User login
Privacy and maternal records
At the undergraduate level, classes on medical ethics tend to focus on the big ticket items like abortion, euthanasia, and social justice. Personally, I find the more interesting clinical cases involve relatively minor issues that accumulate to create problems. Privacy is one example.
A large amount of information in the mother’s prenatal records potentially impacts a newborn’s care. Ideally, the EHR is transferring data to the newborn’s chart, but not everything automatically populates in the newborn record, so there will be times when a pediatrician needs to review the mother’s chart.
- The criteria for selecting which mothers’ charts to review involve racial profiling.
- Access to mental health records involving addiction treatment requires special authorization. State laws and hospital policies will vary.
- Mom is a Hollywood celebrity and, while reviewing her chart, prurient curiosity extends the search to records of her cosmetic surgeries.
In my opinion, most of what is and isn’t permissible is determined by medical custom and not by statutes. The judiciary reserves the power to intervene, so medical custom should be informed by laws and by legal principles. But, the primary basis for these decisions should be a commitment to patient advocacy and to common sense, which in this situation means, “Would the typical reasonable person be upset if she learned I had done something without telling her?” If the answer to that question is yes, or in any way equivocal, I think ethics would dictate obtaining consent or at least assent.
Opiate addiction has quadrupled in the past 15 years. Almost all states now have prescription registries to help detect doctor shopping, multiple prescribers, and misdirection. If you are prescribing an opiate, it is ethically reasonable (and now the law) for you to make writing the prescription contingent on your patient agreeing to your consulting the registry. No consent, no prescription.
I think the facts of that case (writing a prescription) can be distinguished (a legal term) from the case of a neonatologist accessing the narcotic registry of the mother while on a fishing expedition to find evidence that might help the baby. Perhaps it is okay with the mother’s uncoerced consent, but otherwise I think that practice reeks as an unreasonable search. Ethically and legally, it has parallels to Ferguson v. City of Charleston (SCOTUS 2001).
That was a 6-3 Supreme Court decision, so, while I agree with the majority, you may find hospital lawyers who disagree. Overall, I assert that consent and privacy are best considered ethically as advocacy for the patient and not as legalistic forms that the physician must complete.
The reverse situation also occurs. Sometimes maternal health information is placed into the newborn’s chart that doesn’t need to be there. For example, common practice has been to designate mom, after delivery, as G4P2022. This contains the information that mother has had two therapeutic abortions. Does that information belong in a newborn’s chart? Especially in the era of the EHR where this information will hang around forever and will be easily obtained by the baby 16 years later when she can access all her medical information online. Will the mother be upset for her teenage daughter to learn that mom has had two abortions? Is that private information, belonging to the mother, that was given in confidence to her obstetrician? I advocate respecting privacy.
I have similar concerns about STD information being transferred from maternal charts to the newborn’s EHR. A maternal history of gonorrhea treated 8 years previously is unlikely to be relevant and should not populate the newborn’s EHR. I can make an argument that chlamydia detected and treated during the pregnancy might be useful to the baby’s pediatrician because neither treatment nor tests of cure are perfect. Perhaps, it could exist as a Snapchat-type record and disappear from the newborn’s record in a year if no respiratory symptoms occur.
I’m aware of efforts to destigmatize abortion and STDs, but, until that occurs, sensitive information should be handled delicately to preserve privacy. That is a major component of the Hippocratic Oath.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
At the undergraduate level, classes on medical ethics tend to focus on the big ticket items like abortion, euthanasia, and social justice. Personally, I find the more interesting clinical cases involve relatively minor issues that accumulate to create problems. Privacy is one example.
A large amount of information in the mother’s prenatal records potentially impacts a newborn’s care. Ideally, the EHR is transferring data to the newborn’s chart, but not everything automatically populates in the newborn record, so there will be times when a pediatrician needs to review the mother’s chart.
- The criteria for selecting which mothers’ charts to review involve racial profiling.
- Access to mental health records involving addiction treatment requires special authorization. State laws and hospital policies will vary.
- Mom is a Hollywood celebrity and, while reviewing her chart, prurient curiosity extends the search to records of her cosmetic surgeries.
In my opinion, most of what is and isn’t permissible is determined by medical custom and not by statutes. The judiciary reserves the power to intervene, so medical custom should be informed by laws and by legal principles. But, the primary basis for these decisions should be a commitment to patient advocacy and to common sense, which in this situation means, “Would the typical reasonable person be upset if she learned I had done something without telling her?” If the answer to that question is yes, or in any way equivocal, I think ethics would dictate obtaining consent or at least assent.
Opiate addiction has quadrupled in the past 15 years. Almost all states now have prescription registries to help detect doctor shopping, multiple prescribers, and misdirection. If you are prescribing an opiate, it is ethically reasonable (and now the law) for you to make writing the prescription contingent on your patient agreeing to your consulting the registry. No consent, no prescription.
I think the facts of that case (writing a prescription) can be distinguished (a legal term) from the case of a neonatologist accessing the narcotic registry of the mother while on a fishing expedition to find evidence that might help the baby. Perhaps it is okay with the mother’s uncoerced consent, but otherwise I think that practice reeks as an unreasonable search. Ethically and legally, it has parallels to Ferguson v. City of Charleston (SCOTUS 2001).
That was a 6-3 Supreme Court decision, so, while I agree with the majority, you may find hospital lawyers who disagree. Overall, I assert that consent and privacy are best considered ethically as advocacy for the patient and not as legalistic forms that the physician must complete.
The reverse situation also occurs. Sometimes maternal health information is placed into the newborn’s chart that doesn’t need to be there. For example, common practice has been to designate mom, after delivery, as G4P2022. This contains the information that mother has had two therapeutic abortions. Does that information belong in a newborn’s chart? Especially in the era of the EHR where this information will hang around forever and will be easily obtained by the baby 16 years later when she can access all her medical information online. Will the mother be upset for her teenage daughter to learn that mom has had two abortions? Is that private information, belonging to the mother, that was given in confidence to her obstetrician? I advocate respecting privacy.
I have similar concerns about STD information being transferred from maternal charts to the newborn’s EHR. A maternal history of gonorrhea treated 8 years previously is unlikely to be relevant and should not populate the newborn’s EHR. I can make an argument that chlamydia detected and treated during the pregnancy might be useful to the baby’s pediatrician because neither treatment nor tests of cure are perfect. Perhaps, it could exist as a Snapchat-type record and disappear from the newborn’s record in a year if no respiratory symptoms occur.
I’m aware of efforts to destigmatize abortion and STDs, but, until that occurs, sensitive information should be handled delicately to preserve privacy. That is a major component of the Hippocratic Oath.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
At the undergraduate level, classes on medical ethics tend to focus on the big ticket items like abortion, euthanasia, and social justice. Personally, I find the more interesting clinical cases involve relatively minor issues that accumulate to create problems. Privacy is one example.
A large amount of information in the mother’s prenatal records potentially impacts a newborn’s care. Ideally, the EHR is transferring data to the newborn’s chart, but not everything automatically populates in the newborn record, so there will be times when a pediatrician needs to review the mother’s chart.
- The criteria for selecting which mothers’ charts to review involve racial profiling.
- Access to mental health records involving addiction treatment requires special authorization. State laws and hospital policies will vary.
- Mom is a Hollywood celebrity and, while reviewing her chart, prurient curiosity extends the search to records of her cosmetic surgeries.
In my opinion, most of what is and isn’t permissible is determined by medical custom and not by statutes. The judiciary reserves the power to intervene, so medical custom should be informed by laws and by legal principles. But, the primary basis for these decisions should be a commitment to patient advocacy and to common sense, which in this situation means, “Would the typical reasonable person be upset if she learned I had done something without telling her?” If the answer to that question is yes, or in any way equivocal, I think ethics would dictate obtaining consent or at least assent.
Opiate addiction has quadrupled in the past 15 years. Almost all states now have prescription registries to help detect doctor shopping, multiple prescribers, and misdirection. If you are prescribing an opiate, it is ethically reasonable (and now the law) for you to make writing the prescription contingent on your patient agreeing to your consulting the registry. No consent, no prescription.
I think the facts of that case (writing a prescription) can be distinguished (a legal term) from the case of a neonatologist accessing the narcotic registry of the mother while on a fishing expedition to find evidence that might help the baby. Perhaps it is okay with the mother’s uncoerced consent, but otherwise I think that practice reeks as an unreasonable search. Ethically and legally, it has parallels to Ferguson v. City of Charleston (SCOTUS 2001).
That was a 6-3 Supreme Court decision, so, while I agree with the majority, you may find hospital lawyers who disagree. Overall, I assert that consent and privacy are best considered ethically as advocacy for the patient and not as legalistic forms that the physician must complete.
The reverse situation also occurs. Sometimes maternal health information is placed into the newborn’s chart that doesn’t need to be there. For example, common practice has been to designate mom, after delivery, as G4P2022. This contains the information that mother has had two therapeutic abortions. Does that information belong in a newborn’s chart? Especially in the era of the EHR where this information will hang around forever and will be easily obtained by the baby 16 years later when she can access all her medical information online. Will the mother be upset for her teenage daughter to learn that mom has had two abortions? Is that private information, belonging to the mother, that was given in confidence to her obstetrician? I advocate respecting privacy.
I have similar concerns about STD information being transferred from maternal charts to the newborn’s EHR. A maternal history of gonorrhea treated 8 years previously is unlikely to be relevant and should not populate the newborn’s EHR. I can make an argument that chlamydia detected and treated during the pregnancy might be useful to the baby’s pediatrician because neither treatment nor tests of cure are perfect. Perhaps, it could exist as a Snapchat-type record and disappear from the newborn’s record in a year if no respiratory symptoms occur.
I’m aware of efforts to destigmatize abortion and STDs, but, until that occurs, sensitive information should be handled delicately to preserve privacy. That is a major component of the Hippocratic Oath.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
Hepatitis C is a pediatric disease now
The baby looked perfect: healthy term male, weight at the 60th percentile, normal exam. The mother, a 26-year-old diagnosed with hepatitis C virus (HCV) infection during her pregnancy, looked alternately hopeful and horrified as I explained what implications her infection could have for her baby.
“Most babies will be fine,” I explained. “Of all mothers with hepatitis C infection, just under 6% will pass the infection on to their babies.” Transmission rates are twice as high in infants born to women with high HCV viral loads or those coinfected with HIV. The risk of transmission from women with undetectable HCV RNA is almost zero. Unfortunately, this mother did not fall into that category.
At that moment, however, I didn’t have time to be concerned about the numbers. My focus was one mother and her newborn baby.
“What if my baby is one of the unlucky ones who gets infected?” the mother asked, cuddling her infant. “What then?”
We know a lot about the course of hepatitis C in adults. An estimated 75%-86% of those infected will go on to develop chronic infection. Long-term sequelae include cirrhosis, liver failure, and hepatocellular carcinoma.
The course of HCV in children appears to be different. Twenty-five percent to 40% of vertically infected children will spontaneously clear their infection, most by 2 years of age. Occasionally, that might not happen until 7 years of age. Most who are chronically infected experience few symptoms, and fortunately cirrhosis and liver failure rarely present in childhood. In a large cohort of Italian children, half of whom were thought to be infected perinatally, less than 2% progressed to decompensated cirrhosis after 10 years of infection. According to the CDC, most children infected at birth “do well during childhood,” but more research is needed to understand the long-term effects of perinatal hepatitis C in children.
New antivirals have revolutionized the care of HCV-infected adults and now offer the hope of cure for up to 90%. None of these drugs are currently approved for use in children younger than 12 years, although clinical trials are underway. Because most cases of HCV in children are indolent, some children may not require treatment until adulthood.
July 28th was World Hepatitis Day and this year’s theme was Eliminate Hepatitis. To eliminate the problem of hepatitis C in children, pediatricians and others involved in the care of children need to get involved.
We need to know the scope of the problem
Since 2015, Kentucky has mandated reporting of all HCV-infected pregnant women and children through age 60 months, as well as all infants born to all HCV-infected women. At present though, there is substantial variability in state reporting requirements. We likely need a standardized case definition for perinatal HCV and national reporting criteria.
We need some clear guidance about testing during pregnancy
This should come from public health authorities, the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists.
Jonathan Mermin, MD, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, has said, “Women are screened throughout pregnancy for many conditions that threaten their health. An expectant mother at risk for hepatitis C deserves to be tested. Knowing her status is the only way she can access the best hepatitis care and treatment – both for herself and her baby.” Yet, routine hepatitis C testing is not recommended during pregnancy, in part because there are no established interventions to prevent mother-to-child transmission of HCV. Instead, women are to be screened for risk factors and tested if they are present. As we learned with hepatitis B and HIV, risk factor screening is hard and misses individuals who are infected.
We need to ensure that HCV-exposed infants are identified and followed appropriately.
In a study of HCV-exposed infants born to women in Philadelphia, 84% did not receive adequate testing for HCV infection. In human terms, 537 children were born to HCV-positive mothers during the study period and 4 of 84 (5%) children tested were found to be infected. Assuming that 5% of HCV-exposed infants will develop chronic infection, 23 additional children were undiagnosed and, therefore, were not being followed for potential sequelae.
HCV-infected mothers in this study were more likely than non-infected mothers to be socioeconomically disadvantaged – specifically, unmarried, less educated, and publicly insured – suggesting that access to care may have played a role. When you add in drug use as a common risk factor for HCV infection, it is easy to understand why some at-risk infants are lost to follow-up.
Investigators in the Philadelphia study suggested that there might be more to the story. They proposed that pediatricians might be unaware of the need for testing because they had not been alerted to the mother’s HCV status by the obstetrician, the birthing hospital, or the mother herself. Finally, they theorized that many pediatricians “may be unaware or skeptical of the guidelines for testing children exposed to HCV.” This is a problem that we can solve.
I finished the visit with this mother by reassuring her that she could breastfeed her infant as planned as long as she did not have cracked or bleeding nipples. I also explained the schedule for testing. A 2002 National Institutes of Health consensus statement recommends that infants perinatally exposed to HCV have two HCV RNA tests between 2 and 6 months of age and/or be tested for HCV antibodies after 15 months. North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) Practice Guidelines for Diagnosis and Management of Hepatitis C Infection in Infants, Children, and Adolescents recommend testing for HCV antibodies at 18 months of age (J Pediatr Gastroenterol Nutr. 2012 Jun;54[6]:838-55). If a family requests earlier testing, a serum HCV RNA test can be done as early as 2 months of age. If positive, NASPGHAN recommends testing after 12 months of age to evaluate for chronic infection.
My practice has adopted the National Institutes of Health consensus statement approach because many of the families we see experience significant anxiety about the diagnosis, and this mother was no exception. As noted in the expert guidelines, this was a situation in which “early exclusion of HCV infection is reassuring and may be worth the added expense.”
“So first test at 2 months?” she asked. “Until then, we can’t do anything but wait?”
It is estimated that there are 23,000 to 46,000 U.S. children living with HCV. The wait for pediatricians is over. , and we need to educate ourselves about diagnosis and management. A first step might be to begin asking expectant mothers and the mothers of newborns if they know their HCV status.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
The baby looked perfect: healthy term male, weight at the 60th percentile, normal exam. The mother, a 26-year-old diagnosed with hepatitis C virus (HCV) infection during her pregnancy, looked alternately hopeful and horrified as I explained what implications her infection could have for her baby.
“Most babies will be fine,” I explained. “Of all mothers with hepatitis C infection, just under 6% will pass the infection on to their babies.” Transmission rates are twice as high in infants born to women with high HCV viral loads or those coinfected with HIV. The risk of transmission from women with undetectable HCV RNA is almost zero. Unfortunately, this mother did not fall into that category.
At that moment, however, I didn’t have time to be concerned about the numbers. My focus was one mother and her newborn baby.
“What if my baby is one of the unlucky ones who gets infected?” the mother asked, cuddling her infant. “What then?”
We know a lot about the course of hepatitis C in adults. An estimated 75%-86% of those infected will go on to develop chronic infection. Long-term sequelae include cirrhosis, liver failure, and hepatocellular carcinoma.
The course of HCV in children appears to be different. Twenty-five percent to 40% of vertically infected children will spontaneously clear their infection, most by 2 years of age. Occasionally, that might not happen until 7 years of age. Most who are chronically infected experience few symptoms, and fortunately cirrhosis and liver failure rarely present in childhood. In a large cohort of Italian children, half of whom were thought to be infected perinatally, less than 2% progressed to decompensated cirrhosis after 10 years of infection. According to the CDC, most children infected at birth “do well during childhood,” but more research is needed to understand the long-term effects of perinatal hepatitis C in children.
New antivirals have revolutionized the care of HCV-infected adults and now offer the hope of cure for up to 90%. None of these drugs are currently approved for use in children younger than 12 years, although clinical trials are underway. Because most cases of HCV in children are indolent, some children may not require treatment until adulthood.
July 28th was World Hepatitis Day and this year’s theme was Eliminate Hepatitis. To eliminate the problem of hepatitis C in children, pediatricians and others involved in the care of children need to get involved.
We need to know the scope of the problem
Since 2015, Kentucky has mandated reporting of all HCV-infected pregnant women and children through age 60 months, as well as all infants born to all HCV-infected women. At present though, there is substantial variability in state reporting requirements. We likely need a standardized case definition for perinatal HCV and national reporting criteria.
We need some clear guidance about testing during pregnancy
This should come from public health authorities, the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists.
Jonathan Mermin, MD, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, has said, “Women are screened throughout pregnancy for many conditions that threaten their health. An expectant mother at risk for hepatitis C deserves to be tested. Knowing her status is the only way she can access the best hepatitis care and treatment – both for herself and her baby.” Yet, routine hepatitis C testing is not recommended during pregnancy, in part because there are no established interventions to prevent mother-to-child transmission of HCV. Instead, women are to be screened for risk factors and tested if they are present. As we learned with hepatitis B and HIV, risk factor screening is hard and misses individuals who are infected.
We need to ensure that HCV-exposed infants are identified and followed appropriately.
In a study of HCV-exposed infants born to women in Philadelphia, 84% did not receive adequate testing for HCV infection. In human terms, 537 children were born to HCV-positive mothers during the study period and 4 of 84 (5%) children tested were found to be infected. Assuming that 5% of HCV-exposed infants will develop chronic infection, 23 additional children were undiagnosed and, therefore, were not being followed for potential sequelae.
HCV-infected mothers in this study were more likely than non-infected mothers to be socioeconomically disadvantaged – specifically, unmarried, less educated, and publicly insured – suggesting that access to care may have played a role. When you add in drug use as a common risk factor for HCV infection, it is easy to understand why some at-risk infants are lost to follow-up.
Investigators in the Philadelphia study suggested that there might be more to the story. They proposed that pediatricians might be unaware of the need for testing because they had not been alerted to the mother’s HCV status by the obstetrician, the birthing hospital, or the mother herself. Finally, they theorized that many pediatricians “may be unaware or skeptical of the guidelines for testing children exposed to HCV.” This is a problem that we can solve.
I finished the visit with this mother by reassuring her that she could breastfeed her infant as planned as long as she did not have cracked or bleeding nipples. I also explained the schedule for testing. A 2002 National Institutes of Health consensus statement recommends that infants perinatally exposed to HCV have two HCV RNA tests between 2 and 6 months of age and/or be tested for HCV antibodies after 15 months. North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) Practice Guidelines for Diagnosis and Management of Hepatitis C Infection in Infants, Children, and Adolescents recommend testing for HCV antibodies at 18 months of age (J Pediatr Gastroenterol Nutr. 2012 Jun;54[6]:838-55). If a family requests earlier testing, a serum HCV RNA test can be done as early as 2 months of age. If positive, NASPGHAN recommends testing after 12 months of age to evaluate for chronic infection.
My practice has adopted the National Institutes of Health consensus statement approach because many of the families we see experience significant anxiety about the diagnosis, and this mother was no exception. As noted in the expert guidelines, this was a situation in which “early exclusion of HCV infection is reassuring and may be worth the added expense.”
“So first test at 2 months?” she asked. “Until then, we can’t do anything but wait?”
It is estimated that there are 23,000 to 46,000 U.S. children living with HCV. The wait for pediatricians is over. , and we need to educate ourselves about diagnosis and management. A first step might be to begin asking expectant mothers and the mothers of newborns if they know their HCV status.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
The baby looked perfect: healthy term male, weight at the 60th percentile, normal exam. The mother, a 26-year-old diagnosed with hepatitis C virus (HCV) infection during her pregnancy, looked alternately hopeful and horrified as I explained what implications her infection could have for her baby.
“Most babies will be fine,” I explained. “Of all mothers with hepatitis C infection, just under 6% will pass the infection on to their babies.” Transmission rates are twice as high in infants born to women with high HCV viral loads or those coinfected with HIV. The risk of transmission from women with undetectable HCV RNA is almost zero. Unfortunately, this mother did not fall into that category.
At that moment, however, I didn’t have time to be concerned about the numbers. My focus was one mother and her newborn baby.
“What if my baby is one of the unlucky ones who gets infected?” the mother asked, cuddling her infant. “What then?”
We know a lot about the course of hepatitis C in adults. An estimated 75%-86% of those infected will go on to develop chronic infection. Long-term sequelae include cirrhosis, liver failure, and hepatocellular carcinoma.
The course of HCV in children appears to be different. Twenty-five percent to 40% of vertically infected children will spontaneously clear their infection, most by 2 years of age. Occasionally, that might not happen until 7 years of age. Most who are chronically infected experience few symptoms, and fortunately cirrhosis and liver failure rarely present in childhood. In a large cohort of Italian children, half of whom were thought to be infected perinatally, less than 2% progressed to decompensated cirrhosis after 10 years of infection. According to the CDC, most children infected at birth “do well during childhood,” but more research is needed to understand the long-term effects of perinatal hepatitis C in children.
New antivirals have revolutionized the care of HCV-infected adults and now offer the hope of cure for up to 90%. None of these drugs are currently approved for use in children younger than 12 years, although clinical trials are underway. Because most cases of HCV in children are indolent, some children may not require treatment until adulthood.
July 28th was World Hepatitis Day and this year’s theme was Eliminate Hepatitis. To eliminate the problem of hepatitis C in children, pediatricians and others involved in the care of children need to get involved.
We need to know the scope of the problem
Since 2015, Kentucky has mandated reporting of all HCV-infected pregnant women and children through age 60 months, as well as all infants born to all HCV-infected women. At present though, there is substantial variability in state reporting requirements. We likely need a standardized case definition for perinatal HCV and national reporting criteria.
We need some clear guidance about testing during pregnancy
This should come from public health authorities, the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists.
Jonathan Mermin, MD, director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, has said, “Women are screened throughout pregnancy for many conditions that threaten their health. An expectant mother at risk for hepatitis C deserves to be tested. Knowing her status is the only way she can access the best hepatitis care and treatment – both for herself and her baby.” Yet, routine hepatitis C testing is not recommended during pregnancy, in part because there are no established interventions to prevent mother-to-child transmission of HCV. Instead, women are to be screened for risk factors and tested if they are present. As we learned with hepatitis B and HIV, risk factor screening is hard and misses individuals who are infected.
We need to ensure that HCV-exposed infants are identified and followed appropriately.
In a study of HCV-exposed infants born to women in Philadelphia, 84% did not receive adequate testing for HCV infection. In human terms, 537 children were born to HCV-positive mothers during the study period and 4 of 84 (5%) children tested were found to be infected. Assuming that 5% of HCV-exposed infants will develop chronic infection, 23 additional children were undiagnosed and, therefore, were not being followed for potential sequelae.
HCV-infected mothers in this study were more likely than non-infected mothers to be socioeconomically disadvantaged – specifically, unmarried, less educated, and publicly insured – suggesting that access to care may have played a role. When you add in drug use as a common risk factor for HCV infection, it is easy to understand why some at-risk infants are lost to follow-up.
Investigators in the Philadelphia study suggested that there might be more to the story. They proposed that pediatricians might be unaware of the need for testing because they had not been alerted to the mother’s HCV status by the obstetrician, the birthing hospital, or the mother herself. Finally, they theorized that many pediatricians “may be unaware or skeptical of the guidelines for testing children exposed to HCV.” This is a problem that we can solve.
I finished the visit with this mother by reassuring her that she could breastfeed her infant as planned as long as she did not have cracked or bleeding nipples. I also explained the schedule for testing. A 2002 National Institutes of Health consensus statement recommends that infants perinatally exposed to HCV have two HCV RNA tests between 2 and 6 months of age and/or be tested for HCV antibodies after 15 months. North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) Practice Guidelines for Diagnosis and Management of Hepatitis C Infection in Infants, Children, and Adolescents recommend testing for HCV antibodies at 18 months of age (J Pediatr Gastroenterol Nutr. 2012 Jun;54[6]:838-55). If a family requests earlier testing, a serum HCV RNA test can be done as early as 2 months of age. If positive, NASPGHAN recommends testing after 12 months of age to evaluate for chronic infection.
My practice has adopted the National Institutes of Health consensus statement approach because many of the families we see experience significant anxiety about the diagnosis, and this mother was no exception. As noted in the expert guidelines, this was a situation in which “early exclusion of HCV infection is reassuring and may be worth the added expense.”
“So first test at 2 months?” she asked. “Until then, we can’t do anything but wait?”
It is estimated that there are 23,000 to 46,000 U.S. children living with HCV. The wait for pediatricians is over. , and we need to educate ourselves about diagnosis and management. A first step might be to begin asking expectant mothers and the mothers of newborns if they know their HCV status.
Dr. Bryant is a pediatrician specializing in infectious diseases at the University of Louisville (Ky.) and Norton Children’s Hospital, also in Louisville. She said she had no relevant financial disclosures. Email her at [email protected].
The latest news on pediatric migraine
Migraine is the most common disabling neurologic disease, with an estimated 1 billion sufferers worldwide.1 In children aged 5-15 years, migraine prevalence is 10%, and these children miss more school than their peers.2,3 Research specific to the child and adolescent migraine population is imperative, as the findings in adult studies do not always correlate or translate to pediatrics. The American Headache Society (AHS) held its 59th annual scientific meeting in Boston in June 2017, a meeting designed to showcase the latest advances in the field of headache medicine. Several interesting pediatric headache studies were presented.
Pediatric patient, parent goals and preferences for preventive treatment
There is a general consensus among headache specialists that migraine preventive treatment should be instituted when a migraineur has at least four headache days per month. Clinically, and in most research trials, migraine preventive treatment is considered effective when a 50% reduction in headache days or the headache frequency is reduced to no more than four headache days per month.
Perhaps not surprisingly, patients and families expect treatment to result in very few headaches with minimal side effects. It is helpful to understand patient and family treatment goals as clinicians so we can to better provide realistic expectations of care, improve treatment adherence, and reduce patient/parent frustration.
Premonitory symptoms
Migraine is disabling not simply because of the headache but because of the range of symptoms that occur around the headache. Migraine may involve four phases: premonitory, aura, headache, and postdrome. The premonitory phase involves symptoms that may occur hours to days prior to the headache. Functional imaging studies reveal hypothalamic activation during this phase.4 In a large retrospective study, premonitory symptoms occurred in approximately three-quarters of pediatric and adult migraineurs.5 In a prior pediatric chart review, the most common premonitory symptoms in order of decreasing frequency were fatigue, mood change, neck stiffness, and yawning.6
Understanding and identifying premonitory signs is important for better understanding the pathophysiology of migraine and to help our patients recognize when a migraine may be coming.
Mapping pain in pediatric migraine
Diagnosis of migraine is based on the International Classification of Headache Disorders 3rd edition beta (ICHD-3b). For adults with migraine, part of the diagnostic criteria requires at least two of a number of features: unilateral location, pulsating quality, moderate or severe pain intensity, or aggravation by or avoidance of routine physical activity. The comments section of the ICHD-3b mentions that, in children under 18 years, the pain may be bilateral.
This study sought to characterize the location and quality of headache pain in the pediatric and young adult population. Sixty migraineurs were enrolled and divided into three age groups: children (7-11 years), adolescents (12-18), and young adults (19-26). The patients were guided to use a diagram to draw pain location and quality. The pain was bilateral for the majority of patients in all age groups. Of the young adult group, 85% had bilateral headache. This is of interest, as adults with migraine are conventionally thought to have unilateral headache. The main descriptors among all three groups were throbbing, pounding, and pressing. In children, tightening was more common than throbbing.
When diagnosing migraine, it is helpful to take these differences into consideration. Overall, this study provides a better understanding of the quality and location of migraine in the pediatric and young adult population.
Efficacy of zolmitriptan nasal spray in adolescents
Zolmitriptan nasal spray (NS) was approved by the Food and Drug Administration in 2015 for acute migraine treatment in adolescents ages 12-17 years. This was the first triptan NS approved for use in pediatric migraine. The NS route benefits migraineurs who need a rapidly absorbed triptan or those who do not tolerate oral triptans because of significant nausea or emesis with their migraine. The efficacy of zolmitriptan NS in adolescents was established in a multicenter, double-blind, randomized placebo controlled study with 798 participants.7 The primary endpoint of pain freedom at 2 hours after treatment for the 5-mg dose was superior to placebo, 30% vs. 17%, respectively (P less than .001; odds ratio, 2.18; 95% confidence interval, 1.40, 3.39). Patients with migraine going from moderate or severe to mild or no headache at 2 hours post treatment were 51% vs. 39%, respectively (P = .010).
The follow-up study presented at AHS was a subgroup analysis of the above data in younger (12-14 years) and older (15-17 years) adolescents. The primary efficacy endpoint of being pain free at 2 hours post treatment was similarly better for zolmitriptan 5 mg, compared with placebo, in both the younger and older adolescent migraineurs.
This study reinforces that zolmitriptan 5-mg NS is an effective abortive migraine treatment in adolescents and is generally well tolerated.
New migraine treatments
Although not pediatric studies, several presentations addressed exciting new preventive treatments that target one of the main neuropeptides implicated in migraine pathophysiology, calcitonin gene related peptide. Four drug companies have completed phase II and phase III adult trials in which they have developed humanized monoclonal antibodies that bind to CGRP or its receptor. These medications have shown great promise and appear to be very well tolerated. These are the first medications developed specifically for migraine prevention, as opposed to current medications which we borrow from other fields of medicine. It is anticipated they will be available for use in adult migraineurs later this year.
Dr. Qubty is a pediatric headache specialist and an assistant professor of neurology at the University of California, San Francisco, and he is a member of the American Headache Society. He said he had no relevant financial disclosures.
*Correction, 8/10/2017: An earlier version of this article misstated the percentage of pediatric migraine patients who had premonitory signs, and how common premonitory signs were among episodic migraineurs with and without aura.
References
1. Lancet. 2016 Oct 8;388(10053):1545-1602.
2. Dev Med Child Neurol. 2010 Dec;52(12):1088-97.
3. Neurology. 2012 Oct 30;79(18):1881-8.
4. Brain. 2014 Jan;137(Pt 1):232-41.
5. Cephalalgia 2016;36:951-959.
6. J Headache Pain. 2016 Dec;17(1):94.
7. Headache. 2016 Jul;56(7):1107-19.
Migraine is the most common disabling neurologic disease, with an estimated 1 billion sufferers worldwide.1 In children aged 5-15 years, migraine prevalence is 10%, and these children miss more school than their peers.2,3 Research specific to the child and adolescent migraine population is imperative, as the findings in adult studies do not always correlate or translate to pediatrics. The American Headache Society (AHS) held its 59th annual scientific meeting in Boston in June 2017, a meeting designed to showcase the latest advances in the field of headache medicine. Several interesting pediatric headache studies were presented.
Pediatric patient, parent goals and preferences for preventive treatment
There is a general consensus among headache specialists that migraine preventive treatment should be instituted when a migraineur has at least four headache days per month. Clinically, and in most research trials, migraine preventive treatment is considered effective when a 50% reduction in headache days or the headache frequency is reduced to no more than four headache days per month.
Perhaps not surprisingly, patients and families expect treatment to result in very few headaches with minimal side effects. It is helpful to understand patient and family treatment goals as clinicians so we can to better provide realistic expectations of care, improve treatment adherence, and reduce patient/parent frustration.
Premonitory symptoms
Migraine is disabling not simply because of the headache but because of the range of symptoms that occur around the headache. Migraine may involve four phases: premonitory, aura, headache, and postdrome. The premonitory phase involves symptoms that may occur hours to days prior to the headache. Functional imaging studies reveal hypothalamic activation during this phase.4 In a large retrospective study, premonitory symptoms occurred in approximately three-quarters of pediatric and adult migraineurs.5 In a prior pediatric chart review, the most common premonitory symptoms in order of decreasing frequency were fatigue, mood change, neck stiffness, and yawning.6
Understanding and identifying premonitory signs is important for better understanding the pathophysiology of migraine and to help our patients recognize when a migraine may be coming.
Mapping pain in pediatric migraine
Diagnosis of migraine is based on the International Classification of Headache Disorders 3rd edition beta (ICHD-3b). For adults with migraine, part of the diagnostic criteria requires at least two of a number of features: unilateral location, pulsating quality, moderate or severe pain intensity, or aggravation by or avoidance of routine physical activity. The comments section of the ICHD-3b mentions that, in children under 18 years, the pain may be bilateral.
This study sought to characterize the location and quality of headache pain in the pediatric and young adult population. Sixty migraineurs were enrolled and divided into three age groups: children (7-11 years), adolescents (12-18), and young adults (19-26). The patients were guided to use a diagram to draw pain location and quality. The pain was bilateral for the majority of patients in all age groups. Of the young adult group, 85% had bilateral headache. This is of interest, as adults with migraine are conventionally thought to have unilateral headache. The main descriptors among all three groups were throbbing, pounding, and pressing. In children, tightening was more common than throbbing.
When diagnosing migraine, it is helpful to take these differences into consideration. Overall, this study provides a better understanding of the quality and location of migraine in the pediatric and young adult population.
Efficacy of zolmitriptan nasal spray in adolescents
Zolmitriptan nasal spray (NS) was approved by the Food and Drug Administration in 2015 for acute migraine treatment in adolescents ages 12-17 years. This was the first triptan NS approved for use in pediatric migraine. The NS route benefits migraineurs who need a rapidly absorbed triptan or those who do not tolerate oral triptans because of significant nausea or emesis with their migraine. The efficacy of zolmitriptan NS in adolescents was established in a multicenter, double-blind, randomized placebo controlled study with 798 participants.7 The primary endpoint of pain freedom at 2 hours after treatment for the 5-mg dose was superior to placebo, 30% vs. 17%, respectively (P less than .001; odds ratio, 2.18; 95% confidence interval, 1.40, 3.39). Patients with migraine going from moderate or severe to mild or no headache at 2 hours post treatment were 51% vs. 39%, respectively (P = .010).
The follow-up study presented at AHS was a subgroup analysis of the above data in younger (12-14 years) and older (15-17 years) adolescents. The primary efficacy endpoint of being pain free at 2 hours post treatment was similarly better for zolmitriptan 5 mg, compared with placebo, in both the younger and older adolescent migraineurs.
This study reinforces that zolmitriptan 5-mg NS is an effective abortive migraine treatment in adolescents and is generally well tolerated.
New migraine treatments
Although not pediatric studies, several presentations addressed exciting new preventive treatments that target one of the main neuropeptides implicated in migraine pathophysiology, calcitonin gene related peptide. Four drug companies have completed phase II and phase III adult trials in which they have developed humanized monoclonal antibodies that bind to CGRP or its receptor. These medications have shown great promise and appear to be very well tolerated. These are the first medications developed specifically for migraine prevention, as opposed to current medications which we borrow from other fields of medicine. It is anticipated they will be available for use in adult migraineurs later this year.
Dr. Qubty is a pediatric headache specialist and an assistant professor of neurology at the University of California, San Francisco, and he is a member of the American Headache Society. He said he had no relevant financial disclosures.
*Correction, 8/10/2017: An earlier version of this article misstated the percentage of pediatric migraine patients who had premonitory signs, and how common premonitory signs were among episodic migraineurs with and without aura.
References
1. Lancet. 2016 Oct 8;388(10053):1545-1602.
2. Dev Med Child Neurol. 2010 Dec;52(12):1088-97.
3. Neurology. 2012 Oct 30;79(18):1881-8.
4. Brain. 2014 Jan;137(Pt 1):232-41.
5. Cephalalgia 2016;36:951-959.
6. J Headache Pain. 2016 Dec;17(1):94.
7. Headache. 2016 Jul;56(7):1107-19.
Migraine is the most common disabling neurologic disease, with an estimated 1 billion sufferers worldwide.1 In children aged 5-15 years, migraine prevalence is 10%, and these children miss more school than their peers.2,3 Research specific to the child and adolescent migraine population is imperative, as the findings in adult studies do not always correlate or translate to pediatrics. The American Headache Society (AHS) held its 59th annual scientific meeting in Boston in June 2017, a meeting designed to showcase the latest advances in the field of headache medicine. Several interesting pediatric headache studies were presented.
Pediatric patient, parent goals and preferences for preventive treatment
There is a general consensus among headache specialists that migraine preventive treatment should be instituted when a migraineur has at least four headache days per month. Clinically, and in most research trials, migraine preventive treatment is considered effective when a 50% reduction in headache days or the headache frequency is reduced to no more than four headache days per month.
Perhaps not surprisingly, patients and families expect treatment to result in very few headaches with minimal side effects. It is helpful to understand patient and family treatment goals as clinicians so we can to better provide realistic expectations of care, improve treatment adherence, and reduce patient/parent frustration.
Premonitory symptoms
Migraine is disabling not simply because of the headache but because of the range of symptoms that occur around the headache. Migraine may involve four phases: premonitory, aura, headache, and postdrome. The premonitory phase involves symptoms that may occur hours to days prior to the headache. Functional imaging studies reveal hypothalamic activation during this phase.4 In a large retrospective study, premonitory symptoms occurred in approximately three-quarters of pediatric and adult migraineurs.5 In a prior pediatric chart review, the most common premonitory symptoms in order of decreasing frequency were fatigue, mood change, neck stiffness, and yawning.6
Understanding and identifying premonitory signs is important for better understanding the pathophysiology of migraine and to help our patients recognize when a migraine may be coming.
Mapping pain in pediatric migraine
Diagnosis of migraine is based on the International Classification of Headache Disorders 3rd edition beta (ICHD-3b). For adults with migraine, part of the diagnostic criteria requires at least two of a number of features: unilateral location, pulsating quality, moderate or severe pain intensity, or aggravation by or avoidance of routine physical activity. The comments section of the ICHD-3b mentions that, in children under 18 years, the pain may be bilateral.
This study sought to characterize the location and quality of headache pain in the pediatric and young adult population. Sixty migraineurs were enrolled and divided into three age groups: children (7-11 years), adolescents (12-18), and young adults (19-26). The patients were guided to use a diagram to draw pain location and quality. The pain was bilateral for the majority of patients in all age groups. Of the young adult group, 85% had bilateral headache. This is of interest, as adults with migraine are conventionally thought to have unilateral headache. The main descriptors among all three groups were throbbing, pounding, and pressing. In children, tightening was more common than throbbing.
When diagnosing migraine, it is helpful to take these differences into consideration. Overall, this study provides a better understanding of the quality and location of migraine in the pediatric and young adult population.
Efficacy of zolmitriptan nasal spray in adolescents
Zolmitriptan nasal spray (NS) was approved by the Food and Drug Administration in 2015 for acute migraine treatment in adolescents ages 12-17 years. This was the first triptan NS approved for use in pediatric migraine. The NS route benefits migraineurs who need a rapidly absorbed triptan or those who do not tolerate oral triptans because of significant nausea or emesis with their migraine. The efficacy of zolmitriptan NS in adolescents was established in a multicenter, double-blind, randomized placebo controlled study with 798 participants.7 The primary endpoint of pain freedom at 2 hours after treatment for the 5-mg dose was superior to placebo, 30% vs. 17%, respectively (P less than .001; odds ratio, 2.18; 95% confidence interval, 1.40, 3.39). Patients with migraine going from moderate or severe to mild or no headache at 2 hours post treatment were 51% vs. 39%, respectively (P = .010).
The follow-up study presented at AHS was a subgroup analysis of the above data in younger (12-14 years) and older (15-17 years) adolescents. The primary efficacy endpoint of being pain free at 2 hours post treatment was similarly better for zolmitriptan 5 mg, compared with placebo, in both the younger and older adolescent migraineurs.
This study reinforces that zolmitriptan 5-mg NS is an effective abortive migraine treatment in adolescents and is generally well tolerated.
New migraine treatments
Although not pediatric studies, several presentations addressed exciting new preventive treatments that target one of the main neuropeptides implicated in migraine pathophysiology, calcitonin gene related peptide. Four drug companies have completed phase II and phase III adult trials in which they have developed humanized monoclonal antibodies that bind to CGRP or its receptor. These medications have shown great promise and appear to be very well tolerated. These are the first medications developed specifically for migraine prevention, as opposed to current medications which we borrow from other fields of medicine. It is anticipated they will be available for use in adult migraineurs later this year.
Dr. Qubty is a pediatric headache specialist and an assistant professor of neurology at the University of California, San Francisco, and he is a member of the American Headache Society. He said he had no relevant financial disclosures.
*Correction, 8/10/2017: An earlier version of this article misstated the percentage of pediatric migraine patients who had premonitory signs, and how common premonitory signs were among episodic migraineurs with and without aura.
References
1. Lancet. 2016 Oct 8;388(10053):1545-1602.
2. Dev Med Child Neurol. 2010 Dec;52(12):1088-97.
3. Neurology. 2012 Oct 30;79(18):1881-8.
4. Brain. 2014 Jan;137(Pt 1):232-41.
5. Cephalalgia 2016;36:951-959.
6. J Headache Pain. 2016 Dec;17(1):94.
7. Headache. 2016 Jul;56(7):1107-19.
Keep a symptom diary!
A friend sent me an article from the New Yorker called “The Algorithm Will See You Now,” in which Siddhartha Mukherjee, MD, author of the magisterial “The Emperor of All Maladies,” ponders the effect artificial intelligence may have on medicine. One possible outcome may be that computers replace radiologists and dermatologists. (They already beat top humans at Jeopardy, chess, and Go, so why not lick Homo sapiens at pattern recognition?)
No worries for me. When Watson takes over, I will be off somewhere playing shuffleboard.
“It’s a particularly bad case. But, the question is why it appeared now, and why it’s getting worse.” She asked the patient about new hair products or family stress. The man said he’d just lost his job.
“Keep a diary,” she advised. “We can determine if there’s a link.”
Thus was my pedagogic legacy shattered in an instant. I’ve spent decades advising students not to tell patients they have a bad case of anything and never to ask them to keep diaries. Then, a foremost medical writer in a leading cultural journal endorses the reverse of both lessons. What was I thinking all these years?
I counseled students not to call any case “bad” because I saw how patients took it personally if I told them that. No matter how mild their diagnosis – rosacea and seborrhea, maladies less emperors than footmen– patients who heard theirs called “bad” looked sad, even insulted. Sad and insulted patients may give up and don’t follow treatment advice. (With such a bad case, why bother?) I didn’t urge patients to think that way. I just couldn’t ignore that they did. By contrast, assuring people that their case “wasn’t bad at all!” made them light up like Halloween pumpkins.
As for diaries, I’ve filed a few that patients handed me over the years. I showed these detailed chronicles to students to illustrate the lengths to which people will go to explain the unexplainable, like the ups and downs of idiopathic urticaria, eczema, and so forth:
- Thursday, August 6th, had sushi at a restaurant with friends.
- Sunday, September 3rd, watched science-fiction movie, unable to sleep that night.
- Monday, October 2nd, discarded fourth new detergent.
And so on.
In the meantime, several times each working day patients would troop in with randomly reoccurring conditions, atopic dermatitis above all, prompting dialogues like these:
“This is crazy! I never had anything like this before!”
“Well, actually, Ms. Jones, I treated you for the same thing in 2006.”
*********************
“This is bizarre! I never had this, and no one in my family ever did either.”
“I see. Well, here’s a prescription.”
“Come to think of it, my Mom had sensitive skin, and I get these dry patches on my arms and legs every winter.”
********************
“I’ve changed my soap three times and thrown out my makeup four times, and the rash keeps coming back. What should I do?”
“Stop throwing out your soap and makeup?”
And so on and on.
Sometimes, of course, semi-plausible causes seem to surface, such as stress. The question is, How useful is it to point this out? Consider the New Yorker case. Once the doctor “determined there is a link,” how might the conversation go?
“We have found the trigger, Mr. Smith. It’s stress.”
“Great! What should I do?”
“Don’t get laid off.”
No doctor (I hope) would ever say that, but patients present reports like the following all the time:
“As a kid, I was allergic to milk, but I’m not anymore.” (No, he wasn’t – he had infantile eczema that got blamed on milk.)
“Penicillin gave me hives.” (But, the hives lasted 6 weeks after the penicillin was stopped, which showed that the hives were idiopathic.)
“I’m very sensitive. I can’t use any moisturizer, any makeup, or all pills.” (People generate long litanies of sensitivities, piling one spurious correlation on another.)
Who benefits from “determining the link” when there isn’t any? Not the patients I’ve been seeing for forty years. Your patients? Maybe detergent manufacturers?
As to my errant pedagogy, with any luck, my students don’t remember a word I told them, a safe assumption for any teacher.
Either that or they don’t read the New Yorker.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
A friend sent me an article from the New Yorker called “The Algorithm Will See You Now,” in which Siddhartha Mukherjee, MD, author of the magisterial “The Emperor of All Maladies,” ponders the effect artificial intelligence may have on medicine. One possible outcome may be that computers replace radiologists and dermatologists. (They already beat top humans at Jeopardy, chess, and Go, so why not lick Homo sapiens at pattern recognition?)
No worries for me. When Watson takes over, I will be off somewhere playing shuffleboard.
“It’s a particularly bad case. But, the question is why it appeared now, and why it’s getting worse.” She asked the patient about new hair products or family stress. The man said he’d just lost his job.
“Keep a diary,” she advised. “We can determine if there’s a link.”
Thus was my pedagogic legacy shattered in an instant. I’ve spent decades advising students not to tell patients they have a bad case of anything and never to ask them to keep diaries. Then, a foremost medical writer in a leading cultural journal endorses the reverse of both lessons. What was I thinking all these years?
I counseled students not to call any case “bad” because I saw how patients took it personally if I told them that. No matter how mild their diagnosis – rosacea and seborrhea, maladies less emperors than footmen– patients who heard theirs called “bad” looked sad, even insulted. Sad and insulted patients may give up and don’t follow treatment advice. (With such a bad case, why bother?) I didn’t urge patients to think that way. I just couldn’t ignore that they did. By contrast, assuring people that their case “wasn’t bad at all!” made them light up like Halloween pumpkins.
As for diaries, I’ve filed a few that patients handed me over the years. I showed these detailed chronicles to students to illustrate the lengths to which people will go to explain the unexplainable, like the ups and downs of idiopathic urticaria, eczema, and so forth:
- Thursday, August 6th, had sushi at a restaurant with friends.
- Sunday, September 3rd, watched science-fiction movie, unable to sleep that night.
- Monday, October 2nd, discarded fourth new detergent.
And so on.
In the meantime, several times each working day patients would troop in with randomly reoccurring conditions, atopic dermatitis above all, prompting dialogues like these:
“This is crazy! I never had anything like this before!”
“Well, actually, Ms. Jones, I treated you for the same thing in 2006.”
*********************
“This is bizarre! I never had this, and no one in my family ever did either.”
“I see. Well, here’s a prescription.”
“Come to think of it, my Mom had sensitive skin, and I get these dry patches on my arms and legs every winter.”
********************
“I’ve changed my soap three times and thrown out my makeup four times, and the rash keeps coming back. What should I do?”
“Stop throwing out your soap and makeup?”
And so on and on.
Sometimes, of course, semi-plausible causes seem to surface, such as stress. The question is, How useful is it to point this out? Consider the New Yorker case. Once the doctor “determined there is a link,” how might the conversation go?
“We have found the trigger, Mr. Smith. It’s stress.”
“Great! What should I do?”
“Don’t get laid off.”
No doctor (I hope) would ever say that, but patients present reports like the following all the time:
“As a kid, I was allergic to milk, but I’m not anymore.” (No, he wasn’t – he had infantile eczema that got blamed on milk.)
“Penicillin gave me hives.” (But, the hives lasted 6 weeks after the penicillin was stopped, which showed that the hives were idiopathic.)
“I’m very sensitive. I can’t use any moisturizer, any makeup, or all pills.” (People generate long litanies of sensitivities, piling one spurious correlation on another.)
Who benefits from “determining the link” when there isn’t any? Not the patients I’ve been seeing for forty years. Your patients? Maybe detergent manufacturers?
As to my errant pedagogy, with any luck, my students don’t remember a word I told them, a safe assumption for any teacher.
Either that or they don’t read the New Yorker.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
A friend sent me an article from the New Yorker called “The Algorithm Will See You Now,” in which Siddhartha Mukherjee, MD, author of the magisterial “The Emperor of All Maladies,” ponders the effect artificial intelligence may have on medicine. One possible outcome may be that computers replace radiologists and dermatologists. (They already beat top humans at Jeopardy, chess, and Go, so why not lick Homo sapiens at pattern recognition?)
No worries for me. When Watson takes over, I will be off somewhere playing shuffleboard.
“It’s a particularly bad case. But, the question is why it appeared now, and why it’s getting worse.” She asked the patient about new hair products or family stress. The man said he’d just lost his job.
“Keep a diary,” she advised. “We can determine if there’s a link.”
Thus was my pedagogic legacy shattered in an instant. I’ve spent decades advising students not to tell patients they have a bad case of anything and never to ask them to keep diaries. Then, a foremost medical writer in a leading cultural journal endorses the reverse of both lessons. What was I thinking all these years?
I counseled students not to call any case “bad” because I saw how patients took it personally if I told them that. No matter how mild their diagnosis – rosacea and seborrhea, maladies less emperors than footmen– patients who heard theirs called “bad” looked sad, even insulted. Sad and insulted patients may give up and don’t follow treatment advice. (With such a bad case, why bother?) I didn’t urge patients to think that way. I just couldn’t ignore that they did. By contrast, assuring people that their case “wasn’t bad at all!” made them light up like Halloween pumpkins.
As for diaries, I’ve filed a few that patients handed me over the years. I showed these detailed chronicles to students to illustrate the lengths to which people will go to explain the unexplainable, like the ups and downs of idiopathic urticaria, eczema, and so forth:
- Thursday, August 6th, had sushi at a restaurant with friends.
- Sunday, September 3rd, watched science-fiction movie, unable to sleep that night.
- Monday, October 2nd, discarded fourth new detergent.
And so on.
In the meantime, several times each working day patients would troop in with randomly reoccurring conditions, atopic dermatitis above all, prompting dialogues like these:
“This is crazy! I never had anything like this before!”
“Well, actually, Ms. Jones, I treated you for the same thing in 2006.”
*********************
“This is bizarre! I never had this, and no one in my family ever did either.”
“I see. Well, here’s a prescription.”
“Come to think of it, my Mom had sensitive skin, and I get these dry patches on my arms and legs every winter.”
********************
“I’ve changed my soap three times and thrown out my makeup four times, and the rash keeps coming back. What should I do?”
“Stop throwing out your soap and makeup?”
And so on and on.
Sometimes, of course, semi-plausible causes seem to surface, such as stress. The question is, How useful is it to point this out? Consider the New Yorker case. Once the doctor “determined there is a link,” how might the conversation go?
“We have found the trigger, Mr. Smith. It’s stress.”
“Great! What should I do?”
“Don’t get laid off.”
No doctor (I hope) would ever say that, but patients present reports like the following all the time:
“As a kid, I was allergic to milk, but I’m not anymore.” (No, he wasn’t – he had infantile eczema that got blamed on milk.)
“Penicillin gave me hives.” (But, the hives lasted 6 weeks after the penicillin was stopped, which showed that the hives were idiopathic.)
“I’m very sensitive. I can’t use any moisturizer, any makeup, or all pills.” (People generate long litanies of sensitivities, piling one spurious correlation on another.)
Who benefits from “determining the link” when there isn’t any? Not the patients I’ve been seeing for forty years. Your patients? Maybe detergent manufacturers?
As to my errant pedagogy, with any luck, my students don’t remember a word I told them, a safe assumption for any teacher.
Either that or they don’t read the New Yorker.
Dr. Rockoff practices dermatology in Brookline, Mass., and is a longtime contributor to Dermatology News. He serves on the clinical faculty at Tufts University, Boston, and has taught senior medical students and other trainees for 30 years. His second book, “Act Like a Doctor, Think Like a Patient,” is available at amazon.com and barnesandnoble.com. Write to him at [email protected].
Points/Counterpoint: Should surgeons operate on functional tricuspid regurgitation?
Yes, functional TR is worth repairing (David H. Adams, MD)
Functional tricuspid regurgitation is a common finding in patients undergoing degenerative mitral valve repair. Severe tricuspid regurgitation is unusual, and clearly there is little debate on the merits of concomitant tricuspid repair for these patients. Moderate tricuspid regurgitation is identified preoperatively in around 15% of patients undergoing degenerative mitral repair (J Thorac Cardiovasc Surg. 2011;142:608-13), and concomitant tricuspid repair in these patients is certainly supported by both the American and European guidelines (J Am Coll Cardiol. 2017. doi: 10.1016/j.jacc.2017.03.011; Eur Heart J. 2012;33:2451-96).
What experience and evidence has led us to a more aggressive approach? One of the most important influences on our early adoption of tricuspid repair at the time of mitral surgery was linked to observations that tricuspid regurgitation (TR) sometimes progressed after isolated mitral valve repair (MVR), with some patients developing moderate or worse insufficiency. Certainly, the impact of significant tricuspid regurgitation on the quality and length of patients’ lives and the challenges of reoperation for isolated tricuspid regurgitation are well known to all surgeons.
Consequently, the importance of treating significant annular dilatation, even without significant tricuspid regurgitation, is supported by the guidelines. Our own experience with an aggressive approach to functional tricuspid regurgitation (FTR) at the time of mitral surgery put an exclamation point on this (J Am Coll Cardiol. 2015;65:1931-8). We found that concomitant tricuspid repair in patients who were worse off before surgery with more TR and higher rates of atrial fibrillation and right-sided dysfunction, actually did better during 5 years of follow-up than the isolated mitral repair patients who started with completely normal tricuspid valve anatomy and ventricular function.
Benign neglect is always an option (J Thorac Cardiovasc Surg. 2017;154:125-6), but we agree with Roberto Dion, MD – despite our friends’ opinions in Toronto and Rochester – we would much prefer to have minimal TR and a normal sized tricuspid valve after MVR. Ask yourself: would you rather have no TR and a normal sized tricuspid valve after you undergo a mitral operation, or a very dilated annulus and perhaps moderate FTR? I am pretty sure I know the answer, but if you are not sure, read our paper.
Dr. Adams is cardiac surgeon-in-chief, Mount Sinai Health System, and Marie-Josée and Henry R. Kravis Professor and Chairman, department of cardiovascular surgery, Icahn School of Medicine at Mount Sinai and The Mount Sinai Hospital, and president-elect of the American Association for Thoracic Surgery. He disclosed he is the national co-principal investigator for the Medtronic NeoChord trial, and receives royalties from Medtronic and Edwards Lifesciences. The Icahn School of Medicine at Mount Sinai receives royalty payments from Edwards Lifesciences and Medtronic for intellectual property related to Dr. Adams’ involvement in the development of 2 mitral valve repair rings and 1 tricuspid valve repair ring.
No, a patient with FTR does not necessarily need repair (Tirone David, MD)
In our clinic, a patient who undergoes MVR and has FTR generally goes home without an annuloplasty. We now have 12 years or more of follow-up in these patients, and they do not develop TR if their MVR is competent. We have reported that preoperative TR in patients who had MVR is associated with mitral valve disease and often improves after the operation (J Thorac Cardiovasc Surg. 2017;154:110-22). New postoperative TR is uncommon.
Ninety percent of my mitral valve repair patients today have no symptoms. Of those patients, a small proportion have moderate TR.
Dr. David is a professor of surgery at Toronto General Hospital. He reported no financial relationships.
Yes, but repair of FTR requires caution (Gilles Dreyfus, MD)
The controversy surrounding the legitimacy of concomitant tricuspid annuloplasty for functional TR during MVR begs for a clinical trial, but before we can conduct a clinical trial, we must define the primary and secondary endpoints. We’ve seen recent prospective, randomized trials that have reported faulty conclusions because the primary endpoints were wrong.
We need a strong debate to agree on those endpoints. Mortality as an endpoint will probably take a very long time to arrive at.
We’re mixing up many different factors. We’re mixing up TR grading, and we know that grading is unreliable. We have all seen patients with full-fledged TR, and after we put them on Lasix (furosemide, Sanofi), 3 days later they have mild TR. So the same patient with no treatment becomes let’s say a “Dreyfus indication,” and then suddenly in 3 days the patient doesn’t need surgery. At any further stage of his life this patient can experience severe TR again; tricuspid annuloplasty will prevent that from happening.
Moderate TR according to the common definition does not exist. If you look at the reports in echocardiography and if you ask any cardiologist, everything between no TR and severe TR is considered moderate. We have proposed a new staging system for evaluating FTR that uses three factors: TR severity; annular dilatation; and extent of tethering, or mode of leaflet coaptation (J Am Coll Cardiol. 2015;65:2331-6).
Dr. Dreyfus is director of the medical and surgical team at the Cardiothoracic Centre of Monaco in Monte Carlo and professor of cardiothoracic surgery at Paris V University and the Imperial College of London. He disclosed receiving speaker fees from Edwards Lifesciences, LivaNova, and Medtronic.
No, few FTR patients at risk after MVR (Hartzell Schaff, MD)
Echocardiography can provide a great deal of information about when concomitant repair for TR is indicated during MVR. We’ve found that if the patient has no right-sided signs, has normal right atrial pressure, and has mild or mild/moderate TR at the time of repair to the journey mitral valve, the chance of him returning for a tricuspid valve procedure is near zero.
A few patients do return after MVR. They develop atrial fibrillation and may need a pacemaker, but we see very few patients return for tricuspid surgery.
It’s fair to say we cannot demonstrate any benefit of correcting functional mitral regurgitation. Why would we think there’s a benefit of correcting FTR? We can say we’re going to look at grade of TR down the road, or we could look at some other endpoint, but think about it this way: If we cannot prove that correcting functional mitral regurgitation is helpful, why is correcting FTR going to help?
Dr. Schaff is a cardiothoracic surgeon at Mayo Clinic Foundation, Rochester, Minn. He reported no financial relationships.
Yes, functional TR is worth repairing (David H. Adams, MD)
Functional tricuspid regurgitation is a common finding in patients undergoing degenerative mitral valve repair. Severe tricuspid regurgitation is unusual, and clearly there is little debate on the merits of concomitant tricuspid repair for these patients. Moderate tricuspid regurgitation is identified preoperatively in around 15% of patients undergoing degenerative mitral repair (J Thorac Cardiovasc Surg. 2011;142:608-13), and concomitant tricuspid repair in these patients is certainly supported by both the American and European guidelines (J Am Coll Cardiol. 2017. doi: 10.1016/j.jacc.2017.03.011; Eur Heart J. 2012;33:2451-96).
What experience and evidence has led us to a more aggressive approach? One of the most important influences on our early adoption of tricuspid repair at the time of mitral surgery was linked to observations that tricuspid regurgitation (TR) sometimes progressed after isolated mitral valve repair (MVR), with some patients developing moderate or worse insufficiency. Certainly, the impact of significant tricuspid regurgitation on the quality and length of patients’ lives and the challenges of reoperation for isolated tricuspid regurgitation are well known to all surgeons.
Consequently, the importance of treating significant annular dilatation, even without significant tricuspid regurgitation, is supported by the guidelines. Our own experience with an aggressive approach to functional tricuspid regurgitation (FTR) at the time of mitral surgery put an exclamation point on this (J Am Coll Cardiol. 2015;65:1931-8). We found that concomitant tricuspid repair in patients who were worse off before surgery with more TR and higher rates of atrial fibrillation and right-sided dysfunction, actually did better during 5 years of follow-up than the isolated mitral repair patients who started with completely normal tricuspid valve anatomy and ventricular function.
Benign neglect is always an option (J Thorac Cardiovasc Surg. 2017;154:125-6), but we agree with Roberto Dion, MD – despite our friends’ opinions in Toronto and Rochester – we would much prefer to have minimal TR and a normal sized tricuspid valve after MVR. Ask yourself: would you rather have no TR and a normal sized tricuspid valve after you undergo a mitral operation, or a very dilated annulus and perhaps moderate FTR? I am pretty sure I know the answer, but if you are not sure, read our paper.
Dr. Adams is cardiac surgeon-in-chief, Mount Sinai Health System, and Marie-Josée and Henry R. Kravis Professor and Chairman, department of cardiovascular surgery, Icahn School of Medicine at Mount Sinai and The Mount Sinai Hospital, and president-elect of the American Association for Thoracic Surgery. He disclosed he is the national co-principal investigator for the Medtronic NeoChord trial, and receives royalties from Medtronic and Edwards Lifesciences. The Icahn School of Medicine at Mount Sinai receives royalty payments from Edwards Lifesciences and Medtronic for intellectual property related to Dr. Adams’ involvement in the development of 2 mitral valve repair rings and 1 tricuspid valve repair ring.
No, a patient with FTR does not necessarily need repair (Tirone David, MD)
In our clinic, a patient who undergoes MVR and has FTR generally goes home without an annuloplasty. We now have 12 years or more of follow-up in these patients, and they do not develop TR if their MVR is competent. We have reported that preoperative TR in patients who had MVR is associated with mitral valve disease and often improves after the operation (J Thorac Cardiovasc Surg. 2017;154:110-22). New postoperative TR is uncommon.
Ninety percent of my mitral valve repair patients today have no symptoms. Of those patients, a small proportion have moderate TR.
Dr. David is a professor of surgery at Toronto General Hospital. He reported no financial relationships.
Yes, but repair of FTR requires caution (Gilles Dreyfus, MD)
The controversy surrounding the legitimacy of concomitant tricuspid annuloplasty for functional TR during MVR begs for a clinical trial, but before we can conduct a clinical trial, we must define the primary and secondary endpoints. We’ve seen recent prospective, randomized trials that have reported faulty conclusions because the primary endpoints were wrong.
We need a strong debate to agree on those endpoints. Mortality as an endpoint will probably take a very long time to arrive at.
We’re mixing up many different factors. We’re mixing up TR grading, and we know that grading is unreliable. We have all seen patients with full-fledged TR, and after we put them on Lasix (furosemide, Sanofi), 3 days later they have mild TR. So the same patient with no treatment becomes let’s say a “Dreyfus indication,” and then suddenly in 3 days the patient doesn’t need surgery. At any further stage of his life this patient can experience severe TR again; tricuspid annuloplasty will prevent that from happening.
Moderate TR according to the common definition does not exist. If you look at the reports in echocardiography and if you ask any cardiologist, everything between no TR and severe TR is considered moderate. We have proposed a new staging system for evaluating FTR that uses three factors: TR severity; annular dilatation; and extent of tethering, or mode of leaflet coaptation (J Am Coll Cardiol. 2015;65:2331-6).
Dr. Dreyfus is director of the medical and surgical team at the Cardiothoracic Centre of Monaco in Monte Carlo and professor of cardiothoracic surgery at Paris V University and the Imperial College of London. He disclosed receiving speaker fees from Edwards Lifesciences, LivaNova, and Medtronic.
No, few FTR patients at risk after MVR (Hartzell Schaff, MD)
Echocardiography can provide a great deal of information about when concomitant repair for TR is indicated during MVR. We’ve found that if the patient has no right-sided signs, has normal right atrial pressure, and has mild or mild/moderate TR at the time of repair to the journey mitral valve, the chance of him returning for a tricuspid valve procedure is near zero.
A few patients do return after MVR. They develop atrial fibrillation and may need a pacemaker, but we see very few patients return for tricuspid surgery.
It’s fair to say we cannot demonstrate any benefit of correcting functional mitral regurgitation. Why would we think there’s a benefit of correcting FTR? We can say we’re going to look at grade of TR down the road, or we could look at some other endpoint, but think about it this way: If we cannot prove that correcting functional mitral regurgitation is helpful, why is correcting FTR going to help?
Dr. Schaff is a cardiothoracic surgeon at Mayo Clinic Foundation, Rochester, Minn. He reported no financial relationships.
Yes, functional TR is worth repairing (David H. Adams, MD)
Functional tricuspid regurgitation is a common finding in patients undergoing degenerative mitral valve repair. Severe tricuspid regurgitation is unusual, and clearly there is little debate on the merits of concomitant tricuspid repair for these patients. Moderate tricuspid regurgitation is identified preoperatively in around 15% of patients undergoing degenerative mitral repair (J Thorac Cardiovasc Surg. 2011;142:608-13), and concomitant tricuspid repair in these patients is certainly supported by both the American and European guidelines (J Am Coll Cardiol. 2017. doi: 10.1016/j.jacc.2017.03.011; Eur Heart J. 2012;33:2451-96).
What experience and evidence has led us to a more aggressive approach? One of the most important influences on our early adoption of tricuspid repair at the time of mitral surgery was linked to observations that tricuspid regurgitation (TR) sometimes progressed after isolated mitral valve repair (MVR), with some patients developing moderate or worse insufficiency. Certainly, the impact of significant tricuspid regurgitation on the quality and length of patients’ lives and the challenges of reoperation for isolated tricuspid regurgitation are well known to all surgeons.
Consequently, the importance of treating significant annular dilatation, even without significant tricuspid regurgitation, is supported by the guidelines. Our own experience with an aggressive approach to functional tricuspid regurgitation (FTR) at the time of mitral surgery put an exclamation point on this (J Am Coll Cardiol. 2015;65:1931-8). We found that concomitant tricuspid repair in patients who were worse off before surgery with more TR and higher rates of atrial fibrillation and right-sided dysfunction, actually did better during 5 years of follow-up than the isolated mitral repair patients who started with completely normal tricuspid valve anatomy and ventricular function.
Benign neglect is always an option (J Thorac Cardiovasc Surg. 2017;154:125-6), but we agree with Roberto Dion, MD – despite our friends’ opinions in Toronto and Rochester – we would much prefer to have minimal TR and a normal sized tricuspid valve after MVR. Ask yourself: would you rather have no TR and a normal sized tricuspid valve after you undergo a mitral operation, or a very dilated annulus and perhaps moderate FTR? I am pretty sure I know the answer, but if you are not sure, read our paper.
Dr. Adams is cardiac surgeon-in-chief, Mount Sinai Health System, and Marie-Josée and Henry R. Kravis Professor and Chairman, department of cardiovascular surgery, Icahn School of Medicine at Mount Sinai and The Mount Sinai Hospital, and president-elect of the American Association for Thoracic Surgery. He disclosed he is the national co-principal investigator for the Medtronic NeoChord trial, and receives royalties from Medtronic and Edwards Lifesciences. The Icahn School of Medicine at Mount Sinai receives royalty payments from Edwards Lifesciences and Medtronic for intellectual property related to Dr. Adams’ involvement in the development of 2 mitral valve repair rings and 1 tricuspid valve repair ring.
No, a patient with FTR does not necessarily need repair (Tirone David, MD)
In our clinic, a patient who undergoes MVR and has FTR generally goes home without an annuloplasty. We now have 12 years or more of follow-up in these patients, and they do not develop TR if their MVR is competent. We have reported that preoperative TR in patients who had MVR is associated with mitral valve disease and often improves after the operation (J Thorac Cardiovasc Surg. 2017;154:110-22). New postoperative TR is uncommon.
Ninety percent of my mitral valve repair patients today have no symptoms. Of those patients, a small proportion have moderate TR.
Dr. David is a professor of surgery at Toronto General Hospital. He reported no financial relationships.
Yes, but repair of FTR requires caution (Gilles Dreyfus, MD)
The controversy surrounding the legitimacy of concomitant tricuspid annuloplasty for functional TR during MVR begs for a clinical trial, but before we can conduct a clinical trial, we must define the primary and secondary endpoints. We’ve seen recent prospective, randomized trials that have reported faulty conclusions because the primary endpoints were wrong.
We need a strong debate to agree on those endpoints. Mortality as an endpoint will probably take a very long time to arrive at.
We’re mixing up many different factors. We’re mixing up TR grading, and we know that grading is unreliable. We have all seen patients with full-fledged TR, and after we put them on Lasix (furosemide, Sanofi), 3 days later they have mild TR. So the same patient with no treatment becomes let’s say a “Dreyfus indication,” and then suddenly in 3 days the patient doesn’t need surgery. At any further stage of his life this patient can experience severe TR again; tricuspid annuloplasty will prevent that from happening.
Moderate TR according to the common definition does not exist. If you look at the reports in echocardiography and if you ask any cardiologist, everything between no TR and severe TR is considered moderate. We have proposed a new staging system for evaluating FTR that uses three factors: TR severity; annular dilatation; and extent of tethering, or mode of leaflet coaptation (J Am Coll Cardiol. 2015;65:2331-6).
Dr. Dreyfus is director of the medical and surgical team at the Cardiothoracic Centre of Monaco in Monte Carlo and professor of cardiothoracic surgery at Paris V University and the Imperial College of London. He disclosed receiving speaker fees from Edwards Lifesciences, LivaNova, and Medtronic.
No, few FTR patients at risk after MVR (Hartzell Schaff, MD)
Echocardiography can provide a great deal of information about when concomitant repair for TR is indicated during MVR. We’ve found that if the patient has no right-sided signs, has normal right atrial pressure, and has mild or mild/moderate TR at the time of repair to the journey mitral valve, the chance of him returning for a tricuspid valve procedure is near zero.
A few patients do return after MVR. They develop atrial fibrillation and may need a pacemaker, but we see very few patients return for tricuspid surgery.
It’s fair to say we cannot demonstrate any benefit of correcting functional mitral regurgitation. Why would we think there’s a benefit of correcting FTR? We can say we’re going to look at grade of TR down the road, or we could look at some other endpoint, but think about it this way: If we cannot prove that correcting functional mitral regurgitation is helpful, why is correcting FTR going to help?
Dr. Schaff is a cardiothoracic surgeon at Mayo Clinic Foundation, Rochester, Minn. He reported no financial relationships.
AT THE AATS MITRAL CONCLAVE 2017
Want to take action on health care legislation? Here’s how
The U.S. House of Representatives recently passed a revised version of the American Health Care Act (AHCA), which the nonpartisan Congressional Budget Office concluded would result in 14 million people losing coverage by 2018 and 23 million people losing coverage by 2026.
The American Congress of Obstetricians and Gynecologists is opposed to this bill and has stated that it will leave Americans “worse off than they are today” by cutting Medicaid, eliminating Medicaid expansion, allowing states to opt out of covering essential benefits like maternity care, and weakening protections for people with preexisting conditions.
[polldaddy:9770191]
State level
At the state level, the best person to contact is your ACOG section chairman, who can then direct you to your state’s legislative chairman. The legislative chairman will provide you with information on legislative actions that have been taken by the section. If you are interested in women’s health legislation, there may be an advocacy list to join that will provide legislative alerts. You may even choose to tweet about the alerts.
Often the state legislative chairman will send out information about an upcoming bill and ask for ACOG members to provide testimony. If there is a bill of particular interest, you can offer to testify either in person or submit written testimony. Often talking points are made available to help in the preparation of testimony.
Many states also have a Lobby Day, a day when members of the ob.gyn. community meet at the state house to advocate for or oppose legislation. This action can be easier than providing testimony because the time and date are predictable, while legislative hearings may not be.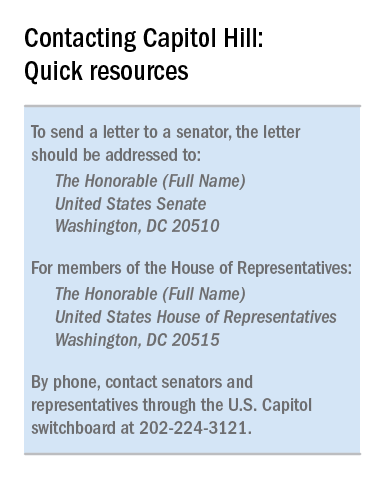
There is a great deal that can be done at the state level in support of women’s health. Perhaps your state does not have a maternal mortality committee, perhaps there needs to be funding for vaccinations, or perhaps you want to support legislation that continues to provide health care for women even if the AHCA becomes law.
National action
Legislative action at the national level mirrors that at the state level, but it is coordinated by the ACOG Government Affairs Department. Contact this department via acog.org. One option is to become an advocate and receive legislative alerts. This alert system informs ACOG members about congressional actions and gives you the option to directly contact your members of Congress through email with a specific message. Some physicians may prefer to send an email different than the one provided by ACOG, while others may tweet using hashtags like #obgynaction or #docs4coverage.
You may prefer to contact your member of Congress by phone. The U.S. Capitol Switchboard number is 202-224-3121. Phone calls typically are taken by staff members. It is reasonable to ask for a staff member who handles the issue you wish to discuss. This person may be referred to as the L.A. (legislative assistant). Inform the staff member that you are a constituent and you would like to leave a brief message for the Senator or Representative. Your comments may be as brief as stating that you support or oppose a particular piece of legislation. As with the letter, you should state the reasons for your opinion and may include a short personal story. If you do not already know it, you should ask for the lawmaker’s position on the bill.
An ideal method of interacting with members of Congress is through town hall meetings. These meetings typically are posted on the member’s website and hearing from constituents in person can have a tremendous impact on legislators. Letters to the Editor, interviews with journalists, and advocating for candidates are also options to consider. In such cases, consider contacting the ACOG Government Affairs Department. They can provide helpful dos and don’ts before an interview is scheduled or an article is written.
Health care policymaking that is not based on scientific or medical evidence is dangerous for our patients. We, as their physicians, need to advocate on their behalf. Stay or get involved to help ensure that our patients can get the health care they need when they need it.
Dr. Bohon is an ob.gyn. in private practice in Washington, and an ACOG state legislative chair from the District of Columbia. She is a member of the Ob.Gyn. News Editorial Advisory Board. Dr. Bohon reported having no relevant financial disclosures.
The U.S. House of Representatives recently passed a revised version of the American Health Care Act (AHCA), which the nonpartisan Congressional Budget Office concluded would result in 14 million people losing coverage by 2018 and 23 million people losing coverage by 2026.
The American Congress of Obstetricians and Gynecologists is opposed to this bill and has stated that it will leave Americans “worse off than they are today” by cutting Medicaid, eliminating Medicaid expansion, allowing states to opt out of covering essential benefits like maternity care, and weakening protections for people with preexisting conditions.
[polldaddy:9770191]
State level
At the state level, the best person to contact is your ACOG section chairman, who can then direct you to your state’s legislative chairman. The legislative chairman will provide you with information on legislative actions that have been taken by the section. If you are interested in women’s health legislation, there may be an advocacy list to join that will provide legislative alerts. You may even choose to tweet about the alerts.
Often the state legislative chairman will send out information about an upcoming bill and ask for ACOG members to provide testimony. If there is a bill of particular interest, you can offer to testify either in person or submit written testimony. Often talking points are made available to help in the preparation of testimony.
Many states also have a Lobby Day, a day when members of the ob.gyn. community meet at the state house to advocate for or oppose legislation. This action can be easier than providing testimony because the time and date are predictable, while legislative hearings may not be.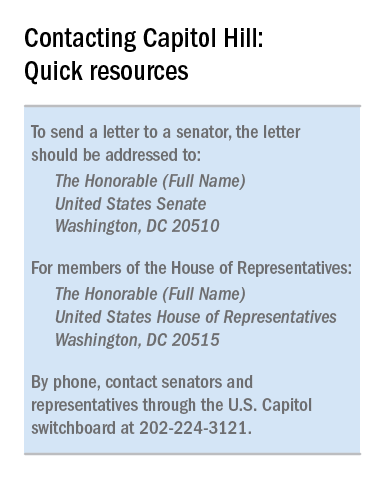
There is a great deal that can be done at the state level in support of women’s health. Perhaps your state does not have a maternal mortality committee, perhaps there needs to be funding for vaccinations, or perhaps you want to support legislation that continues to provide health care for women even if the AHCA becomes law.
National action
Legislative action at the national level mirrors that at the state level, but it is coordinated by the ACOG Government Affairs Department. Contact this department via acog.org. One option is to become an advocate and receive legislative alerts. This alert system informs ACOG members about congressional actions and gives you the option to directly contact your members of Congress through email with a specific message. Some physicians may prefer to send an email different than the one provided by ACOG, while others may tweet using hashtags like #obgynaction or #docs4coverage.
You may prefer to contact your member of Congress by phone. The U.S. Capitol Switchboard number is 202-224-3121. Phone calls typically are taken by staff members. It is reasonable to ask for a staff member who handles the issue you wish to discuss. This person may be referred to as the L.A. (legislative assistant). Inform the staff member that you are a constituent and you would like to leave a brief message for the Senator or Representative. Your comments may be as brief as stating that you support or oppose a particular piece of legislation. As with the letter, you should state the reasons for your opinion and may include a short personal story. If you do not already know it, you should ask for the lawmaker’s position on the bill.
An ideal method of interacting with members of Congress is through town hall meetings. These meetings typically are posted on the member’s website and hearing from constituents in person can have a tremendous impact on legislators. Letters to the Editor, interviews with journalists, and advocating for candidates are also options to consider. In such cases, consider contacting the ACOG Government Affairs Department. They can provide helpful dos and don’ts before an interview is scheduled or an article is written.
Health care policymaking that is not based on scientific or medical evidence is dangerous for our patients. We, as their physicians, need to advocate on their behalf. Stay or get involved to help ensure that our patients can get the health care they need when they need it.
Dr. Bohon is an ob.gyn. in private practice in Washington, and an ACOG state legislative chair from the District of Columbia. She is a member of the Ob.Gyn. News Editorial Advisory Board. Dr. Bohon reported having no relevant financial disclosures.
The U.S. House of Representatives recently passed a revised version of the American Health Care Act (AHCA), which the nonpartisan Congressional Budget Office concluded would result in 14 million people losing coverage by 2018 and 23 million people losing coverage by 2026.
The American Congress of Obstetricians and Gynecologists is opposed to this bill and has stated that it will leave Americans “worse off than they are today” by cutting Medicaid, eliminating Medicaid expansion, allowing states to opt out of covering essential benefits like maternity care, and weakening protections for people with preexisting conditions.
[polldaddy:9770191]
State level
At the state level, the best person to contact is your ACOG section chairman, who can then direct you to your state’s legislative chairman. The legislative chairman will provide you with information on legislative actions that have been taken by the section. If you are interested in women’s health legislation, there may be an advocacy list to join that will provide legislative alerts. You may even choose to tweet about the alerts.
Often the state legislative chairman will send out information about an upcoming bill and ask for ACOG members to provide testimony. If there is a bill of particular interest, you can offer to testify either in person or submit written testimony. Often talking points are made available to help in the preparation of testimony.
Many states also have a Lobby Day, a day when members of the ob.gyn. community meet at the state house to advocate for or oppose legislation. This action can be easier than providing testimony because the time and date are predictable, while legislative hearings may not be.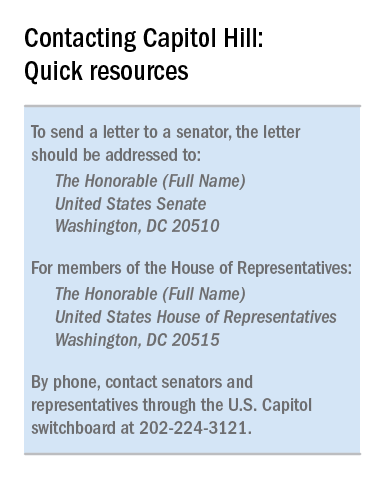
There is a great deal that can be done at the state level in support of women’s health. Perhaps your state does not have a maternal mortality committee, perhaps there needs to be funding for vaccinations, or perhaps you want to support legislation that continues to provide health care for women even if the AHCA becomes law.
National action
Legislative action at the national level mirrors that at the state level, but it is coordinated by the ACOG Government Affairs Department. Contact this department via acog.org. One option is to become an advocate and receive legislative alerts. This alert system informs ACOG members about congressional actions and gives you the option to directly contact your members of Congress through email with a specific message. Some physicians may prefer to send an email different than the one provided by ACOG, while others may tweet using hashtags like #obgynaction or #docs4coverage.
You may prefer to contact your member of Congress by phone. The U.S. Capitol Switchboard number is 202-224-3121. Phone calls typically are taken by staff members. It is reasonable to ask for a staff member who handles the issue you wish to discuss. This person may be referred to as the L.A. (legislative assistant). Inform the staff member that you are a constituent and you would like to leave a brief message for the Senator or Representative. Your comments may be as brief as stating that you support or oppose a particular piece of legislation. As with the letter, you should state the reasons for your opinion and may include a short personal story. If you do not already know it, you should ask for the lawmaker’s position on the bill.
An ideal method of interacting with members of Congress is through town hall meetings. These meetings typically are posted on the member’s website and hearing from constituents in person can have a tremendous impact on legislators. Letters to the Editor, interviews with journalists, and advocating for candidates are also options to consider. In such cases, consider contacting the ACOG Government Affairs Department. They can provide helpful dos and don’ts before an interview is scheduled or an article is written.
Health care policymaking that is not based on scientific or medical evidence is dangerous for our patients. We, as their physicians, need to advocate on their behalf. Stay or get involved to help ensure that our patients can get the health care they need when they need it.
Dr. Bohon is an ob.gyn. in private practice in Washington, and an ACOG state legislative chair from the District of Columbia. She is a member of the Ob.Gyn. News Editorial Advisory Board. Dr. Bohon reported having no relevant financial disclosures.
EHR Report: Don’t let the electronic health record do the driving
The secret to the care of the patient ... is in caring for the patient.
-Francis W. Peabody, MD1
Last month I received a call from a man who was upset about the way he was treated in our office. He had presented with depression and felt insulted by one of our resident physicians in the way he had interacted with him during his visit. I offered to see him the next day.
When I walked into the exam room, I noticed that his eyes were bloodshot and he was fidgeting in his chair. He explained that it was difficult for him to address this issue, but he had been taken aback at his previous visit to our office when the doctor who saw him, after introducing himself, proceeded to sit down, open his computer, and start typing. The patient went on to describe that the physician – while staring at his computer screen – first acknowledged that he was being seen for depression and then immediately asked him if he had any plans to commit suicide. He did not have any suicidal plans, but he felt strongly that being asked about suicide as the first question in the doctor’s interview missed the point of his visit. He was having trouble concentrating, he felt down, and he was having difficulty sleeping at night, all contributing to trouble both at work and in his personal life. Suicide was not a concern of his. He shook his head. He said he understood that we, as doctors, had to put information into the computer, but he also felt that the doctor’s main goal during that visit appeared to be to get through the forms on the computer rather than taking care of him. He admonished that physicians also need to remember that there is a patient in the room and that we should pay attention to the patient first. The computer should be second. I couldn’t have said it better myself. I told him that I would look into what happened, and then we continued with his visit.
You can already see where this discussion is going. The odd thing about the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medicare’s quality payment program, is that, unless we are careful, the result of the program may be the opposite of what it’s intended to accomplish. By leading to an over-focus on documentation of the quality of care, we are at risk of diminishing the quality of care itself. In essence, many of the requirements appear to simply be more advanced versions of the meaningful (meaningless?) use provisions with which we have previously grappled. It is clear that we should assess the quality of care that is given and that physician payment should be influenced by that care. It is also clear that the only reasonable way to measure the care provided is by collecting data from the EHR. The problem is that the sophistication of the EHR has not caught up to the sophistication of our goals.
Our challenge as physicians who care for patients therefore occurs at an individual level for each of us. How do we provide the necessary documentation scattered throughout our digital charts to satisfy reporting requirements, yet still meet the very real needs of patients to have their voices heard and their emotions acknowledged? The Physician Charter by the American Board of Internal Medicine discusses “the primacy of patient welfare” as a core tenant of medical practice. It goes on to state that “administrative exigencies must not compromise this principle.”2 Given competing demands, how do we continue to accomplish these goals which are often in conflict with one another?
We cannot provide an answer to this question because unfortunately – or perhaps fortunately – the answer does not come in the form of a clear algorithm of behaviors or a form that we can click on. However that does not mean that it cannot be done. Simply being mindful of how important personal interaction is to our patients will help us stay focused on patient needs. In fact, one of the most exciting aspects of our digital age (and our use of EHRs) is that the need to actually connect with people is more important than ever, and prioritizing this stands to reward those individuals who continue to pay attention to patients. In a future column, we will discuss suggestions and strategies for integrating the EHR into truly patient-centered care. In the early 1920s, Dr. Francis W. Peabody said, “The treatment of a disease may be entirely impersonal: the care of the patient must be completely personal.”1 Medical competency is essential and documentation is required, but neither alone is sufficient for the care of patients.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
References
1. Peabody FW. The care of the patient. JAMA. 1927;88:877-82.
2. The Physician Charter. American Board of Internal Medicine Foundation at http://abimfoundation.org/what-we-do/physician-charter.
The secret to the care of the patient ... is in caring for the patient.
-Francis W. Peabody, MD1
Last month I received a call from a man who was upset about the way he was treated in our office. He had presented with depression and felt insulted by one of our resident physicians in the way he had interacted with him during his visit. I offered to see him the next day.
When I walked into the exam room, I noticed that his eyes were bloodshot and he was fidgeting in his chair. He explained that it was difficult for him to address this issue, but he had been taken aback at his previous visit to our office when the doctor who saw him, after introducing himself, proceeded to sit down, open his computer, and start typing. The patient went on to describe that the physician – while staring at his computer screen – first acknowledged that he was being seen for depression and then immediately asked him if he had any plans to commit suicide. He did not have any suicidal plans, but he felt strongly that being asked about suicide as the first question in the doctor’s interview missed the point of his visit. He was having trouble concentrating, he felt down, and he was having difficulty sleeping at night, all contributing to trouble both at work and in his personal life. Suicide was not a concern of his. He shook his head. He said he understood that we, as doctors, had to put information into the computer, but he also felt that the doctor’s main goal during that visit appeared to be to get through the forms on the computer rather than taking care of him. He admonished that physicians also need to remember that there is a patient in the room and that we should pay attention to the patient first. The computer should be second. I couldn’t have said it better myself. I told him that I would look into what happened, and then we continued with his visit.
You can already see where this discussion is going. The odd thing about the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medicare’s quality payment program, is that, unless we are careful, the result of the program may be the opposite of what it’s intended to accomplish. By leading to an over-focus on documentation of the quality of care, we are at risk of diminishing the quality of care itself. In essence, many of the requirements appear to simply be more advanced versions of the meaningful (meaningless?) use provisions with which we have previously grappled. It is clear that we should assess the quality of care that is given and that physician payment should be influenced by that care. It is also clear that the only reasonable way to measure the care provided is by collecting data from the EHR. The problem is that the sophistication of the EHR has not caught up to the sophistication of our goals.
Our challenge as physicians who care for patients therefore occurs at an individual level for each of us. How do we provide the necessary documentation scattered throughout our digital charts to satisfy reporting requirements, yet still meet the very real needs of patients to have their voices heard and their emotions acknowledged? The Physician Charter by the American Board of Internal Medicine discusses “the primacy of patient welfare” as a core tenant of medical practice. It goes on to state that “administrative exigencies must not compromise this principle.”2 Given competing demands, how do we continue to accomplish these goals which are often in conflict with one another?
We cannot provide an answer to this question because unfortunately – or perhaps fortunately – the answer does not come in the form of a clear algorithm of behaviors or a form that we can click on. However that does not mean that it cannot be done. Simply being mindful of how important personal interaction is to our patients will help us stay focused on patient needs. In fact, one of the most exciting aspects of our digital age (and our use of EHRs) is that the need to actually connect with people is more important than ever, and prioritizing this stands to reward those individuals who continue to pay attention to patients. In a future column, we will discuss suggestions and strategies for integrating the EHR into truly patient-centered care. In the early 1920s, Dr. Francis W. Peabody said, “The treatment of a disease may be entirely impersonal: the care of the patient must be completely personal.”1 Medical competency is essential and documentation is required, but neither alone is sufficient for the care of patients.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
References
1. Peabody FW. The care of the patient. JAMA. 1927;88:877-82.
2. The Physician Charter. American Board of Internal Medicine Foundation at http://abimfoundation.org/what-we-do/physician-charter.
The secret to the care of the patient ... is in caring for the patient.
-Francis W. Peabody, MD1
Last month I received a call from a man who was upset about the way he was treated in our office. He had presented with depression and felt insulted by one of our resident physicians in the way he had interacted with him during his visit. I offered to see him the next day.
When I walked into the exam room, I noticed that his eyes were bloodshot and he was fidgeting in his chair. He explained that it was difficult for him to address this issue, but he had been taken aback at his previous visit to our office when the doctor who saw him, after introducing himself, proceeded to sit down, open his computer, and start typing. The patient went on to describe that the physician – while staring at his computer screen – first acknowledged that he was being seen for depression and then immediately asked him if he had any plans to commit suicide. He did not have any suicidal plans, but he felt strongly that being asked about suicide as the first question in the doctor’s interview missed the point of his visit. He was having trouble concentrating, he felt down, and he was having difficulty sleeping at night, all contributing to trouble both at work and in his personal life. Suicide was not a concern of his. He shook his head. He said he understood that we, as doctors, had to put information into the computer, but he also felt that the doctor’s main goal during that visit appeared to be to get through the forms on the computer rather than taking care of him. He admonished that physicians also need to remember that there is a patient in the room and that we should pay attention to the patient first. The computer should be second. I couldn’t have said it better myself. I told him that I would look into what happened, and then we continued with his visit.
You can already see where this discussion is going. The odd thing about the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medicare’s quality payment program, is that, unless we are careful, the result of the program may be the opposite of what it’s intended to accomplish. By leading to an over-focus on documentation of the quality of care, we are at risk of diminishing the quality of care itself. In essence, many of the requirements appear to simply be more advanced versions of the meaningful (meaningless?) use provisions with which we have previously grappled. It is clear that we should assess the quality of care that is given and that physician payment should be influenced by that care. It is also clear that the only reasonable way to measure the care provided is by collecting data from the EHR. The problem is that the sophistication of the EHR has not caught up to the sophistication of our goals.
Our challenge as physicians who care for patients therefore occurs at an individual level for each of us. How do we provide the necessary documentation scattered throughout our digital charts to satisfy reporting requirements, yet still meet the very real needs of patients to have their voices heard and their emotions acknowledged? The Physician Charter by the American Board of Internal Medicine discusses “the primacy of patient welfare” as a core tenant of medical practice. It goes on to state that “administrative exigencies must not compromise this principle.”2 Given competing demands, how do we continue to accomplish these goals which are often in conflict with one another?
We cannot provide an answer to this question because unfortunately – or perhaps fortunately – the answer does not come in the form of a clear algorithm of behaviors or a form that we can click on. However that does not mean that it cannot be done. Simply being mindful of how important personal interaction is to our patients will help us stay focused on patient needs. In fact, one of the most exciting aspects of our digital age (and our use of EHRs) is that the need to actually connect with people is more important than ever, and prioritizing this stands to reward those individuals who continue to pay attention to patients. In a future column, we will discuss suggestions and strategies for integrating the EHR into truly patient-centered care. In the early 1920s, Dr. Francis W. Peabody said, “The treatment of a disease may be entirely impersonal: the care of the patient must be completely personal.”1 Medical competency is essential and documentation is required, but neither alone is sufficient for the care of patients.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Notte is a family physician and clinical informaticist for Abington Memorial Hospital. He is also a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records.
References
1. Peabody FW. The care of the patient. JAMA. 1927;88:877-82.
2. The Physician Charter. American Board of Internal Medicine Foundation at http://abimfoundation.org/what-we-do/physician-charter.
An Act of Service, an Act of Love
Since its foundation in 1913 as the premier surgical professional organization in the United States, and one of the most influential in the world, the American College of Surgeons has shaped the policies and molded the education of numerous generations of surgeons. All young surgeons should aspire to be invested as Fellows some day as the highest honor in their career.
Service is an important factor in the decision to become a surgeon. As a Fellow of the ACS, the young surgeon will find many opportunities for service. Active participation as a Fellow is an act of service and can be an act of love for our patients, our colleagues, and our profession. And, with it, comes loyalty, a spirit of dedication, and a sense of unity. In addition, by joining the College we contribute to influencing our society in a positive way to protect our patients and our profession.
Becoming an active participant in the College means serving on committees, attending the Clinical Congress as frequently as feasible, and encouraging colleagues to aspire to become a Fellow.
In the end, being a part of our College and contributing to its growth and legacy is an act of service and, for many, an act of love.
Dr. Oviedo is with Capital Regional Surgical Associates, Tallahassee, Fla., and is Assistant Professor of Surgery, Florida State University College of Medicine. He serves as the ACS Young Fellow Association Liaison.
Since its foundation in 1913 as the premier surgical professional organization in the United States, and one of the most influential in the world, the American College of Surgeons has shaped the policies and molded the education of numerous generations of surgeons. All young surgeons should aspire to be invested as Fellows some day as the highest honor in their career.
Service is an important factor in the decision to become a surgeon. As a Fellow of the ACS, the young surgeon will find many opportunities for service. Active participation as a Fellow is an act of service and can be an act of love for our patients, our colleagues, and our profession. And, with it, comes loyalty, a spirit of dedication, and a sense of unity. In addition, by joining the College we contribute to influencing our society in a positive way to protect our patients and our profession.
Becoming an active participant in the College means serving on committees, attending the Clinical Congress as frequently as feasible, and encouraging colleagues to aspire to become a Fellow.
In the end, being a part of our College and contributing to its growth and legacy is an act of service and, for many, an act of love.
Dr. Oviedo is with Capital Regional Surgical Associates, Tallahassee, Fla., and is Assistant Professor of Surgery, Florida State University College of Medicine. He serves as the ACS Young Fellow Association Liaison.
Since its foundation in 1913 as the premier surgical professional organization in the United States, and one of the most influential in the world, the American College of Surgeons has shaped the policies and molded the education of numerous generations of surgeons. All young surgeons should aspire to be invested as Fellows some day as the highest honor in their career.
Service is an important factor in the decision to become a surgeon. As a Fellow of the ACS, the young surgeon will find many opportunities for service. Active participation as a Fellow is an act of service and can be an act of love for our patients, our colleagues, and our profession. And, with it, comes loyalty, a spirit of dedication, and a sense of unity. In addition, by joining the College we contribute to influencing our society in a positive way to protect our patients and our profession.
Becoming an active participant in the College means serving on committees, attending the Clinical Congress as frequently as feasible, and encouraging colleagues to aspire to become a Fellow.
In the end, being a part of our College and contributing to its growth and legacy is an act of service and, for many, an act of love.
Dr. Oviedo is with Capital Regional Surgical Associates, Tallahassee, Fla., and is Assistant Professor of Surgery, Florida State University College of Medicine. He serves as the ACS Young Fellow Association Liaison.
Commentary—Promising Results Should Prompt Further Study
During the past 20 years, mindfulness-based training has become an increasingly popular treatment for many conditions, including migraine. In the February online issue of the Journal of Headache and Pain, Dr. Grazzi addresses medication overuse chronic migraine (CM-MO) and provides initial evidence for the consideration of mindfulness training to help reduce headache symptoms.
However, the reader should take seriously the authors’ caution that “although our findings are encouraging and suggestive of the independent value of mindfulness for headache care, certain design limitations preclude us [from] making unequivocal claims.”
Since the goal of a noninferiority trial is to assess whether a new therapy is at least as beneficial as standard treatment, extra caution is necessary when interpreting findings from an underpowered feasibility study. In general, a useful approach to noninferiority is to determine whether the confidence intervals include effect sizes that one might consider clinically meaningful. Instead of focusing on whether the mindfulness-based training group performed the same as the comparison group, we should accept the valuable information that is presented. The take away message from this pilot study is threefold. Mindfulness-based training is potentially acceptable to patients with CM-MO. Patients with CM-MO might be amenable to participating in a fully powered randomized controlled trial of mindfulness-based training. Finally, it is possible that mindfulness-based training may show improvement similar in magnitude to pharmaceuticals. Overall, Grazzi et al have laid the groundwork for a fully powered, randomized version of their study.
—Alice R. Pressman, PhD
Director of Analytics and Evaluation
Sutter Health
Walnut Creek, California
During the past 20 years, mindfulness-based training has become an increasingly popular treatment for many conditions, including migraine. In the February online issue of the Journal of Headache and Pain, Dr. Grazzi addresses medication overuse chronic migraine (CM-MO) and provides initial evidence for the consideration of mindfulness training to help reduce headache symptoms.
However, the reader should take seriously the authors’ caution that “although our findings are encouraging and suggestive of the independent value of mindfulness for headache care, certain design limitations preclude us [from] making unequivocal claims.”
Since the goal of a noninferiority trial is to assess whether a new therapy is at least as beneficial as standard treatment, extra caution is necessary when interpreting findings from an underpowered feasibility study. In general, a useful approach to noninferiority is to determine whether the confidence intervals include effect sizes that one might consider clinically meaningful. Instead of focusing on whether the mindfulness-based training group performed the same as the comparison group, we should accept the valuable information that is presented. The take away message from this pilot study is threefold. Mindfulness-based training is potentially acceptable to patients with CM-MO. Patients with CM-MO might be amenable to participating in a fully powered randomized controlled trial of mindfulness-based training. Finally, it is possible that mindfulness-based training may show improvement similar in magnitude to pharmaceuticals. Overall, Grazzi et al have laid the groundwork for a fully powered, randomized version of their study.
—Alice R. Pressman, PhD
Director of Analytics and Evaluation
Sutter Health
Walnut Creek, California
During the past 20 years, mindfulness-based training has become an increasingly popular treatment for many conditions, including migraine. In the February online issue of the Journal of Headache and Pain, Dr. Grazzi addresses medication overuse chronic migraine (CM-MO) and provides initial evidence for the consideration of mindfulness training to help reduce headache symptoms.
However, the reader should take seriously the authors’ caution that “although our findings are encouraging and suggestive of the independent value of mindfulness for headache care, certain design limitations preclude us [from] making unequivocal claims.”
Since the goal of a noninferiority trial is to assess whether a new therapy is at least as beneficial as standard treatment, extra caution is necessary when interpreting findings from an underpowered feasibility study. In general, a useful approach to noninferiority is to determine whether the confidence intervals include effect sizes that one might consider clinically meaningful. Instead of focusing on whether the mindfulness-based training group performed the same as the comparison group, we should accept the valuable information that is presented. The take away message from this pilot study is threefold. Mindfulness-based training is potentially acceptable to patients with CM-MO. Patients with CM-MO might be amenable to participating in a fully powered randomized controlled trial of mindfulness-based training. Finally, it is possible that mindfulness-based training may show improvement similar in magnitude to pharmaceuticals. Overall, Grazzi et al have laid the groundwork for a fully powered, randomized version of their study.
—Alice R. Pressman, PhD
Director of Analytics and Evaluation
Sutter Health
Walnut Creek, California



















