User login
Physician Communications: Avoiding the Blame Game
A recent opinion piece in MedPage Today by an internist about poor communications between emergency physicians (EPs) and primary care physicians (PCPs) was subtitled “We’ve gotten better going from office to ER, but not the other way,” and complained about the lack of a “live, warm handoff” from EPs to PCPs of patients being discharged from EDs. Similar complaints were examined in two recent Emergency Medicine (EM) editorials (Anger Management, 2015;47[4]:149 and Broadside Journalism, 2015;47[6]:244). In the first, we noted that PCPs sometimes are angered when they are not consulted about one of their patients in the ED or about a treatment or disposition plan with which they disagree, while EPs are frustrated by the number of phone calls required to reach some PCPs or a knowledgeable covering physician.
Only 2 months later, we expressed concerns about a New York Times opinion editorial describing a young patient whose vertebral artery dissection had been “diagnosed correctly and acted on in the ED,” but then angrily criticizing an initial recommendation that the patient curtail her physical activities based on what a famous neurologist considered an erroneously interpreted vascular imaging study. (Presumably, the recommendation was by another neurologist and the interpretation by a radiologist, but all of the neurologist’s caustic criticism was directed at the EP and ED.) Although the neurologist subsequently apologized in a letter to his emergency medicine colleagues for “being quoted out of context,” few if any
We concluded the second EM editorial with the suggestion that “all physicians must be very, very careful in framing statements to the media, and should assume that their remarks will not be placed ‘in context’ or nuanced as they may have been intended....Most important, is to not disparage entire specialties or use belittling terms such as ‘ER docs’....[that] heighten...patients’ fears” of being treated in EDs.
Why another editorial about physician-to-physician miscommunications and name-calling? Because patient care is significantly affected.
The Centers for Medicare and Medicaid Services originally classified four medical specialties as “primary care” for reimbursement purposes: family medicine, internal medicine, pediatrics, and obstetrics-gynecology, and the 2010 Affordable Care Act added geriatrics. Although emergency medicine had been considered initially, it has never been categorized as a primary care specialty. That being the case, isn’t it incumbent upon us to learn as much as we can from PCPs about their ill patients en route to the ED for treatment or admission, and afterward ensure that an ED visit is part of a continuum of patient care and not an isolated episode?
In 1996, when I accepted an offer to become New York Presbyterian-Weill Cornell’s first Emergency Physician-in-Chief, I created a new position of full-time “ED follow-up nurse practitioner” to track and report test results to discharged patients and their designated PCPs. When we added a fourth unit to the ED a few years later, I designated an experienced, senior attending EP among the four on duty as the “administrative attending” (AA) who, among other tasks, took all phone calls from PCPs about patients they were sending to the ED and entered the information in the “en route” section of our electronic tracking board. In this way, important patient information, including PCP contact information, was no longer misplaced during shift changes. The AA carried a direct-dial cell phone-like device and eventually all attending EPs and the charge nurse were equipped with such phones. In a short time, most of the communications problems and complaints about incoming patients were eliminated.
But despite numerous attempts, for the reasons mentioned above, systematically ensuring effective communications with PCPs for discharged patients has proven to be a more difficult task. At present, handing off discharged patients to PCPs still depends largely on a combination of judgment, understanding, compassion, and respect.
A recent opinion piece in MedPage Today by an internist about poor communications between emergency physicians (EPs) and primary care physicians (PCPs) was subtitled “We’ve gotten better going from office to ER, but not the other way,” and complained about the lack of a “live, warm handoff” from EPs to PCPs of patients being discharged from EDs. Similar complaints were examined in two recent Emergency Medicine (EM) editorials (Anger Management, 2015;47[4]:149 and Broadside Journalism, 2015;47[6]:244). In the first, we noted that PCPs sometimes are angered when they are not consulted about one of their patients in the ED or about a treatment or disposition plan with which they disagree, while EPs are frustrated by the number of phone calls required to reach some PCPs or a knowledgeable covering physician.
Only 2 months later, we expressed concerns about a New York Times opinion editorial describing a young patient whose vertebral artery dissection had been “diagnosed correctly and acted on in the ED,” but then angrily criticizing an initial recommendation that the patient curtail her physical activities based on what a famous neurologist considered an erroneously interpreted vascular imaging study. (Presumably, the recommendation was by another neurologist and the interpretation by a radiologist, but all of the neurologist’s caustic criticism was directed at the EP and ED.) Although the neurologist subsequently apologized in a letter to his emergency medicine colleagues for “being quoted out of context,” few if any
We concluded the second EM editorial with the suggestion that “all physicians must be very, very careful in framing statements to the media, and should assume that their remarks will not be placed ‘in context’ or nuanced as they may have been intended....Most important, is to not disparage entire specialties or use belittling terms such as ‘ER docs’....[that] heighten...patients’ fears” of being treated in EDs.
Why another editorial about physician-to-physician miscommunications and name-calling? Because patient care is significantly affected.
The Centers for Medicare and Medicaid Services originally classified four medical specialties as “primary care” for reimbursement purposes: family medicine, internal medicine, pediatrics, and obstetrics-gynecology, and the 2010 Affordable Care Act added geriatrics. Although emergency medicine had been considered initially, it has never been categorized as a primary care specialty. That being the case, isn’t it incumbent upon us to learn as much as we can from PCPs about their ill patients en route to the ED for treatment or admission, and afterward ensure that an ED visit is part of a continuum of patient care and not an isolated episode?
In 1996, when I accepted an offer to become New York Presbyterian-Weill Cornell’s first Emergency Physician-in-Chief, I created a new position of full-time “ED follow-up nurse practitioner” to track and report test results to discharged patients and their designated PCPs. When we added a fourth unit to the ED a few years later, I designated an experienced, senior attending EP among the four on duty as the “administrative attending” (AA) who, among other tasks, took all phone calls from PCPs about patients they were sending to the ED and entered the information in the “en route” section of our electronic tracking board. In this way, important patient information, including PCP contact information, was no longer misplaced during shift changes. The AA carried a direct-dial cell phone-like device and eventually all attending EPs and the charge nurse were equipped with such phones. In a short time, most of the communications problems and complaints about incoming patients were eliminated.
But despite numerous attempts, for the reasons mentioned above, systematically ensuring effective communications with PCPs for discharged patients has proven to be a more difficult task. At present, handing off discharged patients to PCPs still depends largely on a combination of judgment, understanding, compassion, and respect.
A recent opinion piece in MedPage Today by an internist about poor communications between emergency physicians (EPs) and primary care physicians (PCPs) was subtitled “We’ve gotten better going from office to ER, but not the other way,” and complained about the lack of a “live, warm handoff” from EPs to PCPs of patients being discharged from EDs. Similar complaints were examined in two recent Emergency Medicine (EM) editorials (Anger Management, 2015;47[4]:149 and Broadside Journalism, 2015;47[6]:244). In the first, we noted that PCPs sometimes are angered when they are not consulted about one of their patients in the ED or about a treatment or disposition plan with which they disagree, while EPs are frustrated by the number of phone calls required to reach some PCPs or a knowledgeable covering physician.
Only 2 months later, we expressed concerns about a New York Times opinion editorial describing a young patient whose vertebral artery dissection had been “diagnosed correctly and acted on in the ED,” but then angrily criticizing an initial recommendation that the patient curtail her physical activities based on what a famous neurologist considered an erroneously interpreted vascular imaging study. (Presumably, the recommendation was by another neurologist and the interpretation by a radiologist, but all of the neurologist’s caustic criticism was directed at the EP and ED.) Although the neurologist subsequently apologized in a letter to his emergency medicine colleagues for “being quoted out of context,” few if any
We concluded the second EM editorial with the suggestion that “all physicians must be very, very careful in framing statements to the media, and should assume that their remarks will not be placed ‘in context’ or nuanced as they may have been intended....Most important, is to not disparage entire specialties or use belittling terms such as ‘ER docs’....[that] heighten...patients’ fears” of being treated in EDs.
Why another editorial about physician-to-physician miscommunications and name-calling? Because patient care is significantly affected.
The Centers for Medicare and Medicaid Services originally classified four medical specialties as “primary care” for reimbursement purposes: family medicine, internal medicine, pediatrics, and obstetrics-gynecology, and the 2010 Affordable Care Act added geriatrics. Although emergency medicine had been considered initially, it has never been categorized as a primary care specialty. That being the case, isn’t it incumbent upon us to learn as much as we can from PCPs about their ill patients en route to the ED for treatment or admission, and afterward ensure that an ED visit is part of a continuum of patient care and not an isolated episode?
In 1996, when I accepted an offer to become New York Presbyterian-Weill Cornell’s first Emergency Physician-in-Chief, I created a new position of full-time “ED follow-up nurse practitioner” to track and report test results to discharged patients and their designated PCPs. When we added a fourth unit to the ED a few years later, I designated an experienced, senior attending EP among the four on duty as the “administrative attending” (AA) who, among other tasks, took all phone calls from PCPs about patients they were sending to the ED and entered the information in the “en route” section of our electronic tracking board. In this way, important patient information, including PCP contact information, was no longer misplaced during shift changes. The AA carried a direct-dial cell phone-like device and eventually all attending EPs and the charge nurse were equipped with such phones. In a short time, most of the communications problems and complaints about incoming patients were eliminated.
But despite numerous attempts, for the reasons mentioned above, systematically ensuring effective communications with PCPs for discharged patients has proven to be a more difficult task. At present, handing off discharged patients to PCPs still depends largely on a combination of judgment, understanding, compassion, and respect.
When to discontinue contact precautions for patients with MRSA
Methicillin-resistant Staphylococcus aureus (MRSA) is a common hospital-acquired infection with significant morbidity and mortality. The CDC currently recommends contact precautions as a mainstay to prevent transmission of MRSA in health care settings. Most hospitals routinely screen patients for MRSA and use contact precautions for those who screen positive. The duration of these precautions vary across hospitals and no standard recommendation exists.
A recent study of members of the Society for Healthcare Epidemiology of America (SHEA) research network indicated that the majority of physicians (94%) and nurses (76%) dislike contact precautions (CP) and most (63%) were in favor of implementing CP in a different way than current practice.1 Patients also report less satisfaction and increased isolation.1
My colleagues and I recently published a study2 in the American Journal of Infection Control to explore the necessary duration of contact precautions for hospitalized patients with MRSA. Our goal was to maintain contact precautions as long as necessary to prevent undesired MRSA infections and colonization but minimize unnecessary days in contact isolation. We also sought to figure out whether patients with positive MRSA surveillance cultures should always remain in isolation and, if not, at what point they could be considered for rescreening and removal of precautions if culture negative.
Our hospital has been performing active surveillance cultures weekly to screen for MRSA among our hospitalized patients for many years; however from 2010 to 2014, we began screening patients who were previously known to be positive for MRSA colonization or infection for at least 1 year. We then assessed medical and demographic factors associated with persistent carriage of MRSA.
In our study, more than 400 patients with known MRSA were rescreened with an active surveillance culture at a subsequent hospital admission. Ultimately 20% of the patients remained MRSA positive on the active surveillance culture. Most patients who were culture positive for MRSA were found on the first active surveillance culture (16.4%) but the remaining positive cultures were found on a second active surveillance culture or a clinical culture.
The amount of time that passed since the patient was culture positive was significantly associated with a lower risk of a positive culture at screening. This continued to drop over time with only 12.5% of patients remaining active surveillance culture positive for MRSA at 5 years after the original positive culture.
Two factors were found to significantly impact the MRSA culture on the multivariate analysis: (1) Female sex reduced the risk of positivity, and (2) Presence of a foreign body increased the risk of positivity.
Most patients who remained positive for an MRSA culture were found with the first active surveillance culture, less than 4% were detected subsequently with a repeat surveillance or clinical culture and this percentage also decreased over time. This indicates that in the absence of a positive active surveillance culture it may be reasonable to discontinue contact precautions, which could result in a substantial cost savings for the hospital and improved patient and provider satisfaction without increasing the risk of MRSA transmission.
We concluded that in the absence of a foreign body and with at least a year from the last known positive culture, patients with known MRSA should be rescreened and, if negative on an active surveillance culture, should be removed from contact precautions.
Lauren Richey, MD, MPH, is assistant professor in the infectious diseases division at the Medical University of South Carolina.
References
1. Morgan DJ, Diekema DJ, Sepkowitz K, Perencevich EN. Adverse outcomes associated with contact precautions: A review of the literature. Am J Infect Control. 2009 Mar;37(2):85-93. doi: 10.1016/j.ajic.2008.04.257.
2. Richey LE, Oh Y, Tchamba DM, Engle M, Formby L, Salgado CD. When should contact precautions be discontinued for patients with Methicillin-resistant Staphylococcus aureus? Am J Infect Control. 2016 Aug 30. doi: 10.1016/j.ajic.2016.05.030.
Methicillin-resistant Staphylococcus aureus (MRSA) is a common hospital-acquired infection with significant morbidity and mortality. The CDC currently recommends contact precautions as a mainstay to prevent transmission of MRSA in health care settings. Most hospitals routinely screen patients for MRSA and use contact precautions for those who screen positive. The duration of these precautions vary across hospitals and no standard recommendation exists.
A recent study of members of the Society for Healthcare Epidemiology of America (SHEA) research network indicated that the majority of physicians (94%) and nurses (76%) dislike contact precautions (CP) and most (63%) were in favor of implementing CP in a different way than current practice.1 Patients also report less satisfaction and increased isolation.1
My colleagues and I recently published a study2 in the American Journal of Infection Control to explore the necessary duration of contact precautions for hospitalized patients with MRSA. Our goal was to maintain contact precautions as long as necessary to prevent undesired MRSA infections and colonization but minimize unnecessary days in contact isolation. We also sought to figure out whether patients with positive MRSA surveillance cultures should always remain in isolation and, if not, at what point they could be considered for rescreening and removal of precautions if culture negative.
Our hospital has been performing active surveillance cultures weekly to screen for MRSA among our hospitalized patients for many years; however from 2010 to 2014, we began screening patients who were previously known to be positive for MRSA colonization or infection for at least 1 year. We then assessed medical and demographic factors associated with persistent carriage of MRSA.
In our study, more than 400 patients with known MRSA were rescreened with an active surveillance culture at a subsequent hospital admission. Ultimately 20% of the patients remained MRSA positive on the active surveillance culture. Most patients who were culture positive for MRSA were found on the first active surveillance culture (16.4%) but the remaining positive cultures were found on a second active surveillance culture or a clinical culture.
The amount of time that passed since the patient was culture positive was significantly associated with a lower risk of a positive culture at screening. This continued to drop over time with only 12.5% of patients remaining active surveillance culture positive for MRSA at 5 years after the original positive culture.
Two factors were found to significantly impact the MRSA culture on the multivariate analysis: (1) Female sex reduced the risk of positivity, and (2) Presence of a foreign body increased the risk of positivity.
Most patients who remained positive for an MRSA culture were found with the first active surveillance culture, less than 4% were detected subsequently with a repeat surveillance or clinical culture and this percentage also decreased over time. This indicates that in the absence of a positive active surveillance culture it may be reasonable to discontinue contact precautions, which could result in a substantial cost savings for the hospital and improved patient and provider satisfaction without increasing the risk of MRSA transmission.
We concluded that in the absence of a foreign body and with at least a year from the last known positive culture, patients with known MRSA should be rescreened and, if negative on an active surveillance culture, should be removed from contact precautions.
Lauren Richey, MD, MPH, is assistant professor in the infectious diseases division at the Medical University of South Carolina.
References
1. Morgan DJ, Diekema DJ, Sepkowitz K, Perencevich EN. Adverse outcomes associated with contact precautions: A review of the literature. Am J Infect Control. 2009 Mar;37(2):85-93. doi: 10.1016/j.ajic.2008.04.257.
2. Richey LE, Oh Y, Tchamba DM, Engle M, Formby L, Salgado CD. When should contact precautions be discontinued for patients with Methicillin-resistant Staphylococcus aureus? Am J Infect Control. 2016 Aug 30. doi: 10.1016/j.ajic.2016.05.030.
Methicillin-resistant Staphylococcus aureus (MRSA) is a common hospital-acquired infection with significant morbidity and mortality. The CDC currently recommends contact precautions as a mainstay to prevent transmission of MRSA in health care settings. Most hospitals routinely screen patients for MRSA and use contact precautions for those who screen positive. The duration of these precautions vary across hospitals and no standard recommendation exists.
A recent study of members of the Society for Healthcare Epidemiology of America (SHEA) research network indicated that the majority of physicians (94%) and nurses (76%) dislike contact precautions (CP) and most (63%) were in favor of implementing CP in a different way than current practice.1 Patients also report less satisfaction and increased isolation.1
My colleagues and I recently published a study2 in the American Journal of Infection Control to explore the necessary duration of contact precautions for hospitalized patients with MRSA. Our goal was to maintain contact precautions as long as necessary to prevent undesired MRSA infections and colonization but minimize unnecessary days in contact isolation. We also sought to figure out whether patients with positive MRSA surveillance cultures should always remain in isolation and, if not, at what point they could be considered for rescreening and removal of precautions if culture negative.
Our hospital has been performing active surveillance cultures weekly to screen for MRSA among our hospitalized patients for many years; however from 2010 to 2014, we began screening patients who were previously known to be positive for MRSA colonization or infection for at least 1 year. We then assessed medical and demographic factors associated with persistent carriage of MRSA.
In our study, more than 400 patients with known MRSA were rescreened with an active surveillance culture at a subsequent hospital admission. Ultimately 20% of the patients remained MRSA positive on the active surveillance culture. Most patients who were culture positive for MRSA were found on the first active surveillance culture (16.4%) but the remaining positive cultures were found on a second active surveillance culture or a clinical culture.
The amount of time that passed since the patient was culture positive was significantly associated with a lower risk of a positive culture at screening. This continued to drop over time with only 12.5% of patients remaining active surveillance culture positive for MRSA at 5 years after the original positive culture.
Two factors were found to significantly impact the MRSA culture on the multivariate analysis: (1) Female sex reduced the risk of positivity, and (2) Presence of a foreign body increased the risk of positivity.
Most patients who remained positive for an MRSA culture were found with the first active surveillance culture, less than 4% were detected subsequently with a repeat surveillance or clinical culture and this percentage also decreased over time. This indicates that in the absence of a positive active surveillance culture it may be reasonable to discontinue contact precautions, which could result in a substantial cost savings for the hospital and improved patient and provider satisfaction without increasing the risk of MRSA transmission.
We concluded that in the absence of a foreign body and with at least a year from the last known positive culture, patients with known MRSA should be rescreened and, if negative on an active surveillance culture, should be removed from contact precautions.
Lauren Richey, MD, MPH, is assistant professor in the infectious diseases division at the Medical University of South Carolina.
References
1. Morgan DJ, Diekema DJ, Sepkowitz K, Perencevich EN. Adverse outcomes associated with contact precautions: A review of the literature. Am J Infect Control. 2009 Mar;37(2):85-93. doi: 10.1016/j.ajic.2008.04.257.
2. Richey LE, Oh Y, Tchamba DM, Engle M, Formby L, Salgado CD. When should contact precautions be discontinued for patients with Methicillin-resistant Staphylococcus aureus? Am J Infect Control. 2016 Aug 30. doi: 10.1016/j.ajic.2016.05.030.
Alexa
How many calories are there in a cheeseburger? (Yes, I too am looking forward to a svelter 2017). The answer, according to my new assistant, is 300 calories. She knows the dose of acetaminophen for a 10-year-old, 65-pound child is 325 mg every 4-6 hours. She also plays George Michael, reorders my Dentyne Ice gum, and turns off the lights. She is Alexa of Amazon’s Echo, the intelligent personal assistant.
Echo and Google Home are popular voice-assisted home appliances. Amazon has built a natural language processing system, so to use it, you simply say, “Alexa,” pause, then ask your question (What’s the weather in New York?) or deliver your command (Play Spotify). It’s hands free, so you can interface while typing, reading, or cooking dinner.
Some medical centers, such as the Boston Children’s Hospital, are leading the way to make voice-assisted technology useful in health care. Their KidsMD app, for example, gives Alexa the “skill” to offer simple health advice regarding their children’s fever and medication dosing. I found this Alexa skill interesting but rudimentary. Most of the advice was reasonable; however, the scope is small and the responses glitchy. For example, when I asked Alexa what to do for a feverish 2-month-old, it advised me to contact my doctor then immediately followed this with recommended antipyretic medication dosing. Although we physicians understand the child must see a doctor, some parents might be confused and choose only to administer the medication. As with any new digital health technology, the team at Boston Children’s are continually iterating and improving based upon feedback.
I found Alexa currently has a few other skills for health care. For example, a skill called Marvee functions as a “care companion” to help aging family members and their caregivers. Another skill, Health Care Genius, helps patients decipher healthcare terminology by asking questions such as, “What is a deductible?”
The potential of voice-assisted technology in clinical and home health care settings is limitless, and I expect this segment to grow dramatically. Here are a few examples:
1. Physicians can ask for real-time help such as: What are treatment options for juvenile dermatomyositis? Order doxycycline 100 mg by mouth, twice daily, quantity sufficient 10 days.
2. Physicians might also use it to dictate notes intelligently, and even extract patient instructions directly from the notes to be emailed to the patient.
3. Surgeons could command an MRI to be viewed without having to scrub out.
4. Bedridden or chronically ill patients could use it to refill medications, make doctor appointments, or contact a caregiver in an emergency.
5. Patients could receive customized instructions, such as the answer to “How often do I change my surgical bandage?”
For all its potential, voice-assisted personal assistants have a long way to go. It would be a mistake to think these won’t be integrated into the entire health care chain from care to wellness, but it will be awhile before we get there.
Interestingly, when I asked my Apple Siri how many calories are in a cheeseburger, she reported 500, which is much more than Alexa’s 300. Which is why, for now, devices like Alexa are ideal for ordering a pizza hands free from your recliner. Just don’t ask how many calories are in it.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]. He has no disclosures related to this column.
How many calories are there in a cheeseburger? (Yes, I too am looking forward to a svelter 2017). The answer, according to my new assistant, is 300 calories. She knows the dose of acetaminophen for a 10-year-old, 65-pound child is 325 mg every 4-6 hours. She also plays George Michael, reorders my Dentyne Ice gum, and turns off the lights. She is Alexa of Amazon’s Echo, the intelligent personal assistant.
Echo and Google Home are popular voice-assisted home appliances. Amazon has built a natural language processing system, so to use it, you simply say, “Alexa,” pause, then ask your question (What’s the weather in New York?) or deliver your command (Play Spotify). It’s hands free, so you can interface while typing, reading, or cooking dinner.
Some medical centers, such as the Boston Children’s Hospital, are leading the way to make voice-assisted technology useful in health care. Their KidsMD app, for example, gives Alexa the “skill” to offer simple health advice regarding their children’s fever and medication dosing. I found this Alexa skill interesting but rudimentary. Most of the advice was reasonable; however, the scope is small and the responses glitchy. For example, when I asked Alexa what to do for a feverish 2-month-old, it advised me to contact my doctor then immediately followed this with recommended antipyretic medication dosing. Although we physicians understand the child must see a doctor, some parents might be confused and choose only to administer the medication. As with any new digital health technology, the team at Boston Children’s are continually iterating and improving based upon feedback.
I found Alexa currently has a few other skills for health care. For example, a skill called Marvee functions as a “care companion” to help aging family members and their caregivers. Another skill, Health Care Genius, helps patients decipher healthcare terminology by asking questions such as, “What is a deductible?”
The potential of voice-assisted technology in clinical and home health care settings is limitless, and I expect this segment to grow dramatically. Here are a few examples:
1. Physicians can ask for real-time help such as: What are treatment options for juvenile dermatomyositis? Order doxycycline 100 mg by mouth, twice daily, quantity sufficient 10 days.
2. Physicians might also use it to dictate notes intelligently, and even extract patient instructions directly from the notes to be emailed to the patient.
3. Surgeons could command an MRI to be viewed without having to scrub out.
4. Bedridden or chronically ill patients could use it to refill medications, make doctor appointments, or contact a caregiver in an emergency.
5. Patients could receive customized instructions, such as the answer to “How often do I change my surgical bandage?”
For all its potential, voice-assisted personal assistants have a long way to go. It would be a mistake to think these won’t be integrated into the entire health care chain from care to wellness, but it will be awhile before we get there.
Interestingly, when I asked my Apple Siri how many calories are in a cheeseburger, she reported 500, which is much more than Alexa’s 300. Which is why, for now, devices like Alexa are ideal for ordering a pizza hands free from your recliner. Just don’t ask how many calories are in it.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]. He has no disclosures related to this column.
How many calories are there in a cheeseburger? (Yes, I too am looking forward to a svelter 2017). The answer, according to my new assistant, is 300 calories. She knows the dose of acetaminophen for a 10-year-old, 65-pound child is 325 mg every 4-6 hours. She also plays George Michael, reorders my Dentyne Ice gum, and turns off the lights. She is Alexa of Amazon’s Echo, the intelligent personal assistant.
Echo and Google Home are popular voice-assisted home appliances. Amazon has built a natural language processing system, so to use it, you simply say, “Alexa,” pause, then ask your question (What’s the weather in New York?) or deliver your command (Play Spotify). It’s hands free, so you can interface while typing, reading, or cooking dinner.
Some medical centers, such as the Boston Children’s Hospital, are leading the way to make voice-assisted technology useful in health care. Their KidsMD app, for example, gives Alexa the “skill” to offer simple health advice regarding their children’s fever and medication dosing. I found this Alexa skill interesting but rudimentary. Most of the advice was reasonable; however, the scope is small and the responses glitchy. For example, when I asked Alexa what to do for a feverish 2-month-old, it advised me to contact my doctor then immediately followed this with recommended antipyretic medication dosing. Although we physicians understand the child must see a doctor, some parents might be confused and choose only to administer the medication. As with any new digital health technology, the team at Boston Children’s are continually iterating and improving based upon feedback.
I found Alexa currently has a few other skills for health care. For example, a skill called Marvee functions as a “care companion” to help aging family members and their caregivers. Another skill, Health Care Genius, helps patients decipher healthcare terminology by asking questions such as, “What is a deductible?”
The potential of voice-assisted technology in clinical and home health care settings is limitless, and I expect this segment to grow dramatically. Here are a few examples:
1. Physicians can ask for real-time help such as: What are treatment options for juvenile dermatomyositis? Order doxycycline 100 mg by mouth, twice daily, quantity sufficient 10 days.
2. Physicians might also use it to dictate notes intelligently, and even extract patient instructions directly from the notes to be emailed to the patient.
3. Surgeons could command an MRI to be viewed without having to scrub out.
4. Bedridden or chronically ill patients could use it to refill medications, make doctor appointments, or contact a caregiver in an emergency.
5. Patients could receive customized instructions, such as the answer to “How often do I change my surgical bandage?”
For all its potential, voice-assisted personal assistants have a long way to go. It would be a mistake to think these won’t be integrated into the entire health care chain from care to wellness, but it will be awhile before we get there.
Interestingly, when I asked my Apple Siri how many calories are in a cheeseburger, she reported 500, which is much more than Alexa’s 300. Which is why, for now, devices like Alexa are ideal for ordering a pizza hands free from your recliner. Just don’t ask how many calories are in it.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected]. He has no disclosures related to this column.
What’s New for Federal Practitioner in 2017?
It has been a long time since a new year has brought as much uncertainty as 2017 promises to bring, making some federal employees excited and others apprehensive. Rumors abound of how the federal health care sector may change: Hiring freezes, manpower cuts, and privatization are all concerns of Federal Practitioner readers. As in the past, we will keep you up-to-date with in-depth interviews of leaders in federal health care, intelligent coverage of news stories impacting your practice, and clinical and research articles about new programs and initiatives.
Also this year, we are pleased to announce several new regular columns that we hope will inform and entertain you. The first is a column on mental health and traumatic brain injury in the DoD and the VA. We are privileged to have U.S. Army COL (Ret) Elspeth Cameron Ritchie, MD, MPH, edit this column. She is widely known and respected and brings her vast experience to the column as an active-duty psychiatrist coupled with her current position as a VA physician. Dr. Ritchie will author articles as well as edit those of her VA and DoD colleagues. Mental health touches almost every aspect of federal practice, and we all will learn our contributions and challenges in this rapidly moving specialty.
Whereas the mental health column looks toward the scientific future, the second column looks back to the humanistic past. We are thrilled that 2 physician-historians of military medicine, Robert Hierholzer, MD, a VA psychiatrist, and John Pierce, MD, a retired U.S. Army pediatrician share the writing and editing for this column, which will debut this spring.
Have you ever wondered who or how VA and military hospitals were named? These 2 historical writers have a wealth of interesting anecdotes and stories about VA and military medical centers. We hope you will enjoy reading the stories of military and veteran health care: the war heroes, devoted clinicians, and groundbreaking researchers who have left their mark on DoD and VA health care.
We also will be launching a new pilot study feature for clinicians and researchers who have a novel or valuable idea but have only a small number of participants or preliminary results. This will be a great way for new investigators, trainees, and young health care practitioners to present their work to the medical community.
These new editorial offerings are just a start—we also want to invite you, your colleagues, and learners to start your own new tradition of writing for Federal Practitioner. For those who have submitted articles in the past, please keep up the habit.We are eager to receive original research, review articles, and clinical cases from DoD, PHS, and VA mid-career and senior clinicians and researchers as well as articles describing innovative programs and modes of health care treatment and delivery. With a print circulation of more than 35,000 readers and very active online presence, consider Federal Practitioner for your next article!
This year my New Year’s resolution as editor-in-chief is to encourage readers to contact either Editor Reid Paul or me if you have an idea for an article you would like to write, a column you would like to see, or if you have an interest in serving as a peer reviewer or joining our Editorial Advisory Association. We want to hear from you about what you want and need from Federal Practitioner.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
It has been a long time since a new year has brought as much uncertainty as 2017 promises to bring, making some federal employees excited and others apprehensive. Rumors abound of how the federal health care sector may change: Hiring freezes, manpower cuts, and privatization are all concerns of Federal Practitioner readers. As in the past, we will keep you up-to-date with in-depth interviews of leaders in federal health care, intelligent coverage of news stories impacting your practice, and clinical and research articles about new programs and initiatives.
Also this year, we are pleased to announce several new regular columns that we hope will inform and entertain you. The first is a column on mental health and traumatic brain injury in the DoD and the VA. We are privileged to have U.S. Army COL (Ret) Elspeth Cameron Ritchie, MD, MPH, edit this column. She is widely known and respected and brings her vast experience to the column as an active-duty psychiatrist coupled with her current position as a VA physician. Dr. Ritchie will author articles as well as edit those of her VA and DoD colleagues. Mental health touches almost every aspect of federal practice, and we all will learn our contributions and challenges in this rapidly moving specialty.
Whereas the mental health column looks toward the scientific future, the second column looks back to the humanistic past. We are thrilled that 2 physician-historians of military medicine, Robert Hierholzer, MD, a VA psychiatrist, and John Pierce, MD, a retired U.S. Army pediatrician share the writing and editing for this column, which will debut this spring.
Have you ever wondered who or how VA and military hospitals were named? These 2 historical writers have a wealth of interesting anecdotes and stories about VA and military medical centers. We hope you will enjoy reading the stories of military and veteran health care: the war heroes, devoted clinicians, and groundbreaking researchers who have left their mark on DoD and VA health care.
We also will be launching a new pilot study feature for clinicians and researchers who have a novel or valuable idea but have only a small number of participants or preliminary results. This will be a great way for new investigators, trainees, and young health care practitioners to present their work to the medical community.
These new editorial offerings are just a start—we also want to invite you, your colleagues, and learners to start your own new tradition of writing for Federal Practitioner. For those who have submitted articles in the past, please keep up the habit.We are eager to receive original research, review articles, and clinical cases from DoD, PHS, and VA mid-career and senior clinicians and researchers as well as articles describing innovative programs and modes of health care treatment and delivery. With a print circulation of more than 35,000 readers and very active online presence, consider Federal Practitioner for your next article!
This year my New Year’s resolution as editor-in-chief is to encourage readers to contact either Editor Reid Paul or me if you have an idea for an article you would like to write, a column you would like to see, or if you have an interest in serving as a peer reviewer or joining our Editorial Advisory Association. We want to hear from you about what you want and need from Federal Practitioner.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
It has been a long time since a new year has brought as much uncertainty as 2017 promises to bring, making some federal employees excited and others apprehensive. Rumors abound of how the federal health care sector may change: Hiring freezes, manpower cuts, and privatization are all concerns of Federal Practitioner readers. As in the past, we will keep you up-to-date with in-depth interviews of leaders in federal health care, intelligent coverage of news stories impacting your practice, and clinical and research articles about new programs and initiatives.
Also this year, we are pleased to announce several new regular columns that we hope will inform and entertain you. The first is a column on mental health and traumatic brain injury in the DoD and the VA. We are privileged to have U.S. Army COL (Ret) Elspeth Cameron Ritchie, MD, MPH, edit this column. She is widely known and respected and brings her vast experience to the column as an active-duty psychiatrist coupled with her current position as a VA physician. Dr. Ritchie will author articles as well as edit those of her VA and DoD colleagues. Mental health touches almost every aspect of federal practice, and we all will learn our contributions and challenges in this rapidly moving specialty.
Whereas the mental health column looks toward the scientific future, the second column looks back to the humanistic past. We are thrilled that 2 physician-historians of military medicine, Robert Hierholzer, MD, a VA psychiatrist, and John Pierce, MD, a retired U.S. Army pediatrician share the writing and editing for this column, which will debut this spring.
Have you ever wondered who or how VA and military hospitals were named? These 2 historical writers have a wealth of interesting anecdotes and stories about VA and military medical centers. We hope you will enjoy reading the stories of military and veteran health care: the war heroes, devoted clinicians, and groundbreaking researchers who have left their mark on DoD and VA health care.
We also will be launching a new pilot study feature for clinicians and researchers who have a novel or valuable idea but have only a small number of participants or preliminary results. This will be a great way for new investigators, trainees, and young health care practitioners to present their work to the medical community.
These new editorial offerings are just a start—we also want to invite you, your colleagues, and learners to start your own new tradition of writing for Federal Practitioner. For those who have submitted articles in the past, please keep up the habit.We are eager to receive original research, review articles, and clinical cases from DoD, PHS, and VA mid-career and senior clinicians and researchers as well as articles describing innovative programs and modes of health care treatment and delivery. With a print circulation of more than 35,000 readers and very active online presence, consider Federal Practitioner for your next article!
This year my New Year’s resolution as editor-in-chief is to encourage readers to contact either Editor Reid Paul or me if you have an idea for an article you would like to write, a column you would like to see, or if you have an interest in serving as a peer reviewer or joining our Editorial Advisory Association. We want to hear from you about what you want and need from Federal Practitioner.
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Personality disorders on the acute care unit
We all know these patients:
The young man who, when his name shows up on the ED board, everyone lets out a little groan, knowing his hospital stay will be long and tumultuous.
The middle-aged woman who seems to do want your care and attention and yet rebuffs your attempts to help her, meanwhile, making constant demands on nursing staff.
The older man who trusts no one and will not cooperate with any of his needed care, frustrating staff and physicians alike.
Caring for the patient is integral to the art of doctoring, and yet, there are some people for whom this is incredibly hard to do. They frustrate even the most seasoned professional and work their way under our skin. While their disruptive acts may feel volitional to those of us attempting to provide care, these individuals may suffer from a personality disorder.
In the hospital, a patient must to relate to, and cooperate with, a revolving team of care providers all while under some degree of physical and emotional distress. While this can be destabilizing for even the most resilient patient, for those with personality disorders, it is nearly inevitable that conflict will arise. In a recent article in the Journal of Hospital Medicine, my colleagues and I discussed the management of such patients, with a focus on evidence-based interventions (doi: 10.1002/jhm.2643).2
While the behaviors associated with personality disorders can feel deliberate and even manipulative, research shows that these disorders arise from a complex set of genetic and environmental factors. Alterations found in the serotonin system and regions of the brain involved in emotional reactivity and social processing suggest an underlying neurophysiology contributing to difficulties with interpersonal relationships seen in these disorders.3-9
Many do not realize that having a personality disorder has real implications for an individual’s healthcare outcomes; those with a personality disorder have a life expectancy nearly two decades shorter than the general population.10 While there are a number of factors that likely contribute to the effect on mortality, it has been suggested that dysfunctional personality structures may interfere with the individual’s ability to access and utilize care, resulting in higher morbidity and mortality.11
Although it can be difficult to make a formal diagnosis of a personality disorder on the acute care unit, we provide guideline for recognizing individuals based on the way in which they interact with others. Specifically, we propose a team should consider a personality disorder when the following features are present:
The patient elicits a strong emotional reaction from providers; these may vary markedly between providers
The patient’s emotional responses may appear disproportionate to the inciting event
The patient is on a number of different psychiatric medications with little relief of symptoms
The patient takes up an disproportionate amount of providers’ time
The patient externalizes blame, seeing others as the source of discomfort or distress and therefore sees others as the solution.2
When the team suspects a patient’s behavior may be driven by an underlying dysfunctional personality structure, there are a number of steps that can be taken to help facilitate care and shape behaviors. Key among these is recognizing our own complicated responses to these individuals. These patients evoke strong responses and no team member – from nurses and aides to residents and senior attendings – is immune.12-15
Reactions can range from a need to care for and protect the patient to feelings of futility or contempt.15 Other important behavioral interventions include providing consistency, reinforcing desired behaviors, offering empathy, and providing boundaries while also recognizing the importance of picking your battles.2 Of note, while medications may offer some help, there is limited evidence for use of pharmacological interventions. Although they may be somewhat helpful in addressing particular features of these disorders, such as impulsivity, affective dysregulation or cognitive-perceptual symptoms16, many of these patients end up on a cocktail of psychotropic medications with minimal evidence for their use or efficacy. Thus behavioral management remains the cornerstone of treatment.
While care of the patient with personality disorders can present unique challenges, it offers the opportunity for therapeutic intervention. By appreciating the underlying genetic and environmental factors, we are in a better position to offer empathy and support. For these patients, managing their personality disorder can be just as important as managing any of their other medical comorbidities. By taking an approach that acknowledges the emotional responses of the team while also reinforcing and facilitating positive behaviors of the patient, the hospital stay can prove therapeutic, helping these individuals to develop new skills while also getting their physical needs addressed.
Megan Riddle, MD, PhD, is based in the department of psychiatry and behavioral sciences at the University of Washington, Seattle.
NOTES
1. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. Arlington, VA: American Psychiatric Association; 2013.
2. Riddle M, Meeks T, Alvarez C, Dubovsky A. When personality is the problem: Managing patients with difficult personalities on the acute care unit. J Hosp Med. 2016 Dec;11(12):873-878.
3. Bukh JD, Bock C, Kessing LV. Association between genetic polymorphisms in the serotonergic system and comorbid personality disorders among patients with first-episode depression. J Pers Disord. 2014 Jun;28(3):365-378.
4. Perez-Rodriguez MM, Weinstein S, New AS, et al. Tryptophan-hydroxylase 2 haplotype association with borderline personality disorder and aggression in a sample of patients with personality disorders and healthy controls. J Psychiatr Res. 2010 Nov; 44(15):1075-1081.
5. Checknita D, Maussion G, Labonte B, et al. Monoamine oxidase: A gene promoter methylation and transcriptional downregulation in an offender population with antisocial personality disorder. Br J Psychiatry. 2015 Mar;206(3):216-222.
6. Boen E, Westlye LT, Elvsashagen T, et al. Regional cortical thinning may be a biological marker for borderline personality disorder. Acta Psychiatr Scand. 2014 Sep;130(3):193-204.
7. Thoma P, Friedmann C, Suchan B. Empathy and social problem solving in alcohol dependence, mood disorders and selected personality disorders. Neurosci Biobehav Rev. 2013 Mar;37(3):448-470.
8. Liu H, Liao J, Jiang W, Wang W. Changes in low-frequency fluctuations in patients with antisocial personality disorder revealed by resting-state functional MRI. PLoS One. 2014 Mar 5;9(3):e89790.
9. Yang Y, Raine A. Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: A meta-analysis. Psychiatry Res. 2009 Nov 30;174(2):81-88.
10. Fok ML, Hayes RD, Chang CK, Stewart R, Callard FJ, Moran P. Life expectancy at birth and all-cause mortality among people with personality disorder. J Psychosom Res. 2012 Aug;73(2):104-107.
11. Tyrer P, Reed GM, Crawford MJ. Classification, assessment, prevalence, and effect of personality disorder. Lancet. 2015 Feb 21;385:717-726.
12. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978 Apr 20; 298:883-887.
13. Groves JE. Management of the borderline patient on a medical or surgical ward: The psychiatric consultant’s role. Int J Psychiatry Med. 1975;6(3):337-348.
14. Bodner E, Cohen-Fridel S, Mashiah M, et al. The attitudes of psychiatric hospital staff toward hospitalization and treatment of patients with borderline personality disorder. BMC psychiatry. 2015 Jan 22;15:2.
15. Colli A, Tanzilli A, Dimaggio G, Lingiardi V. Patient personality and therapist response: An empirical investigation. Am J Psychiatry. 2014 Jan;171(1):102-108.
16. Ingenhoven T, Lafay P, Rinne T, Passchier J, Duivenvoorden H. Effectiveness of pharmacotherapy for severe personality disorders: Meta-analyses of randomized controlled trials. J Clin Psychiatry. 2010 Jan;71(1):14-25.
We all know these patients:
The young man who, when his name shows up on the ED board, everyone lets out a little groan, knowing his hospital stay will be long and tumultuous.
The middle-aged woman who seems to do want your care and attention and yet rebuffs your attempts to help her, meanwhile, making constant demands on nursing staff.
The older man who trusts no one and will not cooperate with any of his needed care, frustrating staff and physicians alike.
Caring for the patient is integral to the art of doctoring, and yet, there are some people for whom this is incredibly hard to do. They frustrate even the most seasoned professional and work their way under our skin. While their disruptive acts may feel volitional to those of us attempting to provide care, these individuals may suffer from a personality disorder.
In the hospital, a patient must to relate to, and cooperate with, a revolving team of care providers all while under some degree of physical and emotional distress. While this can be destabilizing for even the most resilient patient, for those with personality disorders, it is nearly inevitable that conflict will arise. In a recent article in the Journal of Hospital Medicine, my colleagues and I discussed the management of such patients, with a focus on evidence-based interventions (doi: 10.1002/jhm.2643).2
While the behaviors associated with personality disorders can feel deliberate and even manipulative, research shows that these disorders arise from a complex set of genetic and environmental factors. Alterations found in the serotonin system and regions of the brain involved in emotional reactivity and social processing suggest an underlying neurophysiology contributing to difficulties with interpersonal relationships seen in these disorders.3-9
Many do not realize that having a personality disorder has real implications for an individual’s healthcare outcomes; those with a personality disorder have a life expectancy nearly two decades shorter than the general population.10 While there are a number of factors that likely contribute to the effect on mortality, it has been suggested that dysfunctional personality structures may interfere with the individual’s ability to access and utilize care, resulting in higher morbidity and mortality.11
Although it can be difficult to make a formal diagnosis of a personality disorder on the acute care unit, we provide guideline for recognizing individuals based on the way in which they interact with others. Specifically, we propose a team should consider a personality disorder when the following features are present:
The patient elicits a strong emotional reaction from providers; these may vary markedly between providers
The patient’s emotional responses may appear disproportionate to the inciting event
The patient is on a number of different psychiatric medications with little relief of symptoms
The patient takes up an disproportionate amount of providers’ time
The patient externalizes blame, seeing others as the source of discomfort or distress and therefore sees others as the solution.2
When the team suspects a patient’s behavior may be driven by an underlying dysfunctional personality structure, there are a number of steps that can be taken to help facilitate care and shape behaviors. Key among these is recognizing our own complicated responses to these individuals. These patients evoke strong responses and no team member – from nurses and aides to residents and senior attendings – is immune.12-15
Reactions can range from a need to care for and protect the patient to feelings of futility or contempt.15 Other important behavioral interventions include providing consistency, reinforcing desired behaviors, offering empathy, and providing boundaries while also recognizing the importance of picking your battles.2 Of note, while medications may offer some help, there is limited evidence for use of pharmacological interventions. Although they may be somewhat helpful in addressing particular features of these disorders, such as impulsivity, affective dysregulation or cognitive-perceptual symptoms16, many of these patients end up on a cocktail of psychotropic medications with minimal evidence for their use or efficacy. Thus behavioral management remains the cornerstone of treatment.
While care of the patient with personality disorders can present unique challenges, it offers the opportunity for therapeutic intervention. By appreciating the underlying genetic and environmental factors, we are in a better position to offer empathy and support. For these patients, managing their personality disorder can be just as important as managing any of their other medical comorbidities. By taking an approach that acknowledges the emotional responses of the team while also reinforcing and facilitating positive behaviors of the patient, the hospital stay can prove therapeutic, helping these individuals to develop new skills while also getting their physical needs addressed.
Megan Riddle, MD, PhD, is based in the department of psychiatry and behavioral sciences at the University of Washington, Seattle.
NOTES
1. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. Arlington, VA: American Psychiatric Association; 2013.
2. Riddle M, Meeks T, Alvarez C, Dubovsky A. When personality is the problem: Managing patients with difficult personalities on the acute care unit. J Hosp Med. 2016 Dec;11(12):873-878.
3. Bukh JD, Bock C, Kessing LV. Association between genetic polymorphisms in the serotonergic system and comorbid personality disorders among patients with first-episode depression. J Pers Disord. 2014 Jun;28(3):365-378.
4. Perez-Rodriguez MM, Weinstein S, New AS, et al. Tryptophan-hydroxylase 2 haplotype association with borderline personality disorder and aggression in a sample of patients with personality disorders and healthy controls. J Psychiatr Res. 2010 Nov; 44(15):1075-1081.
5. Checknita D, Maussion G, Labonte B, et al. Monoamine oxidase: A gene promoter methylation and transcriptional downregulation in an offender population with antisocial personality disorder. Br J Psychiatry. 2015 Mar;206(3):216-222.
6. Boen E, Westlye LT, Elvsashagen T, et al. Regional cortical thinning may be a biological marker for borderline personality disorder. Acta Psychiatr Scand. 2014 Sep;130(3):193-204.
7. Thoma P, Friedmann C, Suchan B. Empathy and social problem solving in alcohol dependence, mood disorders and selected personality disorders. Neurosci Biobehav Rev. 2013 Mar;37(3):448-470.
8. Liu H, Liao J, Jiang W, Wang W. Changes in low-frequency fluctuations in patients with antisocial personality disorder revealed by resting-state functional MRI. PLoS One. 2014 Mar 5;9(3):e89790.
9. Yang Y, Raine A. Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: A meta-analysis. Psychiatry Res. 2009 Nov 30;174(2):81-88.
10. Fok ML, Hayes RD, Chang CK, Stewart R, Callard FJ, Moran P. Life expectancy at birth and all-cause mortality among people with personality disorder. J Psychosom Res. 2012 Aug;73(2):104-107.
11. Tyrer P, Reed GM, Crawford MJ. Classification, assessment, prevalence, and effect of personality disorder. Lancet. 2015 Feb 21;385:717-726.
12. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978 Apr 20; 298:883-887.
13. Groves JE. Management of the borderline patient on a medical or surgical ward: The psychiatric consultant’s role. Int J Psychiatry Med. 1975;6(3):337-348.
14. Bodner E, Cohen-Fridel S, Mashiah M, et al. The attitudes of psychiatric hospital staff toward hospitalization and treatment of patients with borderline personality disorder. BMC psychiatry. 2015 Jan 22;15:2.
15. Colli A, Tanzilli A, Dimaggio G, Lingiardi V. Patient personality and therapist response: An empirical investigation. Am J Psychiatry. 2014 Jan;171(1):102-108.
16. Ingenhoven T, Lafay P, Rinne T, Passchier J, Duivenvoorden H. Effectiveness of pharmacotherapy for severe personality disorders: Meta-analyses of randomized controlled trials. J Clin Psychiatry. 2010 Jan;71(1):14-25.
We all know these patients:
The young man who, when his name shows up on the ED board, everyone lets out a little groan, knowing his hospital stay will be long and tumultuous.
The middle-aged woman who seems to do want your care and attention and yet rebuffs your attempts to help her, meanwhile, making constant demands on nursing staff.
The older man who trusts no one and will not cooperate with any of his needed care, frustrating staff and physicians alike.
Caring for the patient is integral to the art of doctoring, and yet, there are some people for whom this is incredibly hard to do. They frustrate even the most seasoned professional and work their way under our skin. While their disruptive acts may feel volitional to those of us attempting to provide care, these individuals may suffer from a personality disorder.
In the hospital, a patient must to relate to, and cooperate with, a revolving team of care providers all while under some degree of physical and emotional distress. While this can be destabilizing for even the most resilient patient, for those with personality disorders, it is nearly inevitable that conflict will arise. In a recent article in the Journal of Hospital Medicine, my colleagues and I discussed the management of such patients, with a focus on evidence-based interventions (doi: 10.1002/jhm.2643).2
While the behaviors associated with personality disorders can feel deliberate and even manipulative, research shows that these disorders arise from a complex set of genetic and environmental factors. Alterations found in the serotonin system and regions of the brain involved in emotional reactivity and social processing suggest an underlying neurophysiology contributing to difficulties with interpersonal relationships seen in these disorders.3-9
Many do not realize that having a personality disorder has real implications for an individual’s healthcare outcomes; those with a personality disorder have a life expectancy nearly two decades shorter than the general population.10 While there are a number of factors that likely contribute to the effect on mortality, it has been suggested that dysfunctional personality structures may interfere with the individual’s ability to access and utilize care, resulting in higher morbidity and mortality.11
Although it can be difficult to make a formal diagnosis of a personality disorder on the acute care unit, we provide guideline for recognizing individuals based on the way in which they interact with others. Specifically, we propose a team should consider a personality disorder when the following features are present:
The patient elicits a strong emotional reaction from providers; these may vary markedly between providers
The patient’s emotional responses may appear disproportionate to the inciting event
The patient is on a number of different psychiatric medications with little relief of symptoms
The patient takes up an disproportionate amount of providers’ time
The patient externalizes blame, seeing others as the source of discomfort or distress and therefore sees others as the solution.2
When the team suspects a patient’s behavior may be driven by an underlying dysfunctional personality structure, there are a number of steps that can be taken to help facilitate care and shape behaviors. Key among these is recognizing our own complicated responses to these individuals. These patients evoke strong responses and no team member – from nurses and aides to residents and senior attendings – is immune.12-15
Reactions can range from a need to care for and protect the patient to feelings of futility or contempt.15 Other important behavioral interventions include providing consistency, reinforcing desired behaviors, offering empathy, and providing boundaries while also recognizing the importance of picking your battles.2 Of note, while medications may offer some help, there is limited evidence for use of pharmacological interventions. Although they may be somewhat helpful in addressing particular features of these disorders, such as impulsivity, affective dysregulation or cognitive-perceptual symptoms16, many of these patients end up on a cocktail of psychotropic medications with minimal evidence for their use or efficacy. Thus behavioral management remains the cornerstone of treatment.
While care of the patient with personality disorders can present unique challenges, it offers the opportunity for therapeutic intervention. By appreciating the underlying genetic and environmental factors, we are in a better position to offer empathy and support. For these patients, managing their personality disorder can be just as important as managing any of their other medical comorbidities. By taking an approach that acknowledges the emotional responses of the team while also reinforcing and facilitating positive behaviors of the patient, the hospital stay can prove therapeutic, helping these individuals to develop new skills while also getting their physical needs addressed.
Megan Riddle, MD, PhD, is based in the department of psychiatry and behavioral sciences at the University of Washington, Seattle.
NOTES
1. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. Arlington, VA: American Psychiatric Association; 2013.
2. Riddle M, Meeks T, Alvarez C, Dubovsky A. When personality is the problem: Managing patients with difficult personalities on the acute care unit. J Hosp Med. 2016 Dec;11(12):873-878.
3. Bukh JD, Bock C, Kessing LV. Association between genetic polymorphisms in the serotonergic system and comorbid personality disorders among patients with first-episode depression. J Pers Disord. 2014 Jun;28(3):365-378.
4. Perez-Rodriguez MM, Weinstein S, New AS, et al. Tryptophan-hydroxylase 2 haplotype association with borderline personality disorder and aggression in a sample of patients with personality disorders and healthy controls. J Psychiatr Res. 2010 Nov; 44(15):1075-1081.
5. Checknita D, Maussion G, Labonte B, et al. Monoamine oxidase: A gene promoter methylation and transcriptional downregulation in an offender population with antisocial personality disorder. Br J Psychiatry. 2015 Mar;206(3):216-222.
6. Boen E, Westlye LT, Elvsashagen T, et al. Regional cortical thinning may be a biological marker for borderline personality disorder. Acta Psychiatr Scand. 2014 Sep;130(3):193-204.
7. Thoma P, Friedmann C, Suchan B. Empathy and social problem solving in alcohol dependence, mood disorders and selected personality disorders. Neurosci Biobehav Rev. 2013 Mar;37(3):448-470.
8. Liu H, Liao J, Jiang W, Wang W. Changes in low-frequency fluctuations in patients with antisocial personality disorder revealed by resting-state functional MRI. PLoS One. 2014 Mar 5;9(3):e89790.
9. Yang Y, Raine A. Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: A meta-analysis. Psychiatry Res. 2009 Nov 30;174(2):81-88.
10. Fok ML, Hayes RD, Chang CK, Stewart R, Callard FJ, Moran P. Life expectancy at birth and all-cause mortality among people with personality disorder. J Psychosom Res. 2012 Aug;73(2):104-107.
11. Tyrer P, Reed GM, Crawford MJ. Classification, assessment, prevalence, and effect of personality disorder. Lancet. 2015 Feb 21;385:717-726.
12. Groves JE. Taking care of the hateful patient. N Engl J Med. 1978 Apr 20; 298:883-887.
13. Groves JE. Management of the borderline patient on a medical or surgical ward: The psychiatric consultant’s role. Int J Psychiatry Med. 1975;6(3):337-348.
14. Bodner E, Cohen-Fridel S, Mashiah M, et al. The attitudes of psychiatric hospital staff toward hospitalization and treatment of patients with borderline personality disorder. BMC psychiatry. 2015 Jan 22;15:2.
15. Colli A, Tanzilli A, Dimaggio G, Lingiardi V. Patient personality and therapist response: An empirical investigation. Am J Psychiatry. 2014 Jan;171(1):102-108.
16. Ingenhoven T, Lafay P, Rinne T, Passchier J, Duivenvoorden H. Effectiveness of pharmacotherapy for severe personality disorders: Meta-analyses of randomized controlled trials. J Clin Psychiatry. 2010 Jan;71(1):14-25.
ACL injuries: Why are teen females at greater risk?
Over the last 2 decades, the number of teen females involved in competitive sports has skyrocketed. Research studies continue to show that girls involved in sports have better self-esteem and reduce the risk of obesity.But this involvement in competitive sports has not come without a cost. Recent studies have shown that females are four to six times more likely to tear their anterior cruciate ligament (ACL) than are their male counterparts playing the same sport.1,2 But why is this? And can it be prevented?
Researchers have spent countless hours studying videos to better determine why females are at greater risk. Their findings showed that there were many contributing factors for the difference between the sexes. The general mechanics that put the ACL at risk are landing on an extended knee, the center of mass being off the base, and internal rotation and adduction of the knee. These combined movements put the ACL at its most vulnerable position.
Hormones are another contributing factor. Estrogen and relaxin give strength and flexibility to the ligaments. But during surges of these hormones – such as during menses or a growth spurt – there is laxity within the ligament, putting it at further risk of injury.1 Testosterone increases muscle mass and strength. For males, this is protective because they rely less on their ligaments during jumping and deceleration. Puberty also contributes to the increased risk by accelerating the body mass index quickly over a short period, and therefore, greater strength is needed.1,3
Core strength, which helps with balance, is another contributing factor. Females tend to have lower core strength, which puts them at greater risk for rotational forces, especially when landing on one foot.1,4 As core strength improves, athletes can change direction more efficiently and hold their bodies upright on a single limb, which prevents the torsion that contributes to injury.
Prevention for ACL injuries occurs through very specific training in repetitive jumping and balance exercises are known as plyometric exercises. Neuromuscular training (NMT) includes plyometric training along with strengthening exercises such as lunges, squats, and plank exercises.4 One can reduce the risk of injury by 72% with 6-8 weeks of training by a professional experienced in NMT.5
Educating parents on the increased risk of injury to the ACL in females and importance of proper training can reduce injury and the risk of degenerative joint disease in later years.6 The Institute for Sports Medicine has a website that offers a knee injury prevention program you can refer families to for more information to prevent knee injuries. Sportsmetrics can help locate an NMT professional near them. Knowledge is power!
Reference
1. Pediatrics. 2014 May;133(5):e1437-50
2. Bull Hosp Jt Dis. 2000;59(4):217-26
3. Clin Biomech (Bristol, Avon). 2006 Dec;21(10):1060-6
4. Am J Phys Med Rehabil. 2005 Feb;84(2):122-30
5. Am J Sports Med. 2008 Aug;36(8):1476-83
6. Curr Womens Health Rep. 2001 Dec;1(3):218-24
Dr. Pearce is a pediatrician in Frankfort, Ill. Email her at [email protected].
Over the last 2 decades, the number of teen females involved in competitive sports has skyrocketed. Research studies continue to show that girls involved in sports have better self-esteem and reduce the risk of obesity.But this involvement in competitive sports has not come without a cost. Recent studies have shown that females are four to six times more likely to tear their anterior cruciate ligament (ACL) than are their male counterparts playing the same sport.1,2 But why is this? And can it be prevented?
Researchers have spent countless hours studying videos to better determine why females are at greater risk. Their findings showed that there were many contributing factors for the difference between the sexes. The general mechanics that put the ACL at risk are landing on an extended knee, the center of mass being off the base, and internal rotation and adduction of the knee. These combined movements put the ACL at its most vulnerable position.
Hormones are another contributing factor. Estrogen and relaxin give strength and flexibility to the ligaments. But during surges of these hormones – such as during menses or a growth spurt – there is laxity within the ligament, putting it at further risk of injury.1 Testosterone increases muscle mass and strength. For males, this is protective because they rely less on their ligaments during jumping and deceleration. Puberty also contributes to the increased risk by accelerating the body mass index quickly over a short period, and therefore, greater strength is needed.1,3
Core strength, which helps with balance, is another contributing factor. Females tend to have lower core strength, which puts them at greater risk for rotational forces, especially when landing on one foot.1,4 As core strength improves, athletes can change direction more efficiently and hold their bodies upright on a single limb, which prevents the torsion that contributes to injury.
Prevention for ACL injuries occurs through very specific training in repetitive jumping and balance exercises are known as plyometric exercises. Neuromuscular training (NMT) includes plyometric training along with strengthening exercises such as lunges, squats, and plank exercises.4 One can reduce the risk of injury by 72% with 6-8 weeks of training by a professional experienced in NMT.5
Educating parents on the increased risk of injury to the ACL in females and importance of proper training can reduce injury and the risk of degenerative joint disease in later years.6 The Institute for Sports Medicine has a website that offers a knee injury prevention program you can refer families to for more information to prevent knee injuries. Sportsmetrics can help locate an NMT professional near them. Knowledge is power!
Reference
1. Pediatrics. 2014 May;133(5):e1437-50
2. Bull Hosp Jt Dis. 2000;59(4):217-26
3. Clin Biomech (Bristol, Avon). 2006 Dec;21(10):1060-6
4. Am J Phys Med Rehabil. 2005 Feb;84(2):122-30
5. Am J Sports Med. 2008 Aug;36(8):1476-83
6. Curr Womens Health Rep. 2001 Dec;1(3):218-24
Dr. Pearce is a pediatrician in Frankfort, Ill. Email her at [email protected].
Over the last 2 decades, the number of teen females involved in competitive sports has skyrocketed. Research studies continue to show that girls involved in sports have better self-esteem and reduce the risk of obesity.But this involvement in competitive sports has not come without a cost. Recent studies have shown that females are four to six times more likely to tear their anterior cruciate ligament (ACL) than are their male counterparts playing the same sport.1,2 But why is this? And can it be prevented?
Researchers have spent countless hours studying videos to better determine why females are at greater risk. Their findings showed that there were many contributing factors for the difference between the sexes. The general mechanics that put the ACL at risk are landing on an extended knee, the center of mass being off the base, and internal rotation and adduction of the knee. These combined movements put the ACL at its most vulnerable position.
Hormones are another contributing factor. Estrogen and relaxin give strength and flexibility to the ligaments. But during surges of these hormones – such as during menses or a growth spurt – there is laxity within the ligament, putting it at further risk of injury.1 Testosterone increases muscle mass and strength. For males, this is protective because they rely less on their ligaments during jumping and deceleration. Puberty also contributes to the increased risk by accelerating the body mass index quickly over a short period, and therefore, greater strength is needed.1,3
Core strength, which helps with balance, is another contributing factor. Females tend to have lower core strength, which puts them at greater risk for rotational forces, especially when landing on one foot.1,4 As core strength improves, athletes can change direction more efficiently and hold their bodies upright on a single limb, which prevents the torsion that contributes to injury.
Prevention for ACL injuries occurs through very specific training in repetitive jumping and balance exercises are known as plyometric exercises. Neuromuscular training (NMT) includes plyometric training along with strengthening exercises such as lunges, squats, and plank exercises.4 One can reduce the risk of injury by 72% with 6-8 weeks of training by a professional experienced in NMT.5
Educating parents on the increased risk of injury to the ACL in females and importance of proper training can reduce injury and the risk of degenerative joint disease in later years.6 The Institute for Sports Medicine has a website that offers a knee injury prevention program you can refer families to for more information to prevent knee injuries. Sportsmetrics can help locate an NMT professional near them. Knowledge is power!
Reference
1. Pediatrics. 2014 May;133(5):e1437-50
2. Bull Hosp Jt Dis. 2000;59(4):217-26
3. Clin Biomech (Bristol, Avon). 2006 Dec;21(10):1060-6
4. Am J Phys Med Rehabil. 2005 Feb;84(2):122-30
5. Am J Sports Med. 2008 Aug;36(8):1476-83
6. Curr Womens Health Rep. 2001 Dec;1(3):218-24
Dr. Pearce is a pediatrician in Frankfort, Ill. Email her at [email protected].
Reye’s syndrome: Time to remind the parents
It is that time of year again. We are in the midst of flu season, which means that it is time to remind our patients’ parents about the importance of using acetaminophen instead of aspirin. This fact became evident when several guardians of our patients came in within a few days of each other in late November to early December unaware of the dangers of giving their children aspirin and other salicylate medications.
Case 1: A 4-year-old boy presented with mild diarrhea, but otherwise was clinically well. The diarrhea started while visiting family in Mexico. The mother took out a small bottle of Pepto-Bismol (bismuth subsalicylate) liquid, which she gave him 2 days previously. The bottle did have, in small font, a warning about Reye’s syndrome on the label, which the mother did not notice. She also did not think it pertained to her son anyway. During the visit, she was counseled on this being early influenza season and the avoidance of salicylate products since the 1980s in children, with the exception of cardiac uses.
Case 2: A 16-year-old male presented with his grandmother with a few scattered vesicles and low-grade fever. He had plans to go to Florida in a few days with friends and wished to know if he would be able to go. He had one dose of varicella vaccine when he was a toddler. Varicella IgM and IgG were ordered. When asked, the grandmother stated that she did not remember the warning signs about Reye’s syndrome posted in the pharmacies 30 years ago. In addition, she vaguely remembered baby aspirin not being made anymore, but she could not remember the reason why.
Case 3: An 18-year-old female with a medical history of occasional migraines controlled with over-the-counter products presented for a school form. Her mother mentioned that a relative had influenza symptoms. When we looked up the migraine medication, it was a generic aspirin/caffeine product. When counseled on Reye’s syndrome, the mother did not remember it at all, even though she was a teenager in the 1980s; she stated that she did remember her mom using only Tylenol for her illnesses.
Reye’s syndrome, a rare but serious condition causing liver degeneration and encephalopathy presenting in children younger than 18 years, was first described in 1963.1 Symptoms include mental confusion, vomiting, and even coma. The cause is unknown; however, salicylates have been implicated as a possible causative agent.
Products containing salicylate include but are not limited to aspirin and Pepto-Bismol. Studies linked Reye’s syndrome epidemiologically to recent illness with influenza or varicella and the use of aspirin. In 1978, the Centers for Disease Control and Prevention was informed that several children developed Reye’s syndrome during an influenza outbreak, and by 1980, the CDC demonstrated a link between those patients and the administration of salicylate-containing medications.2 Around the same time, more studies came out to support these findings. In 1980, 555 cases of Reye’s syndrome were reported in the United States. To decrease the occurrence, the CDC, American Academy of Pediatrics, and the U.S. Surgeon General tried to raise awareness of the association between Reye’s syndrome and aspirin by publishing journals, releasing warning statements, and including a “Black Box” warning in 1986 informing parents to not give aspirin to children and teenagers with influenza or chicken pox. Baby aspirin was removed from use for routine fevers in the mid-1980s and large warning signs would be found in every pharmacy for about 10 years. These warning signs are gone now.
As pediatricians and other primary care physicians, we have so many topics that we must address in the limited time we have allotted for each patient. However, we need to remind our patients and their parents about Reye’s syndrome and the importance of avoiding aspirin and salicylate products in children. Due to the public awareness of Reye’s syndrome in the 1980s and into the 1990s, the incidence decreased.2 From 1987 to 1993, fewer than 37 cases were reported in the United States and from 1994 to 1997, fewer than 2 cases were reported.
This demonstrates the importance of educating our patients and their parents about this syndrome and ways to avoid it. Based on the three clinical cases presented, it is clear that at least some of our patient’s guardians are unaware of this threat to their children. As physicians, it is our responsibility to educate our patient populations, but we should also ask our friends at our local supermarkets and pharmacies to dust off those old warning signs and help spread the word. While we are in flu season, let’s not forget to take a few minutes to inform our patients about this awful, but preventable syndrome.
References
1. Pediatrics. 1980 Dec;66(6):859-64.
2. J Gen Intern Med. 2012 Dec;27(12):1697-703.
Rachel Masia is a third-year medical student at Rowan University School of Osteopathic Medicine, Stratford, N.J. Dr. Alan Masia, Ms. Masia’s father, has a practice in Toms River, N.J. They said they had no relevant financial disclosures.
It is that time of year again. We are in the midst of flu season, which means that it is time to remind our patients’ parents about the importance of using acetaminophen instead of aspirin. This fact became evident when several guardians of our patients came in within a few days of each other in late November to early December unaware of the dangers of giving their children aspirin and other salicylate medications.
Case 1: A 4-year-old boy presented with mild diarrhea, but otherwise was clinically well. The diarrhea started while visiting family in Mexico. The mother took out a small bottle of Pepto-Bismol (bismuth subsalicylate) liquid, which she gave him 2 days previously. The bottle did have, in small font, a warning about Reye’s syndrome on the label, which the mother did not notice. She also did not think it pertained to her son anyway. During the visit, she was counseled on this being early influenza season and the avoidance of salicylate products since the 1980s in children, with the exception of cardiac uses.
Case 2: A 16-year-old male presented with his grandmother with a few scattered vesicles and low-grade fever. He had plans to go to Florida in a few days with friends and wished to know if he would be able to go. He had one dose of varicella vaccine when he was a toddler. Varicella IgM and IgG were ordered. When asked, the grandmother stated that she did not remember the warning signs about Reye’s syndrome posted in the pharmacies 30 years ago. In addition, she vaguely remembered baby aspirin not being made anymore, but she could not remember the reason why.
Case 3: An 18-year-old female with a medical history of occasional migraines controlled with over-the-counter products presented for a school form. Her mother mentioned that a relative had influenza symptoms. When we looked up the migraine medication, it was a generic aspirin/caffeine product. When counseled on Reye’s syndrome, the mother did not remember it at all, even though she was a teenager in the 1980s; she stated that she did remember her mom using only Tylenol for her illnesses.
Reye’s syndrome, a rare but serious condition causing liver degeneration and encephalopathy presenting in children younger than 18 years, was first described in 1963.1 Symptoms include mental confusion, vomiting, and even coma. The cause is unknown; however, salicylates have been implicated as a possible causative agent.
Products containing salicylate include but are not limited to aspirin and Pepto-Bismol. Studies linked Reye’s syndrome epidemiologically to recent illness with influenza or varicella and the use of aspirin. In 1978, the Centers for Disease Control and Prevention was informed that several children developed Reye’s syndrome during an influenza outbreak, and by 1980, the CDC demonstrated a link between those patients and the administration of salicylate-containing medications.2 Around the same time, more studies came out to support these findings. In 1980, 555 cases of Reye’s syndrome were reported in the United States. To decrease the occurrence, the CDC, American Academy of Pediatrics, and the U.S. Surgeon General tried to raise awareness of the association between Reye’s syndrome and aspirin by publishing journals, releasing warning statements, and including a “Black Box” warning in 1986 informing parents to not give aspirin to children and teenagers with influenza or chicken pox. Baby aspirin was removed from use for routine fevers in the mid-1980s and large warning signs would be found in every pharmacy for about 10 years. These warning signs are gone now.
As pediatricians and other primary care physicians, we have so many topics that we must address in the limited time we have allotted for each patient. However, we need to remind our patients and their parents about Reye’s syndrome and the importance of avoiding aspirin and salicylate products in children. Due to the public awareness of Reye’s syndrome in the 1980s and into the 1990s, the incidence decreased.2 From 1987 to 1993, fewer than 37 cases were reported in the United States and from 1994 to 1997, fewer than 2 cases were reported.
This demonstrates the importance of educating our patients and their parents about this syndrome and ways to avoid it. Based on the three clinical cases presented, it is clear that at least some of our patient’s guardians are unaware of this threat to their children. As physicians, it is our responsibility to educate our patient populations, but we should also ask our friends at our local supermarkets and pharmacies to dust off those old warning signs and help spread the word. While we are in flu season, let’s not forget to take a few minutes to inform our patients about this awful, but preventable syndrome.
References
1. Pediatrics. 1980 Dec;66(6):859-64.
2. J Gen Intern Med. 2012 Dec;27(12):1697-703.
Rachel Masia is a third-year medical student at Rowan University School of Osteopathic Medicine, Stratford, N.J. Dr. Alan Masia, Ms. Masia’s father, has a practice in Toms River, N.J. They said they had no relevant financial disclosures.
It is that time of year again. We are in the midst of flu season, which means that it is time to remind our patients’ parents about the importance of using acetaminophen instead of aspirin. This fact became evident when several guardians of our patients came in within a few days of each other in late November to early December unaware of the dangers of giving their children aspirin and other salicylate medications.
Case 1: A 4-year-old boy presented with mild diarrhea, but otherwise was clinically well. The diarrhea started while visiting family in Mexico. The mother took out a small bottle of Pepto-Bismol (bismuth subsalicylate) liquid, which she gave him 2 days previously. The bottle did have, in small font, a warning about Reye’s syndrome on the label, which the mother did not notice. She also did not think it pertained to her son anyway. During the visit, she was counseled on this being early influenza season and the avoidance of salicylate products since the 1980s in children, with the exception of cardiac uses.
Case 2: A 16-year-old male presented with his grandmother with a few scattered vesicles and low-grade fever. He had plans to go to Florida in a few days with friends and wished to know if he would be able to go. He had one dose of varicella vaccine when he was a toddler. Varicella IgM and IgG were ordered. When asked, the grandmother stated that she did not remember the warning signs about Reye’s syndrome posted in the pharmacies 30 years ago. In addition, she vaguely remembered baby aspirin not being made anymore, but she could not remember the reason why.
Case 3: An 18-year-old female with a medical history of occasional migraines controlled with over-the-counter products presented for a school form. Her mother mentioned that a relative had influenza symptoms. When we looked up the migraine medication, it was a generic aspirin/caffeine product. When counseled on Reye’s syndrome, the mother did not remember it at all, even though she was a teenager in the 1980s; she stated that she did remember her mom using only Tylenol for her illnesses.
Reye’s syndrome, a rare but serious condition causing liver degeneration and encephalopathy presenting in children younger than 18 years, was first described in 1963.1 Symptoms include mental confusion, vomiting, and even coma. The cause is unknown; however, salicylates have been implicated as a possible causative agent.
Products containing salicylate include but are not limited to aspirin and Pepto-Bismol. Studies linked Reye’s syndrome epidemiologically to recent illness with influenza or varicella and the use of aspirin. In 1978, the Centers for Disease Control and Prevention was informed that several children developed Reye’s syndrome during an influenza outbreak, and by 1980, the CDC demonstrated a link between those patients and the administration of salicylate-containing medications.2 Around the same time, more studies came out to support these findings. In 1980, 555 cases of Reye’s syndrome were reported in the United States. To decrease the occurrence, the CDC, American Academy of Pediatrics, and the U.S. Surgeon General tried to raise awareness of the association between Reye’s syndrome and aspirin by publishing journals, releasing warning statements, and including a “Black Box” warning in 1986 informing parents to not give aspirin to children and teenagers with influenza or chicken pox. Baby aspirin was removed from use for routine fevers in the mid-1980s and large warning signs would be found in every pharmacy for about 10 years. These warning signs are gone now.
As pediatricians and other primary care physicians, we have so many topics that we must address in the limited time we have allotted for each patient. However, we need to remind our patients and their parents about Reye’s syndrome and the importance of avoiding aspirin and salicylate products in children. Due to the public awareness of Reye’s syndrome in the 1980s and into the 1990s, the incidence decreased.2 From 1987 to 1993, fewer than 37 cases were reported in the United States and from 1994 to 1997, fewer than 2 cases were reported.
This demonstrates the importance of educating our patients and their parents about this syndrome and ways to avoid it. Based on the three clinical cases presented, it is clear that at least some of our patient’s guardians are unaware of this threat to their children. As physicians, it is our responsibility to educate our patient populations, but we should also ask our friends at our local supermarkets and pharmacies to dust off those old warning signs and help spread the word. While we are in flu season, let’s not forget to take a few minutes to inform our patients about this awful, but preventable syndrome.
References
1. Pediatrics. 1980 Dec;66(6):859-64.
2. J Gen Intern Med. 2012 Dec;27(12):1697-703.
Rachel Masia is a third-year medical student at Rowan University School of Osteopathic Medicine, Stratford, N.J. Dr. Alan Masia, Ms. Masia’s father, has a practice in Toms River, N.J. They said they had no relevant financial disclosures.
Distinguishing Dependence From Addiction
Four years ago, I left my career at a large urban VA hospital due to cancer; residual effects of my treatment have prevented my return. I share this as it reflects my personal experience with pain management.
As a Certified Addiction Registered Nurse–Advance Practice, I worked in a substance abuse clinic for 15 years, providing everything from primary care to detoxification and opiate replacement maintenance. I also consulted on cases throughout the facility and advocated for patients with substance abuse histories in regard to care management concerns, including pain. I spent a great deal of time educating staff from all areas on proper care for patients with a variety of substance abuse and addiction concerns.
In order to better address the conundrum of appropriate pain management, a fine distinction needs to be made between dependence and addiction. Chemical dependence is a physiologic status and a medical diagnosis; reduction or discontinuation of a culprit drug will result in symptoms of physiologic withdrawal. Addiction, on the other hand, is a legitimate brain disease that might be better thought of as a mental health disorder. It manifests signs and symptoms very similar to those of chemical dependence.
Perhaps the distinction is best revealed by example: A 65-year-old woman who is on opioid-based pain management for two weeks due to a complicated orthopedic injury will need to be tapered off to avoid physiologic symptoms of withdrawal. Yet, she is not considered a drug addict.
The behavioral characteristics of addiction are familiar: drug-seeking, illicit use, presentation with unexplained withdrawal symptoms, etc. Additionally, process addictions involve the same neurochemical pathways as chemical addictions. When they abstain, gamblers, sex addicts, and television addicts manifest the same anxiety and psychologic or even physical symptoms of withdrawal. The pathophysiology of the addiction process is established in addiction medicine literature.
The problem is that this knowledge has not been extended to practice. In my experience, poorly managed pain has a much greater risk for unintended negative consequences than aggressive management with opiods and adjuncts in a patient with a history of heroin addiction. Pseudo-addiction is real, and patients present with signs and symptoms similar to those of addiction: demanding, making specific requests, history of multiple providers (doctor shopping), and elevated anxiety.
Anyone who has experienced poorly managed severe pain will share stories of the drive to get relief at almost any cost. These people are not drug addicts. They are patients in need of informed, aggressive, and compassionate care.
Fear-based inadequate pain management creates instability and desperation in patients. Their intensive search for relief is nothing but rational. A clinician’s withholding of adequate care due to social prejudice, fear (of the DEA), and/or ignorance in a field where knowledge and tools are widely available is bad care at best and negligent incompetence at worst. Ultimately, it is the patient who suffers the consequences.
The well-known but often denied chasm between medicine and mental health has gone on too long. Medical practitioners need to
- Be better able to identify and distinguish between potential and current chemical dependence and true addiction.
- Be willing to treat pain aggressively in patients with a known history of addiction in order to prevent relapse or exacerbation of their addictive use.
- Develop a working knowledge of strategies to treat pain while minimizing risk for addiction and dependence.
- Commit to the intensity of practice that is required for effective pain management in any population.
Yes, my suggestions imply a labor-intensive approach. But there are no 20-minute appointments with a heroin addict. And time spent appropriately assessing patient risk for substance abuse, treating legitimate pain management needs, and intensively following up will reduce the medical and mental health costs associated with poorly managed pain in low-risk patients, and the hugely expensive and potentially tragic outcomes associated with poorly treated drug addicts.
L. Henry Beazlie, RN, CCRN, CARN-AP, MSN, MA (retired)
Akron, OH
Four years ago, I left my career at a large urban VA hospital due to cancer; residual effects of my treatment have prevented my return. I share this as it reflects my personal experience with pain management.
As a Certified Addiction Registered Nurse–Advance Practice, I worked in a substance abuse clinic for 15 years, providing everything from primary care to detoxification and opiate replacement maintenance. I also consulted on cases throughout the facility and advocated for patients with substance abuse histories in regard to care management concerns, including pain. I spent a great deal of time educating staff from all areas on proper care for patients with a variety of substance abuse and addiction concerns.
In order to better address the conundrum of appropriate pain management, a fine distinction needs to be made between dependence and addiction. Chemical dependence is a physiologic status and a medical diagnosis; reduction or discontinuation of a culprit drug will result in symptoms of physiologic withdrawal. Addiction, on the other hand, is a legitimate brain disease that might be better thought of as a mental health disorder. It manifests signs and symptoms very similar to those of chemical dependence.
Perhaps the distinction is best revealed by example: A 65-year-old woman who is on opioid-based pain management for two weeks due to a complicated orthopedic injury will need to be tapered off to avoid physiologic symptoms of withdrawal. Yet, she is not considered a drug addict.
The behavioral characteristics of addiction are familiar: drug-seeking, illicit use, presentation with unexplained withdrawal symptoms, etc. Additionally, process addictions involve the same neurochemical pathways as chemical addictions. When they abstain, gamblers, sex addicts, and television addicts manifest the same anxiety and psychologic or even physical symptoms of withdrawal. The pathophysiology of the addiction process is established in addiction medicine literature.
The problem is that this knowledge has not been extended to practice. In my experience, poorly managed pain has a much greater risk for unintended negative consequences than aggressive management with opiods and adjuncts in a patient with a history of heroin addiction. Pseudo-addiction is real, and patients present with signs and symptoms similar to those of addiction: demanding, making specific requests, history of multiple providers (doctor shopping), and elevated anxiety.
Anyone who has experienced poorly managed severe pain will share stories of the drive to get relief at almost any cost. These people are not drug addicts. They are patients in need of informed, aggressive, and compassionate care.
Fear-based inadequate pain management creates instability and desperation in patients. Their intensive search for relief is nothing but rational. A clinician’s withholding of adequate care due to social prejudice, fear (of the DEA), and/or ignorance in a field where knowledge and tools are widely available is bad care at best and negligent incompetence at worst. Ultimately, it is the patient who suffers the consequences.
The well-known but often denied chasm between medicine and mental health has gone on too long. Medical practitioners need to
- Be better able to identify and distinguish between potential and current chemical dependence and true addiction.
- Be willing to treat pain aggressively in patients with a known history of addiction in order to prevent relapse or exacerbation of their addictive use.
- Develop a working knowledge of strategies to treat pain while minimizing risk for addiction and dependence.
- Commit to the intensity of practice that is required for effective pain management in any population.
Yes, my suggestions imply a labor-intensive approach. But there are no 20-minute appointments with a heroin addict. And time spent appropriately assessing patient risk for substance abuse, treating legitimate pain management needs, and intensively following up will reduce the medical and mental health costs associated with poorly managed pain in low-risk patients, and the hugely expensive and potentially tragic outcomes associated with poorly treated drug addicts.
L. Henry Beazlie, RN, CCRN, CARN-AP, MSN, MA (retired)
Akron, OH
Four years ago, I left my career at a large urban VA hospital due to cancer; residual effects of my treatment have prevented my return. I share this as it reflects my personal experience with pain management.
As a Certified Addiction Registered Nurse–Advance Practice, I worked in a substance abuse clinic for 15 years, providing everything from primary care to detoxification and opiate replacement maintenance. I also consulted on cases throughout the facility and advocated for patients with substance abuse histories in regard to care management concerns, including pain. I spent a great deal of time educating staff from all areas on proper care for patients with a variety of substance abuse and addiction concerns.
In order to better address the conundrum of appropriate pain management, a fine distinction needs to be made between dependence and addiction. Chemical dependence is a physiologic status and a medical diagnosis; reduction or discontinuation of a culprit drug will result in symptoms of physiologic withdrawal. Addiction, on the other hand, is a legitimate brain disease that might be better thought of as a mental health disorder. It manifests signs and symptoms very similar to those of chemical dependence.
Perhaps the distinction is best revealed by example: A 65-year-old woman who is on opioid-based pain management for two weeks due to a complicated orthopedic injury will need to be tapered off to avoid physiologic symptoms of withdrawal. Yet, she is not considered a drug addict.
The behavioral characteristics of addiction are familiar: drug-seeking, illicit use, presentation with unexplained withdrawal symptoms, etc. Additionally, process addictions involve the same neurochemical pathways as chemical addictions. When they abstain, gamblers, sex addicts, and television addicts manifest the same anxiety and psychologic or even physical symptoms of withdrawal. The pathophysiology of the addiction process is established in addiction medicine literature.
The problem is that this knowledge has not been extended to practice. In my experience, poorly managed pain has a much greater risk for unintended negative consequences than aggressive management with opiods and adjuncts in a patient with a history of heroin addiction. Pseudo-addiction is real, and patients present with signs and symptoms similar to those of addiction: demanding, making specific requests, history of multiple providers (doctor shopping), and elevated anxiety.
Anyone who has experienced poorly managed severe pain will share stories of the drive to get relief at almost any cost. These people are not drug addicts. They are patients in need of informed, aggressive, and compassionate care.
Fear-based inadequate pain management creates instability and desperation in patients. Their intensive search for relief is nothing but rational. A clinician’s withholding of adequate care due to social prejudice, fear (of the DEA), and/or ignorance in a field where knowledge and tools are widely available is bad care at best and negligent incompetence at worst. Ultimately, it is the patient who suffers the consequences.
The well-known but often denied chasm between medicine and mental health has gone on too long. Medical practitioners need to
- Be better able to identify and distinguish between potential and current chemical dependence and true addiction.
- Be willing to treat pain aggressively in patients with a known history of addiction in order to prevent relapse or exacerbation of their addictive use.
- Develop a working knowledge of strategies to treat pain while minimizing risk for addiction and dependence.
- Commit to the intensity of practice that is required for effective pain management in any population.
Yes, my suggestions imply a labor-intensive approach. But there are no 20-minute appointments with a heroin addict. And time spent appropriately assessing patient risk for substance abuse, treating legitimate pain management needs, and intensively following up will reduce the medical and mental health costs associated with poorly managed pain in low-risk patients, and the hugely expensive and potentially tragic outcomes associated with poorly treated drug addicts.
L. Henry Beazlie, RN, CCRN, CARN-AP, MSN, MA (retired)
Akron, OH
Keeping Pain A Priority
Before pain was introduced as the “fifth vital sign” and the Joint Commission issued its standards, more than a decade’s worth of international research indicated that pain was largely ignored, untreated, or undertreated. The best tools available to treat pain (opioids) were reserved for patients on their deathbed. The horrific results of the SUPPORT study at the nation’s leading hospitals revealed that most patients had severe, uncontrolled pain up until their final days of life.1 Unfortunately, research suggests we are still reserving opioids for the last days or weeks of life.2
In 1992 and 1994, the Department of Health and Human Services issued clinical practice guidelines highlighting the huge gap between the availability of evidence-based pain control methods and the lack of pain assessment and treatment in practice.3 When these guidelines failed to change practice, the Joint Commission added “attending to pain” to its standards—the first effort to require that evidence-based practices be utilized. Twenty years later, the National Academy of Science issued a report stating that, despite transient improvements, the current state is inadequate since pain is the leading reason people seek health care. Patients with pain report an inability to get help, which is “viewed worldwide as poor medicine, unethical practice, and an abrogation of a fundamental human right.”4 Since I started working as an NP in 1983, I have never seen as many patients with pain stigmatized, ignored, labeled, and denied access to treatment as I have in the past year.
Pain afflicts more than 100 million Americans and is the leading cause of disability worldwide.5 Acute pain that is not effectively treated progresses to chronic pain in 51% of cases.6 An estimated 23 million Americans report frequent intense pain, 25 million endure daily chronic pain, and 40 million adults have high-impact, disabling, chronic pain that degrades health and requires health care intervention.6,7 The most notable damage is to the structure and function of the central nervous system.8 Brain remodeling and loss of gray matter occurs, producing changes in the brain similar to those observed with 10 to 20 years of aging; this explains why some of the learning, memory, and emotional difficulties endured by many with ongoing pain can be partially reversed with effective treatment.9 Left untreated, pain can result in significant biopsychosocial problems, frailty, financial ruin, and premature death.10-14
Prescription drug misuse and addiction also affect millions and have been a largely ignored public health problem for decades. Trying to fix the pain problem without attending equally to the problems of nonmedical drug use, addiction, and overdose deaths has contributed to the escalation of health problems to “epidemic” and “crisis” proportions. Although most patients who are prescribed medically indicated opioids for pain do not misuse their medications or become addicted, the failure to subsequently identify and properly treat an emergent substance use disorder is a problem in our current system.15 Unfortunately, making prescription opioids inaccessible to patients forces some to abuse alcohol or seek drugs from illicit sources, which only exacerbates the situation.16 A national study performed over a five-year period revealed that only 10% of patients admitted for prescription opioid treatment were referred from their health care providers.17 So, health care providers may have been part of the problem but have not been fully engaged in the solution.
Although opioids are neither the firstline, nor only, treatment option in our current evidence-based treatment toolbox, their prudent use does not cause addiction. Only 1% of patients who receive postoperative opioids go on to develop chronic opioid use, and adolescents treated with medically necessary opioids have no greater risk for future addiction than unexposed children. It is the nonmedical use of opioids, rather than proper medical use, that predisposes people to addiction.18,19 Discharging or not treating patients suspected of “drug-seeking” exacerbates the problem. Rates of opioid prescription have declined, while overdoses of illicitly manufactured fentanyl increased by 79% in 27 states from 2013 to 2014.20 In Massachusetts, only 8% of people who fatally overdosed had a prescription, while illicit fentanyl accounted for 54% of overdose deaths in 2015 and more than 74% in the third quarter of 2016.21 We need to screen for nonmedical use, drug misuse, and addiction before, during, and after we treat with this particular tool.
Unfortunately, the prevalence of pain and addiction are both increasing, especially for women and minorities—but there are safe, effective medications and non-drug approaches available to combat this.22-24 These problems will not go away on their own, and every health care professional must choose to be part of the solution rather than perpetuate the problem. A good place to start is to become familiar with the Surgeon General’s Report and the National Pain Strategy. Educate your patients, colleagues, and policy makers about the true nature of these problems. Take a public health approach to primary, secondary, and tertiary prevention by recognizing and treating these conditions in an expedient and effective matter. When problems persist, expand the treatment team to include specialists who can develop a patient-centered, multimodal treatment plan that treats co-occurring conditions. If we continue to ignore these problems, or focus on one at the expense of the other, both problems will worsen and our patients will suffer serious consequences.
Paul Arnstein, PhD, NP-C, FAAN, FNP-C
Boston, MA
1. Lynn J, Teno JM, Phillips RS, et al; SUPPORT Investigators. Perceptions by family members of the dying experience of older and seriously ill patients. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 1997;126(2):97-106.
2. Ziegler L, Mulvey M, Blenkinsopp A, et al. Opioid prescribing for patients with cancer in the last year of life: a longitudinal population cohort study. Pain. 2016;157(11):2445-2451.
3. Agency for Health Care Policy and Research [AHCPR]. Acute Pain Management: Operative or Medical Procedures and Trauma. Rockville, MD: US Department of Health and Human Services, Public Health Service; 1992.
4. Institute of Medicine (IOM). Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington DC: The National Academies Press; 2011.
5. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016; 388(10053):1545-1602.
6. Macfarlane GJ. The epidemiology of chronic pain. Pain. 2016;157(10):2158-2159.
7. Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain. 2015;16(8):769-780.
8. Pozek JP, Beausang D, Baratta JL, Viscusi ER. The acute to chronic pain transition: can chronic pain be prevented? Med Clin North Am. 2016;100(1):17-30.
9. Seminowicz DA, Wideman TH, Naso L, et al. Effective treatment of chronic low back pain in humans reverses abnormal brain anatomy and function. J Neurosci. 2011; 31(20):7540-7550.
10. Wade KF, Lee DM, McBeth J, et al. Chronic widespread pain is associated with worsening frailty in European men. Age Ageing. 2016;45(2):268-274.
11. Torrance N, Elliott A, Lee AJ, Smith BH. Severe chronic pain is associated with increased 10 year mortality. A cohort record linkage study. Eur J Pain. 2010;14(4):380-386.
12. Tang NK, Beckwith P, Ashworth P. Mental defeat is associated with suicide intent in patients with chronic pain. Clin J Pain. 2016;32(5):411-419.
13. Schaefer C, Sadosky A, Mann R, et al. Pain severity and the economic burden of neuropathic pain in the United States: BEAT Neuropathic Pain Observational Study. Clinicoecon Outcomes Res. 2014;6:483-496.
14. Schofield D, Kelly S, Shrestha R, et al. The impact of back problems on retirement wealth. Pain. 2012;153(1):203-210.
15. Chou R, Deyo R, Devine B, et al. The effectiveness and risks of long-term opioid treatment of chronic pain. AHRQ Report No. 218. Agency for Healthcare Research and Quality; September 2014. www.effectivehealthcare.ahrq.gov/ehc/products/557/1988/chronic-pain-opioid-treat ment-executive-141022.pdf. Accessed December 2, 2016.
16. Alford DP, German JS, Samet JH, et al. Primary care patients with drug use report chronic pain and self-medicate with alcohol and other drugs. J Gen Intern Med. 2016;31(5):486-491.
17. St. Marie BJ, Sahker E, Arndt S. Referrals and treatment completion for prescription opioid admissions: five years of national data. J Subst Abus Treat. 2015;59:109-114.
18. Sun EC, Darnall B, Baker LC, et al. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016; 176(9):1286-1293.
19. McCabe SE, Veliz P, Schulenberg JE. Adolescent context of exposure to prescription opioids and substance use disorder (SUD) symptoms at age 35: a national longitudinal study. Pain. 2016;157(10):2171-2178.
20. Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths—27 states, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65(33):837-843.
21. Massachusetts Department of Public Health. Data Brief: Opioid-related Overdose Deaths Among Massachusetts Residents. www.mass.gov/eohhs/docs/dph/quality/drugcontrol/county-level-pmp/data-brief-overdose-deaths-may-2016.pdf. Accessed December 2, 2016.
22. Barbour KE, Boring M, Helmick CG, et al. Prevalence of severe joint pain among adults with doctor-diagnosed arthritis—United States, 2002–2014. MMWR Morb Mortal Wkly Rep. 2016;65(39):1052-1056.
23. US Department of Health and Human Services (HHS), Office of the Surgeon General. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health, Executive Summary. Washington, DC: HHS; 2016. https://addiction.surgeongeneral.gov/executive-summary.pdf. Accessed December 2, 2016.
24. Herndon CM, Arnstein P, Darnall B, et al. Principles of Analgesic Use. 7th ed. Chicago, IL: American Pain Society Press; 2016.
Before pain was introduced as the “fifth vital sign” and the Joint Commission issued its standards, more than a decade’s worth of international research indicated that pain was largely ignored, untreated, or undertreated. The best tools available to treat pain (opioids) were reserved for patients on their deathbed. The horrific results of the SUPPORT study at the nation’s leading hospitals revealed that most patients had severe, uncontrolled pain up until their final days of life.1 Unfortunately, research suggests we are still reserving opioids for the last days or weeks of life.2
In 1992 and 1994, the Department of Health and Human Services issued clinical practice guidelines highlighting the huge gap between the availability of evidence-based pain control methods and the lack of pain assessment and treatment in practice.3 When these guidelines failed to change practice, the Joint Commission added “attending to pain” to its standards—the first effort to require that evidence-based practices be utilized. Twenty years later, the National Academy of Science issued a report stating that, despite transient improvements, the current state is inadequate since pain is the leading reason people seek health care. Patients with pain report an inability to get help, which is “viewed worldwide as poor medicine, unethical practice, and an abrogation of a fundamental human right.”4 Since I started working as an NP in 1983, I have never seen as many patients with pain stigmatized, ignored, labeled, and denied access to treatment as I have in the past year.
Pain afflicts more than 100 million Americans and is the leading cause of disability worldwide.5 Acute pain that is not effectively treated progresses to chronic pain in 51% of cases.6 An estimated 23 million Americans report frequent intense pain, 25 million endure daily chronic pain, and 40 million adults have high-impact, disabling, chronic pain that degrades health and requires health care intervention.6,7 The most notable damage is to the structure and function of the central nervous system.8 Brain remodeling and loss of gray matter occurs, producing changes in the brain similar to those observed with 10 to 20 years of aging; this explains why some of the learning, memory, and emotional difficulties endured by many with ongoing pain can be partially reversed with effective treatment.9 Left untreated, pain can result in significant biopsychosocial problems, frailty, financial ruin, and premature death.10-14
Prescription drug misuse and addiction also affect millions and have been a largely ignored public health problem for decades. Trying to fix the pain problem without attending equally to the problems of nonmedical drug use, addiction, and overdose deaths has contributed to the escalation of health problems to “epidemic” and “crisis” proportions. Although most patients who are prescribed medically indicated opioids for pain do not misuse their medications or become addicted, the failure to subsequently identify and properly treat an emergent substance use disorder is a problem in our current system.15 Unfortunately, making prescription opioids inaccessible to patients forces some to abuse alcohol or seek drugs from illicit sources, which only exacerbates the situation.16 A national study performed over a five-year period revealed that only 10% of patients admitted for prescription opioid treatment were referred from their health care providers.17 So, health care providers may have been part of the problem but have not been fully engaged in the solution.
Although opioids are neither the firstline, nor only, treatment option in our current evidence-based treatment toolbox, their prudent use does not cause addiction. Only 1% of patients who receive postoperative opioids go on to develop chronic opioid use, and adolescents treated with medically necessary opioids have no greater risk for future addiction than unexposed children. It is the nonmedical use of opioids, rather than proper medical use, that predisposes people to addiction.18,19 Discharging or not treating patients suspected of “drug-seeking” exacerbates the problem. Rates of opioid prescription have declined, while overdoses of illicitly manufactured fentanyl increased by 79% in 27 states from 2013 to 2014.20 In Massachusetts, only 8% of people who fatally overdosed had a prescription, while illicit fentanyl accounted for 54% of overdose deaths in 2015 and more than 74% in the third quarter of 2016.21 We need to screen for nonmedical use, drug misuse, and addiction before, during, and after we treat with this particular tool.
Unfortunately, the prevalence of pain and addiction are both increasing, especially for women and minorities—but there are safe, effective medications and non-drug approaches available to combat this.22-24 These problems will not go away on their own, and every health care professional must choose to be part of the solution rather than perpetuate the problem. A good place to start is to become familiar with the Surgeon General’s Report and the National Pain Strategy. Educate your patients, colleagues, and policy makers about the true nature of these problems. Take a public health approach to primary, secondary, and tertiary prevention by recognizing and treating these conditions in an expedient and effective matter. When problems persist, expand the treatment team to include specialists who can develop a patient-centered, multimodal treatment plan that treats co-occurring conditions. If we continue to ignore these problems, or focus on one at the expense of the other, both problems will worsen and our patients will suffer serious consequences.
Paul Arnstein, PhD, NP-C, FAAN, FNP-C
Boston, MA
Before pain was introduced as the “fifth vital sign” and the Joint Commission issued its standards, more than a decade’s worth of international research indicated that pain was largely ignored, untreated, or undertreated. The best tools available to treat pain (opioids) were reserved for patients on their deathbed. The horrific results of the SUPPORT study at the nation’s leading hospitals revealed that most patients had severe, uncontrolled pain up until their final days of life.1 Unfortunately, research suggests we are still reserving opioids for the last days or weeks of life.2
In 1992 and 1994, the Department of Health and Human Services issued clinical practice guidelines highlighting the huge gap between the availability of evidence-based pain control methods and the lack of pain assessment and treatment in practice.3 When these guidelines failed to change practice, the Joint Commission added “attending to pain” to its standards—the first effort to require that evidence-based practices be utilized. Twenty years later, the National Academy of Science issued a report stating that, despite transient improvements, the current state is inadequate since pain is the leading reason people seek health care. Patients with pain report an inability to get help, which is “viewed worldwide as poor medicine, unethical practice, and an abrogation of a fundamental human right.”4 Since I started working as an NP in 1983, I have never seen as many patients with pain stigmatized, ignored, labeled, and denied access to treatment as I have in the past year.
Pain afflicts more than 100 million Americans and is the leading cause of disability worldwide.5 Acute pain that is not effectively treated progresses to chronic pain in 51% of cases.6 An estimated 23 million Americans report frequent intense pain, 25 million endure daily chronic pain, and 40 million adults have high-impact, disabling, chronic pain that degrades health and requires health care intervention.6,7 The most notable damage is to the structure and function of the central nervous system.8 Brain remodeling and loss of gray matter occurs, producing changes in the brain similar to those observed with 10 to 20 years of aging; this explains why some of the learning, memory, and emotional difficulties endured by many with ongoing pain can be partially reversed with effective treatment.9 Left untreated, pain can result in significant biopsychosocial problems, frailty, financial ruin, and premature death.10-14
Prescription drug misuse and addiction also affect millions and have been a largely ignored public health problem for decades. Trying to fix the pain problem without attending equally to the problems of nonmedical drug use, addiction, and overdose deaths has contributed to the escalation of health problems to “epidemic” and “crisis” proportions. Although most patients who are prescribed medically indicated opioids for pain do not misuse their medications or become addicted, the failure to subsequently identify and properly treat an emergent substance use disorder is a problem in our current system.15 Unfortunately, making prescription opioids inaccessible to patients forces some to abuse alcohol or seek drugs from illicit sources, which only exacerbates the situation.16 A national study performed over a five-year period revealed that only 10% of patients admitted for prescription opioid treatment were referred from their health care providers.17 So, health care providers may have been part of the problem but have not been fully engaged in the solution.
Although opioids are neither the firstline, nor only, treatment option in our current evidence-based treatment toolbox, their prudent use does not cause addiction. Only 1% of patients who receive postoperative opioids go on to develop chronic opioid use, and adolescents treated with medically necessary opioids have no greater risk for future addiction than unexposed children. It is the nonmedical use of opioids, rather than proper medical use, that predisposes people to addiction.18,19 Discharging or not treating patients suspected of “drug-seeking” exacerbates the problem. Rates of opioid prescription have declined, while overdoses of illicitly manufactured fentanyl increased by 79% in 27 states from 2013 to 2014.20 In Massachusetts, only 8% of people who fatally overdosed had a prescription, while illicit fentanyl accounted for 54% of overdose deaths in 2015 and more than 74% in the third quarter of 2016.21 We need to screen for nonmedical use, drug misuse, and addiction before, during, and after we treat with this particular tool.
Unfortunately, the prevalence of pain and addiction are both increasing, especially for women and minorities—but there are safe, effective medications and non-drug approaches available to combat this.22-24 These problems will not go away on their own, and every health care professional must choose to be part of the solution rather than perpetuate the problem. A good place to start is to become familiar with the Surgeon General’s Report and the National Pain Strategy. Educate your patients, colleagues, and policy makers about the true nature of these problems. Take a public health approach to primary, secondary, and tertiary prevention by recognizing and treating these conditions in an expedient and effective matter. When problems persist, expand the treatment team to include specialists who can develop a patient-centered, multimodal treatment plan that treats co-occurring conditions. If we continue to ignore these problems, or focus on one at the expense of the other, both problems will worsen and our patients will suffer serious consequences.
Paul Arnstein, PhD, NP-C, FAAN, FNP-C
Boston, MA
1. Lynn J, Teno JM, Phillips RS, et al; SUPPORT Investigators. Perceptions by family members of the dying experience of older and seriously ill patients. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 1997;126(2):97-106.
2. Ziegler L, Mulvey M, Blenkinsopp A, et al. Opioid prescribing for patients with cancer in the last year of life: a longitudinal population cohort study. Pain. 2016;157(11):2445-2451.
3. Agency for Health Care Policy and Research [AHCPR]. Acute Pain Management: Operative or Medical Procedures and Trauma. Rockville, MD: US Department of Health and Human Services, Public Health Service; 1992.
4. Institute of Medicine (IOM). Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington DC: The National Academies Press; 2011.
5. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016; 388(10053):1545-1602.
6. Macfarlane GJ. The epidemiology of chronic pain. Pain. 2016;157(10):2158-2159.
7. Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain. 2015;16(8):769-780.
8. Pozek JP, Beausang D, Baratta JL, Viscusi ER. The acute to chronic pain transition: can chronic pain be prevented? Med Clin North Am. 2016;100(1):17-30.
9. Seminowicz DA, Wideman TH, Naso L, et al. Effective treatment of chronic low back pain in humans reverses abnormal brain anatomy and function. J Neurosci. 2011; 31(20):7540-7550.
10. Wade KF, Lee DM, McBeth J, et al. Chronic widespread pain is associated with worsening frailty in European men. Age Ageing. 2016;45(2):268-274.
11. Torrance N, Elliott A, Lee AJ, Smith BH. Severe chronic pain is associated with increased 10 year mortality. A cohort record linkage study. Eur J Pain. 2010;14(4):380-386.
12. Tang NK, Beckwith P, Ashworth P. Mental defeat is associated with suicide intent in patients with chronic pain. Clin J Pain. 2016;32(5):411-419.
13. Schaefer C, Sadosky A, Mann R, et al. Pain severity and the economic burden of neuropathic pain in the United States: BEAT Neuropathic Pain Observational Study. Clinicoecon Outcomes Res. 2014;6:483-496.
14. Schofield D, Kelly S, Shrestha R, et al. The impact of back problems on retirement wealth. Pain. 2012;153(1):203-210.
15. Chou R, Deyo R, Devine B, et al. The effectiveness and risks of long-term opioid treatment of chronic pain. AHRQ Report No. 218. Agency for Healthcare Research and Quality; September 2014. www.effectivehealthcare.ahrq.gov/ehc/products/557/1988/chronic-pain-opioid-treat ment-executive-141022.pdf. Accessed December 2, 2016.
16. Alford DP, German JS, Samet JH, et al. Primary care patients with drug use report chronic pain and self-medicate with alcohol and other drugs. J Gen Intern Med. 2016;31(5):486-491.
17. St. Marie BJ, Sahker E, Arndt S. Referrals and treatment completion for prescription opioid admissions: five years of national data. J Subst Abus Treat. 2015;59:109-114.
18. Sun EC, Darnall B, Baker LC, et al. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016; 176(9):1286-1293.
19. McCabe SE, Veliz P, Schulenberg JE. Adolescent context of exposure to prescription opioids and substance use disorder (SUD) symptoms at age 35: a national longitudinal study. Pain. 2016;157(10):2171-2178.
20. Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths—27 states, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65(33):837-843.
21. Massachusetts Department of Public Health. Data Brief: Opioid-related Overdose Deaths Among Massachusetts Residents. www.mass.gov/eohhs/docs/dph/quality/drugcontrol/county-level-pmp/data-brief-overdose-deaths-may-2016.pdf. Accessed December 2, 2016.
22. Barbour KE, Boring M, Helmick CG, et al. Prevalence of severe joint pain among adults with doctor-diagnosed arthritis—United States, 2002–2014. MMWR Morb Mortal Wkly Rep. 2016;65(39):1052-1056.
23. US Department of Health and Human Services (HHS), Office of the Surgeon General. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health, Executive Summary. Washington, DC: HHS; 2016. https://addiction.surgeongeneral.gov/executive-summary.pdf. Accessed December 2, 2016.
24. Herndon CM, Arnstein P, Darnall B, et al. Principles of Analgesic Use. 7th ed. Chicago, IL: American Pain Society Press; 2016.
1. Lynn J, Teno JM, Phillips RS, et al; SUPPORT Investigators. Perceptions by family members of the dying experience of older and seriously ill patients. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 1997;126(2):97-106.
2. Ziegler L, Mulvey M, Blenkinsopp A, et al. Opioid prescribing for patients with cancer in the last year of life: a longitudinal population cohort study. Pain. 2016;157(11):2445-2451.
3. Agency for Health Care Policy and Research [AHCPR]. Acute Pain Management: Operative or Medical Procedures and Trauma. Rockville, MD: US Department of Health and Human Services, Public Health Service; 1992.
4. Institute of Medicine (IOM). Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington DC: The National Academies Press; 2011.
5. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016; 388(10053):1545-1602.
6. Macfarlane GJ. The epidemiology of chronic pain. Pain. 2016;157(10):2158-2159.
7. Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain. 2015;16(8):769-780.
8. Pozek JP, Beausang D, Baratta JL, Viscusi ER. The acute to chronic pain transition: can chronic pain be prevented? Med Clin North Am. 2016;100(1):17-30.
9. Seminowicz DA, Wideman TH, Naso L, et al. Effective treatment of chronic low back pain in humans reverses abnormal brain anatomy and function. J Neurosci. 2011; 31(20):7540-7550.
10. Wade KF, Lee DM, McBeth J, et al. Chronic widespread pain is associated with worsening frailty in European men. Age Ageing. 2016;45(2):268-274.
11. Torrance N, Elliott A, Lee AJ, Smith BH. Severe chronic pain is associated with increased 10 year mortality. A cohort record linkage study. Eur J Pain. 2010;14(4):380-386.
12. Tang NK, Beckwith P, Ashworth P. Mental defeat is associated with suicide intent in patients with chronic pain. Clin J Pain. 2016;32(5):411-419.
13. Schaefer C, Sadosky A, Mann R, et al. Pain severity and the economic burden of neuropathic pain in the United States: BEAT Neuropathic Pain Observational Study. Clinicoecon Outcomes Res. 2014;6:483-496.
14. Schofield D, Kelly S, Shrestha R, et al. The impact of back problems on retirement wealth. Pain. 2012;153(1):203-210.
15. Chou R, Deyo R, Devine B, et al. The effectiveness and risks of long-term opioid treatment of chronic pain. AHRQ Report No. 218. Agency for Healthcare Research and Quality; September 2014. www.effectivehealthcare.ahrq.gov/ehc/products/557/1988/chronic-pain-opioid-treat ment-executive-141022.pdf. Accessed December 2, 2016.
16. Alford DP, German JS, Samet JH, et al. Primary care patients with drug use report chronic pain and self-medicate with alcohol and other drugs. J Gen Intern Med. 2016;31(5):486-491.
17. St. Marie BJ, Sahker E, Arndt S. Referrals and treatment completion for prescription opioid admissions: five years of national data. J Subst Abus Treat. 2015;59:109-114.
18. Sun EC, Darnall B, Baker LC, et al. Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016; 176(9):1286-1293.
19. McCabe SE, Veliz P, Schulenberg JE. Adolescent context of exposure to prescription opioids and substance use disorder (SUD) symptoms at age 35: a national longitudinal study. Pain. 2016;157(10):2171-2178.
20. Gladden RM, Martinez P, Seth P. Fentanyl law enforcement submissions and increases in synthetic opioid-involved overdose deaths—27 states, 2013-2014. MMWR Morb Mortal Wkly Rep. 2016;65(33):837-843.
21. Massachusetts Department of Public Health. Data Brief: Opioid-related Overdose Deaths Among Massachusetts Residents. www.mass.gov/eohhs/docs/dph/quality/drugcontrol/county-level-pmp/data-brief-overdose-deaths-may-2016.pdf. Accessed December 2, 2016.
22. Barbour KE, Boring M, Helmick CG, et al. Prevalence of severe joint pain among adults with doctor-diagnosed arthritis—United States, 2002–2014. MMWR Morb Mortal Wkly Rep. 2016;65(39):1052-1056.
23. US Department of Health and Human Services (HHS), Office of the Surgeon General. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health, Executive Summary. Washington, DC: HHS; 2016. https://addiction.surgeongeneral.gov/executive-summary.pdf. Accessed December 2, 2016.
24. Herndon CM, Arnstein P, Darnall B, et al. Principles of Analgesic Use. 7th ed. Chicago, IL: American Pain Society Press; 2016.
Enterovirus D68 – An emerging threat to child health
In August 2014, we first heard of increased pediatric cases of severe respiratory tract disease, many requiring management in the ICU, and of acute flaccid myelitis/paralysis (AFM) of unknown etiology from many states across the United States. Concurrently with this outbreak in the United States, similar clinical cases were reported in Canada and Europe. Subsequently, enterovirus D68 was confirmed in some, but not all, of the paralyzed children. Although new to many of us, enterovirus D68 was already known as an atypical enterovirus sharing many of its structural and chemical properties with rhinovirus. For example, it most often was reported from respiratory samples and less common from stool samples. It also had been associated with clusters of respiratory disease since 2000 and a 2008 case of fatal AFM.
There were 120 cases of AFM, coinciding with the nationwide outbreak of enteroviral D68 disease, reported in 2014. The Centers for Disease Control and Prevention has evaluated the cerebrospinal fluid in many of these cases, and no pathogen has consistently been detected. The children were mostly school age, aged 7-11 years, presented with acute, febrile respiratory illness followed by acute onset of cranial nerve dysfunction or flaccid paralysis of one or more limbs. The CSF revealed mild pleocytosis, most often with mild elevation of protein and a normal glucose. However, the MRI was distinctly abnormal with focal lesion in the cranial nerve nuclei (in those with bulbar dysfunction) and/or in the anterior horn or spinal cord gray matter. Long-term prognosis is unknown, although most patients have persistent weakness, despite some improvement, to date.
In 2016, the CDC has reported an increase in cases after a decline in 2015 despite the absence of epidemic respiratory tract disease in the United States from enterovirus D68. In the Netherlands, an increase in respiratory disease from enterovirus D68 in children and adults also has been reported since June 2016. Respiratory disease has been observed in children as young as 3 months of age, and most of the children have underlying comorbidity, many with asthma or other pulmonary conditions. Thirteen of 17 (77%) cases in children have required ICU admission, while most of the adult cases were mild and influenzalike. One child developed bulbar dysfunction and limb weakness.
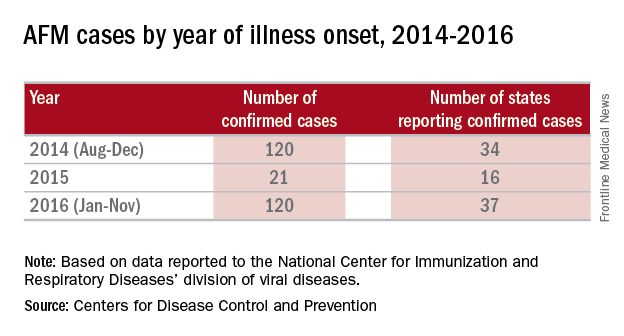
Enterovirus D68 infection should be suspected in children with moderate to severe respiratory tract infection or acute onset bulbar or flaccid paralysis of unknown etiology, especially in summer and fall. In such cases, respiratory specimens (nasopharyngeal or oral swabs or wash, tracheal secretions or bronchoalveolar lavage) should be obtained. Increasingly, hospitals and laboratories can perform multiplex polymerase chain reaction testing for enterovirus/rhinovirus. However, most do not determine the specific enterovirus. CDC and some state health departments use real-time reverse transcription polymerase chain reaction (rRT-PCR), which enables reporting of specific enterovirus species within days. CDC recommends that clinicians consider enterovirus D68 testing for children with unknown, severe respiratory illness or AFM. Details for sending specimens should be available from your state’s Department of Public Health website or the CDC.
Prevention strategies may be critical for limiting the spread of enterovirus D68 in the community. The CDC recommends:
- Wash your hands often with soap and water for 20 seconds.
- Avoid touching your eyes, nose and mouth with unwashed hands.
- Avoid close contact such as kissing, hugging, and sharing cups with people who are ill.
- Cover your coughs and sneezes with a tissue or shirt sleeve, not your hands.
- Clean and disinfect frequently touched surfaces, such as toys and doorknobs, especially if someone is sick.
- Stay home when you are ill.
In 2014, it was speculated that the epidemic might have been a one-time event. It now appears more likely that enterovirus D68 activity has been increasing since 2000, and that children and immunocompromised hosts will be at greatest risk because of a lack of neutralizing antibody. Ongoing enterovirus surveillance will be critical to understand the potential for severe respiratory disease as will the development of new and effective antivirals. A vaccine for enterovirus 71 recently demonstrated efficacy against hand, foot, and mouth disease in children and may provide insights into the development of vaccines against enterovirus D68.
References
Lancet Infect Dis. 2016 May;16(5):e64-75
Emerg Infect Dis. 2017 Jan;23(1):140-3.
J Med Virol. 2016 May;88(5):739-45
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. Dr. Pelton said he had no relevant financial disclosures. Email him at [email protected].
In August 2014, we first heard of increased pediatric cases of severe respiratory tract disease, many requiring management in the ICU, and of acute flaccid myelitis/paralysis (AFM) of unknown etiology from many states across the United States. Concurrently with this outbreak in the United States, similar clinical cases were reported in Canada and Europe. Subsequently, enterovirus D68 was confirmed in some, but not all, of the paralyzed children. Although new to many of us, enterovirus D68 was already known as an atypical enterovirus sharing many of its structural and chemical properties with rhinovirus. For example, it most often was reported from respiratory samples and less common from stool samples. It also had been associated with clusters of respiratory disease since 2000 and a 2008 case of fatal AFM.
There were 120 cases of AFM, coinciding with the nationwide outbreak of enteroviral D68 disease, reported in 2014. The Centers for Disease Control and Prevention has evaluated the cerebrospinal fluid in many of these cases, and no pathogen has consistently been detected. The children were mostly school age, aged 7-11 years, presented with acute, febrile respiratory illness followed by acute onset of cranial nerve dysfunction or flaccid paralysis of one or more limbs. The CSF revealed mild pleocytosis, most often with mild elevation of protein and a normal glucose. However, the MRI was distinctly abnormal with focal lesion in the cranial nerve nuclei (in those with bulbar dysfunction) and/or in the anterior horn or spinal cord gray matter. Long-term prognosis is unknown, although most patients have persistent weakness, despite some improvement, to date.
In 2016, the CDC has reported an increase in cases after a decline in 2015 despite the absence of epidemic respiratory tract disease in the United States from enterovirus D68. In the Netherlands, an increase in respiratory disease from enterovirus D68 in children and adults also has been reported since June 2016. Respiratory disease has been observed in children as young as 3 months of age, and most of the children have underlying comorbidity, many with asthma or other pulmonary conditions. Thirteen of 17 (77%) cases in children have required ICU admission, while most of the adult cases were mild and influenzalike. One child developed bulbar dysfunction and limb weakness.
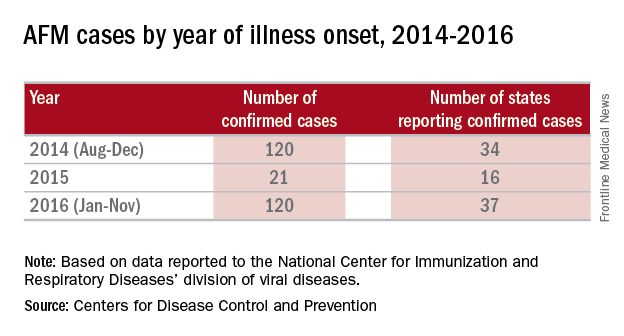
Enterovirus D68 infection should be suspected in children with moderate to severe respiratory tract infection or acute onset bulbar or flaccid paralysis of unknown etiology, especially in summer and fall. In such cases, respiratory specimens (nasopharyngeal or oral swabs or wash, tracheal secretions or bronchoalveolar lavage) should be obtained. Increasingly, hospitals and laboratories can perform multiplex polymerase chain reaction testing for enterovirus/rhinovirus. However, most do not determine the specific enterovirus. CDC and some state health departments use real-time reverse transcription polymerase chain reaction (rRT-PCR), which enables reporting of specific enterovirus species within days. CDC recommends that clinicians consider enterovirus D68 testing for children with unknown, severe respiratory illness or AFM. Details for sending specimens should be available from your state’s Department of Public Health website or the CDC.
Prevention strategies may be critical for limiting the spread of enterovirus D68 in the community. The CDC recommends:
- Wash your hands often with soap and water for 20 seconds.
- Avoid touching your eyes, nose and mouth with unwashed hands.
- Avoid close contact such as kissing, hugging, and sharing cups with people who are ill.
- Cover your coughs and sneezes with a tissue or shirt sleeve, not your hands.
- Clean and disinfect frequently touched surfaces, such as toys and doorknobs, especially if someone is sick.
- Stay home when you are ill.
In 2014, it was speculated that the epidemic might have been a one-time event. It now appears more likely that enterovirus D68 activity has been increasing since 2000, and that children and immunocompromised hosts will be at greatest risk because of a lack of neutralizing antibody. Ongoing enterovirus surveillance will be critical to understand the potential for severe respiratory disease as will the development of new and effective antivirals. A vaccine for enterovirus 71 recently demonstrated efficacy against hand, foot, and mouth disease in children and may provide insights into the development of vaccines against enterovirus D68.
References
Lancet Infect Dis. 2016 May;16(5):e64-75
Emerg Infect Dis. 2017 Jan;23(1):140-3.
J Med Virol. 2016 May;88(5):739-45
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. Dr. Pelton said he had no relevant financial disclosures. Email him at [email protected].
In August 2014, we first heard of increased pediatric cases of severe respiratory tract disease, many requiring management in the ICU, and of acute flaccid myelitis/paralysis (AFM) of unknown etiology from many states across the United States. Concurrently with this outbreak in the United States, similar clinical cases were reported in Canada and Europe. Subsequently, enterovirus D68 was confirmed in some, but not all, of the paralyzed children. Although new to many of us, enterovirus D68 was already known as an atypical enterovirus sharing many of its structural and chemical properties with rhinovirus. For example, it most often was reported from respiratory samples and less common from stool samples. It also had been associated with clusters of respiratory disease since 2000 and a 2008 case of fatal AFM.
There were 120 cases of AFM, coinciding with the nationwide outbreak of enteroviral D68 disease, reported in 2014. The Centers for Disease Control and Prevention has evaluated the cerebrospinal fluid in many of these cases, and no pathogen has consistently been detected. The children were mostly school age, aged 7-11 years, presented with acute, febrile respiratory illness followed by acute onset of cranial nerve dysfunction or flaccid paralysis of one or more limbs. The CSF revealed mild pleocytosis, most often with mild elevation of protein and a normal glucose. However, the MRI was distinctly abnormal with focal lesion in the cranial nerve nuclei (in those with bulbar dysfunction) and/or in the anterior horn or spinal cord gray matter. Long-term prognosis is unknown, although most patients have persistent weakness, despite some improvement, to date.
In 2016, the CDC has reported an increase in cases after a decline in 2015 despite the absence of epidemic respiratory tract disease in the United States from enterovirus D68. In the Netherlands, an increase in respiratory disease from enterovirus D68 in children and adults also has been reported since June 2016. Respiratory disease has been observed in children as young as 3 months of age, and most of the children have underlying comorbidity, many with asthma or other pulmonary conditions. Thirteen of 17 (77%) cases in children have required ICU admission, while most of the adult cases were mild and influenzalike. One child developed bulbar dysfunction and limb weakness.
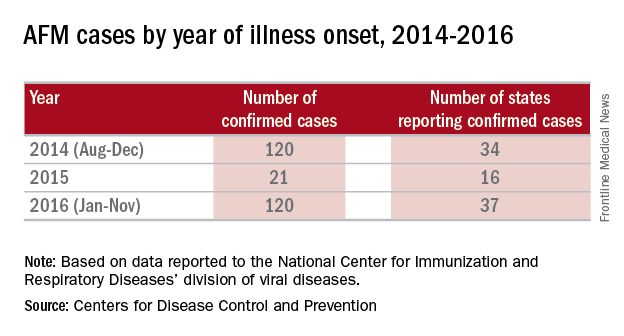
Enterovirus D68 infection should be suspected in children with moderate to severe respiratory tract infection or acute onset bulbar or flaccid paralysis of unknown etiology, especially in summer and fall. In such cases, respiratory specimens (nasopharyngeal or oral swabs or wash, tracheal secretions or bronchoalveolar lavage) should be obtained. Increasingly, hospitals and laboratories can perform multiplex polymerase chain reaction testing for enterovirus/rhinovirus. However, most do not determine the specific enterovirus. CDC and some state health departments use real-time reverse transcription polymerase chain reaction (rRT-PCR), which enables reporting of specific enterovirus species within days. CDC recommends that clinicians consider enterovirus D68 testing for children with unknown, severe respiratory illness or AFM. Details for sending specimens should be available from your state’s Department of Public Health website or the CDC.
Prevention strategies may be critical for limiting the spread of enterovirus D68 in the community. The CDC recommends:
- Wash your hands often with soap and water for 20 seconds.
- Avoid touching your eyes, nose and mouth with unwashed hands.
- Avoid close contact such as kissing, hugging, and sharing cups with people who are ill.
- Cover your coughs and sneezes with a tissue or shirt sleeve, not your hands.
- Clean and disinfect frequently touched surfaces, such as toys and doorknobs, especially if someone is sick.
- Stay home when you are ill.
In 2014, it was speculated that the epidemic might have been a one-time event. It now appears more likely that enterovirus D68 activity has been increasing since 2000, and that children and immunocompromised hosts will be at greatest risk because of a lack of neutralizing antibody. Ongoing enterovirus surveillance will be critical to understand the potential for severe respiratory disease as will the development of new and effective antivirals. A vaccine for enterovirus 71 recently demonstrated efficacy against hand, foot, and mouth disease in children and may provide insights into the development of vaccines against enterovirus D68.
References
Lancet Infect Dis. 2016 May;16(5):e64-75
Emerg Infect Dis. 2017 Jan;23(1):140-3.
J Med Virol. 2016 May;88(5):739-45
Dr. Pelton is chief of pediatric infectious disease and coordinator of the maternal-child HIV program at Boston Medical Center. Dr. Pelton said he had no relevant financial disclosures. Email him at [email protected].