User login
Virotherapy shows activity against MM

Credit: CDC
Results of a proof-of-principle study suggest virotherapy can be effective against multiple myeloma (MM).
The study included 2 MM patients who each received a single dose of a measles virus engineered to target myeloma plasma cells (MV-NIS).
Both patients responded to the treatment, with initial reductions in M protein and complete resolution of bone marrow plasmacytosis. One of the patients achieved a complete remission that lasted 9 months.
The patients did experience adverse effects associated with MV-NIS, but all were resolved with appropriate treatment.
“This is the first study to establish the feasibility of systemic oncolytic virotherapy for disseminated cancer,” said Stephen Russell, MD, PhD, of the Mayo Clinic in Rochester, Minnesota.
“These patients were not responsive to other therapies and had experienced several recurrences of their disease.”
Dr Russell and his colleagues described this research in Mayo Clinic Proceedings.
Patient characteristics, treatment
The researchers explained that the 2 patients described in this report were the first to receive MV-NIS at the highest possible dose. They both received the virus at a dose of 1011 TCID50, infused into a superficial arm vein in 100 mL of normal saline over 60 minutes.
Both patients had limited previous exposure to measles (and therefore fewer antibodies to the virus) and essentially no remaining treatment options.
The first patient was a 49-year-old woman with heavily pretreated, light chain MM. Her last relapse was 9 months after her second autologous stem cell transplant, while she was not receiving therapy.
The second patient was a 65-year-old woman with relapsing IgA k MM that was refractory to all approved antimyeloma drugs. Her disease had progressed while she was receiving carfilzomib, pomalidomide, and dexamethasone therapy.
Adverse events
Patient 1 experienced a number of adverse effects related to MV-NIS, including a severe headache during treatment that required clinicians to temporarily stop her infusion.
This was followed by fever, tachycardia, hypotension, severe nausea and vomiting, and a superficial venous thrombosis extending from the wrist to the upper humerus. But all of these events responded to treatment.
Patient 2 also experienced adverse effects related to MV-NIS, including fever, tachycardia, hypotension, and headache. She responded to treatment for these events, and her recurring fever resolved spontaneously after a few hours.
Treatment response
Both patients’ disease responded to MV-NIS. They experienced initial reductions in M protein and complete resolution of bone marrow plasmacytosis at 6 weeks after treatment.
Patient 1 achieved a complete remission that lasted 9 months. A scan at 6 weeks showed the patient had experienced substantial improvement in all 5 of her previously identified lesions.
Although patient 2 initially responded to treatment, her plasmacytomas were progressing at the 6-week mark, and her free light chain level was increasing. Her 6-week scan revealed increased size and FDG uptake in most soft tissue lesions, although a few lesions did show varying degrees of improvement. ![]()

Credit: CDC
Results of a proof-of-principle study suggest virotherapy can be effective against multiple myeloma (MM).
The study included 2 MM patients who each received a single dose of a measles virus engineered to target myeloma plasma cells (MV-NIS).
Both patients responded to the treatment, with initial reductions in M protein and complete resolution of bone marrow plasmacytosis. One of the patients achieved a complete remission that lasted 9 months.
The patients did experience adverse effects associated with MV-NIS, but all were resolved with appropriate treatment.
“This is the first study to establish the feasibility of systemic oncolytic virotherapy for disseminated cancer,” said Stephen Russell, MD, PhD, of the Mayo Clinic in Rochester, Minnesota.
“These patients were not responsive to other therapies and had experienced several recurrences of their disease.”
Dr Russell and his colleagues described this research in Mayo Clinic Proceedings.
Patient characteristics, treatment
The researchers explained that the 2 patients described in this report were the first to receive MV-NIS at the highest possible dose. They both received the virus at a dose of 1011 TCID50, infused into a superficial arm vein in 100 mL of normal saline over 60 minutes.
Both patients had limited previous exposure to measles (and therefore fewer antibodies to the virus) and essentially no remaining treatment options.
The first patient was a 49-year-old woman with heavily pretreated, light chain MM. Her last relapse was 9 months after her second autologous stem cell transplant, while she was not receiving therapy.
The second patient was a 65-year-old woman with relapsing IgA k MM that was refractory to all approved antimyeloma drugs. Her disease had progressed while she was receiving carfilzomib, pomalidomide, and dexamethasone therapy.
Adverse events
Patient 1 experienced a number of adverse effects related to MV-NIS, including a severe headache during treatment that required clinicians to temporarily stop her infusion.
This was followed by fever, tachycardia, hypotension, severe nausea and vomiting, and a superficial venous thrombosis extending from the wrist to the upper humerus. But all of these events responded to treatment.
Patient 2 also experienced adverse effects related to MV-NIS, including fever, tachycardia, hypotension, and headache. She responded to treatment for these events, and her recurring fever resolved spontaneously after a few hours.
Treatment response
Both patients’ disease responded to MV-NIS. They experienced initial reductions in M protein and complete resolution of bone marrow plasmacytosis at 6 weeks after treatment.
Patient 1 achieved a complete remission that lasted 9 months. A scan at 6 weeks showed the patient had experienced substantial improvement in all 5 of her previously identified lesions.
Although patient 2 initially responded to treatment, her plasmacytomas were progressing at the 6-week mark, and her free light chain level was increasing. Her 6-week scan revealed increased size and FDG uptake in most soft tissue lesions, although a few lesions did show varying degrees of improvement. ![]()

Credit: CDC
Results of a proof-of-principle study suggest virotherapy can be effective against multiple myeloma (MM).
The study included 2 MM patients who each received a single dose of a measles virus engineered to target myeloma plasma cells (MV-NIS).
Both patients responded to the treatment, with initial reductions in M protein and complete resolution of bone marrow plasmacytosis. One of the patients achieved a complete remission that lasted 9 months.
The patients did experience adverse effects associated with MV-NIS, but all were resolved with appropriate treatment.
“This is the first study to establish the feasibility of systemic oncolytic virotherapy for disseminated cancer,” said Stephen Russell, MD, PhD, of the Mayo Clinic in Rochester, Minnesota.
“These patients were not responsive to other therapies and had experienced several recurrences of their disease.”
Dr Russell and his colleagues described this research in Mayo Clinic Proceedings.
Patient characteristics, treatment
The researchers explained that the 2 patients described in this report were the first to receive MV-NIS at the highest possible dose. They both received the virus at a dose of 1011 TCID50, infused into a superficial arm vein in 100 mL of normal saline over 60 minutes.
Both patients had limited previous exposure to measles (and therefore fewer antibodies to the virus) and essentially no remaining treatment options.
The first patient was a 49-year-old woman with heavily pretreated, light chain MM. Her last relapse was 9 months after her second autologous stem cell transplant, while she was not receiving therapy.
The second patient was a 65-year-old woman with relapsing IgA k MM that was refractory to all approved antimyeloma drugs. Her disease had progressed while she was receiving carfilzomib, pomalidomide, and dexamethasone therapy.
Adverse events
Patient 1 experienced a number of adverse effects related to MV-NIS, including a severe headache during treatment that required clinicians to temporarily stop her infusion.
This was followed by fever, tachycardia, hypotension, severe nausea and vomiting, and a superficial venous thrombosis extending from the wrist to the upper humerus. But all of these events responded to treatment.
Patient 2 also experienced adverse effects related to MV-NIS, including fever, tachycardia, hypotension, and headache. She responded to treatment for these events, and her recurring fever resolved spontaneously after a few hours.
Treatment response
Both patients’ disease responded to MV-NIS. They experienced initial reductions in M protein and complete resolution of bone marrow plasmacytosis at 6 weeks after treatment.
Patient 1 achieved a complete remission that lasted 9 months. A scan at 6 weeks showed the patient had experienced substantial improvement in all 5 of her previously identified lesions.
Although patient 2 initially responded to treatment, her plasmacytomas were progressing at the 6-week mark, and her free light chain level was increasing. Her 6-week scan revealed increased size and FDG uptake in most soft tissue lesions, although a few lesions did show varying degrees of improvement. ![]()
Device allows for single-cell analysis
Credit: Duke University
Using components similar to those that control electrons in microchips, engineers have designed a device that can sort, store, and retrieve individual cells for study.
The team hopes this chip-like device could be scaled up to sort and store hundreds of thousands of individual living cells in a matter of minutes.
Benjamin Yellen, PhD, of Duke University in Durham, North Carolina, and his colleagues described the device in Nature Communications.
The team created the device by printing thin electromagnetic components, like those found on microchips, onto a slide. These patterns create magnetic tracks and elements like switches, transistors, and diodes that guide magnetic beads and single cells tagged with magnetic nanoparticles through a thin, liquid film.
Like a series of small conveyer belts, localized rotating magnetic fields move the beads and cells along specific directions etched into a track, while built-in switches direct traffic to storage sites on the chip. The result is an integrated circuit that controls small magnetic objects much the way electrons are controlled on computer chips.
The engineers showed that a grid of 9 compartments—3 across by 3 down—allows the magnetic beads to enter but not leave. By tagging cells with magnetic particles and directing them to different compartments, the cells can be separated, sorted, stored, studied, and retrieved.
“You need to analyze thousands of cells to get the statistics necessary to understand which genes are being turned on and off in response to pharmaceuticals or other stimuli,” Dr Yellen said. “And if you’re looking for cells exhibiting rare behavior, which might be one cell out of a thousand, then you need arrays that can control hundreds of thousands of cells.”
As an example, Dr Yellen pointed to cells affected by cancers. Most afflicted cells are active and can be targeted by therapeutics. But a few rare cells remain dormant, biding their time and avoiding destruction before activating and bringing the disease out of remission.
With the new technology, Dr Yellen and his colleagues hope to watch millions of individual cells, pick out the few that become dormant, quickly retrieve them, and analyze their genetic activity.
“Our technology can offer new tools to improve our basic understanding of cancer metastasis at the single-cell level, how cancer cells respond to chemical and physical stimuli, and to test new concepts for gene delivery and metabolite transfer during cell division and growth,” said study author CheolGi Kim, PhD, of the Daegu Gyeongbuk Institute of Science and Technology in the Republic of Korea.
The researchers now plan to demonstrate a larger grid of 8-by-8 or 16-by-16 compartments with cells, and then to scale it up to hundreds of thousands of compartments.
“Our idea is a simple one,” Dr Kim said. “Because it is a system similar to electronics and is based on the same technology, it would be easy to fabricate. That makes the system relevant to commercialization.”
“There’s another technique paper we need to do as a follow-up before we get to actual biological applications,” Dr Yellen added. “But they’re on their way.” ![]()
Credit: Duke University
Using components similar to those that control electrons in microchips, engineers have designed a device that can sort, store, and retrieve individual cells for study.
The team hopes this chip-like device could be scaled up to sort and store hundreds of thousands of individual living cells in a matter of minutes.
Benjamin Yellen, PhD, of Duke University in Durham, North Carolina, and his colleagues described the device in Nature Communications.
The team created the device by printing thin electromagnetic components, like those found on microchips, onto a slide. These patterns create magnetic tracks and elements like switches, transistors, and diodes that guide magnetic beads and single cells tagged with magnetic nanoparticles through a thin, liquid film.
Like a series of small conveyer belts, localized rotating magnetic fields move the beads and cells along specific directions etched into a track, while built-in switches direct traffic to storage sites on the chip. The result is an integrated circuit that controls small magnetic objects much the way electrons are controlled on computer chips.
The engineers showed that a grid of 9 compartments—3 across by 3 down—allows the magnetic beads to enter but not leave. By tagging cells with magnetic particles and directing them to different compartments, the cells can be separated, sorted, stored, studied, and retrieved.
“You need to analyze thousands of cells to get the statistics necessary to understand which genes are being turned on and off in response to pharmaceuticals or other stimuli,” Dr Yellen said. “And if you’re looking for cells exhibiting rare behavior, which might be one cell out of a thousand, then you need arrays that can control hundreds of thousands of cells.”
As an example, Dr Yellen pointed to cells affected by cancers. Most afflicted cells are active and can be targeted by therapeutics. But a few rare cells remain dormant, biding their time and avoiding destruction before activating and bringing the disease out of remission.
With the new technology, Dr Yellen and his colleagues hope to watch millions of individual cells, pick out the few that become dormant, quickly retrieve them, and analyze their genetic activity.
“Our technology can offer new tools to improve our basic understanding of cancer metastasis at the single-cell level, how cancer cells respond to chemical and physical stimuli, and to test new concepts for gene delivery and metabolite transfer during cell division and growth,” said study author CheolGi Kim, PhD, of the Daegu Gyeongbuk Institute of Science and Technology in the Republic of Korea.
The researchers now plan to demonstrate a larger grid of 8-by-8 or 16-by-16 compartments with cells, and then to scale it up to hundreds of thousands of compartments.
“Our idea is a simple one,” Dr Kim said. “Because it is a system similar to electronics and is based on the same technology, it would be easy to fabricate. That makes the system relevant to commercialization.”
“There’s another technique paper we need to do as a follow-up before we get to actual biological applications,” Dr Yellen added. “But they’re on their way.” ![]()
Credit: Duke University
Using components similar to those that control electrons in microchips, engineers have designed a device that can sort, store, and retrieve individual cells for study.
The team hopes this chip-like device could be scaled up to sort and store hundreds of thousands of individual living cells in a matter of minutes.
Benjamin Yellen, PhD, of Duke University in Durham, North Carolina, and his colleagues described the device in Nature Communications.
The team created the device by printing thin electromagnetic components, like those found on microchips, onto a slide. These patterns create magnetic tracks and elements like switches, transistors, and diodes that guide magnetic beads and single cells tagged with magnetic nanoparticles through a thin, liquid film.
Like a series of small conveyer belts, localized rotating magnetic fields move the beads and cells along specific directions etched into a track, while built-in switches direct traffic to storage sites on the chip. The result is an integrated circuit that controls small magnetic objects much the way electrons are controlled on computer chips.
The engineers showed that a grid of 9 compartments—3 across by 3 down—allows the magnetic beads to enter but not leave. By tagging cells with magnetic particles and directing them to different compartments, the cells can be separated, sorted, stored, studied, and retrieved.
“You need to analyze thousands of cells to get the statistics necessary to understand which genes are being turned on and off in response to pharmaceuticals or other stimuli,” Dr Yellen said. “And if you’re looking for cells exhibiting rare behavior, which might be one cell out of a thousand, then you need arrays that can control hundreds of thousands of cells.”
As an example, Dr Yellen pointed to cells affected by cancers. Most afflicted cells are active and can be targeted by therapeutics. But a few rare cells remain dormant, biding their time and avoiding destruction before activating and bringing the disease out of remission.
With the new technology, Dr Yellen and his colleagues hope to watch millions of individual cells, pick out the few that become dormant, quickly retrieve them, and analyze their genetic activity.
“Our technology can offer new tools to improve our basic understanding of cancer metastasis at the single-cell level, how cancer cells respond to chemical and physical stimuli, and to test new concepts for gene delivery and metabolite transfer during cell division and growth,” said study author CheolGi Kim, PhD, of the Daegu Gyeongbuk Institute of Science and Technology in the Republic of Korea.
The researchers now plan to demonstrate a larger grid of 8-by-8 or 16-by-16 compartments with cells, and then to scale it up to hundreds of thousands of compartments.
“Our idea is a simple one,” Dr Kim said. “Because it is a system similar to electronics and is based on the same technology, it would be easy to fabricate. That makes the system relevant to commercialization.”
“There’s another technique paper we need to do as a follow-up before we get to actual biological applications,” Dr Yellen added. “But they’re on their way.” ![]()
Early Goal-Directed Therapy in Septic Shock Does Not Reduce Deaths (ProCESS)
Clinical question
Does use of protocol-based early goal-directed therapy with central venous monitoring decrease mortality in patients presenting with septic shock?
Bottom line
Protocol-based care for resuscitation in septic shock, with or without the use of central venous monitoring, does not confer a mortality advantage over care provided according to a physician’s bedside judgment. (LOE = 1b)
Reference
The ProCESS Investigators. A randomized trial of protocol-based care for early septic shock. N Engl J Med 2014 Mar 18. [Epub ahead of print]
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Concealed
Setting
Inpatient (any location)
Synopsis
Previous research suggested that a 6-hour protocol of early goal-directed therapy (EGDT) using central hemodynamic monitoring to guide the use of intravenous fluids, vasopressors, inotropes, and transfusions reduces mortality in patients who present with septic shock. In the current study, investigators randomized 1341 patients, using concealed allocation, to 1 of 3 groups: (1) protocol-based EGDT, (2) protocol-based standard therapy, or (3) usual care. Protocol-based standard therapy required peripheral venous access only with the administration of fluids and vasopressors to maintain blood pressure, optimize fluid status, and address hypoperfusion. In the usual care group, care was at the discretion of the bedside physicians. Both protocol-based groups had approximately 90% or greater adherence to the protocols. Notably, although central venous catheter placement was not required in the protocol-based standard therapy or usual care groups, the majority of patients in each had such catheters placed, though only 4% were used for actual central venous monitoring. Analysis was by intention to treat. During the first 6 hours of resuscitation, more patients in the 2 protocol-based groups received vasopressors than patients in the usual care group. Patients in the EGDT group were also more likely to receive dobutamine and red-cell transfusions. Between 6 hours and 72 hours, however, the 3 groups had similar use of intravenous fluids, vasopressors, and transfusions. For the primary outcome of 60-day in-hospital mortality, there were no significant differences among the 3 groups. Patients in the protocol-based standard therapy group were slightly more likely to require renal replacement therapy (6% vs 3% in the other 2 groups; P = .04), whereas patients in the EGDT group were more likely to require intensive care unit admission (90% vs 85% in the other 2 groups; P = .01). Serious adverse events were rare and did not differ among the groups.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Does use of protocol-based early goal-directed therapy with central venous monitoring decrease mortality in patients presenting with septic shock?
Bottom line
Protocol-based care for resuscitation in septic shock, with or without the use of central venous monitoring, does not confer a mortality advantage over care provided according to a physician’s bedside judgment. (LOE = 1b)
Reference
The ProCESS Investigators. A randomized trial of protocol-based care for early septic shock. N Engl J Med 2014 Mar 18. [Epub ahead of print]
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Concealed
Setting
Inpatient (any location)
Synopsis
Previous research suggested that a 6-hour protocol of early goal-directed therapy (EGDT) using central hemodynamic monitoring to guide the use of intravenous fluids, vasopressors, inotropes, and transfusions reduces mortality in patients who present with septic shock. In the current study, investigators randomized 1341 patients, using concealed allocation, to 1 of 3 groups: (1) protocol-based EGDT, (2) protocol-based standard therapy, or (3) usual care. Protocol-based standard therapy required peripheral venous access only with the administration of fluids and vasopressors to maintain blood pressure, optimize fluid status, and address hypoperfusion. In the usual care group, care was at the discretion of the bedside physicians. Both protocol-based groups had approximately 90% or greater adherence to the protocols. Notably, although central venous catheter placement was not required in the protocol-based standard therapy or usual care groups, the majority of patients in each had such catheters placed, though only 4% were used for actual central venous monitoring. Analysis was by intention to treat. During the first 6 hours of resuscitation, more patients in the 2 protocol-based groups received vasopressors than patients in the usual care group. Patients in the EGDT group were also more likely to receive dobutamine and red-cell transfusions. Between 6 hours and 72 hours, however, the 3 groups had similar use of intravenous fluids, vasopressors, and transfusions. For the primary outcome of 60-day in-hospital mortality, there were no significant differences among the 3 groups. Patients in the protocol-based standard therapy group were slightly more likely to require renal replacement therapy (6% vs 3% in the other 2 groups; P = .04), whereas patients in the EGDT group were more likely to require intensive care unit admission (90% vs 85% in the other 2 groups; P = .01). Serious adverse events were rare and did not differ among the groups.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Does use of protocol-based early goal-directed therapy with central venous monitoring decrease mortality in patients presenting with septic shock?
Bottom line
Protocol-based care for resuscitation in septic shock, with or without the use of central venous monitoring, does not confer a mortality advantage over care provided according to a physician’s bedside judgment. (LOE = 1b)
Reference
The ProCESS Investigators. A randomized trial of protocol-based care for early septic shock. N Engl J Med 2014 Mar 18. [Epub ahead of print]
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Concealed
Setting
Inpatient (any location)
Synopsis
Previous research suggested that a 6-hour protocol of early goal-directed therapy (EGDT) using central hemodynamic monitoring to guide the use of intravenous fluids, vasopressors, inotropes, and transfusions reduces mortality in patients who present with septic shock. In the current study, investigators randomized 1341 patients, using concealed allocation, to 1 of 3 groups: (1) protocol-based EGDT, (2) protocol-based standard therapy, or (3) usual care. Protocol-based standard therapy required peripheral venous access only with the administration of fluids and vasopressors to maintain blood pressure, optimize fluid status, and address hypoperfusion. In the usual care group, care was at the discretion of the bedside physicians. Both protocol-based groups had approximately 90% or greater adherence to the protocols. Notably, although central venous catheter placement was not required in the protocol-based standard therapy or usual care groups, the majority of patients in each had such catheters placed, though only 4% were used for actual central venous monitoring. Analysis was by intention to treat. During the first 6 hours of resuscitation, more patients in the 2 protocol-based groups received vasopressors than patients in the usual care group. Patients in the EGDT group were also more likely to receive dobutamine and red-cell transfusions. Between 6 hours and 72 hours, however, the 3 groups had similar use of intravenous fluids, vasopressors, and transfusions. For the primary outcome of 60-day in-hospital mortality, there were no significant differences among the 3 groups. Patients in the protocol-based standard therapy group were slightly more likely to require renal replacement therapy (6% vs 3% in the other 2 groups; P = .04), whereas patients in the EGDT group were more likely to require intensive care unit admission (90% vs 85% in the other 2 groups; P = .01). Serious adverse events were rare and did not differ among the groups.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
No Mortality Benefit with Albumin Administration in Severe Sepsis (ALBIOS)
Clinical question
Does albumin administration reduce mortality in critically ill patients with sepsis?
Bottom line
The use of albumin along with crystalloid solutions in patients with severe sepsis does not affect mortality. (LOE = 1b-)
Reference
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Concealed
Setting
Inpatient (ICU only)
Synopsis
Using concealed allocation, these investigators randomized adult patients in the intensive care unit (ICU) with severe sepsis within the previous 24 hours to receive either 300 mL of 20% albumin plus crystalloid solution or crystalloid solution alone. The treatment group received albumin daily from randomization through day 28 or until discharge from the ICU. Crystalloid solution was administered as clinically indicated in both groups. Baseline characteristics of the 2 groups were similar and analysis was by intention to treat. There were no significant differences detected in either 28-day or 90-day mortality between the groups, although a lower-than-expected mortality rate in the control group may have underpowered the study. Secondary outcomes were also similar, including number of new organ failures, hospital and ICU lengths of stay, and need for renal replacement therapy. The albumin group had a shorter time to suspension of vasopressor/inotropic agents (3 vs 4 days; P = .007), indicating a decreased use of these agents. Finally, a post-hoc subgroup analysis of those patients with confirmed septic shock suggested decreased mortality at 90 days in the albumin group. However, this type of analysis, since it is not prespecified, is very susceptible to bias.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Does albumin administration reduce mortality in critically ill patients with sepsis?
Bottom line
The use of albumin along with crystalloid solutions in patients with severe sepsis does not affect mortality. (LOE = 1b-)
Reference
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Concealed
Setting
Inpatient (ICU only)
Synopsis
Using concealed allocation, these investigators randomized adult patients in the intensive care unit (ICU) with severe sepsis within the previous 24 hours to receive either 300 mL of 20% albumin plus crystalloid solution or crystalloid solution alone. The treatment group received albumin daily from randomization through day 28 or until discharge from the ICU. Crystalloid solution was administered as clinically indicated in both groups. Baseline characteristics of the 2 groups were similar and analysis was by intention to treat. There were no significant differences detected in either 28-day or 90-day mortality between the groups, although a lower-than-expected mortality rate in the control group may have underpowered the study. Secondary outcomes were also similar, including number of new organ failures, hospital and ICU lengths of stay, and need for renal replacement therapy. The albumin group had a shorter time to suspension of vasopressor/inotropic agents (3 vs 4 days; P = .007), indicating a decreased use of these agents. Finally, a post-hoc subgroup analysis of those patients with confirmed septic shock suggested decreased mortality at 90 days in the albumin group. However, this type of analysis, since it is not prespecified, is very susceptible to bias.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Does albumin administration reduce mortality in critically ill patients with sepsis?
Bottom line
The use of albumin along with crystalloid solutions in patients with severe sepsis does not affect mortality. (LOE = 1b-)
Reference
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Concealed
Setting
Inpatient (ICU only)
Synopsis
Using concealed allocation, these investigators randomized adult patients in the intensive care unit (ICU) with severe sepsis within the previous 24 hours to receive either 300 mL of 20% albumin plus crystalloid solution or crystalloid solution alone. The treatment group received albumin daily from randomization through day 28 or until discharge from the ICU. Crystalloid solution was administered as clinically indicated in both groups. Baseline characteristics of the 2 groups were similar and analysis was by intention to treat. There were no significant differences detected in either 28-day or 90-day mortality between the groups, although a lower-than-expected mortality rate in the control group may have underpowered the study. Secondary outcomes were also similar, including number of new organ failures, hospital and ICU lengths of stay, and need for renal replacement therapy. The albumin group had a shorter time to suspension of vasopressor/inotropic agents (3 vs 4 days; P = .007), indicating a decreased use of these agents. Finally, a post-hoc subgroup analysis of those patients with confirmed septic shock suggested decreased mortality at 90 days in the albumin group. However, this type of analysis, since it is not prespecified, is very susceptible to bias.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Can medication reduce crime?
Lately, I've been busy wading through a heavily publicized study that was published this month in the Lancet. In their paper, "Antipsychotics, mood stabilisers and risk of violent crime," Dr. Seena Fazel and his associates linked Swedish national registers to compare rates of violent crime among 82,647 male and female psychiatric patients to assess the effect of medication on this outcome.
The study made quite a splash in the news, because the outcome was almost too good to be true. There was a 64% reduction in violent crime among patients who had been prescribed any antipsychotic or mood stabilizer, compared with those taking other psychotropics. The reduction in violence for those taking neuroleptics and mood stabilizers was 45% and 24%, respectively. Selective serotonin reuptake inhibitors (SSRIs) had no apparent effect on crime (Lancet 2014 [doi:10.1016/S0140-6736(14)60379-2]).
Given our American anxiety over spree shooters and other high-profile crimes allegedly committed by untreated psychiatric patients, this study clearly deserves some scrutiny to thoroughly understand the findings, limitations, and other factors that could limit generalizability to the United States.
The authors compared mental health treatment registries with the national criminal history database. They looked at the rate and types of crimes committed by psychiatric patients when they were in and out of treatment. The "in-treatment" time interval was defined as the time between two or more prescriptions, as long as the prescriptions were no more than 4 months apart. Individuals who had only been given one script [prescription] were excluded. The outcome measure was any criminal conviction. The conviction outcome was based upon the date the offense took place, not the date of conviction. Individuals were excluded if the offense date was unknown.
A within-individual analysis showed significant reduction in all crimes, including violent crime, drug-related crime, and less severe crimes, during times when patients were prescribed medication, compared with medication-free intervals. When medicated, the rate of violent crime did not differ between patients with and without a history of violent offenses when diagnosis was not considered. When the analysis was limited to people with schizophrenia, bipolar disorder, or other psychotic disorders, the prescription of neuroleptics significantly reduced violent crime for both men and women.
For bipolar disorder, mood stabilizing medication reduced violent crime for men but not for women. The SSRI-medicated group was used as a control, to account for the general effect of contact with the mental health system and non-medication interventions related to this, and there was no effect on violent crime with this class of medication.
Now on to the limitations. Medication adherence was not assessed and could not be verified apart from patients given depot neuroleptics. The overall rate of violent crime was low, as would be expected. Only 6% of men and 1% of the women committed a violent crime. The numbers were so low that the study could not statistically assess the impact of violent crime history among patients diagnosed with psychosis. This is a small but crucial finding that did not make the traditional media coverage of this study.
Also, only 40% of those patients taking antipsychotics and mood stabilizers had a diagnosis of schizophrenia, other psychosis, or bipolar disorder, suggesting that, in Sweden, these medications might be prescribed for other indications such as characterologic low frustration tolerance or irritability. The analysis did not look at impact on violent crime by personality disorder diagnosis.
The authors acknowledged that their research could not prove a causal link between psychiatric illness and violence, another important conclusion that was not mentioned in traditional media coverage. In Sweden, mental illness cannot be used to prevent or mitigate a criminal conviction, so any connection between psychiatric symptoms and crime in this population can't be determined. The study also did not consider which subjects, if any, were taking medication or in treatment under court-mandated conditions.
As legislators and advocacy groups push to strengthen involuntary treatment laws, there is a risk that "bottom line" media coverage of research like this may inappropriately sway public opinion. Psychiatrists should be prepared to respond to proposed policies based on inaccurate interpretation of research.
Dr. Hanson is a forensic psychiatrist and coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: The Johns Hopkins University Press, 2011). The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson's employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
Lately, I've been busy wading through a heavily publicized study that was published this month in the Lancet. In their paper, "Antipsychotics, mood stabilisers and risk of violent crime," Dr. Seena Fazel and his associates linked Swedish national registers to compare rates of violent crime among 82,647 male and female psychiatric patients to assess the effect of medication on this outcome.
The study made quite a splash in the news, because the outcome was almost too good to be true. There was a 64% reduction in violent crime among patients who had been prescribed any antipsychotic or mood stabilizer, compared with those taking other psychotropics. The reduction in violence for those taking neuroleptics and mood stabilizers was 45% and 24%, respectively. Selective serotonin reuptake inhibitors (SSRIs) had no apparent effect on crime (Lancet 2014 [doi:10.1016/S0140-6736(14)60379-2]).
Given our American anxiety over spree shooters and other high-profile crimes allegedly committed by untreated psychiatric patients, this study clearly deserves some scrutiny to thoroughly understand the findings, limitations, and other factors that could limit generalizability to the United States.
The authors compared mental health treatment registries with the national criminal history database. They looked at the rate and types of crimes committed by psychiatric patients when they were in and out of treatment. The "in-treatment" time interval was defined as the time between two or more prescriptions, as long as the prescriptions were no more than 4 months apart. Individuals who had only been given one script [prescription] were excluded. The outcome measure was any criminal conviction. The conviction outcome was based upon the date the offense took place, not the date of conviction. Individuals were excluded if the offense date was unknown.
A within-individual analysis showed significant reduction in all crimes, including violent crime, drug-related crime, and less severe crimes, during times when patients were prescribed medication, compared with medication-free intervals. When medicated, the rate of violent crime did not differ between patients with and without a history of violent offenses when diagnosis was not considered. When the analysis was limited to people with schizophrenia, bipolar disorder, or other psychotic disorders, the prescription of neuroleptics significantly reduced violent crime for both men and women.
For bipolar disorder, mood stabilizing medication reduced violent crime for men but not for women. The SSRI-medicated group was used as a control, to account for the general effect of contact with the mental health system and non-medication interventions related to this, and there was no effect on violent crime with this class of medication.
Now on to the limitations. Medication adherence was not assessed and could not be verified apart from patients given depot neuroleptics. The overall rate of violent crime was low, as would be expected. Only 6% of men and 1% of the women committed a violent crime. The numbers were so low that the study could not statistically assess the impact of violent crime history among patients diagnosed with psychosis. This is a small but crucial finding that did not make the traditional media coverage of this study.
Also, only 40% of those patients taking antipsychotics and mood stabilizers had a diagnosis of schizophrenia, other psychosis, or bipolar disorder, suggesting that, in Sweden, these medications might be prescribed for other indications such as characterologic low frustration tolerance or irritability. The analysis did not look at impact on violent crime by personality disorder diagnosis.
The authors acknowledged that their research could not prove a causal link between psychiatric illness and violence, another important conclusion that was not mentioned in traditional media coverage. In Sweden, mental illness cannot be used to prevent or mitigate a criminal conviction, so any connection between psychiatric symptoms and crime in this population can't be determined. The study also did not consider which subjects, if any, were taking medication or in treatment under court-mandated conditions.
As legislators and advocacy groups push to strengthen involuntary treatment laws, there is a risk that "bottom line" media coverage of research like this may inappropriately sway public opinion. Psychiatrists should be prepared to respond to proposed policies based on inaccurate interpretation of research.
Dr. Hanson is a forensic psychiatrist and coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: The Johns Hopkins University Press, 2011). The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson's employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
Lately, I've been busy wading through a heavily publicized study that was published this month in the Lancet. In their paper, "Antipsychotics, mood stabilisers and risk of violent crime," Dr. Seena Fazel and his associates linked Swedish national registers to compare rates of violent crime among 82,647 male and female psychiatric patients to assess the effect of medication on this outcome.
The study made quite a splash in the news, because the outcome was almost too good to be true. There was a 64% reduction in violent crime among patients who had been prescribed any antipsychotic or mood stabilizer, compared with those taking other psychotropics. The reduction in violence for those taking neuroleptics and mood stabilizers was 45% and 24%, respectively. Selective serotonin reuptake inhibitors (SSRIs) had no apparent effect on crime (Lancet 2014 [doi:10.1016/S0140-6736(14)60379-2]).
Given our American anxiety over spree shooters and other high-profile crimes allegedly committed by untreated psychiatric patients, this study clearly deserves some scrutiny to thoroughly understand the findings, limitations, and other factors that could limit generalizability to the United States.
The authors compared mental health treatment registries with the national criminal history database. They looked at the rate and types of crimes committed by psychiatric patients when they were in and out of treatment. The "in-treatment" time interval was defined as the time between two or more prescriptions, as long as the prescriptions were no more than 4 months apart. Individuals who had only been given one script [prescription] were excluded. The outcome measure was any criminal conviction. The conviction outcome was based upon the date the offense took place, not the date of conviction. Individuals were excluded if the offense date was unknown.
A within-individual analysis showed significant reduction in all crimes, including violent crime, drug-related crime, and less severe crimes, during times when patients were prescribed medication, compared with medication-free intervals. When medicated, the rate of violent crime did not differ between patients with and without a history of violent offenses when diagnosis was not considered. When the analysis was limited to people with schizophrenia, bipolar disorder, or other psychotic disorders, the prescription of neuroleptics significantly reduced violent crime for both men and women.
For bipolar disorder, mood stabilizing medication reduced violent crime for men but not for women. The SSRI-medicated group was used as a control, to account for the general effect of contact with the mental health system and non-medication interventions related to this, and there was no effect on violent crime with this class of medication.
Now on to the limitations. Medication adherence was not assessed and could not be verified apart from patients given depot neuroleptics. The overall rate of violent crime was low, as would be expected. Only 6% of men and 1% of the women committed a violent crime. The numbers were so low that the study could not statistically assess the impact of violent crime history among patients diagnosed with psychosis. This is a small but crucial finding that did not make the traditional media coverage of this study.
Also, only 40% of those patients taking antipsychotics and mood stabilizers had a diagnosis of schizophrenia, other psychosis, or bipolar disorder, suggesting that, in Sweden, these medications might be prescribed for other indications such as characterologic low frustration tolerance or irritability. The analysis did not look at impact on violent crime by personality disorder diagnosis.
The authors acknowledged that their research could not prove a causal link between psychiatric illness and violence, another important conclusion that was not mentioned in traditional media coverage. In Sweden, mental illness cannot be used to prevent or mitigate a criminal conviction, so any connection between psychiatric symptoms and crime in this population can't be determined. The study also did not consider which subjects, if any, were taking medication or in treatment under court-mandated conditions.
As legislators and advocacy groups push to strengthen involuntary treatment laws, there is a risk that "bottom line" media coverage of research like this may inappropriately sway public opinion. Psychiatrists should be prepared to respond to proposed policies based on inaccurate interpretation of research.
Dr. Hanson is a forensic psychiatrist and coauthor of "Shrink Rap: Three Psychiatrists Explain Their Work" (Baltimore: The Johns Hopkins University Press, 2011). The opinions expressed are those of the author only, and do not represent those of any of Dr. Hanson's employers or consultees, including the Maryland Department of Health and Mental Hygiene or the Maryland Division of Correction.
RealSelf
If you have patients who express interest in cosmetic procedures, and especially if you are a cosmetic dermatologist or a plastic surgeon, you might want to familiarize yourself with RealSelf.com. Founded in 2006, RealSelf is an online community for learning and sharing information about cosmetic surgery, dermatology, dentistry, and other elective treatments. In 2013, the site had 36 million unique visitors, and it is expected to grow.
Why might RealSelf be relevant for you? Simply put, it’s another channel to market you and your practice. It works by allowing physicians to answer users’ questions about cosmetic procedures ranging from rhinoplasty and liposuction to tattoo removal and Botox. Over time, your participation can lead to new consultations at your practice.
To ensure credibility, physicians must be board-certified in order to join RealSelf’s physician community. There is an element of game mechanics: The more active the physician, the more exposure his or her profile and practice receives. Similarly, paid subscriptions lead to more exposure than free subscriptions (more on this later.) Although this model does not appeal to some physicians, many of them do like the platform, and see it as a way to build a reputation as an expert and to market their practices.
Unlike doctor review sites that focus on the physician, RealSelf focuses on the procedure. For each procedure, users will find actual patient reviews and before and after photos, as well as Q&A’s with board-certified physicians. Users will also find licensed physicians in their area as well as the average cost for the procedure. RealSelf believes that patients value transparency, and including prices creates transparency.
Since most patients genuinely want to help other patients make informed medical decisions, the reviews tend to be thoughtful and thorough, and many of them contain multiple before-and-after photos. As a physician perusing the patient reviews, you’ll start to notice that most of them are reasonable. For example, customer satisfaction with laser treatment for melasma was 51%, whereas satisfaction for laser treatment for rosacea was 80%.
Patients and prospective patients are flocking to the site because it allows them to share their experiences, interact with other patients, and gain access to physician experts in the field. Many patients have difficulty making decisions about cosmetic procedures; RealSelf aims to alleviate their fears and help them "make confident health and beauty decisions." If a prospective patient wants to see a video of tattoo removal or Botox injections, he or she can. If a patient wants to ask physicians their opinions, he or she can. According to RealSelf, physicians have answered over 500,000 questions on the site.
Of course, all this isn’t free for physicians. RealSelf is a business. They have a tiered membership – free, pro, and spotlight. To obtain free membership, you simply visit the site and follow the prompts to "claim your profile." Once your profile is completed, you will have access to a "doctor advisor" who can help you "optimize your visibility on the site." Both "pro" and "spotlight" offer additional benefits, such as integrating patient reviews on your practice website, promotions on Facebook and Twitter, extended directory listings, and exposure in your local area. RealSelf does not discuss costs of membership until you have claimed your profile.
Only you can determine if RealSelf is beneficial to you and your practice. If, for example, you’re not looking for new patients, then you might find it unnecessary. But at the very least, you’ll know what RealSelf is the next time a fellow cosmetic physician brings it up at a conference. And it’s never a bad idea to be familiar with current social technologies that may affect your livelihood.
If you’ve used RealSelf, let us know what you think. For more information, visit RealSelf.com.
Disclaimer: I have no financial interest in RealSelf and am not an active member.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @Dermdoc on Twitter.
If you have patients who express interest in cosmetic procedures, and especially if you are a cosmetic dermatologist or a plastic surgeon, you might want to familiarize yourself with RealSelf.com. Founded in 2006, RealSelf is an online community for learning and sharing information about cosmetic surgery, dermatology, dentistry, and other elective treatments. In 2013, the site had 36 million unique visitors, and it is expected to grow.
Why might RealSelf be relevant for you? Simply put, it’s another channel to market you and your practice. It works by allowing physicians to answer users’ questions about cosmetic procedures ranging from rhinoplasty and liposuction to tattoo removal and Botox. Over time, your participation can lead to new consultations at your practice.
To ensure credibility, physicians must be board-certified in order to join RealSelf’s physician community. There is an element of game mechanics: The more active the physician, the more exposure his or her profile and practice receives. Similarly, paid subscriptions lead to more exposure than free subscriptions (more on this later.) Although this model does not appeal to some physicians, many of them do like the platform, and see it as a way to build a reputation as an expert and to market their practices.
Unlike doctor review sites that focus on the physician, RealSelf focuses on the procedure. For each procedure, users will find actual patient reviews and before and after photos, as well as Q&A’s with board-certified physicians. Users will also find licensed physicians in their area as well as the average cost for the procedure. RealSelf believes that patients value transparency, and including prices creates transparency.
Since most patients genuinely want to help other patients make informed medical decisions, the reviews tend to be thoughtful and thorough, and many of them contain multiple before-and-after photos. As a physician perusing the patient reviews, you’ll start to notice that most of them are reasonable. For example, customer satisfaction with laser treatment for melasma was 51%, whereas satisfaction for laser treatment for rosacea was 80%.
Patients and prospective patients are flocking to the site because it allows them to share their experiences, interact with other patients, and gain access to physician experts in the field. Many patients have difficulty making decisions about cosmetic procedures; RealSelf aims to alleviate their fears and help them "make confident health and beauty decisions." If a prospective patient wants to see a video of tattoo removal or Botox injections, he or she can. If a patient wants to ask physicians their opinions, he or she can. According to RealSelf, physicians have answered over 500,000 questions on the site.
Of course, all this isn’t free for physicians. RealSelf is a business. They have a tiered membership – free, pro, and spotlight. To obtain free membership, you simply visit the site and follow the prompts to "claim your profile." Once your profile is completed, you will have access to a "doctor advisor" who can help you "optimize your visibility on the site." Both "pro" and "spotlight" offer additional benefits, such as integrating patient reviews on your practice website, promotions on Facebook and Twitter, extended directory listings, and exposure in your local area. RealSelf does not discuss costs of membership until you have claimed your profile.
Only you can determine if RealSelf is beneficial to you and your practice. If, for example, you’re not looking for new patients, then you might find it unnecessary. But at the very least, you’ll know what RealSelf is the next time a fellow cosmetic physician brings it up at a conference. And it’s never a bad idea to be familiar with current social technologies that may affect your livelihood.
If you’ve used RealSelf, let us know what you think. For more information, visit RealSelf.com.
Disclaimer: I have no financial interest in RealSelf and am not an active member.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @Dermdoc on Twitter.
If you have patients who express interest in cosmetic procedures, and especially if you are a cosmetic dermatologist or a plastic surgeon, you might want to familiarize yourself with RealSelf.com. Founded in 2006, RealSelf is an online community for learning and sharing information about cosmetic surgery, dermatology, dentistry, and other elective treatments. In 2013, the site had 36 million unique visitors, and it is expected to grow.
Why might RealSelf be relevant for you? Simply put, it’s another channel to market you and your practice. It works by allowing physicians to answer users’ questions about cosmetic procedures ranging from rhinoplasty and liposuction to tattoo removal and Botox. Over time, your participation can lead to new consultations at your practice.
To ensure credibility, physicians must be board-certified in order to join RealSelf’s physician community. There is an element of game mechanics: The more active the physician, the more exposure his or her profile and practice receives. Similarly, paid subscriptions lead to more exposure than free subscriptions (more on this later.) Although this model does not appeal to some physicians, many of them do like the platform, and see it as a way to build a reputation as an expert and to market their practices.
Unlike doctor review sites that focus on the physician, RealSelf focuses on the procedure. For each procedure, users will find actual patient reviews and before and after photos, as well as Q&A’s with board-certified physicians. Users will also find licensed physicians in their area as well as the average cost for the procedure. RealSelf believes that patients value transparency, and including prices creates transparency.
Since most patients genuinely want to help other patients make informed medical decisions, the reviews tend to be thoughtful and thorough, and many of them contain multiple before-and-after photos. As a physician perusing the patient reviews, you’ll start to notice that most of them are reasonable. For example, customer satisfaction with laser treatment for melasma was 51%, whereas satisfaction for laser treatment for rosacea was 80%.
Patients and prospective patients are flocking to the site because it allows them to share their experiences, interact with other patients, and gain access to physician experts in the field. Many patients have difficulty making decisions about cosmetic procedures; RealSelf aims to alleviate their fears and help them "make confident health and beauty decisions." If a prospective patient wants to see a video of tattoo removal or Botox injections, he or she can. If a patient wants to ask physicians their opinions, he or she can. According to RealSelf, physicians have answered over 500,000 questions on the site.
Of course, all this isn’t free for physicians. RealSelf is a business. They have a tiered membership – free, pro, and spotlight. To obtain free membership, you simply visit the site and follow the prompts to "claim your profile." Once your profile is completed, you will have access to a "doctor advisor" who can help you "optimize your visibility on the site." Both "pro" and "spotlight" offer additional benefits, such as integrating patient reviews on your practice website, promotions on Facebook and Twitter, extended directory listings, and exposure in your local area. RealSelf does not discuss costs of membership until you have claimed your profile.
Only you can determine if RealSelf is beneficial to you and your practice. If, for example, you’re not looking for new patients, then you might find it unnecessary. But at the very least, you’ll know what RealSelf is the next time a fellow cosmetic physician brings it up at a conference. And it’s never a bad idea to be familiar with current social technologies that may affect your livelihood.
If you’ve used RealSelf, let us know what you think. For more information, visit RealSelf.com.
Disclaimer: I have no financial interest in RealSelf and am not an active member.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @Dermdoc on Twitter.
Cosmeceutical Critique: Benzoyl peroxide
Benzoyl peroxide (BPO) has been used for more than 45 years for the treatment of acne, and has recently been enjoying renewed popularity, thanks to its performance in recent studies of both prescription and over-the-counter formulations (J. Drugs Dermatol. 2013;12:180-5). In fact, BPO is one of the two most common ingredients in OTC acne products (Semin. Cutan. Med. Surg. 2008;27:170-6). The prescription form is used alone or in combination with tretinoin, adapalene, or clindamycin. BPO, originally sourced from the coal tar component chlorhydroxyquinoline, is now typically prepared by treating hydrogen peroxide with benzoyl chloride (Dermatol. Clin. 2009;27:17-24). Because it can generate reactive oxygen species and commonly leads to skin irritation, its use is somewhat limited.
Antibacterial uses
BPO imparts bactericidal activity by releasing highly reactive oxygen (free radicals) that can oxidize proteins in bacterial cell membranes. It also exhibits antibacterial action against Propionibacterium acnes and Corynebacterium acnes, the bacteria implicated in the pathophysiology of acne (Dermatol. Ther. 2012;25:6-11), as well as Staphylococcus capitis, S. epidermis, S. hominis, P. avidum, P. granulosum, and the yeast Pityrosporum ovale (J. Appl. Bacteriol. 1983;54:379-82).
Acne
Many studies over the years have shown that topically applied BPO effectively treats acne (Expert Opin. Pharmacother. 2009;10:2555-62). These ameliorative results, which include enhancing the benefits of other topical antimicrobials, are thought to arise because BPO, a highly lipophilic molecule, penetrates through the sebum and into the pilosebaceous unit, and exerts bactericidal, keratolytic, and anti-inflammatory activity (Skin Pharmacol. Physiol. 2006;19:283-9). BPO may contribute to the antiacne efficacy of other antimicrobials by preventing bacterial resistance and promoting penetration into the sebum, keratin, and polysaccharides to reach the target bacteria. Specifically, the oxidative activity of BPO helps eliminate the biofilm polysaccharides secreted by P. acnes, thus expediting the delivery of other agents to the bacteria (Int. J. Dermatol. 2006;45:872; Int. J. Dermatol. 2003;42:925-7).
Not surprisingly, several studies have shown that the antiacne efficacy of a combination of BPO with other antimicrobials, such as clindamycin, is greater than that of either agent used alone. Simpson et al. demonstrated that the use of clindamycin and BPO together led to a 61% decline in inflammatory lesions after 3 months, as compared with 39% and 35%, respectively, when the agents were used alone (J. Am. Acad. Dermatol. 1997;37:590-5). BPO is frequently paired with salicylic acid to treat acne (Clin. Exp. Dermatol. 2011;36:840-3).
Acne often improves more rapidly with BPO treatment than with retinoids and other acne therapies, and data suggest that the faster clearing of acne lesions and comedones is most likely because of its keratolytic activity (Dermatol. Clin. 2009;27:17-24; J. Dermatolog. Treat. 2003;14:166-71). However, the dryness and irritation associated with BPO usage may undermine patient compliance. Several studies have suggested that BPO is effective in cleanser formulations, which seem to reduce irritation (Clin. Exp. Dermatol. 2011;36:840-3).
Photocarcinogenicity
Reports that BPO predisposed mice to skin cancer, particularly when they were exposed to ultraviolet radiation, prompted the Food and Drug Administration to form an advisory committee in 1992 to review the safety of BPO. The committee called for additional photocarcinogenicity studies while suggesting that BPO products include animal safety data on the labels. BPO-containing acne products were kept on the market. In the ensuing two decades, newer safety studies have led the FDA to change the classification of BPO to category I, deeming the OTC topical treatment of acne to be generally recognized as safe and effective (GRASE) (Fed. Regist. 2010;75:9767-77).
Photoaging
When BPO breaks down into benzoic acid in the skin, benzoyloxy, a free radical, forms as an intermediate (Prog. Clin. Biol. Res. 1995;391:245). Benzoyloxy can decarboxylate into a phenyl radical. These free radicals produce oxidative stress, which may cause DNA strand breaks in keratinocytes or may harm proteins or lipids. In addition to becoming a free radical, BPO depletes membrane and cytosolic antioxidants (Toxicology 2001;165:225-34). No retrospective trials looking at the effects of long-term use of BP on photoaging have been performed, so the role of BPO in photoaging is not clear. One study in mice found that topical BP has some of the same effects on skin as UVB (J. Invest. Dermatol. 1999;112:933-38).
Other safety issues
Acne is not uncommon among pregnant women. Although safety studies of BPO use by pregnant women have not been performed, various authors suggest that only about 5% of topically applied BPO is absorbed systemically, implying that topical BPO can be safely used during pregnancy (Int. J. Dermatol. 2002;41:197-203; Can. Fam. Physician 2011;57:665-7; Drugs 2013;73:779-87; Dermatol. Ther. 2013;26:302-11).
In approximately 1% of patients, topical BPO causes contact or irritant dermatitis (Contact Dermatitis 1999;41:233; Contact Dermatitis 1996;34:68-9). The use of barrier repair moisturizers may reduce the incidence of irritation, though this has not been proven.
Usage considerations
BPO use for acne is linked to a reduction in antibiotic resistance (J. Drugs Dermatol. 2013;12:s73-6). Because BPO, a potent oxidizer, eliminates bacteria by generating reactive oxygen species in the sebaceous follicle, it is important to consider the chemical compatibility of BPO with other agents (J. Am. Acad. Dermatol. 1981;4:31-7). Martin et al. showed that BPO tends to degrade tretinoin to about 80% of initial content, an effect that is markedly enhanced by indoor light. However, even in the presence of light, adapalene is not degraded by BPO (Br. J. Dermatol. 1998;139 Suppl 52:8-11). But the order in which products are applied is important, given that BPO can inactivate other ingredients.
Studies have demonstrated that the use of BPO in body washes leads to greater efficacy when the product is left on for 5 minutes before rinsing (J. Drugs Dermatol. 2010;9:622-5; J. Clin. Aesthet. Dermatol. 2010;3:26-9). Notably, the efficacy of BPO in cleansing products is comparable to that observed in leave-on products, but BPO provokes less irritation than leave-on formulations (J. Drugs Dermatol. 2009;8:657-61; Skinmed. 2005;4:370).
Conclusion
BPO remains quite effective in acne therapy, and it is one of the few acne medications available both over the counter and by prescription in the United States. BPO helps prevent antibiotic resistance to erythromycin and clindamycin, which makes it an important ingredient in many acne skin care regimens. However, it is pro-oxidant, and clinicians and patients should take into account the risk of BPO contributing to skin aging because of the free radicals it produces.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, April 2002), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever.
Benzoyl peroxide (BPO) has been used for more than 45 years for the treatment of acne, and has recently been enjoying renewed popularity, thanks to its performance in recent studies of both prescription and over-the-counter formulations (J. Drugs Dermatol. 2013;12:180-5). In fact, BPO is one of the two most common ingredients in OTC acne products (Semin. Cutan. Med. Surg. 2008;27:170-6). The prescription form is used alone or in combination with tretinoin, adapalene, or clindamycin. BPO, originally sourced from the coal tar component chlorhydroxyquinoline, is now typically prepared by treating hydrogen peroxide with benzoyl chloride (Dermatol. Clin. 2009;27:17-24). Because it can generate reactive oxygen species and commonly leads to skin irritation, its use is somewhat limited.
Antibacterial uses
BPO imparts bactericidal activity by releasing highly reactive oxygen (free radicals) that can oxidize proteins in bacterial cell membranes. It also exhibits antibacterial action against Propionibacterium acnes and Corynebacterium acnes, the bacteria implicated in the pathophysiology of acne (Dermatol. Ther. 2012;25:6-11), as well as Staphylococcus capitis, S. epidermis, S. hominis, P. avidum, P. granulosum, and the yeast Pityrosporum ovale (J. Appl. Bacteriol. 1983;54:379-82).
Acne
Many studies over the years have shown that topically applied BPO effectively treats acne (Expert Opin. Pharmacother. 2009;10:2555-62). These ameliorative results, which include enhancing the benefits of other topical antimicrobials, are thought to arise because BPO, a highly lipophilic molecule, penetrates through the sebum and into the pilosebaceous unit, and exerts bactericidal, keratolytic, and anti-inflammatory activity (Skin Pharmacol. Physiol. 2006;19:283-9). BPO may contribute to the antiacne efficacy of other antimicrobials by preventing bacterial resistance and promoting penetration into the sebum, keratin, and polysaccharides to reach the target bacteria. Specifically, the oxidative activity of BPO helps eliminate the biofilm polysaccharides secreted by P. acnes, thus expediting the delivery of other agents to the bacteria (Int. J. Dermatol. 2006;45:872; Int. J. Dermatol. 2003;42:925-7).
Not surprisingly, several studies have shown that the antiacne efficacy of a combination of BPO with other antimicrobials, such as clindamycin, is greater than that of either agent used alone. Simpson et al. demonstrated that the use of clindamycin and BPO together led to a 61% decline in inflammatory lesions after 3 months, as compared with 39% and 35%, respectively, when the agents were used alone (J. Am. Acad. Dermatol. 1997;37:590-5). BPO is frequently paired with salicylic acid to treat acne (Clin. Exp. Dermatol. 2011;36:840-3).
Acne often improves more rapidly with BPO treatment than with retinoids and other acne therapies, and data suggest that the faster clearing of acne lesions and comedones is most likely because of its keratolytic activity (Dermatol. Clin. 2009;27:17-24; J. Dermatolog. Treat. 2003;14:166-71). However, the dryness and irritation associated with BPO usage may undermine patient compliance. Several studies have suggested that BPO is effective in cleanser formulations, which seem to reduce irritation (Clin. Exp. Dermatol. 2011;36:840-3).
Photocarcinogenicity
Reports that BPO predisposed mice to skin cancer, particularly when they were exposed to ultraviolet radiation, prompted the Food and Drug Administration to form an advisory committee in 1992 to review the safety of BPO. The committee called for additional photocarcinogenicity studies while suggesting that BPO products include animal safety data on the labels. BPO-containing acne products were kept on the market. In the ensuing two decades, newer safety studies have led the FDA to change the classification of BPO to category I, deeming the OTC topical treatment of acne to be generally recognized as safe and effective (GRASE) (Fed. Regist. 2010;75:9767-77).
Photoaging
When BPO breaks down into benzoic acid in the skin, benzoyloxy, a free radical, forms as an intermediate (Prog. Clin. Biol. Res. 1995;391:245). Benzoyloxy can decarboxylate into a phenyl radical. These free radicals produce oxidative stress, which may cause DNA strand breaks in keratinocytes or may harm proteins or lipids. In addition to becoming a free radical, BPO depletes membrane and cytosolic antioxidants (Toxicology 2001;165:225-34). No retrospective trials looking at the effects of long-term use of BP on photoaging have been performed, so the role of BPO in photoaging is not clear. One study in mice found that topical BP has some of the same effects on skin as UVB (J. Invest. Dermatol. 1999;112:933-38).
Other safety issues
Acne is not uncommon among pregnant women. Although safety studies of BPO use by pregnant women have not been performed, various authors suggest that only about 5% of topically applied BPO is absorbed systemically, implying that topical BPO can be safely used during pregnancy (Int. J. Dermatol. 2002;41:197-203; Can. Fam. Physician 2011;57:665-7; Drugs 2013;73:779-87; Dermatol. Ther. 2013;26:302-11).
In approximately 1% of patients, topical BPO causes contact or irritant dermatitis (Contact Dermatitis 1999;41:233; Contact Dermatitis 1996;34:68-9). The use of barrier repair moisturizers may reduce the incidence of irritation, though this has not been proven.
Usage considerations
BPO use for acne is linked to a reduction in antibiotic resistance (J. Drugs Dermatol. 2013;12:s73-6). Because BPO, a potent oxidizer, eliminates bacteria by generating reactive oxygen species in the sebaceous follicle, it is important to consider the chemical compatibility of BPO with other agents (J. Am. Acad. Dermatol. 1981;4:31-7). Martin et al. showed that BPO tends to degrade tretinoin to about 80% of initial content, an effect that is markedly enhanced by indoor light. However, even in the presence of light, adapalene is not degraded by BPO (Br. J. Dermatol. 1998;139 Suppl 52:8-11). But the order in which products are applied is important, given that BPO can inactivate other ingredients.
Studies have demonstrated that the use of BPO in body washes leads to greater efficacy when the product is left on for 5 minutes before rinsing (J. Drugs Dermatol. 2010;9:622-5; J. Clin. Aesthet. Dermatol. 2010;3:26-9). Notably, the efficacy of BPO in cleansing products is comparable to that observed in leave-on products, but BPO provokes less irritation than leave-on formulations (J. Drugs Dermatol. 2009;8:657-61; Skinmed. 2005;4:370).
Conclusion
BPO remains quite effective in acne therapy, and it is one of the few acne medications available both over the counter and by prescription in the United States. BPO helps prevent antibiotic resistance to erythromycin and clindamycin, which makes it an important ingredient in many acne skin care regimens. However, it is pro-oxidant, and clinicians and patients should take into account the risk of BPO contributing to skin aging because of the free radicals it produces.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, April 2002), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever.
Benzoyl peroxide (BPO) has been used for more than 45 years for the treatment of acne, and has recently been enjoying renewed popularity, thanks to its performance in recent studies of both prescription and over-the-counter formulations (J. Drugs Dermatol. 2013;12:180-5). In fact, BPO is one of the two most common ingredients in OTC acne products (Semin. Cutan. Med. Surg. 2008;27:170-6). The prescription form is used alone or in combination with tretinoin, adapalene, or clindamycin. BPO, originally sourced from the coal tar component chlorhydroxyquinoline, is now typically prepared by treating hydrogen peroxide with benzoyl chloride (Dermatol. Clin. 2009;27:17-24). Because it can generate reactive oxygen species and commonly leads to skin irritation, its use is somewhat limited.
Antibacterial uses
BPO imparts bactericidal activity by releasing highly reactive oxygen (free radicals) that can oxidize proteins in bacterial cell membranes. It also exhibits antibacterial action against Propionibacterium acnes and Corynebacterium acnes, the bacteria implicated in the pathophysiology of acne (Dermatol. Ther. 2012;25:6-11), as well as Staphylococcus capitis, S. epidermis, S. hominis, P. avidum, P. granulosum, and the yeast Pityrosporum ovale (J. Appl. Bacteriol. 1983;54:379-82).
Acne
Many studies over the years have shown that topically applied BPO effectively treats acne (Expert Opin. Pharmacother. 2009;10:2555-62). These ameliorative results, which include enhancing the benefits of other topical antimicrobials, are thought to arise because BPO, a highly lipophilic molecule, penetrates through the sebum and into the pilosebaceous unit, and exerts bactericidal, keratolytic, and anti-inflammatory activity (Skin Pharmacol. Physiol. 2006;19:283-9). BPO may contribute to the antiacne efficacy of other antimicrobials by preventing bacterial resistance and promoting penetration into the sebum, keratin, and polysaccharides to reach the target bacteria. Specifically, the oxidative activity of BPO helps eliminate the biofilm polysaccharides secreted by P. acnes, thus expediting the delivery of other agents to the bacteria (Int. J. Dermatol. 2006;45:872; Int. J. Dermatol. 2003;42:925-7).
Not surprisingly, several studies have shown that the antiacne efficacy of a combination of BPO with other antimicrobials, such as clindamycin, is greater than that of either agent used alone. Simpson et al. demonstrated that the use of clindamycin and BPO together led to a 61% decline in inflammatory lesions after 3 months, as compared with 39% and 35%, respectively, when the agents were used alone (J. Am. Acad. Dermatol. 1997;37:590-5). BPO is frequently paired with salicylic acid to treat acne (Clin. Exp. Dermatol. 2011;36:840-3).
Acne often improves more rapidly with BPO treatment than with retinoids and other acne therapies, and data suggest that the faster clearing of acne lesions and comedones is most likely because of its keratolytic activity (Dermatol. Clin. 2009;27:17-24; J. Dermatolog. Treat. 2003;14:166-71). However, the dryness and irritation associated with BPO usage may undermine patient compliance. Several studies have suggested that BPO is effective in cleanser formulations, which seem to reduce irritation (Clin. Exp. Dermatol. 2011;36:840-3).
Photocarcinogenicity
Reports that BPO predisposed mice to skin cancer, particularly when they were exposed to ultraviolet radiation, prompted the Food and Drug Administration to form an advisory committee in 1992 to review the safety of BPO. The committee called for additional photocarcinogenicity studies while suggesting that BPO products include animal safety data on the labels. BPO-containing acne products were kept on the market. In the ensuing two decades, newer safety studies have led the FDA to change the classification of BPO to category I, deeming the OTC topical treatment of acne to be generally recognized as safe and effective (GRASE) (Fed. Regist. 2010;75:9767-77).
Photoaging
When BPO breaks down into benzoic acid in the skin, benzoyloxy, a free radical, forms as an intermediate (Prog. Clin. Biol. Res. 1995;391:245). Benzoyloxy can decarboxylate into a phenyl radical. These free radicals produce oxidative stress, which may cause DNA strand breaks in keratinocytes or may harm proteins or lipids. In addition to becoming a free radical, BPO depletes membrane and cytosolic antioxidants (Toxicology 2001;165:225-34). No retrospective trials looking at the effects of long-term use of BP on photoaging have been performed, so the role of BPO in photoaging is not clear. One study in mice found that topical BP has some of the same effects on skin as UVB (J. Invest. Dermatol. 1999;112:933-38).
Other safety issues
Acne is not uncommon among pregnant women. Although safety studies of BPO use by pregnant women have not been performed, various authors suggest that only about 5% of topically applied BPO is absorbed systemically, implying that topical BPO can be safely used during pregnancy (Int. J. Dermatol. 2002;41:197-203; Can. Fam. Physician 2011;57:665-7; Drugs 2013;73:779-87; Dermatol. Ther. 2013;26:302-11).
In approximately 1% of patients, topical BPO causes contact or irritant dermatitis (Contact Dermatitis 1999;41:233; Contact Dermatitis 1996;34:68-9). The use of barrier repair moisturizers may reduce the incidence of irritation, though this has not been proven.
Usage considerations
BPO use for acne is linked to a reduction in antibiotic resistance (J. Drugs Dermatol. 2013;12:s73-6). Because BPO, a potent oxidizer, eliminates bacteria by generating reactive oxygen species in the sebaceous follicle, it is important to consider the chemical compatibility of BPO with other agents (J. Am. Acad. Dermatol. 1981;4:31-7). Martin et al. showed that BPO tends to degrade tretinoin to about 80% of initial content, an effect that is markedly enhanced by indoor light. However, even in the presence of light, adapalene is not degraded by BPO (Br. J. Dermatol. 1998;139 Suppl 52:8-11). But the order in which products are applied is important, given that BPO can inactivate other ingredients.
Studies have demonstrated that the use of BPO in body washes leads to greater efficacy when the product is left on for 5 minutes before rinsing (J. Drugs Dermatol. 2010;9:622-5; J. Clin. Aesthet. Dermatol. 2010;3:26-9). Notably, the efficacy of BPO in cleansing products is comparable to that observed in leave-on products, but BPO provokes less irritation than leave-on formulations (J. Drugs Dermatol. 2009;8:657-61; Skinmed. 2005;4:370).
Conclusion
BPO remains quite effective in acne therapy, and it is one of the few acne medications available both over the counter and by prescription in the United States. BPO helps prevent antibiotic resistance to erythromycin and clindamycin, which makes it an important ingredient in many acne skin care regimens. However, it is pro-oxidant, and clinicians and patients should take into account the risk of BPO contributing to skin aging because of the free radicals it produces.
Dr. Baumann is chief executive officer of the Baumann Cosmetic & Research Institute in Miami Beach. She founded the cosmetic dermatology center at the University of Miami in 1997. Dr. Baumann wrote the textbook "Cosmetic Dermatology: Principles and Practice" (McGraw-Hill, April 2002), and a book for consumers, "The Skin Type Solution" (Bantam, 2006). She has contributed to the Cosmeceutical Critique column in Skin & Allergy News since January 2001 and joined the editorial advisory board in 2004. Dr. Baumann has received funding for clinical grants from Allergan, Aveeno, Avon Products, Galderma, Mary Kay, Medicis Pharmaceuticals, Neutrogena, Philosophy, Stiefel, Topix Pharmaceuticals, and Unilever.
Longer-term opioid use in workers’ comp cases highest in Louisiana
In Louisiana, opioid use lasted more than 6 months in 17% of nonsurgical workers’ compensation claims involving employees who received at least one prescription for pain medication, the Workers Compensation Research Institute reported.
In cases with more than 7 days of lost time, that was the highest rate seen among the 25 states in the study, with New York second at 12% and Pennsylvania and Texas tied for third at 11%. There were four states tied for the lowest rate, at 4%: Missouri, New Jersey, Indiana, and Wisconsin, according to the WCRI report.
Overall, use of narcotics for pain relief by injured workers in such cases ranged from 60% in New Jersey to 88% in Arkansas (median, 76%), while use of any pain medication ranged from 85% in Minnesota to 95% in Florida, Georgia, Tennessee, and Texas (median, 94%), the report showed.
The study involved claims with injuries that occurred from Oct. 1, 2009, through Sept. 30, 2010, with prescriptions filled through March 31, 2012. Longer-term users received a prescription for opioids within 3 months of their injury and had three or more visits to fill opioid prescriptions between the 7th and the 12th month after the injury.
The 25 states in the study "represent more than 70% of the workers’ compensation benefits paid in the United States," the WCRI noted.
The study was based on approximately 264,000 nonsurgical claims and more than 1.5 million prescriptions for pain medications. Data were extracted from the WCRI Detailed Benchmark/Evaluation database and consisted of detailed prescription transactions "collected from workers’ compensation payers and their medical bill review and pharmacy benefit management vendors," the report noted.
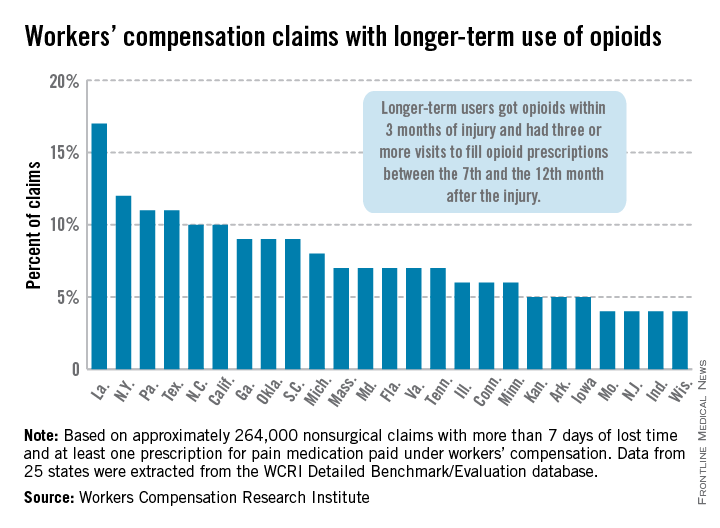
In Louisiana, opioid use lasted more than 6 months in 17% of nonsurgical workers’ compensation claims involving employees who received at least one prescription for pain medication, the Workers Compensation Research Institute reported.
In cases with more than 7 days of lost time, that was the highest rate seen among the 25 states in the study, with New York second at 12% and Pennsylvania and Texas tied for third at 11%. There were four states tied for the lowest rate, at 4%: Missouri, New Jersey, Indiana, and Wisconsin, according to the WCRI report.
Overall, use of narcotics for pain relief by injured workers in such cases ranged from 60% in New Jersey to 88% in Arkansas (median, 76%), while use of any pain medication ranged from 85% in Minnesota to 95% in Florida, Georgia, Tennessee, and Texas (median, 94%), the report showed.
The study involved claims with injuries that occurred from Oct. 1, 2009, through Sept. 30, 2010, with prescriptions filled through March 31, 2012. Longer-term users received a prescription for opioids within 3 months of their injury and had three or more visits to fill opioid prescriptions between the 7th and the 12th month after the injury.
The 25 states in the study "represent more than 70% of the workers’ compensation benefits paid in the United States," the WCRI noted.
The study was based on approximately 264,000 nonsurgical claims and more than 1.5 million prescriptions for pain medications. Data were extracted from the WCRI Detailed Benchmark/Evaluation database and consisted of detailed prescription transactions "collected from workers’ compensation payers and their medical bill review and pharmacy benefit management vendors," the report noted.
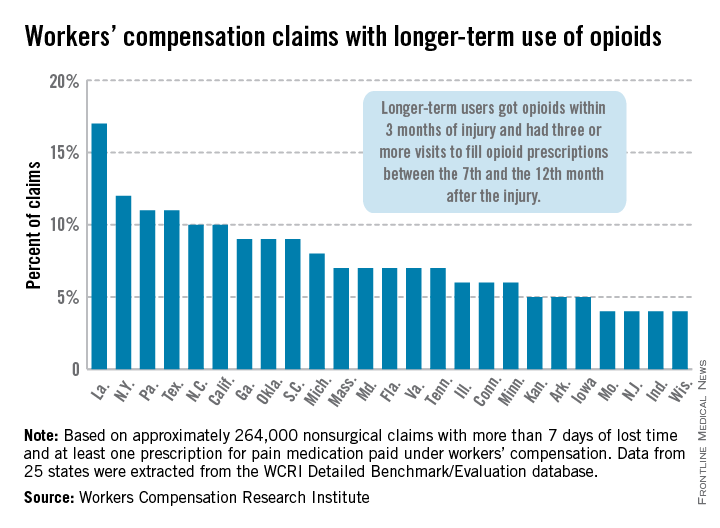
In Louisiana, opioid use lasted more than 6 months in 17% of nonsurgical workers’ compensation claims involving employees who received at least one prescription for pain medication, the Workers Compensation Research Institute reported.
In cases with more than 7 days of lost time, that was the highest rate seen among the 25 states in the study, with New York second at 12% and Pennsylvania and Texas tied for third at 11%. There were four states tied for the lowest rate, at 4%: Missouri, New Jersey, Indiana, and Wisconsin, according to the WCRI report.
Overall, use of narcotics for pain relief by injured workers in such cases ranged from 60% in New Jersey to 88% in Arkansas (median, 76%), while use of any pain medication ranged from 85% in Minnesota to 95% in Florida, Georgia, Tennessee, and Texas (median, 94%), the report showed.
The study involved claims with injuries that occurred from Oct. 1, 2009, through Sept. 30, 2010, with prescriptions filled through March 31, 2012. Longer-term users received a prescription for opioids within 3 months of their injury and had three or more visits to fill opioid prescriptions between the 7th and the 12th month after the injury.
The 25 states in the study "represent more than 70% of the workers’ compensation benefits paid in the United States," the WCRI noted.
The study was based on approximately 264,000 nonsurgical claims and more than 1.5 million prescriptions for pain medications. Data were extracted from the WCRI Detailed Benchmark/Evaluation database and consisted of detailed prescription transactions "collected from workers’ compensation payers and their medical bill review and pharmacy benefit management vendors," the report noted.
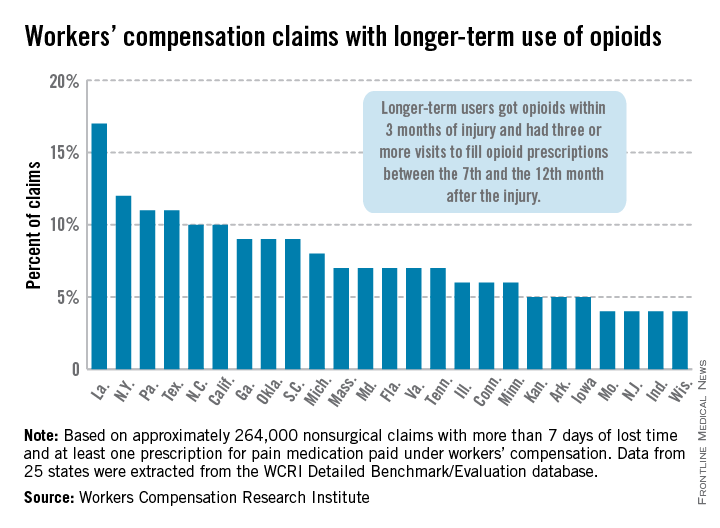
Management of Papillary Thyroid Cancer: An Overview for the Primary Care Physician
From the Yale School of Medicine, New Haven, CT.
ABSTRACT
• Objective: To review management of papillary thyroid cancer.
• Methods: Review of the literature.
• Results: Papillary thyroid cancer is the most common endocrine malignancy. The standard treatment for papillary thyroid cancer is thyroidectomy. Adjuvant therapy includes lifelong thyroid-stimulating hormone suppression and radioiodine therapy. Local recurrence is common and is normally treated with surgery and/or radioiodine. Metastatic radioiodine-resistant disease is a more infrequent event.
• Conclusion: The incidence of papillary thyroid cancer is rapidly increasing. Surgery remains the cornerstone of treatment.
Papillary thyroid cancer is the most common endocrine malignancy and accounts for the majority of cancers of the thyroid. The incidence of papillary thyroid cancer is rapidly increasing [1]. Although increasing detection has been proposed as a possible factor [2], some studies reject this hypothesis, reporting increase in the incidence of larger tumors [3]. Papillary thyroid cancer is characterized by a low mortality but a high recurrence rate [1], posing challenges not only to the endocrinologist and oncologist but also to the general practitioner.
The most frequent presentation of papillary thyroid cancer is a palpable thyroid nodule, cervical lymphadenopathy, or incidental detection on imaging. Locally advanced disease can present with hoarseness or voice alteration. Common risks factors include history of radiation exposure during childhood (the most important risk factor), thyroid cancer in a first-degree relative, family history of a thyroid cancer syndrome (such as Werner syndrome, Cowden syndrome, Carney complex, or familial polyposis), and female sex (2.5:1). Thyroid nodules in the context of an autoimmune thyroiditis may have a higher risk of malignancy [4].
CASE STUDY
Initial Presentation
A 49-year-old man with no significant past medical history presents with a painless mass in the anterior part of his neck.
History, Physical Examination, and Initial Investigations
He has no other symptoms, no weight changes, no history of radiation exposure to the neck, and no family history of malignancy. Physical exam shows a mass in the left thyroid lobe. There is no evidence of cardiac arrhythmias, tremors, or ophthalmologic abnormalities. Thyroid-stimulating hormone (TSH) level is 2.8 mIU/L (normal range, 0.4–4.5 mIU/L) and free thyroxine (T4) level is 1.1 ng/dL (normal range, 0.8–1.5 ng/dL). An ultrasound scan of the neck shows enlargement of the left lobe of thyroid gland, containing multiple complex lesions, the largest measuring 2 x 3 cm, with calcification as well as 3 enlarged lymph nodes in the left level IV. Fine-needle aspiration of the thyroid mass is positive for papillary carcinoma.
• What is the approach to the initial evaluation of a thyroid nodule?
Initial diagnostic evaluation includes history, physical examination, and TSH measurement; nonfunctioning nodules, associated with normal or high values of TSH, carry a higher risk of malignancy [5]. Cervical ultrasound should be performed in all patients with nodules. Fine-needle aspiration (FNA) should be used to evaluate nonfunctioning nodules > 1 cm or subcentimeter nodules with suspicious ultrasound features or if the patient has major risk factors (history of ionizing radiation exposure, external beam radiation exposure, family or personal history of papillary thyroid cancer, or FDG-PET [fluorinated glucose positron emission tomography]–positive thyroid nodules). Scintigraphy can be used to evaluate the need for ultrasound and FNA in patients with low TSH values [6,7]; hyperfunctioning nodules are at low risk for malignancy and do not require biopsy.
• What is initial treatment of papillary thyroid cancer?
Surgery is the primary treatment for papillary thyroid cancer. Unlike for many cancers, surgical removal of the primary tumor is indicated even in the presence of metastatic disease [8]. Total or near-total thyroidectomy is used to treat patients with tumors > 1 cm or with tumors < 1 cm and associated risk factors (eg, contralateral nodules, affected lymph nodes, metastasis, history of radiation, first-degree family history of papillary thyroid cancer, or age > 45 years) [6]. There is a lower risk of recurrence in patients treated with total thyroidectomy versus lobectomy in papillary thyroid cancer [9,10]. Thyroid lobectomy may be used in small (< 1 cm) unifocal tumors without the presence of the associated risk factors listed above.
Patients with central or lateral neck lymph node involvement should also undergo central-compartment (level VI) neck dissection. Therapeutic lateral neck compartmental lymph node dissection is recommended in patients with biopsy-proven metastatic lateral cervical adenopathy [6,7]. The role of unilateral or bilateral prophylactic central-compartment nodal dissection (PCND), that is, lymph node dissection in the level VI compartment of neck in patients without evidence of lymphadenopathy, is controversial. The data for the possible benefit of PCND are inconclusive [11] although the ATA recommends the procedure for locally invasive T3 and T4 tumors [6].
The American Thyroid Association (ATA) and National Comprehensive Cancer Network (NCCN) guidelines [6,7] recommend a preoperative cervical ultrasound in patients with biopsy-proven papillary thyroid cancer to evaluate the presence of disease in the cervical lymph nodes, especially in the lateral and central compartments, and in the contralateral thyroid lobe. If suspicious lymph nodes are found, FNA confirmation is necessary only if this would change management. Systematic use of other preoperative imaging studies, such as CT or MRI, is not recommended [6,7].
Surgical Treatment
The patient underwent a total thyroidectomy with bilateral central neck dissection and selective supraclavicular left-sided lateral neck dissection. Lymph nodes on both sides of the neck (paratracheal nodes) as well as the left supraclavicular nodes were removed. Pathology showed multifocal papillary cancer with extracapsular extension to the paratracheal soft tissue, 14/14 lymph nodes affected, stage IVA T4N1bM0.
• How is papillary thyroid cancer staged?
• How should this patient be treated after surgery? Is any adjuvant therapy indicated?
TSH Suppression
In an effort to reduce risk of recurrence, patients should receive lifelong suppression of TSH using supraphysiologic doses of levothyroxine after total thyroidectomy. This is based upon the hypothesis that TSH is a growth factor for thyroid cancer cells [12,13]. Although a meta-analysis [14] supports the efficacy of TSH suppression therapy, some authors have questioned its widespread use, especially in light of the adverse effects of its use over the long term [15]. Many support its use only in high-risk patients [16], arguing that there is no evidence of benefit for low-risk patients [17]. This view is reflected in the ATA guidelines, which recommend TSH suppression below 0.1 mU/L for high-risk and intermediate-risk patients, while normal or slightly below normal TSH levels are recommended for low-risk patients [6].
Adverse effects of TSH suppression therapy are derived from the induced mild thyrotoxicosis, including cardiovascular and skeletal manifestations. Notably, elderly patients have a higher risk of cardiovascular side effects [18] such as atrial fibrillation, diastolic dysfunction, tachyarrhythmias, increased heart rate or increased left ventricular mass. Likewise, postmenopausal women are most susceptible for skeletal effects such as decreased mineral bone density and fractures [19].
Radioiodine Ablative Therapy
Radioactive iodine (RAI or radioiodine) therapy is based on the capacity of thyroid tissue to take up and retain iodine, specifically, radioiodine. This capacity is present but reduced in papillary and follicular cancer cells.
Radioiodine remnant ablation is performed after surgery, acting as adjuvant therapy by destroying remnant pathological or normal thyroid tissue. The destruction of normal thyroid tissue is useful as it increases the reliability of thyroglobulin testing and radioiodine scanning in the detection of recurrent or metastatic disease. Moreover, remnant ablation has been shown to prevent new thyroid neoplasias in high-risk patients (ie, those with history of radiation exposure). Radioiodine ablative therapy has been shown to reduce recurrence and cause-specific mortality [20] in certain subgroups; however, patients with low mortality risk do not seem to benefit from this therapy [21,22]. Its use is recommended in patients with distant metastases, tumors > 4 cm, or with extrathyroidal extension. It is also recommended for selected patients with tumors 1–4 cm who have high-risk features (such as lymph node involvement, history of radiation, or others previously mentioned) when there is an intermediate to high risk of recurrence or death from thyroid cancer [6]. Lymph node involvement can occur in up to 50% of cases [39] and normally responds to radioiodine therapy.
Since TSH increases radioiodine uptake by normal or pathological thyroid cells, TSH stimulation is required for radioiodine therapy. This can be done by endogenous TSH elevation or by recombinant human TSH (rhTSH). The former can be achieved by either stopping thyroxine 2 to 3 weeks prior to the remnant ablation, or by withdrawing thyroxine and switching to liothyronine for 2 to 3 weeks followed by a discontinuation of liothyronine for 2 weeks. Both approaches seem to produce the same incidence of hypothyroid symptoms [23]. Thyroxine therapy can be resumed 2 to 3 days after radioiodine ablative therapy. Recombinant human TSH can be used with equal efficacy in place of thyroxine withdrawal [24], with the advantage of not producing transitory hypothyroidism. It is especially recommended for patients who are unable to tolerate hypothyroidism or who cannot achieve an adequate TSH level. Short-term recurrence rates are similar in patients treated with rhTSH or thyroxine withdrawal [25].
In addition, a low-iodine diet for 1 or 2 weeks is recommended for patients undergoing radioiodine remnant ablation. The rationale is that a high-iodine diet or iodine exposure (ie, amiodarone treatment or intravenous contrast) can decrease radioiodine uptake by papillary cancer cells due to further dilution of radioactive iodine in an expanded endogenous non-radioactive iodine pool. Patients with suspected high iodine levels can be screened using spot urinary levels [26].
Commonly, a diagnostic scan using low activities of iodine-131 is performed prior to radioablation to avoid the controversial “stunning effect” [27] from any exposure to sublethal radiation in a diagnostic dose. In stunning, the diagnostic RAI dose decreases uptake of a subsequent therapeutic dose. Alternatively, we use [I-123] radioiodine at very low dose (1.4 mCi) in pre-ablation patients. Uptake in the thyroid bed occurs in 75% to 100% of patients, commonly due to remnant normal thyroid tissue [28].
The typical activity used for RAI ablative therapy is 30–100 mCi. The administration of high activities (150–200 mCi) of [I-131] radioiodine has been used to treat recurrent or metastatic disease. This treatment can be very effective, especially in young patients [29].
Side Effects and Contraindications
Common side effects of radioiodine treatment include sialadenitis, radiation thyroiditis, tumor hemorrhage or edema, nausea, transient oligospermia or amenorrhea and nasolacrimal duct obstruction. Moreover, patients treated with radioiodine have a modest increased risk of developing other malignancies [30].
[I-131]Radioiodine must be avoided in pregnancy and in breastfeeding [31]. Indeed, breast tissue has a strong tendency to uptake iodine so breastfeeding should be stopped 5 to 8 weeks before radioiodine treatment, otherwise it can lead to a false-positive radioiodine scan in the chest [32], or worse, deliver radioiodine to the baby with detrimental effects and potential ablation to the baby’s thyroid gland.
Patients treated with radioiodine are advised to drink abundant water after the treatment in order to increase its renal elimination. If no stool elimination occurs in 14 to 24 hours, laxatives may be indicated to eliminate radioiodine from the gastrointestinal track. In addition, patients are advised to avoid sexual contact, avoid sharing bed, utensils, towels, toothbrushes, razors, and avoid public transportation and public places among other measures to avoid exposing the population to radiation [33]. The duration of this restriction depends on the dose administered.
Adjuvant Treatment in this Patient
As the patient was at high risk for recurrence, he received TSH suppression therapy to levels < 0.1 mIU/L. He was referred to nuclear medicine for I-131 treatment. However, at 3 months following thyroidectomy, thyroglobulin measurement showed an elevation (40.5 ng/mL). Ultrasound showed enlarged lymph nodes at level II at the right and at level II at the left. A FNA of left neck node was positive for papillary thyroid cancer.
• How should the patient be treated now?
Treatment of Locoregional Metastatic Disease
The best treatment for residual disease or local recurrences is surgery. ATA guidelines recommend compartmental lateral and/or central neck dissection for patients with persistent or recurrent disease confined to the neck [6]. Radioiodine can be an alternative when recurrent disease is not visible on imaging. Other treatments that can be used for local recurrences or isolated metastases when surgery is not possible are radiofrequency ablation [34], chemo-embolization [35], or ethanol ablation [36]. External beam radiotherapy, which is discussed later, could also be used in selected cases.
Further Treatment
The patient underwent a bilateral modified radical neck dissection followed by adjunctive radioiodine therapy. His initial radioiodine scan showed mild uptake in the neck at the site of his prior surgery. He received treatment with 215 mCi, then 6 months later he was treated with 250 mCi, as his scan showed continued mild uptake. Eleven months later his radioiodine scan showed no uptake and thyroglobulin levels remained stable at 14.4 ng/mL.
One year later, in a follow-up blood analysis he was found to have an elevated thyroglobulin level (90.4 ng/mL). A PET/CT scan showed multiple bone metastases. A neck ultrasound revealed enlarged lymph nodes in the right thyroid bed.
• How common is radioiodine-refractory thyroid cancer?
Radioiodine-refractory thyroid cancer in patients with progression of disease despite radioiodine therapy, or with non-radioiodine-avid lesions [37], is uncommon. It has a poor prognosis with a median survival of 3 to 6 years after diagnosis. It is more frequent in older patients. These lesions are often hypermetabolic and hence [F-18]FDG-avid [38], with a worse prognosis. In one study of patients with metastatic differentiated thyroid cancer, the 10-year overall survival rate was 56% in patients with radioiodine-avid lesions but only 10% in patients with non-radioiodine-avid lesions [38].
• Is the bone a common place for metastasis? Where else should we expect to find a lesion?
Metastatic Pattern
The most common sites for distant metastasis of papillary thyroid cancer are the lungs and the bone. The 10-year survival rate of papillary thyroid cancer patients with lung metastases is between 30% and 50% [38,39]; the prog-nosis is better in patients < 45 years and with radiodine uptake [40]; indeed, patients with pulmonary metastasis seen only in 131-I scans and not on CT or chest x-ray have a longer survival [41]. Pulmonary metastasis can be treated with radioiodine if they are radioiodine-avid. With this treatment complete remission is possible, although it is extremely difficult to achieve in macronodular metastasis.
Bones are the second most common place for distant metastases. Bone metastases seem to have a worse response to treatment with an unfavorable prognosis [42]. Pamidronate (a biphosphonate) and denosumab (a RANK ligand inhibitor) have been used to prevent skeletal related events, including pathologic fractures and cord compression, in bone metastases from other cancers such as breast and prostate, and may also be useful in thyroid cancer, although this has not yet been studied [43,44]. Moreover, surgical resection of isolated bone metastasis seems to improve survival [45].
Skin, liver, and brain metastasis, although uncommon, can also occur. There are also reported rare cases of metastasis in the breast, parotid, larynx, pharynx, adrenal glands, pituitary, kidney, liver, orbit, the sphenoid sinus, choroid plexus, pancreas, and skeletal muscles [46].
• Which treatments can we offer to a patient with metastatic disease refractory to radioiodine?
Chemotherapy and Treatment of Radioiodine-Resistant Disease
Therapeutic options for patients with metastatic papillary thyroid cancer resistant to radioiodine and TSH suppression are limited. Cytotoxic drugs do not play a major role in the treatment of refractory metastatic papillary thyroid cancer, and new research is mainly focused on tyrosine kinase inhibitors (TKIs) with a considerable number of clinical trials either completed or ongoing.
Tyrosine kinases are enzymes that transfer phosphate groups from adenosine triphosphate to proteins. In tumor cells their signaling paths promote proliferation, avoidance of apoptosis, invasion, angiogenesis, and metastasis. TKIs are small molecules that are able to inhibit tyrosine kinase function even at very low intracellullar concentrations. Some of them inhibit various tyrosine kinases and are known as multi-kinase inhibitors (MKIs).
Sorafenib
Sorafenib (400 mg twice daily) is an oral MKI that targets RAF, platelet-derived growth factor receptor, vascular endothelial growth factor receptors 2 and 3, RET and c-Kit [47]. It was approved in November 2013 for patients with radioiodine-refractory differentiated thyroid cancer [48]. Three phase II studies had previously evaluated sorafenib in papillary thyroid cancer, showing a partial response in 15% to 31% of patients and a progression-free survival up to 79 weeks [49–51]. Common adverse effects included weight loss, fatigue, rash, hypertension and the main dose-limiting toxicity—a hand-foot syndrome consisting of swelling, reddening, numbness, and desquamation on palms and soles [52].
Approval of the drug was based on the DECISION trial [52]. A total of 417 patients were randomized (207 to sorafenib and 210 to placebo), of which 57% had papillary thyroid cancer. The primary endpoint of progression-free survival (PFS) was significantly higher in the sorafenib arm, (median, 10.8 months) compared with placebo (median, 5.8 months) (hazard ratio [HR] 0.58, 95% confidence interval [CI] 0.45–0.75, P < 0.001). Median overall survival had not been reached in either arm [52]. The PFS of 5.8 months in the placebo arm confirmed that the group of patients in this study had a rapidly progressing disease, unlike the majority of patients with RAI-sensitive disease.
Selumetinib
Radioiodine re-sensitization was addressed in a study using selumitinib, an inhibitor of mitogen-activated protein kinase kinase (MAPK kinase or MEK). Preclinical models had shown that radioiodine-refractory tumors exposed to inhibitors of this enzyme were able to uptake radioiodine again. Twenty patients with radioiodine-refractory thyroid cancers were treated with selumetinib for 4 weeks and 12 showed increased radioiodine uptake following the treatment. Furthermore, 8 of these patients went on to show responses clinically to retreatment with radioiodine [53].Further studies with this agent will be needed to determine its place in treating patients with differentiated thyroid cancer.
External Beam Radiotherapy and Local Treatment for Metastases
The role of external beam radiotherapy in papillary thyroid cancer is mainly for symptom management. Local radiation can be used in patients with refractory metastatic disease or in lesions that do not uptake radioiodine. Examples include painful bone metastasis or brain metastasis that cannot be treated with surgery. In addition, radiofrequency ablation, chemo-embolization, or ethanol ablation can be used in certain patients.
Sequence of Treatments
In the setting of symptomatic metastatic, radioiodine-resistant disease, we prefer to use a TKI, normally sorafenib, as a first-line treatment. For second-line treatments, enrollment in a clinical trial is an option. Over 70% of patients with metastatic papillary thyroid cancer have mutations of the enzyme BRAF kinase. Vemurafenib is an inhibitor of this enzyme and appears to have some activity in patients with RAI-refractory thyroid cancer in early clinical trials [54–58]. Other TKIs such as sunitinib can also be used. Doxorubicin is only used in cases when a patient is not eligible for a trial and the off-label use of another TKI is contraindicated.
Further Treatment in this Patient
The patient received a trial of sorafenib. He showed disease stabilization that lasted 5 months. The treatment was stopped due to adverse effects (loss of weight and vomiting) and progression of the disease. He was then enrolled in a trial of vemurafenib. He stopped treatment because of adverse events related to the medication and currently has stable disease.
Summary
Papillary thyroid cancer is the most common endocrine malignancy. It is characterized by low mortality but high recurrence rate and can have a considerable impact on quality of life. Any anterior neck nodule, especially in a patient with a history of neck irradiation, should raise concern for this disease. Surgery remains the cornerstone of treatment. Adjuvant therapy includes lifelong TSH suppression and radioiodine therapy. Local recurrence is common and is normally treated with surgery and/or radioiodine. Metastatic radioiodine-resistant disease is a more infrequent event. Thyroid cancer has a tendency to metastasize to the bones and lungs. Metastatic radioiodine-resistant disease is often treated with TKIs such as sorafenib. Enrollment in clinical trials is recommended as second-line therapy in radioiodine-resistant metastatic disease.
Corresponding author: Hari A. Deshpande, MD, Yale Cancer Center, FMP 124, 333 Cedar St., New Haven, CT 06520, [email protected]
Financial disclosures: Dr. Deshpande reports that he is on the advisory board of Bayer/Onyx.
Author contributions: conception and design, PT, EHH, GGC, HAD; drafting of article, PT, EHH, GGC, HAD; critical revision of the article, EHH, GGC, HAD.
REFERENCES
1. Howlader N, Noone AM, Krapcho M, et al (eds). SEER Cancer Statistics Review, 1975-2010, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2010.
2. Katoh R, Sasaki J, Kurihara H, et al. Multiple thyroid involvement (intraglandular metastasis) in papillary thyroid carcinoma: a clinicopathologic study of 105 consecutive patients. Cancer 1992;70:1585–90.
3. Morris LG, Myssiorek D. Improved detection does not fully explain the rising incidence of well-differentiated thyroid cancer: a population-based analysis. Am J Surg 2010;200:454–61.
4. Fiore E, Rago T, Latrofa F, et al. Hashimoto’s thyroiditis is associated with papillary thyroid carcinoma: role of TSH and of treatment with Lthyroxine. Endocr Relat Cancer 2011;18:429–37.
5. Haymart MR, Repplinger DJ, Leverson GE, et al. Higher serum thyroid stimulating hormone level in thyroid nodule patients is associated with greater risks of differentiated thyroid cancer and advanced tumor stage. J Clin Endocrinol Metab 2008;93:809–14.
6. Cooper DS, Doherty GM, Haugen BR, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167–214.
7. National Comprehensive Cancer Network guidelines. Available at www.nccn.org/professionals/physician_gls/pdf/thyroid. pdf.
8. Stephenson BM, Wheeler MH, Clark OH. The role of total thyroidectomy in the management of differentiated thyroid cancer. Curr Opin Gen Surg 1994 53–9.
9. Bilimoria KY, Bentrem DJ, Ko CY, et al. Extent of surgery affects survival for papillary thyroid cancer. Ann Surg 2007;246:375–81.
10. Hay ID, Grant CS, Bergstralh EJ, et al. Unilateral total lobectomy: is it sufficient surgical treatment for patients with AMES low-risk papillary thyroid carcinoma? Surgery 1998;124:958–64.
11. McLeod DS, Sawka AM, Cooper DS. Controversies in primarytreatment of low-risk papillary thyroid cancer. Lancet 2013;381:1046–57.
12. Brabant G. 2008 Thyrotropin suppressive therapy in thyroid carcinoma: what are the targets? J Clin Endocrinol Metab 2008;93:1167–9.
13. Kim HK, Yoon JH, Kim SJ, Cho JS. Higher TSH level is a risk factor for differentiated thyroid cancer. Clin Endocrinol (Oxf) 2013;78:472–7.
14. McGriff NJ, Csako G, Gourgiotis L, et al. Effects of thyroid hormone suppression therapy on adverse clinical outcomes in thyroid cancer. Ann Med 2002;34:554–64.
15. Zafón C. TSH-suppressive treatment in differentiated thyroid cancer. A dogma under review. Endocrin Nutr 2012;59:125–30.
16. Cooper DS, Specker B, Ho M, et al. Thyrotropin suppression and disease progression in patients with differentiated thyroid cancer: Results from the National Thyroid Cancer Treatment Cooperative Registry. Thyroid 1998;8:737-44.
17. Jonklaas J, Sarlis NJ, Litofsky D, et al. Outcomes of patients with differentiated thyroid carcinoma following initial therapy. Thyroid 2006;16:1229–42.
18. Sawin CT, Geller A, Wolf PA, et al. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N Engl J Med 1994;33:1249–52.
19. Kung AW, Yeung SS. Prevention of bone loss induced by thyroxine suppressive therapy in postmenopausal women: the effect of calcium and calcitonin. J Clin Endocrinol Metab 1996;81:1232–36.
20. Samaan NA, Schultz PN, Hickey RC, et al. The results of various modalities of treatment of well differentiated thyroid carcinomas: a retrospective review of 1599 patients. J Clin Endocrinol Metab 1992;75:714–20.
21. Sugitani I, Fujimoto Y. Symptomatic versus asymptomatic papillary thyroid microcarcinoma: a retrospective analysis of surgical outcome and prognostic factors. Endocr J 1999;46:209–16.
22. Kim S, Wei JP, Braveman JM, Brams DM. Predictingoutcome and directing therapy for papillary thyroid carcinoma. Arch Surg 2004;139:390–4.
23. Leboeuf R, Perron P, Carpentier AC, et al. L-T3 preparation for whole-body scintigraphy: a randomized-controlled trial. Clin Endocrinol (Oxf ) 2007;67:839–44.
24. Pacini F, Ladenson PW, Schlumberger M, et al. Radioiodine ablation of thyroid remnants after preparation with recombinant human thyrotropin in differentiated thyroid carcinoma: results of an international, randomized, controlled study. J Clin Endocrinol Metab 2006;91:926–32.
25. Tuttle RM, Brokhin M, Omry G, et al. Recombinant human TSH-assisted radioactive iodine remnant ablation achieves short-term clinical recurrence rates similar to those of traditional thyroid hormone withdrawal. J Nucl Med 2008;49:764–70.
26. Pluijmen MJ, Eustatia-Rutten C, Goslings BM, et al. Effects of low-iodide diet on postsurgical radioiodide ablation therapy in patients with differentiated thyroid carcinoma. Clin Endocrinol (Oxf ) 2003;58:428–35.
27. Park HM. Stunned thyroid after high-dose I-131 imaging. Clin Nucl Med 1992; 17:501–2.
28. Salvatori M, Raffaelli M, Castaldi P, et al. Evaluation of the surgical completeness after total thyroidectomy for differentiated thyroid carcinoma. Eur J Surg Oncol 2007;33:648–54.
29. Durante C, Haddy N, Baudin E, et al. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab 2006;91:2892–9.
30. Lang BH, Wong IO, Wong KP, et al. Risk of second primary malignancy in differentiated thyroid carcinoma treated with radioactive iodine therapy. Surgery 2012;151:844–50.
31. Rubow S, Klopper J. Excretion of radioiodine in human milk following a therapeutic dose of I-131. Eur J Nucl Med 1988;14:632–3.
32. Bakheet SM, Hammami MM. Patterns of radioiodine uptake by the lactating breast. Eur J Nucl Med 1994;21:604–8.
33. American Thyroid Association Taskforce on Radioiodine Safety, Sisson JC, Freitas J, et al. Radiation safety in the treatment of patients with thyroid diseases by radioiodine 131I: practice recommendations of the American Thyroid Association. Thyroid 2011;21:335–46.
34. Dupuy DE, Monchik JM, Decrea C, Pisharodi L. Radiofrequency ablation of regional recurrence from welldifferentiated thyroid malignancy. Surgery 2001;130:971–7.
35. Eustatia-Rutten CF, Romijn JA, Guijt MJ, et al. Outcome of palliative embolization of bone metastases in differentiated thyroid carcinoma. J Clin Endocrinol Metab 2003;88:3184–9.
36. Lewis BD, Hay ID, Charboneau JW, et al. Percutaneous ethanol injection for treatment of cervical lymph node metastases in patients with papillary thyroid carcinoma. Am J Roentgenol 2002;178:699–704.
37. Xing MM, Haugen B, Schlumberger M. Progress in molecular based management of differentiated thyroid cancer. Lancet 2013;381:1058–69.
38. Durante C, Haddy N, Baudin E, et al. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab 2006;91:2892–99.
39. Haq M, Harmer C. Differentiated thyroid carcinoma with distant metastases at presentation: prognostic factors and outcome Clin Endoc 2005;63:87–93.
40. Ronga G, Filesi M, Montesano T, et al. Lung metastases from differentiated thyroid carcinoma. A 40 years’ experience. Q J Nucl Med Mol Imaging 2004;48:12–19.
41. Samaan NA, Schultz PN, Haynie TP, Ordonez NG. Pulmonary metastasis of differentiated thyroid carcinoma: treatment results in 101 patients. J Clin Endocrinol Metab 1985;60:376–80.
42. Lang BH, Wong KP, Cheung CY, et al. Evaluating the prognostic factors associated with cancer-specific survival of differentiated thyroid carcinoma presenting with distant metastasis. Ann Surg Oncol 2013;20:1329–35.
43. Hortobagyi GN, Theriault RL, Porter L, et al. Efficacy of pamidronate in reducing skeletal complications in patients with breast cancer and lytic bone metastases. N Engl J Med 1996;335:1785–92.
44. Smith MR, Saad F, Coleman R, et al. Denosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: Results of a phase 3, randomised, placebocontrolled trial. Lancet 379:39–46.
45. Zettinig G, Fueger BJ, Passler C, et al. Long-term follow-up of patients with bone metastases from differentiated thyroid carcinoma—surgery or conventional therapy? Clin Endocrinol (Oxf ) 2002;56:377–82.
46. Song H-J, Xue Y-L, Xu Y-H, et al. Rare metastases of differentiated thyroid carcinoma: pictorial review Endocr Relat Cancer 2011;18:R165–R174.
47. Wilhelm SM, Carter C, Tang L, et al. BAY 43-9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res 2004;64:7099–109.
48. www.fda.gov/NewsEvents/Newsroom/PresAnnouncements/ucm376443.htm.
49. Kloos RT, Ringel MD, Knopp MV et al. Phase II trial of sorafenib in metastatic thyroid cancer. J Clin Oncol 2009;27:1675–84.
50. Gupta-Abramson V, Troxel AB, Nellore A, et al. Phase II trial of sorafenib in advanced thyroid cancer. J Clin Oncol 2008;26:4714–9.
51. Schneider TC, Abdulrahman RM, Corssmit EP, et al. Longterm analysis of the efficacy and tolerability of sorafenib in advanced radio-iodine refractory differentiated thyroid carcinoma: final results of a phase II trial. Eur J Endocrinol 2012;167:643–50.
52. Brose MS, Nutting CM, Jarzab B, et al. Sorafenib in locally advanced or metastatic patients with radioactive iodine refractory differentiated thyroid cancer: The phase III DECISION trial. J Clin Oncol 2013;31(Suppl, abstr 4).
53. Ho AL, Grewal RK, Leboeuf R, et al. Selumetinib-enhanced radioiodine uptake in advanced thyroid cancer. N Engl J Med 2013;368:623–32.
54. Henderson YC, Shellenberger TD, Williams MD, et al. High rate of BRAF and RET/PTC dual mutations associated with recurrent papillary thyroid carcinoma. Clin Cancer Res 2009;15:485–91.
55. Kim TY, Kim WB, Rhee YS, et al. The BRAF mutation is useful for prediction of clinical recurrence in low-risk patients with conventional papillary thyroid carcinoma. Clin Endocrinol (Oxf) 2006;65:364–8.
56. Elisei R, Ugolini C, Viola D, et al. BRAF (V600E) mutation and outcome of patients with papillary thyroid carcinoma: a 15-year median follow-up study. J Clin Endocrinol Metab 2008;93:3943–9.
57. Xing M, Alzahrani AS, Carson KA, et al. Association between BRAFV600E mutation and mortality in patients with papillary thyroid cancer. JAMA 2103;309:1493–501.
58. Kim KB, Cabanillas ME, Lazar AJ, et al. Clinical responses to vemurafenib in patients with metastatic papillary thyroid cancer harboring
From the Yale School of Medicine, New Haven, CT.
ABSTRACT
• Objective: To review management of papillary thyroid cancer.
• Methods: Review of the literature.
• Results: Papillary thyroid cancer is the most common endocrine malignancy. The standard treatment for papillary thyroid cancer is thyroidectomy. Adjuvant therapy includes lifelong thyroid-stimulating hormone suppression and radioiodine therapy. Local recurrence is common and is normally treated with surgery and/or radioiodine. Metastatic radioiodine-resistant disease is a more infrequent event.
• Conclusion: The incidence of papillary thyroid cancer is rapidly increasing. Surgery remains the cornerstone of treatment.
Papillary thyroid cancer is the most common endocrine malignancy and accounts for the majority of cancers of the thyroid. The incidence of papillary thyroid cancer is rapidly increasing [1]. Although increasing detection has been proposed as a possible factor [2], some studies reject this hypothesis, reporting increase in the incidence of larger tumors [3]. Papillary thyroid cancer is characterized by a low mortality but a high recurrence rate [1], posing challenges not only to the endocrinologist and oncologist but also to the general practitioner.
The most frequent presentation of papillary thyroid cancer is a palpable thyroid nodule, cervical lymphadenopathy, or incidental detection on imaging. Locally advanced disease can present with hoarseness or voice alteration. Common risks factors include history of radiation exposure during childhood (the most important risk factor), thyroid cancer in a first-degree relative, family history of a thyroid cancer syndrome (such as Werner syndrome, Cowden syndrome, Carney complex, or familial polyposis), and female sex (2.5:1). Thyroid nodules in the context of an autoimmune thyroiditis may have a higher risk of malignancy [4].
CASE STUDY
Initial Presentation
A 49-year-old man with no significant past medical history presents with a painless mass in the anterior part of his neck.
History, Physical Examination, and Initial Investigations
He has no other symptoms, no weight changes, no history of radiation exposure to the neck, and no family history of malignancy. Physical exam shows a mass in the left thyroid lobe. There is no evidence of cardiac arrhythmias, tremors, or ophthalmologic abnormalities. Thyroid-stimulating hormone (TSH) level is 2.8 mIU/L (normal range, 0.4–4.5 mIU/L) and free thyroxine (T4) level is 1.1 ng/dL (normal range, 0.8–1.5 ng/dL). An ultrasound scan of the neck shows enlargement of the left lobe of thyroid gland, containing multiple complex lesions, the largest measuring 2 x 3 cm, with calcification as well as 3 enlarged lymph nodes in the left level IV. Fine-needle aspiration of the thyroid mass is positive for papillary carcinoma.
• What is the approach to the initial evaluation of a thyroid nodule?
Initial diagnostic evaluation includes history, physical examination, and TSH measurement; nonfunctioning nodules, associated with normal or high values of TSH, carry a higher risk of malignancy [5]. Cervical ultrasound should be performed in all patients with nodules. Fine-needle aspiration (FNA) should be used to evaluate nonfunctioning nodules > 1 cm or subcentimeter nodules with suspicious ultrasound features or if the patient has major risk factors (history of ionizing radiation exposure, external beam radiation exposure, family or personal history of papillary thyroid cancer, or FDG-PET [fluorinated glucose positron emission tomography]–positive thyroid nodules). Scintigraphy can be used to evaluate the need for ultrasound and FNA in patients with low TSH values [6,7]; hyperfunctioning nodules are at low risk for malignancy and do not require biopsy.
• What is initial treatment of papillary thyroid cancer?
Surgery is the primary treatment for papillary thyroid cancer. Unlike for many cancers, surgical removal of the primary tumor is indicated even in the presence of metastatic disease [8]. Total or near-total thyroidectomy is used to treat patients with tumors > 1 cm or with tumors < 1 cm and associated risk factors (eg, contralateral nodules, affected lymph nodes, metastasis, history of radiation, first-degree family history of papillary thyroid cancer, or age > 45 years) [6]. There is a lower risk of recurrence in patients treated with total thyroidectomy versus lobectomy in papillary thyroid cancer [9,10]. Thyroid lobectomy may be used in small (< 1 cm) unifocal tumors without the presence of the associated risk factors listed above.
Patients with central or lateral neck lymph node involvement should also undergo central-compartment (level VI) neck dissection. Therapeutic lateral neck compartmental lymph node dissection is recommended in patients with biopsy-proven metastatic lateral cervical adenopathy [6,7]. The role of unilateral or bilateral prophylactic central-compartment nodal dissection (PCND), that is, lymph node dissection in the level VI compartment of neck in patients without evidence of lymphadenopathy, is controversial. The data for the possible benefit of PCND are inconclusive [11] although the ATA recommends the procedure for locally invasive T3 and T4 tumors [6].
The American Thyroid Association (ATA) and National Comprehensive Cancer Network (NCCN) guidelines [6,7] recommend a preoperative cervical ultrasound in patients with biopsy-proven papillary thyroid cancer to evaluate the presence of disease in the cervical lymph nodes, especially in the lateral and central compartments, and in the contralateral thyroid lobe. If suspicious lymph nodes are found, FNA confirmation is necessary only if this would change management. Systematic use of other preoperative imaging studies, such as CT or MRI, is not recommended [6,7].
Surgical Treatment
The patient underwent a total thyroidectomy with bilateral central neck dissection and selective supraclavicular left-sided lateral neck dissection. Lymph nodes on both sides of the neck (paratracheal nodes) as well as the left supraclavicular nodes were removed. Pathology showed multifocal papillary cancer with extracapsular extension to the paratracheal soft tissue, 14/14 lymph nodes affected, stage IVA T4N1bM0.
• How is papillary thyroid cancer staged?
• How should this patient be treated after surgery? Is any adjuvant therapy indicated?
TSH Suppression
In an effort to reduce risk of recurrence, patients should receive lifelong suppression of TSH using supraphysiologic doses of levothyroxine after total thyroidectomy. This is based upon the hypothesis that TSH is a growth factor for thyroid cancer cells [12,13]. Although a meta-analysis [14] supports the efficacy of TSH suppression therapy, some authors have questioned its widespread use, especially in light of the adverse effects of its use over the long term [15]. Many support its use only in high-risk patients [16], arguing that there is no evidence of benefit for low-risk patients [17]. This view is reflected in the ATA guidelines, which recommend TSH suppression below 0.1 mU/L for high-risk and intermediate-risk patients, while normal or slightly below normal TSH levels are recommended for low-risk patients [6].
Adverse effects of TSH suppression therapy are derived from the induced mild thyrotoxicosis, including cardiovascular and skeletal manifestations. Notably, elderly patients have a higher risk of cardiovascular side effects [18] such as atrial fibrillation, diastolic dysfunction, tachyarrhythmias, increased heart rate or increased left ventricular mass. Likewise, postmenopausal women are most susceptible for skeletal effects such as decreased mineral bone density and fractures [19].
Radioiodine Ablative Therapy
Radioactive iodine (RAI or radioiodine) therapy is based on the capacity of thyroid tissue to take up and retain iodine, specifically, radioiodine. This capacity is present but reduced in papillary and follicular cancer cells.
Radioiodine remnant ablation is performed after surgery, acting as adjuvant therapy by destroying remnant pathological or normal thyroid tissue. The destruction of normal thyroid tissue is useful as it increases the reliability of thyroglobulin testing and radioiodine scanning in the detection of recurrent or metastatic disease. Moreover, remnant ablation has been shown to prevent new thyroid neoplasias in high-risk patients (ie, those with history of radiation exposure). Radioiodine ablative therapy has been shown to reduce recurrence and cause-specific mortality [20] in certain subgroups; however, patients with low mortality risk do not seem to benefit from this therapy [21,22]. Its use is recommended in patients with distant metastases, tumors > 4 cm, or with extrathyroidal extension. It is also recommended for selected patients with tumors 1–4 cm who have high-risk features (such as lymph node involvement, history of radiation, or others previously mentioned) when there is an intermediate to high risk of recurrence or death from thyroid cancer [6]. Lymph node involvement can occur in up to 50% of cases [39] and normally responds to radioiodine therapy.
Since TSH increases radioiodine uptake by normal or pathological thyroid cells, TSH stimulation is required for radioiodine therapy. This can be done by endogenous TSH elevation or by recombinant human TSH (rhTSH). The former can be achieved by either stopping thyroxine 2 to 3 weeks prior to the remnant ablation, or by withdrawing thyroxine and switching to liothyronine for 2 to 3 weeks followed by a discontinuation of liothyronine for 2 weeks. Both approaches seem to produce the same incidence of hypothyroid symptoms [23]. Thyroxine therapy can be resumed 2 to 3 days after radioiodine ablative therapy. Recombinant human TSH can be used with equal efficacy in place of thyroxine withdrawal [24], with the advantage of not producing transitory hypothyroidism. It is especially recommended for patients who are unable to tolerate hypothyroidism or who cannot achieve an adequate TSH level. Short-term recurrence rates are similar in patients treated with rhTSH or thyroxine withdrawal [25].
In addition, a low-iodine diet for 1 or 2 weeks is recommended for patients undergoing radioiodine remnant ablation. The rationale is that a high-iodine diet or iodine exposure (ie, amiodarone treatment or intravenous contrast) can decrease radioiodine uptake by papillary cancer cells due to further dilution of radioactive iodine in an expanded endogenous non-radioactive iodine pool. Patients with suspected high iodine levels can be screened using spot urinary levels [26].
Commonly, a diagnostic scan using low activities of iodine-131 is performed prior to radioablation to avoid the controversial “stunning effect” [27] from any exposure to sublethal radiation in a diagnostic dose. In stunning, the diagnostic RAI dose decreases uptake of a subsequent therapeutic dose. Alternatively, we use [I-123] radioiodine at very low dose (1.4 mCi) in pre-ablation patients. Uptake in the thyroid bed occurs in 75% to 100% of patients, commonly due to remnant normal thyroid tissue [28].
The typical activity used for RAI ablative therapy is 30–100 mCi. The administration of high activities (150–200 mCi) of [I-131] radioiodine has been used to treat recurrent or metastatic disease. This treatment can be very effective, especially in young patients [29].
Side Effects and Contraindications
Common side effects of radioiodine treatment include sialadenitis, radiation thyroiditis, tumor hemorrhage or edema, nausea, transient oligospermia or amenorrhea and nasolacrimal duct obstruction. Moreover, patients treated with radioiodine have a modest increased risk of developing other malignancies [30].
[I-131]Radioiodine must be avoided in pregnancy and in breastfeeding [31]. Indeed, breast tissue has a strong tendency to uptake iodine so breastfeeding should be stopped 5 to 8 weeks before radioiodine treatment, otherwise it can lead to a false-positive radioiodine scan in the chest [32], or worse, deliver radioiodine to the baby with detrimental effects and potential ablation to the baby’s thyroid gland.
Patients treated with radioiodine are advised to drink abundant water after the treatment in order to increase its renal elimination. If no stool elimination occurs in 14 to 24 hours, laxatives may be indicated to eliminate radioiodine from the gastrointestinal track. In addition, patients are advised to avoid sexual contact, avoid sharing bed, utensils, towels, toothbrushes, razors, and avoid public transportation and public places among other measures to avoid exposing the population to radiation [33]. The duration of this restriction depends on the dose administered.
Adjuvant Treatment in this Patient
As the patient was at high risk for recurrence, he received TSH suppression therapy to levels < 0.1 mIU/L. He was referred to nuclear medicine for I-131 treatment. However, at 3 months following thyroidectomy, thyroglobulin measurement showed an elevation (40.5 ng/mL). Ultrasound showed enlarged lymph nodes at level II at the right and at level II at the left. A FNA of left neck node was positive for papillary thyroid cancer.
• How should the patient be treated now?
Treatment of Locoregional Metastatic Disease
The best treatment for residual disease or local recurrences is surgery. ATA guidelines recommend compartmental lateral and/or central neck dissection for patients with persistent or recurrent disease confined to the neck [6]. Radioiodine can be an alternative when recurrent disease is not visible on imaging. Other treatments that can be used for local recurrences or isolated metastases when surgery is not possible are radiofrequency ablation [34], chemo-embolization [35], or ethanol ablation [36]. External beam radiotherapy, which is discussed later, could also be used in selected cases.
Further Treatment
The patient underwent a bilateral modified radical neck dissection followed by adjunctive radioiodine therapy. His initial radioiodine scan showed mild uptake in the neck at the site of his prior surgery. He received treatment with 215 mCi, then 6 months later he was treated with 250 mCi, as his scan showed continued mild uptake. Eleven months later his radioiodine scan showed no uptake and thyroglobulin levels remained stable at 14.4 ng/mL.
One year later, in a follow-up blood analysis he was found to have an elevated thyroglobulin level (90.4 ng/mL). A PET/CT scan showed multiple bone metastases. A neck ultrasound revealed enlarged lymph nodes in the right thyroid bed.
• How common is radioiodine-refractory thyroid cancer?
Radioiodine-refractory thyroid cancer in patients with progression of disease despite radioiodine therapy, or with non-radioiodine-avid lesions [37], is uncommon. It has a poor prognosis with a median survival of 3 to 6 years after diagnosis. It is more frequent in older patients. These lesions are often hypermetabolic and hence [F-18]FDG-avid [38], with a worse prognosis. In one study of patients with metastatic differentiated thyroid cancer, the 10-year overall survival rate was 56% in patients with radioiodine-avid lesions but only 10% in patients with non-radioiodine-avid lesions [38].
• Is the bone a common place for metastasis? Where else should we expect to find a lesion?
Metastatic Pattern
The most common sites for distant metastasis of papillary thyroid cancer are the lungs and the bone. The 10-year survival rate of papillary thyroid cancer patients with lung metastases is between 30% and 50% [38,39]; the prog-nosis is better in patients < 45 years and with radiodine uptake [40]; indeed, patients with pulmonary metastasis seen only in 131-I scans and not on CT or chest x-ray have a longer survival [41]. Pulmonary metastasis can be treated with radioiodine if they are radioiodine-avid. With this treatment complete remission is possible, although it is extremely difficult to achieve in macronodular metastasis.
Bones are the second most common place for distant metastases. Bone metastases seem to have a worse response to treatment with an unfavorable prognosis [42]. Pamidronate (a biphosphonate) and denosumab (a RANK ligand inhibitor) have been used to prevent skeletal related events, including pathologic fractures and cord compression, in bone metastases from other cancers such as breast and prostate, and may also be useful in thyroid cancer, although this has not yet been studied [43,44]. Moreover, surgical resection of isolated bone metastasis seems to improve survival [45].
Skin, liver, and brain metastasis, although uncommon, can also occur. There are also reported rare cases of metastasis in the breast, parotid, larynx, pharynx, adrenal glands, pituitary, kidney, liver, orbit, the sphenoid sinus, choroid plexus, pancreas, and skeletal muscles [46].
• Which treatments can we offer to a patient with metastatic disease refractory to radioiodine?
Chemotherapy and Treatment of Radioiodine-Resistant Disease
Therapeutic options for patients with metastatic papillary thyroid cancer resistant to radioiodine and TSH suppression are limited. Cytotoxic drugs do not play a major role in the treatment of refractory metastatic papillary thyroid cancer, and new research is mainly focused on tyrosine kinase inhibitors (TKIs) with a considerable number of clinical trials either completed or ongoing.
Tyrosine kinases are enzymes that transfer phosphate groups from adenosine triphosphate to proteins. In tumor cells their signaling paths promote proliferation, avoidance of apoptosis, invasion, angiogenesis, and metastasis. TKIs are small molecules that are able to inhibit tyrosine kinase function even at very low intracellullar concentrations. Some of them inhibit various tyrosine kinases and are known as multi-kinase inhibitors (MKIs).
Sorafenib
Sorafenib (400 mg twice daily) is an oral MKI that targets RAF, platelet-derived growth factor receptor, vascular endothelial growth factor receptors 2 and 3, RET and c-Kit [47]. It was approved in November 2013 for patients with radioiodine-refractory differentiated thyroid cancer [48]. Three phase II studies had previously evaluated sorafenib in papillary thyroid cancer, showing a partial response in 15% to 31% of patients and a progression-free survival up to 79 weeks [49–51]. Common adverse effects included weight loss, fatigue, rash, hypertension and the main dose-limiting toxicity—a hand-foot syndrome consisting of swelling, reddening, numbness, and desquamation on palms and soles [52].
Approval of the drug was based on the DECISION trial [52]. A total of 417 patients were randomized (207 to sorafenib and 210 to placebo), of which 57% had papillary thyroid cancer. The primary endpoint of progression-free survival (PFS) was significantly higher in the sorafenib arm, (median, 10.8 months) compared with placebo (median, 5.8 months) (hazard ratio [HR] 0.58, 95% confidence interval [CI] 0.45–0.75, P < 0.001). Median overall survival had not been reached in either arm [52]. The PFS of 5.8 months in the placebo arm confirmed that the group of patients in this study had a rapidly progressing disease, unlike the majority of patients with RAI-sensitive disease.
Selumetinib
Radioiodine re-sensitization was addressed in a study using selumitinib, an inhibitor of mitogen-activated protein kinase kinase (MAPK kinase or MEK). Preclinical models had shown that radioiodine-refractory tumors exposed to inhibitors of this enzyme were able to uptake radioiodine again. Twenty patients with radioiodine-refractory thyroid cancers were treated with selumetinib for 4 weeks and 12 showed increased radioiodine uptake following the treatment. Furthermore, 8 of these patients went on to show responses clinically to retreatment with radioiodine [53].Further studies with this agent will be needed to determine its place in treating patients with differentiated thyroid cancer.
External Beam Radiotherapy and Local Treatment for Metastases
The role of external beam radiotherapy in papillary thyroid cancer is mainly for symptom management. Local radiation can be used in patients with refractory metastatic disease or in lesions that do not uptake radioiodine. Examples include painful bone metastasis or brain metastasis that cannot be treated with surgery. In addition, radiofrequency ablation, chemo-embolization, or ethanol ablation can be used in certain patients.
Sequence of Treatments
In the setting of symptomatic metastatic, radioiodine-resistant disease, we prefer to use a TKI, normally sorafenib, as a first-line treatment. For second-line treatments, enrollment in a clinical trial is an option. Over 70% of patients with metastatic papillary thyroid cancer have mutations of the enzyme BRAF kinase. Vemurafenib is an inhibitor of this enzyme and appears to have some activity in patients with RAI-refractory thyroid cancer in early clinical trials [54–58]. Other TKIs such as sunitinib can also be used. Doxorubicin is only used in cases when a patient is not eligible for a trial and the off-label use of another TKI is contraindicated.
Further Treatment in this Patient
The patient received a trial of sorafenib. He showed disease stabilization that lasted 5 months. The treatment was stopped due to adverse effects (loss of weight and vomiting) and progression of the disease. He was then enrolled in a trial of vemurafenib. He stopped treatment because of adverse events related to the medication and currently has stable disease.
Summary
Papillary thyroid cancer is the most common endocrine malignancy. It is characterized by low mortality but high recurrence rate and can have a considerable impact on quality of life. Any anterior neck nodule, especially in a patient with a history of neck irradiation, should raise concern for this disease. Surgery remains the cornerstone of treatment. Adjuvant therapy includes lifelong TSH suppression and radioiodine therapy. Local recurrence is common and is normally treated with surgery and/or radioiodine. Metastatic radioiodine-resistant disease is a more infrequent event. Thyroid cancer has a tendency to metastasize to the bones and lungs. Metastatic radioiodine-resistant disease is often treated with TKIs such as sorafenib. Enrollment in clinical trials is recommended as second-line therapy in radioiodine-resistant metastatic disease.
Corresponding author: Hari A. Deshpande, MD, Yale Cancer Center, FMP 124, 333 Cedar St., New Haven, CT 06520, [email protected]
Financial disclosures: Dr. Deshpande reports that he is on the advisory board of Bayer/Onyx.
Author contributions: conception and design, PT, EHH, GGC, HAD; drafting of article, PT, EHH, GGC, HAD; critical revision of the article, EHH, GGC, HAD.
REFERENCES
1. Howlader N, Noone AM, Krapcho M, et al (eds). SEER Cancer Statistics Review, 1975-2010, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2010.
2. Katoh R, Sasaki J, Kurihara H, et al. Multiple thyroid involvement (intraglandular metastasis) in papillary thyroid carcinoma: a clinicopathologic study of 105 consecutive patients. Cancer 1992;70:1585–90.
3. Morris LG, Myssiorek D. Improved detection does not fully explain the rising incidence of well-differentiated thyroid cancer: a population-based analysis. Am J Surg 2010;200:454–61.
4. Fiore E, Rago T, Latrofa F, et al. Hashimoto’s thyroiditis is associated with papillary thyroid carcinoma: role of TSH and of treatment with Lthyroxine. Endocr Relat Cancer 2011;18:429–37.
5. Haymart MR, Repplinger DJ, Leverson GE, et al. Higher serum thyroid stimulating hormone level in thyroid nodule patients is associated with greater risks of differentiated thyroid cancer and advanced tumor stage. J Clin Endocrinol Metab 2008;93:809–14.
6. Cooper DS, Doherty GM, Haugen BR, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167–214.
7. National Comprehensive Cancer Network guidelines. Available at www.nccn.org/professionals/physician_gls/pdf/thyroid. pdf.
8. Stephenson BM, Wheeler MH, Clark OH. The role of total thyroidectomy in the management of differentiated thyroid cancer. Curr Opin Gen Surg 1994 53–9.
9. Bilimoria KY, Bentrem DJ, Ko CY, et al. Extent of surgery affects survival for papillary thyroid cancer. Ann Surg 2007;246:375–81.
10. Hay ID, Grant CS, Bergstralh EJ, et al. Unilateral total lobectomy: is it sufficient surgical treatment for patients with AMES low-risk papillary thyroid carcinoma? Surgery 1998;124:958–64.
11. McLeod DS, Sawka AM, Cooper DS. Controversies in primarytreatment of low-risk papillary thyroid cancer. Lancet 2013;381:1046–57.
12. Brabant G. 2008 Thyrotropin suppressive therapy in thyroid carcinoma: what are the targets? J Clin Endocrinol Metab 2008;93:1167–9.
13. Kim HK, Yoon JH, Kim SJ, Cho JS. Higher TSH level is a risk factor for differentiated thyroid cancer. Clin Endocrinol (Oxf) 2013;78:472–7.
14. McGriff NJ, Csako G, Gourgiotis L, et al. Effects of thyroid hormone suppression therapy on adverse clinical outcomes in thyroid cancer. Ann Med 2002;34:554–64.
15. Zafón C. TSH-suppressive treatment in differentiated thyroid cancer. A dogma under review. Endocrin Nutr 2012;59:125–30.
16. Cooper DS, Specker B, Ho M, et al. Thyrotropin suppression and disease progression in patients with differentiated thyroid cancer: Results from the National Thyroid Cancer Treatment Cooperative Registry. Thyroid 1998;8:737-44.
17. Jonklaas J, Sarlis NJ, Litofsky D, et al. Outcomes of patients with differentiated thyroid carcinoma following initial therapy. Thyroid 2006;16:1229–42.
18. Sawin CT, Geller A, Wolf PA, et al. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N Engl J Med 1994;33:1249–52.
19. Kung AW, Yeung SS. Prevention of bone loss induced by thyroxine suppressive therapy in postmenopausal women: the effect of calcium and calcitonin. J Clin Endocrinol Metab 1996;81:1232–36.
20. Samaan NA, Schultz PN, Hickey RC, et al. The results of various modalities of treatment of well differentiated thyroid carcinomas: a retrospective review of 1599 patients. J Clin Endocrinol Metab 1992;75:714–20.
21. Sugitani I, Fujimoto Y. Symptomatic versus asymptomatic papillary thyroid microcarcinoma: a retrospective analysis of surgical outcome and prognostic factors. Endocr J 1999;46:209–16.
22. Kim S, Wei JP, Braveman JM, Brams DM. Predictingoutcome and directing therapy for papillary thyroid carcinoma. Arch Surg 2004;139:390–4.
23. Leboeuf R, Perron P, Carpentier AC, et al. L-T3 preparation for whole-body scintigraphy: a randomized-controlled trial. Clin Endocrinol (Oxf ) 2007;67:839–44.
24. Pacini F, Ladenson PW, Schlumberger M, et al. Radioiodine ablation of thyroid remnants after preparation with recombinant human thyrotropin in differentiated thyroid carcinoma: results of an international, randomized, controlled study. J Clin Endocrinol Metab 2006;91:926–32.
25. Tuttle RM, Brokhin M, Omry G, et al. Recombinant human TSH-assisted radioactive iodine remnant ablation achieves short-term clinical recurrence rates similar to those of traditional thyroid hormone withdrawal. J Nucl Med 2008;49:764–70.
26. Pluijmen MJ, Eustatia-Rutten C, Goslings BM, et al. Effects of low-iodide diet on postsurgical radioiodide ablation therapy in patients with differentiated thyroid carcinoma. Clin Endocrinol (Oxf ) 2003;58:428–35.
27. Park HM. Stunned thyroid after high-dose I-131 imaging. Clin Nucl Med 1992; 17:501–2.
28. Salvatori M, Raffaelli M, Castaldi P, et al. Evaluation of the surgical completeness after total thyroidectomy for differentiated thyroid carcinoma. Eur J Surg Oncol 2007;33:648–54.
29. Durante C, Haddy N, Baudin E, et al. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab 2006;91:2892–9.
30. Lang BH, Wong IO, Wong KP, et al. Risk of second primary malignancy in differentiated thyroid carcinoma treated with radioactive iodine therapy. Surgery 2012;151:844–50.
31. Rubow S, Klopper J. Excretion of radioiodine in human milk following a therapeutic dose of I-131. Eur J Nucl Med 1988;14:632–3.
32. Bakheet SM, Hammami MM. Patterns of radioiodine uptake by the lactating breast. Eur J Nucl Med 1994;21:604–8.
33. American Thyroid Association Taskforce on Radioiodine Safety, Sisson JC, Freitas J, et al. Radiation safety in the treatment of patients with thyroid diseases by radioiodine 131I: practice recommendations of the American Thyroid Association. Thyroid 2011;21:335–46.
34. Dupuy DE, Monchik JM, Decrea C, Pisharodi L. Radiofrequency ablation of regional recurrence from welldifferentiated thyroid malignancy. Surgery 2001;130:971–7.
35. Eustatia-Rutten CF, Romijn JA, Guijt MJ, et al. Outcome of palliative embolization of bone metastases in differentiated thyroid carcinoma. J Clin Endocrinol Metab 2003;88:3184–9.
36. Lewis BD, Hay ID, Charboneau JW, et al. Percutaneous ethanol injection for treatment of cervical lymph node metastases in patients with papillary thyroid carcinoma. Am J Roentgenol 2002;178:699–704.
37. Xing MM, Haugen B, Schlumberger M. Progress in molecular based management of differentiated thyroid cancer. Lancet 2013;381:1058–69.
38. Durante C, Haddy N, Baudin E, et al. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab 2006;91:2892–99.
39. Haq M, Harmer C. Differentiated thyroid carcinoma with distant metastases at presentation: prognostic factors and outcome Clin Endoc 2005;63:87–93.
40. Ronga G, Filesi M, Montesano T, et al. Lung metastases from differentiated thyroid carcinoma. A 40 years’ experience. Q J Nucl Med Mol Imaging 2004;48:12–19.
41. Samaan NA, Schultz PN, Haynie TP, Ordonez NG. Pulmonary metastasis of differentiated thyroid carcinoma: treatment results in 101 patients. J Clin Endocrinol Metab 1985;60:376–80.
42. Lang BH, Wong KP, Cheung CY, et al. Evaluating the prognostic factors associated with cancer-specific survival of differentiated thyroid carcinoma presenting with distant metastasis. Ann Surg Oncol 2013;20:1329–35.
43. Hortobagyi GN, Theriault RL, Porter L, et al. Efficacy of pamidronate in reducing skeletal complications in patients with breast cancer and lytic bone metastases. N Engl J Med 1996;335:1785–92.
44. Smith MR, Saad F, Coleman R, et al. Denosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: Results of a phase 3, randomised, placebocontrolled trial. Lancet 379:39–46.
45. Zettinig G, Fueger BJ, Passler C, et al. Long-term follow-up of patients with bone metastases from differentiated thyroid carcinoma—surgery or conventional therapy? Clin Endocrinol (Oxf ) 2002;56:377–82.
46. Song H-J, Xue Y-L, Xu Y-H, et al. Rare metastases of differentiated thyroid carcinoma: pictorial review Endocr Relat Cancer 2011;18:R165–R174.
47. Wilhelm SM, Carter C, Tang L, et al. BAY 43-9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res 2004;64:7099–109.
48. www.fda.gov/NewsEvents/Newsroom/PresAnnouncements/ucm376443.htm.
49. Kloos RT, Ringel MD, Knopp MV et al. Phase II trial of sorafenib in metastatic thyroid cancer. J Clin Oncol 2009;27:1675–84.
50. Gupta-Abramson V, Troxel AB, Nellore A, et al. Phase II trial of sorafenib in advanced thyroid cancer. J Clin Oncol 2008;26:4714–9.
51. Schneider TC, Abdulrahman RM, Corssmit EP, et al. Longterm analysis of the efficacy and tolerability of sorafenib in advanced radio-iodine refractory differentiated thyroid carcinoma: final results of a phase II trial. Eur J Endocrinol 2012;167:643–50.
52. Brose MS, Nutting CM, Jarzab B, et al. Sorafenib in locally advanced or metastatic patients with radioactive iodine refractory differentiated thyroid cancer: The phase III DECISION trial. J Clin Oncol 2013;31(Suppl, abstr 4).
53. Ho AL, Grewal RK, Leboeuf R, et al. Selumetinib-enhanced radioiodine uptake in advanced thyroid cancer. N Engl J Med 2013;368:623–32.
54. Henderson YC, Shellenberger TD, Williams MD, et al. High rate of BRAF and RET/PTC dual mutations associated with recurrent papillary thyroid carcinoma. Clin Cancer Res 2009;15:485–91.
55. Kim TY, Kim WB, Rhee YS, et al. The BRAF mutation is useful for prediction of clinical recurrence in low-risk patients with conventional papillary thyroid carcinoma. Clin Endocrinol (Oxf) 2006;65:364–8.
56. Elisei R, Ugolini C, Viola D, et al. BRAF (V600E) mutation and outcome of patients with papillary thyroid carcinoma: a 15-year median follow-up study. J Clin Endocrinol Metab 2008;93:3943–9.
57. Xing M, Alzahrani AS, Carson KA, et al. Association between BRAFV600E mutation and mortality in patients with papillary thyroid cancer. JAMA 2103;309:1493–501.
58. Kim KB, Cabanillas ME, Lazar AJ, et al. Clinical responses to vemurafenib in patients with metastatic papillary thyroid cancer harboring
From the Yale School of Medicine, New Haven, CT.
ABSTRACT
• Objective: To review management of papillary thyroid cancer.
• Methods: Review of the literature.
• Results: Papillary thyroid cancer is the most common endocrine malignancy. The standard treatment for papillary thyroid cancer is thyroidectomy. Adjuvant therapy includes lifelong thyroid-stimulating hormone suppression and radioiodine therapy. Local recurrence is common and is normally treated with surgery and/or radioiodine. Metastatic radioiodine-resistant disease is a more infrequent event.
• Conclusion: The incidence of papillary thyroid cancer is rapidly increasing. Surgery remains the cornerstone of treatment.
Papillary thyroid cancer is the most common endocrine malignancy and accounts for the majority of cancers of the thyroid. The incidence of papillary thyroid cancer is rapidly increasing [1]. Although increasing detection has been proposed as a possible factor [2], some studies reject this hypothesis, reporting increase in the incidence of larger tumors [3]. Papillary thyroid cancer is characterized by a low mortality but a high recurrence rate [1], posing challenges not only to the endocrinologist and oncologist but also to the general practitioner.
The most frequent presentation of papillary thyroid cancer is a palpable thyroid nodule, cervical lymphadenopathy, or incidental detection on imaging. Locally advanced disease can present with hoarseness or voice alteration. Common risks factors include history of radiation exposure during childhood (the most important risk factor), thyroid cancer in a first-degree relative, family history of a thyroid cancer syndrome (such as Werner syndrome, Cowden syndrome, Carney complex, or familial polyposis), and female sex (2.5:1). Thyroid nodules in the context of an autoimmune thyroiditis may have a higher risk of malignancy [4].
CASE STUDY
Initial Presentation
A 49-year-old man with no significant past medical history presents with a painless mass in the anterior part of his neck.
History, Physical Examination, and Initial Investigations
He has no other symptoms, no weight changes, no history of radiation exposure to the neck, and no family history of malignancy. Physical exam shows a mass in the left thyroid lobe. There is no evidence of cardiac arrhythmias, tremors, or ophthalmologic abnormalities. Thyroid-stimulating hormone (TSH) level is 2.8 mIU/L (normal range, 0.4–4.5 mIU/L) and free thyroxine (T4) level is 1.1 ng/dL (normal range, 0.8–1.5 ng/dL). An ultrasound scan of the neck shows enlargement of the left lobe of thyroid gland, containing multiple complex lesions, the largest measuring 2 x 3 cm, with calcification as well as 3 enlarged lymph nodes in the left level IV. Fine-needle aspiration of the thyroid mass is positive for papillary carcinoma.
• What is the approach to the initial evaluation of a thyroid nodule?
Initial diagnostic evaluation includes history, physical examination, and TSH measurement; nonfunctioning nodules, associated with normal or high values of TSH, carry a higher risk of malignancy [5]. Cervical ultrasound should be performed in all patients with nodules. Fine-needle aspiration (FNA) should be used to evaluate nonfunctioning nodules > 1 cm or subcentimeter nodules with suspicious ultrasound features or if the patient has major risk factors (history of ionizing radiation exposure, external beam radiation exposure, family or personal history of papillary thyroid cancer, or FDG-PET [fluorinated glucose positron emission tomography]–positive thyroid nodules). Scintigraphy can be used to evaluate the need for ultrasound and FNA in patients with low TSH values [6,7]; hyperfunctioning nodules are at low risk for malignancy and do not require biopsy.
• What is initial treatment of papillary thyroid cancer?
Surgery is the primary treatment for papillary thyroid cancer. Unlike for many cancers, surgical removal of the primary tumor is indicated even in the presence of metastatic disease [8]. Total or near-total thyroidectomy is used to treat patients with tumors > 1 cm or with tumors < 1 cm and associated risk factors (eg, contralateral nodules, affected lymph nodes, metastasis, history of radiation, first-degree family history of papillary thyroid cancer, or age > 45 years) [6]. There is a lower risk of recurrence in patients treated with total thyroidectomy versus lobectomy in papillary thyroid cancer [9,10]. Thyroid lobectomy may be used in small (< 1 cm) unifocal tumors without the presence of the associated risk factors listed above.
Patients with central or lateral neck lymph node involvement should also undergo central-compartment (level VI) neck dissection. Therapeutic lateral neck compartmental lymph node dissection is recommended in patients with biopsy-proven metastatic lateral cervical adenopathy [6,7]. The role of unilateral or bilateral prophylactic central-compartment nodal dissection (PCND), that is, lymph node dissection in the level VI compartment of neck in patients without evidence of lymphadenopathy, is controversial. The data for the possible benefit of PCND are inconclusive [11] although the ATA recommends the procedure for locally invasive T3 and T4 tumors [6].
The American Thyroid Association (ATA) and National Comprehensive Cancer Network (NCCN) guidelines [6,7] recommend a preoperative cervical ultrasound in patients with biopsy-proven papillary thyroid cancer to evaluate the presence of disease in the cervical lymph nodes, especially in the lateral and central compartments, and in the contralateral thyroid lobe. If suspicious lymph nodes are found, FNA confirmation is necessary only if this would change management. Systematic use of other preoperative imaging studies, such as CT or MRI, is not recommended [6,7].
Surgical Treatment
The patient underwent a total thyroidectomy with bilateral central neck dissection and selective supraclavicular left-sided lateral neck dissection. Lymph nodes on both sides of the neck (paratracheal nodes) as well as the left supraclavicular nodes were removed. Pathology showed multifocal papillary cancer with extracapsular extension to the paratracheal soft tissue, 14/14 lymph nodes affected, stage IVA T4N1bM0.
• How is papillary thyroid cancer staged?
• How should this patient be treated after surgery? Is any adjuvant therapy indicated?
TSH Suppression
In an effort to reduce risk of recurrence, patients should receive lifelong suppression of TSH using supraphysiologic doses of levothyroxine after total thyroidectomy. This is based upon the hypothesis that TSH is a growth factor for thyroid cancer cells [12,13]. Although a meta-analysis [14] supports the efficacy of TSH suppression therapy, some authors have questioned its widespread use, especially in light of the adverse effects of its use over the long term [15]. Many support its use only in high-risk patients [16], arguing that there is no evidence of benefit for low-risk patients [17]. This view is reflected in the ATA guidelines, which recommend TSH suppression below 0.1 mU/L for high-risk and intermediate-risk patients, while normal or slightly below normal TSH levels are recommended for low-risk patients [6].
Adverse effects of TSH suppression therapy are derived from the induced mild thyrotoxicosis, including cardiovascular and skeletal manifestations. Notably, elderly patients have a higher risk of cardiovascular side effects [18] such as atrial fibrillation, diastolic dysfunction, tachyarrhythmias, increased heart rate or increased left ventricular mass. Likewise, postmenopausal women are most susceptible for skeletal effects such as decreased mineral bone density and fractures [19].
Radioiodine Ablative Therapy
Radioactive iodine (RAI or radioiodine) therapy is based on the capacity of thyroid tissue to take up and retain iodine, specifically, radioiodine. This capacity is present but reduced in papillary and follicular cancer cells.
Radioiodine remnant ablation is performed after surgery, acting as adjuvant therapy by destroying remnant pathological or normal thyroid tissue. The destruction of normal thyroid tissue is useful as it increases the reliability of thyroglobulin testing and radioiodine scanning in the detection of recurrent or metastatic disease. Moreover, remnant ablation has been shown to prevent new thyroid neoplasias in high-risk patients (ie, those with history of radiation exposure). Radioiodine ablative therapy has been shown to reduce recurrence and cause-specific mortality [20] in certain subgroups; however, patients with low mortality risk do not seem to benefit from this therapy [21,22]. Its use is recommended in patients with distant metastases, tumors > 4 cm, or with extrathyroidal extension. It is also recommended for selected patients with tumors 1–4 cm who have high-risk features (such as lymph node involvement, history of radiation, or others previously mentioned) when there is an intermediate to high risk of recurrence or death from thyroid cancer [6]. Lymph node involvement can occur in up to 50% of cases [39] and normally responds to radioiodine therapy.
Since TSH increases radioiodine uptake by normal or pathological thyroid cells, TSH stimulation is required for radioiodine therapy. This can be done by endogenous TSH elevation or by recombinant human TSH (rhTSH). The former can be achieved by either stopping thyroxine 2 to 3 weeks prior to the remnant ablation, or by withdrawing thyroxine and switching to liothyronine for 2 to 3 weeks followed by a discontinuation of liothyronine for 2 weeks. Both approaches seem to produce the same incidence of hypothyroid symptoms [23]. Thyroxine therapy can be resumed 2 to 3 days after radioiodine ablative therapy. Recombinant human TSH can be used with equal efficacy in place of thyroxine withdrawal [24], with the advantage of not producing transitory hypothyroidism. It is especially recommended for patients who are unable to tolerate hypothyroidism or who cannot achieve an adequate TSH level. Short-term recurrence rates are similar in patients treated with rhTSH or thyroxine withdrawal [25].
In addition, a low-iodine diet for 1 or 2 weeks is recommended for patients undergoing radioiodine remnant ablation. The rationale is that a high-iodine diet or iodine exposure (ie, amiodarone treatment or intravenous contrast) can decrease radioiodine uptake by papillary cancer cells due to further dilution of radioactive iodine in an expanded endogenous non-radioactive iodine pool. Patients with suspected high iodine levels can be screened using spot urinary levels [26].
Commonly, a diagnostic scan using low activities of iodine-131 is performed prior to radioablation to avoid the controversial “stunning effect” [27] from any exposure to sublethal radiation in a diagnostic dose. In stunning, the diagnostic RAI dose decreases uptake of a subsequent therapeutic dose. Alternatively, we use [I-123] radioiodine at very low dose (1.4 mCi) in pre-ablation patients. Uptake in the thyroid bed occurs in 75% to 100% of patients, commonly due to remnant normal thyroid tissue [28].
The typical activity used for RAI ablative therapy is 30–100 mCi. The administration of high activities (150–200 mCi) of [I-131] radioiodine has been used to treat recurrent or metastatic disease. This treatment can be very effective, especially in young patients [29].
Side Effects and Contraindications
Common side effects of radioiodine treatment include sialadenitis, radiation thyroiditis, tumor hemorrhage or edema, nausea, transient oligospermia or amenorrhea and nasolacrimal duct obstruction. Moreover, patients treated with radioiodine have a modest increased risk of developing other malignancies [30].
[I-131]Radioiodine must be avoided in pregnancy and in breastfeeding [31]. Indeed, breast tissue has a strong tendency to uptake iodine so breastfeeding should be stopped 5 to 8 weeks before radioiodine treatment, otherwise it can lead to a false-positive radioiodine scan in the chest [32], or worse, deliver radioiodine to the baby with detrimental effects and potential ablation to the baby’s thyroid gland.
Patients treated with radioiodine are advised to drink abundant water after the treatment in order to increase its renal elimination. If no stool elimination occurs in 14 to 24 hours, laxatives may be indicated to eliminate radioiodine from the gastrointestinal track. In addition, patients are advised to avoid sexual contact, avoid sharing bed, utensils, towels, toothbrushes, razors, and avoid public transportation and public places among other measures to avoid exposing the population to radiation [33]. The duration of this restriction depends on the dose administered.
Adjuvant Treatment in this Patient
As the patient was at high risk for recurrence, he received TSH suppression therapy to levels < 0.1 mIU/L. He was referred to nuclear medicine for I-131 treatment. However, at 3 months following thyroidectomy, thyroglobulin measurement showed an elevation (40.5 ng/mL). Ultrasound showed enlarged lymph nodes at level II at the right and at level II at the left. A FNA of left neck node was positive for papillary thyroid cancer.
• How should the patient be treated now?
Treatment of Locoregional Metastatic Disease
The best treatment for residual disease or local recurrences is surgery. ATA guidelines recommend compartmental lateral and/or central neck dissection for patients with persistent or recurrent disease confined to the neck [6]. Radioiodine can be an alternative when recurrent disease is not visible on imaging. Other treatments that can be used for local recurrences or isolated metastases when surgery is not possible are radiofrequency ablation [34], chemo-embolization [35], or ethanol ablation [36]. External beam radiotherapy, which is discussed later, could also be used in selected cases.
Further Treatment
The patient underwent a bilateral modified radical neck dissection followed by adjunctive radioiodine therapy. His initial radioiodine scan showed mild uptake in the neck at the site of his prior surgery. He received treatment with 215 mCi, then 6 months later he was treated with 250 mCi, as his scan showed continued mild uptake. Eleven months later his radioiodine scan showed no uptake and thyroglobulin levels remained stable at 14.4 ng/mL.
One year later, in a follow-up blood analysis he was found to have an elevated thyroglobulin level (90.4 ng/mL). A PET/CT scan showed multiple bone metastases. A neck ultrasound revealed enlarged lymph nodes in the right thyroid bed.
• How common is radioiodine-refractory thyroid cancer?
Radioiodine-refractory thyroid cancer in patients with progression of disease despite radioiodine therapy, or with non-radioiodine-avid lesions [37], is uncommon. It has a poor prognosis with a median survival of 3 to 6 years after diagnosis. It is more frequent in older patients. These lesions are often hypermetabolic and hence [F-18]FDG-avid [38], with a worse prognosis. In one study of patients with metastatic differentiated thyroid cancer, the 10-year overall survival rate was 56% in patients with radioiodine-avid lesions but only 10% in patients with non-radioiodine-avid lesions [38].
• Is the bone a common place for metastasis? Where else should we expect to find a lesion?
Metastatic Pattern
The most common sites for distant metastasis of papillary thyroid cancer are the lungs and the bone. The 10-year survival rate of papillary thyroid cancer patients with lung metastases is between 30% and 50% [38,39]; the prog-nosis is better in patients < 45 years and with radiodine uptake [40]; indeed, patients with pulmonary metastasis seen only in 131-I scans and not on CT or chest x-ray have a longer survival [41]. Pulmonary metastasis can be treated with radioiodine if they are radioiodine-avid. With this treatment complete remission is possible, although it is extremely difficult to achieve in macronodular metastasis.
Bones are the second most common place for distant metastases. Bone metastases seem to have a worse response to treatment with an unfavorable prognosis [42]. Pamidronate (a biphosphonate) and denosumab (a RANK ligand inhibitor) have been used to prevent skeletal related events, including pathologic fractures and cord compression, in bone metastases from other cancers such as breast and prostate, and may also be useful in thyroid cancer, although this has not yet been studied [43,44]. Moreover, surgical resection of isolated bone metastasis seems to improve survival [45].
Skin, liver, and brain metastasis, although uncommon, can also occur. There are also reported rare cases of metastasis in the breast, parotid, larynx, pharynx, adrenal glands, pituitary, kidney, liver, orbit, the sphenoid sinus, choroid plexus, pancreas, and skeletal muscles [46].
• Which treatments can we offer to a patient with metastatic disease refractory to radioiodine?
Chemotherapy and Treatment of Radioiodine-Resistant Disease
Therapeutic options for patients with metastatic papillary thyroid cancer resistant to radioiodine and TSH suppression are limited. Cytotoxic drugs do not play a major role in the treatment of refractory metastatic papillary thyroid cancer, and new research is mainly focused on tyrosine kinase inhibitors (TKIs) with a considerable number of clinical trials either completed or ongoing.
Tyrosine kinases are enzymes that transfer phosphate groups from adenosine triphosphate to proteins. In tumor cells their signaling paths promote proliferation, avoidance of apoptosis, invasion, angiogenesis, and metastasis. TKIs are small molecules that are able to inhibit tyrosine kinase function even at very low intracellullar concentrations. Some of them inhibit various tyrosine kinases and are known as multi-kinase inhibitors (MKIs).
Sorafenib
Sorafenib (400 mg twice daily) is an oral MKI that targets RAF, platelet-derived growth factor receptor, vascular endothelial growth factor receptors 2 and 3, RET and c-Kit [47]. It was approved in November 2013 for patients with radioiodine-refractory differentiated thyroid cancer [48]. Three phase II studies had previously evaluated sorafenib in papillary thyroid cancer, showing a partial response in 15% to 31% of patients and a progression-free survival up to 79 weeks [49–51]. Common adverse effects included weight loss, fatigue, rash, hypertension and the main dose-limiting toxicity—a hand-foot syndrome consisting of swelling, reddening, numbness, and desquamation on palms and soles [52].
Approval of the drug was based on the DECISION trial [52]. A total of 417 patients were randomized (207 to sorafenib and 210 to placebo), of which 57% had papillary thyroid cancer. The primary endpoint of progression-free survival (PFS) was significantly higher in the sorafenib arm, (median, 10.8 months) compared with placebo (median, 5.8 months) (hazard ratio [HR] 0.58, 95% confidence interval [CI] 0.45–0.75, P < 0.001). Median overall survival had not been reached in either arm [52]. The PFS of 5.8 months in the placebo arm confirmed that the group of patients in this study had a rapidly progressing disease, unlike the majority of patients with RAI-sensitive disease.
Selumetinib
Radioiodine re-sensitization was addressed in a study using selumitinib, an inhibitor of mitogen-activated protein kinase kinase (MAPK kinase or MEK). Preclinical models had shown that radioiodine-refractory tumors exposed to inhibitors of this enzyme were able to uptake radioiodine again. Twenty patients with radioiodine-refractory thyroid cancers were treated with selumetinib for 4 weeks and 12 showed increased radioiodine uptake following the treatment. Furthermore, 8 of these patients went on to show responses clinically to retreatment with radioiodine [53].Further studies with this agent will be needed to determine its place in treating patients with differentiated thyroid cancer.
External Beam Radiotherapy and Local Treatment for Metastases
The role of external beam radiotherapy in papillary thyroid cancer is mainly for symptom management. Local radiation can be used in patients with refractory metastatic disease or in lesions that do not uptake radioiodine. Examples include painful bone metastasis or brain metastasis that cannot be treated with surgery. In addition, radiofrequency ablation, chemo-embolization, or ethanol ablation can be used in certain patients.
Sequence of Treatments
In the setting of symptomatic metastatic, radioiodine-resistant disease, we prefer to use a TKI, normally sorafenib, as a first-line treatment. For second-line treatments, enrollment in a clinical trial is an option. Over 70% of patients with metastatic papillary thyroid cancer have mutations of the enzyme BRAF kinase. Vemurafenib is an inhibitor of this enzyme and appears to have some activity in patients with RAI-refractory thyroid cancer in early clinical trials [54–58]. Other TKIs such as sunitinib can also be used. Doxorubicin is only used in cases when a patient is not eligible for a trial and the off-label use of another TKI is contraindicated.
Further Treatment in this Patient
The patient received a trial of sorafenib. He showed disease stabilization that lasted 5 months. The treatment was stopped due to adverse effects (loss of weight and vomiting) and progression of the disease. He was then enrolled in a trial of vemurafenib. He stopped treatment because of adverse events related to the medication and currently has stable disease.
Summary
Papillary thyroid cancer is the most common endocrine malignancy. It is characterized by low mortality but high recurrence rate and can have a considerable impact on quality of life. Any anterior neck nodule, especially in a patient with a history of neck irradiation, should raise concern for this disease. Surgery remains the cornerstone of treatment. Adjuvant therapy includes lifelong TSH suppression and radioiodine therapy. Local recurrence is common and is normally treated with surgery and/or radioiodine. Metastatic radioiodine-resistant disease is a more infrequent event. Thyroid cancer has a tendency to metastasize to the bones and lungs. Metastatic radioiodine-resistant disease is often treated with TKIs such as sorafenib. Enrollment in clinical trials is recommended as second-line therapy in radioiodine-resistant metastatic disease.
Corresponding author: Hari A. Deshpande, MD, Yale Cancer Center, FMP 124, 333 Cedar St., New Haven, CT 06520, [email protected]
Financial disclosures: Dr. Deshpande reports that he is on the advisory board of Bayer/Onyx.
Author contributions: conception and design, PT, EHH, GGC, HAD; drafting of article, PT, EHH, GGC, HAD; critical revision of the article, EHH, GGC, HAD.
REFERENCES
1. Howlader N, Noone AM, Krapcho M, et al (eds). SEER Cancer Statistics Review, 1975-2010, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2010.
2. Katoh R, Sasaki J, Kurihara H, et al. Multiple thyroid involvement (intraglandular metastasis) in papillary thyroid carcinoma: a clinicopathologic study of 105 consecutive patients. Cancer 1992;70:1585–90.
3. Morris LG, Myssiorek D. Improved detection does not fully explain the rising incidence of well-differentiated thyroid cancer: a population-based analysis. Am J Surg 2010;200:454–61.
4. Fiore E, Rago T, Latrofa F, et al. Hashimoto’s thyroiditis is associated with papillary thyroid carcinoma: role of TSH and of treatment with Lthyroxine. Endocr Relat Cancer 2011;18:429–37.
5. Haymart MR, Repplinger DJ, Leverson GE, et al. Higher serum thyroid stimulating hormone level in thyroid nodule patients is associated with greater risks of differentiated thyroid cancer and advanced tumor stage. J Clin Endocrinol Metab 2008;93:809–14.
6. Cooper DS, Doherty GM, Haugen BR, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167–214.
7. National Comprehensive Cancer Network guidelines. Available at www.nccn.org/professionals/physician_gls/pdf/thyroid. pdf.
8. Stephenson BM, Wheeler MH, Clark OH. The role of total thyroidectomy in the management of differentiated thyroid cancer. Curr Opin Gen Surg 1994 53–9.
9. Bilimoria KY, Bentrem DJ, Ko CY, et al. Extent of surgery affects survival for papillary thyroid cancer. Ann Surg 2007;246:375–81.
10. Hay ID, Grant CS, Bergstralh EJ, et al. Unilateral total lobectomy: is it sufficient surgical treatment for patients with AMES low-risk papillary thyroid carcinoma? Surgery 1998;124:958–64.
11. McLeod DS, Sawka AM, Cooper DS. Controversies in primarytreatment of low-risk papillary thyroid cancer. Lancet 2013;381:1046–57.
12. Brabant G. 2008 Thyrotropin suppressive therapy in thyroid carcinoma: what are the targets? J Clin Endocrinol Metab 2008;93:1167–9.
13. Kim HK, Yoon JH, Kim SJ, Cho JS. Higher TSH level is a risk factor for differentiated thyroid cancer. Clin Endocrinol (Oxf) 2013;78:472–7.
14. McGriff NJ, Csako G, Gourgiotis L, et al. Effects of thyroid hormone suppression therapy on adverse clinical outcomes in thyroid cancer. Ann Med 2002;34:554–64.
15. Zafón C. TSH-suppressive treatment in differentiated thyroid cancer. A dogma under review. Endocrin Nutr 2012;59:125–30.
16. Cooper DS, Specker B, Ho M, et al. Thyrotropin suppression and disease progression in patients with differentiated thyroid cancer: Results from the National Thyroid Cancer Treatment Cooperative Registry. Thyroid 1998;8:737-44.
17. Jonklaas J, Sarlis NJ, Litofsky D, et al. Outcomes of patients with differentiated thyroid carcinoma following initial therapy. Thyroid 2006;16:1229–42.
18. Sawin CT, Geller A, Wolf PA, et al. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N Engl J Med 1994;33:1249–52.
19. Kung AW, Yeung SS. Prevention of bone loss induced by thyroxine suppressive therapy in postmenopausal women: the effect of calcium and calcitonin. J Clin Endocrinol Metab 1996;81:1232–36.
20. Samaan NA, Schultz PN, Hickey RC, et al. The results of various modalities of treatment of well differentiated thyroid carcinomas: a retrospective review of 1599 patients. J Clin Endocrinol Metab 1992;75:714–20.
21. Sugitani I, Fujimoto Y. Symptomatic versus asymptomatic papillary thyroid microcarcinoma: a retrospective analysis of surgical outcome and prognostic factors. Endocr J 1999;46:209–16.
22. Kim S, Wei JP, Braveman JM, Brams DM. Predictingoutcome and directing therapy for papillary thyroid carcinoma. Arch Surg 2004;139:390–4.
23. Leboeuf R, Perron P, Carpentier AC, et al. L-T3 preparation for whole-body scintigraphy: a randomized-controlled trial. Clin Endocrinol (Oxf ) 2007;67:839–44.
24. Pacini F, Ladenson PW, Schlumberger M, et al. Radioiodine ablation of thyroid remnants after preparation with recombinant human thyrotropin in differentiated thyroid carcinoma: results of an international, randomized, controlled study. J Clin Endocrinol Metab 2006;91:926–32.
25. Tuttle RM, Brokhin M, Omry G, et al. Recombinant human TSH-assisted radioactive iodine remnant ablation achieves short-term clinical recurrence rates similar to those of traditional thyroid hormone withdrawal. J Nucl Med 2008;49:764–70.
26. Pluijmen MJ, Eustatia-Rutten C, Goslings BM, et al. Effects of low-iodide diet on postsurgical radioiodide ablation therapy in patients with differentiated thyroid carcinoma. Clin Endocrinol (Oxf ) 2003;58:428–35.
27. Park HM. Stunned thyroid after high-dose I-131 imaging. Clin Nucl Med 1992; 17:501–2.
28. Salvatori M, Raffaelli M, Castaldi P, et al. Evaluation of the surgical completeness after total thyroidectomy for differentiated thyroid carcinoma. Eur J Surg Oncol 2007;33:648–54.
29. Durante C, Haddy N, Baudin E, et al. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab 2006;91:2892–9.
30. Lang BH, Wong IO, Wong KP, et al. Risk of second primary malignancy in differentiated thyroid carcinoma treated with radioactive iodine therapy. Surgery 2012;151:844–50.
31. Rubow S, Klopper J. Excretion of radioiodine in human milk following a therapeutic dose of I-131. Eur J Nucl Med 1988;14:632–3.
32. Bakheet SM, Hammami MM. Patterns of radioiodine uptake by the lactating breast. Eur J Nucl Med 1994;21:604–8.
33. American Thyroid Association Taskforce on Radioiodine Safety, Sisson JC, Freitas J, et al. Radiation safety in the treatment of patients with thyroid diseases by radioiodine 131I: practice recommendations of the American Thyroid Association. Thyroid 2011;21:335–46.
34. Dupuy DE, Monchik JM, Decrea C, Pisharodi L. Radiofrequency ablation of regional recurrence from welldifferentiated thyroid malignancy. Surgery 2001;130:971–7.
35. Eustatia-Rutten CF, Romijn JA, Guijt MJ, et al. Outcome of palliative embolization of bone metastases in differentiated thyroid carcinoma. J Clin Endocrinol Metab 2003;88:3184–9.
36. Lewis BD, Hay ID, Charboneau JW, et al. Percutaneous ethanol injection for treatment of cervical lymph node metastases in patients with papillary thyroid carcinoma. Am J Roentgenol 2002;178:699–704.
37. Xing MM, Haugen B, Schlumberger M. Progress in molecular based management of differentiated thyroid cancer. Lancet 2013;381:1058–69.
38. Durante C, Haddy N, Baudin E, et al. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab 2006;91:2892–99.
39. Haq M, Harmer C. Differentiated thyroid carcinoma with distant metastases at presentation: prognostic factors and outcome Clin Endoc 2005;63:87–93.
40. Ronga G, Filesi M, Montesano T, et al. Lung metastases from differentiated thyroid carcinoma. A 40 years’ experience. Q J Nucl Med Mol Imaging 2004;48:12–19.
41. Samaan NA, Schultz PN, Haynie TP, Ordonez NG. Pulmonary metastasis of differentiated thyroid carcinoma: treatment results in 101 patients. J Clin Endocrinol Metab 1985;60:376–80.
42. Lang BH, Wong KP, Cheung CY, et al. Evaluating the prognostic factors associated with cancer-specific survival of differentiated thyroid carcinoma presenting with distant metastasis. Ann Surg Oncol 2013;20:1329–35.
43. Hortobagyi GN, Theriault RL, Porter L, et al. Efficacy of pamidronate in reducing skeletal complications in patients with breast cancer and lytic bone metastases. N Engl J Med 1996;335:1785–92.
44. Smith MR, Saad F, Coleman R, et al. Denosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: Results of a phase 3, randomised, placebocontrolled trial. Lancet 379:39–46.
45. Zettinig G, Fueger BJ, Passler C, et al. Long-term follow-up of patients with bone metastases from differentiated thyroid carcinoma—surgery or conventional therapy? Clin Endocrinol (Oxf ) 2002;56:377–82.
46. Song H-J, Xue Y-L, Xu Y-H, et al. Rare metastases of differentiated thyroid carcinoma: pictorial review Endocr Relat Cancer 2011;18:R165–R174.
47. Wilhelm SM, Carter C, Tang L, et al. BAY 43-9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res 2004;64:7099–109.
48. www.fda.gov/NewsEvents/Newsroom/PresAnnouncements/ucm376443.htm.
49. Kloos RT, Ringel MD, Knopp MV et al. Phase II trial of sorafenib in metastatic thyroid cancer. J Clin Oncol 2009;27:1675–84.
50. Gupta-Abramson V, Troxel AB, Nellore A, et al. Phase II trial of sorafenib in advanced thyroid cancer. J Clin Oncol 2008;26:4714–9.
51. Schneider TC, Abdulrahman RM, Corssmit EP, et al. Longterm analysis of the efficacy and tolerability of sorafenib in advanced radio-iodine refractory differentiated thyroid carcinoma: final results of a phase II trial. Eur J Endocrinol 2012;167:643–50.
52. Brose MS, Nutting CM, Jarzab B, et al. Sorafenib in locally advanced or metastatic patients with radioactive iodine refractory differentiated thyroid cancer: The phase III DECISION trial. J Clin Oncol 2013;31(Suppl, abstr 4).
53. Ho AL, Grewal RK, Leboeuf R, et al. Selumetinib-enhanced radioiodine uptake in advanced thyroid cancer. N Engl J Med 2013;368:623–32.
54. Henderson YC, Shellenberger TD, Williams MD, et al. High rate of BRAF and RET/PTC dual mutations associated with recurrent papillary thyroid carcinoma. Clin Cancer Res 2009;15:485–91.
55. Kim TY, Kim WB, Rhee YS, et al. The BRAF mutation is useful for prediction of clinical recurrence in low-risk patients with conventional papillary thyroid carcinoma. Clin Endocrinol (Oxf) 2006;65:364–8.
56. Elisei R, Ugolini C, Viola D, et al. BRAF (V600E) mutation and outcome of patients with papillary thyroid carcinoma: a 15-year median follow-up study. J Clin Endocrinol Metab 2008;93:3943–9.
57. Xing M, Alzahrani AS, Carson KA, et al. Association between BRAFV600E mutation and mortality in patients with papillary thyroid cancer. JAMA 2103;309:1493–501.
58. Kim KB, Cabanillas ME, Lazar AJ, et al. Clinical responses to vemurafenib in patients with metastatic papillary thyroid cancer harboring
Another Win for Veggies
Study Overview
Objective. To determine the association between a vegetarian diet and blood pressure (BP).
Design. Systematic review and meta-analysis of controlled clinical trials and observational studies.
Setting and participants. MEDLINE and Web of Science were respectively searched for English articles published between 1946 to October 2013 and 1900 to November 2013. Inclusion criteria were age > 20 years and vegetarian diet. This included a vegan diet (omitting all animal products), ovo/lacto/pesco vegetarian diet (including eggs/dairy/fish), or semi-vegetarian diet (meat or fish rarely). Exclusion criteria included studies of twins, a multipronged intervention, describing only categorical BP, and reliance on a case series. A total of 258 records were identified. Seven clinical trials and 32 observational studies met inclusion criteria. The 7 clinical trials encompassed 311 participants (median, 38; range, 11–113) with a mean age of 44.5 years (range, 38.0–54.3). All were open-label, 6 were randomized, and 6 provided food to participants. The 32 observational studies included 21,604 participants (median, 152; range, 20–9242) with a mean age of 46.6 years (range, 28.8–68.4 years). Fifteen of these studies included mixed diet types (vegan, lacto, ovolacto, pesca, and/or semivegetarian).
Main outcome measures. The primary outcome was BP. Differences in systolic BP (SBP) and diastolic BP (DBP) between groups consuming vegetarian or comparison diets were pooled using a random effects model. The study compared clinical trials and observational studies separately. Funnel plots, the Egger test, and the trim-and-fill method were all used to assess and correct for publication bias.
Results. Vegetarian diets in clinical trials were associated with a mean SBP reduction of −4.8 mm Hg (95% confidence interval [CI], −6.6 to −3.1; P < 0.001; I2 = 0; P = 0.45 for heterogeneity) and DBP reduction of −2.2 mm Hg (95% CI, −3.5 to −1.0; P < 0.001; I2 = 0; P= 0.43 for heterogeneity) when compared with omnivorous diets. Observational studies had larger reductions but significant heterogeneity: SBP −6.9 mm Hg (95% CI, −9.1 to −4.7; P < 0.001; I2 = 91.4; P < 0.001 for heterogeneity) and DBP −4.7 mm Hg (95% CI, −6.3 to −3.1; P < 0.001; I2 = 92.6; P < 0.001 for heterogeneity). This heterogeneity was best explained by proportion of men (β −0.03; P < 0.001), baseline SBP (β −0.13; P = 0.003), baseline DBP (β −0.30; P < 0.001), sample size (β 0.001; P< 0.001), and BMI (β −0.46; P = 0.02). This suggests that vegetarian diets and lower BP are more strongly associated in men and those with higher baseline BP and BMI.
Subgroup analysis included stratification by age, gender, BMI, diet type, sample size, diet duration, BP medication use, baseline BP, and geographic region. In subgroup analysis of clinical trials, no statistically significant difference between group variation or heterogeneity existed. In comparison, subgroup analysis of observational studies reduced heterogeneity and often effect size. For example, lower SBP was evident in the majority male subgroups (mean SBP/DBP: –18.5 mm Hg/–10.1 mm Hg).
Publication bias existed for both clinical trials and observational studies. According to trim-and-fill methodology, 3 clinical trials of smaller size and larger BP reduction likely were missing (Egger P = 0.04). Their addition shifted mean SBP reduction from −4.8 mm Hg (−6.6 to −3.1) to −5.2 mm Hg (−6.9 to −3.5). Observational studies lacked medium sized negative trials and were overrepresented by larger positive trials (Egger P < 0.001), although this was not confirmed by trim-and-fill (yet this method performs less well under heterogeneous conditions) [1].
Conclusion. Vegetarian diets, when compared with omnivorous diets, are associated with reductions in BP.
Commentary
Several studies show that dietary modifications are effective in preventing and managing hypertension [2,3]. Landmark randomized trials, including the DASH diet [4], DASH-sodium diet [5], and OmniHeart diets [6], all of which emphasize fruit and vegetable intake but are not vegetarian, have led to SBP and DBP reductions ranging from 5.5 to 9.5 mm Hg and 3.0 to 5.2, respectively. However, the impact of a vegetarian diet still remains debated, particularly given disparate findings among randomized controlled trials (RCTs). For example, findings in the early- and mid-1980s of small RCTs with ovolactovegetarians (a vegetarian who consumes eggs and dairy products but not animal flesh) suggested reductions similar to the pooled SBP reduction of –4.8 mm Hg Yokoyama et al report [7,8]. In contrast, one RCT comparing ovolactovegetarian with lean meat diets failed to show a BP benefit [9]. Striking is the dearth of RCTs in the last 20 years to assist in better estimating this impact, particularly given its continual recommendation in the scientific [10] and lay communities [11]. To the authors’ credit, this is the first meta-analysis and second systematic review of this important relationship [12].
A vegetarian diet likely supports BP reductions through a variety of mechanisms, most notably via an abundance of potassium [13]. Potassium likely promotes vasodilation, which facilitates glomerular filtration, allowing decreased renal sodium reabsorption and decreased platelet aggregation. Other more controversial hypotheses include decreased energy density leading to reduced BMI [14], decreased sodium intake [15], reduced blood viscosity [16], and high polyunsaturated with low saturated fat content [17].
Strengths of this analysis include the large observational sample size, the separate analysis of clinical trials and observational studies, the lengthy search time-frame, the subgroup analyses, and the adjustment for publication bias. Although the overall association was robust throughout, we agree with the authors that large heterogeneity among observational studies, small clinical trial sample sizes, and the variation in what “vegetarian” represents throughout the world and in individual studies all represent limitations. The participants in many of the observational studies could have technically eaten meat with unclear and undefined frequency, and this may have explained the heterogeneity of these studies. Correspondingly, the lack of heterogeneity observed in the clinical trials may be due to the fact that participants were provided meals in 6 out of 7 studies.
It was surprising that only 7 clinical trials were found. The authors utilized 2 databases, but perhaps searching additional databases such as EMBASE or CINAHL would have yielded other pertinent studies. The authors also did not use a bias assessment tool such as that proposed by the Cochrane bias methods group, which could have better discriminated high- from low-quality trials and made for useful subgroup analyses [1]. Similarly, reporting on both attrition and adherence could have assisted in decreasing heterogeneity during subgroup analyses and determining high-quality from low-quality studies. For example, adherence in Ferdowsian et al (vegan diet) was determined by unannounced dietician phone calls and found that only 57% of participants abstained from animal products. This may have been secondary to the study’s design, in that “providing meals” included simply making them an available option at the company cafeteria instead of requiring consumption of a study-specific vegetarian meal [18].
Applications for Clinical Practice
In this meta-analysis, vegetarian diets were associated with –4.8 mm Hg SBP and −2.2 mm Hg DBP reductions, indicating that providers can recommend a vegetarian diet as on par with other lifestyle changes, including low-sodium diet, weight loss, and exercise. A vegetarian diet may be comparable to pharmacologic therapy in magnitude of BP change. Short- and long-term pharmacologic therapy is associated with respective SBP/DBP reductions of –8.3/–3.8 and –5.4/–2.3, not altogether different from reductions seen with vegetarian or vegetable-heavy diets [19].
Although there are barriers to a vegetarian diet, including provider attitudes [20], cost [21], poor culinary skill [22], palatability, and adherence, pharmacologic BP treatment also presents barriers: adherence to BP medications is estimated to be 50% to 70% [23], and harm due to side effects can preclude use. Thus, providers can present a vegetarian diet as a potentially effective option, depending on patient preference and ability to adhere.
—David M. Levine, MD, MA, New York University
School of Medicine, and Melanie Jay, MD, MS
References
1. Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available at http://handbook.cochrane.org/chapter_10/10_4_4_2_trim_and_fill.htm.
2. Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2013 Nov 12. [Epub ahead of print]
3. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20.
4. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117–24.
5. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N Engl J Med 2001;344:3–10.
6. Appel LJ, Sacks FM, Carey VJ, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids. JAMA 2005;294:2455–64.
7. Rouse IL, Beilin LJ, Armstrong BK, Vandongen R. Blood-pressure–lowering effect of a vegetarian diet: controlled trial in normotensive subjects. Lancet 1983;321:5–10.
8. Margetts BM, Beilin LJ, Vandongen R, Armstrong BK. Vegetarian diet in mild hypertension: a randomised controlled trial. BMJ 1986;293:1468–71.
9. Kestin M, Rouse IL, Correll RA, Nestel PJ. Cardiovascular disease risk factors in free-living men: comparison of two prudent diets, one based on lactoovovegetarianism and the other allowing lean meat. Am J Clin Nutr 1989;50:280–7.
10. Alpert JS. Nutritional advice for the patient with heart disease: what diet should we recommend for our patients? Circulation 2011;124:e258–e260.
11. Gordinier J. Making vegan a new normal. New York Times. 26 Sept 2012. Page D1.
12. Berkow SE, Barnard ND. Blood pressure regulation and vegetarian diets. Nutr Rev 2005;63:1–8.
13. Aburto NJ, Hanson S, Gutierrez H, et al. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ 2013;346:f1378.
14. Berkow SE, Barnard N. Vegetarian diets and weight status. Nutr Rev 2006;64:175–88.
15. Larsson CL, Johansson GK. Dietary intake and nutritional status of young vegans and omnivores in Sweden. Am J Clin Nutr 2002;76:100–6.
16. Ernst E, Pietsch L, Matrai A, Eisenberg J. Blood rheology in vegetarians. Br J Nutr 1986;56:555–60.
17. Iacono JM, Dougherty RM. Effects of polyunsaturated fats on blood pressure. Annu Rev Nutr 1993;13:243–60.
18. Ferdowsian HR, Barnard ND, Hoover VJ, et al. A multicomponent intervention reduces body weight and cardiovascular risk at a GEICO corporate site. Am J Health Promot 2010;24:384–7.
19. Brugts JJ, Ninomiya T, Boersma E, et al. The consistency of the treatment effect of an ACE-inhibitor based treatment regimen in patients with vascular disease or high risk of vascular disease: a combined analysis of individual data of ADVANCE, EUROPA, and PROGRESS trials. Eur Heart J 2009;30:1385–94.
20. Berman BM, Singh BB, Hartnoll SM, et al. Primary care physicians and complementary-alternative medicine: training, attitudes, and practice patterns. Am Board Fam Pract 1998;11:272–81.
21. Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr 2005;82(1 Suppl):265S-273S.
22. Lea EJ, Crawford D, Worsley A. Public views of the benefits and barriers to the consumption of a plant-based diet. Eur J Clin Nutr 2006;60:828–37.
23. Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressure–lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med 2004;164:722–32.
Study Overview
Objective. To determine the association between a vegetarian diet and blood pressure (BP).
Design. Systematic review and meta-analysis of controlled clinical trials and observational studies.
Setting and participants. MEDLINE and Web of Science were respectively searched for English articles published between 1946 to October 2013 and 1900 to November 2013. Inclusion criteria were age > 20 years and vegetarian diet. This included a vegan diet (omitting all animal products), ovo/lacto/pesco vegetarian diet (including eggs/dairy/fish), or semi-vegetarian diet (meat or fish rarely). Exclusion criteria included studies of twins, a multipronged intervention, describing only categorical BP, and reliance on a case series. A total of 258 records were identified. Seven clinical trials and 32 observational studies met inclusion criteria. The 7 clinical trials encompassed 311 participants (median, 38; range, 11–113) with a mean age of 44.5 years (range, 38.0–54.3). All were open-label, 6 were randomized, and 6 provided food to participants. The 32 observational studies included 21,604 participants (median, 152; range, 20–9242) with a mean age of 46.6 years (range, 28.8–68.4 years). Fifteen of these studies included mixed diet types (vegan, lacto, ovolacto, pesca, and/or semivegetarian).
Main outcome measures. The primary outcome was BP. Differences in systolic BP (SBP) and diastolic BP (DBP) between groups consuming vegetarian or comparison diets were pooled using a random effects model. The study compared clinical trials and observational studies separately. Funnel plots, the Egger test, and the trim-and-fill method were all used to assess and correct for publication bias.
Results. Vegetarian diets in clinical trials were associated with a mean SBP reduction of −4.8 mm Hg (95% confidence interval [CI], −6.6 to −3.1; P < 0.001; I2 = 0; P = 0.45 for heterogeneity) and DBP reduction of −2.2 mm Hg (95% CI, −3.5 to −1.0; P < 0.001; I2 = 0; P= 0.43 for heterogeneity) when compared with omnivorous diets. Observational studies had larger reductions but significant heterogeneity: SBP −6.9 mm Hg (95% CI, −9.1 to −4.7; P < 0.001; I2 = 91.4; P < 0.001 for heterogeneity) and DBP −4.7 mm Hg (95% CI, −6.3 to −3.1; P < 0.001; I2 = 92.6; P < 0.001 for heterogeneity). This heterogeneity was best explained by proportion of men (β −0.03; P < 0.001), baseline SBP (β −0.13; P = 0.003), baseline DBP (β −0.30; P < 0.001), sample size (β 0.001; P< 0.001), and BMI (β −0.46; P = 0.02). This suggests that vegetarian diets and lower BP are more strongly associated in men and those with higher baseline BP and BMI.
Subgroup analysis included stratification by age, gender, BMI, diet type, sample size, diet duration, BP medication use, baseline BP, and geographic region. In subgroup analysis of clinical trials, no statistically significant difference between group variation or heterogeneity existed. In comparison, subgroup analysis of observational studies reduced heterogeneity and often effect size. For example, lower SBP was evident in the majority male subgroups (mean SBP/DBP: –18.5 mm Hg/–10.1 mm Hg).
Publication bias existed for both clinical trials and observational studies. According to trim-and-fill methodology, 3 clinical trials of smaller size and larger BP reduction likely were missing (Egger P = 0.04). Their addition shifted mean SBP reduction from −4.8 mm Hg (−6.6 to −3.1) to −5.2 mm Hg (−6.9 to −3.5). Observational studies lacked medium sized negative trials and were overrepresented by larger positive trials (Egger P < 0.001), although this was not confirmed by trim-and-fill (yet this method performs less well under heterogeneous conditions) [1].
Conclusion. Vegetarian diets, when compared with omnivorous diets, are associated with reductions in BP.
Commentary
Several studies show that dietary modifications are effective in preventing and managing hypertension [2,3]. Landmark randomized trials, including the DASH diet [4], DASH-sodium diet [5], and OmniHeart diets [6], all of which emphasize fruit and vegetable intake but are not vegetarian, have led to SBP and DBP reductions ranging from 5.5 to 9.5 mm Hg and 3.0 to 5.2, respectively. However, the impact of a vegetarian diet still remains debated, particularly given disparate findings among randomized controlled trials (RCTs). For example, findings in the early- and mid-1980s of small RCTs with ovolactovegetarians (a vegetarian who consumes eggs and dairy products but not animal flesh) suggested reductions similar to the pooled SBP reduction of –4.8 mm Hg Yokoyama et al report [7,8]. In contrast, one RCT comparing ovolactovegetarian with lean meat diets failed to show a BP benefit [9]. Striking is the dearth of RCTs in the last 20 years to assist in better estimating this impact, particularly given its continual recommendation in the scientific [10] and lay communities [11]. To the authors’ credit, this is the first meta-analysis and second systematic review of this important relationship [12].
A vegetarian diet likely supports BP reductions through a variety of mechanisms, most notably via an abundance of potassium [13]. Potassium likely promotes vasodilation, which facilitates glomerular filtration, allowing decreased renal sodium reabsorption and decreased platelet aggregation. Other more controversial hypotheses include decreased energy density leading to reduced BMI [14], decreased sodium intake [15], reduced blood viscosity [16], and high polyunsaturated with low saturated fat content [17].
Strengths of this analysis include the large observational sample size, the separate analysis of clinical trials and observational studies, the lengthy search time-frame, the subgroup analyses, and the adjustment for publication bias. Although the overall association was robust throughout, we agree with the authors that large heterogeneity among observational studies, small clinical trial sample sizes, and the variation in what “vegetarian” represents throughout the world and in individual studies all represent limitations. The participants in many of the observational studies could have technically eaten meat with unclear and undefined frequency, and this may have explained the heterogeneity of these studies. Correspondingly, the lack of heterogeneity observed in the clinical trials may be due to the fact that participants were provided meals in 6 out of 7 studies.
It was surprising that only 7 clinical trials were found. The authors utilized 2 databases, but perhaps searching additional databases such as EMBASE or CINAHL would have yielded other pertinent studies. The authors also did not use a bias assessment tool such as that proposed by the Cochrane bias methods group, which could have better discriminated high- from low-quality trials and made for useful subgroup analyses [1]. Similarly, reporting on both attrition and adherence could have assisted in decreasing heterogeneity during subgroup analyses and determining high-quality from low-quality studies. For example, adherence in Ferdowsian et al (vegan diet) was determined by unannounced dietician phone calls and found that only 57% of participants abstained from animal products. This may have been secondary to the study’s design, in that “providing meals” included simply making them an available option at the company cafeteria instead of requiring consumption of a study-specific vegetarian meal [18].
Applications for Clinical Practice
In this meta-analysis, vegetarian diets were associated with –4.8 mm Hg SBP and −2.2 mm Hg DBP reductions, indicating that providers can recommend a vegetarian diet as on par with other lifestyle changes, including low-sodium diet, weight loss, and exercise. A vegetarian diet may be comparable to pharmacologic therapy in magnitude of BP change. Short- and long-term pharmacologic therapy is associated with respective SBP/DBP reductions of –8.3/–3.8 and –5.4/–2.3, not altogether different from reductions seen with vegetarian or vegetable-heavy diets [19].
Although there are barriers to a vegetarian diet, including provider attitudes [20], cost [21], poor culinary skill [22], palatability, and adherence, pharmacologic BP treatment also presents barriers: adherence to BP medications is estimated to be 50% to 70% [23], and harm due to side effects can preclude use. Thus, providers can present a vegetarian diet as a potentially effective option, depending on patient preference and ability to adhere.
—David M. Levine, MD, MA, New York University
School of Medicine, and Melanie Jay, MD, MS
References
1. Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available at http://handbook.cochrane.org/chapter_10/10_4_4_2_trim_and_fill.htm.
2. Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2013 Nov 12. [Epub ahead of print]
3. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20.
4. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117–24.
5. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N Engl J Med 2001;344:3–10.
6. Appel LJ, Sacks FM, Carey VJ, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids. JAMA 2005;294:2455–64.
7. Rouse IL, Beilin LJ, Armstrong BK, Vandongen R. Blood-pressure–lowering effect of a vegetarian diet: controlled trial in normotensive subjects. Lancet 1983;321:5–10.
8. Margetts BM, Beilin LJ, Vandongen R, Armstrong BK. Vegetarian diet in mild hypertension: a randomised controlled trial. BMJ 1986;293:1468–71.
9. Kestin M, Rouse IL, Correll RA, Nestel PJ. Cardiovascular disease risk factors in free-living men: comparison of two prudent diets, one based on lactoovovegetarianism and the other allowing lean meat. Am J Clin Nutr 1989;50:280–7.
10. Alpert JS. Nutritional advice for the patient with heart disease: what diet should we recommend for our patients? Circulation 2011;124:e258–e260.
11. Gordinier J. Making vegan a new normal. New York Times. 26 Sept 2012. Page D1.
12. Berkow SE, Barnard ND. Blood pressure regulation and vegetarian diets. Nutr Rev 2005;63:1–8.
13. Aburto NJ, Hanson S, Gutierrez H, et al. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ 2013;346:f1378.
14. Berkow SE, Barnard N. Vegetarian diets and weight status. Nutr Rev 2006;64:175–88.
15. Larsson CL, Johansson GK. Dietary intake and nutritional status of young vegans and omnivores in Sweden. Am J Clin Nutr 2002;76:100–6.
16. Ernst E, Pietsch L, Matrai A, Eisenberg J. Blood rheology in vegetarians. Br J Nutr 1986;56:555–60.
17. Iacono JM, Dougherty RM. Effects of polyunsaturated fats on blood pressure. Annu Rev Nutr 1993;13:243–60.
18. Ferdowsian HR, Barnard ND, Hoover VJ, et al. A multicomponent intervention reduces body weight and cardiovascular risk at a GEICO corporate site. Am J Health Promot 2010;24:384–7.
19. Brugts JJ, Ninomiya T, Boersma E, et al. The consistency of the treatment effect of an ACE-inhibitor based treatment regimen in patients with vascular disease or high risk of vascular disease: a combined analysis of individual data of ADVANCE, EUROPA, and PROGRESS trials. Eur Heart J 2009;30:1385–94.
20. Berman BM, Singh BB, Hartnoll SM, et al. Primary care physicians and complementary-alternative medicine: training, attitudes, and practice patterns. Am Board Fam Pract 1998;11:272–81.
21. Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr 2005;82(1 Suppl):265S-273S.
22. Lea EJ, Crawford D, Worsley A. Public views of the benefits and barriers to the consumption of a plant-based diet. Eur J Clin Nutr 2006;60:828–37.
23. Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressure–lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med 2004;164:722–32.
Study Overview
Objective. To determine the association between a vegetarian diet and blood pressure (BP).
Design. Systematic review and meta-analysis of controlled clinical trials and observational studies.
Setting and participants. MEDLINE and Web of Science were respectively searched for English articles published between 1946 to October 2013 and 1900 to November 2013. Inclusion criteria were age > 20 years and vegetarian diet. This included a vegan diet (omitting all animal products), ovo/lacto/pesco vegetarian diet (including eggs/dairy/fish), or semi-vegetarian diet (meat or fish rarely). Exclusion criteria included studies of twins, a multipronged intervention, describing only categorical BP, and reliance on a case series. A total of 258 records were identified. Seven clinical trials and 32 observational studies met inclusion criteria. The 7 clinical trials encompassed 311 participants (median, 38; range, 11–113) with a mean age of 44.5 years (range, 38.0–54.3). All were open-label, 6 were randomized, and 6 provided food to participants. The 32 observational studies included 21,604 participants (median, 152; range, 20–9242) with a mean age of 46.6 years (range, 28.8–68.4 years). Fifteen of these studies included mixed diet types (vegan, lacto, ovolacto, pesca, and/or semivegetarian).
Main outcome measures. The primary outcome was BP. Differences in systolic BP (SBP) and diastolic BP (DBP) between groups consuming vegetarian or comparison diets were pooled using a random effects model. The study compared clinical trials and observational studies separately. Funnel plots, the Egger test, and the trim-and-fill method were all used to assess and correct for publication bias.
Results. Vegetarian diets in clinical trials were associated with a mean SBP reduction of −4.8 mm Hg (95% confidence interval [CI], −6.6 to −3.1; P < 0.001; I2 = 0; P = 0.45 for heterogeneity) and DBP reduction of −2.2 mm Hg (95% CI, −3.5 to −1.0; P < 0.001; I2 = 0; P= 0.43 for heterogeneity) when compared with omnivorous diets. Observational studies had larger reductions but significant heterogeneity: SBP −6.9 mm Hg (95% CI, −9.1 to −4.7; P < 0.001; I2 = 91.4; P < 0.001 for heterogeneity) and DBP −4.7 mm Hg (95% CI, −6.3 to −3.1; P < 0.001; I2 = 92.6; P < 0.001 for heterogeneity). This heterogeneity was best explained by proportion of men (β −0.03; P < 0.001), baseline SBP (β −0.13; P = 0.003), baseline DBP (β −0.30; P < 0.001), sample size (β 0.001; P< 0.001), and BMI (β −0.46; P = 0.02). This suggests that vegetarian diets and lower BP are more strongly associated in men and those with higher baseline BP and BMI.
Subgroup analysis included stratification by age, gender, BMI, diet type, sample size, diet duration, BP medication use, baseline BP, and geographic region. In subgroup analysis of clinical trials, no statistically significant difference between group variation or heterogeneity existed. In comparison, subgroup analysis of observational studies reduced heterogeneity and often effect size. For example, lower SBP was evident in the majority male subgroups (mean SBP/DBP: –18.5 mm Hg/–10.1 mm Hg).
Publication bias existed for both clinical trials and observational studies. According to trim-and-fill methodology, 3 clinical trials of smaller size and larger BP reduction likely were missing (Egger P = 0.04). Their addition shifted mean SBP reduction from −4.8 mm Hg (−6.6 to −3.1) to −5.2 mm Hg (−6.9 to −3.5). Observational studies lacked medium sized negative trials and were overrepresented by larger positive trials (Egger P < 0.001), although this was not confirmed by trim-and-fill (yet this method performs less well under heterogeneous conditions) [1].
Conclusion. Vegetarian diets, when compared with omnivorous diets, are associated with reductions in BP.
Commentary
Several studies show that dietary modifications are effective in preventing and managing hypertension [2,3]. Landmark randomized trials, including the DASH diet [4], DASH-sodium diet [5], and OmniHeart diets [6], all of which emphasize fruit and vegetable intake but are not vegetarian, have led to SBP and DBP reductions ranging from 5.5 to 9.5 mm Hg and 3.0 to 5.2, respectively. However, the impact of a vegetarian diet still remains debated, particularly given disparate findings among randomized controlled trials (RCTs). For example, findings in the early- and mid-1980s of small RCTs with ovolactovegetarians (a vegetarian who consumes eggs and dairy products but not animal flesh) suggested reductions similar to the pooled SBP reduction of –4.8 mm Hg Yokoyama et al report [7,8]. In contrast, one RCT comparing ovolactovegetarian with lean meat diets failed to show a BP benefit [9]. Striking is the dearth of RCTs in the last 20 years to assist in better estimating this impact, particularly given its continual recommendation in the scientific [10] and lay communities [11]. To the authors’ credit, this is the first meta-analysis and second systematic review of this important relationship [12].
A vegetarian diet likely supports BP reductions through a variety of mechanisms, most notably via an abundance of potassium [13]. Potassium likely promotes vasodilation, which facilitates glomerular filtration, allowing decreased renal sodium reabsorption and decreased platelet aggregation. Other more controversial hypotheses include decreased energy density leading to reduced BMI [14], decreased sodium intake [15], reduced blood viscosity [16], and high polyunsaturated with low saturated fat content [17].
Strengths of this analysis include the large observational sample size, the separate analysis of clinical trials and observational studies, the lengthy search time-frame, the subgroup analyses, and the adjustment for publication bias. Although the overall association was robust throughout, we agree with the authors that large heterogeneity among observational studies, small clinical trial sample sizes, and the variation in what “vegetarian” represents throughout the world and in individual studies all represent limitations. The participants in many of the observational studies could have technically eaten meat with unclear and undefined frequency, and this may have explained the heterogeneity of these studies. Correspondingly, the lack of heterogeneity observed in the clinical trials may be due to the fact that participants were provided meals in 6 out of 7 studies.
It was surprising that only 7 clinical trials were found. The authors utilized 2 databases, but perhaps searching additional databases such as EMBASE or CINAHL would have yielded other pertinent studies. The authors also did not use a bias assessment tool such as that proposed by the Cochrane bias methods group, which could have better discriminated high- from low-quality trials and made for useful subgroup analyses [1]. Similarly, reporting on both attrition and adherence could have assisted in decreasing heterogeneity during subgroup analyses and determining high-quality from low-quality studies. For example, adherence in Ferdowsian et al (vegan diet) was determined by unannounced dietician phone calls and found that only 57% of participants abstained from animal products. This may have been secondary to the study’s design, in that “providing meals” included simply making them an available option at the company cafeteria instead of requiring consumption of a study-specific vegetarian meal [18].
Applications for Clinical Practice
In this meta-analysis, vegetarian diets were associated with –4.8 mm Hg SBP and −2.2 mm Hg DBP reductions, indicating that providers can recommend a vegetarian diet as on par with other lifestyle changes, including low-sodium diet, weight loss, and exercise. A vegetarian diet may be comparable to pharmacologic therapy in magnitude of BP change. Short- and long-term pharmacologic therapy is associated with respective SBP/DBP reductions of –8.3/–3.8 and –5.4/–2.3, not altogether different from reductions seen with vegetarian or vegetable-heavy diets [19].
Although there are barriers to a vegetarian diet, including provider attitudes [20], cost [21], poor culinary skill [22], palatability, and adherence, pharmacologic BP treatment also presents barriers: adherence to BP medications is estimated to be 50% to 70% [23], and harm due to side effects can preclude use. Thus, providers can present a vegetarian diet as a potentially effective option, depending on patient preference and ability to adhere.
—David M. Levine, MD, MA, New York University
School of Medicine, and Melanie Jay, MD, MS
References
1. Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available at http://handbook.cochrane.org/chapter_10/10_4_4_2_trim_and_fill.htm.
2. Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2013 Nov 12. [Epub ahead of print]
3. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20.
4. Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117–24.
5. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N Engl J Med 2001;344:3–10.
6. Appel LJ, Sacks FM, Carey VJ, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids. JAMA 2005;294:2455–64.
7. Rouse IL, Beilin LJ, Armstrong BK, Vandongen R. Blood-pressure–lowering effect of a vegetarian diet: controlled trial in normotensive subjects. Lancet 1983;321:5–10.
8. Margetts BM, Beilin LJ, Vandongen R, Armstrong BK. Vegetarian diet in mild hypertension: a randomised controlled trial. BMJ 1986;293:1468–71.
9. Kestin M, Rouse IL, Correll RA, Nestel PJ. Cardiovascular disease risk factors in free-living men: comparison of two prudent diets, one based on lactoovovegetarianism and the other allowing lean meat. Am J Clin Nutr 1989;50:280–7.
10. Alpert JS. Nutritional advice for the patient with heart disease: what diet should we recommend for our patients? Circulation 2011;124:e258–e260.
11. Gordinier J. Making vegan a new normal. New York Times. 26 Sept 2012. Page D1.
12. Berkow SE, Barnard ND. Blood pressure regulation and vegetarian diets. Nutr Rev 2005;63:1–8.
13. Aburto NJ, Hanson S, Gutierrez H, et al. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ 2013;346:f1378.
14. Berkow SE, Barnard N. Vegetarian diets and weight status. Nutr Rev 2006;64:175–88.
15. Larsson CL, Johansson GK. Dietary intake and nutritional status of young vegans and omnivores in Sweden. Am J Clin Nutr 2002;76:100–6.
16. Ernst E, Pietsch L, Matrai A, Eisenberg J. Blood rheology in vegetarians. Br J Nutr 1986;56:555–60.
17. Iacono JM, Dougherty RM. Effects of polyunsaturated fats on blood pressure. Annu Rev Nutr 1993;13:243–60.
18. Ferdowsian HR, Barnard ND, Hoover VJ, et al. A multicomponent intervention reduces body weight and cardiovascular risk at a GEICO corporate site. Am J Health Promot 2010;24:384–7.
19. Brugts JJ, Ninomiya T, Boersma E, et al. The consistency of the treatment effect of an ACE-inhibitor based treatment regimen in patients with vascular disease or high risk of vascular disease: a combined analysis of individual data of ADVANCE, EUROPA, and PROGRESS trials. Eur Heart J 2009;30:1385–94.
20. Berman BM, Singh BB, Hartnoll SM, et al. Primary care physicians and complementary-alternative medicine: training, attitudes, and practice patterns. Am Board Fam Pract 1998;11:272–81.
21. Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr 2005;82(1 Suppl):265S-273S.
22. Lea EJ, Crawford D, Worsley A. Public views of the benefits and barriers to the consumption of a plant-based diet. Eur J Clin Nutr 2006;60:828–37.
23. Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressure–lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med 2004;164:722–32.




