User login
Shakespeare and suicide
The medical knowledge that William Shakespeare possessed has awed scholars for centuries. Theories about the provenance of his knowledge abound (such as his son-in-law being a physician), and the inclusion of medical terms and ailments throughout his plays suggests a broad knowledge of disease and sickness. Scholars have noted how he sprinkles references to dermatologic, neurologic, orthopedic, and metabolic ailments throughout his plays, mentioning carbuncles, fistulas, corpulence, rhinophyma, scurvy, ague, enuresis, kyphosis, epilepsy, and parkinsonism.1 What seems to strike post-Enlightenment audiences—and what sets Shakespeare apart from many of his contemporaries—is his portrayal of “complex” characters, those with what we envision as rich interior worlds and with whom a modern audience can resonate. There is a reason psychiatrists such as Sigmund Freud have rushed back to Shakespeare and (sometimes anachronistically) found in his characters various psychiatric diagnoses such as depression, anxiety, paranoia, jealous delusions, and obsessive-compulsive disorder. Suicide and suicidal ideation are prevalent themes in some of Shakespeare’s most well-known characters.
A surprisingly common theme
The gravest outcome of a psychiatric illness is death by suicide, which occurs in 13 of Shakespeare’s characters.2 There are additional characters who exhibit suicidal ideation without a completed act. Shakespearean characters whose lives end in suicide are variably portrayed, dying by various means and circumstances. Hamlet (who dies at the hand of his foe, Laertes), famously soliloquizes the theme of suicide and the afterlife. He ponders “tak[ing] arms against a sea of troubles.” Ophelia dies ambiguously. Immediately after, her mother and brother recount her death in a brook—having had “too much of water” when her garments “heavy with their drink, | pull’d the poor wretch from her melodious lay | To muddy death.” The 2 clowns/gravediggers then debate whether Ophelia deserves a Christian burial and if her death should be considered a suicide: did the water drown her, or did she drown herself?3
Lady Macbeth’s suicide is offstage, punctuated by a “night-shriek.” Romeo drinks poison and dies “with a kiss.” Juliet quickly follows, making her body the sword’s sheath which “there rust, and let [her] die.” Othello stabs himself after requesting that his peers will “speak of me as I am.” One of King Lear’s daughters poisons her sister “and after [slays] herself.” Timon dies by his cave, “entomb’d upon the very hem o’ the sea.” In Antony and Cleopatra, after being told that Cleopatra has killed herself with Antony’s name on her lips, Antony begs to be stabbed and then stabs himself; he is not defeated by Caesar, but rather conquered by himself: “none but Antony | Should conquer Antony.” Cleopatra and her lady-in-waiting, Charmian, kill themselves with an asp. In Julius Caesar, Brutus runs upon his sword. Cassius begs for his own death, asking that “this good sword, | That ran through Caesar’s bowels, search this bosom.” Portia, it is reported, “swallowed fire.”
Shakespeare uses specific stylized language to portray characters in psychological anguish and suicidal states. Scholars have discussed how he uses certain stylistic language to highlight the anguish that happens during solitary, solipsistic moments of contemplation.4 Moments of anguish and suicidal ideation are marked by verbal repetition. An example of this repetition comes in Hamlet’s speech after he returns to the kingdom where his uncle has usurped his father, when he laments that he cannot end his own life. He says:
O, that this too too sullied flesh would melt,
Thaw, and resolve itself into a dew!
Or that the Everlasting had not fix’d
His canon ’gainst self-slaughter! O God, God,
How weary, stale, flat, and unprofitable
Seem to me all the uses of this world.
In these 6 lines, there are 2 instances of verbal repetition: “too too” and “God, God.” In this moment of solitude and despair, Hamlet’s speech fractures; his fractured speech reflects his fractured psyche. While Hamlet speaks of staleness and stagnation in the world, his words represent a sterile excess. No meaning is elicited by their repetition; there is no forward momentum to his speech. The words reflect the extent to which Hamlet is stuck and divided in this moment. Something similar happens in Macbeth’s “Tomorrow and tomorrow and tomorrow” speech. The words march on, and with each repetition they become increasingly hollow and brittle.
Why does this discussion of suicide in Shakespeare hold value for a contemporary psychiatrist? First, there is no single prototypical suicidal character in Shakespeare. His characters who are suicidal vary in their demographics and incentives for ending their lives. In this way, he provides a rich framework, one with which many people can engage. Second, this discussion fits into an existing paradigm for using art therapy (specifically Shakespeare) as a treatment modality for trauma.5 Programs such as DE-CRUIT have used the recitation of Shakespearean verse as a means of processing trauma in veterans.5 While Shakespeare does not mention a remedy for suicide in his plays, perhaps the text can serve as medicine. Third, the repetitive speech that Shakespeare uses in times of anguish could be a fairly accurate reflection of speech patterns in patients who are suicidal. Research that completed a spoken language analysis of patients who were suicidal has found “mechanical and repetitive phrasing” as a quality of these patients’ speech.6,7
For hundreds of years, critics have searched beyond the text for Shakespeare’s voice and opinion; what did he himself think of melancholy, despair, or suicide? We cannot know. We, as readers, are invited to explore a nuanced and multifaceted view of suicide, one that neither chides nor valorizes the act, and provides ambiguity rather than condemnation.
1. Paciaroni M, Bogousslavsky J. William Shakespeare’s neurology. Prog Brain Res. 2013;206:3-18.
2. Kirkland LR. To end itself by death: suicide in Shakespeare’s tragedies. South Med J. 1999;92(7):660-666.
3. Sale C. The “Amending Hand”: Hales v. Petit, Eyston v. Studd, and Equitable Action in Hamlet. In: Jordan C, Cunningham K, eds. The Law in Shakespeare. Early Modern Literature in History. Palgrave Macmillan; 2007:189-207. https://doi.org/10.1057/9780230626348_11
4. Langley E. Narcissism and Suicide in Shakespeare and His Contemporaries. Oxford University Press; 2009.
5. Ali A, Wolfert S, Lam I, et al. Intersecting modes of aesthetic distance and mimetic induction in therapeutic process: examining a drama-based treatment for military-related traumatic stress. Drama Therapy Review. 2018;4(2):153-165.
6. Belouali A, Gupta S, Sourirajan V, et al. Acoustic and language analysis of speech for suicidal ideation among US veterans. BioData Min. 2021;14(1):11. doi:10.1186/s13040-021-00245-y
7. Cummins N, Scherer S, Krajewski J, et al. A review of depression and suicide risk assessment using speech analysis. Speech Commun. 2015;71:10-49.
The medical knowledge that William Shakespeare possessed has awed scholars for centuries. Theories about the provenance of his knowledge abound (such as his son-in-law being a physician), and the inclusion of medical terms and ailments throughout his plays suggests a broad knowledge of disease and sickness. Scholars have noted how he sprinkles references to dermatologic, neurologic, orthopedic, and metabolic ailments throughout his plays, mentioning carbuncles, fistulas, corpulence, rhinophyma, scurvy, ague, enuresis, kyphosis, epilepsy, and parkinsonism.1 What seems to strike post-Enlightenment audiences—and what sets Shakespeare apart from many of his contemporaries—is his portrayal of “complex” characters, those with what we envision as rich interior worlds and with whom a modern audience can resonate. There is a reason psychiatrists such as Sigmund Freud have rushed back to Shakespeare and (sometimes anachronistically) found in his characters various psychiatric diagnoses such as depression, anxiety, paranoia, jealous delusions, and obsessive-compulsive disorder. Suicide and suicidal ideation are prevalent themes in some of Shakespeare’s most well-known characters.
A surprisingly common theme
The gravest outcome of a psychiatric illness is death by suicide, which occurs in 13 of Shakespeare’s characters.2 There are additional characters who exhibit suicidal ideation without a completed act. Shakespearean characters whose lives end in suicide are variably portrayed, dying by various means and circumstances. Hamlet (who dies at the hand of his foe, Laertes), famously soliloquizes the theme of suicide and the afterlife. He ponders “tak[ing] arms against a sea of troubles.” Ophelia dies ambiguously. Immediately after, her mother and brother recount her death in a brook—having had “too much of water” when her garments “heavy with their drink, | pull’d the poor wretch from her melodious lay | To muddy death.” The 2 clowns/gravediggers then debate whether Ophelia deserves a Christian burial and if her death should be considered a suicide: did the water drown her, or did she drown herself?3
Lady Macbeth’s suicide is offstage, punctuated by a “night-shriek.” Romeo drinks poison and dies “with a kiss.” Juliet quickly follows, making her body the sword’s sheath which “there rust, and let [her] die.” Othello stabs himself after requesting that his peers will “speak of me as I am.” One of King Lear’s daughters poisons her sister “and after [slays] herself.” Timon dies by his cave, “entomb’d upon the very hem o’ the sea.” In Antony and Cleopatra, after being told that Cleopatra has killed herself with Antony’s name on her lips, Antony begs to be stabbed and then stabs himself; he is not defeated by Caesar, but rather conquered by himself: “none but Antony | Should conquer Antony.” Cleopatra and her lady-in-waiting, Charmian, kill themselves with an asp. In Julius Caesar, Brutus runs upon his sword. Cassius begs for his own death, asking that “this good sword, | That ran through Caesar’s bowels, search this bosom.” Portia, it is reported, “swallowed fire.”
Shakespeare uses specific stylized language to portray characters in psychological anguish and suicidal states. Scholars have discussed how he uses certain stylistic language to highlight the anguish that happens during solitary, solipsistic moments of contemplation.4 Moments of anguish and suicidal ideation are marked by verbal repetition. An example of this repetition comes in Hamlet’s speech after he returns to the kingdom where his uncle has usurped his father, when he laments that he cannot end his own life. He says:
O, that this too too sullied flesh would melt,
Thaw, and resolve itself into a dew!
Or that the Everlasting had not fix’d
His canon ’gainst self-slaughter! O God, God,
How weary, stale, flat, and unprofitable
Seem to me all the uses of this world.
In these 6 lines, there are 2 instances of verbal repetition: “too too” and “God, God.” In this moment of solitude and despair, Hamlet’s speech fractures; his fractured speech reflects his fractured psyche. While Hamlet speaks of staleness and stagnation in the world, his words represent a sterile excess. No meaning is elicited by their repetition; there is no forward momentum to his speech. The words reflect the extent to which Hamlet is stuck and divided in this moment. Something similar happens in Macbeth’s “Tomorrow and tomorrow and tomorrow” speech. The words march on, and with each repetition they become increasingly hollow and brittle.
Why does this discussion of suicide in Shakespeare hold value for a contemporary psychiatrist? First, there is no single prototypical suicidal character in Shakespeare. His characters who are suicidal vary in their demographics and incentives for ending their lives. In this way, he provides a rich framework, one with which many people can engage. Second, this discussion fits into an existing paradigm for using art therapy (specifically Shakespeare) as a treatment modality for trauma.5 Programs such as DE-CRUIT have used the recitation of Shakespearean verse as a means of processing trauma in veterans.5 While Shakespeare does not mention a remedy for suicide in his plays, perhaps the text can serve as medicine. Third, the repetitive speech that Shakespeare uses in times of anguish could be a fairly accurate reflection of speech patterns in patients who are suicidal. Research that completed a spoken language analysis of patients who were suicidal has found “mechanical and repetitive phrasing” as a quality of these patients’ speech.6,7
For hundreds of years, critics have searched beyond the text for Shakespeare’s voice and opinion; what did he himself think of melancholy, despair, or suicide? We cannot know. We, as readers, are invited to explore a nuanced and multifaceted view of suicide, one that neither chides nor valorizes the act, and provides ambiguity rather than condemnation.
The medical knowledge that William Shakespeare possessed has awed scholars for centuries. Theories about the provenance of his knowledge abound (such as his son-in-law being a physician), and the inclusion of medical terms and ailments throughout his plays suggests a broad knowledge of disease and sickness. Scholars have noted how he sprinkles references to dermatologic, neurologic, orthopedic, and metabolic ailments throughout his plays, mentioning carbuncles, fistulas, corpulence, rhinophyma, scurvy, ague, enuresis, kyphosis, epilepsy, and parkinsonism.1 What seems to strike post-Enlightenment audiences—and what sets Shakespeare apart from many of his contemporaries—is his portrayal of “complex” characters, those with what we envision as rich interior worlds and with whom a modern audience can resonate. There is a reason psychiatrists such as Sigmund Freud have rushed back to Shakespeare and (sometimes anachronistically) found in his characters various psychiatric diagnoses such as depression, anxiety, paranoia, jealous delusions, and obsessive-compulsive disorder. Suicide and suicidal ideation are prevalent themes in some of Shakespeare’s most well-known characters.
A surprisingly common theme
The gravest outcome of a psychiatric illness is death by suicide, which occurs in 13 of Shakespeare’s characters.2 There are additional characters who exhibit suicidal ideation without a completed act. Shakespearean characters whose lives end in suicide are variably portrayed, dying by various means and circumstances. Hamlet (who dies at the hand of his foe, Laertes), famously soliloquizes the theme of suicide and the afterlife. He ponders “tak[ing] arms against a sea of troubles.” Ophelia dies ambiguously. Immediately after, her mother and brother recount her death in a brook—having had “too much of water” when her garments “heavy with their drink, | pull’d the poor wretch from her melodious lay | To muddy death.” The 2 clowns/gravediggers then debate whether Ophelia deserves a Christian burial and if her death should be considered a suicide: did the water drown her, or did she drown herself?3
Lady Macbeth’s suicide is offstage, punctuated by a “night-shriek.” Romeo drinks poison and dies “with a kiss.” Juliet quickly follows, making her body the sword’s sheath which “there rust, and let [her] die.” Othello stabs himself after requesting that his peers will “speak of me as I am.” One of King Lear’s daughters poisons her sister “and after [slays] herself.” Timon dies by his cave, “entomb’d upon the very hem o’ the sea.” In Antony and Cleopatra, after being told that Cleopatra has killed herself with Antony’s name on her lips, Antony begs to be stabbed and then stabs himself; he is not defeated by Caesar, but rather conquered by himself: “none but Antony | Should conquer Antony.” Cleopatra and her lady-in-waiting, Charmian, kill themselves with an asp. In Julius Caesar, Brutus runs upon his sword. Cassius begs for his own death, asking that “this good sword, | That ran through Caesar’s bowels, search this bosom.” Portia, it is reported, “swallowed fire.”
Shakespeare uses specific stylized language to portray characters in psychological anguish and suicidal states. Scholars have discussed how he uses certain stylistic language to highlight the anguish that happens during solitary, solipsistic moments of contemplation.4 Moments of anguish and suicidal ideation are marked by verbal repetition. An example of this repetition comes in Hamlet’s speech after he returns to the kingdom where his uncle has usurped his father, when he laments that he cannot end his own life. He says:
O, that this too too sullied flesh would melt,
Thaw, and resolve itself into a dew!
Or that the Everlasting had not fix’d
His canon ’gainst self-slaughter! O God, God,
How weary, stale, flat, and unprofitable
Seem to me all the uses of this world.
In these 6 lines, there are 2 instances of verbal repetition: “too too” and “God, God.” In this moment of solitude and despair, Hamlet’s speech fractures; his fractured speech reflects his fractured psyche. While Hamlet speaks of staleness and stagnation in the world, his words represent a sterile excess. No meaning is elicited by their repetition; there is no forward momentum to his speech. The words reflect the extent to which Hamlet is stuck and divided in this moment. Something similar happens in Macbeth’s “Tomorrow and tomorrow and tomorrow” speech. The words march on, and with each repetition they become increasingly hollow and brittle.
Why does this discussion of suicide in Shakespeare hold value for a contemporary psychiatrist? First, there is no single prototypical suicidal character in Shakespeare. His characters who are suicidal vary in their demographics and incentives for ending their lives. In this way, he provides a rich framework, one with which many people can engage. Second, this discussion fits into an existing paradigm for using art therapy (specifically Shakespeare) as a treatment modality for trauma.5 Programs such as DE-CRUIT have used the recitation of Shakespearean verse as a means of processing trauma in veterans.5 While Shakespeare does not mention a remedy for suicide in his plays, perhaps the text can serve as medicine. Third, the repetitive speech that Shakespeare uses in times of anguish could be a fairly accurate reflection of speech patterns in patients who are suicidal. Research that completed a spoken language analysis of patients who were suicidal has found “mechanical and repetitive phrasing” as a quality of these patients’ speech.6,7
For hundreds of years, critics have searched beyond the text for Shakespeare’s voice and opinion; what did he himself think of melancholy, despair, or suicide? We cannot know. We, as readers, are invited to explore a nuanced and multifaceted view of suicide, one that neither chides nor valorizes the act, and provides ambiguity rather than condemnation.
1. Paciaroni M, Bogousslavsky J. William Shakespeare’s neurology. Prog Brain Res. 2013;206:3-18.
2. Kirkland LR. To end itself by death: suicide in Shakespeare’s tragedies. South Med J. 1999;92(7):660-666.
3. Sale C. The “Amending Hand”: Hales v. Petit, Eyston v. Studd, and Equitable Action in Hamlet. In: Jordan C, Cunningham K, eds. The Law in Shakespeare. Early Modern Literature in History. Palgrave Macmillan; 2007:189-207. https://doi.org/10.1057/9780230626348_11
4. Langley E. Narcissism and Suicide in Shakespeare and His Contemporaries. Oxford University Press; 2009.
5. Ali A, Wolfert S, Lam I, et al. Intersecting modes of aesthetic distance and mimetic induction in therapeutic process: examining a drama-based treatment for military-related traumatic stress. Drama Therapy Review. 2018;4(2):153-165.
6. Belouali A, Gupta S, Sourirajan V, et al. Acoustic and language analysis of speech for suicidal ideation among US veterans. BioData Min. 2021;14(1):11. doi:10.1186/s13040-021-00245-y
7. Cummins N, Scherer S, Krajewski J, et al. A review of depression and suicide risk assessment using speech analysis. Speech Commun. 2015;71:10-49.
1. Paciaroni M, Bogousslavsky J. William Shakespeare’s neurology. Prog Brain Res. 2013;206:3-18.
2. Kirkland LR. To end itself by death: suicide in Shakespeare’s tragedies. South Med J. 1999;92(7):660-666.
3. Sale C. The “Amending Hand”: Hales v. Petit, Eyston v. Studd, and Equitable Action in Hamlet. In: Jordan C, Cunningham K, eds. The Law in Shakespeare. Early Modern Literature in History. Palgrave Macmillan; 2007:189-207. https://doi.org/10.1057/9780230626348_11
4. Langley E. Narcissism and Suicide in Shakespeare and His Contemporaries. Oxford University Press; 2009.
5. Ali A, Wolfert S, Lam I, et al. Intersecting modes of aesthetic distance and mimetic induction in therapeutic process: examining a drama-based treatment for military-related traumatic stress. Drama Therapy Review. 2018;4(2):153-165.
6. Belouali A, Gupta S, Sourirajan V, et al. Acoustic and language analysis of speech for suicidal ideation among US veterans. BioData Min. 2021;14(1):11. doi:10.1186/s13040-021-00245-y
7. Cummins N, Scherer S, Krajewski J, et al. A review of depression and suicide risk assessment using speech analysis. Speech Commun. 2015;71:10-49.
Valedictory
All that’s bright must fade,
The brightest still the fleetest;
All that’s sweet was made
But to be lost when sweetest.
Thomas Moore
I sometimes hold it half a sin
To put in words the grief I feel;
For words, like Nature, half reveal
And half conceal the Soul within.
Alfred, Lord Tennyson, In Memoriam
Dear Readers,
I have sad news to share with you. This is the last issue of
During my travels around the country over the past 2 decades, countless psychiatrists have told me that
As the saying goes: All good things eventually come to an end. I am so grateful to have had the opportunity to collaborate with a wonderful, highly competent editorial staff, as well as with outstanding colleagues who served on the editorial board all those years. A special shout-out to Jeff Bauer, the publishing staff editor, with whom I worked so closely. I very much appreciated all the authors and peer reviewers who contributed timely clinical articles month after month and made
This has been a unique journey for all of us who strived to transform
All that’s bright must fade,
The brightest still the fleetest;
All that’s sweet was made
But to be lost when sweetest.
Thomas Moore
I sometimes hold it half a sin
To put in words the grief I feel;
For words, like Nature, half reveal
And half conceal the Soul within.
Alfred, Lord Tennyson, In Memoriam
Dear Readers,
I have sad news to share with you. This is the last issue of
During my travels around the country over the past 2 decades, countless psychiatrists have told me that
As the saying goes: All good things eventually come to an end. I am so grateful to have had the opportunity to collaborate with a wonderful, highly competent editorial staff, as well as with outstanding colleagues who served on the editorial board all those years. A special shout-out to Jeff Bauer, the publishing staff editor, with whom I worked so closely. I very much appreciated all the authors and peer reviewers who contributed timely clinical articles month after month and made
This has been a unique journey for all of us who strived to transform
All that’s bright must fade,
The brightest still the fleetest;
All that’s sweet was made
But to be lost when sweetest.
Thomas Moore
I sometimes hold it half a sin
To put in words the grief I feel;
For words, like Nature, half reveal
And half conceal the Soul within.
Alfred, Lord Tennyson, In Memoriam
Dear Readers,
I have sad news to share with you. This is the last issue of
During my travels around the country over the past 2 decades, countless psychiatrists have told me that
As the saying goes: All good things eventually come to an end. I am so grateful to have had the opportunity to collaborate with a wonderful, highly competent editorial staff, as well as with outstanding colleagues who served on the editorial board all those years. A special shout-out to Jeff Bauer, the publishing staff editor, with whom I worked so closely. I very much appreciated all the authors and peer reviewers who contributed timely clinical articles month after month and made
This has been a unique journey for all of us who strived to transform
More on treating chronic insomnia
In “Treating chronic insomnia: An alternating medication strategy” (
Leslie Citrome, MD, MPH
Valhalla, New York
1. Rosenberg R, Citrome L, Drake CL. Advances in the treatment of chronic insomnia: a narrative review of new nonpharmacologic and pharmacologic therapies. Neuropsychiatr Dis Treat. 2021;17:2549-2566.
2. Citrome L. Dissecting clinical trials with ‘number needed to treat.’ Current Psychiatry. 2007;6(3):66-71.
3. Citrome L. Suvorexant for insomnia: a systematic review of the efficacy and safety profile for this newly approved hypnotic - what is the number needed to treat, number needed to harm and likelihood to be helped or harmed? Int J Clin Pract. 2014;68(12):1429-1441.
4. Citrome L, Juday TR, Frech F, et al. Lemborexant for the treatment of insomnia: direct and indirect comparisons with other hypnotics using number needed to treat, number needed to harm, and likelihood to be helped or harmed. J Clin Psychiatry. 2021;82:20m13795. doi:10.4088/JCP.20m13795
5. Citrome L, Juday TR, Lundwall C. Lemborexant and daridorexant for the treatment of insomnia: an indirect comparison using number needed to treat, number needed to harm, and likelihood to be helped or harmed. J Clin Psychiatry. 2023;84(6):23m14851. doi:10.4088/JCP.23m14851
In “Treating chronic insomnia: An alternating medication strategy” (
Leslie Citrome, MD, MPH
Valhalla, New York
In “Treating chronic insomnia: An alternating medication strategy” (
Leslie Citrome, MD, MPH
Valhalla, New York
1. Rosenberg R, Citrome L, Drake CL. Advances in the treatment of chronic insomnia: a narrative review of new nonpharmacologic and pharmacologic therapies. Neuropsychiatr Dis Treat. 2021;17:2549-2566.
2. Citrome L. Dissecting clinical trials with ‘number needed to treat.’ Current Psychiatry. 2007;6(3):66-71.
3. Citrome L. Suvorexant for insomnia: a systematic review of the efficacy and safety profile for this newly approved hypnotic - what is the number needed to treat, number needed to harm and likelihood to be helped or harmed? Int J Clin Pract. 2014;68(12):1429-1441.
4. Citrome L, Juday TR, Frech F, et al. Lemborexant for the treatment of insomnia: direct and indirect comparisons with other hypnotics using number needed to treat, number needed to harm, and likelihood to be helped or harmed. J Clin Psychiatry. 2021;82:20m13795. doi:10.4088/JCP.20m13795
5. Citrome L, Juday TR, Lundwall C. Lemborexant and daridorexant for the treatment of insomnia: an indirect comparison using number needed to treat, number needed to harm, and likelihood to be helped or harmed. J Clin Psychiatry. 2023;84(6):23m14851. doi:10.4088/JCP.23m14851
1. Rosenberg R, Citrome L, Drake CL. Advances in the treatment of chronic insomnia: a narrative review of new nonpharmacologic and pharmacologic therapies. Neuropsychiatr Dis Treat. 2021;17:2549-2566.
2. Citrome L. Dissecting clinical trials with ‘number needed to treat.’ Current Psychiatry. 2007;6(3):66-71.
3. Citrome L. Suvorexant for insomnia: a systematic review of the efficacy and safety profile for this newly approved hypnotic - what is the number needed to treat, number needed to harm and likelihood to be helped or harmed? Int J Clin Pract. 2014;68(12):1429-1441.
4. Citrome L, Juday TR, Frech F, et al. Lemborexant for the treatment of insomnia: direct and indirect comparisons with other hypnotics using number needed to treat, number needed to harm, and likelihood to be helped or harmed. J Clin Psychiatry. 2021;82:20m13795. doi:10.4088/JCP.20m13795
5. Citrome L, Juday TR, Lundwall C. Lemborexant and daridorexant for the treatment of insomnia: an indirect comparison using number needed to treat, number needed to harm, and likelihood to be helped or harmed. J Clin Psychiatry. 2023;84(6):23m14851. doi:10.4088/JCP.23m14851
Worsening mania while receiving low-dose quetiapine: A case report
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
The second-generation antipsychotic quetiapine is commonly used to treat several psychiatric disorders, including bipolar disorder (BD) and insomnia. In this case report, we discuss a patient with a history of unipolar depression and initial signs of mania who experienced an exacerbation of manic symptoms following administration of low-dose quetiapine. This case underscores the need for careful monitoring of patients receiving quetiapine, especially at lower doses, and the potential limitations of its efficacy in controlling manic symptoms.
Depressed with racing thoughts
Mr. X, age 58, is an Army veteran who lives with his wife of 29 years and works as a contractor. He has a history of depression and a suicide attempt 10 years ago by self-inflicted gunshot wound to the head, which left him with a bullet lodged in his sinus cavity and residual dysarthria after tongue surgery. After the suicide attempt, Mr. X was medically hospitalized, but not psychiatrically hospitalized. Shortly after, he self-discontinued all psychotropic medications and follow-up.
Mr. X has no other medical history and takes no other medications or supplements. His family history includes a mother with schizoaffective disorder, 1 brother with BD, and another brother with developmental delay.
Mr. X remained euthymic until his brother died. Soon after, he began to experience low mood, heightened anxiety, racing thoughts, tearfulness, and mild insomnia. He was prescribed quetiapine 25 mg/d at bedtime and instructed to titrate up to 50 mg/d.
Ten days later, Mr. X was brought to the hospital by his wife, who reported that after starting quetiapine, her husband began to act erratically. He had disorganized and racing thoughts, loose associations, labile affect, hyperactivity/restlessness, and was not sleeping. In the morning before presenting to the hospital, Mr. X had gone to work, laid down on the floor, began mumbling to himself, and would not respond to coworkers. Upon evaluation, Mr. X was noted to have pressured speech, disorganized speech, delusions, anxiety, and hallucinations. A CT scan of his head was normal, and a complete blood count, comprehensive metabolic panel, thyroid-stimulating hormone, B12, folate, and hemoglobin A1c were within normal limits. Mr. X’s vitamin D level was low at 22 ng/mL, and a syphilis screen was negative.
Mr. X was admitted to the hospital for his safety. The treatment team discontinued quetiapine and started risperidone 3 mg twice a day for psychotic symptoms and mood stabilization. At the time of discharge 7 days later, Mr. X was no longer experiencing any hallucinations or delusions, his thought process was linear and goal-directed, his mood was stable, and his insomnia had improved. Based on the temporal relationship between the initiation of quetiapine and the onset of Mr. X’s manic symptoms, along with an absence of organic causes, the treatment team suspected Mr. X had experienced a worsening of manic symptoms induced by quetiapine. Before starting quetiapine, he had presented with an initial manic symptom of racing thoughts.
At his next outpatient appointment, Mr. X exhibited significant akathisia. The treatment team initiated propranolol 20 mg twice a day but Mr. X did not experience much improvement. Risperidone was reduced to 1 mg twice a day and Mr. X was started on clonazepam 0.5 mg twice a day. The akathisia resolved. The treatment team decided to discontinue all medications and observe Mr. X for any recurrence of symptoms. One year after his manic episode. Mr. X remained euthymic. He was able to resume full-time work and began psychotherapy to process the grief over the loss of his brother.
Quetiapine’s unique profile
This case sheds light on the potential limitations of quetiapine, especially at lower doses, for managing manic symptoms. Quetiapine exhibits antidepressant effects, even at doses as low as 50 mg/d.1 At higher doses, quetiapine acts as an antagonist at serotonin (5-HT1A and 5-HT2A), dopamine (D1 and D2), histamine H1, and adrenergic receptors.2 At doses <300 mg/d, there is an absence of dopamine receptor blockade and a higher affinity for 5-HT2A receptors, which could explain why higher doses are generally necessary for treating mania and psychotic symptoms.3-5 High 5-HT2A antagonism may disinhibit the dopaminergic system and paradoxically increase dopaminergic activity, which could be the mechanism responsible for lack of control of manic symptoms with low doses of quetiapine.2 Another possible explanation is that the metabolite of quetiapine, N-desalkylquetiapine, acts as a norepinephrine reuptake blocker and partial 5-HT1A antagonist, which acts as an antidepressant, and antidepressants are known to induce mania in vulnerable patients.4
The antimanic property of most antipsychotics (except possibly clozapine) is attributed to their D2 antagonistic potency. Because quetiapine is among the weaker D2 antagonists, its inability to prevent the progression of mania, especially at 50 mg/d, is not unexpected. Mr. X’s subsequent need for a stronger D2 antagonist—risperidone—at a significant dose further supports this observation. A common misconception is that quetiapine’s sedating effects make it effective for treating mania, but that is not the case. Clinicians should be cautious when prescribing quetiapine, especially at lower doses, to patients who exhibit signs of mania. Given the potential risk, clinicians should consider alternative treatments before resorting to low-dose quetiapine for insomnia. Regular monitoring for manic symptoms is crucial for all patients receiving quetiapine. If patients present with signs of mania or hypomania, a therapeutic dose range of 600 to 800 mg/d is recommended.6
- Weisler R, Joyce M, McGill L, et al. Extended release quetiapine fumarate monotherapy for major depressive disorder: results of a double-blind, randomized, placebo-controlled study. CNS Spectr. 2009;14(6):299-313. doi:10.1017/s1092852900020307
- Khalil RB, Baddoura C. Quetiapine induced hypomania: a case report and a review of the literature. Curr Drug Saf. 2012;7(3):250-253. doi:10.2174/157488612803251333
- Benyamina A, Samalin L. Atypical antipsychotic-induced mania/hypomania: a review of recent case reports and clinical studies. Int J Psychiatry Clin Pract. 2012;16(1):2-7. doi:10.3109/13651501.2011.605957
- Gnanavel S. Quetiapine-induced manic episode: a paradox for contemplation. BMJ Case Rep. 2013;2013:bcr2013201761. doi:10.1136/bcr-2013-201761
- Pacchiarotti I, Manfredi G, Kotzalidis GD, et al. Quetiapine-induced mania. Aust N Z J Psychiatry. 2003;37(5):626.
- Millard HY, Wilson BA, Noordsy DL. Low-dose quetiapine induced or worsened mania in the context of possible undertreatment. J Am Board Fam Med. 2015;28(1):154-158. doi:10.3122/jabfm.2015.01.140105
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
The second-generation antipsychotic quetiapine is commonly used to treat several psychiatric disorders, including bipolar disorder (BD) and insomnia. In this case report, we discuss a patient with a history of unipolar depression and initial signs of mania who experienced an exacerbation of manic symptoms following administration of low-dose quetiapine. This case underscores the need for careful monitoring of patients receiving quetiapine, especially at lower doses, and the potential limitations of its efficacy in controlling manic symptoms.
Depressed with racing thoughts
Mr. X, age 58, is an Army veteran who lives with his wife of 29 years and works as a contractor. He has a history of depression and a suicide attempt 10 years ago by self-inflicted gunshot wound to the head, which left him with a bullet lodged in his sinus cavity and residual dysarthria after tongue surgery. After the suicide attempt, Mr. X was medically hospitalized, but not psychiatrically hospitalized. Shortly after, he self-discontinued all psychotropic medications and follow-up.
Mr. X has no other medical history and takes no other medications or supplements. His family history includes a mother with schizoaffective disorder, 1 brother with BD, and another brother with developmental delay.
Mr. X remained euthymic until his brother died. Soon after, he began to experience low mood, heightened anxiety, racing thoughts, tearfulness, and mild insomnia. He was prescribed quetiapine 25 mg/d at bedtime and instructed to titrate up to 50 mg/d.
Ten days later, Mr. X was brought to the hospital by his wife, who reported that after starting quetiapine, her husband began to act erratically. He had disorganized and racing thoughts, loose associations, labile affect, hyperactivity/restlessness, and was not sleeping. In the morning before presenting to the hospital, Mr. X had gone to work, laid down on the floor, began mumbling to himself, and would not respond to coworkers. Upon evaluation, Mr. X was noted to have pressured speech, disorganized speech, delusions, anxiety, and hallucinations. A CT scan of his head was normal, and a complete blood count, comprehensive metabolic panel, thyroid-stimulating hormone, B12, folate, and hemoglobin A1c were within normal limits. Mr. X’s vitamin D level was low at 22 ng/mL, and a syphilis screen was negative.
Mr. X was admitted to the hospital for his safety. The treatment team discontinued quetiapine and started risperidone 3 mg twice a day for psychotic symptoms and mood stabilization. At the time of discharge 7 days later, Mr. X was no longer experiencing any hallucinations or delusions, his thought process was linear and goal-directed, his mood was stable, and his insomnia had improved. Based on the temporal relationship between the initiation of quetiapine and the onset of Mr. X’s manic symptoms, along with an absence of organic causes, the treatment team suspected Mr. X had experienced a worsening of manic symptoms induced by quetiapine. Before starting quetiapine, he had presented with an initial manic symptom of racing thoughts.
At his next outpatient appointment, Mr. X exhibited significant akathisia. The treatment team initiated propranolol 20 mg twice a day but Mr. X did not experience much improvement. Risperidone was reduced to 1 mg twice a day and Mr. X was started on clonazepam 0.5 mg twice a day. The akathisia resolved. The treatment team decided to discontinue all medications and observe Mr. X for any recurrence of symptoms. One year after his manic episode. Mr. X remained euthymic. He was able to resume full-time work and began psychotherapy to process the grief over the loss of his brother.
Quetiapine’s unique profile
This case sheds light on the potential limitations of quetiapine, especially at lower doses, for managing manic symptoms. Quetiapine exhibits antidepressant effects, even at doses as low as 50 mg/d.1 At higher doses, quetiapine acts as an antagonist at serotonin (5-HT1A and 5-HT2A), dopamine (D1 and D2), histamine H1, and adrenergic receptors.2 At doses <300 mg/d, there is an absence of dopamine receptor blockade and a higher affinity for 5-HT2A receptors, which could explain why higher doses are generally necessary for treating mania and psychotic symptoms.3-5 High 5-HT2A antagonism may disinhibit the dopaminergic system and paradoxically increase dopaminergic activity, which could be the mechanism responsible for lack of control of manic symptoms with low doses of quetiapine.2 Another possible explanation is that the metabolite of quetiapine, N-desalkylquetiapine, acts as a norepinephrine reuptake blocker and partial 5-HT1A antagonist, which acts as an antidepressant, and antidepressants are known to induce mania in vulnerable patients.4
The antimanic property of most antipsychotics (except possibly clozapine) is attributed to their D2 antagonistic potency. Because quetiapine is among the weaker D2 antagonists, its inability to prevent the progression of mania, especially at 50 mg/d, is not unexpected. Mr. X’s subsequent need for a stronger D2 antagonist—risperidone—at a significant dose further supports this observation. A common misconception is that quetiapine’s sedating effects make it effective for treating mania, but that is not the case. Clinicians should be cautious when prescribing quetiapine, especially at lower doses, to patients who exhibit signs of mania. Given the potential risk, clinicians should consider alternative treatments before resorting to low-dose quetiapine for insomnia. Regular monitoring for manic symptoms is crucial for all patients receiving quetiapine. If patients present with signs of mania or hypomania, a therapeutic dose range of 600 to 800 mg/d is recommended.6
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
The second-generation antipsychotic quetiapine is commonly used to treat several psychiatric disorders, including bipolar disorder (BD) and insomnia. In this case report, we discuss a patient with a history of unipolar depression and initial signs of mania who experienced an exacerbation of manic symptoms following administration of low-dose quetiapine. This case underscores the need for careful monitoring of patients receiving quetiapine, especially at lower doses, and the potential limitations of its efficacy in controlling manic symptoms.
Depressed with racing thoughts
Mr. X, age 58, is an Army veteran who lives with his wife of 29 years and works as a contractor. He has a history of depression and a suicide attempt 10 years ago by self-inflicted gunshot wound to the head, which left him with a bullet lodged in his sinus cavity and residual dysarthria after tongue surgery. After the suicide attempt, Mr. X was medically hospitalized, but not psychiatrically hospitalized. Shortly after, he self-discontinued all psychotropic medications and follow-up.
Mr. X has no other medical history and takes no other medications or supplements. His family history includes a mother with schizoaffective disorder, 1 brother with BD, and another brother with developmental delay.
Mr. X remained euthymic until his brother died. Soon after, he began to experience low mood, heightened anxiety, racing thoughts, tearfulness, and mild insomnia. He was prescribed quetiapine 25 mg/d at bedtime and instructed to titrate up to 50 mg/d.
Ten days later, Mr. X was brought to the hospital by his wife, who reported that after starting quetiapine, her husband began to act erratically. He had disorganized and racing thoughts, loose associations, labile affect, hyperactivity/restlessness, and was not sleeping. In the morning before presenting to the hospital, Mr. X had gone to work, laid down on the floor, began mumbling to himself, and would not respond to coworkers. Upon evaluation, Mr. X was noted to have pressured speech, disorganized speech, delusions, anxiety, and hallucinations. A CT scan of his head was normal, and a complete blood count, comprehensive metabolic panel, thyroid-stimulating hormone, B12, folate, and hemoglobin A1c were within normal limits. Mr. X’s vitamin D level was low at 22 ng/mL, and a syphilis screen was negative.
Mr. X was admitted to the hospital for his safety. The treatment team discontinued quetiapine and started risperidone 3 mg twice a day for psychotic symptoms and mood stabilization. At the time of discharge 7 days later, Mr. X was no longer experiencing any hallucinations or delusions, his thought process was linear and goal-directed, his mood was stable, and his insomnia had improved. Based on the temporal relationship between the initiation of quetiapine and the onset of Mr. X’s manic symptoms, along with an absence of organic causes, the treatment team suspected Mr. X had experienced a worsening of manic symptoms induced by quetiapine. Before starting quetiapine, he had presented with an initial manic symptom of racing thoughts.
At his next outpatient appointment, Mr. X exhibited significant akathisia. The treatment team initiated propranolol 20 mg twice a day but Mr. X did not experience much improvement. Risperidone was reduced to 1 mg twice a day and Mr. X was started on clonazepam 0.5 mg twice a day. The akathisia resolved. The treatment team decided to discontinue all medications and observe Mr. X for any recurrence of symptoms. One year after his manic episode. Mr. X remained euthymic. He was able to resume full-time work and began psychotherapy to process the grief over the loss of his brother.
Quetiapine’s unique profile
This case sheds light on the potential limitations of quetiapine, especially at lower doses, for managing manic symptoms. Quetiapine exhibits antidepressant effects, even at doses as low as 50 mg/d.1 At higher doses, quetiapine acts as an antagonist at serotonin (5-HT1A and 5-HT2A), dopamine (D1 and D2), histamine H1, and adrenergic receptors.2 At doses <300 mg/d, there is an absence of dopamine receptor blockade and a higher affinity for 5-HT2A receptors, which could explain why higher doses are generally necessary for treating mania and psychotic symptoms.3-5 High 5-HT2A antagonism may disinhibit the dopaminergic system and paradoxically increase dopaminergic activity, which could be the mechanism responsible for lack of control of manic symptoms with low doses of quetiapine.2 Another possible explanation is that the metabolite of quetiapine, N-desalkylquetiapine, acts as a norepinephrine reuptake blocker and partial 5-HT1A antagonist, which acts as an antidepressant, and antidepressants are known to induce mania in vulnerable patients.4
The antimanic property of most antipsychotics (except possibly clozapine) is attributed to their D2 antagonistic potency. Because quetiapine is among the weaker D2 antagonists, its inability to prevent the progression of mania, especially at 50 mg/d, is not unexpected. Mr. X’s subsequent need for a stronger D2 antagonist—risperidone—at a significant dose further supports this observation. A common misconception is that quetiapine’s sedating effects make it effective for treating mania, but that is not the case. Clinicians should be cautious when prescribing quetiapine, especially at lower doses, to patients who exhibit signs of mania. Given the potential risk, clinicians should consider alternative treatments before resorting to low-dose quetiapine for insomnia. Regular monitoring for manic symptoms is crucial for all patients receiving quetiapine. If patients present with signs of mania or hypomania, a therapeutic dose range of 600 to 800 mg/d is recommended.6
- Weisler R, Joyce M, McGill L, et al. Extended release quetiapine fumarate monotherapy for major depressive disorder: results of a double-blind, randomized, placebo-controlled study. CNS Spectr. 2009;14(6):299-313. doi:10.1017/s1092852900020307
- Khalil RB, Baddoura C. Quetiapine induced hypomania: a case report and a review of the literature. Curr Drug Saf. 2012;7(3):250-253. doi:10.2174/157488612803251333
- Benyamina A, Samalin L. Atypical antipsychotic-induced mania/hypomania: a review of recent case reports and clinical studies. Int J Psychiatry Clin Pract. 2012;16(1):2-7. doi:10.3109/13651501.2011.605957
- Gnanavel S. Quetiapine-induced manic episode: a paradox for contemplation. BMJ Case Rep. 2013;2013:bcr2013201761. doi:10.1136/bcr-2013-201761
- Pacchiarotti I, Manfredi G, Kotzalidis GD, et al. Quetiapine-induced mania. Aust N Z J Psychiatry. 2003;37(5):626.
- Millard HY, Wilson BA, Noordsy DL. Low-dose quetiapine induced or worsened mania in the context of possible undertreatment. J Am Board Fam Med. 2015;28(1):154-158. doi:10.3122/jabfm.2015.01.140105
- Weisler R, Joyce M, McGill L, et al. Extended release quetiapine fumarate monotherapy for major depressive disorder: results of a double-blind, randomized, placebo-controlled study. CNS Spectr. 2009;14(6):299-313. doi:10.1017/s1092852900020307
- Khalil RB, Baddoura C. Quetiapine induced hypomania: a case report and a review of the literature. Curr Drug Saf. 2012;7(3):250-253. doi:10.2174/157488612803251333
- Benyamina A, Samalin L. Atypical antipsychotic-induced mania/hypomania: a review of recent case reports and clinical studies. Int J Psychiatry Clin Pract. 2012;16(1):2-7. doi:10.3109/13651501.2011.605957
- Gnanavel S. Quetiapine-induced manic episode: a paradox for contemplation. BMJ Case Rep. 2013;2013:bcr2013201761. doi:10.1136/bcr-2013-201761
- Pacchiarotti I, Manfredi G, Kotzalidis GD, et al. Quetiapine-induced mania. Aust N Z J Psychiatry. 2003;37(5):626.
- Millard HY, Wilson BA, Noordsy DL. Low-dose quetiapine induced or worsened mania in the context of possible undertreatment. J Am Board Fam Med. 2015;28(1):154-158. doi:10.3122/jabfm.2015.01.140105
Navigating the challenges of patients with substance use disorders who leave AMA
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
Working closely with individuals with substance use disorders (SUDs), we’ve observed a worrisome trend of patients leaving the hospital against medical advice (AMA). This issue is not only prevalent in psychiatric settings, but also in emergency departments, medical and surgical floors, and even intensive care units.1
Compared to individuals without such disorders, individuals with SUDs—particularly those with opioid use disorders—are up to 3 times more likely to leave the hospital AMA.1,2 Leaving AMA can lead to multiple complications, including an increased risk of readmission, suboptimal treatment outcomes, and an increased use of health care resources.1-3
It is critical to understand why patients elect to leave a hospital AMA. In a qualitative study, Simon et al1 found that individuals with SUDs often leave AMA due to uncontrolled withdrawal symptoms and pain, perceived stigma and discrimination, and dissatisfaction with care. Predictors of patients leaving the hospital AMA include the severity of their drug dependence and previous negative treatment experiences.4 A systematic review found housing instability and a lack of social support influence an individual’s decision to leave AMA.5
Recommendations for managing patients who leave AMA
Enhancing your understanding of withdrawal symptoms may allow you to offer patients more effective symptom control, possibly with methadone or buprenorphine.2 Injectable opioid agonist treatment may also help to retain a patient in care. In a case report, a 47-year-old man with a severe opioid use disorder who had left the hospital AMA due to uncontrolled opioid withdrawal was readmitted, treated with IV hydromorphone, and enrolled in ongoing community injectable opioid agonist treatment.6
Clinicians must address the stigma and discrimination patients with SUDs often face in health care institutions. Additional training for clinicians to improve their understanding of these disorders and foster a more compassionate and nonjudgmental approach to care may be beneficial.
Like most medicolegal conflicts, leaving AMA is often a clinical and interpersonal problem disguised as a legal one. When assessing these patients’ decision-making capacity, we often find they are angry and dissatisfied with the care they have (or have not) received. The most useful intervention may be to restore communication between the patient and their treatment team.
Even after a patient leaves AMA, the treatment team may experience countertransference issues, such as heightened emotional reactions or biases, that could compromise their clinical judgment. Addressing these dynamics may require team debriefings, supervision, or further training in managing transference and countertransference, particularly since patients who leave AMA may return for subsequent care.7
Integrated care models, which feature close collaboration between clinicians from different specialties, can help ensure that a patient’s diverse health needs are met and reduce the likelihood of them leaving AMA. Integrated care models may be particularly effective for patients with co-occurring conditions such as HIV and SUDs.8
Implementing these recommendations can be challenging. Barriers to addressing AMA departures span several domains, including patient-specific barriers (eg, stigma and discrimination), clinical barriers (eg, lack of resources and training for clinicians), institutional hurdles (eg, systemic inefficiencies), and broader social barriers (eg, housing instability and inadequate social support). Overcoming these barriers requires a multifaceted approach involving clinicians, policymakers, and the community that considers medical, psychological, and social factors.
1. Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: a qualitative study. Subst Abus. 2020;41(4):519-525.
2. Kenne DR, Boros AP, Fischbein RL. Characteristics of opiate users leaving detoxification treatment against medical advice. J Addict Dis. 2010;29(3):383-394.
3. Mahajan RK, Gautam PL, Paul G, et al. Retrospective evaluation of patients leaving against medical advice in a tertiary care teaching hospital. Indian J Crit Care Med. 2019;23(3):139-142.
4. Armenian SH, Chutuape MA, Stitzer ML. Predictors of discharges against medical advice from a short-term hospital detoxification unit. Drug Alcohol Depend. 1999;56(1):1-8.
5. Ti L, Ti L. Leaving the hospital against medical advice among people who use illicit drugs: a systematic review. Am J Public Health. 2015;105(12):e53-e59.
6. McAdam M, Brar R, Young S. Initiation of injectable opioid agonist treatment in hospital: a case report. Drug Alcohol Rev. 2020;39(2):138-141.
7. Schouten R, Weintraub BR. Legal aspects of consultation. In: Stern TA, Freudenreich O, Smith FA, et al, eds. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 7th ed. Elsevier; 2018:578-579.
8. Vallecillo G, Robles MJ, Fonseca F, et al. Integrated care on leaving hospital against medical advice among HIV-infected people with substance use disorders. AIDS Res Hum Retroviruses. 2018;34(12):1044-1049.
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
Working closely with individuals with substance use disorders (SUDs), we’ve observed a worrisome trend of patients leaving the hospital against medical advice (AMA). This issue is not only prevalent in psychiatric settings, but also in emergency departments, medical and surgical floors, and even intensive care units.1
Compared to individuals without such disorders, individuals with SUDs—particularly those with opioid use disorders—are up to 3 times more likely to leave the hospital AMA.1,2 Leaving AMA can lead to multiple complications, including an increased risk of readmission, suboptimal treatment outcomes, and an increased use of health care resources.1-3
It is critical to understand why patients elect to leave a hospital AMA. In a qualitative study, Simon et al1 found that individuals with SUDs often leave AMA due to uncontrolled withdrawal symptoms and pain, perceived stigma and discrimination, and dissatisfaction with care. Predictors of patients leaving the hospital AMA include the severity of their drug dependence and previous negative treatment experiences.4 A systematic review found housing instability and a lack of social support influence an individual’s decision to leave AMA.5
Recommendations for managing patients who leave AMA
Enhancing your understanding of withdrawal symptoms may allow you to offer patients more effective symptom control, possibly with methadone or buprenorphine.2 Injectable opioid agonist treatment may also help to retain a patient in care. In a case report, a 47-year-old man with a severe opioid use disorder who had left the hospital AMA due to uncontrolled opioid withdrawal was readmitted, treated with IV hydromorphone, and enrolled in ongoing community injectable opioid agonist treatment.6
Clinicians must address the stigma and discrimination patients with SUDs often face in health care institutions. Additional training for clinicians to improve their understanding of these disorders and foster a more compassionate and nonjudgmental approach to care may be beneficial.
Like most medicolegal conflicts, leaving AMA is often a clinical and interpersonal problem disguised as a legal one. When assessing these patients’ decision-making capacity, we often find they are angry and dissatisfied with the care they have (or have not) received. The most useful intervention may be to restore communication between the patient and their treatment team.
Even after a patient leaves AMA, the treatment team may experience countertransference issues, such as heightened emotional reactions or biases, that could compromise their clinical judgment. Addressing these dynamics may require team debriefings, supervision, or further training in managing transference and countertransference, particularly since patients who leave AMA may return for subsequent care.7
Integrated care models, which feature close collaboration between clinicians from different specialties, can help ensure that a patient’s diverse health needs are met and reduce the likelihood of them leaving AMA. Integrated care models may be particularly effective for patients with co-occurring conditions such as HIV and SUDs.8
Implementing these recommendations can be challenging. Barriers to addressing AMA departures span several domains, including patient-specific barriers (eg, stigma and discrimination), clinical barriers (eg, lack of resources and training for clinicians), institutional hurdles (eg, systemic inefficiencies), and broader social barriers (eg, housing instability and inadequate social support). Overcoming these barriers requires a multifaceted approach involving clinicians, policymakers, and the community that considers medical, psychological, and social factors.
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
Working closely with individuals with substance use disorders (SUDs), we’ve observed a worrisome trend of patients leaving the hospital against medical advice (AMA). This issue is not only prevalent in psychiatric settings, but also in emergency departments, medical and surgical floors, and even intensive care units.1
Compared to individuals without such disorders, individuals with SUDs—particularly those with opioid use disorders—are up to 3 times more likely to leave the hospital AMA.1,2 Leaving AMA can lead to multiple complications, including an increased risk of readmission, suboptimal treatment outcomes, and an increased use of health care resources.1-3
It is critical to understand why patients elect to leave a hospital AMA. In a qualitative study, Simon et al1 found that individuals with SUDs often leave AMA due to uncontrolled withdrawal symptoms and pain, perceived stigma and discrimination, and dissatisfaction with care. Predictors of patients leaving the hospital AMA include the severity of their drug dependence and previous negative treatment experiences.4 A systematic review found housing instability and a lack of social support influence an individual’s decision to leave AMA.5
Recommendations for managing patients who leave AMA
Enhancing your understanding of withdrawal symptoms may allow you to offer patients more effective symptom control, possibly with methadone or buprenorphine.2 Injectable opioid agonist treatment may also help to retain a patient in care. In a case report, a 47-year-old man with a severe opioid use disorder who had left the hospital AMA due to uncontrolled opioid withdrawal was readmitted, treated with IV hydromorphone, and enrolled in ongoing community injectable opioid agonist treatment.6
Clinicians must address the stigma and discrimination patients with SUDs often face in health care institutions. Additional training for clinicians to improve their understanding of these disorders and foster a more compassionate and nonjudgmental approach to care may be beneficial.
Like most medicolegal conflicts, leaving AMA is often a clinical and interpersonal problem disguised as a legal one. When assessing these patients’ decision-making capacity, we often find they are angry and dissatisfied with the care they have (or have not) received. The most useful intervention may be to restore communication between the patient and their treatment team.
Even after a patient leaves AMA, the treatment team may experience countertransference issues, such as heightened emotional reactions or biases, that could compromise their clinical judgment. Addressing these dynamics may require team debriefings, supervision, or further training in managing transference and countertransference, particularly since patients who leave AMA may return for subsequent care.7
Integrated care models, which feature close collaboration between clinicians from different specialties, can help ensure that a patient’s diverse health needs are met and reduce the likelihood of them leaving AMA. Integrated care models may be particularly effective for patients with co-occurring conditions such as HIV and SUDs.8
Implementing these recommendations can be challenging. Barriers to addressing AMA departures span several domains, including patient-specific barriers (eg, stigma and discrimination), clinical barriers (eg, lack of resources and training for clinicians), institutional hurdles (eg, systemic inefficiencies), and broader social barriers (eg, housing instability and inadequate social support). Overcoming these barriers requires a multifaceted approach involving clinicians, policymakers, and the community that considers medical, psychological, and social factors.
1. Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: a qualitative study. Subst Abus. 2020;41(4):519-525.
2. Kenne DR, Boros AP, Fischbein RL. Characteristics of opiate users leaving detoxification treatment against medical advice. J Addict Dis. 2010;29(3):383-394.
3. Mahajan RK, Gautam PL, Paul G, et al. Retrospective evaluation of patients leaving against medical advice in a tertiary care teaching hospital. Indian J Crit Care Med. 2019;23(3):139-142.
4. Armenian SH, Chutuape MA, Stitzer ML. Predictors of discharges against medical advice from a short-term hospital detoxification unit. Drug Alcohol Depend. 1999;56(1):1-8.
5. Ti L, Ti L. Leaving the hospital against medical advice among people who use illicit drugs: a systematic review. Am J Public Health. 2015;105(12):e53-e59.
6. McAdam M, Brar R, Young S. Initiation of injectable opioid agonist treatment in hospital: a case report. Drug Alcohol Rev. 2020;39(2):138-141.
7. Schouten R, Weintraub BR. Legal aspects of consultation. In: Stern TA, Freudenreich O, Smith FA, et al, eds. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 7th ed. Elsevier; 2018:578-579.
8. Vallecillo G, Robles MJ, Fonseca F, et al. Integrated care on leaving hospital against medical advice among HIV-infected people with substance use disorders. AIDS Res Hum Retroviruses. 2018;34(12):1044-1049.
1. Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: a qualitative study. Subst Abus. 2020;41(4):519-525.
2. Kenne DR, Boros AP, Fischbein RL. Characteristics of opiate users leaving detoxification treatment against medical advice. J Addict Dis. 2010;29(3):383-394.
3. Mahajan RK, Gautam PL, Paul G, et al. Retrospective evaluation of patients leaving against medical advice in a tertiary care teaching hospital. Indian J Crit Care Med. 2019;23(3):139-142.
4. Armenian SH, Chutuape MA, Stitzer ML. Predictors of discharges against medical advice from a short-term hospital detoxification unit. Drug Alcohol Depend. 1999;56(1):1-8.
5. Ti L, Ti L. Leaving the hospital against medical advice among people who use illicit drugs: a systematic review. Am J Public Health. 2015;105(12):e53-e59.
6. McAdam M, Brar R, Young S. Initiation of injectable opioid agonist treatment in hospital: a case report. Drug Alcohol Rev. 2020;39(2):138-141.
7. Schouten R, Weintraub BR. Legal aspects of consultation. In: Stern TA, Freudenreich O, Smith FA, et al, eds. Massachusetts General Hospital Handbook of General Hospital Psychiatry. 7th ed. Elsevier; 2018:578-579.
8. Vallecillo G, Robles MJ, Fonseca F, et al. Integrated care on leaving hospital against medical advice among HIV-infected people with substance use disorders. AIDS Res Hum Retroviruses. 2018;34(12):1044-1049.
Is air filtration the best public health intervention against respiratory viruses?
This transcript has been edited for clarity.
When it comes to the public health fight against respiratory viruses – COVID, flu, RSV, and so on – it has always struck me as strange how staunchly basically any intervention is opposed. Masking was, of course, the prototypical entrenched warfare of opposing ideologies, with advocates pointing to studies suggesting the efficacy of masking to prevent transmission and advocating for broad masking recommendations, and detractors citing studies that suggested masks were ineffective and characterizing masking policies as fascist overreach. I’ll admit that I was always perplexed by this a bit, as that particular intervention seemed so benign – a bit annoying, I guess, but not crazy.
I have come to appreciate what I call status quo bias, which is the tendency to reject any policy, advice, or intervention that would force you, as an individual, to change your usual behavior. We just don’t like to do that. It has made me think that the most successful public health interventions might be the ones that take the individual out of the loop. And air quality control seems an ideal fit here. Here is a potential intervention where you, the individual, have to do precisely nothing. The status quo is preserved. We just, you know, have cleaner indoor air.
But even the suggestion of air treatment systems as a bulwark against respiratory virus transmission has been met with not just skepticism but cynicism, and perhaps even defeatism. It seems that there are those out there who think there really is nothing we can do. Sickness is interpreted in a Calvinistic framework: You become ill because it is your pre-destiny. But maybe air treatment could actually work. It seems like it might, if a new paper from PLOS One is to be believed.
What we’re talking about is a study titled “Bipolar Ionization Rapidly Inactivates Real-World, Airborne Concentrations of Infective Respiratory Viruses” – a highly controlled, laboratory-based analysis of a bipolar ionization system which seems to rapidly reduce viral counts in the air.
The proposed mechanism of action is pretty simple. The ionization system – which, don’t worry, has been shown not to produce ozone – spits out positively and negatively charged particles, which float around the test chamber, designed to look like a pretty standard room that you might find in an office or a school.
Virus is then injected into the chamber through an aerosolization machine, to achieve concentrations on the order of what you might get standing within 6 feet or so of someone actively infected with COVID while they are breathing and talking.
The idea is that those ions stick to the virus particles, similar to how a balloon sticks to the wall after you rub it on your hair, and that tends to cause them to clump together and settle on surfaces more rapidly, and thus get farther away from their ports of entry to the human system: nose, mouth, and eyes. But the ions may also interfere with viruses’ ability to bind to cellular receptors, even in the air.
To quantify viral infectivity, the researchers used a biological system. Basically, you take air samples and expose a petri dish of cells to them and see how many cells die. Fewer cells dying, less infective. Under control conditions, you can see that virus infectivity does decrease over time. Time zero here is the end of a SARS-CoV-2 aerosolization.
This may simply reflect the fact that virus particles settle out of the air. But As you can see, within about an hour, you have almost no infective virus detectable. That’s fairly impressive.
Now, I’m not saying that this is a panacea, but it is certainly worth considering the use of technologies like these if we are going to revamp the infrastructure of our offices and schools. And, of course, it would be nice to see this tested in a rigorous clinical trial with actual infected people, not cells, as the outcome. But I continue to be encouraged by interventions like this which, to be honest, ask very little of us as individuals. Maybe it’s time we accept the things, or people, that we cannot change.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
When it comes to the public health fight against respiratory viruses – COVID, flu, RSV, and so on – it has always struck me as strange how staunchly basically any intervention is opposed. Masking was, of course, the prototypical entrenched warfare of opposing ideologies, with advocates pointing to studies suggesting the efficacy of masking to prevent transmission and advocating for broad masking recommendations, and detractors citing studies that suggested masks were ineffective and characterizing masking policies as fascist overreach. I’ll admit that I was always perplexed by this a bit, as that particular intervention seemed so benign – a bit annoying, I guess, but not crazy.
I have come to appreciate what I call status quo bias, which is the tendency to reject any policy, advice, or intervention that would force you, as an individual, to change your usual behavior. We just don’t like to do that. It has made me think that the most successful public health interventions might be the ones that take the individual out of the loop. And air quality control seems an ideal fit here. Here is a potential intervention where you, the individual, have to do precisely nothing. The status quo is preserved. We just, you know, have cleaner indoor air.
But even the suggestion of air treatment systems as a bulwark against respiratory virus transmission has been met with not just skepticism but cynicism, and perhaps even defeatism. It seems that there are those out there who think there really is nothing we can do. Sickness is interpreted in a Calvinistic framework: You become ill because it is your pre-destiny. But maybe air treatment could actually work. It seems like it might, if a new paper from PLOS One is to be believed.
What we’re talking about is a study titled “Bipolar Ionization Rapidly Inactivates Real-World, Airborne Concentrations of Infective Respiratory Viruses” – a highly controlled, laboratory-based analysis of a bipolar ionization system which seems to rapidly reduce viral counts in the air.
The proposed mechanism of action is pretty simple. The ionization system – which, don’t worry, has been shown not to produce ozone – spits out positively and negatively charged particles, which float around the test chamber, designed to look like a pretty standard room that you might find in an office or a school.
Virus is then injected into the chamber through an aerosolization machine, to achieve concentrations on the order of what you might get standing within 6 feet or so of someone actively infected with COVID while they are breathing and talking.
The idea is that those ions stick to the virus particles, similar to how a balloon sticks to the wall after you rub it on your hair, and that tends to cause them to clump together and settle on surfaces more rapidly, and thus get farther away from their ports of entry to the human system: nose, mouth, and eyes. But the ions may also interfere with viruses’ ability to bind to cellular receptors, even in the air.
To quantify viral infectivity, the researchers used a biological system. Basically, you take air samples and expose a petri dish of cells to them and see how many cells die. Fewer cells dying, less infective. Under control conditions, you can see that virus infectivity does decrease over time. Time zero here is the end of a SARS-CoV-2 aerosolization.
This may simply reflect the fact that virus particles settle out of the air. But As you can see, within about an hour, you have almost no infective virus detectable. That’s fairly impressive.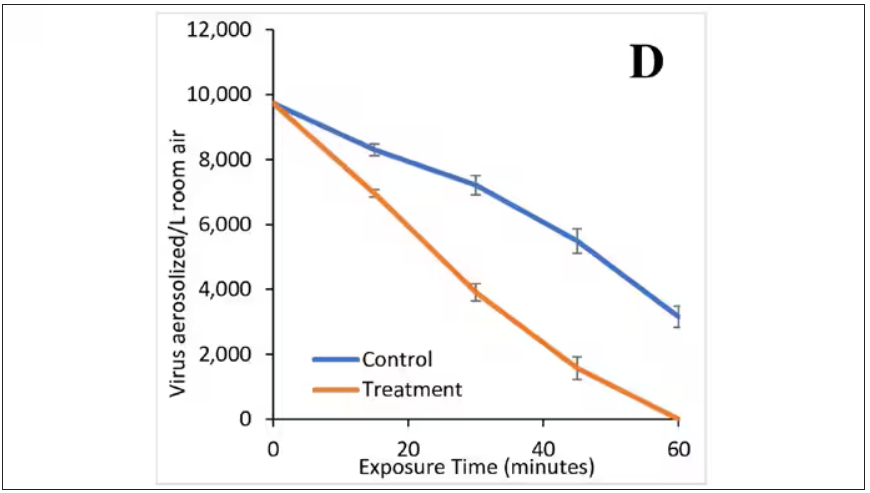
Now, I’m not saying that this is a panacea, but it is certainly worth considering the use of technologies like these if we are going to revamp the infrastructure of our offices and schools. And, of course, it would be nice to see this tested in a rigorous clinical trial with actual infected people, not cells, as the outcome. But I continue to be encouraged by interventions like this which, to be honest, ask very little of us as individuals. Maybe it’s time we accept the things, or people, that we cannot change.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
When it comes to the public health fight against respiratory viruses – COVID, flu, RSV, and so on – it has always struck me as strange how staunchly basically any intervention is opposed. Masking was, of course, the prototypical entrenched warfare of opposing ideologies, with advocates pointing to studies suggesting the efficacy of masking to prevent transmission and advocating for broad masking recommendations, and detractors citing studies that suggested masks were ineffective and characterizing masking policies as fascist overreach. I’ll admit that I was always perplexed by this a bit, as that particular intervention seemed so benign – a bit annoying, I guess, but not crazy.
I have come to appreciate what I call status quo bias, which is the tendency to reject any policy, advice, or intervention that would force you, as an individual, to change your usual behavior. We just don’t like to do that. It has made me think that the most successful public health interventions might be the ones that take the individual out of the loop. And air quality control seems an ideal fit here. Here is a potential intervention where you, the individual, have to do precisely nothing. The status quo is preserved. We just, you know, have cleaner indoor air.
But even the suggestion of air treatment systems as a bulwark against respiratory virus transmission has been met with not just skepticism but cynicism, and perhaps even defeatism. It seems that there are those out there who think there really is nothing we can do. Sickness is interpreted in a Calvinistic framework: You become ill because it is your pre-destiny. But maybe air treatment could actually work. It seems like it might, if a new paper from PLOS One is to be believed.
What we’re talking about is a study titled “Bipolar Ionization Rapidly Inactivates Real-World, Airborne Concentrations of Infective Respiratory Viruses” – a highly controlled, laboratory-based analysis of a bipolar ionization system which seems to rapidly reduce viral counts in the air.
The proposed mechanism of action is pretty simple. The ionization system – which, don’t worry, has been shown not to produce ozone – spits out positively and negatively charged particles, which float around the test chamber, designed to look like a pretty standard room that you might find in an office or a school.
Virus is then injected into the chamber through an aerosolization machine, to achieve concentrations on the order of what you might get standing within 6 feet or so of someone actively infected with COVID while they are breathing and talking.
The idea is that those ions stick to the virus particles, similar to how a balloon sticks to the wall after you rub it on your hair, and that tends to cause them to clump together and settle on surfaces more rapidly, and thus get farther away from their ports of entry to the human system: nose, mouth, and eyes. But the ions may also interfere with viruses’ ability to bind to cellular receptors, even in the air.
To quantify viral infectivity, the researchers used a biological system. Basically, you take air samples and expose a petri dish of cells to them and see how many cells die. Fewer cells dying, less infective. Under control conditions, you can see that virus infectivity does decrease over time. Time zero here is the end of a SARS-CoV-2 aerosolization.
This may simply reflect the fact that virus particles settle out of the air. But As you can see, within about an hour, you have almost no infective virus detectable. That’s fairly impressive.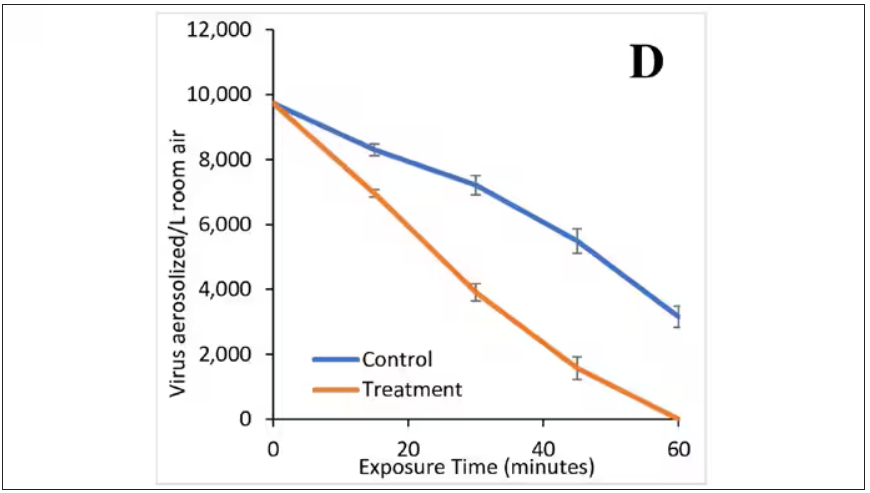
Now, I’m not saying that this is a panacea, but it is certainly worth considering the use of technologies like these if we are going to revamp the infrastructure of our offices and schools. And, of course, it would be nice to see this tested in a rigorous clinical trial with actual infected people, not cells, as the outcome. But I continue to be encouraged by interventions like this which, to be honest, ask very little of us as individuals. Maybe it’s time we accept the things, or people, that we cannot change.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Physicians: Don’t ignore sexuality in your dying patients
I have a long history of being interested in conversations that others avoid. In medical school, I felt that we didn’t talk enough about death, so I organized a lecture series on end-of-life care for my fellow students. Now, as a sexual medicine specialist, I have other conversations from which many medical providers shy away. So, buckle up!
A key question in palliative care is: How do you want to live the life you have left? And where does the wide range of human pleasures fit in? In her book The Pleasure Zone, sex therapist Stella Resnick describes eight kinds of pleasure:
- pain relief
- play, humor, movement, and sound
- mental
- emotional
- sensual
- spiritual
- primal (just being)
- sexual
At the end of life, both medically and culturally, we pay attention to many of these pleasures. But sexuality is often ignored.
Sexuality – which can be defined as the experience of oneself as a sexual being – may include how sex is experienced in relationships or with oneself, sexual orientation, body image, gender expression and identity, as well as sexual satisfaction and pleasure. People may have different priorities at different times regarding their sexuality, but sexuality is a key aspect of feeling fully alive and human across the lifespan. At the end of life, sexuality, sexual expression, and physical connection may play even more important roles than previously.
‘I just want to be able to have sex with my husband again’
Z was a 75-year-old woman who came to me for help with vaginal stenosis. Her cancer treatments were not going well. I asked her one of my typical questions: “What does sex mean to you?”
Sexual pleasure was “glue” – a critical way for her to connect with her sense of self and with her husband, a man of few words. She described transcendent experiences with partnered sex during her life. Finally, she explained, she was saddened by the idea of not experiencing that again before she died.
As medical providers, we don’t all need to be sex experts, but our patients should be able to have open and shame-free conversations with us about these issues at all stages of life. Up to 86% of palliative care patients want the chance to discuss their sexual concerns with a skilled clinician, and many consider this issue important to their psychological well-being. And yet, 91% reported that sexuality had not been addressed in their care.
In a Canadian study of 10 palliative care patients (and their partners), all but one felt that their medical providers should initiate conversations about sexuality and the effect of illness on sexual experience. They felt that this communication should be an integral component of care. The one person who disagreed said it was appropriate for clinicians to ask patients whether they wanted to talk about sexuality.
Before this study, sexuality had been discussed with only one participant. Here’s the magic part: Several of the patients reported that the study itself was therapeutic. This is my clinical experience as well. More often than not, open and shame-free clinical discussions about sexuality led to patients reflecting: “I’ve never been able to say this to another person, and now I feel so much better.”
One study of palliative care nurses found that while the nurses acknowledged the importance of addressing sexuality, their way of addressing sexuality followed cultural myths and norms or relied on their own experience rather than knowledge-based guidelines. Why? One explanation could be that clinicians raised and educated in North America probably did not get adequate training on this topic. We need to do better.
Second, cultural concepts that equate sexuality with healthy and able bodies who are partnered, young, cisgender, and heterosexual make it hard to conceive of how to relate sexuality to other bodies. We’ve been steeped in the biases of our culture.
Some medical providers avoid the topic because they feel vulnerable, fearful that a conversation about sexuality with a patient will reveal something about themselves. Others may simply deny the possibility that sexual function changes in the face of serious illness or that this could be a priority for their patients. Of course, we have a million other things to talk about – I get it.
Views on sex and sexuality affect how clinicians approach these conversations as well. A study of palliative care professionals described themes among those who did and did not address the topic. The professionals who did not discuss sexuality endorsed a narrow definition of sex based on genital sexual acts between two partners, usually heterosexual. Among these clinicians, when the issue came up, patients had raised the topic. They talked about sex using jokes and euphemisms (“are you still enjoying ‘good moments’ with your partner?”), perhaps to ease their own discomfort.
On the other hand, professionals who more frequently discussed sexuality with their patients endorsed a more holistic concept of sexuality: including genital and nongenital contact as well as nonphysical components like verbal communication and emotions. These clinicians found sexuality applicable to all individuals across the lifespan. They were more likely to initiate discussions about the effect of medications or illness on sexual function and address the need for equipment, such as a larger hospital bed.
I’m hoping that you might one day find yourself in the second group. Our patients at the end of life need our help in accessing the full range of pleasure in their lives. We need better medical education on how to help with sexual concerns when they arise (an article for another day), but we can start right now by simply initiating open, shame-free sexual health conversations. This is often the most important therapeutic intervention.
Dr. Kranz, Clinical Assistant Professor of Obstetrics/Gynecology and Family Medicine, University of Rochester (N.Y.) Medical Center, has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
I have a long history of being interested in conversations that others avoid. In medical school, I felt that we didn’t talk enough about death, so I organized a lecture series on end-of-life care for my fellow students. Now, as a sexual medicine specialist, I have other conversations from which many medical providers shy away. So, buckle up!
A key question in palliative care is: How do you want to live the life you have left? And where does the wide range of human pleasures fit in? In her book The Pleasure Zone, sex therapist Stella Resnick describes eight kinds of pleasure:
- pain relief
- play, humor, movement, and sound
- mental
- emotional
- sensual
- spiritual
- primal (just being)
- sexual
At the end of life, both medically and culturally, we pay attention to many of these pleasures. But sexuality is often ignored.
Sexuality – which can be defined as the experience of oneself as a sexual being – may include how sex is experienced in relationships or with oneself, sexual orientation, body image, gender expression and identity, as well as sexual satisfaction and pleasure. People may have different priorities at different times regarding their sexuality, but sexuality is a key aspect of feeling fully alive and human across the lifespan. At the end of life, sexuality, sexual expression, and physical connection may play even more important roles than previously.
‘I just want to be able to have sex with my husband again’
Z was a 75-year-old woman who came to me for help with vaginal stenosis. Her cancer treatments were not going well. I asked her one of my typical questions: “What does sex mean to you?”
Sexual pleasure was “glue” – a critical way for her to connect with her sense of self and with her husband, a man of few words. She described transcendent experiences with partnered sex during her life. Finally, she explained, she was saddened by the idea of not experiencing that again before she died.
As medical providers, we don’t all need to be sex experts, but our patients should be able to have open and shame-free conversations with us about these issues at all stages of life. Up to 86% of palliative care patients want the chance to discuss their sexual concerns with a skilled clinician, and many consider this issue important to their psychological well-being. And yet, 91% reported that sexuality had not been addressed in their care.
In a Canadian study of 10 palliative care patients (and their partners), all but one felt that their medical providers should initiate conversations about sexuality and the effect of illness on sexual experience. They felt that this communication should be an integral component of care. The one person who disagreed said it was appropriate for clinicians to ask patients whether they wanted to talk about sexuality.
Before this study, sexuality had been discussed with only one participant. Here’s the magic part: Several of the patients reported that the study itself was therapeutic. This is my clinical experience as well. More often than not, open and shame-free clinical discussions about sexuality led to patients reflecting: “I’ve never been able to say this to another person, and now I feel so much better.”
One study of palliative care nurses found that while the nurses acknowledged the importance of addressing sexuality, their way of addressing sexuality followed cultural myths and norms or relied on their own experience rather than knowledge-based guidelines. Why? One explanation could be that clinicians raised and educated in North America probably did not get adequate training on this topic. We need to do better.
Second, cultural concepts that equate sexuality with healthy and able bodies who are partnered, young, cisgender, and heterosexual make it hard to conceive of how to relate sexuality to other bodies. We’ve been steeped in the biases of our culture.
Some medical providers avoid the topic because they feel vulnerable, fearful that a conversation about sexuality with a patient will reveal something about themselves. Others may simply deny the possibility that sexual function changes in the face of serious illness or that this could be a priority for their patients. Of course, we have a million other things to talk about – I get it.
Views on sex and sexuality affect how clinicians approach these conversations as well. A study of palliative care professionals described themes among those who did and did not address the topic. The professionals who did not discuss sexuality endorsed a narrow definition of sex based on genital sexual acts between two partners, usually heterosexual. Among these clinicians, when the issue came up, patients had raised the topic. They talked about sex using jokes and euphemisms (“are you still enjoying ‘good moments’ with your partner?”), perhaps to ease their own discomfort.
On the other hand, professionals who more frequently discussed sexuality with their patients endorsed a more holistic concept of sexuality: including genital and nongenital contact as well as nonphysical components like verbal communication and emotions. These clinicians found sexuality applicable to all individuals across the lifespan. They were more likely to initiate discussions about the effect of medications or illness on sexual function and address the need for equipment, such as a larger hospital bed.
I’m hoping that you might one day find yourself in the second group. Our patients at the end of life need our help in accessing the full range of pleasure in their lives. We need better medical education on how to help with sexual concerns when they arise (an article for another day), but we can start right now by simply initiating open, shame-free sexual health conversations. This is often the most important therapeutic intervention.
Dr. Kranz, Clinical Assistant Professor of Obstetrics/Gynecology and Family Medicine, University of Rochester (N.Y.) Medical Center, has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
I have a long history of being interested in conversations that others avoid. In medical school, I felt that we didn’t talk enough about death, so I organized a lecture series on end-of-life care for my fellow students. Now, as a sexual medicine specialist, I have other conversations from which many medical providers shy away. So, buckle up!
A key question in palliative care is: How do you want to live the life you have left? And where does the wide range of human pleasures fit in? In her book The Pleasure Zone, sex therapist Stella Resnick describes eight kinds of pleasure:
- pain relief
- play, humor, movement, and sound
- mental
- emotional
- sensual
- spiritual
- primal (just being)
- sexual
At the end of life, both medically and culturally, we pay attention to many of these pleasures. But sexuality is often ignored.
Sexuality – which can be defined as the experience of oneself as a sexual being – may include how sex is experienced in relationships or with oneself, sexual orientation, body image, gender expression and identity, as well as sexual satisfaction and pleasure. People may have different priorities at different times regarding their sexuality, but sexuality is a key aspect of feeling fully alive and human across the lifespan. At the end of life, sexuality, sexual expression, and physical connection may play even more important roles than previously.
‘I just want to be able to have sex with my husband again’
Z was a 75-year-old woman who came to me for help with vaginal stenosis. Her cancer treatments were not going well. I asked her one of my typical questions: “What does sex mean to you?”
Sexual pleasure was “glue” – a critical way for her to connect with her sense of self and with her husband, a man of few words. She described transcendent experiences with partnered sex during her life. Finally, she explained, she was saddened by the idea of not experiencing that again before she died.
As medical providers, we don’t all need to be sex experts, but our patients should be able to have open and shame-free conversations with us about these issues at all stages of life. Up to 86% of palliative care patients want the chance to discuss their sexual concerns with a skilled clinician, and many consider this issue important to their psychological well-being. And yet, 91% reported that sexuality had not been addressed in their care.
In a Canadian study of 10 palliative care patients (and their partners), all but one felt that their medical providers should initiate conversations about sexuality and the effect of illness on sexual experience. They felt that this communication should be an integral component of care. The one person who disagreed said it was appropriate for clinicians to ask patients whether they wanted to talk about sexuality.
Before this study, sexuality had been discussed with only one participant. Here’s the magic part: Several of the patients reported that the study itself was therapeutic. This is my clinical experience as well. More often than not, open and shame-free clinical discussions about sexuality led to patients reflecting: “I’ve never been able to say this to another person, and now I feel so much better.”
One study of palliative care nurses found that while the nurses acknowledged the importance of addressing sexuality, their way of addressing sexuality followed cultural myths and norms or relied on their own experience rather than knowledge-based guidelines. Why? One explanation could be that clinicians raised and educated in North America probably did not get adequate training on this topic. We need to do better.
Second, cultural concepts that equate sexuality with healthy and able bodies who are partnered, young, cisgender, and heterosexual make it hard to conceive of how to relate sexuality to other bodies. We’ve been steeped in the biases of our culture.
Some medical providers avoid the topic because they feel vulnerable, fearful that a conversation about sexuality with a patient will reveal something about themselves. Others may simply deny the possibility that sexual function changes in the face of serious illness or that this could be a priority for their patients. Of course, we have a million other things to talk about – I get it.
Views on sex and sexuality affect how clinicians approach these conversations as well. A study of palliative care professionals described themes among those who did and did not address the topic. The professionals who did not discuss sexuality endorsed a narrow definition of sex based on genital sexual acts between two partners, usually heterosexual. Among these clinicians, when the issue came up, patients had raised the topic. They talked about sex using jokes and euphemisms (“are you still enjoying ‘good moments’ with your partner?”), perhaps to ease their own discomfort.
On the other hand, professionals who more frequently discussed sexuality with their patients endorsed a more holistic concept of sexuality: including genital and nongenital contact as well as nonphysical components like verbal communication and emotions. These clinicians found sexuality applicable to all individuals across the lifespan. They were more likely to initiate discussions about the effect of medications or illness on sexual function and address the need for equipment, such as a larger hospital bed.
I’m hoping that you might one day find yourself in the second group. Our patients at the end of life need our help in accessing the full range of pleasure in their lives. We need better medical education on how to help with sexual concerns when they arise (an article for another day), but we can start right now by simply initiating open, shame-free sexual health conversations. This is often the most important therapeutic intervention.
Dr. Kranz, Clinical Assistant Professor of Obstetrics/Gynecology and Family Medicine, University of Rochester (N.Y.) Medical Center, has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Is metabolically healthy obesity an ‘illusion’?
I cock my head at my “new” patient, Sherri, who heads into my consultation room at 8:30 on a rainy Monday morning. She looks vaguely familiar but I can’t quite place her face. “Dr. Messer,” she cries, “don’t you remember me? I was one of your very first patients 15 years ago in Westchester. You had just finished training.” Suddenly it all comes back to me.
Meeting Sherri reminded me of the lesson in humility that my mentor, Dr. Alice Levine, taught our crowded lecture hall so many years ago. Once upon a time, she prided herself on being an infinitely important doctor. One day, she met a patient with empty sella syndrome (literally missing his whole pituitary gland – MRI proven). She fully expected to swoop in to save the patient’s life by expertly replacing each absconded pituitary hormone, but to her shock and delight, an invisible little sliver of pituitary left in his brain allowed him to magically eek out completely normal hormone levels.
Sherri walked into my office so many years ago with a body mass index in the mid-40s. In laymen’s terms, she was morbidly obese. I settled in to discuss her hypertension, diabetes, high cholesterol, fatty liver, polycystic ovary syndrome, etc., but to my shock and delight, her blood pressure and blood work were completely normal. I struggled to keep a neutral face. She was there to discuss hair loss. I had just met my first patient with metabolically healthy obesity (MHO), and I was floored.
Fast-forward 15 years. Sherri sits down across the desk from me and hands me her blood work. Her formerly pristine labs are now peppered with red exclamation points and critically high lab values. Sherri had transitioned from MHO to metabolically unhealthy obesity (MUO).
Early clinical trials concluded that it was possible to have obesity but be metabolically healthy. Approximately 15% of patients living with obesity lack any of the comorbidities typically associated with this phenotype. These findings contributed to the de-emphasis on obesity as a true disease state.
In retrospect, the MHO subtype appears to be much more common in the younger and more active population and is typically quite transient. A new study published in Diabetes, Obesity and Metabolism revealed that people with MHO are 1.5 times more likely to develop diabetes vs. metabolically healthy normal-weight individuals. In addition, people living with obesity and no known metabolic complications still had a 50% higher risk for coronary artery disease. The study also showed that over 50% of people initially characterized as MHO eventually became MUO after a 16-year follow-up.
So once again, all roads lead to semaglutide (Wegovy), the most effective U.S. Food and Drug Administration–approved weight loss medication to date. The incretin class of medications not only helps patients lose 15% or more of their body weight, but it also helps reverse insulin resistance, lower the risk for heart disease, melt away fatty liver, and lower cholesterol levels and blood pressures. While an emphasis on lifestyle changes is always important, these medications are critical adjuncts to conventional therapies.
Fifteen years ago, I discussed her hair loss for 45 minutes and never mentioned the looming issue. Of course, back then there was no semaglutide or tirzepatide, which was just approved for obesity.
Sherri left our most recent visit with a prescription for Wegovy as well as appointments with a complimentary trainer and dietitian. Now that we have the tools we need, let’s commit to helping our patients achieve true metabolic health. Unlike the magical pituitary patient, metabolically healthy obesity is an illusion – and we owe it to our patients to treat it as such.
Dr. Messer is a clinical assistant professor at Mount Sinai School of Medicine, New York, and an associate professor at Hofstra University, Hempstead, N.Y. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
I cock my head at my “new” patient, Sherri, who heads into my consultation room at 8:30 on a rainy Monday morning. She looks vaguely familiar but I can’t quite place her face. “Dr. Messer,” she cries, “don’t you remember me? I was one of your very first patients 15 years ago in Westchester. You had just finished training.” Suddenly it all comes back to me.
Meeting Sherri reminded me of the lesson in humility that my mentor, Dr. Alice Levine, taught our crowded lecture hall so many years ago. Once upon a time, she prided herself on being an infinitely important doctor. One day, she met a patient with empty sella syndrome (literally missing his whole pituitary gland – MRI proven). She fully expected to swoop in to save the patient’s life by expertly replacing each absconded pituitary hormone, but to her shock and delight, an invisible little sliver of pituitary left in his brain allowed him to magically eek out completely normal hormone levels.
Sherri walked into my office so many years ago with a body mass index in the mid-40s. In laymen’s terms, she was morbidly obese. I settled in to discuss her hypertension, diabetes, high cholesterol, fatty liver, polycystic ovary syndrome, etc., but to my shock and delight, her blood pressure and blood work were completely normal. I struggled to keep a neutral face. She was there to discuss hair loss. I had just met my first patient with metabolically healthy obesity (MHO), and I was floored.
Fast-forward 15 years. Sherri sits down across the desk from me and hands me her blood work. Her formerly pristine labs are now peppered with red exclamation points and critically high lab values. Sherri had transitioned from MHO to metabolically unhealthy obesity (MUO).
Early clinical trials concluded that it was possible to have obesity but be metabolically healthy. Approximately 15% of patients living with obesity lack any of the comorbidities typically associated with this phenotype. These findings contributed to the de-emphasis on obesity as a true disease state.
In retrospect, the MHO subtype appears to be much more common in the younger and more active population and is typically quite transient. A new study published in Diabetes, Obesity and Metabolism revealed that people with MHO are 1.5 times more likely to develop diabetes vs. metabolically healthy normal-weight individuals. In addition, people living with obesity and no known metabolic complications still had a 50% higher risk for coronary artery disease. The study also showed that over 50% of people initially characterized as MHO eventually became MUO after a 16-year follow-up.
So once again, all roads lead to semaglutide (Wegovy), the most effective U.S. Food and Drug Administration–approved weight loss medication to date. The incretin class of medications not only helps patients lose 15% or more of their body weight, but it also helps reverse insulin resistance, lower the risk for heart disease, melt away fatty liver, and lower cholesterol levels and blood pressures. While an emphasis on lifestyle changes is always important, these medications are critical adjuncts to conventional therapies.
Fifteen years ago, I discussed her hair loss for 45 minutes and never mentioned the looming issue. Of course, back then there was no semaglutide or tirzepatide, which was just approved for obesity.
Sherri left our most recent visit with a prescription for Wegovy as well as appointments with a complimentary trainer and dietitian. Now that we have the tools we need, let’s commit to helping our patients achieve true metabolic health. Unlike the magical pituitary patient, metabolically healthy obesity is an illusion – and we owe it to our patients to treat it as such.
Dr. Messer is a clinical assistant professor at Mount Sinai School of Medicine, New York, and an associate professor at Hofstra University, Hempstead, N.Y. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
I cock my head at my “new” patient, Sherri, who heads into my consultation room at 8:30 on a rainy Monday morning. She looks vaguely familiar but I can’t quite place her face. “Dr. Messer,” she cries, “don’t you remember me? I was one of your very first patients 15 years ago in Westchester. You had just finished training.” Suddenly it all comes back to me.
Meeting Sherri reminded me of the lesson in humility that my mentor, Dr. Alice Levine, taught our crowded lecture hall so many years ago. Once upon a time, she prided herself on being an infinitely important doctor. One day, she met a patient with empty sella syndrome (literally missing his whole pituitary gland – MRI proven). She fully expected to swoop in to save the patient’s life by expertly replacing each absconded pituitary hormone, but to her shock and delight, an invisible little sliver of pituitary left in his brain allowed him to magically eek out completely normal hormone levels.
Sherri walked into my office so many years ago with a body mass index in the mid-40s. In laymen’s terms, she was morbidly obese. I settled in to discuss her hypertension, diabetes, high cholesterol, fatty liver, polycystic ovary syndrome, etc., but to my shock and delight, her blood pressure and blood work were completely normal. I struggled to keep a neutral face. She was there to discuss hair loss. I had just met my first patient with metabolically healthy obesity (MHO), and I was floored.
Fast-forward 15 years. Sherri sits down across the desk from me and hands me her blood work. Her formerly pristine labs are now peppered with red exclamation points and critically high lab values. Sherri had transitioned from MHO to metabolically unhealthy obesity (MUO).
Early clinical trials concluded that it was possible to have obesity but be metabolically healthy. Approximately 15% of patients living with obesity lack any of the comorbidities typically associated with this phenotype. These findings contributed to the de-emphasis on obesity as a true disease state.
In retrospect, the MHO subtype appears to be much more common in the younger and more active population and is typically quite transient. A new study published in Diabetes, Obesity and Metabolism revealed that people with MHO are 1.5 times more likely to develop diabetes vs. metabolically healthy normal-weight individuals. In addition, people living with obesity and no known metabolic complications still had a 50% higher risk for coronary artery disease. The study also showed that over 50% of people initially characterized as MHO eventually became MUO after a 16-year follow-up.
So once again, all roads lead to semaglutide (Wegovy), the most effective U.S. Food and Drug Administration–approved weight loss medication to date. The incretin class of medications not only helps patients lose 15% or more of their body weight, but it also helps reverse insulin resistance, lower the risk for heart disease, melt away fatty liver, and lower cholesterol levels and blood pressures. While an emphasis on lifestyle changes is always important, these medications are critical adjuncts to conventional therapies.
Fifteen years ago, I discussed her hair loss for 45 minutes and never mentioned the looming issue. Of course, back then there was no semaglutide or tirzepatide, which was just approved for obesity.
Sherri left our most recent visit with a prescription for Wegovy as well as appointments with a complimentary trainer and dietitian. Now that we have the tools we need, let’s commit to helping our patients achieve true metabolic health. Unlike the magical pituitary patient, metabolically healthy obesity is an illusion – and we owe it to our patients to treat it as such.
Dr. Messer is a clinical assistant professor at Mount Sinai School of Medicine, New York, and an associate professor at Hofstra University, Hempstead, N.Y. She disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Is most Parkinson’s disease man-made and therefore preventable?
This transcript has been edited for clarity.
Indu Subramanian, MD: It’s my pleasure to have Ray Dorsey on our program today. Ray is a professor of neurology at the University of Rochester and has been doing some amazing advocacy work in largely the space of trying to end Parkinson’s disease.
E. Ray Dorsey, MD: Thanks very much for having me, Indu. I’m delighted to be with you.
Trichloroethylene and PD
Dr. Subramanian: I wanted to first that we talk about as something that is in pretty much everywhere. This paper came out, and you wrote a commentary in JAMA Neurology as well. Perhaps we can summarize the paper and its findings.
Dr. Dorsey: Like most people, I didn’t know what TCE was until about 5 or 6 years ago. TCE is a very simple molecule. It’s got six atoms – two carbon atoms, one hydrogen atom, and three chlorine atoms — hence, its name “trichloroethylene.” There’s a very similar chemical called perchloroethylene, which is widely used in dry cleaning. It’s got one additional chlorine atom, and the prefix “per-” means “four.” I’ll talk about TCE predominantly, but both of these chemicals probably have similar toxicity with respect to Parkinson’s disease.
Research done by Dr. Carlie Tanner and Dr. Sam Goldman about a decade ago showed that in twins who were exposed to this through their work (it’s widely used as a degreasing agent) or hobbies (it’s used in printing and painting, by varnish workers, or by anyone that needs it as a solvent) had a 500% increased risk of developing Parkinson’s disease. Importantly, in that study, they showed that there was a lag time of 10-40 years between exposure to that chemical and the diagnosis of the disease. Because TCE was so widely used, they said that public health implications could be substantial.
What’s Camp Lejeune? Camp Lejeune is a Marine base in North Carolina where many Marines are trained. Between 1953 and 1987 at that Marine base, the drinking water was contaminated with TCE, perchloroethylene, and other toxic chemicals. The reason Camp Lejeune is so infamous is because the Marines knew about the contamination for many years and covered it up.
Indeed, this story only came to the forefront because Jennie Ensminger, the daughter of a Marine drill instructor, developed leukemia at age 6 and died at age 9. Her father, Jerry Ensminger, a retired master sergeant, found out after the fact that these cancer-causing chemicals, including TCE, a known carcinogen, were found at the Marine base and could be an explanation for why his daughter developed and died of leukemia.
Dr. Sam Goldman and Dr. Carlie Tanner and colleagues from UCSF looked at the rates of Parkinson’s among Marines who served at Camp Lejeune during the 1970s and compared that with rates in Marines who served Camp Pendleton on the West Coast. It turned out that the Marines who served at Camp Lejeune had a 70% higher risk of developing Parkinson’s disease than the Marines who served at Camp Pendleton.
Importantly, these Marines, by definition, were healthy. They were young. They were only 20 years old, on average, when they were at Camp Lejeune. They stayed at a Marine base for a short period of time, so on average, they were only there for 2 years. Yet 30 years later, they had a 70% increased risk of developing Parkinson’s disease.
Ending Parkinson’s disease
Dr. Subramanian: Wow, that’s pretty profound. You’ve done a large amount of work, and in fact you, along with some of our colleagues wrote a book about ending Parkinson’s disease. I read that book when it came out a couple of years ago, and I was really struck by a few things. Parkinson’s has doubled in the past 40 years and is going to double again in the next 20 years. Can you tell me a little bit about that statistic and why that is? It’s not just because people are aging. What is the sense of that? How do we interpret that?
Dr. Dorsey: According to the Global Burden of Disease study, which I was fortunate to be part of, the number of people with Parkinson’s disease has more than doubled in the past 25 years. A conservative projection based on aging alone suggests that it’s going to double again unless we change something about it. It’s now the world’s fastest-growing brain disease, and it is growing faster than can be explained by aging alone.
If you look at the map of Parkinson’s disease, if you thought it was purely genetic, you would have a relatively uniform map of rates of Parkinson’s disease. In fact, we don’t see that. Rates of Parkinson’s are five times higher in industrialized parts of the world, like the United States and Canada, than they are in sub-Saharan Africa. Rates of Parkinson’s disease are increasing most rapidly in areas of world that are undergoing the most rapid industrialization, such as India and China, where adjusted for age, the rates of Parkinson’s have more than doubled in the past 25 years.
The thesis of our book is that much of Parkinson’s disease is man-made. Work done by your colleagues at UCLA, including Jeff Bronstein and Beate Ritz, have demonstrated that air pollution and certain pesticides are likely fueling the rise of Parkinson’s disease.
Given that in the United States, rates of Parkinson’s disease are actually higher in urban and suburban areas than they are in rural areas, I think that this dry-cleaning chemical – which was widely used in the 1970s in everything from typewriter correction fluid to decaffeinated coffee and [over] 2 pounds per American [was produced] – could be one of the most important causes or contributing factors to Parkinson’s disease.
What to tell patients
Dr. Subramanian: For the general neurologists or practitioners out there watching this, what can they do? If you have a patient whom you suspect may have been exposed to toxins, what should we tell people who aren’t patients yet who are at risk? What are some things that you think would be helpful?
Dr. Dorsey: I think one of the shortcomings of American medicine is that we often just go from diagnosis to treatment. You’re depressed, you get an antidepressant; you have Parkinson’s disease, you get levodopa; you have seizures, you get put on an antiepileptic medication.
I think we need to spend a couple of minutes at least, maybe at the beginning, to go to the diagnosis of the condition and why you have this disease. If you just do a brief occupational history, after you start the exam – things like finding out what people do for a living or did for a living or how they spend their time – I think you’ll find many of these risk factors are actually present.
It’s pretty easy to identify whether people grew up in a rural area and drank well water, which is prone to be contaminated with pesticides. We know that people who drink [contaminated] well water have about a 75% increased risk of developing Parkinson’s disease. I think you can find for people, especially when they grew up, when they were young, that the most relevant exposure might be that when people were young children.
It’s a little bit harder to identify all exposure to TCE. The Marines at Camp Lejeune didn’t know they were drinking the water that was contaminated with this and only found out about it after the fact because Jerry Ensminger launched a 26-year campaign to bring justice for the Marines and their dependents.
Some people who know that they work with chemicals or with solvents might know about this. In New York City, these chemicals are widely used in dry cleaning. They’re readily volatile. These chemicals can evaporate from dry-cleaning buildings and go into the indoor air of apartments above dry cleaners, for example, in New York City. That can be in toxic levels. These readily dissolve in fat, hence their use in degreasing.
There have been studies, for example, in Germany, that found that supermarkets that are simply near a dry cleaner will have TCE or perchloroethylene in the butter and the cheese that they’re selling.
It gets even worse. For example, you bring your daughter into the dry-cleaning building and she’s eating an ice cream cone. When she leaves, she’s eating perchloroethylene and TCE.
It’s a little bit harder to find it, but I think it’s relevant because some people might be still being exposed and some people might still be drinking well water and they rarely have their well tested. For those people, I recommend they get their well tested and I recommend all my patients to get a carbon filter to decrease exposure to pesticides and chemicals. A carbon filter is just like what Brita and Pure and other brands are.
Because they’re chemicals known to cause cancer, I get a little bit concerned about cancer screening. This is most strongly tied to non-Hodgkin lymphoma, liver cancer, and renal cancer. It’s also linked to multiple myeloma, prostate cancer, probably brain cancer, and probably breast cancer, especially in men.
I tell people to be concerned about those, and then I tell people to avoid pesticides if they have Parkinson’s disease in all its forms, not only in the drinking water but in the produce you buy, the food you eat, what you put on your lawn, what’s on the golf course where you play, and the like.
Dr. Subramanian: I would say, just from the wellness perspective, if people are at risk for degenerative disease in terms of their brain health, things like sleep, mind-body practices, exercise, diet (Mediterranean or organic, if you can), and avoiding pesticides are all important. Social connection is important as well – the things that we think are helpful in general as people age and to prevent Alzheimer’s and other things like that.
Dr. Dorsey: These are fantastic ways to modify disease course. The evidence for them is only increasing. There’s an analogy I like to use. If someone is diagnosed with lung cancer, the first thing we tell them to do is to stop smoking. If someone’s diagnosed with Parkinson’s, we don’t tell them to stop getting exposure to pesticides. We don’t tell them to stop dry cleaning their clothes. We don’t tell them to avoid air pollution. These are all risk factors that are increasingly well established for Parkinson’s disease.
I think Parkinson’s disease, fundamentally for the vast majority of people, is an entirely preventable disease. We’re not taking actions to prevent people from getting this very disabling and very deadly disease.
Advocacy work
Dr. Subramanian: You and I are quite interested in the sense of being advocates as neurologists, and I think it fuels our passion and helps us to wake up every morning feeling like we have something that is meaningful and purposeful in our lives. Could you describe this as your passion and how it may prevent burnout and what it’s given you as a neurologist?
Dr. Dorsey: The credit for much of this is Dr. Carlie Tanner at UC San Francisco. I had the gift of sabbatical and I started reading the literature, I started reading her literature, and I came away with that, over the past 25 years, she detailed these environmental risk factors that are linked to Parkinson’s disease. Pesticides, these dry-cleaning chemicals, and air pollution. When I read it, I just realized that this was the case.
The same time I was reading her work, I read this book called “How to Survive a Plague,” by David France, who was a member of a group called Act Up, which was a group of men in New York City who reacted to the emergence of HIV in the 1980s. If you remember the 1980s, there was no federal response to HIV. People were blamed for the diseases that they were developing. It was only because brave men and women in New York City and in San Francisco banded together and organized that they changed the course of HIV.
They didn’t just do it for themselves. They did it for all of us. You and I and many people may not have HIV because of their courage. They made HIV a treatable condition. It’s actually more treatable than Parkinson’s disease. It’s associated with a near-normal life expectancy. They also made it a preventable disease. Thousands, if not millions, of us don’t have HIV because of their work. It’s an increasingly less common disease. Rates of HIV are actually decreasing, which is something that you or I would never have expected when we were in medical training.
I can’t think of a better outcome for a neurologist or any physician than to make the diseases that they’re caring for nonexistent ... than if we lived in a world that didn’t have HIV, we lived in a world where lung cancer largely didn’t exist. We’ve had worlds in the past where Parkinson’s probably didn’t exist or existed in extremely small numbers. That might be true for diffuse Lewy body disease and others, and if these diseases are preventable, we can take actions as individuals and as a society to lower our risk.
What a wonderful gift for future generations and many generations to come, hopefully, to live in a world that’s largely devoid of Parkinson’s disease. Just like we live in a world free of typhus. We live in a world free of smallpox. We live in a world where polio is extraordinarily uncommon. We don’t even have treatments for polio because we just don’t have polio. I think we can do the same thing for Parkinson’s disease for the vast majority.
Dr. Subramanian: Thank you so much, Ray, for your advocacy. We’re getting to the point in neurology, which is exciting to me, of possibly primary prevention of some of these disorders. I think we have a role in that, which is exciting for the future.
Dr. Dorsey: Absolutely.
Dr. Subramanian is clinical professor, department of neurology, University of California Los Angeles, and director of PADRECC (Parkinson’s Disease Research, Education, and Clinical Centers), West Los Angeles Veterans Association, Los Angeles. She disclosed ties with Acorda Pharma. Dr. Dorsey is the David M. Levy Professor of Neurology, University of Rochester (N.Y.). He disclosed ties to Abbott, AbbVie, Acadia, Acorda Therapeutics, Averitas Pharma, Biogen, BioSensics, Boehringer Ingelheim, Burroughs Wellcome Fund, Caraway Therapeutics, CuraSen, DConsult2, Denali Therapeutics, Eli Lilly, Genentech, Health & Wellness Partners, HMP Education, Included Health, Karger, KOL Groups, Life Sciences, Mediflix, Medrhythms, Merck; MJH Holdings, North American Center for Continuing Medical Education, Novartis, Otsuka, Pfizer, Photopharmics, Praxis Medicine, Roche, Safra Foundation, Sanofi, Seelos Therapeutics, SemCap, Spark Therapeutics, Springer Healthcare, Synapticure, Theravance Biopharmaceuticals, and WebMD.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Indu Subramanian, MD: It’s my pleasure to have Ray Dorsey on our program today. Ray is a professor of neurology at the University of Rochester and has been doing some amazing advocacy work in largely the space of trying to end Parkinson’s disease.
E. Ray Dorsey, MD: Thanks very much for having me, Indu. I’m delighted to be with you.
Trichloroethylene and PD
Dr. Subramanian: I wanted to first that we talk about as something that is in pretty much everywhere. This paper came out, and you wrote a commentary in JAMA Neurology as well. Perhaps we can summarize the paper and its findings.
Dr. Dorsey: Like most people, I didn’t know what TCE was until about 5 or 6 years ago. TCE is a very simple molecule. It’s got six atoms – two carbon atoms, one hydrogen atom, and three chlorine atoms — hence, its name “trichloroethylene.” There’s a very similar chemical called perchloroethylene, which is widely used in dry cleaning. It’s got one additional chlorine atom, and the prefix “per-” means “four.” I’ll talk about TCE predominantly, but both of these chemicals probably have similar toxicity with respect to Parkinson’s disease.
Research done by Dr. Carlie Tanner and Dr. Sam Goldman about a decade ago showed that in twins who were exposed to this through their work (it’s widely used as a degreasing agent) or hobbies (it’s used in printing and painting, by varnish workers, or by anyone that needs it as a solvent) had a 500% increased risk of developing Parkinson’s disease. Importantly, in that study, they showed that there was a lag time of 10-40 years between exposure to that chemical and the diagnosis of the disease. Because TCE was so widely used, they said that public health implications could be substantial.
What’s Camp Lejeune? Camp Lejeune is a Marine base in North Carolina where many Marines are trained. Between 1953 and 1987 at that Marine base, the drinking water was contaminated with TCE, perchloroethylene, and other toxic chemicals. The reason Camp Lejeune is so infamous is because the Marines knew about the contamination for many years and covered it up.
Indeed, this story only came to the forefront because Jennie Ensminger, the daughter of a Marine drill instructor, developed leukemia at age 6 and died at age 9. Her father, Jerry Ensminger, a retired master sergeant, found out after the fact that these cancer-causing chemicals, including TCE, a known carcinogen, were found at the Marine base and could be an explanation for why his daughter developed and died of leukemia.
Dr. Sam Goldman and Dr. Carlie Tanner and colleagues from UCSF looked at the rates of Parkinson’s among Marines who served at Camp Lejeune during the 1970s and compared that with rates in Marines who served Camp Pendleton on the West Coast. It turned out that the Marines who served at Camp Lejeune had a 70% higher risk of developing Parkinson’s disease than the Marines who served at Camp Pendleton.
Importantly, these Marines, by definition, were healthy. They were young. They were only 20 years old, on average, when they were at Camp Lejeune. They stayed at a Marine base for a short period of time, so on average, they were only there for 2 years. Yet 30 years later, they had a 70% increased risk of developing Parkinson’s disease.
Ending Parkinson’s disease
Dr. Subramanian: Wow, that’s pretty profound. You’ve done a large amount of work, and in fact you, along with some of our colleagues wrote a book about ending Parkinson’s disease. I read that book when it came out a couple of years ago, and I was really struck by a few things. Parkinson’s has doubled in the past 40 years and is going to double again in the next 20 years. Can you tell me a little bit about that statistic and why that is? It’s not just because people are aging. What is the sense of that? How do we interpret that?
Dr. Dorsey: According to the Global Burden of Disease study, which I was fortunate to be part of, the number of people with Parkinson’s disease has more than doubled in the past 25 years. A conservative projection based on aging alone suggests that it’s going to double again unless we change something about it. It’s now the world’s fastest-growing brain disease, and it is growing faster than can be explained by aging alone.
If you look at the map of Parkinson’s disease, if you thought it was purely genetic, you would have a relatively uniform map of rates of Parkinson’s disease. In fact, we don’t see that. Rates of Parkinson’s are five times higher in industrialized parts of the world, like the United States and Canada, than they are in sub-Saharan Africa. Rates of Parkinson’s disease are increasing most rapidly in areas of world that are undergoing the most rapid industrialization, such as India and China, where adjusted for age, the rates of Parkinson’s have more than doubled in the past 25 years.
The thesis of our book is that much of Parkinson’s disease is man-made. Work done by your colleagues at UCLA, including Jeff Bronstein and Beate Ritz, have demonstrated that air pollution and certain pesticides are likely fueling the rise of Parkinson’s disease.
Given that in the United States, rates of Parkinson’s disease are actually higher in urban and suburban areas than they are in rural areas, I think that this dry-cleaning chemical – which was widely used in the 1970s in everything from typewriter correction fluid to decaffeinated coffee and [over] 2 pounds per American [was produced] – could be one of the most important causes or contributing factors to Parkinson’s disease.
What to tell patients
Dr. Subramanian: For the general neurologists or practitioners out there watching this, what can they do? If you have a patient whom you suspect may have been exposed to toxins, what should we tell people who aren’t patients yet who are at risk? What are some things that you think would be helpful?
Dr. Dorsey: I think one of the shortcomings of American medicine is that we often just go from diagnosis to treatment. You’re depressed, you get an antidepressant; you have Parkinson’s disease, you get levodopa; you have seizures, you get put on an antiepileptic medication.
I think we need to spend a couple of minutes at least, maybe at the beginning, to go to the diagnosis of the condition and why you have this disease. If you just do a brief occupational history, after you start the exam – things like finding out what people do for a living or did for a living or how they spend their time – I think you’ll find many of these risk factors are actually present.
It’s pretty easy to identify whether people grew up in a rural area and drank well water, which is prone to be contaminated with pesticides. We know that people who drink [contaminated] well water have about a 75% increased risk of developing Parkinson’s disease. I think you can find for people, especially when they grew up, when they were young, that the most relevant exposure might be that when people were young children.
It’s a little bit harder to identify all exposure to TCE. The Marines at Camp Lejeune didn’t know they were drinking the water that was contaminated with this and only found out about it after the fact because Jerry Ensminger launched a 26-year campaign to bring justice for the Marines and their dependents.
Some people who know that they work with chemicals or with solvents might know about this. In New York City, these chemicals are widely used in dry cleaning. They’re readily volatile. These chemicals can evaporate from dry-cleaning buildings and go into the indoor air of apartments above dry cleaners, for example, in New York City. That can be in toxic levels. These readily dissolve in fat, hence their use in degreasing.
There have been studies, for example, in Germany, that found that supermarkets that are simply near a dry cleaner will have TCE or perchloroethylene in the butter and the cheese that they’re selling.
It gets even worse. For example, you bring your daughter into the dry-cleaning building and she’s eating an ice cream cone. When she leaves, she’s eating perchloroethylene and TCE.
It’s a little bit harder to find it, but I think it’s relevant because some people might be still being exposed and some people might still be drinking well water and they rarely have their well tested. For those people, I recommend they get their well tested and I recommend all my patients to get a carbon filter to decrease exposure to pesticides and chemicals. A carbon filter is just like what Brita and Pure and other brands are.
Because they’re chemicals known to cause cancer, I get a little bit concerned about cancer screening. This is most strongly tied to non-Hodgkin lymphoma, liver cancer, and renal cancer. It’s also linked to multiple myeloma, prostate cancer, probably brain cancer, and probably breast cancer, especially in men.
I tell people to be concerned about those, and then I tell people to avoid pesticides if they have Parkinson’s disease in all its forms, not only in the drinking water but in the produce you buy, the food you eat, what you put on your lawn, what’s on the golf course where you play, and the like.
Dr. Subramanian: I would say, just from the wellness perspective, if people are at risk for degenerative disease in terms of their brain health, things like sleep, mind-body practices, exercise, diet (Mediterranean or organic, if you can), and avoiding pesticides are all important. Social connection is important as well – the things that we think are helpful in general as people age and to prevent Alzheimer’s and other things like that.
Dr. Dorsey: These are fantastic ways to modify disease course. The evidence for them is only increasing. There’s an analogy I like to use. If someone is diagnosed with lung cancer, the first thing we tell them to do is to stop smoking. If someone’s diagnosed with Parkinson’s, we don’t tell them to stop getting exposure to pesticides. We don’t tell them to stop dry cleaning their clothes. We don’t tell them to avoid air pollution. These are all risk factors that are increasingly well established for Parkinson’s disease.
I think Parkinson’s disease, fundamentally for the vast majority of people, is an entirely preventable disease. We’re not taking actions to prevent people from getting this very disabling and very deadly disease.
Advocacy work
Dr. Subramanian: You and I are quite interested in the sense of being advocates as neurologists, and I think it fuels our passion and helps us to wake up every morning feeling like we have something that is meaningful and purposeful in our lives. Could you describe this as your passion and how it may prevent burnout and what it’s given you as a neurologist?
Dr. Dorsey: The credit for much of this is Dr. Carlie Tanner at UC San Francisco. I had the gift of sabbatical and I started reading the literature, I started reading her literature, and I came away with that, over the past 25 years, she detailed these environmental risk factors that are linked to Parkinson’s disease. Pesticides, these dry-cleaning chemicals, and air pollution. When I read it, I just realized that this was the case.
The same time I was reading her work, I read this book called “How to Survive a Plague,” by David France, who was a member of a group called Act Up, which was a group of men in New York City who reacted to the emergence of HIV in the 1980s. If you remember the 1980s, there was no federal response to HIV. People were blamed for the diseases that they were developing. It was only because brave men and women in New York City and in San Francisco banded together and organized that they changed the course of HIV.
They didn’t just do it for themselves. They did it for all of us. You and I and many people may not have HIV because of their courage. They made HIV a treatable condition. It’s actually more treatable than Parkinson’s disease. It’s associated with a near-normal life expectancy. They also made it a preventable disease. Thousands, if not millions, of us don’t have HIV because of their work. It’s an increasingly less common disease. Rates of HIV are actually decreasing, which is something that you or I would never have expected when we were in medical training.
I can’t think of a better outcome for a neurologist or any physician than to make the diseases that they’re caring for nonexistent ... than if we lived in a world that didn’t have HIV, we lived in a world where lung cancer largely didn’t exist. We’ve had worlds in the past where Parkinson’s probably didn’t exist or existed in extremely small numbers. That might be true for diffuse Lewy body disease and others, and if these diseases are preventable, we can take actions as individuals and as a society to lower our risk.
What a wonderful gift for future generations and many generations to come, hopefully, to live in a world that’s largely devoid of Parkinson’s disease. Just like we live in a world free of typhus. We live in a world free of smallpox. We live in a world where polio is extraordinarily uncommon. We don’t even have treatments for polio because we just don’t have polio. I think we can do the same thing for Parkinson’s disease for the vast majority.
Dr. Subramanian: Thank you so much, Ray, for your advocacy. We’re getting to the point in neurology, which is exciting to me, of possibly primary prevention of some of these disorders. I think we have a role in that, which is exciting for the future.
Dr. Dorsey: Absolutely.
Dr. Subramanian is clinical professor, department of neurology, University of California Los Angeles, and director of PADRECC (Parkinson’s Disease Research, Education, and Clinical Centers), West Los Angeles Veterans Association, Los Angeles. She disclosed ties with Acorda Pharma. Dr. Dorsey is the David M. Levy Professor of Neurology, University of Rochester (N.Y.). He disclosed ties to Abbott, AbbVie, Acadia, Acorda Therapeutics, Averitas Pharma, Biogen, BioSensics, Boehringer Ingelheim, Burroughs Wellcome Fund, Caraway Therapeutics, CuraSen, DConsult2, Denali Therapeutics, Eli Lilly, Genentech, Health & Wellness Partners, HMP Education, Included Health, Karger, KOL Groups, Life Sciences, Mediflix, Medrhythms, Merck; MJH Holdings, North American Center for Continuing Medical Education, Novartis, Otsuka, Pfizer, Photopharmics, Praxis Medicine, Roche, Safra Foundation, Sanofi, Seelos Therapeutics, SemCap, Spark Therapeutics, Springer Healthcare, Synapticure, Theravance Biopharmaceuticals, and WebMD.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Indu Subramanian, MD: It’s my pleasure to have Ray Dorsey on our program today. Ray is a professor of neurology at the University of Rochester and has been doing some amazing advocacy work in largely the space of trying to end Parkinson’s disease.
E. Ray Dorsey, MD: Thanks very much for having me, Indu. I’m delighted to be with you.
Trichloroethylene and PD
Dr. Subramanian: I wanted to first that we talk about as something that is in pretty much everywhere. This paper came out, and you wrote a commentary in JAMA Neurology as well. Perhaps we can summarize the paper and its findings.
Dr. Dorsey: Like most people, I didn’t know what TCE was until about 5 or 6 years ago. TCE is a very simple molecule. It’s got six atoms – two carbon atoms, one hydrogen atom, and three chlorine atoms — hence, its name “trichloroethylene.” There’s a very similar chemical called perchloroethylene, which is widely used in dry cleaning. It’s got one additional chlorine atom, and the prefix “per-” means “four.” I’ll talk about TCE predominantly, but both of these chemicals probably have similar toxicity with respect to Parkinson’s disease.
Research done by Dr. Carlie Tanner and Dr. Sam Goldman about a decade ago showed that in twins who were exposed to this through their work (it’s widely used as a degreasing agent) or hobbies (it’s used in printing and painting, by varnish workers, or by anyone that needs it as a solvent) had a 500% increased risk of developing Parkinson’s disease. Importantly, in that study, they showed that there was a lag time of 10-40 years between exposure to that chemical and the diagnosis of the disease. Because TCE was so widely used, they said that public health implications could be substantial.
What’s Camp Lejeune? Camp Lejeune is a Marine base in North Carolina where many Marines are trained. Between 1953 and 1987 at that Marine base, the drinking water was contaminated with TCE, perchloroethylene, and other toxic chemicals. The reason Camp Lejeune is so infamous is because the Marines knew about the contamination for many years and covered it up.
Indeed, this story only came to the forefront because Jennie Ensminger, the daughter of a Marine drill instructor, developed leukemia at age 6 and died at age 9. Her father, Jerry Ensminger, a retired master sergeant, found out after the fact that these cancer-causing chemicals, including TCE, a known carcinogen, were found at the Marine base and could be an explanation for why his daughter developed and died of leukemia.
Dr. Sam Goldman and Dr. Carlie Tanner and colleagues from UCSF looked at the rates of Parkinson’s among Marines who served at Camp Lejeune during the 1970s and compared that with rates in Marines who served Camp Pendleton on the West Coast. It turned out that the Marines who served at Camp Lejeune had a 70% higher risk of developing Parkinson’s disease than the Marines who served at Camp Pendleton.
Importantly, these Marines, by definition, were healthy. They were young. They were only 20 years old, on average, when they were at Camp Lejeune. They stayed at a Marine base for a short period of time, so on average, they were only there for 2 years. Yet 30 years later, they had a 70% increased risk of developing Parkinson’s disease.
Ending Parkinson’s disease
Dr. Subramanian: Wow, that’s pretty profound. You’ve done a large amount of work, and in fact you, along with some of our colleagues wrote a book about ending Parkinson’s disease. I read that book when it came out a couple of years ago, and I was really struck by a few things. Parkinson’s has doubled in the past 40 years and is going to double again in the next 20 years. Can you tell me a little bit about that statistic and why that is? It’s not just because people are aging. What is the sense of that? How do we interpret that?
Dr. Dorsey: According to the Global Burden of Disease study, which I was fortunate to be part of, the number of people with Parkinson’s disease has more than doubled in the past 25 years. A conservative projection based on aging alone suggests that it’s going to double again unless we change something about it. It’s now the world’s fastest-growing brain disease, and it is growing faster than can be explained by aging alone.
If you look at the map of Parkinson’s disease, if you thought it was purely genetic, you would have a relatively uniform map of rates of Parkinson’s disease. In fact, we don’t see that. Rates of Parkinson’s are five times higher in industrialized parts of the world, like the United States and Canada, than they are in sub-Saharan Africa. Rates of Parkinson’s disease are increasing most rapidly in areas of world that are undergoing the most rapid industrialization, such as India and China, where adjusted for age, the rates of Parkinson’s have more than doubled in the past 25 years.
The thesis of our book is that much of Parkinson’s disease is man-made. Work done by your colleagues at UCLA, including Jeff Bronstein and Beate Ritz, have demonstrated that air pollution and certain pesticides are likely fueling the rise of Parkinson’s disease.
Given that in the United States, rates of Parkinson’s disease are actually higher in urban and suburban areas than they are in rural areas, I think that this dry-cleaning chemical – which was widely used in the 1970s in everything from typewriter correction fluid to decaffeinated coffee and [over] 2 pounds per American [was produced] – could be one of the most important causes or contributing factors to Parkinson’s disease.
What to tell patients
Dr. Subramanian: For the general neurologists or practitioners out there watching this, what can they do? If you have a patient whom you suspect may have been exposed to toxins, what should we tell people who aren’t patients yet who are at risk? What are some things that you think would be helpful?
Dr. Dorsey: I think one of the shortcomings of American medicine is that we often just go from diagnosis to treatment. You’re depressed, you get an antidepressant; you have Parkinson’s disease, you get levodopa; you have seizures, you get put on an antiepileptic medication.
I think we need to spend a couple of minutes at least, maybe at the beginning, to go to the diagnosis of the condition and why you have this disease. If you just do a brief occupational history, after you start the exam – things like finding out what people do for a living or did for a living or how they spend their time – I think you’ll find many of these risk factors are actually present.
It’s pretty easy to identify whether people grew up in a rural area and drank well water, which is prone to be contaminated with pesticides. We know that people who drink [contaminated] well water have about a 75% increased risk of developing Parkinson’s disease. I think you can find for people, especially when they grew up, when they were young, that the most relevant exposure might be that when people were young children.
It’s a little bit harder to identify all exposure to TCE. The Marines at Camp Lejeune didn’t know they were drinking the water that was contaminated with this and only found out about it after the fact because Jerry Ensminger launched a 26-year campaign to bring justice for the Marines and their dependents.
Some people who know that they work with chemicals or with solvents might know about this. In New York City, these chemicals are widely used in dry cleaning. They’re readily volatile. These chemicals can evaporate from dry-cleaning buildings and go into the indoor air of apartments above dry cleaners, for example, in New York City. That can be in toxic levels. These readily dissolve in fat, hence their use in degreasing.
There have been studies, for example, in Germany, that found that supermarkets that are simply near a dry cleaner will have TCE or perchloroethylene in the butter and the cheese that they’re selling.
It gets even worse. For example, you bring your daughter into the dry-cleaning building and she’s eating an ice cream cone. When she leaves, she’s eating perchloroethylene and TCE.
It’s a little bit harder to find it, but I think it’s relevant because some people might be still being exposed and some people might still be drinking well water and they rarely have their well tested. For those people, I recommend they get their well tested and I recommend all my patients to get a carbon filter to decrease exposure to pesticides and chemicals. A carbon filter is just like what Brita and Pure and other brands are.
Because they’re chemicals known to cause cancer, I get a little bit concerned about cancer screening. This is most strongly tied to non-Hodgkin lymphoma, liver cancer, and renal cancer. It’s also linked to multiple myeloma, prostate cancer, probably brain cancer, and probably breast cancer, especially in men.
I tell people to be concerned about those, and then I tell people to avoid pesticides if they have Parkinson’s disease in all its forms, not only in the drinking water but in the produce you buy, the food you eat, what you put on your lawn, what’s on the golf course where you play, and the like.
Dr. Subramanian: I would say, just from the wellness perspective, if people are at risk for degenerative disease in terms of their brain health, things like sleep, mind-body practices, exercise, diet (Mediterranean or organic, if you can), and avoiding pesticides are all important. Social connection is important as well – the things that we think are helpful in general as people age and to prevent Alzheimer’s and other things like that.
Dr. Dorsey: These are fantastic ways to modify disease course. The evidence for them is only increasing. There’s an analogy I like to use. If someone is diagnosed with lung cancer, the first thing we tell them to do is to stop smoking. If someone’s diagnosed with Parkinson’s, we don’t tell them to stop getting exposure to pesticides. We don’t tell them to stop dry cleaning their clothes. We don’t tell them to avoid air pollution. These are all risk factors that are increasingly well established for Parkinson’s disease.
I think Parkinson’s disease, fundamentally for the vast majority of people, is an entirely preventable disease. We’re not taking actions to prevent people from getting this very disabling and very deadly disease.
Advocacy work
Dr. Subramanian: You and I are quite interested in the sense of being advocates as neurologists, and I think it fuels our passion and helps us to wake up every morning feeling like we have something that is meaningful and purposeful in our lives. Could you describe this as your passion and how it may prevent burnout and what it’s given you as a neurologist?
Dr. Dorsey: The credit for much of this is Dr. Carlie Tanner at UC San Francisco. I had the gift of sabbatical and I started reading the literature, I started reading her literature, and I came away with that, over the past 25 years, she detailed these environmental risk factors that are linked to Parkinson’s disease. Pesticides, these dry-cleaning chemicals, and air pollution. When I read it, I just realized that this was the case.
The same time I was reading her work, I read this book called “How to Survive a Plague,” by David France, who was a member of a group called Act Up, which was a group of men in New York City who reacted to the emergence of HIV in the 1980s. If you remember the 1980s, there was no federal response to HIV. People were blamed for the diseases that they were developing. It was only because brave men and women in New York City and in San Francisco banded together and organized that they changed the course of HIV.
They didn’t just do it for themselves. They did it for all of us. You and I and many people may not have HIV because of their courage. They made HIV a treatable condition. It’s actually more treatable than Parkinson’s disease. It’s associated with a near-normal life expectancy. They also made it a preventable disease. Thousands, if not millions, of us don’t have HIV because of their work. It’s an increasingly less common disease. Rates of HIV are actually decreasing, which is something that you or I would never have expected when we were in medical training.
I can’t think of a better outcome for a neurologist or any physician than to make the diseases that they’re caring for nonexistent ... than if we lived in a world that didn’t have HIV, we lived in a world where lung cancer largely didn’t exist. We’ve had worlds in the past where Parkinson’s probably didn’t exist or existed in extremely small numbers. That might be true for diffuse Lewy body disease and others, and if these diseases are preventable, we can take actions as individuals and as a society to lower our risk.
What a wonderful gift for future generations and many generations to come, hopefully, to live in a world that’s largely devoid of Parkinson’s disease. Just like we live in a world free of typhus. We live in a world free of smallpox. We live in a world where polio is extraordinarily uncommon. We don’t even have treatments for polio because we just don’t have polio. I think we can do the same thing for Parkinson’s disease for the vast majority.
Dr. Subramanian: Thank you so much, Ray, for your advocacy. We’re getting to the point in neurology, which is exciting to me, of possibly primary prevention of some of these disorders. I think we have a role in that, which is exciting for the future.
Dr. Dorsey: Absolutely.
Dr. Subramanian is clinical professor, department of neurology, University of California Los Angeles, and director of PADRECC (Parkinson’s Disease Research, Education, and Clinical Centers), West Los Angeles Veterans Association, Los Angeles. She disclosed ties with Acorda Pharma. Dr. Dorsey is the David M. Levy Professor of Neurology, University of Rochester (N.Y.). He disclosed ties to Abbott, AbbVie, Acadia, Acorda Therapeutics, Averitas Pharma, Biogen, BioSensics, Boehringer Ingelheim, Burroughs Wellcome Fund, Caraway Therapeutics, CuraSen, DConsult2, Denali Therapeutics, Eli Lilly, Genentech, Health & Wellness Partners, HMP Education, Included Health, Karger, KOL Groups, Life Sciences, Mediflix, Medrhythms, Merck; MJH Holdings, North American Center for Continuing Medical Education, Novartis, Otsuka, Pfizer, Photopharmics, Praxis Medicine, Roche, Safra Foundation, Sanofi, Seelos Therapeutics, SemCap, Spark Therapeutics, Springer Healthcare, Synapticure, Theravance Biopharmaceuticals, and WebMD.
A version of this article appeared on Medscape.com.