User login
Locking Plate Fixation for Proximal Humerus Fractures
4 EKG Abnormalities: What Are the Lifesaving Diagnoses?
› Consider placement of an automatic implantable cardioverter-defibrillator for all patients with a type 1 Brugada pattern on EKG accompanied by syncope, documented ventricular arrhythmia, or aborted sudden cardiac death. B
› Always look for EKG findings suggestive of Wolff-Parkinson-White syndrome in otherwise healthy patients presenting with syncope. C
› Refer all patients with suspected hypertrophic cardiomyopathy to Cardiology for a transthoracic echocardiogram. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
When evaluating a patient with a history of chest pain, palpitations, syncope, and/or new-onset seizures, an electrocardiogram (EKG) may be the key to
identifying a potentially life-threatening condition. Here we present 4 cases in which EKG findings were the clue to underlying medical conditions that, if left untreated, could be fatal. Because each of these conditions may not have associated findings on a physical exam, early recognition of these EKG findings can be lifesaving.
CASE 1 › A 15-year-old boy suddenly collapses while walking, and bystanders report seizure-like activity. The patient doesn’t remember the event. Vital signs and physical exam are normal, and his blood glucose level is 86 mg/dL (normal: 70-100 mg/dL). He doesn’t take any medications and denies illicit drug use or recent illness.
What EKG abnormality (FIGURE 1) likely explains the cause of the patient’s collapse?
The EKG abnormality and diagnosis. The patient’s EKG revealed a prolonged QT interval (FIGURE 1, BRACKETS). His QTc (QT interval corrected for heart rate) was .470 seconds, which is at the high end of the normal range for his age and gender.1 The patient had no family history of syncope, sudden cardiac death (SCD), or seizure disorder. Evaluation uncovered a calcium level of 4.4 mEq/L (normal: 4.5-5.5 mEq/L) and a phosphate level of 7.8 mg/dL (normal: 2.4-4.1 mg/dL).
This patient had a low parathyroid hormone from primary hypoparathyroidism. His conduction abnormality was treated with both oral calcium and vitamin D supplements.
Etiology and epidemiology. A prolonged QT interval may be the result of a primary long QT syndrome (LQTS) or an acquired condition from electrolyte imbalance, medication effect, or toxin exposure.
In the United States, the incidence of a genetic mutation that causes LQTS is 1 in 2500 people.2 Patients with LQTS usually remain asymptomatic unless the QT interval is further prolonged by a condition or medication. There are several hundred congenital LQTS subtypes based on specific ion channel defects; the most common is LQTS1, with an inherited defect in the KCNQ1 gene, which regulates the slow potassium ion channel.
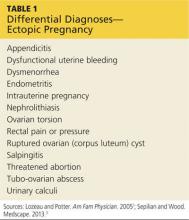
Acquired LQTS is much more common than congenital LQTS.3 Many drugs have been linked to an increased risk of LQTS, including certain antiarrhythmics, antibiotics, and antipsychotics (TABLE 1).4 In addition, electrolyte disturbances such as hypokalemia, hypocalcemia, and hypomagnesemia can be etiologic factors.
Be aware that an acquired LQTS may mask an underlying congenital LQTS. Therefore, patients in whom the offending agent or condition is corrected should still have a follow-up EKG. Screening family members for LQTS is worthwhile, even in those without symptoms.
Clinical features. Patients with symptomatic LQTS may have dizziness, palpitations, and syncope. SCD also is possible. These signs and symptoms may be triggered by strong emotions (in LQTS2) or physical activity (in LQTS1). They likely are caused by torsades de pointes and ventricular fibrillation. A brief aura may precede these arrhythmias, and patients may experience urinary or fecal incontinence.5
The key to making a diagnosis of LQTS is correctly measuring the QT interval. The QT interval is measured from the beginning of the Q-wave to the end of the T-wave as measured from the intersection of a line tangent to the downslope of the T-wave and the isoelectric line. This can be difficult to determine in EKGs showing bundle branch block or an irregular rhythm, such as atrial fibrillation (AF).6,7 A common error in measuring the QT interval occurs when clinicians inadvertently include a U-wave in the measurement.1 Some EKG machines may provide QT interval and QTc measurements. Normal QT intervals are ≤.450 seconds for men and ≤.470 seconds for women.8
It is essential to confirm the QT interval by using the Bazett formula (QTc equals the QT in seconds divided by the square root of the RR interval in seconds) for all patients with a history that suggests a possible arrhythmia.
Our patient had hypocalcemia, which on an EKG can cause T-wave widening with a normal ST segment, rather than a normal T-wave with a long ST segment, as is typically seen in LQTS. This distinction may be difficult to discern and should not preclude the search for either an acquired prolonged QTc or an underlying LQTS.9
Treatment. First rule out or treat any causes of acquired LQTS by taking a careful medication history and evaluating the patient’s electrolytes. Once these have been addressed, a beta-blocker is first-line therapy for symptomatic patients.5
Unfortunately, up to 20% of individuals treated with beta-blockers may continue to have syncope.5 For these patients, options include a left cardiac sympathetic denervation (LCSD) or placement of an automatic implantable cardioverter-defibrillator (AICD). An LCSD involves removal of the left-sided stellate and/or thoracic ganglia. This procedure can be used instead of, or in addition to, beta-blockers. If the patient’s syncope persists, AICDs are an option. AICDs can be lifesaving, but patients run the risk of adverse effects that include inappropriate shocks and infection.10 As the result of these therapies, mortality associated with LQTS has dropped to approximately 1%.11
CASE 2 › A 14-year-old boy has a syncopal episode while at rest. A similar event occurred 3 years earlier; at that time, an echocardiogram and EKG were normal. For 2 days, he’s had a cough and low-grade fever. His temperature is 102ºF and he has a productive cough. Based on this EKG (FIGURE 2), what is the likely diagnosis? What is the significance of his fever?
The EKG abnormality and diagnosis. This patient’s EKG showed a type 1 Brugada pattern (FIGURE 2, ARROWS), which strongly supported the diagnosis of Brugada syndrome (BS). BS is an inherited condition caused by a genetic defect in cardiac ion channel function that leads to characteristic EKG changes and a predisposition to ventricular fibrillation.12 In this case, the fever likely unmasked these EKG findings.
The patient was transferred to a local hospital for treatment of community-acquired pneumonia, and ultimately received an AICD.
Etiology and epidemiology. BS was first described in 199213 and is a major cause of SCD, responsible for up to 4% of all cases of SCD, and 20% of cases of patients without structural heart disease.14 BS is more common in men, and the mean age of diagnosis is 40 to 45.15-18
Mutations in at least 17 cardiac ion channel genes have been linked to BS.19 The SCN5A gene—a cardiac sodium channel—is the most commonly implicated, but accounts for only 11% to 24% of all BS cases.15
Clinical features. Patients with BS may present with syncope, nocturnal agonal respirations, or ventricular arrhythmias.12 EKG findings include partial or complete right bundle branch block (RBBB) and ST segment elevation in right precordial leads V1 to V3.12 There are 2 Brugada EKG patterns, a type 1 cloved pattern as seen in our patient’s EKG and a type 2 saddleback pattern.20 EKG findings are dynamic over time and may alternate between normal, type 1, and type 2.20 Factors that modulate EKG appearance include fever, intoxication, vagal tone, electrolyte imbalance, and sodium channel blockade.12,20
Diagnosis requires a type 1 Brugada pattern on EKG plus a family history of BS, documented ventricular arrhythmia, or arrhythmia-related symptoms such as syncope.12 Patients with a type 2 Brugada pattern may undergo electrophysiology (EP) testing with Class I antiarrhythmic drugs to induce a diagnostic type 1 Brugada pattern.12,21 Patients who have Brugada EKG findings but none of the other diagnostic criteria are considered to have a Brugada pattern (rather than Brugada syndrome).12
The most concerning outcome of BS is ventricular fibrillation. The estimated annual rate of cardiac events is 7.7% among patients who have experienced an aborted SCD, 1.9% among those who have experienced syncope, and 0.5% in asymptomatic patients.18
Treatment. The only effective treatment for BS is placement of an AICD; however, complications of AICD placement cause significant morbidity.6 Ten years after AICD placement, 37% of patients experienced inappropriate shocks and 29% experienced lead failure.22 Recent modifications in device programming and the addition of remote monitoring have decreased complication rates.12,22
The decision to place an AICD is based on the patient’s prior symptoms, EKG findings, and other factors. Recent guidelines recommend an AICD for all patients with a type 1 Brugada pattern (spontaneous or induced) who also have had an aborted SCD, syncope, or documented ventricular arrhythmia.12
Management of asymptomatic patients with type 1 Brugada pattern remains controversial because the rate of cardiac events is low, although such events can be fatal. Asymptomatic patients with type 1 Brugada findings should undergo further EP testing, and should receive AICD only upon demonstration of inducible ventricular arrhythmia.12
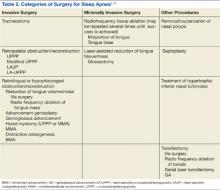
TABLE 2
Arrhythmias associated with Wolff-Parkinson-White syndrome23
| Arrhythmia | EKG findings | Treatment—unstable patients | Treatment—stable patients (in preferred treatment order) |
| PSVT, orthodromic | Narrow QRS, loss of delta wave, rate 160-260 beats/min | Synchronized cardioversion | Vagal maneuvers, adenosine, calcium channel blockers, beta-blockers, digoxin, procainamide |
| PSVT, antidromic | Wide complex tachycardia | Synchronized cardioversion | Procainamide |
| Atrial fibrillation | Irregularly irregular (RR interval variable with no pattern), ventricular rates that can exceed 300 beats/min | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Atrial flutter | Flutter waves, rate normal to tachycardic depending on conduction rate | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Ventricular fibrillation | Rapid, erratic electrical impulses | Defibrillation | N/A |
EKG, electrocardiogram; N/A, not applicable; PSVT, paroxysmal supraventricular tachycardia.
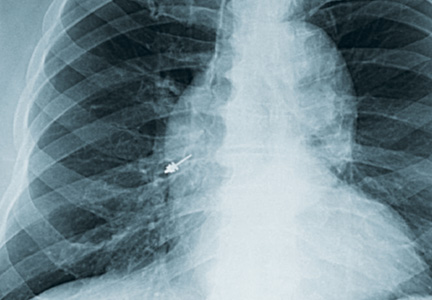
CASE 3 › A 21-year-old man with no medical history presents with sudden onset of lightheadedness followed by syncope. He denies any chest pain or other associated symptoms. At the time of evaluation, he is asymptomatic. His EKG (FIGURE 3) is diagnostic of what syndrome?
The EKG abnormality and diagnosis. The patient had a classic presentation for Wolff-Parkinson-White (WPW) syndrome, a common congenital disorder that alters normal cardiac conduction. He described 2 past instances of unexplained light-headedness and palpitations. Subsequent EP studies demonstrated that the patient had an accessory atrioventricular (AV) tract, causing electrical activity in the heart to bypass the AV node, resulting in a delta wave on EKG (FIGURE 3, GREEN ARROWS).
The patient opted for ablation therapy, which successfully eliminated the delta wave on EKG. Five years later he has had no recurrences.
Epidemiology. The prevalence of WPW syndrome is .1% to 3%.23 Accessory AV tracts are found in men twice as often as in women. Only half of individuals with confirmed tracts develop a tachyarrhythmia. The estimated risk of sudden death due to WPW syndrome is .5% to 4%.24
Pathophysiology. Normally cardiac conduction originates from the sinus node and travels to the AV node, where conduction is slowed, and then proceeds to the His-Purkinje system, and finally to the rest of the ventricular myocardium. In WPW syndrome, ventricular depolarization occurs first by an accessory AV tract called the bundle of Kent, followed shortly thereafter by the His-Purkinje system. This sequence of depolarization is what leads to the EKG findings characteristic of WPW syndrome: a PR interval <.12 seconds, presence of a delta wave, widened QRS complex (>.12 seconds), and repolarization changes seen as ST segment and T-wave changes discordant to (opposite direction) the delta wave and QRS complex (FIGURE 3, RED ARROW).
Factors that influence electrical conduction through the bundle of Kent include cardioactive medications, physiological stress, circulating catecholamines, coronary ischemia, and aging. The end result is a propensity for the heart to convert to one of 4 arrhythmias: paroxysmal supraventricular tachycardia (PSVT), AF, atrial flutter, or ventricular fibrillation (TABLE 2).23
The most common arrhythmia in WPW syndrome is PSVT.23 This rhythm is induced by the formation of a reentry circuit—a pattern in which the heart’s electrical signal loops back on itself—involving the normal conduction pathway and the bundle of Kent. Reentry progressing down the His-Purkinje system and traveling up the bundle of Kent is referred to as orthodromic (anterograde) PSVT. Antidromic (retrograde) PSVT is due to a reentry circuit conducting from the bundle of Kent to the ventricles, and then retrograde through the His-Purkinje system and AV node to the atria.
Clinical features. Under normal circumstances, patients with WPW syndrome are asymptomatic. As was the case with our patient, individuals who develop one of the 4 characteristic arrhythmias can experience light-headedness and syncope.
Treatment. An unstable patient who is experiencing PSVT, AF, or atrial flutter should receive synchronized cardioversion; those experiencing ventricular fibrillation should receive defibrillation (TABLE 2).23 For stable patients, therapy is tailored to the type of arrhythmia. Calcium channel blockers, beta-blockers, and adenosine might be appropriate for patients with orthodromic PSVT but should be avoided in patients with antidromic PSVT, AF, or atrial flutter because these medications block AV node conduction and thus facilitate conduction down the bundle of Kent, which can result in potentially unstable arrhythmias. In general, the longer an arrhythmia has been present, the less effective the pharmacologic intervention because of the increasing sympathetic tone.
Preventive long-term therapies for WPW patients who have experienced arrhythmia include antiarrhythmic medications or ablative procedures. Long-term antiarrhythmic therapy often is reserved for older, more sedentary individuals with less frequent arrhythmias that are not life-threatening. Radiofrequency ablation is a popular option, with long-term success rates as high as 95% and complication rates <1%.23 Patients in whom a WPW pattern is identified incidentally on EKG should be referred to cardiology for EP studies and risk stratification.25
CASE 4 › A 61-year-old woman has an episode of substernal exertional chest pressure that lasted approximately 2 hours but resolved before she arrived at her physician’s office. She also experienced mild nausea. She has no history of coronary artery disease but says that she has experienced similar episodes of chest pressure. What abnormality is seen on her EKG (FIGURE 4)? What is the most likely cause of her symptoms?
The EKG abnormality and diagnosis. Although classically associated with syncope, hypertrophic cardiomyopathy (HCM) often presents similarly to acute coronary syndromes, with chest pain and dyspnea on exertion.26 This patient had no history of cardiac disease or family history of SCD or cardiomyopathy; however, her EKG showed changes indicating left ventricular hypertrophy (LVH), which is consistent with HCM (FIGURE 4, ARROWS). Echocardiography identified myocardial hypertrophy, normal left ventricular ejection fraction, but severe left ventricular outflow obstruction and mild diastolic dysfunction. She was treated with metoprolol and verapamil.
Etiology and epidemiology. Hypertrophic cardiomyopathy is an autosomal dominant intrinsic myocardial disorder resulting in LVH that is commonly associated with SCD during extreme physical activity.26,27 The prevalence of HCM is approximately 1 in 500.26 Although it can present at any age, it is the most common cause of SCD in young people (under age 30), responsible for 33% of deaths during athletic events.28
TABLE 3
4 diagnoses and what you'll see on EKG
| Diagnosis | EKG finding |
| Prolonged QT interval | QTc interval >.450 sec (men) or >.470 sec (women) |
| Brugada syndrome | Partial or complete RBBB, and ST segment elevation in right precordial leads V1-V3 |
| Wolff-Parkinson-White syndrome | Delta wave, widened QRS, short PR interval, ST segment and T-wave changes |
| Hypertrophic cardiomyopathy | No definitive finding; may have left ventricular hypertrophy or abnormal Q-waves |
EKG, electrocardiogram; RBBB, right bundle branch block.
Clinical features. The severity of HCM ranges from asymptomatic to fatal. Symptoms of HCM include chest pain, dyspnea, and syncope. The disorder causes morbidity and mortality in at least one of 3 ways: ventricular tachyarrhythmias (often in younger patients), heart failure (from left ventricular outflow obstruction), and/or thromboembolism.27
Although echocardiography typically is used to make the diagnosis,27 an EKG often is the initial screening tool. EKG changes are seen in 75% to 95% of affected patients and include the presence of Q-waves and increased voltages related to LVH.27,29 Infarct-like patterns may be present before wall thickening on echocardiogram. Abnormal Q-waves are found in 20% to 50% of HCM patients, and are more common in younger patients. Konno et al30 have shown that Q-waves >3 mm in depth and/or >.040 seconds in duration in at least 2 leads other than aVR is specific (90%) in identifying carriers of HCM genes before they develop clinical symptoms.
Ambulatory monitoring may be useful for risk stratifying HCM patients; those with nonsustained ventricular tachycardia (NSVT) are at higher risk of SCD. Holter monitoring is recommended in initial evaluation because evidence of ventricular tachyarrhythmias may warrant AICD placement.26
Treatment. The risk of SCD in HCM is approximately 1%, but higher in those with a family history of SCD, syncope, NSVT, hypotension during exercise, or severe LVH (left ventricle thickness >30 mm).26 AICDs are recommended for HCM patients with prior cardiac arrest, patients with ≥2 of these risk factors, or patients with one risk factor who have experienced syncope related to arrhythmia.26
For patients who are symptomatic but have <2 risk factors, beta-blockers are firstline therapy.26 Verapamil is used as a second line treatment. Both beta-blockers and calcium channel blockers reduce dyspnea, palpitations, and chest pain.27
For patients who don’t respond to medical therapy, septal reduction therapy may be performed, either by septal myectomy or alcohol septal ablation.27 It is also important to consider genetic screening and counseling for the family.
A summary of all 4 diagnoses described in this article, their associated EKG findings, and their pathophysiology appears in TABLE 3.
CORRESPONDENCE
Samir Haydar, DO, MPH, FACEP, Tufts University School of Medicine, Maine Medical Center, Department of Emergency Medicine, 47 Bramhall St., Portland, ME 04103; [email protected]
1. Taggart NW, Haglund CM, Tester DJ, et al. Diagnostic miscues in congenital long-QT syndrome. Circulation. 2007;115:2613-2620.
2. Schwartz PJ, Stramba-Badiale M, Crotti L, et al. Prevalance of the congenital long QT syndrome. Circulation. 2009;120:1761-1767.
3. van Noord C, Eijgelsheim M, Stricker BH. Drug- and nondrug-associated QT interval prolongation. Br J Clin Pharmacol. 2010;70:16-23.
4. Credible Meds Web site. Available at: http://crediblemeds.org. Accessed April 8, 2014.
5. Schwartz PJ, Priori SG, Spazzolini C, et al. Genotype-phenotype correlation in the long QT syndrome: gene specific triggers for life threatening arrhythmias. Circulation. 2001;103:89.
6. Chiladakis JK, Kalogeropoulos A, Koutsogiannis N, et al. Optimal QT/JT interval assessment in patients with complete bundle branch block. Ann Noninvasive Electrocardiol. 2012;17:268-276.
7. Ercan S, Altunbas G, Oylumlu M, et al. Congenital long QT syndrome masked by atrial fibrillation and unmasked by hypokalemia. Am J Emerg Med. 2013;31:451.e3-451.e6.
8. Goldenberg I, Moss AJ, Zareba W. QT interval: how to measure it and what is “normal.” J Cardiovasc Electrophysiol. 2006;17:333-336.
9. Podrid PJ. ECG Response: August 20, 2013. Circulation. 2013;128:869.
10. Olde Nordkamp LR, Wilde AA, Tijssen JG, et al. The ICD for primary prevention in patients with inherited cardiac diseases: indications, use, and outcome: a comparison with secondary prevention. Circ Arrhythm Electrophysiol. 2013;6:91-100.
11. Schwartz PJ. Pharmacological and non-pharmacological management of the congenital long QT syndrome: the rationale. Pharmacol Ther. 2011;131:171-177.
12. Berne P, Brugada J. Brugada syndrome 2012. Circ J. 2012;76:1563-1571.
13. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391-1396.
14. Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005;111:659-670.
15. Brugada J, Brugada R, Antzelevitch C, et al. Long-term followup of individuals with the electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3. Circulation. 2002;105:73-78.
16. Eckardt L, Probst V, Smits JP, et al. Long-term prognosis of individuals with right precordial ST-segment-elevation Brugada syndrome. Circulation. 2005;111:257-263.
17. Giustetto C, Drago S, Demarchi PG, et al; Italian Association of Arrhythmology and Cardiostimulation (AIAC)-Piedmont Section. Risk stratification of the patients with Brugada type electrocardiogram: a community-based prospective study. Europace. 2009;11:507-513.
18. Probst V, Veltmann C, Eckardt L, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: Results from the FINGER Brugada Syndrome Registry. Circulation. 2010;121:635-643.
19. Nielsen MW, Holst AG, Olesen SP, et al. The genetic component of Brugada syndrome. Front Physiol. 2013;4:179.
20. Bayés de Luna A, Brugada J, Baranchuk A, et al. Current electrocardiographic criteria for diagnosis of Brugada pattern: a consensus report. J Electrocardiol. 2012;45:433-442.
21. Veltmann C, Schimpf R, Echternach C, et al. A prospective study on spontaneous fluctuations between diagnostic and non-diagnostic ECGs in Brugada syndrome: implications for correct phenotyping and risk stratification. Eur Heart J. 2006;27:2544-2552.
22. Sacher F, Probst V, Maury P, et al. Outcome after implantation of a cardioverter-defibrillator in patients with Brugada syndrome: a multicenter study-part 2. Circulation. 2013;128:1739-1747.
23. Rosner MH, Brady WJ Jr, Kefer MP, et al. Electrocardiography in the patient with the Wolff-Parkinson-White syndrome: diagnostic and initial therapeutic issues. Am J Emerg Med. 1999;17:705-714.
24. Keating L, Morris FP, Brady WJ. Electrocardiographic features of Wolff-Parkinson-White syndrome. Emerg Med J. 2003;20:491-493.
25. Blomström-Lundqvist C, Scheinman MM, Aliot EM, et al; European Society of Cardiology Committee, NASPE-Heart Rhythm Society. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias—executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003;42:1493-1531.
26. Ho CY. Hypertrophic cardiomyopathy in 2012. Circulation. 2012;125:1432-1438.
27. Gersh BJ, Maron BJ, Bonow RO, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American Society of Echocardiography; American Society of Nuclear Cardiology; Heart Failure Society of America; Heart Rhythm Society; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:e783-e831.
28. Paterick TE, Jan MF, Paterick ZR, et al. Cardiac evaluation of collegiate student athletes: a medical and legal perspective. Am J Med. 2012;125:742-752.
29. Maron BJ. Hypertrophic cardiomyopathy. In: Bonow RO, Mann DL, Zipes DP, et al (eds). Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Philadelphia, PA: Saunders; 2011:1582-1594.
30. Konno T, Shimizu M, Ino H, et al. Diagnostic value of abnormal Q waves for identification of preclinical carriers of hypertrophic cardiomyopathy based on molecular genetic diagnosis. Eur Heart J. 2004;25:246-251.
› Consider placement of an automatic implantable cardioverter-defibrillator for all patients with a type 1 Brugada pattern on EKG accompanied by syncope, documented ventricular arrhythmia, or aborted sudden cardiac death. B
› Always look for EKG findings suggestive of Wolff-Parkinson-White syndrome in otherwise healthy patients presenting with syncope. C
› Refer all patients with suspected hypertrophic cardiomyopathy to Cardiology for a transthoracic echocardiogram. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
When evaluating a patient with a history of chest pain, palpitations, syncope, and/or new-onset seizures, an electrocardiogram (EKG) may be the key to
identifying a potentially life-threatening condition. Here we present 4 cases in which EKG findings were the clue to underlying medical conditions that, if left untreated, could be fatal. Because each of these conditions may not have associated findings on a physical exam, early recognition of these EKG findings can be lifesaving.
CASE 1 › A 15-year-old boy suddenly collapses while walking, and bystanders report seizure-like activity. The patient doesn’t remember the event. Vital signs and physical exam are normal, and his blood glucose level is 86 mg/dL (normal: 70-100 mg/dL). He doesn’t take any medications and denies illicit drug use or recent illness.
What EKG abnormality (FIGURE 1) likely explains the cause of the patient’s collapse?
The EKG abnormality and diagnosis. The patient’s EKG revealed a prolonged QT interval (FIGURE 1, BRACKETS). His QTc (QT interval corrected for heart rate) was .470 seconds, which is at the high end of the normal range for his age and gender.1 The patient had no family history of syncope, sudden cardiac death (SCD), or seizure disorder. Evaluation uncovered a calcium level of 4.4 mEq/L (normal: 4.5-5.5 mEq/L) and a phosphate level of 7.8 mg/dL (normal: 2.4-4.1 mg/dL).
This patient had a low parathyroid hormone from primary hypoparathyroidism. His conduction abnormality was treated with both oral calcium and vitamin D supplements.
Etiology and epidemiology. A prolonged QT interval may be the result of a primary long QT syndrome (LQTS) or an acquired condition from electrolyte imbalance, medication effect, or toxin exposure.
In the United States, the incidence of a genetic mutation that causes LQTS is 1 in 2500 people.2 Patients with LQTS usually remain asymptomatic unless the QT interval is further prolonged by a condition or medication. There are several hundred congenital LQTS subtypes based on specific ion channel defects; the most common is LQTS1, with an inherited defect in the KCNQ1 gene, which regulates the slow potassium ion channel.
Acquired LQTS is much more common than congenital LQTS.3 Many drugs have been linked to an increased risk of LQTS, including certain antiarrhythmics, antibiotics, and antipsychotics (TABLE 1).4 In addition, electrolyte disturbances such as hypokalemia, hypocalcemia, and hypomagnesemia can be etiologic factors.
Be aware that an acquired LQTS may mask an underlying congenital LQTS. Therefore, patients in whom the offending agent or condition is corrected should still have a follow-up EKG. Screening family members for LQTS is worthwhile, even in those without symptoms.
Clinical features. Patients with symptomatic LQTS may have dizziness, palpitations, and syncope. SCD also is possible. These signs and symptoms may be triggered by strong emotions (in LQTS2) or physical activity (in LQTS1). They likely are caused by torsades de pointes and ventricular fibrillation. A brief aura may precede these arrhythmias, and patients may experience urinary or fecal incontinence.5
The key to making a diagnosis of LQTS is correctly measuring the QT interval. The QT interval is measured from the beginning of the Q-wave to the end of the T-wave as measured from the intersection of a line tangent to the downslope of the T-wave and the isoelectric line. This can be difficult to determine in EKGs showing bundle branch block or an irregular rhythm, such as atrial fibrillation (AF).6,7 A common error in measuring the QT interval occurs when clinicians inadvertently include a U-wave in the measurement.1 Some EKG machines may provide QT interval and QTc measurements. Normal QT intervals are ≤.450 seconds for men and ≤.470 seconds for women.8
It is essential to confirm the QT interval by using the Bazett formula (QTc equals the QT in seconds divided by the square root of the RR interval in seconds) for all patients with a history that suggests a possible arrhythmia.
Our patient had hypocalcemia, which on an EKG can cause T-wave widening with a normal ST segment, rather than a normal T-wave with a long ST segment, as is typically seen in LQTS. This distinction may be difficult to discern and should not preclude the search for either an acquired prolonged QTc or an underlying LQTS.9
Treatment. First rule out or treat any causes of acquired LQTS by taking a careful medication history and evaluating the patient’s electrolytes. Once these have been addressed, a beta-blocker is first-line therapy for symptomatic patients.5
Unfortunately, up to 20% of individuals treated with beta-blockers may continue to have syncope.5 For these patients, options include a left cardiac sympathetic denervation (LCSD) or placement of an automatic implantable cardioverter-defibrillator (AICD). An LCSD involves removal of the left-sided stellate and/or thoracic ganglia. This procedure can be used instead of, or in addition to, beta-blockers. If the patient’s syncope persists, AICDs are an option. AICDs can be lifesaving, but patients run the risk of adverse effects that include inappropriate shocks and infection.10 As the result of these therapies, mortality associated with LQTS has dropped to approximately 1%.11
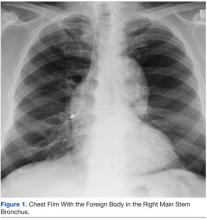
CASE 2 › A 14-year-old boy has a syncopal episode while at rest. A similar event occurred 3 years earlier; at that time, an echocardiogram and EKG were normal. For 2 days, he’s had a cough and low-grade fever. His temperature is 102ºF and he has a productive cough. Based on this EKG (FIGURE 2), what is the likely diagnosis? What is the significance of his fever?
The EKG abnormality and diagnosis. This patient’s EKG showed a type 1 Brugada pattern (FIGURE 2, ARROWS), which strongly supported the diagnosis of Brugada syndrome (BS). BS is an inherited condition caused by a genetic defect in cardiac ion channel function that leads to characteristic EKG changes and a predisposition to ventricular fibrillation.12 In this case, the fever likely unmasked these EKG findings.
The patient was transferred to a local hospital for treatment of community-acquired pneumonia, and ultimately received an AICD.
Etiology and epidemiology. BS was first described in 199213 and is a major cause of SCD, responsible for up to 4% of all cases of SCD, and 20% of cases of patients without structural heart disease.14 BS is more common in men, and the mean age of diagnosis is 40 to 45.15-18
Mutations in at least 17 cardiac ion channel genes have been linked to BS.19 The SCN5A gene—a cardiac sodium channel—is the most commonly implicated, but accounts for only 11% to 24% of all BS cases.15
Clinical features. Patients with BS may present with syncope, nocturnal agonal respirations, or ventricular arrhythmias.12 EKG findings include partial or complete right bundle branch block (RBBB) and ST segment elevation in right precordial leads V1 to V3.12 There are 2 Brugada EKG patterns, a type 1 cloved pattern as seen in our patient’s EKG and a type 2 saddleback pattern.20 EKG findings are dynamic over time and may alternate between normal, type 1, and type 2.20 Factors that modulate EKG appearance include fever, intoxication, vagal tone, electrolyte imbalance, and sodium channel blockade.12,20
Diagnosis requires a type 1 Brugada pattern on EKG plus a family history of BS, documented ventricular arrhythmia, or arrhythmia-related symptoms such as syncope.12 Patients with a type 2 Brugada pattern may undergo electrophysiology (EP) testing with Class I antiarrhythmic drugs to induce a diagnostic type 1 Brugada pattern.12,21 Patients who have Brugada EKG findings but none of the other diagnostic criteria are considered to have a Brugada pattern (rather than Brugada syndrome).12
The most concerning outcome of BS is ventricular fibrillation. The estimated annual rate of cardiac events is 7.7% among patients who have experienced an aborted SCD, 1.9% among those who have experienced syncope, and 0.5% in asymptomatic patients.18
Treatment. The only effective treatment for BS is placement of an AICD; however, complications of AICD placement cause significant morbidity.6 Ten years after AICD placement, 37% of patients experienced inappropriate shocks and 29% experienced lead failure.22 Recent modifications in device programming and the addition of remote monitoring have decreased complication rates.12,22
The decision to place an AICD is based on the patient’s prior symptoms, EKG findings, and other factors. Recent guidelines recommend an AICD for all patients with a type 1 Brugada pattern (spontaneous or induced) who also have had an aborted SCD, syncope, or documented ventricular arrhythmia.12
Management of asymptomatic patients with type 1 Brugada pattern remains controversial because the rate of cardiac events is low, although such events can be fatal. Asymptomatic patients with type 1 Brugada findings should undergo further EP testing, and should receive AICD only upon demonstration of inducible ventricular arrhythmia.12
TABLE 2
Arrhythmias associated with Wolff-Parkinson-White syndrome23
| Arrhythmia | EKG findings | Treatment—unstable patients | Treatment—stable patients (in preferred treatment order) |
| PSVT, orthodromic | Narrow QRS, loss of delta wave, rate 160-260 beats/min | Synchronized cardioversion | Vagal maneuvers, adenosine, calcium channel blockers, beta-blockers, digoxin, procainamide |
| PSVT, antidromic | Wide complex tachycardia | Synchronized cardioversion | Procainamide |
| Atrial fibrillation | Irregularly irregular (RR interval variable with no pattern), ventricular rates that can exceed 300 beats/min | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Atrial flutter | Flutter waves, rate normal to tachycardic depending on conduction rate | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Ventricular fibrillation | Rapid, erratic electrical impulses | Defibrillation | N/A |
EKG, electrocardiogram; N/A, not applicable; PSVT, paroxysmal supraventricular tachycardia.
CASE 3 › A 21-year-old man with no medical history presents with sudden onset of lightheadedness followed by syncope. He denies any chest pain or other associated symptoms. At the time of evaluation, he is asymptomatic. His EKG (FIGURE 3) is diagnostic of what syndrome?
The EKG abnormality and diagnosis. The patient had a classic presentation for Wolff-Parkinson-White (WPW) syndrome, a common congenital disorder that alters normal cardiac conduction. He described 2 past instances of unexplained light-headedness and palpitations. Subsequent EP studies demonstrated that the patient had an accessory atrioventricular (AV) tract, causing electrical activity in the heart to bypass the AV node, resulting in a delta wave on EKG (FIGURE 3, GREEN ARROWS).
The patient opted for ablation therapy, which successfully eliminated the delta wave on EKG. Five years later he has had no recurrences.
Epidemiology. The prevalence of WPW syndrome is .1% to 3%.23 Accessory AV tracts are found in men twice as often as in women. Only half of individuals with confirmed tracts develop a tachyarrhythmia. The estimated risk of sudden death due to WPW syndrome is .5% to 4%.24
Pathophysiology. Normally cardiac conduction originates from the sinus node and travels to the AV node, where conduction is slowed, and then proceeds to the His-Purkinje system, and finally to the rest of the ventricular myocardium. In WPW syndrome, ventricular depolarization occurs first by an accessory AV tract called the bundle of Kent, followed shortly thereafter by the His-Purkinje system. This sequence of depolarization is what leads to the EKG findings characteristic of WPW syndrome: a PR interval <.12 seconds, presence of a delta wave, widened QRS complex (>.12 seconds), and repolarization changes seen as ST segment and T-wave changes discordant to (opposite direction) the delta wave and QRS complex (FIGURE 3, RED ARROW).
Factors that influence electrical conduction through the bundle of Kent include cardioactive medications, physiological stress, circulating catecholamines, coronary ischemia, and aging. The end result is a propensity for the heart to convert to one of 4 arrhythmias: paroxysmal supraventricular tachycardia (PSVT), AF, atrial flutter, or ventricular fibrillation (TABLE 2).23
The most common arrhythmia in WPW syndrome is PSVT.23 This rhythm is induced by the formation of a reentry circuit—a pattern in which the heart’s electrical signal loops back on itself—involving the normal conduction pathway and the bundle of Kent. Reentry progressing down the His-Purkinje system and traveling up the bundle of Kent is referred to as orthodromic (anterograde) PSVT. Antidromic (retrograde) PSVT is due to a reentry circuit conducting from the bundle of Kent to the ventricles, and then retrograde through the His-Purkinje system and AV node to the atria.
Clinical features. Under normal circumstances, patients with WPW syndrome are asymptomatic. As was the case with our patient, individuals who develop one of the 4 characteristic arrhythmias can experience light-headedness and syncope.
Treatment. An unstable patient who is experiencing PSVT, AF, or atrial flutter should receive synchronized cardioversion; those experiencing ventricular fibrillation should receive defibrillation (TABLE 2).23 For stable patients, therapy is tailored to the type of arrhythmia. Calcium channel blockers, beta-blockers, and adenosine might be appropriate for patients with orthodromic PSVT but should be avoided in patients with antidromic PSVT, AF, or atrial flutter because these medications block AV node conduction and thus facilitate conduction down the bundle of Kent, which can result in potentially unstable arrhythmias. In general, the longer an arrhythmia has been present, the less effective the pharmacologic intervention because of the increasing sympathetic tone.
Preventive long-term therapies for WPW patients who have experienced arrhythmia include antiarrhythmic medications or ablative procedures. Long-term antiarrhythmic therapy often is reserved for older, more sedentary individuals with less frequent arrhythmias that are not life-threatening. Radiofrequency ablation is a popular option, with long-term success rates as high as 95% and complication rates <1%.23 Patients in whom a WPW pattern is identified incidentally on EKG should be referred to cardiology for EP studies and risk stratification.25
CASE 4 › A 61-year-old woman has an episode of substernal exertional chest pressure that lasted approximately 2 hours but resolved before she arrived at her physician’s office. She also experienced mild nausea. She has no history of coronary artery disease but says that she has experienced similar episodes of chest pressure. What abnormality is seen on her EKG (FIGURE 4)? What is the most likely cause of her symptoms?
The EKG abnormality and diagnosis. Although classically associated with syncope, hypertrophic cardiomyopathy (HCM) often presents similarly to acute coronary syndromes, with chest pain and dyspnea on exertion.26 This patient had no history of cardiac disease or family history of SCD or cardiomyopathy; however, her EKG showed changes indicating left ventricular hypertrophy (LVH), which is consistent with HCM (FIGURE 4, ARROWS). Echocardiography identified myocardial hypertrophy, normal left ventricular ejection fraction, but severe left ventricular outflow obstruction and mild diastolic dysfunction. She was treated with metoprolol and verapamil.
Etiology and epidemiology. Hypertrophic cardiomyopathy is an autosomal dominant intrinsic myocardial disorder resulting in LVH that is commonly associated with SCD during extreme physical activity.26,27 The prevalence of HCM is approximately 1 in 500.26 Although it can present at any age, it is the most common cause of SCD in young people (under age 30), responsible for 33% of deaths during athletic events.28
TABLE 3
4 diagnoses and what you'll see on EKG
| Diagnosis | EKG finding |
| Prolonged QT interval | QTc interval >.450 sec (men) or >.470 sec (women) |
| Brugada syndrome | Partial or complete RBBB, and ST segment elevation in right precordial leads V1-V3 |
| Wolff-Parkinson-White syndrome | Delta wave, widened QRS, short PR interval, ST segment and T-wave changes |
| Hypertrophic cardiomyopathy | No definitive finding; may have left ventricular hypertrophy or abnormal Q-waves |
EKG, electrocardiogram; RBBB, right bundle branch block.
Clinical features. The severity of HCM ranges from asymptomatic to fatal. Symptoms of HCM include chest pain, dyspnea, and syncope. The disorder causes morbidity and mortality in at least one of 3 ways: ventricular tachyarrhythmias (often in younger patients), heart failure (from left ventricular outflow obstruction), and/or thromboembolism.27
Although echocardiography typically is used to make the diagnosis,27 an EKG often is the initial screening tool. EKG changes are seen in 75% to 95% of affected patients and include the presence of Q-waves and increased voltages related to LVH.27,29 Infarct-like patterns may be present before wall thickening on echocardiogram. Abnormal Q-waves are found in 20% to 50% of HCM patients, and are more common in younger patients. Konno et al30 have shown that Q-waves >3 mm in depth and/or >.040 seconds in duration in at least 2 leads other than aVR is specific (90%) in identifying carriers of HCM genes before they develop clinical symptoms.
Ambulatory monitoring may be useful for risk stratifying HCM patients; those with nonsustained ventricular tachycardia (NSVT) are at higher risk of SCD. Holter monitoring is recommended in initial evaluation because evidence of ventricular tachyarrhythmias may warrant AICD placement.26
Treatment. The risk of SCD in HCM is approximately 1%, but higher in those with a family history of SCD, syncope, NSVT, hypotension during exercise, or severe LVH (left ventricle thickness >30 mm).26 AICDs are recommended for HCM patients with prior cardiac arrest, patients with ≥2 of these risk factors, or patients with one risk factor who have experienced syncope related to arrhythmia.26
For patients who are symptomatic but have <2 risk factors, beta-blockers are firstline therapy.26 Verapamil is used as a second line treatment. Both beta-blockers and calcium channel blockers reduce dyspnea, palpitations, and chest pain.27
For patients who don’t respond to medical therapy, septal reduction therapy may be performed, either by septal myectomy or alcohol septal ablation.27 It is also important to consider genetic screening and counseling for the family.
A summary of all 4 diagnoses described in this article, their associated EKG findings, and their pathophysiology appears in TABLE 3.
CORRESPONDENCE
Samir Haydar, DO, MPH, FACEP, Tufts University School of Medicine, Maine Medical Center, Department of Emergency Medicine, 47 Bramhall St., Portland, ME 04103; [email protected]
› Consider placement of an automatic implantable cardioverter-defibrillator for all patients with a type 1 Brugada pattern on EKG accompanied by syncope, documented ventricular arrhythmia, or aborted sudden cardiac death. B
› Always look for EKG findings suggestive of Wolff-Parkinson-White syndrome in otherwise healthy patients presenting with syncope. C
› Refer all patients with suspected hypertrophic cardiomyopathy to Cardiology for a transthoracic echocardiogram. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
When evaluating a patient with a history of chest pain, palpitations, syncope, and/or new-onset seizures, an electrocardiogram (EKG) may be the key to
identifying a potentially life-threatening condition. Here we present 4 cases in which EKG findings were the clue to underlying medical conditions that, if left untreated, could be fatal. Because each of these conditions may not have associated findings on a physical exam, early recognition of these EKG findings can be lifesaving.
CASE 1 › A 15-year-old boy suddenly collapses while walking, and bystanders report seizure-like activity. The patient doesn’t remember the event. Vital signs and physical exam are normal, and his blood glucose level is 86 mg/dL (normal: 70-100 mg/dL). He doesn’t take any medications and denies illicit drug use or recent illness.
What EKG abnormality (FIGURE 1) likely explains the cause of the patient’s collapse?
The EKG abnormality and diagnosis. The patient’s EKG revealed a prolonged QT interval (FIGURE 1, BRACKETS). His QTc (QT interval corrected for heart rate) was .470 seconds, which is at the high end of the normal range for his age and gender.1 The patient had no family history of syncope, sudden cardiac death (SCD), or seizure disorder. Evaluation uncovered a calcium level of 4.4 mEq/L (normal: 4.5-5.5 mEq/L) and a phosphate level of 7.8 mg/dL (normal: 2.4-4.1 mg/dL).
This patient had a low parathyroid hormone from primary hypoparathyroidism. His conduction abnormality was treated with both oral calcium and vitamin D supplements.
Etiology and epidemiology. A prolonged QT interval may be the result of a primary long QT syndrome (LQTS) or an acquired condition from electrolyte imbalance, medication effect, or toxin exposure.
In the United States, the incidence of a genetic mutation that causes LQTS is 1 in 2500 people.2 Patients with LQTS usually remain asymptomatic unless the QT interval is further prolonged by a condition or medication. There are several hundred congenital LQTS subtypes based on specific ion channel defects; the most common is LQTS1, with an inherited defect in the KCNQ1 gene, which regulates the slow potassium ion channel.
Acquired LQTS is much more common than congenital LQTS.3 Many drugs have been linked to an increased risk of LQTS, including certain antiarrhythmics, antibiotics, and antipsychotics (TABLE 1).4 In addition, electrolyte disturbances such as hypokalemia, hypocalcemia, and hypomagnesemia can be etiologic factors.
Be aware that an acquired LQTS may mask an underlying congenital LQTS. Therefore, patients in whom the offending agent or condition is corrected should still have a follow-up EKG. Screening family members for LQTS is worthwhile, even in those without symptoms.
Clinical features. Patients with symptomatic LQTS may have dizziness, palpitations, and syncope. SCD also is possible. These signs and symptoms may be triggered by strong emotions (in LQTS2) or physical activity (in LQTS1). They likely are caused by torsades de pointes and ventricular fibrillation. A brief aura may precede these arrhythmias, and patients may experience urinary or fecal incontinence.5
The key to making a diagnosis of LQTS is correctly measuring the QT interval. The QT interval is measured from the beginning of the Q-wave to the end of the T-wave as measured from the intersection of a line tangent to the downslope of the T-wave and the isoelectric line. This can be difficult to determine in EKGs showing bundle branch block or an irregular rhythm, such as atrial fibrillation (AF).6,7 A common error in measuring the QT interval occurs when clinicians inadvertently include a U-wave in the measurement.1 Some EKG machines may provide QT interval and QTc measurements. Normal QT intervals are ≤.450 seconds for men and ≤.470 seconds for women.8
It is essential to confirm the QT interval by using the Bazett formula (QTc equals the QT in seconds divided by the square root of the RR interval in seconds) for all patients with a history that suggests a possible arrhythmia.
Our patient had hypocalcemia, which on an EKG can cause T-wave widening with a normal ST segment, rather than a normal T-wave with a long ST segment, as is typically seen in LQTS. This distinction may be difficult to discern and should not preclude the search for either an acquired prolonged QTc or an underlying LQTS.9
Treatment. First rule out or treat any causes of acquired LQTS by taking a careful medication history and evaluating the patient’s electrolytes. Once these have been addressed, a beta-blocker is first-line therapy for symptomatic patients.5
Unfortunately, up to 20% of individuals treated with beta-blockers may continue to have syncope.5 For these patients, options include a left cardiac sympathetic denervation (LCSD) or placement of an automatic implantable cardioverter-defibrillator (AICD). An LCSD involves removal of the left-sided stellate and/or thoracic ganglia. This procedure can be used instead of, or in addition to, beta-blockers. If the patient’s syncope persists, AICDs are an option. AICDs can be lifesaving, but patients run the risk of adverse effects that include inappropriate shocks and infection.10 As the result of these therapies, mortality associated with LQTS has dropped to approximately 1%.11
CASE 2 › A 14-year-old boy has a syncopal episode while at rest. A similar event occurred 3 years earlier; at that time, an echocardiogram and EKG were normal. For 2 days, he’s had a cough and low-grade fever. His temperature is 102ºF and he has a productive cough. Based on this EKG (FIGURE 2), what is the likely diagnosis? What is the significance of his fever?
The EKG abnormality and diagnosis. This patient’s EKG showed a type 1 Brugada pattern (FIGURE 2, ARROWS), which strongly supported the diagnosis of Brugada syndrome (BS). BS is an inherited condition caused by a genetic defect in cardiac ion channel function that leads to characteristic EKG changes and a predisposition to ventricular fibrillation.12 In this case, the fever likely unmasked these EKG findings.
The patient was transferred to a local hospital for treatment of community-acquired pneumonia, and ultimately received an AICD.
Etiology and epidemiology. BS was first described in 199213 and is a major cause of SCD, responsible for up to 4% of all cases of SCD, and 20% of cases of patients without structural heart disease.14 BS is more common in men, and the mean age of diagnosis is 40 to 45.15-18
Mutations in at least 17 cardiac ion channel genes have been linked to BS.19 The SCN5A gene—a cardiac sodium channel—is the most commonly implicated, but accounts for only 11% to 24% of all BS cases.15
Clinical features. Patients with BS may present with syncope, nocturnal agonal respirations, or ventricular arrhythmias.12 EKG findings include partial or complete right bundle branch block (RBBB) and ST segment elevation in right precordial leads V1 to V3.12 There are 2 Brugada EKG patterns, a type 1 cloved pattern as seen in our patient’s EKG and a type 2 saddleback pattern.20 EKG findings are dynamic over time and may alternate between normal, type 1, and type 2.20 Factors that modulate EKG appearance include fever, intoxication, vagal tone, electrolyte imbalance, and sodium channel blockade.12,20
Diagnosis requires a type 1 Brugada pattern on EKG plus a family history of BS, documented ventricular arrhythmia, or arrhythmia-related symptoms such as syncope.12 Patients with a type 2 Brugada pattern may undergo electrophysiology (EP) testing with Class I antiarrhythmic drugs to induce a diagnostic type 1 Brugada pattern.12,21 Patients who have Brugada EKG findings but none of the other diagnostic criteria are considered to have a Brugada pattern (rather than Brugada syndrome).12
The most concerning outcome of BS is ventricular fibrillation. The estimated annual rate of cardiac events is 7.7% among patients who have experienced an aborted SCD, 1.9% among those who have experienced syncope, and 0.5% in asymptomatic patients.18
Treatment. The only effective treatment for BS is placement of an AICD; however, complications of AICD placement cause significant morbidity.6 Ten years after AICD placement, 37% of patients experienced inappropriate shocks and 29% experienced lead failure.22 Recent modifications in device programming and the addition of remote monitoring have decreased complication rates.12,22
The decision to place an AICD is based on the patient’s prior symptoms, EKG findings, and other factors. Recent guidelines recommend an AICD for all patients with a type 1 Brugada pattern (spontaneous or induced) who also have had an aborted SCD, syncope, or documented ventricular arrhythmia.12
Management of asymptomatic patients with type 1 Brugada pattern remains controversial because the rate of cardiac events is low, although such events can be fatal. Asymptomatic patients with type 1 Brugada findings should undergo further EP testing, and should receive AICD only upon demonstration of inducible ventricular arrhythmia.12
TABLE 2
Arrhythmias associated with Wolff-Parkinson-White syndrome23
| Arrhythmia | EKG findings | Treatment—unstable patients | Treatment—stable patients (in preferred treatment order) |
| PSVT, orthodromic | Narrow QRS, loss of delta wave, rate 160-260 beats/min | Synchronized cardioversion | Vagal maneuvers, adenosine, calcium channel blockers, beta-blockers, digoxin, procainamide |
| PSVT, antidromic | Wide complex tachycardia | Synchronized cardioversion | Procainamide |
| Atrial fibrillation | Irregularly irregular (RR interval variable with no pattern), ventricular rates that can exceed 300 beats/min | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Atrial flutter | Flutter waves, rate normal to tachycardic depending on conduction rate | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Ventricular fibrillation | Rapid, erratic electrical impulses | Defibrillation | N/A |
EKG, electrocardiogram; N/A, not applicable; PSVT, paroxysmal supraventricular tachycardia.
CASE 3 › A 21-year-old man with no medical history presents with sudden onset of lightheadedness followed by syncope. He denies any chest pain or other associated symptoms. At the time of evaluation, he is asymptomatic. His EKG (FIGURE 3) is diagnostic of what syndrome?
The EKG abnormality and diagnosis. The patient had a classic presentation for Wolff-Parkinson-White (WPW) syndrome, a common congenital disorder that alters normal cardiac conduction. He described 2 past instances of unexplained light-headedness and palpitations. Subsequent EP studies demonstrated that the patient had an accessory atrioventricular (AV) tract, causing electrical activity in the heart to bypass the AV node, resulting in a delta wave on EKG (FIGURE 3, GREEN ARROWS).
The patient opted for ablation therapy, which successfully eliminated the delta wave on EKG. Five years later he has had no recurrences.
Epidemiology. The prevalence of WPW syndrome is .1% to 3%.23 Accessory AV tracts are found in men twice as often as in women. Only half of individuals with confirmed tracts develop a tachyarrhythmia. The estimated risk of sudden death due to WPW syndrome is .5% to 4%.24
Pathophysiology. Normally cardiac conduction originates from the sinus node and travels to the AV node, where conduction is slowed, and then proceeds to the His-Purkinje system, and finally to the rest of the ventricular myocardium. In WPW syndrome, ventricular depolarization occurs first by an accessory AV tract called the bundle of Kent, followed shortly thereafter by the His-Purkinje system. This sequence of depolarization is what leads to the EKG findings characteristic of WPW syndrome: a PR interval <.12 seconds, presence of a delta wave, widened QRS complex (>.12 seconds), and repolarization changes seen as ST segment and T-wave changes discordant to (opposite direction) the delta wave and QRS complex (FIGURE 3, RED ARROW).
Factors that influence electrical conduction through the bundle of Kent include cardioactive medications, physiological stress, circulating catecholamines, coronary ischemia, and aging. The end result is a propensity for the heart to convert to one of 4 arrhythmias: paroxysmal supraventricular tachycardia (PSVT), AF, atrial flutter, or ventricular fibrillation (TABLE 2).23
The most common arrhythmia in WPW syndrome is PSVT.23 This rhythm is induced by the formation of a reentry circuit—a pattern in which the heart’s electrical signal loops back on itself—involving the normal conduction pathway and the bundle of Kent. Reentry progressing down the His-Purkinje system and traveling up the bundle of Kent is referred to as orthodromic (anterograde) PSVT. Antidromic (retrograde) PSVT is due to a reentry circuit conducting from the bundle of Kent to the ventricles, and then retrograde through the His-Purkinje system and AV node to the atria.
Clinical features. Under normal circumstances, patients with WPW syndrome are asymptomatic. As was the case with our patient, individuals who develop one of the 4 characteristic arrhythmias can experience light-headedness and syncope.
Treatment. An unstable patient who is experiencing PSVT, AF, or atrial flutter should receive synchronized cardioversion; those experiencing ventricular fibrillation should receive defibrillation (TABLE 2).23 For stable patients, therapy is tailored to the type of arrhythmia. Calcium channel blockers, beta-blockers, and adenosine might be appropriate for patients with orthodromic PSVT but should be avoided in patients with antidromic PSVT, AF, or atrial flutter because these medications block AV node conduction and thus facilitate conduction down the bundle of Kent, which can result in potentially unstable arrhythmias. In general, the longer an arrhythmia has been present, the less effective the pharmacologic intervention because of the increasing sympathetic tone.
Preventive long-term therapies for WPW patients who have experienced arrhythmia include antiarrhythmic medications or ablative procedures. Long-term antiarrhythmic therapy often is reserved for older, more sedentary individuals with less frequent arrhythmias that are not life-threatening. Radiofrequency ablation is a popular option, with long-term success rates as high as 95% and complication rates <1%.23 Patients in whom a WPW pattern is identified incidentally on EKG should be referred to cardiology for EP studies and risk stratification.25
CASE 4 › A 61-year-old woman has an episode of substernal exertional chest pressure that lasted approximately 2 hours but resolved before she arrived at her physician’s office. She also experienced mild nausea. She has no history of coronary artery disease but says that she has experienced similar episodes of chest pressure. What abnormality is seen on her EKG (FIGURE 4)? What is the most likely cause of her symptoms?
The EKG abnormality and diagnosis. Although classically associated with syncope, hypertrophic cardiomyopathy (HCM) often presents similarly to acute coronary syndromes, with chest pain and dyspnea on exertion.26 This patient had no history of cardiac disease or family history of SCD or cardiomyopathy; however, her EKG showed changes indicating left ventricular hypertrophy (LVH), which is consistent with HCM (FIGURE 4, ARROWS). Echocardiography identified myocardial hypertrophy, normal left ventricular ejection fraction, but severe left ventricular outflow obstruction and mild diastolic dysfunction. She was treated with metoprolol and verapamil.
Etiology and epidemiology. Hypertrophic cardiomyopathy is an autosomal dominant intrinsic myocardial disorder resulting in LVH that is commonly associated with SCD during extreme physical activity.26,27 The prevalence of HCM is approximately 1 in 500.26 Although it can present at any age, it is the most common cause of SCD in young people (under age 30), responsible for 33% of deaths during athletic events.28
TABLE 3
4 diagnoses and what you'll see on EKG
| Diagnosis | EKG finding |
| Prolonged QT interval | QTc interval >.450 sec (men) or >.470 sec (women) |
| Brugada syndrome | Partial or complete RBBB, and ST segment elevation in right precordial leads V1-V3 |
| Wolff-Parkinson-White syndrome | Delta wave, widened QRS, short PR interval, ST segment and T-wave changes |
| Hypertrophic cardiomyopathy | No definitive finding; may have left ventricular hypertrophy or abnormal Q-waves |
EKG, electrocardiogram; RBBB, right bundle branch block.
Clinical features. The severity of HCM ranges from asymptomatic to fatal. Symptoms of HCM include chest pain, dyspnea, and syncope. The disorder causes morbidity and mortality in at least one of 3 ways: ventricular tachyarrhythmias (often in younger patients), heart failure (from left ventricular outflow obstruction), and/or thromboembolism.27
Although echocardiography typically is used to make the diagnosis,27 an EKG often is the initial screening tool. EKG changes are seen in 75% to 95% of affected patients and include the presence of Q-waves and increased voltages related to LVH.27,29 Infarct-like patterns may be present before wall thickening on echocardiogram. Abnormal Q-waves are found in 20% to 50% of HCM patients, and are more common in younger patients. Konno et al30 have shown that Q-waves >3 mm in depth and/or >.040 seconds in duration in at least 2 leads other than aVR is specific (90%) in identifying carriers of HCM genes before they develop clinical symptoms.
Ambulatory monitoring may be useful for risk stratifying HCM patients; those with nonsustained ventricular tachycardia (NSVT) are at higher risk of SCD. Holter monitoring is recommended in initial evaluation because evidence of ventricular tachyarrhythmias may warrant AICD placement.26
Treatment. The risk of SCD in HCM is approximately 1%, but higher in those with a family history of SCD, syncope, NSVT, hypotension during exercise, or severe LVH (left ventricle thickness >30 mm).26 AICDs are recommended for HCM patients with prior cardiac arrest, patients with ≥2 of these risk factors, or patients with one risk factor who have experienced syncope related to arrhythmia.26
For patients who are symptomatic but have <2 risk factors, beta-blockers are firstline therapy.26 Verapamil is used as a second line treatment. Both beta-blockers and calcium channel blockers reduce dyspnea, palpitations, and chest pain.27
For patients who don’t respond to medical therapy, septal reduction therapy may be performed, either by septal myectomy or alcohol septal ablation.27 It is also important to consider genetic screening and counseling for the family.
A summary of all 4 diagnoses described in this article, their associated EKG findings, and their pathophysiology appears in TABLE 3.
CORRESPONDENCE
Samir Haydar, DO, MPH, FACEP, Tufts University School of Medicine, Maine Medical Center, Department of Emergency Medicine, 47 Bramhall St., Portland, ME 04103; [email protected]
1. Taggart NW, Haglund CM, Tester DJ, et al. Diagnostic miscues in congenital long-QT syndrome. Circulation. 2007;115:2613-2620.
2. Schwartz PJ, Stramba-Badiale M, Crotti L, et al. Prevalance of the congenital long QT syndrome. Circulation. 2009;120:1761-1767.
3. van Noord C, Eijgelsheim M, Stricker BH. Drug- and nondrug-associated QT interval prolongation. Br J Clin Pharmacol. 2010;70:16-23.
4. Credible Meds Web site. Available at: http://crediblemeds.org. Accessed April 8, 2014.
5. Schwartz PJ, Priori SG, Spazzolini C, et al. Genotype-phenotype correlation in the long QT syndrome: gene specific triggers for life threatening arrhythmias. Circulation. 2001;103:89.
6. Chiladakis JK, Kalogeropoulos A, Koutsogiannis N, et al. Optimal QT/JT interval assessment in patients with complete bundle branch block. Ann Noninvasive Electrocardiol. 2012;17:268-276.
7. Ercan S, Altunbas G, Oylumlu M, et al. Congenital long QT syndrome masked by atrial fibrillation and unmasked by hypokalemia. Am J Emerg Med. 2013;31:451.e3-451.e6.
8. Goldenberg I, Moss AJ, Zareba W. QT interval: how to measure it and what is “normal.” J Cardiovasc Electrophysiol. 2006;17:333-336.
9. Podrid PJ. ECG Response: August 20, 2013. Circulation. 2013;128:869.
10. Olde Nordkamp LR, Wilde AA, Tijssen JG, et al. The ICD for primary prevention in patients with inherited cardiac diseases: indications, use, and outcome: a comparison with secondary prevention. Circ Arrhythm Electrophysiol. 2013;6:91-100.
11. Schwartz PJ. Pharmacological and non-pharmacological management of the congenital long QT syndrome: the rationale. Pharmacol Ther. 2011;131:171-177.
12. Berne P, Brugada J. Brugada syndrome 2012. Circ J. 2012;76:1563-1571.
13. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391-1396.
14. Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005;111:659-670.
15. Brugada J, Brugada R, Antzelevitch C, et al. Long-term followup of individuals with the electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3. Circulation. 2002;105:73-78.
16. Eckardt L, Probst V, Smits JP, et al. Long-term prognosis of individuals with right precordial ST-segment-elevation Brugada syndrome. Circulation. 2005;111:257-263.
17. Giustetto C, Drago S, Demarchi PG, et al; Italian Association of Arrhythmology and Cardiostimulation (AIAC)-Piedmont Section. Risk stratification of the patients with Brugada type electrocardiogram: a community-based prospective study. Europace. 2009;11:507-513.
18. Probst V, Veltmann C, Eckardt L, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: Results from the FINGER Brugada Syndrome Registry. Circulation. 2010;121:635-643.
19. Nielsen MW, Holst AG, Olesen SP, et al. The genetic component of Brugada syndrome. Front Physiol. 2013;4:179.
20. Bayés de Luna A, Brugada J, Baranchuk A, et al. Current electrocardiographic criteria for diagnosis of Brugada pattern: a consensus report. J Electrocardiol. 2012;45:433-442.
21. Veltmann C, Schimpf R, Echternach C, et al. A prospective study on spontaneous fluctuations between diagnostic and non-diagnostic ECGs in Brugada syndrome: implications for correct phenotyping and risk stratification. Eur Heart J. 2006;27:2544-2552.
22. Sacher F, Probst V, Maury P, et al. Outcome after implantation of a cardioverter-defibrillator in patients with Brugada syndrome: a multicenter study-part 2. Circulation. 2013;128:1739-1747.
23. Rosner MH, Brady WJ Jr, Kefer MP, et al. Electrocardiography in the patient with the Wolff-Parkinson-White syndrome: diagnostic and initial therapeutic issues. Am J Emerg Med. 1999;17:705-714.
24. Keating L, Morris FP, Brady WJ. Electrocardiographic features of Wolff-Parkinson-White syndrome. Emerg Med J. 2003;20:491-493.
25. Blomström-Lundqvist C, Scheinman MM, Aliot EM, et al; European Society of Cardiology Committee, NASPE-Heart Rhythm Society. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias—executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003;42:1493-1531.
26. Ho CY. Hypertrophic cardiomyopathy in 2012. Circulation. 2012;125:1432-1438.
27. Gersh BJ, Maron BJ, Bonow RO, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American Society of Echocardiography; American Society of Nuclear Cardiology; Heart Failure Society of America; Heart Rhythm Society; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:e783-e831.
28. Paterick TE, Jan MF, Paterick ZR, et al. Cardiac evaluation of collegiate student athletes: a medical and legal perspective. Am J Med. 2012;125:742-752.
29. Maron BJ. Hypertrophic cardiomyopathy. In: Bonow RO, Mann DL, Zipes DP, et al (eds). Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Philadelphia, PA: Saunders; 2011:1582-1594.
30. Konno T, Shimizu M, Ino H, et al. Diagnostic value of abnormal Q waves for identification of preclinical carriers of hypertrophic cardiomyopathy based on molecular genetic diagnosis. Eur Heart J. 2004;25:246-251.
1. Taggart NW, Haglund CM, Tester DJ, et al. Diagnostic miscues in congenital long-QT syndrome. Circulation. 2007;115:2613-2620.
2. Schwartz PJ, Stramba-Badiale M, Crotti L, et al. Prevalance of the congenital long QT syndrome. Circulation. 2009;120:1761-1767.
3. van Noord C, Eijgelsheim M, Stricker BH. Drug- and nondrug-associated QT interval prolongation. Br J Clin Pharmacol. 2010;70:16-23.
4. Credible Meds Web site. Available at: http://crediblemeds.org. Accessed April 8, 2014.
5. Schwartz PJ, Priori SG, Spazzolini C, et al. Genotype-phenotype correlation in the long QT syndrome: gene specific triggers for life threatening arrhythmias. Circulation. 2001;103:89.
6. Chiladakis JK, Kalogeropoulos A, Koutsogiannis N, et al. Optimal QT/JT interval assessment in patients with complete bundle branch block. Ann Noninvasive Electrocardiol. 2012;17:268-276.
7. Ercan S, Altunbas G, Oylumlu M, et al. Congenital long QT syndrome masked by atrial fibrillation and unmasked by hypokalemia. Am J Emerg Med. 2013;31:451.e3-451.e6.
8. Goldenberg I, Moss AJ, Zareba W. QT interval: how to measure it and what is “normal.” J Cardiovasc Electrophysiol. 2006;17:333-336.
9. Podrid PJ. ECG Response: August 20, 2013. Circulation. 2013;128:869.
10. Olde Nordkamp LR, Wilde AA, Tijssen JG, et al. The ICD for primary prevention in patients with inherited cardiac diseases: indications, use, and outcome: a comparison with secondary prevention. Circ Arrhythm Electrophysiol. 2013;6:91-100.
11. Schwartz PJ. Pharmacological and non-pharmacological management of the congenital long QT syndrome: the rationale. Pharmacol Ther. 2011;131:171-177.
12. Berne P, Brugada J. Brugada syndrome 2012. Circ J. 2012;76:1563-1571.
13. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391-1396.
14. Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005;111:659-670.
15. Brugada J, Brugada R, Antzelevitch C, et al. Long-term followup of individuals with the electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3. Circulation. 2002;105:73-78.
16. Eckardt L, Probst V, Smits JP, et al. Long-term prognosis of individuals with right precordial ST-segment-elevation Brugada syndrome. Circulation. 2005;111:257-263.
17. Giustetto C, Drago S, Demarchi PG, et al; Italian Association of Arrhythmology and Cardiostimulation (AIAC)-Piedmont Section. Risk stratification of the patients with Brugada type electrocardiogram: a community-based prospective study. Europace. 2009;11:507-513.
18. Probst V, Veltmann C, Eckardt L, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: Results from the FINGER Brugada Syndrome Registry. Circulation. 2010;121:635-643.
19. Nielsen MW, Holst AG, Olesen SP, et al. The genetic component of Brugada syndrome. Front Physiol. 2013;4:179.
20. Bayés de Luna A, Brugada J, Baranchuk A, et al. Current electrocardiographic criteria for diagnosis of Brugada pattern: a consensus report. J Electrocardiol. 2012;45:433-442.
21. Veltmann C, Schimpf R, Echternach C, et al. A prospective study on spontaneous fluctuations between diagnostic and non-diagnostic ECGs in Brugada syndrome: implications for correct phenotyping and risk stratification. Eur Heart J. 2006;27:2544-2552.
22. Sacher F, Probst V, Maury P, et al. Outcome after implantation of a cardioverter-defibrillator in patients with Brugada syndrome: a multicenter study-part 2. Circulation. 2013;128:1739-1747.
23. Rosner MH, Brady WJ Jr, Kefer MP, et al. Electrocardiography in the patient with the Wolff-Parkinson-White syndrome: diagnostic and initial therapeutic issues. Am J Emerg Med. 1999;17:705-714.
24. Keating L, Morris FP, Brady WJ. Electrocardiographic features of Wolff-Parkinson-White syndrome. Emerg Med J. 2003;20:491-493.
25. Blomström-Lundqvist C, Scheinman MM, Aliot EM, et al; European Society of Cardiology Committee, NASPE-Heart Rhythm Society. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias—executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003;42:1493-1531.
26. Ho CY. Hypertrophic cardiomyopathy in 2012. Circulation. 2012;125:1432-1438.
27. Gersh BJ, Maron BJ, Bonow RO, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American Society of Echocardiography; American Society of Nuclear Cardiology; Heart Failure Society of America; Heart Rhythm Society; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:e783-e831.
28. Paterick TE, Jan MF, Paterick ZR, et al. Cardiac evaluation of collegiate student athletes: a medical and legal perspective. Am J Med. 2012;125:742-752.
29. Maron BJ. Hypertrophic cardiomyopathy. In: Bonow RO, Mann DL, Zipes DP, et al (eds). Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Philadelphia, PA: Saunders; 2011:1582-1594.
30. Konno T, Shimizu M, Ino H, et al. Diagnostic value of abnormal Q waves for identification of preclinical carriers of hypertrophic cardiomyopathy based on molecular genetic diagnosis. Eur Heart J. 2004;25:246-251.
Q&A: “Code Black” Offers Insider Look at ED Challenges
Interview by Mary Ellen Schneider
“Code Black,” the award-winning documentary about working in the ED at Los Angeles County Hospital, opened in theaters in 40 US cities this summer.
It’s the film debut for emergency physician Ryan McGarry, who both stars in and directs the feature-length documentary. It highlights the thrills and challenges of working in a busy ED through the eyes of senior residents, including Dr McGarry, who completed his training while working on the film. The young doctors start the film as fresh-faced idealists in the “C-Booth” trauma bay at LA County Hospital, the famed birthplace of emergency medicine. Later they move to the county’s newly built hospital, which, though state-of-the-art, lacks some of the camaraderie of the original ED.
“Code Black” was the Best Documentary winner at the Los Angeles Film Festival and the Hamptons International Film Festival. And it was the Audience Award winner at both the Starz Denver Film Festival and the Aspen Filmfest.
Dr McGarry, who is now an attending physician at New York-Presbyterian Hospital in New York City, discussed why he made the film and how it is likely to impact the health care debate.
Question: What inspired you to make this film?
Dr McGarry: As documentaries go, this one was kind of an accident in the sense of its narrative development. I set out to capture what I thought was a phenomenally intense, and in some ways, dated and brutal trauma bay. At this point, most people associate modern health care with a lot of sterility and technology and white and blue spaces that are kind of contained. And this shows the opposite. This looks like battlefield medicine. To my surprise, it was working very well. Of course, at the time I was a young medical student, so my basis for evaluating that matured along with the film. As time went on, we migrated from the old L.A. County Hospital to a newer space. So in the course of filming, they closed down an 80-year-old structure in favor of a brand new, billion-dollar, shining, technology-laden palace. What we found was that as we were brought up to speed on modern health care, and of course regulation, the care became much more complicated.
Question: What do you want the audience to take away from the film?
Dr McGarry: It’s hopefully a primer for health care discussion that has not yet existed. There are plenty of films that ride the political undertones of health care very well and, I think, if anything, they seem to keep people in their camps. They don’t really bring people to the middle. They may make discussion more satisfying for people who are politically charged, but from the provider’s point of view, I’m not sure if they get us anywhere. “Code Black” does not have a call to action, as they call it in the documentary world. That’s on purpose. What we’re hoping for is for people to watch it and be a bit more primed when we talk about health care. My prediction—this could be wrong—is that the real discussion for the next quarter-century, as we improve access with the [Affordable Care Act], is going to be the patient-doctor connection and some deregulation. There are just too many barriers right now. The equation is too complicated. The healing and listening that people want are not happening.
Question: So would you like to see policy makers ease up on some of the health care regulations?
Dr McGarry: We all want safety. But as a scientist would say, these regulations ought to be evidence based. What we know as physicians is that any evidence-based truth is a hard thing to prove, period. I think a lot of these regulations are well intentioned. Nobody doubts that. But yesterday, the Joint Commission visited our hospital. Everybody was working hard on a shift trying to move patients through, trying to provide both quick and safe care, and one of the things that [the regulators] were watching out for was keeping the employee bags and coffee off the computer desks. Meanwhile, I have patients with chest pain, patients with stroke, patients with fractures, who are not getting the attention they need because we’re totally focused on pleasing the federal regulators that our bags and coffee aren’t out.
Question: The film is from the perspective of young doctors and talks a lot about their initial idealism. Do you think the messages in the film will also resonate with older doctors?
Dr McGarry: One of the more surprising aspects of “Code Black” is the nostalgia factor, that fact that both physicians who have been working for a while and those who have become administrators watched this film. We thought it would be offensive to them—especially people from private hospitals, whom we are sort of tough on in the movie. We thought that they would find us a little unrealistic and idealistic. Interestingly, they all watched it and they said, “I long for the day in my residency when all I had to worry about was just getting the science right, getting that patient connection right.”
Question: Working in C-Booth was a great experience for ED physicians in training. Can you ever recapture that feeling in the new, heavily regulated environment?
Dr McGarry: One thing we wouldn’t want to return to would be the lack of privacy. The biggest aspect of C-Booth that probably we wouldn’t be proud of is the lack of privacy. I’m definitely for privacy and for a dignified experience. After that, I feel like things are quite undefined. I think we have expectations that technology, in particular, is a huge answer to medicine. But we know it can be expensive and it can be dangerous. And in the case of electronic medical records, it certainly doesn’t make things faster. We know that every institution that has gone from paper charts to an EMR has found not just an immediate slowing of care, but a permanent slowing. And yet there are benefits with being able to quickly look up old medical information. But what about when my patient is waiting 20 minutes for pain medicine because it takes almost that long to get them in the computer, pull up the order, select the medicine, and go through all these stupid hard stops that are built in? Before, I could just write it down on a piece of paper, communicate it to the nurse, and get it done. If you’re the one in pain, is [the EMR] worth it? I don’t know.
Question: How did you find the time to make this movie?
Dr McGarry: There were a lot of consequences. I probably pushed it from a health perspective. I really found myself in a unique position as both a filmmaker and subject. For almost 3 years, I would do every ounce of my residency and then would race from the hospital to the edit room and would live and breathe it for 3 years. You would imagine there’s a cost to that. Lost a girlfriend. Didn’t sleep. Happily, I came through without any major damage, but that’s a heck of a lot of emergency medicine.
Question: What are you doing next? Are you working on another film and how are you balancing your new project with your day job in medicine?
Dr McGarry: This is a different game than it was in residency. I have an option for a scripted series, so basically it means that producers have identified it as a viable project for a fiction series like you would see on HBO. That’s in active development. We just shot a 3-minute spot with the New York and L.A. ballets, which involves these dancers in the old abandoned general hospital. As far as balancing all this, I’m so lucky in that Cornell/New York-Presbyterian and Dr Neal Flomenbaum have been incredibly supportive of me, allowing me to be full time there but with the work flexibility to jump on these projects as they come.
On Twitter @maryellenny
Interview by Mary Ellen Schneider
“Code Black,” the award-winning documentary about working in the ED at Los Angeles County Hospital, opened in theaters in 40 US cities this summer.
It’s the film debut for emergency physician Ryan McGarry, who both stars in and directs the feature-length documentary. It highlights the thrills and challenges of working in a busy ED through the eyes of senior residents, including Dr McGarry, who completed his training while working on the film. The young doctors start the film as fresh-faced idealists in the “C-Booth” trauma bay at LA County Hospital, the famed birthplace of emergency medicine. Later they move to the county’s newly built hospital, which, though state-of-the-art, lacks some of the camaraderie of the original ED.
“Code Black” was the Best Documentary winner at the Los Angeles Film Festival and the Hamptons International Film Festival. And it was the Audience Award winner at both the Starz Denver Film Festival and the Aspen Filmfest.
Dr McGarry, who is now an attending physician at New York-Presbyterian Hospital in New York City, discussed why he made the film and how it is likely to impact the health care debate.
Question: What inspired you to make this film?
Dr McGarry: As documentaries go, this one was kind of an accident in the sense of its narrative development. I set out to capture what I thought was a phenomenally intense, and in some ways, dated and brutal trauma bay. At this point, most people associate modern health care with a lot of sterility and technology and white and blue spaces that are kind of contained. And this shows the opposite. This looks like battlefield medicine. To my surprise, it was working very well. Of course, at the time I was a young medical student, so my basis for evaluating that matured along with the film. As time went on, we migrated from the old L.A. County Hospital to a newer space. So in the course of filming, they closed down an 80-year-old structure in favor of a brand new, billion-dollar, shining, technology-laden palace. What we found was that as we were brought up to speed on modern health care, and of course regulation, the care became much more complicated.
Question: What do you want the audience to take away from the film?
Dr McGarry: It’s hopefully a primer for health care discussion that has not yet existed. There are plenty of films that ride the political undertones of health care very well and, I think, if anything, they seem to keep people in their camps. They don’t really bring people to the middle. They may make discussion more satisfying for people who are politically charged, but from the provider’s point of view, I’m not sure if they get us anywhere. “Code Black” does not have a call to action, as they call it in the documentary world. That’s on purpose. What we’re hoping for is for people to watch it and be a bit more primed when we talk about health care. My prediction—this could be wrong—is that the real discussion for the next quarter-century, as we improve access with the [Affordable Care Act], is going to be the patient-doctor connection and some deregulation. There are just too many barriers right now. The equation is too complicated. The healing and listening that people want are not happening.
Question: So would you like to see policy makers ease up on some of the health care regulations?
Dr McGarry: We all want safety. But as a scientist would say, these regulations ought to be evidence based. What we know as physicians is that any evidence-based truth is a hard thing to prove, period. I think a lot of these regulations are well intentioned. Nobody doubts that. But yesterday, the Joint Commission visited our hospital. Everybody was working hard on a shift trying to move patients through, trying to provide both quick and safe care, and one of the things that [the regulators] were watching out for was keeping the employee bags and coffee off the computer desks. Meanwhile, I have patients with chest pain, patients with stroke, patients with fractures, who are not getting the attention they need because we’re totally focused on pleasing the federal regulators that our bags and coffee aren’t out.
Question: The film is from the perspective of young doctors and talks a lot about their initial idealism. Do you think the messages in the film will also resonate with older doctors?
Dr McGarry: One of the more surprising aspects of “Code Black” is the nostalgia factor, that fact that both physicians who have been working for a while and those who have become administrators watched this film. We thought it would be offensive to them—especially people from private hospitals, whom we are sort of tough on in the movie. We thought that they would find us a little unrealistic and idealistic. Interestingly, they all watched it and they said, “I long for the day in my residency when all I had to worry about was just getting the science right, getting that patient connection right.”
Question: Working in C-Booth was a great experience for ED physicians in training. Can you ever recapture that feeling in the new, heavily regulated environment?
Dr McGarry: One thing we wouldn’t want to return to would be the lack of privacy. The biggest aspect of C-Booth that probably we wouldn’t be proud of is the lack of privacy. I’m definitely for privacy and for a dignified experience. After that, I feel like things are quite undefined. I think we have expectations that technology, in particular, is a huge answer to medicine. But we know it can be expensive and it can be dangerous. And in the case of electronic medical records, it certainly doesn’t make things faster. We know that every institution that has gone from paper charts to an EMR has found not just an immediate slowing of care, but a permanent slowing. And yet there are benefits with being able to quickly look up old medical information. But what about when my patient is waiting 20 minutes for pain medicine because it takes almost that long to get them in the computer, pull up the order, select the medicine, and go through all these stupid hard stops that are built in? Before, I could just write it down on a piece of paper, communicate it to the nurse, and get it done. If you’re the one in pain, is [the EMR] worth it? I don’t know.
Question: How did you find the time to make this movie?
Dr McGarry: There were a lot of consequences. I probably pushed it from a health perspective. I really found myself in a unique position as both a filmmaker and subject. For almost 3 years, I would do every ounce of my residency and then would race from the hospital to the edit room and would live and breathe it for 3 years. You would imagine there’s a cost to that. Lost a girlfriend. Didn’t sleep. Happily, I came through without any major damage, but that’s a heck of a lot of emergency medicine.
Question: What are you doing next? Are you working on another film and how are you balancing your new project with your day job in medicine?
Dr McGarry: This is a different game than it was in residency. I have an option for a scripted series, so basically it means that producers have identified it as a viable project for a fiction series like you would see on HBO. That’s in active development. We just shot a 3-minute spot with the New York and L.A. ballets, which involves these dancers in the old abandoned general hospital. As far as balancing all this, I’m so lucky in that Cornell/New York-Presbyterian and Dr Neal Flomenbaum have been incredibly supportive of me, allowing me to be full time there but with the work flexibility to jump on these projects as they come.
On Twitter @maryellenny
Interview by Mary Ellen Schneider
“Code Black,” the award-winning documentary about working in the ED at Los Angeles County Hospital, opened in theaters in 40 US cities this summer.
It’s the film debut for emergency physician Ryan McGarry, who both stars in and directs the feature-length documentary. It highlights the thrills and challenges of working in a busy ED through the eyes of senior residents, including Dr McGarry, who completed his training while working on the film. The young doctors start the film as fresh-faced idealists in the “C-Booth” trauma bay at LA County Hospital, the famed birthplace of emergency medicine. Later they move to the county’s newly built hospital, which, though state-of-the-art, lacks some of the camaraderie of the original ED.
“Code Black” was the Best Documentary winner at the Los Angeles Film Festival and the Hamptons International Film Festival. And it was the Audience Award winner at both the Starz Denver Film Festival and the Aspen Filmfest.
Dr McGarry, who is now an attending physician at New York-Presbyterian Hospital in New York City, discussed why he made the film and how it is likely to impact the health care debate.
Question: What inspired you to make this film?
Dr McGarry: As documentaries go, this one was kind of an accident in the sense of its narrative development. I set out to capture what I thought was a phenomenally intense, and in some ways, dated and brutal trauma bay. At this point, most people associate modern health care with a lot of sterility and technology and white and blue spaces that are kind of contained. And this shows the opposite. This looks like battlefield medicine. To my surprise, it was working very well. Of course, at the time I was a young medical student, so my basis for evaluating that matured along with the film. As time went on, we migrated from the old L.A. County Hospital to a newer space. So in the course of filming, they closed down an 80-year-old structure in favor of a brand new, billion-dollar, shining, technology-laden palace. What we found was that as we were brought up to speed on modern health care, and of course regulation, the care became much more complicated.
Question: What do you want the audience to take away from the film?
Dr McGarry: It’s hopefully a primer for health care discussion that has not yet existed. There are plenty of films that ride the political undertones of health care very well and, I think, if anything, they seem to keep people in their camps. They don’t really bring people to the middle. They may make discussion more satisfying for people who are politically charged, but from the provider’s point of view, I’m not sure if they get us anywhere. “Code Black” does not have a call to action, as they call it in the documentary world. That’s on purpose. What we’re hoping for is for people to watch it and be a bit more primed when we talk about health care. My prediction—this could be wrong—is that the real discussion for the next quarter-century, as we improve access with the [Affordable Care Act], is going to be the patient-doctor connection and some deregulation. There are just too many barriers right now. The equation is too complicated. The healing and listening that people want are not happening.
Question: So would you like to see policy makers ease up on some of the health care regulations?
Dr McGarry: We all want safety. But as a scientist would say, these regulations ought to be evidence based. What we know as physicians is that any evidence-based truth is a hard thing to prove, period. I think a lot of these regulations are well intentioned. Nobody doubts that. But yesterday, the Joint Commission visited our hospital. Everybody was working hard on a shift trying to move patients through, trying to provide both quick and safe care, and one of the things that [the regulators] were watching out for was keeping the employee bags and coffee off the computer desks. Meanwhile, I have patients with chest pain, patients with stroke, patients with fractures, who are not getting the attention they need because we’re totally focused on pleasing the federal regulators that our bags and coffee aren’t out.
Question: The film is from the perspective of young doctors and talks a lot about their initial idealism. Do you think the messages in the film will also resonate with older doctors?
Dr McGarry: One of the more surprising aspects of “Code Black” is the nostalgia factor, that fact that both physicians who have been working for a while and those who have become administrators watched this film. We thought it would be offensive to them—especially people from private hospitals, whom we are sort of tough on in the movie. We thought that they would find us a little unrealistic and idealistic. Interestingly, they all watched it and they said, “I long for the day in my residency when all I had to worry about was just getting the science right, getting that patient connection right.”
Question: Working in C-Booth was a great experience for ED physicians in training. Can you ever recapture that feeling in the new, heavily regulated environment?
Dr McGarry: One thing we wouldn’t want to return to would be the lack of privacy. The biggest aspect of C-Booth that probably we wouldn’t be proud of is the lack of privacy. I’m definitely for privacy and for a dignified experience. After that, I feel like things are quite undefined. I think we have expectations that technology, in particular, is a huge answer to medicine. But we know it can be expensive and it can be dangerous. And in the case of electronic medical records, it certainly doesn’t make things faster. We know that every institution that has gone from paper charts to an EMR has found not just an immediate slowing of care, but a permanent slowing. And yet there are benefits with being able to quickly look up old medical information. But what about when my patient is waiting 20 minutes for pain medicine because it takes almost that long to get them in the computer, pull up the order, select the medicine, and go through all these stupid hard stops that are built in? Before, I could just write it down on a piece of paper, communicate it to the nurse, and get it done. If you’re the one in pain, is [the EMR] worth it? I don’t know.
Question: How did you find the time to make this movie?
Dr McGarry: There were a lot of consequences. I probably pushed it from a health perspective. I really found myself in a unique position as both a filmmaker and subject. For almost 3 years, I would do every ounce of my residency and then would race from the hospital to the edit room and would live and breathe it for 3 years. You would imagine there’s a cost to that. Lost a girlfriend. Didn’t sleep. Happily, I came through without any major damage, but that’s a heck of a lot of emergency medicine.
Question: What are you doing next? Are you working on another film and how are you balancing your new project with your day job in medicine?
Dr McGarry: This is a different game than it was in residency. I have an option for a scripted series, so basically it means that producers have identified it as a viable project for a fiction series like you would see on HBO. That’s in active development. We just shot a 3-minute spot with the New York and L.A. ballets, which involves these dancers in the old abandoned general hospital. As far as balancing all this, I’m so lucky in that Cornell/New York-Presbyterian and Dr Neal Flomenbaum have been incredibly supportive of me, allowing me to be full time there but with the work flexibility to jump on these projects as they come.
On Twitter @maryellenny
Cutaneous Melanoma
Series Editor: Arthur T. Skarin, MD, FACP, FCCP
Melanoma is the sixth most common cancer in the United States and the leading cause of deaths among all cutaneous malignancies. In 2012, it was estimated that approximately 75,000 individuals were diagnosed with melanoma and more than 9000 died. The incidence of melanoma is rising the fastest among all major malignancies, and the lifetime risk of melanoma among men and women now exceeds 1 in 68, as compared with 1:1500 in 1930.4 The incidence of melanoma is predicted to continue increasing, and there has been no corresponding decrease in mortality. This case-based review summarizes the etiology, risk factors, clinical presentation, and management of cutaneous melanomas, which comprise the majority of melanoma cases. The biology and management for other noncutaneous melanomas (such as mucosal or ocular melanomas) are beyond the scope of this review.
To read the full article in PDF:
Series Editor: Arthur T. Skarin, MD, FACP, FCCP
Melanoma is the sixth most common cancer in the United States and the leading cause of deaths among all cutaneous malignancies. In 2012, it was estimated that approximately 75,000 individuals were diagnosed with melanoma and more than 9000 died. The incidence of melanoma is rising the fastest among all major malignancies, and the lifetime risk of melanoma among men and women now exceeds 1 in 68, as compared with 1:1500 in 1930.4 The incidence of melanoma is predicted to continue increasing, and there has been no corresponding decrease in mortality. This case-based review summarizes the etiology, risk factors, clinical presentation, and management of cutaneous melanomas, which comprise the majority of melanoma cases. The biology and management for other noncutaneous melanomas (such as mucosal or ocular melanomas) are beyond the scope of this review.
To read the full article in PDF:
Series Editor: Arthur T. Skarin, MD, FACP, FCCP
Melanoma is the sixth most common cancer in the United States and the leading cause of deaths among all cutaneous malignancies. In 2012, it was estimated that approximately 75,000 individuals were diagnosed with melanoma and more than 9000 died. The incidence of melanoma is rising the fastest among all major malignancies, and the lifetime risk of melanoma among men and women now exceeds 1 in 68, as compared with 1:1500 in 1930.4 The incidence of melanoma is predicted to continue increasing, and there has been no corresponding decrease in mortality. This case-based review summarizes the etiology, risk factors, clinical presentation, and management of cutaneous melanomas, which comprise the majority of melanoma cases. The biology and management for other noncutaneous melanomas (such as mucosal or ocular melanomas) are beyond the scope of this review.
To read the full article in PDF:
Personality and Risk of Alzheimer Disease
Being agreeable can help with social interaction, according to researchers from the National Institute on Aging and Johns Hopkins University, both in Baltimore, Maryland; and Florida State University College of Medicine in Tallahassee, Florida. The researchers say agreeableness may also lower the risk of Alzheimer disease (AD).
The researchers examined the association between personality traits and risk of AD, using data from 1,671 adults who were followed for up to 22 years in the Baltimore Longitudinal Study of Aging (BLSA), one of the longest running studies in the U.S. The researchers also did a meta-analysis on pooled results from prospective studies involving 5,054 participants.
Participants underwent a series of tests, including a neuropsychological battery, neurologic examination, medication review, and structured interview. They also completed the self-report version of the revised NEO Personality Inventory (NEO-PI-R), a 240-item questionnaire. The NEO-PI-R assesses 5 major dimensions of personality: neuroticism (the tendency to experience negative emotions such as anxiety, anger, and sadness); extraversion (being sociable, assertive, enthusiastic, and energetic); openness (being imaginative, unconventional, curious, and emotionally and artistically sensitive); agreeableness (being altruistic, trusting, and cooperative); and conscientiousness (being organized, strong-willed, persistent, reliable, and a follower of rules and ethical principles). Based on previous research, the researchers expected that people with high conscientiousness (ie, organized and self-disciplined) and low neuroticism (less likely to be anxious, depressed, and vulnerable to stress) would have a lower risk of AD.
Onset of AD was diagnosed in 90 participants within 8 years, on average, from baseline. The researchers found that for each standard deviation (SD) increase in neuroticism, the risk of incident AD increased by > 30%. The risk was 3 times higher for the group in the highest quartile of neuroticism. Moreover, > 10% of the AD cases in the population could be attributed to high neuroticism. The results were similar for conscientiousness. The risk of incident AD was 3 times higher for the lowest quartile, and about 10% of AD cases could be attributed to low conscientiousness. The results remained the same when the researchers excluded people aged < 50 years at baseline or those who developed AD within 2 years of the baseline personality assessment.
Among the neurotic tendencies, anxiety, anger, hostility, and depression increased the risk of AD by > 30%. On the conscientiousness scale, self-discipline had the strongest association, followed by competence, order, and dutifulness. Risk of AD was reduced by > 30% for each SD higher score on any of those facets.
The researchers say low conscientiousness and high neuroticism are also related to inflammatory markers such as interleukin 6 and C-reactive protein. But neuroticism could also be a signifier for a variety of lifestyle behaviors that have been separately linked to AD. For instance, low conscientiousness and high neuroticism are associated with cigarette smoking, physical inactivity, obesity, and depression—all risk factors for dementia.
Personality traits are also related to coping skills, the researchers note. Chronic stress throughout the lifespan may contribute to the inability to cope with the neurodegenerative process underlying AD, for instance, and self-discipline (including the ability to achieve a goal) plays a role in limiting health-risk behavior.
Openness to ideas was particularly revealing, being associated significantly with about a 25% reduced risk of AD for each SD higher score. The meta-analysis, with 607 cases of incident AD, also revealed significant associations for openness. It may be a logical extension that openness is related to lower risk of AD. The hallmarks of the open personality include being intellectually engaged and performing well on cognitive measures. Aspects of intelligence and education are associated with greater cognitive reserve and reduced risk of AD.
But, the researchers say, their novel finding that agreeable people have a reduced risk of AD should be interpreted with caution: None of the studies, including BLSA, found a significant association. Still, they point out, agreeableness measures interpersonal tendencies, and an inclination to be altruistic and cooperative “might facilitate the formation of interpersonal connections and the stability of social networks.” Physiologically speaking, the converse might be that people who score low on agreeableness tend to be aggressive, competitive, and antagonistic, which increases the risk of cardiovascular disease and, thus, AD.
Source
Terracciano A, Sutin AR, An Y, et al. Alzheimers Dement. 2014;10(2):179-186.
doi: 10.1016/j.jalz.2013.03.002.
Being agreeable can help with social interaction, according to researchers from the National Institute on Aging and Johns Hopkins University, both in Baltimore, Maryland; and Florida State University College of Medicine in Tallahassee, Florida. The researchers say agreeableness may also lower the risk of Alzheimer disease (AD).
The researchers examined the association between personality traits and risk of AD, using data from 1,671 adults who were followed for up to 22 years in the Baltimore Longitudinal Study of Aging (BLSA), one of the longest running studies in the U.S. The researchers also did a meta-analysis on pooled results from prospective studies involving 5,054 participants.
Participants underwent a series of tests, including a neuropsychological battery, neurologic examination, medication review, and structured interview. They also completed the self-report version of the revised NEO Personality Inventory (NEO-PI-R), a 240-item questionnaire. The NEO-PI-R assesses 5 major dimensions of personality: neuroticism (the tendency to experience negative emotions such as anxiety, anger, and sadness); extraversion (being sociable, assertive, enthusiastic, and energetic); openness (being imaginative, unconventional, curious, and emotionally and artistically sensitive); agreeableness (being altruistic, trusting, and cooperative); and conscientiousness (being organized, strong-willed, persistent, reliable, and a follower of rules and ethical principles). Based on previous research, the researchers expected that people with high conscientiousness (ie, organized and self-disciplined) and low neuroticism (less likely to be anxious, depressed, and vulnerable to stress) would have a lower risk of AD.
Onset of AD was diagnosed in 90 participants within 8 years, on average, from baseline. The researchers found that for each standard deviation (SD) increase in neuroticism, the risk of incident AD increased by > 30%. The risk was 3 times higher for the group in the highest quartile of neuroticism. Moreover, > 10% of the AD cases in the population could be attributed to high neuroticism. The results were similar for conscientiousness. The risk of incident AD was 3 times higher for the lowest quartile, and about 10% of AD cases could be attributed to low conscientiousness. The results remained the same when the researchers excluded people aged < 50 years at baseline or those who developed AD within 2 years of the baseline personality assessment.
Among the neurotic tendencies, anxiety, anger, hostility, and depression increased the risk of AD by > 30%. On the conscientiousness scale, self-discipline had the strongest association, followed by competence, order, and dutifulness. Risk of AD was reduced by > 30% for each SD higher score on any of those facets.
The researchers say low conscientiousness and high neuroticism are also related to inflammatory markers such as interleukin 6 and C-reactive protein. But neuroticism could also be a signifier for a variety of lifestyle behaviors that have been separately linked to AD. For instance, low conscientiousness and high neuroticism are associated with cigarette smoking, physical inactivity, obesity, and depression—all risk factors for dementia.
Personality traits are also related to coping skills, the researchers note. Chronic stress throughout the lifespan may contribute to the inability to cope with the neurodegenerative process underlying AD, for instance, and self-discipline (including the ability to achieve a goal) plays a role in limiting health-risk behavior.
Openness to ideas was particularly revealing, being associated significantly with about a 25% reduced risk of AD for each SD higher score. The meta-analysis, with 607 cases of incident AD, also revealed significant associations for openness. It may be a logical extension that openness is related to lower risk of AD. The hallmarks of the open personality include being intellectually engaged and performing well on cognitive measures. Aspects of intelligence and education are associated with greater cognitive reserve and reduced risk of AD.
But, the researchers say, their novel finding that agreeable people have a reduced risk of AD should be interpreted with caution: None of the studies, including BLSA, found a significant association. Still, they point out, agreeableness measures interpersonal tendencies, and an inclination to be altruistic and cooperative “might facilitate the formation of interpersonal connections and the stability of social networks.” Physiologically speaking, the converse might be that people who score low on agreeableness tend to be aggressive, competitive, and antagonistic, which increases the risk of cardiovascular disease and, thus, AD.
Source
Terracciano A, Sutin AR, An Y, et al. Alzheimers Dement. 2014;10(2):179-186.
doi: 10.1016/j.jalz.2013.03.002.
Being agreeable can help with social interaction, according to researchers from the National Institute on Aging and Johns Hopkins University, both in Baltimore, Maryland; and Florida State University College of Medicine in Tallahassee, Florida. The researchers say agreeableness may also lower the risk of Alzheimer disease (AD).
The researchers examined the association between personality traits and risk of AD, using data from 1,671 adults who were followed for up to 22 years in the Baltimore Longitudinal Study of Aging (BLSA), one of the longest running studies in the U.S. The researchers also did a meta-analysis on pooled results from prospective studies involving 5,054 participants.
Participants underwent a series of tests, including a neuropsychological battery, neurologic examination, medication review, and structured interview. They also completed the self-report version of the revised NEO Personality Inventory (NEO-PI-R), a 240-item questionnaire. The NEO-PI-R assesses 5 major dimensions of personality: neuroticism (the tendency to experience negative emotions such as anxiety, anger, and sadness); extraversion (being sociable, assertive, enthusiastic, and energetic); openness (being imaginative, unconventional, curious, and emotionally and artistically sensitive); agreeableness (being altruistic, trusting, and cooperative); and conscientiousness (being organized, strong-willed, persistent, reliable, and a follower of rules and ethical principles). Based on previous research, the researchers expected that people with high conscientiousness (ie, organized and self-disciplined) and low neuroticism (less likely to be anxious, depressed, and vulnerable to stress) would have a lower risk of AD.
Onset of AD was diagnosed in 90 participants within 8 years, on average, from baseline. The researchers found that for each standard deviation (SD) increase in neuroticism, the risk of incident AD increased by > 30%. The risk was 3 times higher for the group in the highest quartile of neuroticism. Moreover, > 10% of the AD cases in the population could be attributed to high neuroticism. The results were similar for conscientiousness. The risk of incident AD was 3 times higher for the lowest quartile, and about 10% of AD cases could be attributed to low conscientiousness. The results remained the same when the researchers excluded people aged < 50 years at baseline or those who developed AD within 2 years of the baseline personality assessment.
Among the neurotic tendencies, anxiety, anger, hostility, and depression increased the risk of AD by > 30%. On the conscientiousness scale, self-discipline had the strongest association, followed by competence, order, and dutifulness. Risk of AD was reduced by > 30% for each SD higher score on any of those facets.
The researchers say low conscientiousness and high neuroticism are also related to inflammatory markers such as interleukin 6 and C-reactive protein. But neuroticism could also be a signifier for a variety of lifestyle behaviors that have been separately linked to AD. For instance, low conscientiousness and high neuroticism are associated with cigarette smoking, physical inactivity, obesity, and depression—all risk factors for dementia.
Personality traits are also related to coping skills, the researchers note. Chronic stress throughout the lifespan may contribute to the inability to cope with the neurodegenerative process underlying AD, for instance, and self-discipline (including the ability to achieve a goal) plays a role in limiting health-risk behavior.
Openness to ideas was particularly revealing, being associated significantly with about a 25% reduced risk of AD for each SD higher score. The meta-analysis, with 607 cases of incident AD, also revealed significant associations for openness. It may be a logical extension that openness is related to lower risk of AD. The hallmarks of the open personality include being intellectually engaged and performing well on cognitive measures. Aspects of intelligence and education are associated with greater cognitive reserve and reduced risk of AD.
But, the researchers say, their novel finding that agreeable people have a reduced risk of AD should be interpreted with caution: None of the studies, including BLSA, found a significant association. Still, they point out, agreeableness measures interpersonal tendencies, and an inclination to be altruistic and cooperative “might facilitate the formation of interpersonal connections and the stability of social networks.” Physiologically speaking, the converse might be that people who score low on agreeableness tend to be aggressive, competitive, and antagonistic, which increases the risk of cardiovascular disease and, thus, AD.
Source
Terracciano A, Sutin AR, An Y, et al. Alzheimers Dement. 2014;10(2):179-186.
doi: 10.1016/j.jalz.2013.03.002.
Medical Management of Ectopic Pregnancy: Early Diagnosis is Key
Ectopic pregnancy is a significant health risk to women during their childbearing years; approximately 6% of all pregnancy-related deaths are due to ectopic pregnancy.1-3 Some 1% to 2% of all pregnancies in the United States each year—approximately 100,000 cases—are ectopic, with an estimated annual cost of care approaching $1.1 billion.4 The incidence of ectopic pregnancy has increased in the past 20 years; in one analysis, ectopic pregnancy was diagnosed in 18% of women who presented to an emergency department (ED) with first trimester vaginal bleeding, abdominal pain, or both.5 This growing prevalence is attributed to a number of factors, including the sensitivity of current diagnostic methods in detecting early ectopic pregnancy, the greater incidence of salpingitis, and the growing use of assisted reproductive technologies.2,6
While the number of ectopic pregnancies is on the rise, the proportion of patients requiring hospitalization for surgical treatment of ectopic pregnancy has decreased significantly. Today, for appropriate patients, many clinicians manage ectopic pregnancy on an outpatient basis using the drug methotrexate.6
In this article, we will present an overview of the current status of medical management of ectopic pregnancy, along with a case study. The case study describes a patient diagnosed with an unruptured ectopic pregnancy who was managed medically with methotrexate. It illustrates how, with early diagnosis, clinicians can intervene to make medical management an effective treatment option in selected situations.
The patient reported a history of oral contraceptive use until approximately three months prior to this pregnancy. She was taking no medications and had no known drug allergies. Her previous pregnancies included two uncomplicated vaginal births at term and one miscarriage at six to seven weeks’ gestation two years ago. She also reported a dilation and curettage after the miscarriage. Her medical, surgical, and gynecologic histories were otherwise noncontributory. A review of systems was otherwise negative.
Sexual history revealed that the patient was married and monogamous with her husband of five years. She disclosed four previous sexual partners and inconsistent use of condoms with those partners; no current condom use was reported. Seven years ago, she tested positive for gonorrhea and chlamydia and was treated concurrently with her partner. Subsequent diagnostics were negative. She reported vaginal intercourse but no oral sex and denied any other sexual contact. All partners had been male.
On the next page: Diagnosis and case continuation >>
DIAGNOSIS
There is some variation in the presentation of women experiencing ectopic pregnancy; this may be due to differences in the pathologic mechanisms of ectopic pregnancy. Patients may be asymptomatic, hemodynamically compromised, or somewhere in between.3 Typical clinical signs include abdominal pain, amenorrhea, and vaginal bleeding. Approximately 40% to 50% of patients present with vaginal bleeding, 50% may have a palpable adnexal mass, and 75% may have abdominal tenderness.3 Only about 50% of women with ectopic pregnancies present with these typical symptoms.3
The patient may also experience common symptoms of early pregnancy, such as nausea, fatigue, and breast fullness. Worrisome signs and symptoms, including abdominal guarding, hypotension, tachycardia, shock, shoulder pain from peritoneal irritation, dizziness, fever, and vomiting, may also be present.3,7 Approximately 20% of patients with ectopic pregnancies are hemodynamically compromised at presentation, which is highly suggestive of rupture.3
Risk factors
Risk factors for ectopic pregnancy include previous ectopic pregnancy; previous tubal procedures; history of sexually transmitted disease or genital infections; infertility; use of assisted reproductive technology; previous abdominal or pelvic surgery; smoking; pelvic inflammatory disease; exposure in utero to diethylstilbestrol; and previous intrauterine device use.2,5,7,8 Knowledge of these risk factors can help identify a patient with an ectopic pregnancy.
The diagnosis of ectopic pregnancy is most certainly a clinical challenge. The differential diagnosis is based upon history and physical findings; the list can be lengthy if both vaginal bleeding and abdominal pain (nonspecific symptoms common in women who miscarry) are present.7 Prompt completion of diagnostic testing is critical in making a definitive diagnosis. Possible diagnoses are listed in Table 1.
CASE Upon examination, the patient appeared comfortable and relaxed, and there were no signs of distress. Blood pressure was 100/65 mm Hg, pulse rate was 72 beats/min, and temperature was 99.0°F. There was no tenderness upon abdominal examination. Pelvic examination revealed a small amount of brown vaginal discharge but no active bleeding or pooled blood, clots, or tissue. The cervical os was closed, and positive Chadwick sign was present. Bimanual examination revealed no cervical motion tenderness. The uterus was soft, mobile, and nontender, and consistent in size with a gestation at eight weeks. There were no palpable adnexa, ovaries, or masses. There was no pain with bimanual examination and no evidence of tenderness at the posterior fornix. The remainder of the physical examination was unremarkable.
It is important to note that examination results in the case patient are not unusual in a woman with a small, unruptured ectopic pregnancy. All findings were normal except for the scant brown vaginal discharge. Abdominal and adnexal tenderness are common, as is a palpable adnexal mass; but absence of a detectable mass does not exclude ectopic pregnancy.1 Pathologic findings may include severe abdominal tenderness and pain, significant vaginal bleeding, passage of clots, tachycardia, and orthostatic hypotension.
Diagnostic workup
Laboratory tests are critical to making an accurate diagnosis for women whose history and physical examination results are consistent with ectopic pregnancy. Assessment for ectopic pregnancy should include a urine pregnancy test, transvaginal ultrasound, measurement of serum ß-human chorionic gonadotropin (ß-hCG) level, and occasionally, diagnostic curettage.1 Once the diagnosis is confirmed, a complete blood count (CBC) is necessary to assess anemia and platelet functioning. Coagulation tests may be required for worrisome bleeding. Blood type, Rh status, and antibody screen are also necessary to determine whether a patient who is Rh D-negative will require Rh immune globulin. See Table 2 for the patient’s laboratory test results.
In a patient with a ß-hCG level greater than the discriminatory cutoff value of 1,500 to 1,800 mIU/mL, the level above which an intrauterine gestational sac is visible on transvaginal ultrasound in a normal pregnancy, an empty uterus is considered an ectopic pregnancy until proven otherwise.3 In a definite intrauterine pregnancy of about six weeks’ gestation, transvaginal ultrasound reveals a gestational sac that contains a yolk sac and a fetal pole.3
CASE The patient’s presenting symptoms, combined with a positive pregnancy test, ß-hCG level of 1,850 mIU/mL, and a complex adnexal mass in the right fallopian tube, were highly suggestive of an unruptured ectopic pregnancy (see Table 3 for the patient’s transvaginal ultrasound findings). There was also a secondary finding of a corpus luteum cyst. Other diagnoses were ruled out, and the patient was diagnosed with an unruptured ectopic pregnancy.
On the next page: Treatment >>
TREATMENT
A patient with an ectopic pregnancy who presents with pain and hemodynamic instability should be referred immediately for appropriate surgical care.7 Otherwise, once the diagnosis of ectopic pregnancy is confirmed, the patient should be referred to an obstetric specialist. Treatments for ectopic pregnancy include expectant management and surgery—which will be discussed briefly—and medical management, which is the focus of this review.5
Expectant management
Most ectopic pregnancies are diagnosed early as a result of accurate, minimally invasive and noninvasive diagnostic tools and greater awareness of risk factors. Since the natural course of early ectopic pregnancy is often self-limited, eventually resulting in tubal abortion or reabsorption, expectant management is a viable option.9
This treatment option may be considered if the patient is asymptomatic; ß-hCG is < 200 mIU/mL; the ectopic mass is < 3 cm; and no fetal heartbeat is present.1,2 With this approach, patients must be willing to accept the risk for tubal rupture and agree to close monitoring of ß-hCG levels. The ß-hCG level must be measured every 24 to 48 hours in order to determine if it is declining adequately, plateauing, or increasing.2,5
Surgery
For the hemodynamically unstable patient, the treatment decision is relatively straightforward. Optimal treatment for a ruptured ectopic pregnancy is immediate surgery, which may include salpingostomy or salpingectomy.10 Surgery may also be considered for hemodynamically stable patients with nonruptured ectopic pregnancies; in addition to her clinical presentation, overall management may be driven by a patient’s preferences.5 Salpingostomy and salpingectomy can be performed either laparoscopically or via laparotomy, depending on the specific situation.
Medical management
The use of methotrexate for the management of unruptured ectopic pregnancy was introduced in the early 1980s.11 Initially, protocols called for multiple doses administered during the course of an inpatient stay. Further research led to revised treatment recommendations and today, medical management most often consists of a single dose of methotrexate with outpatient follow-up.3
Methotrexate is a folic acid antagonist often used as an antimetabolite chemotherapeutic agent. In ectopic pregnancy, it inhibits growth of the rapidly dividing trophoblastic cells and ultimately ends the pregnancy.2 Outcomes of medical management are comparable to those of surgical treatment, including the potential for future normal pregnancies.2,5
An analysis of US trends in ectopic pregnancy management from 2002-2007 revealed that the use of methotrexate increased from 11.1% to 35.1% during that time, while the use of surgical approaches declined from 90% to 65%.10 Medical management of ectopic pregnancy eliminates the costs of surgery, anesthesia, and hospitalization and avoids potential complications of surgery and anesthesia.
Appropriate candidates
A hemodynamically stable patient with a confirmed or high clinical suspicion of ectopic pregnancy, an unruptured mass, no active bleeding, and low ß-hCG levels (< 5,000 mIU/mL) can be considered for methotrexate therapy.2,3,9 It is critical that medically managed patients be willing and able to adhere to all follow-up appointments.9 Before initiating treatment, normal serum creatinine and transaminase levels should be confirmed, and there should be no evidence of significant anemia, leukopenia, or thrombocytopenia.2 To detect any adverse effects of methotrexate on renal, hepatic, and hematologic functioning, these tests are repeated one week after administration.2
Contraindications
Contraindications to methotrexate treatment include breastfeeding, immunodeficiency, alcoholism, alcoholic liver disease or other chronic liver disease, preexisting blood dyscrasias (eg, bone marrow hypoplasia, leukopenia, thrombocytopenia, or significant anemia), known sensitivity to methotrexate, active pulmonary disease, peptic ulcer, and hepatic, renal, or hematologic dysfunction. Relative contraindications are a gestational sac larger than 3.5 cm and embryonic cardiac motion.2
On the next page: Patient education >>
PATIENT EDUCATION AND INFORMED CONSENT
A diagnosis of unruptured ectopic pregnancy requires patient education about the condition and its treatment options. The clinician should explain what an ectopic pregnancy is and distinguish between unruptured and ruptured. A discussion of the benefits and risks of each treatment option for which the patient is an appropriate candidate, as well as what to anticipate during treatment, is needed. Emotional support for impending pregnancy loss should also be provided.
For patients who choose medical management, education includes methotrexate-specific information and written instructions to follow after methotrexate administration. Patients must be instructed about the use of safety precautions after treatment (eg, the toilet should be double-flushed with the lid closed during the first 72 hours after treatment to prevent exposing others to methotrexate in urine and stool), the need for adherence to follow-up visits, and warning signs of a possible rupture.5 These warning signs are listed in Table 4.
The most common adverse effects of methotrexate are gastrointestinal (nausea, vomiting, stomatitis). Patients should be advised to avoid alcohol, NSAIDs, folic acid supplements, excessive sun exposure (due to photosensitivity), strenuous exercise, and sexual intercourse until ß-hCG has returned to nonpregnant levels. Other adverse effects may include a temporary elevation in liver enzymes and rarely, alopecia. Abdominal pain may occur a few days after methotrexate administration, likely from the cytotoxic effects of the drug on the trophoblastic tissue.
Informed consent is required prior to methotrexate administration. The patient must be advised of the potential risks of medical management with methotrexate, including rupture of the ectopic pregnancy during treatment, inadvertent administration of methotrexate in the presence of an early intrauterine embryo, allergic reaction to methotrexate, and methotrexate-induced pneumonitis.5
CASE After lengthy discussion of the treatment options, the patient chose medical management with methotrexate. She verbalized her understanding of the teaching provided and signed an informed consent document.
METHOTREXATE REGIMENS
Protocols for single-dose, two-dose, and fixed multidose methotrexate regimens are described in the medical literature, according to a 2008 American Congress of Obstetricians and Gynecologists practice bulletin.2 A 2013 practice committee opinion of the American Society for Reproductive Medicine (ASRM) indicates that single-dose and multiple-dose regimens are used most often.12
With methotrexate treatment, complete resolution of ectopic pregnancy usually occurs in two to three weeks but may require up to six to eight weeks, depending on how high the ß-hCG level is when treatment begins.12
Single-dose
In the single-dose regimen, an intramuscular (IM) injection of methotrexate 50 mg/m2 is administered on day 1. The ß-hCG levels are measured on days 4 and 7 after administration; a decrease of at least 15% in the ß-hCG level should be observed. The ß-hCG level is then measured weekly until it reaches < 2 mIU/mL or is undetectable.2 If the level does not decline, a repeat dose of methotrexate can be given, with measurement of ß-hCG on days 4 and 7 after the repeat dose. If the ß-hCG level fails to decrease, additional methotrexate or surgical intervention should be considered.
The single-dose regimen is more frequently used and is most successful when ß-hCG levels are low (< 5,000 mIU/mL), the ectopic mass is small
(< 3.5 cm), and embryonic cardiac activity is not observed on ultrasound.2,3 Patients with ß-hCG levels > 5,000 mIU/mL may be appropriate candidates for additional doses of methotrexate.2 In fact, the single-dose protocol provides for repeat doses of methotrexate if the ß-hCG level is not decreasing adequately.12
Multiple-dose
With the multiple-dose regimen, methotrexate 1 mg/kg IM is administered on days 1, 3, 5, and 7; on days 2, 4, 6, and 8, the patient receives leucovorin (folinic acid) 0.1 mg/kg IM. The ß-hCG level is measured on days methotrexate is administered; once the minimum 15% decline is observed, ß-hCG is measured weekly until a nonpregnant level is reached.12
The patient received a single dose of methotrexate 50 mg/m2 IM on day 1 and returned to the clinic for follow-up on days 4 and 7 posttreatment. On day 4, her ß-hCG level was 1,060 mIU/mL; on day 7, it was 470 mIU/mL. Also on day 7, blood was drawn for a CBC and comprehensive metabolic panel; results were within normal limits. The patient continued weekly follow-up until her ß-hCG level decreased to < 2 mIU/mL.
On the next page: Follow-up and conclusion >>
FOLLOW-UP AND REFERRALS
Close monitoring of ß-hCG levels, as described previously, is essential after methotrexate treatment in order to confirm that the pregnancy has been terminated and reduce the risk for tubal rupture. Clinicians should also be sensitive to the sequelae of loss of a pregnancy and refer patients as needed to appropriate health care professionals for grief support.
CASE The patient was referred to an obstetrics clinic and reported for all scheduled follow-up appointments. She was discharged from care after a full reduction in her ß-hCG to nonpregnant levels. While at the clinic, the patient was referred to social services for psychosocial counseling.
CONCLUSION
Ectopic implantation is a serious complication that may occur during the first trimester of pregnancy. Worldwide, it is the leading cause of maternal death in the first trimester. For women who meet specific criteria, outpatient treatment of early ectopic pregnancy with methotrexate avoids surgery and decreases the overall cost of care. Medical management and conservative surgical management offer the patient comparable outcomes for tubal patency preservation and risk for ectopic pregnancy recurrence.11
REFERENCES
1. Lozeau AM, Potter B. Diagnosis and management of ectopic pregnancy. Am Fam Physician. 2005;72(9):1707-1714.
2. American Congress of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 94: medical management of ectopic pregnancy. Obstet Gynecol. 2008;111(6):1479-1485.
3. Sepilian VP, Wood E. Ectopic pregnancy. http://emedicine.medscape.com/article/2041923-overview. Medscape. Accessed June 19, 2014.
4. Stein JC, Wang R, Adler N, et al. Emergency physician ultrasonography for evaluating patients at risk for ectopic pregnancy: a meta-analysis. Ann Emerg Med. 2010;56(6):674-683.
5. Murtaza UI, Ortmann MJ, Mando-Vandrick J, Lee ASD. Management of first-trimester complications in the emergency department. Am J Health Syst Pharm. 2013;70(2):99-111.
6. Sewell CA, Cundiff GW. Trends for inpatient treatment of tubal pregnancy in Maryland. Am J Obstet Gynecol. 2002;186(3):404-408.
7. Nama V, Manyonda I. Tubal ectopic pregnancy: diagnosis and management. Arch Gynecol Obstet. 2009;279(4):443-453.
8. Barnhart KT, Sammel MD, Gracia CR, et al. Risk factors for ectopic pregnancy in women with symptomatic first-trimester pregnancies. Fertil Steril. 2006;86(1):36-43.
9. Hajenius PJ, Mol F, Mol BW, et al. Interventions for tubal ectopic pregnancy. Cochrane Database Syst Rev. 2007;(1):CD000324.
10. Hoover KW, Tao G, Kent CK. Trends in the diagnosis and treatment of ectopic pregnancy in the United States. Obstet Gynecol. 2010;115(3): 495-502.
11. Autry A. Medical treatment of ectopic pregnancy: is there something new? Obstet Gynecol. 2013;122(4):733.
12. The Practice Committee of the American Society for Reproductive Medicine. Medical treatment of ectopic pregnancy: a committee opinion. Fertil Steril. 2013;100(3):638-644.
Ectopic pregnancy is a significant health risk to women during their childbearing years; approximately 6% of all pregnancy-related deaths are due to ectopic pregnancy.1-3 Some 1% to 2% of all pregnancies in the United States each year—approximately 100,000 cases—are ectopic, with an estimated annual cost of care approaching $1.1 billion.4 The incidence of ectopic pregnancy has increased in the past 20 years; in one analysis, ectopic pregnancy was diagnosed in 18% of women who presented to an emergency department (ED) with first trimester vaginal bleeding, abdominal pain, or both.5 This growing prevalence is attributed to a number of factors, including the sensitivity of current diagnostic methods in detecting early ectopic pregnancy, the greater incidence of salpingitis, and the growing use of assisted reproductive technologies.2,6
While the number of ectopic pregnancies is on the rise, the proportion of patients requiring hospitalization for surgical treatment of ectopic pregnancy has decreased significantly. Today, for appropriate patients, many clinicians manage ectopic pregnancy on an outpatient basis using the drug methotrexate.6
In this article, we will present an overview of the current status of medical management of ectopic pregnancy, along with a case study. The case study describes a patient diagnosed with an unruptured ectopic pregnancy who was managed medically with methotrexate. It illustrates how, with early diagnosis, clinicians can intervene to make medical management an effective treatment option in selected situations.
The patient reported a history of oral contraceptive use until approximately three months prior to this pregnancy. She was taking no medications and had no known drug allergies. Her previous pregnancies included two uncomplicated vaginal births at term and one miscarriage at six to seven weeks’ gestation two years ago. She also reported a dilation and curettage after the miscarriage. Her medical, surgical, and gynecologic histories were otherwise noncontributory. A review of systems was otherwise negative.
Sexual history revealed that the patient was married and monogamous with her husband of five years. She disclosed four previous sexual partners and inconsistent use of condoms with those partners; no current condom use was reported. Seven years ago, she tested positive for gonorrhea and chlamydia and was treated concurrently with her partner. Subsequent diagnostics were negative. She reported vaginal intercourse but no oral sex and denied any other sexual contact. All partners had been male.
On the next page: Diagnosis and case continuation >>
DIAGNOSIS
There is some variation in the presentation of women experiencing ectopic pregnancy; this may be due to differences in the pathologic mechanisms of ectopic pregnancy. Patients may be asymptomatic, hemodynamically compromised, or somewhere in between.3 Typical clinical signs include abdominal pain, amenorrhea, and vaginal bleeding. Approximately 40% to 50% of patients present with vaginal bleeding, 50% may have a palpable adnexal mass, and 75% may have abdominal tenderness.3 Only about 50% of women with ectopic pregnancies present with these typical symptoms.3
The patient may also experience common symptoms of early pregnancy, such as nausea, fatigue, and breast fullness. Worrisome signs and symptoms, including abdominal guarding, hypotension, tachycardia, shock, shoulder pain from peritoneal irritation, dizziness, fever, and vomiting, may also be present.3,7 Approximately 20% of patients with ectopic pregnancies are hemodynamically compromised at presentation, which is highly suggestive of rupture.3
Risk factors
Risk factors for ectopic pregnancy include previous ectopic pregnancy; previous tubal procedures; history of sexually transmitted disease or genital infections; infertility; use of assisted reproductive technology; previous abdominal or pelvic surgery; smoking; pelvic inflammatory disease; exposure in utero to diethylstilbestrol; and previous intrauterine device use.2,5,7,8 Knowledge of these risk factors can help identify a patient with an ectopic pregnancy.
The diagnosis of ectopic pregnancy is most certainly a clinical challenge. The differential diagnosis is based upon history and physical findings; the list can be lengthy if both vaginal bleeding and abdominal pain (nonspecific symptoms common in women who miscarry) are present.7 Prompt completion of diagnostic testing is critical in making a definitive diagnosis. Possible diagnoses are listed in Table 1.
CASE Upon examination, the patient appeared comfortable and relaxed, and there were no signs of distress. Blood pressure was 100/65 mm Hg, pulse rate was 72 beats/min, and temperature was 99.0°F. There was no tenderness upon abdominal examination. Pelvic examination revealed a small amount of brown vaginal discharge but no active bleeding or pooled blood, clots, or tissue. The cervical os was closed, and positive Chadwick sign was present. Bimanual examination revealed no cervical motion tenderness. The uterus was soft, mobile, and nontender, and consistent in size with a gestation at eight weeks. There were no palpable adnexa, ovaries, or masses. There was no pain with bimanual examination and no evidence of tenderness at the posterior fornix. The remainder of the physical examination was unremarkable.
It is important to note that examination results in the case patient are not unusual in a woman with a small, unruptured ectopic pregnancy. All findings were normal except for the scant brown vaginal discharge. Abdominal and adnexal tenderness are common, as is a palpable adnexal mass; but absence of a detectable mass does not exclude ectopic pregnancy.1 Pathologic findings may include severe abdominal tenderness and pain, significant vaginal bleeding, passage of clots, tachycardia, and orthostatic hypotension.
Diagnostic workup
Laboratory tests are critical to making an accurate diagnosis for women whose history and physical examination results are consistent with ectopic pregnancy. Assessment for ectopic pregnancy should include a urine pregnancy test, transvaginal ultrasound, measurement of serum ß-human chorionic gonadotropin (ß-hCG) level, and occasionally, diagnostic curettage.1 Once the diagnosis is confirmed, a complete blood count (CBC) is necessary to assess anemia and platelet functioning. Coagulation tests may be required for worrisome bleeding. Blood type, Rh status, and antibody screen are also necessary to determine whether a patient who is Rh D-negative will require Rh immune globulin. See Table 2 for the patient’s laboratory test results.
In a patient with a ß-hCG level greater than the discriminatory cutoff value of 1,500 to 1,800 mIU/mL, the level above which an intrauterine gestational sac is visible on transvaginal ultrasound in a normal pregnancy, an empty uterus is considered an ectopic pregnancy until proven otherwise.3 In a definite intrauterine pregnancy of about six weeks’ gestation, transvaginal ultrasound reveals a gestational sac that contains a yolk sac and a fetal pole.3
CASE The patient’s presenting symptoms, combined with a positive pregnancy test, ß-hCG level of 1,850 mIU/mL, and a complex adnexal mass in the right fallopian tube, were highly suggestive of an unruptured ectopic pregnancy (see Table 3 for the patient’s transvaginal ultrasound findings). There was also a secondary finding of a corpus luteum cyst. Other diagnoses were ruled out, and the patient was diagnosed with an unruptured ectopic pregnancy.
On the next page: Treatment >>
TREATMENT
A patient with an ectopic pregnancy who presents with pain and hemodynamic instability should be referred immediately for appropriate surgical care.7 Otherwise, once the diagnosis of ectopic pregnancy is confirmed, the patient should be referred to an obstetric specialist. Treatments for ectopic pregnancy include expectant management and surgery—which will be discussed briefly—and medical management, which is the focus of this review.5
Expectant management
Most ectopic pregnancies are diagnosed early as a result of accurate, minimally invasive and noninvasive diagnostic tools and greater awareness of risk factors. Since the natural course of early ectopic pregnancy is often self-limited, eventually resulting in tubal abortion or reabsorption, expectant management is a viable option.9
This treatment option may be considered if the patient is asymptomatic; ß-hCG is < 200 mIU/mL; the ectopic mass is < 3 cm; and no fetal heartbeat is present.1,2 With this approach, patients must be willing to accept the risk for tubal rupture and agree to close monitoring of ß-hCG levels. The ß-hCG level must be measured every 24 to 48 hours in order to determine if it is declining adequately, plateauing, or increasing.2,5
Surgery
For the hemodynamically unstable patient, the treatment decision is relatively straightforward. Optimal treatment for a ruptured ectopic pregnancy is immediate surgery, which may include salpingostomy or salpingectomy.10 Surgery may also be considered for hemodynamically stable patients with nonruptured ectopic pregnancies; in addition to her clinical presentation, overall management may be driven by a patient’s preferences.5 Salpingostomy and salpingectomy can be performed either laparoscopically or via laparotomy, depending on the specific situation.
Medical management
The use of methotrexate for the management of unruptured ectopic pregnancy was introduced in the early 1980s.11 Initially, protocols called for multiple doses administered during the course of an inpatient stay. Further research led to revised treatment recommendations and today, medical management most often consists of a single dose of methotrexate with outpatient follow-up.3
Methotrexate is a folic acid antagonist often used as an antimetabolite chemotherapeutic agent. In ectopic pregnancy, it inhibits growth of the rapidly dividing trophoblastic cells and ultimately ends the pregnancy.2 Outcomes of medical management are comparable to those of surgical treatment, including the potential for future normal pregnancies.2,5
An analysis of US trends in ectopic pregnancy management from 2002-2007 revealed that the use of methotrexate increased from 11.1% to 35.1% during that time, while the use of surgical approaches declined from 90% to 65%.10 Medical management of ectopic pregnancy eliminates the costs of surgery, anesthesia, and hospitalization and avoids potential complications of surgery and anesthesia.
Appropriate candidates
A hemodynamically stable patient with a confirmed or high clinical suspicion of ectopic pregnancy, an unruptured mass, no active bleeding, and low ß-hCG levels (< 5,000 mIU/mL) can be considered for methotrexate therapy.2,3,9 It is critical that medically managed patients be willing and able to adhere to all follow-up appointments.9 Before initiating treatment, normal serum creatinine and transaminase levels should be confirmed, and there should be no evidence of significant anemia, leukopenia, or thrombocytopenia.2 To detect any adverse effects of methotrexate on renal, hepatic, and hematologic functioning, these tests are repeated one week after administration.2
Contraindications
Contraindications to methotrexate treatment include breastfeeding, immunodeficiency, alcoholism, alcoholic liver disease or other chronic liver disease, preexisting blood dyscrasias (eg, bone marrow hypoplasia, leukopenia, thrombocytopenia, or significant anemia), known sensitivity to methotrexate, active pulmonary disease, peptic ulcer, and hepatic, renal, or hematologic dysfunction. Relative contraindications are a gestational sac larger than 3.5 cm and embryonic cardiac motion.2
On the next page: Patient education >>
PATIENT EDUCATION AND INFORMED CONSENT
A diagnosis of unruptured ectopic pregnancy requires patient education about the condition and its treatment options. The clinician should explain what an ectopic pregnancy is and distinguish between unruptured and ruptured. A discussion of the benefits and risks of each treatment option for which the patient is an appropriate candidate, as well as what to anticipate during treatment, is needed. Emotional support for impending pregnancy loss should also be provided.
For patients who choose medical management, education includes methotrexate-specific information and written instructions to follow after methotrexate administration. Patients must be instructed about the use of safety precautions after treatment (eg, the toilet should be double-flushed with the lid closed during the first 72 hours after treatment to prevent exposing others to methotrexate in urine and stool), the need for adherence to follow-up visits, and warning signs of a possible rupture.5 These warning signs are listed in Table 4.
The most common adverse effects of methotrexate are gastrointestinal (nausea, vomiting, stomatitis). Patients should be advised to avoid alcohol, NSAIDs, folic acid supplements, excessive sun exposure (due to photosensitivity), strenuous exercise, and sexual intercourse until ß-hCG has returned to nonpregnant levels. Other adverse effects may include a temporary elevation in liver enzymes and rarely, alopecia. Abdominal pain may occur a few days after methotrexate administration, likely from the cytotoxic effects of the drug on the trophoblastic tissue.
Informed consent is required prior to methotrexate administration. The patient must be advised of the potential risks of medical management with methotrexate, including rupture of the ectopic pregnancy during treatment, inadvertent administration of methotrexate in the presence of an early intrauterine embryo, allergic reaction to methotrexate, and methotrexate-induced pneumonitis.5
CASE After lengthy discussion of the treatment options, the patient chose medical management with methotrexate. She verbalized her understanding of the teaching provided and signed an informed consent document.
METHOTREXATE REGIMENS
Protocols for single-dose, two-dose, and fixed multidose methotrexate regimens are described in the medical literature, according to a 2008 American Congress of Obstetricians and Gynecologists practice bulletin.2 A 2013 practice committee opinion of the American Society for Reproductive Medicine (ASRM) indicates that single-dose and multiple-dose regimens are used most often.12
With methotrexate treatment, complete resolution of ectopic pregnancy usually occurs in two to three weeks but may require up to six to eight weeks, depending on how high the ß-hCG level is when treatment begins.12
Single-dose
In the single-dose regimen, an intramuscular (IM) injection of methotrexate 50 mg/m2 is administered on day 1. The ß-hCG levels are measured on days 4 and 7 after administration; a decrease of at least 15% in the ß-hCG level should be observed. The ß-hCG level is then measured weekly until it reaches < 2 mIU/mL or is undetectable.2 If the level does not decline, a repeat dose of methotrexate can be given, with measurement of ß-hCG on days 4 and 7 after the repeat dose. If the ß-hCG level fails to decrease, additional methotrexate or surgical intervention should be considered.
The single-dose regimen is more frequently used and is most successful when ß-hCG levels are low (< 5,000 mIU/mL), the ectopic mass is small
(< 3.5 cm), and embryonic cardiac activity is not observed on ultrasound.2,3 Patients with ß-hCG levels > 5,000 mIU/mL may be appropriate candidates for additional doses of methotrexate.2 In fact, the single-dose protocol provides for repeat doses of methotrexate if the ß-hCG level is not decreasing adequately.12
Multiple-dose
With the multiple-dose regimen, methotrexate 1 mg/kg IM is administered on days 1, 3, 5, and 7; on days 2, 4, 6, and 8, the patient receives leucovorin (folinic acid) 0.1 mg/kg IM. The ß-hCG level is measured on days methotrexate is administered; once the minimum 15% decline is observed, ß-hCG is measured weekly until a nonpregnant level is reached.12
The patient received a single dose of methotrexate 50 mg/m2 IM on day 1 and returned to the clinic for follow-up on days 4 and 7 posttreatment. On day 4, her ß-hCG level was 1,060 mIU/mL; on day 7, it was 470 mIU/mL. Also on day 7, blood was drawn for a CBC and comprehensive metabolic panel; results were within normal limits. The patient continued weekly follow-up until her ß-hCG level decreased to < 2 mIU/mL.
On the next page: Follow-up and conclusion >>
FOLLOW-UP AND REFERRALS
Close monitoring of ß-hCG levels, as described previously, is essential after methotrexate treatment in order to confirm that the pregnancy has been terminated and reduce the risk for tubal rupture. Clinicians should also be sensitive to the sequelae of loss of a pregnancy and refer patients as needed to appropriate health care professionals for grief support.
CASE The patient was referred to an obstetrics clinic and reported for all scheduled follow-up appointments. She was discharged from care after a full reduction in her ß-hCG to nonpregnant levels. While at the clinic, the patient was referred to social services for psychosocial counseling.
CONCLUSION
Ectopic implantation is a serious complication that may occur during the first trimester of pregnancy. Worldwide, it is the leading cause of maternal death in the first trimester. For women who meet specific criteria, outpatient treatment of early ectopic pregnancy with methotrexate avoids surgery and decreases the overall cost of care. Medical management and conservative surgical management offer the patient comparable outcomes for tubal patency preservation and risk for ectopic pregnancy recurrence.11
REFERENCES
1. Lozeau AM, Potter B. Diagnosis and management of ectopic pregnancy. Am Fam Physician. 2005;72(9):1707-1714.
2. American Congress of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 94: medical management of ectopic pregnancy. Obstet Gynecol. 2008;111(6):1479-1485.
3. Sepilian VP, Wood E. Ectopic pregnancy. http://emedicine.medscape.com/article/2041923-overview. Medscape. Accessed June 19, 2014.
4. Stein JC, Wang R, Adler N, et al. Emergency physician ultrasonography for evaluating patients at risk for ectopic pregnancy: a meta-analysis. Ann Emerg Med. 2010;56(6):674-683.
5. Murtaza UI, Ortmann MJ, Mando-Vandrick J, Lee ASD. Management of first-trimester complications in the emergency department. Am J Health Syst Pharm. 2013;70(2):99-111.
6. Sewell CA, Cundiff GW. Trends for inpatient treatment of tubal pregnancy in Maryland. Am J Obstet Gynecol. 2002;186(3):404-408.
7. Nama V, Manyonda I. Tubal ectopic pregnancy: diagnosis and management. Arch Gynecol Obstet. 2009;279(4):443-453.
8. Barnhart KT, Sammel MD, Gracia CR, et al. Risk factors for ectopic pregnancy in women with symptomatic first-trimester pregnancies. Fertil Steril. 2006;86(1):36-43.
9. Hajenius PJ, Mol F, Mol BW, et al. Interventions for tubal ectopic pregnancy. Cochrane Database Syst Rev. 2007;(1):CD000324.
10. Hoover KW, Tao G, Kent CK. Trends in the diagnosis and treatment of ectopic pregnancy in the United States. Obstet Gynecol. 2010;115(3): 495-502.
11. Autry A. Medical treatment of ectopic pregnancy: is there something new? Obstet Gynecol. 2013;122(4):733.
12. The Practice Committee of the American Society for Reproductive Medicine. Medical treatment of ectopic pregnancy: a committee opinion. Fertil Steril. 2013;100(3):638-644.
Ectopic pregnancy is a significant health risk to women during their childbearing years; approximately 6% of all pregnancy-related deaths are due to ectopic pregnancy.1-3 Some 1% to 2% of all pregnancies in the United States each year—approximately 100,000 cases—are ectopic, with an estimated annual cost of care approaching $1.1 billion.4 The incidence of ectopic pregnancy has increased in the past 20 years; in one analysis, ectopic pregnancy was diagnosed in 18% of women who presented to an emergency department (ED) with first trimester vaginal bleeding, abdominal pain, or both.5 This growing prevalence is attributed to a number of factors, including the sensitivity of current diagnostic methods in detecting early ectopic pregnancy, the greater incidence of salpingitis, and the growing use of assisted reproductive technologies.2,6
While the number of ectopic pregnancies is on the rise, the proportion of patients requiring hospitalization for surgical treatment of ectopic pregnancy has decreased significantly. Today, for appropriate patients, many clinicians manage ectopic pregnancy on an outpatient basis using the drug methotrexate.6
In this article, we will present an overview of the current status of medical management of ectopic pregnancy, along with a case study. The case study describes a patient diagnosed with an unruptured ectopic pregnancy who was managed medically with methotrexate. It illustrates how, with early diagnosis, clinicians can intervene to make medical management an effective treatment option in selected situations.
The patient reported a history of oral contraceptive use until approximately three months prior to this pregnancy. She was taking no medications and had no known drug allergies. Her previous pregnancies included two uncomplicated vaginal births at term and one miscarriage at six to seven weeks’ gestation two years ago. She also reported a dilation and curettage after the miscarriage. Her medical, surgical, and gynecologic histories were otherwise noncontributory. A review of systems was otherwise negative.
Sexual history revealed that the patient was married and monogamous with her husband of five years. She disclosed four previous sexual partners and inconsistent use of condoms with those partners; no current condom use was reported. Seven years ago, she tested positive for gonorrhea and chlamydia and was treated concurrently with her partner. Subsequent diagnostics were negative. She reported vaginal intercourse but no oral sex and denied any other sexual contact. All partners had been male.
On the next page: Diagnosis and case continuation >>
DIAGNOSIS
There is some variation in the presentation of women experiencing ectopic pregnancy; this may be due to differences in the pathologic mechanisms of ectopic pregnancy. Patients may be asymptomatic, hemodynamically compromised, or somewhere in between.3 Typical clinical signs include abdominal pain, amenorrhea, and vaginal bleeding. Approximately 40% to 50% of patients present with vaginal bleeding, 50% may have a palpable adnexal mass, and 75% may have abdominal tenderness.3 Only about 50% of women with ectopic pregnancies present with these typical symptoms.3
The patient may also experience common symptoms of early pregnancy, such as nausea, fatigue, and breast fullness. Worrisome signs and symptoms, including abdominal guarding, hypotension, tachycardia, shock, shoulder pain from peritoneal irritation, dizziness, fever, and vomiting, may also be present.3,7 Approximately 20% of patients with ectopic pregnancies are hemodynamically compromised at presentation, which is highly suggestive of rupture.3
Risk factors
Risk factors for ectopic pregnancy include previous ectopic pregnancy; previous tubal procedures; history of sexually transmitted disease or genital infections; infertility; use of assisted reproductive technology; previous abdominal or pelvic surgery; smoking; pelvic inflammatory disease; exposure in utero to diethylstilbestrol; and previous intrauterine device use.2,5,7,8 Knowledge of these risk factors can help identify a patient with an ectopic pregnancy.
The diagnosis of ectopic pregnancy is most certainly a clinical challenge. The differential diagnosis is based upon history and physical findings; the list can be lengthy if both vaginal bleeding and abdominal pain (nonspecific symptoms common in women who miscarry) are present.7 Prompt completion of diagnostic testing is critical in making a definitive diagnosis. Possible diagnoses are listed in Table 1.
CASE Upon examination, the patient appeared comfortable and relaxed, and there were no signs of distress. Blood pressure was 100/65 mm Hg, pulse rate was 72 beats/min, and temperature was 99.0°F. There was no tenderness upon abdominal examination. Pelvic examination revealed a small amount of brown vaginal discharge but no active bleeding or pooled blood, clots, or tissue. The cervical os was closed, and positive Chadwick sign was present. Bimanual examination revealed no cervical motion tenderness. The uterus was soft, mobile, and nontender, and consistent in size with a gestation at eight weeks. There were no palpable adnexa, ovaries, or masses. There was no pain with bimanual examination and no evidence of tenderness at the posterior fornix. The remainder of the physical examination was unremarkable.
It is important to note that examination results in the case patient are not unusual in a woman with a small, unruptured ectopic pregnancy. All findings were normal except for the scant brown vaginal discharge. Abdominal and adnexal tenderness are common, as is a palpable adnexal mass; but absence of a detectable mass does not exclude ectopic pregnancy.1 Pathologic findings may include severe abdominal tenderness and pain, significant vaginal bleeding, passage of clots, tachycardia, and orthostatic hypotension.
Diagnostic workup
Laboratory tests are critical to making an accurate diagnosis for women whose history and physical examination results are consistent with ectopic pregnancy. Assessment for ectopic pregnancy should include a urine pregnancy test, transvaginal ultrasound, measurement of serum ß-human chorionic gonadotropin (ß-hCG) level, and occasionally, diagnostic curettage.1 Once the diagnosis is confirmed, a complete blood count (CBC) is necessary to assess anemia and platelet functioning. Coagulation tests may be required for worrisome bleeding. Blood type, Rh status, and antibody screen are also necessary to determine whether a patient who is Rh D-negative will require Rh immune globulin. See Table 2 for the patient’s laboratory test results.
In a patient with a ß-hCG level greater than the discriminatory cutoff value of 1,500 to 1,800 mIU/mL, the level above which an intrauterine gestational sac is visible on transvaginal ultrasound in a normal pregnancy, an empty uterus is considered an ectopic pregnancy until proven otherwise.3 In a definite intrauterine pregnancy of about six weeks’ gestation, transvaginal ultrasound reveals a gestational sac that contains a yolk sac and a fetal pole.3
CASE The patient’s presenting symptoms, combined with a positive pregnancy test, ß-hCG level of 1,850 mIU/mL, and a complex adnexal mass in the right fallopian tube, were highly suggestive of an unruptured ectopic pregnancy (see Table 3 for the patient’s transvaginal ultrasound findings). There was also a secondary finding of a corpus luteum cyst. Other diagnoses were ruled out, and the patient was diagnosed with an unruptured ectopic pregnancy.
On the next page: Treatment >>
TREATMENT
A patient with an ectopic pregnancy who presents with pain and hemodynamic instability should be referred immediately for appropriate surgical care.7 Otherwise, once the diagnosis of ectopic pregnancy is confirmed, the patient should be referred to an obstetric specialist. Treatments for ectopic pregnancy include expectant management and surgery—which will be discussed briefly—and medical management, which is the focus of this review.5
Expectant management
Most ectopic pregnancies are diagnosed early as a result of accurate, minimally invasive and noninvasive diagnostic tools and greater awareness of risk factors. Since the natural course of early ectopic pregnancy is often self-limited, eventually resulting in tubal abortion or reabsorption, expectant management is a viable option.9
This treatment option may be considered if the patient is asymptomatic; ß-hCG is < 200 mIU/mL; the ectopic mass is < 3 cm; and no fetal heartbeat is present.1,2 With this approach, patients must be willing to accept the risk for tubal rupture and agree to close monitoring of ß-hCG levels. The ß-hCG level must be measured every 24 to 48 hours in order to determine if it is declining adequately, plateauing, or increasing.2,5
Surgery
For the hemodynamically unstable patient, the treatment decision is relatively straightforward. Optimal treatment for a ruptured ectopic pregnancy is immediate surgery, which may include salpingostomy or salpingectomy.10 Surgery may also be considered for hemodynamically stable patients with nonruptured ectopic pregnancies; in addition to her clinical presentation, overall management may be driven by a patient’s preferences.5 Salpingostomy and salpingectomy can be performed either laparoscopically or via laparotomy, depending on the specific situation.
Medical management
The use of methotrexate for the management of unruptured ectopic pregnancy was introduced in the early 1980s.11 Initially, protocols called for multiple doses administered during the course of an inpatient stay. Further research led to revised treatment recommendations and today, medical management most often consists of a single dose of methotrexate with outpatient follow-up.3
Methotrexate is a folic acid antagonist often used as an antimetabolite chemotherapeutic agent. In ectopic pregnancy, it inhibits growth of the rapidly dividing trophoblastic cells and ultimately ends the pregnancy.2 Outcomes of medical management are comparable to those of surgical treatment, including the potential for future normal pregnancies.2,5
An analysis of US trends in ectopic pregnancy management from 2002-2007 revealed that the use of methotrexate increased from 11.1% to 35.1% during that time, while the use of surgical approaches declined from 90% to 65%.10 Medical management of ectopic pregnancy eliminates the costs of surgery, anesthesia, and hospitalization and avoids potential complications of surgery and anesthesia.
Appropriate candidates
A hemodynamically stable patient with a confirmed or high clinical suspicion of ectopic pregnancy, an unruptured mass, no active bleeding, and low ß-hCG levels (< 5,000 mIU/mL) can be considered for methotrexate therapy.2,3,9 It is critical that medically managed patients be willing and able to adhere to all follow-up appointments.9 Before initiating treatment, normal serum creatinine and transaminase levels should be confirmed, and there should be no evidence of significant anemia, leukopenia, or thrombocytopenia.2 To detect any adverse effects of methotrexate on renal, hepatic, and hematologic functioning, these tests are repeated one week after administration.2
Contraindications
Contraindications to methotrexate treatment include breastfeeding, immunodeficiency, alcoholism, alcoholic liver disease or other chronic liver disease, preexisting blood dyscrasias (eg, bone marrow hypoplasia, leukopenia, thrombocytopenia, or significant anemia), known sensitivity to methotrexate, active pulmonary disease, peptic ulcer, and hepatic, renal, or hematologic dysfunction. Relative contraindications are a gestational sac larger than 3.5 cm and embryonic cardiac motion.2
On the next page: Patient education >>
PATIENT EDUCATION AND INFORMED CONSENT
A diagnosis of unruptured ectopic pregnancy requires patient education about the condition and its treatment options. The clinician should explain what an ectopic pregnancy is and distinguish between unruptured and ruptured. A discussion of the benefits and risks of each treatment option for which the patient is an appropriate candidate, as well as what to anticipate during treatment, is needed. Emotional support for impending pregnancy loss should also be provided.
For patients who choose medical management, education includes methotrexate-specific information and written instructions to follow after methotrexate administration. Patients must be instructed about the use of safety precautions after treatment (eg, the toilet should be double-flushed with the lid closed during the first 72 hours after treatment to prevent exposing others to methotrexate in urine and stool), the need for adherence to follow-up visits, and warning signs of a possible rupture.5 These warning signs are listed in Table 4.
The most common adverse effects of methotrexate are gastrointestinal (nausea, vomiting, stomatitis). Patients should be advised to avoid alcohol, NSAIDs, folic acid supplements, excessive sun exposure (due to photosensitivity), strenuous exercise, and sexual intercourse until ß-hCG has returned to nonpregnant levels. Other adverse effects may include a temporary elevation in liver enzymes and rarely, alopecia. Abdominal pain may occur a few days after methotrexate administration, likely from the cytotoxic effects of the drug on the trophoblastic tissue.
Informed consent is required prior to methotrexate administration. The patient must be advised of the potential risks of medical management with methotrexate, including rupture of the ectopic pregnancy during treatment, inadvertent administration of methotrexate in the presence of an early intrauterine embryo, allergic reaction to methotrexate, and methotrexate-induced pneumonitis.5
CASE After lengthy discussion of the treatment options, the patient chose medical management with methotrexate. She verbalized her understanding of the teaching provided and signed an informed consent document.
METHOTREXATE REGIMENS
Protocols for single-dose, two-dose, and fixed multidose methotrexate regimens are described in the medical literature, according to a 2008 American Congress of Obstetricians and Gynecologists practice bulletin.2 A 2013 practice committee opinion of the American Society for Reproductive Medicine (ASRM) indicates that single-dose and multiple-dose regimens are used most often.12
With methotrexate treatment, complete resolution of ectopic pregnancy usually occurs in two to three weeks but may require up to six to eight weeks, depending on how high the ß-hCG level is when treatment begins.12
Single-dose
In the single-dose regimen, an intramuscular (IM) injection of methotrexate 50 mg/m2 is administered on day 1. The ß-hCG levels are measured on days 4 and 7 after administration; a decrease of at least 15% in the ß-hCG level should be observed. The ß-hCG level is then measured weekly until it reaches < 2 mIU/mL or is undetectable.2 If the level does not decline, a repeat dose of methotrexate can be given, with measurement of ß-hCG on days 4 and 7 after the repeat dose. If the ß-hCG level fails to decrease, additional methotrexate or surgical intervention should be considered.
The single-dose regimen is more frequently used and is most successful when ß-hCG levels are low (< 5,000 mIU/mL), the ectopic mass is small
(< 3.5 cm), and embryonic cardiac activity is not observed on ultrasound.2,3 Patients with ß-hCG levels > 5,000 mIU/mL may be appropriate candidates for additional doses of methotrexate.2 In fact, the single-dose protocol provides for repeat doses of methotrexate if the ß-hCG level is not decreasing adequately.12
Multiple-dose
With the multiple-dose regimen, methotrexate 1 mg/kg IM is administered on days 1, 3, 5, and 7; on days 2, 4, 6, and 8, the patient receives leucovorin (folinic acid) 0.1 mg/kg IM. The ß-hCG level is measured on days methotrexate is administered; once the minimum 15% decline is observed, ß-hCG is measured weekly until a nonpregnant level is reached.12
The patient received a single dose of methotrexate 50 mg/m2 IM on day 1 and returned to the clinic for follow-up on days 4 and 7 posttreatment. On day 4, her ß-hCG level was 1,060 mIU/mL; on day 7, it was 470 mIU/mL. Also on day 7, blood was drawn for a CBC and comprehensive metabolic panel; results were within normal limits. The patient continued weekly follow-up until her ß-hCG level decreased to < 2 mIU/mL.
On the next page: Follow-up and conclusion >>
FOLLOW-UP AND REFERRALS
Close monitoring of ß-hCG levels, as described previously, is essential after methotrexate treatment in order to confirm that the pregnancy has been terminated and reduce the risk for tubal rupture. Clinicians should also be sensitive to the sequelae of loss of a pregnancy and refer patients as needed to appropriate health care professionals for grief support.
CASE The patient was referred to an obstetrics clinic and reported for all scheduled follow-up appointments. She was discharged from care after a full reduction in her ß-hCG to nonpregnant levels. While at the clinic, the patient was referred to social services for psychosocial counseling.
CONCLUSION
Ectopic implantation is a serious complication that may occur during the first trimester of pregnancy. Worldwide, it is the leading cause of maternal death in the first trimester. For women who meet specific criteria, outpatient treatment of early ectopic pregnancy with methotrexate avoids surgery and decreases the overall cost of care. Medical management and conservative surgical management offer the patient comparable outcomes for tubal patency preservation and risk for ectopic pregnancy recurrence.11
REFERENCES
1. Lozeau AM, Potter B. Diagnosis and management of ectopic pregnancy. Am Fam Physician. 2005;72(9):1707-1714.
2. American Congress of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 94: medical management of ectopic pregnancy. Obstet Gynecol. 2008;111(6):1479-1485.
3. Sepilian VP, Wood E. Ectopic pregnancy. http://emedicine.medscape.com/article/2041923-overview. Medscape. Accessed June 19, 2014.
4. Stein JC, Wang R, Adler N, et al. Emergency physician ultrasonography for evaluating patients at risk for ectopic pregnancy: a meta-analysis. Ann Emerg Med. 2010;56(6):674-683.
5. Murtaza UI, Ortmann MJ, Mando-Vandrick J, Lee ASD. Management of first-trimester complications in the emergency department. Am J Health Syst Pharm. 2013;70(2):99-111.
6. Sewell CA, Cundiff GW. Trends for inpatient treatment of tubal pregnancy in Maryland. Am J Obstet Gynecol. 2002;186(3):404-408.
7. Nama V, Manyonda I. Tubal ectopic pregnancy: diagnosis and management. Arch Gynecol Obstet. 2009;279(4):443-453.
8. Barnhart KT, Sammel MD, Gracia CR, et al. Risk factors for ectopic pregnancy in women with symptomatic first-trimester pregnancies. Fertil Steril. 2006;86(1):36-43.
9. Hajenius PJ, Mol F, Mol BW, et al. Interventions for tubal ectopic pregnancy. Cochrane Database Syst Rev. 2007;(1):CD000324.
10. Hoover KW, Tao G, Kent CK. Trends in the diagnosis and treatment of ectopic pregnancy in the United States. Obstet Gynecol. 2010;115(3): 495-502.
11. Autry A. Medical treatment of ectopic pregnancy: is there something new? Obstet Gynecol. 2013;122(4):733.
12. The Practice Committee of the American Society for Reproductive Medicine. Medical treatment of ectopic pregnancy: a committee opinion. Fertil Steril. 2013;100(3):638-644.
Aspiration of a Dental Tool During a Crown Placement Procedure
There are many reports in the medical and dental literature of complications arising from a routine delivery of dental care. One complication can include physical injury from swallowing or aspirating foreign objects.1 However, a review of such literature presents a scarcity of documented instances and no long-term evaluation of the aforementioned events.2,3
This report presents the case of a patient who aspirated a hex driver tool during a procedure to place a crown on a dental implant. The aspirated object was subsequently removed through flexible fiberoptic bronchoscopy without complications.
Case Report
An 83-year-old man was referred to the Pulmonary and Critical Care Department of the VA Caribbean Healthcare System in San Juan, Puerto Rico, after a hex driver tool was lost during a procedure to place a crown on a dental implant, performed under topical anesthesia. It was first thought that the patient swallowed the hex driver, since he never experienced or complained of coughing or shortness of breath. A chest radiograph revealed a metal object lying within the right main stem bronchus, for which the patient was referred to the Pulmonary and Critical Care Department (Figure 1).
The patient’s past medical history was remarkable for hypertension and hypercholesterolemia. Outpatient medications included hydrochlorothiazide, simvastatin, aspirin, felodipine, and lorazepam. He had no previous history of dysphagia or neurologic disease. A physical examination revealed expiratory and inspiratory wheezing localized to the right lower lobe without associated rhonchi or crackles. No distress, shortness of breath, or coughing was noted.
A flexible fiberoptic bronchoscopy was performed under conscious sedation with 3 mg of IV midazolam and topical anesthesia with nebulized 4% lidocaine. No mucosal edema, hyperemia, or structural damage was noted during direct visualization of both the right and left bronchopulmonary segments. A metallic object was visualized at the entrance of the right lower lobe. The foreign object had irregular borders, providing multiple edges that made it suitable to be embraced (Figure 2).
Using a radial jaw single-use biopsy forceps 1.8 mm, the physician clinched and retrieved the object through the bronchoscope. The object was retrieved on the same day of the dental procedure almost 5 hours after it was aspirated. The patient tolerated the procedure well; no coughing, oxygen desaturation, or bleeding occurred during the procedure.
After a few hours of observation, a postprocedural radiograph confirmed the removal of the foreign body without evidence of pneumothorax. The patient was discharged, and 24 hours after the incident remained asymptomatic without chest pain, cough, hemoptysis, sputum production, or fever.
Discussion
Foreign-body aspiration and inadvertent swallowing remains underrecognized by clinicians. In the U.S., more than 2,700 people, including more than 300 children, die of foreign-body aspiration each year.4,5 Aspiration or ingestion of a foreign body during a dental procedure is serious and potentially fatal.6 Some of the consequences of an aspirated object are complete or partial airway obstruction, respiratory distress and failure, pneumothorax, and hemorrhage.7 In addition, inadvertent aspiration of foreign objects in asymptomatic patients may not be evident for months, resulting in late complications as postobstructive pneumonia, bronchiectasis, or lung abscess.8 Early recognition and diagnosis of these events are crucial to prevent complications.
Accidental aspiration of foreign objects during dental procedures is not as common as is swallowing. In the normal population, the foreign object enters the gastrointestinal tract in about 92.5% of the time, and the tracheobronchial tree in 7.5% of these instances.
A 10-year review done at the School of Dentistry of the University of North Carolina reported 36 incidents of lost instruments during dental procedures. In only 1 case, an object was aspirated, 25 of the 36 cases were secondary to ingestion, and in the remaining 10 incidents, swallowing or aspiration was ruled out by radiography or after the object’s removal from the patient’s mouth.2 Previous reviews about foreign-body aspiration in adults have reported dental appliances as the second most commonly aspirated foreign objects.4 Of all aspirated objects, the most common site of impaction is the right lower lobe; however, aspiration has been reported in all pulmonary lobes.6
Available literature recognizes that impaction of aspirated objects occurred in 56% of instances within the right lower lobe and 33% in the left lower lobe.7,9 Identification of risk factors for aspiration is important for any patient who will undergo dental procedures, such as advanced age (ie, elderly patients may have a decreased gag reflex); neurologic conditions, such as stroke; dementia and other degenerative diseases; the use of topical anesthesia; and altered states of consciousness associated with the use of IV sedation.1,2
The key sign that most dentists recognize when patients aspirate an object during a dental procedure is coughing. It has been reported that coughing resulting from aspiration of foreign objects may range from mild to severe. In this case, the patient was completely asymptomatic during the procedure. The only clue of possible object aspiration was the reported tool loss by the dentist. It is important to always examine, account for, and review all equipment used during dental procedures. Assessment for any lost objects or missing parts of instruments should be done promptly with a high degree of suspicion for possible swallowing or aspiration if an object is missing.
It has been recommended to use a gauze throat screen and rubber dam and to avoid a supine position during a procedure, among other techniques, to minimize risk of ingestion or aspiration.2 Imaging studies should be used for further evaluation of the patient; however, some instruments, such as dental pieces and impression material, may not be identified by plain films. In those cases, further evaluation with more sophisticated imaging techniques, such as computed tomography (CT), should be considered.1-10
In a previous case report of a patient who aspirated a third molar during a dental procedure, a chest film failed to identify it. A chest CT was performed, and the object showed in the right main stem bronchus. In another instance, aspiration of impression material in a 45-year-old man was not observed by chest radiography. In this case, the history of coughing and respiratory symptoms days after the procedure pointed toward aspiration of an object as the culprit, with subsequent identification and removal by flexible fiberoptic bronchoscopy.1-11
Bronchoscopy is the treatment of choice for extraction of aspirated foreign bodies; however, there is still a debate about whether to use flexible or rigid bronchoscopy. The decision is usually made based on the object size, localization, medical facility, and personnel expertise. The rigid bronchoscope has the advantages of offering better control and visualization of the airway and easier use of removal instruments. Its primary disadvantage is that the procedure needs to be done in the operating room under general anesthesia. Flexible fiberoptic bronchoscopy done under conscious sedation and topical anesthesia may be as effective as rigid bronchoscopy and even superior in the case of smaller and more distal impacted objects.10-14
In this case, flexible fiberoptic bronchoscopy was used successfully for the removal of the foreign object. Biopsy forceps were used to grasp the object and retrieve it from the airway without complication.
Conclusion
Aspiration of foreign objects during a dental procedure is a potential life-threatening complication. A high-level of suspicion is needed for early diagnosis and referral of the patient for extraction of the object and further avoidance of complications. Flexible fiberoptic bronchoscopy is a feasible procedure for removal of objects within the airway.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc. , the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Cameron SM, Whitlock WL, Tabor MS. Foreign body aspiration in dentistry: A review. J Am Dent Assoc. 1996;127(8):1224-1229.
2. Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: A 10-year institutional review. J Am Dent Assoc. 2004;135(9):1287-1291.
3. Susini G, Pommel L, Camps J. Accidental ingestion and aspiration of root canal instruments and other dental foreign bodies in a French population. Int Endod J. 2007;40(8):585-589.
4. Fields RT Jr, Schow SR. Aspiration and ingestion of foreign bodies in oral and maxillofacial surgery: A review of the literature and report of five cases. J Oral Maxillofac Surg. 1998;56(9):1091-1098.
5. Black RE, Johnson DG, Matlak ME. Bronchoscopic removal of aspirated foreign bodies in children. J Pediatr Surg. 1994;29(5):682-684.
6. Limper AH, Prakash UBS. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990;112(8):604-609.
7. Bas¸oglu OK, Buduneli N, Cagirici U, Turhan K, Aysan T. Pulmonary aspiration of a two-unit bridge during a deep sleep. J Oral Rehabil. 2005;32(6):461-463.
8. Mahmoud M, Imam S, Patel H, King M. Foreign body aspiration of a dental bridge in the left main stem bronchus. Case Rep Med. 2012;2012:1-4.
9. Jackson C, Jackson CL. Diseases of the Air and Food Passages of Foreign-Body Origin. Philadelphia, PA: Saunders; 1936.
10. Zitzmann NU, Elsasser S, Fried R, Marinello CP. Foreign body ingestion and aspiration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(6):657-660.
11. Elgazzar RF, Abdelhady AI, Sadakah AA. Aspiration of an impacted lower third molar during its surgical removal under local anaesthesia. Int J Oral Maxillofac Surg. 2007;36(4):362-364.
12. Tu CY, Chen HJ, Chen W, Liu YH, Chen CH. A feasible approach for extraction of dental prostheses from the airway by flexible bronchoscopy in concert with wire loops snares. Laryngoscope. 2007;117(7):1280-1282.
13. Ospina JC, Ludemann JP. Aspiration of an extracted molar: Case report. J Can Dent Assoc. 2005;71(8):581-583.
14. Cohen S, Pine H, Drake A. Use of rigid and flexible bronchoscopy among pediatric otolaryngologists. Arch Otoralyngol Head Neck Surg. 2001;127(5):505-509.
There are many reports in the medical and dental literature of complications arising from a routine delivery of dental care. One complication can include physical injury from swallowing or aspirating foreign objects.1 However, a review of such literature presents a scarcity of documented instances and no long-term evaluation of the aforementioned events.2,3
This report presents the case of a patient who aspirated a hex driver tool during a procedure to place a crown on a dental implant. The aspirated object was subsequently removed through flexible fiberoptic bronchoscopy without complications.
Case Report
An 83-year-old man was referred to the Pulmonary and Critical Care Department of the VA Caribbean Healthcare System in San Juan, Puerto Rico, after a hex driver tool was lost during a procedure to place a crown on a dental implant, performed under topical anesthesia. It was first thought that the patient swallowed the hex driver, since he never experienced or complained of coughing or shortness of breath. A chest radiograph revealed a metal object lying within the right main stem bronchus, for which the patient was referred to the Pulmonary and Critical Care Department (Figure 1).
The patient’s past medical history was remarkable for hypertension and hypercholesterolemia. Outpatient medications included hydrochlorothiazide, simvastatin, aspirin, felodipine, and lorazepam. He had no previous history of dysphagia or neurologic disease. A physical examination revealed expiratory and inspiratory wheezing localized to the right lower lobe without associated rhonchi or crackles. No distress, shortness of breath, or coughing was noted.
A flexible fiberoptic bronchoscopy was performed under conscious sedation with 3 mg of IV midazolam and topical anesthesia with nebulized 4% lidocaine. No mucosal edema, hyperemia, or structural damage was noted during direct visualization of both the right and left bronchopulmonary segments. A metallic object was visualized at the entrance of the right lower lobe. The foreign object had irregular borders, providing multiple edges that made it suitable to be embraced (Figure 2).
Using a radial jaw single-use biopsy forceps 1.8 mm, the physician clinched and retrieved the object through the bronchoscope. The object was retrieved on the same day of the dental procedure almost 5 hours after it was aspirated. The patient tolerated the procedure well; no coughing, oxygen desaturation, or bleeding occurred during the procedure.
After a few hours of observation, a postprocedural radiograph confirmed the removal of the foreign body without evidence of pneumothorax. The patient was discharged, and 24 hours after the incident remained asymptomatic without chest pain, cough, hemoptysis, sputum production, or fever.
Discussion
Foreign-body aspiration and inadvertent swallowing remains underrecognized by clinicians. In the U.S., more than 2,700 people, including more than 300 children, die of foreign-body aspiration each year.4,5 Aspiration or ingestion of a foreign body during a dental procedure is serious and potentially fatal.6 Some of the consequences of an aspirated object are complete or partial airway obstruction, respiratory distress and failure, pneumothorax, and hemorrhage.7 In addition, inadvertent aspiration of foreign objects in asymptomatic patients may not be evident for months, resulting in late complications as postobstructive pneumonia, bronchiectasis, or lung abscess.8 Early recognition and diagnosis of these events are crucial to prevent complications.
Accidental aspiration of foreign objects during dental procedures is not as common as is swallowing. In the normal population, the foreign object enters the gastrointestinal tract in about 92.5% of the time, and the tracheobronchial tree in 7.5% of these instances.
A 10-year review done at the School of Dentistry of the University of North Carolina reported 36 incidents of lost instruments during dental procedures. In only 1 case, an object was aspirated, 25 of the 36 cases were secondary to ingestion, and in the remaining 10 incidents, swallowing or aspiration was ruled out by radiography or after the object’s removal from the patient’s mouth.2 Previous reviews about foreign-body aspiration in adults have reported dental appliances as the second most commonly aspirated foreign objects.4 Of all aspirated objects, the most common site of impaction is the right lower lobe; however, aspiration has been reported in all pulmonary lobes.6
Available literature recognizes that impaction of aspirated objects occurred in 56% of instances within the right lower lobe and 33% in the left lower lobe.7,9 Identification of risk factors for aspiration is important for any patient who will undergo dental procedures, such as advanced age (ie, elderly patients may have a decreased gag reflex); neurologic conditions, such as stroke; dementia and other degenerative diseases; the use of topical anesthesia; and altered states of consciousness associated with the use of IV sedation.1,2
The key sign that most dentists recognize when patients aspirate an object during a dental procedure is coughing. It has been reported that coughing resulting from aspiration of foreign objects may range from mild to severe. In this case, the patient was completely asymptomatic during the procedure. The only clue of possible object aspiration was the reported tool loss by the dentist. It is important to always examine, account for, and review all equipment used during dental procedures. Assessment for any lost objects or missing parts of instruments should be done promptly with a high degree of suspicion for possible swallowing or aspiration if an object is missing.
It has been recommended to use a gauze throat screen and rubber dam and to avoid a supine position during a procedure, among other techniques, to minimize risk of ingestion or aspiration.2 Imaging studies should be used for further evaluation of the patient; however, some instruments, such as dental pieces and impression material, may not be identified by plain films. In those cases, further evaluation with more sophisticated imaging techniques, such as computed tomography (CT), should be considered.1-10
In a previous case report of a patient who aspirated a third molar during a dental procedure, a chest film failed to identify it. A chest CT was performed, and the object showed in the right main stem bronchus. In another instance, aspiration of impression material in a 45-year-old man was not observed by chest radiography. In this case, the history of coughing and respiratory symptoms days after the procedure pointed toward aspiration of an object as the culprit, with subsequent identification and removal by flexible fiberoptic bronchoscopy.1-11
Bronchoscopy is the treatment of choice for extraction of aspirated foreign bodies; however, there is still a debate about whether to use flexible or rigid bronchoscopy. The decision is usually made based on the object size, localization, medical facility, and personnel expertise. The rigid bronchoscope has the advantages of offering better control and visualization of the airway and easier use of removal instruments. Its primary disadvantage is that the procedure needs to be done in the operating room under general anesthesia. Flexible fiberoptic bronchoscopy done under conscious sedation and topical anesthesia may be as effective as rigid bronchoscopy and even superior in the case of smaller and more distal impacted objects.10-14
In this case, flexible fiberoptic bronchoscopy was used successfully for the removal of the foreign object. Biopsy forceps were used to grasp the object and retrieve it from the airway without complication.
Conclusion
Aspiration of foreign objects during a dental procedure is a potential life-threatening complication. A high-level of suspicion is needed for early diagnosis and referral of the patient for extraction of the object and further avoidance of complications. Flexible fiberoptic bronchoscopy is a feasible procedure for removal of objects within the airway.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc. , the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
There are many reports in the medical and dental literature of complications arising from a routine delivery of dental care. One complication can include physical injury from swallowing or aspirating foreign objects.1 However, a review of such literature presents a scarcity of documented instances and no long-term evaluation of the aforementioned events.2,3
This report presents the case of a patient who aspirated a hex driver tool during a procedure to place a crown on a dental implant. The aspirated object was subsequently removed through flexible fiberoptic bronchoscopy without complications.
Case Report
An 83-year-old man was referred to the Pulmonary and Critical Care Department of the VA Caribbean Healthcare System in San Juan, Puerto Rico, after a hex driver tool was lost during a procedure to place a crown on a dental implant, performed under topical anesthesia. It was first thought that the patient swallowed the hex driver, since he never experienced or complained of coughing or shortness of breath. A chest radiograph revealed a metal object lying within the right main stem bronchus, for which the patient was referred to the Pulmonary and Critical Care Department (Figure 1).
The patient’s past medical history was remarkable for hypertension and hypercholesterolemia. Outpatient medications included hydrochlorothiazide, simvastatin, aspirin, felodipine, and lorazepam. He had no previous history of dysphagia or neurologic disease. A physical examination revealed expiratory and inspiratory wheezing localized to the right lower lobe without associated rhonchi or crackles. No distress, shortness of breath, or coughing was noted.
A flexible fiberoptic bronchoscopy was performed under conscious sedation with 3 mg of IV midazolam and topical anesthesia with nebulized 4% lidocaine. No mucosal edema, hyperemia, or structural damage was noted during direct visualization of both the right and left bronchopulmonary segments. A metallic object was visualized at the entrance of the right lower lobe. The foreign object had irregular borders, providing multiple edges that made it suitable to be embraced (Figure 2).
Using a radial jaw single-use biopsy forceps 1.8 mm, the physician clinched and retrieved the object through the bronchoscope. The object was retrieved on the same day of the dental procedure almost 5 hours after it was aspirated. The patient tolerated the procedure well; no coughing, oxygen desaturation, or bleeding occurred during the procedure.
After a few hours of observation, a postprocedural radiograph confirmed the removal of the foreign body without evidence of pneumothorax. The patient was discharged, and 24 hours after the incident remained asymptomatic without chest pain, cough, hemoptysis, sputum production, or fever.
Discussion
Foreign-body aspiration and inadvertent swallowing remains underrecognized by clinicians. In the U.S., more than 2,700 people, including more than 300 children, die of foreign-body aspiration each year.4,5 Aspiration or ingestion of a foreign body during a dental procedure is serious and potentially fatal.6 Some of the consequences of an aspirated object are complete or partial airway obstruction, respiratory distress and failure, pneumothorax, and hemorrhage.7 In addition, inadvertent aspiration of foreign objects in asymptomatic patients may not be evident for months, resulting in late complications as postobstructive pneumonia, bronchiectasis, or lung abscess.8 Early recognition and diagnosis of these events are crucial to prevent complications.
Accidental aspiration of foreign objects during dental procedures is not as common as is swallowing. In the normal population, the foreign object enters the gastrointestinal tract in about 92.5% of the time, and the tracheobronchial tree in 7.5% of these instances.
A 10-year review done at the School of Dentistry of the University of North Carolina reported 36 incidents of lost instruments during dental procedures. In only 1 case, an object was aspirated, 25 of the 36 cases were secondary to ingestion, and in the remaining 10 incidents, swallowing or aspiration was ruled out by radiography or after the object’s removal from the patient’s mouth.2 Previous reviews about foreign-body aspiration in adults have reported dental appliances as the second most commonly aspirated foreign objects.4 Of all aspirated objects, the most common site of impaction is the right lower lobe; however, aspiration has been reported in all pulmonary lobes.6
Available literature recognizes that impaction of aspirated objects occurred in 56% of instances within the right lower lobe and 33% in the left lower lobe.7,9 Identification of risk factors for aspiration is important for any patient who will undergo dental procedures, such as advanced age (ie, elderly patients may have a decreased gag reflex); neurologic conditions, such as stroke; dementia and other degenerative diseases; the use of topical anesthesia; and altered states of consciousness associated with the use of IV sedation.1,2
The key sign that most dentists recognize when patients aspirate an object during a dental procedure is coughing. It has been reported that coughing resulting from aspiration of foreign objects may range from mild to severe. In this case, the patient was completely asymptomatic during the procedure. The only clue of possible object aspiration was the reported tool loss by the dentist. It is important to always examine, account for, and review all equipment used during dental procedures. Assessment for any lost objects or missing parts of instruments should be done promptly with a high degree of suspicion for possible swallowing or aspiration if an object is missing.
It has been recommended to use a gauze throat screen and rubber dam and to avoid a supine position during a procedure, among other techniques, to minimize risk of ingestion or aspiration.2 Imaging studies should be used for further evaluation of the patient; however, some instruments, such as dental pieces and impression material, may not be identified by plain films. In those cases, further evaluation with more sophisticated imaging techniques, such as computed tomography (CT), should be considered.1-10
In a previous case report of a patient who aspirated a third molar during a dental procedure, a chest film failed to identify it. A chest CT was performed, and the object showed in the right main stem bronchus. In another instance, aspiration of impression material in a 45-year-old man was not observed by chest radiography. In this case, the history of coughing and respiratory symptoms days after the procedure pointed toward aspiration of an object as the culprit, with subsequent identification and removal by flexible fiberoptic bronchoscopy.1-11
Bronchoscopy is the treatment of choice for extraction of aspirated foreign bodies; however, there is still a debate about whether to use flexible or rigid bronchoscopy. The decision is usually made based on the object size, localization, medical facility, and personnel expertise. The rigid bronchoscope has the advantages of offering better control and visualization of the airway and easier use of removal instruments. Its primary disadvantage is that the procedure needs to be done in the operating room under general anesthesia. Flexible fiberoptic bronchoscopy done under conscious sedation and topical anesthesia may be as effective as rigid bronchoscopy and even superior in the case of smaller and more distal impacted objects.10-14
In this case, flexible fiberoptic bronchoscopy was used successfully for the removal of the foreign object. Biopsy forceps were used to grasp the object and retrieve it from the airway without complication.
Conclusion
Aspiration of foreign objects during a dental procedure is a potential life-threatening complication. A high-level of suspicion is needed for early diagnosis and referral of the patient for extraction of the object and further avoidance of complications. Flexible fiberoptic bronchoscopy is a feasible procedure for removal of objects within the airway.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc. , the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Cameron SM, Whitlock WL, Tabor MS. Foreign body aspiration in dentistry: A review. J Am Dent Assoc. 1996;127(8):1224-1229.
2. Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: A 10-year institutional review. J Am Dent Assoc. 2004;135(9):1287-1291.
3. Susini G, Pommel L, Camps J. Accidental ingestion and aspiration of root canal instruments and other dental foreign bodies in a French population. Int Endod J. 2007;40(8):585-589.
4. Fields RT Jr, Schow SR. Aspiration and ingestion of foreign bodies in oral and maxillofacial surgery: A review of the literature and report of five cases. J Oral Maxillofac Surg. 1998;56(9):1091-1098.
5. Black RE, Johnson DG, Matlak ME. Bronchoscopic removal of aspirated foreign bodies in children. J Pediatr Surg. 1994;29(5):682-684.
6. Limper AH, Prakash UBS. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990;112(8):604-609.
7. Bas¸oglu OK, Buduneli N, Cagirici U, Turhan K, Aysan T. Pulmonary aspiration of a two-unit bridge during a deep sleep. J Oral Rehabil. 2005;32(6):461-463.
8. Mahmoud M, Imam S, Patel H, King M. Foreign body aspiration of a dental bridge in the left main stem bronchus. Case Rep Med. 2012;2012:1-4.
9. Jackson C, Jackson CL. Diseases of the Air and Food Passages of Foreign-Body Origin. Philadelphia, PA: Saunders; 1936.
10. Zitzmann NU, Elsasser S, Fried R, Marinello CP. Foreign body ingestion and aspiration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(6):657-660.
11. Elgazzar RF, Abdelhady AI, Sadakah AA. Aspiration of an impacted lower third molar during its surgical removal under local anaesthesia. Int J Oral Maxillofac Surg. 2007;36(4):362-364.
12. Tu CY, Chen HJ, Chen W, Liu YH, Chen CH. A feasible approach for extraction of dental prostheses from the airway by flexible bronchoscopy in concert with wire loops snares. Laryngoscope. 2007;117(7):1280-1282.
13. Ospina JC, Ludemann JP. Aspiration of an extracted molar: Case report. J Can Dent Assoc. 2005;71(8):581-583.
14. Cohen S, Pine H, Drake A. Use of rigid and flexible bronchoscopy among pediatric otolaryngologists. Arch Otoralyngol Head Neck Surg. 2001;127(5):505-509.
1. Cameron SM, Whitlock WL, Tabor MS. Foreign body aspiration in dentistry: A review. J Am Dent Assoc. 1996;127(8):1224-1229.
2. Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: A 10-year institutional review. J Am Dent Assoc. 2004;135(9):1287-1291.
3. Susini G, Pommel L, Camps J. Accidental ingestion and aspiration of root canal instruments and other dental foreign bodies in a French population. Int Endod J. 2007;40(8):585-589.
4. Fields RT Jr, Schow SR. Aspiration and ingestion of foreign bodies in oral and maxillofacial surgery: A review of the literature and report of five cases. J Oral Maxillofac Surg. 1998;56(9):1091-1098.
5. Black RE, Johnson DG, Matlak ME. Bronchoscopic removal of aspirated foreign bodies in children. J Pediatr Surg. 1994;29(5):682-684.
6. Limper AH, Prakash UBS. Tracheobronchial foreign bodies in adults. Ann Intern Med. 1990;112(8):604-609.
7. Bas¸oglu OK, Buduneli N, Cagirici U, Turhan K, Aysan T. Pulmonary aspiration of a two-unit bridge during a deep sleep. J Oral Rehabil. 2005;32(6):461-463.
8. Mahmoud M, Imam S, Patel H, King M. Foreign body aspiration of a dental bridge in the left main stem bronchus. Case Rep Med. 2012;2012:1-4.
9. Jackson C, Jackson CL. Diseases of the Air and Food Passages of Foreign-Body Origin. Philadelphia, PA: Saunders; 1936.
10. Zitzmann NU, Elsasser S, Fried R, Marinello CP. Foreign body ingestion and aspiration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(6):657-660.
11. Elgazzar RF, Abdelhady AI, Sadakah AA. Aspiration of an impacted lower third molar during its surgical removal under local anaesthesia. Int J Oral Maxillofac Surg. 2007;36(4):362-364.
12. Tu CY, Chen HJ, Chen W, Liu YH, Chen CH. A feasible approach for extraction of dental prostheses from the airway by flexible bronchoscopy in concert with wire loops snares. Laryngoscope. 2007;117(7):1280-1282.
13. Ospina JC, Ludemann JP. Aspiration of an extracted molar: Case report. J Can Dent Assoc. 2005;71(8):581-583.
14. Cohen S, Pine H, Drake A. Use of rigid and flexible bronchoscopy among pediatric otolaryngologists. Arch Otoralyngol Head Neck Surg. 2001;127(5):505-509.
Minimally Invasive Surgical Treatments for Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is recognized primarily as a problem of the upper airway. Although narrowing or actual obstruction of the airway during the night can be found in only 1 or 2 areas of the upper airway, most often sleep apnea involves the entire pharyngeal upper airway passages. Three regions are considered to be of major concern: the nasal cavity region, the retropalatal region, and the retrolingual region. As the level of these 3 regions descends, the volume of tissue from the nose to the base of the tongue increases significantly. This leads to increased difficulty treating OSA with each descending region as well as to a lower success rate overall. Sometimes, the problem causing OSA is limited to only 1 region but may involve 2 or even all 3 regions.1
Continuous positive airway pressure (CPAP) therapy and other positive airway pressure (PAP) therapies have been considered a safe and effective treatment for OSA. Unfortunately, compliance rates, even among patients who use it to successfully eliminate their symptoms, can vary from 50% to 70%. Complaints about using CPAP and other PAP therapies range from skin irritation, discomfort to the nose or nasal passages, and eye problems to claustrophobia from wearing a mask. Patients who are unable or unwilling to use CPAP therapy can be candidates for surgical treatment of OSA.2
This article discusses surgical options for adult patients who have OSA who choose not to use CPAP therapy, the reasons to perform surgery for adults who have OSA, and the desired outcomes of surgery for OSA with a focus on minimally invasive procedures. Interventions for pediatric patients are not addressed.
Treatment Options
Treatments other than CPAP can help lessen the severity of OSA. Noninvasive treatments include weight loss, positional treatment (avoiding sleeping on one’s back), and oral appliances. Practice parameters from the American Academy of Sleep Medicine (AASM) for the treatment of OSA include dietary weight loss in addition to the primary therapy. An improvement in the apnea-hypopnea index (AHI) may occur with dietary weight loss.3
Major weight loss through the use of bariatric surgery has been shown to be effective in treating OSA and obesity hypoventilation syndrome (OHS), which is defined as daytime hypercapnia and hypoxemia (PaCO2 > 45 mm Hg and PaO2 < 70 mm Hg at sea level) in an obese patient (body mass index [BMI] > 30 kg/m2) with sleep-disordered breathing in the absence of any other cause of hypoventilation.4 Some individuals may have both conditions. However, CPAP therapy should not be discontinued even when major weight loss occurs until repeat polysomnography has been performed. Major weight loss may cure OHS and help improve the severity of OSA but will not totally resolve the condition.4 According to Woodson, sleep apnea in patients who are morbidly obese may be different from traditional OSA as rapid eye movement (REM), REM-related apneas, and hypoventilation occur more often in this population. Although weight loss is strongly recommended for patients with OSA, bariatric surgery is not recommended as the sole treatment for traditional OSA.5
Positional therapy, wherein the patient avoids the supine position, can be effective as a secondary or supplemental therapy in addition to treatment with CPAP. Guidelines recommend this primarily for individuals who have a lower AHI when in the nonsupine position than when lying on their backs. Patients who benefit from positional therapy tend to be younger, less obese, and with a less severe condition. The AASM practice parameter was based on 3 level II studies—randomized trials with high alpha and beta levels.6 One of the level II studies compared supine with an upright position, stating: “Because not all patients normalize AHI when non-supine, the committee’s opinion is that correction of OSA by position should be documented with an appropriate test.” Special pillows have been described in 2 papers reviewed by AASM, which seemed to improve OSA.6
The AASM guidelines state that oral appliances are indicated for some patients, although they are not as efficacious in treating OSA as CPAP therapy. Oral appliances are recommended for patients with mild to moderate OSA who have not responded to CPAP therapy, cannot tolerate CPAP therapy, are not appropriate for treatment with CPAP for some reason, or fail treatment with CPAP along with other behavioral measures, such as weight loss or positional therapy.6
In addition, the AASM guidelines recommend that patients with severe OSA, “should have an initial trial of nasal CPAP because greater effectiveness has been shown with this intervention than with the use of oral appliances. Upper airway surgery (including tonsillectomy and adenoidectomy, craniofacial operations, and tracheostomy) may also supersede use of oral appliances in patients for whom these operations are predicted to be highly effective in treating sleep apnea.”6
Nasal expiratory positive end pressure (EPAP) devices may be helpful in treating OSA in some patients. These devices contain a mechanical valve with very low inspiratory resistance but high expiratory resistance. The device has an adhesive and is applied by the patient to create a seal. Exhalation causes a high expiratory resistance that splints the upper airway open. This increases the resistance of the airway to close on inspiration.7 An EPAP device is recommended for potential use in mild to moderate OSA for patients who either have an intolerance to CPAP therapy or have failed to respond to it.8
Finally, there are major surgeries performed by oral surgeons that can benefit some patients with OSA. One of these is maxillomandibular advancement (MMA). According to the AASM practice parameter: MMA “involves simultaneous advancement of the maxilla and mandible through sagittal split osteotomies. It provides enlargement of the retrolingual airway and some advancement of the retropalatal airway.”9 It is indicated as a surgical treatment for patients with severe OSA who are either unwilling or do not tolerate CPAP treatment. These individuals would not benefit from an oral appliance (recommended for mild to moderate OSA) or would find it undesirable.9
There is also stepwise or multilevel surgery (MLS) that can be performed. These include a number of combined procedures, which address multiple sites with narrowing in the upper airway. Frequently, MLS will consist of
2 phases: the first involves use of the uvulopalatopharyngoplasty (UPPP) procedure “and or genioglossus advancement and hyoid myotomy (GAHM). The second phase surgeries consist of utilizing maxillary and mandibular advancement osteotomy (MMO), offered to those failing Phase I surgeries.”9
OSA Surgical Procedures
Tracheostomies are first estimated to have been performed in 2000 BC.10 Performing a tracheostomy to bypass the upper airway was used in the 1960s and 1970s for the treatment of OSA and for many years was the only treatment available for people with Pickwickian syndrome (OHS) and nocturnal upper airway obstruction. The procedure was generally not tolerated or accepted by patients, even though it improved their quality of life and added to their life expectancy. Once CPAP treatment proved successful for OSA, tracheostomy has rarely been necessary.11
Uvulopalatopharyngoplasty surgery was introduced in 1981. The aim of this surgery is to decrease snoring and treat OSA by removing obstructive tissues, enlarging the cross-sectional portion of the upper airway, and bypassing the upper airway. Tissue that is removed includes the tonsils, uvula, and the distal portion of the soft palate.12
Woodson considers surgery for OSA to be the third-line of treatment. The first-line treatment would be CPAP therapy, and second-line therapy would include oral appliances to enlarge the airway or retain the tongue (if the individual has no dentition). The intent of surgery falls into 3 categories: curative, salvage, and ancillary.
In a chronic disease such as OSA, “many may question whether a cure exists.” Instead of eliminating OSA, the curative intent is definitively to reduce symptoms and disease morbidity for long periods. The criteria for defining a responder or cure to surgery for OSA are found in Table 1.5
Surgery for salvage aims at treating patients who have failed CPAP therapy. Successful treatment with the intent of salvage can occur with a lessening of disease severity, including morbidity and mortality, but not necessarily totally eliminating the symptoms. Finally, ancillary surgery for OSA aims to combine a surgical procedure with the first-line therapy (positive pressure) to add an additional therapeutic benefit. The combination of CPAP and ancillary procedures may be of the most benefit to patients with OSA.5
As mentioned previously, the AASM has developed practice parameters for the treatment of OSA, including surgery. Desired outcomes of treatment for OSA include the resolution of symptoms and clinical signs, normalization of the quality of sleep, AHI, and levels of oxyhemoglobin saturation. It is recognized that normalization of the AHI may not reverse all the components of OSA, and up to 22% of patients continue to have residual hypersomnia with CPAP therapy.9
Despite this, most studies that show significant benefits in lowering cardiovascular risk, mortality rates, symptoms, and neurocognitive effects have also shown significant reductions in the AHI.9 Therefore, the AASM puts a high value on treating OSA with the goal of normalization of the AHI. There exists a lack of quality studies and good evidence regarding the effectiveness of surgical procedures of the upper airway as treatment for OSA. Despite this, the AASM recommendation is that “all reasonable treatment alternatives for OSA be discussed in a manner that allows the patient to make an informed decision.”9
Types of OSA Surgeries
Surgery for OSA can be divided into 2 categories, invasive surgery and minimally invasive surgery (Table 2). Invasive surgeries for OSA have a higher risk of complications and postoperative pain.9
Invasive Surgery
The UPPP surgery is perhaps the best-known invasive procedure for treating OSA. A meta-analysis of 15 studies on UPPP outcomes found overall improvement in AHI of 33% but with postoperative AHI remaining elevated at an average of 29.8 events per hour.13
Adverse effects for the procedure include changes in taste, dysphagia, nasal regurgitation, and voice alterations. Seven of the 15 studies reported at least 1 death following the UPPP procedure. The effects of UPPP surgery on systemic and cardiovascular sequelae of OSA are not fully known and need to be further researched. 13
Another invasive procedure that is similar to the UPPP is the laser-assisted uvulopalatoplasty (LAUP) procedure. First reported in 1990, LAUP was developed as a procedure to eliminate snoring and was found to be effective. Other studies have been conducted since then, but there are inconsistencies in the specific types of procedures performed and a lack of detailed data analysis.
Adverse effects of the LAUP procedure include minor bleeding, globus sensation, local infection, minor dysphagia and dysphonia, and transient velopharyngeal insufficiency.14 However, studies have also shown that about one-quarter of the participants developed persistent dysphagia or mild to moderate scar fibrosis. Postoperative swelling can reduce an already narrow airway, and the use of sedatives or narcotics can make this problem worse. Some studies have noted structural changes following this procedure that lower airway resistance, resulting in the collapse of the upper airway and the narrowing of the airway during inhalation with worsening OSA.13,14
Practice parameters for the LAUP procedure were developed by the AASM in 1994. The AASM recommended against using LAUP to treat OSA (and other sleep-related breathing disorders) and against substituting LAUP for UPPP surgery. The AASM also suggested criteria for choosing candidates for LAUP and urged that patients be given full information about the procedure and a preoperative evaluation from their provider.5,14
Minimally Invasive Surgery
Radiofrequency surgery and soft palate implants are considered minimally invasive procedures, according to the criteria established in a study by Maurer.11 Various nasal surgeries (eg, septoplasty, adenoidectomy, and polyp removal) could also be considered minimally invasive and are often performed in patients with OSA to improve tolerance of CPAP by improving the ability to breathe nasally. However, nasal surgery with improvement of nasal breathing has not been found to have a significant impact on adults who have OSA. An advantage of nasal surgery is that some studies have shown longer use of CPAP therapy, up to 2 hours longer per night.5
With radiofrequency of the tongue base, high-frequency radio waves, either monopolar or bipolar, are used to coagulate the interstitial tissue at the base of the tongue. This, in turn, leads to necrosis and scarring, which then leads to stiffening of the tissue and in some cases, volume reduction. The surgeon controls the temperature to avoid overdosing and tissue carbonization. A number of lesions are produced during a session and the number of sessions necessary for full treatment varies per surgeon and the technical system used in procedures.
Although radiofrequency ablation (RFA) has been used on the tonsils and soft palate, RFA is currently available only to patients with OSA on the tongue base. A reduction in AHI of 33% on average was achieved in a review of 6 studies, and the reduction was stable over a 2-year period.11 The average presurgery AHI was 39.5, and the average postsurgery AHI was 28.7. In this same review, the average Epworth Sleepiness Scale (ESS) (a commonly used subjective tool to measure levels of daytime sleepiness) score was 10.4 presurgery and 4.5 postsurgery.11
A Chinese study looked at complications from RFA of the tongue base. According to the abstract (the article was written in Chinese), 1 patient (n = 193) developed a fatal arrhythmia. The authors’ recommendation was for close monitoring after surgery until the swelling subsided.15
With soft palate implants, small cylinders of woven polyester (“polyethylene terephthalate, commonly marketed as Dacron polyester”) yarn, 18 mm long by 2 mm diameter, are inserted at the junction of the hard palate and soft palate. Placed into the proximal soft palate tissue, these implants are designed to stiffen the soft palate “through fibrotic tissue encapsulation and tissue ingrowth over time.” Many patients with only snoring or mild to moderate OSA have found improvement with this procedure. Improved reduction of snoring was found in 1 study (n = 79), which looked at the use of Pillar implants to reduce snoring (Figure 1). This reduction of snoring occurred in patients with lower AHI levels before the procedure.16 Mauer reviewed 3 studies of the palatal implants and found a pooled reduction of 26% in AHI after placement.11
Criteria for Surgery
The mechanism that causes collapse of a patient’s airway will vary from one person to the next. Variables include age, body weight, anatomy, and body position. Thus, different findings will require different surgical techniques, and there is no one-size-fits-all surgery for OSA.11
A thorough physical examination of the upper airway is important. Maurer recommends considering the use of videoendoscopy under sedation, which allows a view of the mechanism and site of obstruction, with pressure catheters inserted to collect data. This procedure was developed in the 1990s to improve the analysis of obstruction within the upper airway. Unfortunately, the data are unclear about whether this aids in the surgical outcome.11 Powell stated that sleep endoscopy is currently considered investigational because medication-induced sleep may differ from natural sleep without medication.1
Nasopharyngoscopy, using fiberoptics, and lateral cephalometric analysis have been used for several years as primary diagnostic tools for patients being considered for a surgical procedure for OSA. Some new imaging procedures (eg, 3-D imaging coupled with advanced software programs) have been developed that may be helpful to assess regions that are constricted as well as provide a more exact measurement of the airway from the nose to the larynx.1
Risks and Complications of Surgery
The higher risk of anesthesia-related complications during or after surgery related to OSA is one reason that surgery is usually considered to be the third-line of treatment. Patients with OSA commonly have hypertension and other cardiovascular disease, which adds to the risk of anesthesia-related complications. Patients who have anatomical abnormalities of the jaw or portions of the upper airway will also be at a higher risk. Initial intubation and providing anesthesia during procedures may be more difficult for patients with these jaw or airway abnormalities. Postsurgical pain management with opioids contributes to the higher rate of apnea. After extubation, the incidence of apnea has been found to be higher in the population with OSA as well.17
A study published in 2001 used a case-control matched population methodology to examine patients who were undergoing elective surgeries for either hip or knee joint replacements. Significant differences in overall complication rates were found among the patients with OSA (n = 101) compared with those of the control group (n = 101). These differences were not related to the type of anesthesia, narcotic use after surgery, or the type of operation performed. The OSA group had a significantly higher number of patients who required higher flow rates of oxygen postoperatively and for a longer period. Serious complications, including the reintubation of 2 patients and unplanned intensive care unit (ICU) transfers, were noted in the patients with OSA (24%) compared with the control group (P = .004). The mean length of hospital stay was significantly longer for patients with OSA (6.8 + 2.8 days) compared with those in the control group (5.1 + 4.1 days, P = .007).18
The OSA group in the aforementioned study was divided into 2 types during this investigation: one group (n = 36) included patients undiagnosed with OSA until after their surgery (mean 1.8 years); the other group (n = 65) had a confirmed diagnosis at the time of surgery. All 36 in the first group and 32 from the second group with diagnosed OSA did not use CPAP therapy at home; a total of 68 patients (67.3%) who had not received therapy before the surgery. The 33 patients with diagnosed OSA (32.7%) who did use CPAP therapy before surgery had lower complication rates, including shorter hospital stays (6.0 + 2.1 days) compared with their counterparts with untreated OSA (7.2 + 3.1 days). The authors surmised that there might be a carryover protective effect at least for the first postoperative day.18
A retrospective study examined patients with OSA who had outpatient surgical procedures performed under either major regional anesthesia (central neuraxial) or general anesthesia. The study looked at the first outpatient surgical procedure for the patient with OSA following the diagnosis except for otorhinolaryngologic surgeries, which were excluded from the study. The 234 patients with OSA were then matched to the same number of control patients who had also had outpatient surgical procedures (excluding the otorhinolaryngologic procedures). The researchers noted a higher incidence of endotracheal intubation in the OSA group (79.9% vs 73.9% in the control group, P = .017).
The OSA group was less likely to have a laryngeal mask airway used during surgery for their airway management (5.1% vs 10.7% in the control group, P = .017). The only significantly different complication between the 2 groups was unplanned admissions to an ICU in the postoperative period (although numbers/percentages were not listed in the article). However, there was no difference in the overall unplanned hospital admission rate between the 2 groups. One limitation to this study was that the control group had not been tested for OSA, and therefore, it was possible that some in the control group might have had undiagnosed OSA.19
It is recommended that the surgeon and anesthesiologist ask about a diagnosis of OSA or sleep apnea symptoms during the preanesthesia assessment for any surgery. The provider performing the preoperative physical examination should pay attention to the circumference of the neck, chin-throat length, Mallampati classification, mandible position, and BMI. Any findings that suggest undiagnosed OSA should prompt further evaluation before any elective surgery.
Those who are at risk of OSA anesthesia-related complications should be offered regional anesthesia if possible. It is undesirable to premedicate with sedatives or opioids for this population. The sniffing position during surgery has been found to reduce the collapsibility of the airway and improve its dimensions. All patients who use CPAP therapy at home should have this therapy available for use in the recovery room with the lateral position preferred.17
Outpatient surgery using sedation and local anesthetics can also be a higher risk for patients with OSA. The unprotected, potentially problematic airway is still a serious concern. Patients requiring short procedures may do well with titrated sedation if well positioned and appropriately selected for this before the procedure. Clinicians must be prepared to handle any complications that occur. One complication that occurs commonly in obese patients related to a smaller functional residual capacity is rapid oxygen desaturation.17
A Chinese study evaluated complications in patients who had received tongue base reduction through RFA. Complications, both intraoperative and postoperative, included hematoma of the tongue base, bleeding, altered taste, an abscess at the base of the tongue, speech dysfunction, numbness, and deviation of the tongue extension movement. One cardiac death occurred 37 hours following surgery related to swelling of the tongue base and pain, which aggravated sleep apnea and nocturnal hypoxemia and induced a fatal arrhythmia.15
The Future of OSA Treatments
Research is underway to evaluate the effectiveness of an implanted system to stimulate the hypoglossal nerve with the intent of activating the upper airway musculature. A small study of 8 patients found improvement in the degree of upper airway collapsibility and the severity of OSA. Continued research on the device is focusing on the parameters for the nerve stimulation. The criteria for patient selection are also being established.20
Another study of hypoglossal nerve stimulation (HNS) evaluated 21 patients who were unable to tolerate CPAP therapy. The researchers found significant improvement in AHI (43.1 + 17.5 to 19.5 + 16.7); Functional Outcomes of Sleep Questionnaire (14.4 + 2.0 to 16.7 + 2.2); ESS (12.1 + 4.7 to 8.1 + 4.4); Beck Depression Inventory (15.8 + 9.0 to 9.7 + 7.6); and the Calgary Sleep Apnea Quality of Life Index (3.2 + 1.0 to 4.9 to 4.9 + 1.3). The researchers concluded HNS decreased OSA-related symptoms and the severity of OSA.21 At least one of these devices, the Inspire device, has been approved for use in Europe (Figure 2).22 In addition, the FDA has approve the Inspire Upper Airway Stimulation therapy for use in a subset of patients with moderate to severe OSA who are unable to use CPAP.23
A recent study investigated the effect of HNS on the severity of OSA among patients who had moderate to severe OSA and had not had a response to CPAP therapy. The HNS was associated with significant improvement in reducing the frequency of respiratory events. The median AHI at 12 months decreased from 29.3 events per hour to 9.0 events per hour (P < .001), and the number of times per hour of sleep that the blood oxygen level dropped by ≥ 4% from the baseline (oxygen desaturation index score) decreased from 25.4 to 7.4 events per hour (P < .001).24
Another area being studied is the development of a device to advance the tongue. Forty-two patients had mandibular bone anchors inserted with a flexible tether connected to a surgically inserted anchor in the posterior tongue. Unfortunately, 31% of the participants developed tissue anchor barb fractures that were asymptomatic and detected through radiography. At this time, the failure rate does not warrant clinical use. However, some patients showed significant improvement in multiple measures for sleep apnea, and more research is ongoing with the device.25
Similarly, a surgically inserted tongue pin that connects to an oral device during sleep has been studied. This pin prevents the tongue from moving back and obstructing the upper airway. Polysomnographies were performed both before and after and showed an increased rate of apnea in the 10 subjects. Visualization with magnetic resonance imaging showed that the upper airway was not kept open by this fixation device. Additional research with a modified design for the device is recommended.26
Reshaping of the epiglottis using a CO2 laser has been studied with cadaver specimens. The researchers believe scar formation following the reshaping would aid in retraction of the epiglottis anteriorly. Studies with animals are being conducted with different laser types. Future studies involving selected patients with OSA who have epiglottis malformations would be the next step.27
More studies about both minimally invasive and invasive surgeries for OSA are needed. There are many unanswered questions, including the timing of follow-up assessments, how long to observe a patient after surgery, whether the use of multilevel surgery affects the rate of relapse, and what are the best follow-up tools to use. Research needs to be performed in diverse populations, including gender, race/ethnicity, and age groups. Complications of surgical procedures need to be studied and clarified over both short- and long-term periods.9
Conclusions
Although there have been some successes in using surgical procedures to treat OSA, CPAP therapy remains the first-line treatment. Invasive surgeries have higher rates of complications and risks than do those of minimally invasive procedures. There are also additional risks related to the use of anesthesia both during and after surgery. Referrals for surgery should include information about a diagnosis of OSA, and patients should be instructed to discuss this with the anesthesiologist or certified nurse anesthetist.
With careful selection by the surgeon and sleep providers, patients who do not tolerate CPAP therapy or respond to other noninvasive interventions can benefit from a surgical procedure. Minimally invasive surgeries are less risky for the patient and should be considered.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
WEB EXCLUSIVE CASE STUDY
A Physical Examination of the Upper Airway by an Ear, Nose, and Throat Physician
1. Powell NB. Contemporary surgery for obstructive sleep apnea syndrome. Clin Exp Otorhinolaryngol. 2009;2(3):107-114.
2. Shine NP, Lewis RH. Transpalatal advancement paryngoplasty for obstructive sleep apnea syndrome: Results and analysis of failures. Arch Otolaryngol Head Neck Surg. 2009;135(5): 434-438.
3. Morgenthaler TI, Kapen S, Lee-Chiong T; American Academy of Sleep Medicine. Practice parameters for the medical therapy of obstructive sleep apnea. Sleep. 2006;29(8):1031-1035.
4. Aigner MJ, Sikka P, Whitfield P. Obesity hypoventilation syndrome: What is it? How is it treated? Is there a cure? Bariatric Nursing and Surgical Patient Care. 2009;4(2):109-113.
5. Woodson BT. Non-pressure therapies for obstructive sleep apnea: Surgery and oral appliances. Respir Care. 2010;55(10):1314-1321.
6. Kushida CA, Morgenthaler TI, Littner MR, et al; American Academy of Sleep Medicine. Practice parameters for the treatment of snoring and Obstructive Sleep Apnea with oral appliances: An update for 2005. Sleep. 2006;29(2):240-243.
7. Berry RB, Kryger MH, Massie CA. A novel nasal expiratory positive airway pressure (EPAP) device for the treatment of obstructive sleep apnea: A randomized controlled trial. Sleep. 2011;34(4):479-485.
8. Kryger MH, Berry RB, Massie CA. Long-term use of a nasal expiratory positive airway pressure (EPAP) device as a treatment of obstructive sleep apnea (OSA). J Clin Sleep Med. 2011;7(5):449-453.
9. Aurora RN, Casey KR, Kristo D, et al; American Academy of Sleep Medicine. Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults. Sleep. 2010;33(10):1408-1413.
10. Szmuk P, Ezri T, Evron S, Roth Y, Katz J. A brief history of tracheostomy and tracheal intubation, from the Bronze Age to the space age. Intensive Care Med. 2008;34(2):222-228.
11. Maurer JT. Update on surgical treatment for sleep apnoea. Swiss Med Wkly. 2009;139(43-44):624-629.
12. Franklin KA, Anttila H, Axelsson S, et al. Effects and side-effects of surgery for snoring and obsructive sleep apnea—a systematic review. Sleep. 2009;32(1):27-36.
13. Caples SM, Rowley JA, Prinsell JR, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: A systematic review and meta-analysis. Sleep. 2010; 33(10):1396-1407.
14. Littner M, Kushida CA, Hartse K, et al. Practice parameters for the use of laser-assisted uvulopalatoplasty: An update for 2000. Sleep. 2001;24(5):603-619.
15. Chen JH, Luo ZH, Yang XL, Zhu MW, Tao ZZ. Complications of tongue base reduction with radiofrequency tissue ablation on obstructive sleep apnea hypopnea syndrome. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2010;45(7):574-577. (Abstract, full text in Chinese.)
16. Gillespie MB, Smith JE, Clarke J, Nguyen SA. Effectiveness of Pillar palatal implants for snoring management. Otolaryngol Head Neck Surg. 2009;140(3):363-368.
17. Ephros HD, Madani M, Yalamanchili SC. Surgical treatment of snoring and obstructive sleep apnoea. Indian J Med Res. 2010;131:267-276.
18. Gupta RM, Parvizi J, Hanssen AD, Gay PC. Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: A case-control study. Mayo Clin Proc. 2001;76(9):897-905.
19. Sabers C, Plevak DJ, Schroeder DR, Warner DO. The diagnosis of obstructive sleep apnea as a risk factor for unanticipated admissions in outpatient surgery. Anesth Analg. 2003;96(5):1328-1335.
20. Kerzirian EJ, Boudewyns A, Eisele DW, et al. Electrical stimulation of the hypoglossal nerve in the treatment of obstructive sleep apnea. Sleep Med Rev. 2010;14(5):299-305.
21. Eastwood PR, Barnes M, Walsh JH, et al. Treating obstructive sleep apnea with hypoglossal nerve stimulation. Sleep. 2011;34(11):1479-1486.
22. Inspire Medical. STAR Trial. Inspire Medical Website. http://www.inspiresleep.com/star-trial.php. Accessed May 7, 2014.
23. FDA approves Inspire Upper Airway Stimulation (UAS) therapy for obstructive sleep apnea [press release]. Inspire Medical Website. http://www.inspiresleep.com/pdf/FDA-Approval-Press-Release-final-20140501.pdf.
Accessed May 29, 2014.
24. Strollo PJ Jr, Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139-149.
25. Woodson BT, Steward DL, Mickelson S, Huntley T, Goldberg A. Multicenter study of a novel adjustable tongue-advancement device for obstructive sleep apnea. Otolaryngol Head Neck Surg. 2010;143(4):585-590.
26. Punke C, Schöentag C, Hortian B, et al. Tongue fixation system for therapy of sleeping disorders. A feasibility study. HNO. 2010;58(12):1184-1189. (Abstract, full text in German).
27. Bourolinas C, Hajiioannou J, Sobol E, Velegrakis G, Helidonis E. Epiglottis reshaping using CO2: A minimally invasive technique and its potential applications. Head Face Med. 2008;4:15.
Obstructive sleep apnea (OSA) is recognized primarily as a problem of the upper airway. Although narrowing or actual obstruction of the airway during the night can be found in only 1 or 2 areas of the upper airway, most often sleep apnea involves the entire pharyngeal upper airway passages. Three regions are considered to be of major concern: the nasal cavity region, the retropalatal region, and the retrolingual region. As the level of these 3 regions descends, the volume of tissue from the nose to the base of the tongue increases significantly. This leads to increased difficulty treating OSA with each descending region as well as to a lower success rate overall. Sometimes, the problem causing OSA is limited to only 1 region but may involve 2 or even all 3 regions.1
Continuous positive airway pressure (CPAP) therapy and other positive airway pressure (PAP) therapies have been considered a safe and effective treatment for OSA. Unfortunately, compliance rates, even among patients who use it to successfully eliminate their symptoms, can vary from 50% to 70%. Complaints about using CPAP and other PAP therapies range from skin irritation, discomfort to the nose or nasal passages, and eye problems to claustrophobia from wearing a mask. Patients who are unable or unwilling to use CPAP therapy can be candidates for surgical treatment of OSA.2
This article discusses surgical options for adult patients who have OSA who choose not to use CPAP therapy, the reasons to perform surgery for adults who have OSA, and the desired outcomes of surgery for OSA with a focus on minimally invasive procedures. Interventions for pediatric patients are not addressed.
Treatment Options
Treatments other than CPAP can help lessen the severity of OSA. Noninvasive treatments include weight loss, positional treatment (avoiding sleeping on one’s back), and oral appliances. Practice parameters from the American Academy of Sleep Medicine (AASM) for the treatment of OSA include dietary weight loss in addition to the primary therapy. An improvement in the apnea-hypopnea index (AHI) may occur with dietary weight loss.3
Major weight loss through the use of bariatric surgery has been shown to be effective in treating OSA and obesity hypoventilation syndrome (OHS), which is defined as daytime hypercapnia and hypoxemia (PaCO2 > 45 mm Hg and PaO2 < 70 mm Hg at sea level) in an obese patient (body mass index [BMI] > 30 kg/m2) with sleep-disordered breathing in the absence of any other cause of hypoventilation.4 Some individuals may have both conditions. However, CPAP therapy should not be discontinued even when major weight loss occurs until repeat polysomnography has been performed. Major weight loss may cure OHS and help improve the severity of OSA but will not totally resolve the condition.4 According to Woodson, sleep apnea in patients who are morbidly obese may be different from traditional OSA as rapid eye movement (REM), REM-related apneas, and hypoventilation occur more often in this population. Although weight loss is strongly recommended for patients with OSA, bariatric surgery is not recommended as the sole treatment for traditional OSA.5
Positional therapy, wherein the patient avoids the supine position, can be effective as a secondary or supplemental therapy in addition to treatment with CPAP. Guidelines recommend this primarily for individuals who have a lower AHI when in the nonsupine position than when lying on their backs. Patients who benefit from positional therapy tend to be younger, less obese, and with a less severe condition. The AASM practice parameter was based on 3 level II studies—randomized trials with high alpha and beta levels.6 One of the level II studies compared supine with an upright position, stating: “Because not all patients normalize AHI when non-supine, the committee’s opinion is that correction of OSA by position should be documented with an appropriate test.” Special pillows have been described in 2 papers reviewed by AASM, which seemed to improve OSA.6
The AASM guidelines state that oral appliances are indicated for some patients, although they are not as efficacious in treating OSA as CPAP therapy. Oral appliances are recommended for patients with mild to moderate OSA who have not responded to CPAP therapy, cannot tolerate CPAP therapy, are not appropriate for treatment with CPAP for some reason, or fail treatment with CPAP along with other behavioral measures, such as weight loss or positional therapy.6
In addition, the AASM guidelines recommend that patients with severe OSA, “should have an initial trial of nasal CPAP because greater effectiveness has been shown with this intervention than with the use of oral appliances. Upper airway surgery (including tonsillectomy and adenoidectomy, craniofacial operations, and tracheostomy) may also supersede use of oral appliances in patients for whom these operations are predicted to be highly effective in treating sleep apnea.”6
Nasal expiratory positive end pressure (EPAP) devices may be helpful in treating OSA in some patients. These devices contain a mechanical valve with very low inspiratory resistance but high expiratory resistance. The device has an adhesive and is applied by the patient to create a seal. Exhalation causes a high expiratory resistance that splints the upper airway open. This increases the resistance of the airway to close on inspiration.7 An EPAP device is recommended for potential use in mild to moderate OSA for patients who either have an intolerance to CPAP therapy or have failed to respond to it.8
Finally, there are major surgeries performed by oral surgeons that can benefit some patients with OSA. One of these is maxillomandibular advancement (MMA). According to the AASM practice parameter: MMA “involves simultaneous advancement of the maxilla and mandible through sagittal split osteotomies. It provides enlargement of the retrolingual airway and some advancement of the retropalatal airway.”9 It is indicated as a surgical treatment for patients with severe OSA who are either unwilling or do not tolerate CPAP treatment. These individuals would not benefit from an oral appliance (recommended for mild to moderate OSA) or would find it undesirable.9
There is also stepwise or multilevel surgery (MLS) that can be performed. These include a number of combined procedures, which address multiple sites with narrowing in the upper airway. Frequently, MLS will consist of
2 phases: the first involves use of the uvulopalatopharyngoplasty (UPPP) procedure “and or genioglossus advancement and hyoid myotomy (GAHM). The second phase surgeries consist of utilizing maxillary and mandibular advancement osteotomy (MMO), offered to those failing Phase I surgeries.”9
OSA Surgical Procedures
Tracheostomies are first estimated to have been performed in 2000 BC.10 Performing a tracheostomy to bypass the upper airway was used in the 1960s and 1970s for the treatment of OSA and for many years was the only treatment available for people with Pickwickian syndrome (OHS) and nocturnal upper airway obstruction. The procedure was generally not tolerated or accepted by patients, even though it improved their quality of life and added to their life expectancy. Once CPAP treatment proved successful for OSA, tracheostomy has rarely been necessary.11
Uvulopalatopharyngoplasty surgery was introduced in 1981. The aim of this surgery is to decrease snoring and treat OSA by removing obstructive tissues, enlarging the cross-sectional portion of the upper airway, and bypassing the upper airway. Tissue that is removed includes the tonsils, uvula, and the distal portion of the soft palate.12
Woodson considers surgery for OSA to be the third-line of treatment. The first-line treatment would be CPAP therapy, and second-line therapy would include oral appliances to enlarge the airway or retain the tongue (if the individual has no dentition). The intent of surgery falls into 3 categories: curative, salvage, and ancillary.
In a chronic disease such as OSA, “many may question whether a cure exists.” Instead of eliminating OSA, the curative intent is definitively to reduce symptoms and disease morbidity for long periods. The criteria for defining a responder or cure to surgery for OSA are found in Table 1.5
Surgery for salvage aims at treating patients who have failed CPAP therapy. Successful treatment with the intent of salvage can occur with a lessening of disease severity, including morbidity and mortality, but not necessarily totally eliminating the symptoms. Finally, ancillary surgery for OSA aims to combine a surgical procedure with the first-line therapy (positive pressure) to add an additional therapeutic benefit. The combination of CPAP and ancillary procedures may be of the most benefit to patients with OSA.5
As mentioned previously, the AASM has developed practice parameters for the treatment of OSA, including surgery. Desired outcomes of treatment for OSA include the resolution of symptoms and clinical signs, normalization of the quality of sleep, AHI, and levels of oxyhemoglobin saturation. It is recognized that normalization of the AHI may not reverse all the components of OSA, and up to 22% of patients continue to have residual hypersomnia with CPAP therapy.9
Despite this, most studies that show significant benefits in lowering cardiovascular risk, mortality rates, symptoms, and neurocognitive effects have also shown significant reductions in the AHI.9 Therefore, the AASM puts a high value on treating OSA with the goal of normalization of the AHI. There exists a lack of quality studies and good evidence regarding the effectiveness of surgical procedures of the upper airway as treatment for OSA. Despite this, the AASM recommendation is that “all reasonable treatment alternatives for OSA be discussed in a manner that allows the patient to make an informed decision.”9
Types of OSA Surgeries
Surgery for OSA can be divided into 2 categories, invasive surgery and minimally invasive surgery (Table 2). Invasive surgeries for OSA have a higher risk of complications and postoperative pain.9
Invasive Surgery
The UPPP surgery is perhaps the best-known invasive procedure for treating OSA. A meta-analysis of 15 studies on UPPP outcomes found overall improvement in AHI of 33% but with postoperative AHI remaining elevated at an average of 29.8 events per hour.13
Adverse effects for the procedure include changes in taste, dysphagia, nasal regurgitation, and voice alterations. Seven of the 15 studies reported at least 1 death following the UPPP procedure. The effects of UPPP surgery on systemic and cardiovascular sequelae of OSA are not fully known and need to be further researched. 13
Another invasive procedure that is similar to the UPPP is the laser-assisted uvulopalatoplasty (LAUP) procedure. First reported in 1990, LAUP was developed as a procedure to eliminate snoring and was found to be effective. Other studies have been conducted since then, but there are inconsistencies in the specific types of procedures performed and a lack of detailed data analysis.
Adverse effects of the LAUP procedure include minor bleeding, globus sensation, local infection, minor dysphagia and dysphonia, and transient velopharyngeal insufficiency.14 However, studies have also shown that about one-quarter of the participants developed persistent dysphagia or mild to moderate scar fibrosis. Postoperative swelling can reduce an already narrow airway, and the use of sedatives or narcotics can make this problem worse. Some studies have noted structural changes following this procedure that lower airway resistance, resulting in the collapse of the upper airway and the narrowing of the airway during inhalation with worsening OSA.13,14
Practice parameters for the LAUP procedure were developed by the AASM in 1994. The AASM recommended against using LAUP to treat OSA (and other sleep-related breathing disorders) and against substituting LAUP for UPPP surgery. The AASM also suggested criteria for choosing candidates for LAUP and urged that patients be given full information about the procedure and a preoperative evaluation from their provider.5,14
Minimally Invasive Surgery
Radiofrequency surgery and soft palate implants are considered minimally invasive procedures, according to the criteria established in a study by Maurer.11 Various nasal surgeries (eg, septoplasty, adenoidectomy, and polyp removal) could also be considered minimally invasive and are often performed in patients with OSA to improve tolerance of CPAP by improving the ability to breathe nasally. However, nasal surgery with improvement of nasal breathing has not been found to have a significant impact on adults who have OSA. An advantage of nasal surgery is that some studies have shown longer use of CPAP therapy, up to 2 hours longer per night.5
With radiofrequency of the tongue base, high-frequency radio waves, either monopolar or bipolar, are used to coagulate the interstitial tissue at the base of the tongue. This, in turn, leads to necrosis and scarring, which then leads to stiffening of the tissue and in some cases, volume reduction. The surgeon controls the temperature to avoid overdosing and tissue carbonization. A number of lesions are produced during a session and the number of sessions necessary for full treatment varies per surgeon and the technical system used in procedures.
Although radiofrequency ablation (RFA) has been used on the tonsils and soft palate, RFA is currently available only to patients with OSA on the tongue base. A reduction in AHI of 33% on average was achieved in a review of 6 studies, and the reduction was stable over a 2-year period.11 The average presurgery AHI was 39.5, and the average postsurgery AHI was 28.7. In this same review, the average Epworth Sleepiness Scale (ESS) (a commonly used subjective tool to measure levels of daytime sleepiness) score was 10.4 presurgery and 4.5 postsurgery.11
A Chinese study looked at complications from RFA of the tongue base. According to the abstract (the article was written in Chinese), 1 patient (n = 193) developed a fatal arrhythmia. The authors’ recommendation was for close monitoring after surgery until the swelling subsided.15
With soft palate implants, small cylinders of woven polyester (“polyethylene terephthalate, commonly marketed as Dacron polyester”) yarn, 18 mm long by 2 mm diameter, are inserted at the junction of the hard palate and soft palate. Placed into the proximal soft palate tissue, these implants are designed to stiffen the soft palate “through fibrotic tissue encapsulation and tissue ingrowth over time.” Many patients with only snoring or mild to moderate OSA have found improvement with this procedure. Improved reduction of snoring was found in 1 study (n = 79), which looked at the use of Pillar implants to reduce snoring (Figure 1). This reduction of snoring occurred in patients with lower AHI levels before the procedure.16 Mauer reviewed 3 studies of the palatal implants and found a pooled reduction of 26% in AHI after placement.11
Criteria for Surgery
The mechanism that causes collapse of a patient’s airway will vary from one person to the next. Variables include age, body weight, anatomy, and body position. Thus, different findings will require different surgical techniques, and there is no one-size-fits-all surgery for OSA.11
A thorough physical examination of the upper airway is important. Maurer recommends considering the use of videoendoscopy under sedation, which allows a view of the mechanism and site of obstruction, with pressure catheters inserted to collect data. This procedure was developed in the 1990s to improve the analysis of obstruction within the upper airway. Unfortunately, the data are unclear about whether this aids in the surgical outcome.11 Powell stated that sleep endoscopy is currently considered investigational because medication-induced sleep may differ from natural sleep without medication.1
Nasopharyngoscopy, using fiberoptics, and lateral cephalometric analysis have been used for several years as primary diagnostic tools for patients being considered for a surgical procedure for OSA. Some new imaging procedures (eg, 3-D imaging coupled with advanced software programs) have been developed that may be helpful to assess regions that are constricted as well as provide a more exact measurement of the airway from the nose to the larynx.1
Risks and Complications of Surgery
The higher risk of anesthesia-related complications during or after surgery related to OSA is one reason that surgery is usually considered to be the third-line of treatment. Patients with OSA commonly have hypertension and other cardiovascular disease, which adds to the risk of anesthesia-related complications. Patients who have anatomical abnormalities of the jaw or portions of the upper airway will also be at a higher risk. Initial intubation and providing anesthesia during procedures may be more difficult for patients with these jaw or airway abnormalities. Postsurgical pain management with opioids contributes to the higher rate of apnea. After extubation, the incidence of apnea has been found to be higher in the population with OSA as well.17
A study published in 2001 used a case-control matched population methodology to examine patients who were undergoing elective surgeries for either hip or knee joint replacements. Significant differences in overall complication rates were found among the patients with OSA (n = 101) compared with those of the control group (n = 101). These differences were not related to the type of anesthesia, narcotic use after surgery, or the type of operation performed. The OSA group had a significantly higher number of patients who required higher flow rates of oxygen postoperatively and for a longer period. Serious complications, including the reintubation of 2 patients and unplanned intensive care unit (ICU) transfers, were noted in the patients with OSA (24%) compared with the control group (P = .004). The mean length of hospital stay was significantly longer for patients with OSA (6.8 + 2.8 days) compared with those in the control group (5.1 + 4.1 days, P = .007).18
The OSA group in the aforementioned study was divided into 2 types during this investigation: one group (n = 36) included patients undiagnosed with OSA until after their surgery (mean 1.8 years); the other group (n = 65) had a confirmed diagnosis at the time of surgery. All 36 in the first group and 32 from the second group with diagnosed OSA did not use CPAP therapy at home; a total of 68 patients (67.3%) who had not received therapy before the surgery. The 33 patients with diagnosed OSA (32.7%) who did use CPAP therapy before surgery had lower complication rates, including shorter hospital stays (6.0 + 2.1 days) compared with their counterparts with untreated OSA (7.2 + 3.1 days). The authors surmised that there might be a carryover protective effect at least for the first postoperative day.18
A retrospective study examined patients with OSA who had outpatient surgical procedures performed under either major regional anesthesia (central neuraxial) or general anesthesia. The study looked at the first outpatient surgical procedure for the patient with OSA following the diagnosis except for otorhinolaryngologic surgeries, which were excluded from the study. The 234 patients with OSA were then matched to the same number of control patients who had also had outpatient surgical procedures (excluding the otorhinolaryngologic procedures). The researchers noted a higher incidence of endotracheal intubation in the OSA group (79.9% vs 73.9% in the control group, P = .017).
The OSA group was less likely to have a laryngeal mask airway used during surgery for their airway management (5.1% vs 10.7% in the control group, P = .017). The only significantly different complication between the 2 groups was unplanned admissions to an ICU in the postoperative period (although numbers/percentages were not listed in the article). However, there was no difference in the overall unplanned hospital admission rate between the 2 groups. One limitation to this study was that the control group had not been tested for OSA, and therefore, it was possible that some in the control group might have had undiagnosed OSA.19
It is recommended that the surgeon and anesthesiologist ask about a diagnosis of OSA or sleep apnea symptoms during the preanesthesia assessment for any surgery. The provider performing the preoperative physical examination should pay attention to the circumference of the neck, chin-throat length, Mallampati classification, mandible position, and BMI. Any findings that suggest undiagnosed OSA should prompt further evaluation before any elective surgery.
Those who are at risk of OSA anesthesia-related complications should be offered regional anesthesia if possible. It is undesirable to premedicate with sedatives or opioids for this population. The sniffing position during surgery has been found to reduce the collapsibility of the airway and improve its dimensions. All patients who use CPAP therapy at home should have this therapy available for use in the recovery room with the lateral position preferred.17
Outpatient surgery using sedation and local anesthetics can also be a higher risk for patients with OSA. The unprotected, potentially problematic airway is still a serious concern. Patients requiring short procedures may do well with titrated sedation if well positioned and appropriately selected for this before the procedure. Clinicians must be prepared to handle any complications that occur. One complication that occurs commonly in obese patients related to a smaller functional residual capacity is rapid oxygen desaturation.17
A Chinese study evaluated complications in patients who had received tongue base reduction through RFA. Complications, both intraoperative and postoperative, included hematoma of the tongue base, bleeding, altered taste, an abscess at the base of the tongue, speech dysfunction, numbness, and deviation of the tongue extension movement. One cardiac death occurred 37 hours following surgery related to swelling of the tongue base and pain, which aggravated sleep apnea and nocturnal hypoxemia and induced a fatal arrhythmia.15
The Future of OSA Treatments
Research is underway to evaluate the effectiveness of an implanted system to stimulate the hypoglossal nerve with the intent of activating the upper airway musculature. A small study of 8 patients found improvement in the degree of upper airway collapsibility and the severity of OSA. Continued research on the device is focusing on the parameters for the nerve stimulation. The criteria for patient selection are also being established.20
Another study of hypoglossal nerve stimulation (HNS) evaluated 21 patients who were unable to tolerate CPAP therapy. The researchers found significant improvement in AHI (43.1 + 17.5 to 19.5 + 16.7); Functional Outcomes of Sleep Questionnaire (14.4 + 2.0 to 16.7 + 2.2); ESS (12.1 + 4.7 to 8.1 + 4.4); Beck Depression Inventory (15.8 + 9.0 to 9.7 + 7.6); and the Calgary Sleep Apnea Quality of Life Index (3.2 + 1.0 to 4.9 to 4.9 + 1.3). The researchers concluded HNS decreased OSA-related symptoms and the severity of OSA.21 At least one of these devices, the Inspire device, has been approved for use in Europe (Figure 2).22 In addition, the FDA has approve the Inspire Upper Airway Stimulation therapy for use in a subset of patients with moderate to severe OSA who are unable to use CPAP.23
A recent study investigated the effect of HNS on the severity of OSA among patients who had moderate to severe OSA and had not had a response to CPAP therapy. The HNS was associated with significant improvement in reducing the frequency of respiratory events. The median AHI at 12 months decreased from 29.3 events per hour to 9.0 events per hour (P < .001), and the number of times per hour of sleep that the blood oxygen level dropped by ≥ 4% from the baseline (oxygen desaturation index score) decreased from 25.4 to 7.4 events per hour (P < .001).24
Another area being studied is the development of a device to advance the tongue. Forty-two patients had mandibular bone anchors inserted with a flexible tether connected to a surgically inserted anchor in the posterior tongue. Unfortunately, 31% of the participants developed tissue anchor barb fractures that were asymptomatic and detected through radiography. At this time, the failure rate does not warrant clinical use. However, some patients showed significant improvement in multiple measures for sleep apnea, and more research is ongoing with the device.25
Similarly, a surgically inserted tongue pin that connects to an oral device during sleep has been studied. This pin prevents the tongue from moving back and obstructing the upper airway. Polysomnographies were performed both before and after and showed an increased rate of apnea in the 10 subjects. Visualization with magnetic resonance imaging showed that the upper airway was not kept open by this fixation device. Additional research with a modified design for the device is recommended.26
Reshaping of the epiglottis using a CO2 laser has been studied with cadaver specimens. The researchers believe scar formation following the reshaping would aid in retraction of the epiglottis anteriorly. Studies with animals are being conducted with different laser types. Future studies involving selected patients with OSA who have epiglottis malformations would be the next step.27
More studies about both minimally invasive and invasive surgeries for OSA are needed. There are many unanswered questions, including the timing of follow-up assessments, how long to observe a patient after surgery, whether the use of multilevel surgery affects the rate of relapse, and what are the best follow-up tools to use. Research needs to be performed in diverse populations, including gender, race/ethnicity, and age groups. Complications of surgical procedures need to be studied and clarified over both short- and long-term periods.9
Conclusions
Although there have been some successes in using surgical procedures to treat OSA, CPAP therapy remains the first-line treatment. Invasive surgeries have higher rates of complications and risks than do those of minimally invasive procedures. There are also additional risks related to the use of anesthesia both during and after surgery. Referrals for surgery should include information about a diagnosis of OSA, and patients should be instructed to discuss this with the anesthesiologist or certified nurse anesthetist.
With careful selection by the surgeon and sleep providers, patients who do not tolerate CPAP therapy or respond to other noninvasive interventions can benefit from a surgical procedure. Minimally invasive surgeries are less risky for the patient and should be considered.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
WEB EXCLUSIVE CASE STUDY
A Physical Examination of the Upper Airway by an Ear, Nose, and Throat Physician
Obstructive sleep apnea (OSA) is recognized primarily as a problem of the upper airway. Although narrowing or actual obstruction of the airway during the night can be found in only 1 or 2 areas of the upper airway, most often sleep apnea involves the entire pharyngeal upper airway passages. Three regions are considered to be of major concern: the nasal cavity region, the retropalatal region, and the retrolingual region. As the level of these 3 regions descends, the volume of tissue from the nose to the base of the tongue increases significantly. This leads to increased difficulty treating OSA with each descending region as well as to a lower success rate overall. Sometimes, the problem causing OSA is limited to only 1 region but may involve 2 or even all 3 regions.1
Continuous positive airway pressure (CPAP) therapy and other positive airway pressure (PAP) therapies have been considered a safe and effective treatment for OSA. Unfortunately, compliance rates, even among patients who use it to successfully eliminate their symptoms, can vary from 50% to 70%. Complaints about using CPAP and other PAP therapies range from skin irritation, discomfort to the nose or nasal passages, and eye problems to claustrophobia from wearing a mask. Patients who are unable or unwilling to use CPAP therapy can be candidates for surgical treatment of OSA.2
This article discusses surgical options for adult patients who have OSA who choose not to use CPAP therapy, the reasons to perform surgery for adults who have OSA, and the desired outcomes of surgery for OSA with a focus on minimally invasive procedures. Interventions for pediatric patients are not addressed.
Treatment Options
Treatments other than CPAP can help lessen the severity of OSA. Noninvasive treatments include weight loss, positional treatment (avoiding sleeping on one’s back), and oral appliances. Practice parameters from the American Academy of Sleep Medicine (AASM) for the treatment of OSA include dietary weight loss in addition to the primary therapy. An improvement in the apnea-hypopnea index (AHI) may occur with dietary weight loss.3
Major weight loss through the use of bariatric surgery has been shown to be effective in treating OSA and obesity hypoventilation syndrome (OHS), which is defined as daytime hypercapnia and hypoxemia (PaCO2 > 45 mm Hg and PaO2 < 70 mm Hg at sea level) in an obese patient (body mass index [BMI] > 30 kg/m2) with sleep-disordered breathing in the absence of any other cause of hypoventilation.4 Some individuals may have both conditions. However, CPAP therapy should not be discontinued even when major weight loss occurs until repeat polysomnography has been performed. Major weight loss may cure OHS and help improve the severity of OSA but will not totally resolve the condition.4 According to Woodson, sleep apnea in patients who are morbidly obese may be different from traditional OSA as rapid eye movement (REM), REM-related apneas, and hypoventilation occur more often in this population. Although weight loss is strongly recommended for patients with OSA, bariatric surgery is not recommended as the sole treatment for traditional OSA.5
Positional therapy, wherein the patient avoids the supine position, can be effective as a secondary or supplemental therapy in addition to treatment with CPAP. Guidelines recommend this primarily for individuals who have a lower AHI when in the nonsupine position than when lying on their backs. Patients who benefit from positional therapy tend to be younger, less obese, and with a less severe condition. The AASM practice parameter was based on 3 level II studies—randomized trials with high alpha and beta levels.6 One of the level II studies compared supine with an upright position, stating: “Because not all patients normalize AHI when non-supine, the committee’s opinion is that correction of OSA by position should be documented with an appropriate test.” Special pillows have been described in 2 papers reviewed by AASM, which seemed to improve OSA.6
The AASM guidelines state that oral appliances are indicated for some patients, although they are not as efficacious in treating OSA as CPAP therapy. Oral appliances are recommended for patients with mild to moderate OSA who have not responded to CPAP therapy, cannot tolerate CPAP therapy, are not appropriate for treatment with CPAP for some reason, or fail treatment with CPAP along with other behavioral measures, such as weight loss or positional therapy.6
In addition, the AASM guidelines recommend that patients with severe OSA, “should have an initial trial of nasal CPAP because greater effectiveness has been shown with this intervention than with the use of oral appliances. Upper airway surgery (including tonsillectomy and adenoidectomy, craniofacial operations, and tracheostomy) may also supersede use of oral appliances in patients for whom these operations are predicted to be highly effective in treating sleep apnea.”6
Nasal expiratory positive end pressure (EPAP) devices may be helpful in treating OSA in some patients. These devices contain a mechanical valve with very low inspiratory resistance but high expiratory resistance. The device has an adhesive and is applied by the patient to create a seal. Exhalation causes a high expiratory resistance that splints the upper airway open. This increases the resistance of the airway to close on inspiration.7 An EPAP device is recommended for potential use in mild to moderate OSA for patients who either have an intolerance to CPAP therapy or have failed to respond to it.8
Finally, there are major surgeries performed by oral surgeons that can benefit some patients with OSA. One of these is maxillomandibular advancement (MMA). According to the AASM practice parameter: MMA “involves simultaneous advancement of the maxilla and mandible through sagittal split osteotomies. It provides enlargement of the retrolingual airway and some advancement of the retropalatal airway.”9 It is indicated as a surgical treatment for patients with severe OSA who are either unwilling or do not tolerate CPAP treatment. These individuals would not benefit from an oral appliance (recommended for mild to moderate OSA) or would find it undesirable.9
There is also stepwise or multilevel surgery (MLS) that can be performed. These include a number of combined procedures, which address multiple sites with narrowing in the upper airway. Frequently, MLS will consist of
2 phases: the first involves use of the uvulopalatopharyngoplasty (UPPP) procedure “and or genioglossus advancement and hyoid myotomy (GAHM). The second phase surgeries consist of utilizing maxillary and mandibular advancement osteotomy (MMO), offered to those failing Phase I surgeries.”9
OSA Surgical Procedures
Tracheostomies are first estimated to have been performed in 2000 BC.10 Performing a tracheostomy to bypass the upper airway was used in the 1960s and 1970s for the treatment of OSA and for many years was the only treatment available for people with Pickwickian syndrome (OHS) and nocturnal upper airway obstruction. The procedure was generally not tolerated or accepted by patients, even though it improved their quality of life and added to their life expectancy. Once CPAP treatment proved successful for OSA, tracheostomy has rarely been necessary.11
Uvulopalatopharyngoplasty surgery was introduced in 1981. The aim of this surgery is to decrease snoring and treat OSA by removing obstructive tissues, enlarging the cross-sectional portion of the upper airway, and bypassing the upper airway. Tissue that is removed includes the tonsils, uvula, and the distal portion of the soft palate.12
Woodson considers surgery for OSA to be the third-line of treatment. The first-line treatment would be CPAP therapy, and second-line therapy would include oral appliances to enlarge the airway or retain the tongue (if the individual has no dentition). The intent of surgery falls into 3 categories: curative, salvage, and ancillary.
In a chronic disease such as OSA, “many may question whether a cure exists.” Instead of eliminating OSA, the curative intent is definitively to reduce symptoms and disease morbidity for long periods. The criteria for defining a responder or cure to surgery for OSA are found in Table 1.5
Surgery for salvage aims at treating patients who have failed CPAP therapy. Successful treatment with the intent of salvage can occur with a lessening of disease severity, including morbidity and mortality, but not necessarily totally eliminating the symptoms. Finally, ancillary surgery for OSA aims to combine a surgical procedure with the first-line therapy (positive pressure) to add an additional therapeutic benefit. The combination of CPAP and ancillary procedures may be of the most benefit to patients with OSA.5
As mentioned previously, the AASM has developed practice parameters for the treatment of OSA, including surgery. Desired outcomes of treatment for OSA include the resolution of symptoms and clinical signs, normalization of the quality of sleep, AHI, and levels of oxyhemoglobin saturation. It is recognized that normalization of the AHI may not reverse all the components of OSA, and up to 22% of patients continue to have residual hypersomnia with CPAP therapy.9
Despite this, most studies that show significant benefits in lowering cardiovascular risk, mortality rates, symptoms, and neurocognitive effects have also shown significant reductions in the AHI.9 Therefore, the AASM puts a high value on treating OSA with the goal of normalization of the AHI. There exists a lack of quality studies and good evidence regarding the effectiveness of surgical procedures of the upper airway as treatment for OSA. Despite this, the AASM recommendation is that “all reasonable treatment alternatives for OSA be discussed in a manner that allows the patient to make an informed decision.”9
Types of OSA Surgeries
Surgery for OSA can be divided into 2 categories, invasive surgery and minimally invasive surgery (Table 2). Invasive surgeries for OSA have a higher risk of complications and postoperative pain.9
Invasive Surgery
The UPPP surgery is perhaps the best-known invasive procedure for treating OSA. A meta-analysis of 15 studies on UPPP outcomes found overall improvement in AHI of 33% but with postoperative AHI remaining elevated at an average of 29.8 events per hour.13
Adverse effects for the procedure include changes in taste, dysphagia, nasal regurgitation, and voice alterations. Seven of the 15 studies reported at least 1 death following the UPPP procedure. The effects of UPPP surgery on systemic and cardiovascular sequelae of OSA are not fully known and need to be further researched. 13
Another invasive procedure that is similar to the UPPP is the laser-assisted uvulopalatoplasty (LAUP) procedure. First reported in 1990, LAUP was developed as a procedure to eliminate snoring and was found to be effective. Other studies have been conducted since then, but there are inconsistencies in the specific types of procedures performed and a lack of detailed data analysis.
Adverse effects of the LAUP procedure include minor bleeding, globus sensation, local infection, minor dysphagia and dysphonia, and transient velopharyngeal insufficiency.14 However, studies have also shown that about one-quarter of the participants developed persistent dysphagia or mild to moderate scar fibrosis. Postoperative swelling can reduce an already narrow airway, and the use of sedatives or narcotics can make this problem worse. Some studies have noted structural changes following this procedure that lower airway resistance, resulting in the collapse of the upper airway and the narrowing of the airway during inhalation with worsening OSA.13,14
Practice parameters for the LAUP procedure were developed by the AASM in 1994. The AASM recommended against using LAUP to treat OSA (and other sleep-related breathing disorders) and against substituting LAUP for UPPP surgery. The AASM also suggested criteria for choosing candidates for LAUP and urged that patients be given full information about the procedure and a preoperative evaluation from their provider.5,14
Minimally Invasive Surgery
Radiofrequency surgery and soft palate implants are considered minimally invasive procedures, according to the criteria established in a study by Maurer.11 Various nasal surgeries (eg, septoplasty, adenoidectomy, and polyp removal) could also be considered minimally invasive and are often performed in patients with OSA to improve tolerance of CPAP by improving the ability to breathe nasally. However, nasal surgery with improvement of nasal breathing has not been found to have a significant impact on adults who have OSA. An advantage of nasal surgery is that some studies have shown longer use of CPAP therapy, up to 2 hours longer per night.5
With radiofrequency of the tongue base, high-frequency radio waves, either monopolar or bipolar, are used to coagulate the interstitial tissue at the base of the tongue. This, in turn, leads to necrosis and scarring, which then leads to stiffening of the tissue and in some cases, volume reduction. The surgeon controls the temperature to avoid overdosing and tissue carbonization. A number of lesions are produced during a session and the number of sessions necessary for full treatment varies per surgeon and the technical system used in procedures.
Although radiofrequency ablation (RFA) has been used on the tonsils and soft palate, RFA is currently available only to patients with OSA on the tongue base. A reduction in AHI of 33% on average was achieved in a review of 6 studies, and the reduction was stable over a 2-year period.11 The average presurgery AHI was 39.5, and the average postsurgery AHI was 28.7. In this same review, the average Epworth Sleepiness Scale (ESS) (a commonly used subjective tool to measure levels of daytime sleepiness) score was 10.4 presurgery and 4.5 postsurgery.11
A Chinese study looked at complications from RFA of the tongue base. According to the abstract (the article was written in Chinese), 1 patient (n = 193) developed a fatal arrhythmia. The authors’ recommendation was for close monitoring after surgery until the swelling subsided.15
With soft palate implants, small cylinders of woven polyester (“polyethylene terephthalate, commonly marketed as Dacron polyester”) yarn, 18 mm long by 2 mm diameter, are inserted at the junction of the hard palate and soft palate. Placed into the proximal soft palate tissue, these implants are designed to stiffen the soft palate “through fibrotic tissue encapsulation and tissue ingrowth over time.” Many patients with only snoring or mild to moderate OSA have found improvement with this procedure. Improved reduction of snoring was found in 1 study (n = 79), which looked at the use of Pillar implants to reduce snoring (Figure 1). This reduction of snoring occurred in patients with lower AHI levels before the procedure.16 Mauer reviewed 3 studies of the palatal implants and found a pooled reduction of 26% in AHI after placement.11
Criteria for Surgery
The mechanism that causes collapse of a patient’s airway will vary from one person to the next. Variables include age, body weight, anatomy, and body position. Thus, different findings will require different surgical techniques, and there is no one-size-fits-all surgery for OSA.11
A thorough physical examination of the upper airway is important. Maurer recommends considering the use of videoendoscopy under sedation, which allows a view of the mechanism and site of obstruction, with pressure catheters inserted to collect data. This procedure was developed in the 1990s to improve the analysis of obstruction within the upper airway. Unfortunately, the data are unclear about whether this aids in the surgical outcome.11 Powell stated that sleep endoscopy is currently considered investigational because medication-induced sleep may differ from natural sleep without medication.1
Nasopharyngoscopy, using fiberoptics, and lateral cephalometric analysis have been used for several years as primary diagnostic tools for patients being considered for a surgical procedure for OSA. Some new imaging procedures (eg, 3-D imaging coupled with advanced software programs) have been developed that may be helpful to assess regions that are constricted as well as provide a more exact measurement of the airway from the nose to the larynx.1
Risks and Complications of Surgery
The higher risk of anesthesia-related complications during or after surgery related to OSA is one reason that surgery is usually considered to be the third-line of treatment. Patients with OSA commonly have hypertension and other cardiovascular disease, which adds to the risk of anesthesia-related complications. Patients who have anatomical abnormalities of the jaw or portions of the upper airway will also be at a higher risk. Initial intubation and providing anesthesia during procedures may be more difficult for patients with these jaw or airway abnormalities. Postsurgical pain management with opioids contributes to the higher rate of apnea. After extubation, the incidence of apnea has been found to be higher in the population with OSA as well.17
A study published in 2001 used a case-control matched population methodology to examine patients who were undergoing elective surgeries for either hip or knee joint replacements. Significant differences in overall complication rates were found among the patients with OSA (n = 101) compared with those of the control group (n = 101). These differences were not related to the type of anesthesia, narcotic use after surgery, or the type of operation performed. The OSA group had a significantly higher number of patients who required higher flow rates of oxygen postoperatively and for a longer period. Serious complications, including the reintubation of 2 patients and unplanned intensive care unit (ICU) transfers, were noted in the patients with OSA (24%) compared with the control group (P = .004). The mean length of hospital stay was significantly longer for patients with OSA (6.8 + 2.8 days) compared with those in the control group (5.1 + 4.1 days, P = .007).18
The OSA group in the aforementioned study was divided into 2 types during this investigation: one group (n = 36) included patients undiagnosed with OSA until after their surgery (mean 1.8 years); the other group (n = 65) had a confirmed diagnosis at the time of surgery. All 36 in the first group and 32 from the second group with diagnosed OSA did not use CPAP therapy at home; a total of 68 patients (67.3%) who had not received therapy before the surgery. The 33 patients with diagnosed OSA (32.7%) who did use CPAP therapy before surgery had lower complication rates, including shorter hospital stays (6.0 + 2.1 days) compared with their counterparts with untreated OSA (7.2 + 3.1 days). The authors surmised that there might be a carryover protective effect at least for the first postoperative day.18
A retrospective study examined patients with OSA who had outpatient surgical procedures performed under either major regional anesthesia (central neuraxial) or general anesthesia. The study looked at the first outpatient surgical procedure for the patient with OSA following the diagnosis except for otorhinolaryngologic surgeries, which were excluded from the study. The 234 patients with OSA were then matched to the same number of control patients who had also had outpatient surgical procedures (excluding the otorhinolaryngologic procedures). The researchers noted a higher incidence of endotracheal intubation in the OSA group (79.9% vs 73.9% in the control group, P = .017).
The OSA group was less likely to have a laryngeal mask airway used during surgery for their airway management (5.1% vs 10.7% in the control group, P = .017). The only significantly different complication between the 2 groups was unplanned admissions to an ICU in the postoperative period (although numbers/percentages were not listed in the article). However, there was no difference in the overall unplanned hospital admission rate between the 2 groups. One limitation to this study was that the control group had not been tested for OSA, and therefore, it was possible that some in the control group might have had undiagnosed OSA.19
It is recommended that the surgeon and anesthesiologist ask about a diagnosis of OSA or sleep apnea symptoms during the preanesthesia assessment for any surgery. The provider performing the preoperative physical examination should pay attention to the circumference of the neck, chin-throat length, Mallampati classification, mandible position, and BMI. Any findings that suggest undiagnosed OSA should prompt further evaluation before any elective surgery.
Those who are at risk of OSA anesthesia-related complications should be offered regional anesthesia if possible. It is undesirable to premedicate with sedatives or opioids for this population. The sniffing position during surgery has been found to reduce the collapsibility of the airway and improve its dimensions. All patients who use CPAP therapy at home should have this therapy available for use in the recovery room with the lateral position preferred.17
Outpatient surgery using sedation and local anesthetics can also be a higher risk for patients with OSA. The unprotected, potentially problematic airway is still a serious concern. Patients requiring short procedures may do well with titrated sedation if well positioned and appropriately selected for this before the procedure. Clinicians must be prepared to handle any complications that occur. One complication that occurs commonly in obese patients related to a smaller functional residual capacity is rapid oxygen desaturation.17
A Chinese study evaluated complications in patients who had received tongue base reduction through RFA. Complications, both intraoperative and postoperative, included hematoma of the tongue base, bleeding, altered taste, an abscess at the base of the tongue, speech dysfunction, numbness, and deviation of the tongue extension movement. One cardiac death occurred 37 hours following surgery related to swelling of the tongue base and pain, which aggravated sleep apnea and nocturnal hypoxemia and induced a fatal arrhythmia.15
The Future of OSA Treatments
Research is underway to evaluate the effectiveness of an implanted system to stimulate the hypoglossal nerve with the intent of activating the upper airway musculature. A small study of 8 patients found improvement in the degree of upper airway collapsibility and the severity of OSA. Continued research on the device is focusing on the parameters for the nerve stimulation. The criteria for patient selection are also being established.20
Another study of hypoglossal nerve stimulation (HNS) evaluated 21 patients who were unable to tolerate CPAP therapy. The researchers found significant improvement in AHI (43.1 + 17.5 to 19.5 + 16.7); Functional Outcomes of Sleep Questionnaire (14.4 + 2.0 to 16.7 + 2.2); ESS (12.1 + 4.7 to 8.1 + 4.4); Beck Depression Inventory (15.8 + 9.0 to 9.7 + 7.6); and the Calgary Sleep Apnea Quality of Life Index (3.2 + 1.0 to 4.9 to 4.9 + 1.3). The researchers concluded HNS decreased OSA-related symptoms and the severity of OSA.21 At least one of these devices, the Inspire device, has been approved for use in Europe (Figure 2).22 In addition, the FDA has approve the Inspire Upper Airway Stimulation therapy for use in a subset of patients with moderate to severe OSA who are unable to use CPAP.23
A recent study investigated the effect of HNS on the severity of OSA among patients who had moderate to severe OSA and had not had a response to CPAP therapy. The HNS was associated with significant improvement in reducing the frequency of respiratory events. The median AHI at 12 months decreased from 29.3 events per hour to 9.0 events per hour (P < .001), and the number of times per hour of sleep that the blood oxygen level dropped by ≥ 4% from the baseline (oxygen desaturation index score) decreased from 25.4 to 7.4 events per hour (P < .001).24
Another area being studied is the development of a device to advance the tongue. Forty-two patients had mandibular bone anchors inserted with a flexible tether connected to a surgically inserted anchor in the posterior tongue. Unfortunately, 31% of the participants developed tissue anchor barb fractures that were asymptomatic and detected through radiography. At this time, the failure rate does not warrant clinical use. However, some patients showed significant improvement in multiple measures for sleep apnea, and more research is ongoing with the device.25
Similarly, a surgically inserted tongue pin that connects to an oral device during sleep has been studied. This pin prevents the tongue from moving back and obstructing the upper airway. Polysomnographies were performed both before and after and showed an increased rate of apnea in the 10 subjects. Visualization with magnetic resonance imaging showed that the upper airway was not kept open by this fixation device. Additional research with a modified design for the device is recommended.26
Reshaping of the epiglottis using a CO2 laser has been studied with cadaver specimens. The researchers believe scar formation following the reshaping would aid in retraction of the epiglottis anteriorly. Studies with animals are being conducted with different laser types. Future studies involving selected patients with OSA who have epiglottis malformations would be the next step.27
More studies about both minimally invasive and invasive surgeries for OSA are needed. There are many unanswered questions, including the timing of follow-up assessments, how long to observe a patient after surgery, whether the use of multilevel surgery affects the rate of relapse, and what are the best follow-up tools to use. Research needs to be performed in diverse populations, including gender, race/ethnicity, and age groups. Complications of surgical procedures need to be studied and clarified over both short- and long-term periods.9
Conclusions
Although there have been some successes in using surgical procedures to treat OSA, CPAP therapy remains the first-line treatment. Invasive surgeries have higher rates of complications and risks than do those of minimally invasive procedures. There are also additional risks related to the use of anesthesia both during and after surgery. Referrals for surgery should include information about a diagnosis of OSA, and patients should be instructed to discuss this with the anesthesiologist or certified nurse anesthetist.
With careful selection by the surgeon and sleep providers, patients who do not tolerate CPAP therapy or respond to other noninvasive interventions can benefit from a surgical procedure. Minimally invasive surgeries are less risky for the patient and should be considered.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
WEB EXCLUSIVE CASE STUDY
A Physical Examination of the Upper Airway by an Ear, Nose, and Throat Physician
1. Powell NB. Contemporary surgery for obstructive sleep apnea syndrome. Clin Exp Otorhinolaryngol. 2009;2(3):107-114.
2. Shine NP, Lewis RH. Transpalatal advancement paryngoplasty for obstructive sleep apnea syndrome: Results and analysis of failures. Arch Otolaryngol Head Neck Surg. 2009;135(5): 434-438.
3. Morgenthaler TI, Kapen S, Lee-Chiong T; American Academy of Sleep Medicine. Practice parameters for the medical therapy of obstructive sleep apnea. Sleep. 2006;29(8):1031-1035.
4. Aigner MJ, Sikka P, Whitfield P. Obesity hypoventilation syndrome: What is it? How is it treated? Is there a cure? Bariatric Nursing and Surgical Patient Care. 2009;4(2):109-113.
5. Woodson BT. Non-pressure therapies for obstructive sleep apnea: Surgery and oral appliances. Respir Care. 2010;55(10):1314-1321.
6. Kushida CA, Morgenthaler TI, Littner MR, et al; American Academy of Sleep Medicine. Practice parameters for the treatment of snoring and Obstructive Sleep Apnea with oral appliances: An update for 2005. Sleep. 2006;29(2):240-243.
7. Berry RB, Kryger MH, Massie CA. A novel nasal expiratory positive airway pressure (EPAP) device for the treatment of obstructive sleep apnea: A randomized controlled trial. Sleep. 2011;34(4):479-485.
8. Kryger MH, Berry RB, Massie CA. Long-term use of a nasal expiratory positive airway pressure (EPAP) device as a treatment of obstructive sleep apnea (OSA). J Clin Sleep Med. 2011;7(5):449-453.
9. Aurora RN, Casey KR, Kristo D, et al; American Academy of Sleep Medicine. Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults. Sleep. 2010;33(10):1408-1413.
10. Szmuk P, Ezri T, Evron S, Roth Y, Katz J. A brief history of tracheostomy and tracheal intubation, from the Bronze Age to the space age. Intensive Care Med. 2008;34(2):222-228.
11. Maurer JT. Update on surgical treatment for sleep apnoea. Swiss Med Wkly. 2009;139(43-44):624-629.
12. Franklin KA, Anttila H, Axelsson S, et al. Effects and side-effects of surgery for snoring and obsructive sleep apnea—a systematic review. Sleep. 2009;32(1):27-36.
13. Caples SM, Rowley JA, Prinsell JR, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: A systematic review and meta-analysis. Sleep. 2010; 33(10):1396-1407.
14. Littner M, Kushida CA, Hartse K, et al. Practice parameters for the use of laser-assisted uvulopalatoplasty: An update for 2000. Sleep. 2001;24(5):603-619.
15. Chen JH, Luo ZH, Yang XL, Zhu MW, Tao ZZ. Complications of tongue base reduction with radiofrequency tissue ablation on obstructive sleep apnea hypopnea syndrome. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2010;45(7):574-577. (Abstract, full text in Chinese.)
16. Gillespie MB, Smith JE, Clarke J, Nguyen SA. Effectiveness of Pillar palatal implants for snoring management. Otolaryngol Head Neck Surg. 2009;140(3):363-368.
17. Ephros HD, Madani M, Yalamanchili SC. Surgical treatment of snoring and obstructive sleep apnoea. Indian J Med Res. 2010;131:267-276.
18. Gupta RM, Parvizi J, Hanssen AD, Gay PC. Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: A case-control study. Mayo Clin Proc. 2001;76(9):897-905.
19. Sabers C, Plevak DJ, Schroeder DR, Warner DO. The diagnosis of obstructive sleep apnea as a risk factor for unanticipated admissions in outpatient surgery. Anesth Analg. 2003;96(5):1328-1335.
20. Kerzirian EJ, Boudewyns A, Eisele DW, et al. Electrical stimulation of the hypoglossal nerve in the treatment of obstructive sleep apnea. Sleep Med Rev. 2010;14(5):299-305.
21. Eastwood PR, Barnes M, Walsh JH, et al. Treating obstructive sleep apnea with hypoglossal nerve stimulation. Sleep. 2011;34(11):1479-1486.
22. Inspire Medical. STAR Trial. Inspire Medical Website. http://www.inspiresleep.com/star-trial.php. Accessed May 7, 2014.
23. FDA approves Inspire Upper Airway Stimulation (UAS) therapy for obstructive sleep apnea [press release]. Inspire Medical Website. http://www.inspiresleep.com/pdf/FDA-Approval-Press-Release-final-20140501.pdf.
Accessed May 29, 2014.
24. Strollo PJ Jr, Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139-149.
25. Woodson BT, Steward DL, Mickelson S, Huntley T, Goldberg A. Multicenter study of a novel adjustable tongue-advancement device for obstructive sleep apnea. Otolaryngol Head Neck Surg. 2010;143(4):585-590.
26. Punke C, Schöentag C, Hortian B, et al. Tongue fixation system for therapy of sleeping disorders. A feasibility study. HNO. 2010;58(12):1184-1189. (Abstract, full text in German).
27. Bourolinas C, Hajiioannou J, Sobol E, Velegrakis G, Helidonis E. Epiglottis reshaping using CO2: A minimally invasive technique and its potential applications. Head Face Med. 2008;4:15.
1. Powell NB. Contemporary surgery for obstructive sleep apnea syndrome. Clin Exp Otorhinolaryngol. 2009;2(3):107-114.
2. Shine NP, Lewis RH. Transpalatal advancement paryngoplasty for obstructive sleep apnea syndrome: Results and analysis of failures. Arch Otolaryngol Head Neck Surg. 2009;135(5): 434-438.
3. Morgenthaler TI, Kapen S, Lee-Chiong T; American Academy of Sleep Medicine. Practice parameters for the medical therapy of obstructive sleep apnea. Sleep. 2006;29(8):1031-1035.
4. Aigner MJ, Sikka P, Whitfield P. Obesity hypoventilation syndrome: What is it? How is it treated? Is there a cure? Bariatric Nursing and Surgical Patient Care. 2009;4(2):109-113.
5. Woodson BT. Non-pressure therapies for obstructive sleep apnea: Surgery and oral appliances. Respir Care. 2010;55(10):1314-1321.
6. Kushida CA, Morgenthaler TI, Littner MR, et al; American Academy of Sleep Medicine. Practice parameters for the treatment of snoring and Obstructive Sleep Apnea with oral appliances: An update for 2005. Sleep. 2006;29(2):240-243.
7. Berry RB, Kryger MH, Massie CA. A novel nasal expiratory positive airway pressure (EPAP) device for the treatment of obstructive sleep apnea: A randomized controlled trial. Sleep. 2011;34(4):479-485.
8. Kryger MH, Berry RB, Massie CA. Long-term use of a nasal expiratory positive airway pressure (EPAP) device as a treatment of obstructive sleep apnea (OSA). J Clin Sleep Med. 2011;7(5):449-453.
9. Aurora RN, Casey KR, Kristo D, et al; American Academy of Sleep Medicine. Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults. Sleep. 2010;33(10):1408-1413.
10. Szmuk P, Ezri T, Evron S, Roth Y, Katz J. A brief history of tracheostomy and tracheal intubation, from the Bronze Age to the space age. Intensive Care Med. 2008;34(2):222-228.
11. Maurer JT. Update on surgical treatment for sleep apnoea. Swiss Med Wkly. 2009;139(43-44):624-629.
12. Franklin KA, Anttila H, Axelsson S, et al. Effects and side-effects of surgery for snoring and obsructive sleep apnea—a systematic review. Sleep. 2009;32(1):27-36.
13. Caples SM, Rowley JA, Prinsell JR, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: A systematic review and meta-analysis. Sleep. 2010; 33(10):1396-1407.
14. Littner M, Kushida CA, Hartse K, et al. Practice parameters for the use of laser-assisted uvulopalatoplasty: An update for 2000. Sleep. 2001;24(5):603-619.
15. Chen JH, Luo ZH, Yang XL, Zhu MW, Tao ZZ. Complications of tongue base reduction with radiofrequency tissue ablation on obstructive sleep apnea hypopnea syndrome. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2010;45(7):574-577. (Abstract, full text in Chinese.)
16. Gillespie MB, Smith JE, Clarke J, Nguyen SA. Effectiveness of Pillar palatal implants for snoring management. Otolaryngol Head Neck Surg. 2009;140(3):363-368.
17. Ephros HD, Madani M, Yalamanchili SC. Surgical treatment of snoring and obstructive sleep apnoea. Indian J Med Res. 2010;131:267-276.
18. Gupta RM, Parvizi J, Hanssen AD, Gay PC. Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: A case-control study. Mayo Clin Proc. 2001;76(9):897-905.
19. Sabers C, Plevak DJ, Schroeder DR, Warner DO. The diagnosis of obstructive sleep apnea as a risk factor for unanticipated admissions in outpatient surgery. Anesth Analg. 2003;96(5):1328-1335.
20. Kerzirian EJ, Boudewyns A, Eisele DW, et al. Electrical stimulation of the hypoglossal nerve in the treatment of obstructive sleep apnea. Sleep Med Rev. 2010;14(5):299-305.
21. Eastwood PR, Barnes M, Walsh JH, et al. Treating obstructive sleep apnea with hypoglossal nerve stimulation. Sleep. 2011;34(11):1479-1486.
22. Inspire Medical. STAR Trial. Inspire Medical Website. http://www.inspiresleep.com/star-trial.php. Accessed May 7, 2014.
23. FDA approves Inspire Upper Airway Stimulation (UAS) therapy for obstructive sleep apnea [press release]. Inspire Medical Website. http://www.inspiresleep.com/pdf/FDA-Approval-Press-Release-final-20140501.pdf.
Accessed May 29, 2014.
24. Strollo PJ Jr, Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139-149.
25. Woodson BT, Steward DL, Mickelson S, Huntley T, Goldberg A. Multicenter study of a novel adjustable tongue-advancement device for obstructive sleep apnea. Otolaryngol Head Neck Surg. 2010;143(4):585-590.
26. Punke C, Schöentag C, Hortian B, et al. Tongue fixation system for therapy of sleeping disorders. A feasibility study. HNO. 2010;58(12):1184-1189. (Abstract, full text in German).
27. Bourolinas C, Hajiioannou J, Sobol E, Velegrakis G, Helidonis E. Epiglottis reshaping using CO2: A minimally invasive technique and its potential applications. Head Face Med. 2008;4:15.
Antimicrobial Stewardship in an Outpatient Parenteral Antibiotic Therapy Program
Antimicrobial stewardship activities have been in place at the Edward Hines, Jr. VA Hospital in Hines, Illinois, since 1988. Initial activities, including antimicrobial restriction and the start of an outpatient-infusion program justified and led to dedicated funding for hiring the first infectious diseases (ID) clinical pharmacist. This position was initiated in 1992 and has been maintained since then. The committed multidisciplinary team, including ID physicians, ID clinical pharmacists, venous access nurses (VAN), microbiologists, infection control practitioners, and an outpatient-infusion coordinator have led stewardship activities at this VA.
One of the first efforts of the team was the development of the outpatient parenteral antibiotic therapy (OPAT) program.1 The program began in 1989 and has served more than 1,200 veterans. Outpatient parenteral antibiotic therapy is only one component of the stewardship program, which provides safe, effective, and cost-minimizing care for veterans, and is the focus of this article.
Background
Complex medical care and escalating costs have pushed all but the most seriously ill patients out of the hospital setting for care delivery. The reality is that patients who might have received care for non–life-threatening problems in a hospital bed are now relegated to an outpatient status. Beginning in the 1970s, OPAT has been used to facilitate the cost-effective, safe administration of antibiotics as an alternative to an extensive, expensive hospital stay.2 Initially developed for use in a nonhospital health care setting, the administration of antibiotics under the guidance of a health care provider (HCP) has now been extended to a self-administered infusion program.3,4 Under the latter, patients and caregivers are educated to safely administer IV antibiotics for extended periods at home.
This program uses elements of both health care–associated OPAT and self-administered OPAT (S-OPAT) to accomplish its goals: (1) safe, effective administration of antibiotic therapy to a variety of patients; (2) reduction in bed days of care (BDOC); (3) reduction of the economic burden to the hospitals’ global budgets; and (4) reduction in the incidence of common nosocomially-acquired infections, including those caused by Clostridium difficile (C difficile), methicillin-resistant Staphylococcus aureus, and vancomycin-resistant enterococcus.3
The advantages of S-OPAT have been fully realized in a variety of countries, enabling patients to receive necessary therapy in the comfort of their homes and providing them with the ability to lead normal lives without the confinement of a protracted hospital stay.5-7
Description of OPAT
The outpatient-infusion team provides specialized care for patients in accordance with the OPAT national guidelines from patient screening to program discharge.8 The dedicated staff include the OPAT nurse coordinator, VAN, pharmacists, and ID consultants. The VAN places the venous access device (VAD), educates the patient and caregiver in the care and safety of the catheter, aseptic technique, and infusion of the selected antimicrobial agent, and monitors the laboratory work. The VA may contract an outside nursing agency to provide support and reinforcement of IV administration for the patient and caregiver.
The pharmacists oversee the pharmacokinetics and pharmacodynamics of the antimicrobials as well as monitor for any toxicities that could potentially arise during and after therapy. The ID consultants identify the infection, collaborate with the pharmacists to select the most appropriate antimicrobial regimen, and determine the duration of required therapy. The team then regularly monitors the patient in the ID clinic until there is evidence of infection resolution.
Primary care providers who want to enroll patients in the OPAT program place a formal electronic consult to the ID team for antibiotic recommendation, to the outpatient infusion team for assessment of potential outpatient therapy, and to the venous access team for insertion of the VAD. The consults are completed after receiving consent from the patient, developing a patient-centered treatment plan, and determining the patient’s ability to comprehend and adhere to the program requirements. The patient or caregiver must be able to competently demonstrate aseptic technique for IV administration prior to discharge. The pharmacist educates the patient or caregiver about the stability, storage requirements, and potential adverse drug reactions of the antimicrobial.
Eligible patients must have resolved their acute medical problems and require > 1 week of therapy to treat their infection. Patients chosen for OPAT or S-OPAT must have a suitable living environment with access to a refrigerator, a telephone, and transportation to return to the hospital for follow-up. Most patients and caregivers are eager to learn and recognize the advantages of home-based care.
The VANs are a central component of the program. They maintain open communication with the patient during the entire treatment course and help triage issues to the appropriate HCP. In addition, they are responsible for submitting catheter-related bloodstream infection (CRBSI) information to the hospital administration, which then gets reported to the National Healthcare Safety Network (NHSN).
Not all patients qualify for S-OPAT. Other options include returning to the hospital daily for infusions, being discharged to a skilled care facility, or arranging for a VA-contracted agency to provide nursing care while the VA provides all required medications and supplies.
On completion of OPAT, patients are asked to evaluate the program. The anonymous survey includes open-ended questions for patients to better express their experience with the program and staff. Patients are given the opportunity to suggest improvements and provide overall feedback. The team for quality assurance and patient satisfaction reviews every survey, which is used as a tool to improve team functions.
Data are also collected in the OPAT program to measure efficacy and monitor for safety. Data obtained from the start of the program in February 1989 through fiscal year (FY) 2011 include the number of patients who were candidates for outpatient-infusion therapy, type of infection, antibiotic selection, CRBSIs, hospital readmission rates, cost savings, and patient satisfaction.
Results
The Edward Hines, Jr. VA Hospital has a proven, successful OPAT program. Most of the patients in the program during the study period were men, which reflects a typical VA population. Patients with spinal cord injury comprised a large portion of those treated. Table 1 provides the number of patients treated and lists the frequency of infections. The data are divided into 3 periods. From 1989 to September 30, 1995, OPAT used other VADs before using peripherally inserted central catheters. During the second period (October 1, 1995-September 30, 2003), patients remained with a VAD for an average of 48.6 days; whereas in Period 3 (October 1, 2003-September 30, 2011), the patients had a VAD average of 34.7 days. Consequently, with fewer VAD days, there was a decreased incidence of complications (Table 2).
Osteomyelitis accounted for the majority of the infections (40.6%), which required ≥ 6 weeks of therapy. Complicated urinary tract infection (UTI), including pyelonephritis, perinephric abscess, and complicated cystitis, was the next most common (14.9%). Bacteremia was the third most common infection (7.9%), whereas abscesses of a diverse variety affected 6.2%, including brain, liver, intra-abdominal, soft tissue, and epidural abscesses. Endocarditis and septic arthritis accounted for 4.4% and 4.7%, respectively, of infected patients.
Three periods of the OPAT program were selected at random (1996, 2003, and 2011) to examine trends in antimicrobial selection. Overall, ceftriaxone was the most commonly used antibiotic (35%). Vancomycin was the next most commonly prescribed (27%). Since its 2001 FDA approval, ertapenem has become the third most commonly prescribed antibiotic for the OPAT program (11%). As expected, antimicrobial agents that have to be dosed more frequently than twice a day were rarely used for OPAT. In addition, there was low usage of aminoglycosides due to the need for the close monitoring of levels and potential toxicity.
Outcomes
Catheter Complications
The majority of catheter complications occurring in the first period were multifactorial, relating to nursing education, product selection, program development, insertion techniques, and a less comprehensive infection control program.
Hospital Readmissions
A snapshot of FY 2011 data was used to evaluate hospital readmissions. One hundred one patients were reviewed. Of these patients, 9 (9%) were readmitted to the hospital at some point after being discharged from OPAT. Readmission due to complications of OPAT was found in 2 of the 9 patients. One was due to an adverse drug reaction from the antibiotic; the other was due to a possible relapse of a hip osteomyelitis.
Cost Analysis
The OPAT program has resulted in a total savings to the global hospital budget from the deferred BDOC of more than $65 million (Table 3) since 1989. The OPAT program eliminated > 47,000 days of inpatient care. In FY 2009 the program cost the hospital $691.35 for each of the 106 patients enrolled (total cost: $73,283.10). This included all IV supplies, antimicrobials, visiting nurse costs when applicable, as well as nursing and pharmacy time dedicated to training the patient and making therapeutic decisions. Expenses for 3,109 BDOC would have cost about $6,218,000. The outpatient-infusion program saved the hospital nearly $6 million in 2009 alone.
Patient Satisfaction
About 60% of the patients discharged from the OPAT program responded to an evaluation survey. The feedback was overwhelmingly positive with about 99% of respondents reporting satisfaction relating to an improved quality of life. Most of the positive comments were directed toward the outpatient-infusion coordinator for resolving issues, being easily accessible, and acting as a patient advocate.
Discussion
The number and types of reasons for OPAT have grown with the knowledge that it is a safe, cost-effective method for the delivery of parenteral antimicrobials. In the early years of the program, before effective antiretroviral therapy was available, cytomegalovirus retinitis was the second most commonly treated infection of the OPAT program. In recent years, the rise of multidrug-resistant organisms has led to limited oral treatment options for UTIs, which are now the second most commonly treated infection of OPAT. Osteomyelitis clearly remains the top indication for OPAT because it requires long-term therapy. Ceftriaxone remains the drug of choice due to once-daily dosing, spectrum of activity, overall safety, and cost-effectiveness.
Catheter complication rates in the OPAT program were lower than those reported in the literature. According to the 2009 NHSN report, the catheter complication rate in the inpatient long-term care units was 1.0 CRBSI/1,000 catheter days.9 Moreover, this program has been instrumental in providing care that otherwise would be administered through the use of home health agencies.
In the private sector, OPAT is frequently contracted to agencies that provide the same type of service to outpatients who have insurance. These agencies charge for the antimicrobials, IV supplies, nursing visits, and laboratory costs for patient-safety monitoring. Use of an agency could raise expenses by a factor of 8-fold or more above the cost of a hospital-based OPAT program, an estimate based on a comparison with a local federally contracted home-infusion agency that provides specialized home-infusion services at a cost.
Although costs related to hospital readmissions were not factored in to the cost savings calculations, the rate of readmission was low in the snapshot analysis that was conducted at the Edward Hines, Jr. VA Hospital. It is believed that this is the result of the close follow-up and continuity of care that the patients in this OPAT program received.
In addition to cost containment, the data reflect the safe, effective care that resulted from treatment outside the hospital setting. One of the key attributes that has made the Edward Hines, Jr. VA Hospital OPAT program unique is that it is recognized in the community as the only VA facility in the area to provide OPAT as an option for the veteran patient. Other VA facilities in the area contract with home-infusion agencies, which are responsible for supplying the antibiotics and nursing care. The Edward Hines, Jr. VA Hospital is the only VA hospital in VISN 12 that has a facility-supported program that provides all supplies and antimicrobials from the VA—a major contributing factor to the cost savings. Continuity of care is provided to the patient who transitions from inpatient to outpatient status with the same team of providers contributing to the significant patient satisfaction that the program has engendered.
Conclusions
One of the main benefits realized with this transition of antibiotic therapy to the home setting is the avoidance of newly acquired nosocomial infections, including C difficile infection, fungal, and multidrug-resistant bacterial infections. Other benefits include early IV to oral switch in therapy when the patient is deemed a candidate, the ability to go back to work sooner, and the ability to receive treatment in the comfort of the patient’s home. Plans for data collection may include a more in-depth review of repeat admissions due to unresolved infections and the number of patients who are unable to complete OPAT at home.
The Edward Hines, Jr. VA Hospital OPAT program has shown that in a large, federally-funded hospital, OPAT is safe, cost-effective, convenient and leads to increased patient satisfaction in a diverse group of veterans.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Lentino JR, Pachucki CT, Byrne R, Lau MT, Bayer D. Parenteral antibiotic therapy: A home-based program. Fed Pract. 2000;17(4):10-15.
2. Paladino JA, Poretz D. Outpatient parenteral antimicrobial therapy today. Clin Infect Dis. 2010;51(suppl 2):S198-S208.
3. Matthews PC, Conlon CP, Berendt AR, et al. Outpatient parenteral antimicrobial therapy (OPAT): Is it safe for selected patients to self-administer at home? A retrospective analysis of a large cohort over 13 years. J Antimicrob Chemother. 2007;60(2):356-362.
4. Ingram PR, Sulaiman Z, Chua A, Fisher DA. Comment on: Outpatient parenteral antibiotic therapy (OPAT): Is it safe for selected patients to self-administer at home? A retrospective analysis of a large cohort over 13 years. J Antimicrob Chemother. 2008;61(1):226-227.
5. Bernard L, El-Hajj, Pron B, et al. Outpatient parenteral antimicrobial therapy (OPAT) for the treatment of osteomyelitis: Evaluation of efficacy, tolerance and cost. J Clin Pharm Ther. 2001;26(6):445-451.
6. Yong C, Fisher DA, Sklar GE, Li SC. A cost analysis of outpatient parenteral antibiotic therapy (OPAT): An Asian perspective. Int J Antimicrob Agents. 2009;33(1):46-51.
7. Tice AD, Hoaglund PA, Nolet B, McKinnon PS, Mozaffari E. Cost perspectives for outpatient intravenous antimicrobial therapy. Pharmacotherapy. 2002;22(2 Pt 2):63S-70S.
8. Tice AD, Rehm SJ, Dalovisio JR, et al. Practice guidelines for outpatient parenteral antimicrobial therapy. Clin Infect Dis. 2004;38(12):1651-1672.
9. Edwards JR, Peterson KD, Mu Y, et al. National Healthcare Safety Network (NHSN) report: Data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009;37(10):783-805.
Antimicrobial stewardship activities have been in place at the Edward Hines, Jr. VA Hospital in Hines, Illinois, since 1988. Initial activities, including antimicrobial restriction and the start of an outpatient-infusion program justified and led to dedicated funding for hiring the first infectious diseases (ID) clinical pharmacist. This position was initiated in 1992 and has been maintained since then. The committed multidisciplinary team, including ID physicians, ID clinical pharmacists, venous access nurses (VAN), microbiologists, infection control practitioners, and an outpatient-infusion coordinator have led stewardship activities at this VA.
One of the first efforts of the team was the development of the outpatient parenteral antibiotic therapy (OPAT) program.1 The program began in 1989 and has served more than 1,200 veterans. Outpatient parenteral antibiotic therapy is only one component of the stewardship program, which provides safe, effective, and cost-minimizing care for veterans, and is the focus of this article.
Background
Complex medical care and escalating costs have pushed all but the most seriously ill patients out of the hospital setting for care delivery. The reality is that patients who might have received care for non–life-threatening problems in a hospital bed are now relegated to an outpatient status. Beginning in the 1970s, OPAT has been used to facilitate the cost-effective, safe administration of antibiotics as an alternative to an extensive, expensive hospital stay.2 Initially developed for use in a nonhospital health care setting, the administration of antibiotics under the guidance of a health care provider (HCP) has now been extended to a self-administered infusion program.3,4 Under the latter, patients and caregivers are educated to safely administer IV antibiotics for extended periods at home.
This program uses elements of both health care–associated OPAT and self-administered OPAT (S-OPAT) to accomplish its goals: (1) safe, effective administration of antibiotic therapy to a variety of patients; (2) reduction in bed days of care (BDOC); (3) reduction of the economic burden to the hospitals’ global budgets; and (4) reduction in the incidence of common nosocomially-acquired infections, including those caused by Clostridium difficile (C difficile), methicillin-resistant Staphylococcus aureus, and vancomycin-resistant enterococcus.3
The advantages of S-OPAT have been fully realized in a variety of countries, enabling patients to receive necessary therapy in the comfort of their homes and providing them with the ability to lead normal lives without the confinement of a protracted hospital stay.5-7
Description of OPAT
The outpatient-infusion team provides specialized care for patients in accordance with the OPAT national guidelines from patient screening to program discharge.8 The dedicated staff include the OPAT nurse coordinator, VAN, pharmacists, and ID consultants. The VAN places the venous access device (VAD), educates the patient and caregiver in the care and safety of the catheter, aseptic technique, and infusion of the selected antimicrobial agent, and monitors the laboratory work. The VA may contract an outside nursing agency to provide support and reinforcement of IV administration for the patient and caregiver.
The pharmacists oversee the pharmacokinetics and pharmacodynamics of the antimicrobials as well as monitor for any toxicities that could potentially arise during and after therapy. The ID consultants identify the infection, collaborate with the pharmacists to select the most appropriate antimicrobial regimen, and determine the duration of required therapy. The team then regularly monitors the patient in the ID clinic until there is evidence of infection resolution.
Primary care providers who want to enroll patients in the OPAT program place a formal electronic consult to the ID team for antibiotic recommendation, to the outpatient infusion team for assessment of potential outpatient therapy, and to the venous access team for insertion of the VAD. The consults are completed after receiving consent from the patient, developing a patient-centered treatment plan, and determining the patient’s ability to comprehend and adhere to the program requirements. The patient or caregiver must be able to competently demonstrate aseptic technique for IV administration prior to discharge. The pharmacist educates the patient or caregiver about the stability, storage requirements, and potential adverse drug reactions of the antimicrobial.
Eligible patients must have resolved their acute medical problems and require > 1 week of therapy to treat their infection. Patients chosen for OPAT or S-OPAT must have a suitable living environment with access to a refrigerator, a telephone, and transportation to return to the hospital for follow-up. Most patients and caregivers are eager to learn and recognize the advantages of home-based care.
The VANs are a central component of the program. They maintain open communication with the patient during the entire treatment course and help triage issues to the appropriate HCP. In addition, they are responsible for submitting catheter-related bloodstream infection (CRBSI) information to the hospital administration, which then gets reported to the National Healthcare Safety Network (NHSN).
Not all patients qualify for S-OPAT. Other options include returning to the hospital daily for infusions, being discharged to a skilled care facility, or arranging for a VA-contracted agency to provide nursing care while the VA provides all required medications and supplies.
On completion of OPAT, patients are asked to evaluate the program. The anonymous survey includes open-ended questions for patients to better express their experience with the program and staff. Patients are given the opportunity to suggest improvements and provide overall feedback. The team for quality assurance and patient satisfaction reviews every survey, which is used as a tool to improve team functions.
Data are also collected in the OPAT program to measure efficacy and monitor for safety. Data obtained from the start of the program in February 1989 through fiscal year (FY) 2011 include the number of patients who were candidates for outpatient-infusion therapy, type of infection, antibiotic selection, CRBSIs, hospital readmission rates, cost savings, and patient satisfaction.
Results
The Edward Hines, Jr. VA Hospital has a proven, successful OPAT program. Most of the patients in the program during the study period were men, which reflects a typical VA population. Patients with spinal cord injury comprised a large portion of those treated. Table 1 provides the number of patients treated and lists the frequency of infections. The data are divided into 3 periods. From 1989 to September 30, 1995, OPAT used other VADs before using peripherally inserted central catheters. During the second period (October 1, 1995-September 30, 2003), patients remained with a VAD for an average of 48.6 days; whereas in Period 3 (October 1, 2003-September 30, 2011), the patients had a VAD average of 34.7 days. Consequently, with fewer VAD days, there was a decreased incidence of complications (Table 2).
Osteomyelitis accounted for the majority of the infections (40.6%), which required ≥ 6 weeks of therapy. Complicated urinary tract infection (UTI), including pyelonephritis, perinephric abscess, and complicated cystitis, was the next most common (14.9%). Bacteremia was the third most common infection (7.9%), whereas abscesses of a diverse variety affected 6.2%, including brain, liver, intra-abdominal, soft tissue, and epidural abscesses. Endocarditis and septic arthritis accounted for 4.4% and 4.7%, respectively, of infected patients.
Three periods of the OPAT program were selected at random (1996, 2003, and 2011) to examine trends in antimicrobial selection. Overall, ceftriaxone was the most commonly used antibiotic (35%). Vancomycin was the next most commonly prescribed (27%). Since its 2001 FDA approval, ertapenem has become the third most commonly prescribed antibiotic for the OPAT program (11%). As expected, antimicrobial agents that have to be dosed more frequently than twice a day were rarely used for OPAT. In addition, there was low usage of aminoglycosides due to the need for the close monitoring of levels and potential toxicity.
Outcomes
Catheter Complications
The majority of catheter complications occurring in the first period were multifactorial, relating to nursing education, product selection, program development, insertion techniques, and a less comprehensive infection control program.
Hospital Readmissions
A snapshot of FY 2011 data was used to evaluate hospital readmissions. One hundred one patients were reviewed. Of these patients, 9 (9%) were readmitted to the hospital at some point after being discharged from OPAT. Readmission due to complications of OPAT was found in 2 of the 9 patients. One was due to an adverse drug reaction from the antibiotic; the other was due to a possible relapse of a hip osteomyelitis.
Cost Analysis
The OPAT program has resulted in a total savings to the global hospital budget from the deferred BDOC of more than $65 million (Table 3) since 1989. The OPAT program eliminated > 47,000 days of inpatient care. In FY 2009 the program cost the hospital $691.35 for each of the 106 patients enrolled (total cost: $73,283.10). This included all IV supplies, antimicrobials, visiting nurse costs when applicable, as well as nursing and pharmacy time dedicated to training the patient and making therapeutic decisions. Expenses for 3,109 BDOC would have cost about $6,218,000. The outpatient-infusion program saved the hospital nearly $6 million in 2009 alone.
Patient Satisfaction
About 60% of the patients discharged from the OPAT program responded to an evaluation survey. The feedback was overwhelmingly positive with about 99% of respondents reporting satisfaction relating to an improved quality of life. Most of the positive comments were directed toward the outpatient-infusion coordinator for resolving issues, being easily accessible, and acting as a patient advocate.
Discussion
The number and types of reasons for OPAT have grown with the knowledge that it is a safe, cost-effective method for the delivery of parenteral antimicrobials. In the early years of the program, before effective antiretroviral therapy was available, cytomegalovirus retinitis was the second most commonly treated infection of the OPAT program. In recent years, the rise of multidrug-resistant organisms has led to limited oral treatment options for UTIs, which are now the second most commonly treated infection of OPAT. Osteomyelitis clearly remains the top indication for OPAT because it requires long-term therapy. Ceftriaxone remains the drug of choice due to once-daily dosing, spectrum of activity, overall safety, and cost-effectiveness.
Catheter complication rates in the OPAT program were lower than those reported in the literature. According to the 2009 NHSN report, the catheter complication rate in the inpatient long-term care units was 1.0 CRBSI/1,000 catheter days.9 Moreover, this program has been instrumental in providing care that otherwise would be administered through the use of home health agencies.
In the private sector, OPAT is frequently contracted to agencies that provide the same type of service to outpatients who have insurance. These agencies charge for the antimicrobials, IV supplies, nursing visits, and laboratory costs for patient-safety monitoring. Use of an agency could raise expenses by a factor of 8-fold or more above the cost of a hospital-based OPAT program, an estimate based on a comparison with a local federally contracted home-infusion agency that provides specialized home-infusion services at a cost.
Although costs related to hospital readmissions were not factored in to the cost savings calculations, the rate of readmission was low in the snapshot analysis that was conducted at the Edward Hines, Jr. VA Hospital. It is believed that this is the result of the close follow-up and continuity of care that the patients in this OPAT program received.
In addition to cost containment, the data reflect the safe, effective care that resulted from treatment outside the hospital setting. One of the key attributes that has made the Edward Hines, Jr. VA Hospital OPAT program unique is that it is recognized in the community as the only VA facility in the area to provide OPAT as an option for the veteran patient. Other VA facilities in the area contract with home-infusion agencies, which are responsible for supplying the antibiotics and nursing care. The Edward Hines, Jr. VA Hospital is the only VA hospital in VISN 12 that has a facility-supported program that provides all supplies and antimicrobials from the VA—a major contributing factor to the cost savings. Continuity of care is provided to the patient who transitions from inpatient to outpatient status with the same team of providers contributing to the significant patient satisfaction that the program has engendered.
Conclusions
One of the main benefits realized with this transition of antibiotic therapy to the home setting is the avoidance of newly acquired nosocomial infections, including C difficile infection, fungal, and multidrug-resistant bacterial infections. Other benefits include early IV to oral switch in therapy when the patient is deemed a candidate, the ability to go back to work sooner, and the ability to receive treatment in the comfort of the patient’s home. Plans for data collection may include a more in-depth review of repeat admissions due to unresolved infections and the number of patients who are unable to complete OPAT at home.
The Edward Hines, Jr. VA Hospital OPAT program has shown that in a large, federally-funded hospital, OPAT is safe, cost-effective, convenient and leads to increased patient satisfaction in a diverse group of veterans.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Antimicrobial stewardship activities have been in place at the Edward Hines, Jr. VA Hospital in Hines, Illinois, since 1988. Initial activities, including antimicrobial restriction and the start of an outpatient-infusion program justified and led to dedicated funding for hiring the first infectious diseases (ID) clinical pharmacist. This position was initiated in 1992 and has been maintained since then. The committed multidisciplinary team, including ID physicians, ID clinical pharmacists, venous access nurses (VAN), microbiologists, infection control practitioners, and an outpatient-infusion coordinator have led stewardship activities at this VA.
One of the first efforts of the team was the development of the outpatient parenteral antibiotic therapy (OPAT) program.1 The program began in 1989 and has served more than 1,200 veterans. Outpatient parenteral antibiotic therapy is only one component of the stewardship program, which provides safe, effective, and cost-minimizing care for veterans, and is the focus of this article.
Background
Complex medical care and escalating costs have pushed all but the most seriously ill patients out of the hospital setting for care delivery. The reality is that patients who might have received care for non–life-threatening problems in a hospital bed are now relegated to an outpatient status. Beginning in the 1970s, OPAT has been used to facilitate the cost-effective, safe administration of antibiotics as an alternative to an extensive, expensive hospital stay.2 Initially developed for use in a nonhospital health care setting, the administration of antibiotics under the guidance of a health care provider (HCP) has now been extended to a self-administered infusion program.3,4 Under the latter, patients and caregivers are educated to safely administer IV antibiotics for extended periods at home.
This program uses elements of both health care–associated OPAT and self-administered OPAT (S-OPAT) to accomplish its goals: (1) safe, effective administration of antibiotic therapy to a variety of patients; (2) reduction in bed days of care (BDOC); (3) reduction of the economic burden to the hospitals’ global budgets; and (4) reduction in the incidence of common nosocomially-acquired infections, including those caused by Clostridium difficile (C difficile), methicillin-resistant Staphylococcus aureus, and vancomycin-resistant enterococcus.3
The advantages of S-OPAT have been fully realized in a variety of countries, enabling patients to receive necessary therapy in the comfort of their homes and providing them with the ability to lead normal lives without the confinement of a protracted hospital stay.5-7
Description of OPAT
The outpatient-infusion team provides specialized care for patients in accordance with the OPAT national guidelines from patient screening to program discharge.8 The dedicated staff include the OPAT nurse coordinator, VAN, pharmacists, and ID consultants. The VAN places the venous access device (VAD), educates the patient and caregiver in the care and safety of the catheter, aseptic technique, and infusion of the selected antimicrobial agent, and monitors the laboratory work. The VA may contract an outside nursing agency to provide support and reinforcement of IV administration for the patient and caregiver.
The pharmacists oversee the pharmacokinetics and pharmacodynamics of the antimicrobials as well as monitor for any toxicities that could potentially arise during and after therapy. The ID consultants identify the infection, collaborate with the pharmacists to select the most appropriate antimicrobial regimen, and determine the duration of required therapy. The team then regularly monitors the patient in the ID clinic until there is evidence of infection resolution.
Primary care providers who want to enroll patients in the OPAT program place a formal electronic consult to the ID team for antibiotic recommendation, to the outpatient infusion team for assessment of potential outpatient therapy, and to the venous access team for insertion of the VAD. The consults are completed after receiving consent from the patient, developing a patient-centered treatment plan, and determining the patient’s ability to comprehend and adhere to the program requirements. The patient or caregiver must be able to competently demonstrate aseptic technique for IV administration prior to discharge. The pharmacist educates the patient or caregiver about the stability, storage requirements, and potential adverse drug reactions of the antimicrobial.
Eligible patients must have resolved their acute medical problems and require > 1 week of therapy to treat their infection. Patients chosen for OPAT or S-OPAT must have a suitable living environment with access to a refrigerator, a telephone, and transportation to return to the hospital for follow-up. Most patients and caregivers are eager to learn and recognize the advantages of home-based care.
The VANs are a central component of the program. They maintain open communication with the patient during the entire treatment course and help triage issues to the appropriate HCP. In addition, they are responsible for submitting catheter-related bloodstream infection (CRBSI) information to the hospital administration, which then gets reported to the National Healthcare Safety Network (NHSN).
Not all patients qualify for S-OPAT. Other options include returning to the hospital daily for infusions, being discharged to a skilled care facility, or arranging for a VA-contracted agency to provide nursing care while the VA provides all required medications and supplies.
On completion of OPAT, patients are asked to evaluate the program. The anonymous survey includes open-ended questions for patients to better express their experience with the program and staff. Patients are given the opportunity to suggest improvements and provide overall feedback. The team for quality assurance and patient satisfaction reviews every survey, which is used as a tool to improve team functions.
Data are also collected in the OPAT program to measure efficacy and monitor for safety. Data obtained from the start of the program in February 1989 through fiscal year (FY) 2011 include the number of patients who were candidates for outpatient-infusion therapy, type of infection, antibiotic selection, CRBSIs, hospital readmission rates, cost savings, and patient satisfaction.
Results
The Edward Hines, Jr. VA Hospital has a proven, successful OPAT program. Most of the patients in the program during the study period were men, which reflects a typical VA population. Patients with spinal cord injury comprised a large portion of those treated. Table 1 provides the number of patients treated and lists the frequency of infections. The data are divided into 3 periods. From 1989 to September 30, 1995, OPAT used other VADs before using peripherally inserted central catheters. During the second period (October 1, 1995-September 30, 2003), patients remained with a VAD for an average of 48.6 days; whereas in Period 3 (October 1, 2003-September 30, 2011), the patients had a VAD average of 34.7 days. Consequently, with fewer VAD days, there was a decreased incidence of complications (Table 2).
Osteomyelitis accounted for the majority of the infections (40.6%), which required ≥ 6 weeks of therapy. Complicated urinary tract infection (UTI), including pyelonephritis, perinephric abscess, and complicated cystitis, was the next most common (14.9%). Bacteremia was the third most common infection (7.9%), whereas abscesses of a diverse variety affected 6.2%, including brain, liver, intra-abdominal, soft tissue, and epidural abscesses. Endocarditis and septic arthritis accounted for 4.4% and 4.7%, respectively, of infected patients.
Three periods of the OPAT program were selected at random (1996, 2003, and 2011) to examine trends in antimicrobial selection. Overall, ceftriaxone was the most commonly used antibiotic (35%). Vancomycin was the next most commonly prescribed (27%). Since its 2001 FDA approval, ertapenem has become the third most commonly prescribed antibiotic for the OPAT program (11%). As expected, antimicrobial agents that have to be dosed more frequently than twice a day were rarely used for OPAT. In addition, there was low usage of aminoglycosides due to the need for the close monitoring of levels and potential toxicity.
Outcomes
Catheter Complications
The majority of catheter complications occurring in the first period were multifactorial, relating to nursing education, product selection, program development, insertion techniques, and a less comprehensive infection control program.
Hospital Readmissions
A snapshot of FY 2011 data was used to evaluate hospital readmissions. One hundred one patients were reviewed. Of these patients, 9 (9%) were readmitted to the hospital at some point after being discharged from OPAT. Readmission due to complications of OPAT was found in 2 of the 9 patients. One was due to an adverse drug reaction from the antibiotic; the other was due to a possible relapse of a hip osteomyelitis.
Cost Analysis
The OPAT program has resulted in a total savings to the global hospital budget from the deferred BDOC of more than $65 million (Table 3) since 1989. The OPAT program eliminated > 47,000 days of inpatient care. In FY 2009 the program cost the hospital $691.35 for each of the 106 patients enrolled (total cost: $73,283.10). This included all IV supplies, antimicrobials, visiting nurse costs when applicable, as well as nursing and pharmacy time dedicated to training the patient and making therapeutic decisions. Expenses for 3,109 BDOC would have cost about $6,218,000. The outpatient-infusion program saved the hospital nearly $6 million in 2009 alone.
Patient Satisfaction
About 60% of the patients discharged from the OPAT program responded to an evaluation survey. The feedback was overwhelmingly positive with about 99% of respondents reporting satisfaction relating to an improved quality of life. Most of the positive comments were directed toward the outpatient-infusion coordinator for resolving issues, being easily accessible, and acting as a patient advocate.
Discussion
The number and types of reasons for OPAT have grown with the knowledge that it is a safe, cost-effective method for the delivery of parenteral antimicrobials. In the early years of the program, before effective antiretroviral therapy was available, cytomegalovirus retinitis was the second most commonly treated infection of the OPAT program. In recent years, the rise of multidrug-resistant organisms has led to limited oral treatment options for UTIs, which are now the second most commonly treated infection of OPAT. Osteomyelitis clearly remains the top indication for OPAT because it requires long-term therapy. Ceftriaxone remains the drug of choice due to once-daily dosing, spectrum of activity, overall safety, and cost-effectiveness.
Catheter complication rates in the OPAT program were lower than those reported in the literature. According to the 2009 NHSN report, the catheter complication rate in the inpatient long-term care units was 1.0 CRBSI/1,000 catheter days.9 Moreover, this program has been instrumental in providing care that otherwise would be administered through the use of home health agencies.
In the private sector, OPAT is frequently contracted to agencies that provide the same type of service to outpatients who have insurance. These agencies charge for the antimicrobials, IV supplies, nursing visits, and laboratory costs for patient-safety monitoring. Use of an agency could raise expenses by a factor of 8-fold or more above the cost of a hospital-based OPAT program, an estimate based on a comparison with a local federally contracted home-infusion agency that provides specialized home-infusion services at a cost.
Although costs related to hospital readmissions were not factored in to the cost savings calculations, the rate of readmission was low in the snapshot analysis that was conducted at the Edward Hines, Jr. VA Hospital. It is believed that this is the result of the close follow-up and continuity of care that the patients in this OPAT program received.
In addition to cost containment, the data reflect the safe, effective care that resulted from treatment outside the hospital setting. One of the key attributes that has made the Edward Hines, Jr. VA Hospital OPAT program unique is that it is recognized in the community as the only VA facility in the area to provide OPAT as an option for the veteran patient. Other VA facilities in the area contract with home-infusion agencies, which are responsible for supplying the antibiotics and nursing care. The Edward Hines, Jr. VA Hospital is the only VA hospital in VISN 12 that has a facility-supported program that provides all supplies and antimicrobials from the VA—a major contributing factor to the cost savings. Continuity of care is provided to the patient who transitions from inpatient to outpatient status with the same team of providers contributing to the significant patient satisfaction that the program has engendered.
Conclusions
One of the main benefits realized with this transition of antibiotic therapy to the home setting is the avoidance of newly acquired nosocomial infections, including C difficile infection, fungal, and multidrug-resistant bacterial infections. Other benefits include early IV to oral switch in therapy when the patient is deemed a candidate, the ability to go back to work sooner, and the ability to receive treatment in the comfort of the patient’s home. Plans for data collection may include a more in-depth review of repeat admissions due to unresolved infections and the number of patients who are unable to complete OPAT at home.
The Edward Hines, Jr. VA Hospital OPAT program has shown that in a large, federally-funded hospital, OPAT is safe, cost-effective, convenient and leads to increased patient satisfaction in a diverse group of veterans.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Lentino JR, Pachucki CT, Byrne R, Lau MT, Bayer D. Parenteral antibiotic therapy: A home-based program. Fed Pract. 2000;17(4):10-15.
2. Paladino JA, Poretz D. Outpatient parenteral antimicrobial therapy today. Clin Infect Dis. 2010;51(suppl 2):S198-S208.
3. Matthews PC, Conlon CP, Berendt AR, et al. Outpatient parenteral antimicrobial therapy (OPAT): Is it safe for selected patients to self-administer at home? A retrospective analysis of a large cohort over 13 years. J Antimicrob Chemother. 2007;60(2):356-362.
4. Ingram PR, Sulaiman Z, Chua A, Fisher DA. Comment on: Outpatient parenteral antibiotic therapy (OPAT): Is it safe for selected patients to self-administer at home? A retrospective analysis of a large cohort over 13 years. J Antimicrob Chemother. 2008;61(1):226-227.
5. Bernard L, El-Hajj, Pron B, et al. Outpatient parenteral antimicrobial therapy (OPAT) for the treatment of osteomyelitis: Evaluation of efficacy, tolerance and cost. J Clin Pharm Ther. 2001;26(6):445-451.
6. Yong C, Fisher DA, Sklar GE, Li SC. A cost analysis of outpatient parenteral antibiotic therapy (OPAT): An Asian perspective. Int J Antimicrob Agents. 2009;33(1):46-51.
7. Tice AD, Hoaglund PA, Nolet B, McKinnon PS, Mozaffari E. Cost perspectives for outpatient intravenous antimicrobial therapy. Pharmacotherapy. 2002;22(2 Pt 2):63S-70S.
8. Tice AD, Rehm SJ, Dalovisio JR, et al. Practice guidelines for outpatient parenteral antimicrobial therapy. Clin Infect Dis. 2004;38(12):1651-1672.
9. Edwards JR, Peterson KD, Mu Y, et al. National Healthcare Safety Network (NHSN) report: Data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009;37(10):783-805.
1. Lentino JR, Pachucki CT, Byrne R, Lau MT, Bayer D. Parenteral antibiotic therapy: A home-based program. Fed Pract. 2000;17(4):10-15.
2. Paladino JA, Poretz D. Outpatient parenteral antimicrobial therapy today. Clin Infect Dis. 2010;51(suppl 2):S198-S208.
3. Matthews PC, Conlon CP, Berendt AR, et al. Outpatient parenteral antimicrobial therapy (OPAT): Is it safe for selected patients to self-administer at home? A retrospective analysis of a large cohort over 13 years. J Antimicrob Chemother. 2007;60(2):356-362.
4. Ingram PR, Sulaiman Z, Chua A, Fisher DA. Comment on: Outpatient parenteral antibiotic therapy (OPAT): Is it safe for selected patients to self-administer at home? A retrospective analysis of a large cohort over 13 years. J Antimicrob Chemother. 2008;61(1):226-227.
5. Bernard L, El-Hajj, Pron B, et al. Outpatient parenteral antimicrobial therapy (OPAT) for the treatment of osteomyelitis: Evaluation of efficacy, tolerance and cost. J Clin Pharm Ther. 2001;26(6):445-451.
6. Yong C, Fisher DA, Sklar GE, Li SC. A cost analysis of outpatient parenteral antibiotic therapy (OPAT): An Asian perspective. Int J Antimicrob Agents. 2009;33(1):46-51.
7. Tice AD, Hoaglund PA, Nolet B, McKinnon PS, Mozaffari E. Cost perspectives for outpatient intravenous antimicrobial therapy. Pharmacotherapy. 2002;22(2 Pt 2):63S-70S.
8. Tice AD, Rehm SJ, Dalovisio JR, et al. Practice guidelines for outpatient parenteral antimicrobial therapy. Clin Infect Dis. 2004;38(12):1651-1672.
9. Edwards JR, Peterson KD, Mu Y, et al. National Healthcare Safety Network (NHSN) report: Data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009;37(10):783-805.
Psychogenic Nonepileptic Seizures
From the Department of Neurology, University of Maryland School of Medicine, Baltimore, MD.
Abstracts
- Objective: To provide a review of psychogenic nonepileptic seizures, including a discussion of the diagnosis, treatment, and clinical significance of the disorder.
- Methods: Review of the relevant literature.
- Results: Psychogenic nonepileptic seizures are a common and potentially disabling neurologic disorder. They are most prevalent in young adults, and more commonly seen in women versus men. Certain psychosocial variables may impact the development of the condition. The diagnosis is made through a detailed history and observation of clinical events in conjunction with video EEG monitoring. Neuropsychological testing is an important component in the evaluation. Treatment includes establishment of an accurate diagnosis, management of any underlying psychiatric diagnoses, and regular follow-up with a neurologist or trained care provider.
- Conclusion: Psychogenic nonepileptic seizures represent a complex interaction between neurologic and psychological factors. Obtaining an accurate diagnosis through the use of video EEG monitoring and clinical observation is an important initial step in treatment and improved quality of life in this patient population.
Psychogenic nonepileptic seizures (PNES) are commonly encountered in outpatient specialty epilepsy clinics as well as inpatient epilepsy monitoring units. They comprise approximately 20% of all refractory seizure disorders referred to specialty epilepsy centers [1–4]. PNES are thought to be psychological in origin as opposed to arising from abnormal electrical discharges as in epileptic seizures. PNES may be more frequent and disabling than epileptic seizures, and patients with PNES may report worse outcomes [5,6]. Increased utilization of long-term video EEG monitoring along with greater recognition of psychogenic neurologic disorders has allowed for improved diagnosis of PNES. However, many diagnostic and therapeutic challenges remain. There are often delays in obtaining an accurate diagnosis, and optimal management remains challenging, often leading to inappropriate, ineffective, and costly treatment, sometimes for many years [6–8].
Epidemiology
PNES are seen across the spectrum of age-groups, from children [9,10] to elderly persons, but they most often occur in young adults between the ages of 15 to 35 years [1,8]. Caution should be used when considering this diagnosis in infants or young children, in whom it is more common to see physiologic events that may mimic epileptic seizures, including gastroesophageal reflux, shuddering, night terrors, or breath holding spells [1,9,10].
PNES are prevalent within epilepsy practices. Patients with PNES comprise approximately 5% to 20% patients thought to have intractable epilepsy seen in outpatient centers, and within epilepsy monitoring units they account for 10% to 40% of patients [1,2,6,8]. A population-based study approximates the incidence of PNES at 1.4 per 100,000 people and 3.4 per 100,000 people between the ages of 15 to 24 years [4].
There is a female preponderance in PNES, which is similar to other conversion and somatoform disorders. Overall, women comprise approximately 70% to 80% of patients with the PNES diagnosis [1,2,6]. There are psychosocial variables that are seen in some patients with this disorder. An important factor that has been described is past history of sexual or physical abuse. In one series, there was a history of sexual abuse in almost 25% of patients with PNES, and history of either sexual abuse, physical abuse, or both in 32% of patients [11]. A history of sexual and/or physical abuse is not exclusive to these patients, and can certainly be seen in patients with epilepsy as well. For example, in a control population of epilepsy patients, there was a reported rate of past sexual or physical abuse approaching 9% [12].
A prior history of head trauma, often of a relatively mild degree, has been described as a potential inciting factor for some cases of PNES [6,13]. In the literature, studies report that as many as 20% of PNES patients attributed their seizures to head trauma, often rather mild head trauma [6,14].
Historcial Context
Historically, what today are called PNES originate with the concept of hysteria, a medical diagnosis in women that can be traced to antiquity [15,16]. By the late 1800s, one of the founders of neurology, Jean Charcot, established hysterical seizures as an important clinical entity with his detailed, elegant descriptions of patients. Charcot formulated clinical methods for distinguishing hysteria and particularly hysterical seizures from epilepsy. He presumed that hysteria and epilepsy were closely related, and he termed seizures due to hysteria as “hysteroepilepsy” or “epileptiform” hysteria. Charcot proposed that hysterical seizures were organic disorders of the brain, like other forms of seizures and epilepsy, and emphasized their relation to disturbance of the female reproductive system [17,18]. Charcot utilized techniques such as manipulation of “hysterogenic zones” and ovarian compression as well as suggestion to both treat and provoke hysteria and hysterical seizures, which he described and documented [17,18]. One of Charcot’s most celebrated students, Sigmund Freud, observed Charcot’s demonstrations but drew different conclusions. He theorized that hysteria and hysterical seizures were not organic disorders of the brain as Charcot proposed, but were rather emotional disorders of the unconscious mind due to repressed energies or drives. Based largely the theories of Freud and Charcot, individuals with hysteria were distinguished from those with epilepsy, with hysterical seizures related to psychological dysfunction while epileptic seizures were associated with physical or organic brain disorders [15,16].
With the introduction of EEG recording in the 1930s, it became possible to characterize epilepsy as an electrical disorder of the brain with associated EEG changes and more effectively distinguish it from hysterical seizures, which did not have such abnormalities. In addition, in the first half of the 20th century, the nature of hysteria as seen and diagnosed by physicians seemed to change. The dramatic, theatrical convulsions described by Charcot and his contemporaries appeared less commonly, while disorders such as chronic pain seemed to increase [1,19].
However, by the 1960s, several reports confirmed that hysterical seizures were actually still prevalent. Newer terms like “pseudoseizures” were used to describe these disorders because the term “hysteria” was thought to be somewhat derogatory, anti-feminist, and antiquated [20,21]. In the 1970s and thereafter, with the increasing availability of video EEG monitoring and growth of inpatient epilepsy monitoring units, it was discovered that these hysterical, pseudo-, or what were also by then termed psychogenic seizures, were actually still common [1,22].
More recently, it has been recognized that the pendulum in some cases may have swung too far in regard to the diagnosis of this disorder. Some rare patients with seizures initially diagnosed as PNES may actually have forms of epileptic seizures such as frontal lobe epilepsy or related physiological disorders rather than psychogenic causes for their episodes [1,23]. These types of epileptic seizures can be very difficult to diagnose properly unless one appreciates how they present and manifest and remains vigilant for them during evaluation [1,23].
Terminology
There is an ongoing debate regarding the appropriate terminology for psychogenic events, and there is no uniform standardized definition or classification at this time. The term that is currently preferred within the epilepsy community for seizures of psychological origin that are thought to be associated with conversion, somatization, or dissociative disorders is “psychogenic nonepileptic seizures” (PNES). This terminology is felt to be non-disparaging and more neutral as compared with other terms such as pseudoseizures, which were previously favored. Nonepileptic seizures or nonepileptic events are broader terms meant to incorporate both physiologic and psychological causes for disorders that are mistaken for epilepsy. PNES are widely defined as paroxysmal events that appear similar to epileptic seizures but are not due to abnormal electrical discharges in the brain and as noted, are typically thought to be related or caused by conversion, somatization, or dissociative disorders.
Physiologic nonepileptic events are another category of physical disorders that may be mistaken for epilepsy. The underlying causes differ between age-groups, and can include conditions such as cardiac arrhythmias, migraine variants, syncope, or metabolic abnormalities. Physiologic nonepileptic seizures account for only a small proportion of all patients with nonepileptic seizures or events [1]. In general, any patient with a psychological disorder that causes symptoms that are mistaken for epilepsy can be said to have PNES.
Clinical Characteristics And Presentation
The duration of PNES is often significantly longer than that seen in epileptic seizures, which usually last less than 3 minutes, excluding the postictal period. PNES may also exhibit waxing and waning convulsive activity, although this finding can certainly be seen in epileptic seizures as well. PNES may be shown to have distractibility with external stimuli. Additionally, the movements in PNES may appear asymmetric, asynchronous, or purposeful, although this is not diagnostic for this disorder. This may contrast with the well-defined, synchronous tonic-clonic activity typically seen in epileptic seizures [1,24,25]. Back arching and pelvic thrusting movements can also be seen in PNES. Despite these differences, it may still be challenging to distinguish the semi-purposeful behaviors of PNES from the automatisms of certain focal epileptic seizures. The often bizarre-appearing, hypermotor activity that can be seen in frontal lobe seizures is often especially difficult to differentiate from PNES [1,23].
Another important consideration is that consciousness is preserved in PNES, while consciousness and responsiveness are frequently impaired in epileptic seizures. Patients with PNES are often apparently unresponsive during events, although there is no true impairment of awareness. Other characteristics that are more commonly seen in PNES are crying and eye closure [26]. Self-injury and incontinence may be reported, but they are less often clearly witnessed or documented [27,28]. Additionally, although patients may at times appear to be asleep at seizure onset, EEG recordings document the patient to actually be asleep in less than 1% of cases [29]. While epileptic seizures often respond well to antiepileptic medications, PNES characteristically do not [1,3,6,8].
In certain situations, provocation maneuvers may be utilized in order to reproduce PNES in patients undergoing EEG monitoring. In comparison to epileptic seizures, suggestion and emotional stimuli are more likely to trigger psychogenic events [1]. Methods utilized to provoke PNES may include saline injections, placement of a tuning fork on the head or body, or even hypnosis, when a suggestion is concurrently provided that such maneuvers can trigger the patient’s seizures [1,30,31]. When evaluating seizures that are provoked in such a manner, it is important to consider whether or not the event captured is in fact a typical event for the patient, or whether the provocation has uncovered a different, atypical event. Given that PNES and epileptic seizures can co-exist within the same patient, care should be taken to avoid making a diagnosis based on capturing an atypical event, or capturing only a subset of a patient’s seizure types. This could result in failure to make an accurate and thorough diagnosis [23]. There is debate regarding the ethics of provoking seizures by way of suggestion. Some members of the epilepsy community feel that provoking seizures through suggestion is inherently deceitful, and therefore can damage the physician-patient relationship. Others assert that such provocative testing can be undertaken in an honest manner, and can ultimately help achieve an accurate diagnosis for the patient [32].
As previously mentioned, there is a proportion of patients who have co-existing epileptic seizures and PNES, and obtaining an accurate diagnosis can be especially challenging in this group. Studies have reported that around 10% to 40% of patients with PNES also have epilepsy [1,22,23,33]. Care must be taken to distinguish between differences in seizure types and if necessary, video EEG monitoring may be needed to capture both seizure types for an accurate diagnosis. This testing can then be useful in education with families and caregivers who may be shown the videos with consent from the patient in order to guide future care.
Evaluation And Diagnosis
As in much of neurology, a thorough history, along with detailed clinical observation remains essential in the diagnosis of patients with PNES and for distinguishing these events from epilepsy. Video EEG monitoring of seizures is a key adjunct to the history and clinical observation in diagnosing this condition [1,2]. Long-term video EEG monitoring is considered the “gold standard” in the characterization and differential diagnosis of seizures. Additional potentially helpful diagnostic techniques include video EEG-monitored seizure provocation, serum prolactin levels, single photon emission computed tomography, and neuropsychological testing.
Video EEG Monitoring
EEG monitoring for characterization of clinical events can be conducted on an ambulatory or outpatient basis or in dedicated inpatient epilepsy monitoring units. Ambulatory monitoring can be useful in the case of patients who report seizures that are more frequent in their home environment or in patients with frequent events. If events are infrequent, then inpatient monitoring may be more efficacious [1]. With longer-term inpatient monitoring, antiepileptic medications can be withdrawn in a supervised setting, in order to lower the seizure threshold as well as to safely discontinue medications that may not be necessary. Such medication titrations are typically not safe in an unsupervised outpatient setting. Some ambulatory EEG monitoring systems do allow for simultaneous video and EEG recording. However, an advantage to inpatient monitoring, which is not afforded in the outpatient setting, is the ability for nursing staff or physicians to perform clinical testing during events to assess for patient responsiveness and other features. Additionally, with inpatient monitoring, EEG technicians can routinely assess for any technical problems with the electrodes or recording system.
Another benefit of video EEG monitoring is that the state (waking, drowsy, or asleep) of the patient at the onset of an event can be established. While epileptic seizures can arise from any state, PNES most often occur from wakefulness. Patients with PNES may appear to be asleep at the onset of events, and they may report seizures from sleep. Video EEG monitoring can help to establish the waking or sleep state of the patient that may aid in diagnosis [29].
Prolactin Levels
Serum prolactin levels may be helpful in the diagnosis of PNES [35,36]. Following generalized tonic-clonic or complex partial epileptic seizures, the serum prolactin can rise from two to threefold to five to tenfold [37]. The maximal rise in serum prolactin occurs in the initial 20 to 60 minutes after the seizure [35–37]. A similar rise in serum prolactin would not be expected in PNES. Although prolactin levels may have some utility in diagnosis, they are not currently routinely ordered as part of a standard admission to most inpatient epilepsy monitoring units. This may be due in part to the fact that false-positive and false-negative results can occur with these levels [37–39]. For example, there may not be a rise in the prolactin level after a simple partial seizure or more subtle complex partial seizure.
Neuropsychological Testing
Neuropsychological testing is also a key component in the evaluation and diagnosis of PNES. Ideally, a mental health provider with a background in psychological assessment and neuropsychological intervention for patients with psychogenic disorders would perform the evaluation [40,41].
The goal of the evaluation should not solely focused on whether the patient suffers from nonepileptic or epileptic seizures. An epileptologist upon review of clinical, electrographic, and neuropsychological data better makes this determination. Moreover, neuropsychological testing cannot in itself either diagnose or exclude the possibility that a seizure disorder is nonepileptic because of the considerable overlap between epileptic and nonepileptic test results [40,41]. Neuropsychological evaluations aid this assessment by (1) determining the potential or likelihood of significant contributing psychopathology or cognitive difficulties, (2) defining the nature of the associated psychological or psychosocial issues, and (3) assessing how a patient might benefit from various psychologically based interventions [1]. The testing may identify psychological problems that can guide treatment after diagnosis.
Delays in Diagnosis
Correct and prompt diagnosis is essential for patients with PNES as is appropriate referral to a knowledgeable trained mental health professional. On average, patients with PNES are diagnosed 7.2 years after manifestation (SD 9.3 years), with mean delay of 5 to 7 years. Younger age, interictal epileptiform potentials in the EEG, and anticonvulsant treatment are associated with longer delays [42,43]. Delays are also thought to occur because of problems with “ownership” of these patients. Although typically neurologists are involved in the diagnosis of PNES, often using video EEG monitoring done in an inpatient setting, the next step is often a referral to a psychiatrist or mental health care provider. There are sometimes delays in the initial referral to the neurologist, delays in referral to specialists for video EEG testing, and also to the physicians, psychologists or social workers who may provide treatment. Another disconnect can occur if patients are “lost to follow-up” if they receive a referral for mental health care and either do not follow up on this on their own, or if the reason for this care is not fully explained. In addition, many mental health professionals are not trained in the evaluation and treatment of psychogenic symptoms and may even feel uncomfortable in dealing with these patients [13,44].
Many studies have been suggestive that delays in diagnosis may result in poorer outcomes [45,46], while other studies have suggested that patients who have an acute diagnosis of PNES upon presentation may do particularly well [8,47–49]. Some of the most recent large outcome studies suggest that there may be no worsening of outcome associated with delays in diagnosis and that outcome was predicted by other factors [50–52].
Management
Management of patients with PNES is similar to that for patients with other types of so-called abnormal illness behavior, although there remains a relative paucity of evidence for specific treatment strategies for PNES [1]. The first consideration should be the manner in which the diagnosis of PNES is presented to the patient and family. It is important to be honest with the patient and demonstrate a positive approach to the diagnosis [53]. The physician should emphasize as favorable or good news the fact that the patient does not have epilepsy, and should also stress that the disorder, although serious and "real," does not require treatment with antiepileptic medications and that once stress or emotional issues are resolved, the patient has the potential to gain better control of these events [1,54,55]. Nevertheless, not all patients readily accept the diagnosis or this type of approach. Some patients may seek other opinions, and this should not be discouraged. An adversarial relationship with the patient should be avoided. The patient should be encouraged to return if desired, and records should be made available to other health care providers to avoid duplication of services.
After the diagnosis of PNES is presented, supportive measures should be initiated. PNES patients may benefit from education and support that can be provided by the neurologist or primary care physician [1]. If the neuropsychological assessment suggests a clinical profile that requires a professional mental health intervention, then an appropriate referral should be made. Regular follow-up visits for the patient with the neurologist are useful even if a mental health professional is involved [49,56]. This allows the patient to get medical attention without demonstrating illness behavior. Patient education and support are stressed at these visits. Because family issues are often important contributing factors, physicians should consider involving family members in visits with consent of the patient [1].
A variety of treatment strategies are employed for the management of PNES including cognitive behavioral therapy (CBT), group and family therapy, antidepressant medication, and other forms of rehabilitation [5,57,58]. A 2007 Cochrane review that identified 608 references for non-medication PNES treatments found that only 3 studies met criteria for a randomized controlled trial. One of the more recently favored treatment options for PNES that has been applied to the treatment of various somatoform disorders and other psychiatric disorders in the past is CBT [57,59,60]. This form of psychotherapy can be administered by trained personnel in a time-limited fashion using defined protocols. The basis of this treatment is that the patient learns to increase awareness of their dysfunctional thoughts and learns new ways to respond to them [57,58]. To date, several groups have reported results of nonrandomized trials as well as case reports and case series which have established the utility of this treatment. There have been reports of significant reductions in seizure frequency and this treatment strategy appears very promising [61–65]. Preliminary randomized controlled trials have also been piloted and are also suggestive that this may be a validated treatment approach [66].
Prognosis
The outcomes of patients with PNES vary. Long-term follow-up studies show that about half of all patients with PNES function reasonably well following their diagnosis. However, only approximately one-third of patients will completely stop having seizures or related problems, and approximately 50% percent have poor functional outcomes [1,2,50]. When the diagnosis of PNES is based on reliable criteria such a video EEG monitoring, misdiagnosis is unlikely. Instead, the usual cause for a poor outcome is related to a patient’s chronic psychological and social problems[1,8,22,50].
It is noteworthy that children with PNES appear to have a much better prognosis than adults [9,10]. In fact, the etiology in children may be related more to transient stress and coping disorders, while adults are more likely to have PNES within the context of more chronic psychological maladjustment, such as personality disorders [10]. Another factor that accounts for the better outcomes in children is that they are usually properly diagnosed earlier in the course of their disorder [9,10].
Patients with milder psychopathology respond better to supportive educational or behavioral therapeutic approaches. In contrast, patients with more severe psychopathology and factitious disorders more often have associated chronic personality problems and correspondingly, a poorer prognosis [1,50]. Also it appears that patients who continue to be followed by the diagnosing neurologist or center do better than patients who are not seen after diagnosis [49,67]. As knowledge about the nature of PNES and their associated psychopathology is gained, better treatment strategies can be developed that will improve the care and prognosis of these difficult and challenging patients.
A large study of 164 patients who were followed for 10 years were considered to have “poor outcome” in general but favorable factors included higher education, younger age of onset and diagnosis, and less “dramatic” attacks, defined as lack of “positive motor features, no ictal incontinence or tongue biting.” These findings were consistent with prior studies [52,68].
In addition, the patients who tended to have less seizures and do better long term, had less somatoform and dissociative symptoms on psychometric testing [51]. These findings are often explained by the theory that patients who do not do well have poor coping strategies to deal with stress and anxiety and that in a sense, these patients have emotional dysregulation.
Special Issues
Coexisting Epileptic and Psychogenic Nonepileptic Seizures
A complicating factor in diagnosis is that both PNES and epileptic seizures may occur in a single patient. Indeed, approximately 10% to 40% of patients identified to have PNES also have been reported to have epileptic seizures [1,23,33,56]. There are several possible explanations for this. Some patients with epilepsy may learn that seizures result in attention and fill certain psychological needs. Alternatively, they may have concomitant neurologic problems, personality disorders, cognitive deficits, or impaired coping mechanisms that predispose them to psychogenic symptoms [69–71]. Fortunately, in such patients with combined seizure disorders, the epileptic seizures are usually well controlled or of only historical relevance at the time a patient develops PNES [1,22,23,33,72–74].
In other patients, both epileptic and PNES may start simultaneously, making management even more complex. In such patients, we have found it particularly helpful to focus on the semiology of seizure manifestations as recorded by video EEG monitoring to distinguish PNES from the epileptic seizures. We then direct our treatment of the patient according to the semiology manifesting at that time. We also have found it useful to show the videos of seizures to family members or caregivers with patient consent to help them understand how to respond best to a patient’s symptoms when epileptic and PNES co-exist.
Misdiagnosis of Psychogenic Nonepileptic Seizures
Sometimes events that are initially diagnosed as nonepileptic actually prove to be epileptic. Such events can be called “pseudo-pseudo” or “epileptic-nonepileptic” seizures [1]. Frontal lobe seizures in particular may not be associated with significant EEG changes ictally and therefore misdiagnosed as PNES [23,75,76]. Clinical presentation and proper diagnosis of these types of events warrant emphasis.
Notable manifestations of frontal lobe seizures that may easily be confused with hysterical behavior include shouting, laughing, cursing, clapping, snapping, genital manipulation, pelvic thrusting, pedaling, running, kicking, and thrashing [23,75–77]. Not all of these behaviors are specific for frontal lobe seizures. For example, bicycling leg movements have also been reported in seizures originating from the temporal lobe [78].
Summary
PNES represent a common yet challenging problem within neurology. This is due to the difficulty in diagnosis as well as lack of effective and widely available treatment options. Overall outcomes of patients with PNES vary, and may relate to an individual patient’s chronic psychological and social problems. However, an accurate and timely diagnosis remains critical and can help provide direction for implementing appropriate treatment.
Corresponding author: Jennifer Hopp, MD, Department of Neurology, University of Maryland Medical Center, Room S12C09, 22 South Greene Street, Baltimore, MD 21201, [email protected].
Financial disclosures: None.
1. Krumholz A. Nonepileptic seizures: diagnosis and management. Neurology 1999;S76–83.
2. Meierkord H, Will B, Fish D, Shorvon S. The clinical features and prognosis of pseudoseizures diagnosed using video-EEG telemetry. Neurology 1991;41:1643–6.
3. Lesser RP. Psychogenic seizures. Neurology 1996;46:1499–1507.
4. Sigurdardottir KR, Olafsson E. Incidence of psychogenic seizures in adults: a population-based study in Iceland. Epilepsia 1998;39:857–62.
5. Szaflarski JP, Szaflarski M, Hughes C, et al. Psychopathology and quality of life: psychogenic non-epileptic seizures versus epilepsy. Med Sci Monit 2003 9:CR113–8.
6. Barry E, Krumholz A, Bergey C, et al. Nonepileptic posttraumatic seizures. Epilepsia 1998;39:427–31.
7. Pakalnis A, Drake ME, Phillips B. Neuropsychiatric aspects of psychogenic status epilepticus. Neurology 1991;41;1104–6.
8. Walzack TS, Papacostas S, Williams DT, et al. Outcome after the diagnosis of psychogenic nonepileptic seizures. Epilepsia 1995;36:1131–7.
9. Metrick ME, Ritter FJ, Gates JR, et al. Nonepileptic events in childhood. Epilepsia 1991;32:322–8.
10. Wyllie E, Friedman D, Luders H, et al. Outcome of psychogenic seizures in children and adolescents compared to adults. Neurology 1991;41:742–4.
11. Duncan R, Oto M. Predictors of antecedent factors in psychogenic nonepileptic attacks: multivariate analysis. Neurology 2008;71:1000–5.
12. Alper K, Devinsky O, Perrine K, et al. Nonepileptic seizures and childhood sexual and physical abuse. Neurology 1993; 43:1950–3.
13. LaFrance WC Jr, Devinsky O. The treatment of nonepileptic seizures: historical perspectives and future directions. Epilepsia 2004;45 Suppl 2:15–21.
14. Westbrook LE, Devinsky O, Geocadin R. Nonepileptic seizures after head injury. Epilepsia 1998;39:978–82.
15. Slavney PR. Perspectives on hysteria. Baltimore: Johns Hopkins University Press; 1990.
16. Veith I. Hysteria: the history of a disease. Chicago: University of Chicago Press; 1965.
17. Goetz CG. Charcot the clinician. The Tuesday lessons. New York: Raven Press; 1987.
18. Massey EW, McHenry LC. Hysteroepilepsy in the nineteenth century: Charcot and Gowers. Neurology 1986;36:65–7.
19. Zeigler FJ, Imboden JB, Meyer E. Contemporary conversion reactions: a clinical study. Am J Psychiatry 1960;116:901–10.
20. Liske E, Forster FM. Pseudoseizures: a problem in the diagnosis and management of epileptic patients. Neurology 1964;14:41–9.
21. Diagnostic and statistical manual of mental disorders. DSM-IV 4th ed. American Psychiatric Association. Washington, DC; 1995.
22. Krumholz A, Niedermeyer, E. Psychogenic seizures: a clinical study with follow-up data. Neurology 1983; 33:498-502.
23. Krumholz A, Ting T. Co-existing epileptic and nonepileptic seizures. in imitators of epilepsy. 2nd ed. In: Kaplan PW, Fisher RS, editors. New York: Demos Medical Publishing; 2005:261–76.
24. Gates JR, Ramani V, Whalen S, Loewenson R. Ictal characteristics of pseudoseizures. Arch Neurol 1985;42:1183–87.
25. Leis AA, Ross MA, Summers AK. Psychogenic seizures: Ictal characteristics and diagnostic pitfalls. Neurology 1992;42:95–9.
26. Walczak TS, Bogolioubov. Weeping during psychogenic nonepileptic seizures. Epilepsia 1996;37:207–10.
27. Bergen D, Ristanovic R. Weeping is a common element during psychogenic nonepileptic seizures. Arch Neurol 1993;50:1059–60.
28. Peguero E, Abou-Khalil B, Fakhoury, Mathews G. Self-injury and incontinence in psychogenic seizures. Epilepsia 1995;36:586–91.
29. Orbach D, Ritaccio A, Devinsky O. Psychogenic, nonepileptic seizures associated with video-EEG-verified sleep. Epilepsia 2003;44:64–8.
30. Walczak TS, Williams DT, Berton W. Utility and reliability of placebo infusion in the evaluation of patients with seizures. Neurology 1994;44:394–99.
31. Bazil CW, Kothari M, Luciano D, et al. Provocation of nonepileptic seizures by suggestion in a general seizure population. Epilepsia 1994;35:768–70.
32. Devinsky O, Fisher RS. Ethical use of placebos and provocative testing in diagnosing nonepileptic seizures. Neurology 1996;47:866–70.
33. Lesser RP, Lueders H, Dinner DS. Evidence for epilepsy is rare in patients with psychogenic seizures. Neurology 1983; 33:502–4.
34. Barre MA, Burnstine TH, Fisher RS, Lesser RP. Electroencephalographic changes during simple partial seizures. Epilepsia 1994;35:715–20.
35. Trimble MR. Serum prolactin levels in epilepsy and hysteria. BMJ 1978;2:1682.
36. Laxer KD, Mullooly JP, Howell B. Prolactin changes after seizures classified by EEG monitoring. Neurology 1985; 35:31–5.
37. Pritchard PB, Wannamaker BB, Sagel J, et al. Endocrine function following complex partial seizures. Ann Neurol 1983;14:27–32.
38. Malkowicz DE, Legido A, Jackel RA, et al. Prolactin secretion following repetitive seizures. Neurology 1995;45:448–52.
39. Oribe E, Rohullah A, Nissenbaum E, Boal B. Serum prolactin concentrations are elevated after syncope. Neurology 1996;47:60–2.
40. Henrichs TF, Tucker DM, Farha J, Novelly RA. MMPI indices in the identification of patients evidencing pseudoseizures. Epilepsia 1988;29:184–8.
41. Wilkus RJ, Dodrill CB. Factors affecting the outcome of MMPI and neuropsychological assessments of psychogenic and epileptic seizure patients. Epilepsia 1989;30:339–47.
42. DeTimary P, Fouchet P, Sylin M, et al. Non–epileptic seizures: delayed diagnosis in patients presenting with electroencephalographic (EEG) or clinical signs of epileptic seizures. Seizure 2002;11:193–7.
43. Reuber M, Fernandez G, et al. Diagnostic delay in psychogenic nonepileptic seizures. Neurology 2002;58:493–5.
44. Rosenbaum DH, et al. Outpatient multidisciplinary management of non-epileptic seizures. In: Rowan AJ, Gates Jr, editors. Non-epileptic seizures. 1st ed. Stoneham, MA: Butterworth-Heinemann; 1993:275–83.
45. Lempert T, Schmidt D. Natural history and outcome of psychogenic seizures: a clinical study in 50 patients. J Neurol 1990;237:35–8.
46. Selwa LM, Geyer J, Nikakhtar N, et al. Nonepileptic seizure outcome varies by type of spell and duration of illness. Epilepsia 2000;41:1330–4.
47. Buchanan N, Snars J. Pseudoseizures (non epileptic attack disorder): clinical management and outcome in 50 patients. Seizure 1993;2:141–6.
48. Kanner AM. More controversies on the treatment of psychogenic pseudoseizures: an addendum. Epilepsy Behav 2003;4:360–4.
49. Aboukasm A, Mahr G, Gahry BR, et al. Retrospective analysis of the effects of psychotherapeutic interventions on outcomes of psychogenic nonepileptic seizures. Epilepsia 1998;39:470–3.
50. Reuber M, Pukrop T, Bauer J, et al. Outcome in psychogenic nonepileptic seizures: 1 to 10-year follow-up in 164 patients. Ann Neurol 2003;53:305–11.
51. McKenzie P, Oto M, Russell A, Pelosi A, Duncan R. Early outcomes and predictors in 260 patients with psychogenic nonepileptic seizures (PNES). Neurology 2010;74:64–9.
52. Kanner AM, Parra J, Frey M, et al. Psychiatric and neurologic predictors of psychogenic pseudoseizure outcome. Neurology 1999;53:933–8.
53. Shen W, Bowman ES, Markand ON. Presenting the diagnosis of pseudoseizure. Neurology 1990; 40:756–9.
54. Friedman JH, LaFrance Jr WC. Psychogenic disorders: the need to speak plainly. Arch Neurol 2010;67:753–5.
55. LaFrance Jr WC. Psychogenic nonepileptic “seizures” or “attacks”? It’s not just semantics: “Seizures.” Neurology 2010;75: 87–8.
56. Ramsay RE, Cohen A, Brown MC. Coexisting epilepsy and non-epileptic seizures. In: Non-epileptic seizures. Butterworth-Heinemann; 1998:47–54.
57. Stone J, Carson A, Sharpe M. Functional symptoms in neurology: management. J Neurol Neurosurg Psychiatry. 2005;6(Suppl 1):i13–i21.
58. LaFrance WC Jr, Bjornaes H. Designing treatment plans based on etiology of psychogenic nonepileptic seizures. In: Schachter SC, LaFrance WC Jr, editors. Gates and Rowan’s nonepileptic seizures. 3rd ed. New York: Cambridge University Press; 2010:266–80.
59. Kroenke K, Swindle R. Cognitive-behavioral therapy for somatization and symptom syndromes: a critical review of controlled clinical trials. Psychother Psychosom 200;69:205–15.
60. Kroenke K. Efficacy of treatment of somatoform disorders: a review of randomized controlled trials. Psychosom Med 2007:69:881–8.
61. LaFrance WC Jr, Miller IW, Ryan CE, et al. Cognitive behavioral therapy for psychogenic nonepileptic seizures. Epilepsy Behav 2009;14:591–6.
62. Chalder T. Non-epileptic attacks: a cognitive behavioral approach in a single case with a four-year follow-up. Clin Psychol Psychother 1996;3:291–7.
63. Betts T, Duffy N. Non-epileptic attack disorder (pseudoseizures) and sexual abuse: a review. In: Gram L, Johannessen SI, Osterman PE, et al, editors. Pseudo-epileptic seizures. Petersfield, UK: Wrightson Biomedical Publishing; 1993:55–66.
64. Lesser RP. Treatment and outcome of psychogenic nonepileptic seizures. Epilepsy Currents 2003;3:198–200.
65. Ramani V. Review of psychiatric treatment strategies in non-epileptic seizures. In: Rowan AJ, Gates JR, eds. Non-epileptic Seizures. 1st ed. Stoneham, MA: Butterworth Heinemann; 1993:259–67.
66. Goldstein LH, Chalder T, Chigwedere C, et al. Cognitive-behavioral therapy for psychogenic nonepileptic seizures: a pilot RCT. Neurology 2010;74:1986–94.
67. Bennet C, So NM, Smith WB, Thompson K. Structured treatment improves the outcome of nonepileptic events. Epilepsia 1997;38(Suppl 8):214.
68. McDade G, Brown SW. Non-epileptic seizures: management and predictive factors of outcome. Seizure 1992;1:7–10.
69. Bowman ES. Etiology and clinical course of pseudoseizures: relationship to trauma, depression, and dissociation. Psychosomatics 1993;34:333–42.
70. Bowman ES, Markand ON. Psychodynamics and psychiatric diagnoses of pseudoseizure subjects. Am J Psychiatry 1996;153:57–63.
71. Vanderzant CW, Giordani B, Berent S, et al. Personality of patients with pseudoseizures. Neurology 1986;36:664–8.
72. Benbadis SR, Agrawal V, Tatum WO. How many patients with psychogenic nonepileptic seizures also have epilepsy? Neurology 2001; 57:915–7.
73. Glosser G, Roberts D, et al. Nonepileptic seizures after resective epilepsy surgery. Epilepsia 1999; 40:1750–4.
74. Reuber M, Kral T. New-onset psychogenic seizures after intracranial neurosurgery. Acta Neurochir (Wien) 2002; 144:901–7.
75. Williamson P, Spencer D, Spencer S, et al. Complex partial seizures of frontal lobe origin. Ann Neurol 1985;18:497–504.
76. Saygi S, Katz A, Marks D, et al. Frontal lobe partial seizures and psychogenic seizures: comparison of clinical and ictal characteristics. Neurology 1992;42:1274–7.
77. Waterman K, Purves S, Kosaka B, et al. An epileptic syndrome caused by mesial frontal lobe seizure foci. Neurology 1987; 37:577–82.
78. Sussman N, Jackel R, Kaplan L, et al. Bicycling movements as a manifestation of complex partial seizures of temporal lobe origin. Epilepsia 1989;30:527–31.
From the Department of Neurology, University of Maryland School of Medicine, Baltimore, MD.
Abstracts
- Objective: To provide a review of psychogenic nonepileptic seizures, including a discussion of the diagnosis, treatment, and clinical significance of the disorder.
- Methods: Review of the relevant literature.
- Results: Psychogenic nonepileptic seizures are a common and potentially disabling neurologic disorder. They are most prevalent in young adults, and more commonly seen in women versus men. Certain psychosocial variables may impact the development of the condition. The diagnosis is made through a detailed history and observation of clinical events in conjunction with video EEG monitoring. Neuropsychological testing is an important component in the evaluation. Treatment includes establishment of an accurate diagnosis, management of any underlying psychiatric diagnoses, and regular follow-up with a neurologist or trained care provider.
- Conclusion: Psychogenic nonepileptic seizures represent a complex interaction between neurologic and psychological factors. Obtaining an accurate diagnosis through the use of video EEG monitoring and clinical observation is an important initial step in treatment and improved quality of life in this patient population.
Psychogenic nonepileptic seizures (PNES) are commonly encountered in outpatient specialty epilepsy clinics as well as inpatient epilepsy monitoring units. They comprise approximately 20% of all refractory seizure disorders referred to specialty epilepsy centers [1–4]. PNES are thought to be psychological in origin as opposed to arising from abnormal electrical discharges as in epileptic seizures. PNES may be more frequent and disabling than epileptic seizures, and patients with PNES may report worse outcomes [5,6]. Increased utilization of long-term video EEG monitoring along with greater recognition of psychogenic neurologic disorders has allowed for improved diagnosis of PNES. However, many diagnostic and therapeutic challenges remain. There are often delays in obtaining an accurate diagnosis, and optimal management remains challenging, often leading to inappropriate, ineffective, and costly treatment, sometimes for many years [6–8].
Epidemiology
PNES are seen across the spectrum of age-groups, from children [9,10] to elderly persons, but they most often occur in young adults between the ages of 15 to 35 years [1,8]. Caution should be used when considering this diagnosis in infants or young children, in whom it is more common to see physiologic events that may mimic epileptic seizures, including gastroesophageal reflux, shuddering, night terrors, or breath holding spells [1,9,10].
PNES are prevalent within epilepsy practices. Patients with PNES comprise approximately 5% to 20% patients thought to have intractable epilepsy seen in outpatient centers, and within epilepsy monitoring units they account for 10% to 40% of patients [1,2,6,8]. A population-based study approximates the incidence of PNES at 1.4 per 100,000 people and 3.4 per 100,000 people between the ages of 15 to 24 years [4].
There is a female preponderance in PNES, which is similar to other conversion and somatoform disorders. Overall, women comprise approximately 70% to 80% of patients with the PNES diagnosis [1,2,6]. There are psychosocial variables that are seen in some patients with this disorder. An important factor that has been described is past history of sexual or physical abuse. In one series, there was a history of sexual abuse in almost 25% of patients with PNES, and history of either sexual abuse, physical abuse, or both in 32% of patients [11]. A history of sexual and/or physical abuse is not exclusive to these patients, and can certainly be seen in patients with epilepsy as well. For example, in a control population of epilepsy patients, there was a reported rate of past sexual or physical abuse approaching 9% [12].
A prior history of head trauma, often of a relatively mild degree, has been described as a potential inciting factor for some cases of PNES [6,13]. In the literature, studies report that as many as 20% of PNES patients attributed their seizures to head trauma, often rather mild head trauma [6,14].
Historcial Context
Historically, what today are called PNES originate with the concept of hysteria, a medical diagnosis in women that can be traced to antiquity [15,16]. By the late 1800s, one of the founders of neurology, Jean Charcot, established hysterical seizures as an important clinical entity with his detailed, elegant descriptions of patients. Charcot formulated clinical methods for distinguishing hysteria and particularly hysterical seizures from epilepsy. He presumed that hysteria and epilepsy were closely related, and he termed seizures due to hysteria as “hysteroepilepsy” or “epileptiform” hysteria. Charcot proposed that hysterical seizures were organic disorders of the brain, like other forms of seizures and epilepsy, and emphasized their relation to disturbance of the female reproductive system [17,18]. Charcot utilized techniques such as manipulation of “hysterogenic zones” and ovarian compression as well as suggestion to both treat and provoke hysteria and hysterical seizures, which he described and documented [17,18]. One of Charcot’s most celebrated students, Sigmund Freud, observed Charcot’s demonstrations but drew different conclusions. He theorized that hysteria and hysterical seizures were not organic disorders of the brain as Charcot proposed, but were rather emotional disorders of the unconscious mind due to repressed energies or drives. Based largely the theories of Freud and Charcot, individuals with hysteria were distinguished from those with epilepsy, with hysterical seizures related to psychological dysfunction while epileptic seizures were associated with physical or organic brain disorders [15,16].
With the introduction of EEG recording in the 1930s, it became possible to characterize epilepsy as an electrical disorder of the brain with associated EEG changes and more effectively distinguish it from hysterical seizures, which did not have such abnormalities. In addition, in the first half of the 20th century, the nature of hysteria as seen and diagnosed by physicians seemed to change. The dramatic, theatrical convulsions described by Charcot and his contemporaries appeared less commonly, while disorders such as chronic pain seemed to increase [1,19].
However, by the 1960s, several reports confirmed that hysterical seizures were actually still prevalent. Newer terms like “pseudoseizures” were used to describe these disorders because the term “hysteria” was thought to be somewhat derogatory, anti-feminist, and antiquated [20,21]. In the 1970s and thereafter, with the increasing availability of video EEG monitoring and growth of inpatient epilepsy monitoring units, it was discovered that these hysterical, pseudo-, or what were also by then termed psychogenic seizures, were actually still common [1,22].
More recently, it has been recognized that the pendulum in some cases may have swung too far in regard to the diagnosis of this disorder. Some rare patients with seizures initially diagnosed as PNES may actually have forms of epileptic seizures such as frontal lobe epilepsy or related physiological disorders rather than psychogenic causes for their episodes [1,23]. These types of epileptic seizures can be very difficult to diagnose properly unless one appreciates how they present and manifest and remains vigilant for them during evaluation [1,23].
Terminology
There is an ongoing debate regarding the appropriate terminology for psychogenic events, and there is no uniform standardized definition or classification at this time. The term that is currently preferred within the epilepsy community for seizures of psychological origin that are thought to be associated with conversion, somatization, or dissociative disorders is “psychogenic nonepileptic seizures” (PNES). This terminology is felt to be non-disparaging and more neutral as compared with other terms such as pseudoseizures, which were previously favored. Nonepileptic seizures or nonepileptic events are broader terms meant to incorporate both physiologic and psychological causes for disorders that are mistaken for epilepsy. PNES are widely defined as paroxysmal events that appear similar to epileptic seizures but are not due to abnormal electrical discharges in the brain and as noted, are typically thought to be related or caused by conversion, somatization, or dissociative disorders.
Physiologic nonepileptic events are another category of physical disorders that may be mistaken for epilepsy. The underlying causes differ between age-groups, and can include conditions such as cardiac arrhythmias, migraine variants, syncope, or metabolic abnormalities. Physiologic nonepileptic seizures account for only a small proportion of all patients with nonepileptic seizures or events [1]. In general, any patient with a psychological disorder that causes symptoms that are mistaken for epilepsy can be said to have PNES.
Clinical Characteristics And Presentation
The duration of PNES is often significantly longer than that seen in epileptic seizures, which usually last less than 3 minutes, excluding the postictal period. PNES may also exhibit waxing and waning convulsive activity, although this finding can certainly be seen in epileptic seizures as well. PNES may be shown to have distractibility with external stimuli. Additionally, the movements in PNES may appear asymmetric, asynchronous, or purposeful, although this is not diagnostic for this disorder. This may contrast with the well-defined, synchronous tonic-clonic activity typically seen in epileptic seizures [1,24,25]. Back arching and pelvic thrusting movements can also be seen in PNES. Despite these differences, it may still be challenging to distinguish the semi-purposeful behaviors of PNES from the automatisms of certain focal epileptic seizures. The often bizarre-appearing, hypermotor activity that can be seen in frontal lobe seizures is often especially difficult to differentiate from PNES [1,23].
Another important consideration is that consciousness is preserved in PNES, while consciousness and responsiveness are frequently impaired in epileptic seizures. Patients with PNES are often apparently unresponsive during events, although there is no true impairment of awareness. Other characteristics that are more commonly seen in PNES are crying and eye closure [26]. Self-injury and incontinence may be reported, but they are less often clearly witnessed or documented [27,28]. Additionally, although patients may at times appear to be asleep at seizure onset, EEG recordings document the patient to actually be asleep in less than 1% of cases [29]. While epileptic seizures often respond well to antiepileptic medications, PNES characteristically do not [1,3,6,8].
In certain situations, provocation maneuvers may be utilized in order to reproduce PNES in patients undergoing EEG monitoring. In comparison to epileptic seizures, suggestion and emotional stimuli are more likely to trigger psychogenic events [1]. Methods utilized to provoke PNES may include saline injections, placement of a tuning fork on the head or body, or even hypnosis, when a suggestion is concurrently provided that such maneuvers can trigger the patient’s seizures [1,30,31]. When evaluating seizures that are provoked in such a manner, it is important to consider whether or not the event captured is in fact a typical event for the patient, or whether the provocation has uncovered a different, atypical event. Given that PNES and epileptic seizures can co-exist within the same patient, care should be taken to avoid making a diagnosis based on capturing an atypical event, or capturing only a subset of a patient’s seizure types. This could result in failure to make an accurate and thorough diagnosis [23]. There is debate regarding the ethics of provoking seizures by way of suggestion. Some members of the epilepsy community feel that provoking seizures through suggestion is inherently deceitful, and therefore can damage the physician-patient relationship. Others assert that such provocative testing can be undertaken in an honest manner, and can ultimately help achieve an accurate diagnosis for the patient [32].
As previously mentioned, there is a proportion of patients who have co-existing epileptic seizures and PNES, and obtaining an accurate diagnosis can be especially challenging in this group. Studies have reported that around 10% to 40% of patients with PNES also have epilepsy [1,22,23,33]. Care must be taken to distinguish between differences in seizure types and if necessary, video EEG monitoring may be needed to capture both seizure types for an accurate diagnosis. This testing can then be useful in education with families and caregivers who may be shown the videos with consent from the patient in order to guide future care.
Evaluation And Diagnosis
As in much of neurology, a thorough history, along with detailed clinical observation remains essential in the diagnosis of patients with PNES and for distinguishing these events from epilepsy. Video EEG monitoring of seizures is a key adjunct to the history and clinical observation in diagnosing this condition [1,2]. Long-term video EEG monitoring is considered the “gold standard” in the characterization and differential diagnosis of seizures. Additional potentially helpful diagnostic techniques include video EEG-monitored seizure provocation, serum prolactin levels, single photon emission computed tomography, and neuropsychological testing.
Video EEG Monitoring
EEG monitoring for characterization of clinical events can be conducted on an ambulatory or outpatient basis or in dedicated inpatient epilepsy monitoring units. Ambulatory monitoring can be useful in the case of patients who report seizures that are more frequent in their home environment or in patients with frequent events. If events are infrequent, then inpatient monitoring may be more efficacious [1]. With longer-term inpatient monitoring, antiepileptic medications can be withdrawn in a supervised setting, in order to lower the seizure threshold as well as to safely discontinue medications that may not be necessary. Such medication titrations are typically not safe in an unsupervised outpatient setting. Some ambulatory EEG monitoring systems do allow for simultaneous video and EEG recording. However, an advantage to inpatient monitoring, which is not afforded in the outpatient setting, is the ability for nursing staff or physicians to perform clinical testing during events to assess for patient responsiveness and other features. Additionally, with inpatient monitoring, EEG technicians can routinely assess for any technical problems with the electrodes or recording system.
Another benefit of video EEG monitoring is that the state (waking, drowsy, or asleep) of the patient at the onset of an event can be established. While epileptic seizures can arise from any state, PNES most often occur from wakefulness. Patients with PNES may appear to be asleep at the onset of events, and they may report seizures from sleep. Video EEG monitoring can help to establish the waking or sleep state of the patient that may aid in diagnosis [29].
Prolactin Levels
Serum prolactin levels may be helpful in the diagnosis of PNES [35,36]. Following generalized tonic-clonic or complex partial epileptic seizures, the serum prolactin can rise from two to threefold to five to tenfold [37]. The maximal rise in serum prolactin occurs in the initial 20 to 60 minutes after the seizure [35–37]. A similar rise in serum prolactin would not be expected in PNES. Although prolactin levels may have some utility in diagnosis, they are not currently routinely ordered as part of a standard admission to most inpatient epilepsy monitoring units. This may be due in part to the fact that false-positive and false-negative results can occur with these levels [37–39]. For example, there may not be a rise in the prolactin level after a simple partial seizure or more subtle complex partial seizure.
Neuropsychological Testing
Neuropsychological testing is also a key component in the evaluation and diagnosis of PNES. Ideally, a mental health provider with a background in psychological assessment and neuropsychological intervention for patients with psychogenic disorders would perform the evaluation [40,41].
The goal of the evaluation should not solely focused on whether the patient suffers from nonepileptic or epileptic seizures. An epileptologist upon review of clinical, electrographic, and neuropsychological data better makes this determination. Moreover, neuropsychological testing cannot in itself either diagnose or exclude the possibility that a seizure disorder is nonepileptic because of the considerable overlap between epileptic and nonepileptic test results [40,41]. Neuropsychological evaluations aid this assessment by (1) determining the potential or likelihood of significant contributing psychopathology or cognitive difficulties, (2) defining the nature of the associated psychological or psychosocial issues, and (3) assessing how a patient might benefit from various psychologically based interventions [1]. The testing may identify psychological problems that can guide treatment after diagnosis.
Delays in Diagnosis
Correct and prompt diagnosis is essential for patients with PNES as is appropriate referral to a knowledgeable trained mental health professional. On average, patients with PNES are diagnosed 7.2 years after manifestation (SD 9.3 years), with mean delay of 5 to 7 years. Younger age, interictal epileptiform potentials in the EEG, and anticonvulsant treatment are associated with longer delays [42,43]. Delays are also thought to occur because of problems with “ownership” of these patients. Although typically neurologists are involved in the diagnosis of PNES, often using video EEG monitoring done in an inpatient setting, the next step is often a referral to a psychiatrist or mental health care provider. There are sometimes delays in the initial referral to the neurologist, delays in referral to specialists for video EEG testing, and also to the physicians, psychologists or social workers who may provide treatment. Another disconnect can occur if patients are “lost to follow-up” if they receive a referral for mental health care and either do not follow up on this on their own, or if the reason for this care is not fully explained. In addition, many mental health professionals are not trained in the evaluation and treatment of psychogenic symptoms and may even feel uncomfortable in dealing with these patients [13,44].
Many studies have been suggestive that delays in diagnosis may result in poorer outcomes [45,46], while other studies have suggested that patients who have an acute diagnosis of PNES upon presentation may do particularly well [8,47–49]. Some of the most recent large outcome studies suggest that there may be no worsening of outcome associated with delays in diagnosis and that outcome was predicted by other factors [50–52].
Management
Management of patients with PNES is similar to that for patients with other types of so-called abnormal illness behavior, although there remains a relative paucity of evidence for specific treatment strategies for PNES [1]. The first consideration should be the manner in which the diagnosis of PNES is presented to the patient and family. It is important to be honest with the patient and demonstrate a positive approach to the diagnosis [53]. The physician should emphasize as favorable or good news the fact that the patient does not have epilepsy, and should also stress that the disorder, although serious and "real," does not require treatment with antiepileptic medications and that once stress or emotional issues are resolved, the patient has the potential to gain better control of these events [1,54,55]. Nevertheless, not all patients readily accept the diagnosis or this type of approach. Some patients may seek other opinions, and this should not be discouraged. An adversarial relationship with the patient should be avoided. The patient should be encouraged to return if desired, and records should be made available to other health care providers to avoid duplication of services.
After the diagnosis of PNES is presented, supportive measures should be initiated. PNES patients may benefit from education and support that can be provided by the neurologist or primary care physician [1]. If the neuropsychological assessment suggests a clinical profile that requires a professional mental health intervention, then an appropriate referral should be made. Regular follow-up visits for the patient with the neurologist are useful even if a mental health professional is involved [49,56]. This allows the patient to get medical attention without demonstrating illness behavior. Patient education and support are stressed at these visits. Because family issues are often important contributing factors, physicians should consider involving family members in visits with consent of the patient [1].
A variety of treatment strategies are employed for the management of PNES including cognitive behavioral therapy (CBT), group and family therapy, antidepressant medication, and other forms of rehabilitation [5,57,58]. A 2007 Cochrane review that identified 608 references for non-medication PNES treatments found that only 3 studies met criteria for a randomized controlled trial. One of the more recently favored treatment options for PNES that has been applied to the treatment of various somatoform disorders and other psychiatric disorders in the past is CBT [57,59,60]. This form of psychotherapy can be administered by trained personnel in a time-limited fashion using defined protocols. The basis of this treatment is that the patient learns to increase awareness of their dysfunctional thoughts and learns new ways to respond to them [57,58]. To date, several groups have reported results of nonrandomized trials as well as case reports and case series which have established the utility of this treatment. There have been reports of significant reductions in seizure frequency and this treatment strategy appears very promising [61–65]. Preliminary randomized controlled trials have also been piloted and are also suggestive that this may be a validated treatment approach [66].
Prognosis
The outcomes of patients with PNES vary. Long-term follow-up studies show that about half of all patients with PNES function reasonably well following their diagnosis. However, only approximately one-third of patients will completely stop having seizures or related problems, and approximately 50% percent have poor functional outcomes [1,2,50]. When the diagnosis of PNES is based on reliable criteria such a video EEG monitoring, misdiagnosis is unlikely. Instead, the usual cause for a poor outcome is related to a patient’s chronic psychological and social problems[1,8,22,50].
It is noteworthy that children with PNES appear to have a much better prognosis than adults [9,10]. In fact, the etiology in children may be related more to transient stress and coping disorders, while adults are more likely to have PNES within the context of more chronic psychological maladjustment, such as personality disorders [10]. Another factor that accounts for the better outcomes in children is that they are usually properly diagnosed earlier in the course of their disorder [9,10].
Patients with milder psychopathology respond better to supportive educational or behavioral therapeutic approaches. In contrast, patients with more severe psychopathology and factitious disorders more often have associated chronic personality problems and correspondingly, a poorer prognosis [1,50]. Also it appears that patients who continue to be followed by the diagnosing neurologist or center do better than patients who are not seen after diagnosis [49,67]. As knowledge about the nature of PNES and their associated psychopathology is gained, better treatment strategies can be developed that will improve the care and prognosis of these difficult and challenging patients.
A large study of 164 patients who were followed for 10 years were considered to have “poor outcome” in general but favorable factors included higher education, younger age of onset and diagnosis, and less “dramatic” attacks, defined as lack of “positive motor features, no ictal incontinence or tongue biting.” These findings were consistent with prior studies [52,68].
In addition, the patients who tended to have less seizures and do better long term, had less somatoform and dissociative symptoms on psychometric testing [51]. These findings are often explained by the theory that patients who do not do well have poor coping strategies to deal with stress and anxiety and that in a sense, these patients have emotional dysregulation.
Special Issues
Coexisting Epileptic and Psychogenic Nonepileptic Seizures
A complicating factor in diagnosis is that both PNES and epileptic seizures may occur in a single patient. Indeed, approximately 10% to 40% of patients identified to have PNES also have been reported to have epileptic seizures [1,23,33,56]. There are several possible explanations for this. Some patients with epilepsy may learn that seizures result in attention and fill certain psychological needs. Alternatively, they may have concomitant neurologic problems, personality disorders, cognitive deficits, or impaired coping mechanisms that predispose them to psychogenic symptoms [69–71]. Fortunately, in such patients with combined seizure disorders, the epileptic seizures are usually well controlled or of only historical relevance at the time a patient develops PNES [1,22,23,33,72–74].
In other patients, both epileptic and PNES may start simultaneously, making management even more complex. In such patients, we have found it particularly helpful to focus on the semiology of seizure manifestations as recorded by video EEG monitoring to distinguish PNES from the epileptic seizures. We then direct our treatment of the patient according to the semiology manifesting at that time. We also have found it useful to show the videos of seizures to family members or caregivers with patient consent to help them understand how to respond best to a patient’s symptoms when epileptic and PNES co-exist.
Misdiagnosis of Psychogenic Nonepileptic Seizures
Sometimes events that are initially diagnosed as nonepileptic actually prove to be epileptic. Such events can be called “pseudo-pseudo” or “epileptic-nonepileptic” seizures [1]. Frontal lobe seizures in particular may not be associated with significant EEG changes ictally and therefore misdiagnosed as PNES [23,75,76]. Clinical presentation and proper diagnosis of these types of events warrant emphasis.
Notable manifestations of frontal lobe seizures that may easily be confused with hysterical behavior include shouting, laughing, cursing, clapping, snapping, genital manipulation, pelvic thrusting, pedaling, running, kicking, and thrashing [23,75–77]. Not all of these behaviors are specific for frontal lobe seizures. For example, bicycling leg movements have also been reported in seizures originating from the temporal lobe [78].
Summary
PNES represent a common yet challenging problem within neurology. This is due to the difficulty in diagnosis as well as lack of effective and widely available treatment options. Overall outcomes of patients with PNES vary, and may relate to an individual patient’s chronic psychological and social problems. However, an accurate and timely diagnosis remains critical and can help provide direction for implementing appropriate treatment.
Corresponding author: Jennifer Hopp, MD, Department of Neurology, University of Maryland Medical Center, Room S12C09, 22 South Greene Street, Baltimore, MD 21201, [email protected].
Financial disclosures: None.
From the Department of Neurology, University of Maryland School of Medicine, Baltimore, MD.
Abstracts
- Objective: To provide a review of psychogenic nonepileptic seizures, including a discussion of the diagnosis, treatment, and clinical significance of the disorder.
- Methods: Review of the relevant literature.
- Results: Psychogenic nonepileptic seizures are a common and potentially disabling neurologic disorder. They are most prevalent in young adults, and more commonly seen in women versus men. Certain psychosocial variables may impact the development of the condition. The diagnosis is made through a detailed history and observation of clinical events in conjunction with video EEG monitoring. Neuropsychological testing is an important component in the evaluation. Treatment includes establishment of an accurate diagnosis, management of any underlying psychiatric diagnoses, and regular follow-up with a neurologist or trained care provider.
- Conclusion: Psychogenic nonepileptic seizures represent a complex interaction between neurologic and psychological factors. Obtaining an accurate diagnosis through the use of video EEG monitoring and clinical observation is an important initial step in treatment and improved quality of life in this patient population.
Psychogenic nonepileptic seizures (PNES) are commonly encountered in outpatient specialty epilepsy clinics as well as inpatient epilepsy monitoring units. They comprise approximately 20% of all refractory seizure disorders referred to specialty epilepsy centers [1–4]. PNES are thought to be psychological in origin as opposed to arising from abnormal electrical discharges as in epileptic seizures. PNES may be more frequent and disabling than epileptic seizures, and patients with PNES may report worse outcomes [5,6]. Increased utilization of long-term video EEG monitoring along with greater recognition of psychogenic neurologic disorders has allowed for improved diagnosis of PNES. However, many diagnostic and therapeutic challenges remain. There are often delays in obtaining an accurate diagnosis, and optimal management remains challenging, often leading to inappropriate, ineffective, and costly treatment, sometimes for many years [6–8].
Epidemiology
PNES are seen across the spectrum of age-groups, from children [9,10] to elderly persons, but they most often occur in young adults between the ages of 15 to 35 years [1,8]. Caution should be used when considering this diagnosis in infants or young children, in whom it is more common to see physiologic events that may mimic epileptic seizures, including gastroesophageal reflux, shuddering, night terrors, or breath holding spells [1,9,10].
PNES are prevalent within epilepsy practices. Patients with PNES comprise approximately 5% to 20% patients thought to have intractable epilepsy seen in outpatient centers, and within epilepsy monitoring units they account for 10% to 40% of patients [1,2,6,8]. A population-based study approximates the incidence of PNES at 1.4 per 100,000 people and 3.4 per 100,000 people between the ages of 15 to 24 years [4].
There is a female preponderance in PNES, which is similar to other conversion and somatoform disorders. Overall, women comprise approximately 70% to 80% of patients with the PNES diagnosis [1,2,6]. There are psychosocial variables that are seen in some patients with this disorder. An important factor that has been described is past history of sexual or physical abuse. In one series, there was a history of sexual abuse in almost 25% of patients with PNES, and history of either sexual abuse, physical abuse, or both in 32% of patients [11]. A history of sexual and/or physical abuse is not exclusive to these patients, and can certainly be seen in patients with epilepsy as well. For example, in a control population of epilepsy patients, there was a reported rate of past sexual or physical abuse approaching 9% [12].
A prior history of head trauma, often of a relatively mild degree, has been described as a potential inciting factor for some cases of PNES [6,13]. In the literature, studies report that as many as 20% of PNES patients attributed their seizures to head trauma, often rather mild head trauma [6,14].
Historcial Context
Historically, what today are called PNES originate with the concept of hysteria, a medical diagnosis in women that can be traced to antiquity [15,16]. By the late 1800s, one of the founders of neurology, Jean Charcot, established hysterical seizures as an important clinical entity with his detailed, elegant descriptions of patients. Charcot formulated clinical methods for distinguishing hysteria and particularly hysterical seizures from epilepsy. He presumed that hysteria and epilepsy were closely related, and he termed seizures due to hysteria as “hysteroepilepsy” or “epileptiform” hysteria. Charcot proposed that hysterical seizures were organic disorders of the brain, like other forms of seizures and epilepsy, and emphasized their relation to disturbance of the female reproductive system [17,18]. Charcot utilized techniques such as manipulation of “hysterogenic zones” and ovarian compression as well as suggestion to both treat and provoke hysteria and hysterical seizures, which he described and documented [17,18]. One of Charcot’s most celebrated students, Sigmund Freud, observed Charcot’s demonstrations but drew different conclusions. He theorized that hysteria and hysterical seizures were not organic disorders of the brain as Charcot proposed, but were rather emotional disorders of the unconscious mind due to repressed energies or drives. Based largely the theories of Freud and Charcot, individuals with hysteria were distinguished from those with epilepsy, with hysterical seizures related to psychological dysfunction while epileptic seizures were associated with physical or organic brain disorders [15,16].
With the introduction of EEG recording in the 1930s, it became possible to characterize epilepsy as an electrical disorder of the brain with associated EEG changes and more effectively distinguish it from hysterical seizures, which did not have such abnormalities. In addition, in the first half of the 20th century, the nature of hysteria as seen and diagnosed by physicians seemed to change. The dramatic, theatrical convulsions described by Charcot and his contemporaries appeared less commonly, while disorders such as chronic pain seemed to increase [1,19].
However, by the 1960s, several reports confirmed that hysterical seizures were actually still prevalent. Newer terms like “pseudoseizures” were used to describe these disorders because the term “hysteria” was thought to be somewhat derogatory, anti-feminist, and antiquated [20,21]. In the 1970s and thereafter, with the increasing availability of video EEG monitoring and growth of inpatient epilepsy monitoring units, it was discovered that these hysterical, pseudo-, or what were also by then termed psychogenic seizures, were actually still common [1,22].
More recently, it has been recognized that the pendulum in some cases may have swung too far in regard to the diagnosis of this disorder. Some rare patients with seizures initially diagnosed as PNES may actually have forms of epileptic seizures such as frontal lobe epilepsy or related physiological disorders rather than psychogenic causes for their episodes [1,23]. These types of epileptic seizures can be very difficult to diagnose properly unless one appreciates how they present and manifest and remains vigilant for them during evaluation [1,23].
Terminology
There is an ongoing debate regarding the appropriate terminology for psychogenic events, and there is no uniform standardized definition or classification at this time. The term that is currently preferred within the epilepsy community for seizures of psychological origin that are thought to be associated with conversion, somatization, or dissociative disorders is “psychogenic nonepileptic seizures” (PNES). This terminology is felt to be non-disparaging and more neutral as compared with other terms such as pseudoseizures, which were previously favored. Nonepileptic seizures or nonepileptic events are broader terms meant to incorporate both physiologic and psychological causes for disorders that are mistaken for epilepsy. PNES are widely defined as paroxysmal events that appear similar to epileptic seizures but are not due to abnormal electrical discharges in the brain and as noted, are typically thought to be related or caused by conversion, somatization, or dissociative disorders.
Physiologic nonepileptic events are another category of physical disorders that may be mistaken for epilepsy. The underlying causes differ between age-groups, and can include conditions such as cardiac arrhythmias, migraine variants, syncope, or metabolic abnormalities. Physiologic nonepileptic seizures account for only a small proportion of all patients with nonepileptic seizures or events [1]. In general, any patient with a psychological disorder that causes symptoms that are mistaken for epilepsy can be said to have PNES.
Clinical Characteristics And Presentation
The duration of PNES is often significantly longer than that seen in epileptic seizures, which usually last less than 3 minutes, excluding the postictal period. PNES may also exhibit waxing and waning convulsive activity, although this finding can certainly be seen in epileptic seizures as well. PNES may be shown to have distractibility with external stimuli. Additionally, the movements in PNES may appear asymmetric, asynchronous, or purposeful, although this is not diagnostic for this disorder. This may contrast with the well-defined, synchronous tonic-clonic activity typically seen in epileptic seizures [1,24,25]. Back arching and pelvic thrusting movements can also be seen in PNES. Despite these differences, it may still be challenging to distinguish the semi-purposeful behaviors of PNES from the automatisms of certain focal epileptic seizures. The often bizarre-appearing, hypermotor activity that can be seen in frontal lobe seizures is often especially difficult to differentiate from PNES [1,23].
Another important consideration is that consciousness is preserved in PNES, while consciousness and responsiveness are frequently impaired in epileptic seizures. Patients with PNES are often apparently unresponsive during events, although there is no true impairment of awareness. Other characteristics that are more commonly seen in PNES are crying and eye closure [26]. Self-injury and incontinence may be reported, but they are less often clearly witnessed or documented [27,28]. Additionally, although patients may at times appear to be asleep at seizure onset, EEG recordings document the patient to actually be asleep in less than 1% of cases [29]. While epileptic seizures often respond well to antiepileptic medications, PNES characteristically do not [1,3,6,8].
In certain situations, provocation maneuvers may be utilized in order to reproduce PNES in patients undergoing EEG monitoring. In comparison to epileptic seizures, suggestion and emotional stimuli are more likely to trigger psychogenic events [1]. Methods utilized to provoke PNES may include saline injections, placement of a tuning fork on the head or body, or even hypnosis, when a suggestion is concurrently provided that such maneuvers can trigger the patient’s seizures [1,30,31]. When evaluating seizures that are provoked in such a manner, it is important to consider whether or not the event captured is in fact a typical event for the patient, or whether the provocation has uncovered a different, atypical event. Given that PNES and epileptic seizures can co-exist within the same patient, care should be taken to avoid making a diagnosis based on capturing an atypical event, or capturing only a subset of a patient’s seizure types. This could result in failure to make an accurate and thorough diagnosis [23]. There is debate regarding the ethics of provoking seizures by way of suggestion. Some members of the epilepsy community feel that provoking seizures through suggestion is inherently deceitful, and therefore can damage the physician-patient relationship. Others assert that such provocative testing can be undertaken in an honest manner, and can ultimately help achieve an accurate diagnosis for the patient [32].
As previously mentioned, there is a proportion of patients who have co-existing epileptic seizures and PNES, and obtaining an accurate diagnosis can be especially challenging in this group. Studies have reported that around 10% to 40% of patients with PNES also have epilepsy [1,22,23,33]. Care must be taken to distinguish between differences in seizure types and if necessary, video EEG monitoring may be needed to capture both seizure types for an accurate diagnosis. This testing can then be useful in education with families and caregivers who may be shown the videos with consent from the patient in order to guide future care.
Evaluation And Diagnosis
As in much of neurology, a thorough history, along with detailed clinical observation remains essential in the diagnosis of patients with PNES and for distinguishing these events from epilepsy. Video EEG monitoring of seizures is a key adjunct to the history and clinical observation in diagnosing this condition [1,2]. Long-term video EEG monitoring is considered the “gold standard” in the characterization and differential diagnosis of seizures. Additional potentially helpful diagnostic techniques include video EEG-monitored seizure provocation, serum prolactin levels, single photon emission computed tomography, and neuropsychological testing.
Video EEG Monitoring
EEG monitoring for characterization of clinical events can be conducted on an ambulatory or outpatient basis or in dedicated inpatient epilepsy monitoring units. Ambulatory monitoring can be useful in the case of patients who report seizures that are more frequent in their home environment or in patients with frequent events. If events are infrequent, then inpatient monitoring may be more efficacious [1]. With longer-term inpatient monitoring, antiepileptic medications can be withdrawn in a supervised setting, in order to lower the seizure threshold as well as to safely discontinue medications that may not be necessary. Such medication titrations are typically not safe in an unsupervised outpatient setting. Some ambulatory EEG monitoring systems do allow for simultaneous video and EEG recording. However, an advantage to inpatient monitoring, which is not afforded in the outpatient setting, is the ability for nursing staff or physicians to perform clinical testing during events to assess for patient responsiveness and other features. Additionally, with inpatient monitoring, EEG technicians can routinely assess for any technical problems with the electrodes or recording system.
Another benefit of video EEG monitoring is that the state (waking, drowsy, or asleep) of the patient at the onset of an event can be established. While epileptic seizures can arise from any state, PNES most often occur from wakefulness. Patients with PNES may appear to be asleep at the onset of events, and they may report seizures from sleep. Video EEG monitoring can help to establish the waking or sleep state of the patient that may aid in diagnosis [29].
Prolactin Levels
Serum prolactin levels may be helpful in the diagnosis of PNES [35,36]. Following generalized tonic-clonic or complex partial epileptic seizures, the serum prolactin can rise from two to threefold to five to tenfold [37]. The maximal rise in serum prolactin occurs in the initial 20 to 60 minutes after the seizure [35–37]. A similar rise in serum prolactin would not be expected in PNES. Although prolactin levels may have some utility in diagnosis, they are not currently routinely ordered as part of a standard admission to most inpatient epilepsy monitoring units. This may be due in part to the fact that false-positive and false-negative results can occur with these levels [37–39]. For example, there may not be a rise in the prolactin level after a simple partial seizure or more subtle complex partial seizure.
Neuropsychological Testing
Neuropsychological testing is also a key component in the evaluation and diagnosis of PNES. Ideally, a mental health provider with a background in psychological assessment and neuropsychological intervention for patients with psychogenic disorders would perform the evaluation [40,41].
The goal of the evaluation should not solely focused on whether the patient suffers from nonepileptic or epileptic seizures. An epileptologist upon review of clinical, electrographic, and neuropsychological data better makes this determination. Moreover, neuropsychological testing cannot in itself either diagnose or exclude the possibility that a seizure disorder is nonepileptic because of the considerable overlap between epileptic and nonepileptic test results [40,41]. Neuropsychological evaluations aid this assessment by (1) determining the potential or likelihood of significant contributing psychopathology or cognitive difficulties, (2) defining the nature of the associated psychological or psychosocial issues, and (3) assessing how a patient might benefit from various psychologically based interventions [1]. The testing may identify psychological problems that can guide treatment after diagnosis.
Delays in Diagnosis
Correct and prompt diagnosis is essential for patients with PNES as is appropriate referral to a knowledgeable trained mental health professional. On average, patients with PNES are diagnosed 7.2 years after manifestation (SD 9.3 years), with mean delay of 5 to 7 years. Younger age, interictal epileptiform potentials in the EEG, and anticonvulsant treatment are associated with longer delays [42,43]. Delays are also thought to occur because of problems with “ownership” of these patients. Although typically neurologists are involved in the diagnosis of PNES, often using video EEG monitoring done in an inpatient setting, the next step is often a referral to a psychiatrist or mental health care provider. There are sometimes delays in the initial referral to the neurologist, delays in referral to specialists for video EEG testing, and also to the physicians, psychologists or social workers who may provide treatment. Another disconnect can occur if patients are “lost to follow-up” if they receive a referral for mental health care and either do not follow up on this on their own, or if the reason for this care is not fully explained. In addition, many mental health professionals are not trained in the evaluation and treatment of psychogenic symptoms and may even feel uncomfortable in dealing with these patients [13,44].
Many studies have been suggestive that delays in diagnosis may result in poorer outcomes [45,46], while other studies have suggested that patients who have an acute diagnosis of PNES upon presentation may do particularly well [8,47–49]. Some of the most recent large outcome studies suggest that there may be no worsening of outcome associated with delays in diagnosis and that outcome was predicted by other factors [50–52].
Management
Management of patients with PNES is similar to that for patients with other types of so-called abnormal illness behavior, although there remains a relative paucity of evidence for specific treatment strategies for PNES [1]. The first consideration should be the manner in which the diagnosis of PNES is presented to the patient and family. It is important to be honest with the patient and demonstrate a positive approach to the diagnosis [53]. The physician should emphasize as favorable or good news the fact that the patient does not have epilepsy, and should also stress that the disorder, although serious and "real," does not require treatment with antiepileptic medications and that once stress or emotional issues are resolved, the patient has the potential to gain better control of these events [1,54,55]. Nevertheless, not all patients readily accept the diagnosis or this type of approach. Some patients may seek other opinions, and this should not be discouraged. An adversarial relationship with the patient should be avoided. The patient should be encouraged to return if desired, and records should be made available to other health care providers to avoid duplication of services.
After the diagnosis of PNES is presented, supportive measures should be initiated. PNES patients may benefit from education and support that can be provided by the neurologist or primary care physician [1]. If the neuropsychological assessment suggests a clinical profile that requires a professional mental health intervention, then an appropriate referral should be made. Regular follow-up visits for the patient with the neurologist are useful even if a mental health professional is involved [49,56]. This allows the patient to get medical attention without demonstrating illness behavior. Patient education and support are stressed at these visits. Because family issues are often important contributing factors, physicians should consider involving family members in visits with consent of the patient [1].
A variety of treatment strategies are employed for the management of PNES including cognitive behavioral therapy (CBT), group and family therapy, antidepressant medication, and other forms of rehabilitation [5,57,58]. A 2007 Cochrane review that identified 608 references for non-medication PNES treatments found that only 3 studies met criteria for a randomized controlled trial. One of the more recently favored treatment options for PNES that has been applied to the treatment of various somatoform disorders and other psychiatric disorders in the past is CBT [57,59,60]. This form of psychotherapy can be administered by trained personnel in a time-limited fashion using defined protocols. The basis of this treatment is that the patient learns to increase awareness of their dysfunctional thoughts and learns new ways to respond to them [57,58]. To date, several groups have reported results of nonrandomized trials as well as case reports and case series which have established the utility of this treatment. There have been reports of significant reductions in seizure frequency and this treatment strategy appears very promising [61–65]. Preliminary randomized controlled trials have also been piloted and are also suggestive that this may be a validated treatment approach [66].
Prognosis
The outcomes of patients with PNES vary. Long-term follow-up studies show that about half of all patients with PNES function reasonably well following their diagnosis. However, only approximately one-third of patients will completely stop having seizures or related problems, and approximately 50% percent have poor functional outcomes [1,2,50]. When the diagnosis of PNES is based on reliable criteria such a video EEG monitoring, misdiagnosis is unlikely. Instead, the usual cause for a poor outcome is related to a patient’s chronic psychological and social problems[1,8,22,50].
It is noteworthy that children with PNES appear to have a much better prognosis than adults [9,10]. In fact, the etiology in children may be related more to transient stress and coping disorders, while adults are more likely to have PNES within the context of more chronic psychological maladjustment, such as personality disorders [10]. Another factor that accounts for the better outcomes in children is that they are usually properly diagnosed earlier in the course of their disorder [9,10].
Patients with milder psychopathology respond better to supportive educational or behavioral therapeutic approaches. In contrast, patients with more severe psychopathology and factitious disorders more often have associated chronic personality problems and correspondingly, a poorer prognosis [1,50]. Also it appears that patients who continue to be followed by the diagnosing neurologist or center do better than patients who are not seen after diagnosis [49,67]. As knowledge about the nature of PNES and their associated psychopathology is gained, better treatment strategies can be developed that will improve the care and prognosis of these difficult and challenging patients.
A large study of 164 patients who were followed for 10 years were considered to have “poor outcome” in general but favorable factors included higher education, younger age of onset and diagnosis, and less “dramatic” attacks, defined as lack of “positive motor features, no ictal incontinence or tongue biting.” These findings were consistent with prior studies [52,68].
In addition, the patients who tended to have less seizures and do better long term, had less somatoform and dissociative symptoms on psychometric testing [51]. These findings are often explained by the theory that patients who do not do well have poor coping strategies to deal with stress and anxiety and that in a sense, these patients have emotional dysregulation.
Special Issues
Coexisting Epileptic and Psychogenic Nonepileptic Seizures
A complicating factor in diagnosis is that both PNES and epileptic seizures may occur in a single patient. Indeed, approximately 10% to 40% of patients identified to have PNES also have been reported to have epileptic seizures [1,23,33,56]. There are several possible explanations for this. Some patients with epilepsy may learn that seizures result in attention and fill certain psychological needs. Alternatively, they may have concomitant neurologic problems, personality disorders, cognitive deficits, or impaired coping mechanisms that predispose them to psychogenic symptoms [69–71]. Fortunately, in such patients with combined seizure disorders, the epileptic seizures are usually well controlled or of only historical relevance at the time a patient develops PNES [1,22,23,33,72–74].
In other patients, both epileptic and PNES may start simultaneously, making management even more complex. In such patients, we have found it particularly helpful to focus on the semiology of seizure manifestations as recorded by video EEG monitoring to distinguish PNES from the epileptic seizures. We then direct our treatment of the patient according to the semiology manifesting at that time. We also have found it useful to show the videos of seizures to family members or caregivers with patient consent to help them understand how to respond best to a patient’s symptoms when epileptic and PNES co-exist.
Misdiagnosis of Psychogenic Nonepileptic Seizures
Sometimes events that are initially diagnosed as nonepileptic actually prove to be epileptic. Such events can be called “pseudo-pseudo” or “epileptic-nonepileptic” seizures [1]. Frontal lobe seizures in particular may not be associated with significant EEG changes ictally and therefore misdiagnosed as PNES [23,75,76]. Clinical presentation and proper diagnosis of these types of events warrant emphasis.
Notable manifestations of frontal lobe seizures that may easily be confused with hysterical behavior include shouting, laughing, cursing, clapping, snapping, genital manipulation, pelvic thrusting, pedaling, running, kicking, and thrashing [23,75–77]. Not all of these behaviors are specific for frontal lobe seizures. For example, bicycling leg movements have also been reported in seizures originating from the temporal lobe [78].
Summary
PNES represent a common yet challenging problem within neurology. This is due to the difficulty in diagnosis as well as lack of effective and widely available treatment options. Overall outcomes of patients with PNES vary, and may relate to an individual patient’s chronic psychological and social problems. However, an accurate and timely diagnosis remains critical and can help provide direction for implementing appropriate treatment.
Corresponding author: Jennifer Hopp, MD, Department of Neurology, University of Maryland Medical Center, Room S12C09, 22 South Greene Street, Baltimore, MD 21201, [email protected].
Financial disclosures: None.
1. Krumholz A. Nonepileptic seizures: diagnosis and management. Neurology 1999;S76–83.
2. Meierkord H, Will B, Fish D, Shorvon S. The clinical features and prognosis of pseudoseizures diagnosed using video-EEG telemetry. Neurology 1991;41:1643–6.
3. Lesser RP. Psychogenic seizures. Neurology 1996;46:1499–1507.
4. Sigurdardottir KR, Olafsson E. Incidence of psychogenic seizures in adults: a population-based study in Iceland. Epilepsia 1998;39:857–62.
5. Szaflarski JP, Szaflarski M, Hughes C, et al. Psychopathology and quality of life: psychogenic non-epileptic seizures versus epilepsy. Med Sci Monit 2003 9:CR113–8.
6. Barry E, Krumholz A, Bergey C, et al. Nonepileptic posttraumatic seizures. Epilepsia 1998;39:427–31.
7. Pakalnis A, Drake ME, Phillips B. Neuropsychiatric aspects of psychogenic status epilepticus. Neurology 1991;41;1104–6.
8. Walzack TS, Papacostas S, Williams DT, et al. Outcome after the diagnosis of psychogenic nonepileptic seizures. Epilepsia 1995;36:1131–7.
9. Metrick ME, Ritter FJ, Gates JR, et al. Nonepileptic events in childhood. Epilepsia 1991;32:322–8.
10. Wyllie E, Friedman D, Luders H, et al. Outcome of psychogenic seizures in children and adolescents compared to adults. Neurology 1991;41:742–4.
11. Duncan R, Oto M. Predictors of antecedent factors in psychogenic nonepileptic attacks: multivariate analysis. Neurology 2008;71:1000–5.
12. Alper K, Devinsky O, Perrine K, et al. Nonepileptic seizures and childhood sexual and physical abuse. Neurology 1993; 43:1950–3.
13. LaFrance WC Jr, Devinsky O. The treatment of nonepileptic seizures: historical perspectives and future directions. Epilepsia 2004;45 Suppl 2:15–21.
14. Westbrook LE, Devinsky O, Geocadin R. Nonepileptic seizures after head injury. Epilepsia 1998;39:978–82.
15. Slavney PR. Perspectives on hysteria. Baltimore: Johns Hopkins University Press; 1990.
16. Veith I. Hysteria: the history of a disease. Chicago: University of Chicago Press; 1965.
17. Goetz CG. Charcot the clinician. The Tuesday lessons. New York: Raven Press; 1987.
18. Massey EW, McHenry LC. Hysteroepilepsy in the nineteenth century: Charcot and Gowers. Neurology 1986;36:65–7.
19. Zeigler FJ, Imboden JB, Meyer E. Contemporary conversion reactions: a clinical study. Am J Psychiatry 1960;116:901–10.
20. Liske E, Forster FM. Pseudoseizures: a problem in the diagnosis and management of epileptic patients. Neurology 1964;14:41–9.
21. Diagnostic and statistical manual of mental disorders. DSM-IV 4th ed. American Psychiatric Association. Washington, DC; 1995.
22. Krumholz A, Niedermeyer, E. Psychogenic seizures: a clinical study with follow-up data. Neurology 1983; 33:498-502.
23. Krumholz A, Ting T. Co-existing epileptic and nonepileptic seizures. in imitators of epilepsy. 2nd ed. In: Kaplan PW, Fisher RS, editors. New York: Demos Medical Publishing; 2005:261–76.
24. Gates JR, Ramani V, Whalen S, Loewenson R. Ictal characteristics of pseudoseizures. Arch Neurol 1985;42:1183–87.
25. Leis AA, Ross MA, Summers AK. Psychogenic seizures: Ictal characteristics and diagnostic pitfalls. Neurology 1992;42:95–9.
26. Walczak TS, Bogolioubov. Weeping during psychogenic nonepileptic seizures. Epilepsia 1996;37:207–10.
27. Bergen D, Ristanovic R. Weeping is a common element during psychogenic nonepileptic seizures. Arch Neurol 1993;50:1059–60.
28. Peguero E, Abou-Khalil B, Fakhoury, Mathews G. Self-injury and incontinence in psychogenic seizures. Epilepsia 1995;36:586–91.
29. Orbach D, Ritaccio A, Devinsky O. Psychogenic, nonepileptic seizures associated with video-EEG-verified sleep. Epilepsia 2003;44:64–8.
30. Walczak TS, Williams DT, Berton W. Utility and reliability of placebo infusion in the evaluation of patients with seizures. Neurology 1994;44:394–99.
31. Bazil CW, Kothari M, Luciano D, et al. Provocation of nonepileptic seizures by suggestion in a general seizure population. Epilepsia 1994;35:768–70.
32. Devinsky O, Fisher RS. Ethical use of placebos and provocative testing in diagnosing nonepileptic seizures. Neurology 1996;47:866–70.
33. Lesser RP, Lueders H, Dinner DS. Evidence for epilepsy is rare in patients with psychogenic seizures. Neurology 1983; 33:502–4.
34. Barre MA, Burnstine TH, Fisher RS, Lesser RP. Electroencephalographic changes during simple partial seizures. Epilepsia 1994;35:715–20.
35. Trimble MR. Serum prolactin levels in epilepsy and hysteria. BMJ 1978;2:1682.
36. Laxer KD, Mullooly JP, Howell B. Prolactin changes after seizures classified by EEG monitoring. Neurology 1985; 35:31–5.
37. Pritchard PB, Wannamaker BB, Sagel J, et al. Endocrine function following complex partial seizures. Ann Neurol 1983;14:27–32.
38. Malkowicz DE, Legido A, Jackel RA, et al. Prolactin secretion following repetitive seizures. Neurology 1995;45:448–52.
39. Oribe E, Rohullah A, Nissenbaum E, Boal B. Serum prolactin concentrations are elevated after syncope. Neurology 1996;47:60–2.
40. Henrichs TF, Tucker DM, Farha J, Novelly RA. MMPI indices in the identification of patients evidencing pseudoseizures. Epilepsia 1988;29:184–8.
41. Wilkus RJ, Dodrill CB. Factors affecting the outcome of MMPI and neuropsychological assessments of psychogenic and epileptic seizure patients. Epilepsia 1989;30:339–47.
42. DeTimary P, Fouchet P, Sylin M, et al. Non–epileptic seizures: delayed diagnosis in patients presenting with electroencephalographic (EEG) or clinical signs of epileptic seizures. Seizure 2002;11:193–7.
43. Reuber M, Fernandez G, et al. Diagnostic delay in psychogenic nonepileptic seizures. Neurology 2002;58:493–5.
44. Rosenbaum DH, et al. Outpatient multidisciplinary management of non-epileptic seizures. In: Rowan AJ, Gates Jr, editors. Non-epileptic seizures. 1st ed. Stoneham, MA: Butterworth-Heinemann; 1993:275–83.
45. Lempert T, Schmidt D. Natural history and outcome of psychogenic seizures: a clinical study in 50 patients. J Neurol 1990;237:35–8.
46. Selwa LM, Geyer J, Nikakhtar N, et al. Nonepileptic seizure outcome varies by type of spell and duration of illness. Epilepsia 2000;41:1330–4.
47. Buchanan N, Snars J. Pseudoseizures (non epileptic attack disorder): clinical management and outcome in 50 patients. Seizure 1993;2:141–6.
48. Kanner AM. More controversies on the treatment of psychogenic pseudoseizures: an addendum. Epilepsy Behav 2003;4:360–4.
49. Aboukasm A, Mahr G, Gahry BR, et al. Retrospective analysis of the effects of psychotherapeutic interventions on outcomes of psychogenic nonepileptic seizures. Epilepsia 1998;39:470–3.
50. Reuber M, Pukrop T, Bauer J, et al. Outcome in psychogenic nonepileptic seizures: 1 to 10-year follow-up in 164 patients. Ann Neurol 2003;53:305–11.
51. McKenzie P, Oto M, Russell A, Pelosi A, Duncan R. Early outcomes and predictors in 260 patients with psychogenic nonepileptic seizures (PNES). Neurology 2010;74:64–9.
52. Kanner AM, Parra J, Frey M, et al. Psychiatric and neurologic predictors of psychogenic pseudoseizure outcome. Neurology 1999;53:933–8.
53. Shen W, Bowman ES, Markand ON. Presenting the diagnosis of pseudoseizure. Neurology 1990; 40:756–9.
54. Friedman JH, LaFrance Jr WC. Psychogenic disorders: the need to speak plainly. Arch Neurol 2010;67:753–5.
55. LaFrance Jr WC. Psychogenic nonepileptic “seizures” or “attacks”? It’s not just semantics: “Seizures.” Neurology 2010;75: 87–8.
56. Ramsay RE, Cohen A, Brown MC. Coexisting epilepsy and non-epileptic seizures. In: Non-epileptic seizures. Butterworth-Heinemann; 1998:47–54.
57. Stone J, Carson A, Sharpe M. Functional symptoms in neurology: management. J Neurol Neurosurg Psychiatry. 2005;6(Suppl 1):i13–i21.
58. LaFrance WC Jr, Bjornaes H. Designing treatment plans based on etiology of psychogenic nonepileptic seizures. In: Schachter SC, LaFrance WC Jr, editors. Gates and Rowan’s nonepileptic seizures. 3rd ed. New York: Cambridge University Press; 2010:266–80.
59. Kroenke K, Swindle R. Cognitive-behavioral therapy for somatization and symptom syndromes: a critical review of controlled clinical trials. Psychother Psychosom 200;69:205–15.
60. Kroenke K. Efficacy of treatment of somatoform disorders: a review of randomized controlled trials. Psychosom Med 2007:69:881–8.
61. LaFrance WC Jr, Miller IW, Ryan CE, et al. Cognitive behavioral therapy for psychogenic nonepileptic seizures. Epilepsy Behav 2009;14:591–6.
62. Chalder T. Non-epileptic attacks: a cognitive behavioral approach in a single case with a four-year follow-up. Clin Psychol Psychother 1996;3:291–7.
63. Betts T, Duffy N. Non-epileptic attack disorder (pseudoseizures) and sexual abuse: a review. In: Gram L, Johannessen SI, Osterman PE, et al, editors. Pseudo-epileptic seizures. Petersfield, UK: Wrightson Biomedical Publishing; 1993:55–66.
64. Lesser RP. Treatment and outcome of psychogenic nonepileptic seizures. Epilepsy Currents 2003;3:198–200.
65. Ramani V. Review of psychiatric treatment strategies in non-epileptic seizures. In: Rowan AJ, Gates JR, eds. Non-epileptic Seizures. 1st ed. Stoneham, MA: Butterworth Heinemann; 1993:259–67.
66. Goldstein LH, Chalder T, Chigwedere C, et al. Cognitive-behavioral therapy for psychogenic nonepileptic seizures: a pilot RCT. Neurology 2010;74:1986–94.
67. Bennet C, So NM, Smith WB, Thompson K. Structured treatment improves the outcome of nonepileptic events. Epilepsia 1997;38(Suppl 8):214.
68. McDade G, Brown SW. Non-epileptic seizures: management and predictive factors of outcome. Seizure 1992;1:7–10.
69. Bowman ES. Etiology and clinical course of pseudoseizures: relationship to trauma, depression, and dissociation. Psychosomatics 1993;34:333–42.
70. Bowman ES, Markand ON. Psychodynamics and psychiatric diagnoses of pseudoseizure subjects. Am J Psychiatry 1996;153:57–63.
71. Vanderzant CW, Giordani B, Berent S, et al. Personality of patients with pseudoseizures. Neurology 1986;36:664–8.
72. Benbadis SR, Agrawal V, Tatum WO. How many patients with psychogenic nonepileptic seizures also have epilepsy? Neurology 2001; 57:915–7.
73. Glosser G, Roberts D, et al. Nonepileptic seizures after resective epilepsy surgery. Epilepsia 1999; 40:1750–4.
74. Reuber M, Kral T. New-onset psychogenic seizures after intracranial neurosurgery. Acta Neurochir (Wien) 2002; 144:901–7.
75. Williamson P, Spencer D, Spencer S, et al. Complex partial seizures of frontal lobe origin. Ann Neurol 1985;18:497–504.
76. Saygi S, Katz A, Marks D, et al. Frontal lobe partial seizures and psychogenic seizures: comparison of clinical and ictal characteristics. Neurology 1992;42:1274–7.
77. Waterman K, Purves S, Kosaka B, et al. An epileptic syndrome caused by mesial frontal lobe seizure foci. Neurology 1987; 37:577–82.
78. Sussman N, Jackel R, Kaplan L, et al. Bicycling movements as a manifestation of complex partial seizures of temporal lobe origin. Epilepsia 1989;30:527–31.
1. Krumholz A. Nonepileptic seizures: diagnosis and management. Neurology 1999;S76–83.
2. Meierkord H, Will B, Fish D, Shorvon S. The clinical features and prognosis of pseudoseizures diagnosed using video-EEG telemetry. Neurology 1991;41:1643–6.
3. Lesser RP. Psychogenic seizures. Neurology 1996;46:1499–1507.
4. Sigurdardottir KR, Olafsson E. Incidence of psychogenic seizures in adults: a population-based study in Iceland. Epilepsia 1998;39:857–62.
5. Szaflarski JP, Szaflarski M, Hughes C, et al. Psychopathology and quality of life: psychogenic non-epileptic seizures versus epilepsy. Med Sci Monit 2003 9:CR113–8.
6. Barry E, Krumholz A, Bergey C, et al. Nonepileptic posttraumatic seizures. Epilepsia 1998;39:427–31.
7. Pakalnis A, Drake ME, Phillips B. Neuropsychiatric aspects of psychogenic status epilepticus. Neurology 1991;41;1104–6.
8. Walzack TS, Papacostas S, Williams DT, et al. Outcome after the diagnosis of psychogenic nonepileptic seizures. Epilepsia 1995;36:1131–7.
9. Metrick ME, Ritter FJ, Gates JR, et al. Nonepileptic events in childhood. Epilepsia 1991;32:322–8.
10. Wyllie E, Friedman D, Luders H, et al. Outcome of psychogenic seizures in children and adolescents compared to adults. Neurology 1991;41:742–4.
11. Duncan R, Oto M. Predictors of antecedent factors in psychogenic nonepileptic attacks: multivariate analysis. Neurology 2008;71:1000–5.
12. Alper K, Devinsky O, Perrine K, et al. Nonepileptic seizures and childhood sexual and physical abuse. Neurology 1993; 43:1950–3.
13. LaFrance WC Jr, Devinsky O. The treatment of nonepileptic seizures: historical perspectives and future directions. Epilepsia 2004;45 Suppl 2:15–21.
14. Westbrook LE, Devinsky O, Geocadin R. Nonepileptic seizures after head injury. Epilepsia 1998;39:978–82.
15. Slavney PR. Perspectives on hysteria. Baltimore: Johns Hopkins University Press; 1990.
16. Veith I. Hysteria: the history of a disease. Chicago: University of Chicago Press; 1965.
17. Goetz CG. Charcot the clinician. The Tuesday lessons. New York: Raven Press; 1987.
18. Massey EW, McHenry LC. Hysteroepilepsy in the nineteenth century: Charcot and Gowers. Neurology 1986;36:65–7.
19. Zeigler FJ, Imboden JB, Meyer E. Contemporary conversion reactions: a clinical study. Am J Psychiatry 1960;116:901–10.
20. Liske E, Forster FM. Pseudoseizures: a problem in the diagnosis and management of epileptic patients. Neurology 1964;14:41–9.
21. Diagnostic and statistical manual of mental disorders. DSM-IV 4th ed. American Psychiatric Association. Washington, DC; 1995.
22. Krumholz A, Niedermeyer, E. Psychogenic seizures: a clinical study with follow-up data. Neurology 1983; 33:498-502.
23. Krumholz A, Ting T. Co-existing epileptic and nonepileptic seizures. in imitators of epilepsy. 2nd ed. In: Kaplan PW, Fisher RS, editors. New York: Demos Medical Publishing; 2005:261–76.
24. Gates JR, Ramani V, Whalen S, Loewenson R. Ictal characteristics of pseudoseizures. Arch Neurol 1985;42:1183–87.
25. Leis AA, Ross MA, Summers AK. Psychogenic seizures: Ictal characteristics and diagnostic pitfalls. Neurology 1992;42:95–9.
26. Walczak TS, Bogolioubov. Weeping during psychogenic nonepileptic seizures. Epilepsia 1996;37:207–10.
27. Bergen D, Ristanovic R. Weeping is a common element during psychogenic nonepileptic seizures. Arch Neurol 1993;50:1059–60.
28. Peguero E, Abou-Khalil B, Fakhoury, Mathews G. Self-injury and incontinence in psychogenic seizures. Epilepsia 1995;36:586–91.
29. Orbach D, Ritaccio A, Devinsky O. Psychogenic, nonepileptic seizures associated with video-EEG-verified sleep. Epilepsia 2003;44:64–8.
30. Walczak TS, Williams DT, Berton W. Utility and reliability of placebo infusion in the evaluation of patients with seizures. Neurology 1994;44:394–99.
31. Bazil CW, Kothari M, Luciano D, et al. Provocation of nonepileptic seizures by suggestion in a general seizure population. Epilepsia 1994;35:768–70.
32. Devinsky O, Fisher RS. Ethical use of placebos and provocative testing in diagnosing nonepileptic seizures. Neurology 1996;47:866–70.
33. Lesser RP, Lueders H, Dinner DS. Evidence for epilepsy is rare in patients with psychogenic seizures. Neurology 1983; 33:502–4.
34. Barre MA, Burnstine TH, Fisher RS, Lesser RP. Electroencephalographic changes during simple partial seizures. Epilepsia 1994;35:715–20.
35. Trimble MR. Serum prolactin levels in epilepsy and hysteria. BMJ 1978;2:1682.
36. Laxer KD, Mullooly JP, Howell B. Prolactin changes after seizures classified by EEG monitoring. Neurology 1985; 35:31–5.
37. Pritchard PB, Wannamaker BB, Sagel J, et al. Endocrine function following complex partial seizures. Ann Neurol 1983;14:27–32.
38. Malkowicz DE, Legido A, Jackel RA, et al. Prolactin secretion following repetitive seizures. Neurology 1995;45:448–52.
39. Oribe E, Rohullah A, Nissenbaum E, Boal B. Serum prolactin concentrations are elevated after syncope. Neurology 1996;47:60–2.
40. Henrichs TF, Tucker DM, Farha J, Novelly RA. MMPI indices in the identification of patients evidencing pseudoseizures. Epilepsia 1988;29:184–8.
41. Wilkus RJ, Dodrill CB. Factors affecting the outcome of MMPI and neuropsychological assessments of psychogenic and epileptic seizure patients. Epilepsia 1989;30:339–47.
42. DeTimary P, Fouchet P, Sylin M, et al. Non–epileptic seizures: delayed diagnosis in patients presenting with electroencephalographic (EEG) or clinical signs of epileptic seizures. Seizure 2002;11:193–7.
43. Reuber M, Fernandez G, et al. Diagnostic delay in psychogenic nonepileptic seizures. Neurology 2002;58:493–5.
44. Rosenbaum DH, et al. Outpatient multidisciplinary management of non-epileptic seizures. In: Rowan AJ, Gates Jr, editors. Non-epileptic seizures. 1st ed. Stoneham, MA: Butterworth-Heinemann; 1993:275–83.
45. Lempert T, Schmidt D. Natural history and outcome of psychogenic seizures: a clinical study in 50 patients. J Neurol 1990;237:35–8.
46. Selwa LM, Geyer J, Nikakhtar N, et al. Nonepileptic seizure outcome varies by type of spell and duration of illness. Epilepsia 2000;41:1330–4.
47. Buchanan N, Snars J. Pseudoseizures (non epileptic attack disorder): clinical management and outcome in 50 patients. Seizure 1993;2:141–6.
48. Kanner AM. More controversies on the treatment of psychogenic pseudoseizures: an addendum. Epilepsy Behav 2003;4:360–4.
49. Aboukasm A, Mahr G, Gahry BR, et al. Retrospective analysis of the effects of psychotherapeutic interventions on outcomes of psychogenic nonepileptic seizures. Epilepsia 1998;39:470–3.
50. Reuber M, Pukrop T, Bauer J, et al. Outcome in psychogenic nonepileptic seizures: 1 to 10-year follow-up in 164 patients. Ann Neurol 2003;53:305–11.
51. McKenzie P, Oto M, Russell A, Pelosi A, Duncan R. Early outcomes and predictors in 260 patients with psychogenic nonepileptic seizures (PNES). Neurology 2010;74:64–9.
52. Kanner AM, Parra J, Frey M, et al. Psychiatric and neurologic predictors of psychogenic pseudoseizure outcome. Neurology 1999;53:933–8.
53. Shen W, Bowman ES, Markand ON. Presenting the diagnosis of pseudoseizure. Neurology 1990; 40:756–9.
54. Friedman JH, LaFrance Jr WC. Psychogenic disorders: the need to speak plainly. Arch Neurol 2010;67:753–5.
55. LaFrance Jr WC. Psychogenic nonepileptic “seizures” or “attacks”? It’s not just semantics: “Seizures.” Neurology 2010;75: 87–8.
56. Ramsay RE, Cohen A, Brown MC. Coexisting epilepsy and non-epileptic seizures. In: Non-epileptic seizures. Butterworth-Heinemann; 1998:47–54.
57. Stone J, Carson A, Sharpe M. Functional symptoms in neurology: management. J Neurol Neurosurg Psychiatry. 2005;6(Suppl 1):i13–i21.
58. LaFrance WC Jr, Bjornaes H. Designing treatment plans based on etiology of psychogenic nonepileptic seizures. In: Schachter SC, LaFrance WC Jr, editors. Gates and Rowan’s nonepileptic seizures. 3rd ed. New York: Cambridge University Press; 2010:266–80.
59. Kroenke K, Swindle R. Cognitive-behavioral therapy for somatization and symptom syndromes: a critical review of controlled clinical trials. Psychother Psychosom 200;69:205–15.
60. Kroenke K. Efficacy of treatment of somatoform disorders: a review of randomized controlled trials. Psychosom Med 2007:69:881–8.
61. LaFrance WC Jr, Miller IW, Ryan CE, et al. Cognitive behavioral therapy for psychogenic nonepileptic seizures. Epilepsy Behav 2009;14:591–6.
62. Chalder T. Non-epileptic attacks: a cognitive behavioral approach in a single case with a four-year follow-up. Clin Psychol Psychother 1996;3:291–7.
63. Betts T, Duffy N. Non-epileptic attack disorder (pseudoseizures) and sexual abuse: a review. In: Gram L, Johannessen SI, Osterman PE, et al, editors. Pseudo-epileptic seizures. Petersfield, UK: Wrightson Biomedical Publishing; 1993:55–66.
64. Lesser RP. Treatment and outcome of psychogenic nonepileptic seizures. Epilepsy Currents 2003;3:198–200.
65. Ramani V. Review of psychiatric treatment strategies in non-epileptic seizures. In: Rowan AJ, Gates JR, eds. Non-epileptic Seizures. 1st ed. Stoneham, MA: Butterworth Heinemann; 1993:259–67.
66. Goldstein LH, Chalder T, Chigwedere C, et al. Cognitive-behavioral therapy for psychogenic nonepileptic seizures: a pilot RCT. Neurology 2010;74:1986–94.
67. Bennet C, So NM, Smith WB, Thompson K. Structured treatment improves the outcome of nonepileptic events. Epilepsia 1997;38(Suppl 8):214.
68. McDade G, Brown SW. Non-epileptic seizures: management and predictive factors of outcome. Seizure 1992;1:7–10.
69. Bowman ES. Etiology and clinical course of pseudoseizures: relationship to trauma, depression, and dissociation. Psychosomatics 1993;34:333–42.
70. Bowman ES, Markand ON. Psychodynamics and psychiatric diagnoses of pseudoseizure subjects. Am J Psychiatry 1996;153:57–63.
71. Vanderzant CW, Giordani B, Berent S, et al. Personality of patients with pseudoseizures. Neurology 1986;36:664–8.
72. Benbadis SR, Agrawal V, Tatum WO. How many patients with psychogenic nonepileptic seizures also have epilepsy? Neurology 2001; 57:915–7.
73. Glosser G, Roberts D, et al. Nonepileptic seizures after resective epilepsy surgery. Epilepsia 1999; 40:1750–4.
74. Reuber M, Kral T. New-onset psychogenic seizures after intracranial neurosurgery. Acta Neurochir (Wien) 2002; 144:901–7.
75. Williamson P, Spencer D, Spencer S, et al. Complex partial seizures of frontal lobe origin. Ann Neurol 1985;18:497–504.
76. Saygi S, Katz A, Marks D, et al. Frontal lobe partial seizures and psychogenic seizures: comparison of clinical and ictal characteristics. Neurology 1992;42:1274–7.
77. Waterman K, Purves S, Kosaka B, et al. An epileptic syndrome caused by mesial frontal lobe seizure foci. Neurology 1987; 37:577–82.
78. Sussman N, Jackel R, Kaplan L, et al. Bicycling movements as a manifestation of complex partial seizures of temporal lobe origin. Epilepsia 1989;30:527–31.