User login
Surgical management of borderline ovarian tumors, part 1
Borderline ovarian tumors (BOTs) are estimated to comprise 10%-15% of all epithelial tumors of the ovary. They are characterized by their behavior, which falls somewhere between benign ovarian masses and frank carcinomas. They have cytologic characteristics suggesting malignancy, such as higher cellular proliferation and more variable nuclear atypia, but, unlike carcinomas, they lack destructive stromal invasion. For decades after their recognition by the International Federation of Gynecology and Obstetrics in 1971, these tumors were classified as being of low malignant potential (and subsequently referred to as LMP tumors of the ovary). Beginning with the 2014 World Health Organization classification, the recommended terminology is now borderline tumor of the ovary.
The primary treatment for BOTs is surgery. With a mean age at diagnosis in the fifth decade, many patients with BOTs desire ovarian preservation to maintain fertility and/or prevent surgical menopause. This raises multiple questions regarding the use of fertility-sparing surgery for BOTs: What types of procedures are safe and should be offered? For those patients who undergo fertility-sparing surgery initially, is additional surgery indicated after completion of childbearing or at an age closer to natural menopause? What should this completion surgery include?
Ovarian-sparing surgery
The diagnosis of a BOT is frequently only confirmed after the decision for ovarian conservation has been made. What should be considered before electing to proceed with ovarian cystectomy instead of unilateral salpingo-oophorectomy (USO)?
Is the risk of recurrence higher with cystectomy versus oophorectomy?
Yes. The risk of recurrence of BOT appears to be higher after cystectomy than it is after oophorectomy. There is a large range reported in the literature, with the risk of recurrence after cystectomy described as between 12% and 58%. Most studies report recurrences between 25% and 35% of patients who undergo cystectomy. In contrast, the risk of recurrence after USO is often reported to be approximately 10%. Higher risk of recurrence after cystectomy is speculated to be due to leaving some BOT at the time of initial surgery.
Multiple meta-analyses have found an increased risk of recurrence after cystectomy. The risk of recurrence after unilateral cystectomy was 19.4%, compared with 9.1% after USO, in 2,145 patients included in a 2017 meta-analysis.1 Similarly, a 2021 meta-analysis found a significantly higher rate of BOT recurrence in patients who underwent unilateral or bilateral cystectomy compared with USO (odds ratio, 2.02; 95% confidence interval, 1.59-2.57).2
Does the higher recurrence risk translate into a difference in long-term outcomes?
No. Despite an increased risk of recurrence after cystectomy, ovarian-sparing surgery does not appear to alter patients’ survival. The pooled mortality estimate was 1.6% for those undergoing fertility-sparing surgery (95% CI, 0.011-0.023), compared with 2.0% for those undergoing radical surgery (95% CI, 0.014-0.029), in a 2015 meta-analysis of over 5,100 patients. The analysis included studies in which patients underwent unilateral cystectomy, bilateral cystectomy, USO, or USO plus contralateral cystectomy. The low mortality rate did not allow for comparison between the different types of fertility-sparing surgeries.3
Do we accept a higher risk of recurrence with ovarian sparing surgery to improve fertility?
Data are mixed. When we examine studies describing fertility rates after conservative surgery, there are significant limitations to interpreting the data available. Some studies do not differentiate among patients who underwent fertility-sparing surgery, or between those who had cystectomy versus USO. Other studies do not report the number of patients who tried to achieve pregnancy after surgery. Conception rates are reported to be as high as 88.2%, which was in 116 patients who were able to be reached after fertility-sparing surgery (retained at least one ovary). Of the 51 patients who tried to conceive, 45 were successful.4
Multiple studies and meta-analyses have shown no difference in postoperative pregnancy rates when comparing oophorectomy to cystectomy. For instance, in a 2021 meta-analysis, there was no significant difference noted in pregnancy rates between patients who underwent USO versus cystectomy (OR, 0.92; 95% CI, 0.60-1.42).
There are some data that support improved postoperative pregnancy rates in more conservative surgery, especially in the setting of bilateral BOT. In a small study of 32 patients who had laparoscopic staging for bilateral BOTs, patients were randomized to unilateral oophorectomy plus contralateral cystectomy or to bilateral cystectomy, which was referred to as ultraconservative surgery. The time to first recurrence was shorter in the ultraconservative group (although this lost significance when regression analysis was performed), but the time to first live birth was shorter and the relative chance of having a baby was higher in the bilateral cystectomy group.5
Ovarian-sparing procedures should be offered to patients in the setting of BOT. With ovarian-sparing surgery, it is important to counsel patients about the increased risk of recurrence and need for long-term follow-up. Pregnancy rates are generally good after fertility-sparing surgery. Surgery to conserve both ovaries does not seem to improve pregnancy rates in the setting of unilateral BOTs.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Jiao X et al. Int J Gynecol Cancer. 2017 Nov;27(9):1833-41.
2. Wang P and Fang L. World J Surg Oncol. 2021 Apr 21;19(1):132.
3. Vasconcelos I and de Sousa Mendes M. Eur J Cancer. 2015 Mar;51(5):620-31.
4. Song T et al. Int J Gynecol Cancer. 2011 May;21(4):640-6.
5. Palomba S et al. Hum Reprod. 2010 Aug;25(8):1966-72.
Borderline ovarian tumors (BOTs) are estimated to comprise 10%-15% of all epithelial tumors of the ovary. They are characterized by their behavior, which falls somewhere between benign ovarian masses and frank carcinomas. They have cytologic characteristics suggesting malignancy, such as higher cellular proliferation and more variable nuclear atypia, but, unlike carcinomas, they lack destructive stromal invasion. For decades after their recognition by the International Federation of Gynecology and Obstetrics in 1971, these tumors were classified as being of low malignant potential (and subsequently referred to as LMP tumors of the ovary). Beginning with the 2014 World Health Organization classification, the recommended terminology is now borderline tumor of the ovary.
The primary treatment for BOTs is surgery. With a mean age at diagnosis in the fifth decade, many patients with BOTs desire ovarian preservation to maintain fertility and/or prevent surgical menopause. This raises multiple questions regarding the use of fertility-sparing surgery for BOTs: What types of procedures are safe and should be offered? For those patients who undergo fertility-sparing surgery initially, is additional surgery indicated after completion of childbearing or at an age closer to natural menopause? What should this completion surgery include?
Ovarian-sparing surgery
The diagnosis of a BOT is frequently only confirmed after the decision for ovarian conservation has been made. What should be considered before electing to proceed with ovarian cystectomy instead of unilateral salpingo-oophorectomy (USO)?
Is the risk of recurrence higher with cystectomy versus oophorectomy?
Yes. The risk of recurrence of BOT appears to be higher after cystectomy than it is after oophorectomy. There is a large range reported in the literature, with the risk of recurrence after cystectomy described as between 12% and 58%. Most studies report recurrences between 25% and 35% of patients who undergo cystectomy. In contrast, the risk of recurrence after USO is often reported to be approximately 10%. Higher risk of recurrence after cystectomy is speculated to be due to leaving some BOT at the time of initial surgery.
Multiple meta-analyses have found an increased risk of recurrence after cystectomy. The risk of recurrence after unilateral cystectomy was 19.4%, compared with 9.1% after USO, in 2,145 patients included in a 2017 meta-analysis.1 Similarly, a 2021 meta-analysis found a significantly higher rate of BOT recurrence in patients who underwent unilateral or bilateral cystectomy compared with USO (odds ratio, 2.02; 95% confidence interval, 1.59-2.57).2
Does the higher recurrence risk translate into a difference in long-term outcomes?
No. Despite an increased risk of recurrence after cystectomy, ovarian-sparing surgery does not appear to alter patients’ survival. The pooled mortality estimate was 1.6% for those undergoing fertility-sparing surgery (95% CI, 0.011-0.023), compared with 2.0% for those undergoing radical surgery (95% CI, 0.014-0.029), in a 2015 meta-analysis of over 5,100 patients. The analysis included studies in which patients underwent unilateral cystectomy, bilateral cystectomy, USO, or USO plus contralateral cystectomy. The low mortality rate did not allow for comparison between the different types of fertility-sparing surgeries.3
Do we accept a higher risk of recurrence with ovarian sparing surgery to improve fertility?
Data are mixed. When we examine studies describing fertility rates after conservative surgery, there are significant limitations to interpreting the data available. Some studies do not differentiate among patients who underwent fertility-sparing surgery, or between those who had cystectomy versus USO. Other studies do not report the number of patients who tried to achieve pregnancy after surgery. Conception rates are reported to be as high as 88.2%, which was in 116 patients who were able to be reached after fertility-sparing surgery (retained at least one ovary). Of the 51 patients who tried to conceive, 45 were successful.4
Multiple studies and meta-analyses have shown no difference in postoperative pregnancy rates when comparing oophorectomy to cystectomy. For instance, in a 2021 meta-analysis, there was no significant difference noted in pregnancy rates between patients who underwent USO versus cystectomy (OR, 0.92; 95% CI, 0.60-1.42).
There are some data that support improved postoperative pregnancy rates in more conservative surgery, especially in the setting of bilateral BOT. In a small study of 32 patients who had laparoscopic staging for bilateral BOTs, patients were randomized to unilateral oophorectomy plus contralateral cystectomy or to bilateral cystectomy, which was referred to as ultraconservative surgery. The time to first recurrence was shorter in the ultraconservative group (although this lost significance when regression analysis was performed), but the time to first live birth was shorter and the relative chance of having a baby was higher in the bilateral cystectomy group.5
Ovarian-sparing procedures should be offered to patients in the setting of BOT. With ovarian-sparing surgery, it is important to counsel patients about the increased risk of recurrence and need for long-term follow-up. Pregnancy rates are generally good after fertility-sparing surgery. Surgery to conserve both ovaries does not seem to improve pregnancy rates in the setting of unilateral BOTs.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Jiao X et al. Int J Gynecol Cancer. 2017 Nov;27(9):1833-41.
2. Wang P and Fang L. World J Surg Oncol. 2021 Apr 21;19(1):132.
3. Vasconcelos I and de Sousa Mendes M. Eur J Cancer. 2015 Mar;51(5):620-31.
4. Song T et al. Int J Gynecol Cancer. 2011 May;21(4):640-6.
5. Palomba S et al. Hum Reprod. 2010 Aug;25(8):1966-72.
Borderline ovarian tumors (BOTs) are estimated to comprise 10%-15% of all epithelial tumors of the ovary. They are characterized by their behavior, which falls somewhere between benign ovarian masses and frank carcinomas. They have cytologic characteristics suggesting malignancy, such as higher cellular proliferation and more variable nuclear atypia, but, unlike carcinomas, they lack destructive stromal invasion. For decades after their recognition by the International Federation of Gynecology and Obstetrics in 1971, these tumors were classified as being of low malignant potential (and subsequently referred to as LMP tumors of the ovary). Beginning with the 2014 World Health Organization classification, the recommended terminology is now borderline tumor of the ovary.
The primary treatment for BOTs is surgery. With a mean age at diagnosis in the fifth decade, many patients with BOTs desire ovarian preservation to maintain fertility and/or prevent surgical menopause. This raises multiple questions regarding the use of fertility-sparing surgery for BOTs: What types of procedures are safe and should be offered? For those patients who undergo fertility-sparing surgery initially, is additional surgery indicated after completion of childbearing or at an age closer to natural menopause? What should this completion surgery include?
Ovarian-sparing surgery
The diagnosis of a BOT is frequently only confirmed after the decision for ovarian conservation has been made. What should be considered before electing to proceed with ovarian cystectomy instead of unilateral salpingo-oophorectomy (USO)?
Is the risk of recurrence higher with cystectomy versus oophorectomy?
Yes. The risk of recurrence of BOT appears to be higher after cystectomy than it is after oophorectomy. There is a large range reported in the literature, with the risk of recurrence after cystectomy described as between 12% and 58%. Most studies report recurrences between 25% and 35% of patients who undergo cystectomy. In contrast, the risk of recurrence after USO is often reported to be approximately 10%. Higher risk of recurrence after cystectomy is speculated to be due to leaving some BOT at the time of initial surgery.
Multiple meta-analyses have found an increased risk of recurrence after cystectomy. The risk of recurrence after unilateral cystectomy was 19.4%, compared with 9.1% after USO, in 2,145 patients included in a 2017 meta-analysis.1 Similarly, a 2021 meta-analysis found a significantly higher rate of BOT recurrence in patients who underwent unilateral or bilateral cystectomy compared with USO (odds ratio, 2.02; 95% confidence interval, 1.59-2.57).2
Does the higher recurrence risk translate into a difference in long-term outcomes?
No. Despite an increased risk of recurrence after cystectomy, ovarian-sparing surgery does not appear to alter patients’ survival. The pooled mortality estimate was 1.6% for those undergoing fertility-sparing surgery (95% CI, 0.011-0.023), compared with 2.0% for those undergoing radical surgery (95% CI, 0.014-0.029), in a 2015 meta-analysis of over 5,100 patients. The analysis included studies in which patients underwent unilateral cystectomy, bilateral cystectomy, USO, or USO plus contralateral cystectomy. The low mortality rate did not allow for comparison between the different types of fertility-sparing surgeries.3
Do we accept a higher risk of recurrence with ovarian sparing surgery to improve fertility?
Data are mixed. When we examine studies describing fertility rates after conservative surgery, there are significant limitations to interpreting the data available. Some studies do not differentiate among patients who underwent fertility-sparing surgery, or between those who had cystectomy versus USO. Other studies do not report the number of patients who tried to achieve pregnancy after surgery. Conception rates are reported to be as high as 88.2%, which was in 116 patients who were able to be reached after fertility-sparing surgery (retained at least one ovary). Of the 51 patients who tried to conceive, 45 were successful.4
Multiple studies and meta-analyses have shown no difference in postoperative pregnancy rates when comparing oophorectomy to cystectomy. For instance, in a 2021 meta-analysis, there was no significant difference noted in pregnancy rates between patients who underwent USO versus cystectomy (OR, 0.92; 95% CI, 0.60-1.42).
There are some data that support improved postoperative pregnancy rates in more conservative surgery, especially in the setting of bilateral BOT. In a small study of 32 patients who had laparoscopic staging for bilateral BOTs, patients were randomized to unilateral oophorectomy plus contralateral cystectomy or to bilateral cystectomy, which was referred to as ultraconservative surgery. The time to first recurrence was shorter in the ultraconservative group (although this lost significance when regression analysis was performed), but the time to first live birth was shorter and the relative chance of having a baby was higher in the bilateral cystectomy group.5
Ovarian-sparing procedures should be offered to patients in the setting of BOT. With ovarian-sparing surgery, it is important to counsel patients about the increased risk of recurrence and need for long-term follow-up. Pregnancy rates are generally good after fertility-sparing surgery. Surgery to conserve both ovaries does not seem to improve pregnancy rates in the setting of unilateral BOTs.
Dr. Tucker is assistant professor of gynecologic oncology at the University of North Carolina at Chapel Hill.
References
1. Jiao X et al. Int J Gynecol Cancer. 2017 Nov;27(9):1833-41.
2. Wang P and Fang L. World J Surg Oncol. 2021 Apr 21;19(1):132.
3. Vasconcelos I and de Sousa Mendes M. Eur J Cancer. 2015 Mar;51(5):620-31.
4. Song T et al. Int J Gynecol Cancer. 2011 May;21(4):640-6.
5. Palomba S et al. Hum Reprod. 2010 Aug;25(8):1966-72.
FDA approves OTC naloxone, but will cost be a barrier?
Greater access to the drug should mean more lives saved. However, it’s unclear how much the nasal spray will cost and whether pharmacies will stock the product openly on shelves.
Currently, major pharmacy chains such as CVS and Walgreens make naloxone available without prescription, but consumers have to ask a pharmacist to dispense the drug.
“The major question is what is it going to cost,” Brian Hurley, MD, MBA, president-elect of the American Society of Addiction Medicine, said in an interview. “In order for people to access it they have to be able to afford it.”
“We won’t accomplish much if people can’t afford to buy Narcan,” said Chuck Ingoglia, president and CEO of the National Council for Mental Wellbeing, in a statement. Still, he applauded the FDA.
“No single approach will end overdose deaths but making Narcan easy to obtain and widely available likely will save countless lives annually,” he said.
“The timeline for availability and price of this OTC product is determined by the manufacturer,” the FDA said in a statement.
Commissioner Robert M. Califf, MD, called for the drug’s manufacturer to “make accessibility to the product a priority by making it available as soon as possible and at an affordable price.”
Emergent BioSolutions did not comment on cost. It said in a statement that the spray “will be available on U.S. shelves and at online retailers by the late summer,” after it has adapted Narcan for direct-to-consumer use, including more consumer-oriented packaging.
Naloxone’s cost varies, depending on geographic location and whether it is generic. According to GoodRX, a box containing two doses of generic naloxone costs $31-$100, depending on location and coupon availability.
A two-dose box of Narcan costs $135-$140. Emergent reported a 14% decline in naloxone sales in 2022 – to $373.7 million – blaming it in part on the introduction of generic formulations.
Dr. Hurley said he expects those who purchase Narcan at a drug store will primarily already be shopping there. It may or may not be those who most often experience overdose, such as people leaving incarceration or experiencing homelessness.
Having Narcan available over-the-counter “is an important supplement but it doesn’t replace the existing array of naloxone distribution programs,” Dr. Hurley said.
The FDA has encouraged naloxone manufacturers to seek OTC approval for the medication since at least 2019, when it designed a model label for a theoretical OTC product.
In November, the agency said it had determined that some naloxone products had the potential to be safe and effective for OTC use and again urged drugmakers to seek such an approval.
Emergent BioSolutions was the first to pursue OTC approval, but another manufacturer – the nonprofit Harm Reduction Therapeutics – is awaiting approval of its application to sell its spray directly to consumers.
Scott Gottlieb, MD, who was the FDA commissioner from 2017 to 2019, said in a tweet that more work needed to be done.
“This regulatory move should be followed by a strong push by elected officials to support wider deployment of Narcan, getting more doses into the hands of at risk households and frontline workers,” he tweeted.
Mr. Ingoglia said that “Narcan represents a second chance. By giving people a second chance, we also give them an opportunity to enter treatment if they so choose. You can’t recover if you’re dead, and we shouldn’t turn our backs on those who may choose a pathway to recovery that includes treatment.”
A version of this article first appeared on Medscape.com.
Greater access to the drug should mean more lives saved. However, it’s unclear how much the nasal spray will cost and whether pharmacies will stock the product openly on shelves.
Currently, major pharmacy chains such as CVS and Walgreens make naloxone available without prescription, but consumers have to ask a pharmacist to dispense the drug.
“The major question is what is it going to cost,” Brian Hurley, MD, MBA, president-elect of the American Society of Addiction Medicine, said in an interview. “In order for people to access it they have to be able to afford it.”
“We won’t accomplish much if people can’t afford to buy Narcan,” said Chuck Ingoglia, president and CEO of the National Council for Mental Wellbeing, in a statement. Still, he applauded the FDA.
“No single approach will end overdose deaths but making Narcan easy to obtain and widely available likely will save countless lives annually,” he said.
“The timeline for availability and price of this OTC product is determined by the manufacturer,” the FDA said in a statement.
Commissioner Robert M. Califf, MD, called for the drug’s manufacturer to “make accessibility to the product a priority by making it available as soon as possible and at an affordable price.”
Emergent BioSolutions did not comment on cost. It said in a statement that the spray “will be available on U.S. shelves and at online retailers by the late summer,” after it has adapted Narcan for direct-to-consumer use, including more consumer-oriented packaging.
Naloxone’s cost varies, depending on geographic location and whether it is generic. According to GoodRX, a box containing two doses of generic naloxone costs $31-$100, depending on location and coupon availability.
A two-dose box of Narcan costs $135-$140. Emergent reported a 14% decline in naloxone sales in 2022 – to $373.7 million – blaming it in part on the introduction of generic formulations.
Dr. Hurley said he expects those who purchase Narcan at a drug store will primarily already be shopping there. It may or may not be those who most often experience overdose, such as people leaving incarceration or experiencing homelessness.
Having Narcan available over-the-counter “is an important supplement but it doesn’t replace the existing array of naloxone distribution programs,” Dr. Hurley said.
The FDA has encouraged naloxone manufacturers to seek OTC approval for the medication since at least 2019, when it designed a model label for a theoretical OTC product.
In November, the agency said it had determined that some naloxone products had the potential to be safe and effective for OTC use and again urged drugmakers to seek such an approval.
Emergent BioSolutions was the first to pursue OTC approval, but another manufacturer – the nonprofit Harm Reduction Therapeutics – is awaiting approval of its application to sell its spray directly to consumers.
Scott Gottlieb, MD, who was the FDA commissioner from 2017 to 2019, said in a tweet that more work needed to be done.
“This regulatory move should be followed by a strong push by elected officials to support wider deployment of Narcan, getting more doses into the hands of at risk households and frontline workers,” he tweeted.
Mr. Ingoglia said that “Narcan represents a second chance. By giving people a second chance, we also give them an opportunity to enter treatment if they so choose. You can’t recover if you’re dead, and we shouldn’t turn our backs on those who may choose a pathway to recovery that includes treatment.”
A version of this article first appeared on Medscape.com.
Greater access to the drug should mean more lives saved. However, it’s unclear how much the nasal spray will cost and whether pharmacies will stock the product openly on shelves.
Currently, major pharmacy chains such as CVS and Walgreens make naloxone available without prescription, but consumers have to ask a pharmacist to dispense the drug.
“The major question is what is it going to cost,” Brian Hurley, MD, MBA, president-elect of the American Society of Addiction Medicine, said in an interview. “In order for people to access it they have to be able to afford it.”
“We won’t accomplish much if people can’t afford to buy Narcan,” said Chuck Ingoglia, president and CEO of the National Council for Mental Wellbeing, in a statement. Still, he applauded the FDA.
“No single approach will end overdose deaths but making Narcan easy to obtain and widely available likely will save countless lives annually,” he said.
“The timeline for availability and price of this OTC product is determined by the manufacturer,” the FDA said in a statement.
Commissioner Robert M. Califf, MD, called for the drug’s manufacturer to “make accessibility to the product a priority by making it available as soon as possible and at an affordable price.”
Emergent BioSolutions did not comment on cost. It said in a statement that the spray “will be available on U.S. shelves and at online retailers by the late summer,” after it has adapted Narcan for direct-to-consumer use, including more consumer-oriented packaging.
Naloxone’s cost varies, depending on geographic location and whether it is generic. According to GoodRX, a box containing two doses of generic naloxone costs $31-$100, depending on location and coupon availability.
A two-dose box of Narcan costs $135-$140. Emergent reported a 14% decline in naloxone sales in 2022 – to $373.7 million – blaming it in part on the introduction of generic formulations.
Dr. Hurley said he expects those who purchase Narcan at a drug store will primarily already be shopping there. It may or may not be those who most often experience overdose, such as people leaving incarceration or experiencing homelessness.
Having Narcan available over-the-counter “is an important supplement but it doesn’t replace the existing array of naloxone distribution programs,” Dr. Hurley said.
The FDA has encouraged naloxone manufacturers to seek OTC approval for the medication since at least 2019, when it designed a model label for a theoretical OTC product.
In November, the agency said it had determined that some naloxone products had the potential to be safe and effective for OTC use and again urged drugmakers to seek such an approval.
Emergent BioSolutions was the first to pursue OTC approval, but another manufacturer – the nonprofit Harm Reduction Therapeutics – is awaiting approval of its application to sell its spray directly to consumers.
Scott Gottlieb, MD, who was the FDA commissioner from 2017 to 2019, said in a tweet that more work needed to be done.
“This regulatory move should be followed by a strong push by elected officials to support wider deployment of Narcan, getting more doses into the hands of at risk households and frontline workers,” he tweeted.
Mr. Ingoglia said that “Narcan represents a second chance. By giving people a second chance, we also give them an opportunity to enter treatment if they so choose. You can’t recover if you’re dead, and we shouldn’t turn our backs on those who may choose a pathway to recovery that includes treatment.”
A version of this article first appeared on Medscape.com.
Breast conservation safe even with multiple-site tumors
BOSTON – , as new data show a low risk of recurrence at 5 years when they are treated with breast-conserving therapy and radiation.
“[The study] proves the oncologic safety of breast conservation in women with two or three sites of disease, making this a very reasonable option for (previously reluctant) surgeons to present to patients,” first author Kari Rosenkranz, MD, an associate professor at Dartmouth Health in Norwich, Vt., said in an interview.
The findings were presented here at the International Conference on Surgical Cancer Care (SSO 2023), and were published online in the Journal of Clinical Oncology.
Commenting on the study, Hiram S. Cody III, MD, an attending surgeon and professor of surgery at Weill Cornell Medicine, Memorial Sloan Kettering Cancer Center, in New York, said the findings provide valuable new evidence on the issue.
“This is an important study confirming that breast conservation is feasible and safe for women with multiple ipsilateral breast cancers, with excellent results comparable to those for women with unifocal (single site) disease,” he said in an interview.
Although there have been as many as seven previous randomized trials that have shown identical outcomes in survival and local control of disease with breast-conserving therapy versus mastectomy, all those studies excluded patients with more than one site of disease.
At present, many surgeons and guidelines continue to recommend mastectomy for women with multiple-site tumors, based on older data that showed higher recurrence rates.
That is why the new study is so important, Dr. Cody explained. “Here, we see in a prospective trial that breast-conserving therapy is feasible for those with more than one site of disease as well, with high survival and very low rates of local recurrence,” he emphasized.
Dr. Cody noted that “the ideal candidate would be a woman with relatively small tumor size and a breast large enough that the multiple excisions could be performed with a good cosmetic result.”
“We have followed this approach for some time and hope that with the publication of these results more surgeons will recommend this approach for suitable patients,” he said.
The new results were also highlighted in a press release from Mayo Clinic highlighting the Journal of Clinical Oncology publication. Lead author of the article, surgical oncologist Judy Boughey, MD, from the Mayo Clinic in Rochester, Minn., commented: “I am excited about these findings because it will empower patients and the multidisciplinary care teams caring for patients to be thinking about this option for women who may want to preserve their breast.”
This study showed the rate of cancer local recurrence was 3.1%, she noted. This is an excellent outcome and is similar to the local recurrence rate for patients with a single tumor in a breast who had breast-conserving therapy, Dr. Boughey said.
Historically, women with multiple tumors in one breast have been advised to have a mastectomy. Now, patients can be offered a less invasive option with faster recovery, resulting in better patient satisfaction and cosmetic outcomes, she added.
Study details
This study, known as the ACOSOG (Alliance) Z11102 trial, was a phase 2 trial conducted in 204 patients enrolled between 2012 and 2016 who had two or three sites of biopsy-proven breast cancer (each site less rhan 5 cm in size, with cN0 or cN1 disease).
These patients were a median age of 61 years, and 83.5% were ER-positive/HER2-negative, 11.5% were HER2-positive, 5.0% were ER-negative/HER2-negative, and 77.5% were node-negative.
All patients were treated with breast conservation surgery, including lumpectomy resected to negative margins, followed by whole breast radiation with a cavity boost to all lumpectomy beds.
With a median follow-up of 66.4 months, six patients developed local recurrence, with five of the recurrences occurring in the ipsilateral breast and one in the chest wall.
For the primary endpoint, the six recurrences represented an estimated cumulative incidence of local recurrence of 3.1% (95% CI, 1.3-6.4), well below the cutoff of 8% that was determined to be the acceptable 5-year local recurrence rate based on historic recurrence rates for unifocal disease, Dr. Rosenkranz explained.
There were no cases of synchronous local and distant recurrences, six contralateral breast cancers, and three new primary nonbreast cancers. Eight patients died, including one related to breast cancer.
There were no significant associations between risk of local recurrence and factors including patient age, number of sites of preoperative biopsy-proven breast cancer, HER2 status, and pathologic T and N category.
In terms of secondary endpoints, 14 patients (7.1%) converted to mastectomy because of positive margins, while 67.6% achieved margin-negative excision in a single operation.
Regarding cosmesis, 70.6% of patients reported good or excellent cosmetic outcomes at 2 years.
In terms of adherence, the whole breast radiation therapy protocol was feasible in most patients.
Of note, among patients without a breast preoperative MRI, the 5-year rate of local recurrence was significantly higher, at 22.6% (n = 14) at 5 years, compared with 1.7% among the 180 patients who did have a preoperative MRI (P = .002). However, Dr. Rosenkranz said these differences should be interpreted with caution.
“We may look at these data and think we should consider preoperative breast MRI in patients who do have known multiple ipsilateral breast cancer, although I think this cohort was certainly much too small to draw definitive conclusions, and this was not a planned secondary endpoint of the trial,” she said during her presentation.
Most prefer breast conservation, when possible
Overall, the findings are important considering the array of known benefits of breast conservation over mastectomy, Dr. Rosenkranz concluded.
“The reason this is so important is that we know that patients who undergo breast conservation report improved quality of life, self-esteem, and body image, and therefore it’s incumbent on us as surgeons to expand the indications for breast conservation where we can,” she told the audience.
Speaking with this news organization, she added that the decision-making around breast conservation versus mastectomy can be complicated, and some women do opt for mastectomy because of a variety of factors; therefore, “tailoring therapy to the individual goals and priorities in addition to the disease characteristics is critical.”
That said, she added that “the majority of patients who are eligible for breast conservation do prefer this option.”
Dr. Rosenkranz and Dr. Cody have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
BOSTON – , as new data show a low risk of recurrence at 5 years when they are treated with breast-conserving therapy and radiation.
“[The study] proves the oncologic safety of breast conservation in women with two or three sites of disease, making this a very reasonable option for (previously reluctant) surgeons to present to patients,” first author Kari Rosenkranz, MD, an associate professor at Dartmouth Health in Norwich, Vt., said in an interview.
The findings were presented here at the International Conference on Surgical Cancer Care (SSO 2023), and were published online in the Journal of Clinical Oncology.
Commenting on the study, Hiram S. Cody III, MD, an attending surgeon and professor of surgery at Weill Cornell Medicine, Memorial Sloan Kettering Cancer Center, in New York, said the findings provide valuable new evidence on the issue.
“This is an important study confirming that breast conservation is feasible and safe for women with multiple ipsilateral breast cancers, with excellent results comparable to those for women with unifocal (single site) disease,” he said in an interview.
Although there have been as many as seven previous randomized trials that have shown identical outcomes in survival and local control of disease with breast-conserving therapy versus mastectomy, all those studies excluded patients with more than one site of disease.
At present, many surgeons and guidelines continue to recommend mastectomy for women with multiple-site tumors, based on older data that showed higher recurrence rates.
That is why the new study is so important, Dr. Cody explained. “Here, we see in a prospective trial that breast-conserving therapy is feasible for those with more than one site of disease as well, with high survival and very low rates of local recurrence,” he emphasized.
Dr. Cody noted that “the ideal candidate would be a woman with relatively small tumor size and a breast large enough that the multiple excisions could be performed with a good cosmetic result.”
“We have followed this approach for some time and hope that with the publication of these results more surgeons will recommend this approach for suitable patients,” he said.
The new results were also highlighted in a press release from Mayo Clinic highlighting the Journal of Clinical Oncology publication. Lead author of the article, surgical oncologist Judy Boughey, MD, from the Mayo Clinic in Rochester, Minn., commented: “I am excited about these findings because it will empower patients and the multidisciplinary care teams caring for patients to be thinking about this option for women who may want to preserve their breast.”
This study showed the rate of cancer local recurrence was 3.1%, she noted. This is an excellent outcome and is similar to the local recurrence rate for patients with a single tumor in a breast who had breast-conserving therapy, Dr. Boughey said.
Historically, women with multiple tumors in one breast have been advised to have a mastectomy. Now, patients can be offered a less invasive option with faster recovery, resulting in better patient satisfaction and cosmetic outcomes, she added.
Study details
This study, known as the ACOSOG (Alliance) Z11102 trial, was a phase 2 trial conducted in 204 patients enrolled between 2012 and 2016 who had two or three sites of biopsy-proven breast cancer (each site less rhan 5 cm in size, with cN0 or cN1 disease).
These patients were a median age of 61 years, and 83.5% were ER-positive/HER2-negative, 11.5% were HER2-positive, 5.0% were ER-negative/HER2-negative, and 77.5% were node-negative.
All patients were treated with breast conservation surgery, including lumpectomy resected to negative margins, followed by whole breast radiation with a cavity boost to all lumpectomy beds.
With a median follow-up of 66.4 months, six patients developed local recurrence, with five of the recurrences occurring in the ipsilateral breast and one in the chest wall.
For the primary endpoint, the six recurrences represented an estimated cumulative incidence of local recurrence of 3.1% (95% CI, 1.3-6.4), well below the cutoff of 8% that was determined to be the acceptable 5-year local recurrence rate based on historic recurrence rates for unifocal disease, Dr. Rosenkranz explained.
There were no cases of synchronous local and distant recurrences, six contralateral breast cancers, and three new primary nonbreast cancers. Eight patients died, including one related to breast cancer.
There were no significant associations between risk of local recurrence and factors including patient age, number of sites of preoperative biopsy-proven breast cancer, HER2 status, and pathologic T and N category.
In terms of secondary endpoints, 14 patients (7.1%) converted to mastectomy because of positive margins, while 67.6% achieved margin-negative excision in a single operation.
Regarding cosmesis, 70.6% of patients reported good or excellent cosmetic outcomes at 2 years.
In terms of adherence, the whole breast radiation therapy protocol was feasible in most patients.
Of note, among patients without a breast preoperative MRI, the 5-year rate of local recurrence was significantly higher, at 22.6% (n = 14) at 5 years, compared with 1.7% among the 180 patients who did have a preoperative MRI (P = .002). However, Dr. Rosenkranz said these differences should be interpreted with caution.
“We may look at these data and think we should consider preoperative breast MRI in patients who do have known multiple ipsilateral breast cancer, although I think this cohort was certainly much too small to draw definitive conclusions, and this was not a planned secondary endpoint of the trial,” she said during her presentation.
Most prefer breast conservation, when possible
Overall, the findings are important considering the array of known benefits of breast conservation over mastectomy, Dr. Rosenkranz concluded.
“The reason this is so important is that we know that patients who undergo breast conservation report improved quality of life, self-esteem, and body image, and therefore it’s incumbent on us as surgeons to expand the indications for breast conservation where we can,” she told the audience.
Speaking with this news organization, she added that the decision-making around breast conservation versus mastectomy can be complicated, and some women do opt for mastectomy because of a variety of factors; therefore, “tailoring therapy to the individual goals and priorities in addition to the disease characteristics is critical.”
That said, she added that “the majority of patients who are eligible for breast conservation do prefer this option.”
Dr. Rosenkranz and Dr. Cody have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
BOSTON – , as new data show a low risk of recurrence at 5 years when they are treated with breast-conserving therapy and radiation.
“[The study] proves the oncologic safety of breast conservation in women with two or three sites of disease, making this a very reasonable option for (previously reluctant) surgeons to present to patients,” first author Kari Rosenkranz, MD, an associate professor at Dartmouth Health in Norwich, Vt., said in an interview.
The findings were presented here at the International Conference on Surgical Cancer Care (SSO 2023), and were published online in the Journal of Clinical Oncology.
Commenting on the study, Hiram S. Cody III, MD, an attending surgeon and professor of surgery at Weill Cornell Medicine, Memorial Sloan Kettering Cancer Center, in New York, said the findings provide valuable new evidence on the issue.
“This is an important study confirming that breast conservation is feasible and safe for women with multiple ipsilateral breast cancers, with excellent results comparable to those for women with unifocal (single site) disease,” he said in an interview.
Although there have been as many as seven previous randomized trials that have shown identical outcomes in survival and local control of disease with breast-conserving therapy versus mastectomy, all those studies excluded patients with more than one site of disease.
At present, many surgeons and guidelines continue to recommend mastectomy for women with multiple-site tumors, based on older data that showed higher recurrence rates.
That is why the new study is so important, Dr. Cody explained. “Here, we see in a prospective trial that breast-conserving therapy is feasible for those with more than one site of disease as well, with high survival and very low rates of local recurrence,” he emphasized.
Dr. Cody noted that “the ideal candidate would be a woman with relatively small tumor size and a breast large enough that the multiple excisions could be performed with a good cosmetic result.”
“We have followed this approach for some time and hope that with the publication of these results more surgeons will recommend this approach for suitable patients,” he said.
The new results were also highlighted in a press release from Mayo Clinic highlighting the Journal of Clinical Oncology publication. Lead author of the article, surgical oncologist Judy Boughey, MD, from the Mayo Clinic in Rochester, Minn., commented: “I am excited about these findings because it will empower patients and the multidisciplinary care teams caring for patients to be thinking about this option for women who may want to preserve their breast.”
This study showed the rate of cancer local recurrence was 3.1%, she noted. This is an excellent outcome and is similar to the local recurrence rate for patients with a single tumor in a breast who had breast-conserving therapy, Dr. Boughey said.
Historically, women with multiple tumors in one breast have been advised to have a mastectomy. Now, patients can be offered a less invasive option with faster recovery, resulting in better patient satisfaction and cosmetic outcomes, she added.
Study details
This study, known as the ACOSOG (Alliance) Z11102 trial, was a phase 2 trial conducted in 204 patients enrolled between 2012 and 2016 who had two or three sites of biopsy-proven breast cancer (each site less rhan 5 cm in size, with cN0 or cN1 disease).
These patients were a median age of 61 years, and 83.5% were ER-positive/HER2-negative, 11.5% were HER2-positive, 5.0% were ER-negative/HER2-negative, and 77.5% were node-negative.
All patients were treated with breast conservation surgery, including lumpectomy resected to negative margins, followed by whole breast radiation with a cavity boost to all lumpectomy beds.
With a median follow-up of 66.4 months, six patients developed local recurrence, with five of the recurrences occurring in the ipsilateral breast and one in the chest wall.
For the primary endpoint, the six recurrences represented an estimated cumulative incidence of local recurrence of 3.1% (95% CI, 1.3-6.4), well below the cutoff of 8% that was determined to be the acceptable 5-year local recurrence rate based on historic recurrence rates for unifocal disease, Dr. Rosenkranz explained.
There were no cases of synchronous local and distant recurrences, six contralateral breast cancers, and three new primary nonbreast cancers. Eight patients died, including one related to breast cancer.
There were no significant associations between risk of local recurrence and factors including patient age, number of sites of preoperative biopsy-proven breast cancer, HER2 status, and pathologic T and N category.
In terms of secondary endpoints, 14 patients (7.1%) converted to mastectomy because of positive margins, while 67.6% achieved margin-negative excision in a single operation.
Regarding cosmesis, 70.6% of patients reported good or excellent cosmetic outcomes at 2 years.
In terms of adherence, the whole breast radiation therapy protocol was feasible in most patients.
Of note, among patients without a breast preoperative MRI, the 5-year rate of local recurrence was significantly higher, at 22.6% (n = 14) at 5 years, compared with 1.7% among the 180 patients who did have a preoperative MRI (P = .002). However, Dr. Rosenkranz said these differences should be interpreted with caution.
“We may look at these data and think we should consider preoperative breast MRI in patients who do have known multiple ipsilateral breast cancer, although I think this cohort was certainly much too small to draw definitive conclusions, and this was not a planned secondary endpoint of the trial,” she said during her presentation.
Most prefer breast conservation, when possible
Overall, the findings are important considering the array of known benefits of breast conservation over mastectomy, Dr. Rosenkranz concluded.
“The reason this is so important is that we know that patients who undergo breast conservation report improved quality of life, self-esteem, and body image, and therefore it’s incumbent on us as surgeons to expand the indications for breast conservation where we can,” she told the audience.
Speaking with this news organization, she added that the decision-making around breast conservation versus mastectomy can be complicated, and some women do opt for mastectomy because of a variety of factors; therefore, “tailoring therapy to the individual goals and priorities in addition to the disease characteristics is critical.”
That said, she added that “the majority of patients who are eligible for breast conservation do prefer this option.”
Dr. Rosenkranz and Dr. Cody have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM SSO 2023
Brain stimulation can improve prognosis following a stroke and other neurological diseases
HAMBURG, GERMANY – Around 86 billion nerve cells in our brain work together in complex dynamic networks to control almost every sensorimotor and cognitive process. However, the way in which the information is processed in the different regions of the brain is still unclear. There are already some promising approaches to specifically influence the dynamics of neuronal networks to treat neurological and psychiatric diseases.
One of the main topics at the Congress for Clinical Neuroscience of the German Society for Clinical Neurophysiology and Functional Neuroimaging (DGKN), recently held in Hamburg, Germany, was the dynamics of cerebral networks in sensorimotor and cognitive processes, as well as disruptions to network dynamics in neurological and psychiatric diseases.
“We will be unable to develop innovative therapies for widespread neurological and psychiatric diseases until we understand neuronal functions on every level of complexity,” Andreas K. Engel, PhD, director of the Institute for Neurophysiology and Pathophysiology at the University Hospital of Hamburg-Eppendorf, president of the DGKN, and congress president, said during an online press conference.
Characterizing states of consciousness
For more than 30 years, it has been known that neuronal signals in the brain are dynamically coupled. Despite intensive research, the functional significance of this coupling on information processing is still largely unknown.
Neuroimaging methods such as electroencephalography (EEG), magnetoencephalography (MEG), structural and functional magnetic resonance imaging (MRI), and electrophysiological examinations were used. Model calculations of the data suggest that dynamic couplings of signals in the cortex play a crucial role in memory performance, thinking processes, and developing perception, among other things.
It has already been shown that the network dynamics of neuronal signals could possibly characterize states of consciousness. Neuronal signals and coupling patterns differ significantly between healthy individuals in a waking state and those who are asleep, under general anesthetic, or in a vegetative state. In Dr. Engel’s view, it may be possible in the future for machine learning algorithms to be used to classify states of consciousness.
Changes in brain activity as a biomarker?
The differences in the dynamics of neuronal signals between healthy individuals and patients with psychiatric diseases such as schizophrenia appear much more important for clinical practice. “The characteristic changes in brain activity in the primary auditory cortex could be considered a potential biomarker and used to predict the clinical course of psychiatric diseases, such as psychoses,” reported Dr. Engel.
The gamma-band activity in the auditory cortex could be a potential marker for schizophrenia. According to MEG examinations, the values are decreased both in people at increased risk of psychosis and experiencing first symptoms compared with controls.
Activation or inhibition of cerebral networks as new therapeutic approaches
New therapeutic approaches based on the activation or inhibition of cerebral networks are currently areas of intensive research. Close interdisciplinary collaboration between basic science researchers and clinicians is necessary, stressed Dr. Engel. The use of noninvasive brain stimulation is already within reach for the neurorehabilitation of stroke patients. “I am optimistic that in a few years brain stimulation will be established as an integral element of stroke therapy,” said Christian Grefkes-Hermann, MD, PhD, director of the department of neurology at University Hospital of Frankfurt and first vice president of the DGKN.
Despite great advances in acute stroke therapy, many patients must endure permanent deficits in their everyday life, he said. According to Dr. Grefkes-Hermann, rehabilitation procedures often have a dissatisfactory effect, and results greatly vary. He hopes that in the future it may be possible to personalize therapy by using network patterns, thereby improving results.
“The most important factor for functional recovery after a stroke is neuronal reorganization,” said Dr. Grefkes-Hermann. With the new methods of neurorehabilitation, network-connectivity disruptions, which are associated with motor function deficits, are first visualized using functional MRI (fMRI).
The imaging or the EEG makes visible the area of the brain that may benefit most from neurostimulation. Subsequently, nerve cells in this region may be precisely stimulated with TMS. Because the healthy hemisphere of the brain is usually overactive after a stroke, there are simultaneous attempts to inhibit the contralesional motor cortex.
Initial results are hopeful. In the initial period after a stroke, TMS can be used in some patients to correct pathological connectivities and thereby improve motor deficits, reported Dr. Grefkes-Hermann. The fMRI pattern can also be used to predict recovery and intervention effects on an individual basis. A phase 3 trial is currently underway of 150 patients who have had a stroke and aims to study the efficacy of the new procedure.
Combined TMS and EEG
With the combination of TMS and the simultaneous measurement of EEG activity, a further development of fMRI connectivity analyses is currently being tested. Dr. Grefkes-Hermann believes that this procedure, which is more cost-effective, has higher temporal resolution, can be used directly at the bedside, and has more potential for personalized therapy planning in clinical practice.
The TMS-EEG procedure also makes it possible to predict the risk of post-stroke delirium, which affects around 30% of stroke patients and greatly worsens the outcome, underlined Ulf Ziemann, MD, medical director of the department of neurology at Tübingen (Germany) University Hospital. In a study of 33 patients with acute stroke, the onset of post-stroke delirium could be predicted with a high degree of accuracy by using the TMS-EEG procedure no later than 48 hours after the event.
Other promising, noninvasive methods for neuron activation mentioned by Dr. Ziemann include transcranial focused ultrasound stimulation (tFUS) with low intensity, which is being studied for chronic pain, dementia, epilepsy, traumatic brain injury, and depression, as well as transcranial pulse stimulation (TPS), which is also based on ultrasound. In a pilot study of 35 patients with Alzheimer’s disease, use of TPS within 3 months had positive effects on cognition. However, the study was not controlled and therefore further assessments are needed.
Custom deep brain stimulation
For deep brain stimulation (DBS), an established therapy for Parkinson’s disease and other movement disorders, the aim is individualized, symptom-related network stimulation, reported Andrea Kühn, MD, head of the movement disorders and neuromodulation section in the department of neurology at Charité University Hospital Berlin.
At the panregional collaborative research center ReTune, which has been supported for 4 years now by €10 million from the German Research Foundation (DFG), imaging and computer-assisted programming algorithms are being developed for DBS. They will greatly simplify the time-consuming standard procedure for the best possible setting of the stimulation parameters, which requires a hospital stay of several days.
A randomized crossover study of 35 patients with Parkinson’s disease proved the equivalence of the fast, algorithm-assisted DBS for the control of motor symptoms compared with standard procedures.
The new methods have the potential to considerably improve the outcome of patients with neurological and psychiatric diseases, according to scientists. However, the positive data must still be validated in further studies.
This article was translated from Medscape’s German edition. A version of this article appeared on Medscape.com.
HAMBURG, GERMANY – Around 86 billion nerve cells in our brain work together in complex dynamic networks to control almost every sensorimotor and cognitive process. However, the way in which the information is processed in the different regions of the brain is still unclear. There are already some promising approaches to specifically influence the dynamics of neuronal networks to treat neurological and psychiatric diseases.
One of the main topics at the Congress for Clinical Neuroscience of the German Society for Clinical Neurophysiology and Functional Neuroimaging (DGKN), recently held in Hamburg, Germany, was the dynamics of cerebral networks in sensorimotor and cognitive processes, as well as disruptions to network dynamics in neurological and psychiatric diseases.
“We will be unable to develop innovative therapies for widespread neurological and psychiatric diseases until we understand neuronal functions on every level of complexity,” Andreas K. Engel, PhD, director of the Institute for Neurophysiology and Pathophysiology at the University Hospital of Hamburg-Eppendorf, president of the DGKN, and congress president, said during an online press conference.
Characterizing states of consciousness
For more than 30 years, it has been known that neuronal signals in the brain are dynamically coupled. Despite intensive research, the functional significance of this coupling on information processing is still largely unknown.
Neuroimaging methods such as electroencephalography (EEG), magnetoencephalography (MEG), structural and functional magnetic resonance imaging (MRI), and electrophysiological examinations were used. Model calculations of the data suggest that dynamic couplings of signals in the cortex play a crucial role in memory performance, thinking processes, and developing perception, among other things.
It has already been shown that the network dynamics of neuronal signals could possibly characterize states of consciousness. Neuronal signals and coupling patterns differ significantly between healthy individuals in a waking state and those who are asleep, under general anesthetic, or in a vegetative state. In Dr. Engel’s view, it may be possible in the future for machine learning algorithms to be used to classify states of consciousness.
Changes in brain activity as a biomarker?
The differences in the dynamics of neuronal signals between healthy individuals and patients with psychiatric diseases such as schizophrenia appear much more important for clinical practice. “The characteristic changes in brain activity in the primary auditory cortex could be considered a potential biomarker and used to predict the clinical course of psychiatric diseases, such as psychoses,” reported Dr. Engel.
The gamma-band activity in the auditory cortex could be a potential marker for schizophrenia. According to MEG examinations, the values are decreased both in people at increased risk of psychosis and experiencing first symptoms compared with controls.
Activation or inhibition of cerebral networks as new therapeutic approaches
New therapeutic approaches based on the activation or inhibition of cerebral networks are currently areas of intensive research. Close interdisciplinary collaboration between basic science researchers and clinicians is necessary, stressed Dr. Engel. The use of noninvasive brain stimulation is already within reach for the neurorehabilitation of stroke patients. “I am optimistic that in a few years brain stimulation will be established as an integral element of stroke therapy,” said Christian Grefkes-Hermann, MD, PhD, director of the department of neurology at University Hospital of Frankfurt and first vice president of the DGKN.
Despite great advances in acute stroke therapy, many patients must endure permanent deficits in their everyday life, he said. According to Dr. Grefkes-Hermann, rehabilitation procedures often have a dissatisfactory effect, and results greatly vary. He hopes that in the future it may be possible to personalize therapy by using network patterns, thereby improving results.
“The most important factor for functional recovery after a stroke is neuronal reorganization,” said Dr. Grefkes-Hermann. With the new methods of neurorehabilitation, network-connectivity disruptions, which are associated with motor function deficits, are first visualized using functional MRI (fMRI).
The imaging or the EEG makes visible the area of the brain that may benefit most from neurostimulation. Subsequently, nerve cells in this region may be precisely stimulated with TMS. Because the healthy hemisphere of the brain is usually overactive after a stroke, there are simultaneous attempts to inhibit the contralesional motor cortex.
Initial results are hopeful. In the initial period after a stroke, TMS can be used in some patients to correct pathological connectivities and thereby improve motor deficits, reported Dr. Grefkes-Hermann. The fMRI pattern can also be used to predict recovery and intervention effects on an individual basis. A phase 3 trial is currently underway of 150 patients who have had a stroke and aims to study the efficacy of the new procedure.
Combined TMS and EEG
With the combination of TMS and the simultaneous measurement of EEG activity, a further development of fMRI connectivity analyses is currently being tested. Dr. Grefkes-Hermann believes that this procedure, which is more cost-effective, has higher temporal resolution, can be used directly at the bedside, and has more potential for personalized therapy planning in clinical practice.
The TMS-EEG procedure also makes it possible to predict the risk of post-stroke delirium, which affects around 30% of stroke patients and greatly worsens the outcome, underlined Ulf Ziemann, MD, medical director of the department of neurology at Tübingen (Germany) University Hospital. In a study of 33 patients with acute stroke, the onset of post-stroke delirium could be predicted with a high degree of accuracy by using the TMS-EEG procedure no later than 48 hours after the event.
Other promising, noninvasive methods for neuron activation mentioned by Dr. Ziemann include transcranial focused ultrasound stimulation (tFUS) with low intensity, which is being studied for chronic pain, dementia, epilepsy, traumatic brain injury, and depression, as well as transcranial pulse stimulation (TPS), which is also based on ultrasound. In a pilot study of 35 patients with Alzheimer’s disease, use of TPS within 3 months had positive effects on cognition. However, the study was not controlled and therefore further assessments are needed.
Custom deep brain stimulation
For deep brain stimulation (DBS), an established therapy for Parkinson’s disease and other movement disorders, the aim is individualized, symptom-related network stimulation, reported Andrea Kühn, MD, head of the movement disorders and neuromodulation section in the department of neurology at Charité University Hospital Berlin.
At the panregional collaborative research center ReTune, which has been supported for 4 years now by €10 million from the German Research Foundation (DFG), imaging and computer-assisted programming algorithms are being developed for DBS. They will greatly simplify the time-consuming standard procedure for the best possible setting of the stimulation parameters, which requires a hospital stay of several days.
A randomized crossover study of 35 patients with Parkinson’s disease proved the equivalence of the fast, algorithm-assisted DBS for the control of motor symptoms compared with standard procedures.
The new methods have the potential to considerably improve the outcome of patients with neurological and psychiatric diseases, according to scientists. However, the positive data must still be validated in further studies.
This article was translated from Medscape’s German edition. A version of this article appeared on Medscape.com.
HAMBURG, GERMANY – Around 86 billion nerve cells in our brain work together in complex dynamic networks to control almost every sensorimotor and cognitive process. However, the way in which the information is processed in the different regions of the brain is still unclear. There are already some promising approaches to specifically influence the dynamics of neuronal networks to treat neurological and psychiatric diseases.
One of the main topics at the Congress for Clinical Neuroscience of the German Society for Clinical Neurophysiology and Functional Neuroimaging (DGKN), recently held in Hamburg, Germany, was the dynamics of cerebral networks in sensorimotor and cognitive processes, as well as disruptions to network dynamics in neurological and psychiatric diseases.
“We will be unable to develop innovative therapies for widespread neurological and psychiatric diseases until we understand neuronal functions on every level of complexity,” Andreas K. Engel, PhD, director of the Institute for Neurophysiology and Pathophysiology at the University Hospital of Hamburg-Eppendorf, president of the DGKN, and congress president, said during an online press conference.
Characterizing states of consciousness
For more than 30 years, it has been known that neuronal signals in the brain are dynamically coupled. Despite intensive research, the functional significance of this coupling on information processing is still largely unknown.
Neuroimaging methods such as electroencephalography (EEG), magnetoencephalography (MEG), structural and functional magnetic resonance imaging (MRI), and electrophysiological examinations were used. Model calculations of the data suggest that dynamic couplings of signals in the cortex play a crucial role in memory performance, thinking processes, and developing perception, among other things.
It has already been shown that the network dynamics of neuronal signals could possibly characterize states of consciousness. Neuronal signals and coupling patterns differ significantly between healthy individuals in a waking state and those who are asleep, under general anesthetic, or in a vegetative state. In Dr. Engel’s view, it may be possible in the future for machine learning algorithms to be used to classify states of consciousness.
Changes in brain activity as a biomarker?
The differences in the dynamics of neuronal signals between healthy individuals and patients with psychiatric diseases such as schizophrenia appear much more important for clinical practice. “The characteristic changes in brain activity in the primary auditory cortex could be considered a potential biomarker and used to predict the clinical course of psychiatric diseases, such as psychoses,” reported Dr. Engel.
The gamma-band activity in the auditory cortex could be a potential marker for schizophrenia. According to MEG examinations, the values are decreased both in people at increased risk of psychosis and experiencing first symptoms compared with controls.
Activation or inhibition of cerebral networks as new therapeutic approaches
New therapeutic approaches based on the activation or inhibition of cerebral networks are currently areas of intensive research. Close interdisciplinary collaboration between basic science researchers and clinicians is necessary, stressed Dr. Engel. The use of noninvasive brain stimulation is already within reach for the neurorehabilitation of stroke patients. “I am optimistic that in a few years brain stimulation will be established as an integral element of stroke therapy,” said Christian Grefkes-Hermann, MD, PhD, director of the department of neurology at University Hospital of Frankfurt and first vice president of the DGKN.
Despite great advances in acute stroke therapy, many patients must endure permanent deficits in their everyday life, he said. According to Dr. Grefkes-Hermann, rehabilitation procedures often have a dissatisfactory effect, and results greatly vary. He hopes that in the future it may be possible to personalize therapy by using network patterns, thereby improving results.
“The most important factor for functional recovery after a stroke is neuronal reorganization,” said Dr. Grefkes-Hermann. With the new methods of neurorehabilitation, network-connectivity disruptions, which are associated with motor function deficits, are first visualized using functional MRI (fMRI).
The imaging or the EEG makes visible the area of the brain that may benefit most from neurostimulation. Subsequently, nerve cells in this region may be precisely stimulated with TMS. Because the healthy hemisphere of the brain is usually overactive after a stroke, there are simultaneous attempts to inhibit the contralesional motor cortex.
Initial results are hopeful. In the initial period after a stroke, TMS can be used in some patients to correct pathological connectivities and thereby improve motor deficits, reported Dr. Grefkes-Hermann. The fMRI pattern can also be used to predict recovery and intervention effects on an individual basis. A phase 3 trial is currently underway of 150 patients who have had a stroke and aims to study the efficacy of the new procedure.
Combined TMS and EEG
With the combination of TMS and the simultaneous measurement of EEG activity, a further development of fMRI connectivity analyses is currently being tested. Dr. Grefkes-Hermann believes that this procedure, which is more cost-effective, has higher temporal resolution, can be used directly at the bedside, and has more potential for personalized therapy planning in clinical practice.
The TMS-EEG procedure also makes it possible to predict the risk of post-stroke delirium, which affects around 30% of stroke patients and greatly worsens the outcome, underlined Ulf Ziemann, MD, medical director of the department of neurology at Tübingen (Germany) University Hospital. In a study of 33 patients with acute stroke, the onset of post-stroke delirium could be predicted with a high degree of accuracy by using the TMS-EEG procedure no later than 48 hours after the event.
Other promising, noninvasive methods for neuron activation mentioned by Dr. Ziemann include transcranial focused ultrasound stimulation (tFUS) with low intensity, which is being studied for chronic pain, dementia, epilepsy, traumatic brain injury, and depression, as well as transcranial pulse stimulation (TPS), which is also based on ultrasound. In a pilot study of 35 patients with Alzheimer’s disease, use of TPS within 3 months had positive effects on cognition. However, the study was not controlled and therefore further assessments are needed.
Custom deep brain stimulation
For deep brain stimulation (DBS), an established therapy for Parkinson’s disease and other movement disorders, the aim is individualized, symptom-related network stimulation, reported Andrea Kühn, MD, head of the movement disorders and neuromodulation section in the department of neurology at Charité University Hospital Berlin.
At the panregional collaborative research center ReTune, which has been supported for 4 years now by €10 million from the German Research Foundation (DFG), imaging and computer-assisted programming algorithms are being developed for DBS. They will greatly simplify the time-consuming standard procedure for the best possible setting of the stimulation parameters, which requires a hospital stay of several days.
A randomized crossover study of 35 patients with Parkinson’s disease proved the equivalence of the fast, algorithm-assisted DBS for the control of motor symptoms compared with standard procedures.
The new methods have the potential to considerably improve the outcome of patients with neurological and psychiatric diseases, according to scientists. However, the positive data must still be validated in further studies.
This article was translated from Medscape’s German edition. A version of this article appeared on Medscape.com.
Optimal Use of CDK4/6 Inhibitors in Breast Cancer
Cyclin-dependent kinase 4/6 (CDK4/6) inhibitors have become integral to the treatment of HR+/HER2- breast cancer. Approved in 2015 for use in the metastatic setting and most recently in the adjuvant setting, CDK4/6 inhibitors have revolutionized treatment in both endocrine-sensitive and endocrine-resistant settings and in pre- and postmenopausal women.
But many questions remain regarding the optimal use of these medications in clinical practice.
In this ReCAP, Dr Virginia Kaklamani from the University of Texas Health Sciences Center in San Antonio, Texas, and Dr Harold Burstein from Dana-Farber Cancer Institute, Boston, Massachusetts, begin their discussion by examining the potential role of adjuvant CDK4/6 inhibitor therapy in early, high-risk breast cancer.
They discuss the three main studies that looked at the role of adjuvant CDK4/6 inhibitors, including the PALLAS and PENELOPE-B trials, in which palbociclib showed no benefit in invasive disease-free survival. In contrast, in the monarchE trial, abemaciclib showed a robust benefit in preventing recurrence, which was sustained after longer follow-up, as reported at the San Antonio Breast Cancer Symposium 2022.
Turning to the metastatic setting, the panelists discuss the varied side effect profiles of the three approved CDK4/6 inhibitors, palbociclib, ribociclib, and abemaciclib. They also discuss current research into the continuation of these agents beyond progression and whether sequencing of CDK4/6 inhibitors may provide benefit.
--
Virginia Kaklamani, MD, Professor of Medicine, Division of Hematology/Oncology, University of Texas Health Sciences Center; Leader, Breast Oncology Program, University of Texas Health MD Anderson Cancer Center, San Antonio, Texas
Virginia Kaklamani, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Gilead; Menarini; Pfizer; Novartis; Lilly; AstraZeneca; Genentech; Daichii; Seagen
Harold J. Burstein, MD, PhD, Professor, Department of Medicine, Harvard Medical School; Medical Oncologist, Dana-Farber Cancer Institute, Boston, Massachusetts
Harold J. Burstein, MD, PhD, has disclosed no relevant financial relationships.
Cyclin-dependent kinase 4/6 (CDK4/6) inhibitors have become integral to the treatment of HR+/HER2- breast cancer. Approved in 2015 for use in the metastatic setting and most recently in the adjuvant setting, CDK4/6 inhibitors have revolutionized treatment in both endocrine-sensitive and endocrine-resistant settings and in pre- and postmenopausal women.
But many questions remain regarding the optimal use of these medications in clinical practice.
In this ReCAP, Dr Virginia Kaklamani from the University of Texas Health Sciences Center in San Antonio, Texas, and Dr Harold Burstein from Dana-Farber Cancer Institute, Boston, Massachusetts, begin their discussion by examining the potential role of adjuvant CDK4/6 inhibitor therapy in early, high-risk breast cancer.
They discuss the three main studies that looked at the role of adjuvant CDK4/6 inhibitors, including the PALLAS and PENELOPE-B trials, in which palbociclib showed no benefit in invasive disease-free survival. In contrast, in the monarchE trial, abemaciclib showed a robust benefit in preventing recurrence, which was sustained after longer follow-up, as reported at the San Antonio Breast Cancer Symposium 2022.
Turning to the metastatic setting, the panelists discuss the varied side effect profiles of the three approved CDK4/6 inhibitors, palbociclib, ribociclib, and abemaciclib. They also discuss current research into the continuation of these agents beyond progression and whether sequencing of CDK4/6 inhibitors may provide benefit.
--
Virginia Kaklamani, MD, Professor of Medicine, Division of Hematology/Oncology, University of Texas Health Sciences Center; Leader, Breast Oncology Program, University of Texas Health MD Anderson Cancer Center, San Antonio, Texas
Virginia Kaklamani, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Gilead; Menarini; Pfizer; Novartis; Lilly; AstraZeneca; Genentech; Daichii; Seagen
Harold J. Burstein, MD, PhD, Professor, Department of Medicine, Harvard Medical School; Medical Oncologist, Dana-Farber Cancer Institute, Boston, Massachusetts
Harold J. Burstein, MD, PhD, has disclosed no relevant financial relationships.
Cyclin-dependent kinase 4/6 (CDK4/6) inhibitors have become integral to the treatment of HR+/HER2- breast cancer. Approved in 2015 for use in the metastatic setting and most recently in the adjuvant setting, CDK4/6 inhibitors have revolutionized treatment in both endocrine-sensitive and endocrine-resistant settings and in pre- and postmenopausal women.
But many questions remain regarding the optimal use of these medications in clinical practice.
In this ReCAP, Dr Virginia Kaklamani from the University of Texas Health Sciences Center in San Antonio, Texas, and Dr Harold Burstein from Dana-Farber Cancer Institute, Boston, Massachusetts, begin their discussion by examining the potential role of adjuvant CDK4/6 inhibitor therapy in early, high-risk breast cancer.
They discuss the three main studies that looked at the role of adjuvant CDK4/6 inhibitors, including the PALLAS and PENELOPE-B trials, in which palbociclib showed no benefit in invasive disease-free survival. In contrast, in the monarchE trial, abemaciclib showed a robust benefit in preventing recurrence, which was sustained after longer follow-up, as reported at the San Antonio Breast Cancer Symposium 2022.
Turning to the metastatic setting, the panelists discuss the varied side effect profiles of the three approved CDK4/6 inhibitors, palbociclib, ribociclib, and abemaciclib. They also discuss current research into the continuation of these agents beyond progression and whether sequencing of CDK4/6 inhibitors may provide benefit.
--
Virginia Kaklamani, MD, Professor of Medicine, Division of Hematology/Oncology, University of Texas Health Sciences Center; Leader, Breast Oncology Program, University of Texas Health MD Anderson Cancer Center, San Antonio, Texas
Virginia Kaklamani, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Gilead; Menarini; Pfizer; Novartis; Lilly; AstraZeneca; Genentech; Daichii; Seagen
Harold J. Burstein, MD, PhD, Professor, Department of Medicine, Harvard Medical School; Medical Oncologist, Dana-Farber Cancer Institute, Boston, Massachusetts
Harold J. Burstein, MD, PhD, has disclosed no relevant financial relationships.

Osteoarthritis adjunctive therapies offer negligible added benefit to exercise
DENVER – Adding therapies such as acupuncture, electrophysical stimulation, or other interventions to standard exercise therapy does not appear to offer much benefit in pain relief or physical function for patients with knee osteoarthritis, according to a study presented at the OARSI 2023 World Congress. The findings were also published in the Cochrane Database of Systematic Reviews in October 2022.
“The results do not support the use of adjunctive therapies when we add them to exercise for pain, physical function, or quality of life, when compared against placebo, adjunctive therapy, and exercise,” Helen P. French, PhD, told attendees at the meeting sponsored by the Osteoarthritis Research Society International. The findings were similar for pain and physical function when comparing adjunctive therapies with exercise against exercise alone, said Dr. French, an associate professor in physiotherapy at the Royal College of Surgeons, Dublin, except that patients using adjunctive therapies reported feeling greater improvement in their global assessments.
Exercise is recommended as a core treatment for osteoarthritis, but some patients or clinicians may be interested in supplementing that therapy with acupuncture, heat therapy, electromagnetic fields, transcutaneous electrical nerve stimulation, braces/orthotics, and other interventions. Various Cochrane Reviews of the evidence exist for these interventions in treating chronic pain in general but not for their use as adjunctive therapies in addition to exercise for osteoarthritis pain.
Researchers therefore assessed the evidence for improvement in pain, physical function, and quality of life for two sets of comparisons: adjunctive therapies plus exercise versus exercise alone, and adjunctive therapies with exercise versus placebo adjunctive therapy with exercise. The review excluded studies looking at medications or supplements.
Pain was assessed with the Numeric Pain Rating Scale (NPRS, 0-10), with an improvement of at least 2 points (15% improvement) representing the minimum clinically important difference (MCID). Physical function was assessed with the Western Ontario and McMaster Universities Arthritis Index (WOMAC, 0-68), with 6 points (15%) considered the MCID, and quality of life was assessed with the SF-36 (0-100), with 6 points (12%) as the MCID.
The researchers identified trials on knee osteoarthritis that included an overall 6,508 participants with an average age ranging from 52 to 83 years. A total of 36 studies evaluated electrophysical agents. Another seven looked at manual therapies; four looked at acupuncture/dry needling or taping; three looked at psychological, dietary, or “whole body vibration” therapies; and two evaluated spa or peloid therapy. Only one trial evaluated foot insoles.
Nearly all the studies (98%) assessed pain, and most (87%) assessed physical function. Only about one in five (21%) assessed quality of life. The improvement in pain from adding adjunctive therapies to exercise, compared with placebo therapies plus exercise, was 0.77 points, or just under a 10% improvement, which fell short of the 15% MCID. Physical function improvement similarly fell short, with an average improvement of 5 points (12%).
In comparisons of exercise plus adjunctive therapies against exercise alone, the improvement from the additional interventions was even lower. Pain improvement was 0.41 points (7%), and physical function improvement was 2.8 points (9%). However, patients’ perceptions told a different story: 37% more patients who were using an adjunctive therapy reported feeling that the therapies were successful, compared with patients undergoing exercise therapy alone.
Adverse events were poorly reported in the trials, with only 10 trials reporting them at all, and the researchers found no significant difference in adverse events among the studies reporting them. The most common adverse events were increased pain in the joint with the osteoarthritis, pain elsewhere, or swelling and inflammation. It’s unclear, however, whether the pain, swelling, and inflammation were related to the interventions and how serious these effects might have been.
Michelle Hall, PhD, an associate professor in the department of physiotherapy at the University of Melbourne, comoderated the session with this presentation and found it interesting that more than one-third of patients perceived that they did better with the additional therapies even though improvement didn’t bear out in their pain or physical function assessments.
“But the other part of that was that the studies were of poor quality, so we can’t say with confidence, ‘Don’t do this therapy because it’s not going to work,’ ” Dr. Hall said in an interview. She said she personally would probably discourage patients from those therapies, “but I don’t think the evidence is there for everybody to do that,” she added.
Martin Van Der Esch, PhD, of Reade Centre of Rehabilitation and Rheumatology in Amsterdam, also comoderated the discussion and had more concerns about the use of adjunctive therapies in light of the study’s findings. He said in an interview that he tended to believe the patients’ overall self-reported improvement is likely a placebo effect, and he sees potential harm in that effect. If the pain is not truly decreasing as patients continue using those therapies, then the pain may become a more stable part of the nervous system, “so I think they need to do an intervention which really has evidence in reducing pain, an active approach that means exercising in the right way,” Dr. Van Der Esch said. If patients are undergoing therapy whose primary benefit is a placebo effect, “the pain will prolong and become more fixed in the nervous system,” shifting the patients toward greater risk of the pain becoming chronic, he said.
“I want to emphasize that we have an ethical role to our management, and it’s not ethical to give treatments which have no response and no pain relief except that the patient or the professional believes it will have an effect,” Dr. Van Der Esch said.
The research did not involve outside funding. Dr. French, Dr. Hall, and Dr. Van Der Esch reported having no relevant financial relationships.
DENVER – Adding therapies such as acupuncture, electrophysical stimulation, or other interventions to standard exercise therapy does not appear to offer much benefit in pain relief or physical function for patients with knee osteoarthritis, according to a study presented at the OARSI 2023 World Congress. The findings were also published in the Cochrane Database of Systematic Reviews in October 2022.
“The results do not support the use of adjunctive therapies when we add them to exercise for pain, physical function, or quality of life, when compared against placebo, adjunctive therapy, and exercise,” Helen P. French, PhD, told attendees at the meeting sponsored by the Osteoarthritis Research Society International. The findings were similar for pain and physical function when comparing adjunctive therapies with exercise against exercise alone, said Dr. French, an associate professor in physiotherapy at the Royal College of Surgeons, Dublin, except that patients using adjunctive therapies reported feeling greater improvement in their global assessments.
Exercise is recommended as a core treatment for osteoarthritis, but some patients or clinicians may be interested in supplementing that therapy with acupuncture, heat therapy, electromagnetic fields, transcutaneous electrical nerve stimulation, braces/orthotics, and other interventions. Various Cochrane Reviews of the evidence exist for these interventions in treating chronic pain in general but not for their use as adjunctive therapies in addition to exercise for osteoarthritis pain.
Researchers therefore assessed the evidence for improvement in pain, physical function, and quality of life for two sets of comparisons: adjunctive therapies plus exercise versus exercise alone, and adjunctive therapies with exercise versus placebo adjunctive therapy with exercise. The review excluded studies looking at medications or supplements.
Pain was assessed with the Numeric Pain Rating Scale (NPRS, 0-10), with an improvement of at least 2 points (15% improvement) representing the minimum clinically important difference (MCID). Physical function was assessed with the Western Ontario and McMaster Universities Arthritis Index (WOMAC, 0-68), with 6 points (15%) considered the MCID, and quality of life was assessed with the SF-36 (0-100), with 6 points (12%) as the MCID.
The researchers identified trials on knee osteoarthritis that included an overall 6,508 participants with an average age ranging from 52 to 83 years. A total of 36 studies evaluated electrophysical agents. Another seven looked at manual therapies; four looked at acupuncture/dry needling or taping; three looked at psychological, dietary, or “whole body vibration” therapies; and two evaluated spa or peloid therapy. Only one trial evaluated foot insoles.
Nearly all the studies (98%) assessed pain, and most (87%) assessed physical function. Only about one in five (21%) assessed quality of life. The improvement in pain from adding adjunctive therapies to exercise, compared with placebo therapies plus exercise, was 0.77 points, or just under a 10% improvement, which fell short of the 15% MCID. Physical function improvement similarly fell short, with an average improvement of 5 points (12%).
In comparisons of exercise plus adjunctive therapies against exercise alone, the improvement from the additional interventions was even lower. Pain improvement was 0.41 points (7%), and physical function improvement was 2.8 points (9%). However, patients’ perceptions told a different story: 37% more patients who were using an adjunctive therapy reported feeling that the therapies were successful, compared with patients undergoing exercise therapy alone.
Adverse events were poorly reported in the trials, with only 10 trials reporting them at all, and the researchers found no significant difference in adverse events among the studies reporting them. The most common adverse events were increased pain in the joint with the osteoarthritis, pain elsewhere, or swelling and inflammation. It’s unclear, however, whether the pain, swelling, and inflammation were related to the interventions and how serious these effects might have been.
Michelle Hall, PhD, an associate professor in the department of physiotherapy at the University of Melbourne, comoderated the session with this presentation and found it interesting that more than one-third of patients perceived that they did better with the additional therapies even though improvement didn’t bear out in their pain or physical function assessments.
“But the other part of that was that the studies were of poor quality, so we can’t say with confidence, ‘Don’t do this therapy because it’s not going to work,’ ” Dr. Hall said in an interview. She said she personally would probably discourage patients from those therapies, “but I don’t think the evidence is there for everybody to do that,” she added.
Martin Van Der Esch, PhD, of Reade Centre of Rehabilitation and Rheumatology in Amsterdam, also comoderated the discussion and had more concerns about the use of adjunctive therapies in light of the study’s findings. He said in an interview that he tended to believe the patients’ overall self-reported improvement is likely a placebo effect, and he sees potential harm in that effect. If the pain is not truly decreasing as patients continue using those therapies, then the pain may become a more stable part of the nervous system, “so I think they need to do an intervention which really has evidence in reducing pain, an active approach that means exercising in the right way,” Dr. Van Der Esch said. If patients are undergoing therapy whose primary benefit is a placebo effect, “the pain will prolong and become more fixed in the nervous system,” shifting the patients toward greater risk of the pain becoming chronic, he said.
“I want to emphasize that we have an ethical role to our management, and it’s not ethical to give treatments which have no response and no pain relief except that the patient or the professional believes it will have an effect,” Dr. Van Der Esch said.
The research did not involve outside funding. Dr. French, Dr. Hall, and Dr. Van Der Esch reported having no relevant financial relationships.
DENVER – Adding therapies such as acupuncture, electrophysical stimulation, or other interventions to standard exercise therapy does not appear to offer much benefit in pain relief or physical function for patients with knee osteoarthritis, according to a study presented at the OARSI 2023 World Congress. The findings were also published in the Cochrane Database of Systematic Reviews in October 2022.
“The results do not support the use of adjunctive therapies when we add them to exercise for pain, physical function, or quality of life, when compared against placebo, adjunctive therapy, and exercise,” Helen P. French, PhD, told attendees at the meeting sponsored by the Osteoarthritis Research Society International. The findings were similar for pain and physical function when comparing adjunctive therapies with exercise against exercise alone, said Dr. French, an associate professor in physiotherapy at the Royal College of Surgeons, Dublin, except that patients using adjunctive therapies reported feeling greater improvement in their global assessments.
Exercise is recommended as a core treatment for osteoarthritis, but some patients or clinicians may be interested in supplementing that therapy with acupuncture, heat therapy, electromagnetic fields, transcutaneous electrical nerve stimulation, braces/orthotics, and other interventions. Various Cochrane Reviews of the evidence exist for these interventions in treating chronic pain in general but not for their use as adjunctive therapies in addition to exercise for osteoarthritis pain.
Researchers therefore assessed the evidence for improvement in pain, physical function, and quality of life for two sets of comparisons: adjunctive therapies plus exercise versus exercise alone, and adjunctive therapies with exercise versus placebo adjunctive therapy with exercise. The review excluded studies looking at medications or supplements.
Pain was assessed with the Numeric Pain Rating Scale (NPRS, 0-10), with an improvement of at least 2 points (15% improvement) representing the minimum clinically important difference (MCID). Physical function was assessed with the Western Ontario and McMaster Universities Arthritis Index (WOMAC, 0-68), with 6 points (15%) considered the MCID, and quality of life was assessed with the SF-36 (0-100), with 6 points (12%) as the MCID.
The researchers identified trials on knee osteoarthritis that included an overall 6,508 participants with an average age ranging from 52 to 83 years. A total of 36 studies evaluated electrophysical agents. Another seven looked at manual therapies; four looked at acupuncture/dry needling or taping; three looked at psychological, dietary, or “whole body vibration” therapies; and two evaluated spa or peloid therapy. Only one trial evaluated foot insoles.
Nearly all the studies (98%) assessed pain, and most (87%) assessed physical function. Only about one in five (21%) assessed quality of life. The improvement in pain from adding adjunctive therapies to exercise, compared with placebo therapies plus exercise, was 0.77 points, or just under a 10% improvement, which fell short of the 15% MCID. Physical function improvement similarly fell short, with an average improvement of 5 points (12%).
In comparisons of exercise plus adjunctive therapies against exercise alone, the improvement from the additional interventions was even lower. Pain improvement was 0.41 points (7%), and physical function improvement was 2.8 points (9%). However, patients’ perceptions told a different story: 37% more patients who were using an adjunctive therapy reported feeling that the therapies were successful, compared with patients undergoing exercise therapy alone.
Adverse events were poorly reported in the trials, with only 10 trials reporting them at all, and the researchers found no significant difference in adverse events among the studies reporting them. The most common adverse events were increased pain in the joint with the osteoarthritis, pain elsewhere, or swelling and inflammation. It’s unclear, however, whether the pain, swelling, and inflammation were related to the interventions and how serious these effects might have been.
Michelle Hall, PhD, an associate professor in the department of physiotherapy at the University of Melbourne, comoderated the session with this presentation and found it interesting that more than one-third of patients perceived that they did better with the additional therapies even though improvement didn’t bear out in their pain or physical function assessments.
“But the other part of that was that the studies were of poor quality, so we can’t say with confidence, ‘Don’t do this therapy because it’s not going to work,’ ” Dr. Hall said in an interview. She said she personally would probably discourage patients from those therapies, “but I don’t think the evidence is there for everybody to do that,” she added.
Martin Van Der Esch, PhD, of Reade Centre of Rehabilitation and Rheumatology in Amsterdam, also comoderated the discussion and had more concerns about the use of adjunctive therapies in light of the study’s findings. He said in an interview that he tended to believe the patients’ overall self-reported improvement is likely a placebo effect, and he sees potential harm in that effect. If the pain is not truly decreasing as patients continue using those therapies, then the pain may become a more stable part of the nervous system, “so I think they need to do an intervention which really has evidence in reducing pain, an active approach that means exercising in the right way,” Dr. Van Der Esch said. If patients are undergoing therapy whose primary benefit is a placebo effect, “the pain will prolong and become more fixed in the nervous system,” shifting the patients toward greater risk of the pain becoming chronic, he said.
“I want to emphasize that we have an ethical role to our management, and it’s not ethical to give treatments which have no response and no pain relief except that the patient or the professional believes it will have an effect,” Dr. Van Der Esch said.
The research did not involve outside funding. Dr. French, Dr. Hall, and Dr. Van Der Esch reported having no relevant financial relationships.
AT OARSI 2023
Commotio cordis underrecognized, undertreated outside of sports
Sudden cardiac arrest (SCA) due to commotio cordis occurs more frequently in non–sport-related settings than is commonly thought, resulting in lower rates of resuscitation and increased mortality, especially among young women, a new review suggests.
The condition is rare, caused by an often fatal arrhythmia secondary to a blunt, nonpenetrating impact over the precordium, without direct structural damage to the heart itself. Common causes in nonsport settings include assault, motor vehicle accidents (MVAs), and daily activities such as occupational accidents.
“We found a stark difference in mortality outcomes between non–sport-related commotio cordis compared to sport-related events,” at 88% vs. 66%, Han S. Lim, MBBS, PhD, of the University of Melbourne, and Austin Health, Heidelberg, Australia, told this news organization. “Rates of cardiopulmonary resuscitation (CPR) (27% vs. 97%) and defibrillation (17% vs. 81%) were considerably lower in the non–sport-related events.”
“Although still being male-predominant, of concern, we saw a higher proportion of females in non–sport-related commotio cordis due to assault, MVAs, and other activities,” he noted. Such events may occur “in secluded domestic settings, may not be witnessed, or may occur as intentional harm, whereby the witness could also be the perpetrator, reducing the likelihood of prompt diagnosis, CPR, and defibrillation administration.”
The study was published online in JACC: Clinical Electrophysiology.
Young women affected
Dr. Lim and colleagues searched the literature through 2021 for all cases of commotio cordis. Three hundred and thirty-four cases from among 53 citations were included in the analysis; of those, 121 (36%) occurred in non–sport-related settings, including assault (76%), MVAs (7%), and daily activities (16%). “Daily activities” comprised activities that were expected in a person’s day-to-day routine such as falls, play fighting (in children), and occupational accidents.
Non–sport-related cases primarily involved nonprojectile etiologies (95%), including bodily contact (79%), such as impacts from fists, feet, and knees; impacts with handlebars or steering wheels; and solid stick-like weapons and flat surfaces.
Sport-related cases involved a significantly higher proportion of projectiles (94% vs. 5%) and occurred across a range of sports, mostly at the competitive level (66%).
Both sport-related and non–sport-related commotio cordis affected a similar younger demographic (mean age, 19; mostly males). No statistically significant differences between the two groups were seen with regard to previous cardiac history or family history of cardiac disease, or in arrhythmias on electrocardiogram, biomarkers, or imaging findings.
However, in non–sport-related events, the proportion of females affected was significantly higher (13% vs. 2%), as was mortality (88% vs. 66%). Rates were lower for CPR (27% vs. 97%) and defibrillation use (17% vs. 81%), and resuscitation was more commonly delayed beyond 3 minutes (80% vs. 5%).
The finding that more than a third of reported cases were non–sport-related “is higher than previously reported, and included data from 15 different countries,” the authors noted.
Study limitations included the use of data only from published studies, inclusion of a case series limited to fatal cases, small sample sizes, and lack of consistent reporting of demographic data, mechanisms, investigation results, management, and outcomes.
Increased awareness ‘essential’
Dr. Lim and colleagues concluded that increased awareness of non–sport-related commotio cordis is “essential” for early recognition, resuscitation, and mortality reduction.
Jim Cheung, MD, chair of the American College of Cardiology’s electrophysiology section, “completely agrees.” Greater awareness among the general population could reduce barriers to CPR and automated external defibrillator (AED) use, he said, which in turn, can lead to improved survival.
Furthermore, Dr. Cheung added, “This study underscores the importance of ensuring that non–cardiology-trained physicians such as emergency medicine physicians and trauma surgeons who might encounter patients with non–sports-related commotio cordis recognize the entity during the course of treatment.”
Because the review relied only on published cases, “it may not represent the true breadth of cases that are occurring in the real world,” he noted. “I suspect that cases that occur outside of sports-related activities, such as MVAs and assault, are more likely to be underreported and that the true proportion of non–sports-related commotio cordis may be significantly higher than 36%.” Increased reporting of cases as part of an international commotio cordis registry would help provide additional insights, he suggested.
“There is a common misperception that SCA only occurs among older patients and patients with known coronary artery disease or heart failure,” he said. “For us to move the needle on improving SCA survival, we will need to tackle the problem from multiple angles including increasing public awareness, training the public on CPR and AED use, and improving access to AEDs by addressing structural barriers.”
Dr. Cheung pointed to ongoing efforts by nonprofit, patient-driven organizations such as the SADS Foundation and Omar Carter Foundation, and professional societies such as the American College of Cardiology, the American Heart Association, and Heart Rhythm Society, to direct public awareness campaigns and legislative proposals to address this problem.
Similar efforts are underway among cardiac societies and SCA awareness groups in Australia, Dr. Lim said.
No funding or relevant financial relationships were disclosed.
A version of this article first appeared on Medscape.com.
Sudden cardiac arrest (SCA) due to commotio cordis occurs more frequently in non–sport-related settings than is commonly thought, resulting in lower rates of resuscitation and increased mortality, especially among young women, a new review suggests.
The condition is rare, caused by an often fatal arrhythmia secondary to a blunt, nonpenetrating impact over the precordium, without direct structural damage to the heart itself. Common causes in nonsport settings include assault, motor vehicle accidents (MVAs), and daily activities such as occupational accidents.
“We found a stark difference in mortality outcomes between non–sport-related commotio cordis compared to sport-related events,” at 88% vs. 66%, Han S. Lim, MBBS, PhD, of the University of Melbourne, and Austin Health, Heidelberg, Australia, told this news organization. “Rates of cardiopulmonary resuscitation (CPR) (27% vs. 97%) and defibrillation (17% vs. 81%) were considerably lower in the non–sport-related events.”
“Although still being male-predominant, of concern, we saw a higher proportion of females in non–sport-related commotio cordis due to assault, MVAs, and other activities,” he noted. Such events may occur “in secluded domestic settings, may not be witnessed, or may occur as intentional harm, whereby the witness could also be the perpetrator, reducing the likelihood of prompt diagnosis, CPR, and defibrillation administration.”
The study was published online in JACC: Clinical Electrophysiology.
Young women affected
Dr. Lim and colleagues searched the literature through 2021 for all cases of commotio cordis. Three hundred and thirty-four cases from among 53 citations were included in the analysis; of those, 121 (36%) occurred in non–sport-related settings, including assault (76%), MVAs (7%), and daily activities (16%). “Daily activities” comprised activities that were expected in a person’s day-to-day routine such as falls, play fighting (in children), and occupational accidents.
Non–sport-related cases primarily involved nonprojectile etiologies (95%), including bodily contact (79%), such as impacts from fists, feet, and knees; impacts with handlebars or steering wheels; and solid stick-like weapons and flat surfaces.
Sport-related cases involved a significantly higher proportion of projectiles (94% vs. 5%) and occurred across a range of sports, mostly at the competitive level (66%).
Both sport-related and non–sport-related commotio cordis affected a similar younger demographic (mean age, 19; mostly males). No statistically significant differences between the two groups were seen with regard to previous cardiac history or family history of cardiac disease, or in arrhythmias on electrocardiogram, biomarkers, or imaging findings.
However, in non–sport-related events, the proportion of females affected was significantly higher (13% vs. 2%), as was mortality (88% vs. 66%). Rates were lower for CPR (27% vs. 97%) and defibrillation use (17% vs. 81%), and resuscitation was more commonly delayed beyond 3 minutes (80% vs. 5%).
The finding that more than a third of reported cases were non–sport-related “is higher than previously reported, and included data from 15 different countries,” the authors noted.
Study limitations included the use of data only from published studies, inclusion of a case series limited to fatal cases, small sample sizes, and lack of consistent reporting of demographic data, mechanisms, investigation results, management, and outcomes.
Increased awareness ‘essential’
Dr. Lim and colleagues concluded that increased awareness of non–sport-related commotio cordis is “essential” for early recognition, resuscitation, and mortality reduction.
Jim Cheung, MD, chair of the American College of Cardiology’s electrophysiology section, “completely agrees.” Greater awareness among the general population could reduce barriers to CPR and automated external defibrillator (AED) use, he said, which in turn, can lead to improved survival.
Furthermore, Dr. Cheung added, “This study underscores the importance of ensuring that non–cardiology-trained physicians such as emergency medicine physicians and trauma surgeons who might encounter patients with non–sports-related commotio cordis recognize the entity during the course of treatment.”
Because the review relied only on published cases, “it may not represent the true breadth of cases that are occurring in the real world,” he noted. “I suspect that cases that occur outside of sports-related activities, such as MVAs and assault, are more likely to be underreported and that the true proportion of non–sports-related commotio cordis may be significantly higher than 36%.” Increased reporting of cases as part of an international commotio cordis registry would help provide additional insights, he suggested.
“There is a common misperception that SCA only occurs among older patients and patients with known coronary artery disease or heart failure,” he said. “For us to move the needle on improving SCA survival, we will need to tackle the problem from multiple angles including increasing public awareness, training the public on CPR and AED use, and improving access to AEDs by addressing structural barriers.”
Dr. Cheung pointed to ongoing efforts by nonprofit, patient-driven organizations such as the SADS Foundation and Omar Carter Foundation, and professional societies such as the American College of Cardiology, the American Heart Association, and Heart Rhythm Society, to direct public awareness campaigns and legislative proposals to address this problem.
Similar efforts are underway among cardiac societies and SCA awareness groups in Australia, Dr. Lim said.
No funding or relevant financial relationships were disclosed.
A version of this article first appeared on Medscape.com.
Sudden cardiac arrest (SCA) due to commotio cordis occurs more frequently in non–sport-related settings than is commonly thought, resulting in lower rates of resuscitation and increased mortality, especially among young women, a new review suggests.
The condition is rare, caused by an often fatal arrhythmia secondary to a blunt, nonpenetrating impact over the precordium, without direct structural damage to the heart itself. Common causes in nonsport settings include assault, motor vehicle accidents (MVAs), and daily activities such as occupational accidents.
“We found a stark difference in mortality outcomes between non–sport-related commotio cordis compared to sport-related events,” at 88% vs. 66%, Han S. Lim, MBBS, PhD, of the University of Melbourne, and Austin Health, Heidelberg, Australia, told this news organization. “Rates of cardiopulmonary resuscitation (CPR) (27% vs. 97%) and defibrillation (17% vs. 81%) were considerably lower in the non–sport-related events.”
“Although still being male-predominant, of concern, we saw a higher proportion of females in non–sport-related commotio cordis due to assault, MVAs, and other activities,” he noted. Such events may occur “in secluded domestic settings, may not be witnessed, or may occur as intentional harm, whereby the witness could also be the perpetrator, reducing the likelihood of prompt diagnosis, CPR, and defibrillation administration.”
The study was published online in JACC: Clinical Electrophysiology.
Young women affected
Dr. Lim and colleagues searched the literature through 2021 for all cases of commotio cordis. Three hundred and thirty-four cases from among 53 citations were included in the analysis; of those, 121 (36%) occurred in non–sport-related settings, including assault (76%), MVAs (7%), and daily activities (16%). “Daily activities” comprised activities that were expected in a person’s day-to-day routine such as falls, play fighting (in children), and occupational accidents.
Non–sport-related cases primarily involved nonprojectile etiologies (95%), including bodily contact (79%), such as impacts from fists, feet, and knees; impacts with handlebars or steering wheels; and solid stick-like weapons and flat surfaces.
Sport-related cases involved a significantly higher proportion of projectiles (94% vs. 5%) and occurred across a range of sports, mostly at the competitive level (66%).
Both sport-related and non–sport-related commotio cordis affected a similar younger demographic (mean age, 19; mostly males). No statistically significant differences between the two groups were seen with regard to previous cardiac history or family history of cardiac disease, or in arrhythmias on electrocardiogram, biomarkers, or imaging findings.
However, in non–sport-related events, the proportion of females affected was significantly higher (13% vs. 2%), as was mortality (88% vs. 66%). Rates were lower for CPR (27% vs. 97%) and defibrillation use (17% vs. 81%), and resuscitation was more commonly delayed beyond 3 minutes (80% vs. 5%).
The finding that more than a third of reported cases were non–sport-related “is higher than previously reported, and included data from 15 different countries,” the authors noted.
Study limitations included the use of data only from published studies, inclusion of a case series limited to fatal cases, small sample sizes, and lack of consistent reporting of demographic data, mechanisms, investigation results, management, and outcomes.
Increased awareness ‘essential’
Dr. Lim and colleagues concluded that increased awareness of non–sport-related commotio cordis is “essential” for early recognition, resuscitation, and mortality reduction.
Jim Cheung, MD, chair of the American College of Cardiology’s electrophysiology section, “completely agrees.” Greater awareness among the general population could reduce barriers to CPR and automated external defibrillator (AED) use, he said, which in turn, can lead to improved survival.
Furthermore, Dr. Cheung added, “This study underscores the importance of ensuring that non–cardiology-trained physicians such as emergency medicine physicians and trauma surgeons who might encounter patients with non–sports-related commotio cordis recognize the entity during the course of treatment.”
Because the review relied only on published cases, “it may not represent the true breadth of cases that are occurring in the real world,” he noted. “I suspect that cases that occur outside of sports-related activities, such as MVAs and assault, are more likely to be underreported and that the true proportion of non–sports-related commotio cordis may be significantly higher than 36%.” Increased reporting of cases as part of an international commotio cordis registry would help provide additional insights, he suggested.
“There is a common misperception that SCA only occurs among older patients and patients with known coronary artery disease or heart failure,” he said. “For us to move the needle on improving SCA survival, we will need to tackle the problem from multiple angles including increasing public awareness, training the public on CPR and AED use, and improving access to AEDs by addressing structural barriers.”
Dr. Cheung pointed to ongoing efforts by nonprofit, patient-driven organizations such as the SADS Foundation and Omar Carter Foundation, and professional societies such as the American College of Cardiology, the American Heart Association, and Heart Rhythm Society, to direct public awareness campaigns and legislative proposals to address this problem.
Similar efforts are underway among cardiac societies and SCA awareness groups in Australia, Dr. Lim said.
No funding or relevant financial relationships were disclosed.
A version of this article first appeared on Medscape.com.
FROM JACC: CLINICAL ELECTROPHYSIOLOGY
Plant-based diets not always healthy; quality is key
The prospective cohort study used data from more than 120,000 middle-aged adults followed for over 10 years in the UK Biobank. Those who consumed a healthful plant-based diet – with higher amounts of foods such as fruits, vegetables, legumes, whole grains, and nuts – and lower intakes of animal products, sugary drinks, and refined grains had a 16% lower risk of dying during follow-up, compared with those with the lowest intakes of the healthful plant-based foods.
By contrast, an unhealthy plant-based diet was associated with a 23% higher total mortality risk.
“Not all plant-based diets are created equally. Our data provide evidence to support the notion that for health benefits the plant-based sources need to be whole grains, fruits and vegetables, legumes, nuts, etc., rather than processed plant-based foods,” study coauthor Aedín Cassidy, PhD, of Queen’s University, Belfast, Northern Ireland, said in an interview.
She added: “We do not necessarily need to radically shift diets to vegan or vegetarian regimens, but rather to switch proportions on the plate to incorporate more healthful plant-based foods, fish, and leaner cuts of meat into our habitual diet. This would have benefits for both individual health and planetary health.”
The findings were published online in JAMA Network Open by Alysha S. Thompson, MSc, also at Queen’s University, and colleagues.
High- vs. low-quality plant-based diets linked to better outcomes
The UK Biobank is a population-based, prospective study that included more than 500,000 participants aged 40-69 years at the time of recruitment between 2006 and 2010 at 22 centers in England, Scotland, and Wales. The current study included 126,395 individuals; slightly over half (55.9%) are women.
Food intake data were collected for at least two 24-hour periods to create both “healthful” and “unhealthful” plant-based diet indexes (PDIs). These included 17 food groups: whole grains, fruits, vegetables, nuts, legumes and vegetarian protein alternatives, tea and coffee, fruit juices, refined grains, potatoes, sugar-sweetened beverages, sweets and desserts, animal fat, dairy, eggs, fish or seafood, meat, and miscellaneous animal-derived foods. Data on oils weren’t available.
Higher scores on the healthful PDI and unhealthful PDI were scored positively or negatively based on quantities of those foods consumed.
Participants were then ranked in quartiles for portions of each food group and assigned scores between 2 (lowest-intake category) and 5 (highest).
During a follow-up of 10.6-12.2 years, there were 698 deaths attributed to cardiovascular disease, 3,275 deaths caused by cancer, 6,890 individuals who experienced a cardiovascular incident, and 8,939 with incident cancer.
Another 4,751 experienced an incident fracture, which was evaluated because of the concern that diets low in animal protein might lead to insufficient vitamin B and calcium intake.
After adjustment for confounding factors, the hazard ratio for all-cause mortality in individuals with the highest healthful PDI score quartile compared with the lowest quartile was 0.84.
At the same time, the HR for all-cause mortality for those with the highest versus lowest unhealthful PDI scores was 1.23, and for cancer-related mortality was 1.19. All were statistically significant (P = .004).
Similarly, greater healthy plant-based diet adherence was associated with a significantly lower risk of being diagnosed with any cancer (HR, 0.93; P = .03), while higher unhealthful PDI scores yielded a higher risk (HR, 1.10; P = .004).
Moreover, higher healthy PDI scores were associated with lower risks for total cardiovascular incident risks (HR, 0.92; P = .007), as well as for the individual events of ischemic stroke (HR, 0.84; P = .08) and MI (HR, 0.86; P = .004). Higher unhealthy PDI scores were similarly associated with greater risks for those outcomes, with an overall HR of 1.21 (P = .004).
No associations were found between either healthful PDI or unhealthful PDI and total or site-specific fracture risk.
And because 91.3% of the UK Biobank study population was White, “future studies among more racially, ethnically, and culturally diverse populations are needed to assess the risk of major chronic disease in relation to [plant-based diets],” the authors wrote.
Dr. Cassidy and Ms. Thompson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The prospective cohort study used data from more than 120,000 middle-aged adults followed for over 10 years in the UK Biobank. Those who consumed a healthful plant-based diet – with higher amounts of foods such as fruits, vegetables, legumes, whole grains, and nuts – and lower intakes of animal products, sugary drinks, and refined grains had a 16% lower risk of dying during follow-up, compared with those with the lowest intakes of the healthful plant-based foods.
By contrast, an unhealthy plant-based diet was associated with a 23% higher total mortality risk.
“Not all plant-based diets are created equally. Our data provide evidence to support the notion that for health benefits the plant-based sources need to be whole grains, fruits and vegetables, legumes, nuts, etc., rather than processed plant-based foods,” study coauthor Aedín Cassidy, PhD, of Queen’s University, Belfast, Northern Ireland, said in an interview.
She added: “We do not necessarily need to radically shift diets to vegan or vegetarian regimens, but rather to switch proportions on the plate to incorporate more healthful plant-based foods, fish, and leaner cuts of meat into our habitual diet. This would have benefits for both individual health and planetary health.”
The findings were published online in JAMA Network Open by Alysha S. Thompson, MSc, also at Queen’s University, and colleagues.
High- vs. low-quality plant-based diets linked to better outcomes
The UK Biobank is a population-based, prospective study that included more than 500,000 participants aged 40-69 years at the time of recruitment between 2006 and 2010 at 22 centers in England, Scotland, and Wales. The current study included 126,395 individuals; slightly over half (55.9%) are women.
Food intake data were collected for at least two 24-hour periods to create both “healthful” and “unhealthful” plant-based diet indexes (PDIs). These included 17 food groups: whole grains, fruits, vegetables, nuts, legumes and vegetarian protein alternatives, tea and coffee, fruit juices, refined grains, potatoes, sugar-sweetened beverages, sweets and desserts, animal fat, dairy, eggs, fish or seafood, meat, and miscellaneous animal-derived foods. Data on oils weren’t available.
Higher scores on the healthful PDI and unhealthful PDI were scored positively or negatively based on quantities of those foods consumed.
Participants were then ranked in quartiles for portions of each food group and assigned scores between 2 (lowest-intake category) and 5 (highest).
During a follow-up of 10.6-12.2 years, there were 698 deaths attributed to cardiovascular disease, 3,275 deaths caused by cancer, 6,890 individuals who experienced a cardiovascular incident, and 8,939 with incident cancer.
Another 4,751 experienced an incident fracture, which was evaluated because of the concern that diets low in animal protein might lead to insufficient vitamin B and calcium intake.
After adjustment for confounding factors, the hazard ratio for all-cause mortality in individuals with the highest healthful PDI score quartile compared with the lowest quartile was 0.84.
At the same time, the HR for all-cause mortality for those with the highest versus lowest unhealthful PDI scores was 1.23, and for cancer-related mortality was 1.19. All were statistically significant (P = .004).
Similarly, greater healthy plant-based diet adherence was associated with a significantly lower risk of being diagnosed with any cancer (HR, 0.93; P = .03), while higher unhealthful PDI scores yielded a higher risk (HR, 1.10; P = .004).
Moreover, higher healthy PDI scores were associated with lower risks for total cardiovascular incident risks (HR, 0.92; P = .007), as well as for the individual events of ischemic stroke (HR, 0.84; P = .08) and MI (HR, 0.86; P = .004). Higher unhealthy PDI scores were similarly associated with greater risks for those outcomes, with an overall HR of 1.21 (P = .004).
No associations were found between either healthful PDI or unhealthful PDI and total or site-specific fracture risk.
And because 91.3% of the UK Biobank study population was White, “future studies among more racially, ethnically, and culturally diverse populations are needed to assess the risk of major chronic disease in relation to [plant-based diets],” the authors wrote.
Dr. Cassidy and Ms. Thompson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The prospective cohort study used data from more than 120,000 middle-aged adults followed for over 10 years in the UK Biobank. Those who consumed a healthful plant-based diet – with higher amounts of foods such as fruits, vegetables, legumes, whole grains, and nuts – and lower intakes of animal products, sugary drinks, and refined grains had a 16% lower risk of dying during follow-up, compared with those with the lowest intakes of the healthful plant-based foods.
By contrast, an unhealthy plant-based diet was associated with a 23% higher total mortality risk.
“Not all plant-based diets are created equally. Our data provide evidence to support the notion that for health benefits the plant-based sources need to be whole grains, fruits and vegetables, legumes, nuts, etc., rather than processed plant-based foods,” study coauthor Aedín Cassidy, PhD, of Queen’s University, Belfast, Northern Ireland, said in an interview.
She added: “We do not necessarily need to radically shift diets to vegan or vegetarian regimens, but rather to switch proportions on the plate to incorporate more healthful plant-based foods, fish, and leaner cuts of meat into our habitual diet. This would have benefits for both individual health and planetary health.”
The findings were published online in JAMA Network Open by Alysha S. Thompson, MSc, also at Queen’s University, and colleagues.
High- vs. low-quality plant-based diets linked to better outcomes
The UK Biobank is a population-based, prospective study that included more than 500,000 participants aged 40-69 years at the time of recruitment between 2006 and 2010 at 22 centers in England, Scotland, and Wales. The current study included 126,395 individuals; slightly over half (55.9%) are women.
Food intake data were collected for at least two 24-hour periods to create both “healthful” and “unhealthful” plant-based diet indexes (PDIs). These included 17 food groups: whole grains, fruits, vegetables, nuts, legumes and vegetarian protein alternatives, tea and coffee, fruit juices, refined grains, potatoes, sugar-sweetened beverages, sweets and desserts, animal fat, dairy, eggs, fish or seafood, meat, and miscellaneous animal-derived foods. Data on oils weren’t available.
Higher scores on the healthful PDI and unhealthful PDI were scored positively or negatively based on quantities of those foods consumed.
Participants were then ranked in quartiles for portions of each food group and assigned scores between 2 (lowest-intake category) and 5 (highest).
During a follow-up of 10.6-12.2 years, there were 698 deaths attributed to cardiovascular disease, 3,275 deaths caused by cancer, 6,890 individuals who experienced a cardiovascular incident, and 8,939 with incident cancer.
Another 4,751 experienced an incident fracture, which was evaluated because of the concern that diets low in animal protein might lead to insufficient vitamin B and calcium intake.
After adjustment for confounding factors, the hazard ratio for all-cause mortality in individuals with the highest healthful PDI score quartile compared with the lowest quartile was 0.84.
At the same time, the HR for all-cause mortality for those with the highest versus lowest unhealthful PDI scores was 1.23, and for cancer-related mortality was 1.19. All were statistically significant (P = .004).
Similarly, greater healthy plant-based diet adherence was associated with a significantly lower risk of being diagnosed with any cancer (HR, 0.93; P = .03), while higher unhealthful PDI scores yielded a higher risk (HR, 1.10; P = .004).
Moreover, higher healthy PDI scores were associated with lower risks for total cardiovascular incident risks (HR, 0.92; P = .007), as well as for the individual events of ischemic stroke (HR, 0.84; P = .08) and MI (HR, 0.86; P = .004). Higher unhealthy PDI scores were similarly associated with greater risks for those outcomes, with an overall HR of 1.21 (P = .004).
No associations were found between either healthful PDI or unhealthful PDI and total or site-specific fracture risk.
And because 91.3% of the UK Biobank study population was White, “future studies among more racially, ethnically, and culturally diverse populations are needed to assess the risk of major chronic disease in relation to [plant-based diets],” the authors wrote.
Dr. Cassidy and Ms. Thompson reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
One or two high-step days may reduce mortality risks
Taking 8,000 steps or more for just 1 or 2 days a week was linked to a significant reduction in all-cause and cardiovascular mortality, according to a study of about 3,000 adults.
Previous research has shown lower mortality rates among individuals who walk consistently, especially those who log at least 8,000 steps daily, but the benefit of intense walking just once or twice a week on long-term health outcomes has not been examined, wrote Kosuke Inoue, MD, of Kyoto University, Japan, and colleagues.
In a study published in JAMA Network Open, the researchers reviewed 10-year follow-up data for 3,101 adults aged 20 years and older who were part of the 2005 and 2006 National Health and Nutrition Examination Survey (NHANES).
The participants were asked to wear accelerometers to track their steps for 7 consecutive days. The researchers assessed the dose-response relationship between days of taking 8,000 steps or more (about 4 miles) during 1 week, and the primary outcome of all-cause mortality risk after 10 years. Cardiovascular mortality risk after 10 years was a secondary outcome.
The mean age of the participants was 50.5 years and 51% were women. The breakdown by ethnicity was 51% White, 21% Black, 24% Hispanic, and 4% other races/ethnicities. A total of 632 individuals took 8,000 steps or more 0 days a week, 532 took at least 8,000 steps 1-2 days per week, and 1,937 took at least 8,000 steps 3-7 days a week.
During the 10-year follow-up period, overall all-cause mortality was 14.2% and cardiovascular mortality was 5.3% across all step groups.
In an adjusted analysis, individuals who took at least 8,000 steps 1-2 days a week had a 14.9% lower all-cause mortality risk compared with those who never reached 8,000 daily steps. This difference was similar to the 16.5% reduced mortality risk for those who took at least 8,000 steps 3-7 days a week.
Similarly, compared with the group with no days of at least 8,000 steps, cardiovascular mortality risk was 8.1% lower for those who took 8,000 steps 1-2 days per week and 8.4% lower for those who took at least 8,000 steps 3-7 days per week. The decreased mortality risk plateaued at 3-4 days.
These patterns in reduced all-cause mortality risk persisted in a stratified analysis by age (younger than 65 years and 65 years and older) and sex. Similar patterns in reduced mortality also emerged when the researchers used different thresholds of daily steps, such as a minimum of 10,000 steps instead of 8,000. The adjusted all-cause mortality for groups who took at least 10,000 steps 1-2 days a week, 3-7 days a week, and no days a week were 8.1%, 7.3%, and 16.7%, respectively, with corresponding cardiovascular mortality risks of 2.4%, 2.3%, and 7.0%, respectively.
“Given the simplicity and ease of counting daily steps, our findings indicate that the recommended number of steps taken on as few as 1 to 2 days per week may be a feasible option for individuals who are striving to achieve some health benefits through adhering to a recommended daily step count but are unable to accomplish this on a daily basis,” the researchers wrote in their discussion.
The findings were limited by several factors including the use daily step measures for 1 week only at baseline, with no data on how physical activity changes might impact mortality risk, the researchers noted. Other limitations included possible accelerometer error and misclassification of activity, possible selection bias, and lack of data on cause-specific mortality outside of cardiovascular death, they said.
However, the results were strengthened by the use of accelerometers as objective measures of activity and by the availability of 10-year follow-up data for nearly 100% of the participants, they said.
“Although our findings might suffer from residual confounding that should be addressed in future research, they suggest that people may receive substantial health benefits even if a sufficient number of steps are taken on only a couple days of the week,” they concluded.
Proceed with caution
The current study findings should be interpreted cautiously in light of the potential unmeasured confounding factors and selection bias that often occur in studies of physical activity, James Sawalla Guseh, MD, of Massachusetts General Hospital, and Jose F. Figueroa, MD, of Harvard T.H. Chan School of Public Health, Boston, wrote in an accompanying editorial.
The results support previous studies showing some longevity benefits with “weekend warrior” patterns of intense physical activity for only a couple of days; however, “the body of evidence for sporadic activity is not as robust as the evidence for sustained and regular aerobic activity,” the authors emphasized.
The editorial authors also highlighted the limitations of the current study, including the observational design and significant differences in demographics and comorbidities between the 1- to 2-days of 8,000 steps exercise group and the 0-day group, as well as the reliance on only a week’s worth of data to infer 10 years’ mortality.
Although the data are consistent with previous observations that increased exercise volume reduces mortality, more research is needed, as the current study findings may not reflect other dimensions of health, including neurological health, they said.
Despite the need for cautious interpretation of the results, the current study “supports the emerging and popular idea that step counting, which does not require consideration of exercise duration or intensity, can offer guidance toward robust and favorable health outcomes,” and may inform step-based activity goals to improve public health, the editorialists wrote.
The study was supported by the Japan Agency for Medical Research and Development, the Japan Society for the Promotion of Science, the Japan Endocrine Society, and the Meiji Yasuda Life Foundation of Health and Welfare. Dr. Inoue also was supported by the Program for the Development of Next-Generation Leading Scientists With Global Insight sponsored by the Ministry of Education, Culture, Sports, Science and Technology, Japan. The other researchers had no relevant financial conflicts to disclose. The editorial authors had no financial conflicts to disclose.
Taking 8,000 steps or more for just 1 or 2 days a week was linked to a significant reduction in all-cause and cardiovascular mortality, according to a study of about 3,000 adults.
Previous research has shown lower mortality rates among individuals who walk consistently, especially those who log at least 8,000 steps daily, but the benefit of intense walking just once or twice a week on long-term health outcomes has not been examined, wrote Kosuke Inoue, MD, of Kyoto University, Japan, and colleagues.
In a study published in JAMA Network Open, the researchers reviewed 10-year follow-up data for 3,101 adults aged 20 years and older who were part of the 2005 and 2006 National Health and Nutrition Examination Survey (NHANES).
The participants were asked to wear accelerometers to track their steps for 7 consecutive days. The researchers assessed the dose-response relationship between days of taking 8,000 steps or more (about 4 miles) during 1 week, and the primary outcome of all-cause mortality risk after 10 years. Cardiovascular mortality risk after 10 years was a secondary outcome.
The mean age of the participants was 50.5 years and 51% were women. The breakdown by ethnicity was 51% White, 21% Black, 24% Hispanic, and 4% other races/ethnicities. A total of 632 individuals took 8,000 steps or more 0 days a week, 532 took at least 8,000 steps 1-2 days per week, and 1,937 took at least 8,000 steps 3-7 days a week.
During the 10-year follow-up period, overall all-cause mortality was 14.2% and cardiovascular mortality was 5.3% across all step groups.
In an adjusted analysis, individuals who took at least 8,000 steps 1-2 days a week had a 14.9% lower all-cause mortality risk compared with those who never reached 8,000 daily steps. This difference was similar to the 16.5% reduced mortality risk for those who took at least 8,000 steps 3-7 days a week.
Similarly, compared with the group with no days of at least 8,000 steps, cardiovascular mortality risk was 8.1% lower for those who took 8,000 steps 1-2 days per week and 8.4% lower for those who took at least 8,000 steps 3-7 days per week. The decreased mortality risk plateaued at 3-4 days.
These patterns in reduced all-cause mortality risk persisted in a stratified analysis by age (younger than 65 years and 65 years and older) and sex. Similar patterns in reduced mortality also emerged when the researchers used different thresholds of daily steps, such as a minimum of 10,000 steps instead of 8,000. The adjusted all-cause mortality for groups who took at least 10,000 steps 1-2 days a week, 3-7 days a week, and no days a week were 8.1%, 7.3%, and 16.7%, respectively, with corresponding cardiovascular mortality risks of 2.4%, 2.3%, and 7.0%, respectively.
“Given the simplicity and ease of counting daily steps, our findings indicate that the recommended number of steps taken on as few as 1 to 2 days per week may be a feasible option for individuals who are striving to achieve some health benefits through adhering to a recommended daily step count but are unable to accomplish this on a daily basis,” the researchers wrote in their discussion.
The findings were limited by several factors including the use daily step measures for 1 week only at baseline, with no data on how physical activity changes might impact mortality risk, the researchers noted. Other limitations included possible accelerometer error and misclassification of activity, possible selection bias, and lack of data on cause-specific mortality outside of cardiovascular death, they said.
However, the results were strengthened by the use of accelerometers as objective measures of activity and by the availability of 10-year follow-up data for nearly 100% of the participants, they said.
“Although our findings might suffer from residual confounding that should be addressed in future research, they suggest that people may receive substantial health benefits even if a sufficient number of steps are taken on only a couple days of the week,” they concluded.
Proceed with caution
The current study findings should be interpreted cautiously in light of the potential unmeasured confounding factors and selection bias that often occur in studies of physical activity, James Sawalla Guseh, MD, of Massachusetts General Hospital, and Jose F. Figueroa, MD, of Harvard T.H. Chan School of Public Health, Boston, wrote in an accompanying editorial.
The results support previous studies showing some longevity benefits with “weekend warrior” patterns of intense physical activity for only a couple of days; however, “the body of evidence for sporadic activity is not as robust as the evidence for sustained and regular aerobic activity,” the authors emphasized.
The editorial authors also highlighted the limitations of the current study, including the observational design and significant differences in demographics and comorbidities between the 1- to 2-days of 8,000 steps exercise group and the 0-day group, as well as the reliance on only a week’s worth of data to infer 10 years’ mortality.
Although the data are consistent with previous observations that increased exercise volume reduces mortality, more research is needed, as the current study findings may not reflect other dimensions of health, including neurological health, they said.
Despite the need for cautious interpretation of the results, the current study “supports the emerging and popular idea that step counting, which does not require consideration of exercise duration or intensity, can offer guidance toward robust and favorable health outcomes,” and may inform step-based activity goals to improve public health, the editorialists wrote.
The study was supported by the Japan Agency for Medical Research and Development, the Japan Society for the Promotion of Science, the Japan Endocrine Society, and the Meiji Yasuda Life Foundation of Health and Welfare. Dr. Inoue also was supported by the Program for the Development of Next-Generation Leading Scientists With Global Insight sponsored by the Ministry of Education, Culture, Sports, Science and Technology, Japan. The other researchers had no relevant financial conflicts to disclose. The editorial authors had no financial conflicts to disclose.
Taking 8,000 steps or more for just 1 or 2 days a week was linked to a significant reduction in all-cause and cardiovascular mortality, according to a study of about 3,000 adults.
Previous research has shown lower mortality rates among individuals who walk consistently, especially those who log at least 8,000 steps daily, but the benefit of intense walking just once or twice a week on long-term health outcomes has not been examined, wrote Kosuke Inoue, MD, of Kyoto University, Japan, and colleagues.
In a study published in JAMA Network Open, the researchers reviewed 10-year follow-up data for 3,101 adults aged 20 years and older who were part of the 2005 and 2006 National Health and Nutrition Examination Survey (NHANES).
The participants were asked to wear accelerometers to track their steps for 7 consecutive days. The researchers assessed the dose-response relationship between days of taking 8,000 steps or more (about 4 miles) during 1 week, and the primary outcome of all-cause mortality risk after 10 years. Cardiovascular mortality risk after 10 years was a secondary outcome.
The mean age of the participants was 50.5 years and 51% were women. The breakdown by ethnicity was 51% White, 21% Black, 24% Hispanic, and 4% other races/ethnicities. A total of 632 individuals took 8,000 steps or more 0 days a week, 532 took at least 8,000 steps 1-2 days per week, and 1,937 took at least 8,000 steps 3-7 days a week.
During the 10-year follow-up period, overall all-cause mortality was 14.2% and cardiovascular mortality was 5.3% across all step groups.
In an adjusted analysis, individuals who took at least 8,000 steps 1-2 days a week had a 14.9% lower all-cause mortality risk compared with those who never reached 8,000 daily steps. This difference was similar to the 16.5% reduced mortality risk for those who took at least 8,000 steps 3-7 days a week.
Similarly, compared with the group with no days of at least 8,000 steps, cardiovascular mortality risk was 8.1% lower for those who took 8,000 steps 1-2 days per week and 8.4% lower for those who took at least 8,000 steps 3-7 days per week. The decreased mortality risk plateaued at 3-4 days.
These patterns in reduced all-cause mortality risk persisted in a stratified analysis by age (younger than 65 years and 65 years and older) and sex. Similar patterns in reduced mortality also emerged when the researchers used different thresholds of daily steps, such as a minimum of 10,000 steps instead of 8,000. The adjusted all-cause mortality for groups who took at least 10,000 steps 1-2 days a week, 3-7 days a week, and no days a week were 8.1%, 7.3%, and 16.7%, respectively, with corresponding cardiovascular mortality risks of 2.4%, 2.3%, and 7.0%, respectively.
“Given the simplicity and ease of counting daily steps, our findings indicate that the recommended number of steps taken on as few as 1 to 2 days per week may be a feasible option for individuals who are striving to achieve some health benefits through adhering to a recommended daily step count but are unable to accomplish this on a daily basis,” the researchers wrote in their discussion.
The findings were limited by several factors including the use daily step measures for 1 week only at baseline, with no data on how physical activity changes might impact mortality risk, the researchers noted. Other limitations included possible accelerometer error and misclassification of activity, possible selection bias, and lack of data on cause-specific mortality outside of cardiovascular death, they said.
However, the results were strengthened by the use of accelerometers as objective measures of activity and by the availability of 10-year follow-up data for nearly 100% of the participants, they said.
“Although our findings might suffer from residual confounding that should be addressed in future research, they suggest that people may receive substantial health benefits even if a sufficient number of steps are taken on only a couple days of the week,” they concluded.
Proceed with caution
The current study findings should be interpreted cautiously in light of the potential unmeasured confounding factors and selection bias that often occur in studies of physical activity, James Sawalla Guseh, MD, of Massachusetts General Hospital, and Jose F. Figueroa, MD, of Harvard T.H. Chan School of Public Health, Boston, wrote in an accompanying editorial.
The results support previous studies showing some longevity benefits with “weekend warrior” patterns of intense physical activity for only a couple of days; however, “the body of evidence for sporadic activity is not as robust as the evidence for sustained and regular aerobic activity,” the authors emphasized.
The editorial authors also highlighted the limitations of the current study, including the observational design and significant differences in demographics and comorbidities between the 1- to 2-days of 8,000 steps exercise group and the 0-day group, as well as the reliance on only a week’s worth of data to infer 10 years’ mortality.
Although the data are consistent with previous observations that increased exercise volume reduces mortality, more research is needed, as the current study findings may not reflect other dimensions of health, including neurological health, they said.
Despite the need for cautious interpretation of the results, the current study “supports the emerging and popular idea that step counting, which does not require consideration of exercise duration or intensity, can offer guidance toward robust and favorable health outcomes,” and may inform step-based activity goals to improve public health, the editorialists wrote.
The study was supported by the Japan Agency for Medical Research and Development, the Japan Society for the Promotion of Science, the Japan Endocrine Society, and the Meiji Yasuda Life Foundation of Health and Welfare. Dr. Inoue also was supported by the Program for the Development of Next-Generation Leading Scientists With Global Insight sponsored by the Ministry of Education, Culture, Sports, Science and Technology, Japan. The other researchers had no relevant financial conflicts to disclose. The editorial authors had no financial conflicts to disclose.
FROM JAMA NETWORK OPEN
Annular Erythematous Plaques With Central Hypopigmentation on Sun-Exposed Skin
A biopsy showed a markedly elastotic dermis consisting of a palisading granulomatous inflammatory infiltrate and numerous multinucleated histiocytes (Figure). These histopathologic findings along with the clinical presentation confirmed a diagnosis of annular elastolytic granuloma (AEG). Treatment consisting of 3 months of oral minocycline, 2 months of oral doxycycline, and clobetasol ointment all failed. At that point, oral hydroxychloroquine was recommended. Our patient was lost to follow-up by dermatology, then subsequently was placed on hydroxychloroquine by rheumatology to treat both the osteoarthritis and AEG. A follow-up appointment with dermatology was planned for 3 months to monitor hydroxychloroquine treatment and monitor treatment progress; however, she did not follow-up or seek further treatment.
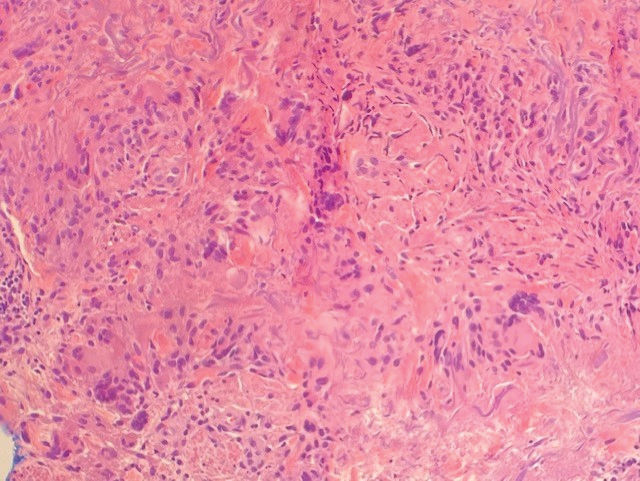
Annular elastolytic granuloma clinically is similar to granuloma annulare (GA), with both presenting as annular plaques surrounded by an elevated border.1 Although AEG clinically is distinct with hypopigmented atrophied plaque centers,2 a biopsy is required to confirm the lack of elastic tissue in zones of atrophy and the presence of multinucleated histiocytes.1,3 Lesions most commonly are seen clinically on sun-exposed areas in middle-aged White women; however, they rarely have been seen on frequently covered skin.4 Our case illustrates the striking photodistribution of AEG, especially on the posterior neck area. The clinical diagnoses of AEG, annular elastolytic giant cell granuloma, and GA in sun-exposed areas are synonymous and can be used interchangeably.5,6
Pathologies considered in the diagnosis of AEG include but are not limited to tinea corporis, annular lichen planus, erythema annulare centrifugum, and necrobiosis lipoidica. Scaling typically is absent in AEG, while tinea corporis presents with hyphae within the stratum corneum of the plaques.7 Papules along the periphery of annular lesions are more typical of annular lichen planus than AEG, and they tend to have a more purple hue.8 Erythema annulare centrifugum has annular erythematous plaques similar to those found in AEG but differs with scaling on the inner margins of these plaques. Histopathology presenting with a lymphocytic infiltrate surrounding vasculature and no indication of elastolytic degradation would further indicate a diagnosis of erythema annulare centrifugum.9 Histopathology showing necrobiosis, lipid depositions, and vascular wall thickenings is indicative of necrobiosis lipoidica.10
Similar to GA,11 the cause of AEG is idiopathic.2 Annular elastolytic granuloma and GA differ in the fact that elastin degradation is characteristic of AEG compared to collagen degradation in GA. It is suspected that elastin degradation in AEG patients is caused by an immune response triggering phagocytosis of elastin by multinucleated histiocytes.2 Actinic damage also is considered a possible cause of elastin fiber degradation in AEG.12 Granuloma annulare can be ruled out and the diagnosis of AEG confirmed with the absence of elastin fibers and mucin on pathology.13
Although there is no established first-line treatment of AEG, successful treatment has been achieved with antimalarial drugs paired with topical steroids.14 Treatment recommendations for AEG include minocycline, chloroquine, hydroxychloroquine, tranilast, and oral retinoids, as well as oral and topical steroids. In clinical cases where AEG occurs in the setting of a chronic disease such as diabetes mellitus, vascular occlusion, arthritis, or hypertension, treatment of underlying disease has been shown to resolve AEG symptoms.14
Although light therapy is not common for AEG, UV light radiation has demonstrated success in treating AEG.15,16 One study showed complete clearance of granulomatous papules after narrowband UVB treatment.15 Another study showed that 2 patients treated with psoralen plus UVA therapy reached complete clearance of AEG lasting at least 3 months after treatment.16
1. Lai JH, Murray SJ, Walsh NM. Evolution of granuloma annulare to mid-dermal elastolysis: report of a case and review of the literature. J Cutan Pathol. 2014;41:462-468. doi:10.1111/cup.12292 2. Klemke CD, Siebold D, Dippel E, et al. Generalised annular elastolytic giant cell granuloma. Dermatology. 2003;207:420-422. doi:10.1159/000074132 3. Limas C. The spectrum of primary cutaneous elastolytic granulomas and their distinction from granuloma annulare: a clinicopathological analysis. Histopathology. 2004;44:277-282. doi:10.1111/j.0309-0167.2004.01755.x 4. Revenga F, Rovira I, Pimentel J, et al. Annular elastolytic giant cell granuloma—actinic granuloma? Clin Exp Dermatol. 1996;21:51-53. 5. Hawryluk EB, Izikson L, English JC 3rd. Non-infectious granulomatous diseases of the skin and their associated systemic diseases: an evidence-based update to important clinical questions. Am J Clin Dermatol. 2010;11:171-181. doi:10.2165/11530080-000000000-00000 6. Berliner JG, Haemel A, LeBoit PE, et al. The sarcoidal variant of annular elastolytic granuloma. J Cutan Pathol. 2013;40:918-920. doi:10.1111/cup.12237 7. Pflederer RT, Ahmed S, Tonkovic-Capin V, et al. Annular polycyclic plaques on the chest and upper back [published online April 24, 2018]. JAAD Case Rep. 2018;4:405-407. doi:10.1016/j.jdcr.2017.07.022 8. Trayes KP, Savage K, Studdiford JS. Annular lesions: diagnosis and treatment. Am Fam Physician. 2018;98:283-291. 9. Weyers W, Diaz-Cascajo C, Weyers I. Erythema annulare centrifugum: results of a clinicopathologic study of 73 patients. Am J Dermatopathol. 2003;25:451-462. doi:10.1097/00000372-200312000-00001 10. Dowling GB, Jones EW. Atypical (annular) necrobiosis lipoidica of the face and scalp. a report of the clinical and histological features of 7 cases. Dermatologica. 1967;135:11-26. doi:10.1159/000254156 11. Piette EW, Rosenbach M. Granuloma annulare: pathogenesis, disease associations and triggers, and therapeutic options. J Am Acad Dermatol. 2016;75:467-479. doi:10.1016/j.jaad.2015 .03.055 12. O’Brien JP, Regan W. Actinically degenerate elastic tissue is the likely antigenic basis of actinic granuloma of the skin and of temporal arteritis [published correction appears in J Am Acad Dermatol. 2000; 42(1 pt 1):148]. J Am Acad Dermatol. 1999;40(2 pt 1):214-222. doi:10.1016/s0190-9622(99)70191-x 13. Rencic A, Nousari CH. Other rheumatologic diseases. In: Bolognia JL, Jorizzo JL, Rapini RP, et al, eds. Dermatology. 2nd ed. Elsevier Limited; 2008:600-601. 14. Burlando M, Herzum A, Cozzani E, et al. Can methotrexate be a successful treatment for unresponsive generalized annular elastolytic giant cell granuloma? case report and review of the literature. Dermatol Ther. 2021;34:E14705. doi:10.1111/dth.14705 15. Takata T, Ikeda M, Kodama H, et al. Regression of papular elastolytic giant cell granuloma using narrow-band UVB irradiation. Dermatology. 2006;212:77-79. doi:10.1159/000089028 16. Pérez-Pérez L, García-Gavín J, Allegue F, et al. Successful treatment of generalized elastolytic giant cell granuloma with psoralenultraviolet A. Photodermatol Photoimmunol Photomed. 2012;28:264-266. doi:10.1111/j.1600-0781.2012.00680.x
A biopsy showed a markedly elastotic dermis consisting of a palisading granulomatous inflammatory infiltrate and numerous multinucleated histiocytes (Figure). These histopathologic findings along with the clinical presentation confirmed a diagnosis of annular elastolytic granuloma (AEG). Treatment consisting of 3 months of oral minocycline, 2 months of oral doxycycline, and clobetasol ointment all failed. At that point, oral hydroxychloroquine was recommended. Our patient was lost to follow-up by dermatology, then subsequently was placed on hydroxychloroquine by rheumatology to treat both the osteoarthritis and AEG. A follow-up appointment with dermatology was planned for 3 months to monitor hydroxychloroquine treatment and monitor treatment progress; however, she did not follow-up or seek further treatment.
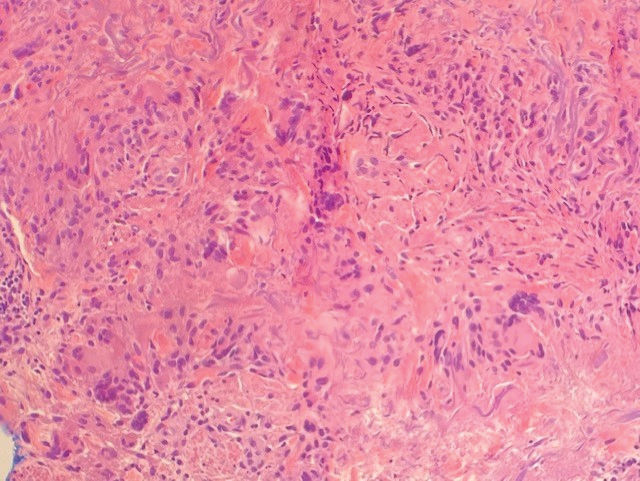
Annular elastolytic granuloma clinically is similar to granuloma annulare (GA), with both presenting as annular plaques surrounded by an elevated border.1 Although AEG clinically is distinct with hypopigmented atrophied plaque centers,2 a biopsy is required to confirm the lack of elastic tissue in zones of atrophy and the presence of multinucleated histiocytes.1,3 Lesions most commonly are seen clinically on sun-exposed areas in middle-aged White women; however, they rarely have been seen on frequently covered skin.4 Our case illustrates the striking photodistribution of AEG, especially on the posterior neck area. The clinical diagnoses of AEG, annular elastolytic giant cell granuloma, and GA in sun-exposed areas are synonymous and can be used interchangeably.5,6
Pathologies considered in the diagnosis of AEG include but are not limited to tinea corporis, annular lichen planus, erythema annulare centrifugum, and necrobiosis lipoidica. Scaling typically is absent in AEG, while tinea corporis presents with hyphae within the stratum corneum of the plaques.7 Papules along the periphery of annular lesions are more typical of annular lichen planus than AEG, and they tend to have a more purple hue.8 Erythema annulare centrifugum has annular erythematous plaques similar to those found in AEG but differs with scaling on the inner margins of these plaques. Histopathology presenting with a lymphocytic infiltrate surrounding vasculature and no indication of elastolytic degradation would further indicate a diagnosis of erythema annulare centrifugum.9 Histopathology showing necrobiosis, lipid depositions, and vascular wall thickenings is indicative of necrobiosis lipoidica.10
Similar to GA,11 the cause of AEG is idiopathic.2 Annular elastolytic granuloma and GA differ in the fact that elastin degradation is characteristic of AEG compared to collagen degradation in GA. It is suspected that elastin degradation in AEG patients is caused by an immune response triggering phagocytosis of elastin by multinucleated histiocytes.2 Actinic damage also is considered a possible cause of elastin fiber degradation in AEG.12 Granuloma annulare can be ruled out and the diagnosis of AEG confirmed with the absence of elastin fibers and mucin on pathology.13
Although there is no established first-line treatment of AEG, successful treatment has been achieved with antimalarial drugs paired with topical steroids.14 Treatment recommendations for AEG include minocycline, chloroquine, hydroxychloroquine, tranilast, and oral retinoids, as well as oral and topical steroids. In clinical cases where AEG occurs in the setting of a chronic disease such as diabetes mellitus, vascular occlusion, arthritis, or hypertension, treatment of underlying disease has been shown to resolve AEG symptoms.14
Although light therapy is not common for AEG, UV light radiation has demonstrated success in treating AEG.15,16 One study showed complete clearance of granulomatous papules after narrowband UVB treatment.15 Another study showed that 2 patients treated with psoralen plus UVA therapy reached complete clearance of AEG lasting at least 3 months after treatment.16
A biopsy showed a markedly elastotic dermis consisting of a palisading granulomatous inflammatory infiltrate and numerous multinucleated histiocytes (Figure). These histopathologic findings along with the clinical presentation confirmed a diagnosis of annular elastolytic granuloma (AEG). Treatment consisting of 3 months of oral minocycline, 2 months of oral doxycycline, and clobetasol ointment all failed. At that point, oral hydroxychloroquine was recommended. Our patient was lost to follow-up by dermatology, then subsequently was placed on hydroxychloroquine by rheumatology to treat both the osteoarthritis and AEG. A follow-up appointment with dermatology was planned for 3 months to monitor hydroxychloroquine treatment and monitor treatment progress; however, she did not follow-up or seek further treatment.
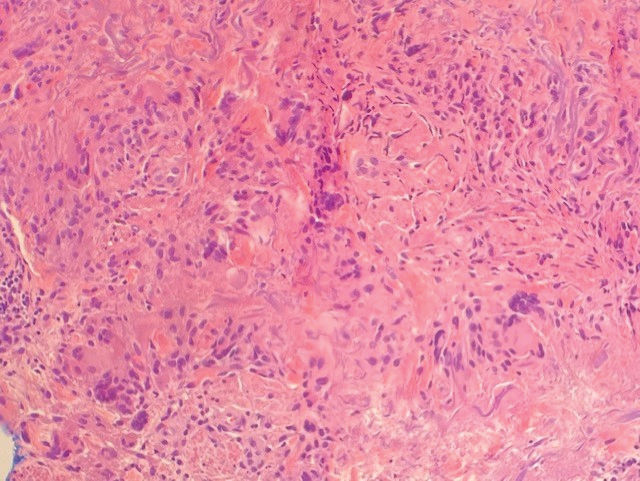
Annular elastolytic granuloma clinically is similar to granuloma annulare (GA), with both presenting as annular plaques surrounded by an elevated border.1 Although AEG clinically is distinct with hypopigmented atrophied plaque centers,2 a biopsy is required to confirm the lack of elastic tissue in zones of atrophy and the presence of multinucleated histiocytes.1,3 Lesions most commonly are seen clinically on sun-exposed areas in middle-aged White women; however, they rarely have been seen on frequently covered skin.4 Our case illustrates the striking photodistribution of AEG, especially on the posterior neck area. The clinical diagnoses of AEG, annular elastolytic giant cell granuloma, and GA in sun-exposed areas are synonymous and can be used interchangeably.5,6
Pathologies considered in the diagnosis of AEG include but are not limited to tinea corporis, annular lichen planus, erythema annulare centrifugum, and necrobiosis lipoidica. Scaling typically is absent in AEG, while tinea corporis presents with hyphae within the stratum corneum of the plaques.7 Papules along the periphery of annular lesions are more typical of annular lichen planus than AEG, and they tend to have a more purple hue.8 Erythema annulare centrifugum has annular erythematous plaques similar to those found in AEG but differs with scaling on the inner margins of these plaques. Histopathology presenting with a lymphocytic infiltrate surrounding vasculature and no indication of elastolytic degradation would further indicate a diagnosis of erythema annulare centrifugum.9 Histopathology showing necrobiosis, lipid depositions, and vascular wall thickenings is indicative of necrobiosis lipoidica.10
Similar to GA,11 the cause of AEG is idiopathic.2 Annular elastolytic granuloma and GA differ in the fact that elastin degradation is characteristic of AEG compared to collagen degradation in GA. It is suspected that elastin degradation in AEG patients is caused by an immune response triggering phagocytosis of elastin by multinucleated histiocytes.2 Actinic damage also is considered a possible cause of elastin fiber degradation in AEG.12 Granuloma annulare can be ruled out and the diagnosis of AEG confirmed with the absence of elastin fibers and mucin on pathology.13
Although there is no established first-line treatment of AEG, successful treatment has been achieved with antimalarial drugs paired with topical steroids.14 Treatment recommendations for AEG include minocycline, chloroquine, hydroxychloroquine, tranilast, and oral retinoids, as well as oral and topical steroids. In clinical cases where AEG occurs in the setting of a chronic disease such as diabetes mellitus, vascular occlusion, arthritis, or hypertension, treatment of underlying disease has been shown to resolve AEG symptoms.14
Although light therapy is not common for AEG, UV light radiation has demonstrated success in treating AEG.15,16 One study showed complete clearance of granulomatous papules after narrowband UVB treatment.15 Another study showed that 2 patients treated with psoralen plus UVA therapy reached complete clearance of AEG lasting at least 3 months after treatment.16
1. Lai JH, Murray SJ, Walsh NM. Evolution of granuloma annulare to mid-dermal elastolysis: report of a case and review of the literature. J Cutan Pathol. 2014;41:462-468. doi:10.1111/cup.12292 2. Klemke CD, Siebold D, Dippel E, et al. Generalised annular elastolytic giant cell granuloma. Dermatology. 2003;207:420-422. doi:10.1159/000074132 3. Limas C. The spectrum of primary cutaneous elastolytic granulomas and their distinction from granuloma annulare: a clinicopathological analysis. Histopathology. 2004;44:277-282. doi:10.1111/j.0309-0167.2004.01755.x 4. Revenga F, Rovira I, Pimentel J, et al. Annular elastolytic giant cell granuloma—actinic granuloma? Clin Exp Dermatol. 1996;21:51-53. 5. Hawryluk EB, Izikson L, English JC 3rd. Non-infectious granulomatous diseases of the skin and their associated systemic diseases: an evidence-based update to important clinical questions. Am J Clin Dermatol. 2010;11:171-181. doi:10.2165/11530080-000000000-00000 6. Berliner JG, Haemel A, LeBoit PE, et al. The sarcoidal variant of annular elastolytic granuloma. J Cutan Pathol. 2013;40:918-920. doi:10.1111/cup.12237 7. Pflederer RT, Ahmed S, Tonkovic-Capin V, et al. Annular polycyclic plaques on the chest and upper back [published online April 24, 2018]. JAAD Case Rep. 2018;4:405-407. doi:10.1016/j.jdcr.2017.07.022 8. Trayes KP, Savage K, Studdiford JS. Annular lesions: diagnosis and treatment. Am Fam Physician. 2018;98:283-291. 9. Weyers W, Diaz-Cascajo C, Weyers I. Erythema annulare centrifugum: results of a clinicopathologic study of 73 patients. Am J Dermatopathol. 2003;25:451-462. doi:10.1097/00000372-200312000-00001 10. Dowling GB, Jones EW. Atypical (annular) necrobiosis lipoidica of the face and scalp. a report of the clinical and histological features of 7 cases. Dermatologica. 1967;135:11-26. doi:10.1159/000254156 11. Piette EW, Rosenbach M. Granuloma annulare: pathogenesis, disease associations and triggers, and therapeutic options. J Am Acad Dermatol. 2016;75:467-479. doi:10.1016/j.jaad.2015 .03.055 12. O’Brien JP, Regan W. Actinically degenerate elastic tissue is the likely antigenic basis of actinic granuloma of the skin and of temporal arteritis [published correction appears in J Am Acad Dermatol. 2000; 42(1 pt 1):148]. J Am Acad Dermatol. 1999;40(2 pt 1):214-222. doi:10.1016/s0190-9622(99)70191-x 13. Rencic A, Nousari CH. Other rheumatologic diseases. In: Bolognia JL, Jorizzo JL, Rapini RP, et al, eds. Dermatology. 2nd ed. Elsevier Limited; 2008:600-601. 14. Burlando M, Herzum A, Cozzani E, et al. Can methotrexate be a successful treatment for unresponsive generalized annular elastolytic giant cell granuloma? case report and review of the literature. Dermatol Ther. 2021;34:E14705. doi:10.1111/dth.14705 15. Takata T, Ikeda M, Kodama H, et al. Regression of papular elastolytic giant cell granuloma using narrow-band UVB irradiation. Dermatology. 2006;212:77-79. doi:10.1159/000089028 16. Pérez-Pérez L, García-Gavín J, Allegue F, et al. Successful treatment of generalized elastolytic giant cell granuloma with psoralenultraviolet A. Photodermatol Photoimmunol Photomed. 2012;28:264-266. doi:10.1111/j.1600-0781.2012.00680.x
1. Lai JH, Murray SJ, Walsh NM. Evolution of granuloma annulare to mid-dermal elastolysis: report of a case and review of the literature. J Cutan Pathol. 2014;41:462-468. doi:10.1111/cup.12292 2. Klemke CD, Siebold D, Dippel E, et al. Generalised annular elastolytic giant cell granuloma. Dermatology. 2003;207:420-422. doi:10.1159/000074132 3. Limas C. The spectrum of primary cutaneous elastolytic granulomas and their distinction from granuloma annulare: a clinicopathological analysis. Histopathology. 2004;44:277-282. doi:10.1111/j.0309-0167.2004.01755.x 4. Revenga F, Rovira I, Pimentel J, et al. Annular elastolytic giant cell granuloma—actinic granuloma? Clin Exp Dermatol. 1996;21:51-53. 5. Hawryluk EB, Izikson L, English JC 3rd. Non-infectious granulomatous diseases of the skin and their associated systemic diseases: an evidence-based update to important clinical questions. Am J Clin Dermatol. 2010;11:171-181. doi:10.2165/11530080-000000000-00000 6. Berliner JG, Haemel A, LeBoit PE, et al. The sarcoidal variant of annular elastolytic granuloma. J Cutan Pathol. 2013;40:918-920. doi:10.1111/cup.12237 7. Pflederer RT, Ahmed S, Tonkovic-Capin V, et al. Annular polycyclic plaques on the chest and upper back [published online April 24, 2018]. JAAD Case Rep. 2018;4:405-407. doi:10.1016/j.jdcr.2017.07.022 8. Trayes KP, Savage K, Studdiford JS. Annular lesions: diagnosis and treatment. Am Fam Physician. 2018;98:283-291. 9. Weyers W, Diaz-Cascajo C, Weyers I. Erythema annulare centrifugum: results of a clinicopathologic study of 73 patients. Am J Dermatopathol. 2003;25:451-462. doi:10.1097/00000372-200312000-00001 10. Dowling GB, Jones EW. Atypical (annular) necrobiosis lipoidica of the face and scalp. a report of the clinical and histological features of 7 cases. Dermatologica. 1967;135:11-26. doi:10.1159/000254156 11. Piette EW, Rosenbach M. Granuloma annulare: pathogenesis, disease associations and triggers, and therapeutic options. J Am Acad Dermatol. 2016;75:467-479. doi:10.1016/j.jaad.2015 .03.055 12. O’Brien JP, Regan W. Actinically degenerate elastic tissue is the likely antigenic basis of actinic granuloma of the skin and of temporal arteritis [published correction appears in J Am Acad Dermatol. 2000; 42(1 pt 1):148]. J Am Acad Dermatol. 1999;40(2 pt 1):214-222. doi:10.1016/s0190-9622(99)70191-x 13. Rencic A, Nousari CH. Other rheumatologic diseases. In: Bolognia JL, Jorizzo JL, Rapini RP, et al, eds. Dermatology. 2nd ed. Elsevier Limited; 2008:600-601. 14. Burlando M, Herzum A, Cozzani E, et al. Can methotrexate be a successful treatment for unresponsive generalized annular elastolytic giant cell granuloma? case report and review of the literature. Dermatol Ther. 2021;34:E14705. doi:10.1111/dth.14705 15. Takata T, Ikeda M, Kodama H, et al. Regression of papular elastolytic giant cell granuloma using narrow-band UVB irradiation. Dermatology. 2006;212:77-79. doi:10.1159/000089028 16. Pérez-Pérez L, García-Gavín J, Allegue F, et al. Successful treatment of generalized elastolytic giant cell granuloma with psoralenultraviolet A. Photodermatol Photoimmunol Photomed. 2012;28:264-266. doi:10.1111/j.1600-0781.2012.00680.x
A 67-year-old White woman presented to our dermatology clinic with pruritic annular erythematous plaques with central hypopigmentation on the forearms, dorsal aspect of the hands, neck, and fingers of 3 to 4 months’ duration. The patient rated the severity of pruritus an 8 on a 10-point scale. A review of symptoms was positive for fatigue, joint pain, and headache. The patient had a history of type 2 diabetes mellitus, osteoarthritis, thyroid disease, and stage 3 renal failure. A punch biopsy from the left forearm was performed.





