User login
Opioid prescribing laws having an impact
State laws capping initial opioid prescriptions to 7 days or less have led to a reduction in opioid prescribing, a new analysis of Medicare data shows.
While overall opioid prescribing has decreased, the reduction in states with legislation restricting opioid prescribing was “significantly greater than in states without such legislation,” study investigator Michael Brenner, MD, University of Michigan, Ann Arbor, said in an interview.
The study was published online August 9 in JAMA Internal Medicine.
Significant but limited effect
Because of rising concern around the opioid crisis, 23 states representing 43% of the U.S. population passed laws from 2016 through 2018 limiting initial opioid prescription to 7 days or less.
Using Medicare data from 2013 through 2018, Dr. Brenner and colleagues conducted a before-and-after study to assess the effect of these laws.
They found that on average, the number of days an opioid was prescribed for each Medicare beneficiary decreased by 11.6 days (from 44.2 days in 2013 to 32.7 days in 2018) in states that imposed duration limits, compared with 10.1 days in states without these laws (from 43.4 days in 2013 to 33.3 days in 2018).
Prior to the start of duration limits in 2016, days an opioid was prescribed were comparable among states.
After adjusting for state-level differences in race, urbanization, median income, tobacco and alcohol use, serious mental illness, and other factors, state laws limiting opioid prescriptions to 7 days or less were associated with a reduction in prescribing of 1.7 days per enrollee, “suggesting a significant but limited outcome” for these laws, the researchers note.
, but this was not significantly different in states with limit laws versus those without. However, state laws limiting duration led to a significant reduction in days of opioid prescribed among surgeons, dentists, pain specialists, and other specialists.
Inadequate pain control?
The researchers note the study was limited to Medicare beneficiaries; however, excess opioid prescribing is prevalent across all patient populations.
In addition, it’s not possible to tell from the data whether acute pain was adequately controlled with fewer pills.
“The question of adequacy of pain control is a crucial one that has been investigated extensively in prior work but was not possible to evaluate in this particular study,” said Dr. Brenner.
However, “ample evidence supports a role for reducing opioid prescribing and that such reduction can be achieved while ensuring that pain is adequately controlled with fewer pills,” he noted.
“A persistent misconception is that opioids are uniquely powerful and effective for controlling pain. Patients may perceive that effective analgesia is being withheld when opioids are not included in a regimen,” Dr. Brenner added.
“Yet, the evidence from meta-analyses derived from large numbers of randomized clinical trials finds that [nonsteroidal anti-inflammatory drugs] NSAIDS combined with acetaminophen provide similar or improved acute pain when compared to commonly prescribed opioid regimens, based on number-needed-to-treat analyses,” he added.
In a related editorial, Deborah Grady, MD, MPH, with University of California, San Francisco, and Mitchell H. Katz, MD, president and CEO of NYC Health + Hospitals, say the decrease in opioid prescribing with duration limits was “small but probably meaningful.”
Restricting initial prescriptions to seven or fewer days is “reasonable because patients with new onset of pain should be re-evaluated in a week if the pain continues,” they write.
However, Dr. Grady and Dr. Katz “worry” that restricting initial prescriptions to shorter periods, such as 3 or 5 days, as has occurred in six states, “may result in patients with acute pain going untreated or having to go to extraordinary effort to obtain adequate pain relief.”
In their view, the data from this study suggest that limiting initial prescriptions to seven or fewer days is “helpful, but we would not restrict any further given that we do not know how it affected patients with acute pain.”
The study had no specific funding. Dr. Brenner, Dr. Grady, and Dr. Katz have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
State laws capping initial opioid prescriptions to 7 days or less have led to a reduction in opioid prescribing, a new analysis of Medicare data shows.
While overall opioid prescribing has decreased, the reduction in states with legislation restricting opioid prescribing was “significantly greater than in states without such legislation,” study investigator Michael Brenner, MD, University of Michigan, Ann Arbor, said in an interview.
The study was published online August 9 in JAMA Internal Medicine.
Significant but limited effect
Because of rising concern around the opioid crisis, 23 states representing 43% of the U.S. population passed laws from 2016 through 2018 limiting initial opioid prescription to 7 days or less.
Using Medicare data from 2013 through 2018, Dr. Brenner and colleagues conducted a before-and-after study to assess the effect of these laws.
They found that on average, the number of days an opioid was prescribed for each Medicare beneficiary decreased by 11.6 days (from 44.2 days in 2013 to 32.7 days in 2018) in states that imposed duration limits, compared with 10.1 days in states without these laws (from 43.4 days in 2013 to 33.3 days in 2018).
Prior to the start of duration limits in 2016, days an opioid was prescribed were comparable among states.
After adjusting for state-level differences in race, urbanization, median income, tobacco and alcohol use, serious mental illness, and other factors, state laws limiting opioid prescriptions to 7 days or less were associated with a reduction in prescribing of 1.7 days per enrollee, “suggesting a significant but limited outcome” for these laws, the researchers note.
, but this was not significantly different in states with limit laws versus those without. However, state laws limiting duration led to a significant reduction in days of opioid prescribed among surgeons, dentists, pain specialists, and other specialists.
Inadequate pain control?
The researchers note the study was limited to Medicare beneficiaries; however, excess opioid prescribing is prevalent across all patient populations.
In addition, it’s not possible to tell from the data whether acute pain was adequately controlled with fewer pills.
“The question of adequacy of pain control is a crucial one that has been investigated extensively in prior work but was not possible to evaluate in this particular study,” said Dr. Brenner.
However, “ample evidence supports a role for reducing opioid prescribing and that such reduction can be achieved while ensuring that pain is adequately controlled with fewer pills,” he noted.
“A persistent misconception is that opioids are uniquely powerful and effective for controlling pain. Patients may perceive that effective analgesia is being withheld when opioids are not included in a regimen,” Dr. Brenner added.
“Yet, the evidence from meta-analyses derived from large numbers of randomized clinical trials finds that [nonsteroidal anti-inflammatory drugs] NSAIDS combined with acetaminophen provide similar or improved acute pain when compared to commonly prescribed opioid regimens, based on number-needed-to-treat analyses,” he added.
In a related editorial, Deborah Grady, MD, MPH, with University of California, San Francisco, and Mitchell H. Katz, MD, president and CEO of NYC Health + Hospitals, say the decrease in opioid prescribing with duration limits was “small but probably meaningful.”
Restricting initial prescriptions to seven or fewer days is “reasonable because patients with new onset of pain should be re-evaluated in a week if the pain continues,” they write.
However, Dr. Grady and Dr. Katz “worry” that restricting initial prescriptions to shorter periods, such as 3 or 5 days, as has occurred in six states, “may result in patients with acute pain going untreated or having to go to extraordinary effort to obtain adequate pain relief.”
In their view, the data from this study suggest that limiting initial prescriptions to seven or fewer days is “helpful, but we would not restrict any further given that we do not know how it affected patients with acute pain.”
The study had no specific funding. Dr. Brenner, Dr. Grady, and Dr. Katz have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
State laws capping initial opioid prescriptions to 7 days or less have led to a reduction in opioid prescribing, a new analysis of Medicare data shows.
While overall opioid prescribing has decreased, the reduction in states with legislation restricting opioid prescribing was “significantly greater than in states without such legislation,” study investigator Michael Brenner, MD, University of Michigan, Ann Arbor, said in an interview.
The study was published online August 9 in JAMA Internal Medicine.
Significant but limited effect
Because of rising concern around the opioid crisis, 23 states representing 43% of the U.S. population passed laws from 2016 through 2018 limiting initial opioid prescription to 7 days or less.
Using Medicare data from 2013 through 2018, Dr. Brenner and colleagues conducted a before-and-after study to assess the effect of these laws.
They found that on average, the number of days an opioid was prescribed for each Medicare beneficiary decreased by 11.6 days (from 44.2 days in 2013 to 32.7 days in 2018) in states that imposed duration limits, compared with 10.1 days in states without these laws (from 43.4 days in 2013 to 33.3 days in 2018).
Prior to the start of duration limits in 2016, days an opioid was prescribed were comparable among states.
After adjusting for state-level differences in race, urbanization, median income, tobacco and alcohol use, serious mental illness, and other factors, state laws limiting opioid prescriptions to 7 days or less were associated with a reduction in prescribing of 1.7 days per enrollee, “suggesting a significant but limited outcome” for these laws, the researchers note.
, but this was not significantly different in states with limit laws versus those without. However, state laws limiting duration led to a significant reduction in days of opioid prescribed among surgeons, dentists, pain specialists, and other specialists.
Inadequate pain control?
The researchers note the study was limited to Medicare beneficiaries; however, excess opioid prescribing is prevalent across all patient populations.
In addition, it’s not possible to tell from the data whether acute pain was adequately controlled with fewer pills.
“The question of adequacy of pain control is a crucial one that has been investigated extensively in prior work but was not possible to evaluate in this particular study,” said Dr. Brenner.
However, “ample evidence supports a role for reducing opioid prescribing and that such reduction can be achieved while ensuring that pain is adequately controlled with fewer pills,” he noted.
“A persistent misconception is that opioids are uniquely powerful and effective for controlling pain. Patients may perceive that effective analgesia is being withheld when opioids are not included in a regimen,” Dr. Brenner added.
“Yet, the evidence from meta-analyses derived from large numbers of randomized clinical trials finds that [nonsteroidal anti-inflammatory drugs] NSAIDS combined with acetaminophen provide similar or improved acute pain when compared to commonly prescribed opioid regimens, based on number-needed-to-treat analyses,” he added.
In a related editorial, Deborah Grady, MD, MPH, with University of California, San Francisco, and Mitchell H. Katz, MD, president and CEO of NYC Health + Hospitals, say the decrease in opioid prescribing with duration limits was “small but probably meaningful.”
Restricting initial prescriptions to seven or fewer days is “reasonable because patients with new onset of pain should be re-evaluated in a week if the pain continues,” they write.
However, Dr. Grady and Dr. Katz “worry” that restricting initial prescriptions to shorter periods, such as 3 or 5 days, as has occurred in six states, “may result in patients with acute pain going untreated or having to go to extraordinary effort to obtain adequate pain relief.”
In their view, the data from this study suggest that limiting initial prescriptions to seven or fewer days is “helpful, but we would not restrict any further given that we do not know how it affected patients with acute pain.”
The study had no specific funding. Dr. Brenner, Dr. Grady, and Dr. Katz have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID-19 mitigation measures led to shifts in typical annual respiratory virus patterns
Nonpharmaceutical interventions, such as masking, staying home, limiting travel, and social distancing, have been doing more than reducing the risk for COVID-19. They’re also having an impact on infection rates and the timing of seasonal surges of other common respiratory diseases, according to an article published July 23 in Morbidity and Mortality Weekly Report.
Typically, respiratory pathogens such as respiratory syncytial virus (RSV), common cold coronaviruses, parainfluenza viruses, and respiratory adenoviruses increase in the fall and remain high throughout winter, following the same basic patterns as influenza. Although the historically low rates of influenza remained low into spring 2021, that’s not the case for several other common respiratory viruses.
“Clinicians should be aware of increases in some respiratory virus activity and remain vigilant for off-season increases,” wrote Sonja J. Olsen, PhD, and her colleagues at the Centers for Disease Control and Prevention. She told this news organization that clinicians should use multipathogen testing to help guide treatment.
The authors also underscore the importance of fall influenza vaccination campaigns for anyone aged 6 months or older.
Timothy Brewer, MD, MPH, a professor of medicine in the Division of Infectious Diseases at the University of California, Los Angeles (UCLA), and of epidemiology at the UCLA Fielding School of Public Health, agreed that it’s important for health care professionals to consider off-season illnesses in their patients.
“Practitioners should be aware that if they see a sick child in the summer, outside of what normally might be influenza season, but they look like they have influenza, consider potentially influenza and test for it, because it might be possible that we may have disrupted that natural pattern,” Dr. Brewer told this news organization. Dr. Brewer, who was not involved in the CDC research, said it’s also “critically important” to encourage influenza vaccination as the season approaches.
The CDC researchers used the U.S. World Health Organization Collaborating Laboratories System and the CDC’s National Respiratory and Enteric Virus Surveillance System to analyze virologic data from Oct. 3, 2020, to May 22, 2021, for influenza and Jan. 4, 2020, to May 22, 2021, for other respiratory viruses. The authors compared virus circulation during these periods to circulation during the same dates from four previous years.
Data to calculate influenza and RSV hospitalization rates came from the Influenza Hospitalization Surveillance Network and RSV Hospitalization Surveillance Network.
The authors report that flu activity dropped dramatically in March 2020 to its lowest levels since 1997, the earliest season for which data are available. Only 0.2% of more than 1 million specimens tested positive for influenza; the rate of hospitalizations for lab-confirmed flu was 0.8 per 100,000 people. Flu levels remained low through the summer, fall, and on to May 2021.
A potential drawback to this low activity, however, is a more prevalent and severe upcoming flu season, the authors write. The repeated exposure to flu viruses every year often “does not lead to illness, but it does serve to boost our immune response to influenza viruses,” Dr. Olsen said in an interview. “The absence of influenza viruses in the community over the last year means that we are not getting these regular boosts to our immune system. When we finally get exposed, our body may mount a weak response, and this could mean we develop a more clinically severe illness.”
Children are most susceptible to that phenomenon because they haven’t had a lifetime of exposure to flu viruses, Dr. Olsen said.
“An immunologically naive child may be more likely to develop a severe illness than someone who has lived through several influenza seasons,” she said. “This is why it is especially important for everyone 6 months and older to get vaccinated against influenza this season.”
Rhinovirus and enterovirus infections rebounded fairly quickly after their decline in March 2020 and started increasing in May 2020 until they reached “near prepandemic seasonal levels,” the authors write.
RSV infections dropped from 15.3% of weekly positive results in January 2020 to 1.4% by April and then stayed below 1% through the end of 2020. In past years, weekly positive results climbed to 3% in October and peaked at 12.5% to 16.7% in late December. Instead, RSV weekly positive results began increasing in April 2021, rising from 1.1% to 2.8% in May.
The “unusually timed” late spring increase in RSV “is probably associated with various nonpharmaceutical measures that have been in place but are now relaxing,” Dr. Olsen stated.
The RSV hospitalization rate was 0.3 per 100,000 people from October 2020 to April 2021, compared to 27.1 and 33.4 per 100,000 people in the previous 2 years. Of all RSV hospitalizations in the past year, 76.5% occurred in April-May 2021.
Rates of illness caused by the four common human coronaviruses (OC43, NL63, 229E, and HKU1) dropped from 7.5% of weekly positive results in January 2020 to 1.3% in April 2020 and stayed below 1% through February 2021. Then they climbed to 6.6% by May 2021. Infection rates of parainfluenza viruses types 1-4 similarly dropped from 2.6% in January 2020 to 1% in March 2020 and stayed below 1% until April 2021. Since then, rates of the common coronaviruses increased to 6.6% and parainfluenza viruses to 10.9% in May 2021.
Normally, parainfluenza viruses peak in October-November and May-June, so “the current increase could represent a return to prepandemic seasonality,” the authors write.
Human pneumoviruses’ weekly positive results initially increased from 4.2% in January 2020 to 7% in March and then fell to 1.9% the second week of April and remained below 1% through May 2021. In typical years, these viruses peak from 6.2% to 7.7% in March-April. Respiratory adenovirus activity similarly dropped to historically low levels in April 2021 and then began increasing to reach 3% by May 2021, the usual level for that month.
“The different circulation patterns observed across respiratory viruses probably also reflect differences in the virus transmission routes and how effective various nonpharmaceutical measures are at stopping transmission,” Dr. Olsen said in an interview. “As pandemic mitigation measures continue to be adjusted, we expect to see more changes in the circulation of these viruses, including a return to prepandemic circulation, as seen for rhinoviruses and enteroviruses.”
Rhinovirus and enterovirus rates dropped from 14.9% in March 2020 to 3.2% in May – lower than typical – and then climbed to a peak in October 2020. The peak (21.7% weekly positive results) was, however, still lower than the usual median of 32.8%. After dropping to 9.9% in January 2021, it then rose 19.1% in May, potentially reflecting “the usual spring peak that has occurred in previous years,” the authors write.
The authors note that it’s not yet clear how the COVID-19 pandemic and related mitigation measures will continue to affect respiratory virus circulation.
The authors hypothesize that the reasons for a seeming return to seasonal activity of respiratory adenoviruses, rhinoviruses, and enteroviruses could involve “different transmission mechanisms, the role of asymptomatic transmission, and prolonged survival of these nonenveloped viruses on surfaces, all of which might make these viruses less susceptible to nonpharmaceutical interventions.”
Dr. Brewer, of UCLA, agreed.
All the viruses basically “flatline except for adenoviruses and enteroviruses, and they behave a little differently in terms of how they spread,” he said. “Enteroviruses are much more likely to be fecal-oral spread than the other viruses [in the study].”
The delayed circulation of parainfluenza and human coronaviruses may have resulted from suspension of in-person classes through late winter 2020, they write, but that doesn’t explain the relative absence of pneumovirus activity, which usually affects the same young pediatric populations as RSV.
Dr. Brewer said California is seeing a surge of RSV right now, as are many states, especially throughout in the South. He’s not surprised by RSV’s deferred season, because those most affected – children younger than 2 years – are less likely to wear masks now and were “not going to daycare, not being out in public” in 2020. “As people are doing more activities, that’s probably why RSV has been starting to go up since April,” he said.
Despite the fact that, unlike many East Asian cultures, the United States has not traditionally been a mask-wearing culture, Dr. Brewer wouldn’t be surprised if more Americans begin wearing masks during flu season. “Hopefully another thing that will come out of this is better hand hygiene, with people just getting used to washing their hands more, particularly after they come home from being out,” he added.
Dr. Brewer similarly emphasized the importance of flu vaccination for the upcoming season, especially for younger children who may have poorer natural immunity to influenza, owing to its low circulation rates in 2020-2021.
The study was funded by the CDC. Dr. Brewer and Dr. Olsen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Nonpharmaceutical interventions, such as masking, staying home, limiting travel, and social distancing, have been doing more than reducing the risk for COVID-19. They’re also having an impact on infection rates and the timing of seasonal surges of other common respiratory diseases, according to an article published July 23 in Morbidity and Mortality Weekly Report.
Typically, respiratory pathogens such as respiratory syncytial virus (RSV), common cold coronaviruses, parainfluenza viruses, and respiratory adenoviruses increase in the fall and remain high throughout winter, following the same basic patterns as influenza. Although the historically low rates of influenza remained low into spring 2021, that’s not the case for several other common respiratory viruses.
“Clinicians should be aware of increases in some respiratory virus activity and remain vigilant for off-season increases,” wrote Sonja J. Olsen, PhD, and her colleagues at the Centers for Disease Control and Prevention. She told this news organization that clinicians should use multipathogen testing to help guide treatment.
The authors also underscore the importance of fall influenza vaccination campaigns for anyone aged 6 months or older.
Timothy Brewer, MD, MPH, a professor of medicine in the Division of Infectious Diseases at the University of California, Los Angeles (UCLA), and of epidemiology at the UCLA Fielding School of Public Health, agreed that it’s important for health care professionals to consider off-season illnesses in their patients.
“Practitioners should be aware that if they see a sick child in the summer, outside of what normally might be influenza season, but they look like they have influenza, consider potentially influenza and test for it, because it might be possible that we may have disrupted that natural pattern,” Dr. Brewer told this news organization. Dr. Brewer, who was not involved in the CDC research, said it’s also “critically important” to encourage influenza vaccination as the season approaches.
The CDC researchers used the U.S. World Health Organization Collaborating Laboratories System and the CDC’s National Respiratory and Enteric Virus Surveillance System to analyze virologic data from Oct. 3, 2020, to May 22, 2021, for influenza and Jan. 4, 2020, to May 22, 2021, for other respiratory viruses. The authors compared virus circulation during these periods to circulation during the same dates from four previous years.
Data to calculate influenza and RSV hospitalization rates came from the Influenza Hospitalization Surveillance Network and RSV Hospitalization Surveillance Network.
The authors report that flu activity dropped dramatically in March 2020 to its lowest levels since 1997, the earliest season for which data are available. Only 0.2% of more than 1 million specimens tested positive for influenza; the rate of hospitalizations for lab-confirmed flu was 0.8 per 100,000 people. Flu levels remained low through the summer, fall, and on to May 2021.
A potential drawback to this low activity, however, is a more prevalent and severe upcoming flu season, the authors write. The repeated exposure to flu viruses every year often “does not lead to illness, but it does serve to boost our immune response to influenza viruses,” Dr. Olsen said in an interview. “The absence of influenza viruses in the community over the last year means that we are not getting these regular boosts to our immune system. When we finally get exposed, our body may mount a weak response, and this could mean we develop a more clinically severe illness.”
Children are most susceptible to that phenomenon because they haven’t had a lifetime of exposure to flu viruses, Dr. Olsen said.
“An immunologically naive child may be more likely to develop a severe illness than someone who has lived through several influenza seasons,” she said. “This is why it is especially important for everyone 6 months and older to get vaccinated against influenza this season.”
Rhinovirus and enterovirus infections rebounded fairly quickly after their decline in March 2020 and started increasing in May 2020 until they reached “near prepandemic seasonal levels,” the authors write.
RSV infections dropped from 15.3% of weekly positive results in January 2020 to 1.4% by April and then stayed below 1% through the end of 2020. In past years, weekly positive results climbed to 3% in October and peaked at 12.5% to 16.7% in late December. Instead, RSV weekly positive results began increasing in April 2021, rising from 1.1% to 2.8% in May.
The “unusually timed” late spring increase in RSV “is probably associated with various nonpharmaceutical measures that have been in place but are now relaxing,” Dr. Olsen stated.
The RSV hospitalization rate was 0.3 per 100,000 people from October 2020 to April 2021, compared to 27.1 and 33.4 per 100,000 people in the previous 2 years. Of all RSV hospitalizations in the past year, 76.5% occurred in April-May 2021.
Rates of illness caused by the four common human coronaviruses (OC43, NL63, 229E, and HKU1) dropped from 7.5% of weekly positive results in January 2020 to 1.3% in April 2020 and stayed below 1% through February 2021. Then they climbed to 6.6% by May 2021. Infection rates of parainfluenza viruses types 1-4 similarly dropped from 2.6% in January 2020 to 1% in March 2020 and stayed below 1% until April 2021. Since then, rates of the common coronaviruses increased to 6.6% and parainfluenza viruses to 10.9% in May 2021.
Normally, parainfluenza viruses peak in October-November and May-June, so “the current increase could represent a return to prepandemic seasonality,” the authors write.
Human pneumoviruses’ weekly positive results initially increased from 4.2% in January 2020 to 7% in March and then fell to 1.9% the second week of April and remained below 1% through May 2021. In typical years, these viruses peak from 6.2% to 7.7% in March-April. Respiratory adenovirus activity similarly dropped to historically low levels in April 2021 and then began increasing to reach 3% by May 2021, the usual level for that month.
“The different circulation patterns observed across respiratory viruses probably also reflect differences in the virus transmission routes and how effective various nonpharmaceutical measures are at stopping transmission,” Dr. Olsen said in an interview. “As pandemic mitigation measures continue to be adjusted, we expect to see more changes in the circulation of these viruses, including a return to prepandemic circulation, as seen for rhinoviruses and enteroviruses.”
Rhinovirus and enterovirus rates dropped from 14.9% in March 2020 to 3.2% in May – lower than typical – and then climbed to a peak in October 2020. The peak (21.7% weekly positive results) was, however, still lower than the usual median of 32.8%. After dropping to 9.9% in January 2021, it then rose 19.1% in May, potentially reflecting “the usual spring peak that has occurred in previous years,” the authors write.
The authors note that it’s not yet clear how the COVID-19 pandemic and related mitigation measures will continue to affect respiratory virus circulation.
The authors hypothesize that the reasons for a seeming return to seasonal activity of respiratory adenoviruses, rhinoviruses, and enteroviruses could involve “different transmission mechanisms, the role of asymptomatic transmission, and prolonged survival of these nonenveloped viruses on surfaces, all of which might make these viruses less susceptible to nonpharmaceutical interventions.”
Dr. Brewer, of UCLA, agreed.
All the viruses basically “flatline except for adenoviruses and enteroviruses, and they behave a little differently in terms of how they spread,” he said. “Enteroviruses are much more likely to be fecal-oral spread than the other viruses [in the study].”
The delayed circulation of parainfluenza and human coronaviruses may have resulted from suspension of in-person classes through late winter 2020, they write, but that doesn’t explain the relative absence of pneumovirus activity, which usually affects the same young pediatric populations as RSV.
Dr. Brewer said California is seeing a surge of RSV right now, as are many states, especially throughout in the South. He’s not surprised by RSV’s deferred season, because those most affected – children younger than 2 years – are less likely to wear masks now and were “not going to daycare, not being out in public” in 2020. “As people are doing more activities, that’s probably why RSV has been starting to go up since April,” he said.
Despite the fact that, unlike many East Asian cultures, the United States has not traditionally been a mask-wearing culture, Dr. Brewer wouldn’t be surprised if more Americans begin wearing masks during flu season. “Hopefully another thing that will come out of this is better hand hygiene, with people just getting used to washing their hands more, particularly after they come home from being out,” he added.
Dr. Brewer similarly emphasized the importance of flu vaccination for the upcoming season, especially for younger children who may have poorer natural immunity to influenza, owing to its low circulation rates in 2020-2021.
The study was funded by the CDC. Dr. Brewer and Dr. Olsen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Nonpharmaceutical interventions, such as masking, staying home, limiting travel, and social distancing, have been doing more than reducing the risk for COVID-19. They’re also having an impact on infection rates and the timing of seasonal surges of other common respiratory diseases, according to an article published July 23 in Morbidity and Mortality Weekly Report.
Typically, respiratory pathogens such as respiratory syncytial virus (RSV), common cold coronaviruses, parainfluenza viruses, and respiratory adenoviruses increase in the fall and remain high throughout winter, following the same basic patterns as influenza. Although the historically low rates of influenza remained low into spring 2021, that’s not the case for several other common respiratory viruses.
“Clinicians should be aware of increases in some respiratory virus activity and remain vigilant for off-season increases,” wrote Sonja J. Olsen, PhD, and her colleagues at the Centers for Disease Control and Prevention. She told this news organization that clinicians should use multipathogen testing to help guide treatment.
The authors also underscore the importance of fall influenza vaccination campaigns for anyone aged 6 months or older.
Timothy Brewer, MD, MPH, a professor of medicine in the Division of Infectious Diseases at the University of California, Los Angeles (UCLA), and of epidemiology at the UCLA Fielding School of Public Health, agreed that it’s important for health care professionals to consider off-season illnesses in their patients.
“Practitioners should be aware that if they see a sick child in the summer, outside of what normally might be influenza season, but they look like they have influenza, consider potentially influenza and test for it, because it might be possible that we may have disrupted that natural pattern,” Dr. Brewer told this news organization. Dr. Brewer, who was not involved in the CDC research, said it’s also “critically important” to encourage influenza vaccination as the season approaches.
The CDC researchers used the U.S. World Health Organization Collaborating Laboratories System and the CDC’s National Respiratory and Enteric Virus Surveillance System to analyze virologic data from Oct. 3, 2020, to May 22, 2021, for influenza and Jan. 4, 2020, to May 22, 2021, for other respiratory viruses. The authors compared virus circulation during these periods to circulation during the same dates from four previous years.
Data to calculate influenza and RSV hospitalization rates came from the Influenza Hospitalization Surveillance Network and RSV Hospitalization Surveillance Network.
The authors report that flu activity dropped dramatically in March 2020 to its lowest levels since 1997, the earliest season for which data are available. Only 0.2% of more than 1 million specimens tested positive for influenza; the rate of hospitalizations for lab-confirmed flu was 0.8 per 100,000 people. Flu levels remained low through the summer, fall, and on to May 2021.
A potential drawback to this low activity, however, is a more prevalent and severe upcoming flu season, the authors write. The repeated exposure to flu viruses every year often “does not lead to illness, but it does serve to boost our immune response to influenza viruses,” Dr. Olsen said in an interview. “The absence of influenza viruses in the community over the last year means that we are not getting these regular boosts to our immune system. When we finally get exposed, our body may mount a weak response, and this could mean we develop a more clinically severe illness.”
Children are most susceptible to that phenomenon because they haven’t had a lifetime of exposure to flu viruses, Dr. Olsen said.
“An immunologically naive child may be more likely to develop a severe illness than someone who has lived through several influenza seasons,” she said. “This is why it is especially important for everyone 6 months and older to get vaccinated against influenza this season.”
Rhinovirus and enterovirus infections rebounded fairly quickly after their decline in March 2020 and started increasing in May 2020 until they reached “near prepandemic seasonal levels,” the authors write.
RSV infections dropped from 15.3% of weekly positive results in January 2020 to 1.4% by April and then stayed below 1% through the end of 2020. In past years, weekly positive results climbed to 3% in October and peaked at 12.5% to 16.7% in late December. Instead, RSV weekly positive results began increasing in April 2021, rising from 1.1% to 2.8% in May.
The “unusually timed” late spring increase in RSV “is probably associated with various nonpharmaceutical measures that have been in place but are now relaxing,” Dr. Olsen stated.
The RSV hospitalization rate was 0.3 per 100,000 people from October 2020 to April 2021, compared to 27.1 and 33.4 per 100,000 people in the previous 2 years. Of all RSV hospitalizations in the past year, 76.5% occurred in April-May 2021.
Rates of illness caused by the four common human coronaviruses (OC43, NL63, 229E, and HKU1) dropped from 7.5% of weekly positive results in January 2020 to 1.3% in April 2020 and stayed below 1% through February 2021. Then they climbed to 6.6% by May 2021. Infection rates of parainfluenza viruses types 1-4 similarly dropped from 2.6% in January 2020 to 1% in March 2020 and stayed below 1% until April 2021. Since then, rates of the common coronaviruses increased to 6.6% and parainfluenza viruses to 10.9% in May 2021.
Normally, parainfluenza viruses peak in October-November and May-June, so “the current increase could represent a return to prepandemic seasonality,” the authors write.
Human pneumoviruses’ weekly positive results initially increased from 4.2% in January 2020 to 7% in March and then fell to 1.9% the second week of April and remained below 1% through May 2021. In typical years, these viruses peak from 6.2% to 7.7% in March-April. Respiratory adenovirus activity similarly dropped to historically low levels in April 2021 and then began increasing to reach 3% by May 2021, the usual level for that month.
“The different circulation patterns observed across respiratory viruses probably also reflect differences in the virus transmission routes and how effective various nonpharmaceutical measures are at stopping transmission,” Dr. Olsen said in an interview. “As pandemic mitigation measures continue to be adjusted, we expect to see more changes in the circulation of these viruses, including a return to prepandemic circulation, as seen for rhinoviruses and enteroviruses.”
Rhinovirus and enterovirus rates dropped from 14.9% in March 2020 to 3.2% in May – lower than typical – and then climbed to a peak in October 2020. The peak (21.7% weekly positive results) was, however, still lower than the usual median of 32.8%. After dropping to 9.9% in January 2021, it then rose 19.1% in May, potentially reflecting “the usual spring peak that has occurred in previous years,” the authors write.
The authors note that it’s not yet clear how the COVID-19 pandemic and related mitigation measures will continue to affect respiratory virus circulation.
The authors hypothesize that the reasons for a seeming return to seasonal activity of respiratory adenoviruses, rhinoviruses, and enteroviruses could involve “different transmission mechanisms, the role of asymptomatic transmission, and prolonged survival of these nonenveloped viruses on surfaces, all of which might make these viruses less susceptible to nonpharmaceutical interventions.”
Dr. Brewer, of UCLA, agreed.
All the viruses basically “flatline except for adenoviruses and enteroviruses, and they behave a little differently in terms of how they spread,” he said. “Enteroviruses are much more likely to be fecal-oral spread than the other viruses [in the study].”
The delayed circulation of parainfluenza and human coronaviruses may have resulted from suspension of in-person classes through late winter 2020, they write, but that doesn’t explain the relative absence of pneumovirus activity, which usually affects the same young pediatric populations as RSV.
Dr. Brewer said California is seeing a surge of RSV right now, as are many states, especially throughout in the South. He’s not surprised by RSV’s deferred season, because those most affected – children younger than 2 years – are less likely to wear masks now and were “not going to daycare, not being out in public” in 2020. “As people are doing more activities, that’s probably why RSV has been starting to go up since April,” he said.
Despite the fact that, unlike many East Asian cultures, the United States has not traditionally been a mask-wearing culture, Dr. Brewer wouldn’t be surprised if more Americans begin wearing masks during flu season. “Hopefully another thing that will come out of this is better hand hygiene, with people just getting used to washing their hands more, particularly after they come home from being out,” he added.
Dr. Brewer similarly emphasized the importance of flu vaccination for the upcoming season, especially for younger children who may have poorer natural immunity to influenza, owing to its low circulation rates in 2020-2021.
The study was funded by the CDC. Dr. Brewer and Dr. Olsen have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Myocarditis in adolescents after COVID-19 vaccine typically mild
Adolescents can develop mild myocarditis as a rare complication after COVID-19 vaccination, as has been reported in adults, an early case series from Boston confirms.
The adolescents who developed heart inflammation after vaccination typically had a benign course, with symptoms resolving without treatment, although one patient had persistent borderline low left ventricular (LV) function, report Audrey Dionne, MD, and colleagues at Boston Children’s Hospital.
“Despite the risks of myocarditis associated with vaccination, the benefits of vaccination likely outweigh risks in children and adolescents,” they say.
They estimate that for males 12-29 years of age COVID-19 vaccination prevents 11,000 COVID-19 cases, 560 hospitalizations, 138 intensive care unit admissions, and six deaths, compared with 39-47 expected myocarditis cases.
The case series was published online Aug. 10 in JAMA Cardiology.
Long-term risks unknown
Dr. Dionne and colleagues reviewed the results of comprehensive cardiac imaging in 14 boys and 1 girl, 12-18 years of age (median, 15 years), who were hospitalized with myocarditis after receiving the Pfizer-BioNTech messenger RNA COVID-19 vaccine.
Symptoms started 1-6 days after vaccine administration (most after the second dose) and included chest pain in all 15 patients, fever in 10 (67%), myalgia in eight (53%), and headache in six (40%).
On admission, all patients had elevated troponin levels (median, 0.25 ng/mL; range, 0.08-3.15 ng/mL). Troponin levels peaked 0.1-2.3 days after admission.
Echocardiography revealed decreased LV ejection fraction (EF) in three patients (20%) and abnormal global longitudinal or circumferential strain in five patients (33%). No patient had a pericardial effusion.
Cardiac MRI findings were consistent with myocarditis in 13 patients (87%), including late gadolinium enhancement in 12 (80%), regional hyperintensity on T2-weighted imaging in two (13%), elevated extracellular volume fraction in three (20%), and elevated LV global native T1 in two (20%).
The patients remained in the hospital for 1-5 days (median, 2 days) and were discharged. No patient required admission to the intensive care unit.
In follow-up assessments performed 1-13 days after hospital discharge, symptoms of myocarditis had resolved in 11 patients (73%).
One patient (7%) had persistent borderline low LV systolic function on echocardiogram (LVEF, 54%).
Troponin levels remained mildly elevated in three patients (20%). One patient (7%) had nonsustained ventricular tachycardia on ambulatory monitor.
The authors say longitudinal studies of patients with myocarditis after COVID-19 vaccine “will be important to better understand long-term risks.”
In a statement from the UK nonprofit Science Media Centre, Peter Openshaw, FMedSci, Imperial College London, says: “The problem with case series of this type is the lack of comparison groups. How many cases of myocarditis might be seen in normal children, or those given other vaccines (including those that are not for COVID), or in teenagers infected with SARS-CoV-2?”
“As the authors note, myocarditis does happen after other vaccines. The estimated rate (62.8 cases per million) makes this a rare event,” Dr. Openshaw says.
“My view that teenagers should be considered for vaccination is not changed by this new publication,” he adds.
This study was funded by the McCance Foundation. The authors have declared no relevant conflicts of interest. Dr. Openshaw has served on scientific advisory boards for Janssen/J&J, Oxford Immunotech, GSK, Nestle, and Pfizer in relation to immunity to viruses (fees paid to Imperial College London).
A version of this article first appeared on Medscape.com.
Adolescents can develop mild myocarditis as a rare complication after COVID-19 vaccination, as has been reported in adults, an early case series from Boston confirms.
The adolescents who developed heart inflammation after vaccination typically had a benign course, with symptoms resolving without treatment, although one patient had persistent borderline low left ventricular (LV) function, report Audrey Dionne, MD, and colleagues at Boston Children’s Hospital.
“Despite the risks of myocarditis associated with vaccination, the benefits of vaccination likely outweigh risks in children and adolescents,” they say.
They estimate that for males 12-29 years of age COVID-19 vaccination prevents 11,000 COVID-19 cases, 560 hospitalizations, 138 intensive care unit admissions, and six deaths, compared with 39-47 expected myocarditis cases.
The case series was published online Aug. 10 in JAMA Cardiology.
Long-term risks unknown
Dr. Dionne and colleagues reviewed the results of comprehensive cardiac imaging in 14 boys and 1 girl, 12-18 years of age (median, 15 years), who were hospitalized with myocarditis after receiving the Pfizer-BioNTech messenger RNA COVID-19 vaccine.
Symptoms started 1-6 days after vaccine administration (most after the second dose) and included chest pain in all 15 patients, fever in 10 (67%), myalgia in eight (53%), and headache in six (40%).
On admission, all patients had elevated troponin levels (median, 0.25 ng/mL; range, 0.08-3.15 ng/mL). Troponin levels peaked 0.1-2.3 days after admission.
Echocardiography revealed decreased LV ejection fraction (EF) in three patients (20%) and abnormal global longitudinal or circumferential strain in five patients (33%). No patient had a pericardial effusion.
Cardiac MRI findings were consistent with myocarditis in 13 patients (87%), including late gadolinium enhancement in 12 (80%), regional hyperintensity on T2-weighted imaging in two (13%), elevated extracellular volume fraction in three (20%), and elevated LV global native T1 in two (20%).
The patients remained in the hospital for 1-5 days (median, 2 days) and were discharged. No patient required admission to the intensive care unit.
In follow-up assessments performed 1-13 days after hospital discharge, symptoms of myocarditis had resolved in 11 patients (73%).
One patient (7%) had persistent borderline low LV systolic function on echocardiogram (LVEF, 54%).
Troponin levels remained mildly elevated in three patients (20%). One patient (7%) had nonsustained ventricular tachycardia on ambulatory monitor.
The authors say longitudinal studies of patients with myocarditis after COVID-19 vaccine “will be important to better understand long-term risks.”
In a statement from the UK nonprofit Science Media Centre, Peter Openshaw, FMedSci, Imperial College London, says: “The problem with case series of this type is the lack of comparison groups. How many cases of myocarditis might be seen in normal children, or those given other vaccines (including those that are not for COVID), or in teenagers infected with SARS-CoV-2?”
“As the authors note, myocarditis does happen after other vaccines. The estimated rate (62.8 cases per million) makes this a rare event,” Dr. Openshaw says.
“My view that teenagers should be considered for vaccination is not changed by this new publication,” he adds.
This study was funded by the McCance Foundation. The authors have declared no relevant conflicts of interest. Dr. Openshaw has served on scientific advisory boards for Janssen/J&J, Oxford Immunotech, GSK, Nestle, and Pfizer in relation to immunity to viruses (fees paid to Imperial College London).
A version of this article first appeared on Medscape.com.
Adolescents can develop mild myocarditis as a rare complication after COVID-19 vaccination, as has been reported in adults, an early case series from Boston confirms.
The adolescents who developed heart inflammation after vaccination typically had a benign course, with symptoms resolving without treatment, although one patient had persistent borderline low left ventricular (LV) function, report Audrey Dionne, MD, and colleagues at Boston Children’s Hospital.
“Despite the risks of myocarditis associated with vaccination, the benefits of vaccination likely outweigh risks in children and adolescents,” they say.
They estimate that for males 12-29 years of age COVID-19 vaccination prevents 11,000 COVID-19 cases, 560 hospitalizations, 138 intensive care unit admissions, and six deaths, compared with 39-47 expected myocarditis cases.
The case series was published online Aug. 10 in JAMA Cardiology.
Long-term risks unknown
Dr. Dionne and colleagues reviewed the results of comprehensive cardiac imaging in 14 boys and 1 girl, 12-18 years of age (median, 15 years), who were hospitalized with myocarditis after receiving the Pfizer-BioNTech messenger RNA COVID-19 vaccine.
Symptoms started 1-6 days after vaccine administration (most after the second dose) and included chest pain in all 15 patients, fever in 10 (67%), myalgia in eight (53%), and headache in six (40%).
On admission, all patients had elevated troponin levels (median, 0.25 ng/mL; range, 0.08-3.15 ng/mL). Troponin levels peaked 0.1-2.3 days after admission.
Echocardiography revealed decreased LV ejection fraction (EF) in three patients (20%) and abnormal global longitudinal or circumferential strain in five patients (33%). No patient had a pericardial effusion.
Cardiac MRI findings were consistent with myocarditis in 13 patients (87%), including late gadolinium enhancement in 12 (80%), regional hyperintensity on T2-weighted imaging in two (13%), elevated extracellular volume fraction in three (20%), and elevated LV global native T1 in two (20%).
The patients remained in the hospital for 1-5 days (median, 2 days) and were discharged. No patient required admission to the intensive care unit.
In follow-up assessments performed 1-13 days after hospital discharge, symptoms of myocarditis had resolved in 11 patients (73%).
One patient (7%) had persistent borderline low LV systolic function on echocardiogram (LVEF, 54%).
Troponin levels remained mildly elevated in three patients (20%). One patient (7%) had nonsustained ventricular tachycardia on ambulatory monitor.
The authors say longitudinal studies of patients with myocarditis after COVID-19 vaccine “will be important to better understand long-term risks.”
In a statement from the UK nonprofit Science Media Centre, Peter Openshaw, FMedSci, Imperial College London, says: “The problem with case series of this type is the lack of comparison groups. How many cases of myocarditis might be seen in normal children, or those given other vaccines (including those that are not for COVID), or in teenagers infected with SARS-CoV-2?”
“As the authors note, myocarditis does happen after other vaccines. The estimated rate (62.8 cases per million) makes this a rare event,” Dr. Openshaw says.
“My view that teenagers should be considered for vaccination is not changed by this new publication,” he adds.
This study was funded by the McCance Foundation. The authors have declared no relevant conflicts of interest. Dr. Openshaw has served on scientific advisory boards for Janssen/J&J, Oxford Immunotech, GSK, Nestle, and Pfizer in relation to immunity to viruses (fees paid to Imperial College London).
A version of this article first appeared on Medscape.com.
Major musculoskeletal surgery in children with medically complex conditions
A review of the International Committee’s guide
The International Committee on Perioperative Care for Children with Medical Complexity developed an online guide, “Deciding on and Preparing for Major Musculoskeletal Surgery in Children with Cerebral Palsy, Neurodevelopmental Disorders, and Other Medically Complex Conditions,” published on Dec. 20, 2020, detailing how to prepare pediatric patients with medical complexity prior to musculoskeletal surgery. The guide was developed from a dearth of information regarding optimal care practices for these patients.
The multidisciplinary committee included members from orthopedic surgery, general pediatrics, pediatric hospital medicine, anesthesiology, critical care medicine, pain medicine, physiotherapy, developmental and behavioral pediatrics, and families of children with cerebral palsy. Mirna Giordano, MD, FAAP, FHM, associate professor of pediatrics at Columbia University, New York, and International Committee member, helped develop these recommendations to “improve quality of care in the perioperative period for children with medical complexities and neurodisabilities all over the world.”
The guide meticulously details the steps required to successfully prepare for an operation and postoperative recovery. It includes an algorithm and comprehensive assessment plan that can be implemented to assess and optimize the child’s health and wellbeing prior to surgery. It encourages shared decision making and highlights the need for ongoing, open communication between providers, patients, and families to set goals and expectations, discuss potential complications, and describe outcomes and the recovery process.
The module elaborates on several key factors that must be evaluated and addressed long before surgery to ensure success. Baseline nutrition is critical and must be evaluated with body composition and anthropometric measurements. Respiratory health must be assessed with consideration of pulmonology consultation, specific testing, and ventilator or assistive-device optimization. Moreover, children with innate muscular weakness or restrictive lung disease should have baseline physiology evaluated in anticipation of potential postoperative complications, including atelectasis, hypoventilation, and pneumonia. Coexisting chronic medical conditions must also be optimized in anticipation of expected deviations from baseline.
In anticipation of peri- and postoperative care, the medical team should also be aware of details surrounding patients’ indwelling medical devices, such as cardiac implantable devices and tracheostomies. Particular attention should be paid to baclofen pumps, as malfunction or mistitration can lead to periprocedural hypotension or withdrawal.
Of paramount importance is understanding how the child appears and responds when in pain or discomfort, especially for a child with limited verbal communication. The module provides pain assessment tools, tailored to verbal and nonverbal patients in both the inpatient and outpatient settings. The module also shares guidance on establishing communication and goals with the family and within the care team on how the child appears when in distress and how he/she/they respond to pain medications. The pain plan should encompass both pharmacologic and nonpharmacologic therapeutics. Furthermore, as pain and discomfort may present from multiple sources, not limited to the regions involved in the procedure, understanding how the child responds to urinary retention, constipation, dyspnea, and uncomfortable positions is important to care. Postoperative immobilization must also be addressed as it may lead to pressure injury, manifesting as behavioral changes.
The module also presents laboratory testing as part of the preoperative health assessment. It details the utility or lack thereof of several common practices and provides recommendations on components that should be part of each patient’s assessment. It also contains videos showcased from the Courage Parents Network on family and provider perceptions of spinal fusion.
Family and social assessments must not be neglected prior to surgery, as these areas may also affect surgical outcomes. The module shares several screening tools that care team members can use to screen for family and social issues. Challenges to discharge planning are also discussed, including how to approach transportation, medical equipment, and school transitions needs.
The module is available for review in OPEN Pediatrics (www.openpediatrics.org), an online community for pediatric health professionals who share peer-reviewed best practices. “Our aim is to disseminate the recommendations as widely as possible to bring about the maximum good to the most,” Dr. Giordano said. The International Committee on Perioperative Care for Children with Medical Complexity is planning further guides regarding perioperative care, particularly for intraoperative and postoperative considerations.
Dr. Tantoco is a med-peds hospitalist at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital of Chicago, and instructor of medicine (hospital medicine) and pediatrics in Northwestern University, in Chicago. She is also a member of the SHM Pediatrics Special Interest Group Executive Committee. Dr. Bhasin is a med-peds hospitalist at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital, and assistant professor of medicine (hospital medicine) and pediatrics in Northwestern University.
A review of the International Committee’s guide
A review of the International Committee’s guide
The International Committee on Perioperative Care for Children with Medical Complexity developed an online guide, “Deciding on and Preparing for Major Musculoskeletal Surgery in Children with Cerebral Palsy, Neurodevelopmental Disorders, and Other Medically Complex Conditions,” published on Dec. 20, 2020, detailing how to prepare pediatric patients with medical complexity prior to musculoskeletal surgery. The guide was developed from a dearth of information regarding optimal care practices for these patients.
The multidisciplinary committee included members from orthopedic surgery, general pediatrics, pediatric hospital medicine, anesthesiology, critical care medicine, pain medicine, physiotherapy, developmental and behavioral pediatrics, and families of children with cerebral palsy. Mirna Giordano, MD, FAAP, FHM, associate professor of pediatrics at Columbia University, New York, and International Committee member, helped develop these recommendations to “improve quality of care in the perioperative period for children with medical complexities and neurodisabilities all over the world.”
The guide meticulously details the steps required to successfully prepare for an operation and postoperative recovery. It includes an algorithm and comprehensive assessment plan that can be implemented to assess and optimize the child’s health and wellbeing prior to surgery. It encourages shared decision making and highlights the need for ongoing, open communication between providers, patients, and families to set goals and expectations, discuss potential complications, and describe outcomes and the recovery process.
The module elaborates on several key factors that must be evaluated and addressed long before surgery to ensure success. Baseline nutrition is critical and must be evaluated with body composition and anthropometric measurements. Respiratory health must be assessed with consideration of pulmonology consultation, specific testing, and ventilator or assistive-device optimization. Moreover, children with innate muscular weakness or restrictive lung disease should have baseline physiology evaluated in anticipation of potential postoperative complications, including atelectasis, hypoventilation, and pneumonia. Coexisting chronic medical conditions must also be optimized in anticipation of expected deviations from baseline.
In anticipation of peri- and postoperative care, the medical team should also be aware of details surrounding patients’ indwelling medical devices, such as cardiac implantable devices and tracheostomies. Particular attention should be paid to baclofen pumps, as malfunction or mistitration can lead to periprocedural hypotension or withdrawal.
Of paramount importance is understanding how the child appears and responds when in pain or discomfort, especially for a child with limited verbal communication. The module provides pain assessment tools, tailored to verbal and nonverbal patients in both the inpatient and outpatient settings. The module also shares guidance on establishing communication and goals with the family and within the care team on how the child appears when in distress and how he/she/they respond to pain medications. The pain plan should encompass both pharmacologic and nonpharmacologic therapeutics. Furthermore, as pain and discomfort may present from multiple sources, not limited to the regions involved in the procedure, understanding how the child responds to urinary retention, constipation, dyspnea, and uncomfortable positions is important to care. Postoperative immobilization must also be addressed as it may lead to pressure injury, manifesting as behavioral changes.
The module also presents laboratory testing as part of the preoperative health assessment. It details the utility or lack thereof of several common practices and provides recommendations on components that should be part of each patient’s assessment. It also contains videos showcased from the Courage Parents Network on family and provider perceptions of spinal fusion.
Family and social assessments must not be neglected prior to surgery, as these areas may also affect surgical outcomes. The module shares several screening tools that care team members can use to screen for family and social issues. Challenges to discharge planning are also discussed, including how to approach transportation, medical equipment, and school transitions needs.
The module is available for review in OPEN Pediatrics (www.openpediatrics.org), an online community for pediatric health professionals who share peer-reviewed best practices. “Our aim is to disseminate the recommendations as widely as possible to bring about the maximum good to the most,” Dr. Giordano said. The International Committee on Perioperative Care for Children with Medical Complexity is planning further guides regarding perioperative care, particularly for intraoperative and postoperative considerations.
Dr. Tantoco is a med-peds hospitalist at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital of Chicago, and instructor of medicine (hospital medicine) and pediatrics in Northwestern University, in Chicago. She is also a member of the SHM Pediatrics Special Interest Group Executive Committee. Dr. Bhasin is a med-peds hospitalist at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital, and assistant professor of medicine (hospital medicine) and pediatrics in Northwestern University.
The International Committee on Perioperative Care for Children with Medical Complexity developed an online guide, “Deciding on and Preparing for Major Musculoskeletal Surgery in Children with Cerebral Palsy, Neurodevelopmental Disorders, and Other Medically Complex Conditions,” published on Dec. 20, 2020, detailing how to prepare pediatric patients with medical complexity prior to musculoskeletal surgery. The guide was developed from a dearth of information regarding optimal care practices for these patients.
The multidisciplinary committee included members from orthopedic surgery, general pediatrics, pediatric hospital medicine, anesthesiology, critical care medicine, pain medicine, physiotherapy, developmental and behavioral pediatrics, and families of children with cerebral palsy. Mirna Giordano, MD, FAAP, FHM, associate professor of pediatrics at Columbia University, New York, and International Committee member, helped develop these recommendations to “improve quality of care in the perioperative period for children with medical complexities and neurodisabilities all over the world.”
The guide meticulously details the steps required to successfully prepare for an operation and postoperative recovery. It includes an algorithm and comprehensive assessment plan that can be implemented to assess and optimize the child’s health and wellbeing prior to surgery. It encourages shared decision making and highlights the need for ongoing, open communication between providers, patients, and families to set goals and expectations, discuss potential complications, and describe outcomes and the recovery process.
The module elaborates on several key factors that must be evaluated and addressed long before surgery to ensure success. Baseline nutrition is critical and must be evaluated with body composition and anthropometric measurements. Respiratory health must be assessed with consideration of pulmonology consultation, specific testing, and ventilator or assistive-device optimization. Moreover, children with innate muscular weakness or restrictive lung disease should have baseline physiology evaluated in anticipation of potential postoperative complications, including atelectasis, hypoventilation, and pneumonia. Coexisting chronic medical conditions must also be optimized in anticipation of expected deviations from baseline.
In anticipation of peri- and postoperative care, the medical team should also be aware of details surrounding patients’ indwelling medical devices, such as cardiac implantable devices and tracheostomies. Particular attention should be paid to baclofen pumps, as malfunction or mistitration can lead to periprocedural hypotension or withdrawal.
Of paramount importance is understanding how the child appears and responds when in pain or discomfort, especially for a child with limited verbal communication. The module provides pain assessment tools, tailored to verbal and nonverbal patients in both the inpatient and outpatient settings. The module also shares guidance on establishing communication and goals with the family and within the care team on how the child appears when in distress and how he/she/they respond to pain medications. The pain plan should encompass both pharmacologic and nonpharmacologic therapeutics. Furthermore, as pain and discomfort may present from multiple sources, not limited to the regions involved in the procedure, understanding how the child responds to urinary retention, constipation, dyspnea, and uncomfortable positions is important to care. Postoperative immobilization must also be addressed as it may lead to pressure injury, manifesting as behavioral changes.
The module also presents laboratory testing as part of the preoperative health assessment. It details the utility or lack thereof of several common practices and provides recommendations on components that should be part of each patient’s assessment. It also contains videos showcased from the Courage Parents Network on family and provider perceptions of spinal fusion.
Family and social assessments must not be neglected prior to surgery, as these areas may also affect surgical outcomes. The module shares several screening tools that care team members can use to screen for family and social issues. Challenges to discharge planning are also discussed, including how to approach transportation, medical equipment, and school transitions needs.
The module is available for review in OPEN Pediatrics (www.openpediatrics.org), an online community for pediatric health professionals who share peer-reviewed best practices. “Our aim is to disseminate the recommendations as widely as possible to bring about the maximum good to the most,” Dr. Giordano said. The International Committee on Perioperative Care for Children with Medical Complexity is planning further guides regarding perioperative care, particularly for intraoperative and postoperative considerations.
Dr. Tantoco is a med-peds hospitalist at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital of Chicago, and instructor of medicine (hospital medicine) and pediatrics in Northwestern University, in Chicago. She is also a member of the SHM Pediatrics Special Interest Group Executive Committee. Dr. Bhasin is a med-peds hospitalist at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital, and assistant professor of medicine (hospital medicine) and pediatrics in Northwestern University.
Surge of new child COVID cases continues for 6th consecutive week
The current COVID-19 surge has brought new cases in children to their highest level since February, according to a new report.
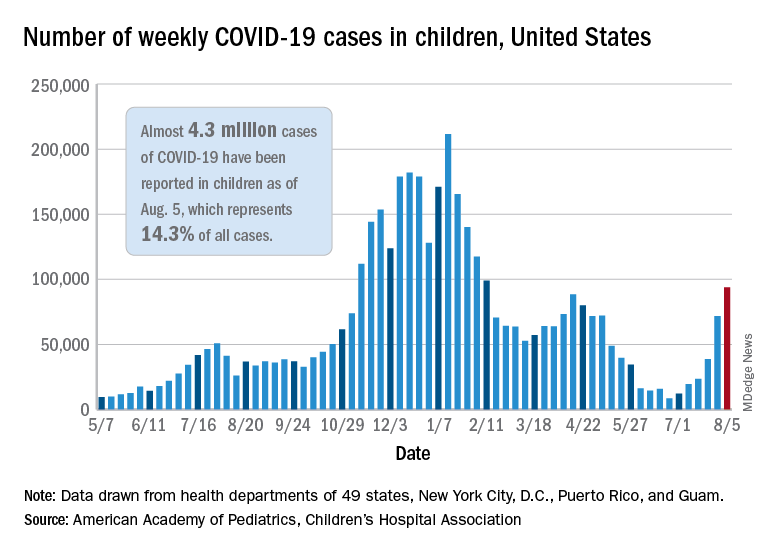
New pediatric cases rose for the 6th straight week, with almost 94,000 reported for the week ending Aug. 5.
That weekly total was up by 31% over the previous week and by over 1,000% since late June, when the new-case figure was at its lowest point (8,447) since early in the pandemic, the American Academy of Pediatrics and the Children’s Hospital Association said. COVID-related deaths – 13 for the week – were also higher than at any time since March 2021.
Almost 4.3 million children have been infected with SARS-CoV-2, which is 14.3% of all cases reported in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. Children represented 15.0% of the new cases reported in those jurisdictions during the week ending Aug. 5, the AAP and CHA said in their weekly report.
Another measure that has been trending upward recently is vaccine initiation among 12- to 15-year-olds, although the latest weekly total is still well below the high of 1.4 million seen in May. First-time vaccinations reached almost 411,000 for the week of Aug. 3-9, marking the fourth consecutive increase in that age group, the Centers for Disease Control and Prevention said on its COVID Data Tracker. Vaccinations also increased, although more modestly, for 16- and 17-year-olds in the most recent week.
Cumulative figures for children aged 12-17 show that almost 10.4 million have received at least one dose and that 7.7 million are fully vaccinated as of Aug. 9. By age group, 42.2% of those aged 12-15 have received at least one dose, and 30.4% have completed the vaccine regimen. Among those aged 16-17 years, 52.2% have gotten their first dose, and 41.4% are fully vaccinated, according to the COVID Data Tracker.
Looking at vaccination rates on the state level shows that only 20% of children aged 12-17 in Wyoming and 21% in Mississippi have gotten at least one dose as of Aug. 4, while Massachusetts is up to 68% and Vermont reports 70%. Rates for full vaccination range from 11% in Mississippi and Alabama to 61% in Vermont, based on an AAP analysis of CDC data, which is not available for Idaho.
The current COVID-19 surge has brought new cases in children to their highest level since February, according to a new report.
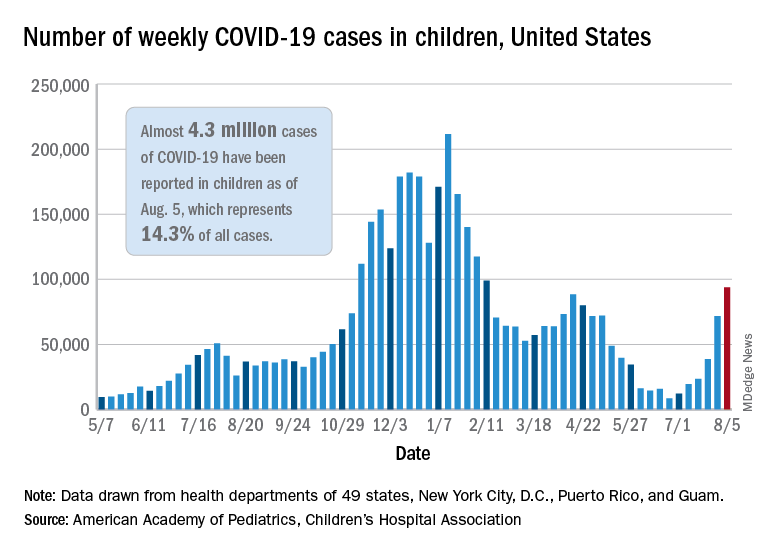
New pediatric cases rose for the 6th straight week, with almost 94,000 reported for the week ending Aug. 5.
That weekly total was up by 31% over the previous week and by over 1,000% since late June, when the new-case figure was at its lowest point (8,447) since early in the pandemic, the American Academy of Pediatrics and the Children’s Hospital Association said. COVID-related deaths – 13 for the week – were also higher than at any time since March 2021.
Almost 4.3 million children have been infected with SARS-CoV-2, which is 14.3% of all cases reported in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. Children represented 15.0% of the new cases reported in those jurisdictions during the week ending Aug. 5, the AAP and CHA said in their weekly report.
Another measure that has been trending upward recently is vaccine initiation among 12- to 15-year-olds, although the latest weekly total is still well below the high of 1.4 million seen in May. First-time vaccinations reached almost 411,000 for the week of Aug. 3-9, marking the fourth consecutive increase in that age group, the Centers for Disease Control and Prevention said on its COVID Data Tracker. Vaccinations also increased, although more modestly, for 16- and 17-year-olds in the most recent week.
Cumulative figures for children aged 12-17 show that almost 10.4 million have received at least one dose and that 7.7 million are fully vaccinated as of Aug. 9. By age group, 42.2% of those aged 12-15 have received at least one dose, and 30.4% have completed the vaccine regimen. Among those aged 16-17 years, 52.2% have gotten their first dose, and 41.4% are fully vaccinated, according to the COVID Data Tracker.
Looking at vaccination rates on the state level shows that only 20% of children aged 12-17 in Wyoming and 21% in Mississippi have gotten at least one dose as of Aug. 4, while Massachusetts is up to 68% and Vermont reports 70%. Rates for full vaccination range from 11% in Mississippi and Alabama to 61% in Vermont, based on an AAP analysis of CDC data, which is not available for Idaho.
The current COVID-19 surge has brought new cases in children to their highest level since February, according to a new report.
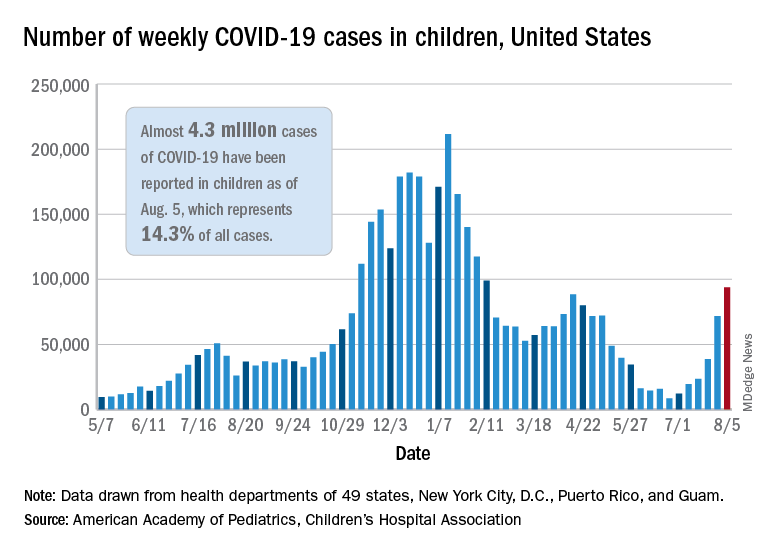
New pediatric cases rose for the 6th straight week, with almost 94,000 reported for the week ending Aug. 5.
That weekly total was up by 31% over the previous week and by over 1,000% since late June, when the new-case figure was at its lowest point (8,447) since early in the pandemic, the American Academy of Pediatrics and the Children’s Hospital Association said. COVID-related deaths – 13 for the week – were also higher than at any time since March 2021.
Almost 4.3 million children have been infected with SARS-CoV-2, which is 14.3% of all cases reported in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. Children represented 15.0% of the new cases reported in those jurisdictions during the week ending Aug. 5, the AAP and CHA said in their weekly report.
Another measure that has been trending upward recently is vaccine initiation among 12- to 15-year-olds, although the latest weekly total is still well below the high of 1.4 million seen in May. First-time vaccinations reached almost 411,000 for the week of Aug. 3-9, marking the fourth consecutive increase in that age group, the Centers for Disease Control and Prevention said on its COVID Data Tracker. Vaccinations also increased, although more modestly, for 16- and 17-year-olds in the most recent week.
Cumulative figures for children aged 12-17 show that almost 10.4 million have received at least one dose and that 7.7 million are fully vaccinated as of Aug. 9. By age group, 42.2% of those aged 12-15 have received at least one dose, and 30.4% have completed the vaccine regimen. Among those aged 16-17 years, 52.2% have gotten their first dose, and 41.4% are fully vaccinated, according to the COVID Data Tracker.
Looking at vaccination rates on the state level shows that only 20% of children aged 12-17 in Wyoming and 21% in Mississippi have gotten at least one dose as of Aug. 4, while Massachusetts is up to 68% and Vermont reports 70%. Rates for full vaccination range from 11% in Mississippi and Alabama to 61% in Vermont, based on an AAP analysis of CDC data, which is not available for Idaho.
Docs fight back after losing hospital privileges, patients, and income
In April, a group of more than a dozen cardiologists at St. Louis Heart and Vascular (SLHV) lost their privileges at SSM Health, an eight-hospital system in St. Louis.
The physicians did not lose their privileges because of a clinical failure. Rather, it was because of SSM’s decision to enter into an exclusive contract with another set of cardiologists.
“The current situation is economically untenable for us,” said Harvey Serota, MD, founder and medical director of SLHV. “This is an existential threat to the practice.”
Because of the exclusive contract, many of SLHV’s patients are now being redirected to SSM-contracted cardiologists. Volume for the group’s new $15 million catheterization lab has plummeted. SLHV is suing SSM to restore its privileges, claiming lack of due process, restraint of trade, interference with its business, and breach of contract.
Losing privileges because a hospital seeks to increase their profits is becoming all too familiar for many independent specialists in fields such as cardiology, orthopedic surgery, and urology, as the hospitals that hosted them become their competitors and forge exclusive contracts with opposing groups.
What can these doctors do if they’re shut out? File a lawsuit, as SLHV has done? Demand a hearing before the medical staff and try to resolve the problem? Or simply give up their privileges and move on?
Unfortunately, none of these approaches offer a quick or certain solution, and each comes with risks.
Generally, courts have upheld hospitals’ use of exclusive contracts, which is also known as economic credentialing, says Barry F. Rosen, a health law attorney at Gordon Feinblatt, in Baltimore.
“Courts have long recognized exclusive contracts, and challenges by excluded doctors usually fail,” he says.
However, Mr. Rosen can cite several examples in which excluded doctors launched legal challenges that prevailed, owing to nuances in the law. The legal field in this area is tangled, and it varies by state.
Can hospitals make exclusive deals?
Hospitals have long used exclusive contracts for hospital-based specialists – anesthesiologists, radiologists, pathologists, emergency physicians, and hospitalists. They say that restricting patients to one group of anesthesiologists or radiologists enhances operational efficiency and that these contracts do not disrupt patients, because patients have no ties to hospital-based physicians. Such contracts are often more profitable for the hospital because of the negotiated rates.
Exclusive contracts in other specialties, however, are less accepted because they involve markedly different strategies and have different effects. In such cases, the hospital is no longer simply enhancing operational efficiency but is competing with physicians on staff, and the arrangement can disrupt the care of patients of the excluded doctors.
In the courts, these concerns might form the basis of an antitrust action or a claim of tortious interference with physicians’ ability to provide care for their patients, but neither claim is easy to win, Mr. Rosen says.
In antitrust cases, “the issue is not whether the excluded doctor was injured but whether the action harmed competition,” Mr. Rosen says. “Will the exclusion lead to higher prices?”
In the case of interference with patient care, “you will always find interference by one entity in the affairs of another,” he says, “but tortious interference applies to situations where something nefarious is going on, such as the other side was out to destroy your business and create a monopoly.”
Hospitals may try to restrict the privileges of physicians who invest in competing facilities such as cath labs and ambulatory surgery centers (ASCs), says Gregory Mertz, managing director of Physician Strategies Group, a consultancy in Virginia Beach.
“However, any revenge that a hospital might take against the doctors who started an ASC would usually not be publicly admitted,” Mr. Mertz says. “Revenge would be exacted in subtle ways.”
In the St. Louis situation, SSM did not cite SLHV’s cath lab as a reason for its exclusive contract. SSM stated in court documents that the decision was based on the recommendations of an expert panel. Furthermore, SSM said the board created the panel in response to a state report that cited the limited experience of some SLHV cardiologists in treating a rare type of heart attack.
Mr. Mertz says the board’s interest in the state’s concern and then its forming the special panel lent a great deal of legitimacy to SSM’s decision to start an exclusive contract. “SSM can show evidence that the board’s decision was based on a clinical matter and not on trying to squeeze out the cardiologists,” he says.
In SLHV’s defense, Dr. Serota says the practice offered to stop taking calls for the type of heart attack that was cited, but the hospital did not respond to its offer. He says SSM should have consulted the hospital’s medical staff to address the state’s concern and to create the exclusive contract, because these decisions involved clinical issues that the medical staff understands better than the board.
The law, however, does not require a hospital board to consult with its medical staff, says Alice G. Gosfield, a health care attorney in Philadelphia. “The board has ultimate legal control of everything in the hospital,” she says. However, the board often delegates certain functions to the medical staff in the hospital bylaws, and depending on the wording of the bylaws, it is still possible that the board violated the bylaws, Ms. Gosfield adds.
Can excluded physicians get peer review?
Can the hospital medical staff help restore the privileges of excluded physicians? Don’t these physicians have the right to peer review – a hearing before the medical staff?
Indeed, the Joint Commission, which accredits hospitals, states that the hospital must have “mechanisms, including a fair hearing and appeal process, for addressing adverse decisions for existing medical staff members and other individuals holding clinical privileges for renewal, revocation, or revision of clinical privileges.”
However, excluded physicians may not have a right to a hearing if they have not been fully stripped of privileges. SSM discontinued adult cardiology privileges for SLHV doctors but retained some doctors’ internal medicine privileges. Dr. Serota says internal medicine privileges are useless to cardiologists, but because the doctors’ privileges had not been fully removed, they cannot ask for a hearing.
More fundamentally, exclusive contracts are not a good fit for peer review. Mr. Rosen says the hearings were designed to review the physicians’ clinical competence or behavior, but excluded physicians do not have these problems. About all the hearing could focus on is the hospital’s policy, which the board would not want to allow. To avoid this, “the hospital might rule out a hearing as contrary to the intent of the bylaws,” Mr. Rosen says.
Furthermore, even if peer review goes forward, “what the medical staff decides is only advisory, and the hospital board makes the final decision,” Mr. Rosen says. He notes that the doctor could challenge the decision in court, but the hospital might still prevail.
Excluded physicians sometimes prevail
Although it is rare for excluded physicians to win a lawsuit against their hospital, it does happen, says Michael R. Callahan, health lawyer at Katten Muchin Rosenman, in Chicago.
Mr. Callahan cites a 2010 decision by the Arkansas Supreme Court that stopped the state’s largest health system from denying physicians’ privileges. Among other things, the hospital was found to have tortiously interfered with the physicians’ contracts with patients.
In a 2007 decision, a West Virginia court ruled that hospitals that have a mission to serve the public cannot exclude physicians for nonquality issues. In addition, some states, such as Texas, limit the economic factors that can be considered when credentialing decisions are made. Other states, such as Ohio, give hospitals a great deal of leeway to alter credentialing.
Dr. Serota is optimistic about his Missouri lawsuit. Although the judge in the case did not immediately grant SLHV’s request for restoration of privileges while the case proceeds, she did grant expedited discovery – allowing SLHV to obtain documents from SSM that could strengthen the doctors’ case – and she agreed to a hearing on SLHV’s request for a temporary restoration of privileges.
Ms. Gosfield says Dr. Serota’s optimism seems justified, but she adds that such cases cost a lot of money and that they may still not be winnable.
Often plaintiffs can settle lawsuits before they go to trial, but Mr. Callahan says hospitals are loath to restore privileges in a settlement because they don’t want to undermine an exclusivity deal. “The exclusive group expects a certain volume, which can’t be reached if the competing doctors are allowed back in,” he says.
Many physicians don’t challenge the exclusion
Quite often, excluded doctors decide not to challenge the decision. For example, Dr. Serota says groups of orthopedic surgeons and urologists have decided not to challenge similar decisions by SSM. “They wanted to move on,” he says.
Mr. Callahan says many excluded doctors also don’t even ask for a hearing. “They expect that the hospital’s decision will be upheld,” he says.
This was the case for Devendra K. Amin, MD, an independent cardiologist in Easton, Pa. Dr. Amin has not had any hospital privileges since July 2020. Even though he is board certified in interventional cardiology, which involves catheterization, Dr. Amin says he cannot perform these procedures because they can only be performed in a hospital in the area.
In the 1990s, Dr. Amin says, he had invasive cardiology privileges at five hospitals, but then those hospitals consolidated, and the remaining ones started constricting his privileges. First he could no longer work in the emergency department, then he could no longer read echocardiograms and interpret stress test results, because that work was assigned exclusively to employed doctors, he says.
Then the one remaining hospital announced that privileges would only be available to physicians by invitation, and he was not invited. Dr. Amin says he could have regained general cardiology privileges if he had accepted employment at the hospital, but he did not want to do this. A recruiter and the head of the cardiology section at the hospital even took him out to dinner 2 years ago to discuss employment, but there was a stipulation that the hospital would not agree to.
“I wanted to get back my interventional privileges back,” Dr. Amin says, “but they told me that would not be possible because they had an exclusive contract with a group.”
Dr. Amin says that now, he can only work as a general cardiologist with reduced volume. He says primary care physicians in the local hospital systems only refer to cardiologists within their systems. “When these patients do come to me, it is only because they specifically requested to see me,” Dr. Amin says.
He does not want to challenge the decisions regarding privileging. “Look, I am 68 years old,” Dr. Amin says. “I’m not retiring yet, but I don’t want to get into a battle with a hospital that has very deep pockets. I’m not a confrontational person to begin with, and I don’t want to spend the next 10 years of my life in litigation.”
Diverging expectations
The law on exclusive contracts does not provide easy answers for excluded doctors, and often it defies physicians’ conception of their own role in the hospital.
Many physicians expect the hospital to be a haven where they can do their work without being cut out by a competitor. This view is reinforced by organizations such as the American Medical Association.
The AMA Council on Medical Service states that privileges “can only be abridged upon recommendation of the medical staff and only for reason related to professional competence, adherence to standards of care, and other parameters agreed to by the medical staff.”
But the courts don’t tend to agree with that position. “Hospitals have a fiduciary duty to protect their own financial interests,” Mr. Callahan says. “This may involve anything that furthers the hospital’s mission to provide high-quality health care services to its patient community.”
At the same time, however, there are plenty of instances in which courts have ruled that exclusive contracts had gone too far. But usually it takes a lawyer experienced in these cases to know what those exceptions are.
A version of this article first appeared on Medscape.com.
In April, a group of more than a dozen cardiologists at St. Louis Heart and Vascular (SLHV) lost their privileges at SSM Health, an eight-hospital system in St. Louis.
The physicians did not lose their privileges because of a clinical failure. Rather, it was because of SSM’s decision to enter into an exclusive contract with another set of cardiologists.
“The current situation is economically untenable for us,” said Harvey Serota, MD, founder and medical director of SLHV. “This is an existential threat to the practice.”
Because of the exclusive contract, many of SLHV’s patients are now being redirected to SSM-contracted cardiologists. Volume for the group’s new $15 million catheterization lab has plummeted. SLHV is suing SSM to restore its privileges, claiming lack of due process, restraint of trade, interference with its business, and breach of contract.
Losing privileges because a hospital seeks to increase their profits is becoming all too familiar for many independent specialists in fields such as cardiology, orthopedic surgery, and urology, as the hospitals that hosted them become their competitors and forge exclusive contracts with opposing groups.
What can these doctors do if they’re shut out? File a lawsuit, as SLHV has done? Demand a hearing before the medical staff and try to resolve the problem? Or simply give up their privileges and move on?
Unfortunately, none of these approaches offer a quick or certain solution, and each comes with risks.
Generally, courts have upheld hospitals’ use of exclusive contracts, which is also known as economic credentialing, says Barry F. Rosen, a health law attorney at Gordon Feinblatt, in Baltimore.
“Courts have long recognized exclusive contracts, and challenges by excluded doctors usually fail,” he says.
However, Mr. Rosen can cite several examples in which excluded doctors launched legal challenges that prevailed, owing to nuances in the law. The legal field in this area is tangled, and it varies by state.
Can hospitals make exclusive deals?
Hospitals have long used exclusive contracts for hospital-based specialists – anesthesiologists, radiologists, pathologists, emergency physicians, and hospitalists. They say that restricting patients to one group of anesthesiologists or radiologists enhances operational efficiency and that these contracts do not disrupt patients, because patients have no ties to hospital-based physicians. Such contracts are often more profitable for the hospital because of the negotiated rates.
Exclusive contracts in other specialties, however, are less accepted because they involve markedly different strategies and have different effects. In such cases, the hospital is no longer simply enhancing operational efficiency but is competing with physicians on staff, and the arrangement can disrupt the care of patients of the excluded doctors.
In the courts, these concerns might form the basis of an antitrust action or a claim of tortious interference with physicians’ ability to provide care for their patients, but neither claim is easy to win, Mr. Rosen says.
In antitrust cases, “the issue is not whether the excluded doctor was injured but whether the action harmed competition,” Mr. Rosen says. “Will the exclusion lead to higher prices?”
In the case of interference with patient care, “you will always find interference by one entity in the affairs of another,” he says, “but tortious interference applies to situations where something nefarious is going on, such as the other side was out to destroy your business and create a monopoly.”
Hospitals may try to restrict the privileges of physicians who invest in competing facilities such as cath labs and ambulatory surgery centers (ASCs), says Gregory Mertz, managing director of Physician Strategies Group, a consultancy in Virginia Beach.
“However, any revenge that a hospital might take against the doctors who started an ASC would usually not be publicly admitted,” Mr. Mertz says. “Revenge would be exacted in subtle ways.”
In the St. Louis situation, SSM did not cite SLHV’s cath lab as a reason for its exclusive contract. SSM stated in court documents that the decision was based on the recommendations of an expert panel. Furthermore, SSM said the board created the panel in response to a state report that cited the limited experience of some SLHV cardiologists in treating a rare type of heart attack.
Mr. Mertz says the board’s interest in the state’s concern and then its forming the special panel lent a great deal of legitimacy to SSM’s decision to start an exclusive contract. “SSM can show evidence that the board’s decision was based on a clinical matter and not on trying to squeeze out the cardiologists,” he says.
In SLHV’s defense, Dr. Serota says the practice offered to stop taking calls for the type of heart attack that was cited, but the hospital did not respond to its offer. He says SSM should have consulted the hospital’s medical staff to address the state’s concern and to create the exclusive contract, because these decisions involved clinical issues that the medical staff understands better than the board.
The law, however, does not require a hospital board to consult with its medical staff, says Alice G. Gosfield, a health care attorney in Philadelphia. “The board has ultimate legal control of everything in the hospital,” she says. However, the board often delegates certain functions to the medical staff in the hospital bylaws, and depending on the wording of the bylaws, it is still possible that the board violated the bylaws, Ms. Gosfield adds.
Can excluded physicians get peer review?
Can the hospital medical staff help restore the privileges of excluded physicians? Don’t these physicians have the right to peer review – a hearing before the medical staff?
Indeed, the Joint Commission, which accredits hospitals, states that the hospital must have “mechanisms, including a fair hearing and appeal process, for addressing adverse decisions for existing medical staff members and other individuals holding clinical privileges for renewal, revocation, or revision of clinical privileges.”
However, excluded physicians may not have a right to a hearing if they have not been fully stripped of privileges. SSM discontinued adult cardiology privileges for SLHV doctors but retained some doctors’ internal medicine privileges. Dr. Serota says internal medicine privileges are useless to cardiologists, but because the doctors’ privileges had not been fully removed, they cannot ask for a hearing.
More fundamentally, exclusive contracts are not a good fit for peer review. Mr. Rosen says the hearings were designed to review the physicians’ clinical competence or behavior, but excluded physicians do not have these problems. About all the hearing could focus on is the hospital’s policy, which the board would not want to allow. To avoid this, “the hospital might rule out a hearing as contrary to the intent of the bylaws,” Mr. Rosen says.
Furthermore, even if peer review goes forward, “what the medical staff decides is only advisory, and the hospital board makes the final decision,” Mr. Rosen says. He notes that the doctor could challenge the decision in court, but the hospital might still prevail.
Excluded physicians sometimes prevail
Although it is rare for excluded physicians to win a lawsuit against their hospital, it does happen, says Michael R. Callahan, health lawyer at Katten Muchin Rosenman, in Chicago.
Mr. Callahan cites a 2010 decision by the Arkansas Supreme Court that stopped the state’s largest health system from denying physicians’ privileges. Among other things, the hospital was found to have tortiously interfered with the physicians’ contracts with patients.
In a 2007 decision, a West Virginia court ruled that hospitals that have a mission to serve the public cannot exclude physicians for nonquality issues. In addition, some states, such as Texas, limit the economic factors that can be considered when credentialing decisions are made. Other states, such as Ohio, give hospitals a great deal of leeway to alter credentialing.
Dr. Serota is optimistic about his Missouri lawsuit. Although the judge in the case did not immediately grant SLHV’s request for restoration of privileges while the case proceeds, she did grant expedited discovery – allowing SLHV to obtain documents from SSM that could strengthen the doctors’ case – and she agreed to a hearing on SLHV’s request for a temporary restoration of privileges.
Ms. Gosfield says Dr. Serota’s optimism seems justified, but she adds that such cases cost a lot of money and that they may still not be winnable.
Often plaintiffs can settle lawsuits before they go to trial, but Mr. Callahan says hospitals are loath to restore privileges in a settlement because they don’t want to undermine an exclusivity deal. “The exclusive group expects a certain volume, which can’t be reached if the competing doctors are allowed back in,” he says.
Many physicians don’t challenge the exclusion
Quite often, excluded doctors decide not to challenge the decision. For example, Dr. Serota says groups of orthopedic surgeons and urologists have decided not to challenge similar decisions by SSM. “They wanted to move on,” he says.
Mr. Callahan says many excluded doctors also don’t even ask for a hearing. “They expect that the hospital’s decision will be upheld,” he says.
This was the case for Devendra K. Amin, MD, an independent cardiologist in Easton, Pa. Dr. Amin has not had any hospital privileges since July 2020. Even though he is board certified in interventional cardiology, which involves catheterization, Dr. Amin says he cannot perform these procedures because they can only be performed in a hospital in the area.
In the 1990s, Dr. Amin says, he had invasive cardiology privileges at five hospitals, but then those hospitals consolidated, and the remaining ones started constricting his privileges. First he could no longer work in the emergency department, then he could no longer read echocardiograms and interpret stress test results, because that work was assigned exclusively to employed doctors, he says.
Then the one remaining hospital announced that privileges would only be available to physicians by invitation, and he was not invited. Dr. Amin says he could have regained general cardiology privileges if he had accepted employment at the hospital, but he did not want to do this. A recruiter and the head of the cardiology section at the hospital even took him out to dinner 2 years ago to discuss employment, but there was a stipulation that the hospital would not agree to.
“I wanted to get back my interventional privileges back,” Dr. Amin says, “but they told me that would not be possible because they had an exclusive contract with a group.”
Dr. Amin says that now, he can only work as a general cardiologist with reduced volume. He says primary care physicians in the local hospital systems only refer to cardiologists within their systems. “When these patients do come to me, it is only because they specifically requested to see me,” Dr. Amin says.
He does not want to challenge the decisions regarding privileging. “Look, I am 68 years old,” Dr. Amin says. “I’m not retiring yet, but I don’t want to get into a battle with a hospital that has very deep pockets. I’m not a confrontational person to begin with, and I don’t want to spend the next 10 years of my life in litigation.”
Diverging expectations
The law on exclusive contracts does not provide easy answers for excluded doctors, and often it defies physicians’ conception of their own role in the hospital.
Many physicians expect the hospital to be a haven where they can do their work without being cut out by a competitor. This view is reinforced by organizations such as the American Medical Association.
The AMA Council on Medical Service states that privileges “can only be abridged upon recommendation of the medical staff and only for reason related to professional competence, adherence to standards of care, and other parameters agreed to by the medical staff.”
But the courts don’t tend to agree with that position. “Hospitals have a fiduciary duty to protect their own financial interests,” Mr. Callahan says. “This may involve anything that furthers the hospital’s mission to provide high-quality health care services to its patient community.”
At the same time, however, there are plenty of instances in which courts have ruled that exclusive contracts had gone too far. But usually it takes a lawyer experienced in these cases to know what those exceptions are.
A version of this article first appeared on Medscape.com.
In April, a group of more than a dozen cardiologists at St. Louis Heart and Vascular (SLHV) lost their privileges at SSM Health, an eight-hospital system in St. Louis.
The physicians did not lose their privileges because of a clinical failure. Rather, it was because of SSM’s decision to enter into an exclusive contract with another set of cardiologists.
“The current situation is economically untenable for us,” said Harvey Serota, MD, founder and medical director of SLHV. “This is an existential threat to the practice.”
Because of the exclusive contract, many of SLHV’s patients are now being redirected to SSM-contracted cardiologists. Volume for the group’s new $15 million catheterization lab has plummeted. SLHV is suing SSM to restore its privileges, claiming lack of due process, restraint of trade, interference with its business, and breach of contract.
Losing privileges because a hospital seeks to increase their profits is becoming all too familiar for many independent specialists in fields such as cardiology, orthopedic surgery, and urology, as the hospitals that hosted them become their competitors and forge exclusive contracts with opposing groups.
What can these doctors do if they’re shut out? File a lawsuit, as SLHV has done? Demand a hearing before the medical staff and try to resolve the problem? Or simply give up their privileges and move on?
Unfortunately, none of these approaches offer a quick or certain solution, and each comes with risks.
Generally, courts have upheld hospitals’ use of exclusive contracts, which is also known as economic credentialing, says Barry F. Rosen, a health law attorney at Gordon Feinblatt, in Baltimore.
“Courts have long recognized exclusive contracts, and challenges by excluded doctors usually fail,” he says.
However, Mr. Rosen can cite several examples in which excluded doctors launched legal challenges that prevailed, owing to nuances in the law. The legal field in this area is tangled, and it varies by state.
Can hospitals make exclusive deals?
Hospitals have long used exclusive contracts for hospital-based specialists – anesthesiologists, radiologists, pathologists, emergency physicians, and hospitalists. They say that restricting patients to one group of anesthesiologists or radiologists enhances operational efficiency and that these contracts do not disrupt patients, because patients have no ties to hospital-based physicians. Such contracts are often more profitable for the hospital because of the negotiated rates.
Exclusive contracts in other specialties, however, are less accepted because they involve markedly different strategies and have different effects. In such cases, the hospital is no longer simply enhancing operational efficiency but is competing with physicians on staff, and the arrangement can disrupt the care of patients of the excluded doctors.
In the courts, these concerns might form the basis of an antitrust action or a claim of tortious interference with physicians’ ability to provide care for their patients, but neither claim is easy to win, Mr. Rosen says.
In antitrust cases, “the issue is not whether the excluded doctor was injured but whether the action harmed competition,” Mr. Rosen says. “Will the exclusion lead to higher prices?”
In the case of interference with patient care, “you will always find interference by one entity in the affairs of another,” he says, “but tortious interference applies to situations where something nefarious is going on, such as the other side was out to destroy your business and create a monopoly.”
Hospitals may try to restrict the privileges of physicians who invest in competing facilities such as cath labs and ambulatory surgery centers (ASCs), says Gregory Mertz, managing director of Physician Strategies Group, a consultancy in Virginia Beach.
“However, any revenge that a hospital might take against the doctors who started an ASC would usually not be publicly admitted,” Mr. Mertz says. “Revenge would be exacted in subtle ways.”
In the St. Louis situation, SSM did not cite SLHV’s cath lab as a reason for its exclusive contract. SSM stated in court documents that the decision was based on the recommendations of an expert panel. Furthermore, SSM said the board created the panel in response to a state report that cited the limited experience of some SLHV cardiologists in treating a rare type of heart attack.
Mr. Mertz says the board’s interest in the state’s concern and then its forming the special panel lent a great deal of legitimacy to SSM’s decision to start an exclusive contract. “SSM can show evidence that the board’s decision was based on a clinical matter and not on trying to squeeze out the cardiologists,” he says.
In SLHV’s defense, Dr. Serota says the practice offered to stop taking calls for the type of heart attack that was cited, but the hospital did not respond to its offer. He says SSM should have consulted the hospital’s medical staff to address the state’s concern and to create the exclusive contract, because these decisions involved clinical issues that the medical staff understands better than the board.
The law, however, does not require a hospital board to consult with its medical staff, says Alice G. Gosfield, a health care attorney in Philadelphia. “The board has ultimate legal control of everything in the hospital,” she says. However, the board often delegates certain functions to the medical staff in the hospital bylaws, and depending on the wording of the bylaws, it is still possible that the board violated the bylaws, Ms. Gosfield adds.
Can excluded physicians get peer review?
Can the hospital medical staff help restore the privileges of excluded physicians? Don’t these physicians have the right to peer review – a hearing before the medical staff?
Indeed, the Joint Commission, which accredits hospitals, states that the hospital must have “mechanisms, including a fair hearing and appeal process, for addressing adverse decisions for existing medical staff members and other individuals holding clinical privileges for renewal, revocation, or revision of clinical privileges.”
However, excluded physicians may not have a right to a hearing if they have not been fully stripped of privileges. SSM discontinued adult cardiology privileges for SLHV doctors but retained some doctors’ internal medicine privileges. Dr. Serota says internal medicine privileges are useless to cardiologists, but because the doctors’ privileges had not been fully removed, they cannot ask for a hearing.
More fundamentally, exclusive contracts are not a good fit for peer review. Mr. Rosen says the hearings were designed to review the physicians’ clinical competence or behavior, but excluded physicians do not have these problems. About all the hearing could focus on is the hospital’s policy, which the board would not want to allow. To avoid this, “the hospital might rule out a hearing as contrary to the intent of the bylaws,” Mr. Rosen says.
Furthermore, even if peer review goes forward, “what the medical staff decides is only advisory, and the hospital board makes the final decision,” Mr. Rosen says. He notes that the doctor could challenge the decision in court, but the hospital might still prevail.
Excluded physicians sometimes prevail
Although it is rare for excluded physicians to win a lawsuit against their hospital, it does happen, says Michael R. Callahan, health lawyer at Katten Muchin Rosenman, in Chicago.
Mr. Callahan cites a 2010 decision by the Arkansas Supreme Court that stopped the state’s largest health system from denying physicians’ privileges. Among other things, the hospital was found to have tortiously interfered with the physicians’ contracts with patients.
In a 2007 decision, a West Virginia court ruled that hospitals that have a mission to serve the public cannot exclude physicians for nonquality issues. In addition, some states, such as Texas, limit the economic factors that can be considered when credentialing decisions are made. Other states, such as Ohio, give hospitals a great deal of leeway to alter credentialing.
Dr. Serota is optimistic about his Missouri lawsuit. Although the judge in the case did not immediately grant SLHV’s request for restoration of privileges while the case proceeds, she did grant expedited discovery – allowing SLHV to obtain documents from SSM that could strengthen the doctors’ case – and she agreed to a hearing on SLHV’s request for a temporary restoration of privileges.
Ms. Gosfield says Dr. Serota’s optimism seems justified, but she adds that such cases cost a lot of money and that they may still not be winnable.
Often plaintiffs can settle lawsuits before they go to trial, but Mr. Callahan says hospitals are loath to restore privileges in a settlement because they don’t want to undermine an exclusivity deal. “The exclusive group expects a certain volume, which can’t be reached if the competing doctors are allowed back in,” he says.
Many physicians don’t challenge the exclusion
Quite often, excluded doctors decide not to challenge the decision. For example, Dr. Serota says groups of orthopedic surgeons and urologists have decided not to challenge similar decisions by SSM. “They wanted to move on,” he says.
Mr. Callahan says many excluded doctors also don’t even ask for a hearing. “They expect that the hospital’s decision will be upheld,” he says.
This was the case for Devendra K. Amin, MD, an independent cardiologist in Easton, Pa. Dr. Amin has not had any hospital privileges since July 2020. Even though he is board certified in interventional cardiology, which involves catheterization, Dr. Amin says he cannot perform these procedures because they can only be performed in a hospital in the area.
In the 1990s, Dr. Amin says, he had invasive cardiology privileges at five hospitals, but then those hospitals consolidated, and the remaining ones started constricting his privileges. First he could no longer work in the emergency department, then he could no longer read echocardiograms and interpret stress test results, because that work was assigned exclusively to employed doctors, he says.
Then the one remaining hospital announced that privileges would only be available to physicians by invitation, and he was not invited. Dr. Amin says he could have regained general cardiology privileges if he had accepted employment at the hospital, but he did not want to do this. A recruiter and the head of the cardiology section at the hospital even took him out to dinner 2 years ago to discuss employment, but there was a stipulation that the hospital would not agree to.
“I wanted to get back my interventional privileges back,” Dr. Amin says, “but they told me that would not be possible because they had an exclusive contract with a group.”
Dr. Amin says that now, he can only work as a general cardiologist with reduced volume. He says primary care physicians in the local hospital systems only refer to cardiologists within their systems. “When these patients do come to me, it is only because they specifically requested to see me,” Dr. Amin says.
He does not want to challenge the decisions regarding privileging. “Look, I am 68 years old,” Dr. Amin says. “I’m not retiring yet, but I don’t want to get into a battle with a hospital that has very deep pockets. I’m not a confrontational person to begin with, and I don’t want to spend the next 10 years of my life in litigation.”
Diverging expectations
The law on exclusive contracts does not provide easy answers for excluded doctors, and often it defies physicians’ conception of their own role in the hospital.
Many physicians expect the hospital to be a haven where they can do their work without being cut out by a competitor. This view is reinforced by organizations such as the American Medical Association.
The AMA Council on Medical Service states that privileges “can only be abridged upon recommendation of the medical staff and only for reason related to professional competence, adherence to standards of care, and other parameters agreed to by the medical staff.”
But the courts don’t tend to agree with that position. “Hospitals have a fiduciary duty to protect their own financial interests,” Mr. Callahan says. “This may involve anything that furthers the hospital’s mission to provide high-quality health care services to its patient community.”
At the same time, however, there are plenty of instances in which courts have ruled that exclusive contracts had gone too far. But usually it takes a lawyer experienced in these cases to know what those exceptions are.
A version of this article first appeared on Medscape.com.
Patients with diabetes more likely to be hospitalized, especially with foot infection
People with diabetes are at increased risk of hospitalization for infection, as well as infection-related mortality, shows a large U.S. study that suggests the risk is even higher in younger and Black individuals.
Michael Fang, PhD, Johns Hopkins University, Baltimore, and colleagues studied more than 12,000 participants in a community cohort study who were followed for an average of 24 years, between 1987-1989 and 2019.
Participants with diabetes faced a 67% increase risk of infection-related hospitalization, compared with those without diabetes.
Of particular note, the risk of hospitalization with foot infection was almost sixfold higher for people with diabetes than those without.
The research, published in Diabetologia on August 4, also suggests that diabetes may be associated with a 72% increased risk of infection-related mortality, although the absolute numbers were small.
Dr. Fang explained to this news organization that they focused on infection-related hospitalization and mortality “because these are comprehensively tracked in administrative data and ... are the most severe types of outcomes.”
However, this is probably just the tip of the iceberg, as people with diabetes are “likely at increased risk for milder infection too,” which can have a “significant adverse impact on people’s well-being and quality of life.”
As a result of their findings, the authors call for “broader guidance on infection prevention and management” in people with diabetes. To achieve this, Dr. Fang said, “we need to better understand why diabetes is associated with an increased risk of infection-related complications.”
“One likely factor is glycemic control: Emerging research suggests patients with diabetes with better glycemic control may be at significantly lower risk of infection-related complications.”
He continued that, in younger patients, a factor for worse outcomes could be that “diabetes tends to be more aggressive when it emerges early in life,” while in Black patients “there is research highlighting Black-White differences in glycemic control, access to care, and beliefs around vaccines.”
Overall, their findings – coupled with recent data showing that diabetes is an important risk factor for adverse outcomes with COVID-19 infection – paint “a common picture,” Dr. Fang said.
“People with diabetes are much more susceptible to infection-related complications, including COVID-related hospitalization and mortality,” which suggests people with diabetes “may need to be especially cautious.”
Adds to existing literature; amputations begin with infections
Robert A. Gabbay, MD, PhD, chief scientific and medical officer for the American Diabetes Association (ADA), said the study “does add to the existing literature by having followed a larger number of people over time and linking them to serious complications from infections.”
“Sadly, we have seen this play out in real-time during the COVID-19 pandemic.”
“One of the sobering bits of data is the significant health disparities that exist in Black Americans and the fact that foot infections remain a significant problem,” he said in an interview.
“Given that amputation rates for [Black Americans] are three times higher than White Americans, amputations begin with infections,” Dr. Gabbay added, noting the ADA “has been taking a strong stand to prevent amputations and address the inequities in health that exist.”
Jamie Hartmann-Boyce, PhD, from the University of Oxford, U.K., who was not involved in the study, commented that diabetes is a “well-known risk factor for worse outcomes from all kinds of infection,” which is why they “are prioritized for flu vaccination every year.”
She told this news organization that the current study “further confirms that people with diabetes are more likely to be hospitalized for infection of any type and most markedly for foot infection.”
“These new data further highlight the need for public health interventions to prevent type 2 diabetes, and for preventive health care in people with diabetes, including access to diabetes medications and support and to vaccinations to prevent infection,” added Dr. Hartmann-Boyce, who is a senior research fellow in health behaviors.
Diabetes is thought to be associated with susceptibility to infection via mechanisms such as impaired neutrophil functioning and humoral immune responses, and studies have shown a link with both common and rare infections.
However, the authors point out that “most” of those included “small clinical populations and were cross-sectional or had short follow-up.”
Guidelines for diabetes management, they note, also “pay less attention” to infectious diseases than they do to the prevention of micro- and macrovascular complications.
ARIC data mined for infections in those with diabetes
The team analyzed data from the ongoing U.S. community-based Atherosclerosis Risk in Communities (ARIC) study.
The National Heart, Lung, and Blood Institute–sponsored cohort was comprised of adults aged 45-64 years from four U.S. communities, recruited between 1987 and 1989 for clinical examinations, medical interviews, and laboratory tests, repeated over five more visits up to 2018-2019.
For the current analysis, the team included 12,739 individuals with a mean age of 54.5 years, of whom 54.3% were female and 24.7% were Black.
Patients were defined as having diabetes if their baseline fasting blood glucose was greater than or equal to 7 mmol/L, or nonfasting glucose was greater than or equal to 11.1 mmol/l, they self-reported a diagnosis of diabetes by a physician, or they were taking glucose-lowering medication at the first study visit. The researchers weren’t able to distinguish between type 1 and type 2 diabetes.
In total, 1,485 individuals had diabetes at baseline. They were more likely to be older, Black, have a low socioeconomic status, and have worse cardiometabolic health than participants without diabetes.
Over an average follow-up of 23.8 years, there were 4,229 incident hospitalizations for infection, at an overall rate of 15.9 per 1,000 person-years.
Individuals with diabetes at baseline had a higher rate of hospitalizations than those without, at 25.4 per 1,000 person-years versus 15.2 per 1,000 person-years.
After taking into account sociodemographic characteristics, socioeconomic status, and cardiometabolic risk factors, this equated to a hazard ratio for hospitalization with any infection of 1.67 (P < .001).
The risk of hospitalization for any infection was significantly higher for younger patients with diabetes, defined as aged less than 55 years (P = .005), and for Black patients (P < .001).
While the increased risk was generally consistent across infection types, it was markedly increased for foot infection, at a hazard ratio of 5.99 (P < .001).
Overall, there were few deaths due to infection in the study, at just 362. The risk of infection mortality was nevertheless significantly increased in people with diabetes, at an adjusted hazard ratio of 1.72 (P < .001).
Dr. Fang has reported being supported by a grant from the National Institutes of Health/National Heart, Lung, and Blood Institute. Dr. Selvin has reported being supported by grants from the National Institutes of Health/National Heart, Lung, and Blood Institute and National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Selvin is an associate editor for Diabetologia and had no role in the peer review of the manuscript.
A version of this article first appeared on Medscape.com.
People with diabetes are at increased risk of hospitalization for infection, as well as infection-related mortality, shows a large U.S. study that suggests the risk is even higher in younger and Black individuals.
Michael Fang, PhD, Johns Hopkins University, Baltimore, and colleagues studied more than 12,000 participants in a community cohort study who were followed for an average of 24 years, between 1987-1989 and 2019.
Participants with diabetes faced a 67% increase risk of infection-related hospitalization, compared with those without diabetes.
Of particular note, the risk of hospitalization with foot infection was almost sixfold higher for people with diabetes than those without.
The research, published in Diabetologia on August 4, also suggests that diabetes may be associated with a 72% increased risk of infection-related mortality, although the absolute numbers were small.
Dr. Fang explained to this news organization that they focused on infection-related hospitalization and mortality “because these are comprehensively tracked in administrative data and ... are the most severe types of outcomes.”
However, this is probably just the tip of the iceberg, as people with diabetes are “likely at increased risk for milder infection too,” which can have a “significant adverse impact on people’s well-being and quality of life.”
As a result of their findings, the authors call for “broader guidance on infection prevention and management” in people with diabetes. To achieve this, Dr. Fang said, “we need to better understand why diabetes is associated with an increased risk of infection-related complications.”
“One likely factor is glycemic control: Emerging research suggests patients with diabetes with better glycemic control may be at significantly lower risk of infection-related complications.”
He continued that, in younger patients, a factor for worse outcomes could be that “diabetes tends to be more aggressive when it emerges early in life,” while in Black patients “there is research highlighting Black-White differences in glycemic control, access to care, and beliefs around vaccines.”
Overall, their findings – coupled with recent data showing that diabetes is an important risk factor for adverse outcomes with COVID-19 infection – paint “a common picture,” Dr. Fang said.
“People with diabetes are much more susceptible to infection-related complications, including COVID-related hospitalization and mortality,” which suggests people with diabetes “may need to be especially cautious.”
Adds to existing literature; amputations begin with infections
Robert A. Gabbay, MD, PhD, chief scientific and medical officer for the American Diabetes Association (ADA), said the study “does add to the existing literature by having followed a larger number of people over time and linking them to serious complications from infections.”
“Sadly, we have seen this play out in real-time during the COVID-19 pandemic.”
“One of the sobering bits of data is the significant health disparities that exist in Black Americans and the fact that foot infections remain a significant problem,” he said in an interview.
“Given that amputation rates for [Black Americans] are three times higher than White Americans, amputations begin with infections,” Dr. Gabbay added, noting the ADA “has been taking a strong stand to prevent amputations and address the inequities in health that exist.”
Jamie Hartmann-Boyce, PhD, from the University of Oxford, U.K., who was not involved in the study, commented that diabetes is a “well-known risk factor for worse outcomes from all kinds of infection,” which is why they “are prioritized for flu vaccination every year.”
She told this news organization that the current study “further confirms that people with diabetes are more likely to be hospitalized for infection of any type and most markedly for foot infection.”
“These new data further highlight the need for public health interventions to prevent type 2 diabetes, and for preventive health care in people with diabetes, including access to diabetes medications and support and to vaccinations to prevent infection,” added Dr. Hartmann-Boyce, who is a senior research fellow in health behaviors.
Diabetes is thought to be associated with susceptibility to infection via mechanisms such as impaired neutrophil functioning and humoral immune responses, and studies have shown a link with both common and rare infections.
However, the authors point out that “most” of those included “small clinical populations and were cross-sectional or had short follow-up.”
Guidelines for diabetes management, they note, also “pay less attention” to infectious diseases than they do to the prevention of micro- and macrovascular complications.
ARIC data mined for infections in those with diabetes
The team analyzed data from the ongoing U.S. community-based Atherosclerosis Risk in Communities (ARIC) study.
The National Heart, Lung, and Blood Institute–sponsored cohort was comprised of adults aged 45-64 years from four U.S. communities, recruited between 1987 and 1989 for clinical examinations, medical interviews, and laboratory tests, repeated over five more visits up to 2018-2019.
For the current analysis, the team included 12,739 individuals with a mean age of 54.5 years, of whom 54.3% were female and 24.7% were Black.
Patients were defined as having diabetes if their baseline fasting blood glucose was greater than or equal to 7 mmol/L, or nonfasting glucose was greater than or equal to 11.1 mmol/l, they self-reported a diagnosis of diabetes by a physician, or they were taking glucose-lowering medication at the first study visit. The researchers weren’t able to distinguish between type 1 and type 2 diabetes.
In total, 1,485 individuals had diabetes at baseline. They were more likely to be older, Black, have a low socioeconomic status, and have worse cardiometabolic health than participants without diabetes.
Over an average follow-up of 23.8 years, there were 4,229 incident hospitalizations for infection, at an overall rate of 15.9 per 1,000 person-years.
Individuals with diabetes at baseline had a higher rate of hospitalizations than those without, at 25.4 per 1,000 person-years versus 15.2 per 1,000 person-years.
After taking into account sociodemographic characteristics, socioeconomic status, and cardiometabolic risk factors, this equated to a hazard ratio for hospitalization with any infection of 1.67 (P < .001).
The risk of hospitalization for any infection was significantly higher for younger patients with diabetes, defined as aged less than 55 years (P = .005), and for Black patients (P < .001).
While the increased risk was generally consistent across infection types, it was markedly increased for foot infection, at a hazard ratio of 5.99 (P < .001).
Overall, there were few deaths due to infection in the study, at just 362. The risk of infection mortality was nevertheless significantly increased in people with diabetes, at an adjusted hazard ratio of 1.72 (P < .001).
Dr. Fang has reported being supported by a grant from the National Institutes of Health/National Heart, Lung, and Blood Institute. Dr. Selvin has reported being supported by grants from the National Institutes of Health/National Heart, Lung, and Blood Institute and National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Selvin is an associate editor for Diabetologia and had no role in the peer review of the manuscript.
A version of this article first appeared on Medscape.com.
People with diabetes are at increased risk of hospitalization for infection, as well as infection-related mortality, shows a large U.S. study that suggests the risk is even higher in younger and Black individuals.
Michael Fang, PhD, Johns Hopkins University, Baltimore, and colleagues studied more than 12,000 participants in a community cohort study who were followed for an average of 24 years, between 1987-1989 and 2019.
Participants with diabetes faced a 67% increase risk of infection-related hospitalization, compared with those without diabetes.
Of particular note, the risk of hospitalization with foot infection was almost sixfold higher for people with diabetes than those without.
The research, published in Diabetologia on August 4, also suggests that diabetes may be associated with a 72% increased risk of infection-related mortality, although the absolute numbers were small.
Dr. Fang explained to this news organization that they focused on infection-related hospitalization and mortality “because these are comprehensively tracked in administrative data and ... are the most severe types of outcomes.”
However, this is probably just the tip of the iceberg, as people with diabetes are “likely at increased risk for milder infection too,” which can have a “significant adverse impact on people’s well-being and quality of life.”
As a result of their findings, the authors call for “broader guidance on infection prevention and management” in people with diabetes. To achieve this, Dr. Fang said, “we need to better understand why diabetes is associated with an increased risk of infection-related complications.”
“One likely factor is glycemic control: Emerging research suggests patients with diabetes with better glycemic control may be at significantly lower risk of infection-related complications.”
He continued that, in younger patients, a factor for worse outcomes could be that “diabetes tends to be more aggressive when it emerges early in life,” while in Black patients “there is research highlighting Black-White differences in glycemic control, access to care, and beliefs around vaccines.”
Overall, their findings – coupled with recent data showing that diabetes is an important risk factor for adverse outcomes with COVID-19 infection – paint “a common picture,” Dr. Fang said.
“People with diabetes are much more susceptible to infection-related complications, including COVID-related hospitalization and mortality,” which suggests people with diabetes “may need to be especially cautious.”
Adds to existing literature; amputations begin with infections
Robert A. Gabbay, MD, PhD, chief scientific and medical officer for the American Diabetes Association (ADA), said the study “does add to the existing literature by having followed a larger number of people over time and linking them to serious complications from infections.”
“Sadly, we have seen this play out in real-time during the COVID-19 pandemic.”
“One of the sobering bits of data is the significant health disparities that exist in Black Americans and the fact that foot infections remain a significant problem,” he said in an interview.
“Given that amputation rates for [Black Americans] are three times higher than White Americans, amputations begin with infections,” Dr. Gabbay added, noting the ADA “has been taking a strong stand to prevent amputations and address the inequities in health that exist.”
Jamie Hartmann-Boyce, PhD, from the University of Oxford, U.K., who was not involved in the study, commented that diabetes is a “well-known risk factor for worse outcomes from all kinds of infection,” which is why they “are prioritized for flu vaccination every year.”
She told this news organization that the current study “further confirms that people with diabetes are more likely to be hospitalized for infection of any type and most markedly for foot infection.”
“These new data further highlight the need for public health interventions to prevent type 2 diabetes, and for preventive health care in people with diabetes, including access to diabetes medications and support and to vaccinations to prevent infection,” added Dr. Hartmann-Boyce, who is a senior research fellow in health behaviors.
Diabetes is thought to be associated with susceptibility to infection via mechanisms such as impaired neutrophil functioning and humoral immune responses, and studies have shown a link with both common and rare infections.
However, the authors point out that “most” of those included “small clinical populations and were cross-sectional or had short follow-up.”
Guidelines for diabetes management, they note, also “pay less attention” to infectious diseases than they do to the prevention of micro- and macrovascular complications.
ARIC data mined for infections in those with diabetes
The team analyzed data from the ongoing U.S. community-based Atherosclerosis Risk in Communities (ARIC) study.
The National Heart, Lung, and Blood Institute–sponsored cohort was comprised of adults aged 45-64 years from four U.S. communities, recruited between 1987 and 1989 for clinical examinations, medical interviews, and laboratory tests, repeated over five more visits up to 2018-2019.
For the current analysis, the team included 12,739 individuals with a mean age of 54.5 years, of whom 54.3% were female and 24.7% were Black.
Patients were defined as having diabetes if their baseline fasting blood glucose was greater than or equal to 7 mmol/L, or nonfasting glucose was greater than or equal to 11.1 mmol/l, they self-reported a diagnosis of diabetes by a physician, or they were taking glucose-lowering medication at the first study visit. The researchers weren’t able to distinguish between type 1 and type 2 diabetes.
In total, 1,485 individuals had diabetes at baseline. They were more likely to be older, Black, have a low socioeconomic status, and have worse cardiometabolic health than participants without diabetes.
Over an average follow-up of 23.8 years, there were 4,229 incident hospitalizations for infection, at an overall rate of 15.9 per 1,000 person-years.
Individuals with diabetes at baseline had a higher rate of hospitalizations than those without, at 25.4 per 1,000 person-years versus 15.2 per 1,000 person-years.
After taking into account sociodemographic characteristics, socioeconomic status, and cardiometabolic risk factors, this equated to a hazard ratio for hospitalization with any infection of 1.67 (P < .001).
The risk of hospitalization for any infection was significantly higher for younger patients with diabetes, defined as aged less than 55 years (P = .005), and for Black patients (P < .001).
While the increased risk was generally consistent across infection types, it was markedly increased for foot infection, at a hazard ratio of 5.99 (P < .001).
Overall, there were few deaths due to infection in the study, at just 362. The risk of infection mortality was nevertheless significantly increased in people with diabetes, at an adjusted hazard ratio of 1.72 (P < .001).
Dr. Fang has reported being supported by a grant from the National Institutes of Health/National Heart, Lung, and Blood Institute. Dr. Selvin has reported being supported by grants from the National Institutes of Health/National Heart, Lung, and Blood Institute and National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Selvin is an associate editor for Diabetologia and had no role in the peer review of the manuscript.
A version of this article first appeared on Medscape.com.
Microlearning during the pandemic
How to become a hospitalist
The vast amounts of information generated this past year related to the COVID-19 pandemic was a feat of wonder – recommendations and guidelines on the hospital level and on the national level came in a flurry, more often overwhelming and confusing than clarifying for the frontline provider. In addition, “routine” hospital care for non-infected patients and improvement processes had to continue as we all dealt with the whirlwind of increasing COVID cases, torrents of new guidelines, and educating our trainees.
Thus, the individual-level question: how does a clinician stay engaged and distill the relentless stream of new information?
In Spring 2020, when the first patients with COVID were admitted, our hospital medicine section was tasked to create a surge plan. This included organizing, orienting, and educating off-service providers on how to become hospitalists. Undoubtedly, the call to arms for our center was heard, and many responded. However, backgrounds were diverse in specialty – clinicians and trainees from psychiatry, general surgery, and various fellowships all answered. It was an exhausting and inefficient effort to produce the material, hold webinars, and schedule training, especially for those who were more removed from a hospital medicine experience. We knew we had to come up with an alternative plan moving forward.
Thus, the systems-level question: how does a health care system educate its clinicians, or any other health care providers, when reallocation of their talents and skills is both necessary, time-sensitive, and occuring during a period where new information is constantly being produced and changing?
To reach the most clinicians as possible, with the most succinct and distilled information, we had to come up with a method to do so. Ultimately, in considering the situation at hand, we had to understand who we were as the provider of the information, and who the recipient would be. We would like to share the initiatives and processes by which we constructed our solution to the two questions – microlearning through hospital podcasting.
Learning from our health care colleagues
With the initial webinars and training sessions for our staff, we assessed our learners’ motivations and background in managing in a hospital medicine capacity. Overall, we discovered that our trainees and clinicians have an innate drive to learn; all of them recognized the importance of keeping up with evidence-based information. However, the difficulty highlighted was the individual time available to dedicate to acquiring new information and awareness of new information being available to the health care sector during the chaotic times of the pandemic.
From our section’s perspective, we had a difficulty with coordinating among multiple professional development groups within our hospital, cost, and resources to execute training. These difficulties between providing knowledge and receiving knowledge have already been expertly analyzed.1
Parallel to this, the pedagogic paradigm shifts as we progress through our careers – the methods and skills we used in school contrast in many ways with those we use on a daily basis when it comes to learning. Instead of dedicating hours at a time to new challenges in our workflow or our interests, we watch videos, search retailers for product solutions, check our email correspondence, and peruse social media accounts several times a day. Information comes at us very quickly, but in small pieces.
One such innovation in pedagogy is the practice of microlearning. This refers to the use of small lesson modules and short-term activities intended to teach and reinforce concepts.2 It is the opposite of “macrolearning,” which is the principle of dedicating reading material, structured coursework, and traditional knowledge evaluation in the form of exams to reinforce learning. Certainly, microlearning has other names as well – “just-in-time,” “just-enough,” and “micro-courses” are a few synonyms seen in the current literature. Though a highly relevant concept for our situation, translating it to an endproduct for our trainees and clinicians required more thought.
From theory to application
Microlearning allows for faster delivery of information – fewer things to write means shorter course distribution times, allowing the learner to respond faster to changing educational goals and training demands. Microlearning is flexible – “micro-courses” can give a broad overview of a subject or cover complex topics broken down into simple parts. In addition, micro-learning promotes retention of key concepts – given the length of each lesson, repetition of the topic by the learner is possible at any point in time. The whole experience is similar to checking your favorite social media application on your smartphone.
Certainly, many examples of the application of microlearning are available in the health care sector – pharmaceutical and nursing training both have utilized the theory extensively.3-4 However, in many instances, individuals were still required to sit at a workstation to complete modules and lessons. We envisioned our application of microlearning to be “on-the-go,” without necessarily requiring a computer workstation or laptop to complete.
In thinking about how social media attracts and influences clinicians, many content creators on social media come to mind. In addition, most, if not all, have branched into various social media platforms – podcasting, blogging, YouTube, for example. In thinking about our colleagues and trainees, we wanted a platform that they could take on the go, without the need to focus their visual attention (such as while driving or running). Ultimately, we believe the podcast would be the best platform to disseminate our information.
Podcasting is not foreign to medicine. A variety of medical podcasts exist, whether produced by major medical journals or by various independent health care practitioners. Both, however, have their drawbacks – the podcasts created by major medical journals are typically a summary of the publication’s content and are less engaging. Alternatively, podcasts produced by independent creators are certainly engaging and entertaining, and have a wealth of information, but the line is often blurred between just that: education and entertainment. In both instances, there is no follow-up or feedback offered to the learner in the form of surveys, or other types of feedback, which is arguably an important piece in any form of pedagogy. Thus, we sought to strike a balance between the two forms for our purposes.
Process of two podcasts
Our section was aware of the two aims during the pandemic – (1) disseminate new information regarding COVID-19 to the rest of our staff members and trainees as quickly as possible, and (2) maintain and improve the current quality of care of our patients. Thus, we sought to apply the reach and efficiency of the podcasting medium to provide ongoing education and feedback with respect to these two aims.
“The Cure” podcast. We recognized the constant flow of new COVID-19 information and updates and we wanted to find a readily accessible platform to reach staff with timely updates. Our marketing & communications team later helped us realize that the content we wanted to share was relevant to our patients and the community, so we formatted the material to be practical and easily digestible- something that may help an individual make decisions at the bedside as well as have conversations at the dinner table. Most recently, we engaged with our human resources department to use our platform in orienting new hires with the goal of helping staff familiarize with the institutions policies, procedures, and job aids that keep staff and patients safe.
“Antibiotry” podcast. Prior to the COVID-19 pandemic, our antibiotic stewardship group noticed an increase in antibiotic use on our medical floors. This is monitored not only through internal metrics by our pharmacy department, but also via the SAAR (standardized antibiotic administration ratio). Both sources demonstrated an increase in antibiotic use, greater than expected. An initiative was formed between our hospital medicine and infectious disease sections, and our pharmacy department to raise awareness of this increase in use, provide education to our trainees, and to create systems solutions for clinicians.
Initially, we sought to hold in-person sessions once a month for our trainees. This was led by a senior resident at the time. Topics of discussion were geared towards clinical decision making regarding empiric antibiotic use on the hospital medicine service. At the same time, our team published empiric antibiotic use guidelines, accessible through our electronic medical record. In addition, the resident leader gave a voluntary survey at the end of the session to assess not only confidence of antibiotic use, but also baseline knowledge regarding antibiotics in various clinical scenarios. This survey was repeated at the end of the resident group’s month-long rotation. Altogether, each in-person session was no longer than 10 minutes.
Unfortunately, the initiative was just gaining momentum when the COVID-19 pandemic was declared. However, we sought to take this challenge and translate it into an opportunity.
We directed our focus towards stewardship during pandemic times. Initially, our resident leader sent out email primers, approximately 3-5 minute reads, as a substitute for the in-person sessions. Our primers’ uniqueness was in its incorporation of prescription pattern data that was developed by our resident leader and our initiative’s data analyst. In doing so, we provided professional feedback regarding our antibiotic use based on the clinical indication. This was a powerful tool to not only engage our learners and staff clinicians, but also as a benchmarking tool for continued quality improvement.
But email primers are not engaging, and despite the ubiquity of teleconferencing, it was difficult to ask our housestaff to break from their morning rounds for a 10 minute tele-meeting. Thus, we devised a podcast method of education – 5-10 minute audio clips with conversation regarding a topic of discussion. This way, our trainees and learners can access episodes of education on their own time throughout the pandemic without disrupting their workflow. Given the brevity of, but high-yield content in, each episode, it would not only be convenient for listeners to access and repeat, but also for the podcaster (our resident leader) to create, as recording of the audio portion takes anywhere between 10-20 minutes for each episode, with postprocessing similarly fast.
The interdisciplinary nature of continued medical education cannot be stressed enough. With the help of our professional development team and their educators, we were able to centralize our podcast and attach surveys and additional graphics for each episode, if appropriate. This additional detail allowed for feedback, engagement with our learners, and the chance to provide additional educational points, if the learner was interested. Given the integrated nature of this platform, quality metrics could easily be recorded in the form of “click” data and various other more conventional metrics, such as listener counts and the duration of each podcast played.
Future applications and initiatives
Thus far, we have had great success in the reception and use of both podcasts within our institution as an application of microlearning. “The Cure” has been widely listened to by all hospital staff from various services; it has caught the attention of state-wide radio programs, and plans to expand it into the community are being discussed.
As for “Antibiotry” podcast, the concept has been lauded by our medical educators. Given its centralization within our institution, we are able to publish institution-based data as a form of professional and educational feedback to our trainees and staff physicians. This is currently coupled with the development of a provider dashboard, visualizing antibiotic prescriptions and narrowing patterns of practice within our medicine department. We plan to expand “Antibiotry” to other services at the hospital.
For both podcasts, the steps it took to achieve the final product from the microlearning concept were possible through a combination of institutional need and a motivated team. We are fortunate to have highly energetic individuals, making the coordination and planning with our hospitalists, various sub-specialists, and professional development teams straightforward. As the team grows with more individuals interested in the initiatives, keen insight into interests, individual clinical expertise, presentation skills, and technical skills ought to be carefully weighed to sustain our podcasts most efficiently, and perhaps expand them through different social media platforms.
Our objective for sustainability is through the continued outreach to and recruitment of residents and medical students, who can play key roles in the development of future projects related to these educational innovations. Both microlearning podcasts were developed through the initial planning, trial and error, and execution by two resident leaders. Their initiative and motivation to educate our institution through these platforms were highly unique; their pathfinding set the foundation for sustainability and expansion to other services.
Of course, one of the key measures we would like to investigate is whether our microlearning platform translates to improved patient outcomes. Regarding “Antibiotry,” we hope to see a decrease in unnecessary broad-spectrum antibiotic use by drawing attention to clinician practice patterns. Quality and outcome metrics will continue to be developed and measured. In addition to patient care metrics, further investigation of pedagogical metrics will be conducted, especially in the evolving realm of graduate and continuing medical education.
Measuring educational quality is neither a new ethical nor philosophical debate – neither does it carry a definitive answer. Further help from education experts may be needed to assess the quality of the information provided and its impact on our learners.
Conclusion
Medicine is ever-changing – the guidelines and criteria for patient care and pathology that we learned in medical school have likely changed. There is no single “best” method of learning new information in medicine, simply due to the breadth and volume of such information generated on a daily basis. This poses both a challenge for present-day clinicians and trainees, and a stimulus for change in the methods of acquiring, absorbing, and applying new information to clinical decision making and practice.
We have found that podcasting is a well-received medium of information transfer that is convenient for both the learner and the content creator. Through the podcast format, we were able to distill non-engaging pieces of education and information and transform them into short-duration lessons that the learner can listen to at their own convenience. This proved to be especially handy during the chaos of the pandemic, not only for dissemination of information regarding the management of COVID-19, but also for sustaining quality improvement goals within our institution.
Further investigation on patient outcomes and information quality are the planned next steps. In addition, expansion of other microlearning media, such as group SMS texting, YouTube videos, and Twitter, ought to be considered. Though many publications discuss the theory, potential benefits, and predicted pitfalls of microlearning, few assess the real-world application of microlearning to the clinical setting for medical education.
So what did we learn? We should think of microlearning as moments when you turn to your smartphone or tablet in order to discover something, answer a question, or complete a task. These are moments when decisions are made and knowledge is reinforced. The goal is to capture these moments and fill them with essential pieces of information.
We offer these suggestions as a place to start. The microlearning platform allows for the collection of data on the interaction between user and course content. The data collected can be used for continuous quality improvement of the curriculum. Microlearning is a dynamic platform where creative ideas are encouraged and a multi-disciplinary approach is valuable to keeping an audience engaged. In the future, we hope to be able to correlate microlearning courses to provider performance and measurable patient outcomes.
Dr. Mercado is medical director at Alice Peck Day Memorial Hospital, and associate hospital epidemiologist, Dartmouth-Hitchcock Medical Center, both in Lebanon, N.H., and assistant professor at the Geisel School of Medicine at Dartmouth, Hanover, N.H. Dr. Feng is a Fellow in the Leadership/Preventive Medicine Program in the Department of Internal Medicine at Dartmouth-Hitchcock Medical Center.
References
1. Duggan F and Banwell L. Constructing a model of effective information dissemination in a crisis. Information Research. 2004;9(3). Paper 178 [Available at http://InformationR.net/ir/9-3/paper178.html].
2. Filipe HP, et al. Microlearning to improve CPD learning objectives. Clin Teach. 2020 Dec;17(6):695-699. doi: 10.1111/tct.13208.
3. Hegerius A, et al. E-Learning in Pharmacovigilance: An Evaluation of Microlearning-Based Modules Developed by Uppsala Monitoring Centre. Drug Saf. 2020 Nov;43(11):1171-1180. doi: 10.1007/s40264-020-00981-w.
4. Orwoll B, et al. Gamification and Microlearning for Engagement With Quality Improvement (GAMEQI): A Bundled Digital Intervention for the Prevention of Central Line-Associated Bloodstream Infection. Am J Med Qual. Jan/Feb 2018;33(1):21-29. doi: 10.1177/1062860617706542.
How to become a hospitalist
How to become a hospitalist
The vast amounts of information generated this past year related to the COVID-19 pandemic was a feat of wonder – recommendations and guidelines on the hospital level and on the national level came in a flurry, more often overwhelming and confusing than clarifying for the frontline provider. In addition, “routine” hospital care for non-infected patients and improvement processes had to continue as we all dealt with the whirlwind of increasing COVID cases, torrents of new guidelines, and educating our trainees.
Thus, the individual-level question: how does a clinician stay engaged and distill the relentless stream of new information?
In Spring 2020, when the first patients with COVID were admitted, our hospital medicine section was tasked to create a surge plan. This included organizing, orienting, and educating off-service providers on how to become hospitalists. Undoubtedly, the call to arms for our center was heard, and many responded. However, backgrounds were diverse in specialty – clinicians and trainees from psychiatry, general surgery, and various fellowships all answered. It was an exhausting and inefficient effort to produce the material, hold webinars, and schedule training, especially for those who were more removed from a hospital medicine experience. We knew we had to come up with an alternative plan moving forward.
Thus, the systems-level question: how does a health care system educate its clinicians, or any other health care providers, when reallocation of their talents and skills is both necessary, time-sensitive, and occuring during a period where new information is constantly being produced and changing?
To reach the most clinicians as possible, with the most succinct and distilled information, we had to come up with a method to do so. Ultimately, in considering the situation at hand, we had to understand who we were as the provider of the information, and who the recipient would be. We would like to share the initiatives and processes by which we constructed our solution to the two questions – microlearning through hospital podcasting.
Learning from our health care colleagues
With the initial webinars and training sessions for our staff, we assessed our learners’ motivations and background in managing in a hospital medicine capacity. Overall, we discovered that our trainees and clinicians have an innate drive to learn; all of them recognized the importance of keeping up with evidence-based information. However, the difficulty highlighted was the individual time available to dedicate to acquiring new information and awareness of new information being available to the health care sector during the chaotic times of the pandemic.
From our section’s perspective, we had a difficulty with coordinating among multiple professional development groups within our hospital, cost, and resources to execute training. These difficulties between providing knowledge and receiving knowledge have already been expertly analyzed.1
Parallel to this, the pedagogic paradigm shifts as we progress through our careers – the methods and skills we used in school contrast in many ways with those we use on a daily basis when it comes to learning. Instead of dedicating hours at a time to new challenges in our workflow or our interests, we watch videos, search retailers for product solutions, check our email correspondence, and peruse social media accounts several times a day. Information comes at us very quickly, but in small pieces.
One such innovation in pedagogy is the practice of microlearning. This refers to the use of small lesson modules and short-term activities intended to teach and reinforce concepts.2 It is the opposite of “macrolearning,” which is the principle of dedicating reading material, structured coursework, and traditional knowledge evaluation in the form of exams to reinforce learning. Certainly, microlearning has other names as well – “just-in-time,” “just-enough,” and “micro-courses” are a few synonyms seen in the current literature. Though a highly relevant concept for our situation, translating it to an endproduct for our trainees and clinicians required more thought.
From theory to application
Microlearning allows for faster delivery of information – fewer things to write means shorter course distribution times, allowing the learner to respond faster to changing educational goals and training demands. Microlearning is flexible – “micro-courses” can give a broad overview of a subject or cover complex topics broken down into simple parts. In addition, micro-learning promotes retention of key concepts – given the length of each lesson, repetition of the topic by the learner is possible at any point in time. The whole experience is similar to checking your favorite social media application on your smartphone.
Certainly, many examples of the application of microlearning are available in the health care sector – pharmaceutical and nursing training both have utilized the theory extensively.3-4 However, in many instances, individuals were still required to sit at a workstation to complete modules and lessons. We envisioned our application of microlearning to be “on-the-go,” without necessarily requiring a computer workstation or laptop to complete.
In thinking about how social media attracts and influences clinicians, many content creators on social media come to mind. In addition, most, if not all, have branched into various social media platforms – podcasting, blogging, YouTube, for example. In thinking about our colleagues and trainees, we wanted a platform that they could take on the go, without the need to focus their visual attention (such as while driving or running). Ultimately, we believe the podcast would be the best platform to disseminate our information.
Podcasting is not foreign to medicine. A variety of medical podcasts exist, whether produced by major medical journals or by various independent health care practitioners. Both, however, have their drawbacks – the podcasts created by major medical journals are typically a summary of the publication’s content and are less engaging. Alternatively, podcasts produced by independent creators are certainly engaging and entertaining, and have a wealth of information, but the line is often blurred between just that: education and entertainment. In both instances, there is no follow-up or feedback offered to the learner in the form of surveys, or other types of feedback, which is arguably an important piece in any form of pedagogy. Thus, we sought to strike a balance between the two forms for our purposes.
Process of two podcasts
Our section was aware of the two aims during the pandemic – (1) disseminate new information regarding COVID-19 to the rest of our staff members and trainees as quickly as possible, and (2) maintain and improve the current quality of care of our patients. Thus, we sought to apply the reach and efficiency of the podcasting medium to provide ongoing education and feedback with respect to these two aims.
“The Cure” podcast. We recognized the constant flow of new COVID-19 information and updates and we wanted to find a readily accessible platform to reach staff with timely updates. Our marketing & communications team later helped us realize that the content we wanted to share was relevant to our patients and the community, so we formatted the material to be practical and easily digestible- something that may help an individual make decisions at the bedside as well as have conversations at the dinner table. Most recently, we engaged with our human resources department to use our platform in orienting new hires with the goal of helping staff familiarize with the institutions policies, procedures, and job aids that keep staff and patients safe.
“Antibiotry” podcast. Prior to the COVID-19 pandemic, our antibiotic stewardship group noticed an increase in antibiotic use on our medical floors. This is monitored not only through internal metrics by our pharmacy department, but also via the SAAR (standardized antibiotic administration ratio). Both sources demonstrated an increase in antibiotic use, greater than expected. An initiative was formed between our hospital medicine and infectious disease sections, and our pharmacy department to raise awareness of this increase in use, provide education to our trainees, and to create systems solutions for clinicians.
Initially, we sought to hold in-person sessions once a month for our trainees. This was led by a senior resident at the time. Topics of discussion were geared towards clinical decision making regarding empiric antibiotic use on the hospital medicine service. At the same time, our team published empiric antibiotic use guidelines, accessible through our electronic medical record. In addition, the resident leader gave a voluntary survey at the end of the session to assess not only confidence of antibiotic use, but also baseline knowledge regarding antibiotics in various clinical scenarios. This survey was repeated at the end of the resident group’s month-long rotation. Altogether, each in-person session was no longer than 10 minutes.
Unfortunately, the initiative was just gaining momentum when the COVID-19 pandemic was declared. However, we sought to take this challenge and translate it into an opportunity.
We directed our focus towards stewardship during pandemic times. Initially, our resident leader sent out email primers, approximately 3-5 minute reads, as a substitute for the in-person sessions. Our primers’ uniqueness was in its incorporation of prescription pattern data that was developed by our resident leader and our initiative’s data analyst. In doing so, we provided professional feedback regarding our antibiotic use based on the clinical indication. This was a powerful tool to not only engage our learners and staff clinicians, but also as a benchmarking tool for continued quality improvement.
But email primers are not engaging, and despite the ubiquity of teleconferencing, it was difficult to ask our housestaff to break from their morning rounds for a 10 minute tele-meeting. Thus, we devised a podcast method of education – 5-10 minute audio clips with conversation regarding a topic of discussion. This way, our trainees and learners can access episodes of education on their own time throughout the pandemic without disrupting their workflow. Given the brevity of, but high-yield content in, each episode, it would not only be convenient for listeners to access and repeat, but also for the podcaster (our resident leader) to create, as recording of the audio portion takes anywhere between 10-20 minutes for each episode, with postprocessing similarly fast.
The interdisciplinary nature of continued medical education cannot be stressed enough. With the help of our professional development team and their educators, we were able to centralize our podcast and attach surveys and additional graphics for each episode, if appropriate. This additional detail allowed for feedback, engagement with our learners, and the chance to provide additional educational points, if the learner was interested. Given the integrated nature of this platform, quality metrics could easily be recorded in the form of “click” data and various other more conventional metrics, such as listener counts and the duration of each podcast played.
Future applications and initiatives
Thus far, we have had great success in the reception and use of both podcasts within our institution as an application of microlearning. “The Cure” has been widely listened to by all hospital staff from various services; it has caught the attention of state-wide radio programs, and plans to expand it into the community are being discussed.
As for “Antibiotry” podcast, the concept has been lauded by our medical educators. Given its centralization within our institution, we are able to publish institution-based data as a form of professional and educational feedback to our trainees and staff physicians. This is currently coupled with the development of a provider dashboard, visualizing antibiotic prescriptions and narrowing patterns of practice within our medicine department. We plan to expand “Antibiotry” to other services at the hospital.
For both podcasts, the steps it took to achieve the final product from the microlearning concept were possible through a combination of institutional need and a motivated team. We are fortunate to have highly energetic individuals, making the coordination and planning with our hospitalists, various sub-specialists, and professional development teams straightforward. As the team grows with more individuals interested in the initiatives, keen insight into interests, individual clinical expertise, presentation skills, and technical skills ought to be carefully weighed to sustain our podcasts most efficiently, and perhaps expand them through different social media platforms.
Our objective for sustainability is through the continued outreach to and recruitment of residents and medical students, who can play key roles in the development of future projects related to these educational innovations. Both microlearning podcasts were developed through the initial planning, trial and error, and execution by two resident leaders. Their initiative and motivation to educate our institution through these platforms were highly unique; their pathfinding set the foundation for sustainability and expansion to other services.
Of course, one of the key measures we would like to investigate is whether our microlearning platform translates to improved patient outcomes. Regarding “Antibiotry,” we hope to see a decrease in unnecessary broad-spectrum antibiotic use by drawing attention to clinician practice patterns. Quality and outcome metrics will continue to be developed and measured. In addition to patient care metrics, further investigation of pedagogical metrics will be conducted, especially in the evolving realm of graduate and continuing medical education.
Measuring educational quality is neither a new ethical nor philosophical debate – neither does it carry a definitive answer. Further help from education experts may be needed to assess the quality of the information provided and its impact on our learners.
Conclusion
Medicine is ever-changing – the guidelines and criteria for patient care and pathology that we learned in medical school have likely changed. There is no single “best” method of learning new information in medicine, simply due to the breadth and volume of such information generated on a daily basis. This poses both a challenge for present-day clinicians and trainees, and a stimulus for change in the methods of acquiring, absorbing, and applying new information to clinical decision making and practice.
We have found that podcasting is a well-received medium of information transfer that is convenient for both the learner and the content creator. Through the podcast format, we were able to distill non-engaging pieces of education and information and transform them into short-duration lessons that the learner can listen to at their own convenience. This proved to be especially handy during the chaos of the pandemic, not only for dissemination of information regarding the management of COVID-19, but also for sustaining quality improvement goals within our institution.
Further investigation on patient outcomes and information quality are the planned next steps. In addition, expansion of other microlearning media, such as group SMS texting, YouTube videos, and Twitter, ought to be considered. Though many publications discuss the theory, potential benefits, and predicted pitfalls of microlearning, few assess the real-world application of microlearning to the clinical setting for medical education.
So what did we learn? We should think of microlearning as moments when you turn to your smartphone or tablet in order to discover something, answer a question, or complete a task. These are moments when decisions are made and knowledge is reinforced. The goal is to capture these moments and fill them with essential pieces of information.
We offer these suggestions as a place to start. The microlearning platform allows for the collection of data on the interaction between user and course content. The data collected can be used for continuous quality improvement of the curriculum. Microlearning is a dynamic platform where creative ideas are encouraged and a multi-disciplinary approach is valuable to keeping an audience engaged. In the future, we hope to be able to correlate microlearning courses to provider performance and measurable patient outcomes.
Dr. Mercado is medical director at Alice Peck Day Memorial Hospital, and associate hospital epidemiologist, Dartmouth-Hitchcock Medical Center, both in Lebanon, N.H., and assistant professor at the Geisel School of Medicine at Dartmouth, Hanover, N.H. Dr. Feng is a Fellow in the Leadership/Preventive Medicine Program in the Department of Internal Medicine at Dartmouth-Hitchcock Medical Center.
References
1. Duggan F and Banwell L. Constructing a model of effective information dissemination in a crisis. Information Research. 2004;9(3). Paper 178 [Available at http://InformationR.net/ir/9-3/paper178.html].
2. Filipe HP, et al. Microlearning to improve CPD learning objectives. Clin Teach. 2020 Dec;17(6):695-699. doi: 10.1111/tct.13208.
3. Hegerius A, et al. E-Learning in Pharmacovigilance: An Evaluation of Microlearning-Based Modules Developed by Uppsala Monitoring Centre. Drug Saf. 2020 Nov;43(11):1171-1180. doi: 10.1007/s40264-020-00981-w.
4. Orwoll B, et al. Gamification and Microlearning for Engagement With Quality Improvement (GAMEQI): A Bundled Digital Intervention for the Prevention of Central Line-Associated Bloodstream Infection. Am J Med Qual. Jan/Feb 2018;33(1):21-29. doi: 10.1177/1062860617706542.
The vast amounts of information generated this past year related to the COVID-19 pandemic was a feat of wonder – recommendations and guidelines on the hospital level and on the national level came in a flurry, more often overwhelming and confusing than clarifying for the frontline provider. In addition, “routine” hospital care for non-infected patients and improvement processes had to continue as we all dealt with the whirlwind of increasing COVID cases, torrents of new guidelines, and educating our trainees.
Thus, the individual-level question: how does a clinician stay engaged and distill the relentless stream of new information?
In Spring 2020, when the first patients with COVID were admitted, our hospital medicine section was tasked to create a surge plan. This included organizing, orienting, and educating off-service providers on how to become hospitalists. Undoubtedly, the call to arms for our center was heard, and many responded. However, backgrounds were diverse in specialty – clinicians and trainees from psychiatry, general surgery, and various fellowships all answered. It was an exhausting and inefficient effort to produce the material, hold webinars, and schedule training, especially for those who were more removed from a hospital medicine experience. We knew we had to come up with an alternative plan moving forward.
Thus, the systems-level question: how does a health care system educate its clinicians, or any other health care providers, when reallocation of their talents and skills is both necessary, time-sensitive, and occuring during a period where new information is constantly being produced and changing?
To reach the most clinicians as possible, with the most succinct and distilled information, we had to come up with a method to do so. Ultimately, in considering the situation at hand, we had to understand who we were as the provider of the information, and who the recipient would be. We would like to share the initiatives and processes by which we constructed our solution to the two questions – microlearning through hospital podcasting.
Learning from our health care colleagues
With the initial webinars and training sessions for our staff, we assessed our learners’ motivations and background in managing in a hospital medicine capacity. Overall, we discovered that our trainees and clinicians have an innate drive to learn; all of them recognized the importance of keeping up with evidence-based information. However, the difficulty highlighted was the individual time available to dedicate to acquiring new information and awareness of new information being available to the health care sector during the chaotic times of the pandemic.
From our section’s perspective, we had a difficulty with coordinating among multiple professional development groups within our hospital, cost, and resources to execute training. These difficulties between providing knowledge and receiving knowledge have already been expertly analyzed.1
Parallel to this, the pedagogic paradigm shifts as we progress through our careers – the methods and skills we used in school contrast in many ways with those we use on a daily basis when it comes to learning. Instead of dedicating hours at a time to new challenges in our workflow or our interests, we watch videos, search retailers for product solutions, check our email correspondence, and peruse social media accounts several times a day. Information comes at us very quickly, but in small pieces.
One such innovation in pedagogy is the practice of microlearning. This refers to the use of small lesson modules and short-term activities intended to teach and reinforce concepts.2 It is the opposite of “macrolearning,” which is the principle of dedicating reading material, structured coursework, and traditional knowledge evaluation in the form of exams to reinforce learning. Certainly, microlearning has other names as well – “just-in-time,” “just-enough,” and “micro-courses” are a few synonyms seen in the current literature. Though a highly relevant concept for our situation, translating it to an endproduct for our trainees and clinicians required more thought.
From theory to application
Microlearning allows for faster delivery of information – fewer things to write means shorter course distribution times, allowing the learner to respond faster to changing educational goals and training demands. Microlearning is flexible – “micro-courses” can give a broad overview of a subject or cover complex topics broken down into simple parts. In addition, micro-learning promotes retention of key concepts – given the length of each lesson, repetition of the topic by the learner is possible at any point in time. The whole experience is similar to checking your favorite social media application on your smartphone.
Certainly, many examples of the application of microlearning are available in the health care sector – pharmaceutical and nursing training both have utilized the theory extensively.3-4 However, in many instances, individuals were still required to sit at a workstation to complete modules and lessons. We envisioned our application of microlearning to be “on-the-go,” without necessarily requiring a computer workstation or laptop to complete.
In thinking about how social media attracts and influences clinicians, many content creators on social media come to mind. In addition, most, if not all, have branched into various social media platforms – podcasting, blogging, YouTube, for example. In thinking about our colleagues and trainees, we wanted a platform that they could take on the go, without the need to focus their visual attention (such as while driving or running). Ultimately, we believe the podcast would be the best platform to disseminate our information.
Podcasting is not foreign to medicine. A variety of medical podcasts exist, whether produced by major medical journals or by various independent health care practitioners. Both, however, have their drawbacks – the podcasts created by major medical journals are typically a summary of the publication’s content and are less engaging. Alternatively, podcasts produced by independent creators are certainly engaging and entertaining, and have a wealth of information, but the line is often blurred between just that: education and entertainment. In both instances, there is no follow-up or feedback offered to the learner in the form of surveys, or other types of feedback, which is arguably an important piece in any form of pedagogy. Thus, we sought to strike a balance between the two forms for our purposes.
Process of two podcasts
Our section was aware of the two aims during the pandemic – (1) disseminate new information regarding COVID-19 to the rest of our staff members and trainees as quickly as possible, and (2) maintain and improve the current quality of care of our patients. Thus, we sought to apply the reach and efficiency of the podcasting medium to provide ongoing education and feedback with respect to these two aims.
“The Cure” podcast. We recognized the constant flow of new COVID-19 information and updates and we wanted to find a readily accessible platform to reach staff with timely updates. Our marketing & communications team later helped us realize that the content we wanted to share was relevant to our patients and the community, so we formatted the material to be practical and easily digestible- something that may help an individual make decisions at the bedside as well as have conversations at the dinner table. Most recently, we engaged with our human resources department to use our platform in orienting new hires with the goal of helping staff familiarize with the institutions policies, procedures, and job aids that keep staff and patients safe.
“Antibiotry” podcast. Prior to the COVID-19 pandemic, our antibiotic stewardship group noticed an increase in antibiotic use on our medical floors. This is monitored not only through internal metrics by our pharmacy department, but also via the SAAR (standardized antibiotic administration ratio). Both sources demonstrated an increase in antibiotic use, greater than expected. An initiative was formed between our hospital medicine and infectious disease sections, and our pharmacy department to raise awareness of this increase in use, provide education to our trainees, and to create systems solutions for clinicians.
Initially, we sought to hold in-person sessions once a month for our trainees. This was led by a senior resident at the time. Topics of discussion were geared towards clinical decision making regarding empiric antibiotic use on the hospital medicine service. At the same time, our team published empiric antibiotic use guidelines, accessible through our electronic medical record. In addition, the resident leader gave a voluntary survey at the end of the session to assess not only confidence of antibiotic use, but also baseline knowledge regarding antibiotics in various clinical scenarios. This survey was repeated at the end of the resident group’s month-long rotation. Altogether, each in-person session was no longer than 10 minutes.
Unfortunately, the initiative was just gaining momentum when the COVID-19 pandemic was declared. However, we sought to take this challenge and translate it into an opportunity.
We directed our focus towards stewardship during pandemic times. Initially, our resident leader sent out email primers, approximately 3-5 minute reads, as a substitute for the in-person sessions. Our primers’ uniqueness was in its incorporation of prescription pattern data that was developed by our resident leader and our initiative’s data analyst. In doing so, we provided professional feedback regarding our antibiotic use based on the clinical indication. This was a powerful tool to not only engage our learners and staff clinicians, but also as a benchmarking tool for continued quality improvement.
But email primers are not engaging, and despite the ubiquity of teleconferencing, it was difficult to ask our housestaff to break from their morning rounds for a 10 minute tele-meeting. Thus, we devised a podcast method of education – 5-10 minute audio clips with conversation regarding a topic of discussion. This way, our trainees and learners can access episodes of education on their own time throughout the pandemic without disrupting their workflow. Given the brevity of, but high-yield content in, each episode, it would not only be convenient for listeners to access and repeat, but also for the podcaster (our resident leader) to create, as recording of the audio portion takes anywhere between 10-20 minutes for each episode, with postprocessing similarly fast.
The interdisciplinary nature of continued medical education cannot be stressed enough. With the help of our professional development team and their educators, we were able to centralize our podcast and attach surveys and additional graphics for each episode, if appropriate. This additional detail allowed for feedback, engagement with our learners, and the chance to provide additional educational points, if the learner was interested. Given the integrated nature of this platform, quality metrics could easily be recorded in the form of “click” data and various other more conventional metrics, such as listener counts and the duration of each podcast played.
Future applications and initiatives
Thus far, we have had great success in the reception and use of both podcasts within our institution as an application of microlearning. “The Cure” has been widely listened to by all hospital staff from various services; it has caught the attention of state-wide radio programs, and plans to expand it into the community are being discussed.
As for “Antibiotry” podcast, the concept has been lauded by our medical educators. Given its centralization within our institution, we are able to publish institution-based data as a form of professional and educational feedback to our trainees and staff physicians. This is currently coupled with the development of a provider dashboard, visualizing antibiotic prescriptions and narrowing patterns of practice within our medicine department. We plan to expand “Antibiotry” to other services at the hospital.
For both podcasts, the steps it took to achieve the final product from the microlearning concept were possible through a combination of institutional need and a motivated team. We are fortunate to have highly energetic individuals, making the coordination and planning with our hospitalists, various sub-specialists, and professional development teams straightforward. As the team grows with more individuals interested in the initiatives, keen insight into interests, individual clinical expertise, presentation skills, and technical skills ought to be carefully weighed to sustain our podcasts most efficiently, and perhaps expand them through different social media platforms.
Our objective for sustainability is through the continued outreach to and recruitment of residents and medical students, who can play key roles in the development of future projects related to these educational innovations. Both microlearning podcasts were developed through the initial planning, trial and error, and execution by two resident leaders. Their initiative and motivation to educate our institution through these platforms were highly unique; their pathfinding set the foundation for sustainability and expansion to other services.
Of course, one of the key measures we would like to investigate is whether our microlearning platform translates to improved patient outcomes. Regarding “Antibiotry,” we hope to see a decrease in unnecessary broad-spectrum antibiotic use by drawing attention to clinician practice patterns. Quality and outcome metrics will continue to be developed and measured. In addition to patient care metrics, further investigation of pedagogical metrics will be conducted, especially in the evolving realm of graduate and continuing medical education.
Measuring educational quality is neither a new ethical nor philosophical debate – neither does it carry a definitive answer. Further help from education experts may be needed to assess the quality of the information provided and its impact on our learners.
Conclusion
Medicine is ever-changing – the guidelines and criteria for patient care and pathology that we learned in medical school have likely changed. There is no single “best” method of learning new information in medicine, simply due to the breadth and volume of such information generated on a daily basis. This poses both a challenge for present-day clinicians and trainees, and a stimulus for change in the methods of acquiring, absorbing, and applying new information to clinical decision making and practice.
We have found that podcasting is a well-received medium of information transfer that is convenient for both the learner and the content creator. Through the podcast format, we were able to distill non-engaging pieces of education and information and transform them into short-duration lessons that the learner can listen to at their own convenience. This proved to be especially handy during the chaos of the pandemic, not only for dissemination of information regarding the management of COVID-19, but also for sustaining quality improvement goals within our institution.
Further investigation on patient outcomes and information quality are the planned next steps. In addition, expansion of other microlearning media, such as group SMS texting, YouTube videos, and Twitter, ought to be considered. Though many publications discuss the theory, potential benefits, and predicted pitfalls of microlearning, few assess the real-world application of microlearning to the clinical setting for medical education.
So what did we learn? We should think of microlearning as moments when you turn to your smartphone or tablet in order to discover something, answer a question, or complete a task. These are moments when decisions are made and knowledge is reinforced. The goal is to capture these moments and fill them with essential pieces of information.
We offer these suggestions as a place to start. The microlearning platform allows for the collection of data on the interaction between user and course content. The data collected can be used for continuous quality improvement of the curriculum. Microlearning is a dynamic platform where creative ideas are encouraged and a multi-disciplinary approach is valuable to keeping an audience engaged. In the future, we hope to be able to correlate microlearning courses to provider performance and measurable patient outcomes.
Dr. Mercado is medical director at Alice Peck Day Memorial Hospital, and associate hospital epidemiologist, Dartmouth-Hitchcock Medical Center, both in Lebanon, N.H., and assistant professor at the Geisel School of Medicine at Dartmouth, Hanover, N.H. Dr. Feng is a Fellow in the Leadership/Preventive Medicine Program in the Department of Internal Medicine at Dartmouth-Hitchcock Medical Center.
References
1. Duggan F and Banwell L. Constructing a model of effective information dissemination in a crisis. Information Research. 2004;9(3). Paper 178 [Available at http://InformationR.net/ir/9-3/paper178.html].
2. Filipe HP, et al. Microlearning to improve CPD learning objectives. Clin Teach. 2020 Dec;17(6):695-699. doi: 10.1111/tct.13208.
3. Hegerius A, et al. E-Learning in Pharmacovigilance: An Evaluation of Microlearning-Based Modules Developed by Uppsala Monitoring Centre. Drug Saf. 2020 Nov;43(11):1171-1180. doi: 10.1007/s40264-020-00981-w.
4. Orwoll B, et al. Gamification and Microlearning for Engagement With Quality Improvement (GAMEQI): A Bundled Digital Intervention for the Prevention of Central Line-Associated Bloodstream Infection. Am J Med Qual. Jan/Feb 2018;33(1):21-29. doi: 10.1177/1062860617706542.
Fauci says ‘unprecedented’ conditions could influence COVID vaccine approval for kids
“From a public health standpoint, I think we have an evolving situation,” said Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, in a moderated session with Lee Beers, MD, president of the American Academy of Pediatrics, at the virtual Pediatric Hospital Medicine annual conference.
The reasons for this shift remain unclear, he said.
Dr. Beers emphasized the ability of pediatric hospitalists to be flexible in the face of uncertainty and the evolving virus, and asked Dr. Fauci to elaborate on the unique traits of the delta variant that make it especially challenging.
“There is no doubt that delta transmits much more efficiently than the alpha variant or any other variant,” Dr. Fauci said. The transmissibility is evident in comparisons of the level of virus in the nasopharynx of the delta variant, compared with the original alpha COVID-19 virus – delta is as much as 1,000 times higher, he explained.
In addition, the level of virus in the nasopharynx of vaccinated individuals who develop breakthrough infections with the delta variant is similar to the levels in unvaccinated individuals who are infected with the delta variant.
The delta variant is “the tough guy on the block” at the moment, Dr. Fauci said.
Dr. Fauci also responded to a question on the lack of winter viruses, such as RSV and the flu, last winter, but the surge in these viruses over the summer.
This winter’s activity remains uncertain, Dr. Fauci said. However, he speculated “with a strong dose of humility and modesty” that viruses tend to have niches, some are seasonal, and the winter viruses that were displaced by COVID-19 hit harder in the summer instead. “If I were a [non-COVID] virus looking for a niche, I would be really confused,” he said. “I don’t know what will happen this winter, but if we get good control over COVID-19 by winter, we could have a very vengeful influenza season,” he said. “This is speculation, I don’t have any data for this,” he cautioned.
Dr. Beers raised the issue of back-to-school safety, and the updated AAP guidance for universal masking for K-12 students. “Our guidance about return to school gets updated as the situation changes and we gain a better understanding of how kids can get to school safely,” she said. A combination of factors affect back-to-school guidance, including the ineligibility of children younger than 12 years to be vaccinated, the number of adolescents who are eligible but have not been vaccinated, and the challenge for educators to navigate which children should wear masks, Dr. Beers said.
“We want to get vaccines for our youngest kids as soon as safely possible,” Dr. Beers emphasized. She noted that the same urgency is needed to provide vaccines for children as for adults, although “we have to do it safely, and be sure and feel confident in the data.”
When asked to comment about the status of FDA authorization of COVID-19 vaccines for younger children, Dr. Fauci described the current situation as one that “might require some unprecedented and unique action” on the part of the FDA, which tends to move cautiously because of safety considerations. However, concerns about adverse events might get in the way of protecting children against what “you are really worried about,” in this case COVID-19 and its variants, he said. Despite the breakthrough infections, “vaccination continues to very adequately protect people from getting severe disease,” he emphasized.
Dr. Fauci also said that he believes the current data support boosters for the immune compromised; however “it is a different story about the general vaccinated population and the vaccinated elderly,” he said. Sooner or later most people will likely need boosters; “the question is who, when, and how soon,” he noted.
Dr. Fauci wrapped up the session with kudos and support for the pediatric health care community. “As a nonpediatrician, I have a great deal of respect for the job you are doing,” he said. “Keep up the great work.”
Dr. Beers echoed this sentiment, saying that she was “continually awed, impressed, and inspired” by how the pediatric hospitalists are navigating the ever-changing pandemic environment.
“From a public health standpoint, I think we have an evolving situation,” said Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, in a moderated session with Lee Beers, MD, president of the American Academy of Pediatrics, at the virtual Pediatric Hospital Medicine annual conference.
The reasons for this shift remain unclear, he said.
Dr. Beers emphasized the ability of pediatric hospitalists to be flexible in the face of uncertainty and the evolving virus, and asked Dr. Fauci to elaborate on the unique traits of the delta variant that make it especially challenging.
“There is no doubt that delta transmits much more efficiently than the alpha variant or any other variant,” Dr. Fauci said. The transmissibility is evident in comparisons of the level of virus in the nasopharynx of the delta variant, compared with the original alpha COVID-19 virus – delta is as much as 1,000 times higher, he explained.
In addition, the level of virus in the nasopharynx of vaccinated individuals who develop breakthrough infections with the delta variant is similar to the levels in unvaccinated individuals who are infected with the delta variant.
The delta variant is “the tough guy on the block” at the moment, Dr. Fauci said.
Dr. Fauci also responded to a question on the lack of winter viruses, such as RSV and the flu, last winter, but the surge in these viruses over the summer.
This winter’s activity remains uncertain, Dr. Fauci said. However, he speculated “with a strong dose of humility and modesty” that viruses tend to have niches, some are seasonal, and the winter viruses that were displaced by COVID-19 hit harder in the summer instead. “If I were a [non-COVID] virus looking for a niche, I would be really confused,” he said. “I don’t know what will happen this winter, but if we get good control over COVID-19 by winter, we could have a very vengeful influenza season,” he said. “This is speculation, I don’t have any data for this,” he cautioned.
Dr. Beers raised the issue of back-to-school safety, and the updated AAP guidance for universal masking for K-12 students. “Our guidance about return to school gets updated as the situation changes and we gain a better understanding of how kids can get to school safely,” she said. A combination of factors affect back-to-school guidance, including the ineligibility of children younger than 12 years to be vaccinated, the number of adolescents who are eligible but have not been vaccinated, and the challenge for educators to navigate which children should wear masks, Dr. Beers said.
“We want to get vaccines for our youngest kids as soon as safely possible,” Dr. Beers emphasized. She noted that the same urgency is needed to provide vaccines for children as for adults, although “we have to do it safely, and be sure and feel confident in the data.”
When asked to comment about the status of FDA authorization of COVID-19 vaccines for younger children, Dr. Fauci described the current situation as one that “might require some unprecedented and unique action” on the part of the FDA, which tends to move cautiously because of safety considerations. However, concerns about adverse events might get in the way of protecting children against what “you are really worried about,” in this case COVID-19 and its variants, he said. Despite the breakthrough infections, “vaccination continues to very adequately protect people from getting severe disease,” he emphasized.
Dr. Fauci also said that he believes the current data support boosters for the immune compromised; however “it is a different story about the general vaccinated population and the vaccinated elderly,” he said. Sooner or later most people will likely need boosters; “the question is who, when, and how soon,” he noted.
Dr. Fauci wrapped up the session with kudos and support for the pediatric health care community. “As a nonpediatrician, I have a great deal of respect for the job you are doing,” he said. “Keep up the great work.”
Dr. Beers echoed this sentiment, saying that she was “continually awed, impressed, and inspired” by how the pediatric hospitalists are navigating the ever-changing pandemic environment.
“From a public health standpoint, I think we have an evolving situation,” said Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, in a moderated session with Lee Beers, MD, president of the American Academy of Pediatrics, at the virtual Pediatric Hospital Medicine annual conference.
The reasons for this shift remain unclear, he said.
Dr. Beers emphasized the ability of pediatric hospitalists to be flexible in the face of uncertainty and the evolving virus, and asked Dr. Fauci to elaborate on the unique traits of the delta variant that make it especially challenging.
“There is no doubt that delta transmits much more efficiently than the alpha variant or any other variant,” Dr. Fauci said. The transmissibility is evident in comparisons of the level of virus in the nasopharynx of the delta variant, compared with the original alpha COVID-19 virus – delta is as much as 1,000 times higher, he explained.
In addition, the level of virus in the nasopharynx of vaccinated individuals who develop breakthrough infections with the delta variant is similar to the levels in unvaccinated individuals who are infected with the delta variant.
The delta variant is “the tough guy on the block” at the moment, Dr. Fauci said.
Dr. Fauci also responded to a question on the lack of winter viruses, such as RSV and the flu, last winter, but the surge in these viruses over the summer.
This winter’s activity remains uncertain, Dr. Fauci said. However, he speculated “with a strong dose of humility and modesty” that viruses tend to have niches, some are seasonal, and the winter viruses that were displaced by COVID-19 hit harder in the summer instead. “If I were a [non-COVID] virus looking for a niche, I would be really confused,” he said. “I don’t know what will happen this winter, but if we get good control over COVID-19 by winter, we could have a very vengeful influenza season,” he said. “This is speculation, I don’t have any data for this,” he cautioned.
Dr. Beers raised the issue of back-to-school safety, and the updated AAP guidance for universal masking for K-12 students. “Our guidance about return to school gets updated as the situation changes and we gain a better understanding of how kids can get to school safely,” she said. A combination of factors affect back-to-school guidance, including the ineligibility of children younger than 12 years to be vaccinated, the number of adolescents who are eligible but have not been vaccinated, and the challenge for educators to navigate which children should wear masks, Dr. Beers said.
“We want to get vaccines for our youngest kids as soon as safely possible,” Dr. Beers emphasized. She noted that the same urgency is needed to provide vaccines for children as for adults, although “we have to do it safely, and be sure and feel confident in the data.”
When asked to comment about the status of FDA authorization of COVID-19 vaccines for younger children, Dr. Fauci described the current situation as one that “might require some unprecedented and unique action” on the part of the FDA, which tends to move cautiously because of safety considerations. However, concerns about adverse events might get in the way of protecting children against what “you are really worried about,” in this case COVID-19 and its variants, he said. Despite the breakthrough infections, “vaccination continues to very adequately protect people from getting severe disease,” he emphasized.
Dr. Fauci also said that he believes the current data support boosters for the immune compromised; however “it is a different story about the general vaccinated population and the vaccinated elderly,” he said. Sooner or later most people will likely need boosters; “the question is who, when, and how soon,” he noted.
Dr. Fauci wrapped up the session with kudos and support for the pediatric health care community. “As a nonpediatrician, I have a great deal of respect for the job you are doing,” he said. “Keep up the great work.”
Dr. Beers echoed this sentiment, saying that she was “continually awed, impressed, and inspired” by how the pediatric hospitalists are navigating the ever-changing pandemic environment.
FROM PHM 2021
Injectable monoclonal antibodies prevent COVID-19 in trial
according to results of a randomized, double-blind, placebo-controlled clinical trial published online August 4, 2021, in the New England Journal of Medicine.
The cocktail of the monoclonal antibodies casirivimab and imdevimab (REGEN-COV, Regeneron Pharmaceuticals) reduced participants’ relative risk of infection by 72%, compared with placebo within the first week. After the first week, risk reduction increased to 93%.
“Long after you would be exposed by your household, there is an enduring effect that prevents you from community spread,” said David Wohl, MD, professor of medicine in the division of infectious diseases at the University of North Carolina at Chapel Hill, who was a site investigator for the trial but not a study author.
Participants were enrolled within 96 hours after someone in their household tested positive for SARS-CoV-2. Participants were randomly assigned to receive 1,200 mg of REGEN-COV subcutaneously or a placebo. Based on serologic testing, study participants showed no evidence of current or previous SARS-CoV-2 infection. The median age of participants was 42.9, but 45% were male teenagers (ages 12-17).
In the group that received REGEN-COV, 11 out of 753 participants developed symptomatic COVID-19, compared with 59 out of 752 participants who received placebo. The relative risk reduction for the study’s 4-week period was 81.4% (P < .001). Of the participants that did develop a SARS-CoV-2 infection, those that received REGEN-COV were less likely to be symptomatic. Asymptomatic infections developed in 25 participants who received REGEN-COV versus 48 in the placebo group. The relative risk of developing any SARS-CoV-2 infection, symptomatic or asymptomatic, was reduced by 66.4% with REGEN-COV (P < .001).
Among the patients who were symptomatic, symptoms subsided within a median of 1.2 weeks for the group that received REGEN-COV, 2 weeks earlier than the placebo group. These patients also had a shorter duration of a high viral load (>104 copies/mL). Few adverse events were reported in the treatment or placebo groups. Monoclonal antibodies “seem to be incredibly safe,” Dr. Wohl said.
“These monoclonal antibodies have proven they can reduce the viral replication in the nose,” said study author Myron Cohen, MD, an infectious disease specialist and professor of epidemiology at the University of North Carolina.
The Food and Drug Administration first granted REGEN-COV emergency use authorization (EUA) in November 2020 for use in patients with mild or moderate COVID-19 who were also at high risk for progressing to severe COVID-19. At that time, the cocktail of monoclonal antibodies was delivered by a single intravenous infusion.
In January, Regeneron first announced the success of this trial of the subcutaneous injection for exposed household contacts based on early results, and in June of 2021, the FDA expanded the EUA to include a subcutaneous delivery when IV is not feasible. On July 30, the EUA was expanded again to include prophylactic use in exposed patients based on these trial results.
The U.S. government has purchased approximately 1.5 million doses of REGEN-COV from Regeneron and has agreed to make the treatments free of charge to patients.
But despite being free, available, and backed by promising data, monoclonal antibodies as a therapeutic answer to COVID-19 still hasn’t really taken off. “The problem is, it first requires knowledge and awareness,” Dr. Wohl said. “A lot [of people] don’t know this exists. To be honest, vaccination has taken up all the oxygen in the room.”
Dr. Cohen agreed. One reason for the slow uptake may be because the drug supply is owned by the government and not a pharmaceutical company. There hasn’t been a typical marketing push to make physicians and consumers aware. Additionally, “the logistics are daunting,” Dr. Cohen said. The office spaces where many physicians care for patients “often aren’t appropriate for patients who think they have SARS-CoV-2.”
“Right now, there’s not a mechanism” to administer the drug to people who could benefit from it, Dr. Wohl said. Eligible patients are either immunocompromised and unlikely to mount a sufficient immune response with vaccination, or not fully vaccinated. They should have been exposed to an infected individual or have a high likelihood of exposure due to where they live, such as in a prison or nursing home. Local doctors are unlikely to be the primary administrators of the drug, Dr. Wohl added. “How do we operationalize this for people who fit the criteria?”
There’s also an issue of timing. REGEN-COV is most effective when given early, Dr. Cohen said. “[Monoclonal antibodies] really only work well in the replication phase.” Many patients who would be eligible delay care until they’ve had symptoms for several days, when REGEN-COV would no longer have the desired effect.
Eventually, Dr. Wohl suspects demand will increase when people realize REGEN-COV can help those with COVID-19 and those who have been exposed. But before then, “we do have to think about how to integrate this into a workflow people can access without being confused.”
The trial was done before there was widespread vaccination, so it’s unclear what the results mean for people who have been vaccinated. Dr. Cohen and Dr. Wohl said there are ongoing conversations about whether monoclonal antibodies could be complementary to vaccination and if there’s potential for continued monthly use of these therapies.
Cohen and Wohl reported no relevant financial relationships. The trial was supported by Regeneron Pharmaceuticals, F. Hoffmann–La Roche, the National Institute of Allergy and Infectious Diseases, NIH, and the COVID-19 Prevention Network.
A version of this article first appeared on Medscape.com.
according to results of a randomized, double-blind, placebo-controlled clinical trial published online August 4, 2021, in the New England Journal of Medicine.
The cocktail of the monoclonal antibodies casirivimab and imdevimab (REGEN-COV, Regeneron Pharmaceuticals) reduced participants’ relative risk of infection by 72%, compared with placebo within the first week. After the first week, risk reduction increased to 93%.
“Long after you would be exposed by your household, there is an enduring effect that prevents you from community spread,” said David Wohl, MD, professor of medicine in the division of infectious diseases at the University of North Carolina at Chapel Hill, who was a site investigator for the trial but not a study author.
Participants were enrolled within 96 hours after someone in their household tested positive for SARS-CoV-2. Participants were randomly assigned to receive 1,200 mg of REGEN-COV subcutaneously or a placebo. Based on serologic testing, study participants showed no evidence of current or previous SARS-CoV-2 infection. The median age of participants was 42.9, but 45% were male teenagers (ages 12-17).
In the group that received REGEN-COV, 11 out of 753 participants developed symptomatic COVID-19, compared with 59 out of 752 participants who received placebo. The relative risk reduction for the study’s 4-week period was 81.4% (P < .001). Of the participants that did develop a SARS-CoV-2 infection, those that received REGEN-COV were less likely to be symptomatic. Asymptomatic infections developed in 25 participants who received REGEN-COV versus 48 in the placebo group. The relative risk of developing any SARS-CoV-2 infection, symptomatic or asymptomatic, was reduced by 66.4% with REGEN-COV (P < .001).
Among the patients who were symptomatic, symptoms subsided within a median of 1.2 weeks for the group that received REGEN-COV, 2 weeks earlier than the placebo group. These patients also had a shorter duration of a high viral load (>104 copies/mL). Few adverse events were reported in the treatment or placebo groups. Monoclonal antibodies “seem to be incredibly safe,” Dr. Wohl said.
“These monoclonal antibodies have proven they can reduce the viral replication in the nose,” said study author Myron Cohen, MD, an infectious disease specialist and professor of epidemiology at the University of North Carolina.
The Food and Drug Administration first granted REGEN-COV emergency use authorization (EUA) in November 2020 for use in patients with mild or moderate COVID-19 who were also at high risk for progressing to severe COVID-19. At that time, the cocktail of monoclonal antibodies was delivered by a single intravenous infusion.
In January, Regeneron first announced the success of this trial of the subcutaneous injection for exposed household contacts based on early results, and in June of 2021, the FDA expanded the EUA to include a subcutaneous delivery when IV is not feasible. On July 30, the EUA was expanded again to include prophylactic use in exposed patients based on these trial results.
The U.S. government has purchased approximately 1.5 million doses of REGEN-COV from Regeneron and has agreed to make the treatments free of charge to patients.
But despite being free, available, and backed by promising data, monoclonal antibodies as a therapeutic answer to COVID-19 still hasn’t really taken off. “The problem is, it first requires knowledge and awareness,” Dr. Wohl said. “A lot [of people] don’t know this exists. To be honest, vaccination has taken up all the oxygen in the room.”
Dr. Cohen agreed. One reason for the slow uptake may be because the drug supply is owned by the government and not a pharmaceutical company. There hasn’t been a typical marketing push to make physicians and consumers aware. Additionally, “the logistics are daunting,” Dr. Cohen said. The office spaces where many physicians care for patients “often aren’t appropriate for patients who think they have SARS-CoV-2.”
“Right now, there’s not a mechanism” to administer the drug to people who could benefit from it, Dr. Wohl said. Eligible patients are either immunocompromised and unlikely to mount a sufficient immune response with vaccination, or not fully vaccinated. They should have been exposed to an infected individual or have a high likelihood of exposure due to where they live, such as in a prison or nursing home. Local doctors are unlikely to be the primary administrators of the drug, Dr. Wohl added. “How do we operationalize this for people who fit the criteria?”
There’s also an issue of timing. REGEN-COV is most effective when given early, Dr. Cohen said. “[Monoclonal antibodies] really only work well in the replication phase.” Many patients who would be eligible delay care until they’ve had symptoms for several days, when REGEN-COV would no longer have the desired effect.
Eventually, Dr. Wohl suspects demand will increase when people realize REGEN-COV can help those with COVID-19 and those who have been exposed. But before then, “we do have to think about how to integrate this into a workflow people can access without being confused.”
The trial was done before there was widespread vaccination, so it’s unclear what the results mean for people who have been vaccinated. Dr. Cohen and Dr. Wohl said there are ongoing conversations about whether monoclonal antibodies could be complementary to vaccination and if there’s potential for continued monthly use of these therapies.
Cohen and Wohl reported no relevant financial relationships. The trial was supported by Regeneron Pharmaceuticals, F. Hoffmann–La Roche, the National Institute of Allergy and Infectious Diseases, NIH, and the COVID-19 Prevention Network.
A version of this article first appeared on Medscape.com.
according to results of a randomized, double-blind, placebo-controlled clinical trial published online August 4, 2021, in the New England Journal of Medicine.
The cocktail of the monoclonal antibodies casirivimab and imdevimab (REGEN-COV, Regeneron Pharmaceuticals) reduced participants’ relative risk of infection by 72%, compared with placebo within the first week. After the first week, risk reduction increased to 93%.
“Long after you would be exposed by your household, there is an enduring effect that prevents you from community spread,” said David Wohl, MD, professor of medicine in the division of infectious diseases at the University of North Carolina at Chapel Hill, who was a site investigator for the trial but not a study author.
Participants were enrolled within 96 hours after someone in their household tested positive for SARS-CoV-2. Participants were randomly assigned to receive 1,200 mg of REGEN-COV subcutaneously or a placebo. Based on serologic testing, study participants showed no evidence of current or previous SARS-CoV-2 infection. The median age of participants was 42.9, but 45% were male teenagers (ages 12-17).
In the group that received REGEN-COV, 11 out of 753 participants developed symptomatic COVID-19, compared with 59 out of 752 participants who received placebo. The relative risk reduction for the study’s 4-week period was 81.4% (P < .001). Of the participants that did develop a SARS-CoV-2 infection, those that received REGEN-COV were less likely to be symptomatic. Asymptomatic infections developed in 25 participants who received REGEN-COV versus 48 in the placebo group. The relative risk of developing any SARS-CoV-2 infection, symptomatic or asymptomatic, was reduced by 66.4% with REGEN-COV (P < .001).
Among the patients who were symptomatic, symptoms subsided within a median of 1.2 weeks for the group that received REGEN-COV, 2 weeks earlier than the placebo group. These patients also had a shorter duration of a high viral load (>104 copies/mL). Few adverse events were reported in the treatment or placebo groups. Monoclonal antibodies “seem to be incredibly safe,” Dr. Wohl said.
“These monoclonal antibodies have proven they can reduce the viral replication in the nose,” said study author Myron Cohen, MD, an infectious disease specialist and professor of epidemiology at the University of North Carolina.
The Food and Drug Administration first granted REGEN-COV emergency use authorization (EUA) in November 2020 for use in patients with mild or moderate COVID-19 who were also at high risk for progressing to severe COVID-19. At that time, the cocktail of monoclonal antibodies was delivered by a single intravenous infusion.
In January, Regeneron first announced the success of this trial of the subcutaneous injection for exposed household contacts based on early results, and in June of 2021, the FDA expanded the EUA to include a subcutaneous delivery when IV is not feasible. On July 30, the EUA was expanded again to include prophylactic use in exposed patients based on these trial results.
The U.S. government has purchased approximately 1.5 million doses of REGEN-COV from Regeneron and has agreed to make the treatments free of charge to patients.
But despite being free, available, and backed by promising data, monoclonal antibodies as a therapeutic answer to COVID-19 still hasn’t really taken off. “The problem is, it first requires knowledge and awareness,” Dr. Wohl said. “A lot [of people] don’t know this exists. To be honest, vaccination has taken up all the oxygen in the room.”
Dr. Cohen agreed. One reason for the slow uptake may be because the drug supply is owned by the government and not a pharmaceutical company. There hasn’t been a typical marketing push to make physicians and consumers aware. Additionally, “the logistics are daunting,” Dr. Cohen said. The office spaces where many physicians care for patients “often aren’t appropriate for patients who think they have SARS-CoV-2.”
“Right now, there’s not a mechanism” to administer the drug to people who could benefit from it, Dr. Wohl said. Eligible patients are either immunocompromised and unlikely to mount a sufficient immune response with vaccination, or not fully vaccinated. They should have been exposed to an infected individual or have a high likelihood of exposure due to where they live, such as in a prison or nursing home. Local doctors are unlikely to be the primary administrators of the drug, Dr. Wohl added. “How do we operationalize this for people who fit the criteria?”
There’s also an issue of timing. REGEN-COV is most effective when given early, Dr. Cohen said. “[Monoclonal antibodies] really only work well in the replication phase.” Many patients who would be eligible delay care until they’ve had symptoms for several days, when REGEN-COV would no longer have the desired effect.
Eventually, Dr. Wohl suspects demand will increase when people realize REGEN-COV can help those with COVID-19 and those who have been exposed. But before then, “we do have to think about how to integrate this into a workflow people can access without being confused.”
The trial was done before there was widespread vaccination, so it’s unclear what the results mean for people who have been vaccinated. Dr. Cohen and Dr. Wohl said there are ongoing conversations about whether monoclonal antibodies could be complementary to vaccination and if there’s potential for continued monthly use of these therapies.
Cohen and Wohl reported no relevant financial relationships. The trial was supported by Regeneron Pharmaceuticals, F. Hoffmann–La Roche, the National Institute of Allergy and Infectious Diseases, NIH, and the COVID-19 Prevention Network.
A version of this article first appeared on Medscape.com.