User login
Risk Factors and Management of Skin Cancer Among Active-Duty Servicemembers and Veterans
Melanoma Risk for Servicemembers
Dr. Dunn: Active-duty jobs are quite diverse. We have had almost every civilian occupation category—everything from clerical to food service to outdoor construction workers. Federal service and active-duty military service could lead to assignments that involve high sunlight exposure and subsequently higher risk for melanoma and nonmelanoma skin cancer.
Dr. Miller: I found 2 articles on the topic. The first published in June 2018 reviewed melanoma and nonmelanoma skin cancers in the military.1 Riemenschneider and colleagues1 looked at 9 studies. Statistically, there was increased risk of melanoma associated with service and/or prisoner-of-war status. In World War II, they found tropical environments had the highest risk. And the highest rates were in the US Air Force.
The other article provided US Department of Defense data on skin cancer incidence rates, incidence rates of malignant melanoma in relation to years of military service overall, and the rates for differing military occupational groups.2 The researchers demonstrated that fixed-wing pilots and crew members had the highest rates of developing melanoma. The general trend was that the incidence rate was exponentially higher with more missions flown in relation to years of active service, which I thought was rather interesting.
For other occupational categories, the rate increase was not as great as those involved in aviation. Yes, it’s probably related to exposure. Flying at 40,000 feet on a transcontinental airplane trip is equivalent to the radiation dosage of a chest X-ray. Given all the training time and operational flying for the Air Force, it is anticipated that that mutagenic radiation would increase rates. An aircraft does not offer a lot of protection, especially in the cockpit.
We just had the anniversary of the Apollo 11 mission. Those astronauts received the equivalent of about 40 chest X-rays going to the moon and back. Exposure to UV and at higher altitudes cosmic radiation explains why we would see that more in Air Force personnel.
Dr. Bandino: At high altitude there is less ozone protecting you, although the shielding in a cockpit is better in modern aircraft. As an Air Force member, that was one of the first things I thought about was that an aviator has increased skin cancer risk. But it’s apt to think of military service in general as an occupational risk because there are so many contingency operations and deployments. Regarding sun exposure, sunscreen is provided nowadays and there is more sun awareness, but there is still a stigma and reluctance to apply the sunscreen. It leaves people’s skin feeling greasy, which is not ideal when one has to handle a firearm. It can also get in someone’s eyes and affect vision and performance during combat operations. In other words, there are many reasons that would reduce the desire to wear sunscreen and therefore increase exposure to the elements.
A great current example is coronavirus disease 2019 (COVID-19) operations. Although I’m a dermatologist and typically work inside, I’ve been tasked to run a COVID-19 screening tent in the middle of a field in San Antonio, and thus I’ve got to make sure I take my sunscreen out there every day. The general population may not have that variability in their work cycle and sudden change in occupational UV exposure.
Dr. Miller: I was deployed in a combat zone for operations Desert Shield and Desert Storm. I was with the 2nd Armored Division of the US Army deployed to the desert. There really wasn’t an emphasis on photoprotection. It’s just the logistics. The commanders have a lot more important things to think about, and that’s something, usually, that doesn’t get a high priority. The US military is deploying to more places near the equator, so from an operational sense, there’s probably something to brief the commanders about in terms of the long-term consequences of radiation exposure for military servicemembers.
Dr. Dunn: If you look at deployments over the past 2 decades, we have been putting tens of thousands of individuals in high UV exposure regions. Then you have to look at the long-term consequence of the increased incidence of skin cancer in those individuals. What is the cost of that when it comes to treatment of precancerous lesions and skin cancer throughout a life expectancy of 80-plus years?
Dr. Bandino: With most skin cancers there is such long lag time between exposures and development. I wish there were some better data and research out there that really showed whether military service truly is an independent risk factor or if it’s just specific occupation types within the military. I have family members who both work in contracting services and had served in the military. Would their skin cancer risk be the same as others who are doing similar jobs without the military service?
Dr. Dunn: I have had county employees present for skin cancer surgery and with them comes a form that relates to disability. For groundskeepers or police, we assumed that skin cancer is occupation related due to the patient’s increased sun exposure. Their cancers may be unrelated to their actual years of service, but it seems that many light-skinned individuals in the military are going to develop basal cell and squamous cell skin cancer in the coming decades, which likely is going to be attributed to their years of federal service, even though they may have had other significant recreational exposure outside of work. So, my gut feeling is that we are going to see skin cancer as a disability tied to federal service, which is going to cost us.
Dr. Logemann: Yes, I think there are always going to be confounders—what if the servicemembers used tanning beds, or they were avid surfers? It’s going to be difficult to always parse that out.
Dr. Miller: In talking about melanoma, you really have to parse out the subsets. Is it melanoma in situ, is it superficial, is it acral, is it nodular? They all have different initiation events.
Nodular melanomas probably don’t need UV light to initiate a tumor. Another risk factor is having more than 100 moles or many atypical moles, which puts that person in a higher risk category. Perhaps when soldiers, airmen, and navy personnel get inducted, they should be screened for their mole population because that is a risk factor for developing melanoma, and then we can intervene a little bit and have them watch their UV exposure.
Dr. Jarell: You can’t overstate the importance of how heterogeneous melanoma is as a disease. While there are clearly some types of melanoma that are caused by UV radiation, there are also many types that aren’t. We don’t understand why someone gets melanoma on the inner thigh, bottom of the foot, top of the sole, inside the mouth, or in the genital region—these aren’t places of high sun exposure.
Lentigo maligna, as an example, is clearly caused by UV radiation in most cases. But there are so many other different types of melanoma that you can’t just attribute to UV radiation, and so you get into this whole other discussion as to why people are getting melanoma—military or not.
Dr. Bandino: When volunteering for military service, there’s the DoDMERB (Department of Defense Medical Examination Review Board) system that screens individuals for medical issues incompatible with military service such as severe psoriasis or atopic dermatitis. But to my knowledge, the DoDMERB process focuses more on current or past issues and does little to investigate for future risk of disease. A cutaneous example would be assessing quantity of dysplastic nevi, Fitzpatrick scale 1 phenotype, and family history of melanoma to determine risk of developing melanoma in someone who may have more UV exposure during their military service than a civilian. This dermatological future risk assessment was certainly not something I was trained to do as a flight surgeon when performing basic trainee flight physicals prior to becoming a dermatologist.
Dr. Jarell: I am a little bit hard-pressed to generalize the military as high occupational risk for melanoma. There are clearly other professions—landscapers, fishermen—that are probably at much higher risk than, say, your general military all-comers. Us physicians in the military were probably not at increased risk compared to other physicians in the United States. We have to be careful not to go down a slippery slope and designate all MOSs (military occupational specialties) as at increased risk for skin cancer, in particular melanoma. Nonmelanoma skin cancer, such as basal cell and squamous cell carcinoma, is clearly related to the proportional amount of UV exposure. But melanoma is quite a diverse cancer that has many, many disparate etiologies.
Dr. Dunn: The entry physical into the military is an opportunity to make an impact on the number of nonmelanoma skin cancers that would arise in that population. There is an educational opportunity to tell inductees that nonmelanoma skin cancer is going to occur on convex surfaces of the sun-exposed skin—nose, ears, forehead, chin, tops of the shoulders. If offered sun protection for those areas and you stretch the potential impact of that information over tens of thousands of military members over decades, you might actually come up with a big number of people that not only decreases their morbidity but also dramatically decreased the cost to the system as a whole.
Dr. Jarell: You also have to factor in ethnicity and the role it plays in someone’s likelihood to get skin cancer—melanoma or nonmelanoma skin cancer. Darker-skinned people are at certainly decreased risk for different types of skin cancers.
Dr. Dunn: Yes, that would have to be part of the education and should be. If you have light skin and freckles, then you’re at much higher risk for nonmelanoma skin cancer and need to know the high-risk areas that can be protected by sunblock and clothing.
Dr. Logemann: One thing that might be a little bit unique in the military is that you’re living in San Antonio one minute, and then the next minute you’re over in Afghanistan with a different climate and different environment. When you’re deployed overseas, you might have a little bit less control over your situation; you might not have a lot of sunscreen in a field hospital in Afghanistan. Whereas if you were just living in San Antonio, you could go down to the store and buy it.
Dr. Miller: Is sunblock now encouraged or available to individuals in deployment situations or training situations where they’re going to have prolonged sun exposure every day? Is it part of the regimen, just like carrying extra water because of the risk for dehydration?
Dr. Logemann: To the best of my knowledge, it is not always included in your normal rations or uniform and it may be up to the servicemember to procure sunscreen.
Dr. Bandino: There have been improvements, and usually you at least have access to sunscreen. In many deployed locations, for example, you have the equivalent of a small PX (post exchange) or BX (base exchange), where they have a variety of products for sale from toothbrushes to flip-flops, and now also sunscreen. Of course, the type and quality of the sunscreen may not be that great. It’s likely going to be basic SPF (sun protection factor) 15 or 30 in small tubes. As a recent example, I participated in a humanitarian medical exercise in South America last summer and was actually issued sunscreen combined with DEET, which is great but it was only SPF 30. The combination product is a good idea for tropical locations, but in addition to people just not wanting to wear it, the DEET combination tends to burn and sting a little bit more; you can get a heat sensation from the DEET; and the DEET can damage plastic surfaces, which may not be ideal for deployed equipment.
The other problem is quantity. We all learned in residency the appropriate sunscreen quantity of at least 1 fl oz for the average adult body, and that’s what we counsel our patients on, but what they issued me was 1 small 2- to 3-fl oz tube. It fit in the palm of my hand, and that was my sunscreen for the trip.
So, I do think, even though there have been some improvements, much of sun protection will still fall on the individual servicemember. And, as mentioned, depending on your ethnicity, some people may need it more than others. But it is an area where there probably could be continued improvements.
Dr. Logemann: In addition to sunscreen, I think that maybe we should be taking into consideration some simple measures. For example, is it necessary for people to stand out in formation at 2
Dr. Dunn: I think we all kind of agree that the military service is diverse and that many of the subcategories of occupations within the military lead to increased sun exposure by mandate. We advise sun protection by physical barriers and sunblock.
Diagnosis of Skin Cancer Via Telemedicine
Dr. Dunn: I have friends who remain in the VA (US Department of Veterans Affairs) system, and they are involved with telemedicine in dermatology, which can reduce waiting time and increase the number of patients seen by the dermatologist. In-person and teledermatology visits now are available to servicemembers on active duty and retirees.
Dr. Bandino: At our residency program (San Antonio Uniformed Services Health Education Consortium), we’ve had asynchronous teledermatology for over a decade, even before I was a resident. We provide it primarily as a service for patients at small bases without access to dermatology. Some bases also use it as part of their prescreening process prior to authorizing an in-person dermatology consultation.
Certainly, with the coronavirus pandemic, civilian dermatology is seeing a boom in the teledermatology world that had been slowly increasing in popularity for the last few years. In our residency program, teledermatology has traditionally been just for active-duty servicemembers or their dependents, but now due to the coronavirus pandemic, our teledermatology services have significantly expanded to include adding synchronous capability. We have patients take pictures before their virtual appointment and/or FaceTime during the appointment. Even after the pandemic, there will likely be more integration of synchronous teledermatology going forward as we’re seeing some of the value. Of course, I’m sure we would all agree that accurate diagnosis of pigmented lesions can be very challenging with teledermatology, not to mention other diagnostic limitations. But I think there is still utility and it should only get better with time as technology improves. So, I’m hopeful that we can incorporate more of it in the military.
Dr. Logemann: I’m definitely aware that we have different telehealth opportunities available, even using some newer modalities that are command approved in recent weeks. My experience has been for more complicated dermatology, so people are in remote locations, and they’re being seen by a nondermatologist, and they have questions about how to approach management. But I’m not aware of telemedicine as a screening tool for skin cancer in the military or among my civilian colleagues. I would hope that it could be someday because we’re developing these total-body photography machines as well. It could be a way for a nondermatologist who identifies a lesion to have it triaged by a dermatologist. To say, “Oh yeah, that looks like a melanoma. They need to get in sooner vs later,” but not on a large-scale sort of screening modality.
Dr. Bandino: In my recent experience, it has definitely been a helpful triage tool. In the military, this form of triage can be particularly helpful if someone is overseas to determine whether he/she needs to evacuated and evaluated in-person right away.
Dr. Jarell: It’s been useful in looking at benign things. People have shown me in the past few weeks a lot of seborrheic keratoses and a lot of benign dermal nevus-type things, and I say, “Don’t worry about that.” And you can tell if the resolution is good enough. But a lot of people have shown me things in the past few weeks that have clearly been basal cell carcinoma, which we can probably let that ride out for a few more weeks, but I’m not sure if maybe somebody has an amelanotic melanoma. Maybe you need to come in and get that biopsied ASAP. Or something that looks like a melanoma. The patient should probably come in and get that biopsied.
Dr. Miller: I think we can rely on teledermatology. It’s all predicated on the resolution because we’re all trained in pattern recognition. I think it’s very useful to screen for things that look clinically benign. We have to understand that most dermatology is practiced by nondermatologists in the United States, and many studies show that their diagnostic accuracy is 20%, at best maybe 50%. So, they do need to reach out to a dermatologist and perhaps get some guidance on what to do. I think it could be a very useful tool if used appropriately.
Dr. Dunn: If used appropriately, teledermatology could function in a couple of ways. One, it could allow us to declare lesions to be wholly benign, and only should a lesion change would it need attention. The second is that it would allow us to accelerate the process of getting a patient to us—physically in front of us—for a biopsy if a suspicious lesion is seen. A by-product of that process would be that if patients who have wholly benign, nonworrisome lesions could be screened by telemedicine, then physical appointments where a patient is in front of the doctor would be more open. In other words, let’s say if 25% of all lesional visits could be declared benign via telemedicine that would allow dermatology to preserve its face-to-face appointments for patients who are more likely to have cancer and require procedures like skin biopsy.
Love it or hate it, I think we’re getting it no matter what now. Telemedicine creeped along forever and within 6 weeks it’s become ubiquitous. It’s phenomenal how fast we had to adapt to a system or perish in private practice. Sometimes these episodes that we go through have good consequences as well as bad consequences. Telemedicine probably has been needed for a long time and the insurers were not covering it very well, but suddenly a stay-at-home mandate has unveiled valuable technology—something that we probably should have been able to use more and be adequately reimbursed.
Surgical Treatment of Skin Cancer
Dr. Dunn: Treatment historically has been surgical for nonmelanoma and melanoma skin cancers. Some radiation devices have gained popularity again in the past decade or so, but excisional surgery remains the standard treatment for skin cancer. Nonmelanoma skin cancers almost all are probably treated surgically still, with a small percentage treated with superficial radiation.
Access to care is important to discuss. Are Mohs surgeons readily available, or are plastic surgeons, general surgeons, or vascular surgeons in the federal system contributing to the care of skin cancer? Are they doing excisional surgery after biopsies are done? Are they doing excisional biopsies with the intent of cure?
Dr. Logemann: For active duty, I don’t see any issues getting access to the medical center for Mohs micrographic surgery. Sometimes, if we have a lot of volume, some patients may get deferred to the network, but in my experience, it would not typically be an active-duty servicemember. An active-duty servicemember would get care rendered at one of the medical centers for Mohs surgery. Typically the active-duty–aged population isn’t getting much skin cancer. It certainly does happen, but most of the skin cancers frequently that are treated at medical centers are not infrequently retirees.
Dr. Bandino: Because of our residency program, we are required to have Mohs surgery capability to be ACGME (Accreditation Council for Graduate Medical Education) accredited. We typically have 3 Mohs surgeons, so we never have a problem with access.
In the military, I just refer cases to our Mohs surgeons and everything is taken care of in-house. In fact, this is an area where we may even have better access than the civilian world because there are no insurance hurdles or significant delay in care since our Mohs surgeons aren’t typically booked up for 3 to 4 months like many civilian Mohs surgeons. This is especially true for complex cases since we provide hospital-based care with all specialty services under the same umbrella. So, for example, if the Mohs surgeons have an extensive and complex case requiring multidisciplinary care such as ENT (ear, nose, and throat), facial plastics, or radiation-oncology, they’re all in-house with no insurance issues to navigate. This of course is not usual for most military bases and is only capable at bases attached to a large medical center. There are some similar scenarios in the civilian world with university medical centers and managed care organizations, but we may still have a slight advantage in accessibility and cost.
Dr. Dunn: There are guidelines from the National Comprehensive Cancer Network as to how to treat nonmelanoma and melanoma skin cancer. Almost all of them are surgical and almost all of them are safe, outpatient, local anesthetic procedures with a high cure rate. The vast majority of melanoma and nonmelanoma skin cancers can be handled safely and effectively with minimal morbidity and almost no known mortalities from the treatments themselves. Some of the cancers have been identified as high risk for metastasis and mortality, but they’re relatively uncommon still. The good news about skin cancer is that the risk of death remains very small.
- Riemenschneider K, Liu J, Powers JG. Skin cancer in the military: a systematic review of melanoma and nonmelanoma skin cancer incidence, prevention, and screening among active duty and veteran personnel.J Am Acad Dermatol. 2018;78:1185-1192.
- Brundage JF, Williams VF, Stahlman S, et al. Incidence rates of malignant melanoma in relation to years of military service, overall and in selected military occupational groups, active component, U.S. Armed Forces, 2001-2015. MSMR. 2017;24:8-14.
Melanoma Risk for Servicemembers
Dr. Dunn: Active-duty jobs are quite diverse. We have had almost every civilian occupation category—everything from clerical to food service to outdoor construction workers. Federal service and active-duty military service could lead to assignments that involve high sunlight exposure and subsequently higher risk for melanoma and nonmelanoma skin cancer.
Dr. Miller: I found 2 articles on the topic. The first published in June 2018 reviewed melanoma and nonmelanoma skin cancers in the military.1 Riemenschneider and colleagues1 looked at 9 studies. Statistically, there was increased risk of melanoma associated with service and/or prisoner-of-war status. In World War II, they found tropical environments had the highest risk. And the highest rates were in the US Air Force.
The other article provided US Department of Defense data on skin cancer incidence rates, incidence rates of malignant melanoma in relation to years of military service overall, and the rates for differing military occupational groups.2 The researchers demonstrated that fixed-wing pilots and crew members had the highest rates of developing melanoma. The general trend was that the incidence rate was exponentially higher with more missions flown in relation to years of active service, which I thought was rather interesting.
For other occupational categories, the rate increase was not as great as those involved in aviation. Yes, it’s probably related to exposure. Flying at 40,000 feet on a transcontinental airplane trip is equivalent to the radiation dosage of a chest X-ray. Given all the training time and operational flying for the Air Force, it is anticipated that that mutagenic radiation would increase rates. An aircraft does not offer a lot of protection, especially in the cockpit.
We just had the anniversary of the Apollo 11 mission. Those astronauts received the equivalent of about 40 chest X-rays going to the moon and back. Exposure to UV and at higher altitudes cosmic radiation explains why we would see that more in Air Force personnel.
Dr. Bandino: At high altitude there is less ozone protecting you, although the shielding in a cockpit is better in modern aircraft. As an Air Force member, that was one of the first things I thought about was that an aviator has increased skin cancer risk. But it’s apt to think of military service in general as an occupational risk because there are so many contingency operations and deployments. Regarding sun exposure, sunscreen is provided nowadays and there is more sun awareness, but there is still a stigma and reluctance to apply the sunscreen. It leaves people’s skin feeling greasy, which is not ideal when one has to handle a firearm. It can also get in someone’s eyes and affect vision and performance during combat operations. In other words, there are many reasons that would reduce the desire to wear sunscreen and therefore increase exposure to the elements.
A great current example is coronavirus disease 2019 (COVID-19) operations. Although I’m a dermatologist and typically work inside, I’ve been tasked to run a COVID-19 screening tent in the middle of a field in San Antonio, and thus I’ve got to make sure I take my sunscreen out there every day. The general population may not have that variability in their work cycle and sudden change in occupational UV exposure.
Dr. Miller: I was deployed in a combat zone for operations Desert Shield and Desert Storm. I was with the 2nd Armored Division of the US Army deployed to the desert. There really wasn’t an emphasis on photoprotection. It’s just the logistics. The commanders have a lot more important things to think about, and that’s something, usually, that doesn’t get a high priority. The US military is deploying to more places near the equator, so from an operational sense, there’s probably something to brief the commanders about in terms of the long-term consequences of radiation exposure for military servicemembers.
Dr. Dunn: If you look at deployments over the past 2 decades, we have been putting tens of thousands of individuals in high UV exposure regions. Then you have to look at the long-term consequence of the increased incidence of skin cancer in those individuals. What is the cost of that when it comes to treatment of precancerous lesions and skin cancer throughout a life expectancy of 80-plus years?
Dr. Bandino: With most skin cancers there is such long lag time between exposures and development. I wish there were some better data and research out there that really showed whether military service truly is an independent risk factor or if it’s just specific occupation types within the military. I have family members who both work in contracting services and had served in the military. Would their skin cancer risk be the same as others who are doing similar jobs without the military service?
Dr. Dunn: I have had county employees present for skin cancer surgery and with them comes a form that relates to disability. For groundskeepers or police, we assumed that skin cancer is occupation related due to the patient’s increased sun exposure. Their cancers may be unrelated to their actual years of service, but it seems that many light-skinned individuals in the military are going to develop basal cell and squamous cell skin cancer in the coming decades, which likely is going to be attributed to their years of federal service, even though they may have had other significant recreational exposure outside of work. So, my gut feeling is that we are going to see skin cancer as a disability tied to federal service, which is going to cost us.
Dr. Logemann: Yes, I think there are always going to be confounders—what if the servicemembers used tanning beds, or they were avid surfers? It’s going to be difficult to always parse that out.
Dr. Miller: In talking about melanoma, you really have to parse out the subsets. Is it melanoma in situ, is it superficial, is it acral, is it nodular? They all have different initiation events.
Nodular melanomas probably don’t need UV light to initiate a tumor. Another risk factor is having more than 100 moles or many atypical moles, which puts that person in a higher risk category. Perhaps when soldiers, airmen, and navy personnel get inducted, they should be screened for their mole population because that is a risk factor for developing melanoma, and then we can intervene a little bit and have them watch their UV exposure.
Dr. Jarell: You can’t overstate the importance of how heterogeneous melanoma is as a disease. While there are clearly some types of melanoma that are caused by UV radiation, there are also many types that aren’t. We don’t understand why someone gets melanoma on the inner thigh, bottom of the foot, top of the sole, inside the mouth, or in the genital region—these aren’t places of high sun exposure.
Lentigo maligna, as an example, is clearly caused by UV radiation in most cases. But there are so many other different types of melanoma that you can’t just attribute to UV radiation, and so you get into this whole other discussion as to why people are getting melanoma—military or not.
Dr. Bandino: When volunteering for military service, there’s the DoDMERB (Department of Defense Medical Examination Review Board) system that screens individuals for medical issues incompatible with military service such as severe psoriasis or atopic dermatitis. But to my knowledge, the DoDMERB process focuses more on current or past issues and does little to investigate for future risk of disease. A cutaneous example would be assessing quantity of dysplastic nevi, Fitzpatrick scale 1 phenotype, and family history of melanoma to determine risk of developing melanoma in someone who may have more UV exposure during their military service than a civilian. This dermatological future risk assessment was certainly not something I was trained to do as a flight surgeon when performing basic trainee flight physicals prior to becoming a dermatologist.
Dr. Jarell: I am a little bit hard-pressed to generalize the military as high occupational risk for melanoma. There are clearly other professions—landscapers, fishermen—that are probably at much higher risk than, say, your general military all-comers. Us physicians in the military were probably not at increased risk compared to other physicians in the United States. We have to be careful not to go down a slippery slope and designate all MOSs (military occupational specialties) as at increased risk for skin cancer, in particular melanoma. Nonmelanoma skin cancer, such as basal cell and squamous cell carcinoma, is clearly related to the proportional amount of UV exposure. But melanoma is quite a diverse cancer that has many, many disparate etiologies.
Dr. Dunn: The entry physical into the military is an opportunity to make an impact on the number of nonmelanoma skin cancers that would arise in that population. There is an educational opportunity to tell inductees that nonmelanoma skin cancer is going to occur on convex surfaces of the sun-exposed skin—nose, ears, forehead, chin, tops of the shoulders. If offered sun protection for those areas and you stretch the potential impact of that information over tens of thousands of military members over decades, you might actually come up with a big number of people that not only decreases their morbidity but also dramatically decreased the cost to the system as a whole.
Dr. Jarell: You also have to factor in ethnicity and the role it plays in someone’s likelihood to get skin cancer—melanoma or nonmelanoma skin cancer. Darker-skinned people are at certainly decreased risk for different types of skin cancers.
Dr. Dunn: Yes, that would have to be part of the education and should be. If you have light skin and freckles, then you’re at much higher risk for nonmelanoma skin cancer and need to know the high-risk areas that can be protected by sunblock and clothing.
Dr. Logemann: One thing that might be a little bit unique in the military is that you’re living in San Antonio one minute, and then the next minute you’re over in Afghanistan with a different climate and different environment. When you’re deployed overseas, you might have a little bit less control over your situation; you might not have a lot of sunscreen in a field hospital in Afghanistan. Whereas if you were just living in San Antonio, you could go down to the store and buy it.
Dr. Miller: Is sunblock now encouraged or available to individuals in deployment situations or training situations where they’re going to have prolonged sun exposure every day? Is it part of the regimen, just like carrying extra water because of the risk for dehydration?
Dr. Logemann: To the best of my knowledge, it is not always included in your normal rations or uniform and it may be up to the servicemember to procure sunscreen.
Dr. Bandino: There have been improvements, and usually you at least have access to sunscreen. In many deployed locations, for example, you have the equivalent of a small PX (post exchange) or BX (base exchange), where they have a variety of products for sale from toothbrushes to flip-flops, and now also sunscreen. Of course, the type and quality of the sunscreen may not be that great. It’s likely going to be basic SPF (sun protection factor) 15 or 30 in small tubes. As a recent example, I participated in a humanitarian medical exercise in South America last summer and was actually issued sunscreen combined with DEET, which is great but it was only SPF 30. The combination product is a good idea for tropical locations, but in addition to people just not wanting to wear it, the DEET combination tends to burn and sting a little bit more; you can get a heat sensation from the DEET; and the DEET can damage plastic surfaces, which may not be ideal for deployed equipment.
The other problem is quantity. We all learned in residency the appropriate sunscreen quantity of at least 1 fl oz for the average adult body, and that’s what we counsel our patients on, but what they issued me was 1 small 2- to 3-fl oz tube. It fit in the palm of my hand, and that was my sunscreen for the trip.
So, I do think, even though there have been some improvements, much of sun protection will still fall on the individual servicemember. And, as mentioned, depending on your ethnicity, some people may need it more than others. But it is an area where there probably could be continued improvements.
Dr. Logemann: In addition to sunscreen, I think that maybe we should be taking into consideration some simple measures. For example, is it necessary for people to stand out in formation at 2
Dr. Dunn: I think we all kind of agree that the military service is diverse and that many of the subcategories of occupations within the military lead to increased sun exposure by mandate. We advise sun protection by physical barriers and sunblock.
Diagnosis of Skin Cancer Via Telemedicine
Dr. Dunn: I have friends who remain in the VA (US Department of Veterans Affairs) system, and they are involved with telemedicine in dermatology, which can reduce waiting time and increase the number of patients seen by the dermatologist. In-person and teledermatology visits now are available to servicemembers on active duty and retirees.
Dr. Bandino: At our residency program (San Antonio Uniformed Services Health Education Consortium), we’ve had asynchronous teledermatology for over a decade, even before I was a resident. We provide it primarily as a service for patients at small bases without access to dermatology. Some bases also use it as part of their prescreening process prior to authorizing an in-person dermatology consultation.
Certainly, with the coronavirus pandemic, civilian dermatology is seeing a boom in the teledermatology world that had been slowly increasing in popularity for the last few years. In our residency program, teledermatology has traditionally been just for active-duty servicemembers or their dependents, but now due to the coronavirus pandemic, our teledermatology services have significantly expanded to include adding synchronous capability. We have patients take pictures before their virtual appointment and/or FaceTime during the appointment. Even after the pandemic, there will likely be more integration of synchronous teledermatology going forward as we’re seeing some of the value. Of course, I’m sure we would all agree that accurate diagnosis of pigmented lesions can be very challenging with teledermatology, not to mention other diagnostic limitations. But I think there is still utility and it should only get better with time as technology improves. So, I’m hopeful that we can incorporate more of it in the military.
Dr. Logemann: I’m definitely aware that we have different telehealth opportunities available, even using some newer modalities that are command approved in recent weeks. My experience has been for more complicated dermatology, so people are in remote locations, and they’re being seen by a nondermatologist, and they have questions about how to approach management. But I’m not aware of telemedicine as a screening tool for skin cancer in the military or among my civilian colleagues. I would hope that it could be someday because we’re developing these total-body photography machines as well. It could be a way for a nondermatologist who identifies a lesion to have it triaged by a dermatologist. To say, “Oh yeah, that looks like a melanoma. They need to get in sooner vs later,” but not on a large-scale sort of screening modality.
Dr. Bandino: In my recent experience, it has definitely been a helpful triage tool. In the military, this form of triage can be particularly helpful if someone is overseas to determine whether he/she needs to evacuated and evaluated in-person right away.
Dr. Jarell: It’s been useful in looking at benign things. People have shown me in the past few weeks a lot of seborrheic keratoses and a lot of benign dermal nevus-type things, and I say, “Don’t worry about that.” And you can tell if the resolution is good enough. But a lot of people have shown me things in the past few weeks that have clearly been basal cell carcinoma, which we can probably let that ride out for a few more weeks, but I’m not sure if maybe somebody has an amelanotic melanoma. Maybe you need to come in and get that biopsied ASAP. Or something that looks like a melanoma. The patient should probably come in and get that biopsied.
Dr. Miller: I think we can rely on teledermatology. It’s all predicated on the resolution because we’re all trained in pattern recognition. I think it’s very useful to screen for things that look clinically benign. We have to understand that most dermatology is practiced by nondermatologists in the United States, and many studies show that their diagnostic accuracy is 20%, at best maybe 50%. So, they do need to reach out to a dermatologist and perhaps get some guidance on what to do. I think it could be a very useful tool if used appropriately.
Dr. Dunn: If used appropriately, teledermatology could function in a couple of ways. One, it could allow us to declare lesions to be wholly benign, and only should a lesion change would it need attention. The second is that it would allow us to accelerate the process of getting a patient to us—physically in front of us—for a biopsy if a suspicious lesion is seen. A by-product of that process would be that if patients who have wholly benign, nonworrisome lesions could be screened by telemedicine, then physical appointments where a patient is in front of the doctor would be more open. In other words, let’s say if 25% of all lesional visits could be declared benign via telemedicine that would allow dermatology to preserve its face-to-face appointments for patients who are more likely to have cancer and require procedures like skin biopsy.
Love it or hate it, I think we’re getting it no matter what now. Telemedicine creeped along forever and within 6 weeks it’s become ubiquitous. It’s phenomenal how fast we had to adapt to a system or perish in private practice. Sometimes these episodes that we go through have good consequences as well as bad consequences. Telemedicine probably has been needed for a long time and the insurers were not covering it very well, but suddenly a stay-at-home mandate has unveiled valuable technology—something that we probably should have been able to use more and be adequately reimbursed.
Surgical Treatment of Skin Cancer
Dr. Dunn: Treatment historically has been surgical for nonmelanoma and melanoma skin cancers. Some radiation devices have gained popularity again in the past decade or so, but excisional surgery remains the standard treatment for skin cancer. Nonmelanoma skin cancers almost all are probably treated surgically still, with a small percentage treated with superficial radiation.
Access to care is important to discuss. Are Mohs surgeons readily available, or are plastic surgeons, general surgeons, or vascular surgeons in the federal system contributing to the care of skin cancer? Are they doing excisional surgery after biopsies are done? Are they doing excisional biopsies with the intent of cure?
Dr. Logemann: For active duty, I don’t see any issues getting access to the medical center for Mohs micrographic surgery. Sometimes, if we have a lot of volume, some patients may get deferred to the network, but in my experience, it would not typically be an active-duty servicemember. An active-duty servicemember would get care rendered at one of the medical centers for Mohs surgery. Typically the active-duty–aged population isn’t getting much skin cancer. It certainly does happen, but most of the skin cancers frequently that are treated at medical centers are not infrequently retirees.
Dr. Bandino: Because of our residency program, we are required to have Mohs surgery capability to be ACGME (Accreditation Council for Graduate Medical Education) accredited. We typically have 3 Mohs surgeons, so we never have a problem with access.
In the military, I just refer cases to our Mohs surgeons and everything is taken care of in-house. In fact, this is an area where we may even have better access than the civilian world because there are no insurance hurdles or significant delay in care since our Mohs surgeons aren’t typically booked up for 3 to 4 months like many civilian Mohs surgeons. This is especially true for complex cases since we provide hospital-based care with all specialty services under the same umbrella. So, for example, if the Mohs surgeons have an extensive and complex case requiring multidisciplinary care such as ENT (ear, nose, and throat), facial plastics, or radiation-oncology, they’re all in-house with no insurance issues to navigate. This of course is not usual for most military bases and is only capable at bases attached to a large medical center. There are some similar scenarios in the civilian world with university medical centers and managed care organizations, but we may still have a slight advantage in accessibility and cost.
Dr. Dunn: There are guidelines from the National Comprehensive Cancer Network as to how to treat nonmelanoma and melanoma skin cancer. Almost all of them are surgical and almost all of them are safe, outpatient, local anesthetic procedures with a high cure rate. The vast majority of melanoma and nonmelanoma skin cancers can be handled safely and effectively with minimal morbidity and almost no known mortalities from the treatments themselves. Some of the cancers have been identified as high risk for metastasis and mortality, but they’re relatively uncommon still. The good news about skin cancer is that the risk of death remains very small.
Melanoma Risk for Servicemembers
Dr. Dunn: Active-duty jobs are quite diverse. We have had almost every civilian occupation category—everything from clerical to food service to outdoor construction workers. Federal service and active-duty military service could lead to assignments that involve high sunlight exposure and subsequently higher risk for melanoma and nonmelanoma skin cancer.
Dr. Miller: I found 2 articles on the topic. The first published in June 2018 reviewed melanoma and nonmelanoma skin cancers in the military.1 Riemenschneider and colleagues1 looked at 9 studies. Statistically, there was increased risk of melanoma associated with service and/or prisoner-of-war status. In World War II, they found tropical environments had the highest risk. And the highest rates were in the US Air Force.
The other article provided US Department of Defense data on skin cancer incidence rates, incidence rates of malignant melanoma in relation to years of military service overall, and the rates for differing military occupational groups.2 The researchers demonstrated that fixed-wing pilots and crew members had the highest rates of developing melanoma. The general trend was that the incidence rate was exponentially higher with more missions flown in relation to years of active service, which I thought was rather interesting.
For other occupational categories, the rate increase was not as great as those involved in aviation. Yes, it’s probably related to exposure. Flying at 40,000 feet on a transcontinental airplane trip is equivalent to the radiation dosage of a chest X-ray. Given all the training time and operational flying for the Air Force, it is anticipated that that mutagenic radiation would increase rates. An aircraft does not offer a lot of protection, especially in the cockpit.
We just had the anniversary of the Apollo 11 mission. Those astronauts received the equivalent of about 40 chest X-rays going to the moon and back. Exposure to UV and at higher altitudes cosmic radiation explains why we would see that more in Air Force personnel.
Dr. Bandino: At high altitude there is less ozone protecting you, although the shielding in a cockpit is better in modern aircraft. As an Air Force member, that was one of the first things I thought about was that an aviator has increased skin cancer risk. But it’s apt to think of military service in general as an occupational risk because there are so many contingency operations and deployments. Regarding sun exposure, sunscreen is provided nowadays and there is more sun awareness, but there is still a stigma and reluctance to apply the sunscreen. It leaves people’s skin feeling greasy, which is not ideal when one has to handle a firearm. It can also get in someone’s eyes and affect vision and performance during combat operations. In other words, there are many reasons that would reduce the desire to wear sunscreen and therefore increase exposure to the elements.
A great current example is coronavirus disease 2019 (COVID-19) operations. Although I’m a dermatologist and typically work inside, I’ve been tasked to run a COVID-19 screening tent in the middle of a field in San Antonio, and thus I’ve got to make sure I take my sunscreen out there every day. The general population may not have that variability in their work cycle and sudden change in occupational UV exposure.
Dr. Miller: I was deployed in a combat zone for operations Desert Shield and Desert Storm. I was with the 2nd Armored Division of the US Army deployed to the desert. There really wasn’t an emphasis on photoprotection. It’s just the logistics. The commanders have a lot more important things to think about, and that’s something, usually, that doesn’t get a high priority. The US military is deploying to more places near the equator, so from an operational sense, there’s probably something to brief the commanders about in terms of the long-term consequences of radiation exposure for military servicemembers.
Dr. Dunn: If you look at deployments over the past 2 decades, we have been putting tens of thousands of individuals in high UV exposure regions. Then you have to look at the long-term consequence of the increased incidence of skin cancer in those individuals. What is the cost of that when it comes to treatment of precancerous lesions and skin cancer throughout a life expectancy of 80-plus years?
Dr. Bandino: With most skin cancers there is such long lag time between exposures and development. I wish there were some better data and research out there that really showed whether military service truly is an independent risk factor or if it’s just specific occupation types within the military. I have family members who both work in contracting services and had served in the military. Would their skin cancer risk be the same as others who are doing similar jobs without the military service?
Dr. Dunn: I have had county employees present for skin cancer surgery and with them comes a form that relates to disability. For groundskeepers or police, we assumed that skin cancer is occupation related due to the patient’s increased sun exposure. Their cancers may be unrelated to their actual years of service, but it seems that many light-skinned individuals in the military are going to develop basal cell and squamous cell skin cancer in the coming decades, which likely is going to be attributed to their years of federal service, even though they may have had other significant recreational exposure outside of work. So, my gut feeling is that we are going to see skin cancer as a disability tied to federal service, which is going to cost us.
Dr. Logemann: Yes, I think there are always going to be confounders—what if the servicemembers used tanning beds, or they were avid surfers? It’s going to be difficult to always parse that out.
Dr. Miller: In talking about melanoma, you really have to parse out the subsets. Is it melanoma in situ, is it superficial, is it acral, is it nodular? They all have different initiation events.
Nodular melanomas probably don’t need UV light to initiate a tumor. Another risk factor is having more than 100 moles or many atypical moles, which puts that person in a higher risk category. Perhaps when soldiers, airmen, and navy personnel get inducted, they should be screened for their mole population because that is a risk factor for developing melanoma, and then we can intervene a little bit and have them watch their UV exposure.
Dr. Jarell: You can’t overstate the importance of how heterogeneous melanoma is as a disease. While there are clearly some types of melanoma that are caused by UV radiation, there are also many types that aren’t. We don’t understand why someone gets melanoma on the inner thigh, bottom of the foot, top of the sole, inside the mouth, or in the genital region—these aren’t places of high sun exposure.
Lentigo maligna, as an example, is clearly caused by UV radiation in most cases. But there are so many other different types of melanoma that you can’t just attribute to UV radiation, and so you get into this whole other discussion as to why people are getting melanoma—military or not.
Dr. Bandino: When volunteering for military service, there’s the DoDMERB (Department of Defense Medical Examination Review Board) system that screens individuals for medical issues incompatible with military service such as severe psoriasis or atopic dermatitis. But to my knowledge, the DoDMERB process focuses more on current or past issues and does little to investigate for future risk of disease. A cutaneous example would be assessing quantity of dysplastic nevi, Fitzpatrick scale 1 phenotype, and family history of melanoma to determine risk of developing melanoma in someone who may have more UV exposure during their military service than a civilian. This dermatological future risk assessment was certainly not something I was trained to do as a flight surgeon when performing basic trainee flight physicals prior to becoming a dermatologist.
Dr. Jarell: I am a little bit hard-pressed to generalize the military as high occupational risk for melanoma. There are clearly other professions—landscapers, fishermen—that are probably at much higher risk than, say, your general military all-comers. Us physicians in the military were probably not at increased risk compared to other physicians in the United States. We have to be careful not to go down a slippery slope and designate all MOSs (military occupational specialties) as at increased risk for skin cancer, in particular melanoma. Nonmelanoma skin cancer, such as basal cell and squamous cell carcinoma, is clearly related to the proportional amount of UV exposure. But melanoma is quite a diverse cancer that has many, many disparate etiologies.
Dr. Dunn: The entry physical into the military is an opportunity to make an impact on the number of nonmelanoma skin cancers that would arise in that population. There is an educational opportunity to tell inductees that nonmelanoma skin cancer is going to occur on convex surfaces of the sun-exposed skin—nose, ears, forehead, chin, tops of the shoulders. If offered sun protection for those areas and you stretch the potential impact of that information over tens of thousands of military members over decades, you might actually come up with a big number of people that not only decreases their morbidity but also dramatically decreased the cost to the system as a whole.
Dr. Jarell: You also have to factor in ethnicity and the role it plays in someone’s likelihood to get skin cancer—melanoma or nonmelanoma skin cancer. Darker-skinned people are at certainly decreased risk for different types of skin cancers.
Dr. Dunn: Yes, that would have to be part of the education and should be. If you have light skin and freckles, then you’re at much higher risk for nonmelanoma skin cancer and need to know the high-risk areas that can be protected by sunblock and clothing.
Dr. Logemann: One thing that might be a little bit unique in the military is that you’re living in San Antonio one minute, and then the next minute you’re over in Afghanistan with a different climate and different environment. When you’re deployed overseas, you might have a little bit less control over your situation; you might not have a lot of sunscreen in a field hospital in Afghanistan. Whereas if you were just living in San Antonio, you could go down to the store and buy it.
Dr. Miller: Is sunblock now encouraged or available to individuals in deployment situations or training situations where they’re going to have prolonged sun exposure every day? Is it part of the regimen, just like carrying extra water because of the risk for dehydration?
Dr. Logemann: To the best of my knowledge, it is not always included in your normal rations or uniform and it may be up to the servicemember to procure sunscreen.
Dr. Bandino: There have been improvements, and usually you at least have access to sunscreen. In many deployed locations, for example, you have the equivalent of a small PX (post exchange) or BX (base exchange), where they have a variety of products for sale from toothbrushes to flip-flops, and now also sunscreen. Of course, the type and quality of the sunscreen may not be that great. It’s likely going to be basic SPF (sun protection factor) 15 or 30 in small tubes. As a recent example, I participated in a humanitarian medical exercise in South America last summer and was actually issued sunscreen combined with DEET, which is great but it was only SPF 30. The combination product is a good idea for tropical locations, but in addition to people just not wanting to wear it, the DEET combination tends to burn and sting a little bit more; you can get a heat sensation from the DEET; and the DEET can damage plastic surfaces, which may not be ideal for deployed equipment.
The other problem is quantity. We all learned in residency the appropriate sunscreen quantity of at least 1 fl oz for the average adult body, and that’s what we counsel our patients on, but what they issued me was 1 small 2- to 3-fl oz tube. It fit in the palm of my hand, and that was my sunscreen for the trip.
So, I do think, even though there have been some improvements, much of sun protection will still fall on the individual servicemember. And, as mentioned, depending on your ethnicity, some people may need it more than others. But it is an area where there probably could be continued improvements.
Dr. Logemann: In addition to sunscreen, I think that maybe we should be taking into consideration some simple measures. For example, is it necessary for people to stand out in formation at 2
Dr. Dunn: I think we all kind of agree that the military service is diverse and that many of the subcategories of occupations within the military lead to increased sun exposure by mandate. We advise sun protection by physical barriers and sunblock.
Diagnosis of Skin Cancer Via Telemedicine
Dr. Dunn: I have friends who remain in the VA (US Department of Veterans Affairs) system, and they are involved with telemedicine in dermatology, which can reduce waiting time and increase the number of patients seen by the dermatologist. In-person and teledermatology visits now are available to servicemembers on active duty and retirees.
Dr. Bandino: At our residency program (San Antonio Uniformed Services Health Education Consortium), we’ve had asynchronous teledermatology for over a decade, even before I was a resident. We provide it primarily as a service for patients at small bases without access to dermatology. Some bases also use it as part of their prescreening process prior to authorizing an in-person dermatology consultation.
Certainly, with the coronavirus pandemic, civilian dermatology is seeing a boom in the teledermatology world that had been slowly increasing in popularity for the last few years. In our residency program, teledermatology has traditionally been just for active-duty servicemembers or their dependents, but now due to the coronavirus pandemic, our teledermatology services have significantly expanded to include adding synchronous capability. We have patients take pictures before their virtual appointment and/or FaceTime during the appointment. Even after the pandemic, there will likely be more integration of synchronous teledermatology going forward as we’re seeing some of the value. Of course, I’m sure we would all agree that accurate diagnosis of pigmented lesions can be very challenging with teledermatology, not to mention other diagnostic limitations. But I think there is still utility and it should only get better with time as technology improves. So, I’m hopeful that we can incorporate more of it in the military.
Dr. Logemann: I’m definitely aware that we have different telehealth opportunities available, even using some newer modalities that are command approved in recent weeks. My experience has been for more complicated dermatology, so people are in remote locations, and they’re being seen by a nondermatologist, and they have questions about how to approach management. But I’m not aware of telemedicine as a screening tool for skin cancer in the military or among my civilian colleagues. I would hope that it could be someday because we’re developing these total-body photography machines as well. It could be a way for a nondermatologist who identifies a lesion to have it triaged by a dermatologist. To say, “Oh yeah, that looks like a melanoma. They need to get in sooner vs later,” but not on a large-scale sort of screening modality.
Dr. Bandino: In my recent experience, it has definitely been a helpful triage tool. In the military, this form of triage can be particularly helpful if someone is overseas to determine whether he/she needs to evacuated and evaluated in-person right away.
Dr. Jarell: It’s been useful in looking at benign things. People have shown me in the past few weeks a lot of seborrheic keratoses and a lot of benign dermal nevus-type things, and I say, “Don’t worry about that.” And you can tell if the resolution is good enough. But a lot of people have shown me things in the past few weeks that have clearly been basal cell carcinoma, which we can probably let that ride out for a few more weeks, but I’m not sure if maybe somebody has an amelanotic melanoma. Maybe you need to come in and get that biopsied ASAP. Or something that looks like a melanoma. The patient should probably come in and get that biopsied.
Dr. Miller: I think we can rely on teledermatology. It’s all predicated on the resolution because we’re all trained in pattern recognition. I think it’s very useful to screen for things that look clinically benign. We have to understand that most dermatology is practiced by nondermatologists in the United States, and many studies show that their diagnostic accuracy is 20%, at best maybe 50%. So, they do need to reach out to a dermatologist and perhaps get some guidance on what to do. I think it could be a very useful tool if used appropriately.
Dr. Dunn: If used appropriately, teledermatology could function in a couple of ways. One, it could allow us to declare lesions to be wholly benign, and only should a lesion change would it need attention. The second is that it would allow us to accelerate the process of getting a patient to us—physically in front of us—for a biopsy if a suspicious lesion is seen. A by-product of that process would be that if patients who have wholly benign, nonworrisome lesions could be screened by telemedicine, then physical appointments where a patient is in front of the doctor would be more open. In other words, let’s say if 25% of all lesional visits could be declared benign via telemedicine that would allow dermatology to preserve its face-to-face appointments for patients who are more likely to have cancer and require procedures like skin biopsy.
Love it or hate it, I think we’re getting it no matter what now. Telemedicine creeped along forever and within 6 weeks it’s become ubiquitous. It’s phenomenal how fast we had to adapt to a system or perish in private practice. Sometimes these episodes that we go through have good consequences as well as bad consequences. Telemedicine probably has been needed for a long time and the insurers were not covering it very well, but suddenly a stay-at-home mandate has unveiled valuable technology—something that we probably should have been able to use more and be adequately reimbursed.
Surgical Treatment of Skin Cancer
Dr. Dunn: Treatment historically has been surgical for nonmelanoma and melanoma skin cancers. Some radiation devices have gained popularity again in the past decade or so, but excisional surgery remains the standard treatment for skin cancer. Nonmelanoma skin cancers almost all are probably treated surgically still, with a small percentage treated with superficial radiation.
Access to care is important to discuss. Are Mohs surgeons readily available, or are plastic surgeons, general surgeons, or vascular surgeons in the federal system contributing to the care of skin cancer? Are they doing excisional surgery after biopsies are done? Are they doing excisional biopsies with the intent of cure?
Dr. Logemann: For active duty, I don’t see any issues getting access to the medical center for Mohs micrographic surgery. Sometimes, if we have a lot of volume, some patients may get deferred to the network, but in my experience, it would not typically be an active-duty servicemember. An active-duty servicemember would get care rendered at one of the medical centers for Mohs surgery. Typically the active-duty–aged population isn’t getting much skin cancer. It certainly does happen, but most of the skin cancers frequently that are treated at medical centers are not infrequently retirees.
Dr. Bandino: Because of our residency program, we are required to have Mohs surgery capability to be ACGME (Accreditation Council for Graduate Medical Education) accredited. We typically have 3 Mohs surgeons, so we never have a problem with access.
In the military, I just refer cases to our Mohs surgeons and everything is taken care of in-house. In fact, this is an area where we may even have better access than the civilian world because there are no insurance hurdles or significant delay in care since our Mohs surgeons aren’t typically booked up for 3 to 4 months like many civilian Mohs surgeons. This is especially true for complex cases since we provide hospital-based care with all specialty services under the same umbrella. So, for example, if the Mohs surgeons have an extensive and complex case requiring multidisciplinary care such as ENT (ear, nose, and throat), facial plastics, or radiation-oncology, they’re all in-house with no insurance issues to navigate. This of course is not usual for most military bases and is only capable at bases attached to a large medical center. There are some similar scenarios in the civilian world with university medical centers and managed care organizations, but we may still have a slight advantage in accessibility and cost.
Dr. Dunn: There are guidelines from the National Comprehensive Cancer Network as to how to treat nonmelanoma and melanoma skin cancer. Almost all of them are surgical and almost all of them are safe, outpatient, local anesthetic procedures with a high cure rate. The vast majority of melanoma and nonmelanoma skin cancers can be handled safely and effectively with minimal morbidity and almost no known mortalities from the treatments themselves. Some of the cancers have been identified as high risk for metastasis and mortality, but they’re relatively uncommon still. The good news about skin cancer is that the risk of death remains very small.
- Riemenschneider K, Liu J, Powers JG. Skin cancer in the military: a systematic review of melanoma and nonmelanoma skin cancer incidence, prevention, and screening among active duty and veteran personnel.J Am Acad Dermatol. 2018;78:1185-1192.
- Brundage JF, Williams VF, Stahlman S, et al. Incidence rates of malignant melanoma in relation to years of military service, overall and in selected military occupational groups, active component, U.S. Armed Forces, 2001-2015. MSMR. 2017;24:8-14.
- Riemenschneider K, Liu J, Powers JG. Skin cancer in the military: a systematic review of melanoma and nonmelanoma skin cancer incidence, prevention, and screening among active duty and veteran personnel.J Am Acad Dermatol. 2018;78:1185-1192.
- Brundage JF, Williams VF, Stahlman S, et al. Incidence rates of malignant melanoma in relation to years of military service, overall and in selected military occupational groups, active component, U.S. Armed Forces, 2001-2015. MSMR. 2017;24:8-14.
When you see something ...
Over the last several decades science has fallen off this country’s radar screen. Yes, STEM (science, technology, engineering, and mathematics) has recently had a brief moment in the spotlight as a buzzword de jour. But the critical importance of careful and systematic investigation into the world around us using observation and trial and error is a tough sell to a large segment of our population.
The COVID-19 pandemic is providing an excellent opportunity for science and medicine to showcase their star qualities. Of course some people in leadership positions persist in disregarding the value of scientific investigation. But I get the feeling that the fear generated by the pandemic is creating some converts among many previous science skeptics. This gathering enthusiasm among the general population is a predictably slow process because that’s the way science works. It often doesn’t provide quick answers. And it is difficult for the nonscientist to see the beauty in the reality that the things we thought were true 2 months ago are likely to be proven wrong today as more observations accumulate.
A recent New York Times article examines the career of one such unscrupulous physician/scientist whose recent exploits threaten to undo much of the positive image the pandemic has cast on science (“The Doctor Behind the Disputed Covid Data,” by Ellen Gabler and Roni Caryn Rabin, The New York Times, July 27, 2020). The subject of the article is the physician who was responsible for providing some of the large data sets on which several papers were published about the apparent ineffectiveness and danger of using hydroxychloroquine in COVID-19 patients. The authenticity of the data sets recently has been seriously questioned, and the articles have been retracted by the journals in which they had appeared.
Based on numerous interviews with coworkers, the Times reporters present a strong case that this individual’s long history of unreliability make his association with allegedly fraudulent data set not surprising but maybe even predictable. At one point in his training, there appears to have been serious questions about advancing the physician to the next level. Despite these concerns, he was allowed to continue and complete his specialty training. It is of note that in his last year of clinical practice, the physician became the subject of three serious malpractice claims that question his competence.
I suspect that some of you have crossed paths with physicians whose competence and/or moral character you found concerning. Were they peers? Were you the individual’s supervisor or was he or she your mentor? How did you respond? Did anyone respond at all?
There has been a lot written and said in recent months about how and when to respond to respond to sexual harassment in the workplace. But I don’t recall reading any articles that discuss how one should respond to incompetence. Of course competency can be a relative term, but in most cases significant incompetence is hard to miss because it tends to be repeated.
It is easy for the airports and subway systems to post signs that say “If you see something say something.” It’s a different story for hospitals and medical schools that may have systems in place for reporting and following up on poor practice. But my sense is that there are too many cases that slip through the cracks.
This is another example of a problem for which I don’t have a solution. However, if this column prompts just one of you who sees something to say something then I have had a good day.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Over the last several decades science has fallen off this country’s radar screen. Yes, STEM (science, technology, engineering, and mathematics) has recently had a brief moment in the spotlight as a buzzword de jour. But the critical importance of careful and systematic investigation into the world around us using observation and trial and error is a tough sell to a large segment of our population.
The COVID-19 pandemic is providing an excellent opportunity for science and medicine to showcase their star qualities. Of course some people in leadership positions persist in disregarding the value of scientific investigation. But I get the feeling that the fear generated by the pandemic is creating some converts among many previous science skeptics. This gathering enthusiasm among the general population is a predictably slow process because that’s the way science works. It often doesn’t provide quick answers. And it is difficult for the nonscientist to see the beauty in the reality that the things we thought were true 2 months ago are likely to be proven wrong today as more observations accumulate.
A recent New York Times article examines the career of one such unscrupulous physician/scientist whose recent exploits threaten to undo much of the positive image the pandemic has cast on science (“The Doctor Behind the Disputed Covid Data,” by Ellen Gabler and Roni Caryn Rabin, The New York Times, July 27, 2020). The subject of the article is the physician who was responsible for providing some of the large data sets on which several papers were published about the apparent ineffectiveness and danger of using hydroxychloroquine in COVID-19 patients. The authenticity of the data sets recently has been seriously questioned, and the articles have been retracted by the journals in which they had appeared.
Based on numerous interviews with coworkers, the Times reporters present a strong case that this individual’s long history of unreliability make his association with allegedly fraudulent data set not surprising but maybe even predictable. At one point in his training, there appears to have been serious questions about advancing the physician to the next level. Despite these concerns, he was allowed to continue and complete his specialty training. It is of note that in his last year of clinical practice, the physician became the subject of three serious malpractice claims that question his competence.
I suspect that some of you have crossed paths with physicians whose competence and/or moral character you found concerning. Were they peers? Were you the individual’s supervisor or was he or she your mentor? How did you respond? Did anyone respond at all?
There has been a lot written and said in recent months about how and when to respond to respond to sexual harassment in the workplace. But I don’t recall reading any articles that discuss how one should respond to incompetence. Of course competency can be a relative term, but in most cases significant incompetence is hard to miss because it tends to be repeated.
It is easy for the airports and subway systems to post signs that say “If you see something say something.” It’s a different story for hospitals and medical schools that may have systems in place for reporting and following up on poor practice. But my sense is that there are too many cases that slip through the cracks.
This is another example of a problem for which I don’t have a solution. However, if this column prompts just one of you who sees something to say something then I have had a good day.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Over the last several decades science has fallen off this country’s radar screen. Yes, STEM (science, technology, engineering, and mathematics) has recently had a brief moment in the spotlight as a buzzword de jour. But the critical importance of careful and systematic investigation into the world around us using observation and trial and error is a tough sell to a large segment of our population.
The COVID-19 pandemic is providing an excellent opportunity for science and medicine to showcase their star qualities. Of course some people in leadership positions persist in disregarding the value of scientific investigation. But I get the feeling that the fear generated by the pandemic is creating some converts among many previous science skeptics. This gathering enthusiasm among the general population is a predictably slow process because that’s the way science works. It often doesn’t provide quick answers. And it is difficult for the nonscientist to see the beauty in the reality that the things we thought were true 2 months ago are likely to be proven wrong today as more observations accumulate.
A recent New York Times article examines the career of one such unscrupulous physician/scientist whose recent exploits threaten to undo much of the positive image the pandemic has cast on science (“The Doctor Behind the Disputed Covid Data,” by Ellen Gabler and Roni Caryn Rabin, The New York Times, July 27, 2020). The subject of the article is the physician who was responsible for providing some of the large data sets on which several papers were published about the apparent ineffectiveness and danger of using hydroxychloroquine in COVID-19 patients. The authenticity of the data sets recently has been seriously questioned, and the articles have been retracted by the journals in which they had appeared.
Based on numerous interviews with coworkers, the Times reporters present a strong case that this individual’s long history of unreliability make his association with allegedly fraudulent data set not surprising but maybe even predictable. At one point in his training, there appears to have been serious questions about advancing the physician to the next level. Despite these concerns, he was allowed to continue and complete his specialty training. It is of note that in his last year of clinical practice, the physician became the subject of three serious malpractice claims that question his competence.
I suspect that some of you have crossed paths with physicians whose competence and/or moral character you found concerning. Were they peers? Were you the individual’s supervisor or was he or she your mentor? How did you respond? Did anyone respond at all?
There has been a lot written and said in recent months about how and when to respond to respond to sexual harassment in the workplace. But I don’t recall reading any articles that discuss how one should respond to incompetence. Of course competency can be a relative term, but in most cases significant incompetence is hard to miss because it tends to be repeated.
It is easy for the airports and subway systems to post signs that say “If you see something say something.” It’s a different story for hospitals and medical schools that may have systems in place for reporting and following up on poor practice. But my sense is that there are too many cases that slip through the cracks.
This is another example of a problem for which I don’t have a solution. However, if this column prompts just one of you who sees something to say something then I have had a good day.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Exploring cannabis use by older adults
Older Americans – people aged 65 or older – make up 15% of the U.S. population, according to the Census Bureau. By the end of this decade, or the year 2030, this proportion will increase to 21% – and all “baby boomers,” those born between 1946 and 1964, will be older than 65.1 Those demographic developments are occurring alongside a change in societal, legal, and public attitudes on cannabis.
Liberalization of cannabis laws across the United States allows for ever easier access to medicinal and recreational cannabis. Traditionally, cannabis use, its effects, and related considerations in the adolescent and young adult populations have commanded significant research attention. Cannabis use in older adults, however, is not as well studied.2 An exploration of trends in cannabis use by older adults and potential impact in terms of health is timely and important.
According to data from the National Survey on Drug Use and Health, cannabis use in adults aged 65 years and older appears to have been increasing steadily over the past 2 decades. Use among this group rose from 0.4% in 2006 and 2007, to 2.9% in 2015 and 2016.2 And, most recently, use climbed from 3.7% in 2017 to 4.2% in 2018.2
Cannabis use also has risen among other adults. For those aged 50-64, cannabis use increased from 2.8% in 2006-2007 to 4.8% in 2012-2013.2,3 Meanwhile, from 2015 to 2016, that number increased to 9.0%.3,4
Past-year cannabis use in the groups of those aged 50-64 and those aged 65 and older appears to be higher in individuals with mental health problems, alcohol use disorder, and nicotine dependence.5,6 Being male and being unmarried appear to be correlated with past-year cannabis use. Multimorbidity does not appear to be associated with past-year cannabis use. Those using cannabis tend to be long-term users and have first use at a much younger age, typically before age 21.
Older adults use cannabis for both recreational and perceived medical benefits. Arthritis, chronic back pain, anxiety, depression, relaxation, stress reduction, and enhancement in terms of creativity are all purported reasons for use. However, there is limited to no evidence for the efficacy of cannabis in helping with those conditions and purposes. Clinical trials have shown that cannabis can be beneficial in managing pain and nausea, but those trials have not been conducted in older adults.7,8
There is a real risk of cannabis use having a negative impact on the health of older adults. To begin with, the cannabis consumed today is significantly higher in potency than the cannabis that baby boomers were introduced to in their youth. The higher potency, combined with an age-related decline in function experienced by some older adults, makes them vulnerable to its known side effects, such as anxiety, dry mouth, tachycardia, high blood pressure, palpitations, wheezing, confusion, and dizziness.
Cannabis use is reported to bring a fourfold increase in cardiac events within the first hour of ingestion.9 Cognitive decline and memory impairment are well known adverse effects of cannabis use. Research has shown significant self-reported cognitive decline in older adults in relation to cannabis use.Cannabis metabolites are known to have an effect on cytochrome P450 enzymes, affecting the metabolism of medication, and increasing the susceptibility of older adults who use cannabis to adverse effects of polypharmacy. Finally, as research on emergency department visits by older adults shows, cannabis use can increase the risk of injury among this cohort.
As in the United States, cannabis use among older adults in Canada has increased significantly. The percentage of older adults who use cannabis in the Canadian province of Ontario, for example, reportedly doubled from 2005 to 2015. In response to this increase, and in anticipation of a rise in problematic use of cannabis and cannabis use disorder in older adults, the Canadian Coalition for Seniors’ Mental Health (through financial support from Substance Use and Addictions Program of Health Canada) has created guidelines on the prevention, assessment, and management of cannabis use disorder in older adults.
In the absence of a set of guidelines specific to the United States, the recommendations made by the coalition should be helpful in the care of older Americans. Among other recommendations, the guidelines highlight the needs for primary care physicians to build a better knowledge base around the use of cannabis in older adults, to screen older adults for cannabis use, and to educate older adults and their families about the risk of cannabis use.9
Cannabis use is increasingly popular among older adults10 for both medicinal and recreational purposes. Research and data supporting its medical benefits are limited, and the potential of harm from its use among older adults is present and significant. Importantly, many older adults who use marijuana have co-occurring mental health issues and substance use disorder(s).
Often, our older patients learn about benefits and harms of cannabis from friends and the Internet rather than from physicians and other clinicians.9 We must do our part to make sure that older patients understand the potential negative health impact that cannabis can have on their health. Physicians should screen older adults for marijuana use. Building a better knowledge base around changing trends and views in/on the use and accessibility of cannabis will help physicians better address cannabis use in older adults.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University College of Medicine, Mount Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in vulnerable populations.
References
1. Vespa J et al. Demographic turning points for the United States: Population projections for 2020 to 2060. Current Population Reports. Washington: U.S. Census Bureau. 2020 Feb.
2. Han BH et al. Addiction. 2016 Oct 21. doi: 10.1111/add.13670.
3. Han BH and Palamar JJ. Drug Alcohol Depend. 2018 Oct;191:374-81.
4. Han BH and Palamar JJ. JAMA Intern Med. 2020 Feb 4;180(4):609-11.
5. Choi NG et al. Drug Alcohol Abuse. 2018;44(2):215-23.
6. Reynolds IR et al. J Am Griatr Soc. 2018 Nov;66(11):2167-71.
7. Ahmed AIA et al. J Am Geriatr Soc. 2014 Feb;62(2):410-1.
8. Lum HD et al. Gerontol Geriatr Med. 2019 Jan-Dec;5:2333721419843707.
9. Bertram JR et al. Can Geriatr J. 2020 Mar;23(1):135-42.
10. Baumbusch J and Yip IS. Clin Gerontol. 2020 Mar 29;1-7.
Older Americans – people aged 65 or older – make up 15% of the U.S. population, according to the Census Bureau. By the end of this decade, or the year 2030, this proportion will increase to 21% – and all “baby boomers,” those born between 1946 and 1964, will be older than 65.1 Those demographic developments are occurring alongside a change in societal, legal, and public attitudes on cannabis.
Liberalization of cannabis laws across the United States allows for ever easier access to medicinal and recreational cannabis. Traditionally, cannabis use, its effects, and related considerations in the adolescent and young adult populations have commanded significant research attention. Cannabis use in older adults, however, is not as well studied.2 An exploration of trends in cannabis use by older adults and potential impact in terms of health is timely and important.
According to data from the National Survey on Drug Use and Health, cannabis use in adults aged 65 years and older appears to have been increasing steadily over the past 2 decades. Use among this group rose from 0.4% in 2006 and 2007, to 2.9% in 2015 and 2016.2 And, most recently, use climbed from 3.7% in 2017 to 4.2% in 2018.2
Cannabis use also has risen among other adults. For those aged 50-64, cannabis use increased from 2.8% in 2006-2007 to 4.8% in 2012-2013.2,3 Meanwhile, from 2015 to 2016, that number increased to 9.0%.3,4
Past-year cannabis use in the groups of those aged 50-64 and those aged 65 and older appears to be higher in individuals with mental health problems, alcohol use disorder, and nicotine dependence.5,6 Being male and being unmarried appear to be correlated with past-year cannabis use. Multimorbidity does not appear to be associated with past-year cannabis use. Those using cannabis tend to be long-term users and have first use at a much younger age, typically before age 21.
Older adults use cannabis for both recreational and perceived medical benefits. Arthritis, chronic back pain, anxiety, depression, relaxation, stress reduction, and enhancement in terms of creativity are all purported reasons for use. However, there is limited to no evidence for the efficacy of cannabis in helping with those conditions and purposes. Clinical trials have shown that cannabis can be beneficial in managing pain and nausea, but those trials have not been conducted in older adults.7,8
There is a real risk of cannabis use having a negative impact on the health of older adults. To begin with, the cannabis consumed today is significantly higher in potency than the cannabis that baby boomers were introduced to in their youth. The higher potency, combined with an age-related decline in function experienced by some older adults, makes them vulnerable to its known side effects, such as anxiety, dry mouth, tachycardia, high blood pressure, palpitations, wheezing, confusion, and dizziness.
Cannabis use is reported to bring a fourfold increase in cardiac events within the first hour of ingestion.9 Cognitive decline and memory impairment are well known adverse effects of cannabis use. Research has shown significant self-reported cognitive decline in older adults in relation to cannabis use.Cannabis metabolites are known to have an effect on cytochrome P450 enzymes, affecting the metabolism of medication, and increasing the susceptibility of older adults who use cannabis to adverse effects of polypharmacy. Finally, as research on emergency department visits by older adults shows, cannabis use can increase the risk of injury among this cohort.
As in the United States, cannabis use among older adults in Canada has increased significantly. The percentage of older adults who use cannabis in the Canadian province of Ontario, for example, reportedly doubled from 2005 to 2015. In response to this increase, and in anticipation of a rise in problematic use of cannabis and cannabis use disorder in older adults, the Canadian Coalition for Seniors’ Mental Health (through financial support from Substance Use and Addictions Program of Health Canada) has created guidelines on the prevention, assessment, and management of cannabis use disorder in older adults.
In the absence of a set of guidelines specific to the United States, the recommendations made by the coalition should be helpful in the care of older Americans. Among other recommendations, the guidelines highlight the needs for primary care physicians to build a better knowledge base around the use of cannabis in older adults, to screen older adults for cannabis use, and to educate older adults and their families about the risk of cannabis use.9
Cannabis use is increasingly popular among older adults10 for both medicinal and recreational purposes. Research and data supporting its medical benefits are limited, and the potential of harm from its use among older adults is present and significant. Importantly, many older adults who use marijuana have co-occurring mental health issues and substance use disorder(s).
Often, our older patients learn about benefits and harms of cannabis from friends and the Internet rather than from physicians and other clinicians.9 We must do our part to make sure that older patients understand the potential negative health impact that cannabis can have on their health. Physicians should screen older adults for marijuana use. Building a better knowledge base around changing trends and views in/on the use and accessibility of cannabis will help physicians better address cannabis use in older adults.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University College of Medicine, Mount Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in vulnerable populations.
References
1. Vespa J et al. Demographic turning points for the United States: Population projections for 2020 to 2060. Current Population Reports. Washington: U.S. Census Bureau. 2020 Feb.
2. Han BH et al. Addiction. 2016 Oct 21. doi: 10.1111/add.13670.
3. Han BH and Palamar JJ. Drug Alcohol Depend. 2018 Oct;191:374-81.
4. Han BH and Palamar JJ. JAMA Intern Med. 2020 Feb 4;180(4):609-11.
5. Choi NG et al. Drug Alcohol Abuse. 2018;44(2):215-23.
6. Reynolds IR et al. J Am Griatr Soc. 2018 Nov;66(11):2167-71.
7. Ahmed AIA et al. J Am Geriatr Soc. 2014 Feb;62(2):410-1.
8. Lum HD et al. Gerontol Geriatr Med. 2019 Jan-Dec;5:2333721419843707.
9. Bertram JR et al. Can Geriatr J. 2020 Mar;23(1):135-42.
10. Baumbusch J and Yip IS. Clin Gerontol. 2020 Mar 29;1-7.
Older Americans – people aged 65 or older – make up 15% of the U.S. population, according to the Census Bureau. By the end of this decade, or the year 2030, this proportion will increase to 21% – and all “baby boomers,” those born between 1946 and 1964, will be older than 65.1 Those demographic developments are occurring alongside a change in societal, legal, and public attitudes on cannabis.
Liberalization of cannabis laws across the United States allows for ever easier access to medicinal and recreational cannabis. Traditionally, cannabis use, its effects, and related considerations in the adolescent and young adult populations have commanded significant research attention. Cannabis use in older adults, however, is not as well studied.2 An exploration of trends in cannabis use by older adults and potential impact in terms of health is timely and important.
According to data from the National Survey on Drug Use and Health, cannabis use in adults aged 65 years and older appears to have been increasing steadily over the past 2 decades. Use among this group rose from 0.4% in 2006 and 2007, to 2.9% in 2015 and 2016.2 And, most recently, use climbed from 3.7% in 2017 to 4.2% in 2018.2
Cannabis use also has risen among other adults. For those aged 50-64, cannabis use increased from 2.8% in 2006-2007 to 4.8% in 2012-2013.2,3 Meanwhile, from 2015 to 2016, that number increased to 9.0%.3,4
Past-year cannabis use in the groups of those aged 50-64 and those aged 65 and older appears to be higher in individuals with mental health problems, alcohol use disorder, and nicotine dependence.5,6 Being male and being unmarried appear to be correlated with past-year cannabis use. Multimorbidity does not appear to be associated with past-year cannabis use. Those using cannabis tend to be long-term users and have first use at a much younger age, typically before age 21.
Older adults use cannabis for both recreational and perceived medical benefits. Arthritis, chronic back pain, anxiety, depression, relaxation, stress reduction, and enhancement in terms of creativity are all purported reasons for use. However, there is limited to no evidence for the efficacy of cannabis in helping with those conditions and purposes. Clinical trials have shown that cannabis can be beneficial in managing pain and nausea, but those trials have not been conducted in older adults.7,8
There is a real risk of cannabis use having a negative impact on the health of older adults. To begin with, the cannabis consumed today is significantly higher in potency than the cannabis that baby boomers were introduced to in their youth. The higher potency, combined with an age-related decline in function experienced by some older adults, makes them vulnerable to its known side effects, such as anxiety, dry mouth, tachycardia, high blood pressure, palpitations, wheezing, confusion, and dizziness.
Cannabis use is reported to bring a fourfold increase in cardiac events within the first hour of ingestion.9 Cognitive decline and memory impairment are well known adverse effects of cannabis use. Research has shown significant self-reported cognitive decline in older adults in relation to cannabis use.Cannabis metabolites are known to have an effect on cytochrome P450 enzymes, affecting the metabolism of medication, and increasing the susceptibility of older adults who use cannabis to adverse effects of polypharmacy. Finally, as research on emergency department visits by older adults shows, cannabis use can increase the risk of injury among this cohort.
As in the United States, cannabis use among older adults in Canada has increased significantly. The percentage of older adults who use cannabis in the Canadian province of Ontario, for example, reportedly doubled from 2005 to 2015. In response to this increase, and in anticipation of a rise in problematic use of cannabis and cannabis use disorder in older adults, the Canadian Coalition for Seniors’ Mental Health (through financial support from Substance Use and Addictions Program of Health Canada) has created guidelines on the prevention, assessment, and management of cannabis use disorder in older adults.
In the absence of a set of guidelines specific to the United States, the recommendations made by the coalition should be helpful in the care of older Americans. Among other recommendations, the guidelines highlight the needs for primary care physicians to build a better knowledge base around the use of cannabis in older adults, to screen older adults for cannabis use, and to educate older adults and their families about the risk of cannabis use.9
Cannabis use is increasingly popular among older adults10 for both medicinal and recreational purposes. Research and data supporting its medical benefits are limited, and the potential of harm from its use among older adults is present and significant. Importantly, many older adults who use marijuana have co-occurring mental health issues and substance use disorder(s).
Often, our older patients learn about benefits and harms of cannabis from friends and the Internet rather than from physicians and other clinicians.9 We must do our part to make sure that older patients understand the potential negative health impact that cannabis can have on their health. Physicians should screen older adults for marijuana use. Building a better knowledge base around changing trends and views in/on the use and accessibility of cannabis will help physicians better address cannabis use in older adults.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University College of Medicine, Mount Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in vulnerable populations.
References
1. Vespa J et al. Demographic turning points for the United States: Population projections for 2020 to 2060. Current Population Reports. Washington: U.S. Census Bureau. 2020 Feb.
2. Han BH et al. Addiction. 2016 Oct 21. doi: 10.1111/add.13670.
3. Han BH and Palamar JJ. Drug Alcohol Depend. 2018 Oct;191:374-81.
4. Han BH and Palamar JJ. JAMA Intern Med. 2020 Feb 4;180(4):609-11.
5. Choi NG et al. Drug Alcohol Abuse. 2018;44(2):215-23.
6. Reynolds IR et al. J Am Griatr Soc. 2018 Nov;66(11):2167-71.
7. Ahmed AIA et al. J Am Geriatr Soc. 2014 Feb;62(2):410-1.
8. Lum HD et al. Gerontol Geriatr Med. 2019 Jan-Dec;5:2333721419843707.
9. Bertram JR et al. Can Geriatr J. 2020 Mar;23(1):135-42.
10. Baumbusch J and Yip IS. Clin Gerontol. 2020 Mar 29;1-7.
A doctor conquers his demons
Adam B. Hill, MD, is home on a “staycation” this week. Today, he took a 3-hour nap. I know this because I follow Dr. Hill on Twitter, where he has an active feed, a lot of posts, retweets, and more than 20,000 followers.
I also know from Twitter that he is married and has three young children, that he was once suicidal, and has been treated for major depression and alcoholism. As a palliative care doctor, Dr. Hill was required by his state medical board to blow into a breathalyzer several times a day for 5 years – something he felt quite shamed by – and while I’ve never met him, I felt just a little bit proud of this stranger when he was released from the medical board’s oversight.
Dr. Hill’s memoir, “Long Walk Out of the Woods: A Physician’s Story of Addiction, Depression, Hope, and Recovery” (Central Recovery Press, 2019) is the culmination of his efforts to use his difficulties as a way of offering hope and connection to anyone who struggled as he has, or to anyone who has struggled at all. Like his Twitter feed, it is a display of vulnerability and gratitude by someone who has been through dark times then returned to conquer his monsters.
He begins by setting the stage for us. “My name is Adam,” he announces in the preface. He tells us his various titles: human being, husband, father, physician, recovering alcoholic, and psychiatric patient. “In the midst of these struggles, working in modern medicine fractured my identity, stole my authenticity, and left me a shell of the person I wanted to be.”
We learn that he tried to buy a gun, but there was a waiting period and he could not purchase the firearm. Instead, he walked into the woods to drink himself to death, with sleeping pills as an add-on – obviously, he didn’t die, and his journey back from his failed suicidal mission is the meat of the book.
Dr. Hill was a quiet and timid child, and he was bullied at school in a way that has lingered on. He struggles with perfectionism and with a sense of never quite belonging. He was a good student, and later a competitive tennis player who was destined for a regional competition until he broke his ankle after drinking just days before the competition. He did well in college, felt more accepted, and went on to medical school after getting in from the wait list. He went on to do a pediatrics residency, and he and his wife moved from Indiana to North Carolina so he could do a hematology oncology fellowship. It was toward the end of his 2-year fellowship when he tried to purchase a gun, then walked into those woods.
His wife called, asked him to come to dinner, and he left the woods before he’d overdosed. After a meeting with his wife, parents, and sister, he returned to psychiatric care, restarted antidepressants, went to Alcoholics Anonymous, and told his employer that he had a problem. This admission started a distressing series of events, including years of being monitored by state medical boards and being labeled an “impaired physician.”
This is the only thing I didn’t like about Dr. Hill’s memoir: As open as he is about his emotional life, there were pieces missing with respect to what actually happened. At this point, I was befuddled as to why he self-reported his difficulties, and it wasn’t until he talked about starting a second fellowship in palliative care in his home state of Indiana that I could fill in some missing pieces. Dr. Hill and his wife purchased a house, and in November, he started his fellowship. The timing was off from the usual start in July, and I realized that perhaps he had gone to an inpatient setting for a number of months – his disclosure to his employer was voluntary, but his treatment likely interfered with his training and couldn’t be hidden. What else transpired he hints at: bottles hidden, driving while intoxicated, a nurse who gave him IV hydration when he came to work with a hangover.
From here, Dr. Hill’s story becomes every doctor’s nightmare. Settled into his new house and weeks into his fellowship, he is called in and fired: His application for a medical license in Indiana has been denied because of his addiction history. He met with a friend of his father’s who worked in a large pediatrics practice. The meeting went well, but the group felt he was too much of a malpractice risk.
He now needs to pay his mortgage and student loans, so he takes a position in Oklahoma with the Indian Health Service. He’s 700 miles from home, living alone in a hotel room, feeling like the work is beneath him, and the chapter is titled “Exile.” His new boss greets him with, “Listen, we all had our own stories that led us here.” Surprisingly, he likes the work and feels supported. If only it weren’t for all that loneliness, and not surprisingly, he relapses despite the mandated breathalyzer. Six beers later, and Dr. Hill is off to Chicago for a rehab program, then back to Oklahoma to finish off his stint.
What happens next is the second time I wondered about the plot of his life: Through “connections and concession,” he returns to Indiana for the palliative care fellowship, and goes on to work at Riley Children’s Hospital.
When a colleague unexpectedly dies from suicide, Dr. Hill tells others that he, too, once entertained suicidal thoughts. The story from here gets better and better: – to conquer their shame, to share their stories, to feel less alone. He and his wife become parents, he remains sober and healthy, and therapy leads him to a place of self-discovery and success.
Intertwined with telling his story, Dr. Hill takes on some of the institutional issues surrounding addiction and mental illness. He feels shamed and punished by the state medical board that mandates the terms of his medical license. Any physician who reads this book will think twice about revealing a diagnosis of depression or substance use disorder. It’s not a new idea that to protect the public, medical boards should ask about current impairments, not a past history or conditions that have been successfully treated. They should encourage treatment, not punish those who seek care.
Dr. Hill writes about how helpful it has been to allow himself to be vulnerable in the aftermath:
In my experience, the more vulnerability I show, the more opportunities I have to connect to other people. I learned the hard way that when I hide my true self from others, I spiral toward shame. Conversely, when I bury my shame, I begin to accept myself as a beautifully flawed human being, and my perspective on the world reflects that. A turn of the vulnerability dial has opened up connections to other people, while turning away pity, judgment, fear, and shame. Meanwhile, when I am to create spaces for vulnerability, permission is granted to have open and honest conversations about mental health conditions on a larger scale. But I would never have learned these lessons without having been humbled by this disease.
Perhaps the thing I liked best about Dr. Hill’s memoir is that he proposes some solutions. He talks about the importance of fighting stigma, how he finds it everywhere, and how the medical field equates mental illnesses with weakness, thereby perpetuating a self-deprecating cycle in those who have them.
In palliative care, there is an acronym – SPIKES (Set up, Perception, Invitation, Knowledge, Explore emotions, and Summary) that provides guidelines for how to deliver bad news to a family. Dr. Hill suggests using this format to discuss mental health and addictions with patients, colleagues, students. He talks about having “Compassion Rounds” to provide a safe space for his colleagues to talk about their emotional reactions to treating very ill children. And he talks about providing mental health care for trainees as an “opt out” – he schedules all his residents for a counseling session – they can cancel without repercussion, but this serves to “normalize” seeking care. I love the idea that each resident might have someone they’ve met with at least once whom they can call if the going gets rough. “As a result,” Dr. Hill writes, “once secretive conversations about attending counseling happen openly, and the physicians actually feel more comfortable going.”
Adam Hill’s memoir is short, it’s an engaging read, his openness is refreshing, and his plea to let doctors be human beings with human problems is so needed in medicine today. Thank you, Adam.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatry Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. Dr. Miller has no disclosures.
Adam B. Hill, MD, is home on a “staycation” this week. Today, he took a 3-hour nap. I know this because I follow Dr. Hill on Twitter, where he has an active feed, a lot of posts, retweets, and more than 20,000 followers.
I also know from Twitter that he is married and has three young children, that he was once suicidal, and has been treated for major depression and alcoholism. As a palliative care doctor, Dr. Hill was required by his state medical board to blow into a breathalyzer several times a day for 5 years – something he felt quite shamed by – and while I’ve never met him, I felt just a little bit proud of this stranger when he was released from the medical board’s oversight.
Dr. Hill’s memoir, “Long Walk Out of the Woods: A Physician’s Story of Addiction, Depression, Hope, and Recovery” (Central Recovery Press, 2019) is the culmination of his efforts to use his difficulties as a way of offering hope and connection to anyone who struggled as he has, or to anyone who has struggled at all. Like his Twitter feed, it is a display of vulnerability and gratitude by someone who has been through dark times then returned to conquer his monsters.
He begins by setting the stage for us. “My name is Adam,” he announces in the preface. He tells us his various titles: human being, husband, father, physician, recovering alcoholic, and psychiatric patient. “In the midst of these struggles, working in modern medicine fractured my identity, stole my authenticity, and left me a shell of the person I wanted to be.”
We learn that he tried to buy a gun, but there was a waiting period and he could not purchase the firearm. Instead, he walked into the woods to drink himself to death, with sleeping pills as an add-on – obviously, he didn’t die, and his journey back from his failed suicidal mission is the meat of the book.
Dr. Hill was a quiet and timid child, and he was bullied at school in a way that has lingered on. He struggles with perfectionism and with a sense of never quite belonging. He was a good student, and later a competitive tennis player who was destined for a regional competition until he broke his ankle after drinking just days before the competition. He did well in college, felt more accepted, and went on to medical school after getting in from the wait list. He went on to do a pediatrics residency, and he and his wife moved from Indiana to North Carolina so he could do a hematology oncology fellowship. It was toward the end of his 2-year fellowship when he tried to purchase a gun, then walked into those woods.
His wife called, asked him to come to dinner, and he left the woods before he’d overdosed. After a meeting with his wife, parents, and sister, he returned to psychiatric care, restarted antidepressants, went to Alcoholics Anonymous, and told his employer that he had a problem. This admission started a distressing series of events, including years of being monitored by state medical boards and being labeled an “impaired physician.”
This is the only thing I didn’t like about Dr. Hill’s memoir: As open as he is about his emotional life, there were pieces missing with respect to what actually happened. At this point, I was befuddled as to why he self-reported his difficulties, and it wasn’t until he talked about starting a second fellowship in palliative care in his home state of Indiana that I could fill in some missing pieces. Dr. Hill and his wife purchased a house, and in November, he started his fellowship. The timing was off from the usual start in July, and I realized that perhaps he had gone to an inpatient setting for a number of months – his disclosure to his employer was voluntary, but his treatment likely interfered with his training and couldn’t be hidden. What else transpired he hints at: bottles hidden, driving while intoxicated, a nurse who gave him IV hydration when he came to work with a hangover.
From here, Dr. Hill’s story becomes every doctor’s nightmare. Settled into his new house and weeks into his fellowship, he is called in and fired: His application for a medical license in Indiana has been denied because of his addiction history. He met with a friend of his father’s who worked in a large pediatrics practice. The meeting went well, but the group felt he was too much of a malpractice risk.
He now needs to pay his mortgage and student loans, so he takes a position in Oklahoma with the Indian Health Service. He’s 700 miles from home, living alone in a hotel room, feeling like the work is beneath him, and the chapter is titled “Exile.” His new boss greets him with, “Listen, we all had our own stories that led us here.” Surprisingly, he likes the work and feels supported. If only it weren’t for all that loneliness, and not surprisingly, he relapses despite the mandated breathalyzer. Six beers later, and Dr. Hill is off to Chicago for a rehab program, then back to Oklahoma to finish off his stint.
What happens next is the second time I wondered about the plot of his life: Through “connections and concession,” he returns to Indiana for the palliative care fellowship, and goes on to work at Riley Children’s Hospital.
When a colleague unexpectedly dies from suicide, Dr. Hill tells others that he, too, once entertained suicidal thoughts. The story from here gets better and better: – to conquer their shame, to share their stories, to feel less alone. He and his wife become parents, he remains sober and healthy, and therapy leads him to a place of self-discovery and success.
Intertwined with telling his story, Dr. Hill takes on some of the institutional issues surrounding addiction and mental illness. He feels shamed and punished by the state medical board that mandates the terms of his medical license. Any physician who reads this book will think twice about revealing a diagnosis of depression or substance use disorder. It’s not a new idea that to protect the public, medical boards should ask about current impairments, not a past history or conditions that have been successfully treated. They should encourage treatment, not punish those who seek care.
Dr. Hill writes about how helpful it has been to allow himself to be vulnerable in the aftermath:
In my experience, the more vulnerability I show, the more opportunities I have to connect to other people. I learned the hard way that when I hide my true self from others, I spiral toward shame. Conversely, when I bury my shame, I begin to accept myself as a beautifully flawed human being, and my perspective on the world reflects that. A turn of the vulnerability dial has opened up connections to other people, while turning away pity, judgment, fear, and shame. Meanwhile, when I am to create spaces for vulnerability, permission is granted to have open and honest conversations about mental health conditions on a larger scale. But I would never have learned these lessons without having been humbled by this disease.
Perhaps the thing I liked best about Dr. Hill’s memoir is that he proposes some solutions. He talks about the importance of fighting stigma, how he finds it everywhere, and how the medical field equates mental illnesses with weakness, thereby perpetuating a self-deprecating cycle in those who have them.
In palliative care, there is an acronym – SPIKES (Set up, Perception, Invitation, Knowledge, Explore emotions, and Summary) that provides guidelines for how to deliver bad news to a family. Dr. Hill suggests using this format to discuss mental health and addictions with patients, colleagues, students. He talks about having “Compassion Rounds” to provide a safe space for his colleagues to talk about their emotional reactions to treating very ill children. And he talks about providing mental health care for trainees as an “opt out” – he schedules all his residents for a counseling session – they can cancel without repercussion, but this serves to “normalize” seeking care. I love the idea that each resident might have someone they’ve met with at least once whom they can call if the going gets rough. “As a result,” Dr. Hill writes, “once secretive conversations about attending counseling happen openly, and the physicians actually feel more comfortable going.”
Adam Hill’s memoir is short, it’s an engaging read, his openness is refreshing, and his plea to let doctors be human beings with human problems is so needed in medicine today. Thank you, Adam.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatry Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. Dr. Miller has no disclosures.
Adam B. Hill, MD, is home on a “staycation” this week. Today, he took a 3-hour nap. I know this because I follow Dr. Hill on Twitter, where he has an active feed, a lot of posts, retweets, and more than 20,000 followers.
I also know from Twitter that he is married and has three young children, that he was once suicidal, and has been treated for major depression and alcoholism. As a palliative care doctor, Dr. Hill was required by his state medical board to blow into a breathalyzer several times a day for 5 years – something he felt quite shamed by – and while I’ve never met him, I felt just a little bit proud of this stranger when he was released from the medical board’s oversight.
Dr. Hill’s memoir, “Long Walk Out of the Woods: A Physician’s Story of Addiction, Depression, Hope, and Recovery” (Central Recovery Press, 2019) is the culmination of his efforts to use his difficulties as a way of offering hope and connection to anyone who struggled as he has, or to anyone who has struggled at all. Like his Twitter feed, it is a display of vulnerability and gratitude by someone who has been through dark times then returned to conquer his monsters.
He begins by setting the stage for us. “My name is Adam,” he announces in the preface. He tells us his various titles: human being, husband, father, physician, recovering alcoholic, and psychiatric patient. “In the midst of these struggles, working in modern medicine fractured my identity, stole my authenticity, and left me a shell of the person I wanted to be.”
We learn that he tried to buy a gun, but there was a waiting period and he could not purchase the firearm. Instead, he walked into the woods to drink himself to death, with sleeping pills as an add-on – obviously, he didn’t die, and his journey back from his failed suicidal mission is the meat of the book.
Dr. Hill was a quiet and timid child, and he was bullied at school in a way that has lingered on. He struggles with perfectionism and with a sense of never quite belonging. He was a good student, and later a competitive tennis player who was destined for a regional competition until he broke his ankle after drinking just days before the competition. He did well in college, felt more accepted, and went on to medical school after getting in from the wait list. He went on to do a pediatrics residency, and he and his wife moved from Indiana to North Carolina so he could do a hematology oncology fellowship. It was toward the end of his 2-year fellowship when he tried to purchase a gun, then walked into those woods.
His wife called, asked him to come to dinner, and he left the woods before he’d overdosed. After a meeting with his wife, parents, and sister, he returned to psychiatric care, restarted antidepressants, went to Alcoholics Anonymous, and told his employer that he had a problem. This admission started a distressing series of events, including years of being monitored by state medical boards and being labeled an “impaired physician.”
This is the only thing I didn’t like about Dr. Hill’s memoir: As open as he is about his emotional life, there were pieces missing with respect to what actually happened. At this point, I was befuddled as to why he self-reported his difficulties, and it wasn’t until he talked about starting a second fellowship in palliative care in his home state of Indiana that I could fill in some missing pieces. Dr. Hill and his wife purchased a house, and in November, he started his fellowship. The timing was off from the usual start in July, and I realized that perhaps he had gone to an inpatient setting for a number of months – his disclosure to his employer was voluntary, but his treatment likely interfered with his training and couldn’t be hidden. What else transpired he hints at: bottles hidden, driving while intoxicated, a nurse who gave him IV hydration when he came to work with a hangover.
From here, Dr. Hill’s story becomes every doctor’s nightmare. Settled into his new house and weeks into his fellowship, he is called in and fired: His application for a medical license in Indiana has been denied because of his addiction history. He met with a friend of his father’s who worked in a large pediatrics practice. The meeting went well, but the group felt he was too much of a malpractice risk.
He now needs to pay his mortgage and student loans, so he takes a position in Oklahoma with the Indian Health Service. He’s 700 miles from home, living alone in a hotel room, feeling like the work is beneath him, and the chapter is titled “Exile.” His new boss greets him with, “Listen, we all had our own stories that led us here.” Surprisingly, he likes the work and feels supported. If only it weren’t for all that loneliness, and not surprisingly, he relapses despite the mandated breathalyzer. Six beers later, and Dr. Hill is off to Chicago for a rehab program, then back to Oklahoma to finish off his stint.
What happens next is the second time I wondered about the plot of his life: Through “connections and concession,” he returns to Indiana for the palliative care fellowship, and goes on to work at Riley Children’s Hospital.
When a colleague unexpectedly dies from suicide, Dr. Hill tells others that he, too, once entertained suicidal thoughts. The story from here gets better and better: – to conquer their shame, to share their stories, to feel less alone. He and his wife become parents, he remains sober and healthy, and therapy leads him to a place of self-discovery and success.
Intertwined with telling his story, Dr. Hill takes on some of the institutional issues surrounding addiction and mental illness. He feels shamed and punished by the state medical board that mandates the terms of his medical license. Any physician who reads this book will think twice about revealing a diagnosis of depression or substance use disorder. It’s not a new idea that to protect the public, medical boards should ask about current impairments, not a past history or conditions that have been successfully treated. They should encourage treatment, not punish those who seek care.
Dr. Hill writes about how helpful it has been to allow himself to be vulnerable in the aftermath:
In my experience, the more vulnerability I show, the more opportunities I have to connect to other people. I learned the hard way that when I hide my true self from others, I spiral toward shame. Conversely, when I bury my shame, I begin to accept myself as a beautifully flawed human being, and my perspective on the world reflects that. A turn of the vulnerability dial has opened up connections to other people, while turning away pity, judgment, fear, and shame. Meanwhile, when I am to create spaces for vulnerability, permission is granted to have open and honest conversations about mental health conditions on a larger scale. But I would never have learned these lessons without having been humbled by this disease.
Perhaps the thing I liked best about Dr. Hill’s memoir is that he proposes some solutions. He talks about the importance of fighting stigma, how he finds it everywhere, and how the medical field equates mental illnesses with weakness, thereby perpetuating a self-deprecating cycle in those who have them.
In palliative care, there is an acronym – SPIKES (Set up, Perception, Invitation, Knowledge, Explore emotions, and Summary) that provides guidelines for how to deliver bad news to a family. Dr. Hill suggests using this format to discuss mental health and addictions with patients, colleagues, students. He talks about having “Compassion Rounds” to provide a safe space for his colleagues to talk about their emotional reactions to treating very ill children. And he talks about providing mental health care for trainees as an “opt out” – he schedules all his residents for a counseling session – they can cancel without repercussion, but this serves to “normalize” seeking care. I love the idea that each resident might have someone they’ve met with at least once whom they can call if the going gets rough. “As a result,” Dr. Hill writes, “once secretive conversations about attending counseling happen openly, and the physicians actually feel more comfortable going.”
Adam Hill’s memoir is short, it’s an engaging read, his openness is refreshing, and his plea to let doctors be human beings with human problems is so needed in medicine today. Thank you, Adam.
Dr. Miller is coauthor of “Committed: The Battle Over Involuntary Psychiatry Care” (Baltimore: Johns Hopkins University Press, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore. Dr. Miller has no disclosures.
Enduring the ordeal of a quadruple threat is especially arduous for psychiatric patients
These are unusually stressful days for everyone, especially our patients. We are all experiencing a turbulent mix of emotions as we try to cope with a confluence of threats to both our lives and to life as we know it. Peace of mind has become so elusive due to the relentless overlapping waves of fear, sadness, anger, and uncertainty. We are all grieving in a different way, but our psychiatric patients are suffering the most.
Fear. It only takes 1 traumatic event to trigger posttraumatic stress disorder (PTSD). Yet over the past few months, we have been afflicted by 4 jarring traumatic events, individually and as a society. Just a few months ago, it would have been impossible to imagine the conflux of 4 concurrent seismic threats to our well-being. A toxic political zeitgeist was the backdrop, which we bemoaned and tried to compartmentalize, despite the corrosive political environment shrouding the country. Then the deadly coronavirus disease 2019 (COVID-19) pandemic suddenly arrived, imposing draconian health-preserving measures that impacted every individual’s daily life in countless detrimental ways. Fear prevailed as we all sheltered at home, stopped commuting to work, canceled all trips, distanced ourselves from our friends and relatives, and watched depressing and anxiety-provoking television and read online news throughout our waking hours. Hoarding food and household supplies became endemic due to fear about survival.
Sadness. The agonizing prospect of a national financial necrosis followed the threat of serious illness or death. The economy came to a screeching halt, hemorrhaging millions of jobs. Unemployed parents stayed home with their morose children whose schools were shuttered, leaving them deprived of socializing with their friends. The government hurried with financial chemotherapy, printing trillions of dollars to prevent economic collapse, to avert potential poverty and hunger for many. The fear of the pandemic became coupled with sadness over the loss of livelihoods and grief for the loss of liberty and the ability to pursue happiness, or even small pleasures.
Anger. Then a tsunami of anger was generated by the brutal and sadistic death of a black man in police custody. This was a spark that ignited a massive amount of previously dormant racial tension dating back to the dark days of slavery. Peaceful protests were marred by destructive riots. The explosive fury was perhaps intensified by the protestors having been being locked up for weeks and having to wear masks, both of which were symbolic of being held down and “unable to breathe,” like the murdered Mr. George Floyd.
An epidemic of destroying statues followed. Heavy statues that appeared invincible for decades were dismantled from their plinth in a matter of minutes, signifying extreme frustration with the social injustice that remains despite the transformational laws of the Civil Rights Acts of 1960 and 1964. Suddenly—like falling dominoes—statues, flags, names of military bases, and previously venerated monuments were removed, changed, vandalized, or threatened with destruction. The founders of the republic were also maligned because they were slave owners 2 centuries ago. The paradigm shift spawned by the rage over racial inequality was disconcerting and dramatic. The anger and rampage spawned a sense that a tipping point in our society has been reached.
Uncertainty. The confluence of political instability, a deadly pandemic, economic collapse, and racial tensions were like the 4 horsemen of mass PTSD. The result was an agonizing uncertainty about the impact of these changes, and whether a sense of normalcy will ever return. It became apparent to all of us that our social structure has changed forever across multiple fundamental domains: public health, social, political, and financial. The wait for a vaccine for COVID-19 seems interminable, and racial healing and harmony seems elusive. Economic recovery may be possible, but political detoxification appears unlikely. The fate of police departments, condemned because of the deplorable and illegal acts of a few, and the safety of citizens, usually guaranteed by law and order, seem uncertain. Like COVID-19, angst has rapidly spread across the population.
The price our patients pay
The ingredients of a large-scale societal PTSD, similar to what probably happens during a world war, are now in place. Even resilient individuals may buckle during quadruple ordeals such as this one. So imagine what is happening to our patients, rendered fragile and vulnerable to threats by their pre-existing psychiatric illness. They all pay a heavy price. Patients with anxiety disorders will decompensate, with more panic attacks. Patients burdened by depression will worsen, with more hopelessness, despair, and suicidal ideation due to anxiety and loneliness. Patients with bipolar disorder will become more labile and irritable, and their comorbid anxiety will intensify. Patients with schizophrenia will become more paranoid, depressed, and anxious. Patients with autism will become more agitated and aggressive because their cherished daily routines are disrupted. Patients with obsessive-compulsive disorder will react to their germaphobia by washing their hands and cleaning everything around them even more frequently, and they (along with everyone else) will become hoarders.
Hope and healing
As psychiatrists, we are determined to transcend our own stress, rise above it all, and attend to the pervasive sadness, grief, anger, and uncertainty all around us, but especially among our patients, for whom the anguish of a psychiatric disorder is further compounded by 4 additional ordeals. This is our moment of truth as healers of our patients’ souls, because they look to us to provide them with hope to help navigate these trying times into full health. And we psychiatrists, along with fellow mental health professionals, are up to this unprecedented challenge.
These are unusually stressful days for everyone, especially our patients. We are all experiencing a turbulent mix of emotions as we try to cope with a confluence of threats to both our lives and to life as we know it. Peace of mind has become so elusive due to the relentless overlapping waves of fear, sadness, anger, and uncertainty. We are all grieving in a different way, but our psychiatric patients are suffering the most.
Fear. It only takes 1 traumatic event to trigger posttraumatic stress disorder (PTSD). Yet over the past few months, we have been afflicted by 4 jarring traumatic events, individually and as a society. Just a few months ago, it would have been impossible to imagine the conflux of 4 concurrent seismic threats to our well-being. A toxic political zeitgeist was the backdrop, which we bemoaned and tried to compartmentalize, despite the corrosive political environment shrouding the country. Then the deadly coronavirus disease 2019 (COVID-19) pandemic suddenly arrived, imposing draconian health-preserving measures that impacted every individual’s daily life in countless detrimental ways. Fear prevailed as we all sheltered at home, stopped commuting to work, canceled all trips, distanced ourselves from our friends and relatives, and watched depressing and anxiety-provoking television and read online news throughout our waking hours. Hoarding food and household supplies became endemic due to fear about survival.
Sadness. The agonizing prospect of a national financial necrosis followed the threat of serious illness or death. The economy came to a screeching halt, hemorrhaging millions of jobs. Unemployed parents stayed home with their morose children whose schools were shuttered, leaving them deprived of socializing with their friends. The government hurried with financial chemotherapy, printing trillions of dollars to prevent economic collapse, to avert potential poverty and hunger for many. The fear of the pandemic became coupled with sadness over the loss of livelihoods and grief for the loss of liberty and the ability to pursue happiness, or even small pleasures.
Anger. Then a tsunami of anger was generated by the brutal and sadistic death of a black man in police custody. This was a spark that ignited a massive amount of previously dormant racial tension dating back to the dark days of slavery. Peaceful protests were marred by destructive riots. The explosive fury was perhaps intensified by the protestors having been being locked up for weeks and having to wear masks, both of which were symbolic of being held down and “unable to breathe,” like the murdered Mr. George Floyd.
An epidemic of destroying statues followed. Heavy statues that appeared invincible for decades were dismantled from their plinth in a matter of minutes, signifying extreme frustration with the social injustice that remains despite the transformational laws of the Civil Rights Acts of 1960 and 1964. Suddenly—like falling dominoes—statues, flags, names of military bases, and previously venerated monuments were removed, changed, vandalized, or threatened with destruction. The founders of the republic were also maligned because they were slave owners 2 centuries ago. The paradigm shift spawned by the rage over racial inequality was disconcerting and dramatic. The anger and rampage spawned a sense that a tipping point in our society has been reached.
Uncertainty. The confluence of political instability, a deadly pandemic, economic collapse, and racial tensions were like the 4 horsemen of mass PTSD. The result was an agonizing uncertainty about the impact of these changes, and whether a sense of normalcy will ever return. It became apparent to all of us that our social structure has changed forever across multiple fundamental domains: public health, social, political, and financial. The wait for a vaccine for COVID-19 seems interminable, and racial healing and harmony seems elusive. Economic recovery may be possible, but political detoxification appears unlikely. The fate of police departments, condemned because of the deplorable and illegal acts of a few, and the safety of citizens, usually guaranteed by law and order, seem uncertain. Like COVID-19, angst has rapidly spread across the population.
The price our patients pay
The ingredients of a large-scale societal PTSD, similar to what probably happens during a world war, are now in place. Even resilient individuals may buckle during quadruple ordeals such as this one. So imagine what is happening to our patients, rendered fragile and vulnerable to threats by their pre-existing psychiatric illness. They all pay a heavy price. Patients with anxiety disorders will decompensate, with more panic attacks. Patients burdened by depression will worsen, with more hopelessness, despair, and suicidal ideation due to anxiety and loneliness. Patients with bipolar disorder will become more labile and irritable, and their comorbid anxiety will intensify. Patients with schizophrenia will become more paranoid, depressed, and anxious. Patients with autism will become more agitated and aggressive because their cherished daily routines are disrupted. Patients with obsessive-compulsive disorder will react to their germaphobia by washing their hands and cleaning everything around them even more frequently, and they (along with everyone else) will become hoarders.
Hope and healing
As psychiatrists, we are determined to transcend our own stress, rise above it all, and attend to the pervasive sadness, grief, anger, and uncertainty all around us, but especially among our patients, for whom the anguish of a psychiatric disorder is further compounded by 4 additional ordeals. This is our moment of truth as healers of our patients’ souls, because they look to us to provide them with hope to help navigate these trying times into full health. And we psychiatrists, along with fellow mental health professionals, are up to this unprecedented challenge.
These are unusually stressful days for everyone, especially our patients. We are all experiencing a turbulent mix of emotions as we try to cope with a confluence of threats to both our lives and to life as we know it. Peace of mind has become so elusive due to the relentless overlapping waves of fear, sadness, anger, and uncertainty. We are all grieving in a different way, but our psychiatric patients are suffering the most.
Fear. It only takes 1 traumatic event to trigger posttraumatic stress disorder (PTSD). Yet over the past few months, we have been afflicted by 4 jarring traumatic events, individually and as a society. Just a few months ago, it would have been impossible to imagine the conflux of 4 concurrent seismic threats to our well-being. A toxic political zeitgeist was the backdrop, which we bemoaned and tried to compartmentalize, despite the corrosive political environment shrouding the country. Then the deadly coronavirus disease 2019 (COVID-19) pandemic suddenly arrived, imposing draconian health-preserving measures that impacted every individual’s daily life in countless detrimental ways. Fear prevailed as we all sheltered at home, stopped commuting to work, canceled all trips, distanced ourselves from our friends and relatives, and watched depressing and anxiety-provoking television and read online news throughout our waking hours. Hoarding food and household supplies became endemic due to fear about survival.
Sadness. The agonizing prospect of a national financial necrosis followed the threat of serious illness or death. The economy came to a screeching halt, hemorrhaging millions of jobs. Unemployed parents stayed home with their morose children whose schools were shuttered, leaving them deprived of socializing with their friends. The government hurried with financial chemotherapy, printing trillions of dollars to prevent economic collapse, to avert potential poverty and hunger for many. The fear of the pandemic became coupled with sadness over the loss of livelihoods and grief for the loss of liberty and the ability to pursue happiness, or even small pleasures.
Anger. Then a tsunami of anger was generated by the brutal and sadistic death of a black man in police custody. This was a spark that ignited a massive amount of previously dormant racial tension dating back to the dark days of slavery. Peaceful protests were marred by destructive riots. The explosive fury was perhaps intensified by the protestors having been being locked up for weeks and having to wear masks, both of which were symbolic of being held down and “unable to breathe,” like the murdered Mr. George Floyd.
An epidemic of destroying statues followed. Heavy statues that appeared invincible for decades were dismantled from their plinth in a matter of minutes, signifying extreme frustration with the social injustice that remains despite the transformational laws of the Civil Rights Acts of 1960 and 1964. Suddenly—like falling dominoes—statues, flags, names of military bases, and previously venerated monuments were removed, changed, vandalized, or threatened with destruction. The founders of the republic were also maligned because they were slave owners 2 centuries ago. The paradigm shift spawned by the rage over racial inequality was disconcerting and dramatic. The anger and rampage spawned a sense that a tipping point in our society has been reached.
Uncertainty. The confluence of political instability, a deadly pandemic, economic collapse, and racial tensions were like the 4 horsemen of mass PTSD. The result was an agonizing uncertainty about the impact of these changes, and whether a sense of normalcy will ever return. It became apparent to all of us that our social structure has changed forever across multiple fundamental domains: public health, social, political, and financial. The wait for a vaccine for COVID-19 seems interminable, and racial healing and harmony seems elusive. Economic recovery may be possible, but political detoxification appears unlikely. The fate of police departments, condemned because of the deplorable and illegal acts of a few, and the safety of citizens, usually guaranteed by law and order, seem uncertain. Like COVID-19, angst has rapidly spread across the population.
The price our patients pay
The ingredients of a large-scale societal PTSD, similar to what probably happens during a world war, are now in place. Even resilient individuals may buckle during quadruple ordeals such as this one. So imagine what is happening to our patients, rendered fragile and vulnerable to threats by their pre-existing psychiatric illness. They all pay a heavy price. Patients with anxiety disorders will decompensate, with more panic attacks. Patients burdened by depression will worsen, with more hopelessness, despair, and suicidal ideation due to anxiety and loneliness. Patients with bipolar disorder will become more labile and irritable, and their comorbid anxiety will intensify. Patients with schizophrenia will become more paranoid, depressed, and anxious. Patients with autism will become more agitated and aggressive because their cherished daily routines are disrupted. Patients with obsessive-compulsive disorder will react to their germaphobia by washing their hands and cleaning everything around them even more frequently, and they (along with everyone else) will become hoarders.
Hope and healing
As psychiatrists, we are determined to transcend our own stress, rise above it all, and attend to the pervasive sadness, grief, anger, and uncertainty all around us, but especially among our patients, for whom the anguish of a psychiatric disorder is further compounded by 4 additional ordeals. This is our moment of truth as healers of our patients’ souls, because they look to us to provide them with hope to help navigate these trying times into full health. And we psychiatrists, along with fellow mental health professionals, are up to this unprecedented challenge.
Differing views of ‘behavioral health’
In the wake of Dr. Nasrallah’s recent editorial “Stop calling it ‘behavioral health:’ Psychiatry is much more” (From the Editor,
Naming a field, institute, department, or group of collaborators is crucially important, and must be undertaken with care. We all are familiar with Departments of Psychiatry, Departments of Psychiatry and Psychology, and Institutes for everything from Behavioral Health to Living. Even within the discipline of psychiatry, there have been adjustments over time in subspecialties (as seen with consultation-liaison psychiatry becoming psychosomatic medicine and then back again).
In our hospital system, we have recently adopted the term “Behavioral Health Institute” to denote the work and worth of significant numbers of caregivers (psychiatrists, psychologists, chemical dependency counselors, social workers, child life workers, advanced practice nurses, and others) who strive to improve the health and well-being of patients with both substance abuse and mental illness. We endeavor to remain mindful that a diversity of providers are involved in caring for and about our patients, and that “psychiatry” cannot—and should not—be the extent of how we conceptualize our services.
We submit that the modern view of behavioral health is ahead of other fields of medicine in recognizing that concepts, such as teamwork and diversity, are key to achieving positive patient outcomes. By identifying our providers as part of a Behavioral Health Institute, we acknowledge that not all mental distress is psychiatric illness but may still benefit from intervention and, importantly, that psychiatrists are not the center of the mental health (behavioral health) world. Treatments ranging from medication management to psychiatric procedures to psychotherapeutic modalities show the depth and breadth of our field, and the multiplicity of providers and modalities should be considered laudable. Recognizing the complexities inherent in behavioral health and its varied treatment options does not diminish but, in fact, elevates the field of psychiatry—and psychiatrists themselves.
Further, we note that behavioral health is not the only term that casts a larger net than the physician in a respective field. Does the term “primary care” insult internal medicine, family medicine, and pediatric physicians? Physicians and health care teams join in partnership with patients and families, either to cure or learn how to manage disease. We believe that constructing a health care system centered on physicians and their identities, rather than on patients and treatment outcomes, has been foolish. To that end, the tenor of Dr. Nasrallah’s editorial runs counter to the overall efforts of our field to improve collaboration, and, at its extreme, such articles promote the antiquated notion of physician elitism.
The editorial’s historical context is of course important, and the caution not to water down what “we” do (as psychiatrists) is appropriate. However, instead of comporting ourselves in a psychiatry-centric way, the use of the term behavioral health allows all of us to acknowledge (with appreciation and humility) the many contributors who work in our field. The use of a broad-minded, inclusive term neither minimizes nor trivializes psychiatry as a medical specialty. Rather, accepting this term and this mindset can place psychiatrists in the unique role of being innovators for the rest of medicine, because we embrace multidisciplinary teams and the value that interdisciplinary care can bring to patients and colleagues alike.
Jeanne Lackamp, MD, DFAPA, FACLP
Director, Pain Management Institute
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Patrick Runnels, MD, MBA
Chief Medical Officer, Population Health – Behavioral Health
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Lori Locke, RN, MSN
Director, Psychiatry Service Line and Nursing Practice
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Erum Ahmad, MD
Director, Child and Adolescent Psychiatry Unit
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Robert Ronis, MD, MPH
Douglas Danford Bond Professor and Chairman
Psychiatrist-in-Chief
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Continue to: Dr. Nasrallah responds
Dr. Nasrallah responds
I thank my Cleveland colleagues for their letter, and I welcome their disagreement with the tenets of my editorial. I still insist that the term “behavioral health” has a very narrow meaning that is not equivalent to psychiatry or psychology or social work or psychiatric nursing practice. This term should not be conflated with the widely used “mental health,” which is used as an overarching term for all professionals involved in the care of psychiatric brain disorders that manifest as various mental illnesses and substance use disorders.
While I am an advocate for multidisciplinary collaborations that benefit our patients, I will always uphold psychiatry as a medical specialty whose unique identity should not be sacrificed on the altar of politically correct egalitarianism of the mental health disciplines. Call it elitist if you like, but the fact is that the extensive medical school, residency, and fellowship training of psychiatrists stand out among all the other mental health disciplines. Psychiatrists are the best trained in all components of the biopsychosocial model (which I acquired many years ago from the father of the concept, George Engel, one of my teachers at the University of Rochester Residency Program).
You bring up primary care as an analogy for behavioral health. I assure you, none of the medical specialists included under that umbrella term refer to themselves as primary care physicians (PCPs) (or, God forbid, providers!). They identify themselves as family physicians, internists, pediatricians, and gynecologists. It is for the convenience of the health care systems and insurance companies that clinicians are called PCPs, which homogenizes them into a fuzzy amalgam and disguises their true medical identities as specialists.
So we agree to disagree. Diversity of opinions is a sacred principle. But I still think that a more accurate name for your Behavioral Health Institute would be “Institute of Psychiatric Medicine and Brain Health.” Behavioral health, which actually refers to educating people about implementing principles of evidence-based healthy habits and behaviors that prevent or reduce the risk of mental illness and/or substance use, is a small sliver of your overall mission. As you’ll notice from the other letters we’ve received, the vast majority of our readers agree that psychiatric medicine is far more than behavioral health.
Henry A. Nasrallah, MD
Professor of Psychiatry, Neurology, and Neuroscience
Medical Director: Neuropsychiatry
Director, Schizophrenia and Neuropsychiatry Programs
University of Cincinnati College of Medicine
Cincinnati, Ohio
Professor Emeritus, Saint Louis University
St. Louis, Missouri
Continue to: I thoroughly enjoyed...
I thoroughly enjoyed Dr. Nasrallah’s editorial and agree completely. Veterans Affairs, my employer for the last 12 years, has fully bought into the use of “behavioral health” and its implications for its many psychiatrists. I have grown very tired of the constant minimization of psychiatric practice, and it is so good to hear from an affirming voice.
Barbara Day, MD
US Department of Veterans Affairs
Ann Arbor, Michigan
Dr. Nasrallah’s editorial made my heart sing! I have been practicing psychiatry since 1979, and have always bristled when called a “provider” or any of the other terms Dr. Nasrallah described. As a graduate of Johns Hopkins Medical School, I had professors who themselves had been taught by Harry Stack Sullivan and Frida Fromm Reichman, and during my residency at the University of Chicago, I sat in discussions with both Bruno Bettelheim and Heinz Kohut. I felt part of an honorable tradition, and even though biological psychiatry was on the ascendency, these analytical luminaries were part of my learning the “art” of psychiatry. It is not so easy to feel good about a specialty that has had such a history as ours, but my own experiences could never be reduced to being called a behavioral health provider. Dr. Nasrallah’s thoughts are very encouraging, and I thank him!
John Engers, MD
Private psychiatric practice (retired)
Fremont, California
Dr. Nasrallah’s editorial resonated with one of my pet peeves. I’ve been telling my medical students for years that we psychiatrists treat disorders of thinking, emotions, and behavior associated with mental illness, and that the term “behavioral health,” though possibly well intentioned, is a euphemism to reduce stigma.
Irl Extein, MD
Private psychiatric practice
Delray Beach, Florida
Clinical Affiliate Associate Professor, Florida
Atlantic University College of Medicine
Boca Raton, Florida
Continue to: I enjoyed...
I enjoyed Dr. Nasrallah’s editorial regarding “behavioral health.” In New England, we have very clear delineation among psychiatry, mental health, and behavioral health. Only physicians can practice psychiatry because it is a medical specialty. Nurse practitioners and psychologists, on the other hand, are specialists in the field of mental health, as are psychiatrists, so mental health is a more encompassing term. Behavioral health encompasses all of the above plus counselors. Because insurers generally pay counselors, nurse practitioners, and psychiatrists, they use the term behavioral health because it wouldn’t be right for them to pay a counselor for a psychiatric intervention. So as a psychiatrist, I respond when being referred to as a psychiatrist, mental health specialist, or behavioral health specialist. And thankfully, per American Medical Association policy, psychiatrists are not providers.
Stu Gitlow, MD, MPH
Executive Director
Annenberg Physician Training Program in Addictive Disease
Woonsocket, Rhode Island
I was grateful for Dr. Nasrallah’s editorial regarding the misnomer of referring to psychiatry as “behavioral health.” Until this editorial, I had wondered if I was the only one bothered by the term. Many people are under the assumption that behavioral health is a politically correct term that helps to lessen stigmatism. I completely disagree. Without question, it adds to the stigmatism. The term behavioral health is belittling to our patients. For example, calling a psychiatric inpatient unit a “behavioral health unit” implies that if patients would just change their behaviors, they wouldn’t have serious biological psychiatric illness. It insinuates that the patients cause and perpetuate their illnesses, such as schizophrenia or bipolar disorder, by behaving poorly. Granted, we teach behavior modification to help manage psychiatric illness, but so, too, do our colleagues in other medical fields teach behavior modification to manage other organ-related illnesses. Some nearly ubiquitous examples include doctors advising patients to lower stress, modify diet, exercise, and take medications as prescribed. Yet, for example, in the case of a patient with diabetes, we don’t refer to diabetic ketoacidosis treatment as behavioral health treatment, though the patient’s behavior no doubt contributes to this condition. And we certainly would never call the ICU or stepdown unit the “behavioral health unit,” even though adequate holistic treatment in these settings includes counseling the patient with diabetes on changing his/her behaviors that led to the ketoacidosis. Just as in diabetes, the underlying basis of psychiatric illness is biologic processes gone awry. First and foremost, a psychiatric medical illness requires complicated and often precarious medications to treat. As in other medical specialties, modifying behavior does not treat the illness, but merely serves to help transmute the course.
In sum, I wholly agree with Dr. Nasrallah’s eloquent assessment regarding the problems with the title behavioral health in lieu of psychiatry. I also might have taken the discussion a step a further: Because psychiatric illness affects every aspect of a person’s life—such as work, social, and personal—it requires a terminology commensurate with the medical gravity it warrants. So in addition to not referring to the specialty as behavioral health, I have wondered if the name psychiatry could be replaced with a more medical-sounding term such as “cerebrology” or something of the sort. But one step at time.
Stacie Lauro, MD, ABPN
Attending in Psychiatry, Emergency Room, and Consultation Liaison
Mindcare Solutions
Tampa, Florida
The evolution within our field of the use of “behavioral health” has disturbed me to the same extent it has for Dr. Nasrallah. I founded and direct a psychiatric treatment facility in Florida. We are a teaching facility affiliated with 3 psychiatric residencies, 8 medical schools, and 60 physician assistant (PA) schools. In all of the literature (eg, evaluations) from the PA schools, they refer to their rotation with my program as “behavioral health.” I have been attempting to correct them for years! I teach all residents and students to correctly use the terms “psychiatry” and “psychiatric.” I understand there may be stigma associated with the latter terms, but the field reinforces that stigma by avoiding the use of these terms.
Robert A. Moran, MD, FAPA, FASAM
CEO and Medical Director, Family Center for Recovery
Lantana, Florida
Continue to: Pre-authorization and 'hold harmless' clauses
Pre-authorization and ‘hold harmless’ clauses
Regarding Dr. Nasrallah’s editorial “Pre-authorization is illegal, unethical, and adversely disrupts patient care” (From the Editor,
Recently to my surprise, while navigating a pre-authorization request for a young patient with bipolar disorder who had accepted the inclusion of lurasidone in his treatment regimen while hospitalized, I found that the CoverMyMeds Business Associate Agreement is required for a user to accomplish pre-authorization online. Having a little extra time for due diligence that day, I read this lengthy agreement carefully. The CoverMyMeds user agreement purports not to offer “medical advice, does not determine medical necessity, insurance coverage or copays and does not otherwise engage in the practice of medicine” (see www.covermymeds.com/main/about/privacy/tos/). Interestingly, the agreement goes on to purport that the whole process is for informational purposes only, not a substitute for clinicians, professional medical judgment, or for individual patient assessments and examinations. Of course, another factor is that the information provided by the process is “solely at the user’s and health care provider’s own risk.” Finally, the agreement requires the user to agree to “indemnify, defend, and hold harmless CoverMyMeds and its affiliates … from any demands, claims, damages, liabilities, expenses, or harms (including attorneys’ fees) arising out of or related to your use of our Services or breach of these Terms of Service.”
Throughout my 25 years of solo private practice, I have refused to sign hold harmless clauses and I refused to sign the CoverMyMeds user agreement. I have made it my practice never to obtain pre-authorization unless the patient is with me in the room during an appointment because the process of navigating pre-authorization does become part of the treatment, however unfortunately. As an alternative, for my patient with bipolar disorder, I was able to use a phone number to talk to a representative of the pharmacy benefit plan that was contracted with CoverMyMeds. Without signing on to be a Business Associate, we accomplished the goal of continuing with the medication as recommended and implemented for 2 preceding months (often pre-authorization actually means continuing authorization, doesn’t it?). I believe if all psychiatrists were to adopt this kind of stance, we could make a change. I know there are anti-trust considerations involved in fee negotiations, but when it comes to the egregious practices of managed care, pre-authorization, and hold harmless clauses, it seems to me that we can mount a counteroffensive to great effect.
Further, I want to stand in strong support of Dr. Nasrallah’s editorial “Stop calling it ‘behavioral health’: Psychiatry is much more.” When I began my first job post-fellowship, I was alarmed to find that our outpatient offices had been named a “counseling center.” Due to such misleading, stigmatizing characterizations, as Dr. Nasrallah pointed out, we have only slid further down the slope into the realm of “providers of behavioral health services.” As an old hand working psychiatric locum tenens told me, we psychiatrists had long since missed the chance to “band together like musk oxen” to defend our profession.
However, I believe it is not too late. With the strength of Dr. Nasrallah’s leadership and a more overt, collective stubbornness coupled with an undying commitment to excellence, we can and must push hard against the insurance and hospital entities, which continue to profiteer from the practice of medicine without a license—using the tools of hold harmless clauses, anti-trust laws in their favor, and misinformation about the scope and efficacy of practicing psychiatry per se. The challenge is to figure out exactly how to proceed.
Although some manage to thrive in independent practice, collectively our struggle seems considerable, but not insurmountable.
David B. Robinson, MD, MPH
Diplomate, American Board of Psychiatry and Neurology in Child, Adolescent and Adult Psychiatry
Fellow, American Psychiatric Association
Private psychiatric practice
Alaska Psychiatric Concepts
Juneau, Alaska
In the wake of Dr. Nasrallah’s recent editorial “Stop calling it ‘behavioral health:’ Psychiatry is much more” (From the Editor,
Naming a field, institute, department, or group of collaborators is crucially important, and must be undertaken with care. We all are familiar with Departments of Psychiatry, Departments of Psychiatry and Psychology, and Institutes for everything from Behavioral Health to Living. Even within the discipline of psychiatry, there have been adjustments over time in subspecialties (as seen with consultation-liaison psychiatry becoming psychosomatic medicine and then back again).
In our hospital system, we have recently adopted the term “Behavioral Health Institute” to denote the work and worth of significant numbers of caregivers (psychiatrists, psychologists, chemical dependency counselors, social workers, child life workers, advanced practice nurses, and others) who strive to improve the health and well-being of patients with both substance abuse and mental illness. We endeavor to remain mindful that a diversity of providers are involved in caring for and about our patients, and that “psychiatry” cannot—and should not—be the extent of how we conceptualize our services.
We submit that the modern view of behavioral health is ahead of other fields of medicine in recognizing that concepts, such as teamwork and diversity, are key to achieving positive patient outcomes. By identifying our providers as part of a Behavioral Health Institute, we acknowledge that not all mental distress is psychiatric illness but may still benefit from intervention and, importantly, that psychiatrists are not the center of the mental health (behavioral health) world. Treatments ranging from medication management to psychiatric procedures to psychotherapeutic modalities show the depth and breadth of our field, and the multiplicity of providers and modalities should be considered laudable. Recognizing the complexities inherent in behavioral health and its varied treatment options does not diminish but, in fact, elevates the field of psychiatry—and psychiatrists themselves.
Further, we note that behavioral health is not the only term that casts a larger net than the physician in a respective field. Does the term “primary care” insult internal medicine, family medicine, and pediatric physicians? Physicians and health care teams join in partnership with patients and families, either to cure or learn how to manage disease. We believe that constructing a health care system centered on physicians and their identities, rather than on patients and treatment outcomes, has been foolish. To that end, the tenor of Dr. Nasrallah’s editorial runs counter to the overall efforts of our field to improve collaboration, and, at its extreme, such articles promote the antiquated notion of physician elitism.
The editorial’s historical context is of course important, and the caution not to water down what “we” do (as psychiatrists) is appropriate. However, instead of comporting ourselves in a psychiatry-centric way, the use of the term behavioral health allows all of us to acknowledge (with appreciation and humility) the many contributors who work in our field. The use of a broad-minded, inclusive term neither minimizes nor trivializes psychiatry as a medical specialty. Rather, accepting this term and this mindset can place psychiatrists in the unique role of being innovators for the rest of medicine, because we embrace multidisciplinary teams and the value that interdisciplinary care can bring to patients and colleagues alike.
Jeanne Lackamp, MD, DFAPA, FACLP
Director, Pain Management Institute
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Patrick Runnels, MD, MBA
Chief Medical Officer, Population Health – Behavioral Health
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Lori Locke, RN, MSN
Director, Psychiatry Service Line and Nursing Practice
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Erum Ahmad, MD
Director, Child and Adolescent Psychiatry Unit
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Robert Ronis, MD, MPH
Douglas Danford Bond Professor and Chairman
Psychiatrist-in-Chief
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Continue to: Dr. Nasrallah responds
Dr. Nasrallah responds
I thank my Cleveland colleagues for their letter, and I welcome their disagreement with the tenets of my editorial. I still insist that the term “behavioral health” has a very narrow meaning that is not equivalent to psychiatry or psychology or social work or psychiatric nursing practice. This term should not be conflated with the widely used “mental health,” which is used as an overarching term for all professionals involved in the care of psychiatric brain disorders that manifest as various mental illnesses and substance use disorders.
While I am an advocate for multidisciplinary collaborations that benefit our patients, I will always uphold psychiatry as a medical specialty whose unique identity should not be sacrificed on the altar of politically correct egalitarianism of the mental health disciplines. Call it elitist if you like, but the fact is that the extensive medical school, residency, and fellowship training of psychiatrists stand out among all the other mental health disciplines. Psychiatrists are the best trained in all components of the biopsychosocial model (which I acquired many years ago from the father of the concept, George Engel, one of my teachers at the University of Rochester Residency Program).
You bring up primary care as an analogy for behavioral health. I assure you, none of the medical specialists included under that umbrella term refer to themselves as primary care physicians (PCPs) (or, God forbid, providers!). They identify themselves as family physicians, internists, pediatricians, and gynecologists. It is for the convenience of the health care systems and insurance companies that clinicians are called PCPs, which homogenizes them into a fuzzy amalgam and disguises their true medical identities as specialists.
So we agree to disagree. Diversity of opinions is a sacred principle. But I still think that a more accurate name for your Behavioral Health Institute would be “Institute of Psychiatric Medicine and Brain Health.” Behavioral health, which actually refers to educating people about implementing principles of evidence-based healthy habits and behaviors that prevent or reduce the risk of mental illness and/or substance use, is a small sliver of your overall mission. As you’ll notice from the other letters we’ve received, the vast majority of our readers agree that psychiatric medicine is far more than behavioral health.
Henry A. Nasrallah, MD
Professor of Psychiatry, Neurology, and Neuroscience
Medical Director: Neuropsychiatry
Director, Schizophrenia and Neuropsychiatry Programs
University of Cincinnati College of Medicine
Cincinnati, Ohio
Professor Emeritus, Saint Louis University
St. Louis, Missouri
Continue to: I thoroughly enjoyed...
I thoroughly enjoyed Dr. Nasrallah’s editorial and agree completely. Veterans Affairs, my employer for the last 12 years, has fully bought into the use of “behavioral health” and its implications for its many psychiatrists. I have grown very tired of the constant minimization of psychiatric practice, and it is so good to hear from an affirming voice.
Barbara Day, MD
US Department of Veterans Affairs
Ann Arbor, Michigan
Dr. Nasrallah’s editorial made my heart sing! I have been practicing psychiatry since 1979, and have always bristled when called a “provider” or any of the other terms Dr. Nasrallah described. As a graduate of Johns Hopkins Medical School, I had professors who themselves had been taught by Harry Stack Sullivan and Frida Fromm Reichman, and during my residency at the University of Chicago, I sat in discussions with both Bruno Bettelheim and Heinz Kohut. I felt part of an honorable tradition, and even though biological psychiatry was on the ascendency, these analytical luminaries were part of my learning the “art” of psychiatry. It is not so easy to feel good about a specialty that has had such a history as ours, but my own experiences could never be reduced to being called a behavioral health provider. Dr. Nasrallah’s thoughts are very encouraging, and I thank him!
John Engers, MD
Private psychiatric practice (retired)
Fremont, California
Dr. Nasrallah’s editorial resonated with one of my pet peeves. I’ve been telling my medical students for years that we psychiatrists treat disorders of thinking, emotions, and behavior associated with mental illness, and that the term “behavioral health,” though possibly well intentioned, is a euphemism to reduce stigma.
Irl Extein, MD
Private psychiatric practice
Delray Beach, Florida
Clinical Affiliate Associate Professor, Florida
Atlantic University College of Medicine
Boca Raton, Florida
Continue to: I enjoyed...
I enjoyed Dr. Nasrallah’s editorial regarding “behavioral health.” In New England, we have very clear delineation among psychiatry, mental health, and behavioral health. Only physicians can practice psychiatry because it is a medical specialty. Nurse practitioners and psychologists, on the other hand, are specialists in the field of mental health, as are psychiatrists, so mental health is a more encompassing term. Behavioral health encompasses all of the above plus counselors. Because insurers generally pay counselors, nurse practitioners, and psychiatrists, they use the term behavioral health because it wouldn’t be right for them to pay a counselor for a psychiatric intervention. So as a psychiatrist, I respond when being referred to as a psychiatrist, mental health specialist, or behavioral health specialist. And thankfully, per American Medical Association policy, psychiatrists are not providers.
Stu Gitlow, MD, MPH
Executive Director
Annenberg Physician Training Program in Addictive Disease
Woonsocket, Rhode Island
I was grateful for Dr. Nasrallah’s editorial regarding the misnomer of referring to psychiatry as “behavioral health.” Until this editorial, I had wondered if I was the only one bothered by the term. Many people are under the assumption that behavioral health is a politically correct term that helps to lessen stigmatism. I completely disagree. Without question, it adds to the stigmatism. The term behavioral health is belittling to our patients. For example, calling a psychiatric inpatient unit a “behavioral health unit” implies that if patients would just change their behaviors, they wouldn’t have serious biological psychiatric illness. It insinuates that the patients cause and perpetuate their illnesses, such as schizophrenia or bipolar disorder, by behaving poorly. Granted, we teach behavior modification to help manage psychiatric illness, but so, too, do our colleagues in other medical fields teach behavior modification to manage other organ-related illnesses. Some nearly ubiquitous examples include doctors advising patients to lower stress, modify diet, exercise, and take medications as prescribed. Yet, for example, in the case of a patient with diabetes, we don’t refer to diabetic ketoacidosis treatment as behavioral health treatment, though the patient’s behavior no doubt contributes to this condition. And we certainly would never call the ICU or stepdown unit the “behavioral health unit,” even though adequate holistic treatment in these settings includes counseling the patient with diabetes on changing his/her behaviors that led to the ketoacidosis. Just as in diabetes, the underlying basis of psychiatric illness is biologic processes gone awry. First and foremost, a psychiatric medical illness requires complicated and often precarious medications to treat. As in other medical specialties, modifying behavior does not treat the illness, but merely serves to help transmute the course.
In sum, I wholly agree with Dr. Nasrallah’s eloquent assessment regarding the problems with the title behavioral health in lieu of psychiatry. I also might have taken the discussion a step a further: Because psychiatric illness affects every aspect of a person’s life—such as work, social, and personal—it requires a terminology commensurate with the medical gravity it warrants. So in addition to not referring to the specialty as behavioral health, I have wondered if the name psychiatry could be replaced with a more medical-sounding term such as “cerebrology” or something of the sort. But one step at time.
Stacie Lauro, MD, ABPN
Attending in Psychiatry, Emergency Room, and Consultation Liaison
Mindcare Solutions
Tampa, Florida
The evolution within our field of the use of “behavioral health” has disturbed me to the same extent it has for Dr. Nasrallah. I founded and direct a psychiatric treatment facility in Florida. We are a teaching facility affiliated with 3 psychiatric residencies, 8 medical schools, and 60 physician assistant (PA) schools. In all of the literature (eg, evaluations) from the PA schools, they refer to their rotation with my program as “behavioral health.” I have been attempting to correct them for years! I teach all residents and students to correctly use the terms “psychiatry” and “psychiatric.” I understand there may be stigma associated with the latter terms, but the field reinforces that stigma by avoiding the use of these terms.
Robert A. Moran, MD, FAPA, FASAM
CEO and Medical Director, Family Center for Recovery
Lantana, Florida
Continue to: Pre-authorization and 'hold harmless' clauses
Pre-authorization and ‘hold harmless’ clauses
Regarding Dr. Nasrallah’s editorial “Pre-authorization is illegal, unethical, and adversely disrupts patient care” (From the Editor,
Recently to my surprise, while navigating a pre-authorization request for a young patient with bipolar disorder who had accepted the inclusion of lurasidone in his treatment regimen while hospitalized, I found that the CoverMyMeds Business Associate Agreement is required for a user to accomplish pre-authorization online. Having a little extra time for due diligence that day, I read this lengthy agreement carefully. The CoverMyMeds user agreement purports not to offer “medical advice, does not determine medical necessity, insurance coverage or copays and does not otherwise engage in the practice of medicine” (see www.covermymeds.com/main/about/privacy/tos/). Interestingly, the agreement goes on to purport that the whole process is for informational purposes only, not a substitute for clinicians, professional medical judgment, or for individual patient assessments and examinations. Of course, another factor is that the information provided by the process is “solely at the user’s and health care provider’s own risk.” Finally, the agreement requires the user to agree to “indemnify, defend, and hold harmless CoverMyMeds and its affiliates … from any demands, claims, damages, liabilities, expenses, or harms (including attorneys’ fees) arising out of or related to your use of our Services or breach of these Terms of Service.”
Throughout my 25 years of solo private practice, I have refused to sign hold harmless clauses and I refused to sign the CoverMyMeds user agreement. I have made it my practice never to obtain pre-authorization unless the patient is with me in the room during an appointment because the process of navigating pre-authorization does become part of the treatment, however unfortunately. As an alternative, for my patient with bipolar disorder, I was able to use a phone number to talk to a representative of the pharmacy benefit plan that was contracted with CoverMyMeds. Without signing on to be a Business Associate, we accomplished the goal of continuing with the medication as recommended and implemented for 2 preceding months (often pre-authorization actually means continuing authorization, doesn’t it?). I believe if all psychiatrists were to adopt this kind of stance, we could make a change. I know there are anti-trust considerations involved in fee negotiations, but when it comes to the egregious practices of managed care, pre-authorization, and hold harmless clauses, it seems to me that we can mount a counteroffensive to great effect.
Further, I want to stand in strong support of Dr. Nasrallah’s editorial “Stop calling it ‘behavioral health’: Psychiatry is much more.” When I began my first job post-fellowship, I was alarmed to find that our outpatient offices had been named a “counseling center.” Due to such misleading, stigmatizing characterizations, as Dr. Nasrallah pointed out, we have only slid further down the slope into the realm of “providers of behavioral health services.” As an old hand working psychiatric locum tenens told me, we psychiatrists had long since missed the chance to “band together like musk oxen” to defend our profession.
However, I believe it is not too late. With the strength of Dr. Nasrallah’s leadership and a more overt, collective stubbornness coupled with an undying commitment to excellence, we can and must push hard against the insurance and hospital entities, which continue to profiteer from the practice of medicine without a license—using the tools of hold harmless clauses, anti-trust laws in their favor, and misinformation about the scope and efficacy of practicing psychiatry per se. The challenge is to figure out exactly how to proceed.
Although some manage to thrive in independent practice, collectively our struggle seems considerable, but not insurmountable.
David B. Robinson, MD, MPH
Diplomate, American Board of Psychiatry and Neurology in Child, Adolescent and Adult Psychiatry
Fellow, American Psychiatric Association
Private psychiatric practice
Alaska Psychiatric Concepts
Juneau, Alaska
In the wake of Dr. Nasrallah’s recent editorial “Stop calling it ‘behavioral health:’ Psychiatry is much more” (From the Editor,
Naming a field, institute, department, or group of collaborators is crucially important, and must be undertaken with care. We all are familiar with Departments of Psychiatry, Departments of Psychiatry and Psychology, and Institutes for everything from Behavioral Health to Living. Even within the discipline of psychiatry, there have been adjustments over time in subspecialties (as seen with consultation-liaison psychiatry becoming psychosomatic medicine and then back again).
In our hospital system, we have recently adopted the term “Behavioral Health Institute” to denote the work and worth of significant numbers of caregivers (psychiatrists, psychologists, chemical dependency counselors, social workers, child life workers, advanced practice nurses, and others) who strive to improve the health and well-being of patients with both substance abuse and mental illness. We endeavor to remain mindful that a diversity of providers are involved in caring for and about our patients, and that “psychiatry” cannot—and should not—be the extent of how we conceptualize our services.
We submit that the modern view of behavioral health is ahead of other fields of medicine in recognizing that concepts, such as teamwork and diversity, are key to achieving positive patient outcomes. By identifying our providers as part of a Behavioral Health Institute, we acknowledge that not all mental distress is psychiatric illness but may still benefit from intervention and, importantly, that psychiatrists are not the center of the mental health (behavioral health) world. Treatments ranging from medication management to psychiatric procedures to psychotherapeutic modalities show the depth and breadth of our field, and the multiplicity of providers and modalities should be considered laudable. Recognizing the complexities inherent in behavioral health and its varied treatment options does not diminish but, in fact, elevates the field of psychiatry—and psychiatrists themselves.
Further, we note that behavioral health is not the only term that casts a larger net than the physician in a respective field. Does the term “primary care” insult internal medicine, family medicine, and pediatric physicians? Physicians and health care teams join in partnership with patients and families, either to cure or learn how to manage disease. We believe that constructing a health care system centered on physicians and their identities, rather than on patients and treatment outcomes, has been foolish. To that end, the tenor of Dr. Nasrallah’s editorial runs counter to the overall efforts of our field to improve collaboration, and, at its extreme, such articles promote the antiquated notion of physician elitism.
The editorial’s historical context is of course important, and the caution not to water down what “we” do (as psychiatrists) is appropriate. However, instead of comporting ourselves in a psychiatry-centric way, the use of the term behavioral health allows all of us to acknowledge (with appreciation and humility) the many contributors who work in our field. The use of a broad-minded, inclusive term neither minimizes nor trivializes psychiatry as a medical specialty. Rather, accepting this term and this mindset can place psychiatrists in the unique role of being innovators for the rest of medicine, because we embrace multidisciplinary teams and the value that interdisciplinary care can bring to patients and colleagues alike.
Jeanne Lackamp, MD, DFAPA, FACLP
Director, Pain Management Institute
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Patrick Runnels, MD, MBA
Chief Medical Officer, Population Health – Behavioral Health
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Lori Locke, RN, MSN
Director, Psychiatry Service Line and Nursing Practice
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Erum Ahmad, MD
Director, Child and Adolescent Psychiatry Unit
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Robert Ronis, MD, MPH
Douglas Danford Bond Professor and Chairman
Psychiatrist-in-Chief
University Hospitals Health System
Case Western Reserve University School of Medicine
Cleveland, Ohio
Continue to: Dr. Nasrallah responds
Dr. Nasrallah responds
I thank my Cleveland colleagues for their letter, and I welcome their disagreement with the tenets of my editorial. I still insist that the term “behavioral health” has a very narrow meaning that is not equivalent to psychiatry or psychology or social work or psychiatric nursing practice. This term should not be conflated with the widely used “mental health,” which is used as an overarching term for all professionals involved in the care of psychiatric brain disorders that manifest as various mental illnesses and substance use disorders.
While I am an advocate for multidisciplinary collaborations that benefit our patients, I will always uphold psychiatry as a medical specialty whose unique identity should not be sacrificed on the altar of politically correct egalitarianism of the mental health disciplines. Call it elitist if you like, but the fact is that the extensive medical school, residency, and fellowship training of psychiatrists stand out among all the other mental health disciplines. Psychiatrists are the best trained in all components of the biopsychosocial model (which I acquired many years ago from the father of the concept, George Engel, one of my teachers at the University of Rochester Residency Program).
You bring up primary care as an analogy for behavioral health. I assure you, none of the medical specialists included under that umbrella term refer to themselves as primary care physicians (PCPs) (or, God forbid, providers!). They identify themselves as family physicians, internists, pediatricians, and gynecologists. It is for the convenience of the health care systems and insurance companies that clinicians are called PCPs, which homogenizes them into a fuzzy amalgam and disguises their true medical identities as specialists.
So we agree to disagree. Diversity of opinions is a sacred principle. But I still think that a more accurate name for your Behavioral Health Institute would be “Institute of Psychiatric Medicine and Brain Health.” Behavioral health, which actually refers to educating people about implementing principles of evidence-based healthy habits and behaviors that prevent or reduce the risk of mental illness and/or substance use, is a small sliver of your overall mission. As you’ll notice from the other letters we’ve received, the vast majority of our readers agree that psychiatric medicine is far more than behavioral health.
Henry A. Nasrallah, MD
Professor of Psychiatry, Neurology, and Neuroscience
Medical Director: Neuropsychiatry
Director, Schizophrenia and Neuropsychiatry Programs
University of Cincinnati College of Medicine
Cincinnati, Ohio
Professor Emeritus, Saint Louis University
St. Louis, Missouri
Continue to: I thoroughly enjoyed...
I thoroughly enjoyed Dr. Nasrallah’s editorial and agree completely. Veterans Affairs, my employer for the last 12 years, has fully bought into the use of “behavioral health” and its implications for its many psychiatrists. I have grown very tired of the constant minimization of psychiatric practice, and it is so good to hear from an affirming voice.
Barbara Day, MD
US Department of Veterans Affairs
Ann Arbor, Michigan
Dr. Nasrallah’s editorial made my heart sing! I have been practicing psychiatry since 1979, and have always bristled when called a “provider” or any of the other terms Dr. Nasrallah described. As a graduate of Johns Hopkins Medical School, I had professors who themselves had been taught by Harry Stack Sullivan and Frida Fromm Reichman, and during my residency at the University of Chicago, I sat in discussions with both Bruno Bettelheim and Heinz Kohut. I felt part of an honorable tradition, and even though biological psychiatry was on the ascendency, these analytical luminaries were part of my learning the “art” of psychiatry. It is not so easy to feel good about a specialty that has had such a history as ours, but my own experiences could never be reduced to being called a behavioral health provider. Dr. Nasrallah’s thoughts are very encouraging, and I thank him!
John Engers, MD
Private psychiatric practice (retired)
Fremont, California
Dr. Nasrallah’s editorial resonated with one of my pet peeves. I’ve been telling my medical students for years that we psychiatrists treat disorders of thinking, emotions, and behavior associated with mental illness, and that the term “behavioral health,” though possibly well intentioned, is a euphemism to reduce stigma.
Irl Extein, MD
Private psychiatric practice
Delray Beach, Florida
Clinical Affiliate Associate Professor, Florida
Atlantic University College of Medicine
Boca Raton, Florida
Continue to: I enjoyed...
I enjoyed Dr. Nasrallah’s editorial regarding “behavioral health.” In New England, we have very clear delineation among psychiatry, mental health, and behavioral health. Only physicians can practice psychiatry because it is a medical specialty. Nurse practitioners and psychologists, on the other hand, are specialists in the field of mental health, as are psychiatrists, so mental health is a more encompassing term. Behavioral health encompasses all of the above plus counselors. Because insurers generally pay counselors, nurse practitioners, and psychiatrists, they use the term behavioral health because it wouldn’t be right for them to pay a counselor for a psychiatric intervention. So as a psychiatrist, I respond when being referred to as a psychiatrist, mental health specialist, or behavioral health specialist. And thankfully, per American Medical Association policy, psychiatrists are not providers.
Stu Gitlow, MD, MPH
Executive Director
Annenberg Physician Training Program in Addictive Disease
Woonsocket, Rhode Island
I was grateful for Dr. Nasrallah’s editorial regarding the misnomer of referring to psychiatry as “behavioral health.” Until this editorial, I had wondered if I was the only one bothered by the term. Many people are under the assumption that behavioral health is a politically correct term that helps to lessen stigmatism. I completely disagree. Without question, it adds to the stigmatism. The term behavioral health is belittling to our patients. For example, calling a psychiatric inpatient unit a “behavioral health unit” implies that if patients would just change their behaviors, they wouldn’t have serious biological psychiatric illness. It insinuates that the patients cause and perpetuate their illnesses, such as schizophrenia or bipolar disorder, by behaving poorly. Granted, we teach behavior modification to help manage psychiatric illness, but so, too, do our colleagues in other medical fields teach behavior modification to manage other organ-related illnesses. Some nearly ubiquitous examples include doctors advising patients to lower stress, modify diet, exercise, and take medications as prescribed. Yet, for example, in the case of a patient with diabetes, we don’t refer to diabetic ketoacidosis treatment as behavioral health treatment, though the patient’s behavior no doubt contributes to this condition. And we certainly would never call the ICU or stepdown unit the “behavioral health unit,” even though adequate holistic treatment in these settings includes counseling the patient with diabetes on changing his/her behaviors that led to the ketoacidosis. Just as in diabetes, the underlying basis of psychiatric illness is biologic processes gone awry. First and foremost, a psychiatric medical illness requires complicated and often precarious medications to treat. As in other medical specialties, modifying behavior does not treat the illness, but merely serves to help transmute the course.
In sum, I wholly agree with Dr. Nasrallah’s eloquent assessment regarding the problems with the title behavioral health in lieu of psychiatry. I also might have taken the discussion a step a further: Because psychiatric illness affects every aspect of a person’s life—such as work, social, and personal—it requires a terminology commensurate with the medical gravity it warrants. So in addition to not referring to the specialty as behavioral health, I have wondered if the name psychiatry could be replaced with a more medical-sounding term such as “cerebrology” or something of the sort. But one step at time.
Stacie Lauro, MD, ABPN
Attending in Psychiatry, Emergency Room, and Consultation Liaison
Mindcare Solutions
Tampa, Florida
The evolution within our field of the use of “behavioral health” has disturbed me to the same extent it has for Dr. Nasrallah. I founded and direct a psychiatric treatment facility in Florida. We are a teaching facility affiliated with 3 psychiatric residencies, 8 medical schools, and 60 physician assistant (PA) schools. In all of the literature (eg, evaluations) from the PA schools, they refer to their rotation with my program as “behavioral health.” I have been attempting to correct them for years! I teach all residents and students to correctly use the terms “psychiatry” and “psychiatric.” I understand there may be stigma associated with the latter terms, but the field reinforces that stigma by avoiding the use of these terms.
Robert A. Moran, MD, FAPA, FASAM
CEO and Medical Director, Family Center for Recovery
Lantana, Florida
Continue to: Pre-authorization and 'hold harmless' clauses
Pre-authorization and ‘hold harmless’ clauses
Regarding Dr. Nasrallah’s editorial “Pre-authorization is illegal, unethical, and adversely disrupts patient care” (From the Editor,
Recently to my surprise, while navigating a pre-authorization request for a young patient with bipolar disorder who had accepted the inclusion of lurasidone in his treatment regimen while hospitalized, I found that the CoverMyMeds Business Associate Agreement is required for a user to accomplish pre-authorization online. Having a little extra time for due diligence that day, I read this lengthy agreement carefully. The CoverMyMeds user agreement purports not to offer “medical advice, does not determine medical necessity, insurance coverage or copays and does not otherwise engage in the practice of medicine” (see www.covermymeds.com/main/about/privacy/tos/). Interestingly, the agreement goes on to purport that the whole process is for informational purposes only, not a substitute for clinicians, professional medical judgment, or for individual patient assessments and examinations. Of course, another factor is that the information provided by the process is “solely at the user’s and health care provider’s own risk.” Finally, the agreement requires the user to agree to “indemnify, defend, and hold harmless CoverMyMeds and its affiliates … from any demands, claims, damages, liabilities, expenses, or harms (including attorneys’ fees) arising out of or related to your use of our Services or breach of these Terms of Service.”
Throughout my 25 years of solo private practice, I have refused to sign hold harmless clauses and I refused to sign the CoverMyMeds user agreement. I have made it my practice never to obtain pre-authorization unless the patient is with me in the room during an appointment because the process of navigating pre-authorization does become part of the treatment, however unfortunately. As an alternative, for my patient with bipolar disorder, I was able to use a phone number to talk to a representative of the pharmacy benefit plan that was contracted with CoverMyMeds. Without signing on to be a Business Associate, we accomplished the goal of continuing with the medication as recommended and implemented for 2 preceding months (often pre-authorization actually means continuing authorization, doesn’t it?). I believe if all psychiatrists were to adopt this kind of stance, we could make a change. I know there are anti-trust considerations involved in fee negotiations, but when it comes to the egregious practices of managed care, pre-authorization, and hold harmless clauses, it seems to me that we can mount a counteroffensive to great effect.
Further, I want to stand in strong support of Dr. Nasrallah’s editorial “Stop calling it ‘behavioral health’: Psychiatry is much more.” When I began my first job post-fellowship, I was alarmed to find that our outpatient offices had been named a “counseling center.” Due to such misleading, stigmatizing characterizations, as Dr. Nasrallah pointed out, we have only slid further down the slope into the realm of “providers of behavioral health services.” As an old hand working psychiatric locum tenens told me, we psychiatrists had long since missed the chance to “band together like musk oxen” to defend our profession.
However, I believe it is not too late. With the strength of Dr. Nasrallah’s leadership and a more overt, collective stubbornness coupled with an undying commitment to excellence, we can and must push hard against the insurance and hospital entities, which continue to profiteer from the practice of medicine without a license—using the tools of hold harmless clauses, anti-trust laws in their favor, and misinformation about the scope and efficacy of practicing psychiatry per se. The challenge is to figure out exactly how to proceed.
Although some manage to thrive in independent practice, collectively our struggle seems considerable, but not insurmountable.
David B. Robinson, MD, MPH
Diplomate, American Board of Psychiatry and Neurology in Child, Adolescent and Adult Psychiatry
Fellow, American Psychiatric Association
Private psychiatric practice
Alaska Psychiatric Concepts
Juneau, Alaska
What to tell parents whose child saw them having sex
Many parents find themselves in a difficult situation when their child accidentally sees them having sex. These patients may ask us, as their clinicians, if they should discuss the incident with their child, and if so, what to say. If parents do not address the subject appropriately, their child might be confused and uncomfortable with his/her interpretation of the encounter.1 Some older research suggests that after witnessing their parents in a sexual encounter, children may have difficulty with affectional love, fears of being alone, or feelings of vulnerability.2,3 Clinicians may find themselves at a loss when parents ask them how to handle these situations. Although there are no evidence-based guidelines to consult, consider the following suggestions:
Relax. For patients who have not yet experienced this situation, tell them it is important not to panic if their child witnesses them having sex. They should cover their bodies and calmly respond to their child’s presence. Calm responsiveness is a key to diffusing this awkward situation. Otherwise, children may sense their parents’ embarrassment and conclude that sex is shameful. Parents should gently explain to their child that they are having a private, adult moment. They should ask their child if something is needed immediately, or if it could wait.
Accept that it happened. Parents should not avoid discussing the incident, but should promptly follow up with their child at an appropriate time and place. Waiting for a child to raise the topic puts the responsibility on him/her, instead of on the parent. Although some forthright children may ask questions, others may feel too ashamed or nervous to broach the topic and will prefer their parents to take the lead.
Discuss what happened. Tell parents to explore their child’s impression of what he/she saw. Tailoring the discussion to the child’s age is important. For example, a 3-year-old might wonder if anyone was harmed, and might need reassurance, whereas a 12-year-old is likely to have a better understanding of sex but still feel uncomfortable. Educational conversations about sexuality might be appropriate for children age 8 to 12. The parents’ goal should be to answer questions honestly without oversharing, and to leave the door open—so to speak—for future conversations.
Recommend that parents use plain, factual language to answer any questions their child asks. Statements such as “We were having a private, adult moment” can be helpful. Parents can categorize sex as a universal activity that is not harmful or scary by telling their child something such as, “This is what all parents do.” Parents should avoid providing unnecessary information or answering questions their child is not asking. The Table4 offers guidance on how parents might handle such conversations.
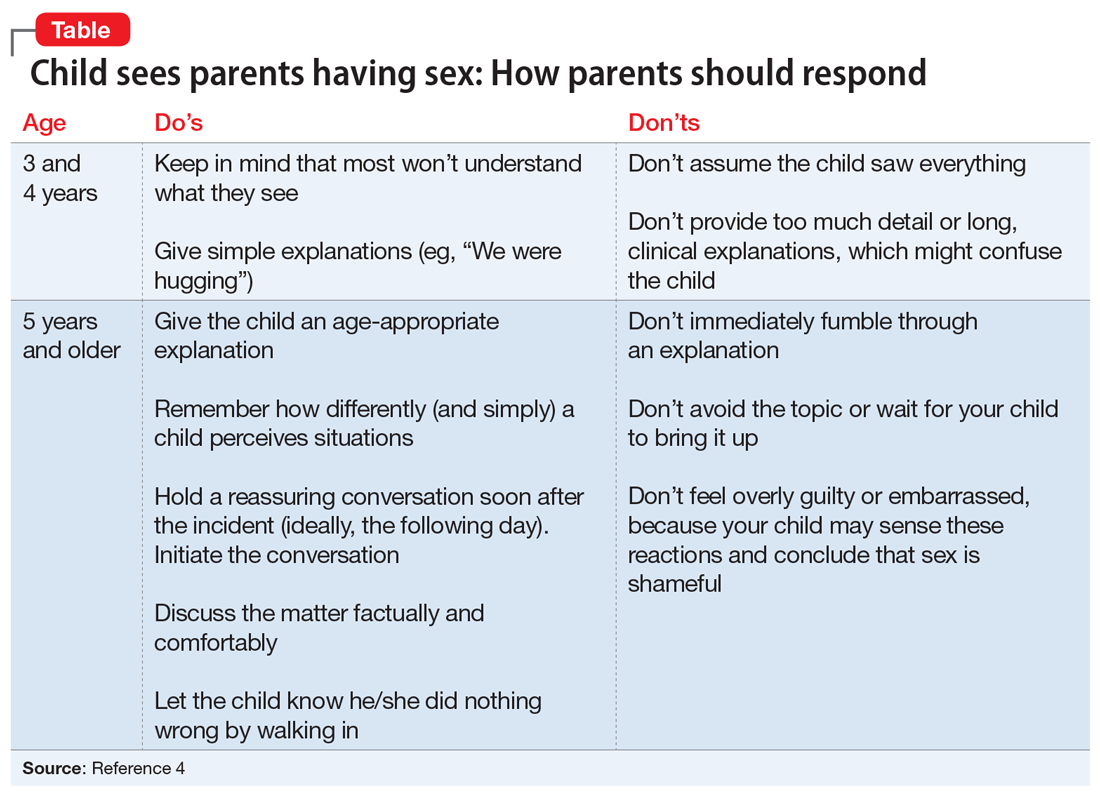
Consider potentially positive outcomes. Although parents may feel guilty or describe this as a terrible situation, remind them that there are some potentially healthy outcomes. For example, such incidents may help reassure the child that their parents love each other, which might give him/her a sense of happiness and security.
Take steps to prevent this from happening again. Advise parents to lock the door when having sex. Remind them to consider the proximity of rooms because their child might hear noises and become curious.
1. Blum HP. On the concept and consequences of the primal scene. Psychoanal Q. 1979;48(1):27-47.
2. Hoyt MF. On the psychology and psychopathology of primal-scene experience. J Am Acad Psychoanal. 1980;8(3):311-335.
3. Ikonen P, Rechardt E. On the universal nature of primal scene fantasies. Int J Psychoanal. 1984;65(pt 1):63-72.
4. Pelly J. Four things my four-year-old already knows about sex. Today’s Parent. https://www.todaysparent.com/family/parenting/4-things-my-4-year-old-already-knows-about-sex/. Published February 1, 2020. Accessed June 20, 2020.
Many parents find themselves in a difficult situation when their child accidentally sees them having sex. These patients may ask us, as their clinicians, if they should discuss the incident with their child, and if so, what to say. If parents do not address the subject appropriately, their child might be confused and uncomfortable with his/her interpretation of the encounter.1 Some older research suggests that after witnessing their parents in a sexual encounter, children may have difficulty with affectional love, fears of being alone, or feelings of vulnerability.2,3 Clinicians may find themselves at a loss when parents ask them how to handle these situations. Although there are no evidence-based guidelines to consult, consider the following suggestions:
Relax. For patients who have not yet experienced this situation, tell them it is important not to panic if their child witnesses them having sex. They should cover their bodies and calmly respond to their child’s presence. Calm responsiveness is a key to diffusing this awkward situation. Otherwise, children may sense their parents’ embarrassment and conclude that sex is shameful. Parents should gently explain to their child that they are having a private, adult moment. They should ask their child if something is needed immediately, or if it could wait.
Accept that it happened. Parents should not avoid discussing the incident, but should promptly follow up with their child at an appropriate time and place. Waiting for a child to raise the topic puts the responsibility on him/her, instead of on the parent. Although some forthright children may ask questions, others may feel too ashamed or nervous to broach the topic and will prefer their parents to take the lead.
Discuss what happened. Tell parents to explore their child’s impression of what he/she saw. Tailoring the discussion to the child’s age is important. For example, a 3-year-old might wonder if anyone was harmed, and might need reassurance, whereas a 12-year-old is likely to have a better understanding of sex but still feel uncomfortable. Educational conversations about sexuality might be appropriate for children age 8 to 12. The parents’ goal should be to answer questions honestly without oversharing, and to leave the door open—so to speak—for future conversations.
Recommend that parents use plain, factual language to answer any questions their child asks. Statements such as “We were having a private, adult moment” can be helpful. Parents can categorize sex as a universal activity that is not harmful or scary by telling their child something such as, “This is what all parents do.” Parents should avoid providing unnecessary information or answering questions their child is not asking. The Table4 offers guidance on how parents might handle such conversations.
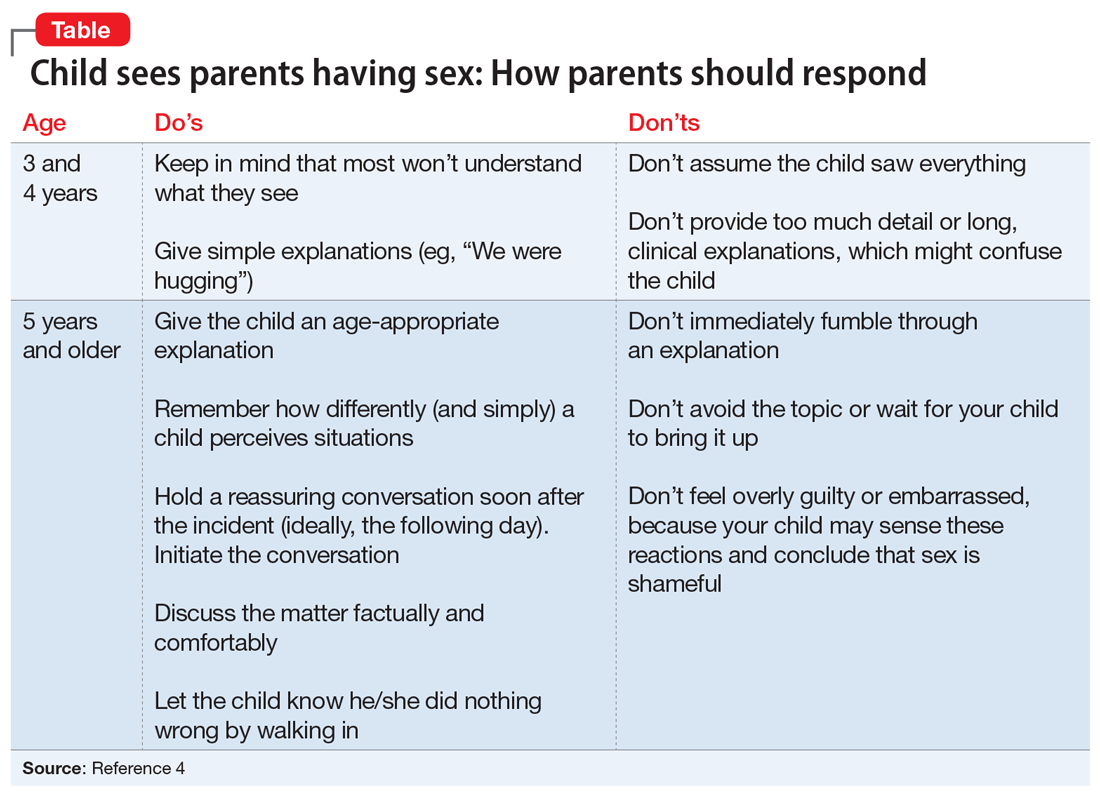
Consider potentially positive outcomes. Although parents may feel guilty or describe this as a terrible situation, remind them that there are some potentially healthy outcomes. For example, such incidents may help reassure the child that their parents love each other, which might give him/her a sense of happiness and security.
Take steps to prevent this from happening again. Advise parents to lock the door when having sex. Remind them to consider the proximity of rooms because their child might hear noises and become curious.
Many parents find themselves in a difficult situation when their child accidentally sees them having sex. These patients may ask us, as their clinicians, if they should discuss the incident with their child, and if so, what to say. If parents do not address the subject appropriately, their child might be confused and uncomfortable with his/her interpretation of the encounter.1 Some older research suggests that after witnessing their parents in a sexual encounter, children may have difficulty with affectional love, fears of being alone, or feelings of vulnerability.2,3 Clinicians may find themselves at a loss when parents ask them how to handle these situations. Although there are no evidence-based guidelines to consult, consider the following suggestions:
Relax. For patients who have not yet experienced this situation, tell them it is important not to panic if their child witnesses them having sex. They should cover their bodies and calmly respond to their child’s presence. Calm responsiveness is a key to diffusing this awkward situation. Otherwise, children may sense their parents’ embarrassment and conclude that sex is shameful. Parents should gently explain to their child that they are having a private, adult moment. They should ask their child if something is needed immediately, or if it could wait.
Accept that it happened. Parents should not avoid discussing the incident, but should promptly follow up with their child at an appropriate time and place. Waiting for a child to raise the topic puts the responsibility on him/her, instead of on the parent. Although some forthright children may ask questions, others may feel too ashamed or nervous to broach the topic and will prefer their parents to take the lead.
Discuss what happened. Tell parents to explore their child’s impression of what he/she saw. Tailoring the discussion to the child’s age is important. For example, a 3-year-old might wonder if anyone was harmed, and might need reassurance, whereas a 12-year-old is likely to have a better understanding of sex but still feel uncomfortable. Educational conversations about sexuality might be appropriate for children age 8 to 12. The parents’ goal should be to answer questions honestly without oversharing, and to leave the door open—so to speak—for future conversations.
Recommend that parents use plain, factual language to answer any questions their child asks. Statements such as “We were having a private, adult moment” can be helpful. Parents can categorize sex as a universal activity that is not harmful or scary by telling their child something such as, “This is what all parents do.” Parents should avoid providing unnecessary information or answering questions their child is not asking. The Table4 offers guidance on how parents might handle such conversations.
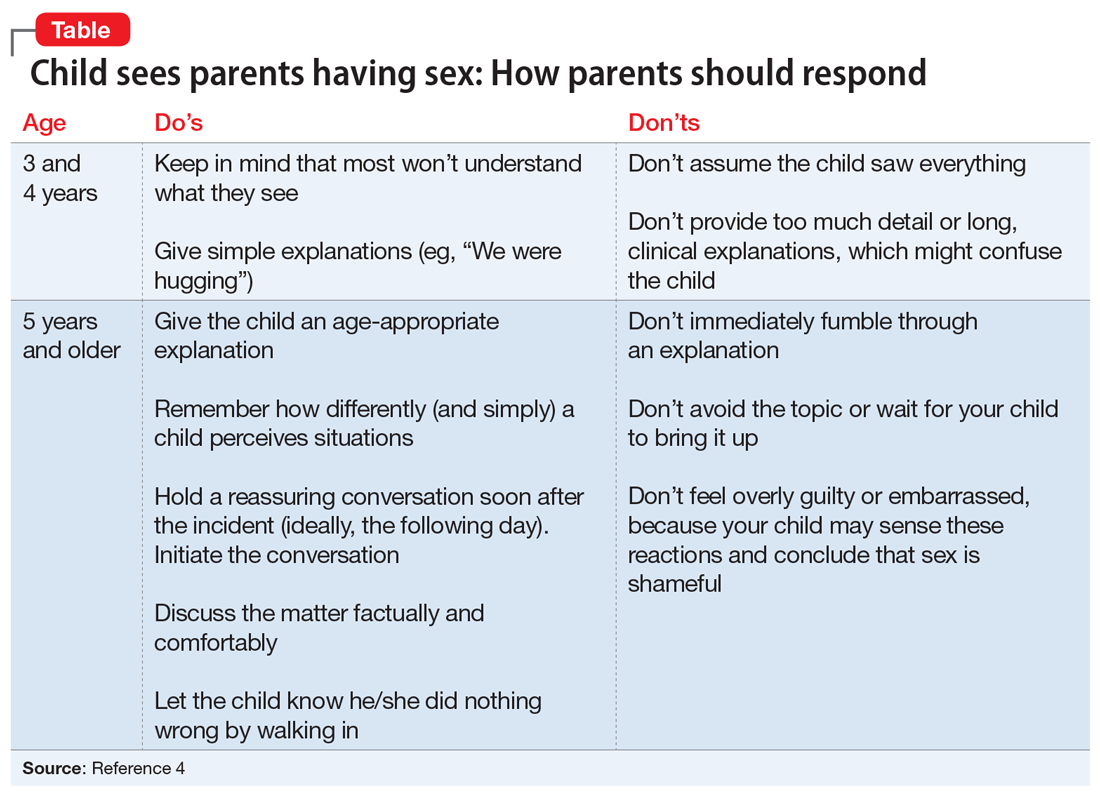
Consider potentially positive outcomes. Although parents may feel guilty or describe this as a terrible situation, remind them that there are some potentially healthy outcomes. For example, such incidents may help reassure the child that their parents love each other, which might give him/her a sense of happiness and security.
Take steps to prevent this from happening again. Advise parents to lock the door when having sex. Remind them to consider the proximity of rooms because their child might hear noises and become curious.
1. Blum HP. On the concept and consequences of the primal scene. Psychoanal Q. 1979;48(1):27-47.
2. Hoyt MF. On the psychology and psychopathology of primal-scene experience. J Am Acad Psychoanal. 1980;8(3):311-335.
3. Ikonen P, Rechardt E. On the universal nature of primal scene fantasies. Int J Psychoanal. 1984;65(pt 1):63-72.
4. Pelly J. Four things my four-year-old already knows about sex. Today’s Parent. https://www.todaysparent.com/family/parenting/4-things-my-4-year-old-already-knows-about-sex/. Published February 1, 2020. Accessed June 20, 2020.
1. Blum HP. On the concept and consequences of the primal scene. Psychoanal Q. 1979;48(1):27-47.
2. Hoyt MF. On the psychology and psychopathology of primal-scene experience. J Am Acad Psychoanal. 1980;8(3):311-335.
3. Ikonen P, Rechardt E. On the universal nature of primal scene fantasies. Int J Psychoanal. 1984;65(pt 1):63-72.
4. Pelly J. Four things my four-year-old already knows about sex. Today’s Parent. https://www.todaysparent.com/family/parenting/4-things-my-4-year-old-already-knows-about-sex/. Published February 1, 2020. Accessed June 20, 2020.
Kleptomania: 4 Tips for better diagnosis and treatment
Kleptomania is characterized by a recurrent failure to resist impulses to steal objects that are not needed for personal use or their monetary value.1 It is a rare disorder; an estimated 0.3% to 0.6% of the general population meet DSM-5 criteria for kleptomania (Table 1).1 Kleptomania usually begins in early adolescence and is more common among females than males (3:1).1 Although DSM-5 does not outline how long symptoms need to be present for patients to meet the diagnostic criteria, the disorder may persist for years, even when patients face legal consequences.1
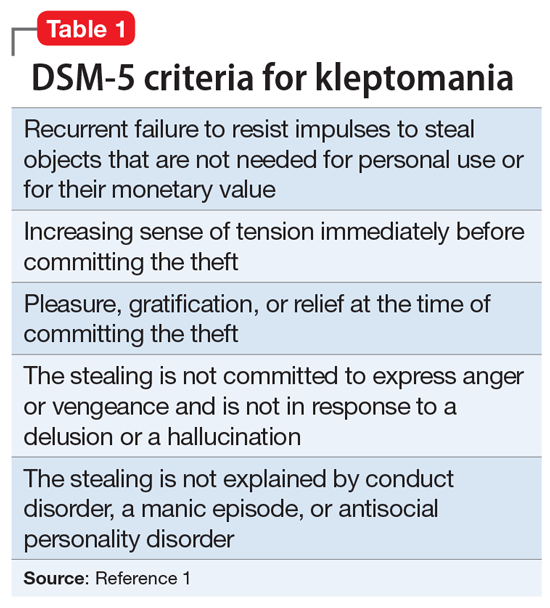
Due to the clinical ambiguities surrounding kleptomania, it remains one of psychiatry’s most poorly understood diagnoses2 and regularly goes undiagnosed and untreated. Here we provide 4 tips for better diagnosis and treatment of this condition.
1. Screen for kleptomania in patients with other psychiatric disorders because kleptomania often is comorbid with other mental illnesses. Patients who present for evaluation of a mood disorder, substance use, anxiety disorders, eating disorders, impulse control disorders, conduct disorder, and obsessive-compulsive disorder should be screened for kleptomania.1,3,4 Patients with kleptomania often are reluctant to discuss their stealing because they may experience humiliation and guilt related to theft.1,4 Undiagnosed kleptomania can be fatal; a study of suicide attempts in 107 individuals with kleptomania found that 92% of the patients attributed their attempt specifically to kleptomania.5 Table 21 offers screening questions based on the DSM-5 criteria for kleptomania.
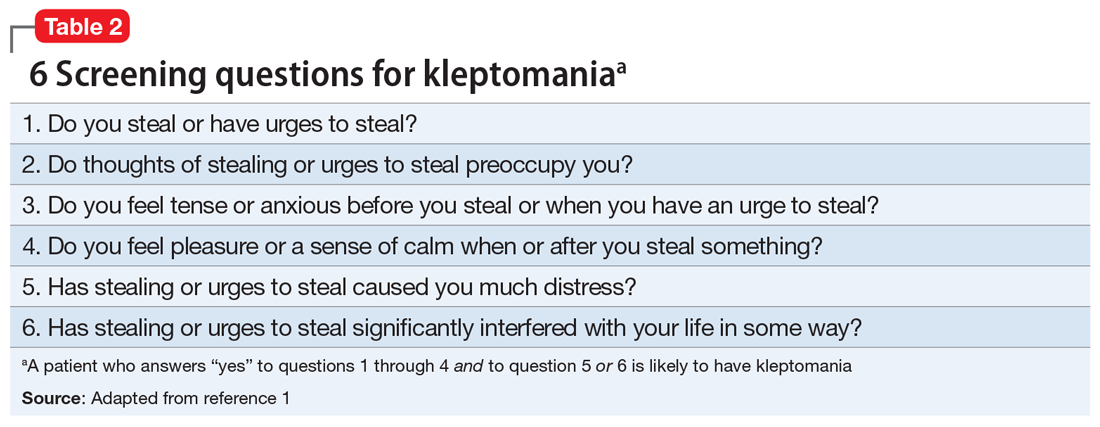
2. Distinguish kleptomania from other diagnoses that can include stealing. Because stealing can be a symptom of several other psychiatric disorders, misdiagnosis is fairly common.1 The differential can include bipolar disorder, borderline personality disorder, antisocial personality disorder, and eating disorder. Table 31,3 describes how to differentiate these diagnoses from kleptomania.
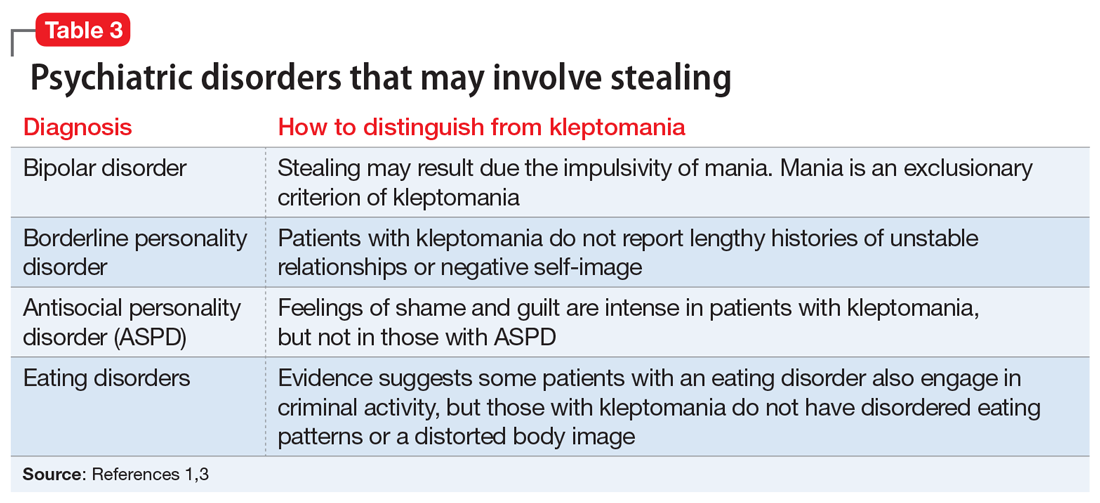
3. Select an appropriate treatment. There are no FDA-approved medications for kleptomania, but some agents may help. In an 8-week, double-blind, placebo-controlled trial, 25 patients with kleptomania who received naltrexone (50 to 150 mg/d) demonstrated significant reductions in stealing urges and behavior.6 Some evidence suggests a combination of pharmacologic and behavioral therapy (cognitive-behavioral therapy, covert sensitization, and systemic desensitization) may be the optimal treatment strategy for kleptomania.4
4. Monitor progress. After initiating treatment, use the Kleptomania Symptom Assessment Scale7 (K-SAS) to determine treatment efficacy. The K-SAS is an 11-item self-report questionnaire that assesses the severity of kleptomania symptoms during the past week.
1. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Goldman MJ. Kleptomania: making sense of the nonsensical. Am J Psychiatry. 1991;148:986-996.
3. Yao S, Kuja‐Halkola R, Thornton LM, et al. Risk of being convicted of theft and other crimes in anorexia nervosa and bulimia nervosa: a prospective cohort study in a Swedish female population. Int J Eat Disord. 2017;50(9):1095-1103.
4. Grant JE, Kim SW. Clinical characteristics and associated psychopathology of 22 patients of kleptomania. Compr Psychiatry. 2002;43(5):378-384.
5. Odlaug BL, Grant JE, Kim SW. Suicide attempts in 107 adolescents and adults with kleptomania. Arch Suicide Res. 2012;16(4):348-359.
6. Grant JE, Kim SW, Odlaug BL. A double-blind, placebo-controlled study of the opiate antagonist, naltrexone, in the treatment of kleptomania. Biol Psychiatry. 2009;65(7):600-606.
7. Grant JE, Odlaug BL, Kim SW. Kleptomania: clinical characteristics and relationship to substance use disorders. Am J Drug Alcohol Abuse. 2010;36(5):291-295.
Kleptomania is characterized by a recurrent failure to resist impulses to steal objects that are not needed for personal use or their monetary value.1 It is a rare disorder; an estimated 0.3% to 0.6% of the general population meet DSM-5 criteria for kleptomania (Table 1).1 Kleptomania usually begins in early adolescence and is more common among females than males (3:1).1 Although DSM-5 does not outline how long symptoms need to be present for patients to meet the diagnostic criteria, the disorder may persist for years, even when patients face legal consequences.1
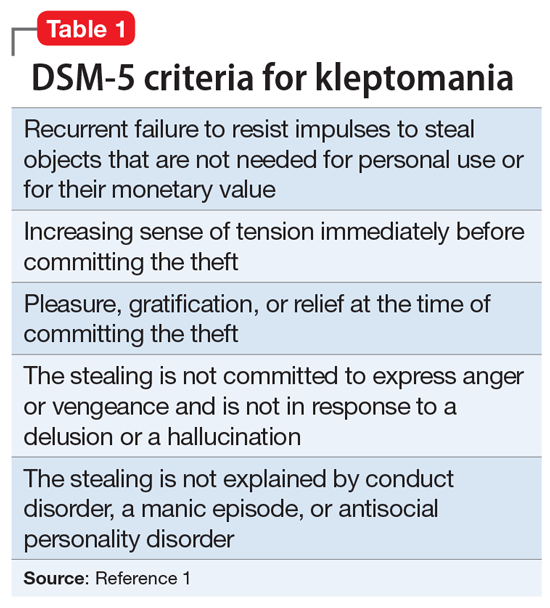
Due to the clinical ambiguities surrounding kleptomania, it remains one of psychiatry’s most poorly understood diagnoses2 and regularly goes undiagnosed and untreated. Here we provide 4 tips for better diagnosis and treatment of this condition.
1. Screen for kleptomania in patients with other psychiatric disorders because kleptomania often is comorbid with other mental illnesses. Patients who present for evaluation of a mood disorder, substance use, anxiety disorders, eating disorders, impulse control disorders, conduct disorder, and obsessive-compulsive disorder should be screened for kleptomania.1,3,4 Patients with kleptomania often are reluctant to discuss their stealing because they may experience humiliation and guilt related to theft.1,4 Undiagnosed kleptomania can be fatal; a study of suicide attempts in 107 individuals with kleptomania found that 92% of the patients attributed their attempt specifically to kleptomania.5 Table 21 offers screening questions based on the DSM-5 criteria for kleptomania.
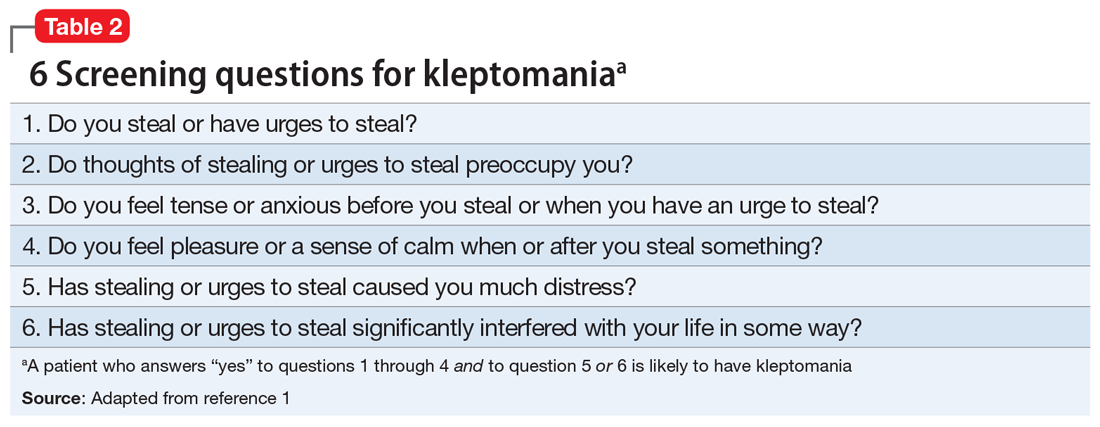
2. Distinguish kleptomania from other diagnoses that can include stealing. Because stealing can be a symptom of several other psychiatric disorders, misdiagnosis is fairly common.1 The differential can include bipolar disorder, borderline personality disorder, antisocial personality disorder, and eating disorder. Table 31,3 describes how to differentiate these diagnoses from kleptomania.
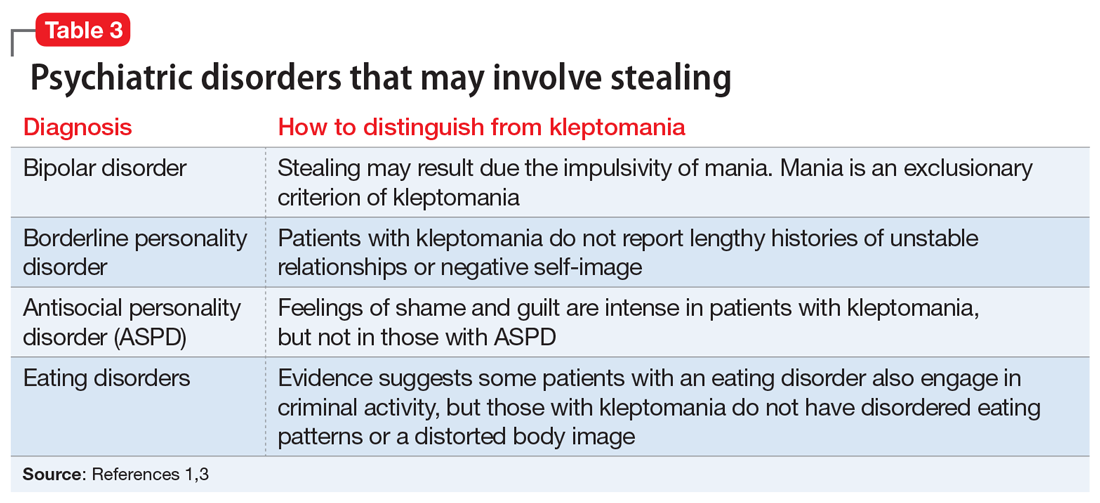
3. Select an appropriate treatment. There are no FDA-approved medications for kleptomania, but some agents may help. In an 8-week, double-blind, placebo-controlled trial, 25 patients with kleptomania who received naltrexone (50 to 150 mg/d) demonstrated significant reductions in stealing urges and behavior.6 Some evidence suggests a combination of pharmacologic and behavioral therapy (cognitive-behavioral therapy, covert sensitization, and systemic desensitization) may be the optimal treatment strategy for kleptomania.4
4. Monitor progress. After initiating treatment, use the Kleptomania Symptom Assessment Scale7 (K-SAS) to determine treatment efficacy. The K-SAS is an 11-item self-report questionnaire that assesses the severity of kleptomania symptoms during the past week.
Kleptomania is characterized by a recurrent failure to resist impulses to steal objects that are not needed for personal use or their monetary value.1 It is a rare disorder; an estimated 0.3% to 0.6% of the general population meet DSM-5 criteria for kleptomania (Table 1).1 Kleptomania usually begins in early adolescence and is more common among females than males (3:1).1 Although DSM-5 does not outline how long symptoms need to be present for patients to meet the diagnostic criteria, the disorder may persist for years, even when patients face legal consequences.1
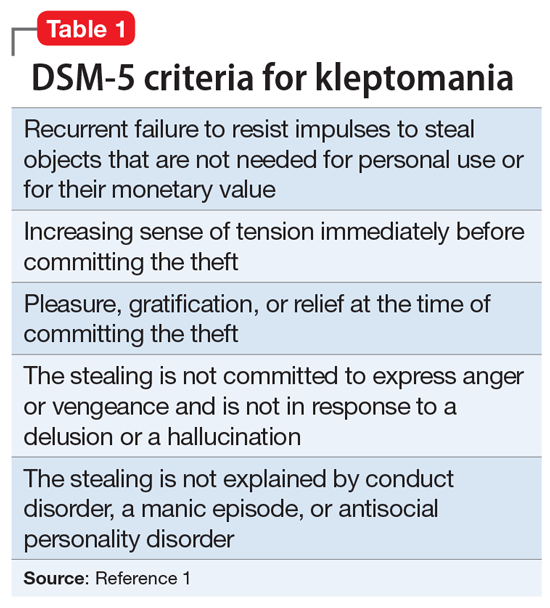
Due to the clinical ambiguities surrounding kleptomania, it remains one of psychiatry’s most poorly understood diagnoses2 and regularly goes undiagnosed and untreated. Here we provide 4 tips for better diagnosis and treatment of this condition.
1. Screen for kleptomania in patients with other psychiatric disorders because kleptomania often is comorbid with other mental illnesses. Patients who present for evaluation of a mood disorder, substance use, anxiety disorders, eating disorders, impulse control disorders, conduct disorder, and obsessive-compulsive disorder should be screened for kleptomania.1,3,4 Patients with kleptomania often are reluctant to discuss their stealing because they may experience humiliation and guilt related to theft.1,4 Undiagnosed kleptomania can be fatal; a study of suicide attempts in 107 individuals with kleptomania found that 92% of the patients attributed their attempt specifically to kleptomania.5 Table 21 offers screening questions based on the DSM-5 criteria for kleptomania.
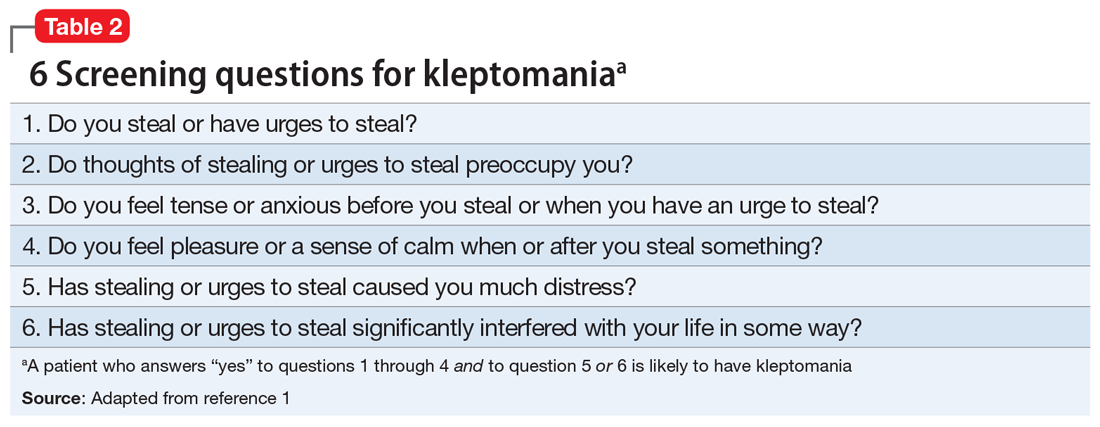
2. Distinguish kleptomania from other diagnoses that can include stealing. Because stealing can be a symptom of several other psychiatric disorders, misdiagnosis is fairly common.1 The differential can include bipolar disorder, borderline personality disorder, antisocial personality disorder, and eating disorder. Table 31,3 describes how to differentiate these diagnoses from kleptomania.
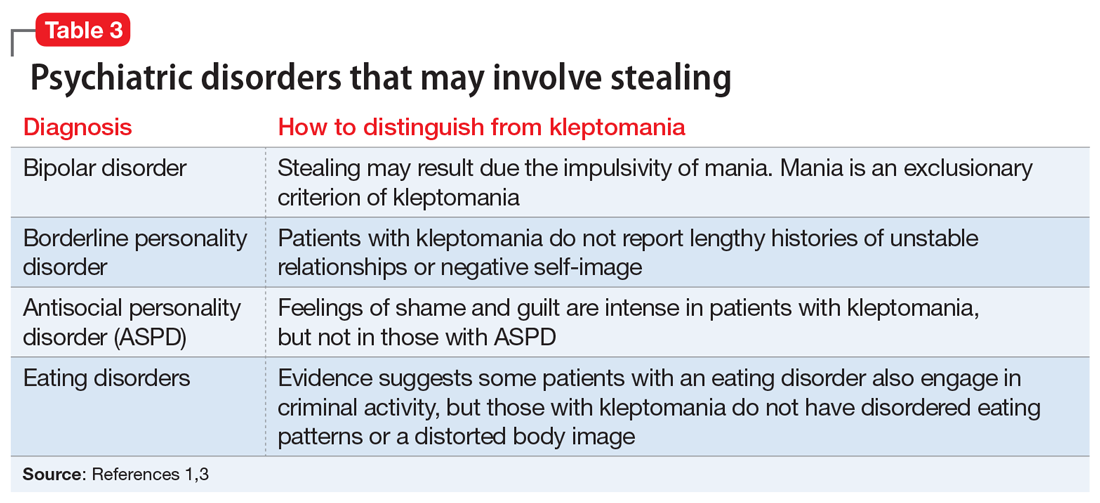
3. Select an appropriate treatment. There are no FDA-approved medications for kleptomania, but some agents may help. In an 8-week, double-blind, placebo-controlled trial, 25 patients with kleptomania who received naltrexone (50 to 150 mg/d) demonstrated significant reductions in stealing urges and behavior.6 Some evidence suggests a combination of pharmacologic and behavioral therapy (cognitive-behavioral therapy, covert sensitization, and systemic desensitization) may be the optimal treatment strategy for kleptomania.4
4. Monitor progress. After initiating treatment, use the Kleptomania Symptom Assessment Scale7 (K-SAS) to determine treatment efficacy. The K-SAS is an 11-item self-report questionnaire that assesses the severity of kleptomania symptoms during the past week.
1. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Goldman MJ. Kleptomania: making sense of the nonsensical. Am J Psychiatry. 1991;148:986-996.
3. Yao S, Kuja‐Halkola R, Thornton LM, et al. Risk of being convicted of theft and other crimes in anorexia nervosa and bulimia nervosa: a prospective cohort study in a Swedish female population. Int J Eat Disord. 2017;50(9):1095-1103.
4. Grant JE, Kim SW. Clinical characteristics and associated psychopathology of 22 patients of kleptomania. Compr Psychiatry. 2002;43(5):378-384.
5. Odlaug BL, Grant JE, Kim SW. Suicide attempts in 107 adolescents and adults with kleptomania. Arch Suicide Res. 2012;16(4):348-359.
6. Grant JE, Kim SW, Odlaug BL. A double-blind, placebo-controlled study of the opiate antagonist, naltrexone, in the treatment of kleptomania. Biol Psychiatry. 2009;65(7):600-606.
7. Grant JE, Odlaug BL, Kim SW. Kleptomania: clinical characteristics and relationship to substance use disorders. Am J Drug Alcohol Abuse. 2010;36(5):291-295.
1. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Goldman MJ. Kleptomania: making sense of the nonsensical. Am J Psychiatry. 1991;148:986-996.
3. Yao S, Kuja‐Halkola R, Thornton LM, et al. Risk of being convicted of theft and other crimes in anorexia nervosa and bulimia nervosa: a prospective cohort study in a Swedish female population. Int J Eat Disord. 2017;50(9):1095-1103.
4. Grant JE, Kim SW. Clinical characteristics and associated psychopathology of 22 patients of kleptomania. Compr Psychiatry. 2002;43(5):378-384.
5. Odlaug BL, Grant JE, Kim SW. Suicide attempts in 107 adolescents and adults with kleptomania. Arch Suicide Res. 2012;16(4):348-359.
6. Grant JE, Kim SW, Odlaug BL. A double-blind, placebo-controlled study of the opiate antagonist, naltrexone, in the treatment of kleptomania. Biol Psychiatry. 2009;65(7):600-606.
7. Grant JE, Odlaug BL, Kim SW. Kleptomania: clinical characteristics and relationship to substance use disorders. Am J Drug Alcohol Abuse. 2010;36(5):291-295.
Improving your experience with electronic health records
The electronic health record (EHR) was introduced to improve how clinicians document patient information, contribute to medical research, and allow for medical records to be universally transferable.1 However, many clinicians find EHRs to be burdensome, time-consuming, and inefficient. Clinicians often spend multiple hours each day navigating their EHR system, which reduces the amount of time they spend interacting with patients and contributes to physician burnout.1-3 For example, in a study of 142 family medicine physicians, clinicians reported that they spent approximately 6 hours per work day interacting with their EHR.3
Clearly, the EHR needs a fundamental revision. In the meantime, how can we adapt to improve the situation? Here I suggest practical steps clinicians can take to improve their experience with their EHR system.4-8
Steps to take during patient visits
Because entering information into the EHR can be distracting, be prepared to multitask during each clinical encounter.1-7 Be ready to address pertinent inquiries and issues your patient raises, and provide instructions on therapies and interventions. Because interpersonal relations are important during clinical encounters, establish interaction with your patient by acknowledging them and maintaining frequent eye contact.7 Consider allowing your patient to view the EHR screen because doing so might increase his/her involvement in the visit.
So that you can pay closer attention to your patient, consider taking notes during the visit and entering the information into the EHR later. Consider improving your typing skills to increase the speed of your note-taking. Alternatively, using a voice-recognition recording tool to transcribe your notes via speech might help you spend less time on note-taking.3 Whenever possible, finish charting for one patient before meeting with the next because doing so will save time and help you to better remember details.7
In addition, lowering your overall stress might help reduce the burden of using the EHR.3-5 Adopt healthy behaviors, including good sleep, nutrition, exercise, and hobbies, and strive for balance in your routines. Attend to any personal medical or psychiatric conditions, and avoid misusing alcohol, medications, or other substances.
Optimize how your practice functions
With your clinical group and colleagues, create a comfortable environment, good patient-to-doctor interactions, and a smooth flow within the practice. Simplify registration. Ask patients to complete screening forms before an appointment; this information could be entered directly into their EHR.3 Consider using physician-extender staff and other personnel, such as scribes, to complete documentation into the EHR.3,8 This may help reduce burnout, create more time for clinical care, and improve face-to-face patient interactions.8 Employing scribes can allow doctors to be better able to directly attend to their patients while complying with record-keeping needs. Although scribes make charting easier, they are an additional expense, and must be trained.
Consider EHR training
EHR training sessions can teach you how to use your EHR system more efficiently.6 Such education may help boost confidence, aid documentation, and reduce the amount of time spent correcting coding errors. In a study of 3,500 physicians who underwent a 3-day intensive EHR training course, 85% to 98% reported having improved the quality, readability, and clinical accuracy of their documentation.6
Help shape future EHRs
Individual doctors and professional groups can promote EHR improvements through their state, regional, and/or national organizations and medical societies. These bodies should deliver EHR revision recommendations to government officials, who can craft laws and regulations, and can influence regulators and/or insurance companies. Clinicians also can communicate with EHR developers on ways to simplify the usability of these tools, such as reducing the amount of steps the EHR’s interface requires.5 With a more efficient EHR, we can better concentrate on patient care, which will reduce expenses and should yield better outcomes.
1. Ehrenfeld JM, Wonderer JP. Technology as friend or foe? Do electronic health records increase burnout? Curr Opin Anesthesiol. 2018;31(3):357-360.
2. Meigs SL, Solomon M. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag. 2016;13:1d.
3. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419-426.
4. Fogarty CT, Winters P, Farah S. Improving patient-centered communication while using an electronic health record: report from a curriculum evaluation. Int J Psych Med. 2016;51(4):379-389.
5. Guo U, Chen L, Mehta PH. Electronic health record innovations: helping physicians - one less click at a time. Health Inf Manag. 2017;46(3):140-144.
6. Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine. 2018;91(38):e123419. doi: 10.1097/MD.0000000000012319.
7. Fogarty CT. Getting your notes done on time. Fam Pract Manag. 2016;23(2):40.
8. DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes. 2019;3(4):384-408.
The electronic health record (EHR) was introduced to improve how clinicians document patient information, contribute to medical research, and allow for medical records to be universally transferable.1 However, many clinicians find EHRs to be burdensome, time-consuming, and inefficient. Clinicians often spend multiple hours each day navigating their EHR system, which reduces the amount of time they spend interacting with patients and contributes to physician burnout.1-3 For example, in a study of 142 family medicine physicians, clinicians reported that they spent approximately 6 hours per work day interacting with their EHR.3
Clearly, the EHR needs a fundamental revision. In the meantime, how can we adapt to improve the situation? Here I suggest practical steps clinicians can take to improve their experience with their EHR system.4-8
Steps to take during patient visits
Because entering information into the EHR can be distracting, be prepared to multitask during each clinical encounter.1-7 Be ready to address pertinent inquiries and issues your patient raises, and provide instructions on therapies and interventions. Because interpersonal relations are important during clinical encounters, establish interaction with your patient by acknowledging them and maintaining frequent eye contact.7 Consider allowing your patient to view the EHR screen because doing so might increase his/her involvement in the visit.
So that you can pay closer attention to your patient, consider taking notes during the visit and entering the information into the EHR later. Consider improving your typing skills to increase the speed of your note-taking. Alternatively, using a voice-recognition recording tool to transcribe your notes via speech might help you spend less time on note-taking.3 Whenever possible, finish charting for one patient before meeting with the next because doing so will save time and help you to better remember details.7
In addition, lowering your overall stress might help reduce the burden of using the EHR.3-5 Adopt healthy behaviors, including good sleep, nutrition, exercise, and hobbies, and strive for balance in your routines. Attend to any personal medical or psychiatric conditions, and avoid misusing alcohol, medications, or other substances.
Optimize how your practice functions
With your clinical group and colleagues, create a comfortable environment, good patient-to-doctor interactions, and a smooth flow within the practice. Simplify registration. Ask patients to complete screening forms before an appointment; this information could be entered directly into their EHR.3 Consider using physician-extender staff and other personnel, such as scribes, to complete documentation into the EHR.3,8 This may help reduce burnout, create more time for clinical care, and improve face-to-face patient interactions.8 Employing scribes can allow doctors to be better able to directly attend to their patients while complying with record-keeping needs. Although scribes make charting easier, they are an additional expense, and must be trained.
Consider EHR training
EHR training sessions can teach you how to use your EHR system more efficiently.6 Such education may help boost confidence, aid documentation, and reduce the amount of time spent correcting coding errors. In a study of 3,500 physicians who underwent a 3-day intensive EHR training course, 85% to 98% reported having improved the quality, readability, and clinical accuracy of their documentation.6
Help shape future EHRs
Individual doctors and professional groups can promote EHR improvements through their state, regional, and/or national organizations and medical societies. These bodies should deliver EHR revision recommendations to government officials, who can craft laws and regulations, and can influence regulators and/or insurance companies. Clinicians also can communicate with EHR developers on ways to simplify the usability of these tools, such as reducing the amount of steps the EHR’s interface requires.5 With a more efficient EHR, we can better concentrate on patient care, which will reduce expenses and should yield better outcomes.
The electronic health record (EHR) was introduced to improve how clinicians document patient information, contribute to medical research, and allow for medical records to be universally transferable.1 However, many clinicians find EHRs to be burdensome, time-consuming, and inefficient. Clinicians often spend multiple hours each day navigating their EHR system, which reduces the amount of time they spend interacting with patients and contributes to physician burnout.1-3 For example, in a study of 142 family medicine physicians, clinicians reported that they spent approximately 6 hours per work day interacting with their EHR.3
Clearly, the EHR needs a fundamental revision. In the meantime, how can we adapt to improve the situation? Here I suggest practical steps clinicians can take to improve their experience with their EHR system.4-8
Steps to take during patient visits
Because entering information into the EHR can be distracting, be prepared to multitask during each clinical encounter.1-7 Be ready to address pertinent inquiries and issues your patient raises, and provide instructions on therapies and interventions. Because interpersonal relations are important during clinical encounters, establish interaction with your patient by acknowledging them and maintaining frequent eye contact.7 Consider allowing your patient to view the EHR screen because doing so might increase his/her involvement in the visit.
So that you can pay closer attention to your patient, consider taking notes during the visit and entering the information into the EHR later. Consider improving your typing skills to increase the speed of your note-taking. Alternatively, using a voice-recognition recording tool to transcribe your notes via speech might help you spend less time on note-taking.3 Whenever possible, finish charting for one patient before meeting with the next because doing so will save time and help you to better remember details.7
In addition, lowering your overall stress might help reduce the burden of using the EHR.3-5 Adopt healthy behaviors, including good sleep, nutrition, exercise, and hobbies, and strive for balance in your routines. Attend to any personal medical or psychiatric conditions, and avoid misusing alcohol, medications, or other substances.
Optimize how your practice functions
With your clinical group and colleagues, create a comfortable environment, good patient-to-doctor interactions, and a smooth flow within the practice. Simplify registration. Ask patients to complete screening forms before an appointment; this information could be entered directly into their EHR.3 Consider using physician-extender staff and other personnel, such as scribes, to complete documentation into the EHR.3,8 This may help reduce burnout, create more time for clinical care, and improve face-to-face patient interactions.8 Employing scribes can allow doctors to be better able to directly attend to their patients while complying with record-keeping needs. Although scribes make charting easier, they are an additional expense, and must be trained.
Consider EHR training
EHR training sessions can teach you how to use your EHR system more efficiently.6 Such education may help boost confidence, aid documentation, and reduce the amount of time spent correcting coding errors. In a study of 3,500 physicians who underwent a 3-day intensive EHR training course, 85% to 98% reported having improved the quality, readability, and clinical accuracy of their documentation.6
Help shape future EHRs
Individual doctors and professional groups can promote EHR improvements through their state, regional, and/or national organizations and medical societies. These bodies should deliver EHR revision recommendations to government officials, who can craft laws and regulations, and can influence regulators and/or insurance companies. Clinicians also can communicate with EHR developers on ways to simplify the usability of these tools, such as reducing the amount of steps the EHR’s interface requires.5 With a more efficient EHR, we can better concentrate on patient care, which will reduce expenses and should yield better outcomes.
1. Ehrenfeld JM, Wonderer JP. Technology as friend or foe? Do electronic health records increase burnout? Curr Opin Anesthesiol. 2018;31(3):357-360.
2. Meigs SL, Solomon M. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag. 2016;13:1d.
3. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419-426.
4. Fogarty CT, Winters P, Farah S. Improving patient-centered communication while using an electronic health record: report from a curriculum evaluation. Int J Psych Med. 2016;51(4):379-389.
5. Guo U, Chen L, Mehta PH. Electronic health record innovations: helping physicians - one less click at a time. Health Inf Manag. 2017;46(3):140-144.
6. Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine. 2018;91(38):e123419. doi: 10.1097/MD.0000000000012319.
7. Fogarty CT. Getting your notes done on time. Fam Pract Manag. 2016;23(2):40.
8. DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes. 2019;3(4):384-408.
1. Ehrenfeld JM, Wonderer JP. Technology as friend or foe? Do electronic health records increase burnout? Curr Opin Anesthesiol. 2018;31(3):357-360.
2. Meigs SL, Solomon M. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag. 2016;13:1d.
3. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419-426.
4. Fogarty CT, Winters P, Farah S. Improving patient-centered communication while using an electronic health record: report from a curriculum evaluation. Int J Psych Med. 2016;51(4):379-389.
5. Guo U, Chen L, Mehta PH. Electronic health record innovations: helping physicians - one less click at a time. Health Inf Manag. 2017;46(3):140-144.
6. Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine. 2018;91(38):e123419. doi: 10.1097/MD.0000000000012319.
7. Fogarty CT. Getting your notes done on time. Fam Pract Manag. 2016;23(2):40.
8. DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes. 2019;3(4):384-408.
Letter from the Editor: Stay safe and, please, wear a mask
“Beginning immediately, the University of Michigan will require all students, staff, faculty, and visitors to wear a face covering that covers the mouth and nose while anywhere on campus grounds.” (Mark S. Schlissel MD, PhD – President, University of Michigan – July 15).
Executive Order 2020-147 (Michigan’s Governor Whitmer) mandated appropriate facial covering for all indoor spaces and crowded outdoor spaces. Additionally, businesses will be held responsible if they allow entry to anyone not wearing a mask.
While enforcement is proving to be a nightmare, masking combined with social distancing, hand washing, and staying home are the only effective levers we have to slow the spread of COVID-19. As of today, 138,000 Americans have died, and we anticipate 240,000 deaths by November 1. By now, most of us (myself included) have had a friend or relative die of this virus. America is not winning this battle and we have yet to see an effective, coordinated national response. Four forces are killing our citizens: COVID-19, structural racism, economic/health inequities, and divisive politics. We should do better.
Although Michigan and Minnesota (my home states) have slowed the virus enough to maintain resource capacity, just last weekend a single house party in a suburb near Ann Arbor resulted in 40 new infections. Thirty-nine states have rising case numbers, hospitalizations, and deaths. We are still in the early innings of this game. Michigan Medicine is actively planning our response to a second surge, which will be combined with increases of influenza and RSV infections.
This month we continue to cover the rapidly emerging information about COVID-19 and digestive implications. There are other interesting articles, including guidance around BRCA risk for colorectal cancer, eosinophilic esophagitis, probiotics, and the emerging impact of AI on endoscopy. Enjoy – stay safe, wash hands, socially distance, and please, wear a mask.
“Respect science, respect nature, respect each other” (Thomas Friedman).
John I. Allen, MD, MBA, AGAF
Editor in Chief
“Beginning immediately, the University of Michigan will require all students, staff, faculty, and visitors to wear a face covering that covers the mouth and nose while anywhere on campus grounds.” (Mark S. Schlissel MD, PhD – President, University of Michigan – July 15).
Executive Order 2020-147 (Michigan’s Governor Whitmer) mandated appropriate facial covering for all indoor spaces and crowded outdoor spaces. Additionally, businesses will be held responsible if they allow entry to anyone not wearing a mask.
While enforcement is proving to be a nightmare, masking combined with social distancing, hand washing, and staying home are the only effective levers we have to slow the spread of COVID-19. As of today, 138,000 Americans have died, and we anticipate 240,000 deaths by November 1. By now, most of us (myself included) have had a friend or relative die of this virus. America is not winning this battle and we have yet to see an effective, coordinated national response. Four forces are killing our citizens: COVID-19, structural racism, economic/health inequities, and divisive politics. We should do better.
Although Michigan and Minnesota (my home states) have slowed the virus enough to maintain resource capacity, just last weekend a single house party in a suburb near Ann Arbor resulted in 40 new infections. Thirty-nine states have rising case numbers, hospitalizations, and deaths. We are still in the early innings of this game. Michigan Medicine is actively planning our response to a second surge, which will be combined with increases of influenza and RSV infections.
This month we continue to cover the rapidly emerging information about COVID-19 and digestive implications. There are other interesting articles, including guidance around BRCA risk for colorectal cancer, eosinophilic esophagitis, probiotics, and the emerging impact of AI on endoscopy. Enjoy – stay safe, wash hands, socially distance, and please, wear a mask.
“Respect science, respect nature, respect each other” (Thomas Friedman).
John I. Allen, MD, MBA, AGAF
Editor in Chief
“Beginning immediately, the University of Michigan will require all students, staff, faculty, and visitors to wear a face covering that covers the mouth and nose while anywhere on campus grounds.” (Mark S. Schlissel MD, PhD – President, University of Michigan – July 15).
Executive Order 2020-147 (Michigan’s Governor Whitmer) mandated appropriate facial covering for all indoor spaces and crowded outdoor spaces. Additionally, businesses will be held responsible if they allow entry to anyone not wearing a mask.
While enforcement is proving to be a nightmare, masking combined with social distancing, hand washing, and staying home are the only effective levers we have to slow the spread of COVID-19. As of today, 138,000 Americans have died, and we anticipate 240,000 deaths by November 1. By now, most of us (myself included) have had a friend or relative die of this virus. America is not winning this battle and we have yet to see an effective, coordinated national response. Four forces are killing our citizens: COVID-19, structural racism, economic/health inequities, and divisive politics. We should do better.
Although Michigan and Minnesota (my home states) have slowed the virus enough to maintain resource capacity, just last weekend a single house party in a suburb near Ann Arbor resulted in 40 new infections. Thirty-nine states have rising case numbers, hospitalizations, and deaths. We are still in the early innings of this game. Michigan Medicine is actively planning our response to a second surge, which will be combined with increases of influenza and RSV infections.
This month we continue to cover the rapidly emerging information about COVID-19 and digestive implications. There are other interesting articles, including guidance around BRCA risk for colorectal cancer, eosinophilic esophagitis, probiotics, and the emerging impact of AI on endoscopy. Enjoy – stay safe, wash hands, socially distance, and please, wear a mask.
“Respect science, respect nature, respect each other” (Thomas Friedman).
John I. Allen, MD, MBA, AGAF
Editor in Chief