User login
Oncologists’ income and net worth rise despite pandemic
Overall, oncologists’ average annual income rose from $377,000 in 2020 to $403,000 this year.
Although many offices closed for periods during 2020, some physicians used the Paycheck Protection Program. Others found other methods to keep their earnings relatively stable, such as switching to telehealth, cutting staff, and renegotiating leases.
The overall net worth of oncologists also increased. This year, 55% reported a net worth of $1.5 million, compared to 42% last year. A contributing factor is the rise in home prices, suggested Joel Greenwald, MD, CFP, a wealth management advisor for physicians.
The rise in the stock market also played a role, he noted. “And I’ve seen clients accumulate cash, which has added to their net worth. They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on.”
The percentage of oncologists (16%) with a net worth of more than $5 million stayed pretty much the same. Oncology remained in the upper half of the list of wealthy specialties. Topping that list are dermatology (28%), orthopedics and orthopedic surgery (25%), and plastic surgery (24%).
On the flip side, the percentage of oncologists on the lower end of the net worth scale declined from last year. Oncology was the specialty with the lowest percentage of practitioners (16%) reporting a net worth of under $500,000.
Expenses and debts
Similar to reports from previous years, this latest survey found that more than half of oncologists (56%) said they are paying off a mortgage on a primary residence. About a third (32%) are paying off a car loan. Credit card debt (19%), college or medical school loans (17%), childcare (14%), and medical expenses for themselves or a loved one (12%) were also reported.
When it comes to paying off school loans, oncology was near the bottom of the list of 29 medical specialties, along with nephrology, gastroenterology, and diabetes and endocrinology. Emergency medicine topped that list, followed by family medicine, pediatrics, physical medicine, and rehabilitation (all 31%).
Although the vast majority of oncologists (94%) were able to keep up with their bills, the pandemic did take a toll on some. Six percent said that they were unable to keep up with their bills, and 3% could not meet their mortgage. This is far superior to the American population at large – a quarter of adults missed a mortgage payment or rent payment because of challenges associated with the pandemic.
Saving and losses
Most oncologists did not take any extra steps to curtail spending – 77% reported that they had not done anything to reduce major expenses. About a quarter of respondents took significant steps to lower their expenses, such as deferring or refinancing loans (11%), switching to a different type of car (6%), or moving to a different home (5%).
Savings for tax deferred accounts this year was a mixed bag. More than half (56%) of oncologists said that they put aside the same amount every month, give or take; 11% do not regularly put money into a 401(k) retirement account or tax-deferred savings account. Compared to last year, 32% put less money into their savings accounts. Having fewer patients or working fewer hours during the pandemic may have resulted in oncologists needing more of their income, or even their full income, to pay their bills.
Similar results were seen with taxable savings. Half of oncologists were putting the same amount into bank accounts; 20% reported that they do not regularly put money into this type of account. Compared to last year, 29% put less money into taxable savings.
Most oncologists (75%) reported that they did not experience any significant financial losses during the past year. This was similar to last year (77%). The percentage of those who had losses related to their practice rose from 3% to 8%. Much of this increase was due to COVID-19.
Living within their means
The vast majority of oncologists live within or below their means (94%). “There are certainly folks who believe that as long as they pay their credit card every month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” said Dr. Greenwald. “I would say living within one’s means is having a 3 to 6 months’ emergency fund and saving at least 20% of gross income toward retirement.”
Although most oncologists live within their means, they also have a higher than average number of credit cards. More than half (54%) have at least five; the average American has four. Nineteen percent of oncologists reported having seven or more credit cards, and none said they had no credit cards.
Mortgage payments varied considerably among respondents, from less than $100,000 (16%) to more than half a million (21%). More than a third (37%) reported having no mortgage at all. According to the Mortgage Bankers Association, the overall average size of a home mortgage loan was $344,556 in March 2020.
For household finances, 57% reported that they pool incomes to pay the bills, regardless of how much each person earns. A quarter said that they do not have joint finances with a spouse or partner, and for 13%, the person with the higher income paid a larger share.
A version of this article first appeared on Medscape.com.
Overall, oncologists’ average annual income rose from $377,000 in 2020 to $403,000 this year.
Although many offices closed for periods during 2020, some physicians used the Paycheck Protection Program. Others found other methods to keep their earnings relatively stable, such as switching to telehealth, cutting staff, and renegotiating leases.
The overall net worth of oncologists also increased. This year, 55% reported a net worth of $1.5 million, compared to 42% last year. A contributing factor is the rise in home prices, suggested Joel Greenwald, MD, CFP, a wealth management advisor for physicians.
The rise in the stock market also played a role, he noted. “And I’ve seen clients accumulate cash, which has added to their net worth. They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on.”
The percentage of oncologists (16%) with a net worth of more than $5 million stayed pretty much the same. Oncology remained in the upper half of the list of wealthy specialties. Topping that list are dermatology (28%), orthopedics and orthopedic surgery (25%), and plastic surgery (24%).
On the flip side, the percentage of oncologists on the lower end of the net worth scale declined from last year. Oncology was the specialty with the lowest percentage of practitioners (16%) reporting a net worth of under $500,000.
Expenses and debts
Similar to reports from previous years, this latest survey found that more than half of oncologists (56%) said they are paying off a mortgage on a primary residence. About a third (32%) are paying off a car loan. Credit card debt (19%), college or medical school loans (17%), childcare (14%), and medical expenses for themselves or a loved one (12%) were also reported.
When it comes to paying off school loans, oncology was near the bottom of the list of 29 medical specialties, along with nephrology, gastroenterology, and diabetes and endocrinology. Emergency medicine topped that list, followed by family medicine, pediatrics, physical medicine, and rehabilitation (all 31%).
Although the vast majority of oncologists (94%) were able to keep up with their bills, the pandemic did take a toll on some. Six percent said that they were unable to keep up with their bills, and 3% could not meet their mortgage. This is far superior to the American population at large – a quarter of adults missed a mortgage payment or rent payment because of challenges associated with the pandemic.
Saving and losses
Most oncologists did not take any extra steps to curtail spending – 77% reported that they had not done anything to reduce major expenses. About a quarter of respondents took significant steps to lower their expenses, such as deferring or refinancing loans (11%), switching to a different type of car (6%), or moving to a different home (5%).
Savings for tax deferred accounts this year was a mixed bag. More than half (56%) of oncologists said that they put aside the same amount every month, give or take; 11% do not regularly put money into a 401(k) retirement account or tax-deferred savings account. Compared to last year, 32% put less money into their savings accounts. Having fewer patients or working fewer hours during the pandemic may have resulted in oncologists needing more of their income, or even their full income, to pay their bills.
Similar results were seen with taxable savings. Half of oncologists were putting the same amount into bank accounts; 20% reported that they do not regularly put money into this type of account. Compared to last year, 29% put less money into taxable savings.
Most oncologists (75%) reported that they did not experience any significant financial losses during the past year. This was similar to last year (77%). The percentage of those who had losses related to their practice rose from 3% to 8%. Much of this increase was due to COVID-19.
Living within their means
The vast majority of oncologists live within or below their means (94%). “There are certainly folks who believe that as long as they pay their credit card every month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” said Dr. Greenwald. “I would say living within one’s means is having a 3 to 6 months’ emergency fund and saving at least 20% of gross income toward retirement.”
Although most oncologists live within their means, they also have a higher than average number of credit cards. More than half (54%) have at least five; the average American has four. Nineteen percent of oncologists reported having seven or more credit cards, and none said they had no credit cards.
Mortgage payments varied considerably among respondents, from less than $100,000 (16%) to more than half a million (21%). More than a third (37%) reported having no mortgage at all. According to the Mortgage Bankers Association, the overall average size of a home mortgage loan was $344,556 in March 2020.
For household finances, 57% reported that they pool incomes to pay the bills, regardless of how much each person earns. A quarter said that they do not have joint finances with a spouse or partner, and for 13%, the person with the higher income paid a larger share.
A version of this article first appeared on Medscape.com.
Overall, oncologists’ average annual income rose from $377,000 in 2020 to $403,000 this year.
Although many offices closed for periods during 2020, some physicians used the Paycheck Protection Program. Others found other methods to keep their earnings relatively stable, such as switching to telehealth, cutting staff, and renegotiating leases.
The overall net worth of oncologists also increased. This year, 55% reported a net worth of $1.5 million, compared to 42% last year. A contributing factor is the rise in home prices, suggested Joel Greenwald, MD, CFP, a wealth management advisor for physicians.
The rise in the stock market also played a role, he noted. “And I’ve seen clients accumulate cash, which has added to their net worth. They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on.”
The percentage of oncologists (16%) with a net worth of more than $5 million stayed pretty much the same. Oncology remained in the upper half of the list of wealthy specialties. Topping that list are dermatology (28%), orthopedics and orthopedic surgery (25%), and plastic surgery (24%).
On the flip side, the percentage of oncologists on the lower end of the net worth scale declined from last year. Oncology was the specialty with the lowest percentage of practitioners (16%) reporting a net worth of under $500,000.
Expenses and debts
Similar to reports from previous years, this latest survey found that more than half of oncologists (56%) said they are paying off a mortgage on a primary residence. About a third (32%) are paying off a car loan. Credit card debt (19%), college or medical school loans (17%), childcare (14%), and medical expenses for themselves or a loved one (12%) were also reported.
When it comes to paying off school loans, oncology was near the bottom of the list of 29 medical specialties, along with nephrology, gastroenterology, and diabetes and endocrinology. Emergency medicine topped that list, followed by family medicine, pediatrics, physical medicine, and rehabilitation (all 31%).
Although the vast majority of oncologists (94%) were able to keep up with their bills, the pandemic did take a toll on some. Six percent said that they were unable to keep up with their bills, and 3% could not meet their mortgage. This is far superior to the American population at large – a quarter of adults missed a mortgage payment or rent payment because of challenges associated with the pandemic.
Saving and losses
Most oncologists did not take any extra steps to curtail spending – 77% reported that they had not done anything to reduce major expenses. About a quarter of respondents took significant steps to lower their expenses, such as deferring or refinancing loans (11%), switching to a different type of car (6%), or moving to a different home (5%).
Savings for tax deferred accounts this year was a mixed bag. More than half (56%) of oncologists said that they put aside the same amount every month, give or take; 11% do not regularly put money into a 401(k) retirement account or tax-deferred savings account. Compared to last year, 32% put less money into their savings accounts. Having fewer patients or working fewer hours during the pandemic may have resulted in oncologists needing more of their income, or even their full income, to pay their bills.
Similar results were seen with taxable savings. Half of oncologists were putting the same amount into bank accounts; 20% reported that they do not regularly put money into this type of account. Compared to last year, 29% put less money into taxable savings.
Most oncologists (75%) reported that they did not experience any significant financial losses during the past year. This was similar to last year (77%). The percentage of those who had losses related to their practice rose from 3% to 8%. Much of this increase was due to COVID-19.
Living within their means
The vast majority of oncologists live within or below their means (94%). “There are certainly folks who believe that as long as they pay their credit card every month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” said Dr. Greenwald. “I would say living within one’s means is having a 3 to 6 months’ emergency fund and saving at least 20% of gross income toward retirement.”
Although most oncologists live within their means, they also have a higher than average number of credit cards. More than half (54%) have at least five; the average American has four. Nineteen percent of oncologists reported having seven or more credit cards, and none said they had no credit cards.
Mortgage payments varied considerably among respondents, from less than $100,000 (16%) to more than half a million (21%). More than a third (37%) reported having no mortgage at all. According to the Mortgage Bankers Association, the overall average size of a home mortgage loan was $344,556 in March 2020.
For household finances, 57% reported that they pool incomes to pay the bills, regardless of how much each person earns. A quarter said that they do not have joint finances with a spouse or partner, and for 13%, the person with the higher income paid a larger share.
A version of this article first appeared on Medscape.com.
Progressive disability in MS explained?
Results from a retrospective study show that complete resolution of brain lesions on MRI was more common among patients with myelin-oligodendrocyte-glycoprotein-IgG-associated disorder (MOGAD). Complete resolution occurred in 72% of the group with MOGAD, versus 17% of those with MS and 14% of those with aquaporin-4-positive neuromyelitis optica spectrum disorder (AQP4+ NMOSD).
“What we found was, with MOGAD in particular, many of the lesions resolved completely,” said co-investigator Eoin Flanagan, MBBCh, neurologist, Mayo Clinic, Rochester, Minn. “That fits with MOGAD having a fairly good prognosis and patients not developing much long-term disability with that disease,” he said.
The researchers also studied whether scarring may account for the absence of slowly progressive disability among patients with AQP4+ NMOSD and MOGAD compared with patients with MS. “The differences in scarring that we found will help physicians distinguish these three diseases more easily to aid in diagnosis. More importantly, our findings improve our understanding of the mechanisms of nerve damage in these three diseases and may suggest an important role of such scars in the development of long-term disability in MS,” Dr. Flanagan said in a statement.
The findings were published online July 14 in Neurology.
Lesion evolution
MOGAD, AQP4+ NMOSD, and MS are inflammatory demyelinating disorders that share certain manifestations. However, these disorders differ in important ways, including the severity of attacks and their clinical course.
Although patients with MOGAD and AQP4+ NMOSD generally have severe attacks that bring major disability, the clinical course of these disorders is better than initial attacks would suggest. In contrast, patients with MS have comparatively mild attacks that are associated with a high risk for progressive disability.
Previous studies of these demyelinating disorders have examined the shape and location of lesions but not change over time. Observing these lesions’ development and resolution could provide information about disease course and influence treatment and the monitoring of disease activity, the current researchers noted.
They retrospectively identified consecutive patients with MOGAD, AQP4+ NMOSD, or MS who presented to the Mayo Clinic between January 2000 and August 2019. Data from a cohort of patients with MS in Olmsted County, Minn., were also included.
Eligible participants had experienced a first brain or myelitis attack, had undergone MRI of the brain or spinal cord within 6 weeks of the attack nadir, and had undergone a follow-up MRI 6 months after the attack.
Patients who experienced a relapse during follow-up in the same region as the initial attack were excluded. Concomitant brain and myelitis attacks were analyzed separately.
An index lesion was identified for each patient. The index lesion was defined as an acute lesion that provided an anatomic explanation for the clinical symptoms. If multiple lesions were present, the largest of them was chosen as the index lesion. MRIs were examined by neuroradiologists who were blinded to patients’ diagnoses and serology results.
Among the 156 participants, 67 had MS (76% women), 51 had AQP4+ NMOSD (80% women), and 38 had MOGAD (45% women). The median age at first attack for the groups was 37, 53, and 25 years, respectively.
In addition, 63 patients had relapsing-remitting MS, two had a single attack of progressive MS, and two had clinically isolated syndrome. No patients with NMOSD or MOGAD had developed progressive disease at final follow-up.
Participants experienced a total of 81 brain attacks and 91 myelitis attacks. Sixteen patients had experienced both a brain attack and a myelitis attack.
Symptoms corresponding to the index brain lesions were brainstem or cerebellar syndrome (56), encephalopathy or focal symptoms (12), or combinations of these (13). Among patients with an index myelitis attack, 31 had cervical involvement, 21 had thoracic involvement, and 39 had involvement of both regions.
Complete resolution
Results showed that 72% of patients with MOGAD experienced complete resolution of the brain index lesion, compared with 17% of patients with MS and 14% of patients with NMOSD (P < .001).
Similarly, 79% of the MOGAD group experienced complete resolution of the myelitis index lesion, compared with no members of the MS or NMOSD groups (P < .001 for both comparisons).
Complete resolution of all T2-abnormalities at MRI follow-up was more common in the MOGAD group than in the other two groups.
For brain attacks, complete resolution occurred in 39% of patients with MOGAD, 10% of patients with NMOSD, and 5% of patients with MS. For spinal cord attacks, complete resolution occurred in 79% of patients with MOGAD, versus none of the patients with NMOSD or MS.
Median reduction in T2 lesion area on follow-up axial brain MRI was larger in patients with MOGAD (213 mm2) than in those with NMOSD (104 mm2; P = .02) or MS (36 mm2; P < .001).
Reductions in lesion size on sagittal spine MRI follow-up were similar between the MOGAD (262 mm2) and NMOSD (309 mm2) groups; both experienced greater reductions than the MS group (23 mm2; P < .001).
Lesion prevention
Dr. Flanagan noted that the diagnosis of MOGAD is based on a test for MOG antibody, but sometimes false positive results occur. “A single follow-up MRI can be useful, showing that if all the lesions went away, you would be more confident that it would be MOGAD,” he said.
Study participants with MS experienced less lesion healing than the patients with MOGAD or NMOSD.
“We now have very effective medications in MS to prevent new lesions from occurring,” Dr. Flanagan said. The study highlights the importance of lesion prevention, “because when you do get a lesion, it does tend to stay and not recover completely,” he added.
He noted that the resolution of lesions in the study population may reflect remyelination. Future research examining whether remyelination is more efficient in MOGAD than in the other disorders could possibly lead to new approaches for MS treatment, said Dr. Flanagan.
“Maybe some of the MOGAD lesions are from edema. When we use steroids, that tends to resolve and not leave a scar. So, that’s another possibility. We’d like to better understand that,” he said.
Differences in pathology
Commenting on the findings, Bruce Cree, MD, PhD, professor of neurology, Weill Institute for Neurosciences, University of California, San Francisco, noted that the study is one of the first to systematically examine and compare MRI lesion evolution across three disease states.
“What they put their finger on are differences in the fundamental pathology of these three different diseases,” said Dr. Cree, who was not involved with the research.
The study’s cross-sectional comparison was its main strength, he noted.
“The main weakness, from my point of view, is that in these three disorders, optic nerve involvement is very common,” Dr. Cree said. “In this paper, no analysis of optic nerve lesions by MRI was performed.”
The researchers acknowledge this limitation and explain that they did not have consistent, dedicated orbital imaging for such an analysis.
Dr. Cree noted that the findings also provide a reminder that the pathogenesis of MOGAD is not yet clear.
“We know that these anti-MOG antibodies are associated with this demyelinating disorder, but whether these antibodies have a pathogenic role has yet to be clearly demonstrated,” said Dr. Cree. “What is actually going on within these lesions [is also] not fully understood.”
The finding that MOGAD lesions can resolve completely suggests that repair mechanisms are at work within the brain and spinal cord, he noted.
Being able to understand and comprehend what those mechanisms at work are and why they occur in MOGAD but not in NMOSD or MS “would be of enormous clinical advantage,” he said.
The current study also highlights the importance of incorporating imaging into clinical trials that study these rare disorders, especially serial imaging for MOGAD, Dr. Cree added.
This imaging is vital not only for developing new treatments but also for understanding the clinical impact of a given medication. “We really need rigorous imaging to be applied to these rare disorders, just as was done with MS,” Dr. Cree concluded.
The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Flanagan has received research support from MedImmune/Viela Bio. Dr. Cree is working with two of the researchers on the steering committee for the N-MOmentum trial of inebilizumab in patients with NMOSD. He has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from a retrospective study show that complete resolution of brain lesions on MRI was more common among patients with myelin-oligodendrocyte-glycoprotein-IgG-associated disorder (MOGAD). Complete resolution occurred in 72% of the group with MOGAD, versus 17% of those with MS and 14% of those with aquaporin-4-positive neuromyelitis optica spectrum disorder (AQP4+ NMOSD).
“What we found was, with MOGAD in particular, many of the lesions resolved completely,” said co-investigator Eoin Flanagan, MBBCh, neurologist, Mayo Clinic, Rochester, Minn. “That fits with MOGAD having a fairly good prognosis and patients not developing much long-term disability with that disease,” he said.
The researchers also studied whether scarring may account for the absence of slowly progressive disability among patients with AQP4+ NMOSD and MOGAD compared with patients with MS. “The differences in scarring that we found will help physicians distinguish these three diseases more easily to aid in diagnosis. More importantly, our findings improve our understanding of the mechanisms of nerve damage in these three diseases and may suggest an important role of such scars in the development of long-term disability in MS,” Dr. Flanagan said in a statement.
The findings were published online July 14 in Neurology.
Lesion evolution
MOGAD, AQP4+ NMOSD, and MS are inflammatory demyelinating disorders that share certain manifestations. However, these disorders differ in important ways, including the severity of attacks and their clinical course.
Although patients with MOGAD and AQP4+ NMOSD generally have severe attacks that bring major disability, the clinical course of these disorders is better than initial attacks would suggest. In contrast, patients with MS have comparatively mild attacks that are associated with a high risk for progressive disability.
Previous studies of these demyelinating disorders have examined the shape and location of lesions but not change over time. Observing these lesions’ development and resolution could provide information about disease course and influence treatment and the monitoring of disease activity, the current researchers noted.
They retrospectively identified consecutive patients with MOGAD, AQP4+ NMOSD, or MS who presented to the Mayo Clinic between January 2000 and August 2019. Data from a cohort of patients with MS in Olmsted County, Minn., were also included.
Eligible participants had experienced a first brain or myelitis attack, had undergone MRI of the brain or spinal cord within 6 weeks of the attack nadir, and had undergone a follow-up MRI 6 months after the attack.
Patients who experienced a relapse during follow-up in the same region as the initial attack were excluded. Concomitant brain and myelitis attacks were analyzed separately.
An index lesion was identified for each patient. The index lesion was defined as an acute lesion that provided an anatomic explanation for the clinical symptoms. If multiple lesions were present, the largest of them was chosen as the index lesion. MRIs were examined by neuroradiologists who were blinded to patients’ diagnoses and serology results.
Among the 156 participants, 67 had MS (76% women), 51 had AQP4+ NMOSD (80% women), and 38 had MOGAD (45% women). The median age at first attack for the groups was 37, 53, and 25 years, respectively.
In addition, 63 patients had relapsing-remitting MS, two had a single attack of progressive MS, and two had clinically isolated syndrome. No patients with NMOSD or MOGAD had developed progressive disease at final follow-up.
Participants experienced a total of 81 brain attacks and 91 myelitis attacks. Sixteen patients had experienced both a brain attack and a myelitis attack.
Symptoms corresponding to the index brain lesions were brainstem or cerebellar syndrome (56), encephalopathy or focal symptoms (12), or combinations of these (13). Among patients with an index myelitis attack, 31 had cervical involvement, 21 had thoracic involvement, and 39 had involvement of both regions.
Complete resolution
Results showed that 72% of patients with MOGAD experienced complete resolution of the brain index lesion, compared with 17% of patients with MS and 14% of patients with NMOSD (P < .001).
Similarly, 79% of the MOGAD group experienced complete resolution of the myelitis index lesion, compared with no members of the MS or NMOSD groups (P < .001 for both comparisons).
Complete resolution of all T2-abnormalities at MRI follow-up was more common in the MOGAD group than in the other two groups.
For brain attacks, complete resolution occurred in 39% of patients with MOGAD, 10% of patients with NMOSD, and 5% of patients with MS. For spinal cord attacks, complete resolution occurred in 79% of patients with MOGAD, versus none of the patients with NMOSD or MS.
Median reduction in T2 lesion area on follow-up axial brain MRI was larger in patients with MOGAD (213 mm2) than in those with NMOSD (104 mm2; P = .02) or MS (36 mm2; P < .001).
Reductions in lesion size on sagittal spine MRI follow-up were similar between the MOGAD (262 mm2) and NMOSD (309 mm2) groups; both experienced greater reductions than the MS group (23 mm2; P < .001).
Lesion prevention
Dr. Flanagan noted that the diagnosis of MOGAD is based on a test for MOG antibody, but sometimes false positive results occur. “A single follow-up MRI can be useful, showing that if all the lesions went away, you would be more confident that it would be MOGAD,” he said.
Study participants with MS experienced less lesion healing than the patients with MOGAD or NMOSD.
“We now have very effective medications in MS to prevent new lesions from occurring,” Dr. Flanagan said. The study highlights the importance of lesion prevention, “because when you do get a lesion, it does tend to stay and not recover completely,” he added.
He noted that the resolution of lesions in the study population may reflect remyelination. Future research examining whether remyelination is more efficient in MOGAD than in the other disorders could possibly lead to new approaches for MS treatment, said Dr. Flanagan.
“Maybe some of the MOGAD lesions are from edema. When we use steroids, that tends to resolve and not leave a scar. So, that’s another possibility. We’d like to better understand that,” he said.
Differences in pathology
Commenting on the findings, Bruce Cree, MD, PhD, professor of neurology, Weill Institute for Neurosciences, University of California, San Francisco, noted that the study is one of the first to systematically examine and compare MRI lesion evolution across three disease states.
“What they put their finger on are differences in the fundamental pathology of these three different diseases,” said Dr. Cree, who was not involved with the research.
The study’s cross-sectional comparison was its main strength, he noted.
“The main weakness, from my point of view, is that in these three disorders, optic nerve involvement is very common,” Dr. Cree said. “In this paper, no analysis of optic nerve lesions by MRI was performed.”
The researchers acknowledge this limitation and explain that they did not have consistent, dedicated orbital imaging for such an analysis.
Dr. Cree noted that the findings also provide a reminder that the pathogenesis of MOGAD is not yet clear.
“We know that these anti-MOG antibodies are associated with this demyelinating disorder, but whether these antibodies have a pathogenic role has yet to be clearly demonstrated,” said Dr. Cree. “What is actually going on within these lesions [is also] not fully understood.”
The finding that MOGAD lesions can resolve completely suggests that repair mechanisms are at work within the brain and spinal cord, he noted.
Being able to understand and comprehend what those mechanisms at work are and why they occur in MOGAD but not in NMOSD or MS “would be of enormous clinical advantage,” he said.
The current study also highlights the importance of incorporating imaging into clinical trials that study these rare disorders, especially serial imaging for MOGAD, Dr. Cree added.
This imaging is vital not only for developing new treatments but also for understanding the clinical impact of a given medication. “We really need rigorous imaging to be applied to these rare disorders, just as was done with MS,” Dr. Cree concluded.
The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Flanagan has received research support from MedImmune/Viela Bio. Dr. Cree is working with two of the researchers on the steering committee for the N-MOmentum trial of inebilizumab in patients with NMOSD. He has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from a retrospective study show that complete resolution of brain lesions on MRI was more common among patients with myelin-oligodendrocyte-glycoprotein-IgG-associated disorder (MOGAD). Complete resolution occurred in 72% of the group with MOGAD, versus 17% of those with MS and 14% of those with aquaporin-4-positive neuromyelitis optica spectrum disorder (AQP4+ NMOSD).
“What we found was, with MOGAD in particular, many of the lesions resolved completely,” said co-investigator Eoin Flanagan, MBBCh, neurologist, Mayo Clinic, Rochester, Minn. “That fits with MOGAD having a fairly good prognosis and patients not developing much long-term disability with that disease,” he said.
The researchers also studied whether scarring may account for the absence of slowly progressive disability among patients with AQP4+ NMOSD and MOGAD compared with patients with MS. “The differences in scarring that we found will help physicians distinguish these three diseases more easily to aid in diagnosis. More importantly, our findings improve our understanding of the mechanisms of nerve damage in these three diseases and may suggest an important role of such scars in the development of long-term disability in MS,” Dr. Flanagan said in a statement.
The findings were published online July 14 in Neurology.
Lesion evolution
MOGAD, AQP4+ NMOSD, and MS are inflammatory demyelinating disorders that share certain manifestations. However, these disorders differ in important ways, including the severity of attacks and their clinical course.
Although patients with MOGAD and AQP4+ NMOSD generally have severe attacks that bring major disability, the clinical course of these disorders is better than initial attacks would suggest. In contrast, patients with MS have comparatively mild attacks that are associated with a high risk for progressive disability.
Previous studies of these demyelinating disorders have examined the shape and location of lesions but not change over time. Observing these lesions’ development and resolution could provide information about disease course and influence treatment and the monitoring of disease activity, the current researchers noted.
They retrospectively identified consecutive patients with MOGAD, AQP4+ NMOSD, or MS who presented to the Mayo Clinic between January 2000 and August 2019. Data from a cohort of patients with MS in Olmsted County, Minn., were also included.
Eligible participants had experienced a first brain or myelitis attack, had undergone MRI of the brain or spinal cord within 6 weeks of the attack nadir, and had undergone a follow-up MRI 6 months after the attack.
Patients who experienced a relapse during follow-up in the same region as the initial attack were excluded. Concomitant brain and myelitis attacks were analyzed separately.
An index lesion was identified for each patient. The index lesion was defined as an acute lesion that provided an anatomic explanation for the clinical symptoms. If multiple lesions were present, the largest of them was chosen as the index lesion. MRIs were examined by neuroradiologists who were blinded to patients’ diagnoses and serology results.
Among the 156 participants, 67 had MS (76% women), 51 had AQP4+ NMOSD (80% women), and 38 had MOGAD (45% women). The median age at first attack for the groups was 37, 53, and 25 years, respectively.
In addition, 63 patients had relapsing-remitting MS, two had a single attack of progressive MS, and two had clinically isolated syndrome. No patients with NMOSD or MOGAD had developed progressive disease at final follow-up.
Participants experienced a total of 81 brain attacks and 91 myelitis attacks. Sixteen patients had experienced both a brain attack and a myelitis attack.
Symptoms corresponding to the index brain lesions were brainstem or cerebellar syndrome (56), encephalopathy or focal symptoms (12), or combinations of these (13). Among patients with an index myelitis attack, 31 had cervical involvement, 21 had thoracic involvement, and 39 had involvement of both regions.
Complete resolution
Results showed that 72% of patients with MOGAD experienced complete resolution of the brain index lesion, compared with 17% of patients with MS and 14% of patients with NMOSD (P < .001).
Similarly, 79% of the MOGAD group experienced complete resolution of the myelitis index lesion, compared with no members of the MS or NMOSD groups (P < .001 for both comparisons).
Complete resolution of all T2-abnormalities at MRI follow-up was more common in the MOGAD group than in the other two groups.
For brain attacks, complete resolution occurred in 39% of patients with MOGAD, 10% of patients with NMOSD, and 5% of patients with MS. For spinal cord attacks, complete resolution occurred in 79% of patients with MOGAD, versus none of the patients with NMOSD or MS.
Median reduction in T2 lesion area on follow-up axial brain MRI was larger in patients with MOGAD (213 mm2) than in those with NMOSD (104 mm2; P = .02) or MS (36 mm2; P < .001).
Reductions in lesion size on sagittal spine MRI follow-up were similar between the MOGAD (262 mm2) and NMOSD (309 mm2) groups; both experienced greater reductions than the MS group (23 mm2; P < .001).
Lesion prevention
Dr. Flanagan noted that the diagnosis of MOGAD is based on a test for MOG antibody, but sometimes false positive results occur. “A single follow-up MRI can be useful, showing that if all the lesions went away, you would be more confident that it would be MOGAD,” he said.
Study participants with MS experienced less lesion healing than the patients with MOGAD or NMOSD.
“We now have very effective medications in MS to prevent new lesions from occurring,” Dr. Flanagan said. The study highlights the importance of lesion prevention, “because when you do get a lesion, it does tend to stay and not recover completely,” he added.
He noted that the resolution of lesions in the study population may reflect remyelination. Future research examining whether remyelination is more efficient in MOGAD than in the other disorders could possibly lead to new approaches for MS treatment, said Dr. Flanagan.
“Maybe some of the MOGAD lesions are from edema. When we use steroids, that tends to resolve and not leave a scar. So, that’s another possibility. We’d like to better understand that,” he said.
Differences in pathology
Commenting on the findings, Bruce Cree, MD, PhD, professor of neurology, Weill Institute for Neurosciences, University of California, San Francisco, noted that the study is one of the first to systematically examine and compare MRI lesion evolution across three disease states.
“What they put their finger on are differences in the fundamental pathology of these three different diseases,” said Dr. Cree, who was not involved with the research.
The study’s cross-sectional comparison was its main strength, he noted.
“The main weakness, from my point of view, is that in these three disorders, optic nerve involvement is very common,” Dr. Cree said. “In this paper, no analysis of optic nerve lesions by MRI was performed.”
The researchers acknowledge this limitation and explain that they did not have consistent, dedicated orbital imaging for such an analysis.
Dr. Cree noted that the findings also provide a reminder that the pathogenesis of MOGAD is not yet clear.
“We know that these anti-MOG antibodies are associated with this demyelinating disorder, but whether these antibodies have a pathogenic role has yet to be clearly demonstrated,” said Dr. Cree. “What is actually going on within these lesions [is also] not fully understood.”
The finding that MOGAD lesions can resolve completely suggests that repair mechanisms are at work within the brain and spinal cord, he noted.
Being able to understand and comprehend what those mechanisms at work are and why they occur in MOGAD but not in NMOSD or MS “would be of enormous clinical advantage,” he said.
The current study also highlights the importance of incorporating imaging into clinical trials that study these rare disorders, especially serial imaging for MOGAD, Dr. Cree added.
This imaging is vital not only for developing new treatments but also for understanding the clinical impact of a given medication. “We really need rigorous imaging to be applied to these rare disorders, just as was done with MS,” Dr. Cree concluded.
The study was funded by the National Institute of Neurological Disorders and Stroke. Dr. Flanagan has received research support from MedImmune/Viela Bio. Dr. Cree is working with two of the researchers on the steering committee for the N-MOmentum trial of inebilizumab in patients with NMOSD. He has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
From Neurology
Better to binge drink than regularly tipple, suggests GI cancer study
When weekly levels are similar
Alcohol use is a known risk factor for gastrointestinal (GI) cancers. Now, new research indicates that this risk is more associated with frequent drinking – even in smaller amounts – compared with higher amounts or binge drinking, given similar weekly levels.
“The novel finding of the current study is that frequent drinking may be more dangerous than binge drinking with regard to GI cancers. Alcohol use is a known risk factor for gastrointestinal (GI) cancers. Now, new research indicates that this risk is more associated with frequent drinking – even in smaller amounts -- compared with higher amounts or binge drinking, given similar weekly levels.” first author Jung Eun Yook, MD, of Seoul (South Korea) National University Hospital, and colleagues reported in an article published Aug. 18, 2021, in JAMA Network Open (doi: 10.1001/jamanetworkopen.2021.20382).
“This finding suggests that repeated alcohol consumption events even at lower amounts of alcohol may have a greater carcinogenic effect on GI organs than the consumption of larger amounts of alcohol at a lower frequency,” the investigators wrote.
A possible reason behind the difference in risk may be that the chronic “carcinogenic insult” from regular alcohol use may promote cancer development, whereas less frequent, episodic alcohol exposures may allow physiologic recovery, said the authors.
The results are from a population-based study that involved 11,737,467 participants in the Korean National Health System database who did not have cancer and who took part in a national screening program between January 2009 and December 2010.
They were followed from the year after their screening until either they had received a diagnosis of a GI cancer, death occurred, or the end of December 2017.
During a median follow-up of 6.4 years, 319,202 (2.7%) of those in the study developed a GI cancer.
The increase in the risk associated with alcohol consumption was dose dependent.
Compared with those who did not consume alcohol, the risk of developing GI cancer was higher for mild drinkers (adjusted hazard ratio, 1.04; 95% confidence interval, 1.03-1.05), moderate drinkers (aHR, 1.14; 95% CI, 1.12-1.15), and heavy drinkers (aHR, 1.28; 95% CI, 1.26-1.29), after adjusting for age, sex, income, smoking status with intensity, regular exercise, body mass index, diabetes, hypertension, and dyslipidemia.
There was a linear association between the frequency of drinking and GI cancer risk, with an aHR of 1.39 for individuals who reported drinking every day (95% CI, 1.36-1.41). The risk for GI cancer increased with consumption of five to seven units per occasion (aHR, 1.15). Notably, there were no similar increases with higher intake, including intake of 8-14 units per occasion (aHR, 1.11; 95% CI, 1.09-1.12), and even up to more than 14 units per occasion (aHR, 1.11; 95%CI, 1.08-1.14), in comparison with an intake of 5-7 units per occasion.
“Given similar weekly alcohol consumption levels, the risk of GI cancer increased with a higher frequency of drinking and decreased with a higher amount per occasion,” the authors write.
“Most previous studies just assess alcohol consumption as a total amount, [such as] drinks per occasion times occasion per week equals drinks per week [and] grams per week,” coauthor Dong Wook Shin, MD, DrPH, Samsung Medical Center, Sungkyunkwan University, Seoul, South Korea, said in an interview.
“But it was not known whether frequent drinking with small amount is more harmful than binge drinking, given a similar level of total drinking,” Dr. Shin said.
The increased risk associated with frequent drinking was generally similar with respect to esophageal, gastric, colorectal, biliary, and pancreatic cancer.
An exception was liver cancer, which showed a slightly decreased risk among mild drinkers (aHR, 0.91; 95% CI, 0.89-0.93).
Of note, the association between alcohol intake and the incidence of GI cancer was lower among women than men in terms of weekly consumption, frequency, and amount of alcohol consumed per occasion.
The associations between drinking and cancer type in terms of esophageal and liver cancers were similar between men and women. However, the alcohol-related risk for colorectal, biliary, and pancreatic cancers was less prominent for women.
Possible mechanisms related to regular drinking
A factor that might account for the increase in GI cancer risk with frequent drinking is that regular alcohol consumption “promotes the accumulation of cell divisions in the stem cells that maintain tissues in homeostasis,” the authors explained.
Another possible explanation is that long-term alcohol exposure may promote carcinogenesis, whereas less frequent exposure might allow “physiological homeostasis,” the authors wrote, adding that in vivo experiments have shown that duration and dose of alcohol exposure have been linked to cancer development.
Importantly, the findings support the importance of reducing the frequency of alcohol use to prevent cancer, the authors noted.
“Alcohol users who have a glass of wine or beer during dinner every day may develop more cancer than people who occasionally consume several drinks,” they cautioned.
Genetics, self-reporting considerations
In a related commentary, John D. Potter, MBBS, PhD, of the Research Center for Hauora and Health, Massey University, Wellington, New Zealand, noted that, in addition to supporting the known link between alcohol and cancers of the esophagus, colorectum, and liver, the study “strengthens evidence for a role of alcohol in stomach, biliary tract, and pancreas cancers.”
In comparison with nondrinkers, those who reported heavy drinking were much more likely to be smokers (51.6% vs. 9.0%); however, the study adjusted for smoking.
“Because the researchers were able to control for tobacco, this last finding [regarding the association with cancers of the stomach, biliary tract, and pancreas] is particularly informative,” Dr. Potter noted.
An important caveat is that more than a quarter of the Korean population is known to have an inactive form of the aldehyde dehydrogenase gene (ALDH2), which could have effects on alcohol metabolism as well as the risk for cancer, Dr. Potter wrote.
“This common polymorphism in ALDH2 (ALDH2 rs671 [c.1510G>A (Glu504Lys)]) has paradoxical effects,” he wrote.
“It increases the level of acetaldehyde in the blood of drinkers, which in turn increases the risk of cancer because acetaldehyde is a key player in the carcinogenicity of alcoholic beverages,” Dr. Potter explained. “On the other hand, the accumulation of acetaldehyde and the resultant flushing response are sufficiently unpleasant that they tend to reduce alcohol consumption among those with the Lys allele.”
The study results may therefore not be generalizable to a population in which the distribution of the variation in the ALDH2 enzyme differs, Dr. Potter added.
The lower prevalence of the inactive form (in North America, for instance) would mean that this lower prevalence was not a constraint on individuals’ drinking behavior as it is for some in Korea, Dr. Potter explained.
He noted another consideration: the underreporting of alcohol use is a well-known limitation of studies involving the assessment of alcohol consumption.
Dr. Shin agreed that underreporting is a limitation.
“People tend to underestimate their alcohol use,” Dr. Shin said in an interview.
However, he noted that “our study participants are health-screening participants aged 40 years and older, [and] people who participate in health screening tend to have higher awareness and better health behavior than nonparticipants.”
The authors and Dr. Potter disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When weekly levels are similar
When weekly levels are similar
Alcohol use is a known risk factor for gastrointestinal (GI) cancers. Now, new research indicates that this risk is more associated with frequent drinking – even in smaller amounts – compared with higher amounts or binge drinking, given similar weekly levels.
“The novel finding of the current study is that frequent drinking may be more dangerous than binge drinking with regard to GI cancers. Alcohol use is a known risk factor for gastrointestinal (GI) cancers. Now, new research indicates that this risk is more associated with frequent drinking – even in smaller amounts -- compared with higher amounts or binge drinking, given similar weekly levels.” first author Jung Eun Yook, MD, of Seoul (South Korea) National University Hospital, and colleagues reported in an article published Aug. 18, 2021, in JAMA Network Open (doi: 10.1001/jamanetworkopen.2021.20382).
“This finding suggests that repeated alcohol consumption events even at lower amounts of alcohol may have a greater carcinogenic effect on GI organs than the consumption of larger amounts of alcohol at a lower frequency,” the investigators wrote.
A possible reason behind the difference in risk may be that the chronic “carcinogenic insult” from regular alcohol use may promote cancer development, whereas less frequent, episodic alcohol exposures may allow physiologic recovery, said the authors.
The results are from a population-based study that involved 11,737,467 participants in the Korean National Health System database who did not have cancer and who took part in a national screening program between January 2009 and December 2010.
They were followed from the year after their screening until either they had received a diagnosis of a GI cancer, death occurred, or the end of December 2017.
During a median follow-up of 6.4 years, 319,202 (2.7%) of those in the study developed a GI cancer.
The increase in the risk associated with alcohol consumption was dose dependent.
Compared with those who did not consume alcohol, the risk of developing GI cancer was higher for mild drinkers (adjusted hazard ratio, 1.04; 95% confidence interval, 1.03-1.05), moderate drinkers (aHR, 1.14; 95% CI, 1.12-1.15), and heavy drinkers (aHR, 1.28; 95% CI, 1.26-1.29), after adjusting for age, sex, income, smoking status with intensity, regular exercise, body mass index, diabetes, hypertension, and dyslipidemia.
There was a linear association between the frequency of drinking and GI cancer risk, with an aHR of 1.39 for individuals who reported drinking every day (95% CI, 1.36-1.41). The risk for GI cancer increased with consumption of five to seven units per occasion (aHR, 1.15). Notably, there were no similar increases with higher intake, including intake of 8-14 units per occasion (aHR, 1.11; 95% CI, 1.09-1.12), and even up to more than 14 units per occasion (aHR, 1.11; 95%CI, 1.08-1.14), in comparison with an intake of 5-7 units per occasion.
“Given similar weekly alcohol consumption levels, the risk of GI cancer increased with a higher frequency of drinking and decreased with a higher amount per occasion,” the authors write.
“Most previous studies just assess alcohol consumption as a total amount, [such as] drinks per occasion times occasion per week equals drinks per week [and] grams per week,” coauthor Dong Wook Shin, MD, DrPH, Samsung Medical Center, Sungkyunkwan University, Seoul, South Korea, said in an interview.
“But it was not known whether frequent drinking with small amount is more harmful than binge drinking, given a similar level of total drinking,” Dr. Shin said.
The increased risk associated with frequent drinking was generally similar with respect to esophageal, gastric, colorectal, biliary, and pancreatic cancer.
An exception was liver cancer, which showed a slightly decreased risk among mild drinkers (aHR, 0.91; 95% CI, 0.89-0.93).
Of note, the association between alcohol intake and the incidence of GI cancer was lower among women than men in terms of weekly consumption, frequency, and amount of alcohol consumed per occasion.
The associations between drinking and cancer type in terms of esophageal and liver cancers were similar between men and women. However, the alcohol-related risk for colorectal, biliary, and pancreatic cancers was less prominent for women.
Possible mechanisms related to regular drinking
A factor that might account for the increase in GI cancer risk with frequent drinking is that regular alcohol consumption “promotes the accumulation of cell divisions in the stem cells that maintain tissues in homeostasis,” the authors explained.
Another possible explanation is that long-term alcohol exposure may promote carcinogenesis, whereas less frequent exposure might allow “physiological homeostasis,” the authors wrote, adding that in vivo experiments have shown that duration and dose of alcohol exposure have been linked to cancer development.
Importantly, the findings support the importance of reducing the frequency of alcohol use to prevent cancer, the authors noted.
“Alcohol users who have a glass of wine or beer during dinner every day may develop more cancer than people who occasionally consume several drinks,” they cautioned.
Genetics, self-reporting considerations
In a related commentary, John D. Potter, MBBS, PhD, of the Research Center for Hauora and Health, Massey University, Wellington, New Zealand, noted that, in addition to supporting the known link between alcohol and cancers of the esophagus, colorectum, and liver, the study “strengthens evidence for a role of alcohol in stomach, biliary tract, and pancreas cancers.”
In comparison with nondrinkers, those who reported heavy drinking were much more likely to be smokers (51.6% vs. 9.0%); however, the study adjusted for smoking.
“Because the researchers were able to control for tobacco, this last finding [regarding the association with cancers of the stomach, biliary tract, and pancreas] is particularly informative,” Dr. Potter noted.
An important caveat is that more than a quarter of the Korean population is known to have an inactive form of the aldehyde dehydrogenase gene (ALDH2), which could have effects on alcohol metabolism as well as the risk for cancer, Dr. Potter wrote.
“This common polymorphism in ALDH2 (ALDH2 rs671 [c.1510G>A (Glu504Lys)]) has paradoxical effects,” he wrote.
“It increases the level of acetaldehyde in the blood of drinkers, which in turn increases the risk of cancer because acetaldehyde is a key player in the carcinogenicity of alcoholic beverages,” Dr. Potter explained. “On the other hand, the accumulation of acetaldehyde and the resultant flushing response are sufficiently unpleasant that they tend to reduce alcohol consumption among those with the Lys allele.”
The study results may therefore not be generalizable to a population in which the distribution of the variation in the ALDH2 enzyme differs, Dr. Potter added.
The lower prevalence of the inactive form (in North America, for instance) would mean that this lower prevalence was not a constraint on individuals’ drinking behavior as it is for some in Korea, Dr. Potter explained.
He noted another consideration: the underreporting of alcohol use is a well-known limitation of studies involving the assessment of alcohol consumption.
Dr. Shin agreed that underreporting is a limitation.
“People tend to underestimate their alcohol use,” Dr. Shin said in an interview.
However, he noted that “our study participants are health-screening participants aged 40 years and older, [and] people who participate in health screening tend to have higher awareness and better health behavior than nonparticipants.”
The authors and Dr. Potter disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alcohol use is a known risk factor for gastrointestinal (GI) cancers. Now, new research indicates that this risk is more associated with frequent drinking – even in smaller amounts – compared with higher amounts or binge drinking, given similar weekly levels.
“The novel finding of the current study is that frequent drinking may be more dangerous than binge drinking with regard to GI cancers. Alcohol use is a known risk factor for gastrointestinal (GI) cancers. Now, new research indicates that this risk is more associated with frequent drinking – even in smaller amounts -- compared with higher amounts or binge drinking, given similar weekly levels.” first author Jung Eun Yook, MD, of Seoul (South Korea) National University Hospital, and colleagues reported in an article published Aug. 18, 2021, in JAMA Network Open (doi: 10.1001/jamanetworkopen.2021.20382).
“This finding suggests that repeated alcohol consumption events even at lower amounts of alcohol may have a greater carcinogenic effect on GI organs than the consumption of larger amounts of alcohol at a lower frequency,” the investigators wrote.
A possible reason behind the difference in risk may be that the chronic “carcinogenic insult” from regular alcohol use may promote cancer development, whereas less frequent, episodic alcohol exposures may allow physiologic recovery, said the authors.
The results are from a population-based study that involved 11,737,467 participants in the Korean National Health System database who did not have cancer and who took part in a national screening program between January 2009 and December 2010.
They were followed from the year after their screening until either they had received a diagnosis of a GI cancer, death occurred, or the end of December 2017.
During a median follow-up of 6.4 years, 319,202 (2.7%) of those in the study developed a GI cancer.
The increase in the risk associated with alcohol consumption was dose dependent.
Compared with those who did not consume alcohol, the risk of developing GI cancer was higher for mild drinkers (adjusted hazard ratio, 1.04; 95% confidence interval, 1.03-1.05), moderate drinkers (aHR, 1.14; 95% CI, 1.12-1.15), and heavy drinkers (aHR, 1.28; 95% CI, 1.26-1.29), after adjusting for age, sex, income, smoking status with intensity, regular exercise, body mass index, diabetes, hypertension, and dyslipidemia.
There was a linear association between the frequency of drinking and GI cancer risk, with an aHR of 1.39 for individuals who reported drinking every day (95% CI, 1.36-1.41). The risk for GI cancer increased with consumption of five to seven units per occasion (aHR, 1.15). Notably, there were no similar increases with higher intake, including intake of 8-14 units per occasion (aHR, 1.11; 95% CI, 1.09-1.12), and even up to more than 14 units per occasion (aHR, 1.11; 95%CI, 1.08-1.14), in comparison with an intake of 5-7 units per occasion.
“Given similar weekly alcohol consumption levels, the risk of GI cancer increased with a higher frequency of drinking and decreased with a higher amount per occasion,” the authors write.
“Most previous studies just assess alcohol consumption as a total amount, [such as] drinks per occasion times occasion per week equals drinks per week [and] grams per week,” coauthor Dong Wook Shin, MD, DrPH, Samsung Medical Center, Sungkyunkwan University, Seoul, South Korea, said in an interview.
“But it was not known whether frequent drinking with small amount is more harmful than binge drinking, given a similar level of total drinking,” Dr. Shin said.
The increased risk associated with frequent drinking was generally similar with respect to esophageal, gastric, colorectal, biliary, and pancreatic cancer.
An exception was liver cancer, which showed a slightly decreased risk among mild drinkers (aHR, 0.91; 95% CI, 0.89-0.93).
Of note, the association between alcohol intake and the incidence of GI cancer was lower among women than men in terms of weekly consumption, frequency, and amount of alcohol consumed per occasion.
The associations between drinking and cancer type in terms of esophageal and liver cancers were similar between men and women. However, the alcohol-related risk for colorectal, biliary, and pancreatic cancers was less prominent for women.
Possible mechanisms related to regular drinking
A factor that might account for the increase in GI cancer risk with frequent drinking is that regular alcohol consumption “promotes the accumulation of cell divisions in the stem cells that maintain tissues in homeostasis,” the authors explained.
Another possible explanation is that long-term alcohol exposure may promote carcinogenesis, whereas less frequent exposure might allow “physiological homeostasis,” the authors wrote, adding that in vivo experiments have shown that duration and dose of alcohol exposure have been linked to cancer development.
Importantly, the findings support the importance of reducing the frequency of alcohol use to prevent cancer, the authors noted.
“Alcohol users who have a glass of wine or beer during dinner every day may develop more cancer than people who occasionally consume several drinks,” they cautioned.
Genetics, self-reporting considerations
In a related commentary, John D. Potter, MBBS, PhD, of the Research Center for Hauora and Health, Massey University, Wellington, New Zealand, noted that, in addition to supporting the known link between alcohol and cancers of the esophagus, colorectum, and liver, the study “strengthens evidence for a role of alcohol in stomach, biliary tract, and pancreas cancers.”
In comparison with nondrinkers, those who reported heavy drinking were much more likely to be smokers (51.6% vs. 9.0%); however, the study adjusted for smoking.
“Because the researchers were able to control for tobacco, this last finding [regarding the association with cancers of the stomach, biliary tract, and pancreas] is particularly informative,” Dr. Potter noted.
An important caveat is that more than a quarter of the Korean population is known to have an inactive form of the aldehyde dehydrogenase gene (ALDH2), which could have effects on alcohol metabolism as well as the risk for cancer, Dr. Potter wrote.
“This common polymorphism in ALDH2 (ALDH2 rs671 [c.1510G>A (Glu504Lys)]) has paradoxical effects,” he wrote.
“It increases the level of acetaldehyde in the blood of drinkers, which in turn increases the risk of cancer because acetaldehyde is a key player in the carcinogenicity of alcoholic beverages,” Dr. Potter explained. “On the other hand, the accumulation of acetaldehyde and the resultant flushing response are sufficiently unpleasant that they tend to reduce alcohol consumption among those with the Lys allele.”
The study results may therefore not be generalizable to a population in which the distribution of the variation in the ALDH2 enzyme differs, Dr. Potter added.
The lower prevalence of the inactive form (in North America, for instance) would mean that this lower prevalence was not a constraint on individuals’ drinking behavior as it is for some in Korea, Dr. Potter explained.
He noted another consideration: the underreporting of alcohol use is a well-known limitation of studies involving the assessment of alcohol consumption.
Dr. Shin agreed that underreporting is a limitation.
“People tend to underestimate their alcohol use,” Dr. Shin said in an interview.
However, he noted that “our study participants are health-screening participants aged 40 years and older, [and] people who participate in health screening tend to have higher awareness and better health behavior than nonparticipants.”
The authors and Dr. Potter disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Use and Toxicity of Checkpoint Inhibitors for Solid Tumor Treatment in a Veteran Population
Due to the high cost of newer chemotherapy agents, institutions search for strategies to minimize drug cost and drug waste. Programmed death-1 (PD-1) inhibitors, nivolumab and pembrolizumab, are commonly used in the treatment of solid tumors; however, the agents cost thousands of dollars per dose. Nivolumab and pembrolizumab were initially approved using weight-based dosing, but package labeling for both agents now includes fixed dosing.1,2 A combination of these 2 dosing strategies could be used by institutions depending on individual patient’s weight to maximize cost savings, minimize drug waste, and maintain safety and efficacy of PD-1 inhibitors. Irrespective of dosing strategy, the development of immune-related adverse events (IrAEs) has been demonstrated with PD-1 inhibitors as a result of the mechanism of action.
PD-1 expression suppresses T cell activity to prevent the development of autoimmunity; however, this is also a mechanism in which tumor cells can evade the host immune system.3-5 Binding of PD-1 and programmed death-ligand 1 (PD-L1) suppresses T cell activity, whereas the inhibition of PD-1 and PD-L1 results in T cell activation.4,5 Increased T cell activity elicits the anticancer effect, but also contributes to the development of IrAEs.4,5 Hypothyroidism is one of the most common IrAEs, with a reported incidence of 9% with nivolumab therapy and 8.5% with pembrolizumab.1,2
Data from the US Department of Veterans Affairs (VA) medical centers is stored in the centralized Corporate Data Warehouse (CDW). VA researchers can obtain approval to use CDW data, which allows for large scale retrospective review of veterans who have received care at VA medical centers (VAMCs). This study aimed to describe the PD-1 inhibitor dosing used within VAMCs and identify actual and potential cost savings. Due to the frequency of immunemediated hypothyroidism and objective data that can be obtained from CDW reports, the study estimated the incidence of immune-mediated hypothyroidism within the veteran population as a safety outcome.
Background
The US Food and Drug Administration (FDA) initially approved dosing for IV nivolumab at 3 mg/kg of patient body weight every 2 weeks and for IV pembrolizumab 2 mg/kg of patient body weight every 3 weeks.1,2 Subsequent pharmacokinetic studies found that these agents have similar exposure and efficacy with fixed doses of nivolumab 240 mg IV every 2 weeks and pembrolizumab 200 mg IV every 3 weeks; in 2016, FDA labeling shifted from weight-based dosing to fixed dosing for most solid tumor indications.6-9 Depending on patient weight, a combination of weightbased and fixed dosing could be used by institutions to maximize cost-savings opportunities, minimize drug waste, and maintain clinical efficacy with PD-1 inhibitors. For example, a patient initiating nivolumab who weighs 80 kg would receive 240 mg for both weight-based (3 mg/kg x 80 kg = 240 mg) and fixed dosing; therefore, no cost-savings opportunities would be available. However, for a patient who weighs ≤ 73.3 kg, it would be more costeffective to use weight-based dosing vs the fixed dose. Since nivolumab is available in 40- mg, 100-mg, and 240-mg vials with similar unit prices, a combination of vial sizes could be used to minimize drug waste. Alternatively, for a patient who weighs ≥ 86.7 kg, it would be more cost-effective to administer the fixed, 240 mg dose when compared with the weightbased dose. Pembrolizumab is available only in a 100-mg vial; therefore, weight-based dosing may result in drug waste.
IrAEs can be seen with PD-1 inhibitors due to increased T cell activity, which is independent of dosing strategy and can affect any organ system. However, immune-mediated hypothyroidism has been commonly seen with PD-1 inhibitors. For patients with immunemediated hypothyroidism, levothyroxine can be considered for asymptomatic patients with thyroid- stimulating hormone (TSH) > 10 uIU/mL with normal thyroxine (T4), or patients with clinical primary hypothyroidism (TSH > 10 uIU/mL with low free T4 and clinical symptoms). Additionally, since hypothyroidism usually follows immunotherapy induced thyrotoxicosis, thyroid function tests should be monitored and levothyroxine initiated if TSH is > 10 uIU/mL for these patients.10,11
Hypothyroidism also can be graded according to the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events. Hypothyroidism is considered grade 1 when hypothyroidism is demonstrated through clinical or diagnostic observations only and the patient is asymptomatic and no intervention needed. Grade 2 occurs when the patient is symptomatic and limits instrumental activities of daily living (ADLs), prompting thyroid replacement therapy. In grade 3, patients experience severe symptoms that restrict self-care ADLs, and hospitalization is indicated. Grade 4 has life-threatening consequences, and urgent intervention is indicated. Grade 5 results in the death of the patient.12
Electronic health records (EHRs) of veterans who receive care at a VAMC are stored in CDW and available through the VA Informatics and Computing Infrastructure (VINCI), which provides access to data while ensuring veterans’ privacy and data security. This feature of the VA EHR allows for analysis of data across the VA health care system, and larger data sets can be used for retrospective chart reviews.
Using reports from CDW, the primary objective of this study was to describe the dosing strategy used for PD-1 inhibitors, and the primary safety outcome was to determine the incidence of immune-mediated hypothyroidism. The secondary objective was to estimate potential cost-savings opportunities using a combination of PD-1 inhibitor dosing strategies.
Methods
This was a retrospective study including data stored in CDW. The study was approved by the Durham VA Health Care System Institutional Review Board and VINCI/Data Access request tracker. Data were limited to nivolumab and pembrolizumab because they received earlier FDA approval, had multiple solid tumor indications, and 2 FDA-approved dosing strategies. The incidence of IrAEs was limited to hypothyroidism, which could be objectively verified with laboratory monitoring of thyroid function tests, including TSH, free or total T4, and triiodothyronine (T3), all of which were available in CDW data. Additionally, most patients with hypothyroidism initiate treatment with levothyroxine. Prescription refill history could also be retrieved using CDW reports.
Hypothyroidism was defined as T4 below lower limit of normal (LLN), TSH above upper limit of normal (ULN), or any increase in levothyroxine dosage. Patients were excluded if they received PD-1 inhibitor for an indication other than solid tumor treatment, such as hematologic malignancy, or if dosing did not follow weight-based or fixed-dosing strategies, such as nivolumab 1 mg/kg when used in combination with ipilimumab, or pembrolizumab 10 mg/kg. The primary endpoint was the percentage of orders for each dosing strategy, and the primary safety outcome was the incidence of immune-mediated hypothyroidism. Secondary endpoints included estimated cost savings and cost-savings opportunities through nivolumab dose rounding and incidence of levothyroxine initiation or dose change. Descriptive statistics were used for the primary and secondary endpoints.
A report in CDW identified patients who received a dose of nivolumab or pembrolizumab between January 1, 2015 and July 1, 2017 at any VAMC. The CDW report obtained weight at time of PD-1 inhibitor therapy initiation, dose of PD-1 inhibitor given, administration date of PD-1 inhibitor, and VA site. Depending on PD-1 inhibitor administered, weight in kg was multiplied by 3 mg/kg or 2 mg/kg to obtain patient’s anticipated weight-based nivolumab and pembrolizumab dose, respectively. The calculated weight-based dose, fixed dose, and administered dose were compared to infer dosing strategy used at the time of ordering. If the patient’s weight-based dose was within 10% of the fixed dose, the order was categorized as converging because the doses were too similar to determine which dosing strategy was intended.
After determination of dosing strategy, the nivolumab orders were evaluated for actual vs missed cost savings. The cost-savings evaluation included only nivolumab orders because nivolumab is available in a 40-mg, 100-mg, and 240-mg vials and, therefore, has more potential for dose-rounding opportunities with minimal drug waste compared with pembrolizumab, which is available only in a 100-mg vial. Actual cost savings included patients who weighed ≤ 73.3 kg and received nivolumab dose based on 3 mg/kg or patients who weighed ≥ 86.7 kg and received nivolumab 240 mg (fixed dose). Missed cost savings comprised patients who weighed ≤ 73.3 kg who received 240 mg nivolumab or patients who weighed ≥ 86.7 kg and received a nivolumab dose > 240 mg. The cost difference between the dose given and theoretical cost-effective dose was calculated to determine actual and potential cost savings. Converging orders were not included in the cost-savings analysis as the intended nivolumab dose could not be determined. An additional cost analysis of nivolumab orders prescribed between September 1, 2016 and July 1, 2017 was also performed because nivolumab fixed dosing was FDA-approved for most solid tumor indications in September 2016.
To determine the incidence of immunemediated hypothyroidism for patients who received a dose of a PD-1 inhibitor at a VAMC, a CDW report with thyroid function laboratory values (TSH, T4, or T3), including reference range values based on specific VA site, and levothyroxine prescriptions issued during PD-1 inhibitor therapy was obtained. A patient was considered to have experienced immune-mediated hypothyroidism if the patient’s laboratory values demonstrated T4 below the LLN, TSH above the ULN, or if the medication fill history demonstrated levothyroxine initiation or a levothyroxine dose increase.
Results
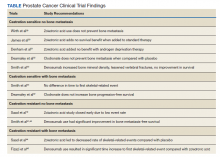
The CDW report identified 32,769 total PD-1 inhibitor orders. There were 3982 orders that did not meet inclusion criteria or inadequate data were obtained with CDW report and were excluded (Figure). The remaining 28,787 PD-1 inhibitor orders were evaluated for actual or missed cost savings. The distribution of dosing strategies can be found in Table 1.
Nivolumab accounted for 81.5% of all PD-1 inhibitor orders. Using the most cost-effective nivolumab dosing, the actual cost savings was estimated to be $8,514,300 with potential additional $5,591,250 of missed cost-savings opportunities. There were 8013 nivolumab orders written between September 1, 2016 and July 1, 2017. Cost-effective dosing was used in 4687 of these orders, which accounted for a cost savings of $5,198,570. The remaining 3326 orders had a missed cost-savings opportunity, which accounted for an additional $2,907,180 potential cost savings (Table 2).
PD-1 inhibitors were used for the treatment of 3249 unique patients. Based on abnormal thyroid function tests and levothyroxine initiation or dose increase, it is estimated that 514 (15.8%) patients experienced hypothyroidism during PD-1 inhibitor therapy. However, prior to PD-1 inhibitor therapy, 274 patients were receiving levothyroxine, suggesting baseline thyroid dysfunction. Of these patients, 152 (55.5%) patients maintained the same levothyroxine dose during PD-1 inhibitor therapy, but 91 (33.2%) required a levothyroxine dose increase. There were 187 patients who initiated levothyroxine during PD-1 inhibitor therapy (Table 3).
Discussion
Changes in FDA-approved dosing for PD-1 inhibitors allowed a combination of dosing strategies. Depending on patient weight, a weight-based or fixed-dosing strategy can be used to reduce drug cost while maintaining equivalent efficacy. This study evaluated use of dose rounding for PD-1 inhibitors within the VA health care system to identify actual and potential cost savings. To our knowledge, this is the first study to demonstrate cost savings through use of a combination of PD-1 inhibitor dosing strategies. Using CDW, researchers were able to review PD-1 dosing from all VAMCs and include a larger number of orders in a single retrospective study.
Nivolumab was the primary agent used within VAMCs. Depending on the indication, pembrolizumab requires PD-1 expression testing prior to its use in several solid tumor indications. Consequently, additional testing and patient eligibility is needed prior to use. Both PD-1 inhibitors were primarily dosed based on patient weight since this was the first FDAapproved dosing strategy. Nivolumab had more orders categorized as converging, which may be due to the therapeutic weight-based dose of 3 mg/kg for nivolumab vs 2 mg/kg for pembrolizumab. The calculated weight-based dose of nivolumab for an 80-kg patient is 240 mg, which also is the fixed dose. A 80-kg patient on pembrolizumab at 2 mg/kg would receive a 160-mg dose, whereas the fixed dose of pembrolizumab is 200 mg. Pembrolizumab is available only in a 100-mg vial, which limits opportunities for dose rounding without drug waste and could explain the higher amount of pembrolizumab orders in the fixed-dose category.
In this review of PD-1 inhibitor orders over approximately a 2.5-year study period, we identified $8,514,300 estimated cost savings with $5,591,250 estimated missed cost savings. When looking at orders administered after FDA approval for nivolumab-fixed dosing in September 2016, there was substantial cost savings of $5,198,570 with the potential for an additional $2,907,180 missed cost savings. Due to lower drug acquisition costs within the VA health care system, there may be higher cost-savings opportunities within other health care systems.
Through review of abnormal thyroid laboratory values and levothyroxine initiation or dose changes, this study estimated the incidence of hypothyroidism in patients receiving PD-1 inhibitor therapy at the VA. The incidence of primary hypothyroidism identified in this study was slightly higher at 15.8% compared with the 8.5 to 9.0% incidence reported from clinical trials.1,2 There are several reasons why the incidence of hypothyroidism appeared higher in this study. Abnormal laboratory values were not assessed for the degree of deviation from the reference range; any TSH above the ULN, T4 below the LLN, or levothyroxine dose increase was included as thyroid dysfunction in this review. There is also the potential for endogenous age-related thyroid fluctuation, and the development of hypothyroidism may not have been related to PD-1 inhibitor therapy. Within this patient population, 8.4% were receiving levothyroxine prior to PD-1 inhibitor initiation indicating baseline thyroid dysfunction, and it is unclear whether levothyroxine dose increases were due to PD-1 inhibitor or endogenous fluctuation.
Limitations
There are several limitations to acknowledge. The dosing strategy and apparent dose rounding was determined by investigator inference and may not accurately represent the intended dosing strategy. This study did not address efficacy of PD-1 inhibitor and dosing strategy; however, clinical trials have demonstrated equivalent efficacy to generate the change in FDA-approved dosing. Additionally, FDA approval for nivolumab fixed dosing was indication specific. Starting in September 2016, many solid tumor indications had fixed dosing approved, but this approval was not necessarily all encompassing.
While the use of CDW allowed for a greater number of PD-1 inhibitor orders to be included in retrospective review, there also were limitations of the CDW report. The patient weight was limited to weight at time of therapy initiation. Due to the potential for weight changes, nivolumab dosing may have seemed inappropriate to investigators, and thereby excluded. Based on data available from CDW reports, hypothyroidism could not be graded according to NCI Common Terminology Criteria for Adverse Events, and the incidence of clinically significant hypothyroidism could not be determined.
Conclusions
With increasing drug acquisition costs, particularly among antineoplastic agents, health care systems frequently seek out cost-savings opportunities. Using a combination of weightbased and fixed-dosing strategies for PD-1 inhibitors can be a mechanism to achieve costsavings. Through the identification of the dosing strategy used for PD-1 inhibitors, we were able to identify and report instances for potential cost-savings opportunities among veterans treated within VA health care system. Use of CDW allows for data from all VAMCs to be evaluated in a single retrospective chart review, which allows for the inclusion of a larger sample size. This study identified a substantial cost savings for nivolumab through a combination of weight-based and fixed-dosing strategies. Due to the novel mechanism of action, ongoing realworld evaluation of adverse events and IrAEs is warranted.
Dosing strategies with nivolumab and pembrolizumab continue to evolve. In March 2018, nivolumab 480 mg IV every 4 weeks was FDA approved and in April 2020, pembrolizumab 400 mg IV every 6 weeks was FDA approved.13,14 While the drug costs will remain the same, extended interval dosing strategies have cost avoidance such as fewer clinic appointments, resulting in decreased staffing costs and decreased patient travel. Additional studies will be needed to evaluate the cost and safety of the recently approved dosing strategies
1. OPDIVO (nivolumab) injection, for intravenous infusion. Package Insert. Princeton, NJ: Bristol-Myers Squibb Company; 2014.
2. Keytruda (pembrolizumab) injection, for intravenous infusion. Package Insert. Whitehouse Station, NJ: Merck & Co, Inc; 2016
3. Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12(4):252-264. doi:10.1038/nrc3239
4. Yao H, Wang H, Li C, Fang J-Y, Xu J. Cancer cellintrinsic PD-1 and implications in combinatorial immunotherapy. Front Immunol. 2018;9:1774. doi:10.3389/fimmu.2018.01774
5. Wang Y, Wang H, Yao H, Li C, Fang J-Y, Xu J. Regulation of PD-L1: emerging routes for targeting tumor immune evasion. Front Pharmacol. 2018;9:536. doi:10.3389/fphar.2018.00536
6. Patnaik A, Kang SP, Rasco D, et al. Phase I study of pembrolizumab (MK-3475; anti-PD-1 monocolonal antibody) in patients with advanced solid tumors. Clin Cancer Res. 2015;21(19):4286-4293. doi:10.1158/1078-0432.CCR-14-2607
7. Zhao X, Suryawanshi S, Hruska M, et al. Assessment of nivolumab benefit-risk profile of a 240-mg flat dose relative to a 3-mg/kg dosing regimen in patients with advanced tumors. Ann Oncol. 2017;28(8):2002-2008. doi:10.1093/annonc/mdx235
8. Freshwater T, Kondic A, Ahamadi M, et al. Evaluation of dosing strategy for pembrolizumab for oncology indications. J Immunother Cancer. 2017;5:43. doi:10.1186/s40425-017-0242-5
9. US Food and Drug Administration. Modification of the dosage regimen for nivolumab. Updated September 15, 2016. Accessed July 8, 2021. https://www.fda.gov/drugs /resources-information-approved-drugs/modification -dosage-regimen-nivolumab
10. Brahmer JR, Lacchetti C, Schneider BJ, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2018;36(17):1714-1768. doi:10.1200/JCO.2017.77.6385
11. National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology: Management of immunotherapy- related toxicities. version 3.2021. Updated May 14, 2021. Accessed July 8,2021.https://www.nccn.org/professionals/physician_gls/pdf/immunotherapy.pdf
12. National Institutes of Health, National Cancer Institute. Common terminology criteria for adverse events (CTCAE) version 5.0. Updated November 17, 2017. Accessed July 8, 2021. https://ctep.cancer.gov /protocoldevelopment/electronic_applications/docs /CTCAE_v5_Quick_Reference_8.5x11.pdf
13. Zhao X, Ivaturi V, Gopalakrishnan M, Shen J, et al. A model-based exposure-response (E-R) assessment of a nivolumab (NIVO) 4-weekly dosing schedule across multiple tumor types. Abstract presented at: American Association of Cancer Research Annual Meeting 2017; April 1-5, 2017; Washington, DC. doi:10.1158/1538-7445.AM2017-CT101
14. US Food and Drug Administration approves new dosing regimen for pembrolizumab. Updated April 29, 2020. Accessed July 8, 2021. https://www.fda.gov/drugs/drug -approvals-and-databases/fda-approves-new-dosing -regimen-pembrolizumab
Due to the high cost of newer chemotherapy agents, institutions search for strategies to minimize drug cost and drug waste. Programmed death-1 (PD-1) inhibitors, nivolumab and pembrolizumab, are commonly used in the treatment of solid tumors; however, the agents cost thousands of dollars per dose. Nivolumab and pembrolizumab were initially approved using weight-based dosing, but package labeling for both agents now includes fixed dosing.1,2 A combination of these 2 dosing strategies could be used by institutions depending on individual patient’s weight to maximize cost savings, minimize drug waste, and maintain safety and efficacy of PD-1 inhibitors. Irrespective of dosing strategy, the development of immune-related adverse events (IrAEs) has been demonstrated with PD-1 inhibitors as a result of the mechanism of action.
PD-1 expression suppresses T cell activity to prevent the development of autoimmunity; however, this is also a mechanism in which tumor cells can evade the host immune system.3-5 Binding of PD-1 and programmed death-ligand 1 (PD-L1) suppresses T cell activity, whereas the inhibition of PD-1 and PD-L1 results in T cell activation.4,5 Increased T cell activity elicits the anticancer effect, but also contributes to the development of IrAEs.4,5 Hypothyroidism is one of the most common IrAEs, with a reported incidence of 9% with nivolumab therapy and 8.5% with pembrolizumab.1,2
Data from the US Department of Veterans Affairs (VA) medical centers is stored in the centralized Corporate Data Warehouse (CDW). VA researchers can obtain approval to use CDW data, which allows for large scale retrospective review of veterans who have received care at VA medical centers (VAMCs). This study aimed to describe the PD-1 inhibitor dosing used within VAMCs and identify actual and potential cost savings. Due to the frequency of immunemediated hypothyroidism and objective data that can be obtained from CDW reports, the study estimated the incidence of immune-mediated hypothyroidism within the veteran population as a safety outcome.
Background
The US Food and Drug Administration (FDA) initially approved dosing for IV nivolumab at 3 mg/kg of patient body weight every 2 weeks and for IV pembrolizumab 2 mg/kg of patient body weight every 3 weeks.1,2 Subsequent pharmacokinetic studies found that these agents have similar exposure and efficacy with fixed doses of nivolumab 240 mg IV every 2 weeks and pembrolizumab 200 mg IV every 3 weeks; in 2016, FDA labeling shifted from weight-based dosing to fixed dosing for most solid tumor indications.6-9 Depending on patient weight, a combination of weightbased and fixed dosing could be used by institutions to maximize cost-savings opportunities, minimize drug waste, and maintain clinical efficacy with PD-1 inhibitors. For example, a patient initiating nivolumab who weighs 80 kg would receive 240 mg for both weight-based (3 mg/kg x 80 kg = 240 mg) and fixed dosing; therefore, no cost-savings opportunities would be available. However, for a patient who weighs ≤ 73.3 kg, it would be more costeffective to use weight-based dosing vs the fixed dose. Since nivolumab is available in 40- mg, 100-mg, and 240-mg vials with similar unit prices, a combination of vial sizes could be used to minimize drug waste. Alternatively, for a patient who weighs ≥ 86.7 kg, it would be more cost-effective to administer the fixed, 240 mg dose when compared with the weightbased dose. Pembrolizumab is available only in a 100-mg vial; therefore, weight-based dosing may result in drug waste.
IrAEs can be seen with PD-1 inhibitors due to increased T cell activity, which is independent of dosing strategy and can affect any organ system. However, immune-mediated hypothyroidism has been commonly seen with PD-1 inhibitors. For patients with immunemediated hypothyroidism, levothyroxine can be considered for asymptomatic patients with thyroid- stimulating hormone (TSH) > 10 uIU/mL with normal thyroxine (T4), or patients with clinical primary hypothyroidism (TSH > 10 uIU/mL with low free T4 and clinical symptoms). Additionally, since hypothyroidism usually follows immunotherapy induced thyrotoxicosis, thyroid function tests should be monitored and levothyroxine initiated if TSH is > 10 uIU/mL for these patients.10,11
Hypothyroidism also can be graded according to the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events. Hypothyroidism is considered grade 1 when hypothyroidism is demonstrated through clinical or diagnostic observations only and the patient is asymptomatic and no intervention needed. Grade 2 occurs when the patient is symptomatic and limits instrumental activities of daily living (ADLs), prompting thyroid replacement therapy. In grade 3, patients experience severe symptoms that restrict self-care ADLs, and hospitalization is indicated. Grade 4 has life-threatening consequences, and urgent intervention is indicated. Grade 5 results in the death of the patient.12
Electronic health records (EHRs) of veterans who receive care at a VAMC are stored in CDW and available through the VA Informatics and Computing Infrastructure (VINCI), which provides access to data while ensuring veterans’ privacy and data security. This feature of the VA EHR allows for analysis of data across the VA health care system, and larger data sets can be used for retrospective chart reviews.
Using reports from CDW, the primary objective of this study was to describe the dosing strategy used for PD-1 inhibitors, and the primary safety outcome was to determine the incidence of immune-mediated hypothyroidism. The secondary objective was to estimate potential cost-savings opportunities using a combination of PD-1 inhibitor dosing strategies.
Methods
This was a retrospective study including data stored in CDW. The study was approved by the Durham VA Health Care System Institutional Review Board and VINCI/Data Access request tracker. Data were limited to nivolumab and pembrolizumab because they received earlier FDA approval, had multiple solid tumor indications, and 2 FDA-approved dosing strategies. The incidence of IrAEs was limited to hypothyroidism, which could be objectively verified with laboratory monitoring of thyroid function tests, including TSH, free or total T4, and triiodothyronine (T3), all of which were available in CDW data. Additionally, most patients with hypothyroidism initiate treatment with levothyroxine. Prescription refill history could also be retrieved using CDW reports.
Hypothyroidism was defined as T4 below lower limit of normal (LLN), TSH above upper limit of normal (ULN), or any increase in levothyroxine dosage. Patients were excluded if they received PD-1 inhibitor for an indication other than solid tumor treatment, such as hematologic malignancy, or if dosing did not follow weight-based or fixed-dosing strategies, such as nivolumab 1 mg/kg when used in combination with ipilimumab, or pembrolizumab 10 mg/kg. The primary endpoint was the percentage of orders for each dosing strategy, and the primary safety outcome was the incidence of immune-mediated hypothyroidism. Secondary endpoints included estimated cost savings and cost-savings opportunities through nivolumab dose rounding and incidence of levothyroxine initiation or dose change. Descriptive statistics were used for the primary and secondary endpoints.
A report in CDW identified patients who received a dose of nivolumab or pembrolizumab between January 1, 2015 and July 1, 2017 at any VAMC. The CDW report obtained weight at time of PD-1 inhibitor therapy initiation, dose of PD-1 inhibitor given, administration date of PD-1 inhibitor, and VA site. Depending on PD-1 inhibitor administered, weight in kg was multiplied by 3 mg/kg or 2 mg/kg to obtain patient’s anticipated weight-based nivolumab and pembrolizumab dose, respectively. The calculated weight-based dose, fixed dose, and administered dose were compared to infer dosing strategy used at the time of ordering. If the patient’s weight-based dose was within 10% of the fixed dose, the order was categorized as converging because the doses were too similar to determine which dosing strategy was intended.
After determination of dosing strategy, the nivolumab orders were evaluated for actual vs missed cost savings. The cost-savings evaluation included only nivolumab orders because nivolumab is available in a 40-mg, 100-mg, and 240-mg vials and, therefore, has more potential for dose-rounding opportunities with minimal drug waste compared with pembrolizumab, which is available only in a 100-mg vial. Actual cost savings included patients who weighed ≤ 73.3 kg and received nivolumab dose based on 3 mg/kg or patients who weighed ≥ 86.7 kg and received nivolumab 240 mg (fixed dose). Missed cost savings comprised patients who weighed ≤ 73.3 kg who received 240 mg nivolumab or patients who weighed ≥ 86.7 kg and received a nivolumab dose > 240 mg. The cost difference between the dose given and theoretical cost-effective dose was calculated to determine actual and potential cost savings. Converging orders were not included in the cost-savings analysis as the intended nivolumab dose could not be determined. An additional cost analysis of nivolumab orders prescribed between September 1, 2016 and July 1, 2017 was also performed because nivolumab fixed dosing was FDA-approved for most solid tumor indications in September 2016.
To determine the incidence of immunemediated hypothyroidism for patients who received a dose of a PD-1 inhibitor at a VAMC, a CDW report with thyroid function laboratory values (TSH, T4, or T3), including reference range values based on specific VA site, and levothyroxine prescriptions issued during PD-1 inhibitor therapy was obtained. A patient was considered to have experienced immune-mediated hypothyroidism if the patient’s laboratory values demonstrated T4 below the LLN, TSH above the ULN, or if the medication fill history demonstrated levothyroxine initiation or a levothyroxine dose increase.
Results
The CDW report identified 32,769 total PD-1 inhibitor orders. There were 3982 orders that did not meet inclusion criteria or inadequate data were obtained with CDW report and were excluded (Figure). The remaining 28,787 PD-1 inhibitor orders were evaluated for actual or missed cost savings. The distribution of dosing strategies can be found in Table 1.
Nivolumab accounted for 81.5% of all PD-1 inhibitor orders. Using the most cost-effective nivolumab dosing, the actual cost savings was estimated to be $8,514,300 with potential additional $5,591,250 of missed cost-savings opportunities. There were 8013 nivolumab orders written between September 1, 2016 and July 1, 2017. Cost-effective dosing was used in 4687 of these orders, which accounted for a cost savings of $5,198,570. The remaining 3326 orders had a missed cost-savings opportunity, which accounted for an additional $2,907,180 potential cost savings (Table 2).
PD-1 inhibitors were used for the treatment of 3249 unique patients. Based on abnormal thyroid function tests and levothyroxine initiation or dose increase, it is estimated that 514 (15.8%) patients experienced hypothyroidism during PD-1 inhibitor therapy. However, prior to PD-1 inhibitor therapy, 274 patients were receiving levothyroxine, suggesting baseline thyroid dysfunction. Of these patients, 152 (55.5%) patients maintained the same levothyroxine dose during PD-1 inhibitor therapy, but 91 (33.2%) required a levothyroxine dose increase. There were 187 patients who initiated levothyroxine during PD-1 inhibitor therapy (Table 3).
Discussion
Changes in FDA-approved dosing for PD-1 inhibitors allowed a combination of dosing strategies. Depending on patient weight, a weight-based or fixed-dosing strategy can be used to reduce drug cost while maintaining equivalent efficacy. This study evaluated use of dose rounding for PD-1 inhibitors within the VA health care system to identify actual and potential cost savings. To our knowledge, this is the first study to demonstrate cost savings through use of a combination of PD-1 inhibitor dosing strategies. Using CDW, researchers were able to review PD-1 dosing from all VAMCs and include a larger number of orders in a single retrospective study.
Nivolumab was the primary agent used within VAMCs. Depending on the indication, pembrolizumab requires PD-1 expression testing prior to its use in several solid tumor indications. Consequently, additional testing and patient eligibility is needed prior to use. Both PD-1 inhibitors were primarily dosed based on patient weight since this was the first FDAapproved dosing strategy. Nivolumab had more orders categorized as converging, which may be due to the therapeutic weight-based dose of 3 mg/kg for nivolumab vs 2 mg/kg for pembrolizumab. The calculated weight-based dose of nivolumab for an 80-kg patient is 240 mg, which also is the fixed dose. A 80-kg patient on pembrolizumab at 2 mg/kg would receive a 160-mg dose, whereas the fixed dose of pembrolizumab is 200 mg. Pembrolizumab is available only in a 100-mg vial, which limits opportunities for dose rounding without drug waste and could explain the higher amount of pembrolizumab orders in the fixed-dose category.
In this review of PD-1 inhibitor orders over approximately a 2.5-year study period, we identified $8,514,300 estimated cost savings with $5,591,250 estimated missed cost savings. When looking at orders administered after FDA approval for nivolumab-fixed dosing in September 2016, there was substantial cost savings of $5,198,570 with the potential for an additional $2,907,180 missed cost savings. Due to lower drug acquisition costs within the VA health care system, there may be higher cost-savings opportunities within other health care systems.
Through review of abnormal thyroid laboratory values and levothyroxine initiation or dose changes, this study estimated the incidence of hypothyroidism in patients receiving PD-1 inhibitor therapy at the VA. The incidence of primary hypothyroidism identified in this study was slightly higher at 15.8% compared with the 8.5 to 9.0% incidence reported from clinical trials.1,2 There are several reasons why the incidence of hypothyroidism appeared higher in this study. Abnormal laboratory values were not assessed for the degree of deviation from the reference range; any TSH above the ULN, T4 below the LLN, or levothyroxine dose increase was included as thyroid dysfunction in this review. There is also the potential for endogenous age-related thyroid fluctuation, and the development of hypothyroidism may not have been related to PD-1 inhibitor therapy. Within this patient population, 8.4% were receiving levothyroxine prior to PD-1 inhibitor initiation indicating baseline thyroid dysfunction, and it is unclear whether levothyroxine dose increases were due to PD-1 inhibitor or endogenous fluctuation.
Limitations
There are several limitations to acknowledge. The dosing strategy and apparent dose rounding was determined by investigator inference and may not accurately represent the intended dosing strategy. This study did not address efficacy of PD-1 inhibitor and dosing strategy; however, clinical trials have demonstrated equivalent efficacy to generate the change in FDA-approved dosing. Additionally, FDA approval for nivolumab fixed dosing was indication specific. Starting in September 2016, many solid tumor indications had fixed dosing approved, but this approval was not necessarily all encompassing.
While the use of CDW allowed for a greater number of PD-1 inhibitor orders to be included in retrospective review, there also were limitations of the CDW report. The patient weight was limited to weight at time of therapy initiation. Due to the potential for weight changes, nivolumab dosing may have seemed inappropriate to investigators, and thereby excluded. Based on data available from CDW reports, hypothyroidism could not be graded according to NCI Common Terminology Criteria for Adverse Events, and the incidence of clinically significant hypothyroidism could not be determined.
Conclusions
With increasing drug acquisition costs, particularly among antineoplastic agents, health care systems frequently seek out cost-savings opportunities. Using a combination of weightbased and fixed-dosing strategies for PD-1 inhibitors can be a mechanism to achieve costsavings. Through the identification of the dosing strategy used for PD-1 inhibitors, we were able to identify and report instances for potential cost-savings opportunities among veterans treated within VA health care system. Use of CDW allows for data from all VAMCs to be evaluated in a single retrospective chart review, which allows for the inclusion of a larger sample size. This study identified a substantial cost savings for nivolumab through a combination of weight-based and fixed-dosing strategies. Due to the novel mechanism of action, ongoing realworld evaluation of adverse events and IrAEs is warranted.
Dosing strategies with nivolumab and pembrolizumab continue to evolve. In March 2018, nivolumab 480 mg IV every 4 weeks was FDA approved and in April 2020, pembrolizumab 400 mg IV every 6 weeks was FDA approved.13,14 While the drug costs will remain the same, extended interval dosing strategies have cost avoidance such as fewer clinic appointments, resulting in decreased staffing costs and decreased patient travel. Additional studies will be needed to evaluate the cost and safety of the recently approved dosing strategies
Due to the high cost of newer chemotherapy agents, institutions search for strategies to minimize drug cost and drug waste. Programmed death-1 (PD-1) inhibitors, nivolumab and pembrolizumab, are commonly used in the treatment of solid tumors; however, the agents cost thousands of dollars per dose. Nivolumab and pembrolizumab were initially approved using weight-based dosing, but package labeling for both agents now includes fixed dosing.1,2 A combination of these 2 dosing strategies could be used by institutions depending on individual patient’s weight to maximize cost savings, minimize drug waste, and maintain safety and efficacy of PD-1 inhibitors. Irrespective of dosing strategy, the development of immune-related adverse events (IrAEs) has been demonstrated with PD-1 inhibitors as a result of the mechanism of action.
PD-1 expression suppresses T cell activity to prevent the development of autoimmunity; however, this is also a mechanism in which tumor cells can evade the host immune system.3-5 Binding of PD-1 and programmed death-ligand 1 (PD-L1) suppresses T cell activity, whereas the inhibition of PD-1 and PD-L1 results in T cell activation.4,5 Increased T cell activity elicits the anticancer effect, but also contributes to the development of IrAEs.4,5 Hypothyroidism is one of the most common IrAEs, with a reported incidence of 9% with nivolumab therapy and 8.5% with pembrolizumab.1,2
Data from the US Department of Veterans Affairs (VA) medical centers is stored in the centralized Corporate Data Warehouse (CDW). VA researchers can obtain approval to use CDW data, which allows for large scale retrospective review of veterans who have received care at VA medical centers (VAMCs). This study aimed to describe the PD-1 inhibitor dosing used within VAMCs and identify actual and potential cost savings. Due to the frequency of immunemediated hypothyroidism and objective data that can be obtained from CDW reports, the study estimated the incidence of immune-mediated hypothyroidism within the veteran population as a safety outcome.
Background
The US Food and Drug Administration (FDA) initially approved dosing for IV nivolumab at 3 mg/kg of patient body weight every 2 weeks and for IV pembrolizumab 2 mg/kg of patient body weight every 3 weeks.1,2 Subsequent pharmacokinetic studies found that these agents have similar exposure and efficacy with fixed doses of nivolumab 240 mg IV every 2 weeks and pembrolizumab 200 mg IV every 3 weeks; in 2016, FDA labeling shifted from weight-based dosing to fixed dosing for most solid tumor indications.6-9 Depending on patient weight, a combination of weightbased and fixed dosing could be used by institutions to maximize cost-savings opportunities, minimize drug waste, and maintain clinical efficacy with PD-1 inhibitors. For example, a patient initiating nivolumab who weighs 80 kg would receive 240 mg for both weight-based (3 mg/kg x 80 kg = 240 mg) and fixed dosing; therefore, no cost-savings opportunities would be available. However, for a patient who weighs ≤ 73.3 kg, it would be more costeffective to use weight-based dosing vs the fixed dose. Since nivolumab is available in 40- mg, 100-mg, and 240-mg vials with similar unit prices, a combination of vial sizes could be used to minimize drug waste. Alternatively, for a patient who weighs ≥ 86.7 kg, it would be more cost-effective to administer the fixed, 240 mg dose when compared with the weightbased dose. Pembrolizumab is available only in a 100-mg vial; therefore, weight-based dosing may result in drug waste.
IrAEs can be seen with PD-1 inhibitors due to increased T cell activity, which is independent of dosing strategy and can affect any organ system. However, immune-mediated hypothyroidism has been commonly seen with PD-1 inhibitors. For patients with immunemediated hypothyroidism, levothyroxine can be considered for asymptomatic patients with thyroid- stimulating hormone (TSH) > 10 uIU/mL with normal thyroxine (T4), or patients with clinical primary hypothyroidism (TSH > 10 uIU/mL with low free T4 and clinical symptoms). Additionally, since hypothyroidism usually follows immunotherapy induced thyrotoxicosis, thyroid function tests should be monitored and levothyroxine initiated if TSH is > 10 uIU/mL for these patients.10,11
Hypothyroidism also can be graded according to the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events. Hypothyroidism is considered grade 1 when hypothyroidism is demonstrated through clinical or diagnostic observations only and the patient is asymptomatic and no intervention needed. Grade 2 occurs when the patient is symptomatic and limits instrumental activities of daily living (ADLs), prompting thyroid replacement therapy. In grade 3, patients experience severe symptoms that restrict self-care ADLs, and hospitalization is indicated. Grade 4 has life-threatening consequences, and urgent intervention is indicated. Grade 5 results in the death of the patient.12
Electronic health records (EHRs) of veterans who receive care at a VAMC are stored in CDW and available through the VA Informatics and Computing Infrastructure (VINCI), which provides access to data while ensuring veterans’ privacy and data security. This feature of the VA EHR allows for analysis of data across the VA health care system, and larger data sets can be used for retrospective chart reviews.
Using reports from CDW, the primary objective of this study was to describe the dosing strategy used for PD-1 inhibitors, and the primary safety outcome was to determine the incidence of immune-mediated hypothyroidism. The secondary objective was to estimate potential cost-savings opportunities using a combination of PD-1 inhibitor dosing strategies.
Methods
This was a retrospective study including data stored in CDW. The study was approved by the Durham VA Health Care System Institutional Review Board and VINCI/Data Access request tracker. Data were limited to nivolumab and pembrolizumab because they received earlier FDA approval, had multiple solid tumor indications, and 2 FDA-approved dosing strategies. The incidence of IrAEs was limited to hypothyroidism, which could be objectively verified with laboratory monitoring of thyroid function tests, including TSH, free or total T4, and triiodothyronine (T3), all of which were available in CDW data. Additionally, most patients with hypothyroidism initiate treatment with levothyroxine. Prescription refill history could also be retrieved using CDW reports.
Hypothyroidism was defined as T4 below lower limit of normal (LLN), TSH above upper limit of normal (ULN), or any increase in levothyroxine dosage. Patients were excluded if they received PD-1 inhibitor for an indication other than solid tumor treatment, such as hematologic malignancy, or if dosing did not follow weight-based or fixed-dosing strategies, such as nivolumab 1 mg/kg when used in combination with ipilimumab, or pembrolizumab 10 mg/kg. The primary endpoint was the percentage of orders for each dosing strategy, and the primary safety outcome was the incidence of immune-mediated hypothyroidism. Secondary endpoints included estimated cost savings and cost-savings opportunities through nivolumab dose rounding and incidence of levothyroxine initiation or dose change. Descriptive statistics were used for the primary and secondary endpoints.
A report in CDW identified patients who received a dose of nivolumab or pembrolizumab between January 1, 2015 and July 1, 2017 at any VAMC. The CDW report obtained weight at time of PD-1 inhibitor therapy initiation, dose of PD-1 inhibitor given, administration date of PD-1 inhibitor, and VA site. Depending on PD-1 inhibitor administered, weight in kg was multiplied by 3 mg/kg or 2 mg/kg to obtain patient’s anticipated weight-based nivolumab and pembrolizumab dose, respectively. The calculated weight-based dose, fixed dose, and administered dose were compared to infer dosing strategy used at the time of ordering. If the patient’s weight-based dose was within 10% of the fixed dose, the order was categorized as converging because the doses were too similar to determine which dosing strategy was intended.
After determination of dosing strategy, the nivolumab orders were evaluated for actual vs missed cost savings. The cost-savings evaluation included only nivolumab orders because nivolumab is available in a 40-mg, 100-mg, and 240-mg vials and, therefore, has more potential for dose-rounding opportunities with minimal drug waste compared with pembrolizumab, which is available only in a 100-mg vial. Actual cost savings included patients who weighed ≤ 73.3 kg and received nivolumab dose based on 3 mg/kg or patients who weighed ≥ 86.7 kg and received nivolumab 240 mg (fixed dose). Missed cost savings comprised patients who weighed ≤ 73.3 kg who received 240 mg nivolumab or patients who weighed ≥ 86.7 kg and received a nivolumab dose > 240 mg. The cost difference between the dose given and theoretical cost-effective dose was calculated to determine actual and potential cost savings. Converging orders were not included in the cost-savings analysis as the intended nivolumab dose could not be determined. An additional cost analysis of nivolumab orders prescribed between September 1, 2016 and July 1, 2017 was also performed because nivolumab fixed dosing was FDA-approved for most solid tumor indications in September 2016.
To determine the incidence of immunemediated hypothyroidism for patients who received a dose of a PD-1 inhibitor at a VAMC, a CDW report with thyroid function laboratory values (TSH, T4, or T3), including reference range values based on specific VA site, and levothyroxine prescriptions issued during PD-1 inhibitor therapy was obtained. A patient was considered to have experienced immune-mediated hypothyroidism if the patient’s laboratory values demonstrated T4 below the LLN, TSH above the ULN, or if the medication fill history demonstrated levothyroxine initiation or a levothyroxine dose increase.
Results
The CDW report identified 32,769 total PD-1 inhibitor orders. There were 3982 orders that did not meet inclusion criteria or inadequate data were obtained with CDW report and were excluded (Figure). The remaining 28,787 PD-1 inhibitor orders were evaluated for actual or missed cost savings. The distribution of dosing strategies can be found in Table 1.
Nivolumab accounted for 81.5% of all PD-1 inhibitor orders. Using the most cost-effective nivolumab dosing, the actual cost savings was estimated to be $8,514,300 with potential additional $5,591,250 of missed cost-savings opportunities. There were 8013 nivolumab orders written between September 1, 2016 and July 1, 2017. Cost-effective dosing was used in 4687 of these orders, which accounted for a cost savings of $5,198,570. The remaining 3326 orders had a missed cost-savings opportunity, which accounted for an additional $2,907,180 potential cost savings (Table 2).
PD-1 inhibitors were used for the treatment of 3249 unique patients. Based on abnormal thyroid function tests and levothyroxine initiation or dose increase, it is estimated that 514 (15.8%) patients experienced hypothyroidism during PD-1 inhibitor therapy. However, prior to PD-1 inhibitor therapy, 274 patients were receiving levothyroxine, suggesting baseline thyroid dysfunction. Of these patients, 152 (55.5%) patients maintained the same levothyroxine dose during PD-1 inhibitor therapy, but 91 (33.2%) required a levothyroxine dose increase. There were 187 patients who initiated levothyroxine during PD-1 inhibitor therapy (Table 3).
Discussion
Changes in FDA-approved dosing for PD-1 inhibitors allowed a combination of dosing strategies. Depending on patient weight, a weight-based or fixed-dosing strategy can be used to reduce drug cost while maintaining equivalent efficacy. This study evaluated use of dose rounding for PD-1 inhibitors within the VA health care system to identify actual and potential cost savings. To our knowledge, this is the first study to demonstrate cost savings through use of a combination of PD-1 inhibitor dosing strategies. Using CDW, researchers were able to review PD-1 dosing from all VAMCs and include a larger number of orders in a single retrospective study.
Nivolumab was the primary agent used within VAMCs. Depending on the indication, pembrolizumab requires PD-1 expression testing prior to its use in several solid tumor indications. Consequently, additional testing and patient eligibility is needed prior to use. Both PD-1 inhibitors were primarily dosed based on patient weight since this was the first FDAapproved dosing strategy. Nivolumab had more orders categorized as converging, which may be due to the therapeutic weight-based dose of 3 mg/kg for nivolumab vs 2 mg/kg for pembrolizumab. The calculated weight-based dose of nivolumab for an 80-kg patient is 240 mg, which also is the fixed dose. A 80-kg patient on pembrolizumab at 2 mg/kg would receive a 160-mg dose, whereas the fixed dose of pembrolizumab is 200 mg. Pembrolizumab is available only in a 100-mg vial, which limits opportunities for dose rounding without drug waste and could explain the higher amount of pembrolizumab orders in the fixed-dose category.
In this review of PD-1 inhibitor orders over approximately a 2.5-year study period, we identified $8,514,300 estimated cost savings with $5,591,250 estimated missed cost savings. When looking at orders administered after FDA approval for nivolumab-fixed dosing in September 2016, there was substantial cost savings of $5,198,570 with the potential for an additional $2,907,180 missed cost savings. Due to lower drug acquisition costs within the VA health care system, there may be higher cost-savings opportunities within other health care systems.
Through review of abnormal thyroid laboratory values and levothyroxine initiation or dose changes, this study estimated the incidence of hypothyroidism in patients receiving PD-1 inhibitor therapy at the VA. The incidence of primary hypothyroidism identified in this study was slightly higher at 15.8% compared with the 8.5 to 9.0% incidence reported from clinical trials.1,2 There are several reasons why the incidence of hypothyroidism appeared higher in this study. Abnormal laboratory values were not assessed for the degree of deviation from the reference range; any TSH above the ULN, T4 below the LLN, or levothyroxine dose increase was included as thyroid dysfunction in this review. There is also the potential for endogenous age-related thyroid fluctuation, and the development of hypothyroidism may not have been related to PD-1 inhibitor therapy. Within this patient population, 8.4% were receiving levothyroxine prior to PD-1 inhibitor initiation indicating baseline thyroid dysfunction, and it is unclear whether levothyroxine dose increases were due to PD-1 inhibitor or endogenous fluctuation.
Limitations
There are several limitations to acknowledge. The dosing strategy and apparent dose rounding was determined by investigator inference and may not accurately represent the intended dosing strategy. This study did not address efficacy of PD-1 inhibitor and dosing strategy; however, clinical trials have demonstrated equivalent efficacy to generate the change in FDA-approved dosing. Additionally, FDA approval for nivolumab fixed dosing was indication specific. Starting in September 2016, many solid tumor indications had fixed dosing approved, but this approval was not necessarily all encompassing.
While the use of CDW allowed for a greater number of PD-1 inhibitor orders to be included in retrospective review, there also were limitations of the CDW report. The patient weight was limited to weight at time of therapy initiation. Due to the potential for weight changes, nivolumab dosing may have seemed inappropriate to investigators, and thereby excluded. Based on data available from CDW reports, hypothyroidism could not be graded according to NCI Common Terminology Criteria for Adverse Events, and the incidence of clinically significant hypothyroidism could not be determined.
Conclusions
With increasing drug acquisition costs, particularly among antineoplastic agents, health care systems frequently seek out cost-savings opportunities. Using a combination of weightbased and fixed-dosing strategies for PD-1 inhibitors can be a mechanism to achieve costsavings. Through the identification of the dosing strategy used for PD-1 inhibitors, we were able to identify and report instances for potential cost-savings opportunities among veterans treated within VA health care system. Use of CDW allows for data from all VAMCs to be evaluated in a single retrospective chart review, which allows for the inclusion of a larger sample size. This study identified a substantial cost savings for nivolumab through a combination of weight-based and fixed-dosing strategies. Due to the novel mechanism of action, ongoing realworld evaluation of adverse events and IrAEs is warranted.
Dosing strategies with nivolumab and pembrolizumab continue to evolve. In March 2018, nivolumab 480 mg IV every 4 weeks was FDA approved and in April 2020, pembrolizumab 400 mg IV every 6 weeks was FDA approved.13,14 While the drug costs will remain the same, extended interval dosing strategies have cost avoidance such as fewer clinic appointments, resulting in decreased staffing costs and decreased patient travel. Additional studies will be needed to evaluate the cost and safety of the recently approved dosing strategies
1. OPDIVO (nivolumab) injection, for intravenous infusion. Package Insert. Princeton, NJ: Bristol-Myers Squibb Company; 2014.
2. Keytruda (pembrolizumab) injection, for intravenous infusion. Package Insert. Whitehouse Station, NJ: Merck & Co, Inc; 2016
3. Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12(4):252-264. doi:10.1038/nrc3239
4. Yao H, Wang H, Li C, Fang J-Y, Xu J. Cancer cellintrinsic PD-1 and implications in combinatorial immunotherapy. Front Immunol. 2018;9:1774. doi:10.3389/fimmu.2018.01774
5. Wang Y, Wang H, Yao H, Li C, Fang J-Y, Xu J. Regulation of PD-L1: emerging routes for targeting tumor immune evasion. Front Pharmacol. 2018;9:536. doi:10.3389/fphar.2018.00536
6. Patnaik A, Kang SP, Rasco D, et al. Phase I study of pembrolizumab (MK-3475; anti-PD-1 monocolonal antibody) in patients with advanced solid tumors. Clin Cancer Res. 2015;21(19):4286-4293. doi:10.1158/1078-0432.CCR-14-2607
7. Zhao X, Suryawanshi S, Hruska M, et al. Assessment of nivolumab benefit-risk profile of a 240-mg flat dose relative to a 3-mg/kg dosing regimen in patients with advanced tumors. Ann Oncol. 2017;28(8):2002-2008. doi:10.1093/annonc/mdx235
8. Freshwater T, Kondic A, Ahamadi M, et al. Evaluation of dosing strategy for pembrolizumab for oncology indications. J Immunother Cancer. 2017;5:43. doi:10.1186/s40425-017-0242-5
9. US Food and Drug Administration. Modification of the dosage regimen for nivolumab. Updated September 15, 2016. Accessed July 8, 2021. https://www.fda.gov/drugs /resources-information-approved-drugs/modification -dosage-regimen-nivolumab
10. Brahmer JR, Lacchetti C, Schneider BJ, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2018;36(17):1714-1768. doi:10.1200/JCO.2017.77.6385
11. National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology: Management of immunotherapy- related toxicities. version 3.2021. Updated May 14, 2021. Accessed July 8,2021.https://www.nccn.org/professionals/physician_gls/pdf/immunotherapy.pdf
12. National Institutes of Health, National Cancer Institute. Common terminology criteria for adverse events (CTCAE) version 5.0. Updated November 17, 2017. Accessed July 8, 2021. https://ctep.cancer.gov /protocoldevelopment/electronic_applications/docs /CTCAE_v5_Quick_Reference_8.5x11.pdf
13. Zhao X, Ivaturi V, Gopalakrishnan M, Shen J, et al. A model-based exposure-response (E-R) assessment of a nivolumab (NIVO) 4-weekly dosing schedule across multiple tumor types. Abstract presented at: American Association of Cancer Research Annual Meeting 2017; April 1-5, 2017; Washington, DC. doi:10.1158/1538-7445.AM2017-CT101
14. US Food and Drug Administration approves new dosing regimen for pembrolizumab. Updated April 29, 2020. Accessed July 8, 2021. https://www.fda.gov/drugs/drug -approvals-and-databases/fda-approves-new-dosing -regimen-pembrolizumab
1. OPDIVO (nivolumab) injection, for intravenous infusion. Package Insert. Princeton, NJ: Bristol-Myers Squibb Company; 2014.
2. Keytruda (pembrolizumab) injection, for intravenous infusion. Package Insert. Whitehouse Station, NJ: Merck & Co, Inc; 2016
3. Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12(4):252-264. doi:10.1038/nrc3239
4. Yao H, Wang H, Li C, Fang J-Y, Xu J. Cancer cellintrinsic PD-1 and implications in combinatorial immunotherapy. Front Immunol. 2018;9:1774. doi:10.3389/fimmu.2018.01774
5. Wang Y, Wang H, Yao H, Li C, Fang J-Y, Xu J. Regulation of PD-L1: emerging routes for targeting tumor immune evasion. Front Pharmacol. 2018;9:536. doi:10.3389/fphar.2018.00536
6. Patnaik A, Kang SP, Rasco D, et al. Phase I study of pembrolizumab (MK-3475; anti-PD-1 monocolonal antibody) in patients with advanced solid tumors. Clin Cancer Res. 2015;21(19):4286-4293. doi:10.1158/1078-0432.CCR-14-2607
7. Zhao X, Suryawanshi S, Hruska M, et al. Assessment of nivolumab benefit-risk profile of a 240-mg flat dose relative to a 3-mg/kg dosing regimen in patients with advanced tumors. Ann Oncol. 2017;28(8):2002-2008. doi:10.1093/annonc/mdx235
8. Freshwater T, Kondic A, Ahamadi M, et al. Evaluation of dosing strategy for pembrolizumab for oncology indications. J Immunother Cancer. 2017;5:43. doi:10.1186/s40425-017-0242-5
9. US Food and Drug Administration. Modification of the dosage regimen for nivolumab. Updated September 15, 2016. Accessed July 8, 2021. https://www.fda.gov/drugs /resources-information-approved-drugs/modification -dosage-regimen-nivolumab
10. Brahmer JR, Lacchetti C, Schneider BJ, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2018;36(17):1714-1768. doi:10.1200/JCO.2017.77.6385
11. National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology: Management of immunotherapy- related toxicities. version 3.2021. Updated May 14, 2021. Accessed July 8,2021.https://www.nccn.org/professionals/physician_gls/pdf/immunotherapy.pdf
12. National Institutes of Health, National Cancer Institute. Common terminology criteria for adverse events (CTCAE) version 5.0. Updated November 17, 2017. Accessed July 8, 2021. https://ctep.cancer.gov /protocoldevelopment/electronic_applications/docs /CTCAE_v5_Quick_Reference_8.5x11.pdf
13. Zhao X, Ivaturi V, Gopalakrishnan M, Shen J, et al. A model-based exposure-response (E-R) assessment of a nivolumab (NIVO) 4-weekly dosing schedule across multiple tumor types. Abstract presented at: American Association of Cancer Research Annual Meeting 2017; April 1-5, 2017; Washington, DC. doi:10.1158/1538-7445.AM2017-CT101
14. US Food and Drug Administration approves new dosing regimen for pembrolizumab. Updated April 29, 2020. Accessed July 8, 2021. https://www.fda.gov/drugs/drug -approvals-and-databases/fda-approves-new-dosing -regimen-pembrolizumab
COVID booster may benefit active-treatment cancer patients
A COVID-19 booster shot may be beneficial for patients with cancer who are undergoing treatment, according to new findings from an Israeli case-control study.
The seropositivity rate among the patients with cancer remained high (87%) about 4 months after the patients had received the second BNT162b2 (Pfizer/BioNTech) vaccination. However, the median IgG titer in the patients and the control persons who were without cancer decreased over time. Notably, in a previous analysis that the authors conducted and in the current one, the IgG titers were statistically significantly lower in the patients with cancer as compared to control persons.
The correlation between antibody levels following vaccination and clinical protection has yet to be proven, but the accumulating evidence supports antibody response as a possible correlate of disease protection.
“Our data can’t predict if a third booster dose is necessary,” said study author Salomon M. Stemmer, MD, professor at the Institute of Oncology of Rabin Medical Center, Petah Tikva, Israel. “It does seem quite logical that a booster dose will cause an increase in IgG levels.”
The findings were published Aug. 11, 2021, in a research letter in JAMA Oncology.
In their previous study, Dr. Stemmer and colleagues compared the rates of anti–spike antibody response to the initial shot of the BNT162b2 vaccine among 102 adults with solid-tumor cancers who were undergoing treatment with that of 78 healthy control persons. They found that a high percentage of patients undergoing treatment for cancer (90%) achieved a sufficient antibody response to the BNT162b2 vaccine.
Booster endorsed
Responses to COVID-19 vaccination have varied among patients with cancer. For patients with solid tumors, responses have been good even while the patients were receiving systemic therapy. However, among patients with blood cancers, particularly those receiving immunosuppressive therapies, responses have been poor. Studies have identified factors associated with a poor response, but it has been unclear whether to recommend booster shots.
In August the Food and Drug Administration authorized a third dose of either the Pfizer or the Moderna COVID-19 vaccine for all individuals with compromised immune systems. Those eligible for a third dose include solid-organ transplant recipients, those undergoing cancer treatments, and people with autoimmune diseases that suppress their immune systems.
IgG titers lower in cancer patients
In the current analysis, the authors evaluated the anti-S response in the patients with cancer approximately 4 months after they had received the second vaccine dose. They compared the responses in those patients with the responses in a control group.
The cohort included 95 patients from the prior study and 66 control persons. The most common malignancies were gastrointestinal (26%), lung (25%), and breast (18%).
All patients were receiving systemic therapy. Chemotherapy was the most common (28%), followed by immunotherapy (21%) and combination chemotherapy/biological therapy (20%).
At a median of 123 days after the second vaccination, 83 patients with cancer (87%) and all of the control patients (100%) were seropositive for anti-S IgG antibodies. The median titer levels were significantly lower among case patients as compared with control patients (417 AU/mL [interquartile range, 136-895] vs. 1,220 AU/mL [IQR, 588-1,987]; P < .001)
There was a 3.6-fold range in median titer values across tumor types and an even wider range (8.8-fold) across the different types of treatment. The lowest titers were observed among patients who had received immunotherapy plus chemotherapy/biological therapy (median [IQR], 94.4 [49.4-191] AU/mL vs. 147 [62.8-339] AU/mL).
In an exploratory multivariable analysis, treatments with chemotherapy plus immunotherapy and immunotherapy plus biological therapy were significantly associated with lower IgG titers.
No downside for cancer patients
The Biden administration announced a plan to begin booster COVID-19 vaccinations for all American adults in September, with recommendations that the third vaccine be given at least 8 months after the second mRNA vaccine dose.
Jeremy M. Levin, DPhil, the chairman and CEO of Ovid Therapeutics, explained that, concerning boosters, “it is inconceivable that we will have all data at this stage.
“Knowledge about how boosters work and don’t work and when you should ideally have them is imperfect,” he told this news organization. “However, we can have a lot of confidence in the fact that hundreds of millions of people have received the vaccine, so we know a lot about the safety and efficacy.”
Immunocompromised adults represent less than 5% of the total population, and most of the available data on vaccination are from patients who have undergone solid-organ transplant, Dr. Levin explained. Studies have shown that their response is less robust to vaccination in comparison with adults in the general population.
“Although it is still preliminary, the strongest data come from Israel,” he said, “where they found that the booster was highly effective and doubled the number of transplant patients who developed antibodies.”
But data are not yet available in the setting of cancer. “But even though we don’t have the data yet, the answer is that no matter, the booster process is essential,” he said. “The evidence we have is that boosters raise the immune response, and it is the best data we have now.”
Martin J. Edelman, MD, chair, department of hematology/oncology, Fox Chase Cancer Center, Philadelphia, noted that the current recommendation is that patients who are immunocompromised receive a booster immediately.
At his health system, this is interpreted to include patients who have undergone the following treatments: Transplant (solid-organ and bone marrow transplant), hemodialysis, hematologic malignancy treatment, active immunosuppressive (chemotherapy, chemoimmunotherapy, and nonhormonal or single-agent immunotherapy) treatment, rheumatology treatments, and high-dose steroids.
“As for cancer patients, we are making arrangements to vaccinate patients who meet the above criteria now,” he said. “There is no known downside to receiving booster immediately. While there may be less of a response than waiting for completion of treatment, we know that patients on active therapy are frequently able to mount a response, and any response is better than none.”
Dr. Edelman added that this area is changing very rapidly. “We will modify our approach as information and guidance from appropriate organizations, such as the FDA and CDC, become available.”
Dr. Stemmer has received institutional research grants from CAN-FITE, AstraZeneca, Bioline RX, BMS, Halozyme, Clovis Oncology, CTG Pharma, Exelixis, Geicam, Incyte, Lilly, Moderna, Teva Pharmaceuticals, and Roche, and owns stocks and options in CTG Pharma, DocBoxMD, Tyrnovo, VYPE, Cytora, and CAN-FITE. Dr. Edelman has received personal fees and other compensation from Windmil, Biomarker Strategies, AstraZeneca, Takeda, GlaxoSmithKline, Apexigen, Nektar, Bristol-Myers Squibb, Armo, Bergen Bio, and Apexigen outside the submitted work. He has submitted a patent for epigenetic modifications to increase susceptibility to radiopharmaceuticals and is a paid adviser for Kanaph and Flame. Dr. Levin is chairman and CEO of Ovid Therapeutics.
A version of this article first appeared on Medscape.com.
A COVID-19 booster shot may be beneficial for patients with cancer who are undergoing treatment, according to new findings from an Israeli case-control study.
The seropositivity rate among the patients with cancer remained high (87%) about 4 months after the patients had received the second BNT162b2 (Pfizer/BioNTech) vaccination. However, the median IgG titer in the patients and the control persons who were without cancer decreased over time. Notably, in a previous analysis that the authors conducted and in the current one, the IgG titers were statistically significantly lower in the patients with cancer as compared to control persons.
The correlation between antibody levels following vaccination and clinical protection has yet to be proven, but the accumulating evidence supports antibody response as a possible correlate of disease protection.
“Our data can’t predict if a third booster dose is necessary,” said study author Salomon M. Stemmer, MD, professor at the Institute of Oncology of Rabin Medical Center, Petah Tikva, Israel. “It does seem quite logical that a booster dose will cause an increase in IgG levels.”
The findings were published Aug. 11, 2021, in a research letter in JAMA Oncology.
In their previous study, Dr. Stemmer and colleagues compared the rates of anti–spike antibody response to the initial shot of the BNT162b2 vaccine among 102 adults with solid-tumor cancers who were undergoing treatment with that of 78 healthy control persons. They found that a high percentage of patients undergoing treatment for cancer (90%) achieved a sufficient antibody response to the BNT162b2 vaccine.
Booster endorsed
Responses to COVID-19 vaccination have varied among patients with cancer. For patients with solid tumors, responses have been good even while the patients were receiving systemic therapy. However, among patients with blood cancers, particularly those receiving immunosuppressive therapies, responses have been poor. Studies have identified factors associated with a poor response, but it has been unclear whether to recommend booster shots.
In August the Food and Drug Administration authorized a third dose of either the Pfizer or the Moderna COVID-19 vaccine for all individuals with compromised immune systems. Those eligible for a third dose include solid-organ transplant recipients, those undergoing cancer treatments, and people with autoimmune diseases that suppress their immune systems.
IgG titers lower in cancer patients
In the current analysis, the authors evaluated the anti-S response in the patients with cancer approximately 4 months after they had received the second vaccine dose. They compared the responses in those patients with the responses in a control group.
The cohort included 95 patients from the prior study and 66 control persons. The most common malignancies were gastrointestinal (26%), lung (25%), and breast (18%).
All patients were receiving systemic therapy. Chemotherapy was the most common (28%), followed by immunotherapy (21%) and combination chemotherapy/biological therapy (20%).
At a median of 123 days after the second vaccination, 83 patients with cancer (87%) and all of the control patients (100%) were seropositive for anti-S IgG antibodies. The median titer levels were significantly lower among case patients as compared with control patients (417 AU/mL [interquartile range, 136-895] vs. 1,220 AU/mL [IQR, 588-1,987]; P < .001)
There was a 3.6-fold range in median titer values across tumor types and an even wider range (8.8-fold) across the different types of treatment. The lowest titers were observed among patients who had received immunotherapy plus chemotherapy/biological therapy (median [IQR], 94.4 [49.4-191] AU/mL vs. 147 [62.8-339] AU/mL).
In an exploratory multivariable analysis, treatments with chemotherapy plus immunotherapy and immunotherapy plus biological therapy were significantly associated with lower IgG titers.
No downside for cancer patients
The Biden administration announced a plan to begin booster COVID-19 vaccinations for all American adults in September, with recommendations that the third vaccine be given at least 8 months after the second mRNA vaccine dose.
Jeremy M. Levin, DPhil, the chairman and CEO of Ovid Therapeutics, explained that, concerning boosters, “it is inconceivable that we will have all data at this stage.
“Knowledge about how boosters work and don’t work and when you should ideally have them is imperfect,” he told this news organization. “However, we can have a lot of confidence in the fact that hundreds of millions of people have received the vaccine, so we know a lot about the safety and efficacy.”
Immunocompromised adults represent less than 5% of the total population, and most of the available data on vaccination are from patients who have undergone solid-organ transplant, Dr. Levin explained. Studies have shown that their response is less robust to vaccination in comparison with adults in the general population.
“Although it is still preliminary, the strongest data come from Israel,” he said, “where they found that the booster was highly effective and doubled the number of transplant patients who developed antibodies.”
But data are not yet available in the setting of cancer. “But even though we don’t have the data yet, the answer is that no matter, the booster process is essential,” he said. “The evidence we have is that boosters raise the immune response, and it is the best data we have now.”
Martin J. Edelman, MD, chair, department of hematology/oncology, Fox Chase Cancer Center, Philadelphia, noted that the current recommendation is that patients who are immunocompromised receive a booster immediately.
At his health system, this is interpreted to include patients who have undergone the following treatments: Transplant (solid-organ and bone marrow transplant), hemodialysis, hematologic malignancy treatment, active immunosuppressive (chemotherapy, chemoimmunotherapy, and nonhormonal or single-agent immunotherapy) treatment, rheumatology treatments, and high-dose steroids.
“As for cancer patients, we are making arrangements to vaccinate patients who meet the above criteria now,” he said. “There is no known downside to receiving booster immediately. While there may be less of a response than waiting for completion of treatment, we know that patients on active therapy are frequently able to mount a response, and any response is better than none.”
Dr. Edelman added that this area is changing very rapidly. “We will modify our approach as information and guidance from appropriate organizations, such as the FDA and CDC, become available.”
Dr. Stemmer has received institutional research grants from CAN-FITE, AstraZeneca, Bioline RX, BMS, Halozyme, Clovis Oncology, CTG Pharma, Exelixis, Geicam, Incyte, Lilly, Moderna, Teva Pharmaceuticals, and Roche, and owns stocks and options in CTG Pharma, DocBoxMD, Tyrnovo, VYPE, Cytora, and CAN-FITE. Dr. Edelman has received personal fees and other compensation from Windmil, Biomarker Strategies, AstraZeneca, Takeda, GlaxoSmithKline, Apexigen, Nektar, Bristol-Myers Squibb, Armo, Bergen Bio, and Apexigen outside the submitted work. He has submitted a patent for epigenetic modifications to increase susceptibility to radiopharmaceuticals and is a paid adviser for Kanaph and Flame. Dr. Levin is chairman and CEO of Ovid Therapeutics.
A version of this article first appeared on Medscape.com.
A COVID-19 booster shot may be beneficial for patients with cancer who are undergoing treatment, according to new findings from an Israeli case-control study.
The seropositivity rate among the patients with cancer remained high (87%) about 4 months after the patients had received the second BNT162b2 (Pfizer/BioNTech) vaccination. However, the median IgG titer in the patients and the control persons who were without cancer decreased over time. Notably, in a previous analysis that the authors conducted and in the current one, the IgG titers were statistically significantly lower in the patients with cancer as compared to control persons.
The correlation between antibody levels following vaccination and clinical protection has yet to be proven, but the accumulating evidence supports antibody response as a possible correlate of disease protection.
“Our data can’t predict if a third booster dose is necessary,” said study author Salomon M. Stemmer, MD, professor at the Institute of Oncology of Rabin Medical Center, Petah Tikva, Israel. “It does seem quite logical that a booster dose will cause an increase in IgG levels.”
The findings were published Aug. 11, 2021, in a research letter in JAMA Oncology.
In their previous study, Dr. Stemmer and colleagues compared the rates of anti–spike antibody response to the initial shot of the BNT162b2 vaccine among 102 adults with solid-tumor cancers who were undergoing treatment with that of 78 healthy control persons. They found that a high percentage of patients undergoing treatment for cancer (90%) achieved a sufficient antibody response to the BNT162b2 vaccine.
Booster endorsed
Responses to COVID-19 vaccination have varied among patients with cancer. For patients with solid tumors, responses have been good even while the patients were receiving systemic therapy. However, among patients with blood cancers, particularly those receiving immunosuppressive therapies, responses have been poor. Studies have identified factors associated with a poor response, but it has been unclear whether to recommend booster shots.
In August the Food and Drug Administration authorized a third dose of either the Pfizer or the Moderna COVID-19 vaccine for all individuals with compromised immune systems. Those eligible for a third dose include solid-organ transplant recipients, those undergoing cancer treatments, and people with autoimmune diseases that suppress their immune systems.
IgG titers lower in cancer patients
In the current analysis, the authors evaluated the anti-S response in the patients with cancer approximately 4 months after they had received the second vaccine dose. They compared the responses in those patients with the responses in a control group.
The cohort included 95 patients from the prior study and 66 control persons. The most common malignancies were gastrointestinal (26%), lung (25%), and breast (18%).
All patients were receiving systemic therapy. Chemotherapy was the most common (28%), followed by immunotherapy (21%) and combination chemotherapy/biological therapy (20%).
At a median of 123 days after the second vaccination, 83 patients with cancer (87%) and all of the control patients (100%) were seropositive for anti-S IgG antibodies. The median titer levels were significantly lower among case patients as compared with control patients (417 AU/mL [interquartile range, 136-895] vs. 1,220 AU/mL [IQR, 588-1,987]; P < .001)
There was a 3.6-fold range in median titer values across tumor types and an even wider range (8.8-fold) across the different types of treatment. The lowest titers were observed among patients who had received immunotherapy plus chemotherapy/biological therapy (median [IQR], 94.4 [49.4-191] AU/mL vs. 147 [62.8-339] AU/mL).
In an exploratory multivariable analysis, treatments with chemotherapy plus immunotherapy and immunotherapy plus biological therapy were significantly associated with lower IgG titers.
No downside for cancer patients
The Biden administration announced a plan to begin booster COVID-19 vaccinations for all American adults in September, with recommendations that the third vaccine be given at least 8 months after the second mRNA vaccine dose.
Jeremy M. Levin, DPhil, the chairman and CEO of Ovid Therapeutics, explained that, concerning boosters, “it is inconceivable that we will have all data at this stage.
“Knowledge about how boosters work and don’t work and when you should ideally have them is imperfect,” he told this news organization. “However, we can have a lot of confidence in the fact that hundreds of millions of people have received the vaccine, so we know a lot about the safety and efficacy.”
Immunocompromised adults represent less than 5% of the total population, and most of the available data on vaccination are from patients who have undergone solid-organ transplant, Dr. Levin explained. Studies have shown that their response is less robust to vaccination in comparison with adults in the general population.
“Although it is still preliminary, the strongest data come from Israel,” he said, “where they found that the booster was highly effective and doubled the number of transplant patients who developed antibodies.”
But data are not yet available in the setting of cancer. “But even though we don’t have the data yet, the answer is that no matter, the booster process is essential,” he said. “The evidence we have is that boosters raise the immune response, and it is the best data we have now.”
Martin J. Edelman, MD, chair, department of hematology/oncology, Fox Chase Cancer Center, Philadelphia, noted that the current recommendation is that patients who are immunocompromised receive a booster immediately.
At his health system, this is interpreted to include patients who have undergone the following treatments: Transplant (solid-organ and bone marrow transplant), hemodialysis, hematologic malignancy treatment, active immunosuppressive (chemotherapy, chemoimmunotherapy, and nonhormonal or single-agent immunotherapy) treatment, rheumatology treatments, and high-dose steroids.
“As for cancer patients, we are making arrangements to vaccinate patients who meet the above criteria now,” he said. “There is no known downside to receiving booster immediately. While there may be less of a response than waiting for completion of treatment, we know that patients on active therapy are frequently able to mount a response, and any response is better than none.”
Dr. Edelman added that this area is changing very rapidly. “We will modify our approach as information and guidance from appropriate organizations, such as the FDA and CDC, become available.”
Dr. Stemmer has received institutional research grants from CAN-FITE, AstraZeneca, Bioline RX, BMS, Halozyme, Clovis Oncology, CTG Pharma, Exelixis, Geicam, Incyte, Lilly, Moderna, Teva Pharmaceuticals, and Roche, and owns stocks and options in CTG Pharma, DocBoxMD, Tyrnovo, VYPE, Cytora, and CAN-FITE. Dr. Edelman has received personal fees and other compensation from Windmil, Biomarker Strategies, AstraZeneca, Takeda, GlaxoSmithKline, Apexigen, Nektar, Bristol-Myers Squibb, Armo, Bergen Bio, and Apexigen outside the submitted work. He has submitted a patent for epigenetic modifications to increase susceptibility to radiopharmaceuticals and is a paid adviser for Kanaph and Flame. Dr. Levin is chairman and CEO of Ovid Therapeutics.
A version of this article first appeared on Medscape.com.
Polygenic breast cancer risk scores strive to overcome racial bias
The potential of polygenic risk scores (PRSs) to become key components in the assessment of individual risk for disease in the clinical setting is inching closer to fruition; however, the technology is plagued by one glaring omission of most existing PRSs – the lack of applicability to those of non-European ancestry.
Polygenic risk scores predict an individual’s risk of disease based on common genetic variants identified in large genomewide association studies (GWASs). They have gained ground in research, as well as in the unregulated realm of the direct-to-consumer market where they are sold as add-ons to DNA ancestry kits such as 23andMe and MyHeritage.com.
While the risk scores show strong validation in estimating risk among people of European descent, their striking caveat is the lack of applicability to other ancestries, particularly African, and their use in practice outside of clinical trials is discouraged in National Comprehensive Cancer Network guidelines.
Study underscores need for ethnically diverse datasets
In a recent study published in JAMA Network Open, researchers evaluated the use of polygenic risk scores’ models in a clinical setting. Researchers tested 7 PRSs models for breast cancer risk against the medical records data of 39,591 women of European, African, and Latinx ancestry.
The PRSs models – all used only for research purposes – included three models involving European ancestry cohorts, two from Latinx cohorts, and two from women African descent.
After adjusting for factors including age, breast cancer family history, and ancestry, the PRSs from women with European ancestry highly corresponded to breast cancer risk, with a mean odds ratio of 1.46 per standard deviation increase in the score.
PRSs were also generalized relatively well among women of Latinx ancestry with a mean OR of 1.31. The authors noted that association is likely caused by Latinx individuals in the United States having a greater proportion of European ancestry than individuals with African ancestry. Importantly, however, the effect size was lower for women of African ancestry with a highest OR of 1.19 per standard deviation.
In the highest percentiles of breast cancer risk, women of European descent had odds ratio as high as 2.19-2.48, suggesting a statistically significant association with overall breast cancer risk. No statistically significant associations were found among women of Latinx and African-ancestry.
The PRSs models were smaller for women of non-European ancestry and included fewer genetic variants for women of non-European ancestry were notably smaller and hence reflected fewer genetic variants. Of the two risk scores involving African ancestry, the Women’s Health Initiative for Women with African ancestry risk score had just 75 variants, while the African diaspora study (ROOT) had 34 variants, compared with 3,820 and 5,218 in the two largest European ancestry PRSs, the Breast Cancer Association Consortium and the UK Biobank, respectively.
“These results highlight the need to improve representation of diverse population groups, particularly women with African ancestry, in genomic research cohorts,” the authors wrote.
First author, Cong Liu, PhD, of Columbia University Irving Medical Center, New York, said that efforts are underway to improve the inclusivity in the Electronic Medical Records and Genomics network data set used in this study.
“Until well-developed and validated PRSs for women with non-European ancestry become available, the current PRSs based on cohorts with European ancestry could be adapted for Latinx women, but not women with African ancestry until additional data sets become available in this important and high-risk group,” Dr. Liu and colleagues wrote.
In a commentary published with the study, Payal D. Shah, MD, of the Basser Center for BRCA at the University of Pennsylvania, Philadelphia, said that PRSs are “disproportionately applicable to patients with European ancestry and are insufficiently vetted and developed in other populations. If an instrument exists that has clinical utility in informing effective cancer risk mitigation strategies, then we must strive to ensure that it is available and applicable to all.”
Higher morality among African American women
While American Cancer Society data shows women with African ancestry generally have incidence rates of breast cancer similar to White women, they have significantly higher mortality from the disease in part because of later-stage diagnosis and health care barriers.
Anne Marie McCarthy, PhD, of the University of Pennsylvania, and Katrina Armstrong, MD, of Harvard Medical School, Boston, wrote in the Journal of the National Cancer Institute that African American women “have 42% higher breast cancer mortality than white women, despite having lower disease incidence, and are more likely to be diagnosed with triple-negative breast cancer, which has poorer prognosis than other molecular subtypes.”
Dr. McCarthy and Dr. Armstrong wrote that African American women are chronically underrepresented in breast cancer studies. And as such, it is impossible to know the extent of the prevalence of mutations and risk.
Failing to address the lack of diversity in genomic studies may worsen health disparities for women with African ancestry, Dr. Liu and colleagues wrote. The higher mortality “underscores the urgent need to increase diversity in genomic studies so that future clinical applications of the PRS do not exacerbate existing health disparities. These results highlight the need to improve representation of diverse population groups, particularly women with African ancestry, in genomic research cohorts.”
Potential PRS benefits underscore need to eliminate bias
The potentially important benefits of PRSs as risk prediction tools used in combination with family history, reproductive history and other factors, should provide strong incentive to push for improvement, Dr. Shah wrote.
For instance, if an individual is estrogen receptor positive and shows elevations in breast cancer risk on a reliable PRS, “this may inform antiestrogen chemoprevention strategies,” she wrote.
A risk score could furthermore influence the age at which breast cancer screening should begin or factor into whether a patient should also receive surveillance breast MRI.
Importantly, PRSs could also add to other risk factors to provide more precise risk estimates and inform management of women with a pathogenic variant in a breast cancer risk predisposition gene, Dr. Shah wrote.
Confluence project
Among the most promising developments in research is the National Cancer Institute’s Confluence Project, a large research resource aiming to include approximately 300,000 breast cancer cases and 300,000 controls of different races/ethnicities, utilizing the confluence of existing GWAS and new genomewide genotyping data.
Having started enrollment in 2018, the project is approaching implementation, said Montserrat García-Closas, MD, MPH, DrPH, deputy director of cancer epidemiology and genetics with the National Cancer Institute.
“We expect genotyping to be completed by the end of 2022 and for the data to be made available to the research community soon after that,” she said.
Among the project’s key objectives are the development of PRSs to be integrated with known risk factors to provide a personalized risk assessment for breast cancer, overall and by ancestral subtype.
“We plan to apply novel methods to derive multiancestry PRS that will account for differences and similarities in genetic architecture across ethnic/racial groups to develop breast cancer PRSs that can be applied in multiethnic/racial populations,” she said.
NCI is working with investigators in Africa, Central and South America, and Asia, and reaching out to non-European organizations such as AORTIC for studies of African populations.
Direct-to-consumer global PRS
In the commercial PRS market, efforts to address diversity shortcomings are also gaining momentum, with Myriad Genetics touting a first-of-its kind “global PRS.”
The PRS, a recalibrated version the company’s riskScore PRS, sold as part of its Myriad myRisk Hereditary Cancer test, will reportedly apply to all ethnicities in estimating an individual’s 5-year and lifetime risk of breast cancer.
A study presented in June at the American Society of Clinical Oncology meeting, describes the development of the model with the use of three large ancestry-specific PRSs based on African American, Asian, and European cohorts, with the system including a total of 149 single-nucleotide polymorphisms, including 93 well established for breast cancer and 56 that are ancestry specific.
In validation of the data in an independent cohort of 62,707 individuals, the global PRS was strongly associated with breast cancer in the full combined validation cohort as well as in all three of the ancestry subcohorts.
However, the effect size among women with African ancestry was still the lowest of all of the groups, with a mean OR of 1.24 per standard deviation, versus the highest rate of mixed ancestry (OR, 1.59).
According to senior author Holly Pederson, MD, director of medical breast services at the Cleveland Clinic, the applicability of the PRS to women with African ancestry is expected to further improve as additional data become available.
“The discriminatory power in women of African descent was significantly improved but still suboptimal,” she said. “The need for more data, particularly in Black women, is challenging not only because there is likely more diversity in the genomic landscape of women of African descent, but also because the barriers created by historical, cultural, institutional and interpersonal dynamics result in the paucity of this data.”
“We must be committed to ending bias resulting in health care disparities,” Dr. Pederson said. She noted that the global PRS is nevertheless “still clinically useful in Black women,” and recommended that clinicians be up front with patients on the status of the research challenges.
“As with any clinical shared decision-making conversation between a patient and her provider, it is important for Black women to know that data is limited in the African American population, particularly given the vast genomic diversity of the African continent,” she said. “This model, as models that have gone before it, will improve with additional data, particularly in this population.”
Commercial PRSs may benefit research
While the commercial marketing of PRSs in a direct-to-consumer fashion have raised some concerns, such as how individuals respond to their risk scores, there could be important benefits as well, commented Megan C. Roberts, PhD.
“There may be an opportunity to learn from these companies about how to engage diverse communities in genomic testing,” said Dr. Roberts, an assistant professor and director of implementation science in precision health and society at the University of North Carolina at Chapel Hill. “Moreover, the data they collect from their customers often can be used for research purposes as well.”
In a recent perspective, Dr. Roberts and colleagues addressed the role of health disparities in PRSs. She’ll be joining international precision public health researchers in October in hosting a free virtual conference at UNC on the topic.
“There is a huge need to improve racial and ethnic diversity in our genomic datasets,” Dr. Roberts said. “Without this, we will not be able to return on the promise of precision medicine and prevention for improving the health of our whole population.”
Dr. Pederson disclosed that she is a consultant for Myriad Genetics.
The potential of polygenic risk scores (PRSs) to become key components in the assessment of individual risk for disease in the clinical setting is inching closer to fruition; however, the technology is plagued by one glaring omission of most existing PRSs – the lack of applicability to those of non-European ancestry.
Polygenic risk scores predict an individual’s risk of disease based on common genetic variants identified in large genomewide association studies (GWASs). They have gained ground in research, as well as in the unregulated realm of the direct-to-consumer market where they are sold as add-ons to DNA ancestry kits such as 23andMe and MyHeritage.com.
While the risk scores show strong validation in estimating risk among people of European descent, their striking caveat is the lack of applicability to other ancestries, particularly African, and their use in practice outside of clinical trials is discouraged in National Comprehensive Cancer Network guidelines.
Study underscores need for ethnically diverse datasets
In a recent study published in JAMA Network Open, researchers evaluated the use of polygenic risk scores’ models in a clinical setting. Researchers tested 7 PRSs models for breast cancer risk against the medical records data of 39,591 women of European, African, and Latinx ancestry.
The PRSs models – all used only for research purposes – included three models involving European ancestry cohorts, two from Latinx cohorts, and two from women African descent.
After adjusting for factors including age, breast cancer family history, and ancestry, the PRSs from women with European ancestry highly corresponded to breast cancer risk, with a mean odds ratio of 1.46 per standard deviation increase in the score.
PRSs were also generalized relatively well among women of Latinx ancestry with a mean OR of 1.31. The authors noted that association is likely caused by Latinx individuals in the United States having a greater proportion of European ancestry than individuals with African ancestry. Importantly, however, the effect size was lower for women of African ancestry with a highest OR of 1.19 per standard deviation.
In the highest percentiles of breast cancer risk, women of European descent had odds ratio as high as 2.19-2.48, suggesting a statistically significant association with overall breast cancer risk. No statistically significant associations were found among women of Latinx and African-ancestry.
The PRSs models were smaller for women of non-European ancestry and included fewer genetic variants for women of non-European ancestry were notably smaller and hence reflected fewer genetic variants. Of the two risk scores involving African ancestry, the Women’s Health Initiative for Women with African ancestry risk score had just 75 variants, while the African diaspora study (ROOT) had 34 variants, compared with 3,820 and 5,218 in the two largest European ancestry PRSs, the Breast Cancer Association Consortium and the UK Biobank, respectively.
“These results highlight the need to improve representation of diverse population groups, particularly women with African ancestry, in genomic research cohorts,” the authors wrote.
First author, Cong Liu, PhD, of Columbia University Irving Medical Center, New York, said that efforts are underway to improve the inclusivity in the Electronic Medical Records and Genomics network data set used in this study.
“Until well-developed and validated PRSs for women with non-European ancestry become available, the current PRSs based on cohorts with European ancestry could be adapted for Latinx women, but not women with African ancestry until additional data sets become available in this important and high-risk group,” Dr. Liu and colleagues wrote.
In a commentary published with the study, Payal D. Shah, MD, of the Basser Center for BRCA at the University of Pennsylvania, Philadelphia, said that PRSs are “disproportionately applicable to patients with European ancestry and are insufficiently vetted and developed in other populations. If an instrument exists that has clinical utility in informing effective cancer risk mitigation strategies, then we must strive to ensure that it is available and applicable to all.”
Higher morality among African American women
While American Cancer Society data shows women with African ancestry generally have incidence rates of breast cancer similar to White women, they have significantly higher mortality from the disease in part because of later-stage diagnosis and health care barriers.
Anne Marie McCarthy, PhD, of the University of Pennsylvania, and Katrina Armstrong, MD, of Harvard Medical School, Boston, wrote in the Journal of the National Cancer Institute that African American women “have 42% higher breast cancer mortality than white women, despite having lower disease incidence, and are more likely to be diagnosed with triple-negative breast cancer, which has poorer prognosis than other molecular subtypes.”
Dr. McCarthy and Dr. Armstrong wrote that African American women are chronically underrepresented in breast cancer studies. And as such, it is impossible to know the extent of the prevalence of mutations and risk.
Failing to address the lack of diversity in genomic studies may worsen health disparities for women with African ancestry, Dr. Liu and colleagues wrote. The higher mortality “underscores the urgent need to increase diversity in genomic studies so that future clinical applications of the PRS do not exacerbate existing health disparities. These results highlight the need to improve representation of diverse population groups, particularly women with African ancestry, in genomic research cohorts.”
Potential PRS benefits underscore need to eliminate bias
The potentially important benefits of PRSs as risk prediction tools used in combination with family history, reproductive history and other factors, should provide strong incentive to push for improvement, Dr. Shah wrote.
For instance, if an individual is estrogen receptor positive and shows elevations in breast cancer risk on a reliable PRS, “this may inform antiestrogen chemoprevention strategies,” she wrote.
A risk score could furthermore influence the age at which breast cancer screening should begin or factor into whether a patient should also receive surveillance breast MRI.
Importantly, PRSs could also add to other risk factors to provide more precise risk estimates and inform management of women with a pathogenic variant in a breast cancer risk predisposition gene, Dr. Shah wrote.
Confluence project
Among the most promising developments in research is the National Cancer Institute’s Confluence Project, a large research resource aiming to include approximately 300,000 breast cancer cases and 300,000 controls of different races/ethnicities, utilizing the confluence of existing GWAS and new genomewide genotyping data.
Having started enrollment in 2018, the project is approaching implementation, said Montserrat García-Closas, MD, MPH, DrPH, deputy director of cancer epidemiology and genetics with the National Cancer Institute.
“We expect genotyping to be completed by the end of 2022 and for the data to be made available to the research community soon after that,” she said.
Among the project’s key objectives are the development of PRSs to be integrated with known risk factors to provide a personalized risk assessment for breast cancer, overall and by ancestral subtype.
“We plan to apply novel methods to derive multiancestry PRS that will account for differences and similarities in genetic architecture across ethnic/racial groups to develop breast cancer PRSs that can be applied in multiethnic/racial populations,” she said.
NCI is working with investigators in Africa, Central and South America, and Asia, and reaching out to non-European organizations such as AORTIC for studies of African populations.
Direct-to-consumer global PRS
In the commercial PRS market, efforts to address diversity shortcomings are also gaining momentum, with Myriad Genetics touting a first-of-its kind “global PRS.”
The PRS, a recalibrated version the company’s riskScore PRS, sold as part of its Myriad myRisk Hereditary Cancer test, will reportedly apply to all ethnicities in estimating an individual’s 5-year and lifetime risk of breast cancer.
A study presented in June at the American Society of Clinical Oncology meeting, describes the development of the model with the use of three large ancestry-specific PRSs based on African American, Asian, and European cohorts, with the system including a total of 149 single-nucleotide polymorphisms, including 93 well established for breast cancer and 56 that are ancestry specific.
In validation of the data in an independent cohort of 62,707 individuals, the global PRS was strongly associated with breast cancer in the full combined validation cohort as well as in all three of the ancestry subcohorts.
However, the effect size among women with African ancestry was still the lowest of all of the groups, with a mean OR of 1.24 per standard deviation, versus the highest rate of mixed ancestry (OR, 1.59).
According to senior author Holly Pederson, MD, director of medical breast services at the Cleveland Clinic, the applicability of the PRS to women with African ancestry is expected to further improve as additional data become available.
“The discriminatory power in women of African descent was significantly improved but still suboptimal,” she said. “The need for more data, particularly in Black women, is challenging not only because there is likely more diversity in the genomic landscape of women of African descent, but also because the barriers created by historical, cultural, institutional and interpersonal dynamics result in the paucity of this data.”
“We must be committed to ending bias resulting in health care disparities,” Dr. Pederson said. She noted that the global PRS is nevertheless “still clinically useful in Black women,” and recommended that clinicians be up front with patients on the status of the research challenges.
“As with any clinical shared decision-making conversation between a patient and her provider, it is important for Black women to know that data is limited in the African American population, particularly given the vast genomic diversity of the African continent,” she said. “This model, as models that have gone before it, will improve with additional data, particularly in this population.”
Commercial PRSs may benefit research
While the commercial marketing of PRSs in a direct-to-consumer fashion have raised some concerns, such as how individuals respond to their risk scores, there could be important benefits as well, commented Megan C. Roberts, PhD.
“There may be an opportunity to learn from these companies about how to engage diverse communities in genomic testing,” said Dr. Roberts, an assistant professor and director of implementation science in precision health and society at the University of North Carolina at Chapel Hill. “Moreover, the data they collect from their customers often can be used for research purposes as well.”
In a recent perspective, Dr. Roberts and colleagues addressed the role of health disparities in PRSs. She’ll be joining international precision public health researchers in October in hosting a free virtual conference at UNC on the topic.
“There is a huge need to improve racial and ethnic diversity in our genomic datasets,” Dr. Roberts said. “Without this, we will not be able to return on the promise of precision medicine and prevention for improving the health of our whole population.”
Dr. Pederson disclosed that she is a consultant for Myriad Genetics.
The potential of polygenic risk scores (PRSs) to become key components in the assessment of individual risk for disease in the clinical setting is inching closer to fruition; however, the technology is plagued by one glaring omission of most existing PRSs – the lack of applicability to those of non-European ancestry.
Polygenic risk scores predict an individual’s risk of disease based on common genetic variants identified in large genomewide association studies (GWASs). They have gained ground in research, as well as in the unregulated realm of the direct-to-consumer market where they are sold as add-ons to DNA ancestry kits such as 23andMe and MyHeritage.com.
While the risk scores show strong validation in estimating risk among people of European descent, their striking caveat is the lack of applicability to other ancestries, particularly African, and their use in practice outside of clinical trials is discouraged in National Comprehensive Cancer Network guidelines.
Study underscores need for ethnically diverse datasets
In a recent study published in JAMA Network Open, researchers evaluated the use of polygenic risk scores’ models in a clinical setting. Researchers tested 7 PRSs models for breast cancer risk against the medical records data of 39,591 women of European, African, and Latinx ancestry.
The PRSs models – all used only for research purposes – included three models involving European ancestry cohorts, two from Latinx cohorts, and two from women African descent.
After adjusting for factors including age, breast cancer family history, and ancestry, the PRSs from women with European ancestry highly corresponded to breast cancer risk, with a mean odds ratio of 1.46 per standard deviation increase in the score.
PRSs were also generalized relatively well among women of Latinx ancestry with a mean OR of 1.31. The authors noted that association is likely caused by Latinx individuals in the United States having a greater proportion of European ancestry than individuals with African ancestry. Importantly, however, the effect size was lower for women of African ancestry with a highest OR of 1.19 per standard deviation.
In the highest percentiles of breast cancer risk, women of European descent had odds ratio as high as 2.19-2.48, suggesting a statistically significant association with overall breast cancer risk. No statistically significant associations were found among women of Latinx and African-ancestry.
The PRSs models were smaller for women of non-European ancestry and included fewer genetic variants for women of non-European ancestry were notably smaller and hence reflected fewer genetic variants. Of the two risk scores involving African ancestry, the Women’s Health Initiative for Women with African ancestry risk score had just 75 variants, while the African diaspora study (ROOT) had 34 variants, compared with 3,820 and 5,218 in the two largest European ancestry PRSs, the Breast Cancer Association Consortium and the UK Biobank, respectively.
“These results highlight the need to improve representation of diverse population groups, particularly women with African ancestry, in genomic research cohorts,” the authors wrote.
First author, Cong Liu, PhD, of Columbia University Irving Medical Center, New York, said that efforts are underway to improve the inclusivity in the Electronic Medical Records and Genomics network data set used in this study.
“Until well-developed and validated PRSs for women with non-European ancestry become available, the current PRSs based on cohorts with European ancestry could be adapted for Latinx women, but not women with African ancestry until additional data sets become available in this important and high-risk group,” Dr. Liu and colleagues wrote.
In a commentary published with the study, Payal D. Shah, MD, of the Basser Center for BRCA at the University of Pennsylvania, Philadelphia, said that PRSs are “disproportionately applicable to patients with European ancestry and are insufficiently vetted and developed in other populations. If an instrument exists that has clinical utility in informing effective cancer risk mitigation strategies, then we must strive to ensure that it is available and applicable to all.”
Higher morality among African American women
While American Cancer Society data shows women with African ancestry generally have incidence rates of breast cancer similar to White women, they have significantly higher mortality from the disease in part because of later-stage diagnosis and health care barriers.
Anne Marie McCarthy, PhD, of the University of Pennsylvania, and Katrina Armstrong, MD, of Harvard Medical School, Boston, wrote in the Journal of the National Cancer Institute that African American women “have 42% higher breast cancer mortality than white women, despite having lower disease incidence, and are more likely to be diagnosed with triple-negative breast cancer, which has poorer prognosis than other molecular subtypes.”
Dr. McCarthy and Dr. Armstrong wrote that African American women are chronically underrepresented in breast cancer studies. And as such, it is impossible to know the extent of the prevalence of mutations and risk.
Failing to address the lack of diversity in genomic studies may worsen health disparities for women with African ancestry, Dr. Liu and colleagues wrote. The higher mortality “underscores the urgent need to increase diversity in genomic studies so that future clinical applications of the PRS do not exacerbate existing health disparities. These results highlight the need to improve representation of diverse population groups, particularly women with African ancestry, in genomic research cohorts.”
Potential PRS benefits underscore need to eliminate bias
The potentially important benefits of PRSs as risk prediction tools used in combination with family history, reproductive history and other factors, should provide strong incentive to push for improvement, Dr. Shah wrote.
For instance, if an individual is estrogen receptor positive and shows elevations in breast cancer risk on a reliable PRS, “this may inform antiestrogen chemoprevention strategies,” she wrote.
A risk score could furthermore influence the age at which breast cancer screening should begin or factor into whether a patient should also receive surveillance breast MRI.
Importantly, PRSs could also add to other risk factors to provide more precise risk estimates and inform management of women with a pathogenic variant in a breast cancer risk predisposition gene, Dr. Shah wrote.
Confluence project
Among the most promising developments in research is the National Cancer Institute’s Confluence Project, a large research resource aiming to include approximately 300,000 breast cancer cases and 300,000 controls of different races/ethnicities, utilizing the confluence of existing GWAS and new genomewide genotyping data.
Having started enrollment in 2018, the project is approaching implementation, said Montserrat García-Closas, MD, MPH, DrPH, deputy director of cancer epidemiology and genetics with the National Cancer Institute.
“We expect genotyping to be completed by the end of 2022 and for the data to be made available to the research community soon after that,” she said.
Among the project’s key objectives are the development of PRSs to be integrated with known risk factors to provide a personalized risk assessment for breast cancer, overall and by ancestral subtype.
“We plan to apply novel methods to derive multiancestry PRS that will account for differences and similarities in genetic architecture across ethnic/racial groups to develop breast cancer PRSs that can be applied in multiethnic/racial populations,” she said.
NCI is working with investigators in Africa, Central and South America, and Asia, and reaching out to non-European organizations such as AORTIC for studies of African populations.
Direct-to-consumer global PRS
In the commercial PRS market, efforts to address diversity shortcomings are also gaining momentum, with Myriad Genetics touting a first-of-its kind “global PRS.”
The PRS, a recalibrated version the company’s riskScore PRS, sold as part of its Myriad myRisk Hereditary Cancer test, will reportedly apply to all ethnicities in estimating an individual’s 5-year and lifetime risk of breast cancer.
A study presented in June at the American Society of Clinical Oncology meeting, describes the development of the model with the use of three large ancestry-specific PRSs based on African American, Asian, and European cohorts, with the system including a total of 149 single-nucleotide polymorphisms, including 93 well established for breast cancer and 56 that are ancestry specific.
In validation of the data in an independent cohort of 62,707 individuals, the global PRS was strongly associated with breast cancer in the full combined validation cohort as well as in all three of the ancestry subcohorts.
However, the effect size among women with African ancestry was still the lowest of all of the groups, with a mean OR of 1.24 per standard deviation, versus the highest rate of mixed ancestry (OR, 1.59).
According to senior author Holly Pederson, MD, director of medical breast services at the Cleveland Clinic, the applicability of the PRS to women with African ancestry is expected to further improve as additional data become available.
“The discriminatory power in women of African descent was significantly improved but still suboptimal,” she said. “The need for more data, particularly in Black women, is challenging not only because there is likely more diversity in the genomic landscape of women of African descent, but also because the barriers created by historical, cultural, institutional and interpersonal dynamics result in the paucity of this data.”
“We must be committed to ending bias resulting in health care disparities,” Dr. Pederson said. She noted that the global PRS is nevertheless “still clinically useful in Black women,” and recommended that clinicians be up front with patients on the status of the research challenges.
“As with any clinical shared decision-making conversation between a patient and her provider, it is important for Black women to know that data is limited in the African American population, particularly given the vast genomic diversity of the African continent,” she said. “This model, as models that have gone before it, will improve with additional data, particularly in this population.”
Commercial PRSs may benefit research
While the commercial marketing of PRSs in a direct-to-consumer fashion have raised some concerns, such as how individuals respond to their risk scores, there could be important benefits as well, commented Megan C. Roberts, PhD.
“There may be an opportunity to learn from these companies about how to engage diverse communities in genomic testing,” said Dr. Roberts, an assistant professor and director of implementation science in precision health and society at the University of North Carolina at Chapel Hill. “Moreover, the data they collect from their customers often can be used for research purposes as well.”
In a recent perspective, Dr. Roberts and colleagues addressed the role of health disparities in PRSs. She’ll be joining international precision public health researchers in October in hosting a free virtual conference at UNC on the topic.
“There is a huge need to improve racial and ethnic diversity in our genomic datasets,” Dr. Roberts said. “Without this, we will not be able to return on the promise of precision medicine and prevention for improving the health of our whole population.”
Dr. Pederson disclosed that she is a consultant for Myriad Genetics.
FROM JAMA NETWORK OPEN
Devices for the treatment of migraine
Remote upper arm neuromodulation and combined occipital and trigeminal neuromodulation lead the way as the newest entries to the field, followed by 8 other devices that are now available or are expected to be soon.
The increasing array of prescription medications for the treatment of migraine are welcome additions for patients who suffer from this life-altering condition and the clinicians who treat it; but not all individuals tolerate oral and injectable therapies, and others face the risk of adverse events and medication overuse headache.1 Fortunately, there are a number of devices available to consider, and still others are awaiting approval from the US Food and Drug Administration (FDA).
Two of the most promising devices are remote upper arm neuromodulation (REN) and combined occipital and trigeminal neuromodulation. Here we highlight data from pivotal trials evaluating these 2 treatment options and provide information about other devices worth consideration.
Remote Upper Arm Neuromodulation (REN)
Nerivio was initially authorized by the FDA for the acute treatment of episodic migraine. Available by prescription, the device is administered by the patient at home.2 It stimulates upper arm peripheral nerves, which induces conditioned pain modulation (CPM) that inhibits pain in remote parts of the body. In other words, a descending, endogenous analgesic “pain inhibits pain” mechanism is used.
The initial authorization was based on the results of a randomized, double-blind, sham-controlled, multicenter study involving 252 individuals who were experiencing 2 to 8 migraine headaches per month. Participants were assigned to either a treatment group (n=126), where the device was applied for 30 to 45 minutes within an hour of a migraine attack, or to a sham treatment group (n=126). Investigators looked at migraine pain levels at baseline and at 2 and 48 hours post-treatment, as well as patient-reported most bothersome symptoms. They found that REN provided superior, clinically meaningful relief from migraine pain and the most bothersome symptoms, as follows3:
- 67% of patients in the active treatment group achieved a response at 2 hours vs 39% of individuals in the sham-treatment group
- Pain-free rates at 2 hours in each group were 37% and 18%, respectively
- Most bothersome symptom relief rates at 2 hours were 46% and 22%, respectively
Additionally, pain relief and pain-free responses were sustained at 48 hours. Nearly 40% of active treatment participants still reported pain relief at 48 hours, with pain-free rates at 48 hours in each group of 21% and 8%, respectively. The adverse event rate was low. The most commonly reported adverse event in the active-treatment group was a sensation of warmth (2.4%). Arm pain (1.6%), redness (1.6%), and numbness (0.8%) were also reported in those receiving active treatment.3
In 2020, REN received authorization for the acute treatment of chronic migraine in adults, and the following year authorization was expanded to include adolescent migraine. This development offered a nonpharmacologic treatment approach for migraine sufferers who experience 15 or more headache days per month, which is significant because it reduces the likelihood of medication overuse headache.
Approval for chronic migraine was based on results of an open-label, single-arm, dual-center study involving 38 individuals with chronic migraine. Participants used the device over 4 weeks within 1 hour of a migraine attack. Investigators assessed pain levels at 2 and 24 hours after use; they defined consistency of response as response to at least half of the treatments. The study demonstrated the following4:
- 74% of patients attained pain relief at 2 hours
- 26% were pain free at 2 hours
- 84% achieved sustained pain relief at 24 hours
- 45% achieved sustained pain relief at 24 hours in at least half of their treated attacks
- <2% of participants experienced device-related adverse events
The authors concluded that REN could be used for a series of migraine attacks and is a safe and effective nonpharmacologic approach for individuals who suffer from chronic migraine.4
The findings from these trials are supported by a subsequent trial published earlier this year. This open-label, single-arm study evaluated 91 individuals with chronic migraine who were treated with REN for 4 weeks. Investigators assessed pain levels, associated pain symptoms, and functional disability at baseline as well as at 2 and 24 hours post-treatment. Of the patients in this study5:
- At 2 hours, 59% achieved pain relief, and 21% reported that their pain disappeared
- 73% noted sustained pain relief at 24 hours
- REN was shown to impact nausea, photophobia, and phonophobia favorably, and patients’ functional ability also improved after use
Results from 2 additional trials were also recently released. One study involving 35 adolescents treated with either REN or standard-of-care medications showed REN to be superior with regard to pain freedom (37% vs 9%), consistency of pain freedom (40% vs 9%), pain relief (71% vs 57%), and consistency of pain relief (80% vs 57%).6 The other study included 91 women with a history of menstrual migraine and at least 4 REN treatments. Nearly 75% of patients reported Nerivio to be at least moderately effective, 45% said they were satisfied with the treatment, and all participants noted that it was at least moderately tolerable.7
Combined Occipital and Trigeminal Neuromodulation
In March 2021, the FDA authorized combined occipital and trigeminal neuromodulation (Relivion) for self-treatment of acute migraine.8 It is not yet commercially available, but it will require a prescription. The headset-like device stimulates the occipital and trigeminal nerves by delivering precise modulated pulses simultaneously to 6 branches of the occipital and trigeminal nerves via 3 adaptive output channels. The occipital and trigeminal nerves conduct the signals directly to the brainstem, which maximizes the synergistic effect.9
The results of 2 clinical trials led to FDA approval. These studies have not yet been published in a peer-reviewed journal. The first study, presented at the 61st Annual Scientific Meeting of the American Headache Society in 2019, was a prospective, randomized, double-blind, parallel-group, sham-controlled clinical study involving 55 individuals with chronic or episodic migraine. Participants administered the device for 1 hour soon after migraine onset or administered a sham treatment. Researchers looked at pain score change from baseline to 1 hour post-treatment, as well as pain intensity at baseline and at 1, 2, and 24 hours post-treatment. The study showed that 76% of participants in the active-treatment group experienced headache relief at 2 hours vs 32% in the sham-treatment contingent. No serious adverse events were reported.10 The investigators hypothesized that the positive results observed were a result of the synergistic neuromodulatory effect elicited by concurrent activation of the occipital and trigeminal neural pathways.
Following this study, there was a multi-center, prospective, randomized, double-blind, placebo-controlled clinical trial involving 131 individuals with migraine with or without aura. Participants were assigned to either active treatment or placebo. Investigators assessed reported migraine pain reduction at 2 hours, as well as improvement in most bothersome symptoms after 2 hours, reported pain reduction at 1 hour, and being pain-free at 2 hours. At 2 hours post-treatment11:
- 46% of individuals who were actively treated reached complete freedom from pain vs 12% in the control group
- 75% of active-treatment participants reported being completely free of their most bothersome symptom vs 47% of control patients
- The rates of complete freedom from migraine symptoms were 47% and 11%, respectively
- The rates of pain relief after 2 hours were 60% and 37%, respectively
- No serious adverse events were noted
A systematic review and meta-analysis of 13 studies involving 221 individuals published earlier this year looked at changes in pain scores and response rates to implantable peripheral nerve stimulation for trigeminal neuropathic pain. The response rate to neuromodulation therapy was 61%, the reduction in overall pain scores (2.363) was significant, and a subgroup assessment revealed that the stimulation target (peripheral branch, trigeminal ganglion, or trigeminal nerve root) was responsible for heterogeneity across the studies analyzed. Furthermore, stimulating the trigeminal peripheral branch resulted in better clinical outcomes. The authors noted that their findings reinforce the promise of implantable therapy, particularly for individuals who do not tolerate traditional therapies.12
Looking forward, new data are scheduled to be presented at the International Headache Virtual Congress in September 2021 showing that neuromodulation therapy is highly effective in reducing monthly headache days in individuals who suffer from difficult-to-treat migraine. A larger-scale, double-blind, sham-controlled study is planned to further establish these findings.
Other FDA-Approved Therapies
A number of other devices are available for treatment of migraine headache, including:
- Transcranial magnetic stimulation (TMS). In a randomized trial involving 164 individuals with migraine, 39% of the individuals receiving treatment were pain-free at 2 hours vs 22% of those given sham treatment13
- Noninvasive vagal nerve stimulation (nVNS). This is performed using a handheld device that is controlled by the patient, which preferentially activates afferent A and large B fibers. In a randomized trial involving 243 individuals, pain-free rates at 30, 60, and 120 minutes for patients receiving active treatment were 13%, 21%, and 30%, respectively. Rates for those receiving sham treatment were 4%, 10%, and 20%, respectively.14
- Sumatriptan nasal spray (10 mg) with a permeation enhancer. A randomized phase 2 trial involving 107 individuals found that 44% of participants in the treatment group achieved pain freedom at 2 hours vs 23% who received placebo. The spray appears to work quickly and with fewer adverse events than generic sumatriptan 20 mg nasal spray.15
- Transcutaneous supraorbital nerve stimulation (tSNS). Available without a prescription, there are 3 devices that can treat acute migraine; prevent acute migraine; or both.
Therapies Awaiting FDA Approval
There are several therapeutic options in the pipeline that have not yet been authorized by the FDA.
- Zavegepant (formerly known as vazegepant) nasal spray.16 This third-generation small molecule calcitonin gene-related peptide (CGRP) receptor antagonist has been demonstrated to work as a nasal spray in individuals with migraine. In a phase 1 study, the spray was shown to reach maximal concentration earlier than with other CGRP receptor antagonists.17 A phase 2/3 placebo-controlled trial demonstrated sustained pain freedom from 2 to 48 hours with 5-mg, 10-mg, and 20-mg dosages. The 10-mg and 20-mg doses were statistically superior to placebo on the co-primary endpoints of pain freedom and freedom from most bothersome symptom at 2 hours using a single dose. Sustained pain relief from 2 to 48 hours was seen with the 5-mg and 10-mg dosages18
- Sphenopalatine ganglion (SPG) stimulation. This is a microstimulator that is inserted orally, designed to fit the face, and directly targets SPG. Stimulation is active and controlled by the patient. A randomized, sham-controlled trial evaluated acute pain relief as well as pain freedom and found that those receiving treatment were more than twice as likely to experience pain relief and pain freedom19
- Adhesive dermally applied microneedle system (ADAM). This is a transdermal patch containing microprojections, which can be coated with both large and small molecules. In a randomized trial, 42% of treated participants reported being pain free at 2 hours vs 14% of placebo-treated patients. Rates of freedom from most bothersome symptom were 68% and 43%, respectively20
- Dihydroergotamine (DHE) nasal powder spray and intranasal liquid. Both therapies are awaiting FDA approval. The mucoadhesive powder formulation facilitates rapid drug absorption and is offered in a single-use nasal delivery device. In clinical trials, the spray demonstrated the device’s simplicity, reliability, and ease of use.21 The intranasal liquid is designed to deliver the drug into the vascular-rich upper nasal space. In the phase 3 trial that included 354 patients, 66.3% of patients reported pain relief, 38% of patients reported pain freedom, and 52% had freedom from their most bothersome migraine symptom at 2 hours following their first dose.22
References
1. Rapoport AM. Medication overuse headache: preventive treatment with or without detoxification? Published May 24, 2021. Accessed August 13, 2021. https://www.mdedge.com/migraine-icymi/article/240472/headache-migraine/medication-overuse-headache-preventive-treatment-or
2. How to prescribe Nerivio. Theranica. Accessed August 13, 2021. https://nerivio.co/prescribe/
3. Yarnitsky D, Dodick DW, Grosberg BM, et al. Remote electrical neuromodulation (REN) relieves acute migraine: a randomized, double-blind, placebo-controlled, multicenter trial. Headache. 2019;59(8):1240-1252.
4. Nierenburg H, Vieira JR, Lev N, et al. Remote electrical neuromodulation for the acute treatment of migraine in patients with chronic migraine: an open-label pilot study. Pain Ther. 2020;9(2):531-543.
5. Grosberg B, Lin T, Vizel M, Schim J. Remote electrical neuromodulation for the acute treatment of chronic migraine (2007). Neurology. 2021;96(15 Suppl) 2007.
6. Hershey AD, Irwin S, Rabany L, et al. Comparison of remote electrical neuromodulation (REN) and standard-care medications for acute treatment of migraine in adolescents: a post-hoc analysis. Pain Med. 2021 June 29;pnab197. doi: 10.1093/pm/pnab197. [Epub ahead of print].
7. Nierenburg H, Rabany L, Lin T, et al. Remote electrical neuromodulation (REN) for the acute treatment of menstrual migraine: a retrospective survey study of effectiveness and tolerability. Pain Ther. 2021 Jun 17. doi: 10.1007/s40122-021-00276-7. [Epub ahead of print].
8. Brooks M. FDA clears neuromodulation device for acute migraine pain. Published March 2, 2021. Accessed August 13, 2021. https://www.medscape.com/viewarticle/946700
9. A new ecosystem for brain neuromodulation. Neurolief. Accessed August 13, 2021. https://www.neurolief.com/technology/
10. Daniel O, Tepper SJ. First non-invasive combined occipital & trigeminal nerve stimulation digital therapeutics system for treatment of migraine: a randomized, sham-controlled, double-blind clinical trial. Published 2019. Accessed August 13, 2021. https://www.neurolief.com/wp-content/uploads/2019/07/American-Headache-Society2019-Abstract-Oved-Daniel-Stewart-Tepper.pdf
11. Neurolief announces positive results from RIME clinical study of its brain neuromodulation system for treating acute migraine. BusinessWire. Published January 6, 2021. Accessed August 13, 2021. https://www.businesswire.com/news/home/20210106005510/en/Neurolief-Announces-Positive-Results-From-RIME-Clinical-Study-of-Its-Brain-Neuromodulation-System-for-Treating-Acute-Migraine
12. Ni Y, Yang L, Han R, et al. Implantable peripheral nerve stimulation for trigeminal neuropathic pain: a systematic review and meta-analysis. Neuromodulation. 2021 May 18. doi: 10.1111/ner.13421. [Epub ahead of print].
13. Lipton RB, Dodick DW, Silberstein SD, et al. Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: a randomized, double-blind, parallel-group, sham-controlled trial. Lancet Neurol. 2010;9(4):373-380.
14. PRESTO clinical trial overview. electroCore. Published 2018. Accessed August 13, 2021. https://www.electrocore.com/wp-content/themes/wp-starter/includes/images/PRESTO_Clinical_Trial_Fact_Sheet_3.29.18.pdf
15. Lipton RB, Munjal S, Brand-Schieber E, Rapoport AM. DFN-02 (sumatriptan 10 mg with a permeation enhancer) nasal spray vs placebo in the acute treatment of migraine: a double-blind, placebo-controlled study. Headache. 2018;58(5):676-687.
16. Clinical trials. Biohaven Pharmaceuticals. Accessed August 14, 2021. https://www.biohavenpharma.com/science-pipeline/resources/clinical-trials
17. Biohaven achieves targeted therapeutic exposures of BHV-3500, a third-generation small molecule CGRP receptor antagonist. Biohaven Pharmaceuticals. Published February 4, 2019. Accessed August 14, 2021. https://www.biohavenpharma.com/investors/news-events/press-releases/02-04-2019
18. Biohaven achieves positive topline results in pivotal phase 2/3 study of vazegepant, the first and only intranasal CGRP receptor antagonist in clinical development for the acute treatment of migraine. Biospace. Published December 17, 2019. Accessed August 14, 2021. https://www.biospace.com/article/releases/biohaven-achieves-positive-topline-results-in-pivotal-phase-2-3-study-of-vazegepant-the-first-and-only-intranasal-cgrp-receptor-antagonist-in-clinical-development-for-the-acute-treatment-of-migraine/
19. Schoenen J, Jensen RH, Lantéri-Minet M, et al. Stimulation of the sphenopalatine ganglion (SPG) for cluster headache treatment. Pathway CH-1: a randomized, sham-controlled study. Cephalalgia. 2013;33(10):816-830.
20. Spierings EL, Brandes JL, Kudrow DB, et al. Randomized, double-blind, placebo-controlled, parallel-group, multi-center study of the safety and efficacy of ADAM zolmitriptan for the acute treatment of migraine. Cephalalgia. 2018;38(2):215-224.
21. STS101 (DHE Nasal Powder). Satsuma Pharmaceuticals. Accessed August 14, 2021. https://www.satsumarx.com/our-research/sts101/
22. Impel NeuroPharma announces U.S. Food & Drug Administration acceptance of new drug application for INP104 for the acute treatment of migraine. PRNewswire. Published January 20, 2021. Accessed August 14, 2021. https://www.prnewswire.com/news-releases/impel-neuropharma-announces-us-food--drug-administration-acceptance-of-new-drug-application-for-inp104-for-the-acute-treatment-of-migraine-301211380.html
Remote upper arm neuromodulation and combined occipital and trigeminal neuromodulation lead the way as the newest entries to the field, followed by 8 other devices that are now available or are expected to be soon.
The increasing array of prescription medications for the treatment of migraine are welcome additions for patients who suffer from this life-altering condition and the clinicians who treat it; but not all individuals tolerate oral and injectable therapies, and others face the risk of adverse events and medication overuse headache.1 Fortunately, there are a number of devices available to consider, and still others are awaiting approval from the US Food and Drug Administration (FDA).
Two of the most promising devices are remote upper arm neuromodulation (REN) and combined occipital and trigeminal neuromodulation. Here we highlight data from pivotal trials evaluating these 2 treatment options and provide information about other devices worth consideration.
Remote Upper Arm Neuromodulation (REN)
Nerivio was initially authorized by the FDA for the acute treatment of episodic migraine. Available by prescription, the device is administered by the patient at home.2 It stimulates upper arm peripheral nerves, which induces conditioned pain modulation (CPM) that inhibits pain in remote parts of the body. In other words, a descending, endogenous analgesic “pain inhibits pain” mechanism is used.
The initial authorization was based on the results of a randomized, double-blind, sham-controlled, multicenter study involving 252 individuals who were experiencing 2 to 8 migraine headaches per month. Participants were assigned to either a treatment group (n=126), where the device was applied for 30 to 45 minutes within an hour of a migraine attack, or to a sham treatment group (n=126). Investigators looked at migraine pain levels at baseline and at 2 and 48 hours post-treatment, as well as patient-reported most bothersome symptoms. They found that REN provided superior, clinically meaningful relief from migraine pain and the most bothersome symptoms, as follows3:
- 67% of patients in the active treatment group achieved a response at 2 hours vs 39% of individuals in the sham-treatment group
- Pain-free rates at 2 hours in each group were 37% and 18%, respectively
- Most bothersome symptom relief rates at 2 hours were 46% and 22%, respectively
Additionally, pain relief and pain-free responses were sustained at 48 hours. Nearly 40% of active treatment participants still reported pain relief at 48 hours, with pain-free rates at 48 hours in each group of 21% and 8%, respectively. The adverse event rate was low. The most commonly reported adverse event in the active-treatment group was a sensation of warmth (2.4%). Arm pain (1.6%), redness (1.6%), and numbness (0.8%) were also reported in those receiving active treatment.3
In 2020, REN received authorization for the acute treatment of chronic migraine in adults, and the following year authorization was expanded to include adolescent migraine. This development offered a nonpharmacologic treatment approach for migraine sufferers who experience 15 or more headache days per month, which is significant because it reduces the likelihood of medication overuse headache.
Approval for chronic migraine was based on results of an open-label, single-arm, dual-center study involving 38 individuals with chronic migraine. Participants used the device over 4 weeks within 1 hour of a migraine attack. Investigators assessed pain levels at 2 and 24 hours after use; they defined consistency of response as response to at least half of the treatments. The study demonstrated the following4:
- 74% of patients attained pain relief at 2 hours
- 26% were pain free at 2 hours
- 84% achieved sustained pain relief at 24 hours
- 45% achieved sustained pain relief at 24 hours in at least half of their treated attacks
- <2% of participants experienced device-related adverse events
The authors concluded that REN could be used for a series of migraine attacks and is a safe and effective nonpharmacologic approach for individuals who suffer from chronic migraine.4
The findings from these trials are supported by a subsequent trial published earlier this year. This open-label, single-arm study evaluated 91 individuals with chronic migraine who were treated with REN for 4 weeks. Investigators assessed pain levels, associated pain symptoms, and functional disability at baseline as well as at 2 and 24 hours post-treatment. Of the patients in this study5:
- At 2 hours, 59% achieved pain relief, and 21% reported that their pain disappeared
- 73% noted sustained pain relief at 24 hours
- REN was shown to impact nausea, photophobia, and phonophobia favorably, and patients’ functional ability also improved after use
Results from 2 additional trials were also recently released. One study involving 35 adolescents treated with either REN or standard-of-care medications showed REN to be superior with regard to pain freedom (37% vs 9%), consistency of pain freedom (40% vs 9%), pain relief (71% vs 57%), and consistency of pain relief (80% vs 57%).6 The other study included 91 women with a history of menstrual migraine and at least 4 REN treatments. Nearly 75% of patients reported Nerivio to be at least moderately effective, 45% said they were satisfied with the treatment, and all participants noted that it was at least moderately tolerable.7
Combined Occipital and Trigeminal Neuromodulation
In March 2021, the FDA authorized combined occipital and trigeminal neuromodulation (Relivion) for self-treatment of acute migraine.8 It is not yet commercially available, but it will require a prescription. The headset-like device stimulates the occipital and trigeminal nerves by delivering precise modulated pulses simultaneously to 6 branches of the occipital and trigeminal nerves via 3 adaptive output channels. The occipital and trigeminal nerves conduct the signals directly to the brainstem, which maximizes the synergistic effect.9
The results of 2 clinical trials led to FDA approval. These studies have not yet been published in a peer-reviewed journal. The first study, presented at the 61st Annual Scientific Meeting of the American Headache Society in 2019, was a prospective, randomized, double-blind, parallel-group, sham-controlled clinical study involving 55 individuals with chronic or episodic migraine. Participants administered the device for 1 hour soon after migraine onset or administered a sham treatment. Researchers looked at pain score change from baseline to 1 hour post-treatment, as well as pain intensity at baseline and at 1, 2, and 24 hours post-treatment. The study showed that 76% of participants in the active-treatment group experienced headache relief at 2 hours vs 32% in the sham-treatment contingent. No serious adverse events were reported.10 The investigators hypothesized that the positive results observed were a result of the synergistic neuromodulatory effect elicited by concurrent activation of the occipital and trigeminal neural pathways.
Following this study, there was a multi-center, prospective, randomized, double-blind, placebo-controlled clinical trial involving 131 individuals with migraine with or without aura. Participants were assigned to either active treatment or placebo. Investigators assessed reported migraine pain reduction at 2 hours, as well as improvement in most bothersome symptoms after 2 hours, reported pain reduction at 1 hour, and being pain-free at 2 hours. At 2 hours post-treatment11:
- 46% of individuals who were actively treated reached complete freedom from pain vs 12% in the control group
- 75% of active-treatment participants reported being completely free of their most bothersome symptom vs 47% of control patients
- The rates of complete freedom from migraine symptoms were 47% and 11%, respectively
- The rates of pain relief after 2 hours were 60% and 37%, respectively
- No serious adverse events were noted
A systematic review and meta-analysis of 13 studies involving 221 individuals published earlier this year looked at changes in pain scores and response rates to implantable peripheral nerve stimulation for trigeminal neuropathic pain. The response rate to neuromodulation therapy was 61%, the reduction in overall pain scores (2.363) was significant, and a subgroup assessment revealed that the stimulation target (peripheral branch, trigeminal ganglion, or trigeminal nerve root) was responsible for heterogeneity across the studies analyzed. Furthermore, stimulating the trigeminal peripheral branch resulted in better clinical outcomes. The authors noted that their findings reinforce the promise of implantable therapy, particularly for individuals who do not tolerate traditional therapies.12
Looking forward, new data are scheduled to be presented at the International Headache Virtual Congress in September 2021 showing that neuromodulation therapy is highly effective in reducing monthly headache days in individuals who suffer from difficult-to-treat migraine. A larger-scale, double-blind, sham-controlled study is planned to further establish these findings.
Other FDA-Approved Therapies
A number of other devices are available for treatment of migraine headache, including:
- Transcranial magnetic stimulation (TMS). In a randomized trial involving 164 individuals with migraine, 39% of the individuals receiving treatment were pain-free at 2 hours vs 22% of those given sham treatment13
- Noninvasive vagal nerve stimulation (nVNS). This is performed using a handheld device that is controlled by the patient, which preferentially activates afferent A and large B fibers. In a randomized trial involving 243 individuals, pain-free rates at 30, 60, and 120 minutes for patients receiving active treatment were 13%, 21%, and 30%, respectively. Rates for those receiving sham treatment were 4%, 10%, and 20%, respectively.14
- Sumatriptan nasal spray (10 mg) with a permeation enhancer. A randomized phase 2 trial involving 107 individuals found that 44% of participants in the treatment group achieved pain freedom at 2 hours vs 23% who received placebo. The spray appears to work quickly and with fewer adverse events than generic sumatriptan 20 mg nasal spray.15
- Transcutaneous supraorbital nerve stimulation (tSNS). Available without a prescription, there are 3 devices that can treat acute migraine; prevent acute migraine; or both.
Therapies Awaiting FDA Approval
There are several therapeutic options in the pipeline that have not yet been authorized by the FDA.
- Zavegepant (formerly known as vazegepant) nasal spray.16 This third-generation small molecule calcitonin gene-related peptide (CGRP) receptor antagonist has been demonstrated to work as a nasal spray in individuals with migraine. In a phase 1 study, the spray was shown to reach maximal concentration earlier than with other CGRP receptor antagonists.17 A phase 2/3 placebo-controlled trial demonstrated sustained pain freedom from 2 to 48 hours with 5-mg, 10-mg, and 20-mg dosages. The 10-mg and 20-mg doses were statistically superior to placebo on the co-primary endpoints of pain freedom and freedom from most bothersome symptom at 2 hours using a single dose. Sustained pain relief from 2 to 48 hours was seen with the 5-mg and 10-mg dosages18
- Sphenopalatine ganglion (SPG) stimulation. This is a microstimulator that is inserted orally, designed to fit the face, and directly targets SPG. Stimulation is active and controlled by the patient. A randomized, sham-controlled trial evaluated acute pain relief as well as pain freedom and found that those receiving treatment were more than twice as likely to experience pain relief and pain freedom19
- Adhesive dermally applied microneedle system (ADAM). This is a transdermal patch containing microprojections, which can be coated with both large and small molecules. In a randomized trial, 42% of treated participants reported being pain free at 2 hours vs 14% of placebo-treated patients. Rates of freedom from most bothersome symptom were 68% and 43%, respectively20
- Dihydroergotamine (DHE) nasal powder spray and intranasal liquid. Both therapies are awaiting FDA approval. The mucoadhesive powder formulation facilitates rapid drug absorption and is offered in a single-use nasal delivery device. In clinical trials, the spray demonstrated the device’s simplicity, reliability, and ease of use.21 The intranasal liquid is designed to deliver the drug into the vascular-rich upper nasal space. In the phase 3 trial that included 354 patients, 66.3% of patients reported pain relief, 38% of patients reported pain freedom, and 52% had freedom from their most bothersome migraine symptom at 2 hours following their first dose.22
Remote upper arm neuromodulation and combined occipital and trigeminal neuromodulation lead the way as the newest entries to the field, followed by 8 other devices that are now available or are expected to be soon.
The increasing array of prescription medications for the treatment of migraine are welcome additions for patients who suffer from this life-altering condition and the clinicians who treat it; but not all individuals tolerate oral and injectable therapies, and others face the risk of adverse events and medication overuse headache.1 Fortunately, there are a number of devices available to consider, and still others are awaiting approval from the US Food and Drug Administration (FDA).
Two of the most promising devices are remote upper arm neuromodulation (REN) and combined occipital and trigeminal neuromodulation. Here we highlight data from pivotal trials evaluating these 2 treatment options and provide information about other devices worth consideration.
Remote Upper Arm Neuromodulation (REN)
Nerivio was initially authorized by the FDA for the acute treatment of episodic migraine. Available by prescription, the device is administered by the patient at home.2 It stimulates upper arm peripheral nerves, which induces conditioned pain modulation (CPM) that inhibits pain in remote parts of the body. In other words, a descending, endogenous analgesic “pain inhibits pain” mechanism is used.
The initial authorization was based on the results of a randomized, double-blind, sham-controlled, multicenter study involving 252 individuals who were experiencing 2 to 8 migraine headaches per month. Participants were assigned to either a treatment group (n=126), where the device was applied for 30 to 45 minutes within an hour of a migraine attack, or to a sham treatment group (n=126). Investigators looked at migraine pain levels at baseline and at 2 and 48 hours post-treatment, as well as patient-reported most bothersome symptoms. They found that REN provided superior, clinically meaningful relief from migraine pain and the most bothersome symptoms, as follows3:
- 67% of patients in the active treatment group achieved a response at 2 hours vs 39% of individuals in the sham-treatment group
- Pain-free rates at 2 hours in each group were 37% and 18%, respectively
- Most bothersome symptom relief rates at 2 hours were 46% and 22%, respectively
Additionally, pain relief and pain-free responses were sustained at 48 hours. Nearly 40% of active treatment participants still reported pain relief at 48 hours, with pain-free rates at 48 hours in each group of 21% and 8%, respectively. The adverse event rate was low. The most commonly reported adverse event in the active-treatment group was a sensation of warmth (2.4%). Arm pain (1.6%), redness (1.6%), and numbness (0.8%) were also reported in those receiving active treatment.3
In 2020, REN received authorization for the acute treatment of chronic migraine in adults, and the following year authorization was expanded to include adolescent migraine. This development offered a nonpharmacologic treatment approach for migraine sufferers who experience 15 or more headache days per month, which is significant because it reduces the likelihood of medication overuse headache.
Approval for chronic migraine was based on results of an open-label, single-arm, dual-center study involving 38 individuals with chronic migraine. Participants used the device over 4 weeks within 1 hour of a migraine attack. Investigators assessed pain levels at 2 and 24 hours after use; they defined consistency of response as response to at least half of the treatments. The study demonstrated the following4:
- 74% of patients attained pain relief at 2 hours
- 26% were pain free at 2 hours
- 84% achieved sustained pain relief at 24 hours
- 45% achieved sustained pain relief at 24 hours in at least half of their treated attacks
- <2% of participants experienced device-related adverse events
The authors concluded that REN could be used for a series of migraine attacks and is a safe and effective nonpharmacologic approach for individuals who suffer from chronic migraine.4
The findings from these trials are supported by a subsequent trial published earlier this year. This open-label, single-arm study evaluated 91 individuals with chronic migraine who were treated with REN for 4 weeks. Investigators assessed pain levels, associated pain symptoms, and functional disability at baseline as well as at 2 and 24 hours post-treatment. Of the patients in this study5:
- At 2 hours, 59% achieved pain relief, and 21% reported that their pain disappeared
- 73% noted sustained pain relief at 24 hours
- REN was shown to impact nausea, photophobia, and phonophobia favorably, and patients’ functional ability also improved after use
Results from 2 additional trials were also recently released. One study involving 35 adolescents treated with either REN or standard-of-care medications showed REN to be superior with regard to pain freedom (37% vs 9%), consistency of pain freedom (40% vs 9%), pain relief (71% vs 57%), and consistency of pain relief (80% vs 57%).6 The other study included 91 women with a history of menstrual migraine and at least 4 REN treatments. Nearly 75% of patients reported Nerivio to be at least moderately effective, 45% said they were satisfied with the treatment, and all participants noted that it was at least moderately tolerable.7
Combined Occipital and Trigeminal Neuromodulation
In March 2021, the FDA authorized combined occipital and trigeminal neuromodulation (Relivion) for self-treatment of acute migraine.8 It is not yet commercially available, but it will require a prescription. The headset-like device stimulates the occipital and trigeminal nerves by delivering precise modulated pulses simultaneously to 6 branches of the occipital and trigeminal nerves via 3 adaptive output channels. The occipital and trigeminal nerves conduct the signals directly to the brainstem, which maximizes the synergistic effect.9
The results of 2 clinical trials led to FDA approval. These studies have not yet been published in a peer-reviewed journal. The first study, presented at the 61st Annual Scientific Meeting of the American Headache Society in 2019, was a prospective, randomized, double-blind, parallel-group, sham-controlled clinical study involving 55 individuals with chronic or episodic migraine. Participants administered the device for 1 hour soon after migraine onset or administered a sham treatment. Researchers looked at pain score change from baseline to 1 hour post-treatment, as well as pain intensity at baseline and at 1, 2, and 24 hours post-treatment. The study showed that 76% of participants in the active-treatment group experienced headache relief at 2 hours vs 32% in the sham-treatment contingent. No serious adverse events were reported.10 The investigators hypothesized that the positive results observed were a result of the synergistic neuromodulatory effect elicited by concurrent activation of the occipital and trigeminal neural pathways.
Following this study, there was a multi-center, prospective, randomized, double-blind, placebo-controlled clinical trial involving 131 individuals with migraine with or without aura. Participants were assigned to either active treatment or placebo. Investigators assessed reported migraine pain reduction at 2 hours, as well as improvement in most bothersome symptoms after 2 hours, reported pain reduction at 1 hour, and being pain-free at 2 hours. At 2 hours post-treatment11:
- 46% of individuals who were actively treated reached complete freedom from pain vs 12% in the control group
- 75% of active-treatment participants reported being completely free of their most bothersome symptom vs 47% of control patients
- The rates of complete freedom from migraine symptoms were 47% and 11%, respectively
- The rates of pain relief after 2 hours were 60% and 37%, respectively
- No serious adverse events were noted
A systematic review and meta-analysis of 13 studies involving 221 individuals published earlier this year looked at changes in pain scores and response rates to implantable peripheral nerve stimulation for trigeminal neuropathic pain. The response rate to neuromodulation therapy was 61%, the reduction in overall pain scores (2.363) was significant, and a subgroup assessment revealed that the stimulation target (peripheral branch, trigeminal ganglion, or trigeminal nerve root) was responsible for heterogeneity across the studies analyzed. Furthermore, stimulating the trigeminal peripheral branch resulted in better clinical outcomes. The authors noted that their findings reinforce the promise of implantable therapy, particularly for individuals who do not tolerate traditional therapies.12
Looking forward, new data are scheduled to be presented at the International Headache Virtual Congress in September 2021 showing that neuromodulation therapy is highly effective in reducing monthly headache days in individuals who suffer from difficult-to-treat migraine. A larger-scale, double-blind, sham-controlled study is planned to further establish these findings.
Other FDA-Approved Therapies
A number of other devices are available for treatment of migraine headache, including:
- Transcranial magnetic stimulation (TMS). In a randomized trial involving 164 individuals with migraine, 39% of the individuals receiving treatment were pain-free at 2 hours vs 22% of those given sham treatment13
- Noninvasive vagal nerve stimulation (nVNS). This is performed using a handheld device that is controlled by the patient, which preferentially activates afferent A and large B fibers. In a randomized trial involving 243 individuals, pain-free rates at 30, 60, and 120 minutes for patients receiving active treatment were 13%, 21%, and 30%, respectively. Rates for those receiving sham treatment were 4%, 10%, and 20%, respectively.14
- Sumatriptan nasal spray (10 mg) with a permeation enhancer. A randomized phase 2 trial involving 107 individuals found that 44% of participants in the treatment group achieved pain freedom at 2 hours vs 23% who received placebo. The spray appears to work quickly and with fewer adverse events than generic sumatriptan 20 mg nasal spray.15
- Transcutaneous supraorbital nerve stimulation (tSNS). Available without a prescription, there are 3 devices that can treat acute migraine; prevent acute migraine; or both.
Therapies Awaiting FDA Approval
There are several therapeutic options in the pipeline that have not yet been authorized by the FDA.
- Zavegepant (formerly known as vazegepant) nasal spray.16 This third-generation small molecule calcitonin gene-related peptide (CGRP) receptor antagonist has been demonstrated to work as a nasal spray in individuals with migraine. In a phase 1 study, the spray was shown to reach maximal concentration earlier than with other CGRP receptor antagonists.17 A phase 2/3 placebo-controlled trial demonstrated sustained pain freedom from 2 to 48 hours with 5-mg, 10-mg, and 20-mg dosages. The 10-mg and 20-mg doses were statistically superior to placebo on the co-primary endpoints of pain freedom and freedom from most bothersome symptom at 2 hours using a single dose. Sustained pain relief from 2 to 48 hours was seen with the 5-mg and 10-mg dosages18
- Sphenopalatine ganglion (SPG) stimulation. This is a microstimulator that is inserted orally, designed to fit the face, and directly targets SPG. Stimulation is active and controlled by the patient. A randomized, sham-controlled trial evaluated acute pain relief as well as pain freedom and found that those receiving treatment were more than twice as likely to experience pain relief and pain freedom19
- Adhesive dermally applied microneedle system (ADAM). This is a transdermal patch containing microprojections, which can be coated with both large and small molecules. In a randomized trial, 42% of treated participants reported being pain free at 2 hours vs 14% of placebo-treated patients. Rates of freedom from most bothersome symptom were 68% and 43%, respectively20
- Dihydroergotamine (DHE) nasal powder spray and intranasal liquid. Both therapies are awaiting FDA approval. The mucoadhesive powder formulation facilitates rapid drug absorption and is offered in a single-use nasal delivery device. In clinical trials, the spray demonstrated the device’s simplicity, reliability, and ease of use.21 The intranasal liquid is designed to deliver the drug into the vascular-rich upper nasal space. In the phase 3 trial that included 354 patients, 66.3% of patients reported pain relief, 38% of patients reported pain freedom, and 52% had freedom from their most bothersome migraine symptom at 2 hours following their first dose.22
References
1. Rapoport AM. Medication overuse headache: preventive treatment with or without detoxification? Published May 24, 2021. Accessed August 13, 2021. https://www.mdedge.com/migraine-icymi/article/240472/headache-migraine/medication-overuse-headache-preventive-treatment-or
2. How to prescribe Nerivio. Theranica. Accessed August 13, 2021. https://nerivio.co/prescribe/
3. Yarnitsky D, Dodick DW, Grosberg BM, et al. Remote electrical neuromodulation (REN) relieves acute migraine: a randomized, double-blind, placebo-controlled, multicenter trial. Headache. 2019;59(8):1240-1252.
4. Nierenburg H, Vieira JR, Lev N, et al. Remote electrical neuromodulation for the acute treatment of migraine in patients with chronic migraine: an open-label pilot study. Pain Ther. 2020;9(2):531-543.
5. Grosberg B, Lin T, Vizel M, Schim J. Remote electrical neuromodulation for the acute treatment of chronic migraine (2007). Neurology. 2021;96(15 Suppl) 2007.
6. Hershey AD, Irwin S, Rabany L, et al. Comparison of remote electrical neuromodulation (REN) and standard-care medications for acute treatment of migraine in adolescents: a post-hoc analysis. Pain Med. 2021 June 29;pnab197. doi: 10.1093/pm/pnab197. [Epub ahead of print].
7. Nierenburg H, Rabany L, Lin T, et al. Remote electrical neuromodulation (REN) for the acute treatment of menstrual migraine: a retrospective survey study of effectiveness and tolerability. Pain Ther. 2021 Jun 17. doi: 10.1007/s40122-021-00276-7. [Epub ahead of print].
8. Brooks M. FDA clears neuromodulation device for acute migraine pain. Published March 2, 2021. Accessed August 13, 2021. https://www.medscape.com/viewarticle/946700
9. A new ecosystem for brain neuromodulation. Neurolief. Accessed August 13, 2021. https://www.neurolief.com/technology/
10. Daniel O, Tepper SJ. First non-invasive combined occipital & trigeminal nerve stimulation digital therapeutics system for treatment of migraine: a randomized, sham-controlled, double-blind clinical trial. Published 2019. Accessed August 13, 2021. https://www.neurolief.com/wp-content/uploads/2019/07/American-Headache-Society2019-Abstract-Oved-Daniel-Stewart-Tepper.pdf
11. Neurolief announces positive results from RIME clinical study of its brain neuromodulation system for treating acute migraine. BusinessWire. Published January 6, 2021. Accessed August 13, 2021. https://www.businesswire.com/news/home/20210106005510/en/Neurolief-Announces-Positive-Results-From-RIME-Clinical-Study-of-Its-Brain-Neuromodulation-System-for-Treating-Acute-Migraine
12. Ni Y, Yang L, Han R, et al. Implantable peripheral nerve stimulation for trigeminal neuropathic pain: a systematic review and meta-analysis. Neuromodulation. 2021 May 18. doi: 10.1111/ner.13421. [Epub ahead of print].
13. Lipton RB, Dodick DW, Silberstein SD, et al. Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: a randomized, double-blind, parallel-group, sham-controlled trial. Lancet Neurol. 2010;9(4):373-380.
14. PRESTO clinical trial overview. electroCore. Published 2018. Accessed August 13, 2021. https://www.electrocore.com/wp-content/themes/wp-starter/includes/images/PRESTO_Clinical_Trial_Fact_Sheet_3.29.18.pdf
15. Lipton RB, Munjal S, Brand-Schieber E, Rapoport AM. DFN-02 (sumatriptan 10 mg with a permeation enhancer) nasal spray vs placebo in the acute treatment of migraine: a double-blind, placebo-controlled study. Headache. 2018;58(5):676-687.
16. Clinical trials. Biohaven Pharmaceuticals. Accessed August 14, 2021. https://www.biohavenpharma.com/science-pipeline/resources/clinical-trials
17. Biohaven achieves targeted therapeutic exposures of BHV-3500, a third-generation small molecule CGRP receptor antagonist. Biohaven Pharmaceuticals. Published February 4, 2019. Accessed August 14, 2021. https://www.biohavenpharma.com/investors/news-events/press-releases/02-04-2019
18. Biohaven achieves positive topline results in pivotal phase 2/3 study of vazegepant, the first and only intranasal CGRP receptor antagonist in clinical development for the acute treatment of migraine. Biospace. Published December 17, 2019. Accessed August 14, 2021. https://www.biospace.com/article/releases/biohaven-achieves-positive-topline-results-in-pivotal-phase-2-3-study-of-vazegepant-the-first-and-only-intranasal-cgrp-receptor-antagonist-in-clinical-development-for-the-acute-treatment-of-migraine/
19. Schoenen J, Jensen RH, Lantéri-Minet M, et al. Stimulation of the sphenopalatine ganglion (SPG) for cluster headache treatment. Pathway CH-1: a randomized, sham-controlled study. Cephalalgia. 2013;33(10):816-830.
20. Spierings EL, Brandes JL, Kudrow DB, et al. Randomized, double-blind, placebo-controlled, parallel-group, multi-center study of the safety and efficacy of ADAM zolmitriptan for the acute treatment of migraine. Cephalalgia. 2018;38(2):215-224.
21. STS101 (DHE Nasal Powder). Satsuma Pharmaceuticals. Accessed August 14, 2021. https://www.satsumarx.com/our-research/sts101/
22. Impel NeuroPharma announces U.S. Food & Drug Administration acceptance of new drug application for INP104 for the acute treatment of migraine. PRNewswire. Published January 20, 2021. Accessed August 14, 2021. https://www.prnewswire.com/news-releases/impel-neuropharma-announces-us-food--drug-administration-acceptance-of-new-drug-application-for-inp104-for-the-acute-treatment-of-migraine-301211380.html
References
1. Rapoport AM. Medication overuse headache: preventive treatment with or without detoxification? Published May 24, 2021. Accessed August 13, 2021. https://www.mdedge.com/migraine-icymi/article/240472/headache-migraine/medication-overuse-headache-preventive-treatment-or
2. How to prescribe Nerivio. Theranica. Accessed August 13, 2021. https://nerivio.co/prescribe/
3. Yarnitsky D, Dodick DW, Grosberg BM, et al. Remote electrical neuromodulation (REN) relieves acute migraine: a randomized, double-blind, placebo-controlled, multicenter trial. Headache. 2019;59(8):1240-1252.
4. Nierenburg H, Vieira JR, Lev N, et al. Remote electrical neuromodulation for the acute treatment of migraine in patients with chronic migraine: an open-label pilot study. Pain Ther. 2020;9(2):531-543.
5. Grosberg B, Lin T, Vizel M, Schim J. Remote electrical neuromodulation for the acute treatment of chronic migraine (2007). Neurology. 2021;96(15 Suppl) 2007.
6. Hershey AD, Irwin S, Rabany L, et al. Comparison of remote electrical neuromodulation (REN) and standard-care medications for acute treatment of migraine in adolescents: a post-hoc analysis. Pain Med. 2021 June 29;pnab197. doi: 10.1093/pm/pnab197. [Epub ahead of print].
7. Nierenburg H, Rabany L, Lin T, et al. Remote electrical neuromodulation (REN) for the acute treatment of menstrual migraine: a retrospective survey study of effectiveness and tolerability. Pain Ther. 2021 Jun 17. doi: 10.1007/s40122-021-00276-7. [Epub ahead of print].
8. Brooks M. FDA clears neuromodulation device for acute migraine pain. Published March 2, 2021. Accessed August 13, 2021. https://www.medscape.com/viewarticle/946700
9. A new ecosystem for brain neuromodulation. Neurolief. Accessed August 13, 2021. https://www.neurolief.com/technology/
10. Daniel O, Tepper SJ. First non-invasive combined occipital & trigeminal nerve stimulation digital therapeutics system for treatment of migraine: a randomized, sham-controlled, double-blind clinical trial. Published 2019. Accessed August 13, 2021. https://www.neurolief.com/wp-content/uploads/2019/07/American-Headache-Society2019-Abstract-Oved-Daniel-Stewart-Tepper.pdf
11. Neurolief announces positive results from RIME clinical study of its brain neuromodulation system for treating acute migraine. BusinessWire. Published January 6, 2021. Accessed August 13, 2021. https://www.businesswire.com/news/home/20210106005510/en/Neurolief-Announces-Positive-Results-From-RIME-Clinical-Study-of-Its-Brain-Neuromodulation-System-for-Treating-Acute-Migraine
12. Ni Y, Yang L, Han R, et al. Implantable peripheral nerve stimulation for trigeminal neuropathic pain: a systematic review and meta-analysis. Neuromodulation. 2021 May 18. doi: 10.1111/ner.13421. [Epub ahead of print].
13. Lipton RB, Dodick DW, Silberstein SD, et al. Single-pulse transcranial magnetic stimulation for acute treatment of migraine with aura: a randomized, double-blind, parallel-group, sham-controlled trial. Lancet Neurol. 2010;9(4):373-380.
14. PRESTO clinical trial overview. electroCore. Published 2018. Accessed August 13, 2021. https://www.electrocore.com/wp-content/themes/wp-starter/includes/images/PRESTO_Clinical_Trial_Fact_Sheet_3.29.18.pdf
15. Lipton RB, Munjal S, Brand-Schieber E, Rapoport AM. DFN-02 (sumatriptan 10 mg with a permeation enhancer) nasal spray vs placebo in the acute treatment of migraine: a double-blind, placebo-controlled study. Headache. 2018;58(5):676-687.
16. Clinical trials. Biohaven Pharmaceuticals. Accessed August 14, 2021. https://www.biohavenpharma.com/science-pipeline/resources/clinical-trials
17. Biohaven achieves targeted therapeutic exposures of BHV-3500, a third-generation small molecule CGRP receptor antagonist. Biohaven Pharmaceuticals. Published February 4, 2019. Accessed August 14, 2021. https://www.biohavenpharma.com/investors/news-events/press-releases/02-04-2019
18. Biohaven achieves positive topline results in pivotal phase 2/3 study of vazegepant, the first and only intranasal CGRP receptor antagonist in clinical development for the acute treatment of migraine. Biospace. Published December 17, 2019. Accessed August 14, 2021. https://www.biospace.com/article/releases/biohaven-achieves-positive-topline-results-in-pivotal-phase-2-3-study-of-vazegepant-the-first-and-only-intranasal-cgrp-receptor-antagonist-in-clinical-development-for-the-acute-treatment-of-migraine/
19. Schoenen J, Jensen RH, Lantéri-Minet M, et al. Stimulation of the sphenopalatine ganglion (SPG) for cluster headache treatment. Pathway CH-1: a randomized, sham-controlled study. Cephalalgia. 2013;33(10):816-830.
20. Spierings EL, Brandes JL, Kudrow DB, et al. Randomized, double-blind, placebo-controlled, parallel-group, multi-center study of the safety and efficacy of ADAM zolmitriptan for the acute treatment of migraine. Cephalalgia. 2018;38(2):215-224.
21. STS101 (DHE Nasal Powder). Satsuma Pharmaceuticals. Accessed August 14, 2021. https://www.satsumarx.com/our-research/sts101/
22. Impel NeuroPharma announces U.S. Food & Drug Administration acceptance of new drug application for INP104 for the acute treatment of migraine. PRNewswire. Published January 20, 2021. Accessed August 14, 2021. https://www.prnewswire.com/news-releases/impel-neuropharma-announces-us-food--drug-administration-acceptance-of-new-drug-application-for-inp104-for-the-acute-treatment-of-migraine-301211380.html
Guidance on additional COVID-19 vaccine dose for MS patients
Patients aged 12 years and older with multiple sclerosis (MS) who are fully immunized against COVID-19 with either the Pfizer-BioNTech or Moderna mRNA vaccine may be eligible to receive an additional dose now, the National Multiple Sclerosis Society has announced.
New guidance, which is “based on available data from studies and expert consensus opinion” by a panel of MS neurologists and experts, was published Aug. 19 on the organization’s website.
The Food and Drug Administration has authorized an additional dose of the coronavirus vaccine for patients who are expected to not have a normal or adequate immune response to the first two doses. Patients with MS who use certain treatments have a reduced or absent antibody response to the vaccine, according to recent data.
“We want people living with MS to be aware of this additional dose and discuss when they need an additional dose or booster dose with their health care provider,” Julie Fiol, RN, MSW, associate vice president of health care access, National MS Society, said in an interview.
Those who may benefit from an additional dose include patients with MS who use sphingosine 1-phosphate receptor modulators, anti-CD20 monoclonal antibodies, or alemtuzumab (Lemtrada), the National MS Society noted. These particular disease modifying therapies (DMTs) have a stronger effect on the immune system than do other treatments.
Protecting ‘the most vulnerable’
Sphingosine 1-phosphate receptor modulators include fingolimod (Gilenya), siponimod (Mayzent), ozanimod (Zeposia), and ponesimod (Ponvory).
Anti-CD20 monoclonal antibodies include ocrelizumab (Ocrevus), ofatumumab (Kesimpta), rituximab (Rituxan), and corresponding biosimilars.
Current data do not support an additional dose for immunocompromised patients who received the Johnson & Johnson vaccine. The FDA and the Centers for Disease Control and Prevention are developing recommendations for these patients, and the National MS Society will update its guidance as needed, the organization noted in its statement.
“Like other medical decisions, the decision to get an additional dose is best made in partnership with your health care provider,” said Ms. Fiol. “Talk to your MS health care provider to determine what is best for you.”
MS itself does not compromise the immune system, but some MS therapies alter the immune system and reduce the body’s response to vaccination. Patients with MS who use B cell-depleting therapies have a better antibody response when they receive the vaccine 3 months or more after the last dose of MS therapy, according to the National MS Society.
Data suggest that patients with MS are not more susceptible to COVID-19 infection, severe illness, or death than are patients without MS. However, certain groups of patients with MS, such as those who receive B cell-depleting treatments, are more susceptible to having a severe case of COVID-19.
That said, “everyone will need a booster at some point. Those who take DMTs that have greater impact on the immune system are the most urgent need now,” the organization noted.
“Vaccination against COVID-19 is critical for public safety and, especially, the safety of the most vulnerable among us,” said Ms. Fiol. “We encourage everyone with MS get vaccinated.”
A version of this article first appeared on Medscape.com.
Patients aged 12 years and older with multiple sclerosis (MS) who are fully immunized against COVID-19 with either the Pfizer-BioNTech or Moderna mRNA vaccine may be eligible to receive an additional dose now, the National Multiple Sclerosis Society has announced.
New guidance, which is “based on available data from studies and expert consensus opinion” by a panel of MS neurologists and experts, was published Aug. 19 on the organization’s website.
The Food and Drug Administration has authorized an additional dose of the coronavirus vaccine for patients who are expected to not have a normal or adequate immune response to the first two doses. Patients with MS who use certain treatments have a reduced or absent antibody response to the vaccine, according to recent data.
“We want people living with MS to be aware of this additional dose and discuss when they need an additional dose or booster dose with their health care provider,” Julie Fiol, RN, MSW, associate vice president of health care access, National MS Society, said in an interview.
Those who may benefit from an additional dose include patients with MS who use sphingosine 1-phosphate receptor modulators, anti-CD20 monoclonal antibodies, or alemtuzumab (Lemtrada), the National MS Society noted. These particular disease modifying therapies (DMTs) have a stronger effect on the immune system than do other treatments.
Protecting ‘the most vulnerable’
Sphingosine 1-phosphate receptor modulators include fingolimod (Gilenya), siponimod (Mayzent), ozanimod (Zeposia), and ponesimod (Ponvory).
Anti-CD20 monoclonal antibodies include ocrelizumab (Ocrevus), ofatumumab (Kesimpta), rituximab (Rituxan), and corresponding biosimilars.
Current data do not support an additional dose for immunocompromised patients who received the Johnson & Johnson vaccine. The FDA and the Centers for Disease Control and Prevention are developing recommendations for these patients, and the National MS Society will update its guidance as needed, the organization noted in its statement.
“Like other medical decisions, the decision to get an additional dose is best made in partnership with your health care provider,” said Ms. Fiol. “Talk to your MS health care provider to determine what is best for you.”
MS itself does not compromise the immune system, but some MS therapies alter the immune system and reduce the body’s response to vaccination. Patients with MS who use B cell-depleting therapies have a better antibody response when they receive the vaccine 3 months or more after the last dose of MS therapy, according to the National MS Society.
Data suggest that patients with MS are not more susceptible to COVID-19 infection, severe illness, or death than are patients without MS. However, certain groups of patients with MS, such as those who receive B cell-depleting treatments, are more susceptible to having a severe case of COVID-19.
That said, “everyone will need a booster at some point. Those who take DMTs that have greater impact on the immune system are the most urgent need now,” the organization noted.
“Vaccination against COVID-19 is critical for public safety and, especially, the safety of the most vulnerable among us,” said Ms. Fiol. “We encourage everyone with MS get vaccinated.”
A version of this article first appeared on Medscape.com.
Patients aged 12 years and older with multiple sclerosis (MS) who are fully immunized against COVID-19 with either the Pfizer-BioNTech or Moderna mRNA vaccine may be eligible to receive an additional dose now, the National Multiple Sclerosis Society has announced.
New guidance, which is “based on available data from studies and expert consensus opinion” by a panel of MS neurologists and experts, was published Aug. 19 on the organization’s website.
The Food and Drug Administration has authorized an additional dose of the coronavirus vaccine for patients who are expected to not have a normal or adequate immune response to the first two doses. Patients with MS who use certain treatments have a reduced or absent antibody response to the vaccine, according to recent data.
“We want people living with MS to be aware of this additional dose and discuss when they need an additional dose or booster dose with their health care provider,” Julie Fiol, RN, MSW, associate vice president of health care access, National MS Society, said in an interview.
Those who may benefit from an additional dose include patients with MS who use sphingosine 1-phosphate receptor modulators, anti-CD20 monoclonal antibodies, or alemtuzumab (Lemtrada), the National MS Society noted. These particular disease modifying therapies (DMTs) have a stronger effect on the immune system than do other treatments.
Protecting ‘the most vulnerable’
Sphingosine 1-phosphate receptor modulators include fingolimod (Gilenya), siponimod (Mayzent), ozanimod (Zeposia), and ponesimod (Ponvory).
Anti-CD20 monoclonal antibodies include ocrelizumab (Ocrevus), ofatumumab (Kesimpta), rituximab (Rituxan), and corresponding biosimilars.
Current data do not support an additional dose for immunocompromised patients who received the Johnson & Johnson vaccine. The FDA and the Centers for Disease Control and Prevention are developing recommendations for these patients, and the National MS Society will update its guidance as needed, the organization noted in its statement.
“Like other medical decisions, the decision to get an additional dose is best made in partnership with your health care provider,” said Ms. Fiol. “Talk to your MS health care provider to determine what is best for you.”
MS itself does not compromise the immune system, but some MS therapies alter the immune system and reduce the body’s response to vaccination. Patients with MS who use B cell-depleting therapies have a better antibody response when they receive the vaccine 3 months or more after the last dose of MS therapy, according to the National MS Society.
Data suggest that patients with MS are not more susceptible to COVID-19 infection, severe illness, or death than are patients without MS. However, certain groups of patients with MS, such as those who receive B cell-depleting treatments, are more susceptible to having a severe case of COVID-19.
That said, “everyone will need a booster at some point. Those who take DMTs that have greater impact on the immune system are the most urgent need now,” the organization noted.
“Vaccination against COVID-19 is critical for public safety and, especially, the safety of the most vulnerable among us,” said Ms. Fiol. “We encourage everyone with MS get vaccinated.”
A version of this article first appeared on Medscape.com.
Bone Health in Patients With Prostate Cancer: An Evidence-Based Algorithm
Prostate cancer (PC) is the most commonly and newly diagnosed nonskin cancer and the second leading cause of cancer death in men in the United States. About 191,930 cases and about 33,330 deaths from PC were expected for the year 2020.1 About 1 in 41 men will die of PC. Most men diagnosed with PC are aged > 65 years and do not die of their disease. The 5-year survival rate of localized and regional disease is nearly 100%, and disease with distant metastases is 31%. As a result, more than 3.1 million men in the United States who have been diagnosed with PC are still alive today.1 Among veterans, there is a substantial population living with PC. Skolarus and Hawley reported in 2014 that an estimated 200,000 veterans with PC were survivors and 12,000 were newly diagnosed.2
In PC, skeletal strength can be affected by several factors, such as aging, malnutrition, androgen-deprivation therapy (ADT), and bone metastasis.3,4 In fact, most men can live the rest of their life with PC by using strategies to monitor and treat it, once it shows either radiographic or chemical signs of progression.5 ADT is the standard of care to treat hormone-sensitive PC, which is associated with significant skeletal-related adverse effects (AEs).6,7
Men undergoing ADT are 4 times more likely to develop substantial bone deficiency, Shahinian and colleagues found that in men surviving 5 years after PC diagnosis, 19.4% of those who received ADT had a fracture compared with 12% in men who did not (P < .001). The authors established a significant relation between the number of doses of gonadotropin-releasing hormone given in the first 12 months and the risk of fracture.8 Of those who progressed to metastatic disease, the first metastatic nonnodal site is most commonly to the bone.9 Advanced PC is characterized by increased bone turnover, which further raises concerns for bone health and patient performance.10
Skeletal-related events (SREs) include pathologic fracture, spinal cord compression, palliative radiation, or surgery to bone, and change in antineoplastic therapy secondary to bone pain. The concept of bone health refers to the prevention, diagnosis, and treatment of idiopathic, pathogenic, and treatment-related bone loss and delay or prevention of SREs.6,11 Guidelines and expert groups have recommended screening for osteoporosis at the start of ADT with bone mineral density testing, ensuring adequate calcium and vitamin D intake, modifying lifestyle behaviors (smoking cessation, alcohol moderation, and regular exercise), and prescribing bisphosphonates or receptor-activated nuclear factor κ-B ligand inhibitor, denosumab, for men with osteoporosis or who are at general high-fracture risk.12,13 The overuse of these medications results in undue cost to patients as well as AEs, such as osteonecrosis of the jaw (ONJ), hypocalcemia, and bone/joint pains.14-17 There are evidence-based guidelines for appropriate use of bisphosphonates and denosumab for delay and prevention of SREs in the setting of advanced PC.18 These doses also typically differ in frequency to those of osteoporosis.19 We summarize the evidence and guidance for health care providers who care for patients with PC at various stages and complications from both disease-related and treatment-related comorbidities.
Bone-Strengthening Agents
Overall, there is evidence to support the use of bone-strengthening agents in patients with osteopenia/osteoporosis in the prevention of SREs with significant risk factors for progressive bone demineralization, such as lifestyle factors and, in particular, treatments such as ADT. Bone-remodeling agents for treatment of bony metastasis have been shown to provide therapeutic advantage only in limited instances in the castration-resistant PC (CRPC) setting. Hence, in patients with hormone-sensitive PC due to medication-related AEs, treatment with bone-strengthening agents is indicated only if the patient has a significant preexisting risk for fracture from osteopenia/osteoporosis (Table). The Figure depicts an algorithm for the management of bone health in men with PC who are being treated with ADT.
Denosumab and bisphosphonates have an established role in preventing SREs in metastatic CRPC.20 The choice of denosumab or a bisphosphonate typically varies based on the indication, possible AEs, and cost of therapy. There are multiple studies involving initiation of these agents at various stages of disease to improve both time to progression as well as management of SREs. There is a lack of evidence that bisphosphonates prevent metastatic-bone lesions in castration-sensitive PC; therefore, prophylactic use of this agent is not recommended in patients unless they have significant bone demineralization.21,22
Medication-induced ONJ is a severe AE of both denosumab and bisphosphonate therapies. Data from recent trials showed that higher dosing and prolonged duration of denosumab and bisphosphonate therapies further increased risk of ONJ by 1.8% and 1.3%, respectively.15 Careful history taking and discussions with the patient and if possible their dentist on how to reduce risk are recommended. It is good practice for the patient to complete a dental evaluation prior to starting IV bisphosphonates or denosumab. Dental evaluations should be performed routinely at 3- to 12-month intervals throughout therapy based on individualized risk assessment.23 The benefits of using bisphosphonates to prevent fractures associated with osteoporosis outweigh the risk of ONJ in high-risk populations, but not in all patients with PC. A case-by-case basis and evaluation of risk factors should be performed prior to administering bone-modifying therapy. The long-term safety of IV bisphosphonates has not been adequately studied in controlled trials, and concerns regarding long-term complications, including renal toxicity, ONJ, and atypical femoral fractures, remain with prolonged therapy.24,25
The CALGB 70604 (Alliance) trial compared 3-month dosing to monthly treatment with zoledronic acid (ZA), showing no inferiority to lower frequency dosing.26 A Cochrane review of clinical trials found that in patients with advanced PC, bisphosphonates were found to provide roughly 58 fewer SREs per 1000 on average.27 A phase 3 study showed a modest benefit to denosumab vs ZA in the CRPC group regarding incidence of SREs. The rates of SREs were 289 of 951 patients in the bisphosphonate group, and 241 of 950 patients in the denosumab group (30.4% vs 25.3%; hazard ratio [HR], 0.78; 95% CI, 0.66-0.93; P = .005).28 In 2020, the American Society of Clinical Oncology endorsed the Cancer Care Ontario guidelines for prostate bone health care.18 Adequate supplementation is necessary in all patients treated with a bisphosphonate or denosumab to prevent treatment-related hypocalcemia. Typically, daily supplementation with a minimum of calcium 500 mg and vitamin D 400 IU is recommended.16
Bone Health in Patients
Nonmetastatic Hormone-Sensitive PC
ADT forms the backbone of treatment for patients with local and advanced metastatic castration-sensitive PC along with surgical and focal radiotherapy options. Cancer treatment-induced bone loss is known to occur with prolonged use of ADT. The ZEUS trial found no prevention of bone metastasis in patients with high-risk localized PC with the use of ZA in the absence of bone metastasis. A Kaplan-Meier estimated proportion of bone metastases after a median follow-up of 4.8 years was found to be not statistically significant: 14.7% in the ZA group vs 13.2% in the control/placebo group.29 The STAMPEDE trial showed no significant overall survival (OS) benefit with the addition of ZA to ADT vs ADT alone (HR, 0.94; 95% CI, 0.79-1.11; P = .45), 5-year survival with ADT alone was 55% compared to ADT plus ZA with 57% 5-year survival.30 The RADAR trial showed that at 5 years in high Gleason score patients, use of ZA in the absence of bone metastasis was beneficial, but not in low- or intermediate-risk patients. However, at 10-year analysis there was no significant difference in any of the high-stratified groups with or without ZA.31
The PR04 trial showed no effect on OS with clodronate compared with placebo in nonmetastatic castration-sensitive PC, with a HR of 1.12 (95% CI, 0.89-1.42; P = .94). The estimated 5-year survival was 80% with placebo and 78% with clodronate; 10-year survival rates were 51% with placebo and 48% with clodronate.32 Data from the HALT trial showed an increased bone mineral density and reduced risk of new vertebral fractures vs placebo (1.5% vs 3.9%, respectively) in the absence of metastatic bone lesions and a reduction in new vertebral fractures in patients with nonmetastatic PC.33 Most of these studies showed no benefit with the addition of ZA to nonmetastatic PC; although, the HALT trial provides evidence to support use of denosumab in patients with nonmetastatic PC for preventing vertebral fragility fractures in men receiving ADT.
Metastatic Hormone-Sensitive PC
ZA is often used to treat men with metastatic castration-sensitive PC despite limited efficacy and safety data. The CALGB 90202 (Alliance) trial authors found that the early use of ZA was not associated with increased time to first SRE. The median time to first SRE was 31.9 months in the ZA group (95% CI, 24.2-40.3) and 29.8 months in the placebo group (stratified HR, 0.97; 95% CI, 0-1.17; 1-sided stratified log-rank P = .39).34 OS was similar between the groups (HR, 0.88; 95% CI, 0.70-1.12; P = .29) as were reported AEs.34 Results from these studies suggest limited benefit in treating patients with metastatic hormone-sensitive PC with bisphosphonates without other medical indications for use. Additional studies suggest similar results for treatment with denosumab to that of bisphosphonate therapies.35
Nonmetastatic CRPC
Reasonable interest among treating clinicians exists to be able to delay or prevent the development of metastatic bone disease in patients who are showing biochemical signs of castration resistance but have not yet developed distant metastatic disease. Time to progression on ADT to castration resistance usually occurs 2 to 3 years following initiation of treatment. This typically occurs in patients with rising prostate-specific antigen (PSA). As per the Prostate Cancer Working Group 3, in the absence of radiologic progression, CRPC is defined by a 25% increase from the nadir (considering a starting value of ≥ 1 ng/mL), with a minimum rise of 2 ng/mL in the setting of castrate serum testosterone < 50 ng/dL despite good adherence to an ADT regimen, with proven serologic castration either by undetectable or a near undetectable nadir of serum testosterone concentration. Therapeutic implications include prevention of SREs as well as time to metastatic bone lesions. The Zometa 704 trial examined the use of ZA to reduce time to first metastatic bone lesion in the setting of patients with nonmetastatic CRPC.36 The trial was discontinued prematurely due to low patient accrual, but initial analysis provided information on the natural history of a rising PSA in this patient population. At 2 years, one-third of patients had developed bone metastases. Median bone metastasis-free survival was 30 months. Median time to first bone metastasis and OS were not reached. Baseline PSA and PSA velocity independently predicted a shorter time to first bone metastasis, metastasis-free survival, and OS.36
Denosumab was also studied in the setting of nonmetastatic CRPC in the Denosumab 147 trial. The study enrolled 1432 patients and found a significantly increased bone metastasis-free survival by a median of 4.2 months over placebo (HR, 0.85; 95% CI, 0.73-0.98; P = .03). Denosumab significantly delayed time to first bone metastasis (HR, 0.84; 95% CI, 0.71-0.98; P = .03). OS was similar between groups (HR, 1.01; 95% CI, 0.85-1.20; P = .91). Rates of AEs and serious AEs were similar between groups, except for ONJ and hypocalcemia. The rates of ONJ for denosumab were 1%, 3%, 4% in years 1,2, 3, respectively; overall, < 5% (n = 33). Hypocalcemia occurred in < 2% (n = 12) in denosumab-treated patients. The authors concluded that in men with CRPC, denosumab significantly prolonged bone metastasis–free survival and delayed time-to-bone metastasis.37 These 2 studies suggest a role of receptor-activated nuclear factor κ-B ligand inhibitor denosumab in patients with nonmetastatic CRPC in the appropriate setting. There were delays in bony metastatic disease, but no difference in OS. Rare denosumab treatment–related specific AEs were noted. Hence, denosumab is not recommended for use in this setting.
Metastatic CRPC
Castration resistance typically occurs 2 to 3 years following initiation of ADT and the most common extranodal site of disease is within the bone in metastatic PC. Disease progression within bones after ADT can be challenging given both the nature of progressive cancer with osteoblastic metastatic lesions and the prolonged effects of ADT on unaffected bone. The Zometa 039 study compared ZA with placebo and found a significant difference in SREs (38% and 49%, respectively; P .03). No survival benefit was observed with the addition of ZA. Use of other bisphosphonates pamidronate and clodronate did not have a similar degree of benefit.38,39
A phase 3 study of 1904 patients found that denosumab was superior to ZA in delaying the time to first on-study SRE (HR, 0.82; 95% CI, 0.71-0.95) and reducing rates of multiple SREs (HR, 0.82; 95% CI, 0.71-0.94).40 This was later confirmed with an additional study that demonstrated treatment with denosumab significantly reduced the risk of developing a first symptomatic SRE, defined as a pathologic fracture, spinal cord compression, necessity for radiation, or surgery (HR, 0.78; 95% CI, 0.66-0.93; P = .005) and first and subsequent symptomatic SREs (rate ratio, 0.78; 95% CI, 0.65-0.92; P = .004) compared with ZA.28 These findings suggest a continued role of denosumab in the treatment of advanced metastatic CRPC from both control of bone disease as well as quality of life and palliation of cancer-related symptoms.
Radium-223 dichloride (radium-223) is an α-emitting radionuclide for treatment of metastatic CRPC with bone metastasis, but otherwise no additional metastatic sites. Radium-223 is a calcium-mimetic that preferentially accumulates into areas of high-bone turnover, such as where bone metastases tend to occur. Radium-223 induces apoptosis of tumor cells through double-stranded DNA breaks. Studies have shown radium-223 to prolong OS and time-to-first symptomatic SRE.41 The ERA-223 trial showed that when radium-223 was combined with abiraterone acetate, there was an increase in fragility fracture risk compared with placebo combined with abiraterone. Data from the study revealed that the median symptomatic SRE-free survival was 22.3 months (95% CI, 20.4-24.8) in the radium-223 group and 26.0 months (21.8-28.3) in the placebo group. Concurrent treatment with abiraterone acetate plus prednisone or prednisolone and radium-223 was associated with increased fracture risk. Osteoporotic fractures were the most common type of fracture in the radium-223 group and of all fracture types, differed the most between the study groups.42
Conclusions
Convincing evidence supports the ongoing use of bisphosphonates and denosumab in patients with osteoporosis, significant osteopenia with risk factors, and in patients with CRPC with bone metastasis. Bone metastases can cause considerable morbidity and mortality among men with advanced PC. Pain, fracture, and neurologic injury can occur with metastatic bone lesions as well as with ADT-related bone loss. Prevention of SREs in patients with PC is a reasonable goal in PC survivors while being mindful of managing the risks of these therapies.
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7-30. doi:10.3322/caac.21590
2. Skolarus TA, Hawley ST. Prostate cancer survivorship care in the Veterans Health Administration. Fed Pract. 2014;31(8):10-17.
3. Gartrell BA, Coleman R, Efstathiou E, et al. Metastatic prostate cancer and the bone: significance and therapeutic options. Eur Urol. 2015;68(5):850-858. doi:10.1016/j.eururo.2015.06.039
4. Bolla M, de Reijke TM, Van Tienhoven G, et al. Duration of androgen suppression in the treatment of prostate cancer. N Engl J Med. 2009;360(24):2516-2527. doi:10.1056/NEJMoa0810095
5. Welch HG, Albertsen PC. Reconsidering Prostate cancer mortality—The future of PSA screening. N Engl J Med. 2020;382(16):1557-1563. doi:10.1056/NEJMms1914228
6. Coleman R, Body JJ, Aapro M, Hadji P, Herrstedt J; ESMO Guidelines Working Group. Bone health in cancer patients: ESMO Clinical Practice Guidelines. Ann Oncol. 2014;25 (suppl 3):iii124-137. doi:10.1093/annonc/mdu103
7. Saylor PJ, Smith MR. Adverse effects of androgen deprivation therapy: defining the problem and promoting health among men with prostate cancer. J Natl Compr Canc Netw. 2010;8(2):211-223. doi:10.6004/jnccn.2010.0014
8. Shahinian VB, Kuo Y-F, Freeman JL, Goodwin JS. Risk of fracture after androgen deprivation for prostate cancer. N Engl J Med. 2005;352(2):154-164. doi:10.1056/NEJMoa041943
9. Sartor O, de Bono JS. Metastatic prostate cancer. N Engl J Med. 2018;378(7):645-657. doi:10.1056/NEJMra1701695
10. Saad F, Eastham JA, Smith MR. Biochemical markers of bone turnover and clinical outcomes in men with prostate cancer. Urol Oncol. 2012;30(4):369-378. doi:10.1016/j.urolonc.2010.08.007
11. Cosman F, de Beur SJ, LeBoff MS, et al; National Osteoporosis Foundation. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-2381. doi:10.1007/s00198-014-2794-2
12. Alibhai SMH, Zukotynski K, Walker-Dilks C, et al; Cancer Care Ontario Genitourinary Cancer Disease Site Group. Bone health and bone-targeted therapies for prostate cancer: a programme in evidence-based care - Cancer Care Ontario Clinical Practice Guideline. Clin Oncol (R Coll Radiol). 2017;29(6):348-355. doi:10.1016/j.clon.2017.01.007
13. LEE CE. A comprehensive bone-health management approach with men with prostate cancer recieving androgen deprivation therapy. Curr Oncol. 2011;18(4):e163-172. doi:10.3747/co.v18i4.746
14. Kennel KA, Drake MT. Adverse effects of bisphosphonates: Implications for osteoporosis management. Mayo Clin Proc. 2009;84(7):632-638. doi:10.1016/S0025-6196(11)60752-0
15. Saad F, Brown JE, Van Poznak C, et al. Incidence, risk factors, and outcomes of osteonecrosis of the jaw: integrated analysis from three blinded active-controlled phase III trials in cancer patients with bone metastases. Ann Oncol. 2012;23(5):1341-1347. doi:10.1093/annonc/mdr435
16. Body J-J, Bone HG, de Boer RH, et al. Hypocalcaemia in patients with metastatic bone disease treated with denosumab. Eur J Cancer. 2015;51(13):1812-1821. doi:10.1016/j.ejca.2015.05.016
17. Wysowski DK, Chang JT. Alendronate and risedronate: reports of severe bone, joint, and muscle pain. Arch Intern Med. 2005;165(3):346-347. doi:10.1001/archinte.165.3.346-b
18. Saylor PJ, Rumble RB, Tagawa S, et al. Bone health and bone-targeted therapies for prostate cancer: ASCO endorsement of a cancer care Ontario guideline. J Clin Oncol. 2020;38(15):1736-1743. doi:10.1200/JCO.19.03148
19. Saad F, Gleason DM, Murray R, et al; Zoledronic Acid Prostate Cancer Study Group. Long-term efficacy of zoledronic acid for the prevention of skeletal complications in patients with metastatic hormone-refractory prostate cancer. J Natl Cancer Inst. 2004;96(11):879-882. doi:10.1093/jnci/djh141
20. Saad F, Gleason DM, Murray R, et al; Zoledronic Acid Prostate Cancer Study Group. A randomized, placebo-controlled trial of zoledronic zcid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst. 2002;94(19):1458-1468. doi:10.1093/jnci/94.19.1458
21. Aapro M, Saad F. Bone-modifying agents in the treatment of bone metastases in patients with advanced genitourinary malignancies: a focus on zoledronic acid. Ther Adv Urol. 2012;4(2):85-101. doi:10.1177/1756287212441234
22. Cianferotti L, Bertoldo F, Carini M, et al. The prevention of fragility fractures in patients with non-metastatic prostate cancer: a position statement by the international osteoporosis foundation. Oncotarget. 2017;8(43):75646-75663. doi:10.18632/oncotarget.17980
23. Ruggiero S, Gralow J, Marx RE, et al. Practical guidelines for the prevention, diagnosis, and treatment of osteonecrosis of the jaw in patients with cancer. J Oncol Pract. 2006;2(1):7-14. doi:10.1200/JOP.2006.2.1.7
24. Corraini P, Heide-Jørgensen U, Schøodt M, et al. Osteonecrosis of the jaw and survival of patients with cancer: a nationwide cohort study in Denmark. Cancer Med. 2017;6(10):2271-2277. doi:10.1002/cam4.1173
25. Watts NB, Diab DL. Long-term use of bisphosphonates in osteoporosis. J Clin Endocrinol Metab. 2010;95(4):1555-1565. doi:10.1210/jc.2009-1947
26. Himelstein AL, Foster JC, Khatcheressian JL, et al. Effect of longer interval vs standard dosing of zoledronic acid on skeletal events in patients with bone metastases: a randomized clinical trial. JAMA. 2017;317(1):48-58. doi:10.1001/jama.2016.19425
27. Macherey S, Monsef I, Jahn F, et al. Bisphosphonates for advanced prostate cancer. Cochrane Database Syst Rev. 2017;12(12):CD006250. doi:10.1002/14651858.CD006250.pub2
28. Smith MR, Coleman RE, Klotz L, et al. Denosumab for the prevention of skeletal complications in metastatic castration-resistant prostate cancer: comparison of skeletal-related events and symptomatic skeletal events. Ann Oncol. 2015;26(2):368-374. doi:10.1093/annonc/mdu519
29. Wirth M, Tammela T, Cicalese V, et al. Prevention of bone metastases in patients with high-risk nonmetastatic prostate cancer treated with zoledronic acid: efficacy and safety results of the Zometa European Study (ZEUS). Eur Urol. 2015;67(3):482-491. doi:10.1016/j.eururo.2014.02.014
30. James ND, Sydes MR, Clarke NW, et al; STAMPEDE Investigators. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016;387(10024):1163-1177. doi:10.1016/S0140-6736(15)01037-5
31. Denham JW, Joseph D, Lamb DS, et al. Short-term androgen suppression and radiotherapy versus intermediate-term androgen suppression and radiotherapy, with or without zoledronic acid, in men with locally advanced prostate cancer (TROG 03.04 RADAR): 10-year results from a randomised, phase 3, factorial trial. Lancet Oncol. 2019;20(2):267-281. doi:10.1016/S1470-2045(18)30757-5
32. Dearnaley DP, Mason MD, Parmar MK, Sanders K, Sydes MR. Adjuvant therapy with oral sodium clodronate in locally advanced and metastatic prostate cancer: long-term overall survival results from the MRC PR04 and PR05 randomised controlled trials. Lancet Oncol. 2009;10(9):872-876. doi:10.1016/S1470-2045(09)70201-3
33. Smith MR, Egerdie B, Toriz NH, et al; Denosumab HALT Prostate Cancer Study Group. Denosumab in men receiving androgen-deprivation therapy for prostate Cancer. N Engl J Med. 2009;361(8):745-755. doi:10.1056/NEJMoa0809003
34. Smith MR, Halabi S, Ryan CJ, et al. Randomized controlled trial of early zoledronic acid in men with castration-sensitive prostate cancer and bone metastases: results of CALGB 90202 (alliance). J Clin Oncol. 2014;32(11):1143-1150. doi:10.1200/JCO.2013.51.6500
35. Kozyrakis D, Paridis D, Perikleous S, Malizos K, Zarkadas A, Tsagkalis A. The current role of osteoclast inhibitors in patients with prostate cancer. Adv Urol. 2018;2018:1525832. doi:10.1155/2018/1525832
36. Smith MR, Kabbinavar F, Saad F, et al. Natural history of rising serum prostate-specific antigen in men with castrate nonmetastatic prostate cancer. J Clin Oncol. 2005;23(13):2918-2925. doi:10.1200/JCO.2005.01.529
37. Smith MR, Saad F, Coleman R, et al. Denosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: results of a phase 3, randomised, placebo-controlled trial. Lancet. 2012;379(9810):39-46. doi:10.1016/S0140-6736(11)61226-9
38. Small EJ, Smith MR, Seaman JJ, Petrone S, Kowalski MO. Combined analysis of two multicenter, randomized, placebo-controlled studies of pamidronate disodium for the palliation of bone pain in men with metastatic prostate cancer. J Clin Oncol. 2003;21(23):4277-4284. doi:10.1200/JCO.2003.05.147
39. Ernst DS, Tannock IF, Winquist EW, et al. Randomized, double-blind, controlled trial of mitoxantrone/prednisone and clodronate versus mitoxantrone/prednisone and placebo in patients with hormone-refractory prostate cancer and pain. J Clin Oncol. 2003;21(17):3335-3342. doi:10.1200/JCO.2003.03.042
40. Fizazi K, Carducci M, Smith M, et al. Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet. 2011;377(9768):813-822. doi:10.1016/S0140-6736(10)62344-6
41. Parker C, Nilsson S, Heinrich D, et al; ALSYMPCA Investigators Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369(3):213-223. doi:10.1056/NEJMoa1213755
42. Smith M, Parker C, Saad F, et al. Addition of radium-223 to abiraterone acetate and prednisone or prednisolone in patients with castration-resistant prostate cancer and bone metastases (ERA 223): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(3):408-419. doi:10.1016/S1470-2045(18)30860-X
43. Smith MR, Saad F, Shore ND, et al. Effect of denosumab on prolonging bone-metastasis-free survival (BMFS) in men with nonmetastatic castrate-resistant prostate cancer (CRPC) presenting with aggressive PSA kinetics. J Clin Oncol. 2012;30(5_suppl):6-6.
44. Saad F, Gleason DM, Murray R, et al; Zoledronic Acid Prostate Cancer Study Group. A randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst. 2002;94(19):1458-1468. doi:10.1093/jnci/94.19.1458
Prostate cancer (PC) is the most commonly and newly diagnosed nonskin cancer and the second leading cause of cancer death in men in the United States. About 191,930 cases and about 33,330 deaths from PC were expected for the year 2020.1 About 1 in 41 men will die of PC. Most men diagnosed with PC are aged > 65 years and do not die of their disease. The 5-year survival rate of localized and regional disease is nearly 100%, and disease with distant metastases is 31%. As a result, more than 3.1 million men in the United States who have been diagnosed with PC are still alive today.1 Among veterans, there is a substantial population living with PC. Skolarus and Hawley reported in 2014 that an estimated 200,000 veterans with PC were survivors and 12,000 were newly diagnosed.2
In PC, skeletal strength can be affected by several factors, such as aging, malnutrition, androgen-deprivation therapy (ADT), and bone metastasis.3,4 In fact, most men can live the rest of their life with PC by using strategies to monitor and treat it, once it shows either radiographic or chemical signs of progression.5 ADT is the standard of care to treat hormone-sensitive PC, which is associated with significant skeletal-related adverse effects (AEs).6,7
Men undergoing ADT are 4 times more likely to develop substantial bone deficiency, Shahinian and colleagues found that in men surviving 5 years after PC diagnosis, 19.4% of those who received ADT had a fracture compared with 12% in men who did not (P < .001). The authors established a significant relation between the number of doses of gonadotropin-releasing hormone given in the first 12 months and the risk of fracture.8 Of those who progressed to metastatic disease, the first metastatic nonnodal site is most commonly to the bone.9 Advanced PC is characterized by increased bone turnover, which further raises concerns for bone health and patient performance.10
Skeletal-related events (SREs) include pathologic fracture, spinal cord compression, palliative radiation, or surgery to bone, and change in antineoplastic therapy secondary to bone pain. The concept of bone health refers to the prevention, diagnosis, and treatment of idiopathic, pathogenic, and treatment-related bone loss and delay or prevention of SREs.6,11 Guidelines and expert groups have recommended screening for osteoporosis at the start of ADT with bone mineral density testing, ensuring adequate calcium and vitamin D intake, modifying lifestyle behaviors (smoking cessation, alcohol moderation, and regular exercise), and prescribing bisphosphonates or receptor-activated nuclear factor κ-B ligand inhibitor, denosumab, for men with osteoporosis or who are at general high-fracture risk.12,13 The overuse of these medications results in undue cost to patients as well as AEs, such as osteonecrosis of the jaw (ONJ), hypocalcemia, and bone/joint pains.14-17 There are evidence-based guidelines for appropriate use of bisphosphonates and denosumab for delay and prevention of SREs in the setting of advanced PC.18 These doses also typically differ in frequency to those of osteoporosis.19 We summarize the evidence and guidance for health care providers who care for patients with PC at various stages and complications from both disease-related and treatment-related comorbidities.
Bone-Strengthening Agents
Overall, there is evidence to support the use of bone-strengthening agents in patients with osteopenia/osteoporosis in the prevention of SREs with significant risk factors for progressive bone demineralization, such as lifestyle factors and, in particular, treatments such as ADT. Bone-remodeling agents for treatment of bony metastasis have been shown to provide therapeutic advantage only in limited instances in the castration-resistant PC (CRPC) setting. Hence, in patients with hormone-sensitive PC due to medication-related AEs, treatment with bone-strengthening agents is indicated only if the patient has a significant preexisting risk for fracture from osteopenia/osteoporosis (Table). The Figure depicts an algorithm for the management of bone health in men with PC who are being treated with ADT.
Denosumab and bisphosphonates have an established role in preventing SREs in metastatic CRPC.20 The choice of denosumab or a bisphosphonate typically varies based on the indication, possible AEs, and cost of therapy. There are multiple studies involving initiation of these agents at various stages of disease to improve both time to progression as well as management of SREs. There is a lack of evidence that bisphosphonates prevent metastatic-bone lesions in castration-sensitive PC; therefore, prophylactic use of this agent is not recommended in patients unless they have significant bone demineralization.21,22
Medication-induced ONJ is a severe AE of both denosumab and bisphosphonate therapies. Data from recent trials showed that higher dosing and prolonged duration of denosumab and bisphosphonate therapies further increased risk of ONJ by 1.8% and 1.3%, respectively.15 Careful history taking and discussions with the patient and if possible their dentist on how to reduce risk are recommended. It is good practice for the patient to complete a dental evaluation prior to starting IV bisphosphonates or denosumab. Dental evaluations should be performed routinely at 3- to 12-month intervals throughout therapy based on individualized risk assessment.23 The benefits of using bisphosphonates to prevent fractures associated with osteoporosis outweigh the risk of ONJ in high-risk populations, but not in all patients with PC. A case-by-case basis and evaluation of risk factors should be performed prior to administering bone-modifying therapy. The long-term safety of IV bisphosphonates has not been adequately studied in controlled trials, and concerns regarding long-term complications, including renal toxicity, ONJ, and atypical femoral fractures, remain with prolonged therapy.24,25
The CALGB 70604 (Alliance) trial compared 3-month dosing to monthly treatment with zoledronic acid (ZA), showing no inferiority to lower frequency dosing.26 A Cochrane review of clinical trials found that in patients with advanced PC, bisphosphonates were found to provide roughly 58 fewer SREs per 1000 on average.27 A phase 3 study showed a modest benefit to denosumab vs ZA in the CRPC group regarding incidence of SREs. The rates of SREs were 289 of 951 patients in the bisphosphonate group, and 241 of 950 patients in the denosumab group (30.4% vs 25.3%; hazard ratio [HR], 0.78; 95% CI, 0.66-0.93; P = .005).28 In 2020, the American Society of Clinical Oncology endorsed the Cancer Care Ontario guidelines for prostate bone health care.18 Adequate supplementation is necessary in all patients treated with a bisphosphonate or denosumab to prevent treatment-related hypocalcemia. Typically, daily supplementation with a minimum of calcium 500 mg and vitamin D 400 IU is recommended.16
Bone Health in Patients
Nonmetastatic Hormone-Sensitive PC
ADT forms the backbone of treatment for patients with local and advanced metastatic castration-sensitive PC along with surgical and focal radiotherapy options. Cancer treatment-induced bone loss is known to occur with prolonged use of ADT. The ZEUS trial found no prevention of bone metastasis in patients with high-risk localized PC with the use of ZA in the absence of bone metastasis. A Kaplan-Meier estimated proportion of bone metastases after a median follow-up of 4.8 years was found to be not statistically significant: 14.7% in the ZA group vs 13.2% in the control/placebo group.29 The STAMPEDE trial showed no significant overall survival (OS) benefit with the addition of ZA to ADT vs ADT alone (HR, 0.94; 95% CI, 0.79-1.11; P = .45), 5-year survival with ADT alone was 55% compared to ADT plus ZA with 57% 5-year survival.30 The RADAR trial showed that at 5 years in high Gleason score patients, use of ZA in the absence of bone metastasis was beneficial, but not in low- or intermediate-risk patients. However, at 10-year analysis there was no significant difference in any of the high-stratified groups with or without ZA.31
The PR04 trial showed no effect on OS with clodronate compared with placebo in nonmetastatic castration-sensitive PC, with a HR of 1.12 (95% CI, 0.89-1.42; P = .94). The estimated 5-year survival was 80% with placebo and 78% with clodronate; 10-year survival rates were 51% with placebo and 48% with clodronate.32 Data from the HALT trial showed an increased bone mineral density and reduced risk of new vertebral fractures vs placebo (1.5% vs 3.9%, respectively) in the absence of metastatic bone lesions and a reduction in new vertebral fractures in patients with nonmetastatic PC.33 Most of these studies showed no benefit with the addition of ZA to nonmetastatic PC; although, the HALT trial provides evidence to support use of denosumab in patients with nonmetastatic PC for preventing vertebral fragility fractures in men receiving ADT.
Metastatic Hormone-Sensitive PC
ZA is often used to treat men with metastatic castration-sensitive PC despite limited efficacy and safety data. The CALGB 90202 (Alliance) trial authors found that the early use of ZA was not associated with increased time to first SRE. The median time to first SRE was 31.9 months in the ZA group (95% CI, 24.2-40.3) and 29.8 months in the placebo group (stratified HR, 0.97; 95% CI, 0-1.17; 1-sided stratified log-rank P = .39).34 OS was similar between the groups (HR, 0.88; 95% CI, 0.70-1.12; P = .29) as were reported AEs.34 Results from these studies suggest limited benefit in treating patients with metastatic hormone-sensitive PC with bisphosphonates without other medical indications for use. Additional studies suggest similar results for treatment with denosumab to that of bisphosphonate therapies.35
Nonmetastatic CRPC
Reasonable interest among treating clinicians exists to be able to delay or prevent the development of metastatic bone disease in patients who are showing biochemical signs of castration resistance but have not yet developed distant metastatic disease. Time to progression on ADT to castration resistance usually occurs 2 to 3 years following initiation of treatment. This typically occurs in patients with rising prostate-specific antigen (PSA). As per the Prostate Cancer Working Group 3, in the absence of radiologic progression, CRPC is defined by a 25% increase from the nadir (considering a starting value of ≥ 1 ng/mL), with a minimum rise of 2 ng/mL in the setting of castrate serum testosterone < 50 ng/dL despite good adherence to an ADT regimen, with proven serologic castration either by undetectable or a near undetectable nadir of serum testosterone concentration. Therapeutic implications include prevention of SREs as well as time to metastatic bone lesions. The Zometa 704 trial examined the use of ZA to reduce time to first metastatic bone lesion in the setting of patients with nonmetastatic CRPC.36 The trial was discontinued prematurely due to low patient accrual, but initial analysis provided information on the natural history of a rising PSA in this patient population. At 2 years, one-third of patients had developed bone metastases. Median bone metastasis-free survival was 30 months. Median time to first bone metastasis and OS were not reached. Baseline PSA and PSA velocity independently predicted a shorter time to first bone metastasis, metastasis-free survival, and OS.36
Denosumab was also studied in the setting of nonmetastatic CRPC in the Denosumab 147 trial. The study enrolled 1432 patients and found a significantly increased bone metastasis-free survival by a median of 4.2 months over placebo (HR, 0.85; 95% CI, 0.73-0.98; P = .03). Denosumab significantly delayed time to first bone metastasis (HR, 0.84; 95% CI, 0.71-0.98; P = .03). OS was similar between groups (HR, 1.01; 95% CI, 0.85-1.20; P = .91). Rates of AEs and serious AEs were similar between groups, except for ONJ and hypocalcemia. The rates of ONJ for denosumab were 1%, 3%, 4% in years 1,2, 3, respectively; overall, < 5% (n = 33). Hypocalcemia occurred in < 2% (n = 12) in denosumab-treated patients. The authors concluded that in men with CRPC, denosumab significantly prolonged bone metastasis–free survival and delayed time-to-bone metastasis.37 These 2 studies suggest a role of receptor-activated nuclear factor κ-B ligand inhibitor denosumab in patients with nonmetastatic CRPC in the appropriate setting. There were delays in bony metastatic disease, but no difference in OS. Rare denosumab treatment–related specific AEs were noted. Hence, denosumab is not recommended for use in this setting.
Metastatic CRPC
Castration resistance typically occurs 2 to 3 years following initiation of ADT and the most common extranodal site of disease is within the bone in metastatic PC. Disease progression within bones after ADT can be challenging given both the nature of progressive cancer with osteoblastic metastatic lesions and the prolonged effects of ADT on unaffected bone. The Zometa 039 study compared ZA with placebo and found a significant difference in SREs (38% and 49%, respectively; P .03). No survival benefit was observed with the addition of ZA. Use of other bisphosphonates pamidronate and clodronate did not have a similar degree of benefit.38,39
A phase 3 study of 1904 patients found that denosumab was superior to ZA in delaying the time to first on-study SRE (HR, 0.82; 95% CI, 0.71-0.95) and reducing rates of multiple SREs (HR, 0.82; 95% CI, 0.71-0.94).40 This was later confirmed with an additional study that demonstrated treatment with denosumab significantly reduced the risk of developing a first symptomatic SRE, defined as a pathologic fracture, spinal cord compression, necessity for radiation, or surgery (HR, 0.78; 95% CI, 0.66-0.93; P = .005) and first and subsequent symptomatic SREs (rate ratio, 0.78; 95% CI, 0.65-0.92; P = .004) compared with ZA.28 These findings suggest a continued role of denosumab in the treatment of advanced metastatic CRPC from both control of bone disease as well as quality of life and palliation of cancer-related symptoms.
Radium-223 dichloride (radium-223) is an α-emitting radionuclide for treatment of metastatic CRPC with bone metastasis, but otherwise no additional metastatic sites. Radium-223 is a calcium-mimetic that preferentially accumulates into areas of high-bone turnover, such as where bone metastases tend to occur. Radium-223 induces apoptosis of tumor cells through double-stranded DNA breaks. Studies have shown radium-223 to prolong OS and time-to-first symptomatic SRE.41 The ERA-223 trial showed that when radium-223 was combined with abiraterone acetate, there was an increase in fragility fracture risk compared with placebo combined with abiraterone. Data from the study revealed that the median symptomatic SRE-free survival was 22.3 months (95% CI, 20.4-24.8) in the radium-223 group and 26.0 months (21.8-28.3) in the placebo group. Concurrent treatment with abiraterone acetate plus prednisone or prednisolone and radium-223 was associated with increased fracture risk. Osteoporotic fractures were the most common type of fracture in the radium-223 group and of all fracture types, differed the most between the study groups.42
Conclusions
Convincing evidence supports the ongoing use of bisphosphonates and denosumab in patients with osteoporosis, significant osteopenia with risk factors, and in patients with CRPC with bone metastasis. Bone metastases can cause considerable morbidity and mortality among men with advanced PC. Pain, fracture, and neurologic injury can occur with metastatic bone lesions as well as with ADT-related bone loss. Prevention of SREs in patients with PC is a reasonable goal in PC survivors while being mindful of managing the risks of these therapies.
Prostate cancer (PC) is the most commonly and newly diagnosed nonskin cancer and the second leading cause of cancer death in men in the United States. About 191,930 cases and about 33,330 deaths from PC were expected for the year 2020.1 About 1 in 41 men will die of PC. Most men diagnosed with PC are aged > 65 years and do not die of their disease. The 5-year survival rate of localized and regional disease is nearly 100%, and disease with distant metastases is 31%. As a result, more than 3.1 million men in the United States who have been diagnosed with PC are still alive today.1 Among veterans, there is a substantial population living with PC. Skolarus and Hawley reported in 2014 that an estimated 200,000 veterans with PC were survivors and 12,000 were newly diagnosed.2
In PC, skeletal strength can be affected by several factors, such as aging, malnutrition, androgen-deprivation therapy (ADT), and bone metastasis.3,4 In fact, most men can live the rest of their life with PC by using strategies to monitor and treat it, once it shows either radiographic or chemical signs of progression.5 ADT is the standard of care to treat hormone-sensitive PC, which is associated with significant skeletal-related adverse effects (AEs).6,7
Men undergoing ADT are 4 times more likely to develop substantial bone deficiency, Shahinian and colleagues found that in men surviving 5 years after PC diagnosis, 19.4% of those who received ADT had a fracture compared with 12% in men who did not (P < .001). The authors established a significant relation between the number of doses of gonadotropin-releasing hormone given in the first 12 months and the risk of fracture.8 Of those who progressed to metastatic disease, the first metastatic nonnodal site is most commonly to the bone.9 Advanced PC is characterized by increased bone turnover, which further raises concerns for bone health and patient performance.10
Skeletal-related events (SREs) include pathologic fracture, spinal cord compression, palliative radiation, or surgery to bone, and change in antineoplastic therapy secondary to bone pain. The concept of bone health refers to the prevention, diagnosis, and treatment of idiopathic, pathogenic, and treatment-related bone loss and delay or prevention of SREs.6,11 Guidelines and expert groups have recommended screening for osteoporosis at the start of ADT with bone mineral density testing, ensuring adequate calcium and vitamin D intake, modifying lifestyle behaviors (smoking cessation, alcohol moderation, and regular exercise), and prescribing bisphosphonates or receptor-activated nuclear factor κ-B ligand inhibitor, denosumab, for men with osteoporosis or who are at general high-fracture risk.12,13 The overuse of these medications results in undue cost to patients as well as AEs, such as osteonecrosis of the jaw (ONJ), hypocalcemia, and bone/joint pains.14-17 There are evidence-based guidelines for appropriate use of bisphosphonates and denosumab for delay and prevention of SREs in the setting of advanced PC.18 These doses also typically differ in frequency to those of osteoporosis.19 We summarize the evidence and guidance for health care providers who care for patients with PC at various stages and complications from both disease-related and treatment-related comorbidities.
Bone-Strengthening Agents
Overall, there is evidence to support the use of bone-strengthening agents in patients with osteopenia/osteoporosis in the prevention of SREs with significant risk factors for progressive bone demineralization, such as lifestyle factors and, in particular, treatments such as ADT. Bone-remodeling agents for treatment of bony metastasis have been shown to provide therapeutic advantage only in limited instances in the castration-resistant PC (CRPC) setting. Hence, in patients with hormone-sensitive PC due to medication-related AEs, treatment with bone-strengthening agents is indicated only if the patient has a significant preexisting risk for fracture from osteopenia/osteoporosis (Table). The Figure depicts an algorithm for the management of bone health in men with PC who are being treated with ADT.
Denosumab and bisphosphonates have an established role in preventing SREs in metastatic CRPC.20 The choice of denosumab or a bisphosphonate typically varies based on the indication, possible AEs, and cost of therapy. There are multiple studies involving initiation of these agents at various stages of disease to improve both time to progression as well as management of SREs. There is a lack of evidence that bisphosphonates prevent metastatic-bone lesions in castration-sensitive PC; therefore, prophylactic use of this agent is not recommended in patients unless they have significant bone demineralization.21,22
Medication-induced ONJ is a severe AE of both denosumab and bisphosphonate therapies. Data from recent trials showed that higher dosing and prolonged duration of denosumab and bisphosphonate therapies further increased risk of ONJ by 1.8% and 1.3%, respectively.15 Careful history taking and discussions with the patient and if possible their dentist on how to reduce risk are recommended. It is good practice for the patient to complete a dental evaluation prior to starting IV bisphosphonates or denosumab. Dental evaluations should be performed routinely at 3- to 12-month intervals throughout therapy based on individualized risk assessment.23 The benefits of using bisphosphonates to prevent fractures associated with osteoporosis outweigh the risk of ONJ in high-risk populations, but not in all patients with PC. A case-by-case basis and evaluation of risk factors should be performed prior to administering bone-modifying therapy. The long-term safety of IV bisphosphonates has not been adequately studied in controlled trials, and concerns regarding long-term complications, including renal toxicity, ONJ, and atypical femoral fractures, remain with prolonged therapy.24,25
The CALGB 70604 (Alliance) trial compared 3-month dosing to monthly treatment with zoledronic acid (ZA), showing no inferiority to lower frequency dosing.26 A Cochrane review of clinical trials found that in patients with advanced PC, bisphosphonates were found to provide roughly 58 fewer SREs per 1000 on average.27 A phase 3 study showed a modest benefit to denosumab vs ZA in the CRPC group regarding incidence of SREs. The rates of SREs were 289 of 951 patients in the bisphosphonate group, and 241 of 950 patients in the denosumab group (30.4% vs 25.3%; hazard ratio [HR], 0.78; 95% CI, 0.66-0.93; P = .005).28 In 2020, the American Society of Clinical Oncology endorsed the Cancer Care Ontario guidelines for prostate bone health care.18 Adequate supplementation is necessary in all patients treated with a bisphosphonate or denosumab to prevent treatment-related hypocalcemia. Typically, daily supplementation with a minimum of calcium 500 mg and vitamin D 400 IU is recommended.16
Bone Health in Patients
Nonmetastatic Hormone-Sensitive PC
ADT forms the backbone of treatment for patients with local and advanced metastatic castration-sensitive PC along with surgical and focal radiotherapy options. Cancer treatment-induced bone loss is known to occur with prolonged use of ADT. The ZEUS trial found no prevention of bone metastasis in patients with high-risk localized PC with the use of ZA in the absence of bone metastasis. A Kaplan-Meier estimated proportion of bone metastases after a median follow-up of 4.8 years was found to be not statistically significant: 14.7% in the ZA group vs 13.2% in the control/placebo group.29 The STAMPEDE trial showed no significant overall survival (OS) benefit with the addition of ZA to ADT vs ADT alone (HR, 0.94; 95% CI, 0.79-1.11; P = .45), 5-year survival with ADT alone was 55% compared to ADT plus ZA with 57% 5-year survival.30 The RADAR trial showed that at 5 years in high Gleason score patients, use of ZA in the absence of bone metastasis was beneficial, but not in low- or intermediate-risk patients. However, at 10-year analysis there was no significant difference in any of the high-stratified groups with or without ZA.31
The PR04 trial showed no effect on OS with clodronate compared with placebo in nonmetastatic castration-sensitive PC, with a HR of 1.12 (95% CI, 0.89-1.42; P = .94). The estimated 5-year survival was 80% with placebo and 78% with clodronate; 10-year survival rates were 51% with placebo and 48% with clodronate.32 Data from the HALT trial showed an increased bone mineral density and reduced risk of new vertebral fractures vs placebo (1.5% vs 3.9%, respectively) in the absence of metastatic bone lesions and a reduction in new vertebral fractures in patients with nonmetastatic PC.33 Most of these studies showed no benefit with the addition of ZA to nonmetastatic PC; although, the HALT trial provides evidence to support use of denosumab in patients with nonmetastatic PC for preventing vertebral fragility fractures in men receiving ADT.
Metastatic Hormone-Sensitive PC
ZA is often used to treat men with metastatic castration-sensitive PC despite limited efficacy and safety data. The CALGB 90202 (Alliance) trial authors found that the early use of ZA was not associated with increased time to first SRE. The median time to first SRE was 31.9 months in the ZA group (95% CI, 24.2-40.3) and 29.8 months in the placebo group (stratified HR, 0.97; 95% CI, 0-1.17; 1-sided stratified log-rank P = .39).34 OS was similar between the groups (HR, 0.88; 95% CI, 0.70-1.12; P = .29) as were reported AEs.34 Results from these studies suggest limited benefit in treating patients with metastatic hormone-sensitive PC with bisphosphonates without other medical indications for use. Additional studies suggest similar results for treatment with denosumab to that of bisphosphonate therapies.35
Nonmetastatic CRPC
Reasonable interest among treating clinicians exists to be able to delay or prevent the development of metastatic bone disease in patients who are showing biochemical signs of castration resistance but have not yet developed distant metastatic disease. Time to progression on ADT to castration resistance usually occurs 2 to 3 years following initiation of treatment. This typically occurs in patients with rising prostate-specific antigen (PSA). As per the Prostate Cancer Working Group 3, in the absence of radiologic progression, CRPC is defined by a 25% increase from the nadir (considering a starting value of ≥ 1 ng/mL), with a minimum rise of 2 ng/mL in the setting of castrate serum testosterone < 50 ng/dL despite good adherence to an ADT regimen, with proven serologic castration either by undetectable or a near undetectable nadir of serum testosterone concentration. Therapeutic implications include prevention of SREs as well as time to metastatic bone lesions. The Zometa 704 trial examined the use of ZA to reduce time to first metastatic bone lesion in the setting of patients with nonmetastatic CRPC.36 The trial was discontinued prematurely due to low patient accrual, but initial analysis provided information on the natural history of a rising PSA in this patient population. At 2 years, one-third of patients had developed bone metastases. Median bone metastasis-free survival was 30 months. Median time to first bone metastasis and OS were not reached. Baseline PSA and PSA velocity independently predicted a shorter time to first bone metastasis, metastasis-free survival, and OS.36
Denosumab was also studied in the setting of nonmetastatic CRPC in the Denosumab 147 trial. The study enrolled 1432 patients and found a significantly increased bone metastasis-free survival by a median of 4.2 months over placebo (HR, 0.85; 95% CI, 0.73-0.98; P = .03). Denosumab significantly delayed time to first bone metastasis (HR, 0.84; 95% CI, 0.71-0.98; P = .03). OS was similar between groups (HR, 1.01; 95% CI, 0.85-1.20; P = .91). Rates of AEs and serious AEs were similar between groups, except for ONJ and hypocalcemia. The rates of ONJ for denosumab were 1%, 3%, 4% in years 1,2, 3, respectively; overall, < 5% (n = 33). Hypocalcemia occurred in < 2% (n = 12) in denosumab-treated patients. The authors concluded that in men with CRPC, denosumab significantly prolonged bone metastasis–free survival and delayed time-to-bone metastasis.37 These 2 studies suggest a role of receptor-activated nuclear factor κ-B ligand inhibitor denosumab in patients with nonmetastatic CRPC in the appropriate setting. There were delays in bony metastatic disease, but no difference in OS. Rare denosumab treatment–related specific AEs were noted. Hence, denosumab is not recommended for use in this setting.
Metastatic CRPC
Castration resistance typically occurs 2 to 3 years following initiation of ADT and the most common extranodal site of disease is within the bone in metastatic PC. Disease progression within bones after ADT can be challenging given both the nature of progressive cancer with osteoblastic metastatic lesions and the prolonged effects of ADT on unaffected bone. The Zometa 039 study compared ZA with placebo and found a significant difference in SREs (38% and 49%, respectively; P .03). No survival benefit was observed with the addition of ZA. Use of other bisphosphonates pamidronate and clodronate did not have a similar degree of benefit.38,39
A phase 3 study of 1904 patients found that denosumab was superior to ZA in delaying the time to first on-study SRE (HR, 0.82; 95% CI, 0.71-0.95) and reducing rates of multiple SREs (HR, 0.82; 95% CI, 0.71-0.94).40 This was later confirmed with an additional study that demonstrated treatment with denosumab significantly reduced the risk of developing a first symptomatic SRE, defined as a pathologic fracture, spinal cord compression, necessity for radiation, or surgery (HR, 0.78; 95% CI, 0.66-0.93; P = .005) and first and subsequent symptomatic SREs (rate ratio, 0.78; 95% CI, 0.65-0.92; P = .004) compared with ZA.28 These findings suggest a continued role of denosumab in the treatment of advanced metastatic CRPC from both control of bone disease as well as quality of life and palliation of cancer-related symptoms.
Radium-223 dichloride (radium-223) is an α-emitting radionuclide for treatment of metastatic CRPC with bone metastasis, but otherwise no additional metastatic sites. Radium-223 is a calcium-mimetic that preferentially accumulates into areas of high-bone turnover, such as where bone metastases tend to occur. Radium-223 induces apoptosis of tumor cells through double-stranded DNA breaks. Studies have shown radium-223 to prolong OS and time-to-first symptomatic SRE.41 The ERA-223 trial showed that when radium-223 was combined with abiraterone acetate, there was an increase in fragility fracture risk compared with placebo combined with abiraterone. Data from the study revealed that the median symptomatic SRE-free survival was 22.3 months (95% CI, 20.4-24.8) in the radium-223 group and 26.0 months (21.8-28.3) in the placebo group. Concurrent treatment with abiraterone acetate plus prednisone or prednisolone and radium-223 was associated with increased fracture risk. Osteoporotic fractures were the most common type of fracture in the radium-223 group and of all fracture types, differed the most between the study groups.42
Conclusions
Convincing evidence supports the ongoing use of bisphosphonates and denosumab in patients with osteoporosis, significant osteopenia with risk factors, and in patients with CRPC with bone metastasis. Bone metastases can cause considerable morbidity and mortality among men with advanced PC. Pain, fracture, and neurologic injury can occur with metastatic bone lesions as well as with ADT-related bone loss. Prevention of SREs in patients with PC is a reasonable goal in PC survivors while being mindful of managing the risks of these therapies.
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7-30. doi:10.3322/caac.21590
2. Skolarus TA, Hawley ST. Prostate cancer survivorship care in the Veterans Health Administration. Fed Pract. 2014;31(8):10-17.
3. Gartrell BA, Coleman R, Efstathiou E, et al. Metastatic prostate cancer and the bone: significance and therapeutic options. Eur Urol. 2015;68(5):850-858. doi:10.1016/j.eururo.2015.06.039
4. Bolla M, de Reijke TM, Van Tienhoven G, et al. Duration of androgen suppression in the treatment of prostate cancer. N Engl J Med. 2009;360(24):2516-2527. doi:10.1056/NEJMoa0810095
5. Welch HG, Albertsen PC. Reconsidering Prostate cancer mortality—The future of PSA screening. N Engl J Med. 2020;382(16):1557-1563. doi:10.1056/NEJMms1914228
6. Coleman R, Body JJ, Aapro M, Hadji P, Herrstedt J; ESMO Guidelines Working Group. Bone health in cancer patients: ESMO Clinical Practice Guidelines. Ann Oncol. 2014;25 (suppl 3):iii124-137. doi:10.1093/annonc/mdu103
7. Saylor PJ, Smith MR. Adverse effects of androgen deprivation therapy: defining the problem and promoting health among men with prostate cancer. J Natl Compr Canc Netw. 2010;8(2):211-223. doi:10.6004/jnccn.2010.0014
8. Shahinian VB, Kuo Y-F, Freeman JL, Goodwin JS. Risk of fracture after androgen deprivation for prostate cancer. N Engl J Med. 2005;352(2):154-164. doi:10.1056/NEJMoa041943
9. Sartor O, de Bono JS. Metastatic prostate cancer. N Engl J Med. 2018;378(7):645-657. doi:10.1056/NEJMra1701695
10. Saad F, Eastham JA, Smith MR. Biochemical markers of bone turnover and clinical outcomes in men with prostate cancer. Urol Oncol. 2012;30(4):369-378. doi:10.1016/j.urolonc.2010.08.007
11. Cosman F, de Beur SJ, LeBoff MS, et al; National Osteoporosis Foundation. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-2381. doi:10.1007/s00198-014-2794-2
12. Alibhai SMH, Zukotynski K, Walker-Dilks C, et al; Cancer Care Ontario Genitourinary Cancer Disease Site Group. Bone health and bone-targeted therapies for prostate cancer: a programme in evidence-based care - Cancer Care Ontario Clinical Practice Guideline. Clin Oncol (R Coll Radiol). 2017;29(6):348-355. doi:10.1016/j.clon.2017.01.007
13. LEE CE. A comprehensive bone-health management approach with men with prostate cancer recieving androgen deprivation therapy. Curr Oncol. 2011;18(4):e163-172. doi:10.3747/co.v18i4.746
14. Kennel KA, Drake MT. Adverse effects of bisphosphonates: Implications for osteoporosis management. Mayo Clin Proc. 2009;84(7):632-638. doi:10.1016/S0025-6196(11)60752-0
15. Saad F, Brown JE, Van Poznak C, et al. Incidence, risk factors, and outcomes of osteonecrosis of the jaw: integrated analysis from three blinded active-controlled phase III trials in cancer patients with bone metastases. Ann Oncol. 2012;23(5):1341-1347. doi:10.1093/annonc/mdr435
16. Body J-J, Bone HG, de Boer RH, et al. Hypocalcaemia in patients with metastatic bone disease treated with denosumab. Eur J Cancer. 2015;51(13):1812-1821. doi:10.1016/j.ejca.2015.05.016
17. Wysowski DK, Chang JT. Alendronate and risedronate: reports of severe bone, joint, and muscle pain. Arch Intern Med. 2005;165(3):346-347. doi:10.1001/archinte.165.3.346-b
18. Saylor PJ, Rumble RB, Tagawa S, et al. Bone health and bone-targeted therapies for prostate cancer: ASCO endorsement of a cancer care Ontario guideline. J Clin Oncol. 2020;38(15):1736-1743. doi:10.1200/JCO.19.03148
19. Saad F, Gleason DM, Murray R, et al; Zoledronic Acid Prostate Cancer Study Group. Long-term efficacy of zoledronic acid for the prevention of skeletal complications in patients with metastatic hormone-refractory prostate cancer. J Natl Cancer Inst. 2004;96(11):879-882. doi:10.1093/jnci/djh141
20. Saad F, Gleason DM, Murray R, et al; Zoledronic Acid Prostate Cancer Study Group. A randomized, placebo-controlled trial of zoledronic zcid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst. 2002;94(19):1458-1468. doi:10.1093/jnci/94.19.1458
21. Aapro M, Saad F. Bone-modifying agents in the treatment of bone metastases in patients with advanced genitourinary malignancies: a focus on zoledronic acid. Ther Adv Urol. 2012;4(2):85-101. doi:10.1177/1756287212441234
22. Cianferotti L, Bertoldo F, Carini M, et al. The prevention of fragility fractures in patients with non-metastatic prostate cancer: a position statement by the international osteoporosis foundation. Oncotarget. 2017;8(43):75646-75663. doi:10.18632/oncotarget.17980
23. Ruggiero S, Gralow J, Marx RE, et al. Practical guidelines for the prevention, diagnosis, and treatment of osteonecrosis of the jaw in patients with cancer. J Oncol Pract. 2006;2(1):7-14. doi:10.1200/JOP.2006.2.1.7
24. Corraini P, Heide-Jørgensen U, Schøodt M, et al. Osteonecrosis of the jaw and survival of patients with cancer: a nationwide cohort study in Denmark. Cancer Med. 2017;6(10):2271-2277. doi:10.1002/cam4.1173
25. Watts NB, Diab DL. Long-term use of bisphosphonates in osteoporosis. J Clin Endocrinol Metab. 2010;95(4):1555-1565. doi:10.1210/jc.2009-1947
26. Himelstein AL, Foster JC, Khatcheressian JL, et al. Effect of longer interval vs standard dosing of zoledronic acid on skeletal events in patients with bone metastases: a randomized clinical trial. JAMA. 2017;317(1):48-58. doi:10.1001/jama.2016.19425
27. Macherey S, Monsef I, Jahn F, et al. Bisphosphonates for advanced prostate cancer. Cochrane Database Syst Rev. 2017;12(12):CD006250. doi:10.1002/14651858.CD006250.pub2
28. Smith MR, Coleman RE, Klotz L, et al. Denosumab for the prevention of skeletal complications in metastatic castration-resistant prostate cancer: comparison of skeletal-related events and symptomatic skeletal events. Ann Oncol. 2015;26(2):368-374. doi:10.1093/annonc/mdu519
29. Wirth M, Tammela T, Cicalese V, et al. Prevention of bone metastases in patients with high-risk nonmetastatic prostate cancer treated with zoledronic acid: efficacy and safety results of the Zometa European Study (ZEUS). Eur Urol. 2015;67(3):482-491. doi:10.1016/j.eururo.2014.02.014
30. James ND, Sydes MR, Clarke NW, et al; STAMPEDE Investigators. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016;387(10024):1163-1177. doi:10.1016/S0140-6736(15)01037-5
31. Denham JW, Joseph D, Lamb DS, et al. Short-term androgen suppression and radiotherapy versus intermediate-term androgen suppression and radiotherapy, with or without zoledronic acid, in men with locally advanced prostate cancer (TROG 03.04 RADAR): 10-year results from a randomised, phase 3, factorial trial. Lancet Oncol. 2019;20(2):267-281. doi:10.1016/S1470-2045(18)30757-5
32. Dearnaley DP, Mason MD, Parmar MK, Sanders K, Sydes MR. Adjuvant therapy with oral sodium clodronate in locally advanced and metastatic prostate cancer: long-term overall survival results from the MRC PR04 and PR05 randomised controlled trials. Lancet Oncol. 2009;10(9):872-876. doi:10.1016/S1470-2045(09)70201-3
33. Smith MR, Egerdie B, Toriz NH, et al; Denosumab HALT Prostate Cancer Study Group. Denosumab in men receiving androgen-deprivation therapy for prostate Cancer. N Engl J Med. 2009;361(8):745-755. doi:10.1056/NEJMoa0809003
34. Smith MR, Halabi S, Ryan CJ, et al. Randomized controlled trial of early zoledronic acid in men with castration-sensitive prostate cancer and bone metastases: results of CALGB 90202 (alliance). J Clin Oncol. 2014;32(11):1143-1150. doi:10.1200/JCO.2013.51.6500
35. Kozyrakis D, Paridis D, Perikleous S, Malizos K, Zarkadas A, Tsagkalis A. The current role of osteoclast inhibitors in patients with prostate cancer. Adv Urol. 2018;2018:1525832. doi:10.1155/2018/1525832
36. Smith MR, Kabbinavar F, Saad F, et al. Natural history of rising serum prostate-specific antigen in men with castrate nonmetastatic prostate cancer. J Clin Oncol. 2005;23(13):2918-2925. doi:10.1200/JCO.2005.01.529
37. Smith MR, Saad F, Coleman R, et al. Denosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: results of a phase 3, randomised, placebo-controlled trial. Lancet. 2012;379(9810):39-46. doi:10.1016/S0140-6736(11)61226-9
38. Small EJ, Smith MR, Seaman JJ, Petrone S, Kowalski MO. Combined analysis of two multicenter, randomized, placebo-controlled studies of pamidronate disodium for the palliation of bone pain in men with metastatic prostate cancer. J Clin Oncol. 2003;21(23):4277-4284. doi:10.1200/JCO.2003.05.147
39. Ernst DS, Tannock IF, Winquist EW, et al. Randomized, double-blind, controlled trial of mitoxantrone/prednisone and clodronate versus mitoxantrone/prednisone and placebo in patients with hormone-refractory prostate cancer and pain. J Clin Oncol. 2003;21(17):3335-3342. doi:10.1200/JCO.2003.03.042
40. Fizazi K, Carducci M, Smith M, et al. Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet. 2011;377(9768):813-822. doi:10.1016/S0140-6736(10)62344-6
41. Parker C, Nilsson S, Heinrich D, et al; ALSYMPCA Investigators Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369(3):213-223. doi:10.1056/NEJMoa1213755
42. Smith M, Parker C, Saad F, et al. Addition of radium-223 to abiraterone acetate and prednisone or prednisolone in patients with castration-resistant prostate cancer and bone metastases (ERA 223): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(3):408-419. doi:10.1016/S1470-2045(18)30860-X
43. Smith MR, Saad F, Shore ND, et al. Effect of denosumab on prolonging bone-metastasis-free survival (BMFS) in men with nonmetastatic castrate-resistant prostate cancer (CRPC) presenting with aggressive PSA kinetics. J Clin Oncol. 2012;30(5_suppl):6-6.
44. Saad F, Gleason DM, Murray R, et al; Zoledronic Acid Prostate Cancer Study Group. A randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst. 2002;94(19):1458-1468. doi:10.1093/jnci/94.19.1458
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7-30. doi:10.3322/caac.21590
2. Skolarus TA, Hawley ST. Prostate cancer survivorship care in the Veterans Health Administration. Fed Pract. 2014;31(8):10-17.
3. Gartrell BA, Coleman R, Efstathiou E, et al. Metastatic prostate cancer and the bone: significance and therapeutic options. Eur Urol. 2015;68(5):850-858. doi:10.1016/j.eururo.2015.06.039
4. Bolla M, de Reijke TM, Van Tienhoven G, et al. Duration of androgen suppression in the treatment of prostate cancer. N Engl J Med. 2009;360(24):2516-2527. doi:10.1056/NEJMoa0810095
5. Welch HG, Albertsen PC. Reconsidering Prostate cancer mortality—The future of PSA screening. N Engl J Med. 2020;382(16):1557-1563. doi:10.1056/NEJMms1914228
6. Coleman R, Body JJ, Aapro M, Hadji P, Herrstedt J; ESMO Guidelines Working Group. Bone health in cancer patients: ESMO Clinical Practice Guidelines. Ann Oncol. 2014;25 (suppl 3):iii124-137. doi:10.1093/annonc/mdu103
7. Saylor PJ, Smith MR. Adverse effects of androgen deprivation therapy: defining the problem and promoting health among men with prostate cancer. J Natl Compr Canc Netw. 2010;8(2):211-223. doi:10.6004/jnccn.2010.0014
8. Shahinian VB, Kuo Y-F, Freeman JL, Goodwin JS. Risk of fracture after androgen deprivation for prostate cancer. N Engl J Med. 2005;352(2):154-164. doi:10.1056/NEJMoa041943
9. Sartor O, de Bono JS. Metastatic prostate cancer. N Engl J Med. 2018;378(7):645-657. doi:10.1056/NEJMra1701695
10. Saad F, Eastham JA, Smith MR. Biochemical markers of bone turnover and clinical outcomes in men with prostate cancer. Urol Oncol. 2012;30(4):369-378. doi:10.1016/j.urolonc.2010.08.007
11. Cosman F, de Beur SJ, LeBoff MS, et al; National Osteoporosis Foundation. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-2381. doi:10.1007/s00198-014-2794-2
12. Alibhai SMH, Zukotynski K, Walker-Dilks C, et al; Cancer Care Ontario Genitourinary Cancer Disease Site Group. Bone health and bone-targeted therapies for prostate cancer: a programme in evidence-based care - Cancer Care Ontario Clinical Practice Guideline. Clin Oncol (R Coll Radiol). 2017;29(6):348-355. doi:10.1016/j.clon.2017.01.007
13. LEE CE. A comprehensive bone-health management approach with men with prostate cancer recieving androgen deprivation therapy. Curr Oncol. 2011;18(4):e163-172. doi:10.3747/co.v18i4.746
14. Kennel KA, Drake MT. Adverse effects of bisphosphonates: Implications for osteoporosis management. Mayo Clin Proc. 2009;84(7):632-638. doi:10.1016/S0025-6196(11)60752-0
15. Saad F, Brown JE, Van Poznak C, et al. Incidence, risk factors, and outcomes of osteonecrosis of the jaw: integrated analysis from three blinded active-controlled phase III trials in cancer patients with bone metastases. Ann Oncol. 2012;23(5):1341-1347. doi:10.1093/annonc/mdr435
16. Body J-J, Bone HG, de Boer RH, et al. Hypocalcaemia in patients with metastatic bone disease treated with denosumab. Eur J Cancer. 2015;51(13):1812-1821. doi:10.1016/j.ejca.2015.05.016
17. Wysowski DK, Chang JT. Alendronate and risedronate: reports of severe bone, joint, and muscle pain. Arch Intern Med. 2005;165(3):346-347. doi:10.1001/archinte.165.3.346-b
18. Saylor PJ, Rumble RB, Tagawa S, et al. Bone health and bone-targeted therapies for prostate cancer: ASCO endorsement of a cancer care Ontario guideline. J Clin Oncol. 2020;38(15):1736-1743. doi:10.1200/JCO.19.03148
19. Saad F, Gleason DM, Murray R, et al; Zoledronic Acid Prostate Cancer Study Group. Long-term efficacy of zoledronic acid for the prevention of skeletal complications in patients with metastatic hormone-refractory prostate cancer. J Natl Cancer Inst. 2004;96(11):879-882. doi:10.1093/jnci/djh141
20. Saad F, Gleason DM, Murray R, et al; Zoledronic Acid Prostate Cancer Study Group. A randomized, placebo-controlled trial of zoledronic zcid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst. 2002;94(19):1458-1468. doi:10.1093/jnci/94.19.1458
21. Aapro M, Saad F. Bone-modifying agents in the treatment of bone metastases in patients with advanced genitourinary malignancies: a focus on zoledronic acid. Ther Adv Urol. 2012;4(2):85-101. doi:10.1177/1756287212441234
22. Cianferotti L, Bertoldo F, Carini M, et al. The prevention of fragility fractures in patients with non-metastatic prostate cancer: a position statement by the international osteoporosis foundation. Oncotarget. 2017;8(43):75646-75663. doi:10.18632/oncotarget.17980
23. Ruggiero S, Gralow J, Marx RE, et al. Practical guidelines for the prevention, diagnosis, and treatment of osteonecrosis of the jaw in patients with cancer. J Oncol Pract. 2006;2(1):7-14. doi:10.1200/JOP.2006.2.1.7
24. Corraini P, Heide-Jørgensen U, Schøodt M, et al. Osteonecrosis of the jaw and survival of patients with cancer: a nationwide cohort study in Denmark. Cancer Med. 2017;6(10):2271-2277. doi:10.1002/cam4.1173
25. Watts NB, Diab DL. Long-term use of bisphosphonates in osteoporosis. J Clin Endocrinol Metab. 2010;95(4):1555-1565. doi:10.1210/jc.2009-1947
26. Himelstein AL, Foster JC, Khatcheressian JL, et al. Effect of longer interval vs standard dosing of zoledronic acid on skeletal events in patients with bone metastases: a randomized clinical trial. JAMA. 2017;317(1):48-58. doi:10.1001/jama.2016.19425
27. Macherey S, Monsef I, Jahn F, et al. Bisphosphonates for advanced prostate cancer. Cochrane Database Syst Rev. 2017;12(12):CD006250. doi:10.1002/14651858.CD006250.pub2
28. Smith MR, Coleman RE, Klotz L, et al. Denosumab for the prevention of skeletal complications in metastatic castration-resistant prostate cancer: comparison of skeletal-related events and symptomatic skeletal events. Ann Oncol. 2015;26(2):368-374. doi:10.1093/annonc/mdu519
29. Wirth M, Tammela T, Cicalese V, et al. Prevention of bone metastases in patients with high-risk nonmetastatic prostate cancer treated with zoledronic acid: efficacy and safety results of the Zometa European Study (ZEUS). Eur Urol. 2015;67(3):482-491. doi:10.1016/j.eururo.2014.02.014
30. James ND, Sydes MR, Clarke NW, et al; STAMPEDE Investigators. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016;387(10024):1163-1177. doi:10.1016/S0140-6736(15)01037-5
31. Denham JW, Joseph D, Lamb DS, et al. Short-term androgen suppression and radiotherapy versus intermediate-term androgen suppression and radiotherapy, with or without zoledronic acid, in men with locally advanced prostate cancer (TROG 03.04 RADAR): 10-year results from a randomised, phase 3, factorial trial. Lancet Oncol. 2019;20(2):267-281. doi:10.1016/S1470-2045(18)30757-5
32. Dearnaley DP, Mason MD, Parmar MK, Sanders K, Sydes MR. Adjuvant therapy with oral sodium clodronate in locally advanced and metastatic prostate cancer: long-term overall survival results from the MRC PR04 and PR05 randomised controlled trials. Lancet Oncol. 2009;10(9):872-876. doi:10.1016/S1470-2045(09)70201-3
33. Smith MR, Egerdie B, Toriz NH, et al; Denosumab HALT Prostate Cancer Study Group. Denosumab in men receiving androgen-deprivation therapy for prostate Cancer. N Engl J Med. 2009;361(8):745-755. doi:10.1056/NEJMoa0809003
34. Smith MR, Halabi S, Ryan CJ, et al. Randomized controlled trial of early zoledronic acid in men with castration-sensitive prostate cancer and bone metastases: results of CALGB 90202 (alliance). J Clin Oncol. 2014;32(11):1143-1150. doi:10.1200/JCO.2013.51.6500
35. Kozyrakis D, Paridis D, Perikleous S, Malizos K, Zarkadas A, Tsagkalis A. The current role of osteoclast inhibitors in patients with prostate cancer. Adv Urol. 2018;2018:1525832. doi:10.1155/2018/1525832
36. Smith MR, Kabbinavar F, Saad F, et al. Natural history of rising serum prostate-specific antigen in men with castrate nonmetastatic prostate cancer. J Clin Oncol. 2005;23(13):2918-2925. doi:10.1200/JCO.2005.01.529
37. Smith MR, Saad F, Coleman R, et al. Denosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: results of a phase 3, randomised, placebo-controlled trial. Lancet. 2012;379(9810):39-46. doi:10.1016/S0140-6736(11)61226-9
38. Small EJ, Smith MR, Seaman JJ, Petrone S, Kowalski MO. Combined analysis of two multicenter, randomized, placebo-controlled studies of pamidronate disodium for the palliation of bone pain in men with metastatic prostate cancer. J Clin Oncol. 2003;21(23):4277-4284. doi:10.1200/JCO.2003.05.147
39. Ernst DS, Tannock IF, Winquist EW, et al. Randomized, double-blind, controlled trial of mitoxantrone/prednisone and clodronate versus mitoxantrone/prednisone and placebo in patients with hormone-refractory prostate cancer and pain. J Clin Oncol. 2003;21(17):3335-3342. doi:10.1200/JCO.2003.03.042
40. Fizazi K, Carducci M, Smith M, et al. Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet. 2011;377(9768):813-822. doi:10.1016/S0140-6736(10)62344-6
41. Parker C, Nilsson S, Heinrich D, et al; ALSYMPCA Investigators Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369(3):213-223. doi:10.1056/NEJMoa1213755
42. Smith M, Parker C, Saad F, et al. Addition of radium-223 to abiraterone acetate and prednisone or prednisolone in patients with castration-resistant prostate cancer and bone metastases (ERA 223): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(3):408-419. doi:10.1016/S1470-2045(18)30860-X
43. Smith MR, Saad F, Shore ND, et al. Effect of denosumab on prolonging bone-metastasis-free survival (BMFS) in men with nonmetastatic castrate-resistant prostate cancer (CRPC) presenting with aggressive PSA kinetics. J Clin Oncol. 2012;30(5_suppl):6-6.
44. Saad F, Gleason DM, Murray R, et al; Zoledronic Acid Prostate Cancer Study Group. A randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst. 2002;94(19):1458-1468. doi:10.1093/jnci/94.19.1458
An Interdisciplinary Approach to Metastatic Pancreatic Cancer and Comorbid Opioid Use Disorder Treatment Within a VA Health Care System
A multidisciplinary approach provided safe and feasible cancer treatment in a patient with advanced pancreatic cancer and coexisting active substance use disorder.
Substance use disorders (SUDs) are an important but understudied aspect of treating patients diagnosed with cancer. Substance use can affect cancer treatment outcomes, including morbidity and mortality.1,2 Additionally, patients with cancer and SUD may have unique psychosocial needs that require close attention and management. There is a paucity of data regarding the best approach to treating such patients. For example, cocaine use may increase the cardiovascular and hematologic risk of some traditional chemotherapy agents.3,4 Newer targeted agents and immunotherapies remain understudied with respect to SUD risk.
Although the US Department of Veterans Affairs (VA) has established helpful clinical practice guidelines for the treatment of SUD, there are no guidelines for treating patients with SUD and cancer.5 Clinicians have limited confidence in treatment approach, and treatment is inconsistent among oncologists nationwide even within the same practice. Furthermore, it can be challenging to safely prescribe opioids for cancer-related pain in individuals with SUD. There is a high risk of SUD and mental health disorders in veterans, making this population particularly vulnerable. We report a case of a male with metastatic pancreatic cancer, severe opioid use disorder (OUD) and moderate cocaine use disorder (CUD) who received pain management and cancer treatment under the direction of a multidisciplinary team approach.
Case Report
A 63-year-old male with a medical history of HIV treated with highly active antiretroviral therapy (HAART), compensated cirrhosis, severe OUD, moderate CUD, and sedative use disorder in sustained remission was admitted to the West Haven campus of the VA Connecticut Healthcare System (VACHS) with abdominal pain, weight loss and fatigue. He used heroin 1 month prior to his admission and reported regular cocaine and marijuana use (Table 1). He was diagnosed with HIV in 1989, and his medical history included herpes zoster and oral candidiasis but no other opportunistic infections. Several months prior to this admission, he had an undetectable viral load and CD4 count of 688.
At the time of this admission, the patient was adherent to methadone treatment. He reported increased abdominal pain. Computed tomography (CT) showed a 2.4-cm mass in the pancreatic uncinate process, multiple liver metastases, retroperitoneal lymphadenopathy, and small lung nodules. A CT-guided liver biopsy showed adenocarcinoma consistent with a primary cancer of the pancreas. Given the complexity of the case, a multidisciplinary team approach was used to treat his cancer and the sequelae safely, including the oncology team, community living center team, palliative care team, and interprofessional opioid reassessment clinic team (ORC).
Cancer Treatment
Chemotherapy with FOLFIRINOX (leucovorin calcium, fluorouracil, irinotecan hydrochloride, and oxaliplatin) was recommended. The first cycle of treatment originally was planned for the outpatient setting, and a peripherally inserted central catheter (PICC) line was placed. However, after a urine toxicology test was positive for cocaine, the PICC line was removed due to concern for possible use of PICC line for nonprescribed substance use. The patient expressed suicidal ideation at the time and was admitted for psychiatric consult and pain control. Cycle 1 FOLFIRINOX was started during this admission. A PICC line was again put in place and then removed before discharge. A celiac plexus block was performed several days after this admission for pain control.
Given concern about cocaine use increasing the risk of cardiac toxicity with FOLFIRINOX treatment, treating providers sconsulted with the community living center (CLC) about possible admission for future chemotherapy administration and pain management. The CLC at VACHS has 38 beds for rehabilitation, long-term care, and hospice with the mission to restore each veteran to his or her highest level of well-being. After discussion with this patient and CLC staff, he agreed to a CLC admission. The patient agreed to remain in the facility, wear a secure care device, and not leave without staff accompaniment. He was able to obtain a 2-hour pass to pay bills and rent. During the 2 months he was admitted to the CLC he would present to the VACHS Cancer Center for chemotherapy every 2 weeks. He completed 6 cycles of chemotherapy while admitted. During the admission, he was transferred to active medical service for 2 days for fever and malaise, and then returned to the CLC. The patient elected to leave the CLC after 2 months as the inability to see close friends was interfering with his quality of life.
Upon being discharged from the CLC, shared decision making took place with the patient to establish a new treatment plan. In collaboration with the patient, a plan was made to admit him every 2 weeks for continued chemotherapy. A PICC line was placed on each day of admission and removed prior to discharge. It was also agreed that treatment would be delayed if a urine drug test was positive for cocaine on the morning of admission. The patient was also seen by ORC every 2 weeks after being discharged from the CLC.
Imaging after cycle 6 showed decreased size of liver metastases, retroperitoneal lymph nodes, and pancreas mass. Cancer antigen 19-9 (CA19-9) tumor marker was reduced from 3513 U/mL pretreatment to 50 U/mL after cycle 7. Chemotherapy cycle 7 was delayed 6 days due to active cocaine and heroin use. A repeat urine was obtained several days later, which was negative for cocaine, and he was admitted for cycle 7 chemotherapy. Using this treatment approach of admissions for every cycle, the patient was able to receive 11 cycles of FOLFIRINOX with clinical benefit.
Palliative Care/Pain Management
Safely treating the patient’s malignant pain in the context of his OUD was critically important. In order to do this the palliative care team worked closely alongside ORC, is a multidisciplinary team consisting of health care providers (HCPs) from addiction psychiatry, internal medicine, health psychology and pharmacy who are consulted to evaluate veterans’ current opioid regimens and make recommendations to optimize both safety and efficacy. ORC followed this particular veteran as an outpatient and consulted on pain issues during his admission. They recommended the continuation of methadone at 120 mg daily and increased oral oxycodone to 30 mg every 6 hours, and then further increased to 45 mg every 6 hours. He continued to have increased pain despite higher doses of oxycodone, and pain medication was changed to oral hydromorphone 28 mg every 6 hours with the continuation of methadone. ORC and the palliative care team obtained consent from the veteran and a release of Information form signed by the patient to contact his community methadone clinic for further collaboration around pain management throughout the time caring for the veteran.
Even with improvement in disease based on imaging and tumor markers, opioid medications could not be decreased in this case. This is likely in part due to the multidimensional nature of pain. Careful assessment of the biologic, emotional, social, and spiritual contributors to pain is needed in the management of pain, especially at end of life.6 Nonpharmacologic pain management strategies used in this case included a transcutaneous electrical nerve stimulation unit, moist heat, celiac plexus block, and emotional support.
Psychosocial Issues/Substance Use
Psychosocial support for the patient was provided by the interdisciplinary palliative care team and the ORC team in both the inpatient and outpatient settings. Despite efforts from case management to get the veteran home services once discharged from the CLC, he declined repeatedly. Thus, the CLC social worker obtained a guardian alert for the veteran on discharge.
Close outpatient follow-up for medical and psychosocial support was very critical. When an outpatient, the veteran was scheduled for biweekly appointments with palliative care or ORC. When admitted to the hospital, the palliative care team medical director and psychologist conducted joint visits with him. Although he denied depressed mood and anxiety throughout his treatment, he often reflected on regrets that he had as he faced the end of his life. Specifically, he shared thoughts about being estranged from his surviving brother given his long struggle with substance use. Although he did not think a relationship was possible with his brother at the end of life, he still cared deeply for him and wanted to make him aware of his pancreatic cancer diagnosis. This was particularly important to him because their late brother had also died of pancreatic cancer. It was the patient’s wish at the end of his life to alert his surviving brother of his diagnosis so he and his children could get adequate screening throughout their lives. Although he had spoken of this desire often, it wasn’t until his disease progressed and he elected to transition to hospice that he felt ready to write the letter. The palliative care team assisted the veteran in writing and mailing a letter to his brother informing him of his diagnosis and transition to hospice as well as communicating that his brother and his family had been in his thoughts at the end of his life. The patient’s brother received this letter and with assistance from the CLC social worker made arrangements to visit the veteran at bedside at the inpatient CLC hospice unit the final days of his life.
Discussion
There are very little data on the safety of cancer-directed therapy in patients with active SUD. The limited studies that have been done showed conflicting results.
A retrospective study among women with co-occurring SUD and locally advanced cervical cancer who were undergoing primary radiation therapy found that SUD was not associated with a difference in toxicity or survival outcomes.7 However, other research suggests that SUD may be associated with an increase in all-cause mortality as well as other adverse outcomes for patients and health care systems (eg, emergency department visits, hospitalizations).8 A retrospective study of patients with a history of SUD and nonsmall cell lung cancer showed that these patients had higher rates of depression, less family support, increased rates of missed appointments, more emergency department visits and more hospitalizations.9 Patients with chronic myeloid leukemia or myelodysplastic syndromes who had long-term cocaine use had a 6-fold increased risk of death, which was not found in patients who had long-term alcohol or marijuana use.2
The limited data highlight the need for careful consideration of ways to mitigate potentially adverse outcomes in this population while still providing clinically indicated cancer treatment. Integrated VA health care systems provide unique resources that can maximize veteran safety during cancer treatment. Utilization of VA resources and close interdisciplinary collaboration across VA HCPs can help to ensure equitable access to state-of-the-art cancer therapies for veterans with comorbid SUD.
VA Services for Patients With Comorbidities
This case highlights several distinct aspects of VA health care that make it possible to safely treat individuals with complex comorbidities. One important aspect of this was collaboration with the CLC to admit the veteran for his initial treatment after a positive cocaine test. CLC admission was nonpunitive and allowed ongoing involvement in the VA community. This provided an essential, safe, and structured environment in which 6 cycles of chemotherapy could be delivered.
Although the patient left the CLC after 2 months due to floor restrictions negatively impacting his quality of life and ability to spend time with close friends, several important events occurred during this stay. First, the patient established close relationships with the CLC staff and the palliative care team; both groups followed him throughout his inpatient and outpatient care. These relationships proved essential throughout his care as they were the foundation of difficult conversations about substance use, treatment adherence, and eventually, transition to hospice.
In addition, the opportunity to administer 6 cycles of chemotherapy at the CLC was enough to lead to clinical benefit and radiographic response to treatment. Clinical benefits while in the CLC included maintenance of a good appetite, 15-lb weight gain and preserved performance status (ECOG [Eastern Cooperative Group]-1), which allowed him to actively participate in multiple social and recreational activities while in the CLC. From early conversations, this patient was clear that he wanted treatment as long as his life could be prolonged with good quality of life. Having evidence of the benefit of treatment, at least initially, increased the patient’s confidence in treatment. There were a few conversations when the challenges of treatment mounted (eg, pain, needs for abstinence from cocaine prior to admission for chemotherapy, frequent doctor appointments), and the patient would remind himself of these data to recommit himself to treatment. The opportunity to admit him to the inpatient VA facility, including bed availability for 3 days during his treatment once he left the CLC was important. This plan to admit the patient following a negative urine toxicology test for cocaine was made collaboratively with the veteran and the oncology and palliative care teams. The plan allowed the patient to achieve his treatment goals while maintaining his safety and reducing theoretical cardiac toxicities with his cancer treatment.
Finally, the availability of a multidisciplinary team approach including palliative care, oncology, psychology, addiction medicine and addiction psychiatry, was critical for addressing the veteran’s malignant pain. Palliative care worked in close collaboration with the ORC to prescribe and renew pain medications. ORC offered ongoing consultation on pain management in the context of OUD. As the veteran’s cancer progressed and functional decline prohibited his daily attendance at the community methadone clinic, palliative care and ORC met with the methadone clinic to arrange a less frequent methadone pickup schedule (the patient previously needed daily pickup). Non-VA settings may not have access to these resources to safely treat the biopsychosocial issues that arise in complex cases.
Substance Use and Cancer Treatments
This case raises several critical questions for oncologic care. Cocaine and fluorouracil are both associated with cardiotoxicity, and many oncologists would not feel it is safe to administer a regimen containing fluorouracil to a patient with active cocaine use. The National Comprehensive Cancer Network (NCCN) panel recommends FOLFIRINOX as a preferred category 1 recommendation for first-line treatment of patients with advanced pancreas cancer with good performance status.10 This recommendation is based on the PRODIGE trial, which has shown improved overall survival (OS): 11.1 vs 6.8 months for patients who received single-agent gemcitabine.11 If patients are not candidates for FOLFIRINOX and have good performance status, the NCCN recommends gemcitabine plus albumin-bound paclitaxel with category 1 level of evidence based on the IMPACT trial, which showed improvement in OS (8.7 vs 6.6 months compared with single-agent gemcitabine).12
Some oncologists may have additional concerns administering fluorouracil treatment alternatives (such as gemcitabine and albumin-bound paclitaxel) to individuals with active SUD because of concerns about altered mental status impacting the ability to report important adverse effects. In the absence of sufficient data, HCPs must determine whether they feel it is safe to administer these agents in individuals with active cocaine use. However, denying these patients the possible benefits of standard-of-care life-prolonging therapies without established data raises concerns regarding the ethics of such practices. There is concern that the stigma surrounding cocaine use might contribute to withholding treatment, while treatment is continued for individuals taking prescribed stimulant medications that also have cardiotoxicity risks. VA health care facilities are uniquely situated to use all available resources to address these issues using interprofessional patient-centered care and determine the most optimal treatment based on a risk/benefit discussion between the patient and the HCP.
Similarly, this case also raised questions among HCPs about the safety of using an indwelling port for treatment in a patient with SUD. In the current case there was concern about keeping in a port for a patient with a history of IV drug use; therefore, a PICC line was initiated and removed at each admission. Without guidelines in these situations, HCPs are left to weigh the risks and benefits of using a port or a PICC for individuals with recent or current substance use without formal data, which can lead to inconsistent access to care. More guidance is needed for these situations.
SUD Screening
This case begs the question of whether oncologists are adequately screening for a range of SUDs, and when they encounter an issue, how they are addressing it. Many oncologists do not receive adequate training on assessment of current or recent substance use. There are health care and systems-level practices that may increase patient safety for individuals with ongoing substance use who are undergoing cancer treatment. Training on obtaining appropriate substance use histories, motivational interviewing to resolve ambivalence about substance use in the direction of change, and shared decision making about treatment options could increase confidence in understanding and addressing substance use issues. It is also important to educate oncologists on how to address patients who return to or continued substance use during treatment. In this case the collaboration from palliative care, psychology, addiction medicine, and addiction psychiatry through the ORC was essential in assisting with ongoing assessment of substance use, guiding difficult conversations about the impact of substance use on the treatment plan, and identifying risk-mitigation strategies. Close collaboration and full utilization of all VA resources allowed this patient to receive first-line treatment for pancreatic cancer in order to reach his goal of prolonging his life while maintaining acceptable quality of life. Table 2 provides best practices for management of patients with comorbid SUD and cancer.
More research is needed into cancer treatment for patients with SUD, especially in the current era of cancer care using novel cancer treatments leading to significantly improved survival in many cancer types. Ideally, oncologists should be routinely or consistently screening patients for substance use, including alcohol. The patient should participate in this decision-making process after being educated about the risks and benefits. These patients can be followed using a multimodal approach to increase their rates of success and improve their quality of life. Although the literature is limited and no formal guidelines are available, VA oncologists are fortunate to have a range of resources available to them to navigate these difficult cases. Veterans have elevated rates of SUD, making this a critical issue to consider in the VA.13 It is the hope that this case can highlight how to take advantage of the many VA resources in order to ensure equitable cancer care for all veterans.
Conclusions
This case demonstrates that cancer-directed treatment is safe and feasible in a patient with advanced pancreatic cancer and coexisting active SUD by using a multidisciplinary approach. The multidisciplinary team included palliative care, oncology, psychology, addiction medicine, and addiction psychiatry. Critical steps for a successful outcome include gathering history about SUD; motivational interviewing to resolve ambivalence about treatment for SUD; shared decision making about cancer treatment; and risk-reduction strategies in pain and SUD management.
Treatment advancements in many cancer types have led to significantly longer survival, and it is critical to develop safe protocols to treat patients with active SUD so they also can derive benefit from these very significant medical advancements.
Acknowledgments
Michal Rose, MD, Director of VACHS Cancer Center, and Chandrika Kumar, MD, Director of VACHS Community Living Center, for their collaboration in care for this veteran.
1. Chang G, Meadows ME, Jones JA, Antin JH, Orav EJ. Substance use and survival after treatment for chronic myelogenous leukemia (CML) or myelodysplastic syndrome (MDS). Am J Drug Alcohol Ab. 2010;36(1):1-6. doi:10.3109/00952990903490758
2. Stagno S, Busby K, Shapiro A, Kotz M. Patients at risk: addressing addiction in patients undergoing hematopoietic SCT. Bone Marrow Transplant. 2008;42(4):221-226. doi:10.1038/bmt.2008.211
3. Arora NP. Cutaneous vasculopathy and neutropenia associated with levamisole-adulterated cocaine. Am J Med Sci. 2013;345(1):45-51. doi:10.1097/MAJ.0b013e31825b2b50
4. Schwartz BG, Rezkalla S, Kloner RA. Cardiovascular effects of cocaine. Circulation. 2010;122(24):2558-2569. doi:10.1161/CIRCULATIONAHA.110.940569
5. US Department of Veterans Affairs, US Department of Defense. VA/DoD clinical practice guideline for the management of substance use disorders. Published 2015. Accessed July 8, 2021. https://www.healthquality.va.gov/guidelines/MH/sud/VADODSUDCPGRevised22216.pdf
6. Mehta A, Chan LS. Understanding of the concept of “total pain”: a prerequisite for pain control. J Hosp Palliat Nurs. 2008;10(1):26-32. doi:10.1097/01.NJH.0000306714.50539.1a
7. Rubinsak LA, Terplan M, Martin CE, Fields EC, McGuire WP, Temkin SM. Co-occurring substance use disorder: The impact on treatment adherence in women with locally advanced cervical cancer. Gynecol Oncol Rep. 2019;28:116-119. Published 2019 Mar 27. doi:10.1016/j.gore.2019.03.016
8. Chhatre S, Metzger DS, Malkowicz SB, Woody G, Jayadevappa R. Substance use disorder and its effects on outcomes in men with advanced-stage prostate cancer. Cancer. 2014;120(21):3338-3345. doi:10.1002/cncr.28861
9. Concannon K, Thayer JH, Hicks R, et al. Outcomes among patients with a history of substance abuse in non-small cell lung cancer: a county hospital experience. J Clin Onc. 2019;37(15)(suppl):e20031-e20031. doi:10.1200/JCO.2019.37.15
10. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: pancreatic adenocarcinoma. Version 2.2021. Updated February 25, 2021. Accessed July 8, 2021. https://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf
11. Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817-1825. doi:10.1056/NEJMoa1011923
12. Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691-1703. doi:10.1056/NEJMoa1304369
13. Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001-2010: Implications for screening, diagnosis and treatment. Drug Alcohol Depend. 2011;116(1-3):93-101. doi:10.1016/j.drugalcdep.2010.11.027
14. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. American Psychiatric Association; 2013.
A multidisciplinary approach provided safe and feasible cancer treatment in a patient with advanced pancreatic cancer and coexisting active substance use disorder.
A multidisciplinary approach provided safe and feasible cancer treatment in a patient with advanced pancreatic cancer and coexisting active substance use disorder.
Substance use disorders (SUDs) are an important but understudied aspect of treating patients diagnosed with cancer. Substance use can affect cancer treatment outcomes, including morbidity and mortality.1,2 Additionally, patients with cancer and SUD may have unique psychosocial needs that require close attention and management. There is a paucity of data regarding the best approach to treating such patients. For example, cocaine use may increase the cardiovascular and hematologic risk of some traditional chemotherapy agents.3,4 Newer targeted agents and immunotherapies remain understudied with respect to SUD risk.
Although the US Department of Veterans Affairs (VA) has established helpful clinical practice guidelines for the treatment of SUD, there are no guidelines for treating patients with SUD and cancer.5 Clinicians have limited confidence in treatment approach, and treatment is inconsistent among oncologists nationwide even within the same practice. Furthermore, it can be challenging to safely prescribe opioids for cancer-related pain in individuals with SUD. There is a high risk of SUD and mental health disorders in veterans, making this population particularly vulnerable. We report a case of a male with metastatic pancreatic cancer, severe opioid use disorder (OUD) and moderate cocaine use disorder (CUD) who received pain management and cancer treatment under the direction of a multidisciplinary team approach.
Case Report
A 63-year-old male with a medical history of HIV treated with highly active antiretroviral therapy (HAART), compensated cirrhosis, severe OUD, moderate CUD, and sedative use disorder in sustained remission was admitted to the West Haven campus of the VA Connecticut Healthcare System (VACHS) with abdominal pain, weight loss and fatigue. He used heroin 1 month prior to his admission and reported regular cocaine and marijuana use (Table 1). He was diagnosed with HIV in 1989, and his medical history included herpes zoster and oral candidiasis but no other opportunistic infections. Several months prior to this admission, he had an undetectable viral load and CD4 count of 688.
At the time of this admission, the patient was adherent to methadone treatment. He reported increased abdominal pain. Computed tomography (CT) showed a 2.4-cm mass in the pancreatic uncinate process, multiple liver metastases, retroperitoneal lymphadenopathy, and small lung nodules. A CT-guided liver biopsy showed adenocarcinoma consistent with a primary cancer of the pancreas. Given the complexity of the case, a multidisciplinary team approach was used to treat his cancer and the sequelae safely, including the oncology team, community living center team, palliative care team, and interprofessional opioid reassessment clinic team (ORC).
Cancer Treatment
Chemotherapy with FOLFIRINOX (leucovorin calcium, fluorouracil, irinotecan hydrochloride, and oxaliplatin) was recommended. The first cycle of treatment originally was planned for the outpatient setting, and a peripherally inserted central catheter (PICC) line was placed. However, after a urine toxicology test was positive for cocaine, the PICC line was removed due to concern for possible use of PICC line for nonprescribed substance use. The patient expressed suicidal ideation at the time and was admitted for psychiatric consult and pain control. Cycle 1 FOLFIRINOX was started during this admission. A PICC line was again put in place and then removed before discharge. A celiac plexus block was performed several days after this admission for pain control.
Given concern about cocaine use increasing the risk of cardiac toxicity with FOLFIRINOX treatment, treating providers sconsulted with the community living center (CLC) about possible admission for future chemotherapy administration and pain management. The CLC at VACHS has 38 beds for rehabilitation, long-term care, and hospice with the mission to restore each veteran to his or her highest level of well-being. After discussion with this patient and CLC staff, he agreed to a CLC admission. The patient agreed to remain in the facility, wear a secure care device, and not leave without staff accompaniment. He was able to obtain a 2-hour pass to pay bills and rent. During the 2 months he was admitted to the CLC he would present to the VACHS Cancer Center for chemotherapy every 2 weeks. He completed 6 cycles of chemotherapy while admitted. During the admission, he was transferred to active medical service for 2 days for fever and malaise, and then returned to the CLC. The patient elected to leave the CLC after 2 months as the inability to see close friends was interfering with his quality of life.
Upon being discharged from the CLC, shared decision making took place with the patient to establish a new treatment plan. In collaboration with the patient, a plan was made to admit him every 2 weeks for continued chemotherapy. A PICC line was placed on each day of admission and removed prior to discharge. It was also agreed that treatment would be delayed if a urine drug test was positive for cocaine on the morning of admission. The patient was also seen by ORC every 2 weeks after being discharged from the CLC.
Imaging after cycle 6 showed decreased size of liver metastases, retroperitoneal lymph nodes, and pancreas mass. Cancer antigen 19-9 (CA19-9) tumor marker was reduced from 3513 U/mL pretreatment to 50 U/mL after cycle 7. Chemotherapy cycle 7 was delayed 6 days due to active cocaine and heroin use. A repeat urine was obtained several days later, which was negative for cocaine, and he was admitted for cycle 7 chemotherapy. Using this treatment approach of admissions for every cycle, the patient was able to receive 11 cycles of FOLFIRINOX with clinical benefit.
Palliative Care/Pain Management
Safely treating the patient’s malignant pain in the context of his OUD was critically important. In order to do this the palliative care team worked closely alongside ORC, is a multidisciplinary team consisting of health care providers (HCPs) from addiction psychiatry, internal medicine, health psychology and pharmacy who are consulted to evaluate veterans’ current opioid regimens and make recommendations to optimize both safety and efficacy. ORC followed this particular veteran as an outpatient and consulted on pain issues during his admission. They recommended the continuation of methadone at 120 mg daily and increased oral oxycodone to 30 mg every 6 hours, and then further increased to 45 mg every 6 hours. He continued to have increased pain despite higher doses of oxycodone, and pain medication was changed to oral hydromorphone 28 mg every 6 hours with the continuation of methadone. ORC and the palliative care team obtained consent from the veteran and a release of Information form signed by the patient to contact his community methadone clinic for further collaboration around pain management throughout the time caring for the veteran.
Even with improvement in disease based on imaging and tumor markers, opioid medications could not be decreased in this case. This is likely in part due to the multidimensional nature of pain. Careful assessment of the biologic, emotional, social, and spiritual contributors to pain is needed in the management of pain, especially at end of life.6 Nonpharmacologic pain management strategies used in this case included a transcutaneous electrical nerve stimulation unit, moist heat, celiac plexus block, and emotional support.
Psychosocial Issues/Substance Use
Psychosocial support for the patient was provided by the interdisciplinary palliative care team and the ORC team in both the inpatient and outpatient settings. Despite efforts from case management to get the veteran home services once discharged from the CLC, he declined repeatedly. Thus, the CLC social worker obtained a guardian alert for the veteran on discharge.
Close outpatient follow-up for medical and psychosocial support was very critical. When an outpatient, the veteran was scheduled for biweekly appointments with palliative care or ORC. When admitted to the hospital, the palliative care team medical director and psychologist conducted joint visits with him. Although he denied depressed mood and anxiety throughout his treatment, he often reflected on regrets that he had as he faced the end of his life. Specifically, he shared thoughts about being estranged from his surviving brother given his long struggle with substance use. Although he did not think a relationship was possible with his brother at the end of life, he still cared deeply for him and wanted to make him aware of his pancreatic cancer diagnosis. This was particularly important to him because their late brother had also died of pancreatic cancer. It was the patient’s wish at the end of his life to alert his surviving brother of his diagnosis so he and his children could get adequate screening throughout their lives. Although he had spoken of this desire often, it wasn’t until his disease progressed and he elected to transition to hospice that he felt ready to write the letter. The palliative care team assisted the veteran in writing and mailing a letter to his brother informing him of his diagnosis and transition to hospice as well as communicating that his brother and his family had been in his thoughts at the end of his life. The patient’s brother received this letter and with assistance from the CLC social worker made arrangements to visit the veteran at bedside at the inpatient CLC hospice unit the final days of his life.
Discussion
There are very little data on the safety of cancer-directed therapy in patients with active SUD. The limited studies that have been done showed conflicting results.
A retrospective study among women with co-occurring SUD and locally advanced cervical cancer who were undergoing primary radiation therapy found that SUD was not associated with a difference in toxicity or survival outcomes.7 However, other research suggests that SUD may be associated with an increase in all-cause mortality as well as other adverse outcomes for patients and health care systems (eg, emergency department visits, hospitalizations).8 A retrospective study of patients with a history of SUD and nonsmall cell lung cancer showed that these patients had higher rates of depression, less family support, increased rates of missed appointments, more emergency department visits and more hospitalizations.9 Patients with chronic myeloid leukemia or myelodysplastic syndromes who had long-term cocaine use had a 6-fold increased risk of death, which was not found in patients who had long-term alcohol or marijuana use.2
The limited data highlight the need for careful consideration of ways to mitigate potentially adverse outcomes in this population while still providing clinically indicated cancer treatment. Integrated VA health care systems provide unique resources that can maximize veteran safety during cancer treatment. Utilization of VA resources and close interdisciplinary collaboration across VA HCPs can help to ensure equitable access to state-of-the-art cancer therapies for veterans with comorbid SUD.
VA Services for Patients With Comorbidities
This case highlights several distinct aspects of VA health care that make it possible to safely treat individuals with complex comorbidities. One important aspect of this was collaboration with the CLC to admit the veteran for his initial treatment after a positive cocaine test. CLC admission was nonpunitive and allowed ongoing involvement in the VA community. This provided an essential, safe, and structured environment in which 6 cycles of chemotherapy could be delivered.
Although the patient left the CLC after 2 months due to floor restrictions negatively impacting his quality of life and ability to spend time with close friends, several important events occurred during this stay. First, the patient established close relationships with the CLC staff and the palliative care team; both groups followed him throughout his inpatient and outpatient care. These relationships proved essential throughout his care as they were the foundation of difficult conversations about substance use, treatment adherence, and eventually, transition to hospice.
In addition, the opportunity to administer 6 cycles of chemotherapy at the CLC was enough to lead to clinical benefit and radiographic response to treatment. Clinical benefits while in the CLC included maintenance of a good appetite, 15-lb weight gain and preserved performance status (ECOG [Eastern Cooperative Group]-1), which allowed him to actively participate in multiple social and recreational activities while in the CLC. From early conversations, this patient was clear that he wanted treatment as long as his life could be prolonged with good quality of life. Having evidence of the benefit of treatment, at least initially, increased the patient’s confidence in treatment. There were a few conversations when the challenges of treatment mounted (eg, pain, needs for abstinence from cocaine prior to admission for chemotherapy, frequent doctor appointments), and the patient would remind himself of these data to recommit himself to treatment. The opportunity to admit him to the inpatient VA facility, including bed availability for 3 days during his treatment once he left the CLC was important. This plan to admit the patient following a negative urine toxicology test for cocaine was made collaboratively with the veteran and the oncology and palliative care teams. The plan allowed the patient to achieve his treatment goals while maintaining his safety and reducing theoretical cardiac toxicities with his cancer treatment.
Finally, the availability of a multidisciplinary team approach including palliative care, oncology, psychology, addiction medicine and addiction psychiatry, was critical for addressing the veteran’s malignant pain. Palliative care worked in close collaboration with the ORC to prescribe and renew pain medications. ORC offered ongoing consultation on pain management in the context of OUD. As the veteran’s cancer progressed and functional decline prohibited his daily attendance at the community methadone clinic, palliative care and ORC met with the methadone clinic to arrange a less frequent methadone pickup schedule (the patient previously needed daily pickup). Non-VA settings may not have access to these resources to safely treat the biopsychosocial issues that arise in complex cases.
Substance Use and Cancer Treatments
This case raises several critical questions for oncologic care. Cocaine and fluorouracil are both associated with cardiotoxicity, and many oncologists would not feel it is safe to administer a regimen containing fluorouracil to a patient with active cocaine use. The National Comprehensive Cancer Network (NCCN) panel recommends FOLFIRINOX as a preferred category 1 recommendation for first-line treatment of patients with advanced pancreas cancer with good performance status.10 This recommendation is based on the PRODIGE trial, which has shown improved overall survival (OS): 11.1 vs 6.8 months for patients who received single-agent gemcitabine.11 If patients are not candidates for FOLFIRINOX and have good performance status, the NCCN recommends gemcitabine plus albumin-bound paclitaxel with category 1 level of evidence based on the IMPACT trial, which showed improvement in OS (8.7 vs 6.6 months compared with single-agent gemcitabine).12
Some oncologists may have additional concerns administering fluorouracil treatment alternatives (such as gemcitabine and albumin-bound paclitaxel) to individuals with active SUD because of concerns about altered mental status impacting the ability to report important adverse effects. In the absence of sufficient data, HCPs must determine whether they feel it is safe to administer these agents in individuals with active cocaine use. However, denying these patients the possible benefits of standard-of-care life-prolonging therapies without established data raises concerns regarding the ethics of such practices. There is concern that the stigma surrounding cocaine use might contribute to withholding treatment, while treatment is continued for individuals taking prescribed stimulant medications that also have cardiotoxicity risks. VA health care facilities are uniquely situated to use all available resources to address these issues using interprofessional patient-centered care and determine the most optimal treatment based on a risk/benefit discussion between the patient and the HCP.
Similarly, this case also raised questions among HCPs about the safety of using an indwelling port for treatment in a patient with SUD. In the current case there was concern about keeping in a port for a patient with a history of IV drug use; therefore, a PICC line was initiated and removed at each admission. Without guidelines in these situations, HCPs are left to weigh the risks and benefits of using a port or a PICC for individuals with recent or current substance use without formal data, which can lead to inconsistent access to care. More guidance is needed for these situations.
SUD Screening
This case begs the question of whether oncologists are adequately screening for a range of SUDs, and when they encounter an issue, how they are addressing it. Many oncologists do not receive adequate training on assessment of current or recent substance use. There are health care and systems-level practices that may increase patient safety for individuals with ongoing substance use who are undergoing cancer treatment. Training on obtaining appropriate substance use histories, motivational interviewing to resolve ambivalence about substance use in the direction of change, and shared decision making about treatment options could increase confidence in understanding and addressing substance use issues. It is also important to educate oncologists on how to address patients who return to or continued substance use during treatment. In this case the collaboration from palliative care, psychology, addiction medicine, and addiction psychiatry through the ORC was essential in assisting with ongoing assessment of substance use, guiding difficult conversations about the impact of substance use on the treatment plan, and identifying risk-mitigation strategies. Close collaboration and full utilization of all VA resources allowed this patient to receive first-line treatment for pancreatic cancer in order to reach his goal of prolonging his life while maintaining acceptable quality of life. Table 2 provides best practices for management of patients with comorbid SUD and cancer.
More research is needed into cancer treatment for patients with SUD, especially in the current era of cancer care using novel cancer treatments leading to significantly improved survival in many cancer types. Ideally, oncologists should be routinely or consistently screening patients for substance use, including alcohol. The patient should participate in this decision-making process after being educated about the risks and benefits. These patients can be followed using a multimodal approach to increase their rates of success and improve their quality of life. Although the literature is limited and no formal guidelines are available, VA oncologists are fortunate to have a range of resources available to them to navigate these difficult cases. Veterans have elevated rates of SUD, making this a critical issue to consider in the VA.13 It is the hope that this case can highlight how to take advantage of the many VA resources in order to ensure equitable cancer care for all veterans.
Conclusions
This case demonstrates that cancer-directed treatment is safe and feasible in a patient with advanced pancreatic cancer and coexisting active SUD by using a multidisciplinary approach. The multidisciplinary team included palliative care, oncology, psychology, addiction medicine, and addiction psychiatry. Critical steps for a successful outcome include gathering history about SUD; motivational interviewing to resolve ambivalence about treatment for SUD; shared decision making about cancer treatment; and risk-reduction strategies in pain and SUD management.
Treatment advancements in many cancer types have led to significantly longer survival, and it is critical to develop safe protocols to treat patients with active SUD so they also can derive benefit from these very significant medical advancements.
Acknowledgments
Michal Rose, MD, Director of VACHS Cancer Center, and Chandrika Kumar, MD, Director of VACHS Community Living Center, for their collaboration in care for this veteran.
Substance use disorders (SUDs) are an important but understudied aspect of treating patients diagnosed with cancer. Substance use can affect cancer treatment outcomes, including morbidity and mortality.1,2 Additionally, patients with cancer and SUD may have unique psychosocial needs that require close attention and management. There is a paucity of data regarding the best approach to treating such patients. For example, cocaine use may increase the cardiovascular and hematologic risk of some traditional chemotherapy agents.3,4 Newer targeted agents and immunotherapies remain understudied with respect to SUD risk.
Although the US Department of Veterans Affairs (VA) has established helpful clinical practice guidelines for the treatment of SUD, there are no guidelines for treating patients with SUD and cancer.5 Clinicians have limited confidence in treatment approach, and treatment is inconsistent among oncologists nationwide even within the same practice. Furthermore, it can be challenging to safely prescribe opioids for cancer-related pain in individuals with SUD. There is a high risk of SUD and mental health disorders in veterans, making this population particularly vulnerable. We report a case of a male with metastatic pancreatic cancer, severe opioid use disorder (OUD) and moderate cocaine use disorder (CUD) who received pain management and cancer treatment under the direction of a multidisciplinary team approach.
Case Report
A 63-year-old male with a medical history of HIV treated with highly active antiretroviral therapy (HAART), compensated cirrhosis, severe OUD, moderate CUD, and sedative use disorder in sustained remission was admitted to the West Haven campus of the VA Connecticut Healthcare System (VACHS) with abdominal pain, weight loss and fatigue. He used heroin 1 month prior to his admission and reported regular cocaine and marijuana use (Table 1). He was diagnosed with HIV in 1989, and his medical history included herpes zoster and oral candidiasis but no other opportunistic infections. Several months prior to this admission, he had an undetectable viral load and CD4 count of 688.
At the time of this admission, the patient was adherent to methadone treatment. He reported increased abdominal pain. Computed tomography (CT) showed a 2.4-cm mass in the pancreatic uncinate process, multiple liver metastases, retroperitoneal lymphadenopathy, and small lung nodules. A CT-guided liver biopsy showed adenocarcinoma consistent with a primary cancer of the pancreas. Given the complexity of the case, a multidisciplinary team approach was used to treat his cancer and the sequelae safely, including the oncology team, community living center team, palliative care team, and interprofessional opioid reassessment clinic team (ORC).
Cancer Treatment
Chemotherapy with FOLFIRINOX (leucovorin calcium, fluorouracil, irinotecan hydrochloride, and oxaliplatin) was recommended. The first cycle of treatment originally was planned for the outpatient setting, and a peripherally inserted central catheter (PICC) line was placed. However, after a urine toxicology test was positive for cocaine, the PICC line was removed due to concern for possible use of PICC line for nonprescribed substance use. The patient expressed suicidal ideation at the time and was admitted for psychiatric consult and pain control. Cycle 1 FOLFIRINOX was started during this admission. A PICC line was again put in place and then removed before discharge. A celiac plexus block was performed several days after this admission for pain control.
Given concern about cocaine use increasing the risk of cardiac toxicity with FOLFIRINOX treatment, treating providers sconsulted with the community living center (CLC) about possible admission for future chemotherapy administration and pain management. The CLC at VACHS has 38 beds for rehabilitation, long-term care, and hospice with the mission to restore each veteran to his or her highest level of well-being. After discussion with this patient and CLC staff, he agreed to a CLC admission. The patient agreed to remain in the facility, wear a secure care device, and not leave without staff accompaniment. He was able to obtain a 2-hour pass to pay bills and rent. During the 2 months he was admitted to the CLC he would present to the VACHS Cancer Center for chemotherapy every 2 weeks. He completed 6 cycles of chemotherapy while admitted. During the admission, he was transferred to active medical service for 2 days for fever and malaise, and then returned to the CLC. The patient elected to leave the CLC after 2 months as the inability to see close friends was interfering with his quality of life.
Upon being discharged from the CLC, shared decision making took place with the patient to establish a new treatment plan. In collaboration with the patient, a plan was made to admit him every 2 weeks for continued chemotherapy. A PICC line was placed on each day of admission and removed prior to discharge. It was also agreed that treatment would be delayed if a urine drug test was positive for cocaine on the morning of admission. The patient was also seen by ORC every 2 weeks after being discharged from the CLC.
Imaging after cycle 6 showed decreased size of liver metastases, retroperitoneal lymph nodes, and pancreas mass. Cancer antigen 19-9 (CA19-9) tumor marker was reduced from 3513 U/mL pretreatment to 50 U/mL after cycle 7. Chemotherapy cycle 7 was delayed 6 days due to active cocaine and heroin use. A repeat urine was obtained several days later, which was negative for cocaine, and he was admitted for cycle 7 chemotherapy. Using this treatment approach of admissions for every cycle, the patient was able to receive 11 cycles of FOLFIRINOX with clinical benefit.
Palliative Care/Pain Management
Safely treating the patient’s malignant pain in the context of his OUD was critically important. In order to do this the palliative care team worked closely alongside ORC, is a multidisciplinary team consisting of health care providers (HCPs) from addiction psychiatry, internal medicine, health psychology and pharmacy who are consulted to evaluate veterans’ current opioid regimens and make recommendations to optimize both safety and efficacy. ORC followed this particular veteran as an outpatient and consulted on pain issues during his admission. They recommended the continuation of methadone at 120 mg daily and increased oral oxycodone to 30 mg every 6 hours, and then further increased to 45 mg every 6 hours. He continued to have increased pain despite higher doses of oxycodone, and pain medication was changed to oral hydromorphone 28 mg every 6 hours with the continuation of methadone. ORC and the palliative care team obtained consent from the veteran and a release of Information form signed by the patient to contact his community methadone clinic for further collaboration around pain management throughout the time caring for the veteran.
Even with improvement in disease based on imaging and tumor markers, opioid medications could not be decreased in this case. This is likely in part due to the multidimensional nature of pain. Careful assessment of the biologic, emotional, social, and spiritual contributors to pain is needed in the management of pain, especially at end of life.6 Nonpharmacologic pain management strategies used in this case included a transcutaneous electrical nerve stimulation unit, moist heat, celiac plexus block, and emotional support.
Psychosocial Issues/Substance Use
Psychosocial support for the patient was provided by the interdisciplinary palliative care team and the ORC team in both the inpatient and outpatient settings. Despite efforts from case management to get the veteran home services once discharged from the CLC, he declined repeatedly. Thus, the CLC social worker obtained a guardian alert for the veteran on discharge.
Close outpatient follow-up for medical and psychosocial support was very critical. When an outpatient, the veteran was scheduled for biweekly appointments with palliative care or ORC. When admitted to the hospital, the palliative care team medical director and psychologist conducted joint visits with him. Although he denied depressed mood and anxiety throughout his treatment, he often reflected on regrets that he had as he faced the end of his life. Specifically, he shared thoughts about being estranged from his surviving brother given his long struggle with substance use. Although he did not think a relationship was possible with his brother at the end of life, he still cared deeply for him and wanted to make him aware of his pancreatic cancer diagnosis. This was particularly important to him because their late brother had also died of pancreatic cancer. It was the patient’s wish at the end of his life to alert his surviving brother of his diagnosis so he and his children could get adequate screening throughout their lives. Although he had spoken of this desire often, it wasn’t until his disease progressed and he elected to transition to hospice that he felt ready to write the letter. The palliative care team assisted the veteran in writing and mailing a letter to his brother informing him of his diagnosis and transition to hospice as well as communicating that his brother and his family had been in his thoughts at the end of his life. The patient’s brother received this letter and with assistance from the CLC social worker made arrangements to visit the veteran at bedside at the inpatient CLC hospice unit the final days of his life.
Discussion
There are very little data on the safety of cancer-directed therapy in patients with active SUD. The limited studies that have been done showed conflicting results.
A retrospective study among women with co-occurring SUD and locally advanced cervical cancer who were undergoing primary radiation therapy found that SUD was not associated with a difference in toxicity or survival outcomes.7 However, other research suggests that SUD may be associated with an increase in all-cause mortality as well as other adverse outcomes for patients and health care systems (eg, emergency department visits, hospitalizations).8 A retrospective study of patients with a history of SUD and nonsmall cell lung cancer showed that these patients had higher rates of depression, less family support, increased rates of missed appointments, more emergency department visits and more hospitalizations.9 Patients with chronic myeloid leukemia or myelodysplastic syndromes who had long-term cocaine use had a 6-fold increased risk of death, which was not found in patients who had long-term alcohol or marijuana use.2
The limited data highlight the need for careful consideration of ways to mitigate potentially adverse outcomes in this population while still providing clinically indicated cancer treatment. Integrated VA health care systems provide unique resources that can maximize veteran safety during cancer treatment. Utilization of VA resources and close interdisciplinary collaboration across VA HCPs can help to ensure equitable access to state-of-the-art cancer therapies for veterans with comorbid SUD.
VA Services for Patients With Comorbidities
This case highlights several distinct aspects of VA health care that make it possible to safely treat individuals with complex comorbidities. One important aspect of this was collaboration with the CLC to admit the veteran for his initial treatment after a positive cocaine test. CLC admission was nonpunitive and allowed ongoing involvement in the VA community. This provided an essential, safe, and structured environment in which 6 cycles of chemotherapy could be delivered.
Although the patient left the CLC after 2 months due to floor restrictions negatively impacting his quality of life and ability to spend time with close friends, several important events occurred during this stay. First, the patient established close relationships with the CLC staff and the palliative care team; both groups followed him throughout his inpatient and outpatient care. These relationships proved essential throughout his care as they were the foundation of difficult conversations about substance use, treatment adherence, and eventually, transition to hospice.
In addition, the opportunity to administer 6 cycles of chemotherapy at the CLC was enough to lead to clinical benefit and radiographic response to treatment. Clinical benefits while in the CLC included maintenance of a good appetite, 15-lb weight gain and preserved performance status (ECOG [Eastern Cooperative Group]-1), which allowed him to actively participate in multiple social and recreational activities while in the CLC. From early conversations, this patient was clear that he wanted treatment as long as his life could be prolonged with good quality of life. Having evidence of the benefit of treatment, at least initially, increased the patient’s confidence in treatment. There were a few conversations when the challenges of treatment mounted (eg, pain, needs for abstinence from cocaine prior to admission for chemotherapy, frequent doctor appointments), and the patient would remind himself of these data to recommit himself to treatment. The opportunity to admit him to the inpatient VA facility, including bed availability for 3 days during his treatment once he left the CLC was important. This plan to admit the patient following a negative urine toxicology test for cocaine was made collaboratively with the veteran and the oncology and palliative care teams. The plan allowed the patient to achieve his treatment goals while maintaining his safety and reducing theoretical cardiac toxicities with his cancer treatment.
Finally, the availability of a multidisciplinary team approach including palliative care, oncology, psychology, addiction medicine and addiction psychiatry, was critical for addressing the veteran’s malignant pain. Palliative care worked in close collaboration with the ORC to prescribe and renew pain medications. ORC offered ongoing consultation on pain management in the context of OUD. As the veteran’s cancer progressed and functional decline prohibited his daily attendance at the community methadone clinic, palliative care and ORC met with the methadone clinic to arrange a less frequent methadone pickup schedule (the patient previously needed daily pickup). Non-VA settings may not have access to these resources to safely treat the biopsychosocial issues that arise in complex cases.
Substance Use and Cancer Treatments
This case raises several critical questions for oncologic care. Cocaine and fluorouracil are both associated with cardiotoxicity, and many oncologists would not feel it is safe to administer a regimen containing fluorouracil to a patient with active cocaine use. The National Comprehensive Cancer Network (NCCN) panel recommends FOLFIRINOX as a preferred category 1 recommendation for first-line treatment of patients with advanced pancreas cancer with good performance status.10 This recommendation is based on the PRODIGE trial, which has shown improved overall survival (OS): 11.1 vs 6.8 months for patients who received single-agent gemcitabine.11 If patients are not candidates for FOLFIRINOX and have good performance status, the NCCN recommends gemcitabine plus albumin-bound paclitaxel with category 1 level of evidence based on the IMPACT trial, which showed improvement in OS (8.7 vs 6.6 months compared with single-agent gemcitabine).12
Some oncologists may have additional concerns administering fluorouracil treatment alternatives (such as gemcitabine and albumin-bound paclitaxel) to individuals with active SUD because of concerns about altered mental status impacting the ability to report important adverse effects. In the absence of sufficient data, HCPs must determine whether they feel it is safe to administer these agents in individuals with active cocaine use. However, denying these patients the possible benefits of standard-of-care life-prolonging therapies without established data raises concerns regarding the ethics of such practices. There is concern that the stigma surrounding cocaine use might contribute to withholding treatment, while treatment is continued for individuals taking prescribed stimulant medications that also have cardiotoxicity risks. VA health care facilities are uniquely situated to use all available resources to address these issues using interprofessional patient-centered care and determine the most optimal treatment based on a risk/benefit discussion between the patient and the HCP.
Similarly, this case also raised questions among HCPs about the safety of using an indwelling port for treatment in a patient with SUD. In the current case there was concern about keeping in a port for a patient with a history of IV drug use; therefore, a PICC line was initiated and removed at each admission. Without guidelines in these situations, HCPs are left to weigh the risks and benefits of using a port or a PICC for individuals with recent or current substance use without formal data, which can lead to inconsistent access to care. More guidance is needed for these situations.
SUD Screening
This case begs the question of whether oncologists are adequately screening for a range of SUDs, and when they encounter an issue, how they are addressing it. Many oncologists do not receive adequate training on assessment of current or recent substance use. There are health care and systems-level practices that may increase patient safety for individuals with ongoing substance use who are undergoing cancer treatment. Training on obtaining appropriate substance use histories, motivational interviewing to resolve ambivalence about substance use in the direction of change, and shared decision making about treatment options could increase confidence in understanding and addressing substance use issues. It is also important to educate oncologists on how to address patients who return to or continued substance use during treatment. In this case the collaboration from palliative care, psychology, addiction medicine, and addiction psychiatry through the ORC was essential in assisting with ongoing assessment of substance use, guiding difficult conversations about the impact of substance use on the treatment plan, and identifying risk-mitigation strategies. Close collaboration and full utilization of all VA resources allowed this patient to receive first-line treatment for pancreatic cancer in order to reach his goal of prolonging his life while maintaining acceptable quality of life. Table 2 provides best practices for management of patients with comorbid SUD and cancer.
More research is needed into cancer treatment for patients with SUD, especially in the current era of cancer care using novel cancer treatments leading to significantly improved survival in many cancer types. Ideally, oncologists should be routinely or consistently screening patients for substance use, including alcohol. The patient should participate in this decision-making process after being educated about the risks and benefits. These patients can be followed using a multimodal approach to increase their rates of success and improve their quality of life. Although the literature is limited and no formal guidelines are available, VA oncologists are fortunate to have a range of resources available to them to navigate these difficult cases. Veterans have elevated rates of SUD, making this a critical issue to consider in the VA.13 It is the hope that this case can highlight how to take advantage of the many VA resources in order to ensure equitable cancer care for all veterans.
Conclusions
This case demonstrates that cancer-directed treatment is safe and feasible in a patient with advanced pancreatic cancer and coexisting active SUD by using a multidisciplinary approach. The multidisciplinary team included palliative care, oncology, psychology, addiction medicine, and addiction psychiatry. Critical steps for a successful outcome include gathering history about SUD; motivational interviewing to resolve ambivalence about treatment for SUD; shared decision making about cancer treatment; and risk-reduction strategies in pain and SUD management.
Treatment advancements in many cancer types have led to significantly longer survival, and it is critical to develop safe protocols to treat patients with active SUD so they also can derive benefit from these very significant medical advancements.
Acknowledgments
Michal Rose, MD, Director of VACHS Cancer Center, and Chandrika Kumar, MD, Director of VACHS Community Living Center, for their collaboration in care for this veteran.
1. Chang G, Meadows ME, Jones JA, Antin JH, Orav EJ. Substance use and survival after treatment for chronic myelogenous leukemia (CML) or myelodysplastic syndrome (MDS). Am J Drug Alcohol Ab. 2010;36(1):1-6. doi:10.3109/00952990903490758
2. Stagno S, Busby K, Shapiro A, Kotz M. Patients at risk: addressing addiction in patients undergoing hematopoietic SCT. Bone Marrow Transplant. 2008;42(4):221-226. doi:10.1038/bmt.2008.211
3. Arora NP. Cutaneous vasculopathy and neutropenia associated with levamisole-adulterated cocaine. Am J Med Sci. 2013;345(1):45-51. doi:10.1097/MAJ.0b013e31825b2b50
4. Schwartz BG, Rezkalla S, Kloner RA. Cardiovascular effects of cocaine. Circulation. 2010;122(24):2558-2569. doi:10.1161/CIRCULATIONAHA.110.940569
5. US Department of Veterans Affairs, US Department of Defense. VA/DoD clinical practice guideline for the management of substance use disorders. Published 2015. Accessed July 8, 2021. https://www.healthquality.va.gov/guidelines/MH/sud/VADODSUDCPGRevised22216.pdf
6. Mehta A, Chan LS. Understanding of the concept of “total pain”: a prerequisite for pain control. J Hosp Palliat Nurs. 2008;10(1):26-32. doi:10.1097/01.NJH.0000306714.50539.1a
7. Rubinsak LA, Terplan M, Martin CE, Fields EC, McGuire WP, Temkin SM. Co-occurring substance use disorder: The impact on treatment adherence in women with locally advanced cervical cancer. Gynecol Oncol Rep. 2019;28:116-119. Published 2019 Mar 27. doi:10.1016/j.gore.2019.03.016
8. Chhatre S, Metzger DS, Malkowicz SB, Woody G, Jayadevappa R. Substance use disorder and its effects on outcomes in men with advanced-stage prostate cancer. Cancer. 2014;120(21):3338-3345. doi:10.1002/cncr.28861
9. Concannon K, Thayer JH, Hicks R, et al. Outcomes among patients with a history of substance abuse in non-small cell lung cancer: a county hospital experience. J Clin Onc. 2019;37(15)(suppl):e20031-e20031. doi:10.1200/JCO.2019.37.15
10. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: pancreatic adenocarcinoma. Version 2.2021. Updated February 25, 2021. Accessed July 8, 2021. https://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf
11. Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817-1825. doi:10.1056/NEJMoa1011923
12. Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691-1703. doi:10.1056/NEJMoa1304369
13. Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001-2010: Implications for screening, diagnosis and treatment. Drug Alcohol Depend. 2011;116(1-3):93-101. doi:10.1016/j.drugalcdep.2010.11.027
14. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. American Psychiatric Association; 2013.
1. Chang G, Meadows ME, Jones JA, Antin JH, Orav EJ. Substance use and survival after treatment for chronic myelogenous leukemia (CML) or myelodysplastic syndrome (MDS). Am J Drug Alcohol Ab. 2010;36(1):1-6. doi:10.3109/00952990903490758
2. Stagno S, Busby K, Shapiro A, Kotz M. Patients at risk: addressing addiction in patients undergoing hematopoietic SCT. Bone Marrow Transplant. 2008;42(4):221-226. doi:10.1038/bmt.2008.211
3. Arora NP. Cutaneous vasculopathy and neutropenia associated with levamisole-adulterated cocaine. Am J Med Sci. 2013;345(1):45-51. doi:10.1097/MAJ.0b013e31825b2b50
4. Schwartz BG, Rezkalla S, Kloner RA. Cardiovascular effects of cocaine. Circulation. 2010;122(24):2558-2569. doi:10.1161/CIRCULATIONAHA.110.940569
5. US Department of Veterans Affairs, US Department of Defense. VA/DoD clinical practice guideline for the management of substance use disorders. Published 2015. Accessed July 8, 2021. https://www.healthquality.va.gov/guidelines/MH/sud/VADODSUDCPGRevised22216.pdf
6. Mehta A, Chan LS. Understanding of the concept of “total pain”: a prerequisite for pain control. J Hosp Palliat Nurs. 2008;10(1):26-32. doi:10.1097/01.NJH.0000306714.50539.1a
7. Rubinsak LA, Terplan M, Martin CE, Fields EC, McGuire WP, Temkin SM. Co-occurring substance use disorder: The impact on treatment adherence in women with locally advanced cervical cancer. Gynecol Oncol Rep. 2019;28:116-119. Published 2019 Mar 27. doi:10.1016/j.gore.2019.03.016
8. Chhatre S, Metzger DS, Malkowicz SB, Woody G, Jayadevappa R. Substance use disorder and its effects on outcomes in men with advanced-stage prostate cancer. Cancer. 2014;120(21):3338-3345. doi:10.1002/cncr.28861
9. Concannon K, Thayer JH, Hicks R, et al. Outcomes among patients with a history of substance abuse in non-small cell lung cancer: a county hospital experience. J Clin Onc. 2019;37(15)(suppl):e20031-e20031. doi:10.1200/JCO.2019.37.15
10. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: pancreatic adenocarcinoma. Version 2.2021. Updated February 25, 2021. Accessed July 8, 2021. https://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf
11. Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817-1825. doi:10.1056/NEJMoa1011923
12. Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691-1703. doi:10.1056/NEJMoa1304369
13. Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001-2010: Implications for screening, diagnosis and treatment. Drug Alcohol Depend. 2011;116(1-3):93-101. doi:10.1016/j.drugalcdep.2010.11.027
14. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. American Psychiatric Association; 2013.