User login
Letter from the Board of Editors: Call to action (again)
This editorial is the first to be published in GI & Hepatology News since the murder of George Floyd in Minneapolis. The corner of 38th and Chicago is 9 miles from my home in Bloomington, Minn. This corner became the epicenter of protests that have spread around the nation and world. Early on, protests were accompanied by widespread riots, looting, and destruction. In the ensuing weeks, this corner has become a memorial for Mr. Floyd and a place where people now go to reflect, pray, pay tribute, and pledge to work for change.
A coalition of willing businesses has formed in the area around 38th and Chicago. The largest employer in the area is Allina Health (I sit on the Governing Board of Allina Health). Our flagship hospital is 8 blocks from the site of George Floyd’s memorial. We will be a change leader by committing funds for local rebuilding, ensuring use of construction firms that promote minority workers (as was done when the Viking’s stadium was built), examining our investment portfolio with racial equity as one guiding principle, increasing our focus on barriers to access, enhancing equity education of our workforce, and working with city and state leaders to promote police reform.
As the Editor in Chief of the official newspaper of the AGA, I invited our board of editors to stand united in our condemnation of the racial injustices that led to the protests we now see. We each agree with the message from the combined Governing Boards of our GI societies (published June 2, 2020) stating “As health care providers, we have dedicated our lives to caring for our fellow human beings. Therefore, we are compelled to speak out against any treatment that results in unacceptable disparities that marginalize the vulnerable among us.”
Our responsibility as editors is to guide the content we deliver, ensuring its relevancy to our readers. In this light, we commit to delivering content that highlights racial injustices and health disparities for all people, as we seek to understand the many factors that result in barriers to health. We will emphasize content that leads to impactful change and will highlight progress we make as a specialty. We hope our collective work will help ensure that George Floyd’s memory, and the memories of all such victims, become a catalyst for permanent cultural change.
Editor in Chief, GI & Hepatology News
John I. Allen, MD, MBA, AGAF
Editor in Chief, The New Gastroenterologist
Vijaya L. Rao, MD
Associate Editors
Megan A. Adams, MD, JD, MSc
Ziad Gellad, MD, MPH, AGAF
Kim L. Isaacs, MD, PhD, AGAF
Charles J. Kahi, MD, MS, AGAF
Gyanprakash A. Ketwaroo, MD, MSc
Larry R. Kosinski, MD, MBA, AGAF
Sonia S. Kupfer, MD
Wajahat Mehal, MD, PhD
This editorial is the first to be published in GI & Hepatology News since the murder of George Floyd in Minneapolis. The corner of 38th and Chicago is 9 miles from my home in Bloomington, Minn. This corner became the epicenter of protests that have spread around the nation and world. Early on, protests were accompanied by widespread riots, looting, and destruction. In the ensuing weeks, this corner has become a memorial for Mr. Floyd and a place where people now go to reflect, pray, pay tribute, and pledge to work for change.
A coalition of willing businesses has formed in the area around 38th and Chicago. The largest employer in the area is Allina Health (I sit on the Governing Board of Allina Health). Our flagship hospital is 8 blocks from the site of George Floyd’s memorial. We will be a change leader by committing funds for local rebuilding, ensuring use of construction firms that promote minority workers (as was done when the Viking’s stadium was built), examining our investment portfolio with racial equity as one guiding principle, increasing our focus on barriers to access, enhancing equity education of our workforce, and working with city and state leaders to promote police reform.
As the Editor in Chief of the official newspaper of the AGA, I invited our board of editors to stand united in our condemnation of the racial injustices that led to the protests we now see. We each agree with the message from the combined Governing Boards of our GI societies (published June 2, 2020) stating “As health care providers, we have dedicated our lives to caring for our fellow human beings. Therefore, we are compelled to speak out against any treatment that results in unacceptable disparities that marginalize the vulnerable among us.”
Our responsibility as editors is to guide the content we deliver, ensuring its relevancy to our readers. In this light, we commit to delivering content that highlights racial injustices and health disparities for all people, as we seek to understand the many factors that result in barriers to health. We will emphasize content that leads to impactful change and will highlight progress we make as a specialty. We hope our collective work will help ensure that George Floyd’s memory, and the memories of all such victims, become a catalyst for permanent cultural change.
Editor in Chief, GI & Hepatology News
John I. Allen, MD, MBA, AGAF
Editor in Chief, The New Gastroenterologist
Vijaya L. Rao, MD
Associate Editors
Megan A. Adams, MD, JD, MSc
Ziad Gellad, MD, MPH, AGAF
Kim L. Isaacs, MD, PhD, AGAF
Charles J. Kahi, MD, MS, AGAF
Gyanprakash A. Ketwaroo, MD, MSc
Larry R. Kosinski, MD, MBA, AGAF
Sonia S. Kupfer, MD
Wajahat Mehal, MD, PhD
This editorial is the first to be published in GI & Hepatology News since the murder of George Floyd in Minneapolis. The corner of 38th and Chicago is 9 miles from my home in Bloomington, Minn. This corner became the epicenter of protests that have spread around the nation and world. Early on, protests were accompanied by widespread riots, looting, and destruction. In the ensuing weeks, this corner has become a memorial for Mr. Floyd and a place where people now go to reflect, pray, pay tribute, and pledge to work for change.
A coalition of willing businesses has formed in the area around 38th and Chicago. The largest employer in the area is Allina Health (I sit on the Governing Board of Allina Health). Our flagship hospital is 8 blocks from the site of George Floyd’s memorial. We will be a change leader by committing funds for local rebuilding, ensuring use of construction firms that promote minority workers (as was done when the Viking’s stadium was built), examining our investment portfolio with racial equity as one guiding principle, increasing our focus on barriers to access, enhancing equity education of our workforce, and working with city and state leaders to promote police reform.
As the Editor in Chief of the official newspaper of the AGA, I invited our board of editors to stand united in our condemnation of the racial injustices that led to the protests we now see. We each agree with the message from the combined Governing Boards of our GI societies (published June 2, 2020) stating “As health care providers, we have dedicated our lives to caring for our fellow human beings. Therefore, we are compelled to speak out against any treatment that results in unacceptable disparities that marginalize the vulnerable among us.”
Our responsibility as editors is to guide the content we deliver, ensuring its relevancy to our readers. In this light, we commit to delivering content that highlights racial injustices and health disparities for all people, as we seek to understand the many factors that result in barriers to health. We will emphasize content that leads to impactful change and will highlight progress we make as a specialty. We hope our collective work will help ensure that George Floyd’s memory, and the memories of all such victims, become a catalyst for permanent cultural change.
Editor in Chief, GI & Hepatology News
John I. Allen, MD, MBA, AGAF
Editor in Chief, The New Gastroenterologist
Vijaya L. Rao, MD
Associate Editors
Megan A. Adams, MD, JD, MSc
Ziad Gellad, MD, MPH, AGAF
Kim L. Isaacs, MD, PhD, AGAF
Charles J. Kahi, MD, MS, AGAF
Gyanprakash A. Ketwaroo, MD, MSc
Larry R. Kosinski, MD, MBA, AGAF
Sonia S. Kupfer, MD
Wajahat Mehal, MD, PhD
COVID-19’s effects on emergency psychiatry
Coronavirus disease 2019 (COVID-19) is affecting every aspect of medical care. Much has been written about overwhelmed hospital settings, the financial devastation to outpatient treatment centers, and an impending pandemic of mental illness that the existing underfunded and fragmented mental health system would not be prepared to weather. Although COVID-19 has undeniably affected the practice of emergency psychiatry, its impact has been surprising and complex. In this article, I describe the effects COVID-19 has had on our psychiatric emergency service, and how the pandemic has affected me personally.
How the pandemic affected our psychiatric ED
The Comprehensive Psychiatric Emergency Program (CPEP) in Buffalo, New York, is part of the emergency department (ED) in the local county hospital and is staffed by faculty from the Department of Psychiatry at the University at Buffalo. It was developed to provide evaluations of acutely psychiatrically ill individuals, to determine their treatment needs and facilitate access to the appropriate level of care.
Before COVID-19, as the only fully staffed psychiatric emergency service in the region, CPEP would routinely be called upon to serve many functions for which it was not designed. For example, people who had difficulty accessing psychiatric care in the community might come to CPEP expecting treatment for chronic conditions. Additionally, due to systemic deficiencies and limited resources, police and other community agencies refer individuals to CPEP who either have illnesses unrelated to current circumstances or who are not psychiatrically ill but unmanageable because of aggression or otherwise unresolvable social challenges such as homelessness, criminal behavior, poor parenting and other family strains, or general dissatisfaction with life. Parents unable to set limits with bored or defiant children might leave them in CPEP, hoping to transfer the parenting role, just as law enforcement officers who feel impotent to apply meaningful sanctions to non-felonious offenders might bring them to CPEP seeking containment. Labeling these problems as psychiatric emergencies has made it more palatable to leave these individuals in our care. These types of visits have contributed to the substantial growth of CPEP in recent years, in terms of annual patient visits, number of children abandoned and their lengths of stay in the CPEP, among other metrics.
The impact of the COVID-19 pandemic on an emergency psychiatry service that is expected to be all things to all people has been interesting. For the first few weeks of the societal shutdown, the patient flow was unchanged. However, during this time, the usual overcrowding created a feeling of vulnerability to contagion that sparked an urgency to minimize the census. Superhuman efforts were fueled by an unspoken sense of impending doom, and wait times dropped from approximately 17 hours to 3 or 4 hours. This state of hypervigilance was impossible to sustain indefinitely, and inevitably those efforts were exhausted. As adrenaline waned, the focus turned toward family and self-preservation. Nursing and social work staff began cancelling shifts, as did part-time physicians who contracted services with our department. Others, however, were drawn to join the front-line fight.
Trends in psychiatric ED usage during the pandemic
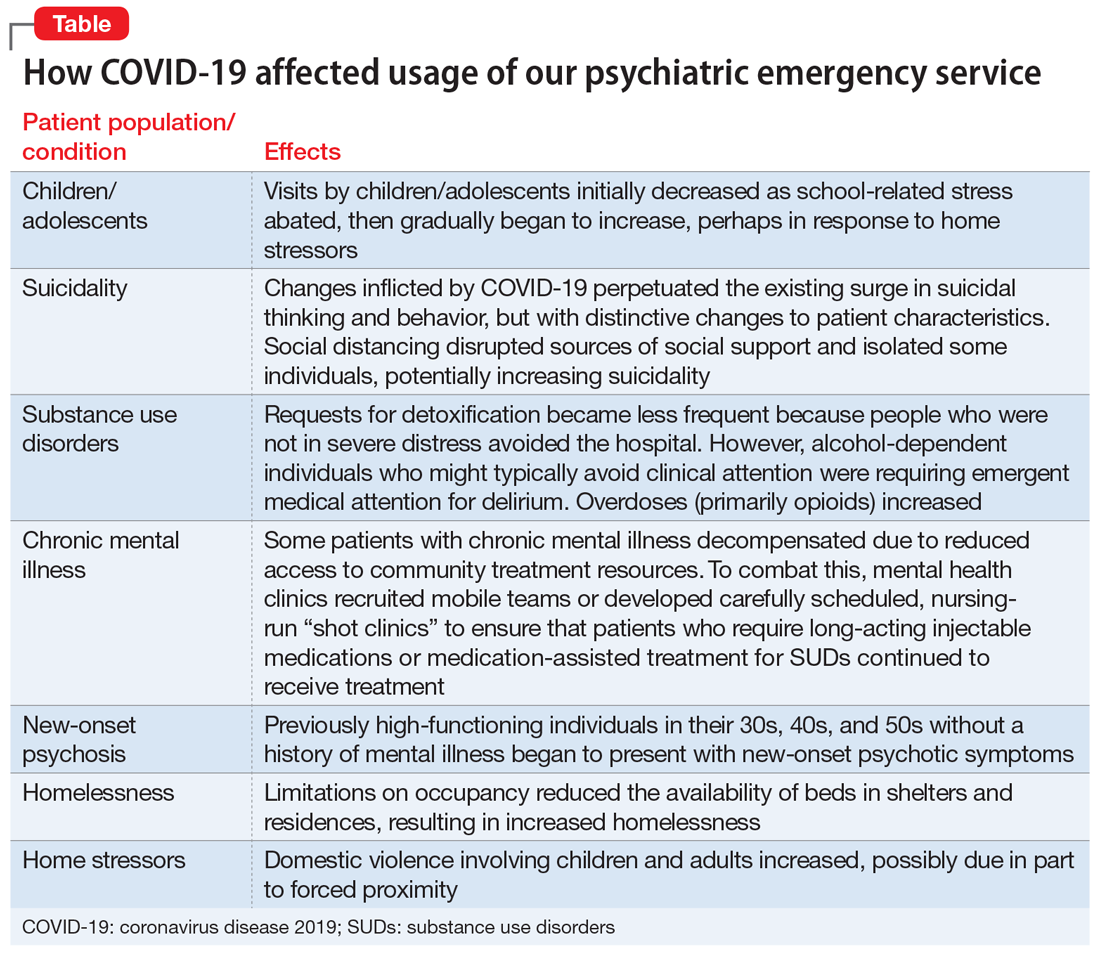
As COVID-19 spread, local media reported the paucity of personal protective equipment (PPE) and created the sense that no one would receive hospital treatment unless they were on the brink of death. Consequently, total visits to the ED began to slow. During April, CPEP saw 25% fewer visits than average. This reduction was partly attributable to cohorting patients with any suspicion of infection in a designated area within the medical ED, with access to remote evaluation by CPEP psychiatrists via telemedicine. In addition, the characteristics and circumstances of patients presenting to CPEP began to change (Table).
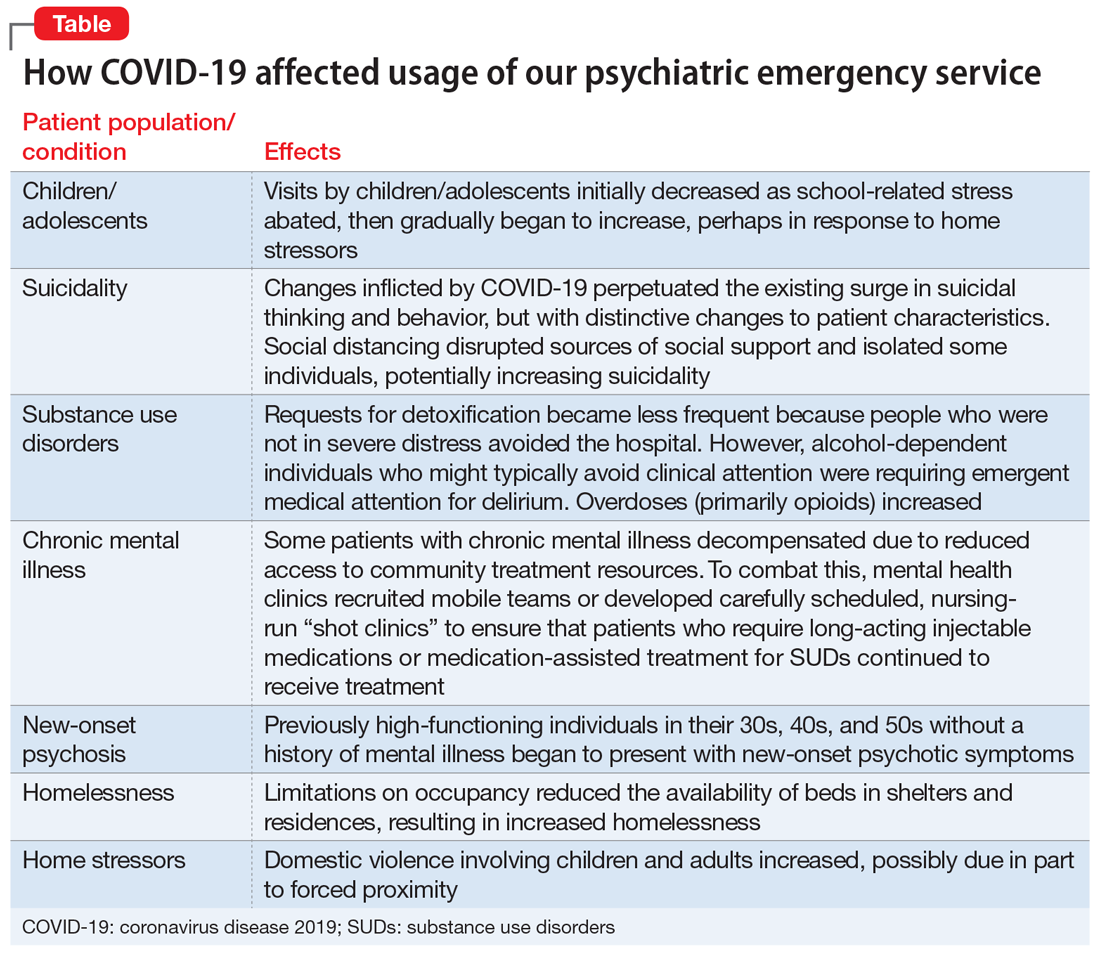
Children/adolescents. In the months before COVID-19’s spread to the United States, there had been an exponential surge in child visits to CPEP, with >200 such visits in January 2020. When schools closed on March 13, school-related stress abruptly abated, and during April, child visits dropped to 89. This reduction might have been due in part to increased access to outpatient treatment via telemedicine or telephone appointments. In our affiliated clinics, both new patient visits and remote attendance to appointments by established patients increased substantially, likely contributing to a decreased reliance on the CPEP for treatment. Limited Family Court operations, though, left already-frustrated police without much recourse when called to intervene with adolescent offenders. CPEP once again served an untraditional role, facilitating the removal of these disruptive individuals from potentially dangerous circumstances, under the guise of behavioral emergencies.
Suicidality. While nonemergent visits declined, presentations related to suicidality persisted. In the United States, suicide rates have increased annually for decades. This trend has also been observed locally, with early evidence suggesting that the changes inflicted by COVID-19 perpetuated the surge in suicidal thinking and behavior, but with a change in character. Some of this is likely related to financial stress and social disruption, though job loss seems more likely to result in increased substance use than suicidality. Even more distressing to those coming to CPEP was anxiety about the illness itself, social isolation, and loss. The death of a loved one is painful enough, but disrupting the grief process by preventing people from visiting family members dying in hospitals or gathering for funerals has been devastating. Reports of increased gun sales undoubtedly associated with fears of social decay caused by the pandemic are concerning with regard to patients with suicidality, because shooting has emerged as the means most likely to result in completed suicide.1 The imposition of social distancing directly isolated some individuals, increasing suicidality. Limitations on gathering in groups disrupted other sources of social support as well, such as religious services, clubhouses, and meetings of 12-step programs such as Alcoholics Anonymous. This could increase suicidality, either directly for more vulnerable patients or indirectly by compromising sobriety and thereby adding to the risk for suicide.
Continue to: Substance use disorders (SUDs)
Substance use disorders (SUDs). Presentations to CPEP by patients with SUDs surged, but the patient profile changed, undoubtedly influenced by the pandemic. Requests for detoxification became less frequent because people who were not in severe distress avoided the hospital. At the same time, alcohol-dependent individuals who might typically avoid clinical attention were requiring emergent medical attention for delirium. This is attributable to a combination of factors, including nutritional depletion, and a lack of access to alcohol leading to abrupt withdrawal or consumption of unconventional sources of alcohol, such as hand sanitizer, or hard liquor (over beer). Amphetamine use appears to have increased, although the observed surge may simply be related to the conspicuousness of stimulant intoxication for someone who is sheltering in place. There was a noticeable uptick in overdoses (primarily with opioids) requiring CPEP evaluation, which was possibly related to a reduction of available beds in inpatient rehabilitation facilities as a result of social distancing rules.
Patients with chronic mental illness. Many experts anticipated an increase in hospital visits by individuals with chronic mental illness expected to decompensate as a result of reduced access to community treatment resources.2 Closing courts did not prevent remote sessions for inpatient retention and treatment over objection, but did result in the expiration of many Assisted Outpatient Treatment orders by restricting renewal hearings, which is circuitously beginning to fulfill this prediction. On the other hand, an impressive community response has managed to continue meeting the needs of most of these patients. Dedicated mental health clinics have recruited mobile teams or developed carefully scheduled, nursing-run “shot clinics” to ensure that patients who require long-acting injectable medications or medication-assisted treatment for SUDs continue to receive treatment.
New-onset psychosis. A new population of patients with acute mania and psychosis also seems to have surfaced during this pandemic. Previously high-functioning individuals in their 30s, 40s, and 50s without a history of mental illness were presenting with new-onset psychotic symptoms. These are individuals who may have been characteristically anxious, or had a “Type A personality,” but were social and employed. The cause is unclear, but given the extreme uncertainty and the political climate COVID-19 brings, it is possible that the pandemic may have triggered these episodes. These individuals and their families now have the stress of learning to navigate the mental health system added to the anxiety COVID-19 brings to most households.
Homelessness. Limitations on occupancy have reduced the availability of beds in shelters and residences, resulting in increased homelessness. Locally, authorities estimated that the homeless population has grown nearly threefold as a result of bussing in from neighboring counties with fewer resources, flight from New York City, and the urgent release from jail of nonviolent offenders, many of whom had no place to go for shelter. New emergency shelter beds have not fully compensated for the relative shortage, leading individuals who had been avoiding the hospital due to fear of infection to CPEP looking for a place to stay.
Home stressors. Whereas CPEP visits by children initially decreased, after 6 weeks, the relief from school pressures appears to have been replaced by weariness from stresses at home, and the number of children presenting with depression, SUDs, and behavioral disruptions has increased. Domestic violence involving children and adults increased. Factors that might be contributing to this include the forced proximity of family members who would typically need intermittent interpersonal distance, and an obligation to care for children who would normally be in school or for disabled loved ones now unable to attend day programs or respite services. After months of enduring the pressure of these conflicts and the resulting emotional strain, patient volumes in CPEP have begun slowly returning toward the expected average, particularly since the perceived threat of coming to the hospital has attenuated.
Continue to: Personal challenges
Personal challenges
For me, COVID-19 has brought the chance to grow and learn, fumbling at times to provide the best care when crisis abounds and when not much can be said to ease the appropriate emotional distress our patients experience. The lines between what is pathological anxiety, what level of anxiety causes functional impairment, and what can realistically be expected to respond to psychiatric treatment have become blurred. At the same time, I have come across some of the sickest patients I have ever encountered.
In some ways, my passion for psychiatry has been rekindled by COVID-19, sparking an enthusiasm to teach and inspire students to pursue careers in this wonderful field of medicine. Helping to care for patients in the absence of a cure can necessitate the application of creativity and thoughtfulness to relieve suffering, thereby teaching the art of healing above offering treatment alone. Unfortunately, replacing actual patient contact with remote learning deprives students of this unique educational opportunity. Residents who attempt to continue training while limiting exposure to patients may mitigate their own risk but could also be missing an opportunity to learn how to balance their needs with making their patients’ well-being a priority. This raises the question of how the next generation of medical students and residents will learn to navigate future crises. Gruesome media depictions of haunting experiences witnessed by medical professionals exposed to an enormity of loss and death, magnified by the suicide deaths of 2 front-line workers in New York City, undoubtedly contribute to the instinct driving the protection of students and residents in this way.
The gratitude the public expresses toward me for simply continuing to do my job brings an expectation of heroism I did not seek, and with which I am uncomfortable. For me, exceptionally poised to analyze and over-analyze myriad aspects of an internal conflict that is exhausting to balance, it all generates frustration and guilt more than anything.
I am theoretically at lower risk than intubating anesthesiologists, emergency medicine physicians, and emergency medical technicians who face patients with active COVID-19. Nevertheless, daily proximity to so many patients naturally generates fear. I convince myself that performing video consultations to the medical ED is an adaptation necessary to preserve PPE, to keep me healthy through reduced exposure, to be available to patients longer, and to support the emotional health of the medical staff who are handing over that headset to patients “under investigation.” At the same time, I am secretly relieved to avoid entering those rooms and taunting death, or even worse, risking exposing my family to the virus. The threat of COVID-19 can be so consuming that it becomes easy to forget that most individuals infected are asymptomatic and therefore difficult to quickly identify.
So I continue to sit with patients face-to-face all day. Many of them are not capable of following masking and distancing recommendations, and are more prone to spitting and biting than their counterparts in the medical ED. I must ignore this threat and convince myself I am safe to be able to place my responsibility to patient care above my own needs and do my job.
Continue to: Most of my colleagues exhibit...
Most of my colleagues exhibit an effortless bravery, even if we all naturally waver briefly at times. I am proud to stand shoulder-to-shoulder every day with these clinicians, and other staff, from police to custodians, as we continue to care for the people of this community. Despite the lower clinical burden, each day we expend significant emotional energy struggling with unexpected and unique challenges, including the burden of facing the unknown. Everyone is under stress right now. For most, the effects will be transient. For some, the damage might be permanent. For others, this stress has brought out the best in us. But knowing that physicians are particularly prone to burnout, how long can the current state of hypervigilance be maintained?
What will the future hold?
The COVID-19 era has brought fewer patients through the door of my psychiatric ED; however, just like everywhere else in the world, everything has changed. The only thing that is certain is that further change is inevitable, and we must adapt to the challenge and learn from it. As unsettling as disruptions to the status quo can be, human behavior dictates that we have the option to seize opportunities created by instability to produce superior outcomes, which can be accomplished only by looking at things anew. The question is whether we will revert to the pre-COVID-19 dysfunctional use of psychiatric emergency services, or can we use what we have learned—particularly about the value of telepsychiatry—to pursue a more effective system based on an improved understanding of the mental health treatment needs of our community. While technology is proving that social distancing requires only space between people, and not necessarily social separation, there is a risk that excessive use of remote treatment could compromise the therapeutic relationship with our patients. Despite emerging opportunities, it is difficult to direct change in a productive way when the future is uncertain.
The continuous outpouring of respect for clinicians is morale-boosting. Behind closed doors, however, news that this county hospital failed to qualify for any of the second round of federal support funding because the management of COVID-19 patients has been too effective brought a new layer of unanticipated stress. This is the only hospital in 7 counties operating a psychiatric emergency service. The mandatory, “voluntary” furloughs expected of nursing and social work staff are only now being scheduled to occur over the next couple of months. And just in time for patient volumes to return to normal. How can we continue to provide quality care, let alone build changes into practice, with reduced nursing and support staff?
It is promising, however, that in the midst of social distancing, the shared experience of endeavoring to overcome COVID-19 has promoted a connectedness among individuals who might otherwise never cross paths. This observation has bolstered my confidence in the capacity for resilience of the mental health system and the individuals within it. The reality is that we are all in this together. Differences should matter less in the face of altered perceptions of mortality. Despite the stress, suicide becomes a less reasonable choice when the value of life is magnified by pandemic circumstances. Maybe there will be even less of a need for psychiatric emergency services in the wake of COVID-19, rather than the anticipated wave of mental health crises. Until we know for sure, it is only through fellowship and continued dedication to healing that the ED experience will continue to be a positive one.
Bottom Line
Coronavirus disease 2019 (COVID-19) led to changes in the characteristics and circumstances of patients presenting to our psychiatric emergency service. Despite a lower clinical burden, each day we expended significant emotional energy struggling with unexpected and unique challenges. We can use what we have learned from COVID-19 to pursue a more effective system based on an improved understanding of the mental health treatment needs of our community.
Related Resource
- American Association for Emergency Psychiatry, American College of Emergency Physicians, American Psychiatric Association, Coalition on Psychiatric Emergencies, Crisis Residential Association, and the Emergency Nurses Association. Joint statement for care of patients with behavioral health emergencies and suspected or confirmed COVID-19. https://aaep.memberclicks.net/assets/joint-statement-covid-behavioral-health.pdf.
1. Wang J, Sumner SA, Simon TR, et al. Trends in the incidence and lethality of suicidal acts in the United States, 2006-2015 [published online April 22, 2020]. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2020.0596.
2. Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019--a perfect storm? [published online April 10, 2020]. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2020.1060.
Coronavirus disease 2019 (COVID-19) is affecting every aspect of medical care. Much has been written about overwhelmed hospital settings, the financial devastation to outpatient treatment centers, and an impending pandemic of mental illness that the existing underfunded and fragmented mental health system would not be prepared to weather. Although COVID-19 has undeniably affected the practice of emergency psychiatry, its impact has been surprising and complex. In this article, I describe the effects COVID-19 has had on our psychiatric emergency service, and how the pandemic has affected me personally.
How the pandemic affected our psychiatric ED
The Comprehensive Psychiatric Emergency Program (CPEP) in Buffalo, New York, is part of the emergency department (ED) in the local county hospital and is staffed by faculty from the Department of Psychiatry at the University at Buffalo. It was developed to provide evaluations of acutely psychiatrically ill individuals, to determine their treatment needs and facilitate access to the appropriate level of care.
Before COVID-19, as the only fully staffed psychiatric emergency service in the region, CPEP would routinely be called upon to serve many functions for which it was not designed. For example, people who had difficulty accessing psychiatric care in the community might come to CPEP expecting treatment for chronic conditions. Additionally, due to systemic deficiencies and limited resources, police and other community agencies refer individuals to CPEP who either have illnesses unrelated to current circumstances or who are not psychiatrically ill but unmanageable because of aggression or otherwise unresolvable social challenges such as homelessness, criminal behavior, poor parenting and other family strains, or general dissatisfaction with life. Parents unable to set limits with bored or defiant children might leave them in CPEP, hoping to transfer the parenting role, just as law enforcement officers who feel impotent to apply meaningful sanctions to non-felonious offenders might bring them to CPEP seeking containment. Labeling these problems as psychiatric emergencies has made it more palatable to leave these individuals in our care. These types of visits have contributed to the substantial growth of CPEP in recent years, in terms of annual patient visits, number of children abandoned and their lengths of stay in the CPEP, among other metrics.
The impact of the COVID-19 pandemic on an emergency psychiatry service that is expected to be all things to all people has been interesting. For the first few weeks of the societal shutdown, the patient flow was unchanged. However, during this time, the usual overcrowding created a feeling of vulnerability to contagion that sparked an urgency to minimize the census. Superhuman efforts were fueled by an unspoken sense of impending doom, and wait times dropped from approximately 17 hours to 3 or 4 hours. This state of hypervigilance was impossible to sustain indefinitely, and inevitably those efforts were exhausted. As adrenaline waned, the focus turned toward family and self-preservation. Nursing and social work staff began cancelling shifts, as did part-time physicians who contracted services with our department. Others, however, were drawn to join the front-line fight.
Trends in psychiatric ED usage during the pandemic
As COVID-19 spread, local media reported the paucity of personal protective equipment (PPE) and created the sense that no one would receive hospital treatment unless they were on the brink of death. Consequently, total visits to the ED began to slow. During April, CPEP saw 25% fewer visits than average. This reduction was partly attributable to cohorting patients with any suspicion of infection in a designated area within the medical ED, with access to remote evaluation by CPEP psychiatrists via telemedicine. In addition, the characteristics and circumstances of patients presenting to CPEP began to change (Table).
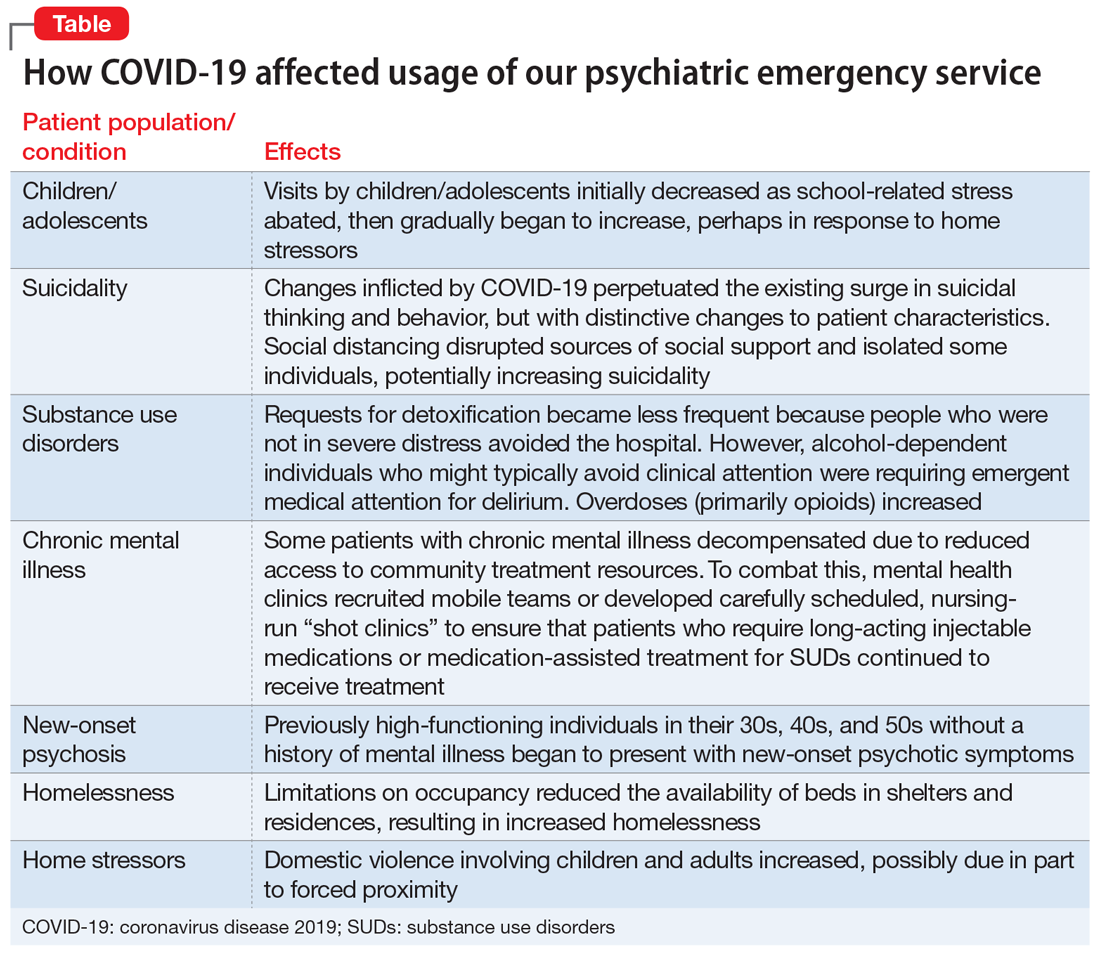
Children/adolescents. In the months before COVID-19’s spread to the United States, there had been an exponential surge in child visits to CPEP, with >200 such visits in January 2020. When schools closed on March 13, school-related stress abruptly abated, and during April, child visits dropped to 89. This reduction might have been due in part to increased access to outpatient treatment via telemedicine or telephone appointments. In our affiliated clinics, both new patient visits and remote attendance to appointments by established patients increased substantially, likely contributing to a decreased reliance on the CPEP for treatment. Limited Family Court operations, though, left already-frustrated police without much recourse when called to intervene with adolescent offenders. CPEP once again served an untraditional role, facilitating the removal of these disruptive individuals from potentially dangerous circumstances, under the guise of behavioral emergencies.
Suicidality. While nonemergent visits declined, presentations related to suicidality persisted. In the United States, suicide rates have increased annually for decades. This trend has also been observed locally, with early evidence suggesting that the changes inflicted by COVID-19 perpetuated the surge in suicidal thinking and behavior, but with a change in character. Some of this is likely related to financial stress and social disruption, though job loss seems more likely to result in increased substance use than suicidality. Even more distressing to those coming to CPEP was anxiety about the illness itself, social isolation, and loss. The death of a loved one is painful enough, but disrupting the grief process by preventing people from visiting family members dying in hospitals or gathering for funerals has been devastating. Reports of increased gun sales undoubtedly associated with fears of social decay caused by the pandemic are concerning with regard to patients with suicidality, because shooting has emerged as the means most likely to result in completed suicide.1 The imposition of social distancing directly isolated some individuals, increasing suicidality. Limitations on gathering in groups disrupted other sources of social support as well, such as religious services, clubhouses, and meetings of 12-step programs such as Alcoholics Anonymous. This could increase suicidality, either directly for more vulnerable patients or indirectly by compromising sobriety and thereby adding to the risk for suicide.
Continue to: Substance use disorders (SUDs)
Substance use disorders (SUDs). Presentations to CPEP by patients with SUDs surged, but the patient profile changed, undoubtedly influenced by the pandemic. Requests for detoxification became less frequent because people who were not in severe distress avoided the hospital. At the same time, alcohol-dependent individuals who might typically avoid clinical attention were requiring emergent medical attention for delirium. This is attributable to a combination of factors, including nutritional depletion, and a lack of access to alcohol leading to abrupt withdrawal or consumption of unconventional sources of alcohol, such as hand sanitizer, or hard liquor (over beer). Amphetamine use appears to have increased, although the observed surge may simply be related to the conspicuousness of stimulant intoxication for someone who is sheltering in place. There was a noticeable uptick in overdoses (primarily with opioids) requiring CPEP evaluation, which was possibly related to a reduction of available beds in inpatient rehabilitation facilities as a result of social distancing rules.
Patients with chronic mental illness. Many experts anticipated an increase in hospital visits by individuals with chronic mental illness expected to decompensate as a result of reduced access to community treatment resources.2 Closing courts did not prevent remote sessions for inpatient retention and treatment over objection, but did result in the expiration of many Assisted Outpatient Treatment orders by restricting renewal hearings, which is circuitously beginning to fulfill this prediction. On the other hand, an impressive community response has managed to continue meeting the needs of most of these patients. Dedicated mental health clinics have recruited mobile teams or developed carefully scheduled, nursing-run “shot clinics” to ensure that patients who require long-acting injectable medications or medication-assisted treatment for SUDs continue to receive treatment.
New-onset psychosis. A new population of patients with acute mania and psychosis also seems to have surfaced during this pandemic. Previously high-functioning individuals in their 30s, 40s, and 50s without a history of mental illness were presenting with new-onset psychotic symptoms. These are individuals who may have been characteristically anxious, or had a “Type A personality,” but were social and employed. The cause is unclear, but given the extreme uncertainty and the political climate COVID-19 brings, it is possible that the pandemic may have triggered these episodes. These individuals and their families now have the stress of learning to navigate the mental health system added to the anxiety COVID-19 brings to most households.
Homelessness. Limitations on occupancy have reduced the availability of beds in shelters and residences, resulting in increased homelessness. Locally, authorities estimated that the homeless population has grown nearly threefold as a result of bussing in from neighboring counties with fewer resources, flight from New York City, and the urgent release from jail of nonviolent offenders, many of whom had no place to go for shelter. New emergency shelter beds have not fully compensated for the relative shortage, leading individuals who had been avoiding the hospital due to fear of infection to CPEP looking for a place to stay.
Home stressors. Whereas CPEP visits by children initially decreased, after 6 weeks, the relief from school pressures appears to have been replaced by weariness from stresses at home, and the number of children presenting with depression, SUDs, and behavioral disruptions has increased. Domestic violence involving children and adults increased. Factors that might be contributing to this include the forced proximity of family members who would typically need intermittent interpersonal distance, and an obligation to care for children who would normally be in school or for disabled loved ones now unable to attend day programs or respite services. After months of enduring the pressure of these conflicts and the resulting emotional strain, patient volumes in CPEP have begun slowly returning toward the expected average, particularly since the perceived threat of coming to the hospital has attenuated.
Continue to: Personal challenges
Personal challenges
For me, COVID-19 has brought the chance to grow and learn, fumbling at times to provide the best care when crisis abounds and when not much can be said to ease the appropriate emotional distress our patients experience. The lines between what is pathological anxiety, what level of anxiety causes functional impairment, and what can realistically be expected to respond to psychiatric treatment have become blurred. At the same time, I have come across some of the sickest patients I have ever encountered.
In some ways, my passion for psychiatry has been rekindled by COVID-19, sparking an enthusiasm to teach and inspire students to pursue careers in this wonderful field of medicine. Helping to care for patients in the absence of a cure can necessitate the application of creativity and thoughtfulness to relieve suffering, thereby teaching the art of healing above offering treatment alone. Unfortunately, replacing actual patient contact with remote learning deprives students of this unique educational opportunity. Residents who attempt to continue training while limiting exposure to patients may mitigate their own risk but could also be missing an opportunity to learn how to balance their needs with making their patients’ well-being a priority. This raises the question of how the next generation of medical students and residents will learn to navigate future crises. Gruesome media depictions of haunting experiences witnessed by medical professionals exposed to an enormity of loss and death, magnified by the suicide deaths of 2 front-line workers in New York City, undoubtedly contribute to the instinct driving the protection of students and residents in this way.
The gratitude the public expresses toward me for simply continuing to do my job brings an expectation of heroism I did not seek, and with which I am uncomfortable. For me, exceptionally poised to analyze and over-analyze myriad aspects of an internal conflict that is exhausting to balance, it all generates frustration and guilt more than anything.
I am theoretically at lower risk than intubating anesthesiologists, emergency medicine physicians, and emergency medical technicians who face patients with active COVID-19. Nevertheless, daily proximity to so many patients naturally generates fear. I convince myself that performing video consultations to the medical ED is an adaptation necessary to preserve PPE, to keep me healthy through reduced exposure, to be available to patients longer, and to support the emotional health of the medical staff who are handing over that headset to patients “under investigation.” At the same time, I am secretly relieved to avoid entering those rooms and taunting death, or even worse, risking exposing my family to the virus. The threat of COVID-19 can be so consuming that it becomes easy to forget that most individuals infected are asymptomatic and therefore difficult to quickly identify.
So I continue to sit with patients face-to-face all day. Many of them are not capable of following masking and distancing recommendations, and are more prone to spitting and biting than their counterparts in the medical ED. I must ignore this threat and convince myself I am safe to be able to place my responsibility to patient care above my own needs and do my job.
Continue to: Most of my colleagues exhibit...
Most of my colleagues exhibit an effortless bravery, even if we all naturally waver briefly at times. I am proud to stand shoulder-to-shoulder every day with these clinicians, and other staff, from police to custodians, as we continue to care for the people of this community. Despite the lower clinical burden, each day we expend significant emotional energy struggling with unexpected and unique challenges, including the burden of facing the unknown. Everyone is under stress right now. For most, the effects will be transient. For some, the damage might be permanent. For others, this stress has brought out the best in us. But knowing that physicians are particularly prone to burnout, how long can the current state of hypervigilance be maintained?
What will the future hold?
The COVID-19 era has brought fewer patients through the door of my psychiatric ED; however, just like everywhere else in the world, everything has changed. The only thing that is certain is that further change is inevitable, and we must adapt to the challenge and learn from it. As unsettling as disruptions to the status quo can be, human behavior dictates that we have the option to seize opportunities created by instability to produce superior outcomes, which can be accomplished only by looking at things anew. The question is whether we will revert to the pre-COVID-19 dysfunctional use of psychiatric emergency services, or can we use what we have learned—particularly about the value of telepsychiatry—to pursue a more effective system based on an improved understanding of the mental health treatment needs of our community. While technology is proving that social distancing requires only space between people, and not necessarily social separation, there is a risk that excessive use of remote treatment could compromise the therapeutic relationship with our patients. Despite emerging opportunities, it is difficult to direct change in a productive way when the future is uncertain.
The continuous outpouring of respect for clinicians is morale-boosting. Behind closed doors, however, news that this county hospital failed to qualify for any of the second round of federal support funding because the management of COVID-19 patients has been too effective brought a new layer of unanticipated stress. This is the only hospital in 7 counties operating a psychiatric emergency service. The mandatory, “voluntary” furloughs expected of nursing and social work staff are only now being scheduled to occur over the next couple of months. And just in time for patient volumes to return to normal. How can we continue to provide quality care, let alone build changes into practice, with reduced nursing and support staff?
It is promising, however, that in the midst of social distancing, the shared experience of endeavoring to overcome COVID-19 has promoted a connectedness among individuals who might otherwise never cross paths. This observation has bolstered my confidence in the capacity for resilience of the mental health system and the individuals within it. The reality is that we are all in this together. Differences should matter less in the face of altered perceptions of mortality. Despite the stress, suicide becomes a less reasonable choice when the value of life is magnified by pandemic circumstances. Maybe there will be even less of a need for psychiatric emergency services in the wake of COVID-19, rather than the anticipated wave of mental health crises. Until we know for sure, it is only through fellowship and continued dedication to healing that the ED experience will continue to be a positive one.
Bottom Line
Coronavirus disease 2019 (COVID-19) led to changes in the characteristics and circumstances of patients presenting to our psychiatric emergency service. Despite a lower clinical burden, each day we expended significant emotional energy struggling with unexpected and unique challenges. We can use what we have learned from COVID-19 to pursue a more effective system based on an improved understanding of the mental health treatment needs of our community.
Related Resource
- American Association for Emergency Psychiatry, American College of Emergency Physicians, American Psychiatric Association, Coalition on Psychiatric Emergencies, Crisis Residential Association, and the Emergency Nurses Association. Joint statement for care of patients with behavioral health emergencies and suspected or confirmed COVID-19. https://aaep.memberclicks.net/assets/joint-statement-covid-behavioral-health.pdf.
Coronavirus disease 2019 (COVID-19) is affecting every aspect of medical care. Much has been written about overwhelmed hospital settings, the financial devastation to outpatient treatment centers, and an impending pandemic of mental illness that the existing underfunded and fragmented mental health system would not be prepared to weather. Although COVID-19 has undeniably affected the practice of emergency psychiatry, its impact has been surprising and complex. In this article, I describe the effects COVID-19 has had on our psychiatric emergency service, and how the pandemic has affected me personally.
How the pandemic affected our psychiatric ED
The Comprehensive Psychiatric Emergency Program (CPEP) in Buffalo, New York, is part of the emergency department (ED) in the local county hospital and is staffed by faculty from the Department of Psychiatry at the University at Buffalo. It was developed to provide evaluations of acutely psychiatrically ill individuals, to determine their treatment needs and facilitate access to the appropriate level of care.
Before COVID-19, as the only fully staffed psychiatric emergency service in the region, CPEP would routinely be called upon to serve many functions for which it was not designed. For example, people who had difficulty accessing psychiatric care in the community might come to CPEP expecting treatment for chronic conditions. Additionally, due to systemic deficiencies and limited resources, police and other community agencies refer individuals to CPEP who either have illnesses unrelated to current circumstances or who are not psychiatrically ill but unmanageable because of aggression or otherwise unresolvable social challenges such as homelessness, criminal behavior, poor parenting and other family strains, or general dissatisfaction with life. Parents unable to set limits with bored or defiant children might leave them in CPEP, hoping to transfer the parenting role, just as law enforcement officers who feel impotent to apply meaningful sanctions to non-felonious offenders might bring them to CPEP seeking containment. Labeling these problems as psychiatric emergencies has made it more palatable to leave these individuals in our care. These types of visits have contributed to the substantial growth of CPEP in recent years, in terms of annual patient visits, number of children abandoned and their lengths of stay in the CPEP, among other metrics.
The impact of the COVID-19 pandemic on an emergency psychiatry service that is expected to be all things to all people has been interesting. For the first few weeks of the societal shutdown, the patient flow was unchanged. However, during this time, the usual overcrowding created a feeling of vulnerability to contagion that sparked an urgency to minimize the census. Superhuman efforts were fueled by an unspoken sense of impending doom, and wait times dropped from approximately 17 hours to 3 or 4 hours. This state of hypervigilance was impossible to sustain indefinitely, and inevitably those efforts were exhausted. As adrenaline waned, the focus turned toward family and self-preservation. Nursing and social work staff began cancelling shifts, as did part-time physicians who contracted services with our department. Others, however, were drawn to join the front-line fight.
Trends in psychiatric ED usage during the pandemic
As COVID-19 spread, local media reported the paucity of personal protective equipment (PPE) and created the sense that no one would receive hospital treatment unless they were on the brink of death. Consequently, total visits to the ED began to slow. During April, CPEP saw 25% fewer visits than average. This reduction was partly attributable to cohorting patients with any suspicion of infection in a designated area within the medical ED, with access to remote evaluation by CPEP psychiatrists via telemedicine. In addition, the characteristics and circumstances of patients presenting to CPEP began to change (Table).
Children/adolescents. In the months before COVID-19’s spread to the United States, there had been an exponential surge in child visits to CPEP, with >200 such visits in January 2020. When schools closed on March 13, school-related stress abruptly abated, and during April, child visits dropped to 89. This reduction might have been due in part to increased access to outpatient treatment via telemedicine or telephone appointments. In our affiliated clinics, both new patient visits and remote attendance to appointments by established patients increased substantially, likely contributing to a decreased reliance on the CPEP for treatment. Limited Family Court operations, though, left already-frustrated police without much recourse when called to intervene with adolescent offenders. CPEP once again served an untraditional role, facilitating the removal of these disruptive individuals from potentially dangerous circumstances, under the guise of behavioral emergencies.
Suicidality. While nonemergent visits declined, presentations related to suicidality persisted. In the United States, suicide rates have increased annually for decades. This trend has also been observed locally, with early evidence suggesting that the changes inflicted by COVID-19 perpetuated the surge in suicidal thinking and behavior, but with a change in character. Some of this is likely related to financial stress and social disruption, though job loss seems more likely to result in increased substance use than suicidality. Even more distressing to those coming to CPEP was anxiety about the illness itself, social isolation, and loss. The death of a loved one is painful enough, but disrupting the grief process by preventing people from visiting family members dying in hospitals or gathering for funerals has been devastating. Reports of increased gun sales undoubtedly associated with fears of social decay caused by the pandemic are concerning with regard to patients with suicidality, because shooting has emerged as the means most likely to result in completed suicide.1 The imposition of social distancing directly isolated some individuals, increasing suicidality. Limitations on gathering in groups disrupted other sources of social support as well, such as religious services, clubhouses, and meetings of 12-step programs such as Alcoholics Anonymous. This could increase suicidality, either directly for more vulnerable patients or indirectly by compromising sobriety and thereby adding to the risk for suicide.
Continue to: Substance use disorders (SUDs)
Substance use disorders (SUDs). Presentations to CPEP by patients with SUDs surged, but the patient profile changed, undoubtedly influenced by the pandemic. Requests for detoxification became less frequent because people who were not in severe distress avoided the hospital. At the same time, alcohol-dependent individuals who might typically avoid clinical attention were requiring emergent medical attention for delirium. This is attributable to a combination of factors, including nutritional depletion, and a lack of access to alcohol leading to abrupt withdrawal or consumption of unconventional sources of alcohol, such as hand sanitizer, or hard liquor (over beer). Amphetamine use appears to have increased, although the observed surge may simply be related to the conspicuousness of stimulant intoxication for someone who is sheltering in place. There was a noticeable uptick in overdoses (primarily with opioids) requiring CPEP evaluation, which was possibly related to a reduction of available beds in inpatient rehabilitation facilities as a result of social distancing rules.
Patients with chronic mental illness. Many experts anticipated an increase in hospital visits by individuals with chronic mental illness expected to decompensate as a result of reduced access to community treatment resources.2 Closing courts did not prevent remote sessions for inpatient retention and treatment over objection, but did result in the expiration of many Assisted Outpatient Treatment orders by restricting renewal hearings, which is circuitously beginning to fulfill this prediction. On the other hand, an impressive community response has managed to continue meeting the needs of most of these patients. Dedicated mental health clinics have recruited mobile teams or developed carefully scheduled, nursing-run “shot clinics” to ensure that patients who require long-acting injectable medications or medication-assisted treatment for SUDs continue to receive treatment.
New-onset psychosis. A new population of patients with acute mania and psychosis also seems to have surfaced during this pandemic. Previously high-functioning individuals in their 30s, 40s, and 50s without a history of mental illness were presenting with new-onset psychotic symptoms. These are individuals who may have been characteristically anxious, or had a “Type A personality,” but were social and employed. The cause is unclear, but given the extreme uncertainty and the political climate COVID-19 brings, it is possible that the pandemic may have triggered these episodes. These individuals and their families now have the stress of learning to navigate the mental health system added to the anxiety COVID-19 brings to most households.
Homelessness. Limitations on occupancy have reduced the availability of beds in shelters and residences, resulting in increased homelessness. Locally, authorities estimated that the homeless population has grown nearly threefold as a result of bussing in from neighboring counties with fewer resources, flight from New York City, and the urgent release from jail of nonviolent offenders, many of whom had no place to go for shelter. New emergency shelter beds have not fully compensated for the relative shortage, leading individuals who had been avoiding the hospital due to fear of infection to CPEP looking for a place to stay.
Home stressors. Whereas CPEP visits by children initially decreased, after 6 weeks, the relief from school pressures appears to have been replaced by weariness from stresses at home, and the number of children presenting with depression, SUDs, and behavioral disruptions has increased. Domestic violence involving children and adults increased. Factors that might be contributing to this include the forced proximity of family members who would typically need intermittent interpersonal distance, and an obligation to care for children who would normally be in school or for disabled loved ones now unable to attend day programs or respite services. After months of enduring the pressure of these conflicts and the resulting emotional strain, patient volumes in CPEP have begun slowly returning toward the expected average, particularly since the perceived threat of coming to the hospital has attenuated.
Continue to: Personal challenges
Personal challenges
For me, COVID-19 has brought the chance to grow and learn, fumbling at times to provide the best care when crisis abounds and when not much can be said to ease the appropriate emotional distress our patients experience. The lines between what is pathological anxiety, what level of anxiety causes functional impairment, and what can realistically be expected to respond to psychiatric treatment have become blurred. At the same time, I have come across some of the sickest patients I have ever encountered.
In some ways, my passion for psychiatry has been rekindled by COVID-19, sparking an enthusiasm to teach and inspire students to pursue careers in this wonderful field of medicine. Helping to care for patients in the absence of a cure can necessitate the application of creativity and thoughtfulness to relieve suffering, thereby teaching the art of healing above offering treatment alone. Unfortunately, replacing actual patient contact with remote learning deprives students of this unique educational opportunity. Residents who attempt to continue training while limiting exposure to patients may mitigate their own risk but could also be missing an opportunity to learn how to balance their needs with making their patients’ well-being a priority. This raises the question of how the next generation of medical students and residents will learn to navigate future crises. Gruesome media depictions of haunting experiences witnessed by medical professionals exposed to an enormity of loss and death, magnified by the suicide deaths of 2 front-line workers in New York City, undoubtedly contribute to the instinct driving the protection of students and residents in this way.
The gratitude the public expresses toward me for simply continuing to do my job brings an expectation of heroism I did not seek, and with which I am uncomfortable. For me, exceptionally poised to analyze and over-analyze myriad aspects of an internal conflict that is exhausting to balance, it all generates frustration and guilt more than anything.
I am theoretically at lower risk than intubating anesthesiologists, emergency medicine physicians, and emergency medical technicians who face patients with active COVID-19. Nevertheless, daily proximity to so many patients naturally generates fear. I convince myself that performing video consultations to the medical ED is an adaptation necessary to preserve PPE, to keep me healthy through reduced exposure, to be available to patients longer, and to support the emotional health of the medical staff who are handing over that headset to patients “under investigation.” At the same time, I am secretly relieved to avoid entering those rooms and taunting death, or even worse, risking exposing my family to the virus. The threat of COVID-19 can be so consuming that it becomes easy to forget that most individuals infected are asymptomatic and therefore difficult to quickly identify.
So I continue to sit with patients face-to-face all day. Many of them are not capable of following masking and distancing recommendations, and are more prone to spitting and biting than their counterparts in the medical ED. I must ignore this threat and convince myself I am safe to be able to place my responsibility to patient care above my own needs and do my job.
Continue to: Most of my colleagues exhibit...
Most of my colleagues exhibit an effortless bravery, even if we all naturally waver briefly at times. I am proud to stand shoulder-to-shoulder every day with these clinicians, and other staff, from police to custodians, as we continue to care for the people of this community. Despite the lower clinical burden, each day we expend significant emotional energy struggling with unexpected and unique challenges, including the burden of facing the unknown. Everyone is under stress right now. For most, the effects will be transient. For some, the damage might be permanent. For others, this stress has brought out the best in us. But knowing that physicians are particularly prone to burnout, how long can the current state of hypervigilance be maintained?
What will the future hold?
The COVID-19 era has brought fewer patients through the door of my psychiatric ED; however, just like everywhere else in the world, everything has changed. The only thing that is certain is that further change is inevitable, and we must adapt to the challenge and learn from it. As unsettling as disruptions to the status quo can be, human behavior dictates that we have the option to seize opportunities created by instability to produce superior outcomes, which can be accomplished only by looking at things anew. The question is whether we will revert to the pre-COVID-19 dysfunctional use of psychiatric emergency services, or can we use what we have learned—particularly about the value of telepsychiatry—to pursue a more effective system based on an improved understanding of the mental health treatment needs of our community. While technology is proving that social distancing requires only space between people, and not necessarily social separation, there is a risk that excessive use of remote treatment could compromise the therapeutic relationship with our patients. Despite emerging opportunities, it is difficult to direct change in a productive way when the future is uncertain.
The continuous outpouring of respect for clinicians is morale-boosting. Behind closed doors, however, news that this county hospital failed to qualify for any of the second round of federal support funding because the management of COVID-19 patients has been too effective brought a new layer of unanticipated stress. This is the only hospital in 7 counties operating a psychiatric emergency service. The mandatory, “voluntary” furloughs expected of nursing and social work staff are only now being scheduled to occur over the next couple of months. And just in time for patient volumes to return to normal. How can we continue to provide quality care, let alone build changes into practice, with reduced nursing and support staff?
It is promising, however, that in the midst of social distancing, the shared experience of endeavoring to overcome COVID-19 has promoted a connectedness among individuals who might otherwise never cross paths. This observation has bolstered my confidence in the capacity for resilience of the mental health system and the individuals within it. The reality is that we are all in this together. Differences should matter less in the face of altered perceptions of mortality. Despite the stress, suicide becomes a less reasonable choice when the value of life is magnified by pandemic circumstances. Maybe there will be even less of a need for psychiatric emergency services in the wake of COVID-19, rather than the anticipated wave of mental health crises. Until we know for sure, it is only through fellowship and continued dedication to healing that the ED experience will continue to be a positive one.
Bottom Line
Coronavirus disease 2019 (COVID-19) led to changes in the characteristics and circumstances of patients presenting to our psychiatric emergency service. Despite a lower clinical burden, each day we expended significant emotional energy struggling with unexpected and unique challenges. We can use what we have learned from COVID-19 to pursue a more effective system based on an improved understanding of the mental health treatment needs of our community.
Related Resource
- American Association for Emergency Psychiatry, American College of Emergency Physicians, American Psychiatric Association, Coalition on Psychiatric Emergencies, Crisis Residential Association, and the Emergency Nurses Association. Joint statement for care of patients with behavioral health emergencies and suspected or confirmed COVID-19. https://aaep.memberclicks.net/assets/joint-statement-covid-behavioral-health.pdf.
1. Wang J, Sumner SA, Simon TR, et al. Trends in the incidence and lethality of suicidal acts in the United States, 2006-2015 [published online April 22, 2020]. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2020.0596.
2. Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019--a perfect storm? [published online April 10, 2020]. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2020.1060.
1. Wang J, Sumner SA, Simon TR, et al. Trends in the incidence and lethality of suicidal acts in the United States, 2006-2015 [published online April 22, 2020]. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2020.0596.
2. Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019--a perfect storm? [published online April 10, 2020]. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2020.1060.
The hidden dangers of supplements: A case of substance-induced psychosis
“You are what you eat,” my mother always said, and structured our dinner plates according to the USDA food pyramid. We dutifully consumed leafy greens, and prior to medical school I invested time and money into healthy diet choices. I drank green smoothies, pureed baby food for my children, read up on the pH balancing diet, grew sprouts on windowsills, bought organic.
With the stressors and time constraints of managing medical school and a family, nutrition tumbled down the ladder of priorities until eventually my family was subsisting on chicken nuggets, pizza, and peanut butter. Intern year has only added the occasional candy bar from the doctors’ lounge. I experienced a vague sense of loss for something I had once valued, but simultaneously felt dismissive of trendy topics such as omega-3 fatty acids and antioxidants in the face of myocardial infarctions and liver failure. A biochemistry professor once scoffed at “the laypeople’s obsession with toxins,” and nutrition received zero attention in our medical school curriculum or board exams.
However, a clinical experience on the inpatient psychiatric unit made me reevaluate the importance nutrition should have in both our personal lives and the practice of medicine. This is the case of an otherwise healthy young man with no psychiatric history who suffered a psychotic break after ingesting an excess of a supplement he purchased online with the purpose of improving his performance at a high-stress job.
CASE REPORT
Mr. K, a 28-year-old computer programmer, was voluntarily admitted to the inpatient psychiatry unit for paranoia and persecutory delusions along with auditory hallucinations. His father reported that Mr. K had been behaving erratically for several days prior to admission and was subsequently found wandering in the street.
On admission, Mr. K was not oriented to place or situation. He was unkempt and guarded, and claimed people were following him. His urine toxicology screen and blood alcohol levels were negative.
While hospitalized, Mr. K was hyperverbal and delusional. He related that at work he had been developing programs to make slaves in the computer, “algorithms for orchestration,” and that he was uncomfortable with the ethical implications. He eventually endorsed having purchased the supplement phenylethylamine (PEA) to improve his focus, and ingesting “two substantial scoops of the crystalline substance.”
We did not initiate any psychiatric medications. On the third day of his hospitalization, Mr. K was alert, oriented, euthymic, relaxed, and had a full range of affect; upon discharge we advised him to discard the PEA and avoid stimulants. He complied, quit his high-stress job, and had no subsequent psychotic symptoms in the 7 months since discharge.
Continue to: Dietary supplements carry risks
Dietary supplements carry risks
According to the FDA, dietary supplements are regulated as food, but many have strong biologic effects or may even contain drugs.1 More than 18% of Americans use herbal or nutritional therapies as part of their health regimen.2 However, many over-the-counter remedies have been found to exhibit psychotropic effects,3 and many more are purported to impact mental and physical health with little to no scientific research into these claims or potential adverse effects.
Phenylethylamine is sold as a nutritional supplement and marketed for its purported beneficial effects on weight loss, mood, and focus.4 However, PEA is known to act as a natural amphetamine and to play a role in the development of neuropsychiatric disorders.5 It is an endogenous psychotogenic molecule that has been previously theorized as a cause for primary psychosis.6 Phenylethylamine interacts with the same receptor ligand that responds to amphetamine and related compounds (such as methamphetamine and 3,4-methylenedioxy-methamphetamine [MDMA]), the genetic coding for which is located in an area of DNA associated with schizophrenia: chromosome 6q23.2.7 While the mechanisms and details of these interactions remain poorly understood, this case of PEA-induced psychosis represents a glimpse into the potential psychoactive properties of this readily available nutritional supplement.
This patient’s cautionary tale has given me pause regarding both my family’s nutrition and the oft-neglected dietary portion of the social history. Also, several subsequent patient experiences hearken back to my mother’s words regarding the importance of healthy eating. A patient with phenylketonuria presented with psychosis after running out of her formula and consuming junk food. Another patient with severely elevated blood glucose levels presented with confusion. I have come to realize that ingestion impacts presentation, or, in other words, you are what you eat.
1. US Food and Drug Administration. Dietary supplements. https://www.fda.gov/consumers/consumer-updates/dietary-supplements. Accessed December 11, 2019.
2. Tindle H, Davis R, Philips R, et al. Trends in use of complementary and alternative medicine by US adults: 1997-2002. Altern Ther Health Med. 2005;11(1):42-49.
3. Sarris J. Herbal medicines in the treatment of psychiatric disorders: 10-year updated review. Phytotherapy Research. 2018;32(7):1147-1162.
4. Irsfeld M, Spadafore M, Prüß BM. β-phenylethylamine, a small molecule with a large impact. WebmedCentral. 2013;4(9):4409.
5. Wolf M, Mosnaim A. Phenylethylamine in neuropsychiatric disorders. Gen Pharmacol. 1983;14(4):385-390.
6. Janssen P, Leysen J, Megens A, et al. Does phenylethylamine act as an endogenous amphetamine in some patients? In J Neuropsychopharmacol. 1999;2(3):229-240.
7. Zucchi R, Chiellini G, Scanlan TS, et al. Trace amine-associated receptors and their ligands. Br J Pharmacol. 2006;149(8):967-978.
“You are what you eat,” my mother always said, and structured our dinner plates according to the USDA food pyramid. We dutifully consumed leafy greens, and prior to medical school I invested time and money into healthy diet choices. I drank green smoothies, pureed baby food for my children, read up on the pH balancing diet, grew sprouts on windowsills, bought organic.
With the stressors and time constraints of managing medical school and a family, nutrition tumbled down the ladder of priorities until eventually my family was subsisting on chicken nuggets, pizza, and peanut butter. Intern year has only added the occasional candy bar from the doctors’ lounge. I experienced a vague sense of loss for something I had once valued, but simultaneously felt dismissive of trendy topics such as omega-3 fatty acids and antioxidants in the face of myocardial infarctions and liver failure. A biochemistry professor once scoffed at “the laypeople’s obsession with toxins,” and nutrition received zero attention in our medical school curriculum or board exams.
However, a clinical experience on the inpatient psychiatric unit made me reevaluate the importance nutrition should have in both our personal lives and the practice of medicine. This is the case of an otherwise healthy young man with no psychiatric history who suffered a psychotic break after ingesting an excess of a supplement he purchased online with the purpose of improving his performance at a high-stress job.
CASE REPORT
Mr. K, a 28-year-old computer programmer, was voluntarily admitted to the inpatient psychiatry unit for paranoia and persecutory delusions along with auditory hallucinations. His father reported that Mr. K had been behaving erratically for several days prior to admission and was subsequently found wandering in the street.
On admission, Mr. K was not oriented to place or situation. He was unkempt and guarded, and claimed people were following him. His urine toxicology screen and blood alcohol levels were negative.
While hospitalized, Mr. K was hyperverbal and delusional. He related that at work he had been developing programs to make slaves in the computer, “algorithms for orchestration,” and that he was uncomfortable with the ethical implications. He eventually endorsed having purchased the supplement phenylethylamine (PEA) to improve his focus, and ingesting “two substantial scoops of the crystalline substance.”
We did not initiate any psychiatric medications. On the third day of his hospitalization, Mr. K was alert, oriented, euthymic, relaxed, and had a full range of affect; upon discharge we advised him to discard the PEA and avoid stimulants. He complied, quit his high-stress job, and had no subsequent psychotic symptoms in the 7 months since discharge.
Continue to: Dietary supplements carry risks
Dietary supplements carry risks
According to the FDA, dietary supplements are regulated as food, but many have strong biologic effects or may even contain drugs.1 More than 18% of Americans use herbal or nutritional therapies as part of their health regimen.2 However, many over-the-counter remedies have been found to exhibit psychotropic effects,3 and many more are purported to impact mental and physical health with little to no scientific research into these claims or potential adverse effects.
Phenylethylamine is sold as a nutritional supplement and marketed for its purported beneficial effects on weight loss, mood, and focus.4 However, PEA is known to act as a natural amphetamine and to play a role in the development of neuropsychiatric disorders.5 It is an endogenous psychotogenic molecule that has been previously theorized as a cause for primary psychosis.6 Phenylethylamine interacts with the same receptor ligand that responds to amphetamine and related compounds (such as methamphetamine and 3,4-methylenedioxy-methamphetamine [MDMA]), the genetic coding for which is located in an area of DNA associated with schizophrenia: chromosome 6q23.2.7 While the mechanisms and details of these interactions remain poorly understood, this case of PEA-induced psychosis represents a glimpse into the potential psychoactive properties of this readily available nutritional supplement.
This patient’s cautionary tale has given me pause regarding both my family’s nutrition and the oft-neglected dietary portion of the social history. Also, several subsequent patient experiences hearken back to my mother’s words regarding the importance of healthy eating. A patient with phenylketonuria presented with psychosis after running out of her formula and consuming junk food. Another patient with severely elevated blood glucose levels presented with confusion. I have come to realize that ingestion impacts presentation, or, in other words, you are what you eat.
“You are what you eat,” my mother always said, and structured our dinner plates according to the USDA food pyramid. We dutifully consumed leafy greens, and prior to medical school I invested time and money into healthy diet choices. I drank green smoothies, pureed baby food for my children, read up on the pH balancing diet, grew sprouts on windowsills, bought organic.
With the stressors and time constraints of managing medical school and a family, nutrition tumbled down the ladder of priorities until eventually my family was subsisting on chicken nuggets, pizza, and peanut butter. Intern year has only added the occasional candy bar from the doctors’ lounge. I experienced a vague sense of loss for something I had once valued, but simultaneously felt dismissive of trendy topics such as omega-3 fatty acids and antioxidants in the face of myocardial infarctions and liver failure. A biochemistry professor once scoffed at “the laypeople’s obsession with toxins,” and nutrition received zero attention in our medical school curriculum or board exams.
However, a clinical experience on the inpatient psychiatric unit made me reevaluate the importance nutrition should have in both our personal lives and the practice of medicine. This is the case of an otherwise healthy young man with no psychiatric history who suffered a psychotic break after ingesting an excess of a supplement he purchased online with the purpose of improving his performance at a high-stress job.
CASE REPORT
Mr. K, a 28-year-old computer programmer, was voluntarily admitted to the inpatient psychiatry unit for paranoia and persecutory delusions along with auditory hallucinations. His father reported that Mr. K had been behaving erratically for several days prior to admission and was subsequently found wandering in the street.
On admission, Mr. K was not oriented to place or situation. He was unkempt and guarded, and claimed people were following him. His urine toxicology screen and blood alcohol levels were negative.
While hospitalized, Mr. K was hyperverbal and delusional. He related that at work he had been developing programs to make slaves in the computer, “algorithms for orchestration,” and that he was uncomfortable with the ethical implications. He eventually endorsed having purchased the supplement phenylethylamine (PEA) to improve his focus, and ingesting “two substantial scoops of the crystalline substance.”
We did not initiate any psychiatric medications. On the third day of his hospitalization, Mr. K was alert, oriented, euthymic, relaxed, and had a full range of affect; upon discharge we advised him to discard the PEA and avoid stimulants. He complied, quit his high-stress job, and had no subsequent psychotic symptoms in the 7 months since discharge.
Continue to: Dietary supplements carry risks
Dietary supplements carry risks
According to the FDA, dietary supplements are regulated as food, but many have strong biologic effects or may even contain drugs.1 More than 18% of Americans use herbal or nutritional therapies as part of their health regimen.2 However, many over-the-counter remedies have been found to exhibit psychotropic effects,3 and many more are purported to impact mental and physical health with little to no scientific research into these claims or potential adverse effects.
Phenylethylamine is sold as a nutritional supplement and marketed for its purported beneficial effects on weight loss, mood, and focus.4 However, PEA is known to act as a natural amphetamine and to play a role in the development of neuropsychiatric disorders.5 It is an endogenous psychotogenic molecule that has been previously theorized as a cause for primary psychosis.6 Phenylethylamine interacts with the same receptor ligand that responds to amphetamine and related compounds (such as methamphetamine and 3,4-methylenedioxy-methamphetamine [MDMA]), the genetic coding for which is located in an area of DNA associated with schizophrenia: chromosome 6q23.2.7 While the mechanisms and details of these interactions remain poorly understood, this case of PEA-induced psychosis represents a glimpse into the potential psychoactive properties of this readily available nutritional supplement.
This patient’s cautionary tale has given me pause regarding both my family’s nutrition and the oft-neglected dietary portion of the social history. Also, several subsequent patient experiences hearken back to my mother’s words regarding the importance of healthy eating. A patient with phenylketonuria presented with psychosis after running out of her formula and consuming junk food. Another patient with severely elevated blood glucose levels presented with confusion. I have come to realize that ingestion impacts presentation, or, in other words, you are what you eat.
1. US Food and Drug Administration. Dietary supplements. https://www.fda.gov/consumers/consumer-updates/dietary-supplements. Accessed December 11, 2019.
2. Tindle H, Davis R, Philips R, et al. Trends in use of complementary and alternative medicine by US adults: 1997-2002. Altern Ther Health Med. 2005;11(1):42-49.
3. Sarris J. Herbal medicines in the treatment of psychiatric disorders: 10-year updated review. Phytotherapy Research. 2018;32(7):1147-1162.
4. Irsfeld M, Spadafore M, Prüß BM. β-phenylethylamine, a small molecule with a large impact. WebmedCentral. 2013;4(9):4409.
5. Wolf M, Mosnaim A. Phenylethylamine in neuropsychiatric disorders. Gen Pharmacol. 1983;14(4):385-390.
6. Janssen P, Leysen J, Megens A, et al. Does phenylethylamine act as an endogenous amphetamine in some patients? In J Neuropsychopharmacol. 1999;2(3):229-240.
7. Zucchi R, Chiellini G, Scanlan TS, et al. Trace amine-associated receptors and their ligands. Br J Pharmacol. 2006;149(8):967-978.
1. US Food and Drug Administration. Dietary supplements. https://www.fda.gov/consumers/consumer-updates/dietary-supplements. Accessed December 11, 2019.
2. Tindle H, Davis R, Philips R, et al. Trends in use of complementary and alternative medicine by US adults: 1997-2002. Altern Ther Health Med. 2005;11(1):42-49.
3. Sarris J. Herbal medicines in the treatment of psychiatric disorders: 10-year updated review. Phytotherapy Research. 2018;32(7):1147-1162.
4. Irsfeld M, Spadafore M, Prüß BM. β-phenylethylamine, a small molecule with a large impact. WebmedCentral. 2013;4(9):4409.
5. Wolf M, Mosnaim A. Phenylethylamine in neuropsychiatric disorders. Gen Pharmacol. 1983;14(4):385-390.
6. Janssen P, Leysen J, Megens A, et al. Does phenylethylamine act as an endogenous amphetamine in some patients? In J Neuropsychopharmacol. 1999;2(3):229-240.
7. Zucchi R, Chiellini G, Scanlan TS, et al. Trace amine-associated receptors and their ligands. Br J Pharmacol. 2006;149(8):967-978.
Rethinking the language of substance abuse
In December 2019, Seattle Seahawks wide receiver Josh Gordon was suspended indefinitely from the NFL for violation of the league’s substance abuse policy. Gordon, once known as one of the most promising wide receivers of the last few decades, had a tumultuous relationship with the NFL as a result of his struggles with substance use. However, the headlines from major sports and news outlets often describe Gordon and other professional and collegiate athletes who struggle with substance use as “violating policies of abuse.” Media coverage of such athletes frequently imposes labels such as “violation” and “abuse,” implying a greater level of personal responsibility and willful misconduct than the biological process of addiction would typically allow. Gordon’s story brought attention not only to the adversity and impairments of substance use, but also the stigmatizing language that often accompanies it.
Shifting to less stigmatizing terminology
In DMS-5, use of the terminology substance use disorder fosters a more biologically-based model of behavior, and encourages recovery-oriented terminology.1 However, for most collegiate and professional sports leagues, the policies regarding substance use often use the term substance abuse, which can perpetuate stigma and a misunderstanding of the underpinnings of substance use, insinuating a sense of personal responsibility, deliberate misconduct, and criminality. When an individual is referred to as an “abuser” of substances, this might suggest that they are willful perpetrators of the disease on themselves, and thus may be undeserving of care.2 Individuals referred to as “substance abusers” rather than having a substance use disorder are more likely to be subjected to negative perceptions and evaluations of their behaviors, particularly by clinicians.
Individuals with substance use disorders are often viewed more negatively than individuals with physical or other psychiatric disorders, and are among the most stigmatized and marginalized groups in health care.4,5 Today, lawmakers, advocates, and health care professionals across the country are working to integrate destigmatizing language into media, policy, and educational settings in order to characterize substance use as a neurobiological process rather than a moral fault.6 For example, legislation in Maine passed in 2018 removed references to stigmatizing terms in policies related to substance use, replacing substance abuse and drug addict with recovery-oriented terminology such as substance use disorder and person with a substance use disorder.7
Individuals with substance use disorders often fear judgment and stigma during clinical encounters, and commonly cite this as a reason to avoid seeking care.8 Words matter, and if we are not careful, the language we use can convey meaning and attitudes that perpetuate the stigma that prevents so many from accessing treatment.9,10 Individuals with a substance use disorder should feel institutionally supported, and the language of policies and the clinicians who treat these patients should reflect this as well.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Wakeman SE. Language and addiction: choosing words wisely. Am J Public Health. 2013;103(4):e1‐e2.
3. Kelly JF, Westerhoff CM. Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. Int J Drug Policy. 2010;21(3):202‐207.
4. Corrigan PW, Kuwabara SA, O’Shaughnessy J. The public stigma of mental illness and drug addiction: findings from a stratified random sample. Journal of Social Work. 2009;9(2):139-147.
5. Barry CL, McGinty EE, Pescosolido BA, et al. Stigma, discrimination, treatment effectiveness, and policy: public views about drug addiction and mental illness. Psychiatr Serv. 2014;65(10):1269‐1272.
6. Office of National Drug Control Policy. Changing the language of addiction. https://www.whitehouse.gov/sites/whitehouse.gov/files/images/Memo%20-%20Changing%20Federal%20Terminology%20Regrading%20Substance%20Use%20and%20Substance%20Use%20Disorders.pdf. Published January 9, 2017. Accessed June 8, 2020.
7. Flaherty N. Why language matters when describing substance use disorder in Maine. http://www.mainepublic.org/post/why-language-matters-when-describing-substance-use-disorder-maine. Published May 16, 2018. Accessed June 8, 2020.
8. Merrill JO, Rhodes LA, Deyo RA, et al. Mutual mistrust in the medical care of drug users: the keys to the “narc” cabinet. J Gen Intern Med. 2002;17(5):327‐333.
9. Yang LH, Wong LY, Grivel MM, et al. Stigma and substance use disorders: an international phenomenon. Curr Opin Psychiatry. 2017;30(5):378‐388.
10. Broyles LM, Binswanger IA, Jenkins JA, et al. Confronting inadvertent stigma and pejorative language in addiction scholarship: a recognition and response. Subst Abus. 2014;35(3):217‐221.
In December 2019, Seattle Seahawks wide receiver Josh Gordon was suspended indefinitely from the NFL for violation of the league’s substance abuse policy. Gordon, once known as one of the most promising wide receivers of the last few decades, had a tumultuous relationship with the NFL as a result of his struggles with substance use. However, the headlines from major sports and news outlets often describe Gordon and other professional and collegiate athletes who struggle with substance use as “violating policies of abuse.” Media coverage of such athletes frequently imposes labels such as “violation” and “abuse,” implying a greater level of personal responsibility and willful misconduct than the biological process of addiction would typically allow. Gordon’s story brought attention not only to the adversity and impairments of substance use, but also the stigmatizing language that often accompanies it.
Shifting to less stigmatizing terminology
In DMS-5, use of the terminology substance use disorder fosters a more biologically-based model of behavior, and encourages recovery-oriented terminology.1 However, for most collegiate and professional sports leagues, the policies regarding substance use often use the term substance abuse, which can perpetuate stigma and a misunderstanding of the underpinnings of substance use, insinuating a sense of personal responsibility, deliberate misconduct, and criminality. When an individual is referred to as an “abuser” of substances, this might suggest that they are willful perpetrators of the disease on themselves, and thus may be undeserving of care.2 Individuals referred to as “substance abusers” rather than having a substance use disorder are more likely to be subjected to negative perceptions and evaluations of their behaviors, particularly by clinicians.
Individuals with substance use disorders are often viewed more negatively than individuals with physical or other psychiatric disorders, and are among the most stigmatized and marginalized groups in health care.4,5 Today, lawmakers, advocates, and health care professionals across the country are working to integrate destigmatizing language into media, policy, and educational settings in order to characterize substance use as a neurobiological process rather than a moral fault.6 For example, legislation in Maine passed in 2018 removed references to stigmatizing terms in policies related to substance use, replacing substance abuse and drug addict with recovery-oriented terminology such as substance use disorder and person with a substance use disorder.7
Individuals with substance use disorders often fear judgment and stigma during clinical encounters, and commonly cite this as a reason to avoid seeking care.8 Words matter, and if we are not careful, the language we use can convey meaning and attitudes that perpetuate the stigma that prevents so many from accessing treatment.9,10 Individuals with a substance use disorder should feel institutionally supported, and the language of policies and the clinicians who treat these patients should reflect this as well.
In December 2019, Seattle Seahawks wide receiver Josh Gordon was suspended indefinitely from the NFL for violation of the league’s substance abuse policy. Gordon, once known as one of the most promising wide receivers of the last few decades, had a tumultuous relationship with the NFL as a result of his struggles with substance use. However, the headlines from major sports and news outlets often describe Gordon and other professional and collegiate athletes who struggle with substance use as “violating policies of abuse.” Media coverage of such athletes frequently imposes labels such as “violation” and “abuse,” implying a greater level of personal responsibility and willful misconduct than the biological process of addiction would typically allow. Gordon’s story brought attention not only to the adversity and impairments of substance use, but also the stigmatizing language that often accompanies it.
Shifting to less stigmatizing terminology
In DMS-5, use of the terminology substance use disorder fosters a more biologically-based model of behavior, and encourages recovery-oriented terminology.1 However, for most collegiate and professional sports leagues, the policies regarding substance use often use the term substance abuse, which can perpetuate stigma and a misunderstanding of the underpinnings of substance use, insinuating a sense of personal responsibility, deliberate misconduct, and criminality. When an individual is referred to as an “abuser” of substances, this might suggest that they are willful perpetrators of the disease on themselves, and thus may be undeserving of care.2 Individuals referred to as “substance abusers” rather than having a substance use disorder are more likely to be subjected to negative perceptions and evaluations of their behaviors, particularly by clinicians.
Individuals with substance use disorders are often viewed more negatively than individuals with physical or other psychiatric disorders, and are among the most stigmatized and marginalized groups in health care.4,5 Today, lawmakers, advocates, and health care professionals across the country are working to integrate destigmatizing language into media, policy, and educational settings in order to characterize substance use as a neurobiological process rather than a moral fault.6 For example, legislation in Maine passed in 2018 removed references to stigmatizing terms in policies related to substance use, replacing substance abuse and drug addict with recovery-oriented terminology such as substance use disorder and person with a substance use disorder.7
Individuals with substance use disorders often fear judgment and stigma during clinical encounters, and commonly cite this as a reason to avoid seeking care.8 Words matter, and if we are not careful, the language we use can convey meaning and attitudes that perpetuate the stigma that prevents so many from accessing treatment.9,10 Individuals with a substance use disorder should feel institutionally supported, and the language of policies and the clinicians who treat these patients should reflect this as well.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Wakeman SE. Language and addiction: choosing words wisely. Am J Public Health. 2013;103(4):e1‐e2.
3. Kelly JF, Westerhoff CM. Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. Int J Drug Policy. 2010;21(3):202‐207.
4. Corrigan PW, Kuwabara SA, O’Shaughnessy J. The public stigma of mental illness and drug addiction: findings from a stratified random sample. Journal of Social Work. 2009;9(2):139-147.
5. Barry CL, McGinty EE, Pescosolido BA, et al. Stigma, discrimination, treatment effectiveness, and policy: public views about drug addiction and mental illness. Psychiatr Serv. 2014;65(10):1269‐1272.
6. Office of National Drug Control Policy. Changing the language of addiction. https://www.whitehouse.gov/sites/whitehouse.gov/files/images/Memo%20-%20Changing%20Federal%20Terminology%20Regrading%20Substance%20Use%20and%20Substance%20Use%20Disorders.pdf. Published January 9, 2017. Accessed June 8, 2020.
7. Flaherty N. Why language matters when describing substance use disorder in Maine. http://www.mainepublic.org/post/why-language-matters-when-describing-substance-use-disorder-maine. Published May 16, 2018. Accessed June 8, 2020.
8. Merrill JO, Rhodes LA, Deyo RA, et al. Mutual mistrust in the medical care of drug users: the keys to the “narc” cabinet. J Gen Intern Med. 2002;17(5):327‐333.
9. Yang LH, Wong LY, Grivel MM, et al. Stigma and substance use disorders: an international phenomenon. Curr Opin Psychiatry. 2017;30(5):378‐388.
10. Broyles LM, Binswanger IA, Jenkins JA, et al. Confronting inadvertent stigma and pejorative language in addiction scholarship: a recognition and response. Subst Abus. 2014;35(3):217‐221.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Wakeman SE. Language and addiction: choosing words wisely. Am J Public Health. 2013;103(4):e1‐e2.
3. Kelly JF, Westerhoff CM. Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. Int J Drug Policy. 2010;21(3):202‐207.
4. Corrigan PW, Kuwabara SA, O’Shaughnessy J. The public stigma of mental illness and drug addiction: findings from a stratified random sample. Journal of Social Work. 2009;9(2):139-147.
5. Barry CL, McGinty EE, Pescosolido BA, et al. Stigma, discrimination, treatment effectiveness, and policy: public views about drug addiction and mental illness. Psychiatr Serv. 2014;65(10):1269‐1272.
6. Office of National Drug Control Policy. Changing the language of addiction. https://www.whitehouse.gov/sites/whitehouse.gov/files/images/Memo%20-%20Changing%20Federal%20Terminology%20Regrading%20Substance%20Use%20and%20Substance%20Use%20Disorders.pdf. Published January 9, 2017. Accessed June 8, 2020.
7. Flaherty N. Why language matters when describing substance use disorder in Maine. http://www.mainepublic.org/post/why-language-matters-when-describing-substance-use-disorder-maine. Published May 16, 2018. Accessed June 8, 2020.
8. Merrill JO, Rhodes LA, Deyo RA, et al. Mutual mistrust in the medical care of drug users: the keys to the “narc” cabinet. J Gen Intern Med. 2002;17(5):327‐333.
9. Yang LH, Wong LY, Grivel MM, et al. Stigma and substance use disorders: an international phenomenon. Curr Opin Psychiatry. 2017;30(5):378‐388.
10. Broyles LM, Binswanger IA, Jenkins JA, et al. Confronting inadvertent stigma and pejorative language in addiction scholarship: a recognition and response. Subst Abus. 2014;35(3):217‐221.
More on the travesty of pre-authorization
We were delighted to read Dr. Nasrallah’s coruscating editorial about the deceptive, unethical, and clinically harmful practice of insurance companies requiring pre-authorization before granting coverage of psychotropic medications that are not on their short list of inexpensive alternatives (“Pre-authorization is illegal, unethical, and adversely disrupts patient care.” From the Editor,
Brian S. Barnett, MD
Staff Psychiatrist
Cleveland Clinic
Lutheran Hospital
Cleveland, Ohio
J. Alexander Bodkin, MD
Chief
Clinical Psychopharmacology
Research Program
McLean Hospital
Harvard Medical School
Belmont, Massachusetts
Disclosures: The authors report no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
I thank Dr. Nasrallah for bringing up the issue of pre-authorization in his editorial and could not agree with him more. As a practicing geriatric psychiatrist—for several decades—I experienced all of what he so nicely summarized, and more. The amount and degree of humiliation, frustration, and (mainly) waste of time have been painful and unacceptable. As he said: It must be stopped! The question is “How?” Hopefully this editorial triggers some activity against pre-authorization. It was time somebody addressed this problem.
Istvan Boksay, MD, PhD
Private psychiatric practice
New York, New York
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Continue to: I thank Dr. Nasrallah...
I thank Dr. Nasrallah for his editorial about pre-authorization, which was well organized and had a perfect headline. In succinct paragraphs, it says what we practitioners have wanted to say for years. If only the American Psychiatric Association and American Medical Association would take up the cause, perhaps some limitations might be put on this corporate intrusion into our practice. Pre-authorization may save insurance companies money, but its cost in time, frustration, and clinical outcomes adds a considerable burden to the financial problems of health care in the United States.
John Buckley, MD
Private psychiatric practice
Glen Arm, Maryland
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
I thank Dr. Nasrallah so much for his editorial. These types of clinically useless administrative tasks are invisible barriers to mental health care access, because the time utilized to complete these tasks can easily be used to see one more patient who needs to be treated. However, I also wonder how we as psychiatrists can move forward so that our psychiatric organizations and legislative bodies can take further action to the real barriers to health care and effective interventions.
Ranvinder Kaur Rai, MD
Private psychiatric practice
Fremont, California
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Continue to: I read with interest...
I read with interest Dr. Nasrallah’s editorials “We are physicians, not providers, and we treat patients, not clients!” (From the Editor,
Dr. Nasrallah’s strong advocacy against the use of the term “provider” is long overdue. I distinctly remember the insidious onset of the use of the terms provider and “consumer” during my years as a medical director of a mental health center. The inception of the provider/consumer terminology can be construed as striving for cultural correctness when psychiatry was going through its own identity crisis in response to deinstitutionalization and the destruction of the so-called myth of psychiatrists as paternalistic and all-powerful. Managed care as the business model of medicine further destroyed the perception of the psychiatric physician as noble and caring, and demythologized the physician–patient relationship. It is amazing how the term provider has persisted and become part of the language of medicine. During the last 20 years or so, psychiatric and medical professional organizations have done little to squash the usage of the term.
Furthermore, the concept of pre-authorization is not new to medicine, but has insidiously become part of the tasks of the psychiatric physician. It has morphed into more than having to obtain approval for using a branded medication over a cheaper generic alternative to having to obtain approval for the use of any medication that does not fall under the approved tier. Even antipsychotics (generally a protected class) have not been immune.
Both the use of the term provider and the concept of pre-authorization require more than the frustration and indignation of a clinical psychiatrist. It requires the determination of professional psychiatric organizations and those with power to fight the gradual but ever-deteriorating authority of medical practice and the role of the psychiatric physician.
Elizabeth A. Varas, MD
Private psychiatric practice
Westwood, New Jersey
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
We were delighted to read Dr. Nasrallah’s coruscating editorial about the deceptive, unethical, and clinically harmful practice of insurance companies requiring pre-authorization before granting coverage of psychotropic medications that are not on their short list of inexpensive alternatives (“Pre-authorization is illegal, unethical, and adversely disrupts patient care.” From the Editor,
Brian S. Barnett, MD
Staff Psychiatrist
Cleveland Clinic
Lutheran Hospital
Cleveland, Ohio
J. Alexander Bodkin, MD
Chief
Clinical Psychopharmacology
Research Program
McLean Hospital
Harvard Medical School
Belmont, Massachusetts
Disclosures: The authors report no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
I thank Dr. Nasrallah for bringing up the issue of pre-authorization in his editorial and could not agree with him more. As a practicing geriatric psychiatrist—for several decades—I experienced all of what he so nicely summarized, and more. The amount and degree of humiliation, frustration, and (mainly) waste of time have been painful and unacceptable. As he said: It must be stopped! The question is “How?” Hopefully this editorial triggers some activity against pre-authorization. It was time somebody addressed this problem.
Istvan Boksay, MD, PhD
Private psychiatric practice
New York, New York
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Continue to: I thank Dr. Nasrallah...
I thank Dr. Nasrallah for his editorial about pre-authorization, which was well organized and had a perfect headline. In succinct paragraphs, it says what we practitioners have wanted to say for years. If only the American Psychiatric Association and American Medical Association would take up the cause, perhaps some limitations might be put on this corporate intrusion into our practice. Pre-authorization may save insurance companies money, but its cost in time, frustration, and clinical outcomes adds a considerable burden to the financial problems of health care in the United States.
John Buckley, MD
Private psychiatric practice
Glen Arm, Maryland
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
I thank Dr. Nasrallah so much for his editorial. These types of clinically useless administrative tasks are invisible barriers to mental health care access, because the time utilized to complete these tasks can easily be used to see one more patient who needs to be treated. However, I also wonder how we as psychiatrists can move forward so that our psychiatric organizations and legislative bodies can take further action to the real barriers to health care and effective interventions.
Ranvinder Kaur Rai, MD
Private psychiatric practice
Fremont, California
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Continue to: I read with interest...
I read with interest Dr. Nasrallah’s editorials “We are physicians, not providers, and we treat patients, not clients!” (From the Editor,
Dr. Nasrallah’s strong advocacy against the use of the term “provider” is long overdue. I distinctly remember the insidious onset of the use of the terms provider and “consumer” during my years as a medical director of a mental health center. The inception of the provider/consumer terminology can be construed as striving for cultural correctness when psychiatry was going through its own identity crisis in response to deinstitutionalization and the destruction of the so-called myth of psychiatrists as paternalistic and all-powerful. Managed care as the business model of medicine further destroyed the perception of the psychiatric physician as noble and caring, and demythologized the physician–patient relationship. It is amazing how the term provider has persisted and become part of the language of medicine. During the last 20 years or so, psychiatric and medical professional organizations have done little to squash the usage of the term.
Furthermore, the concept of pre-authorization is not new to medicine, but has insidiously become part of the tasks of the psychiatric physician. It has morphed into more than having to obtain approval for using a branded medication over a cheaper generic alternative to having to obtain approval for the use of any medication that does not fall under the approved tier. Even antipsychotics (generally a protected class) have not been immune.
Both the use of the term provider and the concept of pre-authorization require more than the frustration and indignation of a clinical psychiatrist. It requires the determination of professional psychiatric organizations and those with power to fight the gradual but ever-deteriorating authority of medical practice and the role of the psychiatric physician.
Elizabeth A. Varas, MD
Private psychiatric practice
Westwood, New Jersey
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
We were delighted to read Dr. Nasrallah’s coruscating editorial about the deceptive, unethical, and clinically harmful practice of insurance companies requiring pre-authorization before granting coverage of psychotropic medications that are not on their short list of inexpensive alternatives (“Pre-authorization is illegal, unethical, and adversely disrupts patient care.” From the Editor,
Brian S. Barnett, MD
Staff Psychiatrist
Cleveland Clinic
Lutheran Hospital
Cleveland, Ohio
J. Alexander Bodkin, MD
Chief
Clinical Psychopharmacology
Research Program
McLean Hospital
Harvard Medical School
Belmont, Massachusetts
Disclosures: The authors report no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
I thank Dr. Nasrallah for bringing up the issue of pre-authorization in his editorial and could not agree with him more. As a practicing geriatric psychiatrist—for several decades—I experienced all of what he so nicely summarized, and more. The amount and degree of humiliation, frustration, and (mainly) waste of time have been painful and unacceptable. As he said: It must be stopped! The question is “How?” Hopefully this editorial triggers some activity against pre-authorization. It was time somebody addressed this problem.
Istvan Boksay, MD, PhD
Private psychiatric practice
New York, New York
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Continue to: I thank Dr. Nasrallah...
I thank Dr. Nasrallah for his editorial about pre-authorization, which was well organized and had a perfect headline. In succinct paragraphs, it says what we practitioners have wanted to say for years. If only the American Psychiatric Association and American Medical Association would take up the cause, perhaps some limitations might be put on this corporate intrusion into our practice. Pre-authorization may save insurance companies money, but its cost in time, frustration, and clinical outcomes adds a considerable burden to the financial problems of health care in the United States.
John Buckley, MD
Private psychiatric practice
Glen Arm, Maryland
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
I thank Dr. Nasrallah so much for his editorial. These types of clinically useless administrative tasks are invisible barriers to mental health care access, because the time utilized to complete these tasks can easily be used to see one more patient who needs to be treated. However, I also wonder how we as psychiatrists can move forward so that our psychiatric organizations and legislative bodies can take further action to the real barriers to health care and effective interventions.
Ranvinder Kaur Rai, MD
Private psychiatric practice
Fremont, California
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
Continue to: I read with interest...
I read with interest Dr. Nasrallah’s editorials “We are physicians, not providers, and we treat patients, not clients!” (From the Editor,
Dr. Nasrallah’s strong advocacy against the use of the term “provider” is long overdue. I distinctly remember the insidious onset of the use of the terms provider and “consumer” during my years as a medical director of a mental health center. The inception of the provider/consumer terminology can be construed as striving for cultural correctness when psychiatry was going through its own identity crisis in response to deinstitutionalization and the destruction of the so-called myth of psychiatrists as paternalistic and all-powerful. Managed care as the business model of medicine further destroyed the perception of the psychiatric physician as noble and caring, and demythologized the physician–patient relationship. It is amazing how the term provider has persisted and become part of the language of medicine. During the last 20 years or so, psychiatric and medical professional organizations have done little to squash the usage of the term.
Furthermore, the concept of pre-authorization is not new to medicine, but has insidiously become part of the tasks of the psychiatric physician. It has morphed into more than having to obtain approval for using a branded medication over a cheaper generic alternative to having to obtain approval for the use of any medication that does not fall under the approved tier. Even antipsychotics (generally a protected class) have not been immune.
Both the use of the term provider and the concept of pre-authorization require more than the frustration and indignation of a clinical psychiatrist. It requires the determination of professional psychiatric organizations and those with power to fight the gradual but ever-deteriorating authority of medical practice and the role of the psychiatric physician.
Elizabeth A. Varas, MD
Private psychiatric practice
Westwood, New Jersey
Disclosure: The author reports no financial relationships with any companies whose products are mentioned in this article, or with manufacturers of competing products.
COVID-19 and the precipitous dismantlement of societal norms
As the life-altering coronavirus disease 2019 (COVID-19) pandemic gradually ebbs, we are all its survivors. Now, we are experiencing COVID-19 fatigue, trying to emerge from its dense fog that pervaded every facet of our lives. We are fully cognizant that there will not be a return to the previous “normal.” The pernicious virus had a transformative effect that did not spare any component of our society. Full recovery will not be easy.
As the uncertainty lingers about another devastating return of the pandemic later this year, we can see the reverberation of this invisible assault on human existence. Although a relatively small fraction of the population lost their lives, the rest of us are valiantly trying to readjust to the multiple ways our world has changed. Consider the following abrupt and sweeping burdens inflicted by the pandemic within a few short weeks:
Mental health. The acute stress of thanatophobia generated a triad of anxiety, depression, and nosophobia on a large scale. The demand for psychiatric care rapidly escalated. Suicide rate increased not only because of the stress of being locked down at home (alien to most people’s lifestyle) but because of the coincidental timing of the pandemic during April and May, the peak time of year for suicide. Animal researchers use immobilization as a paradigm to stress a rat or mouse. Many humans immobilized during the pandemic have developed exquisite empathy towards those rodents! The impact on children may also have long-term effects because playing and socializing with friends is a vital part of their lives. Parents have noticed dysphoria and acting out among their children, and an intense compensatory preoccupation with video games and electronic communications with friends.
Physical health. Medical care focused heavily on COVID-19 victims, to the detriment of all other medical conditions. Non-COVID-19 hospital admissions plummeted, and all elective surgeries and procedures were put on hold, depriving many people of medical care they badly needed. Emergency department (ED) visits also declined dramatically, including the usual flow of heart attacks, stroke, pulmonary embolus, asthma attacks, etc. The minimization of driving greatly reduced the admission of accident victims to EDs. Colonoscopies, cardiac stents, hip replacements, MRIs, mammography, and other procedures that are vital to maintain health and quality of life were halted. Dentists shuttered their practices due to the high risk of infection from exposure to oral secretions and breathing. One can only imagine the suffering of having a toothache with no dental help available, and how that might lead to narcotic abuse.
Social health. The imperative of social distancing disrupted most ordinary human activities, such as dining out, sitting in an auditorium for Grand Rounds or a lecture, visiting friends at their homes, the cherished interactions between grandparents and grandchildren (the lack of which I painfully experienced), and even seeing each other’s smiles behind the ubiquitous masks. And forget about hugging or kissing. The aversion to being near anyone who is coughing or sneezing led to an adaptive social paranoia and the social shunning of anyone who appeared to have an upper respiratory infection, even if it was unrelated to COVID-19.
Redemption for the pharmaceutical industry. The deadly pandemic intensified the public’s awareness of the importance of developing treatments and vaccines for COVID-19. The often-demonized pharmaceutical companies, with their extensive R&D infrastructure, emerged as a major source of hope for discovering an effective treatment for the coronavirus infection, or—better still—one or more vaccines that will enable society to return to its normal functions. It was quite impressive how many pharmaceutical companies “came to the rescue” with clinical trials to repurpose existing medications or to develop new ones. It was very encouraging to see multiple vaccine candidates being developed and expedited for testing around the world. A process that usually takes years was reduced to a few months, thanks to the existing technical infrastructure and thousands of scientists who enable rapid drug development. It is possible that the public may gradually modify its perception of the pharmaceutical industry from a “corporate villain” to an “indispensable health industry” for urgent medical crises such as a pandemic, and also for hundreds of medical diseases that are still in need of safe, effective therapies.
Economic burden. The unimaginable nightmare scenario of a total shutdown of all businesses led to the unprecedented loss of millions of jobs and livelihoods, reflected in miles-long lines of families at food banks. Overnight, the government switched from worrying about its $20-trillion deficit to printing several more trillion dollars to rescue the economy from collapse. The huge magnitude of a trillion can be appreciated if one is aware that it takes roughly 32 years to count to 1 billion, and 32,000 years to count to 1 trillion. Stimulating the economy while the gross domestic product threatens to sink by terrifying percentages (20% to 30%) was urgently needed, even though it meant mortgaging the future, especially when interest rates, and servicing the debt, will inevitably rise from the current zero to much higher levels in the future. The collapse of the once-thriving airline industry (bookings were down an estimated 98%) is an example of why desperate measures were needed to salvage an economy paralyzed by a viral pandemic.
Continue to: Political repercussions
Political repercussions. In our already hyperpartisan country, the COVID-19 crisis created more fissures across party lines. The blame game escalated as each side tried to exploit the crisis for political gain during a presidential election year. None of the leaders, from mayors to governors to the president, had any notion of how to wisely manage an unforeseen catastrophic pandemic. Thus, a political cacophony has developed, further exacerbating the public’s anxiety and uncertainty, especially about how and when the pandemic will end.
Education disruption. Never before have all schools and colleges around the country abruptly closed and sent students of all ages to shelter at home. Massive havoc ensued, with a wholesale switch to solitary online learning, the loss of the unique school and college social experience in the classroom and on campus, and the loss of experiencing commencement to receive a diploma (an important milestone for every graduate). Even medical students were not allowed to complete their clinical rotations and were sent home to attend online classes. A complete paradigm shift emerged about entrance exams: the SAT and ACT were eliminated for college applicants, and the MCAT for medical school applicants. This was unthinkable before the pandemic descended upon us, but benchmarks suddenly evaporated to adjust to the new reality. Then there followed disastrous financial losses by institutions of higher learning as well as academic medical centers and teaching hospitals, all slashing their budgets, furloughing employees, cutting salaries, and eliminating programs. Even the “sacred” tenure of senior faculty became a casualty of the financial “exigency.” Children’s nutrition suffered, especially among those in lower socioeconomic groups for whom the main meal of the day was the school lunch, and was made worse by their parents’ loss of income. For millions of people, the emotional toll was inevitable following the draconian measure of closing all educational institutions to contain the spread of the pandemic.
Family burden. Sheltering at home might have been fun for a few days, but after many weeks, it festered into a major stress, especially for those living in a small house, condominium, or apartment. The resilience of many families was tested as the exercise of freedoms collided with the fear of getting infected. Families were deprived of celebrating birthdays, weddings, funerals, graduation parties, retirement parties, Mother’s Day, Father’s Day, and various religious holidays, including Easter, Passover, and Eid al-Fitr.
Sexual burden. Intimacy and sexual contact between consenting adults living apart were sacrificed on the altar of the pernicious viral pandemic. Mandatory social distancing of 6 feet or more to avoid each other’s droplets emanating from simple speech, not just sneezing or coughing, makes intimacy practically impossible. Thus, physical closeness became taboo, and avoiding another person’s saliva or body secretions became a must to avoid contracting the virus. Being single was quite a lonely experience during this pandemic!
Entertainment deprivation. Americans are known to thrive on an extensive diet of spectator sports. Going to football, basketball, baseball, or hockey games to root for one’s team is intrinsically American. The pursuit of happiness extends to attending concerts, movies, Broadway shows, theme parks, and cruises with thousands of others. The pandemic ripped all those pleasurable leisure activities from our daily lives, leaving a big hole in people’s lives at the precise time fun activities were needed as a useful diversion from the dismal stress of a pandemic. To make things worse, it is uncertain when (if ever) such group activities will be restored, especially if the pandemic returns with another wave. But optimists would hurry to remind us that the “Roaring 20s” blossomed in the decade following the 1918 Spanish Flu pandemic.
Continue to: Legal system
Legal system. Astounding changes were instigated by the pandemic, such as the release of thousands of inmates, including felons, to avoid the spread of the virus in crowded prisons. For us psychiatrists, the silver lining in that unexpected action is that many of those released were patients with mental illness who were incarcerated because of the lack of hospitals that would take them. The police started issuing citations instead of arresting and jailing violators. Enforcement of the law was welcome when it targeted those who gouged the public for personal profit during the scarcity of masks, sanitizers, or even toilet paper and soap.
Medical practice. In addition to delaying medical care for patients, the freeze on so-called elective surgeries or procedures (many of which were actually necessary) was financially ruinous for physicians. Another regrettable consequence of the pandemic is a drop in pediatric vaccinations because parents were reluctant to take their children to the pediatrician. On a more positive note, the massive switch to telehealth was advantageous for both patients and psychiatrists because this technology is well-suited for psychiatric care. Fortunately, regulations that hampered telepsychiatry practice were substantially loosened or eliminated, and even the usually sacrosanct HIPAA regulations were temporarily sidelined.
Medical research. Both human and animal research came to a screeching halt, and many research assistants were furloughed. Data collection was disrupted, and a generation of scientific and medical discoveries became a casualty of the pandemic.
Medical literature. It was stunning to see how quickly COVID-19 occupied most of the pages of prominent journals. The scholarly articles were frankly quite useful, covering topics ranging from risk factors to early symptoms to treatment and pathophysiology across multiple organs. As with other paradigm shifts, there was an accelerated publication push, sometimes with expedited peer reviews to inform health care workers and the public while the pandemic was still raging. However, a couple of very prominent journals had to retract flawed articles that were hastily published without the usual due diligence and rigorous peer review. The pandemic clearly disrupted the science publishing process.
Travel effects. The steep reduction of flights (by 98%) was financially catastrophic, not only for airline companies but to business travel across the country. However, fewer cars on the road resulted in fewer accidents and deaths, and also reduced pollution. Paradoxically, to prevent crowding in subways, trains, and buses, officials reversed their traditional instructions and advised the public to drive their own cars instead of using public transportation!
Continue to: Heroism of front-line medical personnel
Heroism of front-line medical personnel. Everyone saluted and prayed for the health care professionals working at the bedside of highly infectious patients who needed 24/7 intensive care. Many have died while carrying out the noble but hazardous medical duties. Those heroes deserve our lasting respect and admiration.
The COVID-19 pandemic insidiously permeated and altered every aspect of our complex society and revealed how fragile our “normal lifestyle” really is. It is possible that nothing will ever be the same again, and an uneasy sense of vulnerability will engulf us as we cautiously return to a “new normal.” Even our language has expanded with the lexicon of pandemic terminology (Table). We all pray and hope that this plague never returns. And let’s hope one or more vaccines are developed soon so we can manage future recurrences like the annual flu season. In the meantime, keep your masks and sanitizers close by…
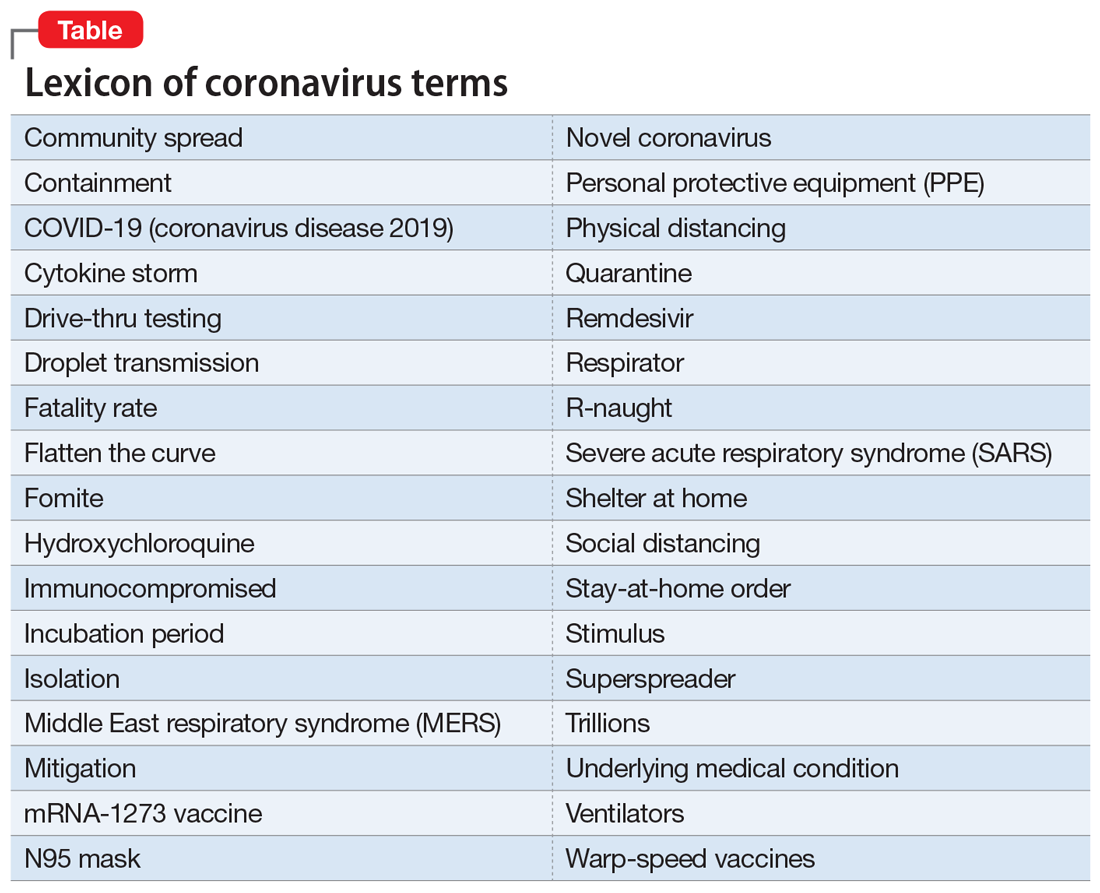
Postscript: Shortly after I completed this editorial, the ongoing COVID-19 plague was overshadowed by the scourge of racism, with massive protests, at times laced by violence, triggered by the death of a black man in custody of the police, under condemnable circumstances. The COVID-19 pandemic and the necessary social distancing it requires were temporarily ignored during the ensuing protests. The combined effect of those overlapping scourges are jarring to the country’s psyche, complicating and perhaps sabotaging the social recovery from the pandemic.
As the life-altering coronavirus disease 2019 (COVID-19) pandemic gradually ebbs, we are all its survivors. Now, we are experiencing COVID-19 fatigue, trying to emerge from its dense fog that pervaded every facet of our lives. We are fully cognizant that there will not be a return to the previous “normal.” The pernicious virus had a transformative effect that did not spare any component of our society. Full recovery will not be easy.
As the uncertainty lingers about another devastating return of the pandemic later this year, we can see the reverberation of this invisible assault on human existence. Although a relatively small fraction of the population lost their lives, the rest of us are valiantly trying to readjust to the multiple ways our world has changed. Consider the following abrupt and sweeping burdens inflicted by the pandemic within a few short weeks:
Mental health. The acute stress of thanatophobia generated a triad of anxiety, depression, and nosophobia on a large scale. The demand for psychiatric care rapidly escalated. Suicide rate increased not only because of the stress of being locked down at home (alien to most people’s lifestyle) but because of the coincidental timing of the pandemic during April and May, the peak time of year for suicide. Animal researchers use immobilization as a paradigm to stress a rat or mouse. Many humans immobilized during the pandemic have developed exquisite empathy towards those rodents! The impact on children may also have long-term effects because playing and socializing with friends is a vital part of their lives. Parents have noticed dysphoria and acting out among their children, and an intense compensatory preoccupation with video games and electronic communications with friends.
Physical health. Medical care focused heavily on COVID-19 victims, to the detriment of all other medical conditions. Non-COVID-19 hospital admissions plummeted, and all elective surgeries and procedures were put on hold, depriving many people of medical care they badly needed. Emergency department (ED) visits also declined dramatically, including the usual flow of heart attacks, stroke, pulmonary embolus, asthma attacks, etc. The minimization of driving greatly reduced the admission of accident victims to EDs. Colonoscopies, cardiac stents, hip replacements, MRIs, mammography, and other procedures that are vital to maintain health and quality of life were halted. Dentists shuttered their practices due to the high risk of infection from exposure to oral secretions and breathing. One can only imagine the suffering of having a toothache with no dental help available, and how that might lead to narcotic abuse.
Social health. The imperative of social distancing disrupted most ordinary human activities, such as dining out, sitting in an auditorium for Grand Rounds or a lecture, visiting friends at their homes, the cherished interactions between grandparents and grandchildren (the lack of which I painfully experienced), and even seeing each other’s smiles behind the ubiquitous masks. And forget about hugging or kissing. The aversion to being near anyone who is coughing or sneezing led to an adaptive social paranoia and the social shunning of anyone who appeared to have an upper respiratory infection, even if it was unrelated to COVID-19.
Redemption for the pharmaceutical industry. The deadly pandemic intensified the public’s awareness of the importance of developing treatments and vaccines for COVID-19. The often-demonized pharmaceutical companies, with their extensive R&D infrastructure, emerged as a major source of hope for discovering an effective treatment for the coronavirus infection, or—better still—one or more vaccines that will enable society to return to its normal functions. It was quite impressive how many pharmaceutical companies “came to the rescue” with clinical trials to repurpose existing medications or to develop new ones. It was very encouraging to see multiple vaccine candidates being developed and expedited for testing around the world. A process that usually takes years was reduced to a few months, thanks to the existing technical infrastructure and thousands of scientists who enable rapid drug development. It is possible that the public may gradually modify its perception of the pharmaceutical industry from a “corporate villain” to an “indispensable health industry” for urgent medical crises such as a pandemic, and also for hundreds of medical diseases that are still in need of safe, effective therapies.
Economic burden. The unimaginable nightmare scenario of a total shutdown of all businesses led to the unprecedented loss of millions of jobs and livelihoods, reflected in miles-long lines of families at food banks. Overnight, the government switched from worrying about its $20-trillion deficit to printing several more trillion dollars to rescue the economy from collapse. The huge magnitude of a trillion can be appreciated if one is aware that it takes roughly 32 years to count to 1 billion, and 32,000 years to count to 1 trillion. Stimulating the economy while the gross domestic product threatens to sink by terrifying percentages (20% to 30%) was urgently needed, even though it meant mortgaging the future, especially when interest rates, and servicing the debt, will inevitably rise from the current zero to much higher levels in the future. The collapse of the once-thriving airline industry (bookings were down an estimated 98%) is an example of why desperate measures were needed to salvage an economy paralyzed by a viral pandemic.
Continue to: Political repercussions
Political repercussions. In our already hyperpartisan country, the COVID-19 crisis created more fissures across party lines. The blame game escalated as each side tried to exploit the crisis for political gain during a presidential election year. None of the leaders, from mayors to governors to the president, had any notion of how to wisely manage an unforeseen catastrophic pandemic. Thus, a political cacophony has developed, further exacerbating the public’s anxiety and uncertainty, especially about how and when the pandemic will end.
Education disruption. Never before have all schools and colleges around the country abruptly closed and sent students of all ages to shelter at home. Massive havoc ensued, with a wholesale switch to solitary online learning, the loss of the unique school and college social experience in the classroom and on campus, and the loss of experiencing commencement to receive a diploma (an important milestone for every graduate). Even medical students were not allowed to complete their clinical rotations and were sent home to attend online classes. A complete paradigm shift emerged about entrance exams: the SAT and ACT were eliminated for college applicants, and the MCAT for medical school applicants. This was unthinkable before the pandemic descended upon us, but benchmarks suddenly evaporated to adjust to the new reality. Then there followed disastrous financial losses by institutions of higher learning as well as academic medical centers and teaching hospitals, all slashing their budgets, furloughing employees, cutting salaries, and eliminating programs. Even the “sacred” tenure of senior faculty became a casualty of the financial “exigency.” Children’s nutrition suffered, especially among those in lower socioeconomic groups for whom the main meal of the day was the school lunch, and was made worse by their parents’ loss of income. For millions of people, the emotional toll was inevitable following the draconian measure of closing all educational institutions to contain the spread of the pandemic.
Family burden. Sheltering at home might have been fun for a few days, but after many weeks, it festered into a major stress, especially for those living in a small house, condominium, or apartment. The resilience of many families was tested as the exercise of freedoms collided with the fear of getting infected. Families were deprived of celebrating birthdays, weddings, funerals, graduation parties, retirement parties, Mother’s Day, Father’s Day, and various religious holidays, including Easter, Passover, and Eid al-Fitr.
Sexual burden. Intimacy and sexual contact between consenting adults living apart were sacrificed on the altar of the pernicious viral pandemic. Mandatory social distancing of 6 feet or more to avoid each other’s droplets emanating from simple speech, not just sneezing or coughing, makes intimacy practically impossible. Thus, physical closeness became taboo, and avoiding another person’s saliva or body secretions became a must to avoid contracting the virus. Being single was quite a lonely experience during this pandemic!
Entertainment deprivation. Americans are known to thrive on an extensive diet of spectator sports. Going to football, basketball, baseball, or hockey games to root for one’s team is intrinsically American. The pursuit of happiness extends to attending concerts, movies, Broadway shows, theme parks, and cruises with thousands of others. The pandemic ripped all those pleasurable leisure activities from our daily lives, leaving a big hole in people’s lives at the precise time fun activities were needed as a useful diversion from the dismal stress of a pandemic. To make things worse, it is uncertain when (if ever) such group activities will be restored, especially if the pandemic returns with another wave. But optimists would hurry to remind us that the “Roaring 20s” blossomed in the decade following the 1918 Spanish Flu pandemic.
Continue to: Legal system
Legal system. Astounding changes were instigated by the pandemic, such as the release of thousands of inmates, including felons, to avoid the spread of the virus in crowded prisons. For us psychiatrists, the silver lining in that unexpected action is that many of those released were patients with mental illness who were incarcerated because of the lack of hospitals that would take them. The police started issuing citations instead of arresting and jailing violators. Enforcement of the law was welcome when it targeted those who gouged the public for personal profit during the scarcity of masks, sanitizers, or even toilet paper and soap.
Medical practice. In addition to delaying medical care for patients, the freeze on so-called elective surgeries or procedures (many of which were actually necessary) was financially ruinous for physicians. Another regrettable consequence of the pandemic is a drop in pediatric vaccinations because parents were reluctant to take their children to the pediatrician. On a more positive note, the massive switch to telehealth was advantageous for both patients and psychiatrists because this technology is well-suited for psychiatric care. Fortunately, regulations that hampered telepsychiatry practice were substantially loosened or eliminated, and even the usually sacrosanct HIPAA regulations were temporarily sidelined.
Medical research. Both human and animal research came to a screeching halt, and many research assistants were furloughed. Data collection was disrupted, and a generation of scientific and medical discoveries became a casualty of the pandemic.
Medical literature. It was stunning to see how quickly COVID-19 occupied most of the pages of prominent journals. The scholarly articles were frankly quite useful, covering topics ranging from risk factors to early symptoms to treatment and pathophysiology across multiple organs. As with other paradigm shifts, there was an accelerated publication push, sometimes with expedited peer reviews to inform health care workers and the public while the pandemic was still raging. However, a couple of very prominent journals had to retract flawed articles that were hastily published without the usual due diligence and rigorous peer review. The pandemic clearly disrupted the science publishing process.
Travel effects. The steep reduction of flights (by 98%) was financially catastrophic, not only for airline companies but to business travel across the country. However, fewer cars on the road resulted in fewer accidents and deaths, and also reduced pollution. Paradoxically, to prevent crowding in subways, trains, and buses, officials reversed their traditional instructions and advised the public to drive their own cars instead of using public transportation!
Continue to: Heroism of front-line medical personnel
Heroism of front-line medical personnel. Everyone saluted and prayed for the health care professionals working at the bedside of highly infectious patients who needed 24/7 intensive care. Many have died while carrying out the noble but hazardous medical duties. Those heroes deserve our lasting respect and admiration.
The COVID-19 pandemic insidiously permeated and altered every aspect of our complex society and revealed how fragile our “normal lifestyle” really is. It is possible that nothing will ever be the same again, and an uneasy sense of vulnerability will engulf us as we cautiously return to a “new normal.” Even our language has expanded with the lexicon of pandemic terminology (Table). We all pray and hope that this plague never returns. And let’s hope one or more vaccines are developed soon so we can manage future recurrences like the annual flu season. In the meantime, keep your masks and sanitizers close by…
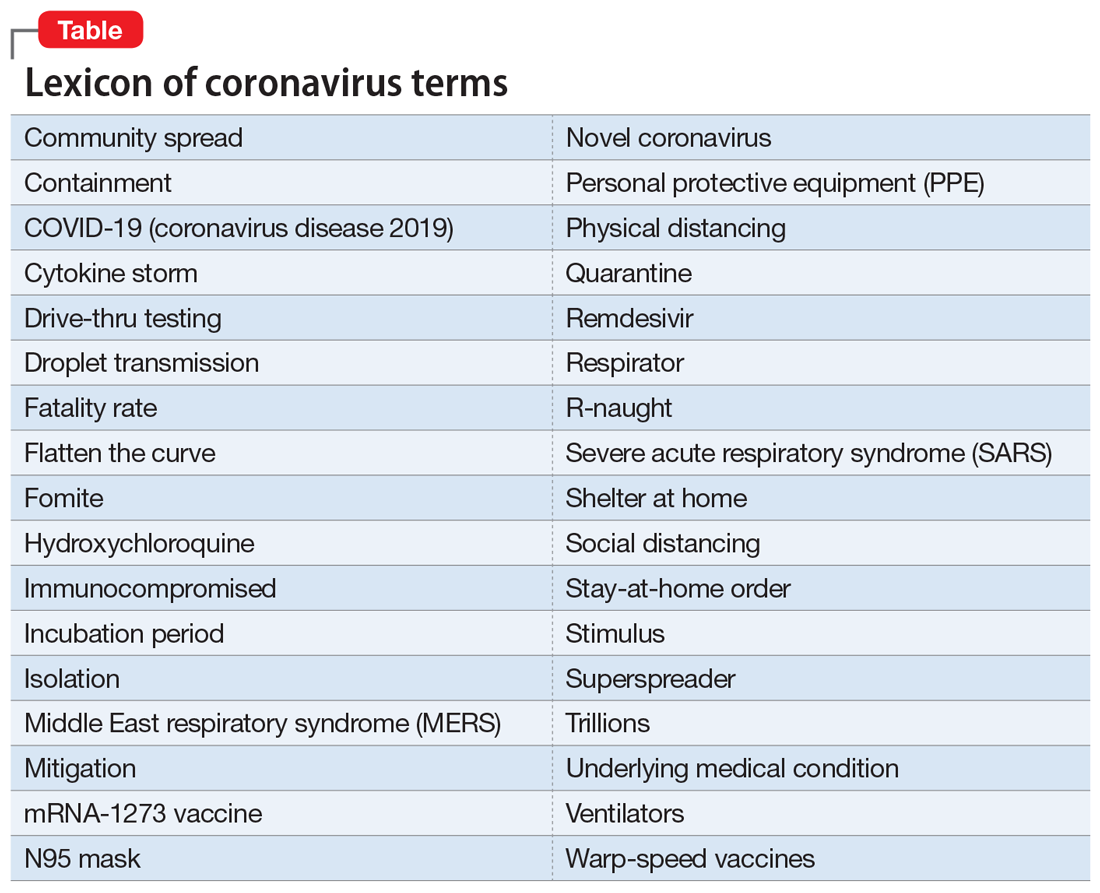
Postscript: Shortly after I completed this editorial, the ongoing COVID-19 plague was overshadowed by the scourge of racism, with massive protests, at times laced by violence, triggered by the death of a black man in custody of the police, under condemnable circumstances. The COVID-19 pandemic and the necessary social distancing it requires were temporarily ignored during the ensuing protests. The combined effect of those overlapping scourges are jarring to the country’s psyche, complicating and perhaps sabotaging the social recovery from the pandemic.
As the life-altering coronavirus disease 2019 (COVID-19) pandemic gradually ebbs, we are all its survivors. Now, we are experiencing COVID-19 fatigue, trying to emerge from its dense fog that pervaded every facet of our lives. We are fully cognizant that there will not be a return to the previous “normal.” The pernicious virus had a transformative effect that did not spare any component of our society. Full recovery will not be easy.
As the uncertainty lingers about another devastating return of the pandemic later this year, we can see the reverberation of this invisible assault on human existence. Although a relatively small fraction of the population lost their lives, the rest of us are valiantly trying to readjust to the multiple ways our world has changed. Consider the following abrupt and sweeping burdens inflicted by the pandemic within a few short weeks:
Mental health. The acute stress of thanatophobia generated a triad of anxiety, depression, and nosophobia on a large scale. The demand for psychiatric care rapidly escalated. Suicide rate increased not only because of the stress of being locked down at home (alien to most people’s lifestyle) but because of the coincidental timing of the pandemic during April and May, the peak time of year for suicide. Animal researchers use immobilization as a paradigm to stress a rat or mouse. Many humans immobilized during the pandemic have developed exquisite empathy towards those rodents! The impact on children may also have long-term effects because playing and socializing with friends is a vital part of their lives. Parents have noticed dysphoria and acting out among their children, and an intense compensatory preoccupation with video games and electronic communications with friends.
Physical health. Medical care focused heavily on COVID-19 victims, to the detriment of all other medical conditions. Non-COVID-19 hospital admissions plummeted, and all elective surgeries and procedures were put on hold, depriving many people of medical care they badly needed. Emergency department (ED) visits also declined dramatically, including the usual flow of heart attacks, stroke, pulmonary embolus, asthma attacks, etc. The minimization of driving greatly reduced the admission of accident victims to EDs. Colonoscopies, cardiac stents, hip replacements, MRIs, mammography, and other procedures that are vital to maintain health and quality of life were halted. Dentists shuttered their practices due to the high risk of infection from exposure to oral secretions and breathing. One can only imagine the suffering of having a toothache with no dental help available, and how that might lead to narcotic abuse.
Social health. The imperative of social distancing disrupted most ordinary human activities, such as dining out, sitting in an auditorium for Grand Rounds or a lecture, visiting friends at their homes, the cherished interactions between grandparents and grandchildren (the lack of which I painfully experienced), and even seeing each other’s smiles behind the ubiquitous masks. And forget about hugging or kissing. The aversion to being near anyone who is coughing or sneezing led to an adaptive social paranoia and the social shunning of anyone who appeared to have an upper respiratory infection, even if it was unrelated to COVID-19.
Redemption for the pharmaceutical industry. The deadly pandemic intensified the public’s awareness of the importance of developing treatments and vaccines for COVID-19. The often-demonized pharmaceutical companies, with their extensive R&D infrastructure, emerged as a major source of hope for discovering an effective treatment for the coronavirus infection, or—better still—one or more vaccines that will enable society to return to its normal functions. It was quite impressive how many pharmaceutical companies “came to the rescue” with clinical trials to repurpose existing medications or to develop new ones. It was very encouraging to see multiple vaccine candidates being developed and expedited for testing around the world. A process that usually takes years was reduced to a few months, thanks to the existing technical infrastructure and thousands of scientists who enable rapid drug development. It is possible that the public may gradually modify its perception of the pharmaceutical industry from a “corporate villain” to an “indispensable health industry” for urgent medical crises such as a pandemic, and also for hundreds of medical diseases that are still in need of safe, effective therapies.
Economic burden. The unimaginable nightmare scenario of a total shutdown of all businesses led to the unprecedented loss of millions of jobs and livelihoods, reflected in miles-long lines of families at food banks. Overnight, the government switched from worrying about its $20-trillion deficit to printing several more trillion dollars to rescue the economy from collapse. The huge magnitude of a trillion can be appreciated if one is aware that it takes roughly 32 years to count to 1 billion, and 32,000 years to count to 1 trillion. Stimulating the economy while the gross domestic product threatens to sink by terrifying percentages (20% to 30%) was urgently needed, even though it meant mortgaging the future, especially when interest rates, and servicing the debt, will inevitably rise from the current zero to much higher levels in the future. The collapse of the once-thriving airline industry (bookings were down an estimated 98%) is an example of why desperate measures were needed to salvage an economy paralyzed by a viral pandemic.
Continue to: Political repercussions
Political repercussions. In our already hyperpartisan country, the COVID-19 crisis created more fissures across party lines. The blame game escalated as each side tried to exploit the crisis for political gain during a presidential election year. None of the leaders, from mayors to governors to the president, had any notion of how to wisely manage an unforeseen catastrophic pandemic. Thus, a political cacophony has developed, further exacerbating the public’s anxiety and uncertainty, especially about how and when the pandemic will end.
Education disruption. Never before have all schools and colleges around the country abruptly closed and sent students of all ages to shelter at home. Massive havoc ensued, with a wholesale switch to solitary online learning, the loss of the unique school and college social experience in the classroom and on campus, and the loss of experiencing commencement to receive a diploma (an important milestone for every graduate). Even medical students were not allowed to complete their clinical rotations and were sent home to attend online classes. A complete paradigm shift emerged about entrance exams: the SAT and ACT were eliminated for college applicants, and the MCAT for medical school applicants. This was unthinkable before the pandemic descended upon us, but benchmarks suddenly evaporated to adjust to the new reality. Then there followed disastrous financial losses by institutions of higher learning as well as academic medical centers and teaching hospitals, all slashing their budgets, furloughing employees, cutting salaries, and eliminating programs. Even the “sacred” tenure of senior faculty became a casualty of the financial “exigency.” Children’s nutrition suffered, especially among those in lower socioeconomic groups for whom the main meal of the day was the school lunch, and was made worse by their parents’ loss of income. For millions of people, the emotional toll was inevitable following the draconian measure of closing all educational institutions to contain the spread of the pandemic.
Family burden. Sheltering at home might have been fun for a few days, but after many weeks, it festered into a major stress, especially for those living in a small house, condominium, or apartment. The resilience of many families was tested as the exercise of freedoms collided with the fear of getting infected. Families were deprived of celebrating birthdays, weddings, funerals, graduation parties, retirement parties, Mother’s Day, Father’s Day, and various religious holidays, including Easter, Passover, and Eid al-Fitr.
Sexual burden. Intimacy and sexual contact between consenting adults living apart were sacrificed on the altar of the pernicious viral pandemic. Mandatory social distancing of 6 feet or more to avoid each other’s droplets emanating from simple speech, not just sneezing or coughing, makes intimacy practically impossible. Thus, physical closeness became taboo, and avoiding another person’s saliva or body secretions became a must to avoid contracting the virus. Being single was quite a lonely experience during this pandemic!
Entertainment deprivation. Americans are known to thrive on an extensive diet of spectator sports. Going to football, basketball, baseball, or hockey games to root for one’s team is intrinsically American. The pursuit of happiness extends to attending concerts, movies, Broadway shows, theme parks, and cruises with thousands of others. The pandemic ripped all those pleasurable leisure activities from our daily lives, leaving a big hole in people’s lives at the precise time fun activities were needed as a useful diversion from the dismal stress of a pandemic. To make things worse, it is uncertain when (if ever) such group activities will be restored, especially if the pandemic returns with another wave. But optimists would hurry to remind us that the “Roaring 20s” blossomed in the decade following the 1918 Spanish Flu pandemic.
Continue to: Legal system
Legal system. Astounding changes were instigated by the pandemic, such as the release of thousands of inmates, including felons, to avoid the spread of the virus in crowded prisons. For us psychiatrists, the silver lining in that unexpected action is that many of those released were patients with mental illness who were incarcerated because of the lack of hospitals that would take them. The police started issuing citations instead of arresting and jailing violators. Enforcement of the law was welcome when it targeted those who gouged the public for personal profit during the scarcity of masks, sanitizers, or even toilet paper and soap.
Medical practice. In addition to delaying medical care for patients, the freeze on so-called elective surgeries or procedures (many of which were actually necessary) was financially ruinous for physicians. Another regrettable consequence of the pandemic is a drop in pediatric vaccinations because parents were reluctant to take their children to the pediatrician. On a more positive note, the massive switch to telehealth was advantageous for both patients and psychiatrists because this technology is well-suited for psychiatric care. Fortunately, regulations that hampered telepsychiatry practice were substantially loosened or eliminated, and even the usually sacrosanct HIPAA regulations were temporarily sidelined.
Medical research. Both human and animal research came to a screeching halt, and many research assistants were furloughed. Data collection was disrupted, and a generation of scientific and medical discoveries became a casualty of the pandemic.
Medical literature. It was stunning to see how quickly COVID-19 occupied most of the pages of prominent journals. The scholarly articles were frankly quite useful, covering topics ranging from risk factors to early symptoms to treatment and pathophysiology across multiple organs. As with other paradigm shifts, there was an accelerated publication push, sometimes with expedited peer reviews to inform health care workers and the public while the pandemic was still raging. However, a couple of very prominent journals had to retract flawed articles that were hastily published without the usual due diligence and rigorous peer review. The pandemic clearly disrupted the science publishing process.
Travel effects. The steep reduction of flights (by 98%) was financially catastrophic, not only for airline companies but to business travel across the country. However, fewer cars on the road resulted in fewer accidents and deaths, and also reduced pollution. Paradoxically, to prevent crowding in subways, trains, and buses, officials reversed their traditional instructions and advised the public to drive their own cars instead of using public transportation!
Continue to: Heroism of front-line medical personnel
Heroism of front-line medical personnel. Everyone saluted and prayed for the health care professionals working at the bedside of highly infectious patients who needed 24/7 intensive care. Many have died while carrying out the noble but hazardous medical duties. Those heroes deserve our lasting respect and admiration.
The COVID-19 pandemic insidiously permeated and altered every aspect of our complex society and revealed how fragile our “normal lifestyle” really is. It is possible that nothing will ever be the same again, and an uneasy sense of vulnerability will engulf us as we cautiously return to a “new normal.” Even our language has expanded with the lexicon of pandemic terminology (Table). We all pray and hope that this plague never returns. And let’s hope one or more vaccines are developed soon so we can manage future recurrences like the annual flu season. In the meantime, keep your masks and sanitizers close by…
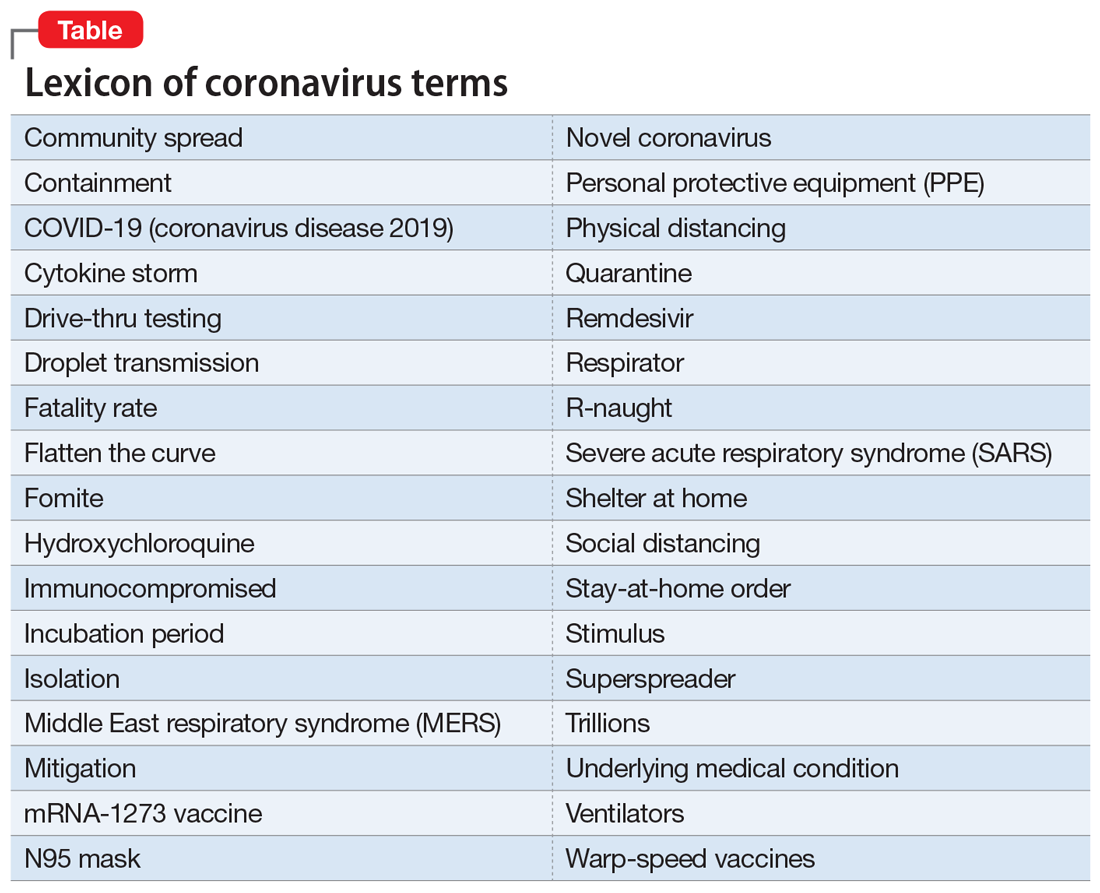
Postscript: Shortly after I completed this editorial, the ongoing COVID-19 plague was overshadowed by the scourge of racism, with massive protests, at times laced by violence, triggered by the death of a black man in custody of the police, under condemnable circumstances. The COVID-19 pandemic and the necessary social distancing it requires were temporarily ignored during the ensuing protests. The combined effect of those overlapping scourges are jarring to the country’s psyche, complicating and perhaps sabotaging the social recovery from the pandemic.
How to best use digital technology to help your patients
As psychiatrists, we are increasingly using digital technology, such as e-mail, video conferencing, social media, and text messaging, to communicate with and even treat our patients.1 The benefits of using digital technology for treating patients include, but are not limited to, enhancing access to psychiatric services that are unavailable due to a patient’s geographical location and/or physical disability; providing more cost‐effective delivery of services; and creating more ways for patients to communicate with their physicians.1 While there are benefits to using digital technology, there are also possible repercussions, such as breaches of confidentiality or boundary violations.2 Although there is no evidence-based guidance about how to best use digital technology in patient care,3 the following approaches can help you protect your patients and minimize your liability.
Assess competence. Determine how familiar and comfortable both you and your patient are with the specific software and/or devices you intend to use. Confirm that your patient can access the technology, and inform them of the benefits and risks of using digital technology in their care.1
Create a written policy about your use of digital technology, and review it with all patients to explain how it will be used in their treatment.1 This policy should include a back-up plan in the event of technology failures.1 It should clearly explain that the information gathered with this technology can become part of the patient’s medical record. It should also prohibit patients from using their devices to record other patients in the waiting room or other areas. Such a policy could enhance the protection of private information and help maintain clear boundaries.1 Review and update your policy as often as needed.
Obtain your patients’ written consent to use digital technology. If you want to post information about your patients on social media, obtain their written consent to do so, and mutually agree as to what information would be posted. This should not include their identity or confidential information.1
Do not accept friend requests or contact requests from current or former patients on any social networking platform. Do not follow your patients’ blogs, Twitter accounts, or any other accounts. Be aware that if you and your patients share the same “friend” network on social media, this may create boundary confusion, inappropriate dual relationships, and potential conflicts of interest.1 Keep personal and professional accounts separate to maintain appropriate boundaries and minimize compromising patient confidentiality. Do not post private information on professional practice accounts, and do not link/sync your personal accounts with professional accounts.
Do not store patient information on your personal electronic devices because these devices could be lost or hacked. Avoid contacting your patients via non-secured platforms because doing so could compromise patient confidentiality. Use encrypted software and firewalls for communicating with your patients and storing their information.1 Also, periodically assess your confidentiality policies and procedures to ensure compliance with appropriate statutes and laws.1
1. Reamer FG. Evolving standards of care in the age of cybertechnology. Behav Sci Law. 2018;36(2):257-269.
2. Ventola CL. Social media and health care professionals: benefits, risks, and best practices. P T. 2014;39(7):491-499, 520.
3. Logghe HJ, Boeck MA, Gusani NJ, et al. Best practices for surgeons’ social media use: statement of the Resident and Associate Society of the American College of Surgeons. J Am Coll Surg. 2018;226(3):317-327.
As psychiatrists, we are increasingly using digital technology, such as e-mail, video conferencing, social media, and text messaging, to communicate with and even treat our patients.1 The benefits of using digital technology for treating patients include, but are not limited to, enhancing access to psychiatric services that are unavailable due to a patient’s geographical location and/or physical disability; providing more cost‐effective delivery of services; and creating more ways for patients to communicate with their physicians.1 While there are benefits to using digital technology, there are also possible repercussions, such as breaches of confidentiality or boundary violations.2 Although there is no evidence-based guidance about how to best use digital technology in patient care,3 the following approaches can help you protect your patients and minimize your liability.
Assess competence. Determine how familiar and comfortable both you and your patient are with the specific software and/or devices you intend to use. Confirm that your patient can access the technology, and inform them of the benefits and risks of using digital technology in their care.1
Create a written policy about your use of digital technology, and review it with all patients to explain how it will be used in their treatment.1 This policy should include a back-up plan in the event of technology failures.1 It should clearly explain that the information gathered with this technology can become part of the patient’s medical record. It should also prohibit patients from using their devices to record other patients in the waiting room or other areas. Such a policy could enhance the protection of private information and help maintain clear boundaries.1 Review and update your policy as often as needed.
Obtain your patients’ written consent to use digital technology. If you want to post information about your patients on social media, obtain their written consent to do so, and mutually agree as to what information would be posted. This should not include their identity or confidential information.1
Do not accept friend requests or contact requests from current or former patients on any social networking platform. Do not follow your patients’ blogs, Twitter accounts, or any other accounts. Be aware that if you and your patients share the same “friend” network on social media, this may create boundary confusion, inappropriate dual relationships, and potential conflicts of interest.1 Keep personal and professional accounts separate to maintain appropriate boundaries and minimize compromising patient confidentiality. Do not post private information on professional practice accounts, and do not link/sync your personal accounts with professional accounts.
Do not store patient information on your personal electronic devices because these devices could be lost or hacked. Avoid contacting your patients via non-secured platforms because doing so could compromise patient confidentiality. Use encrypted software and firewalls for communicating with your patients and storing their information.1 Also, periodically assess your confidentiality policies and procedures to ensure compliance with appropriate statutes and laws.1
As psychiatrists, we are increasingly using digital technology, such as e-mail, video conferencing, social media, and text messaging, to communicate with and even treat our patients.1 The benefits of using digital technology for treating patients include, but are not limited to, enhancing access to psychiatric services that are unavailable due to a patient’s geographical location and/or physical disability; providing more cost‐effective delivery of services; and creating more ways for patients to communicate with their physicians.1 While there are benefits to using digital technology, there are also possible repercussions, such as breaches of confidentiality or boundary violations.2 Although there is no evidence-based guidance about how to best use digital technology in patient care,3 the following approaches can help you protect your patients and minimize your liability.
Assess competence. Determine how familiar and comfortable both you and your patient are with the specific software and/or devices you intend to use. Confirm that your patient can access the technology, and inform them of the benefits and risks of using digital technology in their care.1
Create a written policy about your use of digital technology, and review it with all patients to explain how it will be used in their treatment.1 This policy should include a back-up plan in the event of technology failures.1 It should clearly explain that the information gathered with this technology can become part of the patient’s medical record. It should also prohibit patients from using their devices to record other patients in the waiting room or other areas. Such a policy could enhance the protection of private information and help maintain clear boundaries.1 Review and update your policy as often as needed.
Obtain your patients’ written consent to use digital technology. If you want to post information about your patients on social media, obtain their written consent to do so, and mutually agree as to what information would be posted. This should not include their identity or confidential information.1
Do not accept friend requests or contact requests from current or former patients on any social networking platform. Do not follow your patients’ blogs, Twitter accounts, or any other accounts. Be aware that if you and your patients share the same “friend” network on social media, this may create boundary confusion, inappropriate dual relationships, and potential conflicts of interest.1 Keep personal and professional accounts separate to maintain appropriate boundaries and minimize compromising patient confidentiality. Do not post private information on professional practice accounts, and do not link/sync your personal accounts with professional accounts.
Do not store patient information on your personal electronic devices because these devices could be lost or hacked. Avoid contacting your patients via non-secured platforms because doing so could compromise patient confidentiality. Use encrypted software and firewalls for communicating with your patients and storing their information.1 Also, periodically assess your confidentiality policies and procedures to ensure compliance with appropriate statutes and laws.1
1. Reamer FG. Evolving standards of care in the age of cybertechnology. Behav Sci Law. 2018;36(2):257-269.
2. Ventola CL. Social media and health care professionals: benefits, risks, and best practices. P T. 2014;39(7):491-499, 520.
3. Logghe HJ, Boeck MA, Gusani NJ, et al. Best practices for surgeons’ social media use: statement of the Resident and Associate Society of the American College of Surgeons. J Am Coll Surg. 2018;226(3):317-327.
1. Reamer FG. Evolving standards of care in the age of cybertechnology. Behav Sci Law. 2018;36(2):257-269.
2. Ventola CL. Social media and health care professionals: benefits, risks, and best practices. P T. 2014;39(7):491-499, 520.
3. Logghe HJ, Boeck MA, Gusani NJ, et al. Best practices for surgeons’ social media use: statement of the Resident and Associate Society of the American College of Surgeons. J Am Coll Surg. 2018;226(3):317-327.
Two pandemics
This column is adapted from Dr. Eleryan’s speech at the George Washington University dermatology residency program’s virtual graduation ceremony on June 12.
I’ve been reflecting on my entire residency and the last 2 weeks have stood out the most. I have to admit that I’ve been angry, and so are numerous others who look like me. However, after conversations with a few important people in my life, I’ve realized that people care and are open to listening and changing if I give them the opportunity to see through my lens. I don’t want my legacy to be one of anger, but to be one of change, one of activism, one of heroism, and one of taking a stand in the midst of adversity.
So thank you to everyone who has played a part in my residency and is here to celebrate as I transition to the next step in my career.
But I must pause for a moment to say “I can’t breathe.” I can’t breathe because while I sit here in a place of honor for my accomplishments, I can’t forget that I’m standing in the gap for all of the black men and women who will never have the opportunity to experience a moment like this.
I can’t breathe because George Floyd, Breonna Taylor, Ahmaud Arbery, Tony McDade, Trayvon Martin, Philando Castile, Sandra Bland, Eric Garner, Tamir Rice, Mike Brown, Emmett Till, and so many others will never get to experience a celebratory occasion such as this because of their senseless executions as a likely result of racial bias.
As a black person in “the land of the free,” I have to live with the fact that my life may be taken for simply taking a stroll through a park, jogging through a neighborhood, driving down the street, walking back home from the store, or even sitting in my own home!
As a black physician, I must contend with the very notion that my privilege as a physician does not shield me from discrimination and bias. I recognize that my race walks into the room before I ever do. I know that many of my patients will question my abilities or my title – thinking I am the receptionist, food services worker, or even part of the janitorial staff – simply because of the color of my skin. And what’s even more disturbing is that some of my colleagues will confuse me with another black woman whom I look nothing like or challenge my intelligence and abilities and how I got my position.
All of this boils down to racism – pure and simple. Black people in this country don’t have the privilege of ignoring this truth. We know that this world is not colorblind; neither is anyone in it. We know that this is entrenched racism that for generations has created racial disparities in health care, education, housing, employment, and law enforcement. We weren’t born into a fragile or vulnerable state, yet we were born into a system of dis-enfranchisement, dis-investment, dis-crimination, dis-advantage, and dis-respect.
As physicians, we must recognize and acknowledge the lived experiences that walk through the door with our black patients. And we must understand that black patients walk around with the effects of trauma and toxic stress from just being black in America. That trauma and stress show up in very real ways that contribute to black people experiencing the brunt of chronic diseases and poorer health outcomes. There is no better example than the current COVID-19 pandemic. We are in the midst of a global pandemic from a virus that does not discriminate based on race, but black people are almost three times as likely to be hospitalized as are white people with COVID-19 . And why is that? Because of the “comorbidity” of racism that black people in this country live with. It is not a mere coincidence that the black population is overrepresented in essential jobs and black people are more likely to work in health care than are white people – all positions that increase the risk of infection and death from the virus. So, if we call COVID-19 a pandemic, racism most certainly has been a pandemic that this country has refused to acknowledge, treat, and vaccinate for centuries. We cannot ignore that both have tragically affected black people.
So as Pastor Reginald Sharpe Jr. in Chicago recently said, we’re dealing with two pandemics: One has no vaccination and one has no explanation; one can physiologically take your breath away because it affects the respiratory system, while the second can also take your breath away. Just ask Eric Garner and George Floyd.
As physicians, we must recognize that the mechanisms that tragically resulted in the deaths of George Floyd, Breonna Taylor, Ahmaud Arbery, and so many other black men and women are the same mechanisms that are harming and killing black people in our health care system. It’s not acceptable for institutions that built themselves on black and brown bodies to offer condolences, but to continue to do nothing about the racism that still runs rampant within. It’s not acceptable to do nothing. It’s important to note: Racist systems do not perpetuate themselves – the individuals operating within them do.
Martin Luther King Jr. once said, “He who passively accepts evil is as much involved in it as he who helps to perpetuate it. He who accepts evil without protesting against it is really cooperating with it.” Being well-intentioned, good-hearted, sad, or disheartened is not enough. We won’t be able to tear down the systems and institutions that have been a breeding ground for racism until outrage is met by action, not just from black people and people of color, but also by the white majority.
As physicians it’s time for us to look at how our health care institution – an institution instrumental in the victimization of black people – is affecting the health and well-being of our black patients. (For example, increased maternal mortality among black women.)
Are they being seen and heard? Are they receiving culturally relevant and sensitive care? Are their needs and concerns receiving the same amount of time and attention as other patients? It’s time to understand that, for many black patients, the health care system is another place of injustice that has not proved itself to be trustworthy or inclusive of black culture.
As physicians, we must affirm that the lives and health of black and brown people matter to us, that we see the racism they experience, and that we will use our platform as physicians to eliminate racism not just in the hospitals but in the world our patients live in.
So while I didn’t choose the body that I was born into, I fully embrace it and the challenges that come with it. I’m not here to make people feel comfortable, I’m here to continue the work of my ancestors, accomplish the dreams that they fought and lost their lives for, and most importantly, I’m here to continue the fight against the systems that work to prevent other marginalized persons from getting to where I am and even further.
The author James Baldwin once wrote, “Not everything that is faced can be changed, but nothing can be changed until it is faced.” So, I urge you to be loudly antiracist in every space that you hold. I urge you to educate yourselves about racism and white supremacy and privilege and how it permeates our health care system. I urge you to stand beside black people rather than in front of them. Use your privilege to amplify underheard voices and to challenge the biases of your peers, friends, and family members. Use your platform as physicians to advocate for a more just and equitable health care system.
So let me repeat ... we as physicians have the responsibility to eliminate racial bias in the practice of medicine and recognize racism as a threat to the health and well-being of black people and other people of color.
How do we do this? We are beyond lengthy dialogue and “Black History Month” talks. Now is the time for action. Taking action includes the following:
1. Medical academic institutions committing to having a diverse and inclusive faculty. We know it is critical and vital to the recruitment, success, and matriculation of medical students and residents of color to see faculty, particularly senior level faculty in their specialty, who look like them and can serve as mentors. Every year, these institutions need to set a goal that they will take additional steps to have at least one-third of their faculty be black and another third persons of color. In addition, senior faculty positions – those setting curricula, selecting incoming students and residents – must include at least one-third from underrepresented backgrounds (black, Hispanic, Native American/Indigenous).
2. Hospital administration has to resemble the communities in which the hospital serves. Unfortunately, all too often, we know this is not the case, and as a result, decisions that affect the care of black and brown people are often to their detriment because they perpetuate the racism within the existing system. In order to dismantle racism in the hospital system, hospital administrations must consist of diverse individuals. Therefore, hospitals need to commit to hiring and promoting black and brown staff to ensure one-third of its senior leaderships consists of individuals from underrepresented backgrounds.
3. Improving the pipeline that matriculates black and brown students into medical school and residency programs. Lack of access to mentors within the medical field, lack of funding for travel to/from interviews, and lack of knowledge of the overall application process are a few barriers faced by students of color seeking to enter into the medical field. In addition to current scholarship opportunities, medical schools need to allocate funds to connect underrepresented minority students with a range of lived experiences (not just those from impoverished backgrounds but also those from middle class backgrounds who face difficulty gaining acceptance into medical school and residency programs), such as connecting them with mentors by opening opportunities for them to shadow professionals at a conference, travel to residency interviews with most, if not all, expenses covered up front, and have access to local programs that expose them to physicians in several specialties.
These are just a few examples of the active steps we can take to dismantle racism and reconcile the effects of it in the medical field. So if I may borrow from other movements, “Time’s Up” for silence regarding the existence of racism and white supremacy, and now it’s time to truly show that “We are all in this together.”
It is not just my duty but yours also – to ensure that we never have to hear another black man, woman, or child say “I can’t breathe” at the hands of injustice.
Dr. Eleryan (@skinclusionMD) is a social justice activist and was co-chief resident in dermatology (2019-2020) at George Washington University, Washington, DC, and is an Alpha Omega Alpha inductee (2020). She will be a micrographic surgery and dermatologic oncology fellow at the University of California, Los Angeles, in July 2020.
This column is adapted from Dr. Eleryan’s speech at the George Washington University dermatology residency program’s virtual graduation ceremony on June 12.
I’ve been reflecting on my entire residency and the last 2 weeks have stood out the most. I have to admit that I’ve been angry, and so are numerous others who look like me. However, after conversations with a few important people in my life, I’ve realized that people care and are open to listening and changing if I give them the opportunity to see through my lens. I don’t want my legacy to be one of anger, but to be one of change, one of activism, one of heroism, and one of taking a stand in the midst of adversity.
So thank you to everyone who has played a part in my residency and is here to celebrate as I transition to the next step in my career.
But I must pause for a moment to say “I can’t breathe.” I can’t breathe because while I sit here in a place of honor for my accomplishments, I can’t forget that I’m standing in the gap for all of the black men and women who will never have the opportunity to experience a moment like this.
I can’t breathe because George Floyd, Breonna Taylor, Ahmaud Arbery, Tony McDade, Trayvon Martin, Philando Castile, Sandra Bland, Eric Garner, Tamir Rice, Mike Brown, Emmett Till, and so many others will never get to experience a celebratory occasion such as this because of their senseless executions as a likely result of racial bias.
As a black person in “the land of the free,” I have to live with the fact that my life may be taken for simply taking a stroll through a park, jogging through a neighborhood, driving down the street, walking back home from the store, or even sitting in my own home!
As a black physician, I must contend with the very notion that my privilege as a physician does not shield me from discrimination and bias. I recognize that my race walks into the room before I ever do. I know that many of my patients will question my abilities or my title – thinking I am the receptionist, food services worker, or even part of the janitorial staff – simply because of the color of my skin. And what’s even more disturbing is that some of my colleagues will confuse me with another black woman whom I look nothing like or challenge my intelligence and abilities and how I got my position.
All of this boils down to racism – pure and simple. Black people in this country don’t have the privilege of ignoring this truth. We know that this world is not colorblind; neither is anyone in it. We know that this is entrenched racism that for generations has created racial disparities in health care, education, housing, employment, and law enforcement. We weren’t born into a fragile or vulnerable state, yet we were born into a system of dis-enfranchisement, dis-investment, dis-crimination, dis-advantage, and dis-respect.
As physicians, we must recognize and acknowledge the lived experiences that walk through the door with our black patients. And we must understand that black patients walk around with the effects of trauma and toxic stress from just being black in America. That trauma and stress show up in very real ways that contribute to black people experiencing the brunt of chronic diseases and poorer health outcomes. There is no better example than the current COVID-19 pandemic. We are in the midst of a global pandemic from a virus that does not discriminate based on race, but black people are almost three times as likely to be hospitalized as are white people with COVID-19 . And why is that? Because of the “comorbidity” of racism that black people in this country live with. It is not a mere coincidence that the black population is overrepresented in essential jobs and black people are more likely to work in health care than are white people – all positions that increase the risk of infection and death from the virus. So, if we call COVID-19 a pandemic, racism most certainly has been a pandemic that this country has refused to acknowledge, treat, and vaccinate for centuries. We cannot ignore that both have tragically affected black people.
So as Pastor Reginald Sharpe Jr. in Chicago recently said, we’re dealing with two pandemics: One has no vaccination and one has no explanation; one can physiologically take your breath away because it affects the respiratory system, while the second can also take your breath away. Just ask Eric Garner and George Floyd.
As physicians, we must recognize that the mechanisms that tragically resulted in the deaths of George Floyd, Breonna Taylor, Ahmaud Arbery, and so many other black men and women are the same mechanisms that are harming and killing black people in our health care system. It’s not acceptable for institutions that built themselves on black and brown bodies to offer condolences, but to continue to do nothing about the racism that still runs rampant within. It’s not acceptable to do nothing. It’s important to note: Racist systems do not perpetuate themselves – the individuals operating within them do.
Martin Luther King Jr. once said, “He who passively accepts evil is as much involved in it as he who helps to perpetuate it. He who accepts evil without protesting against it is really cooperating with it.” Being well-intentioned, good-hearted, sad, or disheartened is not enough. We won’t be able to tear down the systems and institutions that have been a breeding ground for racism until outrage is met by action, not just from black people and people of color, but also by the white majority.
As physicians it’s time for us to look at how our health care institution – an institution instrumental in the victimization of black people – is affecting the health and well-being of our black patients. (For example, increased maternal mortality among black women.)
Are they being seen and heard? Are they receiving culturally relevant and sensitive care? Are their needs and concerns receiving the same amount of time and attention as other patients? It’s time to understand that, for many black patients, the health care system is another place of injustice that has not proved itself to be trustworthy or inclusive of black culture.
As physicians, we must affirm that the lives and health of black and brown people matter to us, that we see the racism they experience, and that we will use our platform as physicians to eliminate racism not just in the hospitals but in the world our patients live in.
So while I didn’t choose the body that I was born into, I fully embrace it and the challenges that come with it. I’m not here to make people feel comfortable, I’m here to continue the work of my ancestors, accomplish the dreams that they fought and lost their lives for, and most importantly, I’m here to continue the fight against the systems that work to prevent other marginalized persons from getting to where I am and even further.
The author James Baldwin once wrote, “Not everything that is faced can be changed, but nothing can be changed until it is faced.” So, I urge you to be loudly antiracist in every space that you hold. I urge you to educate yourselves about racism and white supremacy and privilege and how it permeates our health care system. I urge you to stand beside black people rather than in front of them. Use your privilege to amplify underheard voices and to challenge the biases of your peers, friends, and family members. Use your platform as physicians to advocate for a more just and equitable health care system.
So let me repeat ... we as physicians have the responsibility to eliminate racial bias in the practice of medicine and recognize racism as a threat to the health and well-being of black people and other people of color.
How do we do this? We are beyond lengthy dialogue and “Black History Month” talks. Now is the time for action. Taking action includes the following:
1. Medical academic institutions committing to having a diverse and inclusive faculty. We know it is critical and vital to the recruitment, success, and matriculation of medical students and residents of color to see faculty, particularly senior level faculty in their specialty, who look like them and can serve as mentors. Every year, these institutions need to set a goal that they will take additional steps to have at least one-third of their faculty be black and another third persons of color. In addition, senior faculty positions – those setting curricula, selecting incoming students and residents – must include at least one-third from underrepresented backgrounds (black, Hispanic, Native American/Indigenous).
2. Hospital administration has to resemble the communities in which the hospital serves. Unfortunately, all too often, we know this is not the case, and as a result, decisions that affect the care of black and brown people are often to their detriment because they perpetuate the racism within the existing system. In order to dismantle racism in the hospital system, hospital administrations must consist of diverse individuals. Therefore, hospitals need to commit to hiring and promoting black and brown staff to ensure one-third of its senior leaderships consists of individuals from underrepresented backgrounds.
3. Improving the pipeline that matriculates black and brown students into medical school and residency programs. Lack of access to mentors within the medical field, lack of funding for travel to/from interviews, and lack of knowledge of the overall application process are a few barriers faced by students of color seeking to enter into the medical field. In addition to current scholarship opportunities, medical schools need to allocate funds to connect underrepresented minority students with a range of lived experiences (not just those from impoverished backgrounds but also those from middle class backgrounds who face difficulty gaining acceptance into medical school and residency programs), such as connecting them with mentors by opening opportunities for them to shadow professionals at a conference, travel to residency interviews with most, if not all, expenses covered up front, and have access to local programs that expose them to physicians in several specialties.
These are just a few examples of the active steps we can take to dismantle racism and reconcile the effects of it in the medical field. So if I may borrow from other movements, “Time’s Up” for silence regarding the existence of racism and white supremacy, and now it’s time to truly show that “We are all in this together.”
It is not just my duty but yours also – to ensure that we never have to hear another black man, woman, or child say “I can’t breathe” at the hands of injustice.
Dr. Eleryan (@skinclusionMD) is a social justice activist and was co-chief resident in dermatology (2019-2020) at George Washington University, Washington, DC, and is an Alpha Omega Alpha inductee (2020). She will be a micrographic surgery and dermatologic oncology fellow at the University of California, Los Angeles, in July 2020.
This column is adapted from Dr. Eleryan’s speech at the George Washington University dermatology residency program’s virtual graduation ceremony on June 12.
I’ve been reflecting on my entire residency and the last 2 weeks have stood out the most. I have to admit that I’ve been angry, and so are numerous others who look like me. However, after conversations with a few important people in my life, I’ve realized that people care and are open to listening and changing if I give them the opportunity to see through my lens. I don’t want my legacy to be one of anger, but to be one of change, one of activism, one of heroism, and one of taking a stand in the midst of adversity.
So thank you to everyone who has played a part in my residency and is here to celebrate as I transition to the next step in my career.
But I must pause for a moment to say “I can’t breathe.” I can’t breathe because while I sit here in a place of honor for my accomplishments, I can’t forget that I’m standing in the gap for all of the black men and women who will never have the opportunity to experience a moment like this.
I can’t breathe because George Floyd, Breonna Taylor, Ahmaud Arbery, Tony McDade, Trayvon Martin, Philando Castile, Sandra Bland, Eric Garner, Tamir Rice, Mike Brown, Emmett Till, and so many others will never get to experience a celebratory occasion such as this because of their senseless executions as a likely result of racial bias.
As a black person in “the land of the free,” I have to live with the fact that my life may be taken for simply taking a stroll through a park, jogging through a neighborhood, driving down the street, walking back home from the store, or even sitting in my own home!
As a black physician, I must contend with the very notion that my privilege as a physician does not shield me from discrimination and bias. I recognize that my race walks into the room before I ever do. I know that many of my patients will question my abilities or my title – thinking I am the receptionist, food services worker, or even part of the janitorial staff – simply because of the color of my skin. And what’s even more disturbing is that some of my colleagues will confuse me with another black woman whom I look nothing like or challenge my intelligence and abilities and how I got my position.
All of this boils down to racism – pure and simple. Black people in this country don’t have the privilege of ignoring this truth. We know that this world is not colorblind; neither is anyone in it. We know that this is entrenched racism that for generations has created racial disparities in health care, education, housing, employment, and law enforcement. We weren’t born into a fragile or vulnerable state, yet we were born into a system of dis-enfranchisement, dis-investment, dis-crimination, dis-advantage, and dis-respect.
As physicians, we must recognize and acknowledge the lived experiences that walk through the door with our black patients. And we must understand that black patients walk around with the effects of trauma and toxic stress from just being black in America. That trauma and stress show up in very real ways that contribute to black people experiencing the brunt of chronic diseases and poorer health outcomes. There is no better example than the current COVID-19 pandemic. We are in the midst of a global pandemic from a virus that does not discriminate based on race, but black people are almost three times as likely to be hospitalized as are white people with COVID-19 . And why is that? Because of the “comorbidity” of racism that black people in this country live with. It is not a mere coincidence that the black population is overrepresented in essential jobs and black people are more likely to work in health care than are white people – all positions that increase the risk of infection and death from the virus. So, if we call COVID-19 a pandemic, racism most certainly has been a pandemic that this country has refused to acknowledge, treat, and vaccinate for centuries. We cannot ignore that both have tragically affected black people.
So as Pastor Reginald Sharpe Jr. in Chicago recently said, we’re dealing with two pandemics: One has no vaccination and one has no explanation; one can physiologically take your breath away because it affects the respiratory system, while the second can also take your breath away. Just ask Eric Garner and George Floyd.
As physicians, we must recognize that the mechanisms that tragically resulted in the deaths of George Floyd, Breonna Taylor, Ahmaud Arbery, and so many other black men and women are the same mechanisms that are harming and killing black people in our health care system. It’s not acceptable for institutions that built themselves on black and brown bodies to offer condolences, but to continue to do nothing about the racism that still runs rampant within. It’s not acceptable to do nothing. It’s important to note: Racist systems do not perpetuate themselves – the individuals operating within them do.
Martin Luther King Jr. once said, “He who passively accepts evil is as much involved in it as he who helps to perpetuate it. He who accepts evil without protesting against it is really cooperating with it.” Being well-intentioned, good-hearted, sad, or disheartened is not enough. We won’t be able to tear down the systems and institutions that have been a breeding ground for racism until outrage is met by action, not just from black people and people of color, but also by the white majority.
As physicians it’s time for us to look at how our health care institution – an institution instrumental in the victimization of black people – is affecting the health and well-being of our black patients. (For example, increased maternal mortality among black women.)
Are they being seen and heard? Are they receiving culturally relevant and sensitive care? Are their needs and concerns receiving the same amount of time and attention as other patients? It’s time to understand that, for many black patients, the health care system is another place of injustice that has not proved itself to be trustworthy or inclusive of black culture.
As physicians, we must affirm that the lives and health of black and brown people matter to us, that we see the racism they experience, and that we will use our platform as physicians to eliminate racism not just in the hospitals but in the world our patients live in.
So while I didn’t choose the body that I was born into, I fully embrace it and the challenges that come with it. I’m not here to make people feel comfortable, I’m here to continue the work of my ancestors, accomplish the dreams that they fought and lost their lives for, and most importantly, I’m here to continue the fight against the systems that work to prevent other marginalized persons from getting to where I am and even further.
The author James Baldwin once wrote, “Not everything that is faced can be changed, but nothing can be changed until it is faced.” So, I urge you to be loudly antiracist in every space that you hold. I urge you to educate yourselves about racism and white supremacy and privilege and how it permeates our health care system. I urge you to stand beside black people rather than in front of them. Use your privilege to amplify underheard voices and to challenge the biases of your peers, friends, and family members. Use your platform as physicians to advocate for a more just and equitable health care system.
So let me repeat ... we as physicians have the responsibility to eliminate racial bias in the practice of medicine and recognize racism as a threat to the health and well-being of black people and other people of color.
How do we do this? We are beyond lengthy dialogue and “Black History Month” talks. Now is the time for action. Taking action includes the following:
1. Medical academic institutions committing to having a diverse and inclusive faculty. We know it is critical and vital to the recruitment, success, and matriculation of medical students and residents of color to see faculty, particularly senior level faculty in their specialty, who look like them and can serve as mentors. Every year, these institutions need to set a goal that they will take additional steps to have at least one-third of their faculty be black and another third persons of color. In addition, senior faculty positions – those setting curricula, selecting incoming students and residents – must include at least one-third from underrepresented backgrounds (black, Hispanic, Native American/Indigenous).
2. Hospital administration has to resemble the communities in which the hospital serves. Unfortunately, all too often, we know this is not the case, and as a result, decisions that affect the care of black and brown people are often to their detriment because they perpetuate the racism within the existing system. In order to dismantle racism in the hospital system, hospital administrations must consist of diverse individuals. Therefore, hospitals need to commit to hiring and promoting black and brown staff to ensure one-third of its senior leaderships consists of individuals from underrepresented backgrounds.
3. Improving the pipeline that matriculates black and brown students into medical school and residency programs. Lack of access to mentors within the medical field, lack of funding for travel to/from interviews, and lack of knowledge of the overall application process are a few barriers faced by students of color seeking to enter into the medical field. In addition to current scholarship opportunities, medical schools need to allocate funds to connect underrepresented minority students with a range of lived experiences (not just those from impoverished backgrounds but also those from middle class backgrounds who face difficulty gaining acceptance into medical school and residency programs), such as connecting them with mentors by opening opportunities for them to shadow professionals at a conference, travel to residency interviews with most, if not all, expenses covered up front, and have access to local programs that expose them to physicians in several specialties.
These are just a few examples of the active steps we can take to dismantle racism and reconcile the effects of it in the medical field. So if I may borrow from other movements, “Time’s Up” for silence regarding the existence of racism and white supremacy, and now it’s time to truly show that “We are all in this together.”
It is not just my duty but yours also – to ensure that we never have to hear another black man, woman, or child say “I can’t breathe” at the hands of injustice.
Dr. Eleryan (@skinclusionMD) is a social justice activist and was co-chief resident in dermatology (2019-2020) at George Washington University, Washington, DC, and is an Alpha Omega Alpha inductee (2020). She will be a micrographic surgery and dermatologic oncology fellow at the University of California, Los Angeles, in July 2020.
How racism contributes to the effects of SARS-CoV-2
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
It’s been about two months since I volunteered in a hospital in Brooklyn, working in an ICU taking care of patients with COVID-19.
Everyone seems to have forgotten the early days of the pandemic – the time when the ICUs were overrun, we were using FEMA ventilators, and endocrinologists and psychiatrists were acting as intensivists.
Even though things are opening up and people are taking summer vacations in a seemingly amnestic state, having witnessed multiple daily deaths remains a part of my daily consciousness. As I see the case numbers climbing juxtaposed against people being out and about without masks, my anxiety level is rising.
A virus doesn’t discriminate. It can fly through the air, landing on the next available surface. If that virus is SARS-CoV-2 and that surface is a human mucosal membrane, the virus makes itself at home. It orders furniture, buys a fancy mattress and a large high definition TV, hangs art on the walls, and settles in for the long haul. It’s not going anywhere anytime soon.
Even as an equal opportunity virus, what SARS-CoV-2 has done is to hold a mirror up to the healthcare system. It has shown us what was here all along. When people first started noticing that underrepresented minorities were more likely to contract the virus and get sick from it, I heard musings that this was likely because of their preexisting health conditions. For example, commentators on cable news were quick to point out that black people are more likely than other people to have hypertension or diabetes. So doesn’t that explain why they are more affected by this virus?
That certainly is part of the story, but it doesn’t entirely explain the discrepancies we’ve seen. For example, in New York 14% of the population is black, and 25% of those who had a COVID-related death were black patients. Similarly, 19% of the population is Hispanic or Latino, and they made up 26% of COVID-related deaths. On the other hand, 55% of the population in New York is white, and white people account for only 34% of COVID-related deaths.
Working in Brooklyn, I didn’t need to be a keen observer to notice that, out of our entire unit of about 20-25 patients, there was only one patient in a 2-week period who was neither black nor Hispanic.
As others have written, there are other factors at play. I’m not sure how many of those commentators back in March stopped to think about why black patients are more likely to have hypertension and diabetes, but the chronic stress of facing racism on a daily basis surely contributes. Beyond those medical problems, minorities are more likely to live in multigenerational housing, which means that it is harder for them to isolate from others. In addition, their living quarters tend to be further from health care centers and grocery stores, which makes it harder for them to access medical care and healthy food.
As if that weren’t enough to put their health at risk, people of color are also affected by environmental racism . Factories with toxic waste are more likely to be built in or near neighborhoods filled with people of color than in other communities. On top of that, black and Hispanic people are also more likely to be under- or uninsured, meaning they often delay seeking care in order to avoid astronomic healthcare costs.
Black and Hispanic people are also more likely than others to be working in the service industry or other essential services, which means they are less likely to be able to work from home. Consequently, they have to risk more exposures to other people and the virus than do those who have the privilege of working safely from home. They also are less likely to have available paid leave and, therefore, are more likely to work while sick.
With the deck completely stacked against them, underrepresented minorities also face systemic bias and racism when interacting with the health care system. Physicians mistakenly believe black patients experience less pain than other patients, according to some research. Black mothers have significantly worse health care outcomes than do their non-black counterparts, and the infant mortality rate for Black infants is much higher as well.
In my limited time in Brooklyn, taking care of almost exclusively black and Hispanic patients, I saw one physician assistant and one nurse who were black; one nurse practitioner was Hispanic. This mismatch is sadly common. Although 13% of the population of the United States is black, only 5% of physicians in the United States are black. Hispanic people, who make up 18% of the US population, are only 6% of physicians. This undoubtedly contributes to poorer outcomes for underrepresented minority patients who have a hard time finding physicians who look like them and understand them.
So while SARS-CoV-2 may not discriminate, the effects it has on patients depends on all of these other factors. If it flies through the air and lands on the mucosal tract of a person who works from home, has effective health insurance and a primary care physician, and lives in a community with no toxic exposures, that person may be more likely to kick it out before it has a chance to settle in. The reason we have such a huge disparity in outcomes related to COVID-19 by race is that a person meeting that description is less likely to be black or Hispanic. Race is not an independent risk factor; structural racism is.
When I drive by the mall that is now open or the restaurants that are now open with indoor dining, my heart rate quickens just a bit with anxiety. The pandemic fatigue people are experiencing is leading them to act in unsafe ways – gathering with more people, not wearing masks, not keeping a safe distance. I worry about everyone, sure, but I really worry about black and Hispanic people who are most vulnerable as a result of everyone else’s refusal to follow guidelines.
Dr. Salles is a bariatric surgeon and is currently a Scholar in Residence at Stanford (Calif.) University. Find her on Twitter @arghavan_salles.
Endothelial injury may play a major role in COVID-19–associated coagulopathy
A striking clinical feature of illness from SARS-CoV-2 is a marked increase in thrombotic and microvascular complications, or COVID-19–associated coagulopathy (CAC).
A new study suggests endothelial cell injury plays a major role in the pathogenesis of CAC, and blood levels of soluble thrombomodulin correlate with mortality.
George Goshua, MD, of Yale University, New Haven, Conn., presented this study as a late-breaking abstract at the virtual annual congress of the European Hematology Association.
Dr. Goshua cited past research showing CAC to be highly prevalent among hospitalized patients. Venous thromboembolism was found in 17% to 69% of patients, despite thromboprophylaxis.1-4 Arterial thrombosis has been seen in 3.6% to 4.0% of patients,1-3 and autopsy findings have shown microvascular thrombosis in as many as 87% of patients.5-7
For their study, Dr. Goshua and colleagues assessed endothelial cell damage, platelet activation, and hemostatic and fibrinolytic cascade effects of CAC.
The investigators measured markers of endothelial cell injury and platelet activation, plasminogen activation inhibitor 1 (PAI-1), and coagulation factors in stable and critically ill patients hospitalized with COVID-19. In addition, the team sought to identify biomarkers of mortality in hospitalized patients.
Dr. Goshua and colleagues studied 68 adults hospitalized for suspected COVID-19 – 48 in the ICU and 20 outside the ICU. Patients in the ICU received mechanical ventilation, while the non-ICU patients required supplemental oxygen (≤3 L/min per nasal cannula).
There were more men than women (69% vs. 31%) in the ICU population but not in the non-ICU population (40% vs. 60%). There were no statistically significant differences in age or comorbid conditions between the ICU and non-ICU patients.
Results and interpretation
Consistent with augmentation of the coagulation cascade – and as expected – D-dimer and thrombin-antithrombin levels were high in both the ICU and non-ICU populations, but levels were significantly higher (P < .001) among the ICU patients.
Endogenous anticoagulants (antithrombin and proteins C and S) and fibrinolytic enzymes (alpha 2-antiplasmin) were preserved, verifying that CAC is distinct from disseminated intravascular coagulation. Classic fibrinolysis did not occur, as PAI-1 was high in ICU and non-ICU patients, and lysis-30 was normal in nearly all ICU patients (96%).
Von Willebrand factor antigen and activity levels and factor VIII levels were markedly elevated in non-ICU and ICU patients, but they were significantly higher (P < .001) in the ICU cohort. This supports the hypothesis that endothelial cell damage and platelet activation play major roles in CAC.
Similarly, soluble P-selectin, which is shed from endothelial cells and platelets, was dramatically elevated in ICU patients in comparison with controls and non-ICU patients (P < .001 for both comparisons).
Levels of soluble thrombomodulin, which is released from endothelial cells, were not significantly different in ICU patients and controls. However, given thrombomodulin’s significant role in the coagulation cascade, Dr. Goshua and colleagues plotted receiver operating curves to see if soluble thrombomodulin levels were predictive of mortality.
The results showed that soluble thrombomodulin correlated with the probability of survival, both overall and in ICU patients. Soluble thrombomodulin levels greater than 3.26 ng/mL were associated with significantly worse survival in all patients (P = .0087) and ICU patients (P = .0309).
Influence on therapy
Laboratory perturbations were detected in both ICU and non-ICU patients, and otherwise healthy outpatients have exhibited potentially life-threatening CAC, according to Dr. Goshua.
These findings suggest the prothrombotic state occurs early in the pathogenesis of SARS-CoV-2 infection, is driven by platelet activation and endotheliopathy, and becomes more pronounced with worsening severity of infection.
The results of this study prompted a change in how Yale–New Haven Hospital manages COVID-19 patients. Patients without a clinical contraindication now receive aspirin at 81 mg daily in addition to the anticoagulation regimen typically used for all hospitalized COVID-19 patients.
Investigations regarding other medications that can influence platelet-endothelial cell interactions and modulate endothelial cell damage in CAC – such as dipyridamole, defibrotide, and eculizumab – are planned.
Challenges and unanswered questions
Virchow’s triad was described by the eminent German physician, Rudolf Virchow, MD, in the 19th century. It refers to the three broad categories of factors that can predispose patients to thrombosis — circulatory stasis, hypercoagulability, and endothelial injury.
Although all of these elements could be operative in CAC, the current study suggests platelet activation and endothelial cell injury in CAC may be of primary importance.
Because of the limited ability to test critically ill patients and concerns regarding exposure of additional hospital personnel to COVID-19 patients, the current report lacked clarity about the relationship of the detected laboratory abnormalities to confirmed thrombotic events.
It is unknown whether endothelial cells in different organs are damaged uniformly. It is also unclear if the laboratory abnormalities identified in this analysis can be used to monitor response to therapy, to guide follow-up management of discharged patients with CAC, or to identify infected outpatients who should receive prophylactic anticoagulation.
The mechanism by which SARS-CoV-2 injures endothelial cells is not explained by these data. Neutrophil defensins and other prothrombotic peptides or markers of inflammation could play key roles in pathogenesis, assessment of disease severity, or monitoring for therapeutic efficacy.
Today, we have more sophisticated diagnostic tools than Dr. Virchow had. We also have the ability to record and rapidly disseminate information globally. Still, with regard to the COVID-19 pandemic, clinicians face many of the same challenges that confronted Dr. Virchow in his era.
The analysis conducted by Dr. Goshua and colleagues goes a long way toward elucidating some of the mechanisms and therapeutic targets to meet these challenges.
Dr. Goshua disclosed no conflicts of interest.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Goshua G et al. EHA Congress. Abstract LB2605.
References
1. Klok FA et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-50. doi: 10.1016/j.thromres.2020.04.041.
2. Thomas W et al. Thrombotic complications of patients admitted to intensive care with COVID-19 at a teaching hospital in the United Kingdom. Thromb Res. 2020;191:76-7. doi: 10.1016/j.thromres.2020.04.028
3. Lodigiani C et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9-14. doi: 10.1016/j.thromres.2020.04.024
4. Llitjos JF et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients [published online ahead of print, 2020 Apr 22]. J Thromb Haemost. 2020;10.1111/jth.14869. doi: 10.1111/jth.14869
5. Carsana L et al. Pulmonary post-mortem findings in a large series of COVID-19 cases from Northern Italy. medRxiv 2020.04.19.20054262; doi: 10.1101/2020.04.19.20054262v1.
6. Menter T et al. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction [published online ahead of print, 2020 May 4]. Histopathology. 2020;10.1111/his.14134. doi: 10.1111/his.14134
7. Lax SF, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: Results from a prospective, single-center, clinicopathologic case series [published online ahead of print, 2020 May 14]. Ann Intern Med. 2020;M20-2566. doi: 10.7326/M20-2566.
A striking clinical feature of illness from SARS-CoV-2 is a marked increase in thrombotic and microvascular complications, or COVID-19–associated coagulopathy (CAC).
A new study suggests endothelial cell injury plays a major role in the pathogenesis of CAC, and blood levels of soluble thrombomodulin correlate with mortality.
George Goshua, MD, of Yale University, New Haven, Conn., presented this study as a late-breaking abstract at the virtual annual congress of the European Hematology Association.
Dr. Goshua cited past research showing CAC to be highly prevalent among hospitalized patients. Venous thromboembolism was found in 17% to 69% of patients, despite thromboprophylaxis.1-4 Arterial thrombosis has been seen in 3.6% to 4.0% of patients,1-3 and autopsy findings have shown microvascular thrombosis in as many as 87% of patients.5-7
For their study, Dr. Goshua and colleagues assessed endothelial cell damage, platelet activation, and hemostatic and fibrinolytic cascade effects of CAC.
The investigators measured markers of endothelial cell injury and platelet activation, plasminogen activation inhibitor 1 (PAI-1), and coagulation factors in stable and critically ill patients hospitalized with COVID-19. In addition, the team sought to identify biomarkers of mortality in hospitalized patients.
Dr. Goshua and colleagues studied 68 adults hospitalized for suspected COVID-19 – 48 in the ICU and 20 outside the ICU. Patients in the ICU received mechanical ventilation, while the non-ICU patients required supplemental oxygen (≤3 L/min per nasal cannula).
There were more men than women (69% vs. 31%) in the ICU population but not in the non-ICU population (40% vs. 60%). There were no statistically significant differences in age or comorbid conditions between the ICU and non-ICU patients.
Results and interpretation
Consistent with augmentation of the coagulation cascade – and as expected – D-dimer and thrombin-antithrombin levels were high in both the ICU and non-ICU populations, but levels were significantly higher (P < .001) among the ICU patients.
Endogenous anticoagulants (antithrombin and proteins C and S) and fibrinolytic enzymes (alpha 2-antiplasmin) were preserved, verifying that CAC is distinct from disseminated intravascular coagulation. Classic fibrinolysis did not occur, as PAI-1 was high in ICU and non-ICU patients, and lysis-30 was normal in nearly all ICU patients (96%).
Von Willebrand factor antigen and activity levels and factor VIII levels were markedly elevated in non-ICU and ICU patients, but they were significantly higher (P < .001) in the ICU cohort. This supports the hypothesis that endothelial cell damage and platelet activation play major roles in CAC.
Similarly, soluble P-selectin, which is shed from endothelial cells and platelets, was dramatically elevated in ICU patients in comparison with controls and non-ICU patients (P < .001 for both comparisons).
Levels of soluble thrombomodulin, which is released from endothelial cells, were not significantly different in ICU patients and controls. However, given thrombomodulin’s significant role in the coagulation cascade, Dr. Goshua and colleagues plotted receiver operating curves to see if soluble thrombomodulin levels were predictive of mortality.
The results showed that soluble thrombomodulin correlated with the probability of survival, both overall and in ICU patients. Soluble thrombomodulin levels greater than 3.26 ng/mL were associated with significantly worse survival in all patients (P = .0087) and ICU patients (P = .0309).
Influence on therapy
Laboratory perturbations were detected in both ICU and non-ICU patients, and otherwise healthy outpatients have exhibited potentially life-threatening CAC, according to Dr. Goshua.
These findings suggest the prothrombotic state occurs early in the pathogenesis of SARS-CoV-2 infection, is driven by platelet activation and endotheliopathy, and becomes more pronounced with worsening severity of infection.
The results of this study prompted a change in how Yale–New Haven Hospital manages COVID-19 patients. Patients without a clinical contraindication now receive aspirin at 81 mg daily in addition to the anticoagulation regimen typically used for all hospitalized COVID-19 patients.
Investigations regarding other medications that can influence platelet-endothelial cell interactions and modulate endothelial cell damage in CAC – such as dipyridamole, defibrotide, and eculizumab – are planned.
Challenges and unanswered questions
Virchow’s triad was described by the eminent German physician, Rudolf Virchow, MD, in the 19th century. It refers to the three broad categories of factors that can predispose patients to thrombosis — circulatory stasis, hypercoagulability, and endothelial injury.
Although all of these elements could be operative in CAC, the current study suggests platelet activation and endothelial cell injury in CAC may be of primary importance.
Because of the limited ability to test critically ill patients and concerns regarding exposure of additional hospital personnel to COVID-19 patients, the current report lacked clarity about the relationship of the detected laboratory abnormalities to confirmed thrombotic events.
It is unknown whether endothelial cells in different organs are damaged uniformly. It is also unclear if the laboratory abnormalities identified in this analysis can be used to monitor response to therapy, to guide follow-up management of discharged patients with CAC, or to identify infected outpatients who should receive prophylactic anticoagulation.
The mechanism by which SARS-CoV-2 injures endothelial cells is not explained by these data. Neutrophil defensins and other prothrombotic peptides or markers of inflammation could play key roles in pathogenesis, assessment of disease severity, or monitoring for therapeutic efficacy.
Today, we have more sophisticated diagnostic tools than Dr. Virchow had. We also have the ability to record and rapidly disseminate information globally. Still, with regard to the COVID-19 pandemic, clinicians face many of the same challenges that confronted Dr. Virchow in his era.
The analysis conducted by Dr. Goshua and colleagues goes a long way toward elucidating some of the mechanisms and therapeutic targets to meet these challenges.
Dr. Goshua disclosed no conflicts of interest.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Goshua G et al. EHA Congress. Abstract LB2605.
References
1. Klok FA et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-50. doi: 10.1016/j.thromres.2020.04.041.
2. Thomas W et al. Thrombotic complications of patients admitted to intensive care with COVID-19 at a teaching hospital in the United Kingdom. Thromb Res. 2020;191:76-7. doi: 10.1016/j.thromres.2020.04.028
3. Lodigiani C et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9-14. doi: 10.1016/j.thromres.2020.04.024
4. Llitjos JF et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients [published online ahead of print, 2020 Apr 22]. J Thromb Haemost. 2020;10.1111/jth.14869. doi: 10.1111/jth.14869
5. Carsana L et al. Pulmonary post-mortem findings in a large series of COVID-19 cases from Northern Italy. medRxiv 2020.04.19.20054262; doi: 10.1101/2020.04.19.20054262v1.
6. Menter T et al. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction [published online ahead of print, 2020 May 4]. Histopathology. 2020;10.1111/his.14134. doi: 10.1111/his.14134
7. Lax SF, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: Results from a prospective, single-center, clinicopathologic case series [published online ahead of print, 2020 May 14]. Ann Intern Med. 2020;M20-2566. doi: 10.7326/M20-2566.
A striking clinical feature of illness from SARS-CoV-2 is a marked increase in thrombotic and microvascular complications, or COVID-19–associated coagulopathy (CAC).
A new study suggests endothelial cell injury plays a major role in the pathogenesis of CAC, and blood levels of soluble thrombomodulin correlate with mortality.
George Goshua, MD, of Yale University, New Haven, Conn., presented this study as a late-breaking abstract at the virtual annual congress of the European Hematology Association.
Dr. Goshua cited past research showing CAC to be highly prevalent among hospitalized patients. Venous thromboembolism was found in 17% to 69% of patients, despite thromboprophylaxis.1-4 Arterial thrombosis has been seen in 3.6% to 4.0% of patients,1-3 and autopsy findings have shown microvascular thrombosis in as many as 87% of patients.5-7
For their study, Dr. Goshua and colleagues assessed endothelial cell damage, platelet activation, and hemostatic and fibrinolytic cascade effects of CAC.
The investigators measured markers of endothelial cell injury and platelet activation, plasminogen activation inhibitor 1 (PAI-1), and coagulation factors in stable and critically ill patients hospitalized with COVID-19. In addition, the team sought to identify biomarkers of mortality in hospitalized patients.
Dr. Goshua and colleagues studied 68 adults hospitalized for suspected COVID-19 – 48 in the ICU and 20 outside the ICU. Patients in the ICU received mechanical ventilation, while the non-ICU patients required supplemental oxygen (≤3 L/min per nasal cannula).
There were more men than women (69% vs. 31%) in the ICU population but not in the non-ICU population (40% vs. 60%). There were no statistically significant differences in age or comorbid conditions between the ICU and non-ICU patients.
Results and interpretation
Consistent with augmentation of the coagulation cascade – and as expected – D-dimer and thrombin-antithrombin levels were high in both the ICU and non-ICU populations, but levels were significantly higher (P < .001) among the ICU patients.
Endogenous anticoagulants (antithrombin and proteins C and S) and fibrinolytic enzymes (alpha 2-antiplasmin) were preserved, verifying that CAC is distinct from disseminated intravascular coagulation. Classic fibrinolysis did not occur, as PAI-1 was high in ICU and non-ICU patients, and lysis-30 was normal in nearly all ICU patients (96%).
Von Willebrand factor antigen and activity levels and factor VIII levels were markedly elevated in non-ICU and ICU patients, but they were significantly higher (P < .001) in the ICU cohort. This supports the hypothesis that endothelial cell damage and platelet activation play major roles in CAC.
Similarly, soluble P-selectin, which is shed from endothelial cells and platelets, was dramatically elevated in ICU patients in comparison with controls and non-ICU patients (P < .001 for both comparisons).
Levels of soluble thrombomodulin, which is released from endothelial cells, were not significantly different in ICU patients and controls. However, given thrombomodulin’s significant role in the coagulation cascade, Dr. Goshua and colleagues plotted receiver operating curves to see if soluble thrombomodulin levels were predictive of mortality.
The results showed that soluble thrombomodulin correlated with the probability of survival, both overall and in ICU patients. Soluble thrombomodulin levels greater than 3.26 ng/mL were associated with significantly worse survival in all patients (P = .0087) and ICU patients (P = .0309).
Influence on therapy
Laboratory perturbations were detected in both ICU and non-ICU patients, and otherwise healthy outpatients have exhibited potentially life-threatening CAC, according to Dr. Goshua.
These findings suggest the prothrombotic state occurs early in the pathogenesis of SARS-CoV-2 infection, is driven by platelet activation and endotheliopathy, and becomes more pronounced with worsening severity of infection.
The results of this study prompted a change in how Yale–New Haven Hospital manages COVID-19 patients. Patients without a clinical contraindication now receive aspirin at 81 mg daily in addition to the anticoagulation regimen typically used for all hospitalized COVID-19 patients.
Investigations regarding other medications that can influence platelet-endothelial cell interactions and modulate endothelial cell damage in CAC – such as dipyridamole, defibrotide, and eculizumab – are planned.
Challenges and unanswered questions
Virchow’s triad was described by the eminent German physician, Rudolf Virchow, MD, in the 19th century. It refers to the three broad categories of factors that can predispose patients to thrombosis — circulatory stasis, hypercoagulability, and endothelial injury.
Although all of these elements could be operative in CAC, the current study suggests platelet activation and endothelial cell injury in CAC may be of primary importance.
Because of the limited ability to test critically ill patients and concerns regarding exposure of additional hospital personnel to COVID-19 patients, the current report lacked clarity about the relationship of the detected laboratory abnormalities to confirmed thrombotic events.
It is unknown whether endothelial cells in different organs are damaged uniformly. It is also unclear if the laboratory abnormalities identified in this analysis can be used to monitor response to therapy, to guide follow-up management of discharged patients with CAC, or to identify infected outpatients who should receive prophylactic anticoagulation.
The mechanism by which SARS-CoV-2 injures endothelial cells is not explained by these data. Neutrophil defensins and other prothrombotic peptides or markers of inflammation could play key roles in pathogenesis, assessment of disease severity, or monitoring for therapeutic efficacy.
Today, we have more sophisticated diagnostic tools than Dr. Virchow had. We also have the ability to record and rapidly disseminate information globally. Still, with regard to the COVID-19 pandemic, clinicians face many of the same challenges that confronted Dr. Virchow in his era.
The analysis conducted by Dr. Goshua and colleagues goes a long way toward elucidating some of the mechanisms and therapeutic targets to meet these challenges.
Dr. Goshua disclosed no conflicts of interest.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Goshua G et al. EHA Congress. Abstract LB2605.
References
1. Klok FA et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-50. doi: 10.1016/j.thromres.2020.04.041.
2. Thomas W et al. Thrombotic complications of patients admitted to intensive care with COVID-19 at a teaching hospital in the United Kingdom. Thromb Res. 2020;191:76-7. doi: 10.1016/j.thromres.2020.04.028
3. Lodigiani C et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9-14. doi: 10.1016/j.thromres.2020.04.024
4. Llitjos JF et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients [published online ahead of print, 2020 Apr 22]. J Thromb Haemost. 2020;10.1111/jth.14869. doi: 10.1111/jth.14869
5. Carsana L et al. Pulmonary post-mortem findings in a large series of COVID-19 cases from Northern Italy. medRxiv 2020.04.19.20054262; doi: 10.1101/2020.04.19.20054262v1.
6. Menter T et al. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction [published online ahead of print, 2020 May 4]. Histopathology. 2020;10.1111/his.14134. doi: 10.1111/his.14134
7. Lax SF, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: Results from a prospective, single-center, clinicopathologic case series [published online ahead of print, 2020 May 14]. Ann Intern Med. 2020;M20-2566. doi: 10.7326/M20-2566.
FROM EHA CONGRESS