User login
Share supportive care while we wait for an Ebola remedy
While necessary vaccine research proceeds, resource-rich communities need to open their storage closets to send supportive care to where it is needed. Since the outbreak of Ebola in West Africa, and the subsequent introduction of an experimental treatment that may represent a cure for the disease, many have questioned how we expedite this research opportunity, while maximizing the integrity of the data and assisting those who do not have access to treatments.
Both of the Americans and a few others who received the controversial ZMapp treatment have survived. However, two individuals who received it still died. This inconsistency sparked a media campaign that focused on the ineffectiveness of the treatment. The campaign was launched despite the fact that there is currently no way to understand, completely, the reasons some have lived and some have died. That is the purpose of the research.
The accelerated research process sanctioned by the National Institutes of Health and the World Health Organization is an attempt to develop a much-needed vaccine to stop the spread. Unfortunately, research takes time and, if rushed, may result in inaccurate data that may erroneously find the vaccine effective. Exposing people to such a vaccine could cause further harm on many levels (side effects, death, loss of trust in medicine, etc.). Conversely, the hurried research could mistakenly find the vaccine ineffective and prevent entire populations from receiving a lifesaving treatment.
What to do right now
The harmful ramifications of getting this wrong for an already underserved, underprivileged, resource-poor, and extremely vulnerable population would be greater than anyone intends. The panel of experts convened by the World Health Organization determined that expediting the research can be ethically justified due to the emergent nature of the problem. Here we must agree that it should proceed, but insist on it proceeding properly. In the meantime, countries with resources need to determine what actions to take while people are suffering and dying.
The ethically correct action to take is to commit to our responsibilities as members of the global community and offer the supportive assistance that has already been shown to be helpful in managing the symptoms of the disease. Public health workers have enacted preventive strategies to contain the disease and decrease the spread. We in the United States should focus on providing the necessary interventions currently needed to support the masses effectively and less on gearing up to deal with the potential of having one or two people who happen to make it to our borders.
We have the resources in abundance, and it is our ethical duty to play an integral role in protecting others when we can. The media needs to put focus on countries and organizations that are sharing their resources and highlight ways for others to come together in support. We can play an integral part in addressing this crisis while time is taken to work on the research and set a precedent for dealing with such outbreaks in the future, come what may.
Nneka O. Mokwunye, Ph.D., is director of the Center for Ethics, Spiritual Care Department, at MedStar Washington Hospital Center and executive director of its Journal of Hospital Ethics.
While necessary vaccine research proceeds, resource-rich communities need to open their storage closets to send supportive care to where it is needed. Since the outbreak of Ebola in West Africa, and the subsequent introduction of an experimental treatment that may represent a cure for the disease, many have questioned how we expedite this research opportunity, while maximizing the integrity of the data and assisting those who do not have access to treatments.
Both of the Americans and a few others who received the controversial ZMapp treatment have survived. However, two individuals who received it still died. This inconsistency sparked a media campaign that focused on the ineffectiveness of the treatment. The campaign was launched despite the fact that there is currently no way to understand, completely, the reasons some have lived and some have died. That is the purpose of the research.
The accelerated research process sanctioned by the National Institutes of Health and the World Health Organization is an attempt to develop a much-needed vaccine to stop the spread. Unfortunately, research takes time and, if rushed, may result in inaccurate data that may erroneously find the vaccine effective. Exposing people to such a vaccine could cause further harm on many levels (side effects, death, loss of trust in medicine, etc.). Conversely, the hurried research could mistakenly find the vaccine ineffective and prevent entire populations from receiving a lifesaving treatment.
What to do right now
The harmful ramifications of getting this wrong for an already underserved, underprivileged, resource-poor, and extremely vulnerable population would be greater than anyone intends. The panel of experts convened by the World Health Organization determined that expediting the research can be ethically justified due to the emergent nature of the problem. Here we must agree that it should proceed, but insist on it proceeding properly. In the meantime, countries with resources need to determine what actions to take while people are suffering and dying.
The ethically correct action to take is to commit to our responsibilities as members of the global community and offer the supportive assistance that has already been shown to be helpful in managing the symptoms of the disease. Public health workers have enacted preventive strategies to contain the disease and decrease the spread. We in the United States should focus on providing the necessary interventions currently needed to support the masses effectively and less on gearing up to deal with the potential of having one or two people who happen to make it to our borders.
We have the resources in abundance, and it is our ethical duty to play an integral role in protecting others when we can. The media needs to put focus on countries and organizations that are sharing their resources and highlight ways for others to come together in support. We can play an integral part in addressing this crisis while time is taken to work on the research and set a precedent for dealing with such outbreaks in the future, come what may.
Nneka O. Mokwunye, Ph.D., is director of the Center for Ethics, Spiritual Care Department, at MedStar Washington Hospital Center and executive director of its Journal of Hospital Ethics.
While necessary vaccine research proceeds, resource-rich communities need to open their storage closets to send supportive care to where it is needed. Since the outbreak of Ebola in West Africa, and the subsequent introduction of an experimental treatment that may represent a cure for the disease, many have questioned how we expedite this research opportunity, while maximizing the integrity of the data and assisting those who do not have access to treatments.
Both of the Americans and a few others who received the controversial ZMapp treatment have survived. However, two individuals who received it still died. This inconsistency sparked a media campaign that focused on the ineffectiveness of the treatment. The campaign was launched despite the fact that there is currently no way to understand, completely, the reasons some have lived and some have died. That is the purpose of the research.
The accelerated research process sanctioned by the National Institutes of Health and the World Health Organization is an attempt to develop a much-needed vaccine to stop the spread. Unfortunately, research takes time and, if rushed, may result in inaccurate data that may erroneously find the vaccine effective. Exposing people to such a vaccine could cause further harm on many levels (side effects, death, loss of trust in medicine, etc.). Conversely, the hurried research could mistakenly find the vaccine ineffective and prevent entire populations from receiving a lifesaving treatment.
What to do right now
The harmful ramifications of getting this wrong for an already underserved, underprivileged, resource-poor, and extremely vulnerable population would be greater than anyone intends. The panel of experts convened by the World Health Organization determined that expediting the research can be ethically justified due to the emergent nature of the problem. Here we must agree that it should proceed, but insist on it proceeding properly. In the meantime, countries with resources need to determine what actions to take while people are suffering and dying.
The ethically correct action to take is to commit to our responsibilities as members of the global community and offer the supportive assistance that has already been shown to be helpful in managing the symptoms of the disease. Public health workers have enacted preventive strategies to contain the disease and decrease the spread. We in the United States should focus on providing the necessary interventions currently needed to support the masses effectively and less on gearing up to deal with the potential of having one or two people who happen to make it to our borders.
We have the resources in abundance, and it is our ethical duty to play an integral role in protecting others when we can. The media needs to put focus on countries and organizations that are sharing their resources and highlight ways for others to come together in support. We can play an integral part in addressing this crisis while time is taken to work on the research and set a precedent for dealing with such outbreaks in the future, come what may.
Nneka O. Mokwunye, Ph.D., is director of the Center for Ethics, Spiritual Care Department, at MedStar Washington Hospital Center and executive director of its Journal of Hospital Ethics.
Under Pressure
One of the most important elements of a psoriasis patient’s medical history is the medication list. We are aware of the possible association between induction or exacerbation of psoriasis and intake of drugs including beta-blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors, lithium, and nonsteroidal anti-inflammatory drugs. However, we are lacking comprehensive data on these putative relationships.
Wu et al1 evaluated the association of hypertension and antihypertensive medications with risk for psoriasis. The authors pointed out that psoriasis patients have an increased risk for hypertension, and medications for hypertension, especially beta-blockers, have been associated with the development of psoriasis. They noted, however, that there has been no prospective assessment of the association of existing hypertension and antihypertensive medications with risk for incident psoriasis.1
The authors performed a prospective cohort study (June 1996 to June 1998) of 77,728 women from the Nurses’ Health Study who provided biennially updated data on hypertension and antihypertensive medications.1 They documented 843 incidents of psoriasis during 1,066,339 person-years of follow-up. Women with hypertension tended to be older and had a higher body mass index. In addition, they had proportionately higher prevalence rates of cardiovascular disease, type 2 diabetes mellitus, and hypercholesterolemia. They also were less physically active than subjects without hypertension. Compared with those with normal blood pressure, women with hypertension lasting 6 years or more were at higher risk for development of psoriasis (hazard ratio [HR], 1.27; 95% confidence interval [CI], 1.03-1.57). In stratified analysis, the risk for psoriasis was higher among hypertensive women without medication use (HR, 1.49; 95% CI, 1.15-1.92) and among hypertensive women with current medication use (HR, 1.31; 95% CI, 1.10-1.55) when compared with those without hypertension and without medication use.1
Among the individual antihypertensive drugs, only beta-blockers were associated with an increased risk for psoriasis.1 Of interest, this association persisted in a duration-dependent manner, with a higher risk for psoriasis found among women who regularly used beta-blockers with a duration of use of 6 years or more (HR, 1.39; 95% CI, 1.11-1.73; P for trend=.009). No association was found between any other individual hypertension medication and the development of psoriasis.1
The authors concluded that their study provided evidence that a history of long-term hypertension was associated with an increased risk for psoriasis.1 Among the individual medications analyzed in the study, only beta-blockers were linked to an increased risk for psoriasis after long-term regular use (≥6 years). They noted that these findings provided insights into the relationship between hypertension, medications for the condition, and psoriasis. However, further work is necessary to confirm these findings and clarify the biological mechanisms that may explain these links.1
As we further evaluate the associations between psoriasis and systemic comorbidities, we are learning more about the complex interrelationship between these conditions. The findings reported by Wu et al1 serve as another reminder that clinicians should be proactive in having psoriasis patients actively monitor their blood pressure, either with the dermatologist or with the primary care physician. This type of novel prospective information serves as another piece of the puzzle in our comprehensive management of psoriasis.
- Wu S, Han J, Li WQ, et al. Hypertension, antihypertensive medication use, and risk of psoriasis [published online ahead of print July 2, 2014]. JAMA Dermatol. doi:10.1001/jamadermatol.2013.9957.
One of the most important elements of a psoriasis patient’s medical history is the medication list. We are aware of the possible association between induction or exacerbation of psoriasis and intake of drugs including beta-blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors, lithium, and nonsteroidal anti-inflammatory drugs. However, we are lacking comprehensive data on these putative relationships.
Wu et al1 evaluated the association of hypertension and antihypertensive medications with risk for psoriasis. The authors pointed out that psoriasis patients have an increased risk for hypertension, and medications for hypertension, especially beta-blockers, have been associated with the development of psoriasis. They noted, however, that there has been no prospective assessment of the association of existing hypertension and antihypertensive medications with risk for incident psoriasis.1
The authors performed a prospective cohort study (June 1996 to June 1998) of 77,728 women from the Nurses’ Health Study who provided biennially updated data on hypertension and antihypertensive medications.1 They documented 843 incidents of psoriasis during 1,066,339 person-years of follow-up. Women with hypertension tended to be older and had a higher body mass index. In addition, they had proportionately higher prevalence rates of cardiovascular disease, type 2 diabetes mellitus, and hypercholesterolemia. They also were less physically active than subjects without hypertension. Compared with those with normal blood pressure, women with hypertension lasting 6 years or more were at higher risk for development of psoriasis (hazard ratio [HR], 1.27; 95% confidence interval [CI], 1.03-1.57). In stratified analysis, the risk for psoriasis was higher among hypertensive women without medication use (HR, 1.49; 95% CI, 1.15-1.92) and among hypertensive women with current medication use (HR, 1.31; 95% CI, 1.10-1.55) when compared with those without hypertension and without medication use.1
Among the individual antihypertensive drugs, only beta-blockers were associated with an increased risk for psoriasis.1 Of interest, this association persisted in a duration-dependent manner, with a higher risk for psoriasis found among women who regularly used beta-blockers with a duration of use of 6 years or more (HR, 1.39; 95% CI, 1.11-1.73; P for trend=.009). No association was found between any other individual hypertension medication and the development of psoriasis.1
The authors concluded that their study provided evidence that a history of long-term hypertension was associated with an increased risk for psoriasis.1 Among the individual medications analyzed in the study, only beta-blockers were linked to an increased risk for psoriasis after long-term regular use (≥6 years). They noted that these findings provided insights into the relationship between hypertension, medications for the condition, and psoriasis. However, further work is necessary to confirm these findings and clarify the biological mechanisms that may explain these links.1
As we further evaluate the associations between psoriasis and systemic comorbidities, we are learning more about the complex interrelationship between these conditions. The findings reported by Wu et al1 serve as another reminder that clinicians should be proactive in having psoriasis patients actively monitor their blood pressure, either with the dermatologist or with the primary care physician. This type of novel prospective information serves as another piece of the puzzle in our comprehensive management of psoriasis.
One of the most important elements of a psoriasis patient’s medical history is the medication list. We are aware of the possible association between induction or exacerbation of psoriasis and intake of drugs including beta-blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors, lithium, and nonsteroidal anti-inflammatory drugs. However, we are lacking comprehensive data on these putative relationships.
Wu et al1 evaluated the association of hypertension and antihypertensive medications with risk for psoriasis. The authors pointed out that psoriasis patients have an increased risk for hypertension, and medications for hypertension, especially beta-blockers, have been associated with the development of psoriasis. They noted, however, that there has been no prospective assessment of the association of existing hypertension and antihypertensive medications with risk for incident psoriasis.1
The authors performed a prospective cohort study (June 1996 to June 1998) of 77,728 women from the Nurses’ Health Study who provided biennially updated data on hypertension and antihypertensive medications.1 They documented 843 incidents of psoriasis during 1,066,339 person-years of follow-up. Women with hypertension tended to be older and had a higher body mass index. In addition, they had proportionately higher prevalence rates of cardiovascular disease, type 2 diabetes mellitus, and hypercholesterolemia. They also were less physically active than subjects without hypertension. Compared with those with normal blood pressure, women with hypertension lasting 6 years or more were at higher risk for development of psoriasis (hazard ratio [HR], 1.27; 95% confidence interval [CI], 1.03-1.57). In stratified analysis, the risk for psoriasis was higher among hypertensive women without medication use (HR, 1.49; 95% CI, 1.15-1.92) and among hypertensive women with current medication use (HR, 1.31; 95% CI, 1.10-1.55) when compared with those without hypertension and without medication use.1
Among the individual antihypertensive drugs, only beta-blockers were associated with an increased risk for psoriasis.1 Of interest, this association persisted in a duration-dependent manner, with a higher risk for psoriasis found among women who regularly used beta-blockers with a duration of use of 6 years or more (HR, 1.39; 95% CI, 1.11-1.73; P for trend=.009). No association was found between any other individual hypertension medication and the development of psoriasis.1
The authors concluded that their study provided evidence that a history of long-term hypertension was associated with an increased risk for psoriasis.1 Among the individual medications analyzed in the study, only beta-blockers were linked to an increased risk for psoriasis after long-term regular use (≥6 years). They noted that these findings provided insights into the relationship between hypertension, medications for the condition, and psoriasis. However, further work is necessary to confirm these findings and clarify the biological mechanisms that may explain these links.1
As we further evaluate the associations between psoriasis and systemic comorbidities, we are learning more about the complex interrelationship between these conditions. The findings reported by Wu et al1 serve as another reminder that clinicians should be proactive in having psoriasis patients actively monitor their blood pressure, either with the dermatologist or with the primary care physician. This type of novel prospective information serves as another piece of the puzzle in our comprehensive management of psoriasis.
- Wu S, Han J, Li WQ, et al. Hypertension, antihypertensive medication use, and risk of psoriasis [published online ahead of print July 2, 2014]. JAMA Dermatol. doi:10.1001/jamadermatol.2013.9957.
- Wu S, Han J, Li WQ, et al. Hypertension, antihypertensive medication use, and risk of psoriasis [published online ahead of print July 2, 2014]. JAMA Dermatol. doi:10.1001/jamadermatol.2013.9957.
Nostalgic for making diagnoses based on medical history alone? Me, neither
"It is clear that physicians take widely different attitudes towards investigations, some relying on them much more heavily than others."
– J.R. Hampton, et al., British Medical Journal, May 31, 1975
In 1975, a study was published in the British Medical Journal looking at new patients referred to a medical clinic. The study looked specifically at how a diagnosis was made for each new patient, and it concluded that in 66 out of 80 patients, a diagnosis was arrived at based on the history alone, that the physical exam was useful in an additional 7 patients, and that lab testing was useful in the last 7 patients (Br. Med. J. 1975;2:486-9). Since then, medical students have been taught that a good history will lead to the diagnosis about 80% of the time.
One of my professors in my internal medicine class taught me this aphorism. I thought he was brilliant. Surely, anyone who can come up with a diagnosis just by talking to a patient is a minor god? (He is a rheumatologist. He became my mentor, and is, in fact, one of the major influences in my choice of specialty.)
Medical school in the Philippines forces one to think that way anyhow. There is very little government-provided health care; everything else is paid for out of pocket. This means that every CBC I order, every electrolyte panel, every antinuclear antibody, every urinalysis, is charged to the patient. There are not enough hospital beds, ventilators, or MRI machines.
So patients waited a while before seeking medical attention, which means we took full advantage of a history that’s remarkably evolved, with classic, textbook physical exam findings. The general medicine wards were crammed with patients with jaundice, whether from hepatitis or from having the carcass of a dead ascaris worm lodged in their bile ducts. We saw fungating breast masses. Hyperthyroidism is not that hard to identify when the patient is in frank thyrotoxicosis. Patients with pulmonary tuberculosis had massive hemoptysis, buckets of blood, and acid-fast bacilli in the emergency department.
This is the environment in which I trained. Could I say then that I would be able to identify a problem just from taking a history alone? If you had months’, nay, years’ worth of history to work with, you’d be able to identify the problem, too. I’ll bet doctors who practiced in the 1960s and 1970s in the United States had similar experiences, having the benefit of witnessing full-blown cases of anything and everything.
Do I practice this way now? Not at all.
But that isn’t to say I don’t take a good enough history or physical exam, it’s just that patients seek medical attention earlier, and we have so many more resources at our disposal. We have the ability to detect illness before it wreaks havoc. (There are other, less charitable interpretations of this behavior, such as lack of time, patient expectations, etc. But that’s a topic for another time.)
I have a great deal of respect for my mentors who practice with very real limitations. I have no doubt they are better doctors than I am. And, of course, I feel nostalgic for the way we used to do things. It is easy to romanticize the sepia-toned snapshots of my third-world youth. But really, modernity is a blessing. We should celebrate our ability to find things early. Nostalgia is for meals and memories. Medicine is much more pedestrian than that.
Dr. Chan practices rheumatology in Pawtucket, R.I.
"It is clear that physicians take widely different attitudes towards investigations, some relying on them much more heavily than others."
– J.R. Hampton, et al., British Medical Journal, May 31, 1975
In 1975, a study was published in the British Medical Journal looking at new patients referred to a medical clinic. The study looked specifically at how a diagnosis was made for each new patient, and it concluded that in 66 out of 80 patients, a diagnosis was arrived at based on the history alone, that the physical exam was useful in an additional 7 patients, and that lab testing was useful in the last 7 patients (Br. Med. J. 1975;2:486-9). Since then, medical students have been taught that a good history will lead to the diagnosis about 80% of the time.
One of my professors in my internal medicine class taught me this aphorism. I thought he was brilliant. Surely, anyone who can come up with a diagnosis just by talking to a patient is a minor god? (He is a rheumatologist. He became my mentor, and is, in fact, one of the major influences in my choice of specialty.)
Medical school in the Philippines forces one to think that way anyhow. There is very little government-provided health care; everything else is paid for out of pocket. This means that every CBC I order, every electrolyte panel, every antinuclear antibody, every urinalysis, is charged to the patient. There are not enough hospital beds, ventilators, or MRI machines.
So patients waited a while before seeking medical attention, which means we took full advantage of a history that’s remarkably evolved, with classic, textbook physical exam findings. The general medicine wards were crammed with patients with jaundice, whether from hepatitis or from having the carcass of a dead ascaris worm lodged in their bile ducts. We saw fungating breast masses. Hyperthyroidism is not that hard to identify when the patient is in frank thyrotoxicosis. Patients with pulmonary tuberculosis had massive hemoptysis, buckets of blood, and acid-fast bacilli in the emergency department.
This is the environment in which I trained. Could I say then that I would be able to identify a problem just from taking a history alone? If you had months’, nay, years’ worth of history to work with, you’d be able to identify the problem, too. I’ll bet doctors who practiced in the 1960s and 1970s in the United States had similar experiences, having the benefit of witnessing full-blown cases of anything and everything.
Do I practice this way now? Not at all.
But that isn’t to say I don’t take a good enough history or physical exam, it’s just that patients seek medical attention earlier, and we have so many more resources at our disposal. We have the ability to detect illness before it wreaks havoc. (There are other, less charitable interpretations of this behavior, such as lack of time, patient expectations, etc. But that’s a topic for another time.)
I have a great deal of respect for my mentors who practice with very real limitations. I have no doubt they are better doctors than I am. And, of course, I feel nostalgic for the way we used to do things. It is easy to romanticize the sepia-toned snapshots of my third-world youth. But really, modernity is a blessing. We should celebrate our ability to find things early. Nostalgia is for meals and memories. Medicine is much more pedestrian than that.
Dr. Chan practices rheumatology in Pawtucket, R.I.
"It is clear that physicians take widely different attitudes towards investigations, some relying on them much more heavily than others."
– J.R. Hampton, et al., British Medical Journal, May 31, 1975
In 1975, a study was published in the British Medical Journal looking at new patients referred to a medical clinic. The study looked specifically at how a diagnosis was made for each new patient, and it concluded that in 66 out of 80 patients, a diagnosis was arrived at based on the history alone, that the physical exam was useful in an additional 7 patients, and that lab testing was useful in the last 7 patients (Br. Med. J. 1975;2:486-9). Since then, medical students have been taught that a good history will lead to the diagnosis about 80% of the time.
One of my professors in my internal medicine class taught me this aphorism. I thought he was brilliant. Surely, anyone who can come up with a diagnosis just by talking to a patient is a minor god? (He is a rheumatologist. He became my mentor, and is, in fact, one of the major influences in my choice of specialty.)
Medical school in the Philippines forces one to think that way anyhow. There is very little government-provided health care; everything else is paid for out of pocket. This means that every CBC I order, every electrolyte panel, every antinuclear antibody, every urinalysis, is charged to the patient. There are not enough hospital beds, ventilators, or MRI machines.
So patients waited a while before seeking medical attention, which means we took full advantage of a history that’s remarkably evolved, with classic, textbook physical exam findings. The general medicine wards were crammed with patients with jaundice, whether from hepatitis or from having the carcass of a dead ascaris worm lodged in their bile ducts. We saw fungating breast masses. Hyperthyroidism is not that hard to identify when the patient is in frank thyrotoxicosis. Patients with pulmonary tuberculosis had massive hemoptysis, buckets of blood, and acid-fast bacilli in the emergency department.
This is the environment in which I trained. Could I say then that I would be able to identify a problem just from taking a history alone? If you had months’, nay, years’ worth of history to work with, you’d be able to identify the problem, too. I’ll bet doctors who practiced in the 1960s and 1970s in the United States had similar experiences, having the benefit of witnessing full-blown cases of anything and everything.
Do I practice this way now? Not at all.
But that isn’t to say I don’t take a good enough history or physical exam, it’s just that patients seek medical attention earlier, and we have so many more resources at our disposal. We have the ability to detect illness before it wreaks havoc. (There are other, less charitable interpretations of this behavior, such as lack of time, patient expectations, etc. But that’s a topic for another time.)
I have a great deal of respect for my mentors who practice with very real limitations. I have no doubt they are better doctors than I am. And, of course, I feel nostalgic for the way we used to do things. It is easy to romanticize the sepia-toned snapshots of my third-world youth. But really, modernity is a blessing. We should celebrate our ability to find things early. Nostalgia is for meals and memories. Medicine is much more pedestrian than that.
Dr. Chan practices rheumatology in Pawtucket, R.I.
Do not anger the ‘call gods’
"Do you feel lucky?"
It’s one of Clint Eastwood’s iconic lines (probably a notch below "go ahead, make my day") that wasn’t spoken to a home furnishing.
But it’s still a question many of us think of late on a Friday afternoon just before weekend call gets rolled over to us.
Weekend hospital call, like an approaching storm, brings foreboding and dread. You have no control over the circumstances that are about to whack you. If it’s busy, you’re out of luck. Whatever comes in, you have to deal with it.
I try to ameliorate the pain by using a quote from a residency attending: "It’s not busy, it’s profitable." I also often repeat Dory’s line from "Finding Nemo" – "just keep swimming, just keep swimming" – as I round endlessly.
But humans, by nature, are superstitious creatures. Our ancestors across the globe created pantheons of deities to explain the sun, storms, ocean, and other natural phenomenon they couldn’t control and prayed to them to try to do so.
Now we fear a nebulous group of beings named the "call gods."
It’s always plural, and it’s never been established how many there are or if they have individual names. But they’re feared by all who take hospital call. Amongst physicians, I find they’re universal. Doctors who are Christians, Jews, Hindus, Muslims, atheists ... all know and fear them.
The rules of this medical religion have never been put down and are passed on by verbal tradition. The main theme is that you never, ever, ever do anything to make them angry. This primarily involves not saying things like "it’s quiet so far" or "gee, my phone hasn’t rung all day," for doing so will most assuredly bring their wrath down upon you.
Likewise, even if things are quiet, you never say that until 7:01 on Monday morning, when it’s been rolled back over to your call partner. If someone asks, "how’s your call going?" – even if nothing has happened – you still say "steady" or "hopping" just to avoid challenging the unseen deities.
Of course, the call gods aren’t the only ones we fear. There are specialty-specific, and even procedure-specific, deities. Any neurologist attempting a bedside lumbar puncture on a large person will likely say a quick prayer to the LP gods.
Medicine has come a long way, over time, but even a field with a hefty base in science can’t overcome human nature and our inherent fear of forces beyond our control.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
"Do you feel lucky?"
It’s one of Clint Eastwood’s iconic lines (probably a notch below "go ahead, make my day") that wasn’t spoken to a home furnishing.
But it’s still a question many of us think of late on a Friday afternoon just before weekend call gets rolled over to us.
Weekend hospital call, like an approaching storm, brings foreboding and dread. You have no control over the circumstances that are about to whack you. If it’s busy, you’re out of luck. Whatever comes in, you have to deal with it.
I try to ameliorate the pain by using a quote from a residency attending: "It’s not busy, it’s profitable." I also often repeat Dory’s line from "Finding Nemo" – "just keep swimming, just keep swimming" – as I round endlessly.
But humans, by nature, are superstitious creatures. Our ancestors across the globe created pantheons of deities to explain the sun, storms, ocean, and other natural phenomenon they couldn’t control and prayed to them to try to do so.
Now we fear a nebulous group of beings named the "call gods."
It’s always plural, and it’s never been established how many there are or if they have individual names. But they’re feared by all who take hospital call. Amongst physicians, I find they’re universal. Doctors who are Christians, Jews, Hindus, Muslims, atheists ... all know and fear them.
The rules of this medical religion have never been put down and are passed on by verbal tradition. The main theme is that you never, ever, ever do anything to make them angry. This primarily involves not saying things like "it’s quiet so far" or "gee, my phone hasn’t rung all day," for doing so will most assuredly bring their wrath down upon you.
Likewise, even if things are quiet, you never say that until 7:01 on Monday morning, when it’s been rolled back over to your call partner. If someone asks, "how’s your call going?" – even if nothing has happened – you still say "steady" or "hopping" just to avoid challenging the unseen deities.
Of course, the call gods aren’t the only ones we fear. There are specialty-specific, and even procedure-specific, deities. Any neurologist attempting a bedside lumbar puncture on a large person will likely say a quick prayer to the LP gods.
Medicine has come a long way, over time, but even a field with a hefty base in science can’t overcome human nature and our inherent fear of forces beyond our control.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
"Do you feel lucky?"
It’s one of Clint Eastwood’s iconic lines (probably a notch below "go ahead, make my day") that wasn’t spoken to a home furnishing.
But it’s still a question many of us think of late on a Friday afternoon just before weekend call gets rolled over to us.
Weekend hospital call, like an approaching storm, brings foreboding and dread. You have no control over the circumstances that are about to whack you. If it’s busy, you’re out of luck. Whatever comes in, you have to deal with it.
I try to ameliorate the pain by using a quote from a residency attending: "It’s not busy, it’s profitable." I also often repeat Dory’s line from "Finding Nemo" – "just keep swimming, just keep swimming" – as I round endlessly.
But humans, by nature, are superstitious creatures. Our ancestors across the globe created pantheons of deities to explain the sun, storms, ocean, and other natural phenomenon they couldn’t control and prayed to them to try to do so.
Now we fear a nebulous group of beings named the "call gods."
It’s always plural, and it’s never been established how many there are or if they have individual names. But they’re feared by all who take hospital call. Amongst physicians, I find they’re universal. Doctors who are Christians, Jews, Hindus, Muslims, atheists ... all know and fear them.
The rules of this medical religion have never been put down and are passed on by verbal tradition. The main theme is that you never, ever, ever do anything to make them angry. This primarily involves not saying things like "it’s quiet so far" or "gee, my phone hasn’t rung all day," for doing so will most assuredly bring their wrath down upon you.
Likewise, even if things are quiet, you never say that until 7:01 on Monday morning, when it’s been rolled back over to your call partner. If someone asks, "how’s your call going?" – even if nothing has happened – you still say "steady" or "hopping" just to avoid challenging the unseen deities.
Of course, the call gods aren’t the only ones we fear. There are specialty-specific, and even procedure-specific, deities. Any neurologist attempting a bedside lumbar puncture on a large person will likely say a quick prayer to the LP gods.
Medicine has come a long way, over time, but even a field with a hefty base in science can’t overcome human nature and our inherent fear of forces beyond our control.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Should off-pump CABG be abandoned?
YES
I believe on-pump coronary artery bypass graft (CABG) surgery should be our primary operation, with off-pump CABG reserved only for certain situations.
In talking about these two surgical options, there are basically three main issues of interest: procedural outcomes, the quality of revascularization, and long-term effectiveness.
Procedural outcomes: In the 1990s, there was great excitement for the potential for off-pump CABG. We thought survival would be better, stroke less common, neurocognitive outcomes improved, etc., but after several randomized studies and a number of well-controlled observational studies, we found that, in terms of the important procedural outcomes – death, MI, stroke, and acute renal failure – there were actually no differences between off- and on-pump CABG. We saw this in ROOBY, with low-risk patients and less experienced surgeons; in the Canadian CORONARY trial, with experienced off-pump surgeons; and in the European GOPCABE trial, where the surgeons were very experienced and the patients were high risk.
There are some benefits with off-pump CABG in terms of what I call the "reversible" complications of surgery: fewer transfusions, less postoperative atrial fibrillation, fewer respiratory infections; but I believe these things have to be balanced against some of the negative effects of off-pump surgery in terms of its quality of revascularization and long-term effectiveness.
Probably one of the biggest disappointments we’ve had with off-pump CABG is that, in the trials, we didn’t see any major difference in neurocognitive dysfunction. What we learned is that cardiopulmonary bypass really is not that bad in terms of neurocognitive dysfunction after surgery.
One issue that tends to be forgotten is the risk associated with conversion. In a hemodynamically unstable patient, converting from off-pump to on-pump is associated with higher risks of death, bleeding, renal failure, stroke, respiratory failure, and GI complications. In CORONARY, with experienced surgeons, the conversion rate was almost 7.9%, and in GOPCABE, it was 9.7%. Even with experienced surgeons, conversions do occur, and they have negative consequences.
Quality of revascularization: We know that long-term survival is related to completeness of revascularization. The more ischemic myocardium that is left at risk after CABG, the more likely the patients is to have an MI or die, and this has been very clearly demonstrated in the surgical literature as well as the percutaneous coronary intervention literature. It has been shown multiple times that fewer grafts are done in off-pump patients, compared with on-pump patients. Indeed, in a recent Cochrane meta-analysis of more than 7,000 patients in 57 trials, there were significantly more grafts done in on-pump than off-pump cases.
Also in terms of graft patency, again, multiple studies have shown lower graft patency in off-pump patients, either directly or by means of showing a higher reintervention rate after off-pump as compared with on-pump surgery. In both CORONARY and GOPCABE, the repeat revascularization rate at 30 days was higher for off-pump CABG.
Long-term effectiveness: The long-term results from ROOBY are very sobering: significantly higher 1-year cardiac mortality in the off-pump arm and higher 1-year composite adverse events. Again, in the 2012 Cochrane meta-analysis, with more than 10,000 patients in 75 trials, mortality was significantly higher with off-pump patients, compared with on-pump, with a hazard ratio of 1.24 (95% CI, 1.01-1.53). When the authors of the Cochrane meta-analysis removed what they called the "studies with bias," this signal was even stronger. Also in observational studies, such as one published by Racz et al. in 2004 (J. Am. Coll. Cardiol. 2004; 43: 557-64), the best survival was found to be in patients who had on-pump CABG and the worst in those who had undergone off-pump CABG.
In summary, procedural outcomes with off-pump and on-pump CABG are similar, albeit with lower reversible complications in the off-pump patients, but a greater conversion risk, along with its associated complications. The quality of the revascularization is worse in off-pump patients, the completeness of revascularization is less and re-intervention rates are higher, and the bottom line, of course, it that there is higher long-term mortality after off-pump CABG.
"Should off-pump CABG be abandoned?" As our default procedure, yes. The vast majority of our patients are best served with on-pump revascularization.
Dr. Joseph Sabik is the chairman of the department of thoracic and cardiovascular surgery and the Sheik Hamdam Bin Rashid Al Maktoum Distinguished Chair at the Cleveland Clinic. He disclosed that he performs both off-pump and on-pump CABG.
References
Anesthesiology 2005;102:188-203
N. Engl. J. Med. 2009;361:1827-37
N. Engl. J. Med. 2012;366:1489-97
N. Engl. J. Med. 2013;368:1179-88
Cochrane Database Syst. Rev. 2012; Mar 14. 3: CD007224 [doi:10.1002/14651858.CD007224.pub2])
J. Am. Coll. Cardiol. 2004;43:557-64
NO
Should off pump bypass be abandoned? Absolutely not, but let’s do it well.
The rationale for why off-pump CABG should be the preferred strategy is simple: cardiopulmonary bypass (CPB) entails extracorporeal circulation, aortic cannulation and clamping, global MI, hypothermia, and hemodilution, among other potentially deleterious phenomena. There are morbidities that can be attributed to these entities, and off-pump bypass avoids those effects by mechanically stabilizing each coronary artery target individually, while the rest of the heart beats and supports normal physiologic circulation. There is an important caveat to this, however, and that is if – and perhaps only if – a complete revascularization with precise anastomoses can be accomplished off pump, then the patient will in fact benefit.
At Emory University in Atlanta, we did a prospective, randomized trial on my own patients, which we called SMART (Surgical Management of Arterial Revascularization) trial. What we found was that in 200 unselected, consecutive patients undergoing either off- or on-pump CABG, we had lower myocardial enzyme release, fewer transfusions, more rapid extubation, and a shorter length of stay in hospital with off-pump CABG.
Completeness of revascularization is a very important issue. In SMART, the number of grafts per patient was exactly the same: 3.39 per patient with off-pump CABG and 3.4 with on-pump CABG. We coined the phrase "Index of Completeness of Revascularization," which we defined as the number of grafts we planned to do in examining the arteriogram prior to randomization and surgery divided by the number of grafts we actually did. We found no difference here, meaning we were able to do the operation we planned to do (1.00 vs. 1.01; P = not significant). Moreover, for the lateral wall, which is technically more difficult to reach in a beating heart, the number was similar in the off- and on-pump groups (0.97 vs. 0.98; P = not significant). We also used a similar percentage of arterial grafts in both groups.
CPB was an independent predictor of the need for transfusion by multivariate analysis with an odds ratio of 2.42 (P = .0073) and was associated with a longer length of stay by 1 day (5.1 days for off-pump and 6.1 for on-pump; P = .005 Wilcoxon).
Creatine phosphokinase of muscle band and troponin I release was about half as much in the off-pump group as in the on-pump group (P less than .001 Wilcoxon), and the rates of death, stroke, MI, angina, and reintervention were similar at both 30 days and 1 year, as was graft patency and quality of life. Off-pump CABG costs at 1 year were $1,955 less than on-pump, but this difference was not statistically significant (P = .08).
At 8 years, survival in SMART was still similar between groups (P = .33), as was graft patency in the small number of patients who had CT angiograms. PET scan results similarly showed no significant difference in ischemia between these two groups (P = .62). One patient in each group has had a percutaneous reintervention, and none have had a repeat coronary bypass in 10 years.
To see if these results could be replicated nationally, we turned to the STS database and looked at North American centers that performed more than 100 on-pump CABGs and more than 100 off-pump surgeries. This gave us 42,477 patients (16,245 off pump and 26,232 on pump) at 63 North American centers. We included the 2.2% of off-pump cases that were converted to on-pump cases in the off-pump group.
After risk adjustment for 32 variables, for the outcomes of death, stroke, MI, and major adverse cardiac events, off-pump bypass outperformed on-pump bypass in this huge cohort of patients from around the country. Looking at less-significant outcomes – renal failure, dialysis, sternal infection, reoperation, atrial fibrillation, prolonged ventilation, and length of stay greater than 14 days – all of them favored off-pump bypass.
We then looked at the Emory dataset (14,766 consecutive patients, 48% of whom had off-pump CABG and 52% on-pump) to see which patients benefitted more. For patients in the two lower quartiles of predicted risk, there was no difference in operative mortality. In the higher two risk quartiles, there was a mortality benefit with off-pump CABG, with a risk reduction for operative mortality of about 55% in the highest risk patients (P less than 0.001).
Logistic regression confirmed that there was an interaction between surgery type and predicted risk, and we now know that low-risk patients do not have the survival benefit of avoiding CPB. They do fine with on-pump CABG, but higher risk patients have a benefit from avoiding CPB and the higher the predicted risk, the greater the benefit to the patient.
We went back to the STS database and we looked at whether this applies only at some centers or all centers, some surgeons or all surgeons. We looked at almost a million cases, 210,469 of which were at sites that had a large off-pump CABG volume. With the usual adjustments, off-pump CABG was associated with significant reduction of risk of death, stroke, renal failure, any morbidity or mortality or prolonged length of stay, compared with on-pump bypass. This benefit was even more pronounced after adjustment for surgeon effect. Once again, the greater reduction was enjoyed by those patients who had the highest preoperative risk. In all predicted risk quartiles, off pump bypass reduced risk of death and stroke and that magnitude increased with increasing predicted risk of mortality. This was seen in large-volume centers and low-volume centers.
Similar results were seen in a recent multicenter, randomized, prospective trial by Lemma et al. that assigned 411 patients to either off- or on-pump coronary bypass (J. Thorac. Cardiovasc. Surg. 2012;143:625-31). There was reduced early mortality and morbidity among higher-risk patients. Interestingly, in this study, they used an experience-based randomization scheme, in which they had surgeons within each center who like to do off-pump CABG and those who like to do on-pump CABG, and each surgeon had hundreds of cases under his belt. For the primary endpoint, a composite of death, MI, stroke or TIA, renal failure, acute respiratory distress syndrome, or reoperation for bleeding, the rates were 5.8% of off-pump and 13.3% for on-pump patients (odds ratio, 2.5; P = .01).
I think the conclusions are clear, but not everyone has reached these same conclusions. In ROOBY, the results were different. Although the study was well conducted, it enrolled low-risk patients, in whom avoidance of CPB was unlikely to improve the expected excellent outcomes. And the operations were performed by residents, with supervising attendings who themselves only had to do 20 total career off-pump cases to be eligible. I think this lack of experience is well demonstrated by the 12.5% conversion rate from off-pump cases to on-pump in that trial. ROOBY enrolled the wrong patients and used the wrong surgeons.
In the CORONARY trial, conducted by Dr. Lamy in Canada but enrolling patients from 19 countries outside of Canada, there was no difference in the primary endpoint of death, stroke, MI, and renal failure at 30 days, but there was a decrease in transfusion, reoperation for bleeding, acute kidney injury, or respiratory complications. There wasn\'t a difference in stroke, interestingly, but the surgeons in this trial appropriately converted a hundred patients from on pump to off pump to avoid manipulating a calcified aorta. This was a good, well-conducted trial.
However, the primary outcome in CORONARY differed when assessed according to EuroSCORE. When the EuroSCORE was low, on pump outperformed off pump. When the EuroSCORE was high, off pump outperformed on pump.
These two trials offer important perspective: the ROOBY trial, enrolling low-risk patients, was actually in favor of on-pump CABG. The CORONARY trial, enrolling higher-risk patients, had a slight benefit in favor of off-pump CABG, and this was particularly evident in the Canadian cohort of 830 randomized patients, in which the primary outcome was, in fact, statistically significantly better in the off-pump group at 9.2% vs. 13.7%.
At the end of the day, I think it matters in whom you do off-pump CABG and how well you do it. It may not be for every patient or for every surgeon; off-pump CABG requires a focused and sustained effort to master a new set of physical and psychological skills to accomplish precise and complete revascularization. When we can do this, I think, we offer better outcomes for our patients.
Dr. John Puskas is the chairman of the department of cardiac surgery at Mount Sinai Beth Israel in New York. Dr. Puskas disclosed that he also does both on- and off-pump CABG. He received royalties from coronary surgical instruments marketed by Scanlan, as well.
References
JAMA 2004;291:1841-9
Ann. Thorac. Surg. 2009;88:1142-7
N. Engl. J. Med. 2009;361:1827-37
N. Engl. J. Med. 2010;362:851
N. Engl. J. Med. 2012;366:1489-97
N. Engl. J. Med. 2013;368:1179-88
Ann. Thorac. Surg. 2011;91:1836-42
J. Thorac. Cardiovasc. Surg. 2012;143:625-31
YES
I believe on-pump coronary artery bypass graft (CABG) surgery should be our primary operation, with off-pump CABG reserved only for certain situations.
In talking about these two surgical options, there are basically three main issues of interest: procedural outcomes, the quality of revascularization, and long-term effectiveness.
Procedural outcomes: In the 1990s, there was great excitement for the potential for off-pump CABG. We thought survival would be better, stroke less common, neurocognitive outcomes improved, etc., but after several randomized studies and a number of well-controlled observational studies, we found that, in terms of the important procedural outcomes – death, MI, stroke, and acute renal failure – there were actually no differences between off- and on-pump CABG. We saw this in ROOBY, with low-risk patients and less experienced surgeons; in the Canadian CORONARY trial, with experienced off-pump surgeons; and in the European GOPCABE trial, where the surgeons were very experienced and the patients were high risk.
There are some benefits with off-pump CABG in terms of what I call the "reversible" complications of surgery: fewer transfusions, less postoperative atrial fibrillation, fewer respiratory infections; but I believe these things have to be balanced against some of the negative effects of off-pump surgery in terms of its quality of revascularization and long-term effectiveness.
Probably one of the biggest disappointments we’ve had with off-pump CABG is that, in the trials, we didn’t see any major difference in neurocognitive dysfunction. What we learned is that cardiopulmonary bypass really is not that bad in terms of neurocognitive dysfunction after surgery.
One issue that tends to be forgotten is the risk associated with conversion. In a hemodynamically unstable patient, converting from off-pump to on-pump is associated with higher risks of death, bleeding, renal failure, stroke, respiratory failure, and GI complications. In CORONARY, with experienced surgeons, the conversion rate was almost 7.9%, and in GOPCABE, it was 9.7%. Even with experienced surgeons, conversions do occur, and they have negative consequences.
Quality of revascularization: We know that long-term survival is related to completeness of revascularization. The more ischemic myocardium that is left at risk after CABG, the more likely the patients is to have an MI or die, and this has been very clearly demonstrated in the surgical literature as well as the percutaneous coronary intervention literature. It has been shown multiple times that fewer grafts are done in off-pump patients, compared with on-pump patients. Indeed, in a recent Cochrane meta-analysis of more than 7,000 patients in 57 trials, there were significantly more grafts done in on-pump than off-pump cases.
Also in terms of graft patency, again, multiple studies have shown lower graft patency in off-pump patients, either directly or by means of showing a higher reintervention rate after off-pump as compared with on-pump surgery. In both CORONARY and GOPCABE, the repeat revascularization rate at 30 days was higher for off-pump CABG.
Long-term effectiveness: The long-term results from ROOBY are very sobering: significantly higher 1-year cardiac mortality in the off-pump arm and higher 1-year composite adverse events. Again, in the 2012 Cochrane meta-analysis, with more than 10,000 patients in 75 trials, mortality was significantly higher with off-pump patients, compared with on-pump, with a hazard ratio of 1.24 (95% CI, 1.01-1.53). When the authors of the Cochrane meta-analysis removed what they called the "studies with bias," this signal was even stronger. Also in observational studies, such as one published by Racz et al. in 2004 (J. Am. Coll. Cardiol. 2004; 43: 557-64), the best survival was found to be in patients who had on-pump CABG and the worst in those who had undergone off-pump CABG.
In summary, procedural outcomes with off-pump and on-pump CABG are similar, albeit with lower reversible complications in the off-pump patients, but a greater conversion risk, along with its associated complications. The quality of the revascularization is worse in off-pump patients, the completeness of revascularization is less and re-intervention rates are higher, and the bottom line, of course, it that there is higher long-term mortality after off-pump CABG.
"Should off-pump CABG be abandoned?" As our default procedure, yes. The vast majority of our patients are best served with on-pump revascularization.
Dr. Joseph Sabik is the chairman of the department of thoracic and cardiovascular surgery and the Sheik Hamdam Bin Rashid Al Maktoum Distinguished Chair at the Cleveland Clinic. He disclosed that he performs both off-pump and on-pump CABG.
References
Anesthesiology 2005;102:188-203
N. Engl. J. Med. 2009;361:1827-37
N. Engl. J. Med. 2012;366:1489-97
N. Engl. J. Med. 2013;368:1179-88
Cochrane Database Syst. Rev. 2012; Mar 14. 3: CD007224 [doi:10.1002/14651858.CD007224.pub2])
J. Am. Coll. Cardiol. 2004;43:557-64
NO
Should off pump bypass be abandoned? Absolutely not, but let’s do it well.
The rationale for why off-pump CABG should be the preferred strategy is simple: cardiopulmonary bypass (CPB) entails extracorporeal circulation, aortic cannulation and clamping, global MI, hypothermia, and hemodilution, among other potentially deleterious phenomena. There are morbidities that can be attributed to these entities, and off-pump bypass avoids those effects by mechanically stabilizing each coronary artery target individually, while the rest of the heart beats and supports normal physiologic circulation. There is an important caveat to this, however, and that is if – and perhaps only if – a complete revascularization with precise anastomoses can be accomplished off pump, then the patient will in fact benefit.
At Emory University in Atlanta, we did a prospective, randomized trial on my own patients, which we called SMART (Surgical Management of Arterial Revascularization) trial. What we found was that in 200 unselected, consecutive patients undergoing either off- or on-pump CABG, we had lower myocardial enzyme release, fewer transfusions, more rapid extubation, and a shorter length of stay in hospital with off-pump CABG.
Completeness of revascularization is a very important issue. In SMART, the number of grafts per patient was exactly the same: 3.39 per patient with off-pump CABG and 3.4 with on-pump CABG. We coined the phrase "Index of Completeness of Revascularization," which we defined as the number of grafts we planned to do in examining the arteriogram prior to randomization and surgery divided by the number of grafts we actually did. We found no difference here, meaning we were able to do the operation we planned to do (1.00 vs. 1.01; P = not significant). Moreover, for the lateral wall, which is technically more difficult to reach in a beating heart, the number was similar in the off- and on-pump groups (0.97 vs. 0.98; P = not significant). We also used a similar percentage of arterial grafts in both groups.
CPB was an independent predictor of the need for transfusion by multivariate analysis with an odds ratio of 2.42 (P = .0073) and was associated with a longer length of stay by 1 day (5.1 days for off-pump and 6.1 for on-pump; P = .005 Wilcoxon).
Creatine phosphokinase of muscle band and troponin I release was about half as much in the off-pump group as in the on-pump group (P less than .001 Wilcoxon), and the rates of death, stroke, MI, angina, and reintervention were similar at both 30 days and 1 year, as was graft patency and quality of life. Off-pump CABG costs at 1 year were $1,955 less than on-pump, but this difference was not statistically significant (P = .08).
At 8 years, survival in SMART was still similar between groups (P = .33), as was graft patency in the small number of patients who had CT angiograms. PET scan results similarly showed no significant difference in ischemia between these two groups (P = .62). One patient in each group has had a percutaneous reintervention, and none have had a repeat coronary bypass in 10 years.
To see if these results could be replicated nationally, we turned to the STS database and looked at North American centers that performed more than 100 on-pump CABGs and more than 100 off-pump surgeries. This gave us 42,477 patients (16,245 off pump and 26,232 on pump) at 63 North American centers. We included the 2.2% of off-pump cases that were converted to on-pump cases in the off-pump group.
After risk adjustment for 32 variables, for the outcomes of death, stroke, MI, and major adverse cardiac events, off-pump bypass outperformed on-pump bypass in this huge cohort of patients from around the country. Looking at less-significant outcomes – renal failure, dialysis, sternal infection, reoperation, atrial fibrillation, prolonged ventilation, and length of stay greater than 14 days – all of them favored off-pump bypass.
We then looked at the Emory dataset (14,766 consecutive patients, 48% of whom had off-pump CABG and 52% on-pump) to see which patients benefitted more. For patients in the two lower quartiles of predicted risk, there was no difference in operative mortality. In the higher two risk quartiles, there was a mortality benefit with off-pump CABG, with a risk reduction for operative mortality of about 55% in the highest risk patients (P less than 0.001).
Logistic regression confirmed that there was an interaction between surgery type and predicted risk, and we now know that low-risk patients do not have the survival benefit of avoiding CPB. They do fine with on-pump CABG, but higher risk patients have a benefit from avoiding CPB and the higher the predicted risk, the greater the benefit to the patient.
We went back to the STS database and we looked at whether this applies only at some centers or all centers, some surgeons or all surgeons. We looked at almost a million cases, 210,469 of which were at sites that had a large off-pump CABG volume. With the usual adjustments, off-pump CABG was associated with significant reduction of risk of death, stroke, renal failure, any morbidity or mortality or prolonged length of stay, compared with on-pump bypass. This benefit was even more pronounced after adjustment for surgeon effect. Once again, the greater reduction was enjoyed by those patients who had the highest preoperative risk. In all predicted risk quartiles, off pump bypass reduced risk of death and stroke and that magnitude increased with increasing predicted risk of mortality. This was seen in large-volume centers and low-volume centers.
Similar results were seen in a recent multicenter, randomized, prospective trial by Lemma et al. that assigned 411 patients to either off- or on-pump coronary bypass (J. Thorac. Cardiovasc. Surg. 2012;143:625-31). There was reduced early mortality and morbidity among higher-risk patients. Interestingly, in this study, they used an experience-based randomization scheme, in which they had surgeons within each center who like to do off-pump CABG and those who like to do on-pump CABG, and each surgeon had hundreds of cases under his belt. For the primary endpoint, a composite of death, MI, stroke or TIA, renal failure, acute respiratory distress syndrome, or reoperation for bleeding, the rates were 5.8% of off-pump and 13.3% for on-pump patients (odds ratio, 2.5; P = .01).
I think the conclusions are clear, but not everyone has reached these same conclusions. In ROOBY, the results were different. Although the study was well conducted, it enrolled low-risk patients, in whom avoidance of CPB was unlikely to improve the expected excellent outcomes. And the operations were performed by residents, with supervising attendings who themselves only had to do 20 total career off-pump cases to be eligible. I think this lack of experience is well demonstrated by the 12.5% conversion rate from off-pump cases to on-pump in that trial. ROOBY enrolled the wrong patients and used the wrong surgeons.
In the CORONARY trial, conducted by Dr. Lamy in Canada but enrolling patients from 19 countries outside of Canada, there was no difference in the primary endpoint of death, stroke, MI, and renal failure at 30 days, but there was a decrease in transfusion, reoperation for bleeding, acute kidney injury, or respiratory complications. There wasn\'t a difference in stroke, interestingly, but the surgeons in this trial appropriately converted a hundred patients from on pump to off pump to avoid manipulating a calcified aorta. This was a good, well-conducted trial.
However, the primary outcome in CORONARY differed when assessed according to EuroSCORE. When the EuroSCORE was low, on pump outperformed off pump. When the EuroSCORE was high, off pump outperformed on pump.
These two trials offer important perspective: the ROOBY trial, enrolling low-risk patients, was actually in favor of on-pump CABG. The CORONARY trial, enrolling higher-risk patients, had a slight benefit in favor of off-pump CABG, and this was particularly evident in the Canadian cohort of 830 randomized patients, in which the primary outcome was, in fact, statistically significantly better in the off-pump group at 9.2% vs. 13.7%.
At the end of the day, I think it matters in whom you do off-pump CABG and how well you do it. It may not be for every patient or for every surgeon; off-pump CABG requires a focused and sustained effort to master a new set of physical and psychological skills to accomplish precise and complete revascularization. When we can do this, I think, we offer better outcomes for our patients.
Dr. John Puskas is the chairman of the department of cardiac surgery at Mount Sinai Beth Israel in New York. Dr. Puskas disclosed that he also does both on- and off-pump CABG. He received royalties from coronary surgical instruments marketed by Scanlan, as well.
References
JAMA 2004;291:1841-9
Ann. Thorac. Surg. 2009;88:1142-7
N. Engl. J. Med. 2009;361:1827-37
N. Engl. J. Med. 2010;362:851
N. Engl. J. Med. 2012;366:1489-97
N. Engl. J. Med. 2013;368:1179-88
Ann. Thorac. Surg. 2011;91:1836-42
J. Thorac. Cardiovasc. Surg. 2012;143:625-31
YES
I believe on-pump coronary artery bypass graft (CABG) surgery should be our primary operation, with off-pump CABG reserved only for certain situations.
In talking about these two surgical options, there are basically three main issues of interest: procedural outcomes, the quality of revascularization, and long-term effectiveness.
Procedural outcomes: In the 1990s, there was great excitement for the potential for off-pump CABG. We thought survival would be better, stroke less common, neurocognitive outcomes improved, etc., but after several randomized studies and a number of well-controlled observational studies, we found that, in terms of the important procedural outcomes – death, MI, stroke, and acute renal failure – there were actually no differences between off- and on-pump CABG. We saw this in ROOBY, with low-risk patients and less experienced surgeons; in the Canadian CORONARY trial, with experienced off-pump surgeons; and in the European GOPCABE trial, where the surgeons were very experienced and the patients were high risk.
There are some benefits with off-pump CABG in terms of what I call the "reversible" complications of surgery: fewer transfusions, less postoperative atrial fibrillation, fewer respiratory infections; but I believe these things have to be balanced against some of the negative effects of off-pump surgery in terms of its quality of revascularization and long-term effectiveness.
Probably one of the biggest disappointments we’ve had with off-pump CABG is that, in the trials, we didn’t see any major difference in neurocognitive dysfunction. What we learned is that cardiopulmonary bypass really is not that bad in terms of neurocognitive dysfunction after surgery.
One issue that tends to be forgotten is the risk associated with conversion. In a hemodynamically unstable patient, converting from off-pump to on-pump is associated with higher risks of death, bleeding, renal failure, stroke, respiratory failure, and GI complications. In CORONARY, with experienced surgeons, the conversion rate was almost 7.9%, and in GOPCABE, it was 9.7%. Even with experienced surgeons, conversions do occur, and they have negative consequences.
Quality of revascularization: We know that long-term survival is related to completeness of revascularization. The more ischemic myocardium that is left at risk after CABG, the more likely the patients is to have an MI or die, and this has been very clearly demonstrated in the surgical literature as well as the percutaneous coronary intervention literature. It has been shown multiple times that fewer grafts are done in off-pump patients, compared with on-pump patients. Indeed, in a recent Cochrane meta-analysis of more than 7,000 patients in 57 trials, there were significantly more grafts done in on-pump than off-pump cases.
Also in terms of graft patency, again, multiple studies have shown lower graft patency in off-pump patients, either directly or by means of showing a higher reintervention rate after off-pump as compared with on-pump surgery. In both CORONARY and GOPCABE, the repeat revascularization rate at 30 days was higher for off-pump CABG.
Long-term effectiveness: The long-term results from ROOBY are very sobering: significantly higher 1-year cardiac mortality in the off-pump arm and higher 1-year composite adverse events. Again, in the 2012 Cochrane meta-analysis, with more than 10,000 patients in 75 trials, mortality was significantly higher with off-pump patients, compared with on-pump, with a hazard ratio of 1.24 (95% CI, 1.01-1.53). When the authors of the Cochrane meta-analysis removed what they called the "studies with bias," this signal was even stronger. Also in observational studies, such as one published by Racz et al. in 2004 (J. Am. Coll. Cardiol. 2004; 43: 557-64), the best survival was found to be in patients who had on-pump CABG and the worst in those who had undergone off-pump CABG.
In summary, procedural outcomes with off-pump and on-pump CABG are similar, albeit with lower reversible complications in the off-pump patients, but a greater conversion risk, along with its associated complications. The quality of the revascularization is worse in off-pump patients, the completeness of revascularization is less and re-intervention rates are higher, and the bottom line, of course, it that there is higher long-term mortality after off-pump CABG.
"Should off-pump CABG be abandoned?" As our default procedure, yes. The vast majority of our patients are best served with on-pump revascularization.
Dr. Joseph Sabik is the chairman of the department of thoracic and cardiovascular surgery and the Sheik Hamdam Bin Rashid Al Maktoum Distinguished Chair at the Cleveland Clinic. He disclosed that he performs both off-pump and on-pump CABG.
References
Anesthesiology 2005;102:188-203
N. Engl. J. Med. 2009;361:1827-37
N. Engl. J. Med. 2012;366:1489-97
N. Engl. J. Med. 2013;368:1179-88
Cochrane Database Syst. Rev. 2012; Mar 14. 3: CD007224 [doi:10.1002/14651858.CD007224.pub2])
J. Am. Coll. Cardiol. 2004;43:557-64
NO
Should off pump bypass be abandoned? Absolutely not, but let’s do it well.
The rationale for why off-pump CABG should be the preferred strategy is simple: cardiopulmonary bypass (CPB) entails extracorporeal circulation, aortic cannulation and clamping, global MI, hypothermia, and hemodilution, among other potentially deleterious phenomena. There are morbidities that can be attributed to these entities, and off-pump bypass avoids those effects by mechanically stabilizing each coronary artery target individually, while the rest of the heart beats and supports normal physiologic circulation. There is an important caveat to this, however, and that is if – and perhaps only if – a complete revascularization with precise anastomoses can be accomplished off pump, then the patient will in fact benefit.
At Emory University in Atlanta, we did a prospective, randomized trial on my own patients, which we called SMART (Surgical Management of Arterial Revascularization) trial. What we found was that in 200 unselected, consecutive patients undergoing either off- or on-pump CABG, we had lower myocardial enzyme release, fewer transfusions, more rapid extubation, and a shorter length of stay in hospital with off-pump CABG.
Completeness of revascularization is a very important issue. In SMART, the number of grafts per patient was exactly the same: 3.39 per patient with off-pump CABG and 3.4 with on-pump CABG. We coined the phrase "Index of Completeness of Revascularization," which we defined as the number of grafts we planned to do in examining the arteriogram prior to randomization and surgery divided by the number of grafts we actually did. We found no difference here, meaning we were able to do the operation we planned to do (1.00 vs. 1.01; P = not significant). Moreover, for the lateral wall, which is technically more difficult to reach in a beating heart, the number was similar in the off- and on-pump groups (0.97 vs. 0.98; P = not significant). We also used a similar percentage of arterial grafts in both groups.
CPB was an independent predictor of the need for transfusion by multivariate analysis with an odds ratio of 2.42 (P = .0073) and was associated with a longer length of stay by 1 day (5.1 days for off-pump and 6.1 for on-pump; P = .005 Wilcoxon).
Creatine phosphokinase of muscle band and troponin I release was about half as much in the off-pump group as in the on-pump group (P less than .001 Wilcoxon), and the rates of death, stroke, MI, angina, and reintervention were similar at both 30 days and 1 year, as was graft patency and quality of life. Off-pump CABG costs at 1 year were $1,955 less than on-pump, but this difference was not statistically significant (P = .08).
At 8 years, survival in SMART was still similar between groups (P = .33), as was graft patency in the small number of patients who had CT angiograms. PET scan results similarly showed no significant difference in ischemia between these two groups (P = .62). One patient in each group has had a percutaneous reintervention, and none have had a repeat coronary bypass in 10 years.
To see if these results could be replicated nationally, we turned to the STS database and looked at North American centers that performed more than 100 on-pump CABGs and more than 100 off-pump surgeries. This gave us 42,477 patients (16,245 off pump and 26,232 on pump) at 63 North American centers. We included the 2.2% of off-pump cases that were converted to on-pump cases in the off-pump group.
After risk adjustment for 32 variables, for the outcomes of death, stroke, MI, and major adverse cardiac events, off-pump bypass outperformed on-pump bypass in this huge cohort of patients from around the country. Looking at less-significant outcomes – renal failure, dialysis, sternal infection, reoperation, atrial fibrillation, prolonged ventilation, and length of stay greater than 14 days – all of them favored off-pump bypass.
We then looked at the Emory dataset (14,766 consecutive patients, 48% of whom had off-pump CABG and 52% on-pump) to see which patients benefitted more. For patients in the two lower quartiles of predicted risk, there was no difference in operative mortality. In the higher two risk quartiles, there was a mortality benefit with off-pump CABG, with a risk reduction for operative mortality of about 55% in the highest risk patients (P less than 0.001).
Logistic regression confirmed that there was an interaction between surgery type and predicted risk, and we now know that low-risk patients do not have the survival benefit of avoiding CPB. They do fine with on-pump CABG, but higher risk patients have a benefit from avoiding CPB and the higher the predicted risk, the greater the benefit to the patient.
We went back to the STS database and we looked at whether this applies only at some centers or all centers, some surgeons or all surgeons. We looked at almost a million cases, 210,469 of which were at sites that had a large off-pump CABG volume. With the usual adjustments, off-pump CABG was associated with significant reduction of risk of death, stroke, renal failure, any morbidity or mortality or prolonged length of stay, compared with on-pump bypass. This benefit was even more pronounced after adjustment for surgeon effect. Once again, the greater reduction was enjoyed by those patients who had the highest preoperative risk. In all predicted risk quartiles, off pump bypass reduced risk of death and stroke and that magnitude increased with increasing predicted risk of mortality. This was seen in large-volume centers and low-volume centers.
Similar results were seen in a recent multicenter, randomized, prospective trial by Lemma et al. that assigned 411 patients to either off- or on-pump coronary bypass (J. Thorac. Cardiovasc. Surg. 2012;143:625-31). There was reduced early mortality and morbidity among higher-risk patients. Interestingly, in this study, they used an experience-based randomization scheme, in which they had surgeons within each center who like to do off-pump CABG and those who like to do on-pump CABG, and each surgeon had hundreds of cases under his belt. For the primary endpoint, a composite of death, MI, stroke or TIA, renal failure, acute respiratory distress syndrome, or reoperation for bleeding, the rates were 5.8% of off-pump and 13.3% for on-pump patients (odds ratio, 2.5; P = .01).
I think the conclusions are clear, but not everyone has reached these same conclusions. In ROOBY, the results were different. Although the study was well conducted, it enrolled low-risk patients, in whom avoidance of CPB was unlikely to improve the expected excellent outcomes. And the operations were performed by residents, with supervising attendings who themselves only had to do 20 total career off-pump cases to be eligible. I think this lack of experience is well demonstrated by the 12.5% conversion rate from off-pump cases to on-pump in that trial. ROOBY enrolled the wrong patients and used the wrong surgeons.
In the CORONARY trial, conducted by Dr. Lamy in Canada but enrolling patients from 19 countries outside of Canada, there was no difference in the primary endpoint of death, stroke, MI, and renal failure at 30 days, but there was a decrease in transfusion, reoperation for bleeding, acute kidney injury, or respiratory complications. There wasn\'t a difference in stroke, interestingly, but the surgeons in this trial appropriately converted a hundred patients from on pump to off pump to avoid manipulating a calcified aorta. This was a good, well-conducted trial.
However, the primary outcome in CORONARY differed when assessed according to EuroSCORE. When the EuroSCORE was low, on pump outperformed off pump. When the EuroSCORE was high, off pump outperformed on pump.
These two trials offer important perspective: the ROOBY trial, enrolling low-risk patients, was actually in favor of on-pump CABG. The CORONARY trial, enrolling higher-risk patients, had a slight benefit in favor of off-pump CABG, and this was particularly evident in the Canadian cohort of 830 randomized patients, in which the primary outcome was, in fact, statistically significantly better in the off-pump group at 9.2% vs. 13.7%.
At the end of the day, I think it matters in whom you do off-pump CABG and how well you do it. It may not be for every patient or for every surgeon; off-pump CABG requires a focused and sustained effort to master a new set of physical and psychological skills to accomplish precise and complete revascularization. When we can do this, I think, we offer better outcomes for our patients.
Dr. John Puskas is the chairman of the department of cardiac surgery at Mount Sinai Beth Israel in New York. Dr. Puskas disclosed that he also does both on- and off-pump CABG. He received royalties from coronary surgical instruments marketed by Scanlan, as well.
References
JAMA 2004;291:1841-9
Ann. Thorac. Surg. 2009;88:1142-7
N. Engl. J. Med. 2009;361:1827-37
N. Engl. J. Med. 2010;362:851
N. Engl. J. Med. 2012;366:1489-97
N. Engl. J. Med. 2013;368:1179-88
Ann. Thorac. Surg. 2011;91:1836-42
J. Thorac. Cardiovasc. Surg. 2012;143:625-31
ID Consult: National immunization coverage and measles
August was National Immunization Awareness Month. For most pediatricians, it is also a very busy month as patients prepare for the start of the new school year. So how are we doing?
On August 28, 2013, vaccination coverage of U.S. children aged 19-35 months was published in Morbidity and Mortality Weekly Review (2014; 63:741-8) based on results from the National Information Survey (NIS), which provides national, regional, state, and selected local area vaccination coverage estimates. NIS has monitored vaccination coverage since 1994 for all 50 states and assists in tracking the progress of achieving our national goals. It also can identify problem areas that may require special interventions. Survey data was obtained by a random telephone survey using both landline and cellular phones to households that have children born between January 2010 and May 2012. The verbal interview was followed by a survey mailed to the vaccine provider to confirm the verbal vaccine history.
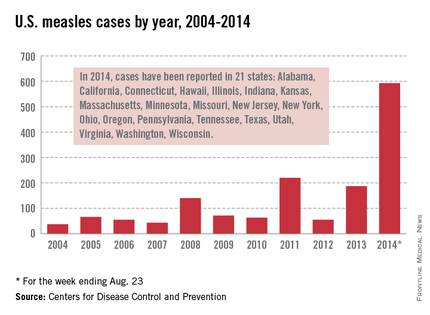
Highlights
Vaccination coverage of at least 90 %, a goal of Healthy People 2020, was achieved for receipt of one or more dose of MMR (91.9%); three or more doses of hepatitis B vaccine (HepB) (90.8 %); three or more doses of poliovirus vaccine (92.7%) and one or more doses of varicella vaccine (91.2%).
Coverage for the following vaccines failed to meet this goal: four or more doses of diphtheria, tetanus, and pertussis vaccine (DTaP) (83.1%); four or more doses of pneumococcal conjugate vaccine (PCV) (82%); and a full series of Haemophilus influenzae type b (Hib) (82%). Coverage for the remaining vaccines also fell short of their respective targeted goals: two or more doses of hepatitis A vaccine (54.7%; target 85%); rotavirus (72.6%; target 80%); and hepatitis B birth dose (74.2%; target 85%).
Compared with 2012, coverage remained stable for the four vaccines that achieved at least 90% coverage. For those that did not, rotavirus was the only vaccine in 2013 that had an increase (4%) in coverage. Of note, there was an increase in the birth dose of 2.6% for Hep B.
Children living at or below the poverty level had lower vaccination coverage, compared with those living at or above this level for several vaccines, including four or more doses of DTaP; full series of Hib vaccine, four or more doses of PCV, and rotavirus vaccine. Coverage was between 8% and 12.6% points lower for these vaccines.
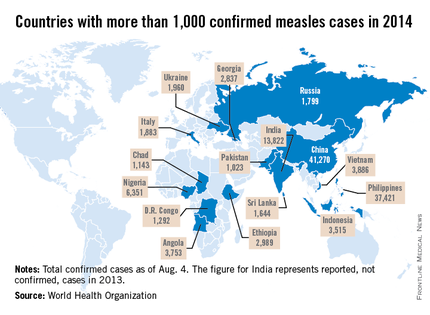
Measles
Let’s take a closer look at measles. Nationally, almost 92 % of children received at least one dose of MMR. However, coverage varied by state – an observation unchanged from 2012. New Hampshire had the highest coverage at 96.3% and three states had coverage of only 86% (Colorado, Ohio, and West Virginia). Overall 17 states had immunization rates less than 90%. Additionally, 1 in 12 children did not receive their first dose of MMR on time. Why the concern? In 2013, there were 187 cases of measles including 11 outbreaks. A total of 82% occurred in unvaccinated individuals, and another 9% were unaware of their immunization status.
As of Aug. 25, 2014, there were 595 cases of measles in the United States in 21 states, according to the Centers for Disease Control and Prevention’s National Center for Immunization and Respiratory Diseases. This is the highest number of cases reported since endemic measles was eliminated in 2000. There were as a result of 18 outbreaks, representing 89% of the reported cases. Cases are occurring even in states where immunization rates are reported to be at least 90% – a reminder that there can be pockets of low or nonimmunizing communities that leave its citizens vulnerable to outbreaks when a highly contagious virus is introduced.
Since endemic measles was eliminated 14 years ago in the United States, many health care providers have never seen a case of measles or may not realize the impact it once had on our public health system. Prior to the initiation of the measles vaccination program in 1963, 3-4 million cases of measles occurred annually in the United States with 400-500 deaths and 48,000 hospitalizations. Approximately another 1,000 individuals were left disabled secondary to measles encephalitis. Once the vaccine was introduced, the incidence of measles declined 98%, according to "Epidemiology and Prevention of Vaccine-Preventable Diseases," 12th ed., second printing. (Washington, D.C: Public Health Foundation, 2012). Between 1989 and 1991, there was a resurgence of measles resulting in approximately 55,000 cases, 11,000 hospitalizations, and 123 deaths. The resurgence was caused primarily by the failure to vaccinate uninsured children at the recommended 12-15 months of age. Children younger than 5 years of age accounted for 45% of all cases. The Vaccines for Children Program was created in 1993 as a direct response to the resurgence of measles. It would ensure that no child would contract a vaccine preventable disease because of inability to pay.
Measles remains endemic in multiple countries worldwide that are travel destinations for many Americans. In 2013, 99% of 159 U.S. cases were import related. An overwhelming majority of infections occurred in unvaccinated individuals. In 2014, this trend continues, with the majority of cases occurring in unvaccinated international travelers who return infected and spread disease to susceptible persons including children in their communities (MMWR 2014:63;496-9). Of the 288 cases reported in by May 23, 2014, 97% were associated with importations from 18 countries.
High immunization coverage must be maintained to prevent and sustain measles elimination in the United States. As a reminder, all children aged 6-11 months should receive one dose of MMR ideally 2 weeks prior to international travel. When the infant is at least 12 months of age, they should receive two additional doses of MMR or MMRV according to the routine immunization schedule. Those children older than 12 months of age should receive two doses of MMR. The second can be administered as soon as 4 weeks after the first dose. It is not uncommon for families to travel internationally and fail to mention it to you. Many have been told their child’s immunizations are up to date, not realizing that international travel may alter that definition. It behooves primary care providers to develop strategies to facilitate discussions regarding sharing international travel plans in a timely manner.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She had no relevant financial disclosures. Write to Dr. Word at [email protected].
August was National Immunization Awareness Month. For most pediatricians, it is also a very busy month as patients prepare for the start of the new school year. So how are we doing?
On August 28, 2013, vaccination coverage of U.S. children aged 19-35 months was published in Morbidity and Mortality Weekly Review (2014; 63:741-8) based on results from the National Information Survey (NIS), which provides national, regional, state, and selected local area vaccination coverage estimates. NIS has monitored vaccination coverage since 1994 for all 50 states and assists in tracking the progress of achieving our national goals. It also can identify problem areas that may require special interventions. Survey data was obtained by a random telephone survey using both landline and cellular phones to households that have children born between January 2010 and May 2012. The verbal interview was followed by a survey mailed to the vaccine provider to confirm the verbal vaccine history.
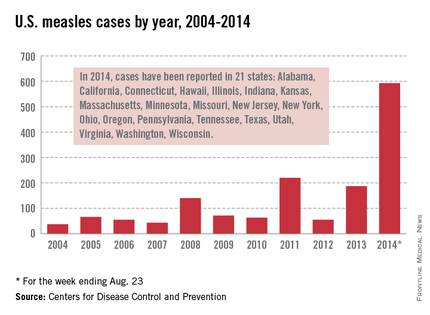
Highlights
Vaccination coverage of at least 90 %, a goal of Healthy People 2020, was achieved for receipt of one or more dose of MMR (91.9%); three or more doses of hepatitis B vaccine (HepB) (90.8 %); three or more doses of poliovirus vaccine (92.7%) and one or more doses of varicella vaccine (91.2%).
Coverage for the following vaccines failed to meet this goal: four or more doses of diphtheria, tetanus, and pertussis vaccine (DTaP) (83.1%); four or more doses of pneumococcal conjugate vaccine (PCV) (82%); and a full series of Haemophilus influenzae type b (Hib) (82%). Coverage for the remaining vaccines also fell short of their respective targeted goals: two or more doses of hepatitis A vaccine (54.7%; target 85%); rotavirus (72.6%; target 80%); and hepatitis B birth dose (74.2%; target 85%).
Compared with 2012, coverage remained stable for the four vaccines that achieved at least 90% coverage. For those that did not, rotavirus was the only vaccine in 2013 that had an increase (4%) in coverage. Of note, there was an increase in the birth dose of 2.6% for Hep B.
Children living at or below the poverty level had lower vaccination coverage, compared with those living at or above this level for several vaccines, including four or more doses of DTaP; full series of Hib vaccine, four or more doses of PCV, and rotavirus vaccine. Coverage was between 8% and 12.6% points lower for these vaccines.
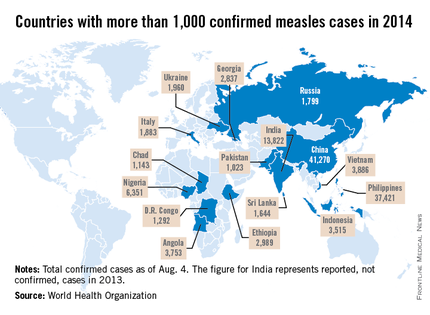
Measles
Let’s take a closer look at measles. Nationally, almost 92 % of children received at least one dose of MMR. However, coverage varied by state – an observation unchanged from 2012. New Hampshire had the highest coverage at 96.3% and three states had coverage of only 86% (Colorado, Ohio, and West Virginia). Overall 17 states had immunization rates less than 90%. Additionally, 1 in 12 children did not receive their first dose of MMR on time. Why the concern? In 2013, there were 187 cases of measles including 11 outbreaks. A total of 82% occurred in unvaccinated individuals, and another 9% were unaware of their immunization status.
As of Aug. 25, 2014, there were 595 cases of measles in the United States in 21 states, according to the Centers for Disease Control and Prevention’s National Center for Immunization and Respiratory Diseases. This is the highest number of cases reported since endemic measles was eliminated in 2000. There were as a result of 18 outbreaks, representing 89% of the reported cases. Cases are occurring even in states where immunization rates are reported to be at least 90% – a reminder that there can be pockets of low or nonimmunizing communities that leave its citizens vulnerable to outbreaks when a highly contagious virus is introduced.
Since endemic measles was eliminated 14 years ago in the United States, many health care providers have never seen a case of measles or may not realize the impact it once had on our public health system. Prior to the initiation of the measles vaccination program in 1963, 3-4 million cases of measles occurred annually in the United States with 400-500 deaths and 48,000 hospitalizations. Approximately another 1,000 individuals were left disabled secondary to measles encephalitis. Once the vaccine was introduced, the incidence of measles declined 98%, according to "Epidemiology and Prevention of Vaccine-Preventable Diseases," 12th ed., second printing. (Washington, D.C: Public Health Foundation, 2012). Between 1989 and 1991, there was a resurgence of measles resulting in approximately 55,000 cases, 11,000 hospitalizations, and 123 deaths. The resurgence was caused primarily by the failure to vaccinate uninsured children at the recommended 12-15 months of age. Children younger than 5 years of age accounted for 45% of all cases. The Vaccines for Children Program was created in 1993 as a direct response to the resurgence of measles. It would ensure that no child would contract a vaccine preventable disease because of inability to pay.
Measles remains endemic in multiple countries worldwide that are travel destinations for many Americans. In 2013, 99% of 159 U.S. cases were import related. An overwhelming majority of infections occurred in unvaccinated individuals. In 2014, this trend continues, with the majority of cases occurring in unvaccinated international travelers who return infected and spread disease to susceptible persons including children in their communities (MMWR 2014:63;496-9). Of the 288 cases reported in by May 23, 2014, 97% were associated with importations from 18 countries.
High immunization coverage must be maintained to prevent and sustain measles elimination in the United States. As a reminder, all children aged 6-11 months should receive one dose of MMR ideally 2 weeks prior to international travel. When the infant is at least 12 months of age, they should receive two additional doses of MMR or MMRV according to the routine immunization schedule. Those children older than 12 months of age should receive two doses of MMR. The second can be administered as soon as 4 weeks after the first dose. It is not uncommon for families to travel internationally and fail to mention it to you. Many have been told their child’s immunizations are up to date, not realizing that international travel may alter that definition. It behooves primary care providers to develop strategies to facilitate discussions regarding sharing international travel plans in a timely manner.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She had no relevant financial disclosures. Write to Dr. Word at [email protected].
August was National Immunization Awareness Month. For most pediatricians, it is also a very busy month as patients prepare for the start of the new school year. So how are we doing?
On August 28, 2013, vaccination coverage of U.S. children aged 19-35 months was published in Morbidity and Mortality Weekly Review (2014; 63:741-8) based on results from the National Information Survey (NIS), which provides national, regional, state, and selected local area vaccination coverage estimates. NIS has monitored vaccination coverage since 1994 for all 50 states and assists in tracking the progress of achieving our national goals. It also can identify problem areas that may require special interventions. Survey data was obtained by a random telephone survey using both landline and cellular phones to households that have children born between January 2010 and May 2012. The verbal interview was followed by a survey mailed to the vaccine provider to confirm the verbal vaccine history.
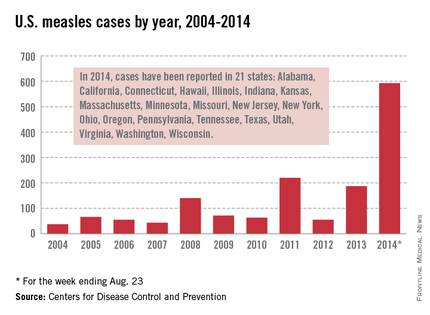
Highlights
Vaccination coverage of at least 90 %, a goal of Healthy People 2020, was achieved for receipt of one or more dose of MMR (91.9%); three or more doses of hepatitis B vaccine (HepB) (90.8 %); three or more doses of poliovirus vaccine (92.7%) and one or more doses of varicella vaccine (91.2%).
Coverage for the following vaccines failed to meet this goal: four or more doses of diphtheria, tetanus, and pertussis vaccine (DTaP) (83.1%); four or more doses of pneumococcal conjugate vaccine (PCV) (82%); and a full series of Haemophilus influenzae type b (Hib) (82%). Coverage for the remaining vaccines also fell short of their respective targeted goals: two or more doses of hepatitis A vaccine (54.7%; target 85%); rotavirus (72.6%; target 80%); and hepatitis B birth dose (74.2%; target 85%).
Compared with 2012, coverage remained stable for the four vaccines that achieved at least 90% coverage. For those that did not, rotavirus was the only vaccine in 2013 that had an increase (4%) in coverage. Of note, there was an increase in the birth dose of 2.6% for Hep B.
Children living at or below the poverty level had lower vaccination coverage, compared with those living at or above this level for several vaccines, including four or more doses of DTaP; full series of Hib vaccine, four or more doses of PCV, and rotavirus vaccine. Coverage was between 8% and 12.6% points lower for these vaccines.
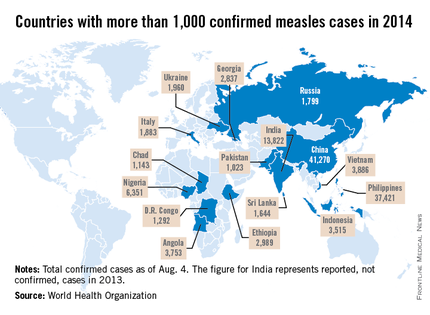
Measles
Let’s take a closer look at measles. Nationally, almost 92 % of children received at least one dose of MMR. However, coverage varied by state – an observation unchanged from 2012. New Hampshire had the highest coverage at 96.3% and three states had coverage of only 86% (Colorado, Ohio, and West Virginia). Overall 17 states had immunization rates less than 90%. Additionally, 1 in 12 children did not receive their first dose of MMR on time. Why the concern? In 2013, there were 187 cases of measles including 11 outbreaks. A total of 82% occurred in unvaccinated individuals, and another 9% were unaware of their immunization status.
As of Aug. 25, 2014, there were 595 cases of measles in the United States in 21 states, according to the Centers for Disease Control and Prevention’s National Center for Immunization and Respiratory Diseases. This is the highest number of cases reported since endemic measles was eliminated in 2000. There were as a result of 18 outbreaks, representing 89% of the reported cases. Cases are occurring even in states where immunization rates are reported to be at least 90% – a reminder that there can be pockets of low or nonimmunizing communities that leave its citizens vulnerable to outbreaks when a highly contagious virus is introduced.
Since endemic measles was eliminated 14 years ago in the United States, many health care providers have never seen a case of measles or may not realize the impact it once had on our public health system. Prior to the initiation of the measles vaccination program in 1963, 3-4 million cases of measles occurred annually in the United States with 400-500 deaths and 48,000 hospitalizations. Approximately another 1,000 individuals were left disabled secondary to measles encephalitis. Once the vaccine was introduced, the incidence of measles declined 98%, according to "Epidemiology and Prevention of Vaccine-Preventable Diseases," 12th ed., second printing. (Washington, D.C: Public Health Foundation, 2012). Between 1989 and 1991, there was a resurgence of measles resulting in approximately 55,000 cases, 11,000 hospitalizations, and 123 deaths. The resurgence was caused primarily by the failure to vaccinate uninsured children at the recommended 12-15 months of age. Children younger than 5 years of age accounted for 45% of all cases. The Vaccines for Children Program was created in 1993 as a direct response to the resurgence of measles. It would ensure that no child would contract a vaccine preventable disease because of inability to pay.
Measles remains endemic in multiple countries worldwide that are travel destinations for many Americans. In 2013, 99% of 159 U.S. cases were import related. An overwhelming majority of infections occurred in unvaccinated individuals. In 2014, this trend continues, with the majority of cases occurring in unvaccinated international travelers who return infected and spread disease to susceptible persons including children in their communities (MMWR 2014:63;496-9). Of the 288 cases reported in by May 23, 2014, 97% were associated with importations from 18 countries.
High immunization coverage must be maintained to prevent and sustain measles elimination in the United States. As a reminder, all children aged 6-11 months should receive one dose of MMR ideally 2 weeks prior to international travel. When the infant is at least 12 months of age, they should receive two additional doses of MMR or MMRV according to the routine immunization schedule. Those children older than 12 months of age should receive two doses of MMR. The second can be administered as soon as 4 weeks after the first dose. It is not uncommon for families to travel internationally and fail to mention it to you. Many have been told their child’s immunizations are up to date, not realizing that international travel may alter that definition. It behooves primary care providers to develop strategies to facilitate discussions regarding sharing international travel plans in a timely manner.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She had no relevant financial disclosures. Write to Dr. Word at [email protected].
C’est la vie
Sometimes in life you just have to do something you’ve always wanted to do. I’ve always wanted to go to the grocery store at 1:00 a.m. in my bathrobe, drink a carton of half-and-half, and pay for it with a check, but after discussing the plan with my wife, I’m instead learning French. Online. For free. I’m sorry, my sweet crème moitié-moitié, maybe next year.
Bank shot
For those of us who, for whatever reason, don’t like children to get preventable deadly diseases, it’s been a depressing year. First came the news that a whooping cough outbreak in Washington state had no effect on pertussis vaccination rates there, then we learned that correcting vaccine misinformation actually makes parents less likely to protect their children than saying nothing. Finally, however, we get a ray of hope, and, like everything else in the vaccine debate, it’s confusing. Like French.
A group of researchers from Indiana appear to have cracked the code to vaccine acceptance, at least for the measles, mumps, rubella (MMR) vaccine: tell parents how the vaccine will help their children. See how simple that was, people? Any questions?
I have one: What did y’all say that we weren’t already saying?! In their Internet-based survey of 802 parents of infants, the investigators gave subjects four different messages about vaccines, all including the standard Centers for Disease Control and Prevention Vaccine Information Statement (VIS). One group got only the VIS. Another group also heard about the vaccine’s benefits to their children; a third group heard about how vaccination protects the community at large, and a fourth group heard about vaccination’s benefits both to children and to the community.
Two of those groups saw increased vaccine acceptance: the two who heard that MMR vaccines would benefit their children. In my own practice, I tend to emphasize how the MMR vaccine helps children avoid some of the common side effects of measles infection, like severe brain damage, or death, but perhaps there are some benefits I’ve been missing. Does the MMR vaccine, say, improve your complexion, burn fat without diet or exercise, or make it easier to learn a foreign language? If so, then I may be due for a booster.
Take a hike
There is good news from the world of summer camp, and it has nothing to do with a decrease in the number of campers infected with Lyme disease since July. No, thanks to a report from a team of psychologists in Los Angeles, we now know that summer camp is where kids learn all sorts of long-forgotten skills, like how to paddle a canoe, how to start a fire, and how to read human facial expressions.
According to well-validated tests of emotional perception, kids aged 11-13 years who spent just 5 days at a summer camp without electronics saw a dramatic leap in their perception of nonverbal communications, compared with kids who did not have to trade in their iPhones for cans of concentrated DEET. A subgroup analysis that has rocked the middle school literature also demonstrated that despite being without their electronics for 5 days, none of the 51 subjects died.
Children in both groups observed photos and short videos demonstrating emotional facial expressions and body language and were then asked to describe the emotions being demonstrated. The kids who had been to camp did remarkably well on the tests. The kids who kept their electronic devices over the same time period found the images perplexing until they were replaced with the following: at which point they started texting each other the answers. The camp kids then stole the control group’s cell phones and paddled them across a river in a bark canoe, where they added them to a bonfire and made s’mores. The control group appeared to be both sad and angry, but having no way to communicate these feelings, they just went home.
Charlatan’s Web
How do I know I’m a pediatrician and not a businessperson? Because when I hear that parents, kids, and coaches are more aware of sports-related concussion, I think “good news,” not, “Hmm, I wonder if I can use this trend to sell someone some useless garbage in a bottle?” Not everyone, however, is a pediatrician, and the U.S. Food and Drug Administration (FDA) has taken notice.
In an announcement last week, the FDA warned the public about unscrupulous dietary supplement companies peddling products that claim to prevent, treat, or cure concussions and traumatic brain injuries because, you know, there’s stuff that can do that. The FDA’s greatest concern is not that athletes and their families may waste money on this snake oil (Was there every a time when rusty snakes were a common problem?) but that young athletes will put themselves at risk by returning to play before they’re fully recovered, believing that they are actually protected from further brain injury. The companies, of course, have found the perfect market, since the more injured someone’s brain is, the more likely that person is to believe their claims.
I certainly hope the FDA is serious when they say they plan to take enforcement actions against these mountebanks. Or, as I say in my online French lessons, “The cow in a hat gives the monkey with a book an apple and an orange.”
David L. Hill, M.D., FAAP, is the author of Dad to Dad: Parenting Like a Pro (AAP Publishing, 2012). He is also vice president of Cape Fear Pediatrics in Wilmington, N.C., and adjunct assistant professor of pediatrics at the University of North Carolina at Chapel Hill. He serves as Program Director for the AAP Council on Communications and Media and as an executive committee member of the North Carolina Pediatric Society. He has recorded commentaries for NPR's All Things Considered and provided content for various print, television, and Internet outlets.
Sometimes in life you just have to do something you’ve always wanted to do. I’ve always wanted to go to the grocery store at 1:00 a.m. in my bathrobe, drink a carton of half-and-half, and pay for it with a check, but after discussing the plan with my wife, I’m instead learning French. Online. For free. I’m sorry, my sweet crème moitié-moitié, maybe next year.
Bank shot
For those of us who, for whatever reason, don’t like children to get preventable deadly diseases, it’s been a depressing year. First came the news that a whooping cough outbreak in Washington state had no effect on pertussis vaccination rates there, then we learned that correcting vaccine misinformation actually makes parents less likely to protect their children than saying nothing. Finally, however, we get a ray of hope, and, like everything else in the vaccine debate, it’s confusing. Like French.
A group of researchers from Indiana appear to have cracked the code to vaccine acceptance, at least for the measles, mumps, rubella (MMR) vaccine: tell parents how the vaccine will help their children. See how simple that was, people? Any questions?
I have one: What did y’all say that we weren’t already saying?! In their Internet-based survey of 802 parents of infants, the investigators gave subjects four different messages about vaccines, all including the standard Centers for Disease Control and Prevention Vaccine Information Statement (VIS). One group got only the VIS. Another group also heard about the vaccine’s benefits to their children; a third group heard about how vaccination protects the community at large, and a fourth group heard about vaccination’s benefits both to children and to the community.
Two of those groups saw increased vaccine acceptance: the two who heard that MMR vaccines would benefit their children. In my own practice, I tend to emphasize how the MMR vaccine helps children avoid some of the common side effects of measles infection, like severe brain damage, or death, but perhaps there are some benefits I’ve been missing. Does the MMR vaccine, say, improve your complexion, burn fat without diet or exercise, or make it easier to learn a foreign language? If so, then I may be due for a booster.
Take a hike
There is good news from the world of summer camp, and it has nothing to do with a decrease in the number of campers infected with Lyme disease since July. No, thanks to a report from a team of psychologists in Los Angeles, we now know that summer camp is where kids learn all sorts of long-forgotten skills, like how to paddle a canoe, how to start a fire, and how to read human facial expressions.
According to well-validated tests of emotional perception, kids aged 11-13 years who spent just 5 days at a summer camp without electronics saw a dramatic leap in their perception of nonverbal communications, compared with kids who did not have to trade in their iPhones for cans of concentrated DEET. A subgroup analysis that has rocked the middle school literature also demonstrated that despite being without their electronics for 5 days, none of the 51 subjects died.
Children in both groups observed photos and short videos demonstrating emotional facial expressions and body language and were then asked to describe the emotions being demonstrated. The kids who had been to camp did remarkably well on the tests. The kids who kept their electronic devices over the same time period found the images perplexing until they were replaced with the following: at which point they started texting each other the answers. The camp kids then stole the control group’s cell phones and paddled them across a river in a bark canoe, where they added them to a bonfire and made s’mores. The control group appeared to be both sad and angry, but having no way to communicate these feelings, they just went home.
Charlatan’s Web
How do I know I’m a pediatrician and not a businessperson? Because when I hear that parents, kids, and coaches are more aware of sports-related concussion, I think “good news,” not, “Hmm, I wonder if I can use this trend to sell someone some useless garbage in a bottle?” Not everyone, however, is a pediatrician, and the U.S. Food and Drug Administration (FDA) has taken notice.
In an announcement last week, the FDA warned the public about unscrupulous dietary supplement companies peddling products that claim to prevent, treat, or cure concussions and traumatic brain injuries because, you know, there’s stuff that can do that. The FDA’s greatest concern is not that athletes and their families may waste money on this snake oil (Was there every a time when rusty snakes were a common problem?) but that young athletes will put themselves at risk by returning to play before they’re fully recovered, believing that they are actually protected from further brain injury. The companies, of course, have found the perfect market, since the more injured someone’s brain is, the more likely that person is to believe their claims.
I certainly hope the FDA is serious when they say they plan to take enforcement actions against these mountebanks. Or, as I say in my online French lessons, “The cow in a hat gives the monkey with a book an apple and an orange.”
David L. Hill, M.D., FAAP, is the author of Dad to Dad: Parenting Like a Pro (AAP Publishing, 2012). He is also vice president of Cape Fear Pediatrics in Wilmington, N.C., and adjunct assistant professor of pediatrics at the University of North Carolina at Chapel Hill. He serves as Program Director for the AAP Council on Communications and Media and as an executive committee member of the North Carolina Pediatric Society. He has recorded commentaries for NPR's All Things Considered and provided content for various print, television, and Internet outlets.
Sometimes in life you just have to do something you’ve always wanted to do. I’ve always wanted to go to the grocery store at 1:00 a.m. in my bathrobe, drink a carton of half-and-half, and pay for it with a check, but after discussing the plan with my wife, I’m instead learning French. Online. For free. I’m sorry, my sweet crème moitié-moitié, maybe next year.
Bank shot
For those of us who, for whatever reason, don’t like children to get preventable deadly diseases, it’s been a depressing year. First came the news that a whooping cough outbreak in Washington state had no effect on pertussis vaccination rates there, then we learned that correcting vaccine misinformation actually makes parents less likely to protect their children than saying nothing. Finally, however, we get a ray of hope, and, like everything else in the vaccine debate, it’s confusing. Like French.
A group of researchers from Indiana appear to have cracked the code to vaccine acceptance, at least for the measles, mumps, rubella (MMR) vaccine: tell parents how the vaccine will help their children. See how simple that was, people? Any questions?
I have one: What did y’all say that we weren’t already saying?! In their Internet-based survey of 802 parents of infants, the investigators gave subjects four different messages about vaccines, all including the standard Centers for Disease Control and Prevention Vaccine Information Statement (VIS). One group got only the VIS. Another group also heard about the vaccine’s benefits to their children; a third group heard about how vaccination protects the community at large, and a fourth group heard about vaccination’s benefits both to children and to the community.
Two of those groups saw increased vaccine acceptance: the two who heard that MMR vaccines would benefit their children. In my own practice, I tend to emphasize how the MMR vaccine helps children avoid some of the common side effects of measles infection, like severe brain damage, or death, but perhaps there are some benefits I’ve been missing. Does the MMR vaccine, say, improve your complexion, burn fat without diet or exercise, or make it easier to learn a foreign language? If so, then I may be due for a booster.
Take a hike
There is good news from the world of summer camp, and it has nothing to do with a decrease in the number of campers infected with Lyme disease since July. No, thanks to a report from a team of psychologists in Los Angeles, we now know that summer camp is where kids learn all sorts of long-forgotten skills, like how to paddle a canoe, how to start a fire, and how to read human facial expressions.
According to well-validated tests of emotional perception, kids aged 11-13 years who spent just 5 days at a summer camp without electronics saw a dramatic leap in their perception of nonverbal communications, compared with kids who did not have to trade in their iPhones for cans of concentrated DEET. A subgroup analysis that has rocked the middle school literature also demonstrated that despite being without their electronics for 5 days, none of the 51 subjects died.
Children in both groups observed photos and short videos demonstrating emotional facial expressions and body language and were then asked to describe the emotions being demonstrated. The kids who had been to camp did remarkably well on the tests. The kids who kept their electronic devices over the same time period found the images perplexing until they were replaced with the following: at which point they started texting each other the answers. The camp kids then stole the control group’s cell phones and paddled them across a river in a bark canoe, where they added them to a bonfire and made s’mores. The control group appeared to be both sad and angry, but having no way to communicate these feelings, they just went home.
Charlatan’s Web
How do I know I’m a pediatrician and not a businessperson? Because when I hear that parents, kids, and coaches are more aware of sports-related concussion, I think “good news,” not, “Hmm, I wonder if I can use this trend to sell someone some useless garbage in a bottle?” Not everyone, however, is a pediatrician, and the U.S. Food and Drug Administration (FDA) has taken notice.
In an announcement last week, the FDA warned the public about unscrupulous dietary supplement companies peddling products that claim to prevent, treat, or cure concussions and traumatic brain injuries because, you know, there’s stuff that can do that. The FDA’s greatest concern is not that athletes and their families may waste money on this snake oil (Was there every a time when rusty snakes were a common problem?) but that young athletes will put themselves at risk by returning to play before they’re fully recovered, believing that they are actually protected from further brain injury. The companies, of course, have found the perfect market, since the more injured someone’s brain is, the more likely that person is to believe their claims.
I certainly hope the FDA is serious when they say they plan to take enforcement actions against these mountebanks. Or, as I say in my online French lessons, “The cow in a hat gives the monkey with a book an apple and an orange.”
David L. Hill, M.D., FAAP, is the author of Dad to Dad: Parenting Like a Pro (AAP Publishing, 2012). He is also vice president of Cape Fear Pediatrics in Wilmington, N.C., and adjunct assistant professor of pediatrics at the University of North Carolina at Chapel Hill. He serves as Program Director for the AAP Council on Communications and Media and as an executive committee member of the North Carolina Pediatric Society. He has recorded commentaries for NPR's All Things Considered and provided content for various print, television, and Internet outlets.
Meaningful use – Stage 2 (Part 1 of 2)
The words "meaningful use" have been making providers cringe for more than 2 years now. Those clinicians who worked hard to demonstrate meaningful use under the stage 1 requirements now must go on to demonstrate meaningful use under the stage 2 requirements. We recently heard one of our colleagues describe stage 2 of meaningful use as reminiscent of the 1978 movie "Jaws 2," the ads for which ran with the tagline: "Just when you thought it was safe to go back in the water..."
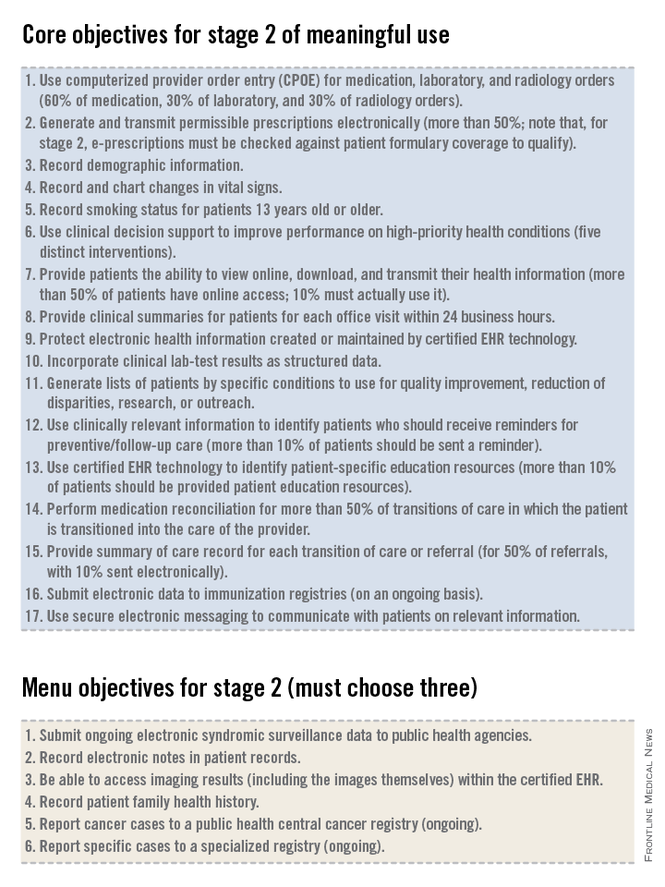
As you may be aware, on August 29th the Department of Health and Human Services published a final rule allowing certain eligible providers the flexibility to continue using the Stage 1 criteria for the 2014 attestation year, even if they were due to start Stage 2. This only applies to those who have been unable to obtain the 2014-certified software in time due to vendor delays. Unfortunately, this flexibility does not extend to those who can’t meet Stage 2 due to measure difficulty or procrastination in purchasing software or adopting new workflows (we recommend speaking with a meaningful use expert or consultant before attempting to take advantage of this flexibility). Regardless of stage or year, everyone is on a 90-day reporting period for 2014, but remember that 2015 will require a full year of reporting (January through December). So even if you qualify for the flexibility and opt to stick with the Stage 1 measures, you’ll need to be ready to hit the ground running with Stage 2 as soon as the ball drops on January 1st, 2015.
The government’s intent with the EHR incentive program is to ensure that practitioners use an EHR to do more than what could otherwise be done on a paper note. As we review the criteria that must be met for stage 2 of meaningful use, we will see the inclusion of menu items and quality measures that are aimed at enhancing actionable decision support to improve the quality of medical care, population management (even for patients who might not come in to the office), and physician-patient communication. By articulating these goals we can see that they are very different from what most practitioners perceive to be the main outcome of the meaningful use rules: the creation of a lot of unnecessary busywork in the office that yields very little benefit for practitioners or patients.
The EHR incentive program consists of three stages.
• Stage 1, which many practitioners have already accomplished and received incentive dollars for completing, focused on basic data capture.
• Stage 2, which focuses on more advanced processes including additional requirements for e-prescribing, incorporating lab results into the record, electronic transmission of patient summaries across systems, and increased patient engagement.
• Stage 3, which will utilize the processes put in place in the first two stages and focus on improved patient outcomes.
For stage 2 of meaningful use, clinicians must meet or exceed the thresholds for the 17 core objectives and 3 menu objectives, as well as report on defined Clinical Quality Measures (CQMs). Many of the objectives in stage 2 are the same as those from stage 1. Some objectives that were in the set of choices in stage 1 are now part of the mandatory core set for stage 2, required for all providers. Some objectives that were in the core set in stage 1 now have higher thresholds or percentages of patients that must meet the criteria in order to qualify for meaningful use in stage 2. The data reported to the Centers for Medicare & Medicaid Services for CQMs must originate from an EHR that has been certified for 2014 standards. This rule requires that clinicians upgrade their EHR to current technology standards, a rule that is good for EHR vendors, makes sense when we look at the system as a whole, but may be very expensive for many practitioners.
In addition to the 17 core objectives, and 3 out of 6 menu objectives, clinicians will need to report on nine CQMs. We will review the details of reporting on CQMs in next month in part 2 of our overview of Meaningful Use Stage 2.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
The words "meaningful use" have been making providers cringe for more than 2 years now. Those clinicians who worked hard to demonstrate meaningful use under the stage 1 requirements now must go on to demonstrate meaningful use under the stage 2 requirements. We recently heard one of our colleagues describe stage 2 of meaningful use as reminiscent of the 1978 movie "Jaws 2," the ads for which ran with the tagline: "Just when you thought it was safe to go back in the water..."
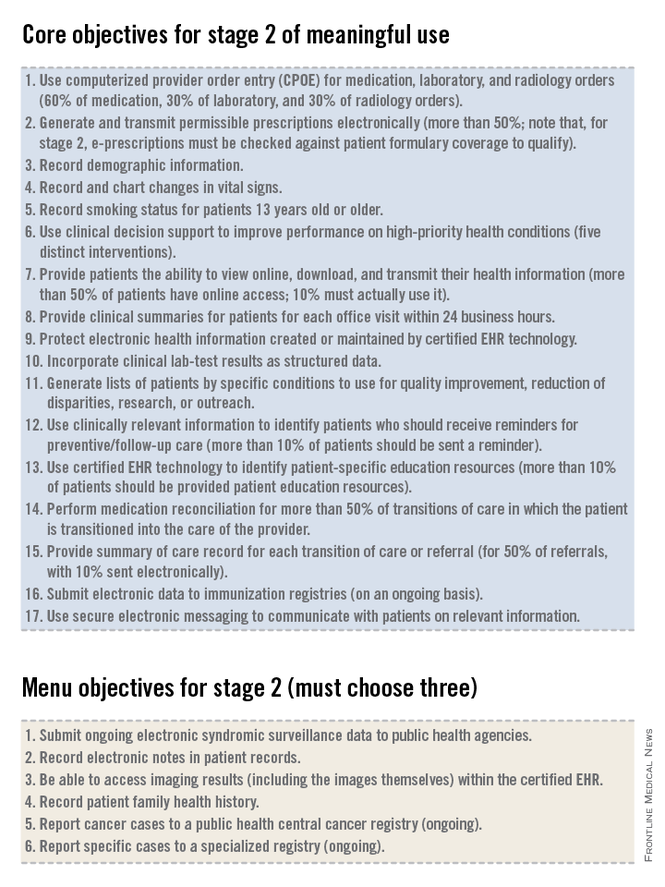
As you may be aware, on August 29th the Department of Health and Human Services published a final rule allowing certain eligible providers the flexibility to continue using the Stage 1 criteria for the 2014 attestation year, even if they were due to start Stage 2. This only applies to those who have been unable to obtain the 2014-certified software in time due to vendor delays. Unfortunately, this flexibility does not extend to those who can’t meet Stage 2 due to measure difficulty or procrastination in purchasing software or adopting new workflows (we recommend speaking with a meaningful use expert or consultant before attempting to take advantage of this flexibility). Regardless of stage or year, everyone is on a 90-day reporting period for 2014, but remember that 2015 will require a full year of reporting (January through December). So even if you qualify for the flexibility and opt to stick with the Stage 1 measures, you’ll need to be ready to hit the ground running with Stage 2 as soon as the ball drops on January 1st, 2015.
The government’s intent with the EHR incentive program is to ensure that practitioners use an EHR to do more than what could otherwise be done on a paper note. As we review the criteria that must be met for stage 2 of meaningful use, we will see the inclusion of menu items and quality measures that are aimed at enhancing actionable decision support to improve the quality of medical care, population management (even for patients who might not come in to the office), and physician-patient communication. By articulating these goals we can see that they are very different from what most practitioners perceive to be the main outcome of the meaningful use rules: the creation of a lot of unnecessary busywork in the office that yields very little benefit for practitioners or patients.
The EHR incentive program consists of three stages.
• Stage 1, which many practitioners have already accomplished and received incentive dollars for completing, focused on basic data capture.
• Stage 2, which focuses on more advanced processes including additional requirements for e-prescribing, incorporating lab results into the record, electronic transmission of patient summaries across systems, and increased patient engagement.
• Stage 3, which will utilize the processes put in place in the first two stages and focus on improved patient outcomes.
For stage 2 of meaningful use, clinicians must meet or exceed the thresholds for the 17 core objectives and 3 menu objectives, as well as report on defined Clinical Quality Measures (CQMs). Many of the objectives in stage 2 are the same as those from stage 1. Some objectives that were in the set of choices in stage 1 are now part of the mandatory core set for stage 2, required for all providers. Some objectives that were in the core set in stage 1 now have higher thresholds or percentages of patients that must meet the criteria in order to qualify for meaningful use in stage 2. The data reported to the Centers for Medicare & Medicaid Services for CQMs must originate from an EHR that has been certified for 2014 standards. This rule requires that clinicians upgrade their EHR to current technology standards, a rule that is good for EHR vendors, makes sense when we look at the system as a whole, but may be very expensive for many practitioners.
In addition to the 17 core objectives, and 3 out of 6 menu objectives, clinicians will need to report on nine CQMs. We will review the details of reporting on CQMs in next month in part 2 of our overview of Meaningful Use Stage 2.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
The words "meaningful use" have been making providers cringe for more than 2 years now. Those clinicians who worked hard to demonstrate meaningful use under the stage 1 requirements now must go on to demonstrate meaningful use under the stage 2 requirements. We recently heard one of our colleagues describe stage 2 of meaningful use as reminiscent of the 1978 movie "Jaws 2," the ads for which ran with the tagline: "Just when you thought it was safe to go back in the water..."
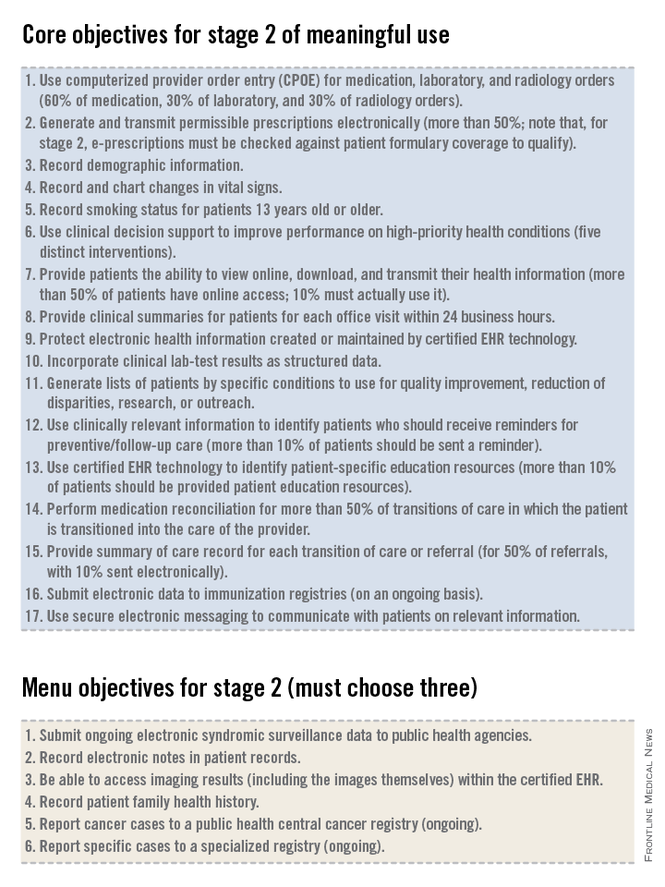
As you may be aware, on August 29th the Department of Health and Human Services published a final rule allowing certain eligible providers the flexibility to continue using the Stage 1 criteria for the 2014 attestation year, even if they were due to start Stage 2. This only applies to those who have been unable to obtain the 2014-certified software in time due to vendor delays. Unfortunately, this flexibility does not extend to those who can’t meet Stage 2 due to measure difficulty or procrastination in purchasing software or adopting new workflows (we recommend speaking with a meaningful use expert or consultant before attempting to take advantage of this flexibility). Regardless of stage or year, everyone is on a 90-day reporting period for 2014, but remember that 2015 will require a full year of reporting (January through December). So even if you qualify for the flexibility and opt to stick with the Stage 1 measures, you’ll need to be ready to hit the ground running with Stage 2 as soon as the ball drops on January 1st, 2015.
The government’s intent with the EHR incentive program is to ensure that practitioners use an EHR to do more than what could otherwise be done on a paper note. As we review the criteria that must be met for stage 2 of meaningful use, we will see the inclusion of menu items and quality measures that are aimed at enhancing actionable decision support to improve the quality of medical care, population management (even for patients who might not come in to the office), and physician-patient communication. By articulating these goals we can see that they are very different from what most practitioners perceive to be the main outcome of the meaningful use rules: the creation of a lot of unnecessary busywork in the office that yields very little benefit for practitioners or patients.
The EHR incentive program consists of three stages.
• Stage 1, which many practitioners have already accomplished and received incentive dollars for completing, focused on basic data capture.
• Stage 2, which focuses on more advanced processes including additional requirements for e-prescribing, incorporating lab results into the record, electronic transmission of patient summaries across systems, and increased patient engagement.
• Stage 3, which will utilize the processes put in place in the first two stages and focus on improved patient outcomes.
For stage 2 of meaningful use, clinicians must meet or exceed the thresholds for the 17 core objectives and 3 menu objectives, as well as report on defined Clinical Quality Measures (CQMs). Many of the objectives in stage 2 are the same as those from stage 1. Some objectives that were in the set of choices in stage 1 are now part of the mandatory core set for stage 2, required for all providers. Some objectives that were in the core set in stage 1 now have higher thresholds or percentages of patients that must meet the criteria in order to qualify for meaningful use in stage 2. The data reported to the Centers for Medicare & Medicaid Services for CQMs must originate from an EHR that has been certified for 2014 standards. This rule requires that clinicians upgrade their EHR to current technology standards, a rule that is good for EHR vendors, makes sense when we look at the system as a whole, but may be very expensive for many practitioners.
In addition to the 17 core objectives, and 3 out of 6 menu objectives, clinicians will need to report on nine CQMs. We will review the details of reporting on CQMs in next month in part 2 of our overview of Meaningful Use Stage 2.
Dr. Notte is a family physician and clinical informaticist for Abington (Pa.) Memorial Hospital. He is a partner in EHR Practice Consultants, a firm that aids physicians in adopting electronic health records. Dr. Skolnik is associate director of the family medicine residency program at Abington Memorial Hospital and professor of family and community medicine at Temple University in Philadelphia.
Management of atrial fibrillation
Atrial fibrillation is a common disorder with a lifetime prevalence of approximately 10%-15%. Risk factors include advancing age, diabetes, myocardial infarction, valvular disease, smoking, hypertension, obstructive sleep apnea, hyperthyroidism, alcohol abuse, illicit drug use, and obesity.
The diagnosis of AF should be based on the patient’s history and physical exam, including an ECG and lab work to evaluate thyroid, renal, and hepatic function, as well as a blood count. Further testing should be individualized and may include exercise testing, Holter monitoring, transesophageal echocardiogram (TEE), electrophysiology study, sleep study, or chest x-ray.
An important consideration in the approach to AF is prevention of thromboembolic events; multiple scoring systems have been developed to help stratify risk. The guideline recommends using the newer CHA2DS2-VASc scoring system, rather than the older CHADS2 scoring system, for patients with nonvalvular AF. Points are awarded as follows: congestive heart failure, 1; hypertension, 1; age of 75 years or older, 2; diabetes mellitus, 1; stroke/transient ischemic attack, 2; vascular disease (myocardial infarction, peripheral arterial disease, or aortic plaque), 1; age 65-74 years, 1; sex category (female), 1; for a maximum of 9 points. The CHA2DS2-VASc system reflects the increased risk attributed to age of 75 years or older, vascular disease, and female sex not accounted for in the CHADS2 system, and it is better than CHADS2 at discriminating among low-risk individuals. The annual risk of stroke ranges from less than 1% for a score of 0, to greater than 15% with a score of 9.
In patients with nonvalvular AF with a CHA2DS2-VASc score of 0, it is reasonable to forego antithrombotic therapy altogether. For patients with nonvalvular AF and a CHA2DS2-VASc score of 1, it is reasonable to choose either no anticoagulation therapy or use of daily aspirin or an oral anticoagulant. For a CHA2DS2-VASc score of 2, using an oral anticoagulant is recommended, either warfarin or a newer agent – dabigatran, rivaroxaban, or apixaban. For patients who have mechanical heart valves, warfarin is the only recommended choice for anticoagulation, with dabigatran specifically noted as causing harm.
Prevention of thromboembolism is just one of the treatment goals in AF. Affected patients generally require either rate- or rhythm-control therapy. Choosing which treatment to pursue depends on multiple individualized factors. The guideline points out that over time, attempting to maintain sinus rhythm results in more hospitalizations than does therapy focused on rate control, with no decrease in mortality. The guidelines state: "Routine use of a rhythm-control strategy is not warranted for some patients." Persistent symptoms are the most important indication for a rhythm-control strategy.
If a rate-control approach is chosen, the guideline recommends choosing a beta-blocker or nondihydropyridine calcium channel blocker as first-line therapy unless contraindicated, regardless of whether the AF is paroxysmal, persistent, or permanent. The dose of these medications should be titrated according to resting heart rate. Previously a target of fewer than 80 bpm was recommended; however, findings from the RACE-II (Rate Control Efficacy in Permanent Atrial Fibrillation) trial demonstrated no higher rates of cardiovascular death, hospitalization for heart failure, stroke, embolism, bleeding, or life-threatening arrhythmic events in patients with permanent AF who were allowed a target heart rate of fewer than 110 bpm.
While it is not clear if the conclusions of the RACE-II trial are applicable to all patients, the guideline recommends that for patients with permanent AF, it is reasonable to use a goal heart rate of fewer than 110 bpm if the patient is still asymptomatic and maintains normal left ventricular function. If rate control cannot be achieved using beta-blockers or calcium channel blockers, amiodarone may be a reasonable choice.
It may be reasonable to pursue restoration of sinus rhythm in patients with persistent, bothersome symptoms, a first episode of AF, or an acute illness or event leading to the onset of AF. Other situations where a rhythm-control approach may be reasonable include young patient age, inadequate rate control despite appropriate therapy, tachycardia-mediated cardiomyopathy, or patient preference.
If considering cardioversion, the length of time the patient has been in AF is critical. If the onset of AF can be reliably pinpointed to fewer than 48 hours ago, the guideline states that cardioversion is reasonable at that point, and preprocedure anticoagulation is not necessary if the patient is at low risk for thromboembolic events. If the duration of AF is 48 hours or unknown, anticoagulation with warfarin or a newer agent for 3 weeks prior to and 4 weeks after cardioversion is recommended. Alternatively, the preprocedure period of anticoagulation can be eliminated if anticoagulation can be established and a TEE performed that shows no thrombus in the left atrium (LA) or left atrium appendage (LAA).
For patients who achieve sinus rhythm, there are several choices of antiarrhythmic agent to be considered for a rhythm-control strategy, including amiodarone, dofetilide, dronedarone, flecainide, propafenone, and sotalol. It is important to note that these medications are reasonable to continue even if the patient experiences episodes of AF, if the medication decreases the number of episodes or the symptoms associated with them. These medications should be stopped, however, if AF becomes permanent.
The bottom line
Atrial fibrillation is a common rhythm disorder that requires ongoing management of thromboembolic risk as well as adherence to either a rate-control or rhythm-control strategy. The choice for anticoagulation should be made jointly between the patient and physician, and should be based on the CHA2DS2-VASc score.
Reference
2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society (Circulation 2014 March 28 [doi: 10.1161/CIR.0000000000000040]).
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. Dr. George-Reichley is a third-year resident in the family medicine residency program at Abington Memorial Hospital.
Atrial fibrillation is a common disorder with a lifetime prevalence of approximately 10%-15%. Risk factors include advancing age, diabetes, myocardial infarction, valvular disease, smoking, hypertension, obstructive sleep apnea, hyperthyroidism, alcohol abuse, illicit drug use, and obesity.
The diagnosis of AF should be based on the patient’s history and physical exam, including an ECG and lab work to evaluate thyroid, renal, and hepatic function, as well as a blood count. Further testing should be individualized and may include exercise testing, Holter monitoring, transesophageal echocardiogram (TEE), electrophysiology study, sleep study, or chest x-ray.
An important consideration in the approach to AF is prevention of thromboembolic events; multiple scoring systems have been developed to help stratify risk. The guideline recommends using the newer CHA2DS2-VASc scoring system, rather than the older CHADS2 scoring system, for patients with nonvalvular AF. Points are awarded as follows: congestive heart failure, 1; hypertension, 1; age of 75 years or older, 2; diabetes mellitus, 1; stroke/transient ischemic attack, 2; vascular disease (myocardial infarction, peripheral arterial disease, or aortic plaque), 1; age 65-74 years, 1; sex category (female), 1; for a maximum of 9 points. The CHA2DS2-VASc system reflects the increased risk attributed to age of 75 years or older, vascular disease, and female sex not accounted for in the CHADS2 system, and it is better than CHADS2 at discriminating among low-risk individuals. The annual risk of stroke ranges from less than 1% for a score of 0, to greater than 15% with a score of 9.
In patients with nonvalvular AF with a CHA2DS2-VASc score of 0, it is reasonable to forego antithrombotic therapy altogether. For patients with nonvalvular AF and a CHA2DS2-VASc score of 1, it is reasonable to choose either no anticoagulation therapy or use of daily aspirin or an oral anticoagulant. For a CHA2DS2-VASc score of 2, using an oral anticoagulant is recommended, either warfarin or a newer agent – dabigatran, rivaroxaban, or apixaban. For patients who have mechanical heart valves, warfarin is the only recommended choice for anticoagulation, with dabigatran specifically noted as causing harm.
Prevention of thromboembolism is just one of the treatment goals in AF. Affected patients generally require either rate- or rhythm-control therapy. Choosing which treatment to pursue depends on multiple individualized factors. The guideline points out that over time, attempting to maintain sinus rhythm results in more hospitalizations than does therapy focused on rate control, with no decrease in mortality. The guidelines state: "Routine use of a rhythm-control strategy is not warranted for some patients." Persistent symptoms are the most important indication for a rhythm-control strategy.
If a rate-control approach is chosen, the guideline recommends choosing a beta-blocker or nondihydropyridine calcium channel blocker as first-line therapy unless contraindicated, regardless of whether the AF is paroxysmal, persistent, or permanent. The dose of these medications should be titrated according to resting heart rate. Previously a target of fewer than 80 bpm was recommended; however, findings from the RACE-II (Rate Control Efficacy in Permanent Atrial Fibrillation) trial demonstrated no higher rates of cardiovascular death, hospitalization for heart failure, stroke, embolism, bleeding, or life-threatening arrhythmic events in patients with permanent AF who were allowed a target heart rate of fewer than 110 bpm.
While it is not clear if the conclusions of the RACE-II trial are applicable to all patients, the guideline recommends that for patients with permanent AF, it is reasonable to use a goal heart rate of fewer than 110 bpm if the patient is still asymptomatic and maintains normal left ventricular function. If rate control cannot be achieved using beta-blockers or calcium channel blockers, amiodarone may be a reasonable choice.
It may be reasonable to pursue restoration of sinus rhythm in patients with persistent, bothersome symptoms, a first episode of AF, or an acute illness or event leading to the onset of AF. Other situations where a rhythm-control approach may be reasonable include young patient age, inadequate rate control despite appropriate therapy, tachycardia-mediated cardiomyopathy, or patient preference.
If considering cardioversion, the length of time the patient has been in AF is critical. If the onset of AF can be reliably pinpointed to fewer than 48 hours ago, the guideline states that cardioversion is reasonable at that point, and preprocedure anticoagulation is not necessary if the patient is at low risk for thromboembolic events. If the duration of AF is 48 hours or unknown, anticoagulation with warfarin or a newer agent for 3 weeks prior to and 4 weeks after cardioversion is recommended. Alternatively, the preprocedure period of anticoagulation can be eliminated if anticoagulation can be established and a TEE performed that shows no thrombus in the left atrium (LA) or left atrium appendage (LAA).
For patients who achieve sinus rhythm, there are several choices of antiarrhythmic agent to be considered for a rhythm-control strategy, including amiodarone, dofetilide, dronedarone, flecainide, propafenone, and sotalol. It is important to note that these medications are reasonable to continue even if the patient experiences episodes of AF, if the medication decreases the number of episodes or the symptoms associated with them. These medications should be stopped, however, if AF becomes permanent.
The bottom line
Atrial fibrillation is a common rhythm disorder that requires ongoing management of thromboembolic risk as well as adherence to either a rate-control or rhythm-control strategy. The choice for anticoagulation should be made jointly between the patient and physician, and should be based on the CHA2DS2-VASc score.
Reference
2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society (Circulation 2014 March 28 [doi: 10.1161/CIR.0000000000000040]).
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. Dr. George-Reichley is a third-year resident in the family medicine residency program at Abington Memorial Hospital.
Atrial fibrillation is a common disorder with a lifetime prevalence of approximately 10%-15%. Risk factors include advancing age, diabetes, myocardial infarction, valvular disease, smoking, hypertension, obstructive sleep apnea, hyperthyroidism, alcohol abuse, illicit drug use, and obesity.
The diagnosis of AF should be based on the patient’s history and physical exam, including an ECG and lab work to evaluate thyroid, renal, and hepatic function, as well as a blood count. Further testing should be individualized and may include exercise testing, Holter monitoring, transesophageal echocardiogram (TEE), electrophysiology study, sleep study, or chest x-ray.
An important consideration in the approach to AF is prevention of thromboembolic events; multiple scoring systems have been developed to help stratify risk. The guideline recommends using the newer CHA2DS2-VASc scoring system, rather than the older CHADS2 scoring system, for patients with nonvalvular AF. Points are awarded as follows: congestive heart failure, 1; hypertension, 1; age of 75 years or older, 2; diabetes mellitus, 1; stroke/transient ischemic attack, 2; vascular disease (myocardial infarction, peripheral arterial disease, or aortic plaque), 1; age 65-74 years, 1; sex category (female), 1; for a maximum of 9 points. The CHA2DS2-VASc system reflects the increased risk attributed to age of 75 years or older, vascular disease, and female sex not accounted for in the CHADS2 system, and it is better than CHADS2 at discriminating among low-risk individuals. The annual risk of stroke ranges from less than 1% for a score of 0, to greater than 15% with a score of 9.
In patients with nonvalvular AF with a CHA2DS2-VASc score of 0, it is reasonable to forego antithrombotic therapy altogether. For patients with nonvalvular AF and a CHA2DS2-VASc score of 1, it is reasonable to choose either no anticoagulation therapy or use of daily aspirin or an oral anticoagulant. For a CHA2DS2-VASc score of 2, using an oral anticoagulant is recommended, either warfarin or a newer agent – dabigatran, rivaroxaban, or apixaban. For patients who have mechanical heart valves, warfarin is the only recommended choice for anticoagulation, with dabigatran specifically noted as causing harm.
Prevention of thromboembolism is just one of the treatment goals in AF. Affected patients generally require either rate- or rhythm-control therapy. Choosing which treatment to pursue depends on multiple individualized factors. The guideline points out that over time, attempting to maintain sinus rhythm results in more hospitalizations than does therapy focused on rate control, with no decrease in mortality. The guidelines state: "Routine use of a rhythm-control strategy is not warranted for some patients." Persistent symptoms are the most important indication for a rhythm-control strategy.
If a rate-control approach is chosen, the guideline recommends choosing a beta-blocker or nondihydropyridine calcium channel blocker as first-line therapy unless contraindicated, regardless of whether the AF is paroxysmal, persistent, or permanent. The dose of these medications should be titrated according to resting heart rate. Previously a target of fewer than 80 bpm was recommended; however, findings from the RACE-II (Rate Control Efficacy in Permanent Atrial Fibrillation) trial demonstrated no higher rates of cardiovascular death, hospitalization for heart failure, stroke, embolism, bleeding, or life-threatening arrhythmic events in patients with permanent AF who were allowed a target heart rate of fewer than 110 bpm.
While it is not clear if the conclusions of the RACE-II trial are applicable to all patients, the guideline recommends that for patients with permanent AF, it is reasonable to use a goal heart rate of fewer than 110 bpm if the patient is still asymptomatic and maintains normal left ventricular function. If rate control cannot be achieved using beta-blockers or calcium channel blockers, amiodarone may be a reasonable choice.
It may be reasonable to pursue restoration of sinus rhythm in patients with persistent, bothersome symptoms, a first episode of AF, or an acute illness or event leading to the onset of AF. Other situations where a rhythm-control approach may be reasonable include young patient age, inadequate rate control despite appropriate therapy, tachycardia-mediated cardiomyopathy, or patient preference.
If considering cardioversion, the length of time the patient has been in AF is critical. If the onset of AF can be reliably pinpointed to fewer than 48 hours ago, the guideline states that cardioversion is reasonable at that point, and preprocedure anticoagulation is not necessary if the patient is at low risk for thromboembolic events. If the duration of AF is 48 hours or unknown, anticoagulation with warfarin or a newer agent for 3 weeks prior to and 4 weeks after cardioversion is recommended. Alternatively, the preprocedure period of anticoagulation can be eliminated if anticoagulation can be established and a TEE performed that shows no thrombus in the left atrium (LA) or left atrium appendage (LAA).
For patients who achieve sinus rhythm, there are several choices of antiarrhythmic agent to be considered for a rhythm-control strategy, including amiodarone, dofetilide, dronedarone, flecainide, propafenone, and sotalol. It is important to note that these medications are reasonable to continue even if the patient experiences episodes of AF, if the medication decreases the number of episodes or the symptoms associated with them. These medications should be stopped, however, if AF becomes permanent.
The bottom line
Atrial fibrillation is a common rhythm disorder that requires ongoing management of thromboembolic risk as well as adherence to either a rate-control or rhythm-control strategy. The choice for anticoagulation should be made jointly between the patient and physician, and should be based on the CHA2DS2-VASc score.
Reference
2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society (Circulation 2014 March 28 [doi: 10.1161/CIR.0000000000000040]).
Dr. Skolnik is associate director of the family medicine residency program at Abington (Pa.) Memorial Hospital and professor of family and community medicine at Temple University, Philadelphia. Dr. George-Reichley is a third-year resident in the family medicine residency program at Abington Memorial Hospital.
The power of the piggy bank
I didn’t have a piggy bank when I was a child. But, I did have a bank. Instead of a porcelain porcine, my coin repository was a fiendishly designed miniature cash register. It would accept pennies, but it only acknowledged the receipt of nickels, dimes, and quarters by revealing the total amount in a window next to the register arm. It was surprisingly complex given that this was many decades prior to the invention of computer chips.
The contents only could be retrieved through a spring-loaded cash drawer that opened when the devilish instrument of torture perceived that it had been fully fed with $10 worth of silver coins. The spring that held the door tight was one tough spring. Trust me, I tried every tool on my dad’s workbench to try to open the door before it was ready. This bank demanded patience, and as a 5-year-old without an allowance, it was painful to wait and then wait and then wait some more until I had accumulated $10.
Once I was in grade school, my classmates and I opened our own accounts with a bank that provided the service to the school. I assume the bank hoped they would harvest a bountiful crop of future customers to whom they could offer mortgages and auto loans. On Wednesdays, we all arrived with our handful of coins, and the teacher recorded the amounts in our little bankbooks. I can’t recall how the interest was calculated, but we all understood that in some mysterious fashion our money was making money.
My diabolical cash register bank and my grade school bank account provided me with an introduction to the concept of saving for the future that has stayed with me to this day. It turns out that those two exercises in financial health may have contributed to my physical health.
In a recent New York Times article ("Your 401(k) Is Healthy. So Maybe You Are, Too." Aug. 16, 2014), I learned about a study published in the journal Psychological Science that found that regular contributors to their 401(k)’s were more likely to take steps to improve their health. Two business school professors at Washington University, St. Louis, studied 200 workers at an industrial laundry business. The subjects were given a baseline health evaluation that included blood tests. When the workers were informed of the results of the evaluation, they also were offered suggestions on how they could address any concerning findings. In follow-up, the regular 401(k) contributors as a group had a 27% improvement in their lab results, while noncontributors continued to suffer health declines (Psychol. Sci. 2014 June 27 [doi: 10.1177/0956797614540467]).
As a pediatrician, wouldn’t you like to know if these healthier investors were born that way? Or, were there factors in their childhood that molded them into adults who will choose to invest in the future, of both their finances and their health? We didn’t talk about money in my family as I was growing up, nor have my wife and I raised the topic with our children. But, we all fund our IRAs and try to lead healthy lifestyles. Were there subliminal messages that my parents conveyed to me and then I passed on to my children?
This country is going through a spell in which saving has slipped out of fashion. This study from St. Louis suggests that it may be linked to our difficulty in getting patients to take better care of themselves. Most of you know that we ask pediatricians to address too many issues at well-child visits. But, maybe we should begin asking every 4-year-old if he or she has a piggy bank. Maybe we even should be giving out piggy banks the way we give out children’s books, and take a moment to discuss the concept of saving. If we can convince this next generation that the future is something worth investing in now, then maybe they will be more receptive to advice about their health when they are adults.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including "How to Say No to Your Toddler." E-mail him at [email protected].
I didn’t have a piggy bank when I was a child. But, I did have a bank. Instead of a porcelain porcine, my coin repository was a fiendishly designed miniature cash register. It would accept pennies, but it only acknowledged the receipt of nickels, dimes, and quarters by revealing the total amount in a window next to the register arm. It was surprisingly complex given that this was many decades prior to the invention of computer chips.
The contents only could be retrieved through a spring-loaded cash drawer that opened when the devilish instrument of torture perceived that it had been fully fed with $10 worth of silver coins. The spring that held the door tight was one tough spring. Trust me, I tried every tool on my dad’s workbench to try to open the door before it was ready. This bank demanded patience, and as a 5-year-old without an allowance, it was painful to wait and then wait and then wait some more until I had accumulated $10.
Once I was in grade school, my classmates and I opened our own accounts with a bank that provided the service to the school. I assume the bank hoped they would harvest a bountiful crop of future customers to whom they could offer mortgages and auto loans. On Wednesdays, we all arrived with our handful of coins, and the teacher recorded the amounts in our little bankbooks. I can’t recall how the interest was calculated, but we all understood that in some mysterious fashion our money was making money.
My diabolical cash register bank and my grade school bank account provided me with an introduction to the concept of saving for the future that has stayed with me to this day. It turns out that those two exercises in financial health may have contributed to my physical health.
In a recent New York Times article ("Your 401(k) Is Healthy. So Maybe You Are, Too." Aug. 16, 2014), I learned about a study published in the journal Psychological Science that found that regular contributors to their 401(k)’s were more likely to take steps to improve their health. Two business school professors at Washington University, St. Louis, studied 200 workers at an industrial laundry business. The subjects were given a baseline health evaluation that included blood tests. When the workers were informed of the results of the evaluation, they also were offered suggestions on how they could address any concerning findings. In follow-up, the regular 401(k) contributors as a group had a 27% improvement in their lab results, while noncontributors continued to suffer health declines (Psychol. Sci. 2014 June 27 [doi: 10.1177/0956797614540467]).
As a pediatrician, wouldn’t you like to know if these healthier investors were born that way? Or, were there factors in their childhood that molded them into adults who will choose to invest in the future, of both their finances and their health? We didn’t talk about money in my family as I was growing up, nor have my wife and I raised the topic with our children. But, we all fund our IRAs and try to lead healthy lifestyles. Were there subliminal messages that my parents conveyed to me and then I passed on to my children?
This country is going through a spell in which saving has slipped out of fashion. This study from St. Louis suggests that it may be linked to our difficulty in getting patients to take better care of themselves. Most of you know that we ask pediatricians to address too many issues at well-child visits. But, maybe we should begin asking every 4-year-old if he or she has a piggy bank. Maybe we even should be giving out piggy banks the way we give out children’s books, and take a moment to discuss the concept of saving. If we can convince this next generation that the future is something worth investing in now, then maybe they will be more receptive to advice about their health when they are adults.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including "How to Say No to Your Toddler." E-mail him at [email protected].
I didn’t have a piggy bank when I was a child. But, I did have a bank. Instead of a porcelain porcine, my coin repository was a fiendishly designed miniature cash register. It would accept pennies, but it only acknowledged the receipt of nickels, dimes, and quarters by revealing the total amount in a window next to the register arm. It was surprisingly complex given that this was many decades prior to the invention of computer chips.
The contents only could be retrieved through a spring-loaded cash drawer that opened when the devilish instrument of torture perceived that it had been fully fed with $10 worth of silver coins. The spring that held the door tight was one tough spring. Trust me, I tried every tool on my dad’s workbench to try to open the door before it was ready. This bank demanded patience, and as a 5-year-old without an allowance, it was painful to wait and then wait and then wait some more until I had accumulated $10.
Once I was in grade school, my classmates and I opened our own accounts with a bank that provided the service to the school. I assume the bank hoped they would harvest a bountiful crop of future customers to whom they could offer mortgages and auto loans. On Wednesdays, we all arrived with our handful of coins, and the teacher recorded the amounts in our little bankbooks. I can’t recall how the interest was calculated, but we all understood that in some mysterious fashion our money was making money.
My diabolical cash register bank and my grade school bank account provided me with an introduction to the concept of saving for the future that has stayed with me to this day. It turns out that those two exercises in financial health may have contributed to my physical health.
In a recent New York Times article ("Your 401(k) Is Healthy. So Maybe You Are, Too." Aug. 16, 2014), I learned about a study published in the journal Psychological Science that found that regular contributors to their 401(k)’s were more likely to take steps to improve their health. Two business school professors at Washington University, St. Louis, studied 200 workers at an industrial laundry business. The subjects were given a baseline health evaluation that included blood tests. When the workers were informed of the results of the evaluation, they also were offered suggestions on how they could address any concerning findings. In follow-up, the regular 401(k) contributors as a group had a 27% improvement in their lab results, while noncontributors continued to suffer health declines (Psychol. Sci. 2014 June 27 [doi: 10.1177/0956797614540467]).
As a pediatrician, wouldn’t you like to know if these healthier investors were born that way? Or, were there factors in their childhood that molded them into adults who will choose to invest in the future, of both their finances and their health? We didn’t talk about money in my family as I was growing up, nor have my wife and I raised the topic with our children. But, we all fund our IRAs and try to lead healthy lifestyles. Were there subliminal messages that my parents conveyed to me and then I passed on to my children?
This country is going through a spell in which saving has slipped out of fashion. This study from St. Louis suggests that it may be linked to our difficulty in getting patients to take better care of themselves. Most of you know that we ask pediatricians to address too many issues at well-child visits. But, maybe we should begin asking every 4-year-old if he or she has a piggy bank. Maybe we even should be giving out piggy banks the way we give out children’s books, and take a moment to discuss the concept of saving. If we can convince this next generation that the future is something worth investing in now, then maybe they will be more receptive to advice about their health when they are adults.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including "How to Say No to Your Toddler." E-mail him at [email protected].