User login
Phialophora verrucosa as a Cause of Deep Infection Following Total Knee Arthroplasty
Osteolytic Psuedotumor After Cemented Total Knee Arthroplasty
Neonatal Seizure: Sepsis or Toxic Syndrome?
A mother presents to the ED with her 4-day-old daughter after noting abnormal jerking movements of the neonate's upper extremities. She states the baby has had watery stools for the past day, but has been tolerating bottle formula feeds without vomiting and having appropriate urinary output. The patient was born full-term via normal spontaneous vaginal delivery, with Apgar scores of 8 at 1 minute and 9 at 5 minutes. The postdelivery course was uncomplicated, and both mother and baby were discharged home 2 days after delivery.
Initial vital signs are: heart rate, 135 beats/min; respiratory rate (RR), 48 breaths/min; and temperature, 98.7°F; blood glucose was normal. On physical examination, the baby is awake and well-appearing, with a nonbulging anterior fontanelle, soft, supple neck, and flexed and symmetrically mobile extremities. Moro, suck, rooting, and grasp reflexes are all intact. No abnormal movements are noted. The remainder of the examination is unremarkable.
Do the jerking movements indicate a focal seizure? What could cause these movements in a neonate?
As the length of the postpartum hospital stay has decreased over the past 20 years, EDs have experienced an increase in neonatal visits for conditions that traditionally manifested in newborn nurseries. While most presentations are for benign reasons (eg, issues related to feeding, irritability), patients with concerning conditions, including central nervous system (CNS) abnormalities, may also initially present to the ED. Causes of such clinical findings may be structural (eg, cerebral malformations, subdural hematomas, herpes encephalitis) and/or metabolic (eg, hypoglycemia, hypocalcemia, inborn errors). Many early-onset neonatal seizures are benign and resolve by several months of age, but it is essential to identify those that are consequential and treatable.
Case Continuation
In the evaluation of the neonatal patient with suspected seizure, it is important to take a detailed maternal and labor history, and to consider a broad differential in the face of nonspecific findings. In this case, the patient's mother disclosed a personal history of chronic pain, for which she took buprenorphine 2 mg orally in the morning and 4 mg orally at bedtime (total daily dose of 6mg/day) throughout her pregnancy.
How does drug withdrawal present in the neonate?
Neonatal abstinence syndrome (NAS) is the clinical syndrome of withdrawal in a newborn exposed in utero to drugs capable of inducing dependence. Agents associated with NAS include opioids, benzodiazepines, ethanol, selective serotonin reuptake inhibitors (SSRIs), mood stabilizers, and nicotine.1,2
Over the past decade, there has been a 330% rise in the diagnosis of opioid-related NAS alone.3 In response to this increase, the US Food and Drug Administration recently added a black-box warning to all extended-release/long-acting opioid preparations detailing this risk.4
Presenting symptoms of NAS are protean, differ from patient to patient, and are a function of drug type, duration, and amount of drug exposure. NAS may mimic other severe life-threatening conditions such as those previously noted, and the inability to obtain an adequate symptom-based medical history from a neonate further complicates the diagnosis. Before making a diagnosis of NAS, other conditions should be carefully considered in the differential.
Neonatal opioid withdrawal manifests primarily with CNS and gastrointestinal (GI) effects since there are high concentrations of opioid receptors in these areas. Although clinical findings are generally similar among opioid agents, the onset and duration following abstinence varies—largely based on individual drug half-life; this helps to differentiate between opioid agents. For example, while babies exposed to heroin in utero present with signs of NAS within 24 hours of birth, those exposed to buprenorphine or methadone tend to present 2 to 6 days after delivery.1 Between 55% to 94% of neonates with in-utero opioid exposure develop NAS.5
Selective Serotonin Reuptake Inhibitors
SSRIs have also been associated with a neonatal syndrome, and largely involve similar signs and symptoms as NAS. Although the specific etiology is not clear, it has been suggested that this syndrome is the result of serotonin toxicity rather than withdrawal; as such, it is often referred to as "serotonin discontinuation syndrome." Clinical findings occur from several hours to several days after birth and usually resolve within 1 to 2 weeks.6
Cocaine Exposure
In-utero cocaine exposure is also associated with neurobehavioral abnormalities in neonates although a withdrawal syndrome is less clearly defined. Findings, however, are consistent with NAS and include increased irritability, tremors, and high-pitched cry—most frequently occurring between 24 and 48 hours postdelivery.6
Neonatal Alcohol Withdrawal Syndrome
Neonatal alcohol withdrawal syndrome, particularly in fetuses exposed to alcohol during the last trimester, is distinct from fetal alcohol syndrome (FAS). The latter is associated with typical dysmorphic features, growth deficiencies, and CNS findings reflective of permanent neurologic sequelae. Neonatal alcohol withdrawal presents with CNS findings similar to those listed for other in-utero exposures—eg, increased irritability, tremors, nystagmus hyperactive reflexes.7
Screening for NAS: The Finnegan Scale
The Finnegan Neonatal Abstinence Scoring System is one of the most commonly employed and validated tools used to screen for NAS. It comprises a 31-item scale, listing the clinical signs and symptoms of NAS, which are scored by severity and organized by system to include neurologic, metabolic, vasomotor, respiratory, and GI disturbances (Figure). Point allocation is based on mild, moderate, or severe symptoms as follows:
- Mild findings (eg, sweating, fever <101°F mottling, nasal stuffiness) each score 1 point.
- Moderate findings (eg, high-pitched cry, hyperactive moro reflex, increased muscle tone, fever >101°F, increased RR >60 with retractions, poor feeding, loose stools) each score 2 points.
- Severe findings (eg, myoclonic jerks, generalized convulsions, projectile vomiting, watery stools) each score 3 points.
While each of the above are independently nonspecific, the constellation of findings, together with the appropriate history, provide for a clinical diagnosis. The Finnegan Scale is therefore designed not only to aid in diagnosis, but also to quantify the severity of NAS and guide management.
Screening for NAS begins at birth in neonates with known in-utero exposure (ie, when risk of NAS is high) or at the time of initial presentation in other circumstances. Scoring is performed every 4 hours; the first two or three scores will determine the need for pharmacotherapy (see below).
| Pharmacotherapy is indicated in the following Finnegan scoring scenarios: |
|
|
|
How is NAS treated?
The two main goals of management in the treatment of opioid-related NAS are to relieve the signs and symptoms of withdrawal and to prevent complications (eg, fever, weight loss, seizures). Therapy should begin with nonpharmacologic measures that minimize excess external stimuli, such as swaddling, gentle handling, and minimizing noise and light. To prevent weight loss, small hypercaloric feeds may be helpful. If pharmacologic treatment is indicated, oral opioid replacement with morphine is considered by many to be the drug of choice. Oral morphine dosing may be guided by NAS severity based on the Finnegan score; alternatively, initial dosing at 0.1 mg/kg orally every 4 hours has also been recommended.1
Other agents, such methadone 0.1 mg/kg orally every 12 hours and buprenorphine 15.9 mcg/kg divided in three doses orally, may also be used. In patients whose symptoms persist despite opioid treatment, use of adjuncts such as phenobarbital and clonidine may be indicated.
Case Conclusion
The patient was admitted to the neonatal intensive care unit where she appropriately underwent a sepsis workup. Laboratory evaluation, including blood and urine cultures, was obtained. A brain ultrasound was unremarkable, and since lumbar puncture was unsuccessful, the patient was started empirically on meningitis doses of the cefotaxime, vancomycin, and acyclovir.
An initial Finnegan score was calculated. With the exception of soft stools, there were no other persistent symptoms, and patient did not achieve a score indicating a need for pharmacologic management. After 48 hours, she remained afebrile and soft stools resolved. All laboratory values, including cultures, were unremarkable. The patient was discharged on hospital day 3, with a scheduled well-baby follow-up appointment.
| Take Home Points |
|
- Cramton RE, Gruchala NE. Babies breaking bad: neonatal and iatrogenic withdrawal syndromes. Curr Opin Pediatr. 2013;25(4): 532-542.
- Kraft WK, Dysart K, Greenspan JS, Gibson E, Kaltenbach K, Ehrlich ME. Revised dose schema of sublingual buprenorphine in the treatment of the neonatal opioid abstinence syndrome. Addiction. 2011;106(3):574-580. http://dx.doi.org/10.1111/j.1360-0443.2010.03170.x Accessed October 24, 2013.
- Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009. JAMA. 2012;307(18):1934-40.
- New safety measures announced for extended-release and long-acting opioids. US Food and Drug Administration Web site. www.fda.gov/Drugs/DrugSafety/InformationbyDrugClass/ucm363722.htm. Accessed October 24, 2013.
- Burgos AE, Burke BL Jr. Neonatal abstinence syndrome. NeoReviews. 2009;10(5):e222-e228. http://dx.doi.org/10.1542/neo.10-5-e222. Accessed October 24, 2013.
- Hudak ML, Tan RC. Committee on Drugs. Committee on Fetus and Newborn. Neonatal drug withdrawal. Pediatrics. 2012;129(2):e540-e560.
- Coles CD, Smith IE, Fernhoff PM, Falek A. Neonatal ethanol withdrawal: Characteristics in clinically normal nondysmorphic neonates. J Pediatr. 1984;105(3):445-451.
A mother presents to the ED with her 4-day-old daughter after noting abnormal jerking movements of the neonate's upper extremities. She states the baby has had watery stools for the past day, but has been tolerating bottle formula feeds without vomiting and having appropriate urinary output. The patient was born full-term via normal spontaneous vaginal delivery, with Apgar scores of 8 at 1 minute and 9 at 5 minutes. The postdelivery course was uncomplicated, and both mother and baby were discharged home 2 days after delivery.
Initial vital signs are: heart rate, 135 beats/min; respiratory rate (RR), 48 breaths/min; and temperature, 98.7°F; blood glucose was normal. On physical examination, the baby is awake and well-appearing, with a nonbulging anterior fontanelle, soft, supple neck, and flexed and symmetrically mobile extremities. Moro, suck, rooting, and grasp reflexes are all intact. No abnormal movements are noted. The remainder of the examination is unremarkable.
Do the jerking movements indicate a focal seizure? What could cause these movements in a neonate?
As the length of the postpartum hospital stay has decreased over the past 20 years, EDs have experienced an increase in neonatal visits for conditions that traditionally manifested in newborn nurseries. While most presentations are for benign reasons (eg, issues related to feeding, irritability), patients with concerning conditions, including central nervous system (CNS) abnormalities, may also initially present to the ED. Causes of such clinical findings may be structural (eg, cerebral malformations, subdural hematomas, herpes encephalitis) and/or metabolic (eg, hypoglycemia, hypocalcemia, inborn errors). Many early-onset neonatal seizures are benign and resolve by several months of age, but it is essential to identify those that are consequential and treatable.
Case Continuation
In the evaluation of the neonatal patient with suspected seizure, it is important to take a detailed maternal and labor history, and to consider a broad differential in the face of nonspecific findings. In this case, the patient's mother disclosed a personal history of chronic pain, for which she took buprenorphine 2 mg orally in the morning and 4 mg orally at bedtime (total daily dose of 6mg/day) throughout her pregnancy.
How does drug withdrawal present in the neonate?
Neonatal abstinence syndrome (NAS) is the clinical syndrome of withdrawal in a newborn exposed in utero to drugs capable of inducing dependence. Agents associated with NAS include opioids, benzodiazepines, ethanol, selective serotonin reuptake inhibitors (SSRIs), mood stabilizers, and nicotine.1,2
Over the past decade, there has been a 330% rise in the diagnosis of opioid-related NAS alone.3 In response to this increase, the US Food and Drug Administration recently added a black-box warning to all extended-release/long-acting opioid preparations detailing this risk.4
Presenting symptoms of NAS are protean, differ from patient to patient, and are a function of drug type, duration, and amount of drug exposure. NAS may mimic other severe life-threatening conditions such as those previously noted, and the inability to obtain an adequate symptom-based medical history from a neonate further complicates the diagnosis. Before making a diagnosis of NAS, other conditions should be carefully considered in the differential.
Neonatal opioid withdrawal manifests primarily with CNS and gastrointestinal (GI) effects since there are high concentrations of opioid receptors in these areas. Although clinical findings are generally similar among opioid agents, the onset and duration following abstinence varies—largely based on individual drug half-life; this helps to differentiate between opioid agents. For example, while babies exposed to heroin in utero present with signs of NAS within 24 hours of birth, those exposed to buprenorphine or methadone tend to present 2 to 6 days after delivery.1 Between 55% to 94% of neonates with in-utero opioid exposure develop NAS.5
Selective Serotonin Reuptake Inhibitors
SSRIs have also been associated with a neonatal syndrome, and largely involve similar signs and symptoms as NAS. Although the specific etiology is not clear, it has been suggested that this syndrome is the result of serotonin toxicity rather than withdrawal; as such, it is often referred to as "serotonin discontinuation syndrome." Clinical findings occur from several hours to several days after birth and usually resolve within 1 to 2 weeks.6
Cocaine Exposure
In-utero cocaine exposure is also associated with neurobehavioral abnormalities in neonates although a withdrawal syndrome is less clearly defined. Findings, however, are consistent with NAS and include increased irritability, tremors, and high-pitched cry—most frequently occurring between 24 and 48 hours postdelivery.6
Neonatal Alcohol Withdrawal Syndrome
Neonatal alcohol withdrawal syndrome, particularly in fetuses exposed to alcohol during the last trimester, is distinct from fetal alcohol syndrome (FAS). The latter is associated with typical dysmorphic features, growth deficiencies, and CNS findings reflective of permanent neurologic sequelae. Neonatal alcohol withdrawal presents with CNS findings similar to those listed for other in-utero exposures—eg, increased irritability, tremors, nystagmus hyperactive reflexes.7
Screening for NAS: The Finnegan Scale
The Finnegan Neonatal Abstinence Scoring System is one of the most commonly employed and validated tools used to screen for NAS. It comprises a 31-item scale, listing the clinical signs and symptoms of NAS, which are scored by severity and organized by system to include neurologic, metabolic, vasomotor, respiratory, and GI disturbances (Figure). Point allocation is based on mild, moderate, or severe symptoms as follows:
- Mild findings (eg, sweating, fever <101°F mottling, nasal stuffiness) each score 1 point.
- Moderate findings (eg, high-pitched cry, hyperactive moro reflex, increased muscle tone, fever >101°F, increased RR >60 with retractions, poor feeding, loose stools) each score 2 points.
- Severe findings (eg, myoclonic jerks, generalized convulsions, projectile vomiting, watery stools) each score 3 points.
While each of the above are independently nonspecific, the constellation of findings, together with the appropriate history, provide for a clinical diagnosis. The Finnegan Scale is therefore designed not only to aid in diagnosis, but also to quantify the severity of NAS and guide management.
Screening for NAS begins at birth in neonates with known in-utero exposure (ie, when risk of NAS is high) or at the time of initial presentation in other circumstances. Scoring is performed every 4 hours; the first two or three scores will determine the need for pharmacotherapy (see below).
| Pharmacotherapy is indicated in the following Finnegan scoring scenarios: |
|
|
|
How is NAS treated?
The two main goals of management in the treatment of opioid-related NAS are to relieve the signs and symptoms of withdrawal and to prevent complications (eg, fever, weight loss, seizures). Therapy should begin with nonpharmacologic measures that minimize excess external stimuli, such as swaddling, gentle handling, and minimizing noise and light. To prevent weight loss, small hypercaloric feeds may be helpful. If pharmacologic treatment is indicated, oral opioid replacement with morphine is considered by many to be the drug of choice. Oral morphine dosing may be guided by NAS severity based on the Finnegan score; alternatively, initial dosing at 0.1 mg/kg orally every 4 hours has also been recommended.1
Other agents, such methadone 0.1 mg/kg orally every 12 hours and buprenorphine 15.9 mcg/kg divided in three doses orally, may also be used. In patients whose symptoms persist despite opioid treatment, use of adjuncts such as phenobarbital and clonidine may be indicated.
Case Conclusion
The patient was admitted to the neonatal intensive care unit where she appropriately underwent a sepsis workup. Laboratory evaluation, including blood and urine cultures, was obtained. A brain ultrasound was unremarkable, and since lumbar puncture was unsuccessful, the patient was started empirically on meningitis doses of the cefotaxime, vancomycin, and acyclovir.
An initial Finnegan score was calculated. With the exception of soft stools, there were no other persistent symptoms, and patient did not achieve a score indicating a need for pharmacologic management. After 48 hours, she remained afebrile and soft stools resolved. All laboratory values, including cultures, were unremarkable. The patient was discharged on hospital day 3, with a scheduled well-baby follow-up appointment.
| Take Home Points |
|
A mother presents to the ED with her 4-day-old daughter after noting abnormal jerking movements of the neonate's upper extremities. She states the baby has had watery stools for the past day, but has been tolerating bottle formula feeds without vomiting and having appropriate urinary output. The patient was born full-term via normal spontaneous vaginal delivery, with Apgar scores of 8 at 1 minute and 9 at 5 minutes. The postdelivery course was uncomplicated, and both mother and baby were discharged home 2 days after delivery.
Initial vital signs are: heart rate, 135 beats/min; respiratory rate (RR), 48 breaths/min; and temperature, 98.7°F; blood glucose was normal. On physical examination, the baby is awake and well-appearing, with a nonbulging anterior fontanelle, soft, supple neck, and flexed and symmetrically mobile extremities. Moro, suck, rooting, and grasp reflexes are all intact. No abnormal movements are noted. The remainder of the examination is unremarkable.
Do the jerking movements indicate a focal seizure? What could cause these movements in a neonate?
As the length of the postpartum hospital stay has decreased over the past 20 years, EDs have experienced an increase in neonatal visits for conditions that traditionally manifested in newborn nurseries. While most presentations are for benign reasons (eg, issues related to feeding, irritability), patients with concerning conditions, including central nervous system (CNS) abnormalities, may also initially present to the ED. Causes of such clinical findings may be structural (eg, cerebral malformations, subdural hematomas, herpes encephalitis) and/or metabolic (eg, hypoglycemia, hypocalcemia, inborn errors). Many early-onset neonatal seizures are benign and resolve by several months of age, but it is essential to identify those that are consequential and treatable.
Case Continuation
In the evaluation of the neonatal patient with suspected seizure, it is important to take a detailed maternal and labor history, and to consider a broad differential in the face of nonspecific findings. In this case, the patient's mother disclosed a personal history of chronic pain, for which she took buprenorphine 2 mg orally in the morning and 4 mg orally at bedtime (total daily dose of 6mg/day) throughout her pregnancy.
How does drug withdrawal present in the neonate?
Neonatal abstinence syndrome (NAS) is the clinical syndrome of withdrawal in a newborn exposed in utero to drugs capable of inducing dependence. Agents associated with NAS include opioids, benzodiazepines, ethanol, selective serotonin reuptake inhibitors (SSRIs), mood stabilizers, and nicotine.1,2
Over the past decade, there has been a 330% rise in the diagnosis of opioid-related NAS alone.3 In response to this increase, the US Food and Drug Administration recently added a black-box warning to all extended-release/long-acting opioid preparations detailing this risk.4
Presenting symptoms of NAS are protean, differ from patient to patient, and are a function of drug type, duration, and amount of drug exposure. NAS may mimic other severe life-threatening conditions such as those previously noted, and the inability to obtain an adequate symptom-based medical history from a neonate further complicates the diagnosis. Before making a diagnosis of NAS, other conditions should be carefully considered in the differential.
Neonatal opioid withdrawal manifests primarily with CNS and gastrointestinal (GI) effects since there are high concentrations of opioid receptors in these areas. Although clinical findings are generally similar among opioid agents, the onset and duration following abstinence varies—largely based on individual drug half-life; this helps to differentiate between opioid agents. For example, while babies exposed to heroin in utero present with signs of NAS within 24 hours of birth, those exposed to buprenorphine or methadone tend to present 2 to 6 days after delivery.1 Between 55% to 94% of neonates with in-utero opioid exposure develop NAS.5
Selective Serotonin Reuptake Inhibitors
SSRIs have also been associated with a neonatal syndrome, and largely involve similar signs and symptoms as NAS. Although the specific etiology is not clear, it has been suggested that this syndrome is the result of serotonin toxicity rather than withdrawal; as such, it is often referred to as "serotonin discontinuation syndrome." Clinical findings occur from several hours to several days after birth and usually resolve within 1 to 2 weeks.6
Cocaine Exposure
In-utero cocaine exposure is also associated with neurobehavioral abnormalities in neonates although a withdrawal syndrome is less clearly defined. Findings, however, are consistent with NAS and include increased irritability, tremors, and high-pitched cry—most frequently occurring between 24 and 48 hours postdelivery.6
Neonatal Alcohol Withdrawal Syndrome
Neonatal alcohol withdrawal syndrome, particularly in fetuses exposed to alcohol during the last trimester, is distinct from fetal alcohol syndrome (FAS). The latter is associated with typical dysmorphic features, growth deficiencies, and CNS findings reflective of permanent neurologic sequelae. Neonatal alcohol withdrawal presents with CNS findings similar to those listed for other in-utero exposures—eg, increased irritability, tremors, nystagmus hyperactive reflexes.7
Screening for NAS: The Finnegan Scale
The Finnegan Neonatal Abstinence Scoring System is one of the most commonly employed and validated tools used to screen for NAS. It comprises a 31-item scale, listing the clinical signs and symptoms of NAS, which are scored by severity and organized by system to include neurologic, metabolic, vasomotor, respiratory, and GI disturbances (Figure). Point allocation is based on mild, moderate, or severe symptoms as follows:
- Mild findings (eg, sweating, fever <101°F mottling, nasal stuffiness) each score 1 point.
- Moderate findings (eg, high-pitched cry, hyperactive moro reflex, increased muscle tone, fever >101°F, increased RR >60 with retractions, poor feeding, loose stools) each score 2 points.
- Severe findings (eg, myoclonic jerks, generalized convulsions, projectile vomiting, watery stools) each score 3 points.
While each of the above are independently nonspecific, the constellation of findings, together with the appropriate history, provide for a clinical diagnosis. The Finnegan Scale is therefore designed not only to aid in diagnosis, but also to quantify the severity of NAS and guide management.
Screening for NAS begins at birth in neonates with known in-utero exposure (ie, when risk of NAS is high) or at the time of initial presentation in other circumstances. Scoring is performed every 4 hours; the first two or three scores will determine the need for pharmacotherapy (see below).
| Pharmacotherapy is indicated in the following Finnegan scoring scenarios: |
|
|
|
How is NAS treated?
The two main goals of management in the treatment of opioid-related NAS are to relieve the signs and symptoms of withdrawal and to prevent complications (eg, fever, weight loss, seizures). Therapy should begin with nonpharmacologic measures that minimize excess external stimuli, such as swaddling, gentle handling, and minimizing noise and light. To prevent weight loss, small hypercaloric feeds may be helpful. If pharmacologic treatment is indicated, oral opioid replacement with morphine is considered by many to be the drug of choice. Oral morphine dosing may be guided by NAS severity based on the Finnegan score; alternatively, initial dosing at 0.1 mg/kg orally every 4 hours has also been recommended.1
Other agents, such methadone 0.1 mg/kg orally every 12 hours and buprenorphine 15.9 mcg/kg divided in three doses orally, may also be used. In patients whose symptoms persist despite opioid treatment, use of adjuncts such as phenobarbital and clonidine may be indicated.
Case Conclusion
The patient was admitted to the neonatal intensive care unit where she appropriately underwent a sepsis workup. Laboratory evaluation, including blood and urine cultures, was obtained. A brain ultrasound was unremarkable, and since lumbar puncture was unsuccessful, the patient was started empirically on meningitis doses of the cefotaxime, vancomycin, and acyclovir.
An initial Finnegan score was calculated. With the exception of soft stools, there were no other persistent symptoms, and patient did not achieve a score indicating a need for pharmacologic management. After 48 hours, she remained afebrile and soft stools resolved. All laboratory values, including cultures, were unremarkable. The patient was discharged on hospital day 3, with a scheduled well-baby follow-up appointment.
| Take Home Points |
|
- Cramton RE, Gruchala NE. Babies breaking bad: neonatal and iatrogenic withdrawal syndromes. Curr Opin Pediatr. 2013;25(4): 532-542.
- Kraft WK, Dysart K, Greenspan JS, Gibson E, Kaltenbach K, Ehrlich ME. Revised dose schema of sublingual buprenorphine in the treatment of the neonatal opioid abstinence syndrome. Addiction. 2011;106(3):574-580. http://dx.doi.org/10.1111/j.1360-0443.2010.03170.x Accessed October 24, 2013.
- Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009. JAMA. 2012;307(18):1934-40.
- New safety measures announced for extended-release and long-acting opioids. US Food and Drug Administration Web site. www.fda.gov/Drugs/DrugSafety/InformationbyDrugClass/ucm363722.htm. Accessed October 24, 2013.
- Burgos AE, Burke BL Jr. Neonatal abstinence syndrome. NeoReviews. 2009;10(5):e222-e228. http://dx.doi.org/10.1542/neo.10-5-e222. Accessed October 24, 2013.
- Hudak ML, Tan RC. Committee on Drugs. Committee on Fetus and Newborn. Neonatal drug withdrawal. Pediatrics. 2012;129(2):e540-e560.
- Coles CD, Smith IE, Fernhoff PM, Falek A. Neonatal ethanol withdrawal: Characteristics in clinically normal nondysmorphic neonates. J Pediatr. 1984;105(3):445-451.
- Cramton RE, Gruchala NE. Babies breaking bad: neonatal and iatrogenic withdrawal syndromes. Curr Opin Pediatr. 2013;25(4): 532-542.
- Kraft WK, Dysart K, Greenspan JS, Gibson E, Kaltenbach K, Ehrlich ME. Revised dose schema of sublingual buprenorphine in the treatment of the neonatal opioid abstinence syndrome. Addiction. 2011;106(3):574-580. http://dx.doi.org/10.1111/j.1360-0443.2010.03170.x Accessed October 24, 2013.
- Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009. JAMA. 2012;307(18):1934-40.
- New safety measures announced for extended-release and long-acting opioids. US Food and Drug Administration Web site. www.fda.gov/Drugs/DrugSafety/InformationbyDrugClass/ucm363722.htm. Accessed October 24, 2013.
- Burgos AE, Burke BL Jr. Neonatal abstinence syndrome. NeoReviews. 2009;10(5):e222-e228. http://dx.doi.org/10.1542/neo.10-5-e222. Accessed October 24, 2013.
- Hudak ML, Tan RC. Committee on Drugs. Committee on Fetus and Newborn. Neonatal drug withdrawal. Pediatrics. 2012;129(2):e540-e560.
- Coles CD, Smith IE, Fernhoff PM, Falek A. Neonatal ethanol withdrawal: Characteristics in clinically normal nondysmorphic neonates. J Pediatr. 1984;105(3):445-451.
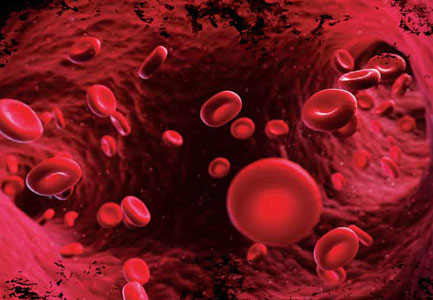
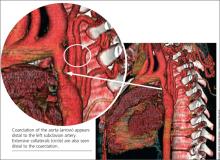
Direct Thrombin and Factor Xa Inhibitors
Parenteral direct thrombin inhibitors (DTI), such as bivalirudin, have been used for more than a decade in the hospital setting. Over the past few years, new DTIs have received US Food and Drug Administration (FDA) approval, most notably dabigatran etexilate, an orally active DTI touted as a viable alternative for anticoagulation in patients previously taking warfarin or enoxaparin. In addition to the DTIs, oral factor Xa (FXa) inhibitors have also received FDA approval. As these drugs begin to appear on the medication lists of many patients in the ED, a review—especially of the newer, oral agents—is essential. This article provides an overview of the parenteral DTIs and oral DTI dabigatran etexilate, as well as the oral FXa inhibitors, with a focus on proper monitoring of anticoagulation and common problems encountered in patients taking these medications.
Parenteral Direct Thrombin Inhibitors
Hirudin
Hirudin, a bivalent DTI, was the first parenteral anticoagulant of its kind approved for use in humans.1 Commercially available analogs, including lepirudin, bivalirudin, and desirudin, have since become available. Anticoagulation in patients taking hirudin can be monitored effectively in the ED via activated partial thromboplastin time (aPTT).2 However, there are significant disadvantages to its use, including high cost, lack of a reversal agent, and the potential development of antibodies to hirudin and its derivatives. In addition, since anaphylactoid reactions have been reported, current recommendations contraindicate its use in patients previously treated with hirudin derivatives.3
Lepirudin
Lepirudin is a hirudin analog derived from yeast cells, and is ideal for patients with heparin-induced thrombocytopenia (HIT). With respect to thromboembolic complications in patients with a previous history of HIT, Greinacher et al,4 demonstrated its relative safety and effectiveness. Their study showed a significant reduction in thromboembolic complications per patient day from 6.1% to 1.3%.4 Bleeding events in study participants occurred at an increased rate compared to controls, but these events were greatly decreased when aPTT levels were maintained between 1.5 to 2.5-fold above baseline.4 Since lepirudin is renally excreted and no reversal agent currently exists, clinicians must use caution when administering it to patients with renal insufficiency.
Bivalirudin
Bivalirudin is another hirudin analog and has an important niche among patients requiring percutaneous coronary intervention, primarily due to its favorable pharmacokinetic profile. In contrast to other DTIs, bivalirudin does not undergo organ-specific clearance, but rather proteolysis—an excellent option for patients with other comorbidities. Additionally, its short half-life of 25 minutes makes it an appropriate choice in cases warranting only a brief period of anticoagulation.5
Argatroban
Argatroban, another parenteral DTI, differs from hirudin, lepirudin, and bivalirudin in that it is a univalent molecule. Anticoagulation is monitored by aPTT, though dose-dependent changes may be seen in prothrombin time (PT). Since argatroban undergoes hepatic clearance, dose adjustments are required in patients with hepatic dysfunction—but not in those with renal insufficiency.6 Similar to lepirudin, argatroban is also indicated for patients with a history of HIT. In recent studies, argatroban achieved patency more frequently than heparin in patients with acute myocardial infarction—without differences in clinical outcomes.7
Dabigatran Etexilate
With the increased number of patients presenting to the ED with venous and arterial thromboembolic disorders, emergency physicians should be familiar with the orally active prodrug, dabigatran. This DTI is taken twice daily and converts to it active form after administration, binding to thrombin with great specificity and affinity.8 Its half-life ranges from 12 to 24 hours in patients with normal renal function; reduced dosing schedules are recommended in patients older than age 75 years and in those with renal impairment. Dabigatran is contraindicated if creatinine clearance is less than 30 mL/min. Even though dabigatran is not cleared by the cytochrome P450 system, it does utilize the P-glycoprotein efflux transporter and is thus vulnerable to both inducers and inhibitors, including systemic antifungals and other medications.9
Monitoring Anticoagulation
Unlike warfarin, dabigatran does not require extensive monitoring. However, thrombin and aPPT assays are often less predictable at supertherapeutic levels of dabigatran, and results vary depending on last administration time of the drug.10 Strangier et al11 identified some weaknesses in aPTT measurement, concluding that while measurement of aPTT may provide a qualitative indication of anticoagulant activity, it is not suitable for the precise quantification of anticoagulant effect—especially at high plasma concentrations of dabigatran.11 Furthermore, since PT time is not significantly affected by DTIs, this assay is a poor monitoring choice for these medications.12
The thrombin time (TT) assay test, which is usually accessible in routine clinical practice, directly assesses thrombin activity, providing a direct measure of dabigatran concentration. The TT is particularly sensitive to the effects of dabigatran and displays a linear dose-response even at supratherapeutic concentrations, making it the most useful and sensitive method for determining the anticoagulation effect of dabigatran.13
When treating patients in the ED who could potentially benefit from thrombolytic agents, monitoring dabigatran anticoagulation can present a challenge. There is very little information regarding the use of tissue plasminogen activator (tPA) in patients on dabigatran, with only one published case on the subject. In this case, intravenous (IV) tPA was administered just less than 4.5 hours after onset of neurologic symptoms and 7 hours after the last intake of dabigatran, with no complications and improved neurology function.14
The Interventional Management Stroke (IMS) III trial has suggested clinicians consider IV tPA in patients with acute stroke if the last dose of dabigatran was greater than 48 hours prior to presentation in the ED.15 Until further evidence becomes available, the decision to administer thrombolytics to stroke patients taking dabigatran should be made on a case-by-case basis and in consultation with a neurologist.
Noninferiority Studies
Dabigatran has been compared to enoxaparin and showed noninferiority for venous thromboembolism (VTE) prophylaxis, with a similar safety profile.16 The RE-COVER study in 2009 demonstrated the noninferiority of dabigatran compared to warfarin. In this study, patients received either the standard dose of dabigatran (150 mg orally, twice daily) or traditional dose-adjusted warfarin. In patients on the dabigatran regimen, recurrent VTE complications occurred at a rate of 2.4%, compared with the 2.1% observed in the warfarin group.17 The safety profile was also similar, with major bleeding episodes occurring in 1.6% and 1.9%, respectively.17
Another study, the RE-LY trial, also sought to prove noninferiority between dabigatran and warfarin, specifically in patients with a known history of atrial fibrillation requiring anticoagulation.18 The authors of the study concluded a clinical net benefit of dabigatran over warfarin with respect to reduction in both hemorrhagic and ischemic stroke and bleeding versus the increase of myocardial infarction.19 Further studies, however, are needed to determine the safety profile of dabigatran.
Dabigatran Reversal
Perhaps the most pressing question for the emergency physician is how to approach the bleeding patient on dabigatran. Although well-known protocols exist for the reversal of other anticoagulants such as warfarin and heparin, no clear, effective reversal agent is currently available for dabigatran. Given its relatively short half-life (12 to 24 hours), the first line of treatment should be to discontinue its use, followed by mechanical pressure or surgical hemostatic, if indicated. Transfusion of blood products (eg, packed red blood cells, fresh frozen plasma, platelets) should be administered based on the extent of the patient’s bleeding.
If these measures fail, dialysis may be considered, particularly in patients with renal insufficiency that may have bleeding secondary to dabigatran toxicity. In cases of suspected overdose, although activated charcoal is still being evaluated, Van Ryn and colleagues noted "preliminary in vitro data indicate that dabigatran etexilate can be successfully adsorbed by classical activated charcoal therapy. However, this has not been tested in vivo or in patients…additional clinically relevant models are required before this can be recommended in patients."10
Managing Dti-Associated Bleeding
Factor VII
Since recombinant activated factor VII directly activates thrombin on the surface of platelets, it is an option in cases of life-threatening DTI-associated bleeding. While laboratory data has supported this use, human studies have been less convincing, with conflicting results in two separate studies.20,21 Moreover, financial considerations may also affect the decision to use factor VII as its dollar cost is in the thousands at most institutions.22 Since the role of factor VII in life-threatening bleeding related to DTIs has yet to be defined, it is prudent to consider this option when other measures fail, understanding the variable rates of success in reversal of anticoagulation.
Prothrombin Complex Concentrates
Prothrombin complex concentrates (PCCs) have a significant place in reversing bleeding in patients on certain anticoagulants. Since these products contain all of the vitamin K-dependent clotting factors and proteins C and S, they have been used in the treatment of warfarin toxicity.
PCCs can be divided into activated and nonactivated categories. Among the nonactivated PCCs are PCC3 and PCC4. Both contain factors II, VII, IX, and X, but PCC3 products have lower concentrations of factor VII. To augment factor VII activity, it has been proposed that fresh frozen plasma or packed red blood cells be given in conjunction with a PCC3.23
Activated prothrombin complex concentrates (APCC) contain activated factor VII, along with inactivated forms of factors II, IX, X, and protein C. Animal studies appear promising for the use of PCCs in DTI-associated bleeding; however, this treatment has not yet been fully evaluated in human studies.24
A recent randomized, placebo-controlled crossover study by Eerenberg et al25 evaluated 12 healthy volunteers treated with PCC4 after receiving either dabigatran or rivaroxaban. While the PCC completely reversed anticoagulation in the rivaroxaban group, there was no reversal of anticoagulation in the dabigatran group.25 The authors made note of the study limitations, which include small sample size and the fact that healthy volunteers were used as surrogates as opposed to patients with major bleeding complications. The authors stated that "although this trial may have important clinical implications, the effect of PCC has yet to be confirmed in patients with bleeding events treated with these anticoagulants."25 This is the only human study available and serves as a starting point from which further human research can be initiated.25
Oral Factor Xa Inhibitors
Apixaban
The FXa inhibitors are a new class of prophylactic anticoagulants. Apixaban, one of the more recent oral FXa inhibitors, has a half-life of approximately 12 hours, predictable pharmacokinetics, and is cleared primarily via the GI tract. Given its hepatic metabolism, patients taking apixaban along with cytochrome P3A4 inhibitors (eg, certain antibiotics and antifungals) may be at increased risk of bleeding.26 As evidenced by the ARISTOTLE trial, compared to standard treatment with warfarin, apixaban is an effective alternative therapy for patients with atrial fibrillation.27 Of note, however, the ADOPT trial showed increased rates of bleeding in patients with comorbid conditions taking apixaban compared to standard enoxaparin dosing.28
Rivaroxaban
Rivaroxaban is another oral FXa inhibitor, with similar pharmacokinetics as apixaban and a half-life ranging from 8 hours in young healthy subjects to 12 hours in elderly patients. Since one third of the drug is renally cleared, rivaroxaban should be prescribed with caution in patients who have impaired creatinine clearance. Moreover, as the remaining two thirds undergo hepatic clearance, as with apixaban, its use is contraindicated in patients taking other cytochrome P-inhibiting medications.29
The MAGELLAN trial found rivaroxaban to be an effective means of DVT prophylaxis compared to control subjects who received enoxaparin injections, but there was in increased rate of clinically significant bleeding in the rivaroxaban group—arguably one of the more important outcome measures for the emergency provider.30 The ROCKET-AF trial, however, showed reduced rates of stroke in patients who received rivaroxaban versus warfarin. Both drugs had similar rates of major and minor bleeding, but rivaroxaban showed a decrease in intracranial hemorrhage and fatal bleeding.31
Monitoring and Reversal
As with the DTIs, monitoring the anticoagulant activity of factor Xa inhibitors can be a challenge, though various factor X assays have been proposed.31 Similar difficulties likewise exist in terms of reversal. There is no specific reversal agent for the FXa inhibitors, and current treatment guidelines recommend the use of PCCs, APCCs, or recombinant factor VIIa—though limited data exist on which agent to base clinical practice. In contrast to the DTIs, neither apixaban nor rivaroxaban are dialyzable.32 The relatively short half-life of these products, however, can prove beneficial, with cessation of the medication being the first line therapy in the case of any clinically significant bleeding.33
Conclusion
Parenteral DTIs have been utilized for years in the ED setting. With the increasing use of newer oral DTIs and FXa inhibitors, emergency physicians must also become familiar with the drug profile of these products, including appropriate anticoagulation monitoring and effective methods to treat DTI- and FXa-associated bleeding. Many questions remain unanswered about these drugs, necessitating further research—specifically in areas of practical monitoring of anticoagulation and possible reversal protocols in the bleeding patient.
Dr Byrne is a clinical instructor in the department of emergency medicine, Eastern Virginia Medical School, Norfolk. Dr Byars is an associate professor in the department of emergency medicine, Eastern Virginia Medical School, Norfolk.
Disclosure: The authors report no conflict of interest.
- Greinacher A, Warkentin TE. The direct thrombin inhibitor hirudin. Thromb Haemost. 2008;99(5):819-829.
- Greinacher A, Eichler P, Albrecht D, Strobel U, Pötzsch B, Eriksson BI. Antihirudin antibodies following low-dose subcutaneous treatment with desirudin for thrombosis prophylaxis after hip-replacement surgery: incidence and clinical relevance. Blood. 2003;101(7):2617-2619.
- Desirudin (Iprivask) for DVT prevention. Med Lett Drugs Ther. 2010;52(1350):85,86.
- Greinacher A, Völpel H, Janssens U, et al. Recombinant hirudin (lepirudin) provides safe and effective anticoagulation in patients with heparin-induced thrombocytopenia: a prospective study. Circulation. 1999;99(1):73-80.
- Warkentin TE, Greinacher A, Koster A. Bivalirudin. Thromb Haemost. 2008;99(5):830-839.
- Swan SK, Hursting MJ. The pharmacokinetics and pharmacodynamics of argatroban: effects of age, gender, and hepatic or renal dysfunction. Pharmacotherapy. 2000;20(3):318-329.
- Jang IK, Brown DF, Giugliano RP, et al. A multicenter, randomized study of argatroban versus heparin as adjunct to tissue plasminogen activator (TPA) in acute myocardial infarction: myocardial infarction with novastan and TPA (MINT) study. J Am Coll Cardiol 1999;33(7):1879-1885.
- Blech S, Ebner T, Ludwig-Schwellinger E, Stangier J, Roth W. The metabolism and disposition of the oral direct thrombin inhibitor, dabigatran, in humans. Drug Metab Dispos. 2008;36(2):386-399.
- Stangier J, Rathgen K, Stähle H, Gansser D, Roth W. The pharmacokinetics, pharmacodynamics and tolerability of dabigatran etexilate, a new oral direct thrombin inhibitor, in healthy male subjects. Br J Clin Pharmacol. 2007;64(3):292-303.
- van Ryn J, Stangier J, Haertter S, et al. Dabigatran etexilate—a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity.Thromb Haemost. 2010;103(6):1116-1127.
- Stangier J, Rathgen K, Stähle H, Mazur D. Influence of renal impairment on the pharmacokinetics and pharmacodynamics of oral dabigatran etexilate: an open-label, parallel-group, single-centre study. Clin Pharmacokinet. 2010;49(4):259-268.
- Nowak G. The ecarin clotting time, a universal method to quantify direct thrombin inhibitors. Pathophysiol Haemost Thromb. 2003;33(4):173-183.
- Watanabe M, Siddiqui FM, Qureshi AI. Incidence and management of ischemic stroke and intracerebral hemorrhage in patients on dabigatran etexilate treatment. Neurocrit Care. 2012;16(1):203-209.
- De Smedt A, De Raedt S, Nieboer K, De Keyser J, Brouns R. Intravenous thrombolysis with recombinant tissue plasminogen activator in a stroke patient treated with dabigatran. Cerebrovasc Dis. 2010;30(5):533,534.
- Broderick J; National Institute of Neurological Disorders and Stroke (NINDS). Interventional management of stroke (IMS) III trial (IMS III). http://clinicaltrials.gov/ct2/show/NCT00359424. Accessed October 29, 2013.
- Wolowacz SE, Roskell NS, Plumb JM, Caprini JA, Eriksson BI. Efficacy and safety of dabigatran etexilate for the prevention of venous thromboembolism following total hip or knee arthoplasty. A meta-analysis. Thromb Haemost. 2009;101(1):77-85.
- Schulman S, Kearon C, Kakkar AK, et al; RE-COVER Study Group. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361(24):2342-2352.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361(12):1139-1151.
- Hughes S. Dabigatran: New data on MI and ischemic events. Medscape. 2012. http://www.theheart.org/article/1338427.do Accessed October 29, 2013.
- Wolzt M, Levi M, Sarich TC, et al. Effect of recombinant factor VIIa on melagatran-induced inhibition of thrombin generation and platelet activation in health volunteers. Thromb Haemost. 2004;91(6):1090-1096.
- Sørensen B, Ingerslev J. A direct thrombin inhibitor studied by dynamic whole blood clot formation. Haemostatic response to ex-vivo addition of recombinant factor VIIa or activated prothrombin complex concentrate. Thromb Haemost. 2006;96(4):446-453.
- Kissela BM, Eckman MH. Cost effectiveness of recombinant factor VIIa for treatment of intracerebral hemorrhage. BMC Neurology. 2008;8:17.
- Dager WE. Using prothrombin complex concentrates to rapidly reverse oral anticoagulant effects. Ann Pharmacother. 2011;45(7-8):1016-1020.
- Uchino K, Hernandez AV. Dabigatran association with higher risk of acute coronary events: meta-analysis of noninferiority randomized controlled trials. Arch Inter Med. 2012;172(5):397-402.
- Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation. 2011;124(14):1573-1579.
- Tahir F, Riaz H, Riaz T, et al. The new oral anti-coagulants and the phase 3 clinical trials - a systematic review of the literature. Thromb J. 2013;11(1):18.
- Granger C, Alexander J, McMurray JJ, et al; ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981-992.
- Goldhaber SZ, Leizorovicz A, Kakkar AK, et al; ADOPT Trial Investigators. Apixaban versus enoxaparin for thromboprophylaxis in medically ill patients. N Engl J Med. 2011;365(23):2167-2177.
- Mueck W, Stampfuss J, Kubitza D, Becka M. Clinical pharmacokinetic and pharmacodynamic profile of rivaroxaban. Clin Pharmacokinet. 2013.
- Cohen AT, Spiro TE, Büller HR, et al; MAGELLAN Investigators. Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med. 2013; 368(6):513-523.
- Patel MR, Mahaffey KW, Garg J, et al; ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883-991.
- Samama MM, Contant G, Spiro TE, et al; Rivaroxaban Anti-Factor Xa Chromogenic Assay Field Trial Laboratories. Evaluation of the anti-factor Xa chromogenic assay for the measurement of rivaroxaban plasma concentrations using calibrators and controls. Thromb Haemost. 2012;107(2):379-387.
- Goldstein P, Elalamy I, Huber K, Danchin N, Wiel E. Rivaroxaban and other non-vitamin K antagonist oral anticoagulants in the emergency treatment of thromboembolism. Int J Emerg Med. 2013;6(1):25.
- Fawole A, Daw HA, Crowther MA. Practical management of bleeding due to the anticoagulants dabigatran, rivaroxaban, and apixaban. Cleve Clin J Med. 2013; 80(7):443-451.
Parenteral direct thrombin inhibitors (DTI), such as bivalirudin, have been used for more than a decade in the hospital setting. Over the past few years, new DTIs have received US Food and Drug Administration (FDA) approval, most notably dabigatran etexilate, an orally active DTI touted as a viable alternative for anticoagulation in patients previously taking warfarin or enoxaparin. In addition to the DTIs, oral factor Xa (FXa) inhibitors have also received FDA approval. As these drugs begin to appear on the medication lists of many patients in the ED, a review—especially of the newer, oral agents—is essential. This article provides an overview of the parenteral DTIs and oral DTI dabigatran etexilate, as well as the oral FXa inhibitors, with a focus on proper monitoring of anticoagulation and common problems encountered in patients taking these medications.
Parenteral Direct Thrombin Inhibitors
Hirudin
Hirudin, a bivalent DTI, was the first parenteral anticoagulant of its kind approved for use in humans.1 Commercially available analogs, including lepirudin, bivalirudin, and desirudin, have since become available. Anticoagulation in patients taking hirudin can be monitored effectively in the ED via activated partial thromboplastin time (aPTT).2 However, there are significant disadvantages to its use, including high cost, lack of a reversal agent, and the potential development of antibodies to hirudin and its derivatives. In addition, since anaphylactoid reactions have been reported, current recommendations contraindicate its use in patients previously treated with hirudin derivatives.3
Lepirudin
Lepirudin is a hirudin analog derived from yeast cells, and is ideal for patients with heparin-induced thrombocytopenia (HIT). With respect to thromboembolic complications in patients with a previous history of HIT, Greinacher et al,4 demonstrated its relative safety and effectiveness. Their study showed a significant reduction in thromboembolic complications per patient day from 6.1% to 1.3%.4 Bleeding events in study participants occurred at an increased rate compared to controls, but these events were greatly decreased when aPTT levels were maintained between 1.5 to 2.5-fold above baseline.4 Since lepirudin is renally excreted and no reversal agent currently exists, clinicians must use caution when administering it to patients with renal insufficiency.
Bivalirudin
Bivalirudin is another hirudin analog and has an important niche among patients requiring percutaneous coronary intervention, primarily due to its favorable pharmacokinetic profile. In contrast to other DTIs, bivalirudin does not undergo organ-specific clearance, but rather proteolysis—an excellent option for patients with other comorbidities. Additionally, its short half-life of 25 minutes makes it an appropriate choice in cases warranting only a brief period of anticoagulation.5
Argatroban
Argatroban, another parenteral DTI, differs from hirudin, lepirudin, and bivalirudin in that it is a univalent molecule. Anticoagulation is monitored by aPTT, though dose-dependent changes may be seen in prothrombin time (PT). Since argatroban undergoes hepatic clearance, dose adjustments are required in patients with hepatic dysfunction—but not in those with renal insufficiency.6 Similar to lepirudin, argatroban is also indicated for patients with a history of HIT. In recent studies, argatroban achieved patency more frequently than heparin in patients with acute myocardial infarction—without differences in clinical outcomes.7
Dabigatran Etexilate
With the increased number of patients presenting to the ED with venous and arterial thromboembolic disorders, emergency physicians should be familiar with the orally active prodrug, dabigatran. This DTI is taken twice daily and converts to it active form after administration, binding to thrombin with great specificity and affinity.8 Its half-life ranges from 12 to 24 hours in patients with normal renal function; reduced dosing schedules are recommended in patients older than age 75 years and in those with renal impairment. Dabigatran is contraindicated if creatinine clearance is less than 30 mL/min. Even though dabigatran is not cleared by the cytochrome P450 system, it does utilize the P-glycoprotein efflux transporter and is thus vulnerable to both inducers and inhibitors, including systemic antifungals and other medications.9
Monitoring Anticoagulation
Unlike warfarin, dabigatran does not require extensive monitoring. However, thrombin and aPPT assays are often less predictable at supertherapeutic levels of dabigatran, and results vary depending on last administration time of the drug.10 Strangier et al11 identified some weaknesses in aPTT measurement, concluding that while measurement of aPTT may provide a qualitative indication of anticoagulant activity, it is not suitable for the precise quantification of anticoagulant effect—especially at high plasma concentrations of dabigatran.11 Furthermore, since PT time is not significantly affected by DTIs, this assay is a poor monitoring choice for these medications.12
The thrombin time (TT) assay test, which is usually accessible in routine clinical practice, directly assesses thrombin activity, providing a direct measure of dabigatran concentration. The TT is particularly sensitive to the effects of dabigatran and displays a linear dose-response even at supratherapeutic concentrations, making it the most useful and sensitive method for determining the anticoagulation effect of dabigatran.13
When treating patients in the ED who could potentially benefit from thrombolytic agents, monitoring dabigatran anticoagulation can present a challenge. There is very little information regarding the use of tissue plasminogen activator (tPA) in patients on dabigatran, with only one published case on the subject. In this case, intravenous (IV) tPA was administered just less than 4.5 hours after onset of neurologic symptoms and 7 hours after the last intake of dabigatran, with no complications and improved neurology function.14
The Interventional Management Stroke (IMS) III trial has suggested clinicians consider IV tPA in patients with acute stroke if the last dose of dabigatran was greater than 48 hours prior to presentation in the ED.15 Until further evidence becomes available, the decision to administer thrombolytics to stroke patients taking dabigatran should be made on a case-by-case basis and in consultation with a neurologist.
Noninferiority Studies
Dabigatran has been compared to enoxaparin and showed noninferiority for venous thromboembolism (VTE) prophylaxis, with a similar safety profile.16 The RE-COVER study in 2009 demonstrated the noninferiority of dabigatran compared to warfarin. In this study, patients received either the standard dose of dabigatran (150 mg orally, twice daily) or traditional dose-adjusted warfarin. In patients on the dabigatran regimen, recurrent VTE complications occurred at a rate of 2.4%, compared with the 2.1% observed in the warfarin group.17 The safety profile was also similar, with major bleeding episodes occurring in 1.6% and 1.9%, respectively.17
Another study, the RE-LY trial, also sought to prove noninferiority between dabigatran and warfarin, specifically in patients with a known history of atrial fibrillation requiring anticoagulation.18 The authors of the study concluded a clinical net benefit of dabigatran over warfarin with respect to reduction in both hemorrhagic and ischemic stroke and bleeding versus the increase of myocardial infarction.19 Further studies, however, are needed to determine the safety profile of dabigatran.
Dabigatran Reversal
Perhaps the most pressing question for the emergency physician is how to approach the bleeding patient on dabigatran. Although well-known protocols exist for the reversal of other anticoagulants such as warfarin and heparin, no clear, effective reversal agent is currently available for dabigatran. Given its relatively short half-life (12 to 24 hours), the first line of treatment should be to discontinue its use, followed by mechanical pressure or surgical hemostatic, if indicated. Transfusion of blood products (eg, packed red blood cells, fresh frozen plasma, platelets) should be administered based on the extent of the patient’s bleeding.
If these measures fail, dialysis may be considered, particularly in patients with renal insufficiency that may have bleeding secondary to dabigatran toxicity. In cases of suspected overdose, although activated charcoal is still being evaluated, Van Ryn and colleagues noted "preliminary in vitro data indicate that dabigatran etexilate can be successfully adsorbed by classical activated charcoal therapy. However, this has not been tested in vivo or in patients…additional clinically relevant models are required before this can be recommended in patients."10
Managing Dti-Associated Bleeding
Factor VII
Since recombinant activated factor VII directly activates thrombin on the surface of platelets, it is an option in cases of life-threatening DTI-associated bleeding. While laboratory data has supported this use, human studies have been less convincing, with conflicting results in two separate studies.20,21 Moreover, financial considerations may also affect the decision to use factor VII as its dollar cost is in the thousands at most institutions.22 Since the role of factor VII in life-threatening bleeding related to DTIs has yet to be defined, it is prudent to consider this option when other measures fail, understanding the variable rates of success in reversal of anticoagulation.
Prothrombin Complex Concentrates
Prothrombin complex concentrates (PCCs) have a significant place in reversing bleeding in patients on certain anticoagulants. Since these products contain all of the vitamin K-dependent clotting factors and proteins C and S, they have been used in the treatment of warfarin toxicity.
PCCs can be divided into activated and nonactivated categories. Among the nonactivated PCCs are PCC3 and PCC4. Both contain factors II, VII, IX, and X, but PCC3 products have lower concentrations of factor VII. To augment factor VII activity, it has been proposed that fresh frozen plasma or packed red blood cells be given in conjunction with a PCC3.23
Activated prothrombin complex concentrates (APCC) contain activated factor VII, along with inactivated forms of factors II, IX, X, and protein C. Animal studies appear promising for the use of PCCs in DTI-associated bleeding; however, this treatment has not yet been fully evaluated in human studies.24
A recent randomized, placebo-controlled crossover study by Eerenberg et al25 evaluated 12 healthy volunteers treated with PCC4 after receiving either dabigatran or rivaroxaban. While the PCC completely reversed anticoagulation in the rivaroxaban group, there was no reversal of anticoagulation in the dabigatran group.25 The authors made note of the study limitations, which include small sample size and the fact that healthy volunteers were used as surrogates as opposed to patients with major bleeding complications. The authors stated that "although this trial may have important clinical implications, the effect of PCC has yet to be confirmed in patients with bleeding events treated with these anticoagulants."25 This is the only human study available and serves as a starting point from which further human research can be initiated.25
Oral Factor Xa Inhibitors
Apixaban
The FXa inhibitors are a new class of prophylactic anticoagulants. Apixaban, one of the more recent oral FXa inhibitors, has a half-life of approximately 12 hours, predictable pharmacokinetics, and is cleared primarily via the GI tract. Given its hepatic metabolism, patients taking apixaban along with cytochrome P3A4 inhibitors (eg, certain antibiotics and antifungals) may be at increased risk of bleeding.26 As evidenced by the ARISTOTLE trial, compared to standard treatment with warfarin, apixaban is an effective alternative therapy for patients with atrial fibrillation.27 Of note, however, the ADOPT trial showed increased rates of bleeding in patients with comorbid conditions taking apixaban compared to standard enoxaparin dosing.28
Rivaroxaban
Rivaroxaban is another oral FXa inhibitor, with similar pharmacokinetics as apixaban and a half-life ranging from 8 hours in young healthy subjects to 12 hours in elderly patients. Since one third of the drug is renally cleared, rivaroxaban should be prescribed with caution in patients who have impaired creatinine clearance. Moreover, as the remaining two thirds undergo hepatic clearance, as with apixaban, its use is contraindicated in patients taking other cytochrome P-inhibiting medications.29
The MAGELLAN trial found rivaroxaban to be an effective means of DVT prophylaxis compared to control subjects who received enoxaparin injections, but there was in increased rate of clinically significant bleeding in the rivaroxaban group—arguably one of the more important outcome measures for the emergency provider.30 The ROCKET-AF trial, however, showed reduced rates of stroke in patients who received rivaroxaban versus warfarin. Both drugs had similar rates of major and minor bleeding, but rivaroxaban showed a decrease in intracranial hemorrhage and fatal bleeding.31
Monitoring and Reversal
As with the DTIs, monitoring the anticoagulant activity of factor Xa inhibitors can be a challenge, though various factor X assays have been proposed.31 Similar difficulties likewise exist in terms of reversal. There is no specific reversal agent for the FXa inhibitors, and current treatment guidelines recommend the use of PCCs, APCCs, or recombinant factor VIIa—though limited data exist on which agent to base clinical practice. In contrast to the DTIs, neither apixaban nor rivaroxaban are dialyzable.32 The relatively short half-life of these products, however, can prove beneficial, with cessation of the medication being the first line therapy in the case of any clinically significant bleeding.33
Conclusion
Parenteral DTIs have been utilized for years in the ED setting. With the increasing use of newer oral DTIs and FXa inhibitors, emergency physicians must also become familiar with the drug profile of these products, including appropriate anticoagulation monitoring and effective methods to treat DTI- and FXa-associated bleeding. Many questions remain unanswered about these drugs, necessitating further research—specifically in areas of practical monitoring of anticoagulation and possible reversal protocols in the bleeding patient.
Dr Byrne is a clinical instructor in the department of emergency medicine, Eastern Virginia Medical School, Norfolk. Dr Byars is an associate professor in the department of emergency medicine, Eastern Virginia Medical School, Norfolk.
Disclosure: The authors report no conflict of interest.
Parenteral direct thrombin inhibitors (DTI), such as bivalirudin, have been used for more than a decade in the hospital setting. Over the past few years, new DTIs have received US Food and Drug Administration (FDA) approval, most notably dabigatran etexilate, an orally active DTI touted as a viable alternative for anticoagulation in patients previously taking warfarin or enoxaparin. In addition to the DTIs, oral factor Xa (FXa) inhibitors have also received FDA approval. As these drugs begin to appear on the medication lists of many patients in the ED, a review—especially of the newer, oral agents—is essential. This article provides an overview of the parenteral DTIs and oral DTI dabigatran etexilate, as well as the oral FXa inhibitors, with a focus on proper monitoring of anticoagulation and common problems encountered in patients taking these medications.
Parenteral Direct Thrombin Inhibitors
Hirudin
Hirudin, a bivalent DTI, was the first parenteral anticoagulant of its kind approved for use in humans.1 Commercially available analogs, including lepirudin, bivalirudin, and desirudin, have since become available. Anticoagulation in patients taking hirudin can be monitored effectively in the ED via activated partial thromboplastin time (aPTT).2 However, there are significant disadvantages to its use, including high cost, lack of a reversal agent, and the potential development of antibodies to hirudin and its derivatives. In addition, since anaphylactoid reactions have been reported, current recommendations contraindicate its use in patients previously treated with hirudin derivatives.3
Lepirudin
Lepirudin is a hirudin analog derived from yeast cells, and is ideal for patients with heparin-induced thrombocytopenia (HIT). With respect to thromboembolic complications in patients with a previous history of HIT, Greinacher et al,4 demonstrated its relative safety and effectiveness. Their study showed a significant reduction in thromboembolic complications per patient day from 6.1% to 1.3%.4 Bleeding events in study participants occurred at an increased rate compared to controls, but these events were greatly decreased when aPTT levels were maintained between 1.5 to 2.5-fold above baseline.4 Since lepirudin is renally excreted and no reversal agent currently exists, clinicians must use caution when administering it to patients with renal insufficiency.
Bivalirudin
Bivalirudin is another hirudin analog and has an important niche among patients requiring percutaneous coronary intervention, primarily due to its favorable pharmacokinetic profile. In contrast to other DTIs, bivalirudin does not undergo organ-specific clearance, but rather proteolysis—an excellent option for patients with other comorbidities. Additionally, its short half-life of 25 minutes makes it an appropriate choice in cases warranting only a brief period of anticoagulation.5
Argatroban
Argatroban, another parenteral DTI, differs from hirudin, lepirudin, and bivalirudin in that it is a univalent molecule. Anticoagulation is monitored by aPTT, though dose-dependent changes may be seen in prothrombin time (PT). Since argatroban undergoes hepatic clearance, dose adjustments are required in patients with hepatic dysfunction—but not in those with renal insufficiency.6 Similar to lepirudin, argatroban is also indicated for patients with a history of HIT. In recent studies, argatroban achieved patency more frequently than heparin in patients with acute myocardial infarction—without differences in clinical outcomes.7
Dabigatran Etexilate
With the increased number of patients presenting to the ED with venous and arterial thromboembolic disorders, emergency physicians should be familiar with the orally active prodrug, dabigatran. This DTI is taken twice daily and converts to it active form after administration, binding to thrombin with great specificity and affinity.8 Its half-life ranges from 12 to 24 hours in patients with normal renal function; reduced dosing schedules are recommended in patients older than age 75 years and in those with renal impairment. Dabigatran is contraindicated if creatinine clearance is less than 30 mL/min. Even though dabigatran is not cleared by the cytochrome P450 system, it does utilize the P-glycoprotein efflux transporter and is thus vulnerable to both inducers and inhibitors, including systemic antifungals and other medications.9
Monitoring Anticoagulation
Unlike warfarin, dabigatran does not require extensive monitoring. However, thrombin and aPPT assays are often less predictable at supertherapeutic levels of dabigatran, and results vary depending on last administration time of the drug.10 Strangier et al11 identified some weaknesses in aPTT measurement, concluding that while measurement of aPTT may provide a qualitative indication of anticoagulant activity, it is not suitable for the precise quantification of anticoagulant effect—especially at high plasma concentrations of dabigatran.11 Furthermore, since PT time is not significantly affected by DTIs, this assay is a poor monitoring choice for these medications.12
The thrombin time (TT) assay test, which is usually accessible in routine clinical practice, directly assesses thrombin activity, providing a direct measure of dabigatran concentration. The TT is particularly sensitive to the effects of dabigatran and displays a linear dose-response even at supratherapeutic concentrations, making it the most useful and sensitive method for determining the anticoagulation effect of dabigatran.13
When treating patients in the ED who could potentially benefit from thrombolytic agents, monitoring dabigatran anticoagulation can present a challenge. There is very little information regarding the use of tissue plasminogen activator (tPA) in patients on dabigatran, with only one published case on the subject. In this case, intravenous (IV) tPA was administered just less than 4.5 hours after onset of neurologic symptoms and 7 hours after the last intake of dabigatran, with no complications and improved neurology function.14
The Interventional Management Stroke (IMS) III trial has suggested clinicians consider IV tPA in patients with acute stroke if the last dose of dabigatran was greater than 48 hours prior to presentation in the ED.15 Until further evidence becomes available, the decision to administer thrombolytics to stroke patients taking dabigatran should be made on a case-by-case basis and in consultation with a neurologist.
Noninferiority Studies
Dabigatran has been compared to enoxaparin and showed noninferiority for venous thromboembolism (VTE) prophylaxis, with a similar safety profile.16 The RE-COVER study in 2009 demonstrated the noninferiority of dabigatran compared to warfarin. In this study, patients received either the standard dose of dabigatran (150 mg orally, twice daily) or traditional dose-adjusted warfarin. In patients on the dabigatran regimen, recurrent VTE complications occurred at a rate of 2.4%, compared with the 2.1% observed in the warfarin group.17 The safety profile was also similar, with major bleeding episodes occurring in 1.6% and 1.9%, respectively.17
Another study, the RE-LY trial, also sought to prove noninferiority between dabigatran and warfarin, specifically in patients with a known history of atrial fibrillation requiring anticoagulation.18 The authors of the study concluded a clinical net benefit of dabigatran over warfarin with respect to reduction in both hemorrhagic and ischemic stroke and bleeding versus the increase of myocardial infarction.19 Further studies, however, are needed to determine the safety profile of dabigatran.
Dabigatran Reversal
Perhaps the most pressing question for the emergency physician is how to approach the bleeding patient on dabigatran. Although well-known protocols exist for the reversal of other anticoagulants such as warfarin and heparin, no clear, effective reversal agent is currently available for dabigatran. Given its relatively short half-life (12 to 24 hours), the first line of treatment should be to discontinue its use, followed by mechanical pressure or surgical hemostatic, if indicated. Transfusion of blood products (eg, packed red blood cells, fresh frozen plasma, platelets) should be administered based on the extent of the patient’s bleeding.
If these measures fail, dialysis may be considered, particularly in patients with renal insufficiency that may have bleeding secondary to dabigatran toxicity. In cases of suspected overdose, although activated charcoal is still being evaluated, Van Ryn and colleagues noted "preliminary in vitro data indicate that dabigatran etexilate can be successfully adsorbed by classical activated charcoal therapy. However, this has not been tested in vivo or in patients…additional clinically relevant models are required before this can be recommended in patients."10
Managing Dti-Associated Bleeding
Factor VII
Since recombinant activated factor VII directly activates thrombin on the surface of platelets, it is an option in cases of life-threatening DTI-associated bleeding. While laboratory data has supported this use, human studies have been less convincing, with conflicting results in two separate studies.20,21 Moreover, financial considerations may also affect the decision to use factor VII as its dollar cost is in the thousands at most institutions.22 Since the role of factor VII in life-threatening bleeding related to DTIs has yet to be defined, it is prudent to consider this option when other measures fail, understanding the variable rates of success in reversal of anticoagulation.
Prothrombin Complex Concentrates
Prothrombin complex concentrates (PCCs) have a significant place in reversing bleeding in patients on certain anticoagulants. Since these products contain all of the vitamin K-dependent clotting factors and proteins C and S, they have been used in the treatment of warfarin toxicity.
PCCs can be divided into activated and nonactivated categories. Among the nonactivated PCCs are PCC3 and PCC4. Both contain factors II, VII, IX, and X, but PCC3 products have lower concentrations of factor VII. To augment factor VII activity, it has been proposed that fresh frozen plasma or packed red blood cells be given in conjunction with a PCC3.23
Activated prothrombin complex concentrates (APCC) contain activated factor VII, along with inactivated forms of factors II, IX, X, and protein C. Animal studies appear promising for the use of PCCs in DTI-associated bleeding; however, this treatment has not yet been fully evaluated in human studies.24
A recent randomized, placebo-controlled crossover study by Eerenberg et al25 evaluated 12 healthy volunteers treated with PCC4 after receiving either dabigatran or rivaroxaban. While the PCC completely reversed anticoagulation in the rivaroxaban group, there was no reversal of anticoagulation in the dabigatran group.25 The authors made note of the study limitations, which include small sample size and the fact that healthy volunteers were used as surrogates as opposed to patients with major bleeding complications. The authors stated that "although this trial may have important clinical implications, the effect of PCC has yet to be confirmed in patients with bleeding events treated with these anticoagulants."25 This is the only human study available and serves as a starting point from which further human research can be initiated.25
Oral Factor Xa Inhibitors
Apixaban
The FXa inhibitors are a new class of prophylactic anticoagulants. Apixaban, one of the more recent oral FXa inhibitors, has a half-life of approximately 12 hours, predictable pharmacokinetics, and is cleared primarily via the GI tract. Given its hepatic metabolism, patients taking apixaban along with cytochrome P3A4 inhibitors (eg, certain antibiotics and antifungals) may be at increased risk of bleeding.26 As evidenced by the ARISTOTLE trial, compared to standard treatment with warfarin, apixaban is an effective alternative therapy for patients with atrial fibrillation.27 Of note, however, the ADOPT trial showed increased rates of bleeding in patients with comorbid conditions taking apixaban compared to standard enoxaparin dosing.28
Rivaroxaban
Rivaroxaban is another oral FXa inhibitor, with similar pharmacokinetics as apixaban and a half-life ranging from 8 hours in young healthy subjects to 12 hours in elderly patients. Since one third of the drug is renally cleared, rivaroxaban should be prescribed with caution in patients who have impaired creatinine clearance. Moreover, as the remaining two thirds undergo hepatic clearance, as with apixaban, its use is contraindicated in patients taking other cytochrome P-inhibiting medications.29
The MAGELLAN trial found rivaroxaban to be an effective means of DVT prophylaxis compared to control subjects who received enoxaparin injections, but there was in increased rate of clinically significant bleeding in the rivaroxaban group—arguably one of the more important outcome measures for the emergency provider.30 The ROCKET-AF trial, however, showed reduced rates of stroke in patients who received rivaroxaban versus warfarin. Both drugs had similar rates of major and minor bleeding, but rivaroxaban showed a decrease in intracranial hemorrhage and fatal bleeding.31
Monitoring and Reversal
As with the DTIs, monitoring the anticoagulant activity of factor Xa inhibitors can be a challenge, though various factor X assays have been proposed.31 Similar difficulties likewise exist in terms of reversal. There is no specific reversal agent for the FXa inhibitors, and current treatment guidelines recommend the use of PCCs, APCCs, or recombinant factor VIIa—though limited data exist on which agent to base clinical practice. In contrast to the DTIs, neither apixaban nor rivaroxaban are dialyzable.32 The relatively short half-life of these products, however, can prove beneficial, with cessation of the medication being the first line therapy in the case of any clinically significant bleeding.33
Conclusion
Parenteral DTIs have been utilized for years in the ED setting. With the increasing use of newer oral DTIs and FXa inhibitors, emergency physicians must also become familiar with the drug profile of these products, including appropriate anticoagulation monitoring and effective methods to treat DTI- and FXa-associated bleeding. Many questions remain unanswered about these drugs, necessitating further research—specifically in areas of practical monitoring of anticoagulation and possible reversal protocols in the bleeding patient.
Dr Byrne is a clinical instructor in the department of emergency medicine, Eastern Virginia Medical School, Norfolk. Dr Byars is an associate professor in the department of emergency medicine, Eastern Virginia Medical School, Norfolk.
Disclosure: The authors report no conflict of interest.
- Greinacher A, Warkentin TE. The direct thrombin inhibitor hirudin. Thromb Haemost. 2008;99(5):819-829.
- Greinacher A, Eichler P, Albrecht D, Strobel U, Pötzsch B, Eriksson BI. Antihirudin antibodies following low-dose subcutaneous treatment with desirudin for thrombosis prophylaxis after hip-replacement surgery: incidence and clinical relevance. Blood. 2003;101(7):2617-2619.
- Desirudin (Iprivask) for DVT prevention. Med Lett Drugs Ther. 2010;52(1350):85,86.
- Greinacher A, Völpel H, Janssens U, et al. Recombinant hirudin (lepirudin) provides safe and effective anticoagulation in patients with heparin-induced thrombocytopenia: a prospective study. Circulation. 1999;99(1):73-80.
- Warkentin TE, Greinacher A, Koster A. Bivalirudin. Thromb Haemost. 2008;99(5):830-839.
- Swan SK, Hursting MJ. The pharmacokinetics and pharmacodynamics of argatroban: effects of age, gender, and hepatic or renal dysfunction. Pharmacotherapy. 2000;20(3):318-329.
- Jang IK, Brown DF, Giugliano RP, et al. A multicenter, randomized study of argatroban versus heparin as adjunct to tissue plasminogen activator (TPA) in acute myocardial infarction: myocardial infarction with novastan and TPA (MINT) study. J Am Coll Cardiol 1999;33(7):1879-1885.
- Blech S, Ebner T, Ludwig-Schwellinger E, Stangier J, Roth W. The metabolism and disposition of the oral direct thrombin inhibitor, dabigatran, in humans. Drug Metab Dispos. 2008;36(2):386-399.
- Stangier J, Rathgen K, Stähle H, Gansser D, Roth W. The pharmacokinetics, pharmacodynamics and tolerability of dabigatran etexilate, a new oral direct thrombin inhibitor, in healthy male subjects. Br J Clin Pharmacol. 2007;64(3):292-303.
- van Ryn J, Stangier J, Haertter S, et al. Dabigatran etexilate—a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity.Thromb Haemost. 2010;103(6):1116-1127.
- Stangier J, Rathgen K, Stähle H, Mazur D. Influence of renal impairment on the pharmacokinetics and pharmacodynamics of oral dabigatran etexilate: an open-label, parallel-group, single-centre study. Clin Pharmacokinet. 2010;49(4):259-268.
- Nowak G. The ecarin clotting time, a universal method to quantify direct thrombin inhibitors. Pathophysiol Haemost Thromb. 2003;33(4):173-183.
- Watanabe M, Siddiqui FM, Qureshi AI. Incidence and management of ischemic stroke and intracerebral hemorrhage in patients on dabigatran etexilate treatment. Neurocrit Care. 2012;16(1):203-209.
- De Smedt A, De Raedt S, Nieboer K, De Keyser J, Brouns R. Intravenous thrombolysis with recombinant tissue plasminogen activator in a stroke patient treated with dabigatran. Cerebrovasc Dis. 2010;30(5):533,534.
- Broderick J; National Institute of Neurological Disorders and Stroke (NINDS). Interventional management of stroke (IMS) III trial (IMS III). http://clinicaltrials.gov/ct2/show/NCT00359424. Accessed October 29, 2013.
- Wolowacz SE, Roskell NS, Plumb JM, Caprini JA, Eriksson BI. Efficacy and safety of dabigatran etexilate for the prevention of venous thromboembolism following total hip or knee arthoplasty. A meta-analysis. Thromb Haemost. 2009;101(1):77-85.
- Schulman S, Kearon C, Kakkar AK, et al; RE-COVER Study Group. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361(24):2342-2352.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361(12):1139-1151.
- Hughes S. Dabigatran: New data on MI and ischemic events. Medscape. 2012. http://www.theheart.org/article/1338427.do Accessed October 29, 2013.
- Wolzt M, Levi M, Sarich TC, et al. Effect of recombinant factor VIIa on melagatran-induced inhibition of thrombin generation and platelet activation in health volunteers. Thromb Haemost. 2004;91(6):1090-1096.
- Sørensen B, Ingerslev J. A direct thrombin inhibitor studied by dynamic whole blood clot formation. Haemostatic response to ex-vivo addition of recombinant factor VIIa or activated prothrombin complex concentrate. Thromb Haemost. 2006;96(4):446-453.
- Kissela BM, Eckman MH. Cost effectiveness of recombinant factor VIIa for treatment of intracerebral hemorrhage. BMC Neurology. 2008;8:17.
- Dager WE. Using prothrombin complex concentrates to rapidly reverse oral anticoagulant effects. Ann Pharmacother. 2011;45(7-8):1016-1020.
- Uchino K, Hernandez AV. Dabigatran association with higher risk of acute coronary events: meta-analysis of noninferiority randomized controlled trials. Arch Inter Med. 2012;172(5):397-402.
- Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation. 2011;124(14):1573-1579.
- Tahir F, Riaz H, Riaz T, et al. The new oral anti-coagulants and the phase 3 clinical trials - a systematic review of the literature. Thromb J. 2013;11(1):18.
- Granger C, Alexander J, McMurray JJ, et al; ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981-992.
- Goldhaber SZ, Leizorovicz A, Kakkar AK, et al; ADOPT Trial Investigators. Apixaban versus enoxaparin for thromboprophylaxis in medically ill patients. N Engl J Med. 2011;365(23):2167-2177.
- Mueck W, Stampfuss J, Kubitza D, Becka M. Clinical pharmacokinetic and pharmacodynamic profile of rivaroxaban. Clin Pharmacokinet. 2013.
- Cohen AT, Spiro TE, Büller HR, et al; MAGELLAN Investigators. Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med. 2013; 368(6):513-523.
- Patel MR, Mahaffey KW, Garg J, et al; ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883-991.
- Samama MM, Contant G, Spiro TE, et al; Rivaroxaban Anti-Factor Xa Chromogenic Assay Field Trial Laboratories. Evaluation of the anti-factor Xa chromogenic assay for the measurement of rivaroxaban plasma concentrations using calibrators and controls. Thromb Haemost. 2012;107(2):379-387.
- Goldstein P, Elalamy I, Huber K, Danchin N, Wiel E. Rivaroxaban and other non-vitamin K antagonist oral anticoagulants in the emergency treatment of thromboembolism. Int J Emerg Med. 2013;6(1):25.
- Fawole A, Daw HA, Crowther MA. Practical management of bleeding due to the anticoagulants dabigatran, rivaroxaban, and apixaban. Cleve Clin J Med. 2013; 80(7):443-451.
- Greinacher A, Warkentin TE. The direct thrombin inhibitor hirudin. Thromb Haemost. 2008;99(5):819-829.
- Greinacher A, Eichler P, Albrecht D, Strobel U, Pötzsch B, Eriksson BI. Antihirudin antibodies following low-dose subcutaneous treatment with desirudin for thrombosis prophylaxis after hip-replacement surgery: incidence and clinical relevance. Blood. 2003;101(7):2617-2619.
- Desirudin (Iprivask) for DVT prevention. Med Lett Drugs Ther. 2010;52(1350):85,86.
- Greinacher A, Völpel H, Janssens U, et al. Recombinant hirudin (lepirudin) provides safe and effective anticoagulation in patients with heparin-induced thrombocytopenia: a prospective study. Circulation. 1999;99(1):73-80.
- Warkentin TE, Greinacher A, Koster A. Bivalirudin. Thromb Haemost. 2008;99(5):830-839.
- Swan SK, Hursting MJ. The pharmacokinetics and pharmacodynamics of argatroban: effects of age, gender, and hepatic or renal dysfunction. Pharmacotherapy. 2000;20(3):318-329.
- Jang IK, Brown DF, Giugliano RP, et al. A multicenter, randomized study of argatroban versus heparin as adjunct to tissue plasminogen activator (TPA) in acute myocardial infarction: myocardial infarction with novastan and TPA (MINT) study. J Am Coll Cardiol 1999;33(7):1879-1885.
- Blech S, Ebner T, Ludwig-Schwellinger E, Stangier J, Roth W. The metabolism and disposition of the oral direct thrombin inhibitor, dabigatran, in humans. Drug Metab Dispos. 2008;36(2):386-399.
- Stangier J, Rathgen K, Stähle H, Gansser D, Roth W. The pharmacokinetics, pharmacodynamics and tolerability of dabigatran etexilate, a new oral direct thrombin inhibitor, in healthy male subjects. Br J Clin Pharmacol. 2007;64(3):292-303.
- van Ryn J, Stangier J, Haertter S, et al. Dabigatran etexilate—a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity.Thromb Haemost. 2010;103(6):1116-1127.
- Stangier J, Rathgen K, Stähle H, Mazur D. Influence of renal impairment on the pharmacokinetics and pharmacodynamics of oral dabigatran etexilate: an open-label, parallel-group, single-centre study. Clin Pharmacokinet. 2010;49(4):259-268.
- Nowak G. The ecarin clotting time, a universal method to quantify direct thrombin inhibitors. Pathophysiol Haemost Thromb. 2003;33(4):173-183.
- Watanabe M, Siddiqui FM, Qureshi AI. Incidence and management of ischemic stroke and intracerebral hemorrhage in patients on dabigatran etexilate treatment. Neurocrit Care. 2012;16(1):203-209.
- De Smedt A, De Raedt S, Nieboer K, De Keyser J, Brouns R. Intravenous thrombolysis with recombinant tissue plasminogen activator in a stroke patient treated with dabigatran. Cerebrovasc Dis. 2010;30(5):533,534.
- Broderick J; National Institute of Neurological Disorders and Stroke (NINDS). Interventional management of stroke (IMS) III trial (IMS III). http://clinicaltrials.gov/ct2/show/NCT00359424. Accessed October 29, 2013.
- Wolowacz SE, Roskell NS, Plumb JM, Caprini JA, Eriksson BI. Efficacy and safety of dabigatran etexilate for the prevention of venous thromboembolism following total hip or knee arthoplasty. A meta-analysis. Thromb Haemost. 2009;101(1):77-85.
- Schulman S, Kearon C, Kakkar AK, et al; RE-COVER Study Group. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361(24):2342-2352.
- Connolly SJ, Ezekowitz MD, Yusuf S, et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361(12):1139-1151.
- Hughes S. Dabigatran: New data on MI and ischemic events. Medscape. 2012. http://www.theheart.org/article/1338427.do Accessed October 29, 2013.
- Wolzt M, Levi M, Sarich TC, et al. Effect of recombinant factor VIIa on melagatran-induced inhibition of thrombin generation and platelet activation in health volunteers. Thromb Haemost. 2004;91(6):1090-1096.
- Sørensen B, Ingerslev J. A direct thrombin inhibitor studied by dynamic whole blood clot formation. Haemostatic response to ex-vivo addition of recombinant factor VIIa or activated prothrombin complex concentrate. Thromb Haemost. 2006;96(4):446-453.
- Kissela BM, Eckman MH. Cost effectiveness of recombinant factor VIIa for treatment of intracerebral hemorrhage. BMC Neurology. 2008;8:17.
- Dager WE. Using prothrombin complex concentrates to rapidly reverse oral anticoagulant effects. Ann Pharmacother. 2011;45(7-8):1016-1020.
- Uchino K, Hernandez AV. Dabigatran association with higher risk of acute coronary events: meta-analysis of noninferiority randomized controlled trials. Arch Inter Med. 2012;172(5):397-402.
- Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation. 2011;124(14):1573-1579.
- Tahir F, Riaz H, Riaz T, et al. The new oral anti-coagulants and the phase 3 clinical trials - a systematic review of the literature. Thromb J. 2013;11(1):18.
- Granger C, Alexander J, McMurray JJ, et al; ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981-992.
- Goldhaber SZ, Leizorovicz A, Kakkar AK, et al; ADOPT Trial Investigators. Apixaban versus enoxaparin for thromboprophylaxis in medically ill patients. N Engl J Med. 2011;365(23):2167-2177.
- Mueck W, Stampfuss J, Kubitza D, Becka M. Clinical pharmacokinetic and pharmacodynamic profile of rivaroxaban. Clin Pharmacokinet. 2013.
- Cohen AT, Spiro TE, Büller HR, et al; MAGELLAN Investigators. Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med. 2013; 368(6):513-523.
- Patel MR, Mahaffey KW, Garg J, et al; ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883-991.
- Samama MM, Contant G, Spiro TE, et al; Rivaroxaban Anti-Factor Xa Chromogenic Assay Field Trial Laboratories. Evaluation of the anti-factor Xa chromogenic assay for the measurement of rivaroxaban plasma concentrations using calibrators and controls. Thromb Haemost. 2012;107(2):379-387.
- Goldstein P, Elalamy I, Huber K, Danchin N, Wiel E. Rivaroxaban and other non-vitamin K antagonist oral anticoagulants in the emergency treatment of thromboembolism. Int J Emerg Med. 2013;6(1):25.
- Fawole A, Daw HA, Crowther MA. Practical management of bleeding due to the anticoagulants dabigatran, rivaroxaban, and apixaban. Cleve Clin J Med. 2013; 80(7):443-451.
Impact of Mild Chronic Hyponatremia on Falls, Fractures, Osteoporosis, and Death
Coarctation of the Aorta
At age 27, a woman with no family history of hypertension was diagnosed with the disease, which was left untreated. Two years later—during her first pregnancy—she was still hypertensive and was prescribed methyldopa, which was switched to lisinopril in the postpartum period. Her blood pressure (BP) remained elevated, despite titration of lisinopril and the addition of a β-blocking agent.
In the same year, the woman went to the emergency department with a severe headache and near-syncope; her BP was 180/100 mm Hg. Her medications were changed, and she was discharged with a prescription for captopril 50 mg bid and the angiotensin receptor blocker (ARB) valsartan 80 mg bid. Over the following six years, her average BP remained around 140/90 mm Hg with no further medication adjustment.
When the patient was 37, she underwent a chest x-ray (CXR), prompted by positive results on a purified protein derivative test at an employment physical; the CXR demonstrated a 3.6-cm mediastinal mass. This finding led to a chest CT exam that demonstrated a severe coarctation distal to the left subclavian artery with diffuse tubular hypoplasia, a collateral reconstitution of the descending aorta, and a true 2.7-cm aneurysm of one of the intercostal arteries.
The gradient between the ascending and descending aorta was 50 mm Hg, and the same wide pressure gradient was present between the upper and lower extremities (50 mm Hg).
Referral to pediatric cardiology was initiated. (It is not uncommon for an adult with a congenital heart lesion to be evaluated by a pediatric cardiologist in centers where adult congenital heart disease [ACHD] specialists are not available.) A cardiac MRI revealed a virtual interruption of the aortic arch in juxta-ductal position with multiple aortic collateral arteries. Subsequent cardiac catheterization demonstrated a transverse aortic arch at 1.2 cm and a narrowing to 7 mm just distal to the left subclavian artery, with a discrete coarctation of 2.5 mm.
With hypertension and a 50–mm Hg resting clinical gradient, corrective treatment was deemed necessary. Subsequently, balloon angioplasty was performed, and a drug-eluting stent was placed in the proximal distal aorta with dilation of the narrowing and a resultant decrease in BP gradient from 50 mm Hg to 7 mm Hg. Following stent placement, the aneurysm thrombosed secondary to reduced blood flow. Clinical reevaluation showed good dorsalis pedis and posterior tibial pulses with improved BP. The ARB was subsequently discontinued, and the patient continued to take captopril for mildly elevated BP (average, 130/85 mm Hg).
The patient did well until three years later, when she developed shortness of breath on exertion, claudication, and fatigue for a period of two weeks. On physical examination, her BP was noted to be elevated at 140/90 mm Hg with a clinical gradient of 20 mm between the upper and lower extremities and an increase in the gradient on echocardiogram to a peak of approximately 46 mm Hg and a mean of 21 mm Hg.
A subsequent chest CT demonstrated a narrowing of the previous stent site, and a right and left cardiac catheterization revealed neo-intimal proliferation affecting the stent with a 3–mm Hg gradient across the transverse arch and a 15–mm Hg gradient across the proximal descending aorta stent. The stent was subsequently redilated, and an additional stent was placed with no residual gradient.
The patient was discharged while taking clopidogrel 75 mg/d in addition to aspirin 325 mg/d for six months; antihypertensive medications were no longer necessary. Clinical evaluation with echocardiography was recommended every three months for the first year, and annually thereafter. At three-month and one-year follow-up, the patient was found to be symptom-free and normotensive (BP, 110/70 mm Hg).
DISCUSSION
Coarctation of the aorta (CoA) is a discrete narrowing of the thoracic aorta at the junction of the ductus arteriosus and the aortic arch, just distal to the subclavian artery. The specific anatomy, severity, and degree of hypoplasia proximal to the aortic coarctation are highly variable. For example, in some instances, coarctation presents as a long segment or a tubular hypoplasia.1
The defect is often associated with other congenital cardiovascular abnormalities, including bicuspid aortic valve (BAV; reported incidence, up to 85%),2,3 intracranial aneurysms (incidence, 3% to 10%),4 intrinsic abnormality in the aorta, aortic arch hypoplasia, ventricular septal defect, patent ductus arteriosus, aortic stenosis at different levels (valvular, subvalvular, or supravalvular), and mitral valve abnormalities.2,5 There is evidence of increased familial risk for CoA and increased prevalence with certain disorders, including Turner syndrome, maternal phenylketonuria syndrome, and Kabuki syndrome.6
CoA accounts for 5% to 8% of all congenital heart disease,2,3 and its incidence is 4 in 10,000 births.1 (Adults presenting with CoA represent either recoarctation or a missed diagnosis of native coarctation.) The mean life expectancy of untreated patients with aortic coarctation is 35 years; 90% die before age 50.1
Reduced life expectancy of patients with untreated CoA is due to systemic hypertension, accelerated coronary artery disease, stroke, heart failure, aortic rupture/dissection, cerebral hemorrhage, infective endarteritis/endocarditis, concomitant aortic valve disease (usually involving a BAV), and sudden cardiac death of presumed arrhythmogenic etiology.4 Even adults whose CoA has been detected early and managed with catheter-based and surgical interventions continue to face lifelong complications, including recoarctation, aneurysm formation, premature coronary artery disease, and cerebrovascular disease—mostly resulting from residual hypertension.3
Persistent hypertension has been reported in 68% of patients with repaired CoA at long-term follow-up. Hypertension may result in recurrence of CoA (incidence ranges from 5% to 50%), a residual CoA, or an idiopathic condition.7
The role of primary care providers is crucial in early detection and prompt referral to specialists in ACHD. For clinicians who manage these patients, increased morbidity and mortality from the associated cardiovascular sequelae pose an ongoing challenge.8
Presentation
Patients with hemodynamically stable coarctation in adolescence or adulthood are usually asymptomatic. Occasionally, a patient may be diagnosed with CoA based on its typical appearance on CXR or may come to medical attention because of an incidental murmur or management of hypertension.4 Symptoms vary in intensity and include headache, epistaxis, claudication, exertional fatigue, heart failure, aortic rupture, or dissection.7 Based on the Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7), and the 2008 American College of Cardiology/American Heart Association (ACC/AHA) guidelines for adults with congenital heart disease, patients with hypertension and/or a history of CoA repair should be evaluated periodically for coarctation.8
Physical Examination
Physical assessment should include simultaneous palpation of the brachial and femoral pulses to assess amplitude and timing, looking for diminished arterial pulses and brachial-femoral delay. Additionally, measurement of supine bilateral arm (brachial artery) BP and right or left supine leg BP is recommended to detect differing pressures.8
The following physical findings may be suggestive of CoA or recoarctation:
• Systolic BP in the right arm higher than in the lower extremities, unless the origin of the right subclavian artery is anomalous and thus is not reliable; the left arm BP may not always be reliable because of the origin of the left subclavian artery, which may vary and may or may not be hypertensive
• Hyperdynamic carotid pulsations
• A pulse delay between the right arm and the femoral or popliteal arteries
• A murmur or bruit heard in the left interscapular position; a systolic ejection click of moderate intensity heard along the left sternal border
• In cases of BAV, an early diastolic decrescendo murmur of aortic regurgitation
Diagnostic Workup
The diagnosis of CoA is usually confirmed by echocardiography or radiographic imaging, including cardiac MRI or CT angiography.8
The initial diagnostic workup should include echocardiography, which may demonstrate left ventricular hypertrophy and secondary ST-T wave abnormalities, and a two-dimensional Doppler echocardiogram, which can establish the diagnosis and severity of the CoA, with possible associated cardiac defects.9 Also recommended is a CXR, which may occasionally reveal rib notching (caused by erosion of the inferior border of the posterior ribs by enlarged intercostal arteries), also known as the 3 sign. Finally, cardiac MRI is used to delineate the coarctation anatomy and to determine whether collateral arteries and/or associated vascular anomalies and flow abnormalities exist.9 If MRI is not possible, CT angiography can be an alternate approach. Subsequently, invasive angiography is required for better assessment of the coarctation gradient and hemodynamic measurement.9
Treatment
Management of CoA requires treatment of hypertension with β-blockers, ACE inhibitors, and/or ARBs as first-line medications. Aortic root size, the presence of aortic regurgitation, or both may influence the choice of antihypertensive agents.3
Intervention is recommended if the peak-to-peak coarctation gradient is ≥ 20 mm Hg, or the peak-to-peak coarctation gradient is < 20 mm Hg, with evidence of significant coarctation and collateral flow on radiologic imaging.8 The choice of treatment (stenting or surgery) should be decided by a team of ACHD cardiologists, interventionalists, and surgeons at an ACHD center.
Surgical intervention via a lateral left thoracotomy approach was first performed in 1944. The most common surgical repair is resection with end-to-end anastomosis, which yields a low mortality and recoarctation rate. Other techniques such as resection with replacement by a tube graft, patch aortoplasty, and bypass graft are used less frequently.10-12 Postsurgical morbidity most commonly includes recoarctation and residual hypertension.
Thoracotomy was the only surgical treatment until 1982, when balloon angioplasty became available as an alternative.13 However, recoarctation, aneurysm formation, and aortic dissection are major disadvantages to balloon angioplasty.13
In the early 1990s, endovascular stents were introduced and have become an alternative approach to surgical repair.14 Aneurysms remain a significant complication in 4% to 7% of patients who undergo stent placement for CoA.14
Currently, there is insufficient evidence to indicate which is the best treatment for CoA: surgical or stent repair. Choice of treatment strategy will continue to depend on the operator’s skills or institutional preference until a prospective randomized controlled clinical trial is performed.13
Follow-Up
Based on recommendations from the ACC/AHA and the 2009 Canadian Cardiovascular Society Consensus Conference on the management of adults with congenital heart disease, lifelong follow-up is recommended for all patients with aortic coarctation (whether repaired or not), including an evaluation by a cardiologist with expertise in ACHD.4,8
A baseline cardiac MRI or CT for complete evaluation of the thoracic aorta and intracranial vessels is required for follow-up. Patients who have previously undergone surgical or interventional CoA repair should be followed annually with echocardiography to assess for potential late complications, such as aortic dilatation and aneurysm formation. Evaluation of the coarctation repair site by MRI and/or CT at intervals of five years or less is also recommended. Moreover, patients should be monitored for recurrent resting or exercise-induced hypertension, which should be treated aggressively after recoarctation is excluded.
The guidelines recommend that every patient with systemic arterial hypertension have the brachial and femoral pulses palpated simultaneously.4,8 This additional physical assessment will help detect significant aortic coarctation by assessing timing and amplitude of both pulses in search for a brachial-femoral delay. Moreover, measuring the differential pressure between bilateral arms (brachial artery) in a supine position and prone right or left supine leg (popliteal artery) BP should be performed.4,8 Initial imaging and hemodynamic evaluation by transthoracic echocardiogram is recommended in suspected aortic coarctation.
CONCLUSION
This case represents a missed CoA and provides an example of recoarctation as a late complication after repair. Unfortunately, the critical need to screen for coarctation was not recognized by the patient’s primary care providers in a timely manner. Had the guidelines for CoA screening been applied, this defect would have been detected earlier, avoiding many years of cardiovascular system stress from the sequelae of hypertension.
Measuring the BP gradient between the upper and lower extremities and searching for brachial-femoral timing delay are simple but crucial steps in the initial application of the clinical guidelines for early detection of CoA and recoarctation.
References
1. Jurcut R, Daraban AM, Lorber A, et al. Coarctation of the aorta in adults: what is the best treatment? Case report and literature review. J Med Life. 2011;4:189-195.
2. Teo LLS, Cannell T, Babu-Narayan SV, et al. Prevalence of associated cardiovascular abnormalities in 500 patients with aortic coarctation referred for cardiovascular magnetic resonance imaging to a tertiary center. Pediatr Cardiol. 2011;32:1120-1127.
3. Canniffe C. Hypertension after repair of aortic coarctation–a systematic review. Int J Cardiol. 2012;167:2456-2461.
4. Silversides CK, Kiess M, Beauchesne L, et al. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: outflow tract obstruction, coarctation of the aorta, tetralogy of Fallot, Ebstein anomaly and Marfan’s syndrome. Can J Cardiol. 2010;26:e80-e97.
5. Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 Guidelines for The Management of Adults With Congenital Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease) Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52:e143-e263.
6. McBride KL, Pignatelli R, Lewin M, et al. Inheritance analysis of congenital left ventricular outflow tract obstruction malformations: segregation, multiplex relative risk, and heritability. Am J Med Genet. Part A. 2005;134:
180-186.
7. Brown JW, Ruzmetov M, Hoyer MH, et al. Recurrent coarctation: is surgical repair of recurrent coarctation of the aorta safe and effective? Ann Thorac Surg. 2009;88:1923-1931.
8. Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: Executive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines for the management of adults with congenital heart disease). Circulation. 2008;118:2395-2451.
9. Darabian S, Zeb I, Rezaeian P, et al. Use of noninvasive imaging in the evaluation of coarctation of aorta. J Comput Assist Tomogr. 2013;37:75-78.
10. Backer CL, Mavroudis C, Zias EA, et al. Repair of coarctation with resection and extended end-to-end anastomosis. Ann Thorac Surg. 1998;66:1365-1370.
11. Cobanoglu A, Thyagarajan GK, Dobbs JL. Surgery for coarctation of the aorta in infants younger than 3 months: end-to-end repair versus subclavian flap angioplasty: is either operation better? Eur J Cardiothorac Surg. 1998;14:19-25.
12. Walhout RJ, Lekkerkerker JC, Oron GH, et al. Comparison of polytetrafluoroethylene patch aortoplasty and end-to-end anastomosis for coarctation of the aorta. J Thorac Cardiovasc Surg. 2003;126:521-528.
13. Pádua LM, Garcia LC, Rubira CJ, de Oliveira Carvalho PE. Stent placement versus surgery for coarctation of the thoracic aorta. Cochrane Database Syst Rev. 2012;5:CD008204.
14. Suárez de Lezo J, Pan M, Romero M, et al. Immediate and follow-up findings after stent treatment for severe coarctation of aorta. Am J Cardiol. 1999;83:400-406.
At age 27, a woman with no family history of hypertension was diagnosed with the disease, which was left untreated. Two years later—during her first pregnancy—she was still hypertensive and was prescribed methyldopa, which was switched to lisinopril in the postpartum period. Her blood pressure (BP) remained elevated, despite titration of lisinopril and the addition of a β-blocking agent.
In the same year, the woman went to the emergency department with a severe headache and near-syncope; her BP was 180/100 mm Hg. Her medications were changed, and she was discharged with a prescription for captopril 50 mg bid and the angiotensin receptor blocker (ARB) valsartan 80 mg bid. Over the following six years, her average BP remained around 140/90 mm Hg with no further medication adjustment.
When the patient was 37, she underwent a chest x-ray (CXR), prompted by positive results on a purified protein derivative test at an employment physical; the CXR demonstrated a 3.6-cm mediastinal mass. This finding led to a chest CT exam that demonstrated a severe coarctation distal to the left subclavian artery with diffuse tubular hypoplasia, a collateral reconstitution of the descending aorta, and a true 2.7-cm aneurysm of one of the intercostal arteries.
The gradient between the ascending and descending aorta was 50 mm Hg, and the same wide pressure gradient was present between the upper and lower extremities (50 mm Hg).
Referral to pediatric cardiology was initiated. (It is not uncommon for an adult with a congenital heart lesion to be evaluated by a pediatric cardiologist in centers where adult congenital heart disease [ACHD] specialists are not available.) A cardiac MRI revealed a virtual interruption of the aortic arch in juxta-ductal position with multiple aortic collateral arteries. Subsequent cardiac catheterization demonstrated a transverse aortic arch at 1.2 cm and a narrowing to 7 mm just distal to the left subclavian artery, with a discrete coarctation of 2.5 mm.
With hypertension and a 50–mm Hg resting clinical gradient, corrective treatment was deemed necessary. Subsequently, balloon angioplasty was performed, and a drug-eluting stent was placed in the proximal distal aorta with dilation of the narrowing and a resultant decrease in BP gradient from 50 mm Hg to 7 mm Hg. Following stent placement, the aneurysm thrombosed secondary to reduced blood flow. Clinical reevaluation showed good dorsalis pedis and posterior tibial pulses with improved BP. The ARB was subsequently discontinued, and the patient continued to take captopril for mildly elevated BP (average, 130/85 mm Hg).
The patient did well until three years later, when she developed shortness of breath on exertion, claudication, and fatigue for a period of two weeks. On physical examination, her BP was noted to be elevated at 140/90 mm Hg with a clinical gradient of 20 mm between the upper and lower extremities and an increase in the gradient on echocardiogram to a peak of approximately 46 mm Hg and a mean of 21 mm Hg.
A subsequent chest CT demonstrated a narrowing of the previous stent site, and a right and left cardiac catheterization revealed neo-intimal proliferation affecting the stent with a 3–mm Hg gradient across the transverse arch and a 15–mm Hg gradient across the proximal descending aorta stent. The stent was subsequently redilated, and an additional stent was placed with no residual gradient.
The patient was discharged while taking clopidogrel 75 mg/d in addition to aspirin 325 mg/d for six months; antihypertensive medications were no longer necessary. Clinical evaluation with echocardiography was recommended every three months for the first year, and annually thereafter. At three-month and one-year follow-up, the patient was found to be symptom-free and normotensive (BP, 110/70 mm Hg).
DISCUSSION
Coarctation of the aorta (CoA) is a discrete narrowing of the thoracic aorta at the junction of the ductus arteriosus and the aortic arch, just distal to the subclavian artery. The specific anatomy, severity, and degree of hypoplasia proximal to the aortic coarctation are highly variable. For example, in some instances, coarctation presents as a long segment or a tubular hypoplasia.1
The defect is often associated with other congenital cardiovascular abnormalities, including bicuspid aortic valve (BAV; reported incidence, up to 85%),2,3 intracranial aneurysms (incidence, 3% to 10%),4 intrinsic abnormality in the aorta, aortic arch hypoplasia, ventricular septal defect, patent ductus arteriosus, aortic stenosis at different levels (valvular, subvalvular, or supravalvular), and mitral valve abnormalities.2,5 There is evidence of increased familial risk for CoA and increased prevalence with certain disorders, including Turner syndrome, maternal phenylketonuria syndrome, and Kabuki syndrome.6
CoA accounts for 5% to 8% of all congenital heart disease,2,3 and its incidence is 4 in 10,000 births.1 (Adults presenting with CoA represent either recoarctation or a missed diagnosis of native coarctation.) The mean life expectancy of untreated patients with aortic coarctation is 35 years; 90% die before age 50.1
Reduced life expectancy of patients with untreated CoA is due to systemic hypertension, accelerated coronary artery disease, stroke, heart failure, aortic rupture/dissection, cerebral hemorrhage, infective endarteritis/endocarditis, concomitant aortic valve disease (usually involving a BAV), and sudden cardiac death of presumed arrhythmogenic etiology.4 Even adults whose CoA has been detected early and managed with catheter-based and surgical interventions continue to face lifelong complications, including recoarctation, aneurysm formation, premature coronary artery disease, and cerebrovascular disease—mostly resulting from residual hypertension.3
Persistent hypertension has been reported in 68% of patients with repaired CoA at long-term follow-up. Hypertension may result in recurrence of CoA (incidence ranges from 5% to 50%), a residual CoA, or an idiopathic condition.7
The role of primary care providers is crucial in early detection and prompt referral to specialists in ACHD. For clinicians who manage these patients, increased morbidity and mortality from the associated cardiovascular sequelae pose an ongoing challenge.8
Presentation
Patients with hemodynamically stable coarctation in adolescence or adulthood are usually asymptomatic. Occasionally, a patient may be diagnosed with CoA based on its typical appearance on CXR or may come to medical attention because of an incidental murmur or management of hypertension.4 Symptoms vary in intensity and include headache, epistaxis, claudication, exertional fatigue, heart failure, aortic rupture, or dissection.7 Based on the Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7), and the 2008 American College of Cardiology/American Heart Association (ACC/AHA) guidelines for adults with congenital heart disease, patients with hypertension and/or a history of CoA repair should be evaluated periodically for coarctation.8
Physical Examination
Physical assessment should include simultaneous palpation of the brachial and femoral pulses to assess amplitude and timing, looking for diminished arterial pulses and brachial-femoral delay. Additionally, measurement of supine bilateral arm (brachial artery) BP and right or left supine leg BP is recommended to detect differing pressures.8
The following physical findings may be suggestive of CoA or recoarctation:
• Systolic BP in the right arm higher than in the lower extremities, unless the origin of the right subclavian artery is anomalous and thus is not reliable; the left arm BP may not always be reliable because of the origin of the left subclavian artery, which may vary and may or may not be hypertensive
• Hyperdynamic carotid pulsations
• A pulse delay between the right arm and the femoral or popliteal arteries
• A murmur or bruit heard in the left interscapular position; a systolic ejection click of moderate intensity heard along the left sternal border
• In cases of BAV, an early diastolic decrescendo murmur of aortic regurgitation
Diagnostic Workup
The diagnosis of CoA is usually confirmed by echocardiography or radiographic imaging, including cardiac MRI or CT angiography.8
The initial diagnostic workup should include echocardiography, which may demonstrate left ventricular hypertrophy and secondary ST-T wave abnormalities, and a two-dimensional Doppler echocardiogram, which can establish the diagnosis and severity of the CoA, with possible associated cardiac defects.9 Also recommended is a CXR, which may occasionally reveal rib notching (caused by erosion of the inferior border of the posterior ribs by enlarged intercostal arteries), also known as the 3 sign. Finally, cardiac MRI is used to delineate the coarctation anatomy and to determine whether collateral arteries and/or associated vascular anomalies and flow abnormalities exist.9 If MRI is not possible, CT angiography can be an alternate approach. Subsequently, invasive angiography is required for better assessment of the coarctation gradient and hemodynamic measurement.9
Treatment
Management of CoA requires treatment of hypertension with β-blockers, ACE inhibitors, and/or ARBs as first-line medications. Aortic root size, the presence of aortic regurgitation, or both may influence the choice of antihypertensive agents.3
Intervention is recommended if the peak-to-peak coarctation gradient is ≥ 20 mm Hg, or the peak-to-peak coarctation gradient is < 20 mm Hg, with evidence of significant coarctation and collateral flow on radiologic imaging.8 The choice of treatment (stenting or surgery) should be decided by a team of ACHD cardiologists, interventionalists, and surgeons at an ACHD center.
Surgical intervention via a lateral left thoracotomy approach was first performed in 1944. The most common surgical repair is resection with end-to-end anastomosis, which yields a low mortality and recoarctation rate. Other techniques such as resection with replacement by a tube graft, patch aortoplasty, and bypass graft are used less frequently.10-12 Postsurgical morbidity most commonly includes recoarctation and residual hypertension.
Thoracotomy was the only surgical treatment until 1982, when balloon angioplasty became available as an alternative.13 However, recoarctation, aneurysm formation, and aortic dissection are major disadvantages to balloon angioplasty.13
In the early 1990s, endovascular stents were introduced and have become an alternative approach to surgical repair.14 Aneurysms remain a significant complication in 4% to 7% of patients who undergo stent placement for CoA.14
Currently, there is insufficient evidence to indicate which is the best treatment for CoA: surgical or stent repair. Choice of treatment strategy will continue to depend on the operator’s skills or institutional preference until a prospective randomized controlled clinical trial is performed.13
Follow-Up
Based on recommendations from the ACC/AHA and the 2009 Canadian Cardiovascular Society Consensus Conference on the management of adults with congenital heart disease, lifelong follow-up is recommended for all patients with aortic coarctation (whether repaired or not), including an evaluation by a cardiologist with expertise in ACHD.4,8
A baseline cardiac MRI or CT for complete evaluation of the thoracic aorta and intracranial vessels is required for follow-up. Patients who have previously undergone surgical or interventional CoA repair should be followed annually with echocardiography to assess for potential late complications, such as aortic dilatation and aneurysm formation. Evaluation of the coarctation repair site by MRI and/or CT at intervals of five years or less is also recommended. Moreover, patients should be monitored for recurrent resting or exercise-induced hypertension, which should be treated aggressively after recoarctation is excluded.
The guidelines recommend that every patient with systemic arterial hypertension have the brachial and femoral pulses palpated simultaneously.4,8 This additional physical assessment will help detect significant aortic coarctation by assessing timing and amplitude of both pulses in search for a brachial-femoral delay. Moreover, measuring the differential pressure between bilateral arms (brachial artery) in a supine position and prone right or left supine leg (popliteal artery) BP should be performed.4,8 Initial imaging and hemodynamic evaluation by transthoracic echocardiogram is recommended in suspected aortic coarctation.
CONCLUSION
This case represents a missed CoA and provides an example of recoarctation as a late complication after repair. Unfortunately, the critical need to screen for coarctation was not recognized by the patient’s primary care providers in a timely manner. Had the guidelines for CoA screening been applied, this defect would have been detected earlier, avoiding many years of cardiovascular system stress from the sequelae of hypertension.
Measuring the BP gradient between the upper and lower extremities and searching for brachial-femoral timing delay are simple but crucial steps in the initial application of the clinical guidelines for early detection of CoA and recoarctation.
References
1. Jurcut R, Daraban AM, Lorber A, et al. Coarctation of the aorta in adults: what is the best treatment? Case report and literature review. J Med Life. 2011;4:189-195.
2. Teo LLS, Cannell T, Babu-Narayan SV, et al. Prevalence of associated cardiovascular abnormalities in 500 patients with aortic coarctation referred for cardiovascular magnetic resonance imaging to a tertiary center. Pediatr Cardiol. 2011;32:1120-1127.
3. Canniffe C. Hypertension after repair of aortic coarctation–a systematic review. Int J Cardiol. 2012;167:2456-2461.
4. Silversides CK, Kiess M, Beauchesne L, et al. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: outflow tract obstruction, coarctation of the aorta, tetralogy of Fallot, Ebstein anomaly and Marfan’s syndrome. Can J Cardiol. 2010;26:e80-e97.
5. Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 Guidelines for The Management of Adults With Congenital Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease) Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52:e143-e263.
6. McBride KL, Pignatelli R, Lewin M, et al. Inheritance analysis of congenital left ventricular outflow tract obstruction malformations: segregation, multiplex relative risk, and heritability. Am J Med Genet. Part A. 2005;134:
180-186.
7. Brown JW, Ruzmetov M, Hoyer MH, et al. Recurrent coarctation: is surgical repair of recurrent coarctation of the aorta safe and effective? Ann Thorac Surg. 2009;88:1923-1931.
8. Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: Executive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines for the management of adults with congenital heart disease). Circulation. 2008;118:2395-2451.
9. Darabian S, Zeb I, Rezaeian P, et al. Use of noninvasive imaging in the evaluation of coarctation of aorta. J Comput Assist Tomogr. 2013;37:75-78.
10. Backer CL, Mavroudis C, Zias EA, et al. Repair of coarctation with resection and extended end-to-end anastomosis. Ann Thorac Surg. 1998;66:1365-1370.
11. Cobanoglu A, Thyagarajan GK, Dobbs JL. Surgery for coarctation of the aorta in infants younger than 3 months: end-to-end repair versus subclavian flap angioplasty: is either operation better? Eur J Cardiothorac Surg. 1998;14:19-25.
12. Walhout RJ, Lekkerkerker JC, Oron GH, et al. Comparison of polytetrafluoroethylene patch aortoplasty and end-to-end anastomosis for coarctation of the aorta. J Thorac Cardiovasc Surg. 2003;126:521-528.
13. Pádua LM, Garcia LC, Rubira CJ, de Oliveira Carvalho PE. Stent placement versus surgery for coarctation of the thoracic aorta. Cochrane Database Syst Rev. 2012;5:CD008204.
14. Suárez de Lezo J, Pan M, Romero M, et al. Immediate and follow-up findings after stent treatment for severe coarctation of aorta. Am J Cardiol. 1999;83:400-406.
At age 27, a woman with no family history of hypertension was diagnosed with the disease, which was left untreated. Two years later—during her first pregnancy—she was still hypertensive and was prescribed methyldopa, which was switched to lisinopril in the postpartum period. Her blood pressure (BP) remained elevated, despite titration of lisinopril and the addition of a β-blocking agent.
In the same year, the woman went to the emergency department with a severe headache and near-syncope; her BP was 180/100 mm Hg. Her medications were changed, and she was discharged with a prescription for captopril 50 mg bid and the angiotensin receptor blocker (ARB) valsartan 80 mg bid. Over the following six years, her average BP remained around 140/90 mm Hg with no further medication adjustment.
When the patient was 37, she underwent a chest x-ray (CXR), prompted by positive results on a purified protein derivative test at an employment physical; the CXR demonstrated a 3.6-cm mediastinal mass. This finding led to a chest CT exam that demonstrated a severe coarctation distal to the left subclavian artery with diffuse tubular hypoplasia, a collateral reconstitution of the descending aorta, and a true 2.7-cm aneurysm of one of the intercostal arteries.
The gradient between the ascending and descending aorta was 50 mm Hg, and the same wide pressure gradient was present between the upper and lower extremities (50 mm Hg).
Referral to pediatric cardiology was initiated. (It is not uncommon for an adult with a congenital heart lesion to be evaluated by a pediatric cardiologist in centers where adult congenital heart disease [ACHD] specialists are not available.) A cardiac MRI revealed a virtual interruption of the aortic arch in juxta-ductal position with multiple aortic collateral arteries. Subsequent cardiac catheterization demonstrated a transverse aortic arch at 1.2 cm and a narrowing to 7 mm just distal to the left subclavian artery, with a discrete coarctation of 2.5 mm.
With hypertension and a 50–mm Hg resting clinical gradient, corrective treatment was deemed necessary. Subsequently, balloon angioplasty was performed, and a drug-eluting stent was placed in the proximal distal aorta with dilation of the narrowing and a resultant decrease in BP gradient from 50 mm Hg to 7 mm Hg. Following stent placement, the aneurysm thrombosed secondary to reduced blood flow. Clinical reevaluation showed good dorsalis pedis and posterior tibial pulses with improved BP. The ARB was subsequently discontinued, and the patient continued to take captopril for mildly elevated BP (average, 130/85 mm Hg).
The patient did well until three years later, when she developed shortness of breath on exertion, claudication, and fatigue for a period of two weeks. On physical examination, her BP was noted to be elevated at 140/90 mm Hg with a clinical gradient of 20 mm between the upper and lower extremities and an increase in the gradient on echocardiogram to a peak of approximately 46 mm Hg and a mean of 21 mm Hg.
A subsequent chest CT demonstrated a narrowing of the previous stent site, and a right and left cardiac catheterization revealed neo-intimal proliferation affecting the stent with a 3–mm Hg gradient across the transverse arch and a 15–mm Hg gradient across the proximal descending aorta stent. The stent was subsequently redilated, and an additional stent was placed with no residual gradient.
The patient was discharged while taking clopidogrel 75 mg/d in addition to aspirin 325 mg/d for six months; antihypertensive medications were no longer necessary. Clinical evaluation with echocardiography was recommended every three months for the first year, and annually thereafter. At three-month and one-year follow-up, the patient was found to be symptom-free and normotensive (BP, 110/70 mm Hg).
DISCUSSION
Coarctation of the aorta (CoA) is a discrete narrowing of the thoracic aorta at the junction of the ductus arteriosus and the aortic arch, just distal to the subclavian artery. The specific anatomy, severity, and degree of hypoplasia proximal to the aortic coarctation are highly variable. For example, in some instances, coarctation presents as a long segment or a tubular hypoplasia.1
The defect is often associated with other congenital cardiovascular abnormalities, including bicuspid aortic valve (BAV; reported incidence, up to 85%),2,3 intracranial aneurysms (incidence, 3% to 10%),4 intrinsic abnormality in the aorta, aortic arch hypoplasia, ventricular septal defect, patent ductus arteriosus, aortic stenosis at different levels (valvular, subvalvular, or supravalvular), and mitral valve abnormalities.2,5 There is evidence of increased familial risk for CoA and increased prevalence with certain disorders, including Turner syndrome, maternal phenylketonuria syndrome, and Kabuki syndrome.6
CoA accounts for 5% to 8% of all congenital heart disease,2,3 and its incidence is 4 in 10,000 births.1 (Adults presenting with CoA represent either recoarctation or a missed diagnosis of native coarctation.) The mean life expectancy of untreated patients with aortic coarctation is 35 years; 90% die before age 50.1
Reduced life expectancy of patients with untreated CoA is due to systemic hypertension, accelerated coronary artery disease, stroke, heart failure, aortic rupture/dissection, cerebral hemorrhage, infective endarteritis/endocarditis, concomitant aortic valve disease (usually involving a BAV), and sudden cardiac death of presumed arrhythmogenic etiology.4 Even adults whose CoA has been detected early and managed with catheter-based and surgical interventions continue to face lifelong complications, including recoarctation, aneurysm formation, premature coronary artery disease, and cerebrovascular disease—mostly resulting from residual hypertension.3
Persistent hypertension has been reported in 68% of patients with repaired CoA at long-term follow-up. Hypertension may result in recurrence of CoA (incidence ranges from 5% to 50%), a residual CoA, or an idiopathic condition.7
The role of primary care providers is crucial in early detection and prompt referral to specialists in ACHD. For clinicians who manage these patients, increased morbidity and mortality from the associated cardiovascular sequelae pose an ongoing challenge.8
Presentation
Patients with hemodynamically stable coarctation in adolescence or adulthood are usually asymptomatic. Occasionally, a patient may be diagnosed with CoA based on its typical appearance on CXR or may come to medical attention because of an incidental murmur or management of hypertension.4 Symptoms vary in intensity and include headache, epistaxis, claudication, exertional fatigue, heart failure, aortic rupture, or dissection.7 Based on the Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7), and the 2008 American College of Cardiology/American Heart Association (ACC/AHA) guidelines for adults with congenital heart disease, patients with hypertension and/or a history of CoA repair should be evaluated periodically for coarctation.8
Physical Examination
Physical assessment should include simultaneous palpation of the brachial and femoral pulses to assess amplitude and timing, looking for diminished arterial pulses and brachial-femoral delay. Additionally, measurement of supine bilateral arm (brachial artery) BP and right or left supine leg BP is recommended to detect differing pressures.8
The following physical findings may be suggestive of CoA or recoarctation:
• Systolic BP in the right arm higher than in the lower extremities, unless the origin of the right subclavian artery is anomalous and thus is not reliable; the left arm BP may not always be reliable because of the origin of the left subclavian artery, which may vary and may or may not be hypertensive
• Hyperdynamic carotid pulsations
• A pulse delay between the right arm and the femoral or popliteal arteries
• A murmur or bruit heard in the left interscapular position; a systolic ejection click of moderate intensity heard along the left sternal border
• In cases of BAV, an early diastolic decrescendo murmur of aortic regurgitation
Diagnostic Workup
The diagnosis of CoA is usually confirmed by echocardiography or radiographic imaging, including cardiac MRI or CT angiography.8
The initial diagnostic workup should include echocardiography, which may demonstrate left ventricular hypertrophy and secondary ST-T wave abnormalities, and a two-dimensional Doppler echocardiogram, which can establish the diagnosis and severity of the CoA, with possible associated cardiac defects.9 Also recommended is a CXR, which may occasionally reveal rib notching (caused by erosion of the inferior border of the posterior ribs by enlarged intercostal arteries), also known as the 3 sign. Finally, cardiac MRI is used to delineate the coarctation anatomy and to determine whether collateral arteries and/or associated vascular anomalies and flow abnormalities exist.9 If MRI is not possible, CT angiography can be an alternate approach. Subsequently, invasive angiography is required for better assessment of the coarctation gradient and hemodynamic measurement.9
Treatment
Management of CoA requires treatment of hypertension with β-blockers, ACE inhibitors, and/or ARBs as first-line medications. Aortic root size, the presence of aortic regurgitation, or both may influence the choice of antihypertensive agents.3
Intervention is recommended if the peak-to-peak coarctation gradient is ≥ 20 mm Hg, or the peak-to-peak coarctation gradient is < 20 mm Hg, with evidence of significant coarctation and collateral flow on radiologic imaging.8 The choice of treatment (stenting or surgery) should be decided by a team of ACHD cardiologists, interventionalists, and surgeons at an ACHD center.
Surgical intervention via a lateral left thoracotomy approach was first performed in 1944. The most common surgical repair is resection with end-to-end anastomosis, which yields a low mortality and recoarctation rate. Other techniques such as resection with replacement by a tube graft, patch aortoplasty, and bypass graft are used less frequently.10-12 Postsurgical morbidity most commonly includes recoarctation and residual hypertension.
Thoracotomy was the only surgical treatment until 1982, when balloon angioplasty became available as an alternative.13 However, recoarctation, aneurysm formation, and aortic dissection are major disadvantages to balloon angioplasty.13
In the early 1990s, endovascular stents were introduced and have become an alternative approach to surgical repair.14 Aneurysms remain a significant complication in 4% to 7% of patients who undergo stent placement for CoA.14
Currently, there is insufficient evidence to indicate which is the best treatment for CoA: surgical or stent repair. Choice of treatment strategy will continue to depend on the operator’s skills or institutional preference until a prospective randomized controlled clinical trial is performed.13
Follow-Up
Based on recommendations from the ACC/AHA and the 2009 Canadian Cardiovascular Society Consensus Conference on the management of adults with congenital heart disease, lifelong follow-up is recommended for all patients with aortic coarctation (whether repaired or not), including an evaluation by a cardiologist with expertise in ACHD.4,8
A baseline cardiac MRI or CT for complete evaluation of the thoracic aorta and intracranial vessels is required for follow-up. Patients who have previously undergone surgical or interventional CoA repair should be followed annually with echocardiography to assess for potential late complications, such as aortic dilatation and aneurysm formation. Evaluation of the coarctation repair site by MRI and/or CT at intervals of five years or less is also recommended. Moreover, patients should be monitored for recurrent resting or exercise-induced hypertension, which should be treated aggressively after recoarctation is excluded.
The guidelines recommend that every patient with systemic arterial hypertension have the brachial and femoral pulses palpated simultaneously.4,8 This additional physical assessment will help detect significant aortic coarctation by assessing timing and amplitude of both pulses in search for a brachial-femoral delay. Moreover, measuring the differential pressure between bilateral arms (brachial artery) in a supine position and prone right or left supine leg (popliteal artery) BP should be performed.4,8 Initial imaging and hemodynamic evaluation by transthoracic echocardiogram is recommended in suspected aortic coarctation.
CONCLUSION
This case represents a missed CoA and provides an example of recoarctation as a late complication after repair. Unfortunately, the critical need to screen for coarctation was not recognized by the patient’s primary care providers in a timely manner. Had the guidelines for CoA screening been applied, this defect would have been detected earlier, avoiding many years of cardiovascular system stress from the sequelae of hypertension.
Measuring the BP gradient between the upper and lower extremities and searching for brachial-femoral timing delay are simple but crucial steps in the initial application of the clinical guidelines for early detection of CoA and recoarctation.
References
1. Jurcut R, Daraban AM, Lorber A, et al. Coarctation of the aorta in adults: what is the best treatment? Case report and literature review. J Med Life. 2011;4:189-195.
2. Teo LLS, Cannell T, Babu-Narayan SV, et al. Prevalence of associated cardiovascular abnormalities in 500 patients with aortic coarctation referred for cardiovascular magnetic resonance imaging to a tertiary center. Pediatr Cardiol. 2011;32:1120-1127.
3. Canniffe C. Hypertension after repair of aortic coarctation–a systematic review. Int J Cardiol. 2012;167:2456-2461.
4. Silversides CK, Kiess M, Beauchesne L, et al. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: outflow tract obstruction, coarctation of the aorta, tetralogy of Fallot, Ebstein anomaly and Marfan’s syndrome. Can J Cardiol. 2010;26:e80-e97.
5. Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 Guidelines for The Management of Adults With Congenital Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease) Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52:e143-e263.
6. McBride KL, Pignatelli R, Lewin M, et al. Inheritance analysis of congenital left ventricular outflow tract obstruction malformations: segregation, multiplex relative risk, and heritability. Am J Med Genet. Part A. 2005;134:
180-186.
7. Brown JW, Ruzmetov M, Hoyer MH, et al. Recurrent coarctation: is surgical repair of recurrent coarctation of the aorta safe and effective? Ann Thorac Surg. 2009;88:1923-1931.
8. Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: Executive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines for the management of adults with congenital heart disease). Circulation. 2008;118:2395-2451.
9. Darabian S, Zeb I, Rezaeian P, et al. Use of noninvasive imaging in the evaluation of coarctation of aorta. J Comput Assist Tomogr. 2013;37:75-78.
10. Backer CL, Mavroudis C, Zias EA, et al. Repair of coarctation with resection and extended end-to-end anastomosis. Ann Thorac Surg. 1998;66:1365-1370.
11. Cobanoglu A, Thyagarajan GK, Dobbs JL. Surgery for coarctation of the aorta in infants younger than 3 months: end-to-end repair versus subclavian flap angioplasty: is either operation better? Eur J Cardiothorac Surg. 1998;14:19-25.
12. Walhout RJ, Lekkerkerker JC, Oron GH, et al. Comparison of polytetrafluoroethylene patch aortoplasty and end-to-end anastomosis for coarctation of the aorta. J Thorac Cardiovasc Surg. 2003;126:521-528.
13. Pádua LM, Garcia LC, Rubira CJ, de Oliveira Carvalho PE. Stent placement versus surgery for coarctation of the thoracic aorta. Cochrane Database Syst Rev. 2012;5:CD008204.
14. Suárez de Lezo J, Pan M, Romero M, et al. Immediate and follow-up findings after stent treatment for severe coarctation of aorta. Am J Cardiol. 1999;83:400-406.
Helping Patients Navigate the Web
How often does this happen to you? You walk into an exam room and ask the patient what brings him in today, and the reply is something like, “Well, doc, I have stomach cancer.” You do a double-take and scan the patient’s chart, looking for test results or notes from a referring provider. Finding nothing, you ask the patient for more information on his diagnosis. To your surprise/dismay/frustration, he says, “Naw, I Googled my symptoms and that’s what I came up with.”
While you can’t control the Web-surfing your patients do before they present, you can influence their information-seeking behavior once you’ve delivered a diagnosis and/or treatment plan. You know they (and their family/caregivers) will have questions about the patient’s condition and how it can be managed for the long term. You hope they’ll come to you for answers. But since they are likely to use the resources at their fingertips, you at least want to ensure the information they receive is accurate and trustworthy.
With that in mind, we asked several Clinician Reviews board members to share the Web sites that they recommend to their patients. Some, including Cathy St. Pierre, PhD, APRN, FNP-BC, FAANP, and Ellen Mandel, DMH, MPA, PA-C, CDE, cited behemoths such as the Mayo Clinic Web site (www.mayoclinic.com/health-information), lauding it for being up to date, easy to access, and “clear and data-driven.” Other board members, as you’ll see below, suggested specialty-specific sites.
Freddi I. Segal-Gidan, PhD, PA, may speak for many clinicians when she explains, “We offer these [resources] to patients and families as part of health education, acknowledging that learning about someone’s condition is the first step to better understanding what they are experiencing and how this may change over time—since most of what we deal with are progressive, lengthy illnesses and chronic disease management.”
If you have reliable Web-based resources that you recommend to your patients, please visit us on Facebook (www.facebook.com/ClinRev) to share them!
Alzheimer’s Disease
ADEAR—Alzheimer’s Disease Education and Referral Center
www.nia.nih.gov/alzheimers
Who recommends it: Freddi I. Segal-Gidan, PA, PhD
Why: Operated by the NIH/National Institute on Aging specifically to provide consumers with current, accurate, state-of-the-art information about Alzheimer’s disease and dementing illness
Also recommended: Alzheimer’s Association (www.alz.org); Family Caregiver Alliance (www.caregiver.org); UCSF Memory Center for information on frontotemporal dementia (www.memory.ucsf.edu/ftd); Foundation for Health in Aging (www.healthinaging.org); Kaiser Family Foundation for information about Medicare, Medicaid, and health policy related to aging (www.kff.org)
Cardiology
Cardiac Arrhythmias Research and Education Foundation, Inc (CARE)
www.longqt.org
Who recommends it: Lyle W. Larson, PhD, PA-C
Why: Provides an overview of long QT syndrome (eg, management, genetics); includes links to a study registry for persons with implantable cardioverters-defibrillators who are participating in sports and a complete list of medications to avoid in this patient population. The information is collated and disseminated by health care experts in this field and is updated continuously as new data emerges.
Also recommended: CredibleMeds™ (www.crediblemeds.org)
Dermatology
American Academy of Dermatology: For the Public
www.aad.org/for-the-public
Who recommends it: Joe R. Monroe, MPAS, PA
Why: Provides patient information about a specific topic or diagnosis that is reliable, up to date, and in understandable language.
eMedicine
http://emedicine.medscape.com
Who recommends it: Joe R. Monroe, MPAS, PA
Why: The information is current and written by authoritative dermatologists or other relevant specialists. References are copious and relevant, and links in the text guide readers to equally good information on related topics.
Caveats: The only problem with eMedicine is that it’s jargon-heavy and meant only for those who are comfortable with the terminology. I reserve this suggestion for more medically erudite patients (eg, nurses or PAs).
Diabetes
DiabetesMine
www.diabetesmine.com/
Who recommends it: Christine Kessler, RN, MN, CNS, ANP, BC-ADM
Why: This is an award-winning blog by an individual with type 1 diabetes, but it has something for every diabetic patient and his/her family. Really awesome. I recommend it to my patients, and some of them blog for it!
Also recommended: American Diabetes Association (www.diabetes.org/)
Nephrology
American Association of Kidney Patients
www.aakp.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: Their information is written for and by kidney patients. It is for all patients with kidney disease, not just dialysis patients. They offer free publications that emphasize living with kidney disease; these pubs are attractive, with realistic information.
Kidney School
www.kidneyschool.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: This site offers about 16 modules, each on a different topic ranging from dialysis options to sexuality. It is for patients and allows them to pick the topic they want and view the module as often as they wish.
National Kidney Foundation
www.kidney.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: The patient section of this site contains recipes and health information. Patients can register for the Kidney Peers Program, in which they match up either as a mentor or a mentee with another kidney patient in the US. It covers the range from moderate kidney disease to kidney failure and transplant.
Also recommended: DaVita (www.davita.com); Fresenius Medical Care (www.ultracare-dialysis.com)
Orthopedics
OrthoInfo
orthoinfo.aaos.org/
Who recommends it: Mike Rudzinski, RPh, RPA-C
Why: Endorsed by the American Academy of Orthopedic Surgeons, this site offers patients information on the most common musculoskeletal conditions. Includes patient education materials with anatomic pictures and discussion. This is my “go to” site for these conditions; it offers an incredible, comprehensive overview of the condition, options for care including potential surgery, and what the patient can do to improve the condition. It is easy to use for the patient—they just click on the anatomic body part involved and a list of conditions comes up.
Rheumatology
American College of Rheumatology
www.rheumatology.org/Practice/Clinical/Patients/Information_for_Patients/
Who recommends it: Rick Pope, MPAS, PA-C, DFAAPA, CPAAPA
Why: Vetted by the American College of Rheumatologists, whose faculty is nationwide, altruistic, and collaborative, it is chock full of resources that are the standard of thinking and care for rheumatic conditions. It includes “scary” diagnoses such as lupus and rheumatoid arthritis, with short, patient-specific resources that can take the sting out of the perceived notions of these diseases. The information is available in Spanish and English. The Spanish information sheets can be provided to our Hispanic population and European populations that speak primarily Spanish. This is an awesome service for those of us on the East Coast and likely more helpful in parts of the country where Spanish is spoken more commonly.
How often does this happen to you? You walk into an exam room and ask the patient what brings him in today, and the reply is something like, “Well, doc, I have stomach cancer.” You do a double-take and scan the patient’s chart, looking for test results or notes from a referring provider. Finding nothing, you ask the patient for more information on his diagnosis. To your surprise/dismay/frustration, he says, “Naw, I Googled my symptoms and that’s what I came up with.”
While you can’t control the Web-surfing your patients do before they present, you can influence their information-seeking behavior once you’ve delivered a diagnosis and/or treatment plan. You know they (and their family/caregivers) will have questions about the patient’s condition and how it can be managed for the long term. You hope they’ll come to you for answers. But since they are likely to use the resources at their fingertips, you at least want to ensure the information they receive is accurate and trustworthy.
With that in mind, we asked several Clinician Reviews board members to share the Web sites that they recommend to their patients. Some, including Cathy St. Pierre, PhD, APRN, FNP-BC, FAANP, and Ellen Mandel, DMH, MPA, PA-C, CDE, cited behemoths such as the Mayo Clinic Web site (www.mayoclinic.com/health-information), lauding it for being up to date, easy to access, and “clear and data-driven.” Other board members, as you’ll see below, suggested specialty-specific sites.
Freddi I. Segal-Gidan, PhD, PA, may speak for many clinicians when she explains, “We offer these [resources] to patients and families as part of health education, acknowledging that learning about someone’s condition is the first step to better understanding what they are experiencing and how this may change over time—since most of what we deal with are progressive, lengthy illnesses and chronic disease management.”
If you have reliable Web-based resources that you recommend to your patients, please visit us on Facebook (www.facebook.com/ClinRev) to share them!
Alzheimer’s Disease
ADEAR—Alzheimer’s Disease Education and Referral Center
www.nia.nih.gov/alzheimers
Who recommends it: Freddi I. Segal-Gidan, PA, PhD
Why: Operated by the NIH/National Institute on Aging specifically to provide consumers with current, accurate, state-of-the-art information about Alzheimer’s disease and dementing illness
Also recommended: Alzheimer’s Association (www.alz.org); Family Caregiver Alliance (www.caregiver.org); UCSF Memory Center for information on frontotemporal dementia (www.memory.ucsf.edu/ftd); Foundation for Health in Aging (www.healthinaging.org); Kaiser Family Foundation for information about Medicare, Medicaid, and health policy related to aging (www.kff.org)
Cardiology
Cardiac Arrhythmias Research and Education Foundation, Inc (CARE)
www.longqt.org
Who recommends it: Lyle W. Larson, PhD, PA-C
Why: Provides an overview of long QT syndrome (eg, management, genetics); includes links to a study registry for persons with implantable cardioverters-defibrillators who are participating in sports and a complete list of medications to avoid in this patient population. The information is collated and disseminated by health care experts in this field and is updated continuously as new data emerges.
Also recommended: CredibleMeds™ (www.crediblemeds.org)
Dermatology
American Academy of Dermatology: For the Public
www.aad.org/for-the-public
Who recommends it: Joe R. Monroe, MPAS, PA
Why: Provides patient information about a specific topic or diagnosis that is reliable, up to date, and in understandable language.
eMedicine
http://emedicine.medscape.com
Who recommends it: Joe R. Monroe, MPAS, PA
Why: The information is current and written by authoritative dermatologists or other relevant specialists. References are copious and relevant, and links in the text guide readers to equally good information on related topics.
Caveats: The only problem with eMedicine is that it’s jargon-heavy and meant only for those who are comfortable with the terminology. I reserve this suggestion for more medically erudite patients (eg, nurses or PAs).
Diabetes
DiabetesMine
www.diabetesmine.com/
Who recommends it: Christine Kessler, RN, MN, CNS, ANP, BC-ADM
Why: This is an award-winning blog by an individual with type 1 diabetes, but it has something for every diabetic patient and his/her family. Really awesome. I recommend it to my patients, and some of them blog for it!
Also recommended: American Diabetes Association (www.diabetes.org/)
Nephrology
American Association of Kidney Patients
www.aakp.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: Their information is written for and by kidney patients. It is for all patients with kidney disease, not just dialysis patients. They offer free publications that emphasize living with kidney disease; these pubs are attractive, with realistic information.
Kidney School
www.kidneyschool.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: This site offers about 16 modules, each on a different topic ranging from dialysis options to sexuality. It is for patients and allows them to pick the topic they want and view the module as often as they wish.
National Kidney Foundation
www.kidney.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: The patient section of this site contains recipes and health information. Patients can register for the Kidney Peers Program, in which they match up either as a mentor or a mentee with another kidney patient in the US. It covers the range from moderate kidney disease to kidney failure and transplant.
Also recommended: DaVita (www.davita.com); Fresenius Medical Care (www.ultracare-dialysis.com)
Orthopedics
OrthoInfo
orthoinfo.aaos.org/
Who recommends it: Mike Rudzinski, RPh, RPA-C
Why: Endorsed by the American Academy of Orthopedic Surgeons, this site offers patients information on the most common musculoskeletal conditions. Includes patient education materials with anatomic pictures and discussion. This is my “go to” site for these conditions; it offers an incredible, comprehensive overview of the condition, options for care including potential surgery, and what the patient can do to improve the condition. It is easy to use for the patient—they just click on the anatomic body part involved and a list of conditions comes up.
Rheumatology
American College of Rheumatology
www.rheumatology.org/Practice/Clinical/Patients/Information_for_Patients/
Who recommends it: Rick Pope, MPAS, PA-C, DFAAPA, CPAAPA
Why: Vetted by the American College of Rheumatologists, whose faculty is nationwide, altruistic, and collaborative, it is chock full of resources that are the standard of thinking and care for rheumatic conditions. It includes “scary” diagnoses such as lupus and rheumatoid arthritis, with short, patient-specific resources that can take the sting out of the perceived notions of these diseases. The information is available in Spanish and English. The Spanish information sheets can be provided to our Hispanic population and European populations that speak primarily Spanish. This is an awesome service for those of us on the East Coast and likely more helpful in parts of the country where Spanish is spoken more commonly.
How often does this happen to you? You walk into an exam room and ask the patient what brings him in today, and the reply is something like, “Well, doc, I have stomach cancer.” You do a double-take and scan the patient’s chart, looking for test results or notes from a referring provider. Finding nothing, you ask the patient for more information on his diagnosis. To your surprise/dismay/frustration, he says, “Naw, I Googled my symptoms and that’s what I came up with.”
While you can’t control the Web-surfing your patients do before they present, you can influence their information-seeking behavior once you’ve delivered a diagnosis and/or treatment plan. You know they (and their family/caregivers) will have questions about the patient’s condition and how it can be managed for the long term. You hope they’ll come to you for answers. But since they are likely to use the resources at their fingertips, you at least want to ensure the information they receive is accurate and trustworthy.
With that in mind, we asked several Clinician Reviews board members to share the Web sites that they recommend to their patients. Some, including Cathy St. Pierre, PhD, APRN, FNP-BC, FAANP, and Ellen Mandel, DMH, MPA, PA-C, CDE, cited behemoths such as the Mayo Clinic Web site (www.mayoclinic.com/health-information), lauding it for being up to date, easy to access, and “clear and data-driven.” Other board members, as you’ll see below, suggested specialty-specific sites.
Freddi I. Segal-Gidan, PhD, PA, may speak for many clinicians when she explains, “We offer these [resources] to patients and families as part of health education, acknowledging that learning about someone’s condition is the first step to better understanding what they are experiencing and how this may change over time—since most of what we deal with are progressive, lengthy illnesses and chronic disease management.”
If you have reliable Web-based resources that you recommend to your patients, please visit us on Facebook (www.facebook.com/ClinRev) to share them!
Alzheimer’s Disease
ADEAR—Alzheimer’s Disease Education and Referral Center
www.nia.nih.gov/alzheimers
Who recommends it: Freddi I. Segal-Gidan, PA, PhD
Why: Operated by the NIH/National Institute on Aging specifically to provide consumers with current, accurate, state-of-the-art information about Alzheimer’s disease and dementing illness
Also recommended: Alzheimer’s Association (www.alz.org); Family Caregiver Alliance (www.caregiver.org); UCSF Memory Center for information on frontotemporal dementia (www.memory.ucsf.edu/ftd); Foundation for Health in Aging (www.healthinaging.org); Kaiser Family Foundation for information about Medicare, Medicaid, and health policy related to aging (www.kff.org)
Cardiology
Cardiac Arrhythmias Research and Education Foundation, Inc (CARE)
www.longqt.org
Who recommends it: Lyle W. Larson, PhD, PA-C
Why: Provides an overview of long QT syndrome (eg, management, genetics); includes links to a study registry for persons with implantable cardioverters-defibrillators who are participating in sports and a complete list of medications to avoid in this patient population. The information is collated and disseminated by health care experts in this field and is updated continuously as new data emerges.
Also recommended: CredibleMeds™ (www.crediblemeds.org)
Dermatology
American Academy of Dermatology: For the Public
www.aad.org/for-the-public
Who recommends it: Joe R. Monroe, MPAS, PA
Why: Provides patient information about a specific topic or diagnosis that is reliable, up to date, and in understandable language.
eMedicine
http://emedicine.medscape.com
Who recommends it: Joe R. Monroe, MPAS, PA
Why: The information is current and written by authoritative dermatologists or other relevant specialists. References are copious and relevant, and links in the text guide readers to equally good information on related topics.
Caveats: The only problem with eMedicine is that it’s jargon-heavy and meant only for those who are comfortable with the terminology. I reserve this suggestion for more medically erudite patients (eg, nurses or PAs).
Diabetes
DiabetesMine
www.diabetesmine.com/
Who recommends it: Christine Kessler, RN, MN, CNS, ANP, BC-ADM
Why: This is an award-winning blog by an individual with type 1 diabetes, but it has something for every diabetic patient and his/her family. Really awesome. I recommend it to my patients, and some of them blog for it!
Also recommended: American Diabetes Association (www.diabetes.org/)
Nephrology
American Association of Kidney Patients
www.aakp.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: Their information is written for and by kidney patients. It is for all patients with kidney disease, not just dialysis patients. They offer free publications that emphasize living with kidney disease; these pubs are attractive, with realistic information.
Kidney School
www.kidneyschool.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: This site offers about 16 modules, each on a different topic ranging from dialysis options to sexuality. It is for patients and allows them to pick the topic they want and view the module as often as they wish.
National Kidney Foundation
www.kidney.org
Who recommends it: Jane S. Davis, DNP, CRNP
Why: The patient section of this site contains recipes and health information. Patients can register for the Kidney Peers Program, in which they match up either as a mentor or a mentee with another kidney patient in the US. It covers the range from moderate kidney disease to kidney failure and transplant.
Also recommended: DaVita (www.davita.com); Fresenius Medical Care (www.ultracare-dialysis.com)
Orthopedics
OrthoInfo
orthoinfo.aaos.org/
Who recommends it: Mike Rudzinski, RPh, RPA-C
Why: Endorsed by the American Academy of Orthopedic Surgeons, this site offers patients information on the most common musculoskeletal conditions. Includes patient education materials with anatomic pictures and discussion. This is my “go to” site for these conditions; it offers an incredible, comprehensive overview of the condition, options for care including potential surgery, and what the patient can do to improve the condition. It is easy to use for the patient—they just click on the anatomic body part involved and a list of conditions comes up.
Rheumatology
American College of Rheumatology
www.rheumatology.org/Practice/Clinical/Patients/Information_for_Patients/
Who recommends it: Rick Pope, MPAS, PA-C, DFAAPA, CPAAPA
Why: Vetted by the American College of Rheumatologists, whose faculty is nationwide, altruistic, and collaborative, it is chock full of resources that are the standard of thinking and care for rheumatic conditions. It includes “scary” diagnoses such as lupus and rheumatoid arthritis, with short, patient-specific resources that can take the sting out of the perceived notions of these diseases. The information is available in Spanish and English. The Spanish information sheets can be provided to our Hispanic population and European populations that speak primarily Spanish. This is an awesome service for those of us on the East Coast and likely more helpful in parts of the country where Spanish is spoken more commonly.
Update on pelvic floor dysfunction: Focus on urinary incontinence
Urinary incontinence (UI) affects almost half of all women in the United States.1,2 Estimates suggest that the prevalence of UI gradually rises during young adult life, comes to a broad plateau in middle age, and then steadily increases from that plateau after age 65. Therefore, over the next 40 years, as the elderly population expands in size, the number of women affected by UI will significantly grow.3
For patients with UI, a multitude of therapeutic options are available. Which option is the best for your patient? In this article, we aim to answer that question by interpreting the results of four randomized trials, each of which directly compare two available treatment options. The first study examines patients with stress urinary incontinence (SUI), comparing the patients’ subjective improvement in urinary leakage and bladder function at 12 months after randomization to treatment with physiotherapy or midurethral sling surgery.
The three other trials examine patients with overactive bladder (OAB) and urgency urinary incontinence (UUI). Each trial directly compares the use of anticholinergic medications to an alternate treatment modality. Currently, anticholinergic medications and behavioral therapy are the recommended first-line therapies for OAB. Unfortunately, anticholinergic medications have poor patient compliance and significant systemic side effects.4 Caution should be used when considering anticholinergic medications in patients with impaired gastric emptying or a history of urinary retention. They also should be used with caution in elderly patients who are extremely frail. Additionally, clearance from an ophthalmologist must be obtained prior to starting anticholinergic medication in patients with narrow-angle glaucoma.5 Due to poor adherence and potential side effects, there is a growing effort to discover alternative treatment modalities that are safe and effective. Therefore, we chose to examine trials comparing: mirabegron versus tolterodine, percutaneous tibial nerve stimulation versus tolterodine, and onabotulinumtoxinA versus anticholingeric medications.
UI defined
Before discussing treatment options, we want to clarify the main types of UI (FIGURE). UI is defined as the complaint of involuntary loss of urine. UI can be subdivided into SUI, OAB/UUI, or mixed urinary incontinence.6 While there are other less common genitourinary etiologies that can lead to UI, nongenitourinary etiologies are prevalent and can aggravate existing SUI or OAB (TABLE).
SUI is the complaint of involuntary loss of urine on effort or physical exertion (such as during sporting activities) or on sneezing or coughing. Often, SUI can be diagnosed by patient report alone and surgery can be considered in symptomatic patients who demonstrate cough leakage on physical examination and normal postvoid residual volumes.
UUI is the involuntary loss of urine associated with urgency; it often occurs in the setting of OAB, which is defined as the syndrome of urinary urgency, usually accompanied by frequency and nocturia, with or without UUI, in the absence of urinary tract infection or other obvious pathology (such as neurologic dysfunction, infection, or urologic neoplasm). OAB-dry is present when patients do not have leakage with urgency, but are bothered by urgency, frequency, and/or nocturia. OAB-wet occurs when a patient has urgencyincontinence.
The presence of both SUI and OAB/UUI is known as mixed urinary incontinence. Stress and urgency urinary symptoms often present together. In fact, 10% to 30% of women with stress symptoms are found to have bladder overactivity on subsequent evaluation.2,7 Therefore, it is important to take a good history and consider urodynamic evaluation to confirm the diagnosis of SUI prior to surgery in women with mixed stress and urge symptoms, a history of a previous surgery for incontinence, or when there is a poor correlation of physical examination findings to reported symptoms.
Is surgery a first-line option for patients with SUI?
Labrie J, Berghmans BL, Fischer K, et al. Surgery versus physiotherapy for stress urinary incontinence. NEJM. 2013;369(12):1124−1133.
Physiotherapy, including pelvic floor muscle training (“Kegel exercises”), is utilized as a first-line treatment option for women with SUI that carries minimal risk for the patient. Midurethral sling surgery is often recommended if an initial trial of conservative treatment fails.7 Up to 50% of women treated with pelvic floor physiotherapy will ultimately undergo surgery to treat their SUI.8
Related article: Does urodynamic testing before surgery for stress incontinence improve outcomes? G. Willy Davila, MD (Examining the Evidence, December 2012)
Details of the study
This was a randomized, multicenter trial of women aged 35 to 80 years with moderate to severe SUI. After excluding women with previous incontinence surgery and stage 2 or higher pelvic organ prolapse, 460 participants were randomly assigned to undergo either a midurethral sling surgery or physiotherapy (pelvic floor muscle training). The primary outcome was subjective improvement in urinary leakage and bladder function at 12 months, as measured by the Patient Global Impression of Improvement (PGI-I), a 7-point Likert scale ranging from “very much worse” to “very much better.”
In an intention-to-treat analysis, subjective improvement at 12 months was significantly higher in women randomized to midurethral sling surgery than in women randomized to physiotherapy (91% vs 64%, respectively).
Ten percent of patients had adverse events (AEs); all were related to surgery. The most common AEs were hematoma, vaginal epithelial perforation, and bladder perforation.
Notably, women had the option to cross over to the other treatment modality if they desired. In the physiotherapy group, 49% of women elected to cross over to surgery, while 11% of those who underwent midurethral sling surgery elected to cross over to physiotherapy during the 12-month follow-up period. When analyzing results by treatment received, the investigators found that the proportion of women who reported improvement was significantly lower among women who underwent physiotherapy only (32%), versus sling only (94%), or sling after physiotherapy (91%).
This randomized trial was well-designed and included a variety of treatment centers (university and general hospitals) with interventions performed by experienced surgeons (all of whom had performed at least 20 sling surgeries) and physiotherapists educated specifically in pelvic floor physiotherapy. The study population was limited to patients with moderate to severe SUI as defined by the Sandvik severity index.9 Therefore, these results may not be applicable to patients with milder symptoms, for whom physiotherapy has been recommended as first-line therapy with consideration of surgery if physiotherapy fails to sufficiently improve symptoms.7
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Women with moderate to severe SUI without significant prolapse or a history of prior incontinence surgery have significantly better outcomes at 12 months after undergoing midurethral sling surgery versus physiotherapy. Physiotherapy carries little to no risk of adverse effects. Women with moderate to severe SUI should be counseled regarding the risks and benefits of both physiotherapy and midurethral sling surgery as initial treatment options.
Because stress and urgency urinary symptoms often present together, it is important to consider urodynamic evaluation to confirm SUI prior to surgery in women with:
• mixed stress and urge symptoms
• a history of a previous surgery for incontinence, or
• poor correlation of physical examination findings to reported symptoms.
Safety and tolerability of mirabegron versus tolterodine for OAB
Chapple CR, Kaplan SA, Mitcheson D, et al. Randomized double-blind, active-controlled phase 3 study to assess 12-month safety and efficacy of mirabegron, a beta(3)-adrenoceptor agonist, in overactive bladder. Eur Urol. 2013;63(2):296−305.
In the bladder, beta3-receptors located within the detrusor smooth muscle facilitate urine storage by relaxing the detrusor, enabling the bladder to fill.10 The activation of beta3-receptors is thought to increase the bladder’s ability to store urine, with the goal of decreasing urgency, frequency, nocturia, and urgency incontinence. An alternative to anticholinergic medications, mirabegron is a beta3-agonist approved by the US Food and Drug Administration (FDA) in 2012 for clinical use in the treatment of OAB.
Details of the study
Chapple and colleagues aimed to assess the 12-month efficacy and safety of mirabegron in a randomized, double-blind active controlled trial. The primary outcome was incidence and severity of treatment-emergent adverse effects (TEAEs); the secondary outcome was the change in OAB symptoms from baseline to up to 12 months. Patients experiencing OAB symptoms for more than 3 months were eligible and were subsequently enrolled if they averaged 8 or more voids per day and 3 or more episodes of urgency with or without incontinence on a 3-day bladder diary. A total of 2,444 patients were randomly assigned in a 1:1:1 fashion to mirabegron 50 mg daily, mirabegron 100 mg daily, or tolterodine extended release (ER) 4 mg daily.
There was a similar incidence (60% to 63%) of TEAEs across all three groups. The most common TEAEs were hypertension (defined as average systolic blood pressure [BP] >140 mm Hg or average diastolic BP >90 mm Hg at two consecutive visits), UTI, headache, nasopharyngitis, and constipation. The adjusted mean changes in BP from baseline to final visit were less than 1 mm Hg for both systolic and diastolic BP for patients taking both doses of mirabegron, as well as for patients taking tolterodine. The incidence of dry mouth was higher in the tolterodine group than the mirabegron groups. Mirabegron 50 mg daily and 100 mg daily improved incontinence symptoms within 1 month of starting therapy; the degree of improvement was similar to that seen in the patients taking tolterodine ER 4 mg daily.
Related article: New overactive bladder treatment approved by the FDA (August 2012)
Some caveats
This study was well-designed to assess the safety and tolerability of mirabegron versus tolterodine. The doses utilized in the study were at or above the FDA-approved dosage of 25 mg to 50 mg daily for OAB treatment. Although investigators found mirabegron to be a safe alternative to anticholinergic medication, the study was not designed or powered to examine the efficacy of mirabegron versus tolterodine. No formal comparison of efficacy was made between mirabegron or tolterodine, or between the 50-mg and 100-mg doses of mirabegron. Moreover, 81% of participants had been treated with mirabegron in earlier Phase 3 studies, so most were not treatment naïve, limiting the applicability of results.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Mirabegron should be considered as a potential treatment option for patients who demonstrate poor tolerance of or response to anticholinergic medications; however, caution should be used in patients with severe uncontrolled high BP, end-stage kidney disease, or severe liver impairment.
Consider percutaneous tibial nerve stimulation over tolterodine for OAB in select patients
Peters KM, Macdiarmid SA, Wooldridge LS, et al. Randomized trial of percutaneous tibial nerve stimulation versus extended-release tolterodine: Results from the overactive bladder innovative therapy trial. J Urol. 2009;182(3):1055−1061.
Neuromodulation utilizes electrical stimulation to improve bladder function and decrease OAB symptoms. First developed in the early 1980s by McGuire and colleagues, percutaneous tibial nerve stimulation (PTNS) was approved by the FDA in 2000 as Urgent PC and provides an outpatient, nonimplantable neuromodulation alternative to medication therapy for patients with OAB.11,12 By directly stimulating the posterior tibial nerve, PTNS works via the S3 sacral nerve plexus to alter the micturition reflex and improve bladder function.
Details of the study
Patients were eligible for the study if they demonstrated 8 or more voids per day on a 3-day bladder diary (whether or not they had a history of previous anticholinergic drug use). A total of 100 ambulatory adults with OAB symptoms were enrolled and randomly assigned to PTNS 30-minutes per week or tolterodine ER 4 mg daily.
At 12 weeks, both groups demonstrated a significant improvement in OAB measures as well as validated symptom severity and quality-of-life questionnaire scores. Subjective assessment of improvement in OAB symptoms was significantly greater in the PTNS group than in the tolterodine group (79.5% vs 54.8%, respectively; P = .01). However, mean reduction of voids for 24 hours was not significantly different between the two groups.
Both treatments were well tolerated, with only 15% to 16% of patients in both groups reporting mild to moderate side effects. The tolterodine group did have a significantly higher risk of dry mouth; however, the risk of constipation was not significantly different between the groups.
Study limitations
The authors performed an important multicenter, nonblinded, randomized, controlled trial, which was one of the first trials to directly compare two OAB therapies. The generalizability of the findings were limited, as the cohort included mostly patients with dry OAB who had no objective measures on UUI episodes. In addition, this trial had a limited observation period of only 12 weeks. Information regarding the effect of treatment after cessation of weekly PTNS therapy was not examined. Therefore, we are not able to determine whether repeat sessions provide adequate maintenance in the long term.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
PTNS 30 minutes daily is as effective as tolterodine ER 4 mg daily for 12 weeks in reducing OAB symptoms. PTNS is a safe alternative that should be considered in patients with OAB who poorly tolerate or have contraindications to medication therapy.
OnabotulinumtoxinA is an effective therapy for OAB
Visco AG, Brubaker L, Richter HE, et al. Anticholinergic therapy vs onabotulinumtoxinA for urgency urinary incontinence. NEJM. 2012;367(19):1803−1813.
The newest therapy for OAB is onabotulinumtoxinA, or Botox, which was FDA approved this year for the treatment of OAB in adults who cannot use or do not tolerate anticholinergic medications. Recommended doses are 100 U onabotulinumtoxinA in patients with idiopathic refractory OAB and 200 U onabotulinumtoxinA for patients with neurogenic OAB.
OnabotulinumtoxinA is a neurotoxin that blocks synaptic transmission at the neuromuscular junction to cause muscle paralysis and atrophy.13 Injecting onabotulinumtoxinA into the detrusor smooth muscle should relax the bladder and decrease sensations of urgency and frequency to achieve a longer duration of time for bladder filling and reduce the risk of urgency incontinence.
Effects of onabotulinumtoxinA appear to wear off over time, and patients may require repeat injections. Side effects of onabotulinumtoxinA therapy include an increased risk of UTI and the potential for urinary retention requiring intermittent self-catheterization.
Related article: Update on Pelvic Floor Dysfunction Autumn L. Edenfield, MD, and Cindy L. Amundsen, MD (October 2012)
Details of the study
The Anticholinergic Versus Botulinum Toxin Comparison (ABC) study was a multicenter, randomized, double-blind, double-placebo–controlled trial conducted in women without known neurologic disease with moderate to severe UUI (defined as >5 UUI episodes on a 3-day bladder diary). Women were randomly assigned to a single intradetrusor injection of 100 U onabotulinumtoxinA plus oral placebo or to a single intradetrusor injection of saline plus solifenacin 5 mg daily (with the option of dose escalation and then switching to trospium XR if no improvement was seen).
Of the 241 women included in the final analysis, approximately 70% in each group reported adequate control of symptoms at 6 months. Adequate control was defined as a response of “agree strongly” or “agree” to the statement: “This treatment has given me adequate control of my urinary leakage.” Women in the onabotulinumtoxinA group were significantly more likely than women in the anticholinergic medication group to report complete resolution of UUI at 6 months (27% vs 13%, P = .003). However, the mean reduction in episodes of UUI per day and the improvements in quality-of-life questionnaire scores were found to be similar. Interestingly, worse baseline UUI was associated with greater reduction in episodes of UUI for both therapies.
This was a rigorous and well-executed double-blind, double-placebo−controlled randomized trial. By utilizing broad inclusion criteria and enrolling patients both with and without previous exposure to anticholinergic medications, the generalizability of study findings are greatly improved. Because this study did not examine the effect or efficacy of repeat injections, these findings have limited applicability to patients undergoing multiple onabotulinumtoxinA injections.
When considering use in your patient population, keep the possible side effects in mind.There were important differences in the side effects experienced with each therapy. Specifically, while the anticholinergic group had a higher frequency of dry mouth (46% anticholinergic vs 31% onabotulinumtoxinA, P = .02), the onabotulinumtoxinA group demonstrated higher rates of incomplete bladder emptying requiring catheterization (peak of 5% at 2 months) and greater risk of UTI (33% onabotulinumtoxinA vs 13% anticholinergic, P <.001).
WHAT THIS EVIDENCE MEANS FOR PRACTICE
This study showed that, among women with UUI, anticholinergic medication and onabotulinumtoxinA are equally effective in reducing UUI episodes and improving quality of life. It is important to consider the side effect profile, determine the patient’s preferences, and weigh the risks and benefits of each therapy when deciding what is the best treatment for your individual patient.
We want to hear from you! Tell us what you think.
- Anger JT, Saigal CS, Litwin MS. The prevalence of urinary incontinence among community dwelling adult women: Results from the National Health and Nutrition Examination Survey. J Urol. 2006;175(2):601–604.
- Dooley Y, Kenton K, Cao G, et al. Urinary incontinence prevalence: Results from the National Health and Nutrition Examination Survey. J Urol. 2008;179(2):656–661.
- Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in U.S. Women: 2010 to 2050. Obstetr Gynecol. 2009;114(6):1278–1283.
- Gormley EA, Lightner DJ, Burgio KL, et al. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU Guideline. Americal Urological Association. http://www.auanet.org/common/pdf/education/clinical-guidance/Overactive-Bladder.pdf. Published 2012. Revised June 11, 2013. Accessed October 21, 2013.
- Yu YF, Nichol MB, Yu AP, Ahn J. Persistence and adherence of medications for chronic overactive bladder/urinary incontinence in the California Medicaid program. Value Health. 2005;8(4):495–505.
- Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26.
- ACOG Practice Bulletin No. 63: Urinary incontinence in women. American College of Obstetricians and Gynecologists. Obstetr Gynecol. 2005;105(6):1533–1545.
- Bo K, Kvarstein B, Nygaard I. Lower urinary tract symptoms and pelvic floor muscle exercise adherence after 15 years. Obstetr Gynecol. 2005;105(5 Pt 1):999–1005.
- Sandvik H, Hunskaar S, Seim A, Hermstad R, Vanvik A, Bratt H. Validation of a severity index in female urinary incontinence and its implementation in an epidemiological survey. J Epidemiol Community Health. 1993;47(6):497–499.
- Fowler CJ, Griffiths D, de Groat WC. The neural control of micturition. Nat Rev Neurosci. 2008;9(6):453–466.
- Levin PJ, Wu JM, Kawasaki A, Weidner AC, Amundsen CL. The efficacy of posterior tibial nerve stimulation for the treatment of overactive bladder in women: a systematic review. Int Urogynecol J. 2012;23(11):1591–1597.
- McGuire EJ, Zhang SC, Horwinski ER, Lytton B. Treatment of motor and sensory detrusor instability by electrical stimulation. J Urol. 1983;129(1):78–79.
- Schiavo G, Santucci A, Dasgupta BR, et al. Botulinum neurotoxins serotypes A and E cleave SNAP-25 at distinct COOH-terminal peptide bonds. FEBS Lett. 1993;335(1):99–103.
Urinary incontinence (UI) affects almost half of all women in the United States.1,2 Estimates suggest that the prevalence of UI gradually rises during young adult life, comes to a broad plateau in middle age, and then steadily increases from that plateau after age 65. Therefore, over the next 40 years, as the elderly population expands in size, the number of women affected by UI will significantly grow.3
For patients with UI, a multitude of therapeutic options are available. Which option is the best for your patient? In this article, we aim to answer that question by interpreting the results of four randomized trials, each of which directly compare two available treatment options. The first study examines patients with stress urinary incontinence (SUI), comparing the patients’ subjective improvement in urinary leakage and bladder function at 12 months after randomization to treatment with physiotherapy or midurethral sling surgery.
The three other trials examine patients with overactive bladder (OAB) and urgency urinary incontinence (UUI). Each trial directly compares the use of anticholinergic medications to an alternate treatment modality. Currently, anticholinergic medications and behavioral therapy are the recommended first-line therapies for OAB. Unfortunately, anticholinergic medications have poor patient compliance and significant systemic side effects.4 Caution should be used when considering anticholinergic medications in patients with impaired gastric emptying or a history of urinary retention. They also should be used with caution in elderly patients who are extremely frail. Additionally, clearance from an ophthalmologist must be obtained prior to starting anticholinergic medication in patients with narrow-angle glaucoma.5 Due to poor adherence and potential side effects, there is a growing effort to discover alternative treatment modalities that are safe and effective. Therefore, we chose to examine trials comparing: mirabegron versus tolterodine, percutaneous tibial nerve stimulation versus tolterodine, and onabotulinumtoxinA versus anticholingeric medications.
UI defined
Before discussing treatment options, we want to clarify the main types of UI (FIGURE). UI is defined as the complaint of involuntary loss of urine. UI can be subdivided into SUI, OAB/UUI, or mixed urinary incontinence.6 While there are other less common genitourinary etiologies that can lead to UI, nongenitourinary etiologies are prevalent and can aggravate existing SUI or OAB (TABLE).
SUI is the complaint of involuntary loss of urine on effort or physical exertion (such as during sporting activities) or on sneezing or coughing. Often, SUI can be diagnosed by patient report alone and surgery can be considered in symptomatic patients who demonstrate cough leakage on physical examination and normal postvoid residual volumes.
UUI is the involuntary loss of urine associated with urgency; it often occurs in the setting of OAB, which is defined as the syndrome of urinary urgency, usually accompanied by frequency and nocturia, with or without UUI, in the absence of urinary tract infection or other obvious pathology (such as neurologic dysfunction, infection, or urologic neoplasm). OAB-dry is present when patients do not have leakage with urgency, but are bothered by urgency, frequency, and/or nocturia. OAB-wet occurs when a patient has urgencyincontinence.
The presence of both SUI and OAB/UUI is known as mixed urinary incontinence. Stress and urgency urinary symptoms often present together. In fact, 10% to 30% of women with stress symptoms are found to have bladder overactivity on subsequent evaluation.2,7 Therefore, it is important to take a good history and consider urodynamic evaluation to confirm the diagnosis of SUI prior to surgery in women with mixed stress and urge symptoms, a history of a previous surgery for incontinence, or when there is a poor correlation of physical examination findings to reported symptoms.
Is surgery a first-line option for patients with SUI?
Labrie J, Berghmans BL, Fischer K, et al. Surgery versus physiotherapy for stress urinary incontinence. NEJM. 2013;369(12):1124−1133.
Physiotherapy, including pelvic floor muscle training (“Kegel exercises”), is utilized as a first-line treatment option for women with SUI that carries minimal risk for the patient. Midurethral sling surgery is often recommended if an initial trial of conservative treatment fails.7 Up to 50% of women treated with pelvic floor physiotherapy will ultimately undergo surgery to treat their SUI.8
Related article: Does urodynamic testing before surgery for stress incontinence improve outcomes? G. Willy Davila, MD (Examining the Evidence, December 2012)
Details of the study
This was a randomized, multicenter trial of women aged 35 to 80 years with moderate to severe SUI. After excluding women with previous incontinence surgery and stage 2 or higher pelvic organ prolapse, 460 participants were randomly assigned to undergo either a midurethral sling surgery or physiotherapy (pelvic floor muscle training). The primary outcome was subjective improvement in urinary leakage and bladder function at 12 months, as measured by the Patient Global Impression of Improvement (PGI-I), a 7-point Likert scale ranging from “very much worse” to “very much better.”
In an intention-to-treat analysis, subjective improvement at 12 months was significantly higher in women randomized to midurethral sling surgery than in women randomized to physiotherapy (91% vs 64%, respectively).
Ten percent of patients had adverse events (AEs); all were related to surgery. The most common AEs were hematoma, vaginal epithelial perforation, and bladder perforation.
Notably, women had the option to cross over to the other treatment modality if they desired. In the physiotherapy group, 49% of women elected to cross over to surgery, while 11% of those who underwent midurethral sling surgery elected to cross over to physiotherapy during the 12-month follow-up period. When analyzing results by treatment received, the investigators found that the proportion of women who reported improvement was significantly lower among women who underwent physiotherapy only (32%), versus sling only (94%), or sling after physiotherapy (91%).
This randomized trial was well-designed and included a variety of treatment centers (university and general hospitals) with interventions performed by experienced surgeons (all of whom had performed at least 20 sling surgeries) and physiotherapists educated specifically in pelvic floor physiotherapy. The study population was limited to patients with moderate to severe SUI as defined by the Sandvik severity index.9 Therefore, these results may not be applicable to patients with milder symptoms, for whom physiotherapy has been recommended as first-line therapy with consideration of surgery if physiotherapy fails to sufficiently improve symptoms.7
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Women with moderate to severe SUI without significant prolapse or a history of prior incontinence surgery have significantly better outcomes at 12 months after undergoing midurethral sling surgery versus physiotherapy. Physiotherapy carries little to no risk of adverse effects. Women with moderate to severe SUI should be counseled regarding the risks and benefits of both physiotherapy and midurethral sling surgery as initial treatment options.
Because stress and urgency urinary symptoms often present together, it is important to consider urodynamic evaluation to confirm SUI prior to surgery in women with:
• mixed stress and urge symptoms
• a history of a previous surgery for incontinence, or
• poor correlation of physical examination findings to reported symptoms.
Safety and tolerability of mirabegron versus tolterodine for OAB
Chapple CR, Kaplan SA, Mitcheson D, et al. Randomized double-blind, active-controlled phase 3 study to assess 12-month safety and efficacy of mirabegron, a beta(3)-adrenoceptor agonist, in overactive bladder. Eur Urol. 2013;63(2):296−305.
In the bladder, beta3-receptors located within the detrusor smooth muscle facilitate urine storage by relaxing the detrusor, enabling the bladder to fill.10 The activation of beta3-receptors is thought to increase the bladder’s ability to store urine, with the goal of decreasing urgency, frequency, nocturia, and urgency incontinence. An alternative to anticholinergic medications, mirabegron is a beta3-agonist approved by the US Food and Drug Administration (FDA) in 2012 for clinical use in the treatment of OAB.
Details of the study
Chapple and colleagues aimed to assess the 12-month efficacy and safety of mirabegron in a randomized, double-blind active controlled trial. The primary outcome was incidence and severity of treatment-emergent adverse effects (TEAEs); the secondary outcome was the change in OAB symptoms from baseline to up to 12 months. Patients experiencing OAB symptoms for more than 3 months were eligible and were subsequently enrolled if they averaged 8 or more voids per day and 3 or more episodes of urgency with or without incontinence on a 3-day bladder diary. A total of 2,444 patients were randomly assigned in a 1:1:1 fashion to mirabegron 50 mg daily, mirabegron 100 mg daily, or tolterodine extended release (ER) 4 mg daily.
There was a similar incidence (60% to 63%) of TEAEs across all three groups. The most common TEAEs were hypertension (defined as average systolic blood pressure [BP] >140 mm Hg or average diastolic BP >90 mm Hg at two consecutive visits), UTI, headache, nasopharyngitis, and constipation. The adjusted mean changes in BP from baseline to final visit were less than 1 mm Hg for both systolic and diastolic BP for patients taking both doses of mirabegron, as well as for patients taking tolterodine. The incidence of dry mouth was higher in the tolterodine group than the mirabegron groups. Mirabegron 50 mg daily and 100 mg daily improved incontinence symptoms within 1 month of starting therapy; the degree of improvement was similar to that seen in the patients taking tolterodine ER 4 mg daily.
Related article: New overactive bladder treatment approved by the FDA (August 2012)
Some caveats
This study was well-designed to assess the safety and tolerability of mirabegron versus tolterodine. The doses utilized in the study were at or above the FDA-approved dosage of 25 mg to 50 mg daily for OAB treatment. Although investigators found mirabegron to be a safe alternative to anticholinergic medication, the study was not designed or powered to examine the efficacy of mirabegron versus tolterodine. No formal comparison of efficacy was made between mirabegron or tolterodine, or between the 50-mg and 100-mg doses of mirabegron. Moreover, 81% of participants had been treated with mirabegron in earlier Phase 3 studies, so most were not treatment naïve, limiting the applicability of results.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Mirabegron should be considered as a potential treatment option for patients who demonstrate poor tolerance of or response to anticholinergic medications; however, caution should be used in patients with severe uncontrolled high BP, end-stage kidney disease, or severe liver impairment.
Consider percutaneous tibial nerve stimulation over tolterodine for OAB in select patients
Peters KM, Macdiarmid SA, Wooldridge LS, et al. Randomized trial of percutaneous tibial nerve stimulation versus extended-release tolterodine: Results from the overactive bladder innovative therapy trial. J Urol. 2009;182(3):1055−1061.
Neuromodulation utilizes electrical stimulation to improve bladder function and decrease OAB symptoms. First developed in the early 1980s by McGuire and colleagues, percutaneous tibial nerve stimulation (PTNS) was approved by the FDA in 2000 as Urgent PC and provides an outpatient, nonimplantable neuromodulation alternative to medication therapy for patients with OAB.11,12 By directly stimulating the posterior tibial nerve, PTNS works via the S3 sacral nerve plexus to alter the micturition reflex and improve bladder function.
Details of the study
Patients were eligible for the study if they demonstrated 8 or more voids per day on a 3-day bladder diary (whether or not they had a history of previous anticholinergic drug use). A total of 100 ambulatory adults with OAB symptoms were enrolled and randomly assigned to PTNS 30-minutes per week or tolterodine ER 4 mg daily.
At 12 weeks, both groups demonstrated a significant improvement in OAB measures as well as validated symptom severity and quality-of-life questionnaire scores. Subjective assessment of improvement in OAB symptoms was significantly greater in the PTNS group than in the tolterodine group (79.5% vs 54.8%, respectively; P = .01). However, mean reduction of voids for 24 hours was not significantly different between the two groups.
Both treatments were well tolerated, with only 15% to 16% of patients in both groups reporting mild to moderate side effects. The tolterodine group did have a significantly higher risk of dry mouth; however, the risk of constipation was not significantly different between the groups.
Study limitations
The authors performed an important multicenter, nonblinded, randomized, controlled trial, which was one of the first trials to directly compare two OAB therapies. The generalizability of the findings were limited, as the cohort included mostly patients with dry OAB who had no objective measures on UUI episodes. In addition, this trial had a limited observation period of only 12 weeks. Information regarding the effect of treatment after cessation of weekly PTNS therapy was not examined. Therefore, we are not able to determine whether repeat sessions provide adequate maintenance in the long term.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
PTNS 30 minutes daily is as effective as tolterodine ER 4 mg daily for 12 weeks in reducing OAB symptoms. PTNS is a safe alternative that should be considered in patients with OAB who poorly tolerate or have contraindications to medication therapy.
OnabotulinumtoxinA is an effective therapy for OAB
Visco AG, Brubaker L, Richter HE, et al. Anticholinergic therapy vs onabotulinumtoxinA for urgency urinary incontinence. NEJM. 2012;367(19):1803−1813.
The newest therapy for OAB is onabotulinumtoxinA, or Botox, which was FDA approved this year for the treatment of OAB in adults who cannot use or do not tolerate anticholinergic medications. Recommended doses are 100 U onabotulinumtoxinA in patients with idiopathic refractory OAB and 200 U onabotulinumtoxinA for patients with neurogenic OAB.
OnabotulinumtoxinA is a neurotoxin that blocks synaptic transmission at the neuromuscular junction to cause muscle paralysis and atrophy.13 Injecting onabotulinumtoxinA into the detrusor smooth muscle should relax the bladder and decrease sensations of urgency and frequency to achieve a longer duration of time for bladder filling and reduce the risk of urgency incontinence.
Effects of onabotulinumtoxinA appear to wear off over time, and patients may require repeat injections. Side effects of onabotulinumtoxinA therapy include an increased risk of UTI and the potential for urinary retention requiring intermittent self-catheterization.
Related article: Update on Pelvic Floor Dysfunction Autumn L. Edenfield, MD, and Cindy L. Amundsen, MD (October 2012)
Details of the study
The Anticholinergic Versus Botulinum Toxin Comparison (ABC) study was a multicenter, randomized, double-blind, double-placebo–controlled trial conducted in women without known neurologic disease with moderate to severe UUI (defined as >5 UUI episodes on a 3-day bladder diary). Women were randomly assigned to a single intradetrusor injection of 100 U onabotulinumtoxinA plus oral placebo or to a single intradetrusor injection of saline plus solifenacin 5 mg daily (with the option of dose escalation and then switching to trospium XR if no improvement was seen).
Of the 241 women included in the final analysis, approximately 70% in each group reported adequate control of symptoms at 6 months. Adequate control was defined as a response of “agree strongly” or “agree” to the statement: “This treatment has given me adequate control of my urinary leakage.” Women in the onabotulinumtoxinA group were significantly more likely than women in the anticholinergic medication group to report complete resolution of UUI at 6 months (27% vs 13%, P = .003). However, the mean reduction in episodes of UUI per day and the improvements in quality-of-life questionnaire scores were found to be similar. Interestingly, worse baseline UUI was associated with greater reduction in episodes of UUI for both therapies.
This was a rigorous and well-executed double-blind, double-placebo−controlled randomized trial. By utilizing broad inclusion criteria and enrolling patients both with and without previous exposure to anticholinergic medications, the generalizability of study findings are greatly improved. Because this study did not examine the effect or efficacy of repeat injections, these findings have limited applicability to patients undergoing multiple onabotulinumtoxinA injections.
When considering use in your patient population, keep the possible side effects in mind.There were important differences in the side effects experienced with each therapy. Specifically, while the anticholinergic group had a higher frequency of dry mouth (46% anticholinergic vs 31% onabotulinumtoxinA, P = .02), the onabotulinumtoxinA group demonstrated higher rates of incomplete bladder emptying requiring catheterization (peak of 5% at 2 months) and greater risk of UTI (33% onabotulinumtoxinA vs 13% anticholinergic, P <.001).
WHAT THIS EVIDENCE MEANS FOR PRACTICE
This study showed that, among women with UUI, anticholinergic medication and onabotulinumtoxinA are equally effective in reducing UUI episodes and improving quality of life. It is important to consider the side effect profile, determine the patient’s preferences, and weigh the risks and benefits of each therapy when deciding what is the best treatment for your individual patient.
We want to hear from you! Tell us what you think.
Urinary incontinence (UI) affects almost half of all women in the United States.1,2 Estimates suggest that the prevalence of UI gradually rises during young adult life, comes to a broad plateau in middle age, and then steadily increases from that plateau after age 65. Therefore, over the next 40 years, as the elderly population expands in size, the number of women affected by UI will significantly grow.3
For patients with UI, a multitude of therapeutic options are available. Which option is the best for your patient? In this article, we aim to answer that question by interpreting the results of four randomized trials, each of which directly compare two available treatment options. The first study examines patients with stress urinary incontinence (SUI), comparing the patients’ subjective improvement in urinary leakage and bladder function at 12 months after randomization to treatment with physiotherapy or midurethral sling surgery.
The three other trials examine patients with overactive bladder (OAB) and urgency urinary incontinence (UUI). Each trial directly compares the use of anticholinergic medications to an alternate treatment modality. Currently, anticholinergic medications and behavioral therapy are the recommended first-line therapies for OAB. Unfortunately, anticholinergic medications have poor patient compliance and significant systemic side effects.4 Caution should be used when considering anticholinergic medications in patients with impaired gastric emptying or a history of urinary retention. They also should be used with caution in elderly patients who are extremely frail. Additionally, clearance from an ophthalmologist must be obtained prior to starting anticholinergic medication in patients with narrow-angle glaucoma.5 Due to poor adherence and potential side effects, there is a growing effort to discover alternative treatment modalities that are safe and effective. Therefore, we chose to examine trials comparing: mirabegron versus tolterodine, percutaneous tibial nerve stimulation versus tolterodine, and onabotulinumtoxinA versus anticholingeric medications.
UI defined
Before discussing treatment options, we want to clarify the main types of UI (FIGURE). UI is defined as the complaint of involuntary loss of urine. UI can be subdivided into SUI, OAB/UUI, or mixed urinary incontinence.6 While there are other less common genitourinary etiologies that can lead to UI, nongenitourinary etiologies are prevalent and can aggravate existing SUI or OAB (TABLE).
SUI is the complaint of involuntary loss of urine on effort or physical exertion (such as during sporting activities) or on sneezing or coughing. Often, SUI can be diagnosed by patient report alone and surgery can be considered in symptomatic patients who demonstrate cough leakage on physical examination and normal postvoid residual volumes.
UUI is the involuntary loss of urine associated with urgency; it often occurs in the setting of OAB, which is defined as the syndrome of urinary urgency, usually accompanied by frequency and nocturia, with or without UUI, in the absence of urinary tract infection or other obvious pathology (such as neurologic dysfunction, infection, or urologic neoplasm). OAB-dry is present when patients do not have leakage with urgency, but are bothered by urgency, frequency, and/or nocturia. OAB-wet occurs when a patient has urgencyincontinence.
The presence of both SUI and OAB/UUI is known as mixed urinary incontinence. Stress and urgency urinary symptoms often present together. In fact, 10% to 30% of women with stress symptoms are found to have bladder overactivity on subsequent evaluation.2,7 Therefore, it is important to take a good history and consider urodynamic evaluation to confirm the diagnosis of SUI prior to surgery in women with mixed stress and urge symptoms, a history of a previous surgery for incontinence, or when there is a poor correlation of physical examination findings to reported symptoms.
Is surgery a first-line option for patients with SUI?
Labrie J, Berghmans BL, Fischer K, et al. Surgery versus physiotherapy for stress urinary incontinence. NEJM. 2013;369(12):1124−1133.
Physiotherapy, including pelvic floor muscle training (“Kegel exercises”), is utilized as a first-line treatment option for women with SUI that carries minimal risk for the patient. Midurethral sling surgery is often recommended if an initial trial of conservative treatment fails.7 Up to 50% of women treated with pelvic floor physiotherapy will ultimately undergo surgery to treat their SUI.8
Related article: Does urodynamic testing before surgery for stress incontinence improve outcomes? G. Willy Davila, MD (Examining the Evidence, December 2012)
Details of the study
This was a randomized, multicenter trial of women aged 35 to 80 years with moderate to severe SUI. After excluding women with previous incontinence surgery and stage 2 or higher pelvic organ prolapse, 460 participants were randomly assigned to undergo either a midurethral sling surgery or physiotherapy (pelvic floor muscle training). The primary outcome was subjective improvement in urinary leakage and bladder function at 12 months, as measured by the Patient Global Impression of Improvement (PGI-I), a 7-point Likert scale ranging from “very much worse” to “very much better.”
In an intention-to-treat analysis, subjective improvement at 12 months was significantly higher in women randomized to midurethral sling surgery than in women randomized to physiotherapy (91% vs 64%, respectively).
Ten percent of patients had adverse events (AEs); all were related to surgery. The most common AEs were hematoma, vaginal epithelial perforation, and bladder perforation.
Notably, women had the option to cross over to the other treatment modality if they desired. In the physiotherapy group, 49% of women elected to cross over to surgery, while 11% of those who underwent midurethral sling surgery elected to cross over to physiotherapy during the 12-month follow-up period. When analyzing results by treatment received, the investigators found that the proportion of women who reported improvement was significantly lower among women who underwent physiotherapy only (32%), versus sling only (94%), or sling after physiotherapy (91%).
This randomized trial was well-designed and included a variety of treatment centers (university and general hospitals) with interventions performed by experienced surgeons (all of whom had performed at least 20 sling surgeries) and physiotherapists educated specifically in pelvic floor physiotherapy. The study population was limited to patients with moderate to severe SUI as defined by the Sandvik severity index.9 Therefore, these results may not be applicable to patients with milder symptoms, for whom physiotherapy has been recommended as first-line therapy with consideration of surgery if physiotherapy fails to sufficiently improve symptoms.7
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Women with moderate to severe SUI without significant prolapse or a history of prior incontinence surgery have significantly better outcomes at 12 months after undergoing midurethral sling surgery versus physiotherapy. Physiotherapy carries little to no risk of adverse effects. Women with moderate to severe SUI should be counseled regarding the risks and benefits of both physiotherapy and midurethral sling surgery as initial treatment options.
Because stress and urgency urinary symptoms often present together, it is important to consider urodynamic evaluation to confirm SUI prior to surgery in women with:
• mixed stress and urge symptoms
• a history of a previous surgery for incontinence, or
• poor correlation of physical examination findings to reported symptoms.
Safety and tolerability of mirabegron versus tolterodine for OAB
Chapple CR, Kaplan SA, Mitcheson D, et al. Randomized double-blind, active-controlled phase 3 study to assess 12-month safety and efficacy of mirabegron, a beta(3)-adrenoceptor agonist, in overactive bladder. Eur Urol. 2013;63(2):296−305.
In the bladder, beta3-receptors located within the detrusor smooth muscle facilitate urine storage by relaxing the detrusor, enabling the bladder to fill.10 The activation of beta3-receptors is thought to increase the bladder’s ability to store urine, with the goal of decreasing urgency, frequency, nocturia, and urgency incontinence. An alternative to anticholinergic medications, mirabegron is a beta3-agonist approved by the US Food and Drug Administration (FDA) in 2012 for clinical use in the treatment of OAB.
Details of the study
Chapple and colleagues aimed to assess the 12-month efficacy and safety of mirabegron in a randomized, double-blind active controlled trial. The primary outcome was incidence and severity of treatment-emergent adverse effects (TEAEs); the secondary outcome was the change in OAB symptoms from baseline to up to 12 months. Patients experiencing OAB symptoms for more than 3 months were eligible and were subsequently enrolled if they averaged 8 or more voids per day and 3 or more episodes of urgency with or without incontinence on a 3-day bladder diary. A total of 2,444 patients were randomly assigned in a 1:1:1 fashion to mirabegron 50 mg daily, mirabegron 100 mg daily, or tolterodine extended release (ER) 4 mg daily.
There was a similar incidence (60% to 63%) of TEAEs across all three groups. The most common TEAEs were hypertension (defined as average systolic blood pressure [BP] >140 mm Hg or average diastolic BP >90 mm Hg at two consecutive visits), UTI, headache, nasopharyngitis, and constipation. The adjusted mean changes in BP from baseline to final visit were less than 1 mm Hg for both systolic and diastolic BP for patients taking both doses of mirabegron, as well as for patients taking tolterodine. The incidence of dry mouth was higher in the tolterodine group than the mirabegron groups. Mirabegron 50 mg daily and 100 mg daily improved incontinence symptoms within 1 month of starting therapy; the degree of improvement was similar to that seen in the patients taking tolterodine ER 4 mg daily.
Related article: New overactive bladder treatment approved by the FDA (August 2012)
Some caveats
This study was well-designed to assess the safety and tolerability of mirabegron versus tolterodine. The doses utilized in the study were at or above the FDA-approved dosage of 25 mg to 50 mg daily for OAB treatment. Although investigators found mirabegron to be a safe alternative to anticholinergic medication, the study was not designed or powered to examine the efficacy of mirabegron versus tolterodine. No formal comparison of efficacy was made between mirabegron or tolterodine, or between the 50-mg and 100-mg doses of mirabegron. Moreover, 81% of participants had been treated with mirabegron in earlier Phase 3 studies, so most were not treatment naïve, limiting the applicability of results.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
Mirabegron should be considered as a potential treatment option for patients who demonstrate poor tolerance of or response to anticholinergic medications; however, caution should be used in patients with severe uncontrolled high BP, end-stage kidney disease, or severe liver impairment.
Consider percutaneous tibial nerve stimulation over tolterodine for OAB in select patients
Peters KM, Macdiarmid SA, Wooldridge LS, et al. Randomized trial of percutaneous tibial nerve stimulation versus extended-release tolterodine: Results from the overactive bladder innovative therapy trial. J Urol. 2009;182(3):1055−1061.
Neuromodulation utilizes electrical stimulation to improve bladder function and decrease OAB symptoms. First developed in the early 1980s by McGuire and colleagues, percutaneous tibial nerve stimulation (PTNS) was approved by the FDA in 2000 as Urgent PC and provides an outpatient, nonimplantable neuromodulation alternative to medication therapy for patients with OAB.11,12 By directly stimulating the posterior tibial nerve, PTNS works via the S3 sacral nerve plexus to alter the micturition reflex and improve bladder function.
Details of the study
Patients were eligible for the study if they demonstrated 8 or more voids per day on a 3-day bladder diary (whether or not they had a history of previous anticholinergic drug use). A total of 100 ambulatory adults with OAB symptoms were enrolled and randomly assigned to PTNS 30-minutes per week or tolterodine ER 4 mg daily.
At 12 weeks, both groups demonstrated a significant improvement in OAB measures as well as validated symptom severity and quality-of-life questionnaire scores. Subjective assessment of improvement in OAB symptoms was significantly greater in the PTNS group than in the tolterodine group (79.5% vs 54.8%, respectively; P = .01). However, mean reduction of voids for 24 hours was not significantly different between the two groups.
Both treatments were well tolerated, with only 15% to 16% of patients in both groups reporting mild to moderate side effects. The tolterodine group did have a significantly higher risk of dry mouth; however, the risk of constipation was not significantly different between the groups.
Study limitations
The authors performed an important multicenter, nonblinded, randomized, controlled trial, which was one of the first trials to directly compare two OAB therapies. The generalizability of the findings were limited, as the cohort included mostly patients with dry OAB who had no objective measures on UUI episodes. In addition, this trial had a limited observation period of only 12 weeks. Information regarding the effect of treatment after cessation of weekly PTNS therapy was not examined. Therefore, we are not able to determine whether repeat sessions provide adequate maintenance in the long term.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
PTNS 30 minutes daily is as effective as tolterodine ER 4 mg daily for 12 weeks in reducing OAB symptoms. PTNS is a safe alternative that should be considered in patients with OAB who poorly tolerate or have contraindications to medication therapy.
OnabotulinumtoxinA is an effective therapy for OAB
Visco AG, Brubaker L, Richter HE, et al. Anticholinergic therapy vs onabotulinumtoxinA for urgency urinary incontinence. NEJM. 2012;367(19):1803−1813.
The newest therapy for OAB is onabotulinumtoxinA, or Botox, which was FDA approved this year for the treatment of OAB in adults who cannot use or do not tolerate anticholinergic medications. Recommended doses are 100 U onabotulinumtoxinA in patients with idiopathic refractory OAB and 200 U onabotulinumtoxinA for patients with neurogenic OAB.
OnabotulinumtoxinA is a neurotoxin that blocks synaptic transmission at the neuromuscular junction to cause muscle paralysis and atrophy.13 Injecting onabotulinumtoxinA into the detrusor smooth muscle should relax the bladder and decrease sensations of urgency and frequency to achieve a longer duration of time for bladder filling and reduce the risk of urgency incontinence.
Effects of onabotulinumtoxinA appear to wear off over time, and patients may require repeat injections. Side effects of onabotulinumtoxinA therapy include an increased risk of UTI and the potential for urinary retention requiring intermittent self-catheterization.
Related article: Update on Pelvic Floor Dysfunction Autumn L. Edenfield, MD, and Cindy L. Amundsen, MD (October 2012)
Details of the study
The Anticholinergic Versus Botulinum Toxin Comparison (ABC) study was a multicenter, randomized, double-blind, double-placebo–controlled trial conducted in women without known neurologic disease with moderate to severe UUI (defined as >5 UUI episodes on a 3-day bladder diary). Women were randomly assigned to a single intradetrusor injection of 100 U onabotulinumtoxinA plus oral placebo or to a single intradetrusor injection of saline plus solifenacin 5 mg daily (with the option of dose escalation and then switching to trospium XR if no improvement was seen).
Of the 241 women included in the final analysis, approximately 70% in each group reported adequate control of symptoms at 6 months. Adequate control was defined as a response of “agree strongly” or “agree” to the statement: “This treatment has given me adequate control of my urinary leakage.” Women in the onabotulinumtoxinA group were significantly more likely than women in the anticholinergic medication group to report complete resolution of UUI at 6 months (27% vs 13%, P = .003). However, the mean reduction in episodes of UUI per day and the improvements in quality-of-life questionnaire scores were found to be similar. Interestingly, worse baseline UUI was associated with greater reduction in episodes of UUI for both therapies.
This was a rigorous and well-executed double-blind, double-placebo−controlled randomized trial. By utilizing broad inclusion criteria and enrolling patients both with and without previous exposure to anticholinergic medications, the generalizability of study findings are greatly improved. Because this study did not examine the effect or efficacy of repeat injections, these findings have limited applicability to patients undergoing multiple onabotulinumtoxinA injections.
When considering use in your patient population, keep the possible side effects in mind.There were important differences in the side effects experienced with each therapy. Specifically, while the anticholinergic group had a higher frequency of dry mouth (46% anticholinergic vs 31% onabotulinumtoxinA, P = .02), the onabotulinumtoxinA group demonstrated higher rates of incomplete bladder emptying requiring catheterization (peak of 5% at 2 months) and greater risk of UTI (33% onabotulinumtoxinA vs 13% anticholinergic, P <.001).
WHAT THIS EVIDENCE MEANS FOR PRACTICE
This study showed that, among women with UUI, anticholinergic medication and onabotulinumtoxinA are equally effective in reducing UUI episodes and improving quality of life. It is important to consider the side effect profile, determine the patient’s preferences, and weigh the risks and benefits of each therapy when deciding what is the best treatment for your individual patient.
We want to hear from you! Tell us what you think.
- Anger JT, Saigal CS, Litwin MS. The prevalence of urinary incontinence among community dwelling adult women: Results from the National Health and Nutrition Examination Survey. J Urol. 2006;175(2):601–604.
- Dooley Y, Kenton K, Cao G, et al. Urinary incontinence prevalence: Results from the National Health and Nutrition Examination Survey. J Urol. 2008;179(2):656–661.
- Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in U.S. Women: 2010 to 2050. Obstetr Gynecol. 2009;114(6):1278–1283.
- Gormley EA, Lightner DJ, Burgio KL, et al. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU Guideline. Americal Urological Association. http://www.auanet.org/common/pdf/education/clinical-guidance/Overactive-Bladder.pdf. Published 2012. Revised June 11, 2013. Accessed October 21, 2013.
- Yu YF, Nichol MB, Yu AP, Ahn J. Persistence and adherence of medications for chronic overactive bladder/urinary incontinence in the California Medicaid program. Value Health. 2005;8(4):495–505.
- Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26.
- ACOG Practice Bulletin No. 63: Urinary incontinence in women. American College of Obstetricians and Gynecologists. Obstetr Gynecol. 2005;105(6):1533–1545.
- Bo K, Kvarstein B, Nygaard I. Lower urinary tract symptoms and pelvic floor muscle exercise adherence after 15 years. Obstetr Gynecol. 2005;105(5 Pt 1):999–1005.
- Sandvik H, Hunskaar S, Seim A, Hermstad R, Vanvik A, Bratt H. Validation of a severity index in female urinary incontinence and its implementation in an epidemiological survey. J Epidemiol Community Health. 1993;47(6):497–499.
- Fowler CJ, Griffiths D, de Groat WC. The neural control of micturition. Nat Rev Neurosci. 2008;9(6):453–466.
- Levin PJ, Wu JM, Kawasaki A, Weidner AC, Amundsen CL. The efficacy of posterior tibial nerve stimulation for the treatment of overactive bladder in women: a systematic review. Int Urogynecol J. 2012;23(11):1591–1597.
- McGuire EJ, Zhang SC, Horwinski ER, Lytton B. Treatment of motor and sensory detrusor instability by electrical stimulation. J Urol. 1983;129(1):78–79.
- Schiavo G, Santucci A, Dasgupta BR, et al. Botulinum neurotoxins serotypes A and E cleave SNAP-25 at distinct COOH-terminal peptide bonds. FEBS Lett. 1993;335(1):99–103.
- Anger JT, Saigal CS, Litwin MS. The prevalence of urinary incontinence among community dwelling adult women: Results from the National Health and Nutrition Examination Survey. J Urol. 2006;175(2):601–604.
- Dooley Y, Kenton K, Cao G, et al. Urinary incontinence prevalence: Results from the National Health and Nutrition Examination Survey. J Urol. 2008;179(2):656–661.
- Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in U.S. Women: 2010 to 2050. Obstetr Gynecol. 2009;114(6):1278–1283.
- Gormley EA, Lightner DJ, Burgio KL, et al. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU Guideline. Americal Urological Association. http://www.auanet.org/common/pdf/education/clinical-guidance/Overactive-Bladder.pdf. Published 2012. Revised June 11, 2013. Accessed October 21, 2013.
- Yu YF, Nichol MB, Yu AP, Ahn J. Persistence and adherence of medications for chronic overactive bladder/urinary incontinence in the California Medicaid program. Value Health. 2005;8(4):495–505.
- Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26.
- ACOG Practice Bulletin No. 63: Urinary incontinence in women. American College of Obstetricians and Gynecologists. Obstetr Gynecol. 2005;105(6):1533–1545.
- Bo K, Kvarstein B, Nygaard I. Lower urinary tract symptoms and pelvic floor muscle exercise adherence after 15 years. Obstetr Gynecol. 2005;105(5 Pt 1):999–1005.
- Sandvik H, Hunskaar S, Seim A, Hermstad R, Vanvik A, Bratt H. Validation of a severity index in female urinary incontinence and its implementation in an epidemiological survey. J Epidemiol Community Health. 1993;47(6):497–499.
- Fowler CJ, Griffiths D, de Groat WC. The neural control of micturition. Nat Rev Neurosci. 2008;9(6):453–466.
- Levin PJ, Wu JM, Kawasaki A, Weidner AC, Amundsen CL. The efficacy of posterior tibial nerve stimulation for the treatment of overactive bladder in women: a systematic review. Int Urogynecol J. 2012;23(11):1591–1597.
- McGuire EJ, Zhang SC, Horwinski ER, Lytton B. Treatment of motor and sensory detrusor instability by electrical stimulation. J Urol. 1983;129(1):78–79.
- Schiavo G, Santucci A, Dasgupta BR, et al. Botulinum neurotoxins serotypes A and E cleave SNAP-25 at distinct COOH-terminal peptide bonds. FEBS Lett. 1993;335(1):99–103.