User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
Hospitalists confront administrative, financial challenges of COVID-19 crisis
Hospitalists nationwide have put in longer hours, played new clinical roles, and stretched beyond their medical specialty and comfort level to meet their hospital’s COVID-19 care demands. Can they expect some kind of financial recognition – perhaps in the form of “hazard pay” for going above and beyond – even though their institutions are experiencing negative financial fallout from the crisis?
Hospitals in regions experiencing a COVID-19 surge have limited elective procedures, discouraged non–COVID-19 admissions, and essentially entered crisis management mode. Other facilities in less hard-hit communities are also standing by, with reduced hospital census, smaller caseloads and less work to do, while trying to prepare their bottom lines for lower demand.
“This crisis has put most hospitals in financial jeopardy and that is likely to trickle down to all employees – including hospitalists,” said Ron Greeno, MD, FCCP, MHM, a past president of SHM and the society’s current senior advisor for government affairs. “But it’s not like hospitals could or would forgo an effective hospitalist program today. Hospitalists will be important players in defining the hospital’s future direction post crisis.”
That doesn’t mean tighter financials, caps on annual salary increases, or higher productivity expectations won’t be part of future conversations between hospital administrators and their hospitalists, Dr. Greeno said. Administrators are starting to look ahead to the post–COVID-19 era even as numbers of cases and rates of growth continue to rise in various regions, and Dr. Greeno sees a lot of uncertainty ahead.
Even prior to the crisis, he noted, hospital margins had been falling, while the cost of labor, including hospitalist labor, was going up. That was pointing toward an inevitable collision, which has only intensified with the new financial crisis facing hospitals – created by SARS-CoV-2 and by policies such as shutting down elective surgeries in anticipation of a COVID-19 patient surge that, for some institutions, may never come.
Brian Harte, MD, MHM, president of Cleveland Clinic Akron General and a past president of SHM, said that the Cleveland Clinic system has been planning since January its response to the coming crisis. “Governor Mike DeWine and the state Department of Health led the way in flattening the curve in Ohio. We engaged our hospitalists in brainstorming solutions. They have been excellent partners,” he said.
Approaching the crisis with a sense of urgency from the outset, the Cleveland Clinic built a COVID-19 surge team and incident command structure, with nursing, infectious diseases, critical care and hospital medicine represented. “We used that time to get ready for what was coming. We worked on streamlining consultant work flows.”
But utilization numbers are off in almost every service line, Dr. Harte said. “It has forced us to look at things we’ve always talked about, including greater use of telemedicine and exploring other ways of caring for patients, such as increased use of evening hours.”
Cleveland Clinic contracts with Sound Physicians of Tacoma, Wash., for its hospitalist coverage. “We have an excellent working relationship with Sound at the local, regional, and national levels, with common goals for quality and utilization. We tried to involve our hospitalists as early as possible in planning. We needed them to step in and role model and lead the way,” Dr. Harte said, for everybody’s anxiety levels.
“We’re still in the process of understanding the long-term financial impact of the epidemic,” Dr. Harte added. “But at this point I see no reason to think our relationship with our hospitalists needs to change. We’re the stewards of long-term finances. We’ll need to keep a close eye on this. But we’re committed to working through this together.”
Hazard pay for frontline health care workers was included in the COVID-19 relief package assembled in mid-May by Democrats in the House of Representatives. The $3 trillion HEROES Act includes $200 billion to award hazard pay to essential workers, including those in the health field, but Senate Majority Leader Mitch McConnell (R-Ky.) declared the legislation “dead on arrival” in the Senate.
Supplementary hazard payments made by hospitals to their hospitalists as a reward for sacrifices they made in the crisis is an interesting question, Dr. Greeno noted, and it’s definitely on the table at some hospitals. “But I think it is going to be a tough ask in these times.”
Dr. Harte said he has not offered nor been asked about hazard pay for hospitalists. Cleveland Clinic Akron General made a strategic decision that hazard pay was not going to be part of its response to the pandemic. Other hospital administrators interviewed for this article concur.
Hospitals respond to the fiscal crisis
Hospitals in other parts of the country also report significant fiscal fallout from the COVID-19 crisis, with predictions that 100 or more hospitals may be forced to close. Jeff Dye, president of the New Mexico Hospital Association, told the Albuquerque Journal on May 1 that hospitals in his state have been squeezed on all sides by increased costs, patients delaying routine care, and public health orders restricting elective surgeries. New Mexico hospitals, especially in rural areas, face incredible financial strain.
The University of Virginia Medical Center, Charlottesville, recently announced 20% reductions in total compensation for its providers through July 31, along with suspension of retirement contributions. Those changes won’t affect team members caring for COVID-19 patients. And the Spectrum Health Medical Group of 15 hospitals in western Michigan, according to Michigan Public Radio, told its doctors they either needed to sign “contract addendums” giving the system more control over their hours – or face a 25% pay cut, or worse.
Cheyenne (Wyo.) Regional Medical Center issued a statement April 24 that it expected losses of $10 million for the month of April. “CRMC, like every other hospital in Wyoming, is certainly feeling the financial impact that COVID-19 is having,” CEO Tim Thornell told the Cowboy State Daily on April 24. That includes a 30% reduction in inpatient care and 50% reduction in outpatient care, while the hospital has only had a handful of COVID-19 patients at any time. Capital projects are now on hold, overtime is limited, and a hiring freeze is in effect.
“We’re certainly prepared for a larger surge, which hasn’t come yet,” Mr. Thornell said in an interview. CRMC’s ICU was split to create a nine-bed dedicated COVID-19 unit. Intensivists see most of the critical care patients, while the hospital’s 15 directly-employed hospitalists are treating all of the non-ICU COVID-19 patients. “Among themselves, the hospitalists volunteered who would work on the unit. We’ve been fortunate enough to have enough volunteers and enough PPE [personal protective equipment],” he said.
Preparing for the COVID-19 pandemic has strengthened the medical center’s relationship with its hospitalists, Mr. Thornell explained. “Hospitalists are key to our operations, involved in so much that happens here. We’re trying to staff to volume with decreased utilization. We’ve scaled back, which only makes fiscal sense. Now, how do we reinfuse patients back into the mix? Our hospitalists are paid by the number of shifts, and as you distribute shift reductions over 15 providers, it shouldn’t be an intolerable burden.” But two open hospitalist positions have not been filled, he noted.
CRMC is trying to approach these changes with a Lean perspective, Mr. Thornell said. “We had already adopted a Lean program, but this has been a chance to go through a life-altering circumstance using the tools of Lean planning and applying them instantaneously.”
Providers step up
At Emory Healthcare in Atlanta, a major center for COVID-19 cases, communication has been essential in the crisis, said Bryce Gartland, MD, SFHM, Emory’s hospital group president and cochief of clinical operations. “Our group was prepared for a significant influx of patients. Like every other institution, we made the decision to postpone elective care, with a resulting plummet in volume,” he said.
As COVID-19 patients entered the Emory system, frontline hospitalists stepped up to care for those patients. “We’ve had ample providers in terms of clinical care. We guaranteed our physicians’ base compensation. They have flexed teams up and down as needed.” Advanced practice professionals also stepped up to bridge gaps.
With regard to the return of volumes of non–COVID-19 patients, the jury’s still out, Dr. Gartland said. “None of us has a crystal ball, and there are tremendous variables and decision points that will have significant impact. We have started to see numbers of time-sensitive and essential cases increase as of the first week of May.”
What lies ahead will likely include some rightsizing to future volumes. On top of that, the broader economic pressures on hospitals from high rates of unemployment, uninsured patients, bad debt, and charity care will push health care systems to significantly address costs and infrastructure, he said. “We’re still early in planning, and striving to maintain flexibility and nimbleness, given the uncertainties to this early understanding of our new normal. No hospital is immune from the financial impact. We’ll see and hear about more of these conversations in the months ahead.”
But the experience has also generated some positives, Dr. Gartland noted. “Things like telehealth, which we’ve been talking about for years but previously faced barriers to widespread adoption.” Now with COVID-19, the federal government issued waivers, and barriers – both internal and external – came down. “With telehealth, what will the role and deployment of hospitalists look like in this new model? How will traditional productivity expectations change, or the numbers and types of providers? This will make the relationship and partnership between hospitalist groups and hospital administrators ever more important as we consider the evolution toward new care models.”
Dr. Gartland said that “one of the great things about hospital medicine as a field is its flexibility and adaptability. Where there have been gaps, hospitalists were quick to step in. As long as hospital medicine continues to embrace those kinds of behaviors, it will be successful.” But if the conversation with hospitals is just about money, it will be harder, he acknowledged. “Where there is this kind of disruption in our usual way of doing things, there are also tremendous opportunities for care model innovation. I would encourage hospitalist groups to try to be true value partners.”
Command center mode
Like other physicians in hospital C-suites, Chad Whelan MD, FACP, SFHM, chief executive officer of Banner–University Medicine in Tucson, Ariz., led his two hospitals into command center mode when the crisis hit, planning for a surge of COVID-19 cases that could overwhelm hospital capacity.
“In terms of our hospitalists, we leaned in to them hard in the beginning, preparing them to supervise other physicians who came in to help if needed,” he said. “Our [non–COVID-19] census is down, revenues are down, and the implications are enormous – like nothing we’ve ever seen before.”
“We’re fortunate that we’re part of the Banner health system. We made a decision that we would essentially keep our physicians financially protected through this crisis,” Dr. Whelan said. “In return, we called on them to step up and be on the front lines and to put in enormous hours for planning. We asked them to consider: How could you contribute if the surge comes?”
He affirmed that hospital medicine has been a major part of his medical center’s planning and implementation. “I’ve been overwhelmed by the degree to which the entire delivery team has rallied around the pandemic, with everybody saying they want to keep people safe and be part of the solution. We have always had hospitalist leaders at the table as we’ve planned our response and as decisions were made,” said Dr. Whelan, a practicing hospitalist and teaching service attending since 2000 until he assumed his current executive position in Arizona 18 months ago.
“While we have kept people whole during the immediate crisis, we have acknowledged that we don’t know what our recovery will look like. What if [non–COVID-19] volume doesn’t return? That keeps me awake at night,” he said. “I have talked to our physician leadership in hospital medicine and more broadly. We need to ask ourselves many questions, including: do we have the right levels of staffing? Is this the time to consider alternate models of staffing, for example, advanced practice providers? And does the compensation plan need adjustments?”
Dr. Whelan thinks that the COVID-19 crisis is an opportunity for hospital medicine to more rapidly explore different models and to ask what additional value hospitalists can bring to the care model. “For example, what would it mean to redefine the hospitalist’s scope of practice as an acute medicine specialist, not defined by the hospital’s four walls?” he noted.
“One of the reasons our smaller hospital reached capacity with COVID-19 patients was the skilled nursing facility located a few hundred feet away that turned into a hot spot. If we had imported the hospital medicine model virtually into that SNF early on, could there have been a different scenario? Have we thought through what that would have even looked like?” Dr. Whelan asked.
He challenges the hospital medicine field, once it gets to the other side of this crisis, to not fall back on old way of doing things. “Instead, let’s use this time to create a better model today,” he said. “That’s what we’re trying to do at a system level at Banner, with our hospital medicine groups partnering with the hospital. I want to see our hospitalists create and thrive in that new model.”
Hospitalists nationwide have put in longer hours, played new clinical roles, and stretched beyond their medical specialty and comfort level to meet their hospital’s COVID-19 care demands. Can they expect some kind of financial recognition – perhaps in the form of “hazard pay” for going above and beyond – even though their institutions are experiencing negative financial fallout from the crisis?
Hospitals in regions experiencing a COVID-19 surge have limited elective procedures, discouraged non–COVID-19 admissions, and essentially entered crisis management mode. Other facilities in less hard-hit communities are also standing by, with reduced hospital census, smaller caseloads and less work to do, while trying to prepare their bottom lines for lower demand.
“This crisis has put most hospitals in financial jeopardy and that is likely to trickle down to all employees – including hospitalists,” said Ron Greeno, MD, FCCP, MHM, a past president of SHM and the society’s current senior advisor for government affairs. “But it’s not like hospitals could or would forgo an effective hospitalist program today. Hospitalists will be important players in defining the hospital’s future direction post crisis.”
That doesn’t mean tighter financials, caps on annual salary increases, or higher productivity expectations won’t be part of future conversations between hospital administrators and their hospitalists, Dr. Greeno said. Administrators are starting to look ahead to the post–COVID-19 era even as numbers of cases and rates of growth continue to rise in various regions, and Dr. Greeno sees a lot of uncertainty ahead.
Even prior to the crisis, he noted, hospital margins had been falling, while the cost of labor, including hospitalist labor, was going up. That was pointing toward an inevitable collision, which has only intensified with the new financial crisis facing hospitals – created by SARS-CoV-2 and by policies such as shutting down elective surgeries in anticipation of a COVID-19 patient surge that, for some institutions, may never come.
Brian Harte, MD, MHM, president of Cleveland Clinic Akron General and a past president of SHM, said that the Cleveland Clinic system has been planning since January its response to the coming crisis. “Governor Mike DeWine and the state Department of Health led the way in flattening the curve in Ohio. We engaged our hospitalists in brainstorming solutions. They have been excellent partners,” he said.
Approaching the crisis with a sense of urgency from the outset, the Cleveland Clinic built a COVID-19 surge team and incident command structure, with nursing, infectious diseases, critical care and hospital medicine represented. “We used that time to get ready for what was coming. We worked on streamlining consultant work flows.”
But utilization numbers are off in almost every service line, Dr. Harte said. “It has forced us to look at things we’ve always talked about, including greater use of telemedicine and exploring other ways of caring for patients, such as increased use of evening hours.”
Cleveland Clinic contracts with Sound Physicians of Tacoma, Wash., for its hospitalist coverage. “We have an excellent working relationship with Sound at the local, regional, and national levels, with common goals for quality and utilization. We tried to involve our hospitalists as early as possible in planning. We needed them to step in and role model and lead the way,” Dr. Harte said, for everybody’s anxiety levels.
“We’re still in the process of understanding the long-term financial impact of the epidemic,” Dr. Harte added. “But at this point I see no reason to think our relationship with our hospitalists needs to change. We’re the stewards of long-term finances. We’ll need to keep a close eye on this. But we’re committed to working through this together.”
Hazard pay for frontline health care workers was included in the COVID-19 relief package assembled in mid-May by Democrats in the House of Representatives. The $3 trillion HEROES Act includes $200 billion to award hazard pay to essential workers, including those in the health field, but Senate Majority Leader Mitch McConnell (R-Ky.) declared the legislation “dead on arrival” in the Senate.
Supplementary hazard payments made by hospitals to their hospitalists as a reward for sacrifices they made in the crisis is an interesting question, Dr. Greeno noted, and it’s definitely on the table at some hospitals. “But I think it is going to be a tough ask in these times.”
Dr. Harte said he has not offered nor been asked about hazard pay for hospitalists. Cleveland Clinic Akron General made a strategic decision that hazard pay was not going to be part of its response to the pandemic. Other hospital administrators interviewed for this article concur.
Hospitals respond to the fiscal crisis
Hospitals in other parts of the country also report significant fiscal fallout from the COVID-19 crisis, with predictions that 100 or more hospitals may be forced to close. Jeff Dye, president of the New Mexico Hospital Association, told the Albuquerque Journal on May 1 that hospitals in his state have been squeezed on all sides by increased costs, patients delaying routine care, and public health orders restricting elective surgeries. New Mexico hospitals, especially in rural areas, face incredible financial strain.
The University of Virginia Medical Center, Charlottesville, recently announced 20% reductions in total compensation for its providers through July 31, along with suspension of retirement contributions. Those changes won’t affect team members caring for COVID-19 patients. And the Spectrum Health Medical Group of 15 hospitals in western Michigan, according to Michigan Public Radio, told its doctors they either needed to sign “contract addendums” giving the system more control over their hours – or face a 25% pay cut, or worse.
Cheyenne (Wyo.) Regional Medical Center issued a statement April 24 that it expected losses of $10 million for the month of April. “CRMC, like every other hospital in Wyoming, is certainly feeling the financial impact that COVID-19 is having,” CEO Tim Thornell told the Cowboy State Daily on April 24. That includes a 30% reduction in inpatient care and 50% reduction in outpatient care, while the hospital has only had a handful of COVID-19 patients at any time. Capital projects are now on hold, overtime is limited, and a hiring freeze is in effect.
“We’re certainly prepared for a larger surge, which hasn’t come yet,” Mr. Thornell said in an interview. CRMC’s ICU was split to create a nine-bed dedicated COVID-19 unit. Intensivists see most of the critical care patients, while the hospital’s 15 directly-employed hospitalists are treating all of the non-ICU COVID-19 patients. “Among themselves, the hospitalists volunteered who would work on the unit. We’ve been fortunate enough to have enough volunteers and enough PPE [personal protective equipment],” he said.
Preparing for the COVID-19 pandemic has strengthened the medical center’s relationship with its hospitalists, Mr. Thornell explained. “Hospitalists are key to our operations, involved in so much that happens here. We’re trying to staff to volume with decreased utilization. We’ve scaled back, which only makes fiscal sense. Now, how do we reinfuse patients back into the mix? Our hospitalists are paid by the number of shifts, and as you distribute shift reductions over 15 providers, it shouldn’t be an intolerable burden.” But two open hospitalist positions have not been filled, he noted.
CRMC is trying to approach these changes with a Lean perspective, Mr. Thornell said. “We had already adopted a Lean program, but this has been a chance to go through a life-altering circumstance using the tools of Lean planning and applying them instantaneously.”
Providers step up
At Emory Healthcare in Atlanta, a major center for COVID-19 cases, communication has been essential in the crisis, said Bryce Gartland, MD, SFHM, Emory’s hospital group president and cochief of clinical operations. “Our group was prepared for a significant influx of patients. Like every other institution, we made the decision to postpone elective care, with a resulting plummet in volume,” he said.
As COVID-19 patients entered the Emory system, frontline hospitalists stepped up to care for those patients. “We’ve had ample providers in terms of clinical care. We guaranteed our physicians’ base compensation. They have flexed teams up and down as needed.” Advanced practice professionals also stepped up to bridge gaps.
With regard to the return of volumes of non–COVID-19 patients, the jury’s still out, Dr. Gartland said. “None of us has a crystal ball, and there are tremendous variables and decision points that will have significant impact. We have started to see numbers of time-sensitive and essential cases increase as of the first week of May.”
What lies ahead will likely include some rightsizing to future volumes. On top of that, the broader economic pressures on hospitals from high rates of unemployment, uninsured patients, bad debt, and charity care will push health care systems to significantly address costs and infrastructure, he said. “We’re still early in planning, and striving to maintain flexibility and nimbleness, given the uncertainties to this early understanding of our new normal. No hospital is immune from the financial impact. We’ll see and hear about more of these conversations in the months ahead.”
But the experience has also generated some positives, Dr. Gartland noted. “Things like telehealth, which we’ve been talking about for years but previously faced barriers to widespread adoption.” Now with COVID-19, the federal government issued waivers, and barriers – both internal and external – came down. “With telehealth, what will the role and deployment of hospitalists look like in this new model? How will traditional productivity expectations change, or the numbers and types of providers? This will make the relationship and partnership between hospitalist groups and hospital administrators ever more important as we consider the evolution toward new care models.”
Dr. Gartland said that “one of the great things about hospital medicine as a field is its flexibility and adaptability. Where there have been gaps, hospitalists were quick to step in. As long as hospital medicine continues to embrace those kinds of behaviors, it will be successful.” But if the conversation with hospitals is just about money, it will be harder, he acknowledged. “Where there is this kind of disruption in our usual way of doing things, there are also tremendous opportunities for care model innovation. I would encourage hospitalist groups to try to be true value partners.”
Command center mode
Like other physicians in hospital C-suites, Chad Whelan MD, FACP, SFHM, chief executive officer of Banner–University Medicine in Tucson, Ariz., led his two hospitals into command center mode when the crisis hit, planning for a surge of COVID-19 cases that could overwhelm hospital capacity.
“In terms of our hospitalists, we leaned in to them hard in the beginning, preparing them to supervise other physicians who came in to help if needed,” he said. “Our [non–COVID-19] census is down, revenues are down, and the implications are enormous – like nothing we’ve ever seen before.”
“We’re fortunate that we’re part of the Banner health system. We made a decision that we would essentially keep our physicians financially protected through this crisis,” Dr. Whelan said. “In return, we called on them to step up and be on the front lines and to put in enormous hours for planning. We asked them to consider: How could you contribute if the surge comes?”
He affirmed that hospital medicine has been a major part of his medical center’s planning and implementation. “I’ve been overwhelmed by the degree to which the entire delivery team has rallied around the pandemic, with everybody saying they want to keep people safe and be part of the solution. We have always had hospitalist leaders at the table as we’ve planned our response and as decisions were made,” said Dr. Whelan, a practicing hospitalist and teaching service attending since 2000 until he assumed his current executive position in Arizona 18 months ago.
“While we have kept people whole during the immediate crisis, we have acknowledged that we don’t know what our recovery will look like. What if [non–COVID-19] volume doesn’t return? That keeps me awake at night,” he said. “I have talked to our physician leadership in hospital medicine and more broadly. We need to ask ourselves many questions, including: do we have the right levels of staffing? Is this the time to consider alternate models of staffing, for example, advanced practice providers? And does the compensation plan need adjustments?”
Dr. Whelan thinks that the COVID-19 crisis is an opportunity for hospital medicine to more rapidly explore different models and to ask what additional value hospitalists can bring to the care model. “For example, what would it mean to redefine the hospitalist’s scope of practice as an acute medicine specialist, not defined by the hospital’s four walls?” he noted.
“One of the reasons our smaller hospital reached capacity with COVID-19 patients was the skilled nursing facility located a few hundred feet away that turned into a hot spot. If we had imported the hospital medicine model virtually into that SNF early on, could there have been a different scenario? Have we thought through what that would have even looked like?” Dr. Whelan asked.
He challenges the hospital medicine field, once it gets to the other side of this crisis, to not fall back on old way of doing things. “Instead, let’s use this time to create a better model today,” he said. “That’s what we’re trying to do at a system level at Banner, with our hospital medicine groups partnering with the hospital. I want to see our hospitalists create and thrive in that new model.”
Hospitalists nationwide have put in longer hours, played new clinical roles, and stretched beyond their medical specialty and comfort level to meet their hospital’s COVID-19 care demands. Can they expect some kind of financial recognition – perhaps in the form of “hazard pay” for going above and beyond – even though their institutions are experiencing negative financial fallout from the crisis?
Hospitals in regions experiencing a COVID-19 surge have limited elective procedures, discouraged non–COVID-19 admissions, and essentially entered crisis management mode. Other facilities in less hard-hit communities are also standing by, with reduced hospital census, smaller caseloads and less work to do, while trying to prepare their bottom lines for lower demand.
“This crisis has put most hospitals in financial jeopardy and that is likely to trickle down to all employees – including hospitalists,” said Ron Greeno, MD, FCCP, MHM, a past president of SHM and the society’s current senior advisor for government affairs. “But it’s not like hospitals could or would forgo an effective hospitalist program today. Hospitalists will be important players in defining the hospital’s future direction post crisis.”
That doesn’t mean tighter financials, caps on annual salary increases, or higher productivity expectations won’t be part of future conversations between hospital administrators and their hospitalists, Dr. Greeno said. Administrators are starting to look ahead to the post–COVID-19 era even as numbers of cases and rates of growth continue to rise in various regions, and Dr. Greeno sees a lot of uncertainty ahead.
Even prior to the crisis, he noted, hospital margins had been falling, while the cost of labor, including hospitalist labor, was going up. That was pointing toward an inevitable collision, which has only intensified with the new financial crisis facing hospitals – created by SARS-CoV-2 and by policies such as shutting down elective surgeries in anticipation of a COVID-19 patient surge that, for some institutions, may never come.
Brian Harte, MD, MHM, president of Cleveland Clinic Akron General and a past president of SHM, said that the Cleveland Clinic system has been planning since January its response to the coming crisis. “Governor Mike DeWine and the state Department of Health led the way in flattening the curve in Ohio. We engaged our hospitalists in brainstorming solutions. They have been excellent partners,” he said.
Approaching the crisis with a sense of urgency from the outset, the Cleveland Clinic built a COVID-19 surge team and incident command structure, with nursing, infectious diseases, critical care and hospital medicine represented. “We used that time to get ready for what was coming. We worked on streamlining consultant work flows.”
But utilization numbers are off in almost every service line, Dr. Harte said. “It has forced us to look at things we’ve always talked about, including greater use of telemedicine and exploring other ways of caring for patients, such as increased use of evening hours.”
Cleveland Clinic contracts with Sound Physicians of Tacoma, Wash., for its hospitalist coverage. “We have an excellent working relationship with Sound at the local, regional, and national levels, with common goals for quality and utilization. We tried to involve our hospitalists as early as possible in planning. We needed them to step in and role model and lead the way,” Dr. Harte said, for everybody’s anxiety levels.
“We’re still in the process of understanding the long-term financial impact of the epidemic,” Dr. Harte added. “But at this point I see no reason to think our relationship with our hospitalists needs to change. We’re the stewards of long-term finances. We’ll need to keep a close eye on this. But we’re committed to working through this together.”
Hazard pay for frontline health care workers was included in the COVID-19 relief package assembled in mid-May by Democrats in the House of Representatives. The $3 trillion HEROES Act includes $200 billion to award hazard pay to essential workers, including those in the health field, but Senate Majority Leader Mitch McConnell (R-Ky.) declared the legislation “dead on arrival” in the Senate.
Supplementary hazard payments made by hospitals to their hospitalists as a reward for sacrifices they made in the crisis is an interesting question, Dr. Greeno noted, and it’s definitely on the table at some hospitals. “But I think it is going to be a tough ask in these times.”
Dr. Harte said he has not offered nor been asked about hazard pay for hospitalists. Cleveland Clinic Akron General made a strategic decision that hazard pay was not going to be part of its response to the pandemic. Other hospital administrators interviewed for this article concur.
Hospitals respond to the fiscal crisis
Hospitals in other parts of the country also report significant fiscal fallout from the COVID-19 crisis, with predictions that 100 or more hospitals may be forced to close. Jeff Dye, president of the New Mexico Hospital Association, told the Albuquerque Journal on May 1 that hospitals in his state have been squeezed on all sides by increased costs, patients delaying routine care, and public health orders restricting elective surgeries. New Mexico hospitals, especially in rural areas, face incredible financial strain.
The University of Virginia Medical Center, Charlottesville, recently announced 20% reductions in total compensation for its providers through July 31, along with suspension of retirement contributions. Those changes won’t affect team members caring for COVID-19 patients. And the Spectrum Health Medical Group of 15 hospitals in western Michigan, according to Michigan Public Radio, told its doctors they either needed to sign “contract addendums” giving the system more control over their hours – or face a 25% pay cut, or worse.
Cheyenne (Wyo.) Regional Medical Center issued a statement April 24 that it expected losses of $10 million for the month of April. “CRMC, like every other hospital in Wyoming, is certainly feeling the financial impact that COVID-19 is having,” CEO Tim Thornell told the Cowboy State Daily on April 24. That includes a 30% reduction in inpatient care and 50% reduction in outpatient care, while the hospital has only had a handful of COVID-19 patients at any time. Capital projects are now on hold, overtime is limited, and a hiring freeze is in effect.
“We’re certainly prepared for a larger surge, which hasn’t come yet,” Mr. Thornell said in an interview. CRMC’s ICU was split to create a nine-bed dedicated COVID-19 unit. Intensivists see most of the critical care patients, while the hospital’s 15 directly-employed hospitalists are treating all of the non-ICU COVID-19 patients. “Among themselves, the hospitalists volunteered who would work on the unit. We’ve been fortunate enough to have enough volunteers and enough PPE [personal protective equipment],” he said.
Preparing for the COVID-19 pandemic has strengthened the medical center’s relationship with its hospitalists, Mr. Thornell explained. “Hospitalists are key to our operations, involved in so much that happens here. We’re trying to staff to volume with decreased utilization. We’ve scaled back, which only makes fiscal sense. Now, how do we reinfuse patients back into the mix? Our hospitalists are paid by the number of shifts, and as you distribute shift reductions over 15 providers, it shouldn’t be an intolerable burden.” But two open hospitalist positions have not been filled, he noted.
CRMC is trying to approach these changes with a Lean perspective, Mr. Thornell said. “We had already adopted a Lean program, but this has been a chance to go through a life-altering circumstance using the tools of Lean planning and applying them instantaneously.”
Providers step up
At Emory Healthcare in Atlanta, a major center for COVID-19 cases, communication has been essential in the crisis, said Bryce Gartland, MD, SFHM, Emory’s hospital group president and cochief of clinical operations. “Our group was prepared for a significant influx of patients. Like every other institution, we made the decision to postpone elective care, with a resulting plummet in volume,” he said.
As COVID-19 patients entered the Emory system, frontline hospitalists stepped up to care for those patients. “We’ve had ample providers in terms of clinical care. We guaranteed our physicians’ base compensation. They have flexed teams up and down as needed.” Advanced practice professionals also stepped up to bridge gaps.
With regard to the return of volumes of non–COVID-19 patients, the jury’s still out, Dr. Gartland said. “None of us has a crystal ball, and there are tremendous variables and decision points that will have significant impact. We have started to see numbers of time-sensitive and essential cases increase as of the first week of May.”
What lies ahead will likely include some rightsizing to future volumes. On top of that, the broader economic pressures on hospitals from high rates of unemployment, uninsured patients, bad debt, and charity care will push health care systems to significantly address costs and infrastructure, he said. “We’re still early in planning, and striving to maintain flexibility and nimbleness, given the uncertainties to this early understanding of our new normal. No hospital is immune from the financial impact. We’ll see and hear about more of these conversations in the months ahead.”
But the experience has also generated some positives, Dr. Gartland noted. “Things like telehealth, which we’ve been talking about for years but previously faced barriers to widespread adoption.” Now with COVID-19, the federal government issued waivers, and barriers – both internal and external – came down. “With telehealth, what will the role and deployment of hospitalists look like in this new model? How will traditional productivity expectations change, or the numbers and types of providers? This will make the relationship and partnership between hospitalist groups and hospital administrators ever more important as we consider the evolution toward new care models.”
Dr. Gartland said that “one of the great things about hospital medicine as a field is its flexibility and adaptability. Where there have been gaps, hospitalists were quick to step in. As long as hospital medicine continues to embrace those kinds of behaviors, it will be successful.” But if the conversation with hospitals is just about money, it will be harder, he acknowledged. “Where there is this kind of disruption in our usual way of doing things, there are also tremendous opportunities for care model innovation. I would encourage hospitalist groups to try to be true value partners.”
Command center mode
Like other physicians in hospital C-suites, Chad Whelan MD, FACP, SFHM, chief executive officer of Banner–University Medicine in Tucson, Ariz., led his two hospitals into command center mode when the crisis hit, planning for a surge of COVID-19 cases that could overwhelm hospital capacity.
“In terms of our hospitalists, we leaned in to them hard in the beginning, preparing them to supervise other physicians who came in to help if needed,” he said. “Our [non–COVID-19] census is down, revenues are down, and the implications are enormous – like nothing we’ve ever seen before.”
“We’re fortunate that we’re part of the Banner health system. We made a decision that we would essentially keep our physicians financially protected through this crisis,” Dr. Whelan said. “In return, we called on them to step up and be on the front lines and to put in enormous hours for planning. We asked them to consider: How could you contribute if the surge comes?”
He affirmed that hospital medicine has been a major part of his medical center’s planning and implementation. “I’ve been overwhelmed by the degree to which the entire delivery team has rallied around the pandemic, with everybody saying they want to keep people safe and be part of the solution. We have always had hospitalist leaders at the table as we’ve planned our response and as decisions were made,” said Dr. Whelan, a practicing hospitalist and teaching service attending since 2000 until he assumed his current executive position in Arizona 18 months ago.
“While we have kept people whole during the immediate crisis, we have acknowledged that we don’t know what our recovery will look like. What if [non–COVID-19] volume doesn’t return? That keeps me awake at night,” he said. “I have talked to our physician leadership in hospital medicine and more broadly. We need to ask ourselves many questions, including: do we have the right levels of staffing? Is this the time to consider alternate models of staffing, for example, advanced practice providers? And does the compensation plan need adjustments?”
Dr. Whelan thinks that the COVID-19 crisis is an opportunity for hospital medicine to more rapidly explore different models and to ask what additional value hospitalists can bring to the care model. “For example, what would it mean to redefine the hospitalist’s scope of practice as an acute medicine specialist, not defined by the hospital’s four walls?” he noted.
“One of the reasons our smaller hospital reached capacity with COVID-19 patients was the skilled nursing facility located a few hundred feet away that turned into a hot spot. If we had imported the hospital medicine model virtually into that SNF early on, could there have been a different scenario? Have we thought through what that would have even looked like?” Dr. Whelan asked.
He challenges the hospital medicine field, once it gets to the other side of this crisis, to not fall back on old way of doing things. “Instead, let’s use this time to create a better model today,” he said. “That’s what we’re trying to do at a system level at Banner, with our hospital medicine groups partnering with the hospital. I want to see our hospitalists create and thrive in that new model.”
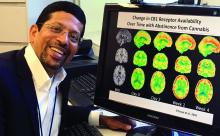
Frequent cannabis use in depression tripled over past decade
Not only are individuals with depression at significantly higher risk for cannabis use, compared with those without depression, this trend has increased dramatically over the last decade, new research shows.
Investigators analyzed data from more than 16,000 U.S. adults between the ages of 20 and 59 years and found that those with depression had almost twice the odds of any past-month cannabis use compared with those without depression. Odds rose from 1.5 in the 2005-2006 period to 2.3 in the 2015-2016 period.
Moreover, the odds ratio for daily or near-daily use almost tripled for those with versus without depression between the two periods.
“Clinicians should screen their depressed patients for cannabis use, since this is becoming more common and could actually make their depressive symptoms worse rather than better,” senior author Deborah Hasin, PhD, professor of epidemiology, Columbia University Irving Medical Center, New York City, told Medscape Medical News.
The results were published online August 18 in JAMA Network Open.
Misleading advertising
“Cannabis use is increasing in the U.S. and the potency of cannabis products is increasing as well,” Dr. Hasin said.
“Misleading media information and advertising suggests that cannabis is a good treatment for depression, although studies show that cannabis use may actually worsen depression symptoms, [so] we were interested in whether U.S. adults were increasingly likely to be cannabis users if they were depressed,” she reported.
To investigate, the researchers assessed data from the National Health and Nutrition Examination Survey (NHANES), with a final study sample consisting of 16,216 U.S. adults. The mean age was 39.12 years, 48.9% were men, 66.4% were non-Hispanic White, 65.6% had at least some college education, and 62.4% had an annual family income of less than $75,000.
Of these participants, 7.5% had “probable depression,” based on the Patient Health Questionnaire–9, the investigators report.
Past-month cannabis use was defined as using cannabis at least once during the past 20 days. Daily or near-daily past-month use was defined as using cannabis at least 20 times in the past 30 days.
Covariates included age, gender, race, education, marital status, annual family income, and past-year use of other substances, such as alcohol, heroin, and methamphetamine.
The researchers note that because the NHANES data were divided into six survey years (2005-2006, 2007-2008, 2009-2010, 2011-2012, 2013-2014, and 2015-2016), their analysis was based on a “new sample weight” that combined the datasets.
Especially pronounced
Results showed that the prevalence of any past-month cannabis use in the overall sample group increased from 12.2% in the 2005-2006 period to 17.3% in the 2015-2016 period (P < .001).
The investigators characterized this change as “significant,” adding that the estimated odds of cannabis use increased by approximately 9% between every 2-year time period.
The change was even more dramatic when the increase was examined across survey time periods (OR, 1.12; P < .001). The estimated odds of daily or near-daily use increased by approximately 12% between every 2-year period.
Interestingly, however, there were no significant changes in odds for depression when consecutive survey years were compared.
When the researchers specifically focused on the association between any past-month cannabis use and depression versus no depression, they found an adjusted OR of 1.90 (95% CI, 1.62-2.12; P < .001).
Individuals with depression also had 2.29 (95% CI, 1.80-2.92) times the odds for daily or near-daily cannabis use, compared with those without depression.
A post-hoc analysis looked at time trends in a sample group that included those missing information on at least one covariate (n = 17,724 participants). It showed similar results to those in the final sample that included no missing data.
People with depression have increased risk of using “most substances that can be abused,” Dr. Hasin said. “However, with the overall rates of cannabis use increasing in the general population, this is becoming especially pronounced for cannabis.”
Clear implications
Commenting on the findings for Medscape Medical News, Deepak D’Souza, MD, professor of psychiatry, Yale University, New Haven, Conn., said there is “concern about the unsubstantiated claims of cannabis having a beneficial effect in psychiatric disorders, the most common being depression.”
Dr. D’Souza, who was not involved with the study, called it “yet another piece of evidence suggesting that over the period of time during which cannabis laws have been liberalized, rates of past-month and daily cannabis use have increased, whereas rates of other substances, including alcohol, have remained stable.”
He suggested that a common limitation of epidemiological studies is that it is difficult to tell the direction of the association, “and it could be bidirectional.”
Nevertheless, there are clear implications for the practicing clinician, he added.
“If people have a history of depression, one should ask patients about the use of cannabis and also remind them about potential psychiatric negative effects of use,” Dr. D’Souza noted.
For the general public, “the point is that there is no good evidence to support cannabis use in depression treatment and, in fact, people with depression might be more likely to use it in problematic way,” he said.
Dr. Hasin agreed that it is “certainly possible that the relationship between cannabis use and depression is bidirectional, but the mechanism of this association requires more study.”
The study was supported by a grant from the National Institute on Drug Abuse to Dr. Hasin and by the New York State Psychiatric Institute. The study authors and Dr. D’Souza disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Not only are individuals with depression at significantly higher risk for cannabis use, compared with those without depression, this trend has increased dramatically over the last decade, new research shows.
Investigators analyzed data from more than 16,000 U.S. adults between the ages of 20 and 59 years and found that those with depression had almost twice the odds of any past-month cannabis use compared with those without depression. Odds rose from 1.5 in the 2005-2006 period to 2.3 in the 2015-2016 period.
Moreover, the odds ratio for daily or near-daily use almost tripled for those with versus without depression between the two periods.
“Clinicians should screen their depressed patients for cannabis use, since this is becoming more common and could actually make their depressive symptoms worse rather than better,” senior author Deborah Hasin, PhD, professor of epidemiology, Columbia University Irving Medical Center, New York City, told Medscape Medical News.
The results were published online August 18 in JAMA Network Open.
Misleading advertising
“Cannabis use is increasing in the U.S. and the potency of cannabis products is increasing as well,” Dr. Hasin said.
“Misleading media information and advertising suggests that cannabis is a good treatment for depression, although studies show that cannabis use may actually worsen depression symptoms, [so] we were interested in whether U.S. adults were increasingly likely to be cannabis users if they were depressed,” she reported.
To investigate, the researchers assessed data from the National Health and Nutrition Examination Survey (NHANES), with a final study sample consisting of 16,216 U.S. adults. The mean age was 39.12 years, 48.9% were men, 66.4% were non-Hispanic White, 65.6% had at least some college education, and 62.4% had an annual family income of less than $75,000.
Of these participants, 7.5% had “probable depression,” based on the Patient Health Questionnaire–9, the investigators report.
Past-month cannabis use was defined as using cannabis at least once during the past 20 days. Daily or near-daily past-month use was defined as using cannabis at least 20 times in the past 30 days.
Covariates included age, gender, race, education, marital status, annual family income, and past-year use of other substances, such as alcohol, heroin, and methamphetamine.
The researchers note that because the NHANES data were divided into six survey years (2005-2006, 2007-2008, 2009-2010, 2011-2012, 2013-2014, and 2015-2016), their analysis was based on a “new sample weight” that combined the datasets.
Especially pronounced
Results showed that the prevalence of any past-month cannabis use in the overall sample group increased from 12.2% in the 2005-2006 period to 17.3% in the 2015-2016 period (P < .001).
The investigators characterized this change as “significant,” adding that the estimated odds of cannabis use increased by approximately 9% between every 2-year time period.
The change was even more dramatic when the increase was examined across survey time periods (OR, 1.12; P < .001). The estimated odds of daily or near-daily use increased by approximately 12% between every 2-year period.
Interestingly, however, there were no significant changes in odds for depression when consecutive survey years were compared.
When the researchers specifically focused on the association between any past-month cannabis use and depression versus no depression, they found an adjusted OR of 1.90 (95% CI, 1.62-2.12; P < .001).
Individuals with depression also had 2.29 (95% CI, 1.80-2.92) times the odds for daily or near-daily cannabis use, compared with those without depression.
A post-hoc analysis looked at time trends in a sample group that included those missing information on at least one covariate (n = 17,724 participants). It showed similar results to those in the final sample that included no missing data.
People with depression have increased risk of using “most substances that can be abused,” Dr. Hasin said. “However, with the overall rates of cannabis use increasing in the general population, this is becoming especially pronounced for cannabis.”
Clear implications
Commenting on the findings for Medscape Medical News, Deepak D’Souza, MD, professor of psychiatry, Yale University, New Haven, Conn., said there is “concern about the unsubstantiated claims of cannabis having a beneficial effect in psychiatric disorders, the most common being depression.”
Dr. D’Souza, who was not involved with the study, called it “yet another piece of evidence suggesting that over the period of time during which cannabis laws have been liberalized, rates of past-month and daily cannabis use have increased, whereas rates of other substances, including alcohol, have remained stable.”
He suggested that a common limitation of epidemiological studies is that it is difficult to tell the direction of the association, “and it could be bidirectional.”
Nevertheless, there are clear implications for the practicing clinician, he added.
“If people have a history of depression, one should ask patients about the use of cannabis and also remind them about potential psychiatric negative effects of use,” Dr. D’Souza noted.
For the general public, “the point is that there is no good evidence to support cannabis use in depression treatment and, in fact, people with depression might be more likely to use it in problematic way,” he said.
Dr. Hasin agreed that it is “certainly possible that the relationship between cannabis use and depression is bidirectional, but the mechanism of this association requires more study.”
The study was supported by a grant from the National Institute on Drug Abuse to Dr. Hasin and by the New York State Psychiatric Institute. The study authors and Dr. D’Souza disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Not only are individuals with depression at significantly higher risk for cannabis use, compared with those without depression, this trend has increased dramatically over the last decade, new research shows.
Investigators analyzed data from more than 16,000 U.S. adults between the ages of 20 and 59 years and found that those with depression had almost twice the odds of any past-month cannabis use compared with those without depression. Odds rose from 1.5 in the 2005-2006 period to 2.3 in the 2015-2016 period.
Moreover, the odds ratio for daily or near-daily use almost tripled for those with versus without depression between the two periods.
“Clinicians should screen their depressed patients for cannabis use, since this is becoming more common and could actually make their depressive symptoms worse rather than better,” senior author Deborah Hasin, PhD, professor of epidemiology, Columbia University Irving Medical Center, New York City, told Medscape Medical News.
The results were published online August 18 in JAMA Network Open.
Misleading advertising
“Cannabis use is increasing in the U.S. and the potency of cannabis products is increasing as well,” Dr. Hasin said.
“Misleading media information and advertising suggests that cannabis is a good treatment for depression, although studies show that cannabis use may actually worsen depression symptoms, [so] we were interested in whether U.S. adults were increasingly likely to be cannabis users if they were depressed,” she reported.
To investigate, the researchers assessed data from the National Health and Nutrition Examination Survey (NHANES), with a final study sample consisting of 16,216 U.S. adults. The mean age was 39.12 years, 48.9% were men, 66.4% were non-Hispanic White, 65.6% had at least some college education, and 62.4% had an annual family income of less than $75,000.
Of these participants, 7.5% had “probable depression,” based on the Patient Health Questionnaire–9, the investigators report.
Past-month cannabis use was defined as using cannabis at least once during the past 20 days. Daily or near-daily past-month use was defined as using cannabis at least 20 times in the past 30 days.
Covariates included age, gender, race, education, marital status, annual family income, and past-year use of other substances, such as alcohol, heroin, and methamphetamine.
The researchers note that because the NHANES data were divided into six survey years (2005-2006, 2007-2008, 2009-2010, 2011-2012, 2013-2014, and 2015-2016), their analysis was based on a “new sample weight” that combined the datasets.
Especially pronounced
Results showed that the prevalence of any past-month cannabis use in the overall sample group increased from 12.2% in the 2005-2006 period to 17.3% in the 2015-2016 period (P < .001).
The investigators characterized this change as “significant,” adding that the estimated odds of cannabis use increased by approximately 9% between every 2-year time period.
The change was even more dramatic when the increase was examined across survey time periods (OR, 1.12; P < .001). The estimated odds of daily or near-daily use increased by approximately 12% between every 2-year period.
Interestingly, however, there were no significant changes in odds for depression when consecutive survey years were compared.
When the researchers specifically focused on the association between any past-month cannabis use and depression versus no depression, they found an adjusted OR of 1.90 (95% CI, 1.62-2.12; P < .001).
Individuals with depression also had 2.29 (95% CI, 1.80-2.92) times the odds for daily or near-daily cannabis use, compared with those without depression.
A post-hoc analysis looked at time trends in a sample group that included those missing information on at least one covariate (n = 17,724 participants). It showed similar results to those in the final sample that included no missing data.
People with depression have increased risk of using “most substances that can be abused,” Dr. Hasin said. “However, with the overall rates of cannabis use increasing in the general population, this is becoming especially pronounced for cannabis.”
Clear implications
Commenting on the findings for Medscape Medical News, Deepak D’Souza, MD, professor of psychiatry, Yale University, New Haven, Conn., said there is “concern about the unsubstantiated claims of cannabis having a beneficial effect in psychiatric disorders, the most common being depression.”
Dr. D’Souza, who was not involved with the study, called it “yet another piece of evidence suggesting that over the period of time during which cannabis laws have been liberalized, rates of past-month and daily cannabis use have increased, whereas rates of other substances, including alcohol, have remained stable.”
He suggested that a common limitation of epidemiological studies is that it is difficult to tell the direction of the association, “and it could be bidirectional.”
Nevertheless, there are clear implications for the practicing clinician, he added.
“If people have a history of depression, one should ask patients about the use of cannabis and also remind them about potential psychiatric negative effects of use,” Dr. D’Souza noted.
For the general public, “the point is that there is no good evidence to support cannabis use in depression treatment and, in fact, people with depression might be more likely to use it in problematic way,” he said.
Dr. Hasin agreed that it is “certainly possible that the relationship between cannabis use and depression is bidirectional, but the mechanism of this association requires more study.”
The study was supported by a grant from the National Institute on Drug Abuse to Dr. Hasin and by the New York State Psychiatric Institute. The study authors and Dr. D’Souza disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The transitions of COVID-19
When I was preparing for the recent birth of my baby, I anticipated a period of transition for myself. As a reproductive psychiatrist, I have treated many women during the perinatal and postpartum periods, and have a unique appreciation for the life changes that accompany birth. What I did not expect, however, was the world transitioning with me.
“The new normal” is an economic phrase that describes the COVID-19 era. The pandemic has engendered economic instability, collapsed industries, challenged health care systems, and has led to many deaths worldwide. The COVID-19 pandemic also has been associated with overall increases in anxiety and depression.1 Emerging research suggests that frontline medical workers are especially at risk for developing psychological distress.2
COVID-19 has also created immense challenges for families. Because of concern for the spread of the virus, schools have been suspended, older grandparents isolated, and many parents continue to work remotely. For families in psychiatric care, this time has also been a time of change. Telepsychiatry might be more accessible, but the transition has been an adjustment for patients and clinicians.
As psychiatrists, how do we best treat families during this time? What are some ways to support our psychiatric colleagues? How do we ensure our own emotional well-being amid the tremendous changes occurring around us?
Background of interpersonal psychotherapy
Interpersonal psychotherapy (IPT) is a form of psychotherapy designed to treat depression following periods of transition. Its main goals include improving interpersonal connection and reducing psychological distress. Originally developed in the 1970s by Gerald Klerman, MD; Myrna Weissman, PhD; and Eugene Paykel, MD, IPT is a structured, time-limited form of psychotherapy.3
Conceptualizing depression as a treatable illness, Pim Cuijpers, PhD, and associates summarized the division of IPT into three phases.4 The initial phase involves history taking, forming an alliance, and choosing an interpersonal focus for treatment. The middle phase focuses on applying interpersonal problem-specific therapeutic techniques. The concluding phase of treatment involves consolidation of gains as well as formulating contingency plans for relapse of symptoms. Over the course of treatment, an IPT clinician focuses on life transitions and emphasizes that isolation and antagonistic relationships increase an individual’s vulnerability for a depressive episode.3
Randomized, controlled trials support IPT’s efficacy as a treatment for depression. Research also suggests it can possibly prevent the development of depression.4 Although IPT initially was designed as an individual form of psychotherapy, it has been adapted to both family and group contexts.5,6 IPT is also an empirically valid form of psychotherapy for postpartum depression.7
Interpersonal psychotherapy for families
Given IPT’s role for treating depression following times of transition, clinicians should consider adapting interpersonal psychotherapy to family treatment during this time. Addressing social isolation, managing complex family relationships, and monitoring the family’s overall emotional health should be prioritized. Families under quarantine or who are grieving the death of family members may especially benefit from improved interpersonal connection. Consistent with the IPT model, contingency plans for the family should also be explored to prepare for potential future waves of the pandemic.
In addition to supporting and strengthening families, psychiatrists can use IPT themes to identify positive changes for families tied to COVID-19. Despite its difficulties, the stay-at-home order provided some families a unique chance to slow down and adapt a more relaxed routine. Busy families were suddenly given the opportunity to spend more time with one another. Although many older grandparents were isolated, creative uses of technology provided a chance for grandparents to remain an integral part of family life. Psychiatrists can assist families in transitioning back to previous schedules, while also exploring ways to incorporate the positive changes gained during this time.
Interpersonal psychotherapy for psychiatrists
An interpersonal focus could also be helpful for clinicians to adapt to changes in psychiatric practice. Many clinicians have been thrust into telepsychiatry practice, some with little to no preparation. Because of the trauma associated with frontline work, some psychiatrists have expanded their patient panel to treat physician colleagues. For consult-liaison psychiatrists, the possible neuropsychiatric effects of COVID-19 are new symptoms to consider when evaluating patients in a medical hospital setting.8 Fundamentally, modern day psychiatrists have never encountered a pandemic nor attempted to treat its psychological implications. Prioritizing seeking support from colleagues and caring for one’s personal relationships are helpful tools for clinicians to maintain their own emotional health during this challenging period.
Personal reflection
When I reflect on my baby’s recent birth, I recognize the importance of interpersonal relationships. COVID-19 developed shortly after I gave birth, during the initial haze of the newborn period. Initially, I felt overwhelmed by the many transitions and emotions that were occurring simultaneously. However, as I began to prioritize socialization for myself and my family (albeit creatively at times while socially distancing), I witnessed its positive effects on my emotional well-being and recognized its value in managing times of transition.
Using IPT for families, colleagues, and ourselves
As general psychiatrists, there are several ways to utilize IPT-related themes during this time:
- Connect with families: Although families may recognize they are struggling emotionally, some may find it difficult to navigate the sea of mental health resources. This is particularly true when a family’s financial situation is also stressed. Reaching out to local religious services and community medical resources or inquiring about the mental health of other family members are ways for psychiatrists to engage more families in mental health treatment.
- Reach out to colleagues: Psychiatrists are not immune to developing psychiatric disorders,and it is important to support each other.9 This is also an unusual time when psychiatrists are treating symptoms in patients that they themselves may be also experiencing. Supporting help groups and hot lines, reaching out to colleagues who appear to be struggling and addressing interpersonal conflicts within one’s practice are crucial practices for psychiatrists during this time.
- Explore within ourselves: Evaluating our own interpersonal relationships as well as areas for improvement are critical skills to maintain our own emotional well-being. Setting aside time to connect with friends in a nonclinical setting and prioritizing our family connections are helpful tools. In addition, exploring our reactions to past life transitions could improve our own level of insight into our response to COVID-19.
Conclusion
Conceptualizing COVID-19 as a period of transition and using IPT themes are helpful tools to mitigate the potential adverse psychological effects of COVID-19 on families. Similarly, they can also be helpful in supporting our colleagues and helping ourselves cope during this difficult period.
References
1. Qiu J et al. Gen Psychiatr. 2020 Mar 6;33(2):e100213.
2. Gautam M et al. Psychosomatics. 2020 Apr 20. doi: 10.1016/j.psym.2020.04.009.
3. Markowitz JC, Weissman MM. Clin Psychol Psychother. 2012 Mar-Apr;19(2):99-105.
4. Cuijpers P et al. Am J Psychiatry. 2016 Jul;173(7):680-7.
5. Dietz LJ et al. J Am Acad Child Adolesc Psychiatry. 2015 Mar;54(3):191-9.
6. Verdeli H et al. Child Adolesc Psychiatr Clin N Am. 2008 Jul;17(3):605-24.
7. Stuart S. Clin Psychol Psychother. 2012 Mar-Apr;19(2):134-40.
8. Rogers JP et al. Lancet Psychiatry. 2020 Jul;7(7):611-27.
9. Korkeila JA et al. Scand J Public Health. 2003;31(2):85-91.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital, New York. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care. Dr. Reinstein has no conflicts of interest. Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
When I was preparing for the recent birth of my baby, I anticipated a period of transition for myself. As a reproductive psychiatrist, I have treated many women during the perinatal and postpartum periods, and have a unique appreciation for the life changes that accompany birth. What I did not expect, however, was the world transitioning with me.
“The new normal” is an economic phrase that describes the COVID-19 era. The pandemic has engendered economic instability, collapsed industries, challenged health care systems, and has led to many deaths worldwide. The COVID-19 pandemic also has been associated with overall increases in anxiety and depression.1 Emerging research suggests that frontline medical workers are especially at risk for developing psychological distress.2
COVID-19 has also created immense challenges for families. Because of concern for the spread of the virus, schools have been suspended, older grandparents isolated, and many parents continue to work remotely. For families in psychiatric care, this time has also been a time of change. Telepsychiatry might be more accessible, but the transition has been an adjustment for patients and clinicians.
As psychiatrists, how do we best treat families during this time? What are some ways to support our psychiatric colleagues? How do we ensure our own emotional well-being amid the tremendous changes occurring around us?
Background of interpersonal psychotherapy
Interpersonal psychotherapy (IPT) is a form of psychotherapy designed to treat depression following periods of transition. Its main goals include improving interpersonal connection and reducing psychological distress. Originally developed in the 1970s by Gerald Klerman, MD; Myrna Weissman, PhD; and Eugene Paykel, MD, IPT is a structured, time-limited form of psychotherapy.3
Conceptualizing depression as a treatable illness, Pim Cuijpers, PhD, and associates summarized the division of IPT into three phases.4 The initial phase involves history taking, forming an alliance, and choosing an interpersonal focus for treatment. The middle phase focuses on applying interpersonal problem-specific therapeutic techniques. The concluding phase of treatment involves consolidation of gains as well as formulating contingency plans for relapse of symptoms. Over the course of treatment, an IPT clinician focuses on life transitions and emphasizes that isolation and antagonistic relationships increase an individual’s vulnerability for a depressive episode.3
Randomized, controlled trials support IPT’s efficacy as a treatment for depression. Research also suggests it can possibly prevent the development of depression.4 Although IPT initially was designed as an individual form of psychotherapy, it has been adapted to both family and group contexts.5,6 IPT is also an empirically valid form of psychotherapy for postpartum depression.7
Interpersonal psychotherapy for families
Given IPT’s role for treating depression following times of transition, clinicians should consider adapting interpersonal psychotherapy to family treatment during this time. Addressing social isolation, managing complex family relationships, and monitoring the family’s overall emotional health should be prioritized. Families under quarantine or who are grieving the death of family members may especially benefit from improved interpersonal connection. Consistent with the IPT model, contingency plans for the family should also be explored to prepare for potential future waves of the pandemic.
In addition to supporting and strengthening families, psychiatrists can use IPT themes to identify positive changes for families tied to COVID-19. Despite its difficulties, the stay-at-home order provided some families a unique chance to slow down and adapt a more relaxed routine. Busy families were suddenly given the opportunity to spend more time with one another. Although many older grandparents were isolated, creative uses of technology provided a chance for grandparents to remain an integral part of family life. Psychiatrists can assist families in transitioning back to previous schedules, while also exploring ways to incorporate the positive changes gained during this time.
Interpersonal psychotherapy for psychiatrists
An interpersonal focus could also be helpful for clinicians to adapt to changes in psychiatric practice. Many clinicians have been thrust into telepsychiatry practice, some with little to no preparation. Because of the trauma associated with frontline work, some psychiatrists have expanded their patient panel to treat physician colleagues. For consult-liaison psychiatrists, the possible neuropsychiatric effects of COVID-19 are new symptoms to consider when evaluating patients in a medical hospital setting.8 Fundamentally, modern day psychiatrists have never encountered a pandemic nor attempted to treat its psychological implications. Prioritizing seeking support from colleagues and caring for one’s personal relationships are helpful tools for clinicians to maintain their own emotional health during this challenging period.
Personal reflection
When I reflect on my baby’s recent birth, I recognize the importance of interpersonal relationships. COVID-19 developed shortly after I gave birth, during the initial haze of the newborn period. Initially, I felt overwhelmed by the many transitions and emotions that were occurring simultaneously. However, as I began to prioritize socialization for myself and my family (albeit creatively at times while socially distancing), I witnessed its positive effects on my emotional well-being and recognized its value in managing times of transition.
Using IPT for families, colleagues, and ourselves
As general psychiatrists, there are several ways to utilize IPT-related themes during this time:
- Connect with families: Although families may recognize they are struggling emotionally, some may find it difficult to navigate the sea of mental health resources. This is particularly true when a family’s financial situation is also stressed. Reaching out to local religious services and community medical resources or inquiring about the mental health of other family members are ways for psychiatrists to engage more families in mental health treatment.
- Reach out to colleagues: Psychiatrists are not immune to developing psychiatric disorders,and it is important to support each other.9 This is also an unusual time when psychiatrists are treating symptoms in patients that they themselves may be also experiencing. Supporting help groups and hot lines, reaching out to colleagues who appear to be struggling and addressing interpersonal conflicts within one’s practice are crucial practices for psychiatrists during this time.
- Explore within ourselves: Evaluating our own interpersonal relationships as well as areas for improvement are critical skills to maintain our own emotional well-being. Setting aside time to connect with friends in a nonclinical setting and prioritizing our family connections are helpful tools. In addition, exploring our reactions to past life transitions could improve our own level of insight into our response to COVID-19.
Conclusion
Conceptualizing COVID-19 as a period of transition and using IPT themes are helpful tools to mitigate the potential adverse psychological effects of COVID-19 on families. Similarly, they can also be helpful in supporting our colleagues and helping ourselves cope during this difficult period.
References
1. Qiu J et al. Gen Psychiatr. 2020 Mar 6;33(2):e100213.
2. Gautam M et al. Psychosomatics. 2020 Apr 20. doi: 10.1016/j.psym.2020.04.009.
3. Markowitz JC, Weissman MM. Clin Psychol Psychother. 2012 Mar-Apr;19(2):99-105.
4. Cuijpers P et al. Am J Psychiatry. 2016 Jul;173(7):680-7.
5. Dietz LJ et al. J Am Acad Child Adolesc Psychiatry. 2015 Mar;54(3):191-9.
6. Verdeli H et al. Child Adolesc Psychiatr Clin N Am. 2008 Jul;17(3):605-24.
7. Stuart S. Clin Psychol Psychother. 2012 Mar-Apr;19(2):134-40.
8. Rogers JP et al. Lancet Psychiatry. 2020 Jul;7(7):611-27.
9. Korkeila JA et al. Scand J Public Health. 2003;31(2):85-91.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital, New York. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care. Dr. Reinstein has no conflicts of interest. Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
When I was preparing for the recent birth of my baby, I anticipated a period of transition for myself. As a reproductive psychiatrist, I have treated many women during the perinatal and postpartum periods, and have a unique appreciation for the life changes that accompany birth. What I did not expect, however, was the world transitioning with me.
“The new normal” is an economic phrase that describes the COVID-19 era. The pandemic has engendered economic instability, collapsed industries, challenged health care systems, and has led to many deaths worldwide. The COVID-19 pandemic also has been associated with overall increases in anxiety and depression.1 Emerging research suggests that frontline medical workers are especially at risk for developing psychological distress.2
COVID-19 has also created immense challenges for families. Because of concern for the spread of the virus, schools have been suspended, older grandparents isolated, and many parents continue to work remotely. For families in psychiatric care, this time has also been a time of change. Telepsychiatry might be more accessible, but the transition has been an adjustment for patients and clinicians.
As psychiatrists, how do we best treat families during this time? What are some ways to support our psychiatric colleagues? How do we ensure our own emotional well-being amid the tremendous changes occurring around us?
Background of interpersonal psychotherapy
Interpersonal psychotherapy (IPT) is a form of psychotherapy designed to treat depression following periods of transition. Its main goals include improving interpersonal connection and reducing psychological distress. Originally developed in the 1970s by Gerald Klerman, MD; Myrna Weissman, PhD; and Eugene Paykel, MD, IPT is a structured, time-limited form of psychotherapy.3
Conceptualizing depression as a treatable illness, Pim Cuijpers, PhD, and associates summarized the division of IPT into three phases.4 The initial phase involves history taking, forming an alliance, and choosing an interpersonal focus for treatment. The middle phase focuses on applying interpersonal problem-specific therapeutic techniques. The concluding phase of treatment involves consolidation of gains as well as formulating contingency plans for relapse of symptoms. Over the course of treatment, an IPT clinician focuses on life transitions and emphasizes that isolation and antagonistic relationships increase an individual’s vulnerability for a depressive episode.3
Randomized, controlled trials support IPT’s efficacy as a treatment for depression. Research also suggests it can possibly prevent the development of depression.4 Although IPT initially was designed as an individual form of psychotherapy, it has been adapted to both family and group contexts.5,6 IPT is also an empirically valid form of psychotherapy for postpartum depression.7
Interpersonal psychotherapy for families
Given IPT’s role for treating depression following times of transition, clinicians should consider adapting interpersonal psychotherapy to family treatment during this time. Addressing social isolation, managing complex family relationships, and monitoring the family’s overall emotional health should be prioritized. Families under quarantine or who are grieving the death of family members may especially benefit from improved interpersonal connection. Consistent with the IPT model, contingency plans for the family should also be explored to prepare for potential future waves of the pandemic.
In addition to supporting and strengthening families, psychiatrists can use IPT themes to identify positive changes for families tied to COVID-19. Despite its difficulties, the stay-at-home order provided some families a unique chance to slow down and adapt a more relaxed routine. Busy families were suddenly given the opportunity to spend more time with one another. Although many older grandparents were isolated, creative uses of technology provided a chance for grandparents to remain an integral part of family life. Psychiatrists can assist families in transitioning back to previous schedules, while also exploring ways to incorporate the positive changes gained during this time.
Interpersonal psychotherapy for psychiatrists
An interpersonal focus could also be helpful for clinicians to adapt to changes in psychiatric practice. Many clinicians have been thrust into telepsychiatry practice, some with little to no preparation. Because of the trauma associated with frontline work, some psychiatrists have expanded their patient panel to treat physician colleagues. For consult-liaison psychiatrists, the possible neuropsychiatric effects of COVID-19 are new symptoms to consider when evaluating patients in a medical hospital setting.8 Fundamentally, modern day psychiatrists have never encountered a pandemic nor attempted to treat its psychological implications. Prioritizing seeking support from colleagues and caring for one’s personal relationships are helpful tools for clinicians to maintain their own emotional health during this challenging period.
Personal reflection
When I reflect on my baby’s recent birth, I recognize the importance of interpersonal relationships. COVID-19 developed shortly after I gave birth, during the initial haze of the newborn period. Initially, I felt overwhelmed by the many transitions and emotions that were occurring simultaneously. However, as I began to prioritize socialization for myself and my family (albeit creatively at times while socially distancing), I witnessed its positive effects on my emotional well-being and recognized its value in managing times of transition.
Using IPT for families, colleagues, and ourselves
As general psychiatrists, there are several ways to utilize IPT-related themes during this time:
- Connect with families: Although families may recognize they are struggling emotionally, some may find it difficult to navigate the sea of mental health resources. This is particularly true when a family’s financial situation is also stressed. Reaching out to local religious services and community medical resources or inquiring about the mental health of other family members are ways for psychiatrists to engage more families in mental health treatment.
- Reach out to colleagues: Psychiatrists are not immune to developing psychiatric disorders,and it is important to support each other.9 This is also an unusual time when psychiatrists are treating symptoms in patients that they themselves may be also experiencing. Supporting help groups and hot lines, reaching out to colleagues who appear to be struggling and addressing interpersonal conflicts within one’s practice are crucial practices for psychiatrists during this time.
- Explore within ourselves: Evaluating our own interpersonal relationships as well as areas for improvement are critical skills to maintain our own emotional well-being. Setting aside time to connect with friends in a nonclinical setting and prioritizing our family connections are helpful tools. In addition, exploring our reactions to past life transitions could improve our own level of insight into our response to COVID-19.
Conclusion
Conceptualizing COVID-19 as a period of transition and using IPT themes are helpful tools to mitigate the potential adverse psychological effects of COVID-19 on families. Similarly, they can also be helpful in supporting our colleagues and helping ourselves cope during this difficult period.
References
1. Qiu J et al. Gen Psychiatr. 2020 Mar 6;33(2):e100213.
2. Gautam M et al. Psychosomatics. 2020 Apr 20. doi: 10.1016/j.psym.2020.04.009.
3. Markowitz JC, Weissman MM. Clin Psychol Psychother. 2012 Mar-Apr;19(2):99-105.
4. Cuijpers P et al. Am J Psychiatry. 2016 Jul;173(7):680-7.
5. Dietz LJ et al. J Am Acad Child Adolesc Psychiatry. 2015 Mar;54(3):191-9.
6. Verdeli H et al. Child Adolesc Psychiatr Clin N Am. 2008 Jul;17(3):605-24.
7. Stuart S. Clin Psychol Psychother. 2012 Mar-Apr;19(2):134-40.
8. Rogers JP et al. Lancet Psychiatry. 2020 Jul;7(7):611-27.
9. Korkeila JA et al. Scand J Public Health. 2003;31(2):85-91.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital, New York. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care. Dr. Reinstein has no conflicts of interest. Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
Oleander extract for COVID-19? That’s a hard ‘no’ experts say
“Though renowned for its beauty and use in landscaping, this Mediterranean shrub is responsible for cases of accidental poisoning across the globe. All parts of the plant are poisonous,” Cassandra Quave, PhD, ethnobotanist and herbarium curator at Emory University, Atlanta, cautioned in an article in The Conversation, an independent, not-for-profit publication.
Oleandrin has properties similar to digoxin; the onset of toxicity occurs several hours after consumption.
The first symptoms of oleandrin poisoning may be gastrointestinal, such as nausea, vomiting, abdominal pain, diarrhea (which may contain blood), and loss of appetite.
After these first symptoms, the heart may be affected by tachyarrhythmia, bradyarrhythmia, premature ventricular contractions, or atrioventricular blockage. Xanthopsia (yellow vision), a burning sensation in the eyes, paralysis of the gastrointestinal tract, and respiratory symptoms may also occur.
Oleandrin poisoning may affect the central nervous system, as evidenced by drowsiness, tremors, seizures, collapse, and coma leading to death. When applied to the skin, oleander sap can cause skin irritations and allergic reactions characterized by dermatitis.
Diagnosis of oleandrin poisoning is mainly made on the basis of a description of the plant, how much of it was ingested, how much time has elapsed since ingestion, and symptoms. Confirmation of oleandrin in blood involves fluorescence polarization immunoassay, digoxin immunoassay, or liquid chromatography-electrospray tandem mass spectrometry.
Neither oleander nor oleandrin is approved by regulatory agencies as a prescription drug or dietary supplement.
In vitro study
Oleandrin for COVID-19 made headlines after President Trump met in the Oval Office with Andrew Whitney, vice chairman and director of Phoenix Biotechnology, along with Housing and Urban Development Secretary Ben Carson, MD, and MyPillow founder/CEO Mike Lindell, a strong supporter of Trump and an investor in the biotech company, to learn about oleandrin, which Whitney called a “cure” for COVID-19, Axios reported.
In an in vitro study, researchers from Phoenix Biotechnology and the University of Texas Medical Branch, Galveston, tested oleandrin against SARS-CoV-2 in cultured Vero cells.
“When administered both before and after virus infection, nanogram doses of oleandrin significantly inhibited replication by 45 to 3000-fold,” the researchers said in an article posted on bioRxiv, a free online archive and distribution service for unpublished preprints in the life sciences. The study has not been peer reviewed.
On the basis of these in vitro findings, the researchers said the plant extract has “potential to prevent disease and virus spread in persons recently exposed to SARS-CoV-2, as well as to prevent severe disease in persons at high risk.”
But it’s a far cry from test tube to human, one expert cautioned.
“This is an understatement: Care must be taken when inferring potential therapeutic benefits from in vitro antiviral effects,” Harlan Krumholz, MD, cardiologist and director, Yale New Haven Hospital Center for Outcomes Research and Evaluation, New Haven, Connecticut, told Medscape Medical News.
“There is a chasm between a single in vitro study and any use in humans outside of a protocol. People should be cautioned about that distance and the need [to] avoid such remedies unless part of a credible research project,” said Krumholz.
Yet Lindell told Axios that, in the Oval Office meeting, Trump expressed enthusiasm for the Food and Drug Administration to allow oleandrin to be marketed as a dietary supplement or approved for COVID-19.
“This is really just nonsense and a distraction,” Jonathan Reiner, MD, of George Washington University Medical Center, Washington, DC, said on CNN.
This article first appeared on Medscape.com.
“Though renowned for its beauty and use in landscaping, this Mediterranean shrub is responsible for cases of accidental poisoning across the globe. All parts of the plant are poisonous,” Cassandra Quave, PhD, ethnobotanist and herbarium curator at Emory University, Atlanta, cautioned in an article in The Conversation, an independent, not-for-profit publication.
Oleandrin has properties similar to digoxin; the onset of toxicity occurs several hours after consumption.
The first symptoms of oleandrin poisoning may be gastrointestinal, such as nausea, vomiting, abdominal pain, diarrhea (which may contain blood), and loss of appetite.
After these first symptoms, the heart may be affected by tachyarrhythmia, bradyarrhythmia, premature ventricular contractions, or atrioventricular blockage. Xanthopsia (yellow vision), a burning sensation in the eyes, paralysis of the gastrointestinal tract, and respiratory symptoms may also occur.
Oleandrin poisoning may affect the central nervous system, as evidenced by drowsiness, tremors, seizures, collapse, and coma leading to death. When applied to the skin, oleander sap can cause skin irritations and allergic reactions characterized by dermatitis.
Diagnosis of oleandrin poisoning is mainly made on the basis of a description of the plant, how much of it was ingested, how much time has elapsed since ingestion, and symptoms. Confirmation of oleandrin in blood involves fluorescence polarization immunoassay, digoxin immunoassay, or liquid chromatography-electrospray tandem mass spectrometry.
Neither oleander nor oleandrin is approved by regulatory agencies as a prescription drug or dietary supplement.
In vitro study
Oleandrin for COVID-19 made headlines after President Trump met in the Oval Office with Andrew Whitney, vice chairman and director of Phoenix Biotechnology, along with Housing and Urban Development Secretary Ben Carson, MD, and MyPillow founder/CEO Mike Lindell, a strong supporter of Trump and an investor in the biotech company, to learn about oleandrin, which Whitney called a “cure” for COVID-19, Axios reported.
In an in vitro study, researchers from Phoenix Biotechnology and the University of Texas Medical Branch, Galveston, tested oleandrin against SARS-CoV-2 in cultured Vero cells.
“When administered both before and after virus infection, nanogram doses of oleandrin significantly inhibited replication by 45 to 3000-fold,” the researchers said in an article posted on bioRxiv, a free online archive and distribution service for unpublished preprints in the life sciences. The study has not been peer reviewed.
On the basis of these in vitro findings, the researchers said the plant extract has “potential to prevent disease and virus spread in persons recently exposed to SARS-CoV-2, as well as to prevent severe disease in persons at high risk.”
But it’s a far cry from test tube to human, one expert cautioned.
“This is an understatement: Care must be taken when inferring potential therapeutic benefits from in vitro antiviral effects,” Harlan Krumholz, MD, cardiologist and director, Yale New Haven Hospital Center for Outcomes Research and Evaluation, New Haven, Connecticut, told Medscape Medical News.
“There is a chasm between a single in vitro study and any use in humans outside of a protocol. People should be cautioned about that distance and the need [to] avoid such remedies unless part of a credible research project,” said Krumholz.
Yet Lindell told Axios that, in the Oval Office meeting, Trump expressed enthusiasm for the Food and Drug Administration to allow oleandrin to be marketed as a dietary supplement or approved for COVID-19.
“This is really just nonsense and a distraction,” Jonathan Reiner, MD, of George Washington University Medical Center, Washington, DC, said on CNN.
This article first appeared on Medscape.com.
“Though renowned for its beauty and use in landscaping, this Mediterranean shrub is responsible for cases of accidental poisoning across the globe. All parts of the plant are poisonous,” Cassandra Quave, PhD, ethnobotanist and herbarium curator at Emory University, Atlanta, cautioned in an article in The Conversation, an independent, not-for-profit publication.
Oleandrin has properties similar to digoxin; the onset of toxicity occurs several hours after consumption.
The first symptoms of oleandrin poisoning may be gastrointestinal, such as nausea, vomiting, abdominal pain, diarrhea (which may contain blood), and loss of appetite.
After these first symptoms, the heart may be affected by tachyarrhythmia, bradyarrhythmia, premature ventricular contractions, or atrioventricular blockage. Xanthopsia (yellow vision), a burning sensation in the eyes, paralysis of the gastrointestinal tract, and respiratory symptoms may also occur.
Oleandrin poisoning may affect the central nervous system, as evidenced by drowsiness, tremors, seizures, collapse, and coma leading to death. When applied to the skin, oleander sap can cause skin irritations and allergic reactions characterized by dermatitis.
Diagnosis of oleandrin poisoning is mainly made on the basis of a description of the plant, how much of it was ingested, how much time has elapsed since ingestion, and symptoms. Confirmation of oleandrin in blood involves fluorescence polarization immunoassay, digoxin immunoassay, or liquid chromatography-electrospray tandem mass spectrometry.
Neither oleander nor oleandrin is approved by regulatory agencies as a prescription drug or dietary supplement.
In vitro study
Oleandrin for COVID-19 made headlines after President Trump met in the Oval Office with Andrew Whitney, vice chairman and director of Phoenix Biotechnology, along with Housing and Urban Development Secretary Ben Carson, MD, and MyPillow founder/CEO Mike Lindell, a strong supporter of Trump and an investor in the biotech company, to learn about oleandrin, which Whitney called a “cure” for COVID-19, Axios reported.
In an in vitro study, researchers from Phoenix Biotechnology and the University of Texas Medical Branch, Galveston, tested oleandrin against SARS-CoV-2 in cultured Vero cells.
“When administered both before and after virus infection, nanogram doses of oleandrin significantly inhibited replication by 45 to 3000-fold,” the researchers said in an article posted on bioRxiv, a free online archive and distribution service for unpublished preprints in the life sciences. The study has not been peer reviewed.
On the basis of these in vitro findings, the researchers said the plant extract has “potential to prevent disease and virus spread in persons recently exposed to SARS-CoV-2, as well as to prevent severe disease in persons at high risk.”
But it’s a far cry from test tube to human, one expert cautioned.
“This is an understatement: Care must be taken when inferring potential therapeutic benefits from in vitro antiviral effects,” Harlan Krumholz, MD, cardiologist and director, Yale New Haven Hospital Center for Outcomes Research and Evaluation, New Haven, Connecticut, told Medscape Medical News.
“There is a chasm between a single in vitro study and any use in humans outside of a protocol. People should be cautioned about that distance and the need [to] avoid such remedies unless part of a credible research project,” said Krumholz.
Yet Lindell told Axios that, in the Oval Office meeting, Trump expressed enthusiasm for the Food and Drug Administration to allow oleandrin to be marketed as a dietary supplement or approved for COVID-19.
“This is really just nonsense and a distraction,” Jonathan Reiner, MD, of George Washington University Medical Center, Washington, DC, said on CNN.
This article first appeared on Medscape.com.
Anxiety disorders begin earlier in life, differ by gender
Anxiety disorders start very early in life and may manifest themselves first as other conditions like social anxiety disorder, according to Jeffrey R. Strawn, MD.
An adolescent presenting to a mental health clinician with anxiety at 16 years old, for example has likely struggled with her anxiety for years before visiting a clinic. “That child may have been someone who had separation anxiety earlier in life and who as, even an infant, had behavioral inhibitions, that reluctance or timidness to explore new things, that tendency to retreat from novel stimuli,” Dr. Strawn, associate professor of psychiatry, pediatrics and clinical pharmacology at Cincinnati Children’s Hospital Medical Center, said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. “Anxiety disorders are enduring and persistent, and they begin very early in life.”
Social anxiety disorder is one of the first anxiety disorders that appear in childhood or adolescents, which rises during puberty and during a time in a child’s life when they are dealing with new social pressures and challenges, such as graduating from elementary to middle school, Dr. Strawn noted. Generalized anxiety disorder is usually the next to emerge, followed by panic disorder. On the other hand, agoraphobia, another anxiety disorder that begins in childhood, “often represents behavioral avoidance as opposed to agoraphobia as we classically think about it as adult psychiatrists.”
Onset of anxiety disorders also differ by gender. “In terms of the emergence of these anxiety disorders, another thing that’s important to know is that the onset seems to be a bit different with regard to girls and boys. We see that break there emerging really around the time of puberty or as people are moving into late puberty, at least for girls,” Dr. Strawn said at the meeting presented by Global Academy for Medical Education. .
A shift occurs in amygdala prefrontal circuitry as children age, Dr. Strawn explained. Younger children do not have the ability to modulate the amygdala with their prefrontal cortex, but this amygdala–medial prefrontal cortex functional connectivity will change as children grow. A study by Dylan G. Gee, PhD, and colleagues found positive amygdala–medial prefrontal cortex functional connectivity at younger than 10 years old, and a “steady decline in amygdala activity” from 10-13 years to adulthood at 22 years old (J Neurosci. 2013 Mar 6;33[10]:4584-93).
“In essence, what we’re seeing is that there’s improvement or more effectiveness in terms of that connection between the prefrontal cortex, the amygdala, and that ability to amplify the brake to the amygdala,” Dr. Strawn said.
SSRIs, SNRIs for pediatric patients
Selective serotonin reuptake inhibitors can be effective for pediatric patients with anxiety disorders. Results from the Child/Adolescent Anxiety Multimodal Study (CAMS) show that patients with generalized separation or social anxiety disorder treated with sertraline or cognitive-behavioral therapy (CBT) for 3 months responded better to treatment than placebo. A combination of sertraline and CBT performing best, compared with either intervention alone (N Engl J Med. 2008;359:2753-66).
When examining treatment response in 76 patients from CAMS, the researchers saw improvement at 4 weeks from baseline in patients with anxiety symptoms receiving CBT, but no significant change in improvement after 4 weeks up to 12 weeks (J Child Adolesc Psychopharm. 2017 Aug 1. doi: 10.1089/cap.2016.0198).
“What that actually means is that your improvement at week 4 is better than your improvement at baseline, and your improvement at week 8 is greater than your improvement at week 4. Similarly, in your improvement, week 12 is greater than your improvement at week 8,” Dr. Strawn said.
However, “that’s not the case for aggressively titrated sertraline,” which had no statistically significant difference in improvement at 8 weeks and 12 weeks, he explained. “What this actually means is that, if I have not had improvement by week 8, there is a three-to-one odds against improvement over those next 4 weeks. The take-home message here is really that an adequate trial for an SSRI in pediatric anxiety disorders is probably about 8 weeks – not 12, not longer.”
Serotonin norepinephrine reuptake inhibitors (SNRIs) are also effective in pediatric patients with anxiety disorders.
“Both SNRIs as well as SSRIs have certainly demonstrated efficacy in terms of treating pediatric patients with anxiety, but there is a very important difference here with regard to the trajectory of improvement and also the magnitude of improvement,” Dr. Strawn said. SNRIs like atomoxetine, duloxetine, or venlafaxine “do not improve as rapidly and do not improve to the same extent as kids who are treated with an SSRI.”
Dose is another factor that affects symptom improvement in patients with pediatric anxiety disorders. In a 2018 meta-analysis, Dr. Strawn and colleagues found that patients treated with a higher dose of SSRIs demonstrated more rapid improvement at 2 weeks, compared with patients who received SNRIs (P = .002), but there was no significant difference in overall response trajectory (J Am Acad Child Adolesc Psychiatry. 2018 Apr;57[4]:235-44.E2).
Response to SSRIs can depend a patient’s genotype, Dr. Strawn said. The serotonin transporter promotor polymorphism has received “considerable attention in adults with depressive disorders primarily” but also might play a role in anxiety disorder response in pediatric patients. One study presented by his group at the 2019 annual meeting of the American Academy of Child & Adolescent Psychiatry showed that patients with a short-short copy of the serotonin transporter promoter polymorphism instead of a long copy had “shallower and less improvement over the course of treatment” when taking escitalopram.
“This is something that doesn’t necessarily compel us to use an SNRI over an SSRI, but it’s something that does give us some important information in terms of the trajectory of improvement,” he said.
When it comes to side effects of SNRIs and SSRIs, the profile is “pretty consistent with what we know to be the side effect profile in adults with depressive and anxiety disorders,” Dr. Strawn noted. “SNRIs tend to be a little bit better tolerated, both in terms of adverse event–related discontinuation and also in terms of their likelihood of producing activation.”
Patient and caregiver expectations can further affect response to treatment. “I think this has implications in terms of how we actively manage expectations and discussions about the evidence for interventions with our patients in the clinic.”
Global Academy and this news organization are owned by the same parent company. Dr. Strawn reported receiving research support from Edgemont Pharmaceuticals, Eli Lilly, Forest Research Laboratories, Lundbeck, the National Institutes of Health, Neuronetics, and Shire. He also reported receiving royalties from Springer Publishing, and is a consultant for and receives material support from Assurex/Genesight.
Anxiety disorders start very early in life and may manifest themselves first as other conditions like social anxiety disorder, according to Jeffrey R. Strawn, MD.
An adolescent presenting to a mental health clinician with anxiety at 16 years old, for example has likely struggled with her anxiety for years before visiting a clinic. “That child may have been someone who had separation anxiety earlier in life and who as, even an infant, had behavioral inhibitions, that reluctance or timidness to explore new things, that tendency to retreat from novel stimuli,” Dr. Strawn, associate professor of psychiatry, pediatrics and clinical pharmacology at Cincinnati Children’s Hospital Medical Center, said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. “Anxiety disorders are enduring and persistent, and they begin very early in life.”
Social anxiety disorder is one of the first anxiety disorders that appear in childhood or adolescents, which rises during puberty and during a time in a child’s life when they are dealing with new social pressures and challenges, such as graduating from elementary to middle school, Dr. Strawn noted. Generalized anxiety disorder is usually the next to emerge, followed by panic disorder. On the other hand, agoraphobia, another anxiety disorder that begins in childhood, “often represents behavioral avoidance as opposed to agoraphobia as we classically think about it as adult psychiatrists.”
Onset of anxiety disorders also differ by gender. “In terms of the emergence of these anxiety disorders, another thing that’s important to know is that the onset seems to be a bit different with regard to girls and boys. We see that break there emerging really around the time of puberty or as people are moving into late puberty, at least for girls,” Dr. Strawn said at the meeting presented by Global Academy for Medical Education. .
A shift occurs in amygdala prefrontal circuitry as children age, Dr. Strawn explained. Younger children do not have the ability to modulate the amygdala with their prefrontal cortex, but this amygdala–medial prefrontal cortex functional connectivity will change as children grow. A study by Dylan G. Gee, PhD, and colleagues found positive amygdala–medial prefrontal cortex functional connectivity at younger than 10 years old, and a “steady decline in amygdala activity” from 10-13 years to adulthood at 22 years old (J Neurosci. 2013 Mar 6;33[10]:4584-93).
“In essence, what we’re seeing is that there’s improvement or more effectiveness in terms of that connection between the prefrontal cortex, the amygdala, and that ability to amplify the brake to the amygdala,” Dr. Strawn said.
SSRIs, SNRIs for pediatric patients
Selective serotonin reuptake inhibitors can be effective for pediatric patients with anxiety disorders. Results from the Child/Adolescent Anxiety Multimodal Study (CAMS) show that patients with generalized separation or social anxiety disorder treated with sertraline or cognitive-behavioral therapy (CBT) for 3 months responded better to treatment than placebo. A combination of sertraline and CBT performing best, compared with either intervention alone (N Engl J Med. 2008;359:2753-66).
When examining treatment response in 76 patients from CAMS, the researchers saw improvement at 4 weeks from baseline in patients with anxiety symptoms receiving CBT, but no significant change in improvement after 4 weeks up to 12 weeks (J Child Adolesc Psychopharm. 2017 Aug 1. doi: 10.1089/cap.2016.0198).
“What that actually means is that your improvement at week 4 is better than your improvement at baseline, and your improvement at week 8 is greater than your improvement at week 4. Similarly, in your improvement, week 12 is greater than your improvement at week 8,” Dr. Strawn said.
However, “that’s not the case for aggressively titrated sertraline,” which had no statistically significant difference in improvement at 8 weeks and 12 weeks, he explained. “What this actually means is that, if I have not had improvement by week 8, there is a three-to-one odds against improvement over those next 4 weeks. The take-home message here is really that an adequate trial for an SSRI in pediatric anxiety disorders is probably about 8 weeks – not 12, not longer.”
Serotonin norepinephrine reuptake inhibitors (SNRIs) are also effective in pediatric patients with anxiety disorders.
“Both SNRIs as well as SSRIs have certainly demonstrated efficacy in terms of treating pediatric patients with anxiety, but there is a very important difference here with regard to the trajectory of improvement and also the magnitude of improvement,” Dr. Strawn said. SNRIs like atomoxetine, duloxetine, or venlafaxine “do not improve as rapidly and do not improve to the same extent as kids who are treated with an SSRI.”
Dose is another factor that affects symptom improvement in patients with pediatric anxiety disorders. In a 2018 meta-analysis, Dr. Strawn and colleagues found that patients treated with a higher dose of SSRIs demonstrated more rapid improvement at 2 weeks, compared with patients who received SNRIs (P = .002), but there was no significant difference in overall response trajectory (J Am Acad Child Adolesc Psychiatry. 2018 Apr;57[4]:235-44.E2).
Response to SSRIs can depend a patient’s genotype, Dr. Strawn said. The serotonin transporter promotor polymorphism has received “considerable attention in adults with depressive disorders primarily” but also might play a role in anxiety disorder response in pediatric patients. One study presented by his group at the 2019 annual meeting of the American Academy of Child & Adolescent Psychiatry showed that patients with a short-short copy of the serotonin transporter promoter polymorphism instead of a long copy had “shallower and less improvement over the course of treatment” when taking escitalopram.
“This is something that doesn’t necessarily compel us to use an SNRI over an SSRI, but it’s something that does give us some important information in terms of the trajectory of improvement,” he said.
When it comes to side effects of SNRIs and SSRIs, the profile is “pretty consistent with what we know to be the side effect profile in adults with depressive and anxiety disorders,” Dr. Strawn noted. “SNRIs tend to be a little bit better tolerated, both in terms of adverse event–related discontinuation and also in terms of their likelihood of producing activation.”
Patient and caregiver expectations can further affect response to treatment. “I think this has implications in terms of how we actively manage expectations and discussions about the evidence for interventions with our patients in the clinic.”
Global Academy and this news organization are owned by the same parent company. Dr. Strawn reported receiving research support from Edgemont Pharmaceuticals, Eli Lilly, Forest Research Laboratories, Lundbeck, the National Institutes of Health, Neuronetics, and Shire. He also reported receiving royalties from Springer Publishing, and is a consultant for and receives material support from Assurex/Genesight.
Anxiety disorders start very early in life and may manifest themselves first as other conditions like social anxiety disorder, according to Jeffrey R. Strawn, MD.
An adolescent presenting to a mental health clinician with anxiety at 16 years old, for example has likely struggled with her anxiety for years before visiting a clinic. “That child may have been someone who had separation anxiety earlier in life and who as, even an infant, had behavioral inhibitions, that reluctance or timidness to explore new things, that tendency to retreat from novel stimuli,” Dr. Strawn, associate professor of psychiatry, pediatrics and clinical pharmacology at Cincinnati Children’s Hospital Medical Center, said at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. “Anxiety disorders are enduring and persistent, and they begin very early in life.”
Social anxiety disorder is one of the first anxiety disorders that appear in childhood or adolescents, which rises during puberty and during a time in a child’s life when they are dealing with new social pressures and challenges, such as graduating from elementary to middle school, Dr. Strawn noted. Generalized anxiety disorder is usually the next to emerge, followed by panic disorder. On the other hand, agoraphobia, another anxiety disorder that begins in childhood, “often represents behavioral avoidance as opposed to agoraphobia as we classically think about it as adult psychiatrists.”
Onset of anxiety disorders also differ by gender. “In terms of the emergence of these anxiety disorders, another thing that’s important to know is that the onset seems to be a bit different with regard to girls and boys. We see that break there emerging really around the time of puberty or as people are moving into late puberty, at least for girls,” Dr. Strawn said at the meeting presented by Global Academy for Medical Education. .
A shift occurs in amygdala prefrontal circuitry as children age, Dr. Strawn explained. Younger children do not have the ability to modulate the amygdala with their prefrontal cortex, but this amygdala–medial prefrontal cortex functional connectivity will change as children grow. A study by Dylan G. Gee, PhD, and colleagues found positive amygdala–medial prefrontal cortex functional connectivity at younger than 10 years old, and a “steady decline in amygdala activity” from 10-13 years to adulthood at 22 years old (J Neurosci. 2013 Mar 6;33[10]:4584-93).
“In essence, what we’re seeing is that there’s improvement or more effectiveness in terms of that connection between the prefrontal cortex, the amygdala, and that ability to amplify the brake to the amygdala,” Dr. Strawn said.
SSRIs, SNRIs for pediatric patients
Selective serotonin reuptake inhibitors can be effective for pediatric patients with anxiety disorders. Results from the Child/Adolescent Anxiety Multimodal Study (CAMS) show that patients with generalized separation or social anxiety disorder treated with sertraline or cognitive-behavioral therapy (CBT) for 3 months responded better to treatment than placebo. A combination of sertraline and CBT performing best, compared with either intervention alone (N Engl J Med. 2008;359:2753-66).
When examining treatment response in 76 patients from CAMS, the researchers saw improvement at 4 weeks from baseline in patients with anxiety symptoms receiving CBT, but no significant change in improvement after 4 weeks up to 12 weeks (J Child Adolesc Psychopharm. 2017 Aug 1. doi: 10.1089/cap.2016.0198).
“What that actually means is that your improvement at week 4 is better than your improvement at baseline, and your improvement at week 8 is greater than your improvement at week 4. Similarly, in your improvement, week 12 is greater than your improvement at week 8,” Dr. Strawn said.
However, “that’s not the case for aggressively titrated sertraline,” which had no statistically significant difference in improvement at 8 weeks and 12 weeks, he explained. “What this actually means is that, if I have not had improvement by week 8, there is a three-to-one odds against improvement over those next 4 weeks. The take-home message here is really that an adequate trial for an SSRI in pediatric anxiety disorders is probably about 8 weeks – not 12, not longer.”
Serotonin norepinephrine reuptake inhibitors (SNRIs) are also effective in pediatric patients with anxiety disorders.
“Both SNRIs as well as SSRIs have certainly demonstrated efficacy in terms of treating pediatric patients with anxiety, but there is a very important difference here with regard to the trajectory of improvement and also the magnitude of improvement,” Dr. Strawn said. SNRIs like atomoxetine, duloxetine, or venlafaxine “do not improve as rapidly and do not improve to the same extent as kids who are treated with an SSRI.”
Dose is another factor that affects symptom improvement in patients with pediatric anxiety disorders. In a 2018 meta-analysis, Dr. Strawn and colleagues found that patients treated with a higher dose of SSRIs demonstrated more rapid improvement at 2 weeks, compared with patients who received SNRIs (P = .002), but there was no significant difference in overall response trajectory (J Am Acad Child Adolesc Psychiatry. 2018 Apr;57[4]:235-44.E2).
Response to SSRIs can depend a patient’s genotype, Dr. Strawn said. The serotonin transporter promotor polymorphism has received “considerable attention in adults with depressive disorders primarily” but also might play a role in anxiety disorder response in pediatric patients. One study presented by his group at the 2019 annual meeting of the American Academy of Child & Adolescent Psychiatry showed that patients with a short-short copy of the serotonin transporter promoter polymorphism instead of a long copy had “shallower and less improvement over the course of treatment” when taking escitalopram.
“This is something that doesn’t necessarily compel us to use an SNRI over an SSRI, but it’s something that does give us some important information in terms of the trajectory of improvement,” he said.
When it comes to side effects of SNRIs and SSRIs, the profile is “pretty consistent with what we know to be the side effect profile in adults with depressive and anxiety disorders,” Dr. Strawn noted. “SNRIs tend to be a little bit better tolerated, both in terms of adverse event–related discontinuation and also in terms of their likelihood of producing activation.”
Patient and caregiver expectations can further affect response to treatment. “I think this has implications in terms of how we actively manage expectations and discussions about the evidence for interventions with our patients in the clinic.”
Global Academy and this news organization are owned by the same parent company. Dr. Strawn reported receiving research support from Edgemont Pharmaceuticals, Eli Lilly, Forest Research Laboratories, Lundbeck, the National Institutes of Health, Neuronetics, and Shire. He also reported receiving royalties from Springer Publishing, and is a consultant for and receives material support from Assurex/Genesight.
FROM Focus on Neuropsychiatry 2020
Are aging physicians a burden?
The evaluation of physicians with alleged cognitive decline
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
The evaluation of physicians with alleged cognitive decline
The evaluation of physicians with alleged cognitive decline
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
As forensic evaluators, we are often asked to review and assess the cognition of aging colleagues. The premise often involves a minor mistake, a poor choice of words, or a lapse in judgment. A physician gets reported for having difficulty using a new electronic form, forgetting the dose of a brand new medication, or getting upset in a public setting. Those behaviors often lead to mandatory psychiatric evaluations. Those requirements are often perceived by the provider as an insult, and betrayal by peers despite many years of dedicated work.
Interestingly, we have noticed many independent evaluators and hospital administrators using this opportunity to send many of our colleagues to pasture. There seems to be an unspoken rule among some forensic evaluators that physicians should represent some form of apex of humanity, beyond reproach, and beyond any fault. Those evaluators will point to any mistake on cognitive scales as proof that the aging physician is no longer safe to practice.1 Forgetting that Jill is from Illinois in the Saint Louis University Mental Status Examination test or how to copy a three-dimensional cube on the Montreal Cognitive Assessment can cost someone their license.2 We are also aware of some evaluators even taking the step further and opining that physicians not only need to score adequately but also demonstrate cognition significantly above average to maintain their privileges.
There is certainly significant appeal in setting a high bar for physicians. In many ways, physicians are characterized in society by their astuteness, intelligence, and high ethical standards. Patients place their lives in the hands of physicians and should trust that those physicians have the cognitive tools to heal them. It could almost seem evident that physicians should have high IQs, score perfectly on screening tools for dementia, and complete a mandatory psychiatric evaluation without any reproach. Yet the reality is often more complex.
We have two main concerns about the idea that we should be intransigent with aging physicians. The first one is the vast differential diagnosis for minor mistakes. An aging physician refusing to comply with a new form or yelling at a clerk once when asked to learn a new electronic medical record are inappropriate though not specific assessments for dementia. Similarly, having significant difficulty learning a new electronic medical record system more often is a sign of ageism rather than cognitive impairment. Subsequently, when arriving for their evaluation, forgetting the date is a common sign of anxiety. A relatable analogy would be to compare the mistake with a medical student forgetting part of the anatomy while questioning by an attending during surgery. Imagine such medical students being referred to mandatory psychiatric evaluation when failing to answer a question during rounds.
In our practice, the most common reason for those minor mistakes during our clinical evaluation is anxiety. After all, patients who present for problems completely unrelated to cognitive decline make similar mistakes. Psychological stressors in physicians require no introduction. The concept is so prevalent and pervasive that it has its own name, “burnout.” Imagine having dedicated most of one’s life to a profession then being enumerated a list of complaints, having one’s privileges put on hold, then being told to complete an independent psychiatric evaluation. If burnout is in part caused by a lack of control, unclear job expectations, rapidly changing models of health care, and dysfunctional workplace dynamics, imagine the consequence of such a referral.
The militant evaluator will use jargon to vilify the reviewed physician. If the physician complains too voraciously, he will be described as having signs of frontotemporal dementia. If the physician comes with a written list of rebuttals, he will be described as having memory problems requiring aids. If the physician is demoralized and quiet, he will be described as being withdrawn and apathetic. If the physician refuses to use or has difficulty with new forms or electronic systems, he will be described as having “impaired executive function,” an ominous term that surely should not be associated with a practicing physician.
The second concern arises from problems with the validity and use of diagnoses like mild cognitive impairment (MCI). MCI is considered to be a transition stage when one maintains “normal activities of daily living, and normal general cognitive function.”3 The American Psychiatric Association Textbook of Psychiatry mentions that there are “however, many cases of nonprogressive MCI.” Should a disorder with generally normal cognition and unclear progression to a more severe disorder require one to be dispensed of their privileges? Should any disorder trump an assessment of functioning?
It is our experience that many if not most physicians’ practice of medicine is not a job but a profession that defines who they are. As such, their occupational habits are an overly repeated and ingrained series of maneuvers analogous to so-called muscle memory. This kind of ritualistic pattern is precisely the kind of cognition that may persist as one starts to have some deficits. This requires the evaluator to be particularly sensitive and cognizant that one may still be able to perform professionally despite some mild but notable deficits. While it is facile to diagnose someone with MCI and justify removing their license, a review of their actual clinical skills is, despite being more time consuming, more pertinent to the evaluation.
In practice, we find that many cases lie in a gray area, which is hard to define. Physicians may come to our office for an evaluation after having said something odd at work. Maybe they misdosed a medication on one occasion. Maybe they wrote the wrong year on a chart. However, if the physician was 30 years old, would we consider any one of those incidents significant? As a psychiatrist rather than a physician practicing the specialty in review, it is particularly hard and sometimes unwise to condone or sanction individual incidents.
Evaluators find solace in neuropsychological testing. However the relevance to the safety of patients is unclear. Many of those tests end up being a simple proxy for age. A physicians’ ability to sort words or cards at a certain speed might correlate to cognitive performance but has unclear significance to the ability to care for patients. Using such tests becomes a de facto age limit on the practice of medicine. It seems essential to expand and refine our repertoire of evaluation tools for the assessment of physicians. As when we perform capacity evaluation in the hospital, we enlist the assistance of the treating team in understanding the questions being asked for a patient, medical boards could consider creating independent multidisciplinary teams where psychiatry has a seat along with the relevant specialties of the evaluee. Likewise, the assessment would benefit from a broad review of the physicians’ general practice rather than the more typical review of one or two incidents.
We are promoting a more individualized approach by medical boards to the many issues of the aging physician. Retiring is no longer the dream of older physicians, but rather working in the suitable position where their contributions, clinical experience, and wisdom are positive contributions to patient care. Furthermore, we encourage medical boards to consider more nuanced decisions. A binary approach fits few cases that we see. Surgeons are a prime example of this. A surgeon in the early stages of Parkinsonism may be unfit to perform surgery but very capable of continuing to contribute to the well-being of patients in other forms of clinical work, including postsurgical care that doesn’t involve physical dexterity. Similarly, medical boards could consider other forms of partial restrictions, including a ban on procedures, a ban on hospital privileges, as well as required supervision or working in teams. Accumulated clinical wisdom allows older physicians to be excellent mentors and educators for younger doctors. There is no simple method to predict which physicians may have the early stages of a progressive dementia, and which may have a stable MCI. A yearly reevaluation if there are no further complaints, is the best approach to determine progression of cognitive problems.
Few crises like the current COVID-19 pandemic can better remind us of the importance of the place of medicine in society. Many states have encouraged retired physicians to contribute their knowledge and expertise, putting themselves in particular risk because of their age. It is a good time to be reminded that we owe them significant respect and care when deciding to remove their license. We are encouraged by the diligent efforts of medical boards in supervising our colleagues but warn against zealot evaluators who use this opportunity to force physicians into retirement. We also encourage medical boards to expand their tools and approaches when facing such cases, as mislabeled cognitive diagnoses can be an easy scapegoat of a poor understanding of the more important psychological and biological factors in the evaluation.
References
1. Tariq SH et al. Am J Geriatr Psychiatry. 2006;14:900-10.
2. Nasreddine Z. mocatest.org. Version 2004 Nov 7.
3. Hales RE et al. The American Psychiatric Publishing Textbook of Psychiatry. Washington: American Psychiatric Association Publishing, 2014.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings in chapter 7 in the book “Critical Psychiatry: Controversies and Clinical Implications” (Cham, Switzerland: Springer, 2019). He has no disclosures.
Dr. Abrams is a forensic psychiatrist and attorney in San Diego. He is an expert in addictionology, behavioral toxicology, psychopharmacology and correctional mental health. He holds a teaching positions at the University of California, San Diego. Among his writings are chapters about competency in national textbooks. Dr. Abrams has no disclosures.
Non-COVID-19 clinical trials grind to a halt during pandemic
The COVID-19 pandemic has created unique and unprecedented challenges for the clinical research world, with potentially long-lasting consequences.
A new analysis of the extent of disruption shows that the average rate of stopped trials nearly doubled during the first 5 months of 2020, compared with the 2 previous years.
“Typically, clinical research precedes clinical practice by several years, so this disruption we’re seeing now will be felt for many years to come,” said Mario Guadino, MD, of Weill Cornell Medicine, New York.
The analysis was published online July 31 in the Journal of the American College of Cardiology.
The researchers used Python software to query meta-data from all trials reported on ClinicalTrials.gov. Of 321,218 non-COVID-19 trials queried, 28,672 (8.9%) were reported as stopped, defined as a switch in trial status from “recruiting” to “active and not recruiting,” “completed,” “suspended,” “terminated,” or “withdrawn.”
The average rate of discontinuation was 638 trials/month from January 2017 to December 2019, rising to 1,147 trials/month between January 2020 and May 2020 (P < .001 for trend).
Once stopped (as opposed to paused), restarting a trial is a tricky prospect, said Dr. Guadino. “You can’t stop and restart a trial because it creates a lot of issues, so we should expect many of these stopped trials to never be completed.”
He said these figures likely represent an underestimate of the true impact of the pandemic because there is typically a delay in the updating of the status of a trial on ClinicalTrials.gov.
“We are likely looking only at the tip of the iceberg,” he added. “My impression is that the number of trials that will be affected and even canceled will be very high.”
As for cardiology trials, one of the report’s authors, Deepak Bhatt, MD, Brigham and Women’s Hospital, Boston, without naming specific trials, had this to say: “Several cardiovascular trials were paused, and some were permanently discontinued. It may be a while before we fully appreciate just how much information was lost and how much might be salvaged.”
He’s not worried, however, that upcoming cardiology meetings, which have moved online for the foreseeable future, might get a bit boring. “Fortunately, there is enough good work going on in the cardiovascular and cardiometabolic space that I believe there will still be ample randomized and observational data of high quality to present at the major meetings,” Dr. Bhatt said in an email.
The researchers found a weak correlation between the national population-adjusted numbers of COVID-19 cases and the proportion of non-COVID-19 trials stopped by country.
Even for trials that stopped recruiting for a period of time but are continuing, there are myriad issues involving compliance, data integrity, statistical interpretability, etc.
“Even if there is just a temporary disruption, that will most likely lead to reduced enrollment, missing follow-up visits, and protocol deviations, all things that would be red flags during normal times and impact the quality of the clinical trial,” said Dr. Guadino.
“And if your outcome of interest is mortality, well, how exactly do you measure that during a pandemic?” he added.
Stopped for lack of funding
Besides the logistical issues, another reason trials may be in jeopardy is funding. A warning early in the pandemic from the research community in Canada that funding was quickly drying up, leaving both jobs and data at risk, led to an aid package from the government to keep the lights on.
The National Institutes of Health (NIH), the Canadian Institutes of Health Research, and similar groups “have devoted large sums of money to research in COVID, which is of course very appropriate, but that clearly reduces the amount of funding that is available for other researchers,” said Dr. Guadino.
Some funding agencies around the world have canceled or put on hold all non-COVID-19 clinical trials still at the design state, Dr. Guadino said in an interview.
The NIH, he stressed, has not canceled funding and has been “extremely open and cooperative” in trying to help trialists navigate the many COVID-generated issues. They’ve even issued guidance on how to manage trials during COVID-19.
Of note, in the survey, the majority of the trials stopped (95.4%) had nongovernmental funding.
“The data are not very granular, so we’re only able to make some very simple, descriptive comments, but it does seem like the more fragile trials – those that are smaller and industry-funded – are the ones more likely to be disrupted,” said Dr. Guadino.
In some cases, he said, priorities have shifted to COVID-19. “If a small company is sponsoring a trial and they decide they want to sponsor something related to COVID, or they realize that because of the slow enrollment, the trial becomes too expensive to complete, they may opt to just abandon it,” said Dr. Guadino.
At what cost? It will take years to sort that out, he said.
This study received no funding. Dr. Guadino and Dr. Bhatt are both active trialists, participating in both industry- and government-sponsored clinical research.
A version of this article originally appeared on Medscape.com.
The COVID-19 pandemic has created unique and unprecedented challenges for the clinical research world, with potentially long-lasting consequences.
A new analysis of the extent of disruption shows that the average rate of stopped trials nearly doubled during the first 5 months of 2020, compared with the 2 previous years.
“Typically, clinical research precedes clinical practice by several years, so this disruption we’re seeing now will be felt for many years to come,” said Mario Guadino, MD, of Weill Cornell Medicine, New York.
The analysis was published online July 31 in the Journal of the American College of Cardiology.
The researchers used Python software to query meta-data from all trials reported on ClinicalTrials.gov. Of 321,218 non-COVID-19 trials queried, 28,672 (8.9%) were reported as stopped, defined as a switch in trial status from “recruiting” to “active and not recruiting,” “completed,” “suspended,” “terminated,” or “withdrawn.”
The average rate of discontinuation was 638 trials/month from January 2017 to December 2019, rising to 1,147 trials/month between January 2020 and May 2020 (P < .001 for trend).
Once stopped (as opposed to paused), restarting a trial is a tricky prospect, said Dr. Guadino. “You can’t stop and restart a trial because it creates a lot of issues, so we should expect many of these stopped trials to never be completed.”
He said these figures likely represent an underestimate of the true impact of the pandemic because there is typically a delay in the updating of the status of a trial on ClinicalTrials.gov.
“We are likely looking only at the tip of the iceberg,” he added. “My impression is that the number of trials that will be affected and even canceled will be very high.”
As for cardiology trials, one of the report’s authors, Deepak Bhatt, MD, Brigham and Women’s Hospital, Boston, without naming specific trials, had this to say: “Several cardiovascular trials were paused, and some were permanently discontinued. It may be a while before we fully appreciate just how much information was lost and how much might be salvaged.”
He’s not worried, however, that upcoming cardiology meetings, which have moved online for the foreseeable future, might get a bit boring. “Fortunately, there is enough good work going on in the cardiovascular and cardiometabolic space that I believe there will still be ample randomized and observational data of high quality to present at the major meetings,” Dr. Bhatt said in an email.
The researchers found a weak correlation between the national population-adjusted numbers of COVID-19 cases and the proportion of non-COVID-19 trials stopped by country.
Even for trials that stopped recruiting for a period of time but are continuing, there are myriad issues involving compliance, data integrity, statistical interpretability, etc.
“Even if there is just a temporary disruption, that will most likely lead to reduced enrollment, missing follow-up visits, and protocol deviations, all things that would be red flags during normal times and impact the quality of the clinical trial,” said Dr. Guadino.
“And if your outcome of interest is mortality, well, how exactly do you measure that during a pandemic?” he added.
Stopped for lack of funding
Besides the logistical issues, another reason trials may be in jeopardy is funding. A warning early in the pandemic from the research community in Canada that funding was quickly drying up, leaving both jobs and data at risk, led to an aid package from the government to keep the lights on.
The National Institutes of Health (NIH), the Canadian Institutes of Health Research, and similar groups “have devoted large sums of money to research in COVID, which is of course very appropriate, but that clearly reduces the amount of funding that is available for other researchers,” said Dr. Guadino.
Some funding agencies around the world have canceled or put on hold all non-COVID-19 clinical trials still at the design state, Dr. Guadino said in an interview.
The NIH, he stressed, has not canceled funding and has been “extremely open and cooperative” in trying to help trialists navigate the many COVID-generated issues. They’ve even issued guidance on how to manage trials during COVID-19.
Of note, in the survey, the majority of the trials stopped (95.4%) had nongovernmental funding.
“The data are not very granular, so we’re only able to make some very simple, descriptive comments, but it does seem like the more fragile trials – those that are smaller and industry-funded – are the ones more likely to be disrupted,” said Dr. Guadino.
In some cases, he said, priorities have shifted to COVID-19. “If a small company is sponsoring a trial and they decide they want to sponsor something related to COVID, or they realize that because of the slow enrollment, the trial becomes too expensive to complete, they may opt to just abandon it,” said Dr. Guadino.
At what cost? It will take years to sort that out, he said.
This study received no funding. Dr. Guadino and Dr. Bhatt are both active trialists, participating in both industry- and government-sponsored clinical research.
A version of this article originally appeared on Medscape.com.
The COVID-19 pandemic has created unique and unprecedented challenges for the clinical research world, with potentially long-lasting consequences.
A new analysis of the extent of disruption shows that the average rate of stopped trials nearly doubled during the first 5 months of 2020, compared with the 2 previous years.
“Typically, clinical research precedes clinical practice by several years, so this disruption we’re seeing now will be felt for many years to come,” said Mario Guadino, MD, of Weill Cornell Medicine, New York.
The analysis was published online July 31 in the Journal of the American College of Cardiology.
The researchers used Python software to query meta-data from all trials reported on ClinicalTrials.gov. Of 321,218 non-COVID-19 trials queried, 28,672 (8.9%) were reported as stopped, defined as a switch in trial status from “recruiting” to “active and not recruiting,” “completed,” “suspended,” “terminated,” or “withdrawn.”
The average rate of discontinuation was 638 trials/month from January 2017 to December 2019, rising to 1,147 trials/month between January 2020 and May 2020 (P < .001 for trend).
Once stopped (as opposed to paused), restarting a trial is a tricky prospect, said Dr. Guadino. “You can’t stop and restart a trial because it creates a lot of issues, so we should expect many of these stopped trials to never be completed.”
He said these figures likely represent an underestimate of the true impact of the pandemic because there is typically a delay in the updating of the status of a trial on ClinicalTrials.gov.
“We are likely looking only at the tip of the iceberg,” he added. “My impression is that the number of trials that will be affected and even canceled will be very high.”
As for cardiology trials, one of the report’s authors, Deepak Bhatt, MD, Brigham and Women’s Hospital, Boston, without naming specific trials, had this to say: “Several cardiovascular trials were paused, and some were permanently discontinued. It may be a while before we fully appreciate just how much information was lost and how much might be salvaged.”
He’s not worried, however, that upcoming cardiology meetings, which have moved online for the foreseeable future, might get a bit boring. “Fortunately, there is enough good work going on in the cardiovascular and cardiometabolic space that I believe there will still be ample randomized and observational data of high quality to present at the major meetings,” Dr. Bhatt said in an email.
The researchers found a weak correlation between the national population-adjusted numbers of COVID-19 cases and the proportion of non-COVID-19 trials stopped by country.
Even for trials that stopped recruiting for a period of time but are continuing, there are myriad issues involving compliance, data integrity, statistical interpretability, etc.
“Even if there is just a temporary disruption, that will most likely lead to reduced enrollment, missing follow-up visits, and protocol deviations, all things that would be red flags during normal times and impact the quality of the clinical trial,” said Dr. Guadino.
“And if your outcome of interest is mortality, well, how exactly do you measure that during a pandemic?” he added.
Stopped for lack of funding
Besides the logistical issues, another reason trials may be in jeopardy is funding. A warning early in the pandemic from the research community in Canada that funding was quickly drying up, leaving both jobs and data at risk, led to an aid package from the government to keep the lights on.
The National Institutes of Health (NIH), the Canadian Institutes of Health Research, and similar groups “have devoted large sums of money to research in COVID, which is of course very appropriate, but that clearly reduces the amount of funding that is available for other researchers,” said Dr. Guadino.
Some funding agencies around the world have canceled or put on hold all non-COVID-19 clinical trials still at the design state, Dr. Guadino said in an interview.
The NIH, he stressed, has not canceled funding and has been “extremely open and cooperative” in trying to help trialists navigate the many COVID-generated issues. They’ve even issued guidance on how to manage trials during COVID-19.
Of note, in the survey, the majority of the trials stopped (95.4%) had nongovernmental funding.
“The data are not very granular, so we’re only able to make some very simple, descriptive comments, but it does seem like the more fragile trials – those that are smaller and industry-funded – are the ones more likely to be disrupted,” said Dr. Guadino.
In some cases, he said, priorities have shifted to COVID-19. “If a small company is sponsoring a trial and they decide they want to sponsor something related to COVID, or they realize that because of the slow enrollment, the trial becomes too expensive to complete, they may opt to just abandon it,” said Dr. Guadino.
At what cost? It will take years to sort that out, he said.
This study received no funding. Dr. Guadino and Dr. Bhatt are both active trialists, participating in both industry- and government-sponsored clinical research.
A version of this article originally appeared on Medscape.com.
Send kids to school safely if possible, supplement virtually
The abrupt transition to online learning for American children in kindergarten through 12th grade has left educators and parents unprepared, but virtual learning can be a successful part of education going forward, according to a viewpoint published in JAMA Pediatrics. However, schools also can reopen safely if precautions are taken, and students would benefit in many ways, according to a second viewpoint.
“As policy makers, health care professionals, and parents prepare for the fall semester and as public and private schools grapple with how to make that possible, a better understanding of K-12 virtual learning options and outcomes may facilitate those difficult decisions,” wrote Erik Black, PhD, of the University of Florida, Gainesville; Richard Ferdig, PhD, of Kent State University, Ohio; and Lindsay A. Thompson, MD, of the University of Florida, Gainesville.
“Importantly, K-12 virtual schooling is not suited for all students or all families.”
In a viewpoint published in JAMA Pediatrics, the authors noted that virtual schooling has existed in the United States in various forms for some time. “Just like the myriad options that are available for face-to-face schooling in the U.S., virtual schooling exists in a complex landscape of for-profit, charter, and public options.”
Not all virtual schools are equal
Consequently, not all virtual schools are created equal, they emphasized. Virtual education can be successful for many students when presented by trained online instructors using a curriculum designed to be effective in an online venue.
“Parents need to seek reviews and ask for educational outcomes from each virtual school system to assess the quality of the provided education,” Dr. Black, Dr. Ferdig, and Dr. Thompson emphasized.
Key questions for parents to consider when faced with online learning include the type of technology needed to participate; whether their child can maintain a study schedule and complete assignments with limited supervision; whether their child could ask for help and communicate with teachers through technology including phone, text, email, or video; and whether their child has the basic reading, math, and computer literacy skills to engage in online learning, the authors said. Other questions include the school’s expectations for parents and caregivers, how student information may be shared, and how the virtual school lines up with state standards for K-12 educators (in the case of options outside the public school system).
“The COVID-19 pandemic offers a unique challenge for educators, policymakers, and health care professionals to partner with parents to make the best local and individual decisions for children,” Dr. Black, Dr. Ferdig, and Dr. Thompson concluded.
Schools may be able to open safely
Children continue to make up a low percentage of COVID-19 cases and appear less likely to experience illness, wrote C. Jason Wang, MD, PhD, and Henry Bair, BS, of Stanford (Calif.) University in a second viewpoint also published in JAMA Pediatrics. The impact of long-term school closures extends beyond education and can “exacerbate socioeconomic disparities, amplify existing educational inequalities, and aggravate food insecurity, domestic violence, and mental health disorders,” they wrote.
Dr. Wang and Mr. Bair proposed that school districts “engage key stakeholders to establish a COVID-19 task force, composed of the superintendent, members of the school board, teachers, parents, and health care professionals to develop policies and procedures,” that would allow schools to open safely.
The authors outlined strategies including adapting teaching spaces to accommodate physical distance, with the addition of temporary modular buildings if needed. They advised assigned seating on school buses, and acknowledged the need for the availability of protective equipment, including hand sanitizer and masks, as well as the possible use of transparent barriers on the sides of student desks.
“As the AAP [American Academy of Pediatrics] guidance suggests, teachers who must work closely with students with special needs or with students who are unable to wear masks should wear N95 masks if possible or wear face shields in addition to surgical masks,” Dr. Wang and Mr. Bair noted. Other elements of the AAP guidance include the creation of fixed cohorts of students and teachers to limit virus exposure.
“Even with all the precautions in place, COVID-19 outbreaks within schools are still likely,” they said. “Therefore, schools will need to remain flexible and consider temporary closures if there is an outbreak involving multiple students and/or staff and be ready to transition to online education.”
The AAP guidance does not address operational approaches to identifying signs and symptoms of COVID-19, the authors noted. “To address this, we recommend that schools implement multilevel screening for students and staff.”
“In summary, to maximize health and educational outcomes, school districts should adopt some or all of the measures of the AAP guidance and prioritize them after considering local COVID-19 incidence, key stakeholder input, and budgetary constraints,” Dr. Wang and Mr. Bair concluded.
Schools opening is a regional decision
“The mission of the AAP is to attain optimal physical, mental, and social health and well-being for all infants, children, adolescents, and young adults,” Howard Smart, MD, said in an interview. The question of school reopening “is of national importance, and the AAP has a national role in making recommendations regarding national policy affecting the health of the children.”
“The decision to open schools will be made regionally, but it is important for a nonpolitical national voice to make expert recommendations,” he emphasized.
“Many of the recommendations are ideal goals,” noted Dr. Smart, chairman of the department of pediatrics at the Sharp Rees-Stealy Medical Group in San Diego. “It will be difficult, for example, to implement symptom screening every day before school, no matter where it is performed. Some of the measures may be quite costly, and take time to implement, or require expansion of school staff, for which there may be no budget.”
In addition, “[n]ot all students are likely to comply with masking, distance, and hand-washing recommendations. One student who is noncompliant will be able to infect many other students and staff, as has been seen in other countries.” Also, parental attitudes toward control measures are likely to affect student attitudes, he noted.
“I have interviewed many families at recent checkups, and most have felt that the rush to remote learning that occurred at the end of the last school year resulted in fairly disorganized instruction,” Dr. Smart said. “They are hoping that, having had the summer to plan ahead, the remote teaching will be handled better. Remote learning will certainly work best for self-motivated, organized students with good family support, as noted in the Black, Ferdig, and Thompson article,” he said.
Pediatricians can support the schools by being a source of evidence-based information for parents, Dr. Smart said. “Pediatricians with time and energy might want to volunteer to hold informational video conferences for parents and/or school personnel if they feel they are up to date on current COVID-19 science and want to handle potentially contentious questions.”
The decision parents make to send their children back to school comes down to a risk-benefit calculation. “In some communities this may be left to parents, while in other communities this will a public health decision,” he said. “It is still not clear whether having students attend school in person will result in increased spread of COVID-19 among the students, or in their communities. Although some evidence from early in the pandemic suggests that children may not spread the virus as much as adults, more recent evidence suggests that children 10 years and older do transmit the virus at least as much as adults.”
“The risk to the students and the community, therefore, is unknown,” and difficult to compare with the benefit of in-person schooling, Dr. Smart noted.
“We will learn quite a bit from communities where students do go back to in-person class, as we follow the progression of COVID-19 over the weeks following the resumption of instruction.” Ultimately, advice to parents will need to be tailored to the current conditions of COVID-19 transmission in the community, he concluded.
It’s not just about education
“The AAP released its guidance to ensure that as school districts were contemplating reopening they were considering the full array of risks for children and adolescents. These risks included not only those related to COVID-19, but also those related to the impact of not reopening in-person,” Nathaniel Beers, MD, president of the HSC Health Care System in Washington, said in an interview.
“Students and families are dependent on schools for much more than just an education, and those [elements] need to be factored into the decisions to reopen,” the pediatrician said.
However, “[t]he major barrier for schools is resources to safely reopen,” said Dr. Beers. “The additional staffing and supplies will require additional funding. There are increased demands regardless of whether students are learning in-person or virtually or through hybrid models.”
“Another significant barrier is ensuring that parents and staff are actively engaged in planning for the type of model being used,” he said.
“All of the models require buy-in by staff and parents. This will require significant outreach and strong communication plans. Schools also need to ensure they are planning not just for how to return students to schools, but what will happen when staff or students test positive for COVID-19. Students, families, and staff all will need to know what these plans are up front to feel confident in returning to school,” he emphasized.
“There are students who can thrive in a virtual learning environment,” Dr. Beers said. “There are also students who benefit from the virtual learning environment because of their own risk, or because of a family member’s risk for COVID-19 or the complications from it.”
“However, many children with disabilities have struggled in a virtual environment,” he said. “These students struggle to access the educational services without the adequate supports at home. They often receive additional services in school, such as speech, occupational therapy or physical therapy, or nursing services, that may not have transitioned to home but are critical for their health and development. Many students with disabilities are dependent on family members to successfully access the educational services they need.”
“Pediatricians can play a role in providing feedback on recommendations related to physical distancing and face coverings in particular,” said Dr. Beers. “In addition, they can be helpful in developing plans for children with disabilities as well as what the response plan should be for students who become sick during the school day.”
The Centers for Disease Control and Prevention released a decision tool for parents who are considering whether to send their child to in-person school, and pediatricians can help parents walk through these questions, Dr. Beers noted. “In addition, pediatricians play an important role in helping patients and families think about the risks of COVID for the patient and other family members, and this can be helpful in addressing the anxiety that parents and patients may be experiencing.”
Further information can be found in Return to School During COVID-19, which can be located at HealthyChildren.org, by the American Academy of Pediatrics.
The authors of the viewpoints had no relevant financial disclosures. Dr. Smart, a member of the Pediatric News editorial advisory board, had no relevant financial disclosures. Dr. Beers has served on the editorial advisory board of Pediatric News in the past, but had no relevant financial disclosures.
SOURCES: Black E, Ferdig R, Thompson LA. JAMA Pediatr. 2020 Aug 11. doi: 10.1001/jamapediatrics.2020.3800. Wang CJ and Bair H. JAMA Pediatr. Aug 11. doi: 10.1001/jamapediatrics.2020.3871.
The abrupt transition to online learning for American children in kindergarten through 12th grade has left educators and parents unprepared, but virtual learning can be a successful part of education going forward, according to a viewpoint published in JAMA Pediatrics. However, schools also can reopen safely if precautions are taken, and students would benefit in many ways, according to a second viewpoint.
“As policy makers, health care professionals, and parents prepare for the fall semester and as public and private schools grapple with how to make that possible, a better understanding of K-12 virtual learning options and outcomes may facilitate those difficult decisions,” wrote Erik Black, PhD, of the University of Florida, Gainesville; Richard Ferdig, PhD, of Kent State University, Ohio; and Lindsay A. Thompson, MD, of the University of Florida, Gainesville.
“Importantly, K-12 virtual schooling is not suited for all students or all families.”
In a viewpoint published in JAMA Pediatrics, the authors noted that virtual schooling has existed in the United States in various forms for some time. “Just like the myriad options that are available for face-to-face schooling in the U.S., virtual schooling exists in a complex landscape of for-profit, charter, and public options.”
Not all virtual schools are equal
Consequently, not all virtual schools are created equal, they emphasized. Virtual education can be successful for many students when presented by trained online instructors using a curriculum designed to be effective in an online venue.
“Parents need to seek reviews and ask for educational outcomes from each virtual school system to assess the quality of the provided education,” Dr. Black, Dr. Ferdig, and Dr. Thompson emphasized.
Key questions for parents to consider when faced with online learning include the type of technology needed to participate; whether their child can maintain a study schedule and complete assignments with limited supervision; whether their child could ask for help and communicate with teachers through technology including phone, text, email, or video; and whether their child has the basic reading, math, and computer literacy skills to engage in online learning, the authors said. Other questions include the school’s expectations for parents and caregivers, how student information may be shared, and how the virtual school lines up with state standards for K-12 educators (in the case of options outside the public school system).
“The COVID-19 pandemic offers a unique challenge for educators, policymakers, and health care professionals to partner with parents to make the best local and individual decisions for children,” Dr. Black, Dr. Ferdig, and Dr. Thompson concluded.
Schools may be able to open safely
Children continue to make up a low percentage of COVID-19 cases and appear less likely to experience illness, wrote C. Jason Wang, MD, PhD, and Henry Bair, BS, of Stanford (Calif.) University in a second viewpoint also published in JAMA Pediatrics. The impact of long-term school closures extends beyond education and can “exacerbate socioeconomic disparities, amplify existing educational inequalities, and aggravate food insecurity, domestic violence, and mental health disorders,” they wrote.
Dr. Wang and Mr. Bair proposed that school districts “engage key stakeholders to establish a COVID-19 task force, composed of the superintendent, members of the school board, teachers, parents, and health care professionals to develop policies and procedures,” that would allow schools to open safely.
The authors outlined strategies including adapting teaching spaces to accommodate physical distance, with the addition of temporary modular buildings if needed. They advised assigned seating on school buses, and acknowledged the need for the availability of protective equipment, including hand sanitizer and masks, as well as the possible use of transparent barriers on the sides of student desks.
“As the AAP [American Academy of Pediatrics] guidance suggests, teachers who must work closely with students with special needs or with students who are unable to wear masks should wear N95 masks if possible or wear face shields in addition to surgical masks,” Dr. Wang and Mr. Bair noted. Other elements of the AAP guidance include the creation of fixed cohorts of students and teachers to limit virus exposure.
“Even with all the precautions in place, COVID-19 outbreaks within schools are still likely,” they said. “Therefore, schools will need to remain flexible and consider temporary closures if there is an outbreak involving multiple students and/or staff and be ready to transition to online education.”
The AAP guidance does not address operational approaches to identifying signs and symptoms of COVID-19, the authors noted. “To address this, we recommend that schools implement multilevel screening for students and staff.”
“In summary, to maximize health and educational outcomes, school districts should adopt some or all of the measures of the AAP guidance and prioritize them after considering local COVID-19 incidence, key stakeholder input, and budgetary constraints,” Dr. Wang and Mr. Bair concluded.
Schools opening is a regional decision
“The mission of the AAP is to attain optimal physical, mental, and social health and well-being for all infants, children, adolescents, and young adults,” Howard Smart, MD, said in an interview. The question of school reopening “is of national importance, and the AAP has a national role in making recommendations regarding national policy affecting the health of the children.”
“The decision to open schools will be made regionally, but it is important for a nonpolitical national voice to make expert recommendations,” he emphasized.
“Many of the recommendations are ideal goals,” noted Dr. Smart, chairman of the department of pediatrics at the Sharp Rees-Stealy Medical Group in San Diego. “It will be difficult, for example, to implement symptom screening every day before school, no matter where it is performed. Some of the measures may be quite costly, and take time to implement, or require expansion of school staff, for which there may be no budget.”
In addition, “[n]ot all students are likely to comply with masking, distance, and hand-washing recommendations. One student who is noncompliant will be able to infect many other students and staff, as has been seen in other countries.” Also, parental attitudes toward control measures are likely to affect student attitudes, he noted.
“I have interviewed many families at recent checkups, and most have felt that the rush to remote learning that occurred at the end of the last school year resulted in fairly disorganized instruction,” Dr. Smart said. “They are hoping that, having had the summer to plan ahead, the remote teaching will be handled better. Remote learning will certainly work best for self-motivated, organized students with good family support, as noted in the Black, Ferdig, and Thompson article,” he said.
Pediatricians can support the schools by being a source of evidence-based information for parents, Dr. Smart said. “Pediatricians with time and energy might want to volunteer to hold informational video conferences for parents and/or school personnel if they feel they are up to date on current COVID-19 science and want to handle potentially contentious questions.”
The decision parents make to send their children back to school comes down to a risk-benefit calculation. “In some communities this may be left to parents, while in other communities this will a public health decision,” he said. “It is still not clear whether having students attend school in person will result in increased spread of COVID-19 among the students, or in their communities. Although some evidence from early in the pandemic suggests that children may not spread the virus as much as adults, more recent evidence suggests that children 10 years and older do transmit the virus at least as much as adults.”
“The risk to the students and the community, therefore, is unknown,” and difficult to compare with the benefit of in-person schooling, Dr. Smart noted.
“We will learn quite a bit from communities where students do go back to in-person class, as we follow the progression of COVID-19 over the weeks following the resumption of instruction.” Ultimately, advice to parents will need to be tailored to the current conditions of COVID-19 transmission in the community, he concluded.
It’s not just about education
“The AAP released its guidance to ensure that as school districts were contemplating reopening they were considering the full array of risks for children and adolescents. These risks included not only those related to COVID-19, but also those related to the impact of not reopening in-person,” Nathaniel Beers, MD, president of the HSC Health Care System in Washington, said in an interview.
“Students and families are dependent on schools for much more than just an education, and those [elements] need to be factored into the decisions to reopen,” the pediatrician said.
However, “[t]he major barrier for schools is resources to safely reopen,” said Dr. Beers. “The additional staffing and supplies will require additional funding. There are increased demands regardless of whether students are learning in-person or virtually or through hybrid models.”
“Another significant barrier is ensuring that parents and staff are actively engaged in planning for the type of model being used,” he said.
“All of the models require buy-in by staff and parents. This will require significant outreach and strong communication plans. Schools also need to ensure they are planning not just for how to return students to schools, but what will happen when staff or students test positive for COVID-19. Students, families, and staff all will need to know what these plans are up front to feel confident in returning to school,” he emphasized.
“There are students who can thrive in a virtual learning environment,” Dr. Beers said. “There are also students who benefit from the virtual learning environment because of their own risk, or because of a family member’s risk for COVID-19 or the complications from it.”
“However, many children with disabilities have struggled in a virtual environment,” he said. “These students struggle to access the educational services without the adequate supports at home. They often receive additional services in school, such as speech, occupational therapy or physical therapy, or nursing services, that may not have transitioned to home but are critical for their health and development. Many students with disabilities are dependent on family members to successfully access the educational services they need.”
“Pediatricians can play a role in providing feedback on recommendations related to physical distancing and face coverings in particular,” said Dr. Beers. “In addition, they can be helpful in developing plans for children with disabilities as well as what the response plan should be for students who become sick during the school day.”
The Centers for Disease Control and Prevention released a decision tool for parents who are considering whether to send their child to in-person school, and pediatricians can help parents walk through these questions, Dr. Beers noted. “In addition, pediatricians play an important role in helping patients and families think about the risks of COVID for the patient and other family members, and this can be helpful in addressing the anxiety that parents and patients may be experiencing.”
Further information can be found in Return to School During COVID-19, which can be located at HealthyChildren.org, by the American Academy of Pediatrics.
The authors of the viewpoints had no relevant financial disclosures. Dr. Smart, a member of the Pediatric News editorial advisory board, had no relevant financial disclosures. Dr. Beers has served on the editorial advisory board of Pediatric News in the past, but had no relevant financial disclosures.
SOURCES: Black E, Ferdig R, Thompson LA. JAMA Pediatr. 2020 Aug 11. doi: 10.1001/jamapediatrics.2020.3800. Wang CJ and Bair H. JAMA Pediatr. Aug 11. doi: 10.1001/jamapediatrics.2020.3871.
The abrupt transition to online learning for American children in kindergarten through 12th grade has left educators and parents unprepared, but virtual learning can be a successful part of education going forward, according to a viewpoint published in JAMA Pediatrics. However, schools also can reopen safely if precautions are taken, and students would benefit in many ways, according to a second viewpoint.
“As policy makers, health care professionals, and parents prepare for the fall semester and as public and private schools grapple with how to make that possible, a better understanding of K-12 virtual learning options and outcomes may facilitate those difficult decisions,” wrote Erik Black, PhD, of the University of Florida, Gainesville; Richard Ferdig, PhD, of Kent State University, Ohio; and Lindsay A. Thompson, MD, of the University of Florida, Gainesville.
“Importantly, K-12 virtual schooling is not suited for all students or all families.”
In a viewpoint published in JAMA Pediatrics, the authors noted that virtual schooling has existed in the United States in various forms for some time. “Just like the myriad options that are available for face-to-face schooling in the U.S., virtual schooling exists in a complex landscape of for-profit, charter, and public options.”
Not all virtual schools are equal
Consequently, not all virtual schools are created equal, they emphasized. Virtual education can be successful for many students when presented by trained online instructors using a curriculum designed to be effective in an online venue.
“Parents need to seek reviews and ask for educational outcomes from each virtual school system to assess the quality of the provided education,” Dr. Black, Dr. Ferdig, and Dr. Thompson emphasized.
Key questions for parents to consider when faced with online learning include the type of technology needed to participate; whether their child can maintain a study schedule and complete assignments with limited supervision; whether their child could ask for help and communicate with teachers through technology including phone, text, email, or video; and whether their child has the basic reading, math, and computer literacy skills to engage in online learning, the authors said. Other questions include the school’s expectations for parents and caregivers, how student information may be shared, and how the virtual school lines up with state standards for K-12 educators (in the case of options outside the public school system).
“The COVID-19 pandemic offers a unique challenge for educators, policymakers, and health care professionals to partner with parents to make the best local and individual decisions for children,” Dr. Black, Dr. Ferdig, and Dr. Thompson concluded.
Schools may be able to open safely
Children continue to make up a low percentage of COVID-19 cases and appear less likely to experience illness, wrote C. Jason Wang, MD, PhD, and Henry Bair, BS, of Stanford (Calif.) University in a second viewpoint also published in JAMA Pediatrics. The impact of long-term school closures extends beyond education and can “exacerbate socioeconomic disparities, amplify existing educational inequalities, and aggravate food insecurity, domestic violence, and mental health disorders,” they wrote.
Dr. Wang and Mr. Bair proposed that school districts “engage key stakeholders to establish a COVID-19 task force, composed of the superintendent, members of the school board, teachers, parents, and health care professionals to develop policies and procedures,” that would allow schools to open safely.
The authors outlined strategies including adapting teaching spaces to accommodate physical distance, with the addition of temporary modular buildings if needed. They advised assigned seating on school buses, and acknowledged the need for the availability of protective equipment, including hand sanitizer and masks, as well as the possible use of transparent barriers on the sides of student desks.
“As the AAP [American Academy of Pediatrics] guidance suggests, teachers who must work closely with students with special needs or with students who are unable to wear masks should wear N95 masks if possible or wear face shields in addition to surgical masks,” Dr. Wang and Mr. Bair noted. Other elements of the AAP guidance include the creation of fixed cohorts of students and teachers to limit virus exposure.
“Even with all the precautions in place, COVID-19 outbreaks within schools are still likely,” they said. “Therefore, schools will need to remain flexible and consider temporary closures if there is an outbreak involving multiple students and/or staff and be ready to transition to online education.”
The AAP guidance does not address operational approaches to identifying signs and symptoms of COVID-19, the authors noted. “To address this, we recommend that schools implement multilevel screening for students and staff.”
“In summary, to maximize health and educational outcomes, school districts should adopt some or all of the measures of the AAP guidance and prioritize them after considering local COVID-19 incidence, key stakeholder input, and budgetary constraints,” Dr. Wang and Mr. Bair concluded.
Schools opening is a regional decision
“The mission of the AAP is to attain optimal physical, mental, and social health and well-being for all infants, children, adolescents, and young adults,” Howard Smart, MD, said in an interview. The question of school reopening “is of national importance, and the AAP has a national role in making recommendations regarding national policy affecting the health of the children.”
“The decision to open schools will be made regionally, but it is important for a nonpolitical national voice to make expert recommendations,” he emphasized.
“Many of the recommendations are ideal goals,” noted Dr. Smart, chairman of the department of pediatrics at the Sharp Rees-Stealy Medical Group in San Diego. “It will be difficult, for example, to implement symptom screening every day before school, no matter where it is performed. Some of the measures may be quite costly, and take time to implement, or require expansion of school staff, for which there may be no budget.”
In addition, “[n]ot all students are likely to comply with masking, distance, and hand-washing recommendations. One student who is noncompliant will be able to infect many other students and staff, as has been seen in other countries.” Also, parental attitudes toward control measures are likely to affect student attitudes, he noted.
“I have interviewed many families at recent checkups, and most have felt that the rush to remote learning that occurred at the end of the last school year resulted in fairly disorganized instruction,” Dr. Smart said. “They are hoping that, having had the summer to plan ahead, the remote teaching will be handled better. Remote learning will certainly work best for self-motivated, organized students with good family support, as noted in the Black, Ferdig, and Thompson article,” he said.
Pediatricians can support the schools by being a source of evidence-based information for parents, Dr. Smart said. “Pediatricians with time and energy might want to volunteer to hold informational video conferences for parents and/or school personnel if they feel they are up to date on current COVID-19 science and want to handle potentially contentious questions.”
The decision parents make to send their children back to school comes down to a risk-benefit calculation. “In some communities this may be left to parents, while in other communities this will a public health decision,” he said. “It is still not clear whether having students attend school in person will result in increased spread of COVID-19 among the students, or in their communities. Although some evidence from early in the pandemic suggests that children may not spread the virus as much as adults, more recent evidence suggests that children 10 years and older do transmit the virus at least as much as adults.”
“The risk to the students and the community, therefore, is unknown,” and difficult to compare with the benefit of in-person schooling, Dr. Smart noted.
“We will learn quite a bit from communities where students do go back to in-person class, as we follow the progression of COVID-19 over the weeks following the resumption of instruction.” Ultimately, advice to parents will need to be tailored to the current conditions of COVID-19 transmission in the community, he concluded.
It’s not just about education
“The AAP released its guidance to ensure that as school districts were contemplating reopening they were considering the full array of risks for children and adolescents. These risks included not only those related to COVID-19, but also those related to the impact of not reopening in-person,” Nathaniel Beers, MD, president of the HSC Health Care System in Washington, said in an interview.
“Students and families are dependent on schools for much more than just an education, and those [elements] need to be factored into the decisions to reopen,” the pediatrician said.
However, “[t]he major barrier for schools is resources to safely reopen,” said Dr. Beers. “The additional staffing and supplies will require additional funding. There are increased demands regardless of whether students are learning in-person or virtually or through hybrid models.”
“Another significant barrier is ensuring that parents and staff are actively engaged in planning for the type of model being used,” he said.
“All of the models require buy-in by staff and parents. This will require significant outreach and strong communication plans. Schools also need to ensure they are planning not just for how to return students to schools, but what will happen when staff or students test positive for COVID-19. Students, families, and staff all will need to know what these plans are up front to feel confident in returning to school,” he emphasized.
“There are students who can thrive in a virtual learning environment,” Dr. Beers said. “There are also students who benefit from the virtual learning environment because of their own risk, or because of a family member’s risk for COVID-19 or the complications from it.”
“However, many children with disabilities have struggled in a virtual environment,” he said. “These students struggle to access the educational services without the adequate supports at home. They often receive additional services in school, such as speech, occupational therapy or physical therapy, or nursing services, that may not have transitioned to home but are critical for their health and development. Many students with disabilities are dependent on family members to successfully access the educational services they need.”
“Pediatricians can play a role in providing feedback on recommendations related to physical distancing and face coverings in particular,” said Dr. Beers. “In addition, they can be helpful in developing plans for children with disabilities as well as what the response plan should be for students who become sick during the school day.”
The Centers for Disease Control and Prevention released a decision tool for parents who are considering whether to send their child to in-person school, and pediatricians can help parents walk through these questions, Dr. Beers noted. “In addition, pediatricians play an important role in helping patients and families think about the risks of COVID for the patient and other family members, and this can be helpful in addressing the anxiety that parents and patients may be experiencing.”
Further information can be found in Return to School During COVID-19, which can be located at HealthyChildren.org, by the American Academy of Pediatrics.
The authors of the viewpoints had no relevant financial disclosures. Dr. Smart, a member of the Pediatric News editorial advisory board, had no relevant financial disclosures. Dr. Beers has served on the editorial advisory board of Pediatric News in the past, but had no relevant financial disclosures.
SOURCES: Black E, Ferdig R, Thompson LA. JAMA Pediatr. 2020 Aug 11. doi: 10.1001/jamapediatrics.2020.3800. Wang CJ and Bair H. JAMA Pediatr. Aug 11. doi: 10.1001/jamapediatrics.2020.3871.
FROM JAMA PEDIATRICS
Only 40% of residents said training prepped them for COVID-19
Most residents who were asked whether their training prepared them for COVID-19 in a Medscape survey said it had not or they weren’t sure.
Whereas 40% said they felt prepared, 30% said they did not feel prepared and 31% answered they were unsure. (Numbers were rounded, so some answers pushed above 100%.)
One quarter have $300,000 or more in student debt
The Medscape Residents Salary & Debt Report 2020, with data collected April 3 to June 1, found that nearly one in four residents (24%) had medical school debt of more than $300,000. Half (49%) had more than $200,000.
The data include answers from 1,659 U.S. medical residents.
For the sixth straight year, female residents were more satisfied with their pay than were their male colleagues. This year the satisfaction gap was 45% female compared with 42% male. That imbalance came despite their making nearly the same pay overall ($63,700 for men and $63,000 for women).
Among practicing physicians, the pay gap is much wider: Men make 25% more in primary care and 31% more in specialties.
Ten percent thought they should earn 76%-100% more.
For those not satisfied with pay, the top reasons were feeling the pay was too low for the hours worked (81%) or too low compared with other medical staff, such as physician assistants (PAs) or nurses (77% chose that answer).
As for hours worked, 31% of residents reported they spend more than 60 hours/week seeing patients.
The top-paying specialties, averaging $69,500, were allergy and immunology, hematology, plastic surgery, aesthetic medicine, rheumatology, and specialized surgery. The lowest paid were family medicine residents at $58,500.
In primary care, overall, most residents said they planned to specialize. Only 47% planned to continue to work in primary care. Male residents were much more likely to say they will subspecialize than were their female colleagues (52% vs. 35%).
More than 90% of residents say future pay has influenced their choice of specialty, though more men than women felt that way (93% vs. 86%).
Good relationships with others
Overall, residents reported good relationships with attending physicians and nurses.
Most (88%) said they had good or very good relationships with attending physicians, 10% said the relationships were fair, and 2% said they were poor.
In addition, 89% of residents said the amount of supervision was appropriate, 4% said there was too much, and 7% said there was too little.
Relationships with nurses/PAs were slightly less positive overall: Eighty-two percent reported good or very good relationships with nurses/PAs, 15% said those relationships were fair, and 3% said they were poor.
One respondent said: “Our relationships could be better, but I think everyone is just overwhelmed with COVID-19, so emotions are heightened.”
Another said: “It takes time to earn the respect from nurses.”
Seventy-seven percent said they were satisfied with their learning experience overall, 12% were neutral on the question, and 11% said they were dissatisfied or very dissatisfied.
Work-life balance is the top concern
Work-life balance continues to be the top concern for residents. More than one-quarter (27%) in residency years 1 through 4 listed that as the top concern, and even more (32%) of those in years 5 through 8 agreed.
That was followed by demands on time and fear of failure or making a serious mistake.
The survey indicates that benefit packages for residents have stayed much the same over the past 2 years with health insurance and paid time off for sick leave, vacation, and personal time most commonly reported at 89% and 87%, respectively.
Much less common were benefits including commuter assistance (parking, public transportation) at 24%, housing allowance (8%), and child care (4%).
The vast majority of residents reported doing scut work (unskilled tasks): More than half (54%) reported doing 1-10 hours/week and 22% did 11-20 hours/week. Regardless of the number of hours, however, 62% said the time spent performing these tasks was appropriate.
A version of this article originally appeared on Medscape.com.
Most residents who were asked whether their training prepared them for COVID-19 in a Medscape survey said it had not or they weren’t sure.
Whereas 40% said they felt prepared, 30% said they did not feel prepared and 31% answered they were unsure. (Numbers were rounded, so some answers pushed above 100%.)
One quarter have $300,000 or more in student debt
The Medscape Residents Salary & Debt Report 2020, with data collected April 3 to June 1, found that nearly one in four residents (24%) had medical school debt of more than $300,000. Half (49%) had more than $200,000.
The data include answers from 1,659 U.S. medical residents.
For the sixth straight year, female residents were more satisfied with their pay than were their male colleagues. This year the satisfaction gap was 45% female compared with 42% male. That imbalance came despite their making nearly the same pay overall ($63,700 for men and $63,000 for women).
Among practicing physicians, the pay gap is much wider: Men make 25% more in primary care and 31% more in specialties.
Ten percent thought they should earn 76%-100% more.
For those not satisfied with pay, the top reasons were feeling the pay was too low for the hours worked (81%) or too low compared with other medical staff, such as physician assistants (PAs) or nurses (77% chose that answer).
As for hours worked, 31% of residents reported they spend more than 60 hours/week seeing patients.
The top-paying specialties, averaging $69,500, were allergy and immunology, hematology, plastic surgery, aesthetic medicine, rheumatology, and specialized surgery. The lowest paid were family medicine residents at $58,500.
In primary care, overall, most residents said they planned to specialize. Only 47% planned to continue to work in primary care. Male residents were much more likely to say they will subspecialize than were their female colleagues (52% vs. 35%).
More than 90% of residents say future pay has influenced their choice of specialty, though more men than women felt that way (93% vs. 86%).
Good relationships with others
Overall, residents reported good relationships with attending physicians and nurses.
Most (88%) said they had good or very good relationships with attending physicians, 10% said the relationships were fair, and 2% said they were poor.
In addition, 89% of residents said the amount of supervision was appropriate, 4% said there was too much, and 7% said there was too little.
Relationships with nurses/PAs were slightly less positive overall: Eighty-two percent reported good or very good relationships with nurses/PAs, 15% said those relationships were fair, and 3% said they were poor.
One respondent said: “Our relationships could be better, but I think everyone is just overwhelmed with COVID-19, so emotions are heightened.”
Another said: “It takes time to earn the respect from nurses.”
Seventy-seven percent said they were satisfied with their learning experience overall, 12% were neutral on the question, and 11% said they were dissatisfied or very dissatisfied.
Work-life balance is the top concern
Work-life balance continues to be the top concern for residents. More than one-quarter (27%) in residency years 1 through 4 listed that as the top concern, and even more (32%) of those in years 5 through 8 agreed.
That was followed by demands on time and fear of failure or making a serious mistake.
The survey indicates that benefit packages for residents have stayed much the same over the past 2 years with health insurance and paid time off for sick leave, vacation, and personal time most commonly reported at 89% and 87%, respectively.
Much less common were benefits including commuter assistance (parking, public transportation) at 24%, housing allowance (8%), and child care (4%).
The vast majority of residents reported doing scut work (unskilled tasks): More than half (54%) reported doing 1-10 hours/week and 22% did 11-20 hours/week. Regardless of the number of hours, however, 62% said the time spent performing these tasks was appropriate.
A version of this article originally appeared on Medscape.com.
Most residents who were asked whether their training prepared them for COVID-19 in a Medscape survey said it had not or they weren’t sure.
Whereas 40% said they felt prepared, 30% said they did not feel prepared and 31% answered they were unsure. (Numbers were rounded, so some answers pushed above 100%.)
One quarter have $300,000 or more in student debt
The Medscape Residents Salary & Debt Report 2020, with data collected April 3 to June 1, found that nearly one in four residents (24%) had medical school debt of more than $300,000. Half (49%) had more than $200,000.
The data include answers from 1,659 U.S. medical residents.
For the sixth straight year, female residents were more satisfied with their pay than were their male colleagues. This year the satisfaction gap was 45% female compared with 42% male. That imbalance came despite their making nearly the same pay overall ($63,700 for men and $63,000 for women).
Among practicing physicians, the pay gap is much wider: Men make 25% more in primary care and 31% more in specialties.
Ten percent thought they should earn 76%-100% more.
For those not satisfied with pay, the top reasons were feeling the pay was too low for the hours worked (81%) or too low compared with other medical staff, such as physician assistants (PAs) or nurses (77% chose that answer).
As for hours worked, 31% of residents reported they spend more than 60 hours/week seeing patients.
The top-paying specialties, averaging $69,500, were allergy and immunology, hematology, plastic surgery, aesthetic medicine, rheumatology, and specialized surgery. The lowest paid were family medicine residents at $58,500.
In primary care, overall, most residents said they planned to specialize. Only 47% planned to continue to work in primary care. Male residents were much more likely to say they will subspecialize than were their female colleagues (52% vs. 35%).
More than 90% of residents say future pay has influenced their choice of specialty, though more men than women felt that way (93% vs. 86%).
Good relationships with others
Overall, residents reported good relationships with attending physicians and nurses.
Most (88%) said they had good or very good relationships with attending physicians, 10% said the relationships were fair, and 2% said they were poor.
In addition, 89% of residents said the amount of supervision was appropriate, 4% said there was too much, and 7% said there was too little.
Relationships with nurses/PAs were slightly less positive overall: Eighty-two percent reported good or very good relationships with nurses/PAs, 15% said those relationships were fair, and 3% said they were poor.
One respondent said: “Our relationships could be better, but I think everyone is just overwhelmed with COVID-19, so emotions are heightened.”
Another said: “It takes time to earn the respect from nurses.”
Seventy-seven percent said they were satisfied with their learning experience overall, 12% were neutral on the question, and 11% said they were dissatisfied or very dissatisfied.
Work-life balance is the top concern
Work-life balance continues to be the top concern for residents. More than one-quarter (27%) in residency years 1 through 4 listed that as the top concern, and even more (32%) of those in years 5 through 8 agreed.
That was followed by demands on time and fear of failure or making a serious mistake.
The survey indicates that benefit packages for residents have stayed much the same over the past 2 years with health insurance and paid time off for sick leave, vacation, and personal time most commonly reported at 89% and 87%, respectively.
Much less common were benefits including commuter assistance (parking, public transportation) at 24%, housing allowance (8%), and child care (4%).
The vast majority of residents reported doing scut work (unskilled tasks): More than half (54%) reported doing 1-10 hours/week and 22% did 11-20 hours/week. Regardless of the number of hours, however, 62% said the time spent performing these tasks was appropriate.
A version of this article originally appeared on Medscape.com.
Financial planning in the COVID-19 era
Less than a year ago, I wrote a column on retirement strategies; but that was before COVID-19 took down the economy, putting millions out of work and shuttering many of our offices. Add extraordinary racial tensions and an election year like no other, and 2020 has generated fear and uncertainty on an unprecedented level.
Not surprisingly, my e-mail has been dominated for months by questions about the short- and long-term financial consequences of this annus horribilis on our practices and retirement plans. Most physicians have felt the downturn acutely, of course. Revenues have declined, non-COVID-19-related hospital visits plunged, and only recently have we seen hospitals resuming elective procedures. As I write this, my practice is approaching its prepandemic volume; but many patients have been avoiding hospitals and doctors’ offices for fear of COVID-19 exposure. With no real end in sight, who can say when this trend will finally correct itself?
Long term, the outlook is not nearly so grim. I have always written that downturns – even steep ones – are inevitable; and rather than fear them, you should expect them and plan for them. Younger physicians with riskier investments have plenty of time to rebound. Physicians nearing retirement, if they have done everything right, probably have the least to lose. Ideally, they will be at or near their savings target and will have transitioned to less vulnerable assets. And remember, you don’t need to have 100% of your retirement money to retire; a sound retirement plan will continue to generate investment returns as you move through retirement.
In short, .
By way of a brief review, the basics of a good plan are a budget, an emergency fund, disability insurance, and retiring your debt as quickly as possible. All of these have been covered individually in previous columns.
An essential component of your plan should be a list of long-term goals – and it should be more specific than simply accumulating a pile of cash. What do you plan to accomplish with the money? If it’s travel, helping your grandkids with college expenses, hobbies, or something else, make a list. Review it regularly, and modify it if your goals change.
Time to trot out another hoary old cliché: Saving for retirement is a marathon, not a sprint. If the pandemic has temporarily derailed your retirement strategy – forcing you, for example, to make retirement account withdrawals to cover expenses, or raid your emergency fund – no worries! When things have stabilized, it’s time to recommit to your retirement plan. Once again, with so many other issues to deal with, retaining the services of a qualified financial professional is usually a far better strategy than going it alone.
Many readers have expressed the fear that their retirement savings would never recover from the COVID-19 hit – but my own financial adviser pointed out that as I write this, in August, conservative portfolio values are about level with similar portfolios on Jan. 1, 2020. “Good plans are built to withstand difficult times,” she said. “Sometimes staying the course is the most difficult, disciplined course of action.”
“If your gut tells you that things will only get worse,” writes Kimberly Lankford in AARP’s magazine, “know that your gut is a terrible economic forecaster.” The University of Michigan’s Index of Consumer Sentiment hit rock bottom in 2008, during the Great Recession; yet only 4 months later, the U.S. economy began its longest expansion in modern history. The point is that it is important to maintain a long-term approach, and not make changes based on short-term events.
COVID-19 (or whatever else comes along) then becomes a matter of statement pain, not long-term financial pain. The key to recovery has nothing to do with a financial change, an investment strategy change, or a holding change, and everything to do with realigning your long-term goals.
So, moving on from COVID-19 is actually quite simple: Fill your retirement plan to its legal limit and let it grow, tax-deferred. Then invest for the long term, with your target amount in mind. And once again, the earlier you start and the longer you stick with it, the better.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Less than a year ago, I wrote a column on retirement strategies; but that was before COVID-19 took down the economy, putting millions out of work and shuttering many of our offices. Add extraordinary racial tensions and an election year like no other, and 2020 has generated fear and uncertainty on an unprecedented level.
Not surprisingly, my e-mail has been dominated for months by questions about the short- and long-term financial consequences of this annus horribilis on our practices and retirement plans. Most physicians have felt the downturn acutely, of course. Revenues have declined, non-COVID-19-related hospital visits plunged, and only recently have we seen hospitals resuming elective procedures. As I write this, my practice is approaching its prepandemic volume; but many patients have been avoiding hospitals and doctors’ offices for fear of COVID-19 exposure. With no real end in sight, who can say when this trend will finally correct itself?
Long term, the outlook is not nearly so grim. I have always written that downturns – even steep ones – are inevitable; and rather than fear them, you should expect them and plan for them. Younger physicians with riskier investments have plenty of time to rebound. Physicians nearing retirement, if they have done everything right, probably have the least to lose. Ideally, they will be at or near their savings target and will have transitioned to less vulnerable assets. And remember, you don’t need to have 100% of your retirement money to retire; a sound retirement plan will continue to generate investment returns as you move through retirement.
In short, .
By way of a brief review, the basics of a good plan are a budget, an emergency fund, disability insurance, and retiring your debt as quickly as possible. All of these have been covered individually in previous columns.
An essential component of your plan should be a list of long-term goals – and it should be more specific than simply accumulating a pile of cash. What do you plan to accomplish with the money? If it’s travel, helping your grandkids with college expenses, hobbies, or something else, make a list. Review it regularly, and modify it if your goals change.
Time to trot out another hoary old cliché: Saving for retirement is a marathon, not a sprint. If the pandemic has temporarily derailed your retirement strategy – forcing you, for example, to make retirement account withdrawals to cover expenses, or raid your emergency fund – no worries! When things have stabilized, it’s time to recommit to your retirement plan. Once again, with so many other issues to deal with, retaining the services of a qualified financial professional is usually a far better strategy than going it alone.
Many readers have expressed the fear that their retirement savings would never recover from the COVID-19 hit – but my own financial adviser pointed out that as I write this, in August, conservative portfolio values are about level with similar portfolios on Jan. 1, 2020. “Good plans are built to withstand difficult times,” she said. “Sometimes staying the course is the most difficult, disciplined course of action.”
“If your gut tells you that things will only get worse,” writes Kimberly Lankford in AARP’s magazine, “know that your gut is a terrible economic forecaster.” The University of Michigan’s Index of Consumer Sentiment hit rock bottom in 2008, during the Great Recession; yet only 4 months later, the U.S. economy began its longest expansion in modern history. The point is that it is important to maintain a long-term approach, and not make changes based on short-term events.
COVID-19 (or whatever else comes along) then becomes a matter of statement pain, not long-term financial pain. The key to recovery has nothing to do with a financial change, an investment strategy change, or a holding change, and everything to do with realigning your long-term goals.
So, moving on from COVID-19 is actually quite simple: Fill your retirement plan to its legal limit and let it grow, tax-deferred. Then invest for the long term, with your target amount in mind. And once again, the earlier you start and the longer you stick with it, the better.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Less than a year ago, I wrote a column on retirement strategies; but that was before COVID-19 took down the economy, putting millions out of work and shuttering many of our offices. Add extraordinary racial tensions and an election year like no other, and 2020 has generated fear and uncertainty on an unprecedented level.
Not surprisingly, my e-mail has been dominated for months by questions about the short- and long-term financial consequences of this annus horribilis on our practices and retirement plans. Most physicians have felt the downturn acutely, of course. Revenues have declined, non-COVID-19-related hospital visits plunged, and only recently have we seen hospitals resuming elective procedures. As I write this, my practice is approaching its prepandemic volume; but many patients have been avoiding hospitals and doctors’ offices for fear of COVID-19 exposure. With no real end in sight, who can say when this trend will finally correct itself?
Long term, the outlook is not nearly so grim. I have always written that downturns – even steep ones – are inevitable; and rather than fear them, you should expect them and plan for them. Younger physicians with riskier investments have plenty of time to rebound. Physicians nearing retirement, if they have done everything right, probably have the least to lose. Ideally, they will be at or near their savings target and will have transitioned to less vulnerable assets. And remember, you don’t need to have 100% of your retirement money to retire; a sound retirement plan will continue to generate investment returns as you move through retirement.
In short, .
By way of a brief review, the basics of a good plan are a budget, an emergency fund, disability insurance, and retiring your debt as quickly as possible. All of these have been covered individually in previous columns.
An essential component of your plan should be a list of long-term goals – and it should be more specific than simply accumulating a pile of cash. What do you plan to accomplish with the money? If it’s travel, helping your grandkids with college expenses, hobbies, or something else, make a list. Review it regularly, and modify it if your goals change.
Time to trot out another hoary old cliché: Saving for retirement is a marathon, not a sprint. If the pandemic has temporarily derailed your retirement strategy – forcing you, for example, to make retirement account withdrawals to cover expenses, or raid your emergency fund – no worries! When things have stabilized, it’s time to recommit to your retirement plan. Once again, with so many other issues to deal with, retaining the services of a qualified financial professional is usually a far better strategy than going it alone.
Many readers have expressed the fear that their retirement savings would never recover from the COVID-19 hit – but my own financial adviser pointed out that as I write this, in August, conservative portfolio values are about level with similar portfolios on Jan. 1, 2020. “Good plans are built to withstand difficult times,” she said. “Sometimes staying the course is the most difficult, disciplined course of action.”
“If your gut tells you that things will only get worse,” writes Kimberly Lankford in AARP’s magazine, “know that your gut is a terrible economic forecaster.” The University of Michigan’s Index of Consumer Sentiment hit rock bottom in 2008, during the Great Recession; yet only 4 months later, the U.S. economy began its longest expansion in modern history. The point is that it is important to maintain a long-term approach, and not make changes based on short-term events.
COVID-19 (or whatever else comes along) then becomes a matter of statement pain, not long-term financial pain. The key to recovery has nothing to do with a financial change, an investment strategy change, or a holding change, and everything to do with realigning your long-term goals.
So, moving on from COVID-19 is actually quite simple: Fill your retirement plan to its legal limit and let it grow, tax-deferred. Then invest for the long term, with your target amount in mind. And once again, the earlier you start and the longer you stick with it, the better.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].