User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Rheumatology Match Day results for 2024 follow trends of past years
While adult rheumatology programs continue to have high match rates, pediatric rheumatology programs remain less popular.
The National Residency Matching Program (NRMP) reported on Nov. 29 that rheumatology filled 124 of 127 programs (97.6%), with 273 (98.9%) of 276 positions filled. Comparatively, pediatric rheumatology filled 21 out of 38 programs (55%) and 32 (61.5%) of 52 positions.
This year, the number of programs and positions across all specialties rose by 3%, whereas the number of applications only rose by 0.4% (35 additional applicants).
“The growth of fellowship programs and positions in the Match reflect training opportunities and the future workforce trends of medical subspecialties,” said NRMP President Donna Lamb, DHSc, MBA, BSN, in a statement. “While the increase in applicant numbers did not keep pace with the increase in positions this year, the Match rate for applicants remains strong at 82%.”
In adult rheumatology, matched applicants included 117 MD graduates, 86 foreign applicants, 38 DO graduates, and 32 U.S. citizen international medical graduates. A total of 348 applicants preferred the specialty, and 78% matched to rheumatology, whereas 2% matched to a different specialty. Another 70 applicants (20%) did not match to any program.
In pediatric rheumatology, matched applicants included 23 MD graduates, 6 DO graduates, and 3 foreign applicants. All applicants who preferred pediatric rheumatology matched to a program.
Adult rheumatology was one of several specialties that filled over 95% of positions. The other specialties that matched at that rate were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, critical care medicine, gastroenterology, hematology and oncology, and pulmonary/critical care. Interventional Pulmonology and Oncology was the only specialty to achieve a 100% fill rate.
A version of this article first appeared on Medscape.com.
While adult rheumatology programs continue to have high match rates, pediatric rheumatology programs remain less popular.
The National Residency Matching Program (NRMP) reported on Nov. 29 that rheumatology filled 124 of 127 programs (97.6%), with 273 (98.9%) of 276 positions filled. Comparatively, pediatric rheumatology filled 21 out of 38 programs (55%) and 32 (61.5%) of 52 positions.
This year, the number of programs and positions across all specialties rose by 3%, whereas the number of applications only rose by 0.4% (35 additional applicants).
“The growth of fellowship programs and positions in the Match reflect training opportunities and the future workforce trends of medical subspecialties,” said NRMP President Donna Lamb, DHSc, MBA, BSN, in a statement. “While the increase in applicant numbers did not keep pace with the increase in positions this year, the Match rate for applicants remains strong at 82%.”
In adult rheumatology, matched applicants included 117 MD graduates, 86 foreign applicants, 38 DO graduates, and 32 U.S. citizen international medical graduates. A total of 348 applicants preferred the specialty, and 78% matched to rheumatology, whereas 2% matched to a different specialty. Another 70 applicants (20%) did not match to any program.
In pediatric rheumatology, matched applicants included 23 MD graduates, 6 DO graduates, and 3 foreign applicants. All applicants who preferred pediatric rheumatology matched to a program.
Adult rheumatology was one of several specialties that filled over 95% of positions. The other specialties that matched at that rate were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, critical care medicine, gastroenterology, hematology and oncology, and pulmonary/critical care. Interventional Pulmonology and Oncology was the only specialty to achieve a 100% fill rate.
A version of this article first appeared on Medscape.com.
While adult rheumatology programs continue to have high match rates, pediatric rheumatology programs remain less popular.
The National Residency Matching Program (NRMP) reported on Nov. 29 that rheumatology filled 124 of 127 programs (97.6%), with 273 (98.9%) of 276 positions filled. Comparatively, pediatric rheumatology filled 21 out of 38 programs (55%) and 32 (61.5%) of 52 positions.
This year, the number of programs and positions across all specialties rose by 3%, whereas the number of applications only rose by 0.4% (35 additional applicants).
“The growth of fellowship programs and positions in the Match reflect training opportunities and the future workforce trends of medical subspecialties,” said NRMP President Donna Lamb, DHSc, MBA, BSN, in a statement. “While the increase in applicant numbers did not keep pace with the increase in positions this year, the Match rate for applicants remains strong at 82%.”
In adult rheumatology, matched applicants included 117 MD graduates, 86 foreign applicants, 38 DO graduates, and 32 U.S. citizen international medical graduates. A total of 348 applicants preferred the specialty, and 78% matched to rheumatology, whereas 2% matched to a different specialty. Another 70 applicants (20%) did not match to any program.
In pediatric rheumatology, matched applicants included 23 MD graduates, 6 DO graduates, and 3 foreign applicants. All applicants who preferred pediatric rheumatology matched to a program.
Adult rheumatology was one of several specialties that filled over 95% of positions. The other specialties that matched at that rate were allergy and immunology, cardiovascular disease, clinical cardiac electrophysiology, critical care medicine, gastroenterology, hematology and oncology, and pulmonary/critical care. Interventional Pulmonology and Oncology was the only specialty to achieve a 100% fill rate.
A version of this article first appeared on Medscape.com.
FDA warns of potentially lethal reaction to seizure meds
that can be life threatening if not detected and treated promptly, the Food and Drug Administration warns in an alert.
Known as drug reaction with eosinophilia and systemic symptoms (DRESS), it may start as a rash but can quickly progress and cause injury to internal organs, the need for hospitalization, and death, the FDA notes.
A search of the FDA Adverse Event Reporting System (FAERS) and the medical literature through March 2023 identified 32 serious cases of DRESS worldwide that were associated with levetiracetam.
Three cases occurred in the United States, and 29 occurred abroad. In all 32 cases, the patients were hospitalized and received medical treatment; in 2 cases, the patients died.
The median time to onset of DRESS in the levetiracetam cases was 24 days; times ranged from 7 to 170 days. The reported signs and symptoms included skin rash (n = 22), fever (n = 20), eosinophilia (n = 17), lymph node swelling (n = 9), and atypical lymphocytes (n = 4).
Twenty-two levetiracetam-associated cases of DRESS involved injury to one or more organs, including the liver, lungs, kidneys, and gallbladder.
In 25 of the 29 cases for which information on treatment discontinuation was available, DRESS symptoms resolved when levetiracetam was discontinued.
As for clobazam, a search of FAERS and the medical literature through July 2023 identified 10 serious cases of DRESS worldwide – 1 in the United States and 9 abroad. All 10 patients were hospitalized and received medical treatment. No deaths were reported.
The median time to onset of clobazam-associated DRESS was 21.5 days (range, 7-103 days). The reported signs and symptoms included skin rash (n = 10), fever (n = 8), eosinophilia (n = 7), facial swelling (n = 7), leukocytosis (n = 4), lymph node swelling (n = 4), and leukopenia/thrombocytopenia (n = 1).
In nine cases, there was injury to one or more organs, including the liver, kidneys, and gastrointestinal tract.
DRESS symptoms resolved in all 10 cases when treatment with clobazam was stopped. DRESS and other serious skin reactions reported with clobazam, a benzodiazepine, have not generally been associated with other benzodiazepines, the FDA notes.
Label updates
As a result of these cases, warnings about the risk of DRESS will be added to the prescribing information and patient medication guides for these medicines, the FDA announced.
“Health care professionals should be aware that prompt recognition and early treatment is important for improving DRESS outcomes and decreasing mortality,” the FDA said.
They noted that diagnosis is often difficult because early signs and symptoms, such as fever and swollen lymph nodes, may be present without evidence of a rash.
DRESS may develop 2-8 weeks after starting levetiracetam or clobazam. Symptoms and intensity can vary widely.
DRESS can also be confused with other serious skin reactions, such as Stevens-Johnson syndrome and toxic epidermal necrolysis.
The FDA says patients should be advised of the signs and symptoms of DRESS and be told to stop taking the medicine and seek immediate medical attention if DRESS is suspected during treatment with levetiracetam or clobazam.
Adverse reactions with these medications should be reported to the FDA’s MedWatch program.
A version of this article appeared on Medscape.com.
that can be life threatening if not detected and treated promptly, the Food and Drug Administration warns in an alert.
Known as drug reaction with eosinophilia and systemic symptoms (DRESS), it may start as a rash but can quickly progress and cause injury to internal organs, the need for hospitalization, and death, the FDA notes.
A search of the FDA Adverse Event Reporting System (FAERS) and the medical literature through March 2023 identified 32 serious cases of DRESS worldwide that were associated with levetiracetam.
Three cases occurred in the United States, and 29 occurred abroad. In all 32 cases, the patients were hospitalized and received medical treatment; in 2 cases, the patients died.
The median time to onset of DRESS in the levetiracetam cases was 24 days; times ranged from 7 to 170 days. The reported signs and symptoms included skin rash (n = 22), fever (n = 20), eosinophilia (n = 17), lymph node swelling (n = 9), and atypical lymphocytes (n = 4).
Twenty-two levetiracetam-associated cases of DRESS involved injury to one or more organs, including the liver, lungs, kidneys, and gallbladder.
In 25 of the 29 cases for which information on treatment discontinuation was available, DRESS symptoms resolved when levetiracetam was discontinued.
As for clobazam, a search of FAERS and the medical literature through July 2023 identified 10 serious cases of DRESS worldwide – 1 in the United States and 9 abroad. All 10 patients were hospitalized and received medical treatment. No deaths were reported.
The median time to onset of clobazam-associated DRESS was 21.5 days (range, 7-103 days). The reported signs and symptoms included skin rash (n = 10), fever (n = 8), eosinophilia (n = 7), facial swelling (n = 7), leukocytosis (n = 4), lymph node swelling (n = 4), and leukopenia/thrombocytopenia (n = 1).
In nine cases, there was injury to one or more organs, including the liver, kidneys, and gastrointestinal tract.
DRESS symptoms resolved in all 10 cases when treatment with clobazam was stopped. DRESS and other serious skin reactions reported with clobazam, a benzodiazepine, have not generally been associated with other benzodiazepines, the FDA notes.
Label updates
As a result of these cases, warnings about the risk of DRESS will be added to the prescribing information and patient medication guides for these medicines, the FDA announced.
“Health care professionals should be aware that prompt recognition and early treatment is important for improving DRESS outcomes and decreasing mortality,” the FDA said.
They noted that diagnosis is often difficult because early signs and symptoms, such as fever and swollen lymph nodes, may be present without evidence of a rash.
DRESS may develop 2-8 weeks after starting levetiracetam or clobazam. Symptoms and intensity can vary widely.
DRESS can also be confused with other serious skin reactions, such as Stevens-Johnson syndrome and toxic epidermal necrolysis.
The FDA says patients should be advised of the signs and symptoms of DRESS and be told to stop taking the medicine and seek immediate medical attention if DRESS is suspected during treatment with levetiracetam or clobazam.
Adverse reactions with these medications should be reported to the FDA’s MedWatch program.
A version of this article appeared on Medscape.com.
that can be life threatening if not detected and treated promptly, the Food and Drug Administration warns in an alert.
Known as drug reaction with eosinophilia and systemic symptoms (DRESS), it may start as a rash but can quickly progress and cause injury to internal organs, the need for hospitalization, and death, the FDA notes.
A search of the FDA Adverse Event Reporting System (FAERS) and the medical literature through March 2023 identified 32 serious cases of DRESS worldwide that were associated with levetiracetam.
Three cases occurred in the United States, and 29 occurred abroad. In all 32 cases, the patients were hospitalized and received medical treatment; in 2 cases, the patients died.
The median time to onset of DRESS in the levetiracetam cases was 24 days; times ranged from 7 to 170 days. The reported signs and symptoms included skin rash (n = 22), fever (n = 20), eosinophilia (n = 17), lymph node swelling (n = 9), and atypical lymphocytes (n = 4).
Twenty-two levetiracetam-associated cases of DRESS involved injury to one or more organs, including the liver, lungs, kidneys, and gallbladder.
In 25 of the 29 cases for which information on treatment discontinuation was available, DRESS symptoms resolved when levetiracetam was discontinued.
As for clobazam, a search of FAERS and the medical literature through July 2023 identified 10 serious cases of DRESS worldwide – 1 in the United States and 9 abroad. All 10 patients were hospitalized and received medical treatment. No deaths were reported.
The median time to onset of clobazam-associated DRESS was 21.5 days (range, 7-103 days). The reported signs and symptoms included skin rash (n = 10), fever (n = 8), eosinophilia (n = 7), facial swelling (n = 7), leukocytosis (n = 4), lymph node swelling (n = 4), and leukopenia/thrombocytopenia (n = 1).
In nine cases, there was injury to one or more organs, including the liver, kidneys, and gastrointestinal tract.
DRESS symptoms resolved in all 10 cases when treatment with clobazam was stopped. DRESS and other serious skin reactions reported with clobazam, a benzodiazepine, have not generally been associated with other benzodiazepines, the FDA notes.
Label updates
As a result of these cases, warnings about the risk of DRESS will be added to the prescribing information and patient medication guides for these medicines, the FDA announced.
“Health care professionals should be aware that prompt recognition and early treatment is important for improving DRESS outcomes and decreasing mortality,” the FDA said.
They noted that diagnosis is often difficult because early signs and symptoms, such as fever and swollen lymph nodes, may be present without evidence of a rash.
DRESS may develop 2-8 weeks after starting levetiracetam or clobazam. Symptoms and intensity can vary widely.
DRESS can also be confused with other serious skin reactions, such as Stevens-Johnson syndrome and toxic epidermal necrolysis.
The FDA says patients should be advised of the signs and symptoms of DRESS and be told to stop taking the medicine and seek immediate medical attention if DRESS is suspected during treatment with levetiracetam or clobazam.
Adverse reactions with these medications should be reported to the FDA’s MedWatch program.
A version of this article appeared on Medscape.com.
New consensus guide on rare drug hypersensitivity reaction
TOPLINE:
).
METHODOLOGY:
Data on the evaluation, assessment, and treatment of the rare but potentially life-threatening drug hypersensitivity reaction are lacking.
To support clinicians in diagnosing and managing DRESS, a steering committee conducted a literature review to examine current research, identify evidence, and develop consensus statements. They invited experts from 21 countries across four continents to participate in a Delphi consensus process.
An international panel of 54 experts (including 45 dermatologists) initially assessed 100 statements related to baseline workup, severity of the condition, and treatment. Two more statements were added in the second round.
After revisions and the second round, the group reached consensus for 93 statements overall.
TAKEAWAY:
The statements generating the most disagreement involved diagnosis. The group ultimately supported the value of measuring the viral load of Epstein-Barr virus, cytomegalovirus, and human herpesvirus 6 in all patients with suspected DRESS. The group also agreed on screening for hepatitis A, B, and C in cases of liver involvement and screening for hepatitis B and C before starting systemic therapy.
The group agreed with previous severity criteria that differentiate between mild, moderate, and severe DRESS based on the extent of liver, kidney, and blood involvement and the damage of other organs.
Consensus on treatment was reached for all 12 relevant statements in the first Delphi round. Recommendations included the use of corticosteroids and immediate discontinuation of the drugs causing the reaction.
IN PRACTICE:
“This Delphi exercise aimed to provide a common ground of consensus,” the authors noted. However, “each of the addressed categories needs more in-depth follow-up studies to improve the clinical management of patients.”
SOURCE:
The DRESS Delphi consensus group conducted its exercise under the leadership of Marie-Charlotte Brüggen, MD, of the University Hospital of Zürich. The consensus was published online in the JAMA Dermatology.
LIMITATIONS:
Published evidence was limited because of the low prevalence of DRESS. The consensus statements should therefore be considered with caution and in the context of a clinician’s expertise and available resources. Research gaps also persist in how DRESS may vary with region and ethnicity. The severity thresholds need validation in a revised multicenter statement.
DISCLOSURES:
The consensus review received no outside funding. Dr. Brüggen disclosed relationships with the Swiss National Science Foundation, Christine Kühne – Center for Allergy Research and Education, FreeNovation, LEO Foundation, Olga Mayenfisch Foundation, University of Zürich, LEO Pharma, Pierre Fabre Eczema Foundation, Eli Lilly, AbbVie, GSK, and AstraZeneca. Coauthors disclosed relationships with multiple pharmaceutical companies, foundations, and medical publishing companies.
A version of this article appeared on Medscape.com.
TOPLINE:
).
METHODOLOGY:
Data on the evaluation, assessment, and treatment of the rare but potentially life-threatening drug hypersensitivity reaction are lacking.
To support clinicians in diagnosing and managing DRESS, a steering committee conducted a literature review to examine current research, identify evidence, and develop consensus statements. They invited experts from 21 countries across four continents to participate in a Delphi consensus process.
An international panel of 54 experts (including 45 dermatologists) initially assessed 100 statements related to baseline workup, severity of the condition, and treatment. Two more statements were added in the second round.
After revisions and the second round, the group reached consensus for 93 statements overall.
TAKEAWAY:
The statements generating the most disagreement involved diagnosis. The group ultimately supported the value of measuring the viral load of Epstein-Barr virus, cytomegalovirus, and human herpesvirus 6 in all patients with suspected DRESS. The group also agreed on screening for hepatitis A, B, and C in cases of liver involvement and screening for hepatitis B and C before starting systemic therapy.
The group agreed with previous severity criteria that differentiate between mild, moderate, and severe DRESS based on the extent of liver, kidney, and blood involvement and the damage of other organs.
Consensus on treatment was reached for all 12 relevant statements in the first Delphi round. Recommendations included the use of corticosteroids and immediate discontinuation of the drugs causing the reaction.
IN PRACTICE:
“This Delphi exercise aimed to provide a common ground of consensus,” the authors noted. However, “each of the addressed categories needs more in-depth follow-up studies to improve the clinical management of patients.”
SOURCE:
The DRESS Delphi consensus group conducted its exercise under the leadership of Marie-Charlotte Brüggen, MD, of the University Hospital of Zürich. The consensus was published online in the JAMA Dermatology.
LIMITATIONS:
Published evidence was limited because of the low prevalence of DRESS. The consensus statements should therefore be considered with caution and in the context of a clinician’s expertise and available resources. Research gaps also persist in how DRESS may vary with region and ethnicity. The severity thresholds need validation in a revised multicenter statement.
DISCLOSURES:
The consensus review received no outside funding. Dr. Brüggen disclosed relationships with the Swiss National Science Foundation, Christine Kühne – Center for Allergy Research and Education, FreeNovation, LEO Foundation, Olga Mayenfisch Foundation, University of Zürich, LEO Pharma, Pierre Fabre Eczema Foundation, Eli Lilly, AbbVie, GSK, and AstraZeneca. Coauthors disclosed relationships with multiple pharmaceutical companies, foundations, and medical publishing companies.
A version of this article appeared on Medscape.com.
TOPLINE:
).
METHODOLOGY:
Data on the evaluation, assessment, and treatment of the rare but potentially life-threatening drug hypersensitivity reaction are lacking.
To support clinicians in diagnosing and managing DRESS, a steering committee conducted a literature review to examine current research, identify evidence, and develop consensus statements. They invited experts from 21 countries across four continents to participate in a Delphi consensus process.
An international panel of 54 experts (including 45 dermatologists) initially assessed 100 statements related to baseline workup, severity of the condition, and treatment. Two more statements were added in the second round.
After revisions and the second round, the group reached consensus for 93 statements overall.
TAKEAWAY:
The statements generating the most disagreement involved diagnosis. The group ultimately supported the value of measuring the viral load of Epstein-Barr virus, cytomegalovirus, and human herpesvirus 6 in all patients with suspected DRESS. The group also agreed on screening for hepatitis A, B, and C in cases of liver involvement and screening for hepatitis B and C before starting systemic therapy.
The group agreed with previous severity criteria that differentiate between mild, moderate, and severe DRESS based on the extent of liver, kidney, and blood involvement and the damage of other organs.
Consensus on treatment was reached for all 12 relevant statements in the first Delphi round. Recommendations included the use of corticosteroids and immediate discontinuation of the drugs causing the reaction.
IN PRACTICE:
“This Delphi exercise aimed to provide a common ground of consensus,” the authors noted. However, “each of the addressed categories needs more in-depth follow-up studies to improve the clinical management of patients.”
SOURCE:
The DRESS Delphi consensus group conducted its exercise under the leadership of Marie-Charlotte Brüggen, MD, of the University Hospital of Zürich. The consensus was published online in the JAMA Dermatology.
LIMITATIONS:
Published evidence was limited because of the low prevalence of DRESS. The consensus statements should therefore be considered with caution and in the context of a clinician’s expertise and available resources. Research gaps also persist in how DRESS may vary with region and ethnicity. The severity thresholds need validation in a revised multicenter statement.
DISCLOSURES:
The consensus review received no outside funding. Dr. Brüggen disclosed relationships with the Swiss National Science Foundation, Christine Kühne – Center for Allergy Research and Education, FreeNovation, LEO Foundation, Olga Mayenfisch Foundation, University of Zürich, LEO Pharma, Pierre Fabre Eczema Foundation, Eli Lilly, AbbVie, GSK, and AstraZeneca. Coauthors disclosed relationships with multiple pharmaceutical companies, foundations, and medical publishing companies.
A version of this article appeared on Medscape.com.
Laser epilation may reduce pilonidal disease recurrences when added to standard care
according to the results of a randomized trial.
The study, recently published in JAMA Surgery, enrolled 302 patients ages 11-21 with pilonidal disease. Half of the participants were assigned to receive LE (laser hair removal) plus standard treatment (improved hygiene plus mechanical or chemical hair removal), and half were assigned to receive standard care alone.
At 1 year, 10.4% of the patients who had received LE plus standard treatment had experienced a recurrence of pilonidal disease, compared with 33.6% of patients in the standard treatment group (P < .001). Rates were based on the data available on 96 patients in the LE group and 134 patients in the standard care group.
“These results provide further evidence that laser epilation is safe, well-tolerated, and should be available as an initial treatment option or adjunct treatment modality for all eligible patients,” first author Peter C. Minneci, MD, chair of surgery at Nemours Children’s Health, Delaware Valley, Wilmington, Del, said in a press release reporting the results. “There have been few comparative studies that have investigated recurrence rates after LE versus other treatment modalities,” he and his coauthors wrote in the study, noting that the study “was the first, to our knowledge, to compare LE as an adjunct to standard care versus standard care alone and demonstrate a decrease in recurrence rates.”
Pilonidal disease, a common condition, results when cysts form between the buttocks and is most common in adolescents and young adults. It is thought to recur about 33% of the time, with most cases recurring within 1 year of treatment.
In practice, there are large variations in management strategies for pilonidal disease because evidence for an ideal treatment approach is lacking, Dr. Minneci and coauthors wrote. Although lifestyle modifications and nonepilation hair removal strategies have been linked to a reduced need for surgery, compliance with these strategies is low. Additionally, recurrence contributes to “a high degree of psychosocial stress in patients, who often miss school or sports and may avoid social activities,” Dr. Minneci said in the press release. Therefore, some practitioners have begun using LE – which uses selective thermolysis to remove the hair shaft, follicle, and bulb – as an adjunct to standard treatments in the hopes of avoiding surgery.
A few studies have shown LE is effective in reducing pilonidal disease recurrence, but these studies had small sample sizes, according to the authors.
Study methods
The randomized, nonblinded clinical trial was conducted between 2017 and 2022 at Nationwide Children’s Hospital, Columbus, and enrolled patients aged 11-21 years with a history of pilonidal disease, who did not have active disease.
Those in the control group (151 patients) had an in-person clinic visit where they received education and training about hair removal in the gluteal cleft, and were provided with supplies for hair removal (chemical epilation or shaving) for 6 months (standard of care). Those in the LE group (151 patients) received standard of care therapy, and also received one LE treatment every 4-6 weeks for a total of five treatments. They were encouraged to perform hair removal using chemical or mechanical depilation between visits.
At the 1-year follow-up, data were available in 96 patients in the LE group and 134 patients in the standard care group. At that time, the proportion of those who had a recurrence within 1 year was significantly lower in the LE group than in the standard care group (mean difference, –23.2%; 95% CI, –33.2% to –13.1%; P < .001).
In addition, over the course of a year, those in the LE-treated group had significantly higher Child Attitude Toward Illness scores, indicating that they felt more positively about their illness at 6 months than participants in the standard care group. There were no differences between the groups in terms of patient or caregiver disability days, patient- or caregiver-reported health-related quality of life, health care satisfaction, or perceived stigma. In the LE group, no burns were reported, and no inability to tolerate treatment because of pain.
The study had several limitations, including the potential for participation bias, and because of a loss to follow-up, primary and secondary outcomes were missing data points, which was higher in the LE group. Loss to follow-up in the LE arm increased after 6 months, when laser treatments ended, with many of those patients not completing surveys at 9 and 12 months. The hospital’s pilonidal clinic shut down for 3 months during the COVID-19 pandemic, and when the clinic reopened, 15 patients in the LE arm withdrew from the study.
|In the press release, Dr. Minneci said that confirmation of the effectiveness of LE could help justify insurance coverage for pilonidal disease, noting that LE is usually not covered with insurance, and a course of treatment could cost $800-$1,500.
Dr. Minneci and four of the other six coauthors reported receiving grants from Patient-Centered Outcomes Research Institute during the conduct of the study. One author reported receiving grants from the National Institute on Minority Health and Health Disparities outside the submitted work. The research was funded by a grant from the Patient-Centered Outcomes Research Institute.
according to the results of a randomized trial.
The study, recently published in JAMA Surgery, enrolled 302 patients ages 11-21 with pilonidal disease. Half of the participants were assigned to receive LE (laser hair removal) plus standard treatment (improved hygiene plus mechanical or chemical hair removal), and half were assigned to receive standard care alone.
At 1 year, 10.4% of the patients who had received LE plus standard treatment had experienced a recurrence of pilonidal disease, compared with 33.6% of patients in the standard treatment group (P < .001). Rates were based on the data available on 96 patients in the LE group and 134 patients in the standard care group.
“These results provide further evidence that laser epilation is safe, well-tolerated, and should be available as an initial treatment option or adjunct treatment modality for all eligible patients,” first author Peter C. Minneci, MD, chair of surgery at Nemours Children’s Health, Delaware Valley, Wilmington, Del, said in a press release reporting the results. “There have been few comparative studies that have investigated recurrence rates after LE versus other treatment modalities,” he and his coauthors wrote in the study, noting that the study “was the first, to our knowledge, to compare LE as an adjunct to standard care versus standard care alone and demonstrate a decrease in recurrence rates.”
Pilonidal disease, a common condition, results when cysts form between the buttocks and is most common in adolescents and young adults. It is thought to recur about 33% of the time, with most cases recurring within 1 year of treatment.
In practice, there are large variations in management strategies for pilonidal disease because evidence for an ideal treatment approach is lacking, Dr. Minneci and coauthors wrote. Although lifestyle modifications and nonepilation hair removal strategies have been linked to a reduced need for surgery, compliance with these strategies is low. Additionally, recurrence contributes to “a high degree of psychosocial stress in patients, who often miss school or sports and may avoid social activities,” Dr. Minneci said in the press release. Therefore, some practitioners have begun using LE – which uses selective thermolysis to remove the hair shaft, follicle, and bulb – as an adjunct to standard treatments in the hopes of avoiding surgery.
A few studies have shown LE is effective in reducing pilonidal disease recurrence, but these studies had small sample sizes, according to the authors.
Study methods
The randomized, nonblinded clinical trial was conducted between 2017 and 2022 at Nationwide Children’s Hospital, Columbus, and enrolled patients aged 11-21 years with a history of pilonidal disease, who did not have active disease.
Those in the control group (151 patients) had an in-person clinic visit where they received education and training about hair removal in the gluteal cleft, and were provided with supplies for hair removal (chemical epilation or shaving) for 6 months (standard of care). Those in the LE group (151 patients) received standard of care therapy, and also received one LE treatment every 4-6 weeks for a total of five treatments. They were encouraged to perform hair removal using chemical or mechanical depilation between visits.
At the 1-year follow-up, data were available in 96 patients in the LE group and 134 patients in the standard care group. At that time, the proportion of those who had a recurrence within 1 year was significantly lower in the LE group than in the standard care group (mean difference, –23.2%; 95% CI, –33.2% to –13.1%; P < .001).
In addition, over the course of a year, those in the LE-treated group had significantly higher Child Attitude Toward Illness scores, indicating that they felt more positively about their illness at 6 months than participants in the standard care group. There were no differences between the groups in terms of patient or caregiver disability days, patient- or caregiver-reported health-related quality of life, health care satisfaction, or perceived stigma. In the LE group, no burns were reported, and no inability to tolerate treatment because of pain.
The study had several limitations, including the potential for participation bias, and because of a loss to follow-up, primary and secondary outcomes were missing data points, which was higher in the LE group. Loss to follow-up in the LE arm increased after 6 months, when laser treatments ended, with many of those patients not completing surveys at 9 and 12 months. The hospital’s pilonidal clinic shut down for 3 months during the COVID-19 pandemic, and when the clinic reopened, 15 patients in the LE arm withdrew from the study.
|In the press release, Dr. Minneci said that confirmation of the effectiveness of LE could help justify insurance coverage for pilonidal disease, noting that LE is usually not covered with insurance, and a course of treatment could cost $800-$1,500.
Dr. Minneci and four of the other six coauthors reported receiving grants from Patient-Centered Outcomes Research Institute during the conduct of the study. One author reported receiving grants from the National Institute on Minority Health and Health Disparities outside the submitted work. The research was funded by a grant from the Patient-Centered Outcomes Research Institute.
according to the results of a randomized trial.
The study, recently published in JAMA Surgery, enrolled 302 patients ages 11-21 with pilonidal disease. Half of the participants were assigned to receive LE (laser hair removal) plus standard treatment (improved hygiene plus mechanical or chemical hair removal), and half were assigned to receive standard care alone.
At 1 year, 10.4% of the patients who had received LE plus standard treatment had experienced a recurrence of pilonidal disease, compared with 33.6% of patients in the standard treatment group (P < .001). Rates were based on the data available on 96 patients in the LE group and 134 patients in the standard care group.
“These results provide further evidence that laser epilation is safe, well-tolerated, and should be available as an initial treatment option or adjunct treatment modality for all eligible patients,” first author Peter C. Minneci, MD, chair of surgery at Nemours Children’s Health, Delaware Valley, Wilmington, Del, said in a press release reporting the results. “There have been few comparative studies that have investigated recurrence rates after LE versus other treatment modalities,” he and his coauthors wrote in the study, noting that the study “was the first, to our knowledge, to compare LE as an adjunct to standard care versus standard care alone and demonstrate a decrease in recurrence rates.”
Pilonidal disease, a common condition, results when cysts form between the buttocks and is most common in adolescents and young adults. It is thought to recur about 33% of the time, with most cases recurring within 1 year of treatment.
In practice, there are large variations in management strategies for pilonidal disease because evidence for an ideal treatment approach is lacking, Dr. Minneci and coauthors wrote. Although lifestyle modifications and nonepilation hair removal strategies have been linked to a reduced need for surgery, compliance with these strategies is low. Additionally, recurrence contributes to “a high degree of psychosocial stress in patients, who often miss school or sports and may avoid social activities,” Dr. Minneci said in the press release. Therefore, some practitioners have begun using LE – which uses selective thermolysis to remove the hair shaft, follicle, and bulb – as an adjunct to standard treatments in the hopes of avoiding surgery.
A few studies have shown LE is effective in reducing pilonidal disease recurrence, but these studies had small sample sizes, according to the authors.
Study methods
The randomized, nonblinded clinical trial was conducted between 2017 and 2022 at Nationwide Children’s Hospital, Columbus, and enrolled patients aged 11-21 years with a history of pilonidal disease, who did not have active disease.
Those in the control group (151 patients) had an in-person clinic visit where they received education and training about hair removal in the gluteal cleft, and were provided with supplies for hair removal (chemical epilation or shaving) for 6 months (standard of care). Those in the LE group (151 patients) received standard of care therapy, and also received one LE treatment every 4-6 weeks for a total of five treatments. They were encouraged to perform hair removal using chemical or mechanical depilation between visits.
At the 1-year follow-up, data were available in 96 patients in the LE group and 134 patients in the standard care group. At that time, the proportion of those who had a recurrence within 1 year was significantly lower in the LE group than in the standard care group (mean difference, –23.2%; 95% CI, –33.2% to –13.1%; P < .001).
In addition, over the course of a year, those in the LE-treated group had significantly higher Child Attitude Toward Illness scores, indicating that they felt more positively about their illness at 6 months than participants in the standard care group. There were no differences between the groups in terms of patient or caregiver disability days, patient- or caregiver-reported health-related quality of life, health care satisfaction, or perceived stigma. In the LE group, no burns were reported, and no inability to tolerate treatment because of pain.
The study had several limitations, including the potential for participation bias, and because of a loss to follow-up, primary and secondary outcomes were missing data points, which was higher in the LE group. Loss to follow-up in the LE arm increased after 6 months, when laser treatments ended, with many of those patients not completing surveys at 9 and 12 months. The hospital’s pilonidal clinic shut down for 3 months during the COVID-19 pandemic, and when the clinic reopened, 15 patients in the LE arm withdrew from the study.
|In the press release, Dr. Minneci said that confirmation of the effectiveness of LE could help justify insurance coverage for pilonidal disease, noting that LE is usually not covered with insurance, and a course of treatment could cost $800-$1,500.
Dr. Minneci and four of the other six coauthors reported receiving grants from Patient-Centered Outcomes Research Institute during the conduct of the study. One author reported receiving grants from the National Institute on Minority Health and Health Disparities outside the submitted work. The research was funded by a grant from the Patient-Centered Outcomes Research Institute.
FROM JAMA SURGERY
Novel approach curbs the impact of racism on mental health in Black youth
TOPLINE:
, results of a post hoc analysis of a randomized controlled trial show.
METHODOLOGY:
- SAAF is a 7-week family skills training program delivered at local community centers that targets effective parenting behavior, adolescent self-regulation, and Black pride.
- In the original trial, 472 Black children aged 11-12 years were randomly allocated to SAAF or no treatment control.
- The post hoc analysis investigated changes in adolescent-reported depressive symptoms from age 13 to 14 years using the 20-item Center for Epidemiologic Studies Depression Scale for Children.
TAKEAWAY:
- Exposure to racial discrimination at age 13 years correlated with increased depressive symptoms at age 14 years (P < .001).
- Participation in the SAAF program significantly attenuated the association of racial discrimination at age 13 with increases in depressive symptoms at age 14 (P = .01).
- Racial discrimination was significantly associated with increases in depressive symptoms in the control group (P < .001) but not in the SAAF group.
- This moderating effect was observed using intent-to-treat design; the investigators accounted for family socioeconomic disadvantage and youth gender.
IN PRACTICE:
The findings add to other evidence suggesting that “prevention programs targeting aspects of racial identity, racial socialization processes, and parenting behavior may, to some extent, mitigate the mental health effects associated with racial discrimination. These processes appear to increase positive coping in the aftermath of discrimination, and prevent adolescents internalization of toxic messages regarding racial inferiority,” the authors wrote.
SOURCE:
The study, with first author Steven M. Kogan, PhD, University of Georgia in Athens, was published online in JAMA Network Open with a commentary by Kevin M. Simon, MD, MPH, with Boston Children’s Hospital.
LIMITATIONS:
This was a post hoc analysis of trial data. The sample consisted of Black adolescents from rural areas of Georgia, and the results may not be generalizable to Black adolescents from urban areas or adolescents from other racial groups. Because of the study’s focus on individual-level racial discrimination, the potential for SAAF to buffer the effects of structural and institutional forms of racism is unknown.
DISCLOSURES:
The study had no specific funding. The authors have disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
, results of a post hoc analysis of a randomized controlled trial show.
METHODOLOGY:
- SAAF is a 7-week family skills training program delivered at local community centers that targets effective parenting behavior, adolescent self-regulation, and Black pride.
- In the original trial, 472 Black children aged 11-12 years were randomly allocated to SAAF or no treatment control.
- The post hoc analysis investigated changes in adolescent-reported depressive symptoms from age 13 to 14 years using the 20-item Center for Epidemiologic Studies Depression Scale for Children.
TAKEAWAY:
- Exposure to racial discrimination at age 13 years correlated with increased depressive symptoms at age 14 years (P < .001).
- Participation in the SAAF program significantly attenuated the association of racial discrimination at age 13 with increases in depressive symptoms at age 14 (P = .01).
- Racial discrimination was significantly associated with increases in depressive symptoms in the control group (P < .001) but not in the SAAF group.
- This moderating effect was observed using intent-to-treat design; the investigators accounted for family socioeconomic disadvantage and youth gender.
IN PRACTICE:
The findings add to other evidence suggesting that “prevention programs targeting aspects of racial identity, racial socialization processes, and parenting behavior may, to some extent, mitigate the mental health effects associated with racial discrimination. These processes appear to increase positive coping in the aftermath of discrimination, and prevent adolescents internalization of toxic messages regarding racial inferiority,” the authors wrote.
SOURCE:
The study, with first author Steven M. Kogan, PhD, University of Georgia in Athens, was published online in JAMA Network Open with a commentary by Kevin M. Simon, MD, MPH, with Boston Children’s Hospital.
LIMITATIONS:
This was a post hoc analysis of trial data. The sample consisted of Black adolescents from rural areas of Georgia, and the results may not be generalizable to Black adolescents from urban areas or adolescents from other racial groups. Because of the study’s focus on individual-level racial discrimination, the potential for SAAF to buffer the effects of structural and institutional forms of racism is unknown.
DISCLOSURES:
The study had no specific funding. The authors have disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
, results of a post hoc analysis of a randomized controlled trial show.
METHODOLOGY:
- SAAF is a 7-week family skills training program delivered at local community centers that targets effective parenting behavior, adolescent self-regulation, and Black pride.
- In the original trial, 472 Black children aged 11-12 years were randomly allocated to SAAF or no treatment control.
- The post hoc analysis investigated changes in adolescent-reported depressive symptoms from age 13 to 14 years using the 20-item Center for Epidemiologic Studies Depression Scale for Children.
TAKEAWAY:
- Exposure to racial discrimination at age 13 years correlated with increased depressive symptoms at age 14 years (P < .001).
- Participation in the SAAF program significantly attenuated the association of racial discrimination at age 13 with increases in depressive symptoms at age 14 (P = .01).
- Racial discrimination was significantly associated with increases in depressive symptoms in the control group (P < .001) but not in the SAAF group.
- This moderating effect was observed using intent-to-treat design; the investigators accounted for family socioeconomic disadvantage and youth gender.
IN PRACTICE:
The findings add to other evidence suggesting that “prevention programs targeting aspects of racial identity, racial socialization processes, and parenting behavior may, to some extent, mitigate the mental health effects associated with racial discrimination. These processes appear to increase positive coping in the aftermath of discrimination, and prevent adolescents internalization of toxic messages regarding racial inferiority,” the authors wrote.
SOURCE:
The study, with first author Steven M. Kogan, PhD, University of Georgia in Athens, was published online in JAMA Network Open with a commentary by Kevin M. Simon, MD, MPH, with Boston Children’s Hospital.
LIMITATIONS:
This was a post hoc analysis of trial data. The sample consisted of Black adolescents from rural areas of Georgia, and the results may not be generalizable to Black adolescents from urban areas or adolescents from other racial groups. Because of the study’s focus on individual-level racial discrimination, the potential for SAAF to buffer the effects of structural and institutional forms of racism is unknown.
DISCLOSURES:
The study had no specific funding. The authors have disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
New CDC advisory once again flags BA.2.86 COVID variant
An emerging variant of COVID-19 called BA.2.86 that caused alarm in the summer of 2023 has landed on the Center for Disease Control and Prevention’s radar again.
The variant accounted for nearly 9% of cases during the 2-week period ending Nov. 25, up from 3% during the previous 2 weeks, according to data published Nov. 27 by the CDC. The estimates are not exact, and the CDC indicated the actual percentage of cases may range from 5% to 15%.
The CDC took the unusual step of publishing a specific statement about the rise in BA.2.86 cases. The variant drew worldwide attention during the summer because of how different its makeup is, compared with other prominent variants of the virus that causes COVID-19, raising the potential for the new variant to be more capable of causing infection. But after a flurry of interest in BA.2.86, it didn’t end up being as widespread as expected, so for months it wasn’t listed as a standalone variant on the CDC’s variant tracker list.
“At this time, BA.2.86 does not appear to be driving increases in infections or hospitalizations in the United States,” the CDC wrote in its advisory. “It is not possible at this time to know whether BA.2.86 infection produces different symptoms from other variants. In general, symptoms of COVID-19 tend to be similar across variants. The types of symptoms and how severe they are usually depend more on a person’s immunity than which variant causes the infection.”
BA.2.86 is now the third-most prominent variant circulating the United States, behind HV.1 and EG.5, which combined account for about 45% of all U.S. COVID-19 cases. All three are from the Omicron lineage of the virus.
About 8% of all COVID tests reported to the CDC were positive for the week ending Nov. 18, which is a decline, compared with recent weeks. But indicators for severe cases of the illness have ticked up lately, including rises among ED visits for COVID, hospitalizations, and deaths.
A version of this article appeared on WebMD.com.
An emerging variant of COVID-19 called BA.2.86 that caused alarm in the summer of 2023 has landed on the Center for Disease Control and Prevention’s radar again.
The variant accounted for nearly 9% of cases during the 2-week period ending Nov. 25, up from 3% during the previous 2 weeks, according to data published Nov. 27 by the CDC. The estimates are not exact, and the CDC indicated the actual percentage of cases may range from 5% to 15%.
The CDC took the unusual step of publishing a specific statement about the rise in BA.2.86 cases. The variant drew worldwide attention during the summer because of how different its makeup is, compared with other prominent variants of the virus that causes COVID-19, raising the potential for the new variant to be more capable of causing infection. But after a flurry of interest in BA.2.86, it didn’t end up being as widespread as expected, so for months it wasn’t listed as a standalone variant on the CDC’s variant tracker list.
“At this time, BA.2.86 does not appear to be driving increases in infections or hospitalizations in the United States,” the CDC wrote in its advisory. “It is not possible at this time to know whether BA.2.86 infection produces different symptoms from other variants. In general, symptoms of COVID-19 tend to be similar across variants. The types of symptoms and how severe they are usually depend more on a person’s immunity than which variant causes the infection.”
BA.2.86 is now the third-most prominent variant circulating the United States, behind HV.1 and EG.5, which combined account for about 45% of all U.S. COVID-19 cases. All three are from the Omicron lineage of the virus.
About 8% of all COVID tests reported to the CDC were positive for the week ending Nov. 18, which is a decline, compared with recent weeks. But indicators for severe cases of the illness have ticked up lately, including rises among ED visits for COVID, hospitalizations, and deaths.
A version of this article appeared on WebMD.com.
An emerging variant of COVID-19 called BA.2.86 that caused alarm in the summer of 2023 has landed on the Center for Disease Control and Prevention’s radar again.
The variant accounted for nearly 9% of cases during the 2-week period ending Nov. 25, up from 3% during the previous 2 weeks, according to data published Nov. 27 by the CDC. The estimates are not exact, and the CDC indicated the actual percentage of cases may range from 5% to 15%.
The CDC took the unusual step of publishing a specific statement about the rise in BA.2.86 cases. The variant drew worldwide attention during the summer because of how different its makeup is, compared with other prominent variants of the virus that causes COVID-19, raising the potential for the new variant to be more capable of causing infection. But after a flurry of interest in BA.2.86, it didn’t end up being as widespread as expected, so for months it wasn’t listed as a standalone variant on the CDC’s variant tracker list.
“At this time, BA.2.86 does not appear to be driving increases in infections or hospitalizations in the United States,” the CDC wrote in its advisory. “It is not possible at this time to know whether BA.2.86 infection produces different symptoms from other variants. In general, symptoms of COVID-19 tend to be similar across variants. The types of symptoms and how severe they are usually depend more on a person’s immunity than which variant causes the infection.”
BA.2.86 is now the third-most prominent variant circulating the United States, behind HV.1 and EG.5, which combined account for about 45% of all U.S. COVID-19 cases. All three are from the Omicron lineage of the virus.
About 8% of all COVID tests reported to the CDC were positive for the week ending Nov. 18, which is a decline, compared with recent weeks. But indicators for severe cases of the illness have ticked up lately, including rises among ED visits for COVID, hospitalizations, and deaths.
A version of this article appeared on WebMD.com.
New drug reporting limit may overlook cannabis in children
TOPLINE:
, according to a research letter published online in JAMA Pediatrics.
METHODOLOGY:
- After a laboratory changed its reporting threshold for the metabolite 11-nor-9-carboxy-Δ9-tetrahydrocannabinol (THC-COOH) from 5 ng/mL to 15 ng/mL in 2019 to match federal standards, researchers examined the rate of false positives for the initial urine drug screen and the false-negative rate with LC-MS.
- Their study focused on 976 cannabinoid-positive drug screens conducted at a pediatric hospital between Nov. 18, 2019, and May 31, 2021, that had confirmatory LC-MS to rule out false-positive results.
- Patients had a median age of 16 years.
TAKEAWAY:
- The false-positive rate was 10.1% based on the 15 ng/mL threshold compared with 2% based on the 5 ng/mL limit of quantification.
- About 81% of samples with negative LC-MS reports had detectable concentrations of THC-COOH.
IN PRACTICE:
“Confirming THC-COOH in children’s and adolescents’ urine may be relevant at concentrations less than 15 ng/mL, particularly if child protection is pertinent,” according to the study authors.
“Confirmatory testing should be reserved for select cases and must be interpreted with caution,” they added. “Laboratories should report down to the limit of quantification on request.”
SOURCE:
Christopher J. Watson, MD, emergency medicine physician, Maine Medical Center, Portland, is the study’s corresponding author.
LIMITATIONS:
The researchers lacked information about the clinical context in which patients underwent drug screening.
DISCLOSURES:
A coauthor disclosed royalties from UpToDate outside of the study.
A version of this article appeared on Medscape.com.
TOPLINE:
, according to a research letter published online in JAMA Pediatrics.
METHODOLOGY:
- After a laboratory changed its reporting threshold for the metabolite 11-nor-9-carboxy-Δ9-tetrahydrocannabinol (THC-COOH) from 5 ng/mL to 15 ng/mL in 2019 to match federal standards, researchers examined the rate of false positives for the initial urine drug screen and the false-negative rate with LC-MS.
- Their study focused on 976 cannabinoid-positive drug screens conducted at a pediatric hospital between Nov. 18, 2019, and May 31, 2021, that had confirmatory LC-MS to rule out false-positive results.
- Patients had a median age of 16 years.
TAKEAWAY:
- The false-positive rate was 10.1% based on the 15 ng/mL threshold compared with 2% based on the 5 ng/mL limit of quantification.
- About 81% of samples with negative LC-MS reports had detectable concentrations of THC-COOH.
IN PRACTICE:
“Confirming THC-COOH in children’s and adolescents’ urine may be relevant at concentrations less than 15 ng/mL, particularly if child protection is pertinent,” according to the study authors.
“Confirmatory testing should be reserved for select cases and must be interpreted with caution,” they added. “Laboratories should report down to the limit of quantification on request.”
SOURCE:
Christopher J. Watson, MD, emergency medicine physician, Maine Medical Center, Portland, is the study’s corresponding author.
LIMITATIONS:
The researchers lacked information about the clinical context in which patients underwent drug screening.
DISCLOSURES:
A coauthor disclosed royalties from UpToDate outside of the study.
A version of this article appeared on Medscape.com.
TOPLINE:
, according to a research letter published online in JAMA Pediatrics.
METHODOLOGY:
- After a laboratory changed its reporting threshold for the metabolite 11-nor-9-carboxy-Δ9-tetrahydrocannabinol (THC-COOH) from 5 ng/mL to 15 ng/mL in 2019 to match federal standards, researchers examined the rate of false positives for the initial urine drug screen and the false-negative rate with LC-MS.
- Their study focused on 976 cannabinoid-positive drug screens conducted at a pediatric hospital between Nov. 18, 2019, and May 31, 2021, that had confirmatory LC-MS to rule out false-positive results.
- Patients had a median age of 16 years.
TAKEAWAY:
- The false-positive rate was 10.1% based on the 15 ng/mL threshold compared with 2% based on the 5 ng/mL limit of quantification.
- About 81% of samples with negative LC-MS reports had detectable concentrations of THC-COOH.
IN PRACTICE:
“Confirming THC-COOH in children’s and adolescents’ urine may be relevant at concentrations less than 15 ng/mL, particularly if child protection is pertinent,” according to the study authors.
“Confirmatory testing should be reserved for select cases and must be interpreted with caution,” they added. “Laboratories should report down to the limit of quantification on request.”
SOURCE:
Christopher J. Watson, MD, emergency medicine physician, Maine Medical Center, Portland, is the study’s corresponding author.
LIMITATIONS:
The researchers lacked information about the clinical context in which patients underwent drug screening.
DISCLOSURES:
A coauthor disclosed royalties from UpToDate outside of the study.
A version of this article appeared on Medscape.com.
Quitting medical school
A few weeks ago I shared by concerns about the dwindling numbers of primary care physicians. The early exodus of practicing providers and an obvious disinterest by future physicians in what they see as the unpalatable work/life balance of frontline hands-on medicine are among the causes.
A recent study published in the journal Pediatrics highlights personal finance as a contributor to the drain on the primary care workforce. The investigators found “high self-reported educational debt ($200,000 to < $300,000) was positively associated with training in a positive lifetime earnings potential subspecialty.” In other words, why would a physician who was burdened with student loans enter a subspecialty that would limit his or her ability to pay it off? I suspect that money has always been a factor in career selection, but the ballooning cost of college and medical school has certainly not nudged graduates toward the low lifetime earnings potential of primary care pediatrics.
Another recently released survey adds the perspective of current medical school students to the murky future of the primary health care workforce. The Clinician of the Future 2023: Education Edition, published by Elsevier Health, reports on insights of more than 2,000 nursing and medical school student from around the world. The headline shocker was that while across the board a not surprising 12% of medical students were considering quitting their studies, in the United States this number was 25%.
Overall, more than 60% of the students worried about their future income, how workforce shortages would effect them and whether they would join the ranks of those clinicians suffering from burnout. While the students surveyed acknowledged that artificial intelligence could have some negative repercussions, 62% were excited about its use in their education. Similarly, they anticipated the positive contribution of digital technology while acknowledging its potential downsides.
Given the current mental health climate in this country, I was not surprised that almost a quarter of medical students in this country are considering quitting school. I would like to see a larger sample surveyed and repeated over time. But, the discrepancy between the United States and the rest of the world is troubling.
The number that really jumped out at me was that 54% of medical students (nurses, 62%) viewed “ their current studies as a stepping-stone toward a broader career in health care.” As an example, the authors quoted one medical student who plans to “look for other possibilities where I don’t directly treat patients.”
Whether this disinterest in direct patient care is an attitude that preceded their entry into medical school or a change reflecting a major reversal induced by the realty of face-to-face patient encounters in school was not addressed in the survey. I think the general population would be surprised and maybe disappointed to learn that half the students in medical school weren’t planning on seeing patients.
I went off to medical school with a rather naive Norman Rockwellian view of a physician. I was a little surprised that a few of my classmates seemed to be gravitating toward administrative and research careers, but by far most of us were heading toward opportunities that would place us face to face with patients. Some would become specialists but primary care still had an appeal for many of us.
In my last letter about primary care training, I suggested that traditional medical school was probably a poor investment for the person who shares a bit of my old-school image of the primary care physician. In addition to cost and the time invested, the curriculum would likely be overly broad and deep and not terribly applicable to the patient mix he or she would eventually be seeing. This global survey may suggest that medical students have already discovered, or are just now discovering, this mismatch between medical school and the realities of primary care.
Our challenge is to first deal with deterrent of student debt and then to develop a new, affordable and efficient pathway to primary care that attracts those people who are looking for a face to face style of medicine on the front line. The patients know we need specialists and administrators but they also want a bit more of Norman Rockwell.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
A few weeks ago I shared by concerns about the dwindling numbers of primary care physicians. The early exodus of practicing providers and an obvious disinterest by future physicians in what they see as the unpalatable work/life balance of frontline hands-on medicine are among the causes.
A recent study published in the journal Pediatrics highlights personal finance as a contributor to the drain on the primary care workforce. The investigators found “high self-reported educational debt ($200,000 to < $300,000) was positively associated with training in a positive lifetime earnings potential subspecialty.” In other words, why would a physician who was burdened with student loans enter a subspecialty that would limit his or her ability to pay it off? I suspect that money has always been a factor in career selection, but the ballooning cost of college and medical school has certainly not nudged graduates toward the low lifetime earnings potential of primary care pediatrics.
Another recently released survey adds the perspective of current medical school students to the murky future of the primary health care workforce. The Clinician of the Future 2023: Education Edition, published by Elsevier Health, reports on insights of more than 2,000 nursing and medical school student from around the world. The headline shocker was that while across the board a not surprising 12% of medical students were considering quitting their studies, in the United States this number was 25%.
Overall, more than 60% of the students worried about their future income, how workforce shortages would effect them and whether they would join the ranks of those clinicians suffering from burnout. While the students surveyed acknowledged that artificial intelligence could have some negative repercussions, 62% were excited about its use in their education. Similarly, they anticipated the positive contribution of digital technology while acknowledging its potential downsides.
Given the current mental health climate in this country, I was not surprised that almost a quarter of medical students in this country are considering quitting school. I would like to see a larger sample surveyed and repeated over time. But, the discrepancy between the United States and the rest of the world is troubling.
The number that really jumped out at me was that 54% of medical students (nurses, 62%) viewed “ their current studies as a stepping-stone toward a broader career in health care.” As an example, the authors quoted one medical student who plans to “look for other possibilities where I don’t directly treat patients.”
Whether this disinterest in direct patient care is an attitude that preceded their entry into medical school or a change reflecting a major reversal induced by the realty of face-to-face patient encounters in school was not addressed in the survey. I think the general population would be surprised and maybe disappointed to learn that half the students in medical school weren’t planning on seeing patients.
I went off to medical school with a rather naive Norman Rockwellian view of a physician. I was a little surprised that a few of my classmates seemed to be gravitating toward administrative and research careers, but by far most of us were heading toward opportunities that would place us face to face with patients. Some would become specialists but primary care still had an appeal for many of us.
In my last letter about primary care training, I suggested that traditional medical school was probably a poor investment for the person who shares a bit of my old-school image of the primary care physician. In addition to cost and the time invested, the curriculum would likely be overly broad and deep and not terribly applicable to the patient mix he or she would eventually be seeing. This global survey may suggest that medical students have already discovered, or are just now discovering, this mismatch between medical school and the realities of primary care.
Our challenge is to first deal with deterrent of student debt and then to develop a new, affordable and efficient pathway to primary care that attracts those people who are looking for a face to face style of medicine on the front line. The patients know we need specialists and administrators but they also want a bit more of Norman Rockwell.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
A few weeks ago I shared by concerns about the dwindling numbers of primary care physicians. The early exodus of practicing providers and an obvious disinterest by future physicians in what they see as the unpalatable work/life balance of frontline hands-on medicine are among the causes.
A recent study published in the journal Pediatrics highlights personal finance as a contributor to the drain on the primary care workforce. The investigators found “high self-reported educational debt ($200,000 to < $300,000) was positively associated with training in a positive lifetime earnings potential subspecialty.” In other words, why would a physician who was burdened with student loans enter a subspecialty that would limit his or her ability to pay it off? I suspect that money has always been a factor in career selection, but the ballooning cost of college and medical school has certainly not nudged graduates toward the low lifetime earnings potential of primary care pediatrics.
Another recently released survey adds the perspective of current medical school students to the murky future of the primary health care workforce. The Clinician of the Future 2023: Education Edition, published by Elsevier Health, reports on insights of more than 2,000 nursing and medical school student from around the world. The headline shocker was that while across the board a not surprising 12% of medical students were considering quitting their studies, in the United States this number was 25%.
Overall, more than 60% of the students worried about their future income, how workforce shortages would effect them and whether they would join the ranks of those clinicians suffering from burnout. While the students surveyed acknowledged that artificial intelligence could have some negative repercussions, 62% were excited about its use in their education. Similarly, they anticipated the positive contribution of digital technology while acknowledging its potential downsides.
Given the current mental health climate in this country, I was not surprised that almost a quarter of medical students in this country are considering quitting school. I would like to see a larger sample surveyed and repeated over time. But, the discrepancy between the United States and the rest of the world is troubling.
The number that really jumped out at me was that 54% of medical students (nurses, 62%) viewed “ their current studies as a stepping-stone toward a broader career in health care.” As an example, the authors quoted one medical student who plans to “look for other possibilities where I don’t directly treat patients.”
Whether this disinterest in direct patient care is an attitude that preceded their entry into medical school or a change reflecting a major reversal induced by the realty of face-to-face patient encounters in school was not addressed in the survey. I think the general population would be surprised and maybe disappointed to learn that half the students in medical school weren’t planning on seeing patients.
I went off to medical school with a rather naive Norman Rockwellian view of a physician. I was a little surprised that a few of my classmates seemed to be gravitating toward administrative and research careers, but by far most of us were heading toward opportunities that would place us face to face with patients. Some would become specialists but primary care still had an appeal for many of us.
In my last letter about primary care training, I suggested that traditional medical school was probably a poor investment for the person who shares a bit of my old-school image of the primary care physician. In addition to cost and the time invested, the curriculum would likely be overly broad and deep and not terribly applicable to the patient mix he or she would eventually be seeing. This global survey may suggest that medical students have already discovered, or are just now discovering, this mismatch between medical school and the realities of primary care.
Our challenge is to first deal with deterrent of student debt and then to develop a new, affordable and efficient pathway to primary care that attracts those people who are looking for a face to face style of medicine on the front line. The patients know we need specialists and administrators but they also want a bit more of Norman Rockwell.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
U.S. kids are taking melatonin for sleep, despite evidence gap
according to a recent study.
These findings should prompt clinicians to discuss with parents the various factors that could be driving sleep disturbances, and potential safety issues associated with melatonin usage, lead author Lauren E. Hartstein, PhD, a postdoctoral fellow in the Sleep and Development Lab at the University of Colorado, Boulder, and colleagues reported.
Writing in JAMA Pediatrics, the investigators noted that melatonin products are notorious for mislabeling, with active ingredient quantities as much as three times higher than the labeled amount. This issue is particularly concerning, they added, as calls to poison control for melatonin ingestion jumped more than fivefold from 2012 to 2021, with most cases involving children younger than 5 years. Meanwhile, scant evidence is available to characterize intentional usage in the same population.
“Current data are lacking on the prevalence of melatonin use and the frequency, dosing, and timing of melatonin administration in U.S. youth,” Dr. Hartstein and colleagues wrote.
To address this knowledge gap, the investigators conducted an online survey of parents with children and adolescents aged 1.0-13.9 years. The survey asked parents to report any melatonin usage in their children in the past 30 days.
Parents reporting melatonin usage were asked about frequency, dose, timing of administration before bedtime, and duration of use.
Findings were reported within three age groups: preschool (1-4 years), school aged (5-9 years), and preteen (10-13 years).
The survey revealed that almost one in five children in the older age groups were using melatonin, with a rate of 18.5% in the school-aged group and 19.4% in the preteen group. In comparison, 5.6% of preschool children had received melatonin for sleep in the past 30 days.
A significant uptick in usage
These findings point to a significant uptick in usage, according to Dr. Hartstein and colleagues, who cited a 2017-2018 study that found just 1.3% of U.S. children had taken melatonin in the past 30 days.
In the present study, melatonin was typically administered 30 minutes before bedtime, most often as a gummy (64.3%) or chewable tablet (27.0%).
Frequency of administration was similar between age groups and trended toward a bimodal pattern, with melatonin often given either 1 day per week or 7 days per week.
Median dose increased significantly with age, from 0.5 mg in the preschool group to 1.0 mg in the school-aged group and 2.0 mg in the preteen group. Median duration also showed a significant upward trend, with 12-month, 18-month, and 21-month durations, respectively, for ascending age groups.
The investigators concluded that melatonin usage among U.S. adolescents and children is “exceedingly common,” despite a lack of evidence to support long-term safety or guide optimal dosing.
Is melatonin use masking other sleep issues?
“Widespread melatonin use across developmental stages may suggest a high prevalence of sleep disruption, which deserves accurate diagnosis and effective treatment,” Dr. Hartstein and colleagues wrote. “Dissemination of information regarding safety concerns, such as overdose and supplement mislabeling, is necessary. Clinicians should discuss with parents the factors associated with sleep difficulties and effective behavioral strategies.”
Large-scale, long-term studies are needed, they added, to generate relevant safety and efficacy data, and to characterize the factors driving melatonin administration by parents.
“Studies like these add to our knowledge base and give us insight into what patients or parents may be doing that can impact overall health,” said Alfonso J. Padilla, MD, assistant clinical professor of sleep medicine at the University of California, Los Angeles, in a written comment. “Often, in normal encounters with our patients we may not be able to gather this information easily. It may help open conversations about sleep issues that are not being addressed.”
Dr. Padilla suggested that parents may believe that melatonin is safe because it is not regulated by the Food and Drug Administration, when in fact they could be negatively impacting their children’s sleep. He noted that short-term risks include altered circadian rhythm and vivid dreams or nightmares, while long-term safety remains unclear.
“As a sleep physician, I use melatonin for specific indications only,” Dr. Padilla said. “I may use it in small children that are having difficulty falling asleep, especially in children with autism or special needs. I also use it for help in adjustment in circadian rhythm, especially in adolescents.”
He recommends melatonin, he added, if he has a complete case history, and melatonin is suitable for that patient.
Typically, it’s not.
“Most often a medication is not the answer for the sleep concern that parents are having about their child,” he said.
The investigators disclosed grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Colorado Clinical and Translational Science Award Program of the National Center for Advancing Translational Sciences of the National Institutes of Health. They reported no conflicts of interest.
according to a recent study.
These findings should prompt clinicians to discuss with parents the various factors that could be driving sleep disturbances, and potential safety issues associated with melatonin usage, lead author Lauren E. Hartstein, PhD, a postdoctoral fellow in the Sleep and Development Lab at the University of Colorado, Boulder, and colleagues reported.
Writing in JAMA Pediatrics, the investigators noted that melatonin products are notorious for mislabeling, with active ingredient quantities as much as three times higher than the labeled amount. This issue is particularly concerning, they added, as calls to poison control for melatonin ingestion jumped more than fivefold from 2012 to 2021, with most cases involving children younger than 5 years. Meanwhile, scant evidence is available to characterize intentional usage in the same population.
“Current data are lacking on the prevalence of melatonin use and the frequency, dosing, and timing of melatonin administration in U.S. youth,” Dr. Hartstein and colleagues wrote.
To address this knowledge gap, the investigators conducted an online survey of parents with children and adolescents aged 1.0-13.9 years. The survey asked parents to report any melatonin usage in their children in the past 30 days.
Parents reporting melatonin usage were asked about frequency, dose, timing of administration before bedtime, and duration of use.
Findings were reported within three age groups: preschool (1-4 years), school aged (5-9 years), and preteen (10-13 years).
The survey revealed that almost one in five children in the older age groups were using melatonin, with a rate of 18.5% in the school-aged group and 19.4% in the preteen group. In comparison, 5.6% of preschool children had received melatonin for sleep in the past 30 days.
A significant uptick in usage
These findings point to a significant uptick in usage, according to Dr. Hartstein and colleagues, who cited a 2017-2018 study that found just 1.3% of U.S. children had taken melatonin in the past 30 days.
In the present study, melatonin was typically administered 30 minutes before bedtime, most often as a gummy (64.3%) or chewable tablet (27.0%).
Frequency of administration was similar between age groups and trended toward a bimodal pattern, with melatonin often given either 1 day per week or 7 days per week.
Median dose increased significantly with age, from 0.5 mg in the preschool group to 1.0 mg in the school-aged group and 2.0 mg in the preteen group. Median duration also showed a significant upward trend, with 12-month, 18-month, and 21-month durations, respectively, for ascending age groups.
The investigators concluded that melatonin usage among U.S. adolescents and children is “exceedingly common,” despite a lack of evidence to support long-term safety or guide optimal dosing.
Is melatonin use masking other sleep issues?
“Widespread melatonin use across developmental stages may suggest a high prevalence of sleep disruption, which deserves accurate diagnosis and effective treatment,” Dr. Hartstein and colleagues wrote. “Dissemination of information regarding safety concerns, such as overdose and supplement mislabeling, is necessary. Clinicians should discuss with parents the factors associated with sleep difficulties and effective behavioral strategies.”
Large-scale, long-term studies are needed, they added, to generate relevant safety and efficacy data, and to characterize the factors driving melatonin administration by parents.
“Studies like these add to our knowledge base and give us insight into what patients or parents may be doing that can impact overall health,” said Alfonso J. Padilla, MD, assistant clinical professor of sleep medicine at the University of California, Los Angeles, in a written comment. “Often, in normal encounters with our patients we may not be able to gather this information easily. It may help open conversations about sleep issues that are not being addressed.”
Dr. Padilla suggested that parents may believe that melatonin is safe because it is not regulated by the Food and Drug Administration, when in fact they could be negatively impacting their children’s sleep. He noted that short-term risks include altered circadian rhythm and vivid dreams or nightmares, while long-term safety remains unclear.
“As a sleep physician, I use melatonin for specific indications only,” Dr. Padilla said. “I may use it in small children that are having difficulty falling asleep, especially in children with autism or special needs. I also use it for help in adjustment in circadian rhythm, especially in adolescents.”
He recommends melatonin, he added, if he has a complete case history, and melatonin is suitable for that patient.
Typically, it’s not.
“Most often a medication is not the answer for the sleep concern that parents are having about their child,” he said.
The investigators disclosed grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Colorado Clinical and Translational Science Award Program of the National Center for Advancing Translational Sciences of the National Institutes of Health. They reported no conflicts of interest.
according to a recent study.
These findings should prompt clinicians to discuss with parents the various factors that could be driving sleep disturbances, and potential safety issues associated with melatonin usage, lead author Lauren E. Hartstein, PhD, a postdoctoral fellow in the Sleep and Development Lab at the University of Colorado, Boulder, and colleagues reported.
Writing in JAMA Pediatrics, the investigators noted that melatonin products are notorious for mislabeling, with active ingredient quantities as much as three times higher than the labeled amount. This issue is particularly concerning, they added, as calls to poison control for melatonin ingestion jumped more than fivefold from 2012 to 2021, with most cases involving children younger than 5 years. Meanwhile, scant evidence is available to characterize intentional usage in the same population.
“Current data are lacking on the prevalence of melatonin use and the frequency, dosing, and timing of melatonin administration in U.S. youth,” Dr. Hartstein and colleagues wrote.
To address this knowledge gap, the investigators conducted an online survey of parents with children and adolescents aged 1.0-13.9 years. The survey asked parents to report any melatonin usage in their children in the past 30 days.
Parents reporting melatonin usage were asked about frequency, dose, timing of administration before bedtime, and duration of use.
Findings were reported within three age groups: preschool (1-4 years), school aged (5-9 years), and preteen (10-13 years).
The survey revealed that almost one in five children in the older age groups were using melatonin, with a rate of 18.5% in the school-aged group and 19.4% in the preteen group. In comparison, 5.6% of preschool children had received melatonin for sleep in the past 30 days.
A significant uptick in usage
These findings point to a significant uptick in usage, according to Dr. Hartstein and colleagues, who cited a 2017-2018 study that found just 1.3% of U.S. children had taken melatonin in the past 30 days.
In the present study, melatonin was typically administered 30 minutes before bedtime, most often as a gummy (64.3%) or chewable tablet (27.0%).
Frequency of administration was similar between age groups and trended toward a bimodal pattern, with melatonin often given either 1 day per week or 7 days per week.
Median dose increased significantly with age, from 0.5 mg in the preschool group to 1.0 mg in the school-aged group and 2.0 mg in the preteen group. Median duration also showed a significant upward trend, with 12-month, 18-month, and 21-month durations, respectively, for ascending age groups.
The investigators concluded that melatonin usage among U.S. adolescents and children is “exceedingly common,” despite a lack of evidence to support long-term safety or guide optimal dosing.
Is melatonin use masking other sleep issues?
“Widespread melatonin use across developmental stages may suggest a high prevalence of sleep disruption, which deserves accurate diagnosis and effective treatment,” Dr. Hartstein and colleagues wrote. “Dissemination of information regarding safety concerns, such as overdose and supplement mislabeling, is necessary. Clinicians should discuss with parents the factors associated with sleep difficulties and effective behavioral strategies.”
Large-scale, long-term studies are needed, they added, to generate relevant safety and efficacy data, and to characterize the factors driving melatonin administration by parents.
“Studies like these add to our knowledge base and give us insight into what patients or parents may be doing that can impact overall health,” said Alfonso J. Padilla, MD, assistant clinical professor of sleep medicine at the University of California, Los Angeles, in a written comment. “Often, in normal encounters with our patients we may not be able to gather this information easily. It may help open conversations about sleep issues that are not being addressed.”
Dr. Padilla suggested that parents may believe that melatonin is safe because it is not regulated by the Food and Drug Administration, when in fact they could be negatively impacting their children’s sleep. He noted that short-term risks include altered circadian rhythm and vivid dreams or nightmares, while long-term safety remains unclear.
“As a sleep physician, I use melatonin for specific indications only,” Dr. Padilla said. “I may use it in small children that are having difficulty falling asleep, especially in children with autism or special needs. I also use it for help in adjustment in circadian rhythm, especially in adolescents.”
He recommends melatonin, he added, if he has a complete case history, and melatonin is suitable for that patient.
Typically, it’s not.
“Most often a medication is not the answer for the sleep concern that parents are having about their child,” he said.
The investigators disclosed grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Colorado Clinical and Translational Science Award Program of the National Center for Advancing Translational Sciences of the National Institutes of Health. They reported no conflicts of interest.
FROM JAMA PEDIATRICS
Is air filtration the best public health intervention against respiratory viruses?
This transcript has been edited for clarity.
When it comes to the public health fight against respiratory viruses – COVID, flu, RSV, and so on – it has always struck me as strange how staunchly basically any intervention is opposed. Masking was, of course, the prototypical entrenched warfare of opposing ideologies, with advocates pointing to studies suggesting the efficacy of masking to prevent transmission and advocating for broad masking recommendations, and detractors citing studies that suggested masks were ineffective and characterizing masking policies as fascist overreach. I’ll admit that I was always perplexed by this a bit, as that particular intervention seemed so benign – a bit annoying, I guess, but not crazy.
I have come to appreciate what I call status quo bias, which is the tendency to reject any policy, advice, or intervention that would force you, as an individual, to change your usual behavior. We just don’t like to do that. It has made me think that the most successful public health interventions might be the ones that take the individual out of the loop. And air quality control seems an ideal fit here. Here is a potential intervention where you, the individual, have to do precisely nothing. The status quo is preserved. We just, you know, have cleaner indoor air.
But even the suggestion of air treatment systems as a bulwark against respiratory virus transmission has been met with not just skepticism but cynicism, and perhaps even defeatism. It seems that there are those out there who think there really is nothing we can do. Sickness is interpreted in a Calvinistic framework: You become ill because it is your pre-destiny. But maybe air treatment could actually work. It seems like it might, if a new paper from PLOS One is to be believed.
What we’re talking about is a study titled “Bipolar Ionization Rapidly Inactivates Real-World, Airborne Concentrations of Infective Respiratory Viruses” – a highly controlled, laboratory-based analysis of a bipolar ionization system which seems to rapidly reduce viral counts in the air.
The proposed mechanism of action is pretty simple. The ionization system – which, don’t worry, has been shown not to produce ozone – spits out positively and negatively charged particles, which float around the test chamber, designed to look like a pretty standard room that you might find in an office or a school.
Virus is then injected into the chamber through an aerosolization machine, to achieve concentrations on the order of what you might get standing within 6 feet or so of someone actively infected with COVID while they are breathing and talking.
The idea is that those ions stick to the virus particles, similar to how a balloon sticks to the wall after you rub it on your hair, and that tends to cause them to clump together and settle on surfaces more rapidly, and thus get farther away from their ports of entry to the human system: nose, mouth, and eyes. But the ions may also interfere with viruses’ ability to bind to cellular receptors, even in the air.
To quantify viral infectivity, the researchers used a biological system. Basically, you take air samples and expose a petri dish of cells to them and see how many cells die. Fewer cells dying, less infective. Under control conditions, you can see that virus infectivity does decrease over time. Time zero here is the end of a SARS-CoV-2 aerosolization.
This may simply reflect the fact that virus particles settle out of the air. But As you can see, within about an hour, you have almost no infective virus detectable. That’s fairly impressive.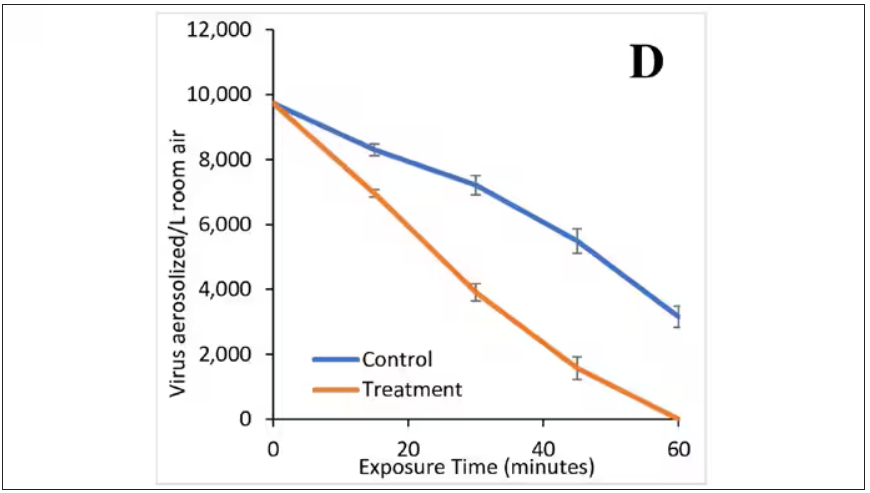
Now, I’m not saying that this is a panacea, but it is certainly worth considering the use of technologies like these if we are going to revamp the infrastructure of our offices and schools. And, of course, it would be nice to see this tested in a rigorous clinical trial with actual infected people, not cells, as the outcome. But I continue to be encouraged by interventions like this which, to be honest, ask very little of us as individuals. Maybe it’s time we accept the things, or people, that we cannot change.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
When it comes to the public health fight against respiratory viruses – COVID, flu, RSV, and so on – it has always struck me as strange how staunchly basically any intervention is opposed. Masking was, of course, the prototypical entrenched warfare of opposing ideologies, with advocates pointing to studies suggesting the efficacy of masking to prevent transmission and advocating for broad masking recommendations, and detractors citing studies that suggested masks were ineffective and characterizing masking policies as fascist overreach. I’ll admit that I was always perplexed by this a bit, as that particular intervention seemed so benign – a bit annoying, I guess, but not crazy.
I have come to appreciate what I call status quo bias, which is the tendency to reject any policy, advice, or intervention that would force you, as an individual, to change your usual behavior. We just don’t like to do that. It has made me think that the most successful public health interventions might be the ones that take the individual out of the loop. And air quality control seems an ideal fit here. Here is a potential intervention where you, the individual, have to do precisely nothing. The status quo is preserved. We just, you know, have cleaner indoor air.
But even the suggestion of air treatment systems as a bulwark against respiratory virus transmission has been met with not just skepticism but cynicism, and perhaps even defeatism. It seems that there are those out there who think there really is nothing we can do. Sickness is interpreted in a Calvinistic framework: You become ill because it is your pre-destiny. But maybe air treatment could actually work. It seems like it might, if a new paper from PLOS One is to be believed.
What we’re talking about is a study titled “Bipolar Ionization Rapidly Inactivates Real-World, Airborne Concentrations of Infective Respiratory Viruses” – a highly controlled, laboratory-based analysis of a bipolar ionization system which seems to rapidly reduce viral counts in the air.
The proposed mechanism of action is pretty simple. The ionization system – which, don’t worry, has been shown not to produce ozone – spits out positively and negatively charged particles, which float around the test chamber, designed to look like a pretty standard room that you might find in an office or a school.
Virus is then injected into the chamber through an aerosolization machine, to achieve concentrations on the order of what you might get standing within 6 feet or so of someone actively infected with COVID while they are breathing and talking.
The idea is that those ions stick to the virus particles, similar to how a balloon sticks to the wall after you rub it on your hair, and that tends to cause them to clump together and settle on surfaces more rapidly, and thus get farther away from their ports of entry to the human system: nose, mouth, and eyes. But the ions may also interfere with viruses’ ability to bind to cellular receptors, even in the air.
To quantify viral infectivity, the researchers used a biological system. Basically, you take air samples and expose a petri dish of cells to them and see how many cells die. Fewer cells dying, less infective. Under control conditions, you can see that virus infectivity does decrease over time. Time zero here is the end of a SARS-CoV-2 aerosolization.
This may simply reflect the fact that virus particles settle out of the air. But As you can see, within about an hour, you have almost no infective virus detectable. That’s fairly impressive.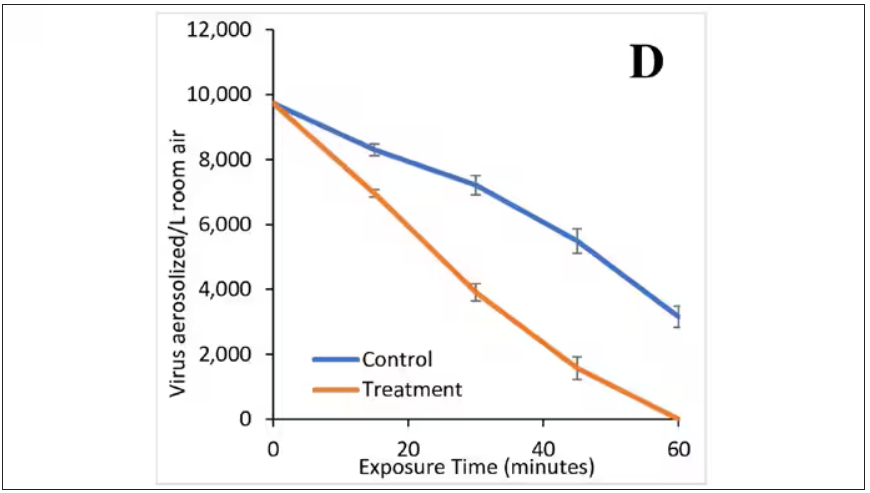
Now, I’m not saying that this is a panacea, but it is certainly worth considering the use of technologies like these if we are going to revamp the infrastructure of our offices and schools. And, of course, it would be nice to see this tested in a rigorous clinical trial with actual infected people, not cells, as the outcome. But I continue to be encouraged by interventions like this which, to be honest, ask very little of us as individuals. Maybe it’s time we accept the things, or people, that we cannot change.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
When it comes to the public health fight against respiratory viruses – COVID, flu, RSV, and so on – it has always struck me as strange how staunchly basically any intervention is opposed. Masking was, of course, the prototypical entrenched warfare of opposing ideologies, with advocates pointing to studies suggesting the efficacy of masking to prevent transmission and advocating for broad masking recommendations, and detractors citing studies that suggested masks were ineffective and characterizing masking policies as fascist overreach. I’ll admit that I was always perplexed by this a bit, as that particular intervention seemed so benign – a bit annoying, I guess, but not crazy.
I have come to appreciate what I call status quo bias, which is the tendency to reject any policy, advice, or intervention that would force you, as an individual, to change your usual behavior. We just don’t like to do that. It has made me think that the most successful public health interventions might be the ones that take the individual out of the loop. And air quality control seems an ideal fit here. Here is a potential intervention where you, the individual, have to do precisely nothing. The status quo is preserved. We just, you know, have cleaner indoor air.
But even the suggestion of air treatment systems as a bulwark against respiratory virus transmission has been met with not just skepticism but cynicism, and perhaps even defeatism. It seems that there are those out there who think there really is nothing we can do. Sickness is interpreted in a Calvinistic framework: You become ill because it is your pre-destiny. But maybe air treatment could actually work. It seems like it might, if a new paper from PLOS One is to be believed.
What we’re talking about is a study titled “Bipolar Ionization Rapidly Inactivates Real-World, Airborne Concentrations of Infective Respiratory Viruses” – a highly controlled, laboratory-based analysis of a bipolar ionization system which seems to rapidly reduce viral counts in the air.
The proposed mechanism of action is pretty simple. The ionization system – which, don’t worry, has been shown not to produce ozone – spits out positively and negatively charged particles, which float around the test chamber, designed to look like a pretty standard room that you might find in an office or a school.
Virus is then injected into the chamber through an aerosolization machine, to achieve concentrations on the order of what you might get standing within 6 feet or so of someone actively infected with COVID while they are breathing and talking.
The idea is that those ions stick to the virus particles, similar to how a balloon sticks to the wall after you rub it on your hair, and that tends to cause them to clump together and settle on surfaces more rapidly, and thus get farther away from their ports of entry to the human system: nose, mouth, and eyes. But the ions may also interfere with viruses’ ability to bind to cellular receptors, even in the air.
To quantify viral infectivity, the researchers used a biological system. Basically, you take air samples and expose a petri dish of cells to them and see how many cells die. Fewer cells dying, less infective. Under control conditions, you can see that virus infectivity does decrease over time. Time zero here is the end of a SARS-CoV-2 aerosolization.
This may simply reflect the fact that virus particles settle out of the air. But As you can see, within about an hour, you have almost no infective virus detectable. That’s fairly impressive.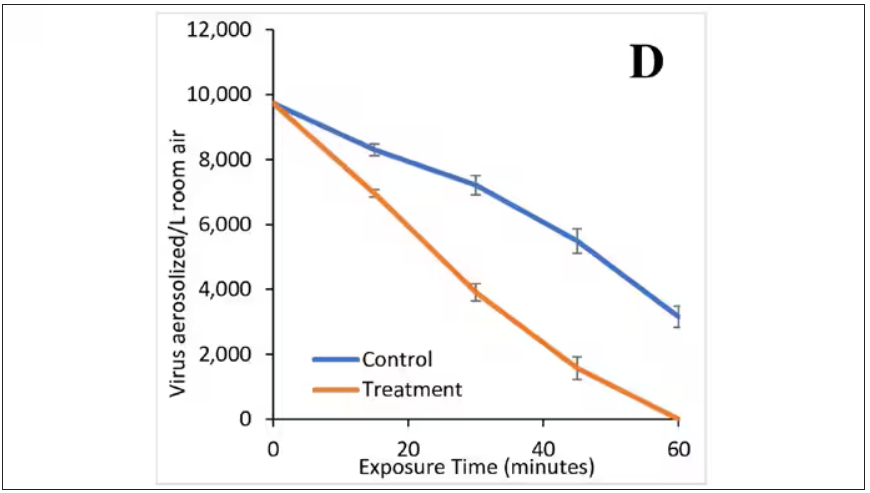
Now, I’m not saying that this is a panacea, but it is certainly worth considering the use of technologies like these if we are going to revamp the infrastructure of our offices and schools. And, of course, it would be nice to see this tested in a rigorous clinical trial with actual infected people, not cells, as the outcome. But I continue to be encouraged by interventions like this which, to be honest, ask very little of us as individuals. Maybe it’s time we accept the things, or people, that we cannot change.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.




