User login
Trientine reduces NT-proBNP up to 8 weeks in HFrEF: TRACER-HF
In models of HF, intracellular copper depletion is associated with myocardial hypertrophy and fibrosis, and thus an increased risk for cardiac remodeling, James Januzzi, MD, of Massachusetts General Hospital and Harvard Medical School in Boston, told attendees at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) 2023 sessions.
Although trientine has been used for over 40 years to treat Wilson disease – a rare inherited disease characterized by copper overload – “paradoxically, it acts as a copper chaperone and can restore intracellular copper concentrations at low doses,” Dr. Januzzi explained during his presentation of the TRACER-HF results.
Although the dose-ranging study found that at 300 mg twice daily trientine effectively reduced NT-proBNP levels at 4 and 8 weeks, by 12 weeks, the effect had disappeared.
Nevertheless, Dr. Januzzi told the meeting attendees that the same dose was “most consistently” associated with most favorable Kansas City Cardiomyopathy Questionnaire Overall Summary Score (KCCQ-OSS) changes, as well as improvements in left ventricular (LV) function and 6-minute walk distance.
‘Challenging is an understatement’
Asked why the improvement in NT-proBNP levels was no longer evident at week 12, Dr. Januzzi acknowledged, “We just don’t know.” However, the team speculates that the disrupted nature of the study might play a role.
The phase 2, placebo-controlled trial started recruiting at 27 sites in North America in 2019. When the pandemic hit in 2020, enrollment was suspended, then pivoted to China in 2021. A total of 190 participants were ultimately enrolled.
However, 91% of participants in China were finishing their follow-up in late 2022, when the country was hit by a COVID-19 surge, which might have affected the 12-week outcomes – though this is speculation for now.
Overall, participants had a mean age of 57 years; about 80% were men; 91% were Asian; the mean left ventricular ejection fraction (LVEF) was 30%; and most (77%) were New York Heart Association class II. All were stable on optimal drug therapy, including chronic loop diuretics.
All had elevated NT-proBNP: ≥ 400 pg/mL without atrial fibrillation or flutter, or ≥ 1200 pg/mL with atrial fibrillation or flutter.
Participants were randomized to placebo or twice-daily trientine doses of 50 mg, 150 mg, or 300 mg.
The primary endpoint was the proportional change in NT-proBNP from baseline to 12 weeks. Key secondary endpoints included the effect of trientine compared with placebo on mechanistic outcomes such as change in cardiac remodeling indices, 6-minute walk distance, and the KCCQ-OSS.
As noted, the greatest reduction in NT-proBNP at 4 and 8 weeks was in the 300-mg group, with a geometric mean ratio of 0.82 at week 4 vs. 1.03 for placebo; 0.92 for 50 mg; and 0.83 for 150 mg; and 0.79 at week 8 vs 1.02 for placebo; 0.85 for 50 mg; and 0.91 for 150 mg.
LV volumes improved at all doses, though by the most at 50 mg (–11.7 mL).
The change in 6-minute walk distance was greatest at the 300-mg dose at 42 meters.
The responder analysis showed that 300 mg was most consistently associated with most of the favorable KCCQ changes.
From a safety standpoint, trientine was well tolerated without any adverse outcomes. Notably, Dr. Januzzi told meeting attendees, blood pressure and heart rate were not affected by the addition of trientine to background medical care.
In addition, a post hoc interaction was identified between treatment response and a baseline LVEF ≤ 30%, data that, for now, are “compelling but hypothesis-generating,” he said. Data on secondary endpoints specifically for that group “are forthcoming.”
Looking ahead
Dr. Januzzi said in an interview that the team is now finalizing the main report “and will turn our attention to the interaction analyses suggesting exaggerated benefit in those with lower LVEF.
“We are examining all possible options for this novel therapy, which may include progressing to phase 3,” he said.
Challenges going forward include the need to understand which patients are most appropriate for the drug. “Given that it does not affect blood pressure or heart rate, it is an attractive consideration for any patient on guideline-directed medical therapy, but we need to have more clarity about the mechanism of benefit and understanding about the subgroup interactions that we have detected.
“Even in a well-managed population of patients with heart failure, there may still be room for therapies with benefit,” he concluded.
Danyaal Moin, MD, assistant professor of medicine at NYU Langone Health in New York and a specialist in advanced heart failure and transplantation, commented on these findings for this article.
“It is always exciting to consider new pathways to treat patients with systolic dysfunction, given the residual risk even for patients on contemporary quadruple therapy for HFrEF,” he said. “However, certain challenges with this phase 2 study will need to be addressed in an eventual phase 3 clinical trial.
“The study sample was predominately recruited in China and is not necessarily representative of a heart failure population in many clinical practices,” he said.
“It would be important that future studies with trientine-HCL assess endpoints such as heart failure hospitalizations and mortality that would help elucidate where this therapy would stand relative to current established heart failure therapies.”
Longer follow-up is needed and, he noted, “while it appears the investigators will ultimately favor the 300-mg dosage, it is interesting that left ventricular volume indices changed most favorably with the 50-mg dose of the therapy.”
The study was sponsored by Innolife Pharmaceuticals and coordinated by the Baim Institute for Clinical Research in Boston. Dr. Januzzi has received grant support from Innolife. Dr. Moin declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In models of HF, intracellular copper depletion is associated with myocardial hypertrophy and fibrosis, and thus an increased risk for cardiac remodeling, James Januzzi, MD, of Massachusetts General Hospital and Harvard Medical School in Boston, told attendees at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) 2023 sessions.
Although trientine has been used for over 40 years to treat Wilson disease – a rare inherited disease characterized by copper overload – “paradoxically, it acts as a copper chaperone and can restore intracellular copper concentrations at low doses,” Dr. Januzzi explained during his presentation of the TRACER-HF results.
Although the dose-ranging study found that at 300 mg twice daily trientine effectively reduced NT-proBNP levels at 4 and 8 weeks, by 12 weeks, the effect had disappeared.
Nevertheless, Dr. Januzzi told the meeting attendees that the same dose was “most consistently” associated with most favorable Kansas City Cardiomyopathy Questionnaire Overall Summary Score (KCCQ-OSS) changes, as well as improvements in left ventricular (LV) function and 6-minute walk distance.
‘Challenging is an understatement’
Asked why the improvement in NT-proBNP levels was no longer evident at week 12, Dr. Januzzi acknowledged, “We just don’t know.” However, the team speculates that the disrupted nature of the study might play a role.
The phase 2, placebo-controlled trial started recruiting at 27 sites in North America in 2019. When the pandemic hit in 2020, enrollment was suspended, then pivoted to China in 2021. A total of 190 participants were ultimately enrolled.
However, 91% of participants in China were finishing their follow-up in late 2022, when the country was hit by a COVID-19 surge, which might have affected the 12-week outcomes – though this is speculation for now.
Overall, participants had a mean age of 57 years; about 80% were men; 91% were Asian; the mean left ventricular ejection fraction (LVEF) was 30%; and most (77%) were New York Heart Association class II. All were stable on optimal drug therapy, including chronic loop diuretics.
All had elevated NT-proBNP: ≥ 400 pg/mL without atrial fibrillation or flutter, or ≥ 1200 pg/mL with atrial fibrillation or flutter.
Participants were randomized to placebo or twice-daily trientine doses of 50 mg, 150 mg, or 300 mg.
The primary endpoint was the proportional change in NT-proBNP from baseline to 12 weeks. Key secondary endpoints included the effect of trientine compared with placebo on mechanistic outcomes such as change in cardiac remodeling indices, 6-minute walk distance, and the KCCQ-OSS.
As noted, the greatest reduction in NT-proBNP at 4 and 8 weeks was in the 300-mg group, with a geometric mean ratio of 0.82 at week 4 vs. 1.03 for placebo; 0.92 for 50 mg; and 0.83 for 150 mg; and 0.79 at week 8 vs 1.02 for placebo; 0.85 for 50 mg; and 0.91 for 150 mg.
LV volumes improved at all doses, though by the most at 50 mg (–11.7 mL).
The change in 6-minute walk distance was greatest at the 300-mg dose at 42 meters.
The responder analysis showed that 300 mg was most consistently associated with most of the favorable KCCQ changes.
From a safety standpoint, trientine was well tolerated without any adverse outcomes. Notably, Dr. Januzzi told meeting attendees, blood pressure and heart rate were not affected by the addition of trientine to background medical care.
In addition, a post hoc interaction was identified between treatment response and a baseline LVEF ≤ 30%, data that, for now, are “compelling but hypothesis-generating,” he said. Data on secondary endpoints specifically for that group “are forthcoming.”
Looking ahead
Dr. Januzzi said in an interview that the team is now finalizing the main report “and will turn our attention to the interaction analyses suggesting exaggerated benefit in those with lower LVEF.
“We are examining all possible options for this novel therapy, which may include progressing to phase 3,” he said.
Challenges going forward include the need to understand which patients are most appropriate for the drug. “Given that it does not affect blood pressure or heart rate, it is an attractive consideration for any patient on guideline-directed medical therapy, but we need to have more clarity about the mechanism of benefit and understanding about the subgroup interactions that we have detected.
“Even in a well-managed population of patients with heart failure, there may still be room for therapies with benefit,” he concluded.
Danyaal Moin, MD, assistant professor of medicine at NYU Langone Health in New York and a specialist in advanced heart failure and transplantation, commented on these findings for this article.
“It is always exciting to consider new pathways to treat patients with systolic dysfunction, given the residual risk even for patients on contemporary quadruple therapy for HFrEF,” he said. “However, certain challenges with this phase 2 study will need to be addressed in an eventual phase 3 clinical trial.
“The study sample was predominately recruited in China and is not necessarily representative of a heart failure population in many clinical practices,” he said.
“It would be important that future studies with trientine-HCL assess endpoints such as heart failure hospitalizations and mortality that would help elucidate where this therapy would stand relative to current established heart failure therapies.”
Longer follow-up is needed and, he noted, “while it appears the investigators will ultimately favor the 300-mg dosage, it is interesting that left ventricular volume indices changed most favorably with the 50-mg dose of the therapy.”
The study was sponsored by Innolife Pharmaceuticals and coordinated by the Baim Institute for Clinical Research in Boston. Dr. Januzzi has received grant support from Innolife. Dr. Moin declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In models of HF, intracellular copper depletion is associated with myocardial hypertrophy and fibrosis, and thus an increased risk for cardiac remodeling, James Januzzi, MD, of Massachusetts General Hospital and Harvard Medical School in Boston, told attendees at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) 2023 sessions.
Although trientine has been used for over 40 years to treat Wilson disease – a rare inherited disease characterized by copper overload – “paradoxically, it acts as a copper chaperone and can restore intracellular copper concentrations at low doses,” Dr. Januzzi explained during his presentation of the TRACER-HF results.
Although the dose-ranging study found that at 300 mg twice daily trientine effectively reduced NT-proBNP levels at 4 and 8 weeks, by 12 weeks, the effect had disappeared.
Nevertheless, Dr. Januzzi told the meeting attendees that the same dose was “most consistently” associated with most favorable Kansas City Cardiomyopathy Questionnaire Overall Summary Score (KCCQ-OSS) changes, as well as improvements in left ventricular (LV) function and 6-minute walk distance.
‘Challenging is an understatement’
Asked why the improvement in NT-proBNP levels was no longer evident at week 12, Dr. Januzzi acknowledged, “We just don’t know.” However, the team speculates that the disrupted nature of the study might play a role.
The phase 2, placebo-controlled trial started recruiting at 27 sites in North America in 2019. When the pandemic hit in 2020, enrollment was suspended, then pivoted to China in 2021. A total of 190 participants were ultimately enrolled.
However, 91% of participants in China were finishing their follow-up in late 2022, when the country was hit by a COVID-19 surge, which might have affected the 12-week outcomes – though this is speculation for now.
Overall, participants had a mean age of 57 years; about 80% were men; 91% were Asian; the mean left ventricular ejection fraction (LVEF) was 30%; and most (77%) were New York Heart Association class II. All were stable on optimal drug therapy, including chronic loop diuretics.
All had elevated NT-proBNP: ≥ 400 pg/mL without atrial fibrillation or flutter, or ≥ 1200 pg/mL with atrial fibrillation or flutter.
Participants were randomized to placebo or twice-daily trientine doses of 50 mg, 150 mg, or 300 mg.
The primary endpoint was the proportional change in NT-proBNP from baseline to 12 weeks. Key secondary endpoints included the effect of trientine compared with placebo on mechanistic outcomes such as change in cardiac remodeling indices, 6-minute walk distance, and the KCCQ-OSS.
As noted, the greatest reduction in NT-proBNP at 4 and 8 weeks was in the 300-mg group, with a geometric mean ratio of 0.82 at week 4 vs. 1.03 for placebo; 0.92 for 50 mg; and 0.83 for 150 mg; and 0.79 at week 8 vs 1.02 for placebo; 0.85 for 50 mg; and 0.91 for 150 mg.
LV volumes improved at all doses, though by the most at 50 mg (–11.7 mL).
The change in 6-minute walk distance was greatest at the 300-mg dose at 42 meters.
The responder analysis showed that 300 mg was most consistently associated with most of the favorable KCCQ changes.
From a safety standpoint, trientine was well tolerated without any adverse outcomes. Notably, Dr. Januzzi told meeting attendees, blood pressure and heart rate were not affected by the addition of trientine to background medical care.
In addition, a post hoc interaction was identified between treatment response and a baseline LVEF ≤ 30%, data that, for now, are “compelling but hypothesis-generating,” he said. Data on secondary endpoints specifically for that group “are forthcoming.”
Looking ahead
Dr. Januzzi said in an interview that the team is now finalizing the main report “and will turn our attention to the interaction analyses suggesting exaggerated benefit in those with lower LVEF.
“We are examining all possible options for this novel therapy, which may include progressing to phase 3,” he said.
Challenges going forward include the need to understand which patients are most appropriate for the drug. “Given that it does not affect blood pressure or heart rate, it is an attractive consideration for any patient on guideline-directed medical therapy, but we need to have more clarity about the mechanism of benefit and understanding about the subgroup interactions that we have detected.
“Even in a well-managed population of patients with heart failure, there may still be room for therapies with benefit,” he concluded.
Danyaal Moin, MD, assistant professor of medicine at NYU Langone Health in New York and a specialist in advanced heart failure and transplantation, commented on these findings for this article.
“It is always exciting to consider new pathways to treat patients with systolic dysfunction, given the residual risk even for patients on contemporary quadruple therapy for HFrEF,” he said. “However, certain challenges with this phase 2 study will need to be addressed in an eventual phase 3 clinical trial.
“The study sample was predominately recruited in China and is not necessarily representative of a heart failure population in many clinical practices,” he said.
“It would be important that future studies with trientine-HCL assess endpoints such as heart failure hospitalizations and mortality that would help elucidate where this therapy would stand relative to current established heart failure therapies.”
Longer follow-up is needed and, he noted, “while it appears the investigators will ultimately favor the 300-mg dosage, it is interesting that left ventricular volume indices changed most favorably with the 50-mg dose of the therapy.”
The study was sponsored by Innolife Pharmaceuticals and coordinated by the Baim Institute for Clinical Research in Boston. Dr. Januzzi has received grant support from Innolife. Dr. Moin declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ESC HEART FAILURE 2023
Diabetes, cholesterol meds use drops after bariatric surgery
compared with patients with obesity who did not have such an operation. However, these declines didn’t extend to cardiovascular medication use.
“In this study, undergoing bariatric surgery was associated with a substantial and long-lasting reduction in the use of lipid-lowering and antidiabetic medications, compared with no surgery for obesity, while for cardiovascular medications this reduction was only transient,” the authors report in research published in JAMA Surgery.
“The results can aid in informed decision-making when considering bariatric surgery for patients with morbid obesity and inform patients and professionals about the expected long-term effects of medication use for obesity-related comorbidities,” they write.
The study “highlights the benefits of mandated databases that report metabolic bariatric surgery, obesity-related comorbidities, and medications,” writes Paulina Salminen, MD, in an accompanying editorial.
However, key limitations include a lack of weight data, which is important in light of previous studies showing that suboptimal weight loss after bariatric surgery is linked to a higher incidence of type 2 diabetes, dyslipidemia, and hypertension, note Dr. Salminen, of the department of digestive surgery, University Hospital, Turku, Finland, and colleagues.
Swedish, Finnish obesity data probed
When significant weight loss is achieved, bariatric surgery has been well documented to be associated with improvements in a variety of comorbidities, quality of life, and even life expectancy.
Key comorbidities shown to improve with the surgery include hyperlipidemia, cardiovascular disease, and type 2 diabetes.
However, data are lacking on the association between bariatric surgery and the use of medications for those conditions, particularly compared with people with obesity who don’t have bariatric surgery.
To investigate, first author Joonas H. Kauppila, MD, PhD, of Upper Gastrointestinal Surgery, Karolinska University Hospital, Stockholm, and colleagues conducted a population-based cohort study, evaluating data on 26,396 patients who underwent bariatric surgery with gastric bypass or sleeve gastrectomy in Sweden between 2005 and 2020 or Finland between 1995 and 2018.
Overall, 66.4% of patients were women and their median age was 50.
They were compared with five times as many matched controls with obesity who had not had bariatric surgery from the same population databases, representing a total of 131,980 patients who were matched based on age, country, sex, calendar year, and medication use.
In terms of lipid-lowering medication, rates of use after bariatric surgery decreased from 20.3% at baseline to 12.9% after 2 years and bounced back somewhat to 17.6% after 15 years. Comparatively, in the no surgery group, baseline lipid-lowering medication use of 21.0% increased to 44.6% after 15 years, more than twice the rate of usage in the bariatric surgery group in the same period.
Antidiabetic medications were used by 27.7% of patients in the bariatric surgery group at baseline, with a drop to 10.0% after 2 years, followed by an increase to 23.5% after 15 years. In the no surgery group, the rate of antidiabetic medication use steadily increased from 27.7% at baseline to 54.2% after 15 years, which again was nearly double the rate of antidiabetic medication use in the bariatric surgery group at 15 years.
Meanwhile, cardiovascular medications were used by 60.2% of patients receiving bariatric surgery at baseline, with the rate decreasing to 43.2% after 2 years but increasing to 74.6% after 15 years. Among the nonbariatric surgery patients, use of cardiovascular medications increased from 54.4% at baseline to 83.3% after 15 years.
Causes?
As for the cause of the lack of any decline in use of cardiovascular medications versus other medications in the surgery patients, the authors speculate that the effect “may be related to aging and regain of weight over time after bariatric surgery, a phenomenon caused by hormonal, dietary, physical, and behavioral factors.”
“In contrast, as expected, a gradual increase in the use of all three medication groups was observed over time among the patients treated with no surgery for obesity,” they note.
The lower medication use with bariatric surgery can also translate to economic benefits, the authors add.
“Economically, the long-lasting reductions in medication use for hyperlipidemia, cardiovascular morbidity, and diabetes suggest that surgical treatment of morbid obesity may infer savings in medication expenses for patients, health care, and society,” they report.
“Future research may focus on subgroups that are most likely to benefit from bariatric surgery, including resolution and severity of comorbidities,” they continue.
In their editorial, Dr. Salminen and colleagues note that previous research has shown remission of dyslipidemia in up to 70% of patients after bariatric surgery that was independent of weight loss, which appears to support the sustained reduction in lipid-lowering medications following surgery observed in the current study, suggesting some benefits on lipids beyond weight loss.
Other limitations, however, include that the bariatric surgery group in the study was older and had more comorbidities than those in previous bariatric surgery studies.
“Future studies should assess this in a younger cohort with less disease at baseline and differentiation within cardiovascular disease regarding at least hypertension, ischemic heart disease, and heart failure,” the authors conclude.
The authors have reported no relevant financial relationships. Dr. Salminen has reported receiving grants from the Sigrid Jusélius Foundation, Academy of Finland, Government Research Grant Foundation, and the University of Turku (Finland).
A version of this article first appeared on Medscape.com.
compared with patients with obesity who did not have such an operation. However, these declines didn’t extend to cardiovascular medication use.
“In this study, undergoing bariatric surgery was associated with a substantial and long-lasting reduction in the use of lipid-lowering and antidiabetic medications, compared with no surgery for obesity, while for cardiovascular medications this reduction was only transient,” the authors report in research published in JAMA Surgery.
“The results can aid in informed decision-making when considering bariatric surgery for patients with morbid obesity and inform patients and professionals about the expected long-term effects of medication use for obesity-related comorbidities,” they write.
The study “highlights the benefits of mandated databases that report metabolic bariatric surgery, obesity-related comorbidities, and medications,” writes Paulina Salminen, MD, in an accompanying editorial.
However, key limitations include a lack of weight data, which is important in light of previous studies showing that suboptimal weight loss after bariatric surgery is linked to a higher incidence of type 2 diabetes, dyslipidemia, and hypertension, note Dr. Salminen, of the department of digestive surgery, University Hospital, Turku, Finland, and colleagues.
Swedish, Finnish obesity data probed
When significant weight loss is achieved, bariatric surgery has been well documented to be associated with improvements in a variety of comorbidities, quality of life, and even life expectancy.
Key comorbidities shown to improve with the surgery include hyperlipidemia, cardiovascular disease, and type 2 diabetes.
However, data are lacking on the association between bariatric surgery and the use of medications for those conditions, particularly compared with people with obesity who don’t have bariatric surgery.
To investigate, first author Joonas H. Kauppila, MD, PhD, of Upper Gastrointestinal Surgery, Karolinska University Hospital, Stockholm, and colleagues conducted a population-based cohort study, evaluating data on 26,396 patients who underwent bariatric surgery with gastric bypass or sleeve gastrectomy in Sweden between 2005 and 2020 or Finland between 1995 and 2018.
Overall, 66.4% of patients were women and their median age was 50.
They were compared with five times as many matched controls with obesity who had not had bariatric surgery from the same population databases, representing a total of 131,980 patients who were matched based on age, country, sex, calendar year, and medication use.
In terms of lipid-lowering medication, rates of use after bariatric surgery decreased from 20.3% at baseline to 12.9% after 2 years and bounced back somewhat to 17.6% after 15 years. Comparatively, in the no surgery group, baseline lipid-lowering medication use of 21.0% increased to 44.6% after 15 years, more than twice the rate of usage in the bariatric surgery group in the same period.
Antidiabetic medications were used by 27.7% of patients in the bariatric surgery group at baseline, with a drop to 10.0% after 2 years, followed by an increase to 23.5% after 15 years. In the no surgery group, the rate of antidiabetic medication use steadily increased from 27.7% at baseline to 54.2% after 15 years, which again was nearly double the rate of antidiabetic medication use in the bariatric surgery group at 15 years.
Meanwhile, cardiovascular medications were used by 60.2% of patients receiving bariatric surgery at baseline, with the rate decreasing to 43.2% after 2 years but increasing to 74.6% after 15 years. Among the nonbariatric surgery patients, use of cardiovascular medications increased from 54.4% at baseline to 83.3% after 15 years.
Causes?
As for the cause of the lack of any decline in use of cardiovascular medications versus other medications in the surgery patients, the authors speculate that the effect “may be related to aging and regain of weight over time after bariatric surgery, a phenomenon caused by hormonal, dietary, physical, and behavioral factors.”
“In contrast, as expected, a gradual increase in the use of all three medication groups was observed over time among the patients treated with no surgery for obesity,” they note.
The lower medication use with bariatric surgery can also translate to economic benefits, the authors add.
“Economically, the long-lasting reductions in medication use for hyperlipidemia, cardiovascular morbidity, and diabetes suggest that surgical treatment of morbid obesity may infer savings in medication expenses for patients, health care, and society,” they report.
“Future research may focus on subgroups that are most likely to benefit from bariatric surgery, including resolution and severity of comorbidities,” they continue.
In their editorial, Dr. Salminen and colleagues note that previous research has shown remission of dyslipidemia in up to 70% of patients after bariatric surgery that was independent of weight loss, which appears to support the sustained reduction in lipid-lowering medications following surgery observed in the current study, suggesting some benefits on lipids beyond weight loss.
Other limitations, however, include that the bariatric surgery group in the study was older and had more comorbidities than those in previous bariatric surgery studies.
“Future studies should assess this in a younger cohort with less disease at baseline and differentiation within cardiovascular disease regarding at least hypertension, ischemic heart disease, and heart failure,” the authors conclude.
The authors have reported no relevant financial relationships. Dr. Salminen has reported receiving grants from the Sigrid Jusélius Foundation, Academy of Finland, Government Research Grant Foundation, and the University of Turku (Finland).
A version of this article first appeared on Medscape.com.
compared with patients with obesity who did not have such an operation. However, these declines didn’t extend to cardiovascular medication use.
“In this study, undergoing bariatric surgery was associated with a substantial and long-lasting reduction in the use of lipid-lowering and antidiabetic medications, compared with no surgery for obesity, while for cardiovascular medications this reduction was only transient,” the authors report in research published in JAMA Surgery.
“The results can aid in informed decision-making when considering bariatric surgery for patients with morbid obesity and inform patients and professionals about the expected long-term effects of medication use for obesity-related comorbidities,” they write.
The study “highlights the benefits of mandated databases that report metabolic bariatric surgery, obesity-related comorbidities, and medications,” writes Paulina Salminen, MD, in an accompanying editorial.
However, key limitations include a lack of weight data, which is important in light of previous studies showing that suboptimal weight loss after bariatric surgery is linked to a higher incidence of type 2 diabetes, dyslipidemia, and hypertension, note Dr. Salminen, of the department of digestive surgery, University Hospital, Turku, Finland, and colleagues.
Swedish, Finnish obesity data probed
When significant weight loss is achieved, bariatric surgery has been well documented to be associated with improvements in a variety of comorbidities, quality of life, and even life expectancy.
Key comorbidities shown to improve with the surgery include hyperlipidemia, cardiovascular disease, and type 2 diabetes.
However, data are lacking on the association between bariatric surgery and the use of medications for those conditions, particularly compared with people with obesity who don’t have bariatric surgery.
To investigate, first author Joonas H. Kauppila, MD, PhD, of Upper Gastrointestinal Surgery, Karolinska University Hospital, Stockholm, and colleagues conducted a population-based cohort study, evaluating data on 26,396 patients who underwent bariatric surgery with gastric bypass or sleeve gastrectomy in Sweden between 2005 and 2020 or Finland between 1995 and 2018.
Overall, 66.4% of patients were women and their median age was 50.
They were compared with five times as many matched controls with obesity who had not had bariatric surgery from the same population databases, representing a total of 131,980 patients who were matched based on age, country, sex, calendar year, and medication use.
In terms of lipid-lowering medication, rates of use after bariatric surgery decreased from 20.3% at baseline to 12.9% after 2 years and bounced back somewhat to 17.6% after 15 years. Comparatively, in the no surgery group, baseline lipid-lowering medication use of 21.0% increased to 44.6% after 15 years, more than twice the rate of usage in the bariatric surgery group in the same period.
Antidiabetic medications were used by 27.7% of patients in the bariatric surgery group at baseline, with a drop to 10.0% after 2 years, followed by an increase to 23.5% after 15 years. In the no surgery group, the rate of antidiabetic medication use steadily increased from 27.7% at baseline to 54.2% after 15 years, which again was nearly double the rate of antidiabetic medication use in the bariatric surgery group at 15 years.
Meanwhile, cardiovascular medications were used by 60.2% of patients receiving bariatric surgery at baseline, with the rate decreasing to 43.2% after 2 years but increasing to 74.6% after 15 years. Among the nonbariatric surgery patients, use of cardiovascular medications increased from 54.4% at baseline to 83.3% after 15 years.
Causes?
As for the cause of the lack of any decline in use of cardiovascular medications versus other medications in the surgery patients, the authors speculate that the effect “may be related to aging and regain of weight over time after bariatric surgery, a phenomenon caused by hormonal, dietary, physical, and behavioral factors.”
“In contrast, as expected, a gradual increase in the use of all three medication groups was observed over time among the patients treated with no surgery for obesity,” they note.
The lower medication use with bariatric surgery can also translate to economic benefits, the authors add.
“Economically, the long-lasting reductions in medication use for hyperlipidemia, cardiovascular morbidity, and diabetes suggest that surgical treatment of morbid obesity may infer savings in medication expenses for patients, health care, and society,” they report.
“Future research may focus on subgroups that are most likely to benefit from bariatric surgery, including resolution and severity of comorbidities,” they continue.
In their editorial, Dr. Salminen and colleagues note that previous research has shown remission of dyslipidemia in up to 70% of patients after bariatric surgery that was independent of weight loss, which appears to support the sustained reduction in lipid-lowering medications following surgery observed in the current study, suggesting some benefits on lipids beyond weight loss.
Other limitations, however, include that the bariatric surgery group in the study was older and had more comorbidities than those in previous bariatric surgery studies.
“Future studies should assess this in a younger cohort with less disease at baseline and differentiation within cardiovascular disease regarding at least hypertension, ischemic heart disease, and heart failure,” the authors conclude.
The authors have reported no relevant financial relationships. Dr. Salminen has reported receiving grants from the Sigrid Jusélius Foundation, Academy of Finland, Government Research Grant Foundation, and the University of Turku (Finland).
A version of this article first appeared on Medscape.com.
FROM JAMA SURGERY
Severe hydroxychloroquine nonadherence linked to worse SLE outcomes
SEOUL, SOUTH KOREA – Regular testing of hydroxychloroquine levels in patients with systemic lupus erythematosus – especially those who are experiencing a disease flare – could help to identify patients who are not taking their treatment and are at risk of worse outcomes.
Data presented at an international congress on systemic lupus erythematosus showed that 7.3% of patients with SLE are severely nonadherent to their medication and have a higher risk of flare, early damage, and mortality.
Rheumatologist Nathalie Costedoat-Chalumeau, MD, PhD, professor of internal medicine at Cochin Hospital, Paris, presented data from 660 patients enrolled in the international longitudinal SLICC Inception Cohort, who had all been on hydroxychloroquine therapy for at least 3 months at baseline.
Patients’ serum hydroxychloroquine levels were measured at baseline and follow-up, and severe nonadherence was defined as below 106 ng/mL for those on 400 mg/day or 53 ng/mL for those on 200 mg/day.
Dr. Costedoat-Chalumeau said that those thresholds were chosen based on earlier work that analyzed the blood concentration of hydroxychloroquine in a group of patients and identified a group with very low concentrations corresponding to severe nonadherence.
“Since then, it has been reproduced by others with the same threshold,” she said. “When you have very low levels of hydroxychloroquine in their blood, you know that your patients don’t take their treatment.”
In the present study, the 7.3% of patients who met the criteria for severe nonadherence had a significant 3.3-fold higher risk of disease flare within a year of enrollment than did those who were adherent. They also had significantly higher mortality at 5 years after enrollment.
While the study didn’t show a significant difference in the level of damage at 5 years – defined as a worsening of their SLICC damage index – Dr. Costedoat-Chalumeau said they saw significantly greater damage occurring at 1, 2, and 3 years after enrollment among those who were severely nonadherent.
The challenge with recognizing these nonadherent patients is that they have no obvious differences at baseline from those who are adherent, Dr. Costedoat-Chalumeau said. The rates of nonadherence were similar regardless of what dose the patient was on, their ethnicity, gender, education level, or other demographic variables.
“I believe strongly that there is a benefit of testing hydroxychloroquine levels in the blood or serum to detect severe nonadherence,” she said.
At Dr. Costedoat-Chalumeau’s clinic, patients’ hydroxychloroquine levels are tested at every clinic visit, she said in an interview, and especially if they are experiencing a disease flare. “We want to know if the flare is because the patient is not taking the treatment or if it’s because the treatment is not effective, which is very different in terms of management,” she said. She recommended waiting at least 1 month after patients start treatment before measuring their hydroxychloroquine levels.
As to why some patients choose to stop taking their medication, Dr. Costedoat-Chalumeau said sometimes it was because patients were worried about side effects, but others were also unclear about why they needed to keep taking hydroxychloroquine.
“They think steroids are effective because when they take it they are better, but they don’t see the effect of hydroxychloroquine,” she said. “You have to explain that it doesn’t work the same.”
Commenting on the findings, session chair Joan Merrill, MD, professor of medicine at the University of Oklahoma Health Sciences Center, Oklahoma City, said the data show that severe nonadherence does have prognostic significance. “Many patients with SLE have low-grade disease or inflammation in the blood vessels that may not be clinically apparent and which hydroxychloroquine can help, so it might be wise to routinely get blood levels,” she said.
Dr. Costedoat-Chalumeau reported no relevant financial relationships apart from unrestricted institutional research grants from UCB and Roche.
SEOUL, SOUTH KOREA – Regular testing of hydroxychloroquine levels in patients with systemic lupus erythematosus – especially those who are experiencing a disease flare – could help to identify patients who are not taking their treatment and are at risk of worse outcomes.
Data presented at an international congress on systemic lupus erythematosus showed that 7.3% of patients with SLE are severely nonadherent to their medication and have a higher risk of flare, early damage, and mortality.
Rheumatologist Nathalie Costedoat-Chalumeau, MD, PhD, professor of internal medicine at Cochin Hospital, Paris, presented data from 660 patients enrolled in the international longitudinal SLICC Inception Cohort, who had all been on hydroxychloroquine therapy for at least 3 months at baseline.
Patients’ serum hydroxychloroquine levels were measured at baseline and follow-up, and severe nonadherence was defined as below 106 ng/mL for those on 400 mg/day or 53 ng/mL for those on 200 mg/day.
Dr. Costedoat-Chalumeau said that those thresholds were chosen based on earlier work that analyzed the blood concentration of hydroxychloroquine in a group of patients and identified a group with very low concentrations corresponding to severe nonadherence.
“Since then, it has been reproduced by others with the same threshold,” she said. “When you have very low levels of hydroxychloroquine in their blood, you know that your patients don’t take their treatment.”
In the present study, the 7.3% of patients who met the criteria for severe nonadherence had a significant 3.3-fold higher risk of disease flare within a year of enrollment than did those who were adherent. They also had significantly higher mortality at 5 years after enrollment.
While the study didn’t show a significant difference in the level of damage at 5 years – defined as a worsening of their SLICC damage index – Dr. Costedoat-Chalumeau said they saw significantly greater damage occurring at 1, 2, and 3 years after enrollment among those who were severely nonadherent.
The challenge with recognizing these nonadherent patients is that they have no obvious differences at baseline from those who are adherent, Dr. Costedoat-Chalumeau said. The rates of nonadherence were similar regardless of what dose the patient was on, their ethnicity, gender, education level, or other demographic variables.
“I believe strongly that there is a benefit of testing hydroxychloroquine levels in the blood or serum to detect severe nonadherence,” she said.
At Dr. Costedoat-Chalumeau’s clinic, patients’ hydroxychloroquine levels are tested at every clinic visit, she said in an interview, and especially if they are experiencing a disease flare. “We want to know if the flare is because the patient is not taking the treatment or if it’s because the treatment is not effective, which is very different in terms of management,” she said. She recommended waiting at least 1 month after patients start treatment before measuring their hydroxychloroquine levels.
As to why some patients choose to stop taking their medication, Dr. Costedoat-Chalumeau said sometimes it was because patients were worried about side effects, but others were also unclear about why they needed to keep taking hydroxychloroquine.
“They think steroids are effective because when they take it they are better, but they don’t see the effect of hydroxychloroquine,” she said. “You have to explain that it doesn’t work the same.”
Commenting on the findings, session chair Joan Merrill, MD, professor of medicine at the University of Oklahoma Health Sciences Center, Oklahoma City, said the data show that severe nonadherence does have prognostic significance. “Many patients with SLE have low-grade disease or inflammation in the blood vessels that may not be clinically apparent and which hydroxychloroquine can help, so it might be wise to routinely get blood levels,” she said.
Dr. Costedoat-Chalumeau reported no relevant financial relationships apart from unrestricted institutional research grants from UCB and Roche.
SEOUL, SOUTH KOREA – Regular testing of hydroxychloroquine levels in patients with systemic lupus erythematosus – especially those who are experiencing a disease flare – could help to identify patients who are not taking their treatment and are at risk of worse outcomes.
Data presented at an international congress on systemic lupus erythematosus showed that 7.3% of patients with SLE are severely nonadherent to their medication and have a higher risk of flare, early damage, and mortality.
Rheumatologist Nathalie Costedoat-Chalumeau, MD, PhD, professor of internal medicine at Cochin Hospital, Paris, presented data from 660 patients enrolled in the international longitudinal SLICC Inception Cohort, who had all been on hydroxychloroquine therapy for at least 3 months at baseline.
Patients’ serum hydroxychloroquine levels were measured at baseline and follow-up, and severe nonadherence was defined as below 106 ng/mL for those on 400 mg/day or 53 ng/mL for those on 200 mg/day.
Dr. Costedoat-Chalumeau said that those thresholds were chosen based on earlier work that analyzed the blood concentration of hydroxychloroquine in a group of patients and identified a group with very low concentrations corresponding to severe nonadherence.
“Since then, it has been reproduced by others with the same threshold,” she said. “When you have very low levels of hydroxychloroquine in their blood, you know that your patients don’t take their treatment.”
In the present study, the 7.3% of patients who met the criteria for severe nonadherence had a significant 3.3-fold higher risk of disease flare within a year of enrollment than did those who were adherent. They also had significantly higher mortality at 5 years after enrollment.
While the study didn’t show a significant difference in the level of damage at 5 years – defined as a worsening of their SLICC damage index – Dr. Costedoat-Chalumeau said they saw significantly greater damage occurring at 1, 2, and 3 years after enrollment among those who were severely nonadherent.
The challenge with recognizing these nonadherent patients is that they have no obvious differences at baseline from those who are adherent, Dr. Costedoat-Chalumeau said. The rates of nonadherence were similar regardless of what dose the patient was on, their ethnicity, gender, education level, or other demographic variables.
“I believe strongly that there is a benefit of testing hydroxychloroquine levels in the blood or serum to detect severe nonadherence,” she said.
At Dr. Costedoat-Chalumeau’s clinic, patients’ hydroxychloroquine levels are tested at every clinic visit, she said in an interview, and especially if they are experiencing a disease flare. “We want to know if the flare is because the patient is not taking the treatment or if it’s because the treatment is not effective, which is very different in terms of management,” she said. She recommended waiting at least 1 month after patients start treatment before measuring their hydroxychloroquine levels.
As to why some patients choose to stop taking their medication, Dr. Costedoat-Chalumeau said sometimes it was because patients were worried about side effects, but others were also unclear about why they needed to keep taking hydroxychloroquine.
“They think steroids are effective because when they take it they are better, but they don’t see the effect of hydroxychloroquine,” she said. “You have to explain that it doesn’t work the same.”
Commenting on the findings, session chair Joan Merrill, MD, professor of medicine at the University of Oklahoma Health Sciences Center, Oklahoma City, said the data show that severe nonadherence does have prognostic significance. “Many patients with SLE have low-grade disease or inflammation in the blood vessels that may not be clinically apparent and which hydroxychloroquine can help, so it might be wise to routinely get blood levels,” she said.
Dr. Costedoat-Chalumeau reported no relevant financial relationships apart from unrestricted institutional research grants from UCB and Roche.
AT LUPUS 2023
Investigating the etiology of recurrent pregnancy loss
With attention to the timing of loss
Introduction: Reassurance through pregnancy loss and workups
Pregnancy loss is not an uncommon complication but it can be associated with significant stress among parents and loved ones when it occurs. Especially when recurrent, it also becomes a medical dilemma for physicians and nurses because the cause is not always obvious immediately, and even with exploration, the cause may not always be found.
First and foremost, it is important that physicians provide counseling and reassurance to families experiencing loss, and that they encourage a level of patience while the investigation for loss is done. Investigations tend not to be linear. One must look at a number of diagnostic areas including genetics, anatomy, immunology, and infections.
Even with an extensive workup, what often is found are potential associations rather than precise causes. For instance, one may find that certain antibodies or certain conditions are present, or that certain anatomic structures are abnormal. While such findings are not necessarily causative, there are therapeutic interventions that we can offer to address many of the conditions (e.g., surgical correction of the septate uterus, and low-dose aspirin and heparin for antiphospholipid syndrome).
Less than 1% of couples experience recurrent pregnancy loss (traditionally defined as three or more losses), so parents who experience one loss should be given reassurance that their loss was likely a sporadic miscarriage and that chances of recurrence will be low. Even as workups proceed, reassurance is important.
For this month’s Master Class in Obstetrics we’ve invited Wendy L. Kinzler, MD, and Anthony Vintzileos, MD, both of whom have expertise in the area of recurrent pregnancy loss, to review the potential causes and the management approach. They focus on the first trimester, when genetic causes predominate, and the early second trimester, when undetected uterine factors can be at play. They explain that the gestational age at which recurrent losses occur is an important factor in decoding etiology and management.
Dr. Kinzler is associate dean, graduate medical education, and professor of obstetrics and gynecology at NYU Long Island School of Medicine, Mineola, N.Y., and Dr. Vintzileos is chief patient safety officer for obstetrics, Northwell Health–Western Region, and professor in the department of obstetrics and gynecology in the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, N.Y. Dr. Kinzler and Dr. Vintzileos reported no relevant disclosures.
E. Albert Reece, MD, PhD, MBA, a maternal-fetal medicine specialist, is dean emeritus of the University of Maryland School of Medicine, former university executive vice president; currently the endowed professor and director of the Center for Advanced Research Training and Innovation (CARTI), and senior scientist in the Center for Birth Defects Research. Dr. Reece reported no relevant disclosures. He is the medical editor of this column. Contact him at [email protected].
Investigating the etiology of recurrent pregnancy loss
Pregnancy loss is defined as a loss occurring at < 20 weeks’ gestation.
Consideration of the timing of the pregnancy loss can provide a useful guide to this evaluation, as etiologies vary depending on when in gestation losses occur. In this Master Class, we will address the evaluation of pregnancy loss at < 20 weeks’ gestation, with particular attention to first trimester and early second trimester causes. Literature on the role of the cervix and intra-amniotic infection in midtrimester loss is extensive and will not be covered here.
Although early first trimester miscarriage is common, occurring in approximately 15% of clinically recognized pregnancies, only 2%-3% of couples experience two or more miscarriages and 0.5%-1% experience three or more.
When to begin a diagnostic workup should be part of a shared decision-making process, taking into consideration future family planning, parity, number of previous losses, and notably, the gestational age at which loss(es) occurred. Recurrence rates for first trimester miscarriage are similar after two versus three consecutive losses and either situation usually prompts an evaluation, whereas any second-trimester loss should be evaluated.
Increasingly, we are appreciating the value of a more targeted, gestational age–driven approach to the evaluation of pregnancy loss in an attempt to provide grieving parents with useful information without subjecting them to a wide array of expensive and unnecessary tests.
Genetic causes
The earlier the pregnancy loss, the more likely it is the result of abnormal fetal genetics. Genetic factors should be considered as the most likely cause for first trimester pregnancy losses (especially those occurring at < 10 weeks’ gestation), the most frequent being autosomal trisomies or monosomy X. The vast majority of trisomy conceptuses are sporadic in nature and are related to the natural aging process of the ovary (increasing the rate of meiotic nondisjunction).
If fetal aneuploidy is identified in a pregnancy loss, couples can be counseled about the definitive cause of the loss and can be counseled about recurrence based on age-related risks and/or tests of ovarian reserve. Recurrent pregnancy loss (RPL) is only rarely associated with a parental translocation (< 5%). Testing parental karyotypes should be reserved for cases in which the fetal karyotypes are unknown or in which an unbalanced translocation was identified in the fetus.
When a first trimester pregnancy loss is diagnosed, chorionic villus sampling (CVS) with microarray testing is the most reliable and comprehensive method for evaluating potential genetic causes. It provides valuable information even when cells are not viable and reduces the risk of maternal cell contamination – two significant limitations to standard karyotype analysis performed on tissue passed spontaneously or at the time of D&C. Studies of products of conception (POC) testing with microarray have documented the detection of abnormalities in an additional 10%-15% of cases compared with traditional karyotype analysis.
When CVS is not feasible, testing maternal serum for cell-free DNA is a reasonable alternative. In a prospective cohort study of 50 maternal blood samples taken after fetal demise, 76% of samples yielded cell-free DNA results, meaning fetal fractions were within the detectable range. The higher the gestational age at the time of loss, the higher the chance of obtaining a result: Findings in the study were possible in 88% of samples when the gestational age was 8 weeks or greater, and in 53% of cases involving a lower gestational age. The time from demise to blood draw did not affect the likelihood of obtaining a result (Obstet Gynecol. 2015 Jun;125[6]:1321-29).
When neither CVS nor cell-free DNA analysis is feasible, analysis of either spontaneously passed tissue or tissue obtained at the time of a D&C may still be worthwhile. Maternal cell contamination, of course, is the main downside.
A paper published in 2020 documented the value of refocusing the initial workup. Researchers reported that 57% of 1,400 cases of recurrent pregnancy loss went unexplained using the 2012 ASRM guidelines, which included parental karyotyping but not POC cytogenetic analysis. When parental karyotypes were omitted from the initial workup and POC analysis with 24-chromosome microarray was added, at least one potential explanation for loss could be identified in 92% of cases. Only 8% were left “unexplained” (Curr Opin Obstet Gynecol. 2020 Oct;32[5]:371-9).
When genetics are ruled out
Issues that are top of mind when we lack genetic information or when genetic causes are ruled out include maternal metabolic disorders (uncontrolled diabetes, obesity, uncontrolled thyroid disease), environmental exposures (smoking), uterine abnormalities, and antiphospholipid syndrome.
Thorough evaluation of the uterine cavity after recurrent first trimester miscarriage – or after any second trimester loss – is too often a missing element of investigation. It is a vital component of the evaluation, and information about uterine structure is easily obtained.
A saline infusion sonogram (SIS) allows us to look at the external contour of the uterus, assess the myometrium for muscular abnormalities, visualize the uterine lining, and assess uterine orientation. Performed in the nonpregnant state, and ideally coupled with 3D technology, this relatively simple test can identify congenital uterine anomalies, intracavitary abnormalities (such as fibroids, polyps, or synechiae) which can surgically be removed prior to another pregnancy, a retroverted uterus that may be predisposed to incarceration during pregnancy, and other potentially impactful conditions, such as adenomyosis.
Structural anomalies
Congenital uterine anomalies are associated with first trimester miscarriage, second trimester pregnancy loss, and preterm birth. A uterine septum is of particular concern for early miscarriage, as the early embryo can implant on the relatively avascular septum.
Other congenital uterine anomalies (bicornuate, didelphys, unicornuate) can be associated with concomitant cervical structural abnormalities leading to cervical insufficiency and/or result in pathologic uterine stretch of a space-limited cavity, leading to midtrimester loss or preterm birth. The diagnosis of these anomalies is an important part of the evaluation of pregnancy loss, as it can guide monitoring in future pregnancies, or can be surgically corrected, as in the case of a uterine septum, significantly improving pregnancy outcomes.
A short cervix can result either congenitally or from injury or trauma and may also be associated with cervical insufficiency and miscarriage. It can be evaluated and monitored by ultrasound and, in some cases, treated by surgical cerclage. Pregnancy losses due to cervical insufficiency usually occur after 16 weeks of gestation and frequently are associated with intra-amniotic infections.
Incarcerated uterus and adenomyosis
Other uterine factors that can contribute to pregnancy loss and that are largely underdiagnosed or undiagnosed are an incarcerated retroverted uterus and adenomyosis.
Most of the time, a retroverted uterus naturally assumes an anteverted position by the late first trimester or early second trimester, allowing for continued growth of the uterus and developing fetus. In approximately 10% of cases, however, the retroverted uterus becomes “stuck” or incarcerated in the posterior pelvis. This is more likely if there are large uterine fibroids or in the presence of pelvic adhesions due to endometriosis or previous pelvic surgery.
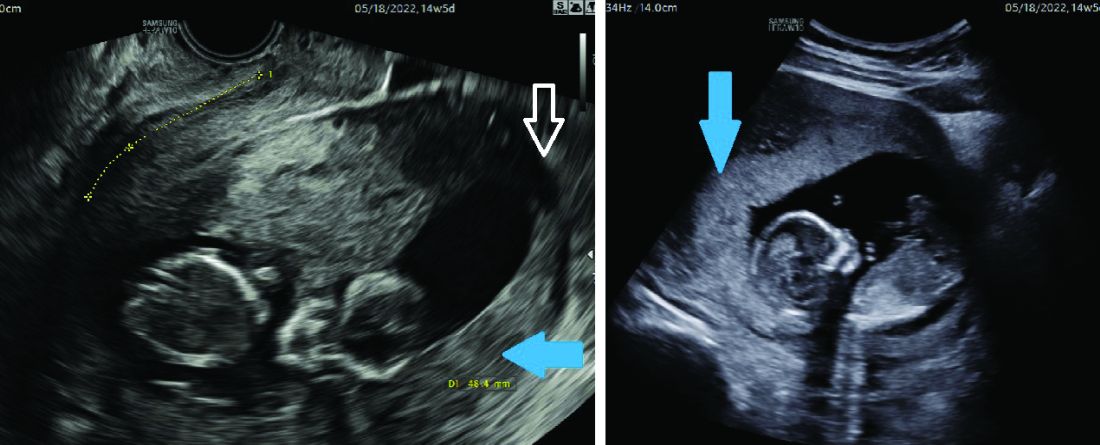
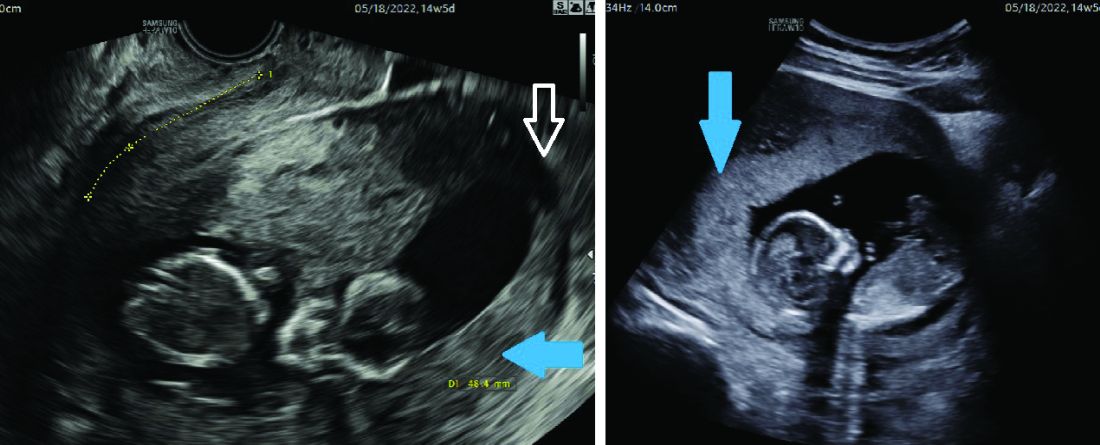
When this occurs, the fundus is wedged on the sacral promontory (may cause pelvic discomfort and constipation) and the cervix is markedly displaced anteriorly under the pubic symphysis (causing bladder outlet obstruction and urinary retention).
It is critical that ob.gyns. and emergency medicine providers are aware of this condition, which typically presents between 12 and 16 weeks’ gestation. The most frequent complaint is lower abdominal discomfort due to distended bladder and inability to void, which usually leads to bladder catheterization with drainage of large amounts of urine. An incarcerated uterus can predispose to pregnancy loss during this time (few other conditions cause loss during this time window), presumably due to impaired uterine artery blood flow.
Once the diagnosis is made, uterine incarceration may be corrected by elevating the gravid uterus out of the pelvis either manually, or by using a transvaginal ultrasound probe. (The latter minimally invasive approach was described in March at the American Institute of Ultrasound in Medicine’s annual conference by Martin Chavez, MD, and coinvestigators. More invasive approaches are rarely required but include CO2 intraperitoneal insufflation, as used prior to laparoscopy, or laparotomy.
The later in gestation the condition is allowed to persist, the less likely correction will be possible due to the enlarging fundus. Correction between 14 and 16 weeks, or earlier if symptoms develop, is recommended.
Adenomyosis, another poorly understood condition impacting pregnancy outcomes, has been associated with increased rates of miscarriage after in vitro fertilization (in addition to lower implantation rates); a meta-analysis published almost a decade ago found a risk ratio of miscarriage of 2.12 (95% confidence interval, 1.2-3.75) in women with adenomyosis versus those without (Hum Reprod. 2014 May;29[5]:964-77). However, outside of reproductive endocrinology, its impact on pregnancy outcomes in the obstetrical literature is not well recognized.
Although more research is necessary, we believe that adenomyosis should be considered a risk factor for pregnancy loss in the second trimester. The presence of endometrial glands within the myometrium, predisposing for an inflammatory environment, can lead to abnormal implantation, poor uterine distensibility, sterile inflammation, and early cervical insufficiency. As the prevalence of adenomyosis increases with age and maternal ages are increasing, this is an important condition to consider.
Diagnosis is typically made with MRI (although pathology of a hysterectomy specimen is the gold standard). Ultrasound findings consistent with adenomyosis are not routinely assessed and have not been studied in a gravid uterus. Nonetheless, a heightened sense of awareness about this possible contributor to pregnancy loss is very important.
A word about antiphospholipid syndrome
Antiphospholipid syndrome can cause a variety of adverse pregnancy outcomes, including first and second trimester pregnancy loss, fetal demise, fetal growth restriction, preeclampsia, preterm birth, and maternal thromboembolism. The classical presentation of miscarriage due to untreated antiphospholipid antibody syndrome is early severe fetal growth restriction, oligohydramnios, and IUFD in the second trimester.
The diagnosis requires at least one clinical criterion and one laboratory criterion. The mere presence of low level antibodies does not make the diagnosis of antiphospholipid antibody syndrome, and care should be taken to consider both the clinical and laboratory diagnostic criteria to make an accurate diagnosis.
When present, close maternal and fetal surveillance and a combination of low-dose aspirin and heparin are mainstays of treatment. The majority of studies suggest that low-molecular weight heparin (LMWH) and unfractionated heparin have comparable clinical efficacy. However, if a recurrent loss is experienced despite treatment with LMWH, the use of unfractionated heparin in a subsequent pregnancy should be considered.
With attention to the timing of loss
With attention to the timing of loss
Introduction: Reassurance through pregnancy loss and workups
Pregnancy loss is not an uncommon complication but it can be associated with significant stress among parents and loved ones when it occurs. Especially when recurrent, it also becomes a medical dilemma for physicians and nurses because the cause is not always obvious immediately, and even with exploration, the cause may not always be found.
First and foremost, it is important that physicians provide counseling and reassurance to families experiencing loss, and that they encourage a level of patience while the investigation for loss is done. Investigations tend not to be linear. One must look at a number of diagnostic areas including genetics, anatomy, immunology, and infections.
Even with an extensive workup, what often is found are potential associations rather than precise causes. For instance, one may find that certain antibodies or certain conditions are present, or that certain anatomic structures are abnormal. While such findings are not necessarily causative, there are therapeutic interventions that we can offer to address many of the conditions (e.g., surgical correction of the septate uterus, and low-dose aspirin and heparin for antiphospholipid syndrome).
Less than 1% of couples experience recurrent pregnancy loss (traditionally defined as three or more losses), so parents who experience one loss should be given reassurance that their loss was likely a sporadic miscarriage and that chances of recurrence will be low. Even as workups proceed, reassurance is important.
For this month’s Master Class in Obstetrics we’ve invited Wendy L. Kinzler, MD, and Anthony Vintzileos, MD, both of whom have expertise in the area of recurrent pregnancy loss, to review the potential causes and the management approach. They focus on the first trimester, when genetic causes predominate, and the early second trimester, when undetected uterine factors can be at play. They explain that the gestational age at which recurrent losses occur is an important factor in decoding etiology and management.
Dr. Kinzler is associate dean, graduate medical education, and professor of obstetrics and gynecology at NYU Long Island School of Medicine, Mineola, N.Y., and Dr. Vintzileos is chief patient safety officer for obstetrics, Northwell Health–Western Region, and professor in the department of obstetrics and gynecology in the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, N.Y. Dr. Kinzler and Dr. Vintzileos reported no relevant disclosures.
E. Albert Reece, MD, PhD, MBA, a maternal-fetal medicine specialist, is dean emeritus of the University of Maryland School of Medicine, former university executive vice president; currently the endowed professor and director of the Center for Advanced Research Training and Innovation (CARTI), and senior scientist in the Center for Birth Defects Research. Dr. Reece reported no relevant disclosures. He is the medical editor of this column. Contact him at [email protected].
Investigating the etiology of recurrent pregnancy loss
Pregnancy loss is defined as a loss occurring at < 20 weeks’ gestation.
Consideration of the timing of the pregnancy loss can provide a useful guide to this evaluation, as etiologies vary depending on when in gestation losses occur. In this Master Class, we will address the evaluation of pregnancy loss at < 20 weeks’ gestation, with particular attention to first trimester and early second trimester causes. Literature on the role of the cervix and intra-amniotic infection in midtrimester loss is extensive and will not be covered here.
Although early first trimester miscarriage is common, occurring in approximately 15% of clinically recognized pregnancies, only 2%-3% of couples experience two or more miscarriages and 0.5%-1% experience three or more.
When to begin a diagnostic workup should be part of a shared decision-making process, taking into consideration future family planning, parity, number of previous losses, and notably, the gestational age at which loss(es) occurred. Recurrence rates for first trimester miscarriage are similar after two versus three consecutive losses and either situation usually prompts an evaluation, whereas any second-trimester loss should be evaluated.
Increasingly, we are appreciating the value of a more targeted, gestational age–driven approach to the evaluation of pregnancy loss in an attempt to provide grieving parents with useful information without subjecting them to a wide array of expensive and unnecessary tests.
Genetic causes
The earlier the pregnancy loss, the more likely it is the result of abnormal fetal genetics. Genetic factors should be considered as the most likely cause for first trimester pregnancy losses (especially those occurring at < 10 weeks’ gestation), the most frequent being autosomal trisomies or monosomy X. The vast majority of trisomy conceptuses are sporadic in nature and are related to the natural aging process of the ovary (increasing the rate of meiotic nondisjunction).
If fetal aneuploidy is identified in a pregnancy loss, couples can be counseled about the definitive cause of the loss and can be counseled about recurrence based on age-related risks and/or tests of ovarian reserve. Recurrent pregnancy loss (RPL) is only rarely associated with a parental translocation (< 5%). Testing parental karyotypes should be reserved for cases in which the fetal karyotypes are unknown or in which an unbalanced translocation was identified in the fetus.
When a first trimester pregnancy loss is diagnosed, chorionic villus sampling (CVS) with microarray testing is the most reliable and comprehensive method for evaluating potential genetic causes. It provides valuable information even when cells are not viable and reduces the risk of maternal cell contamination – two significant limitations to standard karyotype analysis performed on tissue passed spontaneously or at the time of D&C. Studies of products of conception (POC) testing with microarray have documented the detection of abnormalities in an additional 10%-15% of cases compared with traditional karyotype analysis.
When CVS is not feasible, testing maternal serum for cell-free DNA is a reasonable alternative. In a prospective cohort study of 50 maternal blood samples taken after fetal demise, 76% of samples yielded cell-free DNA results, meaning fetal fractions were within the detectable range. The higher the gestational age at the time of loss, the higher the chance of obtaining a result: Findings in the study were possible in 88% of samples when the gestational age was 8 weeks or greater, and in 53% of cases involving a lower gestational age. The time from demise to blood draw did not affect the likelihood of obtaining a result (Obstet Gynecol. 2015 Jun;125[6]:1321-29).
When neither CVS nor cell-free DNA analysis is feasible, analysis of either spontaneously passed tissue or tissue obtained at the time of a D&C may still be worthwhile. Maternal cell contamination, of course, is the main downside.
A paper published in 2020 documented the value of refocusing the initial workup. Researchers reported that 57% of 1,400 cases of recurrent pregnancy loss went unexplained using the 2012 ASRM guidelines, which included parental karyotyping but not POC cytogenetic analysis. When parental karyotypes were omitted from the initial workup and POC analysis with 24-chromosome microarray was added, at least one potential explanation for loss could be identified in 92% of cases. Only 8% were left “unexplained” (Curr Opin Obstet Gynecol. 2020 Oct;32[5]:371-9).
When genetics are ruled out
Issues that are top of mind when we lack genetic information or when genetic causes are ruled out include maternal metabolic disorders (uncontrolled diabetes, obesity, uncontrolled thyroid disease), environmental exposures (smoking), uterine abnormalities, and antiphospholipid syndrome.
Thorough evaluation of the uterine cavity after recurrent first trimester miscarriage – or after any second trimester loss – is too often a missing element of investigation. It is a vital component of the evaluation, and information about uterine structure is easily obtained.
A saline infusion sonogram (SIS) allows us to look at the external contour of the uterus, assess the myometrium for muscular abnormalities, visualize the uterine lining, and assess uterine orientation. Performed in the nonpregnant state, and ideally coupled with 3D technology, this relatively simple test can identify congenital uterine anomalies, intracavitary abnormalities (such as fibroids, polyps, or synechiae) which can surgically be removed prior to another pregnancy, a retroverted uterus that may be predisposed to incarceration during pregnancy, and other potentially impactful conditions, such as adenomyosis.
Structural anomalies
Congenital uterine anomalies are associated with first trimester miscarriage, second trimester pregnancy loss, and preterm birth. A uterine septum is of particular concern for early miscarriage, as the early embryo can implant on the relatively avascular septum.
Other congenital uterine anomalies (bicornuate, didelphys, unicornuate) can be associated with concomitant cervical structural abnormalities leading to cervical insufficiency and/or result in pathologic uterine stretch of a space-limited cavity, leading to midtrimester loss or preterm birth. The diagnosis of these anomalies is an important part of the evaluation of pregnancy loss, as it can guide monitoring in future pregnancies, or can be surgically corrected, as in the case of a uterine septum, significantly improving pregnancy outcomes.
A short cervix can result either congenitally or from injury or trauma and may also be associated with cervical insufficiency and miscarriage. It can be evaluated and monitored by ultrasound and, in some cases, treated by surgical cerclage. Pregnancy losses due to cervical insufficiency usually occur after 16 weeks of gestation and frequently are associated with intra-amniotic infections.
Incarcerated uterus and adenomyosis
Other uterine factors that can contribute to pregnancy loss and that are largely underdiagnosed or undiagnosed are an incarcerated retroverted uterus and adenomyosis.
Most of the time, a retroverted uterus naturally assumes an anteverted position by the late first trimester or early second trimester, allowing for continued growth of the uterus and developing fetus. In approximately 10% of cases, however, the retroverted uterus becomes “stuck” or incarcerated in the posterior pelvis. This is more likely if there are large uterine fibroids or in the presence of pelvic adhesions due to endometriosis or previous pelvic surgery.
When this occurs, the fundus is wedged on the sacral promontory (may cause pelvic discomfort and constipation) and the cervix is markedly displaced anteriorly under the pubic symphysis (causing bladder outlet obstruction and urinary retention).
It is critical that ob.gyns. and emergency medicine providers are aware of this condition, which typically presents between 12 and 16 weeks’ gestation. The most frequent complaint is lower abdominal discomfort due to distended bladder and inability to void, which usually leads to bladder catheterization with drainage of large amounts of urine. An incarcerated uterus can predispose to pregnancy loss during this time (few other conditions cause loss during this time window), presumably due to impaired uterine artery blood flow.
Once the diagnosis is made, uterine incarceration may be corrected by elevating the gravid uterus out of the pelvis either manually, or by using a transvaginal ultrasound probe. (The latter minimally invasive approach was described in March at the American Institute of Ultrasound in Medicine’s annual conference by Martin Chavez, MD, and coinvestigators. More invasive approaches are rarely required but include CO2 intraperitoneal insufflation, as used prior to laparoscopy, or laparotomy.
The later in gestation the condition is allowed to persist, the less likely correction will be possible due to the enlarging fundus. Correction between 14 and 16 weeks, or earlier if symptoms develop, is recommended.
Adenomyosis, another poorly understood condition impacting pregnancy outcomes, has been associated with increased rates of miscarriage after in vitro fertilization (in addition to lower implantation rates); a meta-analysis published almost a decade ago found a risk ratio of miscarriage of 2.12 (95% confidence interval, 1.2-3.75) in women with adenomyosis versus those without (Hum Reprod. 2014 May;29[5]:964-77). However, outside of reproductive endocrinology, its impact on pregnancy outcomes in the obstetrical literature is not well recognized.
Although more research is necessary, we believe that adenomyosis should be considered a risk factor for pregnancy loss in the second trimester. The presence of endometrial glands within the myometrium, predisposing for an inflammatory environment, can lead to abnormal implantation, poor uterine distensibility, sterile inflammation, and early cervical insufficiency. As the prevalence of adenomyosis increases with age and maternal ages are increasing, this is an important condition to consider.
Diagnosis is typically made with MRI (although pathology of a hysterectomy specimen is the gold standard). Ultrasound findings consistent with adenomyosis are not routinely assessed and have not been studied in a gravid uterus. Nonetheless, a heightened sense of awareness about this possible contributor to pregnancy loss is very important.
A word about antiphospholipid syndrome
Antiphospholipid syndrome can cause a variety of adverse pregnancy outcomes, including first and second trimester pregnancy loss, fetal demise, fetal growth restriction, preeclampsia, preterm birth, and maternal thromboembolism. The classical presentation of miscarriage due to untreated antiphospholipid antibody syndrome is early severe fetal growth restriction, oligohydramnios, and IUFD in the second trimester.
The diagnosis requires at least one clinical criterion and one laboratory criterion. The mere presence of low level antibodies does not make the diagnosis of antiphospholipid antibody syndrome, and care should be taken to consider both the clinical and laboratory diagnostic criteria to make an accurate diagnosis.
When present, close maternal and fetal surveillance and a combination of low-dose aspirin and heparin are mainstays of treatment. The majority of studies suggest that low-molecular weight heparin (LMWH) and unfractionated heparin have comparable clinical efficacy. However, if a recurrent loss is experienced despite treatment with LMWH, the use of unfractionated heparin in a subsequent pregnancy should be considered.
Introduction: Reassurance through pregnancy loss and workups
Pregnancy loss is not an uncommon complication but it can be associated with significant stress among parents and loved ones when it occurs. Especially when recurrent, it also becomes a medical dilemma for physicians and nurses because the cause is not always obvious immediately, and even with exploration, the cause may not always be found.
First and foremost, it is important that physicians provide counseling and reassurance to families experiencing loss, and that they encourage a level of patience while the investigation for loss is done. Investigations tend not to be linear. One must look at a number of diagnostic areas including genetics, anatomy, immunology, and infections.
Even with an extensive workup, what often is found are potential associations rather than precise causes. For instance, one may find that certain antibodies or certain conditions are present, or that certain anatomic structures are abnormal. While such findings are not necessarily causative, there are therapeutic interventions that we can offer to address many of the conditions (e.g., surgical correction of the septate uterus, and low-dose aspirin and heparin for antiphospholipid syndrome).
Less than 1% of couples experience recurrent pregnancy loss (traditionally defined as three or more losses), so parents who experience one loss should be given reassurance that their loss was likely a sporadic miscarriage and that chances of recurrence will be low. Even as workups proceed, reassurance is important.
For this month’s Master Class in Obstetrics we’ve invited Wendy L. Kinzler, MD, and Anthony Vintzileos, MD, both of whom have expertise in the area of recurrent pregnancy loss, to review the potential causes and the management approach. They focus on the first trimester, when genetic causes predominate, and the early second trimester, when undetected uterine factors can be at play. They explain that the gestational age at which recurrent losses occur is an important factor in decoding etiology and management.
Dr. Kinzler is associate dean, graduate medical education, and professor of obstetrics and gynecology at NYU Long Island School of Medicine, Mineola, N.Y., and Dr. Vintzileos is chief patient safety officer for obstetrics, Northwell Health–Western Region, and professor in the department of obstetrics and gynecology in the Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, N.Y. Dr. Kinzler and Dr. Vintzileos reported no relevant disclosures.
E. Albert Reece, MD, PhD, MBA, a maternal-fetal medicine specialist, is dean emeritus of the University of Maryland School of Medicine, former university executive vice president; currently the endowed professor and director of the Center for Advanced Research Training and Innovation (CARTI), and senior scientist in the Center for Birth Defects Research. Dr. Reece reported no relevant disclosures. He is the medical editor of this column. Contact him at [email protected].
Investigating the etiology of recurrent pregnancy loss
Pregnancy loss is defined as a loss occurring at < 20 weeks’ gestation.
Consideration of the timing of the pregnancy loss can provide a useful guide to this evaluation, as etiologies vary depending on when in gestation losses occur. In this Master Class, we will address the evaluation of pregnancy loss at < 20 weeks’ gestation, with particular attention to first trimester and early second trimester causes. Literature on the role of the cervix and intra-amniotic infection in midtrimester loss is extensive and will not be covered here.
Although early first trimester miscarriage is common, occurring in approximately 15% of clinically recognized pregnancies, only 2%-3% of couples experience two or more miscarriages and 0.5%-1% experience three or more.
When to begin a diagnostic workup should be part of a shared decision-making process, taking into consideration future family planning, parity, number of previous losses, and notably, the gestational age at which loss(es) occurred. Recurrence rates for first trimester miscarriage are similar after two versus three consecutive losses and either situation usually prompts an evaluation, whereas any second-trimester loss should be evaluated.
Increasingly, we are appreciating the value of a more targeted, gestational age–driven approach to the evaluation of pregnancy loss in an attempt to provide grieving parents with useful information without subjecting them to a wide array of expensive and unnecessary tests.
Genetic causes
The earlier the pregnancy loss, the more likely it is the result of abnormal fetal genetics. Genetic factors should be considered as the most likely cause for first trimester pregnancy losses (especially those occurring at < 10 weeks’ gestation), the most frequent being autosomal trisomies or monosomy X. The vast majority of trisomy conceptuses are sporadic in nature and are related to the natural aging process of the ovary (increasing the rate of meiotic nondisjunction).
If fetal aneuploidy is identified in a pregnancy loss, couples can be counseled about the definitive cause of the loss and can be counseled about recurrence based on age-related risks and/or tests of ovarian reserve. Recurrent pregnancy loss (RPL) is only rarely associated with a parental translocation (< 5%). Testing parental karyotypes should be reserved for cases in which the fetal karyotypes are unknown or in which an unbalanced translocation was identified in the fetus.
When a first trimester pregnancy loss is diagnosed, chorionic villus sampling (CVS) with microarray testing is the most reliable and comprehensive method for evaluating potential genetic causes. It provides valuable information even when cells are not viable and reduces the risk of maternal cell contamination – two significant limitations to standard karyotype analysis performed on tissue passed spontaneously or at the time of D&C. Studies of products of conception (POC) testing with microarray have documented the detection of abnormalities in an additional 10%-15% of cases compared with traditional karyotype analysis.
When CVS is not feasible, testing maternal serum for cell-free DNA is a reasonable alternative. In a prospective cohort study of 50 maternal blood samples taken after fetal demise, 76% of samples yielded cell-free DNA results, meaning fetal fractions were within the detectable range. The higher the gestational age at the time of loss, the higher the chance of obtaining a result: Findings in the study were possible in 88% of samples when the gestational age was 8 weeks or greater, and in 53% of cases involving a lower gestational age. The time from demise to blood draw did not affect the likelihood of obtaining a result (Obstet Gynecol. 2015 Jun;125[6]:1321-29).
When neither CVS nor cell-free DNA analysis is feasible, analysis of either spontaneously passed tissue or tissue obtained at the time of a D&C may still be worthwhile. Maternal cell contamination, of course, is the main downside.
A paper published in 2020 documented the value of refocusing the initial workup. Researchers reported that 57% of 1,400 cases of recurrent pregnancy loss went unexplained using the 2012 ASRM guidelines, which included parental karyotyping but not POC cytogenetic analysis. When parental karyotypes were omitted from the initial workup and POC analysis with 24-chromosome microarray was added, at least one potential explanation for loss could be identified in 92% of cases. Only 8% were left “unexplained” (Curr Opin Obstet Gynecol. 2020 Oct;32[5]:371-9).
When genetics are ruled out
Issues that are top of mind when we lack genetic information or when genetic causes are ruled out include maternal metabolic disorders (uncontrolled diabetes, obesity, uncontrolled thyroid disease), environmental exposures (smoking), uterine abnormalities, and antiphospholipid syndrome.
Thorough evaluation of the uterine cavity after recurrent first trimester miscarriage – or after any second trimester loss – is too often a missing element of investigation. It is a vital component of the evaluation, and information about uterine structure is easily obtained.
A saline infusion sonogram (SIS) allows us to look at the external contour of the uterus, assess the myometrium for muscular abnormalities, visualize the uterine lining, and assess uterine orientation. Performed in the nonpregnant state, and ideally coupled with 3D technology, this relatively simple test can identify congenital uterine anomalies, intracavitary abnormalities (such as fibroids, polyps, or synechiae) which can surgically be removed prior to another pregnancy, a retroverted uterus that may be predisposed to incarceration during pregnancy, and other potentially impactful conditions, such as adenomyosis.
Structural anomalies
Congenital uterine anomalies are associated with first trimester miscarriage, second trimester pregnancy loss, and preterm birth. A uterine septum is of particular concern for early miscarriage, as the early embryo can implant on the relatively avascular septum.
Other congenital uterine anomalies (bicornuate, didelphys, unicornuate) can be associated with concomitant cervical structural abnormalities leading to cervical insufficiency and/or result in pathologic uterine stretch of a space-limited cavity, leading to midtrimester loss or preterm birth. The diagnosis of these anomalies is an important part of the evaluation of pregnancy loss, as it can guide monitoring in future pregnancies, or can be surgically corrected, as in the case of a uterine septum, significantly improving pregnancy outcomes.
A short cervix can result either congenitally or from injury or trauma and may also be associated with cervical insufficiency and miscarriage. It can be evaluated and monitored by ultrasound and, in some cases, treated by surgical cerclage. Pregnancy losses due to cervical insufficiency usually occur after 16 weeks of gestation and frequently are associated with intra-amniotic infections.
Incarcerated uterus and adenomyosis
Other uterine factors that can contribute to pregnancy loss and that are largely underdiagnosed or undiagnosed are an incarcerated retroverted uterus and adenomyosis.
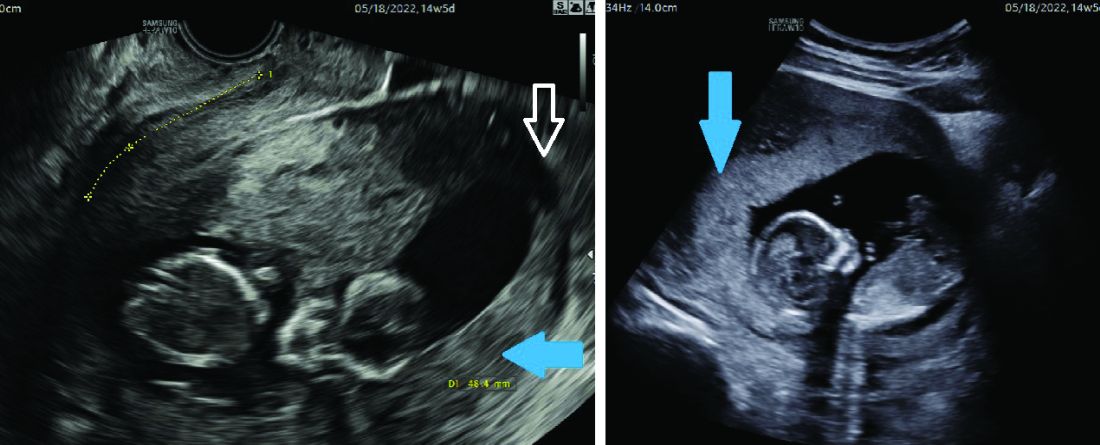
Most of the time, a retroverted uterus naturally assumes an anteverted position by the late first trimester or early second trimester, allowing for continued growth of the uterus and developing fetus. In approximately 10% of cases, however, the retroverted uterus becomes “stuck” or incarcerated in the posterior pelvis. This is more likely if there are large uterine fibroids or in the presence of pelvic adhesions due to endometriosis or previous pelvic surgery.
When this occurs, the fundus is wedged on the sacral promontory (may cause pelvic discomfort and constipation) and the cervix is markedly displaced anteriorly under the pubic symphysis (causing bladder outlet obstruction and urinary retention).
It is critical that ob.gyns. and emergency medicine providers are aware of this condition, which typically presents between 12 and 16 weeks’ gestation. The most frequent complaint is lower abdominal discomfort due to distended bladder and inability to void, which usually leads to bladder catheterization with drainage of large amounts of urine. An incarcerated uterus can predispose to pregnancy loss during this time (few other conditions cause loss during this time window), presumably due to impaired uterine artery blood flow.
Once the diagnosis is made, uterine incarceration may be corrected by elevating the gravid uterus out of the pelvis either manually, or by using a transvaginal ultrasound probe. (The latter minimally invasive approach was described in March at the American Institute of Ultrasound in Medicine’s annual conference by Martin Chavez, MD, and coinvestigators. More invasive approaches are rarely required but include CO2 intraperitoneal insufflation, as used prior to laparoscopy, or laparotomy.
The later in gestation the condition is allowed to persist, the less likely correction will be possible due to the enlarging fundus. Correction between 14 and 16 weeks, or earlier if symptoms develop, is recommended.
Adenomyosis, another poorly understood condition impacting pregnancy outcomes, has been associated with increased rates of miscarriage after in vitro fertilization (in addition to lower implantation rates); a meta-analysis published almost a decade ago found a risk ratio of miscarriage of 2.12 (95% confidence interval, 1.2-3.75) in women with adenomyosis versus those without (Hum Reprod. 2014 May;29[5]:964-77). However, outside of reproductive endocrinology, its impact on pregnancy outcomes in the obstetrical literature is not well recognized.
Although more research is necessary, we believe that adenomyosis should be considered a risk factor for pregnancy loss in the second trimester. The presence of endometrial glands within the myometrium, predisposing for an inflammatory environment, can lead to abnormal implantation, poor uterine distensibility, sterile inflammation, and early cervical insufficiency. As the prevalence of adenomyosis increases with age and maternal ages are increasing, this is an important condition to consider.
Diagnosis is typically made with MRI (although pathology of a hysterectomy specimen is the gold standard). Ultrasound findings consistent with adenomyosis are not routinely assessed and have not been studied in a gravid uterus. Nonetheless, a heightened sense of awareness about this possible contributor to pregnancy loss is very important.
A word about antiphospholipid syndrome
Antiphospholipid syndrome can cause a variety of adverse pregnancy outcomes, including first and second trimester pregnancy loss, fetal demise, fetal growth restriction, preeclampsia, preterm birth, and maternal thromboembolism. The classical presentation of miscarriage due to untreated antiphospholipid antibody syndrome is early severe fetal growth restriction, oligohydramnios, and IUFD in the second trimester.
The diagnosis requires at least one clinical criterion and one laboratory criterion. The mere presence of low level antibodies does not make the diagnosis of antiphospholipid antibody syndrome, and care should be taken to consider both the clinical and laboratory diagnostic criteria to make an accurate diagnosis.
When present, close maternal and fetal surveillance and a combination of low-dose aspirin and heparin are mainstays of treatment. The majority of studies suggest that low-molecular weight heparin (LMWH) and unfractionated heparin have comparable clinical efficacy. However, if a recurrent loss is experienced despite treatment with LMWH, the use of unfractionated heparin in a subsequent pregnancy should be considered.
Younger age of type 2 diabetes onset linked to dementia risk
, new findings suggest.
Moreover, the new data from the prospective Atherosclerosis Risk in Communities (ARIC) cohort also suggest that the previously identified increased risk for dementia among people with prediabetes appears to be entirely explained by the subset who go on to develop type 2 diabetes.
“Our findings suggest that preventing prediabetes progression, especially in younger individuals, may be an important way to reduce the dementia burden,” wrote PhD student Jiaqi Hu of Johns Hopkins University, Baltimore, and colleagues. Their article was published online in Diabetologia.
The result builds on previous findings linking dysglycemia and cognitive decline, the study’s lead author, Elizabeth Selvin, PhD, of the Bloomberg School of Public Health at Johns Hopkins, said in an interview.
“Our prior work in the ARIC study suggests that improving glucose control could help prevent dementia in later life,” she said.
Other studies have also linked higher A1c levels and diabetes in midlife to increased rates of cognitive decline. In addition, Dr. Selvin noted, “There is growing evidence that focusing on vascular health, especially focusing on diabetes and blood pressure, in midlife can stave off dementia in later life.”
This new study is the first to examine the effect of diabetes in the relationship between prediabetes and dementia, as well as the age of diabetes onset on subsequent dementia.
Prediabetes linked to dementia via diabetes development
Of the 11,656 ARIC participants without diabetes at baseline during 1990-1992 (age 46-70 years), 20.0% had prediabetes (defined as A1c 5.7%-6.4% or 39-46 mmol/mol). During a median follow-up of 15.9 years, 3,143 participants developed diabetes. The proportions of patients who developed diabetes were 44.6% among those with prediabetes at baseline versus 22.5% of those without.
Dementia developed in 2,247 participants over a median follow-up of 24.7 years. The cumulative incidence of dementia was 23.9% among those who developed diabetes versus 20.5% among those who did not.
After adjustment for demographics and for the Alzheimer’s disease–linked apolipoprotein E (APOE) gene, prediabetes was significantly associated with incident dementia (hazard ratio [HR], 1.19). However, significance disappeared after adjustment for incident diabetes (HR, 1.09), the researchers reported.
Younger age at diabetes diagnosis raises dementia risk
Age at diabetes diagnosis made a difference in dementia risk. With adjustments for lifestyle, demographic, and clinical factors, those diagnosed with diabetes before age 60 years had a nearly threefold increased risk for dementia compared with those who never developed diabetes (HR, 2.92; P < .001).
The dementia risk was also significantly increased, although to a lesser degree, among those aged 60-69 years at diabetes diagnosis (HR, 1.73; P < .001) and age 70-79 years at diabetes diagnosis (HR, 1.23; P < .001). The relationship was not significant for those aged 80 years and older (HR, 1.13).
“Prevention efforts in people with diabetes diagnosed younger than 65 years should be a high priority,” the authors urged.
Taken together, the data suggest that prolonged exposure to hyperglycemia plays a major role in dementia development.
“Putative mechanisms include acute and chronic hyperglycemia, glucose toxicity, insulin resistance, and microvascular dysfunction of the central nervous system. ... Glucose toxicity and microvascular dysfunction are associated with increased inflammatory and oxidative stress, leading to increased blood–brain permeability,” the researchers wrote.
Dr. Selvin said that her group is pursuing further work in this area using continuous glucose monitoring. “We plan to look at ... how glycemic control and different patterns of glucose in older adults may be linked to cognitive decline and other neurocognitive outcomes.”
The researchers reported no relevant financial relationships. Dr. Selvin has reported being on the advisory board for Diabetologia; she had no role in peer review of the manuscript.
A version of this article first appeared on Medscape.com.
, new findings suggest.
Moreover, the new data from the prospective Atherosclerosis Risk in Communities (ARIC) cohort also suggest that the previously identified increased risk for dementia among people with prediabetes appears to be entirely explained by the subset who go on to develop type 2 diabetes.
“Our findings suggest that preventing prediabetes progression, especially in younger individuals, may be an important way to reduce the dementia burden,” wrote PhD student Jiaqi Hu of Johns Hopkins University, Baltimore, and colleagues. Their article was published online in Diabetologia.
The result builds on previous findings linking dysglycemia and cognitive decline, the study’s lead author, Elizabeth Selvin, PhD, of the Bloomberg School of Public Health at Johns Hopkins, said in an interview.
“Our prior work in the ARIC study suggests that improving glucose control could help prevent dementia in later life,” she said.
Other studies have also linked higher A1c levels and diabetes in midlife to increased rates of cognitive decline. In addition, Dr. Selvin noted, “There is growing evidence that focusing on vascular health, especially focusing on diabetes and blood pressure, in midlife can stave off dementia in later life.”
This new study is the first to examine the effect of diabetes in the relationship between prediabetes and dementia, as well as the age of diabetes onset on subsequent dementia.
Prediabetes linked to dementia via diabetes development
Of the 11,656 ARIC participants without diabetes at baseline during 1990-1992 (age 46-70 years), 20.0% had prediabetes (defined as A1c 5.7%-6.4% or 39-46 mmol/mol). During a median follow-up of 15.9 years, 3,143 participants developed diabetes. The proportions of patients who developed diabetes were 44.6% among those with prediabetes at baseline versus 22.5% of those without.
Dementia developed in 2,247 participants over a median follow-up of 24.7 years. The cumulative incidence of dementia was 23.9% among those who developed diabetes versus 20.5% among those who did not.
After adjustment for demographics and for the Alzheimer’s disease–linked apolipoprotein E (APOE) gene, prediabetes was significantly associated with incident dementia (hazard ratio [HR], 1.19). However, significance disappeared after adjustment for incident diabetes (HR, 1.09), the researchers reported.
Younger age at diabetes diagnosis raises dementia risk
Age at diabetes diagnosis made a difference in dementia risk. With adjustments for lifestyle, demographic, and clinical factors, those diagnosed with diabetes before age 60 years had a nearly threefold increased risk for dementia compared with those who never developed diabetes (HR, 2.92; P < .001).
The dementia risk was also significantly increased, although to a lesser degree, among those aged 60-69 years at diabetes diagnosis (HR, 1.73; P < .001) and age 70-79 years at diabetes diagnosis (HR, 1.23; P < .001). The relationship was not significant for those aged 80 years and older (HR, 1.13).
“Prevention efforts in people with diabetes diagnosed younger than 65 years should be a high priority,” the authors urged.
Taken together, the data suggest that prolonged exposure to hyperglycemia plays a major role in dementia development.
“Putative mechanisms include acute and chronic hyperglycemia, glucose toxicity, insulin resistance, and microvascular dysfunction of the central nervous system. ... Glucose toxicity and microvascular dysfunction are associated with increased inflammatory and oxidative stress, leading to increased blood–brain permeability,” the researchers wrote.
Dr. Selvin said that her group is pursuing further work in this area using continuous glucose monitoring. “We plan to look at ... how glycemic control and different patterns of glucose in older adults may be linked to cognitive decline and other neurocognitive outcomes.”
The researchers reported no relevant financial relationships. Dr. Selvin has reported being on the advisory board for Diabetologia; she had no role in peer review of the manuscript.
A version of this article first appeared on Medscape.com.
, new findings suggest.
Moreover, the new data from the prospective Atherosclerosis Risk in Communities (ARIC) cohort also suggest that the previously identified increased risk for dementia among people with prediabetes appears to be entirely explained by the subset who go on to develop type 2 diabetes.
“Our findings suggest that preventing prediabetes progression, especially in younger individuals, may be an important way to reduce the dementia burden,” wrote PhD student Jiaqi Hu of Johns Hopkins University, Baltimore, and colleagues. Their article was published online in Diabetologia.
The result builds on previous findings linking dysglycemia and cognitive decline, the study’s lead author, Elizabeth Selvin, PhD, of the Bloomberg School of Public Health at Johns Hopkins, said in an interview.
“Our prior work in the ARIC study suggests that improving glucose control could help prevent dementia in later life,” she said.
Other studies have also linked higher A1c levels and diabetes in midlife to increased rates of cognitive decline. In addition, Dr. Selvin noted, “There is growing evidence that focusing on vascular health, especially focusing on diabetes and blood pressure, in midlife can stave off dementia in later life.”
This new study is the first to examine the effect of diabetes in the relationship between prediabetes and dementia, as well as the age of diabetes onset on subsequent dementia.
Prediabetes linked to dementia via diabetes development
Of the 11,656 ARIC participants without diabetes at baseline during 1990-1992 (age 46-70 years), 20.0% had prediabetes (defined as A1c 5.7%-6.4% or 39-46 mmol/mol). During a median follow-up of 15.9 years, 3,143 participants developed diabetes. The proportions of patients who developed diabetes were 44.6% among those with prediabetes at baseline versus 22.5% of those without.
Dementia developed in 2,247 participants over a median follow-up of 24.7 years. The cumulative incidence of dementia was 23.9% among those who developed diabetes versus 20.5% among those who did not.
After adjustment for demographics and for the Alzheimer’s disease–linked apolipoprotein E (APOE) gene, prediabetes was significantly associated with incident dementia (hazard ratio [HR], 1.19). However, significance disappeared after adjustment for incident diabetes (HR, 1.09), the researchers reported.
Younger age at diabetes diagnosis raises dementia risk
Age at diabetes diagnosis made a difference in dementia risk. With adjustments for lifestyle, demographic, and clinical factors, those diagnosed with diabetes before age 60 years had a nearly threefold increased risk for dementia compared with those who never developed diabetes (HR, 2.92; P < .001).
The dementia risk was also significantly increased, although to a lesser degree, among those aged 60-69 years at diabetes diagnosis (HR, 1.73; P < .001) and age 70-79 years at diabetes diagnosis (HR, 1.23; P < .001). The relationship was not significant for those aged 80 years and older (HR, 1.13).
“Prevention efforts in people with diabetes diagnosed younger than 65 years should be a high priority,” the authors urged.
Taken together, the data suggest that prolonged exposure to hyperglycemia plays a major role in dementia development.
“Putative mechanisms include acute and chronic hyperglycemia, glucose toxicity, insulin resistance, and microvascular dysfunction of the central nervous system. ... Glucose toxicity and microvascular dysfunction are associated with increased inflammatory and oxidative stress, leading to increased blood–brain permeability,” the researchers wrote.
Dr. Selvin said that her group is pursuing further work in this area using continuous glucose monitoring. “We plan to look at ... how glycemic control and different patterns of glucose in older adults may be linked to cognitive decline and other neurocognitive outcomes.”
The researchers reported no relevant financial relationships. Dr. Selvin has reported being on the advisory board for Diabetologia; she had no role in peer review of the manuscript.
A version of this article first appeared on Medscape.com.
FROM DIABETOLOGIA
Real-world data validate ESC risk model in NSTE-ACS
ESC model appropriately identifies risk
A real-world study of more than 12,000 cases over 7 years has validated the predictive ability of the proposed guidelines for stratifying thrombotic risks at 1 year for patients with non–ST-elevated acute coronary syndrome (NSTE-ACS) undergoing percutaneous coronary intervention (PCI).
In research presented at the Society for Cardiovascular Angiography & Interventions annual scientific sessions, George Dangas, MD, PhD, current SCAI president and professor of cardiology and vascular surgery at the Icahn School of Medicine at Mount Sinai, New York, reported that the European Society of Cardiology risk stratification criteria appropriately predicted risk in 12,538 patients treated from 2012 to 2019.
Despite these proposed guidelines put forward by the ESC in 2020, no consensus exists on criteria for ischemic or thrombotic risk in NSTE-ACS patients, Dr. Dangas noted.
The new study shows that the 1-year major adverse cardiovascular events (MACE) risk was four times greater in patients classified as medium risk (hazard ratio, 4.31; 95% confidence interval, 2.47-7.52) and six times greater in high-risk patients (HR, 6.16; 95% CI, 3.52-10.8), compared with the low-risk group, mostly because of higher rates of all-cause death and myocardial infarction, Dr. Dangas said in an interview.
“Indeed, we found some good correlation between the three risk categories and gradation of risk that validates essentially, but with the statistical testing that we need, that this classification is meaningful if not perfect,” Dr. Dangas said. “In the future we may perform calibrations to enhance its performance.”
The study used data on consecutive patients from the Angioplasty and Stent Procedures Database of Mount Sinai, grouping them into low, medium, and high thrombotic risk based on the proposed ESC guidelines for the management of NSTE-ACS.
The guidelines included a subset of criteria to identify patients with increased thrombotic risk who may benefit from extended treatment with a second antithrombotic agent.
This study aimed to evaluate the value of the criteria to identify patients at higher risk of ischemic events. “That’s why we went to our database to see how this might work,” Dr. Dangas said.
The researchers also found that high-risk patients had about a 40% greater risk of major bleeding (HR, 1.39; 95% CI, 1.06-1.84). Bleeding risks were similar between the low- and moderate-risk groups.
The risk categories reflected the rates of all-cause death, myocardial infarction, or stroke: 5.4%, 4.1%, and 1.6% in the high-, moderate-, and low-risks groups, respectively (P < .001).
“This identification of ischemic risks worked very well for all-cause mortality,” Dr. Dangas said. “I feel this is a strength because mortality is a leader of outcomes. And of course, we’ve had some associations with all events like mortality, myocardial infarction, repeat revascularization, which are interesting and valid, but I think a study result that indicates the mortality itself is known to be unidirectional and a very good correlation makes the result more robust.”
Critical role
Risk prediction models such as the proposed ESC guidelines will play a critical role as individualized medicine continues to evolve, Somjot Brar, MD, MPH, director of the regional department of cardiac catheterization at Kaiser Permanente, Los Angeles Medical Center, and associate clinical professor at the University of California, Los Angeles, said in an interview.
“This study highlights again the importance of the value for predictive and precision medicine,” Dr. Brar said. “Everything is moving in this direction where we make decisions that are more appropriate for a given patient as opposed to a population of patients.”
Study strengths are the large sample size in a real-world setting and thorough 1-year follow-up, Dr. Brar said.
A limitation is the three risk categories the guidelines proposed. “These are still pretty big boxes,” he said. “The low-, moderate- and high-risk categorization is still very, very broad and can be very vague.”
The relatively low percentage of low-risk patients – 12% versus 56% and 32% for the moderate- and high-risk groups – in this data set may also skew results, Dr. Brar said.
“As we move toward predictive analytics and medicine, we want to make these boxes smaller and smaller and smaller to be able to better understand which treatments should be administered to which patients to maximize the benefit against the risk,” he said. That would be a focus for future analyses, Dr. Brar said.
Dr. Dangas and Dr. Brar have no relevant financial disclosures.
ESC model appropriately identifies risk
ESC model appropriately identifies risk
A real-world study of more than 12,000 cases over 7 years has validated the predictive ability of the proposed guidelines for stratifying thrombotic risks at 1 year for patients with non–ST-elevated acute coronary syndrome (NSTE-ACS) undergoing percutaneous coronary intervention (PCI).
In research presented at the Society for Cardiovascular Angiography & Interventions annual scientific sessions, George Dangas, MD, PhD, current SCAI president and professor of cardiology and vascular surgery at the Icahn School of Medicine at Mount Sinai, New York, reported that the European Society of Cardiology risk stratification criteria appropriately predicted risk in 12,538 patients treated from 2012 to 2019.
Despite these proposed guidelines put forward by the ESC in 2020, no consensus exists on criteria for ischemic or thrombotic risk in NSTE-ACS patients, Dr. Dangas noted.
The new study shows that the 1-year major adverse cardiovascular events (MACE) risk was four times greater in patients classified as medium risk (hazard ratio, 4.31; 95% confidence interval, 2.47-7.52) and six times greater in high-risk patients (HR, 6.16; 95% CI, 3.52-10.8), compared with the low-risk group, mostly because of higher rates of all-cause death and myocardial infarction, Dr. Dangas said in an interview.
“Indeed, we found some good correlation between the three risk categories and gradation of risk that validates essentially, but with the statistical testing that we need, that this classification is meaningful if not perfect,” Dr. Dangas said. “In the future we may perform calibrations to enhance its performance.”
The study used data on consecutive patients from the Angioplasty and Stent Procedures Database of Mount Sinai, grouping them into low, medium, and high thrombotic risk based on the proposed ESC guidelines for the management of NSTE-ACS.
The guidelines included a subset of criteria to identify patients with increased thrombotic risk who may benefit from extended treatment with a second antithrombotic agent.
This study aimed to evaluate the value of the criteria to identify patients at higher risk of ischemic events. “That’s why we went to our database to see how this might work,” Dr. Dangas said.
The researchers also found that high-risk patients had about a 40% greater risk of major bleeding (HR, 1.39; 95% CI, 1.06-1.84). Bleeding risks were similar between the low- and moderate-risk groups.
The risk categories reflected the rates of all-cause death, myocardial infarction, or stroke: 5.4%, 4.1%, and 1.6% in the high-, moderate-, and low-risks groups, respectively (P < .001).
“This identification of ischemic risks worked very well for all-cause mortality,” Dr. Dangas said. “I feel this is a strength because mortality is a leader of outcomes. And of course, we’ve had some associations with all events like mortality, myocardial infarction, repeat revascularization, which are interesting and valid, but I think a study result that indicates the mortality itself is known to be unidirectional and a very good correlation makes the result more robust.”
Critical role
Risk prediction models such as the proposed ESC guidelines will play a critical role as individualized medicine continues to evolve, Somjot Brar, MD, MPH, director of the regional department of cardiac catheterization at Kaiser Permanente, Los Angeles Medical Center, and associate clinical professor at the University of California, Los Angeles, said in an interview.
“This study highlights again the importance of the value for predictive and precision medicine,” Dr. Brar said. “Everything is moving in this direction where we make decisions that are more appropriate for a given patient as opposed to a population of patients.”
Study strengths are the large sample size in a real-world setting and thorough 1-year follow-up, Dr. Brar said.
A limitation is the three risk categories the guidelines proposed. “These are still pretty big boxes,” he said. “The low-, moderate- and high-risk categorization is still very, very broad and can be very vague.”
The relatively low percentage of low-risk patients – 12% versus 56% and 32% for the moderate- and high-risk groups – in this data set may also skew results, Dr. Brar said.
“As we move toward predictive analytics and medicine, we want to make these boxes smaller and smaller and smaller to be able to better understand which treatments should be administered to which patients to maximize the benefit against the risk,” he said. That would be a focus for future analyses, Dr. Brar said.
Dr. Dangas and Dr. Brar have no relevant financial disclosures.
A real-world study of more than 12,000 cases over 7 years has validated the predictive ability of the proposed guidelines for stratifying thrombotic risks at 1 year for patients with non–ST-elevated acute coronary syndrome (NSTE-ACS) undergoing percutaneous coronary intervention (PCI).
In research presented at the Society for Cardiovascular Angiography & Interventions annual scientific sessions, George Dangas, MD, PhD, current SCAI president and professor of cardiology and vascular surgery at the Icahn School of Medicine at Mount Sinai, New York, reported that the European Society of Cardiology risk stratification criteria appropriately predicted risk in 12,538 patients treated from 2012 to 2019.
Despite these proposed guidelines put forward by the ESC in 2020, no consensus exists on criteria for ischemic or thrombotic risk in NSTE-ACS patients, Dr. Dangas noted.
The new study shows that the 1-year major adverse cardiovascular events (MACE) risk was four times greater in patients classified as medium risk (hazard ratio, 4.31; 95% confidence interval, 2.47-7.52) and six times greater in high-risk patients (HR, 6.16; 95% CI, 3.52-10.8), compared with the low-risk group, mostly because of higher rates of all-cause death and myocardial infarction, Dr. Dangas said in an interview.
“Indeed, we found some good correlation between the three risk categories and gradation of risk that validates essentially, but with the statistical testing that we need, that this classification is meaningful if not perfect,” Dr. Dangas said. “In the future we may perform calibrations to enhance its performance.”
The study used data on consecutive patients from the Angioplasty and Stent Procedures Database of Mount Sinai, grouping them into low, medium, and high thrombotic risk based on the proposed ESC guidelines for the management of NSTE-ACS.
The guidelines included a subset of criteria to identify patients with increased thrombotic risk who may benefit from extended treatment with a second antithrombotic agent.
This study aimed to evaluate the value of the criteria to identify patients at higher risk of ischemic events. “That’s why we went to our database to see how this might work,” Dr. Dangas said.
The researchers also found that high-risk patients had about a 40% greater risk of major bleeding (HR, 1.39; 95% CI, 1.06-1.84). Bleeding risks were similar between the low- and moderate-risk groups.
The risk categories reflected the rates of all-cause death, myocardial infarction, or stroke: 5.4%, 4.1%, and 1.6% in the high-, moderate-, and low-risks groups, respectively (P < .001).
“This identification of ischemic risks worked very well for all-cause mortality,” Dr. Dangas said. “I feel this is a strength because mortality is a leader of outcomes. And of course, we’ve had some associations with all events like mortality, myocardial infarction, repeat revascularization, which are interesting and valid, but I think a study result that indicates the mortality itself is known to be unidirectional and a very good correlation makes the result more robust.”
Critical role
Risk prediction models such as the proposed ESC guidelines will play a critical role as individualized medicine continues to evolve, Somjot Brar, MD, MPH, director of the regional department of cardiac catheterization at Kaiser Permanente, Los Angeles Medical Center, and associate clinical professor at the University of California, Los Angeles, said in an interview.
“This study highlights again the importance of the value for predictive and precision medicine,” Dr. Brar said. “Everything is moving in this direction where we make decisions that are more appropriate for a given patient as opposed to a population of patients.”
Study strengths are the large sample size in a real-world setting and thorough 1-year follow-up, Dr. Brar said.
A limitation is the three risk categories the guidelines proposed. “These are still pretty big boxes,” he said. “The low-, moderate- and high-risk categorization is still very, very broad and can be very vague.”
The relatively low percentage of low-risk patients – 12% versus 56% and 32% for the moderate- and high-risk groups – in this data set may also skew results, Dr. Brar said.
“As we move toward predictive analytics and medicine, we want to make these boxes smaller and smaller and smaller to be able to better understand which treatments should be administered to which patients to maximize the benefit against the risk,” he said. That would be a focus for future analyses, Dr. Brar said.
Dr. Dangas and Dr. Brar have no relevant financial disclosures.
FROM SCAI 2023
FDA approves buprenorphine injection for opioid use disorder
The medication comes in two formulations: a weekly and a monthly version. The weekly treatment is indicated in patients who have initiated treatment with a single dose of transmucosal buprenorphine or who are already being treated with the drug. The monthly version is for patients already receiving buprenorphine.
“Buprenorphine is an important treatment option for opioid use disorder. Today’s approval expands dosing options and provides people with opioid use disorder a greater opportunity to sustain long-term recovery,” said FDA Commissioner Robert M. Califf, MD, in a release. “The FDA will continue to take the critical steps necessary to pursue efforts that advance evidence-based treatments for substance use disorders, which is a strategic priority under the FDA’s Overdose Prevention Framework,” Dr. Califf added.
The Substance Abuse and Mental Health Services Administration reports that patients receiving medication for OUD have their risk for all-cause mortality cut by 50%.
In its release, the FDA said that it remains committed to increasing treatment options for OUD. Earlier this month, the agency issued a joint letter with SAMHSA to underscore the importance of counseling and other services as part of a comprehensive treatment plan the disorder. It also emphasized that receiving buprenorphine should not be contingent on participating in such services.
Brixadi is approved in both weekly and monthly subcutaneous injectable formulations at varying doses, including lower doses that may be appropriate for patients who do not tolerate higher doses of extended-release buprenorphine that are currently available.
The drug will be available through a Risk Evaluation and Mitigation Strategy program and administered only by health care providers in a health care setting.
The most common adverse reactions associated with the drug include injection-site pain, headache, constipation, nausea, injection-site erythema, injection-site pruritus, insomnia, and urinary tract infections. The FDA reports that such side effects occur in at least 5% of patients.
A version of this article originally appeared on Medscape.com.
The medication comes in two formulations: a weekly and a monthly version. The weekly treatment is indicated in patients who have initiated treatment with a single dose of transmucosal buprenorphine or who are already being treated with the drug. The monthly version is for patients already receiving buprenorphine.
“Buprenorphine is an important treatment option for opioid use disorder. Today’s approval expands dosing options and provides people with opioid use disorder a greater opportunity to sustain long-term recovery,” said FDA Commissioner Robert M. Califf, MD, in a release. “The FDA will continue to take the critical steps necessary to pursue efforts that advance evidence-based treatments for substance use disorders, which is a strategic priority under the FDA’s Overdose Prevention Framework,” Dr. Califf added.
The Substance Abuse and Mental Health Services Administration reports that patients receiving medication for OUD have their risk for all-cause mortality cut by 50%.
In its release, the FDA said that it remains committed to increasing treatment options for OUD. Earlier this month, the agency issued a joint letter with SAMHSA to underscore the importance of counseling and other services as part of a comprehensive treatment plan the disorder. It also emphasized that receiving buprenorphine should not be contingent on participating in such services.
Brixadi is approved in both weekly and monthly subcutaneous injectable formulations at varying doses, including lower doses that may be appropriate for patients who do not tolerate higher doses of extended-release buprenorphine that are currently available.
The drug will be available through a Risk Evaluation and Mitigation Strategy program and administered only by health care providers in a health care setting.
The most common adverse reactions associated with the drug include injection-site pain, headache, constipation, nausea, injection-site erythema, injection-site pruritus, insomnia, and urinary tract infections. The FDA reports that such side effects occur in at least 5% of patients.
A version of this article originally appeared on Medscape.com.
The medication comes in two formulations: a weekly and a monthly version. The weekly treatment is indicated in patients who have initiated treatment with a single dose of transmucosal buprenorphine or who are already being treated with the drug. The monthly version is for patients already receiving buprenorphine.
“Buprenorphine is an important treatment option for opioid use disorder. Today’s approval expands dosing options and provides people with opioid use disorder a greater opportunity to sustain long-term recovery,” said FDA Commissioner Robert M. Califf, MD, in a release. “The FDA will continue to take the critical steps necessary to pursue efforts that advance evidence-based treatments for substance use disorders, which is a strategic priority under the FDA’s Overdose Prevention Framework,” Dr. Califf added.
The Substance Abuse and Mental Health Services Administration reports that patients receiving medication for OUD have their risk for all-cause mortality cut by 50%.
In its release, the FDA said that it remains committed to increasing treatment options for OUD. Earlier this month, the agency issued a joint letter with SAMHSA to underscore the importance of counseling and other services as part of a comprehensive treatment plan the disorder. It also emphasized that receiving buprenorphine should not be contingent on participating in such services.
Brixadi is approved in both weekly and monthly subcutaneous injectable formulations at varying doses, including lower doses that may be appropriate for patients who do not tolerate higher doses of extended-release buprenorphine that are currently available.
The drug will be available through a Risk Evaluation and Mitigation Strategy program and administered only by health care providers in a health care setting.
The most common adverse reactions associated with the drug include injection-site pain, headache, constipation, nausea, injection-site erythema, injection-site pruritus, insomnia, and urinary tract infections. The FDA reports that such side effects occur in at least 5% of patients.
A version of this article originally appeared on Medscape.com.
Female sexual pleasure: Is it in the water?
BALTIMORE – , according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. In a secondary analysis also presented at the meeting, the lubricants were found not to alter the vaginal microbiome.
Using these types of lubricants during vaginal intercourse at least once a week over a 4-week period resulted in a statistically significant increase of over four points in the 36-point Female Sexual Function Index (FSFI), a self-reported measure of sexual functioning, for participants, said Michael Krychman, MD, executive director of the Southern California Center for Sexual Health and Survivorship Medicine, Newport Beach, the senior author of the study. Statistically significant improvements also were observed in individual areas such as sexual desire and arousal, orgasm, and satisfaction. Results of the study have been published in the Journal of Sexual Medicine.
In the open-label, five-arm, parallel study conducted in Germany, 174 women aged 18-65 years were randomly assigned to use one of five lubricants from three popular brands. After a 4-week run-in period with no use of lubricants, participants were shown how to apply the products and instructed to use the substances during vaginal intercourse at least once a week over a 4-week period.
Participants reported experiencing mild to moderate vaginal dryness and dyspareunia during vaginal intercourse within the previous 3 months.
Statistically significant improvements were seen across all six individual domain scores of the FSFI (desire, arousal, lubrication, orgasm, satisfaction, and pain reduction) from baseline to week 4 with all five lubricants (P < .0001 for lubrication and pain reduction; P < .05 for desire, arousal, orgasm, and satisfaction), according to the researchers.
After 4 weeks, a clinically meaningful improvement in the total FSFI score was observed for four lubricants among premenopausal women and for all lubricants among postmenopausal women. The percentage of participants with sexual function as defined as a score of at least 26.55 on the FSFI was significantly greater after treatment (76.9%) than before treatment (20.8%; P < .0001).
“You would assume if you’re using lubricant it would improve the dryness, but what was very exciting for us is that it improved desire, it improved orgasm, it improved arousal,” Dr. Krychman said in an interview. Like concentric overlapping circles of female sexual function, he said, “if you improve one aspect, you improve the other.”
Nearly 80 nonserious adverse effects occurred in 43 participants, five of which were thought to be possibly attributed to the products, such as vulvovaginal burning, itching, or discomfort. In questionnaires, most women agreed that using the lubricants made sex more enjoyable and provided an overall pleasant experience.
One limitation of the study is that because most participants were Caucasian, the results may not be generalizable to all populations, according to the researchers. Further research is required to fully determine safety and efficacy in patients of all races and ethnicities, they reported, especially given that vaginal dryness has been reported more frequently in non-White ethnic groups.
In a companion presentation, Dr. Krychman discussed another aspect of the study looking at the lubricants’ effects on the vaginal microbiome. Repeated application of the products did not significantly alter the vaginal microbiome for up to 4 weeks, and vaginal pH slightly increased in all treatment groups shortly after use but was restored in most cases after a day.
Water-based lubricants are recommended by the WHO for use with condoms because they do not erode latex, said Karen Adams, MD, professor emeritus of obstetrics and gynecology and founding director of the Menopause and Sexual Medicine Program at Oregon Health & Science University, Portland. Guidelines from the group recommend lubricants should have an osmolality that is as close to normal vaginal secretions as possible to decrease the likelihood of irritation or other side effects, she said. Some available lubricants have four to six times that osmolality, which potentially could dehydrate cells, achieving the opposite of the desired effect.
“The reason this is important is they’re trying to develop lubricants that are more ‘vaginal friendly’ and more in line with the WHO guidelines,” said Dr. Adams, who is joining Stanford (Calif.) University in July to create and lead a new program in menopause and healthy aging. “They came up with four formulas consistent with WHO guidelines to see if these new ones worked at least as well [as commercially available products with higher osmolality], and it turns out they did,” she said. “They worked just fine.”
The study was funded by Reckitt Healthcare. Dr. Krychman is a paid medical consultant for the company. Dr. Adams disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
BALTIMORE – , according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. In a secondary analysis also presented at the meeting, the lubricants were found not to alter the vaginal microbiome.
Using these types of lubricants during vaginal intercourse at least once a week over a 4-week period resulted in a statistically significant increase of over four points in the 36-point Female Sexual Function Index (FSFI), a self-reported measure of sexual functioning, for participants, said Michael Krychman, MD, executive director of the Southern California Center for Sexual Health and Survivorship Medicine, Newport Beach, the senior author of the study. Statistically significant improvements also were observed in individual areas such as sexual desire and arousal, orgasm, and satisfaction. Results of the study have been published in the Journal of Sexual Medicine.
In the open-label, five-arm, parallel study conducted in Germany, 174 women aged 18-65 years were randomly assigned to use one of five lubricants from three popular brands. After a 4-week run-in period with no use of lubricants, participants were shown how to apply the products and instructed to use the substances during vaginal intercourse at least once a week over a 4-week period.
Participants reported experiencing mild to moderate vaginal dryness and dyspareunia during vaginal intercourse within the previous 3 months.
Statistically significant improvements were seen across all six individual domain scores of the FSFI (desire, arousal, lubrication, orgasm, satisfaction, and pain reduction) from baseline to week 4 with all five lubricants (P < .0001 for lubrication and pain reduction; P < .05 for desire, arousal, orgasm, and satisfaction), according to the researchers.
After 4 weeks, a clinically meaningful improvement in the total FSFI score was observed for four lubricants among premenopausal women and for all lubricants among postmenopausal women. The percentage of participants with sexual function as defined as a score of at least 26.55 on the FSFI was significantly greater after treatment (76.9%) than before treatment (20.8%; P < .0001).
“You would assume if you’re using lubricant it would improve the dryness, but what was very exciting for us is that it improved desire, it improved orgasm, it improved arousal,” Dr. Krychman said in an interview. Like concentric overlapping circles of female sexual function, he said, “if you improve one aspect, you improve the other.”
Nearly 80 nonserious adverse effects occurred in 43 participants, five of which were thought to be possibly attributed to the products, such as vulvovaginal burning, itching, or discomfort. In questionnaires, most women agreed that using the lubricants made sex more enjoyable and provided an overall pleasant experience.
One limitation of the study is that because most participants were Caucasian, the results may not be generalizable to all populations, according to the researchers. Further research is required to fully determine safety and efficacy in patients of all races and ethnicities, they reported, especially given that vaginal dryness has been reported more frequently in non-White ethnic groups.
In a companion presentation, Dr. Krychman discussed another aspect of the study looking at the lubricants’ effects on the vaginal microbiome. Repeated application of the products did not significantly alter the vaginal microbiome for up to 4 weeks, and vaginal pH slightly increased in all treatment groups shortly after use but was restored in most cases after a day.
Water-based lubricants are recommended by the WHO for use with condoms because they do not erode latex, said Karen Adams, MD, professor emeritus of obstetrics and gynecology and founding director of the Menopause and Sexual Medicine Program at Oregon Health & Science University, Portland. Guidelines from the group recommend lubricants should have an osmolality that is as close to normal vaginal secretions as possible to decrease the likelihood of irritation or other side effects, she said. Some available lubricants have four to six times that osmolality, which potentially could dehydrate cells, achieving the opposite of the desired effect.
“The reason this is important is they’re trying to develop lubricants that are more ‘vaginal friendly’ and more in line with the WHO guidelines,” said Dr. Adams, who is joining Stanford (Calif.) University in July to create and lead a new program in menopause and healthy aging. “They came up with four formulas consistent with WHO guidelines to see if these new ones worked at least as well [as commercially available products with higher osmolality], and it turns out they did,” she said. “They worked just fine.”
The study was funded by Reckitt Healthcare. Dr. Krychman is a paid medical consultant for the company. Dr. Adams disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
BALTIMORE – , according to research presented at the annual clinical and scientific meeting of the American College of Obstetricians and Gynecologists. In a secondary analysis also presented at the meeting, the lubricants were found not to alter the vaginal microbiome.
Using these types of lubricants during vaginal intercourse at least once a week over a 4-week period resulted in a statistically significant increase of over four points in the 36-point Female Sexual Function Index (FSFI), a self-reported measure of sexual functioning, for participants, said Michael Krychman, MD, executive director of the Southern California Center for Sexual Health and Survivorship Medicine, Newport Beach, the senior author of the study. Statistically significant improvements also were observed in individual areas such as sexual desire and arousal, orgasm, and satisfaction. Results of the study have been published in the Journal of Sexual Medicine.
In the open-label, five-arm, parallel study conducted in Germany, 174 women aged 18-65 years were randomly assigned to use one of five lubricants from three popular brands. After a 4-week run-in period with no use of lubricants, participants were shown how to apply the products and instructed to use the substances during vaginal intercourse at least once a week over a 4-week period.
Participants reported experiencing mild to moderate vaginal dryness and dyspareunia during vaginal intercourse within the previous 3 months.
Statistically significant improvements were seen across all six individual domain scores of the FSFI (desire, arousal, lubrication, orgasm, satisfaction, and pain reduction) from baseline to week 4 with all five lubricants (P < .0001 for lubrication and pain reduction; P < .05 for desire, arousal, orgasm, and satisfaction), according to the researchers.
After 4 weeks, a clinically meaningful improvement in the total FSFI score was observed for four lubricants among premenopausal women and for all lubricants among postmenopausal women. The percentage of participants with sexual function as defined as a score of at least 26.55 on the FSFI was significantly greater after treatment (76.9%) than before treatment (20.8%; P < .0001).
“You would assume if you’re using lubricant it would improve the dryness, but what was very exciting for us is that it improved desire, it improved orgasm, it improved arousal,” Dr. Krychman said in an interview. Like concentric overlapping circles of female sexual function, he said, “if you improve one aspect, you improve the other.”
Nearly 80 nonserious adverse effects occurred in 43 participants, five of which were thought to be possibly attributed to the products, such as vulvovaginal burning, itching, or discomfort. In questionnaires, most women agreed that using the lubricants made sex more enjoyable and provided an overall pleasant experience.
One limitation of the study is that because most participants were Caucasian, the results may not be generalizable to all populations, according to the researchers. Further research is required to fully determine safety and efficacy in patients of all races and ethnicities, they reported, especially given that vaginal dryness has been reported more frequently in non-White ethnic groups.
In a companion presentation, Dr. Krychman discussed another aspect of the study looking at the lubricants’ effects on the vaginal microbiome. Repeated application of the products did not significantly alter the vaginal microbiome for up to 4 weeks, and vaginal pH slightly increased in all treatment groups shortly after use but was restored in most cases after a day.
Water-based lubricants are recommended by the WHO for use with condoms because they do not erode latex, said Karen Adams, MD, professor emeritus of obstetrics and gynecology and founding director of the Menopause and Sexual Medicine Program at Oregon Health & Science University, Portland. Guidelines from the group recommend lubricants should have an osmolality that is as close to normal vaginal secretions as possible to decrease the likelihood of irritation or other side effects, she said. Some available lubricants have four to six times that osmolality, which potentially could dehydrate cells, achieving the opposite of the desired effect.
“The reason this is important is they’re trying to develop lubricants that are more ‘vaginal friendly’ and more in line with the WHO guidelines,” said Dr. Adams, who is joining Stanford (Calif.) University in July to create and lead a new program in menopause and healthy aging. “They came up with four formulas consistent with WHO guidelines to see if these new ones worked at least as well [as commercially available products with higher osmolality], and it turns out they did,” she said. “They worked just fine.”
The study was funded by Reckitt Healthcare. Dr. Krychman is a paid medical consultant for the company. Dr. Adams disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
AT ACOG 2023
Can online mindfulness and self-compassion training improve quality of life for patients with atopic dermatitis?
, according to results of a small randomized controlled trial in Japan.
“We found that skin disease–specific QOL improved over time with a large effect size,” lead study author Sanae Kishimoto, MHS, MPH, of the School of Public Health, Graduate School of Medicine at Kyoto University and colleagues write in JAMA Dermatology. “These findings suggest that mindfulness and self-compassion training is an effective treatment option for adults with AD.”
A bothersome disease that worsens quality of life
AD, a chronic, relapsing, inflammatory, multifactorial skin disease involving intense itching, affects an estimated 15%-30% of children and 2%-10% of adults, with the incidence increasing in industrialized countries, the authors state.
Measured by disability-adjusted life years, AD has the highest disease burden among skin diseases, and people with AD commonly have anxiety, depression, and sleep problems. Treatments include medications, other skin care, and lifestyle changes. New biologics appear to be effective but are expensive and need to be studied for their long-term safety, the authors add.
“Stress can make the skin worse, but at the same time the skin disease and symptoms cause stress,” Peter A. Lio, MD, who was not involved in the study, told this news organization by email. “This vicious cycle contributes greatly to impairing quality of life.”
A program focused on wise, kind self-care
In the SMiLE study, the authors recruited adults with moderate to severe AD and Dermatology Life Quality Index (DLQI) score above 6 from dermatology clinics and through online announcements over 1 year beginning in July 2019.
Participants averaged 36.3 years of age, 80% were women, and their mean AD duration was 26.6 years. Everyone was allowed to receive usual care during the study, except for dupilumab (a newly marketed drug when the study started), psychotherapy, or other mindfulness training.
The researchers randomly assigned 56 adults to receive mindfulness training in addition to their usual care and 51 to the wait list plus usual care. Those in the training group received eight weekly 90-minute online mindfulness and self-compassion sessions. Each group-based session was conducted at the same time and day of the week and included meditation, informal psychoeducation, inquiry, and a short lecture, along with an optional 1-day silent meditation retreat at week 7 and an optional 2-hour videoconferencing booster session at week 13.
The intervention encouraged a nonjudgmental relationship with stress using mindfulness-based stress reduction (MBSR) and emphasized a compassionate relationship with oneself during suffering using mindful self-compassion (MSC). The program was developed and taught by lead author Dr. Kishimoto, a Japanese licensed clinical psychologist who has a history of AD, the paper notes.
At 13 weeks, after completing electronic assessments, patients in the training group showed greater improvement in the DLQI score than those on the wait list (between-group difference estimate, –6.34; 95% confidence interval, –8.27 to –4.41; P < .001). The standardized effect size (Cohen’s d) at 13 weeks was –1.06 (95% CI, –1.39 to –0.74).
Patients in the training group also improved more in all secondary outcomes: severity, itch- and scratch-related visual analog scales, self-compassion, mindfulness, psychological symptoms, and adherence to dermatologist-advised treatments.
They were also more likely to follow their dermatologist’s medical treatment plans, including moisturizer and topical steroid use.
One serious adverse event, endometrial cancer in one patient, was judged to be unrelated to the intervention.
Online format may give more patients access to treatment
“With relatively limited data in the literature, this particularly well-done, important study is likely to positively shape thinking around this topic,” said Dr. Lio, of the departments of dermatology and pediatrics at Northwestern University, Chicago. “This study nicely demonstrates that an online approach can be effective.
“In theory, these methods or techniques could democratize treatments like this, and open them up to many more patients,” he added. He would like to see partially or entirely automated apps (free of cost), similar to meditation “apps,” to treat patients more cost-effectively.
Dr. Lio explained that excluding participants on dupilumab (Dupixent) makes the results slightly less generalizable to patients with moderate to severe AD, who may have the most serious QOL challenges and who are often candidates for dupilumab.
“However, given that we almost never have all the known variables for a study, we are generally comfortable extrapolating that the intervention would likely be helpful for patients taking dupilumab as well, despite it not being specifically evaluated in that group,” he said.
Susan Massick, MD, of the department of dermatology at the Ohio State University Wexner Medical Center in Columbus, advises clinicians to take a multipronged approach to treating the physical and behavioral components of AD and to embrace therapies beyond prescription medications.
“Self-compassion training is another tool in our toolbox toward finding the right fix for our patients,” Dr. Massick said by email. She was not involved with this research.
“I applaud the focus of this study on behavioral health training as a means toward wellness and improved mindfulness,” she added. “I was impressed by the extent to which these simple measures helped improve the quality of life for patients who used the training.”
U.S. patients can benefit from these findings
“My sense is that AD patients the world over have many similar characteristics and concerns, so I would anticipate that the results would be comparable in a U.S. population,” Dr. Lio said. “Other studies performed in the U.S. also support this line of thinking.”
Although the study involved highly motivated patients in Japan, the suffering that patients with AD experience is universal regardless of race or ethnicity, Dr. Massick said. “Americans may be even more willing to embrace mindfulness and self-compassion training as a path toward better health and wellness.”
The study was funded by the Japan Agency for Medical Research and Development and the Mental Health Okamoto Memorial Foundation, the KDDI Foundation, the Pfizer Health Research Foundation, and the Japan Society for the Promotion of Science.
Dr. Kishimoto and several coauthors report relevant financial relationships with pharmaceutical companies. Dr. Lio reports financial relationships with Sanofi and Regeneron, the joint developers of dupilumab. Dr. Massick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to results of a small randomized controlled trial in Japan.
“We found that skin disease–specific QOL improved over time with a large effect size,” lead study author Sanae Kishimoto, MHS, MPH, of the School of Public Health, Graduate School of Medicine at Kyoto University and colleagues write in JAMA Dermatology. “These findings suggest that mindfulness and self-compassion training is an effective treatment option for adults with AD.”
A bothersome disease that worsens quality of life
AD, a chronic, relapsing, inflammatory, multifactorial skin disease involving intense itching, affects an estimated 15%-30% of children and 2%-10% of adults, with the incidence increasing in industrialized countries, the authors state.
Measured by disability-adjusted life years, AD has the highest disease burden among skin diseases, and people with AD commonly have anxiety, depression, and sleep problems. Treatments include medications, other skin care, and lifestyle changes. New biologics appear to be effective but are expensive and need to be studied for their long-term safety, the authors add.
“Stress can make the skin worse, but at the same time the skin disease and symptoms cause stress,” Peter A. Lio, MD, who was not involved in the study, told this news organization by email. “This vicious cycle contributes greatly to impairing quality of life.”
A program focused on wise, kind self-care
In the SMiLE study, the authors recruited adults with moderate to severe AD and Dermatology Life Quality Index (DLQI) score above 6 from dermatology clinics and through online announcements over 1 year beginning in July 2019.
Participants averaged 36.3 years of age, 80% were women, and their mean AD duration was 26.6 years. Everyone was allowed to receive usual care during the study, except for dupilumab (a newly marketed drug when the study started), psychotherapy, or other mindfulness training.
The researchers randomly assigned 56 adults to receive mindfulness training in addition to their usual care and 51 to the wait list plus usual care. Those in the training group received eight weekly 90-minute online mindfulness and self-compassion sessions. Each group-based session was conducted at the same time and day of the week and included meditation, informal psychoeducation, inquiry, and a short lecture, along with an optional 1-day silent meditation retreat at week 7 and an optional 2-hour videoconferencing booster session at week 13.
The intervention encouraged a nonjudgmental relationship with stress using mindfulness-based stress reduction (MBSR) and emphasized a compassionate relationship with oneself during suffering using mindful self-compassion (MSC). The program was developed and taught by lead author Dr. Kishimoto, a Japanese licensed clinical psychologist who has a history of AD, the paper notes.
At 13 weeks, after completing electronic assessments, patients in the training group showed greater improvement in the DLQI score than those on the wait list (between-group difference estimate, –6.34; 95% confidence interval, –8.27 to –4.41; P < .001). The standardized effect size (Cohen’s d) at 13 weeks was –1.06 (95% CI, –1.39 to –0.74).
Patients in the training group also improved more in all secondary outcomes: severity, itch- and scratch-related visual analog scales, self-compassion, mindfulness, psychological symptoms, and adherence to dermatologist-advised treatments.
They were also more likely to follow their dermatologist’s medical treatment plans, including moisturizer and topical steroid use.
One serious adverse event, endometrial cancer in one patient, was judged to be unrelated to the intervention.
Online format may give more patients access to treatment
“With relatively limited data in the literature, this particularly well-done, important study is likely to positively shape thinking around this topic,” said Dr. Lio, of the departments of dermatology and pediatrics at Northwestern University, Chicago. “This study nicely demonstrates that an online approach can be effective.
“In theory, these methods or techniques could democratize treatments like this, and open them up to many more patients,” he added. He would like to see partially or entirely automated apps (free of cost), similar to meditation “apps,” to treat patients more cost-effectively.
Dr. Lio explained that excluding participants on dupilumab (Dupixent) makes the results slightly less generalizable to patients with moderate to severe AD, who may have the most serious QOL challenges and who are often candidates for dupilumab.
“However, given that we almost never have all the known variables for a study, we are generally comfortable extrapolating that the intervention would likely be helpful for patients taking dupilumab as well, despite it not being specifically evaluated in that group,” he said.
Susan Massick, MD, of the department of dermatology at the Ohio State University Wexner Medical Center in Columbus, advises clinicians to take a multipronged approach to treating the physical and behavioral components of AD and to embrace therapies beyond prescription medications.
“Self-compassion training is another tool in our toolbox toward finding the right fix for our patients,” Dr. Massick said by email. She was not involved with this research.
“I applaud the focus of this study on behavioral health training as a means toward wellness and improved mindfulness,” she added. “I was impressed by the extent to which these simple measures helped improve the quality of life for patients who used the training.”
U.S. patients can benefit from these findings
“My sense is that AD patients the world over have many similar characteristics and concerns, so I would anticipate that the results would be comparable in a U.S. population,” Dr. Lio said. “Other studies performed in the U.S. also support this line of thinking.”
Although the study involved highly motivated patients in Japan, the suffering that patients with AD experience is universal regardless of race or ethnicity, Dr. Massick said. “Americans may be even more willing to embrace mindfulness and self-compassion training as a path toward better health and wellness.”
The study was funded by the Japan Agency for Medical Research and Development and the Mental Health Okamoto Memorial Foundation, the KDDI Foundation, the Pfizer Health Research Foundation, and the Japan Society for the Promotion of Science.
Dr. Kishimoto and several coauthors report relevant financial relationships with pharmaceutical companies. Dr. Lio reports financial relationships with Sanofi and Regeneron, the joint developers of dupilumab. Dr. Massick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to results of a small randomized controlled trial in Japan.
“We found that skin disease–specific QOL improved over time with a large effect size,” lead study author Sanae Kishimoto, MHS, MPH, of the School of Public Health, Graduate School of Medicine at Kyoto University and colleagues write in JAMA Dermatology. “These findings suggest that mindfulness and self-compassion training is an effective treatment option for adults with AD.”
A bothersome disease that worsens quality of life
AD, a chronic, relapsing, inflammatory, multifactorial skin disease involving intense itching, affects an estimated 15%-30% of children and 2%-10% of adults, with the incidence increasing in industrialized countries, the authors state.
Measured by disability-adjusted life years, AD has the highest disease burden among skin diseases, and people with AD commonly have anxiety, depression, and sleep problems. Treatments include medications, other skin care, and lifestyle changes. New biologics appear to be effective but are expensive and need to be studied for their long-term safety, the authors add.
“Stress can make the skin worse, but at the same time the skin disease and symptoms cause stress,” Peter A. Lio, MD, who was not involved in the study, told this news organization by email. “This vicious cycle contributes greatly to impairing quality of life.”
A program focused on wise, kind self-care
In the SMiLE study, the authors recruited adults with moderate to severe AD and Dermatology Life Quality Index (DLQI) score above 6 from dermatology clinics and through online announcements over 1 year beginning in July 2019.
Participants averaged 36.3 years of age, 80% were women, and their mean AD duration was 26.6 years. Everyone was allowed to receive usual care during the study, except for dupilumab (a newly marketed drug when the study started), psychotherapy, or other mindfulness training.
The researchers randomly assigned 56 adults to receive mindfulness training in addition to their usual care and 51 to the wait list plus usual care. Those in the training group received eight weekly 90-minute online mindfulness and self-compassion sessions. Each group-based session was conducted at the same time and day of the week and included meditation, informal psychoeducation, inquiry, and a short lecture, along with an optional 1-day silent meditation retreat at week 7 and an optional 2-hour videoconferencing booster session at week 13.
The intervention encouraged a nonjudgmental relationship with stress using mindfulness-based stress reduction (MBSR) and emphasized a compassionate relationship with oneself during suffering using mindful self-compassion (MSC). The program was developed and taught by lead author Dr. Kishimoto, a Japanese licensed clinical psychologist who has a history of AD, the paper notes.
At 13 weeks, after completing electronic assessments, patients in the training group showed greater improvement in the DLQI score than those on the wait list (between-group difference estimate, –6.34; 95% confidence interval, –8.27 to –4.41; P < .001). The standardized effect size (Cohen’s d) at 13 weeks was –1.06 (95% CI, –1.39 to –0.74).
Patients in the training group also improved more in all secondary outcomes: severity, itch- and scratch-related visual analog scales, self-compassion, mindfulness, psychological symptoms, and adherence to dermatologist-advised treatments.
They were also more likely to follow their dermatologist’s medical treatment plans, including moisturizer and topical steroid use.
One serious adverse event, endometrial cancer in one patient, was judged to be unrelated to the intervention.
Online format may give more patients access to treatment
“With relatively limited data in the literature, this particularly well-done, important study is likely to positively shape thinking around this topic,” said Dr. Lio, of the departments of dermatology and pediatrics at Northwestern University, Chicago. “This study nicely demonstrates that an online approach can be effective.
“In theory, these methods or techniques could democratize treatments like this, and open them up to many more patients,” he added. He would like to see partially or entirely automated apps (free of cost), similar to meditation “apps,” to treat patients more cost-effectively.
Dr. Lio explained that excluding participants on dupilumab (Dupixent) makes the results slightly less generalizable to patients with moderate to severe AD, who may have the most serious QOL challenges and who are often candidates for dupilumab.
“However, given that we almost never have all the known variables for a study, we are generally comfortable extrapolating that the intervention would likely be helpful for patients taking dupilumab as well, despite it not being specifically evaluated in that group,” he said.
Susan Massick, MD, of the department of dermatology at the Ohio State University Wexner Medical Center in Columbus, advises clinicians to take a multipronged approach to treating the physical and behavioral components of AD and to embrace therapies beyond prescription medications.
“Self-compassion training is another tool in our toolbox toward finding the right fix for our patients,” Dr. Massick said by email. She was not involved with this research.
“I applaud the focus of this study on behavioral health training as a means toward wellness and improved mindfulness,” she added. “I was impressed by the extent to which these simple measures helped improve the quality of life for patients who used the training.”
U.S. patients can benefit from these findings
“My sense is that AD patients the world over have many similar characteristics and concerns, so I would anticipate that the results would be comparable in a U.S. population,” Dr. Lio said. “Other studies performed in the U.S. also support this line of thinking.”
Although the study involved highly motivated patients in Japan, the suffering that patients with AD experience is universal regardless of race or ethnicity, Dr. Massick said. “Americans may be even more willing to embrace mindfulness and self-compassion training as a path toward better health and wellness.”
The study was funded by the Japan Agency for Medical Research and Development and the Mental Health Okamoto Memorial Foundation, the KDDI Foundation, the Pfizer Health Research Foundation, and the Japan Society for the Promotion of Science.
Dr. Kishimoto and several coauthors report relevant financial relationships with pharmaceutical companies. Dr. Lio reports financial relationships with Sanofi and Regeneron, the joint developers of dupilumab. Dr. Massick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA DERMATOLOGY
Cut in AFib burden gains traction as gauge of ablation success: PULSED-AF
suggests a new analysis.
It’s the first study tying those outcomes to residual AFib burden after ablation achieved using the emerging pulsed-field ablation (PFA) technology, say researchers. These associations are already established for cath ablation using traditional radiofrequency energy or cryoablation.
The new findings come from a secondary analysis of the recently published PULSED-AF study, which highlighted the ablation efficacy of Medtronic’s investigational PulseSelect PFA system in patients with either paroxysmal AFib (PAF) or persistent AFib.
The trial had entered 300 adult candidates for catheter ablation of recurrent, symptomatic PAF or persistent AFib at 41 centers in Australia, Canada, Europe, Japan, and the United States.
After ablation, 69% of PAF patients and 62% of those who had persistent AFib showed no sign of atrial arrhythmia (AA) over 12 months, based on the trial’s method for estimating AA burden.
Residual AA burden less than 10% was seen in 87% and 82% of those initially with PAF and persistent AFib, respectively. Burdens in that lowest range, compared with greater AA burden, predicted a “clinically meaningful” improvement in QoL scores in PAF patients.
Those who entered the study with persistent AFib showed such improvement – defined as a more than 19-point gain on the Atrial Fibrillation Effect on Quality-of-Life Questionnaire – regardless of postablation AA burden.
Moreover, patients initially with either type of AFib and residual burdens in the lowest range went on to have fewer cardioversions and repeat ablations (P < .01), Atul Verma, MD, McGill University Health Centre, Montreal, reported at the annual scientific sessions of the Heart Rhythm Society.
Dr. Verma, the trial’s principal investigator, is also lead author on the same-day publication of the secondary analysis in Heart Rhythm.
Binary endpoint lacks relevance
The PULSED-AF primary analysis defined ablation efficacy partly as freedom from AA recurrence lasting at least 30 seconds, with or without symptoms, a traditional AFib-ablation trial endpoint that is nonetheless considered clinically unhelpful.
The secondary analysis recasts that binary endpoint as degree of reduction in AFib burden, a continuous variable. That potentially allows AFib ablation efficacy to be assessed in a more nuanced way likely to be more meaningful to patients and the health care system, observed Dr. Verma and colleagues.
The “30-second endpoint” is limited in clinical usefulness and “doesn’t mean much to the patient,” he said at a press conference on the analysis before formally presenting it at the HRS sessions.
Recent AFib ablation trials have explored AA burden as possibly a superior way to assess the procedure’s success “but also to see if it’s better correlated with quality of life and health care outcomes,” Dr. Verma said. “So that’s exactly what we’ve tried to do here using the PULSED-AF data.”
In the secondary analysis, he said, patients’ rate of freedom from the 30-second endpoint was about 70%, but “more than 85% of them had an AFib burden of less than 10%.”
“This efficacy endpoint of 30 seconds of atrial arrhythmia has been challenged and has been seen clinically as insignificant,” agreed Rajeev Pathak, MBBS, PhD, of Australian National University and director of cardiac electrophysiology at Canberra (Australia) Hospital.
In AFib radiofrequency ablation and cryoablation studies “there is clear disconnect between these 30-second episodes of atrial arrhythmias we see and the clinical relevance of health care utilization and quality of life,” said Dr. Pathak, invited discussant for Dr. Verma’s presentation at the sessions.
Now an AFib ablation trial using PFA catheters has yielded similar results, finding AA burden to be “a more objective and relevant measure of success,” he said. “A 30-second endpoint is arbitrary, lacks significance, and is highly dependent on the monitoring strategy.”
The more you look, the more you see
The new secondary analysis included a demonstration that success rates based on the 30-second endpoint indeed vary depending on how subsequent arrhythmias are monitored.
As described by Dr. Verma, PULSED-AF data were assessed for the 30-second endpoint captured using three separate intermittent monitoring strategies that it and other recent ablation trials have used:
- Strategy A: Transtelephonic monitoring weekly and in the event of symptoms, plus 24-hour Holter monitoring at 6 and 12 months and 12-lead ECG at 3, 6, and 12 months
- Strategy B: Transtelephonic monitoring weekly and at symptoms for 3-6 months followed by monthly and at symptoms from 6 to 12 months, plus 24-hour Holter monitoring at 6 and 12 months, plus 12-lead ECG at 3, 6, and 12 months
- Strategy C: The median of two 24-hour Holter monitoring sessions per patient over 12 months
As Dr. Verma reported, rates of freedom from the 30-second endpoint climbed with successive monitoring strategies. The rates for PAF and persistent AFib patients, respectively, were: Strategy A – 70% and 62%, Strategy B – 71% and 68%, Strategy C – 91% and 86%.
“If you’re using the ‘freedom-from-30-seconds’ endpoint, the results that you are going to get are highly dependent on the monitoring strategy,” Dr. Verma said. “The more you look, the more you see.”
Valid estimation of burden
For the main PULSED-AF secondary analysis, the investigators defined AA burden according to findings on either Holter monitoring or the 12-lead ECG. “So as not to bias these results,” Dr. Verma said, “for every patient, we picked the method that gave us the highest atrial arrhythmia burden.”
Ideally, Dr. Verma said in an interview, arrhythmia burden would be determined using devices such as implantable loop recorders. “The problem is, this is expensive and not practical” in both clinical practice and many trials, so PULSED-AF investigators went with the intermittent monitoring strategy to estimate burdens.
Their method appears valid, he said, given that the study identified a statistically relevant 10% AA burden cut off for predicting quality of life improvement or less health care resource use.
“If their residual atrial arrhythmia burden was greater than 10%, they did not have a statistically significant improvement in quality of life,” Dr. Verma observed. And “very few” of them had cardioversions or repeat ablation.
“I couldn’t agree more” that residual AA burden is preferable to the 30-second endpoint for gauging AFib ablation success, Kenneth Ellenbogen, MD, Virginia Commonwealth University Medical Center, Richmond, said in an interview. Dr. Ellenbogen is also director of clinical cardiac electrophysiology and pacing at VCU Health Pauley Heart Center and not associated with PULSED-AF.
That AA burden was linked to health care resource use in the study “is absolutely brilliant,” he said, “because that’s what the bean counters really want at the end of the day. And as doctors we care about patients feeling better – improving quality of life.”
PULSED-AF was funded by Medtronic. Dr. Verma disclosed financial relationships with Bayer, Biosense Webster, Medtronic, Thermedical, Kardium, and Galaxy Medical, as well as and research grants from Adagio Medical. Dr. Ellenbogen disclosed financial relationships with Boston Scientific, Medtronic, Kestra, Hylomorph, Biotronik, MediLynx, Impulse Dynamics USA, Abbott, Biosense Webster, Milestone Pharmaceuticals, Sanofi, Medpace, and Elsevier. Dr. Pathak disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
suggests a new analysis.
It’s the first study tying those outcomes to residual AFib burden after ablation achieved using the emerging pulsed-field ablation (PFA) technology, say researchers. These associations are already established for cath ablation using traditional radiofrequency energy or cryoablation.
The new findings come from a secondary analysis of the recently published PULSED-AF study, which highlighted the ablation efficacy of Medtronic’s investigational PulseSelect PFA system in patients with either paroxysmal AFib (PAF) or persistent AFib.
The trial had entered 300 adult candidates for catheter ablation of recurrent, symptomatic PAF or persistent AFib at 41 centers in Australia, Canada, Europe, Japan, and the United States.
After ablation, 69% of PAF patients and 62% of those who had persistent AFib showed no sign of atrial arrhythmia (AA) over 12 months, based on the trial’s method for estimating AA burden.
Residual AA burden less than 10% was seen in 87% and 82% of those initially with PAF and persistent AFib, respectively. Burdens in that lowest range, compared with greater AA burden, predicted a “clinically meaningful” improvement in QoL scores in PAF patients.
Those who entered the study with persistent AFib showed such improvement – defined as a more than 19-point gain on the Atrial Fibrillation Effect on Quality-of-Life Questionnaire – regardless of postablation AA burden.
Moreover, patients initially with either type of AFib and residual burdens in the lowest range went on to have fewer cardioversions and repeat ablations (P < .01), Atul Verma, MD, McGill University Health Centre, Montreal, reported at the annual scientific sessions of the Heart Rhythm Society.
Dr. Verma, the trial’s principal investigator, is also lead author on the same-day publication of the secondary analysis in Heart Rhythm.
Binary endpoint lacks relevance
The PULSED-AF primary analysis defined ablation efficacy partly as freedom from AA recurrence lasting at least 30 seconds, with or without symptoms, a traditional AFib-ablation trial endpoint that is nonetheless considered clinically unhelpful.
The secondary analysis recasts that binary endpoint as degree of reduction in AFib burden, a continuous variable. That potentially allows AFib ablation efficacy to be assessed in a more nuanced way likely to be more meaningful to patients and the health care system, observed Dr. Verma and colleagues.
The “30-second endpoint” is limited in clinical usefulness and “doesn’t mean much to the patient,” he said at a press conference on the analysis before formally presenting it at the HRS sessions.
Recent AFib ablation trials have explored AA burden as possibly a superior way to assess the procedure’s success “but also to see if it’s better correlated with quality of life and health care outcomes,” Dr. Verma said. “So that’s exactly what we’ve tried to do here using the PULSED-AF data.”
In the secondary analysis, he said, patients’ rate of freedom from the 30-second endpoint was about 70%, but “more than 85% of them had an AFib burden of less than 10%.”
“This efficacy endpoint of 30 seconds of atrial arrhythmia has been challenged and has been seen clinically as insignificant,” agreed Rajeev Pathak, MBBS, PhD, of Australian National University and director of cardiac electrophysiology at Canberra (Australia) Hospital.
In AFib radiofrequency ablation and cryoablation studies “there is clear disconnect between these 30-second episodes of atrial arrhythmias we see and the clinical relevance of health care utilization and quality of life,” said Dr. Pathak, invited discussant for Dr. Verma’s presentation at the sessions.
Now an AFib ablation trial using PFA catheters has yielded similar results, finding AA burden to be “a more objective and relevant measure of success,” he said. “A 30-second endpoint is arbitrary, lacks significance, and is highly dependent on the monitoring strategy.”
The more you look, the more you see
The new secondary analysis included a demonstration that success rates based on the 30-second endpoint indeed vary depending on how subsequent arrhythmias are monitored.
As described by Dr. Verma, PULSED-AF data were assessed for the 30-second endpoint captured using three separate intermittent monitoring strategies that it and other recent ablation trials have used:
- Strategy A: Transtelephonic monitoring weekly and in the event of symptoms, plus 24-hour Holter monitoring at 6 and 12 months and 12-lead ECG at 3, 6, and 12 months
- Strategy B: Transtelephonic monitoring weekly and at symptoms for 3-6 months followed by monthly and at symptoms from 6 to 12 months, plus 24-hour Holter monitoring at 6 and 12 months, plus 12-lead ECG at 3, 6, and 12 months
- Strategy C: The median of two 24-hour Holter monitoring sessions per patient over 12 months
As Dr. Verma reported, rates of freedom from the 30-second endpoint climbed with successive monitoring strategies. The rates for PAF and persistent AFib patients, respectively, were: Strategy A – 70% and 62%, Strategy B – 71% and 68%, Strategy C – 91% and 86%.
“If you’re using the ‘freedom-from-30-seconds’ endpoint, the results that you are going to get are highly dependent on the monitoring strategy,” Dr. Verma said. “The more you look, the more you see.”
Valid estimation of burden
For the main PULSED-AF secondary analysis, the investigators defined AA burden according to findings on either Holter monitoring or the 12-lead ECG. “So as not to bias these results,” Dr. Verma said, “for every patient, we picked the method that gave us the highest atrial arrhythmia burden.”
Ideally, Dr. Verma said in an interview, arrhythmia burden would be determined using devices such as implantable loop recorders. “The problem is, this is expensive and not practical” in both clinical practice and many trials, so PULSED-AF investigators went with the intermittent monitoring strategy to estimate burdens.
Their method appears valid, he said, given that the study identified a statistically relevant 10% AA burden cut off for predicting quality of life improvement or less health care resource use.
“If their residual atrial arrhythmia burden was greater than 10%, they did not have a statistically significant improvement in quality of life,” Dr. Verma observed. And “very few” of them had cardioversions or repeat ablation.
“I couldn’t agree more” that residual AA burden is preferable to the 30-second endpoint for gauging AFib ablation success, Kenneth Ellenbogen, MD, Virginia Commonwealth University Medical Center, Richmond, said in an interview. Dr. Ellenbogen is also director of clinical cardiac electrophysiology and pacing at VCU Health Pauley Heart Center and not associated with PULSED-AF.
That AA burden was linked to health care resource use in the study “is absolutely brilliant,” he said, “because that’s what the bean counters really want at the end of the day. And as doctors we care about patients feeling better – improving quality of life.”
PULSED-AF was funded by Medtronic. Dr. Verma disclosed financial relationships with Bayer, Biosense Webster, Medtronic, Thermedical, Kardium, and Galaxy Medical, as well as and research grants from Adagio Medical. Dr. Ellenbogen disclosed financial relationships with Boston Scientific, Medtronic, Kestra, Hylomorph, Biotronik, MediLynx, Impulse Dynamics USA, Abbott, Biosense Webster, Milestone Pharmaceuticals, Sanofi, Medpace, and Elsevier. Dr. Pathak disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
suggests a new analysis.
It’s the first study tying those outcomes to residual AFib burden after ablation achieved using the emerging pulsed-field ablation (PFA) technology, say researchers. These associations are already established for cath ablation using traditional radiofrequency energy or cryoablation.
The new findings come from a secondary analysis of the recently published PULSED-AF study, which highlighted the ablation efficacy of Medtronic’s investigational PulseSelect PFA system in patients with either paroxysmal AFib (PAF) or persistent AFib.
The trial had entered 300 adult candidates for catheter ablation of recurrent, symptomatic PAF or persistent AFib at 41 centers in Australia, Canada, Europe, Japan, and the United States.
After ablation, 69% of PAF patients and 62% of those who had persistent AFib showed no sign of atrial arrhythmia (AA) over 12 months, based on the trial’s method for estimating AA burden.
Residual AA burden less than 10% was seen in 87% and 82% of those initially with PAF and persistent AFib, respectively. Burdens in that lowest range, compared with greater AA burden, predicted a “clinically meaningful” improvement in QoL scores in PAF patients.
Those who entered the study with persistent AFib showed such improvement – defined as a more than 19-point gain on the Atrial Fibrillation Effect on Quality-of-Life Questionnaire – regardless of postablation AA burden.
Moreover, patients initially with either type of AFib and residual burdens in the lowest range went on to have fewer cardioversions and repeat ablations (P < .01), Atul Verma, MD, McGill University Health Centre, Montreal, reported at the annual scientific sessions of the Heart Rhythm Society.
Dr. Verma, the trial’s principal investigator, is also lead author on the same-day publication of the secondary analysis in Heart Rhythm.
Binary endpoint lacks relevance
The PULSED-AF primary analysis defined ablation efficacy partly as freedom from AA recurrence lasting at least 30 seconds, with or without symptoms, a traditional AFib-ablation trial endpoint that is nonetheless considered clinically unhelpful.
The secondary analysis recasts that binary endpoint as degree of reduction in AFib burden, a continuous variable. That potentially allows AFib ablation efficacy to be assessed in a more nuanced way likely to be more meaningful to patients and the health care system, observed Dr. Verma and colleagues.
The “30-second endpoint” is limited in clinical usefulness and “doesn’t mean much to the patient,” he said at a press conference on the analysis before formally presenting it at the HRS sessions.
Recent AFib ablation trials have explored AA burden as possibly a superior way to assess the procedure’s success “but also to see if it’s better correlated with quality of life and health care outcomes,” Dr. Verma said. “So that’s exactly what we’ve tried to do here using the PULSED-AF data.”
In the secondary analysis, he said, patients’ rate of freedom from the 30-second endpoint was about 70%, but “more than 85% of them had an AFib burden of less than 10%.”
“This efficacy endpoint of 30 seconds of atrial arrhythmia has been challenged and has been seen clinically as insignificant,” agreed Rajeev Pathak, MBBS, PhD, of Australian National University and director of cardiac electrophysiology at Canberra (Australia) Hospital.
In AFib radiofrequency ablation and cryoablation studies “there is clear disconnect between these 30-second episodes of atrial arrhythmias we see and the clinical relevance of health care utilization and quality of life,” said Dr. Pathak, invited discussant for Dr. Verma’s presentation at the sessions.
Now an AFib ablation trial using PFA catheters has yielded similar results, finding AA burden to be “a more objective and relevant measure of success,” he said. “A 30-second endpoint is arbitrary, lacks significance, and is highly dependent on the monitoring strategy.”
The more you look, the more you see
The new secondary analysis included a demonstration that success rates based on the 30-second endpoint indeed vary depending on how subsequent arrhythmias are monitored.
As described by Dr. Verma, PULSED-AF data were assessed for the 30-second endpoint captured using three separate intermittent monitoring strategies that it and other recent ablation trials have used:
- Strategy A: Transtelephonic monitoring weekly and in the event of symptoms, plus 24-hour Holter monitoring at 6 and 12 months and 12-lead ECG at 3, 6, and 12 months
- Strategy B: Transtelephonic monitoring weekly and at symptoms for 3-6 months followed by monthly and at symptoms from 6 to 12 months, plus 24-hour Holter monitoring at 6 and 12 months, plus 12-lead ECG at 3, 6, and 12 months
- Strategy C: The median of two 24-hour Holter monitoring sessions per patient over 12 months
As Dr. Verma reported, rates of freedom from the 30-second endpoint climbed with successive monitoring strategies. The rates for PAF and persistent AFib patients, respectively, were: Strategy A – 70% and 62%, Strategy B – 71% and 68%, Strategy C – 91% and 86%.
“If you’re using the ‘freedom-from-30-seconds’ endpoint, the results that you are going to get are highly dependent on the monitoring strategy,” Dr. Verma said. “The more you look, the more you see.”
Valid estimation of burden
For the main PULSED-AF secondary analysis, the investigators defined AA burden according to findings on either Holter monitoring or the 12-lead ECG. “So as not to bias these results,” Dr. Verma said, “for every patient, we picked the method that gave us the highest atrial arrhythmia burden.”
Ideally, Dr. Verma said in an interview, arrhythmia burden would be determined using devices such as implantable loop recorders. “The problem is, this is expensive and not practical” in both clinical practice and many trials, so PULSED-AF investigators went with the intermittent monitoring strategy to estimate burdens.
Their method appears valid, he said, given that the study identified a statistically relevant 10% AA burden cut off for predicting quality of life improvement or less health care resource use.
“If their residual atrial arrhythmia burden was greater than 10%, they did not have a statistically significant improvement in quality of life,” Dr. Verma observed. And “very few” of them had cardioversions or repeat ablation.
“I couldn’t agree more” that residual AA burden is preferable to the 30-second endpoint for gauging AFib ablation success, Kenneth Ellenbogen, MD, Virginia Commonwealth University Medical Center, Richmond, said in an interview. Dr. Ellenbogen is also director of clinical cardiac electrophysiology and pacing at VCU Health Pauley Heart Center and not associated with PULSED-AF.
That AA burden was linked to health care resource use in the study “is absolutely brilliant,” he said, “because that’s what the bean counters really want at the end of the day. And as doctors we care about patients feeling better – improving quality of life.”
PULSED-AF was funded by Medtronic. Dr. Verma disclosed financial relationships with Bayer, Biosense Webster, Medtronic, Thermedical, Kardium, and Galaxy Medical, as well as and research grants from Adagio Medical. Dr. Ellenbogen disclosed financial relationships with Boston Scientific, Medtronic, Kestra, Hylomorph, Biotronik, MediLynx, Impulse Dynamics USA, Abbott, Biosense Webster, Milestone Pharmaceuticals, Sanofi, Medpace, and Elsevier. Dr. Pathak disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HRS 2023


















