User login
Summer is over, more health care changes are afoot
CMS has released its proposed rule (see related articles and a commentary) and included changes as substantial as I have seen in the last two decades. Additionally, the Affordable Care Act has been under continued attack despite its majority support from our citizenry. Loss of the individual mandate, allowance of “skinny” health plans, a rewrite of association plan rules, elimination of cost-sharing reductions and premium support – all have contributed to a shifting away from socialized medical costs and toward a system of individual responsibility for health. Depending on one’s political philosophy (and income), that may be bad or good.
Our article list this month will be interesting to many. The AGA produced a Clinical Practice Update about tumor seeding with endoscopic procedures. This should give us pause and make us reconsider our endoscopic practices. My wife (an endoscopy nurse in Minneapolis) has been asking for years whether pulling a PEG tube past an esophageal cancer might cause tumor seeding, and physicians have reassured her that there is no cause for worry. Turns out she was right (as usual). Deaths from liver disease in the U.S. have seen a dramatic increase since 1999, driven substantially by increasing alcohol use. Fecal transplants in irritable bowel syndrome? Possibly helpful, as reported in an article from Digestive Disease Week.®
As summer comes to an end, we head into a tumultuous fall that will be dominated by November elections.
John I. Allen, MD, MBA, AGAF
Editor in Chief
CMS has released its proposed rule (see related articles and a commentary) and included changes as substantial as I have seen in the last two decades. Additionally, the Affordable Care Act has been under continued attack despite its majority support from our citizenry. Loss of the individual mandate, allowance of “skinny” health plans, a rewrite of association plan rules, elimination of cost-sharing reductions and premium support – all have contributed to a shifting away from socialized medical costs and toward a system of individual responsibility for health. Depending on one’s political philosophy (and income), that may be bad or good.
Our article list this month will be interesting to many. The AGA produced a Clinical Practice Update about tumor seeding with endoscopic procedures. This should give us pause and make us reconsider our endoscopic practices. My wife (an endoscopy nurse in Minneapolis) has been asking for years whether pulling a PEG tube past an esophageal cancer might cause tumor seeding, and physicians have reassured her that there is no cause for worry. Turns out she was right (as usual). Deaths from liver disease in the U.S. have seen a dramatic increase since 1999, driven substantially by increasing alcohol use. Fecal transplants in irritable bowel syndrome? Possibly helpful, as reported in an article from Digestive Disease Week.®
As summer comes to an end, we head into a tumultuous fall that will be dominated by November elections.
John I. Allen, MD, MBA, AGAF
Editor in Chief
CMS has released its proposed rule (see related articles and a commentary) and included changes as substantial as I have seen in the last two decades. Additionally, the Affordable Care Act has been under continued attack despite its majority support from our citizenry. Loss of the individual mandate, allowance of “skinny” health plans, a rewrite of association plan rules, elimination of cost-sharing reductions and premium support – all have contributed to a shifting away from socialized medical costs and toward a system of individual responsibility for health. Depending on one’s political philosophy (and income), that may be bad or good.
Our article list this month will be interesting to many. The AGA produced a Clinical Practice Update about tumor seeding with endoscopic procedures. This should give us pause and make us reconsider our endoscopic practices. My wife (an endoscopy nurse in Minneapolis) has been asking for years whether pulling a PEG tube past an esophageal cancer might cause tumor seeding, and physicians have reassured her that there is no cause for worry. Turns out she was right (as usual). Deaths from liver disease in the U.S. have seen a dramatic increase since 1999, driven substantially by increasing alcohol use. Fecal transplants in irritable bowel syndrome? Possibly helpful, as reported in an article from Digestive Disease Week.®
As summer comes to an end, we head into a tumultuous fall that will be dominated by November elections.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Sometimes talk is useless
“Alex, I understand that you are upset that you left your little bulldozer at home. Let’s try to think of something else you can play with here at the restaurant that is kind of like a bulldozer.”
Sounds like a reasonable strategy to calm an unruly preschooler, and it might have been had it not been the fifth attempt in a 45-minute dialogue between a mother and her overtired, misbehaving 3-year-old. There had been a lot of “I understand how you feel” and “use your words” woven into a gag-worthy and futile effort to forge a collaborative parent-child solution to the problem of an exhausted preschooler who is up past his bedtime in a public place.
My wife and I enjoy a night out with friends and prefer a quiet dining atmosphere. However, some evenings we eat earlier and choose a restaurant we know appeals to families with young children. At those meals, we anticipate being serenaded by a loud background buzz punctuated by the occasional shriek or short bout of crying. We expect a degree of childish behavior to come with the territory, and watching the dramas unfold brings back fond “been there, done that” memories. But, listening to those behaviors being horribly mismanaged can ruin even the most tolerant adult’s appetite in less time than it takes a parent to say, “I can see you’re unhappy, and we need to talk about why.”
In an op-ed piece, a psychotherapist asks the legitimate question, and provides the correct quick answer (“Which Is Better, Rewards or Punishments? Neither,” New York Times, Aug. 21, 2018). I couldn’t agree more. In my experience, rewards have a very short half-life and can become disastrously inflationary in the blink of an eye. On the other hand, punishments can be either too heavy-handed or so irrational that the child fails to make a logical connection between his misbehavior and his sentence.
Unfortunately, many child behavior advisers, including the op-ed author, offer alternatives to rewards and punishment that are unworkable in real-world circumstances, such as the restaurant scenario my wife and I endured.
While it sounds very democratic to ask a 3-year-old why he is misbehaving, more often than not it should be the parent who is asking what he or she could have done differently to avoid the situation. It is likely the child has been allowed to become overtired and/or the parent may be in denial about his/her child’s intolerance for stimulating environments.
Too often the parent takes too long to realize that the water is spilling over the dam and it is time to head for shore. Children who are overtired and having a tantrum can’t participate in a rational discussion about their feelings. If that dialogue needs to happen, and that is seldom, it should be the next day after the parent has time to consider his or her own mistakes.
When it comes to managing misbehaving children, I prefer well-tailored consequences and my favorite is a humanely crafted time-out. When presented and executed properly, a time-out can break the cycle of misbehavior and give both parent and child a chance to reconsider their positions.
But at 7 p.m. on a Friday evening in a busy restaurant, neither a time-out nor philosophizing with a 3-year-old is going to work. It’s time to ask for the check and head home to bed.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
“Alex, I understand that you are upset that you left your little bulldozer at home. Let’s try to think of something else you can play with here at the restaurant that is kind of like a bulldozer.”
Sounds like a reasonable strategy to calm an unruly preschooler, and it might have been had it not been the fifth attempt in a 45-minute dialogue between a mother and her overtired, misbehaving 3-year-old. There had been a lot of “I understand how you feel” and “use your words” woven into a gag-worthy and futile effort to forge a collaborative parent-child solution to the problem of an exhausted preschooler who is up past his bedtime in a public place.
My wife and I enjoy a night out with friends and prefer a quiet dining atmosphere. However, some evenings we eat earlier and choose a restaurant we know appeals to families with young children. At those meals, we anticipate being serenaded by a loud background buzz punctuated by the occasional shriek or short bout of crying. We expect a degree of childish behavior to come with the territory, and watching the dramas unfold brings back fond “been there, done that” memories. But, listening to those behaviors being horribly mismanaged can ruin even the most tolerant adult’s appetite in less time than it takes a parent to say, “I can see you’re unhappy, and we need to talk about why.”
In an op-ed piece, a psychotherapist asks the legitimate question, and provides the correct quick answer (“Which Is Better, Rewards or Punishments? Neither,” New York Times, Aug. 21, 2018). I couldn’t agree more. In my experience, rewards have a very short half-life and can become disastrously inflationary in the blink of an eye. On the other hand, punishments can be either too heavy-handed or so irrational that the child fails to make a logical connection between his misbehavior and his sentence.
Unfortunately, many child behavior advisers, including the op-ed author, offer alternatives to rewards and punishment that are unworkable in real-world circumstances, such as the restaurant scenario my wife and I endured.
While it sounds very democratic to ask a 3-year-old why he is misbehaving, more often than not it should be the parent who is asking what he or she could have done differently to avoid the situation. It is likely the child has been allowed to become overtired and/or the parent may be in denial about his/her child’s intolerance for stimulating environments.
Too often the parent takes too long to realize that the water is spilling over the dam and it is time to head for shore. Children who are overtired and having a tantrum can’t participate in a rational discussion about their feelings. If that dialogue needs to happen, and that is seldom, it should be the next day after the parent has time to consider his or her own mistakes.
When it comes to managing misbehaving children, I prefer well-tailored consequences and my favorite is a humanely crafted time-out. When presented and executed properly, a time-out can break the cycle of misbehavior and give both parent and child a chance to reconsider their positions.
But at 7 p.m. on a Friday evening in a busy restaurant, neither a time-out nor philosophizing with a 3-year-old is going to work. It’s time to ask for the check and head home to bed.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
“Alex, I understand that you are upset that you left your little bulldozer at home. Let’s try to think of something else you can play with here at the restaurant that is kind of like a bulldozer.”
Sounds like a reasonable strategy to calm an unruly preschooler, and it might have been had it not been the fifth attempt in a 45-minute dialogue between a mother and her overtired, misbehaving 3-year-old. There had been a lot of “I understand how you feel” and “use your words” woven into a gag-worthy and futile effort to forge a collaborative parent-child solution to the problem of an exhausted preschooler who is up past his bedtime in a public place.
My wife and I enjoy a night out with friends and prefer a quiet dining atmosphere. However, some evenings we eat earlier and choose a restaurant we know appeals to families with young children. At those meals, we anticipate being serenaded by a loud background buzz punctuated by the occasional shriek or short bout of crying. We expect a degree of childish behavior to come with the territory, and watching the dramas unfold brings back fond “been there, done that” memories. But, listening to those behaviors being horribly mismanaged can ruin even the most tolerant adult’s appetite in less time than it takes a parent to say, “I can see you’re unhappy, and we need to talk about why.”
In an op-ed piece, a psychotherapist asks the legitimate question, and provides the correct quick answer (“Which Is Better, Rewards or Punishments? Neither,” New York Times, Aug. 21, 2018). I couldn’t agree more. In my experience, rewards have a very short half-life and can become disastrously inflationary in the blink of an eye. On the other hand, punishments can be either too heavy-handed or so irrational that the child fails to make a logical connection between his misbehavior and his sentence.
Unfortunately, many child behavior advisers, including the op-ed author, offer alternatives to rewards and punishment that are unworkable in real-world circumstances, such as the restaurant scenario my wife and I endured.
While it sounds very democratic to ask a 3-year-old why he is misbehaving, more often than not it should be the parent who is asking what he or she could have done differently to avoid the situation. It is likely the child has been allowed to become overtired and/or the parent may be in denial about his/her child’s intolerance for stimulating environments.
Too often the parent takes too long to realize that the water is spilling over the dam and it is time to head for shore. Children who are overtired and having a tantrum can’t participate in a rational discussion about their feelings. If that dialogue needs to happen, and that is seldom, it should be the next day after the parent has time to consider his or her own mistakes.
When it comes to managing misbehaving children, I prefer well-tailored consequences and my favorite is a humanely crafted time-out. When presented and executed properly, a time-out can break the cycle of misbehavior and give both parent and child a chance to reconsider their positions.
But at 7 p.m. on a Friday evening in a busy restaurant, neither a time-out nor philosophizing with a 3-year-old is going to work. It’s time to ask for the check and head home to bed.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Artificial Intelligence for Clinical Decision Support
There is abundant research being conducted on the use of artificial intelligence (AI) to improve diagnosis in dermatology. Recently, convolutional neural networks trained using large image libraries have achieved parity with dermatologists in discriminating between benign and malignant lesions.1 There are expectations that these systems, as they improve and are implemented in mobile electronic devices, will revolutionize diagnosis. Substantially less attention has been given to the use of AI to guide management options following a diagnosis. There are several reasons this area lends itself to the application of AI.
In 2015, the National Library of Medicine indexed more than 800,000 articles.2 Medical literature is growing at an overwhelming pace that makes it challenging for health care professionals to read, retain, and appropriately implement the latest research into their care. One survey found that physicians spend no more than 4 hours per week reading medical journals, and for the majority of articles, only the abstracts are read.3 Conversely, AI networks today are able to interpret millions of pages of data within seconds. It is worth investigating how AI can be used to improve treatment and management decisions made by physicians.
Cognitive computing is a modern approach to AI that incorporates natural language processing, machine learning, and other techniques to answer questions. One cognitive computing system developed by IBM research in 2007, Watson, can interpret a user’s query using natural language processing and then generate hypotheses. It searches data sources extensively to find and score evidence for each candidate hypothesis.4 This information is synthesized to provide a simple output: ranked answers with associated confidence scores. Machine learning is used to improve the answers with feedback, training, and repetition.4,5
Watson Oncology, an ongoing collaboration between IBM and Memorial Sloan Kettering Cancer Center, is an application of cognitive computing to medicine. At Memorial Sloan Kettering, Watson has been trained by expert clinicians to provide an individualized, evidence-based list of therapeutic options for oncologists and patients to discuss. Furthermore, Watson is capable of taking patient preferences into consideration.4
In the near future, there also may be a role that cognitive computing could play in aiding dermatologists. Dermatologists manage a multitude of conditions requiring systemic therapies such as chemotherapeutics, biologics, and immunosuppressant medications. Frequently, the patient population has a complicated medical history with multiple comorbidities. Although current electronic health record (EHR) systems are able to assist physicians with structured numerical data such as vitals and laboratory results, cognitive computing systems could interpret the natural language of journal articles, textbooks, and published guidelines, as well as the narrative components of EHR notes. Outcomes from similar patients also could be used as inputs. With enough data, cognitive computing systems may be able to identify associations and epidemiologic trends that would not otherwise be noticed. As described by Miotto et al,6 one system, “deep patient,” was able to accurately predict the development of schizophrenia, diabetes mellitus, and various cancers based on EHR data. Patient genetic information also could one day be used to generate new insights into pharmacogenomics.
The benefit of a cognitive computing decision support system is that ineffective treatments and adverse reactions could be minimized, which may improve outcomes and reduce costs. Artificial intelligence also could help to decrease work burden so that physicians can spend more time with their patients, resulting in improved patient satisfaction and overall increased access to the specialty.
As with other clinical decision support systems, a number of challenges exist with the integration of cognitive computing into real care. One obstacle unique to machine learning algorithms is the black box problem. For instance, the skin lesion–identifying neural network cannot be questioned to determine which factors it used to arrive at its diagnosis. This shortcoming can lead to dangerous situations, such as the one reported by Caruana et al.7 A predictive model classified patients with pneumonia and a history of asthma as having a lower mortality risk than those with pneumonia alone because the model was unable to recognize the confounder that asthmatic patients were preemptively admitted to the intensive care unit and treated more aggressively, which is another reason that AI recommendations must always be evaluated by a physician.7 Physician and patient input also will be integral to incorporate contextual and qualitative information that may not be accessible to computers.8
As cognitive computing decision support systems are primarily used in oncology, they will need to be adjusted to optimize them for dermatologic conditions. It also will be up to health care providers to benchmark the performance of these systems.
Current clinical decision support systems that do not use AI have struggled to improve major patient outcomes such as mortality. These systems have been hobbled by poor usability and human-computer integration. Clinicians find their alerts and warnings to be a nuisance. The adoption of cognitive computing systems has the potential to give clinicians an intelligent partner. Their natural language processing, ability to comprehend questions, and easily understandable output give them an inherent ease of use that simplifies interactions with clinicians. Rather than replacing physicians, these systems will free clinicians to spend more of their time on the components of care that only a human can provide.
- Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542:115-118.
- The National Library of Medicine fact sheet. U.S. National Library of Medicine website https://www.nlm.nih.gov/pubs/factsheets/nlm.html. Updated October 20, 2016. Accessed June 18, 2018.
- Saint S, Christakis DA, Saha S, et al. Journal reading habits of internists. J Gen Intern Med. 2000;15:881-884.
- Kelly JE III, Hamm S. Smart Machines: IBM’s Watson and the Era of Cognitive Computing. New York, NY: Columbia University Press; 2013.
- Ferrucci D, Levas A, Bagchi S, et al. Watson: beyond Jeopardy! Artificial Intelligence. 2013;199:93-105.
- Miotto R, Li L, Kidd BA, et al. Deep patient: an unsupervised representation to predict the future of patients from the electronic health records. Sci Rep. 2016;6:26094.
- Caruana R, Lou Y, Gehrke J, et al. Intelligible models for healthcare: predicting pneumonia risk and hospital 30-day readmission. Paper presented at: 21st ACM SIGKDD International Conference on Knowledge Discovery and Data Mining 2015; August 10-13, 2015; Sydney, Australia.
- Verghese A, Shah NH, Harrington RA. What this computer needs is a physician: humanism and artificial intelligence. JAMA. 2018;319:19-20.
There is abundant research being conducted on the use of artificial intelligence (AI) to improve diagnosis in dermatology. Recently, convolutional neural networks trained using large image libraries have achieved parity with dermatologists in discriminating between benign and malignant lesions.1 There are expectations that these systems, as they improve and are implemented in mobile electronic devices, will revolutionize diagnosis. Substantially less attention has been given to the use of AI to guide management options following a diagnosis. There are several reasons this area lends itself to the application of AI.
In 2015, the National Library of Medicine indexed more than 800,000 articles.2 Medical literature is growing at an overwhelming pace that makes it challenging for health care professionals to read, retain, and appropriately implement the latest research into their care. One survey found that physicians spend no more than 4 hours per week reading medical journals, and for the majority of articles, only the abstracts are read.3 Conversely, AI networks today are able to interpret millions of pages of data within seconds. It is worth investigating how AI can be used to improve treatment and management decisions made by physicians.
Cognitive computing is a modern approach to AI that incorporates natural language processing, machine learning, and other techniques to answer questions. One cognitive computing system developed by IBM research in 2007, Watson, can interpret a user’s query using natural language processing and then generate hypotheses. It searches data sources extensively to find and score evidence for each candidate hypothesis.4 This information is synthesized to provide a simple output: ranked answers with associated confidence scores. Machine learning is used to improve the answers with feedback, training, and repetition.4,5
Watson Oncology, an ongoing collaboration between IBM and Memorial Sloan Kettering Cancer Center, is an application of cognitive computing to medicine. At Memorial Sloan Kettering, Watson has been trained by expert clinicians to provide an individualized, evidence-based list of therapeutic options for oncologists and patients to discuss. Furthermore, Watson is capable of taking patient preferences into consideration.4
In the near future, there also may be a role that cognitive computing could play in aiding dermatologists. Dermatologists manage a multitude of conditions requiring systemic therapies such as chemotherapeutics, biologics, and immunosuppressant medications. Frequently, the patient population has a complicated medical history with multiple comorbidities. Although current electronic health record (EHR) systems are able to assist physicians with structured numerical data such as vitals and laboratory results, cognitive computing systems could interpret the natural language of journal articles, textbooks, and published guidelines, as well as the narrative components of EHR notes. Outcomes from similar patients also could be used as inputs. With enough data, cognitive computing systems may be able to identify associations and epidemiologic trends that would not otherwise be noticed. As described by Miotto et al,6 one system, “deep patient,” was able to accurately predict the development of schizophrenia, diabetes mellitus, and various cancers based on EHR data. Patient genetic information also could one day be used to generate new insights into pharmacogenomics.
The benefit of a cognitive computing decision support system is that ineffective treatments and adverse reactions could be minimized, which may improve outcomes and reduce costs. Artificial intelligence also could help to decrease work burden so that physicians can spend more time with their patients, resulting in improved patient satisfaction and overall increased access to the specialty.
As with other clinical decision support systems, a number of challenges exist with the integration of cognitive computing into real care. One obstacle unique to machine learning algorithms is the black box problem. For instance, the skin lesion–identifying neural network cannot be questioned to determine which factors it used to arrive at its diagnosis. This shortcoming can lead to dangerous situations, such as the one reported by Caruana et al.7 A predictive model classified patients with pneumonia and a history of asthma as having a lower mortality risk than those with pneumonia alone because the model was unable to recognize the confounder that asthmatic patients were preemptively admitted to the intensive care unit and treated more aggressively, which is another reason that AI recommendations must always be evaluated by a physician.7 Physician and patient input also will be integral to incorporate contextual and qualitative information that may not be accessible to computers.8
As cognitive computing decision support systems are primarily used in oncology, they will need to be adjusted to optimize them for dermatologic conditions. It also will be up to health care providers to benchmark the performance of these systems.
Current clinical decision support systems that do not use AI have struggled to improve major patient outcomes such as mortality. These systems have been hobbled by poor usability and human-computer integration. Clinicians find their alerts and warnings to be a nuisance. The adoption of cognitive computing systems has the potential to give clinicians an intelligent partner. Their natural language processing, ability to comprehend questions, and easily understandable output give them an inherent ease of use that simplifies interactions with clinicians. Rather than replacing physicians, these systems will free clinicians to spend more of their time on the components of care that only a human can provide.
There is abundant research being conducted on the use of artificial intelligence (AI) to improve diagnosis in dermatology. Recently, convolutional neural networks trained using large image libraries have achieved parity with dermatologists in discriminating between benign and malignant lesions.1 There are expectations that these systems, as they improve and are implemented in mobile electronic devices, will revolutionize diagnosis. Substantially less attention has been given to the use of AI to guide management options following a diagnosis. There are several reasons this area lends itself to the application of AI.
In 2015, the National Library of Medicine indexed more than 800,000 articles.2 Medical literature is growing at an overwhelming pace that makes it challenging for health care professionals to read, retain, and appropriately implement the latest research into their care. One survey found that physicians spend no more than 4 hours per week reading medical journals, and for the majority of articles, only the abstracts are read.3 Conversely, AI networks today are able to interpret millions of pages of data within seconds. It is worth investigating how AI can be used to improve treatment and management decisions made by physicians.
Cognitive computing is a modern approach to AI that incorporates natural language processing, machine learning, and other techniques to answer questions. One cognitive computing system developed by IBM research in 2007, Watson, can interpret a user’s query using natural language processing and then generate hypotheses. It searches data sources extensively to find and score evidence for each candidate hypothesis.4 This information is synthesized to provide a simple output: ranked answers with associated confidence scores. Machine learning is used to improve the answers with feedback, training, and repetition.4,5
Watson Oncology, an ongoing collaboration between IBM and Memorial Sloan Kettering Cancer Center, is an application of cognitive computing to medicine. At Memorial Sloan Kettering, Watson has been trained by expert clinicians to provide an individualized, evidence-based list of therapeutic options for oncologists and patients to discuss. Furthermore, Watson is capable of taking patient preferences into consideration.4
In the near future, there also may be a role that cognitive computing could play in aiding dermatologists. Dermatologists manage a multitude of conditions requiring systemic therapies such as chemotherapeutics, biologics, and immunosuppressant medications. Frequently, the patient population has a complicated medical history with multiple comorbidities. Although current electronic health record (EHR) systems are able to assist physicians with structured numerical data such as vitals and laboratory results, cognitive computing systems could interpret the natural language of journal articles, textbooks, and published guidelines, as well as the narrative components of EHR notes. Outcomes from similar patients also could be used as inputs. With enough data, cognitive computing systems may be able to identify associations and epidemiologic trends that would not otherwise be noticed. As described by Miotto et al,6 one system, “deep patient,” was able to accurately predict the development of schizophrenia, diabetes mellitus, and various cancers based on EHR data. Patient genetic information also could one day be used to generate new insights into pharmacogenomics.
The benefit of a cognitive computing decision support system is that ineffective treatments and adverse reactions could be minimized, which may improve outcomes and reduce costs. Artificial intelligence also could help to decrease work burden so that physicians can spend more time with their patients, resulting in improved patient satisfaction and overall increased access to the specialty.
As with other clinical decision support systems, a number of challenges exist with the integration of cognitive computing into real care. One obstacle unique to machine learning algorithms is the black box problem. For instance, the skin lesion–identifying neural network cannot be questioned to determine which factors it used to arrive at its diagnosis. This shortcoming can lead to dangerous situations, such as the one reported by Caruana et al.7 A predictive model classified patients with pneumonia and a history of asthma as having a lower mortality risk than those with pneumonia alone because the model was unable to recognize the confounder that asthmatic patients were preemptively admitted to the intensive care unit and treated more aggressively, which is another reason that AI recommendations must always be evaluated by a physician.7 Physician and patient input also will be integral to incorporate contextual and qualitative information that may not be accessible to computers.8
As cognitive computing decision support systems are primarily used in oncology, they will need to be adjusted to optimize them for dermatologic conditions. It also will be up to health care providers to benchmark the performance of these systems.
Current clinical decision support systems that do not use AI have struggled to improve major patient outcomes such as mortality. These systems have been hobbled by poor usability and human-computer integration. Clinicians find their alerts and warnings to be a nuisance. The adoption of cognitive computing systems has the potential to give clinicians an intelligent partner. Their natural language processing, ability to comprehend questions, and easily understandable output give them an inherent ease of use that simplifies interactions with clinicians. Rather than replacing physicians, these systems will free clinicians to spend more of their time on the components of care that only a human can provide.
- Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542:115-118.
- The National Library of Medicine fact sheet. U.S. National Library of Medicine website https://www.nlm.nih.gov/pubs/factsheets/nlm.html. Updated October 20, 2016. Accessed June 18, 2018.
- Saint S, Christakis DA, Saha S, et al. Journal reading habits of internists. J Gen Intern Med. 2000;15:881-884.
- Kelly JE III, Hamm S. Smart Machines: IBM’s Watson and the Era of Cognitive Computing. New York, NY: Columbia University Press; 2013.
- Ferrucci D, Levas A, Bagchi S, et al. Watson: beyond Jeopardy! Artificial Intelligence. 2013;199:93-105.
- Miotto R, Li L, Kidd BA, et al. Deep patient: an unsupervised representation to predict the future of patients from the electronic health records. Sci Rep. 2016;6:26094.
- Caruana R, Lou Y, Gehrke J, et al. Intelligible models for healthcare: predicting pneumonia risk and hospital 30-day readmission. Paper presented at: 21st ACM SIGKDD International Conference on Knowledge Discovery and Data Mining 2015; August 10-13, 2015; Sydney, Australia.
- Verghese A, Shah NH, Harrington RA. What this computer needs is a physician: humanism and artificial intelligence. JAMA. 2018;319:19-20.
- Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542:115-118.
- The National Library of Medicine fact sheet. U.S. National Library of Medicine website https://www.nlm.nih.gov/pubs/factsheets/nlm.html. Updated October 20, 2016. Accessed June 18, 2018.
- Saint S, Christakis DA, Saha S, et al. Journal reading habits of internists. J Gen Intern Med. 2000;15:881-884.
- Kelly JE III, Hamm S. Smart Machines: IBM’s Watson and the Era of Cognitive Computing. New York, NY: Columbia University Press; 2013.
- Ferrucci D, Levas A, Bagchi S, et al. Watson: beyond Jeopardy! Artificial Intelligence. 2013;199:93-105.
- Miotto R, Li L, Kidd BA, et al. Deep patient: an unsupervised representation to predict the future of patients from the electronic health records. Sci Rep. 2016;6:26094.
- Caruana R, Lou Y, Gehrke J, et al. Intelligible models for healthcare: predicting pneumonia risk and hospital 30-day readmission. Paper presented at: 21st ACM SIGKDD International Conference on Knowledge Discovery and Data Mining 2015; August 10-13, 2015; Sydney, Australia.
- Verghese A, Shah NH, Harrington RA. What this computer needs is a physician: humanism and artificial intelligence. JAMA. 2018;319:19-20.
Outcomes Associated With Shorter Wait Times at a County Hospital Outpatient Dermatology Clinic
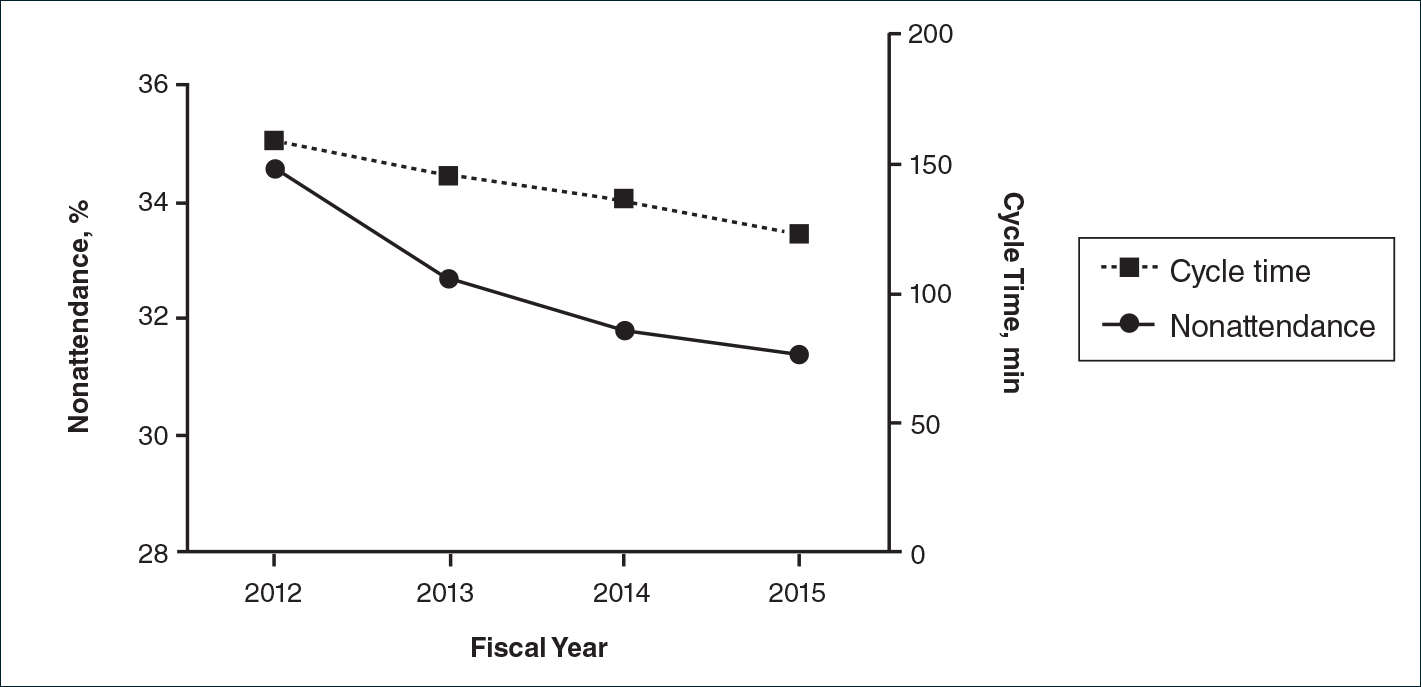
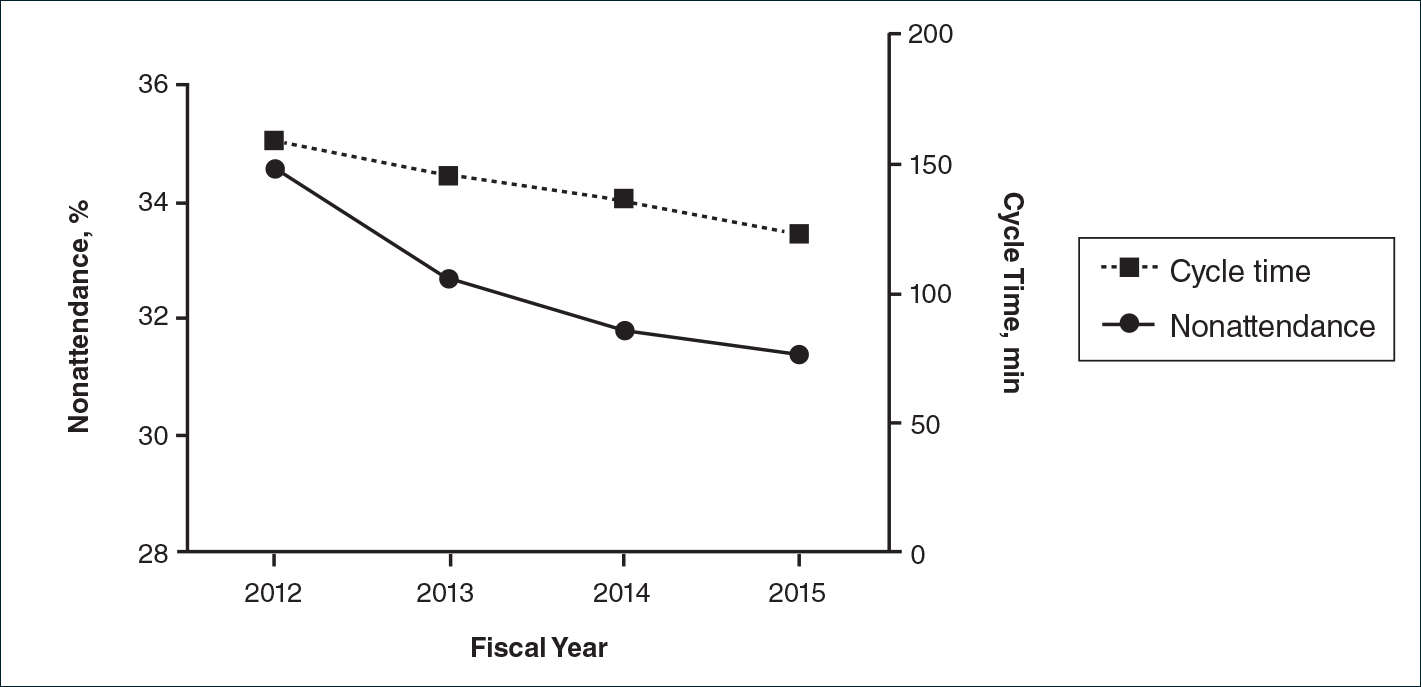
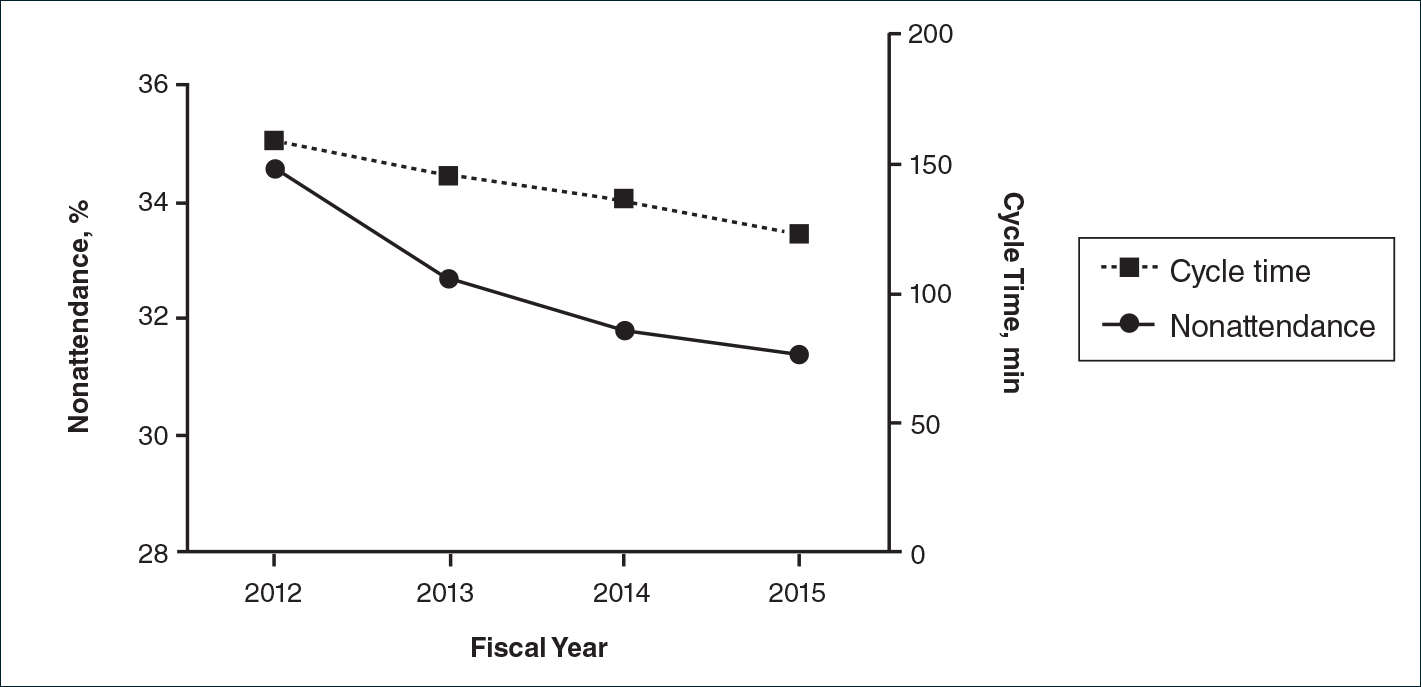
Maximizing productivity is prudent for outpatient subspecialty clinics to improve access to care. The outpatient dermatology clinic at Parkland Health and Hospital System in Dallas, Texas, which is a safety-net hospital in Dallas County, decreased wait times for new patients (from 377 to 48 days) and follow-up patients (from 95 to 34 days) from May 2012 to September 2015.1 Changes in clinic productivity measures that occur with decreased wait times are not well characterized; therefore, we sought to address this knowledge gap. We propose that decreased wait times are associated with improvement in additional clinic productivity measures, specifically decreases in nonattendance and cycle times (defined as time between patient check-in and discharge) as well as increases in referrals.
In our retrospective cohort study of patients seen in the Parkland outpatient dermatology clinic between fiscal year (FY) 2012 and FY 2015 (between October 2011 and September 2015), we collected data on patient nonattendance rates, cycle times, and referral volumes. Categorical variables were compared using χ2 tests, and changes in cycle times were analyzed using 2-way analysis of variance. P<.05 was considered statistically significant.
There were 52,775 scheduled clinic visits from FY 2012 to FY 2015. The overall proportion of patient nonattendance rates decreased from 34.6% (4202/12,141) to 31.4% (4429/14,119)(P<.001)(Figure), despite an increase in completed patient visits during the study period (7939 vs 9690). New patient nonattendance rates decreased from 42.9% (1831/4269) to 30.2% (1474/4874)(P<.001). The number of completed visits for new patients increased from 2438 in FY 2012 to 3400 in FY 2015. Follow-up nonattendance rates increased from 30.1% (2371/7872) to 32.0% (2955/9245)(P<.001). Follow-up completed visits increased from 5501 in FY 2012 to 6290 in FY 2015. Overall, average cycle time showed a trend to decrease from 159 to 123 minutes (22.6%)(Figure). Average cycle times were reduced from 159 to 128 minutes (19.5%) for new patients and from 161 to 115 minutes (28.6%) for follow-up patients (P=.02). Overall, referrals increased by 14.1% (816/5799)(P<.001), which was largely due to the increase in volume of referrals observed between FY 2014 (n=5770) and FY 2015 (n=6615).
We have demonstrated that decreased wait times can be associated with improvements in clinic productivity measures, namely decreased nonattendance rates and cycle times and increased referrals. Patient nonattendance is a burden on clinic resources and has been described in the dermatology clinic setting.2-6 Increased likelihood of nonattendance has been associated with prolonged wait times.3,7 We propose that decreased wait times can lead to diminished nonattendance rates, as patients are more likely to keep their appointments rather than seek other providers for dermatologic care. The difference in trends between new patient and follow-up nonattendance rates may be attributed to the larger relative increase in completed new patient visits compared to follow-ups during the study period.
Furthermore, the decrease in average cycle time reflected our clinic’s ability to see a larger number of patients per clinic, with subsequently shorter wait times. The greater reduction in cycle times for follow-up patients may be attributed to the increased continuity of providers who had previously seen these patients. Although the cycle times may seem high in our clinic compared to other practice settings, we believe that this marker of productivity is widely applicable to various clinic settings, including private practices and other outpatient specialty clinics. Increased clinic referrals can be a downstream effect of decreased wait times due to improvements in access to care, as shown in other specialty clinics.8 Effects of confounding variables on referral volumes, including nationwide health insurance changes during our study period, could not be ruled out.
Limitations of this study include unavailable data on patient and provider satisfaction and changes in patients’ health insurance. This study provides evidence of changes in clinical productivity measures associated with decreased wait times that can demonstrate widespread benefits to the health system.
Acknowledgments
The authors would like to thank Michael Estabrooks, RN, and Trung Vu for providing aggregate data, as well as Linda Hynan, PhD, for statistical advice (all Dallas, Texas).
- O’Brien JC, Chong BF. Reducing outpatient dermatology clinic wait times in a safety net health system in Dallas, Texas. J Am Acad Dermatol. 2016;75:631-632.
- Canizares MJ, Penneys NS. The incidence of nonattendance at an urgent care dermatology clinic. J Am Acad Dermatol. 2002;46:457-459.
- Cohen AD, Dreiher J, Vardy DA, et al. Nonattendance in a dermatology clinic—a large sample analysis. J Eur Acad Dermatol Venereol. 2008;22:1178-1183.
- Resneck JS Jr, Lipton S, Pletcher MJ. Short wait times for patients seeking cosmetic botulinum toxin appointments with dermatologists. J Am Acad Dermatol. 2007;57:985-989.
- Tsang MW, Resneck JS Jr. Even patients with changing moles face long dermatology appointment wait-times: a study of simulated patient calls to dermatologists. J Am Acad Dermatol. 2006;55:54-58.
- Rosenbach M, Kagan S, Leventhal S. Dermatology urgent care clinic: a survey of referring physician satisfaction. J Am Acad Dermatol. 2013;69:1067-1069.e1.
- Dickey W, Morrow JI. Can outpatient non-attendance be predicted from the referral letter? an audit of default at neurology clinics. J R Soc Med. 1991;8:662-663.
- Bungard TJ, Smigorowsky MJ, Lalonde LD, et al. Cardiac EASE (Ensuring Access and Speedy Evaluation)—the impact of a single-point-of-entry multidisciplinary outpatient cardiology consultation program on wait times in Canada. Can J Cardiol. 2009;25:697-702.
Maximizing productivity is prudent for outpatient subspecialty clinics to improve access to care. The outpatient dermatology clinic at Parkland Health and Hospital System in Dallas, Texas, which is a safety-net hospital in Dallas County, decreased wait times for new patients (from 377 to 48 days) and follow-up patients (from 95 to 34 days) from May 2012 to September 2015.1 Changes in clinic productivity measures that occur with decreased wait times are not well characterized; therefore, we sought to address this knowledge gap. We propose that decreased wait times are associated with improvement in additional clinic productivity measures, specifically decreases in nonattendance and cycle times (defined as time between patient check-in and discharge) as well as increases in referrals.
In our retrospective cohort study of patients seen in the Parkland outpatient dermatology clinic between fiscal year (FY) 2012 and FY 2015 (between October 2011 and September 2015), we collected data on patient nonattendance rates, cycle times, and referral volumes. Categorical variables were compared using χ2 tests, and changes in cycle times were analyzed using 2-way analysis of variance. P<.05 was considered statistically significant.
There were 52,775 scheduled clinic visits from FY 2012 to FY 2015. The overall proportion of patient nonattendance rates decreased from 34.6% (4202/12,141) to 31.4% (4429/14,119)(P<.001)(Figure), despite an increase in completed patient visits during the study period (7939 vs 9690). New patient nonattendance rates decreased from 42.9% (1831/4269) to 30.2% (1474/4874)(P<.001). The number of completed visits for new patients increased from 2438 in FY 2012 to 3400 in FY 2015. Follow-up nonattendance rates increased from 30.1% (2371/7872) to 32.0% (2955/9245)(P<.001). Follow-up completed visits increased from 5501 in FY 2012 to 6290 in FY 2015. Overall, average cycle time showed a trend to decrease from 159 to 123 minutes (22.6%)(Figure). Average cycle times were reduced from 159 to 128 minutes (19.5%) for new patients and from 161 to 115 minutes (28.6%) for follow-up patients (P=.02). Overall, referrals increased by 14.1% (816/5799)(P<.001), which was largely due to the increase in volume of referrals observed between FY 2014 (n=5770) and FY 2015 (n=6615).
We have demonstrated that decreased wait times can be associated with improvements in clinic productivity measures, namely decreased nonattendance rates and cycle times and increased referrals. Patient nonattendance is a burden on clinic resources and has been described in the dermatology clinic setting.2-6 Increased likelihood of nonattendance has been associated with prolonged wait times.3,7 We propose that decreased wait times can lead to diminished nonattendance rates, as patients are more likely to keep their appointments rather than seek other providers for dermatologic care. The difference in trends between new patient and follow-up nonattendance rates may be attributed to the larger relative increase in completed new patient visits compared to follow-ups during the study period.
Furthermore, the decrease in average cycle time reflected our clinic’s ability to see a larger number of patients per clinic, with subsequently shorter wait times. The greater reduction in cycle times for follow-up patients may be attributed to the increased continuity of providers who had previously seen these patients. Although the cycle times may seem high in our clinic compared to other practice settings, we believe that this marker of productivity is widely applicable to various clinic settings, including private practices and other outpatient specialty clinics. Increased clinic referrals can be a downstream effect of decreased wait times due to improvements in access to care, as shown in other specialty clinics.8 Effects of confounding variables on referral volumes, including nationwide health insurance changes during our study period, could not be ruled out.
Limitations of this study include unavailable data on patient and provider satisfaction and changes in patients’ health insurance. This study provides evidence of changes in clinical productivity measures associated with decreased wait times that can demonstrate widespread benefits to the health system.
Acknowledgments
The authors would like to thank Michael Estabrooks, RN, and Trung Vu for providing aggregate data, as well as Linda Hynan, PhD, for statistical advice (all Dallas, Texas).
Maximizing productivity is prudent for outpatient subspecialty clinics to improve access to care. The outpatient dermatology clinic at Parkland Health and Hospital System in Dallas, Texas, which is a safety-net hospital in Dallas County, decreased wait times for new patients (from 377 to 48 days) and follow-up patients (from 95 to 34 days) from May 2012 to September 2015.1 Changes in clinic productivity measures that occur with decreased wait times are not well characterized; therefore, we sought to address this knowledge gap. We propose that decreased wait times are associated with improvement in additional clinic productivity measures, specifically decreases in nonattendance and cycle times (defined as time between patient check-in and discharge) as well as increases in referrals.
In our retrospective cohort study of patients seen in the Parkland outpatient dermatology clinic between fiscal year (FY) 2012 and FY 2015 (between October 2011 and September 2015), we collected data on patient nonattendance rates, cycle times, and referral volumes. Categorical variables were compared using χ2 tests, and changes in cycle times were analyzed using 2-way analysis of variance. P<.05 was considered statistically significant.
There were 52,775 scheduled clinic visits from FY 2012 to FY 2015. The overall proportion of patient nonattendance rates decreased from 34.6% (4202/12,141) to 31.4% (4429/14,119)(P<.001)(Figure), despite an increase in completed patient visits during the study period (7939 vs 9690). New patient nonattendance rates decreased from 42.9% (1831/4269) to 30.2% (1474/4874)(P<.001). The number of completed visits for new patients increased from 2438 in FY 2012 to 3400 in FY 2015. Follow-up nonattendance rates increased from 30.1% (2371/7872) to 32.0% (2955/9245)(P<.001). Follow-up completed visits increased from 5501 in FY 2012 to 6290 in FY 2015. Overall, average cycle time showed a trend to decrease from 159 to 123 minutes (22.6%)(Figure). Average cycle times were reduced from 159 to 128 minutes (19.5%) for new patients and from 161 to 115 minutes (28.6%) for follow-up patients (P=.02). Overall, referrals increased by 14.1% (816/5799)(P<.001), which was largely due to the increase in volume of referrals observed between FY 2014 (n=5770) and FY 2015 (n=6615).
We have demonstrated that decreased wait times can be associated with improvements in clinic productivity measures, namely decreased nonattendance rates and cycle times and increased referrals. Patient nonattendance is a burden on clinic resources and has been described in the dermatology clinic setting.2-6 Increased likelihood of nonattendance has been associated with prolonged wait times.3,7 We propose that decreased wait times can lead to diminished nonattendance rates, as patients are more likely to keep their appointments rather than seek other providers for dermatologic care. The difference in trends between new patient and follow-up nonattendance rates may be attributed to the larger relative increase in completed new patient visits compared to follow-ups during the study period.
Furthermore, the decrease in average cycle time reflected our clinic’s ability to see a larger number of patients per clinic, with subsequently shorter wait times. The greater reduction in cycle times for follow-up patients may be attributed to the increased continuity of providers who had previously seen these patients. Although the cycle times may seem high in our clinic compared to other practice settings, we believe that this marker of productivity is widely applicable to various clinic settings, including private practices and other outpatient specialty clinics. Increased clinic referrals can be a downstream effect of decreased wait times due to improvements in access to care, as shown in other specialty clinics.8 Effects of confounding variables on referral volumes, including nationwide health insurance changes during our study period, could not be ruled out.
Limitations of this study include unavailable data on patient and provider satisfaction and changes in patients’ health insurance. This study provides evidence of changes in clinical productivity measures associated with decreased wait times that can demonstrate widespread benefits to the health system.
Acknowledgments
The authors would like to thank Michael Estabrooks, RN, and Trung Vu for providing aggregate data, as well as Linda Hynan, PhD, for statistical advice (all Dallas, Texas).
- O’Brien JC, Chong BF. Reducing outpatient dermatology clinic wait times in a safety net health system in Dallas, Texas. J Am Acad Dermatol. 2016;75:631-632.
- Canizares MJ, Penneys NS. The incidence of nonattendance at an urgent care dermatology clinic. J Am Acad Dermatol. 2002;46:457-459.
- Cohen AD, Dreiher J, Vardy DA, et al. Nonattendance in a dermatology clinic—a large sample analysis. J Eur Acad Dermatol Venereol. 2008;22:1178-1183.
- Resneck JS Jr, Lipton S, Pletcher MJ. Short wait times for patients seeking cosmetic botulinum toxin appointments with dermatologists. J Am Acad Dermatol. 2007;57:985-989.
- Tsang MW, Resneck JS Jr. Even patients with changing moles face long dermatology appointment wait-times: a study of simulated patient calls to dermatologists. J Am Acad Dermatol. 2006;55:54-58.
- Rosenbach M, Kagan S, Leventhal S. Dermatology urgent care clinic: a survey of referring physician satisfaction. J Am Acad Dermatol. 2013;69:1067-1069.e1.
- Dickey W, Morrow JI. Can outpatient non-attendance be predicted from the referral letter? an audit of default at neurology clinics. J R Soc Med. 1991;8:662-663.
- Bungard TJ, Smigorowsky MJ, Lalonde LD, et al. Cardiac EASE (Ensuring Access and Speedy Evaluation)—the impact of a single-point-of-entry multidisciplinary outpatient cardiology consultation program on wait times in Canada. Can J Cardiol. 2009;25:697-702.
- O’Brien JC, Chong BF. Reducing outpatient dermatology clinic wait times in a safety net health system in Dallas, Texas. J Am Acad Dermatol. 2016;75:631-632.
- Canizares MJ, Penneys NS. The incidence of nonattendance at an urgent care dermatology clinic. J Am Acad Dermatol. 2002;46:457-459.
- Cohen AD, Dreiher J, Vardy DA, et al. Nonattendance in a dermatology clinic—a large sample analysis. J Eur Acad Dermatol Venereol. 2008;22:1178-1183.
- Resneck JS Jr, Lipton S, Pletcher MJ. Short wait times for patients seeking cosmetic botulinum toxin appointments with dermatologists. J Am Acad Dermatol. 2007;57:985-989.
- Tsang MW, Resneck JS Jr. Even patients with changing moles face long dermatology appointment wait-times: a study of simulated patient calls to dermatologists. J Am Acad Dermatol. 2006;55:54-58.
- Rosenbach M, Kagan S, Leventhal S. Dermatology urgent care clinic: a survey of referring physician satisfaction. J Am Acad Dermatol. 2013;69:1067-1069.e1.
- Dickey W, Morrow JI. Can outpatient non-attendance be predicted from the referral letter? an audit of default at neurology clinics. J R Soc Med. 1991;8:662-663.
- Bungard TJ, Smigorowsky MJ, Lalonde LD, et al. Cardiac EASE (Ensuring Access and Speedy Evaluation)—the impact of a single-point-of-entry multidisciplinary outpatient cardiology consultation program on wait times in Canada. Can J Cardiol. 2009;25:697-702.
Atopic Dermatitis Pipeline
Just when you might have thought dermatologic therapies were peaking, along came another banner year in atopic dermatitis (AD). Last year we saw the landmark launch of dupilumab, the first US Food and Drug Administration (FDA)–approved biologic therapy for AD. Dupilumab addresses a novel mechanism of AD in adults by blocking IL-4 and IL-13, which both play a central role in the type 2 helper T cell (TH2) axis on the dual development of barrier-impaired skin and aberrant immune response including IgE to cutaneous aggravating agents with resultant inflammation. Additional information has shown direct effects to reduce itch in AD.1 A 12-week study of dupilumab monotherapy showed that 85% (47/55) of treated patients had at least a 50% reduction in Eczema Area and Severity Index (EASI) score and 40% (22/55) were clear or almost clear on the investigator global assessment. With concomitant corticosteroid therapy, 100% of patients achieved EASI-50.2 Also notable, 2017 ushered in the appearance of a novel iteration of the 30-year-old concept of phosphodiesterase inhibition with the approval of the topical agent crisaborole for AD treatment in patients 2 years and older, which has been shown to be effective in both children and adults.3,4 However, despite these leaps of advancement in the care of AD, by no means has the condition been cured.
Atopic dermatitis has remained an incurable disease due to many factors: (1) variable immunologic and environmental triggers and patient disease course; (2) intolerance to therapeutic agents, including an enhanced sense of stinging and/or reactivity; (3) poor access to novel therapies among underserved patient populations; (4) lack of available data and information on variable treatment response by ethnicity and race; and (5) the absence of biologic treatments for severe childhood AD to modify long-term recurrence and progression of atopy, which is probably the most important issue, as the majority of AD cases start in children 5 years and younger.
Instituting a treatment today to provide children with disease-free skin for a lifetime truly is the Holy Grail in pediatric dermatology. To aid in the progress toward this goal, a deeper understanding of the manifestation of pediatric versus adult AD is now being investigated. It is clear that with adult chronicity, type 1 helper T cell (TH1) axis activity and prolonged defects are triggered in barrier maturation; however, recent data have started to demonstrate that the youngest patients have different issues in lipid maturation and lack TH1 activation. In particular, fatty acyl-CoA reductase 2 and fatty acid 2-hydroxylase is preferentially downregulated in children.5 It appears that the young immune system may be ripe for immune modification, which previously has been demonstrated with wild-type viral infections of varicella in children.6 However, future research will focus on what kind of tweaks to the immune system are required.
To encapsulate the AD pipeline, we will review drug trials that are in active recruitment as well as recently published data, which constitute an exciting group full of modifications of current therapies and agents with novel mechanisms of action.
Therapies targeting new mechanisms of action include Janus kinase (JAK) inhibitors, which have shown promising results for alopecia areata and vitiligo vulgaris. These agents may create selective modification of the immune system and are being tested topically and orally (Clinicaltrials.gov identifier NCT03011892).
Another mechanism that currently is being studied includes a topical IL-4 and IL-13 inhibitor, which would hopefully mimic the efficacy of dupilumab, antioxidant therapies, and antimicrobials (NCT03351777, NCT03381625, NCT02910011).
Data on the outcome of a phase 3 trial of dupilumab in adolescents has been released but not yet published by the manufacturer and shows promising results in children aged 12 to 17 years, both in reduction of EASI score and in achieving clear or almost clear skin.11 Interestingly, limited data available from a press release reported similar results with dupilumab injection every 2 weeks versus every 4 weeks, which may give alternative dosing regimens in this age group once approved11; however, publication has yet to occur for the latter data.
Other mechanistic agents include blockade of cytokines and interleukins, particularly those involved in type 2 helper T cell (TH2) activity, such as thymic stromal lymphopoietin (a cytokine), as well as targeted single inhibition of IL-4, IL-5, IL-13, and IL-31 and/or their receptors. Nemolizumab, an anti–IL-31 receptor A antibody, is showing promise in the control of AD-associated itch and reduction in EASI
The future of AD therapy is anyone’s guess. Having entered the biologic era with dupilumab, we have a high bar set for efficacy and safety of AD therapies, yet there remains a core group of AD patients who have not yet achieved clearance or refuse injectables; therefore, adjunctive or alternative therapeutics are still needed. Furthermore, we still have not identified who will best benefit long-term from systemic intervention and how to best effect long-term disease control with biologics or novel agents, and choosing the therapy based on patient disease characteristics or serotyping has not yet come of age. It is exciting to think about what next year will bring!
- Xu X, Zheng Y, Zhang X, et al. Efficacy and safety of dupilumab for the treatment of moderate-to-severe atopic dermatitis in adults. Oncotarget. 2017;8:108480-108491.
- Beck LA, Thaçi D, Hamilton JD, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med. 2014;371:130-139.
- Murrell D, Gebauer K, Spelman L, et al. Crisaborole topical ointment, 2% in adults with atopic dermatitis: a phase 2a, vehicle-controlled, proof-of-concept study. J Drugs Dermatol. 2015;14:1108-1112.
- Paller AS, Tom WL, Lebwohl MG, et al. Efficacy and safety of crisaborole ointment, a novel, nonsteroidal phosphodiesterase 4 (PDE4) inhibitor for the topical treatment of atopic dermatitis (AD) in children and adults. J Am Acad Dermatol. 2016;75:494-503.e6.
- Brunner PM, Israel A, Zhang N, et al. Early-onset pediatric atopic dermatitis is characterized by TH2/TH17/TH22-centered inflammation and lipid alterations. J Allergy Clin Immunol. 2018;141:2094-2106.
- Silverberg JI, Kleiman E, Silverberg NB, et al. Chickenpox in childhood is associated with decreased atopic disorders, IgE, allergic sensitization, and leukocyte subsets. Pediatr Allergy Immunol. 2012;23:50-58.
- Paller AS, Kabashima K, Bieber T. Therapeutic pipeline for atopic dermatitis: end of the drought? Allergy Clin Immunol. 2017;140:633-643.
- Renert-Yuval Y, Guttman-Yassky E. Systemic therapies in atopic dermatitis: the pipeline. Clin Dermatol. 2017;35:387-397.
- Bissonnette R, Papp KA, Poulin Y, et al. Topical tofacitinib for atopic dermatitis: a phase IIa randomized trial. Br J Dermatol. 2016;175:902-911.
- Guttman-Yassky E, Silverberg JI, Nemoto O, et al. Baricitinib in adult patients with moderate-to-severe atopic dermatitis: a phase 2 parallel, double-blinded, randomized placebo-controlled multiple-dose study [published online February 1, 2018]. J Am Acad Dermatol. doi: 10.1016/j.jaad.2018.01.018.
- Dupixent (dupilumab) showed positive phase 3 results in adolescents with inadequately controlled moderate-to-severe atopic dermatitis [press release]. Tarrytown, NY: Sanofi; May 16, 2018. https://www.prnewswire.com/news-releases/dupixent-dupilumab-showed-positive-phase-3-results-in-adolescents-with-inadequately-controlled-moderate-to-severe-atopic-dermatitis-300649146.html. Accessed July 11, 2018.
- Ruzicka T, Hanifin JM, Furue M, et al. Anti–interleukin-31 receptor A antibody for atopic dermatitis. N Engl J Med. 2017;376:826-835.
Just when you might have thought dermatologic therapies were peaking, along came another banner year in atopic dermatitis (AD). Last year we saw the landmark launch of dupilumab, the first US Food and Drug Administration (FDA)–approved biologic therapy for AD. Dupilumab addresses a novel mechanism of AD in adults by blocking IL-4 and IL-13, which both play a central role in the type 2 helper T cell (TH2) axis on the dual development of barrier-impaired skin and aberrant immune response including IgE to cutaneous aggravating agents with resultant inflammation. Additional information has shown direct effects to reduce itch in AD.1 A 12-week study of dupilumab monotherapy showed that 85% (47/55) of treated patients had at least a 50% reduction in Eczema Area and Severity Index (EASI) score and 40% (22/55) were clear or almost clear on the investigator global assessment. With concomitant corticosteroid therapy, 100% of patients achieved EASI-50.2 Also notable, 2017 ushered in the appearance of a novel iteration of the 30-year-old concept of phosphodiesterase inhibition with the approval of the topical agent crisaborole for AD treatment in patients 2 years and older, which has been shown to be effective in both children and adults.3,4 However, despite these leaps of advancement in the care of AD, by no means has the condition been cured.
Atopic dermatitis has remained an incurable disease due to many factors: (1) variable immunologic and environmental triggers and patient disease course; (2) intolerance to therapeutic agents, including an enhanced sense of stinging and/or reactivity; (3) poor access to novel therapies among underserved patient populations; (4) lack of available data and information on variable treatment response by ethnicity and race; and (5) the absence of biologic treatments for severe childhood AD to modify long-term recurrence and progression of atopy, which is probably the most important issue, as the majority of AD cases start in children 5 years and younger.
Instituting a treatment today to provide children with disease-free skin for a lifetime truly is the Holy Grail in pediatric dermatology. To aid in the progress toward this goal, a deeper understanding of the manifestation of pediatric versus adult AD is now being investigated. It is clear that with adult chronicity, type 1 helper T cell (TH1) axis activity and prolonged defects are triggered in barrier maturation; however, recent data have started to demonstrate that the youngest patients have different issues in lipid maturation and lack TH1 activation. In particular, fatty acyl-CoA reductase 2 and fatty acid 2-hydroxylase is preferentially downregulated in children.5 It appears that the young immune system may be ripe for immune modification, which previously has been demonstrated with wild-type viral infections of varicella in children.6 However, future research will focus on what kind of tweaks to the immune system are required.
To encapsulate the AD pipeline, we will review drug trials that are in active recruitment as well as recently published data, which constitute an exciting group full of modifications of current therapies and agents with novel mechanisms of action.
Therapies targeting new mechanisms of action include Janus kinase (JAK) inhibitors, which have shown promising results for alopecia areata and vitiligo vulgaris. These agents may create selective modification of the immune system and are being tested topically and orally (Clinicaltrials.gov identifier NCT03011892).
Another mechanism that currently is being studied includes a topical IL-4 and IL-13 inhibitor, which would hopefully mimic the efficacy of dupilumab, antioxidant therapies, and antimicrobials (NCT03351777, NCT03381625, NCT02910011).
Data on the outcome of a phase 3 trial of dupilumab in adolescents has been released but not yet published by the manufacturer and shows promising results in children aged 12 to 17 years, both in reduction of EASI score and in achieving clear or almost clear skin.11 Interestingly, limited data available from a press release reported similar results with dupilumab injection every 2 weeks versus every 4 weeks, which may give alternative dosing regimens in this age group once approved11; however, publication has yet to occur for the latter data.
Other mechanistic agents include blockade of cytokines and interleukins, particularly those involved in type 2 helper T cell (TH2) activity, such as thymic stromal lymphopoietin (a cytokine), as well as targeted single inhibition of IL-4, IL-5, IL-13, and IL-31 and/or their receptors. Nemolizumab, an anti–IL-31 receptor A antibody, is showing promise in the control of AD-associated itch and reduction in EASI
The future of AD therapy is anyone’s guess. Having entered the biologic era with dupilumab, we have a high bar set for efficacy and safety of AD therapies, yet there remains a core group of AD patients who have not yet achieved clearance or refuse injectables; therefore, adjunctive or alternative therapeutics are still needed. Furthermore, we still have not identified who will best benefit long-term from systemic intervention and how to best effect long-term disease control with biologics or novel agents, and choosing the therapy based on patient disease characteristics or serotyping has not yet come of age. It is exciting to think about what next year will bring!
Just when you might have thought dermatologic therapies were peaking, along came another banner year in atopic dermatitis (AD). Last year we saw the landmark launch of dupilumab, the first US Food and Drug Administration (FDA)–approved biologic therapy for AD. Dupilumab addresses a novel mechanism of AD in adults by blocking IL-4 and IL-13, which both play a central role in the type 2 helper T cell (TH2) axis on the dual development of barrier-impaired skin and aberrant immune response including IgE to cutaneous aggravating agents with resultant inflammation. Additional information has shown direct effects to reduce itch in AD.1 A 12-week study of dupilumab monotherapy showed that 85% (47/55) of treated patients had at least a 50% reduction in Eczema Area and Severity Index (EASI) score and 40% (22/55) were clear or almost clear on the investigator global assessment. With concomitant corticosteroid therapy, 100% of patients achieved EASI-50.2 Also notable, 2017 ushered in the appearance of a novel iteration of the 30-year-old concept of phosphodiesterase inhibition with the approval of the topical agent crisaborole for AD treatment in patients 2 years and older, which has been shown to be effective in both children and adults.3,4 However, despite these leaps of advancement in the care of AD, by no means has the condition been cured.
Atopic dermatitis has remained an incurable disease due to many factors: (1) variable immunologic and environmental triggers and patient disease course; (2) intolerance to therapeutic agents, including an enhanced sense of stinging and/or reactivity; (3) poor access to novel therapies among underserved patient populations; (4) lack of available data and information on variable treatment response by ethnicity and race; and (5) the absence of biologic treatments for severe childhood AD to modify long-term recurrence and progression of atopy, which is probably the most important issue, as the majority of AD cases start in children 5 years and younger.
Instituting a treatment today to provide children with disease-free skin for a lifetime truly is the Holy Grail in pediatric dermatology. To aid in the progress toward this goal, a deeper understanding of the manifestation of pediatric versus adult AD is now being investigated. It is clear that with adult chronicity, type 1 helper T cell (TH1) axis activity and prolonged defects are triggered in barrier maturation; however, recent data have started to demonstrate that the youngest patients have different issues in lipid maturation and lack TH1 activation. In particular, fatty acyl-CoA reductase 2 and fatty acid 2-hydroxylase is preferentially downregulated in children.5 It appears that the young immune system may be ripe for immune modification, which previously has been demonstrated with wild-type viral infections of varicella in children.6 However, future research will focus on what kind of tweaks to the immune system are required.
To encapsulate the AD pipeline, we will review drug trials that are in active recruitment as well as recently published data, which constitute an exciting group full of modifications of current therapies and agents with novel mechanisms of action.
Therapies targeting new mechanisms of action include Janus kinase (JAK) inhibitors, which have shown promising results for alopecia areata and vitiligo vulgaris. These agents may create selective modification of the immune system and are being tested topically and orally (Clinicaltrials.gov identifier NCT03011892).
Another mechanism that currently is being studied includes a topical IL-4 and IL-13 inhibitor, which would hopefully mimic the efficacy of dupilumab, antioxidant therapies, and antimicrobials (NCT03351777, NCT03381625, NCT02910011).
Data on the outcome of a phase 3 trial of dupilumab in adolescents has been released but not yet published by the manufacturer and shows promising results in children aged 12 to 17 years, both in reduction of EASI score and in achieving clear or almost clear skin.11 Interestingly, limited data available from a press release reported similar results with dupilumab injection every 2 weeks versus every 4 weeks, which may give alternative dosing regimens in this age group once approved11; however, publication has yet to occur for the latter data.
Other mechanistic agents include blockade of cytokines and interleukins, particularly those involved in type 2 helper T cell (TH2) activity, such as thymic stromal lymphopoietin (a cytokine), as well as targeted single inhibition of IL-4, IL-5, IL-13, and IL-31 and/or their receptors. Nemolizumab, an anti–IL-31 receptor A antibody, is showing promise in the control of AD-associated itch and reduction in EASI
The future of AD therapy is anyone’s guess. Having entered the biologic era with dupilumab, we have a high bar set for efficacy and safety of AD therapies, yet there remains a core group of AD patients who have not yet achieved clearance or refuse injectables; therefore, adjunctive or alternative therapeutics are still needed. Furthermore, we still have not identified who will best benefit long-term from systemic intervention and how to best effect long-term disease control with biologics or novel agents, and choosing the therapy based on patient disease characteristics or serotyping has not yet come of age. It is exciting to think about what next year will bring!
- Xu X, Zheng Y, Zhang X, et al. Efficacy and safety of dupilumab for the treatment of moderate-to-severe atopic dermatitis in adults. Oncotarget. 2017;8:108480-108491.
- Beck LA, Thaçi D, Hamilton JD, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med. 2014;371:130-139.
- Murrell D, Gebauer K, Spelman L, et al. Crisaborole topical ointment, 2% in adults with atopic dermatitis: a phase 2a, vehicle-controlled, proof-of-concept study. J Drugs Dermatol. 2015;14:1108-1112.
- Paller AS, Tom WL, Lebwohl MG, et al. Efficacy and safety of crisaborole ointment, a novel, nonsteroidal phosphodiesterase 4 (PDE4) inhibitor for the topical treatment of atopic dermatitis (AD) in children and adults. J Am Acad Dermatol. 2016;75:494-503.e6.
- Brunner PM, Israel A, Zhang N, et al. Early-onset pediatric atopic dermatitis is characterized by TH2/TH17/TH22-centered inflammation and lipid alterations. J Allergy Clin Immunol. 2018;141:2094-2106.
- Silverberg JI, Kleiman E, Silverberg NB, et al. Chickenpox in childhood is associated with decreased atopic disorders, IgE, allergic sensitization, and leukocyte subsets. Pediatr Allergy Immunol. 2012;23:50-58.
- Paller AS, Kabashima K, Bieber T. Therapeutic pipeline for atopic dermatitis: end of the drought? Allergy Clin Immunol. 2017;140:633-643.
- Renert-Yuval Y, Guttman-Yassky E. Systemic therapies in atopic dermatitis: the pipeline. Clin Dermatol. 2017;35:387-397.
- Bissonnette R, Papp KA, Poulin Y, et al. Topical tofacitinib for atopic dermatitis: a phase IIa randomized trial. Br J Dermatol. 2016;175:902-911.
- Guttman-Yassky E, Silverberg JI, Nemoto O, et al. Baricitinib in adult patients with moderate-to-severe atopic dermatitis: a phase 2 parallel, double-blinded, randomized placebo-controlled multiple-dose study [published online February 1, 2018]. J Am Acad Dermatol. doi: 10.1016/j.jaad.2018.01.018.
- Dupixent (dupilumab) showed positive phase 3 results in adolescents with inadequately controlled moderate-to-severe atopic dermatitis [press release]. Tarrytown, NY: Sanofi; May 16, 2018. https://www.prnewswire.com/news-releases/dupixent-dupilumab-showed-positive-phase-3-results-in-adolescents-with-inadequately-controlled-moderate-to-severe-atopic-dermatitis-300649146.html. Accessed July 11, 2018.
- Ruzicka T, Hanifin JM, Furue M, et al. Anti–interleukin-31 receptor A antibody for atopic dermatitis. N Engl J Med. 2017;376:826-835.
- Xu X, Zheng Y, Zhang X, et al. Efficacy and safety of dupilumab for the treatment of moderate-to-severe atopic dermatitis in adults. Oncotarget. 2017;8:108480-108491.
- Beck LA, Thaçi D, Hamilton JD, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med. 2014;371:130-139.
- Murrell D, Gebauer K, Spelman L, et al. Crisaborole topical ointment, 2% in adults with atopic dermatitis: a phase 2a, vehicle-controlled, proof-of-concept study. J Drugs Dermatol. 2015;14:1108-1112.
- Paller AS, Tom WL, Lebwohl MG, et al. Efficacy and safety of crisaborole ointment, a novel, nonsteroidal phosphodiesterase 4 (PDE4) inhibitor for the topical treatment of atopic dermatitis (AD) in children and adults. J Am Acad Dermatol. 2016;75:494-503.e6.
- Brunner PM, Israel A, Zhang N, et al. Early-onset pediatric atopic dermatitis is characterized by TH2/TH17/TH22-centered inflammation and lipid alterations. J Allergy Clin Immunol. 2018;141:2094-2106.
- Silverberg JI, Kleiman E, Silverberg NB, et al. Chickenpox in childhood is associated with decreased atopic disorders, IgE, allergic sensitization, and leukocyte subsets. Pediatr Allergy Immunol. 2012;23:50-58.
- Paller AS, Kabashima K, Bieber T. Therapeutic pipeline for atopic dermatitis: end of the drought? Allergy Clin Immunol. 2017;140:633-643.
- Renert-Yuval Y, Guttman-Yassky E. Systemic therapies in atopic dermatitis: the pipeline. Clin Dermatol. 2017;35:387-397.
- Bissonnette R, Papp KA, Poulin Y, et al. Topical tofacitinib for atopic dermatitis: a phase IIa randomized trial. Br J Dermatol. 2016;175:902-911.
- Guttman-Yassky E, Silverberg JI, Nemoto O, et al. Baricitinib in adult patients with moderate-to-severe atopic dermatitis: a phase 2 parallel, double-blinded, randomized placebo-controlled multiple-dose study [published online February 1, 2018]. J Am Acad Dermatol. doi: 10.1016/j.jaad.2018.01.018.
- Dupixent (dupilumab) showed positive phase 3 results in adolescents with inadequately controlled moderate-to-severe atopic dermatitis [press release]. Tarrytown, NY: Sanofi; May 16, 2018. https://www.prnewswire.com/news-releases/dupixent-dupilumab-showed-positive-phase-3-results-in-adolescents-with-inadequately-controlled-moderate-to-severe-atopic-dermatitis-300649146.html. Accessed July 11, 2018.
- Ruzicka T, Hanifin JM, Furue M, et al. Anti–interleukin-31 receptor A antibody for atopic dermatitis. N Engl J Med. 2017;376:826-835.
Speaking the unspeakable: Talking to children about parental mental illness
You probably think you know how to talk with a child about death. But somehow talking about a parent’s mental illness may seem more difficult. Even medical professionals, as most people, can find themselves feeling more judgmental or uneasy talking about mental illness than about physical problems. But with a prevalence of about one in four people having mental disorders, we need to be prepared for this discussion.
Sometimes family members, or even parents themselves, have asked me to tell a child about a parent’s mental illness or substance use. They know the child is confused and scared but don’t know what to say about this still-hushed issue. Other times, children’s behaviors show that they are struggling – by their aggression, depression, decline in school performance, anger, anxiety, or running away – and I find out only by asking that they are experiencing life with a mentally ill parent.
Both are times to get more information about the nature of the parent’s symptoms, what is being done about it; what the child has seen, heard, or experienced; the child’s safety; and what intrinsic or cultural attitudes the family has about the problem. It is best if the affected parents themselves are able to talk realistically about the illness with the child. Sometimes we, as pediatric professionals, can help get the conversation started or may need to step in.
Teens can understand the nature of mental illness as a brain disorder, but often have acquired misinformation from peers, the other parent who is hurt and angry, or the Internet that needs to be respectfully corrected. They may be less willing to have such a discussion than would younger children, as they may have experienced verbal or physical aggression from the parent, embarrassment in front of peers, or teasing by classmates. They may have developed coping strategies of writing off the parent, defiance, aggressive responses, or denial.
It is important to find a relaxed moment and begin by saying, “May I ask what you have noticed about your parent’s behavior?” and “What did you make of it?” If they do not answer, you could add, “You know, like acting different or strange.” It is very valuable to be able to name it, if you know the diagnosis, to make the illness more objective. Teens are typically egocentric and wonder if they are prone to develop a similar condition, as well as anxious about who will be there for them if the parent does not get better; both are good questions to address.
Both adolescents and school-aged children are very attuned to when things in life are “unfair,” and having an ill parent certainly qualifies. It is important for whoever has this discussion to empathize, and to acknowledge that it is unfair and that feeling angry, sad, or confused is natural – without giving them permission for misbehavior. It may be easier for some children to have a journal in which to write questions to have an adult answer later. Any child can be given hope by knowing that the parent is getting help (or that you will work on this), especially if the parents themselves say they are trying to get better. The children need to know that although mental illness tends to get better and worse at unexpected times, mental health can be improved. It is essential that children of school age and older have a clear plan for what to do if the parent loses control or is in danger. This might include getting out of the house and calling the parent’s partner, a trusted neighbor, or 911.
While teens may feel guilty about their anger or things they might have said or done in reaction to the ill parent, school-aged and preschool children are more likely to feel guilty that they somehow contributed to the parent’s condition through misbehavior or some imagined influence. Eliciting these thoughts may simply require asking, “What thoughts have you had about why this happened?” or having another family member prompting them by saying, “I have been wondering if there is something I should have done. Have you wondered about that, too?”
What is harder to explain is the impression children may get that their depressed or psychotic or drug-abusing parents no longer love them; and the parents may have said hurtful things to them. School-aged children can be told and can understand an illness of “the feelings and thinking parts of the brain” as being similar to other physical illnesses, such as the flu, that “make people act tired or grouchy or say things they do not mean.” Children of all ages need to be reassured that, inside, their parents still love them, and “it is the illness talking” if they act or speak otherwise. In the case of substance abuse disorders, which might seem more of a choice by the parent than would other mental illnesses, it can be helpful to point out that “drugs and alcohol can be stronger than people and can take over their brains.” The National Alliance on Mental Illness (www.nami.org) offers support programs that may be helpful for older children.
Sometimes families may resist telling a child about parental mental illness because of personal beliefs, cultural stigma, or privacy concerns. I try to emphasize that by being honest in giving children an understanding of their parents’ mental illness, one is helping them trust the adults in their lives. They need the truth and also to practice formulating things to say to counter those who have incorrect ideas, or who insult or make fun of them. They need the truth about mental illness to make sense of their experiences so they can feel lovable and hopeful about their own futures and can recognize illness symptoms in themselves. Giving them words, ensuring their safety and support, and strengthening their coping can help buffer the impact of this common adverse childhood experience to help prevent long-term negative effects.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
You probably think you know how to talk with a child about death. But somehow talking about a parent’s mental illness may seem more difficult. Even medical professionals, as most people, can find themselves feeling more judgmental or uneasy talking about mental illness than about physical problems. But with a prevalence of about one in four people having mental disorders, we need to be prepared for this discussion.
Sometimes family members, or even parents themselves, have asked me to tell a child about a parent’s mental illness or substance use. They know the child is confused and scared but don’t know what to say about this still-hushed issue. Other times, children’s behaviors show that they are struggling – by their aggression, depression, decline in school performance, anger, anxiety, or running away – and I find out only by asking that they are experiencing life with a mentally ill parent.
Both are times to get more information about the nature of the parent’s symptoms, what is being done about it; what the child has seen, heard, or experienced; the child’s safety; and what intrinsic or cultural attitudes the family has about the problem. It is best if the affected parents themselves are able to talk realistically about the illness with the child. Sometimes we, as pediatric professionals, can help get the conversation started or may need to step in.
Teens can understand the nature of mental illness as a brain disorder, but often have acquired misinformation from peers, the other parent who is hurt and angry, or the Internet that needs to be respectfully corrected. They may be less willing to have such a discussion than would younger children, as they may have experienced verbal or physical aggression from the parent, embarrassment in front of peers, or teasing by classmates. They may have developed coping strategies of writing off the parent, defiance, aggressive responses, or denial.
It is important to find a relaxed moment and begin by saying, “May I ask what you have noticed about your parent’s behavior?” and “What did you make of it?” If they do not answer, you could add, “You know, like acting different or strange.” It is very valuable to be able to name it, if you know the diagnosis, to make the illness more objective. Teens are typically egocentric and wonder if they are prone to develop a similar condition, as well as anxious about who will be there for them if the parent does not get better; both are good questions to address.
Both adolescents and school-aged children are very attuned to when things in life are “unfair,” and having an ill parent certainly qualifies. It is important for whoever has this discussion to empathize, and to acknowledge that it is unfair and that feeling angry, sad, or confused is natural – without giving them permission for misbehavior. It may be easier for some children to have a journal in which to write questions to have an adult answer later. Any child can be given hope by knowing that the parent is getting help (or that you will work on this), especially if the parents themselves say they are trying to get better. The children need to know that although mental illness tends to get better and worse at unexpected times, mental health can be improved. It is essential that children of school age and older have a clear plan for what to do if the parent loses control or is in danger. This might include getting out of the house and calling the parent’s partner, a trusted neighbor, or 911.
While teens may feel guilty about their anger or things they might have said or done in reaction to the ill parent, school-aged and preschool children are more likely to feel guilty that they somehow contributed to the parent’s condition through misbehavior or some imagined influence. Eliciting these thoughts may simply require asking, “What thoughts have you had about why this happened?” or having another family member prompting them by saying, “I have been wondering if there is something I should have done. Have you wondered about that, too?”
What is harder to explain is the impression children may get that their depressed or psychotic or drug-abusing parents no longer love them; and the parents may have said hurtful things to them. School-aged children can be told and can understand an illness of “the feelings and thinking parts of the brain” as being similar to other physical illnesses, such as the flu, that “make people act tired or grouchy or say things they do not mean.” Children of all ages need to be reassured that, inside, their parents still love them, and “it is the illness talking” if they act or speak otherwise. In the case of substance abuse disorders, which might seem more of a choice by the parent than would other mental illnesses, it can be helpful to point out that “drugs and alcohol can be stronger than people and can take over their brains.” The National Alliance on Mental Illness (www.nami.org) offers support programs that may be helpful for older children.
Sometimes families may resist telling a child about parental mental illness because of personal beliefs, cultural stigma, or privacy concerns. I try to emphasize that by being honest in giving children an understanding of their parents’ mental illness, one is helping them trust the adults in their lives. They need the truth and also to practice formulating things to say to counter those who have incorrect ideas, or who insult or make fun of them. They need the truth about mental illness to make sense of their experiences so they can feel lovable and hopeful about their own futures and can recognize illness symptoms in themselves. Giving them words, ensuring their safety and support, and strengthening their coping can help buffer the impact of this common adverse childhood experience to help prevent long-term negative effects.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
You probably think you know how to talk with a child about death. But somehow talking about a parent’s mental illness may seem more difficult. Even medical professionals, as most people, can find themselves feeling more judgmental or uneasy talking about mental illness than about physical problems. But with a prevalence of about one in four people having mental disorders, we need to be prepared for this discussion.
Sometimes family members, or even parents themselves, have asked me to tell a child about a parent’s mental illness or substance use. They know the child is confused and scared but don’t know what to say about this still-hushed issue. Other times, children’s behaviors show that they are struggling – by their aggression, depression, decline in school performance, anger, anxiety, or running away – and I find out only by asking that they are experiencing life with a mentally ill parent.
Both are times to get more information about the nature of the parent’s symptoms, what is being done about it; what the child has seen, heard, or experienced; the child’s safety; and what intrinsic or cultural attitudes the family has about the problem. It is best if the affected parents themselves are able to talk realistically about the illness with the child. Sometimes we, as pediatric professionals, can help get the conversation started or may need to step in.
Teens can understand the nature of mental illness as a brain disorder, but often have acquired misinformation from peers, the other parent who is hurt and angry, or the Internet that needs to be respectfully corrected. They may be less willing to have such a discussion than would younger children, as they may have experienced verbal or physical aggression from the parent, embarrassment in front of peers, or teasing by classmates. They may have developed coping strategies of writing off the parent, defiance, aggressive responses, or denial.
It is important to find a relaxed moment and begin by saying, “May I ask what you have noticed about your parent’s behavior?” and “What did you make of it?” If they do not answer, you could add, “You know, like acting different or strange.” It is very valuable to be able to name it, if you know the diagnosis, to make the illness more objective. Teens are typically egocentric and wonder if they are prone to develop a similar condition, as well as anxious about who will be there for them if the parent does not get better; both are good questions to address.
Both adolescents and school-aged children are very attuned to when things in life are “unfair,” and having an ill parent certainly qualifies. It is important for whoever has this discussion to empathize, and to acknowledge that it is unfair and that feeling angry, sad, or confused is natural – without giving them permission for misbehavior. It may be easier for some children to have a journal in which to write questions to have an adult answer later. Any child can be given hope by knowing that the parent is getting help (or that you will work on this), especially if the parents themselves say they are trying to get better. The children need to know that although mental illness tends to get better and worse at unexpected times, mental health can be improved. It is essential that children of school age and older have a clear plan for what to do if the parent loses control or is in danger. This might include getting out of the house and calling the parent’s partner, a trusted neighbor, or 911.
While teens may feel guilty about their anger or things they might have said or done in reaction to the ill parent, school-aged and preschool children are more likely to feel guilty that they somehow contributed to the parent’s condition through misbehavior or some imagined influence. Eliciting these thoughts may simply require asking, “What thoughts have you had about why this happened?” or having another family member prompting them by saying, “I have been wondering if there is something I should have done. Have you wondered about that, too?”
What is harder to explain is the impression children may get that their depressed or psychotic or drug-abusing parents no longer love them; and the parents may have said hurtful things to them. School-aged children can be told and can understand an illness of “the feelings and thinking parts of the brain” as being similar to other physical illnesses, such as the flu, that “make people act tired or grouchy or say things they do not mean.” Children of all ages need to be reassured that, inside, their parents still love them, and “it is the illness talking” if they act or speak otherwise. In the case of substance abuse disorders, which might seem more of a choice by the parent than would other mental illnesses, it can be helpful to point out that “drugs and alcohol can be stronger than people and can take over their brains.” The National Alliance on Mental Illness (www.nami.org) offers support programs that may be helpful for older children.
Sometimes families may resist telling a child about parental mental illness because of personal beliefs, cultural stigma, or privacy concerns. I try to emphasize that by being honest in giving children an understanding of their parents’ mental illness, one is helping them trust the adults in their lives. They need the truth and also to practice formulating things to say to counter those who have incorrect ideas, or who insult or make fun of them. They need the truth about mental illness to make sense of their experiences so they can feel lovable and hopeful about their own futures and can recognize illness symptoms in themselves. Giving them words, ensuring their safety and support, and strengthening their coping can help buffer the impact of this common adverse childhood experience to help prevent long-term negative effects.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
Am I My Brother’s/Sister’s Keeper?
Adherents of the Abrahamic faiths or students of the Bible as literature will easily recall the circumstances of this famous quotation from the Hebrew Scriptures. Cain has killed his brother Abel, earning the disrepute of committing the first murder in biblical history. Scholars of ethics have answered Cain’s sardonic question in the affirmative: avowing that while the individual is primarily responsible for his conduct and its consequences, the community also bears a responsibility.1
Many of you will have seen news clips of yet another Department of Veteran Affairs (VA) scandal: This one involving an impaired pathologist. I have purposely not used the pathologist’s name to emphasize that our shared obligation to protect patients from impaired members of the profession goes far beyond this single outrage. Although we might believe we could never be that individual; none of us are immune from depression, dementia, or physical disabilities that diminish our ability to care for patients. Although it is worth noting that having read or watched everything I could find on the story, the “facts” are few and far between, which I will argue later only underscores the problems with professional accountability especially in a large bureaucratic organization.
This column is not meant to impugn or exculpate anyone but to encourage us to reflect on our ethical awareness and response to hints that there might be an impaired practitioner among us. The Fayetteville VA Medical Center (VAMC) in North Carolina—ground zero for this incident—held several town halls in which anxious and angry veterans demanded an explanation for how an impaired pathologist could have placed in harm’s way nearly 19,000 patients.2 Of this cohort, 5,250 patients have died since 2005. The VA leadership, including the VISN 16 network director and the interim medical director of the Fayetteville VAMC indicated that out of 911 pathology reports that had undergone expert peer review, an incorrect diagnosis was identified in at least 7 with 1 possible associated death.3
The VA officials estimate that the entire review may involve more than 30,000 cases. The allegations are that the pathologist was impaired due to a substance use disorder, in this case alcohol. In interviews, the physician has admitted the alcohol problem and receiving treatment for it but denied he was ever impaired on duty.4 This denial directly contradicts the VA reports that he was intoxicated on duty at least twice.
We do know that the physician in question was enrolled in the Mississippi Physician Health Program (PHP). The Federation of State Physician Health Programs (FSPHP), of which the Mississippi program is a member, provides confidential initial evaluation, ongoing treatment, and monitoring for state licensed health care practitioners with a substance use or other mental health disorder or other condition that could potentially impair their fitness for duty. The PHPs have been career saving for many physicians and other health care professionals. The incentives to return to the practice of medicine are powerful, leading to a higher recovery rate than that of the general population.5
According to FSPHP, “While both PHPs and state licensing boards are engaged in patient safety efforts, PHPs primary focus is on improving the health of the physician, and the licensing board’s primary duty is to protect the public.”6 This potential conflict of interest has been criticized recently.7 News reports suggest that the ambiguity of this relationship between PHP and licensing board may have left a “who’s minding the store” mentality. But here are the facts of this particular case.
In March 2016, an employee reported that the pathologist was intoxicated on duty, and he was immediately removed from service. Of the many elephants in the room, the biggest moral pachyderm is why, given the chronic and progressive nature of substance use disorders did it take 11 years for a formal report leading to action?
Having been in circles of leadership, I know well that often there is much discussed that cannot be disclosed, which frequently contributes to staff demoralization. Dozens of medical center employees over decades must have seen behaviors; some of those employees likely reported their observations. The news reports are silent on this point except for attributing it to “fear of retaliation.” In our current VA climate this is a major intimidator of staff trying to tell the truth and leaders seeking to do what is right. Yet research has identified myriad other motives for not reporting impaired colleagues, including loyalty, collusion, denial, indifference, scarcity of resources, and overwork.8
In October 2017, the pathologist was again found intoxicated on the job, attributing it to a migraine headache. The hospital investigated, but the pathologist may have continued working in some capacity. Finally, after the pathologist was arrested for driving while intoxicated March 1 of this year, the interim VAMC director contacted the Mississippi licensing board, declaring that the pathologist “had failed to meet standards of practice” and indicted that he “constituted an imminent threat to patient welfare.” The Arkansas Medical Foundation then rescinded its support of the pathologist, citing the pathologist’s failure to adhere to monitoring and reporting requirements. The Mississippi program followed suit on June 20, and the medical board rescinded his license.
All employees at whatever level are owed due process and respect for their rights, but Congress recently saw fit to legislate further limits on federal employee protections. Most health care administrators still standing in the chaos of today’s VA would tell you that survival is all about when did you know and what did you do about it? But it is not just administrators, the code of ethics of almost every health care profession includes an obligation to report impaired practitioners. Principle II of the American Medical Association Code of Ethics states, “A physician shall uphold the standards of professionalism, be honest in all professional interactions, and strive to report physicians deficient in character or competence, or engaging in fraud or deception, to appropriate entities.”9
If one is in private practice in a small town, it is easier to pull your friend aside on the golf course and say you seem to be having a problem, counsel your friend to get help, often through a PHP. Then if the gentler approach fails, take the harder action of reporting to the medical board or other authority. To report takes moral courage. It takes seeing that the practitioner is not betraying the “white line” of health care professions but honoring the highest commitment of professionalism to the patient.
The last thing we need in our current suspicious and fearful environment is to turn VAMCs and clinics into a dystopia.Yet reporting in a large organization with rules and red tape can seem terrifying, overwhelming, and confusing. A fair, safe, transparent, clear, and consistent means for staff to discharge their ethical obligations is sorely needed. Or else we will be reading about another tragic scandal and asking each other, “How could this have happened?”
1. Morreim EH. Am I my brother’s warden? Responding to the unethical or incompetent colleague. Hastings Cent Rep. 1993;23(3):19-27
2. Worrell T. Veterans question VA over report of ‘impaired’ pathologist at town hall. http://www.joplinglobe.com/news /local_news/veterans-question-va-over-report-of-impaired-pathologist-at-town/article_9281a9d8-8354-5739-b21e-d38e2f28137c.html. Published July 9, 2018. Accessed July 25, 2018 .
3. Wornell T. Fayetteville VA hospital: ‘impaired’ pathologist misdiagnosed some patients. http://www.joplinglobe.com/news/local_news/fayetteville-va-hospital-impaired-pathologist-misdiagnosed-some-patients/article_519f6adc-2109-5ff1-a9ca-98ba9403d6a7.html. Published June 18, 2018. Accessed July 25, 2018.
4. Merlo LLJ, Teitelbaum SA, Thompson K. Substance use disorders in physicians: assessment and treatment. https://www.uptodate.com/contents/substance-use-disorders-in-physicians-assessment-and-treatment. Last updated July 13, 2017. Accessed July 25, 2018.
5. Grabenstein H. Former VA pathologist denies being impaired on duty. https://www.apnews.com/8ca77da8f7ce40868ffbc091608ee681. Published July 9, 2018. Accessed July 25, 2018.
6. Federation of State Physician Health Programs. Frequently asked questions. https://www.fsphp.org/about/faqs. Accessed July 25, 2018.
7. Anderson P. Physician health programs: more harm than good? https://www.medscape.com/viewarticle/849772. Published August 19, 2015. Accessed July 25, 2018.
8. DesRoches CM, Rao SR, Fromson JA, et al. Physicians’ perceptions, preparedness for reporting, and experiences related to impaired and incompetent colleagues. JAMA. 2010;304(2):187-193.
9. American Medical Association. Code of Medical Ethics 2014-2015. https://commerce.ama-assn.org/store/catalog/productDetail.jsp?product_id=prod2510003&sku_id=sku2510003&navAction=push. Accessed July 25, 2018.
Adherents of the Abrahamic faiths or students of the Bible as literature will easily recall the circumstances of this famous quotation from the Hebrew Scriptures. Cain has killed his brother Abel, earning the disrepute of committing the first murder in biblical history. Scholars of ethics have answered Cain’s sardonic question in the affirmative: avowing that while the individual is primarily responsible for his conduct and its consequences, the community also bears a responsibility.1
Many of you will have seen news clips of yet another Department of Veteran Affairs (VA) scandal: This one involving an impaired pathologist. I have purposely not used the pathologist’s name to emphasize that our shared obligation to protect patients from impaired members of the profession goes far beyond this single outrage. Although we might believe we could never be that individual; none of us are immune from depression, dementia, or physical disabilities that diminish our ability to care for patients. Although it is worth noting that having read or watched everything I could find on the story, the “facts” are few and far between, which I will argue later only underscores the problems with professional accountability especially in a large bureaucratic organization.
This column is not meant to impugn or exculpate anyone but to encourage us to reflect on our ethical awareness and response to hints that there might be an impaired practitioner among us. The Fayetteville VA Medical Center (VAMC) in North Carolina—ground zero for this incident—held several town halls in which anxious and angry veterans demanded an explanation for how an impaired pathologist could have placed in harm’s way nearly 19,000 patients.2 Of this cohort, 5,250 patients have died since 2005. The VA leadership, including the VISN 16 network director and the interim medical director of the Fayetteville VAMC indicated that out of 911 pathology reports that had undergone expert peer review, an incorrect diagnosis was identified in at least 7 with 1 possible associated death.3
The VA officials estimate that the entire review may involve more than 30,000 cases. The allegations are that the pathologist was impaired due to a substance use disorder, in this case alcohol. In interviews, the physician has admitted the alcohol problem and receiving treatment for it but denied he was ever impaired on duty.4 This denial directly contradicts the VA reports that he was intoxicated on duty at least twice.
We do know that the physician in question was enrolled in the Mississippi Physician Health Program (PHP). The Federation of State Physician Health Programs (FSPHP), of which the Mississippi program is a member, provides confidential initial evaluation, ongoing treatment, and monitoring for state licensed health care practitioners with a substance use or other mental health disorder or other condition that could potentially impair their fitness for duty. The PHPs have been career saving for many physicians and other health care professionals. The incentives to return to the practice of medicine are powerful, leading to a higher recovery rate than that of the general population.5
According to FSPHP, “While both PHPs and state licensing boards are engaged in patient safety efforts, PHPs primary focus is on improving the health of the physician, and the licensing board’s primary duty is to protect the public.”6 This potential conflict of interest has been criticized recently.7 News reports suggest that the ambiguity of this relationship between PHP and licensing board may have left a “who’s minding the store” mentality. But here are the facts of this particular case.
In March 2016, an employee reported that the pathologist was intoxicated on duty, and he was immediately removed from service. Of the many elephants in the room, the biggest moral pachyderm is why, given the chronic and progressive nature of substance use disorders did it take 11 years for a formal report leading to action?
Having been in circles of leadership, I know well that often there is much discussed that cannot be disclosed, which frequently contributes to staff demoralization. Dozens of medical center employees over decades must have seen behaviors; some of those employees likely reported their observations. The news reports are silent on this point except for attributing it to “fear of retaliation.” In our current VA climate this is a major intimidator of staff trying to tell the truth and leaders seeking to do what is right. Yet research has identified myriad other motives for not reporting impaired colleagues, including loyalty, collusion, denial, indifference, scarcity of resources, and overwork.8
In October 2017, the pathologist was again found intoxicated on the job, attributing it to a migraine headache. The hospital investigated, but the pathologist may have continued working in some capacity. Finally, after the pathologist was arrested for driving while intoxicated March 1 of this year, the interim VAMC director contacted the Mississippi licensing board, declaring that the pathologist “had failed to meet standards of practice” and indicted that he “constituted an imminent threat to patient welfare.” The Arkansas Medical Foundation then rescinded its support of the pathologist, citing the pathologist’s failure to adhere to monitoring and reporting requirements. The Mississippi program followed suit on June 20, and the medical board rescinded his license.
All employees at whatever level are owed due process and respect for their rights, but Congress recently saw fit to legislate further limits on federal employee protections. Most health care administrators still standing in the chaos of today’s VA would tell you that survival is all about when did you know and what did you do about it? But it is not just administrators, the code of ethics of almost every health care profession includes an obligation to report impaired practitioners. Principle II of the American Medical Association Code of Ethics states, “A physician shall uphold the standards of professionalism, be honest in all professional interactions, and strive to report physicians deficient in character or competence, or engaging in fraud or deception, to appropriate entities.”9
If one is in private practice in a small town, it is easier to pull your friend aside on the golf course and say you seem to be having a problem, counsel your friend to get help, often through a PHP. Then if the gentler approach fails, take the harder action of reporting to the medical board or other authority. To report takes moral courage. It takes seeing that the practitioner is not betraying the “white line” of health care professions but honoring the highest commitment of professionalism to the patient.
The last thing we need in our current suspicious and fearful environment is to turn VAMCs and clinics into a dystopia.Yet reporting in a large organization with rules and red tape can seem terrifying, overwhelming, and confusing. A fair, safe, transparent, clear, and consistent means for staff to discharge their ethical obligations is sorely needed. Or else we will be reading about another tragic scandal and asking each other, “How could this have happened?”
Adherents of the Abrahamic faiths or students of the Bible as literature will easily recall the circumstances of this famous quotation from the Hebrew Scriptures. Cain has killed his brother Abel, earning the disrepute of committing the first murder in biblical history. Scholars of ethics have answered Cain’s sardonic question in the affirmative: avowing that while the individual is primarily responsible for his conduct and its consequences, the community also bears a responsibility.1
Many of you will have seen news clips of yet another Department of Veteran Affairs (VA) scandal: This one involving an impaired pathologist. I have purposely not used the pathologist’s name to emphasize that our shared obligation to protect patients from impaired members of the profession goes far beyond this single outrage. Although we might believe we could never be that individual; none of us are immune from depression, dementia, or physical disabilities that diminish our ability to care for patients. Although it is worth noting that having read or watched everything I could find on the story, the “facts” are few and far between, which I will argue later only underscores the problems with professional accountability especially in a large bureaucratic organization.
This column is not meant to impugn or exculpate anyone but to encourage us to reflect on our ethical awareness and response to hints that there might be an impaired practitioner among us. The Fayetteville VA Medical Center (VAMC) in North Carolina—ground zero for this incident—held several town halls in which anxious and angry veterans demanded an explanation for how an impaired pathologist could have placed in harm’s way nearly 19,000 patients.2 Of this cohort, 5,250 patients have died since 2005. The VA leadership, including the VISN 16 network director and the interim medical director of the Fayetteville VAMC indicated that out of 911 pathology reports that had undergone expert peer review, an incorrect diagnosis was identified in at least 7 with 1 possible associated death.3
The VA officials estimate that the entire review may involve more than 30,000 cases. The allegations are that the pathologist was impaired due to a substance use disorder, in this case alcohol. In interviews, the physician has admitted the alcohol problem and receiving treatment for it but denied he was ever impaired on duty.4 This denial directly contradicts the VA reports that he was intoxicated on duty at least twice.
We do know that the physician in question was enrolled in the Mississippi Physician Health Program (PHP). The Federation of State Physician Health Programs (FSPHP), of which the Mississippi program is a member, provides confidential initial evaluation, ongoing treatment, and monitoring for state licensed health care practitioners with a substance use or other mental health disorder or other condition that could potentially impair their fitness for duty. The PHPs have been career saving for many physicians and other health care professionals. The incentives to return to the practice of medicine are powerful, leading to a higher recovery rate than that of the general population.5
According to FSPHP, “While both PHPs and state licensing boards are engaged in patient safety efforts, PHPs primary focus is on improving the health of the physician, and the licensing board’s primary duty is to protect the public.”6 This potential conflict of interest has been criticized recently.7 News reports suggest that the ambiguity of this relationship between PHP and licensing board may have left a “who’s minding the store” mentality. But here are the facts of this particular case.
In March 2016, an employee reported that the pathologist was intoxicated on duty, and he was immediately removed from service. Of the many elephants in the room, the biggest moral pachyderm is why, given the chronic and progressive nature of substance use disorders did it take 11 years for a formal report leading to action?
Having been in circles of leadership, I know well that often there is much discussed that cannot be disclosed, which frequently contributes to staff demoralization. Dozens of medical center employees over decades must have seen behaviors; some of those employees likely reported their observations. The news reports are silent on this point except for attributing it to “fear of retaliation.” In our current VA climate this is a major intimidator of staff trying to tell the truth and leaders seeking to do what is right. Yet research has identified myriad other motives for not reporting impaired colleagues, including loyalty, collusion, denial, indifference, scarcity of resources, and overwork.8
In October 2017, the pathologist was again found intoxicated on the job, attributing it to a migraine headache. The hospital investigated, but the pathologist may have continued working in some capacity. Finally, after the pathologist was arrested for driving while intoxicated March 1 of this year, the interim VAMC director contacted the Mississippi licensing board, declaring that the pathologist “had failed to meet standards of practice” and indicted that he “constituted an imminent threat to patient welfare.” The Arkansas Medical Foundation then rescinded its support of the pathologist, citing the pathologist’s failure to adhere to monitoring and reporting requirements. The Mississippi program followed suit on June 20, and the medical board rescinded his license.
All employees at whatever level are owed due process and respect for their rights, but Congress recently saw fit to legislate further limits on federal employee protections. Most health care administrators still standing in the chaos of today’s VA would tell you that survival is all about when did you know and what did you do about it? But it is not just administrators, the code of ethics of almost every health care profession includes an obligation to report impaired practitioners. Principle II of the American Medical Association Code of Ethics states, “A physician shall uphold the standards of professionalism, be honest in all professional interactions, and strive to report physicians deficient in character or competence, or engaging in fraud or deception, to appropriate entities.”9
If one is in private practice in a small town, it is easier to pull your friend aside on the golf course and say you seem to be having a problem, counsel your friend to get help, often through a PHP. Then if the gentler approach fails, take the harder action of reporting to the medical board or other authority. To report takes moral courage. It takes seeing that the practitioner is not betraying the “white line” of health care professions but honoring the highest commitment of professionalism to the patient.
The last thing we need in our current suspicious and fearful environment is to turn VAMCs and clinics into a dystopia.Yet reporting in a large organization with rules and red tape can seem terrifying, overwhelming, and confusing. A fair, safe, transparent, clear, and consistent means for staff to discharge their ethical obligations is sorely needed. Or else we will be reading about another tragic scandal and asking each other, “How could this have happened?”
1. Morreim EH. Am I my brother’s warden? Responding to the unethical or incompetent colleague. Hastings Cent Rep. 1993;23(3):19-27
2. Worrell T. Veterans question VA over report of ‘impaired’ pathologist at town hall. http://www.joplinglobe.com/news /local_news/veterans-question-va-over-report-of-impaired-pathologist-at-town/article_9281a9d8-8354-5739-b21e-d38e2f28137c.html. Published July 9, 2018. Accessed July 25, 2018 .
3. Wornell T. Fayetteville VA hospital: ‘impaired’ pathologist misdiagnosed some patients. http://www.joplinglobe.com/news/local_news/fayetteville-va-hospital-impaired-pathologist-misdiagnosed-some-patients/article_519f6adc-2109-5ff1-a9ca-98ba9403d6a7.html. Published June 18, 2018. Accessed July 25, 2018.
4. Merlo LLJ, Teitelbaum SA, Thompson K. Substance use disorders in physicians: assessment and treatment. https://www.uptodate.com/contents/substance-use-disorders-in-physicians-assessment-and-treatment. Last updated July 13, 2017. Accessed July 25, 2018.
5. Grabenstein H. Former VA pathologist denies being impaired on duty. https://www.apnews.com/8ca77da8f7ce40868ffbc091608ee681. Published July 9, 2018. Accessed July 25, 2018.
6. Federation of State Physician Health Programs. Frequently asked questions. https://www.fsphp.org/about/faqs. Accessed July 25, 2018.
7. Anderson P. Physician health programs: more harm than good? https://www.medscape.com/viewarticle/849772. Published August 19, 2015. Accessed July 25, 2018.
8. DesRoches CM, Rao SR, Fromson JA, et al. Physicians’ perceptions, preparedness for reporting, and experiences related to impaired and incompetent colleagues. JAMA. 2010;304(2):187-193.
9. American Medical Association. Code of Medical Ethics 2014-2015. https://commerce.ama-assn.org/store/catalog/productDetail.jsp?product_id=prod2510003&sku_id=sku2510003&navAction=push. Accessed July 25, 2018.
1. Morreim EH. Am I my brother’s warden? Responding to the unethical or incompetent colleague. Hastings Cent Rep. 1993;23(3):19-27
2. Worrell T. Veterans question VA over report of ‘impaired’ pathologist at town hall. http://www.joplinglobe.com/news /local_news/veterans-question-va-over-report-of-impaired-pathologist-at-town/article_9281a9d8-8354-5739-b21e-d38e2f28137c.html. Published July 9, 2018. Accessed July 25, 2018 .
3. Wornell T. Fayetteville VA hospital: ‘impaired’ pathologist misdiagnosed some patients. http://www.joplinglobe.com/news/local_news/fayetteville-va-hospital-impaired-pathologist-misdiagnosed-some-patients/article_519f6adc-2109-5ff1-a9ca-98ba9403d6a7.html. Published June 18, 2018. Accessed July 25, 2018.
4. Merlo LLJ, Teitelbaum SA, Thompson K. Substance use disorders in physicians: assessment and treatment. https://www.uptodate.com/contents/substance-use-disorders-in-physicians-assessment-and-treatment. Last updated July 13, 2017. Accessed July 25, 2018.
5. Grabenstein H. Former VA pathologist denies being impaired on duty. https://www.apnews.com/8ca77da8f7ce40868ffbc091608ee681. Published July 9, 2018. Accessed July 25, 2018.
6. Federation of State Physician Health Programs. Frequently asked questions. https://www.fsphp.org/about/faqs. Accessed July 25, 2018.
7. Anderson P. Physician health programs: more harm than good? https://www.medscape.com/viewarticle/849772. Published August 19, 2015. Accessed July 25, 2018.
8. DesRoches CM, Rao SR, Fromson JA, et al. Physicians’ perceptions, preparedness for reporting, and experiences related to impaired and incompetent colleagues. JAMA. 2010;304(2):187-193.
9. American Medical Association. Code of Medical Ethics 2014-2015. https://commerce.ama-assn.org/store/catalog/productDetail.jsp?product_id=prod2510003&sku_id=sku2510003&navAction=push. Accessed July 25, 2018.
Principles for freshly minted psychiatrists
I just finished reading Dr. Nasrallah’s editorial “The DNA of psychiatric practice: A covenant with our patients” (From the Editor,
David W. Goodman, MD, FAPA
Assistant Professor
Department of Psychiatry and Behavioral Sciences
Johns Hopkins School of Medicine
Baltimore, Maryland
Unfortunately, there is no way a physician who uses an electronic medical record can “Maintain total and unimpeachable confidentiality” as the “The medical record is a clinical, billing, legal, and research document.” Since 2003, patients no longer need to give consent for their medical records to be seen by the many staff members who work in treatment, payment, and health care operations, as long as these individuals follow the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Even de-identified data is no longer safe because re-identification is still possible with all the databases available for cross-referencing (ie, Facebook and hospitals as one instance).
So, when a patient finally tells you about a history of sexual abuse, do you make it clear to him or her that although this information is no longer private, it can be expected to be kept confidential by all the business associates, covered entities, government agencies, etc., who see their records?
Maybe there also would be fewer physician suicides if they could be assured of receiving truly private, off-the-grid psychiatric treatment.
Susan Israel, MD
Private psychiatric practice (retired)
Woodbridge, Connecticut
I just read your excellent and exhaustive May editorial, which offered advice for new psychiatrists. I was surprised to see that nowhere on the list was “Please remember to practice what you preach and be vigilant about self-care. We have become increasingly aware of the high rates of burnout among physicians. Know your own limitations so that you can appreciate the work that you do.”
Hal D. Cash, MD
Private psychiatric practice (retired)
Mica Collaborative
Wellesley, Massachusetts
Continue to: Dr. Nasrallah's editorial should have...
Dr. Nasrallah’s editorial should have listed something about the terms of payment for the psychiatrist who “provides” his or her clinical services to patients. This is an ethical issue. As you know, usually a corporation, rather than a patient, pays the psychiatrist. This payment may come from a health insurance company, government program, or (increasingly) a large clinic. When an organization pays the psychiatrist, it calls the tune for both the doctor’s employment and the patient’s access to quality care. Contracts between the hiring organization and psychiatrists are crucial, and therefore, most young doctors must join a hiring organization for financial reasons after completing their psychiatric residency. The young psychiatrists with whom I speak tell me they have no alternative but to be a “corporate dependent” in the world of 2018 psychiatric practice. They are aware of your (and my) noble principles, which should govern their relationships with patients. But the boss often does not agree with such principles.
In my book Passion for Patients1 and as President of the 501(c)3 Minnesota Physician-Patient Alliance think tank (www.physician-patient.org), I argue for empowering patients with the means to direct payments to their physicians. Allowing patients this option is especially important for forming and maintaining strong relationship-based psychiatric and other medical treatments. In 1996, I was fed up with being a psychiatric medical director for 5 years at a large Minnesota Preferred Provider Organization. For me, the saving grace was being able to have an independent, private psychiatric practice. Most of my patients agreed.Therefore, I suggest another principle: “Build and maintain an independent psychiatric practice as an escape option no matter what you do should you decide the ethical practice of psychiatry is not possible if you are employed by a given organization.”
Lee Beecher, MD
Member
Editorial Advisory Board
Clinical Psychiatry News
Adjunct Professor of Psychiatry
University of Minnesota
Minneapolis, Minnesota
Reference
1. Beecher L, Racer D. Passion for patients. St. Paul, MN: Alethos Press; 2017.
I agree with Dr. Nasrallah’s guiding principles of psychiatry, which he proposes to govern the relationships of psychiatrists with their patients. However, there is one glaring omission. The first principle should be “to appropriately diagnose the patient’s condition,” which may or may not be based in psychiatry. Misdiagnoses and inappropriate pharmacologic therapy have ruined the lives of some very good friends of mine, and the need to first do no harm by misdiagnosing the patient, especially in psychiatric emergency rooms and on inpatient units, cannot be overemphasized.
These situations may not rear their head in the everyday practice of psychiatry. However, medical malpractice, especially in the field of psychiatry, is a constant caution that all new physicians need to watch for.
I would like to thank Dr. Nasrallah for his efforts to strengthen the patient–psychiatrist contract.
Rama Kasturi, PhD
Associate Professor (retired)
Department of Pharmacology and Cell Biophysics
Director (1999 to 2013)
Medical Pharmacology Tutorial Program University of Cincinnati, College of Medicine
Cincinnati, Ohio
Continue to: Dr. Nasrallah responds
Dr. Nasrallah responds
I thank my 5 colleagues for their perspectives on my editorial. You all made cogent points.
I agree with Dr. Israel that our patients’ records are now accessible by many entities due to the drastic changes in our health care delivery system. However, while I regard the basic psychiatric signs and symptoms as medical data, like heart disease or cancer, there are personal details that emerge during psychotherapy that should remain confidential and not be included in the written record, and thus are not accessible to billers, health insurance companies, or malpractice lawyers. As for physicians who consider suicide because of fear of the consequences of receiving psychiatric treatment that becomes a matter of record, that is a matter of the unfortunate stigma and ignorance about mental illness and how treatable it can be.
Regarding Dr. Cash’s comments, I agree that psychiatrists should be (and are almost always are) introspective about their vulnerabilities and limitations, and should act accordingly, which includes taking care of their needs to stay healthy and avoid burnout.
As Dr. Beecher pointed out, the employment model for psychiatrists does have many implications and constraints for patient care. I concur that having a small direct-care practice, sometimes called a “cash practice,” provides patients who can afford it the complete privacy they desire, with no one having access to their medical records except for their psychiatrist. Your book is a useful resource in that regard.
Dr. Kasturi is right about the importance of arriving at an accurate diagnosis before embarking on treatment; otherwise, patients will suffer from “therapeutic misadventures.” I have observed this being experienced by some of the patients referred to me because of “treatment resistance.”
Thanks again to my colleagues for their comments and suggestions to the newly minted psychiatrists for whom my editorial was intended.
Henry A. Nasrallah, MD
The Sydney W. Souers Endowed ChairProfessor and Chairman
Department of Psychiatry and Behavioral Neuroscience
Saint Louis University School of Medicine
St. Louis, Missouri
I just finished reading Dr. Nasrallah’s editorial “The DNA of psychiatric practice: A covenant with our patients” (From the Editor,
David W. Goodman, MD, FAPA
Assistant Professor
Department of Psychiatry and Behavioral Sciences
Johns Hopkins School of Medicine
Baltimore, Maryland
Unfortunately, there is no way a physician who uses an electronic medical record can “Maintain total and unimpeachable confidentiality” as the “The medical record is a clinical, billing, legal, and research document.” Since 2003, patients no longer need to give consent for their medical records to be seen by the many staff members who work in treatment, payment, and health care operations, as long as these individuals follow the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Even de-identified data is no longer safe because re-identification is still possible with all the databases available for cross-referencing (ie, Facebook and hospitals as one instance).
So, when a patient finally tells you about a history of sexual abuse, do you make it clear to him or her that although this information is no longer private, it can be expected to be kept confidential by all the business associates, covered entities, government agencies, etc., who see their records?
Maybe there also would be fewer physician suicides if they could be assured of receiving truly private, off-the-grid psychiatric treatment.
Susan Israel, MD
Private psychiatric practice (retired)
Woodbridge, Connecticut
I just read your excellent and exhaustive May editorial, which offered advice for new psychiatrists. I was surprised to see that nowhere on the list was “Please remember to practice what you preach and be vigilant about self-care. We have become increasingly aware of the high rates of burnout among physicians. Know your own limitations so that you can appreciate the work that you do.”
Hal D. Cash, MD
Private psychiatric practice (retired)
Mica Collaborative
Wellesley, Massachusetts
Continue to: Dr. Nasrallah's editorial should have...
Dr. Nasrallah’s editorial should have listed something about the terms of payment for the psychiatrist who “provides” his or her clinical services to patients. This is an ethical issue. As you know, usually a corporation, rather than a patient, pays the psychiatrist. This payment may come from a health insurance company, government program, or (increasingly) a large clinic. When an organization pays the psychiatrist, it calls the tune for both the doctor’s employment and the patient’s access to quality care. Contracts between the hiring organization and psychiatrists are crucial, and therefore, most young doctors must join a hiring organization for financial reasons after completing their psychiatric residency. The young psychiatrists with whom I speak tell me they have no alternative but to be a “corporate dependent” in the world of 2018 psychiatric practice. They are aware of your (and my) noble principles, which should govern their relationships with patients. But the boss often does not agree with such principles.
In my book Passion for Patients1 and as President of the 501(c)3 Minnesota Physician-Patient Alliance think tank (www.physician-patient.org), I argue for empowering patients with the means to direct payments to their physicians. Allowing patients this option is especially important for forming and maintaining strong relationship-based psychiatric and other medical treatments. In 1996, I was fed up with being a psychiatric medical director for 5 years at a large Minnesota Preferred Provider Organization. For me, the saving grace was being able to have an independent, private psychiatric practice. Most of my patients agreed.Therefore, I suggest another principle: “Build and maintain an independent psychiatric practice as an escape option no matter what you do should you decide the ethical practice of psychiatry is not possible if you are employed by a given organization.”
Lee Beecher, MD
Member
Editorial Advisory Board
Clinical Psychiatry News
Adjunct Professor of Psychiatry
University of Minnesota
Minneapolis, Minnesota
Reference
1. Beecher L, Racer D. Passion for patients. St. Paul, MN: Alethos Press; 2017.
I agree with Dr. Nasrallah’s guiding principles of psychiatry, which he proposes to govern the relationships of psychiatrists with their patients. However, there is one glaring omission. The first principle should be “to appropriately diagnose the patient’s condition,” which may or may not be based in psychiatry. Misdiagnoses and inappropriate pharmacologic therapy have ruined the lives of some very good friends of mine, and the need to first do no harm by misdiagnosing the patient, especially in psychiatric emergency rooms and on inpatient units, cannot be overemphasized.
These situations may not rear their head in the everyday practice of psychiatry. However, medical malpractice, especially in the field of psychiatry, is a constant caution that all new physicians need to watch for.
I would like to thank Dr. Nasrallah for his efforts to strengthen the patient–psychiatrist contract.
Rama Kasturi, PhD
Associate Professor (retired)
Department of Pharmacology and Cell Biophysics
Director (1999 to 2013)
Medical Pharmacology Tutorial Program University of Cincinnati, College of Medicine
Cincinnati, Ohio
Continue to: Dr. Nasrallah responds
Dr. Nasrallah responds
I thank my 5 colleagues for their perspectives on my editorial. You all made cogent points.
I agree with Dr. Israel that our patients’ records are now accessible by many entities due to the drastic changes in our health care delivery system. However, while I regard the basic psychiatric signs and symptoms as medical data, like heart disease or cancer, there are personal details that emerge during psychotherapy that should remain confidential and not be included in the written record, and thus are not accessible to billers, health insurance companies, or malpractice lawyers. As for physicians who consider suicide because of fear of the consequences of receiving psychiatric treatment that becomes a matter of record, that is a matter of the unfortunate stigma and ignorance about mental illness and how treatable it can be.
Regarding Dr. Cash’s comments, I agree that psychiatrists should be (and are almost always are) introspective about their vulnerabilities and limitations, and should act accordingly, which includes taking care of their needs to stay healthy and avoid burnout.
As Dr. Beecher pointed out, the employment model for psychiatrists does have many implications and constraints for patient care. I concur that having a small direct-care practice, sometimes called a “cash practice,” provides patients who can afford it the complete privacy they desire, with no one having access to their medical records except for their psychiatrist. Your book is a useful resource in that regard.
Dr. Kasturi is right about the importance of arriving at an accurate diagnosis before embarking on treatment; otherwise, patients will suffer from “therapeutic misadventures.” I have observed this being experienced by some of the patients referred to me because of “treatment resistance.”
Thanks again to my colleagues for their comments and suggestions to the newly minted psychiatrists for whom my editorial was intended.
Henry A. Nasrallah, MD
The Sydney W. Souers Endowed ChairProfessor and Chairman
Department of Psychiatry and Behavioral Neuroscience
Saint Louis University School of Medicine
St. Louis, Missouri
I just finished reading Dr. Nasrallah’s editorial “The DNA of psychiatric practice: A covenant with our patients” (From the Editor,
David W. Goodman, MD, FAPA
Assistant Professor
Department of Psychiatry and Behavioral Sciences
Johns Hopkins School of Medicine
Baltimore, Maryland
Unfortunately, there is no way a physician who uses an electronic medical record can “Maintain total and unimpeachable confidentiality” as the “The medical record is a clinical, billing, legal, and research document.” Since 2003, patients no longer need to give consent for their medical records to be seen by the many staff members who work in treatment, payment, and health care operations, as long as these individuals follow the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Even de-identified data is no longer safe because re-identification is still possible with all the databases available for cross-referencing (ie, Facebook and hospitals as one instance).
So, when a patient finally tells you about a history of sexual abuse, do you make it clear to him or her that although this information is no longer private, it can be expected to be kept confidential by all the business associates, covered entities, government agencies, etc., who see their records?
Maybe there also would be fewer physician suicides if they could be assured of receiving truly private, off-the-grid psychiatric treatment.
Susan Israel, MD
Private psychiatric practice (retired)
Woodbridge, Connecticut
I just read your excellent and exhaustive May editorial, which offered advice for new psychiatrists. I was surprised to see that nowhere on the list was “Please remember to practice what you preach and be vigilant about self-care. We have become increasingly aware of the high rates of burnout among physicians. Know your own limitations so that you can appreciate the work that you do.”
Hal D. Cash, MD
Private psychiatric practice (retired)
Mica Collaborative
Wellesley, Massachusetts
Continue to: Dr. Nasrallah's editorial should have...
Dr. Nasrallah’s editorial should have listed something about the terms of payment for the psychiatrist who “provides” his or her clinical services to patients. This is an ethical issue. As you know, usually a corporation, rather than a patient, pays the psychiatrist. This payment may come from a health insurance company, government program, or (increasingly) a large clinic. When an organization pays the psychiatrist, it calls the tune for both the doctor’s employment and the patient’s access to quality care. Contracts between the hiring organization and psychiatrists are crucial, and therefore, most young doctors must join a hiring organization for financial reasons after completing their psychiatric residency. The young psychiatrists with whom I speak tell me they have no alternative but to be a “corporate dependent” in the world of 2018 psychiatric practice. They are aware of your (and my) noble principles, which should govern their relationships with patients. But the boss often does not agree with such principles.
In my book Passion for Patients1 and as President of the 501(c)3 Minnesota Physician-Patient Alliance think tank (www.physician-patient.org), I argue for empowering patients with the means to direct payments to their physicians. Allowing patients this option is especially important for forming and maintaining strong relationship-based psychiatric and other medical treatments. In 1996, I was fed up with being a psychiatric medical director for 5 years at a large Minnesota Preferred Provider Organization. For me, the saving grace was being able to have an independent, private psychiatric practice. Most of my patients agreed.Therefore, I suggest another principle: “Build and maintain an independent psychiatric practice as an escape option no matter what you do should you decide the ethical practice of psychiatry is not possible if you are employed by a given organization.”
Lee Beecher, MD
Member
Editorial Advisory Board
Clinical Psychiatry News
Adjunct Professor of Psychiatry
University of Minnesota
Minneapolis, Minnesota
Reference
1. Beecher L, Racer D. Passion for patients. St. Paul, MN: Alethos Press; 2017.
I agree with Dr. Nasrallah’s guiding principles of psychiatry, which he proposes to govern the relationships of psychiatrists with their patients. However, there is one glaring omission. The first principle should be “to appropriately diagnose the patient’s condition,” which may or may not be based in psychiatry. Misdiagnoses and inappropriate pharmacologic therapy have ruined the lives of some very good friends of mine, and the need to first do no harm by misdiagnosing the patient, especially in psychiatric emergency rooms and on inpatient units, cannot be overemphasized.
These situations may not rear their head in the everyday practice of psychiatry. However, medical malpractice, especially in the field of psychiatry, is a constant caution that all new physicians need to watch for.
I would like to thank Dr. Nasrallah for his efforts to strengthen the patient–psychiatrist contract.
Rama Kasturi, PhD
Associate Professor (retired)
Department of Pharmacology and Cell Biophysics
Director (1999 to 2013)
Medical Pharmacology Tutorial Program University of Cincinnati, College of Medicine
Cincinnati, Ohio
Continue to: Dr. Nasrallah responds
Dr. Nasrallah responds
I thank my 5 colleagues for their perspectives on my editorial. You all made cogent points.
I agree with Dr. Israel that our patients’ records are now accessible by many entities due to the drastic changes in our health care delivery system. However, while I regard the basic psychiatric signs and symptoms as medical data, like heart disease or cancer, there are personal details that emerge during psychotherapy that should remain confidential and not be included in the written record, and thus are not accessible to billers, health insurance companies, or malpractice lawyers. As for physicians who consider suicide because of fear of the consequences of receiving psychiatric treatment that becomes a matter of record, that is a matter of the unfortunate stigma and ignorance about mental illness and how treatable it can be.
Regarding Dr. Cash’s comments, I agree that psychiatrists should be (and are almost always are) introspective about their vulnerabilities and limitations, and should act accordingly, which includes taking care of their needs to stay healthy and avoid burnout.
As Dr. Beecher pointed out, the employment model for psychiatrists does have many implications and constraints for patient care. I concur that having a small direct-care practice, sometimes called a “cash practice,” provides patients who can afford it the complete privacy they desire, with no one having access to their medical records except for their psychiatrist. Your book is a useful resource in that regard.
Dr. Kasturi is right about the importance of arriving at an accurate diagnosis before embarking on treatment; otherwise, patients will suffer from “therapeutic misadventures.” I have observed this being experienced by some of the patients referred to me because of “treatment resistance.”
Thanks again to my colleagues for their comments and suggestions to the newly minted psychiatrists for whom my editorial was intended.
Henry A. Nasrallah, MD
The Sydney W. Souers Endowed ChairProfessor and Chairman
Department of Psychiatry and Behavioral Neuroscience
Saint Louis University School of Medicine
St. Louis, Missouri
Hand, foot, and mouth disease: From self-limited to fatal
Hand, foot, and mouth disease (HFMD) has become a global challenge since its first description in 1957 in New Zealand and Canada. Clinicians readily recognize the characteristic syndrome in young children: fever associated with a papulovesicular rash affecting the palms or soles, or both, usually in spring, summer, or fall. In most cases the disease is self-limited, and brief. However, aseptic meningitis, brainstem encephalitis, acute flaccid paralysis or autonomic nervous system deregulation or cardiorespiratory failure may complicate the clinical course.
HFMD is caused by enterovirus A (formerly called human enterovirus A) which consists of 25 serotypes including multiple coxsackie A viruses, multiple enteroviruses, simian enteroviruses, and baboon enterovirus A13. The clinical spectrum spans from herpangina, characterized by fever and painful mouth ulcers most prominent in the posterior oral cavity (uvula, tonsils, soft plates, and anterior pharyngeal folds), to HFMD with papulovesicular rash on palms and soles with or without mouth ulcers/vesicles.1 In atypical cases, the rash may be maculopapular and may include the buttocks, knees or elbows.
In the United States, the predominant cause is coxsackie A16. However, coxsackie A6 appears to be emerging; often more than one HFMD causing virus is circulating concurrently and clinically indistinguishable. Globally, especially, in Asia, enterovirus 1 is a major cause of HFMD and more often associated with prominent central nervous system involvement. Disease can be sporadic or epidemic. An outbreak is usually defined as two or more cases within a defined geographic area; global epidemics as large as 1.5 million cases (Taiwan, 1998) have been reported, and outbreaks in China involving tens of thousands with multiple deaths have been reported.
In 2015, an outbreak of HFMD occurred during basic military training at Lackland Air Force Base, Bexar County, Texas, due to coxsackie A6.2 The illness was characterized by prodromal symptoms of fever and malaise followed by erosive stomatitis and a rash that began on the palms and soles. The rate of infection among trainees was 4.7% (50 of 1,054 persons).
The differential diagnosis includes aphthous ulcers and herpetic gingivostomatitis.3 Aphthous ulcers are seen more commonly in older children and adolescents, are often recurrent, are not seasonal, and are not associated with rash. Herpes simplex virus gingivostomatitis usually has a febrile prodrome, perioral lesions are frequent in addition to gum and tongue involvement, and gingival bleeding is common. HFMD usually has an incubation period of 3-5 days and fever, malaise, and myalgia prodrome followed by onset of oral and dermatologic manifestations in sequence. The skin rash has features that may overlap with varicella, erythema multiforme (EM) or drug eruption. Varicella usually involves the face before spreading to the extremities, and the lesions are characterized by umbilication and subsequent crusting. EM is characterized by target lesions and drug eruptions are morbilliform or maculopapular. The majority of cases of HFMD are diagnosed clinically; polymerase chain reaction testing is available and best performed on throat or vesicle specimens. Serologic testing for A16 and enterovirus 71 (IgM) is available. Infected patients shed virus for 2-4 weeks and virus is stable in the environment resulting in fecal-oral or oral-oral transmission.
Atypical features of HFMD include occurrence in the winter (outbreak in Alabama in 2011/2012) or an atypical distribution of rash involving the antecubital and popliteal fossae distribution of rash, or “eczema coxsackium” – the accentuation of rash in areas previously affected by atopic dermatitis. Additional features may include nail dystrophies that manifest as Beau lines (deep grooved lines that run from side to side on the fingernail or the toenail) and nail shedding.
A spectrum of neurologic complications has been observed, more frequently with EV71 and more frequently in Asia. The spectrum includes aseptic meningitis and brainstem encephalitis. Progressive cardiopulmonary failure also can be observed in severe cases. The hallmark of severe disease is often presentation with high fever, sweating, mottled skin, and tachycardia. Early signs of CNS involvement include myoclonic jerks, ataxia, and “wandering eyes.”3 Elevated white blood count and/or hyperglycemia may distinguish children with severe disease from benign disease. Anecdotal reports of response to treatment with high-dose methylprednisolone and intravenous immune globulin suggest that the neurologic disease may be an autoimmune phenomenon.
The clinician’s primary role is to accurately diagnose HFMD, provide supportive care for fever and dehydration, and identify those with early signs or laboratory features heralding a more severe course of disease.3 The Centers for Disease Control and Prevention recommends frequent hand washing after toileting and changing diapers, disinfecting surfaces such as toys, avoiding close contact with infected individuals or sharing of personal items for all affected patients. No antiviral treatment is available although improvement following early treatment with acyclovir has been reported anecdotally. Intravenous immunoglobulin has been used in severe cases in Asia with retrospective data analysis suggesting a potential for improvement when administered prior to cardiopulmonary arrest.1
Dr. Pelton is professor of pediatrics and epidemiology at Boston University. Dr. Pelton said he had no relevant financial disclosures. Email him at [email protected].
References
1. Cleveland Clinic Journal of Medicine 2014;81(9):537-43.
2. Morbidity and Mortality Weekly Report MMWR. 2016 Jul 8;65(26);678-80.
3. A Guide to clinical management and public health response for hand, foot and mouth disease (HFMD).
Hand, foot, and mouth disease (HFMD) has become a global challenge since its first description in 1957 in New Zealand and Canada. Clinicians readily recognize the characteristic syndrome in young children: fever associated with a papulovesicular rash affecting the palms or soles, or both, usually in spring, summer, or fall. In most cases the disease is self-limited, and brief. However, aseptic meningitis, brainstem encephalitis, acute flaccid paralysis or autonomic nervous system deregulation or cardiorespiratory failure may complicate the clinical course.
HFMD is caused by enterovirus A (formerly called human enterovirus A) which consists of 25 serotypes including multiple coxsackie A viruses, multiple enteroviruses, simian enteroviruses, and baboon enterovirus A13. The clinical spectrum spans from herpangina, characterized by fever and painful mouth ulcers most prominent in the posterior oral cavity (uvula, tonsils, soft plates, and anterior pharyngeal folds), to HFMD with papulovesicular rash on palms and soles with or without mouth ulcers/vesicles.1 In atypical cases, the rash may be maculopapular and may include the buttocks, knees or elbows.
In the United States, the predominant cause is coxsackie A16. However, coxsackie A6 appears to be emerging; often more than one HFMD causing virus is circulating concurrently and clinically indistinguishable. Globally, especially, in Asia, enterovirus 1 is a major cause of HFMD and more often associated with prominent central nervous system involvement. Disease can be sporadic or epidemic. An outbreak is usually defined as two or more cases within a defined geographic area; global epidemics as large as 1.5 million cases (Taiwan, 1998) have been reported, and outbreaks in China involving tens of thousands with multiple deaths have been reported.
In 2015, an outbreak of HFMD occurred during basic military training at Lackland Air Force Base, Bexar County, Texas, due to coxsackie A6.2 The illness was characterized by prodromal symptoms of fever and malaise followed by erosive stomatitis and a rash that began on the palms and soles. The rate of infection among trainees was 4.7% (50 of 1,054 persons).
The differential diagnosis includes aphthous ulcers and herpetic gingivostomatitis.3 Aphthous ulcers are seen more commonly in older children and adolescents, are often recurrent, are not seasonal, and are not associated with rash. Herpes simplex virus gingivostomatitis usually has a febrile prodrome, perioral lesions are frequent in addition to gum and tongue involvement, and gingival bleeding is common. HFMD usually has an incubation period of 3-5 days and fever, malaise, and myalgia prodrome followed by onset of oral and dermatologic manifestations in sequence. The skin rash has features that may overlap with varicella, erythema multiforme (EM) or drug eruption. Varicella usually involves the face before spreading to the extremities, and the lesions are characterized by umbilication and subsequent crusting. EM is characterized by target lesions and drug eruptions are morbilliform or maculopapular. The majority of cases of HFMD are diagnosed clinically; polymerase chain reaction testing is available and best performed on throat or vesicle specimens. Serologic testing for A16 and enterovirus 71 (IgM) is available. Infected patients shed virus for 2-4 weeks and virus is stable in the environment resulting in fecal-oral or oral-oral transmission.
Atypical features of HFMD include occurrence in the winter (outbreak in Alabama in 2011/2012) or an atypical distribution of rash involving the antecubital and popliteal fossae distribution of rash, or “eczema coxsackium” – the accentuation of rash in areas previously affected by atopic dermatitis. Additional features may include nail dystrophies that manifest as Beau lines (deep grooved lines that run from side to side on the fingernail or the toenail) and nail shedding.
A spectrum of neurologic complications has been observed, more frequently with EV71 and more frequently in Asia. The spectrum includes aseptic meningitis and brainstem encephalitis. Progressive cardiopulmonary failure also can be observed in severe cases. The hallmark of severe disease is often presentation with high fever, sweating, mottled skin, and tachycardia. Early signs of CNS involvement include myoclonic jerks, ataxia, and “wandering eyes.”3 Elevated white blood count and/or hyperglycemia may distinguish children with severe disease from benign disease. Anecdotal reports of response to treatment with high-dose methylprednisolone and intravenous immune globulin suggest that the neurologic disease may be an autoimmune phenomenon.
The clinician’s primary role is to accurately diagnose HFMD, provide supportive care for fever and dehydration, and identify those with early signs or laboratory features heralding a more severe course of disease.3 The Centers for Disease Control and Prevention recommends frequent hand washing after toileting and changing diapers, disinfecting surfaces such as toys, avoiding close contact with infected individuals or sharing of personal items for all affected patients. No antiviral treatment is available although improvement following early treatment with acyclovir has been reported anecdotally. Intravenous immunoglobulin has been used in severe cases in Asia with retrospective data analysis suggesting a potential for improvement when administered prior to cardiopulmonary arrest.1
Dr. Pelton is professor of pediatrics and epidemiology at Boston University. Dr. Pelton said he had no relevant financial disclosures. Email him at [email protected].
References
1. Cleveland Clinic Journal of Medicine 2014;81(9):537-43.
2. Morbidity and Mortality Weekly Report MMWR. 2016 Jul 8;65(26);678-80.
3. A Guide to clinical management and public health response for hand, foot and mouth disease (HFMD).
Hand, foot, and mouth disease (HFMD) has become a global challenge since its first description in 1957 in New Zealand and Canada. Clinicians readily recognize the characteristic syndrome in young children: fever associated with a papulovesicular rash affecting the palms or soles, or both, usually in spring, summer, or fall. In most cases the disease is self-limited, and brief. However, aseptic meningitis, brainstem encephalitis, acute flaccid paralysis or autonomic nervous system deregulation or cardiorespiratory failure may complicate the clinical course.
HFMD is caused by enterovirus A (formerly called human enterovirus A) which consists of 25 serotypes including multiple coxsackie A viruses, multiple enteroviruses, simian enteroviruses, and baboon enterovirus A13. The clinical spectrum spans from herpangina, characterized by fever and painful mouth ulcers most prominent in the posterior oral cavity (uvula, tonsils, soft plates, and anterior pharyngeal folds), to HFMD with papulovesicular rash on palms and soles with or without mouth ulcers/vesicles.1 In atypical cases, the rash may be maculopapular and may include the buttocks, knees or elbows.
In the United States, the predominant cause is coxsackie A16. However, coxsackie A6 appears to be emerging; often more than one HFMD causing virus is circulating concurrently and clinically indistinguishable. Globally, especially, in Asia, enterovirus 1 is a major cause of HFMD and more often associated with prominent central nervous system involvement. Disease can be sporadic or epidemic. An outbreak is usually defined as two or more cases within a defined geographic area; global epidemics as large as 1.5 million cases (Taiwan, 1998) have been reported, and outbreaks in China involving tens of thousands with multiple deaths have been reported.
In 2015, an outbreak of HFMD occurred during basic military training at Lackland Air Force Base, Bexar County, Texas, due to coxsackie A6.2 The illness was characterized by prodromal symptoms of fever and malaise followed by erosive stomatitis and a rash that began on the palms and soles. The rate of infection among trainees was 4.7% (50 of 1,054 persons).
The differential diagnosis includes aphthous ulcers and herpetic gingivostomatitis.3 Aphthous ulcers are seen more commonly in older children and adolescents, are often recurrent, are not seasonal, and are not associated with rash. Herpes simplex virus gingivostomatitis usually has a febrile prodrome, perioral lesions are frequent in addition to gum and tongue involvement, and gingival bleeding is common. HFMD usually has an incubation period of 3-5 days and fever, malaise, and myalgia prodrome followed by onset of oral and dermatologic manifestations in sequence. The skin rash has features that may overlap with varicella, erythema multiforme (EM) or drug eruption. Varicella usually involves the face before spreading to the extremities, and the lesions are characterized by umbilication and subsequent crusting. EM is characterized by target lesions and drug eruptions are morbilliform or maculopapular. The majority of cases of HFMD are diagnosed clinically; polymerase chain reaction testing is available and best performed on throat or vesicle specimens. Serologic testing for A16 and enterovirus 71 (IgM) is available. Infected patients shed virus for 2-4 weeks and virus is stable in the environment resulting in fecal-oral or oral-oral transmission.
Atypical features of HFMD include occurrence in the winter (outbreak in Alabama in 2011/2012) or an atypical distribution of rash involving the antecubital and popliteal fossae distribution of rash, or “eczema coxsackium” – the accentuation of rash in areas previously affected by atopic dermatitis. Additional features may include nail dystrophies that manifest as Beau lines (deep grooved lines that run from side to side on the fingernail or the toenail) and nail shedding.
A spectrum of neurologic complications has been observed, more frequently with EV71 and more frequently in Asia. The spectrum includes aseptic meningitis and brainstem encephalitis. Progressive cardiopulmonary failure also can be observed in severe cases. The hallmark of severe disease is often presentation with high fever, sweating, mottled skin, and tachycardia. Early signs of CNS involvement include myoclonic jerks, ataxia, and “wandering eyes.”3 Elevated white blood count and/or hyperglycemia may distinguish children with severe disease from benign disease. Anecdotal reports of response to treatment with high-dose methylprednisolone and intravenous immune globulin suggest that the neurologic disease may be an autoimmune phenomenon.
The clinician’s primary role is to accurately diagnose HFMD, provide supportive care for fever and dehydration, and identify those with early signs or laboratory features heralding a more severe course of disease.3 The Centers for Disease Control and Prevention recommends frequent hand washing after toileting and changing diapers, disinfecting surfaces such as toys, avoiding close contact with infected individuals or sharing of personal items for all affected patients. No antiviral treatment is available although improvement following early treatment with acyclovir has been reported anecdotally. Intravenous immunoglobulin has been used in severe cases in Asia with retrospective data analysis suggesting a potential for improvement when administered prior to cardiopulmonary arrest.1
Dr. Pelton is professor of pediatrics and epidemiology at Boston University. Dr. Pelton said he had no relevant financial disclosures. Email him at [email protected].
References
1. Cleveland Clinic Journal of Medicine 2014;81(9):537-43.
2. Morbidity and Mortality Weekly Report MMWR. 2016 Jul 8;65(26);678-80.
3. A Guide to clinical management and public health response for hand, foot and mouth disease (HFMD).












