User login
Do PFAs Cause Kidney Cancer? VA to Investigate
The US Department of Veterans Affairs (VA) will conduct a scientific assessment to find out in whether kidney cancer should be considered a presumptive service-connected condition for veterans exposed to per- and polyfluoroalkyl substances (PFAs). This assessment is the first step in the VA presumptive condition investigative process, which could allow exposed veterans who were exposed to PFAs during their service to access more VA services.
A class of more than 12,000 chemicals, PFAs have been used in the military since the early 1970s in many items, including military-grade firefighting foam. Studies have already suggested links between the so-called forever chemicals and cancer, particularly kidney cancer.
The US Department of Defense (DoD) is assessing contamination at hundreds of sites, while the National Defense Authorization Act in Fiscal Year 2020 mandated that DoD stop using those foams starting in October and remove all stocks from active and former installations and equipment. That may not happen until next year, though, because the DoD has requested a waiver through October 2025 and may extend it through 2026.
When a condition is considered presumptive, eligible veterans do not need to prove their service caused their disease to receive benefits. As part of the Biden Administration’s efforts to expand benefits and services for toxin-exposed veterans and their families, the VA expedited health care and benefits eligibility under the PACT Act by several years—including extending presumptions for head cancer, neck cancer, gastrointestinal cancer, reproductive cancer, lymphoma, pancreatic cancer, kidney cancer, melanoma, and hypertension for Vietnam era veterans. The VA has also extended presumptions for > 300 new conditions, most recently for male breast cancer, urethral cancer, and cancer of the paraurethral glands.
Whether a condition is an established presumptive condition or not, the VA will consider claims on a case-by-case basis and can grant disability compensation benefits if sufficient evidence of service connection is found. “[M]ake no mistake: Veterans should not wait for the outcome of this review to apply for the benefits and care they deserve,” VA Secretary Denis McDonough said in a release. “If you’re a veteran and believe your military service has negatively impacted your health, we encourage you to apply for VA care and benefits today.”
The public has 30 days to comment on the proposed scientific assessment between PFAs exposure and kidney cancer via the Federal Register. The VA is set to host a listening session on Nov. 19, 2024, to allow individuals to share research and input. Interested individuals may register to participate. The public may also comment via either forum on other conditions that would benefit from review for potential service-connection.
The US Department of Veterans Affairs (VA) will conduct a scientific assessment to find out in whether kidney cancer should be considered a presumptive service-connected condition for veterans exposed to per- and polyfluoroalkyl substances (PFAs). This assessment is the first step in the VA presumptive condition investigative process, which could allow exposed veterans who were exposed to PFAs during their service to access more VA services.
A class of more than 12,000 chemicals, PFAs have been used in the military since the early 1970s in many items, including military-grade firefighting foam. Studies have already suggested links between the so-called forever chemicals and cancer, particularly kidney cancer.
The US Department of Defense (DoD) is assessing contamination at hundreds of sites, while the National Defense Authorization Act in Fiscal Year 2020 mandated that DoD stop using those foams starting in October and remove all stocks from active and former installations and equipment. That may not happen until next year, though, because the DoD has requested a waiver through October 2025 and may extend it through 2026.
When a condition is considered presumptive, eligible veterans do not need to prove their service caused their disease to receive benefits. As part of the Biden Administration’s efforts to expand benefits and services for toxin-exposed veterans and their families, the VA expedited health care and benefits eligibility under the PACT Act by several years—including extending presumptions for head cancer, neck cancer, gastrointestinal cancer, reproductive cancer, lymphoma, pancreatic cancer, kidney cancer, melanoma, and hypertension for Vietnam era veterans. The VA has also extended presumptions for > 300 new conditions, most recently for male breast cancer, urethral cancer, and cancer of the paraurethral glands.
Whether a condition is an established presumptive condition or not, the VA will consider claims on a case-by-case basis and can grant disability compensation benefits if sufficient evidence of service connection is found. “[M]ake no mistake: Veterans should not wait for the outcome of this review to apply for the benefits and care they deserve,” VA Secretary Denis McDonough said in a release. “If you’re a veteran and believe your military service has negatively impacted your health, we encourage you to apply for VA care and benefits today.”
The public has 30 days to comment on the proposed scientific assessment between PFAs exposure and kidney cancer via the Federal Register. The VA is set to host a listening session on Nov. 19, 2024, to allow individuals to share research and input. Interested individuals may register to participate. The public may also comment via either forum on other conditions that would benefit from review for potential service-connection.
The US Department of Veterans Affairs (VA) will conduct a scientific assessment to find out in whether kidney cancer should be considered a presumptive service-connected condition for veterans exposed to per- and polyfluoroalkyl substances (PFAs). This assessment is the first step in the VA presumptive condition investigative process, which could allow exposed veterans who were exposed to PFAs during their service to access more VA services.
A class of more than 12,000 chemicals, PFAs have been used in the military since the early 1970s in many items, including military-grade firefighting foam. Studies have already suggested links between the so-called forever chemicals and cancer, particularly kidney cancer.
The US Department of Defense (DoD) is assessing contamination at hundreds of sites, while the National Defense Authorization Act in Fiscal Year 2020 mandated that DoD stop using those foams starting in October and remove all stocks from active and former installations and equipment. That may not happen until next year, though, because the DoD has requested a waiver through October 2025 and may extend it through 2026.
When a condition is considered presumptive, eligible veterans do not need to prove their service caused their disease to receive benefits. As part of the Biden Administration’s efforts to expand benefits and services for toxin-exposed veterans and their families, the VA expedited health care and benefits eligibility under the PACT Act by several years—including extending presumptions for head cancer, neck cancer, gastrointestinal cancer, reproductive cancer, lymphoma, pancreatic cancer, kidney cancer, melanoma, and hypertension for Vietnam era veterans. The VA has also extended presumptions for > 300 new conditions, most recently for male breast cancer, urethral cancer, and cancer of the paraurethral glands.
Whether a condition is an established presumptive condition or not, the VA will consider claims on a case-by-case basis and can grant disability compensation benefits if sufficient evidence of service connection is found. “[M]ake no mistake: Veterans should not wait for the outcome of this review to apply for the benefits and care they deserve,” VA Secretary Denis McDonough said in a release. “If you’re a veteran and believe your military service has negatively impacted your health, we encourage you to apply for VA care and benefits today.”
The public has 30 days to comment on the proposed scientific assessment between PFAs exposure and kidney cancer via the Federal Register. The VA is set to host a listening session on Nov. 19, 2024, to allow individuals to share research and input. Interested individuals may register to participate. The public may also comment via either forum on other conditions that would benefit from review for potential service-connection.
VA Tele-Emergency Care Program Expanded Nationwide
The US Department of Veterans Affairs (VA) has announced that tele-emergency care (tele-EC) is now available nationwide. According to the VA, the expansion has already helped > 61,000 callers with a 59.4% case resolution rate, meaning veterans’ needs were resolved without them having to travel to urgent care or an emergency department.
Tele-EC does not replace the need for in-person emergency evaluation, but offers quick, virtual triage assessments for veterans in rural areas or those with mobility and transportation challenges when in-person immediate care can be difficult to access. The program is a part of VA Health Connect, which connects the caller to a clinical triage nurse, who connects the veteran to tele-emergency care when clinically appropriate. Tele-EC practitioners evaluate the veteran over the phone or on video and recommend treatment or follow-up, including in-person care if needed. In life-threatening emergencies, the clinical triage nurse will call 911 and stay on the phone with the veteran until help arrives. The VA however, says the best step for a veteran experiencing a life-threatening emergency is to immediately contact 911 as opposed to seeking support via tele-EC.
The program can save time not only through on-the-spot evaluation, but by avoiding drive and wait times. “Sometimes, you’re not sure whether what you’re experiencing is a minor emergency or not — and tele-emergency care can help you resolve those questions,” VA Under Secretary for Health Shereef Elnahal, MD, says. “Veterans can get immediate, virtual triage with a VA medical provider who has direct access to their medical records. This avoids having to potentially drive to the nearest emergency department and wait to be evaluated, if appropriate.”
Veterans enrolled in VA health care can now access tele-EC nationwide by calling VA Health Connect and through the VA Health Chat app. Veterans can find their local VA Health Connect number by searching for their facility.
The US Department of Veterans Affairs (VA) has announced that tele-emergency care (tele-EC) is now available nationwide. According to the VA, the expansion has already helped > 61,000 callers with a 59.4% case resolution rate, meaning veterans’ needs were resolved without them having to travel to urgent care or an emergency department.
Tele-EC does not replace the need for in-person emergency evaluation, but offers quick, virtual triage assessments for veterans in rural areas or those with mobility and transportation challenges when in-person immediate care can be difficult to access. The program is a part of VA Health Connect, which connects the caller to a clinical triage nurse, who connects the veteran to tele-emergency care when clinically appropriate. Tele-EC practitioners evaluate the veteran over the phone or on video and recommend treatment or follow-up, including in-person care if needed. In life-threatening emergencies, the clinical triage nurse will call 911 and stay on the phone with the veteran until help arrives. The VA however, says the best step for a veteran experiencing a life-threatening emergency is to immediately contact 911 as opposed to seeking support via tele-EC.
The program can save time not only through on-the-spot evaluation, but by avoiding drive and wait times. “Sometimes, you’re not sure whether what you’re experiencing is a minor emergency or not — and tele-emergency care can help you resolve those questions,” VA Under Secretary for Health Shereef Elnahal, MD, says. “Veterans can get immediate, virtual triage with a VA medical provider who has direct access to their medical records. This avoids having to potentially drive to the nearest emergency department and wait to be evaluated, if appropriate.”
Veterans enrolled in VA health care can now access tele-EC nationwide by calling VA Health Connect and through the VA Health Chat app. Veterans can find their local VA Health Connect number by searching for their facility.
The US Department of Veterans Affairs (VA) has announced that tele-emergency care (tele-EC) is now available nationwide. According to the VA, the expansion has already helped > 61,000 callers with a 59.4% case resolution rate, meaning veterans’ needs were resolved without them having to travel to urgent care or an emergency department.
Tele-EC does not replace the need for in-person emergency evaluation, but offers quick, virtual triage assessments for veterans in rural areas or those with mobility and transportation challenges when in-person immediate care can be difficult to access. The program is a part of VA Health Connect, which connects the caller to a clinical triage nurse, who connects the veteran to tele-emergency care when clinically appropriate. Tele-EC practitioners evaluate the veteran over the phone or on video and recommend treatment or follow-up, including in-person care if needed. In life-threatening emergencies, the clinical triage nurse will call 911 and stay on the phone with the veteran until help arrives. The VA however, says the best step for a veteran experiencing a life-threatening emergency is to immediately contact 911 as opposed to seeking support via tele-EC.
The program can save time not only through on-the-spot evaluation, but by avoiding drive and wait times. “Sometimes, you’re not sure whether what you’re experiencing is a minor emergency or not — and tele-emergency care can help you resolve those questions,” VA Under Secretary for Health Shereef Elnahal, MD, says. “Veterans can get immediate, virtual triage with a VA medical provider who has direct access to their medical records. This avoids having to potentially drive to the nearest emergency department and wait to be evaluated, if appropriate.”
Veterans enrolled in VA health care can now access tele-EC nationwide by calling VA Health Connect and through the VA Health Chat app. Veterans can find their local VA Health Connect number by searching for their facility.
Reduced Vaccination Rates Contribute to Rising Pertussis Numbers
New data from the Centers for Disease Control and Prevention (CDC) show significant spikes in pertussis cases compared with last year, especially in several urban areas including New York, Illinois, Florida, and Colorado.
Notably, the current pertussis case count in Illinois as of September 21, 2024, was five times higher than the total cases in 2023 (1058 vs 50). New York City alone had reported 624 cases as of September 21, compared with 38 cases in 2023.
Additional data from the CDC on vaccination coverage and exemptions of school-aged children showed an increase from 3.0% last year to 3.3% in 2024 of children who were exempted from recommended vaccination requirements. Although nearly 93% of kindergarteners in the United States received recommended vaccines (including Tdap), similar to last year, this number shows a steady decline from 94% in the 2021-2021 school year and 93% in the 2021-2022 school year, according to previous CDC reports.
What’s Happening in the Clinic
Clinical experience and the most recent CDC data point to under vaccination as a driver of the increased pertussis cases this year, David J. Cennimo, MD, associate professor of medicine and pediatrics in the division of infectious disease at Rutgers New Jersey Medical School, Newark, New Jersey, said in an interview.
Although the pertussis vaccination rates in infancy are still very good, clinicians are seeing a drop-off in school-aged children and adults, and the lingering anti-vaccine efforts from the COVID-19 pandemic period are undoubtedly playing a part, said Dr. Cennimo. “Unfortunately, pertussis is contagious, and the vaccine effectiveness wears off. Having decreased numbers of people protected results in more rapid spread,” he said.
Dr. Cennimo agreed that the number of cases in the United States is underreported, and even higher than the data suggest. “I’m sure of it; the initial clinical presentation may be mistaken for a viral upper respiratory tract infection (common cold),” he told this news organization.
Many older children and adults with pertussis do not manifest the classic “whooping cough” seen in infants and young children, so making a clinical diagnosis can be difficult, he said. “One classical component of the illness is a prolonged cough. I have wondered if some people now reporting a lingering cough had pertussis that was missed,” Dr. Cennimo noted.
“Clinicians should stress the value of boosters in a vaccine-preventable illness where we know immunity wanes overtime,” Dr. Cennimo said. “We have a great remedy in the Tdap vaccine, which we should all be getting very 10 years,” he said.
He also emphasized that clinicians remind pregnant women of the current recommendations to receive the Tdap vaccine for every pregnancy. “Vaccination during pregnancy is the best way to protect both the pregnant person and the newborn.
Even for the vaccine hesitant, this vaccine has a long track record of safety so should not be a significant concern,” he said.
The ultimate take-home message is not a new one, and applies to all illnesses, Dr. Cennimo told this news organization. Simply put, “Stay home if you are sick. Social distancing is not just for COVID-19,” he said.
Dr. Cennimo had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
New data from the Centers for Disease Control and Prevention (CDC) show significant spikes in pertussis cases compared with last year, especially in several urban areas including New York, Illinois, Florida, and Colorado.
Notably, the current pertussis case count in Illinois as of September 21, 2024, was five times higher than the total cases in 2023 (1058 vs 50). New York City alone had reported 624 cases as of September 21, compared with 38 cases in 2023.
Additional data from the CDC on vaccination coverage and exemptions of school-aged children showed an increase from 3.0% last year to 3.3% in 2024 of children who were exempted from recommended vaccination requirements. Although nearly 93% of kindergarteners in the United States received recommended vaccines (including Tdap), similar to last year, this number shows a steady decline from 94% in the 2021-2021 school year and 93% in the 2021-2022 school year, according to previous CDC reports.
What’s Happening in the Clinic
Clinical experience and the most recent CDC data point to under vaccination as a driver of the increased pertussis cases this year, David J. Cennimo, MD, associate professor of medicine and pediatrics in the division of infectious disease at Rutgers New Jersey Medical School, Newark, New Jersey, said in an interview.
Although the pertussis vaccination rates in infancy are still very good, clinicians are seeing a drop-off in school-aged children and adults, and the lingering anti-vaccine efforts from the COVID-19 pandemic period are undoubtedly playing a part, said Dr. Cennimo. “Unfortunately, pertussis is contagious, and the vaccine effectiveness wears off. Having decreased numbers of people protected results in more rapid spread,” he said.
Dr. Cennimo agreed that the number of cases in the United States is underreported, and even higher than the data suggest. “I’m sure of it; the initial clinical presentation may be mistaken for a viral upper respiratory tract infection (common cold),” he told this news organization.
Many older children and adults with pertussis do not manifest the classic “whooping cough” seen in infants and young children, so making a clinical diagnosis can be difficult, he said. “One classical component of the illness is a prolonged cough. I have wondered if some people now reporting a lingering cough had pertussis that was missed,” Dr. Cennimo noted.
“Clinicians should stress the value of boosters in a vaccine-preventable illness where we know immunity wanes overtime,” Dr. Cennimo said. “We have a great remedy in the Tdap vaccine, which we should all be getting very 10 years,” he said.
He also emphasized that clinicians remind pregnant women of the current recommendations to receive the Tdap vaccine for every pregnancy. “Vaccination during pregnancy is the best way to protect both the pregnant person and the newborn.
Even for the vaccine hesitant, this vaccine has a long track record of safety so should not be a significant concern,” he said.
The ultimate take-home message is not a new one, and applies to all illnesses, Dr. Cennimo told this news organization. Simply put, “Stay home if you are sick. Social distancing is not just for COVID-19,” he said.
Dr. Cennimo had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
New data from the Centers for Disease Control and Prevention (CDC) show significant spikes in pertussis cases compared with last year, especially in several urban areas including New York, Illinois, Florida, and Colorado.
Notably, the current pertussis case count in Illinois as of September 21, 2024, was five times higher than the total cases in 2023 (1058 vs 50). New York City alone had reported 624 cases as of September 21, compared with 38 cases in 2023.
Additional data from the CDC on vaccination coverage and exemptions of school-aged children showed an increase from 3.0% last year to 3.3% in 2024 of children who were exempted from recommended vaccination requirements. Although nearly 93% of kindergarteners in the United States received recommended vaccines (including Tdap), similar to last year, this number shows a steady decline from 94% in the 2021-2021 school year and 93% in the 2021-2022 school year, according to previous CDC reports.
What’s Happening in the Clinic
Clinical experience and the most recent CDC data point to under vaccination as a driver of the increased pertussis cases this year, David J. Cennimo, MD, associate professor of medicine and pediatrics in the division of infectious disease at Rutgers New Jersey Medical School, Newark, New Jersey, said in an interview.
Although the pertussis vaccination rates in infancy are still very good, clinicians are seeing a drop-off in school-aged children and adults, and the lingering anti-vaccine efforts from the COVID-19 pandemic period are undoubtedly playing a part, said Dr. Cennimo. “Unfortunately, pertussis is contagious, and the vaccine effectiveness wears off. Having decreased numbers of people protected results in more rapid spread,” he said.
Dr. Cennimo agreed that the number of cases in the United States is underreported, and even higher than the data suggest. “I’m sure of it; the initial clinical presentation may be mistaken for a viral upper respiratory tract infection (common cold),” he told this news organization.
Many older children and adults with pertussis do not manifest the classic “whooping cough” seen in infants and young children, so making a clinical diagnosis can be difficult, he said. “One classical component of the illness is a prolonged cough. I have wondered if some people now reporting a lingering cough had pertussis that was missed,” Dr. Cennimo noted.
“Clinicians should stress the value of boosters in a vaccine-preventable illness where we know immunity wanes overtime,” Dr. Cennimo said. “We have a great remedy in the Tdap vaccine, which we should all be getting very 10 years,” he said.
He also emphasized that clinicians remind pregnant women of the current recommendations to receive the Tdap vaccine for every pregnancy. “Vaccination during pregnancy is the best way to protect both the pregnant person and the newborn.
Even for the vaccine hesitant, this vaccine has a long track record of safety so should not be a significant concern,” he said.
The ultimate take-home message is not a new one, and applies to all illnesses, Dr. Cennimo told this news organization. Simply put, “Stay home if you are sick. Social distancing is not just for COVID-19,” he said.
Dr. Cennimo had no financial conflicts to disclose.
A version of this article first appeared on Medscape.com.
Which Medication Is Best? VA Genetic Tests May Have the Answer
The US Department of Veterans Affairs (VA) now has a permanent pharmacogenomics service that provides genetic tests to give clinicians insight into the best medication options for their patients.
The tests, which have no extra cost, are available to all veterans, said pharmacist Jill S. Bates, PharmD, MS, executive director of the VA National Pharmacogenomics Program, who spoke in an interview and a presentation at the annual meeting of the Association of VA Hematology/Oncology.
Genetic testing is “a tool that can help optimize care that we provide for veterans,” she said. “Pharmacogenomics is additional information to help the clinician make a decision. We know that most veterans—greater than 90%—carry a variant in a pharmacogenomics gene that is actionable.”
The genetic tests can provide insight into the optimal medication for multiple conditions such as mental illness, gastrointestinal disorders, cancer, pain, and heart disease. According to a 2019 analysis of over 6 years of data, more than half of the VA patient population used medications whose efficacy may have been affected by detectable genetic variants.
For instance, Bates said tests can let clinicians know whether patients are susceptible to statin-associated muscle adverse effects if they take simvastatin, the cholesterol medication. An estimated 25.6% of the VA population has this variant.
Elsewhere on the cardiac front, an estimated 58.3% of the VA population has a genetic variant that increases sensitivity to the blood thinner warfarin.
Testing could help psychiatrists determine whether certain medications should not be prescribed—or should be prescribed at lower doses—in patients who’ve had adverse reactions to antidepressants, Bates said.
In cancer, Bates said, genetic testing can identify patients who have a genetic variant that boosts toxicity from fluoropyrimidine chemotherapy treatments, which include capecitabine, floxuridine, and fluorouracil. Meanwhile, an estimated 0.9% will have no reaction or limited reaction to capecitabine and fluorouracil, and 4.8% will have hypersensitivity to carbamazepine and oxcarbazepine.
Tests can also identify a genetic variant that can lead to poor metabolism of the chemotherapy drug irinotecan, which is used to treat colon cancer. “In those patients, you’d want to reduce the dose by 20%,” Bates said. In other cases, alternate drugs may be the best strategy to address genetic variations.
Prior to 2019, clinicians had to order pharmacogenomic tests outside of the VA system, according to Bates. That year, a donation from Sanford Health brought VA pharmacogenomics to 40 pilot sites. Since then, more than 88,000 tests have been performed.
The VA has now made its pharmacogenomic program permanent, Bates said. As of early September, testing was available at 139 VA sites and is coming soon to 4 more. It’s not available at another 23 sites that are scattered across the country.
A tool in the VA electronic health record now reminds clinicians about the availability of genetic testing and allows them to order tests. However, testing isn’t available for patients who have had liver transplants or certain bone marrow transplants.
The VA is working on developing decision-making tools to help clinicians determine when the tests are appropriate, Bates said. It typically takes 2 to 3 weeks to get results, she said, adding that external laboratories provide results. “We eventually would like to bring in all pharmacogenomics testing to be conducted within the VA enterprise.”
Bates reported that she had no disclosures.
The US Department of Veterans Affairs (VA) now has a permanent pharmacogenomics service that provides genetic tests to give clinicians insight into the best medication options for their patients.
The tests, which have no extra cost, are available to all veterans, said pharmacist Jill S. Bates, PharmD, MS, executive director of the VA National Pharmacogenomics Program, who spoke in an interview and a presentation at the annual meeting of the Association of VA Hematology/Oncology.
Genetic testing is “a tool that can help optimize care that we provide for veterans,” she said. “Pharmacogenomics is additional information to help the clinician make a decision. We know that most veterans—greater than 90%—carry a variant in a pharmacogenomics gene that is actionable.”
The genetic tests can provide insight into the optimal medication for multiple conditions such as mental illness, gastrointestinal disorders, cancer, pain, and heart disease. According to a 2019 analysis of over 6 years of data, more than half of the VA patient population used medications whose efficacy may have been affected by detectable genetic variants.
For instance, Bates said tests can let clinicians know whether patients are susceptible to statin-associated muscle adverse effects if they take simvastatin, the cholesterol medication. An estimated 25.6% of the VA population has this variant.
Elsewhere on the cardiac front, an estimated 58.3% of the VA population has a genetic variant that increases sensitivity to the blood thinner warfarin.
Testing could help psychiatrists determine whether certain medications should not be prescribed—or should be prescribed at lower doses—in patients who’ve had adverse reactions to antidepressants, Bates said.
In cancer, Bates said, genetic testing can identify patients who have a genetic variant that boosts toxicity from fluoropyrimidine chemotherapy treatments, which include capecitabine, floxuridine, and fluorouracil. Meanwhile, an estimated 0.9% will have no reaction or limited reaction to capecitabine and fluorouracil, and 4.8% will have hypersensitivity to carbamazepine and oxcarbazepine.
Tests can also identify a genetic variant that can lead to poor metabolism of the chemotherapy drug irinotecan, which is used to treat colon cancer. “In those patients, you’d want to reduce the dose by 20%,” Bates said. In other cases, alternate drugs may be the best strategy to address genetic variations.
Prior to 2019, clinicians had to order pharmacogenomic tests outside of the VA system, according to Bates. That year, a donation from Sanford Health brought VA pharmacogenomics to 40 pilot sites. Since then, more than 88,000 tests have been performed.
The VA has now made its pharmacogenomic program permanent, Bates said. As of early September, testing was available at 139 VA sites and is coming soon to 4 more. It’s not available at another 23 sites that are scattered across the country.
A tool in the VA electronic health record now reminds clinicians about the availability of genetic testing and allows them to order tests. However, testing isn’t available for patients who have had liver transplants or certain bone marrow transplants.
The VA is working on developing decision-making tools to help clinicians determine when the tests are appropriate, Bates said. It typically takes 2 to 3 weeks to get results, she said, adding that external laboratories provide results. “We eventually would like to bring in all pharmacogenomics testing to be conducted within the VA enterprise.”
Bates reported that she had no disclosures.
The US Department of Veterans Affairs (VA) now has a permanent pharmacogenomics service that provides genetic tests to give clinicians insight into the best medication options for their patients.
The tests, which have no extra cost, are available to all veterans, said pharmacist Jill S. Bates, PharmD, MS, executive director of the VA National Pharmacogenomics Program, who spoke in an interview and a presentation at the annual meeting of the Association of VA Hematology/Oncology.
Genetic testing is “a tool that can help optimize care that we provide for veterans,” she said. “Pharmacogenomics is additional information to help the clinician make a decision. We know that most veterans—greater than 90%—carry a variant in a pharmacogenomics gene that is actionable.”
The genetic tests can provide insight into the optimal medication for multiple conditions such as mental illness, gastrointestinal disorders, cancer, pain, and heart disease. According to a 2019 analysis of over 6 years of data, more than half of the VA patient population used medications whose efficacy may have been affected by detectable genetic variants.
For instance, Bates said tests can let clinicians know whether patients are susceptible to statin-associated muscle adverse effects if they take simvastatin, the cholesterol medication. An estimated 25.6% of the VA population has this variant.
Elsewhere on the cardiac front, an estimated 58.3% of the VA population has a genetic variant that increases sensitivity to the blood thinner warfarin.
Testing could help psychiatrists determine whether certain medications should not be prescribed—or should be prescribed at lower doses—in patients who’ve had adverse reactions to antidepressants, Bates said.
In cancer, Bates said, genetic testing can identify patients who have a genetic variant that boosts toxicity from fluoropyrimidine chemotherapy treatments, which include capecitabine, floxuridine, and fluorouracil. Meanwhile, an estimated 0.9% will have no reaction or limited reaction to capecitabine and fluorouracil, and 4.8% will have hypersensitivity to carbamazepine and oxcarbazepine.
Tests can also identify a genetic variant that can lead to poor metabolism of the chemotherapy drug irinotecan, which is used to treat colon cancer. “In those patients, you’d want to reduce the dose by 20%,” Bates said. In other cases, alternate drugs may be the best strategy to address genetic variations.
Prior to 2019, clinicians had to order pharmacogenomic tests outside of the VA system, according to Bates. That year, a donation from Sanford Health brought VA pharmacogenomics to 40 pilot sites. Since then, more than 88,000 tests have been performed.
The VA has now made its pharmacogenomic program permanent, Bates said. As of early September, testing was available at 139 VA sites and is coming soon to 4 more. It’s not available at another 23 sites that are scattered across the country.
A tool in the VA electronic health record now reminds clinicians about the availability of genetic testing and allows them to order tests. However, testing isn’t available for patients who have had liver transplants or certain bone marrow transplants.
The VA is working on developing decision-making tools to help clinicians determine when the tests are appropriate, Bates said. It typically takes 2 to 3 weeks to get results, she said, adding that external laboratories provide results. “We eventually would like to bring in all pharmacogenomics testing to be conducted within the VA enterprise.”
Bates reported that she had no disclosures.
Prominent NIH Neuroscientist Fired Over Alleged Research Misconduct
, the NIH said in a statement.
The misconduct involved “falsification and/or fabrication involving reuse and relabel of figure panels representing different experimental results in two publications,” the NIH said.
The agency said it will notify the two journals of its findings so that appropriate action can be taken.
The NIH reportedly launched its probe into potential research misconduct in May 2023 after it received allegations from the Health and Human Service (HHS) Office of Research Integrity (ORI) that month.
The investigation phase began in December 2023 and concluded on September 15, 2024. The institute subsequently notified HHS ORI of its findings.
Dr. Masliah joined the NIH in the summer of 2016 as director of the Division of Neuroscience at the NIA and an NIH intramural researcher investigating synaptic damage in neurodegenerative disorders, publishing “numerous” papers, the NIH said.
Given the findings of their investigation, the NIH said, Dr. Masliah is no longer serving as director of NIA’s Division of Neuroscience.
NIA deputy director Amy Kelley, MD, is now acting director of NIA’s neuroscience division.
Consistent with NIH policies and procedures, any allegations involving Dr. Masliah’s NIH-supported extramural research prior to joining NIH would be referred to HHS ORI, the NIH said.
The NIH announcement came on the same day that Science magazine published an investigative piece suggesting that Dr. Masliah may have fabricated or falsified images or other information in far more than the two studies NIH cited.
According to the article, “scores” of Dr. Masliah’s lab studies conducted at the NIA and the University of California San Diego are “riddled with apparently falsified Western blots — images used to show the presence of proteins — and micrographs of brain tissue. Numerous images seem to have been inappropriately reused within and across papers, sometimes published years apart in different journals, describing divergent experimental conditions.”
The article noted that a neuroscientist and forensic analysts who had previously worked with Science magazine produced a “300-page dossier revealing a steady stream of suspect images between 1997 and 2023 in 132 of his published research papers.”
They concluded that this “pattern of anomalous data raises a credible concern for research misconduct and calls into question a remarkably large body of scientific work,” the Science article stated.
A version of this article appeared on Medscape.com.
, the NIH said in a statement.
The misconduct involved “falsification and/or fabrication involving reuse and relabel of figure panels representing different experimental results in two publications,” the NIH said.
The agency said it will notify the two journals of its findings so that appropriate action can be taken.
The NIH reportedly launched its probe into potential research misconduct in May 2023 after it received allegations from the Health and Human Service (HHS) Office of Research Integrity (ORI) that month.
The investigation phase began in December 2023 and concluded on September 15, 2024. The institute subsequently notified HHS ORI of its findings.
Dr. Masliah joined the NIH in the summer of 2016 as director of the Division of Neuroscience at the NIA and an NIH intramural researcher investigating synaptic damage in neurodegenerative disorders, publishing “numerous” papers, the NIH said.
Given the findings of their investigation, the NIH said, Dr. Masliah is no longer serving as director of NIA’s Division of Neuroscience.
NIA deputy director Amy Kelley, MD, is now acting director of NIA’s neuroscience division.
Consistent with NIH policies and procedures, any allegations involving Dr. Masliah’s NIH-supported extramural research prior to joining NIH would be referred to HHS ORI, the NIH said.
The NIH announcement came on the same day that Science magazine published an investigative piece suggesting that Dr. Masliah may have fabricated or falsified images or other information in far more than the two studies NIH cited.
According to the article, “scores” of Dr. Masliah’s lab studies conducted at the NIA and the University of California San Diego are “riddled with apparently falsified Western blots — images used to show the presence of proteins — and micrographs of brain tissue. Numerous images seem to have been inappropriately reused within and across papers, sometimes published years apart in different journals, describing divergent experimental conditions.”
The article noted that a neuroscientist and forensic analysts who had previously worked with Science magazine produced a “300-page dossier revealing a steady stream of suspect images between 1997 and 2023 in 132 of his published research papers.”
They concluded that this “pattern of anomalous data raises a credible concern for research misconduct and calls into question a remarkably large body of scientific work,” the Science article stated.
A version of this article appeared on Medscape.com.
, the NIH said in a statement.
The misconduct involved “falsification and/or fabrication involving reuse and relabel of figure panels representing different experimental results in two publications,” the NIH said.
The agency said it will notify the two journals of its findings so that appropriate action can be taken.
The NIH reportedly launched its probe into potential research misconduct in May 2023 after it received allegations from the Health and Human Service (HHS) Office of Research Integrity (ORI) that month.
The investigation phase began in December 2023 and concluded on September 15, 2024. The institute subsequently notified HHS ORI of its findings.
Dr. Masliah joined the NIH in the summer of 2016 as director of the Division of Neuroscience at the NIA and an NIH intramural researcher investigating synaptic damage in neurodegenerative disorders, publishing “numerous” papers, the NIH said.
Given the findings of their investigation, the NIH said, Dr. Masliah is no longer serving as director of NIA’s Division of Neuroscience.
NIA deputy director Amy Kelley, MD, is now acting director of NIA’s neuroscience division.
Consistent with NIH policies and procedures, any allegations involving Dr. Masliah’s NIH-supported extramural research prior to joining NIH would be referred to HHS ORI, the NIH said.
The NIH announcement came on the same day that Science magazine published an investigative piece suggesting that Dr. Masliah may have fabricated or falsified images or other information in far more than the two studies NIH cited.
According to the article, “scores” of Dr. Masliah’s lab studies conducted at the NIA and the University of California San Diego are “riddled with apparently falsified Western blots — images used to show the presence of proteins — and micrographs of brain tissue. Numerous images seem to have been inappropriately reused within and across papers, sometimes published years apart in different journals, describing divergent experimental conditions.”
The article noted that a neuroscientist and forensic analysts who had previously worked with Science magazine produced a “300-page dossier revealing a steady stream of suspect images between 1997 and 2023 in 132 of his published research papers.”
They concluded that this “pattern of anomalous data raises a credible concern for research misconduct and calls into question a remarkably large body of scientific work,” the Science article stated.
A version of this article appeared on Medscape.com.
Expert Calls for Research into GLP-1s for Mental Illness
MILAN — Recent research allaying concerns about suicidality linked to glucagon-like peptide 1 (GLP-1) receptor agonists, along with evidence of these agents’ potential psychiatric and cognitive benefits, has prompted the lead investigator of a major analysis to urge researchers to explore the potential of these drugs for mental illness.
“So far, we’ve been talking about the safety from a neuropsychiatric perspective in diabetes, but there is also the safety and benefit in people with mental disorders,” Riccardo De Giorgi, MD, PhD, from the Department of Psychiatry, University of Oxford in England, said in an interview.
The results of the meta-analysis were previously reported by this news organization and reviewed by Dr. De Giorgi at the 37th European College of Neuropsychopharmacology (ECNP) Congress. Dr. De Giorgi broached
Noting that GLP-1s are not approved for psychiatric disorders, Dr. De Giorgi said it can’t be assumed that the “metabolic or maybe even more general mechanisms that are being modified with these medications in diabetes or even in obesity are the same for people with psychiatric disorders. We’re talking about very different things. From a clinical perspective, you could do real harm,” he told this news organization.
Yet Dr. De Giorgi emphasized the importance of exploring the potential benefits of these medications in psychiatry.
“From a research perspective ... I am very worried about missing an opportunity here. This happened with rimonabant, a cannabis medication that was used for weight loss back in 2012 and was withdrawn quite dramatically in Europe immediately after licensing because it increased suicide risk. Since then, nobody has been touching the cannabinoid system, and that’s a shame because in psychiatry, we don’t have that much we can work on. So we don’t want to miss an opportunity with the GLP-1 system — that’s why we need to be cautious and look at safety first,” he said.
Signal of Efficacy?
Dr. De Giorgi’s research suggested several potential neurobiological effects of GLP-1 inhibition in diabetes research.
“There was a bit of a signal specifically for the big three dementias — vascular, Lewy Body, and frontotemporal — although there was not enough power,” he reported. “We also saw a reduced risk in nicotine misuse, especially amongst other substance use disorders ... and finally a more tentative association for reduced depression.”
He noted that GLP-1s for psychiatric illness likely have limitations and may not cure mental disorders but could help specific subsets of patients. Rather than aiming for large-scale studies, the focus should be on small, incremental studies to advance the research.
Asked by the session chair, John Cryan, PhD, from University College Cork in Ireland, and chair of the ECNP Scientific Committee whether improvement in patients’ mood could be attributed to weight loss, Dr. De Giorgi replied no.
“We now have quite a lot of studies that show that if there is an effect or association it is seen quite a bit earlier than any weight loss. Remember, weight loss takes quite a lot of time, and at quite high doses, but more provocatively, even if that’s the case, does it matter? We as psychiatrists do worry that we need to disentangle these things, but they don’t do that in cardiology, for example. If they see a benefit in mortality they don’t really care if it’s specifically an effect on heart failure or ischemic disease,” said Dr. De Giorgi.
Regardless of their neuropsychiatric potential, the cardiometabolic benefits of GLP-1 inhibitors are sorely needed in the psychiatric population, noted two experts in a recent JAMA Psychiatry viewpoint article.
Sri Mahavir Agarwal, MD, PhD, and Margaret Hahn, MD, PhD, from the University of Toronto and the Schizophrenia Division at the Centre for Addiction and Mental Health, in Toronto, Ontario, Canada, pointed out that “individuals with severe mental illness (SMI) have exceedingly high rates of metabolic comorbidity; three of four are overweight or obese, whereas the prevalence of type 2 diabetes (T2D) is several-fold higher than in the general population. Consequently, individuals with SMI die 15-20 years earlier from cardiovascular disease (CVD) than do those in the general population with CVD,” they noted.
“The arrival of semaglutide has infused significant enthusiasm in the field of mental health research. The proximal effects of weight and related CV comorbidities are significant in themselves. It is plausible that semaglutide could act through neurogenesis or secondary benefits of improving metabolic health on other important outcomes, such as cognitive health and quality of life, thereby filling an unmet need in the treatment of SMI,” Dr. Agarwal and Dr. Hahn added.
An Exciting Opportunity
Current research investigating GLP-1s in psychiatry and neurology is increasingly focused on neuroinflammation, said Dr. De Giorgi.
Research shows significant evidence that certain medications may help reduce dysfunctional inflammatory processes linked to various cognitive and psychiatric disorders, he added.
Many patients with established psychiatric conditions also have physical health issues, which contribute to increased mortality risk, said Dr. De Giorgi. It’s crucial to understand that, if these treatments improve mortality outcomes for psychiatric patients, the specific mechanisms involved are secondary to the results. Psychiatrists must be equipped to prescribe, manage, and initiate these therapies.
“While trials involving psychosis patients are ongoing, we are making progress and should seize this opportunity” said Dr. De Giorgi.
Dr. Cryan agreed: “I think we’ll get there. What these drugs have shown is that you can, through a single mechanism, have multitude effects related to brain-body interactions, and why not focus that on mood and anxiety and cognitive performance? It’s exciting no matter what. We now need to do longitudinal, cross-sectional, placebo-controlled trials in specific patient populations.”
This study received funding from the National Institute for Health and Care Research Oxford Health Biomedical Research Centre and Medical Research Council. Dr. De Giorgi’s coauthors reported receiving funding for other work from Novo Nordisk, Five Lives, Cognetivity Ltd., Cognex, P1vital, Lundbeck, Servier, UCB, Zogenix, Johnson & Johnson, and Syndesi. Dr. Cryan reported no relevant disclosures.
A version of this article appeared on Medscape.com.
MILAN — Recent research allaying concerns about suicidality linked to glucagon-like peptide 1 (GLP-1) receptor agonists, along with evidence of these agents’ potential psychiatric and cognitive benefits, has prompted the lead investigator of a major analysis to urge researchers to explore the potential of these drugs for mental illness.
“So far, we’ve been talking about the safety from a neuropsychiatric perspective in diabetes, but there is also the safety and benefit in people with mental disorders,” Riccardo De Giorgi, MD, PhD, from the Department of Psychiatry, University of Oxford in England, said in an interview.
The results of the meta-analysis were previously reported by this news organization and reviewed by Dr. De Giorgi at the 37th European College of Neuropsychopharmacology (ECNP) Congress. Dr. De Giorgi broached
Noting that GLP-1s are not approved for psychiatric disorders, Dr. De Giorgi said it can’t be assumed that the “metabolic or maybe even more general mechanisms that are being modified with these medications in diabetes or even in obesity are the same for people with psychiatric disorders. We’re talking about very different things. From a clinical perspective, you could do real harm,” he told this news organization.
Yet Dr. De Giorgi emphasized the importance of exploring the potential benefits of these medications in psychiatry.
“From a research perspective ... I am very worried about missing an opportunity here. This happened with rimonabant, a cannabis medication that was used for weight loss back in 2012 and was withdrawn quite dramatically in Europe immediately after licensing because it increased suicide risk. Since then, nobody has been touching the cannabinoid system, and that’s a shame because in psychiatry, we don’t have that much we can work on. So we don’t want to miss an opportunity with the GLP-1 system — that’s why we need to be cautious and look at safety first,” he said.
Signal of Efficacy?
Dr. De Giorgi’s research suggested several potential neurobiological effects of GLP-1 inhibition in diabetes research.
“There was a bit of a signal specifically for the big three dementias — vascular, Lewy Body, and frontotemporal — although there was not enough power,” he reported. “We also saw a reduced risk in nicotine misuse, especially amongst other substance use disorders ... and finally a more tentative association for reduced depression.”
He noted that GLP-1s for psychiatric illness likely have limitations and may not cure mental disorders but could help specific subsets of patients. Rather than aiming for large-scale studies, the focus should be on small, incremental studies to advance the research.
Asked by the session chair, John Cryan, PhD, from University College Cork in Ireland, and chair of the ECNP Scientific Committee whether improvement in patients’ mood could be attributed to weight loss, Dr. De Giorgi replied no.
“We now have quite a lot of studies that show that if there is an effect or association it is seen quite a bit earlier than any weight loss. Remember, weight loss takes quite a lot of time, and at quite high doses, but more provocatively, even if that’s the case, does it matter? We as psychiatrists do worry that we need to disentangle these things, but they don’t do that in cardiology, for example. If they see a benefit in mortality they don’t really care if it’s specifically an effect on heart failure or ischemic disease,” said Dr. De Giorgi.
Regardless of their neuropsychiatric potential, the cardiometabolic benefits of GLP-1 inhibitors are sorely needed in the psychiatric population, noted two experts in a recent JAMA Psychiatry viewpoint article.
Sri Mahavir Agarwal, MD, PhD, and Margaret Hahn, MD, PhD, from the University of Toronto and the Schizophrenia Division at the Centre for Addiction and Mental Health, in Toronto, Ontario, Canada, pointed out that “individuals with severe mental illness (SMI) have exceedingly high rates of metabolic comorbidity; three of four are overweight or obese, whereas the prevalence of type 2 diabetes (T2D) is several-fold higher than in the general population. Consequently, individuals with SMI die 15-20 years earlier from cardiovascular disease (CVD) than do those in the general population with CVD,” they noted.
“The arrival of semaglutide has infused significant enthusiasm in the field of mental health research. The proximal effects of weight and related CV comorbidities are significant in themselves. It is plausible that semaglutide could act through neurogenesis or secondary benefits of improving metabolic health on other important outcomes, such as cognitive health and quality of life, thereby filling an unmet need in the treatment of SMI,” Dr. Agarwal and Dr. Hahn added.
An Exciting Opportunity
Current research investigating GLP-1s in psychiatry and neurology is increasingly focused on neuroinflammation, said Dr. De Giorgi.
Research shows significant evidence that certain medications may help reduce dysfunctional inflammatory processes linked to various cognitive and psychiatric disorders, he added.
Many patients with established psychiatric conditions also have physical health issues, which contribute to increased mortality risk, said Dr. De Giorgi. It’s crucial to understand that, if these treatments improve mortality outcomes for psychiatric patients, the specific mechanisms involved are secondary to the results. Psychiatrists must be equipped to prescribe, manage, and initiate these therapies.
“While trials involving psychosis patients are ongoing, we are making progress and should seize this opportunity” said Dr. De Giorgi.
Dr. Cryan agreed: “I think we’ll get there. What these drugs have shown is that you can, through a single mechanism, have multitude effects related to brain-body interactions, and why not focus that on mood and anxiety and cognitive performance? It’s exciting no matter what. We now need to do longitudinal, cross-sectional, placebo-controlled trials in specific patient populations.”
This study received funding from the National Institute for Health and Care Research Oxford Health Biomedical Research Centre and Medical Research Council. Dr. De Giorgi’s coauthors reported receiving funding for other work from Novo Nordisk, Five Lives, Cognetivity Ltd., Cognex, P1vital, Lundbeck, Servier, UCB, Zogenix, Johnson & Johnson, and Syndesi. Dr. Cryan reported no relevant disclosures.
A version of this article appeared on Medscape.com.
MILAN — Recent research allaying concerns about suicidality linked to glucagon-like peptide 1 (GLP-1) receptor agonists, along with evidence of these agents’ potential psychiatric and cognitive benefits, has prompted the lead investigator of a major analysis to urge researchers to explore the potential of these drugs for mental illness.
“So far, we’ve been talking about the safety from a neuropsychiatric perspective in diabetes, but there is also the safety and benefit in people with mental disorders,” Riccardo De Giorgi, MD, PhD, from the Department of Psychiatry, University of Oxford in England, said in an interview.
The results of the meta-analysis were previously reported by this news organization and reviewed by Dr. De Giorgi at the 37th European College of Neuropsychopharmacology (ECNP) Congress. Dr. De Giorgi broached
Noting that GLP-1s are not approved for psychiatric disorders, Dr. De Giorgi said it can’t be assumed that the “metabolic or maybe even more general mechanisms that are being modified with these medications in diabetes or even in obesity are the same for people with psychiatric disorders. We’re talking about very different things. From a clinical perspective, you could do real harm,” he told this news organization.
Yet Dr. De Giorgi emphasized the importance of exploring the potential benefits of these medications in psychiatry.
“From a research perspective ... I am very worried about missing an opportunity here. This happened with rimonabant, a cannabis medication that was used for weight loss back in 2012 and was withdrawn quite dramatically in Europe immediately after licensing because it increased suicide risk. Since then, nobody has been touching the cannabinoid system, and that’s a shame because in psychiatry, we don’t have that much we can work on. So we don’t want to miss an opportunity with the GLP-1 system — that’s why we need to be cautious and look at safety first,” he said.
Signal of Efficacy?
Dr. De Giorgi’s research suggested several potential neurobiological effects of GLP-1 inhibition in diabetes research.
“There was a bit of a signal specifically for the big three dementias — vascular, Lewy Body, and frontotemporal — although there was not enough power,” he reported. “We also saw a reduced risk in nicotine misuse, especially amongst other substance use disorders ... and finally a more tentative association for reduced depression.”
He noted that GLP-1s for psychiatric illness likely have limitations and may not cure mental disorders but could help specific subsets of patients. Rather than aiming for large-scale studies, the focus should be on small, incremental studies to advance the research.
Asked by the session chair, John Cryan, PhD, from University College Cork in Ireland, and chair of the ECNP Scientific Committee whether improvement in patients’ mood could be attributed to weight loss, Dr. De Giorgi replied no.
“We now have quite a lot of studies that show that if there is an effect or association it is seen quite a bit earlier than any weight loss. Remember, weight loss takes quite a lot of time, and at quite high doses, but more provocatively, even if that’s the case, does it matter? We as psychiatrists do worry that we need to disentangle these things, but they don’t do that in cardiology, for example. If they see a benefit in mortality they don’t really care if it’s specifically an effect on heart failure or ischemic disease,” said Dr. De Giorgi.
Regardless of their neuropsychiatric potential, the cardiometabolic benefits of GLP-1 inhibitors are sorely needed in the psychiatric population, noted two experts in a recent JAMA Psychiatry viewpoint article.
Sri Mahavir Agarwal, MD, PhD, and Margaret Hahn, MD, PhD, from the University of Toronto and the Schizophrenia Division at the Centre for Addiction and Mental Health, in Toronto, Ontario, Canada, pointed out that “individuals with severe mental illness (SMI) have exceedingly high rates of metabolic comorbidity; three of four are overweight or obese, whereas the prevalence of type 2 diabetes (T2D) is several-fold higher than in the general population. Consequently, individuals with SMI die 15-20 years earlier from cardiovascular disease (CVD) than do those in the general population with CVD,” they noted.
“The arrival of semaglutide has infused significant enthusiasm in the field of mental health research. The proximal effects of weight and related CV comorbidities are significant in themselves. It is plausible that semaglutide could act through neurogenesis or secondary benefits of improving metabolic health on other important outcomes, such as cognitive health and quality of life, thereby filling an unmet need in the treatment of SMI,” Dr. Agarwal and Dr. Hahn added.
An Exciting Opportunity
Current research investigating GLP-1s in psychiatry and neurology is increasingly focused on neuroinflammation, said Dr. De Giorgi.
Research shows significant evidence that certain medications may help reduce dysfunctional inflammatory processes linked to various cognitive and psychiatric disorders, he added.
Many patients with established psychiatric conditions also have physical health issues, which contribute to increased mortality risk, said Dr. De Giorgi. It’s crucial to understand that, if these treatments improve mortality outcomes for psychiatric patients, the specific mechanisms involved are secondary to the results. Psychiatrists must be equipped to prescribe, manage, and initiate these therapies.
“While trials involving psychosis patients are ongoing, we are making progress and should seize this opportunity” said Dr. De Giorgi.
Dr. Cryan agreed: “I think we’ll get there. What these drugs have shown is that you can, through a single mechanism, have multitude effects related to brain-body interactions, and why not focus that on mood and anxiety and cognitive performance? It’s exciting no matter what. We now need to do longitudinal, cross-sectional, placebo-controlled trials in specific patient populations.”
This study received funding from the National Institute for Health and Care Research Oxford Health Biomedical Research Centre and Medical Research Council. Dr. De Giorgi’s coauthors reported receiving funding for other work from Novo Nordisk, Five Lives, Cognetivity Ltd., Cognex, P1vital, Lundbeck, Servier, UCB, Zogenix, Johnson & Johnson, and Syndesi. Dr. Cryan reported no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM ECNP CONGRESS 2024
Healthy Lifestyle Mitigates Brain Aging in Diabetes
TOPLINE:
with brain age gaps of 2.29 and 0.50 years, respectively. This association is more pronounced in men and those with poor cardiometabolic health but may be mitigated by a healthy lifestyle.
METHODOLOGY:
- Diabetes is a known risk factor for cognitive impairment, dementia, and global brain atrophy but conflicting results have been reported for prediabetes, and it’s unknown whether a healthy lifestyle can counteract the negative impact of prediabetes.
- Researchers examined the cross-sectional and longitudinal relationship between hyperglycemia and brain aging, as well as the potential mitigating effect of a healthy lifestyle in 31,229 dementia-free adults (mean age, 54.8 years; 53% women) from the UK Biobank, including 13,518 participants with prediabetes and 1149 with diabetes.
- The glycemic status of the participants was determined by their medical history, medication use, and A1c levels.
- The brain age gap was calculated as a difference between chronologic age and brain age estimated from MRI data from six modalities vs several hundred brain MRI phenotypes that were modeled from a subset of healthy individuals.
- The role of sex, cardiometabolic risk factors, and a healthy lifestyle and their association with brain age was also explored, with a healthy lifestyle defined as never smoking, no or light or moderate alcohol consumption, and high physical activity.
TAKEAWAY:
- Prediabetes and diabetes were associated with a higher brain age gap than normoglycemia (beta-coefficient, 0.22 and 2.01; 95% CI, 0.10-0.34 and 1.70-2.32, respectively), and diabetes was more pronounced in men vs women and those with a higher vs lower burden of cardiometabolic risk factors.
- The brain ages of those with prediabetes and diabetes were 0.50 years and 2.29 years older on average than their respective chronologic ages.
- In an exploratory longitudinal analysis of the 2414 participants with two brain MRI scans, diabetes was linked to a 0.27-year annual increase in the brain age gap, and higher A1c, but not prediabetes, was associated with a significant increase in brain age gap.
- A healthy lifestyle attenuated the association between diabetes and a higher brain age gap (P = .003), reducing it by 1.68 years, also with a significant interaction between glycemic status and lifestyle.
IN PRACTICE:
“Our findings highlight diabetes and prediabetes as ideal targets for lifestyle-based interventions to promote brain health,” the authors wrote.
SOURCE:
This study, led by Abigail Dove, Aging Research Center, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Stockholm, Sweden, was published online in Diabetes Care.
LIMITATIONS:
The generalizability of the findings was limited due to a healthy volunteer bias in the UK Biobank. A high proportion of missing data prevented the inclusion of diet in the healthy lifestyle construct. Reverse causality may be possible as an older brain may contribute to the development of prediabetes by making it more difficult to manage medical conditions and adhere to a healthy lifestyle. A1c levels were measured only at baseline, preventing the assessment of changes in glycemic control over time.
DISCLOSURES:
The authors reported receiving funding from the Swedish Research Council; Swedish Research Council for Health, Working Life and Welfare; Karolinska Institutet Board of Research; Riksbankens Jubileumsfond; Marianne and Marcus Wallenberg Foundation; Alzheimerfonden; and Demensfonden. They declared no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
with brain age gaps of 2.29 and 0.50 years, respectively. This association is more pronounced in men and those with poor cardiometabolic health but may be mitigated by a healthy lifestyle.
METHODOLOGY:
- Diabetes is a known risk factor for cognitive impairment, dementia, and global brain atrophy but conflicting results have been reported for prediabetes, and it’s unknown whether a healthy lifestyle can counteract the negative impact of prediabetes.
- Researchers examined the cross-sectional and longitudinal relationship between hyperglycemia and brain aging, as well as the potential mitigating effect of a healthy lifestyle in 31,229 dementia-free adults (mean age, 54.8 years; 53% women) from the UK Biobank, including 13,518 participants with prediabetes and 1149 with diabetes.
- The glycemic status of the participants was determined by their medical history, medication use, and A1c levels.
- The brain age gap was calculated as a difference between chronologic age and brain age estimated from MRI data from six modalities vs several hundred brain MRI phenotypes that were modeled from a subset of healthy individuals.
- The role of sex, cardiometabolic risk factors, and a healthy lifestyle and their association with brain age was also explored, with a healthy lifestyle defined as never smoking, no or light or moderate alcohol consumption, and high physical activity.
TAKEAWAY:
- Prediabetes and diabetes were associated with a higher brain age gap than normoglycemia (beta-coefficient, 0.22 and 2.01; 95% CI, 0.10-0.34 and 1.70-2.32, respectively), and diabetes was more pronounced in men vs women and those with a higher vs lower burden of cardiometabolic risk factors.
- The brain ages of those with prediabetes and diabetes were 0.50 years and 2.29 years older on average than their respective chronologic ages.
- In an exploratory longitudinal analysis of the 2414 participants with two brain MRI scans, diabetes was linked to a 0.27-year annual increase in the brain age gap, and higher A1c, but not prediabetes, was associated with a significant increase in brain age gap.
- A healthy lifestyle attenuated the association between diabetes and a higher brain age gap (P = .003), reducing it by 1.68 years, also with a significant interaction between glycemic status and lifestyle.
IN PRACTICE:
“Our findings highlight diabetes and prediabetes as ideal targets for lifestyle-based interventions to promote brain health,” the authors wrote.
SOURCE:
This study, led by Abigail Dove, Aging Research Center, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Stockholm, Sweden, was published online in Diabetes Care.
LIMITATIONS:
The generalizability of the findings was limited due to a healthy volunteer bias in the UK Biobank. A high proportion of missing data prevented the inclusion of diet in the healthy lifestyle construct. Reverse causality may be possible as an older brain may contribute to the development of prediabetes by making it more difficult to manage medical conditions and adhere to a healthy lifestyle. A1c levels were measured only at baseline, preventing the assessment of changes in glycemic control over time.
DISCLOSURES:
The authors reported receiving funding from the Swedish Research Council; Swedish Research Council for Health, Working Life and Welfare; Karolinska Institutet Board of Research; Riksbankens Jubileumsfond; Marianne and Marcus Wallenberg Foundation; Alzheimerfonden; and Demensfonden. They declared no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
with brain age gaps of 2.29 and 0.50 years, respectively. This association is more pronounced in men and those with poor cardiometabolic health but may be mitigated by a healthy lifestyle.
METHODOLOGY:
- Diabetes is a known risk factor for cognitive impairment, dementia, and global brain atrophy but conflicting results have been reported for prediabetes, and it’s unknown whether a healthy lifestyle can counteract the negative impact of prediabetes.
- Researchers examined the cross-sectional and longitudinal relationship between hyperglycemia and brain aging, as well as the potential mitigating effect of a healthy lifestyle in 31,229 dementia-free adults (mean age, 54.8 years; 53% women) from the UK Biobank, including 13,518 participants with prediabetes and 1149 with diabetes.
- The glycemic status of the participants was determined by their medical history, medication use, and A1c levels.
- The brain age gap was calculated as a difference between chronologic age and brain age estimated from MRI data from six modalities vs several hundred brain MRI phenotypes that were modeled from a subset of healthy individuals.
- The role of sex, cardiometabolic risk factors, and a healthy lifestyle and their association with brain age was also explored, with a healthy lifestyle defined as never smoking, no or light or moderate alcohol consumption, and high physical activity.
TAKEAWAY:
- Prediabetes and diabetes were associated with a higher brain age gap than normoglycemia (beta-coefficient, 0.22 and 2.01; 95% CI, 0.10-0.34 and 1.70-2.32, respectively), and diabetes was more pronounced in men vs women and those with a higher vs lower burden of cardiometabolic risk factors.
- The brain ages of those with prediabetes and diabetes were 0.50 years and 2.29 years older on average than their respective chronologic ages.
- In an exploratory longitudinal analysis of the 2414 participants with two brain MRI scans, diabetes was linked to a 0.27-year annual increase in the brain age gap, and higher A1c, but not prediabetes, was associated with a significant increase in brain age gap.
- A healthy lifestyle attenuated the association between diabetes and a higher brain age gap (P = .003), reducing it by 1.68 years, also with a significant interaction between glycemic status and lifestyle.
IN PRACTICE:
“Our findings highlight diabetes and prediabetes as ideal targets for lifestyle-based interventions to promote brain health,” the authors wrote.
SOURCE:
This study, led by Abigail Dove, Aging Research Center, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Stockholm, Sweden, was published online in Diabetes Care.
LIMITATIONS:
The generalizability of the findings was limited due to a healthy volunteer bias in the UK Biobank. A high proportion of missing data prevented the inclusion of diet in the healthy lifestyle construct. Reverse causality may be possible as an older brain may contribute to the development of prediabetes by making it more difficult to manage medical conditions and adhere to a healthy lifestyle. A1c levels were measured only at baseline, preventing the assessment of changes in glycemic control over time.
DISCLOSURES:
The authors reported receiving funding from the Swedish Research Council; Swedish Research Council for Health, Working Life and Welfare; Karolinska Institutet Board of Research; Riksbankens Jubileumsfond; Marianne and Marcus Wallenberg Foundation; Alzheimerfonden; and Demensfonden. They declared no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Muscle Relaxants for Chronic Pain: Where Is the Greatest Evidence?
TOPLINE:
The long-term use of muscle relaxants may benefit patients with painful spasms or cramps and neck pain, according to a systematic review of clinical studies, but they do not appear to be beneficial for low back pain, fibromyalgia, or headaches and can have adverse effects such as sedation and dry mouth.
METHODOLOGY:
- Researchers conducted a systematic review to evaluate the effectiveness of long-term use (≥ 4 weeks) of muscle relaxants for chronic pain lasting ≥ 3 months.
- They identified 30 randomized clinical trials involving 1314 patients and 14 cohort studies involving 1168 patients, grouped according to the categories of low back pain, fibromyalgia, painful cramps or spasticity, headaches, and other syndromes.
- Baclofen, tizanidine, cyclobenzaprine, eperisone, quinine, carisoprodol, orphenadrine, chlormezanone, and methocarbamol were the muscle relaxants assessed in comparison with placebo, other treatments, or untreated individuals.
TAKEAWAY:
- The long-term use of muscle relaxants reduced pain intensity in those with painful spasms or cramps and neck pain. Baclofen, orphenadrine, carisoprodol, and methocarbamol improved cramp frequency, while the use of eperisone and chlormezanone improved neck pain and enhanced the quality of sleep, respectively, in those with neck osteoarthritis.
- While some studies suggested that muscle relaxants reduced pain intensity in those with back pain and fibromyalgia, between-group differences were not observed. The benefits seen with some medications diminished after their discontinuation.
- Despite tizanidine improving pain severity in headaches, 25% participants dropped out owing to adverse effects. Although certain muscle relaxants demonstrated pain relief, others did not.
- The most common adverse effects of muscle relaxants were somnolence and dry mouth. Other adverse events included vomiting, diarrhea, nausea, weakness, and constipation.
IN PRACTICE:
“For patients already prescribed long-term SMRs [skeletal muscle relaxants], interventions are needed to assist clinicians to engage in shared decision-making with patients about deprescribing SMRs. This may be particularly true for older patients for whom risks of adverse events may be greater,” the authors wrote. “Clinicians should be vigilant for adverse effects and consider deprescribing if pain-related goals are not met.”
SOURCE:
The study, led by Benjamin J. Oldfield, MD, MHS, Yale School of Medicine, New Haven, Connecticut, was published online on September 19, 2024, in JAMA Network Open
LIMITATIONS:
This systematic review was limited to publications written in English, Spanish, and Italian language, potentially excluding studies from other regions. Variations in clinical sites, definitions of pain syndromes, medications, and durations of therapy prevented the possibility of conducting meta-analyses. Only quantitative studies were included, excluding valuable insights into patient experiences offered by qualitative studies.
DISCLOSURES:
The study was supported by the National Institute on Drug Abuse. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
The long-term use of muscle relaxants may benefit patients with painful spasms or cramps and neck pain, according to a systematic review of clinical studies, but they do not appear to be beneficial for low back pain, fibromyalgia, or headaches and can have adverse effects such as sedation and dry mouth.
METHODOLOGY:
- Researchers conducted a systematic review to evaluate the effectiveness of long-term use (≥ 4 weeks) of muscle relaxants for chronic pain lasting ≥ 3 months.
- They identified 30 randomized clinical trials involving 1314 patients and 14 cohort studies involving 1168 patients, grouped according to the categories of low back pain, fibromyalgia, painful cramps or spasticity, headaches, and other syndromes.
- Baclofen, tizanidine, cyclobenzaprine, eperisone, quinine, carisoprodol, orphenadrine, chlormezanone, and methocarbamol were the muscle relaxants assessed in comparison with placebo, other treatments, or untreated individuals.
TAKEAWAY:
- The long-term use of muscle relaxants reduced pain intensity in those with painful spasms or cramps and neck pain. Baclofen, orphenadrine, carisoprodol, and methocarbamol improved cramp frequency, while the use of eperisone and chlormezanone improved neck pain and enhanced the quality of sleep, respectively, in those with neck osteoarthritis.
- While some studies suggested that muscle relaxants reduced pain intensity in those with back pain and fibromyalgia, between-group differences were not observed. The benefits seen with some medications diminished after their discontinuation.
- Despite tizanidine improving pain severity in headaches, 25% participants dropped out owing to adverse effects. Although certain muscle relaxants demonstrated pain relief, others did not.
- The most common adverse effects of muscle relaxants were somnolence and dry mouth. Other adverse events included vomiting, diarrhea, nausea, weakness, and constipation.
IN PRACTICE:
“For patients already prescribed long-term SMRs [skeletal muscle relaxants], interventions are needed to assist clinicians to engage in shared decision-making with patients about deprescribing SMRs. This may be particularly true for older patients for whom risks of adverse events may be greater,” the authors wrote. “Clinicians should be vigilant for adverse effects and consider deprescribing if pain-related goals are not met.”
SOURCE:
The study, led by Benjamin J. Oldfield, MD, MHS, Yale School of Medicine, New Haven, Connecticut, was published online on September 19, 2024, in JAMA Network Open
LIMITATIONS:
This systematic review was limited to publications written in English, Spanish, and Italian language, potentially excluding studies from other regions. Variations in clinical sites, definitions of pain syndromes, medications, and durations of therapy prevented the possibility of conducting meta-analyses. Only quantitative studies were included, excluding valuable insights into patient experiences offered by qualitative studies.
DISCLOSURES:
The study was supported by the National Institute on Drug Abuse. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
The long-term use of muscle relaxants may benefit patients with painful spasms or cramps and neck pain, according to a systematic review of clinical studies, but they do not appear to be beneficial for low back pain, fibromyalgia, or headaches and can have adverse effects such as sedation and dry mouth.
METHODOLOGY:
- Researchers conducted a systematic review to evaluate the effectiveness of long-term use (≥ 4 weeks) of muscle relaxants for chronic pain lasting ≥ 3 months.
- They identified 30 randomized clinical trials involving 1314 patients and 14 cohort studies involving 1168 patients, grouped according to the categories of low back pain, fibromyalgia, painful cramps or spasticity, headaches, and other syndromes.
- Baclofen, tizanidine, cyclobenzaprine, eperisone, quinine, carisoprodol, orphenadrine, chlormezanone, and methocarbamol were the muscle relaxants assessed in comparison with placebo, other treatments, or untreated individuals.
TAKEAWAY:
- The long-term use of muscle relaxants reduced pain intensity in those with painful spasms or cramps and neck pain. Baclofen, orphenadrine, carisoprodol, and methocarbamol improved cramp frequency, while the use of eperisone and chlormezanone improved neck pain and enhanced the quality of sleep, respectively, in those with neck osteoarthritis.
- While some studies suggested that muscle relaxants reduced pain intensity in those with back pain and fibromyalgia, between-group differences were not observed. The benefits seen with some medications diminished after their discontinuation.
- Despite tizanidine improving pain severity in headaches, 25% participants dropped out owing to adverse effects. Although certain muscle relaxants demonstrated pain relief, others did not.
- The most common adverse effects of muscle relaxants were somnolence and dry mouth. Other adverse events included vomiting, diarrhea, nausea, weakness, and constipation.
IN PRACTICE:
“For patients already prescribed long-term SMRs [skeletal muscle relaxants], interventions are needed to assist clinicians to engage in shared decision-making with patients about deprescribing SMRs. This may be particularly true for older patients for whom risks of adverse events may be greater,” the authors wrote. “Clinicians should be vigilant for adverse effects and consider deprescribing if pain-related goals are not met.”
SOURCE:
The study, led by Benjamin J. Oldfield, MD, MHS, Yale School of Medicine, New Haven, Connecticut, was published online on September 19, 2024, in JAMA Network Open
LIMITATIONS:
This systematic review was limited to publications written in English, Spanish, and Italian language, potentially excluding studies from other regions. Variations in clinical sites, definitions of pain syndromes, medications, and durations of therapy prevented the possibility of conducting meta-analyses. Only quantitative studies were included, excluding valuable insights into patient experiences offered by qualitative studies.
DISCLOSURES:
The study was supported by the National Institute on Drug Abuse. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Transgender Women and Prostate Cancer: It’s Complicated
The Veterans Health Administration (VHA) provides care for about 10,000 transgender women, and clinicians must understand their distinctive needs for prostate cancer screening, a urologist told cancer specialists during a presentation at the 2024 annual meeting of the Association of VA Hematology/Oncology in Atlanta.
Even if they’ve undergone gender reassignment surgery, “all transgender women still have a prostate, so therefore they remain at risk of prostate cancer and could still be considered for prostate cancer screening,” said Farnoosh Nik-Ahd, MD, a resident physician at the University of California San Francisco. However, “clinicians and patients may not be aware of prostate cancer risk, so that they may not think [of screening] transgender women.”
Nik-Ahd also noted another complication: The results of prostate screening tests may be misleading in this population.
Transgender women were born biologically male but now identify as female. These individuals may have undergone gender reassignment surgery to remove male genitalia, but the procedures do not remove the prostate. They also might be taking estrogen therapy. “Prostate cancer is a hormonally driven cancer, and the exact impact of gender-affirming hormones on prostate cancer risk and development is unknown,” Nik-Ahd said.
In a 2023 study in JAMA, Nik-Ahd and colleagues identified 155 cases of prostate cancer in transgender women within the VHA (about 14 cases per year) from 2000 to 2022. Of these patients, 116 had never used estrogen, while 17 had used it previously and 22 used it at diagnosis.
The median age of patients was 61 years, 88% identified as White, and the median prostate-specific antigen (PSA) was 6.8 ng/mL. “Given estimates of 10,000 transgender women in the US Department of Veterans Affairs, 33 cases per year would be expected. Instead, only about 14 per year were observed,” the researchers wrote. “Lower rates may stem from less PSA screening owing to barriers including lack of prostate cancer risk awareness or stigma, the suppressive effects of estrogen on prostate cancer development, or prostate cancers being missed in transgender women because of misinterpretation of ‘normal’ PSA levels among those receiving gender-affirming hormone therapies.”
In the presentation, Nik-Ahd said, “PSA density, which is a marker of prostate cancer aggressiveness, was highest in transgender women who were actively on estrogen.”
She noted, “the existing thyrotropin reference ranges, which is what we use to interpret PSA values, are all based on data from cisgender men.” The ranges would be expected to be far lower in transgender women who are taking estrogen, potentially throwing off screening tests, she said, and “ultimately missing clinically significant prostate cancer.”
In the larger picture, there are no specific guidelines about PSA screening in transgender women, she said.
A recent study published in JAMA by Nik-Ahd and colleagues examined PSA levels in 210 transgender women (mean age 60 years) treated within the VHA from 2000 to 2023. All were aged 40 to 80 years, had received estrogen for at least 6 months (mean duration 4.7 years), and didn’t have prostate cancer diagnoses.
“Median (IQR) PSA was 0.02 (0-0.2) ng/mL and the 95th percentile value was 0.6 ng/mL,” the report found. “PSAs were undetectable in 36% of patients (23% and 49% of PSAs in patients without and with orchiectomy, respectively).”
The researchers write that “the historic cut point of 4 ng/mL, often used as a threshold for further evaluation, is likely far too high a threshold for this population.”
Nik-Ahd noted, “clinicians should interpret PSA values in transgender women on estrogen with extreme caution. In this population, normal might actually not be normal, and a value that is considered normal might be very abnormal for somebody who is on estrogen. If you're unsure of whether a PSA value is appropriate for a transgender woman on estrogen, refer that patient to a urologist so they can undergo further evaluation.”
Farnoosh Nik-Ahd discloses consulting for Janssen.
The Veterans Health Administration (VHA) provides care for about 10,000 transgender women, and clinicians must understand their distinctive needs for prostate cancer screening, a urologist told cancer specialists during a presentation at the 2024 annual meeting of the Association of VA Hematology/Oncology in Atlanta.
Even if they’ve undergone gender reassignment surgery, “all transgender women still have a prostate, so therefore they remain at risk of prostate cancer and could still be considered for prostate cancer screening,” said Farnoosh Nik-Ahd, MD, a resident physician at the University of California San Francisco. However, “clinicians and patients may not be aware of prostate cancer risk, so that they may not think [of screening] transgender women.”
Nik-Ahd also noted another complication: The results of prostate screening tests may be misleading in this population.
Transgender women were born biologically male but now identify as female. These individuals may have undergone gender reassignment surgery to remove male genitalia, but the procedures do not remove the prostate. They also might be taking estrogen therapy. “Prostate cancer is a hormonally driven cancer, and the exact impact of gender-affirming hormones on prostate cancer risk and development is unknown,” Nik-Ahd said.
In a 2023 study in JAMA, Nik-Ahd and colleagues identified 155 cases of prostate cancer in transgender women within the VHA (about 14 cases per year) from 2000 to 2022. Of these patients, 116 had never used estrogen, while 17 had used it previously and 22 used it at diagnosis.
The median age of patients was 61 years, 88% identified as White, and the median prostate-specific antigen (PSA) was 6.8 ng/mL. “Given estimates of 10,000 transgender women in the US Department of Veterans Affairs, 33 cases per year would be expected. Instead, only about 14 per year were observed,” the researchers wrote. “Lower rates may stem from less PSA screening owing to barriers including lack of prostate cancer risk awareness or stigma, the suppressive effects of estrogen on prostate cancer development, or prostate cancers being missed in transgender women because of misinterpretation of ‘normal’ PSA levels among those receiving gender-affirming hormone therapies.”
In the presentation, Nik-Ahd said, “PSA density, which is a marker of prostate cancer aggressiveness, was highest in transgender women who were actively on estrogen.”
She noted, “the existing thyrotropin reference ranges, which is what we use to interpret PSA values, are all based on data from cisgender men.” The ranges would be expected to be far lower in transgender women who are taking estrogen, potentially throwing off screening tests, she said, and “ultimately missing clinically significant prostate cancer.”
In the larger picture, there are no specific guidelines about PSA screening in transgender women, she said.
A recent study published in JAMA by Nik-Ahd and colleagues examined PSA levels in 210 transgender women (mean age 60 years) treated within the VHA from 2000 to 2023. All were aged 40 to 80 years, had received estrogen for at least 6 months (mean duration 4.7 years), and didn’t have prostate cancer diagnoses.
“Median (IQR) PSA was 0.02 (0-0.2) ng/mL and the 95th percentile value was 0.6 ng/mL,” the report found. “PSAs were undetectable in 36% of patients (23% and 49% of PSAs in patients without and with orchiectomy, respectively).”
The researchers write that “the historic cut point of 4 ng/mL, often used as a threshold for further evaluation, is likely far too high a threshold for this population.”
Nik-Ahd noted, “clinicians should interpret PSA values in transgender women on estrogen with extreme caution. In this population, normal might actually not be normal, and a value that is considered normal might be very abnormal for somebody who is on estrogen. If you're unsure of whether a PSA value is appropriate for a transgender woman on estrogen, refer that patient to a urologist so they can undergo further evaluation.”
Farnoosh Nik-Ahd discloses consulting for Janssen.
The Veterans Health Administration (VHA) provides care for about 10,000 transgender women, and clinicians must understand their distinctive needs for prostate cancer screening, a urologist told cancer specialists during a presentation at the 2024 annual meeting of the Association of VA Hematology/Oncology in Atlanta.
Even if they’ve undergone gender reassignment surgery, “all transgender women still have a prostate, so therefore they remain at risk of prostate cancer and could still be considered for prostate cancer screening,” said Farnoosh Nik-Ahd, MD, a resident physician at the University of California San Francisco. However, “clinicians and patients may not be aware of prostate cancer risk, so that they may not think [of screening] transgender women.”
Nik-Ahd also noted another complication: The results of prostate screening tests may be misleading in this population.
Transgender women were born biologically male but now identify as female. These individuals may have undergone gender reassignment surgery to remove male genitalia, but the procedures do not remove the prostate. They also might be taking estrogen therapy. “Prostate cancer is a hormonally driven cancer, and the exact impact of gender-affirming hormones on prostate cancer risk and development is unknown,” Nik-Ahd said.
In a 2023 study in JAMA, Nik-Ahd and colleagues identified 155 cases of prostate cancer in transgender women within the VHA (about 14 cases per year) from 2000 to 2022. Of these patients, 116 had never used estrogen, while 17 had used it previously and 22 used it at diagnosis.
The median age of patients was 61 years, 88% identified as White, and the median prostate-specific antigen (PSA) was 6.8 ng/mL. “Given estimates of 10,000 transgender women in the US Department of Veterans Affairs, 33 cases per year would be expected. Instead, only about 14 per year were observed,” the researchers wrote. “Lower rates may stem from less PSA screening owing to barriers including lack of prostate cancer risk awareness or stigma, the suppressive effects of estrogen on prostate cancer development, or prostate cancers being missed in transgender women because of misinterpretation of ‘normal’ PSA levels among those receiving gender-affirming hormone therapies.”
In the presentation, Nik-Ahd said, “PSA density, which is a marker of prostate cancer aggressiveness, was highest in transgender women who were actively on estrogen.”
She noted, “the existing thyrotropin reference ranges, which is what we use to interpret PSA values, are all based on data from cisgender men.” The ranges would be expected to be far lower in transgender women who are taking estrogen, potentially throwing off screening tests, she said, and “ultimately missing clinically significant prostate cancer.”
In the larger picture, there are no specific guidelines about PSA screening in transgender women, she said.
A recent study published in JAMA by Nik-Ahd and colleagues examined PSA levels in 210 transgender women (mean age 60 years) treated within the VHA from 2000 to 2023. All were aged 40 to 80 years, had received estrogen for at least 6 months (mean duration 4.7 years), and didn’t have prostate cancer diagnoses.
“Median (IQR) PSA was 0.02 (0-0.2) ng/mL and the 95th percentile value was 0.6 ng/mL,” the report found. “PSAs were undetectable in 36% of patients (23% and 49% of PSAs in patients without and with orchiectomy, respectively).”
The researchers write that “the historic cut point of 4 ng/mL, often used as a threshold for further evaluation, is likely far too high a threshold for this population.”
Nik-Ahd noted, “clinicians should interpret PSA values in transgender women on estrogen with extreme caution. In this population, normal might actually not be normal, and a value that is considered normal might be very abnormal for somebody who is on estrogen. If you're unsure of whether a PSA value is appropriate for a transgender woman on estrogen, refer that patient to a urologist so they can undergo further evaluation.”
Farnoosh Nik-Ahd discloses consulting for Janssen.
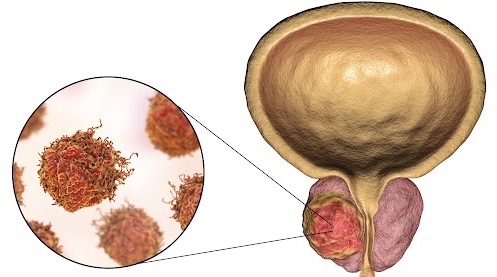
Cancer Risk: Are Pesticides the New Smoking?
Pesticides have transformed modern agriculture by boosting production yields and helping alleviate food insecurity amid rapid global population growth. However, from a public health perspective, exposure to pesticides has been linked to numerous harmful effects, including neurologic disorders like Parkinson’s disease, weakened immune function, and an increased risk for cancer.
thus offering a limited perspective.
A comprehensive assessment of how pesticide use affects cancer risk across a broader population has yet to be conducted.
A recent population-level study aimed to address this gap by evaluating cancer risks in the US population using a model that accounts for pesticide use and adjusts for various factors. The goal was to identify regional disparities in exposure and contribute to the development of public health policies that protect populations from potential harm.
Calculating Cancer Risk
Researchers developed a model using several data sources to estimate the additional cancer risk from agricultural pesticide use. Key data included:
- Pesticide use data from the US Geological Survey in 2019, which covered 69 agricultural pesticides across 3143 counties
- Cancer incidence rates per 100,000 people, which were collected between 2015 and 2019 by the National Institutes of Health and the Centers for Disease Control and Prevention; these data covered various cancers, including bladder, colorectal, leukemia, lung, non-Hodgkin lymphoma, and pancreatic cancers
- Covariates, including smoking prevalence, the Social Vulnerability Index, agricultural land use, and total US population in 2019
Pesticide use profile patterns were developed using latent class analysis, a statistical method used to identify homogeneous subgroups within a heterogeneous population. A generalized linear model then estimated how these pesticide use patterns and the covariates affected cancer incidence.
The model highlighted regions with the highest and lowest “additional” cancer risks linked to pesticide exposure, calculating the estimated increase in cancer cases per year that resulted from variations in agricultural pesticide use.
Midwest Most Affected
While this model doesn’t establish causality or assess individual risk, it reveals regional trends in the association between pesticide use patterns and cancer incidence from a population-based perspective.
The Midwest, known for its high corn production, emerged as the region most affected by pesticide use. Compared with regions with the lowest risk, the Midwest faced an additional 154,541 cancer cases annually across all types. For colorectal and pancreatic cancers, the yearly increases were 20,927 and 3835 cases, respectively. Similar trends were observed for leukemia and non-Hodgkin lymphoma.
Pesticides vs Smoking
The researchers also estimated the additional cancer risk related to smoking, using the same model. They found that pesticides contributed to a higher risk for cancer than smoking in several cases.
The most significant difference was observed with non-Hodgkin lymphoma, where pesticides were linked to 154.1% more cases than smoking. For all cancers combined, as well as bladder cancer and leukemia, the increases were moderate: 18.7%, 19.3%, and 21.0%, respectively.
This result highlights the importance of considering pesticide exposure alongside smoking when studying cancer risks.
Expanding Scope of Research
Some limitations of this study should be noted. Certain counties lacked complete data, and there was heterogeneity in the size and population of the counties studied. The research also did not account for seasonal and migrant workers, who are likely to be heavily exposed. In addition, the data used in the study were not independently validated, and they could not be used to assess individual risk.
The effect of pesticides on human health is a vast and critical field of research, often focusing on a limited range of pesticides or specific cancers. This study stands out by taking a broader, more holistic approach, aiming to highlight regional inequalities and identify less-studied pesticides that could be future research priorities.
Given the significant public health impact, the authors encouraged the authorities to share these findings with the most vulnerable communities to raise awareness.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Pesticides have transformed modern agriculture by boosting production yields and helping alleviate food insecurity amid rapid global population growth. However, from a public health perspective, exposure to pesticides has been linked to numerous harmful effects, including neurologic disorders like Parkinson’s disease, weakened immune function, and an increased risk for cancer.
thus offering a limited perspective.
A comprehensive assessment of how pesticide use affects cancer risk across a broader population has yet to be conducted.
A recent population-level study aimed to address this gap by evaluating cancer risks in the US population using a model that accounts for pesticide use and adjusts for various factors. The goal was to identify regional disparities in exposure and contribute to the development of public health policies that protect populations from potential harm.
Calculating Cancer Risk
Researchers developed a model using several data sources to estimate the additional cancer risk from agricultural pesticide use. Key data included:
- Pesticide use data from the US Geological Survey in 2019, which covered 69 agricultural pesticides across 3143 counties
- Cancer incidence rates per 100,000 people, which were collected between 2015 and 2019 by the National Institutes of Health and the Centers for Disease Control and Prevention; these data covered various cancers, including bladder, colorectal, leukemia, lung, non-Hodgkin lymphoma, and pancreatic cancers
- Covariates, including smoking prevalence, the Social Vulnerability Index, agricultural land use, and total US population in 2019
Pesticide use profile patterns were developed using latent class analysis, a statistical method used to identify homogeneous subgroups within a heterogeneous population. A generalized linear model then estimated how these pesticide use patterns and the covariates affected cancer incidence.
The model highlighted regions with the highest and lowest “additional” cancer risks linked to pesticide exposure, calculating the estimated increase in cancer cases per year that resulted from variations in agricultural pesticide use.
Midwest Most Affected
While this model doesn’t establish causality or assess individual risk, it reveals regional trends in the association between pesticide use patterns and cancer incidence from a population-based perspective.
The Midwest, known for its high corn production, emerged as the region most affected by pesticide use. Compared with regions with the lowest risk, the Midwest faced an additional 154,541 cancer cases annually across all types. For colorectal and pancreatic cancers, the yearly increases were 20,927 and 3835 cases, respectively. Similar trends were observed for leukemia and non-Hodgkin lymphoma.
Pesticides vs Smoking
The researchers also estimated the additional cancer risk related to smoking, using the same model. They found that pesticides contributed to a higher risk for cancer than smoking in several cases.
The most significant difference was observed with non-Hodgkin lymphoma, where pesticides were linked to 154.1% more cases than smoking. For all cancers combined, as well as bladder cancer and leukemia, the increases were moderate: 18.7%, 19.3%, and 21.0%, respectively.
This result highlights the importance of considering pesticide exposure alongside smoking when studying cancer risks.
Expanding Scope of Research
Some limitations of this study should be noted. Certain counties lacked complete data, and there was heterogeneity in the size and population of the counties studied. The research also did not account for seasonal and migrant workers, who are likely to be heavily exposed. In addition, the data used in the study were not independently validated, and they could not be used to assess individual risk.
The effect of pesticides on human health is a vast and critical field of research, often focusing on a limited range of pesticides or specific cancers. This study stands out by taking a broader, more holistic approach, aiming to highlight regional inequalities and identify less-studied pesticides that could be future research priorities.
Given the significant public health impact, the authors encouraged the authorities to share these findings with the most vulnerable communities to raise awareness.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Pesticides have transformed modern agriculture by boosting production yields and helping alleviate food insecurity amid rapid global population growth. However, from a public health perspective, exposure to pesticides has been linked to numerous harmful effects, including neurologic disorders like Parkinson’s disease, weakened immune function, and an increased risk for cancer.
thus offering a limited perspective.
A comprehensive assessment of how pesticide use affects cancer risk across a broader population has yet to be conducted.
A recent population-level study aimed to address this gap by evaluating cancer risks in the US population using a model that accounts for pesticide use and adjusts for various factors. The goal was to identify regional disparities in exposure and contribute to the development of public health policies that protect populations from potential harm.
Calculating Cancer Risk
Researchers developed a model using several data sources to estimate the additional cancer risk from agricultural pesticide use. Key data included:
- Pesticide use data from the US Geological Survey in 2019, which covered 69 agricultural pesticides across 3143 counties
- Cancer incidence rates per 100,000 people, which were collected between 2015 and 2019 by the National Institutes of Health and the Centers for Disease Control and Prevention; these data covered various cancers, including bladder, colorectal, leukemia, lung, non-Hodgkin lymphoma, and pancreatic cancers
- Covariates, including smoking prevalence, the Social Vulnerability Index, agricultural land use, and total US population in 2019
Pesticide use profile patterns were developed using latent class analysis, a statistical method used to identify homogeneous subgroups within a heterogeneous population. A generalized linear model then estimated how these pesticide use patterns and the covariates affected cancer incidence.
The model highlighted regions with the highest and lowest “additional” cancer risks linked to pesticide exposure, calculating the estimated increase in cancer cases per year that resulted from variations in agricultural pesticide use.
Midwest Most Affected
While this model doesn’t establish causality or assess individual risk, it reveals regional trends in the association between pesticide use patterns and cancer incidence from a population-based perspective.
The Midwest, known for its high corn production, emerged as the region most affected by pesticide use. Compared with regions with the lowest risk, the Midwest faced an additional 154,541 cancer cases annually across all types. For colorectal and pancreatic cancers, the yearly increases were 20,927 and 3835 cases, respectively. Similar trends were observed for leukemia and non-Hodgkin lymphoma.
Pesticides vs Smoking
The researchers also estimated the additional cancer risk related to smoking, using the same model. They found that pesticides contributed to a higher risk for cancer than smoking in several cases.
The most significant difference was observed with non-Hodgkin lymphoma, where pesticides were linked to 154.1% more cases than smoking. For all cancers combined, as well as bladder cancer and leukemia, the increases were moderate: 18.7%, 19.3%, and 21.0%, respectively.
This result highlights the importance of considering pesticide exposure alongside smoking when studying cancer risks.
Expanding Scope of Research
Some limitations of this study should be noted. Certain counties lacked complete data, and there was heterogeneity in the size and population of the counties studied. The research also did not account for seasonal and migrant workers, who are likely to be heavily exposed. In addition, the data used in the study were not independently validated, and they could not be used to assess individual risk.
The effect of pesticides on human health is a vast and critical field of research, often focusing on a limited range of pesticides or specific cancers. This study stands out by taking a broader, more holistic approach, aiming to highlight regional inequalities and identify less-studied pesticides that could be future research priorities.
Given the significant public health impact, the authors encouraged the authorities to share these findings with the most vulnerable communities to raise awareness.
This story was translated from JIM using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.