User login
COMMENTARY—EXPEDITION3: A Winding Path to Nowhere
This new phase III trial of solanezumab reveals that the drug is not effective for patients with mild Alzheimer’s disease, despite the hint that it was possibly effective based on post hoc analyses of earlier studies with this drug.
The findings expose the hazards of such post hoc analyses, typically done when the desired results are not observed, in the hope of squeezing lemonade from lemons. Although the subanalysis of patients with mild Alzheimer’s disease in the earlier studies suggested a 34% slowing of cognitive decline, as assessed by ADAS-Cog, an incremental slowing of 11% was seen in the new study that was not even statistically significant. While some secondary end points reached statistical significance, the slowing was so modest as to make no practical difference clinically.
I cannot emphasize enough that such equivocal results as seen in EXPEDITION3 do absolutely nothing to either confirm or deny the amyloid hypothesis. By now, there have been so many of these studies with antiamyloid agents, with little or no hint of efficacy, that we have long passed the definition of insanity: doing the same thing over and over in the hope of getting a different result.
The combination of all these clinical trial failures with the result of imaging studies that have shown amyloid deposition some 20 years before the expected onset of symptoms clearly tells us that antiamyloid agents should only be considered as potential prophylactics. By the time symptoms appear, disease progression is largely independent of amyloid and may be primarily tau-driven, spreading from neuron to neuron even when amyloid is effectively targeted by therapeutics. Even the A4 and DIAN studies are likely initiating treatment too late to make anything more than a modest effect with little practical value clinically. I am not suggesting that we drop amyloid as a target, only that we stop making these incremental changes in clinical trial design in the hope of getting a different result.
—Michael S. Wolfe, PhD
Mathias P. Mertes Professor of Medicinal Chemistry
University of Kansas, Lawrence
This new phase III trial of solanezumab reveals that the drug is not effective for patients with mild Alzheimer’s disease, despite the hint that it was possibly effective based on post hoc analyses of earlier studies with this drug.
The findings expose the hazards of such post hoc analyses, typically done when the desired results are not observed, in the hope of squeezing lemonade from lemons. Although the subanalysis of patients with mild Alzheimer’s disease in the earlier studies suggested a 34% slowing of cognitive decline, as assessed by ADAS-Cog, an incremental slowing of 11% was seen in the new study that was not even statistically significant. While some secondary end points reached statistical significance, the slowing was so modest as to make no practical difference clinically.
I cannot emphasize enough that such equivocal results as seen in EXPEDITION3 do absolutely nothing to either confirm or deny the amyloid hypothesis. By now, there have been so many of these studies with antiamyloid agents, with little or no hint of efficacy, that we have long passed the definition of insanity: doing the same thing over and over in the hope of getting a different result.
The combination of all these clinical trial failures with the result of imaging studies that have shown amyloid deposition some 20 years before the expected onset of symptoms clearly tells us that antiamyloid agents should only be considered as potential prophylactics. By the time symptoms appear, disease progression is largely independent of amyloid and may be primarily tau-driven, spreading from neuron to neuron even when amyloid is effectively targeted by therapeutics. Even the A4 and DIAN studies are likely initiating treatment too late to make anything more than a modest effect with little practical value clinically. I am not suggesting that we drop amyloid as a target, only that we stop making these incremental changes in clinical trial design in the hope of getting a different result.
—Michael S. Wolfe, PhD
Mathias P. Mertes Professor of Medicinal Chemistry
University of Kansas, Lawrence
This new phase III trial of solanezumab reveals that the drug is not effective for patients with mild Alzheimer’s disease, despite the hint that it was possibly effective based on post hoc analyses of earlier studies with this drug.
The findings expose the hazards of such post hoc analyses, typically done when the desired results are not observed, in the hope of squeezing lemonade from lemons. Although the subanalysis of patients with mild Alzheimer’s disease in the earlier studies suggested a 34% slowing of cognitive decline, as assessed by ADAS-Cog, an incremental slowing of 11% was seen in the new study that was not even statistically significant. While some secondary end points reached statistical significance, the slowing was so modest as to make no practical difference clinically.
I cannot emphasize enough that such equivocal results as seen in EXPEDITION3 do absolutely nothing to either confirm or deny the amyloid hypothesis. By now, there have been so many of these studies with antiamyloid agents, with little or no hint of efficacy, that we have long passed the definition of insanity: doing the same thing over and over in the hope of getting a different result.
The combination of all these clinical trial failures with the result of imaging studies that have shown amyloid deposition some 20 years before the expected onset of symptoms clearly tells us that antiamyloid agents should only be considered as potential prophylactics. By the time symptoms appear, disease progression is largely independent of amyloid and may be primarily tau-driven, spreading from neuron to neuron even when amyloid is effectively targeted by therapeutics. Even the A4 and DIAN studies are likely initiating treatment too late to make anything more than a modest effect with little practical value clinically. I am not suggesting that we drop amyloid as a target, only that we stop making these incremental changes in clinical trial design in the hope of getting a different result.
—Michael S. Wolfe, PhD
Mathias P. Mertes Professor of Medicinal Chemistry
University of Kansas, Lawrence
Preventing surgical site infections in hysterectomy
Surgical site infections are a major source of patient morbidity. They are also an important quality metric for surgeons and hospital systems, and are increasingly being linked to reimbursement.
They occur in approximately 2% of the 600,000 women undergoing hysterectomy in the United States each year. The U.S. Centers for Disease Control and Prevention defines surgical site infection (SSI) as an infection that occurs within 30 days of a procedure in the part of the body where the surgery took place. Most SSIs are superficial incisional, but they also include deep incisional or organ or space infections.
Classification
The incidence of SSI varies according to the classification of the wound, as defined by the National Academy of Sciences.1 Most hysterectomies are classified as clean-contaminated wounds because they involve entry into the mucosa of the genitourinary tract. However, hysterectomy with contamination of bowel flora, or in the setting of acute infection (such as suppurative pelvic inflammatory disease) are considered a contaminated wound class, and are associated with even higher rates of SSI.
Risk factors
The risk factors associated with SSI are both modifiable and unmodifiable. Broadly speaking, they include increased risk to endogenous flora (e.g., wound classification), increased exposure to exogenous flora (e.g., inadequate protection of a wound from external pathogens), and impairment of the body’s immune mechanisms to prevent and overcome infection (e.g., hypothermia and hypoglycemia).
Unmodifiable risk factors include increasing age, a history of radiation exposure, vascular disease, and a history of prior SSIs. Modifiable risk factors include obesity, tobacco use, immunosuppressive medications, hypoalbuminemia, route of hysterectomy, hair removal, preoperative infections (such as bacterial vaginosis), surgical scrub, skin and vaginal preparation, antimicrobial prophylaxis (inappropriate choice or timing, inadequate dosing or redosing), operative time, blood transfusion, surgical skill, and operating room characteristics (ventilation, increased OR traffic, and sterilization of surgical equipment).
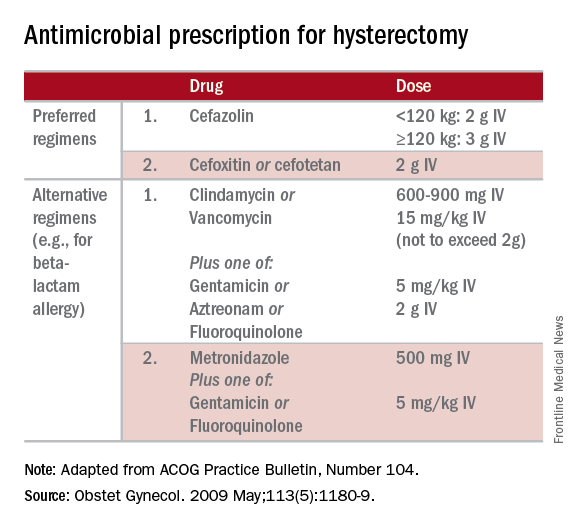
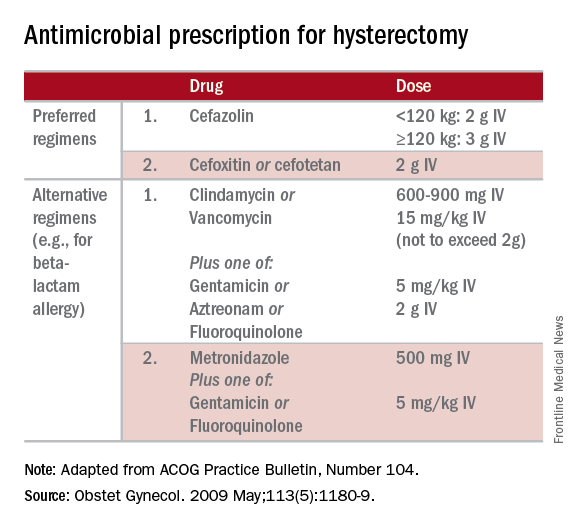
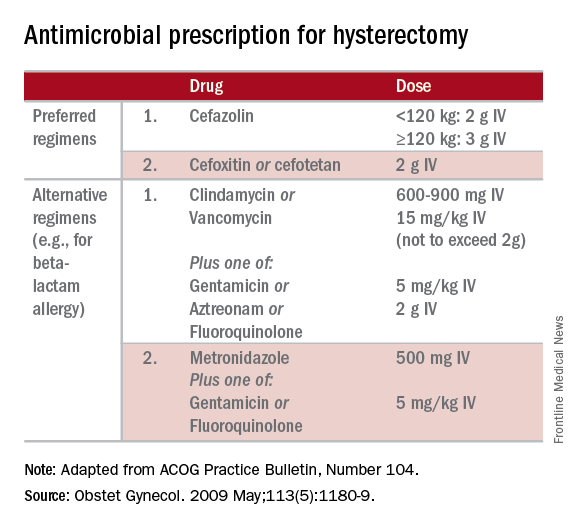
Antimicrobial prophylaxis
The CDC and the American College of Obstetricians and Gynecologists (ACOG) have provided clear guidelines regarding methods to reduce SSI in hysterectomy.3,4 There is strong evidence for using antimicrobial prophylaxis for hysterectomy.
It is important that physicians confirm the validity of beta-lactam allergies with patients because there are higher rates of SSI with the use of non–beta-lactam regimens, even those endorsed by the CDC and ACOG.5
Antibiotics should be administered within 1 hour of skin incision, and ideally within 30 minutes. They should be discontinued within 24 hours. Dosing should be adjusted to weight, and antimicrobials should be redosed for long procedures (at intervals of two half-lives), and for increased blood loss.
Skin preparation
Hair removal should be avoided unless necessary for technical reasons. If it is required, it should be performed outside of the operative space using clippers, not razors. For patients colonized with methicillin-resistant S. aureus, there is supporting evidence for pretreatment with mupirocin ointment to the nares, and chlorhexidine showers for 5-10 days. Patients who have bacterial vaginosis should be treated before surgery to decrease the rate of vaginal cuff SSI.
If there is a planned or potential gastrointestinal procedure as part of the hysterectomy, the surgeon should consider using an impervious plastic wound protector in place of, or in addition to, other retractors. Preoperative oral antimicrobials with mechanical bowel preparation have been associated with decreased SSIs; however, this benefit is not observed with mechanical bowel preparation alone.
Wound closure
Surgical technique and wound closure techniques also impact SSI. Minimally invasive and vaginal hysterectomy routes are preferred, as these are associated with the lowest rates of SSI. Antimicrobial-impregnated suture materials appear to be unnecessary. Surgeons should ensure that there is delicate handling of tissues and closure of dead spaces. If the subcutaneous fat space depth measures more than 2.5 cm, it should be reapproximated with a rapidly-absorbing suture material.
Use of electrosurgery versus a scalpel when creating the incision does not appear to influence infection rates, nor does use of staples versus subcuticular suture during closure.7
Using a dilute iodine lavage in the subcutaneous space, opening a sterile closing tray, and having surgeons change gloves prior to skin closure should be considered. The CDC recommends keeping the skin dressing in place for 24 hours postoperatively.
Other strategies
Hyperglycemia is associated with impaired neutrophil response, and therefore blood glucose should be controlled before surgery (hemoglobin A1c levels of less than 7% preoperatively) and immediately postoperatively (less than 180 mg/dL within 18-24 hours after the end of anesthesia).
It is also important to minimize perioperative hypothermia (less than 35.5° F), as this also impairs the body’s immune response. Keeping operative room ambient temperatures higher, minimizing incision size, warming CO2 gas in minimally invasive procedures, warming fluids, and using extrinsic body warmers can help achieve this.
Excessive blood loss should be minimized because blood transfusion is associated with impaired macrophage function and increased risk for SSI.
In addition to teamwide (including nonsurgeon) strict adherence to hand hygiene, OR personnel should avoid unnecessary operating room traffic. Hospital officials should ensure that the facility’s ventilator systems are well maintained and that there is care and maintenance of air handlers.
Many strategies can be employed perioperatively to decrease SSI rates for hysterectomy. We advocate for a protocol-based approach (known as “bundling” strategies) to achieve consistency of practice and to maximize surgeon and institutional improvements in SSI rates. This is similar to the approach outlined in a recent consensus statement from the Council on Patient Safety in Women’s Health Care.8
A comprehensive multidisciplinary approach throughout the perioperative period is necessary. It is imperative that good communication exist with patients regarding SSIs after hysterectomy and how patients, surgeons, and hospitals can together minimize the risks of SSIs.
References
1. Altemeier WA. “Manual on Control of Infection in Surgical Patients” (Philadelphia: Lippincott Williams & Wilkins, 1984).
2. Rev Infect Dis. 1991 Sep-Oct;13(Suppl 10):S821-41.
3. Infect Control Hosp Epidemiol. 2014 Jun;35(6):605-27.
4. Obstet Gynecol. 2009 May;113(5):1180-9.
5. Obstet Gynecol. 2016 Feb;127(2):321-9.
6. Am J Obstet Gynecol. 2005 Feb;192(2):422-5.
7. J Gastrointest Surg. 2016 Dec;20(12):2083-92.
8. Obstet Gynecol. 2016 Dec 7. doi: 10.1097/AOG.0000000000001751.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Jackson-Moore is an associate professor in gynecologic oncology at UNC. They reported having no relevant financial disclosures.
Surgical site infections are a major source of patient morbidity. They are also an important quality metric for surgeons and hospital systems, and are increasingly being linked to reimbursement.
They occur in approximately 2% of the 600,000 women undergoing hysterectomy in the United States each year. The U.S. Centers for Disease Control and Prevention defines surgical site infection (SSI) as an infection that occurs within 30 days of a procedure in the part of the body where the surgery took place. Most SSIs are superficial incisional, but they also include deep incisional or organ or space infections.
Classification
The incidence of SSI varies according to the classification of the wound, as defined by the National Academy of Sciences.1 Most hysterectomies are classified as clean-contaminated wounds because they involve entry into the mucosa of the genitourinary tract. However, hysterectomy with contamination of bowel flora, or in the setting of acute infection (such as suppurative pelvic inflammatory disease) are considered a contaminated wound class, and are associated with even higher rates of SSI.
Risk factors
The risk factors associated with SSI are both modifiable and unmodifiable. Broadly speaking, they include increased risk to endogenous flora (e.g., wound classification), increased exposure to exogenous flora (e.g., inadequate protection of a wound from external pathogens), and impairment of the body’s immune mechanisms to prevent and overcome infection (e.g., hypothermia and hypoglycemia).
Unmodifiable risk factors include increasing age, a history of radiation exposure, vascular disease, and a history of prior SSIs. Modifiable risk factors include obesity, tobacco use, immunosuppressive medications, hypoalbuminemia, route of hysterectomy, hair removal, preoperative infections (such as bacterial vaginosis), surgical scrub, skin and vaginal preparation, antimicrobial prophylaxis (inappropriate choice or timing, inadequate dosing or redosing), operative time, blood transfusion, surgical skill, and operating room characteristics (ventilation, increased OR traffic, and sterilization of surgical equipment).
Antimicrobial prophylaxis
The CDC and the American College of Obstetricians and Gynecologists (ACOG) have provided clear guidelines regarding methods to reduce SSI in hysterectomy.3,4 There is strong evidence for using antimicrobial prophylaxis for hysterectomy.
It is important that physicians confirm the validity of beta-lactam allergies with patients because there are higher rates of SSI with the use of non–beta-lactam regimens, even those endorsed by the CDC and ACOG.5
Antibiotics should be administered within 1 hour of skin incision, and ideally within 30 minutes. They should be discontinued within 24 hours. Dosing should be adjusted to weight, and antimicrobials should be redosed for long procedures (at intervals of two half-lives), and for increased blood loss.
Skin preparation
Hair removal should be avoided unless necessary for technical reasons. If it is required, it should be performed outside of the operative space using clippers, not razors. For patients colonized with methicillin-resistant S. aureus, there is supporting evidence for pretreatment with mupirocin ointment to the nares, and chlorhexidine showers for 5-10 days. Patients who have bacterial vaginosis should be treated before surgery to decrease the rate of vaginal cuff SSI.
If there is a planned or potential gastrointestinal procedure as part of the hysterectomy, the surgeon should consider using an impervious plastic wound protector in place of, or in addition to, other retractors. Preoperative oral antimicrobials with mechanical bowel preparation have been associated with decreased SSIs; however, this benefit is not observed with mechanical bowel preparation alone.
Wound closure
Surgical technique and wound closure techniques also impact SSI. Minimally invasive and vaginal hysterectomy routes are preferred, as these are associated with the lowest rates of SSI. Antimicrobial-impregnated suture materials appear to be unnecessary. Surgeons should ensure that there is delicate handling of tissues and closure of dead spaces. If the subcutaneous fat space depth measures more than 2.5 cm, it should be reapproximated with a rapidly-absorbing suture material.
Use of electrosurgery versus a scalpel when creating the incision does not appear to influence infection rates, nor does use of staples versus subcuticular suture during closure.7
Using a dilute iodine lavage in the subcutaneous space, opening a sterile closing tray, and having surgeons change gloves prior to skin closure should be considered. The CDC recommends keeping the skin dressing in place for 24 hours postoperatively.
Other strategies
Hyperglycemia is associated with impaired neutrophil response, and therefore blood glucose should be controlled before surgery (hemoglobin A1c levels of less than 7% preoperatively) and immediately postoperatively (less than 180 mg/dL within 18-24 hours after the end of anesthesia).
It is also important to minimize perioperative hypothermia (less than 35.5° F), as this also impairs the body’s immune response. Keeping operative room ambient temperatures higher, minimizing incision size, warming CO2 gas in minimally invasive procedures, warming fluids, and using extrinsic body warmers can help achieve this.
Excessive blood loss should be minimized because blood transfusion is associated with impaired macrophage function and increased risk for SSI.
In addition to teamwide (including nonsurgeon) strict adherence to hand hygiene, OR personnel should avoid unnecessary operating room traffic. Hospital officials should ensure that the facility’s ventilator systems are well maintained and that there is care and maintenance of air handlers.
Many strategies can be employed perioperatively to decrease SSI rates for hysterectomy. We advocate for a protocol-based approach (known as “bundling” strategies) to achieve consistency of practice and to maximize surgeon and institutional improvements in SSI rates. This is similar to the approach outlined in a recent consensus statement from the Council on Patient Safety in Women’s Health Care.8
A comprehensive multidisciplinary approach throughout the perioperative period is necessary. It is imperative that good communication exist with patients regarding SSIs after hysterectomy and how patients, surgeons, and hospitals can together minimize the risks of SSIs.
References
1. Altemeier WA. “Manual on Control of Infection in Surgical Patients” (Philadelphia: Lippincott Williams & Wilkins, 1984).
2. Rev Infect Dis. 1991 Sep-Oct;13(Suppl 10):S821-41.
3. Infect Control Hosp Epidemiol. 2014 Jun;35(6):605-27.
4. Obstet Gynecol. 2009 May;113(5):1180-9.
5. Obstet Gynecol. 2016 Feb;127(2):321-9.
6. Am J Obstet Gynecol. 2005 Feb;192(2):422-5.
7. J Gastrointest Surg. 2016 Dec;20(12):2083-92.
8. Obstet Gynecol. 2016 Dec 7. doi: 10.1097/AOG.0000000000001751.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Jackson-Moore is an associate professor in gynecologic oncology at UNC. They reported having no relevant financial disclosures.
Surgical site infections are a major source of patient morbidity. They are also an important quality metric for surgeons and hospital systems, and are increasingly being linked to reimbursement.
They occur in approximately 2% of the 600,000 women undergoing hysterectomy in the United States each year. The U.S. Centers for Disease Control and Prevention defines surgical site infection (SSI) as an infection that occurs within 30 days of a procedure in the part of the body where the surgery took place. Most SSIs are superficial incisional, but they also include deep incisional or organ or space infections.
Classification
The incidence of SSI varies according to the classification of the wound, as defined by the National Academy of Sciences.1 Most hysterectomies are classified as clean-contaminated wounds because they involve entry into the mucosa of the genitourinary tract. However, hysterectomy with contamination of bowel flora, or in the setting of acute infection (such as suppurative pelvic inflammatory disease) are considered a contaminated wound class, and are associated with even higher rates of SSI.
Risk factors
The risk factors associated with SSI are both modifiable and unmodifiable. Broadly speaking, they include increased risk to endogenous flora (e.g., wound classification), increased exposure to exogenous flora (e.g., inadequate protection of a wound from external pathogens), and impairment of the body’s immune mechanisms to prevent and overcome infection (e.g., hypothermia and hypoglycemia).
Unmodifiable risk factors include increasing age, a history of radiation exposure, vascular disease, and a history of prior SSIs. Modifiable risk factors include obesity, tobacco use, immunosuppressive medications, hypoalbuminemia, route of hysterectomy, hair removal, preoperative infections (such as bacterial vaginosis), surgical scrub, skin and vaginal preparation, antimicrobial prophylaxis (inappropriate choice or timing, inadequate dosing or redosing), operative time, blood transfusion, surgical skill, and operating room characteristics (ventilation, increased OR traffic, and sterilization of surgical equipment).
Antimicrobial prophylaxis
The CDC and the American College of Obstetricians and Gynecologists (ACOG) have provided clear guidelines regarding methods to reduce SSI in hysterectomy.3,4 There is strong evidence for using antimicrobial prophylaxis for hysterectomy.
It is important that physicians confirm the validity of beta-lactam allergies with patients because there are higher rates of SSI with the use of non–beta-lactam regimens, even those endorsed by the CDC and ACOG.5
Antibiotics should be administered within 1 hour of skin incision, and ideally within 30 minutes. They should be discontinued within 24 hours. Dosing should be adjusted to weight, and antimicrobials should be redosed for long procedures (at intervals of two half-lives), and for increased blood loss.
Skin preparation
Hair removal should be avoided unless necessary for technical reasons. If it is required, it should be performed outside of the operative space using clippers, not razors. For patients colonized with methicillin-resistant S. aureus, there is supporting evidence for pretreatment with mupirocin ointment to the nares, and chlorhexidine showers for 5-10 days. Patients who have bacterial vaginosis should be treated before surgery to decrease the rate of vaginal cuff SSI.
If there is a planned or potential gastrointestinal procedure as part of the hysterectomy, the surgeon should consider using an impervious plastic wound protector in place of, or in addition to, other retractors. Preoperative oral antimicrobials with mechanical bowel preparation have been associated with decreased SSIs; however, this benefit is not observed with mechanical bowel preparation alone.
Wound closure
Surgical technique and wound closure techniques also impact SSI. Minimally invasive and vaginal hysterectomy routes are preferred, as these are associated with the lowest rates of SSI. Antimicrobial-impregnated suture materials appear to be unnecessary. Surgeons should ensure that there is delicate handling of tissues and closure of dead spaces. If the subcutaneous fat space depth measures more than 2.5 cm, it should be reapproximated with a rapidly-absorbing suture material.
Use of electrosurgery versus a scalpel when creating the incision does not appear to influence infection rates, nor does use of staples versus subcuticular suture during closure.7
Using a dilute iodine lavage in the subcutaneous space, opening a sterile closing tray, and having surgeons change gloves prior to skin closure should be considered. The CDC recommends keeping the skin dressing in place for 24 hours postoperatively.
Other strategies
Hyperglycemia is associated with impaired neutrophil response, and therefore blood glucose should be controlled before surgery (hemoglobin A1c levels of less than 7% preoperatively) and immediately postoperatively (less than 180 mg/dL within 18-24 hours after the end of anesthesia).
It is also important to minimize perioperative hypothermia (less than 35.5° F), as this also impairs the body’s immune response. Keeping operative room ambient temperatures higher, minimizing incision size, warming CO2 gas in minimally invasive procedures, warming fluids, and using extrinsic body warmers can help achieve this.
Excessive blood loss should be minimized because blood transfusion is associated with impaired macrophage function and increased risk for SSI.
In addition to teamwide (including nonsurgeon) strict adherence to hand hygiene, OR personnel should avoid unnecessary operating room traffic. Hospital officials should ensure that the facility’s ventilator systems are well maintained and that there is care and maintenance of air handlers.
Many strategies can be employed perioperatively to decrease SSI rates for hysterectomy. We advocate for a protocol-based approach (known as “bundling” strategies) to achieve consistency of practice and to maximize surgeon and institutional improvements in SSI rates. This is similar to the approach outlined in a recent consensus statement from the Council on Patient Safety in Women’s Health Care.8
A comprehensive multidisciplinary approach throughout the perioperative period is necessary. It is imperative that good communication exist with patients regarding SSIs after hysterectomy and how patients, surgeons, and hospitals can together minimize the risks of SSIs.
References
1. Altemeier WA. “Manual on Control of Infection in Surgical Patients” (Philadelphia: Lippincott Williams & Wilkins, 1984).
2. Rev Infect Dis. 1991 Sep-Oct;13(Suppl 10):S821-41.
3. Infect Control Hosp Epidemiol. 2014 Jun;35(6):605-27.
4. Obstet Gynecol. 2009 May;113(5):1180-9.
5. Obstet Gynecol. 2016 Feb;127(2):321-9.
6. Am J Obstet Gynecol. 2005 Feb;192(2):422-5.
7. J Gastrointest Surg. 2016 Dec;20(12):2083-92.
8. Obstet Gynecol. 2016 Dec 7. doi: 10.1097/AOG.0000000000001751.
Dr. Rossi is an assistant professor in the division of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Jackson-Moore is an associate professor in gynecologic oncology at UNC. They reported having no relevant financial disclosures.
Letters to the Editor: Benefit of self-administered vaginal lidocaine gel in IUD placement
“BENEFIT OF SELF-ADMINISTERED VAGINAL LIDOCAINE GEL IN IUD PLACEMENT"
ANDREW M. KAUNITZ, MD (COMMENTARY; DECEMBER 2016)
Use anesthesia for in-office GYN procedures
The recent article by Dr. Kaunitz on the use of self-administered lidocaine gel prior to intrauterine device (IUD) placement was excellent. Having been known as the “lidocaine queen” in the Department of ObGyn at the Mayo Clinic, I feel strongly that gynecologic office procedures should always involve some form of anesthesia, whether with topical lidocaine, intracervical lidocaine, or paracervical block. Such anesthesia often makes the procedure a “nonevent” for the patient. While Dr. Kaunitz describes the use of a fine-toothed tenaculum, I have found that after administration of lidocaine gel, an Allis clamp applied superficially to the cervix provides sufficient traction, is often not detected by the patient, and does not leave any holes. It is unusual for it to slip off.
It is important to teach residents that it is not necessary for women to “tolerate” pain to have good health. I use the above techniques for endometrial biopsy and cervical biopsy as well—there is never a reason for a woman’s biopsy to be done without anesthesia.
Ingrid Carlson, MD
Ponte Vedra, Florida
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“BENEFIT OF SELF-ADMINISTERED VAGINAL LIDOCAINE GEL IN IUD PLACEMENT"
ANDREW M. KAUNITZ, MD (COMMENTARY; DECEMBER 2016)
Use anesthesia for in-office GYN procedures
The recent article by Dr. Kaunitz on the use of self-administered lidocaine gel prior to intrauterine device (IUD) placement was excellent. Having been known as the “lidocaine queen” in the Department of ObGyn at the Mayo Clinic, I feel strongly that gynecologic office procedures should always involve some form of anesthesia, whether with topical lidocaine, intracervical lidocaine, or paracervical block. Such anesthesia often makes the procedure a “nonevent” for the patient. While Dr. Kaunitz describes the use of a fine-toothed tenaculum, I have found that after administration of lidocaine gel, an Allis clamp applied superficially to the cervix provides sufficient traction, is often not detected by the patient, and does not leave any holes. It is unusual for it to slip off.
It is important to teach residents that it is not necessary for women to “tolerate” pain to have good health. I use the above techniques for endometrial biopsy and cervical biopsy as well—there is never a reason for a woman’s biopsy to be done without anesthesia.
Ingrid Carlson, MD
Ponte Vedra, Florida
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“BENEFIT OF SELF-ADMINISTERED VAGINAL LIDOCAINE GEL IN IUD PLACEMENT"
ANDREW M. KAUNITZ, MD (COMMENTARY; DECEMBER 2016)
Use anesthesia for in-office GYN procedures
The recent article by Dr. Kaunitz on the use of self-administered lidocaine gel prior to intrauterine device (IUD) placement was excellent. Having been known as the “lidocaine queen” in the Department of ObGyn at the Mayo Clinic, I feel strongly that gynecologic office procedures should always involve some form of anesthesia, whether with topical lidocaine, intracervical lidocaine, or paracervical block. Such anesthesia often makes the procedure a “nonevent” for the patient. While Dr. Kaunitz describes the use of a fine-toothed tenaculum, I have found that after administration of lidocaine gel, an Allis clamp applied superficially to the cervix provides sufficient traction, is often not detected by the patient, and does not leave any holes. It is unusual for it to slip off.
It is important to teach residents that it is not necessary for women to “tolerate” pain to have good health. I use the above techniques for endometrial biopsy and cervical biopsy as well—there is never a reason for a woman’s biopsy to be done without anesthesia.
Ingrid Carlson, MD
Ponte Vedra, Florida
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Letters to the Editor: Avoid uterine vessels when injecting vasopressin
“DO YOU UTILIZE VASOPRESSIN IN YOUR DIFFICULT CESAREAN DELIVERY SURGERIES?”
ROBERT L. BARBIERI, MD (EDITORIAL; NOVEMBER 2016)
Avoid uterine vessels when injecting vasopressin
Thank you for your recent editorial discussing using vasopressin in difficult cesarean deliveries. I am very interested in using vasopressin for our placenta previa cases.
I reviewed the Kato et al article that Dr. Barbieri referenced, and the authors note a risk of injecting vasopressin into a vessel.1 If you are injecting into the placental bed, how can you confirm you are not in a vessel? (When you withdraw, you will get some blood regardless.)
Sara Garmel, MD
Dearborn, Michigan
REFERENCE
- Kato S, Tanabe A, Kanki K, et al. Local injection of vasopressin reduces the blood loss during cesarean section in placenta previa. J Obstet Gynaecol Res. 2014;40(5):1249–1256.
Dr. Barbieri responds
I agree with Dr. Garmel that we should avoid the intravascular injection of vasopressin. As I noted in the editorial, “I prefer to inject vasopressin in the subserosa of the uterus rather than inject it in a highly vascular area such as the subendometrium or near the uterine artery and vein.” Subserosal injection creates a depot bleb of vasopressin that is absorbed over a few minutes. You can visualize the reduced blood flow to the uterus following vasopressin injection because the uterus blanches and the diameter of the uterine vessels decreases significantly.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“DO YOU UTILIZE VASOPRESSIN IN YOUR DIFFICULT CESAREAN DELIVERY SURGERIES?”
ROBERT L. BARBIERI, MD (EDITORIAL; NOVEMBER 2016)
Avoid uterine vessels when injecting vasopressin
Thank you for your recent editorial discussing using vasopressin in difficult cesarean deliveries. I am very interested in using vasopressin for our placenta previa cases.
I reviewed the Kato et al article that Dr. Barbieri referenced, and the authors note a risk of injecting vasopressin into a vessel.1 If you are injecting into the placental bed, how can you confirm you are not in a vessel? (When you withdraw, you will get some blood regardless.)
Sara Garmel, MD
Dearborn, Michigan
REFERENCE
- Kato S, Tanabe A, Kanki K, et al. Local injection of vasopressin reduces the blood loss during cesarean section in placenta previa. J Obstet Gynaecol Res. 2014;40(5):1249–1256.
Dr. Barbieri responds
I agree with Dr. Garmel that we should avoid the intravascular injection of vasopressin. As I noted in the editorial, “I prefer to inject vasopressin in the subserosa of the uterus rather than inject it in a highly vascular area such as the subendometrium or near the uterine artery and vein.” Subserosal injection creates a depot bleb of vasopressin that is absorbed over a few minutes. You can visualize the reduced blood flow to the uterus following vasopressin injection because the uterus blanches and the diameter of the uterine vessels decreases significantly.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“DO YOU UTILIZE VASOPRESSIN IN YOUR DIFFICULT CESAREAN DELIVERY SURGERIES?”
ROBERT L. BARBIERI, MD (EDITORIAL; NOVEMBER 2016)
Avoid uterine vessels when injecting vasopressin
Thank you for your recent editorial discussing using vasopressin in difficult cesarean deliveries. I am very interested in using vasopressin for our placenta previa cases.
I reviewed the Kato et al article that Dr. Barbieri referenced, and the authors note a risk of injecting vasopressin into a vessel.1 If you are injecting into the placental bed, how can you confirm you are not in a vessel? (When you withdraw, you will get some blood regardless.)
Sara Garmel, MD
Dearborn, Michigan
REFERENCE
- Kato S, Tanabe A, Kanki K, et al. Local injection of vasopressin reduces the blood loss during cesarean section in placenta previa. J Obstet Gynaecol Res. 2014;40(5):1249–1256.
Dr. Barbieri responds
I agree with Dr. Garmel that we should avoid the intravascular injection of vasopressin. As I noted in the editorial, “I prefer to inject vasopressin in the subserosa of the uterus rather than inject it in a highly vascular area such as the subendometrium or near the uterine artery and vein.” Subserosal injection creates a depot bleb of vasopressin that is absorbed over a few minutes. You can visualize the reduced blood flow to the uterus following vasopressin injection because the uterus blanches and the diameter of the uterine vessels decreases significantly.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Letters to the Editor: Patient with a breast mass: Why did she pursue litigation?
“PATIENT WITH A BREAST MASS: WHY DID SHE PURSUE LITIGATION?”
JOSEPH S. SANFILIPPO, MD, MBA, AND STEVEN R. SMITH, JD (WHAT'S THE VERDICT?; DECEMBER 2016)
Clear communication is often key to avoiding litigation
Thank you for the article concerning the patient who commenced action for delay in diagnosis of her breast lesion. In my opinion the gynecologist lost control of the situation because of inadequate communication with the patient either on his or her part and/or on the part of the staff.
J. S. Calabrese, MD, JD
Buffalo, New York
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“PATIENT WITH A BREAST MASS: WHY DID SHE PURSUE LITIGATION?”
JOSEPH S. SANFILIPPO, MD, MBA, AND STEVEN R. SMITH, JD (WHAT'S THE VERDICT?; DECEMBER 2016)
Clear communication is often key to avoiding litigation
Thank you for the article concerning the patient who commenced action for delay in diagnosis of her breast lesion. In my opinion the gynecologist lost control of the situation because of inadequate communication with the patient either on his or her part and/or on the part of the staff.
J. S. Calabrese, MD, JD
Buffalo, New York
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
“PATIENT WITH A BREAST MASS: WHY DID SHE PURSUE LITIGATION?”
JOSEPH S. SANFILIPPO, MD, MBA, AND STEVEN R. SMITH, JD (WHAT'S THE VERDICT?; DECEMBER 2016)
Clear communication is often key to avoiding litigation
Thank you for the article concerning the patient who commenced action for delay in diagnosis of her breast lesion. In my opinion the gynecologist lost control of the situation because of inadequate communication with the patient either on his or her part and/or on the part of the staff.
J. S. Calabrese, MD, JD
Buffalo, New York
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Point/Counterpoint: Is limb salvage always best in diabetes?
Salvage limbs at all costs
Aggressive limb salvage in people with diabetes leads to an overall reduction in cost not only economically, but also from the patient’s perspective. The vast majority of diabetic patients with critical ischemia are actually good candidates for limb salvage. Tragically, many of these patients are never referred for evaluation for limb salvage because of misconceptions about the pathophysiology of the disease.
An argument against limb salvage is that primary amputation prevents or shortens the course of wound care and enables patients to become ambulatory, albeit with a prosthesis, faster. However, in the modern era of vascular surgery, revascularization can be performed successfully with minimal mortality and excellent rates of limb salvage, especially when it’s done within a team-based approach.
The mortality in primary amputation is shockingly high, anywhere from 5% to 23% higher than revascularization alone, and the major complication rate of amputation associated with diabetes is also unacceptably high – up to 37%. This is in contrast to a 17% rate in major nonamputation vascular surgery and 1%-5% in endovascular procedures (BMC Nephrol. 2005;6:3).
We can’t ignore the economic burden this places on the country. In 2014, primary amputations cost the health care system $11 billion annually, and that is expected to grow to more than $25 billion in the next several years, according to the SAGE Group. It’s important to keep in mind that Medicare covers over 80% of this cost.
A number of studies have shown that conservative management with wound care and amputation is more cost effective than primary amputation in ambulatory, independent adults. Data can be difficult to interpret because of different recording strategies for all the costs associated with amputation, but a single-institution study concluded that revascularization costs almost $5,280 more than expectant management, but $33,900 less than primary amputation alone (Cardiovasc Surg. 1999;7;62-9).
We must also consider the costs of revision after primary amputation; above-the-knee amputation has a 12% in-hospital revision rate, and below-the-knee amputation about 20%. Endovascular interventions, on the other hand, have a 1%-9% in-hospital revision rate, and only 2%-4% of these patients will go on to require an amputation during the same admission (Eur J Vasc Endovasc Surg. 2006;32:484-90; Arch Phys Med Rehabil. 2005;86:480-6).This does not include the costs of those complications as well as other indirect costs of amputation, such as nursing home care and living situation modification (Int J Behav Med. 2016;23:714-21; Pak J Med Sci. 2014; 30:1044-9). They quickly add up to that $25 billion.
The proponents of primary amputation tell us that it leads to quicker recovery time and an earlier time to ambulation. However, only 47% of patients will actually ambulate after amputation, in contrast to 97% who will ambulate after limb salvage as a primary procedure. In a nonambulatory cohort, 21% of those patients go on to regain functional status that was lost prior to surgery (J Vasc Surg. 1997;25;287-95).
Many question if our success with vascular surgery over the past few decades can translate to helping the most difficult subset of patients. An Italian study reported on a cohort of diabetic vs. nondiabetic patients and determined both groups have similar amputation-free rates after infrainguinal arterial reconstruction for critical limb ischemia, with excellent primary and secondary patency rates and a limb salvage rate of 88% at 5 years (J Vasc Surg. 2014;59:708-19). This tells us that we do have the skill set necessary to save these limbs.
A multidisciplinary limb preservation team is paramount to the success of any limb salvage program. A revascularization team should be in place which uses early intervention to achieve the highest limb salvage rates possible. Wound care needs to be an integrated part of it. Advanced podiatric reconstructive surgery also is key because this can provide complex foot reconstructions and help ambulatory patients return home.
Dr. Trissa A. Babrowski is an assistant professor of surgery, specializing in vascular surgery and endovascular therapy, at the University of Chicago Heart and Vascular Center. She had no financial relationships to disclose.
Primary amputation can be OK
I am not an amputationalist. I do practice limb salvage. In fact I’m probably the most aggressive limb salvage surgeon in my hospital. But primary amputation is a completely acceptable option for a selected group of patients with diabetes. We should not try to do limb salvage “at all costs.”
I do not find this to be a contradictory position. In fact, I think it adds credence to my support of limb salvage that I think primary amputation can be OK. In all honesty, there are very few things in life that should be done at all costs.
A study out of Loma Linda University involving patients with CLI compared primary amputation vs. revascularization; 43% of patients had a primary amputation (Ann Vasc Surg. 2007;21:458-63). A multivariate analysis showed that patients with major tissue loss, end-stage renal disease (ESRD), diabetes and nonambulatory status were more likely to undergo primary amputation rather than revascularization.
While major tissue loss (Rutherford category 6) is certainly an indication for primary amputation, ambulatory status can represent a gray area in determining the best course. ESRD and diabetes are much more nonspecific factors; probably more than 10% of the patients that we see with CLI have ESRD. Also, 50%-70% of these patients with CLI, and in some series even higher percentages, have diabetes. Thus, these factors by themselves do not assist us in determining which patients potentially should be offered primary amputation vs. revascularization.
In general, we know that we can get good results in limb bypass or revascularization in patients with CLI: The PREVENT III multicenter trial, with the use of the vein as the conduit, showed 1-year limb salvage rates of 88% in these high-risk patients (J Vasc Surg. 2006;43:742-51). However, one of the major risk factors that adversely affected outcome was ESRD.
We know that ESRD is a significant predictor of lowering our chances of saving a limb successfully. Knowing the cost of multiple continued episodes of revascularization in these patients prior to proceeding with an amputation, it’s intuitive that these patients would benefit from a more precise process in their treatment from the beginning. A number of papers have concluded that a primary amputation may be the preferred approach in patients with ESRD.
Can we preoperatively predict which patients with CLI will fail operative revascularization? Data from the New England Vascular Quality Initiative identified eight variables associated with failure of revascularization, among them age younger than 59, ESRD, diabetes, CLI, conduit requiring venovenostomy, tarsal target, and nursing home residence (Ann Vasc Surg. 2010;24:57-68). The presence of three or more risk factors has a 27.7% risk of limb loss and/or graft thrombosis within 1 year.
Postponing amputation is a major cost issue. Direct costs of bypass for critical limb ischemia were $3.6 billion in 2004 (J Vasc Surg. 2011;54:1021-31), and we know that a functional outcome can be problematic in this patient group. Factors associated with a poor functional outcome include dementia, dependent-living situation preoperatively and nonambulatory status.
Unfortunately, there are not a lot of data that deal with quality of life outcomes for patients with CLI who have undergone bypass. Using a point system comprised of dialysis (4 points), tissue loss (3 points), age above 75 (2 points), hematocrit less than or equal to 30 (2 points), and coronary artery disease (1 point), a follow-up study of patients in the PREVENT III trial found that a high-risk group (greater than or equal to 8 points) had an amputation-free survival of only 45% (J Vasc Surg. 2009;50:769-75). Again, these results do not justify the effort and costs of limb salvage in this high-risk patient group.
We should consider the following options carefully in selecting a cost-effective patient-focused approach in patients with CLI: wound care, primary amputation, bypass revascularization, or endovascular revascularization. I would argue that the vascular surgeon who is qualified as an expert in all of the above is best positioned to select an appropriate plan of treatment based upon the patient’s risk factors, wound factors, ambulatory ability, pattern of disease, severity of ischemia, and living status.
Thus, upon presentation, a patient with CLI should undergo confirmatory tests and optimize his or her risk factors. The vascular surgeon then has the option, in discussion with the patient and family, to pursue an appropriate treatment plan inclusive of primary amputation – not one of limb salvage “at all costs.”
Primary amputation should be used in situations where there is dementia and nonambulatory status, and in patients who are poor candidates for revascularization because of high risk of failure and limited life expectancy. The recently developed WIfI (wound, ischemia, and foot infection) classification can also be utilized, as stage 4 WIfI classification is associated with high risk of limb loss – 38%-40% at 1 year.
Primary amputation is an option that can result in better care overall, and it is a cost-effective approach for a selected group of patients. We should not try to do limb salvage at all cost. Primary amputation, in selected patients, is OK.
Dr. Timothy J. Nypaver is head of vascular surgery at Henry Ford Hospital, Detroit. He had no financial relationships to disclose.
Salvage limbs at all costs
Aggressive limb salvage in people with diabetes leads to an overall reduction in cost not only economically, but also from the patient’s perspective. The vast majority of diabetic patients with critical ischemia are actually good candidates for limb salvage. Tragically, many of these patients are never referred for evaluation for limb salvage because of misconceptions about the pathophysiology of the disease.
An argument against limb salvage is that primary amputation prevents or shortens the course of wound care and enables patients to become ambulatory, albeit with a prosthesis, faster. However, in the modern era of vascular surgery, revascularization can be performed successfully with minimal mortality and excellent rates of limb salvage, especially when it’s done within a team-based approach.
The mortality in primary amputation is shockingly high, anywhere from 5% to 23% higher than revascularization alone, and the major complication rate of amputation associated with diabetes is also unacceptably high – up to 37%. This is in contrast to a 17% rate in major nonamputation vascular surgery and 1%-5% in endovascular procedures (BMC Nephrol. 2005;6:3).
We can’t ignore the economic burden this places on the country. In 2014, primary amputations cost the health care system $11 billion annually, and that is expected to grow to more than $25 billion in the next several years, according to the SAGE Group. It’s important to keep in mind that Medicare covers over 80% of this cost.
A number of studies have shown that conservative management with wound care and amputation is more cost effective than primary amputation in ambulatory, independent adults. Data can be difficult to interpret because of different recording strategies for all the costs associated with amputation, but a single-institution study concluded that revascularization costs almost $5,280 more than expectant management, but $33,900 less than primary amputation alone (Cardiovasc Surg. 1999;7;62-9).
We must also consider the costs of revision after primary amputation; above-the-knee amputation has a 12% in-hospital revision rate, and below-the-knee amputation about 20%. Endovascular interventions, on the other hand, have a 1%-9% in-hospital revision rate, and only 2%-4% of these patients will go on to require an amputation during the same admission (Eur J Vasc Endovasc Surg. 2006;32:484-90; Arch Phys Med Rehabil. 2005;86:480-6).This does not include the costs of those complications as well as other indirect costs of amputation, such as nursing home care and living situation modification (Int J Behav Med. 2016;23:714-21; Pak J Med Sci. 2014; 30:1044-9). They quickly add up to that $25 billion.
The proponents of primary amputation tell us that it leads to quicker recovery time and an earlier time to ambulation. However, only 47% of patients will actually ambulate after amputation, in contrast to 97% who will ambulate after limb salvage as a primary procedure. In a nonambulatory cohort, 21% of those patients go on to regain functional status that was lost prior to surgery (J Vasc Surg. 1997;25;287-95).
Many question if our success with vascular surgery over the past few decades can translate to helping the most difficult subset of patients. An Italian study reported on a cohort of diabetic vs. nondiabetic patients and determined both groups have similar amputation-free rates after infrainguinal arterial reconstruction for critical limb ischemia, with excellent primary and secondary patency rates and a limb salvage rate of 88% at 5 years (J Vasc Surg. 2014;59:708-19). This tells us that we do have the skill set necessary to save these limbs.
A multidisciplinary limb preservation team is paramount to the success of any limb salvage program. A revascularization team should be in place which uses early intervention to achieve the highest limb salvage rates possible. Wound care needs to be an integrated part of it. Advanced podiatric reconstructive surgery also is key because this can provide complex foot reconstructions and help ambulatory patients return home.
Dr. Trissa A. Babrowski is an assistant professor of surgery, specializing in vascular surgery and endovascular therapy, at the University of Chicago Heart and Vascular Center. She had no financial relationships to disclose.
Primary amputation can be OK
I am not an amputationalist. I do practice limb salvage. In fact I’m probably the most aggressive limb salvage surgeon in my hospital. But primary amputation is a completely acceptable option for a selected group of patients with diabetes. We should not try to do limb salvage “at all costs.”
I do not find this to be a contradictory position. In fact, I think it adds credence to my support of limb salvage that I think primary amputation can be OK. In all honesty, there are very few things in life that should be done at all costs.
A study out of Loma Linda University involving patients with CLI compared primary amputation vs. revascularization; 43% of patients had a primary amputation (Ann Vasc Surg. 2007;21:458-63). A multivariate analysis showed that patients with major tissue loss, end-stage renal disease (ESRD), diabetes and nonambulatory status were more likely to undergo primary amputation rather than revascularization.
While major tissue loss (Rutherford category 6) is certainly an indication for primary amputation, ambulatory status can represent a gray area in determining the best course. ESRD and diabetes are much more nonspecific factors; probably more than 10% of the patients that we see with CLI have ESRD. Also, 50%-70% of these patients with CLI, and in some series even higher percentages, have diabetes. Thus, these factors by themselves do not assist us in determining which patients potentially should be offered primary amputation vs. revascularization.
In general, we know that we can get good results in limb bypass or revascularization in patients with CLI: The PREVENT III multicenter trial, with the use of the vein as the conduit, showed 1-year limb salvage rates of 88% in these high-risk patients (J Vasc Surg. 2006;43:742-51). However, one of the major risk factors that adversely affected outcome was ESRD.
We know that ESRD is a significant predictor of lowering our chances of saving a limb successfully. Knowing the cost of multiple continued episodes of revascularization in these patients prior to proceeding with an amputation, it’s intuitive that these patients would benefit from a more precise process in their treatment from the beginning. A number of papers have concluded that a primary amputation may be the preferred approach in patients with ESRD.
Can we preoperatively predict which patients with CLI will fail operative revascularization? Data from the New England Vascular Quality Initiative identified eight variables associated with failure of revascularization, among them age younger than 59, ESRD, diabetes, CLI, conduit requiring venovenostomy, tarsal target, and nursing home residence (Ann Vasc Surg. 2010;24:57-68). The presence of three or more risk factors has a 27.7% risk of limb loss and/or graft thrombosis within 1 year.
Postponing amputation is a major cost issue. Direct costs of bypass for critical limb ischemia were $3.6 billion in 2004 (J Vasc Surg. 2011;54:1021-31), and we know that a functional outcome can be problematic in this patient group. Factors associated with a poor functional outcome include dementia, dependent-living situation preoperatively and nonambulatory status.
Unfortunately, there are not a lot of data that deal with quality of life outcomes for patients with CLI who have undergone bypass. Using a point system comprised of dialysis (4 points), tissue loss (3 points), age above 75 (2 points), hematocrit less than or equal to 30 (2 points), and coronary artery disease (1 point), a follow-up study of patients in the PREVENT III trial found that a high-risk group (greater than or equal to 8 points) had an amputation-free survival of only 45% (J Vasc Surg. 2009;50:769-75). Again, these results do not justify the effort and costs of limb salvage in this high-risk patient group.
We should consider the following options carefully in selecting a cost-effective patient-focused approach in patients with CLI: wound care, primary amputation, bypass revascularization, or endovascular revascularization. I would argue that the vascular surgeon who is qualified as an expert in all of the above is best positioned to select an appropriate plan of treatment based upon the patient’s risk factors, wound factors, ambulatory ability, pattern of disease, severity of ischemia, and living status.
Thus, upon presentation, a patient with CLI should undergo confirmatory tests and optimize his or her risk factors. The vascular surgeon then has the option, in discussion with the patient and family, to pursue an appropriate treatment plan inclusive of primary amputation – not one of limb salvage “at all costs.”
Primary amputation should be used in situations where there is dementia and nonambulatory status, and in patients who are poor candidates for revascularization because of high risk of failure and limited life expectancy. The recently developed WIfI (wound, ischemia, and foot infection) classification can also be utilized, as stage 4 WIfI classification is associated with high risk of limb loss – 38%-40% at 1 year.
Primary amputation is an option that can result in better care overall, and it is a cost-effective approach for a selected group of patients. We should not try to do limb salvage at all cost. Primary amputation, in selected patients, is OK.
Dr. Timothy J. Nypaver is head of vascular surgery at Henry Ford Hospital, Detroit. He had no financial relationships to disclose.
Salvage limbs at all costs
Aggressive limb salvage in people with diabetes leads to an overall reduction in cost not only economically, but also from the patient’s perspective. The vast majority of diabetic patients with critical ischemia are actually good candidates for limb salvage. Tragically, many of these patients are never referred for evaluation for limb salvage because of misconceptions about the pathophysiology of the disease.
An argument against limb salvage is that primary amputation prevents or shortens the course of wound care and enables patients to become ambulatory, albeit with a prosthesis, faster. However, in the modern era of vascular surgery, revascularization can be performed successfully with minimal mortality and excellent rates of limb salvage, especially when it’s done within a team-based approach.
The mortality in primary amputation is shockingly high, anywhere from 5% to 23% higher than revascularization alone, and the major complication rate of amputation associated with diabetes is also unacceptably high – up to 37%. This is in contrast to a 17% rate in major nonamputation vascular surgery and 1%-5% in endovascular procedures (BMC Nephrol. 2005;6:3).
We can’t ignore the economic burden this places on the country. In 2014, primary amputations cost the health care system $11 billion annually, and that is expected to grow to more than $25 billion in the next several years, according to the SAGE Group. It’s important to keep in mind that Medicare covers over 80% of this cost.
A number of studies have shown that conservative management with wound care and amputation is more cost effective than primary amputation in ambulatory, independent adults. Data can be difficult to interpret because of different recording strategies for all the costs associated with amputation, but a single-institution study concluded that revascularization costs almost $5,280 more than expectant management, but $33,900 less than primary amputation alone (Cardiovasc Surg. 1999;7;62-9).
We must also consider the costs of revision after primary amputation; above-the-knee amputation has a 12% in-hospital revision rate, and below-the-knee amputation about 20%. Endovascular interventions, on the other hand, have a 1%-9% in-hospital revision rate, and only 2%-4% of these patients will go on to require an amputation during the same admission (Eur J Vasc Endovasc Surg. 2006;32:484-90; Arch Phys Med Rehabil. 2005;86:480-6).This does not include the costs of those complications as well as other indirect costs of amputation, such as nursing home care and living situation modification (Int J Behav Med. 2016;23:714-21; Pak J Med Sci. 2014; 30:1044-9). They quickly add up to that $25 billion.
The proponents of primary amputation tell us that it leads to quicker recovery time and an earlier time to ambulation. However, only 47% of patients will actually ambulate after amputation, in contrast to 97% who will ambulate after limb salvage as a primary procedure. In a nonambulatory cohort, 21% of those patients go on to regain functional status that was lost prior to surgery (J Vasc Surg. 1997;25;287-95).
Many question if our success with vascular surgery over the past few decades can translate to helping the most difficult subset of patients. An Italian study reported on a cohort of diabetic vs. nondiabetic patients and determined both groups have similar amputation-free rates after infrainguinal arterial reconstruction for critical limb ischemia, with excellent primary and secondary patency rates and a limb salvage rate of 88% at 5 years (J Vasc Surg. 2014;59:708-19). This tells us that we do have the skill set necessary to save these limbs.
A multidisciplinary limb preservation team is paramount to the success of any limb salvage program. A revascularization team should be in place which uses early intervention to achieve the highest limb salvage rates possible. Wound care needs to be an integrated part of it. Advanced podiatric reconstructive surgery also is key because this can provide complex foot reconstructions and help ambulatory patients return home.
Dr. Trissa A. Babrowski is an assistant professor of surgery, specializing in vascular surgery and endovascular therapy, at the University of Chicago Heart and Vascular Center. She had no financial relationships to disclose.
Primary amputation can be OK
I am not an amputationalist. I do practice limb salvage. In fact I’m probably the most aggressive limb salvage surgeon in my hospital. But primary amputation is a completely acceptable option for a selected group of patients with diabetes. We should not try to do limb salvage “at all costs.”
I do not find this to be a contradictory position. In fact, I think it adds credence to my support of limb salvage that I think primary amputation can be OK. In all honesty, there are very few things in life that should be done at all costs.
A study out of Loma Linda University involving patients with CLI compared primary amputation vs. revascularization; 43% of patients had a primary amputation (Ann Vasc Surg. 2007;21:458-63). A multivariate analysis showed that patients with major tissue loss, end-stage renal disease (ESRD), diabetes and nonambulatory status were more likely to undergo primary amputation rather than revascularization.
While major tissue loss (Rutherford category 6) is certainly an indication for primary amputation, ambulatory status can represent a gray area in determining the best course. ESRD and diabetes are much more nonspecific factors; probably more than 10% of the patients that we see with CLI have ESRD. Also, 50%-70% of these patients with CLI, and in some series even higher percentages, have diabetes. Thus, these factors by themselves do not assist us in determining which patients potentially should be offered primary amputation vs. revascularization.
In general, we know that we can get good results in limb bypass or revascularization in patients with CLI: The PREVENT III multicenter trial, with the use of the vein as the conduit, showed 1-year limb salvage rates of 88% in these high-risk patients (J Vasc Surg. 2006;43:742-51). However, one of the major risk factors that adversely affected outcome was ESRD.
We know that ESRD is a significant predictor of lowering our chances of saving a limb successfully. Knowing the cost of multiple continued episodes of revascularization in these patients prior to proceeding with an amputation, it’s intuitive that these patients would benefit from a more precise process in their treatment from the beginning. A number of papers have concluded that a primary amputation may be the preferred approach in patients with ESRD.
Can we preoperatively predict which patients with CLI will fail operative revascularization? Data from the New England Vascular Quality Initiative identified eight variables associated with failure of revascularization, among them age younger than 59, ESRD, diabetes, CLI, conduit requiring venovenostomy, tarsal target, and nursing home residence (Ann Vasc Surg. 2010;24:57-68). The presence of three or more risk factors has a 27.7% risk of limb loss and/or graft thrombosis within 1 year.
Postponing amputation is a major cost issue. Direct costs of bypass for critical limb ischemia were $3.6 billion in 2004 (J Vasc Surg. 2011;54:1021-31), and we know that a functional outcome can be problematic in this patient group. Factors associated with a poor functional outcome include dementia, dependent-living situation preoperatively and nonambulatory status.
Unfortunately, there are not a lot of data that deal with quality of life outcomes for patients with CLI who have undergone bypass. Using a point system comprised of dialysis (4 points), tissue loss (3 points), age above 75 (2 points), hematocrit less than or equal to 30 (2 points), and coronary artery disease (1 point), a follow-up study of patients in the PREVENT III trial found that a high-risk group (greater than or equal to 8 points) had an amputation-free survival of only 45% (J Vasc Surg. 2009;50:769-75). Again, these results do not justify the effort and costs of limb salvage in this high-risk patient group.
We should consider the following options carefully in selecting a cost-effective patient-focused approach in patients with CLI: wound care, primary amputation, bypass revascularization, or endovascular revascularization. I would argue that the vascular surgeon who is qualified as an expert in all of the above is best positioned to select an appropriate plan of treatment based upon the patient’s risk factors, wound factors, ambulatory ability, pattern of disease, severity of ischemia, and living status.
Thus, upon presentation, a patient with CLI should undergo confirmatory tests and optimize his or her risk factors. The vascular surgeon then has the option, in discussion with the patient and family, to pursue an appropriate treatment plan inclusive of primary amputation – not one of limb salvage “at all costs.”
Primary amputation should be used in situations where there is dementia and nonambulatory status, and in patients who are poor candidates for revascularization because of high risk of failure and limited life expectancy. The recently developed WIfI (wound, ischemia, and foot infection) classification can also be utilized, as stage 4 WIfI classification is associated with high risk of limb loss – 38%-40% at 1 year.
Primary amputation is an option that can result in better care overall, and it is a cost-effective approach for a selected group of patients. We should not try to do limb salvage at all cost. Primary amputation, in selected patients, is OK.
Dr. Timothy J. Nypaver is head of vascular surgery at Henry Ford Hospital, Detroit. He had no financial relationships to disclose.
Transition to adult epilepsy care done right
Has this ever happened to you? You are an adult neurologist who has been asked to take on the care of a pediatric neurology patient. The patient who comes to your clinic is a 20-year-old young woman with a history of moderate developmental delay and intractable epilepsy. She is on numerous medications including valproic acid with a previous trial of the ketogenic diet. You receive a report that she has focal epilepsy and is having frequent seizures and last had an MRI at age 2 years. Prior notes talk about her summer vacations but not much about the future plans for her epilepsy. You see the patient in clinic, and the family is not happy to be in the adult clinic. They are disappointed that you don’t spend more time with them or fill out myriad forms. You find out that they have not obtained legal guardianship for their daughter and have no plan for work placement after school. She also has various other medical comorbidities that were previously addressed by the pediatric neurologist.
There is a not much evidence on the right way to do this. In 2013, the American Epilepsy Society approved a Transition Tool that is helpful in outlining the steps for a successful transition, and in 2016, the Child Neurology Foundation put forth a consensus statement with eight principles to guide a successful transition. Transitions are an expectation of good care and they recommend that a written policy be present for all offices.
Talking about transitioning should start as early as 10-12 years of age and should be discussed every year. Thinking about prognosis and a realistic plan for each child as they enter adult life is important. Patients and families should be able to understand how the disease affects them, what their medications are and how to independently obtain them, what comorbidities are associated with their disease, how to stay healthy, how to improve their quality of life, and how to advocate for themselves. As children become teenagers they should have a concrete plan for ongoing education, work, women’s issues, and an understanding of decision-making capacity and whether legal guardianship or a power of attorney needs to be implemented.
, even if they are still seen in the pediatric setting. A transition packet should be created that includes a summary of the diagnosis, work-up, previous treatments, and considerations for future treatments and emergency care. Also included is a plan for who will continue to address any non–seizure-related diagnoses the pediatric neurologist may have been managing. The patient and family also have an opportunity to review and contribute to this. This packet enables the adult neurologist to easily understand all issues and assume care of the patient, easing this aspect of the transition.
An advance meeting of the patient and family with the adult provider should be arranged whenever possible. To address this, some centers are now creating a transition clinic staffed by both pediatric and adult neurologists and/or nurses. This ideally takes place in the adult setting and is an excellent way to smooth the transition for the patient, family, and providers. Good transition is important to help prevent gaps in care, avoid reinventing the wheel, and improve satisfaction for everyone involved (patient, family, nurses, and neurologists). The key points are that transition discussions start early, patients and families should be involved and empowered in the process, and the creation of a transition packet for the adult provider is very helpful. Care transitions are something we will be hearing a lot more about in the upcoming years. And, hopefully, next time, the patient scenario seen above will go more smoothly!
Dr. Felton is an epilepsy specialist at the University of Wisconsin, Madison, and Dr. Kelley is director of the Pediatric Epilepsy Monitoring Unit at Johns Hopkins University, Baltimore. This editorial reflects the content of a presentation given by Dr. Felton and Dr. Kelley at the annual meeting of the American Epilepsy Society in Houston. The authors report no conflict of interest.
Has this ever happened to you? You are an adult neurologist who has been asked to take on the care of a pediatric neurology patient. The patient who comes to your clinic is a 20-year-old young woman with a history of moderate developmental delay and intractable epilepsy. She is on numerous medications including valproic acid with a previous trial of the ketogenic diet. You receive a report that she has focal epilepsy and is having frequent seizures and last had an MRI at age 2 years. Prior notes talk about her summer vacations but not much about the future plans for her epilepsy. You see the patient in clinic, and the family is not happy to be in the adult clinic. They are disappointed that you don’t spend more time with them or fill out myriad forms. You find out that they have not obtained legal guardianship for their daughter and have no plan for work placement after school. She also has various other medical comorbidities that were previously addressed by the pediatric neurologist.
There is a not much evidence on the right way to do this. In 2013, the American Epilepsy Society approved a Transition Tool that is helpful in outlining the steps for a successful transition, and in 2016, the Child Neurology Foundation put forth a consensus statement with eight principles to guide a successful transition. Transitions are an expectation of good care and they recommend that a written policy be present for all offices.
Talking about transitioning should start as early as 10-12 years of age and should be discussed every year. Thinking about prognosis and a realistic plan for each child as they enter adult life is important. Patients and families should be able to understand how the disease affects them, what their medications are and how to independently obtain them, what comorbidities are associated with their disease, how to stay healthy, how to improve their quality of life, and how to advocate for themselves. As children become teenagers they should have a concrete plan for ongoing education, work, women’s issues, and an understanding of decision-making capacity and whether legal guardianship or a power of attorney needs to be implemented.
, even if they are still seen in the pediatric setting. A transition packet should be created that includes a summary of the diagnosis, work-up, previous treatments, and considerations for future treatments and emergency care. Also included is a plan for who will continue to address any non–seizure-related diagnoses the pediatric neurologist may have been managing. The patient and family also have an opportunity to review and contribute to this. This packet enables the adult neurologist to easily understand all issues and assume care of the patient, easing this aspect of the transition.
An advance meeting of the patient and family with the adult provider should be arranged whenever possible. To address this, some centers are now creating a transition clinic staffed by both pediatric and adult neurologists and/or nurses. This ideally takes place in the adult setting and is an excellent way to smooth the transition for the patient, family, and providers. Good transition is important to help prevent gaps in care, avoid reinventing the wheel, and improve satisfaction for everyone involved (patient, family, nurses, and neurologists). The key points are that transition discussions start early, patients and families should be involved and empowered in the process, and the creation of a transition packet for the adult provider is very helpful. Care transitions are something we will be hearing a lot more about in the upcoming years. And, hopefully, next time, the patient scenario seen above will go more smoothly!
Dr. Felton is an epilepsy specialist at the University of Wisconsin, Madison, and Dr. Kelley is director of the Pediatric Epilepsy Monitoring Unit at Johns Hopkins University, Baltimore. This editorial reflects the content of a presentation given by Dr. Felton and Dr. Kelley at the annual meeting of the American Epilepsy Society in Houston. The authors report no conflict of interest.
Has this ever happened to you? You are an adult neurologist who has been asked to take on the care of a pediatric neurology patient. The patient who comes to your clinic is a 20-year-old young woman with a history of moderate developmental delay and intractable epilepsy. She is on numerous medications including valproic acid with a previous trial of the ketogenic diet. You receive a report that she has focal epilepsy and is having frequent seizures and last had an MRI at age 2 years. Prior notes talk about her summer vacations but not much about the future plans for her epilepsy. You see the patient in clinic, and the family is not happy to be in the adult clinic. They are disappointed that you don’t spend more time with them or fill out myriad forms. You find out that they have not obtained legal guardianship for their daughter and have no plan for work placement after school. She also has various other medical comorbidities that were previously addressed by the pediatric neurologist.
There is a not much evidence on the right way to do this. In 2013, the American Epilepsy Society approved a Transition Tool that is helpful in outlining the steps for a successful transition, and in 2016, the Child Neurology Foundation put forth a consensus statement with eight principles to guide a successful transition. Transitions are an expectation of good care and they recommend that a written policy be present for all offices.
Talking about transitioning should start as early as 10-12 years of age and should be discussed every year. Thinking about prognosis and a realistic plan for each child as they enter adult life is important. Patients and families should be able to understand how the disease affects them, what their medications are and how to independently obtain them, what comorbidities are associated with their disease, how to stay healthy, how to improve their quality of life, and how to advocate for themselves. As children become teenagers they should have a concrete plan for ongoing education, work, women’s issues, and an understanding of decision-making capacity and whether legal guardianship or a power of attorney needs to be implemented.
, even if they are still seen in the pediatric setting. A transition packet should be created that includes a summary of the diagnosis, work-up, previous treatments, and considerations for future treatments and emergency care. Also included is a plan for who will continue to address any non–seizure-related diagnoses the pediatric neurologist may have been managing. The patient and family also have an opportunity to review and contribute to this. This packet enables the adult neurologist to easily understand all issues and assume care of the patient, easing this aspect of the transition.
An advance meeting of the patient and family with the adult provider should be arranged whenever possible. To address this, some centers are now creating a transition clinic staffed by both pediatric and adult neurologists and/or nurses. This ideally takes place in the adult setting and is an excellent way to smooth the transition for the patient, family, and providers. Good transition is important to help prevent gaps in care, avoid reinventing the wheel, and improve satisfaction for everyone involved (patient, family, nurses, and neurologists). The key points are that transition discussions start early, patients and families should be involved and empowered in the process, and the creation of a transition packet for the adult provider is very helpful. Care transitions are something we will be hearing a lot more about in the upcoming years. And, hopefully, next time, the patient scenario seen above will go more smoothly!
Dr. Felton is an epilepsy specialist at the University of Wisconsin, Madison, and Dr. Kelley is director of the Pediatric Epilepsy Monitoring Unit at Johns Hopkins University, Baltimore. This editorial reflects the content of a presentation given by Dr. Felton and Dr. Kelley at the annual meeting of the American Epilepsy Society in Houston. The authors report no conflict of interest.
Scientific skepticism
Contrary to popular belief, great scientists do not spend their days proving that their new ideas are correct. That is just the romantic portrait of the field that is taught to schoolchildren. The reality is that great scientists do everything they can think of to disprove their theories. They exhaustively consider all other plausible explanations, challenge any potential bias in their methodology, rule out random flukes in the data collection, and refine any error in the data measurement. Only after doing all that, when no other conclusion is possible, do true scientists publish their new theories as truth. Then they await confirmation from their peers.
That is the philosophy behind the modern scientific method. In the hard sciences like chemistry and physics, this paradigm is reinforced because a scientist stakes his or her reputation on every publication. Funding from various government agencies often is controlled by peers in the field. If published work is inaccurate, the likelihood of receiving funding is markedly diminished.
Medicine has a long history of being biased by the belief that its therapies work. Even faith healers who consider themselves scientists will cite repeated examples of personal success as evidence that their approach works. However, they were looking for confirmation. To truly be a scientist, one cannot seek to affirm one’s beliefs. One must to the best of one’s ability seek to disprove them.
In 2016, postmodern voices have challenged the very existence of truth. The falsehoods rampant in politics have spilled over into a distrust of science. This distrust is manifest in vaccine deniers and the debate about climate change. There are a few charlatans and mercenaries in every field who sell their soul and skills to the highest bidder. Science is no exception. These disreputable scientists seek to obfuscate rather than clarify. They have been employed by the tobacco industry, the oil industry, and various groups with agendas other than seeking truth. They, with the help of weak journalism, have tainted the perception of science in the public arena. The uproar has prominent scientists defending the scientific method and arguing for science as the determiner of facts. Sen. Daniel Patrick Moynihan once said, “Everyone is entitled to his own opinion, but not to his own facts.”
In the 19th century, hawking snake oil was big business. In the early 20th century, the ethical drug industry was created in the United States. The Pure Food and Drug Act of 1906 and the Federal Food, Drug, and Cosmetic Act of 1938 empowered the Food and Drug Administration to regulate what has become 25% of U.S. industry. Those regulations demand honest labeling, good manufacturing processes, proof of efficacy, and an assessment of safety. The FDA deals with many stakeholders in the process for approving new drugs. The system is an imperfect balance between getting lifesaving new discoveries to market quickly while avoiding disasters. The most recent news has been the head of the FDA defending the need for proof of effectiveness in addition to proof of safety.
Even after a year in which truth seemed elusive and science hit a low point in prestige, it is still bizarre to me that the government would consider turning the drug industry into one in which proof of effectiveness is not a minimum requirement. That is postmodern thinking run amok. But the root of the problem lies deeper. When scientists stop being skeptics and instead focus on finding something publishable, the temptation is already leading them along the road illuminated by Dante Alighieri.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
Contrary to popular belief, great scientists do not spend their days proving that their new ideas are correct. That is just the romantic portrait of the field that is taught to schoolchildren. The reality is that great scientists do everything they can think of to disprove their theories. They exhaustively consider all other plausible explanations, challenge any potential bias in their methodology, rule out random flukes in the data collection, and refine any error in the data measurement. Only after doing all that, when no other conclusion is possible, do true scientists publish their new theories as truth. Then they await confirmation from their peers.
That is the philosophy behind the modern scientific method. In the hard sciences like chemistry and physics, this paradigm is reinforced because a scientist stakes his or her reputation on every publication. Funding from various government agencies often is controlled by peers in the field. If published work is inaccurate, the likelihood of receiving funding is markedly diminished.
Medicine has a long history of being biased by the belief that its therapies work. Even faith healers who consider themselves scientists will cite repeated examples of personal success as evidence that their approach works. However, they were looking for confirmation. To truly be a scientist, one cannot seek to affirm one’s beliefs. One must to the best of one’s ability seek to disprove them.
In 2016, postmodern voices have challenged the very existence of truth. The falsehoods rampant in politics have spilled over into a distrust of science. This distrust is manifest in vaccine deniers and the debate about climate change. There are a few charlatans and mercenaries in every field who sell their soul and skills to the highest bidder. Science is no exception. These disreputable scientists seek to obfuscate rather than clarify. They have been employed by the tobacco industry, the oil industry, and various groups with agendas other than seeking truth. They, with the help of weak journalism, have tainted the perception of science in the public arena. The uproar has prominent scientists defending the scientific method and arguing for science as the determiner of facts. Sen. Daniel Patrick Moynihan once said, “Everyone is entitled to his own opinion, but not to his own facts.”
In the 19th century, hawking snake oil was big business. In the early 20th century, the ethical drug industry was created in the United States. The Pure Food and Drug Act of 1906 and the Federal Food, Drug, and Cosmetic Act of 1938 empowered the Food and Drug Administration to regulate what has become 25% of U.S. industry. Those regulations demand honest labeling, good manufacturing processes, proof of efficacy, and an assessment of safety. The FDA deals with many stakeholders in the process for approving new drugs. The system is an imperfect balance between getting lifesaving new discoveries to market quickly while avoiding disasters. The most recent news has been the head of the FDA defending the need for proof of effectiveness in addition to proof of safety.
Even after a year in which truth seemed elusive and science hit a low point in prestige, it is still bizarre to me that the government would consider turning the drug industry into one in which proof of effectiveness is not a minimum requirement. That is postmodern thinking run amok. But the root of the problem lies deeper. When scientists stop being skeptics and instead focus on finding something publishable, the temptation is already leading them along the road illuminated by Dante Alighieri.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
Contrary to popular belief, great scientists do not spend their days proving that their new ideas are correct. That is just the romantic portrait of the field that is taught to schoolchildren. The reality is that great scientists do everything they can think of to disprove their theories. They exhaustively consider all other plausible explanations, challenge any potential bias in their methodology, rule out random flukes in the data collection, and refine any error in the data measurement. Only after doing all that, when no other conclusion is possible, do true scientists publish their new theories as truth. Then they await confirmation from their peers.
That is the philosophy behind the modern scientific method. In the hard sciences like chemistry and physics, this paradigm is reinforced because a scientist stakes his or her reputation on every publication. Funding from various government agencies often is controlled by peers in the field. If published work is inaccurate, the likelihood of receiving funding is markedly diminished.
Medicine has a long history of being biased by the belief that its therapies work. Even faith healers who consider themselves scientists will cite repeated examples of personal success as evidence that their approach works. However, they were looking for confirmation. To truly be a scientist, one cannot seek to affirm one’s beliefs. One must to the best of one’s ability seek to disprove them.
In 2016, postmodern voices have challenged the very existence of truth. The falsehoods rampant in politics have spilled over into a distrust of science. This distrust is manifest in vaccine deniers and the debate about climate change. There are a few charlatans and mercenaries in every field who sell their soul and skills to the highest bidder. Science is no exception. These disreputable scientists seek to obfuscate rather than clarify. They have been employed by the tobacco industry, the oil industry, and various groups with agendas other than seeking truth. They, with the help of weak journalism, have tainted the perception of science in the public arena. The uproar has prominent scientists defending the scientific method and arguing for science as the determiner of facts. Sen. Daniel Patrick Moynihan once said, “Everyone is entitled to his own opinion, but not to his own facts.”
In the 19th century, hawking snake oil was big business. In the early 20th century, the ethical drug industry was created in the United States. The Pure Food and Drug Act of 1906 and the Federal Food, Drug, and Cosmetic Act of 1938 empowered the Food and Drug Administration to regulate what has become 25% of U.S. industry. Those regulations demand honest labeling, good manufacturing processes, proof of efficacy, and an assessment of safety. The FDA deals with many stakeholders in the process for approving new drugs. The system is an imperfect balance between getting lifesaving new discoveries to market quickly while avoiding disasters. The most recent news has been the head of the FDA defending the need for proof of effectiveness in addition to proof of safety.
Even after a year in which truth seemed elusive and science hit a low point in prestige, it is still bizarre to me that the government would consider turning the drug industry into one in which proof of effectiveness is not a minimum requirement. That is postmodern thinking run amok. But the root of the problem lies deeper. When scientists stop being skeptics and instead focus on finding something publishable, the temptation is already leading them along the road illuminated by Dante Alighieri.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis.
Hip Arthroscopy
Editor’s Note: AJO is fortunate to have Shane Nho, one of the nation’s leading hip arthroscopists, as our Deputy Editor-in-Chief. He has compiled an outstanding update for all orthopedic surgeons who see hip patients. It’s my pleasure to turn this issue over to him. On a side note, we’ve added a new feature for our speed readers. From now on, all articles published in AJO will feature a “Take-Home Points” text box. These points represent the most important items that the authors wish to convey from their article. Please enjoy this month’s issue and keep the feedback coming. We are striving to continuously improve AJO and make it your go-to journal for practical information that you can apply directly to your practice.
—Bryan T. Hanypsiak, MD
Hip arthroscopy has been evolving over the past 2 decades as our techniques have been refined and our clinical outcomes have been reported. We have reached a point in our field to look back at the progress that has been made while also providing our readers with the most up-to-date information on diagnosis, imaging studies, and decision making for appropriate treatment.
Trofa and colleagues provide an excellent overview on intra- and extra-articular pathology of the hip and pelvis in their article, “Mastering the Physical Examination of the Athlete’s Hip”. The authors review common injuries in the athlete and provide physical examination tests to differentiate between adductor strain, athletic pubalgia, osteitis pubis, and femoroacetabular impingement (FAI). Also in this issue, Lewis and colleagues provide a comprehensive review of imaging studies in the “Imaging for Nonarthritic Hip Pathology”. The authors review the most common radiographic measurements to detect FAI as well as describe the role of computed tomography and magnetic resonance imaging.
The mastery of hip arthroscopy for the treatment of FAI has a steep learning curve and the techniques have evolved along with our understanding of the importance of the labrum and capsule. We are fortunate to have an article provided by one of the pioneers in the field, Dr. Marc J. Philippon, describing his role in advancing the field in the article “Treatment of FAI: Labrum, Cartilage, Osseous Deformity, and Capsule”. Kollmorgen and Mather provide the most up-to-date techniques for labrum repair and reconstruction. Friel and colleagues report on capsular repair and plication using the T-capsulotomy and the extensile interportal capsulotomy.
We also have the opportunity to read about a number of clinical studies describing the experiences of multi-center studies and epidemiologic studies on large volumes of data. The ANCHOR group provides a summary of the experiences of some of the most renowned hip surgeons in North America as the treatment of FAI evolved from an open approach to an all-arthroscopic approach. The MASH group is a large multi-center group of hip arthroscopists in the United States who describe their current indications for surgical treatment of FAI.
On AmJOrthopedics.com, Matsuda and colleagues describe the outcomes of borderline dysplasia patients compared to normal controls across multiple centers. Anthony and colleagues report on the complication rates using the National Surgical Quality Improvement Program database.
I believe that our Hip Arthroscopy issue will not disappoint you. It is a comprehensive review of the state-of-the-art in hip arthroscopy from physical examination to current surgical techniques to clinical outcomes from large databases for the treatment of FAI. After reviewing this issue, you will be equipped with the most up-to-date information on the treatment of nonarthritic hip disease.
Am J Orthop. 2017;46(1):8. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Editor’s Note: AJO is fortunate to have Shane Nho, one of the nation’s leading hip arthroscopists, as our Deputy Editor-in-Chief. He has compiled an outstanding update for all orthopedic surgeons who see hip patients. It’s my pleasure to turn this issue over to him. On a side note, we’ve added a new feature for our speed readers. From now on, all articles published in AJO will feature a “Take-Home Points” text box. These points represent the most important items that the authors wish to convey from their article. Please enjoy this month’s issue and keep the feedback coming. We are striving to continuously improve AJO and make it your go-to journal for practical information that you can apply directly to your practice.
—Bryan T. Hanypsiak, MD
Hip arthroscopy has been evolving over the past 2 decades as our techniques have been refined and our clinical outcomes have been reported. We have reached a point in our field to look back at the progress that has been made while also providing our readers with the most up-to-date information on diagnosis, imaging studies, and decision making for appropriate treatment.
Trofa and colleagues provide an excellent overview on intra- and extra-articular pathology of the hip and pelvis in their article, “Mastering the Physical Examination of the Athlete’s Hip”. The authors review common injuries in the athlete and provide physical examination tests to differentiate between adductor strain, athletic pubalgia, osteitis pubis, and femoroacetabular impingement (FAI). Also in this issue, Lewis and colleagues provide a comprehensive review of imaging studies in the “Imaging for Nonarthritic Hip Pathology”. The authors review the most common radiographic measurements to detect FAI as well as describe the role of computed tomography and magnetic resonance imaging.
The mastery of hip arthroscopy for the treatment of FAI has a steep learning curve and the techniques have evolved along with our understanding of the importance of the labrum and capsule. We are fortunate to have an article provided by one of the pioneers in the field, Dr. Marc J. Philippon, describing his role in advancing the field in the article “Treatment of FAI: Labrum, Cartilage, Osseous Deformity, and Capsule”. Kollmorgen and Mather provide the most up-to-date techniques for labrum repair and reconstruction. Friel and colleagues report on capsular repair and plication using the T-capsulotomy and the extensile interportal capsulotomy.
We also have the opportunity to read about a number of clinical studies describing the experiences of multi-center studies and epidemiologic studies on large volumes of data. The ANCHOR group provides a summary of the experiences of some of the most renowned hip surgeons in North America as the treatment of FAI evolved from an open approach to an all-arthroscopic approach. The MASH group is a large multi-center group of hip arthroscopists in the United States who describe their current indications for surgical treatment of FAI.
On AmJOrthopedics.com, Matsuda and colleagues describe the outcomes of borderline dysplasia patients compared to normal controls across multiple centers. Anthony and colleagues report on the complication rates using the National Surgical Quality Improvement Program database.
I believe that our Hip Arthroscopy issue will not disappoint you. It is a comprehensive review of the state-of-the-art in hip arthroscopy from physical examination to current surgical techniques to clinical outcomes from large databases for the treatment of FAI. After reviewing this issue, you will be equipped with the most up-to-date information on the treatment of nonarthritic hip disease.
Am J Orthop. 2017;46(1):8. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Editor’s Note: AJO is fortunate to have Shane Nho, one of the nation’s leading hip arthroscopists, as our Deputy Editor-in-Chief. He has compiled an outstanding update for all orthopedic surgeons who see hip patients. It’s my pleasure to turn this issue over to him. On a side note, we’ve added a new feature for our speed readers. From now on, all articles published in AJO will feature a “Take-Home Points” text box. These points represent the most important items that the authors wish to convey from their article. Please enjoy this month’s issue and keep the feedback coming. We are striving to continuously improve AJO and make it your go-to journal for practical information that you can apply directly to your practice.
—Bryan T. Hanypsiak, MD
Hip arthroscopy has been evolving over the past 2 decades as our techniques have been refined and our clinical outcomes have been reported. We have reached a point in our field to look back at the progress that has been made while also providing our readers with the most up-to-date information on diagnosis, imaging studies, and decision making for appropriate treatment.
Trofa and colleagues provide an excellent overview on intra- and extra-articular pathology of the hip and pelvis in their article, “Mastering the Physical Examination of the Athlete’s Hip”. The authors review common injuries in the athlete and provide physical examination tests to differentiate between adductor strain, athletic pubalgia, osteitis pubis, and femoroacetabular impingement (FAI). Also in this issue, Lewis and colleagues provide a comprehensive review of imaging studies in the “Imaging for Nonarthritic Hip Pathology”. The authors review the most common radiographic measurements to detect FAI as well as describe the role of computed tomography and magnetic resonance imaging.
The mastery of hip arthroscopy for the treatment of FAI has a steep learning curve and the techniques have evolved along with our understanding of the importance of the labrum and capsule. We are fortunate to have an article provided by one of the pioneers in the field, Dr. Marc J. Philippon, describing his role in advancing the field in the article “Treatment of FAI: Labrum, Cartilage, Osseous Deformity, and Capsule”. Kollmorgen and Mather provide the most up-to-date techniques for labrum repair and reconstruction. Friel and colleagues report on capsular repair and plication using the T-capsulotomy and the extensile interportal capsulotomy.
We also have the opportunity to read about a number of clinical studies describing the experiences of multi-center studies and epidemiologic studies on large volumes of data. The ANCHOR group provides a summary of the experiences of some of the most renowned hip surgeons in North America as the treatment of FAI evolved from an open approach to an all-arthroscopic approach. The MASH group is a large multi-center group of hip arthroscopists in the United States who describe their current indications for surgical treatment of FAI.
On AmJOrthopedics.com, Matsuda and colleagues describe the outcomes of borderline dysplasia patients compared to normal controls across multiple centers. Anthony and colleagues report on the complication rates using the National Surgical Quality Improvement Program database.
I believe that our Hip Arthroscopy issue will not disappoint you. It is a comprehensive review of the state-of-the-art in hip arthroscopy from physical examination to current surgical techniques to clinical outcomes from large databases for the treatment of FAI. After reviewing this issue, you will be equipped with the most up-to-date information on the treatment of nonarthritic hip disease.
Am J Orthop. 2017;46(1):8. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.
Clinicians Should Retain the Ability to Choose a Pathologist
As employers search for ways to reduce the cost of providing health care to their employees, there is a growing trend toward narrowed provider networks and exclusive laboratory contracts. In the case of clinical pathology, some of these choices make sense from the employer’s perspective. A complete blood cell count or comprehensive metabolic panel is done on a machine and the result is much the same regardless of the laboratory. So why not have all laboratory tests performed by the lowest bidder?
Laboratories vary in quality and anatomic pathology services are different from blood tests. Each slide must be interpreted by a physician and skill in the interpretation of skin specimens varies widely. Dermatopathology was one of the first subspecialties to be recognized within pathology, as it requires a high level of expertise. Clinicopathological correlation often is key to the accurate interpretation of a specimen. The stakes are high, and a delay in diagnosis of melanoma remains one of the most serious errors in medicine and one of the most common causes for litigation in dermatology.
The accurate interpretation of skin biopsy specimens becomes especially difficult when inadequate or misleading clinical information accompanies the specimen. A study of 589 biopsies submitted by primary care physicians and reported by general pathologists demonstrated a 6.5% error rate. False-negative errors were the most common, but false-positives also were observed.1 A study of pigmented lesions referred to the University of California, San Francisco, demonstrated a discordance rate of 14.3%.2 The degree of discordance would be expected to vary based on the range of diagnoses included in each study.
Board-certified dermatopathologists have varying areas of expertise and there is notable subjectivity in the interpretation of biopsy specimens. In the case of problematic pigmented lesions such as atypical Spitz nevi, there can be low interobserver agreement even among the experts in categorizing lesions as malignant versus nonmalignant (κ=0.30).3 The low concordance among expert dermatopathologists demonstrates that light microscopic features alone often are inadequate for diagnosis. Advanced studies, including immunohistochemical stains, can help to clarify the diagnosis. In the case of atypical Spitz tumors, the contribution of special stains to the final diagnosis is statistically similar to that of hematoxylin and eosin sections and age, suggesting that nothing alone is sufficiently reliable to establish a definitive diagnosis in every case.4 Although helpful, these studies are costly, and savings obtained by sending cases to the lowest bidder can evaporate quickly. Costs are higher when factoring in molecular studies, which can run upwards of $3000 per slide; the cost of litigation related to incorrect diagnoses; or the human costs of an incorrect diagnosis.
As a group, dermatopathologists are highly skilled in the interpretation of skin specimens, but challenging lesions are common in the routine practice of dermatopathology. A study of 1249 pigmented melanocytic lesions demonstrated substantial agreement among expert dermatopathologists for less problematic lesions, though agreement was greater for patients 40 years and older (κ=0.67) than for younger patients (κ=0.49). Agreement was lower for patients with atypical mole syndrome (κ=0.31).5 These discrepancies occur despite the fact that there is good interobserver reproducibility for grading of individual histological features such as asymmetry, circumscription, irregular confluent nests, single melanocytes predominating, absence of maturation, suprabasal melanocytes, symmetrical melanin, deep melanin, cytological atypia, mitoses, dermal lymphocytic infiltrate, and necrosis.6 These results indicate that accurate diagnoses cannot be reliably established simply by grading a list of histological features. Accurate diagnosis requires complex pattern recognition and integration of findings. Conflicting criteria often are present and an accurate interpretation requires considerable judgment as to which features are significant and which are not.
Separation of sebaceous adenoma, sebaceoma, and well-differentiated sebaceous carcinoma is another challenging area, and interobserver consensus can be as low as 11%,7 which suggests notable subjectivity in the criteria for diagnosis of nonmelanocytic tumors and emphasizes the importance of communication between the dermatopathologist and clinician when determining how to manage an ambiguous lesion. The interpretation of inflammatory skin diseases, alopecia, and lymphoid proliferations also can be problematic, and expert consultation often is required.
All dermatologists receive substantial training in dermatopathology, which puts them in an excellent position to interpret ambiguous findings in the context of the clinical presentation. Sometimes the dermatologist who has seen the clinical presentation can be in the best position to make the diagnosis. All clinicians must be wary of bias and an objective set of eyes often can be helpful. Communication is crucial to ensure appropriate care for each patient, and policies that restrict the choice of pathologist can be damaging.
- Trotter MJ, Bruecks AK. Interpretation of skin biopsies by general pathologists: diagnostic discrepancy rate measured by blinded review. Arch Pathol Lab Med. 2003;127:1489-1492.
- Shoo BA, Sagebiel RW, Kashani-Sabet M. Discordance in the histopathologic diagnosis of melanoma at a melanoma referral center [published online March 19, 2010]. J Am Acad Dermatol. 2010;62:751-756.
- Gerami P, Busam K, Cochran A, et al. Histomorphologic assessment and interobserver diagnostic reproducibility of atypical spitzoid melanocytic neoplasms with long-term follow-up. Am J Surg Pathol. 2014;38:934-940.
- Puri PK, Ferringer TC, Tyler WB, et al. Statistical analysis of the concordance of immunohistochemical stains with the final diagnosis in spitzoid neoplasms. Am J Dermatopathol. 2011;33:72-77.
- Braun RP, Gutkowicz-Krusin D, Rabinovitz H, et al. Agreement of dermatopathologists in the evaluation of clinically difficult melanocytic lesions: how golden is the ‘gold standard’? Dermatology. 2012;224:51-58.
- Urso C, Rongioletti F, Innocenzi D, et al. Interobserver reproducibility of histological features in cutaneous malignant melanoma. J Clin Pathol. 2005;58:1194-1198.
- Harvey NT, Budgeon CA, Leecy T, et al. Interobserver variability in the diagnosis of circumscribed sebaceous neoplasms of the skin. Pathology. 2013;45:581-586.
As employers search for ways to reduce the cost of providing health care to their employees, there is a growing trend toward narrowed provider networks and exclusive laboratory contracts. In the case of clinical pathology, some of these choices make sense from the employer’s perspective. A complete blood cell count or comprehensive metabolic panel is done on a machine and the result is much the same regardless of the laboratory. So why not have all laboratory tests performed by the lowest bidder?
Laboratories vary in quality and anatomic pathology services are different from blood tests. Each slide must be interpreted by a physician and skill in the interpretation of skin specimens varies widely. Dermatopathology was one of the first subspecialties to be recognized within pathology, as it requires a high level of expertise. Clinicopathological correlation often is key to the accurate interpretation of a specimen. The stakes are high, and a delay in diagnosis of melanoma remains one of the most serious errors in medicine and one of the most common causes for litigation in dermatology.
The accurate interpretation of skin biopsy specimens becomes especially difficult when inadequate or misleading clinical information accompanies the specimen. A study of 589 biopsies submitted by primary care physicians and reported by general pathologists demonstrated a 6.5% error rate. False-negative errors were the most common, but false-positives also were observed.1 A study of pigmented lesions referred to the University of California, San Francisco, demonstrated a discordance rate of 14.3%.2 The degree of discordance would be expected to vary based on the range of diagnoses included in each study.
Board-certified dermatopathologists have varying areas of expertise and there is notable subjectivity in the interpretation of biopsy specimens. In the case of problematic pigmented lesions such as atypical Spitz nevi, there can be low interobserver agreement even among the experts in categorizing lesions as malignant versus nonmalignant (κ=0.30).3 The low concordance among expert dermatopathologists demonstrates that light microscopic features alone often are inadequate for diagnosis. Advanced studies, including immunohistochemical stains, can help to clarify the diagnosis. In the case of atypical Spitz tumors, the contribution of special stains to the final diagnosis is statistically similar to that of hematoxylin and eosin sections and age, suggesting that nothing alone is sufficiently reliable to establish a definitive diagnosis in every case.4 Although helpful, these studies are costly, and savings obtained by sending cases to the lowest bidder can evaporate quickly. Costs are higher when factoring in molecular studies, which can run upwards of $3000 per slide; the cost of litigation related to incorrect diagnoses; or the human costs of an incorrect diagnosis.
As a group, dermatopathologists are highly skilled in the interpretation of skin specimens, but challenging lesions are common in the routine practice of dermatopathology. A study of 1249 pigmented melanocytic lesions demonstrated substantial agreement among expert dermatopathologists for less problematic lesions, though agreement was greater for patients 40 years and older (κ=0.67) than for younger patients (κ=0.49). Agreement was lower for patients with atypical mole syndrome (κ=0.31).5 These discrepancies occur despite the fact that there is good interobserver reproducibility for grading of individual histological features such as asymmetry, circumscription, irregular confluent nests, single melanocytes predominating, absence of maturation, suprabasal melanocytes, symmetrical melanin, deep melanin, cytological atypia, mitoses, dermal lymphocytic infiltrate, and necrosis.6 These results indicate that accurate diagnoses cannot be reliably established simply by grading a list of histological features. Accurate diagnosis requires complex pattern recognition and integration of findings. Conflicting criteria often are present and an accurate interpretation requires considerable judgment as to which features are significant and which are not.
Separation of sebaceous adenoma, sebaceoma, and well-differentiated sebaceous carcinoma is another challenging area, and interobserver consensus can be as low as 11%,7 which suggests notable subjectivity in the criteria for diagnosis of nonmelanocytic tumors and emphasizes the importance of communication between the dermatopathologist and clinician when determining how to manage an ambiguous lesion. The interpretation of inflammatory skin diseases, alopecia, and lymphoid proliferations also can be problematic, and expert consultation often is required.
All dermatologists receive substantial training in dermatopathology, which puts them in an excellent position to interpret ambiguous findings in the context of the clinical presentation. Sometimes the dermatologist who has seen the clinical presentation can be in the best position to make the diagnosis. All clinicians must be wary of bias and an objective set of eyes often can be helpful. Communication is crucial to ensure appropriate care for each patient, and policies that restrict the choice of pathologist can be damaging.
As employers search for ways to reduce the cost of providing health care to their employees, there is a growing trend toward narrowed provider networks and exclusive laboratory contracts. In the case of clinical pathology, some of these choices make sense from the employer’s perspective. A complete blood cell count or comprehensive metabolic panel is done on a machine and the result is much the same regardless of the laboratory. So why not have all laboratory tests performed by the lowest bidder?
Laboratories vary in quality and anatomic pathology services are different from blood tests. Each slide must be interpreted by a physician and skill in the interpretation of skin specimens varies widely. Dermatopathology was one of the first subspecialties to be recognized within pathology, as it requires a high level of expertise. Clinicopathological correlation often is key to the accurate interpretation of a specimen. The stakes are high, and a delay in diagnosis of melanoma remains one of the most serious errors in medicine and one of the most common causes for litigation in dermatology.
The accurate interpretation of skin biopsy specimens becomes especially difficult when inadequate or misleading clinical information accompanies the specimen. A study of 589 biopsies submitted by primary care physicians and reported by general pathologists demonstrated a 6.5% error rate. False-negative errors were the most common, but false-positives also were observed.1 A study of pigmented lesions referred to the University of California, San Francisco, demonstrated a discordance rate of 14.3%.2 The degree of discordance would be expected to vary based on the range of diagnoses included in each study.
Board-certified dermatopathologists have varying areas of expertise and there is notable subjectivity in the interpretation of biopsy specimens. In the case of problematic pigmented lesions such as atypical Spitz nevi, there can be low interobserver agreement even among the experts in categorizing lesions as malignant versus nonmalignant (κ=0.30).3 The low concordance among expert dermatopathologists demonstrates that light microscopic features alone often are inadequate for diagnosis. Advanced studies, including immunohistochemical stains, can help to clarify the diagnosis. In the case of atypical Spitz tumors, the contribution of special stains to the final diagnosis is statistically similar to that of hematoxylin and eosin sections and age, suggesting that nothing alone is sufficiently reliable to establish a definitive diagnosis in every case.4 Although helpful, these studies are costly, and savings obtained by sending cases to the lowest bidder can evaporate quickly. Costs are higher when factoring in molecular studies, which can run upwards of $3000 per slide; the cost of litigation related to incorrect diagnoses; or the human costs of an incorrect diagnosis.
As a group, dermatopathologists are highly skilled in the interpretation of skin specimens, but challenging lesions are common in the routine practice of dermatopathology. A study of 1249 pigmented melanocytic lesions demonstrated substantial agreement among expert dermatopathologists for less problematic lesions, though agreement was greater for patients 40 years and older (κ=0.67) than for younger patients (κ=0.49). Agreement was lower for patients with atypical mole syndrome (κ=0.31).5 These discrepancies occur despite the fact that there is good interobserver reproducibility for grading of individual histological features such as asymmetry, circumscription, irregular confluent nests, single melanocytes predominating, absence of maturation, suprabasal melanocytes, symmetrical melanin, deep melanin, cytological atypia, mitoses, dermal lymphocytic infiltrate, and necrosis.6 These results indicate that accurate diagnoses cannot be reliably established simply by grading a list of histological features. Accurate diagnosis requires complex pattern recognition and integration of findings. Conflicting criteria often are present and an accurate interpretation requires considerable judgment as to which features are significant and which are not.
Separation of sebaceous adenoma, sebaceoma, and well-differentiated sebaceous carcinoma is another challenging area, and interobserver consensus can be as low as 11%,7 which suggests notable subjectivity in the criteria for diagnosis of nonmelanocytic tumors and emphasizes the importance of communication between the dermatopathologist and clinician when determining how to manage an ambiguous lesion. The interpretation of inflammatory skin diseases, alopecia, and lymphoid proliferations also can be problematic, and expert consultation often is required.
All dermatologists receive substantial training in dermatopathology, which puts them in an excellent position to interpret ambiguous findings in the context of the clinical presentation. Sometimes the dermatologist who has seen the clinical presentation can be in the best position to make the diagnosis. All clinicians must be wary of bias and an objective set of eyes often can be helpful. Communication is crucial to ensure appropriate care for each patient, and policies that restrict the choice of pathologist can be damaging.
- Trotter MJ, Bruecks AK. Interpretation of skin biopsies by general pathologists: diagnostic discrepancy rate measured by blinded review. Arch Pathol Lab Med. 2003;127:1489-1492.
- Shoo BA, Sagebiel RW, Kashani-Sabet M. Discordance in the histopathologic diagnosis of melanoma at a melanoma referral center [published online March 19, 2010]. J Am Acad Dermatol. 2010;62:751-756.
- Gerami P, Busam K, Cochran A, et al. Histomorphologic assessment and interobserver diagnostic reproducibility of atypical spitzoid melanocytic neoplasms with long-term follow-up. Am J Surg Pathol. 2014;38:934-940.
- Puri PK, Ferringer TC, Tyler WB, et al. Statistical analysis of the concordance of immunohistochemical stains with the final diagnosis in spitzoid neoplasms. Am J Dermatopathol. 2011;33:72-77.
- Braun RP, Gutkowicz-Krusin D, Rabinovitz H, et al. Agreement of dermatopathologists in the evaluation of clinically difficult melanocytic lesions: how golden is the ‘gold standard’? Dermatology. 2012;224:51-58.
- Urso C, Rongioletti F, Innocenzi D, et al. Interobserver reproducibility of histological features in cutaneous malignant melanoma. J Clin Pathol. 2005;58:1194-1198.
- Harvey NT, Budgeon CA, Leecy T, et al. Interobserver variability in the diagnosis of circumscribed sebaceous neoplasms of the skin. Pathology. 2013;45:581-586.
- Trotter MJ, Bruecks AK. Interpretation of skin biopsies by general pathologists: diagnostic discrepancy rate measured by blinded review. Arch Pathol Lab Med. 2003;127:1489-1492.
- Shoo BA, Sagebiel RW, Kashani-Sabet M. Discordance in the histopathologic diagnosis of melanoma at a melanoma referral center [published online March 19, 2010]. J Am Acad Dermatol. 2010;62:751-756.
- Gerami P, Busam K, Cochran A, et al. Histomorphologic assessment and interobserver diagnostic reproducibility of atypical spitzoid melanocytic neoplasms with long-term follow-up. Am J Surg Pathol. 2014;38:934-940.
- Puri PK, Ferringer TC, Tyler WB, et al. Statistical analysis of the concordance of immunohistochemical stains with the final diagnosis in spitzoid neoplasms. Am J Dermatopathol. 2011;33:72-77.
- Braun RP, Gutkowicz-Krusin D, Rabinovitz H, et al. Agreement of dermatopathologists in the evaluation of clinically difficult melanocytic lesions: how golden is the ‘gold standard’? Dermatology. 2012;224:51-58.
- Urso C, Rongioletti F, Innocenzi D, et al. Interobserver reproducibility of histological features in cutaneous malignant melanoma. J Clin Pathol. 2005;58:1194-1198.
- Harvey NT, Budgeon CA, Leecy T, et al. Interobserver variability in the diagnosis of circumscribed sebaceous neoplasms of the skin. Pathology. 2013;45:581-586.