User login
Take Your Statins, for Heaven’s Sake
It’s an extremely common scenario. A patient’s screening tests return, showing a significant elevation of the calculated low-density lipoprotein cholesterol (LDL-C), known to the lay public as bad cholesterol. To a physician like myself, someone who prides himself on a modest bit of expertise in lipids, it’s an absolute no-brainer. The patient should be placed on statin therapy pronto to reduce the major risks of heart attack, stroke, and other vascular misfortunes that are clearly associated with an elevated LDL-C level.
The tremendous ability of statins to reduce cardiovascular risk is among the best-demonstrated therapeutic effects of any class of medication in any branch of medical practice. The first major trial to show definitive benefits with the use of statins was the Scandinavian Simvastatin Survival Study, which came out in 1994 and showed a 30% relative reduction in cardiovascular events in a high-risk secondary prevention population, meaning that the subjects already had documented vascular disease before entering the trial.
Related: Did Niacin Get a Bum Rap?
Similar results were reported soon after in primary prevention populations in the WOSCOPS study in the United Kingdom (UK), and from the AFCAPS/TexCAPS studies in the U.S. Then the large UK-based Heart Protection Study showed that statins reduce cardiovascular risk regardless of the initial LDL-C level. Some experts suspected that many of the protective effects of statins were due not only to the LDL-C reduction per se, but also the so-called pleiotropic benefits, which included vasodilation, antithrombotic effects, and improved function of the endothelial cells that line the walls of blood vessels.
A number of additional studies have since markedly expanded the role of statins. The CARDS study showed that patients with diabetes had fewer events on statins. The ASCOT study suggested that statins reduce risk in patients with hypertension. And the SPARCL study revealed fewer recurrent events in patients on statins who had experienced a stroke or transient ischemic attack. Perhaps an even greater advance came with the JUPITER study, which showed that patients with elevated C-reactive protein levels—a marker of systemic inflammation—had fewer cardiovascular events when treated with statins than with placebo.
As you can imagine, there are plenty of times when I reach for my prescription pad (actually, my mouse) with the intention of ordering a statin to reduce a patient’s cardiovascular risk. But unfortunately, many times the patient catches me up short by objecting to such a plan. I can’t tell you how many times a patient responds by asking rather pointedly about the adverse effects (AEs) of statins. Now, I’ll readily admit that a small number of patients ask about AEs with any medication, but I would submit that the question comes up far more commonly with statins than it does with almost any other class of medication. Why?
I firmly believe that a huge driver of my patients’ irrational suspicions of statins is the drivel that is found on countless unreliable and unscientific websites. Antistatin nonsense is readily available, and many patients have thoroughly marinated themselves in a toxic slurry of misinformation and medical fantasy. Most of these sites emphasize known statin AEs, such as myalgias and myopathies, liver damage, and rhabdomyolysis, but then grossly exaggerate the severity and frequency. Other sites hammer on the modest number of patients who are nudged from prediabetes to full-fledged diabetes by the statins or rant about medically unsubstantiated AEs of statins, such as worsened mentation and depression.
Related: Are Statins Safe to Use in Pregnancy? (Clinical Edge)
That’s all bad enough, but what’s even worse is when patients attack the very medical foundation for prescribing statins, claiming that their online “research” causes them to doubt the reported association between LDL-C levels and cardiovascular risk. They also hint darkly at a vast medical-industrial conspiracy to inflate the true importance of LDL-C, thus allowing for more sales of the highly questionable statins and increased drug company profits. No patient has directly accused me of personally benefitting financially by overprescribing statins, but some have certainly hinted at it.
Another large group of patients declines to take the proffered statins by insisting that they would much rather pursue diet and exercise to bring down their high levels of LDL-C. They are invariably surprised when I tell them that even the most aggressive approaches are unlikely to reduce LDL-C by more than a negligible amount. I suspect that they think that their tired old doctor has bought into a reflexive pills-cure-all mentality and does not appreciate the wondrous benefits of a holistic approach.
The most annoying patients tell me they will instead take red yeast rice to bring down their LDL-C, because they prefer a “natural” remedy to some monstrous artificial chemical produced in a pharmaceutical company laboratory. When I try to tell them that red yeast rice contains a varying but unknown amount of a natural inhibitor of hMG-coA reductase, the same enzyme targeted with precisely dosed statins, they gape at me with unhidden disgust for completely missing the point: The naturally occurring remedy is inherently superior, precisely because it is naturally occurring!
Of course, I have to remind myself that a good number of patients simply do not want to take statins because it is a reminder of their vulnerability, status as a cardiac patient, or as a potential future victim of a heart attack or stroke. Some patients find that concept so upsetting that they would rather ignore it altogether.
Reluctantly, I admit that statins are not perfect drugs. But I would still submit that they’re the closest things we have to wonder drugs today. Yes, a fair number of patients do develop myalgias, but these are often mild and transient and can be managed. Very infrequently, patients may manifest some degree of hepatotoxicity, and very rarely rhabdomyolysis can rear its ugly head. Statins can sometimes nudge prediabetes into diabetes, just as thiazide diuretics and beta-blockers will sometimes do. However, on balance, the risk-benefit analysis of taking statins in both primary and secondary prevention settings is very much in favor of taking the drugs.
So my message to my patients (and to your patients as well) is a very simple one. Take advantage of the phenomenal life-saving benefits of these near-wonder drugs, ignore the unscientific online nonsense authored by individuals practicing medicine without a license, and do what your tired but well-meaning doctor urges: take your statins, for Heaven’s sake!
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
It’s an extremely common scenario. A patient’s screening tests return, showing a significant elevation of the calculated low-density lipoprotein cholesterol (LDL-C), known to the lay public as bad cholesterol. To a physician like myself, someone who prides himself on a modest bit of expertise in lipids, it’s an absolute no-brainer. The patient should be placed on statin therapy pronto to reduce the major risks of heart attack, stroke, and other vascular misfortunes that are clearly associated with an elevated LDL-C level.
The tremendous ability of statins to reduce cardiovascular risk is among the best-demonstrated therapeutic effects of any class of medication in any branch of medical practice. The first major trial to show definitive benefits with the use of statins was the Scandinavian Simvastatin Survival Study, which came out in 1994 and showed a 30% relative reduction in cardiovascular events in a high-risk secondary prevention population, meaning that the subjects already had documented vascular disease before entering the trial.
Related: Did Niacin Get a Bum Rap?
Similar results were reported soon after in primary prevention populations in the WOSCOPS study in the United Kingdom (UK), and from the AFCAPS/TexCAPS studies in the U.S. Then the large UK-based Heart Protection Study showed that statins reduce cardiovascular risk regardless of the initial LDL-C level. Some experts suspected that many of the protective effects of statins were due not only to the LDL-C reduction per se, but also the so-called pleiotropic benefits, which included vasodilation, antithrombotic effects, and improved function of the endothelial cells that line the walls of blood vessels.
A number of additional studies have since markedly expanded the role of statins. The CARDS study showed that patients with diabetes had fewer events on statins. The ASCOT study suggested that statins reduce risk in patients with hypertension. And the SPARCL study revealed fewer recurrent events in patients on statins who had experienced a stroke or transient ischemic attack. Perhaps an even greater advance came with the JUPITER study, which showed that patients with elevated C-reactive protein levels—a marker of systemic inflammation—had fewer cardiovascular events when treated with statins than with placebo.
As you can imagine, there are plenty of times when I reach for my prescription pad (actually, my mouse) with the intention of ordering a statin to reduce a patient’s cardiovascular risk. But unfortunately, many times the patient catches me up short by objecting to such a plan. I can’t tell you how many times a patient responds by asking rather pointedly about the adverse effects (AEs) of statins. Now, I’ll readily admit that a small number of patients ask about AEs with any medication, but I would submit that the question comes up far more commonly with statins than it does with almost any other class of medication. Why?
I firmly believe that a huge driver of my patients’ irrational suspicions of statins is the drivel that is found on countless unreliable and unscientific websites. Antistatin nonsense is readily available, and many patients have thoroughly marinated themselves in a toxic slurry of misinformation and medical fantasy. Most of these sites emphasize known statin AEs, such as myalgias and myopathies, liver damage, and rhabdomyolysis, but then grossly exaggerate the severity and frequency. Other sites hammer on the modest number of patients who are nudged from prediabetes to full-fledged diabetes by the statins or rant about medically unsubstantiated AEs of statins, such as worsened mentation and depression.
Related: Are Statins Safe to Use in Pregnancy? (Clinical Edge)
That’s all bad enough, but what’s even worse is when patients attack the very medical foundation for prescribing statins, claiming that their online “research” causes them to doubt the reported association between LDL-C levels and cardiovascular risk. They also hint darkly at a vast medical-industrial conspiracy to inflate the true importance of LDL-C, thus allowing for more sales of the highly questionable statins and increased drug company profits. No patient has directly accused me of personally benefitting financially by overprescribing statins, but some have certainly hinted at it.
Another large group of patients declines to take the proffered statins by insisting that they would much rather pursue diet and exercise to bring down their high levels of LDL-C. They are invariably surprised when I tell them that even the most aggressive approaches are unlikely to reduce LDL-C by more than a negligible amount. I suspect that they think that their tired old doctor has bought into a reflexive pills-cure-all mentality and does not appreciate the wondrous benefits of a holistic approach.
The most annoying patients tell me they will instead take red yeast rice to bring down their LDL-C, because they prefer a “natural” remedy to some monstrous artificial chemical produced in a pharmaceutical company laboratory. When I try to tell them that red yeast rice contains a varying but unknown amount of a natural inhibitor of hMG-coA reductase, the same enzyme targeted with precisely dosed statins, they gape at me with unhidden disgust for completely missing the point: The naturally occurring remedy is inherently superior, precisely because it is naturally occurring!
Of course, I have to remind myself that a good number of patients simply do not want to take statins because it is a reminder of their vulnerability, status as a cardiac patient, or as a potential future victim of a heart attack or stroke. Some patients find that concept so upsetting that they would rather ignore it altogether.
Reluctantly, I admit that statins are not perfect drugs. But I would still submit that they’re the closest things we have to wonder drugs today. Yes, a fair number of patients do develop myalgias, but these are often mild and transient and can be managed. Very infrequently, patients may manifest some degree of hepatotoxicity, and very rarely rhabdomyolysis can rear its ugly head. Statins can sometimes nudge prediabetes into diabetes, just as thiazide diuretics and beta-blockers will sometimes do. However, on balance, the risk-benefit analysis of taking statins in both primary and secondary prevention settings is very much in favor of taking the drugs.
So my message to my patients (and to your patients as well) is a very simple one. Take advantage of the phenomenal life-saving benefits of these near-wonder drugs, ignore the unscientific online nonsense authored by individuals practicing medicine without a license, and do what your tired but well-meaning doctor urges: take your statins, for Heaven’s sake!
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
It’s an extremely common scenario. A patient’s screening tests return, showing a significant elevation of the calculated low-density lipoprotein cholesterol (LDL-C), known to the lay public as bad cholesterol. To a physician like myself, someone who prides himself on a modest bit of expertise in lipids, it’s an absolute no-brainer. The patient should be placed on statin therapy pronto to reduce the major risks of heart attack, stroke, and other vascular misfortunes that are clearly associated with an elevated LDL-C level.
The tremendous ability of statins to reduce cardiovascular risk is among the best-demonstrated therapeutic effects of any class of medication in any branch of medical practice. The first major trial to show definitive benefits with the use of statins was the Scandinavian Simvastatin Survival Study, which came out in 1994 and showed a 30% relative reduction in cardiovascular events in a high-risk secondary prevention population, meaning that the subjects already had documented vascular disease before entering the trial.
Related: Did Niacin Get a Bum Rap?
Similar results were reported soon after in primary prevention populations in the WOSCOPS study in the United Kingdom (UK), and from the AFCAPS/TexCAPS studies in the U.S. Then the large UK-based Heart Protection Study showed that statins reduce cardiovascular risk regardless of the initial LDL-C level. Some experts suspected that many of the protective effects of statins were due not only to the LDL-C reduction per se, but also the so-called pleiotropic benefits, which included vasodilation, antithrombotic effects, and improved function of the endothelial cells that line the walls of blood vessels.
A number of additional studies have since markedly expanded the role of statins. The CARDS study showed that patients with diabetes had fewer events on statins. The ASCOT study suggested that statins reduce risk in patients with hypertension. And the SPARCL study revealed fewer recurrent events in patients on statins who had experienced a stroke or transient ischemic attack. Perhaps an even greater advance came with the JUPITER study, which showed that patients with elevated C-reactive protein levels—a marker of systemic inflammation—had fewer cardiovascular events when treated with statins than with placebo.
As you can imagine, there are plenty of times when I reach for my prescription pad (actually, my mouse) with the intention of ordering a statin to reduce a patient’s cardiovascular risk. But unfortunately, many times the patient catches me up short by objecting to such a plan. I can’t tell you how many times a patient responds by asking rather pointedly about the adverse effects (AEs) of statins. Now, I’ll readily admit that a small number of patients ask about AEs with any medication, but I would submit that the question comes up far more commonly with statins than it does with almost any other class of medication. Why?
I firmly believe that a huge driver of my patients’ irrational suspicions of statins is the drivel that is found on countless unreliable and unscientific websites. Antistatin nonsense is readily available, and many patients have thoroughly marinated themselves in a toxic slurry of misinformation and medical fantasy. Most of these sites emphasize known statin AEs, such as myalgias and myopathies, liver damage, and rhabdomyolysis, but then grossly exaggerate the severity and frequency. Other sites hammer on the modest number of patients who are nudged from prediabetes to full-fledged diabetes by the statins or rant about medically unsubstantiated AEs of statins, such as worsened mentation and depression.
Related: Are Statins Safe to Use in Pregnancy? (Clinical Edge)
That’s all bad enough, but what’s even worse is when patients attack the very medical foundation for prescribing statins, claiming that their online “research” causes them to doubt the reported association between LDL-C levels and cardiovascular risk. They also hint darkly at a vast medical-industrial conspiracy to inflate the true importance of LDL-C, thus allowing for more sales of the highly questionable statins and increased drug company profits. No patient has directly accused me of personally benefitting financially by overprescribing statins, but some have certainly hinted at it.
Another large group of patients declines to take the proffered statins by insisting that they would much rather pursue diet and exercise to bring down their high levels of LDL-C. They are invariably surprised when I tell them that even the most aggressive approaches are unlikely to reduce LDL-C by more than a negligible amount. I suspect that they think that their tired old doctor has bought into a reflexive pills-cure-all mentality and does not appreciate the wondrous benefits of a holistic approach.
The most annoying patients tell me they will instead take red yeast rice to bring down their LDL-C, because they prefer a “natural” remedy to some monstrous artificial chemical produced in a pharmaceutical company laboratory. When I try to tell them that red yeast rice contains a varying but unknown amount of a natural inhibitor of hMG-coA reductase, the same enzyme targeted with precisely dosed statins, they gape at me with unhidden disgust for completely missing the point: The naturally occurring remedy is inherently superior, precisely because it is naturally occurring!
Of course, I have to remind myself that a good number of patients simply do not want to take statins because it is a reminder of their vulnerability, status as a cardiac patient, or as a potential future victim of a heart attack or stroke. Some patients find that concept so upsetting that they would rather ignore it altogether.
Reluctantly, I admit that statins are not perfect drugs. But I would still submit that they’re the closest things we have to wonder drugs today. Yes, a fair number of patients do develop myalgias, but these are often mild and transient and can be managed. Very infrequently, patients may manifest some degree of hepatotoxicity, and very rarely rhabdomyolysis can rear its ugly head. Statins can sometimes nudge prediabetes into diabetes, just as thiazide diuretics and beta-blockers will sometimes do. However, on balance, the risk-benefit analysis of taking statins in both primary and secondary prevention settings is very much in favor of taking the drugs.
So my message to my patients (and to your patients as well) is a very simple one. Take advantage of the phenomenal life-saving benefits of these near-wonder drugs, ignore the unscientific online nonsense authored by individuals practicing medicine without a license, and do what your tired but well-meaning doctor urges: take your statins, for Heaven’s sake!
Author disclosures
The author reports no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the author and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
No Man Is an Island in the Public Health Service
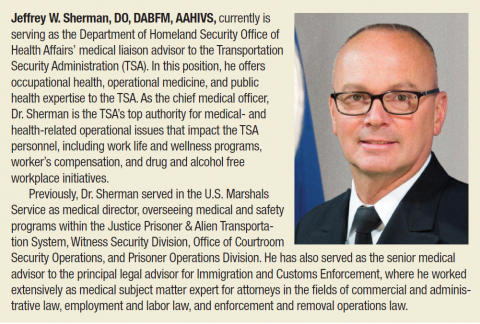
Below is an edited and condensed version of the Federal Practitioner interview with Jeffrey W. Sherman, DO, chief medical officer of the Department of Homeland Security’s Transportation Security Administration. Dr. Sherman recently received the Outstanding Service Medal from PHS. To hear the complete interview, visit: http://www.fedprac.com/multimedia/multimedia-library.html.
The Transportation Security Administration
Jeffrey W. Sherman, DO. I’m primarily responsible for providing expert opinion to the senior leadership of the Transportation Security Administration (TSA) as it relates to occupational health, preventive medicine, and other medical topics. The position of chief medical officer at the TSA has been on the books for quite a while. However, it hasn’t been filled on a permanent basis until the time that I came over from the Office of Health Affairs…. For the most part, the marching orders that I was given from the senior leadership was to take a fairly neutral look at the agency’s ability to manage the health and wellness of its workforce and find both positive areas and areas for improvement where the TSA could impact the welfare of the TSA population.
Related: Committed to Showing Results at the VA
Programs that we were able to identify that were already in existence and working really well for the TSA were in abundance. However, there were a number of programs that I found would probably enhance the TSA’ s ability to manage its workforce better and to provide a more comfortable, safe workplace. The main one was an ability to measure the transportation security officers’ medical capability and aptitude over a period of time, so more or less to manage them periodically and allow us to review the requirements and assessments for that particular workforce from an occupational health standpoint.
Having a Career in the PHS
Dr. Sherman. My previous work with the PHS included being a director for a number of different medical programs in other government agencies, including Immigration and Customs Enforcement (ICE), where I was acting director of the Division of Immigration Health Services for a period of time. I moved on to be the senior medical advisor to the principal legal advisor at ICE; and again, working with the attorneys on various medical issues allowed me to build greater confidence in my ability to manage the interface between what’s appropriate legally from the medical standpoint and what’s appropriate from the clinical practice of medicine in occupational health. So that was very vital and important.
Just prior to coming to the TSA, I was the medical director for a number of programs for the U.S. Marshals Services. Working alongside law enforcement in their unique roles and managing programs that are variously clinical and nonclinical gives good insight as to how to come into a large organization such as the TSA, with more than 48,000 transportation security officers, and put in place programs in a preexisting organization. To retrofit programs into an organization of that size requires some tact and ability. So all that time previously spent has allowed me to gain those skills.
Joining the PHS
Dr. Sherman. We are a group of dedicated professionals; we have a very close connection and a close network of collegial interactions. I was the Professional Advisory Committee (PAC) chair for the Physicians PAC for a year and vice chair before that. Meeting all the individuals and working with them on various cross-agency public health and professional projects has absolutely brought a lot of their wealth into what I do here at the TSA specifically. No man is an island; and certainly, in the PHS, you never feel that way…
Related: Pharmacist Management of Adult Asthma at an Indian Health Service Facility
I was in private practice in rural upstate New York in 2005 when Hurricane Katrina and Hurricane Rita came ashore, and I was part of the National Health Service Corps at that time. Part of my response as a National Health Service Corps Scholar was to join colleagues—some of whom were PHS officers—down in the recovery area in Louisiana; that is where I met my first uniformed Commissioned Corps officer, 2 of them, in fact. I worked with them for several weeks and was so incredibly impressed with the work of the PHS that while I was there, I applied for my commission. So I was hit pretty hard and pretty heavy, and I haven’t looked back…
It’s, of course, very satisfying to hear your uniformed service spoken highly of in a public forum and especially by elected officials such as the president. I mean it’s difficult not to smile when you hear that. I will say, as one of the 7 uniformed services of the U.S., we do take a lot of knuckling under from our sister services that are more well known. But frankly, at the end of the day, we work beside them regardless of the notoriety or note that we get from them or from anyone else.
I’ve served alongside the Navy on the USNS Mercy, and I’ve been out with Air Force and Coast Guard on their vessels as well. So I’m very comfortable, and I think most of the PHS officers are comfortable working with our sister uniformed services. It is nice to hear the recognition.
The PHS Outstanding Service Medal
Dr. Sherman. It’s a real honor and a privilege to have received that medal…. There are things you do in your professional career that you do not do for notoriety; you do it because it’s the right thing to do, and you know it’s in the greater service to your profession.
In this case, our profession is also a uniformed service. And so for the uniformed service itself to take note and to give recognition for what I would do anyway and the manner in which I do it, it’s again, very satisfying; and it’s very humbling.
Mentoring Junior Officers
Dr. Sherman. The PHS has a very robust program of mentoring junior officers; and I think one of the things that has been most satisfying in my time in uniform, outside of the obvious professional things, has really been mentoring junior officers on their way up through the ranks and as they find their pathway forward in a career as a Commissioned Corps officer. And if I can say one thing to any new officer coming into the organization, it’s make sure that you reach out to your senior officers, and make sure you learn from both their successes and their errors so that by the time you finish your career, you can look back and say you’ve done everything you’ve wanted to.
I still maintain relationships with [my] mentors. I don’t think you’re ever too old or ever too experienced to have a mentor. There’s always something you can learn from another individual. So you know, you never stop learning, and you never stop appreciating the people who you’re working beside who come before you and who are coming behind you. And please don’t ask me to state names, because there are too many.
Below is an edited and condensed version of the Federal Practitioner interview with Jeffrey W. Sherman, DO, chief medical officer of the Department of Homeland Security’s Transportation Security Administration. Dr. Sherman recently received the Outstanding Service Medal from PHS. To hear the complete interview, visit: http://www.fedprac.com/multimedia/multimedia-library.html.
The Transportation Security Administration
Jeffrey W. Sherman, DO. I’m primarily responsible for providing expert opinion to the senior leadership of the Transportation Security Administration (TSA) as it relates to occupational health, preventive medicine, and other medical topics. The position of chief medical officer at the TSA has been on the books for quite a while. However, it hasn’t been filled on a permanent basis until the time that I came over from the Office of Health Affairs…. For the most part, the marching orders that I was given from the senior leadership was to take a fairly neutral look at the agency’s ability to manage the health and wellness of its workforce and find both positive areas and areas for improvement where the TSA could impact the welfare of the TSA population.
Related: Committed to Showing Results at the VA
Programs that we were able to identify that were already in existence and working really well for the TSA were in abundance. However, there were a number of programs that I found would probably enhance the TSA’ s ability to manage its workforce better and to provide a more comfortable, safe workplace. The main one was an ability to measure the transportation security officers’ medical capability and aptitude over a period of time, so more or less to manage them periodically and allow us to review the requirements and assessments for that particular workforce from an occupational health standpoint.
Having a Career in the PHS
Dr. Sherman. My previous work with the PHS included being a director for a number of different medical programs in other government agencies, including Immigration and Customs Enforcement (ICE), where I was acting director of the Division of Immigration Health Services for a period of time. I moved on to be the senior medical advisor to the principal legal advisor at ICE; and again, working with the attorneys on various medical issues allowed me to build greater confidence in my ability to manage the interface between what’s appropriate legally from the medical standpoint and what’s appropriate from the clinical practice of medicine in occupational health. So that was very vital and important.
Just prior to coming to the TSA, I was the medical director for a number of programs for the U.S. Marshals Services. Working alongside law enforcement in their unique roles and managing programs that are variously clinical and nonclinical gives good insight as to how to come into a large organization such as the TSA, with more than 48,000 transportation security officers, and put in place programs in a preexisting organization. To retrofit programs into an organization of that size requires some tact and ability. So all that time previously spent has allowed me to gain those skills.
Joining the PHS
Dr. Sherman. We are a group of dedicated professionals; we have a very close connection and a close network of collegial interactions. I was the Professional Advisory Committee (PAC) chair for the Physicians PAC for a year and vice chair before that. Meeting all the individuals and working with them on various cross-agency public health and professional projects has absolutely brought a lot of their wealth into what I do here at the TSA specifically. No man is an island; and certainly, in the PHS, you never feel that way…
Related: Pharmacist Management of Adult Asthma at an Indian Health Service Facility
I was in private practice in rural upstate New York in 2005 when Hurricane Katrina and Hurricane Rita came ashore, and I was part of the National Health Service Corps at that time. Part of my response as a National Health Service Corps Scholar was to join colleagues—some of whom were PHS officers—down in the recovery area in Louisiana; that is where I met my first uniformed Commissioned Corps officer, 2 of them, in fact. I worked with them for several weeks and was so incredibly impressed with the work of the PHS that while I was there, I applied for my commission. So I was hit pretty hard and pretty heavy, and I haven’t looked back…
It’s, of course, very satisfying to hear your uniformed service spoken highly of in a public forum and especially by elected officials such as the president. I mean it’s difficult not to smile when you hear that. I will say, as one of the 7 uniformed services of the U.S., we do take a lot of knuckling under from our sister services that are more well known. But frankly, at the end of the day, we work beside them regardless of the notoriety or note that we get from them or from anyone else.
I’ve served alongside the Navy on the USNS Mercy, and I’ve been out with Air Force and Coast Guard on their vessels as well. So I’m very comfortable, and I think most of the PHS officers are comfortable working with our sister uniformed services. It is nice to hear the recognition.
The PHS Outstanding Service Medal
Dr. Sherman. It’s a real honor and a privilege to have received that medal…. There are things you do in your professional career that you do not do for notoriety; you do it because it’s the right thing to do, and you know it’s in the greater service to your profession.
In this case, our profession is also a uniformed service. And so for the uniformed service itself to take note and to give recognition for what I would do anyway and the manner in which I do it, it’s again, very satisfying; and it’s very humbling.
Mentoring Junior Officers
Dr. Sherman. The PHS has a very robust program of mentoring junior officers; and I think one of the things that has been most satisfying in my time in uniform, outside of the obvious professional things, has really been mentoring junior officers on their way up through the ranks and as they find their pathway forward in a career as a Commissioned Corps officer. And if I can say one thing to any new officer coming into the organization, it’s make sure that you reach out to your senior officers, and make sure you learn from both their successes and their errors so that by the time you finish your career, you can look back and say you’ve done everything you’ve wanted to.
I still maintain relationships with [my] mentors. I don’t think you’re ever too old or ever too experienced to have a mentor. There’s always something you can learn from another individual. So you know, you never stop learning, and you never stop appreciating the people who you’re working beside who come before you and who are coming behind you. And please don’t ask me to state names, because there are too many.
Below is an edited and condensed version of the Federal Practitioner interview with Jeffrey W. Sherman, DO, chief medical officer of the Department of Homeland Security’s Transportation Security Administration. Dr. Sherman recently received the Outstanding Service Medal from PHS. To hear the complete interview, visit: http://www.fedprac.com/multimedia/multimedia-library.html.
The Transportation Security Administration
Jeffrey W. Sherman, DO. I’m primarily responsible for providing expert opinion to the senior leadership of the Transportation Security Administration (TSA) as it relates to occupational health, preventive medicine, and other medical topics. The position of chief medical officer at the TSA has been on the books for quite a while. However, it hasn’t been filled on a permanent basis until the time that I came over from the Office of Health Affairs…. For the most part, the marching orders that I was given from the senior leadership was to take a fairly neutral look at the agency’s ability to manage the health and wellness of its workforce and find both positive areas and areas for improvement where the TSA could impact the welfare of the TSA population.
Related: Committed to Showing Results at the VA
Programs that we were able to identify that were already in existence and working really well for the TSA were in abundance. However, there were a number of programs that I found would probably enhance the TSA’ s ability to manage its workforce better and to provide a more comfortable, safe workplace. The main one was an ability to measure the transportation security officers’ medical capability and aptitude over a period of time, so more or less to manage them periodically and allow us to review the requirements and assessments for that particular workforce from an occupational health standpoint.
Having a Career in the PHS
Dr. Sherman. My previous work with the PHS included being a director for a number of different medical programs in other government agencies, including Immigration and Customs Enforcement (ICE), where I was acting director of the Division of Immigration Health Services for a period of time. I moved on to be the senior medical advisor to the principal legal advisor at ICE; and again, working with the attorneys on various medical issues allowed me to build greater confidence in my ability to manage the interface between what’s appropriate legally from the medical standpoint and what’s appropriate from the clinical practice of medicine in occupational health. So that was very vital and important.
Just prior to coming to the TSA, I was the medical director for a number of programs for the U.S. Marshals Services. Working alongside law enforcement in their unique roles and managing programs that are variously clinical and nonclinical gives good insight as to how to come into a large organization such as the TSA, with more than 48,000 transportation security officers, and put in place programs in a preexisting organization. To retrofit programs into an organization of that size requires some tact and ability. So all that time previously spent has allowed me to gain those skills.
Joining the PHS
Dr. Sherman. We are a group of dedicated professionals; we have a very close connection and a close network of collegial interactions. I was the Professional Advisory Committee (PAC) chair for the Physicians PAC for a year and vice chair before that. Meeting all the individuals and working with them on various cross-agency public health and professional projects has absolutely brought a lot of their wealth into what I do here at the TSA specifically. No man is an island; and certainly, in the PHS, you never feel that way…
Related: Pharmacist Management of Adult Asthma at an Indian Health Service Facility
I was in private practice in rural upstate New York in 2005 when Hurricane Katrina and Hurricane Rita came ashore, and I was part of the National Health Service Corps at that time. Part of my response as a National Health Service Corps Scholar was to join colleagues—some of whom were PHS officers—down in the recovery area in Louisiana; that is where I met my first uniformed Commissioned Corps officer, 2 of them, in fact. I worked with them for several weeks and was so incredibly impressed with the work of the PHS that while I was there, I applied for my commission. So I was hit pretty hard and pretty heavy, and I haven’t looked back…
It’s, of course, very satisfying to hear your uniformed service spoken highly of in a public forum and especially by elected officials such as the president. I mean it’s difficult not to smile when you hear that. I will say, as one of the 7 uniformed services of the U.S., we do take a lot of knuckling under from our sister services that are more well known. But frankly, at the end of the day, we work beside them regardless of the notoriety or note that we get from them or from anyone else.
I’ve served alongside the Navy on the USNS Mercy, and I’ve been out with Air Force and Coast Guard on their vessels as well. So I’m very comfortable, and I think most of the PHS officers are comfortable working with our sister uniformed services. It is nice to hear the recognition.
The PHS Outstanding Service Medal
Dr. Sherman. It’s a real honor and a privilege to have received that medal…. There are things you do in your professional career that you do not do for notoriety; you do it because it’s the right thing to do, and you know it’s in the greater service to your profession.
In this case, our profession is also a uniformed service. And so for the uniformed service itself to take note and to give recognition for what I would do anyway and the manner in which I do it, it’s again, very satisfying; and it’s very humbling.
Mentoring Junior Officers
Dr. Sherman. The PHS has a very robust program of mentoring junior officers; and I think one of the things that has been most satisfying in my time in uniform, outside of the obvious professional things, has really been mentoring junior officers on their way up through the ranks and as they find their pathway forward in a career as a Commissioned Corps officer. And if I can say one thing to any new officer coming into the organization, it’s make sure that you reach out to your senior officers, and make sure you learn from both their successes and their errors so that by the time you finish your career, you can look back and say you’ve done everything you’ve wanted to.
I still maintain relationships with [my] mentors. I don’t think you’re ever too old or ever too experienced to have a mentor. There’s always something you can learn from another individual. So you know, you never stop learning, and you never stop appreciating the people who you’re working beside who come before you and who are coming behind you. And please don’t ask me to state names, because there are too many.
Be true to yourself
How often have nonphysicians told you that they could never work the hours you do?
Most people think physicians are a unique breed, and in some respects, we are. But in important ways we are just like everyone else. When we work long hours under stressful conditions and go without adequate sleep or nourishment, we cannot function at peak performance. Just like everyone else, we can become irritable, grumpy, and cynical when our basic needs are not met. We are human too, and we are at higher risk than most people for burnout, depression, and even suicide.
An article in the Journal of Hospital Medicine in 2014 noted that slightly over 50% of hospitalists were affected by burnout. We scored high on the emotional exhaustion subscale, and 40.3% of us had symptoms of depression, with a surprising 9.2% rate of recent suicidality. Hospital medicine definitely has its advantages over many other fields of medicine, but as this study demonstrates, there is still much to be desired in our “work-life balance.”
Each practice has its own perks and negatives, and what will enhance the lives of hospitalists in one group may make intolerable the lives of members of another group. For instance, it is no surprise that 12-hour shifts with 7-on, 7-off block scheduling can be exhausting. If you have a family, this schedule leaves plenty of fun time on the weeks you are off, but you may still be missing 50% of your family’s life if you leave for work before your kids wake up and return after they go to bed.
Whatever your concerns and stressors may be, rest assured, you are not alone, and if enough of the members of your group have similar issues, you may be successful addressing them with your director or hospital administrator. Retaining good hospitalists is vital to the financial success of many hospitals, and being flexible enough to truly meet their reasonable needs can literally make or break a hospitalist team.
How often have nonphysicians told you that they could never work the hours you do?
Most people think physicians are a unique breed, and in some respects, we are. But in important ways we are just like everyone else. When we work long hours under stressful conditions and go without adequate sleep or nourishment, we cannot function at peak performance. Just like everyone else, we can become irritable, grumpy, and cynical when our basic needs are not met. We are human too, and we are at higher risk than most people for burnout, depression, and even suicide.
An article in the Journal of Hospital Medicine in 2014 noted that slightly over 50% of hospitalists were affected by burnout. We scored high on the emotional exhaustion subscale, and 40.3% of us had symptoms of depression, with a surprising 9.2% rate of recent suicidality. Hospital medicine definitely has its advantages over many other fields of medicine, but as this study demonstrates, there is still much to be desired in our “work-life balance.”
Each practice has its own perks and negatives, and what will enhance the lives of hospitalists in one group may make intolerable the lives of members of another group. For instance, it is no surprise that 12-hour shifts with 7-on, 7-off block scheduling can be exhausting. If you have a family, this schedule leaves plenty of fun time on the weeks you are off, but you may still be missing 50% of your family’s life if you leave for work before your kids wake up and return after they go to bed.
Whatever your concerns and stressors may be, rest assured, you are not alone, and if enough of the members of your group have similar issues, you may be successful addressing them with your director or hospital administrator. Retaining good hospitalists is vital to the financial success of many hospitals, and being flexible enough to truly meet their reasonable needs can literally make or break a hospitalist team.
How often have nonphysicians told you that they could never work the hours you do?
Most people think physicians are a unique breed, and in some respects, we are. But in important ways we are just like everyone else. When we work long hours under stressful conditions and go without adequate sleep or nourishment, we cannot function at peak performance. Just like everyone else, we can become irritable, grumpy, and cynical when our basic needs are not met. We are human too, and we are at higher risk than most people for burnout, depression, and even suicide.
An article in the Journal of Hospital Medicine in 2014 noted that slightly over 50% of hospitalists were affected by burnout. We scored high on the emotional exhaustion subscale, and 40.3% of us had symptoms of depression, with a surprising 9.2% rate of recent suicidality. Hospital medicine definitely has its advantages over many other fields of medicine, but as this study demonstrates, there is still much to be desired in our “work-life balance.”
Each practice has its own perks and negatives, and what will enhance the lives of hospitalists in one group may make intolerable the lives of members of another group. For instance, it is no surprise that 12-hour shifts with 7-on, 7-off block scheduling can be exhausting. If you have a family, this schedule leaves plenty of fun time on the weeks you are off, but you may still be missing 50% of your family’s life if you leave for work before your kids wake up and return after they go to bed.
Whatever your concerns and stressors may be, rest assured, you are not alone, and if enough of the members of your group have similar issues, you may be successful addressing them with your director or hospital administrator. Retaining good hospitalists is vital to the financial success of many hospitals, and being flexible enough to truly meet their reasonable needs can literally make or break a hospitalist team.
Eat slowly to reduce consumed calories
I freely admit I am obsessed with research articles about eating habits. I hold out hope that this will eventually unlock the magic bullet to cure us of the modern plague of obesity. At a certain level, our patients need us to be captivated by such literature. We should feel fairly comfortable with the common knowledge that diets are effective if you stay on them and reducing the caloric density of foods can result in meaningful weight loss.
But what about how quickly we eat? In our fast-paced, heavily caffeinated society, we seem to shovel rather than chew. Ever since I was a medical resident, I have practically inhaled my food. Perchance I am operating under the erroneous and illogical assumption that if I don’t taste the food it won’t register as calories. True science has now enlightened me to the error in my thinking.
Dr. Eric Robinson and his colleagues conducted a brilliant systematic review of the impact of eating rate on energy intake and hunger (Am. J. Clin. Nutr. 2014;100:123-51). They included studies for which there was at least one study arm in which participants ate a meal at a statistically significant slower rate than that of a different arm. Twenty-two studies met the criteria for inclusion.
Available evidence suggests that a slower eating rate is associated with lower intake, compared with faster eating. The effect on caloric intake was observed regardless of the intervention used to modify the eating rate, such as modifying food from soft (fast rate) to hard (slow rate) or verbal instruction. No relationship was observed between eating rate and hunger at the end of the meal or several hours later.
Intriguing to me is the hypothesis that eating rate likely affects intake through the duration and intensity of oral exposure to taste. Previous studies have shown that, when eating rate is held constant, increasing sensory exposure leads to a lower energy intake. This seems to relate to our innate wiring that gives us a “sensory specific satiety.” In my understanding, sensory specific satiety turns off appetitive drive when you have had too much chocolate or too many potato chips and you feel slightly ill. Unfortunately, the food industry is on to this game and they have designed foods to be perfectly balanced to not render satiety. These foods can tragically be eaten ceaselessly.
Take-home message: If your patients cannot control the bad foods they eat, they should try to eat them more slowly.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician.
I freely admit I am obsessed with research articles about eating habits. I hold out hope that this will eventually unlock the magic bullet to cure us of the modern plague of obesity. At a certain level, our patients need us to be captivated by such literature. We should feel fairly comfortable with the common knowledge that diets are effective if you stay on them and reducing the caloric density of foods can result in meaningful weight loss.
But what about how quickly we eat? In our fast-paced, heavily caffeinated society, we seem to shovel rather than chew. Ever since I was a medical resident, I have practically inhaled my food. Perchance I am operating under the erroneous and illogical assumption that if I don’t taste the food it won’t register as calories. True science has now enlightened me to the error in my thinking.
Dr. Eric Robinson and his colleagues conducted a brilliant systematic review of the impact of eating rate on energy intake and hunger (Am. J. Clin. Nutr. 2014;100:123-51). They included studies for which there was at least one study arm in which participants ate a meal at a statistically significant slower rate than that of a different arm. Twenty-two studies met the criteria for inclusion.
Available evidence suggests that a slower eating rate is associated with lower intake, compared with faster eating. The effect on caloric intake was observed regardless of the intervention used to modify the eating rate, such as modifying food from soft (fast rate) to hard (slow rate) or verbal instruction. No relationship was observed between eating rate and hunger at the end of the meal or several hours later.
Intriguing to me is the hypothesis that eating rate likely affects intake through the duration and intensity of oral exposure to taste. Previous studies have shown that, when eating rate is held constant, increasing sensory exposure leads to a lower energy intake. This seems to relate to our innate wiring that gives us a “sensory specific satiety.” In my understanding, sensory specific satiety turns off appetitive drive when you have had too much chocolate or too many potato chips and you feel slightly ill. Unfortunately, the food industry is on to this game and they have designed foods to be perfectly balanced to not render satiety. These foods can tragically be eaten ceaselessly.
Take-home message: If your patients cannot control the bad foods they eat, they should try to eat them more slowly.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician.
I freely admit I am obsessed with research articles about eating habits. I hold out hope that this will eventually unlock the magic bullet to cure us of the modern plague of obesity. At a certain level, our patients need us to be captivated by such literature. We should feel fairly comfortable with the common knowledge that diets are effective if you stay on them and reducing the caloric density of foods can result in meaningful weight loss.
But what about how quickly we eat? In our fast-paced, heavily caffeinated society, we seem to shovel rather than chew. Ever since I was a medical resident, I have practically inhaled my food. Perchance I am operating under the erroneous and illogical assumption that if I don’t taste the food it won’t register as calories. True science has now enlightened me to the error in my thinking.
Dr. Eric Robinson and his colleagues conducted a brilliant systematic review of the impact of eating rate on energy intake and hunger (Am. J. Clin. Nutr. 2014;100:123-51). They included studies for which there was at least one study arm in which participants ate a meal at a statistically significant slower rate than that of a different arm. Twenty-two studies met the criteria for inclusion.
Available evidence suggests that a slower eating rate is associated with lower intake, compared with faster eating. The effect on caloric intake was observed regardless of the intervention used to modify the eating rate, such as modifying food from soft (fast rate) to hard (slow rate) or verbal instruction. No relationship was observed between eating rate and hunger at the end of the meal or several hours later.
Intriguing to me is the hypothesis that eating rate likely affects intake through the duration and intensity of oral exposure to taste. Previous studies have shown that, when eating rate is held constant, increasing sensory exposure leads to a lower energy intake. This seems to relate to our innate wiring that gives us a “sensory specific satiety.” In my understanding, sensory specific satiety turns off appetitive drive when you have had too much chocolate or too many potato chips and you feel slightly ill. Unfortunately, the food industry is on to this game and they have designed foods to be perfectly balanced to not render satiety. These foods can tragically be eaten ceaselessly.
Take-home message: If your patients cannot control the bad foods they eat, they should try to eat them more slowly.
Dr. Ebbert is professor of medicine, a general internist at the Mayo Clinic in Rochester, Minn., and a diplomate of the American Board of Addiction Medicine. The opinions expressed are those of the author and do not necessarily represent the views and opinions of the Mayo Clinic. The opinions expressed in this article should not be used to diagnose or treat any medical condition nor should they be used as a substitute for medical advice from a qualified, board-certified practicing clinician.
Physician Advocacy for Zoster Vaccination
Herpes zoster (HZ) infection occurs when the varicella-zoster virus (VZV) is reactivated due to waning cellular immunity associated with age or immunosuppression. It results in a painful blistering cutaneous eruption.1 The incidence and rate of complications from HZ infection increase with age.2 The most common complication of HZ infection is postherpetic neuralgia (PHN), which can be extremely debilitating.1
In 2006 the US Food and Drug Administration approved a live attenuated HZ vaccine that boosts VZV cell-mediated immunity and largely reduces HZ disease burden. The HZ vaccine contains the same strain of VZV as the varicella vaccine but contains 14 times more virus particles.3 In a study of the efficacy and safety of the HZ vaccine, HZ vaccination was associated with a 51% reduction in HZ incidence, a 61% reduction in HZ disease burden, and a 67% reduction in PHN incidence at 3-year follow-up.4 In adults aged 60 to 69 years, the benefit of the HZ vaccine resulted from the reduction in HZ incidence.5 However, in adults 70 years and older, the benefit resulted from the reduction in PHN incidence and severity. Overall, the absolute benefit of the HZ vaccine was greatest in the older age group, as the severity and incidence of HZ and PHN are highest in these patients.5 Although efficacy declines with time, a long-term persistence substudy demonstrated that the HZ vaccine still reduced the incidence and severity of HZ.6
The HZ vaccine currently is approved for adults aged 50 years or older.3 Antivirals that are active against VZV (eg, acyclovir, valacyclovir, famciclovir) should not be administered 24 hours before or 14 days after vaccination.1 Concurrent administration of the HZ vaccine and the pneumococcal vaccine is not recommended due to risk for reduced immunogenicity of the zoster vaccine.5 Because it is a live vaccine, the HZ vaccine is not recommended in immunocompromised patients. However, the HZ vaccine can be safely given to moderately immunosuppressed patients. The HZ vaccine also is well tolerated and stimulates a strong cell-mediated immune response in adults who have had prior HZ infections. Herpes zoster vaccination is recommended in patients with a history of shingles, though there are no published data showing that it reduces the already low rate of recurrent HZ infections.7
Despite strong efficacy data and established guidelines, a low vaccination rate has been reported8 due to doubts about its long-term efficacy, failure of both physicians and patients to recognize the burden of disease imposed by HZ infection and PHN, and concerns about reimbursement and out-of-pocket costs for the patient.5 Furthermore, many patients who are eligible to receive the HZ vaccine may not do so because they do not remember having chickenpox and therefore do not feel they are at risk for developing shingles.
The HZ vaccine is an important factor in public health prevention strategy, as HZ infection and PHN are common, incurable, and incapacitating. The HZ vaccine is the most efficacious agent currently available on the market for prevention. It is important for dermatologists to educate our patients and encourage them to receive the HZ vaccine to safeguard their long-term health.
1. Sampathkumar P, Drage LA, Martin DP. Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc. 2009;84:274-280.
2. Gilden D. Efficacy of live zoster vaccine in preventing zoster and postherpetic neuralgia. J Intern Med. 2011;269:496-506.
3. Javed S, Javed SA, Trying SK. Varicella vaccines. Curr Open Infect Dis. 2012;25:135-140.
4. Oxman MN, Levin MJ, Johnson GR, et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005;353:2271-2284.
5. Oxman MN. Zoster vaccine: current status and future prospects. Clin Infect Dis. 2010;51:197-213.
6. Keating GM. Shingles (herpes zoster) vaccine (Zostavax®): a review of its use in the prevention of herpes zoster and postherpetic neuralgia in adults aged >50 years. Drugs. 2013;73:1227-1244.
7. Herpes zoster vaccination. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/vaccines/vpd-vac/shingles/hcp-vaccination.htm. Updated March 12, 2015. Accessed April 21, 2015.
8. Langan SM, Smeeth L, Margolis D, et al. Herpes zoster vaccine effectiveness against herpes zoster and post-herpetic neuralgia in an older US population: a cohort study. PLoS Med. 2013;10:e1001420.
Herpes zoster (HZ) infection occurs when the varicella-zoster virus (VZV) is reactivated due to waning cellular immunity associated with age or immunosuppression. It results in a painful blistering cutaneous eruption.1 The incidence and rate of complications from HZ infection increase with age.2 The most common complication of HZ infection is postherpetic neuralgia (PHN), which can be extremely debilitating.1
In 2006 the US Food and Drug Administration approved a live attenuated HZ vaccine that boosts VZV cell-mediated immunity and largely reduces HZ disease burden. The HZ vaccine contains the same strain of VZV as the varicella vaccine but contains 14 times more virus particles.3 In a study of the efficacy and safety of the HZ vaccine, HZ vaccination was associated with a 51% reduction in HZ incidence, a 61% reduction in HZ disease burden, and a 67% reduction in PHN incidence at 3-year follow-up.4 In adults aged 60 to 69 years, the benefit of the HZ vaccine resulted from the reduction in HZ incidence.5 However, in adults 70 years and older, the benefit resulted from the reduction in PHN incidence and severity. Overall, the absolute benefit of the HZ vaccine was greatest in the older age group, as the severity and incidence of HZ and PHN are highest in these patients.5 Although efficacy declines with time, a long-term persistence substudy demonstrated that the HZ vaccine still reduced the incidence and severity of HZ.6
The HZ vaccine currently is approved for adults aged 50 years or older.3 Antivirals that are active against VZV (eg, acyclovir, valacyclovir, famciclovir) should not be administered 24 hours before or 14 days after vaccination.1 Concurrent administration of the HZ vaccine and the pneumococcal vaccine is not recommended due to risk for reduced immunogenicity of the zoster vaccine.5 Because it is a live vaccine, the HZ vaccine is not recommended in immunocompromised patients. However, the HZ vaccine can be safely given to moderately immunosuppressed patients. The HZ vaccine also is well tolerated and stimulates a strong cell-mediated immune response in adults who have had prior HZ infections. Herpes zoster vaccination is recommended in patients with a history of shingles, though there are no published data showing that it reduces the already low rate of recurrent HZ infections.7
Despite strong efficacy data and established guidelines, a low vaccination rate has been reported8 due to doubts about its long-term efficacy, failure of both physicians and patients to recognize the burden of disease imposed by HZ infection and PHN, and concerns about reimbursement and out-of-pocket costs for the patient.5 Furthermore, many patients who are eligible to receive the HZ vaccine may not do so because they do not remember having chickenpox and therefore do not feel they are at risk for developing shingles.
The HZ vaccine is an important factor in public health prevention strategy, as HZ infection and PHN are common, incurable, and incapacitating. The HZ vaccine is the most efficacious agent currently available on the market for prevention. It is important for dermatologists to educate our patients and encourage them to receive the HZ vaccine to safeguard their long-term health.
Herpes zoster (HZ) infection occurs when the varicella-zoster virus (VZV) is reactivated due to waning cellular immunity associated with age or immunosuppression. It results in a painful blistering cutaneous eruption.1 The incidence and rate of complications from HZ infection increase with age.2 The most common complication of HZ infection is postherpetic neuralgia (PHN), which can be extremely debilitating.1
In 2006 the US Food and Drug Administration approved a live attenuated HZ vaccine that boosts VZV cell-mediated immunity and largely reduces HZ disease burden. The HZ vaccine contains the same strain of VZV as the varicella vaccine but contains 14 times more virus particles.3 In a study of the efficacy and safety of the HZ vaccine, HZ vaccination was associated with a 51% reduction in HZ incidence, a 61% reduction in HZ disease burden, and a 67% reduction in PHN incidence at 3-year follow-up.4 In adults aged 60 to 69 years, the benefit of the HZ vaccine resulted from the reduction in HZ incidence.5 However, in adults 70 years and older, the benefit resulted from the reduction in PHN incidence and severity. Overall, the absolute benefit of the HZ vaccine was greatest in the older age group, as the severity and incidence of HZ and PHN are highest in these patients.5 Although efficacy declines with time, a long-term persistence substudy demonstrated that the HZ vaccine still reduced the incidence and severity of HZ.6
The HZ vaccine currently is approved for adults aged 50 years or older.3 Antivirals that are active against VZV (eg, acyclovir, valacyclovir, famciclovir) should not be administered 24 hours before or 14 days after vaccination.1 Concurrent administration of the HZ vaccine and the pneumococcal vaccine is not recommended due to risk for reduced immunogenicity of the zoster vaccine.5 Because it is a live vaccine, the HZ vaccine is not recommended in immunocompromised patients. However, the HZ vaccine can be safely given to moderately immunosuppressed patients. The HZ vaccine also is well tolerated and stimulates a strong cell-mediated immune response in adults who have had prior HZ infections. Herpes zoster vaccination is recommended in patients with a history of shingles, though there are no published data showing that it reduces the already low rate of recurrent HZ infections.7
Despite strong efficacy data and established guidelines, a low vaccination rate has been reported8 due to doubts about its long-term efficacy, failure of both physicians and patients to recognize the burden of disease imposed by HZ infection and PHN, and concerns about reimbursement and out-of-pocket costs for the patient.5 Furthermore, many patients who are eligible to receive the HZ vaccine may not do so because they do not remember having chickenpox and therefore do not feel they are at risk for developing shingles.
The HZ vaccine is an important factor in public health prevention strategy, as HZ infection and PHN are common, incurable, and incapacitating. The HZ vaccine is the most efficacious agent currently available on the market for prevention. It is important for dermatologists to educate our patients and encourage them to receive the HZ vaccine to safeguard their long-term health.
1. Sampathkumar P, Drage LA, Martin DP. Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc. 2009;84:274-280.
2. Gilden D. Efficacy of live zoster vaccine in preventing zoster and postherpetic neuralgia. J Intern Med. 2011;269:496-506.
3. Javed S, Javed SA, Trying SK. Varicella vaccines. Curr Open Infect Dis. 2012;25:135-140.
4. Oxman MN, Levin MJ, Johnson GR, et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005;353:2271-2284.
5. Oxman MN. Zoster vaccine: current status and future prospects. Clin Infect Dis. 2010;51:197-213.
6. Keating GM. Shingles (herpes zoster) vaccine (Zostavax®): a review of its use in the prevention of herpes zoster and postherpetic neuralgia in adults aged >50 years. Drugs. 2013;73:1227-1244.
7. Herpes zoster vaccination. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/vaccines/vpd-vac/shingles/hcp-vaccination.htm. Updated March 12, 2015. Accessed April 21, 2015.
8. Langan SM, Smeeth L, Margolis D, et al. Herpes zoster vaccine effectiveness against herpes zoster and post-herpetic neuralgia in an older US population: a cohort study. PLoS Med. 2013;10:e1001420.
1. Sampathkumar P, Drage LA, Martin DP. Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc. 2009;84:274-280.
2. Gilden D. Efficacy of live zoster vaccine in preventing zoster and postherpetic neuralgia. J Intern Med. 2011;269:496-506.
3. Javed S, Javed SA, Trying SK. Varicella vaccines. Curr Open Infect Dis. 2012;25:135-140.
4. Oxman MN, Levin MJ, Johnson GR, et al. A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005;353:2271-2284.
5. Oxman MN. Zoster vaccine: current status and future prospects. Clin Infect Dis. 2010;51:197-213.
6. Keating GM. Shingles (herpes zoster) vaccine (Zostavax®): a review of its use in the prevention of herpes zoster and postherpetic neuralgia in adults aged >50 years. Drugs. 2013;73:1227-1244.
7. Herpes zoster vaccination. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/vaccines/vpd-vac/shingles/hcp-vaccination.htm. Updated March 12, 2015. Accessed April 21, 2015.
8. Langan SM, Smeeth L, Margolis D, et al. Herpes zoster vaccine effectiveness against herpes zoster and post-herpetic neuralgia in an older US population: a cohort study. PLoS Med. 2013;10:e1001420.
Trauma center verification
Despite the many changes in medicine over the past century, traumatic injury remains a surgical disease.
Trauma injury is a major public health concern in rural areas, where death rates from unintentional injuries are higher than in metropolitan areas (Am. J. Public Health 2004;10:1689-93). The rural surgeon sees more than his or her fair share of victims of automobile accidents, falls, unintentional firearms injuries, and occupational accidents (think tractor accidents and injuries involving machinery and animals).
Another reality of the rural areas of the United States is that the number of broadly trained general surgeons who can treat a wide variety of trauma injuries is shrinking. Aging and retirements of the “old school rural surgeons” are accelerating and precipitating a lack of surgical coverage crisis, including trauma, in rural areas (Arch. Surg. 2005;140:74-9).
These well-documented developments have combined to reduce the availability of rural surgeons to manage injured patients in planned and consistent ways. Because of the current training paradigm of increasing subspecialization, injured rural patients may be cared for at rural hospitals with reduced capabilities and by rural surgeons with limited trauma training and experience.
What is the action plan to help counteract these developments and to provide the highest-quality patient care at facilities staffed by surgeons who have sworn to “serve all with skill and fidelity”?
The most straightforward and well-established action plan to achieve those goals is the verification process developed by the ACS Verification, Review, and Consultation Program (VRC) in 1987 to help hospitals improve trauma care. The process involves a pre-review questionnaire, a site visit, and report of findings. Verification as a trauma center guarantees that the facility has the required resources listed in the current, evidence-based guide, Resources for Optimal Care of the Injured Patient (2014). If successful, the trauma center receives a certificate of verification that is valid for 3 years.
Most rural hospitals are designated as Level III and IV verified trauma centers on the basis of their available resources. ACS verification confirms that these centers have the commitments and capabilities to manage the initial care of injured patients by providing stabilization and instituting life-saving maneuvers. In addition, verification confirms that protocols and agreements with higher-level trauma centers within a system enable the safe and efficient transfer of injured patients.
During many years of practice in the rural hospitals verified as trauma centers, including being the medical director of a Level II and Level III facility, I provided care to injured patients who presented to the emergency departments (EDs). My experiences confirmed the unequivocal value of practicing in those facilities, and I can attest to the benefits of verification within a system, like Iowa’s state program.
The following case report validates such assertions. A helicopter, unable to complete the transfer to a Level I center for a deteriorating patient with a left chest gunshot wound, landed at my Level III hospital. There was a “Hot Off Load,” which was followed by a full trauma alert for the patient in profound shock. After placing a chest tube during a 20-minute ED stay, the patient transferred to the OR for further resuscitation, and stabilization with required operative treatment. With the patient stabilized and fully resuscitated, according to established agreements, I contacted the Level I center from the OR. After 3 hours, the patient returned to the helicopter and completed the transfer to the Level I trauma center. The patient survived because of the local trauma team’s commitment, organization, and skill brought about by the trauma center verification.
Most research to date has focused on higher-level trauma centers, but recent studies have shown that ACS verification was an independent predictor of survival of trauma patients at Level II centers (J. Trauma Acute Care Surg. 2013;75:44-9; J. Trauma Acute Care Surg. 2010;69:1362-6).
I have firsthand experience with the verification process. Following my involvement with the ACS Committee on Trauma, I became a national site surveyor for the ACSVRC. I became an Advanced Trauma Life Support (ATLS) instructor and then worked as a course director. ATLS is an essential component for trauma center verification. It supports the rural surgeon by giving the local trauma team a format for consistent, life-saving care for the most severely injured patients. I subsequently completed the ACS Advanced Trauma Operative Management course and elected to become an instructor.
I have made site visits to many rural hospitals as a part of the ACSVRC process and have met with a wide range of reactions from “Let’s show off how good we are” to “We really don’t know why we’re doing this” to “Just give us the merit badge and then get out of our hair.” I am gratified to note that ACS Fellows are uniformly supportive. They understand the need for organization, standards, and performance improvement.
Opposition to the ACSVRC process by hospitals and staff is no doubt rooted in cost concerns and general resistance to change. But, as most of us know, demonstrated benefits for patient care can be highly persuasive to most medical professionals.
It is also worth noting that in an effort to decrease stress, the ACSVRC takes significant steps to support facilities that seek verification by eliminating ambiguity from application to on-site visit, by defining criteria deficiencies, and by providing evidence for the entire verification process. The complete VRC program along with an FAQ is available on the ACS website (facs.org/quality-programs/trauma/vrc).
For me, trauma care has always been about what is best for the injured patient. I often ask colleagues this question: “What care do you want for an injured member of your family?” I then answer my own question: “I want the best care possible. That means organized, efficient, and life-saving [care] if needed.” Fortunately, I experienced these benefits at my verified trauma center hospital when my second son was in a rollover motor vehicle crash. He survived.
Verified rural trauma centers do indeed offer the best opportunities for high-quality patient care and for support of the rural surgeons who render that care to “serve all with skill and fidelity.” I know. I have been there.
Dr. Caropreso is a general surgeon at Keokuk (Iowa) Area Hospital and clinical professor of surgery at the University of Iowa Carver College of Medicine, Iowa City. He has practiced surgery in the rural communities of Mason City, Iowa; Keokuk, Iowa; and Carthage, Ill., for 37 years.
Despite the many changes in medicine over the past century, traumatic injury remains a surgical disease.
Trauma injury is a major public health concern in rural areas, where death rates from unintentional injuries are higher than in metropolitan areas (Am. J. Public Health 2004;10:1689-93). The rural surgeon sees more than his or her fair share of victims of automobile accidents, falls, unintentional firearms injuries, and occupational accidents (think tractor accidents and injuries involving machinery and animals).
Another reality of the rural areas of the United States is that the number of broadly trained general surgeons who can treat a wide variety of trauma injuries is shrinking. Aging and retirements of the “old school rural surgeons” are accelerating and precipitating a lack of surgical coverage crisis, including trauma, in rural areas (Arch. Surg. 2005;140:74-9).
These well-documented developments have combined to reduce the availability of rural surgeons to manage injured patients in planned and consistent ways. Because of the current training paradigm of increasing subspecialization, injured rural patients may be cared for at rural hospitals with reduced capabilities and by rural surgeons with limited trauma training and experience.
What is the action plan to help counteract these developments and to provide the highest-quality patient care at facilities staffed by surgeons who have sworn to “serve all with skill and fidelity”?
The most straightforward and well-established action plan to achieve those goals is the verification process developed by the ACS Verification, Review, and Consultation Program (VRC) in 1987 to help hospitals improve trauma care. The process involves a pre-review questionnaire, a site visit, and report of findings. Verification as a trauma center guarantees that the facility has the required resources listed in the current, evidence-based guide, Resources for Optimal Care of the Injured Patient (2014). If successful, the trauma center receives a certificate of verification that is valid for 3 years.
Most rural hospitals are designated as Level III and IV verified trauma centers on the basis of their available resources. ACS verification confirms that these centers have the commitments and capabilities to manage the initial care of injured patients by providing stabilization and instituting life-saving maneuvers. In addition, verification confirms that protocols and agreements with higher-level trauma centers within a system enable the safe and efficient transfer of injured patients.
During many years of practice in the rural hospitals verified as trauma centers, including being the medical director of a Level II and Level III facility, I provided care to injured patients who presented to the emergency departments (EDs). My experiences confirmed the unequivocal value of practicing in those facilities, and I can attest to the benefits of verification within a system, like Iowa’s state program.
The following case report validates such assertions. A helicopter, unable to complete the transfer to a Level I center for a deteriorating patient with a left chest gunshot wound, landed at my Level III hospital. There was a “Hot Off Load,” which was followed by a full trauma alert for the patient in profound shock. After placing a chest tube during a 20-minute ED stay, the patient transferred to the OR for further resuscitation, and stabilization with required operative treatment. With the patient stabilized and fully resuscitated, according to established agreements, I contacted the Level I center from the OR. After 3 hours, the patient returned to the helicopter and completed the transfer to the Level I trauma center. The patient survived because of the local trauma team’s commitment, organization, and skill brought about by the trauma center verification.
Most research to date has focused on higher-level trauma centers, but recent studies have shown that ACS verification was an independent predictor of survival of trauma patients at Level II centers (J. Trauma Acute Care Surg. 2013;75:44-9; J. Trauma Acute Care Surg. 2010;69:1362-6).
I have firsthand experience with the verification process. Following my involvement with the ACS Committee on Trauma, I became a national site surveyor for the ACSVRC. I became an Advanced Trauma Life Support (ATLS) instructor and then worked as a course director. ATLS is an essential component for trauma center verification. It supports the rural surgeon by giving the local trauma team a format for consistent, life-saving care for the most severely injured patients. I subsequently completed the ACS Advanced Trauma Operative Management course and elected to become an instructor.
I have made site visits to many rural hospitals as a part of the ACSVRC process and have met with a wide range of reactions from “Let’s show off how good we are” to “We really don’t know why we’re doing this” to “Just give us the merit badge and then get out of our hair.” I am gratified to note that ACS Fellows are uniformly supportive. They understand the need for organization, standards, and performance improvement.
Opposition to the ACSVRC process by hospitals and staff is no doubt rooted in cost concerns and general resistance to change. But, as most of us know, demonstrated benefits for patient care can be highly persuasive to most medical professionals.
It is also worth noting that in an effort to decrease stress, the ACSVRC takes significant steps to support facilities that seek verification by eliminating ambiguity from application to on-site visit, by defining criteria deficiencies, and by providing evidence for the entire verification process. The complete VRC program along with an FAQ is available on the ACS website (facs.org/quality-programs/trauma/vrc).
For me, trauma care has always been about what is best for the injured patient. I often ask colleagues this question: “What care do you want for an injured member of your family?” I then answer my own question: “I want the best care possible. That means organized, efficient, and life-saving [care] if needed.” Fortunately, I experienced these benefits at my verified trauma center hospital when my second son was in a rollover motor vehicle crash. He survived.
Verified rural trauma centers do indeed offer the best opportunities for high-quality patient care and for support of the rural surgeons who render that care to “serve all with skill and fidelity.” I know. I have been there.
Dr. Caropreso is a general surgeon at Keokuk (Iowa) Area Hospital and clinical professor of surgery at the University of Iowa Carver College of Medicine, Iowa City. He has practiced surgery in the rural communities of Mason City, Iowa; Keokuk, Iowa; and Carthage, Ill., for 37 years.
Despite the many changes in medicine over the past century, traumatic injury remains a surgical disease.
Trauma injury is a major public health concern in rural areas, where death rates from unintentional injuries are higher than in metropolitan areas (Am. J. Public Health 2004;10:1689-93). The rural surgeon sees more than his or her fair share of victims of automobile accidents, falls, unintentional firearms injuries, and occupational accidents (think tractor accidents and injuries involving machinery and animals).
Another reality of the rural areas of the United States is that the number of broadly trained general surgeons who can treat a wide variety of trauma injuries is shrinking. Aging and retirements of the “old school rural surgeons” are accelerating and precipitating a lack of surgical coverage crisis, including trauma, in rural areas (Arch. Surg. 2005;140:74-9).
These well-documented developments have combined to reduce the availability of rural surgeons to manage injured patients in planned and consistent ways. Because of the current training paradigm of increasing subspecialization, injured rural patients may be cared for at rural hospitals with reduced capabilities and by rural surgeons with limited trauma training and experience.
What is the action plan to help counteract these developments and to provide the highest-quality patient care at facilities staffed by surgeons who have sworn to “serve all with skill and fidelity”?
The most straightforward and well-established action plan to achieve those goals is the verification process developed by the ACS Verification, Review, and Consultation Program (VRC) in 1987 to help hospitals improve trauma care. The process involves a pre-review questionnaire, a site visit, and report of findings. Verification as a trauma center guarantees that the facility has the required resources listed in the current, evidence-based guide, Resources for Optimal Care of the Injured Patient (2014). If successful, the trauma center receives a certificate of verification that is valid for 3 years.
Most rural hospitals are designated as Level III and IV verified trauma centers on the basis of their available resources. ACS verification confirms that these centers have the commitments and capabilities to manage the initial care of injured patients by providing stabilization and instituting life-saving maneuvers. In addition, verification confirms that protocols and agreements with higher-level trauma centers within a system enable the safe and efficient transfer of injured patients.
During many years of practice in the rural hospitals verified as trauma centers, including being the medical director of a Level II and Level III facility, I provided care to injured patients who presented to the emergency departments (EDs). My experiences confirmed the unequivocal value of practicing in those facilities, and I can attest to the benefits of verification within a system, like Iowa’s state program.
The following case report validates such assertions. A helicopter, unable to complete the transfer to a Level I center for a deteriorating patient with a left chest gunshot wound, landed at my Level III hospital. There was a “Hot Off Load,” which was followed by a full trauma alert for the patient in profound shock. After placing a chest tube during a 20-minute ED stay, the patient transferred to the OR for further resuscitation, and stabilization with required operative treatment. With the patient stabilized and fully resuscitated, according to established agreements, I contacted the Level I center from the OR. After 3 hours, the patient returned to the helicopter and completed the transfer to the Level I trauma center. The patient survived because of the local trauma team’s commitment, organization, and skill brought about by the trauma center verification.
Most research to date has focused on higher-level trauma centers, but recent studies have shown that ACS verification was an independent predictor of survival of trauma patients at Level II centers (J. Trauma Acute Care Surg. 2013;75:44-9; J. Trauma Acute Care Surg. 2010;69:1362-6).
I have firsthand experience with the verification process. Following my involvement with the ACS Committee on Trauma, I became a national site surveyor for the ACSVRC. I became an Advanced Trauma Life Support (ATLS) instructor and then worked as a course director. ATLS is an essential component for trauma center verification. It supports the rural surgeon by giving the local trauma team a format for consistent, life-saving care for the most severely injured patients. I subsequently completed the ACS Advanced Trauma Operative Management course and elected to become an instructor.
I have made site visits to many rural hospitals as a part of the ACSVRC process and have met with a wide range of reactions from “Let’s show off how good we are” to “We really don’t know why we’re doing this” to “Just give us the merit badge and then get out of our hair.” I am gratified to note that ACS Fellows are uniformly supportive. They understand the need for organization, standards, and performance improvement.
Opposition to the ACSVRC process by hospitals and staff is no doubt rooted in cost concerns and general resistance to change. But, as most of us know, demonstrated benefits for patient care can be highly persuasive to most medical professionals.
It is also worth noting that in an effort to decrease stress, the ACSVRC takes significant steps to support facilities that seek verification by eliminating ambiguity from application to on-site visit, by defining criteria deficiencies, and by providing evidence for the entire verification process. The complete VRC program along with an FAQ is available on the ACS website (facs.org/quality-programs/trauma/vrc).
For me, trauma care has always been about what is best for the injured patient. I often ask colleagues this question: “What care do you want for an injured member of your family?” I then answer my own question: “I want the best care possible. That means organized, efficient, and life-saving [care] if needed.” Fortunately, I experienced these benefits at my verified trauma center hospital when my second son was in a rollover motor vehicle crash. He survived.
Verified rural trauma centers do indeed offer the best opportunities for high-quality patient care and for support of the rural surgeons who render that care to “serve all with skill and fidelity.” I know. I have been there.
Dr. Caropreso is a general surgeon at Keokuk (Iowa) Area Hospital and clinical professor of surgery at the University of Iowa Carver College of Medicine, Iowa City. He has practiced surgery in the rural communities of Mason City, Iowa; Keokuk, Iowa; and Carthage, Ill., for 37 years.
From the Washington Office
S…G…R (continued) – It is much to all of our collective delight and relief that the SGR has finally been relegated to the ash heap of history.
In the late evening of April 14, in an act of historic bipartisanship, the Senate voted 92-8 in favor of H.R. 2 thus completing legislative action about which I wrote last month. President Obama signed the bill into law on April 16. As I write, Dave Hoyt, ACS Executive Director, is attending an event at the White House, along with other leaders of the physician community, to celebrate the full and permanent repeal of the SGR.
In the coming months, I will use this column to inform surgeons about various components of the legislation and its attendant policy. To start this process, I would first like to cover the key provisions of what is now known as MACRA – the Medicare Access and CHIP Reauthorization Act.
For starters, MACRA fully and permanently repeals the sustainable growth rate (SGR), thus providing stability to the Medicare physician fee schedule. Such repeal averts a 21% SGR-induced cut scheduled for April 1, 2015. MACRA also provides modest but stable positive updates of 0.5%/year for 5 years. When the legislative template that ultimately became MACRA was negotiated in late 2013 and early 2014, no provision was initially made for a positive update to physician payment. However, as a direct result of objections made by the leadership of the ACS, the legislation was subsequently revised to include the 0.5%/year update.
In addition, MACRA provides for the elimination, in 2018, of the current-law penalties associated with the existing quality programs, namely the Physician Quality Reporting System (PQRS), the Value-Based Modifier (VBM) program, and the Electronic Health Record-Meaningful Use (EHR-MU) program. The monies expected from those penalties will be returned to the pool, thus increasing the amount of funds available for incentive updates.
Beginning in 2019, these three programs will be combined into a single program known as the Merit-Based Incentive Payment System (MIPS). The MIPS makes it possible for all surgeons to receive an annual positive update based on their individual performance in four categories of Quality, Resource Use, Meaningful use of the electronic health record, and Clinical practice improvement activities. Surgeons will receive an annual, individual, single composite score based on their performance in these four categories. This score will be compared to a threshold score, defined as either the mean or median of composite scores from a prior performance period. Those with a score above the threshold will receive a positive adjustment and those with a score below the threshold will receive a negative adjustment.The legislation also provides the opportunity to receive a 5% bonus beginning in 2019 for participation in an Alternative Payment Model (APM). Surgeons who meet the full APM criteria will also be excluded from the MIPS assessment and most EHR-MU requirements. Those who participate in an APM at lower levels will receive credit toward their MIPS score. The bonus payment encourages the development of, testing of, and participation in an alternative payment model.
The passage of MACRA also represents a major victory relative to the College’s efforts to rescind the CMS policy transitioning 10- and 90-day global codes to zero-day global codes. ACS leadership and staff of the D.C. office had direct input into the specific language included in the legislation through multiple exchanges with congressional committee staff. In short, MACRA prohibits CMS from implementing its flawed plan relative to the transitioning of the global codes. Instead, beginning no later than 2017, CMS will collect samples of data on the number and level of postoperative visits furnished during the global period. Beginning in 2019, CMS will use this data to improve the accuracy of the valuation of surgical services. CMS is allowed to withhold 5% of the surgical payment until the sample information is reported at the end of the global period.
While MACRA does not implement broad medical liability reforms, it does include a provision which assures that MIPS participation cannot be used in a medical liability action. Specifically, the legislation specifies that the development, recognition or implementation of any guideline or other standard under any federal health care provision, including Medicare, cannot be construed as to establish the standard of care or duty of care owed by a surgeon to a patient in any medical malpractice claim.
Finally, and of particular interest to pediatric surgeons and other surgeons who care for children, MACRA includes two years of additional funding for the Children’s Health Insurance Program (CHIP) at the level provided under the Affordable Care Act.
Unfortunately, surgeons will need to become familiar with an entire new lexicon of acronyms associated with this new law and its policy. While this may initially seem daunting and confusing, it can be mastered with relative ease. It is my hope to continue to facilitate such with the content provided herein with the June edition of this column.
Until next month …
Dr. Bailey is a pediatric surgeon and Medical Director, Advocacy for the Division of Advocacy and Health Policy in the ACS offices in Washington, DC.
S…G…R (continued) – It is much to all of our collective delight and relief that the SGR has finally been relegated to the ash heap of history.
In the late evening of April 14, in an act of historic bipartisanship, the Senate voted 92-8 in favor of H.R. 2 thus completing legislative action about which I wrote last month. President Obama signed the bill into law on April 16. As I write, Dave Hoyt, ACS Executive Director, is attending an event at the White House, along with other leaders of the physician community, to celebrate the full and permanent repeal of the SGR.
In the coming months, I will use this column to inform surgeons about various components of the legislation and its attendant policy. To start this process, I would first like to cover the key provisions of what is now known as MACRA – the Medicare Access and CHIP Reauthorization Act.
For starters, MACRA fully and permanently repeals the sustainable growth rate (SGR), thus providing stability to the Medicare physician fee schedule. Such repeal averts a 21% SGR-induced cut scheduled for April 1, 2015. MACRA also provides modest but stable positive updates of 0.5%/year for 5 years. When the legislative template that ultimately became MACRA was negotiated in late 2013 and early 2014, no provision was initially made for a positive update to physician payment. However, as a direct result of objections made by the leadership of the ACS, the legislation was subsequently revised to include the 0.5%/year update.
In addition, MACRA provides for the elimination, in 2018, of the current-law penalties associated with the existing quality programs, namely the Physician Quality Reporting System (PQRS), the Value-Based Modifier (VBM) program, and the Electronic Health Record-Meaningful Use (EHR-MU) program. The monies expected from those penalties will be returned to the pool, thus increasing the amount of funds available for incentive updates.
Beginning in 2019, these three programs will be combined into a single program known as the Merit-Based Incentive Payment System (MIPS). The MIPS makes it possible for all surgeons to receive an annual positive update based on their individual performance in four categories of Quality, Resource Use, Meaningful use of the electronic health record, and Clinical practice improvement activities. Surgeons will receive an annual, individual, single composite score based on their performance in these four categories. This score will be compared to a threshold score, defined as either the mean or median of composite scores from a prior performance period. Those with a score above the threshold will receive a positive adjustment and those with a score below the threshold will receive a negative adjustment.The legislation also provides the opportunity to receive a 5% bonus beginning in 2019 for participation in an Alternative Payment Model (APM). Surgeons who meet the full APM criteria will also be excluded from the MIPS assessment and most EHR-MU requirements. Those who participate in an APM at lower levels will receive credit toward their MIPS score. The bonus payment encourages the development of, testing of, and participation in an alternative payment model.
The passage of MACRA also represents a major victory relative to the College’s efforts to rescind the CMS policy transitioning 10- and 90-day global codes to zero-day global codes. ACS leadership and staff of the D.C. office had direct input into the specific language included in the legislation through multiple exchanges with congressional committee staff. In short, MACRA prohibits CMS from implementing its flawed plan relative to the transitioning of the global codes. Instead, beginning no later than 2017, CMS will collect samples of data on the number and level of postoperative visits furnished during the global period. Beginning in 2019, CMS will use this data to improve the accuracy of the valuation of surgical services. CMS is allowed to withhold 5% of the surgical payment until the sample information is reported at the end of the global period.
While MACRA does not implement broad medical liability reforms, it does include a provision which assures that MIPS participation cannot be used in a medical liability action. Specifically, the legislation specifies that the development, recognition or implementation of any guideline or other standard under any federal health care provision, including Medicare, cannot be construed as to establish the standard of care or duty of care owed by a surgeon to a patient in any medical malpractice claim.
Finally, and of particular interest to pediatric surgeons and other surgeons who care for children, MACRA includes two years of additional funding for the Children’s Health Insurance Program (CHIP) at the level provided under the Affordable Care Act.
Unfortunately, surgeons will need to become familiar with an entire new lexicon of acronyms associated with this new law and its policy. While this may initially seem daunting and confusing, it can be mastered with relative ease. It is my hope to continue to facilitate such with the content provided herein with the June edition of this column.
Until next month …
Dr. Bailey is a pediatric surgeon and Medical Director, Advocacy for the Division of Advocacy and Health Policy in the ACS offices in Washington, DC.
S…G…R (continued) – It is much to all of our collective delight and relief that the SGR has finally been relegated to the ash heap of history.
In the late evening of April 14, in an act of historic bipartisanship, the Senate voted 92-8 in favor of H.R. 2 thus completing legislative action about which I wrote last month. President Obama signed the bill into law on April 16. As I write, Dave Hoyt, ACS Executive Director, is attending an event at the White House, along with other leaders of the physician community, to celebrate the full and permanent repeal of the SGR.
In the coming months, I will use this column to inform surgeons about various components of the legislation and its attendant policy. To start this process, I would first like to cover the key provisions of what is now known as MACRA – the Medicare Access and CHIP Reauthorization Act.
For starters, MACRA fully and permanently repeals the sustainable growth rate (SGR), thus providing stability to the Medicare physician fee schedule. Such repeal averts a 21% SGR-induced cut scheduled for April 1, 2015. MACRA also provides modest but stable positive updates of 0.5%/year for 5 years. When the legislative template that ultimately became MACRA was negotiated in late 2013 and early 2014, no provision was initially made for a positive update to physician payment. However, as a direct result of objections made by the leadership of the ACS, the legislation was subsequently revised to include the 0.5%/year update.
In addition, MACRA provides for the elimination, in 2018, of the current-law penalties associated with the existing quality programs, namely the Physician Quality Reporting System (PQRS), the Value-Based Modifier (VBM) program, and the Electronic Health Record-Meaningful Use (EHR-MU) program. The monies expected from those penalties will be returned to the pool, thus increasing the amount of funds available for incentive updates.
Beginning in 2019, these three programs will be combined into a single program known as the Merit-Based Incentive Payment System (MIPS). The MIPS makes it possible for all surgeons to receive an annual positive update based on their individual performance in four categories of Quality, Resource Use, Meaningful use of the electronic health record, and Clinical practice improvement activities. Surgeons will receive an annual, individual, single composite score based on their performance in these four categories. This score will be compared to a threshold score, defined as either the mean or median of composite scores from a prior performance period. Those with a score above the threshold will receive a positive adjustment and those with a score below the threshold will receive a negative adjustment.The legislation also provides the opportunity to receive a 5% bonus beginning in 2019 for participation in an Alternative Payment Model (APM). Surgeons who meet the full APM criteria will also be excluded from the MIPS assessment and most EHR-MU requirements. Those who participate in an APM at lower levels will receive credit toward their MIPS score. The bonus payment encourages the development of, testing of, and participation in an alternative payment model.
The passage of MACRA also represents a major victory relative to the College’s efforts to rescind the CMS policy transitioning 10- and 90-day global codes to zero-day global codes. ACS leadership and staff of the D.C. office had direct input into the specific language included in the legislation through multiple exchanges with congressional committee staff. In short, MACRA prohibits CMS from implementing its flawed plan relative to the transitioning of the global codes. Instead, beginning no later than 2017, CMS will collect samples of data on the number and level of postoperative visits furnished during the global period. Beginning in 2019, CMS will use this data to improve the accuracy of the valuation of surgical services. CMS is allowed to withhold 5% of the surgical payment until the sample information is reported at the end of the global period.
While MACRA does not implement broad medical liability reforms, it does include a provision which assures that MIPS participation cannot be used in a medical liability action. Specifically, the legislation specifies that the development, recognition or implementation of any guideline or other standard under any federal health care provision, including Medicare, cannot be construed as to establish the standard of care or duty of care owed by a surgeon to a patient in any medical malpractice claim.
Finally, and of particular interest to pediatric surgeons and other surgeons who care for children, MACRA includes two years of additional funding for the Children’s Health Insurance Program (CHIP) at the level provided under the Affordable Care Act.
Unfortunately, surgeons will need to become familiar with an entire new lexicon of acronyms associated with this new law and its policy. While this may initially seem daunting and confusing, it can be mastered with relative ease. It is my hope to continue to facilitate such with the content provided herein with the June edition of this column.
Until next month …
Dr. Bailey is a pediatric surgeon and Medical Director, Advocacy for the Division of Advocacy and Health Policy in the ACS offices in Washington, DC.
Lessons from our dying patients
Dying patients teach us to think more carefully about whether or not our surgical interventions will be beneficial.
I work in palliative care, and my surgical colleagues, especially the residents, are often surprised when I call them and ask them to consult on my patients who are very ill and have a “Do Not Resuscitate” order in their charts. I’m also an anesthesiologist working in interventional pain management, and I regularly do procedures on patients who have prognoses that are extremely limited. For other patients, I recommend against any interventions at all.
How do we know when to intervene on patients who are dying? Perhaps more importantly, how do we know when NOT to intervene? Two recent cases of almost identical fractures illustrated for me the need to think beyond the anatomic problem when evaluating options for care.
Last year, I admitted a woman, “Donna,” with widely metastatic breast cancer to our inpatient palliative care service. She had fallen at home and hurt her arm about 2 months prior to admission. She had been confined to her bed for about 6 weeks. She was brought to the hospital because she was becoming delirious. She had many sources of pain that were relatively well controlled when she was lying down, but her worst pain was in her left arm. We found a fracture of her humerus. When her family learned that the fracture would not heal on its own because of the large metastasis there, they demanded surgery to fix it. Shortly thereafter, I re-admitted a patient, “Cindy,” with a very similar story. She also had widely metastatic breast cancer, and her pain had been very difficult to control. We had found a pain regimen that worked well for her on her previous admission, but she had fallen over her walker and broke her humerus after we had discharged her to a rehab facility. When I saw her back in the hospital, I told her that I thought she would need surgery to fix her arm. She was depressed by this setback, she was in pain again, and she told me that she would prefer not to have any intervention because she feared the additional pain that it would cause.
With Donna, we sat down with her and her family to hear what their hopes were for her care. They understood that she did not have further chemotherapy or radiation options for her cancer, but they thought if she got the surgery that at least she would be able to get out of bed and walk again. My colleague carefully explained that yes, he could fix the fracture and that this could mean that the pain in her left arm would improve. He went on to say, however, that he did not think that the surgery would allow her to walk again as she had not been able to walk for a few weeks after the injury. When the family heard that the surgery probably wouldn’t restore her mobility, they decided against the procedure. With Cindy, we had a very different conversation. She was not inclined to have the procedure, but I expressed my concern that she wouldn’t be able to walk again unless she had the procedure because she needed her arms to use her walker. Although she did not have any further chemotherapy or radiation options, her oncologist had told us that her prognosis could be several months. In this case, my surgical colleague explained that he could perform surgery for the fracture and that he thought that it would both help her pain and allow her to use her walker again. We recommended that she have the surgery given her hope to continue to live independently, as she had been, for as long as possible. She ultimately agreed to do so and was able to return home.
These two patients reminded me again of how important it is for us to understand what our patients’ hopes and expectations are for a procedure. It is very distressing for clinicians when desperate families want treatments that likely have little benefit. When patients have limited prognoses, aligning patient goals and procedure goals is especially important as the outcome of the procedure can define the patient’s remaining days.
Donna’s family demanded a surgery expecting a result that was very unlikely, and Cindy initially declined the same surgery that ultimately benefitted her greatly. Our job is to make and execute the medical recommendations that best fit with our patients’ goals and understanding. Sometimes this will mean performing procedures on patients who are extremely ill and have “Do Not Resuscitate” orders, and at other times, it will mean not doing procedures, even if a patient and family want them to be done.
Dr. Rickerson is an anesthesiologist at the Dana-Farber Cancer Institute and Brigham and Women’s Hospital, Boston.
Dying patients teach us to think more carefully about whether or not our surgical interventions will be beneficial.
I work in palliative care, and my surgical colleagues, especially the residents, are often surprised when I call them and ask them to consult on my patients who are very ill and have a “Do Not Resuscitate” order in their charts. I’m also an anesthesiologist working in interventional pain management, and I regularly do procedures on patients who have prognoses that are extremely limited. For other patients, I recommend against any interventions at all.
How do we know when to intervene on patients who are dying? Perhaps more importantly, how do we know when NOT to intervene? Two recent cases of almost identical fractures illustrated for me the need to think beyond the anatomic problem when evaluating options for care.
Last year, I admitted a woman, “Donna,” with widely metastatic breast cancer to our inpatient palliative care service. She had fallen at home and hurt her arm about 2 months prior to admission. She had been confined to her bed for about 6 weeks. She was brought to the hospital because she was becoming delirious. She had many sources of pain that were relatively well controlled when she was lying down, but her worst pain was in her left arm. We found a fracture of her humerus. When her family learned that the fracture would not heal on its own because of the large metastasis there, they demanded surgery to fix it. Shortly thereafter, I re-admitted a patient, “Cindy,” with a very similar story. She also had widely metastatic breast cancer, and her pain had been very difficult to control. We had found a pain regimen that worked well for her on her previous admission, but she had fallen over her walker and broke her humerus after we had discharged her to a rehab facility. When I saw her back in the hospital, I told her that I thought she would need surgery to fix her arm. She was depressed by this setback, she was in pain again, and she told me that she would prefer not to have any intervention because she feared the additional pain that it would cause.
With Donna, we sat down with her and her family to hear what their hopes were for her care. They understood that she did not have further chemotherapy or radiation options for her cancer, but they thought if she got the surgery that at least she would be able to get out of bed and walk again. My colleague carefully explained that yes, he could fix the fracture and that this could mean that the pain in her left arm would improve. He went on to say, however, that he did not think that the surgery would allow her to walk again as she had not been able to walk for a few weeks after the injury. When the family heard that the surgery probably wouldn’t restore her mobility, they decided against the procedure. With Cindy, we had a very different conversation. She was not inclined to have the procedure, but I expressed my concern that she wouldn’t be able to walk again unless she had the procedure because she needed her arms to use her walker. Although she did not have any further chemotherapy or radiation options, her oncologist had told us that her prognosis could be several months. In this case, my surgical colleague explained that he could perform surgery for the fracture and that he thought that it would both help her pain and allow her to use her walker again. We recommended that she have the surgery given her hope to continue to live independently, as she had been, for as long as possible. She ultimately agreed to do so and was able to return home.
These two patients reminded me again of how important it is for us to understand what our patients’ hopes and expectations are for a procedure. It is very distressing for clinicians when desperate families want treatments that likely have little benefit. When patients have limited prognoses, aligning patient goals and procedure goals is especially important as the outcome of the procedure can define the patient’s remaining days.
Donna’s family demanded a surgery expecting a result that was very unlikely, and Cindy initially declined the same surgery that ultimately benefitted her greatly. Our job is to make and execute the medical recommendations that best fit with our patients’ goals and understanding. Sometimes this will mean performing procedures on patients who are extremely ill and have “Do Not Resuscitate” orders, and at other times, it will mean not doing procedures, even if a patient and family want them to be done.
Dr. Rickerson is an anesthesiologist at the Dana-Farber Cancer Institute and Brigham and Women’s Hospital, Boston.
Dying patients teach us to think more carefully about whether or not our surgical interventions will be beneficial.
I work in palliative care, and my surgical colleagues, especially the residents, are often surprised when I call them and ask them to consult on my patients who are very ill and have a “Do Not Resuscitate” order in their charts. I’m also an anesthesiologist working in interventional pain management, and I regularly do procedures on patients who have prognoses that are extremely limited. For other patients, I recommend against any interventions at all.
How do we know when to intervene on patients who are dying? Perhaps more importantly, how do we know when NOT to intervene? Two recent cases of almost identical fractures illustrated for me the need to think beyond the anatomic problem when evaluating options for care.
Last year, I admitted a woman, “Donna,” with widely metastatic breast cancer to our inpatient palliative care service. She had fallen at home and hurt her arm about 2 months prior to admission. She had been confined to her bed for about 6 weeks. She was brought to the hospital because she was becoming delirious. She had many sources of pain that were relatively well controlled when she was lying down, but her worst pain was in her left arm. We found a fracture of her humerus. When her family learned that the fracture would not heal on its own because of the large metastasis there, they demanded surgery to fix it. Shortly thereafter, I re-admitted a patient, “Cindy,” with a very similar story. She also had widely metastatic breast cancer, and her pain had been very difficult to control. We had found a pain regimen that worked well for her on her previous admission, but she had fallen over her walker and broke her humerus after we had discharged her to a rehab facility. When I saw her back in the hospital, I told her that I thought she would need surgery to fix her arm. She was depressed by this setback, she was in pain again, and she told me that she would prefer not to have any intervention because she feared the additional pain that it would cause.
With Donna, we sat down with her and her family to hear what their hopes were for her care. They understood that she did not have further chemotherapy or radiation options for her cancer, but they thought if she got the surgery that at least she would be able to get out of bed and walk again. My colleague carefully explained that yes, he could fix the fracture and that this could mean that the pain in her left arm would improve. He went on to say, however, that he did not think that the surgery would allow her to walk again as she had not been able to walk for a few weeks after the injury. When the family heard that the surgery probably wouldn’t restore her mobility, they decided against the procedure. With Cindy, we had a very different conversation. She was not inclined to have the procedure, but I expressed my concern that she wouldn’t be able to walk again unless she had the procedure because she needed her arms to use her walker. Although she did not have any further chemotherapy or radiation options, her oncologist had told us that her prognosis could be several months. In this case, my surgical colleague explained that he could perform surgery for the fracture and that he thought that it would both help her pain and allow her to use her walker again. We recommended that she have the surgery given her hope to continue to live independently, as she had been, for as long as possible. She ultimately agreed to do so and was able to return home.
These two patients reminded me again of how important it is for us to understand what our patients’ hopes and expectations are for a procedure. It is very distressing for clinicians when desperate families want treatments that likely have little benefit. When patients have limited prognoses, aligning patient goals and procedure goals is especially important as the outcome of the procedure can define the patient’s remaining days.
Donna’s family demanded a surgery expecting a result that was very unlikely, and Cindy initially declined the same surgery that ultimately benefitted her greatly. Our job is to make and execute the medical recommendations that best fit with our patients’ goals and understanding. Sometimes this will mean performing procedures on patients who are extremely ill and have “Do Not Resuscitate” orders, and at other times, it will mean not doing procedures, even if a patient and family want them to be done.
Dr. Rickerson is an anesthesiologist at the Dana-Farber Cancer Institute and Brigham and Women’s Hospital, Boston.
Avoiding metformin in renal insufficiency
A 47-year-old obese male with type 2 diabetes has been on metformin for the last 2 years with good effect (hemoglobin A1c of 6.8), and with exercise has been able to lose 5-10 pounds. His last two blood tests show creatinine levels of 1.5 and 1.6. What do you recommend?
A) Continue with metformin.
B) Stop metformin, start sulfonylurea.
C) Stop metformin, begin glargine.
D) Stop metformin, begin pioglitazone.
Myth: Metformin should not be used in patients with mild to moderate renal insufficiency because of an increased risk of lactic acidosis.
Metformin is the most commonly used oral agent for the treatment of type 2 diabetes in the United States, but the FDA-approved drug label states that it is contraindicated in patients with an abnormal creatinine clearance or serum creatinine of 1.4 in women and 1.5 in men.<sup/>The concern is for development of lactic acidosis in patients because the renally excreted metformin may build up as a result of decreased renal function.
Metformin was approved for use in the United States in 1995, many years after the drug was introduced in Europe. The first drug in its class, phenformin, was removed from the United States and most European markets in 1977 because of a high incidence of lactic acidosis occurring at therapeutic doses. One in 4,000 patients taking phenformin develops lactic acidosis (J. Emerg. Med. 1998;16:881-6). Phenformin has been shown to cause type B lactic acidosis, without evidence of hypoxia or hypoperfusion, and lactic acidosis because of phenformin carried a 50% mortality rate.
Deep concern for the possibility of a similar problem with metformin played an important role in its delay of availability in the United States. It isn’t clear, however, that diabetes patients on metformin have a higher risk of developing lactic acidosis than diabetes patients who are not on metformin.
A Cochrane review of 347 studies, including 70,490 person-years of metformin use, compared with 55,451 person-years in the nonmetformin group, showed no cases of fatal or nonfatal lactic acidosis in either group (Cochrane Database Syst. Rev. 2010 Apr 14:CD002967). More than half the studies included (53%) allowed for the inclusion of patients with creatinine levels greater than 1.5. There were no differences in lactate levels between metformin-treated patients and patients who did not receive metformin.
In a study using the Saskatchewan Health administrative database, which involved 11,797 patients with 22,296 years of metformin exposure, there were two cases of lactic acidosis (Diabetes Care 1999;22:925-7). This calculates to a rate of 9 cases per 100,000 person years, the same rate as in patients with diabetes who are not taking metformin (9.7 cases per 100,000) (Diabetes Care 1998;21:1659-63).
A recent study looked at the incidence of lactic acidosis in patients taking metformin with and without abnormalities in renal function (Diabetes Care 2014;37:2291-5). There was no statistically significant difference in the rates of lactic acidosis in patients who were on metformin with normal renal function, compared with those with varying degrees of renal insufficiency. The overall rate of lactic acidosis was 10.3 per 100,000 patient years, which is almost identical to the rates in the other studies mentioned, and there were no fatalities.
Several recommendations for using metformin in patients with renal insufficiency have been published (see table) (JAMA 2014;312:2668-75; Diabetes Care 2011;34:1431-7). Metformin has shown cardiovascular mortality benefits, compared with sulfonylureas, in the treatment of diabetes (Diabetes Care 2013;36:1304-11). Avoiding its use in patients with mild to moderate renal insufficiency in favor of other treatments that may not be as beneficial and may well lead to worse outcomes.
There is no evidence that metformin increases the lactic acidosis risk in patients with diabetes, but until there is a change in the FDA labeling, physicians will likely continue to be hesitant to use it in patients with renal insufficiency.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is the Rathmann Family Foundation Chair in Patient-Centered Clinical Education. Contact Dr. Paauw at [email protected].
A 47-year-old obese male with type 2 diabetes has been on metformin for the last 2 years with good effect (hemoglobin A1c of 6.8), and with exercise has been able to lose 5-10 pounds. His last two blood tests show creatinine levels of 1.5 and 1.6. What do you recommend?
A) Continue with metformin.
B) Stop metformin, start sulfonylurea.
C) Stop metformin, begin glargine.
D) Stop metformin, begin pioglitazone.
Myth: Metformin should not be used in patients with mild to moderate renal insufficiency because of an increased risk of lactic acidosis.
Metformin is the most commonly used oral agent for the treatment of type 2 diabetes in the United States, but the FDA-approved drug label states that it is contraindicated in patients with an abnormal creatinine clearance or serum creatinine of 1.4 in women and 1.5 in men.<sup/>The concern is for development of lactic acidosis in patients because the renally excreted metformin may build up as a result of decreased renal function.
Metformin was approved for use in the United States in 1995, many years after the drug was introduced in Europe. The first drug in its class, phenformin, was removed from the United States and most European markets in 1977 because of a high incidence of lactic acidosis occurring at therapeutic doses. One in 4,000 patients taking phenformin develops lactic acidosis (J. Emerg. Med. 1998;16:881-6). Phenformin has been shown to cause type B lactic acidosis, without evidence of hypoxia or hypoperfusion, and lactic acidosis because of phenformin carried a 50% mortality rate.
Deep concern for the possibility of a similar problem with metformin played an important role in its delay of availability in the United States. It isn’t clear, however, that diabetes patients on metformin have a higher risk of developing lactic acidosis than diabetes patients who are not on metformin.
A Cochrane review of 347 studies, including 70,490 person-years of metformin use, compared with 55,451 person-years in the nonmetformin group, showed no cases of fatal or nonfatal lactic acidosis in either group (Cochrane Database Syst. Rev. 2010 Apr 14:CD002967). More than half the studies included (53%) allowed for the inclusion of patients with creatinine levels greater than 1.5. There were no differences in lactate levels between metformin-treated patients and patients who did not receive metformin.
In a study using the Saskatchewan Health administrative database, which involved 11,797 patients with 22,296 years of metformin exposure, there were two cases of lactic acidosis (Diabetes Care 1999;22:925-7). This calculates to a rate of 9 cases per 100,000 person years, the same rate as in patients with diabetes who are not taking metformin (9.7 cases per 100,000) (Diabetes Care 1998;21:1659-63).
A recent study looked at the incidence of lactic acidosis in patients taking metformin with and without abnormalities in renal function (Diabetes Care 2014;37:2291-5). There was no statistically significant difference in the rates of lactic acidosis in patients who were on metformin with normal renal function, compared with those with varying degrees of renal insufficiency. The overall rate of lactic acidosis was 10.3 per 100,000 patient years, which is almost identical to the rates in the other studies mentioned, and there were no fatalities.
Several recommendations for using metformin in patients with renal insufficiency have been published (see table) (JAMA 2014;312:2668-75; Diabetes Care 2011;34:1431-7). Metformin has shown cardiovascular mortality benefits, compared with sulfonylureas, in the treatment of diabetes (Diabetes Care 2013;36:1304-11). Avoiding its use in patients with mild to moderate renal insufficiency in favor of other treatments that may not be as beneficial and may well lead to worse outcomes.
There is no evidence that metformin increases the lactic acidosis risk in patients with diabetes, but until there is a change in the FDA labeling, physicians will likely continue to be hesitant to use it in patients with renal insufficiency.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is the Rathmann Family Foundation Chair in Patient-Centered Clinical Education. Contact Dr. Paauw at [email protected].
A 47-year-old obese male with type 2 diabetes has been on metformin for the last 2 years with good effect (hemoglobin A1c of 6.8), and with exercise has been able to lose 5-10 pounds. His last two blood tests show creatinine levels of 1.5 and 1.6. What do you recommend?
A) Continue with metformin.
B) Stop metformin, start sulfonylurea.
C) Stop metformin, begin glargine.
D) Stop metformin, begin pioglitazone.
Myth: Metformin should not be used in patients with mild to moderate renal insufficiency because of an increased risk of lactic acidosis.
Metformin is the most commonly used oral agent for the treatment of type 2 diabetes in the United States, but the FDA-approved drug label states that it is contraindicated in patients with an abnormal creatinine clearance or serum creatinine of 1.4 in women and 1.5 in men.<sup/>The concern is for development of lactic acidosis in patients because the renally excreted metformin may build up as a result of decreased renal function.
Metformin was approved for use in the United States in 1995, many years after the drug was introduced in Europe. The first drug in its class, phenformin, was removed from the United States and most European markets in 1977 because of a high incidence of lactic acidosis occurring at therapeutic doses. One in 4,000 patients taking phenformin develops lactic acidosis (J. Emerg. Med. 1998;16:881-6). Phenformin has been shown to cause type B lactic acidosis, without evidence of hypoxia or hypoperfusion, and lactic acidosis because of phenformin carried a 50% mortality rate.
Deep concern for the possibility of a similar problem with metformin played an important role in its delay of availability in the United States. It isn’t clear, however, that diabetes patients on metformin have a higher risk of developing lactic acidosis than diabetes patients who are not on metformin.
A Cochrane review of 347 studies, including 70,490 person-years of metformin use, compared with 55,451 person-years in the nonmetformin group, showed no cases of fatal or nonfatal lactic acidosis in either group (Cochrane Database Syst. Rev. 2010 Apr 14:CD002967). More than half the studies included (53%) allowed for the inclusion of patients with creatinine levels greater than 1.5. There were no differences in lactate levels between metformin-treated patients and patients who did not receive metformin.
In a study using the Saskatchewan Health administrative database, which involved 11,797 patients with 22,296 years of metformin exposure, there were two cases of lactic acidosis (Diabetes Care 1999;22:925-7). This calculates to a rate of 9 cases per 100,000 person years, the same rate as in patients with diabetes who are not taking metformin (9.7 cases per 100,000) (Diabetes Care 1998;21:1659-63).
A recent study looked at the incidence of lactic acidosis in patients taking metformin with and without abnormalities in renal function (Diabetes Care 2014;37:2291-5). There was no statistically significant difference in the rates of lactic acidosis in patients who were on metformin with normal renal function, compared with those with varying degrees of renal insufficiency. The overall rate of lactic acidosis was 10.3 per 100,000 patient years, which is almost identical to the rates in the other studies mentioned, and there were no fatalities.
Several recommendations for using metformin in patients with renal insufficiency have been published (see table) (JAMA 2014;312:2668-75; Diabetes Care 2011;34:1431-7). Metformin has shown cardiovascular mortality benefits, compared with sulfonylureas, in the treatment of diabetes (Diabetes Care 2013;36:1304-11). Avoiding its use in patients with mild to moderate renal insufficiency in favor of other treatments that may not be as beneficial and may well lead to worse outcomes.
There is no evidence that metformin increases the lactic acidosis risk in patients with diabetes, but until there is a change in the FDA labeling, physicians will likely continue to be hesitant to use it in patients with renal insufficiency.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is the Rathmann Family Foundation Chair in Patient-Centered Clinical Education. Contact Dr. Paauw at [email protected].
Best interest
A dense broth of tedium, a sprinkle of annoyance, and a dash of trepidation – these are the ingredients of the mental soup that simmers in my head when I answer a middle-of-the-night parent phone call.
At least they were until the task of solving the community’s nighttime phone “crises” fell upon the able, eager shoulders of our new interns.
Every now and then, the universe throws up a surprise. One night, my intern was placating a very angry man who was upset with his inconsolable baby. He was the foster father of a baby with neonatal abstinence syndrome (NAS) who had been discharged earlier that day.
“I feel like this baby’s been thrown at us! He wasn’t ready to go home!” he cried. Having never met the baby (foster mom had taken the baby home), this man had returned from a long work shift to find a screaming baby at home. He was aggressive and rude as he ranted at my intern. She empathized and explained that other symptoms might include rapid breathing, irritability, sleep problems, etc.
Although she handled the call with consummate grace and professionalism, afterward an uneasy feeling crept over us. An angry, tired man pushed to his limits, and a very difficult, strange new baby at home was a setup for the perfect storm. Our duty in this situation was clear – we were the protectors of this baby’s best interest. That was all that mattered.
With a rising sense of dread, we juggled frantic phone calls between Child Protective Services, the attending physician, the foster family, and the nearest emergency department. All I could think of was how badly we had failed this baby. Something somewhere had gone horribly wrong for this innocent child to be in danger now.
An hour later, when I finally got through to the foster father, he sounded calmer. “We can’t do this,” he stated simply. He informed me he had called Child Protective Services himself. The baby would come back to us temporarily, while we found him a safe home. Relief swept over us.
Perhaps the baby should never have gone home with this family. Perhaps we had no way of knowing this would happen. Perhaps the family did not realize the responsibility they were assuming. We are all only human. We make mistakes. But we pick up the pieces and we try again, guided by the best interest of the children we swear to protect. This desire to keep trying is what makes all the difference in the world. By making the call himself, this man reaffirmed my faith in the process in which we all play a part. May the quest for the best interest of our children endure forever.
Dr. Behere is a third-year resident in pediatrics at Children’s Hospital at Dartmouth-Hitchcock, Lebanon, N.H. E-mail him at [email protected].
A dense broth of tedium, a sprinkle of annoyance, and a dash of trepidation – these are the ingredients of the mental soup that simmers in my head when I answer a middle-of-the-night parent phone call.
At least they were until the task of solving the community’s nighttime phone “crises” fell upon the able, eager shoulders of our new interns.
Every now and then, the universe throws up a surprise. One night, my intern was placating a very angry man who was upset with his inconsolable baby. He was the foster father of a baby with neonatal abstinence syndrome (NAS) who had been discharged earlier that day.
“I feel like this baby’s been thrown at us! He wasn’t ready to go home!” he cried. Having never met the baby (foster mom had taken the baby home), this man had returned from a long work shift to find a screaming baby at home. He was aggressive and rude as he ranted at my intern. She empathized and explained that other symptoms might include rapid breathing, irritability, sleep problems, etc.
Although she handled the call with consummate grace and professionalism, afterward an uneasy feeling crept over us. An angry, tired man pushed to his limits, and a very difficult, strange new baby at home was a setup for the perfect storm. Our duty in this situation was clear – we were the protectors of this baby’s best interest. That was all that mattered.
With a rising sense of dread, we juggled frantic phone calls between Child Protective Services, the attending physician, the foster family, and the nearest emergency department. All I could think of was how badly we had failed this baby. Something somewhere had gone horribly wrong for this innocent child to be in danger now.
An hour later, when I finally got through to the foster father, he sounded calmer. “We can’t do this,” he stated simply. He informed me he had called Child Protective Services himself. The baby would come back to us temporarily, while we found him a safe home. Relief swept over us.
Perhaps the baby should never have gone home with this family. Perhaps we had no way of knowing this would happen. Perhaps the family did not realize the responsibility they were assuming. We are all only human. We make mistakes. But we pick up the pieces and we try again, guided by the best interest of the children we swear to protect. This desire to keep trying is what makes all the difference in the world. By making the call himself, this man reaffirmed my faith in the process in which we all play a part. May the quest for the best interest of our children endure forever.
Dr. Behere is a third-year resident in pediatrics at Children’s Hospital at Dartmouth-Hitchcock, Lebanon, N.H. E-mail him at [email protected].
A dense broth of tedium, a sprinkle of annoyance, and a dash of trepidation – these are the ingredients of the mental soup that simmers in my head when I answer a middle-of-the-night parent phone call.
At least they were until the task of solving the community’s nighttime phone “crises” fell upon the able, eager shoulders of our new interns.
Every now and then, the universe throws up a surprise. One night, my intern was placating a very angry man who was upset with his inconsolable baby. He was the foster father of a baby with neonatal abstinence syndrome (NAS) who had been discharged earlier that day.
“I feel like this baby’s been thrown at us! He wasn’t ready to go home!” he cried. Having never met the baby (foster mom had taken the baby home), this man had returned from a long work shift to find a screaming baby at home. He was aggressive and rude as he ranted at my intern. She empathized and explained that other symptoms might include rapid breathing, irritability, sleep problems, etc.
Although she handled the call with consummate grace and professionalism, afterward an uneasy feeling crept over us. An angry, tired man pushed to his limits, and a very difficult, strange new baby at home was a setup for the perfect storm. Our duty in this situation was clear – we were the protectors of this baby’s best interest. That was all that mattered.
With a rising sense of dread, we juggled frantic phone calls between Child Protective Services, the attending physician, the foster family, and the nearest emergency department. All I could think of was how badly we had failed this baby. Something somewhere had gone horribly wrong for this innocent child to be in danger now.
An hour later, when I finally got through to the foster father, he sounded calmer. “We can’t do this,” he stated simply. He informed me he had called Child Protective Services himself. The baby would come back to us temporarily, while we found him a safe home. Relief swept over us.
Perhaps the baby should never have gone home with this family. Perhaps we had no way of knowing this would happen. Perhaps the family did not realize the responsibility they were assuming. We are all only human. We make mistakes. But we pick up the pieces and we try again, guided by the best interest of the children we swear to protect. This desire to keep trying is what makes all the difference in the world. By making the call himself, this man reaffirmed my faith in the process in which we all play a part. May the quest for the best interest of our children endure forever.
Dr. Behere is a third-year resident in pediatrics at Children’s Hospital at Dartmouth-Hitchcock, Lebanon, N.H. E-mail him at [email protected].