User login
Does the current age cutoff for screening miss too many cases of cervical cancer in older women?
Cooley JJ, Maguire FB, Morris CR, et al. Cervical cancer stage at diagnosis and survival among women ≥65 years in California. Cancer Epidemiol Biomarkers Prev. 2023;32:91-97. doi:10.1158/1055-9965.EPI-22-0793.
EXPERT COMMENTARY
Cervical cancer screening guidelines recommend screening cessation at age 65 once specific exit criteria are met. (According to the American Cancer Society, individuals aged >65 years who have no history of cervical intraepithelial neoplasia [CIN] grade 2 or more severe disease within the past 25 years, and who have documented adequate negative prior screening in the prior 10 years, discontinue all cervical cancer screening.)1 We know, however, that about one-fifth of all cervical cancer cases are diagnosed among individuals aged 65 or older, and for Black women that proportion is even higher when data are appropriately adjusted to account for the increased rate of hysterectomy among Black versus White women.2-4
Early-stage cervical cancer is largely a curable disease with very high 5-year overall survival rates. Unfortunately, more than half of all cervical cancer is diagnosed at a more advanced stage, and survival rates are much lower for this population.5
Cervical cancer incidence rates plummeted in the United States after the introduction of the Pap test for cervical cancer screening. However, the percentage of women who are not up to date with cervical cancer screening may now be increasing, from 14% in 2005 to 23% in 2019 according to one study from the US Preventive Services Task Force.6 When looking at cervical cancer screening rates by age, researchers from the Centers for Disease Control and Prevention estimate that the proportion of patients who have not been recently screened goes up as patients get older, with approximately 845,000 American women aged 61 to 65 not adequately screened in 2015 alone.7
Details of the study
Cooley and colleagues sought to better characterize the cohort of women diagnosed with cervical cancer at a later age, specifically the stage at diagnosis and survival.8 They used data from the California Cancer Registry (CCR), a large state-mandated, population-based data repository that is affiliated with the Surveillance, Epidemiology, and End Results (SEER) program.
The researchers identified 12,442 womenin the CCR who were newly diagnosed with cervical cancer from 2009 to 2018, 17.4% of whom were age 65 or older. They looked at cancer stage at diagnosis as it relates to relative survival rate (“the ratio of the observed survival rate among those who have cancer divided by the expected survival rate for people of the same sex, race/ethnicity, and age who do not have cancer”), Charlson comorbidity score, socioeconomic status, health insurance status, urbanicity, and race/ethnicity.
Results. In this study, 71% of women aged 65 or older presented with advanced-stage disease (FIGO [International Federation of Gynecology and Obstetrics] stage II–IV) as compared with only 48% in those aged 21 to 64. Five-year relative survival rates also were lower in the older cohort—23% to 37%, compared with 42% to 52% in the younger patients. In a sensitivity analysis, late-stage disease was associated with older age, increasing medical comorbidities, and nonadenocarcinoma histology.
Interestingly, older women of Hispanic ethnicity were less likely to be diagnosed with late-stage disease when compared with non-Hispanic White women.
Study strengths and limitations
Although this study’s conclusions—that patients with advanced-stage cancer are more likely to do poorly than those with early-stage cancer—may seem obvious to some even without the proven data, it is still important to highlight what a clinician may intuit with data to support that intuition. It is particularly important to emphasize this risk in older women in light of the aging population in the United States, with adults older than age 65 expected to account for more than 20% of the nation’s population by 2030.9
The study by Cooley and colleagues adds value to the existing literature due to its large study population, which included more than 12,000 patients diagnosed with cervical cancer.8 And although its results may not be completely generalizable as the data were gathered from only a California-specific population, the sample was diverse with significant portions of Hispanic and Black patients. This study supports previous data that showed high rates of advanced cervical cancer in women older than age 65, with resultant worse 5-year relative survival in this population of older women specifically.4 ●
Cervical cancer is both common and deadly in older women. Although current cervical cancer screening guidelines recommend screening cessation after age 65, remember that this is based on strict exit criteria. Consider screening older women (especially with human papillomavirus [HPV] testing) for cervical cancer if they have risk factors (such as smoking, multiple sexual partners, inconsistent or infrequent screening, history of abnormal Pap or HPV tests), and keep cervical cancer on your differential diagnosis in women who present with postmenopausal bleeding, vaginal discharge, pelvic pain, recurrent urinary tract infections, or other concerning symptoms.
SARAH DILLEY, MD, MPH, AND WARNER HUH, MD
- Fontham ETH, Wolf AMD, Church TR, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020;70:321-346. doi:10.3322/caac.21628.
- Dilley S, Huh W, Blechter B, et al. It’s time to re-evaluate cervical cancer screening after age 65. Gynecol Oncol. 2021;162:200-202. doi:10.1016/j.ygyno.2021.04.027.
- Rositch AF, Nowak RG, Gravitt PE. Increased age and racespecific incidence of cervical cancer after correction for hysterectomy prevalence in the United States from 2000 to 2009. Cancer. 2014;120:2032-2038. doi:10.1002/cncr.28548.
- Beavis AL, Gravitt PE, Rositch AF. Hysterectomy-corrected cervical cancer mortality rates reveal a larger racial disparity in the United States. Cancer. 2017;123:1044-1050. doi:10.1002 /cncr.30507.
- Cancer Stat Facts. National Cancer Institute Surveillance, Epidemiology, and End Results Program. https://seer.cancer .gov/statfacts/html/cervix.html
- Suk R, Hong YR, Rajan SS, et al. Assessment of US Preventive Services Task Force guideline-concordant cervical cancer screening rates and reasons for underscreening by age, race and ethnicity, sexual orientation, rurality, and insurance, 2005 to 2019. JAMA Netw Open. 2022;5:e2143582. doi:10.1001 /jamanetworkopen.2021.43582.
- White MC, Shoemaker ML, Benard VB. Cervical cancer screening and incidence by age: unmet needs near and after the stopping age for screening. Am J Prev Med. 2017;53:392395. doi:10.1016/j.amepre.2017.02.024.
- Cooley JJ, Maguire FB, Morris CR, et al. Cervical cancer stage at diagnosis and survival among women ≥65 years in California. Cancer Epidemiol Biomarkers Prev. 2023;32:91-97. doi:10.1158/1055-9965.EPI-22-0793.
- Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States. May 2014. United States Census Bureau. Accessed April 12, 2023. https://www.census .gov/library/publications/2014/demo/p25-1140.html
Cooley JJ, Maguire FB, Morris CR, et al. Cervical cancer stage at diagnosis and survival among women ≥65 years in California. Cancer Epidemiol Biomarkers Prev. 2023;32:91-97. doi:10.1158/1055-9965.EPI-22-0793.
EXPERT COMMENTARY
Cervical cancer screening guidelines recommend screening cessation at age 65 once specific exit criteria are met. (According to the American Cancer Society, individuals aged >65 years who have no history of cervical intraepithelial neoplasia [CIN] grade 2 or more severe disease within the past 25 years, and who have documented adequate negative prior screening in the prior 10 years, discontinue all cervical cancer screening.)1 We know, however, that about one-fifth of all cervical cancer cases are diagnosed among individuals aged 65 or older, and for Black women that proportion is even higher when data are appropriately adjusted to account for the increased rate of hysterectomy among Black versus White women.2-4
Early-stage cervical cancer is largely a curable disease with very high 5-year overall survival rates. Unfortunately, more than half of all cervical cancer is diagnosed at a more advanced stage, and survival rates are much lower for this population.5
Cervical cancer incidence rates plummeted in the United States after the introduction of the Pap test for cervical cancer screening. However, the percentage of women who are not up to date with cervical cancer screening may now be increasing, from 14% in 2005 to 23% in 2019 according to one study from the US Preventive Services Task Force.6 When looking at cervical cancer screening rates by age, researchers from the Centers for Disease Control and Prevention estimate that the proportion of patients who have not been recently screened goes up as patients get older, with approximately 845,000 American women aged 61 to 65 not adequately screened in 2015 alone.7
Details of the study
Cooley and colleagues sought to better characterize the cohort of women diagnosed with cervical cancer at a later age, specifically the stage at diagnosis and survival.8 They used data from the California Cancer Registry (CCR), a large state-mandated, population-based data repository that is affiliated with the Surveillance, Epidemiology, and End Results (SEER) program.
The researchers identified 12,442 womenin the CCR who were newly diagnosed with cervical cancer from 2009 to 2018, 17.4% of whom were age 65 or older. They looked at cancer stage at diagnosis as it relates to relative survival rate (“the ratio of the observed survival rate among those who have cancer divided by the expected survival rate for people of the same sex, race/ethnicity, and age who do not have cancer”), Charlson comorbidity score, socioeconomic status, health insurance status, urbanicity, and race/ethnicity.
Results. In this study, 71% of women aged 65 or older presented with advanced-stage disease (FIGO [International Federation of Gynecology and Obstetrics] stage II–IV) as compared with only 48% in those aged 21 to 64. Five-year relative survival rates also were lower in the older cohort—23% to 37%, compared with 42% to 52% in the younger patients. In a sensitivity analysis, late-stage disease was associated with older age, increasing medical comorbidities, and nonadenocarcinoma histology.
Interestingly, older women of Hispanic ethnicity were less likely to be diagnosed with late-stage disease when compared with non-Hispanic White women.
Study strengths and limitations
Although this study’s conclusions—that patients with advanced-stage cancer are more likely to do poorly than those with early-stage cancer—may seem obvious to some even without the proven data, it is still important to highlight what a clinician may intuit with data to support that intuition. It is particularly important to emphasize this risk in older women in light of the aging population in the United States, with adults older than age 65 expected to account for more than 20% of the nation’s population by 2030.9
The study by Cooley and colleagues adds value to the existing literature due to its large study population, which included more than 12,000 patients diagnosed with cervical cancer.8 And although its results may not be completely generalizable as the data were gathered from only a California-specific population, the sample was diverse with significant portions of Hispanic and Black patients. This study supports previous data that showed high rates of advanced cervical cancer in women older than age 65, with resultant worse 5-year relative survival in this population of older women specifically.4 ●
Cervical cancer is both common and deadly in older women. Although current cervical cancer screening guidelines recommend screening cessation after age 65, remember that this is based on strict exit criteria. Consider screening older women (especially with human papillomavirus [HPV] testing) for cervical cancer if they have risk factors (such as smoking, multiple sexual partners, inconsistent or infrequent screening, history of abnormal Pap or HPV tests), and keep cervical cancer on your differential diagnosis in women who present with postmenopausal bleeding, vaginal discharge, pelvic pain, recurrent urinary tract infections, or other concerning symptoms.
SARAH DILLEY, MD, MPH, AND WARNER HUH, MD
Cooley JJ, Maguire FB, Morris CR, et al. Cervical cancer stage at diagnosis and survival among women ≥65 years in California. Cancer Epidemiol Biomarkers Prev. 2023;32:91-97. doi:10.1158/1055-9965.EPI-22-0793.
EXPERT COMMENTARY
Cervical cancer screening guidelines recommend screening cessation at age 65 once specific exit criteria are met. (According to the American Cancer Society, individuals aged >65 years who have no history of cervical intraepithelial neoplasia [CIN] grade 2 or more severe disease within the past 25 years, and who have documented adequate negative prior screening in the prior 10 years, discontinue all cervical cancer screening.)1 We know, however, that about one-fifth of all cervical cancer cases are diagnosed among individuals aged 65 or older, and for Black women that proportion is even higher when data are appropriately adjusted to account for the increased rate of hysterectomy among Black versus White women.2-4
Early-stage cervical cancer is largely a curable disease with very high 5-year overall survival rates. Unfortunately, more than half of all cervical cancer is diagnosed at a more advanced stage, and survival rates are much lower for this population.5
Cervical cancer incidence rates plummeted in the United States after the introduction of the Pap test for cervical cancer screening. However, the percentage of women who are not up to date with cervical cancer screening may now be increasing, from 14% in 2005 to 23% in 2019 according to one study from the US Preventive Services Task Force.6 When looking at cervical cancer screening rates by age, researchers from the Centers for Disease Control and Prevention estimate that the proportion of patients who have not been recently screened goes up as patients get older, with approximately 845,000 American women aged 61 to 65 not adequately screened in 2015 alone.7
Details of the study
Cooley and colleagues sought to better characterize the cohort of women diagnosed with cervical cancer at a later age, specifically the stage at diagnosis and survival.8 They used data from the California Cancer Registry (CCR), a large state-mandated, population-based data repository that is affiliated with the Surveillance, Epidemiology, and End Results (SEER) program.
The researchers identified 12,442 womenin the CCR who were newly diagnosed with cervical cancer from 2009 to 2018, 17.4% of whom were age 65 or older. They looked at cancer stage at diagnosis as it relates to relative survival rate (“the ratio of the observed survival rate among those who have cancer divided by the expected survival rate for people of the same sex, race/ethnicity, and age who do not have cancer”), Charlson comorbidity score, socioeconomic status, health insurance status, urbanicity, and race/ethnicity.
Results. In this study, 71% of women aged 65 or older presented with advanced-stage disease (FIGO [International Federation of Gynecology and Obstetrics] stage II–IV) as compared with only 48% in those aged 21 to 64. Five-year relative survival rates also were lower in the older cohort—23% to 37%, compared with 42% to 52% in the younger patients. In a sensitivity analysis, late-stage disease was associated with older age, increasing medical comorbidities, and nonadenocarcinoma histology.
Interestingly, older women of Hispanic ethnicity were less likely to be diagnosed with late-stage disease when compared with non-Hispanic White women.
Study strengths and limitations
Although this study’s conclusions—that patients with advanced-stage cancer are more likely to do poorly than those with early-stage cancer—may seem obvious to some even without the proven data, it is still important to highlight what a clinician may intuit with data to support that intuition. It is particularly important to emphasize this risk in older women in light of the aging population in the United States, with adults older than age 65 expected to account for more than 20% of the nation’s population by 2030.9
The study by Cooley and colleagues adds value to the existing literature due to its large study population, which included more than 12,000 patients diagnosed with cervical cancer.8 And although its results may not be completely generalizable as the data were gathered from only a California-specific population, the sample was diverse with significant portions of Hispanic and Black patients. This study supports previous data that showed high rates of advanced cervical cancer in women older than age 65, with resultant worse 5-year relative survival in this population of older women specifically.4 ●
Cervical cancer is both common and deadly in older women. Although current cervical cancer screening guidelines recommend screening cessation after age 65, remember that this is based on strict exit criteria. Consider screening older women (especially with human papillomavirus [HPV] testing) for cervical cancer if they have risk factors (such as smoking, multiple sexual partners, inconsistent or infrequent screening, history of abnormal Pap or HPV tests), and keep cervical cancer on your differential diagnosis in women who present with postmenopausal bleeding, vaginal discharge, pelvic pain, recurrent urinary tract infections, or other concerning symptoms.
SARAH DILLEY, MD, MPH, AND WARNER HUH, MD
- Fontham ETH, Wolf AMD, Church TR, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020;70:321-346. doi:10.3322/caac.21628.
- Dilley S, Huh W, Blechter B, et al. It’s time to re-evaluate cervical cancer screening after age 65. Gynecol Oncol. 2021;162:200-202. doi:10.1016/j.ygyno.2021.04.027.
- Rositch AF, Nowak RG, Gravitt PE. Increased age and racespecific incidence of cervical cancer after correction for hysterectomy prevalence in the United States from 2000 to 2009. Cancer. 2014;120:2032-2038. doi:10.1002/cncr.28548.
- Beavis AL, Gravitt PE, Rositch AF. Hysterectomy-corrected cervical cancer mortality rates reveal a larger racial disparity in the United States. Cancer. 2017;123:1044-1050. doi:10.1002 /cncr.30507.
- Cancer Stat Facts. National Cancer Institute Surveillance, Epidemiology, and End Results Program. https://seer.cancer .gov/statfacts/html/cervix.html
- Suk R, Hong YR, Rajan SS, et al. Assessment of US Preventive Services Task Force guideline-concordant cervical cancer screening rates and reasons for underscreening by age, race and ethnicity, sexual orientation, rurality, and insurance, 2005 to 2019. JAMA Netw Open. 2022;5:e2143582. doi:10.1001 /jamanetworkopen.2021.43582.
- White MC, Shoemaker ML, Benard VB. Cervical cancer screening and incidence by age: unmet needs near and after the stopping age for screening. Am J Prev Med. 2017;53:392395. doi:10.1016/j.amepre.2017.02.024.
- Cooley JJ, Maguire FB, Morris CR, et al. Cervical cancer stage at diagnosis and survival among women ≥65 years in California. Cancer Epidemiol Biomarkers Prev. 2023;32:91-97. doi:10.1158/1055-9965.EPI-22-0793.
- Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States. May 2014. United States Census Bureau. Accessed April 12, 2023. https://www.census .gov/library/publications/2014/demo/p25-1140.html
- Fontham ETH, Wolf AMD, Church TR, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020;70:321-346. doi:10.3322/caac.21628.
- Dilley S, Huh W, Blechter B, et al. It’s time to re-evaluate cervical cancer screening after age 65. Gynecol Oncol. 2021;162:200-202. doi:10.1016/j.ygyno.2021.04.027.
- Rositch AF, Nowak RG, Gravitt PE. Increased age and racespecific incidence of cervical cancer after correction for hysterectomy prevalence in the United States from 2000 to 2009. Cancer. 2014;120:2032-2038. doi:10.1002/cncr.28548.
- Beavis AL, Gravitt PE, Rositch AF. Hysterectomy-corrected cervical cancer mortality rates reveal a larger racial disparity in the United States. Cancer. 2017;123:1044-1050. doi:10.1002 /cncr.30507.
- Cancer Stat Facts. National Cancer Institute Surveillance, Epidemiology, and End Results Program. https://seer.cancer .gov/statfacts/html/cervix.html
- Suk R, Hong YR, Rajan SS, et al. Assessment of US Preventive Services Task Force guideline-concordant cervical cancer screening rates and reasons for underscreening by age, race and ethnicity, sexual orientation, rurality, and insurance, 2005 to 2019. JAMA Netw Open. 2022;5:e2143582. doi:10.1001 /jamanetworkopen.2021.43582.
- White MC, Shoemaker ML, Benard VB. Cervical cancer screening and incidence by age: unmet needs near and after the stopping age for screening. Am J Prev Med. 2017;53:392395. doi:10.1016/j.amepre.2017.02.024.
- Cooley JJ, Maguire FB, Morris CR, et al. Cervical cancer stage at diagnosis and survival among women ≥65 years in California. Cancer Epidemiol Biomarkers Prev. 2023;32:91-97. doi:10.1158/1055-9965.EPI-22-0793.
- Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States. May 2014. United States Census Bureau. Accessed April 12, 2023. https://www.census .gov/library/publications/2014/demo/p25-1140.html
Doctor spots a gunshot victim staggering down his street
It was a quiet day. I got up around 3 o’clock in the afternoon for my shift at 6 p.m. I was shaking off the cobwebs and making coffee at our front window that overlooked Brown Street in North Philadelphia. There was nobody else around so I went outside to see what was going on.
He was in his 50s or 60s, bleeding and obviously in distress. I had him sit down. Then I ran back inside and grabbed a dish towel and some exam gloves that I had in the house.
I ran back out and assessed him. A bullet had gone through one of his hands, but he had other wounds. I had to expose him, so I trauma stripped him on the sidewalk. I got his pants and his shirt off and saw a gunshot going through his lower pelvis. He was bleeding out from there.
I got the towel and started applying deep pressure down into the iliac vein in case they hit something, which I found out later, they had. I held it there. The man was just lying there begging not to die.
I’m someone who is very calm, maybe abnormally calm, as people tell me. I try to use that during my resuscitations and traumas. Just keeping everybody calm makes the situation easier. Afterwards, people asked me, “Weren’t you worried that you were going to get shot?” That does happen in North Philadelphia. But it didn’t even cross my mind.
I didn’t have to think at all about what I was doing. We saw so many gunshots, especially at Einstein Medical Center. We saw them daily. I’d sometimes get more than half a dozen gunshots in one shift.
So, I was holding pressure and some people started to come over. I got somebody to call 911 and asked the man about his medical history. I found out he had diabetes. Five or 10 minutes later, EMS showed up. They looked pretty stunned when I was able to give the handoff presentation to them. I told them what happened and his back-story. I wanted to make sure they would check his sugar and take extra precautions.
They got him on the stretcher, and he eventually made it to the hospital where he had surgery. They had to have a vascular surgeon work on him. I called later, and they told me, “Yeah, he’s alive.” But that’s about the extent of the update I got.
After the ambulance left, it was kind of chaos. All the neighbors poured out of their houses. People were panicked, talking and getting excited about it. I didn’t know, but everyone else had actually been home the whole time. They didn’t come out until then.
I went back inside and tried to get ready for work. I wasn’t planning on talking to the media, but my next door neighbor just walked the news camera crew over to my house and knocked on my door. I wasn’t exactly dressed to be on TV, but they talked to me on camera, and it was on the news later that night.
I went to work and didn’t say anything about it. To be honest, I was trying to avoid telling anyone. Our team had a close-knit bond, and we would often tease each other when we received any type of recognition.
Naturally one of my attendings saw it on the local news and told everybody. So, I got a lot of happy harassment for quite some time. Someone baked me a cake that said, “Hero of Fairmount” (the Philly neighborhood in which I live). Someone else printed out a photo of me that said, “Stop the Bleed Hero of Fairmount,” and put it on every single computer screen.
The man came to see me about 2 weeks later (a neighbor told him where I lived). The man was very tearful and gave me a big hug. We just embraced for a while, and he said how thankful he was. He brought me a bottle of wine, which I thought was really nice.
He told me what happened to him: There was a lot of construction on our street and he was the contractor overseeing a couple of home remodels and demolitions. Sometimes he paid workers in cash and carried it with him. Somebody had tipped off somebody else that he was going to be there that day. The contractor walked into one of the houses and a guy in a ski mask waited there with a gun. The guy shot him and took the cash. The bullet went through his hand into his pelvis.
I had never had to deal with something that intense before outside of work. Most of it really comes down to the basics – the ABCs and bleeding control. You do whatever you can with what you have. In this case, it was just a dish towel, gloves, and my hands to put as much pressure as possible.
It really was strange that I happened to be looking out the window at that moment. I don’t know if it was just a coincidence. The man told me he believed God had put somebody there at the right place at the right time to save his life. I just felt very fortunate to have been able to help him. I never saw him again.
I think something like this gives you a little confidence that you can actually do something and make a meaningful impact anywhere when it’s needed. It lets you know that you’re capable of doing it. You always think about it, but you don’t know until it happens.
A version of this article first appeared on Medscape.com.
It was a quiet day. I got up around 3 o’clock in the afternoon for my shift at 6 p.m. I was shaking off the cobwebs and making coffee at our front window that overlooked Brown Street in North Philadelphia. There was nobody else around so I went outside to see what was going on.
He was in his 50s or 60s, bleeding and obviously in distress. I had him sit down. Then I ran back inside and grabbed a dish towel and some exam gloves that I had in the house.
I ran back out and assessed him. A bullet had gone through one of his hands, but he had other wounds. I had to expose him, so I trauma stripped him on the sidewalk. I got his pants and his shirt off and saw a gunshot going through his lower pelvis. He was bleeding out from there.
I got the towel and started applying deep pressure down into the iliac vein in case they hit something, which I found out later, they had. I held it there. The man was just lying there begging not to die.
I’m someone who is very calm, maybe abnormally calm, as people tell me. I try to use that during my resuscitations and traumas. Just keeping everybody calm makes the situation easier. Afterwards, people asked me, “Weren’t you worried that you were going to get shot?” That does happen in North Philadelphia. But it didn’t even cross my mind.
I didn’t have to think at all about what I was doing. We saw so many gunshots, especially at Einstein Medical Center. We saw them daily. I’d sometimes get more than half a dozen gunshots in one shift.
So, I was holding pressure and some people started to come over. I got somebody to call 911 and asked the man about his medical history. I found out he had diabetes. Five or 10 minutes later, EMS showed up. They looked pretty stunned when I was able to give the handoff presentation to them. I told them what happened and his back-story. I wanted to make sure they would check his sugar and take extra precautions.
They got him on the stretcher, and he eventually made it to the hospital where he had surgery. They had to have a vascular surgeon work on him. I called later, and they told me, “Yeah, he’s alive.” But that’s about the extent of the update I got.
After the ambulance left, it was kind of chaos. All the neighbors poured out of their houses. People were panicked, talking and getting excited about it. I didn’t know, but everyone else had actually been home the whole time. They didn’t come out until then.
I went back inside and tried to get ready for work. I wasn’t planning on talking to the media, but my next door neighbor just walked the news camera crew over to my house and knocked on my door. I wasn’t exactly dressed to be on TV, but they talked to me on camera, and it was on the news later that night.
I went to work and didn’t say anything about it. To be honest, I was trying to avoid telling anyone. Our team had a close-knit bond, and we would often tease each other when we received any type of recognition.
Naturally one of my attendings saw it on the local news and told everybody. So, I got a lot of happy harassment for quite some time. Someone baked me a cake that said, “Hero of Fairmount” (the Philly neighborhood in which I live). Someone else printed out a photo of me that said, “Stop the Bleed Hero of Fairmount,” and put it on every single computer screen.
The man came to see me about 2 weeks later (a neighbor told him where I lived). The man was very tearful and gave me a big hug. We just embraced for a while, and he said how thankful he was. He brought me a bottle of wine, which I thought was really nice.
He told me what happened to him: There was a lot of construction on our street and he was the contractor overseeing a couple of home remodels and demolitions. Sometimes he paid workers in cash and carried it with him. Somebody had tipped off somebody else that he was going to be there that day. The contractor walked into one of the houses and a guy in a ski mask waited there with a gun. The guy shot him and took the cash. The bullet went through his hand into his pelvis.
I had never had to deal with something that intense before outside of work. Most of it really comes down to the basics – the ABCs and bleeding control. You do whatever you can with what you have. In this case, it was just a dish towel, gloves, and my hands to put as much pressure as possible.
It really was strange that I happened to be looking out the window at that moment. I don’t know if it was just a coincidence. The man told me he believed God had put somebody there at the right place at the right time to save his life. I just felt very fortunate to have been able to help him. I never saw him again.
I think something like this gives you a little confidence that you can actually do something and make a meaningful impact anywhere when it’s needed. It lets you know that you’re capable of doing it. You always think about it, but you don’t know until it happens.
A version of this article first appeared on Medscape.com.
It was a quiet day. I got up around 3 o’clock in the afternoon for my shift at 6 p.m. I was shaking off the cobwebs and making coffee at our front window that overlooked Brown Street in North Philadelphia. There was nobody else around so I went outside to see what was going on.
He was in his 50s or 60s, bleeding and obviously in distress. I had him sit down. Then I ran back inside and grabbed a dish towel and some exam gloves that I had in the house.
I ran back out and assessed him. A bullet had gone through one of his hands, but he had other wounds. I had to expose him, so I trauma stripped him on the sidewalk. I got his pants and his shirt off and saw a gunshot going through his lower pelvis. He was bleeding out from there.
I got the towel and started applying deep pressure down into the iliac vein in case they hit something, which I found out later, they had. I held it there. The man was just lying there begging not to die.
I’m someone who is very calm, maybe abnormally calm, as people tell me. I try to use that during my resuscitations and traumas. Just keeping everybody calm makes the situation easier. Afterwards, people asked me, “Weren’t you worried that you were going to get shot?” That does happen in North Philadelphia. But it didn’t even cross my mind.
I didn’t have to think at all about what I was doing. We saw so many gunshots, especially at Einstein Medical Center. We saw them daily. I’d sometimes get more than half a dozen gunshots in one shift.
So, I was holding pressure and some people started to come over. I got somebody to call 911 and asked the man about his medical history. I found out he had diabetes. Five or 10 minutes later, EMS showed up. They looked pretty stunned when I was able to give the handoff presentation to them. I told them what happened and his back-story. I wanted to make sure they would check his sugar and take extra precautions.
They got him on the stretcher, and he eventually made it to the hospital where he had surgery. They had to have a vascular surgeon work on him. I called later, and they told me, “Yeah, he’s alive.” But that’s about the extent of the update I got.
After the ambulance left, it was kind of chaos. All the neighbors poured out of their houses. People were panicked, talking and getting excited about it. I didn’t know, but everyone else had actually been home the whole time. They didn’t come out until then.
I went back inside and tried to get ready for work. I wasn’t planning on talking to the media, but my next door neighbor just walked the news camera crew over to my house and knocked on my door. I wasn’t exactly dressed to be on TV, but they talked to me on camera, and it was on the news later that night.
I went to work and didn’t say anything about it. To be honest, I was trying to avoid telling anyone. Our team had a close-knit bond, and we would often tease each other when we received any type of recognition.
Naturally one of my attendings saw it on the local news and told everybody. So, I got a lot of happy harassment for quite some time. Someone baked me a cake that said, “Hero of Fairmount” (the Philly neighborhood in which I live). Someone else printed out a photo of me that said, “Stop the Bleed Hero of Fairmount,” and put it on every single computer screen.
The man came to see me about 2 weeks later (a neighbor told him where I lived). The man was very tearful and gave me a big hug. We just embraced for a while, and he said how thankful he was. He brought me a bottle of wine, which I thought was really nice.
He told me what happened to him: There was a lot of construction on our street and he was the contractor overseeing a couple of home remodels and demolitions. Sometimes he paid workers in cash and carried it with him. Somebody had tipped off somebody else that he was going to be there that day. The contractor walked into one of the houses and a guy in a ski mask waited there with a gun. The guy shot him and took the cash. The bullet went through his hand into his pelvis.
I had never had to deal with something that intense before outside of work. Most of it really comes down to the basics – the ABCs and bleeding control. You do whatever you can with what you have. In this case, it was just a dish towel, gloves, and my hands to put as much pressure as possible.
It really was strange that I happened to be looking out the window at that moment. I don’t know if it was just a coincidence. The man told me he believed God had put somebody there at the right place at the right time to save his life. I just felt very fortunate to have been able to help him. I never saw him again.
I think something like this gives you a little confidence that you can actually do something and make a meaningful impact anywhere when it’s needed. It lets you know that you’re capable of doing it. You always think about it, but you don’t know until it happens.
A version of this article first appeared on Medscape.com.
A legacy of unfair admissions
This is where people related to successful alumni and/or big donors can get preferential admission, possibly over more qualified people.
All of us likely experienced this from one side or another, though realistically I haven’t thought about it years. My kids went to the same state school I did, but I’m pretty sure I had nothing to do with their being accepted. I never gave the school a single donation, nor did I call anyone there to try and get them in. Not that anyone would have known who I was if I’d tried. I’m just another one of many who went there, preserved only in some filing cabinet of transcripts somewhere.
I’m all for the legacy system ending, though, for one simple reason: It’s not fair.
If someone is qualified, great. They should be admitted on their own merits. But if they’re not, they shouldn’t get into medical school just because one (or both) of their parents went there, or is a VIP, or paid for a new library wing.
The reason I’m writing this is because the recent reporting did bring back a memory.
A long time ago, when I was in college, I hung out with other premed students. We knew we were all competing with each other for the same spots at the state medical school, but also knew that we wouldn’t all get in there. That didn’t make us enemies, it was just the truth. It’s that point in life where ANY medical school admission is all you want.
Pete (not his real name) was a nice guy, but his grades weren’t the best. His MCAT scores lagged behind the rest of us in the clique, and ... he didn’t care.
Pete’s dad had graduated from the state medical school, and was still on staff there. He was now on the teaching staff ... and on the school’s admissions board. To Pete, tests and grades didn’t matter. His admission was assured.
So it was no surprise when he got in ahead of the rest of us with better qualifications. Most of us, including me, did get in somewhere, so we were still happy. We just had to move farther and pay more, but that’s life.
I really didn’t think much about Pete again after that. I was now in medical school, I had a whole new social group, and more importantly I didn’t really have time to think of much beyond when the next exam was.
Then I moved home, and started residency. During my PGY-2 year we had a changing group of medical students assigned to my wards rotation.
And, as you probably guessed, one of them was Pete.
Pete was in his last year of medical school. But we’d both started in the same year, and now I was 2 years ahead of him. I didn’t ask him what happened, but another medical student told me he wasn’t known to be the best student, but the university refused to drop him, and just kept setting him back a class here, a year there.
Maybe they’d have done the same for anyone, but I doubt it.
I never saw Pete again after that. When I looked him up online tonight he’s not listed as being a doctor, and isn’t even in medicine. Granted, a lot of doctors have left medicine, and maybe he did too.
But the more likely reason is that Pete never should have been there in the first place. He got in as a legacy, taking a medical school slot from someone who may have been more capable and driven.
And that just doesn’t seem right to me. It didn’t then and it doesn’t now.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
This is where people related to successful alumni and/or big donors can get preferential admission, possibly over more qualified people.
All of us likely experienced this from one side or another, though realistically I haven’t thought about it years. My kids went to the same state school I did, but I’m pretty sure I had nothing to do with their being accepted. I never gave the school a single donation, nor did I call anyone there to try and get them in. Not that anyone would have known who I was if I’d tried. I’m just another one of many who went there, preserved only in some filing cabinet of transcripts somewhere.
I’m all for the legacy system ending, though, for one simple reason: It’s not fair.
If someone is qualified, great. They should be admitted on their own merits. But if they’re not, they shouldn’t get into medical school just because one (or both) of their parents went there, or is a VIP, or paid for a new library wing.
The reason I’m writing this is because the recent reporting did bring back a memory.
A long time ago, when I was in college, I hung out with other premed students. We knew we were all competing with each other for the same spots at the state medical school, but also knew that we wouldn’t all get in there. That didn’t make us enemies, it was just the truth. It’s that point in life where ANY medical school admission is all you want.
Pete (not his real name) was a nice guy, but his grades weren’t the best. His MCAT scores lagged behind the rest of us in the clique, and ... he didn’t care.
Pete’s dad had graduated from the state medical school, and was still on staff there. He was now on the teaching staff ... and on the school’s admissions board. To Pete, tests and grades didn’t matter. His admission was assured.
So it was no surprise when he got in ahead of the rest of us with better qualifications. Most of us, including me, did get in somewhere, so we were still happy. We just had to move farther and pay more, but that’s life.
I really didn’t think much about Pete again after that. I was now in medical school, I had a whole new social group, and more importantly I didn’t really have time to think of much beyond when the next exam was.
Then I moved home, and started residency. During my PGY-2 year we had a changing group of medical students assigned to my wards rotation.
And, as you probably guessed, one of them was Pete.
Pete was in his last year of medical school. But we’d both started in the same year, and now I was 2 years ahead of him. I didn’t ask him what happened, but another medical student told me he wasn’t known to be the best student, but the university refused to drop him, and just kept setting him back a class here, a year there.
Maybe they’d have done the same for anyone, but I doubt it.
I never saw Pete again after that. When I looked him up online tonight he’s not listed as being a doctor, and isn’t even in medicine. Granted, a lot of doctors have left medicine, and maybe he did too.
But the more likely reason is that Pete never should have been there in the first place. He got in as a legacy, taking a medical school slot from someone who may have been more capable and driven.
And that just doesn’t seem right to me. It didn’t then and it doesn’t now.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
This is where people related to successful alumni and/or big donors can get preferential admission, possibly over more qualified people.
All of us likely experienced this from one side or another, though realistically I haven’t thought about it years. My kids went to the same state school I did, but I’m pretty sure I had nothing to do with their being accepted. I never gave the school a single donation, nor did I call anyone there to try and get them in. Not that anyone would have known who I was if I’d tried. I’m just another one of many who went there, preserved only in some filing cabinet of transcripts somewhere.
I’m all for the legacy system ending, though, for one simple reason: It’s not fair.
If someone is qualified, great. They should be admitted on their own merits. But if they’re not, they shouldn’t get into medical school just because one (or both) of their parents went there, or is a VIP, or paid for a new library wing.
The reason I’m writing this is because the recent reporting did bring back a memory.
A long time ago, when I was in college, I hung out with other premed students. We knew we were all competing with each other for the same spots at the state medical school, but also knew that we wouldn’t all get in there. That didn’t make us enemies, it was just the truth. It’s that point in life where ANY medical school admission is all you want.
Pete (not his real name) was a nice guy, but his grades weren’t the best. His MCAT scores lagged behind the rest of us in the clique, and ... he didn’t care.
Pete’s dad had graduated from the state medical school, and was still on staff there. He was now on the teaching staff ... and on the school’s admissions board. To Pete, tests and grades didn’t matter. His admission was assured.
So it was no surprise when he got in ahead of the rest of us with better qualifications. Most of us, including me, did get in somewhere, so we were still happy. We just had to move farther and pay more, but that’s life.
I really didn’t think much about Pete again after that. I was now in medical school, I had a whole new social group, and more importantly I didn’t really have time to think of much beyond when the next exam was.
Then I moved home, and started residency. During my PGY-2 year we had a changing group of medical students assigned to my wards rotation.
And, as you probably guessed, one of them was Pete.
Pete was in his last year of medical school. But we’d both started in the same year, and now I was 2 years ahead of him. I didn’t ask him what happened, but another medical student told me he wasn’t known to be the best student, but the university refused to drop him, and just kept setting him back a class here, a year there.
Maybe they’d have done the same for anyone, but I doubt it.
I never saw Pete again after that. When I looked him up online tonight he’s not listed as being a doctor, and isn’t even in medicine. Granted, a lot of doctors have left medicine, and maybe he did too.
But the more likely reason is that Pete never should have been there in the first place. He got in as a legacy, taking a medical school slot from someone who may have been more capable and driven.
And that just doesn’t seem right to me. It didn’t then and it doesn’t now.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Fatigue is a monster for patients with pulmonary disease
If you’re looking for it, you’ll find fatigue almost everywhere. It’s so common that it hides in plain sight, never dealt with because it’s present for good reason: the inevitable consequence of age, whatever disease you’re treating, poor lifestyle choices, and the daily grind of twenty-first–century life. Its impact is so ubiquitous and pernicious that it’s considered acceptable.
Is it though? After all, fatigue can be debilitating. Not every symptom is worthy of a chronic syndrome bearing its name. Furthermore, what if its relationship to the disease you’re treating is bidirectional?
Outside of sleep medicine, I see little focus on fatigue among pulmonologists. This despite the existing data on fatigue related to sarcoidosis, chronic obstructive pulmonary disease (COPD), and interstitial lung disease. Even when we do pay it lip service, “addressing” fatigue or sleep is essentially a euphemism for ordering a sleep study.
As with fatigue, if you look for obstructive sleep apnea, it’ll be there, although with OSA, it’s related to the incredibly low, nonevidence-based threshold the American Academy of Sleep Medicine has established for making the diagnosis. With continuous positive airway pressure (CPAP) in hand, the patient has a new disease to worry about and a difficult behavioral change (wearing, cleaning, and resupplying their CPAP equipment) to make. Too often, the CPAP isn’t used – or is – and the fatigue persists. But it’s okay, because we followed somebody’s guideline.
The American Thoracic Society just published a research statement on cancer-related fatigue. It is comprehensive and highlights the high prevalence and poor recognition of cancer-related fatigue. The authors note that among cancers, those of the lung are associated with a higher comorbid disease burden, older age, and cigarette smoking. All these factors make patients with lung cancer particularly prone to fatigue. Interactions between these factors, lung cancer histology, and specific chemotherapy regimens are poorly understood. True to its title, the “research statement” serves more as a call to action than an evidence-based blueprint for diagnosis and management.
The cancer-related fatigue data that does exist suggests treatment starts with recognition followed by a focus on sleep, exercise, and nutrition. This should surprise no one. The data on fatigue in general (not specific to cancer-related fatigue) shows that although fatigue is not synonymous with poor quality or insufficient sleep, sleep is usually a major factor. The cancer-related conditions affecting sleep include anxiety, depression, insufficient sleep, insomnia, medication side effects, and OSA. The intersecting web is complex, but across underlying conditions (cancer or otherwise), the quickest most efficient method for mitigating fatigue is optimizing sleep.
Exercise and nutrition are also important. Again, across disease processes (interstitial lung disease, COPD, lung cancer, and so on), no drug comes close to aerobic exercise for reducing symptoms, including fatigue. If an exercise prescription could be delivered in pill-form, it’d be a blockbuster. But it can’t be, and the ATS lung cancer–related fatigue research statement nicely outlines the evidence for increased activity levels and the barriers to obtaining support and compliance. As is the case with exercise, support for improving nutrition is limited by cost, access, and patient education.
Perhaps most importantly, sleep, exercise, and nutrition require time for counseling and a behavior change for the physician and patient. Both are in short supply, and commitment is always ephemeral. Incentivization could perhaps be re-structured, but the ATS document notes this will be challenging. With respect to pulmonary rehabilitation (about 50% of patients with lung cancer have comorbid COPD), for example, reimbursement is poor, which serves as a disincentive. Their suggestions? Early integration and repeated introduction to rehabilitation and exercise concepts. Sounds great.
In summary, in my opinion, fatigue doesn’t receive the attention level commensurate with its impact. It’s easy to understand why, but I’m glad the ATS is highlighting the problem. Unbeknownst to me, multiple cancer guidelines already recommend screening for fatigue. The recent sarcoidosis treatment guideline published by the European Respiratory Society dedicated a PICO (Patients, Intervention, Comparison, Outcomes) to the topic and recommended exercise (pulmonary rehabilitation). That said, consensus statements on COPD mention it only in passing in relation to severe disease and end-of-life care, and idiopathic pulmonary fibrosis guidelines ignore it entirely. So, recognition is improving, but we’ve got ways to go.
Dr. Holley is professor of medicine at Uniformed Services University, Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He disclosed ties with Metapharm, CHEST College, and WebMD.
A version of this article originally appeared on Medscape.com.
If you’re looking for it, you’ll find fatigue almost everywhere. It’s so common that it hides in plain sight, never dealt with because it’s present for good reason: the inevitable consequence of age, whatever disease you’re treating, poor lifestyle choices, and the daily grind of twenty-first–century life. Its impact is so ubiquitous and pernicious that it’s considered acceptable.
Is it though? After all, fatigue can be debilitating. Not every symptom is worthy of a chronic syndrome bearing its name. Furthermore, what if its relationship to the disease you’re treating is bidirectional?
Outside of sleep medicine, I see little focus on fatigue among pulmonologists. This despite the existing data on fatigue related to sarcoidosis, chronic obstructive pulmonary disease (COPD), and interstitial lung disease. Even when we do pay it lip service, “addressing” fatigue or sleep is essentially a euphemism for ordering a sleep study.
As with fatigue, if you look for obstructive sleep apnea, it’ll be there, although with OSA, it’s related to the incredibly low, nonevidence-based threshold the American Academy of Sleep Medicine has established for making the diagnosis. With continuous positive airway pressure (CPAP) in hand, the patient has a new disease to worry about and a difficult behavioral change (wearing, cleaning, and resupplying their CPAP equipment) to make. Too often, the CPAP isn’t used – or is – and the fatigue persists. But it’s okay, because we followed somebody’s guideline.
The American Thoracic Society just published a research statement on cancer-related fatigue. It is comprehensive and highlights the high prevalence and poor recognition of cancer-related fatigue. The authors note that among cancers, those of the lung are associated with a higher comorbid disease burden, older age, and cigarette smoking. All these factors make patients with lung cancer particularly prone to fatigue. Interactions between these factors, lung cancer histology, and specific chemotherapy regimens are poorly understood. True to its title, the “research statement” serves more as a call to action than an evidence-based blueprint for diagnosis and management.
The cancer-related fatigue data that does exist suggests treatment starts with recognition followed by a focus on sleep, exercise, and nutrition. This should surprise no one. The data on fatigue in general (not specific to cancer-related fatigue) shows that although fatigue is not synonymous with poor quality or insufficient sleep, sleep is usually a major factor. The cancer-related conditions affecting sleep include anxiety, depression, insufficient sleep, insomnia, medication side effects, and OSA. The intersecting web is complex, but across underlying conditions (cancer or otherwise), the quickest most efficient method for mitigating fatigue is optimizing sleep.
Exercise and nutrition are also important. Again, across disease processes (interstitial lung disease, COPD, lung cancer, and so on), no drug comes close to aerobic exercise for reducing symptoms, including fatigue. If an exercise prescription could be delivered in pill-form, it’d be a blockbuster. But it can’t be, and the ATS lung cancer–related fatigue research statement nicely outlines the evidence for increased activity levels and the barriers to obtaining support and compliance. As is the case with exercise, support for improving nutrition is limited by cost, access, and patient education.
Perhaps most importantly, sleep, exercise, and nutrition require time for counseling and a behavior change for the physician and patient. Both are in short supply, and commitment is always ephemeral. Incentivization could perhaps be re-structured, but the ATS document notes this will be challenging. With respect to pulmonary rehabilitation (about 50% of patients with lung cancer have comorbid COPD), for example, reimbursement is poor, which serves as a disincentive. Their suggestions? Early integration and repeated introduction to rehabilitation and exercise concepts. Sounds great.
In summary, in my opinion, fatigue doesn’t receive the attention level commensurate with its impact. It’s easy to understand why, but I’m glad the ATS is highlighting the problem. Unbeknownst to me, multiple cancer guidelines already recommend screening for fatigue. The recent sarcoidosis treatment guideline published by the European Respiratory Society dedicated a PICO (Patients, Intervention, Comparison, Outcomes) to the topic and recommended exercise (pulmonary rehabilitation). That said, consensus statements on COPD mention it only in passing in relation to severe disease and end-of-life care, and idiopathic pulmonary fibrosis guidelines ignore it entirely. So, recognition is improving, but we’ve got ways to go.
Dr. Holley is professor of medicine at Uniformed Services University, Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He disclosed ties with Metapharm, CHEST College, and WebMD.
A version of this article originally appeared on Medscape.com.
If you’re looking for it, you’ll find fatigue almost everywhere. It’s so common that it hides in plain sight, never dealt with because it’s present for good reason: the inevitable consequence of age, whatever disease you’re treating, poor lifestyle choices, and the daily grind of twenty-first–century life. Its impact is so ubiquitous and pernicious that it’s considered acceptable.
Is it though? After all, fatigue can be debilitating. Not every symptom is worthy of a chronic syndrome bearing its name. Furthermore, what if its relationship to the disease you’re treating is bidirectional?
Outside of sleep medicine, I see little focus on fatigue among pulmonologists. This despite the existing data on fatigue related to sarcoidosis, chronic obstructive pulmonary disease (COPD), and interstitial lung disease. Even when we do pay it lip service, “addressing” fatigue or sleep is essentially a euphemism for ordering a sleep study.
As with fatigue, if you look for obstructive sleep apnea, it’ll be there, although with OSA, it’s related to the incredibly low, nonevidence-based threshold the American Academy of Sleep Medicine has established for making the diagnosis. With continuous positive airway pressure (CPAP) in hand, the patient has a new disease to worry about and a difficult behavioral change (wearing, cleaning, and resupplying their CPAP equipment) to make. Too often, the CPAP isn’t used – or is – and the fatigue persists. But it’s okay, because we followed somebody’s guideline.
The American Thoracic Society just published a research statement on cancer-related fatigue. It is comprehensive and highlights the high prevalence and poor recognition of cancer-related fatigue. The authors note that among cancers, those of the lung are associated with a higher comorbid disease burden, older age, and cigarette smoking. All these factors make patients with lung cancer particularly prone to fatigue. Interactions between these factors, lung cancer histology, and specific chemotherapy regimens are poorly understood. True to its title, the “research statement” serves more as a call to action than an evidence-based blueprint for diagnosis and management.
The cancer-related fatigue data that does exist suggests treatment starts with recognition followed by a focus on sleep, exercise, and nutrition. This should surprise no one. The data on fatigue in general (not specific to cancer-related fatigue) shows that although fatigue is not synonymous with poor quality or insufficient sleep, sleep is usually a major factor. The cancer-related conditions affecting sleep include anxiety, depression, insufficient sleep, insomnia, medication side effects, and OSA. The intersecting web is complex, but across underlying conditions (cancer or otherwise), the quickest most efficient method for mitigating fatigue is optimizing sleep.
Exercise and nutrition are also important. Again, across disease processes (interstitial lung disease, COPD, lung cancer, and so on), no drug comes close to aerobic exercise for reducing symptoms, including fatigue. If an exercise prescription could be delivered in pill-form, it’d be a blockbuster. But it can’t be, and the ATS lung cancer–related fatigue research statement nicely outlines the evidence for increased activity levels and the barriers to obtaining support and compliance. As is the case with exercise, support for improving nutrition is limited by cost, access, and patient education.
Perhaps most importantly, sleep, exercise, and nutrition require time for counseling and a behavior change for the physician and patient. Both are in short supply, and commitment is always ephemeral. Incentivization could perhaps be re-structured, but the ATS document notes this will be challenging. With respect to pulmonary rehabilitation (about 50% of patients with lung cancer have comorbid COPD), for example, reimbursement is poor, which serves as a disincentive. Their suggestions? Early integration and repeated introduction to rehabilitation and exercise concepts. Sounds great.
In summary, in my opinion, fatigue doesn’t receive the attention level commensurate with its impact. It’s easy to understand why, but I’m glad the ATS is highlighting the problem. Unbeknownst to me, multiple cancer guidelines already recommend screening for fatigue. The recent sarcoidosis treatment guideline published by the European Respiratory Society dedicated a PICO (Patients, Intervention, Comparison, Outcomes) to the topic and recommended exercise (pulmonary rehabilitation). That said, consensus statements on COPD mention it only in passing in relation to severe disease and end-of-life care, and idiopathic pulmonary fibrosis guidelines ignore it entirely. So, recognition is improving, but we’ve got ways to go.
Dr. Holley is professor of medicine at Uniformed Services University, Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He disclosed ties with Metapharm, CHEST College, and WebMD.
A version of this article originally appeared on Medscape.com.
Boys may carry the weight, or overweight, of adults’ infertility
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
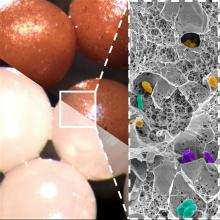
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Nurses: The unsung heroes
Try practicing inpatient medicine without nurses.
You can’t.
We blow in and out of the rooms, write notes, check results and vitals, then move on to the next person.
But the nurses are the ones who actually make this all happen. And, amazingly, can do all that work with a smile.
But in our current postpandemic world, we’re facing a serious shortage. A recent survey of registered nurses found that only 15% of hospital nurses were planning on being there in 1 year. Thirty percent said they were planning on changing careers entirely in the aftermath of the pandemic. Their job satisfaction scores have dropped 15% from 2019 to 2023. Their stress scores, and concerns that the job is affecting their health, have increased 15%-20%.
The problem reflects a combination of things intersecting at a bad time: Staffing shortages resulting in more patients per nurse, hospital administrators cutting corners on staffing and pay, and the ongoing state of incivility.
The last one is a particularly new issue. Difficult patients and their families are nothing new. We all encounter them, and learn to deal with them in our own way. It’s part of the territory.
But since 2020 it’s climbed to a new-level of in-your-face confrontation, rudeness, and aggression, sometimes leading to violence. Physical attacks on people in all jobs have increased, but health care workers are five times more likely to encounter workplace violence than any other field.
Underpaid, overworked, and a sitting duck for violence. Can you blame people for looking elsewhere?
All of this is coming at a time when a whole generation of nurses is retiring, another generation is starting to reach an age of needing more health care, and nursing schools are short on teaching staff, limiting the number of new people that can be trained. Nursing education, like medical school, isn’t a place to cut corners (neither is care, obviously).
These days we toss the word “burnout” around to the point that it’s become almost meaningless, but to those affected by it, the consequences are quite real. And when it causes a loss of staff and impairs the ability of all to provide quality medical care, it quickly becomes everyone’s problem.
Finding solutions for such things isn’t a can you just kick down the road, as governmental agencies have always been so good at doing. These are things that have real-world consequences for all involved, and solutions need to involve private, public, and educational sectors working together.
I don’t have any ideas, but I hope the people who can change this will sit down and work some out.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Try practicing inpatient medicine without nurses.
You can’t.
We blow in and out of the rooms, write notes, check results and vitals, then move on to the next person.
But the nurses are the ones who actually make this all happen. And, amazingly, can do all that work with a smile.
But in our current postpandemic world, we’re facing a serious shortage. A recent survey of registered nurses found that only 15% of hospital nurses were planning on being there in 1 year. Thirty percent said they were planning on changing careers entirely in the aftermath of the pandemic. Their job satisfaction scores have dropped 15% from 2019 to 2023. Their stress scores, and concerns that the job is affecting their health, have increased 15%-20%.
The problem reflects a combination of things intersecting at a bad time: Staffing shortages resulting in more patients per nurse, hospital administrators cutting corners on staffing and pay, and the ongoing state of incivility.
The last one is a particularly new issue. Difficult patients and their families are nothing new. We all encounter them, and learn to deal with them in our own way. It’s part of the territory.
But since 2020 it’s climbed to a new-level of in-your-face confrontation, rudeness, and aggression, sometimes leading to violence. Physical attacks on people in all jobs have increased, but health care workers are five times more likely to encounter workplace violence than any other field.
Underpaid, overworked, and a sitting duck for violence. Can you blame people for looking elsewhere?
All of this is coming at a time when a whole generation of nurses is retiring, another generation is starting to reach an age of needing more health care, and nursing schools are short on teaching staff, limiting the number of new people that can be trained. Nursing education, like medical school, isn’t a place to cut corners (neither is care, obviously).
These days we toss the word “burnout” around to the point that it’s become almost meaningless, but to those affected by it, the consequences are quite real. And when it causes a loss of staff and impairs the ability of all to provide quality medical care, it quickly becomes everyone’s problem.
Finding solutions for such things isn’t a can you just kick down the road, as governmental agencies have always been so good at doing. These are things that have real-world consequences for all involved, and solutions need to involve private, public, and educational sectors working together.
I don’t have any ideas, but I hope the people who can change this will sit down and work some out.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Try practicing inpatient medicine without nurses.
You can’t.
We blow in and out of the rooms, write notes, check results and vitals, then move on to the next person.
But the nurses are the ones who actually make this all happen. And, amazingly, can do all that work with a smile.
But in our current postpandemic world, we’re facing a serious shortage. A recent survey of registered nurses found that only 15% of hospital nurses were planning on being there in 1 year. Thirty percent said they were planning on changing careers entirely in the aftermath of the pandemic. Their job satisfaction scores have dropped 15% from 2019 to 2023. Their stress scores, and concerns that the job is affecting their health, have increased 15%-20%.
The problem reflects a combination of things intersecting at a bad time: Staffing shortages resulting in more patients per nurse, hospital administrators cutting corners on staffing and pay, and the ongoing state of incivility.
The last one is a particularly new issue. Difficult patients and their families are nothing new. We all encounter them, and learn to deal with them in our own way. It’s part of the territory.
But since 2020 it’s climbed to a new-level of in-your-face confrontation, rudeness, and aggression, sometimes leading to violence. Physical attacks on people in all jobs have increased, but health care workers are five times more likely to encounter workplace violence than any other field.
Underpaid, overworked, and a sitting duck for violence. Can you blame people for looking elsewhere?
All of this is coming at a time when a whole generation of nurses is retiring, another generation is starting to reach an age of needing more health care, and nursing schools are short on teaching staff, limiting the number of new people that can be trained. Nursing education, like medical school, isn’t a place to cut corners (neither is care, obviously).
These days we toss the word “burnout” around to the point that it’s become almost meaningless, but to those affected by it, the consequences are quite real. And when it causes a loss of staff and impairs the ability of all to provide quality medical care, it quickly becomes everyone’s problem.
Finding solutions for such things isn’t a can you just kick down the road, as governmental agencies have always been so good at doing. These are things that have real-world consequences for all involved, and solutions need to involve private, public, and educational sectors working together.
I don’t have any ideas, but I hope the people who can change this will sit down and work some out.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Medications that scare me
An 85-year-old woman is brought to the emergency department after a syncopal episode. Her caregivers report a similar episode 2 weeks ago, but she recovered so quickly they did not seek evaluation for her.
Medications: Omeprazole 20 mg, pravastatin 40 mg, citalopram 10 mg, albuterol, donepezil 10 mg, isosorbide mononitrate 60 mg, and calcium. On exam, blood pressure is 100/60 mm Hg, pulse 55. ECG indicates bradycardia with normal intervals. What drug most likely caused her syncope?
A. Citalopram
B. Pravastatin
C. Donepezil
D. Isosorbide
E. Calcium
This woman’s syncope is likely caused by donepezil. Citalopram can lengthen the QT interval, especially in elderly patients, but the normal intervals on ECG eliminate this possibility. Donepezil can cause bradycardia, which can contribute to syncope.
Hernandez and colleagues evaluated a cohort of veterans with dementia over an 8-year period.1 They found that there was a 1.4-fold increased risk of bradycardia in patients with dementia treated with an acetylcholine inhibitor (compared with that in patients who were not taking these medications) and that there was a dose-dependent increase in risk for patients on donepezil.
Park-Wyllie et al. found in a study of 1.4 million older adults a greater than twofold risk of hospitalization for bradycardia in patients treated with a cholinesterase inhibitor.2 Gill and colleagues performed a population-based cohort study of 19,803 elderly patients with dementia who were prescribed cholinesterase inhibitors, and compared them to age-matched controls.3 They found increased hospital visits for syncope in people receiving cholinesterase inhibitors (hazard ratio, 1.76; 95% confidence interval, 1.57-1.98). Other syncope-related events were also more common in people receiving cholinesterase inhibitors, compared with controls: hospital visits for bradycardia (HR, 1.69; 95% CI, 1.32-2.15), permanent pacemaker insertion (HR, 1.49; 95% CI, 1.12-2.00), and hip fracture (HR, 1.18; (95% CI, 1.04-1.34).
Nausea, vomiting, and weight loss are much more common than the rarer side effects of bradycardia and syncope. The frequency of gastroenterological side effects is up to 25%. Cholinesterase inhibitors have modest effects on cognitive function with a high number needed to treat (NNT) of 10, and an NNT as high as 100 for global function. The number needed to harm (NNH) is 4, when gastrointestinal symptoms are added in.4 Another important, problematic side effect of cholinesterase inhibitors is urinary incontinence. This often leads to patients receiving medications, to combat this side effect, that may worsen cognitive function.
Another commonly used medication that scares me in certain circumstances is trimethoprim-sulfamethoxazole. My main concern is when it is used in patients who are elderly, have chronic kidney disease, or are taking other medications that can cause hyperkalemia (ACEIs, ARBs, potassium-sparing diuretics including spironolactone). Hyperkalemia is a real concern in these patient populations. Trimethoprim reduces renal potassium excretion through the competitive inhibition of sodium channels in the distal nephron, in a manner similar to the potassium-sparing diuretic amiloride. Hospitalizations for hyperkalemia are more common in patients who take ACEIs and ARBs and are prescribed trimethoprim-sulfamethoxazole, compared with other antibiotics.5
Sudden cardiac death is also more common in patients who are taking ACEIs or ARBs and receive trimethoprim-sulfamethoxazole.6 Trimethoprim-sulfamethoxazole also has a powerful interaction with warfarin, both displacing warfarin from albumin and inhibiting its metabolism. It raises the INR (international normalized ratio) in warfarin-treated patients much greater than do other antibiotics.7
Pearls
- Think carefully about the use of cholinesterase inhibitors because of the unfavorable NNH vs. NNT.
- Use caution prescribing trimethoprim for patients who are elderly, especially if they are on an ACEI, an ARB, or spironolactone, and in patients with chronic kidney disease.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Hernandez RK et al. J Am Geriatr Soc. 2009;57:1997-2003.
2. Park-Wyllie LY et al. PLoS Med. 2009;6:e1000157.
3. Gill SS et al. Arch Intern Med 2009;169:867-73.
4. Peters KR. J Am Geriatr Soc. 2013 Jul;61(7):1170-4.
5. Antoniou TN et al. Arch Intern Med. 2010;170(12):1045-9.
6. Fralick M et al. BMJ. 2014 Oct 30;349:g6196.
7. Glasheen JJ et al. J Gen Intern Med. 2005 Jul;20(7):653-6.
An 85-year-old woman is brought to the emergency department after a syncopal episode. Her caregivers report a similar episode 2 weeks ago, but she recovered so quickly they did not seek evaluation for her.
Medications: Omeprazole 20 mg, pravastatin 40 mg, citalopram 10 mg, albuterol, donepezil 10 mg, isosorbide mononitrate 60 mg, and calcium. On exam, blood pressure is 100/60 mm Hg, pulse 55. ECG indicates bradycardia with normal intervals. What drug most likely caused her syncope?
A. Citalopram
B. Pravastatin
C. Donepezil
D. Isosorbide
E. Calcium
This woman’s syncope is likely caused by donepezil. Citalopram can lengthen the QT interval, especially in elderly patients, but the normal intervals on ECG eliminate this possibility. Donepezil can cause bradycardia, which can contribute to syncope.
Hernandez and colleagues evaluated a cohort of veterans with dementia over an 8-year period.1 They found that there was a 1.4-fold increased risk of bradycardia in patients with dementia treated with an acetylcholine inhibitor (compared with that in patients who were not taking these medications) and that there was a dose-dependent increase in risk for patients on donepezil.
Park-Wyllie et al. found in a study of 1.4 million older adults a greater than twofold risk of hospitalization for bradycardia in patients treated with a cholinesterase inhibitor.2 Gill and colleagues performed a population-based cohort study of 19,803 elderly patients with dementia who were prescribed cholinesterase inhibitors, and compared them to age-matched controls.3 They found increased hospital visits for syncope in people receiving cholinesterase inhibitors (hazard ratio, 1.76; 95% confidence interval, 1.57-1.98). Other syncope-related events were also more common in people receiving cholinesterase inhibitors, compared with controls: hospital visits for bradycardia (HR, 1.69; 95% CI, 1.32-2.15), permanent pacemaker insertion (HR, 1.49; 95% CI, 1.12-2.00), and hip fracture (HR, 1.18; (95% CI, 1.04-1.34).
Nausea, vomiting, and weight loss are much more common than the rarer side effects of bradycardia and syncope. The frequency of gastroenterological side effects is up to 25%. Cholinesterase inhibitors have modest effects on cognitive function with a high number needed to treat (NNT) of 10, and an NNT as high as 100 for global function. The number needed to harm (NNH) is 4, when gastrointestinal symptoms are added in.4 Another important, problematic side effect of cholinesterase inhibitors is urinary incontinence. This often leads to patients receiving medications, to combat this side effect, that may worsen cognitive function.
Another commonly used medication that scares me in certain circumstances is trimethoprim-sulfamethoxazole. My main concern is when it is used in patients who are elderly, have chronic kidney disease, or are taking other medications that can cause hyperkalemia (ACEIs, ARBs, potassium-sparing diuretics including spironolactone). Hyperkalemia is a real concern in these patient populations. Trimethoprim reduces renal potassium excretion through the competitive inhibition of sodium channels in the distal nephron, in a manner similar to the potassium-sparing diuretic amiloride. Hospitalizations for hyperkalemia are more common in patients who take ACEIs and ARBs and are prescribed trimethoprim-sulfamethoxazole, compared with other antibiotics.5
Sudden cardiac death is also more common in patients who are taking ACEIs or ARBs and receive trimethoprim-sulfamethoxazole.6 Trimethoprim-sulfamethoxazole also has a powerful interaction with warfarin, both displacing warfarin from albumin and inhibiting its metabolism. It raises the INR (international normalized ratio) in warfarin-treated patients much greater than do other antibiotics.7
Pearls
- Think carefully about the use of cholinesterase inhibitors because of the unfavorable NNH vs. NNT.
- Use caution prescribing trimethoprim for patients who are elderly, especially if they are on an ACEI, an ARB, or spironolactone, and in patients with chronic kidney disease.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Hernandez RK et al. J Am Geriatr Soc. 2009;57:1997-2003.
2. Park-Wyllie LY et al. PLoS Med. 2009;6:e1000157.
3. Gill SS et al. Arch Intern Med 2009;169:867-73.
4. Peters KR. J Am Geriatr Soc. 2013 Jul;61(7):1170-4.
5. Antoniou TN et al. Arch Intern Med. 2010;170(12):1045-9.
6. Fralick M et al. BMJ. 2014 Oct 30;349:g6196.
7. Glasheen JJ et al. J Gen Intern Med. 2005 Jul;20(7):653-6.
An 85-year-old woman is brought to the emergency department after a syncopal episode. Her caregivers report a similar episode 2 weeks ago, but she recovered so quickly they did not seek evaluation for her.
Medications: Omeprazole 20 mg, pravastatin 40 mg, citalopram 10 mg, albuterol, donepezil 10 mg, isosorbide mononitrate 60 mg, and calcium. On exam, blood pressure is 100/60 mm Hg, pulse 55. ECG indicates bradycardia with normal intervals. What drug most likely caused her syncope?
A. Citalopram
B. Pravastatin
C. Donepezil
D. Isosorbide
E. Calcium
This woman’s syncope is likely caused by donepezil. Citalopram can lengthen the QT interval, especially in elderly patients, but the normal intervals on ECG eliminate this possibility. Donepezil can cause bradycardia, which can contribute to syncope.
Hernandez and colleagues evaluated a cohort of veterans with dementia over an 8-year period.1 They found that there was a 1.4-fold increased risk of bradycardia in patients with dementia treated with an acetylcholine inhibitor (compared with that in patients who were not taking these medications) and that there was a dose-dependent increase in risk for patients on donepezil.
Park-Wyllie et al. found in a study of 1.4 million older adults a greater than twofold risk of hospitalization for bradycardia in patients treated with a cholinesterase inhibitor.2 Gill and colleagues performed a population-based cohort study of 19,803 elderly patients with dementia who were prescribed cholinesterase inhibitors, and compared them to age-matched controls.3 They found increased hospital visits for syncope in people receiving cholinesterase inhibitors (hazard ratio, 1.76; 95% confidence interval, 1.57-1.98). Other syncope-related events were also more common in people receiving cholinesterase inhibitors, compared with controls: hospital visits for bradycardia (HR, 1.69; 95% CI, 1.32-2.15), permanent pacemaker insertion (HR, 1.49; 95% CI, 1.12-2.00), and hip fracture (HR, 1.18; (95% CI, 1.04-1.34).
Nausea, vomiting, and weight loss are much more common than the rarer side effects of bradycardia and syncope. The frequency of gastroenterological side effects is up to 25%. Cholinesterase inhibitors have modest effects on cognitive function with a high number needed to treat (NNT) of 10, and an NNT as high as 100 for global function. The number needed to harm (NNH) is 4, when gastrointestinal symptoms are added in.4 Another important, problematic side effect of cholinesterase inhibitors is urinary incontinence. This often leads to patients receiving medications, to combat this side effect, that may worsen cognitive function.
Another commonly used medication that scares me in certain circumstances is trimethoprim-sulfamethoxazole. My main concern is when it is used in patients who are elderly, have chronic kidney disease, or are taking other medications that can cause hyperkalemia (ACEIs, ARBs, potassium-sparing diuretics including spironolactone). Hyperkalemia is a real concern in these patient populations. Trimethoprim reduces renal potassium excretion through the competitive inhibition of sodium channels in the distal nephron, in a manner similar to the potassium-sparing diuretic amiloride. Hospitalizations for hyperkalemia are more common in patients who take ACEIs and ARBs and are prescribed trimethoprim-sulfamethoxazole, compared with other antibiotics.5
Sudden cardiac death is also more common in patients who are taking ACEIs or ARBs and receive trimethoprim-sulfamethoxazole.6 Trimethoprim-sulfamethoxazole also has a powerful interaction with warfarin, both displacing warfarin from albumin and inhibiting its metabolism. It raises the INR (international normalized ratio) in warfarin-treated patients much greater than do other antibiotics.7
Pearls
- Think carefully about the use of cholinesterase inhibitors because of the unfavorable NNH vs. NNT.
- Use caution prescribing trimethoprim for patients who are elderly, especially if they are on an ACEI, an ARB, or spironolactone, and in patients with chronic kidney disease.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Hernandez RK et al. J Am Geriatr Soc. 2009;57:1997-2003.
2. Park-Wyllie LY et al. PLoS Med. 2009;6:e1000157.
3. Gill SS et al. Arch Intern Med 2009;169:867-73.
4. Peters KR. J Am Geriatr Soc. 2013 Jul;61(7):1170-4.
5. Antoniou TN et al. Arch Intern Med. 2010;170(12):1045-9.
6. Fralick M et al. BMJ. 2014 Oct 30;349:g6196.
7. Glasheen JJ et al. J Gen Intern Med. 2005 Jul;20(7):653-6.
Overcoming dental phobias
When I was medical student, world famous behaviorist Dr. Joseph Wolpe was my mentor and taught me a great deal about anxiety disorders and phobias in his clinic. I did some of the original research on agoraphobias in the mid-1970s and have used the experience to treat many patients with phobias over the last 40-plus years.
Some of these patients with phobias had marked functional impairments in their social functioning and their adaptive skills. One such example – dental phobia – is a fear of going to the dentist and is commonly found in the general population.
Susan A. Cohen, DMD, a dentist who has practiced for more than 20 years, has seen this fear on a daily basis in her patients, ranging from mild to extreme. She says that most dental patients are able to overcome their fear and panic, but she estimates that about 5% have extreme dental phobias that prevented a patient from visiting the dentist. This can lead to poor dental health, affect self esteem, and destroy relationships.
The causes of dental phobia are multifactorial and as follows:
- Fear of pain and needles.
- Past bad experiences with dental procedures.
- Past history of abuse.
- Fear of loss of control in the dental chair.
- History of other phobias or anxiety disorders.
Dr. Cohen also states that the anticipatory anxiety of going to the dentist can be just as fearful as being in the dental chair. And she further states this anticipatory anxiety causes a great deal of noncompliance in keeping dental appointments. Patients missed dental appointments that were very necessary for their overall health. Dr. Cohen noticed that triggers to this specific dental anxiety are:
- Thoughts of being in the dental office.
- Thoughts of lying in the dental chair.
- Thoughts of hearing sounds of drills or seeing dental instruments.
- The smells of the dental office.
- Dental overhead lights.
Symptoms of dental phobias include chills, dizziness, hyperhidrosis, heart palpitations, shortness of breath, indigestion, and trembling. Dr. Cohen also notes that people with dental phobias can cry before visits, have insomnia, and experience panic attacks. These symptoms can further cause avoidance of visits, and can trigger anxiety and fears that do not match the danger.
Avoidance of treatment often leads to poor dental health, periodontal disease, tooth loss, and decayed teeth, but also may contribute to heart problems, diabetes, and undetected carcinomas. Noncompliance with dental care affects general well being and self esteem, and may cause chronic pain, sleep problems, and embarrassment. It may also affect performance in work and school, and can cause social isolation.
Exposure therapy in vivo and in vitro with systematic desensitization and flooding can decrease significantly the fears, panic, and avoidance some dental patients experience. Cognitive behavioral therapy (CBT) can change the way patients see and respond to the situations that trigger symptoms.
Additionally, acupuncture can reduce the anxiety that patients feel about dental visits, and distraction techniques such as music and television can be very helpful during dental appointments. Guided imagery using deep breathing exercises with relaxation, visualization, and positive suggestion can create a sense of well-being and calmness. Hypnosis has also been shown to decrease the stress of being in a dental office. Nitrous oxide and oral or IV sedation may be a helpful last resort.
It is important for a person with dental phobias to be referred to a caring dentist who is sensitive to anxiety, and choose a dentist who will listen to and help the patient come up with signals, such as raising their hand, to temporarily stop a dental procedure. This technique will help the dental patient to avoid experiencing a total loss of control and help them feel less overwhelmed.
Dr. Cohen also says that it is helpful to visit the dentist at a less busy time of the day so there are fewer dental sounds and anxiety triggers in the office.
I have found that behavior modification with systematic desensitization and flooding in vivo and in vitro is extremely helpful in helping patients with extreme dental phobias overcome their fears and become more compliant with their dental treatments. Through the use of these techniques, dental phobias – and their emotional and physical sequelae – may be alleviated together.
Dr. Richard W. Cohen is a psychiatrist who has been in private practice for more than 40 years and is on the editorial advisory board for Clinical Psychiatry News. Dr. Susan A. Cohen has practiced dentistry for over 20 years. The Cohens, who are married, are based in Philadelphia.
When I was medical student, world famous behaviorist Dr. Joseph Wolpe was my mentor and taught me a great deal about anxiety disorders and phobias in his clinic. I did some of the original research on agoraphobias in the mid-1970s and have used the experience to treat many patients with phobias over the last 40-plus years.
Some of these patients with phobias had marked functional impairments in their social functioning and their adaptive skills. One such example – dental phobia – is a fear of going to the dentist and is commonly found in the general population.
Susan A. Cohen, DMD, a dentist who has practiced for more than 20 years, has seen this fear on a daily basis in her patients, ranging from mild to extreme. She says that most dental patients are able to overcome their fear and panic, but she estimates that about 5% have extreme dental phobias that prevented a patient from visiting the dentist. This can lead to poor dental health, affect self esteem, and destroy relationships.
The causes of dental phobia are multifactorial and as follows:
- Fear of pain and needles.
- Past bad experiences with dental procedures.
- Past history of abuse.
- Fear of loss of control in the dental chair.
- History of other phobias or anxiety disorders.
Dr. Cohen also states that the anticipatory anxiety of going to the dentist can be just as fearful as being in the dental chair. And she further states this anticipatory anxiety causes a great deal of noncompliance in keeping dental appointments. Patients missed dental appointments that were very necessary for their overall health. Dr. Cohen noticed that triggers to this specific dental anxiety are:
- Thoughts of being in the dental office.
- Thoughts of lying in the dental chair.
- Thoughts of hearing sounds of drills or seeing dental instruments.
- The smells of the dental office.
- Dental overhead lights.
Symptoms of dental phobias include chills, dizziness, hyperhidrosis, heart palpitations, shortness of breath, indigestion, and trembling. Dr. Cohen also notes that people with dental phobias can cry before visits, have insomnia, and experience panic attacks. These symptoms can further cause avoidance of visits, and can trigger anxiety and fears that do not match the danger.
Avoidance of treatment often leads to poor dental health, periodontal disease, tooth loss, and decayed teeth, but also may contribute to heart problems, diabetes, and undetected carcinomas. Noncompliance with dental care affects general well being and self esteem, and may cause chronic pain, sleep problems, and embarrassment. It may also affect performance in work and school, and can cause social isolation.
Exposure therapy in vivo and in vitro with systematic desensitization and flooding can decrease significantly the fears, panic, and avoidance some dental patients experience. Cognitive behavioral therapy (CBT) can change the way patients see and respond to the situations that trigger symptoms.
Additionally, acupuncture can reduce the anxiety that patients feel about dental visits, and distraction techniques such as music and television can be very helpful during dental appointments. Guided imagery using deep breathing exercises with relaxation, visualization, and positive suggestion can create a sense of well-being and calmness. Hypnosis has also been shown to decrease the stress of being in a dental office. Nitrous oxide and oral or IV sedation may be a helpful last resort.
It is important for a person with dental phobias to be referred to a caring dentist who is sensitive to anxiety, and choose a dentist who will listen to and help the patient come up with signals, such as raising their hand, to temporarily stop a dental procedure. This technique will help the dental patient to avoid experiencing a total loss of control and help them feel less overwhelmed.
Dr. Cohen also says that it is helpful to visit the dentist at a less busy time of the day so there are fewer dental sounds and anxiety triggers in the office.
I have found that behavior modification with systematic desensitization and flooding in vivo and in vitro is extremely helpful in helping patients with extreme dental phobias overcome their fears and become more compliant with their dental treatments. Through the use of these techniques, dental phobias – and their emotional and physical sequelae – may be alleviated together.
Dr. Richard W. Cohen is a psychiatrist who has been in private practice for more than 40 years and is on the editorial advisory board for Clinical Psychiatry News. Dr. Susan A. Cohen has practiced dentistry for over 20 years. The Cohens, who are married, are based in Philadelphia.
When I was medical student, world famous behaviorist Dr. Joseph Wolpe was my mentor and taught me a great deal about anxiety disorders and phobias in his clinic. I did some of the original research on agoraphobias in the mid-1970s and have used the experience to treat many patients with phobias over the last 40-plus years.
Some of these patients with phobias had marked functional impairments in their social functioning and their adaptive skills. One such example – dental phobia – is a fear of going to the dentist and is commonly found in the general population.
Susan A. Cohen, DMD, a dentist who has practiced for more than 20 years, has seen this fear on a daily basis in her patients, ranging from mild to extreme. She says that most dental patients are able to overcome their fear and panic, but she estimates that about 5% have extreme dental phobias that prevented a patient from visiting the dentist. This can lead to poor dental health, affect self esteem, and destroy relationships.
The causes of dental phobia are multifactorial and as follows:
- Fear of pain and needles.
- Past bad experiences with dental procedures.
- Past history of abuse.
- Fear of loss of control in the dental chair.
- History of other phobias or anxiety disorders.
Dr. Cohen also states that the anticipatory anxiety of going to the dentist can be just as fearful as being in the dental chair. And she further states this anticipatory anxiety causes a great deal of noncompliance in keeping dental appointments. Patients missed dental appointments that were very necessary for their overall health. Dr. Cohen noticed that triggers to this specific dental anxiety are:
- Thoughts of being in the dental office.
- Thoughts of lying in the dental chair.
- Thoughts of hearing sounds of drills or seeing dental instruments.
- The smells of the dental office.
- Dental overhead lights.
Symptoms of dental phobias include chills, dizziness, hyperhidrosis, heart palpitations, shortness of breath, indigestion, and trembling. Dr. Cohen also notes that people with dental phobias can cry before visits, have insomnia, and experience panic attacks. These symptoms can further cause avoidance of visits, and can trigger anxiety and fears that do not match the danger.
Avoidance of treatment often leads to poor dental health, periodontal disease, tooth loss, and decayed teeth, but also may contribute to heart problems, diabetes, and undetected carcinomas. Noncompliance with dental care affects general well being and self esteem, and may cause chronic pain, sleep problems, and embarrassment. It may also affect performance in work and school, and can cause social isolation.
Exposure therapy in vivo and in vitro with systematic desensitization and flooding can decrease significantly the fears, panic, and avoidance some dental patients experience. Cognitive behavioral therapy (CBT) can change the way patients see and respond to the situations that trigger symptoms.
Additionally, acupuncture can reduce the anxiety that patients feel about dental visits, and distraction techniques such as music and television can be very helpful during dental appointments. Guided imagery using deep breathing exercises with relaxation, visualization, and positive suggestion can create a sense of well-being and calmness. Hypnosis has also been shown to decrease the stress of being in a dental office. Nitrous oxide and oral or IV sedation may be a helpful last resort.
It is important for a person with dental phobias to be referred to a caring dentist who is sensitive to anxiety, and choose a dentist who will listen to and help the patient come up with signals, such as raising their hand, to temporarily stop a dental procedure. This technique will help the dental patient to avoid experiencing a total loss of control and help them feel less overwhelmed.
Dr. Cohen also says that it is helpful to visit the dentist at a less busy time of the day so there are fewer dental sounds and anxiety triggers in the office.
I have found that behavior modification with systematic desensitization and flooding in vivo and in vitro is extremely helpful in helping patients with extreme dental phobias overcome their fears and become more compliant with their dental treatments. Through the use of these techniques, dental phobias – and their emotional and physical sequelae – may be alleviated together.
Dr. Richard W. Cohen is a psychiatrist who has been in private practice for more than 40 years and is on the editorial advisory board for Clinical Psychiatry News. Dr. Susan A. Cohen has practiced dentistry for over 20 years. The Cohens, who are married, are based in Philadelphia.
Diversity – We’re not one size fits all
The United States has often been described as a “melting pot,” defined as diverse cultures and ethnicities coming together to form the rich fabric of our nation. These days, it seems that our fabric is a bit frayed.
DEIB (diversity, equity, inclusion, and belonging) is dawning as a significant conversation. Each and every one of us is unique by age, gender, culture/ethnicity, religion, socioeconomic status, geographical location, race, and sexual identity – to name just a few aspects of our identity. Keeping these differences in mind, it is evident that none of us fits a “one size fits all” mold.
Some of these differences, such as cross-cultural cuisine and holidays, are enjoyed and celebrated as wonderful opportunities to learn from others, embrace our distinctions, and have them beneficially contribute to our lives. Other differences, however, are not understood or embraced and are, in fact, belittled and stigmatized. Sexual identity falls into this category. It behooves us as a country to become more aware and educated about this category in our identities, in order to understand it, quell our unfounded fear, learn to support one another, and improve our collective mental health.
Recent reports have shown that exposing students and teachers to sexual identity diversity education has sparked some backlash from parents and communities alike. Those opposed are citing concerns over introducing children to LGBTQ+ information, either embedded in the school curriculum or made available in school library reading materials. “Children should remain innocent” seems to be the message. Perhaps parents prefer to discuss this topic privately, at home. Either way, teaching about diversity does not damage one’s innocence or deprive parents of private conversations. In fact, it educates children by improving their awareness, tolerance, and acceptance of others’ differences, and can serve as a catalyst to further parental conversation.
There are kids everywhere who are starting to develop and understand their identities. Wouldn’t it be wonderful for them to know that whichever way they identify is okay, that they are not ‘weird’ or ‘different,’ but that in fact we are all different? Wouldn’t it be great for them to be able to explore and discuss their identities and journeys openly, and not have to hide for fear of retribution or bullying?
It is important for these children to know that they are not alone, that they have options, and that they don’t need to contemplate suicide because they believe that their identity makes them not worthy of being in this world.
Starting the conversation early on in life can empower our youth by planting the seed that people are not “one size fits all,” which is the element responsible for our being unique and human. Diversity can be woven into the rich fabric that defines our nation, rather than be a factor that unravels it.
April was National Diversity Awareness Month and we took time to celebrate our country’s cultural melting pot. By embracing our differences, we can show our children and ourselves how to better navigate diversity, which can help us all fit in.
Dr. Jarkon is a psychiatrist and director of the Center for Behavioral Health at the New York Institute of Technology College of Osteopathic Medicine in Old Westbury, N.Y.
The United States has often been described as a “melting pot,” defined as diverse cultures and ethnicities coming together to form the rich fabric of our nation. These days, it seems that our fabric is a bit frayed.
DEIB (diversity, equity, inclusion, and belonging) is dawning as a significant conversation. Each and every one of us is unique by age, gender, culture/ethnicity, religion, socioeconomic status, geographical location, race, and sexual identity – to name just a few aspects of our identity. Keeping these differences in mind, it is evident that none of us fits a “one size fits all” mold.
Some of these differences, such as cross-cultural cuisine and holidays, are enjoyed and celebrated as wonderful opportunities to learn from others, embrace our distinctions, and have them beneficially contribute to our lives. Other differences, however, are not understood or embraced and are, in fact, belittled and stigmatized. Sexual identity falls into this category. It behooves us as a country to become more aware and educated about this category in our identities, in order to understand it, quell our unfounded fear, learn to support one another, and improve our collective mental health.
Recent reports have shown that exposing students and teachers to sexual identity diversity education has sparked some backlash from parents and communities alike. Those opposed are citing concerns over introducing children to LGBTQ+ information, either embedded in the school curriculum or made available in school library reading materials. “Children should remain innocent” seems to be the message. Perhaps parents prefer to discuss this topic privately, at home. Either way, teaching about diversity does not damage one’s innocence or deprive parents of private conversations. In fact, it educates children by improving their awareness, tolerance, and acceptance of others’ differences, and can serve as a catalyst to further parental conversation.
There are kids everywhere who are starting to develop and understand their identities. Wouldn’t it be wonderful for them to know that whichever way they identify is okay, that they are not ‘weird’ or ‘different,’ but that in fact we are all different? Wouldn’t it be great for them to be able to explore and discuss their identities and journeys openly, and not have to hide for fear of retribution or bullying?
It is important for these children to know that they are not alone, that they have options, and that they don’t need to contemplate suicide because they believe that their identity makes them not worthy of being in this world.
Starting the conversation early on in life can empower our youth by planting the seed that people are not “one size fits all,” which is the element responsible for our being unique and human. Diversity can be woven into the rich fabric that defines our nation, rather than be a factor that unravels it.
April was National Diversity Awareness Month and we took time to celebrate our country’s cultural melting pot. By embracing our differences, we can show our children and ourselves how to better navigate diversity, which can help us all fit in.
Dr. Jarkon is a psychiatrist and director of the Center for Behavioral Health at the New York Institute of Technology College of Osteopathic Medicine in Old Westbury, N.Y.
The United States has often been described as a “melting pot,” defined as diverse cultures and ethnicities coming together to form the rich fabric of our nation. These days, it seems that our fabric is a bit frayed.
DEIB (diversity, equity, inclusion, and belonging) is dawning as a significant conversation. Each and every one of us is unique by age, gender, culture/ethnicity, religion, socioeconomic status, geographical location, race, and sexual identity – to name just a few aspects of our identity. Keeping these differences in mind, it is evident that none of us fits a “one size fits all” mold.
Some of these differences, such as cross-cultural cuisine and holidays, are enjoyed and celebrated as wonderful opportunities to learn from others, embrace our distinctions, and have them beneficially contribute to our lives. Other differences, however, are not understood or embraced and are, in fact, belittled and stigmatized. Sexual identity falls into this category. It behooves us as a country to become more aware and educated about this category in our identities, in order to understand it, quell our unfounded fear, learn to support one another, and improve our collective mental health.
Recent reports have shown that exposing students and teachers to sexual identity diversity education has sparked some backlash from parents and communities alike. Those opposed are citing concerns over introducing children to LGBTQ+ information, either embedded in the school curriculum or made available in school library reading materials. “Children should remain innocent” seems to be the message. Perhaps parents prefer to discuss this topic privately, at home. Either way, teaching about diversity does not damage one’s innocence or deprive parents of private conversations. In fact, it educates children by improving their awareness, tolerance, and acceptance of others’ differences, and can serve as a catalyst to further parental conversation.
There are kids everywhere who are starting to develop and understand their identities. Wouldn’t it be wonderful for them to know that whichever way they identify is okay, that they are not ‘weird’ or ‘different,’ but that in fact we are all different? Wouldn’t it be great for them to be able to explore and discuss their identities and journeys openly, and not have to hide for fear of retribution or bullying?
It is important for these children to know that they are not alone, that they have options, and that they don’t need to contemplate suicide because they believe that their identity makes them not worthy of being in this world.
Starting the conversation early on in life can empower our youth by planting the seed that people are not “one size fits all,” which is the element responsible for our being unique and human. Diversity can be woven into the rich fabric that defines our nation, rather than be a factor that unravels it.
April was National Diversity Awareness Month and we took time to celebrate our country’s cultural melting pot. By embracing our differences, we can show our children and ourselves how to better navigate diversity, which can help us all fit in.
Dr. Jarkon is a psychiatrist and director of the Center for Behavioral Health at the New York Institute of Technology College of Osteopathic Medicine in Old Westbury, N.Y.
Transcranial magnetic stimulation during pregnancy: An alternative to antidepressant treatment?
A growing number of women ask about nonpharmacologic approaches for either the treatment of acute perinatal depression or for relapse prevention during pregnancy.
The last several decades have brought an increasing level of comfort with respect to antidepressant use during pregnancy, which derives from several factors.
First, it’s been well described that there’s an increased risk of relapse and morbidity associated with discontinuation of antidepressants proximate to pregnancy, particularly in women with histories of recurrent disease (JAMA Psychiatry. 2023;80[5]:441-50 and JAMA. 2006;295[5]:499-507).
Second, there’s an obvious increased confidence about using antidepressants during pregnancy given the robust reproductive safety data about antidepressants with respect to both teratogenesis and risk for organ malformation. Other studies also fail to demonstrate a relationship between fetal exposure to antidepressants and risk for subsequent development of attention-deficit/hyperactivity disorder (ADHD) and autism. These latter studies have been reviewed extensively in systematic reviews of meta-analyses addressing this question.
However, there are women who, as they approach the question of antidepressant use during pregnancy, would prefer a nonpharmacologic approach to managing depression in the setting of either a planned pregnancy, or sometimes in the setting of acute onset of depressive symptoms during pregnancy. Other women are more comfortable with the data in hand regarding the reproductive safety of antidepressants and continue antidepressants that have afforded emotional well-being, particularly if the road to well-being or euthymia has been a long one.
Still, we at Massachusetts General Hospital (MGH) Center for Women’s Mental Health along with multidisciplinary colleagues with whom we engage during our weekly Virtual Rounds community have observed a growing number of women asking about nonpharmacologic approaches for either the treatment of acute perinatal depression or for relapse prevention during pregnancy. They ask about these options for personal reasons, regardless of what we may know (and what we may not know) about existing pharmacologic interventions. In these scenarios, it is important to keep in mind that it is not about what we as clinicians necessarily know about these medicines per se that drives treatment, but rather about the private calculus that women and their partners apply about risk and benefit of pharmacologic treatment during pregnancy.
Nonpharmacologic treatment options
Mindfulness-based cognitive therapy (MBCT), cognitive behavioral therapy (CBT), and behavioral activation are therapies all of which have an evidence base with respect to their effectiveness for either the acute treatment of both depression (and perinatal depression specifically) or for mitigating risk for depressive relapse (MBCT). Several investigations are underway evaluating digital apps that utilize MBCT and CBT in these patient populations as well.
New treatments for which we have none or exceedingly sparse data to support use during pregnancy are neurosteroids. We are asked all the time about the use of neurosteroids such as brexanolone or zuranolone during pregnancy. Given the data on effectiveness of these agents for treatment of postpartum depression, the question about use during pregnancy is intuitive. But at this point in time, absent data, their use during pregnancy cannot be recommended.
With respect to newer nonpharmacologic approaches that have been looked at for treatment of major depressive disorder, the Food and Drug Administration has approved transcranial magnetic stimulation (TMS), a noninvasive form of neuromodulating therapy that use magnetic pulses to stimulate specific regions of the brain that have been implicated in psychiatric illness.
While there are no safety concerns that have been noted about use of TMS, the data regarding its use during pregnancy are still relatively limited, but it has been used to treat certain neurologic conditions during pregnancy. We now have a small randomized controlled study using TMS during pregnancy and multiple small case series suggesting a signal of efficacy in women with perinatal major depressive disorder. Side effects of TMS use during pregnancy have included hypotension, which has sometimes required repositioning of subjects, particularly later in pregnancy. Unlike electroconvulsive therapy, (ECT), often used when clinicians have exhausted other treatment options, TMS has no risk of seizure associated with its use.
TMS is now entering into the clinical arena in a more robust way. In certain settings, insurance companies are reimbursing for TMS treatment more often than was the case previously, making it a more viable option for a larger number of patients. There are also several exciting newer protocols, including theta burst stimulation, a new form of TMS treatment with less of a time commitment, and which may be more cost effective. However, data on this modality of treatment remain limited.
Where TMS fits in treating depression during pregnancy
The real question we are getting asked in clinic, both in person and during virtual rounds with multidisciplinary colleagues from across the world, is where TMS might fit into the algorithm for treating of depression during pregnancy. Where is it appropriate to be thinking about TMS in pregnancy, and where should it perhaps be deferred at this moment (and where is it not appropriate)?
It is probably of limited value (and possibly of potential harm) to switch to TMS in patients who have severe recurrent major depression and who are on maintenance antidepressant, and who believe that a switch to TMS will be effective for relapse prevention; there are simply no data currently suggesting that TMS can be used as a relapse prevention tool, unlike certain other nonpharmacologic interventions.
What about managing relapse of major depressive disorder during pregnancy in a patient who had responded to an antidepressant? We have seen patients with histories of severe recurrent disease who are managed well on antidepressants during pregnancy who then have breakthrough symptoms and inquire about using TMS as an augmentation strategy. Although we don’t have clear data supporting the use of TMS as an adjunct in that setting, in those patients, one could argue that a trial of TMS may be appropriate – as opposed to introducing multiple medicines to recapture euthymia during pregnancy where the benefit is unclear and where more exposure is implied by having to do potentially multiple trials.
Other patients with new onset of depression during pregnancy who, for personal reasons, will not take an antidepressant or pursue other nonpharmacologic interventions will frequently ask about TMS. and the increased availability of TMS in the community in various centers – as opposed to previously where it was more restricted to large academic medical centers.
I think it is a time of excitement in reproductive psychiatry where we have a growing number of tools to treat perinatal depression – from medications to digital tools. These tools – either alone or in combination with medicines that we’ve been using for years – are able to afford women a greater number of choices with respect to the treatment of perinatal depression than was available even 5 years ago. That takes us closer to an ability to use interventions that truly combine patient wishes and “precision perinatal psychiatry,” where we can match effective therapies with the individual clinical presentations and wishes with which patients come to us.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
A growing number of women ask about nonpharmacologic approaches for either the treatment of acute perinatal depression or for relapse prevention during pregnancy.
The last several decades have brought an increasing level of comfort with respect to antidepressant use during pregnancy, which derives from several factors.
First, it’s been well described that there’s an increased risk of relapse and morbidity associated with discontinuation of antidepressants proximate to pregnancy, particularly in women with histories of recurrent disease (JAMA Psychiatry. 2023;80[5]:441-50 and JAMA. 2006;295[5]:499-507).
Second, there’s an obvious increased confidence about using antidepressants during pregnancy given the robust reproductive safety data about antidepressants with respect to both teratogenesis and risk for organ malformation. Other studies also fail to demonstrate a relationship between fetal exposure to antidepressants and risk for subsequent development of attention-deficit/hyperactivity disorder (ADHD) and autism. These latter studies have been reviewed extensively in systematic reviews of meta-analyses addressing this question.
However, there are women who, as they approach the question of antidepressant use during pregnancy, would prefer a nonpharmacologic approach to managing depression in the setting of either a planned pregnancy, or sometimes in the setting of acute onset of depressive symptoms during pregnancy. Other women are more comfortable with the data in hand regarding the reproductive safety of antidepressants and continue antidepressants that have afforded emotional well-being, particularly if the road to well-being or euthymia has been a long one.
Still, we at Massachusetts General Hospital (MGH) Center for Women’s Mental Health along with multidisciplinary colleagues with whom we engage during our weekly Virtual Rounds community have observed a growing number of women asking about nonpharmacologic approaches for either the treatment of acute perinatal depression or for relapse prevention during pregnancy. They ask about these options for personal reasons, regardless of what we may know (and what we may not know) about existing pharmacologic interventions. In these scenarios, it is important to keep in mind that it is not about what we as clinicians necessarily know about these medicines per se that drives treatment, but rather about the private calculus that women and their partners apply about risk and benefit of pharmacologic treatment during pregnancy.
Nonpharmacologic treatment options
Mindfulness-based cognitive therapy (MBCT), cognitive behavioral therapy (CBT), and behavioral activation are therapies all of which have an evidence base with respect to their effectiveness for either the acute treatment of both depression (and perinatal depression specifically) or for mitigating risk for depressive relapse (MBCT). Several investigations are underway evaluating digital apps that utilize MBCT and CBT in these patient populations as well.
New treatments for which we have none or exceedingly sparse data to support use during pregnancy are neurosteroids. We are asked all the time about the use of neurosteroids such as brexanolone or zuranolone during pregnancy. Given the data on effectiveness of these agents for treatment of postpartum depression, the question about use during pregnancy is intuitive. But at this point in time, absent data, their use during pregnancy cannot be recommended.
With respect to newer nonpharmacologic approaches that have been looked at for treatment of major depressive disorder, the Food and Drug Administration has approved transcranial magnetic stimulation (TMS), a noninvasive form of neuromodulating therapy that use magnetic pulses to stimulate specific regions of the brain that have been implicated in psychiatric illness.
While there are no safety concerns that have been noted about use of TMS, the data regarding its use during pregnancy are still relatively limited, but it has been used to treat certain neurologic conditions during pregnancy. We now have a small randomized controlled study using TMS during pregnancy and multiple small case series suggesting a signal of efficacy in women with perinatal major depressive disorder. Side effects of TMS use during pregnancy have included hypotension, which has sometimes required repositioning of subjects, particularly later in pregnancy. Unlike electroconvulsive therapy, (ECT), often used when clinicians have exhausted other treatment options, TMS has no risk of seizure associated with its use.
TMS is now entering into the clinical arena in a more robust way. In certain settings, insurance companies are reimbursing for TMS treatment more often than was the case previously, making it a more viable option for a larger number of patients. There are also several exciting newer protocols, including theta burst stimulation, a new form of TMS treatment with less of a time commitment, and which may be more cost effective. However, data on this modality of treatment remain limited.
Where TMS fits in treating depression during pregnancy
The real question we are getting asked in clinic, both in person and during virtual rounds with multidisciplinary colleagues from across the world, is where TMS might fit into the algorithm for treating of depression during pregnancy. Where is it appropriate to be thinking about TMS in pregnancy, and where should it perhaps be deferred at this moment (and where is it not appropriate)?
It is probably of limited value (and possibly of potential harm) to switch to TMS in patients who have severe recurrent major depression and who are on maintenance antidepressant, and who believe that a switch to TMS will be effective for relapse prevention; there are simply no data currently suggesting that TMS can be used as a relapse prevention tool, unlike certain other nonpharmacologic interventions.
What about managing relapse of major depressive disorder during pregnancy in a patient who had responded to an antidepressant? We have seen patients with histories of severe recurrent disease who are managed well on antidepressants during pregnancy who then have breakthrough symptoms and inquire about using TMS as an augmentation strategy. Although we don’t have clear data supporting the use of TMS as an adjunct in that setting, in those patients, one could argue that a trial of TMS may be appropriate – as opposed to introducing multiple medicines to recapture euthymia during pregnancy where the benefit is unclear and where more exposure is implied by having to do potentially multiple trials.
Other patients with new onset of depression during pregnancy who, for personal reasons, will not take an antidepressant or pursue other nonpharmacologic interventions will frequently ask about TMS. and the increased availability of TMS in the community in various centers – as opposed to previously where it was more restricted to large academic medical centers.
I think it is a time of excitement in reproductive psychiatry where we have a growing number of tools to treat perinatal depression – from medications to digital tools. These tools – either alone or in combination with medicines that we’ve been using for years – are able to afford women a greater number of choices with respect to the treatment of perinatal depression than was available even 5 years ago. That takes us closer to an ability to use interventions that truly combine patient wishes and “precision perinatal psychiatry,” where we can match effective therapies with the individual clinical presentations and wishes with which patients come to us.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].
A growing number of women ask about nonpharmacologic approaches for either the treatment of acute perinatal depression or for relapse prevention during pregnancy.
The last several decades have brought an increasing level of comfort with respect to antidepressant use during pregnancy, which derives from several factors.
First, it’s been well described that there’s an increased risk of relapse and morbidity associated with discontinuation of antidepressants proximate to pregnancy, particularly in women with histories of recurrent disease (JAMA Psychiatry. 2023;80[5]:441-50 and JAMA. 2006;295[5]:499-507).
Second, there’s an obvious increased confidence about using antidepressants during pregnancy given the robust reproductive safety data about antidepressants with respect to both teratogenesis and risk for organ malformation. Other studies also fail to demonstrate a relationship between fetal exposure to antidepressants and risk for subsequent development of attention-deficit/hyperactivity disorder (ADHD) and autism. These latter studies have been reviewed extensively in systematic reviews of meta-analyses addressing this question.
However, there are women who, as they approach the question of antidepressant use during pregnancy, would prefer a nonpharmacologic approach to managing depression in the setting of either a planned pregnancy, or sometimes in the setting of acute onset of depressive symptoms during pregnancy. Other women are more comfortable with the data in hand regarding the reproductive safety of antidepressants and continue antidepressants that have afforded emotional well-being, particularly if the road to well-being or euthymia has been a long one.
Still, we at Massachusetts General Hospital (MGH) Center for Women’s Mental Health along with multidisciplinary colleagues with whom we engage during our weekly Virtual Rounds community have observed a growing number of women asking about nonpharmacologic approaches for either the treatment of acute perinatal depression or for relapse prevention during pregnancy. They ask about these options for personal reasons, regardless of what we may know (and what we may not know) about existing pharmacologic interventions. In these scenarios, it is important to keep in mind that it is not about what we as clinicians necessarily know about these medicines per se that drives treatment, but rather about the private calculus that women and their partners apply about risk and benefit of pharmacologic treatment during pregnancy.
Nonpharmacologic treatment options
Mindfulness-based cognitive therapy (MBCT), cognitive behavioral therapy (CBT), and behavioral activation are therapies all of which have an evidence base with respect to their effectiveness for either the acute treatment of both depression (and perinatal depression specifically) or for mitigating risk for depressive relapse (MBCT). Several investigations are underway evaluating digital apps that utilize MBCT and CBT in these patient populations as well.
New treatments for which we have none or exceedingly sparse data to support use during pregnancy are neurosteroids. We are asked all the time about the use of neurosteroids such as brexanolone or zuranolone during pregnancy. Given the data on effectiveness of these agents for treatment of postpartum depression, the question about use during pregnancy is intuitive. But at this point in time, absent data, their use during pregnancy cannot be recommended.
With respect to newer nonpharmacologic approaches that have been looked at for treatment of major depressive disorder, the Food and Drug Administration has approved transcranial magnetic stimulation (TMS), a noninvasive form of neuromodulating therapy that use magnetic pulses to stimulate specific regions of the brain that have been implicated in psychiatric illness.
While there are no safety concerns that have been noted about use of TMS, the data regarding its use during pregnancy are still relatively limited, but it has been used to treat certain neurologic conditions during pregnancy. We now have a small randomized controlled study using TMS during pregnancy and multiple small case series suggesting a signal of efficacy in women with perinatal major depressive disorder. Side effects of TMS use during pregnancy have included hypotension, which has sometimes required repositioning of subjects, particularly later in pregnancy. Unlike electroconvulsive therapy, (ECT), often used when clinicians have exhausted other treatment options, TMS has no risk of seizure associated with its use.
TMS is now entering into the clinical arena in a more robust way. In certain settings, insurance companies are reimbursing for TMS treatment more often than was the case previously, making it a more viable option for a larger number of patients. There are also several exciting newer protocols, including theta burst stimulation, a new form of TMS treatment with less of a time commitment, and which may be more cost effective. However, data on this modality of treatment remain limited.
Where TMS fits in treating depression during pregnancy
The real question we are getting asked in clinic, both in person and during virtual rounds with multidisciplinary colleagues from across the world, is where TMS might fit into the algorithm for treating of depression during pregnancy. Where is it appropriate to be thinking about TMS in pregnancy, and where should it perhaps be deferred at this moment (and where is it not appropriate)?
It is probably of limited value (and possibly of potential harm) to switch to TMS in patients who have severe recurrent major depression and who are on maintenance antidepressant, and who believe that a switch to TMS will be effective for relapse prevention; there are simply no data currently suggesting that TMS can be used as a relapse prevention tool, unlike certain other nonpharmacologic interventions.
What about managing relapse of major depressive disorder during pregnancy in a patient who had responded to an antidepressant? We have seen patients with histories of severe recurrent disease who are managed well on antidepressants during pregnancy who then have breakthrough symptoms and inquire about using TMS as an augmentation strategy. Although we don’t have clear data supporting the use of TMS as an adjunct in that setting, in those patients, one could argue that a trial of TMS may be appropriate – as opposed to introducing multiple medicines to recapture euthymia during pregnancy where the benefit is unclear and where more exposure is implied by having to do potentially multiple trials.
Other patients with new onset of depression during pregnancy who, for personal reasons, will not take an antidepressant or pursue other nonpharmacologic interventions will frequently ask about TMS. and the increased availability of TMS in the community in various centers – as opposed to previously where it was more restricted to large academic medical centers.
I think it is a time of excitement in reproductive psychiatry where we have a growing number of tools to treat perinatal depression – from medications to digital tools. These tools – either alone or in combination with medicines that we’ve been using for years – are able to afford women a greater number of choices with respect to the treatment of perinatal depression than was available even 5 years ago. That takes us closer to an ability to use interventions that truly combine patient wishes and “precision perinatal psychiatry,” where we can match effective therapies with the individual clinical presentations and wishes with which patients come to us.
Dr. Cohen is the director of the Ammon-Pinizzotto Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information resources and conducts clinical care and research in reproductive mental health. He has been a consultant to manufacturers of psychiatric medications. Email Dr. Cohen at [email protected].