrospective observational database analysis, inpatients of all ages were initially identified who were discharged from a hospital between January 1, 2006 and December 31, 2011 and whose records contained 1 or more International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9) procedural codes or Current Procedural Terminology (CPT‐4) codes signifying CVC placement. The catheter replacement group comprised patients having a catheter replacement during the hospitalization. The alteplase treatment group was identified through patient billing records and by computing the dose administered (2 mg) during the index hospitalization period. Healthcare Common Procedure Coding System J‐codes (J2996, alteplase recombinant injection 10 mg; J2997, alteplase recombinant 1 mg) were also evaluated during the analysis to supplement the search string identification. To account for and eliminate catheter replacement due to mechanical failure rather than occlusion, patients with ICD‐9 diagnosis code 996.1 for mechanical failure were excluded. Patients with an ICD‐9 diagnosis code for infection or who received antibiotics on the day of replacement were excluded as an additional way to narrow the study to patients with occlusion as the reason for catheter replacement. In addition, patients receiving kidney dialysis, a chronic condition prone to greater‐than‐usual risk of catheter occlusion, were excluded. When a patient had multiple hospital stays with CVC insertions or placement during the study period, the first hospitalization with insertions or placement was used in our analyses.
Of the CVC patient population (N=574,252), 36,680 patient discharges resulted in the need for CVC replacement, alteplase therapy, or both. Patients receiving both replacement and alteplase (N=144) were excluded from analysis, resulting in 33,551 patient discharges with alteplase and 1028 patient discharges with CVC replacement.
Outcome Measures
The main outcomes of interest were LOS and hospital costs after occlusion, and readmissions at 30 and 90 days. Secondary measures, as they were thought to play a role in influencing outcomes, included LOS and costs before occlusion, as well as departmental costs such as pharmacy, radiology, and days in the intensive care unit (ICU).
Statistical Analysis
Univariate descriptive statistics were used to characterize the patient population by patient, clinical, and hospital attributes. In addition, subgroup analyses were performed among patients with any cardiology diagnosis (using ICD‐9 diagnosis or procedure codes), heart failure, myocardial infarction, and cancer, which were potentially overlapping categories chosen prior to initiating the analyses. Data measured on a continuous scale were expressed as mean, standard deviation, range, and median. Categorical data were expressed as count/percentages in the categories. In addition, categorical costs were also examined before and after occlusion. Tables of results included P values comparing patients who received CVC replacement with those who received alteplase across all measures. The [2] tests were used to test for differences in categorical variables, and t tests were utilized for differences in continuous variables.
Multivariable regression modeling was conducted to better compare outcomes associated with catheter replacement versus alteplase treatment. Linear regression models were performed to evaluate hospital costs and LOS during the initial hospital discharge. Logistic regression models were performed to evaluate the odds of readmission at 30 and 90 days following discharge. All multivariable models controlled for factors found to be statistically significant in univariate analysis. The covariates varied by model, but generally included age, race, sex, cancer, 3M All Patient Refined Diagnosis Related Group risk of mortality and severity of illness, cerebrovascular disease, renal disease, payer, myocardial infarction, hemiplegia/paraplegia, chronic or acute diabetes, peripheral vascular disease, complication, admission source, admission type, congestive heart failure, dementia, metastatic solid tumor, rheumatic disease, peptic ulcer disease, chronic pulmonary disease, hospital teaching status, urban/rural location, US Census region, and number of hospital beds. Certain of these variables, such as 3M measures of severity and risk, as well as measures of LOS and costs before occlusion, were considered as ways to understand differences in risk of increased costs among patients. For each multivariable model, covariates eligible for inclusion in the models were selected using a backward selection method (logistic used stepwise) until all variables remaining in the model were significant at P0.2.
RESULTS
This study included 34,579 patients who first had a CVC insertion and then were treated for a CVC occlusion by receiving a replacement CVC (n=1028) or by receiving alteplase (2 mg) administration (n=33,551) during the same hospitalization (Table 1). Patients who received alteplase tended to be younger (6019 vs 6220 years old). More than 50% were at least 65 years of age. Twelve percent of alteplase patients were black, whereas 18.5% of catheter‐replacement patients were black.
| Catheter Replacement, n=1,028 | Alteplase Treatment, n=33,551 | |
|---|---|---|
| ||
| Age group, ya | ||
| Under 18 | 29 (2.8%) | 984 (2.9%) |
| 1834 | 84 (8.2%) | 2,479 (7.4%) |
| 3544 | 73 (7.1%) | 2,826 (8.4%) |
| 4554 | 116 (11.3%) | 5,217 (15.5%) |
| 5564 | 210 (20.4%) | 6,761 (20.1%) |
| 6574 | 203 (19.7%) | 6,741 (20.1%) |
| 75+ | 313 (30.4%) | 8,543 (25.5%) |
| Mean (SD) | 62 (20) | 60 (19) |
| Sex | ||
| Female | 565 (55.0%) | 18,172 (54.2%) |
| Male | 463 (45.0%) | 15,378 (45.8%) |
| Unknown | 0 (0%) | 1 (0%) |
| Race/ethnicitya | ||
| Black | 190 (18.5%) | 4,057 (12.1%) |
| Hispanic | 40 (3.9%) | 1,098 (3.3%) |
| Other | 126 (12.3%) | 6,250 (18.6%) |
| White | 672 (65.4%) | 22,146 (66.0%) |
| Comorbid conditions | ||
| Myocardial infarction | 96 (9.3%) | 3,746 (11.2%) |
| Congestive heart failure | 258 (25.1%) | 8,210 (24.5%) |
| Peripheral vascular disease | 104 (10.1%) | 3,451 (10.3%) |
| Cerebrovascular disease | 115 (11.2%) | 3,528 (10.5%) |
| Dementia | 33 (3.2%) | 838 (2.5%) |
| Chronic pulmonary diseasea | 264 (25.7%) | 10,495 (31.3%) |
| Rheumatic disease | 37 (3.6%) | 1,344 (4.0%) |
| Peptic ulcer disease | 41 (4.0%) | 1,068 (3.2%) |
| Mild liver diseasea | 94 (9.1%) | 2,392 (7.1%) |
| Moderate/severe liver diseasea | 29 (2.8%) | 531 (1.6%) |
| Acute diabetes | 255 (24.8%) | 9,185 (27.4%) |
| Chronic diabetesa | 44 (4.3%) | 2,327 (6.9%) |
| Hemiplegia paraplegia | 51 (5.0%) | 1,909 (5.7%) |
| Renal diseasea | 209 (20.3%) | 5,351 (16.0%) |
| Cancera | 207 (20.1%) | 5,685 (16.9%) |
| Metastatic solid tumora | 100 (9.7%) | 2,441 (7.3%) |
| AIDS/HIV | 4 (0.4%) | 244 (0.7%) |
| 3M APR‐DRG Severity of Illnessa | ||
| 1‐minor | 36 (3.5%) | 769 (2.3%) |
| 2‐moderate | 172 (16.7%) | 4,109 (12.2%) |
| 3‐major | 384 (37.3%) | 12,175 (36.3%) |
| 4‐extreme | 436 (42.4%) | 16,497 (49.2%) |
| Unknown | 0 (0%) | 1 (0%) |
| 3M APR‐DRG Risk of Mortalitya | ||
| 1‐minor | 159 (15.5%) | 4,716 (14.1%) |
| 2‐moderate | 253 (24.6%) | 6,746 (20.1%) |
| 3‐major | 313 (30.4%) | 10,569 (31.5%) |
| 4‐mxtreme | 303 (29.5%) | 11,519 (34.3%) |
| Unknown | 0 (0%) | 1 (0%) |
Alteplase patients were significantly more likely to have a diagnosis of chronic pulmonary disease, liver disease, renal disease, chronic diabetes (ie, diabetes with complications), and cancer. There was an equivalent number of urban and rural hospitals across the 2 groups of patients (Table 2); however, there were regional differences including a higher proportion of catheter‐replacement patients from the East North Central and Middle Atlantic areas and a lower proportion of catheter‐replacement patients from Mountain and Pacific states. Catheter‐replacement patients more frequently were treated in teaching hospitals and in hospitals of larger size.
| Catheter Replacement, n=1,028 | Alteplase Treatment, n=33,551 | |
|---|---|---|
| ||
| Provider regiona | ||
| New England | 28 (2.7%) | 976 (2.9%) |
| Middle Atlantic | 227 (22.1%) | 1,944 (5.8%) |
| South Atlantic | 247 (24.0%) | 8,047 (24.0%) |
| East North Central | 153 (14.9%) | 3,015 (9.0%) |
| East South Central | 14 (1.4%) | 1,345 (4.0%) |
| West North Central | 98 (9.5%) | 3,590 (10.7%) |
| West South Central | 112 (10.9%) | 5,096 (15.2%) |
| Mountain | 48 (4.7%) | 3,339 (9.9%) |
| Pacific | 94 (9.1%) | 6,083 (18.1%) |
| Unknown | 7 (0.7%) | 116 (0.3%) |
| Population served | ||
| Rural | 56 (5.4%) | 1,838 (5.5%) |
| Urban | 972 (94.6%) | 31,713 (94.5%) |
| Teaching statusa | ||
| Nonteaching | 431 (41.9%) | 18,598 (55.4%) |
| Teaching | 597 (58.1%) | 14,953 (4.6%) |
| Hospital size, no. of bedsa | ||
| <100 | 4 (0.4%) | 475 (1.4%) |
| 100199 | 56 (5.4%) | 1,725 (5.1%) |
| 200299 | 124 (12.1%) | 5,907 (17.6%) |
| 300499 | 432 (42.0%) | 13,790 (41.1%) |
| 500+ | 412 (40.1%) | 11,654 (34.7%) |
| Primary payora | ||
| Commercial | 50 (4.9%) | 1,779 (5.3%) |
| Managed care | 221 (21.5%) | 6,888 (20.5%) |
| Medicaid | 132 (12.8%) | 4,146 (12.4%) |
| Medicare | 572 (55.6%) | 17,226 (51.3%) |
| Other government programs | 9 (0.9%) | 439 (1.3%) |
| Any other payor | 44 (4.3%) | 3,073 (9.2%) |
| Admission sourcea | ||
| Emergency department | 424 (41.2%) | 12,741 (38.0%) |
| Physician referral | 390 (37.9%) | 14,502 (43.2%) |
| Transfer from another health facility | 154 (15.0%) | 4,109 (12.2%) |
| Unknown | 60 (5.8%) | 2,199 (6.5%) |
| Admission typea | ||
| Elective | 205 (19.9%) | 5,872 (17.5%) |
| Emergency | 613 (59.6%) | 19,660 (58.6%) |
| Newborn | 9 (0.9%) | 37 (0.1%) |
| Trauma center | 3 (0.3%) | 279 (0.8%) |
| Urgent | 192 (18.7%) | 7,573 (22.6%) |
| Unknown | 6 (0.6%) | 130 (0.4%) |
After covariate adjustment for baseline measurements significantly related to each outcome, average daily post occlusion costs were estimated to be $317 lower for alteplase recipients than for patients who received catheter replacement ($317; 95% confidence interval [CI]: $238‐$392; P<0.0001) (Table 3). Average adjusted total post occlusion costs were $1419 lower for alteplase recipients than for patients who received catheter replacement ($1418; 95% CI: $307‐$2458; P=0.012).
| CVC Replace Only, n=1,028 | Alteplase Only, n=33,551 | |
|---|---|---|
| ||
| 30‐day readmission | 24.6% | 23.7% |
| 90‐day readmission | 35.1% | 33.9% |
| Preocclusion | ||
| Mean (SD) length of stay, days | 3.8 (6.7) | 7.3 (6.9) |
| Mean (SD) total cost | $10,485 ($29,088) | $18,546 ($22,658) |
| Mean (SD) cost per day | $2,876 ($3,046) | $2,637 ($1,783) |
| Postocclusion | ||
| Mean (SD) length of stay, days | 8.8 (11.0) | 8.8 (10.0) |
| Mean (SD) total cost | $18,714 ($32,189) | $16,765 ($29,966) |
| Mean (SD) cost per day | $2,146 ($2,995) | $2,058 ($6,585) |
Contributing to the lower cost were certain revenue‐center specific costs (Table 4). Total room and board costs were different between the alteplase and catheter‐replacement groups in both the pre‐ and postocclusion periods; this was related to the difference between the 2 comparison groups in postocclusion LOS of about 0.3 days (Table 5). However, the differences favored alteplase use over catheter replacement. Cardiology/electrocardiography costs were lower for catheter replacement in the preocclusion period but lower for alteplase use in the postocclusion period. Emergency department costs were higher for catheter replacement in both periods, as were respiratory costs in the same manner. Additionally, costs for laboratory tests, nursing, operating room/surgery, pharmacy, radiology, supplies, and ICU room and board were lower in the preocclusion period but higher in the postocclusion period for catheter‐replacement patients. It was unclear why the pharmacy costs after catheter replacement would have increased for catheter‐replacement patients in contrast to the decrease for alteplase‐treated patients, but because this occurred at an average daily basis as well, it appeared that catheter‐replacement patients may have received additional medications. Average adjusted postocclusion LOS was similar for alteplase and catheter‐replacement recipients (P=0.24), suggesting that decreased total costs were due to reasons other than shorter LOS.
| Preocclusiona | Postocclusiona | |||
|---|---|---|---|---|
| CVC Replacement Only, n=1,028 | Alteplase Only, n=33,551 | CVC Replacement Only, n=1,028 | Alteplase Onlyn=33,551 | |
| ||||
| Total room and board cost | ||||
| Mean (SD) total cost | $4,380 ($9,545) | $8,535 ($10,175)b | $8,394 ($14,393) | $8,437 ($18,341)b |
| Mean (SD) cost per day | $693 ($734) | $1,097 ($724)b | $751 ($536) | $983 ($3,250) |
| Cardiology/ECG cost | ||||
| Mean (SD) total cost | $82 ($806) | $154 ($605)b | $124 ($540) | $107 ($735)b |
| Mean (SD) cost per day | $17 ($96) | $26 ($131)b | $17 ($93) | $19 ($217)b |
| Emergency department cost | ||||
| Mean (SD) total cost | $10 ($91) | $36 ($284)b | $10 ($67) | $12 ($195) |
| Mean (SD) cost per day | $4 ($32) | $8 ($65)b | $2 ($19) | $6 ($76) |
| Laboratory cost | ||||
| Mean (SD) total cost | $864 ($2,538) | $1,425 ($3,622)b | $1,471 ($5,614) | $1,175 ($3,961) |
| Mean (SD) cost per day | $140 ($314) | $180 ($269)b | $139 ($313) | $142 ($465)b |
| Nursing Cost | ||||
| Mean (SD) total cost | $218 ($1,497) | $224 ($2,364)b | $432 ($2,538) | $231 ($2,785) |
| Mean (SD) cost per day | $39 ($166) | $24 ($127)b | $35 ($140) | $21 ($112) |
| OR/surgery cost | ||||
| Mean (SD) total cost | $902 ($4,743) | $1,602 ($3,597)b | $1,437 ($3,029) | $847 ($2,701)b |
| Mean (SD) cost per day | $207 ($495) | $267 ($513)b | $302 ($646) | $130 ($827)b |
| Pharmacy cost | ||||
| Mean (SD) total cost | $2,085 ($20,338) | $3,014 ($6,408)b | $3,200 ($16,396) | $2,914 ($8,383)b |
| Mean (SD) cost per day | $263 ($1,509) | $368 ($583)b | $362 ($2,427) | $347 ($853)b |
| Radiology cost | ||||
| Mean (SD) total cost | $470 ($869) | $782 ($1,031)b | $731 ($1,160) | $505 ($1,550)b |
| Mean (SD) cost per day | $133 ($362) | $130 ($189)b | $144 ($293) | $83 ($469)b |
| Respiratory cost | ||||
| Mean (SD) total cost | $391 ($1,442) | $895 ($2,160)b | $673 ($2,209) | $783 ($2,297)b |
| Mean (SD) cost per day | $51 ($121) | $104 ($170)b | $61 ($115) | $81 ($280)b |
| Supply cost | ||||
| Mean (SD) total cost | $834 ($3,221) | $1,408 ($5,871)b | $1,636 ($7,250) | $1,117 ($4,477)b |
| Mean (SD) cost per day | $208 ($1,244) | $211 ($789)b | $264 ($871) | $165 ($1,529)b |
| Other therapy cost | ||||
| Mean (SD) total cost | $179 ($702) | $355 ($815)b | $436 ($837) | $509 ($1,263)b |
| Mean (SD) cost per day | $30 ($81) | $46 ($98)b | $51 ($106) | $66 ($481)b |
| Other departments cost | ||||
| Mean (SD) total cost | $26 ($710) | $1 ($36) | $74 ($1,127) | $3 ($144) b |
| Mean (SD) cost per day | $3 ($56) | $0 ($5) | $6 ($86) | $0 ($13)b |
| Fees cost | ||||
| Mean (SD) total cost | $38 ($370) | $82 ($969)b | $67 ($340) | $86 ($2,704) |
| Mean (SD) cost per day | $7 ($47) | $12 ($77)b | $12 ($120) | $12 ($843) |
| Healthcare services cost | ||||
| Mean (SD) total cost | $5 ($53) | $31 ($1,052)b | $29 ($515) | $35 ($1,162) |
| Mean (SD) cost per day | $1 ($10) | $3 ($65)b | $2 ($11) | $3 ($54) |
| ICU room and board cost | ||||
| Mean (SD) total cost | $2,085 ($7,700) | $4,333 ($8,826)b | $3,158 ($10,767) | $2,884 ($15,863) |
| Mean (SD) cost per day | $293 ($677) | $543 ($854)b | $222 ($512) | $323 ($2,330) |
| Model | Parameter Estimate | Summary Statistic | Estimate (95% CI) |
|---|---|---|---|
| |||
| 30‐day readmissiona | 0.0234 | Odds ratio | 1.048 (0.899 to 1.221) |
| 90‐day readmissionb | 0.0248 | Odds ratio | 1.051 (0.915 to 1.207) |
| Postocclusion total costsc | 0.0842 | Mean differenced | $1,418.69 ($2,458.12 to $307.27)f |
| Postocclusion total cost per daye | 0.1857 | Mean differenced | $317.20 ($392.24 to $238.22)f |
| Post occlusion length of stayg | 0.0313 | Mean differenced | 0.299 (0.196 to 0.820) |
Unadjusted 30‐ and 90‐day readmission rates were 24.6% and 35.1% for CVC replacement and slightly lower at 23.7% and 33.9% for alteplase (Table 3), respectively. Odds of readmission after adjusting for patient and hospital factors were not significantly different at 30 days (odds ratio [OR]: 1.048, 95% CI: 0.899‐1.221; P=0.55) or at 90 days (OR: 1.051, 95% CI: 0.915‐1.207; P=0.48) (Table 5). Subgroup analyses for patients with a diagnosis of heart failure, myocardial infarction, and cancer revealed similar results.
DISCUSSION
The cost of healthcare in the United States has risen at an outstanding rate compared with other countries. Our percentage of gross national product spent on healthcare is on the order of 16% to 18%, almost twice as much as the next most industrialized country in terms of healthcare expenditure.[11] In the current era, finding opportunities to reduce healthcare costs without negatively impacting quality of care is the name of the game. Professional societies have come together under the campaign of Choosing Wisely: An Initiative of the ABIM (American Board of Internal Medicine) Foundation to help educate clinicians and patients on cost‐containment strategies.[12] Research that demonstrates opportunities to reduce cost will help healthcare providers choose wisely among diagnostic and therapeutic options for patients. Our study demonstrated that the use of a drug such as alteplase in clearing CVC catheter obstruction was significantly less costly to the hospital than catheter replacement.
Cathflo Activase (alteplase: Genentech, South San Francisco, CA), the only FDA‐approved thrombolytic for the restoration of central venous catheter function, is the current standard treatment for catheter occlusions in the United States. A dose of 2 mg in 2 mL is instilled in patients weighing 30 kg or 110% of the internal lumen volume of the catheter not to exceed 2 mg in 2 mL for those patients weighing <30 kg. Haire et al. showed that a 2‐mg dose of alteplase was more effective than urokinase (5000 IU) for treating radiographically proven thrombotic occlusion of a CVC after a dwell time of 120 minutes.[13] In the Cardiovascular thrombolytic used to Open Occluded Lines (COOL) trial, one 2‐mg dose of alteplase cleared the catheter occlusion after 120 minutes in 74% of patients, compared with only 17% of patients who received a placebo. Studies have confirmed the safety and efficacy of alteplase administered at various time intervals in different long‐term catheters, including peripherally inserted central catheters, with major hemorrhage reported in 0.3% of patients.[14, 15, 16]
Adding to the knowledge of patient outcomes from clinical studies, many health outcomes studies have demonstrated benefit in cost containment through decreasing LOS, which one can argue is just shifting the cost to an earlier part of the stay. Even though this is highly beneficial, it does not address the core resource utilization within the hospital. Our study found its cost benefit not in the LOS, but in decreasing core resource utilization such as radiology, lab, nursing, and supplies. If patients are admitted for a noncardiovascular condition and have CVC occlusion, using alteplase to clear the CVC occlusion along with implementing strategies to manage the underlying disease to reduce the LOS becomes a powerful opportunity to impact cost. Among patients who may come to the hospital for just the CVC occlusion, the LOS should be short. There may be no significant opportunity to reduce the LOS in those cases, but opportunities to decrease core hospital resource utilization with alteplase make this approach beneficial if the patient can tolerate it.
Limitations of the study include the retrospective and administrative nature of the database used, which is unable to provide certain clinical measures as would be available at the patient's bedside when treatment choices are being made. Had they been available, we might have included them in our assessment of whether patients who underwent CVC replacement were significantly different from those who received alteplase. In addition, not all hospitals in the database had charge masters that facilitated identification of CVC replacements or reinsertions, requiring the use of CPT‐4 codes and evidence of new CVCs being placed or inserted. Certain patients were excluded if there was conflicting information about whether the CVC was new within the hospital stay or dwelling in the patient prior to admission. Also, dialysis patients were excluded because they were not part of any approved indication for alteplase 2 mg, and this group is particularly prone to catheter obstruction. As such, they represent more complicated cases than the norm; this exclusion may have limited the overall generalizability of the study. The study also relied on charge master (billing) data to identify the use of alteplase and other treatments, where there is the potential, albeit minimal, for inaccuracies in the data. Of greater importance, the study relied on ICD‐9 coding to identify comorbid conditions, and as in other studies using similar data sources, such methods are subject to coding errors and omissions. However, many of the listed limitations above were not thought to be different between the comparison groups or more problematic for this study than for other studies based on similar data sources.
CONCLUSION
Among patients treated for an occluded CVC, alteplase‐treated patients had lower daily postocclusion costs and lower total postocclusion costs than patients who received catheter replacement. Differences in costs did not appear to be driven by differences in postocclusion LOS. Readmissions at 30‐ and 90‐day periods were found to be similar between alteplase recipients and catheter‐replacement patients.
Acknowledgements
The authors thank W. Kenne Mountford for his editorial assistance with a prior version of the article and Dima Qato for assistance with the analyses. Additional editorial assistance was provided by Steve Melvin. This assistance was funded by Genentech, Inc.
Disclosures: This study was funded by Genentech, Inc. F. R. Ernst and C. Lipkin are employees of Premier, which was contracted by Genentech to conduct the study covered in this article. E. Chen is an employee of and holds stock in Genentech. D. Tayama is an employee of Genentech. A. N. Amin received research funding from Premier, which was contracted by Genentech to conduct the study covered in this article.
Long‐term central venous catheters (CVCs) facilitate care for patients with chronic illness by providing easy venous access for laboratory tests, administration of medication, and parenteral nutrition. However, several complications resulting from the use of CVCs, including sepsis, extravasation of infusions, and venous thrombosis, can increase associated morbidity and mortality. These complications can also interrupt and delay treatment for the underlying disease and thereby affect outcomes. One of the most common CVC complications is catheter occlusion.[1]
Catheter occlusion occurs in 14% to 36% of patients within 1 to 2 years of catheter placement.[2, 3, 4, 5, 6, 7, 8] A catheter occlusion can be partial or complete, and can occur secondary to a variety of mechanical problems, including an uncommon, but potentially life‐threatening, pinch‐off syndrome. Medication or parenteral nutrition can also cause occlusion, which can be acute or gradual, with increasingly sluggish flow through the catheter. Inappropriate concentrations or incompatible mixtures can cause medications to precipitate within the catheter lumen.
Occlusions are either thrombotic or nonthrombotic. One autopsy study of patients with a long‐term CVC found that a fibrin sheath encased the catheter tip in every case.[9] An occluded catheter may compromise patient care[9, 10]; it may cause cancellation or delay of procedures, it potentially interrupts administration of critical therapies including vesicants, it may result in risk of infection, and it potentially leads to catheter replacement. This can further complicate care, leading to increased length of stay (LOS) and hospital costs.
To better understand resource utilization, LOS, and cost implications of alteplase compared with catheter replacement, we conducted a preplanned, retrospective analysis of hospitalized patients captured between January 2006 and December 2011 in the database maintained by Premier. The Premier database is a large, US hospital‐based, service‐level, all‐payer, comparative database, with information collected primarily from nearly 600 geographically diverse, nonprofit, nongovernment community and teaching hospitals.
METHODS
Data Sources
The Premier database contains information on over 42 million hospital discharges (mean 5.5 million discharges/year)one‐fifth of all US hospitalizationsfrom the year 2000 to the present. The database contains data from standard hospital discharge files, including patient demographic information and disease state. Patients can be tracked, with a unique identifier, across the inpatient and hospital‐based outpatient settings, as well as across visits. In addition to the data elements available in most of the standard hospital discharge files, the Premier database also contains a date‐stamped log of billed items, including procedures, medications, and laboratory, diagnostic, and therapeutic services at the individual patient level. Drug utilization information is available by day of stay and includes quantity, dosing, strength used, and cost.
The Premier database has been used extensively to benchmark hospital clinical and financial performance as well as by the US Food and Drug Administration (FDA) for drug surveillance and by the Centers for Medicare and Medicaid Services to evaluate next‐generation payment models. Preliminary comparisons between patient and hospital characteristics for hospitals that submit data to Premier and those of the probability sample of hospitals and patients selected for the National Hospital Discharge Survey suggest that the patient populations are similar with regard to patient age, gender, LOS, mortality, primary discharge diagnosis, and primary procedure groups.
Patient Population
In this retrospective observational database analysis, inpatients of all ages were initially identified who were discharged from a hospital between January 1, 2006 and December 31, 2011 and whose records contained 1 or more International Classification of Diseases, 9th Revision, Clinical Modification (ICD‐9) procedural codes or Current Procedural Terminology (CPT‐4) codes signifying CVC placement. The catheter replacement group comprised patients having a catheter replacement during the hospitalization. The alteplase treatment group was identified through patient billing records and by computing the dose administered (2 mg) during the index hospitalization period. Healthcare Common Procedure Coding System J‐codes (J2996, alteplase recombinant injection 10 mg; J2997, alteplase recombinant 1 mg) were also evaluated during the analysis to supplement the search string identification. To account for and eliminate catheter replacement due to mechanical failure rather than occlusion, patients with ICD‐9 diagnosis code 996.1 for mechanical failure were excluded. Patients with an ICD‐9 diagnosis code for infection or who received antibiotics on the day of replacement were excluded as an additional way to narrow the study to patients with occlusion as the reason for catheter replacement. In addition, patients receiving kidney dialysis, a chronic condition prone to greater‐than‐usual risk of catheter occlusion, were excluded. When a patient had multiple hospital stays with CVC insertions or placement during the study period, the first hospitalization with insertions or placement was used in our analyses.
Of the CVC patient population (N=574,252), 36,680 patient discharges resulted in the need for CVC replacement, alteplase therapy, or both. Patients receiving both replacement and alteplase (N=144) were excluded from analysis, resulting in 33,551 patient discharges with alteplase and 1028 patient discharges with CVC replacement.
Outcome Measures
The main outcomes of interest were LOS and hospital costs after occlusion, and readmissions at 30 and 90 days. Secondary measures, as they were thought to play a role in influencing outcomes, included LOS and costs before occlusion, as well as departmental costs such as pharmacy, radiology, and days in the intensive care unit (ICU).
Statistical Analysis
Univariate descriptive statistics were used to characterize the patient population by patient, clinical, and hospital attributes. In addition, subgroup analyses were performed among patients with any cardiology diagnosis (using ICD‐9 diagnosis or procedure codes), heart failure, myocardial infarction, and cancer, which were potentially overlapping categories chosen prior to initiating the analyses. Data measured on a continuous scale were expressed as mean, standard deviation, range, and median. Categorical data were expressed as count/percentages in the categories. In addition, categorical costs were also examined before and after occlusion. Tables of results included P values comparing patients who received CVC replacement with those who received alteplase across all measures. The [2] tests were used to test for differences in categorical variables, and t tests were utilized for differences in continuous variables.
Multivariable regression modeling was conducted to better compare outcomes associated with catheter replacement versus alteplase treatment. Linear regression models were performed to evaluate hospital costs and LOS during the initial hospital discharge. Logistic regression models were performed to evaluate the odds of readmission at 30 and 90 days following discharge. All multivariable models controlled for factors found to be statistically significant in univariate analysis. The covariates varied by model, but generally included age, race, sex, cancer, 3M All Patient Refined Diagnosis Related Group risk of mortality and severity of illness, cerebrovascular disease, renal disease, payer, myocardial infarction, hemiplegia/paraplegia, chronic or acute diabetes, peripheral vascular disease, complication, admission source, admission type, congestive heart failure, dementia, metastatic solid tumor, rheumatic disease, peptic ulcer disease, chronic pulmonary disease, hospital teaching status, urban/rural location, US Census region, and number of hospital beds. Certain of these variables, such as 3M measures of severity and risk, as well as measures of LOS and costs before occlusion, were considered as ways to understand differences in risk of increased costs among patients. For each multivariable model, covariates eligible for inclusion in the models were selected using a backward selection method (logistic used stepwise) until all variables remaining in the model were significant at P0.2.
RESULTS
This study included 34,579 patients who first had a CVC insertion and then were treated for a CVC occlusion by receiving a replacement CVC (n=1028) or by receiving alteplase (2 mg) administration (n=33,551) during the same hospitalization (Table 1). Patients who received alteplase tended to be younger (6019 vs 6220 years old). More than 50% were at least 65 years of age. Twelve percent of alteplase patients were black, whereas 18.5% of catheter‐replacement patients were black.
| Catheter Replacement, n=1,028 | Alteplase Treatment, n=33,551 | |
|---|---|---|
| ||
| Age group, ya | ||
| Under 18 | 29 (2.8%) | 984 (2.9%) |
| 1834 | 84 (8.2%) | 2,479 (7.4%) |
| 3544 | 73 (7.1%) | 2,826 (8.4%) |
| 4554 | 116 (11.3%) | 5,217 (15.5%) |
| 5564 | 210 (20.4%) | 6,761 (20.1%) |
| 6574 | 203 (19.7%) | 6,741 (20.1%) |
| 75+ | 313 (30.4%) | 8,543 (25.5%) |
| Mean (SD) | 62 (20) | 60 (19) |
| Sex | ||
| Female | 565 (55.0%) | 18,172 (54.2%) |
| Male | 463 (45.0%) | 15,378 (45.8%) |
| Unknown | 0 (0%) | 1 (0%) |
| Race/ethnicitya | ||
| Black | 190 (18.5%) | 4,057 (12.1%) |
| Hispanic | 40 (3.9%) | 1,098 (3.3%) |
| Other | 126 (12.3%) | 6,250 (18.6%) |
| White | 672 (65.4%) | 22,146 (66.0%) |
| Comorbid conditions | ||
| Myocardial infarction | 96 (9.3%) | 3,746 (11.2%) |
| Congestive heart failure | 258 (25.1%) | 8,210 (24.5%) |
| Peripheral vascular disease | 104 (10.1%) | 3,451 (10.3%) |
| Cerebrovascular disease | 115 (11.2%) | 3,528 (10.5%) |
| Dementia | 33 (3.2%) | 838 (2.5%) |
| Chronic pulmonary diseasea | 264 (25.7%) | 10,495 (31.3%) |
| Rheumatic disease | 37 (3.6%) | 1,344 (4.0%) |
| Peptic ulcer disease | 41 (4.0%) | 1,068 (3.2%) |
| Mild liver diseasea | 94 (9.1%) | 2,392 (7.1%) |
| Moderate/severe liver diseasea | 29 (2.8%) | 531 (1.6%) |
| Acute diabetes | 255 (24.8%) | 9,185 (27.4%) |
| Chronic diabetesa | 44 (4.3%) | 2,327 (6.9%) |
| Hemiplegia paraplegia | 51 (5.0%) | 1,909 (5.7%) |
| Renal diseasea | 209 (20.3%) | 5,351 (16.0%) |
| Cancera | 207 (20.1%) | 5,685 (16.9%) |
| Metastatic solid tumora | 100 (9.7%) | 2,441 (7.3%) |
| AIDS/HIV | 4 (0.4%) | 244 (0.7%) |
| 3M APR‐DRG Severity of Illnessa | ||
| 1‐minor | 36 (3.5%) | 769 (2.3%) |
| 2‐moderate | 172 (16.7%) | 4,109 (12.2%) |
| 3‐major | 384 (37.3%) | 12,175 (36.3%) |
| 4‐extreme | 436 (42.4%) | 16,497 (49.2%) |
| Unknown | 0 (0%) | 1 (0%) |
| 3M APR‐DRG Risk of Mortalitya | ||
| 1‐minor | 159 (15.5%) | 4,716 (14.1%) |
| 2‐moderate | 253 (24.6%) | 6,746 (20.1%) |
| 3‐major | 313 (30.4%) | 10,569 (31.5%) |
| 4‐mxtreme | 303 (29.5%) | 11,519 (34.3%) |
| Unknown | 0 (0%) | 1 (0%) |
Alteplase patients were significantly more likely to have a diagnosis of chronic pulmonary disease, liver disease, renal disease, chronic diabetes (ie, diabetes with complications), and cancer. There was an equivalent number of urban and rural hospitals across the 2 groups of patients (Table 2); however, there were regional differences including a higher proportion of catheter‐replacement patients from the East North Central and Middle Atlantic areas and a lower proportion of catheter‐replacement patients from Mountain and Pacific states. Catheter‐replacement patients more frequently were treated in teaching hospitals and in hospitals of larger size.
| Catheter Replacement, n=1,028 | Alteplase Treatment, n=33,551 | |
|---|---|---|
| ||
| Provider regiona | ||
| New England | 28 (2.7%) | 976 (2.9%) |
| Middle Atlantic | 227 (22.1%) | 1,944 (5.8%) |
| South Atlantic | 247 (24.0%) | 8,047 (24.0%) |
| East North Central | 153 (14.9%) | 3,015 (9.0%) |
| East South Central | 14 (1.4%) | 1,345 (4.0%) |
| West North Central | 98 (9.5%) | 3,590 (10.7%) |
| West South Central | 112 (10.9%) | 5,096 (15.2%) |
| Mountain | 48 (4.7%) | 3,339 (9.9%) |
| Pacific | 94 (9.1%) | 6,083 (18.1%) |
| Unknown | 7 (0.7%) | 116 (0.3%) |
| Population served | ||
| Rural | 56 (5.4%) | 1,838 (5.5%) |
| Urban | 972 (94.6%) | 31,713 (94.5%) |
| Teaching statusa | ||
| Nonteaching | 431 (41.9%) | 18,598 (55.4%) |
| Teaching | 597 (58.1%) | 14,953 (4.6%) |
| Hospital size, no. of bedsa | ||
| <100 | 4 (0.4%) | 475 (1.4%) |
| 100199 | 56 (5.4%) | 1,725 (5.1%) |
| 200299 | 124 (12.1%) | 5,907 (17.6%) |
| 300499 | 432 (42.0%) | 13,790 (41.1%) |
| 500+ | 412 (40.1%) | 11,654 (34.7%) |
| Primary payora | ||
| Commercial | 50 (4.9%) | 1,779 (5.3%) |
| Managed care | 221 (21.5%) | 6,888 (20.5%) |
| Medicaid | 132 (12.8%) | 4,146 (12.4%) |
| Medicare | 572 (55.6%) | 17,226 (51.3%) |
| Other government programs | 9 (0.9%) | 439 (1.3%) |
| Any other payor | 44 (4.3%) | 3,073 (9.2%) |
| Admission sourcea | ||
| Emergency department | 424 (41.2%) | 12,741 (38.0%) |
| Physician referral | 390 (37.9%) | 14,502 (43.2%) |
| Transfer from another health facility | 154 (15.0%) | 4,109 (12.2%) |
| Unknown | 60 (5.8%) | 2,199 (6.5%) |
| Admission typea | ||
| Elective | 205 (19.9%) | 5,872 (17.5%) |
| Emergency | 613 (59.6%) | 19,660 (58.6%) |
| Newborn | 9 (0.9%) | 37 (0.1%) |
| Trauma center | 3 (0.3%) | 279 (0.8%) |
| Urgent | 192 (18.7%) | 7,573 (22.6%) |
| Unknown | 6 (0.6%) | 130 (0.4%) |
After covariate adjustment for baseline measurements significantly related to each outcome, average daily post occlusion costs were estimated to be $317 lower for alteplase recipients than for patients who received catheter replacement ($317; 95% confidence interval [CI]: $238‐$392; P<0.0001) (Table 3). Average adjusted total post occlusion costs were $1419 lower for alteplase recipients than for patients who received catheter replacement ($1418; 95% CI: $307‐$2458; P=0.012).
| CVC Replace Only, n=1,028 | Alteplase Only, n=33,551 | |
|---|---|---|
| ||
| 30‐day readmission | 24.6% | 23.7% |
| 90‐day readmission | 35.1% | 33.9% |
| Preocclusion | ||
| Mean (SD) length of stay, days | 3.8 (6.7) | 7.3 (6.9) |
| Mean (SD) total cost | $10,485 ($29,088) | $18,546 ($22,658) |
| Mean (SD) cost per day | $2,876 ($3,046) | $2,637 ($1,783) |
| Postocclusion | ||
| Mean (SD) length of stay, days | 8.8 (11.0) | 8.8 (10.0) |
| Mean (SD) total cost | $18,714 ($32,189) | $16,765 ($29,966) |
| Mean (SD) cost per day | $2,146 ($2,995) | $2,058 ($6,585) |
Contributing to the lower cost were certain revenue‐center specific costs (Table 4). Total room and board costs were different between the alteplase and catheter‐replacement groups in both the pre‐ and postocclusion periods; this was related to the difference between the 2 comparison groups in postocclusion LOS of about 0.3 days (Table 5). However, the differences favored alteplase use over catheter replacement. Cardiology/electrocardiography costs were lower for catheter replacement in the preocclusion period but lower for alteplase use in the postocclusion period. Emergency department costs were higher for catheter replacement in both periods, as were respiratory costs in the same manner. Additionally, costs for laboratory tests, nursing, operating room/surgery, pharmacy, radiology, supplies, and ICU room and board were lower in the preocclusion period but higher in the postocclusion period for catheter‐replacement patients. It was unclear why the pharmacy costs after catheter replacement would have increased for catheter‐replacement patients in contrast to the decrease for alteplase‐treated patients, but because this occurred at an average daily basis as well, it appeared that catheter‐replacement patients may have received additional medications. Average adjusted postocclusion LOS was similar for alteplase and catheter‐replacement recipients (P=0.24), suggesting that decreased total costs were due to reasons other than shorter LOS.
| Preocclusiona | Postocclusiona | |||
|---|---|---|---|---|
| CVC Replacement Only, n=1,028 | Alteplase Only, n=33,551 | CVC Replacement Only, n=1,028 | Alteplase Onlyn=33,551 | |
| ||||
| Total room and board cost | ||||
| Mean (SD) total cost | $4,380 ($9,545) | $8,535 ($10,175)b | $8,394 ($14,393) | $8,437 ($18,341)b |
| Mean (SD) cost per day | $693 ($734) | $1,097 ($724)b | $751 ($536) | $983 ($3,250) |
| Cardiology/ECG cost | ||||
| Mean (SD) total cost | $82 ($806) | $154 ($605)b | $124 ($540) | $107 ($735)b |
| Mean (SD) cost per day | $17 ($96) | $26 ($131)b | $17 ($93) | $19 ($217)b |
| Emergency department cost | ||||
| Mean (SD) total cost | $10 ($91) | $36 ($284)b | $10 ($67) | $12 ($195) |
| Mean (SD) cost per day | $4 ($32) | $8 ($65)b | $2 ($19) | $6 ($76) |
| Laboratory cost | ||||
| Mean (SD) total cost | $864 ($2,538) | $1,425 ($3,622)b | $1,471 ($5,614) | $1,175 ($3,961) |
| Mean (SD) cost per day | $140 ($314) | $180 ($269)b | $139 ($313) | $142 ($465)b |
| Nursing Cost | ||||
| Mean (SD) total cost | $218 ($1,497) | $224 ($2,364)b | $432 ($2,538) | $231 ($2,785) |
| Mean (SD) cost per day | $39 ($166) | $24 ($127)b | $35 ($140) | $21 ($112) |
| OR/surgery cost | ||||
| Mean (SD) total cost | $902 ($4,743) | $1,602 ($3,597)b | $1,437 ($3,029) | $847 ($2,701)b |
| Mean (SD) cost per day | $207 ($495) | $267 ($513)b | $302 ($646) | $130 ($827)b |
| Pharmacy cost | ||||
| Mean (SD) total cost | $2,085 ($20,338) | $3,014 ($6,408)b | $3,200 ($16,396) | $2,914 ($8,383)b |
| Mean (SD) cost per day | $263 ($1,509) | $368 ($583)b | $362 ($2,427) | $347 ($853)b |
| Radiology cost | ||||
| Mean (SD) total cost | $470 ($869) | $782 ($1,031)b | $731 ($1,160) | $505 ($1,550)b |
| Mean (SD) cost per day | $133 ($362) | $130 ($189)b | $144 ($293) | $83 ($469)b |
| Respiratory cost | ||||
| Mean (SD) total cost | $391 ($1,442) | $895 ($2,160)b | $673 ($2,209) | $783 ($2,297)b |
| Mean (SD) cost per day | $51 ($121) | $104 ($170)b | $61 ($115) | $81 ($280)b |
| Supply cost | ||||
| Mean (SD) total cost | $834 ($3,221) | $1,408 ($5,871)b | $1,636 ($7,250) | $1,117 ($4,477)b |
| Mean (SD) cost per day | $208 ($1,244) | $211 ($789)b | $264 ($871) | $165 ($1,529)b |
| Other therapy cost | ||||
| Mean (SD) total cost | $179 ($702) | $355 ($815)b | $436 ($837) | $509 ($1,263)b |
| Mean (SD) cost per day | $30 ($81) | $46 ($98)b | $51 ($106) | $66 ($481)b |
| Other departments cost | ||||
| Mean (SD) total cost | $26 ($710) | $1 ($36) | $74 ($1,127) | $3 ($144) b |
| Mean (SD) cost per day | $3 ($56) | $0 ($5) | $6 ($86) | $0 ($13)b |
| Fees cost | ||||
| Mean (SD) total cost | $38 ($370) | $82 ($969)b | $67 ($340) | $86 ($2,704) |
| Mean (SD) cost per day | $7 ($47) | $12 ($77)b | $12 ($120) | $12 ($843) |
| Healthcare services cost | ||||
| Mean (SD) total cost | $5 ($53) | $31 ($1,052)b | $29 ($515) | $35 ($1,162) |
| Mean (SD) cost per day | $1 ($10) | $3 ($65)b | $2 ($11) | $3 ($54) |
| ICU room and board cost | ||||
| Mean (SD) total cost | $2,085 ($7,700) | $4,333 ($8,826)b | $3,158 ($10,767) | $2,884 ($15,863) |
| Mean (SD) cost per day | $293 ($677) | $543 ($854)b | $222 ($512) | $323 ($2,330) |
| Model | Parameter Estimate | Summary Statistic | Estimate (95% CI) |
|---|---|---|---|
| |||
| 30‐day readmissiona | 0.0234 | Odds ratio | 1.048 (0.899 to 1.221) |
| 90‐day readmissionb | 0.0248 | Odds ratio | 1.051 (0.915 to 1.207) |
| Postocclusion total costsc | 0.0842 | Mean differenced | $1,418.69 ($2,458.12 to $307.27)f |
| Postocclusion total cost per daye | 0.1857 | Mean differenced | $317.20 ($392.24 to $238.22)f |
| Post occlusion length of stayg | 0.0313 | Mean differenced | 0.299 (0.196 to 0.820) |
Unadjusted 30‐ and 90‐day readmission rates were 24.6% and 35.1% for CVC replacement and slightly lower at 23.7% and 33.9% for alteplase (Table 3), respectively. Odds of readmission after adjusting for patient and hospital factors were not significantly different at 30 days (odds ratio [OR]: 1.048, 95% CI: 0.899‐1.221; P=0.55) or at 90 days (OR: 1.051, 95% CI: 0.915‐1.207; P=0.48) (Table 5). Subgroup analyses for patients with a diagnosis of heart failure, myocardial infarction, and cancer revealed similar results.
DISCUSSION
The cost of healthcare in the United States has risen at an outstanding rate compared with other countries. Our percentage of gross national product spent on healthcare is on the order of 16% to 18%, almost twice as much as the next most industrialized country in terms of healthcare expenditure.[11] In the current era, finding opportunities to reduce healthcare costs without negatively impacting quality of care is the name of the game. Professional societies have come together under the campaign of Choosing Wisely: An Initiative of the ABIM (American Board of Internal Medicine) Foundation to help educate clinicians and patients on cost‐containment strategies.[12] Research that demonstrates opportunities to reduce cost will help healthcare providers choose wisely among diagnostic and therapeutic options for patients. Our study demonstrated that the use of a drug such as alteplase in clearing CVC catheter obstruction was significantly less costly to the hospital than catheter replacement.
Cathflo Activase (alteplase: Genentech, South San Francisco, CA), the only FDA‐approved thrombolytic for the restoration of central venous catheter function, is the current standard treatment for catheter occlusions in the United States. A dose of 2 mg in 2 mL is instilled in patients weighing 30 kg or 110% of the internal lumen volume of the catheter not to exceed 2 mg in 2 mL for those patients weighing <30 kg. Haire et al. showed that a 2‐mg dose of alteplase was more effective than urokinase (5000 IU) for treating radiographically proven thrombotic occlusion of a CVC after a dwell time of 120 minutes.[13] In the Cardiovascular thrombolytic used to Open Occluded Lines (COOL) trial, one 2‐mg dose of alteplase cleared the catheter occlusion after 120 minutes in 74% of patients, compared with only 17% of patients who received a placebo. Studies have confirmed the safety and efficacy of alteplase administered at various time intervals in different long‐term catheters, including peripherally inserted central catheters, with major hemorrhage reported in 0.3% of patients.[14, 15, 16]
Adding to the knowledge of patient outcomes from clinical studies, many health outcomes studies have demonstrated benefit in cost containment through decreasing LOS, which one can argue is just shifting the cost to an earlier part of the stay. Even though this is highly beneficial, it does not address the core resource utilization within the hospital. Our study found its cost benefit not in the LOS, but in decreasing core resource utilization such as radiology, lab, nursing, and supplies. If patients are admitted for a noncardiovascular condition and have CVC occlusion, using alteplase to clear the CVC occlusion along with implementing strategies to manage the underlying disease to reduce the LOS becomes a powerful opportunity to impact cost. Among patients who may come to the hospital for just the CVC occlusion, the LOS should be short. There may be no significant opportunity to reduce the LOS in those cases, but opportunities to decrease core hospital resource utilization with alteplase make this approach beneficial if the patient can tolerate it.
Limitations of the study include the retrospective and administrative nature of the database used, which is unable to provide certain clinical measures as would be available at the patient's bedside when treatment choices are being made. Had they been available, we might have included them in our assessment of whether patients who underwent CVC replacement were significantly different from those who received alteplase. In addition, not all hospitals in the database had charge masters that facilitated identification of CVC replacements or reinsertions, requiring the use of CPT‐4 codes and evidence of new CVCs being placed or inserted. Certain patients were excluded if there was conflicting information about whether the CVC was new within the hospital stay or dwelling in the patient prior to admission. Also, dialysis patients were excluded because they were not part of any approved indication for alteplase 2 mg, and this group is particularly prone to catheter obstruction. As such, they represent more complicated cases than the norm; this exclusion may have limited the overall generalizability of the study. The study also relied on charge master (billing) data to identify the use of alteplase and other treatments, where there is the potential, albeit minimal, for inaccuracies in the data. Of greater importance, the study relied on ICD‐9 coding to identify comorbid conditions, and as in other studies using similar data sources, such methods are subject to coding errors and omissions. However, many of the listed limitations above were not thought to be different between the comparison groups or more problematic for this study than for other studies based on similar data sources.
CONCLUSION
Among patients treated for an occluded CVC, alteplase‐treated patients had lower daily postocclusion costs and lower total postocclusion costs than patients who received catheter replacement. Differences in costs did not appear to be driven by differences in postocclusion LOS. Readmissions at 30‐ and 90‐day periods were found to be similar between alteplase recipients and catheter‐replacement patients.
Acknowledgements
The authors thank W. Kenne Mountford for his editorial assistance with a prior version of the article and Dima Qato for assistance with the analyses. Additional editorial assistance was provided by Steve Melvin. This assistance was funded by Genentech, Inc.
Disclosures: This study was funded by Genentech, Inc. F. R. Ernst and C. Lipkin are employees of Premier, which was contracted by Genentech to conduct the study covered in this article. E. Chen is an employee of and holds stock in Genentech. D. Tayama is an employee of Genentech. A. N. Amin received research funding from Premier, which was contracted by Genentech to conduct the study covered in this article.
- , , , , et al. Management of occlusion and thrombosis associated with long‐term indwelling central venous catheters. Lancet. 2009;374:159–169.
- , , , , , ; Children's Oncology Group. Prophylactic urokinase in the management of long‐term venous access devices in children; a Children's Oncology Group study. J Clin Oncol. 2004;22:2718–2723.
- , , , et al. Central venous catheter‐related complications in children with oncological/hematological diseases: an observational study of 418 devices. Ann Oncol. 1985;16:648–654.
- , , , et al. A cross‐sectional study evaluating post‐thrombotic syndrome in children. Thromb Res. 2003;111:227–233.
- , , , . Complications and management of implanted venous access catheters. J Clin Oncol. 1985;3:710–717.
- . Local installation of small doses of streptokinase for treatment of thrombotic occlusions of long‐term access catheters. J Clin Oncol. 1983;1:572–573.
- , , . Are clinical signs accurate indicators of the cause of central venous catheter occlusion? J Parenter Enteral Nutr. 1995;19:75–79.
- , . Mechanism and management of persistent withdrawal occlusion. Am Surg. 1988;54:326–328.
- . Catheter‐related thrombosis in pediatrics. Pediatr Nurs. 2002;28:97–102, 105–106.
- . Reopen the pipeline. Nursing. 2005;35:54–61.
- , . Chemotherapy extravasation: a consequence of fibrin sheath formation around venous access devices. Oncol Nurs Forum. 1995;22:675–680.
- Organisation for Economic Co‐operation and Development (OECD). Statistics. OECD Health Data 2010, June 2010. http://www.oecd.org/unitedstates/Briefing‐Note‐USA‐2013.pdf. Accessed May 8, 2014.
- ABIM Foundation. Choosing Wisely: An Initiative of the ABIM Foundation. (2013). Available at: http://www.choosingwisely.org. Accessed April 6, 2013.
- , , , . Urokinase versus recombinant tissue plasminogen activator in thrombosed central venous catheters: a double‐blinded, randomized trial. Thromb Haemost. 1994;72:543–547.
- , , , et al. Recombinant tissue plasminogen activator (alteplase) for restoration of flow in occluded central venous access devices: a double‐blind placebo‐controlled trial—the Cardiovascular Thrombolytic to Open Occluded Lines (COOL) efficacy trial. J Vasc Interv Radiol. 2001;12:951–955.
- , , , et al. Safety and efficacy of alteplase for restoring function in occluded central venous catheters: results of the cardiovascular thrombolytic to open occluded lines trial. J Clin Oncol. 2002;20:317–324.
- , , , . Alteplase for treatment of occluded peripherally inserted central catheters: safety and efficacy in 240 patients. J Vasc Interv Radiol. 2004;15:45–49.
- , , , , et al. Management of occlusion and thrombosis associated with long‐term indwelling central venous catheters. Lancet. 2009;374:159–169.
- , , , , , ; Children's Oncology Group. Prophylactic urokinase in the management of long‐term venous access devices in children; a Children's Oncology Group study. J Clin Oncol. 2004;22:2718–2723.
- , , , et al. Central venous catheter‐related complications in children with oncological/hematological diseases: an observational study of 418 devices. Ann Oncol. 1985;16:648–654.
- , , , et al. A cross‐sectional study evaluating post‐thrombotic syndrome in children. Thromb Res. 2003;111:227–233.
- , , , . Complications and management of implanted venous access catheters. J Clin Oncol. 1985;3:710–717.
- . Local installation of small doses of streptokinase for treatment of thrombotic occlusions of long‐term access catheters. J Clin Oncol. 1983;1:572–573.
- , , . Are clinical signs accurate indicators of the cause of central venous catheter occlusion? J Parenter Enteral Nutr. 1995;19:75–79.
- , . Mechanism and management of persistent withdrawal occlusion. Am Surg. 1988;54:326–328.
- . Catheter‐related thrombosis in pediatrics. Pediatr Nurs. 2002;28:97–102, 105–106.
- . Reopen the pipeline. Nursing. 2005;35:54–61.
- , . Chemotherapy extravasation: a consequence of fibrin sheath formation around venous access devices. Oncol Nurs Forum. 1995;22:675–680.
- Organisation for Economic Co‐operation and Development (OECD). Statistics. OECD Health Data 2010, June 2010. http://www.oecd.org/unitedstates/Briefing‐Note‐USA‐2013.pdf. Accessed May 8, 2014.
- ABIM Foundation. Choosing Wisely: An Initiative of the ABIM Foundation. (2013). Available at: http://www.choosingwisely.org. Accessed April 6, 2013.
- , , , . Urokinase versus recombinant tissue plasminogen activator in thrombosed central venous catheters: a double‐blinded, randomized trial. Thromb Haemost. 1994;72:543–547.
- , , , et al. Recombinant tissue plasminogen activator (alteplase) for restoration of flow in occluded central venous access devices: a double‐blind placebo‐controlled trial—the Cardiovascular Thrombolytic to Open Occluded Lines (COOL) efficacy trial. J Vasc Interv Radiol. 2001;12:951–955.
- , , , et al. Safety and efficacy of alteplase for restoring function in occluded central venous catheters: results of the cardiovascular thrombolytic to open occluded lines trial. J Clin Oncol. 2002;20:317–324.
- , , , . Alteplase for treatment of occluded peripherally inserted central catheters: safety and efficacy in 240 patients. J Vasc Interv Radiol. 2004;15:45–49.
Published 2014. The Authors Journal of Hospital Medicine published by Wiley Periodicals, Inc. on behalf of Society of Hospital Medicine
Expert: Choose your sinus surgeon carefully
KEYSTONE, COLO. – Surgical treatment of chronic rhinosinusitis has come a long way from the earlier "grab and tear" days, but referring physicians need to understand that not all otolaryngologists are providing state-of-the-art care.
"I am critical of some of my colleagues," Dr. Todd T. Kingdom said at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
"If I leave you with one message, it’s to set high expectations of your consultants in otolaryngology. You should find colleagues who are interested in sinus disease, who are committed to it, and who are excellent," added Dr. Kingdom, professor and vice chairman of the department of otolaryngology, head and neck surgery, at the University of Colorado, Denver, and immediate past president of the American Rhinologic Society.
One fine source is the pool of graduates of U.S. subspecialty surgical rhinology fellowship programs. Each year, 30 surgeons complete one of these fellowships, he said.
Technical innovations over the past 15 years have driven major advances in endoscopic sinus surgery. Powered microdebriders are used to precisely and efficiently remove hyperplastic mucosal disease and restore mucociliary clearance. Mucosal preservation is now a central tenet. Forward-thinking surgeons place a priority on creating exposure for delivery of topical medications. The procedures are routinely done on an outpatient basis, and they are less invasive than in former times. The outcomes are better, too, with this modern patient-centered, symptom-based approach.
"We have efficient ways now to take care of very severe disease atraumatically," Dr. Kingdom explained.
He emphasized that postoperative care is critical to successful sinus surgery outcomes. "My biggest criticism of my colleagues in otolaryngology is that many of them cut and go. There isn’t an emphasis on postoperative care," he said. "That’s a clear, clear deficiency in our approach.
"My postop schedule is to see patients at 1, 3, and 6 weeks and 3 and 6 months after surgery – and that’s if they’re doing perfectly. My point is you should have your otolaryngologist really fussing over these people. It’s not, ‘Well, it’s been a couple of weeks, you look fine, you can go back to your allergist now, I’ll see you later.’ It shouldn’t be that way," Dr. Kingdom said.
He reported having no financial conflicts of interest.
Dr. Todd T. Kingdom, allergy and respiratory diseases, National Jewish Health, sinus disease, American Rhinologic Society, U.S. subspecialty surgical rhinology fellowship programs, endoscopic sinus surgery, Powered microdebriders, hyperplastic mucosal disease, restore mucociliary clearance, Mucosal preservation,
KEYSTONE, COLO. – Surgical treatment of chronic rhinosinusitis has come a long way from the earlier "grab and tear" days, but referring physicians need to understand that not all otolaryngologists are providing state-of-the-art care.
"I am critical of some of my colleagues," Dr. Todd T. Kingdom said at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
"If I leave you with one message, it’s to set high expectations of your consultants in otolaryngology. You should find colleagues who are interested in sinus disease, who are committed to it, and who are excellent," added Dr. Kingdom, professor and vice chairman of the department of otolaryngology, head and neck surgery, at the University of Colorado, Denver, and immediate past president of the American Rhinologic Society.
One fine source is the pool of graduates of U.S. subspecialty surgical rhinology fellowship programs. Each year, 30 surgeons complete one of these fellowships, he said.
Technical innovations over the past 15 years have driven major advances in endoscopic sinus surgery. Powered microdebriders are used to precisely and efficiently remove hyperplastic mucosal disease and restore mucociliary clearance. Mucosal preservation is now a central tenet. Forward-thinking surgeons place a priority on creating exposure for delivery of topical medications. The procedures are routinely done on an outpatient basis, and they are less invasive than in former times. The outcomes are better, too, with this modern patient-centered, symptom-based approach.
"We have efficient ways now to take care of very severe disease atraumatically," Dr. Kingdom explained.
He emphasized that postoperative care is critical to successful sinus surgery outcomes. "My biggest criticism of my colleagues in otolaryngology is that many of them cut and go. There isn’t an emphasis on postoperative care," he said. "That’s a clear, clear deficiency in our approach.
"My postop schedule is to see patients at 1, 3, and 6 weeks and 3 and 6 months after surgery – and that’s if they’re doing perfectly. My point is you should have your otolaryngologist really fussing over these people. It’s not, ‘Well, it’s been a couple of weeks, you look fine, you can go back to your allergist now, I’ll see you later.’ It shouldn’t be that way," Dr. Kingdom said.
He reported having no financial conflicts of interest.
KEYSTONE, COLO. – Surgical treatment of chronic rhinosinusitis has come a long way from the earlier "grab and tear" days, but referring physicians need to understand that not all otolaryngologists are providing state-of-the-art care.
"I am critical of some of my colleagues," Dr. Todd T. Kingdom said at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
"If I leave you with one message, it’s to set high expectations of your consultants in otolaryngology. You should find colleagues who are interested in sinus disease, who are committed to it, and who are excellent," added Dr. Kingdom, professor and vice chairman of the department of otolaryngology, head and neck surgery, at the University of Colorado, Denver, and immediate past president of the American Rhinologic Society.
One fine source is the pool of graduates of U.S. subspecialty surgical rhinology fellowship programs. Each year, 30 surgeons complete one of these fellowships, he said.
Technical innovations over the past 15 years have driven major advances in endoscopic sinus surgery. Powered microdebriders are used to precisely and efficiently remove hyperplastic mucosal disease and restore mucociliary clearance. Mucosal preservation is now a central tenet. Forward-thinking surgeons place a priority on creating exposure for delivery of topical medications. The procedures are routinely done on an outpatient basis, and they are less invasive than in former times. The outcomes are better, too, with this modern patient-centered, symptom-based approach.
"We have efficient ways now to take care of very severe disease atraumatically," Dr. Kingdom explained.
He emphasized that postoperative care is critical to successful sinus surgery outcomes. "My biggest criticism of my colleagues in otolaryngology is that many of them cut and go. There isn’t an emphasis on postoperative care," he said. "That’s a clear, clear deficiency in our approach.
"My postop schedule is to see patients at 1, 3, and 6 weeks and 3 and 6 months after surgery – and that’s if they’re doing perfectly. My point is you should have your otolaryngologist really fussing over these people. It’s not, ‘Well, it’s been a couple of weeks, you look fine, you can go back to your allergist now, I’ll see you later.’ It shouldn’t be that way," Dr. Kingdom said.
He reported having no financial conflicts of interest.
Dr. Todd T. Kingdom, allergy and respiratory diseases, National Jewish Health, sinus disease, American Rhinologic Society, U.S. subspecialty surgical rhinology fellowship programs, endoscopic sinus surgery, Powered microdebriders, hyperplastic mucosal disease, restore mucociliary clearance, Mucosal preservation,
Dr. Todd T. Kingdom, allergy and respiratory diseases, National Jewish Health, sinus disease, American Rhinologic Society, U.S. subspecialty surgical rhinology fellowship programs, endoscopic sinus surgery, Powered microdebriders, hyperplastic mucosal disease, restore mucociliary clearance, Mucosal preservation,
EXPERT ANALYSIS FROM THE PULMONARY AND ALLERGY UPDATE
Misery, thy name is chronic rhinosinusitis
KEYSTONE, COLO. – Just how lousy do patients with medically refractory chronic rhinosinusitis feel in daily life? A lot worse than you might guess.
Patients who elected to undergo endoscopic sinus surgery after failing medical therapy for chronic rhinosinusitis (CRS) rated their own baseline health state on standardized measures as being well below U.S. population norms. Their degree of impairment was similar to the self-rated scores among age- and gender-matched individuals with end-stage renal disease or Parkinson’s disease, according to Dr. Todd T. Kingdom, professor and vice chairman of the department of otolaryngology, head and neck surgery, at the University of Colorado, Denver, and immediate past president of the American Rhinologic Society.
He cited a 5-year study that prospectively followed 232 adults with CRS who elected to undergo endoscopic sinus surgery (ESS) after failing to improve on medical therapy (Laryngoscope 2011;121:2672-8). Their mean presurgical health state utility value – derived using the Short Form 6D via methods routinely employed by health economists – was 0.65, on a scale in which 0 is death and 1.0 is perfect health.
That was worse than the self-rated scores among patients with heart failure or moderate COPD, as reported in other studies, and only slightly better than the self-rated health of patients awaiting hip replacement or liver transplantation. The U.S. population norm was a score of 0.81, Dr. Kingdom noted at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
When self-rated health status scores were determined again 6 months or longer after ESS, patients who underwent a revision procedure had a statistically and clinically significant 0.06-point improvement on the 0-1 scale, while those with no prior sinus surgery showed an even more robust 0.09-point gain.
Those are markedly larger improvements than documented in other studies following initiation of drug therapy for Parkinson’s disease, for example, or tumor necrosis factor–inhibitor therapy for psoriasis. Of the specific interventions assessed, only total hip replacement and bariatric surgery resulted in greater self-rated gains in health status than ESS.
In this and other studies, a patient’s baseline clinical phenotype didn’t predict the degree of improvement on quality of life measures following ESS, and gender, age, comorbid asthma, or aspirin-exacerbated respiratory disease did not influence how much benefit a patient would receive from ESS.
Patients with baseline self-reported depression, however, were slightly, albeit statistically significantly, less likely than nondepressed patients to experience significant improvement. And patients who presented without nasal polyps showed significantly more improvement in self-reported health status after ESS than did those with polyps.
Dr. Kingdom reported having no financial conflicts of interest.
KEYSTONE, COLO. – Just how lousy do patients with medically refractory chronic rhinosinusitis feel in daily life? A lot worse than you might guess.
Patients who elected to undergo endoscopic sinus surgery after failing medical therapy for chronic rhinosinusitis (CRS) rated their own baseline health state on standardized measures as being well below U.S. population norms. Their degree of impairment was similar to the self-rated scores among age- and gender-matched individuals with end-stage renal disease or Parkinson’s disease, according to Dr. Todd T. Kingdom, professor and vice chairman of the department of otolaryngology, head and neck surgery, at the University of Colorado, Denver, and immediate past president of the American Rhinologic Society.
He cited a 5-year study that prospectively followed 232 adults with CRS who elected to undergo endoscopic sinus surgery (ESS) after failing to improve on medical therapy (Laryngoscope 2011;121:2672-8). Their mean presurgical health state utility value – derived using the Short Form 6D via methods routinely employed by health economists – was 0.65, on a scale in which 0 is death and 1.0 is perfect health.
That was worse than the self-rated scores among patients with heart failure or moderate COPD, as reported in other studies, and only slightly better than the self-rated health of patients awaiting hip replacement or liver transplantation. The U.S. population norm was a score of 0.81, Dr. Kingdom noted at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
When self-rated health status scores were determined again 6 months or longer after ESS, patients who underwent a revision procedure had a statistically and clinically significant 0.06-point improvement on the 0-1 scale, while those with no prior sinus surgery showed an even more robust 0.09-point gain.
Those are markedly larger improvements than documented in other studies following initiation of drug therapy for Parkinson’s disease, for example, or tumor necrosis factor–inhibitor therapy for psoriasis. Of the specific interventions assessed, only total hip replacement and bariatric surgery resulted in greater self-rated gains in health status than ESS.
In this and other studies, a patient’s baseline clinical phenotype didn’t predict the degree of improvement on quality of life measures following ESS, and gender, age, comorbid asthma, or aspirin-exacerbated respiratory disease did not influence how much benefit a patient would receive from ESS.
Patients with baseline self-reported depression, however, were slightly, albeit statistically significantly, less likely than nondepressed patients to experience significant improvement. And patients who presented without nasal polyps showed significantly more improvement in self-reported health status after ESS than did those with polyps.
Dr. Kingdom reported having no financial conflicts of interest.
KEYSTONE, COLO. – Just how lousy do patients with medically refractory chronic rhinosinusitis feel in daily life? A lot worse than you might guess.
Patients who elected to undergo endoscopic sinus surgery after failing medical therapy for chronic rhinosinusitis (CRS) rated their own baseline health state on standardized measures as being well below U.S. population norms. Their degree of impairment was similar to the self-rated scores among age- and gender-matched individuals with end-stage renal disease or Parkinson’s disease, according to Dr. Todd T. Kingdom, professor and vice chairman of the department of otolaryngology, head and neck surgery, at the University of Colorado, Denver, and immediate past president of the American Rhinologic Society.
He cited a 5-year study that prospectively followed 232 adults with CRS who elected to undergo endoscopic sinus surgery (ESS) after failing to improve on medical therapy (Laryngoscope 2011;121:2672-8). Their mean presurgical health state utility value – derived using the Short Form 6D via methods routinely employed by health economists – was 0.65, on a scale in which 0 is death and 1.0 is perfect health.
That was worse than the self-rated scores among patients with heart failure or moderate COPD, as reported in other studies, and only slightly better than the self-rated health of patients awaiting hip replacement or liver transplantation. The U.S. population norm was a score of 0.81, Dr. Kingdom noted at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
When self-rated health status scores were determined again 6 months or longer after ESS, patients who underwent a revision procedure had a statistically and clinically significant 0.06-point improvement on the 0-1 scale, while those with no prior sinus surgery showed an even more robust 0.09-point gain.
Those are markedly larger improvements than documented in other studies following initiation of drug therapy for Parkinson’s disease, for example, or tumor necrosis factor–inhibitor therapy for psoriasis. Of the specific interventions assessed, only total hip replacement and bariatric surgery resulted in greater self-rated gains in health status than ESS.
In this and other studies, a patient’s baseline clinical phenotype didn’t predict the degree of improvement on quality of life measures following ESS, and gender, age, comorbid asthma, or aspirin-exacerbated respiratory disease did not influence how much benefit a patient would receive from ESS.
Patients with baseline self-reported depression, however, were slightly, albeit statistically significantly, less likely than nondepressed patients to experience significant improvement. And patients who presented without nasal polyps showed significantly more improvement in self-reported health status after ESS than did those with polyps.
Dr. Kingdom reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE PULMONARY AND ALLERGY UPDATE
Beware of embezzlement
As the economy continues its slow and uneven recovery, economic crime is on the rise, according to many law enforcement officials around the country.
Despite the current bull market, unemployment remains high and money remains tight.
Tight money increases embezzlement temptations, so this is an excellent time to review your bookkeeping procedures and remove any obvious opportunities for theft by your employees.
Embezzlement is more common than you might think. Discovering it is often easy, because most embezzlers are not particularly skillful at what they do, or adept at covering their tracks. But it often goes undetected, sometimes for years, simply because no one is looking for it.
The experience of a friend of mine was all too typical: His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since she also balanced the checkbook, she got away with it for many months.
"It wasn’t at all clever," he told me. "And I’m somewhat chagrined to admit that it happened to me."
Is it happening to you, too? You won’t know unless you look.
Detecting fraud is an inexact science; there is no textbook approach that one can follow, but a few simple measures can uncover or prevent a large percentage of dishonest behavior:
• Hire honest employees. Check applicants’ references; find out if they are really as good as they look on paper. And for a few dollars, you can screen prospective employees on one of several public information websites to find out whether they have criminal records, or have been sued (or are suing others). My columns on hiring and background checks are in the archives at edermatologynews.com.
• Minimize opportunities for dishonesty. Theft and embezzlement are often products of opportunity, and there are many ways to minimize those opportunities. No one person should be in charge of the entire bookkeeping process. The person who enters charges should not be the one who enters payments. The employee who writes the checks should not balance the checkbook, and so on. Internal audits should occur on a regular basis, and all employees should know that. Your accountant can help with this.
• Reconcile receipts and cash daily. The most common form of embezzlement is simply employees taking cash out of the till. In a typical scenario, a patient pays a $15 copay in cash; the receptionist records the payment as $5 and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the receipts and the cash daily.
• Insist on separate accounting duties. Another common scam – the one to which my friend fell victim – is false invoices. You think you are paying for supplies and services, but the money is going to an employee. Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
• Verify expense reports. False expense reports are another common form of fraud. When an employee asks for reimbursement of expenses, make sure the expenses are real.
• Safeguard your computers. Today’s technology has made embezzlement easier and more tempting. Data are usually concentrated in one place, accounts can be accessed from remote workstations or off-premises servers, and a paper trail is often eliminated. Your computer vendor should be aware of this, and should have safeguards built into your system. Ask about them.
• Look for red flags. Do you have an employee who refuses to take vacations, because someone else will have to look at the books? Does someone insist on approving or entering expenses that are another employee’s responsibility? Is one employee suddenly living beyond his or her means?
• Consider bonding your employees. The mere knowledge that your staff is bonded will frighten off most dishonest applicants, and you will be assured of some measure of recovery should your safeguards fail.
Most embezzlement is not ingenious, or even particularly well concealed. It often sits in full view of physicians who are convinced that theft from within cannot happen to them. It can, and it does, but a little awareness can go a long way toward keeping it from happening to you.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
As the economy continues its slow and uneven recovery, economic crime is on the rise, according to many law enforcement officials around the country.
Despite the current bull market, unemployment remains high and money remains tight.
Tight money increases embezzlement temptations, so this is an excellent time to review your bookkeeping procedures and remove any obvious opportunities for theft by your employees.
Embezzlement is more common than you might think. Discovering it is often easy, because most embezzlers are not particularly skillful at what they do, or adept at covering their tracks. But it often goes undetected, sometimes for years, simply because no one is looking for it.
The experience of a friend of mine was all too typical: His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since she also balanced the checkbook, she got away with it for many months.
"It wasn’t at all clever," he told me. "And I’m somewhat chagrined to admit that it happened to me."
Is it happening to you, too? You won’t know unless you look.
Detecting fraud is an inexact science; there is no textbook approach that one can follow, but a few simple measures can uncover or prevent a large percentage of dishonest behavior:
• Hire honest employees. Check applicants’ references; find out if they are really as good as they look on paper. And for a few dollars, you can screen prospective employees on one of several public information websites to find out whether they have criminal records, or have been sued (or are suing others). My columns on hiring and background checks are in the archives at edermatologynews.com.
• Minimize opportunities for dishonesty. Theft and embezzlement are often products of opportunity, and there are many ways to minimize those opportunities. No one person should be in charge of the entire bookkeeping process. The person who enters charges should not be the one who enters payments. The employee who writes the checks should not balance the checkbook, and so on. Internal audits should occur on a regular basis, and all employees should know that. Your accountant can help with this.
• Reconcile receipts and cash daily. The most common form of embezzlement is simply employees taking cash out of the till. In a typical scenario, a patient pays a $15 copay in cash; the receptionist records the payment as $5 and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the receipts and the cash daily.
• Insist on separate accounting duties. Another common scam – the one to which my friend fell victim – is false invoices. You think you are paying for supplies and services, but the money is going to an employee. Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
• Verify expense reports. False expense reports are another common form of fraud. When an employee asks for reimbursement of expenses, make sure the expenses are real.
• Safeguard your computers. Today’s technology has made embezzlement easier and more tempting. Data are usually concentrated in one place, accounts can be accessed from remote workstations or off-premises servers, and a paper trail is often eliminated. Your computer vendor should be aware of this, and should have safeguards built into your system. Ask about them.
• Look for red flags. Do you have an employee who refuses to take vacations, because someone else will have to look at the books? Does someone insist on approving or entering expenses that are another employee’s responsibility? Is one employee suddenly living beyond his or her means?
• Consider bonding your employees. The mere knowledge that your staff is bonded will frighten off most dishonest applicants, and you will be assured of some measure of recovery should your safeguards fail.
Most embezzlement is not ingenious, or even particularly well concealed. It often sits in full view of physicians who are convinced that theft from within cannot happen to them. It can, and it does, but a little awareness can go a long way toward keeping it from happening to you.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
As the economy continues its slow and uneven recovery, economic crime is on the rise, according to many law enforcement officials around the country.
Despite the current bull market, unemployment remains high and money remains tight.
Tight money increases embezzlement temptations, so this is an excellent time to review your bookkeeping procedures and remove any obvious opportunities for theft by your employees.
Embezzlement is more common than you might think. Discovering it is often easy, because most embezzlers are not particularly skillful at what they do, or adept at covering their tracks. But it often goes undetected, sometimes for years, simply because no one is looking for it.
The experience of a friend of mine was all too typical: His bookkeeper wrote sizable checks to herself, disguising them in the ledger as payments to vendors commonly used by his practice. Since she also balanced the checkbook, she got away with it for many months.
"It wasn’t at all clever," he told me. "And I’m somewhat chagrined to admit that it happened to me."
Is it happening to you, too? You won’t know unless you look.
Detecting fraud is an inexact science; there is no textbook approach that one can follow, but a few simple measures can uncover or prevent a large percentage of dishonest behavior:
• Hire honest employees. Check applicants’ references; find out if they are really as good as they look on paper. And for a few dollars, you can screen prospective employees on one of several public information websites to find out whether they have criminal records, or have been sued (or are suing others). My columns on hiring and background checks are in the archives at edermatologynews.com.
• Minimize opportunities for dishonesty. Theft and embezzlement are often products of opportunity, and there are many ways to minimize those opportunities. No one person should be in charge of the entire bookkeeping process. The person who enters charges should not be the one who enters payments. The employee who writes the checks should not balance the checkbook, and so on. Internal audits should occur on a regular basis, and all employees should know that. Your accountant can help with this.
• Reconcile receipts and cash daily. The most common form of embezzlement is simply employees taking cash out of the till. In a typical scenario, a patient pays a $15 copay in cash; the receptionist records the payment as $5 and pockets the rest. Make sure a receipt is generated for every cash transaction, and that someone other than the person accepting cash reconciles the receipts and the cash daily.
• Insist on separate accounting duties. Another common scam – the one to which my friend fell victim – is false invoices. You think you are paying for supplies and services, but the money is going to an employee. Once again, separation of duties is the key to prevention. One employee should enter invoices into the data system, another should issue the check or make the electronic transfer, and a third should match invoices to goods and services received.
• Verify expense reports. False expense reports are another common form of fraud. When an employee asks for reimbursement of expenses, make sure the expenses are real.
• Safeguard your computers. Today’s technology has made embezzlement easier and more tempting. Data are usually concentrated in one place, accounts can be accessed from remote workstations or off-premises servers, and a paper trail is often eliminated. Your computer vendor should be aware of this, and should have safeguards built into your system. Ask about them.
• Look for red flags. Do you have an employee who refuses to take vacations, because someone else will have to look at the books? Does someone insist on approving or entering expenses that are another employee’s responsibility? Is one employee suddenly living beyond his or her means?
• Consider bonding your employees. The mere knowledge that your staff is bonded will frighten off most dishonest applicants, and you will be assured of some measure of recovery should your safeguards fail.
Most embezzlement is not ingenious, or even particularly well concealed. It often sits in full view of physicians who are convinced that theft from within cannot happen to them. It can, and it does, but a little awareness can go a long way toward keeping it from happening to you.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
Commentary: Preemptive planning is key to palliative care
For decades, surgeons have been at the forefront of the palliative care movement. From the historic utilization of palliative operations to relieve suffering to creation of the American College of Surgeons Palliative Care Task Force, surgeons are often first-line palliative care providers in the management of patients with advanced malignancy.
Palliative care involves paying attention to symptom distress, communicating with patients and families about goals of care in relation to prognosis and patient preferences, planning transitions, and engaging family support. Yet, despite a clear and established role, many surgeons are not prepared to effectively provide palliative care, and they are often resistant to the use of specialty palliative care services.
In my own training, I have witnessed apprehension and failure to use palliative care services. In one instance, I was managing an older patient after a complicated sarcoma resection. The patient suffered complications, which kept him hospitalized and returning to the hospital after short periods at a long-term acute care facility. I suggested that we call palliative care for assistance in management of the patient. He had pain, nausea, and poor oral intake, and he was depressed and anxious about his future. I was told "we don’t want the patient believing we were giving up on him."
After 3 weeks of minimal change, my attending relented. In a short time, the patient’s pain and nausea were better controlled, and we were able to have discussions with the patient and his family to clarify goals of care. Some of the symptom management techniques used methods that I had not yet encountered in my training and that seemed foreign and curious. But seeing the response left no question as to their utility. The patient was able to leave the hospital 2 weeks later with the palliative care service coordinating his management with the primary care provider and surgical team. This was a positive resolution to a significant problem. But what really hindered palliative care use?
Roadblocks include the term palliative having a negative connotation, being equated with "failure." Increased use of quality metrics may deincentivize palliative operations. Also, there is poor training and support for surgeons to provide primary palliative care services themselves. Yet, despite these barriers, there are opportunities for surgeons to improve care of patients with advanced malignancy by improving surgeon-patient communication and giving greater emphasis to advanced care planning prior to operative interventions.
As front-line providers for these patients, surgeons are an ideal conduit for delivery and improved use of early palliative care. My practice includes a discussion of advanced care planning with all of my cancer patients. I introduce this as a normal part of every discussion and refer the patient to the primary care provider or our Quality of Life service to facilitate further conversations and documentation. By destigmatizing the discussion for patients and families, a door is opened to an important part of comprehensive quality care. We must understand that diseases progress and complications occur. Failing to provide preemptive support to patients and families is true failure. With a preemptive approach, patients, families, and caregivers have a better understanding of the medical situation, and the latter can more effectively support the patient.
To standardize the role that surgeons routinely play in management of patients with advanced malignancy, efforts must focus on education and research. The role of education is twofold. First, surgical trainees need adequate tools to perform routine palliative care and an understanding of the appropriate timing to refer for specialized services. There have been multiple national efforts focused on teaching palliative care to varied practitioners. But given the aging population and the paucity of specialist palliative care providers, a renewed effort is needed. Second, surgeons must understand the role that palliative care plays and the benefits their patients can derive from it. Surgeons are routinely involved throughout the course of care of patients with malignancy from diagnosis to the end of life. Recognition of palliative care as a skill along the continuum of care already provided will improve outcomes.
Finally, research must focus on both models of use of palliative care and the quality of current practice. Palliative care as it pertains to surgeons is understudied: What teaching formats are most likely to affect clinical practice? What components of palliative care have an impact in surgical practice? What is the optimal timing and venue for providing palliative care in surgical practice? What health care system changes are needed to support surgeons to provide primary palliative care services?
We are uniquely aware of the complexities of care needed for management of patients with advanced malignancies. We are routinely called on to aid in the management of these patients. Surgical educators and researchers should focus their efforts on what is needed to fully integrate palliative care into patient-centered care already provided by trainees and surgeons.
Dr. Johnston is an assistant professor of surgery in the division of surgical oncology at the Medical College of Wisconsin, Milwaukee. He disclosed no conflicts.
For decades, surgeons have been at the forefront of the palliative care movement. From the historic utilization of palliative operations to relieve suffering to creation of the American College of Surgeons Palliative Care Task Force, surgeons are often first-line palliative care providers in the management of patients with advanced malignancy.
Palliative care involves paying attention to symptom distress, communicating with patients and families about goals of care in relation to prognosis and patient preferences, planning transitions, and engaging family support. Yet, despite a clear and established role, many surgeons are not prepared to effectively provide palliative care, and they are often resistant to the use of specialty palliative care services.
In my own training, I have witnessed apprehension and failure to use palliative care services. In one instance, I was managing an older patient after a complicated sarcoma resection. The patient suffered complications, which kept him hospitalized and returning to the hospital after short periods at a long-term acute care facility. I suggested that we call palliative care for assistance in management of the patient. He had pain, nausea, and poor oral intake, and he was depressed and anxious about his future. I was told "we don’t want the patient believing we were giving up on him."
After 3 weeks of minimal change, my attending relented. In a short time, the patient’s pain and nausea were better controlled, and we were able to have discussions with the patient and his family to clarify goals of care. Some of the symptom management techniques used methods that I had not yet encountered in my training and that seemed foreign and curious. But seeing the response left no question as to their utility. The patient was able to leave the hospital 2 weeks later with the palliative care service coordinating his management with the primary care provider and surgical team. This was a positive resolution to a significant problem. But what really hindered palliative care use?
Roadblocks include the term palliative having a negative connotation, being equated with "failure." Increased use of quality metrics may deincentivize palliative operations. Also, there is poor training and support for surgeons to provide primary palliative care services themselves. Yet, despite these barriers, there are opportunities for surgeons to improve care of patients with advanced malignancy by improving surgeon-patient communication and giving greater emphasis to advanced care planning prior to operative interventions.
As front-line providers for these patients, surgeons are an ideal conduit for delivery and improved use of early palliative care. My practice includes a discussion of advanced care planning with all of my cancer patients. I introduce this as a normal part of every discussion and refer the patient to the primary care provider or our Quality of Life service to facilitate further conversations and documentation. By destigmatizing the discussion for patients and families, a door is opened to an important part of comprehensive quality care. We must understand that diseases progress and complications occur. Failing to provide preemptive support to patients and families is true failure. With a preemptive approach, patients, families, and caregivers have a better understanding of the medical situation, and the latter can more effectively support the patient.
To standardize the role that surgeons routinely play in management of patients with advanced malignancy, efforts must focus on education and research. The role of education is twofold. First, surgical trainees need adequate tools to perform routine palliative care and an understanding of the appropriate timing to refer for specialized services. There have been multiple national efforts focused on teaching palliative care to varied practitioners. But given the aging population and the paucity of specialist palliative care providers, a renewed effort is needed. Second, surgeons must understand the role that palliative care plays and the benefits their patients can derive from it. Surgeons are routinely involved throughout the course of care of patients with malignancy from diagnosis to the end of life. Recognition of palliative care as a skill along the continuum of care already provided will improve outcomes.
Finally, research must focus on both models of use of palliative care and the quality of current practice. Palliative care as it pertains to surgeons is understudied: What teaching formats are most likely to affect clinical practice? What components of palliative care have an impact in surgical practice? What is the optimal timing and venue for providing palliative care in surgical practice? What health care system changes are needed to support surgeons to provide primary palliative care services?
We are uniquely aware of the complexities of care needed for management of patients with advanced malignancies. We are routinely called on to aid in the management of these patients. Surgical educators and researchers should focus their efforts on what is needed to fully integrate palliative care into patient-centered care already provided by trainees and surgeons.
Dr. Johnston is an assistant professor of surgery in the division of surgical oncology at the Medical College of Wisconsin, Milwaukee. He disclosed no conflicts.
For decades, surgeons have been at the forefront of the palliative care movement. From the historic utilization of palliative operations to relieve suffering to creation of the American College of Surgeons Palliative Care Task Force, surgeons are often first-line palliative care providers in the management of patients with advanced malignancy.
Palliative care involves paying attention to symptom distress, communicating with patients and families about goals of care in relation to prognosis and patient preferences, planning transitions, and engaging family support. Yet, despite a clear and established role, many surgeons are not prepared to effectively provide palliative care, and they are often resistant to the use of specialty palliative care services.
In my own training, I have witnessed apprehension and failure to use palliative care services. In one instance, I was managing an older patient after a complicated sarcoma resection. The patient suffered complications, which kept him hospitalized and returning to the hospital after short periods at a long-term acute care facility. I suggested that we call palliative care for assistance in management of the patient. He had pain, nausea, and poor oral intake, and he was depressed and anxious about his future. I was told "we don’t want the patient believing we were giving up on him."
After 3 weeks of minimal change, my attending relented. In a short time, the patient’s pain and nausea were better controlled, and we were able to have discussions with the patient and his family to clarify goals of care. Some of the symptom management techniques used methods that I had not yet encountered in my training and that seemed foreign and curious. But seeing the response left no question as to their utility. The patient was able to leave the hospital 2 weeks later with the palliative care service coordinating his management with the primary care provider and surgical team. This was a positive resolution to a significant problem. But what really hindered palliative care use?
Roadblocks include the term palliative having a negative connotation, being equated with "failure." Increased use of quality metrics may deincentivize palliative operations. Also, there is poor training and support for surgeons to provide primary palliative care services themselves. Yet, despite these barriers, there are opportunities for surgeons to improve care of patients with advanced malignancy by improving surgeon-patient communication and giving greater emphasis to advanced care planning prior to operative interventions.
As front-line providers for these patients, surgeons are an ideal conduit for delivery and improved use of early palliative care. My practice includes a discussion of advanced care planning with all of my cancer patients. I introduce this as a normal part of every discussion and refer the patient to the primary care provider or our Quality of Life service to facilitate further conversations and documentation. By destigmatizing the discussion for patients and families, a door is opened to an important part of comprehensive quality care. We must understand that diseases progress and complications occur. Failing to provide preemptive support to patients and families is true failure. With a preemptive approach, patients, families, and caregivers have a better understanding of the medical situation, and the latter can more effectively support the patient.
To standardize the role that surgeons routinely play in management of patients with advanced malignancy, efforts must focus on education and research. The role of education is twofold. First, surgical trainees need adequate tools to perform routine palliative care and an understanding of the appropriate timing to refer for specialized services. There have been multiple national efforts focused on teaching palliative care to varied practitioners. But given the aging population and the paucity of specialist palliative care providers, a renewed effort is needed. Second, surgeons must understand the role that palliative care plays and the benefits their patients can derive from it. Surgeons are routinely involved throughout the course of care of patients with malignancy from diagnosis to the end of life. Recognition of palliative care as a skill along the continuum of care already provided will improve outcomes.
Finally, research must focus on both models of use of palliative care and the quality of current practice. Palliative care as it pertains to surgeons is understudied: What teaching formats are most likely to affect clinical practice? What components of palliative care have an impact in surgical practice? What is the optimal timing and venue for providing palliative care in surgical practice? What health care system changes are needed to support surgeons to provide primary palliative care services?
We are uniquely aware of the complexities of care needed for management of patients with advanced malignancies. We are routinely called on to aid in the management of these patients. Surgical educators and researchers should focus their efforts on what is needed to fully integrate palliative care into patient-centered care already provided by trainees and surgeons.
Dr. Johnston is an assistant professor of surgery in the division of surgical oncology at the Medical College of Wisconsin, Milwaukee. He disclosed no conflicts.
FDA approves octocog alfa for adults with hemophilia A

The US Food and Drug Administration (FDA) has approved a new indication for the recombinant antihemophilic factor VIII product octocog alfa (Kogenate).
It is now approved for routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adults with hemophilia A.
Octocog alfa was already FDA-approved for the control and prevention of bleeding episodes in adults and children with hemophilia A, for perioperative management in adults and children with hemophilia A, as routine prophylaxis in children with hemophilia A, and to reduce the risk of joint damage in children without pre-existing joint damage.
The FDA’s latest approval is based on data from the SPINART study, in which patients were randomized to receive prophylactic octocog alfa or on-demand treatment. The study was sponsored by Bayer Healthcare, the company developing octocog alfa.
“In Bayer’s SPINART study, adult patients with hemophilia A on the prophylactic regimen experienced significantly fewer bleeding events than those using on-demand treatment,” said Marilyn Manco-Johnson, MD, principal investigator of the study and director at of the Mountain States Regional Hemophilia and Thrombosis Center at the University of Colorado at Denver and Health Sciences Center.
Results of the SPINART study were presented at the World Federation of Hemophilia 2012 World Congress and published in The Journal of Thrombosis and Haemostasis.
The study included 84 patients, ages 15 to 50, with hemophilia A. They were randomized to a prophylaxis regimen of 25 IU/kg 3 times per week (n=42) or on-demand treatment (n=42). Escalation by 5 IU/kg (to 30 or 35 IU/kg maximum) was allowed for subjects with 12 or more annual bleeds after 1 and 2 years.
Patients were stratified based on target joints (presence/absence) and the number of bleeding events in the previous 6 months (≥15 vs <15 annualized bleeds).
Patients who received prophylaxis experienced significantly fewer bleeds (P<0.0001) than patients treated on demand, regardless of factors such as age, bleeding history, and the presence or absence of target joints.
The ratio of the mean bleeding frequency was 15.2 (P<0.0001) for on-demand vs prophylaxis, indicating that patients who received on-demand treatment experienced, on average, 15.2 times as many bleeds as patients treated prophylactically.
The mean annualized bleed rates (bleeds/subject/year) were 37 in the on-demand group versus 2 in the prophylaxis group. The median annualized bleed rate in the on-demand group was 33 versus 0 in the prophylaxis group.
Fifty-two percent (22/42) of prophylaxis subjects experienced no bleeding, and 29% (12/42) of prophylaxis subjects experienced 1 to 2 bleeds during the follow-up period.
Adverse events were consistent with the existing safety profile for octocog alfa. The most common adverse reactions (≥4%) were inhibitor formation in previously untreated and minimally treated patients, skin-related hypersensitivity reactions (eg, rash, pruritus), infusion-site reactions (eg, inflammation, pain), and infections associated with a central venous access device.
Serious adverse reactions associated with octocog alfa include systemic hypersensitivity reactions—bronchospastic reactions and/or hypotension and anaphylaxis—and the development of high-titer inhibitors necessitating alternative treatments to factor VIII.
For more details on octocog alfa, see the full prescribing information. ![]()

The US Food and Drug Administration (FDA) has approved a new indication for the recombinant antihemophilic factor VIII product octocog alfa (Kogenate).
It is now approved for routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adults with hemophilia A.
Octocog alfa was already FDA-approved for the control and prevention of bleeding episodes in adults and children with hemophilia A, for perioperative management in adults and children with hemophilia A, as routine prophylaxis in children with hemophilia A, and to reduce the risk of joint damage in children without pre-existing joint damage.
The FDA’s latest approval is based on data from the SPINART study, in which patients were randomized to receive prophylactic octocog alfa or on-demand treatment. The study was sponsored by Bayer Healthcare, the company developing octocog alfa.
“In Bayer’s SPINART study, adult patients with hemophilia A on the prophylactic regimen experienced significantly fewer bleeding events than those using on-demand treatment,” said Marilyn Manco-Johnson, MD, principal investigator of the study and director at of the Mountain States Regional Hemophilia and Thrombosis Center at the University of Colorado at Denver and Health Sciences Center.
Results of the SPINART study were presented at the World Federation of Hemophilia 2012 World Congress and published in The Journal of Thrombosis and Haemostasis.
The study included 84 patients, ages 15 to 50, with hemophilia A. They were randomized to a prophylaxis regimen of 25 IU/kg 3 times per week (n=42) or on-demand treatment (n=42). Escalation by 5 IU/kg (to 30 or 35 IU/kg maximum) was allowed for subjects with 12 or more annual bleeds after 1 and 2 years.
Patients were stratified based on target joints (presence/absence) and the number of bleeding events in the previous 6 months (≥15 vs <15 annualized bleeds).
Patients who received prophylaxis experienced significantly fewer bleeds (P<0.0001) than patients treated on demand, regardless of factors such as age, bleeding history, and the presence or absence of target joints.
The ratio of the mean bleeding frequency was 15.2 (P<0.0001) for on-demand vs prophylaxis, indicating that patients who received on-demand treatment experienced, on average, 15.2 times as many bleeds as patients treated prophylactically.
The mean annualized bleed rates (bleeds/subject/year) were 37 in the on-demand group versus 2 in the prophylaxis group. The median annualized bleed rate in the on-demand group was 33 versus 0 in the prophylaxis group.
Fifty-two percent (22/42) of prophylaxis subjects experienced no bleeding, and 29% (12/42) of prophylaxis subjects experienced 1 to 2 bleeds during the follow-up period.
Adverse events were consistent with the existing safety profile for octocog alfa. The most common adverse reactions (≥4%) were inhibitor formation in previously untreated and minimally treated patients, skin-related hypersensitivity reactions (eg, rash, pruritus), infusion-site reactions (eg, inflammation, pain), and infections associated with a central venous access device.
Serious adverse reactions associated with octocog alfa include systemic hypersensitivity reactions—bronchospastic reactions and/or hypotension and anaphylaxis—and the development of high-titer inhibitors necessitating alternative treatments to factor VIII.
For more details on octocog alfa, see the full prescribing information. ![]()

The US Food and Drug Administration (FDA) has approved a new indication for the recombinant antihemophilic factor VIII product octocog alfa (Kogenate).
It is now approved for routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adults with hemophilia A.
Octocog alfa was already FDA-approved for the control and prevention of bleeding episodes in adults and children with hemophilia A, for perioperative management in adults and children with hemophilia A, as routine prophylaxis in children with hemophilia A, and to reduce the risk of joint damage in children without pre-existing joint damage.
The FDA’s latest approval is based on data from the SPINART study, in which patients were randomized to receive prophylactic octocog alfa or on-demand treatment. The study was sponsored by Bayer Healthcare, the company developing octocog alfa.
“In Bayer’s SPINART study, adult patients with hemophilia A on the prophylactic regimen experienced significantly fewer bleeding events than those using on-demand treatment,” said Marilyn Manco-Johnson, MD, principal investigator of the study and director at of the Mountain States Regional Hemophilia and Thrombosis Center at the University of Colorado at Denver and Health Sciences Center.
Results of the SPINART study were presented at the World Federation of Hemophilia 2012 World Congress and published in The Journal of Thrombosis and Haemostasis.
The study included 84 patients, ages 15 to 50, with hemophilia A. They were randomized to a prophylaxis regimen of 25 IU/kg 3 times per week (n=42) or on-demand treatment (n=42). Escalation by 5 IU/kg (to 30 or 35 IU/kg maximum) was allowed for subjects with 12 or more annual bleeds after 1 and 2 years.
Patients were stratified based on target joints (presence/absence) and the number of bleeding events in the previous 6 months (≥15 vs <15 annualized bleeds).
Patients who received prophylaxis experienced significantly fewer bleeds (P<0.0001) than patients treated on demand, regardless of factors such as age, bleeding history, and the presence or absence of target joints.
The ratio of the mean bleeding frequency was 15.2 (P<0.0001) for on-demand vs prophylaxis, indicating that patients who received on-demand treatment experienced, on average, 15.2 times as many bleeds as patients treated prophylactically.
The mean annualized bleed rates (bleeds/subject/year) were 37 in the on-demand group versus 2 in the prophylaxis group. The median annualized bleed rate in the on-demand group was 33 versus 0 in the prophylaxis group.
Fifty-two percent (22/42) of prophylaxis subjects experienced no bleeding, and 29% (12/42) of prophylaxis subjects experienced 1 to 2 bleeds during the follow-up period.
Adverse events were consistent with the existing safety profile for octocog alfa. The most common adverse reactions (≥4%) were inhibitor formation in previously untreated and minimally treated patients, skin-related hypersensitivity reactions (eg, rash, pruritus), infusion-site reactions (eg, inflammation, pain), and infections associated with a central venous access device.
Serious adverse reactions associated with octocog alfa include systemic hypersensitivity reactions—bronchospastic reactions and/or hypotension and anaphylaxis—and the development of high-titer inhibitors necessitating alternative treatments to factor VIII.
For more details on octocog alfa, see the full prescribing information. ![]()
Drug delivery vehicle has antimyeloma effects

Credit: PNAS
Researchers have discovered that a solvent used as a drug delivery vehicle has antimyeloma properties.
The team found that N-methyl-2-pyrrolidone (NMP)—long-regarded a basic, stable, and inactive solvent—affects the growth and survival of multiple myeloma (MM) cells and stimulates the immune system to kill these tumors.
Jake Shortt, MBChB, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Australia, described these findings in Cell Reports.
“[W]e found NMP effectively ‘reprograms’ myeloma cells by targeting a class of gene-regulating proteins,” Dr Shortt said. “This reprogramming reawakens thousands of genes that have been silenced in the cancer cells, immediately stopping the myeloma cells from growing, while activating the immune system to respond to the cancer.”
The researchers were surprised by this discovery because they had been using NMP as a vehicle to deliver drugs in mouse models of MM.
“In a routine experiment in 2010, Dr Shortt noticed our preclinical models of myeloma were responding to the control dose of NMP, which was surprising, as this control dose contained none of the novel cancer agents we were actually testing,” said study author Ricky Johnstone, PhD, also of the Peter MacCallum Cancer Centre.
Specifically, the researchers were using NMP as a drug delivery vehicle in mice transplanted with Vk*MYC MM tumors. And they consistently observed antitumor activity in vehicle-only control mice.
The team saw responses to NMP in mice transplanted with multiple, independently derived myelomas; namely, delayed paraprotein progression and improved survival in aggressive clones and sustained regressions in more indolent disease.
Further investigation revealed that NMP is an acetylated lysine mimetic and bromodomain ligand. And NMP shares molecular targets with lenalidomide, including cMYC and IRF4.
Unlike lenalidomide, NMP showed CRBN-independent activity. NMP induced similar growth arrest in CRBN-knockdown MM cells and lenalidomide-resistant MM cells.
Based on these findings, the researchers are planning a phase 1 trial of NMP, which is due to start later this year. The team noted that, because safe levels of NMP in humans are already well-established, the study is in the advanced planning stage.
“We’re at an advantage with this trial because we can immediately start at dosage levels within those recommended under occupational health and safety guidelines,” said David Ritchie, MBChB, PhD, a professor at the Peter MacCallum Cancer Centre and chief investigator of the phase 1 trial.
“It is extremely exciting to have this new insight into NMP, which is comparatively cost-effective and plentiful, compared to novel treatments developed by pharmaceutical companies, and hopefully holds promise for new or improved treatments in other cancer types.” ![]()

Credit: PNAS
Researchers have discovered that a solvent used as a drug delivery vehicle has antimyeloma properties.
The team found that N-methyl-2-pyrrolidone (NMP)—long-regarded a basic, stable, and inactive solvent—affects the growth and survival of multiple myeloma (MM) cells and stimulates the immune system to kill these tumors.
Jake Shortt, MBChB, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Australia, described these findings in Cell Reports.
“[W]e found NMP effectively ‘reprograms’ myeloma cells by targeting a class of gene-regulating proteins,” Dr Shortt said. “This reprogramming reawakens thousands of genes that have been silenced in the cancer cells, immediately stopping the myeloma cells from growing, while activating the immune system to respond to the cancer.”
The researchers were surprised by this discovery because they had been using NMP as a vehicle to deliver drugs in mouse models of MM.
“In a routine experiment in 2010, Dr Shortt noticed our preclinical models of myeloma were responding to the control dose of NMP, which was surprising, as this control dose contained none of the novel cancer agents we were actually testing,” said study author Ricky Johnstone, PhD, also of the Peter MacCallum Cancer Centre.
Specifically, the researchers were using NMP as a drug delivery vehicle in mice transplanted with Vk*MYC MM tumors. And they consistently observed antitumor activity in vehicle-only control mice.
The team saw responses to NMP in mice transplanted with multiple, independently derived myelomas; namely, delayed paraprotein progression and improved survival in aggressive clones and sustained regressions in more indolent disease.
Further investigation revealed that NMP is an acetylated lysine mimetic and bromodomain ligand. And NMP shares molecular targets with lenalidomide, including cMYC and IRF4.
Unlike lenalidomide, NMP showed CRBN-independent activity. NMP induced similar growth arrest in CRBN-knockdown MM cells and lenalidomide-resistant MM cells.
Based on these findings, the researchers are planning a phase 1 trial of NMP, which is due to start later this year. The team noted that, because safe levels of NMP in humans are already well-established, the study is in the advanced planning stage.
“We’re at an advantage with this trial because we can immediately start at dosage levels within those recommended under occupational health and safety guidelines,” said David Ritchie, MBChB, PhD, a professor at the Peter MacCallum Cancer Centre and chief investigator of the phase 1 trial.
“It is extremely exciting to have this new insight into NMP, which is comparatively cost-effective and plentiful, compared to novel treatments developed by pharmaceutical companies, and hopefully holds promise for new or improved treatments in other cancer types.” ![]()

Credit: PNAS
Researchers have discovered that a solvent used as a drug delivery vehicle has antimyeloma properties.
The team found that N-methyl-2-pyrrolidone (NMP)—long-regarded a basic, stable, and inactive solvent—affects the growth and survival of multiple myeloma (MM) cells and stimulates the immune system to kill these tumors.
Jake Shortt, MBChB, PhD, of the Peter MacCallum Cancer Centre in Melbourne, Australia, described these findings in Cell Reports.
“[W]e found NMP effectively ‘reprograms’ myeloma cells by targeting a class of gene-regulating proteins,” Dr Shortt said. “This reprogramming reawakens thousands of genes that have been silenced in the cancer cells, immediately stopping the myeloma cells from growing, while activating the immune system to respond to the cancer.”
The researchers were surprised by this discovery because they had been using NMP as a vehicle to deliver drugs in mouse models of MM.
“In a routine experiment in 2010, Dr Shortt noticed our preclinical models of myeloma were responding to the control dose of NMP, which was surprising, as this control dose contained none of the novel cancer agents we were actually testing,” said study author Ricky Johnstone, PhD, also of the Peter MacCallum Cancer Centre.
Specifically, the researchers were using NMP as a drug delivery vehicle in mice transplanted with Vk*MYC MM tumors. And they consistently observed antitumor activity in vehicle-only control mice.
The team saw responses to NMP in mice transplanted with multiple, independently derived myelomas; namely, delayed paraprotein progression and improved survival in aggressive clones and sustained regressions in more indolent disease.
Further investigation revealed that NMP is an acetylated lysine mimetic and bromodomain ligand. And NMP shares molecular targets with lenalidomide, including cMYC and IRF4.
Unlike lenalidomide, NMP showed CRBN-independent activity. NMP induced similar growth arrest in CRBN-knockdown MM cells and lenalidomide-resistant MM cells.
Based on these findings, the researchers are planning a phase 1 trial of NMP, which is due to start later this year. The team noted that, because safe levels of NMP in humans are already well-established, the study is in the advanced planning stage.
“We’re at an advantage with this trial because we can immediately start at dosage levels within those recommended under occupational health and safety guidelines,” said David Ritchie, MBChB, PhD, a professor at the Peter MacCallum Cancer Centre and chief investigator of the phase 1 trial.
“It is extremely exciting to have this new insight into NMP, which is comparatively cost-effective and plentiful, compared to novel treatments developed by pharmaceutical companies, and hopefully holds promise for new or improved treatments in other cancer types.” ![]()