User login
Recurrent Multidrug Resistant Urinary Tract Infections in Geriatric Patients
Urinary tract infections (UTIs) account for 8.3 million doctor visits, 1 million emergency department (ED) visits, and 100,000 hospitalizations annually, with an estimated cost of $1 billion annually in the U.S.1 Urnary tract infections are the most common bacterial infections found in nursing home residents, accounting for 50% of reported infections in Norwegian nursing homes, 30% to 50% in U.S. nursing homes, and 25% of all infections in the noninstitutionalized elderly in the U.S.2-4 In the geriatric population, UTIs are often found incidentally at the time of hospitalization for other admitting diagnoses, such as mentation changes or falls.5 Asymptomatic pyuria was found in 14.8% of community residents aged ≥ 80 years.6 Woodford and colleague found that 37% of geriatric patients admitted through an ED diagnosed with UTIs had no dysuria or urinary frequency.7
The incidence of UTIs is higher in the elderly due to genitourinary abnormalities, urolithiasis, dehydration, and diabetes, among other causes. These are considered complicated UTIs, defined as those in the presence of factors that predispose to persistent or relapsing infection, such as foreign bodies (calculi, indwelling catheters), obstruction, renal failure, and urinary retention.8
In elderly men, prostate enlargement causes bladder outlet obstruction predisposing them to urinary stasis and UTIs.2 Urinary tract infections are prone to recur when urinary tract abnormalities persist or treatment ineffectively eradicates resistant bacteria. Urinary tract infections are considered recurrent when ≥ 3 occur within 1 year or ≥ 2 occur in a 6-month period. The anticipated recurrence rate of complicated UTIs at 4 to 6 weeks following completion of therapy is 40% to 60%.4
Current practice standards recommend not treating asymptomatic UTIs to avoid contributing to bacterial antibiotic resistance.9 The frequent use of antibiotics, such as quinolones, which are increasingly inactive against these organisms, contributes to the overgrowth of bacteria in the gastrointestinal tract and their appearance in the genitourinary tract.10,11
As UTI-causing bacteria become more resistant to available antibiotics, the need to explore new strategies for managing UTIs is clear.12 The spread of extended spectrum beta-lactamase (ESBL), methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant enterococci (VRE), among other emerging bacterial resistance factors, present increasing treatment cost and poor patient outcomes. This challenge is occurring at a time when the discovery and development of new anti-infective agents is slowing down.13
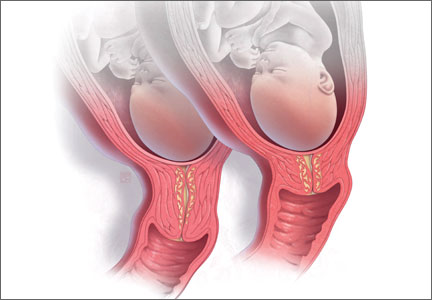
The European Commission Scientific Committee on Health and Environmental Risk reported that in patients receiving up to 4,000 mg/d methenamine for preventive long-term treatment of UTIs, no adverse effects (AEs) were noted (Figure).17
Complicated UTIs in the elderly are difficult to treat due to bacterial resistance. The off-label use of methenamine hippurate for treatment/prophylaxis of MDR-recurrent UTIs is a compelling option, explored further in the following case studies. Four case studies using methenamine for treatment and prevention of recurrent MDR UTIs in geriatric patients are presented.
Treating UTI Patients
Case Study 1
A man aged > 89 years, symptomatic with nocturia due to benign prostatic hypertrophy (BPH) with bladder outlet obstruction had 8 symptomatic UTIs over 15 months. His urine culture tested positive for MDR Providencia stuartia (resistant to ampicillin, chephazolin, gentamycin, tigecycline, tobramycin and sulfamethizole) and Staphylococcus haemolyticus (resistant to ciprofloxacin, levofloxacin, and nitrofurantoin). Postvoid residual urine was identified as the cause for his recurrent UTIs. Self-catheterization was recommended, but the patient declined. Due to his advanced age and preference, surgical intervention was not pursued. His renal function was within normal limits.
Treatment with methenamine hippurate 500 mg bid with 1,000 mg ascorbic acid to acidify the urine was initiated. This reduced dose of 500 mg bid (rather than 1,000 mg bid) was prescribed due to his advanced age and a choice to “err on the side of caution.” Two months later, urinalysis was negative for leukocyte esterase and nitrates, and the growth culture tested negative. Three- and 6-month urinalyses also showed no growth. The patient’s renal function remained stable. He experienced no AEs from the methenamine.
Due to his urinary retention, formaldehyde was able to collect in his bladder for longer than 2 hours, achieving bactericidal levels and effectively preventing recurrence of MDR UTIs.
Case Study 2
A man aged > 89 years with BPH and urinary incontinence managed with an external urinary device worn continuously had a history of 4 UTIs within a 6-month period. His renal function was normal with a creatinine clearance of 37 mg/dL. He was diagnosed with a symptomatic UTI culturing > 100,000 CFU Proteus mirabilis (resistant to ciprofloxacin, nitrofurantoin, and septra).
Due to resistance of the organism to available oral antibiotics, the patient’s desire to avoid hospitalization, and his caregiver’s inability to learn to administer IV antibiotics in the home, methenamine hippurate 500 mg bid was initiated. Within 21 days, the patient’s urinalysis was negative, indicating no bacterial growth. He was treated for 4 months with no recurrence of a UTI. No symptomatic UTIs recurred during the ongoing methenamine treatment.
Case Study 3
A man aged > 89 years with end-stage renal disease and a history of bladder cancer declined dialysis, indicating that his goals for care were palliative. He was followed at home by a hospice team. He had 3 recurrent symptomatic MRSA UTIs in a 9-month period (resistant to ciprofloxacin, levofloxin, penicillin, and oxacillin). The antibiotics the bacteria was sensitive to, nitrofurantoin and septra, could not be given because his creatinine clearance was merely 8 mg/dL. He was prescribed 500 mg methenamine with 1,000 mg ascorbic acid bid. Within 4 weeks, his urinalysis had changed from > 100,000 CFU to > 50,000 CFU (< 100,000 CFU). One month later with the only treatment the methenamine and ascorbic acid, there was no bacterial growth in the patient’s urine culture. He had no recurrence of a symptomatic UTI while receiving methenamine.
Case Study 4
An 89-year-old man with BPH and recurrent MRSA UTIs had 3 hospitalizations within 1 year. He had stage 3 chronic kidney disease with a creatinine clearance of 43 mg/dL. The patient had a symptomatic UTI > 100,000 CFU MRSA. He was treated with 500 mg methenamine and 1,000 mg ascorbic acid bid. Urinalysis results 2 months later revealed the bacterial count had dropped to the colonization range (< 50,000 CFU). His urinalysis was positive for leukocyte esterase with high white blood cell (WBC) counts, but it was negative for nitrites. He continued without recurrent UTIs while receiving the medication.
Discussion
Patients with similar profiles to those discussed in this report were treated with less dramatic results. Several remained free of symptomatic UTIs with urine cultures showing bacterial counts in the colonization range of < 50,000 CFU, as noted in case 4. Frequently, patients treated with methenamine have urinalyses with negative nitrites, positive leukocyte esterase, high WBCs, and few bacteria, but cultures show no growth. Some patients who did not reliably take medications as prescribed had recurrent symptomatic UTIs. Some had a subsequent UTI culturing a different organism or a change in the sensitivity profile of the same organism. This phenomenon suggests that formaldehyde disrupts the manufacture and transmission of the proteins and enzymes responsible for bacterial resistance factors.
Freeman and colleagues conducted a prospective study of 249 men with bacteruria followed for up to 10 years.18 Continuous therapy with methenamine delayed recurrence of bacteruria. Nilsson found that recurrent UTIs were reduced by 25% with long-term treatment (> 3 months) with methenamine.19
Bacteria do not develop resistance to methenamine.20 Reports of AEs are low, and drug interactions are limited to sulfamethizole, which can cause crystallization in the urine. Daily dosing used in studies ranged from 1 g to 4 g daily.21 Nilsson conducted research over 16 months with geriatric patients and found no changes in renal function or crystallization in urine.19
Severe hepatic impairment is also a contraindication, as methenamine can be hydrolyzed to ammonia. Studies have shown a reduced effectiveness with lower urinary tract abnormalities, although those studies administered the medication for short periods of time.21 Because the action of the medication relies on ≥ 2 hours of exposure to urine in the bladder, patients with indwelling catheters or patients who urinate frequently experience little benefit.22 Ideal candidates for methenamine are those with urinary retention and recurrent UTIs.
Although the use of methenamine has increased in Norway and Sweden by 24% since 2000, the use of methenamine in the U.S. remains low, perhaps because of conflicting reports in the literature regarding effectiveness and use with limited populations (ie, noncatheterized patients, those able to retain urine for ≥ 2 hours, and a creatinine clearance > 50 mg/dL).3
Some health care providers use methenamine for UTI prophylaxis, but this practice is less common in the U.S. than it is in Scandinavian countries.3 However, no published studies have explored the action of methenamine on MRSA, ESBL, and VRE bacteria or on the enzymes and proteins that enable and transmit bacterial resistance factors.
Elderly patients with complicated recurrent UTIs due to resistant bacteria are often left with no oral antibiotic options. Costs escalate rapidly when IV antibiotics are given. Administration generally requires hospitalization with close monitoring of renal function and drug levels and the placement of a PICC or midline IV access. If there is no caregiver, then hospitalization followed by an admission to a skilled nursing facility is required.
Lee and colleagues concluded that there is a need for further studies to explore long-duration therapy with methenamine.21 No studies have addressed its use in the geriatric population for long-term use of prevention of recurrent UTIs. No studies have been done on its use for primary treatment of MDR UTIs. The benefits of this drug with a low AE profile and low cost ($60/month for 1 g bid), which has been proven to reduce the incidence and/or delay recurrence of UTIs, is well worth further examination.
Conclusion
Multiple studies over 60 years have shown methenamine hippurate to be a well-tolerated and safe medication. Little data are available about the use of this medication in the elderly in the U.S., despite its wide use in Scandinavian countries. Use of methenamine for MDR UTIs in the geriatric population has been shown to be safe and effective, as presented in these case studies. Substantial cost savings were realized with the use of methenamine in these geriatric patients by reducing hospitalizations and complications due to recurrent MDR UTIs. The use of methenamine for treating MDR UTIs and the prevention of recurrent UTIs in the geriatric population warrants further clinical use and research.
The very interesting changes noted in sensitivity of the same bacteria in subsequent UTIs in patients treated with methenamine raises questions about the action of formaldehyde in the bladder on bacterial resistance factors. Given the worldwide increase in bacterial resistance to currently available antibiotics, this is a most compelling action that demands further study.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Foxman B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am J Med. 2002;113(suppl 1A):5S-13S.
2. Kamel HK. Managing urinary tract infections: Guide for nursing home practitioners. Ann of Long Term Care. 2005;13(9):21-28.
3. Blix HS, Røed J, Sti MO. Large variation in antibacterial use among Norwegian nursing homes. Scand J Infect Dis. 2007;39(6-7):536-541.
4. Nicolle LE. Asymptomatic bacteruria in diabetic women. Diabetes Care. 2000;23(6):722-723.
5. Rhoads J, Clayman A, Nelson S. The relationship of urinary tract infections and falls in a nursing home. Director. 2007;15(1):22-26.
6. Rodhe N, Mølstad S, Englund L, Svärdsudd K. Asymptomatic bacteriuria in a population of elderly residents living in a community setting: Prevalence, characteristics and associated factors. Fam Pract. 2006;23(3):303-307.
7. Woodford HJ, George J. Diagnosis and management of urinary tract infection in hospitalized older people. J Am Geriatr Soc. 2009;57(1):107-114.
8. Levison ME, Kaye D. Treatment of complicated urinary tract infections with an emphasis on drug-resistant gram-negative uropathogens. Curr Infect Dis Rep. 2013;15(2):109-115.
9. Miller LG, Tang AW. Treatment of uncomplicated urinary tract infections in an era of increasing antimicrobial resistance. Mayo Clin Proc. 2004;79(8):1048-1053.
10. Nicoletti J, Kuster SP, Sulser T, et al. Risk factors for urinary tract infections due to ciprofloxacin-resistant Escherichia coli in a tertiary care urology department in Switzerland. Swiss Med Wkly. 2010;140:w13059.
11. Nicolle LE. Urinary tract infection in geriatric and institutionalized patients. Curr Opin Urol. 2002;12(1):51-55.
12. Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7(12):653-660.
13. Spellberg B, Guidos R, Gilbert D, et al; Infectious Diseases Society of America. The epidemic of antibiotic-resistant infections: A call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 2008;46(2):155-164.
14. Dagley S, Dawes EA, Morrison GA. Inhibition of growth of Aerobacter aerogenes: The mode of action of phenols, alcohols, acetone, and ethyl acetate.
J Bacteriol. 1950;60(4):369-379.
15. Neely WB. Action of formaldehyde on microorganisms I. Correlation of activity with formaldehyde metabolism. J Bacteriol. 1963;85(5):1028-1031.
16. Musher DM, Griffith DP. Generation of formaldehyde from methenamine: Effect of pH and concentration, and antibacterial effect. Antimicrob Agents Chemother. 1974;6(6):708-711.
17. Scientific Committee on Health and Environmental Risks. Risk Assessment Report on Methenamine. Brussels, Belgium: European Commission; 2007. CAS 100-97-0.
18. Freeman RB, Smith WM, Richardson JA, et al. Long-term therapy for chronic bacteriuria in men. U.S. Public Health Service cooperative study. Ann Intern Med. 1975;83(2):133-147.
19. Nilsson S. Long-term treatment with methenamine hippurate in recurrent urinary tract infection. Acta Med Scand. 1975;198(1-2):81-85.
20. Drugs.com. Methenamine (systemic). http://www.drugs.com/mmx/methenamine-hippurate.html?printable=1. Updated March 28, 2000. Accessed June 17, 2014.
21. Lee BSB, Simpson JM, Craig JC, Bhuta T. Methenamine hippurate for preventing urinary tract infections. Cochrane Database Syst Rev. 2012;10:CD003265.
22. Lee BB, Haran MJ, Hunt LM, et al. Spinal-injured neuropathic bladder antisepsis (SINBA) trial. Spinal Cord. 2007;45(8):542-550.
Urinary tract infections (UTIs) account for 8.3 million doctor visits, 1 million emergency department (ED) visits, and 100,000 hospitalizations annually, with an estimated cost of $1 billion annually in the U.S.1 Urnary tract infections are the most common bacterial infections found in nursing home residents, accounting for 50% of reported infections in Norwegian nursing homes, 30% to 50% in U.S. nursing homes, and 25% of all infections in the noninstitutionalized elderly in the U.S.2-4 In the geriatric population, UTIs are often found incidentally at the time of hospitalization for other admitting diagnoses, such as mentation changes or falls.5 Asymptomatic pyuria was found in 14.8% of community residents aged ≥ 80 years.6 Woodford and colleague found that 37% of geriatric patients admitted through an ED diagnosed with UTIs had no dysuria or urinary frequency.7
The incidence of UTIs is higher in the elderly due to genitourinary abnormalities, urolithiasis, dehydration, and diabetes, among other causes. These are considered complicated UTIs, defined as those in the presence of factors that predispose to persistent or relapsing infection, such as foreign bodies (calculi, indwelling catheters), obstruction, renal failure, and urinary retention.8
In elderly men, prostate enlargement causes bladder outlet obstruction predisposing them to urinary stasis and UTIs.2 Urinary tract infections are prone to recur when urinary tract abnormalities persist or treatment ineffectively eradicates resistant bacteria. Urinary tract infections are considered recurrent when ≥ 3 occur within 1 year or ≥ 2 occur in a 6-month period. The anticipated recurrence rate of complicated UTIs at 4 to 6 weeks following completion of therapy is 40% to 60%.4
Current practice standards recommend not treating asymptomatic UTIs to avoid contributing to bacterial antibiotic resistance.9 The frequent use of antibiotics, such as quinolones, which are increasingly inactive against these organisms, contributes to the overgrowth of bacteria in the gastrointestinal tract and their appearance in the genitourinary tract.10,11
As UTI-causing bacteria become more resistant to available antibiotics, the need to explore new strategies for managing UTIs is clear.12 The spread of extended spectrum beta-lactamase (ESBL), methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant enterococci (VRE), among other emerging bacterial resistance factors, present increasing treatment cost and poor patient outcomes. This challenge is occurring at a time when the discovery and development of new anti-infective agents is slowing down.13
The European Commission Scientific Committee on Health and Environmental Risk reported that in patients receiving up to 4,000 mg/d methenamine for preventive long-term treatment of UTIs, no adverse effects (AEs) were noted (Figure).17
Complicated UTIs in the elderly are difficult to treat due to bacterial resistance. The off-label use of methenamine hippurate for treatment/prophylaxis of MDR-recurrent UTIs is a compelling option, explored further in the following case studies. Four case studies using methenamine for treatment and prevention of recurrent MDR UTIs in geriatric patients are presented.
Treating UTI Patients
Case Study 1
A man aged > 89 years, symptomatic with nocturia due to benign prostatic hypertrophy (BPH) with bladder outlet obstruction had 8 symptomatic UTIs over 15 months. His urine culture tested positive for MDR Providencia stuartia (resistant to ampicillin, chephazolin, gentamycin, tigecycline, tobramycin and sulfamethizole) and Staphylococcus haemolyticus (resistant to ciprofloxacin, levofloxacin, and nitrofurantoin). Postvoid residual urine was identified as the cause for his recurrent UTIs. Self-catheterization was recommended, but the patient declined. Due to his advanced age and preference, surgical intervention was not pursued. His renal function was within normal limits.
Treatment with methenamine hippurate 500 mg bid with 1,000 mg ascorbic acid to acidify the urine was initiated. This reduced dose of 500 mg bid (rather than 1,000 mg bid) was prescribed due to his advanced age and a choice to “err on the side of caution.” Two months later, urinalysis was negative for leukocyte esterase and nitrates, and the growth culture tested negative. Three- and 6-month urinalyses also showed no growth. The patient’s renal function remained stable. He experienced no AEs from the methenamine.
Due to his urinary retention, formaldehyde was able to collect in his bladder for longer than 2 hours, achieving bactericidal levels and effectively preventing recurrence of MDR UTIs.
Case Study 2
A man aged > 89 years with BPH and urinary incontinence managed with an external urinary device worn continuously had a history of 4 UTIs within a 6-month period. His renal function was normal with a creatinine clearance of 37 mg/dL. He was diagnosed with a symptomatic UTI culturing > 100,000 CFU Proteus mirabilis (resistant to ciprofloxacin, nitrofurantoin, and septra).
Due to resistance of the organism to available oral antibiotics, the patient’s desire to avoid hospitalization, and his caregiver’s inability to learn to administer IV antibiotics in the home, methenamine hippurate 500 mg bid was initiated. Within 21 days, the patient’s urinalysis was negative, indicating no bacterial growth. He was treated for 4 months with no recurrence of a UTI. No symptomatic UTIs recurred during the ongoing methenamine treatment.
Case Study 3
A man aged > 89 years with end-stage renal disease and a history of bladder cancer declined dialysis, indicating that his goals for care were palliative. He was followed at home by a hospice team. He had 3 recurrent symptomatic MRSA UTIs in a 9-month period (resistant to ciprofloxacin, levofloxin, penicillin, and oxacillin). The antibiotics the bacteria was sensitive to, nitrofurantoin and septra, could not be given because his creatinine clearance was merely 8 mg/dL. He was prescribed 500 mg methenamine with 1,000 mg ascorbic acid bid. Within 4 weeks, his urinalysis had changed from > 100,000 CFU to > 50,000 CFU (< 100,000 CFU). One month later with the only treatment the methenamine and ascorbic acid, there was no bacterial growth in the patient’s urine culture. He had no recurrence of a symptomatic UTI while receiving methenamine.
Case Study 4
An 89-year-old man with BPH and recurrent MRSA UTIs had 3 hospitalizations within 1 year. He had stage 3 chronic kidney disease with a creatinine clearance of 43 mg/dL. The patient had a symptomatic UTI > 100,000 CFU MRSA. He was treated with 500 mg methenamine and 1,000 mg ascorbic acid bid. Urinalysis results 2 months later revealed the bacterial count had dropped to the colonization range (< 50,000 CFU). His urinalysis was positive for leukocyte esterase with high white blood cell (WBC) counts, but it was negative for nitrites. He continued without recurrent UTIs while receiving the medication.
Discussion
Patients with similar profiles to those discussed in this report were treated with less dramatic results. Several remained free of symptomatic UTIs with urine cultures showing bacterial counts in the colonization range of < 50,000 CFU, as noted in case 4. Frequently, patients treated with methenamine have urinalyses with negative nitrites, positive leukocyte esterase, high WBCs, and few bacteria, but cultures show no growth. Some patients who did not reliably take medications as prescribed had recurrent symptomatic UTIs. Some had a subsequent UTI culturing a different organism or a change in the sensitivity profile of the same organism. This phenomenon suggests that formaldehyde disrupts the manufacture and transmission of the proteins and enzymes responsible for bacterial resistance factors.
Freeman and colleagues conducted a prospective study of 249 men with bacteruria followed for up to 10 years.18 Continuous therapy with methenamine delayed recurrence of bacteruria. Nilsson found that recurrent UTIs were reduced by 25% with long-term treatment (> 3 months) with methenamine.19
Bacteria do not develop resistance to methenamine.20 Reports of AEs are low, and drug interactions are limited to sulfamethizole, which can cause crystallization in the urine. Daily dosing used in studies ranged from 1 g to 4 g daily.21 Nilsson conducted research over 16 months with geriatric patients and found no changes in renal function or crystallization in urine.19
Severe hepatic impairment is also a contraindication, as methenamine can be hydrolyzed to ammonia. Studies have shown a reduced effectiveness with lower urinary tract abnormalities, although those studies administered the medication for short periods of time.21 Because the action of the medication relies on ≥ 2 hours of exposure to urine in the bladder, patients with indwelling catheters or patients who urinate frequently experience little benefit.22 Ideal candidates for methenamine are those with urinary retention and recurrent UTIs.
Although the use of methenamine has increased in Norway and Sweden by 24% since 2000, the use of methenamine in the U.S. remains low, perhaps because of conflicting reports in the literature regarding effectiveness and use with limited populations (ie, noncatheterized patients, those able to retain urine for ≥ 2 hours, and a creatinine clearance > 50 mg/dL).3
Some health care providers use methenamine for UTI prophylaxis, but this practice is less common in the U.S. than it is in Scandinavian countries.3 However, no published studies have explored the action of methenamine on MRSA, ESBL, and VRE bacteria or on the enzymes and proteins that enable and transmit bacterial resistance factors.
Elderly patients with complicated recurrent UTIs due to resistant bacteria are often left with no oral antibiotic options. Costs escalate rapidly when IV antibiotics are given. Administration generally requires hospitalization with close monitoring of renal function and drug levels and the placement of a PICC or midline IV access. If there is no caregiver, then hospitalization followed by an admission to a skilled nursing facility is required.
Lee and colleagues concluded that there is a need for further studies to explore long-duration therapy with methenamine.21 No studies have addressed its use in the geriatric population for long-term use of prevention of recurrent UTIs. No studies have been done on its use for primary treatment of MDR UTIs. The benefits of this drug with a low AE profile and low cost ($60/month for 1 g bid), which has been proven to reduce the incidence and/or delay recurrence of UTIs, is well worth further examination.
Conclusion
Multiple studies over 60 years have shown methenamine hippurate to be a well-tolerated and safe medication. Little data are available about the use of this medication in the elderly in the U.S., despite its wide use in Scandinavian countries. Use of methenamine for MDR UTIs in the geriatric population has been shown to be safe and effective, as presented in these case studies. Substantial cost savings were realized with the use of methenamine in these geriatric patients by reducing hospitalizations and complications due to recurrent MDR UTIs. The use of methenamine for treating MDR UTIs and the prevention of recurrent UTIs in the geriatric population warrants further clinical use and research.
The very interesting changes noted in sensitivity of the same bacteria in subsequent UTIs in patients treated with methenamine raises questions about the action of formaldehyde in the bladder on bacterial resistance factors. Given the worldwide increase in bacterial resistance to currently available antibiotics, this is a most compelling action that demands further study.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Urinary tract infections (UTIs) account for 8.3 million doctor visits, 1 million emergency department (ED) visits, and 100,000 hospitalizations annually, with an estimated cost of $1 billion annually in the U.S.1 Urnary tract infections are the most common bacterial infections found in nursing home residents, accounting for 50% of reported infections in Norwegian nursing homes, 30% to 50% in U.S. nursing homes, and 25% of all infections in the noninstitutionalized elderly in the U.S.2-4 In the geriatric population, UTIs are often found incidentally at the time of hospitalization for other admitting diagnoses, such as mentation changes or falls.5 Asymptomatic pyuria was found in 14.8% of community residents aged ≥ 80 years.6 Woodford and colleague found that 37% of geriatric patients admitted through an ED diagnosed with UTIs had no dysuria or urinary frequency.7
The incidence of UTIs is higher in the elderly due to genitourinary abnormalities, urolithiasis, dehydration, and diabetes, among other causes. These are considered complicated UTIs, defined as those in the presence of factors that predispose to persistent or relapsing infection, such as foreign bodies (calculi, indwelling catheters), obstruction, renal failure, and urinary retention.8
In elderly men, prostate enlargement causes bladder outlet obstruction predisposing them to urinary stasis and UTIs.2 Urinary tract infections are prone to recur when urinary tract abnormalities persist or treatment ineffectively eradicates resistant bacteria. Urinary tract infections are considered recurrent when ≥ 3 occur within 1 year or ≥ 2 occur in a 6-month period. The anticipated recurrence rate of complicated UTIs at 4 to 6 weeks following completion of therapy is 40% to 60%.4
Current practice standards recommend not treating asymptomatic UTIs to avoid contributing to bacterial antibiotic resistance.9 The frequent use of antibiotics, such as quinolones, which are increasingly inactive against these organisms, contributes to the overgrowth of bacteria in the gastrointestinal tract and their appearance in the genitourinary tract.10,11
As UTI-causing bacteria become more resistant to available antibiotics, the need to explore new strategies for managing UTIs is clear.12 The spread of extended spectrum beta-lactamase (ESBL), methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant enterococci (VRE), among other emerging bacterial resistance factors, present increasing treatment cost and poor patient outcomes. This challenge is occurring at a time when the discovery and development of new anti-infective agents is slowing down.13
The European Commission Scientific Committee on Health and Environmental Risk reported that in patients receiving up to 4,000 mg/d methenamine for preventive long-term treatment of UTIs, no adverse effects (AEs) were noted (Figure).17
Complicated UTIs in the elderly are difficult to treat due to bacterial resistance. The off-label use of methenamine hippurate for treatment/prophylaxis of MDR-recurrent UTIs is a compelling option, explored further in the following case studies. Four case studies using methenamine for treatment and prevention of recurrent MDR UTIs in geriatric patients are presented.
Treating UTI Patients
Case Study 1
A man aged > 89 years, symptomatic with nocturia due to benign prostatic hypertrophy (BPH) with bladder outlet obstruction had 8 symptomatic UTIs over 15 months. His urine culture tested positive for MDR Providencia stuartia (resistant to ampicillin, chephazolin, gentamycin, tigecycline, tobramycin and sulfamethizole) and Staphylococcus haemolyticus (resistant to ciprofloxacin, levofloxacin, and nitrofurantoin). Postvoid residual urine was identified as the cause for his recurrent UTIs. Self-catheterization was recommended, but the patient declined. Due to his advanced age and preference, surgical intervention was not pursued. His renal function was within normal limits.
Treatment with methenamine hippurate 500 mg bid with 1,000 mg ascorbic acid to acidify the urine was initiated. This reduced dose of 500 mg bid (rather than 1,000 mg bid) was prescribed due to his advanced age and a choice to “err on the side of caution.” Two months later, urinalysis was negative for leukocyte esterase and nitrates, and the growth culture tested negative. Three- and 6-month urinalyses also showed no growth. The patient’s renal function remained stable. He experienced no AEs from the methenamine.
Due to his urinary retention, formaldehyde was able to collect in his bladder for longer than 2 hours, achieving bactericidal levels and effectively preventing recurrence of MDR UTIs.
Case Study 2
A man aged > 89 years with BPH and urinary incontinence managed with an external urinary device worn continuously had a history of 4 UTIs within a 6-month period. His renal function was normal with a creatinine clearance of 37 mg/dL. He was diagnosed with a symptomatic UTI culturing > 100,000 CFU Proteus mirabilis (resistant to ciprofloxacin, nitrofurantoin, and septra).
Due to resistance of the organism to available oral antibiotics, the patient’s desire to avoid hospitalization, and his caregiver’s inability to learn to administer IV antibiotics in the home, methenamine hippurate 500 mg bid was initiated. Within 21 days, the patient’s urinalysis was negative, indicating no bacterial growth. He was treated for 4 months with no recurrence of a UTI. No symptomatic UTIs recurred during the ongoing methenamine treatment.
Case Study 3
A man aged > 89 years with end-stage renal disease and a history of bladder cancer declined dialysis, indicating that his goals for care were palliative. He was followed at home by a hospice team. He had 3 recurrent symptomatic MRSA UTIs in a 9-month period (resistant to ciprofloxacin, levofloxin, penicillin, and oxacillin). The antibiotics the bacteria was sensitive to, nitrofurantoin and septra, could not be given because his creatinine clearance was merely 8 mg/dL. He was prescribed 500 mg methenamine with 1,000 mg ascorbic acid bid. Within 4 weeks, his urinalysis had changed from > 100,000 CFU to > 50,000 CFU (< 100,000 CFU). One month later with the only treatment the methenamine and ascorbic acid, there was no bacterial growth in the patient’s urine culture. He had no recurrence of a symptomatic UTI while receiving methenamine.
Case Study 4
An 89-year-old man with BPH and recurrent MRSA UTIs had 3 hospitalizations within 1 year. He had stage 3 chronic kidney disease with a creatinine clearance of 43 mg/dL. The patient had a symptomatic UTI > 100,000 CFU MRSA. He was treated with 500 mg methenamine and 1,000 mg ascorbic acid bid. Urinalysis results 2 months later revealed the bacterial count had dropped to the colonization range (< 50,000 CFU). His urinalysis was positive for leukocyte esterase with high white blood cell (WBC) counts, but it was negative for nitrites. He continued without recurrent UTIs while receiving the medication.
Discussion
Patients with similar profiles to those discussed in this report were treated with less dramatic results. Several remained free of symptomatic UTIs with urine cultures showing bacterial counts in the colonization range of < 50,000 CFU, as noted in case 4. Frequently, patients treated with methenamine have urinalyses with negative nitrites, positive leukocyte esterase, high WBCs, and few bacteria, but cultures show no growth. Some patients who did not reliably take medications as prescribed had recurrent symptomatic UTIs. Some had a subsequent UTI culturing a different organism or a change in the sensitivity profile of the same organism. This phenomenon suggests that formaldehyde disrupts the manufacture and transmission of the proteins and enzymes responsible for bacterial resistance factors.
Freeman and colleagues conducted a prospective study of 249 men with bacteruria followed for up to 10 years.18 Continuous therapy with methenamine delayed recurrence of bacteruria. Nilsson found that recurrent UTIs were reduced by 25% with long-term treatment (> 3 months) with methenamine.19
Bacteria do not develop resistance to methenamine.20 Reports of AEs are low, and drug interactions are limited to sulfamethizole, which can cause crystallization in the urine. Daily dosing used in studies ranged from 1 g to 4 g daily.21 Nilsson conducted research over 16 months with geriatric patients and found no changes in renal function or crystallization in urine.19
Severe hepatic impairment is also a contraindication, as methenamine can be hydrolyzed to ammonia. Studies have shown a reduced effectiveness with lower urinary tract abnormalities, although those studies administered the medication for short periods of time.21 Because the action of the medication relies on ≥ 2 hours of exposure to urine in the bladder, patients with indwelling catheters or patients who urinate frequently experience little benefit.22 Ideal candidates for methenamine are those with urinary retention and recurrent UTIs.
Although the use of methenamine has increased in Norway and Sweden by 24% since 2000, the use of methenamine in the U.S. remains low, perhaps because of conflicting reports in the literature regarding effectiveness and use with limited populations (ie, noncatheterized patients, those able to retain urine for ≥ 2 hours, and a creatinine clearance > 50 mg/dL).3
Some health care providers use methenamine for UTI prophylaxis, but this practice is less common in the U.S. than it is in Scandinavian countries.3 However, no published studies have explored the action of methenamine on MRSA, ESBL, and VRE bacteria or on the enzymes and proteins that enable and transmit bacterial resistance factors.
Elderly patients with complicated recurrent UTIs due to resistant bacteria are often left with no oral antibiotic options. Costs escalate rapidly when IV antibiotics are given. Administration generally requires hospitalization with close monitoring of renal function and drug levels and the placement of a PICC or midline IV access. If there is no caregiver, then hospitalization followed by an admission to a skilled nursing facility is required.
Lee and colleagues concluded that there is a need for further studies to explore long-duration therapy with methenamine.21 No studies have addressed its use in the geriatric population for long-term use of prevention of recurrent UTIs. No studies have been done on its use for primary treatment of MDR UTIs. The benefits of this drug with a low AE profile and low cost ($60/month for 1 g bid), which has been proven to reduce the incidence and/or delay recurrence of UTIs, is well worth further examination.
Conclusion
Multiple studies over 60 years have shown methenamine hippurate to be a well-tolerated and safe medication. Little data are available about the use of this medication in the elderly in the U.S., despite its wide use in Scandinavian countries. Use of methenamine for MDR UTIs in the geriatric population has been shown to be safe and effective, as presented in these case studies. Substantial cost savings were realized with the use of methenamine in these geriatric patients by reducing hospitalizations and complications due to recurrent MDR UTIs. The use of methenamine for treating MDR UTIs and the prevention of recurrent UTIs in the geriatric population warrants further clinical use and research.
The very interesting changes noted in sensitivity of the same bacteria in subsequent UTIs in patients treated with methenamine raises questions about the action of formaldehyde in the bladder on bacterial resistance factors. Given the worldwide increase in bacterial resistance to currently available antibiotics, this is a most compelling action that demands further study.
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
1. Foxman B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am J Med. 2002;113(suppl 1A):5S-13S.
2. Kamel HK. Managing urinary tract infections: Guide for nursing home practitioners. Ann of Long Term Care. 2005;13(9):21-28.
3. Blix HS, Røed J, Sti MO. Large variation in antibacterial use among Norwegian nursing homes. Scand J Infect Dis. 2007;39(6-7):536-541.
4. Nicolle LE. Asymptomatic bacteruria in diabetic women. Diabetes Care. 2000;23(6):722-723.
5. Rhoads J, Clayman A, Nelson S. The relationship of urinary tract infections and falls in a nursing home. Director. 2007;15(1):22-26.
6. Rodhe N, Mølstad S, Englund L, Svärdsudd K. Asymptomatic bacteriuria in a population of elderly residents living in a community setting: Prevalence, characteristics and associated factors. Fam Pract. 2006;23(3):303-307.
7. Woodford HJ, George J. Diagnosis and management of urinary tract infection in hospitalized older people. J Am Geriatr Soc. 2009;57(1):107-114.
8. Levison ME, Kaye D. Treatment of complicated urinary tract infections with an emphasis on drug-resistant gram-negative uropathogens. Curr Infect Dis Rep. 2013;15(2):109-115.
9. Miller LG, Tang AW. Treatment of uncomplicated urinary tract infections in an era of increasing antimicrobial resistance. Mayo Clin Proc. 2004;79(8):1048-1053.
10. Nicoletti J, Kuster SP, Sulser T, et al. Risk factors for urinary tract infections due to ciprofloxacin-resistant Escherichia coli in a tertiary care urology department in Switzerland. Swiss Med Wkly. 2010;140:w13059.
11. Nicolle LE. Urinary tract infection in geriatric and institutionalized patients. Curr Opin Urol. 2002;12(1):51-55.
12. Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7(12):653-660.
13. Spellberg B, Guidos R, Gilbert D, et al; Infectious Diseases Society of America. The epidemic of antibiotic-resistant infections: A call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 2008;46(2):155-164.
14. Dagley S, Dawes EA, Morrison GA. Inhibition of growth of Aerobacter aerogenes: The mode of action of phenols, alcohols, acetone, and ethyl acetate.
J Bacteriol. 1950;60(4):369-379.
15. Neely WB. Action of formaldehyde on microorganisms I. Correlation of activity with formaldehyde metabolism. J Bacteriol. 1963;85(5):1028-1031.
16. Musher DM, Griffith DP. Generation of formaldehyde from methenamine: Effect of pH and concentration, and antibacterial effect. Antimicrob Agents Chemother. 1974;6(6):708-711.
17. Scientific Committee on Health and Environmental Risks. Risk Assessment Report on Methenamine. Brussels, Belgium: European Commission; 2007. CAS 100-97-0.
18. Freeman RB, Smith WM, Richardson JA, et al. Long-term therapy for chronic bacteriuria in men. U.S. Public Health Service cooperative study. Ann Intern Med. 1975;83(2):133-147.
19. Nilsson S. Long-term treatment with methenamine hippurate in recurrent urinary tract infection. Acta Med Scand. 1975;198(1-2):81-85.
20. Drugs.com. Methenamine (systemic). http://www.drugs.com/mmx/methenamine-hippurate.html?printable=1. Updated March 28, 2000. Accessed June 17, 2014.
21. Lee BSB, Simpson JM, Craig JC, Bhuta T. Methenamine hippurate for preventing urinary tract infections. Cochrane Database Syst Rev. 2012;10:CD003265.
22. Lee BB, Haran MJ, Hunt LM, et al. Spinal-injured neuropathic bladder antisepsis (SINBA) trial. Spinal Cord. 2007;45(8):542-550.
1. Foxman B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am J Med. 2002;113(suppl 1A):5S-13S.
2. Kamel HK. Managing urinary tract infections: Guide for nursing home practitioners. Ann of Long Term Care. 2005;13(9):21-28.
3. Blix HS, Røed J, Sti MO. Large variation in antibacterial use among Norwegian nursing homes. Scand J Infect Dis. 2007;39(6-7):536-541.
4. Nicolle LE. Asymptomatic bacteruria in diabetic women. Diabetes Care. 2000;23(6):722-723.
5. Rhoads J, Clayman A, Nelson S. The relationship of urinary tract infections and falls in a nursing home. Director. 2007;15(1):22-26.
6. Rodhe N, Mølstad S, Englund L, Svärdsudd K. Asymptomatic bacteriuria in a population of elderly residents living in a community setting: Prevalence, characteristics and associated factors. Fam Pract. 2006;23(3):303-307.
7. Woodford HJ, George J. Diagnosis and management of urinary tract infection in hospitalized older people. J Am Geriatr Soc. 2009;57(1):107-114.
8. Levison ME, Kaye D. Treatment of complicated urinary tract infections with an emphasis on drug-resistant gram-negative uropathogens. Curr Infect Dis Rep. 2013;15(2):109-115.
9. Miller LG, Tang AW. Treatment of uncomplicated urinary tract infections in an era of increasing antimicrobial resistance. Mayo Clin Proc. 2004;79(8):1048-1053.
10. Nicoletti J, Kuster SP, Sulser T, et al. Risk factors for urinary tract infections due to ciprofloxacin-resistant Escherichia coli in a tertiary care urology department in Switzerland. Swiss Med Wkly. 2010;140:w13059.
11. Nicolle LE. Urinary tract infection in geriatric and institutionalized patients. Curr Opin Urol. 2002;12(1):51-55.
12. Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7(12):653-660.
13. Spellberg B, Guidos R, Gilbert D, et al; Infectious Diseases Society of America. The epidemic of antibiotic-resistant infections: A call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 2008;46(2):155-164.
14. Dagley S, Dawes EA, Morrison GA. Inhibition of growth of Aerobacter aerogenes: The mode of action of phenols, alcohols, acetone, and ethyl acetate.
J Bacteriol. 1950;60(4):369-379.
15. Neely WB. Action of formaldehyde on microorganisms I. Correlation of activity with formaldehyde metabolism. J Bacteriol. 1963;85(5):1028-1031.
16. Musher DM, Griffith DP. Generation of formaldehyde from methenamine: Effect of pH and concentration, and antibacterial effect. Antimicrob Agents Chemother. 1974;6(6):708-711.
17. Scientific Committee on Health and Environmental Risks. Risk Assessment Report on Methenamine. Brussels, Belgium: European Commission; 2007. CAS 100-97-0.
18. Freeman RB, Smith WM, Richardson JA, et al. Long-term therapy for chronic bacteriuria in men. U.S. Public Health Service cooperative study. Ann Intern Med. 1975;83(2):133-147.
19. Nilsson S. Long-term treatment with methenamine hippurate in recurrent urinary tract infection. Acta Med Scand. 1975;198(1-2):81-85.
20. Drugs.com. Methenamine (systemic). http://www.drugs.com/mmx/methenamine-hippurate.html?printable=1. Updated March 28, 2000. Accessed June 17, 2014.
21. Lee BSB, Simpson JM, Craig JC, Bhuta T. Methenamine hippurate for preventing urinary tract infections. Cochrane Database Syst Rev. 2012;10:CD003265.
22. Lee BB, Haran MJ, Hunt LM, et al. Spinal-injured neuropathic bladder antisepsis (SINBA) trial. Spinal Cord. 2007;45(8):542-550.
Experiencing Age-Related Vision and Hearing Impairment: The Psychosocial Dimension
From the University of Education (Dr. Heyl) and Heidelberg University (Dr. Wahl), Heidelberg, Germany.
Abstract
- Objective: To summarize the current state of research regarding the experience of age-related vision and hearing impairment.
- Methods:Review of the literature.
- Results: Negative consequences of age-related vision and hearing impairment manifest in the domains of health and longevity, everyday competence, cognitive functioning, social functioning, and subjective well-being. However, while vision impairment strongly impacts everyday competence, the burden of hearing impairment can mainly be found in the social domain. Psychosocially framed intervention research has shown promising findings, but many studies rely on small samples or do not include a control condition.
- Conclusions: Although more research is needed, it is clear that traditional rehabilitation programs targeting age-related vision and hearing impairments need a strong psychosocial component.
Vision and hearing are essential for person–environment interaction and both are subject to pronounced age-related changes. Ongoing demographic changes and increasing life expectancy is contributing to a significant increase in the number of very old individuals [1]. It is projected that by 2030 about 50% of older Americans may have some significant eye disease, ie, cataract, glaucoma, or age-related macular degeneration [2]. Presbycusis as the major cause of age-related hearing impairment is present in 40% of the American senior citizens [3]. In this narrative review, we review the epidemiological data on age-related vision and hearing impairment, research on its psychosocial impact, and intervention research aimed to improve coping processes and rehabilitative outcomes. We close with future recommendations directed both toward research and clinical practice.
Epidemiology
Vision and hearing impairment is highly prevalent in old age, yet prevalence rates reported in the literature are quite different, depending on the definition of vision and hearing impairment used. A widely used criterion for low vision is the one used by the World Health Organization, ie, visual acuity less than 20/60 and equal to or better than 20/400 in the better eye with best correction. A best corrected visual acuity of less than 20/400 in the better eye is used to define blindness [4]. A disabling hearing impairment is defined by an average hearing loss in decibel (dB HL) of at least 41 dB HL at 500, 1000, 2000, and 4000 Hz. [5]. Translated to everyday life, such hearing impairment mainly manifests in severe difficulties in understanding normal conversation. Besides differing definitions, different methods to assess vision and hearing impairment and heterogenous study populations make comparisons of prevalence rates difficult [6]. In particular, relying solely on self-report data to assess vision and hearing loss seems generally problematic. In addition, the strong focus in vision impairment assessment on visual acuity measures has limitations, as other indicators, such as contrast sensitivity or useful field of vision, may be more important for out-of-home mobility or driving [7].
A recent study on the prevalence of visual impairment (defined as best corrected visual acuity < 20⁄40) in 6 European countries found quite similar prevalence rates as reported for the US: Prevalence of visual impairment was 3% in those aged 65 to 74 years, 13% in those over 75 years and 33% in those over 85 years [8]. At first glance, vision loss seems to be more prevalent among older women than among older men, but this relationship is not sustained in multivariate analyses considering age, health, and social support variables [9].
Regarding hearing loss, Gopinath et al [10] found prevalence rates of 29% among men and 17% among women aged 60 to 69 years. Moreover, for every 10 years of age, the prevalence of hearing loss doubled. In their review of epidemiologic data on prevalence of age-related hearing impairment in Europe, Roth and coauthors [11] report that at the age of 70 years, about 30% of men and 20% of women were found to have a hearing loss of at least 30 dB HL, while at the age of 80 years about 55% of men and 45% of women were affected. Lin et al found that 63% of those 70 years and older had a hearing loss of more than 25 dB in the better ear [12].
According to a recent review by Schneider et al [6], prevalence of impairment in both vision and hearing in older age (dual sensory impairment) varies between 1.6% and 22.5% due to different sample characteristics (eg, size, age) and different definitions and assessments of vision and hearing impairment (see also [13]). However, there is good evidence that dual sensory impairment increases with age, and that it is more common among frailer subpopulations such as older individuals consulting care services [6].
Quality of Life Impact of Vision and Hearing Impairment
Health and Longevity
There is inconsistent evidence that both age-related vision and hearing impairment are accompanied by heightened multimorbidity and an increased mortality rate. For example, while some older as well as more recent studies have found that visual and hearing declines over time predict death in very old age [14–16], other studies have detected no significant relationship after adjusting for confounders such as age, gender, and education [17,18]. Among the hearing impaired, only men seem to have a significant increase in mortality risk [15,19]. Dual sensory impairment appears to be more consistently and more strongly related to increased mortality than vision or hearing impairment alone [19–21].
Everyday Competence
The term everyday competence includes both basic (eg, self-care behaviors) and instrumental (eg, using public transport) activities of daily living (ADL/IADL [22]). Age-related vision impairment has been found to be robustly associated with significantly lower everyday competence, because visual capacity is a critical prerequisite for such behaviors [23,24]. Indeed, lowered everyday competence appeared as the best of a range of variables (including cognitive function and well-being–related measures) used to differentiate between visually impaired and visually unimpaired older adults [18]. Furthermore, vision impairment impacts cross-sectionally as well as longitudinally—more strongly on IADL as compared to ADL—because the execution of IADL is more complex and depends more strongly on environmental enhancing or hindering factors [25–27]. Hence, shrinkage in IADL competence reflects a kind of early behavioral marker of severe vision impairment, whereas significant ADL decrease only happens later in the process of chronic vision loss.
In contrast to vision impairment, age-related hearing loss has been found not to have a major impact in particular on ADL/IADL [28]. However, as has been found elsewhere [29], hearing loss is associated with increased reliance on community and informal supports, suggesting that while IADL function may not deteriorate with hearing loss, the way it is conducted may change (ie, need for support to maintain participation).
It should also be mentioned in this context that assessment strategies have been developed to better consider the specific life conditions of those with vision and hearing impairment. The best-known and frequently applied instruments in this context are the National Eye Institute Visual Function Questionnaire [30] and the Hearing Handicap Inventory for the Elderly [31].
Cognitive Functioning
Previous research largely supports the notion that reduced vision and hearing function is accompanied by a decrease in cognitive performance in older adults. The work of Lindenberger and Baltes, based on the Berlin Aging Study (BASE)—but also including additional studies with a wider age-range—is central in supporting a strong connection among vision, hearing, balance, and cognitive functioning in later life. Lindenberger and Baltes [32] found that general intelligence correlated just as strongly with visual as with auditory ability. In a model conjoining age, sensory function, as well as intelligence, visual and auditory function predicted a large portion of interindividual differences in intelligence and indeed fully mediated the negative correlation between age and intelligence. This finding has meanwhile been replicated by a number of other research groups and may be regarded as rather robust [33,34]. In addition, Baltes and Lindenberger [35] observed that sensory measures were better predictors of intelligence than socio-structural variables such as education or social class. They also showed that the connection among sensory functioning and intelligence was much closer in older adults as compared to adults in early and middle adulthood [34].
No clear difference between the sensory modalities of vision and hearing has been identified regarding their relationship with cognitive performance. On the one hand, there is research supporting the view that both vision and hearing impairment are connected with cognitive decline [12,36,37], while some evidence also supports that the linkage may be stronger with vision [14]. On the other hand, there are also data not supporting a close connection between vision and hearing impairment and cognitive function [38]. Explanations for such inconsistencies may refer to a number of reasons, such as pronounced positive selectivity of samples (which may lead to underestimation of connections among sensory and cognitive function), the application of established cognitive tests not appropriate for sensory impaired older adults (which may lead to overestimation of connections among sensory and cognitive function), and the application of different cut-off scores for significant vision and hearing impairment (possibly, higher cut-offs may lead to higher, lower to lower connections). Longitudinal data using the latest in causal modeling data analysis support the view that the causal dynamics involved in sensory and intelligence change are complex and that each of these variables can drive change in the other across longer periods of later life [39].
Vision status also plays a role when it comes to the connection between cognitive function and everyday competence—a linkage that is generally challenged as people age and that may lead to endpoints such as dependence on others and transition to long-term care. Heyl et al [40] observed that the link between vision status and out-of-home leisure activities is mediated by cognitive status. In a more recent study, able to add to the understanding of such a mediation process, Heyl and Wahl [38,41] showed that the connection between cognitive function and everyday function is much closer in visually and hearing impaired older adults as compared with visually unimpaired older adults, which possibly means that both visually and hearing impaired elders rely more intensely on their cognitive resources. Causality dynamics may however also work in the opposite direction. As Rovner and colleagues [42,43] observed in a study with age-related macular degeneration patients over 64 years of age covering a 3-year observation period and 2 measurement occasions, activity loss over time due to the visual loss led to cognitive decline happening between T1 and T2. This finding fits well with the more general finding in the cognitive aging literature that the exertion of social and leisure activities is important for maintaining cognitive functioning [44].
Social Functioning
Social relations as well as social support have generally been found to be of key importance for older adults [45]. Reinhardt [46] found that visually impaired older adults nominated on average 5.4 persons of intimate relation within their family network, and 3.5 persons within their friendship network, which is similar to sensory-unimpaired older adults, such as those assessed in the BASE [47]. In addition, in Wahl et al’s study [18], visually and hearing impaired older adults nominated practically the same number of persons as being in the most intimate circle of their social network (4.70 versus 4.71); the respective number in a comparison group of visually unimpaired older adults amounted to 5.2 persons, which was not significantly different from both sensory impaired group means.
Neither vision nor hearing impairment seem to affect the experience of loneliness dramatically [18,23,48], although some research did report an increased risk of loneliness in older adults with vision impairment [49]. It is clear however that hearing impairment more strongly than vision impairment negatively impacts social communication and carries a strong stigma for those affected [48,50]. The stigma particularly implies that hearing deficits and concomitant communication disturbances (eg, giving an answer that does not match the question) elicits the view of a cognitively impaired, if not demented older person. In some contrast, vision loss seems to raise rather strong helping impulses and feelings of compassion. The dark side of this tendency is that it seems a challenge to provide visually impaired older adults with the instrumental support needed while at the same time fostering remaining capabilities [51]. Overprotection may put constraints on the visually impaired older adults’ “true” functional capacity and thereby contribute to loss in competence over the longer run due to disuse [52].
Subjective Well Being–related Outcomes and Depression
Visually impaired older adults have shown evidence of diminished well-being as compared with sensory unimpaired older adults [53], although effect sizes were rather small in a respective meta-analysis [54]. Differences in well-being between hearing impaired and unimpaired older adults seem small or nonexistent in some studies [18,55], but considerable in others [56]. The latter study covering a 16-year observational period as well as other longitudinal work (eg, [57]) also support the notion that remaining ADLs and social engagement mediate the linkage between sensory loss and well-being and depression. The “well-being paradox” in old age, pointing to pronounced adaptive resources to maintain well-being in spite of adverse conditions [58], may also apply to sensory impaired older adults [57,59].
At the same time, it is critical to acknowledge that visually impaired older adults represent an at-risk population, in which the positive impact of human adaptation and the drawback of reaching the limits of psychological resilience go hand in hand. Affect balance (ratio of positive and negative affect) has been found to be more toward the negative pole in visually impaired older adults [60] and depression has consistently been found to be significantly increased in visually impaired older adults [61–63]. Rates roughly vary between 15% and 30% and are particularly high in age-related macular degeneration patients [61]. This is also important, because depressive symptoms may accelerate both cognitive decline and decline in everyday competence in age-related macular degeneration patients [42]. Perceived overprotection may also lead to negative consequences in terms of heightened depression and anxiety over time [64].
Regarding the impact of hearing loss on depression, findings are quite inconsistent. Some studies found evidence for a significant relationship between hearing impairment and depressive symptoms among older adults [65, 66], while others did not [67, 68]. Gopinath and co-workers [66] observed that hearing impaired individuals, particularly women, younger than 70 years of age and those who were infrequently using a hearing aid (less than one hour per day) were more likely to suffer from depressive symptoms. According to a population-based study among older Italians, hearing impairment might be more closely related to anxiety symptoms than to depression [69].
Dual Sensory Impairment
Previous research supports the notion that the overall psychosocial situation of those with dual sensory impairment is even worse as compared to those with sole vision or hearing impairment. In particular, higher rates of ADL/IADL impairment, depression and lowered well-being have been found in older adults affected by dual sensory loss [6,13,18,56]. Also, dual sensory impairment has been found to be linked with cognitive decline cross-sectionally [37] as well as longitudinally [36].
Improving Quality of Life in Sensory Impaired Older Adults
The research summary provided in the previous section underscores that the experience of age-related visual and hearing impairment comes with pronounced challenges that deserve evidence-based professional support. In the following, we give an overview and evaluation of major work in the area of psychosocially framed intervention research targeting older adults with vision and hearing loss. By psychosocially framed interventions we mean studies containing programs that focused on psychosocial processes (eg, consultation on how to better cope with sensory impairment, educative components, problem solving strategies, coping with negative affect) and assessed psychosocial outcomes (eg, everyday functioning, depression, emotional stress experiences). Such interventions may have been integrated into regular rehabilitation programs or offered as a separate strategy in addition to classic rehabilitation. We also consider physical activity–related and overall “way of living” interventions such as tai chi and yoga. In doing so, our aim is to highlight the bandwidth of psychosocial interventions and respective outcomes, not comprehensiveness.
Age-related Vision Impairment
Most psychosocially framed interventions could be characterized as self-management– and disease management–like efforts and are promising for visually impaired older adults. Major elements of such programs include stress-reducing strategies (eg, muscle-relaxation exercises), goal-directed problem-solving, strategies to evoke positive affect, activating available resources, and information and consultation. Typically, such programs are conducted in a group format in an eye clinic, bringing together 6 to 8 visually impaired older adults for weekly sessions of 2 to 3 hours over 6 to 8 weeks.
More recent work provides additional support for the usefulness of self-management programs for visually impaired older adults [72,73]. In addition, emerging evidence supports the notion that psychosocially framed interventions may contribute to saving health costs (eg, via reduced psychopharmacy) and may also enhance commitment
It is also obvious that such programs should find a strong liaison with classic high-caliber rehabilitation programs for visually impaired older adults, including effective reading training [75].
Furthermore, physical training programs, which have proven efficiency with old and very old individuals—including those who are cognitively vulnerable—also seem to be of significant advantage for visually impaired older adults. As has been found, such programs not only increase posture, gait, and general physical fitness, they also prevent falls and enhance well-being, self-efficacy, and cognitive function, especially executive control [76]. Postural control has been improved by multimodal balance and strength exercises among older individuals with visual impairments as well [77]. Participation in physical activity and being in better physical condition buffered the relationship between dual sensory impairment and depression, pointing to the importance of physical training programs for the mental health of older persons with dual sensory impairment [78]. According to a randomized control study as well as to some case studies, tai chi seems to be an effective tool to improve balance control in visually impaired older adults, and thus to reduce an important risk factor for falls [79–81]. Visually impaired adults might also benefit from yoga in terms of balance improvement as well as psychosocial improvements [82]. To teach tai chi efficiently, it is necessary to adapt instructions to the needs of the visually impaired seniors by relying on verbal cuing and manual body placement [80]. The need to adapt instructions and to provide an accessible environment (including transportation arrangements) to motivate older individuals with visual impairments to perform regular physical exercises is also highlighted by Surakka and Kivela [83].
Furthermore, there is evidence that state of the art low vision rehabilitation as such also has beneficial effects on psychosocial outcomes, such as general and vision-related quality of life and emotional well-being.
Age-related Hearing Impairment
Interventions concerning older adults with hearing impairment center on amplification and aural rehabilitation, including auditory training [84]. It has been shown that using hearing aids improves the quality of life, in particular hearing-related quality of life, of hearing impaired adults [85]. Yet many older adults who would benefit from hearing aids do not wear them [86]. From the reasons identified in the review by McCormack and Fortnum [86], perceived hearing aid value, in particular poor benefit in noisy situations, fit and comfort, as well as care and maintenance of the hearing aid emerged as most important. Improvements in these areas are necessary to enhance hearing aid usage among older adults with hearing impairment. Meyer and Hickson [87] identified 5 factors increasing the likelihood to seek help for hearing impairment and/or adopt hearing aids: (1) moderate to severe hearing impairment and perceived hearing-related everyday limitations; (2) older age; (3) poor subjective hearing; (4) perceiving more benefits than barriers to amplification; and (5) perceiving significant others as supportive of hearing rehabilitation. Thus, the involvement of family members in the rehabilitation process appears necessary and promising.
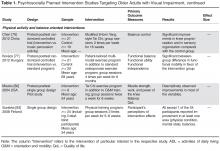
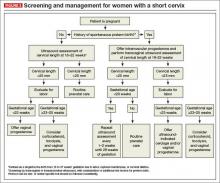
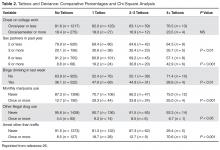
Beyond amplification, aural rehabilitation seeks to improve the situation of hearing impaired older adults by providing listening and communication techniques to enhance communication effectiveness. We have summarized major work in this area in Table 2.
In sum, it seems clear for both vision impairment [95] and hearing impairment [96] that classic rehabilitation strategies, such as fitting a reading device or hearing aid, need significant enrichment by psychosocial training components in order to achieve the best outcomes possible. Furthermore, given the findings on the role of cognitive resources in visually impaired older adults (see respective section above), cognitive training may be an important addition to psychosocial intervention and rehabilitation [38,97]. It must be noted, however, that many of the available studies reveal a number of methodological limitations, such as small sample sizes, missing control condition, and no follow-up assessments to estimate the maintenance of effects.
A significant future need is intervention research addressing older adults with dual sensory impairment. Although we found study protocols related to important trials underway [98,99] and a physical training study with visually impaired older adults that included also some dual sensory impaired individuals [83], it seems that there is not much research in terms of completed interventions and respective findings. Furthermore, it may be important to better involve significant others such as family members and friends in psychosocially framed programs and emerging research with low vision adults has revealed advantages and disadvantages of such an approach [100].
Practical Implications
The older patient is on the way to become the “standard” patient for eye care and hearing specialists and thus a challenge for public health at large. Based on the evidence compiled above, we argue that best practice in medical treatment and traditional rehabilitation of vision and hearing impairment should better consider the psychosocial dimension of age-related vision and hearing impairment. We see different levels at which a stronger psychosocially framed input is needed. First, at the diagnostic level, having a better understanding of everyday competence, the role of cognitive functioning, social resources, and well-being–related dynamics in visually impaired and hearing impaired older adults may significantly enrich the professional background knowledge about the patient. Such knowledge may become important for diagnostic evaluation, treatment decisions, and predictions of long-term outcomes. It seems also critical to have an understanding of the more fundamental mechanisms and systemic inter-relations in older patients (eg, among visual, hearing, mobility, and cognitive impairment), because such evidence helps to evaluate overall vulnerability and likely future trajectories of respective patients.
Second, at the intervention level against the background of the available empirical effectiveness evidence, self-management–oriented and psycho-educative programs should become a regular component of low vision rehabilitation. Similarly, psychosocial programs educating older adults in hearing tactics and hearing loss–oriented coping strategies should become a regular part of hearing rehabilitation. In addition, we argue that cognitive training and physical activity–oriented interventions should have their place in rehabilitation programs designed for older visually and hearing impaired adults. The major reason is that respective programs generally have been found to positively impact quality of life in old age. This impact may be particularly valuable for more vulnerable populations, such as sensory impaired older adults. We therefore recommend implementing psychosocially framed programs as a regular service in eye clinics as well as in ear, nose, and throat clinics, because this seems to be the setting best suited to approach visually and hearing impaired older adults as well as to offer the logistic opportunities to conduct such programs. It would also be critical to extend such programs to in-home services as well as services covering long-term care settings. Older adults with dual sensory impairment bring specific challenges to such interventions, such as the optimal cooperation and combination of rehabilitation and psychosocial expertise related to each domain and traditionally offered side by side. It is also good news that new trials are underway to learn more about psychosocial interventions aimed to address older adults with dual sensory loss [98,99].
In conclusion, we argue for a better implementation of both age-related psycho-ophthalmology as well as psycho-audiology. Although we regard psychologists with a clinical training background as a key profession to be involved in psychosocially framed interventions with older adults with vision and hearing impairment, other professions (eg, occupational therapists, sport scientists) should also play an important role. A multiprofessional enrichment of classic sensory rehabilitation based on the training principles as described above is a major future need.
Corresponding author: Vera Heyl, PhD, Zeppelinstr, 1, D-69121, Heidelberg, Germany, [email protected].
Financial disclosures: None.
1. Oeppen J, Vaupel JW. Broken limits to life expectancy. Science 2002;296:1029–31.
2. Eichenbaum JW. Geriatric vision loss due to cataracts, macular degeneration, and glaucoma. Mt Sinai J Med 2012;79:276–94.
3. Ciorba A, Bianchini C, Pelucchi S, et al. The impact of hearing loss on the quality of life of elderly adults. Clin Interven Aging 2012;7:159–63.
4. WHO - World Health Organization and International Agency for the Prevention of Blindness. Developing an action plan to prevent blindness at national, provincial and district levels. Vision 2020 The right to sight. Geneva: World Health Organization; 2004.
5. WHO - World Health Organizaton. Grades of hearing impairment. Geneva: World Health Organization; 2013.
6. Schneider JM, Gopinath B, McMahon CM, et al. Dual sensory impairment in older age. J Aging Health 2011;23:1309–24.
7. Clay OJ, Wadley VG, Edwards JD, et al. Cumulative meta-analysis of the relationship between useful field of view and driving performance in older adults: current and future implications. Optom Vis Sci 2005;82:724–31.
8. Seland JH, Vingerling JR, Augood CA, et al. Visual Impairment and quality of life in the Older European Population, the EUREYE study. Acta Ophthal 2011;89:608–13.
9. Horowitz A, Brennan M, Reinhardt JP. Prevalence and risk factors for self-reported visual impairment among middle-aged and older adults. Research Aging 2005;27:307–26.
10. Gopinath B, Rochtchina E, Wang JJ, et al. Prevalence of age-related hearing loss in older adults: Blue mountains study. Arch Intern Med 2009;169:415–6.
11. Roth TN, Hanebuth D, Probst R. Prevalence of age-related hearing loss in Europe: a review. Eur Arch Otorhinolaryngol 2011;268:1101–7.
12. Lin FR, Thorpe R, Gordon-Salant S, et al. Hearing loss prevalence and risk factors among older adults in the United States. J Gerontol Series A: Biolog Sci Med Sci 2011;66A:582–90.
13. Brennan M, Horowitz A, Su Y-p. Dual sensory loss and its impact on everyday competence. Gerontologist 2005;45:337–46.
14. Anstey KJ, Luszcz MA, Giles LC, et al. Demographic, health, cognitive, and sensory variables as predictors of mortality in very old adults. Psychol Aging 2001;16:3–11.
15. Appollonio I, Carabellese C, Magni E, et al. Sensory impairments and mortality in an elderly community population: A six-year follow-up study. Age Ageing 1995;24:30–6.
16. McCarty CA, Nanjan MB, Taylor HR. Vision impairment predicts 5 year mortality. Br J Ophthalmol 2001;85:322–6.
17. Ostbye T, Steenhuis R, Wolfson C, et al. Predictors of five-year mortality in older Canadians: the Canadian Study of Health and Aging. J Am Geriatr Soc 1999 47:1249–54.
18. Wahl H-W, Heyl V, Drapaniotis PM, et al. Severe vision and hearing impairment and successful aging: A multidimensional view. Gerontologist 2013;53:950–62.
19. Fisher D, Li C-M, Chiu MS, et al. Impairments in hearing and vision impact on mortality in older people: the AGES-Reykjavik Study. Age Ageing 2013.
20. Bamini G, Schneider J, McMahon CM, et al. Dual sensory impairment in older adults inceases the risk of mortality: A population-based study. PLoS ONE 2013;8:1–6.
21. Lam BL, Lee DJ, Gómez-Marín O, et al. Concurrent visual and hearing impairment and risk of mortality: The National Health Interview Survey. Arch Ophthalmol 2006;124:95–101.
22. Baltes MM, Maas I, Wilms H-U, et al. Everyday competence in old and very old age: Theoretical considerations and empirical findings. In: Baltes PB, Mayer K-U, editors. The Berlin Aging Study Cambridge, UK: Cambridge University Press; 1999: 384–402.
23. Burmedi D, Becker S, Heyl V, et al. Behavioral consequences of age-related low vision: A narrative review. Vis Impair Res 2002;4:15–45.
24. Wahl H-W, Heyl V, Schilling O. Robustness of personality and affect relations under chronic conditions: the case of age-related vision and hearing impairment. J Gerontol B Psycholog Sci Soc Sci 2012;67:687–96.
25. Heyl V, Wahl H-W. On the long-term psychosocial adaptation to vision loss in the later years. In: Wahl H-W, Schulze H-E, editors. On the special needs of blind and low vision seniors: Research and practice concepts. Amsterdam: IOS-Press; 2001: 77–83.
26. Wahl H-W, Schilling O, Oswald F, et al. Psychosocial consequences of age-related visual impairment: Comparison with mobility-impaired older adults and long-term outcome. J Gerontol Psych Sci Soc Sci 1999;54B:P304–P16.
27. Wahl H-W, Becker S, Burmedi D, et al. The role of primary and secondary control in adaptation to age-related vision loss: A study of older adults with macular degeneration Psychol Aging 2004;19:235–9.
28. Rudberg MA, Furner SE, Dunn JE, et al. The relationship of visual and hearing impairments to disability: An analysis using the Longitudinal Study of Aging. J Gerontol Med Sci 1993;48:M261–M5.
29. Schneider J, Gopinath B, Karpa MJ, et al. Hearing loss impacts on the use of community and informal supports. Age Ageing 2010;39:458–64.
30. Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-item National Eye Institute visual function questionnaire. Arch Ophthalmol 2001;119:1050–8.
31. Ventry I, Weinstein B. The hearing handicap inventory for the elderly: A new tool. Ear Hearing 1982;3:128–34.
32. Lindenberger U, Baltes PB. Sensory functioning and intelligence in old age: A strong connection. Psychol Aging 1994;9:339–55.
33. Clay OJ, Edwards JD, Ross LA, et al. Visual function and cognitive speed of processing mediate age-related decline in memory span and fluid intelligence. J Aging Health 2009;21:547–66.
34. Salthouse TA, Hancock HE, Meinz EJ, et al. Interrelations of age, visual acuity, and cognitive functioning. J Gerontol Psychol Sci 1996;51B:P317–P30.
35. Baltes PB, Lindenberger U. Emergence of powerful connection between sensory and cognitive functions across the adult life span: A new window to the study of cognitive aging? Psychol Aging 1997;12:12–21.
36. Lin MY, Gutierrez PR, Stone KL, et al. Vision impairment and combined vision and hearing impairment predict cognitive and functional decline in older women. J Am Geriatr Soc 2004;52:1996–2002.
37. Tay T, Wang JJ, Kifley A, et al. Sensory and cognitive association in older persons: Findings from an older Australian population. Gerontology 2006;52:386–94.
38. Heyl V, Wahl H-W. Managing daily life with age-related sensory loss: Cogni-tive resources gain in importance. Psychol Aging 2012;27:510–21.
39. Lindenberger U, Ghisletta P. Cognitive and sensory declines in old age: Gauging the evidence for a common cause. Psychol Aging 2009;24:1-16.
40. Heyl V, Wahl H-W, Mollenkopf H. Visual capacity, out-of-home activities and emotional well-being in old age: Basic relations and contextual variation. Soc Indicat Res 2005;74:159–89.
41. Heyl V, Wahl H-W. Cognitive ability as a resource for everyday functioning among older adults who are visually impaired. J Vis Impair Blind 2010;104:391–403.
42. Rovner BW, Casten RJ, Leiby BE. Variability in depressive symptoms predicts cognitive decline in age-related macular degeneration. Am J Geriatr Psych 2009;17:574–81
43. Rovner BW, Casten RJ, Leiby BE, et al. Activity loss is associated with cognitive decline in age-related macular degeneration. Thomas Jefferson University, Department of Psychiatry and Human Behavior, Faculty Papers. Paper 5. 2009.
44. Lövdén M, Ghisletta P, Lindenberger U. Social participation attenuates decline in perceptual speed in old and very old age. Psych Aging 2005;20:423–34.
45. Antonucci TC. Social relations. An examination of social networks, social support, and sense of control. In: Birren JE, Schaie KW, editors. Handbook of the psychology of aging. 5th ed. San Diego: Academic Press; 2001: 427–53.
46. Reinhardt JP. The importance of friendship and family support in adaptation to chronic vision impairment. J Gerontol Series B Psychol Sci Soc Sci 1996;51B:P268–P78.
47. Wagner M, Schütze Y, Lang FR. Social relationships in old age. In: Baltes PB, Mayer KU, editors. The Berlin Aging Study Aging from 70 to 100. Cambridge, UK: Cambridge University Press; 1999: 282–301.
48. Wahl H-W, Tesch-Römer C. Aging, sensory loss, and social functioning. In: Charness N, Park D, Sabel B, editors. Aging and communication: Opportunities and challenges of technology. New York: Springer; 2001: 108-26.
49. Nachtegaal J, Smit JH, Smits C, et al. The association between hearing status and psychosocial health before the age of 70 years: Results from an internet-based national survey on hearing. Ear Hearing 2009;30:302-12
50. Wallhagen MI. The stigma of hearing loss. Gerontologist 2010;50:66–75.
51. Cimarolli VR, Boerner K. Social support and well-being in adults who are visually impaired. J Vis Impair Blind 2005 99:521–34.
52. Cicirelli VG. Fear of death in mid-old age. J Gerontol Series B Psychol Sci Soc Sci 2006;61:P75–P81.
53. Horowitz A, Reinhardt JP. Depression among low vision elders. In: Stuen. C, Arditi A, Horowitz A, et al, editors. Vision rehabilitation assessment, intervention and outcomes. Lisse: Swets & Zeitlinger Publishers; 2000: 655–8.
54. Pinquart M, Pfeiffer JP. Psychological well-being in visually impaired and unimpaired individuals: A meta-analysis. Br J Vis Impair 2011;29:27–45.
55. Tesch-Römer C. Schwerhörigkeit im Alter. Belastung, Bewältigung, Rehabilitation. Heidelberg: Median-Verlag; 2001.
56. Kiely KM, Anstey KJ, Luszcz MA. Dual sensory loss and depressive symptoms: the importance of hearing, daily functioning, and activity engagement. Front Hum Neurosci 2013;7:1–13.
57. Schilling OK, Wahl H-W, Horowitz A, et al. The adaptation dynamics of chronic functional impairment: What we can learn from older adults with vision loss. Psychol Aging 2011;26:203–13.
58. Kunzmann U, Little T, Smith J. Is age-related stability of subjective well-being a paradox? Cross-sectional and longitudinal evidence from the Berlin Aging Study. Psychol Aging 2000;15:511-26.
59. Schilling O, Wahl H-W. Modeling late life adaptation in affective well-being under a severe chronic health condition: The case of age-related macular degeneration. Psychol Aging. 2006;21:703–14.
60. Wahl H-W, Schilling O, Becker S, et al. A German research program on the psychosocial adaptation to age-related vision impairment: Recent findings based on a control theory approach. Europ Psychol 2003;8:168-77.
61. Casten R, Rovner B. Depression in age-related macular degeneration. J Visual Impair Blind 2008;102:591-9.
62. Crews JE, Campbell VA. Vision impairment and hearing loss among community-dwelling older Americans: implications for health and functioning. Am J Pub Health 2004;94:823–9.
63. Horowitz A, Reinhardt JP, Boerner K. The effect of rehabilitation on depression among visually disabled older adults. Aging Mental Health 2005;9:563–70.
64. Cimarolli VR. Perceived overprotection and distress in adults with visual impairment. Rehabil Psychol 2006;51:338-45.
65. Ishine M, Okumiya K, Matsubayashi K. A close association between hearing impairment and activities of daily living, depression, and quality of life in community-dwelling older people in Japan. J Am Geriatr Soc 2007;55:316-7.
66. Gopinath B, Wang JJ, Schneider J, et al. Depressive symptoms in older adults with hearing impairments: The Blue Mountains Study. J Am Geriatr Soc 2009;57:1306-8.
67. Chou K-L, Chi I. Combined effect of vision and hearing impairment on depression in elderly Chinese. Int J Geriatr Psych 2004;19:825-32.
68. Tambs K. Moderate effects of hearing loss on mental health and subjective well-being: Results from the Nord-Trøndelag Hearing Loss Study. Psychosom Med 2004;66:776-82.
69. Bernabei V, Morini V, Moretti F, et al. Vision and hearing impairments are associated with depressive--anxiety syndrome in Italian elderly. Aging Ment Health 2011 15:467-74.
70. Wahl H-W, Heyl V, Langer N. Lebensqualität bei Seheinschränkung im Alter: Das Beispiel altersabhängige Makuladegeneration [Quality of life by limited vision in old age: the example of age-related macula degeneration]. Der Ophthalmologe 2008;105:735-43.
71. Wahl H-W, Kämmerer A, Holz F, et al. Psychosocial intervention for age-related macular degeneration: A pilot project. J Vis Impair Blind 2006;100:533-44.
72. Rees G, Keeffe JE, Hassell J, et al. A self-management program for low vision: Program overview and pilot evaluation. Disabil Rehab 2010;32:808-15.
73. Rovner BW, Casten RJ. Preventing late-life depression in age-related macular degeneration. Am J Geriatr Psych 2008;16:454-9
74. Eklund K, Sonn U, Nystedt P, et al. A cost-effectiveness analysis of a health education programme for elderly persons with age-related macular degeneration: A longitudinal study. Disabil Rehab 2005;27:1203-12.
75. Pijnacker J, Verstraten P, van Damme W, et al. Rehabilitation of reading in older individuals with macular degeneration: A review of effective training programs. Aging Neuropsych Cognition. 2011;18:708-32.
76. Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: A meta-analytic study. Psychol Sci 2003;14:125-30.
77. Kovács É, Tóth K, Dénes L, et al. Effects of exercise programs on balance in older women with age-related visual problems: A pilot study. Arch Gerontol Geriatr 2012;55:446-52.
78. McDonnall MC. Physical status as a moderator of depressive symptoms among older adults with dual sensory loss. Rehab Psychol 2011;56:67-76.
79. Chen EW, Fu ASN, Chan KM, et al. The effects of Tai Chi on the balance control of elderly persons with visual impairment: a randomised clinical trial. Age Ageing 2012;41:254-9.
80. Miszko TA, Ramsey VK, Blasch BB. Tai Chi for people with visual impairments: a pilot study. J Vis Impair Blind 2004;98:5-13.
81. Ray C, Horvat M, Keen K, et al. Using Tai Chi as an exercise intervention for improving balance in adults with visual impairments: Two case studies. RE:view 2005;37:17-24.
82. Jeter PE, Dagnelie G, Khalsa SBS, et al. Yoga for persons with severe visual impairment: a feasibility study. Altern Med Stud 2012;2:18-25.
83. Surakka A, Kivela T. Motivating visually impaired and deaf-blind people to perform regular physical exercises. Br J Visual Impair 2008;26:255-68.
84. Li-Korotky H-S. Age-related hearing loss: Quality of care for quality of life. Gerontologist 2012;52:265-71.
85. Chisolm TH, Johnson CE, Danhauer JL, et al. A systematic review of health-related quality of life and hearing aids: Final report of the American Academy of Audiology Task Force on the Health-Related Quality of Life Benefits of Amplification in Adults. J Am Acad Audiol 2007;18:151-83.
86. McCormack A, Fortnum H. Why do people fitted with hearing aids not wear them? Int J Audiol 2013 52:360-8.
87. Meyer C, Hickson L. What factors influence help-seeking for hearing impairment and hearing aid adoption in older adults? Int J Audiol 2012;51:66-74.
88. Andersson G, Green M, Melin L. Behavioural hearing tactics: a controlled trial of a short treatment programme. Behav Res Ther 1997;35:523-30.
89. Andersson G, Melin L, Scott B, et al. Behavioural counselling for subjects with acquired hearing loss. A new approach to hearing tactics. Scandinav Audiol 1994;23:249-56.
90. Burk MH, Humes LE. Effects of long-term training on aided speech-recognition performance in noise in older adults. J Speech Lang Hear Res 2008;51:759-71.
91. Henderson Sabes J, Sweetow RW. Variables predicting outcomes on listening and communication enhancement (LACETM) training. Int J Audiol 2007;46:374-83.
92. Kramer SE, Allessie GH, Dondorp AW, et al. A home education program for older adults with hearing impairment and their significant others: a randomized trial evaluating short- and long-term effects. Int J Audiol 2005;44:255-64.
93. Hickson L, Worrall L, Scarinci N. Measuring outcomes of a communication program for older people with hearing impairment using the International Outcome Inventory. Int J Audiol 2006;45:238-46.
94. Barcroft J, Sommers MS, Tye-Murray N, et al. Tailoring auditory training to patient needs with single and multiple talkers: Transfer-appropriate gains on a four-choice discrimination test. Int J Audiol 2011;50:802-8.
95. Wahl H-W. The psychological challenge of late-life vision impairment: Concepts, Findings, and practical implications. J Ophthalmol 2013.
96. Lin FR. Hearing loss in older adults. Who’s listening? JAMA 2012;307:1147-8.
97. Willis SL, Tennstedt SL, Marsiske M, et al. Long-term effects of cognitive training on everyday functional outcomes in older adults. JAMA 2006;296:2805-14.
98. Roets-Merken LM, Graff MJL, Zuidema SU, et al. Effectiveness of a self-management program for dual sensory impaired seniors in aged care settings: study protocol for a cluster randomized controlled trial. Trials 2013;14.
99. Vreeken HL, van Rens GHMB, Kramer SE, et al. Dual sensory loss: development of a dual sensory loss protocol and design of a randomized controlled trial. BMC Geriatr 2013;13.
100. Rees G, Saw C, Larizza M, et al. Should family and friends be involved in group-based rehabilitation programs for adults with low vision? Br J Visual Impair 2007;25:155-68.
101. Birk T, Hickl S, Wahl H-W, et al. Development and pilot evaluation of a psychosocial intervention program for patients with age-related macular degeneration. Gerontologist 2004;44:836-43.
102. Bradley P, Mitchell J, Bradley C, editors. Peer support for people newly diagnosed with macular degeneration: a pilot study. International Congress Vision 2005 September. London, UK.
103. Brody B, Williams R, Thomas R, et al. Age-related macular degeneration: A randomized clinical trial of a self-management intervention. Ann Behavi Med 1999;21:322-9.
104. Brody BL, Roch-Levecq A-C, Gamst AC, et al. Self-management of age-related macular degeneration and quality of life: a randomized controlled trial. Arch Ophthalmol 2002;120:1477-83.
105. Brody BL, Roch-Levecq A-C, Thomas RG, et al. Self-management of age-related macular degeneration at the 6-month follow-up. a randomized controlled trial. Arch Ophthalmol 2005;123:46-53.
106. Brody BL, Roch-Levecq A-C, Kaplan RM, et al. Age-related macular degeneration: self-management and reduction of depressive symptoms in a randomized, controlled study. J Am Geriatr Soc 2006;54:1557-62.
107. Dahlin-Ivanoff S, Sonn U, Svensson E. A health education program for elderly persons with visual impairments and perceived security in the performance of daily occupations: a randomized study. Am J Occup Thera 2002;56:322-30.
108. Eklund K, Sonn U, Dahlin-Ivanoff S. Long-term evaluation of a health education programme for elderly persons with visual impairment. A randomized study. Disabil Rehab 2004;26:401-9.
109. Eklund K, Dahlin-Ivanoff S. Health education for people with macular degeneration: Learning experiences and the effect on daily occupations. Can J Occup Ther 2006;73:272-80.
110. Eklund K, Sjöstrand J, Dahlin-Ivanoff S. A randomized controlled trial of a health-promotion programme and its effect on ADL dependence and self-reported health problems for the elderly visually impaired. Scand J Occupat Ther 2008;15:68-74.
111. Kämmerer A, Wahl H-W, Becker S, et al. Psychosoziale Unterstützung von älteren Menschen mit einer chronischen Sehbeeinträchtigung: Anwendung und Überprüfung einer problemlöse- und einer emotionsfokussierten Kurzintervention. Zeitschrift für Gesundheitspsychologie 2006;14:95-105.
112. Rovner BW, Casten RJ, Hegel MT, et al. Preventing depression in age-related macular degeneration. Arch Gen Psychiatr 2007;64:886-92.
113. Rovner BW, Casten RJ, Hegel MT, et al. Improving function in age-related macular degeneration: A randomized clinical trial. Ophthalmology 2013;120:1649-55.
114. Barcroft J, Mauzé E, Schroy C, et al. Improving the quality of auditory training by making tasks meaningful. Persp Audiol 2011;7:15-28.
From the University of Education (Dr. Heyl) and Heidelberg University (Dr. Wahl), Heidelberg, Germany.
Abstract
- Objective: To summarize the current state of research regarding the experience of age-related vision and hearing impairment.
- Methods:Review of the literature.
- Results: Negative consequences of age-related vision and hearing impairment manifest in the domains of health and longevity, everyday competence, cognitive functioning, social functioning, and subjective well-being. However, while vision impairment strongly impacts everyday competence, the burden of hearing impairment can mainly be found in the social domain. Psychosocially framed intervention research has shown promising findings, but many studies rely on small samples or do not include a control condition.
- Conclusions: Although more research is needed, it is clear that traditional rehabilitation programs targeting age-related vision and hearing impairments need a strong psychosocial component.
Vision and hearing are essential for person–environment interaction and both are subject to pronounced age-related changes. Ongoing demographic changes and increasing life expectancy is contributing to a significant increase in the number of very old individuals [1]. It is projected that by 2030 about 50% of older Americans may have some significant eye disease, ie, cataract, glaucoma, or age-related macular degeneration [2]. Presbycusis as the major cause of age-related hearing impairment is present in 40% of the American senior citizens [3]. In this narrative review, we review the epidemiological data on age-related vision and hearing impairment, research on its psychosocial impact, and intervention research aimed to improve coping processes and rehabilitative outcomes. We close with future recommendations directed both toward research and clinical practice.
Epidemiology
Vision and hearing impairment is highly prevalent in old age, yet prevalence rates reported in the literature are quite different, depending on the definition of vision and hearing impairment used. A widely used criterion for low vision is the one used by the World Health Organization, ie, visual acuity less than 20/60 and equal to or better than 20/400 in the better eye with best correction. A best corrected visual acuity of less than 20/400 in the better eye is used to define blindness [4]. A disabling hearing impairment is defined by an average hearing loss in decibel (dB HL) of at least 41 dB HL at 500, 1000, 2000, and 4000 Hz. [5]. Translated to everyday life, such hearing impairment mainly manifests in severe difficulties in understanding normal conversation. Besides differing definitions, different methods to assess vision and hearing impairment and heterogenous study populations make comparisons of prevalence rates difficult [6]. In particular, relying solely on self-report data to assess vision and hearing loss seems generally problematic. In addition, the strong focus in vision impairment assessment on visual acuity measures has limitations, as other indicators, such as contrast sensitivity or useful field of vision, may be more important for out-of-home mobility or driving [7].
A recent study on the prevalence of visual impairment (defined as best corrected visual acuity < 20⁄40) in 6 European countries found quite similar prevalence rates as reported for the US: Prevalence of visual impairment was 3% in those aged 65 to 74 years, 13% in those over 75 years and 33% in those over 85 years [8]. At first glance, vision loss seems to be more prevalent among older women than among older men, but this relationship is not sustained in multivariate analyses considering age, health, and social support variables [9].
Regarding hearing loss, Gopinath et al [10] found prevalence rates of 29% among men and 17% among women aged 60 to 69 years. Moreover, for every 10 years of age, the prevalence of hearing loss doubled. In their review of epidemiologic data on prevalence of age-related hearing impairment in Europe, Roth and coauthors [11] report that at the age of 70 years, about 30% of men and 20% of women were found to have a hearing loss of at least 30 dB HL, while at the age of 80 years about 55% of men and 45% of women were affected. Lin et al found that 63% of those 70 years and older had a hearing loss of more than 25 dB in the better ear [12].
According to a recent review by Schneider et al [6], prevalence of impairment in both vision and hearing in older age (dual sensory impairment) varies between 1.6% and 22.5% due to different sample characteristics (eg, size, age) and different definitions and assessments of vision and hearing impairment (see also [13]). However, there is good evidence that dual sensory impairment increases with age, and that it is more common among frailer subpopulations such as older individuals consulting care services [6].
Quality of Life Impact of Vision and Hearing Impairment
Health and Longevity
There is inconsistent evidence that both age-related vision and hearing impairment are accompanied by heightened multimorbidity and an increased mortality rate. For example, while some older as well as more recent studies have found that visual and hearing declines over time predict death in very old age [14–16], other studies have detected no significant relationship after adjusting for confounders such as age, gender, and education [17,18]. Among the hearing impaired, only men seem to have a significant increase in mortality risk [15,19]. Dual sensory impairment appears to be more consistently and more strongly related to increased mortality than vision or hearing impairment alone [19–21].
Everyday Competence
The term everyday competence includes both basic (eg, self-care behaviors) and instrumental (eg, using public transport) activities of daily living (ADL/IADL [22]). Age-related vision impairment has been found to be robustly associated with significantly lower everyday competence, because visual capacity is a critical prerequisite for such behaviors [23,24]. Indeed, lowered everyday competence appeared as the best of a range of variables (including cognitive function and well-being–related measures) used to differentiate between visually impaired and visually unimpaired older adults [18]. Furthermore, vision impairment impacts cross-sectionally as well as longitudinally—more strongly on IADL as compared to ADL—because the execution of IADL is more complex and depends more strongly on environmental enhancing or hindering factors [25–27]. Hence, shrinkage in IADL competence reflects a kind of early behavioral marker of severe vision impairment, whereas significant ADL decrease only happens later in the process of chronic vision loss.
In contrast to vision impairment, age-related hearing loss has been found not to have a major impact in particular on ADL/IADL [28]. However, as has been found elsewhere [29], hearing loss is associated with increased reliance on community and informal supports, suggesting that while IADL function may not deteriorate with hearing loss, the way it is conducted may change (ie, need for support to maintain participation).
It should also be mentioned in this context that assessment strategies have been developed to better consider the specific life conditions of those with vision and hearing impairment. The best-known and frequently applied instruments in this context are the National Eye Institute Visual Function Questionnaire [30] and the Hearing Handicap Inventory for the Elderly [31].
Cognitive Functioning
Previous research largely supports the notion that reduced vision and hearing function is accompanied by a decrease in cognitive performance in older adults. The work of Lindenberger and Baltes, based on the Berlin Aging Study (BASE)—but also including additional studies with a wider age-range—is central in supporting a strong connection among vision, hearing, balance, and cognitive functioning in later life. Lindenberger and Baltes [32] found that general intelligence correlated just as strongly with visual as with auditory ability. In a model conjoining age, sensory function, as well as intelligence, visual and auditory function predicted a large portion of interindividual differences in intelligence and indeed fully mediated the negative correlation between age and intelligence. This finding has meanwhile been replicated by a number of other research groups and may be regarded as rather robust [33,34]. In addition, Baltes and Lindenberger [35] observed that sensory measures were better predictors of intelligence than socio-structural variables such as education or social class. They also showed that the connection among sensory functioning and intelligence was much closer in older adults as compared to adults in early and middle adulthood [34].
No clear difference between the sensory modalities of vision and hearing has been identified regarding their relationship with cognitive performance. On the one hand, there is research supporting the view that both vision and hearing impairment are connected with cognitive decline [12,36,37], while some evidence also supports that the linkage may be stronger with vision [14]. On the other hand, there are also data not supporting a close connection between vision and hearing impairment and cognitive function [38]. Explanations for such inconsistencies may refer to a number of reasons, such as pronounced positive selectivity of samples (which may lead to underestimation of connections among sensory and cognitive function), the application of established cognitive tests not appropriate for sensory impaired older adults (which may lead to overestimation of connections among sensory and cognitive function), and the application of different cut-off scores for significant vision and hearing impairment (possibly, higher cut-offs may lead to higher, lower to lower connections). Longitudinal data using the latest in causal modeling data analysis support the view that the causal dynamics involved in sensory and intelligence change are complex and that each of these variables can drive change in the other across longer periods of later life [39].
Vision status also plays a role when it comes to the connection between cognitive function and everyday competence—a linkage that is generally challenged as people age and that may lead to endpoints such as dependence on others and transition to long-term care. Heyl et al [40] observed that the link between vision status and out-of-home leisure activities is mediated by cognitive status. In a more recent study, able to add to the understanding of such a mediation process, Heyl and Wahl [38,41] showed that the connection between cognitive function and everyday function is much closer in visually and hearing impaired older adults as compared with visually unimpaired older adults, which possibly means that both visually and hearing impaired elders rely more intensely on their cognitive resources. Causality dynamics may however also work in the opposite direction. As Rovner and colleagues [42,43] observed in a study with age-related macular degeneration patients over 64 years of age covering a 3-year observation period and 2 measurement occasions, activity loss over time due to the visual loss led to cognitive decline happening between T1 and T2. This finding fits well with the more general finding in the cognitive aging literature that the exertion of social and leisure activities is important for maintaining cognitive functioning [44].
Social Functioning
Social relations as well as social support have generally been found to be of key importance for older adults [45]. Reinhardt [46] found that visually impaired older adults nominated on average 5.4 persons of intimate relation within their family network, and 3.5 persons within their friendship network, which is similar to sensory-unimpaired older adults, such as those assessed in the BASE [47]. In addition, in Wahl et al’s study [18], visually and hearing impaired older adults nominated practically the same number of persons as being in the most intimate circle of their social network (4.70 versus 4.71); the respective number in a comparison group of visually unimpaired older adults amounted to 5.2 persons, which was not significantly different from both sensory impaired group means.
Neither vision nor hearing impairment seem to affect the experience of loneliness dramatically [18,23,48], although some research did report an increased risk of loneliness in older adults with vision impairment [49]. It is clear however that hearing impairment more strongly than vision impairment negatively impacts social communication and carries a strong stigma for those affected [48,50]. The stigma particularly implies that hearing deficits and concomitant communication disturbances (eg, giving an answer that does not match the question) elicits the view of a cognitively impaired, if not demented older person. In some contrast, vision loss seems to raise rather strong helping impulses and feelings of compassion. The dark side of this tendency is that it seems a challenge to provide visually impaired older adults with the instrumental support needed while at the same time fostering remaining capabilities [51]. Overprotection may put constraints on the visually impaired older adults’ “true” functional capacity and thereby contribute to loss in competence over the longer run due to disuse [52].
Subjective Well Being–related Outcomes and Depression
Visually impaired older adults have shown evidence of diminished well-being as compared with sensory unimpaired older adults [53], although effect sizes were rather small in a respective meta-analysis [54]. Differences in well-being between hearing impaired and unimpaired older adults seem small or nonexistent in some studies [18,55], but considerable in others [56]. The latter study covering a 16-year observational period as well as other longitudinal work (eg, [57]) also support the notion that remaining ADLs and social engagement mediate the linkage between sensory loss and well-being and depression. The “well-being paradox” in old age, pointing to pronounced adaptive resources to maintain well-being in spite of adverse conditions [58], may also apply to sensory impaired older adults [57,59].
At the same time, it is critical to acknowledge that visually impaired older adults represent an at-risk population, in which the positive impact of human adaptation and the drawback of reaching the limits of psychological resilience go hand in hand. Affect balance (ratio of positive and negative affect) has been found to be more toward the negative pole in visually impaired older adults [60] and depression has consistently been found to be significantly increased in visually impaired older adults [61–63]. Rates roughly vary between 15% and 30% and are particularly high in age-related macular degeneration patients [61]. This is also important, because depressive symptoms may accelerate both cognitive decline and decline in everyday competence in age-related macular degeneration patients [42]. Perceived overprotection may also lead to negative consequences in terms of heightened depression and anxiety over time [64].
Regarding the impact of hearing loss on depression, findings are quite inconsistent. Some studies found evidence for a significant relationship between hearing impairment and depressive symptoms among older adults [65, 66], while others did not [67, 68]. Gopinath and co-workers [66] observed that hearing impaired individuals, particularly women, younger than 70 years of age and those who were infrequently using a hearing aid (less than one hour per day) were more likely to suffer from depressive symptoms. According to a population-based study among older Italians, hearing impairment might be more closely related to anxiety symptoms than to depression [69].
Dual Sensory Impairment
Previous research supports the notion that the overall psychosocial situation of those with dual sensory impairment is even worse as compared to those with sole vision or hearing impairment. In particular, higher rates of ADL/IADL impairment, depression and lowered well-being have been found in older adults affected by dual sensory loss [6,13,18,56]. Also, dual sensory impairment has been found to be linked with cognitive decline cross-sectionally [37] as well as longitudinally [36].
Improving Quality of Life in Sensory Impaired Older Adults
The research summary provided in the previous section underscores that the experience of age-related visual and hearing impairment comes with pronounced challenges that deserve evidence-based professional support. In the following, we give an overview and evaluation of major work in the area of psychosocially framed intervention research targeting older adults with vision and hearing loss. By psychosocially framed interventions we mean studies containing programs that focused on psychosocial processes (eg, consultation on how to better cope with sensory impairment, educative components, problem solving strategies, coping with negative affect) and assessed psychosocial outcomes (eg, everyday functioning, depression, emotional stress experiences). Such interventions may have been integrated into regular rehabilitation programs or offered as a separate strategy in addition to classic rehabilitation. We also consider physical activity–related and overall “way of living” interventions such as tai chi and yoga. In doing so, our aim is to highlight the bandwidth of psychosocial interventions and respective outcomes, not comprehensiveness.
Age-related Vision Impairment
Most psychosocially framed interventions could be characterized as self-management– and disease management–like efforts and are promising for visually impaired older adults. Major elements of such programs include stress-reducing strategies (eg, muscle-relaxation exercises), goal-directed problem-solving, strategies to evoke positive affect, activating available resources, and information and consultation. Typically, such programs are conducted in a group format in an eye clinic, bringing together 6 to 8 visually impaired older adults for weekly sessions of 2 to 3 hours over 6 to 8 weeks.
More recent work provides additional support for the usefulness of self-management programs for visually impaired older adults [72,73]. In addition, emerging evidence supports the notion that psychosocially framed interventions may contribute to saving health costs (eg, via reduced psychopharmacy) and may also enhance commitment
It is also obvious that such programs should find a strong liaison with classic high-caliber rehabilitation programs for visually impaired older adults, including effective reading training [75].
Furthermore, physical training programs, which have proven efficiency with old and very old individuals—including those who are cognitively vulnerable—also seem to be of significant advantage for visually impaired older adults. As has been found, such programs not only increase posture, gait, and general physical fitness, they also prevent falls and enhance well-being, self-efficacy, and cognitive function, especially executive control [76]. Postural control has been improved by multimodal balance and strength exercises among older individuals with visual impairments as well [77]. Participation in physical activity and being in better physical condition buffered the relationship between dual sensory impairment and depression, pointing to the importance of physical training programs for the mental health of older persons with dual sensory impairment [78]. According to a randomized control study as well as to some case studies, tai chi seems to be an effective tool to improve balance control in visually impaired older adults, and thus to reduce an important risk factor for falls [79–81]. Visually impaired adults might also benefit from yoga in terms of balance improvement as well as psychosocial improvements [82]. To teach tai chi efficiently, it is necessary to adapt instructions to the needs of the visually impaired seniors by relying on verbal cuing and manual body placement [80]. The need to adapt instructions and to provide an accessible environment (including transportation arrangements) to motivate older individuals with visual impairments to perform regular physical exercises is also highlighted by Surakka and Kivela [83].
Furthermore, there is evidence that state of the art low vision rehabilitation as such also has beneficial effects on psychosocial outcomes, such as general and vision-related quality of life and emotional well-being.
Age-related Hearing Impairment
Interventions concerning older adults with hearing impairment center on amplification and aural rehabilitation, including auditory training [84]. It has been shown that using hearing aids improves the quality of life, in particular hearing-related quality of life, of hearing impaired adults [85]. Yet many older adults who would benefit from hearing aids do not wear them [86]. From the reasons identified in the review by McCormack and Fortnum [86], perceived hearing aid value, in particular poor benefit in noisy situations, fit and comfort, as well as care and maintenance of the hearing aid emerged as most important. Improvements in these areas are necessary to enhance hearing aid usage among older adults with hearing impairment. Meyer and Hickson [87] identified 5 factors increasing the likelihood to seek help for hearing impairment and/or adopt hearing aids: (1) moderate to severe hearing impairment and perceived hearing-related everyday limitations; (2) older age; (3) poor subjective hearing; (4) perceiving more benefits than barriers to amplification; and (5) perceiving significant others as supportive of hearing rehabilitation. Thus, the involvement of family members in the rehabilitation process appears necessary and promising.
Beyond amplification, aural rehabilitation seeks to improve the situation of hearing impaired older adults by providing listening and communication techniques to enhance communication effectiveness. We have summarized major work in this area in Table 2.
In sum, it seems clear for both vision impairment [95] and hearing impairment [96] that classic rehabilitation strategies, such as fitting a reading device or hearing aid, need significant enrichment by psychosocial training components in order to achieve the best outcomes possible. Furthermore, given the findings on the role of cognitive resources in visually impaired older adults (see respective section above), cognitive training may be an important addition to psychosocial intervention and rehabilitation [38,97]. It must be noted, however, that many of the available studies reveal a number of methodological limitations, such as small sample sizes, missing control condition, and no follow-up assessments to estimate the maintenance of effects.
A significant future need is intervention research addressing older adults with dual sensory impairment. Although we found study protocols related to important trials underway [98,99] and a physical training study with visually impaired older adults that included also some dual sensory impaired individuals [83], it seems that there is not much research in terms of completed interventions and respective findings. Furthermore, it may be important to better involve significant others such as family members and friends in psychosocially framed programs and emerging research with low vision adults has revealed advantages and disadvantages of such an approach [100].
Practical Implications
The older patient is on the way to become the “standard” patient for eye care and hearing specialists and thus a challenge for public health at large. Based on the evidence compiled above, we argue that best practice in medical treatment and traditional rehabilitation of vision and hearing impairment should better consider the psychosocial dimension of age-related vision and hearing impairment. We see different levels at which a stronger psychosocially framed input is needed. First, at the diagnostic level, having a better understanding of everyday competence, the role of cognitive functioning, social resources, and well-being–related dynamics in visually impaired and hearing impaired older adults may significantly enrich the professional background knowledge about the patient. Such knowledge may become important for diagnostic evaluation, treatment decisions, and predictions of long-term outcomes. It seems also critical to have an understanding of the more fundamental mechanisms and systemic inter-relations in older patients (eg, among visual, hearing, mobility, and cognitive impairment), because such evidence helps to evaluate overall vulnerability and likely future trajectories of respective patients.
Second, at the intervention level against the background of the available empirical effectiveness evidence, self-management–oriented and psycho-educative programs should become a regular component of low vision rehabilitation. Similarly, psychosocial programs educating older adults in hearing tactics and hearing loss–oriented coping strategies should become a regular part of hearing rehabilitation. In addition, we argue that cognitive training and physical activity–oriented interventions should have their place in rehabilitation programs designed for older visually and hearing impaired adults. The major reason is that respective programs generally have been found to positively impact quality of life in old age. This impact may be particularly valuable for more vulnerable populations, such as sensory impaired older adults. We therefore recommend implementing psychosocially framed programs as a regular service in eye clinics as well as in ear, nose, and throat clinics, because this seems to be the setting best suited to approach visually and hearing impaired older adults as well as to offer the logistic opportunities to conduct such programs. It would also be critical to extend such programs to in-home services as well as services covering long-term care settings. Older adults with dual sensory impairment bring specific challenges to such interventions, such as the optimal cooperation and combination of rehabilitation and psychosocial expertise related to each domain and traditionally offered side by side. It is also good news that new trials are underway to learn more about psychosocial interventions aimed to address older adults with dual sensory loss [98,99].
In conclusion, we argue for a better implementation of both age-related psycho-ophthalmology as well as psycho-audiology. Although we regard psychologists with a clinical training background as a key profession to be involved in psychosocially framed interventions with older adults with vision and hearing impairment, other professions (eg, occupational therapists, sport scientists) should also play an important role. A multiprofessional enrichment of classic sensory rehabilitation based on the training principles as described above is a major future need.
Corresponding author: Vera Heyl, PhD, Zeppelinstr, 1, D-69121, Heidelberg, Germany, [email protected].
Financial disclosures: None.
From the University of Education (Dr. Heyl) and Heidelberg University (Dr. Wahl), Heidelberg, Germany.
Abstract
- Objective: To summarize the current state of research regarding the experience of age-related vision and hearing impairment.
- Methods:Review of the literature.
- Results: Negative consequences of age-related vision and hearing impairment manifest in the domains of health and longevity, everyday competence, cognitive functioning, social functioning, and subjective well-being. However, while vision impairment strongly impacts everyday competence, the burden of hearing impairment can mainly be found in the social domain. Psychosocially framed intervention research has shown promising findings, but many studies rely on small samples or do not include a control condition.
- Conclusions: Although more research is needed, it is clear that traditional rehabilitation programs targeting age-related vision and hearing impairments need a strong psychosocial component.
Vision and hearing are essential for person–environment interaction and both are subject to pronounced age-related changes. Ongoing demographic changes and increasing life expectancy is contributing to a significant increase in the number of very old individuals [1]. It is projected that by 2030 about 50% of older Americans may have some significant eye disease, ie, cataract, glaucoma, or age-related macular degeneration [2]. Presbycusis as the major cause of age-related hearing impairment is present in 40% of the American senior citizens [3]. In this narrative review, we review the epidemiological data on age-related vision and hearing impairment, research on its psychosocial impact, and intervention research aimed to improve coping processes and rehabilitative outcomes. We close with future recommendations directed both toward research and clinical practice.
Epidemiology
Vision and hearing impairment is highly prevalent in old age, yet prevalence rates reported in the literature are quite different, depending on the definition of vision and hearing impairment used. A widely used criterion for low vision is the one used by the World Health Organization, ie, visual acuity less than 20/60 and equal to or better than 20/400 in the better eye with best correction. A best corrected visual acuity of less than 20/400 in the better eye is used to define blindness [4]. A disabling hearing impairment is defined by an average hearing loss in decibel (dB HL) of at least 41 dB HL at 500, 1000, 2000, and 4000 Hz. [5]. Translated to everyday life, such hearing impairment mainly manifests in severe difficulties in understanding normal conversation. Besides differing definitions, different methods to assess vision and hearing impairment and heterogenous study populations make comparisons of prevalence rates difficult [6]. In particular, relying solely on self-report data to assess vision and hearing loss seems generally problematic. In addition, the strong focus in vision impairment assessment on visual acuity measures has limitations, as other indicators, such as contrast sensitivity or useful field of vision, may be more important for out-of-home mobility or driving [7].
A recent study on the prevalence of visual impairment (defined as best corrected visual acuity < 20⁄40) in 6 European countries found quite similar prevalence rates as reported for the US: Prevalence of visual impairment was 3% in those aged 65 to 74 years, 13% in those over 75 years and 33% in those over 85 years [8]. At first glance, vision loss seems to be more prevalent among older women than among older men, but this relationship is not sustained in multivariate analyses considering age, health, and social support variables [9].
Regarding hearing loss, Gopinath et al [10] found prevalence rates of 29% among men and 17% among women aged 60 to 69 years. Moreover, for every 10 years of age, the prevalence of hearing loss doubled. In their review of epidemiologic data on prevalence of age-related hearing impairment in Europe, Roth and coauthors [11] report that at the age of 70 years, about 30% of men and 20% of women were found to have a hearing loss of at least 30 dB HL, while at the age of 80 years about 55% of men and 45% of women were affected. Lin et al found that 63% of those 70 years and older had a hearing loss of more than 25 dB in the better ear [12].
According to a recent review by Schneider et al [6], prevalence of impairment in both vision and hearing in older age (dual sensory impairment) varies between 1.6% and 22.5% due to different sample characteristics (eg, size, age) and different definitions and assessments of vision and hearing impairment (see also [13]). However, there is good evidence that dual sensory impairment increases with age, and that it is more common among frailer subpopulations such as older individuals consulting care services [6].
Quality of Life Impact of Vision and Hearing Impairment
Health and Longevity
There is inconsistent evidence that both age-related vision and hearing impairment are accompanied by heightened multimorbidity and an increased mortality rate. For example, while some older as well as more recent studies have found that visual and hearing declines over time predict death in very old age [14–16], other studies have detected no significant relationship after adjusting for confounders such as age, gender, and education [17,18]. Among the hearing impaired, only men seem to have a significant increase in mortality risk [15,19]. Dual sensory impairment appears to be more consistently and more strongly related to increased mortality than vision or hearing impairment alone [19–21].
Everyday Competence
The term everyday competence includes both basic (eg, self-care behaviors) and instrumental (eg, using public transport) activities of daily living (ADL/IADL [22]). Age-related vision impairment has been found to be robustly associated with significantly lower everyday competence, because visual capacity is a critical prerequisite for such behaviors [23,24]. Indeed, lowered everyday competence appeared as the best of a range of variables (including cognitive function and well-being–related measures) used to differentiate between visually impaired and visually unimpaired older adults [18]. Furthermore, vision impairment impacts cross-sectionally as well as longitudinally—more strongly on IADL as compared to ADL—because the execution of IADL is more complex and depends more strongly on environmental enhancing or hindering factors [25–27]. Hence, shrinkage in IADL competence reflects a kind of early behavioral marker of severe vision impairment, whereas significant ADL decrease only happens later in the process of chronic vision loss.
In contrast to vision impairment, age-related hearing loss has been found not to have a major impact in particular on ADL/IADL [28]. However, as has been found elsewhere [29], hearing loss is associated with increased reliance on community and informal supports, suggesting that while IADL function may not deteriorate with hearing loss, the way it is conducted may change (ie, need for support to maintain participation).
It should also be mentioned in this context that assessment strategies have been developed to better consider the specific life conditions of those with vision and hearing impairment. The best-known and frequently applied instruments in this context are the National Eye Institute Visual Function Questionnaire [30] and the Hearing Handicap Inventory for the Elderly [31].
Cognitive Functioning
Previous research largely supports the notion that reduced vision and hearing function is accompanied by a decrease in cognitive performance in older adults. The work of Lindenberger and Baltes, based on the Berlin Aging Study (BASE)—but also including additional studies with a wider age-range—is central in supporting a strong connection among vision, hearing, balance, and cognitive functioning in later life. Lindenberger and Baltes [32] found that general intelligence correlated just as strongly with visual as with auditory ability. In a model conjoining age, sensory function, as well as intelligence, visual and auditory function predicted a large portion of interindividual differences in intelligence and indeed fully mediated the negative correlation between age and intelligence. This finding has meanwhile been replicated by a number of other research groups and may be regarded as rather robust [33,34]. In addition, Baltes and Lindenberger [35] observed that sensory measures were better predictors of intelligence than socio-structural variables such as education or social class. They also showed that the connection among sensory functioning and intelligence was much closer in older adults as compared to adults in early and middle adulthood [34].
No clear difference between the sensory modalities of vision and hearing has been identified regarding their relationship with cognitive performance. On the one hand, there is research supporting the view that both vision and hearing impairment are connected with cognitive decline [12,36,37], while some evidence also supports that the linkage may be stronger with vision [14]. On the other hand, there are also data not supporting a close connection between vision and hearing impairment and cognitive function [38]. Explanations for such inconsistencies may refer to a number of reasons, such as pronounced positive selectivity of samples (which may lead to underestimation of connections among sensory and cognitive function), the application of established cognitive tests not appropriate for sensory impaired older adults (which may lead to overestimation of connections among sensory and cognitive function), and the application of different cut-off scores for significant vision and hearing impairment (possibly, higher cut-offs may lead to higher, lower to lower connections). Longitudinal data using the latest in causal modeling data analysis support the view that the causal dynamics involved in sensory and intelligence change are complex and that each of these variables can drive change in the other across longer periods of later life [39].
Vision status also plays a role when it comes to the connection between cognitive function and everyday competence—a linkage that is generally challenged as people age and that may lead to endpoints such as dependence on others and transition to long-term care. Heyl et al [40] observed that the link between vision status and out-of-home leisure activities is mediated by cognitive status. In a more recent study, able to add to the understanding of such a mediation process, Heyl and Wahl [38,41] showed that the connection between cognitive function and everyday function is much closer in visually and hearing impaired older adults as compared with visually unimpaired older adults, which possibly means that both visually and hearing impaired elders rely more intensely on their cognitive resources. Causality dynamics may however also work in the opposite direction. As Rovner and colleagues [42,43] observed in a study with age-related macular degeneration patients over 64 years of age covering a 3-year observation period and 2 measurement occasions, activity loss over time due to the visual loss led to cognitive decline happening between T1 and T2. This finding fits well with the more general finding in the cognitive aging literature that the exertion of social and leisure activities is important for maintaining cognitive functioning [44].
Social Functioning
Social relations as well as social support have generally been found to be of key importance for older adults [45]. Reinhardt [46] found that visually impaired older adults nominated on average 5.4 persons of intimate relation within their family network, and 3.5 persons within their friendship network, which is similar to sensory-unimpaired older adults, such as those assessed in the BASE [47]. In addition, in Wahl et al’s study [18], visually and hearing impaired older adults nominated practically the same number of persons as being in the most intimate circle of their social network (4.70 versus 4.71); the respective number in a comparison group of visually unimpaired older adults amounted to 5.2 persons, which was not significantly different from both sensory impaired group means.
Neither vision nor hearing impairment seem to affect the experience of loneliness dramatically [18,23,48], although some research did report an increased risk of loneliness in older adults with vision impairment [49]. It is clear however that hearing impairment more strongly than vision impairment negatively impacts social communication and carries a strong stigma for those affected [48,50]. The stigma particularly implies that hearing deficits and concomitant communication disturbances (eg, giving an answer that does not match the question) elicits the view of a cognitively impaired, if not demented older person. In some contrast, vision loss seems to raise rather strong helping impulses and feelings of compassion. The dark side of this tendency is that it seems a challenge to provide visually impaired older adults with the instrumental support needed while at the same time fostering remaining capabilities [51]. Overprotection may put constraints on the visually impaired older adults’ “true” functional capacity and thereby contribute to loss in competence over the longer run due to disuse [52].
Subjective Well Being–related Outcomes and Depression
Visually impaired older adults have shown evidence of diminished well-being as compared with sensory unimpaired older adults [53], although effect sizes were rather small in a respective meta-analysis [54]. Differences in well-being between hearing impaired and unimpaired older adults seem small or nonexistent in some studies [18,55], but considerable in others [56]. The latter study covering a 16-year observational period as well as other longitudinal work (eg, [57]) also support the notion that remaining ADLs and social engagement mediate the linkage between sensory loss and well-being and depression. The “well-being paradox” in old age, pointing to pronounced adaptive resources to maintain well-being in spite of adverse conditions [58], may also apply to sensory impaired older adults [57,59].
At the same time, it is critical to acknowledge that visually impaired older adults represent an at-risk population, in which the positive impact of human adaptation and the drawback of reaching the limits of psychological resilience go hand in hand. Affect balance (ratio of positive and negative affect) has been found to be more toward the negative pole in visually impaired older adults [60] and depression has consistently been found to be significantly increased in visually impaired older adults [61–63]. Rates roughly vary between 15% and 30% and are particularly high in age-related macular degeneration patients [61]. This is also important, because depressive symptoms may accelerate both cognitive decline and decline in everyday competence in age-related macular degeneration patients [42]. Perceived overprotection may also lead to negative consequences in terms of heightened depression and anxiety over time [64].
Regarding the impact of hearing loss on depression, findings are quite inconsistent. Some studies found evidence for a significant relationship between hearing impairment and depressive symptoms among older adults [65, 66], while others did not [67, 68]. Gopinath and co-workers [66] observed that hearing impaired individuals, particularly women, younger than 70 years of age and those who were infrequently using a hearing aid (less than one hour per day) were more likely to suffer from depressive symptoms. According to a population-based study among older Italians, hearing impairment might be more closely related to anxiety symptoms than to depression [69].
Dual Sensory Impairment
Previous research supports the notion that the overall psychosocial situation of those with dual sensory impairment is even worse as compared to those with sole vision or hearing impairment. In particular, higher rates of ADL/IADL impairment, depression and lowered well-being have been found in older adults affected by dual sensory loss [6,13,18,56]. Also, dual sensory impairment has been found to be linked with cognitive decline cross-sectionally [37] as well as longitudinally [36].
Improving Quality of Life in Sensory Impaired Older Adults
The research summary provided in the previous section underscores that the experience of age-related visual and hearing impairment comes with pronounced challenges that deserve evidence-based professional support. In the following, we give an overview and evaluation of major work in the area of psychosocially framed intervention research targeting older adults with vision and hearing loss. By psychosocially framed interventions we mean studies containing programs that focused on psychosocial processes (eg, consultation on how to better cope with sensory impairment, educative components, problem solving strategies, coping with negative affect) and assessed psychosocial outcomes (eg, everyday functioning, depression, emotional stress experiences). Such interventions may have been integrated into regular rehabilitation programs or offered as a separate strategy in addition to classic rehabilitation. We also consider physical activity–related and overall “way of living” interventions such as tai chi and yoga. In doing so, our aim is to highlight the bandwidth of psychosocial interventions and respective outcomes, not comprehensiveness.
Age-related Vision Impairment
Most psychosocially framed interventions could be characterized as self-management– and disease management–like efforts and are promising for visually impaired older adults. Major elements of such programs include stress-reducing strategies (eg, muscle-relaxation exercises), goal-directed problem-solving, strategies to evoke positive affect, activating available resources, and information and consultation. Typically, such programs are conducted in a group format in an eye clinic, bringing together 6 to 8 visually impaired older adults for weekly sessions of 2 to 3 hours over 6 to 8 weeks.
More recent work provides additional support for the usefulness of self-management programs for visually impaired older adults [72,73]. In addition, emerging evidence supports the notion that psychosocially framed interventions may contribute to saving health costs (eg, via reduced psychopharmacy) and may also enhance commitment
It is also obvious that such programs should find a strong liaison with classic high-caliber rehabilitation programs for visually impaired older adults, including effective reading training [75].
Furthermore, physical training programs, which have proven efficiency with old and very old individuals—including those who are cognitively vulnerable—also seem to be of significant advantage for visually impaired older adults. As has been found, such programs not only increase posture, gait, and general physical fitness, they also prevent falls and enhance well-being, self-efficacy, and cognitive function, especially executive control [76]. Postural control has been improved by multimodal balance and strength exercises among older individuals with visual impairments as well [77]. Participation in physical activity and being in better physical condition buffered the relationship between dual sensory impairment and depression, pointing to the importance of physical training programs for the mental health of older persons with dual sensory impairment [78]. According to a randomized control study as well as to some case studies, tai chi seems to be an effective tool to improve balance control in visually impaired older adults, and thus to reduce an important risk factor for falls [79–81]. Visually impaired adults might also benefit from yoga in terms of balance improvement as well as psychosocial improvements [82]. To teach tai chi efficiently, it is necessary to adapt instructions to the needs of the visually impaired seniors by relying on verbal cuing and manual body placement [80]. The need to adapt instructions and to provide an accessible environment (including transportation arrangements) to motivate older individuals with visual impairments to perform regular physical exercises is also highlighted by Surakka and Kivela [83].
Furthermore, there is evidence that state of the art low vision rehabilitation as such also has beneficial effects on psychosocial outcomes, such as general and vision-related quality of life and emotional well-being.
Age-related Hearing Impairment
Interventions concerning older adults with hearing impairment center on amplification and aural rehabilitation, including auditory training [84]. It has been shown that using hearing aids improves the quality of life, in particular hearing-related quality of life, of hearing impaired adults [85]. Yet many older adults who would benefit from hearing aids do not wear them [86]. From the reasons identified in the review by McCormack and Fortnum [86], perceived hearing aid value, in particular poor benefit in noisy situations, fit and comfort, as well as care and maintenance of the hearing aid emerged as most important. Improvements in these areas are necessary to enhance hearing aid usage among older adults with hearing impairment. Meyer and Hickson [87] identified 5 factors increasing the likelihood to seek help for hearing impairment and/or adopt hearing aids: (1) moderate to severe hearing impairment and perceived hearing-related everyday limitations; (2) older age; (3) poor subjective hearing; (4) perceiving more benefits than barriers to amplification; and (5) perceiving significant others as supportive of hearing rehabilitation. Thus, the involvement of family members in the rehabilitation process appears necessary and promising.
Beyond amplification, aural rehabilitation seeks to improve the situation of hearing impaired older adults by providing listening and communication techniques to enhance communication effectiveness. We have summarized major work in this area in Table 2.
In sum, it seems clear for both vision impairment [95] and hearing impairment [96] that classic rehabilitation strategies, such as fitting a reading device or hearing aid, need significant enrichment by psychosocial training components in order to achieve the best outcomes possible. Furthermore, given the findings on the role of cognitive resources in visually impaired older adults (see respective section above), cognitive training may be an important addition to psychosocial intervention and rehabilitation [38,97]. It must be noted, however, that many of the available studies reveal a number of methodological limitations, such as small sample sizes, missing control condition, and no follow-up assessments to estimate the maintenance of effects.
A significant future need is intervention research addressing older adults with dual sensory impairment. Although we found study protocols related to important trials underway [98,99] and a physical training study with visually impaired older adults that included also some dual sensory impaired individuals [83], it seems that there is not much research in terms of completed interventions and respective findings. Furthermore, it may be important to better involve significant others such as family members and friends in psychosocially framed programs and emerging research with low vision adults has revealed advantages and disadvantages of such an approach [100].
Practical Implications
The older patient is on the way to become the “standard” patient for eye care and hearing specialists and thus a challenge for public health at large. Based on the evidence compiled above, we argue that best practice in medical treatment and traditional rehabilitation of vision and hearing impairment should better consider the psychosocial dimension of age-related vision and hearing impairment. We see different levels at which a stronger psychosocially framed input is needed. First, at the diagnostic level, having a better understanding of everyday competence, the role of cognitive functioning, social resources, and well-being–related dynamics in visually impaired and hearing impaired older adults may significantly enrich the professional background knowledge about the patient. Such knowledge may become important for diagnostic evaluation, treatment decisions, and predictions of long-term outcomes. It seems also critical to have an understanding of the more fundamental mechanisms and systemic inter-relations in older patients (eg, among visual, hearing, mobility, and cognitive impairment), because such evidence helps to evaluate overall vulnerability and likely future trajectories of respective patients.
Second, at the intervention level against the background of the available empirical effectiveness evidence, self-management–oriented and psycho-educative programs should become a regular component of low vision rehabilitation. Similarly, psychosocial programs educating older adults in hearing tactics and hearing loss–oriented coping strategies should become a regular part of hearing rehabilitation. In addition, we argue that cognitive training and physical activity–oriented interventions should have their place in rehabilitation programs designed for older visually and hearing impaired adults. The major reason is that respective programs generally have been found to positively impact quality of life in old age. This impact may be particularly valuable for more vulnerable populations, such as sensory impaired older adults. We therefore recommend implementing psychosocially framed programs as a regular service in eye clinics as well as in ear, nose, and throat clinics, because this seems to be the setting best suited to approach visually and hearing impaired older adults as well as to offer the logistic opportunities to conduct such programs. It would also be critical to extend such programs to in-home services as well as services covering long-term care settings. Older adults with dual sensory impairment bring specific challenges to such interventions, such as the optimal cooperation and combination of rehabilitation and psychosocial expertise related to each domain and traditionally offered side by side. It is also good news that new trials are underway to learn more about psychosocial interventions aimed to address older adults with dual sensory loss [98,99].
In conclusion, we argue for a better implementation of both age-related psycho-ophthalmology as well as psycho-audiology. Although we regard psychologists with a clinical training background as a key profession to be involved in psychosocially framed interventions with older adults with vision and hearing impairment, other professions (eg, occupational therapists, sport scientists) should also play an important role. A multiprofessional enrichment of classic sensory rehabilitation based on the training principles as described above is a major future need.
Corresponding author: Vera Heyl, PhD, Zeppelinstr, 1, D-69121, Heidelberg, Germany, [email protected].
Financial disclosures: None.
1. Oeppen J, Vaupel JW. Broken limits to life expectancy. Science 2002;296:1029–31.
2. Eichenbaum JW. Geriatric vision loss due to cataracts, macular degeneration, and glaucoma. Mt Sinai J Med 2012;79:276–94.
3. Ciorba A, Bianchini C, Pelucchi S, et al. The impact of hearing loss on the quality of life of elderly adults. Clin Interven Aging 2012;7:159–63.
4. WHO - World Health Organization and International Agency for the Prevention of Blindness. Developing an action plan to prevent blindness at national, provincial and district levels. Vision 2020 The right to sight. Geneva: World Health Organization; 2004.
5. WHO - World Health Organizaton. Grades of hearing impairment. Geneva: World Health Organization; 2013.
6. Schneider JM, Gopinath B, McMahon CM, et al. Dual sensory impairment in older age. J Aging Health 2011;23:1309–24.
7. Clay OJ, Wadley VG, Edwards JD, et al. Cumulative meta-analysis of the relationship between useful field of view and driving performance in older adults: current and future implications. Optom Vis Sci 2005;82:724–31.
8. Seland JH, Vingerling JR, Augood CA, et al. Visual Impairment and quality of life in the Older European Population, the EUREYE study. Acta Ophthal 2011;89:608–13.
9. Horowitz A, Brennan M, Reinhardt JP. Prevalence and risk factors for self-reported visual impairment among middle-aged and older adults. Research Aging 2005;27:307–26.
10. Gopinath B, Rochtchina E, Wang JJ, et al. Prevalence of age-related hearing loss in older adults: Blue mountains study. Arch Intern Med 2009;169:415–6.
11. Roth TN, Hanebuth D, Probst R. Prevalence of age-related hearing loss in Europe: a review. Eur Arch Otorhinolaryngol 2011;268:1101–7.
12. Lin FR, Thorpe R, Gordon-Salant S, et al. Hearing loss prevalence and risk factors among older adults in the United States. J Gerontol Series A: Biolog Sci Med Sci 2011;66A:582–90.
13. Brennan M, Horowitz A, Su Y-p. Dual sensory loss and its impact on everyday competence. Gerontologist 2005;45:337–46.
14. Anstey KJ, Luszcz MA, Giles LC, et al. Demographic, health, cognitive, and sensory variables as predictors of mortality in very old adults. Psychol Aging 2001;16:3–11.
15. Appollonio I, Carabellese C, Magni E, et al. Sensory impairments and mortality in an elderly community population: A six-year follow-up study. Age Ageing 1995;24:30–6.
16. McCarty CA, Nanjan MB, Taylor HR. Vision impairment predicts 5 year mortality. Br J Ophthalmol 2001;85:322–6.
17. Ostbye T, Steenhuis R, Wolfson C, et al. Predictors of five-year mortality in older Canadians: the Canadian Study of Health and Aging. J Am Geriatr Soc 1999 47:1249–54.
18. Wahl H-W, Heyl V, Drapaniotis PM, et al. Severe vision and hearing impairment and successful aging: A multidimensional view. Gerontologist 2013;53:950–62.
19. Fisher D, Li C-M, Chiu MS, et al. Impairments in hearing and vision impact on mortality in older people: the AGES-Reykjavik Study. Age Ageing 2013.
20. Bamini G, Schneider J, McMahon CM, et al. Dual sensory impairment in older adults inceases the risk of mortality: A population-based study. PLoS ONE 2013;8:1–6.
21. Lam BL, Lee DJ, Gómez-Marín O, et al. Concurrent visual and hearing impairment and risk of mortality: The National Health Interview Survey. Arch Ophthalmol 2006;124:95–101.
22. Baltes MM, Maas I, Wilms H-U, et al. Everyday competence in old and very old age: Theoretical considerations and empirical findings. In: Baltes PB, Mayer K-U, editors. The Berlin Aging Study Cambridge, UK: Cambridge University Press; 1999: 384–402.
23. Burmedi D, Becker S, Heyl V, et al. Behavioral consequences of age-related low vision: A narrative review. Vis Impair Res 2002;4:15–45.
24. Wahl H-W, Heyl V, Schilling O. Robustness of personality and affect relations under chronic conditions: the case of age-related vision and hearing impairment. J Gerontol B Psycholog Sci Soc Sci 2012;67:687–96.
25. Heyl V, Wahl H-W. On the long-term psychosocial adaptation to vision loss in the later years. In: Wahl H-W, Schulze H-E, editors. On the special needs of blind and low vision seniors: Research and practice concepts. Amsterdam: IOS-Press; 2001: 77–83.
26. Wahl H-W, Schilling O, Oswald F, et al. Psychosocial consequences of age-related visual impairment: Comparison with mobility-impaired older adults and long-term outcome. J Gerontol Psych Sci Soc Sci 1999;54B:P304–P16.
27. Wahl H-W, Becker S, Burmedi D, et al. The role of primary and secondary control in adaptation to age-related vision loss: A study of older adults with macular degeneration Psychol Aging 2004;19:235–9.
28. Rudberg MA, Furner SE, Dunn JE, et al. The relationship of visual and hearing impairments to disability: An analysis using the Longitudinal Study of Aging. J Gerontol Med Sci 1993;48:M261–M5.
29. Schneider J, Gopinath B, Karpa MJ, et al. Hearing loss impacts on the use of community and informal supports. Age Ageing 2010;39:458–64.
30. Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-item National Eye Institute visual function questionnaire. Arch Ophthalmol 2001;119:1050–8.
31. Ventry I, Weinstein B. The hearing handicap inventory for the elderly: A new tool. Ear Hearing 1982;3:128–34.
32. Lindenberger U, Baltes PB. Sensory functioning and intelligence in old age: A strong connection. Psychol Aging 1994;9:339–55.
33. Clay OJ, Edwards JD, Ross LA, et al. Visual function and cognitive speed of processing mediate age-related decline in memory span and fluid intelligence. J Aging Health 2009;21:547–66.
34. Salthouse TA, Hancock HE, Meinz EJ, et al. Interrelations of age, visual acuity, and cognitive functioning. J Gerontol Psychol Sci 1996;51B:P317–P30.
35. Baltes PB, Lindenberger U. Emergence of powerful connection between sensory and cognitive functions across the adult life span: A new window to the study of cognitive aging? Psychol Aging 1997;12:12–21.
36. Lin MY, Gutierrez PR, Stone KL, et al. Vision impairment and combined vision and hearing impairment predict cognitive and functional decline in older women. J Am Geriatr Soc 2004;52:1996–2002.
37. Tay T, Wang JJ, Kifley A, et al. Sensory and cognitive association in older persons: Findings from an older Australian population. Gerontology 2006;52:386–94.
38. Heyl V, Wahl H-W. Managing daily life with age-related sensory loss: Cogni-tive resources gain in importance. Psychol Aging 2012;27:510–21.
39. Lindenberger U, Ghisletta P. Cognitive and sensory declines in old age: Gauging the evidence for a common cause. Psychol Aging 2009;24:1-16.
40. Heyl V, Wahl H-W, Mollenkopf H. Visual capacity, out-of-home activities and emotional well-being in old age: Basic relations and contextual variation. Soc Indicat Res 2005;74:159–89.
41. Heyl V, Wahl H-W. Cognitive ability as a resource for everyday functioning among older adults who are visually impaired. J Vis Impair Blind 2010;104:391–403.
42. Rovner BW, Casten RJ, Leiby BE. Variability in depressive symptoms predicts cognitive decline in age-related macular degeneration. Am J Geriatr Psych 2009;17:574–81
43. Rovner BW, Casten RJ, Leiby BE, et al. Activity loss is associated with cognitive decline in age-related macular degeneration. Thomas Jefferson University, Department of Psychiatry and Human Behavior, Faculty Papers. Paper 5. 2009.
44. Lövdén M, Ghisletta P, Lindenberger U. Social participation attenuates decline in perceptual speed in old and very old age. Psych Aging 2005;20:423–34.
45. Antonucci TC. Social relations. An examination of social networks, social support, and sense of control. In: Birren JE, Schaie KW, editors. Handbook of the psychology of aging. 5th ed. San Diego: Academic Press; 2001: 427–53.
46. Reinhardt JP. The importance of friendship and family support in adaptation to chronic vision impairment. J Gerontol Series B Psychol Sci Soc Sci 1996;51B:P268–P78.
47. Wagner M, Schütze Y, Lang FR. Social relationships in old age. In: Baltes PB, Mayer KU, editors. The Berlin Aging Study Aging from 70 to 100. Cambridge, UK: Cambridge University Press; 1999: 282–301.
48. Wahl H-W, Tesch-Römer C. Aging, sensory loss, and social functioning. In: Charness N, Park D, Sabel B, editors. Aging and communication: Opportunities and challenges of technology. New York: Springer; 2001: 108-26.
49. Nachtegaal J, Smit JH, Smits C, et al. The association between hearing status and psychosocial health before the age of 70 years: Results from an internet-based national survey on hearing. Ear Hearing 2009;30:302-12
50. Wallhagen MI. The stigma of hearing loss. Gerontologist 2010;50:66–75.
51. Cimarolli VR, Boerner K. Social support and well-being in adults who are visually impaired. J Vis Impair Blind 2005 99:521–34.
52. Cicirelli VG. Fear of death in mid-old age. J Gerontol Series B Psychol Sci Soc Sci 2006;61:P75–P81.
53. Horowitz A, Reinhardt JP. Depression among low vision elders. In: Stuen. C, Arditi A, Horowitz A, et al, editors. Vision rehabilitation assessment, intervention and outcomes. Lisse: Swets & Zeitlinger Publishers; 2000: 655–8.
54. Pinquart M, Pfeiffer JP. Psychological well-being in visually impaired and unimpaired individuals: A meta-analysis. Br J Vis Impair 2011;29:27–45.
55. Tesch-Römer C. Schwerhörigkeit im Alter. Belastung, Bewältigung, Rehabilitation. Heidelberg: Median-Verlag; 2001.
56. Kiely KM, Anstey KJ, Luszcz MA. Dual sensory loss and depressive symptoms: the importance of hearing, daily functioning, and activity engagement. Front Hum Neurosci 2013;7:1–13.
57. Schilling OK, Wahl H-W, Horowitz A, et al. The adaptation dynamics of chronic functional impairment: What we can learn from older adults with vision loss. Psychol Aging 2011;26:203–13.
58. Kunzmann U, Little T, Smith J. Is age-related stability of subjective well-being a paradox? Cross-sectional and longitudinal evidence from the Berlin Aging Study. Psychol Aging 2000;15:511-26.
59. Schilling O, Wahl H-W. Modeling late life adaptation in affective well-being under a severe chronic health condition: The case of age-related macular degeneration. Psychol Aging. 2006;21:703–14.
60. Wahl H-W, Schilling O, Becker S, et al. A German research program on the psychosocial adaptation to age-related vision impairment: Recent findings based on a control theory approach. Europ Psychol 2003;8:168-77.
61. Casten R, Rovner B. Depression in age-related macular degeneration. J Visual Impair Blind 2008;102:591-9.
62. Crews JE, Campbell VA. Vision impairment and hearing loss among community-dwelling older Americans: implications for health and functioning. Am J Pub Health 2004;94:823–9.
63. Horowitz A, Reinhardt JP, Boerner K. The effect of rehabilitation on depression among visually disabled older adults. Aging Mental Health 2005;9:563–70.
64. Cimarolli VR. Perceived overprotection and distress in adults with visual impairment. Rehabil Psychol 2006;51:338-45.
65. Ishine M, Okumiya K, Matsubayashi K. A close association between hearing impairment and activities of daily living, depression, and quality of life in community-dwelling older people in Japan. J Am Geriatr Soc 2007;55:316-7.
66. Gopinath B, Wang JJ, Schneider J, et al. Depressive symptoms in older adults with hearing impairments: The Blue Mountains Study. J Am Geriatr Soc 2009;57:1306-8.
67. Chou K-L, Chi I. Combined effect of vision and hearing impairment on depression in elderly Chinese. Int J Geriatr Psych 2004;19:825-32.
68. Tambs K. Moderate effects of hearing loss on mental health and subjective well-being: Results from the Nord-Trøndelag Hearing Loss Study. Psychosom Med 2004;66:776-82.
69. Bernabei V, Morini V, Moretti F, et al. Vision and hearing impairments are associated with depressive--anxiety syndrome in Italian elderly. Aging Ment Health 2011 15:467-74.
70. Wahl H-W, Heyl V, Langer N. Lebensqualität bei Seheinschränkung im Alter: Das Beispiel altersabhängige Makuladegeneration [Quality of life by limited vision in old age: the example of age-related macula degeneration]. Der Ophthalmologe 2008;105:735-43.
71. Wahl H-W, Kämmerer A, Holz F, et al. Psychosocial intervention for age-related macular degeneration: A pilot project. J Vis Impair Blind 2006;100:533-44.
72. Rees G, Keeffe JE, Hassell J, et al. A self-management program for low vision: Program overview and pilot evaluation. Disabil Rehab 2010;32:808-15.
73. Rovner BW, Casten RJ. Preventing late-life depression in age-related macular degeneration. Am J Geriatr Psych 2008;16:454-9
74. Eklund K, Sonn U, Nystedt P, et al. A cost-effectiveness analysis of a health education programme for elderly persons with age-related macular degeneration: A longitudinal study. Disabil Rehab 2005;27:1203-12.
75. Pijnacker J, Verstraten P, van Damme W, et al. Rehabilitation of reading in older individuals with macular degeneration: A review of effective training programs. Aging Neuropsych Cognition. 2011;18:708-32.
76. Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: A meta-analytic study. Psychol Sci 2003;14:125-30.
77. Kovács É, Tóth K, Dénes L, et al. Effects of exercise programs on balance in older women with age-related visual problems: A pilot study. Arch Gerontol Geriatr 2012;55:446-52.
78. McDonnall MC. Physical status as a moderator of depressive symptoms among older adults with dual sensory loss. Rehab Psychol 2011;56:67-76.
79. Chen EW, Fu ASN, Chan KM, et al. The effects of Tai Chi on the balance control of elderly persons with visual impairment: a randomised clinical trial. Age Ageing 2012;41:254-9.
80. Miszko TA, Ramsey VK, Blasch BB. Tai Chi for people with visual impairments: a pilot study. J Vis Impair Blind 2004;98:5-13.
81. Ray C, Horvat M, Keen K, et al. Using Tai Chi as an exercise intervention for improving balance in adults with visual impairments: Two case studies. RE:view 2005;37:17-24.
82. Jeter PE, Dagnelie G, Khalsa SBS, et al. Yoga for persons with severe visual impairment: a feasibility study. Altern Med Stud 2012;2:18-25.
83. Surakka A, Kivela T. Motivating visually impaired and deaf-blind people to perform regular physical exercises. Br J Visual Impair 2008;26:255-68.
84. Li-Korotky H-S. Age-related hearing loss: Quality of care for quality of life. Gerontologist 2012;52:265-71.
85. Chisolm TH, Johnson CE, Danhauer JL, et al. A systematic review of health-related quality of life and hearing aids: Final report of the American Academy of Audiology Task Force on the Health-Related Quality of Life Benefits of Amplification in Adults. J Am Acad Audiol 2007;18:151-83.
86. McCormack A, Fortnum H. Why do people fitted with hearing aids not wear them? Int J Audiol 2013 52:360-8.
87. Meyer C, Hickson L. What factors influence help-seeking for hearing impairment and hearing aid adoption in older adults? Int J Audiol 2012;51:66-74.
88. Andersson G, Green M, Melin L. Behavioural hearing tactics: a controlled trial of a short treatment programme. Behav Res Ther 1997;35:523-30.
89. Andersson G, Melin L, Scott B, et al. Behavioural counselling for subjects with acquired hearing loss. A new approach to hearing tactics. Scandinav Audiol 1994;23:249-56.
90. Burk MH, Humes LE. Effects of long-term training on aided speech-recognition performance in noise in older adults. J Speech Lang Hear Res 2008;51:759-71.
91. Henderson Sabes J, Sweetow RW. Variables predicting outcomes on listening and communication enhancement (LACETM) training. Int J Audiol 2007;46:374-83.
92. Kramer SE, Allessie GH, Dondorp AW, et al. A home education program for older adults with hearing impairment and their significant others: a randomized trial evaluating short- and long-term effects. Int J Audiol 2005;44:255-64.
93. Hickson L, Worrall L, Scarinci N. Measuring outcomes of a communication program for older people with hearing impairment using the International Outcome Inventory. Int J Audiol 2006;45:238-46.
94. Barcroft J, Sommers MS, Tye-Murray N, et al. Tailoring auditory training to patient needs with single and multiple talkers: Transfer-appropriate gains on a four-choice discrimination test. Int J Audiol 2011;50:802-8.
95. Wahl H-W. The psychological challenge of late-life vision impairment: Concepts, Findings, and practical implications. J Ophthalmol 2013.
96. Lin FR. Hearing loss in older adults. Who’s listening? JAMA 2012;307:1147-8.
97. Willis SL, Tennstedt SL, Marsiske M, et al. Long-term effects of cognitive training on everyday functional outcomes in older adults. JAMA 2006;296:2805-14.
98. Roets-Merken LM, Graff MJL, Zuidema SU, et al. Effectiveness of a self-management program for dual sensory impaired seniors in aged care settings: study protocol for a cluster randomized controlled trial. Trials 2013;14.
99. Vreeken HL, van Rens GHMB, Kramer SE, et al. Dual sensory loss: development of a dual sensory loss protocol and design of a randomized controlled trial. BMC Geriatr 2013;13.
100. Rees G, Saw C, Larizza M, et al. Should family and friends be involved in group-based rehabilitation programs for adults with low vision? Br J Visual Impair 2007;25:155-68.
101. Birk T, Hickl S, Wahl H-W, et al. Development and pilot evaluation of a psychosocial intervention program for patients with age-related macular degeneration. Gerontologist 2004;44:836-43.
102. Bradley P, Mitchell J, Bradley C, editors. Peer support for people newly diagnosed with macular degeneration: a pilot study. International Congress Vision 2005 September. London, UK.
103. Brody B, Williams R, Thomas R, et al. Age-related macular degeneration: A randomized clinical trial of a self-management intervention. Ann Behavi Med 1999;21:322-9.
104. Brody BL, Roch-Levecq A-C, Gamst AC, et al. Self-management of age-related macular degeneration and quality of life: a randomized controlled trial. Arch Ophthalmol 2002;120:1477-83.
105. Brody BL, Roch-Levecq A-C, Thomas RG, et al. Self-management of age-related macular degeneration at the 6-month follow-up. a randomized controlled trial. Arch Ophthalmol 2005;123:46-53.
106. Brody BL, Roch-Levecq A-C, Kaplan RM, et al. Age-related macular degeneration: self-management and reduction of depressive symptoms in a randomized, controlled study. J Am Geriatr Soc 2006;54:1557-62.
107. Dahlin-Ivanoff S, Sonn U, Svensson E. A health education program for elderly persons with visual impairments and perceived security in the performance of daily occupations: a randomized study. Am J Occup Thera 2002;56:322-30.
108. Eklund K, Sonn U, Dahlin-Ivanoff S. Long-term evaluation of a health education programme for elderly persons with visual impairment. A randomized study. Disabil Rehab 2004;26:401-9.
109. Eklund K, Dahlin-Ivanoff S. Health education for people with macular degeneration: Learning experiences and the effect on daily occupations. Can J Occup Ther 2006;73:272-80.
110. Eklund K, Sjöstrand J, Dahlin-Ivanoff S. A randomized controlled trial of a health-promotion programme and its effect on ADL dependence and self-reported health problems for the elderly visually impaired. Scand J Occupat Ther 2008;15:68-74.
111. Kämmerer A, Wahl H-W, Becker S, et al. Psychosoziale Unterstützung von älteren Menschen mit einer chronischen Sehbeeinträchtigung: Anwendung und Überprüfung einer problemlöse- und einer emotionsfokussierten Kurzintervention. Zeitschrift für Gesundheitspsychologie 2006;14:95-105.
112. Rovner BW, Casten RJ, Hegel MT, et al. Preventing depression in age-related macular degeneration. Arch Gen Psychiatr 2007;64:886-92.
113. Rovner BW, Casten RJ, Hegel MT, et al. Improving function in age-related macular degeneration: A randomized clinical trial. Ophthalmology 2013;120:1649-55.
114. Barcroft J, Mauzé E, Schroy C, et al. Improving the quality of auditory training by making tasks meaningful. Persp Audiol 2011;7:15-28.
1. Oeppen J, Vaupel JW. Broken limits to life expectancy. Science 2002;296:1029–31.
2. Eichenbaum JW. Geriatric vision loss due to cataracts, macular degeneration, and glaucoma. Mt Sinai J Med 2012;79:276–94.
3. Ciorba A, Bianchini C, Pelucchi S, et al. The impact of hearing loss on the quality of life of elderly adults. Clin Interven Aging 2012;7:159–63.
4. WHO - World Health Organization and International Agency for the Prevention of Blindness. Developing an action plan to prevent blindness at national, provincial and district levels. Vision 2020 The right to sight. Geneva: World Health Organization; 2004.
5. WHO - World Health Organizaton. Grades of hearing impairment. Geneva: World Health Organization; 2013.
6. Schneider JM, Gopinath B, McMahon CM, et al. Dual sensory impairment in older age. J Aging Health 2011;23:1309–24.
7. Clay OJ, Wadley VG, Edwards JD, et al. Cumulative meta-analysis of the relationship between useful field of view and driving performance in older adults: current and future implications. Optom Vis Sci 2005;82:724–31.
8. Seland JH, Vingerling JR, Augood CA, et al. Visual Impairment and quality of life in the Older European Population, the EUREYE study. Acta Ophthal 2011;89:608–13.
9. Horowitz A, Brennan M, Reinhardt JP. Prevalence and risk factors for self-reported visual impairment among middle-aged and older adults. Research Aging 2005;27:307–26.
10. Gopinath B, Rochtchina E, Wang JJ, et al. Prevalence of age-related hearing loss in older adults: Blue mountains study. Arch Intern Med 2009;169:415–6.
11. Roth TN, Hanebuth D, Probst R. Prevalence of age-related hearing loss in Europe: a review. Eur Arch Otorhinolaryngol 2011;268:1101–7.
12. Lin FR, Thorpe R, Gordon-Salant S, et al. Hearing loss prevalence and risk factors among older adults in the United States. J Gerontol Series A: Biolog Sci Med Sci 2011;66A:582–90.
13. Brennan M, Horowitz A, Su Y-p. Dual sensory loss and its impact on everyday competence. Gerontologist 2005;45:337–46.
14. Anstey KJ, Luszcz MA, Giles LC, et al. Demographic, health, cognitive, and sensory variables as predictors of mortality in very old adults. Psychol Aging 2001;16:3–11.
15. Appollonio I, Carabellese C, Magni E, et al. Sensory impairments and mortality in an elderly community population: A six-year follow-up study. Age Ageing 1995;24:30–6.
16. McCarty CA, Nanjan MB, Taylor HR. Vision impairment predicts 5 year mortality. Br J Ophthalmol 2001;85:322–6.
17. Ostbye T, Steenhuis R, Wolfson C, et al. Predictors of five-year mortality in older Canadians: the Canadian Study of Health and Aging. J Am Geriatr Soc 1999 47:1249–54.
18. Wahl H-W, Heyl V, Drapaniotis PM, et al. Severe vision and hearing impairment and successful aging: A multidimensional view. Gerontologist 2013;53:950–62.
19. Fisher D, Li C-M, Chiu MS, et al. Impairments in hearing and vision impact on mortality in older people: the AGES-Reykjavik Study. Age Ageing 2013.
20. Bamini G, Schneider J, McMahon CM, et al. Dual sensory impairment in older adults inceases the risk of mortality: A population-based study. PLoS ONE 2013;8:1–6.
21. Lam BL, Lee DJ, Gómez-Marín O, et al. Concurrent visual and hearing impairment and risk of mortality: The National Health Interview Survey. Arch Ophthalmol 2006;124:95–101.
22. Baltes MM, Maas I, Wilms H-U, et al. Everyday competence in old and very old age: Theoretical considerations and empirical findings. In: Baltes PB, Mayer K-U, editors. The Berlin Aging Study Cambridge, UK: Cambridge University Press; 1999: 384–402.
23. Burmedi D, Becker S, Heyl V, et al. Behavioral consequences of age-related low vision: A narrative review. Vis Impair Res 2002;4:15–45.
24. Wahl H-W, Heyl V, Schilling O. Robustness of personality and affect relations under chronic conditions: the case of age-related vision and hearing impairment. J Gerontol B Psycholog Sci Soc Sci 2012;67:687–96.
25. Heyl V, Wahl H-W. On the long-term psychosocial adaptation to vision loss in the later years. In: Wahl H-W, Schulze H-E, editors. On the special needs of blind and low vision seniors: Research and practice concepts. Amsterdam: IOS-Press; 2001: 77–83.
26. Wahl H-W, Schilling O, Oswald F, et al. Psychosocial consequences of age-related visual impairment: Comparison with mobility-impaired older adults and long-term outcome. J Gerontol Psych Sci Soc Sci 1999;54B:P304–P16.
27. Wahl H-W, Becker S, Burmedi D, et al. The role of primary and secondary control in adaptation to age-related vision loss: A study of older adults with macular degeneration Psychol Aging 2004;19:235–9.
28. Rudberg MA, Furner SE, Dunn JE, et al. The relationship of visual and hearing impairments to disability: An analysis using the Longitudinal Study of Aging. J Gerontol Med Sci 1993;48:M261–M5.
29. Schneider J, Gopinath B, Karpa MJ, et al. Hearing loss impacts on the use of community and informal supports. Age Ageing 2010;39:458–64.
30. Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-item National Eye Institute visual function questionnaire. Arch Ophthalmol 2001;119:1050–8.
31. Ventry I, Weinstein B. The hearing handicap inventory for the elderly: A new tool. Ear Hearing 1982;3:128–34.
32. Lindenberger U, Baltes PB. Sensory functioning and intelligence in old age: A strong connection. Psychol Aging 1994;9:339–55.
33. Clay OJ, Edwards JD, Ross LA, et al. Visual function and cognitive speed of processing mediate age-related decline in memory span and fluid intelligence. J Aging Health 2009;21:547–66.
34. Salthouse TA, Hancock HE, Meinz EJ, et al. Interrelations of age, visual acuity, and cognitive functioning. J Gerontol Psychol Sci 1996;51B:P317–P30.
35. Baltes PB, Lindenberger U. Emergence of powerful connection between sensory and cognitive functions across the adult life span: A new window to the study of cognitive aging? Psychol Aging 1997;12:12–21.
36. Lin MY, Gutierrez PR, Stone KL, et al. Vision impairment and combined vision and hearing impairment predict cognitive and functional decline in older women. J Am Geriatr Soc 2004;52:1996–2002.
37. Tay T, Wang JJ, Kifley A, et al. Sensory and cognitive association in older persons: Findings from an older Australian population. Gerontology 2006;52:386–94.
38. Heyl V, Wahl H-W. Managing daily life with age-related sensory loss: Cogni-tive resources gain in importance. Psychol Aging 2012;27:510–21.
39. Lindenberger U, Ghisletta P. Cognitive and sensory declines in old age: Gauging the evidence for a common cause. Psychol Aging 2009;24:1-16.
40. Heyl V, Wahl H-W, Mollenkopf H. Visual capacity, out-of-home activities and emotional well-being in old age: Basic relations and contextual variation. Soc Indicat Res 2005;74:159–89.
41. Heyl V, Wahl H-W. Cognitive ability as a resource for everyday functioning among older adults who are visually impaired. J Vis Impair Blind 2010;104:391–403.
42. Rovner BW, Casten RJ, Leiby BE. Variability in depressive symptoms predicts cognitive decline in age-related macular degeneration. Am J Geriatr Psych 2009;17:574–81
43. Rovner BW, Casten RJ, Leiby BE, et al. Activity loss is associated with cognitive decline in age-related macular degeneration. Thomas Jefferson University, Department of Psychiatry and Human Behavior, Faculty Papers. Paper 5. 2009.
44. Lövdén M, Ghisletta P, Lindenberger U. Social participation attenuates decline in perceptual speed in old and very old age. Psych Aging 2005;20:423–34.
45. Antonucci TC. Social relations. An examination of social networks, social support, and sense of control. In: Birren JE, Schaie KW, editors. Handbook of the psychology of aging. 5th ed. San Diego: Academic Press; 2001: 427–53.
46. Reinhardt JP. The importance of friendship and family support in adaptation to chronic vision impairment. J Gerontol Series B Psychol Sci Soc Sci 1996;51B:P268–P78.
47. Wagner M, Schütze Y, Lang FR. Social relationships in old age. In: Baltes PB, Mayer KU, editors. The Berlin Aging Study Aging from 70 to 100. Cambridge, UK: Cambridge University Press; 1999: 282–301.
48. Wahl H-W, Tesch-Römer C. Aging, sensory loss, and social functioning. In: Charness N, Park D, Sabel B, editors. Aging and communication: Opportunities and challenges of technology. New York: Springer; 2001: 108-26.
49. Nachtegaal J, Smit JH, Smits C, et al. The association between hearing status and psychosocial health before the age of 70 years: Results from an internet-based national survey on hearing. Ear Hearing 2009;30:302-12
50. Wallhagen MI. The stigma of hearing loss. Gerontologist 2010;50:66–75.
51. Cimarolli VR, Boerner K. Social support and well-being in adults who are visually impaired. J Vis Impair Blind 2005 99:521–34.
52. Cicirelli VG. Fear of death in mid-old age. J Gerontol Series B Psychol Sci Soc Sci 2006;61:P75–P81.
53. Horowitz A, Reinhardt JP. Depression among low vision elders. In: Stuen. C, Arditi A, Horowitz A, et al, editors. Vision rehabilitation assessment, intervention and outcomes. Lisse: Swets & Zeitlinger Publishers; 2000: 655–8.
54. Pinquart M, Pfeiffer JP. Psychological well-being in visually impaired and unimpaired individuals: A meta-analysis. Br J Vis Impair 2011;29:27–45.
55. Tesch-Römer C. Schwerhörigkeit im Alter. Belastung, Bewältigung, Rehabilitation. Heidelberg: Median-Verlag; 2001.
56. Kiely KM, Anstey KJ, Luszcz MA. Dual sensory loss and depressive symptoms: the importance of hearing, daily functioning, and activity engagement. Front Hum Neurosci 2013;7:1–13.
57. Schilling OK, Wahl H-W, Horowitz A, et al. The adaptation dynamics of chronic functional impairment: What we can learn from older adults with vision loss. Psychol Aging 2011;26:203–13.
58. Kunzmann U, Little T, Smith J. Is age-related stability of subjective well-being a paradox? Cross-sectional and longitudinal evidence from the Berlin Aging Study. Psychol Aging 2000;15:511-26.
59. Schilling O, Wahl H-W. Modeling late life adaptation in affective well-being under a severe chronic health condition: The case of age-related macular degeneration. Psychol Aging. 2006;21:703–14.
60. Wahl H-W, Schilling O, Becker S, et al. A German research program on the psychosocial adaptation to age-related vision impairment: Recent findings based on a control theory approach. Europ Psychol 2003;8:168-77.
61. Casten R, Rovner B. Depression in age-related macular degeneration. J Visual Impair Blind 2008;102:591-9.
62. Crews JE, Campbell VA. Vision impairment and hearing loss among community-dwelling older Americans: implications for health and functioning. Am J Pub Health 2004;94:823–9.
63. Horowitz A, Reinhardt JP, Boerner K. The effect of rehabilitation on depression among visually disabled older adults. Aging Mental Health 2005;9:563–70.
64. Cimarolli VR. Perceived overprotection and distress in adults with visual impairment. Rehabil Psychol 2006;51:338-45.
65. Ishine M, Okumiya K, Matsubayashi K. A close association between hearing impairment and activities of daily living, depression, and quality of life in community-dwelling older people in Japan. J Am Geriatr Soc 2007;55:316-7.
66. Gopinath B, Wang JJ, Schneider J, et al. Depressive symptoms in older adults with hearing impairments: The Blue Mountains Study. J Am Geriatr Soc 2009;57:1306-8.
67. Chou K-L, Chi I. Combined effect of vision and hearing impairment on depression in elderly Chinese. Int J Geriatr Psych 2004;19:825-32.
68. Tambs K. Moderate effects of hearing loss on mental health and subjective well-being: Results from the Nord-Trøndelag Hearing Loss Study. Psychosom Med 2004;66:776-82.
69. Bernabei V, Morini V, Moretti F, et al. Vision and hearing impairments are associated with depressive--anxiety syndrome in Italian elderly. Aging Ment Health 2011 15:467-74.
70. Wahl H-W, Heyl V, Langer N. Lebensqualität bei Seheinschränkung im Alter: Das Beispiel altersabhängige Makuladegeneration [Quality of life by limited vision in old age: the example of age-related macula degeneration]. Der Ophthalmologe 2008;105:735-43.
71. Wahl H-W, Kämmerer A, Holz F, et al. Psychosocial intervention for age-related macular degeneration: A pilot project. J Vis Impair Blind 2006;100:533-44.
72. Rees G, Keeffe JE, Hassell J, et al. A self-management program for low vision: Program overview and pilot evaluation. Disabil Rehab 2010;32:808-15.
73. Rovner BW, Casten RJ. Preventing late-life depression in age-related macular degeneration. Am J Geriatr Psych 2008;16:454-9
74. Eklund K, Sonn U, Nystedt P, et al. A cost-effectiveness analysis of a health education programme for elderly persons with age-related macular degeneration: A longitudinal study. Disabil Rehab 2005;27:1203-12.
75. Pijnacker J, Verstraten P, van Damme W, et al. Rehabilitation of reading in older individuals with macular degeneration: A review of effective training programs. Aging Neuropsych Cognition. 2011;18:708-32.
76. Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: A meta-analytic study. Psychol Sci 2003;14:125-30.
77. Kovács É, Tóth K, Dénes L, et al. Effects of exercise programs on balance in older women with age-related visual problems: A pilot study. Arch Gerontol Geriatr 2012;55:446-52.
78. McDonnall MC. Physical status as a moderator of depressive symptoms among older adults with dual sensory loss. Rehab Psychol 2011;56:67-76.
79. Chen EW, Fu ASN, Chan KM, et al. The effects of Tai Chi on the balance control of elderly persons with visual impairment: a randomised clinical trial. Age Ageing 2012;41:254-9.
80. Miszko TA, Ramsey VK, Blasch BB. Tai Chi for people with visual impairments: a pilot study. J Vis Impair Blind 2004;98:5-13.
81. Ray C, Horvat M, Keen K, et al. Using Tai Chi as an exercise intervention for improving balance in adults with visual impairments: Two case studies. RE:view 2005;37:17-24.
82. Jeter PE, Dagnelie G, Khalsa SBS, et al. Yoga for persons with severe visual impairment: a feasibility study. Altern Med Stud 2012;2:18-25.
83. Surakka A, Kivela T. Motivating visually impaired and deaf-blind people to perform regular physical exercises. Br J Visual Impair 2008;26:255-68.
84. Li-Korotky H-S. Age-related hearing loss: Quality of care for quality of life. Gerontologist 2012;52:265-71.
85. Chisolm TH, Johnson CE, Danhauer JL, et al. A systematic review of health-related quality of life and hearing aids: Final report of the American Academy of Audiology Task Force on the Health-Related Quality of Life Benefits of Amplification in Adults. J Am Acad Audiol 2007;18:151-83.
86. McCormack A, Fortnum H. Why do people fitted with hearing aids not wear them? Int J Audiol 2013 52:360-8.
87. Meyer C, Hickson L. What factors influence help-seeking for hearing impairment and hearing aid adoption in older adults? Int J Audiol 2012;51:66-74.
88. Andersson G, Green M, Melin L. Behavioural hearing tactics: a controlled trial of a short treatment programme. Behav Res Ther 1997;35:523-30.
89. Andersson G, Melin L, Scott B, et al. Behavioural counselling for subjects with acquired hearing loss. A new approach to hearing tactics. Scandinav Audiol 1994;23:249-56.
90. Burk MH, Humes LE. Effects of long-term training on aided speech-recognition performance in noise in older adults. J Speech Lang Hear Res 2008;51:759-71.
91. Henderson Sabes J, Sweetow RW. Variables predicting outcomes on listening and communication enhancement (LACETM) training. Int J Audiol 2007;46:374-83.
92. Kramer SE, Allessie GH, Dondorp AW, et al. A home education program for older adults with hearing impairment and their significant others: a randomized trial evaluating short- and long-term effects. Int J Audiol 2005;44:255-64.
93. Hickson L, Worrall L, Scarinci N. Measuring outcomes of a communication program for older people with hearing impairment using the International Outcome Inventory. Int J Audiol 2006;45:238-46.
94. Barcroft J, Sommers MS, Tye-Murray N, et al. Tailoring auditory training to patient needs with single and multiple talkers: Transfer-appropriate gains on a four-choice discrimination test. Int J Audiol 2011;50:802-8.
95. Wahl H-W. The psychological challenge of late-life vision impairment: Concepts, Findings, and practical implications. J Ophthalmol 2013.
96. Lin FR. Hearing loss in older adults. Who’s listening? JAMA 2012;307:1147-8.
97. Willis SL, Tennstedt SL, Marsiske M, et al. Long-term effects of cognitive training on everyday functional outcomes in older adults. JAMA 2006;296:2805-14.
98. Roets-Merken LM, Graff MJL, Zuidema SU, et al. Effectiveness of a self-management program for dual sensory impaired seniors in aged care settings: study protocol for a cluster randomized controlled trial. Trials 2013;14.
99. Vreeken HL, van Rens GHMB, Kramer SE, et al. Dual sensory loss: development of a dual sensory loss protocol and design of a randomized controlled trial. BMC Geriatr 2013;13.
100. Rees G, Saw C, Larizza M, et al. Should family and friends be involved in group-based rehabilitation programs for adults with low vision? Br J Visual Impair 2007;25:155-68.
101. Birk T, Hickl S, Wahl H-W, et al. Development and pilot evaluation of a psychosocial intervention program for patients with age-related macular degeneration. Gerontologist 2004;44:836-43.
102. Bradley P, Mitchell J, Bradley C, editors. Peer support for people newly diagnosed with macular degeneration: a pilot study. International Congress Vision 2005 September. London, UK.
103. Brody B, Williams R, Thomas R, et al. Age-related macular degeneration: A randomized clinical trial of a self-management intervention. Ann Behavi Med 1999;21:322-9.
104. Brody BL, Roch-Levecq A-C, Gamst AC, et al. Self-management of age-related macular degeneration and quality of life: a randomized controlled trial. Arch Ophthalmol 2002;120:1477-83.
105. Brody BL, Roch-Levecq A-C, Thomas RG, et al. Self-management of age-related macular degeneration at the 6-month follow-up. a randomized controlled trial. Arch Ophthalmol 2005;123:46-53.
106. Brody BL, Roch-Levecq A-C, Kaplan RM, et al. Age-related macular degeneration: self-management and reduction of depressive symptoms in a randomized, controlled study. J Am Geriatr Soc 2006;54:1557-62.
107. Dahlin-Ivanoff S, Sonn U, Svensson E. A health education program for elderly persons with visual impairments and perceived security in the performance of daily occupations: a randomized study. Am J Occup Thera 2002;56:322-30.
108. Eklund K, Sonn U, Dahlin-Ivanoff S. Long-term evaluation of a health education programme for elderly persons with visual impairment. A randomized study. Disabil Rehab 2004;26:401-9.
109. Eklund K, Dahlin-Ivanoff S. Health education for people with macular degeneration: Learning experiences and the effect on daily occupations. Can J Occup Ther 2006;73:272-80.
110. Eklund K, Sjöstrand J, Dahlin-Ivanoff S. A randomized controlled trial of a health-promotion programme and its effect on ADL dependence and self-reported health problems for the elderly visually impaired. Scand J Occupat Ther 2008;15:68-74.
111. Kämmerer A, Wahl H-W, Becker S, et al. Psychosoziale Unterstützung von älteren Menschen mit einer chronischen Sehbeeinträchtigung: Anwendung und Überprüfung einer problemlöse- und einer emotionsfokussierten Kurzintervention. Zeitschrift für Gesundheitspsychologie 2006;14:95-105.
112. Rovner BW, Casten RJ, Hegel MT, et al. Preventing depression in age-related macular degeneration. Arch Gen Psychiatr 2007;64:886-92.
113. Rovner BW, Casten RJ, Hegel MT, et al. Improving function in age-related macular degeneration: A randomized clinical trial. Ophthalmology 2013;120:1649-55.
114. Barcroft J, Mauzé E, Schroy C, et al. Improving the quality of auditory training by making tasks meaningful. Persp Audiol 2011;7:15-28.
The short cervix and preterm birth: 8 key questions and evidence-based answers
CASE: NULLIPAROUS WOMAN WITH A SHORT CERVIX
Your ultrasound technician telephones to report that your 32-year-old nulliparous patient, who is currently at 20 weeks’ gestation, was incidentally found to have a short cervix (18 mm) at the time of her routine fetal anatomy survey.
How do you proceed? And how do you counsel the patient? What interventions might reduce the risk of preterm birth (PTB)? Would your recommendations change if she had a history of PTB or was carrying twins?
Preterm birth, defined as delivery prior to 37 weeks’ gestation, is the leading cause of neonatal morbidity and mortality in the United States. The rate of PTB peaked at 12.8% in 2006 and has slowly declined since but remains unacceptably high at 11.5%.1 Most PTBs are spontaneous, arising from the onset of labor or from preterm premature rupture of membranes. Regrettably, tocolytics remain largely ineffective once the process of preterm parturition has begun.
Ideally, women at highest risk for PTB could be identified so that additional screening and interventions could be initiated. Few prognostic tests are available to predict which women will deliver preterm. Generally, the greatest risk factor for spontaneous PTB is a history of spontaneous PTB.2,3 However, women with such a history account for only 10% of all births before 34 weeks’ gestation.
The appearance and length of the cervix during the second trimester appears to be an even better predictor of spontaneous PTB than history alone (FIGURE 1).4,5 For example, in one study of unselected pregnant women at 22 to 24 weeks’ gestation, only 1.7% had a cervical length less than 15 mm, but they accounted for 58% of births before 32 weeks.6 The shorter the cervix, the greater the risk of spontaneous PTB.7 The presence of a short cervix is even more ominous in a woman with a history of spontaneous PTB.8
Optimal pregnancy management after detection of a short cervix remains somewhat unclear and varies, based on the rest of the patient’s clinical picture and obstetric history.
In this article, I address 8 critical questions about diagnosis and management of the short cervix in the second trimester and offer evidence-based answers for clinical practice.
1. How is a short cervix defined?
A cervical length below the 10th centile for gestational age is considered “short.” At 18 to 24 weeks’ gestation, the 10th centile corresponds to a cervical length of less than 25 mm.9
The cervix undergoes physiologic shortening that begins at 28 to 30 weeks of gestation. At 32 weeks, the 50th centile for cervical length is 25 mm. Therefore, cervical-length measurements that appear moderately short between 28 and 32 weeks and beyond are of limited clinical utility, and the clinician should incorporate gestational age into prematurity risk assessment.7
2. Who should be screened?
The question of whether universal cervical-length assessment should be performed is controversial. Several decision analyses in recent years suggest that universal sonographic screening for a short cervix is cost-effective.10,11 Overall, however, the effectiveness of universal cervical-length screening remains clinically understudied, and it is difficult to draw conclusions from decision analyses. Moreover, there is considerable concern about resources and feasibility of implementing universal vaginal cervical-length assessment, as well as significant disagreement about the accuracy of transabdominal cervical-length assessment in the detection of a short cervix.
Transabdominal ultrasound may overestimate cervical length by as much as 10 to 15 mm. One recent study demonstrated that, using a transabdominal cutoff of 30 mm, the sensitivity of detecting a transvaginal cervical length of less than 20 mm was 90%; if the cutoff was increased to 35 mm, sensitivity increased to 100%.12
A collaborative practice guideline on obstetric ultrasound from the American College of Radiology, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, and the Society of Radiologists in Ultrasound recommends that the maternal cervix be examined “as clinically appropriate when technically feasible” during a standard second- or third-trimester ultrasound examination (FIGURE 2).13 The guideline also states that transvaginal or transperineal ultrasound may be considered if the cervix appears shortened or cannot be adequately visualized during the transabdominal ultrasound. However, no specific protocols are suggested.
Given the uncertainty, it is recommended that each practice or ultrasound unit adopt a standard protocol for cervical-length assessment during pregnancy. This protocol can entail either routine abdominal or vaginal assessment of the cervix, or a combination of abdominal and vaginal assessment. Clinical risk factors can be used to help stratify low-risk women when abdominal cervical-length assessment is the initial approach to evaluation.
In my practice, all women undergo cervical-length assessment at the time of the routine anatomy survey (18–22 weeks). Those who are at low risk for PTB are screened initially with transabdominal ultrasound, and a transvaginal examination is performed if the cervix cannot be seen or appears to be less than 30 mm in length.
Women with a history of spontaneous PTB undergo screening by transvaginal cervical-length assessment. Typically, the first measurement is obtained at the time of the fetal anatomic survey (18–22 weeks), when the lower uterine segment is sufficiently developed to accurately measure the cervix. We perform serial cervical-length assessment every 1 or 2 weeks until 28 weeks’ gestation in women with a prior early spontaneous PTB (<34 weeks), those with a history of recurrent PTB, and those who have an initial short cervix. Serial monitoring has been shown to increase the prediction of spontaneous PTB in high-risk women.14
See the algorithm presented in (FIGURE 3) for the screening and treatment of women with singleton gestations.
3. How do I counsel patients about the risk of prematurity?
The risk of spontaneous PTB varies with the gestational age that the short cervix is detected and with the degree of cervical shortening. The earlier in the pregnancy the cervix is found to be short, the higher the risk for spontaneous PTB. For example, results of one large multicenter study of almost 3,000 unselected women pregnant with a singleton gestation across the United States showed that a cervical length of 25 mm was associated with a 15% to 20% incidence of PTB when detected at 28 weeks’ gestation; the incidence rose to 30% to 35% if the short cervix was detected at 20 weeks.9 In this cohort, 84% of women had no history of PTB.
A short cervix and a prior PTB (particularly a very early prior PTB) are two major risk factors for PTB. Together, they significantly increase the risk of an early delivery over individual or single factors alone. Among women who have had a prior PTB and who now have a cervical length of less than 25 mm, the risk of recurrent PTB is 35% to 40%. In contrast, women with a prior PTB and a normal cervical length have a significantly lower risk of recurrence—around 10%.15
If the physical examination is concerning for cervical dilation or prolapsing membranes, women should be counseled about the poor prognosis for the pregnancy, particularly when these findings are detected at a previable or periviable gestational age, regardless of their history of PTB. In these circumstances, in the absence of labor or intra-amniotic infection, a “rescue” cervical cerclage may be considered as a last resort (see page 34 for more on cerclage).
4. What evaluation or monitoring is needed once a short cervix is identified?
Women found to have a short cervix should be evaluated for the presence of preterm labor and intra-amniotic infection. This evaluation may include a sterile speculum examination or digital cervical examination, or both, as well as screening for genitourinary tract infection. Other testing may include a complete blood count with a white blood cell differential and external tocometry with or without fetal heart rate monitoring (based on the gestational age, as appropriate).
For some women with a short cervix, intra-amniotic infection may be a contributing factor (or it may develop if there are exposed membranes in the vagina). The presence of intra-amniotic infection precludes further expectant management of the pregnancy because of the risk of maternal infectious morbidity, including sepsis.
Women who have intra-amniotic infection are not candidates for any intervention such as cerclage or progesterone supplementation.
If the patient is at or beyond the point of fetal viability at the time her short cervix is detected, consider external fetal heart rate monitoring.
Antenatal corticosteroids can be administered, as appropriate, depending on the perceived risk of delivery.
5. Should I place a cerclage?
Numerous studies have examined the efficacy of ultrasound-indicated cerclage, a surgical procedure to stitch the cervix closed once a short cervix has been detected.
In general, placement of a cervical cerclage is not offered past the point of fetal viability, which is generally in the range of 23 to 25 weeks’ gestation, depending on local institutional and neonatal intensive care unit policies. Confirmed or suspected chorioamnionitis is also a contraindication to cerclage placement.
Among women without a history of PTB who are found to have a short cervix, existing data do not suggest a benefit for cerclage, although vaginal progesterone appears to be a reasonable option (see page 36).16,17
As for women with a history of PTB, Owen and colleagues studied 302 patients with a cervical length less than 25 mm and a history of spontaneous PTB before 34 weeks.18 The women were randomly assigned to ultrasound-indicated cerclage or “usual care,” which consisted of recommendations of pelvic rest, physical activity restriction, and education about the symptoms of preterm labor. Otherwise, management was directed by clinical practice at each center. All women treated with cerclage had a reduced risk of previable PTB (<24 weeks’ gestation), and those who had the shortest cervical length (<15 mm) also had a lower risk of delivery before 35 weeks.
The degree of cervical shortening that has “qualified” women for study enrollment has varied between studies, with upper limits ranging from 15 to 25 mm. Berghella and colleagues performed a patient-level meta-analysis to determine whether efficacy of the cerclage varied by cervical length at the time of placement.8 They examined 552 women with singleton gestations from four randomized controlled trials that included 208 women with a short cervix and a history of spontaneous PTB. They found a significant reduction in the rate of preterm delivery before 35 weeks’ gestation among women with singleton pregnancies, a short cervix, and a history of spontaneous PTB; the reduction did not vary by the degree of cervical shortening. However, there was no significant reduction in the rate of PTB among the subset of women without a history of spontaneous PTB.
Berghella and colleagues estimated that, if a cervical cerclage were offered to the 8% of women with a prior spontaneous PTB and a cervical length of less than 25 mm, more than 6,500 newborns would be saved each year from perinatal death associated with prematurity.8
The placement of a “rescue” cerclage in the setting of cervical dilation with or without prolapsing membranes is associated with high rates of maternal and neonatal morbidity, regardless of the patient’s obstetric history. However, cerclage placement in this setting may be associated with better outcomes than expectant management with bed rest alone.19 Patients should be carefully counseled about this procedure, including the risk of infection and the possibility that pregnancy may be prolonged only from a previable to a periviable gestational age. Decisions as to whether a patient is a candidate for rescue cerclage should be made in consultation with a maternal-fetal medicine specialist.20
6. Is a cervical pessary beneficial?
The pessary is another “mechanical” treatment similar to cerclage, and it may be helpful in reducing the incidence of PTB among women with a short cervix. In the largest study of this approach, 16,000 primarily low-risk women with singleton gestations were screened for a short cervix. Of these, 385 women with a cervical length of less than 25 mm were randomly assigned to undergo Arabin pessary placement or expectant management.21
Among those who received the pessary, the odds ratio (OR) for PTB before 34 weeks was significantly reduced (OR, 0.18; 95% confidence interval [CI], 0.08–0.37), and the OR for adverse composite neonatal outcome also was significantly reduced (OR, 0.14; 95% CI, 0.04–0.39).21
The Arabin pessary is not currently approved by the US Food and Drug Administration for this indication in the United States, nor is it available for insertion outside of research studies. Other ring-shaped pessaries are available in the United States, but their use in the setting of a short cervix is considered experimental and off-label. Additional studies of this promising intervention are currently under way.
7. Who is a candidate for supplemental progesterone?
Progesterone is a naturally occurring hormone essential to the maintenance of pregnancy. It has an overall quiescent effect on the myometrium, is known to have anti-inflammatory properties, and inhibits cervical ripening.22 It has been studied in a number of different formulations and doses.
Vaginal progesterone supplementation has been shown to reduce the risk of PTB among women with a shortened cervix regardless of their pregnancy history.16,17,23,24 In the largest trials of unselected general obstetrics populations (including women with and without a history of PTB), use of vaginal progesterone among women with a short cervix reduced the rates of very early spontaneous PTB (<28 and <32 weeks’ gestation) by 40% to 50%.16,17 As expected, progesterone also was associated with a significant reduction in the rates of respiratory distress syndrome and composite neonatal morbidity.
Intramuscular (IM) progesterone supplementation has been shown to reduce the rate of recurrent PTB among women with a history of spontaneous PTB. When caring for a woman with a history of PTB who is found to have a short cervix, IM progesterone should be offered if the woman is not already taking it. IM progesterone has not been proven effective among nulliparous women who are incidentally found to have a short cervix; it should not be offered in this situation.25
8. Should the care of women carrying twins or triplets be managed differently?
Yes. Although women with multiple gestations are at higher risk for PTB than women carrying a singleton fetus, no interventions have proven to be effective in this population. Many studies have been limited to twin gestations as a group, with an inability to perform subgroup analyses or enroll women who also have a short cervix, due to sample size and power issues.
Progesterone in multiple gestations
Although several formulations of progesterone—including IM 17-alpha hydroxyprogesterone caproate, micronized progesterone, and progesterone suppositories—have been studied, no randomized trial data have demonstrated a reduction in PTB or neonatal morbidity.26–29 Individual patient-level data from a meta-analysis of vaginal progesterone in the setting of multiple gestations with a short cervical length suggest trends toward a reduced rate of PTB before 33 weeks’ gestation (relative risk [RR], 0.70; 95% CI, 0.34–1.44) and lower composite neonatal morbidity and mortality (RR, 0.56; 95% CI, 0.30–0.97).30
Mechanical strategies in multiple gestations
No randomized data suggest that a pessary is effective in multiple gestations. In one study of 813 multiple gestations in the Netherlands, women were randomly assigned—regardless of cervical length—to receive a pessary at 16 to 20 weeks versus standard care; no difference in adverse perinatal outcomes was detected between groups.31
As for cerclage, although data are limited, some studies suggest that placement of a cerclage in twin gestations with cervical shortening may increase the rate of PTB.32
Bottom line for multiples
Although women carrying multiple gestations are at higher risk for PTB, data are extremely limited. At present, data do not support routine use of cerclage for a short cervix—and some suggest possible harm. Vaginal progesterone or placement of a pessary may be of benefit but should be used with caution and with the understanding that data are sparse.
CASE RESOLVED
You counsel your nulliparous patient that she has an elevated risk of PTB, based on her cervical length of 18 mm at 20 weeks’ gestation, and evaluate her clinically for evidence of preterm labor. Apart from the short cervix, her examination is unremarkable. You offer her nightly vaginal progesterone suppositories and schedule a visit to reevaluate her cervix in 1 week. If cervical dilation or prolapsing membranes are noted before the age of fetal viability, you will consider placing a “rescue” cervical cerclage.
Had this patient experienced a prior PTB, you would first ensure that she is taking IM 17-alpha hydroxyprogesterone caproate. It also would be reasonable to place an ultrasound-indicated cerclage or begin vaginal progesterone suppositories. Although data are limited on concomitant use of IM and vaginal progesterone, some experts may consider it, on an experimental basis, for patients with a short cervix and a prior PTB.
If this patient were carrying a twin gestation, vaginal progesterone would still be a consideration, provided she is counseled about the limited evidence of its efficacy in this setting. Cerclage would not be appropriate, given the possible risk of harm.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state. Stay in touch! Your feedback is important to us!
1. Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2012. Natl Vital Stat Rep. 2013;62(3):1–20.
2. Adams MM, Elam-Evans LD, Wilson HG, Gilbertz DA. Rates of and factors associated with recurrence of preterm delivery. JAMA. 2000;283(12):1591–1596.
3. Ananth CV, Getahun D, Peltier MR, Salihu HM, Vintzileos AM. Recurrence of spontaneous versus medically indicated preterm birth. Am J Obstet Gynecol 2006;195(3):643–650.
4. To MS, Skentou CA, Royston P, Yu CK, Nicolaides KH. Prediction of patient-specific risk of early preterm delivery using maternal history and sonographic measurement of cervical length: A population-based prospective study. Ultrasound Obstet Gynecol. 2006;27(4):362–367.
5. Guzman ER, Ananth CV. Cervical length and spontaneous prematurity: Laying the foundation for future interventional randomized trials for the short cervix. Ultrasound Obstet Gynecol. 2001;18(3):195–199.
6. Heath VC, Southall TR, Souka AP, Elisseou A, Nicolaides KH. Cervical length at 23 weeks of gestation: Prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol. 1998;12(5):312–317.
7. Berghella V, Roman A, Daskalakis C, Ness A, Baxter JK. Gestational age at cervical length measurement and incidence of preterm birth. Obstet Gynecol. 2007;110(2 Pt 1):311–317.
8. Berghella V, Keeler SM, To MS, Althuisius SM, Rust OA. Effectiveness of cerclage according to severity of cervical length shortening: A meta-analysis. Ultrasound Obstet Gynecol. 2010;35(4):468–473.
9. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334(9):567–572.
10. Werner EF, Han CS, Pettker CM, et al. Universal cervical-length screening to prevent preterm birth: A cost-effectiveness analysis. Ultrasound Obstet Gynecol. 2011;38 (1):32–37.
11. Cahill AG, Odibo AO, Caughey AB, et al. Universal cervical length screening and treatment with vaginal progesterone to prevent preterm birth: A decision and economic analysis. Am J Obstet Gynecol. 2010;202(6):548.e1–e8.
12. Friedman AM, Srinivas SK, Parry S, Elovitz MA, Wang E, Schwartz N. Can transabdominal ultrasound be used as a screening test for short cervical length? Am J Obstet Gynecol. 2013;208(3):190.e1–e7.
13. American College of Radiology, American College of Obstetricians and Gynecologists, American Institute of Ultrasound in Medicine, Society of Radiologists in Ultrasound. ACR–ACOG–AIUM–SRU Practice Guideline for the Performance of Obstetrical Ultrasound. http://www.acr.org/Quality-Safety/Standards-Guidelines/Practice-Guidelines-by-Modality/~/media/ACR/Documents/PGTS/guidelines/US_Obstetrical.pdf. Accessed June 16, 2014.
14. Owen J, Yost N, Berghella V, et al. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA. 2001;286(11):1340–1348.
15. Iams JD, Goldenberg RL, Mercer BM, et al. The Preterm Prediction Study: Recurrence risk of spontaneous preterm birth. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol. 1998;178(5):1035–1040.
16. Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH; Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007;357(5):462–469.
17. Hassan SS, Romero R, Vidyadhari D, et al; PREGNANT Trial. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: A multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2011;38(1):18–31.
18. Owen J, Hankins G, Iams JD, et al. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol. 2009;201(4):375.e1–e8.
19. Namouz S, Porat S, Okun N, Windrim R, Farine D. Emergency cerclage: literature review. Obstet Gynecol Surv. 2013;68(5):379–388.
20. Cockwell HA, Smith GN. Cervical incompetence and the role of emergency cerclage. J Obstet Gynaecol Can. 2005;27(2):123–129.
21. Goya M, Pratcorona L, Merced C, et al. Cervical pessary in pregnant women with a short cervix (PECEP): An open-label randomised controlled trial. Lancet. 2012;379(9828):1800–1806.
22. Mendelson CR. Minireview: fetal-maternal hormonal signaling in pregnancy and labor. Mol Endocrinol. 2009;23(7):947–954.
23. Meis PJ, Klebanoff M, Thom E, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379–2385. Erratum: N England J Med. 2003;349(13):1299.
24. O’Brien JM, Adair CD, Lewis DF, et al. Progesterone vaginal gel for the reduction of recurrent preterm birth: Primary results from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol 2007;30(5):687–696.
25. Grobman WA, Thom EA, Spong CY, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units (MFMU) Network. 17 alpha-hydroxyprogesterone caproate to prevent prematurity in nulliparas with cervical length less than 30 mm. Am J Obstet Gynecol. 2012;207(5):390.e1–e8.
26. Rouse DJ, Caritis SN, Peaceman AM, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. A trial of 17 alpha-hydroxyprogesterone caproate to prevent prematurity in twins. N Engl J Med. 2007;357(5):454–461.
27. Caritis SN, Rouse DJ, Peaceman AM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Maternal-Fetal Medicine Units (MFMU) Network. Prevention of preterm birth in triplets using 17 alpha-hydroxyprogesterone caproate: A randomized controlled trial. Obstet Gynecol. 2009;113(2 Pt 1):285–292.
28. Rode L, Klein K, Nicolaides KH, Krampl-Bettelheim E, Tabor A; PREDICT Group. Prevention of preterm delivery in twin gestations (PREDICT): A multicenter, randomized, placebo-controlled trial on the effect of vaginal micronized progesterone. Ultrasound Obstet Gynecol. 2011;38(3):272–280.
29. Norman JE, Mackenzie F, Owen P, et al. Progesterone for the prevention of preterm birth in twin pregnancy (STOPPIT): A randomised, double-blind, placebo-controlled study and meta-analysis. Lancet. 2009;373(9680):2034–2040.
30. Romero R, Nicolaides K, Conde-Agudelo A, et al. Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: A systematic review and metaanalysis of individual patient data. Am J Obstet Gynecol. 2012;206(2):124.e1–e19.
31. Liem S, Schuit E, Hegeman M, et al. Cervical pessaries for prevention of preterm birth in women with a multiple pregnancy (ProTWIN): A multicentre, open-label randomised controlled trial. Lancet. 2013;382(9901):1341–1349.
32. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: Meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106(1):181–189.
CASE: NULLIPAROUS WOMAN WITH A SHORT CERVIX
Your ultrasound technician telephones to report that your 32-year-old nulliparous patient, who is currently at 20 weeks’ gestation, was incidentally found to have a short cervix (18 mm) at the time of her routine fetal anatomy survey.
How do you proceed? And how do you counsel the patient? What interventions might reduce the risk of preterm birth (PTB)? Would your recommendations change if she had a history of PTB or was carrying twins?
Preterm birth, defined as delivery prior to 37 weeks’ gestation, is the leading cause of neonatal morbidity and mortality in the United States. The rate of PTB peaked at 12.8% in 2006 and has slowly declined since but remains unacceptably high at 11.5%.1 Most PTBs are spontaneous, arising from the onset of labor or from preterm premature rupture of membranes. Regrettably, tocolytics remain largely ineffective once the process of preterm parturition has begun.
Ideally, women at highest risk for PTB could be identified so that additional screening and interventions could be initiated. Few prognostic tests are available to predict which women will deliver preterm. Generally, the greatest risk factor for spontaneous PTB is a history of spontaneous PTB.2,3 However, women with such a history account for only 10% of all births before 34 weeks’ gestation.
The appearance and length of the cervix during the second trimester appears to be an even better predictor of spontaneous PTB than history alone (FIGURE 1).4,5 For example, in one study of unselected pregnant women at 22 to 24 weeks’ gestation, only 1.7% had a cervical length less than 15 mm, but they accounted for 58% of births before 32 weeks.6 The shorter the cervix, the greater the risk of spontaneous PTB.7 The presence of a short cervix is even more ominous in a woman with a history of spontaneous PTB.8
Optimal pregnancy management after detection of a short cervix remains somewhat unclear and varies, based on the rest of the patient’s clinical picture and obstetric history.
In this article, I address 8 critical questions about diagnosis and management of the short cervix in the second trimester and offer evidence-based answers for clinical practice.
1. How is a short cervix defined?
A cervical length below the 10th centile for gestational age is considered “short.” At 18 to 24 weeks’ gestation, the 10th centile corresponds to a cervical length of less than 25 mm.9
The cervix undergoes physiologic shortening that begins at 28 to 30 weeks of gestation. At 32 weeks, the 50th centile for cervical length is 25 mm. Therefore, cervical-length measurements that appear moderately short between 28 and 32 weeks and beyond are of limited clinical utility, and the clinician should incorporate gestational age into prematurity risk assessment.7
2. Who should be screened?
The question of whether universal cervical-length assessment should be performed is controversial. Several decision analyses in recent years suggest that universal sonographic screening for a short cervix is cost-effective.10,11 Overall, however, the effectiveness of universal cervical-length screening remains clinically understudied, and it is difficult to draw conclusions from decision analyses. Moreover, there is considerable concern about resources and feasibility of implementing universal vaginal cervical-length assessment, as well as significant disagreement about the accuracy of transabdominal cervical-length assessment in the detection of a short cervix.
Transabdominal ultrasound may overestimate cervical length by as much as 10 to 15 mm. One recent study demonstrated that, using a transabdominal cutoff of 30 mm, the sensitivity of detecting a transvaginal cervical length of less than 20 mm was 90%; if the cutoff was increased to 35 mm, sensitivity increased to 100%.12
A collaborative practice guideline on obstetric ultrasound from the American College of Radiology, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, and the Society of Radiologists in Ultrasound recommends that the maternal cervix be examined “as clinically appropriate when technically feasible” during a standard second- or third-trimester ultrasound examination (FIGURE 2).13 The guideline also states that transvaginal or transperineal ultrasound may be considered if the cervix appears shortened or cannot be adequately visualized during the transabdominal ultrasound. However, no specific protocols are suggested.
Given the uncertainty, it is recommended that each practice or ultrasound unit adopt a standard protocol for cervical-length assessment during pregnancy. This protocol can entail either routine abdominal or vaginal assessment of the cervix, or a combination of abdominal and vaginal assessment. Clinical risk factors can be used to help stratify low-risk women when abdominal cervical-length assessment is the initial approach to evaluation.
In my practice, all women undergo cervical-length assessment at the time of the routine anatomy survey (18–22 weeks). Those who are at low risk for PTB are screened initially with transabdominal ultrasound, and a transvaginal examination is performed if the cervix cannot be seen or appears to be less than 30 mm in length.
Women with a history of spontaneous PTB undergo screening by transvaginal cervical-length assessment. Typically, the first measurement is obtained at the time of the fetal anatomic survey (18–22 weeks), when the lower uterine segment is sufficiently developed to accurately measure the cervix. We perform serial cervical-length assessment every 1 or 2 weeks until 28 weeks’ gestation in women with a prior early spontaneous PTB (<34 weeks), those with a history of recurrent PTB, and those who have an initial short cervix. Serial monitoring has been shown to increase the prediction of spontaneous PTB in high-risk women.14
See the algorithm presented in (FIGURE 3) for the screening and treatment of women with singleton gestations.
3. How do I counsel patients about the risk of prematurity?
The risk of spontaneous PTB varies with the gestational age that the short cervix is detected and with the degree of cervical shortening. The earlier in the pregnancy the cervix is found to be short, the higher the risk for spontaneous PTB. For example, results of one large multicenter study of almost 3,000 unselected women pregnant with a singleton gestation across the United States showed that a cervical length of 25 mm was associated with a 15% to 20% incidence of PTB when detected at 28 weeks’ gestation; the incidence rose to 30% to 35% if the short cervix was detected at 20 weeks.9 In this cohort, 84% of women had no history of PTB.
A short cervix and a prior PTB (particularly a very early prior PTB) are two major risk factors for PTB. Together, they significantly increase the risk of an early delivery over individual or single factors alone. Among women who have had a prior PTB and who now have a cervical length of less than 25 mm, the risk of recurrent PTB is 35% to 40%. In contrast, women with a prior PTB and a normal cervical length have a significantly lower risk of recurrence—around 10%.15
If the physical examination is concerning for cervical dilation or prolapsing membranes, women should be counseled about the poor prognosis for the pregnancy, particularly when these findings are detected at a previable or periviable gestational age, regardless of their history of PTB. In these circumstances, in the absence of labor or intra-amniotic infection, a “rescue” cervical cerclage may be considered as a last resort (see page 34 for more on cerclage).
4. What evaluation or monitoring is needed once a short cervix is identified?
Women found to have a short cervix should be evaluated for the presence of preterm labor and intra-amniotic infection. This evaluation may include a sterile speculum examination or digital cervical examination, or both, as well as screening for genitourinary tract infection. Other testing may include a complete blood count with a white blood cell differential and external tocometry with or without fetal heart rate monitoring (based on the gestational age, as appropriate).
For some women with a short cervix, intra-amniotic infection may be a contributing factor (or it may develop if there are exposed membranes in the vagina). The presence of intra-amniotic infection precludes further expectant management of the pregnancy because of the risk of maternal infectious morbidity, including sepsis.
Women who have intra-amniotic infection are not candidates for any intervention such as cerclage or progesterone supplementation.
If the patient is at or beyond the point of fetal viability at the time her short cervix is detected, consider external fetal heart rate monitoring.
Antenatal corticosteroids can be administered, as appropriate, depending on the perceived risk of delivery.
5. Should I place a cerclage?
Numerous studies have examined the efficacy of ultrasound-indicated cerclage, a surgical procedure to stitch the cervix closed once a short cervix has been detected.
In general, placement of a cervical cerclage is not offered past the point of fetal viability, which is generally in the range of 23 to 25 weeks’ gestation, depending on local institutional and neonatal intensive care unit policies. Confirmed or suspected chorioamnionitis is also a contraindication to cerclage placement.
Among women without a history of PTB who are found to have a short cervix, existing data do not suggest a benefit for cerclage, although vaginal progesterone appears to be a reasonable option (see page 36).16,17
As for women with a history of PTB, Owen and colleagues studied 302 patients with a cervical length less than 25 mm and a history of spontaneous PTB before 34 weeks.18 The women were randomly assigned to ultrasound-indicated cerclage or “usual care,” which consisted of recommendations of pelvic rest, physical activity restriction, and education about the symptoms of preterm labor. Otherwise, management was directed by clinical practice at each center. All women treated with cerclage had a reduced risk of previable PTB (<24 weeks’ gestation), and those who had the shortest cervical length (<15 mm) also had a lower risk of delivery before 35 weeks.
The degree of cervical shortening that has “qualified” women for study enrollment has varied between studies, with upper limits ranging from 15 to 25 mm. Berghella and colleagues performed a patient-level meta-analysis to determine whether efficacy of the cerclage varied by cervical length at the time of placement.8 They examined 552 women with singleton gestations from four randomized controlled trials that included 208 women with a short cervix and a history of spontaneous PTB. They found a significant reduction in the rate of preterm delivery before 35 weeks’ gestation among women with singleton pregnancies, a short cervix, and a history of spontaneous PTB; the reduction did not vary by the degree of cervical shortening. However, there was no significant reduction in the rate of PTB among the subset of women without a history of spontaneous PTB.
Berghella and colleagues estimated that, if a cervical cerclage were offered to the 8% of women with a prior spontaneous PTB and a cervical length of less than 25 mm, more than 6,500 newborns would be saved each year from perinatal death associated with prematurity.8
The placement of a “rescue” cerclage in the setting of cervical dilation with or without prolapsing membranes is associated with high rates of maternal and neonatal morbidity, regardless of the patient’s obstetric history. However, cerclage placement in this setting may be associated with better outcomes than expectant management with bed rest alone.19 Patients should be carefully counseled about this procedure, including the risk of infection and the possibility that pregnancy may be prolonged only from a previable to a periviable gestational age. Decisions as to whether a patient is a candidate for rescue cerclage should be made in consultation with a maternal-fetal medicine specialist.20
6. Is a cervical pessary beneficial?
The pessary is another “mechanical” treatment similar to cerclage, and it may be helpful in reducing the incidence of PTB among women with a short cervix. In the largest study of this approach, 16,000 primarily low-risk women with singleton gestations were screened for a short cervix. Of these, 385 women with a cervical length of less than 25 mm were randomly assigned to undergo Arabin pessary placement or expectant management.21
Among those who received the pessary, the odds ratio (OR) for PTB before 34 weeks was significantly reduced (OR, 0.18; 95% confidence interval [CI], 0.08–0.37), and the OR for adverse composite neonatal outcome also was significantly reduced (OR, 0.14; 95% CI, 0.04–0.39).21
The Arabin pessary is not currently approved by the US Food and Drug Administration for this indication in the United States, nor is it available for insertion outside of research studies. Other ring-shaped pessaries are available in the United States, but their use in the setting of a short cervix is considered experimental and off-label. Additional studies of this promising intervention are currently under way.
7. Who is a candidate for supplemental progesterone?
Progesterone is a naturally occurring hormone essential to the maintenance of pregnancy. It has an overall quiescent effect on the myometrium, is known to have anti-inflammatory properties, and inhibits cervical ripening.22 It has been studied in a number of different formulations and doses.
Vaginal progesterone supplementation has been shown to reduce the risk of PTB among women with a shortened cervix regardless of their pregnancy history.16,17,23,24 In the largest trials of unselected general obstetrics populations (including women with and without a history of PTB), use of vaginal progesterone among women with a short cervix reduced the rates of very early spontaneous PTB (<28 and <32 weeks’ gestation) by 40% to 50%.16,17 As expected, progesterone also was associated with a significant reduction in the rates of respiratory distress syndrome and composite neonatal morbidity.
Intramuscular (IM) progesterone supplementation has been shown to reduce the rate of recurrent PTB among women with a history of spontaneous PTB. When caring for a woman with a history of PTB who is found to have a short cervix, IM progesterone should be offered if the woman is not already taking it. IM progesterone has not been proven effective among nulliparous women who are incidentally found to have a short cervix; it should not be offered in this situation.25
8. Should the care of women carrying twins or triplets be managed differently?
Yes. Although women with multiple gestations are at higher risk for PTB than women carrying a singleton fetus, no interventions have proven to be effective in this population. Many studies have been limited to twin gestations as a group, with an inability to perform subgroup analyses or enroll women who also have a short cervix, due to sample size and power issues.
Progesterone in multiple gestations
Although several formulations of progesterone—including IM 17-alpha hydroxyprogesterone caproate, micronized progesterone, and progesterone suppositories—have been studied, no randomized trial data have demonstrated a reduction in PTB or neonatal morbidity.26–29 Individual patient-level data from a meta-analysis of vaginal progesterone in the setting of multiple gestations with a short cervical length suggest trends toward a reduced rate of PTB before 33 weeks’ gestation (relative risk [RR], 0.70; 95% CI, 0.34–1.44) and lower composite neonatal morbidity and mortality (RR, 0.56; 95% CI, 0.30–0.97).30
Mechanical strategies in multiple gestations
No randomized data suggest that a pessary is effective in multiple gestations. In one study of 813 multiple gestations in the Netherlands, women were randomly assigned—regardless of cervical length—to receive a pessary at 16 to 20 weeks versus standard care; no difference in adverse perinatal outcomes was detected between groups.31
As for cerclage, although data are limited, some studies suggest that placement of a cerclage in twin gestations with cervical shortening may increase the rate of PTB.32
Bottom line for multiples
Although women carrying multiple gestations are at higher risk for PTB, data are extremely limited. At present, data do not support routine use of cerclage for a short cervix—and some suggest possible harm. Vaginal progesterone or placement of a pessary may be of benefit but should be used with caution and with the understanding that data are sparse.
CASE RESOLVED
You counsel your nulliparous patient that she has an elevated risk of PTB, based on her cervical length of 18 mm at 20 weeks’ gestation, and evaluate her clinically for evidence of preterm labor. Apart from the short cervix, her examination is unremarkable. You offer her nightly vaginal progesterone suppositories and schedule a visit to reevaluate her cervix in 1 week. If cervical dilation or prolapsing membranes are noted before the age of fetal viability, you will consider placing a “rescue” cervical cerclage.
Had this patient experienced a prior PTB, you would first ensure that she is taking IM 17-alpha hydroxyprogesterone caproate. It also would be reasonable to place an ultrasound-indicated cerclage or begin vaginal progesterone suppositories. Although data are limited on concomitant use of IM and vaginal progesterone, some experts may consider it, on an experimental basis, for patients with a short cervix and a prior PTB.
If this patient were carrying a twin gestation, vaginal progesterone would still be a consideration, provided she is counseled about the limited evidence of its efficacy in this setting. Cerclage would not be appropriate, given the possible risk of harm.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state. Stay in touch! Your feedback is important to us!
CASE: NULLIPAROUS WOMAN WITH A SHORT CERVIX
Your ultrasound technician telephones to report that your 32-year-old nulliparous patient, who is currently at 20 weeks’ gestation, was incidentally found to have a short cervix (18 mm) at the time of her routine fetal anatomy survey.
How do you proceed? And how do you counsel the patient? What interventions might reduce the risk of preterm birth (PTB)? Would your recommendations change if she had a history of PTB or was carrying twins?
Preterm birth, defined as delivery prior to 37 weeks’ gestation, is the leading cause of neonatal morbidity and mortality in the United States. The rate of PTB peaked at 12.8% in 2006 and has slowly declined since but remains unacceptably high at 11.5%.1 Most PTBs are spontaneous, arising from the onset of labor or from preterm premature rupture of membranes. Regrettably, tocolytics remain largely ineffective once the process of preterm parturition has begun.
Ideally, women at highest risk for PTB could be identified so that additional screening and interventions could be initiated. Few prognostic tests are available to predict which women will deliver preterm. Generally, the greatest risk factor for spontaneous PTB is a history of spontaneous PTB.2,3 However, women with such a history account for only 10% of all births before 34 weeks’ gestation.
The appearance and length of the cervix during the second trimester appears to be an even better predictor of spontaneous PTB than history alone (FIGURE 1).4,5 For example, in one study of unselected pregnant women at 22 to 24 weeks’ gestation, only 1.7% had a cervical length less than 15 mm, but they accounted for 58% of births before 32 weeks.6 The shorter the cervix, the greater the risk of spontaneous PTB.7 The presence of a short cervix is even more ominous in a woman with a history of spontaneous PTB.8
Optimal pregnancy management after detection of a short cervix remains somewhat unclear and varies, based on the rest of the patient’s clinical picture and obstetric history.
In this article, I address 8 critical questions about diagnosis and management of the short cervix in the second trimester and offer evidence-based answers for clinical practice.
1. How is a short cervix defined?
A cervical length below the 10th centile for gestational age is considered “short.” At 18 to 24 weeks’ gestation, the 10th centile corresponds to a cervical length of less than 25 mm.9
The cervix undergoes physiologic shortening that begins at 28 to 30 weeks of gestation. At 32 weeks, the 50th centile for cervical length is 25 mm. Therefore, cervical-length measurements that appear moderately short between 28 and 32 weeks and beyond are of limited clinical utility, and the clinician should incorporate gestational age into prematurity risk assessment.7
2. Who should be screened?
The question of whether universal cervical-length assessment should be performed is controversial. Several decision analyses in recent years suggest that universal sonographic screening for a short cervix is cost-effective.10,11 Overall, however, the effectiveness of universal cervical-length screening remains clinically understudied, and it is difficult to draw conclusions from decision analyses. Moreover, there is considerable concern about resources and feasibility of implementing universal vaginal cervical-length assessment, as well as significant disagreement about the accuracy of transabdominal cervical-length assessment in the detection of a short cervix.
Transabdominal ultrasound may overestimate cervical length by as much as 10 to 15 mm. One recent study demonstrated that, using a transabdominal cutoff of 30 mm, the sensitivity of detecting a transvaginal cervical length of less than 20 mm was 90%; if the cutoff was increased to 35 mm, sensitivity increased to 100%.12
A collaborative practice guideline on obstetric ultrasound from the American College of Radiology, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, and the Society of Radiologists in Ultrasound recommends that the maternal cervix be examined “as clinically appropriate when technically feasible” during a standard second- or third-trimester ultrasound examination (FIGURE 2).13 The guideline also states that transvaginal or transperineal ultrasound may be considered if the cervix appears shortened or cannot be adequately visualized during the transabdominal ultrasound. However, no specific protocols are suggested.
Given the uncertainty, it is recommended that each practice or ultrasound unit adopt a standard protocol for cervical-length assessment during pregnancy. This protocol can entail either routine abdominal or vaginal assessment of the cervix, or a combination of abdominal and vaginal assessment. Clinical risk factors can be used to help stratify low-risk women when abdominal cervical-length assessment is the initial approach to evaluation.
In my practice, all women undergo cervical-length assessment at the time of the routine anatomy survey (18–22 weeks). Those who are at low risk for PTB are screened initially with transabdominal ultrasound, and a transvaginal examination is performed if the cervix cannot be seen or appears to be less than 30 mm in length.
Women with a history of spontaneous PTB undergo screening by transvaginal cervical-length assessment. Typically, the first measurement is obtained at the time of the fetal anatomic survey (18–22 weeks), when the lower uterine segment is sufficiently developed to accurately measure the cervix. We perform serial cervical-length assessment every 1 or 2 weeks until 28 weeks’ gestation in women with a prior early spontaneous PTB (<34 weeks), those with a history of recurrent PTB, and those who have an initial short cervix. Serial monitoring has been shown to increase the prediction of spontaneous PTB in high-risk women.14
See the algorithm presented in (FIGURE 3) for the screening and treatment of women with singleton gestations.
3. How do I counsel patients about the risk of prematurity?
The risk of spontaneous PTB varies with the gestational age that the short cervix is detected and with the degree of cervical shortening. The earlier in the pregnancy the cervix is found to be short, the higher the risk for spontaneous PTB. For example, results of one large multicenter study of almost 3,000 unselected women pregnant with a singleton gestation across the United States showed that a cervical length of 25 mm was associated with a 15% to 20% incidence of PTB when detected at 28 weeks’ gestation; the incidence rose to 30% to 35% if the short cervix was detected at 20 weeks.9 In this cohort, 84% of women had no history of PTB.
A short cervix and a prior PTB (particularly a very early prior PTB) are two major risk factors for PTB. Together, they significantly increase the risk of an early delivery over individual or single factors alone. Among women who have had a prior PTB and who now have a cervical length of less than 25 mm, the risk of recurrent PTB is 35% to 40%. In contrast, women with a prior PTB and a normal cervical length have a significantly lower risk of recurrence—around 10%.15
If the physical examination is concerning for cervical dilation or prolapsing membranes, women should be counseled about the poor prognosis for the pregnancy, particularly when these findings are detected at a previable or periviable gestational age, regardless of their history of PTB. In these circumstances, in the absence of labor or intra-amniotic infection, a “rescue” cervical cerclage may be considered as a last resort (see page 34 for more on cerclage).
4. What evaluation or monitoring is needed once a short cervix is identified?
Women found to have a short cervix should be evaluated for the presence of preterm labor and intra-amniotic infection. This evaluation may include a sterile speculum examination or digital cervical examination, or both, as well as screening for genitourinary tract infection. Other testing may include a complete blood count with a white blood cell differential and external tocometry with or without fetal heart rate monitoring (based on the gestational age, as appropriate).
For some women with a short cervix, intra-amniotic infection may be a contributing factor (or it may develop if there are exposed membranes in the vagina). The presence of intra-amniotic infection precludes further expectant management of the pregnancy because of the risk of maternal infectious morbidity, including sepsis.
Women who have intra-amniotic infection are not candidates for any intervention such as cerclage or progesterone supplementation.
If the patient is at or beyond the point of fetal viability at the time her short cervix is detected, consider external fetal heart rate monitoring.
Antenatal corticosteroids can be administered, as appropriate, depending on the perceived risk of delivery.
5. Should I place a cerclage?
Numerous studies have examined the efficacy of ultrasound-indicated cerclage, a surgical procedure to stitch the cervix closed once a short cervix has been detected.
In general, placement of a cervical cerclage is not offered past the point of fetal viability, which is generally in the range of 23 to 25 weeks’ gestation, depending on local institutional and neonatal intensive care unit policies. Confirmed or suspected chorioamnionitis is also a contraindication to cerclage placement.
Among women without a history of PTB who are found to have a short cervix, existing data do not suggest a benefit for cerclage, although vaginal progesterone appears to be a reasonable option (see page 36).16,17
As for women with a history of PTB, Owen and colleagues studied 302 patients with a cervical length less than 25 mm and a history of spontaneous PTB before 34 weeks.18 The women were randomly assigned to ultrasound-indicated cerclage or “usual care,” which consisted of recommendations of pelvic rest, physical activity restriction, and education about the symptoms of preterm labor. Otherwise, management was directed by clinical practice at each center. All women treated with cerclage had a reduced risk of previable PTB (<24 weeks’ gestation), and those who had the shortest cervical length (<15 mm) also had a lower risk of delivery before 35 weeks.
The degree of cervical shortening that has “qualified” women for study enrollment has varied between studies, with upper limits ranging from 15 to 25 mm. Berghella and colleagues performed a patient-level meta-analysis to determine whether efficacy of the cerclage varied by cervical length at the time of placement.8 They examined 552 women with singleton gestations from four randomized controlled trials that included 208 women with a short cervix and a history of spontaneous PTB. They found a significant reduction in the rate of preterm delivery before 35 weeks’ gestation among women with singleton pregnancies, a short cervix, and a history of spontaneous PTB; the reduction did not vary by the degree of cervical shortening. However, there was no significant reduction in the rate of PTB among the subset of women without a history of spontaneous PTB.
Berghella and colleagues estimated that, if a cervical cerclage were offered to the 8% of women with a prior spontaneous PTB and a cervical length of less than 25 mm, more than 6,500 newborns would be saved each year from perinatal death associated with prematurity.8
The placement of a “rescue” cerclage in the setting of cervical dilation with or without prolapsing membranes is associated with high rates of maternal and neonatal morbidity, regardless of the patient’s obstetric history. However, cerclage placement in this setting may be associated with better outcomes than expectant management with bed rest alone.19 Patients should be carefully counseled about this procedure, including the risk of infection and the possibility that pregnancy may be prolonged only from a previable to a periviable gestational age. Decisions as to whether a patient is a candidate for rescue cerclage should be made in consultation with a maternal-fetal medicine specialist.20
6. Is a cervical pessary beneficial?
The pessary is another “mechanical” treatment similar to cerclage, and it may be helpful in reducing the incidence of PTB among women with a short cervix. In the largest study of this approach, 16,000 primarily low-risk women with singleton gestations were screened for a short cervix. Of these, 385 women with a cervical length of less than 25 mm were randomly assigned to undergo Arabin pessary placement or expectant management.21
Among those who received the pessary, the odds ratio (OR) for PTB before 34 weeks was significantly reduced (OR, 0.18; 95% confidence interval [CI], 0.08–0.37), and the OR for adverse composite neonatal outcome also was significantly reduced (OR, 0.14; 95% CI, 0.04–0.39).21
The Arabin pessary is not currently approved by the US Food and Drug Administration for this indication in the United States, nor is it available for insertion outside of research studies. Other ring-shaped pessaries are available in the United States, but their use in the setting of a short cervix is considered experimental and off-label. Additional studies of this promising intervention are currently under way.
7. Who is a candidate for supplemental progesterone?
Progesterone is a naturally occurring hormone essential to the maintenance of pregnancy. It has an overall quiescent effect on the myometrium, is known to have anti-inflammatory properties, and inhibits cervical ripening.22 It has been studied in a number of different formulations and doses.
Vaginal progesterone supplementation has been shown to reduce the risk of PTB among women with a shortened cervix regardless of their pregnancy history.16,17,23,24 In the largest trials of unselected general obstetrics populations (including women with and without a history of PTB), use of vaginal progesterone among women with a short cervix reduced the rates of very early spontaneous PTB (<28 and <32 weeks’ gestation) by 40% to 50%.16,17 As expected, progesterone also was associated with a significant reduction in the rates of respiratory distress syndrome and composite neonatal morbidity.
Intramuscular (IM) progesterone supplementation has been shown to reduce the rate of recurrent PTB among women with a history of spontaneous PTB. When caring for a woman with a history of PTB who is found to have a short cervix, IM progesterone should be offered if the woman is not already taking it. IM progesterone has not been proven effective among nulliparous women who are incidentally found to have a short cervix; it should not be offered in this situation.25
8. Should the care of women carrying twins or triplets be managed differently?
Yes. Although women with multiple gestations are at higher risk for PTB than women carrying a singleton fetus, no interventions have proven to be effective in this population. Many studies have been limited to twin gestations as a group, with an inability to perform subgroup analyses or enroll women who also have a short cervix, due to sample size and power issues.
Progesterone in multiple gestations
Although several formulations of progesterone—including IM 17-alpha hydroxyprogesterone caproate, micronized progesterone, and progesterone suppositories—have been studied, no randomized trial data have demonstrated a reduction in PTB or neonatal morbidity.26–29 Individual patient-level data from a meta-analysis of vaginal progesterone in the setting of multiple gestations with a short cervical length suggest trends toward a reduced rate of PTB before 33 weeks’ gestation (relative risk [RR], 0.70; 95% CI, 0.34–1.44) and lower composite neonatal morbidity and mortality (RR, 0.56; 95% CI, 0.30–0.97).30
Mechanical strategies in multiple gestations
No randomized data suggest that a pessary is effective in multiple gestations. In one study of 813 multiple gestations in the Netherlands, women were randomly assigned—regardless of cervical length—to receive a pessary at 16 to 20 weeks versus standard care; no difference in adverse perinatal outcomes was detected between groups.31
As for cerclage, although data are limited, some studies suggest that placement of a cerclage in twin gestations with cervical shortening may increase the rate of PTB.32
Bottom line for multiples
Although women carrying multiple gestations are at higher risk for PTB, data are extremely limited. At present, data do not support routine use of cerclage for a short cervix—and some suggest possible harm. Vaginal progesterone or placement of a pessary may be of benefit but should be used with caution and with the understanding that data are sparse.
CASE RESOLVED
You counsel your nulliparous patient that she has an elevated risk of PTB, based on her cervical length of 18 mm at 20 weeks’ gestation, and evaluate her clinically for evidence of preterm labor. Apart from the short cervix, her examination is unremarkable. You offer her nightly vaginal progesterone suppositories and schedule a visit to reevaluate her cervix in 1 week. If cervical dilation or prolapsing membranes are noted before the age of fetal viability, you will consider placing a “rescue” cervical cerclage.
Had this patient experienced a prior PTB, you would first ensure that she is taking IM 17-alpha hydroxyprogesterone caproate. It also would be reasonable to place an ultrasound-indicated cerclage or begin vaginal progesterone suppositories. Although data are limited on concomitant use of IM and vaginal progesterone, some experts may consider it, on an experimental basis, for patients with a short cervix and a prior PTB.
If this patient were carrying a twin gestation, vaginal progesterone would still be a consideration, provided she is counseled about the limited evidence of its efficacy in this setting. Cerclage would not be appropriate, given the possible risk of harm.
WE WANT TO HEAR FROM YOU!
Drop us a line and let us know what you think about this or other current articles, which topics you'd like to see covered in future issues, and what challenges you face in daily practice. Tell us what you think by emailing us at: [email protected] Please include your name, city and state. Stay in touch! Your feedback is important to us!
1. Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2012. Natl Vital Stat Rep. 2013;62(3):1–20.
2. Adams MM, Elam-Evans LD, Wilson HG, Gilbertz DA. Rates of and factors associated with recurrence of preterm delivery. JAMA. 2000;283(12):1591–1596.
3. Ananth CV, Getahun D, Peltier MR, Salihu HM, Vintzileos AM. Recurrence of spontaneous versus medically indicated preterm birth. Am J Obstet Gynecol 2006;195(3):643–650.
4. To MS, Skentou CA, Royston P, Yu CK, Nicolaides KH. Prediction of patient-specific risk of early preterm delivery using maternal history and sonographic measurement of cervical length: A population-based prospective study. Ultrasound Obstet Gynecol. 2006;27(4):362–367.
5. Guzman ER, Ananth CV. Cervical length and spontaneous prematurity: Laying the foundation for future interventional randomized trials for the short cervix. Ultrasound Obstet Gynecol. 2001;18(3):195–199.
6. Heath VC, Southall TR, Souka AP, Elisseou A, Nicolaides KH. Cervical length at 23 weeks of gestation: Prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol. 1998;12(5):312–317.
7. Berghella V, Roman A, Daskalakis C, Ness A, Baxter JK. Gestational age at cervical length measurement and incidence of preterm birth. Obstet Gynecol. 2007;110(2 Pt 1):311–317.
8. Berghella V, Keeler SM, To MS, Althuisius SM, Rust OA. Effectiveness of cerclage according to severity of cervical length shortening: A meta-analysis. Ultrasound Obstet Gynecol. 2010;35(4):468–473.
9. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334(9):567–572.
10. Werner EF, Han CS, Pettker CM, et al. Universal cervical-length screening to prevent preterm birth: A cost-effectiveness analysis. Ultrasound Obstet Gynecol. 2011;38 (1):32–37.
11. Cahill AG, Odibo AO, Caughey AB, et al. Universal cervical length screening and treatment with vaginal progesterone to prevent preterm birth: A decision and economic analysis. Am J Obstet Gynecol. 2010;202(6):548.e1–e8.
12. Friedman AM, Srinivas SK, Parry S, Elovitz MA, Wang E, Schwartz N. Can transabdominal ultrasound be used as a screening test for short cervical length? Am J Obstet Gynecol. 2013;208(3):190.e1–e7.
13. American College of Radiology, American College of Obstetricians and Gynecologists, American Institute of Ultrasound in Medicine, Society of Radiologists in Ultrasound. ACR–ACOG–AIUM–SRU Practice Guideline for the Performance of Obstetrical Ultrasound. http://www.acr.org/Quality-Safety/Standards-Guidelines/Practice-Guidelines-by-Modality/~/media/ACR/Documents/PGTS/guidelines/US_Obstetrical.pdf. Accessed June 16, 2014.
14. Owen J, Yost N, Berghella V, et al. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA. 2001;286(11):1340–1348.
15. Iams JD, Goldenberg RL, Mercer BM, et al. The Preterm Prediction Study: Recurrence risk of spontaneous preterm birth. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol. 1998;178(5):1035–1040.
16. Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH; Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007;357(5):462–469.
17. Hassan SS, Romero R, Vidyadhari D, et al; PREGNANT Trial. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: A multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2011;38(1):18–31.
18. Owen J, Hankins G, Iams JD, et al. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol. 2009;201(4):375.e1–e8.
19. Namouz S, Porat S, Okun N, Windrim R, Farine D. Emergency cerclage: literature review. Obstet Gynecol Surv. 2013;68(5):379–388.
20. Cockwell HA, Smith GN. Cervical incompetence and the role of emergency cerclage. J Obstet Gynaecol Can. 2005;27(2):123–129.
21. Goya M, Pratcorona L, Merced C, et al. Cervical pessary in pregnant women with a short cervix (PECEP): An open-label randomised controlled trial. Lancet. 2012;379(9828):1800–1806.
22. Mendelson CR. Minireview: fetal-maternal hormonal signaling in pregnancy and labor. Mol Endocrinol. 2009;23(7):947–954.
23. Meis PJ, Klebanoff M, Thom E, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379–2385. Erratum: N England J Med. 2003;349(13):1299.
24. O’Brien JM, Adair CD, Lewis DF, et al. Progesterone vaginal gel for the reduction of recurrent preterm birth: Primary results from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol 2007;30(5):687–696.
25. Grobman WA, Thom EA, Spong CY, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units (MFMU) Network. 17 alpha-hydroxyprogesterone caproate to prevent prematurity in nulliparas with cervical length less than 30 mm. Am J Obstet Gynecol. 2012;207(5):390.e1–e8.
26. Rouse DJ, Caritis SN, Peaceman AM, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. A trial of 17 alpha-hydroxyprogesterone caproate to prevent prematurity in twins. N Engl J Med. 2007;357(5):454–461.
27. Caritis SN, Rouse DJ, Peaceman AM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Maternal-Fetal Medicine Units (MFMU) Network. Prevention of preterm birth in triplets using 17 alpha-hydroxyprogesterone caproate: A randomized controlled trial. Obstet Gynecol. 2009;113(2 Pt 1):285–292.
28. Rode L, Klein K, Nicolaides KH, Krampl-Bettelheim E, Tabor A; PREDICT Group. Prevention of preterm delivery in twin gestations (PREDICT): A multicenter, randomized, placebo-controlled trial on the effect of vaginal micronized progesterone. Ultrasound Obstet Gynecol. 2011;38(3):272–280.
29. Norman JE, Mackenzie F, Owen P, et al. Progesterone for the prevention of preterm birth in twin pregnancy (STOPPIT): A randomised, double-blind, placebo-controlled study and meta-analysis. Lancet. 2009;373(9680):2034–2040.
30. Romero R, Nicolaides K, Conde-Agudelo A, et al. Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: A systematic review and metaanalysis of individual patient data. Am J Obstet Gynecol. 2012;206(2):124.e1–e19.
31. Liem S, Schuit E, Hegeman M, et al. Cervical pessaries for prevention of preterm birth in women with a multiple pregnancy (ProTWIN): A multicentre, open-label randomised controlled trial. Lancet. 2013;382(9901):1341–1349.
32. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: Meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106(1):181–189.
1. Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2012. Natl Vital Stat Rep. 2013;62(3):1–20.
2. Adams MM, Elam-Evans LD, Wilson HG, Gilbertz DA. Rates of and factors associated with recurrence of preterm delivery. JAMA. 2000;283(12):1591–1596.
3. Ananth CV, Getahun D, Peltier MR, Salihu HM, Vintzileos AM. Recurrence of spontaneous versus medically indicated preterm birth. Am J Obstet Gynecol 2006;195(3):643–650.
4. To MS, Skentou CA, Royston P, Yu CK, Nicolaides KH. Prediction of patient-specific risk of early preterm delivery using maternal history and sonographic measurement of cervical length: A population-based prospective study. Ultrasound Obstet Gynecol. 2006;27(4):362–367.
5. Guzman ER, Ananth CV. Cervical length and spontaneous prematurity: Laying the foundation for future interventional randomized trials for the short cervix. Ultrasound Obstet Gynecol. 2001;18(3):195–199.
6. Heath VC, Southall TR, Souka AP, Elisseou A, Nicolaides KH. Cervical length at 23 weeks of gestation: Prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol. 1998;12(5):312–317.
7. Berghella V, Roman A, Daskalakis C, Ness A, Baxter JK. Gestational age at cervical length measurement and incidence of preterm birth. Obstet Gynecol. 2007;110(2 Pt 1):311–317.
8. Berghella V, Keeler SM, To MS, Althuisius SM, Rust OA. Effectiveness of cerclage according to severity of cervical length shortening: A meta-analysis. Ultrasound Obstet Gynecol. 2010;35(4):468–473.
9. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334(9):567–572.
10. Werner EF, Han CS, Pettker CM, et al. Universal cervical-length screening to prevent preterm birth: A cost-effectiveness analysis. Ultrasound Obstet Gynecol. 2011;38 (1):32–37.
11. Cahill AG, Odibo AO, Caughey AB, et al. Universal cervical length screening and treatment with vaginal progesterone to prevent preterm birth: A decision and economic analysis. Am J Obstet Gynecol. 2010;202(6):548.e1–e8.
12. Friedman AM, Srinivas SK, Parry S, Elovitz MA, Wang E, Schwartz N. Can transabdominal ultrasound be used as a screening test for short cervical length? Am J Obstet Gynecol. 2013;208(3):190.e1–e7.
13. American College of Radiology, American College of Obstetricians and Gynecologists, American Institute of Ultrasound in Medicine, Society of Radiologists in Ultrasound. ACR–ACOG–AIUM–SRU Practice Guideline for the Performance of Obstetrical Ultrasound. http://www.acr.org/Quality-Safety/Standards-Guidelines/Practice-Guidelines-by-Modality/~/media/ACR/Documents/PGTS/guidelines/US_Obstetrical.pdf. Accessed June 16, 2014.
14. Owen J, Yost N, Berghella V, et al. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA. 2001;286(11):1340–1348.
15. Iams JD, Goldenberg RL, Mercer BM, et al. The Preterm Prediction Study: Recurrence risk of spontaneous preterm birth. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol. 1998;178(5):1035–1040.
16. Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH; Fetal Medicine Foundation Second Trimester Screening Group. Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med. 2007;357(5):462–469.
17. Hassan SS, Romero R, Vidyadhari D, et al; PREGNANT Trial. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: A multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2011;38(1):18–31.
18. Owen J, Hankins G, Iams JD, et al. Multicenter randomized trial of cerclage for preterm birth prevention in high-risk women with shortened midtrimester cervical length. Am J Obstet Gynecol. 2009;201(4):375.e1–e8.
19. Namouz S, Porat S, Okun N, Windrim R, Farine D. Emergency cerclage: literature review. Obstet Gynecol Surv. 2013;68(5):379–388.
20. Cockwell HA, Smith GN. Cervical incompetence and the role of emergency cerclage. J Obstet Gynaecol Can. 2005;27(2):123–129.
21. Goya M, Pratcorona L, Merced C, et al. Cervical pessary in pregnant women with a short cervix (PECEP): An open-label randomised controlled trial. Lancet. 2012;379(9828):1800–1806.
22. Mendelson CR. Minireview: fetal-maternal hormonal signaling in pregnancy and labor. Mol Endocrinol. 2009;23(7):947–954.
23. Meis PJ, Klebanoff M, Thom E, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379–2385. Erratum: N England J Med. 2003;349(13):1299.
24. O’Brien JM, Adair CD, Lewis DF, et al. Progesterone vaginal gel for the reduction of recurrent preterm birth: Primary results from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol 2007;30(5):687–696.
25. Grobman WA, Thom EA, Spong CY, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units (MFMU) Network. 17 alpha-hydroxyprogesterone caproate to prevent prematurity in nulliparas with cervical length less than 30 mm. Am J Obstet Gynecol. 2012;207(5):390.e1–e8.
26. Rouse DJ, Caritis SN, Peaceman AM, et al; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. A trial of 17 alpha-hydroxyprogesterone caproate to prevent prematurity in twins. N Engl J Med. 2007;357(5):454–461.
27. Caritis SN, Rouse DJ, Peaceman AM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Maternal-Fetal Medicine Units (MFMU) Network. Prevention of preterm birth in triplets using 17 alpha-hydroxyprogesterone caproate: A randomized controlled trial. Obstet Gynecol. 2009;113(2 Pt 1):285–292.
28. Rode L, Klein K, Nicolaides KH, Krampl-Bettelheim E, Tabor A; PREDICT Group. Prevention of preterm delivery in twin gestations (PREDICT): A multicenter, randomized, placebo-controlled trial on the effect of vaginal micronized progesterone. Ultrasound Obstet Gynecol. 2011;38(3):272–280.
29. Norman JE, Mackenzie F, Owen P, et al. Progesterone for the prevention of preterm birth in twin pregnancy (STOPPIT): A randomised, double-blind, placebo-controlled study and meta-analysis. Lancet. 2009;373(9680):2034–2040.
30. Romero R, Nicolaides K, Conde-Agudelo A, et al. Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: A systematic review and metaanalysis of individual patient data. Am J Obstet Gynecol. 2012;206(2):124.e1–e19.
31. Liem S, Schuit E, Hegeman M, et al. Cervical pessaries for prevention of preterm birth in women with a multiple pregnancy (ProTWIN): A multicentre, open-label randomised controlled trial. Lancet. 2013;382(9901):1341–1349.
32. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM. Cerclage for short cervix on ultrasonography: Meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106(1):181–189.
2014 Update on infectious disease
This year I focus on four interesting and clinically relevant studies:
- an article by Huang and colleagues addressing the important issue of how best to reduce the frequency of methicillin-resistant Staphylococcus aureus (MRSA) infection in critically ill patients hospitalized in the intensive care unit (ICU)
- a study by Duggal and colleagues assessing the value of perioperative oxygen supplementation to reduce the frequency of postcesarean infection
- an investigation of diagnostic criteria for urinary tract infection (UTI) by Hooton and colleagues
- an exploration of the association between intra-amniotic inflammation, as distinct from bacterial colonization, and adverse fetal outcomes.
For ICU patients, universal decolonization reduces nosocomial infection more than targeted decolonization
Huang SS, Septimus E, Kleinman K, et al. Targeted versus universal decolonization to prevent ICU infection. N Engl J Med. 2013;368(24):2255–2265.
Infection in general, and nosocomial infection in particular, is common among patients hospitalized in the ICU. Such patients often are severely immunosuppressed and debilitated. They are likely to have multiple indwelling catheters and to require mechanical ventilation—interventions that predispose to life-threatening infection. The longer the duration of care in the ICU, the greater the risk of infection, especially infection caused by organisms that have acquired resistance to multiple antibiotics.
In this cluster-randomized trial, Huang and colleagues compared targeted and universal decolonization of patients treated in an ICU to determine which approach was more effective at preventing nosocomial infection, particularly MRSA infection. They found universal decolonization to be superior to targeted decolonization in reducing these infections.
Details of the studyInvestigators conducted their study in 74 ICUs in 43 hospitals. Each hospital was randomly assigned to one of three interventions:
- Group 1: MRSA screening followed by isolation of colonized patients
- Group 2: MRSA screening followed by isolation and decolonization of MRSA carriers
- Group 3: Universal decolonization (no screening).
The decolonization regimen consisted of twice-daily administration of intranasal mupirocin for 5 days and daily bathing with chlorhexidine-impregnated cloths for the duration of the ICU stay.
The study’s two endpoints were 1) the modeled hazard ratios for MRSA clinical isolates and 2) the hazard ratios for bloodstream infection with any pathogen.
During the intervention period, fewer MRSA isolates were found in the universal decolonization group, compared with the other two groups (P<.01). In addition, the number of bloodstream infections in the universal decolonization group was significantly lower than in the other two groups (P<.001). Fifty-four patients (number needed to treat) needed to undergo decolonization to prevent one bloodstream infection.
What this EVIDENCE means for practiceThe relevance of this investigation for those of us in the field of obstetrics and gynecology is simple and clear: If we have to transfer a patient to an ICU (such as an HIV-infected patient with a serious postcesarean infection, or an oncology patient with a badly infected surgical wound), she should immediately be started on a regimen of twice-daily nasal mupirocin and daily bathing with chlorhexidine. This straightforward intervention will be of great value in reducing the incidence of bacteremia caused by a particularly dangerous pathogen.
Related article: Update on infectious disease. Patrick Duff, MD (July 2013)
The jury is still out on supplemental oxygen to reduce surgical site infection
Duggal N, Poddatorri V, Noroozkhani S, Siddik-Ahman RI, Caughey AB. Perioperative oxygen supplementation and surgical site infection after cesarean delivery. Obstet Gynecol. 2013;122(1):79–84.
In a widely read study published in 2000 in the New England Journal of Medicine, Greif and colleagues demonstrated that, in patients undergoing colorectal surgery, the rate of postoperative wound infection was significantly reduced from 11.2% in patients given 30% supplemental oxygen during surgery to 5.2% in those given 80% supplemental oxygen.1 The oxygen was continued for 2 hours after surgery.
In a later study among general surgery patients, Pryor and colleagues were unable to replicate this finding.2 It was in this setting that Duggal and colleagues undertook their investigation among women undergoing cesarean delivery. These investigators, too, were unable to replicate the 2000 finding of Greif and colleagues.
Related article: Update: Infectious Disease. Patrick Duff, MD (June 2012)
Details of the studyOver 4 years, from 2006 to 2010, Duggal and colleagues conducted a prospective, randomized, double-blinded controlled trial among patients undergoing scheduled, urgent, or emergent cesarean delivery. All patients were given prophylactic antibiotics, usually cefazolin 2 g intravenously after the infant’s umbilical cord was clamped. Surgical technique was reasonably well standardized and included closure of the deep subcutaneous layer of tissue using 2-0 plain gut sutures.
Patients were randomly assigned to receive supplemental oxygen via face mask, at 30% or 80% concentration, during surgery and for 1 hour postoperatively. They were evaluated postoperatively at 2 and 6 weeks. The primary outcome measure was a composite of surgical site infection, endometritis, or both.
A total of 415 women received 30% oxygen and 416 were given 80% oxygen. The two groups were well matched for important confounding variables such as age, race, parity, body mass index, number of prior cesarean deliveries, diabetes, cardiopulmonary disease, anemia, smoking, and chronic steroid use.
The groups did not differ in the frequency of surgical site infection or endometritis, which occurred at a rate of 2.4% in the group receiving 30% oxygen, compared with 2.9% in the group given 80% oxygen.
Rationale for oxygen supplementationAdequate tissue oxygenation has been observed to enhance the bactericidal function of neutrophils. So why were Duggal and colleagues unable to demonstrate a beneficial effect for oxygen therapy?
The most likely explanations:
- Their obstetric patients were less seriously ill than the general surgery patients undergoing colorectal surgery in the study by Greif and colleagues.
- Given the low overall rate of infection, their sample size may have been too small to show a statistically significant difference in outcome (Type II statistical error).
In point of fact, more than 80% of patients in both groups had scheduled cesarean deliveries, presumably prior to the onset of labor and ruptured membranes. The outcome may have been different had the groups included a majority of patients undergoing surgery after labor and ruptured membranes.
What this EVIDENCE means for practiceUntil additional studies are performed, I cannot recommend routine use of perioperative hyperoxygenation as a method of reducing the rate of surgical site infection and/or endometritis. However, we have very good scientific evidence indicating that the following measures significantly reduce the rate of endometritis after both scheduled and unscheduled cesarean delivery:
• administration of prophylactic antibiotics prior to the start of surgery
• removal of the placenta by gentle traction on the umbilical cord rather than by manual extraction.3,4
Similarly, we have sound evidence demonstrating that the following measures significantly reduce the rate of surgical site infection:
• clipping, rather than shaving, the hair at the surgical site just prior to the incision
• preoperative cleansing of the surgical area with chlorhexidine
• administration of prophylactic antibiotics prior to the start of surgery closure of the lower half of the subcutaneous tissue (if it exceeds 2 cm in thickness) using a relatively noninflammatory suture such as polyglactin or polyglycolic acid.
The presence of E coli in a midstream urine specimen is highly predictive of UTI
Hooton TM, Roberts PL, Cox ME, Stapleton AE. Voided midstream urine culture and acute cystitis in premenopausal women. N Engl J Med. 2013;369(20):1883–1891.
Urinary tract infections (UTI) are among the most common infections experienced by women of all ages. Asymptomatic bacteriuria affects 5% to 10% of all sexually active women. During the course of their lifetime, at least 50% of women develop some form of UTI.
Pyelonephritis is not nearly as common as asymptomatic bacteriuria or cystitis, but this infection can be especially dangerous in older, debilitated women who reside in nursing homes and require indwelling catheters.
The most common organisms that cause UTIs in women are the aerobic gram-negative bacilli, principally Escherichia coli, Klebsiella species, and Proteus species. Other Gram-negative bacilli such as Pseudomonas species, Serratia, or Enterobacter are not common uropathogens except in immunosuppressed hosts or patients who have long-term indwelling catheters. Gram-positive organisms such as group B streptococci, enterococci, and staphylococcal species are occasional pathogens but, as Hooton and colleagues demonstrate in this study, perhaps not quite as important as we once thought.
Related articles:
• Update on infectious disease. Alan T. N. Tita, MD, PhD (June 2011)
• Have you tried these innovative alternatives to antibiotics for UTI prevention? Patrick A. Nosti, MD; Kate C. Arnold; Cheryl B. Iglesia, MD (February 2013)
Details of the studyUsing an elegantly simple design, the Hooton team studied women aged 18 to 49 years who had symptoms suggestive of acute cystitis. They collected two urine specimens from each woman for culture—one was collected using the midstream, clean-catch technique and the other by catheterization. They then compared microbial species and colony counts in the paired specimens to determine the positive and negative predictive values of midstream culture results, using the catheterized culture results as the reference standard.
The 226 women in the study experienced 236 clinical episodes suggestive of acute cystitis. One hundred forty-two (70%) of the catheterized specimens were positive for infection; of these, four specimens yielded more than one uropathogen. One hundred fifty-seven (78%) of the midstream specimens were positive for infection.
The presence of E coli in the midstream culture was highly predictive of a positive culture for E coli by catheterization, even when the cutoff was only 100 colonies/mL on the midstream specimen (positive predictive value, 93%). However, neither the presence of enterococci nor the presence of group B streptococci, at any colony count, was predictive of a positive culture by catheterization. Interestingly, among 41 patients who had either enterococci or group B streptococci in their midstream culture, E coli was present in the catheterizedculture in 61% of cases, suggesting that infection with E coli may be the more important cause of the patient’s symptoms.
Hooton and colleagues concluded that the presence of E coli on a midstream culture, even in low colony counts, is predictive of true bladder infection, as determined by catheterization. However, enterococci and group B streptococci were more likely to be vaginal contaminants or associated with coinfection with E coli, or bot.
What this EVIDENCE means for practiceThe findings of Hooton and colleagues have several key implications for practicing clinicians:
• When either a pregnant or nonpregnant patient experiences her first episode of acute cystitis, the overwhelming probability is that E coli is the infecting pathogen. We can reduce costs by empirically treating the initial infection, thereby avoiding the expense of a urine culture.
• For patients with recurrent infections or for immunocompromised patients, a culture and sensitivity test should be performed because other uropathogens are more likely to be involved and may have less predictable antibiotic susceptibility patterns.
• Contamination of supposed “clean-catch” specimens is very common, and the cultures resulting from these specimens can mislead us in our decisions about antibiotic therapy. Enterococci and group B streptococci are more likely than not to be contaminants from the vaginal flora rather than true infecting pathogens. When they are present in the bladder, they are usually associated with E coli. Accordingly, E coli should be the principal target of antibiotic therapy.
• To avoid concerns about contamination of specimens in acutely symptomatic patients, obtain the urine specimen by catheter. In the catheterized specimen, the cutoff for true bladder infection should be ≥100 colonies/mL. The cutoff of ≥100,000 colonies/mLis applicable only for clean-catch specimens obtained from asymptomatic patients.
• Clinical laboratories should embrace the new cutoff and report even seemingly low colony counts when the urine sample has been obtained by catheterization.
In preterm labor, amniotic fluid infection without inflammation does not necessarily predict a poor fetal outcome
Combs CA, Gravett M, Garite TJ, et al. Amniotic fluid infection, inflammation, and colonization in preterm labor with intact membranes. Am J Obstet Gynecol. 2014;210(2):125.e1–e15.
In this very important clinical investigation, Combs and colleagues collected amniotic fluid from 305 women with preterm labor. They then measured the amniotic fluid concentration of interleukin-6 (IL-6) and assessed for the presence of microbial invasion of the amniotic cavity (MIAC) by either culture or detection of microbial 16S ribosomal DNA. Based on these test results, investigators divided the patients into five groups:
- Infection—defined as positive MIAC and IL-6 >11.3 ng/mL
- Severe inflammation—negative MIAC and IL-6 >11.3 ng/mL
- Mild inflammation—no MIAC and IL-6 from 2.6 to 11.2 ng/mL
- Colonization—positive MIAC and IL-6 <2.6 ng/mL
- Negative—no MIAC and IL-6 <2.6 ng/mL.
The end points of the investigation were latency period and composite perinatal morbidity and mortality. Perinatal morbidity included respiratory distress syndrome, grade 3 or 4 intraventricular hemorrhage, necrotizing enterocolitis, and culture-proven neonatal sepsis.
Related article: Does treating asymptomatic bacterial vaginosis reduce preterm delivery? Hyagriv N. Simhan, MD, MSCR (Examining the Evidence; April 2008)
Interestingly, the infection and severe inflammation groups had similar short latency periods (median of <1 and 2 days, respectively) and similar rates of composite perinatal morbidity and mortality (81% and 72%, respectively).
The colonization and negative groups also had similar latency periods (median of 23.5 and 25 days, respectively) and similar rates of composite morbidity and mortality (21% and 25%, respectively).
The mild inflammation group had intermediate outcomes.
When Combs and colleagues used multivariate analysis to adjust for gestational age at enrollment, amniotic fluid IL-6 concentrations greater than 11.3 ng/mL and in the range of 2.6 to 11.3 ng/mL—but not MIAC—were associated with increased composite perinatal morbidity and mortality.
What this EVIDENCE means for practiceThis study offers several critically important take-home messages:
• Bacterial colonization of the amniotic fluid, without actual inflammation, is not necessarily associated with an ominous outcome for the fetus
• Varying degrees of inflammation exist
• The more intense the inflammation, the worse the outcome for the baby
• The logical clinical application of this investigation is to modify our practice so that, when we perform an amniocentesis for patients with preterm labor, we look not only for bacterial growth but for the presence of key inflammatory mediators in the amniotic fluid, such as IL-6
• A rapidly available, inexpensive, and easy-to-perform assay for IL-6 would be invaluable in improving our ability to assess patients for subclinical infection and inflammation
• An important question, of course, is whether early implementation of specific anti-inflammatory therapy could alter the prognosis for the fetus in selected cases.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
1. Greif R, Akca O, Horn EP, Kurz A, Sessler DI; Outcomes Research Group. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med. 2000;342(3):161–167.
2. Pryor KO, Fahey TJ III, Lien CA, Goldstein PA. Surgical site infection and the routine use of perioperative hyperoxia in a general surgery population. JAMA. 2004;291(1):79–87.
3. Duff P. A simple checklist for preventing major complications associated with cesarean delivery. Obstet Gynecol. 2010;116(6):1393–1396.
4. Dahlke JD, Mendez-Figueroa H, Rouse DJ, Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery: An updated systematic review. Am J Obstet Gynecol. 2013;209(4):294–306.
This year I focus on four interesting and clinically relevant studies:
- an article by Huang and colleagues addressing the important issue of how best to reduce the frequency of methicillin-resistant Staphylococcus aureus (MRSA) infection in critically ill patients hospitalized in the intensive care unit (ICU)
- a study by Duggal and colleagues assessing the value of perioperative oxygen supplementation to reduce the frequency of postcesarean infection
- an investigation of diagnostic criteria for urinary tract infection (UTI) by Hooton and colleagues
- an exploration of the association between intra-amniotic inflammation, as distinct from bacterial colonization, and adverse fetal outcomes.
For ICU patients, universal decolonization reduces nosocomial infection more than targeted decolonization
Huang SS, Septimus E, Kleinman K, et al. Targeted versus universal decolonization to prevent ICU infection. N Engl J Med. 2013;368(24):2255–2265.
Infection in general, and nosocomial infection in particular, is common among patients hospitalized in the ICU. Such patients often are severely immunosuppressed and debilitated. They are likely to have multiple indwelling catheters and to require mechanical ventilation—interventions that predispose to life-threatening infection. The longer the duration of care in the ICU, the greater the risk of infection, especially infection caused by organisms that have acquired resistance to multiple antibiotics.
In this cluster-randomized trial, Huang and colleagues compared targeted and universal decolonization of patients treated in an ICU to determine which approach was more effective at preventing nosocomial infection, particularly MRSA infection. They found universal decolonization to be superior to targeted decolonization in reducing these infections.
Details of the studyInvestigators conducted their study in 74 ICUs in 43 hospitals. Each hospital was randomly assigned to one of three interventions:
- Group 1: MRSA screening followed by isolation of colonized patients
- Group 2: MRSA screening followed by isolation and decolonization of MRSA carriers
- Group 3: Universal decolonization (no screening).
The decolonization regimen consisted of twice-daily administration of intranasal mupirocin for 5 days and daily bathing with chlorhexidine-impregnated cloths for the duration of the ICU stay.
The study’s two endpoints were 1) the modeled hazard ratios for MRSA clinical isolates and 2) the hazard ratios for bloodstream infection with any pathogen.
During the intervention period, fewer MRSA isolates were found in the universal decolonization group, compared with the other two groups (P<.01). In addition, the number of bloodstream infections in the universal decolonization group was significantly lower than in the other two groups (P<.001). Fifty-four patients (number needed to treat) needed to undergo decolonization to prevent one bloodstream infection.
What this EVIDENCE means for practiceThe relevance of this investigation for those of us in the field of obstetrics and gynecology is simple and clear: If we have to transfer a patient to an ICU (such as an HIV-infected patient with a serious postcesarean infection, or an oncology patient with a badly infected surgical wound), she should immediately be started on a regimen of twice-daily nasal mupirocin and daily bathing with chlorhexidine. This straightforward intervention will be of great value in reducing the incidence of bacteremia caused by a particularly dangerous pathogen.
Related article: Update on infectious disease. Patrick Duff, MD (July 2013)
The jury is still out on supplemental oxygen to reduce surgical site infection
Duggal N, Poddatorri V, Noroozkhani S, Siddik-Ahman RI, Caughey AB. Perioperative oxygen supplementation and surgical site infection after cesarean delivery. Obstet Gynecol. 2013;122(1):79–84.
In a widely read study published in 2000 in the New England Journal of Medicine, Greif and colleagues demonstrated that, in patients undergoing colorectal surgery, the rate of postoperative wound infection was significantly reduced from 11.2% in patients given 30% supplemental oxygen during surgery to 5.2% in those given 80% supplemental oxygen.1 The oxygen was continued for 2 hours after surgery.
In a later study among general surgery patients, Pryor and colleagues were unable to replicate this finding.2 It was in this setting that Duggal and colleagues undertook their investigation among women undergoing cesarean delivery. These investigators, too, were unable to replicate the 2000 finding of Greif and colleagues.
Related article: Update: Infectious Disease. Patrick Duff, MD (June 2012)
Details of the studyOver 4 years, from 2006 to 2010, Duggal and colleagues conducted a prospective, randomized, double-blinded controlled trial among patients undergoing scheduled, urgent, or emergent cesarean delivery. All patients were given prophylactic antibiotics, usually cefazolin 2 g intravenously after the infant’s umbilical cord was clamped. Surgical technique was reasonably well standardized and included closure of the deep subcutaneous layer of tissue using 2-0 plain gut sutures.
Patients were randomly assigned to receive supplemental oxygen via face mask, at 30% or 80% concentration, during surgery and for 1 hour postoperatively. They were evaluated postoperatively at 2 and 6 weeks. The primary outcome measure was a composite of surgical site infection, endometritis, or both.
A total of 415 women received 30% oxygen and 416 were given 80% oxygen. The two groups were well matched for important confounding variables such as age, race, parity, body mass index, number of prior cesarean deliveries, diabetes, cardiopulmonary disease, anemia, smoking, and chronic steroid use.
The groups did not differ in the frequency of surgical site infection or endometritis, which occurred at a rate of 2.4% in the group receiving 30% oxygen, compared with 2.9% in the group given 80% oxygen.
Rationale for oxygen supplementationAdequate tissue oxygenation has been observed to enhance the bactericidal function of neutrophils. So why were Duggal and colleagues unable to demonstrate a beneficial effect for oxygen therapy?
The most likely explanations:
- Their obstetric patients were less seriously ill than the general surgery patients undergoing colorectal surgery in the study by Greif and colleagues.
- Given the low overall rate of infection, their sample size may have been too small to show a statistically significant difference in outcome (Type II statistical error).
In point of fact, more than 80% of patients in both groups had scheduled cesarean deliveries, presumably prior to the onset of labor and ruptured membranes. The outcome may have been different had the groups included a majority of patients undergoing surgery after labor and ruptured membranes.
What this EVIDENCE means for practiceUntil additional studies are performed, I cannot recommend routine use of perioperative hyperoxygenation as a method of reducing the rate of surgical site infection and/or endometritis. However, we have very good scientific evidence indicating that the following measures significantly reduce the rate of endometritis after both scheduled and unscheduled cesarean delivery:
• administration of prophylactic antibiotics prior to the start of surgery
• removal of the placenta by gentle traction on the umbilical cord rather than by manual extraction.3,4
Similarly, we have sound evidence demonstrating that the following measures significantly reduce the rate of surgical site infection:
• clipping, rather than shaving, the hair at the surgical site just prior to the incision
• preoperative cleansing of the surgical area with chlorhexidine
• administration of prophylactic antibiotics prior to the start of surgery closure of the lower half of the subcutaneous tissue (if it exceeds 2 cm in thickness) using a relatively noninflammatory suture such as polyglactin or polyglycolic acid.
The presence of E coli in a midstream urine specimen is highly predictive of UTI
Hooton TM, Roberts PL, Cox ME, Stapleton AE. Voided midstream urine culture and acute cystitis in premenopausal women. N Engl J Med. 2013;369(20):1883–1891.
Urinary tract infections (UTI) are among the most common infections experienced by women of all ages. Asymptomatic bacteriuria affects 5% to 10% of all sexually active women. During the course of their lifetime, at least 50% of women develop some form of UTI.
Pyelonephritis is not nearly as common as asymptomatic bacteriuria or cystitis, but this infection can be especially dangerous in older, debilitated women who reside in nursing homes and require indwelling catheters.
The most common organisms that cause UTIs in women are the aerobic gram-negative bacilli, principally Escherichia coli, Klebsiella species, and Proteus species. Other Gram-negative bacilli such as Pseudomonas species, Serratia, or Enterobacter are not common uropathogens except in immunosuppressed hosts or patients who have long-term indwelling catheters. Gram-positive organisms such as group B streptococci, enterococci, and staphylococcal species are occasional pathogens but, as Hooton and colleagues demonstrate in this study, perhaps not quite as important as we once thought.
Related articles:
• Update on infectious disease. Alan T. N. Tita, MD, PhD (June 2011)
• Have you tried these innovative alternatives to antibiotics for UTI prevention? Patrick A. Nosti, MD; Kate C. Arnold; Cheryl B. Iglesia, MD (February 2013)
Details of the studyUsing an elegantly simple design, the Hooton team studied women aged 18 to 49 years who had symptoms suggestive of acute cystitis. They collected two urine specimens from each woman for culture—one was collected using the midstream, clean-catch technique and the other by catheterization. They then compared microbial species and colony counts in the paired specimens to determine the positive and negative predictive values of midstream culture results, using the catheterized culture results as the reference standard.
The 226 women in the study experienced 236 clinical episodes suggestive of acute cystitis. One hundred forty-two (70%) of the catheterized specimens were positive for infection; of these, four specimens yielded more than one uropathogen. One hundred fifty-seven (78%) of the midstream specimens were positive for infection.
The presence of E coli in the midstream culture was highly predictive of a positive culture for E coli by catheterization, even when the cutoff was only 100 colonies/mL on the midstream specimen (positive predictive value, 93%). However, neither the presence of enterococci nor the presence of group B streptococci, at any colony count, was predictive of a positive culture by catheterization. Interestingly, among 41 patients who had either enterococci or group B streptococci in their midstream culture, E coli was present in the catheterizedculture in 61% of cases, suggesting that infection with E coli may be the more important cause of the patient’s symptoms.
Hooton and colleagues concluded that the presence of E coli on a midstream culture, even in low colony counts, is predictive of true bladder infection, as determined by catheterization. However, enterococci and group B streptococci were more likely to be vaginal contaminants or associated with coinfection with E coli, or bot.
What this EVIDENCE means for practiceThe findings of Hooton and colleagues have several key implications for practicing clinicians:
• When either a pregnant or nonpregnant patient experiences her first episode of acute cystitis, the overwhelming probability is that E coli is the infecting pathogen. We can reduce costs by empirically treating the initial infection, thereby avoiding the expense of a urine culture.
• For patients with recurrent infections or for immunocompromised patients, a culture and sensitivity test should be performed because other uropathogens are more likely to be involved and may have less predictable antibiotic susceptibility patterns.
• Contamination of supposed “clean-catch” specimens is very common, and the cultures resulting from these specimens can mislead us in our decisions about antibiotic therapy. Enterococci and group B streptococci are more likely than not to be contaminants from the vaginal flora rather than true infecting pathogens. When they are present in the bladder, they are usually associated with E coli. Accordingly, E coli should be the principal target of antibiotic therapy.
• To avoid concerns about contamination of specimens in acutely symptomatic patients, obtain the urine specimen by catheter. In the catheterized specimen, the cutoff for true bladder infection should be ≥100 colonies/mL. The cutoff of ≥100,000 colonies/mLis applicable only for clean-catch specimens obtained from asymptomatic patients.
• Clinical laboratories should embrace the new cutoff and report even seemingly low colony counts when the urine sample has been obtained by catheterization.
In preterm labor, amniotic fluid infection without inflammation does not necessarily predict a poor fetal outcome
Combs CA, Gravett M, Garite TJ, et al. Amniotic fluid infection, inflammation, and colonization in preterm labor with intact membranes. Am J Obstet Gynecol. 2014;210(2):125.e1–e15.
In this very important clinical investigation, Combs and colleagues collected amniotic fluid from 305 women with preterm labor. They then measured the amniotic fluid concentration of interleukin-6 (IL-6) and assessed for the presence of microbial invasion of the amniotic cavity (MIAC) by either culture or detection of microbial 16S ribosomal DNA. Based on these test results, investigators divided the patients into five groups:
- Infection—defined as positive MIAC and IL-6 >11.3 ng/mL
- Severe inflammation—negative MIAC and IL-6 >11.3 ng/mL
- Mild inflammation—no MIAC and IL-6 from 2.6 to 11.2 ng/mL
- Colonization—positive MIAC and IL-6 <2.6 ng/mL
- Negative—no MIAC and IL-6 <2.6 ng/mL.
The end points of the investigation were latency period and composite perinatal morbidity and mortality. Perinatal morbidity included respiratory distress syndrome, grade 3 or 4 intraventricular hemorrhage, necrotizing enterocolitis, and culture-proven neonatal sepsis.
Related article: Does treating asymptomatic bacterial vaginosis reduce preterm delivery? Hyagriv N. Simhan, MD, MSCR (Examining the Evidence; April 2008)
Interestingly, the infection and severe inflammation groups had similar short latency periods (median of <1 and 2 days, respectively) and similar rates of composite perinatal morbidity and mortality (81% and 72%, respectively).
The colonization and negative groups also had similar latency periods (median of 23.5 and 25 days, respectively) and similar rates of composite morbidity and mortality (21% and 25%, respectively).
The mild inflammation group had intermediate outcomes.
When Combs and colleagues used multivariate analysis to adjust for gestational age at enrollment, amniotic fluid IL-6 concentrations greater than 11.3 ng/mL and in the range of 2.6 to 11.3 ng/mL—but not MIAC—were associated with increased composite perinatal morbidity and mortality.
What this EVIDENCE means for practiceThis study offers several critically important take-home messages:
• Bacterial colonization of the amniotic fluid, without actual inflammation, is not necessarily associated with an ominous outcome for the fetus
• Varying degrees of inflammation exist
• The more intense the inflammation, the worse the outcome for the baby
• The logical clinical application of this investigation is to modify our practice so that, when we perform an amniocentesis for patients with preterm labor, we look not only for bacterial growth but for the presence of key inflammatory mediators in the amniotic fluid, such as IL-6
• A rapidly available, inexpensive, and easy-to-perform assay for IL-6 would be invaluable in improving our ability to assess patients for subclinical infection and inflammation
• An important question, of course, is whether early implementation of specific anti-inflammatory therapy could alter the prognosis for the fetus in selected cases.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
This year I focus on four interesting and clinically relevant studies:
- an article by Huang and colleagues addressing the important issue of how best to reduce the frequency of methicillin-resistant Staphylococcus aureus (MRSA) infection in critically ill patients hospitalized in the intensive care unit (ICU)
- a study by Duggal and colleagues assessing the value of perioperative oxygen supplementation to reduce the frequency of postcesarean infection
- an investigation of diagnostic criteria for urinary tract infection (UTI) by Hooton and colleagues
- an exploration of the association between intra-amniotic inflammation, as distinct from bacterial colonization, and adverse fetal outcomes.
For ICU patients, universal decolonization reduces nosocomial infection more than targeted decolonization
Huang SS, Septimus E, Kleinman K, et al. Targeted versus universal decolonization to prevent ICU infection. N Engl J Med. 2013;368(24):2255–2265.
Infection in general, and nosocomial infection in particular, is common among patients hospitalized in the ICU. Such patients often are severely immunosuppressed and debilitated. They are likely to have multiple indwelling catheters and to require mechanical ventilation—interventions that predispose to life-threatening infection. The longer the duration of care in the ICU, the greater the risk of infection, especially infection caused by organisms that have acquired resistance to multiple antibiotics.
In this cluster-randomized trial, Huang and colleagues compared targeted and universal decolonization of patients treated in an ICU to determine which approach was more effective at preventing nosocomial infection, particularly MRSA infection. They found universal decolonization to be superior to targeted decolonization in reducing these infections.
Details of the studyInvestigators conducted their study in 74 ICUs in 43 hospitals. Each hospital was randomly assigned to one of three interventions:
- Group 1: MRSA screening followed by isolation of colonized patients
- Group 2: MRSA screening followed by isolation and decolonization of MRSA carriers
- Group 3: Universal decolonization (no screening).
The decolonization regimen consisted of twice-daily administration of intranasal mupirocin for 5 days and daily bathing with chlorhexidine-impregnated cloths for the duration of the ICU stay.
The study’s two endpoints were 1) the modeled hazard ratios for MRSA clinical isolates and 2) the hazard ratios for bloodstream infection with any pathogen.
During the intervention period, fewer MRSA isolates were found in the universal decolonization group, compared with the other two groups (P<.01). In addition, the number of bloodstream infections in the universal decolonization group was significantly lower than in the other two groups (P<.001). Fifty-four patients (number needed to treat) needed to undergo decolonization to prevent one bloodstream infection.
What this EVIDENCE means for practiceThe relevance of this investigation for those of us in the field of obstetrics and gynecology is simple and clear: If we have to transfer a patient to an ICU (such as an HIV-infected patient with a serious postcesarean infection, or an oncology patient with a badly infected surgical wound), she should immediately be started on a regimen of twice-daily nasal mupirocin and daily bathing with chlorhexidine. This straightforward intervention will be of great value in reducing the incidence of bacteremia caused by a particularly dangerous pathogen.
Related article: Update on infectious disease. Patrick Duff, MD (July 2013)
The jury is still out on supplemental oxygen to reduce surgical site infection
Duggal N, Poddatorri V, Noroozkhani S, Siddik-Ahman RI, Caughey AB. Perioperative oxygen supplementation and surgical site infection after cesarean delivery. Obstet Gynecol. 2013;122(1):79–84.
In a widely read study published in 2000 in the New England Journal of Medicine, Greif and colleagues demonstrated that, in patients undergoing colorectal surgery, the rate of postoperative wound infection was significantly reduced from 11.2% in patients given 30% supplemental oxygen during surgery to 5.2% in those given 80% supplemental oxygen.1 The oxygen was continued for 2 hours after surgery.
In a later study among general surgery patients, Pryor and colleagues were unable to replicate this finding.2 It was in this setting that Duggal and colleagues undertook their investigation among women undergoing cesarean delivery. These investigators, too, were unable to replicate the 2000 finding of Greif and colleagues.
Related article: Update: Infectious Disease. Patrick Duff, MD (June 2012)
Details of the studyOver 4 years, from 2006 to 2010, Duggal and colleagues conducted a prospective, randomized, double-blinded controlled trial among patients undergoing scheduled, urgent, or emergent cesarean delivery. All patients were given prophylactic antibiotics, usually cefazolin 2 g intravenously after the infant’s umbilical cord was clamped. Surgical technique was reasonably well standardized and included closure of the deep subcutaneous layer of tissue using 2-0 plain gut sutures.
Patients were randomly assigned to receive supplemental oxygen via face mask, at 30% or 80% concentration, during surgery and for 1 hour postoperatively. They were evaluated postoperatively at 2 and 6 weeks. The primary outcome measure was a composite of surgical site infection, endometritis, or both.
A total of 415 women received 30% oxygen and 416 were given 80% oxygen. The two groups were well matched for important confounding variables such as age, race, parity, body mass index, number of prior cesarean deliveries, diabetes, cardiopulmonary disease, anemia, smoking, and chronic steroid use.
The groups did not differ in the frequency of surgical site infection or endometritis, which occurred at a rate of 2.4% in the group receiving 30% oxygen, compared with 2.9% in the group given 80% oxygen.
Rationale for oxygen supplementationAdequate tissue oxygenation has been observed to enhance the bactericidal function of neutrophils. So why were Duggal and colleagues unable to demonstrate a beneficial effect for oxygen therapy?
The most likely explanations:
- Their obstetric patients were less seriously ill than the general surgery patients undergoing colorectal surgery in the study by Greif and colleagues.
- Given the low overall rate of infection, their sample size may have been too small to show a statistically significant difference in outcome (Type II statistical error).
In point of fact, more than 80% of patients in both groups had scheduled cesarean deliveries, presumably prior to the onset of labor and ruptured membranes. The outcome may have been different had the groups included a majority of patients undergoing surgery after labor and ruptured membranes.
What this EVIDENCE means for practiceUntil additional studies are performed, I cannot recommend routine use of perioperative hyperoxygenation as a method of reducing the rate of surgical site infection and/or endometritis. However, we have very good scientific evidence indicating that the following measures significantly reduce the rate of endometritis after both scheduled and unscheduled cesarean delivery:
• administration of prophylactic antibiotics prior to the start of surgery
• removal of the placenta by gentle traction on the umbilical cord rather than by manual extraction.3,4
Similarly, we have sound evidence demonstrating that the following measures significantly reduce the rate of surgical site infection:
• clipping, rather than shaving, the hair at the surgical site just prior to the incision
• preoperative cleansing of the surgical area with chlorhexidine
• administration of prophylactic antibiotics prior to the start of surgery closure of the lower half of the subcutaneous tissue (if it exceeds 2 cm in thickness) using a relatively noninflammatory suture such as polyglactin or polyglycolic acid.
The presence of E coli in a midstream urine specimen is highly predictive of UTI
Hooton TM, Roberts PL, Cox ME, Stapleton AE. Voided midstream urine culture and acute cystitis in premenopausal women. N Engl J Med. 2013;369(20):1883–1891.
Urinary tract infections (UTI) are among the most common infections experienced by women of all ages. Asymptomatic bacteriuria affects 5% to 10% of all sexually active women. During the course of their lifetime, at least 50% of women develop some form of UTI.
Pyelonephritis is not nearly as common as asymptomatic bacteriuria or cystitis, but this infection can be especially dangerous in older, debilitated women who reside in nursing homes and require indwelling catheters.
The most common organisms that cause UTIs in women are the aerobic gram-negative bacilli, principally Escherichia coli, Klebsiella species, and Proteus species. Other Gram-negative bacilli such as Pseudomonas species, Serratia, or Enterobacter are not common uropathogens except in immunosuppressed hosts or patients who have long-term indwelling catheters. Gram-positive organisms such as group B streptococci, enterococci, and staphylococcal species are occasional pathogens but, as Hooton and colleagues demonstrate in this study, perhaps not quite as important as we once thought.
Related articles:
• Update on infectious disease. Alan T. N. Tita, MD, PhD (June 2011)
• Have you tried these innovative alternatives to antibiotics for UTI prevention? Patrick A. Nosti, MD; Kate C. Arnold; Cheryl B. Iglesia, MD (February 2013)
Details of the studyUsing an elegantly simple design, the Hooton team studied women aged 18 to 49 years who had symptoms suggestive of acute cystitis. They collected two urine specimens from each woman for culture—one was collected using the midstream, clean-catch technique and the other by catheterization. They then compared microbial species and colony counts in the paired specimens to determine the positive and negative predictive values of midstream culture results, using the catheterized culture results as the reference standard.
The 226 women in the study experienced 236 clinical episodes suggestive of acute cystitis. One hundred forty-two (70%) of the catheterized specimens were positive for infection; of these, four specimens yielded more than one uropathogen. One hundred fifty-seven (78%) of the midstream specimens were positive for infection.
The presence of E coli in the midstream culture was highly predictive of a positive culture for E coli by catheterization, even when the cutoff was only 100 colonies/mL on the midstream specimen (positive predictive value, 93%). However, neither the presence of enterococci nor the presence of group B streptococci, at any colony count, was predictive of a positive culture by catheterization. Interestingly, among 41 patients who had either enterococci or group B streptococci in their midstream culture, E coli was present in the catheterizedculture in 61% of cases, suggesting that infection with E coli may be the more important cause of the patient’s symptoms.
Hooton and colleagues concluded that the presence of E coli on a midstream culture, even in low colony counts, is predictive of true bladder infection, as determined by catheterization. However, enterococci and group B streptococci were more likely to be vaginal contaminants or associated with coinfection with E coli, or bot.
What this EVIDENCE means for practiceThe findings of Hooton and colleagues have several key implications for practicing clinicians:
• When either a pregnant or nonpregnant patient experiences her first episode of acute cystitis, the overwhelming probability is that E coli is the infecting pathogen. We can reduce costs by empirically treating the initial infection, thereby avoiding the expense of a urine culture.
• For patients with recurrent infections or for immunocompromised patients, a culture and sensitivity test should be performed because other uropathogens are more likely to be involved and may have less predictable antibiotic susceptibility patterns.
• Contamination of supposed “clean-catch” specimens is very common, and the cultures resulting from these specimens can mislead us in our decisions about antibiotic therapy. Enterococci and group B streptococci are more likely than not to be contaminants from the vaginal flora rather than true infecting pathogens. When they are present in the bladder, they are usually associated with E coli. Accordingly, E coli should be the principal target of antibiotic therapy.
• To avoid concerns about contamination of specimens in acutely symptomatic patients, obtain the urine specimen by catheter. In the catheterized specimen, the cutoff for true bladder infection should be ≥100 colonies/mL. The cutoff of ≥100,000 colonies/mLis applicable only for clean-catch specimens obtained from asymptomatic patients.
• Clinical laboratories should embrace the new cutoff and report even seemingly low colony counts when the urine sample has been obtained by catheterization.
In preterm labor, amniotic fluid infection without inflammation does not necessarily predict a poor fetal outcome
Combs CA, Gravett M, Garite TJ, et al. Amniotic fluid infection, inflammation, and colonization in preterm labor with intact membranes. Am J Obstet Gynecol. 2014;210(2):125.e1–e15.
In this very important clinical investigation, Combs and colleagues collected amniotic fluid from 305 women with preterm labor. They then measured the amniotic fluid concentration of interleukin-6 (IL-6) and assessed for the presence of microbial invasion of the amniotic cavity (MIAC) by either culture or detection of microbial 16S ribosomal DNA. Based on these test results, investigators divided the patients into five groups:
- Infection—defined as positive MIAC and IL-6 >11.3 ng/mL
- Severe inflammation—negative MIAC and IL-6 >11.3 ng/mL
- Mild inflammation—no MIAC and IL-6 from 2.6 to 11.2 ng/mL
- Colonization—positive MIAC and IL-6 <2.6 ng/mL
- Negative—no MIAC and IL-6 <2.6 ng/mL.
The end points of the investigation were latency period and composite perinatal morbidity and mortality. Perinatal morbidity included respiratory distress syndrome, grade 3 or 4 intraventricular hemorrhage, necrotizing enterocolitis, and culture-proven neonatal sepsis.
Related article: Does treating asymptomatic bacterial vaginosis reduce preterm delivery? Hyagriv N. Simhan, MD, MSCR (Examining the Evidence; April 2008)
Interestingly, the infection and severe inflammation groups had similar short latency periods (median of <1 and 2 days, respectively) and similar rates of composite perinatal morbidity and mortality (81% and 72%, respectively).
The colonization and negative groups also had similar latency periods (median of 23.5 and 25 days, respectively) and similar rates of composite morbidity and mortality (21% and 25%, respectively).
The mild inflammation group had intermediate outcomes.
When Combs and colleagues used multivariate analysis to adjust for gestational age at enrollment, amniotic fluid IL-6 concentrations greater than 11.3 ng/mL and in the range of 2.6 to 11.3 ng/mL—but not MIAC—were associated with increased composite perinatal morbidity and mortality.
What this EVIDENCE means for practiceThis study offers several critically important take-home messages:
• Bacterial colonization of the amniotic fluid, without actual inflammation, is not necessarily associated with an ominous outcome for the fetus
• Varying degrees of inflammation exist
• The more intense the inflammation, the worse the outcome for the baby
• The logical clinical application of this investigation is to modify our practice so that, when we perform an amniocentesis for patients with preterm labor, we look not only for bacterial growth but for the presence of key inflammatory mediators in the amniotic fluid, such as IL-6
• A rapidly available, inexpensive, and easy-to-perform assay for IL-6 would be invaluable in improving our ability to assess patients for subclinical infection and inflammation
• An important question, of course, is whether early implementation of specific anti-inflammatory therapy could alter the prognosis for the fetus in selected cases.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: [email protected]
1. Greif R, Akca O, Horn EP, Kurz A, Sessler DI; Outcomes Research Group. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med. 2000;342(3):161–167.
2. Pryor KO, Fahey TJ III, Lien CA, Goldstein PA. Surgical site infection and the routine use of perioperative hyperoxia in a general surgery population. JAMA. 2004;291(1):79–87.
3. Duff P. A simple checklist for preventing major complications associated with cesarean delivery. Obstet Gynecol. 2010;116(6):1393–1396.
4. Dahlke JD, Mendez-Figueroa H, Rouse DJ, Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery: An updated systematic review. Am J Obstet Gynecol. 2013;209(4):294–306.
1. Greif R, Akca O, Horn EP, Kurz A, Sessler DI; Outcomes Research Group. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med. 2000;342(3):161–167.
2. Pryor KO, Fahey TJ III, Lien CA, Goldstein PA. Surgical site infection and the routine use of perioperative hyperoxia in a general surgery population. JAMA. 2004;291(1):79–87.
3. Duff P. A simple checklist for preventing major complications associated with cesarean delivery. Obstet Gynecol. 2010;116(6):1393–1396.
4. Dahlke JD, Mendez-Figueroa H, Rouse DJ, Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery: An updated systematic review. Am J Obstet Gynecol. 2013;209(4):294–306.
Health Risks Associated with Tattoos and Body Piercing
From the West Virginia University School of Medicine, Morgantown, WV.
Abstract
- Objective: To review the health risks associated with tattoos and body piercing.
- Methods: Review of the literature.
- Results: Tattooing and piercing have become increasingly popular practices in the United States. There are important physical and behavioral risks associated with these forms of body modification. The most common complications from tattooing include skin infections and allergic reactions. Minor complications such as infection and bleeding occur frequently with piercings, but major complications have also been reported. Tattoos and piercings appear to be a marker for risk-taking behavior.
- Conclusion: Clinicians should understand the potential complications of these procedures and be able to counsel patients on how to reduce their health risks.
Tattoos and piercings are ancient practices of body modification that have gained widespread acceptance in modern society, particularly among young adults. Tattoos involve the insertion of colored pigment into the dermal layer of the skin with the goal of creating a permanent marking. They are commonly applied using an electrically powered handheld tattoo machine that moves a needle up and down to inject ink through the epidermis and deposit a drop of ink into the dermis [1]. The cells of the dermis are more stable compared with those of the epidermis, so the ink will mostly stay in place for a person’s lifetime [2].
Body piercing is defined as the insertion of a needle or specially designed piercing gun to create a fistula-like opening into either cartilage or skin for the introduction of decorative ornaments [3]. These ornaments can include jewelry, plastic or wood plugs, beads, or pearls. Body piercing has been part of ritualistic or cultural practices for centuries but is rapidly becoming a worldwide mainstream fashion trend, especially among young women aged 17 to 25 years [4]. Ear piercing has become so well accepted that most studies of body piercing do not include earlobe piercing [5].
There are important physical and behavioral risks associated with body modification. In this paper, we review the epidemiology, potential complications, and behavioral factors associated with tattoos and piercings.
Epidemiology
Tattoos are increasingly popular, with a 2012 Harris poll indicating that 1 in 5 adults has at least 1 tattoo [6], up from 14% in 2008 [7]. In the 2012 poll, adults aged 30 to 39 are most likely to have a tattoo (38%) compared to both those younger (30% of those 25–29 and 22% of those 18–24) and older (27% of those 40–49, 11% of those 50–64 and just 5% of those 65 and older). Women are slightly more likely than men, for the first time since this question was first asked, to have a tattoo (23% versus 19% in men). Current US body piercing rates are approximately 36% [3]. Body piercing is more popular among women than in men [8]. Among adolescents, body piercing is performed considerably earlier than tattooing [9]. The head area is the favored location for piercing, while the most common location for a tattoo is the limb [10].
Associated Health Risks
Tattoos
The most common complications that result from tattooing are skin infections and allergic reactions to the tattoo ink. Extensive skin puncturing can result in bleeding and prolonged leaking of serosanguinous fluid. Pyodermal infections can include temporary inflammation at the site of needle puncture, superficial infections such as impetigo and ecthyma, and deeper infections such as cellulitis, erysipelas, and furunculosis [11]. Unsterile equipment and needles can transmit infectious diseases such as hepatitis [2]. Human immunodeficiency virus is theoretically transmissible this way, but no cases of HIV infection caused by tattooing have been documented [12].
Skin reactions to tattooing include aseptic inflammation and acquired sensitivity to tattoo ink, especially red ink, but also to chromium in green ink, cadmium in yellow ink, and cobalt in blue ink [13]. The reaction can manifest as either allergic contact dermatitis or photo-allergic dermatitis. Cutaneous conditions that localize in tattooed areas include vaccinia, verruca vulgaris, herpes simplex, herpes zoster, psoriasis, lichen planus, keratosis follicularis (Darier disease), chronic discoid lupus erythematosus, and keratoacanthoma. Other possible but less common conditions include keloid, sarcoidal granuloma, erythema multiforme, localized scleroderma, and lymphadenopathy [12].
A recent outbreak of nontuburculous nycobacterial infection was linked to contaminated tattoo inks [14]. Contamination can occur during the manufacturing process due to use of contaminated ingredients or when inks are diluted with nonsterile water by tattoo artists [15]. Investigations of 22 cases of tattoo-associated NTM skin infections in 4 states that occurred during 2011–2012 found that ink was contaminated with NTM before use [16]. M. chelonae, one of several disease-causing NTM species, can cause lung disease, joint infection, eye problems and other organ infections. These infections can be difficult to diagnose and can require treatment lasting 6 months or more [15].
Tattoo laws and regulations vary by state. The inks and ink colorings (pigments) used for tattoos are subject to regulation by the US Food and Drug Administration as cosmetics and color additives. However, the FDA has not traditionally enforced its authority over tattoo inks. The FDA encourages reporting of tattoo-associated complications to its MedWatch program (www.fda.gov/Safety/MedWatch/).
Malignancies reported to develop within tattoos include squamous cell carcinoma, basal cell carcinoma, malignant melanoma, leiomyosarcoma, and dermatofibrosarcoma protuberans [17,18]. These malignancies may be coincidental, but carcinogenicity of the tattoo is as yet unknown. Another concern is that a malignancy within a tattoo is more difficult to identify on skin examination [11,17].
Rarely, tattoos or permanent makeup might cause swelling or burning in the affected areas during magnetic resonance imaging (MRI) exams. The metallic ferric acid pigments used in tattoos can conduct heat on the skin during MRI, resulting in traumatic burns [19]. This has also been reported to occur with tattoos with nonferrous pigments. In some cases, tattoo pigments can interfere with the quality of the image, such as when a person with permanent eyeliner has an MRI of the eye [19].
Patients may self-administer tattoos using sewing needles, forks, paper clips, or pens, and colorants may include charcoal, soot, mascara, or ink. The use of unprofessional tattooists and piercers, who often have limited knowledge of health and hygiene precautions, is more likely to lead to complications [10].
Piercings
While most body piercings are not problematic, the potential for localized infections as well as associated systemic disease is present as long as the piercing site remains open [20]. Bacterial skin infections at or near the site are the most commonly reported complication of body piercings, with causative organisms primarily consisting of Staphylococcus, group A beta-hemolytic Streptococcus, and Pseudomonas [21]. Contributing to the health risks of piercing is the reluctance of patients to seek qualified medical intervention when initial site irritation, pain, or oozing occurs [21].
Systemic infections have been reported. More than 25 infective endocarditis cases in the past decade have come from tongue, navel, earlobe, lower lip, and nipple piercings [21]. Infective endocarditis should be considered in individuals with a new piercing (ie, up to 4 months), with or without a history of congenital heart disease, who present with unexplained fever, night chills, weakness, myalgia, arthralgia, lethargy, or malaise [22]. General complications include allergic contact dermatitis (eg, from nickel or latex), bleeding, scarring and keloid formation, nerve damage, and interference with medical procedures such as intubation and blood/organ donation [20].
Oral piercings may lead to difficulty speaking and eating, excessive salivation, and dental problems. Oral and nasal piercings may be aspirated or become embedded, requiring surgical removal. Tongue piercing, usually performed without anesthesia, may cause damage to teeth and gums, including dental fractures [23] and changes in chewing and speech. Because of the tongue’s vascular nature, prolonged bleeding can result if vessels are punctured during the piercing procedure. In addition, the technique for inserting tongue jewelry may abrade or fracture anterior dentition, and digital manipulation of the jewelry can significantly increase the potential for infection [24]. In fact, complications arising from oral piercing are so numerous—and in some cases life-threatening—that the American Dental Association has issued a formal statement opposing the practice [24].
Behavioral Risk
Several studies have found that those with body modifications engaged in earlier or more frequent sexual activity and had a greater number of sexual partners [26–28]. A study by Deschesnes and colleagues [29] reported that certain “externalized” risk behaviors were more commonly associated with tattooed and pierced youth than with their unmodified counterparts, including the use of drugs, gang affiliation, school truancy, and problem gambling. Other studies of high school youth have found that tattooing was significantly and independently associated with other high-risk behaviors, including sexual intercourse, binge drinking, smoking, marijuana use, gang membership, truancy, and school failure [30]. However, a survey of college students found that, compared to individuals with no body art, individuals with 1 tattoo and less than 4 piercings had no greater likelihood to engage in high-risk behaviors [31].
Conversely, some researchers have attempted to show a positive association for body modification. In a study of women with eating disorders, the authors suggested that body piercing could be seen as reflecting a positive attitude towards the body, an expression of self-care [32]. In addition, people with piercings are more likely to give attention to their physical appearance and are less likely to be overweight than people without piercings [33].
Stirn and Hinz [34] concluded that most people who partake in body modification clearly do not do it because they have any psychological problems. However, for a few, modifications may be utilized as a convenient means to either realize psychopathological inclinations, such as self-injury, or to overcome psychological traumas. The prevalence of self-injury is unknown, though it is believed to be a growing problem. While self-injury is believed to be a low-lethality behavior, teens who hurt themselves are at increased risk for suicide related to their underlying anxiety or depression. Moreover, self-harmers report that they often had their skin tattooed or body pierced to help overcome a negative experience, or simply to experience physical pain. Another clue that self-harm and piercing/tattooing might in some cases be linked derives from the fact that many of the self-harmers said they had ceased cutting themselves after obtaining their first piercing or tattoo [35]. The increasing incidence makes deliberate self-harm a problem that all health care providers dealing with adolescents are likely to encounter.
Given the link between body modification and “externalized risk behaviors” in young people, tattooing and body piercing may serve as clinical markers for health care professionals, potentially identifying those who may be involved in activities that hinder their health and development [29]. For example, closer examination of teens who wear long sleeves or clothing inappropriate for weather could reveal cuts, burns, carvings, or bruises that are self-inflicted.
Patients are more likely to discuss the issue of body art if the clinician does not speak or act judgmentally [1]. Practitioners who are concerned that their tattooed patient might be self-injuring or engaging in other risky behaviors should invite a discussion with the patient, perhaps using general terms, such as “Sometimes people may get involved in self-injury and don’t know where to turn for help. I will try to help you if you are ever worried about that.” As always, if the clinician suspects a patient is engaged in self-harming activities, an immediate referral should be made for mental health evaluation and any necessary intervention.
Preventatively, clinicians should provide targeted and repeated education to transmit the message of effective decision-making and evaluation of risks to children in the early elementary grades, since some students start to obtain body art as early as fifth grade.
Regret and Removal
Over time, many individuals regret getting tattoos and wish to have them removed [35]. In some cases, delayed complications, like the development of allergic, hypersensitivity, or granulomatous reactions, require tattoo removal. On average, tattoo regret occurs 14 years after tattooing and by the age of 40 years.
Removal is more painful and laborious than the tattooing itself, and complete removal, with no scarring, is often not possible. The American Society for Dermatologic Surgery reports that in 2011, its doctors performed nearly 100,000 tattoo removal procedures, up from the 86,000 performed in 2010 [36]. Pulsed lasers have been used to remove tattoos for more than 20 years. With this procedure, pulses of high-intensity laser energy pass through the epidermis and are selectively absorbed by the tattoo pigment. The laser breaks the pigment into smaller particles, which may be metabolized or excreted by the body, or transported to and stored in lymph nodes or other tissues [37].
Other removal techniques include dermabrasion and surgical excision. Do-it-yourself tattoo removal ointments and creams can be purchased online, but they have not been approved by the FDA and there is no clinical evidence that they work. Furthermore, tattoo removal ointments and creams may cause unexpected reactions, such as rashes, burning, scarring, or changes in skin pigmentation [37].
Clinician’s Role
Body art provides a window into an individual’s uniqueness, and acknowledging body modifications can help build trust and develop the physician/patient relationship. The health professional armed with knowledge about body modifications can forge more functional relationships, obtain critical historical information, and provide better treatment and referral for this population [5].
Having a clinician who is a trusted, nonjudgmental source of information and intervention for patients who choose body art will reduce the health risk of complications associated with tattooing and piercing [1]. Unfortunately, only 14% of the population identify health care professionals as a common resource for information on body modification. Instead, young adults endorsed friends (82%), body piercing shops (61%), and tattoo shops (51%) as their top information sources. Clinicians should help patients make informed decisions about body art and counsel them about the importance of universal precautions [35].
Corresponding author: Susannah Grimm Poe, EdD, 176 Gilboa Rd., Fairmont, WV 26554, [email protected].
Financial disclosures: None.
1. Schmidt R, Armstrong M. Tattooing in adolescents and adults. Up to Date 2013. Available at www.uptodate.com.
2. US Food and Drug Administration. Tattoos and permanent makeup. 2009. Available at www.fda.gov/Cosmetics/ProductandIngredientSafety/ProductInformation/ucm108530.htm.
3. Armstrong ML, Koch JR, Saunders JC, et al. The hole picture: risks, decision making, purpose, regulations, and the future of body piercing. Clin Dermatol 2007;25:398-406.
4. Schorzman CM, Gold MA, Downs JS, Murray PJ. Body art: attitudes and practices regarding body piercing among urban undergraduates. J Am Osteopath Assoc 2007;107:432-8.
5. Urdang, M, Mallek, J, Mallon, W. Tattoos and piercings: a review for the emergency physician. West J Emerg Med 2011;12:393–8.
6. Braverman S. One in five US adults now has a tattoo. New York: Harris Interactive; 2012.
7. Corso RA. Nationwide Harris poll. New York: Harris Interactive; 2008.
8. Laumann AE, Derick AJ. Tattoos and body piercings in the United States: a national data set. J Am Acad Dermatol 2006;55:413–21.
9. Antoszewski B, Sitek A, Fijałkowska M, et al. Tattooing and body piercing--what motivates you to do it? Int J Soc Psychiatry. 2010;56:471–9.
10. Quaranta A, Napoli C, Fasano F, et al. Body piercing and tattoos: a survey on young adults’ knowledge of the risks and practices in body art. BMC Public Health 2011;11:774.
11. Glassy C, Glassy M, Aldasoiuqi A. Tattooing: medical uses and problems. Clev Clin J Med 2012;79:761–70.
12. Sperry K. Tattoos and tattooing. Part II: gross pathology, histopathology, medical complications, and applications. Am J Forensic Med Pathol 1992;13:7–17.
13. Kaur RR, Kirby W, Maibach H. Cutaneous allergic reactions to tattoo ink. J Cosmet Dermatol 2009; 8:295–300.
14. Kennedy BS, Bedard B, Younge M, et al. Outbreak of Mycobacterium chelonae infection associated with tattoo ink. N Engl J Med 2012;367:1020–4.
15. CDC. The hidden dangers of getting inked. Available at http://blogs.cdc.gov/publichealthmatters/2012/08/the-hidden-dangers-of-getting-inked.
16. LeBlanc PM, Hollinger KA, Klontz KC. Tattoo ink-related infections—awareness, diagnosis, reporting, and prevention. N Engl J Med 2012;367:985–7.
17. Shinohara MM, Nguyen J, Gardner J, Rosenbach M, Elenitsas R. The histopathologic spectrum of decorative tattoo complications. J Cutan Pathol 2012;39:1110–8.
18. Reddy KK, Hanke CW, Tierney EP. Malignancy arising within cutaneous tattoos: case of dermatofibrosarcoma protuberans and review of literature. J Drugs Dermatol 2011;10:837–42.
19. Tope WD, Shellock FG. Magnetic resonance imaging and permanent cosmetics (tattoos): survey of complications and adverse events. J Magn Reson Imaging 2002;15:180–4.
20. Holbrook, J, Minocha J, Laumann A. Body piercing: complications and prevention of health risks. Am J Clin Dermatol 2012;13:1–17.
21. Hogan L, Armstrong ML. Body piercing: more than skin deep. Skin therapy letter. Available at www.skintherapyletter.com/2009/14.7/2.html.
22. Raja SG, Shad SK, Dreyfus GD. Body piercing: a rare cause of mitral valve endocarditis. J Heart Valve Dis 2004;13:854.
23. Botchway C, Kuc I. Tongue piercing and associated tooth fracture. J Can Dent Assoc 1998;64:803–5.
24. American Dental Association. Statement on intraoral/perioral piercing and tongue splitting. 2012. Available at www.ada.org/prof/resources/positions/statements/piercing.asp.
25. Stirn A. Body piercing: medical consequences and psychological motivations. Lancet 2003;361:1205–15.
26. Koch R, Roberts AE, Armstrong ML, Owen DC. Body art, deviance, and American college students. Soc Sci J 2010;47:151–61.
27. Gueguen N. Tattoos, piercings, and sexual activity. Social Behav Personality 2012;40:1543–7.
28. Skegg K, Nada-Raja S, Paul C, et al. Body piercing, personality, and sexual behavior. Arch Sex Behav 2007; 36:47–54.
29. Deschesnes M, Fines P, Demers S. Are tattooing and body piercing indicators of risk-taking behaviours among high school students? J Adolesc 2006; 29:379–93.
30. Roberts TA, Ryan SA. Tattooing and high-risk behavior in adolescents. Pediatrics 2002;110:1058–63.
31. Owen DC, Armstrong ML, Koch JR, Roberts AE. College students with body art: well-being or high-risk behavior? J Psychosoc Nurs Ment Health Serv 2013;51:20–8.
32. Claes L, Vandereycken W, Vertommen H. Self-care versus self-harm: piercing, tattooing, and self-injuring in eating disorders. Eur Eat Disord Rev 2004;13:11–18.
33. Hicinbothem J, Gonsalves S, Lester D. Body modification and suicidal behavior. Death Stud 2006; 30:351–63.
34. Stirn A, Hinz A. Tattoos, body piercings, and self-injury: Is there a connection? Psychotherapy Res 2008;18:326–33.
35. Burris K, Kim K. Tattoo removal. Clin Dermatol 2007;25:388–92.
36. American Society for Dermatologic Surgery. Unwanted tattoos. Available at www.asds.net/tattooremovalinformation.aspx.
37. US Food and Drug Administration. Inked and regretful: removing tattoos. 2013. Available at www.fda.gov/ForConsumers/ucm336842.htm.
38. Meltzer DI. Complications of body piercing. Am Fam Physician 2005;72:2029–34.
From the West Virginia University School of Medicine, Morgantown, WV.
Abstract
- Objective: To review the health risks associated with tattoos and body piercing.
- Methods: Review of the literature.
- Results: Tattooing and piercing have become increasingly popular practices in the United States. There are important physical and behavioral risks associated with these forms of body modification. The most common complications from tattooing include skin infections and allergic reactions. Minor complications such as infection and bleeding occur frequently with piercings, but major complications have also been reported. Tattoos and piercings appear to be a marker for risk-taking behavior.
- Conclusion: Clinicians should understand the potential complications of these procedures and be able to counsel patients on how to reduce their health risks.
Tattoos and piercings are ancient practices of body modification that have gained widespread acceptance in modern society, particularly among young adults. Tattoos involve the insertion of colored pigment into the dermal layer of the skin with the goal of creating a permanent marking. They are commonly applied using an electrically powered handheld tattoo machine that moves a needle up and down to inject ink through the epidermis and deposit a drop of ink into the dermis [1]. The cells of the dermis are more stable compared with those of the epidermis, so the ink will mostly stay in place for a person’s lifetime [2].
Body piercing is defined as the insertion of a needle or specially designed piercing gun to create a fistula-like opening into either cartilage or skin for the introduction of decorative ornaments [3]. These ornaments can include jewelry, plastic or wood plugs, beads, or pearls. Body piercing has been part of ritualistic or cultural practices for centuries but is rapidly becoming a worldwide mainstream fashion trend, especially among young women aged 17 to 25 years [4]. Ear piercing has become so well accepted that most studies of body piercing do not include earlobe piercing [5].
There are important physical and behavioral risks associated with body modification. In this paper, we review the epidemiology, potential complications, and behavioral factors associated with tattoos and piercings.
Epidemiology
Tattoos are increasingly popular, with a 2012 Harris poll indicating that 1 in 5 adults has at least 1 tattoo [6], up from 14% in 2008 [7]. In the 2012 poll, adults aged 30 to 39 are most likely to have a tattoo (38%) compared to both those younger (30% of those 25–29 and 22% of those 18–24) and older (27% of those 40–49, 11% of those 50–64 and just 5% of those 65 and older). Women are slightly more likely than men, for the first time since this question was first asked, to have a tattoo (23% versus 19% in men). Current US body piercing rates are approximately 36% [3]. Body piercing is more popular among women than in men [8]. Among adolescents, body piercing is performed considerably earlier than tattooing [9]. The head area is the favored location for piercing, while the most common location for a tattoo is the limb [10].
Associated Health Risks
Tattoos
The most common complications that result from tattooing are skin infections and allergic reactions to the tattoo ink. Extensive skin puncturing can result in bleeding and prolonged leaking of serosanguinous fluid. Pyodermal infections can include temporary inflammation at the site of needle puncture, superficial infections such as impetigo and ecthyma, and deeper infections such as cellulitis, erysipelas, and furunculosis [11]. Unsterile equipment and needles can transmit infectious diseases such as hepatitis [2]. Human immunodeficiency virus is theoretically transmissible this way, but no cases of HIV infection caused by tattooing have been documented [12].
Skin reactions to tattooing include aseptic inflammation and acquired sensitivity to tattoo ink, especially red ink, but also to chromium in green ink, cadmium in yellow ink, and cobalt in blue ink [13]. The reaction can manifest as either allergic contact dermatitis or photo-allergic dermatitis. Cutaneous conditions that localize in tattooed areas include vaccinia, verruca vulgaris, herpes simplex, herpes zoster, psoriasis, lichen planus, keratosis follicularis (Darier disease), chronic discoid lupus erythematosus, and keratoacanthoma. Other possible but less common conditions include keloid, sarcoidal granuloma, erythema multiforme, localized scleroderma, and lymphadenopathy [12].
A recent outbreak of nontuburculous nycobacterial infection was linked to contaminated tattoo inks [14]. Contamination can occur during the manufacturing process due to use of contaminated ingredients or when inks are diluted with nonsterile water by tattoo artists [15]. Investigations of 22 cases of tattoo-associated NTM skin infections in 4 states that occurred during 2011–2012 found that ink was contaminated with NTM before use [16]. M. chelonae, one of several disease-causing NTM species, can cause lung disease, joint infection, eye problems and other organ infections. These infections can be difficult to diagnose and can require treatment lasting 6 months or more [15].
Tattoo laws and regulations vary by state. The inks and ink colorings (pigments) used for tattoos are subject to regulation by the US Food and Drug Administration as cosmetics and color additives. However, the FDA has not traditionally enforced its authority over tattoo inks. The FDA encourages reporting of tattoo-associated complications to its MedWatch program (www.fda.gov/Safety/MedWatch/).
Malignancies reported to develop within tattoos include squamous cell carcinoma, basal cell carcinoma, malignant melanoma, leiomyosarcoma, and dermatofibrosarcoma protuberans [17,18]. These malignancies may be coincidental, but carcinogenicity of the tattoo is as yet unknown. Another concern is that a malignancy within a tattoo is more difficult to identify on skin examination [11,17].
Rarely, tattoos or permanent makeup might cause swelling or burning in the affected areas during magnetic resonance imaging (MRI) exams. The metallic ferric acid pigments used in tattoos can conduct heat on the skin during MRI, resulting in traumatic burns [19]. This has also been reported to occur with tattoos with nonferrous pigments. In some cases, tattoo pigments can interfere with the quality of the image, such as when a person with permanent eyeliner has an MRI of the eye [19].
Patients may self-administer tattoos using sewing needles, forks, paper clips, or pens, and colorants may include charcoal, soot, mascara, or ink. The use of unprofessional tattooists and piercers, who often have limited knowledge of health and hygiene precautions, is more likely to lead to complications [10].
Piercings
While most body piercings are not problematic, the potential for localized infections as well as associated systemic disease is present as long as the piercing site remains open [20]. Bacterial skin infections at or near the site are the most commonly reported complication of body piercings, with causative organisms primarily consisting of Staphylococcus, group A beta-hemolytic Streptococcus, and Pseudomonas [21]. Contributing to the health risks of piercing is the reluctance of patients to seek qualified medical intervention when initial site irritation, pain, or oozing occurs [21].
Systemic infections have been reported. More than 25 infective endocarditis cases in the past decade have come from tongue, navel, earlobe, lower lip, and nipple piercings [21]. Infective endocarditis should be considered in individuals with a new piercing (ie, up to 4 months), with or without a history of congenital heart disease, who present with unexplained fever, night chills, weakness, myalgia, arthralgia, lethargy, or malaise [22]. General complications include allergic contact dermatitis (eg, from nickel or latex), bleeding, scarring and keloid formation, nerve damage, and interference with medical procedures such as intubation and blood/organ donation [20].
Oral piercings may lead to difficulty speaking and eating, excessive salivation, and dental problems. Oral and nasal piercings may be aspirated or become embedded, requiring surgical removal. Tongue piercing, usually performed without anesthesia, may cause damage to teeth and gums, including dental fractures [23] and changes in chewing and speech. Because of the tongue’s vascular nature, prolonged bleeding can result if vessels are punctured during the piercing procedure. In addition, the technique for inserting tongue jewelry may abrade or fracture anterior dentition, and digital manipulation of the jewelry can significantly increase the potential for infection [24]. In fact, complications arising from oral piercing are so numerous—and in some cases life-threatening—that the American Dental Association has issued a formal statement opposing the practice [24].
Behavioral Risk
Several studies have found that those with body modifications engaged in earlier or more frequent sexual activity and had a greater number of sexual partners [26–28]. A study by Deschesnes and colleagues [29] reported that certain “externalized” risk behaviors were more commonly associated with tattooed and pierced youth than with their unmodified counterparts, including the use of drugs, gang affiliation, school truancy, and problem gambling. Other studies of high school youth have found that tattooing was significantly and independently associated with other high-risk behaviors, including sexual intercourse, binge drinking, smoking, marijuana use, gang membership, truancy, and school failure [30]. However, a survey of college students found that, compared to individuals with no body art, individuals with 1 tattoo and less than 4 piercings had no greater likelihood to engage in high-risk behaviors [31].
Conversely, some researchers have attempted to show a positive association for body modification. In a study of women with eating disorders, the authors suggested that body piercing could be seen as reflecting a positive attitude towards the body, an expression of self-care [32]. In addition, people with piercings are more likely to give attention to their physical appearance and are less likely to be overweight than people without piercings [33].
Stirn and Hinz [34] concluded that most people who partake in body modification clearly do not do it because they have any psychological problems. However, for a few, modifications may be utilized as a convenient means to either realize psychopathological inclinations, such as self-injury, or to overcome psychological traumas. The prevalence of self-injury is unknown, though it is believed to be a growing problem. While self-injury is believed to be a low-lethality behavior, teens who hurt themselves are at increased risk for suicide related to their underlying anxiety or depression. Moreover, self-harmers report that they often had their skin tattooed or body pierced to help overcome a negative experience, or simply to experience physical pain. Another clue that self-harm and piercing/tattooing might in some cases be linked derives from the fact that many of the self-harmers said they had ceased cutting themselves after obtaining their first piercing or tattoo [35]. The increasing incidence makes deliberate self-harm a problem that all health care providers dealing with adolescents are likely to encounter.
Given the link between body modification and “externalized risk behaviors” in young people, tattooing and body piercing may serve as clinical markers for health care professionals, potentially identifying those who may be involved in activities that hinder their health and development [29]. For example, closer examination of teens who wear long sleeves or clothing inappropriate for weather could reveal cuts, burns, carvings, or bruises that are self-inflicted.
Patients are more likely to discuss the issue of body art if the clinician does not speak or act judgmentally [1]. Practitioners who are concerned that their tattooed patient might be self-injuring or engaging in other risky behaviors should invite a discussion with the patient, perhaps using general terms, such as “Sometimes people may get involved in self-injury and don’t know where to turn for help. I will try to help you if you are ever worried about that.” As always, if the clinician suspects a patient is engaged in self-harming activities, an immediate referral should be made for mental health evaluation and any necessary intervention.
Preventatively, clinicians should provide targeted and repeated education to transmit the message of effective decision-making and evaluation of risks to children in the early elementary grades, since some students start to obtain body art as early as fifth grade.
Regret and Removal
Over time, many individuals regret getting tattoos and wish to have them removed [35]. In some cases, delayed complications, like the development of allergic, hypersensitivity, or granulomatous reactions, require tattoo removal. On average, tattoo regret occurs 14 years after tattooing and by the age of 40 years.
Removal is more painful and laborious than the tattooing itself, and complete removal, with no scarring, is often not possible. The American Society for Dermatologic Surgery reports that in 2011, its doctors performed nearly 100,000 tattoo removal procedures, up from the 86,000 performed in 2010 [36]. Pulsed lasers have been used to remove tattoos for more than 20 years. With this procedure, pulses of high-intensity laser energy pass through the epidermis and are selectively absorbed by the tattoo pigment. The laser breaks the pigment into smaller particles, which may be metabolized or excreted by the body, or transported to and stored in lymph nodes or other tissues [37].
Other removal techniques include dermabrasion and surgical excision. Do-it-yourself tattoo removal ointments and creams can be purchased online, but they have not been approved by the FDA and there is no clinical evidence that they work. Furthermore, tattoo removal ointments and creams may cause unexpected reactions, such as rashes, burning, scarring, or changes in skin pigmentation [37].
Clinician’s Role
Body art provides a window into an individual’s uniqueness, and acknowledging body modifications can help build trust and develop the physician/patient relationship. The health professional armed with knowledge about body modifications can forge more functional relationships, obtain critical historical information, and provide better treatment and referral for this population [5].
Having a clinician who is a trusted, nonjudgmental source of information and intervention for patients who choose body art will reduce the health risk of complications associated with tattooing and piercing [1]. Unfortunately, only 14% of the population identify health care professionals as a common resource for information on body modification. Instead, young adults endorsed friends (82%), body piercing shops (61%), and tattoo shops (51%) as their top information sources. Clinicians should help patients make informed decisions about body art and counsel them about the importance of universal precautions [35].
Corresponding author: Susannah Grimm Poe, EdD, 176 Gilboa Rd., Fairmont, WV 26554, [email protected].
Financial disclosures: None.
From the West Virginia University School of Medicine, Morgantown, WV.
Abstract
- Objective: To review the health risks associated with tattoos and body piercing.
- Methods: Review of the literature.
- Results: Tattooing and piercing have become increasingly popular practices in the United States. There are important physical and behavioral risks associated with these forms of body modification. The most common complications from tattooing include skin infections and allergic reactions. Minor complications such as infection and bleeding occur frequently with piercings, but major complications have also been reported. Tattoos and piercings appear to be a marker for risk-taking behavior.
- Conclusion: Clinicians should understand the potential complications of these procedures and be able to counsel patients on how to reduce their health risks.
Tattoos and piercings are ancient practices of body modification that have gained widespread acceptance in modern society, particularly among young adults. Tattoos involve the insertion of colored pigment into the dermal layer of the skin with the goal of creating a permanent marking. They are commonly applied using an electrically powered handheld tattoo machine that moves a needle up and down to inject ink through the epidermis and deposit a drop of ink into the dermis [1]. The cells of the dermis are more stable compared with those of the epidermis, so the ink will mostly stay in place for a person’s lifetime [2].
Body piercing is defined as the insertion of a needle or specially designed piercing gun to create a fistula-like opening into either cartilage or skin for the introduction of decorative ornaments [3]. These ornaments can include jewelry, plastic or wood plugs, beads, or pearls. Body piercing has been part of ritualistic or cultural practices for centuries but is rapidly becoming a worldwide mainstream fashion trend, especially among young women aged 17 to 25 years [4]. Ear piercing has become so well accepted that most studies of body piercing do not include earlobe piercing [5].
There are important physical and behavioral risks associated with body modification. In this paper, we review the epidemiology, potential complications, and behavioral factors associated with tattoos and piercings.
Epidemiology
Tattoos are increasingly popular, with a 2012 Harris poll indicating that 1 in 5 adults has at least 1 tattoo [6], up from 14% in 2008 [7]. In the 2012 poll, adults aged 30 to 39 are most likely to have a tattoo (38%) compared to both those younger (30% of those 25–29 and 22% of those 18–24) and older (27% of those 40–49, 11% of those 50–64 and just 5% of those 65 and older). Women are slightly more likely than men, for the first time since this question was first asked, to have a tattoo (23% versus 19% in men). Current US body piercing rates are approximately 36% [3]. Body piercing is more popular among women than in men [8]. Among adolescents, body piercing is performed considerably earlier than tattooing [9]. The head area is the favored location for piercing, while the most common location for a tattoo is the limb [10].
Associated Health Risks
Tattoos
The most common complications that result from tattooing are skin infections and allergic reactions to the tattoo ink. Extensive skin puncturing can result in bleeding and prolonged leaking of serosanguinous fluid. Pyodermal infections can include temporary inflammation at the site of needle puncture, superficial infections such as impetigo and ecthyma, and deeper infections such as cellulitis, erysipelas, and furunculosis [11]. Unsterile equipment and needles can transmit infectious diseases such as hepatitis [2]. Human immunodeficiency virus is theoretically transmissible this way, but no cases of HIV infection caused by tattooing have been documented [12].
Skin reactions to tattooing include aseptic inflammation and acquired sensitivity to tattoo ink, especially red ink, but also to chromium in green ink, cadmium in yellow ink, and cobalt in blue ink [13]. The reaction can manifest as either allergic contact dermatitis or photo-allergic dermatitis. Cutaneous conditions that localize in tattooed areas include vaccinia, verruca vulgaris, herpes simplex, herpes zoster, psoriasis, lichen planus, keratosis follicularis (Darier disease), chronic discoid lupus erythematosus, and keratoacanthoma. Other possible but less common conditions include keloid, sarcoidal granuloma, erythema multiforme, localized scleroderma, and lymphadenopathy [12].
A recent outbreak of nontuburculous nycobacterial infection was linked to contaminated tattoo inks [14]. Contamination can occur during the manufacturing process due to use of contaminated ingredients or when inks are diluted with nonsterile water by tattoo artists [15]. Investigations of 22 cases of tattoo-associated NTM skin infections in 4 states that occurred during 2011–2012 found that ink was contaminated with NTM before use [16]. M. chelonae, one of several disease-causing NTM species, can cause lung disease, joint infection, eye problems and other organ infections. These infections can be difficult to diagnose and can require treatment lasting 6 months or more [15].
Tattoo laws and regulations vary by state. The inks and ink colorings (pigments) used for tattoos are subject to regulation by the US Food and Drug Administration as cosmetics and color additives. However, the FDA has not traditionally enforced its authority over tattoo inks. The FDA encourages reporting of tattoo-associated complications to its MedWatch program (www.fda.gov/Safety/MedWatch/).
Malignancies reported to develop within tattoos include squamous cell carcinoma, basal cell carcinoma, malignant melanoma, leiomyosarcoma, and dermatofibrosarcoma protuberans [17,18]. These malignancies may be coincidental, but carcinogenicity of the tattoo is as yet unknown. Another concern is that a malignancy within a tattoo is more difficult to identify on skin examination [11,17].
Rarely, tattoos or permanent makeup might cause swelling or burning in the affected areas during magnetic resonance imaging (MRI) exams. The metallic ferric acid pigments used in tattoos can conduct heat on the skin during MRI, resulting in traumatic burns [19]. This has also been reported to occur with tattoos with nonferrous pigments. In some cases, tattoo pigments can interfere with the quality of the image, such as when a person with permanent eyeliner has an MRI of the eye [19].
Patients may self-administer tattoos using sewing needles, forks, paper clips, or pens, and colorants may include charcoal, soot, mascara, or ink. The use of unprofessional tattooists and piercers, who often have limited knowledge of health and hygiene precautions, is more likely to lead to complications [10].
Piercings
While most body piercings are not problematic, the potential for localized infections as well as associated systemic disease is present as long as the piercing site remains open [20]. Bacterial skin infections at or near the site are the most commonly reported complication of body piercings, with causative organisms primarily consisting of Staphylococcus, group A beta-hemolytic Streptococcus, and Pseudomonas [21]. Contributing to the health risks of piercing is the reluctance of patients to seek qualified medical intervention when initial site irritation, pain, or oozing occurs [21].
Systemic infections have been reported. More than 25 infective endocarditis cases in the past decade have come from tongue, navel, earlobe, lower lip, and nipple piercings [21]. Infective endocarditis should be considered in individuals with a new piercing (ie, up to 4 months), with or without a history of congenital heart disease, who present with unexplained fever, night chills, weakness, myalgia, arthralgia, lethargy, or malaise [22]. General complications include allergic contact dermatitis (eg, from nickel or latex), bleeding, scarring and keloid formation, nerve damage, and interference with medical procedures such as intubation and blood/organ donation [20].
Oral piercings may lead to difficulty speaking and eating, excessive salivation, and dental problems. Oral and nasal piercings may be aspirated or become embedded, requiring surgical removal. Tongue piercing, usually performed without anesthesia, may cause damage to teeth and gums, including dental fractures [23] and changes in chewing and speech. Because of the tongue’s vascular nature, prolonged bleeding can result if vessels are punctured during the piercing procedure. In addition, the technique for inserting tongue jewelry may abrade or fracture anterior dentition, and digital manipulation of the jewelry can significantly increase the potential for infection [24]. In fact, complications arising from oral piercing are so numerous—and in some cases life-threatening—that the American Dental Association has issued a formal statement opposing the practice [24].
Behavioral Risk
Several studies have found that those with body modifications engaged in earlier or more frequent sexual activity and had a greater number of sexual partners [26–28]. A study by Deschesnes and colleagues [29] reported that certain “externalized” risk behaviors were more commonly associated with tattooed and pierced youth than with their unmodified counterparts, including the use of drugs, gang affiliation, school truancy, and problem gambling. Other studies of high school youth have found that tattooing was significantly and independently associated with other high-risk behaviors, including sexual intercourse, binge drinking, smoking, marijuana use, gang membership, truancy, and school failure [30]. However, a survey of college students found that, compared to individuals with no body art, individuals with 1 tattoo and less than 4 piercings had no greater likelihood to engage in high-risk behaviors [31].
Conversely, some researchers have attempted to show a positive association for body modification. In a study of women with eating disorders, the authors suggested that body piercing could be seen as reflecting a positive attitude towards the body, an expression of self-care [32]. In addition, people with piercings are more likely to give attention to their physical appearance and are less likely to be overweight than people without piercings [33].
Stirn and Hinz [34] concluded that most people who partake in body modification clearly do not do it because they have any psychological problems. However, for a few, modifications may be utilized as a convenient means to either realize psychopathological inclinations, such as self-injury, or to overcome psychological traumas. The prevalence of self-injury is unknown, though it is believed to be a growing problem. While self-injury is believed to be a low-lethality behavior, teens who hurt themselves are at increased risk for suicide related to their underlying anxiety or depression. Moreover, self-harmers report that they often had their skin tattooed or body pierced to help overcome a negative experience, or simply to experience physical pain. Another clue that self-harm and piercing/tattooing might in some cases be linked derives from the fact that many of the self-harmers said they had ceased cutting themselves after obtaining their first piercing or tattoo [35]. The increasing incidence makes deliberate self-harm a problem that all health care providers dealing with adolescents are likely to encounter.
Given the link between body modification and “externalized risk behaviors” in young people, tattooing and body piercing may serve as clinical markers for health care professionals, potentially identifying those who may be involved in activities that hinder their health and development [29]. For example, closer examination of teens who wear long sleeves or clothing inappropriate for weather could reveal cuts, burns, carvings, or bruises that are self-inflicted.
Patients are more likely to discuss the issue of body art if the clinician does not speak or act judgmentally [1]. Practitioners who are concerned that their tattooed patient might be self-injuring or engaging in other risky behaviors should invite a discussion with the patient, perhaps using general terms, such as “Sometimes people may get involved in self-injury and don’t know where to turn for help. I will try to help you if you are ever worried about that.” As always, if the clinician suspects a patient is engaged in self-harming activities, an immediate referral should be made for mental health evaluation and any necessary intervention.
Preventatively, clinicians should provide targeted and repeated education to transmit the message of effective decision-making and evaluation of risks to children in the early elementary grades, since some students start to obtain body art as early as fifth grade.
Regret and Removal
Over time, many individuals regret getting tattoos and wish to have them removed [35]. In some cases, delayed complications, like the development of allergic, hypersensitivity, or granulomatous reactions, require tattoo removal. On average, tattoo regret occurs 14 years after tattooing and by the age of 40 years.
Removal is more painful and laborious than the tattooing itself, and complete removal, with no scarring, is often not possible. The American Society for Dermatologic Surgery reports that in 2011, its doctors performed nearly 100,000 tattoo removal procedures, up from the 86,000 performed in 2010 [36]. Pulsed lasers have been used to remove tattoos for more than 20 years. With this procedure, pulses of high-intensity laser energy pass through the epidermis and are selectively absorbed by the tattoo pigment. The laser breaks the pigment into smaller particles, which may be metabolized or excreted by the body, or transported to and stored in lymph nodes or other tissues [37].
Other removal techniques include dermabrasion and surgical excision. Do-it-yourself tattoo removal ointments and creams can be purchased online, but they have not been approved by the FDA and there is no clinical evidence that they work. Furthermore, tattoo removal ointments and creams may cause unexpected reactions, such as rashes, burning, scarring, or changes in skin pigmentation [37].
Clinician’s Role
Body art provides a window into an individual’s uniqueness, and acknowledging body modifications can help build trust and develop the physician/patient relationship. The health professional armed with knowledge about body modifications can forge more functional relationships, obtain critical historical information, and provide better treatment and referral for this population [5].
Having a clinician who is a trusted, nonjudgmental source of information and intervention for patients who choose body art will reduce the health risk of complications associated with tattooing and piercing [1]. Unfortunately, only 14% of the population identify health care professionals as a common resource for information on body modification. Instead, young adults endorsed friends (82%), body piercing shops (61%), and tattoo shops (51%) as their top information sources. Clinicians should help patients make informed decisions about body art and counsel them about the importance of universal precautions [35].
Corresponding author: Susannah Grimm Poe, EdD, 176 Gilboa Rd., Fairmont, WV 26554, [email protected].
Financial disclosures: None.
1. Schmidt R, Armstrong M. Tattooing in adolescents and adults. Up to Date 2013. Available at www.uptodate.com.
2. US Food and Drug Administration. Tattoos and permanent makeup. 2009. Available at www.fda.gov/Cosmetics/ProductandIngredientSafety/ProductInformation/ucm108530.htm.
3. Armstrong ML, Koch JR, Saunders JC, et al. The hole picture: risks, decision making, purpose, regulations, and the future of body piercing. Clin Dermatol 2007;25:398-406.
4. Schorzman CM, Gold MA, Downs JS, Murray PJ. Body art: attitudes and practices regarding body piercing among urban undergraduates. J Am Osteopath Assoc 2007;107:432-8.
5. Urdang, M, Mallek, J, Mallon, W. Tattoos and piercings: a review for the emergency physician. West J Emerg Med 2011;12:393–8.
6. Braverman S. One in five US adults now has a tattoo. New York: Harris Interactive; 2012.
7. Corso RA. Nationwide Harris poll. New York: Harris Interactive; 2008.
8. Laumann AE, Derick AJ. Tattoos and body piercings in the United States: a national data set. J Am Acad Dermatol 2006;55:413–21.
9. Antoszewski B, Sitek A, Fijałkowska M, et al. Tattooing and body piercing--what motivates you to do it? Int J Soc Psychiatry. 2010;56:471–9.
10. Quaranta A, Napoli C, Fasano F, et al. Body piercing and tattoos: a survey on young adults’ knowledge of the risks and practices in body art. BMC Public Health 2011;11:774.
11. Glassy C, Glassy M, Aldasoiuqi A. Tattooing: medical uses and problems. Clev Clin J Med 2012;79:761–70.
12. Sperry K. Tattoos and tattooing. Part II: gross pathology, histopathology, medical complications, and applications. Am J Forensic Med Pathol 1992;13:7–17.
13. Kaur RR, Kirby W, Maibach H. Cutaneous allergic reactions to tattoo ink. J Cosmet Dermatol 2009; 8:295–300.
14. Kennedy BS, Bedard B, Younge M, et al. Outbreak of Mycobacterium chelonae infection associated with tattoo ink. N Engl J Med 2012;367:1020–4.
15. CDC. The hidden dangers of getting inked. Available at http://blogs.cdc.gov/publichealthmatters/2012/08/the-hidden-dangers-of-getting-inked.
16. LeBlanc PM, Hollinger KA, Klontz KC. Tattoo ink-related infections—awareness, diagnosis, reporting, and prevention. N Engl J Med 2012;367:985–7.
17. Shinohara MM, Nguyen J, Gardner J, Rosenbach M, Elenitsas R. The histopathologic spectrum of decorative tattoo complications. J Cutan Pathol 2012;39:1110–8.
18. Reddy KK, Hanke CW, Tierney EP. Malignancy arising within cutaneous tattoos: case of dermatofibrosarcoma protuberans and review of literature. J Drugs Dermatol 2011;10:837–42.
19. Tope WD, Shellock FG. Magnetic resonance imaging and permanent cosmetics (tattoos): survey of complications and adverse events. J Magn Reson Imaging 2002;15:180–4.
20. Holbrook, J, Minocha J, Laumann A. Body piercing: complications and prevention of health risks. Am J Clin Dermatol 2012;13:1–17.
21. Hogan L, Armstrong ML. Body piercing: more than skin deep. Skin therapy letter. Available at www.skintherapyletter.com/2009/14.7/2.html.
22. Raja SG, Shad SK, Dreyfus GD. Body piercing: a rare cause of mitral valve endocarditis. J Heart Valve Dis 2004;13:854.
23. Botchway C, Kuc I. Tongue piercing and associated tooth fracture. J Can Dent Assoc 1998;64:803–5.
24. American Dental Association. Statement on intraoral/perioral piercing and tongue splitting. 2012. Available at www.ada.org/prof/resources/positions/statements/piercing.asp.
25. Stirn A. Body piercing: medical consequences and psychological motivations. Lancet 2003;361:1205–15.
26. Koch R, Roberts AE, Armstrong ML, Owen DC. Body art, deviance, and American college students. Soc Sci J 2010;47:151–61.
27. Gueguen N. Tattoos, piercings, and sexual activity. Social Behav Personality 2012;40:1543–7.
28. Skegg K, Nada-Raja S, Paul C, et al. Body piercing, personality, and sexual behavior. Arch Sex Behav 2007; 36:47–54.
29. Deschesnes M, Fines P, Demers S. Are tattooing and body piercing indicators of risk-taking behaviours among high school students? J Adolesc 2006; 29:379–93.
30. Roberts TA, Ryan SA. Tattooing and high-risk behavior in adolescents. Pediatrics 2002;110:1058–63.
31. Owen DC, Armstrong ML, Koch JR, Roberts AE. College students with body art: well-being or high-risk behavior? J Psychosoc Nurs Ment Health Serv 2013;51:20–8.
32. Claes L, Vandereycken W, Vertommen H. Self-care versus self-harm: piercing, tattooing, and self-injuring in eating disorders. Eur Eat Disord Rev 2004;13:11–18.
33. Hicinbothem J, Gonsalves S, Lester D. Body modification and suicidal behavior. Death Stud 2006; 30:351–63.
34. Stirn A, Hinz A. Tattoos, body piercings, and self-injury: Is there a connection? Psychotherapy Res 2008;18:326–33.
35. Burris K, Kim K. Tattoo removal. Clin Dermatol 2007;25:388–92.
36. American Society for Dermatologic Surgery. Unwanted tattoos. Available at www.asds.net/tattooremovalinformation.aspx.
37. US Food and Drug Administration. Inked and regretful: removing tattoos. 2013. Available at www.fda.gov/ForConsumers/ucm336842.htm.
38. Meltzer DI. Complications of body piercing. Am Fam Physician 2005;72:2029–34.
1. Schmidt R, Armstrong M. Tattooing in adolescents and adults. Up to Date 2013. Available at www.uptodate.com.
2. US Food and Drug Administration. Tattoos and permanent makeup. 2009. Available at www.fda.gov/Cosmetics/ProductandIngredientSafety/ProductInformation/ucm108530.htm.
3. Armstrong ML, Koch JR, Saunders JC, et al. The hole picture: risks, decision making, purpose, regulations, and the future of body piercing. Clin Dermatol 2007;25:398-406.
4. Schorzman CM, Gold MA, Downs JS, Murray PJ. Body art: attitudes and practices regarding body piercing among urban undergraduates. J Am Osteopath Assoc 2007;107:432-8.
5. Urdang, M, Mallek, J, Mallon, W. Tattoos and piercings: a review for the emergency physician. West J Emerg Med 2011;12:393–8.
6. Braverman S. One in five US adults now has a tattoo. New York: Harris Interactive; 2012.
7. Corso RA. Nationwide Harris poll. New York: Harris Interactive; 2008.
8. Laumann AE, Derick AJ. Tattoos and body piercings in the United States: a national data set. J Am Acad Dermatol 2006;55:413–21.
9. Antoszewski B, Sitek A, Fijałkowska M, et al. Tattooing and body piercing--what motivates you to do it? Int J Soc Psychiatry. 2010;56:471–9.
10. Quaranta A, Napoli C, Fasano F, et al. Body piercing and tattoos: a survey on young adults’ knowledge of the risks and practices in body art. BMC Public Health 2011;11:774.
11. Glassy C, Glassy M, Aldasoiuqi A. Tattooing: medical uses and problems. Clev Clin J Med 2012;79:761–70.
12. Sperry K. Tattoos and tattooing. Part II: gross pathology, histopathology, medical complications, and applications. Am J Forensic Med Pathol 1992;13:7–17.
13. Kaur RR, Kirby W, Maibach H. Cutaneous allergic reactions to tattoo ink. J Cosmet Dermatol 2009; 8:295–300.
14. Kennedy BS, Bedard B, Younge M, et al. Outbreak of Mycobacterium chelonae infection associated with tattoo ink. N Engl J Med 2012;367:1020–4.
15. CDC. The hidden dangers of getting inked. Available at http://blogs.cdc.gov/publichealthmatters/2012/08/the-hidden-dangers-of-getting-inked.
16. LeBlanc PM, Hollinger KA, Klontz KC. Tattoo ink-related infections—awareness, diagnosis, reporting, and prevention. N Engl J Med 2012;367:985–7.
17. Shinohara MM, Nguyen J, Gardner J, Rosenbach M, Elenitsas R. The histopathologic spectrum of decorative tattoo complications. J Cutan Pathol 2012;39:1110–8.
18. Reddy KK, Hanke CW, Tierney EP. Malignancy arising within cutaneous tattoos: case of dermatofibrosarcoma protuberans and review of literature. J Drugs Dermatol 2011;10:837–42.
19. Tope WD, Shellock FG. Magnetic resonance imaging and permanent cosmetics (tattoos): survey of complications and adverse events. J Magn Reson Imaging 2002;15:180–4.
20. Holbrook, J, Minocha J, Laumann A. Body piercing: complications and prevention of health risks. Am J Clin Dermatol 2012;13:1–17.
21. Hogan L, Armstrong ML. Body piercing: more than skin deep. Skin therapy letter. Available at www.skintherapyletter.com/2009/14.7/2.html.
22. Raja SG, Shad SK, Dreyfus GD. Body piercing: a rare cause of mitral valve endocarditis. J Heart Valve Dis 2004;13:854.
23. Botchway C, Kuc I. Tongue piercing and associated tooth fracture. J Can Dent Assoc 1998;64:803–5.
24. American Dental Association. Statement on intraoral/perioral piercing and tongue splitting. 2012. Available at www.ada.org/prof/resources/positions/statements/piercing.asp.
25. Stirn A. Body piercing: medical consequences and psychological motivations. Lancet 2003;361:1205–15.
26. Koch R, Roberts AE, Armstrong ML, Owen DC. Body art, deviance, and American college students. Soc Sci J 2010;47:151–61.
27. Gueguen N. Tattoos, piercings, and sexual activity. Social Behav Personality 2012;40:1543–7.
28. Skegg K, Nada-Raja S, Paul C, et al. Body piercing, personality, and sexual behavior. Arch Sex Behav 2007; 36:47–54.
29. Deschesnes M, Fines P, Demers S. Are tattooing and body piercing indicators of risk-taking behaviours among high school students? J Adolesc 2006; 29:379–93.
30. Roberts TA, Ryan SA. Tattooing and high-risk behavior in adolescents. Pediatrics 2002;110:1058–63.
31. Owen DC, Armstrong ML, Koch JR, Roberts AE. College students with body art: well-being or high-risk behavior? J Psychosoc Nurs Ment Health Serv 2013;51:20–8.
32. Claes L, Vandereycken W, Vertommen H. Self-care versus self-harm: piercing, tattooing, and self-injuring in eating disorders. Eur Eat Disord Rev 2004;13:11–18.
33. Hicinbothem J, Gonsalves S, Lester D. Body modification and suicidal behavior. Death Stud 2006; 30:351–63.
34. Stirn A, Hinz A. Tattoos, body piercings, and self-injury: Is there a connection? Psychotherapy Res 2008;18:326–33.
35. Burris K, Kim K. Tattoo removal. Clin Dermatol 2007;25:388–92.
36. American Society for Dermatologic Surgery. Unwanted tattoos. Available at www.asds.net/tattooremovalinformation.aspx.
37. US Food and Drug Administration. Inked and regretful: removing tattoos. 2013. Available at www.fda.gov/ForConsumers/ucm336842.htm.
38. Meltzer DI. Complications of body piercing. Am Fam Physician 2005;72:2029–34.
Locking Plate Fixation for Proximal Humerus Fractures
4 EKG Abnormalities: What Are the Lifesaving Diagnoses?
› Consider placement of an automatic implantable cardioverter-defibrillator for all patients with a type 1 Brugada pattern on EKG accompanied by syncope, documented ventricular arrhythmia, or aborted sudden cardiac death. B
› Always look for EKG findings suggestive of Wolff-Parkinson-White syndrome in otherwise healthy patients presenting with syncope. C
› Refer all patients with suspected hypertrophic cardiomyopathy to Cardiology for a transthoracic echocardiogram. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
When evaluating a patient with a history of chest pain, palpitations, syncope, and/or new-onset seizures, an electrocardiogram (EKG) may be the key to
identifying a potentially life-threatening condition. Here we present 4 cases in which EKG findings were the clue to underlying medical conditions that, if left untreated, could be fatal. Because each of these conditions may not have associated findings on a physical exam, early recognition of these EKG findings can be lifesaving.
CASE 1 › A 15-year-old boy suddenly collapses while walking, and bystanders report seizure-like activity. The patient doesn’t remember the event. Vital signs and physical exam are normal, and his blood glucose level is 86 mg/dL (normal: 70-100 mg/dL). He doesn’t take any medications and denies illicit drug use or recent illness.
What EKG abnormality (FIGURE 1) likely explains the cause of the patient’s collapse?
The EKG abnormality and diagnosis. The patient’s EKG revealed a prolonged QT interval (FIGURE 1, BRACKETS). His QTc (QT interval corrected for heart rate) was .470 seconds, which is at the high end of the normal range for his age and gender.1 The patient had no family history of syncope, sudden cardiac death (SCD), or seizure disorder. Evaluation uncovered a calcium level of 4.4 mEq/L (normal: 4.5-5.5 mEq/L) and a phosphate level of 7.8 mg/dL (normal: 2.4-4.1 mg/dL).
This patient had a low parathyroid hormone from primary hypoparathyroidism. His conduction abnormality was treated with both oral calcium and vitamin D supplements.
Etiology and epidemiology. A prolonged QT interval may be the result of a primary long QT syndrome (LQTS) or an acquired condition from electrolyte imbalance, medication effect, or toxin exposure.
In the United States, the incidence of a genetic mutation that causes LQTS is 1 in 2500 people.2 Patients with LQTS usually remain asymptomatic unless the QT interval is further prolonged by a condition or medication. There are several hundred congenital LQTS subtypes based on specific ion channel defects; the most common is LQTS1, with an inherited defect in the KCNQ1 gene, which regulates the slow potassium ion channel.
Acquired LQTS is much more common than congenital LQTS.3 Many drugs have been linked to an increased risk of LQTS, including certain antiarrhythmics, antibiotics, and antipsychotics (TABLE 1).4 In addition, electrolyte disturbances such as hypokalemia, hypocalcemia, and hypomagnesemia can be etiologic factors.
Be aware that an acquired LQTS may mask an underlying congenital LQTS. Therefore, patients in whom the offending agent or condition is corrected should still have a follow-up EKG. Screening family members for LQTS is worthwhile, even in those without symptoms.
Clinical features. Patients with symptomatic LQTS may have dizziness, palpitations, and syncope. SCD also is possible. These signs and symptoms may be triggered by strong emotions (in LQTS2) or physical activity (in LQTS1). They likely are caused by torsades de pointes and ventricular fibrillation. A brief aura may precede these arrhythmias, and patients may experience urinary or fecal incontinence.5
The key to making a diagnosis of LQTS is correctly measuring the QT interval. The QT interval is measured from the beginning of the Q-wave to the end of the T-wave as measured from the intersection of a line tangent to the downslope of the T-wave and the isoelectric line. This can be difficult to determine in EKGs showing bundle branch block or an irregular rhythm, such as atrial fibrillation (AF).6,7 A common error in measuring the QT interval occurs when clinicians inadvertently include a U-wave in the measurement.1 Some EKG machines may provide QT interval and QTc measurements. Normal QT intervals are ≤.450 seconds for men and ≤.470 seconds for women.8
It is essential to confirm the QT interval by using the Bazett formula (QTc equals the QT in seconds divided by the square root of the RR interval in seconds) for all patients with a history that suggests a possible arrhythmia.
Our patient had hypocalcemia, which on an EKG can cause T-wave widening with a normal ST segment, rather than a normal T-wave with a long ST segment, as is typically seen in LQTS. This distinction may be difficult to discern and should not preclude the search for either an acquired prolonged QTc or an underlying LQTS.9
Treatment. First rule out or treat any causes of acquired LQTS by taking a careful medication history and evaluating the patient’s electrolytes. Once these have been addressed, a beta-blocker is first-line therapy for symptomatic patients.5
Unfortunately, up to 20% of individuals treated with beta-blockers may continue to have syncope.5 For these patients, options include a left cardiac sympathetic denervation (LCSD) or placement of an automatic implantable cardioverter-defibrillator (AICD). An LCSD involves removal of the left-sided stellate and/or thoracic ganglia. This procedure can be used instead of, or in addition to, beta-blockers. If the patient’s syncope persists, AICDs are an option. AICDs can be lifesaving, but patients run the risk of adverse effects that include inappropriate shocks and infection.10 As the result of these therapies, mortality associated with LQTS has dropped to approximately 1%.11
CASE 2 › A 14-year-old boy has a syncopal episode while at rest. A similar event occurred 3 years earlier; at that time, an echocardiogram and EKG were normal. For 2 days, he’s had a cough and low-grade fever. His temperature is 102ºF and he has a productive cough. Based on this EKG (FIGURE 2), what is the likely diagnosis? What is the significance of his fever?
The EKG abnormality and diagnosis. This patient’s EKG showed a type 1 Brugada pattern (FIGURE 2, ARROWS), which strongly supported the diagnosis of Brugada syndrome (BS). BS is an inherited condition caused by a genetic defect in cardiac ion channel function that leads to characteristic EKG changes and a predisposition to ventricular fibrillation.12 In this case, the fever likely unmasked these EKG findings.
The patient was transferred to a local hospital for treatment of community-acquired pneumonia, and ultimately received an AICD.
Etiology and epidemiology. BS was first described in 199213 and is a major cause of SCD, responsible for up to 4% of all cases of SCD, and 20% of cases of patients without structural heart disease.14 BS is more common in men, and the mean age of diagnosis is 40 to 45.15-18
Mutations in at least 17 cardiac ion channel genes have been linked to BS.19 The SCN5A gene—a cardiac sodium channel—is the most commonly implicated, but accounts for only 11% to 24% of all BS cases.15
Clinical features. Patients with BS may present with syncope, nocturnal agonal respirations, or ventricular arrhythmias.12 EKG findings include partial or complete right bundle branch block (RBBB) and ST segment elevation in right precordial leads V1 to V3.12 There are 2 Brugada EKG patterns, a type 1 cloved pattern as seen in our patient’s EKG and a type 2 saddleback pattern.20 EKG findings are dynamic over time and may alternate between normal, type 1, and type 2.20 Factors that modulate EKG appearance include fever, intoxication, vagal tone, electrolyte imbalance, and sodium channel blockade.12,20
Diagnosis requires a type 1 Brugada pattern on EKG plus a family history of BS, documented ventricular arrhythmia, or arrhythmia-related symptoms such as syncope.12 Patients with a type 2 Brugada pattern may undergo electrophysiology (EP) testing with Class I antiarrhythmic drugs to induce a diagnostic type 1 Brugada pattern.12,21 Patients who have Brugada EKG findings but none of the other diagnostic criteria are considered to have a Brugada pattern (rather than Brugada syndrome).12
The most concerning outcome of BS is ventricular fibrillation. The estimated annual rate of cardiac events is 7.7% among patients who have experienced an aborted SCD, 1.9% among those who have experienced syncope, and 0.5% in asymptomatic patients.18
Treatment. The only effective treatment for BS is placement of an AICD; however, complications of AICD placement cause significant morbidity.6 Ten years after AICD placement, 37% of patients experienced inappropriate shocks and 29% experienced lead failure.22 Recent modifications in device programming and the addition of remote monitoring have decreased complication rates.12,22
The decision to place an AICD is based on the patient’s prior symptoms, EKG findings, and other factors. Recent guidelines recommend an AICD for all patients with a type 1 Brugada pattern (spontaneous or induced) who also have had an aborted SCD, syncope, or documented ventricular arrhythmia.12
Management of asymptomatic patients with type 1 Brugada pattern remains controversial because the rate of cardiac events is low, although such events can be fatal. Asymptomatic patients with type 1 Brugada findings should undergo further EP testing, and should receive AICD only upon demonstration of inducible ventricular arrhythmia.12
TABLE 2
Arrhythmias associated with Wolff-Parkinson-White syndrome23
| Arrhythmia | EKG findings | Treatment—unstable patients | Treatment—stable patients (in preferred treatment order) |
| PSVT, orthodromic | Narrow QRS, loss of delta wave, rate 160-260 beats/min | Synchronized cardioversion | Vagal maneuvers, adenosine, calcium channel blockers, beta-blockers, digoxin, procainamide |
| PSVT, antidromic | Wide complex tachycardia | Synchronized cardioversion | Procainamide |
| Atrial fibrillation | Irregularly irregular (RR interval variable with no pattern), ventricular rates that can exceed 300 beats/min | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Atrial flutter | Flutter waves, rate normal to tachycardic depending on conduction rate | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Ventricular fibrillation | Rapid, erratic electrical impulses | Defibrillation | N/A |
EKG, electrocardiogram; N/A, not applicable; PSVT, paroxysmal supraventricular tachycardia.
CASE 3 › A 21-year-old man with no medical history presents with sudden onset of lightheadedness followed by syncope. He denies any chest pain or other associated symptoms. At the time of evaluation, he is asymptomatic. His EKG (FIGURE 3) is diagnostic of what syndrome?
The EKG abnormality and diagnosis. The patient had a classic presentation for Wolff-Parkinson-White (WPW) syndrome, a common congenital disorder that alters normal cardiac conduction. He described 2 past instances of unexplained light-headedness and palpitations. Subsequent EP studies demonstrated that the patient had an accessory atrioventricular (AV) tract, causing electrical activity in the heart to bypass the AV node, resulting in a delta wave on EKG (FIGURE 3, GREEN ARROWS).
The patient opted for ablation therapy, which successfully eliminated the delta wave on EKG. Five years later he has had no recurrences.
Epidemiology. The prevalence of WPW syndrome is .1% to 3%.23 Accessory AV tracts are found in men twice as often as in women. Only half of individuals with confirmed tracts develop a tachyarrhythmia. The estimated risk of sudden death due to WPW syndrome is .5% to 4%.24
Pathophysiology. Normally cardiac conduction originates from the sinus node and travels to the AV node, where conduction is slowed, and then proceeds to the His-Purkinje system, and finally to the rest of the ventricular myocardium. In WPW syndrome, ventricular depolarization occurs first by an accessory AV tract called the bundle of Kent, followed shortly thereafter by the His-Purkinje system. This sequence of depolarization is what leads to the EKG findings characteristic of WPW syndrome: a PR interval <.12 seconds, presence of a delta wave, widened QRS complex (>.12 seconds), and repolarization changes seen as ST segment and T-wave changes discordant to (opposite direction) the delta wave and QRS complex (FIGURE 3, RED ARROW).
Factors that influence electrical conduction through the bundle of Kent include cardioactive medications, physiological stress, circulating catecholamines, coronary ischemia, and aging. The end result is a propensity for the heart to convert to one of 4 arrhythmias: paroxysmal supraventricular tachycardia (PSVT), AF, atrial flutter, or ventricular fibrillation (TABLE 2).23
The most common arrhythmia in WPW syndrome is PSVT.23 This rhythm is induced by the formation of a reentry circuit—a pattern in which the heart’s electrical signal loops back on itself—involving the normal conduction pathway and the bundle of Kent. Reentry progressing down the His-Purkinje system and traveling up the bundle of Kent is referred to as orthodromic (anterograde) PSVT. Antidromic (retrograde) PSVT is due to a reentry circuit conducting from the bundle of Kent to the ventricles, and then retrograde through the His-Purkinje system and AV node to the atria.
Clinical features. Under normal circumstances, patients with WPW syndrome are asymptomatic. As was the case with our patient, individuals who develop one of the 4 characteristic arrhythmias can experience light-headedness and syncope.
Treatment. An unstable patient who is experiencing PSVT, AF, or atrial flutter should receive synchronized cardioversion; those experiencing ventricular fibrillation should receive defibrillation (TABLE 2).23 For stable patients, therapy is tailored to the type of arrhythmia. Calcium channel blockers, beta-blockers, and adenosine might be appropriate for patients with orthodromic PSVT but should be avoided in patients with antidromic PSVT, AF, or atrial flutter because these medications block AV node conduction and thus facilitate conduction down the bundle of Kent, which can result in potentially unstable arrhythmias. In general, the longer an arrhythmia has been present, the less effective the pharmacologic intervention because of the increasing sympathetic tone.
Preventive long-term therapies for WPW patients who have experienced arrhythmia include antiarrhythmic medications or ablative procedures. Long-term antiarrhythmic therapy often is reserved for older, more sedentary individuals with less frequent arrhythmias that are not life-threatening. Radiofrequency ablation is a popular option, with long-term success rates as high as 95% and complication rates <1%.23 Patients in whom a WPW pattern is identified incidentally on EKG should be referred to cardiology for EP studies and risk stratification.25
CASE 4 › A 61-year-old woman has an episode of substernal exertional chest pressure that lasted approximately 2 hours but resolved before she arrived at her physician’s office. She also experienced mild nausea. She has no history of coronary artery disease but says that she has experienced similar episodes of chest pressure. What abnormality is seen on her EKG (FIGURE 4)? What is the most likely cause of her symptoms?
The EKG abnormality and diagnosis. Although classically associated with syncope, hypertrophic cardiomyopathy (HCM) often presents similarly to acute coronary syndromes, with chest pain and dyspnea on exertion.26 This patient had no history of cardiac disease or family history of SCD or cardiomyopathy; however, her EKG showed changes indicating left ventricular hypertrophy (LVH), which is consistent with HCM (FIGURE 4, ARROWS). Echocardiography identified myocardial hypertrophy, normal left ventricular ejection fraction, but severe left ventricular outflow obstruction and mild diastolic dysfunction. She was treated with metoprolol and verapamil.
Etiology and epidemiology. Hypertrophic cardiomyopathy is an autosomal dominant intrinsic myocardial disorder resulting in LVH that is commonly associated with SCD during extreme physical activity.26,27 The prevalence of HCM is approximately 1 in 500.26 Although it can present at any age, it is the most common cause of SCD in young people (under age 30), responsible for 33% of deaths during athletic events.28
TABLE 3
4 diagnoses and what you'll see on EKG
| Diagnosis | EKG finding |
| Prolonged QT interval | QTc interval >.450 sec (men) or >.470 sec (women) |
| Brugada syndrome | Partial or complete RBBB, and ST segment elevation in right precordial leads V1-V3 |
| Wolff-Parkinson-White syndrome | Delta wave, widened QRS, short PR interval, ST segment and T-wave changes |
| Hypertrophic cardiomyopathy | No definitive finding; may have left ventricular hypertrophy or abnormal Q-waves |
EKG, electrocardiogram; RBBB, right bundle branch block.
Clinical features. The severity of HCM ranges from asymptomatic to fatal. Symptoms of HCM include chest pain, dyspnea, and syncope. The disorder causes morbidity and mortality in at least one of 3 ways: ventricular tachyarrhythmias (often in younger patients), heart failure (from left ventricular outflow obstruction), and/or thromboembolism.27
Although echocardiography typically is used to make the diagnosis,27 an EKG often is the initial screening tool. EKG changes are seen in 75% to 95% of affected patients and include the presence of Q-waves and increased voltages related to LVH.27,29 Infarct-like patterns may be present before wall thickening on echocardiogram. Abnormal Q-waves are found in 20% to 50% of HCM patients, and are more common in younger patients. Konno et al30 have shown that Q-waves >3 mm in depth and/or >.040 seconds in duration in at least 2 leads other than aVR is specific (90%) in identifying carriers of HCM genes before they develop clinical symptoms.
Ambulatory monitoring may be useful for risk stratifying HCM patients; those with nonsustained ventricular tachycardia (NSVT) are at higher risk of SCD. Holter monitoring is recommended in initial evaluation because evidence of ventricular tachyarrhythmias may warrant AICD placement.26
Treatment. The risk of SCD in HCM is approximately 1%, but higher in those with a family history of SCD, syncope, NSVT, hypotension during exercise, or severe LVH (left ventricle thickness >30 mm).26 AICDs are recommended for HCM patients with prior cardiac arrest, patients with ≥2 of these risk factors, or patients with one risk factor who have experienced syncope related to arrhythmia.26
For patients who are symptomatic but have <2 risk factors, beta-blockers are firstline therapy.26 Verapamil is used as a second line treatment. Both beta-blockers and calcium channel blockers reduce dyspnea, palpitations, and chest pain.27
For patients who don’t respond to medical therapy, septal reduction therapy may be performed, either by septal myectomy or alcohol septal ablation.27 It is also important to consider genetic screening and counseling for the family.
A summary of all 4 diagnoses described in this article, their associated EKG findings, and their pathophysiology appears in TABLE 3.
CORRESPONDENCE
Samir Haydar, DO, MPH, FACEP, Tufts University School of Medicine, Maine Medical Center, Department of Emergency Medicine, 47 Bramhall St., Portland, ME 04103; [email protected]
1. Taggart NW, Haglund CM, Tester DJ, et al. Diagnostic miscues in congenital long-QT syndrome. Circulation. 2007;115:2613-2620.
2. Schwartz PJ, Stramba-Badiale M, Crotti L, et al. Prevalance of the congenital long QT syndrome. Circulation. 2009;120:1761-1767.
3. van Noord C, Eijgelsheim M, Stricker BH. Drug- and nondrug-associated QT interval prolongation. Br J Clin Pharmacol. 2010;70:16-23.
4. Credible Meds Web site. Available at: http://crediblemeds.org. Accessed April 8, 2014.
5. Schwartz PJ, Priori SG, Spazzolini C, et al. Genotype-phenotype correlation in the long QT syndrome: gene specific triggers for life threatening arrhythmias. Circulation. 2001;103:89.
6. Chiladakis JK, Kalogeropoulos A, Koutsogiannis N, et al. Optimal QT/JT interval assessment in patients with complete bundle branch block. Ann Noninvasive Electrocardiol. 2012;17:268-276.
7. Ercan S, Altunbas G, Oylumlu M, et al. Congenital long QT syndrome masked by atrial fibrillation and unmasked by hypokalemia. Am J Emerg Med. 2013;31:451.e3-451.e6.
8. Goldenberg I, Moss AJ, Zareba W. QT interval: how to measure it and what is “normal.” J Cardiovasc Electrophysiol. 2006;17:333-336.
9. Podrid PJ. ECG Response: August 20, 2013. Circulation. 2013;128:869.
10. Olde Nordkamp LR, Wilde AA, Tijssen JG, et al. The ICD for primary prevention in patients with inherited cardiac diseases: indications, use, and outcome: a comparison with secondary prevention. Circ Arrhythm Electrophysiol. 2013;6:91-100.
11. Schwartz PJ. Pharmacological and non-pharmacological management of the congenital long QT syndrome: the rationale. Pharmacol Ther. 2011;131:171-177.
12. Berne P, Brugada J. Brugada syndrome 2012. Circ J. 2012;76:1563-1571.
13. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391-1396.
14. Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005;111:659-670.
15. Brugada J, Brugada R, Antzelevitch C, et al. Long-term followup of individuals with the electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3. Circulation. 2002;105:73-78.
16. Eckardt L, Probst V, Smits JP, et al. Long-term prognosis of individuals with right precordial ST-segment-elevation Brugada syndrome. Circulation. 2005;111:257-263.
17. Giustetto C, Drago S, Demarchi PG, et al; Italian Association of Arrhythmology and Cardiostimulation (AIAC)-Piedmont Section. Risk stratification of the patients with Brugada type electrocardiogram: a community-based prospective study. Europace. 2009;11:507-513.
18. Probst V, Veltmann C, Eckardt L, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: Results from the FINGER Brugada Syndrome Registry. Circulation. 2010;121:635-643.
19. Nielsen MW, Holst AG, Olesen SP, et al. The genetic component of Brugada syndrome. Front Physiol. 2013;4:179.
20. Bayés de Luna A, Brugada J, Baranchuk A, et al. Current electrocardiographic criteria for diagnosis of Brugada pattern: a consensus report. J Electrocardiol. 2012;45:433-442.
21. Veltmann C, Schimpf R, Echternach C, et al. A prospective study on spontaneous fluctuations between diagnostic and non-diagnostic ECGs in Brugada syndrome: implications for correct phenotyping and risk stratification. Eur Heart J. 2006;27:2544-2552.
22. Sacher F, Probst V, Maury P, et al. Outcome after implantation of a cardioverter-defibrillator in patients with Brugada syndrome: a multicenter study-part 2. Circulation. 2013;128:1739-1747.
23. Rosner MH, Brady WJ Jr, Kefer MP, et al. Electrocardiography in the patient with the Wolff-Parkinson-White syndrome: diagnostic and initial therapeutic issues. Am J Emerg Med. 1999;17:705-714.
24. Keating L, Morris FP, Brady WJ. Electrocardiographic features of Wolff-Parkinson-White syndrome. Emerg Med J. 2003;20:491-493.
25. Blomström-Lundqvist C, Scheinman MM, Aliot EM, et al; European Society of Cardiology Committee, NASPE-Heart Rhythm Society. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias—executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003;42:1493-1531.
26. Ho CY. Hypertrophic cardiomyopathy in 2012. Circulation. 2012;125:1432-1438.
27. Gersh BJ, Maron BJ, Bonow RO, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American Society of Echocardiography; American Society of Nuclear Cardiology; Heart Failure Society of America; Heart Rhythm Society; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:e783-e831.
28. Paterick TE, Jan MF, Paterick ZR, et al. Cardiac evaluation of collegiate student athletes: a medical and legal perspective. Am J Med. 2012;125:742-752.
29. Maron BJ. Hypertrophic cardiomyopathy. In: Bonow RO, Mann DL, Zipes DP, et al (eds). Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Philadelphia, PA: Saunders; 2011:1582-1594.
30. Konno T, Shimizu M, Ino H, et al. Diagnostic value of abnormal Q waves for identification of preclinical carriers of hypertrophic cardiomyopathy based on molecular genetic diagnosis. Eur Heart J. 2004;25:246-251.
› Consider placement of an automatic implantable cardioverter-defibrillator for all patients with a type 1 Brugada pattern on EKG accompanied by syncope, documented ventricular arrhythmia, or aborted sudden cardiac death. B
› Always look for EKG findings suggestive of Wolff-Parkinson-White syndrome in otherwise healthy patients presenting with syncope. C
› Refer all patients with suspected hypertrophic cardiomyopathy to Cardiology for a transthoracic echocardiogram. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
When evaluating a patient with a history of chest pain, palpitations, syncope, and/or new-onset seizures, an electrocardiogram (EKG) may be the key to
identifying a potentially life-threatening condition. Here we present 4 cases in which EKG findings were the clue to underlying medical conditions that, if left untreated, could be fatal. Because each of these conditions may not have associated findings on a physical exam, early recognition of these EKG findings can be lifesaving.
CASE 1 › A 15-year-old boy suddenly collapses while walking, and bystanders report seizure-like activity. The patient doesn’t remember the event. Vital signs and physical exam are normal, and his blood glucose level is 86 mg/dL (normal: 70-100 mg/dL). He doesn’t take any medications and denies illicit drug use or recent illness.
What EKG abnormality (FIGURE 1) likely explains the cause of the patient’s collapse?
The EKG abnormality and diagnosis. The patient’s EKG revealed a prolonged QT interval (FIGURE 1, BRACKETS). His QTc (QT interval corrected for heart rate) was .470 seconds, which is at the high end of the normal range for his age and gender.1 The patient had no family history of syncope, sudden cardiac death (SCD), or seizure disorder. Evaluation uncovered a calcium level of 4.4 mEq/L (normal: 4.5-5.5 mEq/L) and a phosphate level of 7.8 mg/dL (normal: 2.4-4.1 mg/dL).
This patient had a low parathyroid hormone from primary hypoparathyroidism. His conduction abnormality was treated with both oral calcium and vitamin D supplements.
Etiology and epidemiology. A prolonged QT interval may be the result of a primary long QT syndrome (LQTS) or an acquired condition from electrolyte imbalance, medication effect, or toxin exposure.
In the United States, the incidence of a genetic mutation that causes LQTS is 1 in 2500 people.2 Patients with LQTS usually remain asymptomatic unless the QT interval is further prolonged by a condition or medication. There are several hundred congenital LQTS subtypes based on specific ion channel defects; the most common is LQTS1, with an inherited defect in the KCNQ1 gene, which regulates the slow potassium ion channel.
Acquired LQTS is much more common than congenital LQTS.3 Many drugs have been linked to an increased risk of LQTS, including certain antiarrhythmics, antibiotics, and antipsychotics (TABLE 1).4 In addition, electrolyte disturbances such as hypokalemia, hypocalcemia, and hypomagnesemia can be etiologic factors.
Be aware that an acquired LQTS may mask an underlying congenital LQTS. Therefore, patients in whom the offending agent or condition is corrected should still have a follow-up EKG. Screening family members for LQTS is worthwhile, even in those without symptoms.
Clinical features. Patients with symptomatic LQTS may have dizziness, palpitations, and syncope. SCD also is possible. These signs and symptoms may be triggered by strong emotions (in LQTS2) or physical activity (in LQTS1). They likely are caused by torsades de pointes and ventricular fibrillation. A brief aura may precede these arrhythmias, and patients may experience urinary or fecal incontinence.5
The key to making a diagnosis of LQTS is correctly measuring the QT interval. The QT interval is measured from the beginning of the Q-wave to the end of the T-wave as measured from the intersection of a line tangent to the downslope of the T-wave and the isoelectric line. This can be difficult to determine in EKGs showing bundle branch block or an irregular rhythm, such as atrial fibrillation (AF).6,7 A common error in measuring the QT interval occurs when clinicians inadvertently include a U-wave in the measurement.1 Some EKG machines may provide QT interval and QTc measurements. Normal QT intervals are ≤.450 seconds for men and ≤.470 seconds for women.8
It is essential to confirm the QT interval by using the Bazett formula (QTc equals the QT in seconds divided by the square root of the RR interval in seconds) for all patients with a history that suggests a possible arrhythmia.
Our patient had hypocalcemia, which on an EKG can cause T-wave widening with a normal ST segment, rather than a normal T-wave with a long ST segment, as is typically seen in LQTS. This distinction may be difficult to discern and should not preclude the search for either an acquired prolonged QTc or an underlying LQTS.9
Treatment. First rule out or treat any causes of acquired LQTS by taking a careful medication history and evaluating the patient’s electrolytes. Once these have been addressed, a beta-blocker is first-line therapy for symptomatic patients.5
Unfortunately, up to 20% of individuals treated with beta-blockers may continue to have syncope.5 For these patients, options include a left cardiac sympathetic denervation (LCSD) or placement of an automatic implantable cardioverter-defibrillator (AICD). An LCSD involves removal of the left-sided stellate and/or thoracic ganglia. This procedure can be used instead of, or in addition to, beta-blockers. If the patient’s syncope persists, AICDs are an option. AICDs can be lifesaving, but patients run the risk of adverse effects that include inappropriate shocks and infection.10 As the result of these therapies, mortality associated with LQTS has dropped to approximately 1%.11
CASE 2 › A 14-year-old boy has a syncopal episode while at rest. A similar event occurred 3 years earlier; at that time, an echocardiogram and EKG were normal. For 2 days, he’s had a cough and low-grade fever. His temperature is 102ºF and he has a productive cough. Based on this EKG (FIGURE 2), what is the likely diagnosis? What is the significance of his fever?
The EKG abnormality and diagnosis. This patient’s EKG showed a type 1 Brugada pattern (FIGURE 2, ARROWS), which strongly supported the diagnosis of Brugada syndrome (BS). BS is an inherited condition caused by a genetic defect in cardiac ion channel function that leads to characteristic EKG changes and a predisposition to ventricular fibrillation.12 In this case, the fever likely unmasked these EKG findings.
The patient was transferred to a local hospital for treatment of community-acquired pneumonia, and ultimately received an AICD.
Etiology and epidemiology. BS was first described in 199213 and is a major cause of SCD, responsible for up to 4% of all cases of SCD, and 20% of cases of patients without structural heart disease.14 BS is more common in men, and the mean age of diagnosis is 40 to 45.15-18
Mutations in at least 17 cardiac ion channel genes have been linked to BS.19 The SCN5A gene—a cardiac sodium channel—is the most commonly implicated, but accounts for only 11% to 24% of all BS cases.15
Clinical features. Patients with BS may present with syncope, nocturnal agonal respirations, or ventricular arrhythmias.12 EKG findings include partial or complete right bundle branch block (RBBB) and ST segment elevation in right precordial leads V1 to V3.12 There are 2 Brugada EKG patterns, a type 1 cloved pattern as seen in our patient’s EKG and a type 2 saddleback pattern.20 EKG findings are dynamic over time and may alternate between normal, type 1, and type 2.20 Factors that modulate EKG appearance include fever, intoxication, vagal tone, electrolyte imbalance, and sodium channel blockade.12,20
Diagnosis requires a type 1 Brugada pattern on EKG plus a family history of BS, documented ventricular arrhythmia, or arrhythmia-related symptoms such as syncope.12 Patients with a type 2 Brugada pattern may undergo electrophysiology (EP) testing with Class I antiarrhythmic drugs to induce a diagnostic type 1 Brugada pattern.12,21 Patients who have Brugada EKG findings but none of the other diagnostic criteria are considered to have a Brugada pattern (rather than Brugada syndrome).12
The most concerning outcome of BS is ventricular fibrillation. The estimated annual rate of cardiac events is 7.7% among patients who have experienced an aborted SCD, 1.9% among those who have experienced syncope, and 0.5% in asymptomatic patients.18
Treatment. The only effective treatment for BS is placement of an AICD; however, complications of AICD placement cause significant morbidity.6 Ten years after AICD placement, 37% of patients experienced inappropriate shocks and 29% experienced lead failure.22 Recent modifications in device programming and the addition of remote monitoring have decreased complication rates.12,22
The decision to place an AICD is based on the patient’s prior symptoms, EKG findings, and other factors. Recent guidelines recommend an AICD for all patients with a type 1 Brugada pattern (spontaneous or induced) who also have had an aborted SCD, syncope, or documented ventricular arrhythmia.12
Management of asymptomatic patients with type 1 Brugada pattern remains controversial because the rate of cardiac events is low, although such events can be fatal. Asymptomatic patients with type 1 Brugada findings should undergo further EP testing, and should receive AICD only upon demonstration of inducible ventricular arrhythmia.12
TABLE 2
Arrhythmias associated with Wolff-Parkinson-White syndrome23
| Arrhythmia | EKG findings | Treatment—unstable patients | Treatment—stable patients (in preferred treatment order) |
| PSVT, orthodromic | Narrow QRS, loss of delta wave, rate 160-260 beats/min | Synchronized cardioversion | Vagal maneuvers, adenosine, calcium channel blockers, beta-blockers, digoxin, procainamide |
| PSVT, antidromic | Wide complex tachycardia | Synchronized cardioversion | Procainamide |
| Atrial fibrillation | Irregularly irregular (RR interval variable with no pattern), ventricular rates that can exceed 300 beats/min | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Atrial flutter | Flutter waves, rate normal to tachycardic depending on conduction rate | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Ventricular fibrillation | Rapid, erratic electrical impulses | Defibrillation | N/A |
EKG, electrocardiogram; N/A, not applicable; PSVT, paroxysmal supraventricular tachycardia.
CASE 3 › A 21-year-old man with no medical history presents with sudden onset of lightheadedness followed by syncope. He denies any chest pain or other associated symptoms. At the time of evaluation, he is asymptomatic. His EKG (FIGURE 3) is diagnostic of what syndrome?
The EKG abnormality and diagnosis. The patient had a classic presentation for Wolff-Parkinson-White (WPW) syndrome, a common congenital disorder that alters normal cardiac conduction. He described 2 past instances of unexplained light-headedness and palpitations. Subsequent EP studies demonstrated that the patient had an accessory atrioventricular (AV) tract, causing electrical activity in the heart to bypass the AV node, resulting in a delta wave on EKG (FIGURE 3, GREEN ARROWS).
The patient opted for ablation therapy, which successfully eliminated the delta wave on EKG. Five years later he has had no recurrences.
Epidemiology. The prevalence of WPW syndrome is .1% to 3%.23 Accessory AV tracts are found in men twice as often as in women. Only half of individuals with confirmed tracts develop a tachyarrhythmia. The estimated risk of sudden death due to WPW syndrome is .5% to 4%.24
Pathophysiology. Normally cardiac conduction originates from the sinus node and travels to the AV node, where conduction is slowed, and then proceeds to the His-Purkinje system, and finally to the rest of the ventricular myocardium. In WPW syndrome, ventricular depolarization occurs first by an accessory AV tract called the bundle of Kent, followed shortly thereafter by the His-Purkinje system. This sequence of depolarization is what leads to the EKG findings characteristic of WPW syndrome: a PR interval <.12 seconds, presence of a delta wave, widened QRS complex (>.12 seconds), and repolarization changes seen as ST segment and T-wave changes discordant to (opposite direction) the delta wave and QRS complex (FIGURE 3, RED ARROW).
Factors that influence electrical conduction through the bundle of Kent include cardioactive medications, physiological stress, circulating catecholamines, coronary ischemia, and aging. The end result is a propensity for the heart to convert to one of 4 arrhythmias: paroxysmal supraventricular tachycardia (PSVT), AF, atrial flutter, or ventricular fibrillation (TABLE 2).23
The most common arrhythmia in WPW syndrome is PSVT.23 This rhythm is induced by the formation of a reentry circuit—a pattern in which the heart’s electrical signal loops back on itself—involving the normal conduction pathway and the bundle of Kent. Reentry progressing down the His-Purkinje system and traveling up the bundle of Kent is referred to as orthodromic (anterograde) PSVT. Antidromic (retrograde) PSVT is due to a reentry circuit conducting from the bundle of Kent to the ventricles, and then retrograde through the His-Purkinje system and AV node to the atria.
Clinical features. Under normal circumstances, patients with WPW syndrome are asymptomatic. As was the case with our patient, individuals who develop one of the 4 characteristic arrhythmias can experience light-headedness and syncope.
Treatment. An unstable patient who is experiencing PSVT, AF, or atrial flutter should receive synchronized cardioversion; those experiencing ventricular fibrillation should receive defibrillation (TABLE 2).23 For stable patients, therapy is tailored to the type of arrhythmia. Calcium channel blockers, beta-blockers, and adenosine might be appropriate for patients with orthodromic PSVT but should be avoided in patients with antidromic PSVT, AF, or atrial flutter because these medications block AV node conduction and thus facilitate conduction down the bundle of Kent, which can result in potentially unstable arrhythmias. In general, the longer an arrhythmia has been present, the less effective the pharmacologic intervention because of the increasing sympathetic tone.
Preventive long-term therapies for WPW patients who have experienced arrhythmia include antiarrhythmic medications or ablative procedures. Long-term antiarrhythmic therapy often is reserved for older, more sedentary individuals with less frequent arrhythmias that are not life-threatening. Radiofrequency ablation is a popular option, with long-term success rates as high as 95% and complication rates <1%.23 Patients in whom a WPW pattern is identified incidentally on EKG should be referred to cardiology for EP studies and risk stratification.25
CASE 4 › A 61-year-old woman has an episode of substernal exertional chest pressure that lasted approximately 2 hours but resolved before she arrived at her physician’s office. She also experienced mild nausea. She has no history of coronary artery disease but says that she has experienced similar episodes of chest pressure. What abnormality is seen on her EKG (FIGURE 4)? What is the most likely cause of her symptoms?
The EKG abnormality and diagnosis. Although classically associated with syncope, hypertrophic cardiomyopathy (HCM) often presents similarly to acute coronary syndromes, with chest pain and dyspnea on exertion.26 This patient had no history of cardiac disease or family history of SCD or cardiomyopathy; however, her EKG showed changes indicating left ventricular hypertrophy (LVH), which is consistent with HCM (FIGURE 4, ARROWS). Echocardiography identified myocardial hypertrophy, normal left ventricular ejection fraction, but severe left ventricular outflow obstruction and mild diastolic dysfunction. She was treated with metoprolol and verapamil.
Etiology and epidemiology. Hypertrophic cardiomyopathy is an autosomal dominant intrinsic myocardial disorder resulting in LVH that is commonly associated with SCD during extreme physical activity.26,27 The prevalence of HCM is approximately 1 in 500.26 Although it can present at any age, it is the most common cause of SCD in young people (under age 30), responsible for 33% of deaths during athletic events.28
TABLE 3
4 diagnoses and what you'll see on EKG
| Diagnosis | EKG finding |
| Prolonged QT interval | QTc interval >.450 sec (men) or >.470 sec (women) |
| Brugada syndrome | Partial or complete RBBB, and ST segment elevation in right precordial leads V1-V3 |
| Wolff-Parkinson-White syndrome | Delta wave, widened QRS, short PR interval, ST segment and T-wave changes |
| Hypertrophic cardiomyopathy | No definitive finding; may have left ventricular hypertrophy or abnormal Q-waves |
EKG, electrocardiogram; RBBB, right bundle branch block.
Clinical features. The severity of HCM ranges from asymptomatic to fatal. Symptoms of HCM include chest pain, dyspnea, and syncope. The disorder causes morbidity and mortality in at least one of 3 ways: ventricular tachyarrhythmias (often in younger patients), heart failure (from left ventricular outflow obstruction), and/or thromboembolism.27
Although echocardiography typically is used to make the diagnosis,27 an EKG often is the initial screening tool. EKG changes are seen in 75% to 95% of affected patients and include the presence of Q-waves and increased voltages related to LVH.27,29 Infarct-like patterns may be present before wall thickening on echocardiogram. Abnormal Q-waves are found in 20% to 50% of HCM patients, and are more common in younger patients. Konno et al30 have shown that Q-waves >3 mm in depth and/or >.040 seconds in duration in at least 2 leads other than aVR is specific (90%) in identifying carriers of HCM genes before they develop clinical symptoms.
Ambulatory monitoring may be useful for risk stratifying HCM patients; those with nonsustained ventricular tachycardia (NSVT) are at higher risk of SCD. Holter monitoring is recommended in initial evaluation because evidence of ventricular tachyarrhythmias may warrant AICD placement.26
Treatment. The risk of SCD in HCM is approximately 1%, but higher in those with a family history of SCD, syncope, NSVT, hypotension during exercise, or severe LVH (left ventricle thickness >30 mm).26 AICDs are recommended for HCM patients with prior cardiac arrest, patients with ≥2 of these risk factors, or patients with one risk factor who have experienced syncope related to arrhythmia.26
For patients who are symptomatic but have <2 risk factors, beta-blockers are firstline therapy.26 Verapamil is used as a second line treatment. Both beta-blockers and calcium channel blockers reduce dyspnea, palpitations, and chest pain.27
For patients who don’t respond to medical therapy, septal reduction therapy may be performed, either by septal myectomy or alcohol septal ablation.27 It is also important to consider genetic screening and counseling for the family.
A summary of all 4 diagnoses described in this article, their associated EKG findings, and their pathophysiology appears in TABLE 3.
CORRESPONDENCE
Samir Haydar, DO, MPH, FACEP, Tufts University School of Medicine, Maine Medical Center, Department of Emergency Medicine, 47 Bramhall St., Portland, ME 04103; [email protected]
› Consider placement of an automatic implantable cardioverter-defibrillator for all patients with a type 1 Brugada pattern on EKG accompanied by syncope, documented ventricular arrhythmia, or aborted sudden cardiac death. B
› Always look for EKG findings suggestive of Wolff-Parkinson-White syndrome in otherwise healthy patients presenting with syncope. C
› Refer all patients with suspected hypertrophic cardiomyopathy to Cardiology for a transthoracic echocardiogram. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
When evaluating a patient with a history of chest pain, palpitations, syncope, and/or new-onset seizures, an electrocardiogram (EKG) may be the key to
identifying a potentially life-threatening condition. Here we present 4 cases in which EKG findings were the clue to underlying medical conditions that, if left untreated, could be fatal. Because each of these conditions may not have associated findings on a physical exam, early recognition of these EKG findings can be lifesaving.
CASE 1 › A 15-year-old boy suddenly collapses while walking, and bystanders report seizure-like activity. The patient doesn’t remember the event. Vital signs and physical exam are normal, and his blood glucose level is 86 mg/dL (normal: 70-100 mg/dL). He doesn’t take any medications and denies illicit drug use or recent illness.
What EKG abnormality (FIGURE 1) likely explains the cause of the patient’s collapse?
The EKG abnormality and diagnosis. The patient’s EKG revealed a prolonged QT interval (FIGURE 1, BRACKETS). His QTc (QT interval corrected for heart rate) was .470 seconds, which is at the high end of the normal range for his age and gender.1 The patient had no family history of syncope, sudden cardiac death (SCD), or seizure disorder. Evaluation uncovered a calcium level of 4.4 mEq/L (normal: 4.5-5.5 mEq/L) and a phosphate level of 7.8 mg/dL (normal: 2.4-4.1 mg/dL).
This patient had a low parathyroid hormone from primary hypoparathyroidism. His conduction abnormality was treated with both oral calcium and vitamin D supplements.
Etiology and epidemiology. A prolonged QT interval may be the result of a primary long QT syndrome (LQTS) or an acquired condition from electrolyte imbalance, medication effect, or toxin exposure.
In the United States, the incidence of a genetic mutation that causes LQTS is 1 in 2500 people.2 Patients with LQTS usually remain asymptomatic unless the QT interval is further prolonged by a condition or medication. There are several hundred congenital LQTS subtypes based on specific ion channel defects; the most common is LQTS1, with an inherited defect in the KCNQ1 gene, which regulates the slow potassium ion channel.
Acquired LQTS is much more common than congenital LQTS.3 Many drugs have been linked to an increased risk of LQTS, including certain antiarrhythmics, antibiotics, and antipsychotics (TABLE 1).4 In addition, electrolyte disturbances such as hypokalemia, hypocalcemia, and hypomagnesemia can be etiologic factors.
Be aware that an acquired LQTS may mask an underlying congenital LQTS. Therefore, patients in whom the offending agent or condition is corrected should still have a follow-up EKG. Screening family members for LQTS is worthwhile, even in those without symptoms.
Clinical features. Patients with symptomatic LQTS may have dizziness, palpitations, and syncope. SCD also is possible. These signs and symptoms may be triggered by strong emotions (in LQTS2) or physical activity (in LQTS1). They likely are caused by torsades de pointes and ventricular fibrillation. A brief aura may precede these arrhythmias, and patients may experience urinary or fecal incontinence.5
The key to making a diagnosis of LQTS is correctly measuring the QT interval. The QT interval is measured from the beginning of the Q-wave to the end of the T-wave as measured from the intersection of a line tangent to the downslope of the T-wave and the isoelectric line. This can be difficult to determine in EKGs showing bundle branch block or an irregular rhythm, such as atrial fibrillation (AF).6,7 A common error in measuring the QT interval occurs when clinicians inadvertently include a U-wave in the measurement.1 Some EKG machines may provide QT interval and QTc measurements. Normal QT intervals are ≤.450 seconds for men and ≤.470 seconds for women.8
It is essential to confirm the QT interval by using the Bazett formula (QTc equals the QT in seconds divided by the square root of the RR interval in seconds) for all patients with a history that suggests a possible arrhythmia.
Our patient had hypocalcemia, which on an EKG can cause T-wave widening with a normal ST segment, rather than a normal T-wave with a long ST segment, as is typically seen in LQTS. This distinction may be difficult to discern and should not preclude the search for either an acquired prolonged QTc or an underlying LQTS.9
Treatment. First rule out or treat any causes of acquired LQTS by taking a careful medication history and evaluating the patient’s electrolytes. Once these have been addressed, a beta-blocker is first-line therapy for symptomatic patients.5
Unfortunately, up to 20% of individuals treated with beta-blockers may continue to have syncope.5 For these patients, options include a left cardiac sympathetic denervation (LCSD) or placement of an automatic implantable cardioverter-defibrillator (AICD). An LCSD involves removal of the left-sided stellate and/or thoracic ganglia. This procedure can be used instead of, or in addition to, beta-blockers. If the patient’s syncope persists, AICDs are an option. AICDs can be lifesaving, but patients run the risk of adverse effects that include inappropriate shocks and infection.10 As the result of these therapies, mortality associated with LQTS has dropped to approximately 1%.11
CASE 2 › A 14-year-old boy has a syncopal episode while at rest. A similar event occurred 3 years earlier; at that time, an echocardiogram and EKG were normal. For 2 days, he’s had a cough and low-grade fever. His temperature is 102ºF and he has a productive cough. Based on this EKG (FIGURE 2), what is the likely diagnosis? What is the significance of his fever?
The EKG abnormality and diagnosis. This patient’s EKG showed a type 1 Brugada pattern (FIGURE 2, ARROWS), which strongly supported the diagnosis of Brugada syndrome (BS). BS is an inherited condition caused by a genetic defect in cardiac ion channel function that leads to characteristic EKG changes and a predisposition to ventricular fibrillation.12 In this case, the fever likely unmasked these EKG findings.
The patient was transferred to a local hospital for treatment of community-acquired pneumonia, and ultimately received an AICD.
Etiology and epidemiology. BS was first described in 199213 and is a major cause of SCD, responsible for up to 4% of all cases of SCD, and 20% of cases of patients without structural heart disease.14 BS is more common in men, and the mean age of diagnosis is 40 to 45.15-18
Mutations in at least 17 cardiac ion channel genes have been linked to BS.19 The SCN5A gene—a cardiac sodium channel—is the most commonly implicated, but accounts for only 11% to 24% of all BS cases.15
Clinical features. Patients with BS may present with syncope, nocturnal agonal respirations, or ventricular arrhythmias.12 EKG findings include partial or complete right bundle branch block (RBBB) and ST segment elevation in right precordial leads V1 to V3.12 There are 2 Brugada EKG patterns, a type 1 cloved pattern as seen in our patient’s EKG and a type 2 saddleback pattern.20 EKG findings are dynamic over time and may alternate between normal, type 1, and type 2.20 Factors that modulate EKG appearance include fever, intoxication, vagal tone, electrolyte imbalance, and sodium channel blockade.12,20
Diagnosis requires a type 1 Brugada pattern on EKG plus a family history of BS, documented ventricular arrhythmia, or arrhythmia-related symptoms such as syncope.12 Patients with a type 2 Brugada pattern may undergo electrophysiology (EP) testing with Class I antiarrhythmic drugs to induce a diagnostic type 1 Brugada pattern.12,21 Patients who have Brugada EKG findings but none of the other diagnostic criteria are considered to have a Brugada pattern (rather than Brugada syndrome).12
The most concerning outcome of BS is ventricular fibrillation. The estimated annual rate of cardiac events is 7.7% among patients who have experienced an aborted SCD, 1.9% among those who have experienced syncope, and 0.5% in asymptomatic patients.18
Treatment. The only effective treatment for BS is placement of an AICD; however, complications of AICD placement cause significant morbidity.6 Ten years after AICD placement, 37% of patients experienced inappropriate shocks and 29% experienced lead failure.22 Recent modifications in device programming and the addition of remote monitoring have decreased complication rates.12,22
The decision to place an AICD is based on the patient’s prior symptoms, EKG findings, and other factors. Recent guidelines recommend an AICD for all patients with a type 1 Brugada pattern (spontaneous or induced) who also have had an aborted SCD, syncope, or documented ventricular arrhythmia.12
Management of asymptomatic patients with type 1 Brugada pattern remains controversial because the rate of cardiac events is low, although such events can be fatal. Asymptomatic patients with type 1 Brugada findings should undergo further EP testing, and should receive AICD only upon demonstration of inducible ventricular arrhythmia.12
TABLE 2
Arrhythmias associated with Wolff-Parkinson-White syndrome23
| Arrhythmia | EKG findings | Treatment—unstable patients | Treatment—stable patients (in preferred treatment order) |
| PSVT, orthodromic | Narrow QRS, loss of delta wave, rate 160-260 beats/min | Synchronized cardioversion | Vagal maneuvers, adenosine, calcium channel blockers, beta-blockers, digoxin, procainamide |
| PSVT, antidromic | Wide complex tachycardia | Synchronized cardioversion | Procainamide |
| Atrial fibrillation | Irregularly irregular (RR interval variable with no pattern), ventricular rates that can exceed 300 beats/min | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Atrial flutter | Flutter waves, rate normal to tachycardic depending on conduction rate | Synchronized cardioversion | Synchronized cardioversion, procainamide |
| Ventricular fibrillation | Rapid, erratic electrical impulses | Defibrillation | N/A |
EKG, electrocardiogram; N/A, not applicable; PSVT, paroxysmal supraventricular tachycardia.
CASE 3 › A 21-year-old man with no medical history presents with sudden onset of lightheadedness followed by syncope. He denies any chest pain or other associated symptoms. At the time of evaluation, he is asymptomatic. His EKG (FIGURE 3) is diagnostic of what syndrome?
The EKG abnormality and diagnosis. The patient had a classic presentation for Wolff-Parkinson-White (WPW) syndrome, a common congenital disorder that alters normal cardiac conduction. He described 2 past instances of unexplained light-headedness and palpitations. Subsequent EP studies demonstrated that the patient had an accessory atrioventricular (AV) tract, causing electrical activity in the heart to bypass the AV node, resulting in a delta wave on EKG (FIGURE 3, GREEN ARROWS).
The patient opted for ablation therapy, which successfully eliminated the delta wave on EKG. Five years later he has had no recurrences.
Epidemiology. The prevalence of WPW syndrome is .1% to 3%.23 Accessory AV tracts are found in men twice as often as in women. Only half of individuals with confirmed tracts develop a tachyarrhythmia. The estimated risk of sudden death due to WPW syndrome is .5% to 4%.24
Pathophysiology. Normally cardiac conduction originates from the sinus node and travels to the AV node, where conduction is slowed, and then proceeds to the His-Purkinje system, and finally to the rest of the ventricular myocardium. In WPW syndrome, ventricular depolarization occurs first by an accessory AV tract called the bundle of Kent, followed shortly thereafter by the His-Purkinje system. This sequence of depolarization is what leads to the EKG findings characteristic of WPW syndrome: a PR interval <.12 seconds, presence of a delta wave, widened QRS complex (>.12 seconds), and repolarization changes seen as ST segment and T-wave changes discordant to (opposite direction) the delta wave and QRS complex (FIGURE 3, RED ARROW).
Factors that influence electrical conduction through the bundle of Kent include cardioactive medications, physiological stress, circulating catecholamines, coronary ischemia, and aging. The end result is a propensity for the heart to convert to one of 4 arrhythmias: paroxysmal supraventricular tachycardia (PSVT), AF, atrial flutter, or ventricular fibrillation (TABLE 2).23
The most common arrhythmia in WPW syndrome is PSVT.23 This rhythm is induced by the formation of a reentry circuit—a pattern in which the heart’s electrical signal loops back on itself—involving the normal conduction pathway and the bundle of Kent. Reentry progressing down the His-Purkinje system and traveling up the bundle of Kent is referred to as orthodromic (anterograde) PSVT. Antidromic (retrograde) PSVT is due to a reentry circuit conducting from the bundle of Kent to the ventricles, and then retrograde through the His-Purkinje system and AV node to the atria.
Clinical features. Under normal circumstances, patients with WPW syndrome are asymptomatic. As was the case with our patient, individuals who develop one of the 4 characteristic arrhythmias can experience light-headedness and syncope.
Treatment. An unstable patient who is experiencing PSVT, AF, or atrial flutter should receive synchronized cardioversion; those experiencing ventricular fibrillation should receive defibrillation (TABLE 2).23 For stable patients, therapy is tailored to the type of arrhythmia. Calcium channel blockers, beta-blockers, and adenosine might be appropriate for patients with orthodromic PSVT but should be avoided in patients with antidromic PSVT, AF, or atrial flutter because these medications block AV node conduction and thus facilitate conduction down the bundle of Kent, which can result in potentially unstable arrhythmias. In general, the longer an arrhythmia has been present, the less effective the pharmacologic intervention because of the increasing sympathetic tone.
Preventive long-term therapies for WPW patients who have experienced arrhythmia include antiarrhythmic medications or ablative procedures. Long-term antiarrhythmic therapy often is reserved for older, more sedentary individuals with less frequent arrhythmias that are not life-threatening. Radiofrequency ablation is a popular option, with long-term success rates as high as 95% and complication rates <1%.23 Patients in whom a WPW pattern is identified incidentally on EKG should be referred to cardiology for EP studies and risk stratification.25
CASE 4 › A 61-year-old woman has an episode of substernal exertional chest pressure that lasted approximately 2 hours but resolved before she arrived at her physician’s office. She also experienced mild nausea. She has no history of coronary artery disease but says that she has experienced similar episodes of chest pressure. What abnormality is seen on her EKG (FIGURE 4)? What is the most likely cause of her symptoms?
The EKG abnormality and diagnosis. Although classically associated with syncope, hypertrophic cardiomyopathy (HCM) often presents similarly to acute coronary syndromes, with chest pain and dyspnea on exertion.26 This patient had no history of cardiac disease or family history of SCD or cardiomyopathy; however, her EKG showed changes indicating left ventricular hypertrophy (LVH), which is consistent with HCM (FIGURE 4, ARROWS). Echocardiography identified myocardial hypertrophy, normal left ventricular ejection fraction, but severe left ventricular outflow obstruction and mild diastolic dysfunction. She was treated with metoprolol and verapamil.
Etiology and epidemiology. Hypertrophic cardiomyopathy is an autosomal dominant intrinsic myocardial disorder resulting in LVH that is commonly associated with SCD during extreme physical activity.26,27 The prevalence of HCM is approximately 1 in 500.26 Although it can present at any age, it is the most common cause of SCD in young people (under age 30), responsible for 33% of deaths during athletic events.28
TABLE 3
4 diagnoses and what you'll see on EKG
| Diagnosis | EKG finding |
| Prolonged QT interval | QTc interval >.450 sec (men) or >.470 sec (women) |
| Brugada syndrome | Partial or complete RBBB, and ST segment elevation in right precordial leads V1-V3 |
| Wolff-Parkinson-White syndrome | Delta wave, widened QRS, short PR interval, ST segment and T-wave changes |
| Hypertrophic cardiomyopathy | No definitive finding; may have left ventricular hypertrophy or abnormal Q-waves |
EKG, electrocardiogram; RBBB, right bundle branch block.
Clinical features. The severity of HCM ranges from asymptomatic to fatal. Symptoms of HCM include chest pain, dyspnea, and syncope. The disorder causes morbidity and mortality in at least one of 3 ways: ventricular tachyarrhythmias (often in younger patients), heart failure (from left ventricular outflow obstruction), and/or thromboembolism.27
Although echocardiography typically is used to make the diagnosis,27 an EKG often is the initial screening tool. EKG changes are seen in 75% to 95% of affected patients and include the presence of Q-waves and increased voltages related to LVH.27,29 Infarct-like patterns may be present before wall thickening on echocardiogram. Abnormal Q-waves are found in 20% to 50% of HCM patients, and are more common in younger patients. Konno et al30 have shown that Q-waves >3 mm in depth and/or >.040 seconds in duration in at least 2 leads other than aVR is specific (90%) in identifying carriers of HCM genes before they develop clinical symptoms.
Ambulatory monitoring may be useful for risk stratifying HCM patients; those with nonsustained ventricular tachycardia (NSVT) are at higher risk of SCD. Holter monitoring is recommended in initial evaluation because evidence of ventricular tachyarrhythmias may warrant AICD placement.26
Treatment. The risk of SCD in HCM is approximately 1%, but higher in those with a family history of SCD, syncope, NSVT, hypotension during exercise, or severe LVH (left ventricle thickness >30 mm).26 AICDs are recommended for HCM patients with prior cardiac arrest, patients with ≥2 of these risk factors, or patients with one risk factor who have experienced syncope related to arrhythmia.26
For patients who are symptomatic but have <2 risk factors, beta-blockers are firstline therapy.26 Verapamil is used as a second line treatment. Both beta-blockers and calcium channel blockers reduce dyspnea, palpitations, and chest pain.27
For patients who don’t respond to medical therapy, septal reduction therapy may be performed, either by septal myectomy or alcohol septal ablation.27 It is also important to consider genetic screening and counseling for the family.
A summary of all 4 diagnoses described in this article, their associated EKG findings, and their pathophysiology appears in TABLE 3.
CORRESPONDENCE
Samir Haydar, DO, MPH, FACEP, Tufts University School of Medicine, Maine Medical Center, Department of Emergency Medicine, 47 Bramhall St., Portland, ME 04103; [email protected]
1. Taggart NW, Haglund CM, Tester DJ, et al. Diagnostic miscues in congenital long-QT syndrome. Circulation. 2007;115:2613-2620.
2. Schwartz PJ, Stramba-Badiale M, Crotti L, et al. Prevalance of the congenital long QT syndrome. Circulation. 2009;120:1761-1767.
3. van Noord C, Eijgelsheim M, Stricker BH. Drug- and nondrug-associated QT interval prolongation. Br J Clin Pharmacol. 2010;70:16-23.
4. Credible Meds Web site. Available at: http://crediblemeds.org. Accessed April 8, 2014.
5. Schwartz PJ, Priori SG, Spazzolini C, et al. Genotype-phenotype correlation in the long QT syndrome: gene specific triggers for life threatening arrhythmias. Circulation. 2001;103:89.
6. Chiladakis JK, Kalogeropoulos A, Koutsogiannis N, et al. Optimal QT/JT interval assessment in patients with complete bundle branch block. Ann Noninvasive Electrocardiol. 2012;17:268-276.
7. Ercan S, Altunbas G, Oylumlu M, et al. Congenital long QT syndrome masked by atrial fibrillation and unmasked by hypokalemia. Am J Emerg Med. 2013;31:451.e3-451.e6.
8. Goldenberg I, Moss AJ, Zareba W. QT interval: how to measure it and what is “normal.” J Cardiovasc Electrophysiol. 2006;17:333-336.
9. Podrid PJ. ECG Response: August 20, 2013. Circulation. 2013;128:869.
10. Olde Nordkamp LR, Wilde AA, Tijssen JG, et al. The ICD for primary prevention in patients with inherited cardiac diseases: indications, use, and outcome: a comparison with secondary prevention. Circ Arrhythm Electrophysiol. 2013;6:91-100.
11. Schwartz PJ. Pharmacological and non-pharmacological management of the congenital long QT syndrome: the rationale. Pharmacol Ther. 2011;131:171-177.
12. Berne P, Brugada J. Brugada syndrome 2012. Circ J. 2012;76:1563-1571.
13. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391-1396.
14. Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005;111:659-670.
15. Brugada J, Brugada R, Antzelevitch C, et al. Long-term followup of individuals with the electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3. Circulation. 2002;105:73-78.
16. Eckardt L, Probst V, Smits JP, et al. Long-term prognosis of individuals with right precordial ST-segment-elevation Brugada syndrome. Circulation. 2005;111:257-263.
17. Giustetto C, Drago S, Demarchi PG, et al; Italian Association of Arrhythmology and Cardiostimulation (AIAC)-Piedmont Section. Risk stratification of the patients with Brugada type electrocardiogram: a community-based prospective study. Europace. 2009;11:507-513.
18. Probst V, Veltmann C, Eckardt L, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: Results from the FINGER Brugada Syndrome Registry. Circulation. 2010;121:635-643.
19. Nielsen MW, Holst AG, Olesen SP, et al. The genetic component of Brugada syndrome. Front Physiol. 2013;4:179.
20. Bayés de Luna A, Brugada J, Baranchuk A, et al. Current electrocardiographic criteria for diagnosis of Brugada pattern: a consensus report. J Electrocardiol. 2012;45:433-442.
21. Veltmann C, Schimpf R, Echternach C, et al. A prospective study on spontaneous fluctuations between diagnostic and non-diagnostic ECGs in Brugada syndrome: implications for correct phenotyping and risk stratification. Eur Heart J. 2006;27:2544-2552.
22. Sacher F, Probst V, Maury P, et al. Outcome after implantation of a cardioverter-defibrillator in patients with Brugada syndrome: a multicenter study-part 2. Circulation. 2013;128:1739-1747.
23. Rosner MH, Brady WJ Jr, Kefer MP, et al. Electrocardiography in the patient with the Wolff-Parkinson-White syndrome: diagnostic and initial therapeutic issues. Am J Emerg Med. 1999;17:705-714.
24. Keating L, Morris FP, Brady WJ. Electrocardiographic features of Wolff-Parkinson-White syndrome. Emerg Med J. 2003;20:491-493.
25. Blomström-Lundqvist C, Scheinman MM, Aliot EM, et al; European Society of Cardiology Committee, NASPE-Heart Rhythm Society. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias—executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003;42:1493-1531.
26. Ho CY. Hypertrophic cardiomyopathy in 2012. Circulation. 2012;125:1432-1438.
27. Gersh BJ, Maron BJ, Bonow RO, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American Society of Echocardiography; American Society of Nuclear Cardiology; Heart Failure Society of America; Heart Rhythm Society; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:e783-e831.
28. Paterick TE, Jan MF, Paterick ZR, et al. Cardiac evaluation of collegiate student athletes: a medical and legal perspective. Am J Med. 2012;125:742-752.
29. Maron BJ. Hypertrophic cardiomyopathy. In: Bonow RO, Mann DL, Zipes DP, et al (eds). Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Philadelphia, PA: Saunders; 2011:1582-1594.
30. Konno T, Shimizu M, Ino H, et al. Diagnostic value of abnormal Q waves for identification of preclinical carriers of hypertrophic cardiomyopathy based on molecular genetic diagnosis. Eur Heart J. 2004;25:246-251.
1. Taggart NW, Haglund CM, Tester DJ, et al. Diagnostic miscues in congenital long-QT syndrome. Circulation. 2007;115:2613-2620.
2. Schwartz PJ, Stramba-Badiale M, Crotti L, et al. Prevalance of the congenital long QT syndrome. Circulation. 2009;120:1761-1767.
3. van Noord C, Eijgelsheim M, Stricker BH. Drug- and nondrug-associated QT interval prolongation. Br J Clin Pharmacol. 2010;70:16-23.
4. Credible Meds Web site. Available at: http://crediblemeds.org. Accessed April 8, 2014.
5. Schwartz PJ, Priori SG, Spazzolini C, et al. Genotype-phenotype correlation in the long QT syndrome: gene specific triggers for life threatening arrhythmias. Circulation. 2001;103:89.
6. Chiladakis JK, Kalogeropoulos A, Koutsogiannis N, et al. Optimal QT/JT interval assessment in patients with complete bundle branch block. Ann Noninvasive Electrocardiol. 2012;17:268-276.
7. Ercan S, Altunbas G, Oylumlu M, et al. Congenital long QT syndrome masked by atrial fibrillation and unmasked by hypokalemia. Am J Emerg Med. 2013;31:451.e3-451.e6.
8. Goldenberg I, Moss AJ, Zareba W. QT interval: how to measure it and what is “normal.” J Cardiovasc Electrophysiol. 2006;17:333-336.
9. Podrid PJ. ECG Response: August 20, 2013. Circulation. 2013;128:869.
10. Olde Nordkamp LR, Wilde AA, Tijssen JG, et al. The ICD for primary prevention in patients with inherited cardiac diseases: indications, use, and outcome: a comparison with secondary prevention. Circ Arrhythm Electrophysiol. 2013;6:91-100.
11. Schwartz PJ. Pharmacological and non-pharmacological management of the congenital long QT syndrome: the rationale. Pharmacol Ther. 2011;131:171-177.
12. Berne P, Brugada J. Brugada syndrome 2012. Circ J. 2012;76:1563-1571.
13. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391-1396.
14. Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005;111:659-670.
15. Brugada J, Brugada R, Antzelevitch C, et al. Long-term followup of individuals with the electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3. Circulation. 2002;105:73-78.
16. Eckardt L, Probst V, Smits JP, et al. Long-term prognosis of individuals with right precordial ST-segment-elevation Brugada syndrome. Circulation. 2005;111:257-263.
17. Giustetto C, Drago S, Demarchi PG, et al; Italian Association of Arrhythmology and Cardiostimulation (AIAC)-Piedmont Section. Risk stratification of the patients with Brugada type electrocardiogram: a community-based prospective study. Europace. 2009;11:507-513.
18. Probst V, Veltmann C, Eckardt L, et al. Long-term prognosis of patients diagnosed with Brugada syndrome: Results from the FINGER Brugada Syndrome Registry. Circulation. 2010;121:635-643.
19. Nielsen MW, Holst AG, Olesen SP, et al. The genetic component of Brugada syndrome. Front Physiol. 2013;4:179.
20. Bayés de Luna A, Brugada J, Baranchuk A, et al. Current electrocardiographic criteria for diagnosis of Brugada pattern: a consensus report. J Electrocardiol. 2012;45:433-442.
21. Veltmann C, Schimpf R, Echternach C, et al. A prospective study on spontaneous fluctuations between diagnostic and non-diagnostic ECGs in Brugada syndrome: implications for correct phenotyping and risk stratification. Eur Heart J. 2006;27:2544-2552.
22. Sacher F, Probst V, Maury P, et al. Outcome after implantation of a cardioverter-defibrillator in patients with Brugada syndrome: a multicenter study-part 2. Circulation. 2013;128:1739-1747.
23. Rosner MH, Brady WJ Jr, Kefer MP, et al. Electrocardiography in the patient with the Wolff-Parkinson-White syndrome: diagnostic and initial therapeutic issues. Am J Emerg Med. 1999;17:705-714.
24. Keating L, Morris FP, Brady WJ. Electrocardiographic features of Wolff-Parkinson-White syndrome. Emerg Med J. 2003;20:491-493.
25. Blomström-Lundqvist C, Scheinman MM, Aliot EM, et al; European Society of Cardiology Committee, NASPE-Heart Rhythm Society. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias—executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003;42:1493-1531.
26. Ho CY. Hypertrophic cardiomyopathy in 2012. Circulation. 2012;125:1432-1438.
27. Gersh BJ, Maron BJ, Bonow RO, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American Society of Echocardiography; American Society of Nuclear Cardiology; Heart Failure Society of America; Heart Rhythm Society; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;124:e783-e831.
28. Paterick TE, Jan MF, Paterick ZR, et al. Cardiac evaluation of collegiate student athletes: a medical and legal perspective. Am J Med. 2012;125:742-752.
29. Maron BJ. Hypertrophic cardiomyopathy. In: Bonow RO, Mann DL, Zipes DP, et al (eds). Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Philadelphia, PA: Saunders; 2011:1582-1594.
30. Konno T, Shimizu M, Ino H, et al. Diagnostic value of abnormal Q waves for identification of preclinical carriers of hypertrophic cardiomyopathy based on molecular genetic diagnosis. Eur Heart J. 2004;25:246-251.
Q&A: “Code Black” Offers Insider Look at ED Challenges
Interview by Mary Ellen Schneider
“Code Black,” the award-winning documentary about working in the ED at Los Angeles County Hospital, opened in theaters in 40 US cities this summer.
It’s the film debut for emergency physician Ryan McGarry, who both stars in and directs the feature-length documentary. It highlights the thrills and challenges of working in a busy ED through the eyes of senior residents, including Dr McGarry, who completed his training while working on the film. The young doctors start the film as fresh-faced idealists in the “C-Booth” trauma bay at LA County Hospital, the famed birthplace of emergency medicine. Later they move to the county’s newly built hospital, which, though state-of-the-art, lacks some of the camaraderie of the original ED.
“Code Black” was the Best Documentary winner at the Los Angeles Film Festival and the Hamptons International Film Festival. And it was the Audience Award winner at both the Starz Denver Film Festival and the Aspen Filmfest.
Dr McGarry, who is now an attending physician at New York-Presbyterian Hospital in New York City, discussed why he made the film and how it is likely to impact the health care debate.
Question: What inspired you to make this film?
Dr McGarry: As documentaries go, this one was kind of an accident in the sense of its narrative development. I set out to capture what I thought was a phenomenally intense, and in some ways, dated and brutal trauma bay. At this point, most people associate modern health care with a lot of sterility and technology and white and blue spaces that are kind of contained. And this shows the opposite. This looks like battlefield medicine. To my surprise, it was working very well. Of course, at the time I was a young medical student, so my basis for evaluating that matured along with the film. As time went on, we migrated from the old L.A. County Hospital to a newer space. So in the course of filming, they closed down an 80-year-old structure in favor of a brand new, billion-dollar, shining, technology-laden palace. What we found was that as we were brought up to speed on modern health care, and of course regulation, the care became much more complicated.
Question: What do you want the audience to take away from the film?
Dr McGarry: It’s hopefully a primer for health care discussion that has not yet existed. There are plenty of films that ride the political undertones of health care very well and, I think, if anything, they seem to keep people in their camps. They don’t really bring people to the middle. They may make discussion more satisfying for people who are politically charged, but from the provider’s point of view, I’m not sure if they get us anywhere. “Code Black” does not have a call to action, as they call it in the documentary world. That’s on purpose. What we’re hoping for is for people to watch it and be a bit more primed when we talk about health care. My prediction—this could be wrong—is that the real discussion for the next quarter-century, as we improve access with the [Affordable Care Act], is going to be the patient-doctor connection and some deregulation. There are just too many barriers right now. The equation is too complicated. The healing and listening that people want are not happening.
Question: So would you like to see policy makers ease up on some of the health care regulations?
Dr McGarry: We all want safety. But as a scientist would say, these regulations ought to be evidence based. What we know as physicians is that any evidence-based truth is a hard thing to prove, period. I think a lot of these regulations are well intentioned. Nobody doubts that. But yesterday, the Joint Commission visited our hospital. Everybody was working hard on a shift trying to move patients through, trying to provide both quick and safe care, and one of the things that [the regulators] were watching out for was keeping the employee bags and coffee off the computer desks. Meanwhile, I have patients with chest pain, patients with stroke, patients with fractures, who are not getting the attention they need because we’re totally focused on pleasing the federal regulators that our bags and coffee aren’t out.
Question: The film is from the perspective of young doctors and talks a lot about their initial idealism. Do you think the messages in the film will also resonate with older doctors?
Dr McGarry: One of the more surprising aspects of “Code Black” is the nostalgia factor, that fact that both physicians who have been working for a while and those who have become administrators watched this film. We thought it would be offensive to them—especially people from private hospitals, whom we are sort of tough on in the movie. We thought that they would find us a little unrealistic and idealistic. Interestingly, they all watched it and they said, “I long for the day in my residency when all I had to worry about was just getting the science right, getting that patient connection right.”
Question: Working in C-Booth was a great experience for ED physicians in training. Can you ever recapture that feeling in the new, heavily regulated environment?
Dr McGarry: One thing we wouldn’t want to return to would be the lack of privacy. The biggest aspect of C-Booth that probably we wouldn’t be proud of is the lack of privacy. I’m definitely for privacy and for a dignified experience. After that, I feel like things are quite undefined. I think we have expectations that technology, in particular, is a huge answer to medicine. But we know it can be expensive and it can be dangerous. And in the case of electronic medical records, it certainly doesn’t make things faster. We know that every institution that has gone from paper charts to an EMR has found not just an immediate slowing of care, but a permanent slowing. And yet there are benefits with being able to quickly look up old medical information. But what about when my patient is waiting 20 minutes for pain medicine because it takes almost that long to get them in the computer, pull up the order, select the medicine, and go through all these stupid hard stops that are built in? Before, I could just write it down on a piece of paper, communicate it to the nurse, and get it done. If you’re the one in pain, is [the EMR] worth it? I don’t know.
Question: How did you find the time to make this movie?
Dr McGarry: There were a lot of consequences. I probably pushed it from a health perspective. I really found myself in a unique position as both a filmmaker and subject. For almost 3 years, I would do every ounce of my residency and then would race from the hospital to the edit room and would live and breathe it for 3 years. You would imagine there’s a cost to that. Lost a girlfriend. Didn’t sleep. Happily, I came through without any major damage, but that’s a heck of a lot of emergency medicine.
Question: What are you doing next? Are you working on another film and how are you balancing your new project with your day job in medicine?
Dr McGarry: This is a different game than it was in residency. I have an option for a scripted series, so basically it means that producers have identified it as a viable project for a fiction series like you would see on HBO. That’s in active development. We just shot a 3-minute spot with the New York and L.A. ballets, which involves these dancers in the old abandoned general hospital. As far as balancing all this, I’m so lucky in that Cornell/New York-Presbyterian and Dr Neal Flomenbaum have been incredibly supportive of me, allowing me to be full time there but with the work flexibility to jump on these projects as they come.
On Twitter @maryellenny
Interview by Mary Ellen Schneider
“Code Black,” the award-winning documentary about working in the ED at Los Angeles County Hospital, opened in theaters in 40 US cities this summer.
It’s the film debut for emergency physician Ryan McGarry, who both stars in and directs the feature-length documentary. It highlights the thrills and challenges of working in a busy ED through the eyes of senior residents, including Dr McGarry, who completed his training while working on the film. The young doctors start the film as fresh-faced idealists in the “C-Booth” trauma bay at LA County Hospital, the famed birthplace of emergency medicine. Later they move to the county’s newly built hospital, which, though state-of-the-art, lacks some of the camaraderie of the original ED.
“Code Black” was the Best Documentary winner at the Los Angeles Film Festival and the Hamptons International Film Festival. And it was the Audience Award winner at both the Starz Denver Film Festival and the Aspen Filmfest.
Dr McGarry, who is now an attending physician at New York-Presbyterian Hospital in New York City, discussed why he made the film and how it is likely to impact the health care debate.
Question: What inspired you to make this film?
Dr McGarry: As documentaries go, this one was kind of an accident in the sense of its narrative development. I set out to capture what I thought was a phenomenally intense, and in some ways, dated and brutal trauma bay. At this point, most people associate modern health care with a lot of sterility and technology and white and blue spaces that are kind of contained. And this shows the opposite. This looks like battlefield medicine. To my surprise, it was working very well. Of course, at the time I was a young medical student, so my basis for evaluating that matured along with the film. As time went on, we migrated from the old L.A. County Hospital to a newer space. So in the course of filming, they closed down an 80-year-old structure in favor of a brand new, billion-dollar, shining, technology-laden palace. What we found was that as we were brought up to speed on modern health care, and of course regulation, the care became much more complicated.
Question: What do you want the audience to take away from the film?
Dr McGarry: It’s hopefully a primer for health care discussion that has not yet existed. There are plenty of films that ride the political undertones of health care very well and, I think, if anything, they seem to keep people in their camps. They don’t really bring people to the middle. They may make discussion more satisfying for people who are politically charged, but from the provider’s point of view, I’m not sure if they get us anywhere. “Code Black” does not have a call to action, as they call it in the documentary world. That’s on purpose. What we’re hoping for is for people to watch it and be a bit more primed when we talk about health care. My prediction—this could be wrong—is that the real discussion for the next quarter-century, as we improve access with the [Affordable Care Act], is going to be the patient-doctor connection and some deregulation. There are just too many barriers right now. The equation is too complicated. The healing and listening that people want are not happening.
Question: So would you like to see policy makers ease up on some of the health care regulations?
Dr McGarry: We all want safety. But as a scientist would say, these regulations ought to be evidence based. What we know as physicians is that any evidence-based truth is a hard thing to prove, period. I think a lot of these regulations are well intentioned. Nobody doubts that. But yesterday, the Joint Commission visited our hospital. Everybody was working hard on a shift trying to move patients through, trying to provide both quick and safe care, and one of the things that [the regulators] were watching out for was keeping the employee bags and coffee off the computer desks. Meanwhile, I have patients with chest pain, patients with stroke, patients with fractures, who are not getting the attention they need because we’re totally focused on pleasing the federal regulators that our bags and coffee aren’t out.
Question: The film is from the perspective of young doctors and talks a lot about their initial idealism. Do you think the messages in the film will also resonate with older doctors?
Dr McGarry: One of the more surprising aspects of “Code Black” is the nostalgia factor, that fact that both physicians who have been working for a while and those who have become administrators watched this film. We thought it would be offensive to them—especially people from private hospitals, whom we are sort of tough on in the movie. We thought that they would find us a little unrealistic and idealistic. Interestingly, they all watched it and they said, “I long for the day in my residency when all I had to worry about was just getting the science right, getting that patient connection right.”
Question: Working in C-Booth was a great experience for ED physicians in training. Can you ever recapture that feeling in the new, heavily regulated environment?
Dr McGarry: One thing we wouldn’t want to return to would be the lack of privacy. The biggest aspect of C-Booth that probably we wouldn’t be proud of is the lack of privacy. I’m definitely for privacy and for a dignified experience. After that, I feel like things are quite undefined. I think we have expectations that technology, in particular, is a huge answer to medicine. But we know it can be expensive and it can be dangerous. And in the case of electronic medical records, it certainly doesn’t make things faster. We know that every institution that has gone from paper charts to an EMR has found not just an immediate slowing of care, but a permanent slowing. And yet there are benefits with being able to quickly look up old medical information. But what about when my patient is waiting 20 minutes for pain medicine because it takes almost that long to get them in the computer, pull up the order, select the medicine, and go through all these stupid hard stops that are built in? Before, I could just write it down on a piece of paper, communicate it to the nurse, and get it done. If you’re the one in pain, is [the EMR] worth it? I don’t know.
Question: How did you find the time to make this movie?
Dr McGarry: There were a lot of consequences. I probably pushed it from a health perspective. I really found myself in a unique position as both a filmmaker and subject. For almost 3 years, I would do every ounce of my residency and then would race from the hospital to the edit room and would live and breathe it for 3 years. You would imagine there’s a cost to that. Lost a girlfriend. Didn’t sleep. Happily, I came through without any major damage, but that’s a heck of a lot of emergency medicine.
Question: What are you doing next? Are you working on another film and how are you balancing your new project with your day job in medicine?
Dr McGarry: This is a different game than it was in residency. I have an option for a scripted series, so basically it means that producers have identified it as a viable project for a fiction series like you would see on HBO. That’s in active development. We just shot a 3-minute spot with the New York and L.A. ballets, which involves these dancers in the old abandoned general hospital. As far as balancing all this, I’m so lucky in that Cornell/New York-Presbyterian and Dr Neal Flomenbaum have been incredibly supportive of me, allowing me to be full time there but with the work flexibility to jump on these projects as they come.
On Twitter @maryellenny
Interview by Mary Ellen Schneider
“Code Black,” the award-winning documentary about working in the ED at Los Angeles County Hospital, opened in theaters in 40 US cities this summer.
It’s the film debut for emergency physician Ryan McGarry, who both stars in and directs the feature-length documentary. It highlights the thrills and challenges of working in a busy ED through the eyes of senior residents, including Dr McGarry, who completed his training while working on the film. The young doctors start the film as fresh-faced idealists in the “C-Booth” trauma bay at LA County Hospital, the famed birthplace of emergency medicine. Later they move to the county’s newly built hospital, which, though state-of-the-art, lacks some of the camaraderie of the original ED.
“Code Black” was the Best Documentary winner at the Los Angeles Film Festival and the Hamptons International Film Festival. And it was the Audience Award winner at both the Starz Denver Film Festival and the Aspen Filmfest.
Dr McGarry, who is now an attending physician at New York-Presbyterian Hospital in New York City, discussed why he made the film and how it is likely to impact the health care debate.
Question: What inspired you to make this film?
Dr McGarry: As documentaries go, this one was kind of an accident in the sense of its narrative development. I set out to capture what I thought was a phenomenally intense, and in some ways, dated and brutal trauma bay. At this point, most people associate modern health care with a lot of sterility and technology and white and blue spaces that are kind of contained. And this shows the opposite. This looks like battlefield medicine. To my surprise, it was working very well. Of course, at the time I was a young medical student, so my basis for evaluating that matured along with the film. As time went on, we migrated from the old L.A. County Hospital to a newer space. So in the course of filming, they closed down an 80-year-old structure in favor of a brand new, billion-dollar, shining, technology-laden palace. What we found was that as we were brought up to speed on modern health care, and of course regulation, the care became much more complicated.
Question: What do you want the audience to take away from the film?
Dr McGarry: It’s hopefully a primer for health care discussion that has not yet existed. There are plenty of films that ride the political undertones of health care very well and, I think, if anything, they seem to keep people in their camps. They don’t really bring people to the middle. They may make discussion more satisfying for people who are politically charged, but from the provider’s point of view, I’m not sure if they get us anywhere. “Code Black” does not have a call to action, as they call it in the documentary world. That’s on purpose. What we’re hoping for is for people to watch it and be a bit more primed when we talk about health care. My prediction—this could be wrong—is that the real discussion for the next quarter-century, as we improve access with the [Affordable Care Act], is going to be the patient-doctor connection and some deregulation. There are just too many barriers right now. The equation is too complicated. The healing and listening that people want are not happening.
Question: So would you like to see policy makers ease up on some of the health care regulations?
Dr McGarry: We all want safety. But as a scientist would say, these regulations ought to be evidence based. What we know as physicians is that any evidence-based truth is a hard thing to prove, period. I think a lot of these regulations are well intentioned. Nobody doubts that. But yesterday, the Joint Commission visited our hospital. Everybody was working hard on a shift trying to move patients through, trying to provide both quick and safe care, and one of the things that [the regulators] were watching out for was keeping the employee bags and coffee off the computer desks. Meanwhile, I have patients with chest pain, patients with stroke, patients with fractures, who are not getting the attention they need because we’re totally focused on pleasing the federal regulators that our bags and coffee aren’t out.
Question: The film is from the perspective of young doctors and talks a lot about their initial idealism. Do you think the messages in the film will also resonate with older doctors?
Dr McGarry: One of the more surprising aspects of “Code Black” is the nostalgia factor, that fact that both physicians who have been working for a while and those who have become administrators watched this film. We thought it would be offensive to them—especially people from private hospitals, whom we are sort of tough on in the movie. We thought that they would find us a little unrealistic and idealistic. Interestingly, they all watched it and they said, “I long for the day in my residency when all I had to worry about was just getting the science right, getting that patient connection right.”
Question: Working in C-Booth was a great experience for ED physicians in training. Can you ever recapture that feeling in the new, heavily regulated environment?
Dr McGarry: One thing we wouldn’t want to return to would be the lack of privacy. The biggest aspect of C-Booth that probably we wouldn’t be proud of is the lack of privacy. I’m definitely for privacy and for a dignified experience. After that, I feel like things are quite undefined. I think we have expectations that technology, in particular, is a huge answer to medicine. But we know it can be expensive and it can be dangerous. And in the case of electronic medical records, it certainly doesn’t make things faster. We know that every institution that has gone from paper charts to an EMR has found not just an immediate slowing of care, but a permanent slowing. And yet there are benefits with being able to quickly look up old medical information. But what about when my patient is waiting 20 minutes for pain medicine because it takes almost that long to get them in the computer, pull up the order, select the medicine, and go through all these stupid hard stops that are built in? Before, I could just write it down on a piece of paper, communicate it to the nurse, and get it done. If you’re the one in pain, is [the EMR] worth it? I don’t know.
Question: How did you find the time to make this movie?
Dr McGarry: There were a lot of consequences. I probably pushed it from a health perspective. I really found myself in a unique position as both a filmmaker and subject. For almost 3 years, I would do every ounce of my residency and then would race from the hospital to the edit room and would live and breathe it for 3 years. You would imagine there’s a cost to that. Lost a girlfriend. Didn’t sleep. Happily, I came through without any major damage, but that’s a heck of a lot of emergency medicine.
Question: What are you doing next? Are you working on another film and how are you balancing your new project with your day job in medicine?
Dr McGarry: This is a different game than it was in residency. I have an option for a scripted series, so basically it means that producers have identified it as a viable project for a fiction series like you would see on HBO. That’s in active development. We just shot a 3-minute spot with the New York and L.A. ballets, which involves these dancers in the old abandoned general hospital. As far as balancing all this, I’m so lucky in that Cornell/New York-Presbyterian and Dr Neal Flomenbaum have been incredibly supportive of me, allowing me to be full time there but with the work flexibility to jump on these projects as they come.
On Twitter @maryellenny
Cutaneous Melanoma
Series Editor: Arthur T. Skarin, MD, FACP, FCCP
Melanoma is the sixth most common cancer in the United States and the leading cause of deaths among all cutaneous malignancies. In 2012, it was estimated that approximately 75,000 individuals were diagnosed with melanoma and more than 9000 died. The incidence of melanoma is rising the fastest among all major malignancies, and the lifetime risk of melanoma among men and women now exceeds 1 in 68, as compared with 1:1500 in 1930.4 The incidence of melanoma is predicted to continue increasing, and there has been no corresponding decrease in mortality. This case-based review summarizes the etiology, risk factors, clinical presentation, and management of cutaneous melanomas, which comprise the majority of melanoma cases. The biology and management for other noncutaneous melanomas (such as mucosal or ocular melanomas) are beyond the scope of this review.
To read the full article in PDF:
Series Editor: Arthur T. Skarin, MD, FACP, FCCP
Melanoma is the sixth most common cancer in the United States and the leading cause of deaths among all cutaneous malignancies. In 2012, it was estimated that approximately 75,000 individuals were diagnosed with melanoma and more than 9000 died. The incidence of melanoma is rising the fastest among all major malignancies, and the lifetime risk of melanoma among men and women now exceeds 1 in 68, as compared with 1:1500 in 1930.4 The incidence of melanoma is predicted to continue increasing, and there has been no corresponding decrease in mortality. This case-based review summarizes the etiology, risk factors, clinical presentation, and management of cutaneous melanomas, which comprise the majority of melanoma cases. The biology and management for other noncutaneous melanomas (such as mucosal or ocular melanomas) are beyond the scope of this review.
To read the full article in PDF:
Series Editor: Arthur T. Skarin, MD, FACP, FCCP
Melanoma is the sixth most common cancer in the United States and the leading cause of deaths among all cutaneous malignancies. In 2012, it was estimated that approximately 75,000 individuals were diagnosed with melanoma and more than 9000 died. The incidence of melanoma is rising the fastest among all major malignancies, and the lifetime risk of melanoma among men and women now exceeds 1 in 68, as compared with 1:1500 in 1930.4 The incidence of melanoma is predicted to continue increasing, and there has been no corresponding decrease in mortality. This case-based review summarizes the etiology, risk factors, clinical presentation, and management of cutaneous melanomas, which comprise the majority of melanoma cases. The biology and management for other noncutaneous melanomas (such as mucosal or ocular melanomas) are beyond the scope of this review.
To read the full article in PDF:
Personality and Risk of Alzheimer Disease
Being agreeable can help with social interaction, according to researchers from the National Institute on Aging and Johns Hopkins University, both in Baltimore, Maryland; and Florida State University College of Medicine in Tallahassee, Florida. The researchers say agreeableness may also lower the risk of Alzheimer disease (AD).
The researchers examined the association between personality traits and risk of AD, using data from 1,671 adults who were followed for up to 22 years in the Baltimore Longitudinal Study of Aging (BLSA), one of the longest running studies in the U.S. The researchers also did a meta-analysis on pooled results from prospective studies involving 5,054 participants.
Participants underwent a series of tests, including a neuropsychological battery, neurologic examination, medication review, and structured interview. They also completed the self-report version of the revised NEO Personality Inventory (NEO-PI-R), a 240-item questionnaire. The NEO-PI-R assesses 5 major dimensions of personality: neuroticism (the tendency to experience negative emotions such as anxiety, anger, and sadness); extraversion (being sociable, assertive, enthusiastic, and energetic); openness (being imaginative, unconventional, curious, and emotionally and artistically sensitive); agreeableness (being altruistic, trusting, and cooperative); and conscientiousness (being organized, strong-willed, persistent, reliable, and a follower of rules and ethical principles). Based on previous research, the researchers expected that people with high conscientiousness (ie, organized and self-disciplined) and low neuroticism (less likely to be anxious, depressed, and vulnerable to stress) would have a lower risk of AD.
Onset of AD was diagnosed in 90 participants within 8 years, on average, from baseline. The researchers found that for each standard deviation (SD) increase in neuroticism, the risk of incident AD increased by > 30%. The risk was 3 times higher for the group in the highest quartile of neuroticism. Moreover, > 10% of the AD cases in the population could be attributed to high neuroticism. The results were similar for conscientiousness. The risk of incident AD was 3 times higher for the lowest quartile, and about 10% of AD cases could be attributed to low conscientiousness. The results remained the same when the researchers excluded people aged < 50 years at baseline or those who developed AD within 2 years of the baseline personality assessment.
Among the neurotic tendencies, anxiety, anger, hostility, and depression increased the risk of AD by > 30%. On the conscientiousness scale, self-discipline had the strongest association, followed by competence, order, and dutifulness. Risk of AD was reduced by > 30% for each SD higher score on any of those facets.
The researchers say low conscientiousness and high neuroticism are also related to inflammatory markers such as interleukin 6 and C-reactive protein. But neuroticism could also be a signifier for a variety of lifestyle behaviors that have been separately linked to AD. For instance, low conscientiousness and high neuroticism are associated with cigarette smoking, physical inactivity, obesity, and depression—all risk factors for dementia.
Personality traits are also related to coping skills, the researchers note. Chronic stress throughout the lifespan may contribute to the inability to cope with the neurodegenerative process underlying AD, for instance, and self-discipline (including the ability to achieve a goal) plays a role in limiting health-risk behavior.
Openness to ideas was particularly revealing, being associated significantly with about a 25% reduced risk of AD for each SD higher score. The meta-analysis, with 607 cases of incident AD, also revealed significant associations for openness. It may be a logical extension that openness is related to lower risk of AD. The hallmarks of the open personality include being intellectually engaged and performing well on cognitive measures. Aspects of intelligence and education are associated with greater cognitive reserve and reduced risk of AD.
But, the researchers say, their novel finding that agreeable people have a reduced risk of AD should be interpreted with caution: None of the studies, including BLSA, found a significant association. Still, they point out, agreeableness measures interpersonal tendencies, and an inclination to be altruistic and cooperative “might facilitate the formation of interpersonal connections and the stability of social networks.” Physiologically speaking, the converse might be that people who score low on agreeableness tend to be aggressive, competitive, and antagonistic, which increases the risk of cardiovascular disease and, thus, AD.
Source
Terracciano A, Sutin AR, An Y, et al. Alzheimers Dement. 2014;10(2):179-186.
doi: 10.1016/j.jalz.2013.03.002.
Being agreeable can help with social interaction, according to researchers from the National Institute on Aging and Johns Hopkins University, both in Baltimore, Maryland; and Florida State University College of Medicine in Tallahassee, Florida. The researchers say agreeableness may also lower the risk of Alzheimer disease (AD).
The researchers examined the association between personality traits and risk of AD, using data from 1,671 adults who were followed for up to 22 years in the Baltimore Longitudinal Study of Aging (BLSA), one of the longest running studies in the U.S. The researchers also did a meta-analysis on pooled results from prospective studies involving 5,054 participants.
Participants underwent a series of tests, including a neuropsychological battery, neurologic examination, medication review, and structured interview. They also completed the self-report version of the revised NEO Personality Inventory (NEO-PI-R), a 240-item questionnaire. The NEO-PI-R assesses 5 major dimensions of personality: neuroticism (the tendency to experience negative emotions such as anxiety, anger, and sadness); extraversion (being sociable, assertive, enthusiastic, and energetic); openness (being imaginative, unconventional, curious, and emotionally and artistically sensitive); agreeableness (being altruistic, trusting, and cooperative); and conscientiousness (being organized, strong-willed, persistent, reliable, and a follower of rules and ethical principles). Based on previous research, the researchers expected that people with high conscientiousness (ie, organized and self-disciplined) and low neuroticism (less likely to be anxious, depressed, and vulnerable to stress) would have a lower risk of AD.
Onset of AD was diagnosed in 90 participants within 8 years, on average, from baseline. The researchers found that for each standard deviation (SD) increase in neuroticism, the risk of incident AD increased by > 30%. The risk was 3 times higher for the group in the highest quartile of neuroticism. Moreover, > 10% of the AD cases in the population could be attributed to high neuroticism. The results were similar for conscientiousness. The risk of incident AD was 3 times higher for the lowest quartile, and about 10% of AD cases could be attributed to low conscientiousness. The results remained the same when the researchers excluded people aged < 50 years at baseline or those who developed AD within 2 years of the baseline personality assessment.
Among the neurotic tendencies, anxiety, anger, hostility, and depression increased the risk of AD by > 30%. On the conscientiousness scale, self-discipline had the strongest association, followed by competence, order, and dutifulness. Risk of AD was reduced by > 30% for each SD higher score on any of those facets.
The researchers say low conscientiousness and high neuroticism are also related to inflammatory markers such as interleukin 6 and C-reactive protein. But neuroticism could also be a signifier for a variety of lifestyle behaviors that have been separately linked to AD. For instance, low conscientiousness and high neuroticism are associated with cigarette smoking, physical inactivity, obesity, and depression—all risk factors for dementia.
Personality traits are also related to coping skills, the researchers note. Chronic stress throughout the lifespan may contribute to the inability to cope with the neurodegenerative process underlying AD, for instance, and self-discipline (including the ability to achieve a goal) plays a role in limiting health-risk behavior.
Openness to ideas was particularly revealing, being associated significantly with about a 25% reduced risk of AD for each SD higher score. The meta-analysis, with 607 cases of incident AD, also revealed significant associations for openness. It may be a logical extension that openness is related to lower risk of AD. The hallmarks of the open personality include being intellectually engaged and performing well on cognitive measures. Aspects of intelligence and education are associated with greater cognitive reserve and reduced risk of AD.
But, the researchers say, their novel finding that agreeable people have a reduced risk of AD should be interpreted with caution: None of the studies, including BLSA, found a significant association. Still, they point out, agreeableness measures interpersonal tendencies, and an inclination to be altruistic and cooperative “might facilitate the formation of interpersonal connections and the stability of social networks.” Physiologically speaking, the converse might be that people who score low on agreeableness tend to be aggressive, competitive, and antagonistic, which increases the risk of cardiovascular disease and, thus, AD.
Source
Terracciano A, Sutin AR, An Y, et al. Alzheimers Dement. 2014;10(2):179-186.
doi: 10.1016/j.jalz.2013.03.002.
Being agreeable can help with social interaction, according to researchers from the National Institute on Aging and Johns Hopkins University, both in Baltimore, Maryland; and Florida State University College of Medicine in Tallahassee, Florida. The researchers say agreeableness may also lower the risk of Alzheimer disease (AD).
The researchers examined the association between personality traits and risk of AD, using data from 1,671 adults who were followed for up to 22 years in the Baltimore Longitudinal Study of Aging (BLSA), one of the longest running studies in the U.S. The researchers also did a meta-analysis on pooled results from prospective studies involving 5,054 participants.
Participants underwent a series of tests, including a neuropsychological battery, neurologic examination, medication review, and structured interview. They also completed the self-report version of the revised NEO Personality Inventory (NEO-PI-R), a 240-item questionnaire. The NEO-PI-R assesses 5 major dimensions of personality: neuroticism (the tendency to experience negative emotions such as anxiety, anger, and sadness); extraversion (being sociable, assertive, enthusiastic, and energetic); openness (being imaginative, unconventional, curious, and emotionally and artistically sensitive); agreeableness (being altruistic, trusting, and cooperative); and conscientiousness (being organized, strong-willed, persistent, reliable, and a follower of rules and ethical principles). Based on previous research, the researchers expected that people with high conscientiousness (ie, organized and self-disciplined) and low neuroticism (less likely to be anxious, depressed, and vulnerable to stress) would have a lower risk of AD.
Onset of AD was diagnosed in 90 participants within 8 years, on average, from baseline. The researchers found that for each standard deviation (SD) increase in neuroticism, the risk of incident AD increased by > 30%. The risk was 3 times higher for the group in the highest quartile of neuroticism. Moreover, > 10% of the AD cases in the population could be attributed to high neuroticism. The results were similar for conscientiousness. The risk of incident AD was 3 times higher for the lowest quartile, and about 10% of AD cases could be attributed to low conscientiousness. The results remained the same when the researchers excluded people aged < 50 years at baseline or those who developed AD within 2 years of the baseline personality assessment.
Among the neurotic tendencies, anxiety, anger, hostility, and depression increased the risk of AD by > 30%. On the conscientiousness scale, self-discipline had the strongest association, followed by competence, order, and dutifulness. Risk of AD was reduced by > 30% for each SD higher score on any of those facets.
The researchers say low conscientiousness and high neuroticism are also related to inflammatory markers such as interleukin 6 and C-reactive protein. But neuroticism could also be a signifier for a variety of lifestyle behaviors that have been separately linked to AD. For instance, low conscientiousness and high neuroticism are associated with cigarette smoking, physical inactivity, obesity, and depression—all risk factors for dementia.
Personality traits are also related to coping skills, the researchers note. Chronic stress throughout the lifespan may contribute to the inability to cope with the neurodegenerative process underlying AD, for instance, and self-discipline (including the ability to achieve a goal) plays a role in limiting health-risk behavior.
Openness to ideas was particularly revealing, being associated significantly with about a 25% reduced risk of AD for each SD higher score. The meta-analysis, with 607 cases of incident AD, also revealed significant associations for openness. It may be a logical extension that openness is related to lower risk of AD. The hallmarks of the open personality include being intellectually engaged and performing well on cognitive measures. Aspects of intelligence and education are associated with greater cognitive reserve and reduced risk of AD.
But, the researchers say, their novel finding that agreeable people have a reduced risk of AD should be interpreted with caution: None of the studies, including BLSA, found a significant association. Still, they point out, agreeableness measures interpersonal tendencies, and an inclination to be altruistic and cooperative “might facilitate the formation of interpersonal connections and the stability of social networks.” Physiologically speaking, the converse might be that people who score low on agreeableness tend to be aggressive, competitive, and antagonistic, which increases the risk of cardiovascular disease and, thus, AD.
Source
Terracciano A, Sutin AR, An Y, et al. Alzheimers Dement. 2014;10(2):179-186.
doi: 10.1016/j.jalz.2013.03.002.