User login
Noncardiac mortality is not increased by revascularization in a meta-analysis: New data refute recent study
In response to a randomized trial that associated elective revascularization for ischemia with an increase in noncardiac mortality versus medical therapy alone, a meta-analysis with a far larger dataset challenges this assertion, suggesting the initial conclusion is due to a type 1 error.
, reports William Wijns, MD, PhD, professor of interventional cardiology, National University of Ireland, Galway.
The larger pool of data from the meta-analysis was considered compelling by several experts at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions, where it was presented.
“I think these data will close once and forever this controversy,” said Davide Capodanno, MD, PhD, a professor of cardiology and interventional cardiologist at the University of Catania (Italy).
Evidence for an unexpected increased risk of noncardiac mortality was drawn from the ISCHEMIA-EXTEND study, which was published earlier this year. Numerous prior studies comparing percutaneous intervention (PCI) to medical therapy for relief of ischemia had shown no such safety signal.
The ISCHEMIA-EXTEND study provided long-term follow up of patients enrolled in ISCHEMIA, a study that randomized patients with stable coronary disease and moderate or severe ischemia to PCI or a conservative approach. After 3.2 years of follow up, there was no reduction in risk of cardiovascular events or all-cause death. While this lack of benefit was a disappointing result from the perspective of interventional cardiology, there was also no increase in these risks.
In ISCHEMIA-EXTEND, the more than 5,000 patients originally randomized were followed for an additional 2.5 years (total 5.7 years). During this extended period, the estimated 7-year risk of cardiovascular mortality was 22% lower in the group randomized to PCI (hazard ratio, 0.78; 95% confidence interval, 0.63-0.96) but the noncardiac mortality was increased by 44% (HR, 1.44; 95% CI, 1.08-1.91). Because of the counterbalancing effects on survival, all-cause mortality was similar in the two groups.
The newly completed meta-analysis was undertaken to address this surprising result not least because the increased rates of noncardiac death did not have a plausible explanation, according to Dr. Wijns.
When the patients from the 18 randomized trials were compared, noncardiac death occurred in 4.68% of the 8,665 patients assigned to elective revascularization and in 4.17% of the 8,243 patients assigned to medical therapy alone at an average follow up of 5.7 years.
This difference was not significant overall (HR, 1.09; 95% CI, 0.94-1.26; P = .26) or after sensitivity analyses. For example, there was no difference (P = .52) between an invasive or conservative approach after controlling for length of follow up.
There was also no heterogeneity (I2 = 0%) among the studies when ISCHEMIA-EXTEND was excluded.
Absence of negative effect ‘is confirmed’
On the basis of a Bayesian meta-analysis designed to account for residual uncertainty (relative risk, 1.08, 95% CI, 0.90-1.30) and the consistency of results among all studies with the exception of ISCHEMIA-EXTEND (RR, 1.0; 95% CI, 0.84-1;18; P = .7), “the absence of a negative effect of revascularization on noncardiac death was confirmed,” Dr. Wijns reported.
Based on the preponderance of evidence assembled in this meta-analysis, the “noncardiac mortality excess risk observed following revascularization relative to medical therapy was confined to a single large trial and is likely due to a type 1 error,” Dr. Wijns reported. He noted that this study is “the first large-scale meta-analysis study designed to systematically evaluate potential differences in noncardiac mortality between treatment strategies for chronic coronary syndromes.”
Eliano P. Navarese, MD, PhD, an associate professor of interventional cardiology at Nicolaus Copernicus University, Bydgoszcz, Poland, was the lead author of this study and Dr. Wijns was a coinvestigator. The study was published simultaneously in the Journal of the American College of Cardiology at the time of the EuroPCR meeting.
In the late-breaking session where these data were presented, there was a general consensus among invited panelists that the data are convincing. For example, Michael Joner, MD, PhD, director of early clinical trials, German Heart Centre, Munich, agreed that these data “resolve the issue.”
Bernard de Bruyne, MD, PhD, an interventional cardiologist associated with the Cardiovascular Center Aalst, Kraainem, Belgium, also agreed that these data argue convincingly against the concern raised by publication of ISCHEMIA-EXTEND, but he added that this controversy has raised an important issue.
“We should always be reporting all-cause mortality, not just cardiovascular mortality, in our clinical trials,” he said, emphasizing that extending all-cause survival, not just preventing cardiovascular-related events, should be recognized as the goal of invasive strategies.
In an editorial accompanying the publication, Dr. Harvey D. White, MD, Te Whatu Ora-Health New Zealand, Auckland, writes similarly that the current findings, “alert us to the importance of adjudicating causes of death in clinical trials.
“The current trial-level meta-analysis may seem to dispel concerns about increases in noncardiac and cardiovascular deaths seen in some revascularization trials, but paradoxically, it has raised the need for more and careful analysis of causes of death,” Dr. White notes. He feels the signal of increased noncardiac or noncardiovascular death in ISCHEMIA EXTEND and the REVIVED trials is something “that we should pay attention to and explore the possibility that increased radiation doses with PCI may cause increased rates of cancer.”
Further study, including longer follow-up, other datasets, and quality of life data including cognitive function and “patient-focused outcomes such as day alive out of hospital,” is needed, he concludes.
Dr. Navarese has received research grants from Abbott and Amgen and lecture fees/honoraria from Amgen, AstraZeneca, Bayer, Pfizer, and Sanofi-Regeneron. Dr. Wijns reports financial relationships with Argonauts, Corrib Core Laboratory, and Rede Optimus Research. Dr. Capodanno reports financial relationships with Amgen, Daiichi Sankyo, and Sanofi. Dr. de Bruyne and Dr. Joner report financial relationships with multiple pharmaceutical and device manufacturers. Prof. White, as the John Neutze scholar, is supported by the Green Lane Research and Educational Fund. Prof. White has received grant support paid to the institution and fees for serving on steering committees of multiple trials sponsored by various companies.
In response to a randomized trial that associated elective revascularization for ischemia with an increase in noncardiac mortality versus medical therapy alone, a meta-analysis with a far larger dataset challenges this assertion, suggesting the initial conclusion is due to a type 1 error.
, reports William Wijns, MD, PhD, professor of interventional cardiology, National University of Ireland, Galway.
The larger pool of data from the meta-analysis was considered compelling by several experts at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions, where it was presented.
“I think these data will close once and forever this controversy,” said Davide Capodanno, MD, PhD, a professor of cardiology and interventional cardiologist at the University of Catania (Italy).
Evidence for an unexpected increased risk of noncardiac mortality was drawn from the ISCHEMIA-EXTEND study, which was published earlier this year. Numerous prior studies comparing percutaneous intervention (PCI) to medical therapy for relief of ischemia had shown no such safety signal.
The ISCHEMIA-EXTEND study provided long-term follow up of patients enrolled in ISCHEMIA, a study that randomized patients with stable coronary disease and moderate or severe ischemia to PCI or a conservative approach. After 3.2 years of follow up, there was no reduction in risk of cardiovascular events or all-cause death. While this lack of benefit was a disappointing result from the perspective of interventional cardiology, there was also no increase in these risks.
In ISCHEMIA-EXTEND, the more than 5,000 patients originally randomized were followed for an additional 2.5 years (total 5.7 years). During this extended period, the estimated 7-year risk of cardiovascular mortality was 22% lower in the group randomized to PCI (hazard ratio, 0.78; 95% confidence interval, 0.63-0.96) but the noncardiac mortality was increased by 44% (HR, 1.44; 95% CI, 1.08-1.91). Because of the counterbalancing effects on survival, all-cause mortality was similar in the two groups.
The newly completed meta-analysis was undertaken to address this surprising result not least because the increased rates of noncardiac death did not have a plausible explanation, according to Dr. Wijns.
When the patients from the 18 randomized trials were compared, noncardiac death occurred in 4.68% of the 8,665 patients assigned to elective revascularization and in 4.17% of the 8,243 patients assigned to medical therapy alone at an average follow up of 5.7 years.
This difference was not significant overall (HR, 1.09; 95% CI, 0.94-1.26; P = .26) or after sensitivity analyses. For example, there was no difference (P = .52) between an invasive or conservative approach after controlling for length of follow up.
There was also no heterogeneity (I2 = 0%) among the studies when ISCHEMIA-EXTEND was excluded.
Absence of negative effect ‘is confirmed’
On the basis of a Bayesian meta-analysis designed to account for residual uncertainty (relative risk, 1.08, 95% CI, 0.90-1.30) and the consistency of results among all studies with the exception of ISCHEMIA-EXTEND (RR, 1.0; 95% CI, 0.84-1;18; P = .7), “the absence of a negative effect of revascularization on noncardiac death was confirmed,” Dr. Wijns reported.
Based on the preponderance of evidence assembled in this meta-analysis, the “noncardiac mortality excess risk observed following revascularization relative to medical therapy was confined to a single large trial and is likely due to a type 1 error,” Dr. Wijns reported. He noted that this study is “the first large-scale meta-analysis study designed to systematically evaluate potential differences in noncardiac mortality between treatment strategies for chronic coronary syndromes.”
Eliano P. Navarese, MD, PhD, an associate professor of interventional cardiology at Nicolaus Copernicus University, Bydgoszcz, Poland, was the lead author of this study and Dr. Wijns was a coinvestigator. The study was published simultaneously in the Journal of the American College of Cardiology at the time of the EuroPCR meeting.
In the late-breaking session where these data were presented, there was a general consensus among invited panelists that the data are convincing. For example, Michael Joner, MD, PhD, director of early clinical trials, German Heart Centre, Munich, agreed that these data “resolve the issue.”
Bernard de Bruyne, MD, PhD, an interventional cardiologist associated with the Cardiovascular Center Aalst, Kraainem, Belgium, also agreed that these data argue convincingly against the concern raised by publication of ISCHEMIA-EXTEND, but he added that this controversy has raised an important issue.
“We should always be reporting all-cause mortality, not just cardiovascular mortality, in our clinical trials,” he said, emphasizing that extending all-cause survival, not just preventing cardiovascular-related events, should be recognized as the goal of invasive strategies.
In an editorial accompanying the publication, Dr. Harvey D. White, MD, Te Whatu Ora-Health New Zealand, Auckland, writes similarly that the current findings, “alert us to the importance of adjudicating causes of death in clinical trials.
“The current trial-level meta-analysis may seem to dispel concerns about increases in noncardiac and cardiovascular deaths seen in some revascularization trials, but paradoxically, it has raised the need for more and careful analysis of causes of death,” Dr. White notes. He feels the signal of increased noncardiac or noncardiovascular death in ISCHEMIA EXTEND and the REVIVED trials is something “that we should pay attention to and explore the possibility that increased radiation doses with PCI may cause increased rates of cancer.”
Further study, including longer follow-up, other datasets, and quality of life data including cognitive function and “patient-focused outcomes such as day alive out of hospital,” is needed, he concludes.
Dr. Navarese has received research grants from Abbott and Amgen and lecture fees/honoraria from Amgen, AstraZeneca, Bayer, Pfizer, and Sanofi-Regeneron. Dr. Wijns reports financial relationships with Argonauts, Corrib Core Laboratory, and Rede Optimus Research. Dr. Capodanno reports financial relationships with Amgen, Daiichi Sankyo, and Sanofi. Dr. de Bruyne and Dr. Joner report financial relationships with multiple pharmaceutical and device manufacturers. Prof. White, as the John Neutze scholar, is supported by the Green Lane Research and Educational Fund. Prof. White has received grant support paid to the institution and fees for serving on steering committees of multiple trials sponsored by various companies.
In response to a randomized trial that associated elective revascularization for ischemia with an increase in noncardiac mortality versus medical therapy alone, a meta-analysis with a far larger dataset challenges this assertion, suggesting the initial conclusion is due to a type 1 error.
, reports William Wijns, MD, PhD, professor of interventional cardiology, National University of Ireland, Galway.
The larger pool of data from the meta-analysis was considered compelling by several experts at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions, where it was presented.
“I think these data will close once and forever this controversy,” said Davide Capodanno, MD, PhD, a professor of cardiology and interventional cardiologist at the University of Catania (Italy).
Evidence for an unexpected increased risk of noncardiac mortality was drawn from the ISCHEMIA-EXTEND study, which was published earlier this year. Numerous prior studies comparing percutaneous intervention (PCI) to medical therapy for relief of ischemia had shown no such safety signal.
The ISCHEMIA-EXTEND study provided long-term follow up of patients enrolled in ISCHEMIA, a study that randomized patients with stable coronary disease and moderate or severe ischemia to PCI or a conservative approach. After 3.2 years of follow up, there was no reduction in risk of cardiovascular events or all-cause death. While this lack of benefit was a disappointing result from the perspective of interventional cardiology, there was also no increase in these risks.
In ISCHEMIA-EXTEND, the more than 5,000 patients originally randomized were followed for an additional 2.5 years (total 5.7 years). During this extended period, the estimated 7-year risk of cardiovascular mortality was 22% lower in the group randomized to PCI (hazard ratio, 0.78; 95% confidence interval, 0.63-0.96) but the noncardiac mortality was increased by 44% (HR, 1.44; 95% CI, 1.08-1.91). Because of the counterbalancing effects on survival, all-cause mortality was similar in the two groups.
The newly completed meta-analysis was undertaken to address this surprising result not least because the increased rates of noncardiac death did not have a plausible explanation, according to Dr. Wijns.
When the patients from the 18 randomized trials were compared, noncardiac death occurred in 4.68% of the 8,665 patients assigned to elective revascularization and in 4.17% of the 8,243 patients assigned to medical therapy alone at an average follow up of 5.7 years.
This difference was not significant overall (HR, 1.09; 95% CI, 0.94-1.26; P = .26) or after sensitivity analyses. For example, there was no difference (P = .52) between an invasive or conservative approach after controlling for length of follow up.
There was also no heterogeneity (I2 = 0%) among the studies when ISCHEMIA-EXTEND was excluded.
Absence of negative effect ‘is confirmed’
On the basis of a Bayesian meta-analysis designed to account for residual uncertainty (relative risk, 1.08, 95% CI, 0.90-1.30) and the consistency of results among all studies with the exception of ISCHEMIA-EXTEND (RR, 1.0; 95% CI, 0.84-1;18; P = .7), “the absence of a negative effect of revascularization on noncardiac death was confirmed,” Dr. Wijns reported.
Based on the preponderance of evidence assembled in this meta-analysis, the “noncardiac mortality excess risk observed following revascularization relative to medical therapy was confined to a single large trial and is likely due to a type 1 error,” Dr. Wijns reported. He noted that this study is “the first large-scale meta-analysis study designed to systematically evaluate potential differences in noncardiac mortality between treatment strategies for chronic coronary syndromes.”
Eliano P. Navarese, MD, PhD, an associate professor of interventional cardiology at Nicolaus Copernicus University, Bydgoszcz, Poland, was the lead author of this study and Dr. Wijns was a coinvestigator. The study was published simultaneously in the Journal of the American College of Cardiology at the time of the EuroPCR meeting.
In the late-breaking session where these data were presented, there was a general consensus among invited panelists that the data are convincing. For example, Michael Joner, MD, PhD, director of early clinical trials, German Heart Centre, Munich, agreed that these data “resolve the issue.”
Bernard de Bruyne, MD, PhD, an interventional cardiologist associated with the Cardiovascular Center Aalst, Kraainem, Belgium, also agreed that these data argue convincingly against the concern raised by publication of ISCHEMIA-EXTEND, but he added that this controversy has raised an important issue.
“We should always be reporting all-cause mortality, not just cardiovascular mortality, in our clinical trials,” he said, emphasizing that extending all-cause survival, not just preventing cardiovascular-related events, should be recognized as the goal of invasive strategies.
In an editorial accompanying the publication, Dr. Harvey D. White, MD, Te Whatu Ora-Health New Zealand, Auckland, writes similarly that the current findings, “alert us to the importance of adjudicating causes of death in clinical trials.
“The current trial-level meta-analysis may seem to dispel concerns about increases in noncardiac and cardiovascular deaths seen in some revascularization trials, but paradoxically, it has raised the need for more and careful analysis of causes of death,” Dr. White notes. He feels the signal of increased noncardiac or noncardiovascular death in ISCHEMIA EXTEND and the REVIVED trials is something “that we should pay attention to and explore the possibility that increased radiation doses with PCI may cause increased rates of cancer.”
Further study, including longer follow-up, other datasets, and quality of life data including cognitive function and “patient-focused outcomes such as day alive out of hospital,” is needed, he concludes.
Dr. Navarese has received research grants from Abbott and Amgen and lecture fees/honoraria from Amgen, AstraZeneca, Bayer, Pfizer, and Sanofi-Regeneron. Dr. Wijns reports financial relationships with Argonauts, Corrib Core Laboratory, and Rede Optimus Research. Dr. Capodanno reports financial relationships with Amgen, Daiichi Sankyo, and Sanofi. Dr. de Bruyne and Dr. Joner report financial relationships with multiple pharmaceutical and device manufacturers. Prof. White, as the John Neutze scholar, is supported by the Green Lane Research and Educational Fund. Prof. White has received grant support paid to the institution and fees for serving on steering committees of multiple trials sponsored by various companies.
FROM EUROPCR 2023
PTSD, anxiety linked to out-of-hospital cardiac arrest
Investigators compared more than 35,000 OHCA case patients with a similar number of matched control persons and found an almost 1.5 times higher hazard of long-term stress conditions among OHCA case patients, compared with control persons, with a similar hazard for anxiety. Posttraumatic stress disorder was associated with an almost twofold higher risk of OHCA.
The findings applied equally to men and women and were independent of the presence of cardiovascular disease (CVD).
“This study raises awareness of the higher risks of OHCA and early risk monitoring to prevent OHCA in patients with stress-related disorders and anxiety,” write Talip Eroglu, of the department of cardiology, Copenhagen University Hospital, and colleagues.
The study was published online in BMJ Open Heart.
Stress disorders and anxiety overrepresented
OHCA “predominantly arises from lethal cardiac arrhythmias ... that occur most frequently in the setting of coronary heart disease,” the authors write. However, increasing evidence suggests that rates of OHCA may also be increased in association with noncardiac diseases.
Individuals with stress-related disorders and anxiety are “overrepresented” among victims of cardiac arrest as well as those with multiple CVDs. But previous studies of OHCA have been limited by small numbers of cardiac arrests. In addition, those studies involved only data from selected populations or used in-hospital diagnosis to identify cardiac arrest, thereby potentially omitting OHCA patients who died prior to hospital admission.
The researchers therefore turned to data from Danish health registries that include a large, unselected cohort of patients with OHCA to investigate whether long-term stress conditions (that is, PTSD and adjustment disorder) or anxiety disorder were associated with OHCA.
They stratified the cohort according to sex, age, and CVD to identify which risk factor confers the highest risk of OHCA in patients with long-term stress conditions or anxiety, and they conducted sensitivity analyses of potential confounders, such as depression.
The design was a nested-case control model in which records at an individual patient level across registries were cross-linked to data from other national registries and were compared to matched control persons from the general population (35,195 OHCAs and 351,950 matched control persons; median IQR age, 72 [62-81] years; 66.82% men).
The prevalence of comorbidities and use of cardiovascular drugs were higher among OHCA case patients than among non-OHCA control persons.
Keep aware of stress and anxiety as risk factors
Among OHCA and non-OHCA participants, long-term stress conditions were diagnosed in 0.92% and 0.45%, respectively. Anxiety was diagnosed in 0.85% of OHCA case patients and in 0.37% of non-OHCA control persons.
These conditions were associated with a higher rate of OHCA after adjustment for common OHCA risk factors.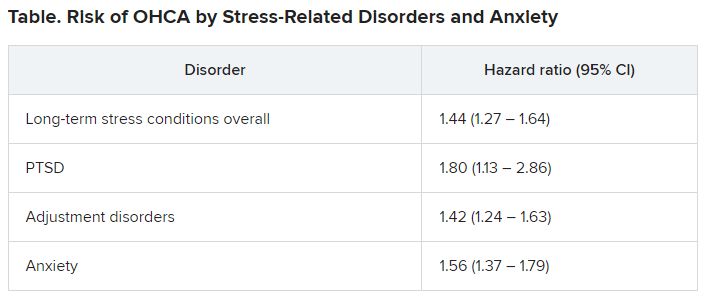
There were no significant differences in results when the researchers adjusted for the use of anxiolytics and antidepressants.
When they examined the prevalence of concomitant medication use or comorbidities, they found that depression was more frequent among patients with long-term stress and anxiety, compared with individuals with neither of those diagnoses. Additionally, patients with long-term stress and anxiety more often used anxiolytics, antidepressants, and QT-prolonging drugs.
Stratification of the analyses according to sex revealed that the OHCA rate was increased in both women and men with long-term stress and anxiety. There were no significant differences between the sexes. There were also no significant differences between the association among different age groups, nor between patients with and those without CVD, ischemic heart disease, or heart failure.
Previous research has shown associations of stress-related disorders or anxiety with cardiovascular outcomes, including myocardial infarction, heart failure, and cerebrovascular disease. These disorders might be “biological mediators in the causal pathway of OHCA” and contribute to the increased OHCA rate associated with stress-related disorders and anxiety, the authors suggest.
Nevertheless, they note, stress-related disorders and anxiety remained significantly associated with OHCA after controlling for these variables, “suggesting that it is unlikely that traditional risk factors of OHCA alone explain this relationship.”
They suggest several potential mechanisms. One is that the relationship is likely mediated by the activity of the sympathetic autonomic nervous system, which “leads to an increase in heart rate, release of neurotransmitters into the circulation, and local release of neurotransmitters in the heart.”
Each of these factors “may potentially influence cardiac electrophysiology and facilitate ventricular arrhythmias and OHCA.”
In addition to a biological mechanism, behavioral and psychosocial factors may also contribute to OHCA risk, since stress-related disorders and anxiety “often lead to unhealthy lifestyle, such as smoking and lower physical activity, which in turn may increase the risk of OHCA.” Given the absence of data on these features in the registries the investigators used, they were unable to account for them.
However, “it is unlikely that knowledge of these factors would have altered our conclusions considering that we have adjusted for all the relevant cardiovascular comorbidities.”
Similarly, other psychiatric disorders, such as depression, can contribute to OHCA risk, but they adjusted for depression in their multivariable analyses.
“Awareness of the higher risks of OHCA in patients with stress-related disorders and anxiety is important when treating these patients,” they conclude.
Detrimental to the heart, not just the psyche
Glenn Levine, MD, master clinician and professor of medicine, Baylor College of Medicine, Houston, called it an “important study in that it is a large, nationwide cohort study and thus provides important information to complement much smaller, focused studies.”
Like those other studies, “it finds that negative psychological health, specifically, long-term stress (as well as anxiety), is associated with a significantly increased risk of out-of-hospital cardiac arrest,” continued Dr. Levine, who is the chief of the cardiology section at Michael E. DeBakey VA Medical Center, Houston, and was not involved with the study.
Dr. Levine thinks the study “does a good job, as best one can for such a study, in trying to control for other factors, and zeroing in specifically on stress (and anxiety), trying to assess their independent contributions to the risk of developing cardiac arrest.”
The take-home message for clinicians and patients “is that negative psychological stress factors, such as stress and anxiety, are not only detrimental to one’s psychological health but likely increase one’s risk for adverse cardiac events, such as cardiac arrest,” he stated.
No specific funding for the study was disclosed. Mr. Eroglu has disclosed no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. Levine reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators compared more than 35,000 OHCA case patients with a similar number of matched control persons and found an almost 1.5 times higher hazard of long-term stress conditions among OHCA case patients, compared with control persons, with a similar hazard for anxiety. Posttraumatic stress disorder was associated with an almost twofold higher risk of OHCA.
The findings applied equally to men and women and were independent of the presence of cardiovascular disease (CVD).
“This study raises awareness of the higher risks of OHCA and early risk monitoring to prevent OHCA in patients with stress-related disorders and anxiety,” write Talip Eroglu, of the department of cardiology, Copenhagen University Hospital, and colleagues.
The study was published online in BMJ Open Heart.
Stress disorders and anxiety overrepresented
OHCA “predominantly arises from lethal cardiac arrhythmias ... that occur most frequently in the setting of coronary heart disease,” the authors write. However, increasing evidence suggests that rates of OHCA may also be increased in association with noncardiac diseases.
Individuals with stress-related disorders and anxiety are “overrepresented” among victims of cardiac arrest as well as those with multiple CVDs. But previous studies of OHCA have been limited by small numbers of cardiac arrests. In addition, those studies involved only data from selected populations or used in-hospital diagnosis to identify cardiac arrest, thereby potentially omitting OHCA patients who died prior to hospital admission.
The researchers therefore turned to data from Danish health registries that include a large, unselected cohort of patients with OHCA to investigate whether long-term stress conditions (that is, PTSD and adjustment disorder) or anxiety disorder were associated with OHCA.
They stratified the cohort according to sex, age, and CVD to identify which risk factor confers the highest risk of OHCA in patients with long-term stress conditions or anxiety, and they conducted sensitivity analyses of potential confounders, such as depression.
The design was a nested-case control model in which records at an individual patient level across registries were cross-linked to data from other national registries and were compared to matched control persons from the general population (35,195 OHCAs and 351,950 matched control persons; median IQR age, 72 [62-81] years; 66.82% men).
The prevalence of comorbidities and use of cardiovascular drugs were higher among OHCA case patients than among non-OHCA control persons.
Keep aware of stress and anxiety as risk factors
Among OHCA and non-OHCA participants, long-term stress conditions were diagnosed in 0.92% and 0.45%, respectively. Anxiety was diagnosed in 0.85% of OHCA case patients and in 0.37% of non-OHCA control persons.
These conditions were associated with a higher rate of OHCA after adjustment for common OHCA risk factors.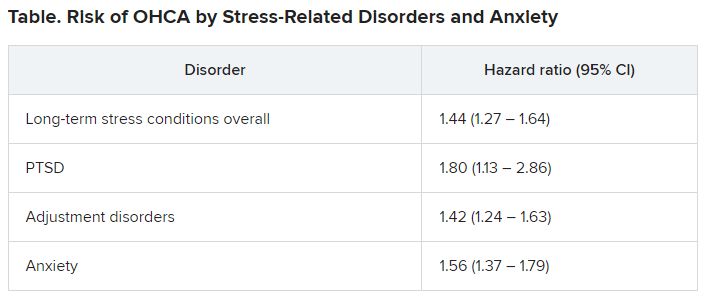
There were no significant differences in results when the researchers adjusted for the use of anxiolytics and antidepressants.
When they examined the prevalence of concomitant medication use or comorbidities, they found that depression was more frequent among patients with long-term stress and anxiety, compared with individuals with neither of those diagnoses. Additionally, patients with long-term stress and anxiety more often used anxiolytics, antidepressants, and QT-prolonging drugs.
Stratification of the analyses according to sex revealed that the OHCA rate was increased in both women and men with long-term stress and anxiety. There were no significant differences between the sexes. There were also no significant differences between the association among different age groups, nor between patients with and those without CVD, ischemic heart disease, or heart failure.
Previous research has shown associations of stress-related disorders or anxiety with cardiovascular outcomes, including myocardial infarction, heart failure, and cerebrovascular disease. These disorders might be “biological mediators in the causal pathway of OHCA” and contribute to the increased OHCA rate associated with stress-related disorders and anxiety, the authors suggest.
Nevertheless, they note, stress-related disorders and anxiety remained significantly associated with OHCA after controlling for these variables, “suggesting that it is unlikely that traditional risk factors of OHCA alone explain this relationship.”
They suggest several potential mechanisms. One is that the relationship is likely mediated by the activity of the sympathetic autonomic nervous system, which “leads to an increase in heart rate, release of neurotransmitters into the circulation, and local release of neurotransmitters in the heart.”
Each of these factors “may potentially influence cardiac electrophysiology and facilitate ventricular arrhythmias and OHCA.”
In addition to a biological mechanism, behavioral and psychosocial factors may also contribute to OHCA risk, since stress-related disorders and anxiety “often lead to unhealthy lifestyle, such as smoking and lower physical activity, which in turn may increase the risk of OHCA.” Given the absence of data on these features in the registries the investigators used, they were unable to account for them.
However, “it is unlikely that knowledge of these factors would have altered our conclusions considering that we have adjusted for all the relevant cardiovascular comorbidities.”
Similarly, other psychiatric disorders, such as depression, can contribute to OHCA risk, but they adjusted for depression in their multivariable analyses.
“Awareness of the higher risks of OHCA in patients with stress-related disorders and anxiety is important when treating these patients,” they conclude.
Detrimental to the heart, not just the psyche
Glenn Levine, MD, master clinician and professor of medicine, Baylor College of Medicine, Houston, called it an “important study in that it is a large, nationwide cohort study and thus provides important information to complement much smaller, focused studies.”
Like those other studies, “it finds that negative psychological health, specifically, long-term stress (as well as anxiety), is associated with a significantly increased risk of out-of-hospital cardiac arrest,” continued Dr. Levine, who is the chief of the cardiology section at Michael E. DeBakey VA Medical Center, Houston, and was not involved with the study.
Dr. Levine thinks the study “does a good job, as best one can for such a study, in trying to control for other factors, and zeroing in specifically on stress (and anxiety), trying to assess their independent contributions to the risk of developing cardiac arrest.”
The take-home message for clinicians and patients “is that negative psychological stress factors, such as stress and anxiety, are not only detrimental to one’s psychological health but likely increase one’s risk for adverse cardiac events, such as cardiac arrest,” he stated.
No specific funding for the study was disclosed. Mr. Eroglu has disclosed no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. Levine reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators compared more than 35,000 OHCA case patients with a similar number of matched control persons and found an almost 1.5 times higher hazard of long-term stress conditions among OHCA case patients, compared with control persons, with a similar hazard for anxiety. Posttraumatic stress disorder was associated with an almost twofold higher risk of OHCA.
The findings applied equally to men and women and were independent of the presence of cardiovascular disease (CVD).
“This study raises awareness of the higher risks of OHCA and early risk monitoring to prevent OHCA in patients with stress-related disorders and anxiety,” write Talip Eroglu, of the department of cardiology, Copenhagen University Hospital, and colleagues.
The study was published online in BMJ Open Heart.
Stress disorders and anxiety overrepresented
OHCA “predominantly arises from lethal cardiac arrhythmias ... that occur most frequently in the setting of coronary heart disease,” the authors write. However, increasing evidence suggests that rates of OHCA may also be increased in association with noncardiac diseases.
Individuals with stress-related disorders and anxiety are “overrepresented” among victims of cardiac arrest as well as those with multiple CVDs. But previous studies of OHCA have been limited by small numbers of cardiac arrests. In addition, those studies involved only data from selected populations or used in-hospital diagnosis to identify cardiac arrest, thereby potentially omitting OHCA patients who died prior to hospital admission.
The researchers therefore turned to data from Danish health registries that include a large, unselected cohort of patients with OHCA to investigate whether long-term stress conditions (that is, PTSD and adjustment disorder) or anxiety disorder were associated with OHCA.
They stratified the cohort according to sex, age, and CVD to identify which risk factor confers the highest risk of OHCA in patients with long-term stress conditions or anxiety, and they conducted sensitivity analyses of potential confounders, such as depression.
The design was a nested-case control model in which records at an individual patient level across registries were cross-linked to data from other national registries and were compared to matched control persons from the general population (35,195 OHCAs and 351,950 matched control persons; median IQR age, 72 [62-81] years; 66.82% men).
The prevalence of comorbidities and use of cardiovascular drugs were higher among OHCA case patients than among non-OHCA control persons.
Keep aware of stress and anxiety as risk factors
Among OHCA and non-OHCA participants, long-term stress conditions were diagnosed in 0.92% and 0.45%, respectively. Anxiety was diagnosed in 0.85% of OHCA case patients and in 0.37% of non-OHCA control persons.
These conditions were associated with a higher rate of OHCA after adjustment for common OHCA risk factors.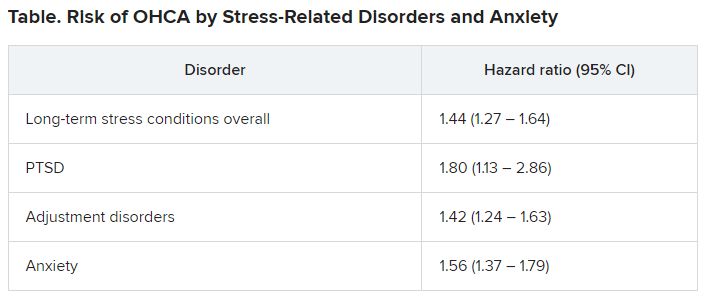
There were no significant differences in results when the researchers adjusted for the use of anxiolytics and antidepressants.
When they examined the prevalence of concomitant medication use or comorbidities, they found that depression was more frequent among patients with long-term stress and anxiety, compared with individuals with neither of those diagnoses. Additionally, patients with long-term stress and anxiety more often used anxiolytics, antidepressants, and QT-prolonging drugs.
Stratification of the analyses according to sex revealed that the OHCA rate was increased in both women and men with long-term stress and anxiety. There were no significant differences between the sexes. There were also no significant differences between the association among different age groups, nor between patients with and those without CVD, ischemic heart disease, or heart failure.
Previous research has shown associations of stress-related disorders or anxiety with cardiovascular outcomes, including myocardial infarction, heart failure, and cerebrovascular disease. These disorders might be “biological mediators in the causal pathway of OHCA” and contribute to the increased OHCA rate associated with stress-related disorders and anxiety, the authors suggest.
Nevertheless, they note, stress-related disorders and anxiety remained significantly associated with OHCA after controlling for these variables, “suggesting that it is unlikely that traditional risk factors of OHCA alone explain this relationship.”
They suggest several potential mechanisms. One is that the relationship is likely mediated by the activity of the sympathetic autonomic nervous system, which “leads to an increase in heart rate, release of neurotransmitters into the circulation, and local release of neurotransmitters in the heart.”
Each of these factors “may potentially influence cardiac electrophysiology and facilitate ventricular arrhythmias and OHCA.”
In addition to a biological mechanism, behavioral and psychosocial factors may also contribute to OHCA risk, since stress-related disorders and anxiety “often lead to unhealthy lifestyle, such as smoking and lower physical activity, which in turn may increase the risk of OHCA.” Given the absence of data on these features in the registries the investigators used, they were unable to account for them.
However, “it is unlikely that knowledge of these factors would have altered our conclusions considering that we have adjusted for all the relevant cardiovascular comorbidities.”
Similarly, other psychiatric disorders, such as depression, can contribute to OHCA risk, but they adjusted for depression in their multivariable analyses.
“Awareness of the higher risks of OHCA in patients with stress-related disorders and anxiety is important when treating these patients,” they conclude.
Detrimental to the heart, not just the psyche
Glenn Levine, MD, master clinician and professor of medicine, Baylor College of Medicine, Houston, called it an “important study in that it is a large, nationwide cohort study and thus provides important information to complement much smaller, focused studies.”
Like those other studies, “it finds that negative psychological health, specifically, long-term stress (as well as anxiety), is associated with a significantly increased risk of out-of-hospital cardiac arrest,” continued Dr. Levine, who is the chief of the cardiology section at Michael E. DeBakey VA Medical Center, Houston, and was not involved with the study.
Dr. Levine thinks the study “does a good job, as best one can for such a study, in trying to control for other factors, and zeroing in specifically on stress (and anxiety), trying to assess their independent contributions to the risk of developing cardiac arrest.”
The take-home message for clinicians and patients “is that negative psychological stress factors, such as stress and anxiety, are not only detrimental to one’s psychological health but likely increase one’s risk for adverse cardiac events, such as cardiac arrest,” he stated.
No specific funding for the study was disclosed. Mr. Eroglu has disclosed no relevant financial relationships. The other authors’ disclosures are listed in the original article. Dr. Levine reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM BMJ OPEN HEART
Can a saliva test predict the best way to manage obesity?
It sounds like a simple solution to a complicated problem: Find out what kind of obesity someone has based on a one-time genetic saliva test. Then patients and their doctor can get a better idea if antiobesity drugs or other treatments are more likely to work for them.
It’s what Mayo Clinic researchers had in mind when they created four phenotypes of obesity.
Obesity experts not affiliated with the research have some concerns and say independent studies are needed to verify the potential of this strategy.
This research could help predict who will respond best to popular antiobesity medications, said Andres Acosta, MD, PhD, cofounder of Phenomix Sciences, the company behind the tests. These medications include glucagonlike peptide–1 (GLP-1) receptor agonists like liraglutide (Saxenda, Victoza) and semaglutide (Ozempic, Wegovy).
“We know that not everyone on a GLP-1 will respond. In reality, about a third of the patients don’t do well with GLP-1s,” said Dr. Acosta, an assistant professor of medicine and researcher in the division of gastroenterology and hepatology at the Mayo Clinic in Rochester, Minn.
Furthest along in development is the “My Phenome Hungry Gut” test for predicting GLP-1 response. People in this Hungry Gut group tend to empty their stomach after a meal faster and are more likely to feel hungry again a short time later, as explained on the company’s website.
A pilot study to test how well it works started in April at three primary care practices. Plans are to expand real-world testing for this and other obesity types later in 2023.
The other obesity categories are:
- “Hungry brain,” where the brain does not recognize signals that the stomach is full
- “Emotional hunger,” where cravings to eat are driven by emotions, anxiety, and negative feelings
- “Slow burn,” where people have a slow metabolism and low energy level
People in these categories might be more likely to benefit from other obesity management strategies, like changes to their diet or placement of an intragastric balloon.
Some things to consider
While applauding their efforts to be more precise in treating people with obesity, not all experts are convinced this saliva test will be the answer. The company’s research might look promising, but verification of results is warranted.
“Can we get better outcomes with things like this? Well, that’s the hope,” said Jaime Almandoz, MD, medical director of weight wellness at the University of Texas Southwestern Medical Center, Dallas.
“We still don’t have randomized trials where we’re looking at obesity phenotyping yet,” said Dr. Almandoz, who is also a spokesperson for the Obesity Society, a professional group of clinicians, researchers, educators, and others focused on obesity science, treatment, and prevention.
There is always concern when a diagnostic test is being developed for commercial use, said Daniel Bessesen, MD, a professor of medicine–endocrinology, metabolism, and diabetes at the University of Colorado at Denver, Aurora. “What they’re talking about doing is super important. But this is a company. This is a company that is, I think, selling a product.”
In an online search, Dr. Bessesen did not find any external studies that showed how well the saliva testing worked. But referring to work by Dr. Acosta and Michael Camilleri, MD, the other cofounder of Phenomix, he said, “I found some papers that they did that I hadn’t read before that are good.”
“These guys are smart guys. And they’ve done a lot of work on [the movement of food through the gut] and how that correlates with obesity and response to some therapies,” said Dr. Bessesen, who is also a spokesperson for the Obesity Society. “So their scientific work does line up with this area.”
Validation of any research is important because the obesity industry has been known for a lot of lose-weight-quick strategies, some with little or no science behind them, he said.
It is also essential, he said, because “anytime you do something commercial in the area of obesity, you have to acknowledge that people with obesity are a vulnerable population. These people face stigma and bias all the time.”
Removing the stigma
If knowing your obesity type ends up making a difference, it could change the conversation people have with their medical provider, Dr. Acosta said. It could also help remove some of the stigma around obesity.
“We’re going to change the conversation because now we can say: ‘Hey, you have obesity because you have ‘Hungry Gut’ phenotype. And because of that, you’re going to respond to this medication,” Dr. Acosta said. The phenotyping suggests a strong genetic tendency – a biologic basis for obesity.
“So it’s not only a way of taking the blame out, but it’s also way of explaining that there’s a reason why you have obesity,” Dr. Acosta said. It tells people: “You’re not a failure.”
More cost-effective treatment?
Targeting obesity treatment could also save on overall health care costs, Dr. Almandoz said. He estimated a cost of $1,400 per month “for forever and ever semaglutide” or at least $1,400 a month for a 3-month trial to see if this medication works in a particular person with obesity.
“That’s a lot of money when you extrapolate that out over the number of people who probably meet the criteria for treatment,” he said. A total 42% of Americans meet the Centers for Disease Control and Prevention definition for obesity.
“You can imagine the potential cost if we were to provide antiobesity therapies to everybody and we were to use what is the most effective class of medication, which is more than a thousand dollars per month, indefinitely,” Dr. Almandoz said. “Not that we should not treat everybody. That’s not the message I’m saying. But if we’re looking at yield or value in terms of treating obesity in a setting with limited resources, it may be best to start with who is most likely to benefit.”
How they created four obesity types
Starting in 2015, Dr. Acosta and colleagues started comparing tests in people with normal weight versus obesity. They used artificial intelligence and machine learning to classify obesity into 11 types at first. They realized this many obesity types were not practical for doctors and people with obesity, so they combined them into four phenotypes.
“The AI machine learning was followed by, as I like to call, HI, or human intelligence,” he said.
The saliva test checks for about 6,000 relevant genetic single-nucleotide polymorphisms. Six thousand genetic changes may sound like a large number to check; however, the average individual carries 5 million and 6 million SNPs in their DNA.
The results are translated to a score that yields a low risk or high risk for Hungry Gut or other types of obesity. “You can have all six thousand genetic mutations, or you can have zero,” Dr. Acosta said.
Moving forward
After the soft launch of Hungry Gut testing in April, Phenomix plans to continue studying their saliva test on other obesity types.
Dr. Acosta is not aware of any direct competitors to Phenomix, although that could change. “I think we’re the only diagnostic company in the space right now. But if it’s really a $14.8 billion market, we’re going to see a lot of diagnostic companies trying to do what we’re doing – if we’re successful,” he said.
An October 2022 report from Polaris Market Research estimates that the global market for obesity treatment – medications, surgery, and all others – was about $14 billion in 2021. The same report predicts the market will grow to $32 billion by 2030.
A version of this article first appeared on WebMD.com.
It sounds like a simple solution to a complicated problem: Find out what kind of obesity someone has based on a one-time genetic saliva test. Then patients and their doctor can get a better idea if antiobesity drugs or other treatments are more likely to work for them.
It’s what Mayo Clinic researchers had in mind when they created four phenotypes of obesity.
Obesity experts not affiliated with the research have some concerns and say independent studies are needed to verify the potential of this strategy.
This research could help predict who will respond best to popular antiobesity medications, said Andres Acosta, MD, PhD, cofounder of Phenomix Sciences, the company behind the tests. These medications include glucagonlike peptide–1 (GLP-1) receptor agonists like liraglutide (Saxenda, Victoza) and semaglutide (Ozempic, Wegovy).
“We know that not everyone on a GLP-1 will respond. In reality, about a third of the patients don’t do well with GLP-1s,” said Dr. Acosta, an assistant professor of medicine and researcher in the division of gastroenterology and hepatology at the Mayo Clinic in Rochester, Minn.
Furthest along in development is the “My Phenome Hungry Gut” test for predicting GLP-1 response. People in this Hungry Gut group tend to empty their stomach after a meal faster and are more likely to feel hungry again a short time later, as explained on the company’s website.
A pilot study to test how well it works started in April at three primary care practices. Plans are to expand real-world testing for this and other obesity types later in 2023.
The other obesity categories are:
- “Hungry brain,” where the brain does not recognize signals that the stomach is full
- “Emotional hunger,” where cravings to eat are driven by emotions, anxiety, and negative feelings
- “Slow burn,” where people have a slow metabolism and low energy level
People in these categories might be more likely to benefit from other obesity management strategies, like changes to their diet or placement of an intragastric balloon.
Some things to consider
While applauding their efforts to be more precise in treating people with obesity, not all experts are convinced this saliva test will be the answer. The company’s research might look promising, but verification of results is warranted.
“Can we get better outcomes with things like this? Well, that’s the hope,” said Jaime Almandoz, MD, medical director of weight wellness at the University of Texas Southwestern Medical Center, Dallas.
“We still don’t have randomized trials where we’re looking at obesity phenotyping yet,” said Dr. Almandoz, who is also a spokesperson for the Obesity Society, a professional group of clinicians, researchers, educators, and others focused on obesity science, treatment, and prevention.
There is always concern when a diagnostic test is being developed for commercial use, said Daniel Bessesen, MD, a professor of medicine–endocrinology, metabolism, and diabetes at the University of Colorado at Denver, Aurora. “What they’re talking about doing is super important. But this is a company. This is a company that is, I think, selling a product.”
In an online search, Dr. Bessesen did not find any external studies that showed how well the saliva testing worked. But referring to work by Dr. Acosta and Michael Camilleri, MD, the other cofounder of Phenomix, he said, “I found some papers that they did that I hadn’t read before that are good.”
“These guys are smart guys. And they’ve done a lot of work on [the movement of food through the gut] and how that correlates with obesity and response to some therapies,” said Dr. Bessesen, who is also a spokesperson for the Obesity Society. “So their scientific work does line up with this area.”
Validation of any research is important because the obesity industry has been known for a lot of lose-weight-quick strategies, some with little or no science behind them, he said.
It is also essential, he said, because “anytime you do something commercial in the area of obesity, you have to acknowledge that people with obesity are a vulnerable population. These people face stigma and bias all the time.”
Removing the stigma
If knowing your obesity type ends up making a difference, it could change the conversation people have with their medical provider, Dr. Acosta said. It could also help remove some of the stigma around obesity.
“We’re going to change the conversation because now we can say: ‘Hey, you have obesity because you have ‘Hungry Gut’ phenotype. And because of that, you’re going to respond to this medication,” Dr. Acosta said. The phenotyping suggests a strong genetic tendency – a biologic basis for obesity.
“So it’s not only a way of taking the blame out, but it’s also way of explaining that there’s a reason why you have obesity,” Dr. Acosta said. It tells people: “You’re not a failure.”
More cost-effective treatment?
Targeting obesity treatment could also save on overall health care costs, Dr. Almandoz said. He estimated a cost of $1,400 per month “for forever and ever semaglutide” or at least $1,400 a month for a 3-month trial to see if this medication works in a particular person with obesity.
“That’s a lot of money when you extrapolate that out over the number of people who probably meet the criteria for treatment,” he said. A total 42% of Americans meet the Centers for Disease Control and Prevention definition for obesity.
“You can imagine the potential cost if we were to provide antiobesity therapies to everybody and we were to use what is the most effective class of medication, which is more than a thousand dollars per month, indefinitely,” Dr. Almandoz said. “Not that we should not treat everybody. That’s not the message I’m saying. But if we’re looking at yield or value in terms of treating obesity in a setting with limited resources, it may be best to start with who is most likely to benefit.”
How they created four obesity types
Starting in 2015, Dr. Acosta and colleagues started comparing tests in people with normal weight versus obesity. They used artificial intelligence and machine learning to classify obesity into 11 types at first. They realized this many obesity types were not practical for doctors and people with obesity, so they combined them into four phenotypes.
“The AI machine learning was followed by, as I like to call, HI, or human intelligence,” he said.
The saliva test checks for about 6,000 relevant genetic single-nucleotide polymorphisms. Six thousand genetic changes may sound like a large number to check; however, the average individual carries 5 million and 6 million SNPs in their DNA.
The results are translated to a score that yields a low risk or high risk for Hungry Gut or other types of obesity. “You can have all six thousand genetic mutations, or you can have zero,” Dr. Acosta said.
Moving forward
After the soft launch of Hungry Gut testing in April, Phenomix plans to continue studying their saliva test on other obesity types.
Dr. Acosta is not aware of any direct competitors to Phenomix, although that could change. “I think we’re the only diagnostic company in the space right now. But if it’s really a $14.8 billion market, we’re going to see a lot of diagnostic companies trying to do what we’re doing – if we’re successful,” he said.
An October 2022 report from Polaris Market Research estimates that the global market for obesity treatment – medications, surgery, and all others – was about $14 billion in 2021. The same report predicts the market will grow to $32 billion by 2030.
A version of this article first appeared on WebMD.com.
It sounds like a simple solution to a complicated problem: Find out what kind of obesity someone has based on a one-time genetic saliva test. Then patients and their doctor can get a better idea if antiobesity drugs or other treatments are more likely to work for them.
It’s what Mayo Clinic researchers had in mind when they created four phenotypes of obesity.
Obesity experts not affiliated with the research have some concerns and say independent studies are needed to verify the potential of this strategy.
This research could help predict who will respond best to popular antiobesity medications, said Andres Acosta, MD, PhD, cofounder of Phenomix Sciences, the company behind the tests. These medications include glucagonlike peptide–1 (GLP-1) receptor agonists like liraglutide (Saxenda, Victoza) and semaglutide (Ozempic, Wegovy).
“We know that not everyone on a GLP-1 will respond. In reality, about a third of the patients don’t do well with GLP-1s,” said Dr. Acosta, an assistant professor of medicine and researcher in the division of gastroenterology and hepatology at the Mayo Clinic in Rochester, Minn.
Furthest along in development is the “My Phenome Hungry Gut” test for predicting GLP-1 response. People in this Hungry Gut group tend to empty their stomach after a meal faster and are more likely to feel hungry again a short time later, as explained on the company’s website.
A pilot study to test how well it works started in April at three primary care practices. Plans are to expand real-world testing for this and other obesity types later in 2023.
The other obesity categories are:
- “Hungry brain,” where the brain does not recognize signals that the stomach is full
- “Emotional hunger,” where cravings to eat are driven by emotions, anxiety, and negative feelings
- “Slow burn,” where people have a slow metabolism and low energy level
People in these categories might be more likely to benefit from other obesity management strategies, like changes to their diet or placement of an intragastric balloon.
Some things to consider
While applauding their efforts to be more precise in treating people with obesity, not all experts are convinced this saliva test will be the answer. The company’s research might look promising, but verification of results is warranted.
“Can we get better outcomes with things like this? Well, that’s the hope,” said Jaime Almandoz, MD, medical director of weight wellness at the University of Texas Southwestern Medical Center, Dallas.
“We still don’t have randomized trials where we’re looking at obesity phenotyping yet,” said Dr. Almandoz, who is also a spokesperson for the Obesity Society, a professional group of clinicians, researchers, educators, and others focused on obesity science, treatment, and prevention.
There is always concern when a diagnostic test is being developed for commercial use, said Daniel Bessesen, MD, a professor of medicine–endocrinology, metabolism, and diabetes at the University of Colorado at Denver, Aurora. “What they’re talking about doing is super important. But this is a company. This is a company that is, I think, selling a product.”
In an online search, Dr. Bessesen did not find any external studies that showed how well the saliva testing worked. But referring to work by Dr. Acosta and Michael Camilleri, MD, the other cofounder of Phenomix, he said, “I found some papers that they did that I hadn’t read before that are good.”
“These guys are smart guys. And they’ve done a lot of work on [the movement of food through the gut] and how that correlates with obesity and response to some therapies,” said Dr. Bessesen, who is also a spokesperson for the Obesity Society. “So their scientific work does line up with this area.”
Validation of any research is important because the obesity industry has been known for a lot of lose-weight-quick strategies, some with little or no science behind them, he said.
It is also essential, he said, because “anytime you do something commercial in the area of obesity, you have to acknowledge that people with obesity are a vulnerable population. These people face stigma and bias all the time.”
Removing the stigma
If knowing your obesity type ends up making a difference, it could change the conversation people have with their medical provider, Dr. Acosta said. It could also help remove some of the stigma around obesity.
“We’re going to change the conversation because now we can say: ‘Hey, you have obesity because you have ‘Hungry Gut’ phenotype. And because of that, you’re going to respond to this medication,” Dr. Acosta said. The phenotyping suggests a strong genetic tendency – a biologic basis for obesity.
“So it’s not only a way of taking the blame out, but it’s also way of explaining that there’s a reason why you have obesity,” Dr. Acosta said. It tells people: “You’re not a failure.”
More cost-effective treatment?
Targeting obesity treatment could also save on overall health care costs, Dr. Almandoz said. He estimated a cost of $1,400 per month “for forever and ever semaglutide” or at least $1,400 a month for a 3-month trial to see if this medication works in a particular person with obesity.
“That’s a lot of money when you extrapolate that out over the number of people who probably meet the criteria for treatment,” he said. A total 42% of Americans meet the Centers for Disease Control and Prevention definition for obesity.
“You can imagine the potential cost if we were to provide antiobesity therapies to everybody and we were to use what is the most effective class of medication, which is more than a thousand dollars per month, indefinitely,” Dr. Almandoz said. “Not that we should not treat everybody. That’s not the message I’m saying. But if we’re looking at yield or value in terms of treating obesity in a setting with limited resources, it may be best to start with who is most likely to benefit.”
How they created four obesity types
Starting in 2015, Dr. Acosta and colleagues started comparing tests in people with normal weight versus obesity. They used artificial intelligence and machine learning to classify obesity into 11 types at first. They realized this many obesity types were not practical for doctors and people with obesity, so they combined them into four phenotypes.
“The AI machine learning was followed by, as I like to call, HI, or human intelligence,” he said.
The saliva test checks for about 6,000 relevant genetic single-nucleotide polymorphisms. Six thousand genetic changes may sound like a large number to check; however, the average individual carries 5 million and 6 million SNPs in their DNA.
The results are translated to a score that yields a low risk or high risk for Hungry Gut or other types of obesity. “You can have all six thousand genetic mutations, or you can have zero,” Dr. Acosta said.
Moving forward
After the soft launch of Hungry Gut testing in April, Phenomix plans to continue studying their saliva test on other obesity types.
Dr. Acosta is not aware of any direct competitors to Phenomix, although that could change. “I think we’re the only diagnostic company in the space right now. But if it’s really a $14.8 billion market, we’re going to see a lot of diagnostic companies trying to do what we’re doing – if we’re successful,” he said.
An October 2022 report from Polaris Market Research estimates that the global market for obesity treatment – medications, surgery, and all others – was about $14 billion in 2021. The same report predicts the market will grow to $32 billion by 2030.
A version of this article first appeared on WebMD.com.
FDA approves new drug, sotagliflozin, for heart failure
Sotagliflozin, a novel agent that inhibits sodium-glucose cotransporter 1 as well as SGLT2, has received marketing approval from the Food and Drug Administration for reducing the risk for cardiovascular death, hospitalization for heart failure, and urgent heart failure visits in patients with heart failure, and also for preventing these same events in patients with type 2 diabetes, chronic kidney disease (CKD), and other cardiovascular disease risk factors.
This puts sotagliflozin in direct competition with two SGLT2 inhibitors, dapagliflozin (Farxiga) and empagliflozin (Jardiance), that already have indications for preventing heart failure hospitalizations in patients with heart failure as well as approvals for type 2 diabetes and preservation of renal function.
Officials at Lexicon Pharmaceuticals, the company that developed and will market sotagliflozin under the trade name Inpefa, said in a press release that they expect U.S. sales of the agent to begin before the end of June 2023. The release also highlighted that the approval broadly covered use in patients with heart failure across the full range of both reduced and preserved left ventricular ejection fractions.
They base this niche target for sotagliflozin on results from the SOLOIST-WHF trial, which randomized 1,222 patients with type 2 diabetes recently hospitalized for worsening heart failure and showed a significant 33% reduction in the rate of deaths from cardiovascular causes and hospitalizations and urgent visits for heart failure, compared with control patients during a median 9 months of follow-up. Nearly half of the enrolled patients received their first dose while still hospitalized, while the other half received their first dose a median of 2 days after hospital discharge. The drug appeared safe.
Cutting heart failure rehospitalizations in half
An exploratory post hoc analysis of SOLOIST-WHF showed that treatment with sotagliflozin cut the rate of rehospitalizations roughly in half after both 30 and 90 days compared with control patients, according to an abstract presented at the 2022 annual scientific sessions of the AHA that has not yet been published in a peer-reviewed journal.
The only SGLT2 inhibitor tested so far when initiated in patients during hospitalization for heart failure is empagliflozin, in the EMPULSE trial, which randomized 530 patients. EMPULSE also showed that starting an SGLT2 inhibitor in this setting was safe and resulted in significant clinical benefit, the study’s primary endpoint, defined as a composite of death from any cause, number of heart failure events, and time to first heart failure event, or a 5-point or greater difference in change from baseline in the Kansas City Cardiomyopathy Questionnaire Total Symptom Score at 90 days.
In the DELIVER trial, which tested dapagliflozin in patients with heart failure with preserved ejection fraction, roughly 10% of patients started study treatment during or within 30 days of heart failure hospitalization, and in this subgroup, dapagliflozin appeared as effective as it was in the other 90% of patients who did not start the drug during an acute or subacute phase.
Despite the SOLOIST-WHF evidence for sotagliflozin’s safety and efficacy in this economically important clinical setting, some experts say the drug faces an uphill path as it contends for market share against two solidly established, albeit dramatically underused, SGLT2 inhibitors. (Recent data document that 20% or fewer of U.S. patients eligible for treatment with an SGLT2 inhibitor receive it, such as a review of 49,000 patients hospitalized during 2021-2022 with heart failure with reduced ejection fraction.)
Others foresee a clear role for sotagliflozin, particularly because of additional facets of the drug’s performance in trials that they perceive give it an edge over dapagliflozin and empagliflozin. This includes evidence that sotagliflozin treatment uniquely (within the SGLT2 inhibitor class) cuts the rate of strokes and myocardial infarctions, as well as evidence of its apparent ability to lower hemoglobin A1c levels in patients with type 2 diabetes and with an estimated glomerular filtration rate below 30 mL/min per 1.73 m2, a property likely linked to inhibition of SGLT1 in the gut that dampens intestinal glucose absorption.
Sotagliflozin uptake ‘will be a challenge’
“It will be a challenge” for sotagliflozin uptake, given the head start that both dapagliflozin and empagliflozin have had as well-documented agents for patients with heart failure, commented Javed Butler, MD, a heart failure clinician and trialist who is president of the Baylor Scott & White Research Institute in Dallas.
Given the position dapagliflozin and empagliflozin currently have in U.S. heart failure management – with the SGLT2 inhibitor class called out in guidelines as foundational for treating patients with heart failure with reduced ejection fraction and likely soon for heart failure with preserved ejection fraction as well – “I can’t imagine [sotagliflozin] will be considered a preferred option,” Dr. Butler said in an interview.
Another expert was even more dismissive of sotagliflozin’s role.
“There is no persuasive evidence that sotagliflozin has any advantages, compared with the SGLT2 inhibitors, for the treatment of heart failure,” said Milton Packer, MD, a heart failure specialist and trialist at Baylor University Medical Center, Dallas. “I do not see why U.S. physicians might pivot from established SGLT2 inhibitors to sotagliflozin,” unless it was priced “at a very meaningful discount to available SGLT2 inhibitors.”
At the time it announced the FDA’s approval, Lexicon did not provide details on how it would price sotagliflozin. Existing retail prices for dapagliflozin and empagliflozin run about $550-$600/month, a price point that has contributed to slow U.S. uptake of the drug class. But experts anticipate a dramatic shake-up of the U.S. market for SGLT2 inhibitors with expected introduction of a generic SGLT2 inhibitor formulation by 2025, a development that could further dampen sotagliflozin’s prospects.
Other experts are more optimistic about the new agent’s uptake, perhaps none more than Deepak L. Bhatt, MD, MPH, who led both pivotal trials that provide the bulk of sotagliflozin’s evidence package.
In addition to SOLOIST-WHF, Dr. Bhatt also headed the SCORED trial, with 10,584 patients with type 2 diabetes, CKD, and risks for cardiovascular disease randomized to sotagliflozin or placebo and followed for a median of 16 months. The primary result showed that sotagliflozin treatment cut the combined rate of deaths from cardiovascular causes, hospitalizations for heart failure, and urgent visits for heart failure by a significant 26% relative to control patients.
A clear MACE benefit
“The data from SOLOIST-WHF and SCORED look at least as good as the data for the SGLT2 inhibitors for heart failure, and what appears to be different are the rates for MI and stroke in SCORED,” said Dr. Bhatt, director of Mount Sinai Heart, New York.
“I believe the rate of major adverse cardiovascular events [MACE] were reduced [in SCORED], and this is different from the SGLT2 inhibitors,” he said in an interview.
In 2022, Dr. Bhatt reported results from a prespecified secondary analysis of SCORED that showed that treatment with sotagliflozin cut the rate of MACE by a significant 21%-26%, compared with placebo. This finding was, in part, driven by the first data to show a substantial benefit from an SGLT inhibitor on stroke rates.
And while SCORED did not report a significant benefit for slowing progression of CKD, subsequent post hoc analyses have suggested this advantage also in as-yet-unpublished findings, Dr. Bhatt added.
But he said he doubted nephrologists will see it as a first-line agent for slowing CKD progression – an indication already held by dapagliflozin, pending for empagliflozin, and also in place for a third SGLT2 inhibitor, canagliflozin (Invokana) – because sotagliflozin lacks clear significant and prespecified evidence for this effect.
Dr. Bhatt also acknowledged the limitation of sotagliflozin compared with the SGLT2 inhibitors as an agent for glucose control, again because of no evidence for this effect from a prospective analysis and no pending indication for type 2 diabetes treatment. But the SCORED data showed a clear A1c benefit, even in patients with severely reduced renal function.
Mostly for cardiologists? ‘Compelling’ reductions in MIs and strokes
That may mean sotagliflozin “won’t get much use by endocrinologists nor by primary care physicians,” commented Carol L. Wysham, MD, an endocrinologist with MultiCare in Spokane, Wash.
Sotagliflozin “will be a cardiology drug,” and will “have a hard time” competing with the SGLT2 inhibitors, she predicted.
Dr. Bhatt agreed that sotagliflozin “will be perceived as a drug for cardiologists to prescribe. I don’t see endocrinologists, nephrologists, and primary care physicians reaching for this drug if it has a heart failure label.” But, he added, “my hope is that the company files for additional indications. It deserves an indication for glycemic control.”
The evidence for a heart failure benefit from sotagliflozin is “valid and compelling,” and “having this option is great,” commented Mikhail N. Kosiborod, MD, a cardiologist, vice president of research at Saint Luke’s Health System, and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo. But, he added, “it will be a reasonably tall task for sotagliflozin to come from behind and be disruptive in a space where there are already two well-established SGLT2 inhibitors” approved for preventing heart failure hospitalizations, “with a lot of data to back them up,”
The feature that sets sotagliflozin apart from the approved SGLT2 inhibitors is the “really compelling decrease” it produced in rates of MIs and strokes “that we simply do not see with SGLT2 inhibitors,” Dr. Kosiborod said in an interview.
He also cited results from SCORED that suggest “a meaningful reduction in A1c” when indirectly compared with SGLT2 inhibitors, especially in patients with more severe CKD. The lack of a dedicated A1c-lowering trial or an approved type 2 diabetes indication “will not be a problem for cardiologists,” he predicted, but also agreed that it is less likely to be used by primary care physicians in low-risk patients.
“I can see myself prescribing sotagliflozin,” said Dr. Kosiborod, a SCORED coinvestigator, especially for patients with coexisting type 2 diabetes, heart failure, CKD, and atherosclerotic cardiovascular disease. These patients may get “more bang for the buck” because of a reduced risk for MI and stroke, making sotagliflozin “a solid consideration in these patients if the economic factors align.”
Like others, Dr. Kosiborod cited the big impact pricing will have, especially if, as expected, a generic SGLT2 inhibitor soon comes onto the U.S. market. “Access and affordability are very important.”
SOLOIST-WHF and SCORED were sponsored initially by Sanofi and later by Lexicon after Sanofi pulled out of sotagliflozin development. Dr. Butler has been a consultant for Lexicon as well as for AstraZeneca (which markets Farxiga), Boehringer Ingelheim and Lilly (which jointly market Jardiance), and Janssen (which markets Invokana), as well as for numerous other companies. Dr. Packer has been a consultant for AstraZeneca, Boehringer Ingelheim, Lilly, and numerous other companies. Dr. Bhatt was lead investigator for SOLOIST-WHF and SCORED and has been an adviser for Boehringer Ingelheim and Janssen and numerous other companies. Dr. Wysham has been an adviser, speaker, and consultant for AstraZeneca, Boehringer Ingelheim, Lilly, Janssen, Novo Nordisk, and Sanofi, an adviser for Abbott, and a speaker for Insulet. Dr. Kosiborod was a member of the SCORED Steering Committee and has been a consultant for Lexicon, AstraZeneca, Boehringer Ingelheim, Janssen, Lilly, Novo Nordisk, and numerous other companies.
A version of this article first appeared on Medscape.com.
Sotagliflozin, a novel agent that inhibits sodium-glucose cotransporter 1 as well as SGLT2, has received marketing approval from the Food and Drug Administration for reducing the risk for cardiovascular death, hospitalization for heart failure, and urgent heart failure visits in patients with heart failure, and also for preventing these same events in patients with type 2 diabetes, chronic kidney disease (CKD), and other cardiovascular disease risk factors.
This puts sotagliflozin in direct competition with two SGLT2 inhibitors, dapagliflozin (Farxiga) and empagliflozin (Jardiance), that already have indications for preventing heart failure hospitalizations in patients with heart failure as well as approvals for type 2 diabetes and preservation of renal function.
Officials at Lexicon Pharmaceuticals, the company that developed and will market sotagliflozin under the trade name Inpefa, said in a press release that they expect U.S. sales of the agent to begin before the end of June 2023. The release also highlighted that the approval broadly covered use in patients with heart failure across the full range of both reduced and preserved left ventricular ejection fractions.
They base this niche target for sotagliflozin on results from the SOLOIST-WHF trial, which randomized 1,222 patients with type 2 diabetes recently hospitalized for worsening heart failure and showed a significant 33% reduction in the rate of deaths from cardiovascular causes and hospitalizations and urgent visits for heart failure, compared with control patients during a median 9 months of follow-up. Nearly half of the enrolled patients received their first dose while still hospitalized, while the other half received their first dose a median of 2 days after hospital discharge. The drug appeared safe.
Cutting heart failure rehospitalizations in half
An exploratory post hoc analysis of SOLOIST-WHF showed that treatment with sotagliflozin cut the rate of rehospitalizations roughly in half after both 30 and 90 days compared with control patients, according to an abstract presented at the 2022 annual scientific sessions of the AHA that has not yet been published in a peer-reviewed journal.
The only SGLT2 inhibitor tested so far when initiated in patients during hospitalization for heart failure is empagliflozin, in the EMPULSE trial, which randomized 530 patients. EMPULSE also showed that starting an SGLT2 inhibitor in this setting was safe and resulted in significant clinical benefit, the study’s primary endpoint, defined as a composite of death from any cause, number of heart failure events, and time to first heart failure event, or a 5-point or greater difference in change from baseline in the Kansas City Cardiomyopathy Questionnaire Total Symptom Score at 90 days.
In the DELIVER trial, which tested dapagliflozin in patients with heart failure with preserved ejection fraction, roughly 10% of patients started study treatment during or within 30 days of heart failure hospitalization, and in this subgroup, dapagliflozin appeared as effective as it was in the other 90% of patients who did not start the drug during an acute or subacute phase.
Despite the SOLOIST-WHF evidence for sotagliflozin’s safety and efficacy in this economically important clinical setting, some experts say the drug faces an uphill path as it contends for market share against two solidly established, albeit dramatically underused, SGLT2 inhibitors. (Recent data document that 20% or fewer of U.S. patients eligible for treatment with an SGLT2 inhibitor receive it, such as a review of 49,000 patients hospitalized during 2021-2022 with heart failure with reduced ejection fraction.)
Others foresee a clear role for sotagliflozin, particularly because of additional facets of the drug’s performance in trials that they perceive give it an edge over dapagliflozin and empagliflozin. This includes evidence that sotagliflozin treatment uniquely (within the SGLT2 inhibitor class) cuts the rate of strokes and myocardial infarctions, as well as evidence of its apparent ability to lower hemoglobin A1c levels in patients with type 2 diabetes and with an estimated glomerular filtration rate below 30 mL/min per 1.73 m2, a property likely linked to inhibition of SGLT1 in the gut that dampens intestinal glucose absorption.
Sotagliflozin uptake ‘will be a challenge’
“It will be a challenge” for sotagliflozin uptake, given the head start that both dapagliflozin and empagliflozin have had as well-documented agents for patients with heart failure, commented Javed Butler, MD, a heart failure clinician and trialist who is president of the Baylor Scott & White Research Institute in Dallas.
Given the position dapagliflozin and empagliflozin currently have in U.S. heart failure management – with the SGLT2 inhibitor class called out in guidelines as foundational for treating patients with heart failure with reduced ejection fraction and likely soon for heart failure with preserved ejection fraction as well – “I can’t imagine [sotagliflozin] will be considered a preferred option,” Dr. Butler said in an interview.
Another expert was even more dismissive of sotagliflozin’s role.
“There is no persuasive evidence that sotagliflozin has any advantages, compared with the SGLT2 inhibitors, for the treatment of heart failure,” said Milton Packer, MD, a heart failure specialist and trialist at Baylor University Medical Center, Dallas. “I do not see why U.S. physicians might pivot from established SGLT2 inhibitors to sotagliflozin,” unless it was priced “at a very meaningful discount to available SGLT2 inhibitors.”
At the time it announced the FDA’s approval, Lexicon did not provide details on how it would price sotagliflozin. Existing retail prices for dapagliflozin and empagliflozin run about $550-$600/month, a price point that has contributed to slow U.S. uptake of the drug class. But experts anticipate a dramatic shake-up of the U.S. market for SGLT2 inhibitors with expected introduction of a generic SGLT2 inhibitor formulation by 2025, a development that could further dampen sotagliflozin’s prospects.
Other experts are more optimistic about the new agent’s uptake, perhaps none more than Deepak L. Bhatt, MD, MPH, who led both pivotal trials that provide the bulk of sotagliflozin’s evidence package.
In addition to SOLOIST-WHF, Dr. Bhatt also headed the SCORED trial, with 10,584 patients with type 2 diabetes, CKD, and risks for cardiovascular disease randomized to sotagliflozin or placebo and followed for a median of 16 months. The primary result showed that sotagliflozin treatment cut the combined rate of deaths from cardiovascular causes, hospitalizations for heart failure, and urgent visits for heart failure by a significant 26% relative to control patients.
A clear MACE benefit
“The data from SOLOIST-WHF and SCORED look at least as good as the data for the SGLT2 inhibitors for heart failure, and what appears to be different are the rates for MI and stroke in SCORED,” said Dr. Bhatt, director of Mount Sinai Heart, New York.
“I believe the rate of major adverse cardiovascular events [MACE] were reduced [in SCORED], and this is different from the SGLT2 inhibitors,” he said in an interview.
In 2022, Dr. Bhatt reported results from a prespecified secondary analysis of SCORED that showed that treatment with sotagliflozin cut the rate of MACE by a significant 21%-26%, compared with placebo. This finding was, in part, driven by the first data to show a substantial benefit from an SGLT inhibitor on stroke rates.
And while SCORED did not report a significant benefit for slowing progression of CKD, subsequent post hoc analyses have suggested this advantage also in as-yet-unpublished findings, Dr. Bhatt added.
But he said he doubted nephrologists will see it as a first-line agent for slowing CKD progression – an indication already held by dapagliflozin, pending for empagliflozin, and also in place for a third SGLT2 inhibitor, canagliflozin (Invokana) – because sotagliflozin lacks clear significant and prespecified evidence for this effect.
Dr. Bhatt also acknowledged the limitation of sotagliflozin compared with the SGLT2 inhibitors as an agent for glucose control, again because of no evidence for this effect from a prospective analysis and no pending indication for type 2 diabetes treatment. But the SCORED data showed a clear A1c benefit, even in patients with severely reduced renal function.
Mostly for cardiologists? ‘Compelling’ reductions in MIs and strokes
That may mean sotagliflozin “won’t get much use by endocrinologists nor by primary care physicians,” commented Carol L. Wysham, MD, an endocrinologist with MultiCare in Spokane, Wash.
Sotagliflozin “will be a cardiology drug,” and will “have a hard time” competing with the SGLT2 inhibitors, she predicted.
Dr. Bhatt agreed that sotagliflozin “will be perceived as a drug for cardiologists to prescribe. I don’t see endocrinologists, nephrologists, and primary care physicians reaching for this drug if it has a heart failure label.” But, he added, “my hope is that the company files for additional indications. It deserves an indication for glycemic control.”
The evidence for a heart failure benefit from sotagliflozin is “valid and compelling,” and “having this option is great,” commented Mikhail N. Kosiborod, MD, a cardiologist, vice president of research at Saint Luke’s Health System, and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo. But, he added, “it will be a reasonably tall task for sotagliflozin to come from behind and be disruptive in a space where there are already two well-established SGLT2 inhibitors” approved for preventing heart failure hospitalizations, “with a lot of data to back them up,”
The feature that sets sotagliflozin apart from the approved SGLT2 inhibitors is the “really compelling decrease” it produced in rates of MIs and strokes “that we simply do not see with SGLT2 inhibitors,” Dr. Kosiborod said in an interview.
He also cited results from SCORED that suggest “a meaningful reduction in A1c” when indirectly compared with SGLT2 inhibitors, especially in patients with more severe CKD. The lack of a dedicated A1c-lowering trial or an approved type 2 diabetes indication “will not be a problem for cardiologists,” he predicted, but also agreed that it is less likely to be used by primary care physicians in low-risk patients.
“I can see myself prescribing sotagliflozin,” said Dr. Kosiborod, a SCORED coinvestigator, especially for patients with coexisting type 2 diabetes, heart failure, CKD, and atherosclerotic cardiovascular disease. These patients may get “more bang for the buck” because of a reduced risk for MI and stroke, making sotagliflozin “a solid consideration in these patients if the economic factors align.”
Like others, Dr. Kosiborod cited the big impact pricing will have, especially if, as expected, a generic SGLT2 inhibitor soon comes onto the U.S. market. “Access and affordability are very important.”
SOLOIST-WHF and SCORED were sponsored initially by Sanofi and later by Lexicon after Sanofi pulled out of sotagliflozin development. Dr. Butler has been a consultant for Lexicon as well as for AstraZeneca (which markets Farxiga), Boehringer Ingelheim and Lilly (which jointly market Jardiance), and Janssen (which markets Invokana), as well as for numerous other companies. Dr. Packer has been a consultant for AstraZeneca, Boehringer Ingelheim, Lilly, and numerous other companies. Dr. Bhatt was lead investigator for SOLOIST-WHF and SCORED and has been an adviser for Boehringer Ingelheim and Janssen and numerous other companies. Dr. Wysham has been an adviser, speaker, and consultant for AstraZeneca, Boehringer Ingelheim, Lilly, Janssen, Novo Nordisk, and Sanofi, an adviser for Abbott, and a speaker for Insulet. Dr. Kosiborod was a member of the SCORED Steering Committee and has been a consultant for Lexicon, AstraZeneca, Boehringer Ingelheim, Janssen, Lilly, Novo Nordisk, and numerous other companies.
A version of this article first appeared on Medscape.com.
Sotagliflozin, a novel agent that inhibits sodium-glucose cotransporter 1 as well as SGLT2, has received marketing approval from the Food and Drug Administration for reducing the risk for cardiovascular death, hospitalization for heart failure, and urgent heart failure visits in patients with heart failure, and also for preventing these same events in patients with type 2 diabetes, chronic kidney disease (CKD), and other cardiovascular disease risk factors.
This puts sotagliflozin in direct competition with two SGLT2 inhibitors, dapagliflozin (Farxiga) and empagliflozin (Jardiance), that already have indications for preventing heart failure hospitalizations in patients with heart failure as well as approvals for type 2 diabetes and preservation of renal function.
Officials at Lexicon Pharmaceuticals, the company that developed and will market sotagliflozin under the trade name Inpefa, said in a press release that they expect U.S. sales of the agent to begin before the end of June 2023. The release also highlighted that the approval broadly covered use in patients with heart failure across the full range of both reduced and preserved left ventricular ejection fractions.
They base this niche target for sotagliflozin on results from the SOLOIST-WHF trial, which randomized 1,222 patients with type 2 diabetes recently hospitalized for worsening heart failure and showed a significant 33% reduction in the rate of deaths from cardiovascular causes and hospitalizations and urgent visits for heart failure, compared with control patients during a median 9 months of follow-up. Nearly half of the enrolled patients received their first dose while still hospitalized, while the other half received their first dose a median of 2 days after hospital discharge. The drug appeared safe.
Cutting heart failure rehospitalizations in half
An exploratory post hoc analysis of SOLOIST-WHF showed that treatment with sotagliflozin cut the rate of rehospitalizations roughly in half after both 30 and 90 days compared with control patients, according to an abstract presented at the 2022 annual scientific sessions of the AHA that has not yet been published in a peer-reviewed journal.
The only SGLT2 inhibitor tested so far when initiated in patients during hospitalization for heart failure is empagliflozin, in the EMPULSE trial, which randomized 530 patients. EMPULSE also showed that starting an SGLT2 inhibitor in this setting was safe and resulted in significant clinical benefit, the study’s primary endpoint, defined as a composite of death from any cause, number of heart failure events, and time to first heart failure event, or a 5-point or greater difference in change from baseline in the Kansas City Cardiomyopathy Questionnaire Total Symptom Score at 90 days.
In the DELIVER trial, which tested dapagliflozin in patients with heart failure with preserved ejection fraction, roughly 10% of patients started study treatment during or within 30 days of heart failure hospitalization, and in this subgroup, dapagliflozin appeared as effective as it was in the other 90% of patients who did not start the drug during an acute or subacute phase.
Despite the SOLOIST-WHF evidence for sotagliflozin’s safety and efficacy in this economically important clinical setting, some experts say the drug faces an uphill path as it contends for market share against two solidly established, albeit dramatically underused, SGLT2 inhibitors. (Recent data document that 20% or fewer of U.S. patients eligible for treatment with an SGLT2 inhibitor receive it, such as a review of 49,000 patients hospitalized during 2021-2022 with heart failure with reduced ejection fraction.)
Others foresee a clear role for sotagliflozin, particularly because of additional facets of the drug’s performance in trials that they perceive give it an edge over dapagliflozin and empagliflozin. This includes evidence that sotagliflozin treatment uniquely (within the SGLT2 inhibitor class) cuts the rate of strokes and myocardial infarctions, as well as evidence of its apparent ability to lower hemoglobin A1c levels in patients with type 2 diabetes and with an estimated glomerular filtration rate below 30 mL/min per 1.73 m2, a property likely linked to inhibition of SGLT1 in the gut that dampens intestinal glucose absorption.
Sotagliflozin uptake ‘will be a challenge’
“It will be a challenge” for sotagliflozin uptake, given the head start that both dapagliflozin and empagliflozin have had as well-documented agents for patients with heart failure, commented Javed Butler, MD, a heart failure clinician and trialist who is president of the Baylor Scott & White Research Institute in Dallas.
Given the position dapagliflozin and empagliflozin currently have in U.S. heart failure management – with the SGLT2 inhibitor class called out in guidelines as foundational for treating patients with heart failure with reduced ejection fraction and likely soon for heart failure with preserved ejection fraction as well – “I can’t imagine [sotagliflozin] will be considered a preferred option,” Dr. Butler said in an interview.
Another expert was even more dismissive of sotagliflozin’s role.
“There is no persuasive evidence that sotagliflozin has any advantages, compared with the SGLT2 inhibitors, for the treatment of heart failure,” said Milton Packer, MD, a heart failure specialist and trialist at Baylor University Medical Center, Dallas. “I do not see why U.S. physicians might pivot from established SGLT2 inhibitors to sotagliflozin,” unless it was priced “at a very meaningful discount to available SGLT2 inhibitors.”
At the time it announced the FDA’s approval, Lexicon did not provide details on how it would price sotagliflozin. Existing retail prices for dapagliflozin and empagliflozin run about $550-$600/month, a price point that has contributed to slow U.S. uptake of the drug class. But experts anticipate a dramatic shake-up of the U.S. market for SGLT2 inhibitors with expected introduction of a generic SGLT2 inhibitor formulation by 2025, a development that could further dampen sotagliflozin’s prospects.
Other experts are more optimistic about the new agent’s uptake, perhaps none more than Deepak L. Bhatt, MD, MPH, who led both pivotal trials that provide the bulk of sotagliflozin’s evidence package.
In addition to SOLOIST-WHF, Dr. Bhatt also headed the SCORED trial, with 10,584 patients with type 2 diabetes, CKD, and risks for cardiovascular disease randomized to sotagliflozin or placebo and followed for a median of 16 months. The primary result showed that sotagliflozin treatment cut the combined rate of deaths from cardiovascular causes, hospitalizations for heart failure, and urgent visits for heart failure by a significant 26% relative to control patients.
A clear MACE benefit
“The data from SOLOIST-WHF and SCORED look at least as good as the data for the SGLT2 inhibitors for heart failure, and what appears to be different are the rates for MI and stroke in SCORED,” said Dr. Bhatt, director of Mount Sinai Heart, New York.
“I believe the rate of major adverse cardiovascular events [MACE] were reduced [in SCORED], and this is different from the SGLT2 inhibitors,” he said in an interview.
In 2022, Dr. Bhatt reported results from a prespecified secondary analysis of SCORED that showed that treatment with sotagliflozin cut the rate of MACE by a significant 21%-26%, compared with placebo. This finding was, in part, driven by the first data to show a substantial benefit from an SGLT inhibitor on stroke rates.
And while SCORED did not report a significant benefit for slowing progression of CKD, subsequent post hoc analyses have suggested this advantage also in as-yet-unpublished findings, Dr. Bhatt added.
But he said he doubted nephrologists will see it as a first-line agent for slowing CKD progression – an indication already held by dapagliflozin, pending for empagliflozin, and also in place for a third SGLT2 inhibitor, canagliflozin (Invokana) – because sotagliflozin lacks clear significant and prespecified evidence for this effect.
Dr. Bhatt also acknowledged the limitation of sotagliflozin compared with the SGLT2 inhibitors as an agent for glucose control, again because of no evidence for this effect from a prospective analysis and no pending indication for type 2 diabetes treatment. But the SCORED data showed a clear A1c benefit, even in patients with severely reduced renal function.
Mostly for cardiologists? ‘Compelling’ reductions in MIs and strokes
That may mean sotagliflozin “won’t get much use by endocrinologists nor by primary care physicians,” commented Carol L. Wysham, MD, an endocrinologist with MultiCare in Spokane, Wash.
Sotagliflozin “will be a cardiology drug,” and will “have a hard time” competing with the SGLT2 inhibitors, she predicted.
Dr. Bhatt agreed that sotagliflozin “will be perceived as a drug for cardiologists to prescribe. I don’t see endocrinologists, nephrologists, and primary care physicians reaching for this drug if it has a heart failure label.” But, he added, “my hope is that the company files for additional indications. It deserves an indication for glycemic control.”
The evidence for a heart failure benefit from sotagliflozin is “valid and compelling,” and “having this option is great,” commented Mikhail N. Kosiborod, MD, a cardiologist, vice president of research at Saint Luke’s Health System, and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo. But, he added, “it will be a reasonably tall task for sotagliflozin to come from behind and be disruptive in a space where there are already two well-established SGLT2 inhibitors” approved for preventing heart failure hospitalizations, “with a lot of data to back them up,”
The feature that sets sotagliflozin apart from the approved SGLT2 inhibitors is the “really compelling decrease” it produced in rates of MIs and strokes “that we simply do not see with SGLT2 inhibitors,” Dr. Kosiborod said in an interview.
He also cited results from SCORED that suggest “a meaningful reduction in A1c” when indirectly compared with SGLT2 inhibitors, especially in patients with more severe CKD. The lack of a dedicated A1c-lowering trial or an approved type 2 diabetes indication “will not be a problem for cardiologists,” he predicted, but also agreed that it is less likely to be used by primary care physicians in low-risk patients.
“I can see myself prescribing sotagliflozin,” said Dr. Kosiborod, a SCORED coinvestigator, especially for patients with coexisting type 2 diabetes, heart failure, CKD, and atherosclerotic cardiovascular disease. These patients may get “more bang for the buck” because of a reduced risk for MI and stroke, making sotagliflozin “a solid consideration in these patients if the economic factors align.”
Like others, Dr. Kosiborod cited the big impact pricing will have, especially if, as expected, a generic SGLT2 inhibitor soon comes onto the U.S. market. “Access and affordability are very important.”
SOLOIST-WHF and SCORED were sponsored initially by Sanofi and later by Lexicon after Sanofi pulled out of sotagliflozin development. Dr. Butler has been a consultant for Lexicon as well as for AstraZeneca (which markets Farxiga), Boehringer Ingelheim and Lilly (which jointly market Jardiance), and Janssen (which markets Invokana), as well as for numerous other companies. Dr. Packer has been a consultant for AstraZeneca, Boehringer Ingelheim, Lilly, and numerous other companies. Dr. Bhatt was lead investigator for SOLOIST-WHF and SCORED and has been an adviser for Boehringer Ingelheim and Janssen and numerous other companies. Dr. Wysham has been an adviser, speaker, and consultant for AstraZeneca, Boehringer Ingelheim, Lilly, Janssen, Novo Nordisk, and Sanofi, an adviser for Abbott, and a speaker for Insulet. Dr. Kosiborod was a member of the SCORED Steering Committee and has been a consultant for Lexicon, AstraZeneca, Boehringer Ingelheim, Janssen, Lilly, Novo Nordisk, and numerous other companies.
A version of this article first appeared on Medscape.com.
Plant-based diet tied to healthier blood lipid levels
, in a new meta-analysis of 30 trials.
The findings suggest that “plant-based diets have the potential to lessen the atherosclerotic burden from atherogenic lipoproteins and thereby reduce the risk of cardiovascular disease,” write Caroline Amelie Koch, a medical student at the University of Copenhagen, and colleagues. Their findings were published online in the European Heart Journal (2023 May 24. doi: 10.1093/eurheartj/ehad211).
“Vegetarian and vegan diets were associated with a 14% reduction in all artery-clogging lipoproteins as indicated by apoB,” senior author Ruth Frikke-Schmidt, DMSc, PhD, Rigshospitalet, Copenhagen, and professor, University of Copenhagen, said in a press release from her university.
“This corresponds to a third of the effect of taking cholesterol-lowering medications such as statins,” she added, “and would result in a 7% reduction in the risk of cardiovascular disease in someone who maintained a plant-based diet for 5 years.”
“Importantly, we found similar results, across continents, ages, different ranges of body mass index, and among people in different states of health,” Dr. Frikke-Schmidt stressed.
And combining statins with plant-based diets would likely produce a synergistic effect, she speculated.
“If people start eating vegetarian or vegan diets from an early age,” she said, “the potential for reducing the risk of cardiovascular disease caused by blocked arteries is substantial.”
In addition, the researchers conclude: “Shifting to plant-based diets at a populational level will reduce emissions of greenhouse gases considerably – together making these diets efficient means [moving] towards a more sustainable development, while at the same time reducing the growing burden of atherosclerotic cardiovascular disease.”
More support for vegan, vegetarian diets
These new findings “add to the body of evidence supporting favorable effects of healthy vegan and vegetarian dietary patterns on circulating levels of LDL-C and atherogenic lipoproteins, which would be expected to reduce ASCVD risk,” Kevin C. Maki, PhD, and Carol Kirkpatrick, PhD, MPH, write in an accompanying editorial.
“While it is not necessary to entirely omit foods such as meat, poultry, and fish/seafood to follow a recommended dietary pattern, reducing consumption of such foods is a reasonable option for those who prefer to do so,” note Dr. Maki, of Indiana University School of Public Health, Bloomington, and Kirkpatrick, of Idaho State University, Pocatello.
Plant-based diet needs to be ‘well-planned’
Several experts who were not involved in this meta-analysis shed light on the study and its implications in comments to the U.K. Science Media Center.
“Although a vegetarian and vegan diet can be very healthy and beneficial with respect to cardiovascular risk, it is important that it is well planned so that nutrients it can be low in are included, including iron, iodine, vitamin B12, and vitamin D,” said Duane Mellor, PhD, a registered dietitian and senior lecturer, Aston Medical School, Aston University, Birmingham, England.
Some people “may find it easier to follow a Mediterranean-style diet that features plenty of fruit, vegetables, pulses, wholegrains, fish, eggs and low-fat dairy, with only small amounts of meat,” Tracy Parker, senior dietitian at the British Heart Foundation, London, suggested.
“There is considerable evidence that this type of diet can help lower your risk of developing heart and circulatory diseases by improving cholesterol and blood pressure levels, reducing inflammation, and controlling blood glucose levels,” she added.
And Aedin Cassidy, PhD, chair in nutrition & preventative medicine, Queen’s University Belfast (Ireland), noted that “not all plant-based diets are equal. Healthy plant-based diets, characterized by fruits, vegetables, and whole grains improve health, but other plant diets (for example, those including refined carbohydrates, processed foods high in fat/salt, etc.) do not.”
This new study shows that plant-based diets have the potential to improve health by improving blood lipids, “but this is one of many potential mechanisms, including impact on blood pressure, weight maintenance, and blood sugars,” she added.
“This work represents a well-conducted analysis of 30 clinical trials involving over two thousand participants and highlights the value of a vegetarian diet in reducing the risk of heart attack or stroke through reduction in blood cholesterol levels,” said Robert Storey, BM, DM, professor of cardiology, University of Sheffield, U.K.
However, it also demonstrates that the impact of diet on an individual’s cholesterol level is relatively limited, he added.
“This is because people inherit the tendency for their livers to produce too much cholesterol, meaning that high cholesterol is more strongly influenced by our genes than by our diet,” he explained.
This is “why statins are needed to block cholesterol production in people who are at higher risk of or have already suffered from a heart attack, stroke, or other illness related to cholesterol build-up in blood vessels.”
Beneficial effect on ApoB, LDL-C, and total cholesterol
ApoB is the main apolipoprotein in LDL-C (“bad” cholesterol), the researchers note. Previous studies have shown that LDL-C and apoB-containing particles are associated with increased risk of ASCVD.
They aimed to estimate the effect of vegetarian or vegan diets on blood levels of total cholesterol, LDL-C, triglycerides, and apoB in people randomized to a vegetarian or vegan diet versus an omnivorous diet (that is, including meat and dairy).
They identified 30 studies published between 1982 and 2022 and conducted in the United States (18 studies), Sweden (2), Finland (2), South Korea (2), Australia (1), Brazil (1), Czech Republic (1), Italy (1), Iran (1), and New Zealand (1).
The diet interventions lasted from 10 days to 5 years with a mean of 29 weeks (15 studies ≤ 3 months; 12 studies 3-12 months; and three studies > 1 year). Nine studies used a crossover design, and the rest used a parallel design whereby participants followed only one diet.
The studies had 11 to 291 participants (mean, 79 participants) with a mean BMI of 21.5-35.1 kg/m2 and a mean age of 20-67 years. Thirteen studies included participants treated with lipid-lowering therapy at baseline.
The dietary intervention was vegetarian in 15 trials (three lacto-vegetarian and 12 lacto-ovo-vegetarian) and vegan in the other 15 trials.
On average, compared with people eating an omnivore diet, people eating a plant-based diet had a 7% reduction in total cholesterol from baseline (–0.34 mmol/L), a 10% reduction in LDL-C from baseline (–0.30 mmol/L), and a 14% reduction in apoB from baseline (–12.9 mg/dL) (all P < .01).
The effects were similar across age, continent, study duration, health status, intervention diet, intervention program, and study design subgroups.
There was no significant difference in triglyceride levels in patients in the omnivore versus plant-based diet groups.
Such diets could considerably reduce greenhouse gases
Senior author Dr. Frikke-Schmidt noted: “Recent systematic reviews have shown that if the populations of high-income countries shift to plant-based diets, this can reduce net emissions of greenhouse gases by between 35% to 49%.”
“Plant-based diets are key instruments for changing food production to more environmentally sustainable forms, while at the same time reducing the burden of cardiovascular disease” in an aging population, she said.
“We should be eating a varied, plant-rich diet, not too much, and quenching our thirst with water,” she concluded.
The study was funded by the Lundbeck Foundation, the Danish Heart Foundation, and the Leducq Foundation. The authors, editorialists, Ms. Parker, Dr. Cassidy, and Dr. Storey have reported no relevant financial relationships. Dr. Mellor has disclosed that he is a vegetarian.
A version of this article first appeared on Medscape.com.
, in a new meta-analysis of 30 trials.
The findings suggest that “plant-based diets have the potential to lessen the atherosclerotic burden from atherogenic lipoproteins and thereby reduce the risk of cardiovascular disease,” write Caroline Amelie Koch, a medical student at the University of Copenhagen, and colleagues. Their findings were published online in the European Heart Journal (2023 May 24. doi: 10.1093/eurheartj/ehad211).
“Vegetarian and vegan diets were associated with a 14% reduction in all artery-clogging lipoproteins as indicated by apoB,” senior author Ruth Frikke-Schmidt, DMSc, PhD, Rigshospitalet, Copenhagen, and professor, University of Copenhagen, said in a press release from her university.
“This corresponds to a third of the effect of taking cholesterol-lowering medications such as statins,” she added, “and would result in a 7% reduction in the risk of cardiovascular disease in someone who maintained a plant-based diet for 5 years.”
“Importantly, we found similar results, across continents, ages, different ranges of body mass index, and among people in different states of health,” Dr. Frikke-Schmidt stressed.
And combining statins with plant-based diets would likely produce a synergistic effect, she speculated.
“If people start eating vegetarian or vegan diets from an early age,” she said, “the potential for reducing the risk of cardiovascular disease caused by blocked arteries is substantial.”
In addition, the researchers conclude: “Shifting to plant-based diets at a populational level will reduce emissions of greenhouse gases considerably – together making these diets efficient means [moving] towards a more sustainable development, while at the same time reducing the growing burden of atherosclerotic cardiovascular disease.”
More support for vegan, vegetarian diets
These new findings “add to the body of evidence supporting favorable effects of healthy vegan and vegetarian dietary patterns on circulating levels of LDL-C and atherogenic lipoproteins, which would be expected to reduce ASCVD risk,” Kevin C. Maki, PhD, and Carol Kirkpatrick, PhD, MPH, write in an accompanying editorial.
“While it is not necessary to entirely omit foods such as meat, poultry, and fish/seafood to follow a recommended dietary pattern, reducing consumption of such foods is a reasonable option for those who prefer to do so,” note Dr. Maki, of Indiana University School of Public Health, Bloomington, and Kirkpatrick, of Idaho State University, Pocatello.
Plant-based diet needs to be ‘well-planned’
Several experts who were not involved in this meta-analysis shed light on the study and its implications in comments to the U.K. Science Media Center.
“Although a vegetarian and vegan diet can be very healthy and beneficial with respect to cardiovascular risk, it is important that it is well planned so that nutrients it can be low in are included, including iron, iodine, vitamin B12, and vitamin D,” said Duane Mellor, PhD, a registered dietitian and senior lecturer, Aston Medical School, Aston University, Birmingham, England.
Some people “may find it easier to follow a Mediterranean-style diet that features plenty of fruit, vegetables, pulses, wholegrains, fish, eggs and low-fat dairy, with only small amounts of meat,” Tracy Parker, senior dietitian at the British Heart Foundation, London, suggested.
“There is considerable evidence that this type of diet can help lower your risk of developing heart and circulatory diseases by improving cholesterol and blood pressure levels, reducing inflammation, and controlling blood glucose levels,” she added.
And Aedin Cassidy, PhD, chair in nutrition & preventative medicine, Queen’s University Belfast (Ireland), noted that “not all plant-based diets are equal. Healthy plant-based diets, characterized by fruits, vegetables, and whole grains improve health, but other plant diets (for example, those including refined carbohydrates, processed foods high in fat/salt, etc.) do not.”
This new study shows that plant-based diets have the potential to improve health by improving blood lipids, “but this is one of many potential mechanisms, including impact on blood pressure, weight maintenance, and blood sugars,” she added.
“This work represents a well-conducted analysis of 30 clinical trials involving over two thousand participants and highlights the value of a vegetarian diet in reducing the risk of heart attack or stroke through reduction in blood cholesterol levels,” said Robert Storey, BM, DM, professor of cardiology, University of Sheffield, U.K.
However, it also demonstrates that the impact of diet on an individual’s cholesterol level is relatively limited, he added.
“This is because people inherit the tendency for their livers to produce too much cholesterol, meaning that high cholesterol is more strongly influenced by our genes than by our diet,” he explained.
This is “why statins are needed to block cholesterol production in people who are at higher risk of or have already suffered from a heart attack, stroke, or other illness related to cholesterol build-up in blood vessels.”
Beneficial effect on ApoB, LDL-C, and total cholesterol
ApoB is the main apolipoprotein in LDL-C (“bad” cholesterol), the researchers note. Previous studies have shown that LDL-C and apoB-containing particles are associated with increased risk of ASCVD.
They aimed to estimate the effect of vegetarian or vegan diets on blood levels of total cholesterol, LDL-C, triglycerides, and apoB in people randomized to a vegetarian or vegan diet versus an omnivorous diet (that is, including meat and dairy).
They identified 30 studies published between 1982 and 2022 and conducted in the United States (18 studies), Sweden (2), Finland (2), South Korea (2), Australia (1), Brazil (1), Czech Republic (1), Italy (1), Iran (1), and New Zealand (1).
The diet interventions lasted from 10 days to 5 years with a mean of 29 weeks (15 studies ≤ 3 months; 12 studies 3-12 months; and three studies > 1 year). Nine studies used a crossover design, and the rest used a parallel design whereby participants followed only one diet.
The studies had 11 to 291 participants (mean, 79 participants) with a mean BMI of 21.5-35.1 kg/m2 and a mean age of 20-67 years. Thirteen studies included participants treated with lipid-lowering therapy at baseline.
The dietary intervention was vegetarian in 15 trials (three lacto-vegetarian and 12 lacto-ovo-vegetarian) and vegan in the other 15 trials.
On average, compared with people eating an omnivore diet, people eating a plant-based diet had a 7% reduction in total cholesterol from baseline (–0.34 mmol/L), a 10% reduction in LDL-C from baseline (–0.30 mmol/L), and a 14% reduction in apoB from baseline (–12.9 mg/dL) (all P < .01).
The effects were similar across age, continent, study duration, health status, intervention diet, intervention program, and study design subgroups.
There was no significant difference in triglyceride levels in patients in the omnivore versus plant-based diet groups.
Such diets could considerably reduce greenhouse gases
Senior author Dr. Frikke-Schmidt noted: “Recent systematic reviews have shown that if the populations of high-income countries shift to plant-based diets, this can reduce net emissions of greenhouse gases by between 35% to 49%.”
“Plant-based diets are key instruments for changing food production to more environmentally sustainable forms, while at the same time reducing the burden of cardiovascular disease” in an aging population, she said.
“We should be eating a varied, plant-rich diet, not too much, and quenching our thirst with water,” she concluded.
The study was funded by the Lundbeck Foundation, the Danish Heart Foundation, and the Leducq Foundation. The authors, editorialists, Ms. Parker, Dr. Cassidy, and Dr. Storey have reported no relevant financial relationships. Dr. Mellor has disclosed that he is a vegetarian.
A version of this article first appeared on Medscape.com.
, in a new meta-analysis of 30 trials.
The findings suggest that “plant-based diets have the potential to lessen the atherosclerotic burden from atherogenic lipoproteins and thereby reduce the risk of cardiovascular disease,” write Caroline Amelie Koch, a medical student at the University of Copenhagen, and colleagues. Their findings were published online in the European Heart Journal (2023 May 24. doi: 10.1093/eurheartj/ehad211).
“Vegetarian and vegan diets were associated with a 14% reduction in all artery-clogging lipoproteins as indicated by apoB,” senior author Ruth Frikke-Schmidt, DMSc, PhD, Rigshospitalet, Copenhagen, and professor, University of Copenhagen, said in a press release from her university.
“This corresponds to a third of the effect of taking cholesterol-lowering medications such as statins,” she added, “and would result in a 7% reduction in the risk of cardiovascular disease in someone who maintained a plant-based diet for 5 years.”
“Importantly, we found similar results, across continents, ages, different ranges of body mass index, and among people in different states of health,” Dr. Frikke-Schmidt stressed.
And combining statins with plant-based diets would likely produce a synergistic effect, she speculated.
“If people start eating vegetarian or vegan diets from an early age,” she said, “the potential for reducing the risk of cardiovascular disease caused by blocked arteries is substantial.”
In addition, the researchers conclude: “Shifting to plant-based diets at a populational level will reduce emissions of greenhouse gases considerably – together making these diets efficient means [moving] towards a more sustainable development, while at the same time reducing the growing burden of atherosclerotic cardiovascular disease.”
More support for vegan, vegetarian diets
These new findings “add to the body of evidence supporting favorable effects of healthy vegan and vegetarian dietary patterns on circulating levels of LDL-C and atherogenic lipoproteins, which would be expected to reduce ASCVD risk,” Kevin C. Maki, PhD, and Carol Kirkpatrick, PhD, MPH, write in an accompanying editorial.
“While it is not necessary to entirely omit foods such as meat, poultry, and fish/seafood to follow a recommended dietary pattern, reducing consumption of such foods is a reasonable option for those who prefer to do so,” note Dr. Maki, of Indiana University School of Public Health, Bloomington, and Kirkpatrick, of Idaho State University, Pocatello.
Plant-based diet needs to be ‘well-planned’
Several experts who were not involved in this meta-analysis shed light on the study and its implications in comments to the U.K. Science Media Center.
“Although a vegetarian and vegan diet can be very healthy and beneficial with respect to cardiovascular risk, it is important that it is well planned so that nutrients it can be low in are included, including iron, iodine, vitamin B12, and vitamin D,” said Duane Mellor, PhD, a registered dietitian and senior lecturer, Aston Medical School, Aston University, Birmingham, England.
Some people “may find it easier to follow a Mediterranean-style diet that features plenty of fruit, vegetables, pulses, wholegrains, fish, eggs and low-fat dairy, with only small amounts of meat,” Tracy Parker, senior dietitian at the British Heart Foundation, London, suggested.
“There is considerable evidence that this type of diet can help lower your risk of developing heart and circulatory diseases by improving cholesterol and blood pressure levels, reducing inflammation, and controlling blood glucose levels,” she added.
And Aedin Cassidy, PhD, chair in nutrition & preventative medicine, Queen’s University Belfast (Ireland), noted that “not all plant-based diets are equal. Healthy plant-based diets, characterized by fruits, vegetables, and whole grains improve health, but other plant diets (for example, those including refined carbohydrates, processed foods high in fat/salt, etc.) do not.”
This new study shows that plant-based diets have the potential to improve health by improving blood lipids, “but this is one of many potential mechanisms, including impact on blood pressure, weight maintenance, and blood sugars,” she added.
“This work represents a well-conducted analysis of 30 clinical trials involving over two thousand participants and highlights the value of a vegetarian diet in reducing the risk of heart attack or stroke through reduction in blood cholesterol levels,” said Robert Storey, BM, DM, professor of cardiology, University of Sheffield, U.K.
However, it also demonstrates that the impact of diet on an individual’s cholesterol level is relatively limited, he added.
“This is because people inherit the tendency for their livers to produce too much cholesterol, meaning that high cholesterol is more strongly influenced by our genes than by our diet,” he explained.
This is “why statins are needed to block cholesterol production in people who are at higher risk of or have already suffered from a heart attack, stroke, or other illness related to cholesterol build-up in blood vessels.”
Beneficial effect on ApoB, LDL-C, and total cholesterol
ApoB is the main apolipoprotein in LDL-C (“bad” cholesterol), the researchers note. Previous studies have shown that LDL-C and apoB-containing particles are associated with increased risk of ASCVD.
They aimed to estimate the effect of vegetarian or vegan diets on blood levels of total cholesterol, LDL-C, triglycerides, and apoB in people randomized to a vegetarian or vegan diet versus an omnivorous diet (that is, including meat and dairy).
They identified 30 studies published between 1982 and 2022 and conducted in the United States (18 studies), Sweden (2), Finland (2), South Korea (2), Australia (1), Brazil (1), Czech Republic (1), Italy (1), Iran (1), and New Zealand (1).
The diet interventions lasted from 10 days to 5 years with a mean of 29 weeks (15 studies ≤ 3 months; 12 studies 3-12 months; and three studies > 1 year). Nine studies used a crossover design, and the rest used a parallel design whereby participants followed only one diet.
The studies had 11 to 291 participants (mean, 79 participants) with a mean BMI of 21.5-35.1 kg/m2 and a mean age of 20-67 years. Thirteen studies included participants treated with lipid-lowering therapy at baseline.
The dietary intervention was vegetarian in 15 trials (three lacto-vegetarian and 12 lacto-ovo-vegetarian) and vegan in the other 15 trials.
On average, compared with people eating an omnivore diet, people eating a plant-based diet had a 7% reduction in total cholesterol from baseline (–0.34 mmol/L), a 10% reduction in LDL-C from baseline (–0.30 mmol/L), and a 14% reduction in apoB from baseline (–12.9 mg/dL) (all P < .01).
The effects were similar across age, continent, study duration, health status, intervention diet, intervention program, and study design subgroups.
There was no significant difference in triglyceride levels in patients in the omnivore versus plant-based diet groups.
Such diets could considerably reduce greenhouse gases
Senior author Dr. Frikke-Schmidt noted: “Recent systematic reviews have shown that if the populations of high-income countries shift to plant-based diets, this can reduce net emissions of greenhouse gases by between 35% to 49%.”
“Plant-based diets are key instruments for changing food production to more environmentally sustainable forms, while at the same time reducing the burden of cardiovascular disease” in an aging population, she said.
“We should be eating a varied, plant-rich diet, not too much, and quenching our thirst with water,” she concluded.
The study was funded by the Lundbeck Foundation, the Danish Heart Foundation, and the Leducq Foundation. The authors, editorialists, Ms. Parker, Dr. Cassidy, and Dr. Storey have reported no relevant financial relationships. Dr. Mellor has disclosed that he is a vegetarian.
A version of this article first appeared on Medscape.com.
FROM EUROPEAN HEART JOURNAL
Ticagrelor, DAPT equal in preventing repeat revascularization
PHOENIX – Post hoc analysis of the randomized TWILIGHT trial comparing ticagrelor alone with ticagrelor plus aspirin in high-risk patients after percutaneous coronary intervention (PCI) shows both regimens were similarly effective in preventing repeat revascularization after 1 year.
In TWILIGHT, the main findings of which were previously published in the New England Journal of Medicine, 7,119 high-risk PCI patients on standard dual antiplatelet therapy (DAPT) of ticagrelor plus aspirin for 3 months were randomized to continuation of DAPT or to ticagrelor plus placebo for 12 months.
The new post hoc analysis included 6,759 patients and shows the rates of clinically driven revascularization were similar between the two groups: 7.1% and 6.6% for the ticagrelor monotherapy and ticagrelor-based DAPT groups, respectively (P = .363).
The findings were presented at the Society for Cardiovascular Angiography & Interventions annual scientific sessions.
Three key findings come from the post hoc analysis, Usman Baber, MD, director of the cardiac catheterization lab and associate professor at the University of Oklahoma Health Sciences Center, Oklahoma City, who presented the findings, said in an interview.
“The first is that, over the 1-year follow-up of our trial, we found that a repeat revascularization event occurred in 6.7% of patients,” he said. “We found that a slight majority of these repeat revascularization events were due to events at the target lesion or target vessel; and we found that most of the repeat revascularization events actually occurred in patients without a concomitant acute coronary syndrome. In other words, these were essentially stable patients when they were getting their repeat revascularization.”
The second major finding was that these high-risk patients who had repeat revascularization were at three times greater risk for major adverse cardiac and cerebrovascular events (MACCE), based on a multivariable adjusted model, Dr. Baber said.
“And then third is that he said.
Repeat revascularization
The goal of the analysis was to focus on clinically driven repeat revascularization as an outcome, Dr. Baber said. The analysis also aimed to understand the association between repeat revascularization and subsequent risk.
Secondary endpoints included target lesion revascularization (TLR); target vessel revascularization (TVR); MACCE, including clinically driven revascularization; and net adverse clinical events (NACE), a composite of MACCE or Bleeding Academic Research Consortium (BARC) 2, 3, or 5 bleeding.
The outcomes of all those endpoints, except for NACE, were similar, Dr. Baber said. “Overall, ticagrelor monotherapy, as expected, reduced rates of bleeding as compared with ticagrelor plus aspirin,” he said. The rates of NACE were 12.2% versus 14.6%, respectively (P = .004). For BARC 2,3, or 5 bleeding, the rates were 3.4% versus 7.1% (P < .001).
The findings validated repeat revascularization as a meaningful endpoint, Dr. Baber said. “Certainly, we don’t elevate repeat revascularization as an endpoint to the same level as death or stroke, but certainly this analysis and some others prior to it highlight the fact that when these patients come back for repeat revascularization, even if they’re stable, they clearly are at elevated risk for future ischemic events,” he said.
One limitation of the analysis is that the data are from a clinical trial, “which renders the findings not as generalizable to the broader patients in a clinical practice,” he said. However, the TWILIGHT data are validated and adjusted for multiple risk factors.
“When patients come in and they have a repeat revascularization, should there be a consideration to placing them on more intensive antithrombotic therapy?” he asked. “Right now, if patients have a repeat revascularization event and they’re stable, guidelines and clinical practice usually calls for continuing clopidogrel, but again our study and others like it indicate these patients are at a higher thrombotic risk, so maybe there’s a rationale for at least a short course of a more potent antiplatelet agent in such patients.”
The post hoc findings confirm those of the primary TWILIGHT trial, Lorenzo Azzalini, MD, PhD, MSc, director of interventional cardiology research at the University of Washington Medical Center, Seattle, said in an interview.
“It’s not surprising to find no difference between the two therapies with regard to unplanned revascularization,” he said. “It’s considered that only stent thrombosis can only actually be mitigated by the drugs being investigated in the trial; all the other ischemic endpoints reflect more chronic ischemia—TLR or known TVR—upon which ticagrelor and aspirin do not play any role.”
However, he added, “I still think this study provides useful information to the community in a period of intense scrutiny on the relative benefits and merits of PCI versus CABG [coronary artery bypass graft], and this study confirms that shortening DAPT to 3 months and then continuing with just ticagrelor does not bring any penalty in terms of ischemic events or repeat revascularization.”
TWILIGHT enrolled high-risk patients, but not “very-high-risk” patients, Dr. Azzalini noted. The enrollment criteria excluded patients on chronic anticoagulation, who had a prior stroke or liver sclerosis, or were on dialysis.
“Future trials should focus more on very-high-risk patients because these are the patients that we deal with on a daily basis in our clinical practice and we need data to inform our decisions,” he said. “I’m not sure I could use the science contained in this study and extrapolate them to patients on dialysis because these patients really have a high risk of restenosis on follow-up.”
Dr. Baber disclosed relationships with Amgen and Abbott. Dr. Azzalini had no relevant disclosures.
PHOENIX – Post hoc analysis of the randomized TWILIGHT trial comparing ticagrelor alone with ticagrelor plus aspirin in high-risk patients after percutaneous coronary intervention (PCI) shows both regimens were similarly effective in preventing repeat revascularization after 1 year.
In TWILIGHT, the main findings of which were previously published in the New England Journal of Medicine, 7,119 high-risk PCI patients on standard dual antiplatelet therapy (DAPT) of ticagrelor plus aspirin for 3 months were randomized to continuation of DAPT or to ticagrelor plus placebo for 12 months.
The new post hoc analysis included 6,759 patients and shows the rates of clinically driven revascularization were similar between the two groups: 7.1% and 6.6% for the ticagrelor monotherapy and ticagrelor-based DAPT groups, respectively (P = .363).
The findings were presented at the Society for Cardiovascular Angiography & Interventions annual scientific sessions.
Three key findings come from the post hoc analysis, Usman Baber, MD, director of the cardiac catheterization lab and associate professor at the University of Oklahoma Health Sciences Center, Oklahoma City, who presented the findings, said in an interview.
“The first is that, over the 1-year follow-up of our trial, we found that a repeat revascularization event occurred in 6.7% of patients,” he said. “We found that a slight majority of these repeat revascularization events were due to events at the target lesion or target vessel; and we found that most of the repeat revascularization events actually occurred in patients without a concomitant acute coronary syndrome. In other words, these were essentially stable patients when they were getting their repeat revascularization.”
The second major finding was that these high-risk patients who had repeat revascularization were at three times greater risk for major adverse cardiac and cerebrovascular events (MACCE), based on a multivariable adjusted model, Dr. Baber said.
“And then third is that he said.
Repeat revascularization
The goal of the analysis was to focus on clinically driven repeat revascularization as an outcome, Dr. Baber said. The analysis also aimed to understand the association between repeat revascularization and subsequent risk.
Secondary endpoints included target lesion revascularization (TLR); target vessel revascularization (TVR); MACCE, including clinically driven revascularization; and net adverse clinical events (NACE), a composite of MACCE or Bleeding Academic Research Consortium (BARC) 2, 3, or 5 bleeding.
The outcomes of all those endpoints, except for NACE, were similar, Dr. Baber said. “Overall, ticagrelor monotherapy, as expected, reduced rates of bleeding as compared with ticagrelor plus aspirin,” he said. The rates of NACE were 12.2% versus 14.6%, respectively (P = .004). For BARC 2,3, or 5 bleeding, the rates were 3.4% versus 7.1% (P < .001).
The findings validated repeat revascularization as a meaningful endpoint, Dr. Baber said. “Certainly, we don’t elevate repeat revascularization as an endpoint to the same level as death or stroke, but certainly this analysis and some others prior to it highlight the fact that when these patients come back for repeat revascularization, even if they’re stable, they clearly are at elevated risk for future ischemic events,” he said.
One limitation of the analysis is that the data are from a clinical trial, “which renders the findings not as generalizable to the broader patients in a clinical practice,” he said. However, the TWILIGHT data are validated and adjusted for multiple risk factors.
“When patients come in and they have a repeat revascularization, should there be a consideration to placing them on more intensive antithrombotic therapy?” he asked. “Right now, if patients have a repeat revascularization event and they’re stable, guidelines and clinical practice usually calls for continuing clopidogrel, but again our study and others like it indicate these patients are at a higher thrombotic risk, so maybe there’s a rationale for at least a short course of a more potent antiplatelet agent in such patients.”
The post hoc findings confirm those of the primary TWILIGHT trial, Lorenzo Azzalini, MD, PhD, MSc, director of interventional cardiology research at the University of Washington Medical Center, Seattle, said in an interview.
“It’s not surprising to find no difference between the two therapies with regard to unplanned revascularization,” he said. “It’s considered that only stent thrombosis can only actually be mitigated by the drugs being investigated in the trial; all the other ischemic endpoints reflect more chronic ischemia—TLR or known TVR—upon which ticagrelor and aspirin do not play any role.”
However, he added, “I still think this study provides useful information to the community in a period of intense scrutiny on the relative benefits and merits of PCI versus CABG [coronary artery bypass graft], and this study confirms that shortening DAPT to 3 months and then continuing with just ticagrelor does not bring any penalty in terms of ischemic events or repeat revascularization.”
TWILIGHT enrolled high-risk patients, but not “very-high-risk” patients, Dr. Azzalini noted. The enrollment criteria excluded patients on chronic anticoagulation, who had a prior stroke or liver sclerosis, or were on dialysis.
“Future trials should focus more on very-high-risk patients because these are the patients that we deal with on a daily basis in our clinical practice and we need data to inform our decisions,” he said. “I’m not sure I could use the science contained in this study and extrapolate them to patients on dialysis because these patients really have a high risk of restenosis on follow-up.”
Dr. Baber disclosed relationships with Amgen and Abbott. Dr. Azzalini had no relevant disclosures.
PHOENIX – Post hoc analysis of the randomized TWILIGHT trial comparing ticagrelor alone with ticagrelor plus aspirin in high-risk patients after percutaneous coronary intervention (PCI) shows both regimens were similarly effective in preventing repeat revascularization after 1 year.
In TWILIGHT, the main findings of which were previously published in the New England Journal of Medicine, 7,119 high-risk PCI patients on standard dual antiplatelet therapy (DAPT) of ticagrelor plus aspirin for 3 months were randomized to continuation of DAPT or to ticagrelor plus placebo for 12 months.
The new post hoc analysis included 6,759 patients and shows the rates of clinically driven revascularization were similar between the two groups: 7.1% and 6.6% for the ticagrelor monotherapy and ticagrelor-based DAPT groups, respectively (P = .363).
The findings were presented at the Society for Cardiovascular Angiography & Interventions annual scientific sessions.
Three key findings come from the post hoc analysis, Usman Baber, MD, director of the cardiac catheterization lab and associate professor at the University of Oklahoma Health Sciences Center, Oklahoma City, who presented the findings, said in an interview.
“The first is that, over the 1-year follow-up of our trial, we found that a repeat revascularization event occurred in 6.7% of patients,” he said. “We found that a slight majority of these repeat revascularization events were due to events at the target lesion or target vessel; and we found that most of the repeat revascularization events actually occurred in patients without a concomitant acute coronary syndrome. In other words, these were essentially stable patients when they were getting their repeat revascularization.”
The second major finding was that these high-risk patients who had repeat revascularization were at three times greater risk for major adverse cardiac and cerebrovascular events (MACCE), based on a multivariable adjusted model, Dr. Baber said.
“And then third is that he said.
Repeat revascularization
The goal of the analysis was to focus on clinically driven repeat revascularization as an outcome, Dr. Baber said. The analysis also aimed to understand the association between repeat revascularization and subsequent risk.
Secondary endpoints included target lesion revascularization (TLR); target vessel revascularization (TVR); MACCE, including clinically driven revascularization; and net adverse clinical events (NACE), a composite of MACCE or Bleeding Academic Research Consortium (BARC) 2, 3, or 5 bleeding.
The outcomes of all those endpoints, except for NACE, were similar, Dr. Baber said. “Overall, ticagrelor monotherapy, as expected, reduced rates of bleeding as compared with ticagrelor plus aspirin,” he said. The rates of NACE were 12.2% versus 14.6%, respectively (P = .004). For BARC 2,3, or 5 bleeding, the rates were 3.4% versus 7.1% (P < .001).
The findings validated repeat revascularization as a meaningful endpoint, Dr. Baber said. “Certainly, we don’t elevate repeat revascularization as an endpoint to the same level as death or stroke, but certainly this analysis and some others prior to it highlight the fact that when these patients come back for repeat revascularization, even if they’re stable, they clearly are at elevated risk for future ischemic events,” he said.
One limitation of the analysis is that the data are from a clinical trial, “which renders the findings not as generalizable to the broader patients in a clinical practice,” he said. However, the TWILIGHT data are validated and adjusted for multiple risk factors.
“When patients come in and they have a repeat revascularization, should there be a consideration to placing them on more intensive antithrombotic therapy?” he asked. “Right now, if patients have a repeat revascularization event and they’re stable, guidelines and clinical practice usually calls for continuing clopidogrel, but again our study and others like it indicate these patients are at a higher thrombotic risk, so maybe there’s a rationale for at least a short course of a more potent antiplatelet agent in such patients.”
The post hoc findings confirm those of the primary TWILIGHT trial, Lorenzo Azzalini, MD, PhD, MSc, director of interventional cardiology research at the University of Washington Medical Center, Seattle, said in an interview.
“It’s not surprising to find no difference between the two therapies with regard to unplanned revascularization,” he said. “It’s considered that only stent thrombosis can only actually be mitigated by the drugs being investigated in the trial; all the other ischemic endpoints reflect more chronic ischemia—TLR or known TVR—upon which ticagrelor and aspirin do not play any role.”
However, he added, “I still think this study provides useful information to the community in a period of intense scrutiny on the relative benefits and merits of PCI versus CABG [coronary artery bypass graft], and this study confirms that shortening DAPT to 3 months and then continuing with just ticagrelor does not bring any penalty in terms of ischemic events or repeat revascularization.”
TWILIGHT enrolled high-risk patients, but not “very-high-risk” patients, Dr. Azzalini noted. The enrollment criteria excluded patients on chronic anticoagulation, who had a prior stroke or liver sclerosis, or were on dialysis.
“Future trials should focus more on very-high-risk patients because these are the patients that we deal with on a daily basis in our clinical practice and we need data to inform our decisions,” he said. “I’m not sure I could use the science contained in this study and extrapolate them to patients on dialysis because these patients really have a high risk of restenosis on follow-up.”
Dr. Baber disclosed relationships with Amgen and Abbott. Dr. Azzalini had no relevant disclosures.
AT SCAI 2023
ECMO signals benefit for cardiogenic shock after MI in halted trial
Data support new randomized trial
At the time that it was halted, a multicenter randomized trial was associating venoarterial extracorporeal membrane oxygenation (VA-ECMO) with an intriguing signal of benefit for patients in cardiogenic shock undergoing percutaneous intervention (PCI) for acute myocardial infarction.
Stopped early because of the pandemic, the EURO SHOCK trial has data on only 35 patients, but all-cause mortality at 30 days was nearly 30% lower in the VA-ECMO arm than in the standard-therapy arm, reported Manel Sabate, MD, PhD, chief of the interventional cardiology unit, Clinic University Hospital, Barcelona.
When patients were followed out to 12 months, the numerical survival advantage appeared to persist.
Yet, because of the early trial termination, “there really are no definite conclusions to be drawn from these results,” acknowledged Dr. Sabate, who noted that less than 10% of the planned enrollment had been reached. In addition, the survival benefit in the VA-ECMO arm was achieved at the cost of a higher rate of complications.
Despite the small numbers, results from the halted trial were presented as a late-breaker at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions. They were also simultaneously published in EuroIntervention.
The interest is based on an important unmet need, said Dr. Sabate. Cardiogenic shock occurs in about 10% of acute MI patients. Of those that continue on to revascularization, the 30-day mortality can approach 50%.
Meanwhile, the potential of mechanical circulatory support to maintain perfusion during cardiogenic shock makes it one of the most attractive, if unproven, approaches for improving outcomes.
Major multicenter trial terminated
The EURO SHOCK trial had a planned enrollment of 428 patients when it was initiated; 15 centers in six European countries participated. Recruitment and the trial were brought to a halt by the COVID-19 pandemic.
When trial recruitment was stopped, 18 patients had been assigned to standard supportive care and 17 patients to VA-ECMO. The primary endpoint of the trial was all-cause mortality at 30 days. Mortality at 12 months along with bleeding complications, cerebrovascular events, and readmission for heart failure, were among secondary endpoints.
At 30 days, the mortality rate was 61.1% among patients randomized to standard care, versus 43.8% among patients randomized to VA ECMO (hazard ratio, 0.56; 95% confidence interval, 0.21-01.45; P = 0.22).
At 12 months, the numerical advantage of VA-ECMO persisted (81.5% vs. 51.8%) with a similar nonsignificant signal for potential benefit despite the small sample size (HR, 0.52; 95% CI, 0.21-1.26; P = 0.14).
There were also numerically lower rates of cardiovascular death, ischemic stroke, recurrent MI, and acute kidney injury among patients in the VA-ECMO group relative to those in the standard-care group, Dr. Sabate reported.
However, VA-ECMO was associated with more vascular complications (21.4% vs. 0%) and bleeding events (35.7% vs. 5.6%).
Furthermore, although quality of life data were limited, Dr. Sabate noted that about half of patients in the VA-ECMO group reported problems with mobility, self-care, or usual activities on the basis of the EQ-5D-3L questionnaire at 30 days. None of the patients in the standard-care group reported any such difficulties.
When standard care was compared with VA-ECMO, rates of readmission for heart failure over 12 months (8.0% vs. 6.9%) were not different.
To be enrolled in this study, patients being treated for MI had to be in cardiogenic shock for at least 30 minutes following primary PCI. The median time from onset of cardiogenic shock to VA-ECMO in the active treatment arm was 4.8 hours.
Patient enrollment was challenging
Even independent of the COVID-19 pandemic, enrolling patients proved to be difficult. The 35 patients enrolled represented about 10% of the 333 patients screened at the participating centers. Unwitnessed out-of-hospital cardiac arrest, cardiogenic shock from a cause other than MI, and recovery from cardiogenic shock after the PCI was performed were among reasons for the high rate of exclusions.
The difficulty of identifying and engaging appropriate candidates for VA-ECMO, along with a substantial crossover rate, should be among lessons for investigators planning the next trial, said Dr. Sabate, who pointed out that 5 of the 17 patients assigned to VA-ECMO were never treated due to complications or patient refusal.
Dr. Sabate said.
Davide Capodanno, MD, PhD, a professor of cardiology and interventional cardiologist at the University of Catania (Italy), agreed.
“It was a good decision to publish these results,” he said. Noting that there were challenges in conducting the trial unrelated to COVID-19, Dr. Capodanno acknowledged the promise of mechanical ventilatory support for a relatively common and life-threatening complication.
“This study must be read for the lessons it will provide for future trials,” he said.
Dr. Sabate reported he has no potential conflicts of interest. Dr. Capodanno reported financial relationships with Amgen, Daiichi Sankyo, and Sanofi.
Data support new randomized trial
Data support new randomized trial
At the time that it was halted, a multicenter randomized trial was associating venoarterial extracorporeal membrane oxygenation (VA-ECMO) with an intriguing signal of benefit for patients in cardiogenic shock undergoing percutaneous intervention (PCI) for acute myocardial infarction.
Stopped early because of the pandemic, the EURO SHOCK trial has data on only 35 patients, but all-cause mortality at 30 days was nearly 30% lower in the VA-ECMO arm than in the standard-therapy arm, reported Manel Sabate, MD, PhD, chief of the interventional cardiology unit, Clinic University Hospital, Barcelona.
When patients were followed out to 12 months, the numerical survival advantage appeared to persist.
Yet, because of the early trial termination, “there really are no definite conclusions to be drawn from these results,” acknowledged Dr. Sabate, who noted that less than 10% of the planned enrollment had been reached. In addition, the survival benefit in the VA-ECMO arm was achieved at the cost of a higher rate of complications.
Despite the small numbers, results from the halted trial were presented as a late-breaker at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions. They were also simultaneously published in EuroIntervention.
The interest is based on an important unmet need, said Dr. Sabate. Cardiogenic shock occurs in about 10% of acute MI patients. Of those that continue on to revascularization, the 30-day mortality can approach 50%.
Meanwhile, the potential of mechanical circulatory support to maintain perfusion during cardiogenic shock makes it one of the most attractive, if unproven, approaches for improving outcomes.
Major multicenter trial terminated
The EURO SHOCK trial had a planned enrollment of 428 patients when it was initiated; 15 centers in six European countries participated. Recruitment and the trial were brought to a halt by the COVID-19 pandemic.
When trial recruitment was stopped, 18 patients had been assigned to standard supportive care and 17 patients to VA-ECMO. The primary endpoint of the trial was all-cause mortality at 30 days. Mortality at 12 months along with bleeding complications, cerebrovascular events, and readmission for heart failure, were among secondary endpoints.
At 30 days, the mortality rate was 61.1% among patients randomized to standard care, versus 43.8% among patients randomized to VA ECMO (hazard ratio, 0.56; 95% confidence interval, 0.21-01.45; P = 0.22).
At 12 months, the numerical advantage of VA-ECMO persisted (81.5% vs. 51.8%) with a similar nonsignificant signal for potential benefit despite the small sample size (HR, 0.52; 95% CI, 0.21-1.26; P = 0.14).
There were also numerically lower rates of cardiovascular death, ischemic stroke, recurrent MI, and acute kidney injury among patients in the VA-ECMO group relative to those in the standard-care group, Dr. Sabate reported.
However, VA-ECMO was associated with more vascular complications (21.4% vs. 0%) and bleeding events (35.7% vs. 5.6%).
Furthermore, although quality of life data were limited, Dr. Sabate noted that about half of patients in the VA-ECMO group reported problems with mobility, self-care, or usual activities on the basis of the EQ-5D-3L questionnaire at 30 days. None of the patients in the standard-care group reported any such difficulties.
When standard care was compared with VA-ECMO, rates of readmission for heart failure over 12 months (8.0% vs. 6.9%) were not different.
To be enrolled in this study, patients being treated for MI had to be in cardiogenic shock for at least 30 minutes following primary PCI. The median time from onset of cardiogenic shock to VA-ECMO in the active treatment arm was 4.8 hours.
Patient enrollment was challenging
Even independent of the COVID-19 pandemic, enrolling patients proved to be difficult. The 35 patients enrolled represented about 10% of the 333 patients screened at the participating centers. Unwitnessed out-of-hospital cardiac arrest, cardiogenic shock from a cause other than MI, and recovery from cardiogenic shock after the PCI was performed were among reasons for the high rate of exclusions.
The difficulty of identifying and engaging appropriate candidates for VA-ECMO, along with a substantial crossover rate, should be among lessons for investigators planning the next trial, said Dr. Sabate, who pointed out that 5 of the 17 patients assigned to VA-ECMO were never treated due to complications or patient refusal.
Dr. Sabate said.
Davide Capodanno, MD, PhD, a professor of cardiology and interventional cardiologist at the University of Catania (Italy), agreed.
“It was a good decision to publish these results,” he said. Noting that there were challenges in conducting the trial unrelated to COVID-19, Dr. Capodanno acknowledged the promise of mechanical ventilatory support for a relatively common and life-threatening complication.
“This study must be read for the lessons it will provide for future trials,” he said.
Dr. Sabate reported he has no potential conflicts of interest. Dr. Capodanno reported financial relationships with Amgen, Daiichi Sankyo, and Sanofi.
At the time that it was halted, a multicenter randomized trial was associating venoarterial extracorporeal membrane oxygenation (VA-ECMO) with an intriguing signal of benefit for patients in cardiogenic shock undergoing percutaneous intervention (PCI) for acute myocardial infarction.
Stopped early because of the pandemic, the EURO SHOCK trial has data on only 35 patients, but all-cause mortality at 30 days was nearly 30% lower in the VA-ECMO arm than in the standard-therapy arm, reported Manel Sabate, MD, PhD, chief of the interventional cardiology unit, Clinic University Hospital, Barcelona.
When patients were followed out to 12 months, the numerical survival advantage appeared to persist.
Yet, because of the early trial termination, “there really are no definite conclusions to be drawn from these results,” acknowledged Dr. Sabate, who noted that less than 10% of the planned enrollment had been reached. In addition, the survival benefit in the VA-ECMO arm was achieved at the cost of a higher rate of complications.
Despite the small numbers, results from the halted trial were presented as a late-breaker at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions. They were also simultaneously published in EuroIntervention.
The interest is based on an important unmet need, said Dr. Sabate. Cardiogenic shock occurs in about 10% of acute MI patients. Of those that continue on to revascularization, the 30-day mortality can approach 50%.
Meanwhile, the potential of mechanical circulatory support to maintain perfusion during cardiogenic shock makes it one of the most attractive, if unproven, approaches for improving outcomes.
Major multicenter trial terminated
The EURO SHOCK trial had a planned enrollment of 428 patients when it was initiated; 15 centers in six European countries participated. Recruitment and the trial were brought to a halt by the COVID-19 pandemic.
When trial recruitment was stopped, 18 patients had been assigned to standard supportive care and 17 patients to VA-ECMO. The primary endpoint of the trial was all-cause mortality at 30 days. Mortality at 12 months along with bleeding complications, cerebrovascular events, and readmission for heart failure, were among secondary endpoints.
At 30 days, the mortality rate was 61.1% among patients randomized to standard care, versus 43.8% among patients randomized to VA ECMO (hazard ratio, 0.56; 95% confidence interval, 0.21-01.45; P = 0.22).
At 12 months, the numerical advantage of VA-ECMO persisted (81.5% vs. 51.8%) with a similar nonsignificant signal for potential benefit despite the small sample size (HR, 0.52; 95% CI, 0.21-1.26; P = 0.14).
There were also numerically lower rates of cardiovascular death, ischemic stroke, recurrent MI, and acute kidney injury among patients in the VA-ECMO group relative to those in the standard-care group, Dr. Sabate reported.
However, VA-ECMO was associated with more vascular complications (21.4% vs. 0%) and bleeding events (35.7% vs. 5.6%).
Furthermore, although quality of life data were limited, Dr. Sabate noted that about half of patients in the VA-ECMO group reported problems with mobility, self-care, or usual activities on the basis of the EQ-5D-3L questionnaire at 30 days. None of the patients in the standard-care group reported any such difficulties.
When standard care was compared with VA-ECMO, rates of readmission for heart failure over 12 months (8.0% vs. 6.9%) were not different.
To be enrolled in this study, patients being treated for MI had to be in cardiogenic shock for at least 30 minutes following primary PCI. The median time from onset of cardiogenic shock to VA-ECMO in the active treatment arm was 4.8 hours.
Patient enrollment was challenging
Even independent of the COVID-19 pandemic, enrolling patients proved to be difficult. The 35 patients enrolled represented about 10% of the 333 patients screened at the participating centers. Unwitnessed out-of-hospital cardiac arrest, cardiogenic shock from a cause other than MI, and recovery from cardiogenic shock after the PCI was performed were among reasons for the high rate of exclusions.
The difficulty of identifying and engaging appropriate candidates for VA-ECMO, along with a substantial crossover rate, should be among lessons for investigators planning the next trial, said Dr. Sabate, who pointed out that 5 of the 17 patients assigned to VA-ECMO were never treated due to complications or patient refusal.
Dr. Sabate said.
Davide Capodanno, MD, PhD, a professor of cardiology and interventional cardiologist at the University of Catania (Italy), agreed.
“It was a good decision to publish these results,” he said. Noting that there were challenges in conducting the trial unrelated to COVID-19, Dr. Capodanno acknowledged the promise of mechanical ventilatory support for a relatively common and life-threatening complication.
“This study must be read for the lessons it will provide for future trials,” he said.
Dr. Sabate reported he has no potential conflicts of interest. Dr. Capodanno reported financial relationships with Amgen, Daiichi Sankyo, and Sanofi.
FROM EUROPCR 2023
Commentary: Trastuzumab, breast density, and extended treatment in BC, June 2023
Among the patients treated with trastuzumab deruxtecan, median progression-free survival was significantly prolonged compared with the physician's choice treatment group (17.8 vs 6.9 months; hazard ratio 0.36; P < .0001). There were no new safety signals reported for trastuzumab deruxtecan. Of interest, drug-related interstitial lung disease occurred in 10% of patients treated with trastuzumab deruxtecan (including two grade 5 death events) compared with < 1% in the physician's-choice treatment group.
Overall, trastuzumab deruxtecan demonstrated a favorable benefit-risk profile in patients with HER2+ BC previously treated with trastuzumab emtansine. This is the first randomized study to show efficacy with an antibody-drug conjugate after a previous antibody-drug conjugate.
Breast density is a known independent risk factor for BC, furthermore, dense breast tissue can make identifying BC on screening mammograms more challenging. The nested case-control cohort study by Jiang and colleagues observed women with no history of any cancer for 10 years, with screening mammograms every 1-2 years. Subsequently, 289 women who developed BC were identified and analyzed along with 658 matched control individuals. BC risk factors were also collected via questionnaires at the time of enrollment. Of note, the BC cases cohort had an overall higher mean body mass index, a higher percentage of Black women, and of women with a family history of BC. The results showed that though women's breast density decreased over time in both cases and controls, the rate of change in breast density was significantly slower in the breast that later developed cancer compared with the cancer-free breast in control individuals (estimate 0.027; P = .04). Enhancing screening modalities to enable assessing for longitudinal changes in breast density may provide an additional tool for evaluating the risk for BC.
Reducing the late BC recurrence risk beyond 5 years is a significant issue in patients with hormone receptor–positive (HR+) BC. This prospective, randomized, phase 3, AERAS trial included 1593 postmenopausal women with HR+ early-stage invasive BC who were disease-free at 5 years after postoperative endocrine therapy. Patients were randomly assigned 1:1 to stop or continue receiving anastrozole for an additional 5 years. Results showed that continuation of anastrozole treatment for an additional 5 years significantly improved 5-year disease-free survival (DFS) (hazard ratio 0.61; 95% CI 0.46-0.82; P < .0010). Furthermore, extended anastrozole treatment reduced the incidence of local recurrence and second primary cancers. However, there was no significant difference in distant DFS. The incidence of grade 3 or higher adverse events was < 1% in both groups, although menopausal or bone-related all-grade adverse events were more frequent among patients in the group that continued with anastrozole, as expected. Results from this study help inform the risks and benefits of extending hormone therapy beyond 5 years.
The RxPONDER trial comparing endocrine therapy (ET) alone to chemotherapy plus endocrine therapy (CET) in patients with one to three positive axillary lymph nodes and recurrence score (RS) ≤ 25 showed that CET did not improve survival outcomes compared with ET alone in postmenopausal women with HR+/HER2- BC. This retrospective cohort study of real-world data from the National Cancer Database included 28,427 women with stage I-III HR+/HER2- BC and one to three positive axillary lymph nodes, of which 26.3% and 73.7% of patients received CET and ET, respectively. Results showed that in patients with RS of 20-25, CET was associated with a significant improvement in overall survival compared with ET alone, in both premenopausal (age ≤ 50 years: hazard ratio 0.334, P = .002) and postmenopausal patients (age > 50 years: hazard ratio 0.521, P = .019). Though these results are inconsistent with the RxPONDER trial results regarding the postmenopausal cohort, they do raise an important finding that is supported by prior published data.1 More studies are needed to validate these findings. At this time, guidelines recommend omitting chemotherapy in patients with HR+/HER2- BC, one to three positive axillary lymph nodes, and an RS of 20-25 per RxPONDER.
Additional Reference
- Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Comparisons between different polychemotherapy regimens for early breast cancer: Meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet. 2012;379:432-444. doi: 10.1016/S0140-6736(11)61625-5
Among the patients treated with trastuzumab deruxtecan, median progression-free survival was significantly prolonged compared with the physician's choice treatment group (17.8 vs 6.9 months; hazard ratio 0.36; P < .0001). There were no new safety signals reported for trastuzumab deruxtecan. Of interest, drug-related interstitial lung disease occurred in 10% of patients treated with trastuzumab deruxtecan (including two grade 5 death events) compared with < 1% in the physician's-choice treatment group.
Overall, trastuzumab deruxtecan demonstrated a favorable benefit-risk profile in patients with HER2+ BC previously treated with trastuzumab emtansine. This is the first randomized study to show efficacy with an antibody-drug conjugate after a previous antibody-drug conjugate.
Breast density is a known independent risk factor for BC, furthermore, dense breast tissue can make identifying BC on screening mammograms more challenging. The nested case-control cohort study by Jiang and colleagues observed women with no history of any cancer for 10 years, with screening mammograms every 1-2 years. Subsequently, 289 women who developed BC were identified and analyzed along with 658 matched control individuals. BC risk factors were also collected via questionnaires at the time of enrollment. Of note, the BC cases cohort had an overall higher mean body mass index, a higher percentage of Black women, and of women with a family history of BC. The results showed that though women's breast density decreased over time in both cases and controls, the rate of change in breast density was significantly slower in the breast that later developed cancer compared with the cancer-free breast in control individuals (estimate 0.027; P = .04). Enhancing screening modalities to enable assessing for longitudinal changes in breast density may provide an additional tool for evaluating the risk for BC.
Reducing the late BC recurrence risk beyond 5 years is a significant issue in patients with hormone receptor–positive (HR+) BC. This prospective, randomized, phase 3, AERAS trial included 1593 postmenopausal women with HR+ early-stage invasive BC who were disease-free at 5 years after postoperative endocrine therapy. Patients were randomly assigned 1:1 to stop or continue receiving anastrozole for an additional 5 years. Results showed that continuation of anastrozole treatment for an additional 5 years significantly improved 5-year disease-free survival (DFS) (hazard ratio 0.61; 95% CI 0.46-0.82; P < .0010). Furthermore, extended anastrozole treatment reduced the incidence of local recurrence and second primary cancers. However, there was no significant difference in distant DFS. The incidence of grade 3 or higher adverse events was < 1% in both groups, although menopausal or bone-related all-grade adverse events were more frequent among patients in the group that continued with anastrozole, as expected. Results from this study help inform the risks and benefits of extending hormone therapy beyond 5 years.
The RxPONDER trial comparing endocrine therapy (ET) alone to chemotherapy plus endocrine therapy (CET) in patients with one to three positive axillary lymph nodes and recurrence score (RS) ≤ 25 showed that CET did not improve survival outcomes compared with ET alone in postmenopausal women with HR+/HER2- BC. This retrospective cohort study of real-world data from the National Cancer Database included 28,427 women with stage I-III HR+/HER2- BC and one to three positive axillary lymph nodes, of which 26.3% and 73.7% of patients received CET and ET, respectively. Results showed that in patients with RS of 20-25, CET was associated with a significant improvement in overall survival compared with ET alone, in both premenopausal (age ≤ 50 years: hazard ratio 0.334, P = .002) and postmenopausal patients (age > 50 years: hazard ratio 0.521, P = .019). Though these results are inconsistent with the RxPONDER trial results regarding the postmenopausal cohort, they do raise an important finding that is supported by prior published data.1 More studies are needed to validate these findings. At this time, guidelines recommend omitting chemotherapy in patients with HR+/HER2- BC, one to three positive axillary lymph nodes, and an RS of 20-25 per RxPONDER.
Additional Reference
- Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Comparisons between different polychemotherapy regimens for early breast cancer: Meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet. 2012;379:432-444. doi: 10.1016/S0140-6736(11)61625-5
Among the patients treated with trastuzumab deruxtecan, median progression-free survival was significantly prolonged compared with the physician's choice treatment group (17.8 vs 6.9 months; hazard ratio 0.36; P < .0001). There were no new safety signals reported for trastuzumab deruxtecan. Of interest, drug-related interstitial lung disease occurred in 10% of patients treated with trastuzumab deruxtecan (including two grade 5 death events) compared with < 1% in the physician's-choice treatment group.
Overall, trastuzumab deruxtecan demonstrated a favorable benefit-risk profile in patients with HER2+ BC previously treated with trastuzumab emtansine. This is the first randomized study to show efficacy with an antibody-drug conjugate after a previous antibody-drug conjugate.
Breast density is a known independent risk factor for BC, furthermore, dense breast tissue can make identifying BC on screening mammograms more challenging. The nested case-control cohort study by Jiang and colleagues observed women with no history of any cancer for 10 years, with screening mammograms every 1-2 years. Subsequently, 289 women who developed BC were identified and analyzed along with 658 matched control individuals. BC risk factors were also collected via questionnaires at the time of enrollment. Of note, the BC cases cohort had an overall higher mean body mass index, a higher percentage of Black women, and of women with a family history of BC. The results showed that though women's breast density decreased over time in both cases and controls, the rate of change in breast density was significantly slower in the breast that later developed cancer compared with the cancer-free breast in control individuals (estimate 0.027; P = .04). Enhancing screening modalities to enable assessing for longitudinal changes in breast density may provide an additional tool for evaluating the risk for BC.
Reducing the late BC recurrence risk beyond 5 years is a significant issue in patients with hormone receptor–positive (HR+) BC. This prospective, randomized, phase 3, AERAS trial included 1593 postmenopausal women with HR+ early-stage invasive BC who were disease-free at 5 years after postoperative endocrine therapy. Patients were randomly assigned 1:1 to stop or continue receiving anastrozole for an additional 5 years. Results showed that continuation of anastrozole treatment for an additional 5 years significantly improved 5-year disease-free survival (DFS) (hazard ratio 0.61; 95% CI 0.46-0.82; P < .0010). Furthermore, extended anastrozole treatment reduced the incidence of local recurrence and second primary cancers. However, there was no significant difference in distant DFS. The incidence of grade 3 or higher adverse events was < 1% in both groups, although menopausal or bone-related all-grade adverse events were more frequent among patients in the group that continued with anastrozole, as expected. Results from this study help inform the risks and benefits of extending hormone therapy beyond 5 years.
The RxPONDER trial comparing endocrine therapy (ET) alone to chemotherapy plus endocrine therapy (CET) in patients with one to three positive axillary lymph nodes and recurrence score (RS) ≤ 25 showed that CET did not improve survival outcomes compared with ET alone in postmenopausal women with HR+/HER2- BC. This retrospective cohort study of real-world data from the National Cancer Database included 28,427 women with stage I-III HR+/HER2- BC and one to three positive axillary lymph nodes, of which 26.3% and 73.7% of patients received CET and ET, respectively. Results showed that in patients with RS of 20-25, CET was associated with a significant improvement in overall survival compared with ET alone, in both premenopausal (age ≤ 50 years: hazard ratio 0.334, P = .002) and postmenopausal patients (age > 50 years: hazard ratio 0.521, P = .019). Though these results are inconsistent with the RxPONDER trial results regarding the postmenopausal cohort, they do raise an important finding that is supported by prior published data.1 More studies are needed to validate these findings. At this time, guidelines recommend omitting chemotherapy in patients with HR+/HER2- BC, one to three positive axillary lymph nodes, and an RS of 20-25 per RxPONDER.
Additional Reference
- Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Comparisons between different polychemotherapy regimens for early breast cancer: Meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet. 2012;379:432-444. doi: 10.1016/S0140-6736(11)61625-5
JAK-inhibitor safety in adolescents with AD: Long-term analyses reported
WASHINGTON – and over 1,000 patient-years of exposure, Lawrence F. Eichenfield, MD, reported at the annual Revolutionizing Atopic Dermatitis conference.
In March 2023, the oral Janus kinase 1 (JAK1) inhibitor was approved by the Food and Drug Administration for treating adolescents aged 12-17 with refractory moderate to severe AD – an expanded indication from the approval in adults in 2022.
The new analysis evaluated data from patients who participated in the phase 3 JADE clinical trials – MONO-1, MONO-2, TEEN, and REGIMEN – and were subsequently enrolled in the ongoing phase 3 extension trial JADE EXTEND. Compared with a previous post hoc analysis in which adolescent patients had approximately 1 year of exposure, this updated analysis includes a sizable portion of patients with more than 96 weeks of exposure.
“We’re starting to get good numbers of [adolescents] who’ve had about 2 years of exposure,” said Dr. Eichenfield, professor of dermatology and pediatrics and vice chair of the department of dermatology at the University of California, San Diego, during a late-breaking research session.
With a data cut for this analysis of September 2021, “we haven’t seen additive long-term [adverse] effects” with longer exposures, he said. In addition, “there were no unique safety concerns related to adolescents compared to the findings observed [in an] integrated safety analysis using the same data cut in which most patients were adults.”
(The analysis in adults covered 3,802 patients with over 5,000 patient-years of exposure, and was presented at the annual American Academy of Dermatology meeting in March 2023.)
Also presented in the late-breaking abstract session at RAD 2023 was a long-term safety study of upadacitinib (Rinvoq), the other JAK1 inhibitor approved for adolescents with AD – approved by the FDA for both adolescents and adults with moderate to severe AD in 2022. The new analysis captures exposure of up to 4 years and shows no “worsening or accumulation of events,” compared with 1-year data, reported Christopher G. Bunick, MD, PhD, of the department of dermatology and the program in translational biomedicine at Yale University, New Haven, Conn.
Abrocitinib in adolescents
For the safety analysis of abrocitinib (Cibinqo), data were pooled into two cohorts: A consistent-dose cohort of 490 adolescents who received the same dose (200 mg or 100 mg) during the entire duration of the qualifying JADE trials, and a variable-dose cohort of 145 adolescents who received different doses (200 mg or 100 mg) during the JADE REGIMEN qualifying trial.
Duration of exposure was 96 weeks or more in 37%-38% of the consistent-dose cohort and 68% of the variable-dose cohort.
In the consistent-dose cohort, adverse events occurred in 243 (84%) and 153 (76%) of patients receiving 200-mg doses and 100-mg doses, respectively. Incidence rates for severe adverse events were 5.87 per 100 patient-years at both doses, and rates for adverse events leading to study discontinuation were 6.96/100 patient-years at 200 mg and 5.13/100 patient-years at 100 mg.
“No meaningful dose-response relationship was observed for serious adverse events, or adverse events leading to discontinuation, or adverse events of special interest,” said Dr. Eichenfield, also chief of pediatric and adolescent dermatology at Rady Children’s Hospital, San Diego.
The IRs of adverse events of special interest were 1.84/100 patient-years and 1.28/100 patient-years for serious infection; 2.11/100 patient-years, and 1.62/100 patient-years for all herpes zoster infections; and 0.69/100 patient-years and 0.32/100 patient-years for opportunistic herpes zoster infections in the 200-mg and 100-mg arms, respectively.
“Other than herpes zoster, there were no opportunistic infections observed and no tuberculosis cases,” he said. “There was one nonfatal venous thromboembolism in an adolescent who had a very strong family history of [pulmonary embolism], one retinal detachment [with a concurrent diagnosis of cataracts and of left eyebrow folliculitis], and no events of nonmelanoma skin cancer or other malignancies, major adverse cardiovascular events, or deaths.” The thromboembolism case was reported in the previous post hoc analysis.
In the variable-dose cohort, data were similar, Dr. Eichenfield said. The IRs for severe adverse events, adverse events leading to study withdrawal, and adverse events of special interest were consistent with those in the other cohort. And similarly, there were no reports of tuberculosis or other opportunistic infections (excluding herpes zoster), and no reports of nonmelanoma skin cancer (NMSC) or other malignancies, major adverse cardiovascular events (MACE), or death. In this cohort, there were no venous thromboembolism (VTE) reports.
Upadacitinib in adolescents, adults
The new analysis looked at up to 4 years of upadacitinib treatment in almost 2,700 adolescents and adults– and over 6,200 patient-years – using integrated data from three ongoing pivotal phase 3 studies: Measure Up 1, Measure Up 2, and AD Up. (Of these patients, 539 were adolescents, Dr. Bunick said after the meeting.)
In the Measure Up studies, patients were randomized 1:1:1 to receive a 15-mg dose, a 30-mg dose, or placebo once daily. In AD Up, patients in each arm received concomitant topical corticosteroids. At week 16, patients receiving the drug continued their assigned treatment during the ongoing blinded extension period, and those receiving placebo were rerandomized to upadacitinib 15 mg or 30 mg.
The exposure-adjusted event rates for any adverse event leading to discontinuation were 4.1/100 patient-years and 4.7/100 patient-years in patients receiving 15 mg and 30 mg, respectively, and the rates of any serious adverse event were 6.5/100 patient-years and 7.5/100 patient-years, Dr. Bunick reported. Three deaths occurred in the 30-mg group; all deaths were related to COVID infection and occurred in adults with cardiovascular risk factors.
Incidence rates of adverse events of special interest were similar to those in a previous 1-year analysis. The rate of serious infections per 100 patient years, for instance, was 2.3 and 2.8 in the 15-mg and 30-mg groups, respectively, compared with 2.2 and 2.8 in the 1-year analysis.
The rate of opportunistic infections, including eczema herpeticum (and excluding TB and herpes zoster), saw a slight bump in the new analysis to 2.4/100 patient-years with the 30-mg dose. Other event rates, across both dosages and durations, were less than 0.1/100 patient-years for active TB; 0.3-0.4/100 patient-years for NMSC, and 0.1/100 patient-years or below for other malignancies, MACE, and VTE. Herpes zoster had the highest event rate in both the 1- and 4-year analyses of between 3.1/100 patient-years and 5.8/100 patient-years, Dr. Bunick reported.
The adverse event rates for adolescents and adults “show consistency and are very low,” Dr. Bunick said. At 4 years, no new safety risks were identified.
‘The more data ... the better’
Data on the safety of new medications in children and adolescents is always important, and with systemic JAK inhibitors in particular, “the more data we can accumulate in [younger] patients with AD ... the better,” said Robert Sidbury, MD, MPH, professor in the department of pediatrics at the University of Washington, Seattle, and chief of the division of dermatology at Seattle Children’s Hospital, who was asked to comment on the two studies.
Dermatologists have taken comfort in the fact that the “daunting” boxed warning on JAK inhibitors “was generated in a very different population than we generally propose to treat, certainly when talking about children and adolescents,” said Dr. Sidbury, who was not involved in either of the new safety analyses.
The JAK inhibitor boxed warning “reflects a study of tofacitinib – a different JAK inhibitor with arguably more risk of adverse effects – in adults over the age of 50 with rheumatoid arthritis and multiple risk factors for comorbidities included in the boxed warning,” he said.
“This allows dermatologists to reasonably conclude that the boxed warning – while critical to discuss and consider in every patient – is likely less concerning than might otherwise by implied.”
With more patient experience, “the more our assessment of risk, and of the ‘legitimacy’ of the boxed warning in our patient population, becomes evidence-based as opposed to extrapolation,” Dr. Sidbury said.
The two studies reported, he said, “detail an experience that is not adverse effect free –I have yet to find that medication – but is a reasonable profile considering the robust efficacy results they accompany.”
The abrocitinib safety analysis was sponsored by Pfizer. Regarding the study of upadacitinib, AbbVie contributed to the design of the safety analysis and participated in data collection. No honoria or payments were made to the authors, according to the study abstract. Dr. Eichenfield is a consultant/advisory board member for Pfizer and other companies, and has served on the speakers bureau/received honoria for Pfizer and other companies. Dr. Bunick is a consultant for AbbVie and other companies, and has served as an speaker/received honoraria or served as an investigator for several companies. Dr. Sidbury disclosed being a consultant/advisory board member for Lilly and Leo and serving on the speakers bureau/honoraria for Beiersdorf. All reported receiving grant/research support from various companies.
WASHINGTON – and over 1,000 patient-years of exposure, Lawrence F. Eichenfield, MD, reported at the annual Revolutionizing Atopic Dermatitis conference.
In March 2023, the oral Janus kinase 1 (JAK1) inhibitor was approved by the Food and Drug Administration for treating adolescents aged 12-17 with refractory moderate to severe AD – an expanded indication from the approval in adults in 2022.
The new analysis evaluated data from patients who participated in the phase 3 JADE clinical trials – MONO-1, MONO-2, TEEN, and REGIMEN – and were subsequently enrolled in the ongoing phase 3 extension trial JADE EXTEND. Compared with a previous post hoc analysis in which adolescent patients had approximately 1 year of exposure, this updated analysis includes a sizable portion of patients with more than 96 weeks of exposure.
“We’re starting to get good numbers of [adolescents] who’ve had about 2 years of exposure,” said Dr. Eichenfield, professor of dermatology and pediatrics and vice chair of the department of dermatology at the University of California, San Diego, during a late-breaking research session.
With a data cut for this analysis of September 2021, “we haven’t seen additive long-term [adverse] effects” with longer exposures, he said. In addition, “there were no unique safety concerns related to adolescents compared to the findings observed [in an] integrated safety analysis using the same data cut in which most patients were adults.”
(The analysis in adults covered 3,802 patients with over 5,000 patient-years of exposure, and was presented at the annual American Academy of Dermatology meeting in March 2023.)
Also presented in the late-breaking abstract session at RAD 2023 was a long-term safety study of upadacitinib (Rinvoq), the other JAK1 inhibitor approved for adolescents with AD – approved by the FDA for both adolescents and adults with moderate to severe AD in 2022. The new analysis captures exposure of up to 4 years and shows no “worsening or accumulation of events,” compared with 1-year data, reported Christopher G. Bunick, MD, PhD, of the department of dermatology and the program in translational biomedicine at Yale University, New Haven, Conn.
Abrocitinib in adolescents
For the safety analysis of abrocitinib (Cibinqo), data were pooled into two cohorts: A consistent-dose cohort of 490 adolescents who received the same dose (200 mg or 100 mg) during the entire duration of the qualifying JADE trials, and a variable-dose cohort of 145 adolescents who received different doses (200 mg or 100 mg) during the JADE REGIMEN qualifying trial.
Duration of exposure was 96 weeks or more in 37%-38% of the consistent-dose cohort and 68% of the variable-dose cohort.
In the consistent-dose cohort, adverse events occurred in 243 (84%) and 153 (76%) of patients receiving 200-mg doses and 100-mg doses, respectively. Incidence rates for severe adverse events were 5.87 per 100 patient-years at both doses, and rates for adverse events leading to study discontinuation were 6.96/100 patient-years at 200 mg and 5.13/100 patient-years at 100 mg.
“No meaningful dose-response relationship was observed for serious adverse events, or adverse events leading to discontinuation, or adverse events of special interest,” said Dr. Eichenfield, also chief of pediatric and adolescent dermatology at Rady Children’s Hospital, San Diego.
The IRs of adverse events of special interest were 1.84/100 patient-years and 1.28/100 patient-years for serious infection; 2.11/100 patient-years, and 1.62/100 patient-years for all herpes zoster infections; and 0.69/100 patient-years and 0.32/100 patient-years for opportunistic herpes zoster infections in the 200-mg and 100-mg arms, respectively.
“Other than herpes zoster, there were no opportunistic infections observed and no tuberculosis cases,” he said. “There was one nonfatal venous thromboembolism in an adolescent who had a very strong family history of [pulmonary embolism], one retinal detachment [with a concurrent diagnosis of cataracts and of left eyebrow folliculitis], and no events of nonmelanoma skin cancer or other malignancies, major adverse cardiovascular events, or deaths.” The thromboembolism case was reported in the previous post hoc analysis.
In the variable-dose cohort, data were similar, Dr. Eichenfield said. The IRs for severe adverse events, adverse events leading to study withdrawal, and adverse events of special interest were consistent with those in the other cohort. And similarly, there were no reports of tuberculosis or other opportunistic infections (excluding herpes zoster), and no reports of nonmelanoma skin cancer (NMSC) or other malignancies, major adverse cardiovascular events (MACE), or death. In this cohort, there were no venous thromboembolism (VTE) reports.
Upadacitinib in adolescents, adults
The new analysis looked at up to 4 years of upadacitinib treatment in almost 2,700 adolescents and adults– and over 6,200 patient-years – using integrated data from three ongoing pivotal phase 3 studies: Measure Up 1, Measure Up 2, and AD Up. (Of these patients, 539 were adolescents, Dr. Bunick said after the meeting.)
In the Measure Up studies, patients were randomized 1:1:1 to receive a 15-mg dose, a 30-mg dose, or placebo once daily. In AD Up, patients in each arm received concomitant topical corticosteroids. At week 16, patients receiving the drug continued their assigned treatment during the ongoing blinded extension period, and those receiving placebo were rerandomized to upadacitinib 15 mg or 30 mg.
The exposure-adjusted event rates for any adverse event leading to discontinuation were 4.1/100 patient-years and 4.7/100 patient-years in patients receiving 15 mg and 30 mg, respectively, and the rates of any serious adverse event were 6.5/100 patient-years and 7.5/100 patient-years, Dr. Bunick reported. Three deaths occurred in the 30-mg group; all deaths were related to COVID infection and occurred in adults with cardiovascular risk factors.
Incidence rates of adverse events of special interest were similar to those in a previous 1-year analysis. The rate of serious infections per 100 patient years, for instance, was 2.3 and 2.8 in the 15-mg and 30-mg groups, respectively, compared with 2.2 and 2.8 in the 1-year analysis.
The rate of opportunistic infections, including eczema herpeticum (and excluding TB and herpes zoster), saw a slight bump in the new analysis to 2.4/100 patient-years with the 30-mg dose. Other event rates, across both dosages and durations, were less than 0.1/100 patient-years for active TB; 0.3-0.4/100 patient-years for NMSC, and 0.1/100 patient-years or below for other malignancies, MACE, and VTE. Herpes zoster had the highest event rate in both the 1- and 4-year analyses of between 3.1/100 patient-years and 5.8/100 patient-years, Dr. Bunick reported.
The adverse event rates for adolescents and adults “show consistency and are very low,” Dr. Bunick said. At 4 years, no new safety risks were identified.
‘The more data ... the better’
Data on the safety of new medications in children and adolescents is always important, and with systemic JAK inhibitors in particular, “the more data we can accumulate in [younger] patients with AD ... the better,” said Robert Sidbury, MD, MPH, professor in the department of pediatrics at the University of Washington, Seattle, and chief of the division of dermatology at Seattle Children’s Hospital, who was asked to comment on the two studies.
Dermatologists have taken comfort in the fact that the “daunting” boxed warning on JAK inhibitors “was generated in a very different population than we generally propose to treat, certainly when talking about children and adolescents,” said Dr. Sidbury, who was not involved in either of the new safety analyses.
The JAK inhibitor boxed warning “reflects a study of tofacitinib – a different JAK inhibitor with arguably more risk of adverse effects – in adults over the age of 50 with rheumatoid arthritis and multiple risk factors for comorbidities included in the boxed warning,” he said.
“This allows dermatologists to reasonably conclude that the boxed warning – while critical to discuss and consider in every patient – is likely less concerning than might otherwise by implied.”
With more patient experience, “the more our assessment of risk, and of the ‘legitimacy’ of the boxed warning in our patient population, becomes evidence-based as opposed to extrapolation,” Dr. Sidbury said.
The two studies reported, he said, “detail an experience that is not adverse effect free –I have yet to find that medication – but is a reasonable profile considering the robust efficacy results they accompany.”
The abrocitinib safety analysis was sponsored by Pfizer. Regarding the study of upadacitinib, AbbVie contributed to the design of the safety analysis and participated in data collection. No honoria or payments were made to the authors, according to the study abstract. Dr. Eichenfield is a consultant/advisory board member for Pfizer and other companies, and has served on the speakers bureau/received honoria for Pfizer and other companies. Dr. Bunick is a consultant for AbbVie and other companies, and has served as an speaker/received honoraria or served as an investigator for several companies. Dr. Sidbury disclosed being a consultant/advisory board member for Lilly and Leo and serving on the speakers bureau/honoraria for Beiersdorf. All reported receiving grant/research support from various companies.
WASHINGTON – and over 1,000 patient-years of exposure, Lawrence F. Eichenfield, MD, reported at the annual Revolutionizing Atopic Dermatitis conference.
In March 2023, the oral Janus kinase 1 (JAK1) inhibitor was approved by the Food and Drug Administration for treating adolescents aged 12-17 with refractory moderate to severe AD – an expanded indication from the approval in adults in 2022.
The new analysis evaluated data from patients who participated in the phase 3 JADE clinical trials – MONO-1, MONO-2, TEEN, and REGIMEN – and were subsequently enrolled in the ongoing phase 3 extension trial JADE EXTEND. Compared with a previous post hoc analysis in which adolescent patients had approximately 1 year of exposure, this updated analysis includes a sizable portion of patients with more than 96 weeks of exposure.
“We’re starting to get good numbers of [adolescents] who’ve had about 2 years of exposure,” said Dr. Eichenfield, professor of dermatology and pediatrics and vice chair of the department of dermatology at the University of California, San Diego, during a late-breaking research session.
With a data cut for this analysis of September 2021, “we haven’t seen additive long-term [adverse] effects” with longer exposures, he said. In addition, “there were no unique safety concerns related to adolescents compared to the findings observed [in an] integrated safety analysis using the same data cut in which most patients were adults.”
(The analysis in adults covered 3,802 patients with over 5,000 patient-years of exposure, and was presented at the annual American Academy of Dermatology meeting in March 2023.)
Also presented in the late-breaking abstract session at RAD 2023 was a long-term safety study of upadacitinib (Rinvoq), the other JAK1 inhibitor approved for adolescents with AD – approved by the FDA for both adolescents and adults with moderate to severe AD in 2022. The new analysis captures exposure of up to 4 years and shows no “worsening or accumulation of events,” compared with 1-year data, reported Christopher G. Bunick, MD, PhD, of the department of dermatology and the program in translational biomedicine at Yale University, New Haven, Conn.
Abrocitinib in adolescents
For the safety analysis of abrocitinib (Cibinqo), data were pooled into two cohorts: A consistent-dose cohort of 490 adolescents who received the same dose (200 mg or 100 mg) during the entire duration of the qualifying JADE trials, and a variable-dose cohort of 145 adolescents who received different doses (200 mg or 100 mg) during the JADE REGIMEN qualifying trial.
Duration of exposure was 96 weeks or more in 37%-38% of the consistent-dose cohort and 68% of the variable-dose cohort.
In the consistent-dose cohort, adverse events occurred in 243 (84%) and 153 (76%) of patients receiving 200-mg doses and 100-mg doses, respectively. Incidence rates for severe adverse events were 5.87 per 100 patient-years at both doses, and rates for adverse events leading to study discontinuation were 6.96/100 patient-years at 200 mg and 5.13/100 patient-years at 100 mg.
“No meaningful dose-response relationship was observed for serious adverse events, or adverse events leading to discontinuation, or adverse events of special interest,” said Dr. Eichenfield, also chief of pediatric and adolescent dermatology at Rady Children’s Hospital, San Diego.
The IRs of adverse events of special interest were 1.84/100 patient-years and 1.28/100 patient-years for serious infection; 2.11/100 patient-years, and 1.62/100 patient-years for all herpes zoster infections; and 0.69/100 patient-years and 0.32/100 patient-years for opportunistic herpes zoster infections in the 200-mg and 100-mg arms, respectively.
“Other than herpes zoster, there were no opportunistic infections observed and no tuberculosis cases,” he said. “There was one nonfatal venous thromboembolism in an adolescent who had a very strong family history of [pulmonary embolism], one retinal detachment [with a concurrent diagnosis of cataracts and of left eyebrow folliculitis], and no events of nonmelanoma skin cancer or other malignancies, major adverse cardiovascular events, or deaths.” The thromboembolism case was reported in the previous post hoc analysis.
In the variable-dose cohort, data were similar, Dr. Eichenfield said. The IRs for severe adverse events, adverse events leading to study withdrawal, and adverse events of special interest were consistent with those in the other cohort. And similarly, there were no reports of tuberculosis or other opportunistic infections (excluding herpes zoster), and no reports of nonmelanoma skin cancer (NMSC) or other malignancies, major adverse cardiovascular events (MACE), or death. In this cohort, there were no venous thromboembolism (VTE) reports.
Upadacitinib in adolescents, adults
The new analysis looked at up to 4 years of upadacitinib treatment in almost 2,700 adolescents and adults– and over 6,200 patient-years – using integrated data from three ongoing pivotal phase 3 studies: Measure Up 1, Measure Up 2, and AD Up. (Of these patients, 539 were adolescents, Dr. Bunick said after the meeting.)
In the Measure Up studies, patients were randomized 1:1:1 to receive a 15-mg dose, a 30-mg dose, or placebo once daily. In AD Up, patients in each arm received concomitant topical corticosteroids. At week 16, patients receiving the drug continued their assigned treatment during the ongoing blinded extension period, and those receiving placebo were rerandomized to upadacitinib 15 mg or 30 mg.
The exposure-adjusted event rates for any adverse event leading to discontinuation were 4.1/100 patient-years and 4.7/100 patient-years in patients receiving 15 mg and 30 mg, respectively, and the rates of any serious adverse event were 6.5/100 patient-years and 7.5/100 patient-years, Dr. Bunick reported. Three deaths occurred in the 30-mg group; all deaths were related to COVID infection and occurred in adults with cardiovascular risk factors.
Incidence rates of adverse events of special interest were similar to those in a previous 1-year analysis. The rate of serious infections per 100 patient years, for instance, was 2.3 and 2.8 in the 15-mg and 30-mg groups, respectively, compared with 2.2 and 2.8 in the 1-year analysis.
The rate of opportunistic infections, including eczema herpeticum (and excluding TB and herpes zoster), saw a slight bump in the new analysis to 2.4/100 patient-years with the 30-mg dose. Other event rates, across both dosages and durations, were less than 0.1/100 patient-years for active TB; 0.3-0.4/100 patient-years for NMSC, and 0.1/100 patient-years or below for other malignancies, MACE, and VTE. Herpes zoster had the highest event rate in both the 1- and 4-year analyses of between 3.1/100 patient-years and 5.8/100 patient-years, Dr. Bunick reported.
The adverse event rates for adolescents and adults “show consistency and are very low,” Dr. Bunick said. At 4 years, no new safety risks were identified.
‘The more data ... the better’
Data on the safety of new medications in children and adolescents is always important, and with systemic JAK inhibitors in particular, “the more data we can accumulate in [younger] patients with AD ... the better,” said Robert Sidbury, MD, MPH, professor in the department of pediatrics at the University of Washington, Seattle, and chief of the division of dermatology at Seattle Children’s Hospital, who was asked to comment on the two studies.
Dermatologists have taken comfort in the fact that the “daunting” boxed warning on JAK inhibitors “was generated in a very different population than we generally propose to treat, certainly when talking about children and adolescents,” said Dr. Sidbury, who was not involved in either of the new safety analyses.
The JAK inhibitor boxed warning “reflects a study of tofacitinib – a different JAK inhibitor with arguably more risk of adverse effects – in adults over the age of 50 with rheumatoid arthritis and multiple risk factors for comorbidities included in the boxed warning,” he said.
“This allows dermatologists to reasonably conclude that the boxed warning – while critical to discuss and consider in every patient – is likely less concerning than might otherwise by implied.”
With more patient experience, “the more our assessment of risk, and of the ‘legitimacy’ of the boxed warning in our patient population, becomes evidence-based as opposed to extrapolation,” Dr. Sidbury said.
The two studies reported, he said, “detail an experience that is not adverse effect free –I have yet to find that medication – but is a reasonable profile considering the robust efficacy results they accompany.”
The abrocitinib safety analysis was sponsored by Pfizer. Regarding the study of upadacitinib, AbbVie contributed to the design of the safety analysis and participated in data collection. No honoria or payments were made to the authors, according to the study abstract. Dr. Eichenfield is a consultant/advisory board member for Pfizer and other companies, and has served on the speakers bureau/received honoria for Pfizer and other companies. Dr. Bunick is a consultant for AbbVie and other companies, and has served as an speaker/received honoraria or served as an investigator for several companies. Dr. Sidbury disclosed being a consultant/advisory board member for Lilly and Leo and serving on the speakers bureau/honoraria for Beiersdorf. All reported receiving grant/research support from various companies.
AT RAD 2023
Talking tobacco with youth? Ask the right questions
There is good news and bad news regarding the use of tobacco products by young people in the United States, according to the recently released findings from the 2021 Youth Risk Behavior Survey (YRBS).1 The use of cigarettes among high school students declined from 36.4% in 1997 to 6.0% in 2019.2 However, young people have replaced cigarettes with other tobacco products, including electronic vapor products (EVPs). So we need to ask specifically about these products.
Known by many names. EVPs are referred to as e-cigarettes, vapes, hookah pens, and mods. They usually contain nicotine, which is highly addictive, can affect brain development, and may lead to smoking of cigarettes.3 The most common reasons young people say they use EVPs are feelings of anxiety, stress, and depression, as well as the “high” associated with nicotine use.4
Use of EVPs among youth. The YRBS, which includes a representative sample of public and private school students in grades 9 to 12 in the 50 states, categorizes the use of EVPs as
- ever use
- current use (≥ 1 use during the 30 days before the survey), and
- daily use (during the 30 days before the survey).
In 2021, 36.2% of young people reported ever use of EVPs (40.9% of females; 32.1% of males), 18% reported current use (21.4% of females; 14.9% of males), and 5% reported daily use (5.6% of females; 4.5% of males). Differences between racial and ethnic groups were minor, except for markedly lower rates in Asian youth (19.5% ever use, 5.5% current use, and 1.2% daily use).5
Current recommendations. The US Preventive Services Task Force (USPSTF) recommends education and brief counseling for school-age children and adolescents to prevent them from starting to use tobacco (including use of EVPs).6 The USPSTF also recommends tobacco cessation using behavioral interventions and/or pharmacotherapy for those ages 18 years and older.7
The USPSTF makes no recommendation on cessation for those younger than 18 years, citing weak evidence. However, it would be reasonable to offer behavioral interventions to younger current users. (Pharmacotherapy is not approved for use in children and adolescents.)
The take-home message. When we ask children and adolescents about use of tobacco products, we need to specifically mention EVPs and advise against their use.
1. CDC. Youth Risk Behavior Surveillance—United States, 2021. MMWR Morb Mortal Wkly Rep. 2023;72(suppl 1):1-93. Accessed May 24, 2023. www.cdc.gov/mmwr/volumes/72/su/pdfs/su7201-h.pdf
2. Creamer MR, Everett Jones S, Gentzke AS, et al. Tobacco product use among high school students—Youth Risk Behavior Survey, United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(suppl 1):56-63. doi: 10.15585/mmwr.su6901a7
3. National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-Cigarettes. Washington, DC: National Academies Press; 2018. Accessed May 24, 2023. https://nap.nationalacademies.org/catalog/24952/public-health-consequences-of-e-cigarettes
4. Gentzke AS, Wang TW, Cornelius M, et al. Tobacco product use and associated factors among middle and high school students—National Youth Tobacco Survey, United States, 2021. MMWR Surveill Summ. 2022;71(no. SS-5):1-29. doi: 10.15585/mmwr.ss7105a1
5. Oliver BE, Jones SE, Hops ED, et al. Electronic vapor product use among high school students—Youth Risk Behavior Survey, United States, 2021. MMWR Morb Mortal Wkly Rep. 2023;72(suppl 1):93-99. doi: 10.15585/mmwr.su7201a11
6. USPSTF. Tobacco use in children and adolescents: primary care interventions. Final recommendation statement. Published April 28, 2020. Accessed May 24, 2023. www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-and-nicotine-use-prevention-in-children-and-adolescents-primary-care-interventions
7. USPSTF. Tobacco smoking cessation in adults, including pregnant persons: interventions. Final recommendation statement. Published January 19, 2021. Accessed May 24, 2023. www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions
There is good news and bad news regarding the use of tobacco products by young people in the United States, according to the recently released findings from the 2021 Youth Risk Behavior Survey (YRBS).1 The use of cigarettes among high school students declined from 36.4% in 1997 to 6.0% in 2019.2 However, young people have replaced cigarettes with other tobacco products, including electronic vapor products (EVPs). So we need to ask specifically about these products.
Known by many names. EVPs are referred to as e-cigarettes, vapes, hookah pens, and mods. They usually contain nicotine, which is highly addictive, can affect brain development, and may lead to smoking of cigarettes.3 The most common reasons young people say they use EVPs are feelings of anxiety, stress, and depression, as well as the “high” associated with nicotine use.4
Use of EVPs among youth. The YRBS, which includes a representative sample of public and private school students in grades 9 to 12 in the 50 states, categorizes the use of EVPs as
- ever use
- current use (≥ 1 use during the 30 days before the survey), and
- daily use (during the 30 days before the survey).
In 2021, 36.2% of young people reported ever use of EVPs (40.9% of females; 32.1% of males), 18% reported current use (21.4% of females; 14.9% of males), and 5% reported daily use (5.6% of females; 4.5% of males). Differences between racial and ethnic groups were minor, except for markedly lower rates in Asian youth (19.5% ever use, 5.5% current use, and 1.2% daily use).5
Current recommendations. The US Preventive Services Task Force (USPSTF) recommends education and brief counseling for school-age children and adolescents to prevent them from starting to use tobacco (including use of EVPs).6 The USPSTF also recommends tobacco cessation using behavioral interventions and/or pharmacotherapy for those ages 18 years and older.7
The USPSTF makes no recommendation on cessation for those younger than 18 years, citing weak evidence. However, it would be reasonable to offer behavioral interventions to younger current users. (Pharmacotherapy is not approved for use in children and adolescents.)
The take-home message. When we ask children and adolescents about use of tobacco products, we need to specifically mention EVPs and advise against their use.
There is good news and bad news regarding the use of tobacco products by young people in the United States, according to the recently released findings from the 2021 Youth Risk Behavior Survey (YRBS).1 The use of cigarettes among high school students declined from 36.4% in 1997 to 6.0% in 2019.2 However, young people have replaced cigarettes with other tobacco products, including electronic vapor products (EVPs). So we need to ask specifically about these products.
Known by many names. EVPs are referred to as e-cigarettes, vapes, hookah pens, and mods. They usually contain nicotine, which is highly addictive, can affect brain development, and may lead to smoking of cigarettes.3 The most common reasons young people say they use EVPs are feelings of anxiety, stress, and depression, as well as the “high” associated with nicotine use.4
Use of EVPs among youth. The YRBS, which includes a representative sample of public and private school students in grades 9 to 12 in the 50 states, categorizes the use of EVPs as
- ever use
- current use (≥ 1 use during the 30 days before the survey), and
- daily use (during the 30 days before the survey).
In 2021, 36.2% of young people reported ever use of EVPs (40.9% of females; 32.1% of males), 18% reported current use (21.4% of females; 14.9% of males), and 5% reported daily use (5.6% of females; 4.5% of males). Differences between racial and ethnic groups were minor, except for markedly lower rates in Asian youth (19.5% ever use, 5.5% current use, and 1.2% daily use).5
Current recommendations. The US Preventive Services Task Force (USPSTF) recommends education and brief counseling for school-age children and adolescents to prevent them from starting to use tobacco (including use of EVPs).6 The USPSTF also recommends tobacco cessation using behavioral interventions and/or pharmacotherapy for those ages 18 years and older.7
The USPSTF makes no recommendation on cessation for those younger than 18 years, citing weak evidence. However, it would be reasonable to offer behavioral interventions to younger current users. (Pharmacotherapy is not approved for use in children and adolescents.)
The take-home message. When we ask children and adolescents about use of tobacco products, we need to specifically mention EVPs and advise against their use.
1. CDC. Youth Risk Behavior Surveillance—United States, 2021. MMWR Morb Mortal Wkly Rep. 2023;72(suppl 1):1-93. Accessed May 24, 2023. www.cdc.gov/mmwr/volumes/72/su/pdfs/su7201-h.pdf
2. Creamer MR, Everett Jones S, Gentzke AS, et al. Tobacco product use among high school students—Youth Risk Behavior Survey, United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(suppl 1):56-63. doi: 10.15585/mmwr.su6901a7
3. National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-Cigarettes. Washington, DC: National Academies Press; 2018. Accessed May 24, 2023. https://nap.nationalacademies.org/catalog/24952/public-health-consequences-of-e-cigarettes
4. Gentzke AS, Wang TW, Cornelius M, et al. Tobacco product use and associated factors among middle and high school students—National Youth Tobacco Survey, United States, 2021. MMWR Surveill Summ. 2022;71(no. SS-5):1-29. doi: 10.15585/mmwr.ss7105a1
5. Oliver BE, Jones SE, Hops ED, et al. Electronic vapor product use among high school students—Youth Risk Behavior Survey, United States, 2021. MMWR Morb Mortal Wkly Rep. 2023;72(suppl 1):93-99. doi: 10.15585/mmwr.su7201a11
6. USPSTF. Tobacco use in children and adolescents: primary care interventions. Final recommendation statement. Published April 28, 2020. Accessed May 24, 2023. www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-and-nicotine-use-prevention-in-children-and-adolescents-primary-care-interventions
7. USPSTF. Tobacco smoking cessation in adults, including pregnant persons: interventions. Final recommendation statement. Published January 19, 2021. Accessed May 24, 2023. www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions
1. CDC. Youth Risk Behavior Surveillance—United States, 2021. MMWR Morb Mortal Wkly Rep. 2023;72(suppl 1):1-93. Accessed May 24, 2023. www.cdc.gov/mmwr/volumes/72/su/pdfs/su7201-h.pdf
2. Creamer MR, Everett Jones S, Gentzke AS, et al. Tobacco product use among high school students—Youth Risk Behavior Survey, United States, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(suppl 1):56-63. doi: 10.15585/mmwr.su6901a7
3. National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-Cigarettes. Washington, DC: National Academies Press; 2018. Accessed May 24, 2023. https://nap.nationalacademies.org/catalog/24952/public-health-consequences-of-e-cigarettes
4. Gentzke AS, Wang TW, Cornelius M, et al. Tobacco product use and associated factors among middle and high school students—National Youth Tobacco Survey, United States, 2021. MMWR Surveill Summ. 2022;71(no. SS-5):1-29. doi: 10.15585/mmwr.ss7105a1
5. Oliver BE, Jones SE, Hops ED, et al. Electronic vapor product use among high school students—Youth Risk Behavior Survey, United States, 2021. MMWR Morb Mortal Wkly Rep. 2023;72(suppl 1):93-99. doi: 10.15585/mmwr.su7201a11
6. USPSTF. Tobacco use in children and adolescents: primary care interventions. Final recommendation statement. Published April 28, 2020. Accessed May 24, 2023. www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-and-nicotine-use-prevention-in-children-and-adolescents-primary-care-interventions
7. USPSTF. Tobacco smoking cessation in adults, including pregnant persons: interventions. Final recommendation statement. Published January 19, 2021. Accessed May 24, 2023. www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions