User login
Rabies: How to respond to parents’ questions
When most families hear the word rabies, they envision a dog foaming at the mouth and think about receiving multiple painful, often intra-abdominal injections. However, the epidemiology of rabies has changed in the United States. Postexposure prophylaxis (PEP) may not always be indicated and for certain persons preexposure prophylaxis (PrEP) is available and recommended.
Rabies is a Lyssavirus that is transmitted through saliva most often from the bite or scratch of an infected animal. Sometimes it’s via direct contact with mucous membranes. Although rare, cases have been described in which an undiagnosed donor passed the virus via transplant to recipients and four cases of aerosolized transmission were documented in two spelunkers and two laboratory technicians working with the virus. Worldwide it’s estimated that rabies causes 59,000 deaths annually.
Most cases (98%) are secondary to canine rabies. Prior to 1960, dogs were the major reservoir in the United States; however, after introduction of leash laws and animal vaccination in 1947, there was a drastic decline in cases caused by the canine rabies virus variant (CRVV). By 2004, CRVV was eliminated in the United States.
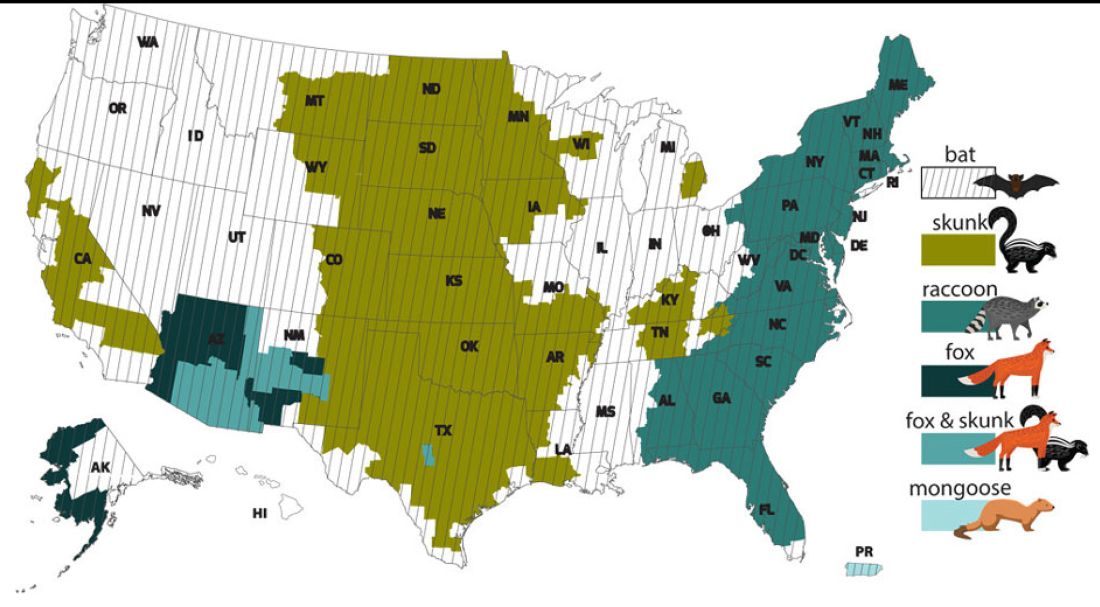
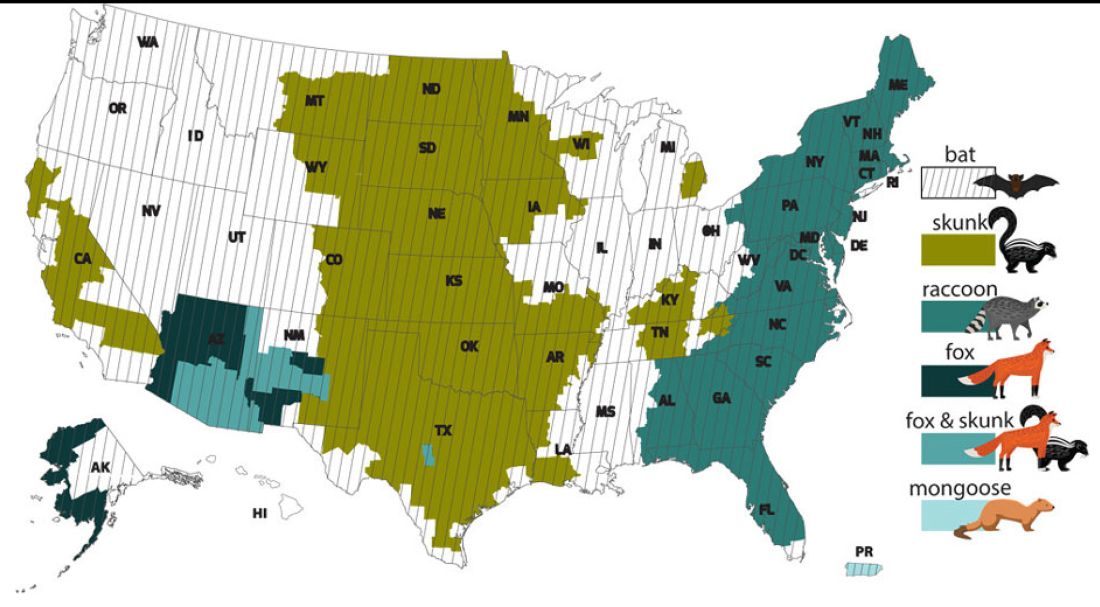
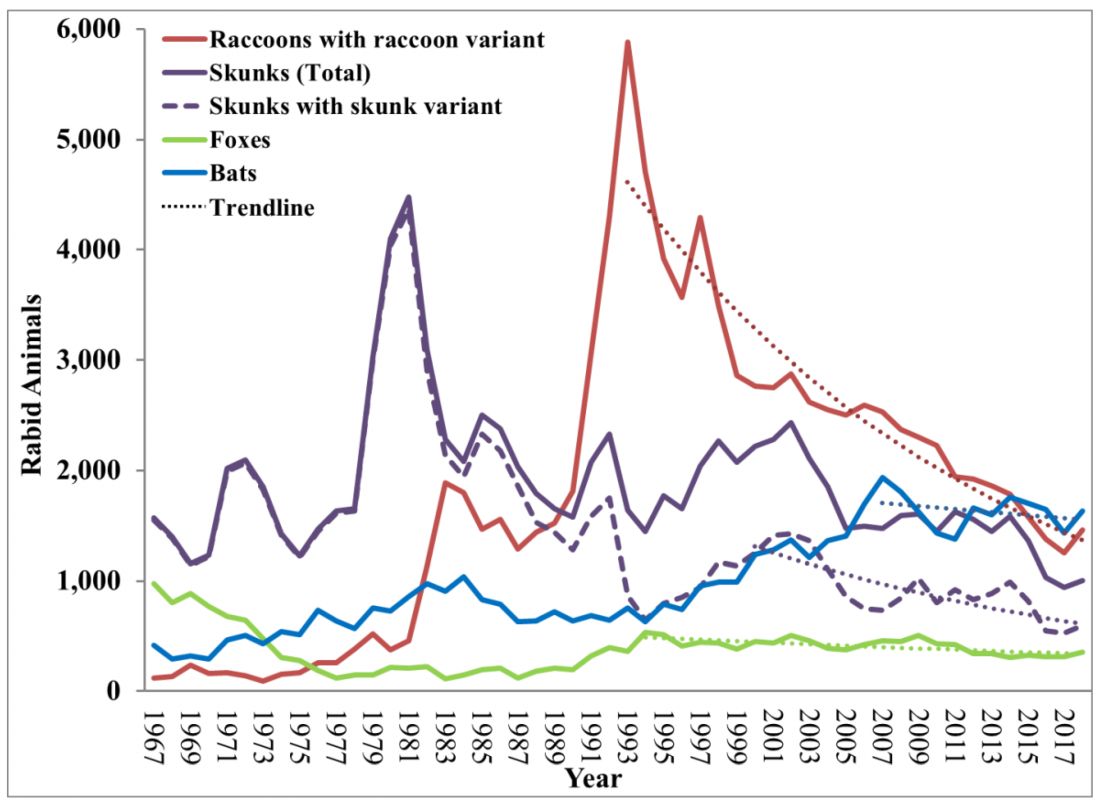
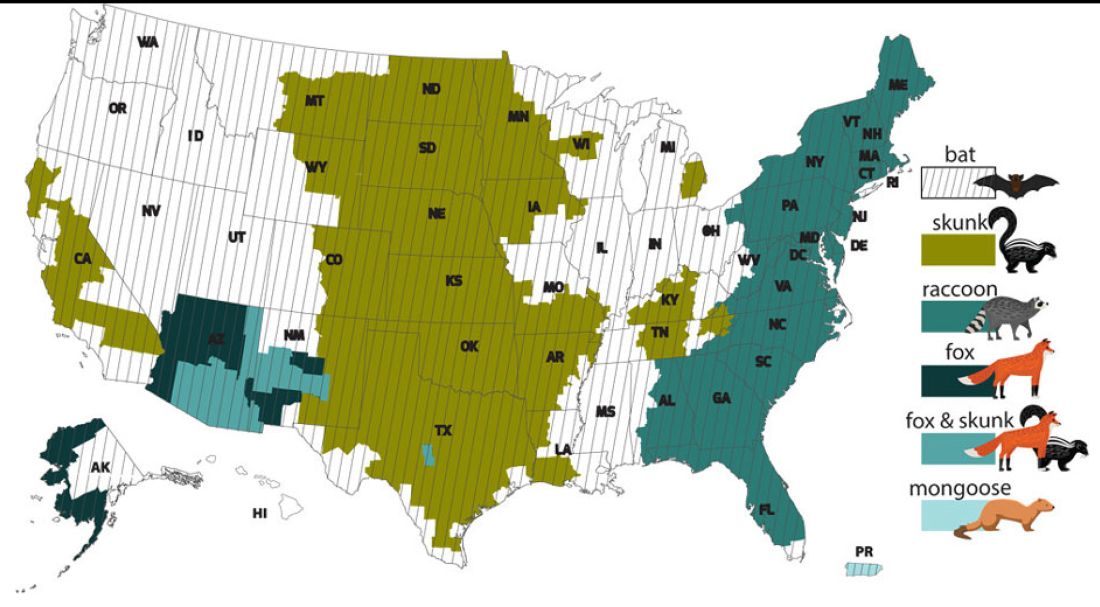
However, the proportion of strains associated with wildlife including raccoons, skunks, foxes, bats, coyotes, and mongoose now account for most of the cases in humans. Wildlife rabies is found in all states except Hawaii. Between 1960 and 2018, 89 cases were acquired in the United States and 62 (70%) were from bat exposure. Dog bites acquired during international travel were the cause of 36 cases.
Once signs and symptoms of disease develop there is no treatment. Regardless of the species variant, rabies virus infection is fatal in over 99% of cases. However, disease can be prevented with prompt initiation of PEP, which includes administration of rabies immune globulin (RIG) and rabies vaccine. Let’s look at a few different scenarios.
1. A delivery person is bitten by your neighbor’s dog while making a delivery. He was told to get rabies vaccine. What should we advise?
Canine rabies has been eliminated in the United States. However, unvaccinated canines can acquire rabies from wildlife. In this situation, you can determine the immunization status of the dog. Contact your local/state health department to assist with enforcement and management. Bites by cats and ferrets should be managed similarly.
Healthy dog:
1. Observe for 10 days.
2. PEP is not indicated unless the animal develops signs/symptoms of rabies. Then euthanize and begin PEP.
Dog appears rabid or suspected to be rabid:
1. Begin PEP.
2. Animal should be euthanized. If immunofluorescent test is negative discontinue PEP.
Dog unavailable:
Contact local/state health department. They are more familiar with rabies surveillance data.
2. Patient relocating to Malaysia for 3-4 years. Rabies PrEP was recommended but the family wants your opinion before receiving the vaccine. What would you advise?
Canine rabies is felt to be the primary cause of rabies outside of the United States. Canines are not routinely vaccinated in many foreign destinations, and the availability of RIG and rabies vaccine is not guaranteed in developing countries. As noted above, dog bites during international travel accounted for 28% of U.S. cases between 1960 and 2018.
In May 2022 recommendations for a modified two-dose PrEP schedule was published that identifies five risk groups and includes specific timing for checking rabies titers. The third rabies dose can now be administered up until year 3 (Morb Mortal Wkly Rep. 2022 May 6;71[18]:619-27). For individuals relocating to countries where CRVV is present, I prefer the traditional three-dose PrEP schedule administered between 21 and 28 days. However, we now have options. If exposure occurs any time after completion of a three-dose PrEP series or within 3 years after completion of a two-dose PrEP series, RIG would not be required. All patients would receive two doses of rabies vaccine (days 0, 3). If exposure occurs after 3 years in a person who received two doses of PrEP who did not have documentation of a protective rabies titer (> 5 IU/mL), treatment will include RIG plus four doses of vaccine (days 0, 3, 7, 14).
For this relocating patient, supporting PrEP would be strongly recommended.
3. A mother tells you she sees bats flying around her home at night and a few have even gotten into the home. This morning she saw one in her child’s room. He was still sleeping. Is there anything she needs to do?
Bats have become the predominant source of rabies in the United States. In addition to the cases noted above, three fatal cases occurred between Sept. 28 and Nov. 10, 2021, after bat exposures in August 2021 (MMWR Morb Mortal Wkly Rep. 2022 Jan 7;71:31-2). All had recognized contact with a bat 3-7 weeks prior to onset of symptoms and died 2-3 weeks after symptom onset. One declined PEP and the other two did not realize the risk for rabies from their exposure or did not notice a scratch or bite. Bites from bats may be small and unnoticed. Exposure to a bat in a closed room while sleeping is considered an exposure. Hawaii is the only state not reporting rabid bats.
PEP is recommended for her child. She should identify potential areas bats may enter the home and seal them in addition to removal of any bat roosts.
4. A parent realizes a house guest has been feeding raccoons in the backyard. What’s your response?
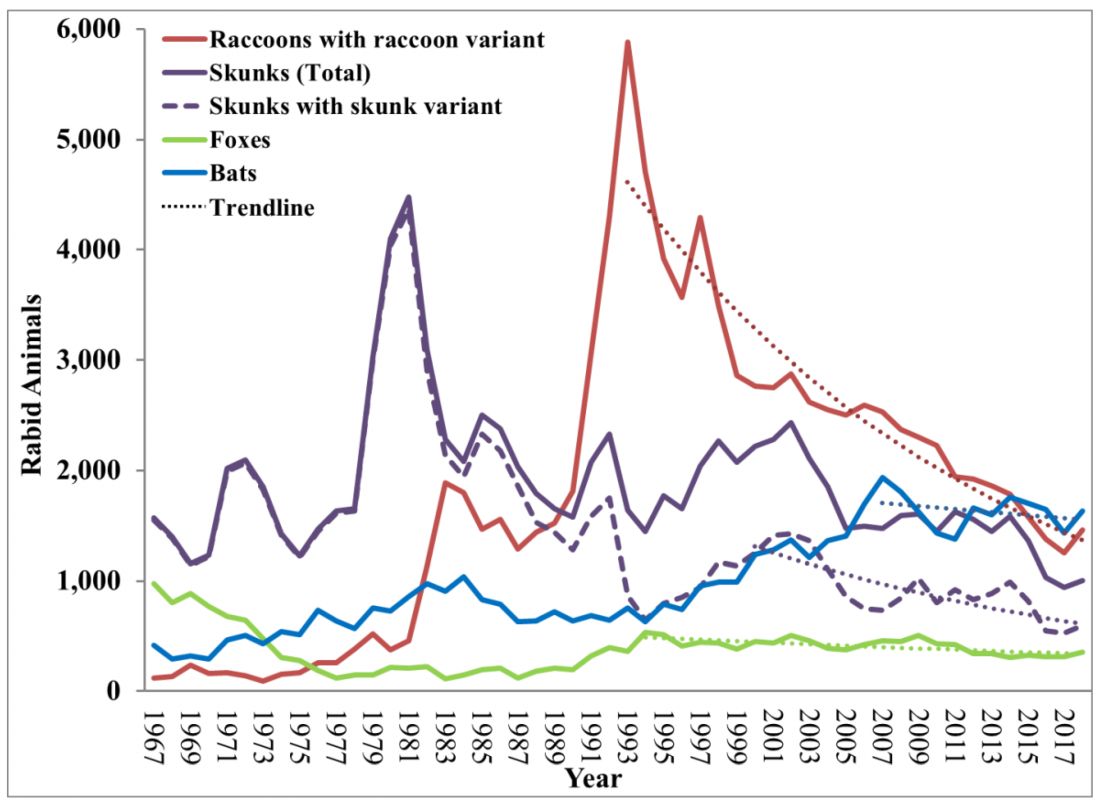
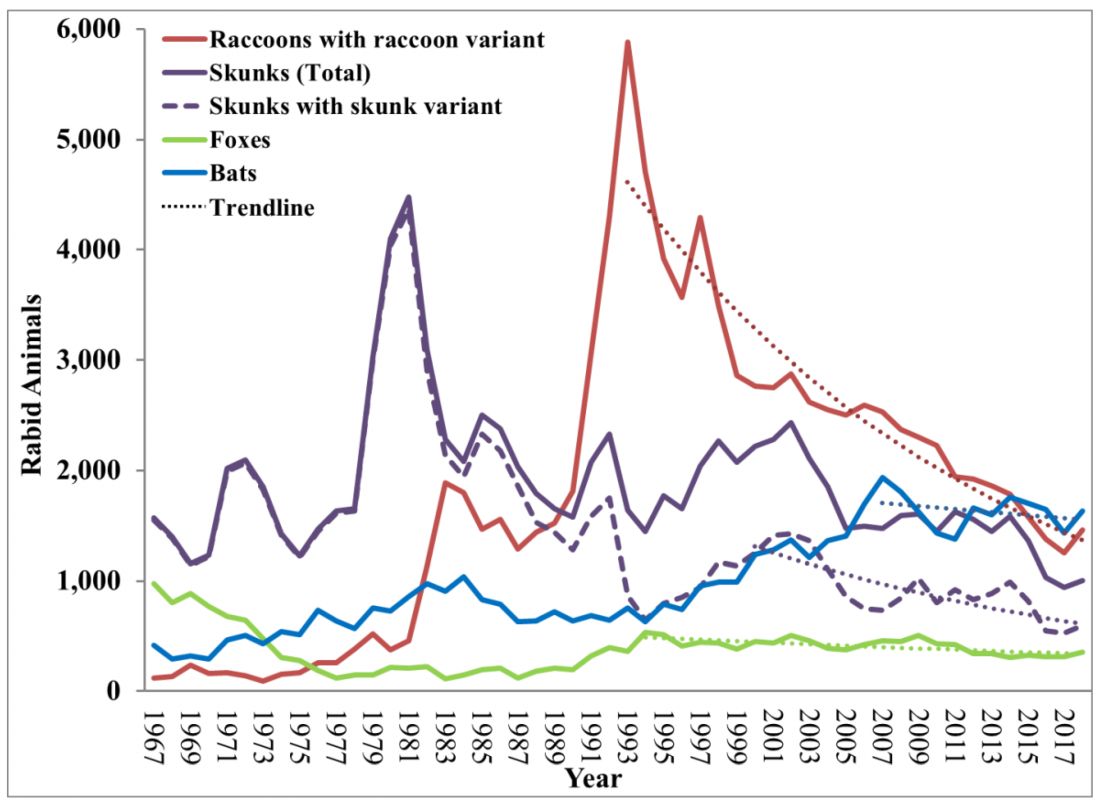
While bat rabies is the predominant variant associated with disease in the United States, as illustrated in Figure 1, other species of wildlife including raccoons are a major source of rabies. The geographic spread of the raccoon variant of rabies has been limited by oral vaccination via bait. In the situation noted here, the raccoons have returned because food was being offered thus increasing the families chance of a potential rabies exposure. Wildlife including skunks, raccoons, coyotes, foxes, and mongooses are always considered rabid until proven negative by laboratory testing.
You recommend to stop feeding wildlife and never to approach them. Have them contact the local rabies control unit and/or state wildlife services to assist with removal of the raccoons. Depending on the locale, pest control may be required at the owners expense. Inform the family to seek PEP if anyone is bitten or scratched by the raccoons.
As per the Centers for Disease Control and Prevention, about 55,000 residents receive PEP annually with health-associated expenditures including diagnostics, prevention, and control estimated between $245 and $510 million annually. Rabies is one of the most fatal diseases that can be prevented by avoiding contact with wild animals, maintenance of high immunization rates in pets, and keeping people informed of potential sources including bats. One can’t determine if an animal has rabies by looking at it. Rabies remains an urgent disease that we have to remember to address with our patients and their families. For additional information go to www.CDC.gov/rabies.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures.
When most families hear the word rabies, they envision a dog foaming at the mouth and think about receiving multiple painful, often intra-abdominal injections. However, the epidemiology of rabies has changed in the United States. Postexposure prophylaxis (PEP) may not always be indicated and for certain persons preexposure prophylaxis (PrEP) is available and recommended.
Rabies is a Lyssavirus that is transmitted through saliva most often from the bite or scratch of an infected animal. Sometimes it’s via direct contact with mucous membranes. Although rare, cases have been described in which an undiagnosed donor passed the virus via transplant to recipients and four cases of aerosolized transmission were documented in two spelunkers and two laboratory technicians working with the virus. Worldwide it’s estimated that rabies causes 59,000 deaths annually.
Most cases (98%) are secondary to canine rabies. Prior to 1960, dogs were the major reservoir in the United States; however, after introduction of leash laws and animal vaccination in 1947, there was a drastic decline in cases caused by the canine rabies virus variant (CRVV). By 2004, CRVV was eliminated in the United States.
However, the proportion of strains associated with wildlife including raccoons, skunks, foxes, bats, coyotes, and mongoose now account for most of the cases in humans. Wildlife rabies is found in all states except Hawaii. Between 1960 and 2018, 89 cases were acquired in the United States and 62 (70%) were from bat exposure. Dog bites acquired during international travel were the cause of 36 cases.
Once signs and symptoms of disease develop there is no treatment. Regardless of the species variant, rabies virus infection is fatal in over 99% of cases. However, disease can be prevented with prompt initiation of PEP, which includes administration of rabies immune globulin (RIG) and rabies vaccine. Let’s look at a few different scenarios.
1. A delivery person is bitten by your neighbor’s dog while making a delivery. He was told to get rabies vaccine. What should we advise?
Canine rabies has been eliminated in the United States. However, unvaccinated canines can acquire rabies from wildlife. In this situation, you can determine the immunization status of the dog. Contact your local/state health department to assist with enforcement and management. Bites by cats and ferrets should be managed similarly.
Healthy dog:
1. Observe for 10 days.
2. PEP is not indicated unless the animal develops signs/symptoms of rabies. Then euthanize and begin PEP.
Dog appears rabid or suspected to be rabid:
1. Begin PEP.
2. Animal should be euthanized. If immunofluorescent test is negative discontinue PEP.
Dog unavailable:
Contact local/state health department. They are more familiar with rabies surveillance data.
2. Patient relocating to Malaysia for 3-4 years. Rabies PrEP was recommended but the family wants your opinion before receiving the vaccine. What would you advise?
Canine rabies is felt to be the primary cause of rabies outside of the United States. Canines are not routinely vaccinated in many foreign destinations, and the availability of RIG and rabies vaccine is not guaranteed in developing countries. As noted above, dog bites during international travel accounted for 28% of U.S. cases between 1960 and 2018.
In May 2022 recommendations for a modified two-dose PrEP schedule was published that identifies five risk groups and includes specific timing for checking rabies titers. The third rabies dose can now be administered up until year 3 (Morb Mortal Wkly Rep. 2022 May 6;71[18]:619-27). For individuals relocating to countries where CRVV is present, I prefer the traditional three-dose PrEP schedule administered between 21 and 28 days. However, we now have options. If exposure occurs any time after completion of a three-dose PrEP series or within 3 years after completion of a two-dose PrEP series, RIG would not be required. All patients would receive two doses of rabies vaccine (days 0, 3). If exposure occurs after 3 years in a person who received two doses of PrEP who did not have documentation of a protective rabies titer (> 5 IU/mL), treatment will include RIG plus four doses of vaccine (days 0, 3, 7, 14).
For this relocating patient, supporting PrEP would be strongly recommended.
3. A mother tells you she sees bats flying around her home at night and a few have even gotten into the home. This morning she saw one in her child’s room. He was still sleeping. Is there anything she needs to do?
Bats have become the predominant source of rabies in the United States. In addition to the cases noted above, three fatal cases occurred between Sept. 28 and Nov. 10, 2021, after bat exposures in August 2021 (MMWR Morb Mortal Wkly Rep. 2022 Jan 7;71:31-2). All had recognized contact with a bat 3-7 weeks prior to onset of symptoms and died 2-3 weeks after symptom onset. One declined PEP and the other two did not realize the risk for rabies from their exposure or did not notice a scratch or bite. Bites from bats may be small and unnoticed. Exposure to a bat in a closed room while sleeping is considered an exposure. Hawaii is the only state not reporting rabid bats.
PEP is recommended for her child. She should identify potential areas bats may enter the home and seal them in addition to removal of any bat roosts.
4. A parent realizes a house guest has been feeding raccoons in the backyard. What’s your response?
While bat rabies is the predominant variant associated with disease in the United States, as illustrated in Figure 1, other species of wildlife including raccoons are a major source of rabies. The geographic spread of the raccoon variant of rabies has been limited by oral vaccination via bait. In the situation noted here, the raccoons have returned because food was being offered thus increasing the families chance of a potential rabies exposure. Wildlife including skunks, raccoons, coyotes, foxes, and mongooses are always considered rabid until proven negative by laboratory testing.
You recommend to stop feeding wildlife and never to approach them. Have them contact the local rabies control unit and/or state wildlife services to assist with removal of the raccoons. Depending on the locale, pest control may be required at the owners expense. Inform the family to seek PEP if anyone is bitten or scratched by the raccoons.
As per the Centers for Disease Control and Prevention, about 55,000 residents receive PEP annually with health-associated expenditures including diagnostics, prevention, and control estimated between $245 and $510 million annually. Rabies is one of the most fatal diseases that can be prevented by avoiding contact with wild animals, maintenance of high immunization rates in pets, and keeping people informed of potential sources including bats. One can’t determine if an animal has rabies by looking at it. Rabies remains an urgent disease that we have to remember to address with our patients and their families. For additional information go to www.CDC.gov/rabies.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures.
When most families hear the word rabies, they envision a dog foaming at the mouth and think about receiving multiple painful, often intra-abdominal injections. However, the epidemiology of rabies has changed in the United States. Postexposure prophylaxis (PEP) may not always be indicated and for certain persons preexposure prophylaxis (PrEP) is available and recommended.
Rabies is a Lyssavirus that is transmitted through saliva most often from the bite or scratch of an infected animal. Sometimes it’s via direct contact with mucous membranes. Although rare, cases have been described in which an undiagnosed donor passed the virus via transplant to recipients and four cases of aerosolized transmission were documented in two spelunkers and two laboratory technicians working with the virus. Worldwide it’s estimated that rabies causes 59,000 deaths annually.
Most cases (98%) are secondary to canine rabies. Prior to 1960, dogs were the major reservoir in the United States; however, after introduction of leash laws and animal vaccination in 1947, there was a drastic decline in cases caused by the canine rabies virus variant (CRVV). By 2004, CRVV was eliminated in the United States.
However, the proportion of strains associated with wildlife including raccoons, skunks, foxes, bats, coyotes, and mongoose now account for most of the cases in humans. Wildlife rabies is found in all states except Hawaii. Between 1960 and 2018, 89 cases were acquired in the United States and 62 (70%) were from bat exposure. Dog bites acquired during international travel were the cause of 36 cases.
Once signs and symptoms of disease develop there is no treatment. Regardless of the species variant, rabies virus infection is fatal in over 99% of cases. However, disease can be prevented with prompt initiation of PEP, which includes administration of rabies immune globulin (RIG) and rabies vaccine. Let’s look at a few different scenarios.
1. A delivery person is bitten by your neighbor’s dog while making a delivery. He was told to get rabies vaccine. What should we advise?
Canine rabies has been eliminated in the United States. However, unvaccinated canines can acquire rabies from wildlife. In this situation, you can determine the immunization status of the dog. Contact your local/state health department to assist with enforcement and management. Bites by cats and ferrets should be managed similarly.
Healthy dog:
1. Observe for 10 days.
2. PEP is not indicated unless the animal develops signs/symptoms of rabies. Then euthanize and begin PEP.
Dog appears rabid or suspected to be rabid:
1. Begin PEP.
2. Animal should be euthanized. If immunofluorescent test is negative discontinue PEP.
Dog unavailable:
Contact local/state health department. They are more familiar with rabies surveillance data.
2. Patient relocating to Malaysia for 3-4 years. Rabies PrEP was recommended but the family wants your opinion before receiving the vaccine. What would you advise?
Canine rabies is felt to be the primary cause of rabies outside of the United States. Canines are not routinely vaccinated in many foreign destinations, and the availability of RIG and rabies vaccine is not guaranteed in developing countries. As noted above, dog bites during international travel accounted for 28% of U.S. cases between 1960 and 2018.
In May 2022 recommendations for a modified two-dose PrEP schedule was published that identifies five risk groups and includes specific timing for checking rabies titers. The third rabies dose can now be administered up until year 3 (Morb Mortal Wkly Rep. 2022 May 6;71[18]:619-27). For individuals relocating to countries where CRVV is present, I prefer the traditional three-dose PrEP schedule administered between 21 and 28 days. However, we now have options. If exposure occurs any time after completion of a three-dose PrEP series or within 3 years after completion of a two-dose PrEP series, RIG would not be required. All patients would receive two doses of rabies vaccine (days 0, 3). If exposure occurs after 3 years in a person who received two doses of PrEP who did not have documentation of a protective rabies titer (> 5 IU/mL), treatment will include RIG plus four doses of vaccine (days 0, 3, 7, 14).
For this relocating patient, supporting PrEP would be strongly recommended.
3. A mother tells you she sees bats flying around her home at night and a few have even gotten into the home. This morning she saw one in her child’s room. He was still sleeping. Is there anything she needs to do?
Bats have become the predominant source of rabies in the United States. In addition to the cases noted above, three fatal cases occurred between Sept. 28 and Nov. 10, 2021, after bat exposures in August 2021 (MMWR Morb Mortal Wkly Rep. 2022 Jan 7;71:31-2). All had recognized contact with a bat 3-7 weeks prior to onset of symptoms and died 2-3 weeks after symptom onset. One declined PEP and the other two did not realize the risk for rabies from their exposure or did not notice a scratch or bite. Bites from bats may be small and unnoticed. Exposure to a bat in a closed room while sleeping is considered an exposure. Hawaii is the only state not reporting rabid bats.
PEP is recommended for her child. She should identify potential areas bats may enter the home and seal them in addition to removal of any bat roosts.
4. A parent realizes a house guest has been feeding raccoons in the backyard. What’s your response?
While bat rabies is the predominant variant associated with disease in the United States, as illustrated in Figure 1, other species of wildlife including raccoons are a major source of rabies. The geographic spread of the raccoon variant of rabies has been limited by oral vaccination via bait. In the situation noted here, the raccoons have returned because food was being offered thus increasing the families chance of a potential rabies exposure. Wildlife including skunks, raccoons, coyotes, foxes, and mongooses are always considered rabid until proven negative by laboratory testing.
You recommend to stop feeding wildlife and never to approach them. Have them contact the local rabies control unit and/or state wildlife services to assist with removal of the raccoons. Depending on the locale, pest control may be required at the owners expense. Inform the family to seek PEP if anyone is bitten or scratched by the raccoons.
As per the Centers for Disease Control and Prevention, about 55,000 residents receive PEP annually with health-associated expenditures including diagnostics, prevention, and control estimated between $245 and $510 million annually. Rabies is one of the most fatal diseases that can be prevented by avoiding contact with wild animals, maintenance of high immunization rates in pets, and keeping people informed of potential sources including bats. One can’t determine if an animal has rabies by looking at it. Rabies remains an urgent disease that we have to remember to address with our patients and their families. For additional information go to www.CDC.gov/rabies.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures.
Cleansing balms
A skin care trend, particularly in the Korean beauty product market and now worldwide, cleansing balms are a soft, yet solid variation of an oil-based cleanser. The solid oily component is combined with a surfactant or emulsifier. The cream balm texture melts into more of an oil texture once warmed with fingertips and applied to facial skin. The oils are effective at breaking down or attracting skin care products, oil, and grime on the skin surface. Once warm water is added, the oil emulsifies, and after it is wiped or rinsed off, what’s left behind is clean, hydrated skin.
They don’t tend to compromise the moisture barrier or disrupt skin pH, thus, resulting in less dry skin and have less potential to cause irritation. These products are particularly useful during drier, colder months, or in dry climates, and for those who have dry skin or eczema.
The popularity of cleansing balms has largely been based on their ability to remove makeup, similar to an oil cleanser, without the need to necessarily “double cleanse” with a regular cleanser afterward.
Alternatives to remove makeup besides cleansing balms, oil cleansers, and regular liquid water-based cleansers include micellar water (oil in water), chemical makeup removing cloths, and nonchemical makeup removing pads used with water. Micellar water is also gentle on the skin; it requires a cotton pad, tip, or cloth to remove makeup, without the need for water or washing. Both are effective, but it may be easier to remove makeup with cleansing balms, without the need for rubbing dry skin, than with micellar water. A study published in 2020 of 20 individuals reported that waterproof sunscreen was more effectively removed with a cleansing oil than a non–oil-based cleanser, with less irritation and dryness. Both were effective at removing non-waterproof sunscreen.
Both cleansing balms and oil-based cleansers need to be kept at room temperature (not in the refrigerator), since they may separate or solidify at low temperatures.
Most cleansing balms can be applied to dry skin, massaged, and rinsed off with warm water, but they are sometimes easier to remove with a wet cloth (typically either cotton or muslin). Many are nonirritating to the eyes, which is important when used to remove eye makeup and mascara on delicate skin. While many cleansing balms are noncomedogenic, residue from balms that are too thick or not rinsed off properly can contribute to comedones or milia. If residue is present after use, then “double-cleansing” with a water-based cleanser is reasonable, but not necessary for most users.
Did the development of Ponds cold cream mark the beginning of this trend? Yes and no. The creation of the first cold cream prototype has been attributed to the Greek physician, Galen (who lived in Rome), a combination of rose water, beeswax, and olive oil in 150 CE. While Ponds also has manufactured a cleansing balm, the original cold cream is a 50% moisturizer in a cleanser. So while similar in containing an oil, water, emulsifier, and thickener, and effective, it is more of a moisturizer and less of a solid oil/balm in its consistency.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Write to her at [email protected]. She had no relevant disclosures.
A skin care trend, particularly in the Korean beauty product market and now worldwide, cleansing balms are a soft, yet solid variation of an oil-based cleanser. The solid oily component is combined with a surfactant or emulsifier. The cream balm texture melts into more of an oil texture once warmed with fingertips and applied to facial skin. The oils are effective at breaking down or attracting skin care products, oil, and grime on the skin surface. Once warm water is added, the oil emulsifies, and after it is wiped or rinsed off, what’s left behind is clean, hydrated skin.
They don’t tend to compromise the moisture barrier or disrupt skin pH, thus, resulting in less dry skin and have less potential to cause irritation. These products are particularly useful during drier, colder months, or in dry climates, and for those who have dry skin or eczema.
The popularity of cleansing balms has largely been based on their ability to remove makeup, similar to an oil cleanser, without the need to necessarily “double cleanse” with a regular cleanser afterward.
Alternatives to remove makeup besides cleansing balms, oil cleansers, and regular liquid water-based cleansers include micellar water (oil in water), chemical makeup removing cloths, and nonchemical makeup removing pads used with water. Micellar water is also gentle on the skin; it requires a cotton pad, tip, or cloth to remove makeup, without the need for water or washing. Both are effective, but it may be easier to remove makeup with cleansing balms, without the need for rubbing dry skin, than with micellar water. A study published in 2020 of 20 individuals reported that waterproof sunscreen was more effectively removed with a cleansing oil than a non–oil-based cleanser, with less irritation and dryness. Both were effective at removing non-waterproof sunscreen.
Both cleansing balms and oil-based cleansers need to be kept at room temperature (not in the refrigerator), since they may separate or solidify at low temperatures.
Most cleansing balms can be applied to dry skin, massaged, and rinsed off with warm water, but they are sometimes easier to remove with a wet cloth (typically either cotton or muslin). Many are nonirritating to the eyes, which is important when used to remove eye makeup and mascara on delicate skin. While many cleansing balms are noncomedogenic, residue from balms that are too thick or not rinsed off properly can contribute to comedones or milia. If residue is present after use, then “double-cleansing” with a water-based cleanser is reasonable, but not necessary for most users.
Did the development of Ponds cold cream mark the beginning of this trend? Yes and no. The creation of the first cold cream prototype has been attributed to the Greek physician, Galen (who lived in Rome), a combination of rose water, beeswax, and olive oil in 150 CE. While Ponds also has manufactured a cleansing balm, the original cold cream is a 50% moisturizer in a cleanser. So while similar in containing an oil, water, emulsifier, and thickener, and effective, it is more of a moisturizer and less of a solid oil/balm in its consistency.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Write to her at [email protected]. She had no relevant disclosures.
A skin care trend, particularly in the Korean beauty product market and now worldwide, cleansing balms are a soft, yet solid variation of an oil-based cleanser. The solid oily component is combined with a surfactant or emulsifier. The cream balm texture melts into more of an oil texture once warmed with fingertips and applied to facial skin. The oils are effective at breaking down or attracting skin care products, oil, and grime on the skin surface. Once warm water is added, the oil emulsifies, and after it is wiped or rinsed off, what’s left behind is clean, hydrated skin.
They don’t tend to compromise the moisture barrier or disrupt skin pH, thus, resulting in less dry skin and have less potential to cause irritation. These products are particularly useful during drier, colder months, or in dry climates, and for those who have dry skin or eczema.
The popularity of cleansing balms has largely been based on their ability to remove makeup, similar to an oil cleanser, without the need to necessarily “double cleanse” with a regular cleanser afterward.
Alternatives to remove makeup besides cleansing balms, oil cleansers, and regular liquid water-based cleansers include micellar water (oil in water), chemical makeup removing cloths, and nonchemical makeup removing pads used with water. Micellar water is also gentle on the skin; it requires a cotton pad, tip, or cloth to remove makeup, without the need for water or washing. Both are effective, but it may be easier to remove makeup with cleansing balms, without the need for rubbing dry skin, than with micellar water. A study published in 2020 of 20 individuals reported that waterproof sunscreen was more effectively removed with a cleansing oil than a non–oil-based cleanser, with less irritation and dryness. Both were effective at removing non-waterproof sunscreen.
Both cleansing balms and oil-based cleansers need to be kept at room temperature (not in the refrigerator), since they may separate or solidify at low temperatures.
Most cleansing balms can be applied to dry skin, massaged, and rinsed off with warm water, but they are sometimes easier to remove with a wet cloth (typically either cotton or muslin). Many are nonirritating to the eyes, which is important when used to remove eye makeup and mascara on delicate skin. While many cleansing balms are noncomedogenic, residue from balms that are too thick or not rinsed off properly can contribute to comedones or milia. If residue is present after use, then “double-cleansing” with a water-based cleanser is reasonable, but not necessary for most users.
Did the development of Ponds cold cream mark the beginning of this trend? Yes and no. The creation of the first cold cream prototype has been attributed to the Greek physician, Galen (who lived in Rome), a combination of rose water, beeswax, and olive oil in 150 CE. While Ponds also has manufactured a cleansing balm, the original cold cream is a 50% moisturizer in a cleanser. So while similar in containing an oil, water, emulsifier, and thickener, and effective, it is more of a moisturizer and less of a solid oil/balm in its consistency.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Write to her at [email protected]. She had no relevant disclosures.
Get action! – Teddy Roosevelt
“Papa! Where donut?” asks my 2½ year-old sitting with her legs dangling and hands folded in a bustling Starbucks. We’ve been waiting for 8 minutes and we’ve reached her limit of tolerance. She’s unimpressed by the queued customers who compliment her curly blonde hair, many of whom have come and gone since we’ve been waiting. I agree – how long does it take to pour a kiddie milk and grab a donut? We can both see it in the case right there!
No one likes to wait. Truly, one of the great benefits of the modern world is that wait times are now incredibly short. Many Starbucks customers, unlike my daughter, ordered their drink ahead and waited exactly 0 minutes to get their drink. What about Amazon? I ordered a bird feeder this morning and it’s already hanging in the yard. It’s still daylight. Feel like Himalayan Momo Dumplings tonight? Your food could arrive in 37 minutes. The modern wait standard has been set impossibly high for us.
Yes, for some. We created a whole room just for waiting. Airlines call theirs “The Platinum Executive Lounge.” Ours is “The waiting room.”
Excess waiting is a significant reason why health care gets beat up in reviews. We’re unable to keep up with the new expectations. Waiting is also a significant cause of distress. Many patients report the most difficult part of their cancer diagnosis was the waiting for results, not the treatment. It’s because when under stress, we are hardwired to take action. Binding patients into inaction while they wait is very uncomfortable.
Fortunately, the psychology of waiting is well understood and there are best practices that can help. First, anxiety makes waiting much worse. Conveying confidence and reassuring patients they are in the right place and that everything will be OK makes the wait time feel shorter for them. Uncertainty also compounds their apprehension. If you believe the diagnosis will be melanoma, tell them that at the time of the biopsy and tell them what you expect next. This is better than saying, “Well, that could be cancer. We’ll see.”
Knowing a wait time is also much better than not. Have your staff advise patients on how much longer they can expect before seeing you (telling them they’re next isn’t as effective). Advise that test results should be back by the end of next week. Of course, under promise and over deliver. When the results are back on Tuesday, you’ve got a pleased patient.
Explaining that you had to add in an urgent patient helps. Even if it’s not your fault, it’s still better to apologize. For example, the 78 highway, the left anterior descending artery to our office, has been closed because of a sinkhole this month (not kidding). I’ve been apologizing to a lot of patients saying that all our patients are arriving late, which is putting us behind. As they can envision the linear parking lot that used to be a highway, it helps.
Lastly, as any child can tell you, waiting has to not only be, but to also appear, fair. The only thing worse than waiting for an appointment, or donut, is seeing someone who came in after you get their donut before you do. If you’re pulling both Mohs and cosmetics patients from the same waiting area, then your surgery patients will see a lot of patients come and go while they are sitting. Demarcating one sitting area for Mohs and one for clinics might help. So does ordering ahead. I’d show my daughter how to use the app so we don’t have to wait so long next week, but she’s 2 and I’m quite sure she already knows.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
“Papa! Where donut?” asks my 2½ year-old sitting with her legs dangling and hands folded in a bustling Starbucks. We’ve been waiting for 8 minutes and we’ve reached her limit of tolerance. She’s unimpressed by the queued customers who compliment her curly blonde hair, many of whom have come and gone since we’ve been waiting. I agree – how long does it take to pour a kiddie milk and grab a donut? We can both see it in the case right there!
No one likes to wait. Truly, one of the great benefits of the modern world is that wait times are now incredibly short. Many Starbucks customers, unlike my daughter, ordered their drink ahead and waited exactly 0 minutes to get their drink. What about Amazon? I ordered a bird feeder this morning and it’s already hanging in the yard. It’s still daylight. Feel like Himalayan Momo Dumplings tonight? Your food could arrive in 37 minutes. The modern wait standard has been set impossibly high for us.
Yes, for some. We created a whole room just for waiting. Airlines call theirs “The Platinum Executive Lounge.” Ours is “The waiting room.”
Excess waiting is a significant reason why health care gets beat up in reviews. We’re unable to keep up with the new expectations. Waiting is also a significant cause of distress. Many patients report the most difficult part of their cancer diagnosis was the waiting for results, not the treatment. It’s because when under stress, we are hardwired to take action. Binding patients into inaction while they wait is very uncomfortable.
Fortunately, the psychology of waiting is well understood and there are best practices that can help. First, anxiety makes waiting much worse. Conveying confidence and reassuring patients they are in the right place and that everything will be OK makes the wait time feel shorter for them. Uncertainty also compounds their apprehension. If you believe the diagnosis will be melanoma, tell them that at the time of the biopsy and tell them what you expect next. This is better than saying, “Well, that could be cancer. We’ll see.”
Knowing a wait time is also much better than not. Have your staff advise patients on how much longer they can expect before seeing you (telling them they’re next isn’t as effective). Advise that test results should be back by the end of next week. Of course, under promise and over deliver. When the results are back on Tuesday, you’ve got a pleased patient.
Explaining that you had to add in an urgent patient helps. Even if it’s not your fault, it’s still better to apologize. For example, the 78 highway, the left anterior descending artery to our office, has been closed because of a sinkhole this month (not kidding). I’ve been apologizing to a lot of patients saying that all our patients are arriving late, which is putting us behind. As they can envision the linear parking lot that used to be a highway, it helps.
Lastly, as any child can tell you, waiting has to not only be, but to also appear, fair. The only thing worse than waiting for an appointment, or donut, is seeing someone who came in after you get their donut before you do. If you’re pulling both Mohs and cosmetics patients from the same waiting area, then your surgery patients will see a lot of patients come and go while they are sitting. Demarcating one sitting area for Mohs and one for clinics might help. So does ordering ahead. I’d show my daughter how to use the app so we don’t have to wait so long next week, but she’s 2 and I’m quite sure she already knows.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
“Papa! Where donut?” asks my 2½ year-old sitting with her legs dangling and hands folded in a bustling Starbucks. We’ve been waiting for 8 minutes and we’ve reached her limit of tolerance. She’s unimpressed by the queued customers who compliment her curly blonde hair, many of whom have come and gone since we’ve been waiting. I agree – how long does it take to pour a kiddie milk and grab a donut? We can both see it in the case right there!
No one likes to wait. Truly, one of the great benefits of the modern world is that wait times are now incredibly short. Many Starbucks customers, unlike my daughter, ordered their drink ahead and waited exactly 0 minutes to get their drink. What about Amazon? I ordered a bird feeder this morning and it’s already hanging in the yard. It’s still daylight. Feel like Himalayan Momo Dumplings tonight? Your food could arrive in 37 minutes. The modern wait standard has been set impossibly high for us.
Yes, for some. We created a whole room just for waiting. Airlines call theirs “The Platinum Executive Lounge.” Ours is “The waiting room.”
Excess waiting is a significant reason why health care gets beat up in reviews. We’re unable to keep up with the new expectations. Waiting is also a significant cause of distress. Many patients report the most difficult part of their cancer diagnosis was the waiting for results, not the treatment. It’s because when under stress, we are hardwired to take action. Binding patients into inaction while they wait is very uncomfortable.
Fortunately, the psychology of waiting is well understood and there are best practices that can help. First, anxiety makes waiting much worse. Conveying confidence and reassuring patients they are in the right place and that everything will be OK makes the wait time feel shorter for them. Uncertainty also compounds their apprehension. If you believe the diagnosis will be melanoma, tell them that at the time of the biopsy and tell them what you expect next. This is better than saying, “Well, that could be cancer. We’ll see.”
Knowing a wait time is also much better than not. Have your staff advise patients on how much longer they can expect before seeing you (telling them they’re next isn’t as effective). Advise that test results should be back by the end of next week. Of course, under promise and over deliver. When the results are back on Tuesday, you’ve got a pleased patient.
Explaining that you had to add in an urgent patient helps. Even if it’s not your fault, it’s still better to apologize. For example, the 78 highway, the left anterior descending artery to our office, has been closed because of a sinkhole this month (not kidding). I’ve been apologizing to a lot of patients saying that all our patients are arriving late, which is putting us behind. As they can envision the linear parking lot that used to be a highway, it helps.
Lastly, as any child can tell you, waiting has to not only be, but to also appear, fair. The only thing worse than waiting for an appointment, or donut, is seeing someone who came in after you get their donut before you do. If you’re pulling both Mohs and cosmetics patients from the same waiting area, then your surgery patients will see a lot of patients come and go while they are sitting. Demarcating one sitting area for Mohs and one for clinics might help. So does ordering ahead. I’d show my daughter how to use the app so we don’t have to wait so long next week, but she’s 2 and I’m quite sure she already knows.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
A 7-month-old male presents with pustules and inflamed papules on the scalp and extremities
The bacterial, fungal, and atypical mycobacterial cultures from the lesions performed at the emergency department were all negative.
Pediatric dermatology was consulted and a punch biopsy of one of the lesions was done. Histopathologic examination showed a mixed perifollicular infiltrate of predominantly eosinophils with some neutrophils and associated microabscesses. Periodic acid Schiff and Fite stains failed to reveal any organisms. CD1 immunostain was negative. Fresh tissue cultures for bacteria, fungi, and atypical mycobacteria were negative.
Given the clinical presentation of chronic recurrent sterile pustules on an infant with associated eosinophilia and the reported histopathologic findings, the patient was diagnosed with eosinophilic pustular folliculitis of infancy (EPFI).
EPFI is a rare and idiopathic cutaneous disorder present in children. About 70% of the cases reported occur in the first 6 month of life and rarely present past 3 years of age. EPF encompasses a group of conditions including the classic adult form, or Ofuji disease. EPF is seen in immunosuppressed patients, mainly HIV positive, and EPF is also seen in infants and children.
In EPFI, males are most commonly affected. The condition presents, as it did in our patient, with recurrent crops of sterile papules and pustules mainly on the scalp, but they can occur in other parts of the body. The lesions go away within a few weeks to months without leaving any scars but it can take months to years to resolve. Histopathologic analysis of the lesions show an eosinophilic infiltrate which can be follicular, perifollicular, or periadnexal with associated flame figures in about 26% of cases.
Aggressive treatment is usually not needed as lesions are self-limited. Lesions can be treated with topical corticosteroids and oral antihistamine medications like cetirizine if symptomatic.
If the lesions start to present during the neonatal period, one may consider in the differential diagnosis, neonatal rashes like transient neonatal pustular melanosis and erythema toxicum neonatorum. Both of these neonatal conditions tend to resolve in the first month of life, compared with EPFI where lesions can come and go for months to years. EPFI lesions can be described as pustules and inflammatory papules, as well as furuncles and vesicles. All of the lesions may be seen in one patient at one time, which will not be typical for transient neonatal pustular melanosis or erythema toxicum. Eosinophils can be seen in erythema toxicum but folliculitis is not present. The inflammatory infiltrate seen in transient neonatal pustular melanosis is polymorphonuclear, not eosinophilic.
Early in the presentation, infectious conditions like staphylococcal or streptococcal folliculitis, cellulitis and furunculosis, tinea capitis, atypical mycobacterial infections, herpes simplex, and parasitic infections like scabies should be considered. In young infants, empiric antibiotic treatment may be started until cultures are finalized. If there is a family history of pruritic papules and pustules, scabies should be considered. A scabies prep can be done to rule out this entity.
Langerhans cell histiocytosis can also present with pustules and papules in early infancy and also has a predilection for the scalp. When this condition is in question, a skin biopsy should be performed which shows a CD1 positive histiocytic infiltrate.
In conclusion, EPFI is a benign rare condition that can present in infants as recurrent pustules and papules, mainly on the scalp, which are self-limited and if symptomatic can be treated with topical corticosteroids and antihistamines.
References
Alonso-Castro L et al. Dermatol Online J. 2012 Oct 15;18(10):6.
Frølunde AS et al. Clin Case Rep. 2021 May 11;9(5):e04167.
Hernández-Martín Á et al. J Am Acad Dermatol. 2013 Jan;68(1):150-5.
The bacterial, fungal, and atypical mycobacterial cultures from the lesions performed at the emergency department were all negative.
Pediatric dermatology was consulted and a punch biopsy of one of the lesions was done. Histopathologic examination showed a mixed perifollicular infiltrate of predominantly eosinophils with some neutrophils and associated microabscesses. Periodic acid Schiff and Fite stains failed to reveal any organisms. CD1 immunostain was negative. Fresh tissue cultures for bacteria, fungi, and atypical mycobacteria were negative.
Given the clinical presentation of chronic recurrent sterile pustules on an infant with associated eosinophilia and the reported histopathologic findings, the patient was diagnosed with eosinophilic pustular folliculitis of infancy (EPFI).
EPFI is a rare and idiopathic cutaneous disorder present in children. About 70% of the cases reported occur in the first 6 month of life and rarely present past 3 years of age. EPF encompasses a group of conditions including the classic adult form, or Ofuji disease. EPF is seen in immunosuppressed patients, mainly HIV positive, and EPF is also seen in infants and children.
In EPFI, males are most commonly affected. The condition presents, as it did in our patient, with recurrent crops of sterile papules and pustules mainly on the scalp, but they can occur in other parts of the body. The lesions go away within a few weeks to months without leaving any scars but it can take months to years to resolve. Histopathologic analysis of the lesions show an eosinophilic infiltrate which can be follicular, perifollicular, or periadnexal with associated flame figures in about 26% of cases.
Aggressive treatment is usually not needed as lesions are self-limited. Lesions can be treated with topical corticosteroids and oral antihistamine medications like cetirizine if symptomatic.
If the lesions start to present during the neonatal period, one may consider in the differential diagnosis, neonatal rashes like transient neonatal pustular melanosis and erythema toxicum neonatorum. Both of these neonatal conditions tend to resolve in the first month of life, compared with EPFI where lesions can come and go for months to years. EPFI lesions can be described as pustules and inflammatory papules, as well as furuncles and vesicles. All of the lesions may be seen in one patient at one time, which will not be typical for transient neonatal pustular melanosis or erythema toxicum. Eosinophils can be seen in erythema toxicum but folliculitis is not present. The inflammatory infiltrate seen in transient neonatal pustular melanosis is polymorphonuclear, not eosinophilic.
Early in the presentation, infectious conditions like staphylococcal or streptococcal folliculitis, cellulitis and furunculosis, tinea capitis, atypical mycobacterial infections, herpes simplex, and parasitic infections like scabies should be considered. In young infants, empiric antibiotic treatment may be started until cultures are finalized. If there is a family history of pruritic papules and pustules, scabies should be considered. A scabies prep can be done to rule out this entity.
Langerhans cell histiocytosis can also present with pustules and papules in early infancy and also has a predilection for the scalp. When this condition is in question, a skin biopsy should be performed which shows a CD1 positive histiocytic infiltrate.
In conclusion, EPFI is a benign rare condition that can present in infants as recurrent pustules and papules, mainly on the scalp, which are self-limited and if symptomatic can be treated with topical corticosteroids and antihistamines.
References
Alonso-Castro L et al. Dermatol Online J. 2012 Oct 15;18(10):6.
Frølunde AS et al. Clin Case Rep. 2021 May 11;9(5):e04167.
Hernández-Martín Á et al. J Am Acad Dermatol. 2013 Jan;68(1):150-5.
The bacterial, fungal, and atypical mycobacterial cultures from the lesions performed at the emergency department were all negative.
Pediatric dermatology was consulted and a punch biopsy of one of the lesions was done. Histopathologic examination showed a mixed perifollicular infiltrate of predominantly eosinophils with some neutrophils and associated microabscesses. Periodic acid Schiff and Fite stains failed to reveal any organisms. CD1 immunostain was negative. Fresh tissue cultures for bacteria, fungi, and atypical mycobacteria were negative.
Given the clinical presentation of chronic recurrent sterile pustules on an infant with associated eosinophilia and the reported histopathologic findings, the patient was diagnosed with eosinophilic pustular folliculitis of infancy (EPFI).
EPFI is a rare and idiopathic cutaneous disorder present in children. About 70% of the cases reported occur in the first 6 month of life and rarely present past 3 years of age. EPF encompasses a group of conditions including the classic adult form, or Ofuji disease. EPF is seen in immunosuppressed patients, mainly HIV positive, and EPF is also seen in infants and children.
In EPFI, males are most commonly affected. The condition presents, as it did in our patient, with recurrent crops of sterile papules and pustules mainly on the scalp, but they can occur in other parts of the body. The lesions go away within a few weeks to months without leaving any scars but it can take months to years to resolve. Histopathologic analysis of the lesions show an eosinophilic infiltrate which can be follicular, perifollicular, or periadnexal with associated flame figures in about 26% of cases.
Aggressive treatment is usually not needed as lesions are self-limited. Lesions can be treated with topical corticosteroids and oral antihistamine medications like cetirizine if symptomatic.
If the lesions start to present during the neonatal period, one may consider in the differential diagnosis, neonatal rashes like transient neonatal pustular melanosis and erythema toxicum neonatorum. Both of these neonatal conditions tend to resolve in the first month of life, compared with EPFI where lesions can come and go for months to years. EPFI lesions can be described as pustules and inflammatory papules, as well as furuncles and vesicles. All of the lesions may be seen in one patient at one time, which will not be typical for transient neonatal pustular melanosis or erythema toxicum. Eosinophils can be seen in erythema toxicum but folliculitis is not present. The inflammatory infiltrate seen in transient neonatal pustular melanosis is polymorphonuclear, not eosinophilic.
Early in the presentation, infectious conditions like staphylococcal or streptococcal folliculitis, cellulitis and furunculosis, tinea capitis, atypical mycobacterial infections, herpes simplex, and parasitic infections like scabies should be considered. In young infants, empiric antibiotic treatment may be started until cultures are finalized. If there is a family history of pruritic papules and pustules, scabies should be considered. A scabies prep can be done to rule out this entity.
Langerhans cell histiocytosis can also present with pustules and papules in early infancy and also has a predilection for the scalp. When this condition is in question, a skin biopsy should be performed which shows a CD1 positive histiocytic infiltrate.
In conclusion, EPFI is a benign rare condition that can present in infants as recurrent pustules and papules, mainly on the scalp, which are self-limited and if symptomatic can be treated with topical corticosteroids and antihistamines.
References
Alonso-Castro L et al. Dermatol Online J. 2012 Oct 15;18(10):6.
Frølunde AS et al. Clin Case Rep. 2021 May 11;9(5):e04167.
Hernández-Martín Á et al. J Am Acad Dermatol. 2013 Jan;68(1):150-5.
A 7-month-old male is brought to the emergency department for evaluation of pustules and inflamed papules on the scalp and extremities for several weeks of duration. The parents report the lesions started about a month prior and he has already been treated with cephalexin, clindamycin, and sulfamethoxazole without any improvement. Cultures sent prior by the child's pediatrician did not reveal any fungus or bacteria. The parents report a low-grade fever for about 3 days.
He was born via natural vaginal delivery with no instrumentation or external monitoring. Mom had prenatal care. Besides the skin lesions, the baby has been healthy and growing well. He has no history of eczema or severe infections. He has not been hospitalized before.
On physical examination the baby was not febrile. On the scalp and forehead, he had diffusely distributed pustules, erythematous papules, and nodules. He also presented with scattered, fine, small, crusted 1-2-mm pink papules on the trunk and extremities. He had no adenopathy or hepatosplenomegaly.
At the emergency department, samples from one of the pustules were sent for bacterial, fungal, and atypical mycobacteria cultures. Laboratory test showed a normal blood count with associated eosinophilia (2.8 x 109 L), and normal liver and kidney function. A head ultrasound showed three ill-defined hypoechoic foci within the scalp.
The patient was admitted for treatment with broad-spectrum antibiotics and dermatology was consulted.
Neuropsychiatric side effects of hormonal contraceptives: More common than you think!
Since its introduction in 1950, the combined oral contraceptive pill has been used by countless women as a method for birth control (Liao P. Can Fam Physician. 2012 Dec; 58[12]:e757-e760).
Hormonal contraception (HC) provides women with both contraceptive and noncontraceptive benefits, most notably a method for avoiding unintended pregnancy. In addition to being an effective method of contraception, oral contraceptive pills (OCPs) are well established for treating conditions such as hirsutism, pain symptoms associated with endometriosis and adenomyosis, and pelvic inflammatory disease, among others (Schindler A. Int J Endocrinol Metab. 2013 Winter;11[1]:41-7).
Combined hormonal contraceptives are also first-line treatment for women with menstrual disorders, and in women with polycystic ovary syndrome, can offer an effective long-term method to regulate their menstrual cycle, decrease androgens, clear up oily skin and acne, and reduce facial hair while also providing them with effective contraception (de Melo et al. Open Access J Contracept. 2017;8:13-23).
Associations between ‘the pill’ and mood effects remain controversial
More than 100 million women worldwide use hormonal contraceptives today, yet despite this, the data are mixed regarding the prevalence and extent of neuropsychiatric symptoms and mood changes associated with use of “the pill.” Some studies show combined oral contraceptives are associated with a decrease in general well-being, but had no effect on depression, in women compared with placebo (Zethraeus N et al. Fertil Steril. 2017 May;107[5]:1238-45).
However, a large Danish study published in JAMA Psychiatry of more than 1 million women found a significant association between use of hormonal contraception and antidepressant use or first diagnosis of depression, with adolescents having a higher rate of first depression diagnosis and antidepressant use compared with women 20–30 years old (Skovlund C et al. JAMA Psychiatry. 2016 Nov 1;73[11]:1154-62).
Studies have also shown long-term exposure to levonorgestrel is significantly associated with anxiety and sleep problems in women without a history of these issues (Slattery J et al. Drug Saf. 2018 Oct;41[10]:951-8). A recent small nationwide cohort study in France suggests this may also be true of levonorgestrel delivered by intrauterine devices (IUD) and the association may be dose-dependent (Roland N et al. JAMA. 2023;329[3]:257-9).
Of note, a study published in the American Journal of Psychiatry found a nearly twofold risk of suicide attempt and over threefold risk of suicide among women taking hormonal contraception compared with women who had never used hormonal contraceptives (Skovlund et al. Am J Psychiatry. 2017 Nov 17:appiajp201717060616).
Knowledge gaps make drawing conclusions difficult
The latest information on use of antidepressant and antianxiety medications in women of reproductive age (18-44 years) is sparse and, in some cases, outdated. According to data from the National Health and Nutrition Examination Survey, 18.6% of adult women 18 years or older reported using antidepressant medications within the last 30 days in 2017-2018, an increase from 13.8% in 2009-2010. Among women aged 15-44 year with private employer–sponsored insurance surveyed during 2008-2013, the results showed 15.4% of women filled a prescription for an antidepressant. We must look back further to find data on antianxiety medication use among women aged 18-44 years where use of antianxiety drugs (anxiolytics, sedatives, and hypnotics) was 4.3% between 2005 and 2008.
A lack of literature in this area is likely due to significant underreporting, and an inability to select patients who are sensitive to or at risk of developing neuropsychiatric symptoms resulting from hormonal contraception use because the true pathophysiology is unknown. Existing studies tend to use varying methods to assess mood changes, and do not usually specify hormonal contraceptive use type in their analyses (Schaffir J et al. Eur J Contracept Reprod Health Care. 2016 Oct;21[5]:347-55).
Studies of this nature also require large sample sizes, but the percentage of women who develop neuropsychiatric symptoms from hormonal contraceptive use has historically been relatively small. In the late 1990s, Rosenberg and colleagues found 46% of 1,657 women discontinued oral contraceptives due to side effects within 6 months of starting a new prescription; of these women, 5% reported mood changes as their reason for discontinuing oral contraceptives (Rosenberg M et al. Am J Obstet Gynecol. 1998 Sep;179[3 Pt 1]:577-82).
One might expect that, as lower dosage combined hormonal contraceptives were developed in the 1980s, that the rate of reporting psychological side effects would continue to decrease as well. Yet greater awareness of the potential for mood changes while on “the pill” as outlined by the lay press and social media may be leading to increased reporting of neuropsychiatric effects in women. In a recent cross-sectional survey of 188 women in New York, 43.6% said they experienced mood changes while on hormonal contraceptives, and 61.2% of women with histories of psychiatric illness reported mood changes they attributed to hormonal contraceptives (Martell S et al. Contracept Reprod Med. 2023;8:9).
Martell and colleagues found 48.3% of women cited side effects as a reason for discontinuing hormonal contraception, and 43 participants mentioned psychological side effects unprompted, including 2 patients with suicidal thoughts. The authors said this suggests “psychological side effects, at least in part, may have impacted” HC users’ decisions to switch from OCPs to an alternative method of contraception.
It is also not clear what risk factors exist for women who develop neuropsychiatric symptoms from hormonal contraceptive use. First, it is important to note that both progestin-only contraceptives and combined hormonal contraceptives are classified by the Centers for Disease Control and Prevention’s US Medical Eligibility Criteria for Contraceptive Use, 2016 as having no restrictions for use, including among patients with depression. While women in a smaller subgroup have significant neuropsychiatric symptoms related to their hormonal contraceptives, the underlying mechanism is unknown, and is thought to be largely related to the progestogen component of combined hormonal contraceptives or progestogen-only contraceptives (Mu E. Aust Prescr. 2022 Jun; 45[3]:75-9). We know that some women are hormone sensitive, while others are less so, and some not at all. Progestogens could affect mood as a direct action of the progestogen, because progestogens can be neurosteroids, or the progestogen effect could be mediated secondarily through a change in that woman’s own production of or bioavailability of androgens or naturally occurring estrogens (Giatti S. J Mol Endocrinol. 2016 Aug;57[2]:R109-26).
Here, we also find that currently available evidence limits our ability to draw firm conclusions. A study by Berry-Bibee and colleagues found a “low concern for clinically significant interactions” between hormonal contraception and psychotropic drugs, but was limited by quality/quantity of evidence (Berry-Bibee E et al. Contraception. 2016 Dec;94[6]:650-67). Interestingly, a study by Robinson and colleagues from the mid-2000s posited based on low evidence that “psychological response to the practice of contraception” was a potential explanation for the side effect profile of hormonal contraception (Robinson S et al. Med Hypotheses. 2004;63[2]:268-73).
Further, it may be that women with premenstrual dysphoric disorder (PMDD) might be selected for oral contraceptives, and they are predisposed to other neuropsychiatric problems. Estimates have placed the prevalence of comorbid psychiatric disorders such as anxiety, major depression, bipolar disorder, and posttraumatic stress disorder as high as 70% for women with PMDD (Sepede G et al. Neuropsychiatr Dis Treat. 2020;16:415-26). This phenomenon is not new, having been characterized in the lay literature nearly 20 years ago, by endocrinologist Geoffrey P. Redmond, MD (Redmond GP. The Hormonally Vulnerable Woman. New York: HarperCollins; 2005).
While the cause is not exactly idiosyncratic, They tend to have an entire spectrum of responses to the progestogens in combined or progestin-only contraceptives, ranging from just a flattened affect – which could easily be explained by their flattened level of endogenous hormones – to frank depression. Their frank depression, in turn, can be demonstrated to include suicidal ideation and actual suicide.
Compounding this issue is a woman’s perception of her sexuality. Some women with low sexual desire or sexual problems who are younger may have more distress about their problems compared with women of older reproductive age. While the reason for that is not clear, it may be that in the sexual arena, it is more important for some younger women to be a sexual person than in perimenopausal women, or that women who are younger are more likely to be partnered than women of older reproductive age. While the European Society of Sexual Medicine concluded in a 2019 position statement that there is inconclusive evidence whether hormonal contraception may be contributing to changes in sexual desire and sexual dysfunction, it appears that “a minority of women” experience “better or worse sexual functioning” from taking combined oral contraceptives (Both S et al. J Sex Med. 2019 Nov;16[11]:1681-95), suggesting that the majority of women report no significant changes.
Practitioners should discuss mood effects during consultation
An ob.gyn., primary care physicians, or others with prescriptive authority (i.e. nurse practitioners and physician assistants) in clinical practice may encounter a patient who seems to have mood side effects owing to progestogen-containing contraceptives that they prescribe. However, many ob.gyns. are likely unaware of the prevalence, or that some of those same patients can have such significant mood effects that they would become or are suicidal.
I believe questioning patients about mood effects during consultation and particularly during follow-up following the initiation of any hormonal contraceptive is worth a passing comment for every patient, which should include mood effects in broader discussion for anyone currently using an antidepressant, patients with a history of antidepressant use, and patients who have considered suicide. As we do with other drugs, these questions can be posed in the form of a questionnaire followed up by the practitioner in counseling.
Practitioners who encounter a patient with mood changes as a result of hormonal contraceptive use can consider changing to a nonhormonal method of birth control, or recommending the patient use a barrier method during sexual activity, as none of these options have neuropsychiatric side effects.
Ultimately, practitioners of all types need to engage in shared decision-making to identify the key benefits and risks of hormonal contraceptive use for each patient, which may involve trial and error to determine the ideal treatment. It is critical that practitioners of all types strike a balance between alleviating patient concerns about potential mood changes, monitoring patients with an appreciable risk of mood changes, and continuing patients on hormonal contraception for whom the benefits outweigh the risks.
Dr. Simon is a clinical professor at George Washington University and the medical director and founder of IntimMedicine Specialists in Washington, which provides patient-focused care for women across the reproductive life cycle. He is a past president of the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Dr. Simon has been a consultant to, received grant and research support from, and served on the speakers bureau for various pharmaceutical companies that develop combination hormonal contraceptives. Email Dr. Simon at [email protected].
Since its introduction in 1950, the combined oral contraceptive pill has been used by countless women as a method for birth control (Liao P. Can Fam Physician. 2012 Dec; 58[12]:e757-e760).
Hormonal contraception (HC) provides women with both contraceptive and noncontraceptive benefits, most notably a method for avoiding unintended pregnancy. In addition to being an effective method of contraception, oral contraceptive pills (OCPs) are well established for treating conditions such as hirsutism, pain symptoms associated with endometriosis and adenomyosis, and pelvic inflammatory disease, among others (Schindler A. Int J Endocrinol Metab. 2013 Winter;11[1]:41-7).
Combined hormonal contraceptives are also first-line treatment for women with menstrual disorders, and in women with polycystic ovary syndrome, can offer an effective long-term method to regulate their menstrual cycle, decrease androgens, clear up oily skin and acne, and reduce facial hair while also providing them with effective contraception (de Melo et al. Open Access J Contracept. 2017;8:13-23).
Associations between ‘the pill’ and mood effects remain controversial
More than 100 million women worldwide use hormonal contraceptives today, yet despite this, the data are mixed regarding the prevalence and extent of neuropsychiatric symptoms and mood changes associated with use of “the pill.” Some studies show combined oral contraceptives are associated with a decrease in general well-being, but had no effect on depression, in women compared with placebo (Zethraeus N et al. Fertil Steril. 2017 May;107[5]:1238-45).
However, a large Danish study published in JAMA Psychiatry of more than 1 million women found a significant association between use of hormonal contraception and antidepressant use or first diagnosis of depression, with adolescents having a higher rate of first depression diagnosis and antidepressant use compared with women 20–30 years old (Skovlund C et al. JAMA Psychiatry. 2016 Nov 1;73[11]:1154-62).
Studies have also shown long-term exposure to levonorgestrel is significantly associated with anxiety and sleep problems in women without a history of these issues (Slattery J et al. Drug Saf. 2018 Oct;41[10]:951-8). A recent small nationwide cohort study in France suggests this may also be true of levonorgestrel delivered by intrauterine devices (IUD) and the association may be dose-dependent (Roland N et al. JAMA. 2023;329[3]:257-9).
Of note, a study published in the American Journal of Psychiatry found a nearly twofold risk of suicide attempt and over threefold risk of suicide among women taking hormonal contraception compared with women who had never used hormonal contraceptives (Skovlund et al. Am J Psychiatry. 2017 Nov 17:appiajp201717060616).
Knowledge gaps make drawing conclusions difficult
The latest information on use of antidepressant and antianxiety medications in women of reproductive age (18-44 years) is sparse and, in some cases, outdated. According to data from the National Health and Nutrition Examination Survey, 18.6% of adult women 18 years or older reported using antidepressant medications within the last 30 days in 2017-2018, an increase from 13.8% in 2009-2010. Among women aged 15-44 year with private employer–sponsored insurance surveyed during 2008-2013, the results showed 15.4% of women filled a prescription for an antidepressant. We must look back further to find data on antianxiety medication use among women aged 18-44 years where use of antianxiety drugs (anxiolytics, sedatives, and hypnotics) was 4.3% between 2005 and 2008.
A lack of literature in this area is likely due to significant underreporting, and an inability to select patients who are sensitive to or at risk of developing neuropsychiatric symptoms resulting from hormonal contraception use because the true pathophysiology is unknown. Existing studies tend to use varying methods to assess mood changes, and do not usually specify hormonal contraceptive use type in their analyses (Schaffir J et al. Eur J Contracept Reprod Health Care. 2016 Oct;21[5]:347-55).
Studies of this nature also require large sample sizes, but the percentage of women who develop neuropsychiatric symptoms from hormonal contraceptive use has historically been relatively small. In the late 1990s, Rosenberg and colleagues found 46% of 1,657 women discontinued oral contraceptives due to side effects within 6 months of starting a new prescription; of these women, 5% reported mood changes as their reason for discontinuing oral contraceptives (Rosenberg M et al. Am J Obstet Gynecol. 1998 Sep;179[3 Pt 1]:577-82).
One might expect that, as lower dosage combined hormonal contraceptives were developed in the 1980s, that the rate of reporting psychological side effects would continue to decrease as well. Yet greater awareness of the potential for mood changes while on “the pill” as outlined by the lay press and social media may be leading to increased reporting of neuropsychiatric effects in women. In a recent cross-sectional survey of 188 women in New York, 43.6% said they experienced mood changes while on hormonal contraceptives, and 61.2% of women with histories of psychiatric illness reported mood changes they attributed to hormonal contraceptives (Martell S et al. Contracept Reprod Med. 2023;8:9).
Martell and colleagues found 48.3% of women cited side effects as a reason for discontinuing hormonal contraception, and 43 participants mentioned psychological side effects unprompted, including 2 patients with suicidal thoughts. The authors said this suggests “psychological side effects, at least in part, may have impacted” HC users’ decisions to switch from OCPs to an alternative method of contraception.
It is also not clear what risk factors exist for women who develop neuropsychiatric symptoms from hormonal contraceptive use. First, it is important to note that both progestin-only contraceptives and combined hormonal contraceptives are classified by the Centers for Disease Control and Prevention’s US Medical Eligibility Criteria for Contraceptive Use, 2016 as having no restrictions for use, including among patients with depression. While women in a smaller subgroup have significant neuropsychiatric symptoms related to their hormonal contraceptives, the underlying mechanism is unknown, and is thought to be largely related to the progestogen component of combined hormonal contraceptives or progestogen-only contraceptives (Mu E. Aust Prescr. 2022 Jun; 45[3]:75-9). We know that some women are hormone sensitive, while others are less so, and some not at all. Progestogens could affect mood as a direct action of the progestogen, because progestogens can be neurosteroids, or the progestogen effect could be mediated secondarily through a change in that woman’s own production of or bioavailability of androgens or naturally occurring estrogens (Giatti S. J Mol Endocrinol. 2016 Aug;57[2]:R109-26).
Here, we also find that currently available evidence limits our ability to draw firm conclusions. A study by Berry-Bibee and colleagues found a “low concern for clinically significant interactions” between hormonal contraception and psychotropic drugs, but was limited by quality/quantity of evidence (Berry-Bibee E et al. Contraception. 2016 Dec;94[6]:650-67). Interestingly, a study by Robinson and colleagues from the mid-2000s posited based on low evidence that “psychological response to the practice of contraception” was a potential explanation for the side effect profile of hormonal contraception (Robinson S et al. Med Hypotheses. 2004;63[2]:268-73).
Further, it may be that women with premenstrual dysphoric disorder (PMDD) might be selected for oral contraceptives, and they are predisposed to other neuropsychiatric problems. Estimates have placed the prevalence of comorbid psychiatric disorders such as anxiety, major depression, bipolar disorder, and posttraumatic stress disorder as high as 70% for women with PMDD (Sepede G et al. Neuropsychiatr Dis Treat. 2020;16:415-26). This phenomenon is not new, having been characterized in the lay literature nearly 20 years ago, by endocrinologist Geoffrey P. Redmond, MD (Redmond GP. The Hormonally Vulnerable Woman. New York: HarperCollins; 2005).
While the cause is not exactly idiosyncratic, They tend to have an entire spectrum of responses to the progestogens in combined or progestin-only contraceptives, ranging from just a flattened affect – which could easily be explained by their flattened level of endogenous hormones – to frank depression. Their frank depression, in turn, can be demonstrated to include suicidal ideation and actual suicide.
Compounding this issue is a woman’s perception of her sexuality. Some women with low sexual desire or sexual problems who are younger may have more distress about their problems compared with women of older reproductive age. While the reason for that is not clear, it may be that in the sexual arena, it is more important for some younger women to be a sexual person than in perimenopausal women, or that women who are younger are more likely to be partnered than women of older reproductive age. While the European Society of Sexual Medicine concluded in a 2019 position statement that there is inconclusive evidence whether hormonal contraception may be contributing to changes in sexual desire and sexual dysfunction, it appears that “a minority of women” experience “better or worse sexual functioning” from taking combined oral contraceptives (Both S et al. J Sex Med. 2019 Nov;16[11]:1681-95), suggesting that the majority of women report no significant changes.
Practitioners should discuss mood effects during consultation
An ob.gyn., primary care physicians, or others with prescriptive authority (i.e. nurse practitioners and physician assistants) in clinical practice may encounter a patient who seems to have mood side effects owing to progestogen-containing contraceptives that they prescribe. However, many ob.gyns. are likely unaware of the prevalence, or that some of those same patients can have such significant mood effects that they would become or are suicidal.
I believe questioning patients about mood effects during consultation and particularly during follow-up following the initiation of any hormonal contraceptive is worth a passing comment for every patient, which should include mood effects in broader discussion for anyone currently using an antidepressant, patients with a history of antidepressant use, and patients who have considered suicide. As we do with other drugs, these questions can be posed in the form of a questionnaire followed up by the practitioner in counseling.
Practitioners who encounter a patient with mood changes as a result of hormonal contraceptive use can consider changing to a nonhormonal method of birth control, or recommending the patient use a barrier method during sexual activity, as none of these options have neuropsychiatric side effects.
Ultimately, practitioners of all types need to engage in shared decision-making to identify the key benefits and risks of hormonal contraceptive use for each patient, which may involve trial and error to determine the ideal treatment. It is critical that practitioners of all types strike a balance between alleviating patient concerns about potential mood changes, monitoring patients with an appreciable risk of mood changes, and continuing patients on hormonal contraception for whom the benefits outweigh the risks.
Dr. Simon is a clinical professor at George Washington University and the medical director and founder of IntimMedicine Specialists in Washington, which provides patient-focused care for women across the reproductive life cycle. He is a past president of the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Dr. Simon has been a consultant to, received grant and research support from, and served on the speakers bureau for various pharmaceutical companies that develop combination hormonal contraceptives. Email Dr. Simon at [email protected].
Since its introduction in 1950, the combined oral contraceptive pill has been used by countless women as a method for birth control (Liao P. Can Fam Physician. 2012 Dec; 58[12]:e757-e760).
Hormonal contraception (HC) provides women with both contraceptive and noncontraceptive benefits, most notably a method for avoiding unintended pregnancy. In addition to being an effective method of contraception, oral contraceptive pills (OCPs) are well established for treating conditions such as hirsutism, pain symptoms associated with endometriosis and adenomyosis, and pelvic inflammatory disease, among others (Schindler A. Int J Endocrinol Metab. 2013 Winter;11[1]:41-7).
Combined hormonal contraceptives are also first-line treatment for women with menstrual disorders, and in women with polycystic ovary syndrome, can offer an effective long-term method to regulate their menstrual cycle, decrease androgens, clear up oily skin and acne, and reduce facial hair while also providing them with effective contraception (de Melo et al. Open Access J Contracept. 2017;8:13-23).
Associations between ‘the pill’ and mood effects remain controversial
More than 100 million women worldwide use hormonal contraceptives today, yet despite this, the data are mixed regarding the prevalence and extent of neuropsychiatric symptoms and mood changes associated with use of “the pill.” Some studies show combined oral contraceptives are associated with a decrease in general well-being, but had no effect on depression, in women compared with placebo (Zethraeus N et al. Fertil Steril. 2017 May;107[5]:1238-45).
However, a large Danish study published in JAMA Psychiatry of more than 1 million women found a significant association between use of hormonal contraception and antidepressant use or first diagnosis of depression, with adolescents having a higher rate of first depression diagnosis and antidepressant use compared with women 20–30 years old (Skovlund C et al. JAMA Psychiatry. 2016 Nov 1;73[11]:1154-62).
Studies have also shown long-term exposure to levonorgestrel is significantly associated with anxiety and sleep problems in women without a history of these issues (Slattery J et al. Drug Saf. 2018 Oct;41[10]:951-8). A recent small nationwide cohort study in France suggests this may also be true of levonorgestrel delivered by intrauterine devices (IUD) and the association may be dose-dependent (Roland N et al. JAMA. 2023;329[3]:257-9).
Of note, a study published in the American Journal of Psychiatry found a nearly twofold risk of suicide attempt and over threefold risk of suicide among women taking hormonal contraception compared with women who had never used hormonal contraceptives (Skovlund et al. Am J Psychiatry. 2017 Nov 17:appiajp201717060616).
Knowledge gaps make drawing conclusions difficult
The latest information on use of antidepressant and antianxiety medications in women of reproductive age (18-44 years) is sparse and, in some cases, outdated. According to data from the National Health and Nutrition Examination Survey, 18.6% of adult women 18 years or older reported using antidepressant medications within the last 30 days in 2017-2018, an increase from 13.8% in 2009-2010. Among women aged 15-44 year with private employer–sponsored insurance surveyed during 2008-2013, the results showed 15.4% of women filled a prescription for an antidepressant. We must look back further to find data on antianxiety medication use among women aged 18-44 years where use of antianxiety drugs (anxiolytics, sedatives, and hypnotics) was 4.3% between 2005 and 2008.
A lack of literature in this area is likely due to significant underreporting, and an inability to select patients who are sensitive to or at risk of developing neuropsychiatric symptoms resulting from hormonal contraception use because the true pathophysiology is unknown. Existing studies tend to use varying methods to assess mood changes, and do not usually specify hormonal contraceptive use type in their analyses (Schaffir J et al. Eur J Contracept Reprod Health Care. 2016 Oct;21[5]:347-55).
Studies of this nature also require large sample sizes, but the percentage of women who develop neuropsychiatric symptoms from hormonal contraceptive use has historically been relatively small. In the late 1990s, Rosenberg and colleagues found 46% of 1,657 women discontinued oral contraceptives due to side effects within 6 months of starting a new prescription; of these women, 5% reported mood changes as their reason for discontinuing oral contraceptives (Rosenberg M et al. Am J Obstet Gynecol. 1998 Sep;179[3 Pt 1]:577-82).
One might expect that, as lower dosage combined hormonal contraceptives were developed in the 1980s, that the rate of reporting psychological side effects would continue to decrease as well. Yet greater awareness of the potential for mood changes while on “the pill” as outlined by the lay press and social media may be leading to increased reporting of neuropsychiatric effects in women. In a recent cross-sectional survey of 188 women in New York, 43.6% said they experienced mood changes while on hormonal contraceptives, and 61.2% of women with histories of psychiatric illness reported mood changes they attributed to hormonal contraceptives (Martell S et al. Contracept Reprod Med. 2023;8:9).
Martell and colleagues found 48.3% of women cited side effects as a reason for discontinuing hormonal contraception, and 43 participants mentioned psychological side effects unprompted, including 2 patients with suicidal thoughts. The authors said this suggests “psychological side effects, at least in part, may have impacted” HC users’ decisions to switch from OCPs to an alternative method of contraception.
It is also not clear what risk factors exist for women who develop neuropsychiatric symptoms from hormonal contraceptive use. First, it is important to note that both progestin-only contraceptives and combined hormonal contraceptives are classified by the Centers for Disease Control and Prevention’s US Medical Eligibility Criteria for Contraceptive Use, 2016 as having no restrictions for use, including among patients with depression. While women in a smaller subgroup have significant neuropsychiatric symptoms related to their hormonal contraceptives, the underlying mechanism is unknown, and is thought to be largely related to the progestogen component of combined hormonal contraceptives or progestogen-only contraceptives (Mu E. Aust Prescr. 2022 Jun; 45[3]:75-9). We know that some women are hormone sensitive, while others are less so, and some not at all. Progestogens could affect mood as a direct action of the progestogen, because progestogens can be neurosteroids, or the progestogen effect could be mediated secondarily through a change in that woman’s own production of or bioavailability of androgens or naturally occurring estrogens (Giatti S. J Mol Endocrinol. 2016 Aug;57[2]:R109-26).
Here, we also find that currently available evidence limits our ability to draw firm conclusions. A study by Berry-Bibee and colleagues found a “low concern for clinically significant interactions” between hormonal contraception and psychotropic drugs, but was limited by quality/quantity of evidence (Berry-Bibee E et al. Contraception. 2016 Dec;94[6]:650-67). Interestingly, a study by Robinson and colleagues from the mid-2000s posited based on low evidence that “psychological response to the practice of contraception” was a potential explanation for the side effect profile of hormonal contraception (Robinson S et al. Med Hypotheses. 2004;63[2]:268-73).
Further, it may be that women with premenstrual dysphoric disorder (PMDD) might be selected for oral contraceptives, and they are predisposed to other neuropsychiatric problems. Estimates have placed the prevalence of comorbid psychiatric disorders such as anxiety, major depression, bipolar disorder, and posttraumatic stress disorder as high as 70% for women with PMDD (Sepede G et al. Neuropsychiatr Dis Treat. 2020;16:415-26). This phenomenon is not new, having been characterized in the lay literature nearly 20 years ago, by endocrinologist Geoffrey P. Redmond, MD (Redmond GP. The Hormonally Vulnerable Woman. New York: HarperCollins; 2005).
While the cause is not exactly idiosyncratic, They tend to have an entire spectrum of responses to the progestogens in combined or progestin-only contraceptives, ranging from just a flattened affect – which could easily be explained by their flattened level of endogenous hormones – to frank depression. Their frank depression, in turn, can be demonstrated to include suicidal ideation and actual suicide.
Compounding this issue is a woman’s perception of her sexuality. Some women with low sexual desire or sexual problems who are younger may have more distress about their problems compared with women of older reproductive age. While the reason for that is not clear, it may be that in the sexual arena, it is more important for some younger women to be a sexual person than in perimenopausal women, or that women who are younger are more likely to be partnered than women of older reproductive age. While the European Society of Sexual Medicine concluded in a 2019 position statement that there is inconclusive evidence whether hormonal contraception may be contributing to changes in sexual desire and sexual dysfunction, it appears that “a minority of women” experience “better or worse sexual functioning” from taking combined oral contraceptives (Both S et al. J Sex Med. 2019 Nov;16[11]:1681-95), suggesting that the majority of women report no significant changes.
Practitioners should discuss mood effects during consultation
An ob.gyn., primary care physicians, or others with prescriptive authority (i.e. nurse practitioners and physician assistants) in clinical practice may encounter a patient who seems to have mood side effects owing to progestogen-containing contraceptives that they prescribe. However, many ob.gyns. are likely unaware of the prevalence, or that some of those same patients can have such significant mood effects that they would become or are suicidal.
I believe questioning patients about mood effects during consultation and particularly during follow-up following the initiation of any hormonal contraceptive is worth a passing comment for every patient, which should include mood effects in broader discussion for anyone currently using an antidepressant, patients with a history of antidepressant use, and patients who have considered suicide. As we do with other drugs, these questions can be posed in the form of a questionnaire followed up by the practitioner in counseling.
Practitioners who encounter a patient with mood changes as a result of hormonal contraceptive use can consider changing to a nonhormonal method of birth control, or recommending the patient use a barrier method during sexual activity, as none of these options have neuropsychiatric side effects.
Ultimately, practitioners of all types need to engage in shared decision-making to identify the key benefits and risks of hormonal contraceptive use for each patient, which may involve trial and error to determine the ideal treatment. It is critical that practitioners of all types strike a balance between alleviating patient concerns about potential mood changes, monitoring patients with an appreciable risk of mood changes, and continuing patients on hormonal contraception for whom the benefits outweigh the risks.
Dr. Simon is a clinical professor at George Washington University and the medical director and founder of IntimMedicine Specialists in Washington, which provides patient-focused care for women across the reproductive life cycle. He is a past president of the International Society for the Study of Women’s Sexual Health and the North American Menopause Society. Dr. Simon has been a consultant to, received grant and research support from, and served on the speakers bureau for various pharmaceutical companies that develop combination hormonal contraceptives. Email Dr. Simon at [email protected].
ChatGPT as a tool in the ob.gyn. office
Artificial intelligence (AI) has recently gained significant public attention, primarily driven by the launch of a noteworthy program by OpenAI called Chat Generative Pre-trained Transformer (ChatGPT). This large language model is an AI system that enables users to interact with it using plain language. In just the first 2 months since its release, over 100 million subscribers have registered to use ChatGPT.
AI is now deeply integrated into our daily lives, pervading a wide array of smart devices such as phones, tablets, and numerous other gadgets that we rely on every day. These sophisticated technologies operate seamlessly in the background, often without us being consciously aware of their presence. Nevertheless, we greatly appreciate the way they enhance our lives by simplifying tasks and streamlining our routines.
A key factor contributing to ChatGPT’s popularity is its ability to accept input in the form of prompts in plain English. Our team published a comprehensive journal article showcasing examples of how this technology can be utilized by general ob.gyn. practitioners. ChatGPT has the potential to streamline work flow, generate letters to insurance companies, draft clinical plans, and assist with various other routine tasks in any ob.gyn. practice environment.
As with any new technology, it is essential for users to familiarize themselves with its capabilities and understand its limitations. A critical aspect to consider with the current version of ChatGPT is that it was developed using information primarily sourced from the Internet up until September 2021. This limitation is especially significant in the field of medicine, where practitioners consistently seek the most up-to-date and current information to inform their decisions.
However, it is expected that, in the near future, these programs will gain access to real-time information from a diverse range of sources, including but not limited to the Internet. This development will enhance the program’s utility and relevance in medical contexts.
Another limitation of ChatGPT is its propensity to “hallucinate.” Large language models are trained to respond to the best of their abilities, occasionally attempting to fill knowledge gaps with fabricated information. Being aware of these limitations enables users to recognize the program’s potential while also understanding the need for careful monitoring.
Our expertise and clinical knowledge are crucial in guiding and refining this technology, ensuring that it serves as a valuable tool in the ever-evolving landscape of medicine.
Another crucial factor to consider is that users must adhere to all guidelines and policies established within their work environment. This entails complying with HIPAA regulations and ensuring that any information generated by these programs is thoroughly examined before being integrated into practice work flows. As an increasing number of organizations develop specific guidelines for such technologies, the aim is to safeguard patients, users, and the organization itself. The individuals utilizing these technologies must exercise utmost caution and refrain from storing or sharing any sensitive or proprietary information.
The aim of this article is not to provide an exhaustive overview, but rather to offer a selection of examples and inspire readers to consider adopting these programs. By doing so, we hope to facilitate the exploration of innovative approaches that can improve the practice of ob.gyn.
The first example illustrates a common scenario that we frequently encounter – the situation in which an insurance company denies coverage for specific care or treatment for a patient. In fact, this was one of the first examples that was demonstrated by others on social media as a possible benefit for this technology. It effectively demonstrated the ability to save time and surmount the challenges of writer’s block that we occasionally encounter.
Prompt input:
“Write a letter to the insurance company who is denying cervical length surveillance for a patient with a short cervix and add references.”
ChatGPT response:
[Your Name]
[Your Address]
[City, State, Zip Code]
[Date]
[Insurance Company Name]
[Claims Department]
[Insurance Company Address]
[City, State, Zip Code]
Re: Request for Reconsideration – Cervical Length Surveillance
Policy Number: [Policy Number]
Insured: [Patient’s Name]
Date of Birth: [Patient’s Date of Birth]
Claim Number: [Claim Number]
Date of Service: [Date of Service]
Dear Claims Reviewer,
I am writing to request a reconsideration of the denial for cervical length surveillance for my patient, [Patient’s Name], who has been diagnosed with a short cervix. As a healthcare provider, I strongly believe that this is a medically necessary service for the patient in order to prevent preterm birth and its associated complications.
A short cervix is a well-established risk factor for preterm birth, and numerous studies have shown the efficacy of cervical length surveillance in the prevention and management of preterm birth. I kindly request that you reconsider the coverage for this essential service and refer to the following authoritative sources:
Berghella, V., & Saccone, G. (2019). Fetal fibronectin testing for reducing the risk of preterm birth. Cochrane Database of Systematic Reviews, 2019(7). doi:10.1002/14651858.CD004843.pub3
American College of Obstetricians and Gynecologists (2016). Practice Bulletin No. 171: Management of Preterm Labor. Obstetrics & Gynecology, 128(4), e155-e164. doi:10.1097/AOG.0000000000001711
Society for Maternal-Fetal Medicine (SMFM), McIntosh, J., Feltovich, H., Berghella, V., & Manuck, T. (2016). The role of routine cervical length screening in selected high- and low-risk women for preterm birth prevention. American Journal of Obstetrics & Gynecology, 215(3), B2-B7. doi:10.1016/j.ajog.2016.03.015
By denying coverage for cervical length surveillance, the insurance company is putting [Patient’s Name] at an increased risk for preterm birth and the numerous health complications that can accompany it, both for the mother and the infant. It is crucial to provide this service in order to improve health outcomes and reduce the risk of costly neonatal intensive care unit (NICU) admissions and long-term medical issues.
I kindly request that you review this case with the provided references and reconsider the coverage for cervical length surveillance for [Patient’s Name]. Thank you for your attention to this matter. Please feel free to contact me if you require any further information or clarification.
Sincerely,
[Your Name]
[Your Title]
[Your Phone Number]
[Your Email Address]
The document took less than 15 seconds to generate, it is well written and concise, and can also be utilized as a template for future use. But as mentioned above, it is important to confirm all the information within the document. For example, references 1 and 3 in the ChatGPT-generated letter above include document objective identifiers that do not correctly correspond to the reference.
Other uses that the reader might consider: patient education, helping to answer a patient question utilizing appropriate grade-level language, dietary plans for a patient - the potential list is endless. Another key aspect of utilizing these types of programs is understanding how to effectively ask a question. This involves providing ample detail about the inquiry you wish to have answered by the program. With some practice and review of guidance on how to do this from the Internet, one can become highly proficient at crafting questions and generating relevant responses. But as mentioned above, it is important to keep in mind that all information generated by this program needs to be vetted prior to utilization.
This groundbreaking technology is not only here to stay but will continue to become increasingly pervasive. It is already being integrated into conventional search engines such as Google and Bing. Microsoft has ambitious plans to incorporate this innovation into its entire suite of Office products. Just imagine working on a document and seeking assistance for editing or rephrasing, effortlessly searching your inbox for all emails containing a specific phrase or topic, or even crafting a PowerPoint presentation for a lecture while receiving help with both content and formatting. These scenarios offer just a glimpse of how AI programs can significantly assist and enhance our workflow.
I also anticipate that our patients will increasingly adopt this type of technology to generate customized lists of questions tailored to their specific medical conditions, which they can then ask their health care providers. Often, our patients express uncertainty about the appropriate questions to ask during a particular visit. Now envision a scenario in which they can effortlessly obtain a comprehensive list of relevant questions, specifically designed for their office consultation. This would empower them to engage more actively in their health care and enhance communication with their clinical team.
I highly recommend that readers explore and experiment with these programs. By doing so, we can provide valuable assistance and guidance not only within our specific medical specialties but also for our patients. In this way, we can effectively harness the power of technology to improve patient care and optimize our office work flow, ultimately benefiting both our patients and our practices.
Dr. Chavez is professor, department of obstetrics and gynecology, at NYU Long Island School of Medicine and director of maternal and fetal medicine at NYU Langone Hospital–Long Island, both in Mineola, N.Y. He has no disclosures.
Artificial intelligence (AI) has recently gained significant public attention, primarily driven by the launch of a noteworthy program by OpenAI called Chat Generative Pre-trained Transformer (ChatGPT). This large language model is an AI system that enables users to interact with it using plain language. In just the first 2 months since its release, over 100 million subscribers have registered to use ChatGPT.
AI is now deeply integrated into our daily lives, pervading a wide array of smart devices such as phones, tablets, and numerous other gadgets that we rely on every day. These sophisticated technologies operate seamlessly in the background, often without us being consciously aware of their presence. Nevertheless, we greatly appreciate the way they enhance our lives by simplifying tasks and streamlining our routines.
A key factor contributing to ChatGPT’s popularity is its ability to accept input in the form of prompts in plain English. Our team published a comprehensive journal article showcasing examples of how this technology can be utilized by general ob.gyn. practitioners. ChatGPT has the potential to streamline work flow, generate letters to insurance companies, draft clinical plans, and assist with various other routine tasks in any ob.gyn. practice environment.
As with any new technology, it is essential for users to familiarize themselves with its capabilities and understand its limitations. A critical aspect to consider with the current version of ChatGPT is that it was developed using information primarily sourced from the Internet up until September 2021. This limitation is especially significant in the field of medicine, where practitioners consistently seek the most up-to-date and current information to inform their decisions.
However, it is expected that, in the near future, these programs will gain access to real-time information from a diverse range of sources, including but not limited to the Internet. This development will enhance the program’s utility and relevance in medical contexts.
Another limitation of ChatGPT is its propensity to “hallucinate.” Large language models are trained to respond to the best of their abilities, occasionally attempting to fill knowledge gaps with fabricated information. Being aware of these limitations enables users to recognize the program’s potential while also understanding the need for careful monitoring.
Our expertise and clinical knowledge are crucial in guiding and refining this technology, ensuring that it serves as a valuable tool in the ever-evolving landscape of medicine.
Another crucial factor to consider is that users must adhere to all guidelines and policies established within their work environment. This entails complying with HIPAA regulations and ensuring that any information generated by these programs is thoroughly examined before being integrated into practice work flows. As an increasing number of organizations develop specific guidelines for such technologies, the aim is to safeguard patients, users, and the organization itself. The individuals utilizing these technologies must exercise utmost caution and refrain from storing or sharing any sensitive or proprietary information.
The aim of this article is not to provide an exhaustive overview, but rather to offer a selection of examples and inspire readers to consider adopting these programs. By doing so, we hope to facilitate the exploration of innovative approaches that can improve the practice of ob.gyn.
The first example illustrates a common scenario that we frequently encounter – the situation in which an insurance company denies coverage for specific care or treatment for a patient. In fact, this was one of the first examples that was demonstrated by others on social media as a possible benefit for this technology. It effectively demonstrated the ability to save time and surmount the challenges of writer’s block that we occasionally encounter.
Prompt input:
“Write a letter to the insurance company who is denying cervical length surveillance for a patient with a short cervix and add references.”
ChatGPT response:
[Your Name]
[Your Address]
[City, State, Zip Code]
[Date]
[Insurance Company Name]
[Claims Department]
[Insurance Company Address]
[City, State, Zip Code]
Re: Request for Reconsideration – Cervical Length Surveillance
Policy Number: [Policy Number]
Insured: [Patient’s Name]
Date of Birth: [Patient’s Date of Birth]
Claim Number: [Claim Number]
Date of Service: [Date of Service]
Dear Claims Reviewer,
I am writing to request a reconsideration of the denial for cervical length surveillance for my patient, [Patient’s Name], who has been diagnosed with a short cervix. As a healthcare provider, I strongly believe that this is a medically necessary service for the patient in order to prevent preterm birth and its associated complications.
A short cervix is a well-established risk factor for preterm birth, and numerous studies have shown the efficacy of cervical length surveillance in the prevention and management of preterm birth. I kindly request that you reconsider the coverage for this essential service and refer to the following authoritative sources:
Berghella, V., & Saccone, G. (2019). Fetal fibronectin testing for reducing the risk of preterm birth. Cochrane Database of Systematic Reviews, 2019(7). doi:10.1002/14651858.CD004843.pub3
American College of Obstetricians and Gynecologists (2016). Practice Bulletin No. 171: Management of Preterm Labor. Obstetrics & Gynecology, 128(4), e155-e164. doi:10.1097/AOG.0000000000001711
Society for Maternal-Fetal Medicine (SMFM), McIntosh, J., Feltovich, H., Berghella, V., & Manuck, T. (2016). The role of routine cervical length screening in selected high- and low-risk women for preterm birth prevention. American Journal of Obstetrics & Gynecology, 215(3), B2-B7. doi:10.1016/j.ajog.2016.03.015
By denying coverage for cervical length surveillance, the insurance company is putting [Patient’s Name] at an increased risk for preterm birth and the numerous health complications that can accompany it, both for the mother and the infant. It is crucial to provide this service in order to improve health outcomes and reduce the risk of costly neonatal intensive care unit (NICU) admissions and long-term medical issues.
I kindly request that you review this case with the provided references and reconsider the coverage for cervical length surveillance for [Patient’s Name]. Thank you for your attention to this matter. Please feel free to contact me if you require any further information or clarification.
Sincerely,
[Your Name]
[Your Title]
[Your Phone Number]
[Your Email Address]
The document took less than 15 seconds to generate, it is well written and concise, and can also be utilized as a template for future use. But as mentioned above, it is important to confirm all the information within the document. For example, references 1 and 3 in the ChatGPT-generated letter above include document objective identifiers that do not correctly correspond to the reference.
Other uses that the reader might consider: patient education, helping to answer a patient question utilizing appropriate grade-level language, dietary plans for a patient - the potential list is endless. Another key aspect of utilizing these types of programs is understanding how to effectively ask a question. This involves providing ample detail about the inquiry you wish to have answered by the program. With some practice and review of guidance on how to do this from the Internet, one can become highly proficient at crafting questions and generating relevant responses. But as mentioned above, it is important to keep in mind that all information generated by this program needs to be vetted prior to utilization.
This groundbreaking technology is not only here to stay but will continue to become increasingly pervasive. It is already being integrated into conventional search engines such as Google and Bing. Microsoft has ambitious plans to incorporate this innovation into its entire suite of Office products. Just imagine working on a document and seeking assistance for editing or rephrasing, effortlessly searching your inbox for all emails containing a specific phrase or topic, or even crafting a PowerPoint presentation for a lecture while receiving help with both content and formatting. These scenarios offer just a glimpse of how AI programs can significantly assist and enhance our workflow.
I also anticipate that our patients will increasingly adopt this type of technology to generate customized lists of questions tailored to their specific medical conditions, which they can then ask their health care providers. Often, our patients express uncertainty about the appropriate questions to ask during a particular visit. Now envision a scenario in which they can effortlessly obtain a comprehensive list of relevant questions, specifically designed for their office consultation. This would empower them to engage more actively in their health care and enhance communication with their clinical team.
I highly recommend that readers explore and experiment with these programs. By doing so, we can provide valuable assistance and guidance not only within our specific medical specialties but also for our patients. In this way, we can effectively harness the power of technology to improve patient care and optimize our office work flow, ultimately benefiting both our patients and our practices.
Dr. Chavez is professor, department of obstetrics and gynecology, at NYU Long Island School of Medicine and director of maternal and fetal medicine at NYU Langone Hospital–Long Island, both in Mineola, N.Y. He has no disclosures.
Artificial intelligence (AI) has recently gained significant public attention, primarily driven by the launch of a noteworthy program by OpenAI called Chat Generative Pre-trained Transformer (ChatGPT). This large language model is an AI system that enables users to interact with it using plain language. In just the first 2 months since its release, over 100 million subscribers have registered to use ChatGPT.
AI is now deeply integrated into our daily lives, pervading a wide array of smart devices such as phones, tablets, and numerous other gadgets that we rely on every day. These sophisticated technologies operate seamlessly in the background, often without us being consciously aware of their presence. Nevertheless, we greatly appreciate the way they enhance our lives by simplifying tasks and streamlining our routines.
A key factor contributing to ChatGPT’s popularity is its ability to accept input in the form of prompts in plain English. Our team published a comprehensive journal article showcasing examples of how this technology can be utilized by general ob.gyn. practitioners. ChatGPT has the potential to streamline work flow, generate letters to insurance companies, draft clinical plans, and assist with various other routine tasks in any ob.gyn. practice environment.
As with any new technology, it is essential for users to familiarize themselves with its capabilities and understand its limitations. A critical aspect to consider with the current version of ChatGPT is that it was developed using information primarily sourced from the Internet up until September 2021. This limitation is especially significant in the field of medicine, where practitioners consistently seek the most up-to-date and current information to inform their decisions.
However, it is expected that, in the near future, these programs will gain access to real-time information from a diverse range of sources, including but not limited to the Internet. This development will enhance the program’s utility and relevance in medical contexts.
Another limitation of ChatGPT is its propensity to “hallucinate.” Large language models are trained to respond to the best of their abilities, occasionally attempting to fill knowledge gaps with fabricated information. Being aware of these limitations enables users to recognize the program’s potential while also understanding the need for careful monitoring.
Our expertise and clinical knowledge are crucial in guiding and refining this technology, ensuring that it serves as a valuable tool in the ever-evolving landscape of medicine.
Another crucial factor to consider is that users must adhere to all guidelines and policies established within their work environment. This entails complying with HIPAA regulations and ensuring that any information generated by these programs is thoroughly examined before being integrated into practice work flows. As an increasing number of organizations develop specific guidelines for such technologies, the aim is to safeguard patients, users, and the organization itself. The individuals utilizing these technologies must exercise utmost caution and refrain from storing or sharing any sensitive or proprietary information.
The aim of this article is not to provide an exhaustive overview, but rather to offer a selection of examples and inspire readers to consider adopting these programs. By doing so, we hope to facilitate the exploration of innovative approaches that can improve the practice of ob.gyn.
The first example illustrates a common scenario that we frequently encounter – the situation in which an insurance company denies coverage for specific care or treatment for a patient. In fact, this was one of the first examples that was demonstrated by others on social media as a possible benefit for this technology. It effectively demonstrated the ability to save time and surmount the challenges of writer’s block that we occasionally encounter.
Prompt input:
“Write a letter to the insurance company who is denying cervical length surveillance for a patient with a short cervix and add references.”
ChatGPT response:
[Your Name]
[Your Address]
[City, State, Zip Code]
[Date]
[Insurance Company Name]
[Claims Department]
[Insurance Company Address]
[City, State, Zip Code]
Re: Request for Reconsideration – Cervical Length Surveillance
Policy Number: [Policy Number]
Insured: [Patient’s Name]
Date of Birth: [Patient’s Date of Birth]
Claim Number: [Claim Number]
Date of Service: [Date of Service]
Dear Claims Reviewer,
I am writing to request a reconsideration of the denial for cervical length surveillance for my patient, [Patient’s Name], who has been diagnosed with a short cervix. As a healthcare provider, I strongly believe that this is a medically necessary service for the patient in order to prevent preterm birth and its associated complications.
A short cervix is a well-established risk factor for preterm birth, and numerous studies have shown the efficacy of cervical length surveillance in the prevention and management of preterm birth. I kindly request that you reconsider the coverage for this essential service and refer to the following authoritative sources:
Berghella, V., & Saccone, G. (2019). Fetal fibronectin testing for reducing the risk of preterm birth. Cochrane Database of Systematic Reviews, 2019(7). doi:10.1002/14651858.CD004843.pub3
American College of Obstetricians and Gynecologists (2016). Practice Bulletin No. 171: Management of Preterm Labor. Obstetrics & Gynecology, 128(4), e155-e164. doi:10.1097/AOG.0000000000001711
Society for Maternal-Fetal Medicine (SMFM), McIntosh, J., Feltovich, H., Berghella, V., & Manuck, T. (2016). The role of routine cervical length screening in selected high- and low-risk women for preterm birth prevention. American Journal of Obstetrics & Gynecology, 215(3), B2-B7. doi:10.1016/j.ajog.2016.03.015
By denying coverage for cervical length surveillance, the insurance company is putting [Patient’s Name] at an increased risk for preterm birth and the numerous health complications that can accompany it, both for the mother and the infant. It is crucial to provide this service in order to improve health outcomes and reduce the risk of costly neonatal intensive care unit (NICU) admissions and long-term medical issues.
I kindly request that you review this case with the provided references and reconsider the coverage for cervical length surveillance for [Patient’s Name]. Thank you for your attention to this matter. Please feel free to contact me if you require any further information or clarification.
Sincerely,
[Your Name]
[Your Title]
[Your Phone Number]
[Your Email Address]
The document took less than 15 seconds to generate, it is well written and concise, and can also be utilized as a template for future use. But as mentioned above, it is important to confirm all the information within the document. For example, references 1 and 3 in the ChatGPT-generated letter above include document objective identifiers that do not correctly correspond to the reference.
Other uses that the reader might consider: patient education, helping to answer a patient question utilizing appropriate grade-level language, dietary plans for a patient - the potential list is endless. Another key aspect of utilizing these types of programs is understanding how to effectively ask a question. This involves providing ample detail about the inquiry you wish to have answered by the program. With some practice and review of guidance on how to do this from the Internet, one can become highly proficient at crafting questions and generating relevant responses. But as mentioned above, it is important to keep in mind that all information generated by this program needs to be vetted prior to utilization.
This groundbreaking technology is not only here to stay but will continue to become increasingly pervasive. It is already being integrated into conventional search engines such as Google and Bing. Microsoft has ambitious plans to incorporate this innovation into its entire suite of Office products. Just imagine working on a document and seeking assistance for editing or rephrasing, effortlessly searching your inbox for all emails containing a specific phrase or topic, or even crafting a PowerPoint presentation for a lecture while receiving help with both content and formatting. These scenarios offer just a glimpse of how AI programs can significantly assist and enhance our workflow.
I also anticipate that our patients will increasingly adopt this type of technology to generate customized lists of questions tailored to their specific medical conditions, which they can then ask their health care providers. Often, our patients express uncertainty about the appropriate questions to ask during a particular visit. Now envision a scenario in which they can effortlessly obtain a comprehensive list of relevant questions, specifically designed for their office consultation. This would empower them to engage more actively in their health care and enhance communication with their clinical team.
I highly recommend that readers explore and experiment with these programs. By doing so, we can provide valuable assistance and guidance not only within our specific medical specialties but also for our patients. In this way, we can effectively harness the power of technology to improve patient care and optimize our office work flow, ultimately benefiting both our patients and our practices.
Dr. Chavez is professor, department of obstetrics and gynecology, at NYU Long Island School of Medicine and director of maternal and fetal medicine at NYU Langone Hospital–Long Island, both in Mineola, N.Y. He has no disclosures.
OSHA revisited
Time for my periodic reminder about your Occupational Health and Safety Administration (OSHA) obligations. The health care field still has the most work-related illness and injury reports of any industry in the United States, and OSHA standards are in place to minimize potential workplace incidents.
Even if you hold regular safety meetings (which all too often is not the case), the occasional comprehensive review is always a good idea, and could save you a bundle in fines.
For starters, do you have an official OSHA poster, enumerating employee rights and explaining how to file complaints? Every office must have one posted in plain sight, and it is the first thing an OSHA inspector will look for. You can download one from OSHA’s website or order one at no charge by calling 800-321-OSHA.
The poster discusses the “general standards” that all workplaces must comply with to avoid work-related illnesses and injuries. The standards most applicable to medical offices are those dealing with personal protective equipment (PPE), bloodborne pathogens, hazard communication, and – increasingly, of late – ionizing radiation.
Physicians have become all too familiar with the PPE standard as a result of the COVID pandemic. Ironically, OSHA considers PPE a less acceptable means of employee protection than the other standards, as safe work practices should always supersede safety equipment. Nevertheless, employers must have a PPE program in place to train employees on what equipment is necessary, and under which conditions.
You also need a written exposure control plan for bloodborne pathogens. It should document your use of such protective equipment as gloves, face and eye protection, needle guards, and gowns, and your implementation of universal precautions – and it is supposed to be updated annually, to reflect changes in technology. You must provide all at-risk employees with hepatitis B vaccine at no cost to them. You also must provide and pay for appropriate medical treatment and follow-up after any exposure to a dangerous pathogen.
You need not adopt every new safety device as it comes on the market, but you should document which ones you are using – and which you pass up – and why. For example, you and your employees may decide not to purchase a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it’s worth; but you should document how you arrived at that decision, and why you feel that your current protocol is as good or better.
The hazard communication (or right-to-know) standard involves compiling a list of hazardous substances, which all employees have a right to know about. Keep in mind that OSHA’s list includes alcohol, hydrogen peroxide, acetone, liquid nitrogen, and other substances that you might not consider particularly dangerous, but are nevertheless classified as “hazardous.” For each substance, your employees must have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific material, and for handling and containing it in a spill or other emergency.
If your office has x-ray equipment, or you are considering one of the new image-guided superficial radiotherapy machines, you must be in compliance with the ionizing radiation standard, which entails shielding, radiation monitors, and clear labeling of equipment.
Other, more general regulations include the physical setup of your office. Everyone must be able to evacuate quickly in case of fire or other emergencies. At a minimum, you (or the owner of the office building) are expected to establish exit routes to accommodate all employees and to post easily visible evacuation diagrams.
Examine all electrical devices and their power sources. All electrically powered equipment – medical, clerical, or anything else in the office – must operate safely. Pay particular attention to the way wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it, and that circuit breakers are present and functioning. And beware the common situation of too many gadgets running off a single circuit.
Other components of the rule include proper containment of regulated medical waste, identification of regulated-waste containers, sharps disposal boxes, and periodic employee training regarding all of these things.
Federal OSHA regulations do not require medical and dental offices to keep an injury and illness log, as other businesses must; but your state may have a requirement that supersedes the federal law. Check with your state, or with your local OSHA office, regarding any such requirements.
It is a mistake to take OSHA regulations lightly; failure to comply with them can result in stiff penalties running into many thousands of dollars. How can you be certain you are complying with all the rules? The easiest and cheapest way is to call your local OSHA office and request an inspection. Why would you do that? Because OSHA issues no citations during voluntary inspections as long as you agree to remedy any violations they find.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Time for my periodic reminder about your Occupational Health and Safety Administration (OSHA) obligations. The health care field still has the most work-related illness and injury reports of any industry in the United States, and OSHA standards are in place to minimize potential workplace incidents.
Even if you hold regular safety meetings (which all too often is not the case), the occasional comprehensive review is always a good idea, and could save you a bundle in fines.
For starters, do you have an official OSHA poster, enumerating employee rights and explaining how to file complaints? Every office must have one posted in plain sight, and it is the first thing an OSHA inspector will look for. You can download one from OSHA’s website or order one at no charge by calling 800-321-OSHA.
The poster discusses the “general standards” that all workplaces must comply with to avoid work-related illnesses and injuries. The standards most applicable to medical offices are those dealing with personal protective equipment (PPE), bloodborne pathogens, hazard communication, and – increasingly, of late – ionizing radiation.
Physicians have become all too familiar with the PPE standard as a result of the COVID pandemic. Ironically, OSHA considers PPE a less acceptable means of employee protection than the other standards, as safe work practices should always supersede safety equipment. Nevertheless, employers must have a PPE program in place to train employees on what equipment is necessary, and under which conditions.
You also need a written exposure control plan for bloodborne pathogens. It should document your use of such protective equipment as gloves, face and eye protection, needle guards, and gowns, and your implementation of universal precautions – and it is supposed to be updated annually, to reflect changes in technology. You must provide all at-risk employees with hepatitis B vaccine at no cost to them. You also must provide and pay for appropriate medical treatment and follow-up after any exposure to a dangerous pathogen.
You need not adopt every new safety device as it comes on the market, but you should document which ones you are using – and which you pass up – and why. For example, you and your employees may decide not to purchase a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it’s worth; but you should document how you arrived at that decision, and why you feel that your current protocol is as good or better.
The hazard communication (or right-to-know) standard involves compiling a list of hazardous substances, which all employees have a right to know about. Keep in mind that OSHA’s list includes alcohol, hydrogen peroxide, acetone, liquid nitrogen, and other substances that you might not consider particularly dangerous, but are nevertheless classified as “hazardous.” For each substance, your employees must have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific material, and for handling and containing it in a spill or other emergency.
If your office has x-ray equipment, or you are considering one of the new image-guided superficial radiotherapy machines, you must be in compliance with the ionizing radiation standard, which entails shielding, radiation monitors, and clear labeling of equipment.
Other, more general regulations include the physical setup of your office. Everyone must be able to evacuate quickly in case of fire or other emergencies. At a minimum, you (or the owner of the office building) are expected to establish exit routes to accommodate all employees and to post easily visible evacuation diagrams.
Examine all electrical devices and their power sources. All electrically powered equipment – medical, clerical, or anything else in the office – must operate safely. Pay particular attention to the way wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it, and that circuit breakers are present and functioning. And beware the common situation of too many gadgets running off a single circuit.
Other components of the rule include proper containment of regulated medical waste, identification of regulated-waste containers, sharps disposal boxes, and periodic employee training regarding all of these things.
Federal OSHA regulations do not require medical and dental offices to keep an injury and illness log, as other businesses must; but your state may have a requirement that supersedes the federal law. Check with your state, or with your local OSHA office, regarding any such requirements.
It is a mistake to take OSHA regulations lightly; failure to comply with them can result in stiff penalties running into many thousands of dollars. How can you be certain you are complying with all the rules? The easiest and cheapest way is to call your local OSHA office and request an inspection. Why would you do that? Because OSHA issues no citations during voluntary inspections as long as you agree to remedy any violations they find.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Time for my periodic reminder about your Occupational Health and Safety Administration (OSHA) obligations. The health care field still has the most work-related illness and injury reports of any industry in the United States, and OSHA standards are in place to minimize potential workplace incidents.
Even if you hold regular safety meetings (which all too often is not the case), the occasional comprehensive review is always a good idea, and could save you a bundle in fines.
For starters, do you have an official OSHA poster, enumerating employee rights and explaining how to file complaints? Every office must have one posted in plain sight, and it is the first thing an OSHA inspector will look for. You can download one from OSHA’s website or order one at no charge by calling 800-321-OSHA.
The poster discusses the “general standards” that all workplaces must comply with to avoid work-related illnesses and injuries. The standards most applicable to medical offices are those dealing with personal protective equipment (PPE), bloodborne pathogens, hazard communication, and – increasingly, of late – ionizing radiation.
Physicians have become all too familiar with the PPE standard as a result of the COVID pandemic. Ironically, OSHA considers PPE a less acceptable means of employee protection than the other standards, as safe work practices should always supersede safety equipment. Nevertheless, employers must have a PPE program in place to train employees on what equipment is necessary, and under which conditions.
You also need a written exposure control plan for bloodborne pathogens. It should document your use of such protective equipment as gloves, face and eye protection, needle guards, and gowns, and your implementation of universal precautions – and it is supposed to be updated annually, to reflect changes in technology. You must provide all at-risk employees with hepatitis B vaccine at no cost to them. You also must provide and pay for appropriate medical treatment and follow-up after any exposure to a dangerous pathogen.
You need not adopt every new safety device as it comes on the market, but you should document which ones you are using – and which you pass up – and why. For example, you and your employees may decide not to purchase a new safety needle because you don’t think it will improve safety, or that it will be more trouble than it’s worth; but you should document how you arrived at that decision, and why you feel that your current protocol is as good or better.
The hazard communication (or right-to-know) standard involves compiling a list of hazardous substances, which all employees have a right to know about. Keep in mind that OSHA’s list includes alcohol, hydrogen peroxide, acetone, liquid nitrogen, and other substances that you might not consider particularly dangerous, but are nevertheless classified as “hazardous.” For each substance, your employees must have access to the manufacturer-supplied Material Safety Data Sheet, which outlines the proper procedures for working with a specific material, and for handling and containing it in a spill or other emergency.
If your office has x-ray equipment, or you are considering one of the new image-guided superficial radiotherapy machines, you must be in compliance with the ionizing radiation standard, which entails shielding, radiation monitors, and clear labeling of equipment.
Other, more general regulations include the physical setup of your office. Everyone must be able to evacuate quickly in case of fire or other emergencies. At a minimum, you (or the owner of the office building) are expected to establish exit routes to accommodate all employees and to post easily visible evacuation diagrams.
Examine all electrical devices and their power sources. All electrically powered equipment – medical, clerical, or anything else in the office – must operate safely. Pay particular attention to the way wall outlets are set up. Make sure each outlet has sufficient power to run the equipment plugged into it, and that circuit breakers are present and functioning. And beware the common situation of too many gadgets running off a single circuit.
Other components of the rule include proper containment of regulated medical waste, identification of regulated-waste containers, sharps disposal boxes, and periodic employee training regarding all of these things.
Federal OSHA regulations do not require medical and dental offices to keep an injury and illness log, as other businesses must; but your state may have a requirement that supersedes the federal law. Check with your state, or with your local OSHA office, regarding any such requirements.
It is a mistake to take OSHA regulations lightly; failure to comply with them can result in stiff penalties running into many thousands of dollars. How can you be certain you are complying with all the rules? The easiest and cheapest way is to call your local OSHA office and request an inspection. Why would you do that? Because OSHA issues no citations during voluntary inspections as long as you agree to remedy any violations they find.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Bergamot
Citrus bergamia (bergamot) is a fruit tree thought to originate in the Mediterranean area; its fruit has been a part of the diet in that region since the early 18th century.1 Bergamot is known to confer antioxidant as well as anti-inflammatory activity, and yields proapoptotic effects in the sebaceous gland.2,3 The plant contains the natural furocoumarin bergapten, which is also known as 5-methoxypsoralen.4
5 In this capacity, bergamot oil has been used for photodynamic therapy of cutaneous conditions such as vitiligo.6 In fact, for several years 5-methoxypsoralen and 8-methoxypsoralen have been used to achieve acceptable clearance rates of psoriasis and vitiligo.7 This column focuses on bergapten, as well as the cutaneous conditions for which bergamot has been shown to have some benefits warranting application or further investigation.
Bergapten
In a 2021 literature review, Liang et al. cited the anti-inflammatory, antimicrobial, anticancer, and other salutary effects associated with bergapten. Based on numerous citations, they also cautioned about the phototoxicity of the compound combined with ultraviolet (UV) light while noting the photoactivation of bergapten for anticancer uses.4
The following year, Quetglas-Llabrés et al. acknowledged, in another literature review, the numerous preclinical and in vitro studies demonstrating the therapeutic activity of bergapten and highlighted clinical trials revealing notable lesion clearance rates of psoriasis or vitiligo imparted by oral or topical bergapten along with UV irradiation. Bergapten was also found to be effective as hypolipemic therapy.5
Anti-inflammatory topical uses
In a 2017 study by Han et al. of 10 essential oils, bergamot was among the investigated oils, all of which exhibited significant anti-proliferative activity in a preinflamed human dermal fibroblast system simulating chronic inflammation. Bergamot was among three essential oils that also suppressed protein molecules involved with inflammation, immune responses, and tissue remodeling, indicating anti-inflammatory and wound healing characteristics.8
More recently, Cristiano et al. reported that ultradeformable nanocarriers containing bergamot essential oil and ammonium glycyrrhizinate were demonstrated in healthy human volunteers to be characterized by the appropriate mean size, size distribution, surface charge, and long-term stability for topical administration. Topical administration on human volunteers also revealed greater activity of the combined agents as compared with a nanosystem loaded only with ammonium glycyrrhizinate. The researchers concluded that this combination of ingredients in ultradeformable vesicles shows potential as topical anti-inflammatory treatment.3
Acne
In a 2020 study using golden hamsters, Sun et al. assessed the effects of the juice and essential oils of bergamot and sweet orange on acne vulgaris engendered by excessive androgen secretion. Among 80 male hamsters randomly divided into 10 groups ranging from low to high doses, all results demonstrated improvement with treatment as seen by decreased growth rates of sebaceous glands, suppressed triglyceride accumulation, lowered inflammatory cytokine release, and apoptosis promotion in sebaceous glands. The authors noted that the essential oils yielded better dose-dependent effects than the juices.2
Psoriasis
In 2019, Perna et al. conducted a literature review on the effects of bergamot essential oil, extract, juice, and polyphenolic fraction on various health metrics. Thirty-one studies (20 involving humans with 1,709 subjects and 11 in rats and mice) were identified. Animal models indicated that bergamot essential oil (10 mg/kg or 20 mg/kg daily for 20 weeks) reduced psoriatic plaques, increased skin collagen content, and fostered hair growth and that bergamot juice (20 mg/kg) diminished proinflammatory cytokines. Human studies showed that bergamot extract and essential oil may reduce blood pressure and improve mental conditions.9
Vitiligo
In 2019, Shaaban et al. prepared elastic nanocarriers (spanlastics) to deliver psoralen-containing bergamot oil along with PUVB with the intention of harnessing melanogenic activity to treat vitiligo. Histopathologic assessment on rat skin was conducted before clinical treatment in patients with vitiligo. The spanlastics were deemed to be of suitable nanosize and deformable, yielding consistent bergamot oil release. The bergamot oil included in the nanocarrier was found to enhance photostability and photodynamic activity, with the researchers concluding that bergamot oil nanospanlastics with psoralen-UVB therapy shows potential as a vitiligo therapy.10
Two years later, Shaaban evaluated bergamot oil formulated in nanostructured lipid carriers as a photosensitizer for photodynamic treatment of vitiligo. The botanical oil was effectively used in the nanostructured lipid carriers with a gel consistency that delivered sustained release of the oil for 24 hours. Preclinical and clinical results in patients were encouraging for the topical photodynamic treatment of vitiligo, with the nanostructured lipid carriers improving the photostability and photodynamic activity of bergamot oil.6
Photoaging, photoprotection, and safety concerns
Three decades ago, an international cooperative study of the photophysical, photomutagenic, and photocarcinogenic characteristics of bergamot oil and the effect of UVA and UVB sunscreens found that UVB and UVA sunscreens at low concentration (0.5%-1%) in perfumes could not inhibit the phototoxicity of bergamot oil on human skin.11
In a 2015 study assessing the impact of 38% bergamot polyphenolic fraction (a highly concentrated Citrus bergamia fruit extract) on UVB-generated photoaging, Nisticò et al. found that the bergamot compound dose-dependently protected HaCaT cells against UVB-caused oxidative stress and photoaging markers. Suggesting that the high-antioxidant bergamot polyphenolic fraction has potential for use in skin care formulations, the researchers added that the extract seems to induce antiproliferative, immune-modulating, and antiaging activity.12In 2022, Alexa et al. performed in vitro tests and found that natural preparations containing bergamot, orange, and clove essential oils do not significantly alter physiological skin parameters and were deemed safe for topical use. An emulsion with bergamot essential oil was also found to reduce the viability of oral squamous cell carcinoma cells.13
Conclusion
As a photosensitizing agent, bergamot has an established role in skin care. Beyond its niche role in treatments for vitiligo and psoriasis, this botanical product appears to show potential as an anti-inflammatory agent as well as an ingredient to combat photoaging and skin cancer. Much more research is needed to elucidate the possible wider benefits of this Mediterranean staple.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a SaaS company used to generate skin care routines in office and as an ecommerce solution. Write to her at [email protected].
References
1. Juber M. Health benefits of bergamot. WebMD. November 29, 2022. Accessed March 21, 2023.
2. Sun P et al. Mediators Inflamm. 2020 Oct 6;2020:8868107.
3. Cristiano MC et al. Biomedicines. 2022 Apr 30;10(5):1039.
4. Liang Y et al. Phytother Res. 2021 Nov;35(11):6131-47.
5. Quetglas-Llabrés MM et al. Oxid Med Cell Longev. 2022 Apr 25;2022:8615242.
6. Shaaban M et al. Expert Opin Drug Deliv. 2021 Jan;18(1):139-50.
7. McNeely W, Goa KL. Drugs. 1998 Oct;56(4):667-90.
8. Han X, Beaumont C, Stevens N. Biochim Open. 2017 Apr 26;5:1-7.
9. Perna S et al. Food Sci Nutr. 2019 Jan 25;7(2):369-84.
10. Shaaban M et al. Drug Deliv Transl Res. 2019 Dec;9(6):1106-16.
11. Dubertret L et al. J Photochem Photobiol B. 1990 Nov;7(2-4):251-9.
12. Nisticò S et al. J Biol Regul Homeost Agents. 2015 Jul-Sep;29(3):723-8.
13. Alexa VT et al. Molecules. 2022 Feb 1;27(3):990.
Citrus bergamia (bergamot) is a fruit tree thought to originate in the Mediterranean area; its fruit has been a part of the diet in that region since the early 18th century.1 Bergamot is known to confer antioxidant as well as anti-inflammatory activity, and yields proapoptotic effects in the sebaceous gland.2,3 The plant contains the natural furocoumarin bergapten, which is also known as 5-methoxypsoralen.4
5 In this capacity, bergamot oil has been used for photodynamic therapy of cutaneous conditions such as vitiligo.6 In fact, for several years 5-methoxypsoralen and 8-methoxypsoralen have been used to achieve acceptable clearance rates of psoriasis and vitiligo.7 This column focuses on bergapten, as well as the cutaneous conditions for which bergamot has been shown to have some benefits warranting application or further investigation.
Bergapten
In a 2021 literature review, Liang et al. cited the anti-inflammatory, antimicrobial, anticancer, and other salutary effects associated with bergapten. Based on numerous citations, they also cautioned about the phototoxicity of the compound combined with ultraviolet (UV) light while noting the photoactivation of bergapten for anticancer uses.4
The following year, Quetglas-Llabrés et al. acknowledged, in another literature review, the numerous preclinical and in vitro studies demonstrating the therapeutic activity of bergapten and highlighted clinical trials revealing notable lesion clearance rates of psoriasis or vitiligo imparted by oral or topical bergapten along with UV irradiation. Bergapten was also found to be effective as hypolipemic therapy.5
Anti-inflammatory topical uses
In a 2017 study by Han et al. of 10 essential oils, bergamot was among the investigated oils, all of which exhibited significant anti-proliferative activity in a preinflamed human dermal fibroblast system simulating chronic inflammation. Bergamot was among three essential oils that also suppressed protein molecules involved with inflammation, immune responses, and tissue remodeling, indicating anti-inflammatory and wound healing characteristics.8
More recently, Cristiano et al. reported that ultradeformable nanocarriers containing bergamot essential oil and ammonium glycyrrhizinate were demonstrated in healthy human volunteers to be characterized by the appropriate mean size, size distribution, surface charge, and long-term stability for topical administration. Topical administration on human volunteers also revealed greater activity of the combined agents as compared with a nanosystem loaded only with ammonium glycyrrhizinate. The researchers concluded that this combination of ingredients in ultradeformable vesicles shows potential as topical anti-inflammatory treatment.3
Acne
In a 2020 study using golden hamsters, Sun et al. assessed the effects of the juice and essential oils of bergamot and sweet orange on acne vulgaris engendered by excessive androgen secretion. Among 80 male hamsters randomly divided into 10 groups ranging from low to high doses, all results demonstrated improvement with treatment as seen by decreased growth rates of sebaceous glands, suppressed triglyceride accumulation, lowered inflammatory cytokine release, and apoptosis promotion in sebaceous glands. The authors noted that the essential oils yielded better dose-dependent effects than the juices.2
Psoriasis
In 2019, Perna et al. conducted a literature review on the effects of bergamot essential oil, extract, juice, and polyphenolic fraction on various health metrics. Thirty-one studies (20 involving humans with 1,709 subjects and 11 in rats and mice) were identified. Animal models indicated that bergamot essential oil (10 mg/kg or 20 mg/kg daily for 20 weeks) reduced psoriatic plaques, increased skin collagen content, and fostered hair growth and that bergamot juice (20 mg/kg) diminished proinflammatory cytokines. Human studies showed that bergamot extract and essential oil may reduce blood pressure and improve mental conditions.9
Vitiligo
In 2019, Shaaban et al. prepared elastic nanocarriers (spanlastics) to deliver psoralen-containing bergamot oil along with PUVB with the intention of harnessing melanogenic activity to treat vitiligo. Histopathologic assessment on rat skin was conducted before clinical treatment in patients with vitiligo. The spanlastics were deemed to be of suitable nanosize and deformable, yielding consistent bergamot oil release. The bergamot oil included in the nanocarrier was found to enhance photostability and photodynamic activity, with the researchers concluding that bergamot oil nanospanlastics with psoralen-UVB therapy shows potential as a vitiligo therapy.10
Two years later, Shaaban evaluated bergamot oil formulated in nanostructured lipid carriers as a photosensitizer for photodynamic treatment of vitiligo. The botanical oil was effectively used in the nanostructured lipid carriers with a gel consistency that delivered sustained release of the oil for 24 hours. Preclinical and clinical results in patients were encouraging for the topical photodynamic treatment of vitiligo, with the nanostructured lipid carriers improving the photostability and photodynamic activity of bergamot oil.6
Photoaging, photoprotection, and safety concerns
Three decades ago, an international cooperative study of the photophysical, photomutagenic, and photocarcinogenic characteristics of bergamot oil and the effect of UVA and UVB sunscreens found that UVB and UVA sunscreens at low concentration (0.5%-1%) in perfumes could not inhibit the phototoxicity of bergamot oil on human skin.11
In a 2015 study assessing the impact of 38% bergamot polyphenolic fraction (a highly concentrated Citrus bergamia fruit extract) on UVB-generated photoaging, Nisticò et al. found that the bergamot compound dose-dependently protected HaCaT cells against UVB-caused oxidative stress and photoaging markers. Suggesting that the high-antioxidant bergamot polyphenolic fraction has potential for use in skin care formulations, the researchers added that the extract seems to induce antiproliferative, immune-modulating, and antiaging activity.12In 2022, Alexa et al. performed in vitro tests and found that natural preparations containing bergamot, orange, and clove essential oils do not significantly alter physiological skin parameters and were deemed safe for topical use. An emulsion with bergamot essential oil was also found to reduce the viability of oral squamous cell carcinoma cells.13
Conclusion
As a photosensitizing agent, bergamot has an established role in skin care. Beyond its niche role in treatments for vitiligo and psoriasis, this botanical product appears to show potential as an anti-inflammatory agent as well as an ingredient to combat photoaging and skin cancer. Much more research is needed to elucidate the possible wider benefits of this Mediterranean staple.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a SaaS company used to generate skin care routines in office and as an ecommerce solution. Write to her at [email protected].
References
1. Juber M. Health benefits of bergamot. WebMD. November 29, 2022. Accessed March 21, 2023.
2. Sun P et al. Mediators Inflamm. 2020 Oct 6;2020:8868107.
3. Cristiano MC et al. Biomedicines. 2022 Apr 30;10(5):1039.
4. Liang Y et al. Phytother Res. 2021 Nov;35(11):6131-47.
5. Quetglas-Llabrés MM et al. Oxid Med Cell Longev. 2022 Apr 25;2022:8615242.
6. Shaaban M et al. Expert Opin Drug Deliv. 2021 Jan;18(1):139-50.
7. McNeely W, Goa KL. Drugs. 1998 Oct;56(4):667-90.
8. Han X, Beaumont C, Stevens N. Biochim Open. 2017 Apr 26;5:1-7.
9. Perna S et al. Food Sci Nutr. 2019 Jan 25;7(2):369-84.
10. Shaaban M et al. Drug Deliv Transl Res. 2019 Dec;9(6):1106-16.
11. Dubertret L et al. J Photochem Photobiol B. 1990 Nov;7(2-4):251-9.
12. Nisticò S et al. J Biol Regul Homeost Agents. 2015 Jul-Sep;29(3):723-8.
13. Alexa VT et al. Molecules. 2022 Feb 1;27(3):990.
Citrus bergamia (bergamot) is a fruit tree thought to originate in the Mediterranean area; its fruit has been a part of the diet in that region since the early 18th century.1 Bergamot is known to confer antioxidant as well as anti-inflammatory activity, and yields proapoptotic effects in the sebaceous gland.2,3 The plant contains the natural furocoumarin bergapten, which is also known as 5-methoxypsoralen.4
5 In this capacity, bergamot oil has been used for photodynamic therapy of cutaneous conditions such as vitiligo.6 In fact, for several years 5-methoxypsoralen and 8-methoxypsoralen have been used to achieve acceptable clearance rates of psoriasis and vitiligo.7 This column focuses on bergapten, as well as the cutaneous conditions for which bergamot has been shown to have some benefits warranting application or further investigation.
Bergapten
In a 2021 literature review, Liang et al. cited the anti-inflammatory, antimicrobial, anticancer, and other salutary effects associated with bergapten. Based on numerous citations, they also cautioned about the phototoxicity of the compound combined with ultraviolet (UV) light while noting the photoactivation of bergapten for anticancer uses.4
The following year, Quetglas-Llabrés et al. acknowledged, in another literature review, the numerous preclinical and in vitro studies demonstrating the therapeutic activity of bergapten and highlighted clinical trials revealing notable lesion clearance rates of psoriasis or vitiligo imparted by oral or topical bergapten along with UV irradiation. Bergapten was also found to be effective as hypolipemic therapy.5
Anti-inflammatory topical uses
In a 2017 study by Han et al. of 10 essential oils, bergamot was among the investigated oils, all of which exhibited significant anti-proliferative activity in a preinflamed human dermal fibroblast system simulating chronic inflammation. Bergamot was among three essential oils that also suppressed protein molecules involved with inflammation, immune responses, and tissue remodeling, indicating anti-inflammatory and wound healing characteristics.8
More recently, Cristiano et al. reported that ultradeformable nanocarriers containing bergamot essential oil and ammonium glycyrrhizinate were demonstrated in healthy human volunteers to be characterized by the appropriate mean size, size distribution, surface charge, and long-term stability for topical administration. Topical administration on human volunteers also revealed greater activity of the combined agents as compared with a nanosystem loaded only with ammonium glycyrrhizinate. The researchers concluded that this combination of ingredients in ultradeformable vesicles shows potential as topical anti-inflammatory treatment.3
Acne
In a 2020 study using golden hamsters, Sun et al. assessed the effects of the juice and essential oils of bergamot and sweet orange on acne vulgaris engendered by excessive androgen secretion. Among 80 male hamsters randomly divided into 10 groups ranging from low to high doses, all results demonstrated improvement with treatment as seen by decreased growth rates of sebaceous glands, suppressed triglyceride accumulation, lowered inflammatory cytokine release, and apoptosis promotion in sebaceous glands. The authors noted that the essential oils yielded better dose-dependent effects than the juices.2
Psoriasis
In 2019, Perna et al. conducted a literature review on the effects of bergamot essential oil, extract, juice, and polyphenolic fraction on various health metrics. Thirty-one studies (20 involving humans with 1,709 subjects and 11 in rats and mice) were identified. Animal models indicated that bergamot essential oil (10 mg/kg or 20 mg/kg daily for 20 weeks) reduced psoriatic plaques, increased skin collagen content, and fostered hair growth and that bergamot juice (20 mg/kg) diminished proinflammatory cytokines. Human studies showed that bergamot extract and essential oil may reduce blood pressure and improve mental conditions.9
Vitiligo
In 2019, Shaaban et al. prepared elastic nanocarriers (spanlastics) to deliver psoralen-containing bergamot oil along with PUVB with the intention of harnessing melanogenic activity to treat vitiligo. Histopathologic assessment on rat skin was conducted before clinical treatment in patients with vitiligo. The spanlastics were deemed to be of suitable nanosize and deformable, yielding consistent bergamot oil release. The bergamot oil included in the nanocarrier was found to enhance photostability and photodynamic activity, with the researchers concluding that bergamot oil nanospanlastics with psoralen-UVB therapy shows potential as a vitiligo therapy.10
Two years later, Shaaban evaluated bergamot oil formulated in nanostructured lipid carriers as a photosensitizer for photodynamic treatment of vitiligo. The botanical oil was effectively used in the nanostructured lipid carriers with a gel consistency that delivered sustained release of the oil for 24 hours. Preclinical and clinical results in patients were encouraging for the topical photodynamic treatment of vitiligo, with the nanostructured lipid carriers improving the photostability and photodynamic activity of bergamot oil.6
Photoaging, photoprotection, and safety concerns
Three decades ago, an international cooperative study of the photophysical, photomutagenic, and photocarcinogenic characteristics of bergamot oil and the effect of UVA and UVB sunscreens found that UVB and UVA sunscreens at low concentration (0.5%-1%) in perfumes could not inhibit the phototoxicity of bergamot oil on human skin.11
In a 2015 study assessing the impact of 38% bergamot polyphenolic fraction (a highly concentrated Citrus bergamia fruit extract) on UVB-generated photoaging, Nisticò et al. found that the bergamot compound dose-dependently protected HaCaT cells against UVB-caused oxidative stress and photoaging markers. Suggesting that the high-antioxidant bergamot polyphenolic fraction has potential for use in skin care formulations, the researchers added that the extract seems to induce antiproliferative, immune-modulating, and antiaging activity.12In 2022, Alexa et al. performed in vitro tests and found that natural preparations containing bergamot, orange, and clove essential oils do not significantly alter physiological skin parameters and were deemed safe for topical use. An emulsion with bergamot essential oil was also found to reduce the viability of oral squamous cell carcinoma cells.13
Conclusion
As a photosensitizing agent, bergamot has an established role in skin care. Beyond its niche role in treatments for vitiligo and psoriasis, this botanical product appears to show potential as an anti-inflammatory agent as well as an ingredient to combat photoaging and skin cancer. Much more research is needed to elucidate the possible wider benefits of this Mediterranean staple.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions Inc., a SaaS company used to generate skin care routines in office and as an ecommerce solution. Write to her at [email protected].
References
1. Juber M. Health benefits of bergamot. WebMD. November 29, 2022. Accessed March 21, 2023.
2. Sun P et al. Mediators Inflamm. 2020 Oct 6;2020:8868107.
3. Cristiano MC et al. Biomedicines. 2022 Apr 30;10(5):1039.
4. Liang Y et al. Phytother Res. 2021 Nov;35(11):6131-47.
5. Quetglas-Llabrés MM et al. Oxid Med Cell Longev. 2022 Apr 25;2022:8615242.
6. Shaaban M et al. Expert Opin Drug Deliv. 2021 Jan;18(1):139-50.
7. McNeely W, Goa KL. Drugs. 1998 Oct;56(4):667-90.
8. Han X, Beaumont C, Stevens N. Biochim Open. 2017 Apr 26;5:1-7.
9. Perna S et al. Food Sci Nutr. 2019 Jan 25;7(2):369-84.
10. Shaaban M et al. Drug Deliv Transl Res. 2019 Dec;9(6):1106-16.
11. Dubertret L et al. J Photochem Photobiol B. 1990 Nov;7(2-4):251-9.
12. Nisticò S et al. J Biol Regul Homeost Agents. 2015 Jul-Sep;29(3):723-8.
13. Alexa VT et al. Molecules. 2022 Feb 1;27(3):990.
Teen girls are in crisis: A call to action resulting from 2021 CDC data
Case: “Where’s my mommy?”
A 13-year-old girl “D” appeared lifeless in her hospital bed, swallowed by tubes, gauze, and crisp white sheets. She seemed fragile next to the giant machines beeping all around her, as they churned and groaned to keep her alive. She was in the pediatric intensive care unit, a place she had only seen once or twice on TV. Her sleeping mother lay next to her in an uncomfortable-looking recliner chair, curled up in a ball. She abruptly woke up when I walked into the room, doing her best to wipe away 5 days’ worth of worry and sadness from her exhausted face. She saw “Child Psychiatrist” written on my hospital badge, desperately searching my face for answers or a sign of hope.
Her daughter – a straight-A middle school student who loved Taylor Swift and soccer – had overdosed on Tylenol after discovering that she did not make the cheerleading team. I reported that her daughter’s liver enzymes were finally trending down and that she would likely not require a liver transplant. She would survive. As tears welled up in this mother’s eyes, I heard a faint whisper from across the room. “Where’s my mommy?” D was awake and frantically searching the room for her mother, someone who could soothe her in this living nightmare. As the two embraced, I felt tears well up in my eyes as I couldn’t help but think of my own 3-year-old daughter at home. How could I protect her from the sadness and despair that this little girl was feeling? How can we collectively protect every little girl from wanting to end their life?
CDC data: Teen girls need help now
The latest biennial Centers for Disease Control and Prevention Youth Risk Behavior Survey, administered in the fall of 2021, resulted in alarming data showing that mental health has worsened for all adolescents, but especially for girls. The survey was administered to more than 17,000 students in 152 public and private schools throughout the United States, showing that “America’s teen girls are engulfed in a growing wave of sadness, violence, and trauma.”1 In particular, rates of sadness, suicidal ideation, suicide attempts, and mental health crisis ED visits among girls are the highest reported in a decade. Nearly 60% of girls felt persistent sadness or hopelessness during the past year, double the rate of boys. More than 25% of girls made a suicide plan; this percentage increased 60% over the past 10 years. Alarmingly, ED visits for suicide attempts for girls increased more than 50% in the past 2 years alone.
Even before the COVID-19 pandemic, experts were sounding the alarm on the growing rates of anxiety and depression in U.S. youth. The pandemic-driven isolation, lack of social connection, and missing of major milestones did not help the situation and only deepened the cracks in a faulty mental health care system. Further, civil unrest and social upheaval in the United States felt – and continues to feel – chaotic and unpredictable. For teens, the current cultural climate represents their not-too-distant future as adults, causing worry and anxiety.
In addition to securing their futures through performance in school and extracurricular activities, teenagers are forming their identities. Establishing a personal identity is a difficult task for all teens, though teenage girls face uniquely difficult challenges in our current society. In particular, teenage girls are expected to conform their behaviors to fit societal expectations that may clash with their desires and self-conceptualization. This conflict is further complicated by heightened beauty standards, online hate and competition, academic pressure, and self-doubt. CDC data show that girls experience sexual harassment and cyberbullying at roughly twice the rate of their male counterparts. Girls also experience higher levels of sexual violence and bullying. Alarmingly, 14% of girls reported being forced to have sex at some point in their lives. The sad truth is that, for every 10 teenage girls you know, at least one of them, and probably more, has likely been raped.
A call to action for providers
As providers, what can we do about these alarming statistics? It’s easy to become overwhelmed by data on a national level. However, regardless of our current clinical practice situation, we cannot lose sight of the humanity behind these numbers. Five extra minutes of truly listening to our patients, normalizing conversations about mental health, and looking for mental health warning signs (that is, increased isolation, declining function in school, maladaptive coping skills such as self-injurious behavior or substance use) can mean the difference between life and death.
As pediatric providers, formally screening for suicide risk is critical. Specifically, the American Academy of Pediatrics recommends that all youth aged 12 years or older be screened for suicide risk.2 In addition to asking families to reduce access to lethal means, it is important to utilize suicide-specific screeners to prevent suicide attempts and deaths in the pediatric community. Pediatric providers must feel prepared to counsel patients and families on suicide prevention and, if this skill set is underdeveloped, appropriate referrals and support must be provided.
At the same time, it is important to note the larger context. This national tragedy has been long-standing and further accelerated by the social isolation and stress of the pandemic. Madigan and colleagues recently showed that the lack of a social outlet resulting from COVID-19 caused an increase in screen time among all children.3 As a result, many teen girls turned to social media to recreate these social connections online.4 This dependence on social media for validation has contributed to increased rates of depression by intensifying unrealistic body standards, comparisons, and competition among peers.5 However, recent pediatric partnership programs have improved mental health access, reduced ED visits, and increased primary care physician’s comfort with managing mental health concerns.6 These programs are called Child Psychiatry Access Programs (CPAPs) and utilize a collaborative care model through which primary care clinicians consult with child and adolescent psychiatrists. CPAPs, while not the entire solution, offer a major step in the right direction toward tackling this mental health crisis in a sustainable, collaborative, and effective way.
As students return to in-person learning, connectedness at school is a powerful protective factor against depression and anxiety. We must infuse resources and support into our schools and teachers, as they stand on the front lines for our children. Specifically, bolstering schools with school counselors and appropriate mental health support staff will help rescue teachers from burnout while also explicitly identifying mental health care as a priority. Finally, modeling positive behavior for families and identifying safe adults at school can help at-risk youth feel more connected. To achieve meaningful improvement in children’s mental health, it is crucial to collaboratively remodel broken systems to ensure that all children are supported early, effectively, and equitably.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences, program director of the child and adolescent psychiatry fellowship, and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior in Los Angeles.
References
1. Centers for Disease Control and Prevention. YRBSS Data Summary & Trends. 2023 Feb 13. https://www.cdc.gov/healthyyouth/data/yrbs/yrbs_data_summary_and_trends.htm
2. American Academy of Pediatrics. Screening for Suicide Risk in Clinical Practice. 2023 Feb 22. https://www.aap.org/en/patient-care/blueprint-for-youth-suicide-prevention/strategies-for-clinical-settings-for-youth-suicide-prevention/screening-for-suicide-risk-in-clinical-practice/
3. Madigan S et al. JAMA Pediatr. 2022;176(12):1188-98. doi: 10.1001/JAMAPEDIATRICS.2022.4116
4. Pew Research Center. Teens, Social Media and Technology 2022. 2022 Aug 10. https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/
5. Hunt MG et al. J Social Clin Psychology. 2018;37(10):751-68. doi: 10.1521/JSCP.2018.37.10.751
6. Godoy L et al. J Pediatr Health Care. 2022 Dec 16. doi: 10.1016/j.pedhc.2022.11.009.
Case: “Where’s my mommy?”
A 13-year-old girl “D” appeared lifeless in her hospital bed, swallowed by tubes, gauze, and crisp white sheets. She seemed fragile next to the giant machines beeping all around her, as they churned and groaned to keep her alive. She was in the pediatric intensive care unit, a place she had only seen once or twice on TV. Her sleeping mother lay next to her in an uncomfortable-looking recliner chair, curled up in a ball. She abruptly woke up when I walked into the room, doing her best to wipe away 5 days’ worth of worry and sadness from her exhausted face. She saw “Child Psychiatrist” written on my hospital badge, desperately searching my face for answers or a sign of hope.
Her daughter – a straight-A middle school student who loved Taylor Swift and soccer – had overdosed on Tylenol after discovering that she did not make the cheerleading team. I reported that her daughter’s liver enzymes were finally trending down and that she would likely not require a liver transplant. She would survive. As tears welled up in this mother’s eyes, I heard a faint whisper from across the room. “Where’s my mommy?” D was awake and frantically searching the room for her mother, someone who could soothe her in this living nightmare. As the two embraced, I felt tears well up in my eyes as I couldn’t help but think of my own 3-year-old daughter at home. How could I protect her from the sadness and despair that this little girl was feeling? How can we collectively protect every little girl from wanting to end their life?
CDC data: Teen girls need help now
The latest biennial Centers for Disease Control and Prevention Youth Risk Behavior Survey, administered in the fall of 2021, resulted in alarming data showing that mental health has worsened for all adolescents, but especially for girls. The survey was administered to more than 17,000 students in 152 public and private schools throughout the United States, showing that “America’s teen girls are engulfed in a growing wave of sadness, violence, and trauma.”1 In particular, rates of sadness, suicidal ideation, suicide attempts, and mental health crisis ED visits among girls are the highest reported in a decade. Nearly 60% of girls felt persistent sadness or hopelessness during the past year, double the rate of boys. More than 25% of girls made a suicide plan; this percentage increased 60% over the past 10 years. Alarmingly, ED visits for suicide attempts for girls increased more than 50% in the past 2 years alone.
Even before the COVID-19 pandemic, experts were sounding the alarm on the growing rates of anxiety and depression in U.S. youth. The pandemic-driven isolation, lack of social connection, and missing of major milestones did not help the situation and only deepened the cracks in a faulty mental health care system. Further, civil unrest and social upheaval in the United States felt – and continues to feel – chaotic and unpredictable. For teens, the current cultural climate represents their not-too-distant future as adults, causing worry and anxiety.
In addition to securing their futures through performance in school and extracurricular activities, teenagers are forming their identities. Establishing a personal identity is a difficult task for all teens, though teenage girls face uniquely difficult challenges in our current society. In particular, teenage girls are expected to conform their behaviors to fit societal expectations that may clash with their desires and self-conceptualization. This conflict is further complicated by heightened beauty standards, online hate and competition, academic pressure, and self-doubt. CDC data show that girls experience sexual harassment and cyberbullying at roughly twice the rate of their male counterparts. Girls also experience higher levels of sexual violence and bullying. Alarmingly, 14% of girls reported being forced to have sex at some point in their lives. The sad truth is that, for every 10 teenage girls you know, at least one of them, and probably more, has likely been raped.
A call to action for providers
As providers, what can we do about these alarming statistics? It’s easy to become overwhelmed by data on a national level. However, regardless of our current clinical practice situation, we cannot lose sight of the humanity behind these numbers. Five extra minutes of truly listening to our patients, normalizing conversations about mental health, and looking for mental health warning signs (that is, increased isolation, declining function in school, maladaptive coping skills such as self-injurious behavior or substance use) can mean the difference between life and death.
As pediatric providers, formally screening for suicide risk is critical. Specifically, the American Academy of Pediatrics recommends that all youth aged 12 years or older be screened for suicide risk.2 In addition to asking families to reduce access to lethal means, it is important to utilize suicide-specific screeners to prevent suicide attempts and deaths in the pediatric community. Pediatric providers must feel prepared to counsel patients and families on suicide prevention and, if this skill set is underdeveloped, appropriate referrals and support must be provided.
At the same time, it is important to note the larger context. This national tragedy has been long-standing and further accelerated by the social isolation and stress of the pandemic. Madigan and colleagues recently showed that the lack of a social outlet resulting from COVID-19 caused an increase in screen time among all children.3 As a result, many teen girls turned to social media to recreate these social connections online.4 This dependence on social media for validation has contributed to increased rates of depression by intensifying unrealistic body standards, comparisons, and competition among peers.5 However, recent pediatric partnership programs have improved mental health access, reduced ED visits, and increased primary care physician’s comfort with managing mental health concerns.6 These programs are called Child Psychiatry Access Programs (CPAPs) and utilize a collaborative care model through which primary care clinicians consult with child and adolescent psychiatrists. CPAPs, while not the entire solution, offer a major step in the right direction toward tackling this mental health crisis in a sustainable, collaborative, and effective way.
As students return to in-person learning, connectedness at school is a powerful protective factor against depression and anxiety. We must infuse resources and support into our schools and teachers, as they stand on the front lines for our children. Specifically, bolstering schools with school counselors and appropriate mental health support staff will help rescue teachers from burnout while also explicitly identifying mental health care as a priority. Finally, modeling positive behavior for families and identifying safe adults at school can help at-risk youth feel more connected. To achieve meaningful improvement in children’s mental health, it is crucial to collaboratively remodel broken systems to ensure that all children are supported early, effectively, and equitably.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences, program director of the child and adolescent psychiatry fellowship, and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior in Los Angeles.
References
1. Centers for Disease Control and Prevention. YRBSS Data Summary & Trends. 2023 Feb 13. https://www.cdc.gov/healthyyouth/data/yrbs/yrbs_data_summary_and_trends.htm
2. American Academy of Pediatrics. Screening for Suicide Risk in Clinical Practice. 2023 Feb 22. https://www.aap.org/en/patient-care/blueprint-for-youth-suicide-prevention/strategies-for-clinical-settings-for-youth-suicide-prevention/screening-for-suicide-risk-in-clinical-practice/
3. Madigan S et al. JAMA Pediatr. 2022;176(12):1188-98. doi: 10.1001/JAMAPEDIATRICS.2022.4116
4. Pew Research Center. Teens, Social Media and Technology 2022. 2022 Aug 10. https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/
5. Hunt MG et al. J Social Clin Psychology. 2018;37(10):751-68. doi: 10.1521/JSCP.2018.37.10.751
6. Godoy L et al. J Pediatr Health Care. 2022 Dec 16. doi: 10.1016/j.pedhc.2022.11.009.
Case: “Where’s my mommy?”
A 13-year-old girl “D” appeared lifeless in her hospital bed, swallowed by tubes, gauze, and crisp white sheets. She seemed fragile next to the giant machines beeping all around her, as they churned and groaned to keep her alive. She was in the pediatric intensive care unit, a place she had only seen once or twice on TV. Her sleeping mother lay next to her in an uncomfortable-looking recliner chair, curled up in a ball. She abruptly woke up when I walked into the room, doing her best to wipe away 5 days’ worth of worry and sadness from her exhausted face. She saw “Child Psychiatrist” written on my hospital badge, desperately searching my face for answers or a sign of hope.
Her daughter – a straight-A middle school student who loved Taylor Swift and soccer – had overdosed on Tylenol after discovering that she did not make the cheerleading team. I reported that her daughter’s liver enzymes were finally trending down and that she would likely not require a liver transplant. She would survive. As tears welled up in this mother’s eyes, I heard a faint whisper from across the room. “Where’s my mommy?” D was awake and frantically searching the room for her mother, someone who could soothe her in this living nightmare. As the two embraced, I felt tears well up in my eyes as I couldn’t help but think of my own 3-year-old daughter at home. How could I protect her from the sadness and despair that this little girl was feeling? How can we collectively protect every little girl from wanting to end their life?
CDC data: Teen girls need help now
The latest biennial Centers for Disease Control and Prevention Youth Risk Behavior Survey, administered in the fall of 2021, resulted in alarming data showing that mental health has worsened for all adolescents, but especially for girls. The survey was administered to more than 17,000 students in 152 public and private schools throughout the United States, showing that “America’s teen girls are engulfed in a growing wave of sadness, violence, and trauma.”1 In particular, rates of sadness, suicidal ideation, suicide attempts, and mental health crisis ED visits among girls are the highest reported in a decade. Nearly 60% of girls felt persistent sadness or hopelessness during the past year, double the rate of boys. More than 25% of girls made a suicide plan; this percentage increased 60% over the past 10 years. Alarmingly, ED visits for suicide attempts for girls increased more than 50% in the past 2 years alone.
Even before the COVID-19 pandemic, experts were sounding the alarm on the growing rates of anxiety and depression in U.S. youth. The pandemic-driven isolation, lack of social connection, and missing of major milestones did not help the situation and only deepened the cracks in a faulty mental health care system. Further, civil unrest and social upheaval in the United States felt – and continues to feel – chaotic and unpredictable. For teens, the current cultural climate represents their not-too-distant future as adults, causing worry and anxiety.
In addition to securing their futures through performance in school and extracurricular activities, teenagers are forming their identities. Establishing a personal identity is a difficult task for all teens, though teenage girls face uniquely difficult challenges in our current society. In particular, teenage girls are expected to conform their behaviors to fit societal expectations that may clash with their desires and self-conceptualization. This conflict is further complicated by heightened beauty standards, online hate and competition, academic pressure, and self-doubt. CDC data show that girls experience sexual harassment and cyberbullying at roughly twice the rate of their male counterparts. Girls also experience higher levels of sexual violence and bullying. Alarmingly, 14% of girls reported being forced to have sex at some point in their lives. The sad truth is that, for every 10 teenage girls you know, at least one of them, and probably more, has likely been raped.
A call to action for providers
As providers, what can we do about these alarming statistics? It’s easy to become overwhelmed by data on a national level. However, regardless of our current clinical practice situation, we cannot lose sight of the humanity behind these numbers. Five extra minutes of truly listening to our patients, normalizing conversations about mental health, and looking for mental health warning signs (that is, increased isolation, declining function in school, maladaptive coping skills such as self-injurious behavior or substance use) can mean the difference between life and death.
As pediatric providers, formally screening for suicide risk is critical. Specifically, the American Academy of Pediatrics recommends that all youth aged 12 years or older be screened for suicide risk.2 In addition to asking families to reduce access to lethal means, it is important to utilize suicide-specific screeners to prevent suicide attempts and deaths in the pediatric community. Pediatric providers must feel prepared to counsel patients and families on suicide prevention and, if this skill set is underdeveloped, appropriate referrals and support must be provided.
At the same time, it is important to note the larger context. This national tragedy has been long-standing and further accelerated by the social isolation and stress of the pandemic. Madigan and colleagues recently showed that the lack of a social outlet resulting from COVID-19 caused an increase in screen time among all children.3 As a result, many teen girls turned to social media to recreate these social connections online.4 This dependence on social media for validation has contributed to increased rates of depression by intensifying unrealistic body standards, comparisons, and competition among peers.5 However, recent pediatric partnership programs have improved mental health access, reduced ED visits, and increased primary care physician’s comfort with managing mental health concerns.6 These programs are called Child Psychiatry Access Programs (CPAPs) and utilize a collaborative care model through which primary care clinicians consult with child and adolescent psychiatrists. CPAPs, while not the entire solution, offer a major step in the right direction toward tackling this mental health crisis in a sustainable, collaborative, and effective way.
As students return to in-person learning, connectedness at school is a powerful protective factor against depression and anxiety. We must infuse resources and support into our schools and teachers, as they stand on the front lines for our children. Specifically, bolstering schools with school counselors and appropriate mental health support staff will help rescue teachers from burnout while also explicitly identifying mental health care as a priority. Finally, modeling positive behavior for families and identifying safe adults at school can help at-risk youth feel more connected. To achieve meaningful improvement in children’s mental health, it is crucial to collaboratively remodel broken systems to ensure that all children are supported early, effectively, and equitably.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences, program director of the child and adolescent psychiatry fellowship, and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior in Los Angeles.
References
1. Centers for Disease Control and Prevention. YRBSS Data Summary & Trends. 2023 Feb 13. https://www.cdc.gov/healthyyouth/data/yrbs/yrbs_data_summary_and_trends.htm
2. American Academy of Pediatrics. Screening for Suicide Risk in Clinical Practice. 2023 Feb 22. https://www.aap.org/en/patient-care/blueprint-for-youth-suicide-prevention/strategies-for-clinical-settings-for-youth-suicide-prevention/screening-for-suicide-risk-in-clinical-practice/
3. Madigan S et al. JAMA Pediatr. 2022;176(12):1188-98. doi: 10.1001/JAMAPEDIATRICS.2022.4116
4. Pew Research Center. Teens, Social Media and Technology 2022. 2022 Aug 10. https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/
5. Hunt MG et al. J Social Clin Psychology. 2018;37(10):751-68. doi: 10.1521/JSCP.2018.37.10.751
6. Godoy L et al. J Pediatr Health Care. 2022 Dec 16. doi: 10.1016/j.pedhc.2022.11.009.
Prior authorizations: Time to rebel?
I imagine I am not alone when I tell you that my blood pressure rises every time I receive an email from CoverMyMeds, or worse, a phone call from a patient to tell me the pharmacist says I need to call their insurance company to get a medication authorized. Prior authorizations (PAs) are the bane of every physician’s existence.
They ask providers to jump through hoops, and no one oversees the placement of these hoops. The process puts patients at risk and sucks the joy from the practice of medicine.
In fall 2021, the legislative committee of the Maryland Psychiatric Society, with the help of Kathy Orellana and Tim Clement from the American Psychiatric Association, drafted a bill to modify the use of PAs. Unfortunately, the bill died in committee during the 2022 Maryland General Assembly legislative session.
Robert Herman, MD, who helped draft the initial legislation, was delighted when he learned that MedChi, the Maryland State Medical Society, had taken the proposed legislation and expanded it. “It was everything we wished for and more,” Dr. Herman said.
During this year’s legislative session, House Bill 305/Senate Bill 308, Health Insurance – Utilization Review – Revisions, was sponsored by 19 delegates and two senators. Fifty medical associations, including dentists and physical therapists, endorsed the bill. Many people, including Dr. Herman, testified before the Health and Government Operations Committee on Feb. 16.
Delegate Kenneth Kerr introduced the legislation to the committee.
“Before I begin, let me make two points. First, the bill does not do away with prior authorization or other utilization review techniques; rather, it tries to make a more balanced approach for both patients and physicians by attempting to reduce the volume that’s subject to prior authorization, by increasing transparency and communication, and by studying how the process can be improved overall. Second, we have over 50 organizations representing health care providers and patient advocacy organizations supporting this legislation. This is a systemic issue across the entire spectrum of healthcare,” said Mr. Kerr.
Mr. Kerr went on to say there were 81,143 denials for treatment in 2021. The three areas with the highest rate of denials were pharmacy, dental, and the combination of labs and radiology.
He further noted that, when consumers filed a complaint with the Maryland Insurance Administration, 72.4% of denials were reversed in 2022.
“This resulted in more benefits that could have, and should have, been given to the patient at the first request. These reversals indicate there is a problem,” Mr. Kerr said. He discussed increased administrative costs, the enormous workload burden this incurs, and the problem of burnout among medical providers.
The proposed legislation includes a ban on PA requirements for generic medications, for dose changes of previously authorized medication, and ends the requirement for yearly authorizations. It requires that a physician of the same specialty be on the panel that denies care and shortens the time periods allowed for responses and appeals.
Testimony began with those supporting the legislation. Doctors highlighted the harm inflicted on their patients by the PA process. An oncologist spoke of how it took weeks to get approval for chemotherapy for a patient with an aggressive cancer, a gastroenterologist discussed a patient who became ill and lost her job when successful treatment for inflammatory bowel disease was stopped while she waited for the yearly medication reapproval, and another physician told of a patient who died of an exacerbation of obstructive lung disease, also while awaiting a yearly reapproval for an effective medication.
A dentist spoke about how he was not authorized to place a crown on a patient’s tooth. Instead, he was instructed to try a filling first, and when the filling failed, he was told he would not be authorized to work on the same tooth twice in one year.
A physical therapist testified that PA was required every two to four sessions, and each request took up half of a session – a significant portion of time that was not used for treatment.
Three people testified in opposition to the bill. Matthew Celantano, executive director of the League of Life and Health Insurers of Maryland, called the legislation “drastic” and testified that the cost would be prohibitive.
“From our end, it’s important for you to hear that prior authorization is care coordination. It’s protection that keeps [patients] safe, but helps control skyrocketing health care costs,” said Mr. Celantano.
Deb Rivkin, vice president of government affairs for CareFirst Blue Cross Blue Shield, testified in favor of using better technology. She cited legislation under consideration in Virginia that would give clinicians more information about the specific medications that require PAs, price information, and real-time authorizations.
Finally, representing the Pharmaceutical Care Management Association, Heather Cascone testified about PAs for generic medications. Her testimony focused on prior authorization for generic medications. She claimed that “... by allowing unrestricted dispensing of generic drugs, or an override based on the subjective opinion of the prescriber, prior authorization can protect patients from drugs with a safety risk; they can catch things like drug-disease contraindications, dosage errors, pregnancy-related contraindications, and a variety of cost-savings protections.”
I found this testimony particularly difficult because the “protector” is generally not a physician and has neither seen, nor examined, the patient. The implication that patients need protection from their doctors who would be unaware aware that they are pregnant, or are ill, was offensive. It also implies that PBMs are lax by not requiring PA on all medications, ignoring the fact that patients often bypass such denials by paying out of pocket for treatment.
If this had been a high school debate, there would be no doubt the enthusiasm for the bill for HB305 was strong, the committee chair was eager, and the arguments in favor of the legislation robust. There are no public minutes for the subsequent meetings with stakeholders, and I was somewhat heartbroken to learn that once again, the bill died in committee.
Annette Hanson, MD, chair of the MPS legislative committee, remains optimistic for the future. “Since then, the APA [American Psychiatric Association] has taken our bill and used it as model legislation now being offered to other district branches. MPS has created something that is going to spread across the country. Change may be slow, but it is not inevitable. And when it happens, I want you to remember that it started here,” she said.
However, the pressure is on. A recent ProPublica article documented how Cigna rejects claims by the batch without ever reviewing them. Soon after that piece was published, it was announced that several of the large insurers, including Cigna, would be cutting back on PA demands. It remains to be seen whether this is a token move to placate legislators, and whether it will provide meaningful relief to physicians and patients. I remain skeptical.
In the meantime, physicians’ ability to help their patients remains compromised and administrative tasks consume valuable time. I have started to wonder whether there may be some other way to push this issue to action. PA is about cost containment, but perhaps there are other ways to economize.
Why do medications cost less in other countries? Why does a medication cost hundreds of dollars more at one pharmacy versus another? Why do medicines sometimes have a copay that is two or three times higher than the cash price? Why do some covered medications have copays of thousands of dollars a year? I wonder if physicians shouldn’t come together and collectively agree not to comply and refuse to complete PAs in organized rebellion.
The fear, of course, is that such an endeavor would hurt patients, but if we all agreed in concert, then for better or for worse, something would have to give. The existing system is already hurting everyone, and physicians, by agreeing to play this awful game, are complicit in letting insurers dictate the care our patients receive.
Dinah Miller, MD, is a coauthor of Committed: The Battle Over Involuntary Psychiatric Care (Johns Hopkins University Press, 2016) and has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore.
A version of this article first appeared on Medscape.com.
I imagine I am not alone when I tell you that my blood pressure rises every time I receive an email from CoverMyMeds, or worse, a phone call from a patient to tell me the pharmacist says I need to call their insurance company to get a medication authorized. Prior authorizations (PAs) are the bane of every physician’s existence.
They ask providers to jump through hoops, and no one oversees the placement of these hoops. The process puts patients at risk and sucks the joy from the practice of medicine.
In fall 2021, the legislative committee of the Maryland Psychiatric Society, with the help of Kathy Orellana and Tim Clement from the American Psychiatric Association, drafted a bill to modify the use of PAs. Unfortunately, the bill died in committee during the 2022 Maryland General Assembly legislative session.
Robert Herman, MD, who helped draft the initial legislation, was delighted when he learned that MedChi, the Maryland State Medical Society, had taken the proposed legislation and expanded it. “It was everything we wished for and more,” Dr. Herman said.
During this year’s legislative session, House Bill 305/Senate Bill 308, Health Insurance – Utilization Review – Revisions, was sponsored by 19 delegates and two senators. Fifty medical associations, including dentists and physical therapists, endorsed the bill. Many people, including Dr. Herman, testified before the Health and Government Operations Committee on Feb. 16.
Delegate Kenneth Kerr introduced the legislation to the committee.
“Before I begin, let me make two points. First, the bill does not do away with prior authorization or other utilization review techniques; rather, it tries to make a more balanced approach for both patients and physicians by attempting to reduce the volume that’s subject to prior authorization, by increasing transparency and communication, and by studying how the process can be improved overall. Second, we have over 50 organizations representing health care providers and patient advocacy organizations supporting this legislation. This is a systemic issue across the entire spectrum of healthcare,” said Mr. Kerr.
Mr. Kerr went on to say there were 81,143 denials for treatment in 2021. The three areas with the highest rate of denials were pharmacy, dental, and the combination of labs and radiology.
He further noted that, when consumers filed a complaint with the Maryland Insurance Administration, 72.4% of denials were reversed in 2022.
“This resulted in more benefits that could have, and should have, been given to the patient at the first request. These reversals indicate there is a problem,” Mr. Kerr said. He discussed increased administrative costs, the enormous workload burden this incurs, and the problem of burnout among medical providers.
The proposed legislation includes a ban on PA requirements for generic medications, for dose changes of previously authorized medication, and ends the requirement for yearly authorizations. It requires that a physician of the same specialty be on the panel that denies care and shortens the time periods allowed for responses and appeals.
Testimony began with those supporting the legislation. Doctors highlighted the harm inflicted on their patients by the PA process. An oncologist spoke of how it took weeks to get approval for chemotherapy for a patient with an aggressive cancer, a gastroenterologist discussed a patient who became ill and lost her job when successful treatment for inflammatory bowel disease was stopped while she waited for the yearly medication reapproval, and another physician told of a patient who died of an exacerbation of obstructive lung disease, also while awaiting a yearly reapproval for an effective medication.
A dentist spoke about how he was not authorized to place a crown on a patient’s tooth. Instead, he was instructed to try a filling first, and when the filling failed, he was told he would not be authorized to work on the same tooth twice in one year.
A physical therapist testified that PA was required every two to four sessions, and each request took up half of a session – a significant portion of time that was not used for treatment.
Three people testified in opposition to the bill. Matthew Celantano, executive director of the League of Life and Health Insurers of Maryland, called the legislation “drastic” and testified that the cost would be prohibitive.
“From our end, it’s important for you to hear that prior authorization is care coordination. It’s protection that keeps [patients] safe, but helps control skyrocketing health care costs,” said Mr. Celantano.
Deb Rivkin, vice president of government affairs for CareFirst Blue Cross Blue Shield, testified in favor of using better technology. She cited legislation under consideration in Virginia that would give clinicians more information about the specific medications that require PAs, price information, and real-time authorizations.
Finally, representing the Pharmaceutical Care Management Association, Heather Cascone testified about PAs for generic medications. Her testimony focused on prior authorization for generic medications. She claimed that “... by allowing unrestricted dispensing of generic drugs, or an override based on the subjective opinion of the prescriber, prior authorization can protect patients from drugs with a safety risk; they can catch things like drug-disease contraindications, dosage errors, pregnancy-related contraindications, and a variety of cost-savings protections.”
I found this testimony particularly difficult because the “protector” is generally not a physician and has neither seen, nor examined, the patient. The implication that patients need protection from their doctors who would be unaware aware that they are pregnant, or are ill, was offensive. It also implies that PBMs are lax by not requiring PA on all medications, ignoring the fact that patients often bypass such denials by paying out of pocket for treatment.
If this had been a high school debate, there would be no doubt the enthusiasm for the bill for HB305 was strong, the committee chair was eager, and the arguments in favor of the legislation robust. There are no public minutes for the subsequent meetings with stakeholders, and I was somewhat heartbroken to learn that once again, the bill died in committee.
Annette Hanson, MD, chair of the MPS legislative committee, remains optimistic for the future. “Since then, the APA [American Psychiatric Association] has taken our bill and used it as model legislation now being offered to other district branches. MPS has created something that is going to spread across the country. Change may be slow, but it is not inevitable. And when it happens, I want you to remember that it started here,” she said.
However, the pressure is on. A recent ProPublica article documented how Cigna rejects claims by the batch without ever reviewing them. Soon after that piece was published, it was announced that several of the large insurers, including Cigna, would be cutting back on PA demands. It remains to be seen whether this is a token move to placate legislators, and whether it will provide meaningful relief to physicians and patients. I remain skeptical.
In the meantime, physicians’ ability to help their patients remains compromised and administrative tasks consume valuable time. I have started to wonder whether there may be some other way to push this issue to action. PA is about cost containment, but perhaps there are other ways to economize.
Why do medications cost less in other countries? Why does a medication cost hundreds of dollars more at one pharmacy versus another? Why do medicines sometimes have a copay that is two or three times higher than the cash price? Why do some covered medications have copays of thousands of dollars a year? I wonder if physicians shouldn’t come together and collectively agree not to comply and refuse to complete PAs in organized rebellion.
The fear, of course, is that such an endeavor would hurt patients, but if we all agreed in concert, then for better or for worse, something would have to give. The existing system is already hurting everyone, and physicians, by agreeing to play this awful game, are complicit in letting insurers dictate the care our patients receive.
Dinah Miller, MD, is a coauthor of Committed: The Battle Over Involuntary Psychiatric Care (Johns Hopkins University Press, 2016) and has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore.
A version of this article first appeared on Medscape.com.
I imagine I am not alone when I tell you that my blood pressure rises every time I receive an email from CoverMyMeds, or worse, a phone call from a patient to tell me the pharmacist says I need to call their insurance company to get a medication authorized. Prior authorizations (PAs) are the bane of every physician’s existence.
They ask providers to jump through hoops, and no one oversees the placement of these hoops. The process puts patients at risk and sucks the joy from the practice of medicine.
In fall 2021, the legislative committee of the Maryland Psychiatric Society, with the help of Kathy Orellana and Tim Clement from the American Psychiatric Association, drafted a bill to modify the use of PAs. Unfortunately, the bill died in committee during the 2022 Maryland General Assembly legislative session.
Robert Herman, MD, who helped draft the initial legislation, was delighted when he learned that MedChi, the Maryland State Medical Society, had taken the proposed legislation and expanded it. “It was everything we wished for and more,” Dr. Herman said.
During this year’s legislative session, House Bill 305/Senate Bill 308, Health Insurance – Utilization Review – Revisions, was sponsored by 19 delegates and two senators. Fifty medical associations, including dentists and physical therapists, endorsed the bill. Many people, including Dr. Herman, testified before the Health and Government Operations Committee on Feb. 16.
Delegate Kenneth Kerr introduced the legislation to the committee.
“Before I begin, let me make two points. First, the bill does not do away with prior authorization or other utilization review techniques; rather, it tries to make a more balanced approach for both patients and physicians by attempting to reduce the volume that’s subject to prior authorization, by increasing transparency and communication, and by studying how the process can be improved overall. Second, we have over 50 organizations representing health care providers and patient advocacy organizations supporting this legislation. This is a systemic issue across the entire spectrum of healthcare,” said Mr. Kerr.
Mr. Kerr went on to say there were 81,143 denials for treatment in 2021. The three areas with the highest rate of denials were pharmacy, dental, and the combination of labs and radiology.
He further noted that, when consumers filed a complaint with the Maryland Insurance Administration, 72.4% of denials were reversed in 2022.
“This resulted in more benefits that could have, and should have, been given to the patient at the first request. These reversals indicate there is a problem,” Mr. Kerr said. He discussed increased administrative costs, the enormous workload burden this incurs, and the problem of burnout among medical providers.
The proposed legislation includes a ban on PA requirements for generic medications, for dose changes of previously authorized medication, and ends the requirement for yearly authorizations. It requires that a physician of the same specialty be on the panel that denies care and shortens the time periods allowed for responses and appeals.
Testimony began with those supporting the legislation. Doctors highlighted the harm inflicted on their patients by the PA process. An oncologist spoke of how it took weeks to get approval for chemotherapy for a patient with an aggressive cancer, a gastroenterologist discussed a patient who became ill and lost her job when successful treatment for inflammatory bowel disease was stopped while she waited for the yearly medication reapproval, and another physician told of a patient who died of an exacerbation of obstructive lung disease, also while awaiting a yearly reapproval for an effective medication.
A dentist spoke about how he was not authorized to place a crown on a patient’s tooth. Instead, he was instructed to try a filling first, and when the filling failed, he was told he would not be authorized to work on the same tooth twice in one year.
A physical therapist testified that PA was required every two to four sessions, and each request took up half of a session – a significant portion of time that was not used for treatment.
Three people testified in opposition to the bill. Matthew Celantano, executive director of the League of Life and Health Insurers of Maryland, called the legislation “drastic” and testified that the cost would be prohibitive.
“From our end, it’s important for you to hear that prior authorization is care coordination. It’s protection that keeps [patients] safe, but helps control skyrocketing health care costs,” said Mr. Celantano.
Deb Rivkin, vice president of government affairs for CareFirst Blue Cross Blue Shield, testified in favor of using better technology. She cited legislation under consideration in Virginia that would give clinicians more information about the specific medications that require PAs, price information, and real-time authorizations.
Finally, representing the Pharmaceutical Care Management Association, Heather Cascone testified about PAs for generic medications. Her testimony focused on prior authorization for generic medications. She claimed that “... by allowing unrestricted dispensing of generic drugs, or an override based on the subjective opinion of the prescriber, prior authorization can protect patients from drugs with a safety risk; they can catch things like drug-disease contraindications, dosage errors, pregnancy-related contraindications, and a variety of cost-savings protections.”
I found this testimony particularly difficult because the “protector” is generally not a physician and has neither seen, nor examined, the patient. The implication that patients need protection from their doctors who would be unaware aware that they are pregnant, or are ill, was offensive. It also implies that PBMs are lax by not requiring PA on all medications, ignoring the fact that patients often bypass such denials by paying out of pocket for treatment.
If this had been a high school debate, there would be no doubt the enthusiasm for the bill for HB305 was strong, the committee chair was eager, and the arguments in favor of the legislation robust. There are no public minutes for the subsequent meetings with stakeholders, and I was somewhat heartbroken to learn that once again, the bill died in committee.
Annette Hanson, MD, chair of the MPS legislative committee, remains optimistic for the future. “Since then, the APA [American Psychiatric Association] has taken our bill and used it as model legislation now being offered to other district branches. MPS has created something that is going to spread across the country. Change may be slow, but it is not inevitable. And when it happens, I want you to remember that it started here,” she said.
However, the pressure is on. A recent ProPublica article documented how Cigna rejects claims by the batch without ever reviewing them. Soon after that piece was published, it was announced that several of the large insurers, including Cigna, would be cutting back on PA demands. It remains to be seen whether this is a token move to placate legislators, and whether it will provide meaningful relief to physicians and patients. I remain skeptical.
In the meantime, physicians’ ability to help their patients remains compromised and administrative tasks consume valuable time. I have started to wonder whether there may be some other way to push this issue to action. PA is about cost containment, but perhaps there are other ways to economize.
Why do medications cost less in other countries? Why does a medication cost hundreds of dollars more at one pharmacy versus another? Why do medicines sometimes have a copay that is two or three times higher than the cash price? Why do some covered medications have copays of thousands of dollars a year? I wonder if physicians shouldn’t come together and collectively agree not to comply and refuse to complete PAs in organized rebellion.
The fear, of course, is that such an endeavor would hurt patients, but if we all agreed in concert, then for better or for worse, something would have to give. The existing system is already hurting everyone, and physicians, by agreeing to play this awful game, are complicit in letting insurers dictate the care our patients receive.
Dinah Miller, MD, is a coauthor of Committed: The Battle Over Involuntary Psychiatric Care (Johns Hopkins University Press, 2016) and has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore.
A version of this article first appeared on Medscape.com.